SOX2 in Cellular Dedifferentiation: Mechanisms, Applications, and Therapeutic Targeting
This article comprehensively examines the transcription factor SOX2, a master regulator of cellular dedifferentiation.
SOX2 in Cellular Dedifferentiation: Mechanisms, Applications, and Therapeutic Targeting
Abstract
This article comprehensively examines the transcription factor SOX2, a master regulator of cellular dedifferentiation. We explore its foundational biology, from its role in embryonic development and the maintenance of pluripotency to its aberrant re-expression in cancer, where it drives the acquisition of stem cell-like properties and therapy resistance. The content details methodological approaches for studying SOX2-mediated dedifferentiation, addresses common challenges in research and therapeutic targeting, and provides a comparative analysis of its functions across different cancer types and normal physiological contexts. Aimed at researchers and drug development professionals, this review synthesizes current knowledge to highlight SOX2's significant potential as a therapeutic target in regenerative medicine and oncology.
The Core Principles of SOX2: From Embryonic Pluripotency to Oncogenic Reprogramming
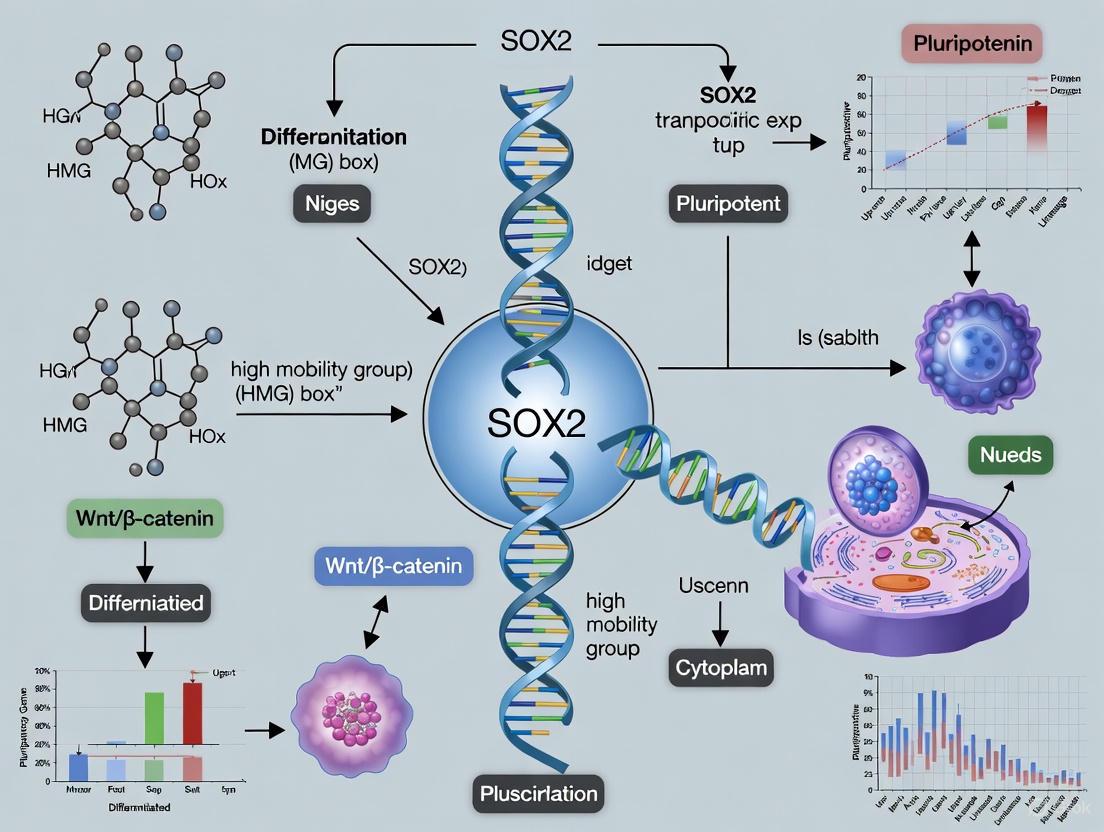
The transcription factor SOX2 (SRY-related HMG-box 2) is a pivotal orchestrator of cellular plasticity, playing indispensable roles in maintaining embryonic stem cell pluripotency, reprogramming somatic cells to induced pluripotent stem cells (iPSCs), and promoting dedifferentiation in cancer contexts [1]. Its ability to impart stem cell-like features makes it a critical focus in regenerative medicine and oncology research. Biochemically, SOX2 executes these complex functions through two principal domains: the high mobility group (HMG) box for specific DNA binding and the intrinsically disordered transactivation domain (TAD) for protein interactions and transcriptional regulation [1] [2]. Understanding the precise biochemical mechanisms of these domains provides fundamental insights into how SOX2 drives cellular dedifferentiation, a process reactivated in tumorigenesis and crucial for regenerative applications.
Structural Architecture of SOX2
SOX2 is a 317-amino acid protein characterized by a central, structured DNA-binding domain flanked by largely unstructured, intrinsically disordered regions (IDRs). The functional organization of these domains is summarized in the diagram below.
- N-Terminal Intrinsically Disordered Region (N-IDR, residues 1-40): This short, low-complexity region is predicted to be disordered and facilitates interactions with other transcription factors [2].
- HMG DNA-Binding Domain (residues 40-123): A structured domain rich in positively charged residues (net charge = +13) that facilitates binding to both DNA and RNA. It contains motifs crucial for nuclear localization (NLS) and nuclear export (NES) [1] [2].
- C-Terminal Intrinsically Disordered Region (C-IDR, residues 124-317): A long, disordered region enriched in methionines, serines, glycines, and prolines. It contains two transcriptional activation domains (AD1 and AD2) and a serine-rich domain that mediates interaction with the transcription factor Nanog [2]. The C-IDR is highly dynamic and its conformation is modulated by interactions with the HMG domain and DNA [2].
The HMG DNA-Binding Domain: Structure and Mechanisms
The HMG domain is the defining feature of SOX proteins, conferring sequence-specific DNA binding through a conserved high mobility group box fold.
DNA Recognition and Binding
The HMG domain folds into a characteristic L-shaped structure composed of three alpha-helices that form a helix-turn-helix motif. This structure preferentially binds to the DNA consensus sequence 5'-(A/T)(A/T)CAA(A/T)G-3', causing a sharp bend of approximately 70-85° in the DNA helix [1] [2]. This bending is thought to facilitate the assembly of enhanceosomes by bringing distal regulatory elements into proximity.
Table 1: Biophysical Properties of SOX2 HMG Domain Nucleic Acid Interactions
| Nucleic Acid Ligand | Structure/Sequence Context | Affinity (K_D,app) | Binding Specificity | Primary Interaction Mediator |
|---|---|---|---|---|
| FGF4 Enhancer DNA | Double-stranded consensus site | 2.1 ± 0.6 nM [3] | High, sequence-specific | HMG domain (full) |
| Non-consensus DNA | Double-stranded, non-specific sequence | >400 nM [3] | Low, non-specific | HMG domain (full) |
| ES2 lncRNA | Double-stranded RNA regions | 18 ± 1 nM [3] | Low, structure-preferential | HMG domain (full) |
| Unstructured ssRNA | Single-stranded, non-structured | >400 nM [3] | Very low, non-specific | HMG domain (full) |
RNA Binding Capacity
Beyond DNA recognition, the HMG domain directly binds RNA with high affinity but low sequence specificity. It primarily interacts with double-stranded RNA regions, as demonstrated by its nanomolar affinity for the ES2 lncRNA (K_D,app = 18 ± 1 nM) [3]. This interaction is mediated by a similar but not identical interaction surface used for DNA binding, employing a partially overlapping set of amino acids for high-affinity binding to each nucleic acid [3]. In vivo, SOX2 directly binds over a thousand RNA targets, suggesting this is a fundamental aspect of its regulatory function [3].
The Transactivation Domain: A Dynamic Interaction Hub
The C-terminal transactivation domain (TAD) of SOX2 is predominantly intrinsically disordered, lacking stable secondary structure. This disorder is not a functional deficiency but rather a key feature enabling dynamic interactions with multiple protein partners.
Structural Dynamics and Ensemble Behavior
Biophysical analyses using single-molecule FRET (smFRET) and NMR spectroscopy reveal that the C-TAD samples a broad ensemble of conformations in solution [2]. The dimensions and dynamics of this domain are guided by weak, dynamic charge interactions between the negatively charged C-TAD and the positively charged surface of the HMG domain. These intramolecular interactions constrain the C-TAD in a more compact state than expected for a random coil polymer [2].
DNA-Induced Redistribution of the Activation Domain
DNA binding triggers a major rearrangement of the C-TAD ensemble. Upon binding DNA, the HMG domain engages with the negatively charged DNA backbone, thereby releasing the C-TAD from its electrostatic interactions with the HMG domain. This leads to a more extended C-TAD conformation with increased accessibility of the two activation domains (AD1 and AD2) for interactions with transcriptional co-regulators [2]. This mechanism likely enhances the recruitment of the transcriptional machinery to target genes.
Protein-Protein Interaction Capabilities
The C-TAD utilizes multiple distinct regions to associate with different protein partners, enabling SOX2 to participate in diverse regulatory complexes. Domain mapping studies demonstrate that SOX2 employs different domains for self-association and interaction with partners like Sall4, HDAC1, and HDAC2 [4]. For instance, while the HMG domain alone can weakly associate with Sall4, stronger interaction requires both the HMG domain and C-terminal regions [4]. This multi-domain interaction strategy allows SOX2 to assemble into complexes of varying sizes and functions, ranging from ~40 kDa to >800 kDa [4].
SOX2 Domain Functions in Dedifferentiation and Stemness
The biochemical properties of SOX2's domains directly underlie its ability to promote dedifferentiation and maintain stem cell-like states, particularly in cancer.
Transcriptional Regulation of Stemness and EMT
In pancreatic cancer, SOX2 expression is aberrantly activated in 19.3% of tumors and is enriched in cancer stem cell (CSC) populations marked by ALDH1, ESA, and CD44 [5] [6]. SOX2 promotes dedifferentiation by directly binding to the promoters of EMT transcription factors Snail, Slug, and Twist, leading to loss of E-cadherin and ZO-1 expression [5]. This HMG domain-mediated transcriptional regulation drives the acquisition of mesenchymal traits and stem-like properties.
Cell Cycle Control and Proliferation
The SOX2 HMG domain directly binds to and represses the promoters of cell cycle inhibitors p21^Cip1^ and p27^Kip1^, thereby promoting S-phase entry and cell proliferation [5]. Knockdown of SOX2 results in cell cycle arrest at G1/S, while overexpression enhances cyclin D3 induction and proliferation [5]. This function is dependent on the DNA-binding capability of the HMG domain and its proper regulation by the transactivation domain.
Cooperation with Pluripotency Factors
SOX2 cooperates with other core pluripotency factors like Nanog through DNA-mediated interactions. Computational models and molecular dynamics simulations reveal that DNA-mediated Nanog-Sox2 cooperativity involves allosteric interactions that influence protein conformational changes and enhance DNA-binding stability [7] [8]. This cooperation is fundamental to the establishment and maintenance of the dedifferentiated state in both physiological and pathological contexts.
Experimental Methodologies for SOX2 Domain Analysis
Key Research Reagent Solutions
Table 2: Essential Research Reagents for SOX2 Domain-Function Studies
| Reagent / Method | Specific Application | Key Function in SOX2 Research |
|---|---|---|
| Chromatin Immunoprecipitation (ChIP) | Mapping SOX2 genomic binding sites [5] | Identifies direct gene targets (e.g., Snail, p21) in dedifferentiation |
| smFRET (single-molecule FRET) | Measuring C-TAD conformational dynamics [2] | Quantifies DNA-induced structural rearrangements in SOX2 ensemble |
| NMR Spectroscopy | Residue-specific analysis of IDR structure [2] | Characterizes transient secondary structure in activation domains |
| Fluorescence Anisotropy | Quantifying nucleic acid binding affinity [3] | Measures K_D for SOX2 interactions with DNA and RNA ligands |
| Lentiviral SOX2 Expression Vectors | Ectopic SOX2 expression and domain mutants [9] | Tools for functional domain mapping and reprogramming studies |
| Co-immunoprecipitation | Identifying SOX2-protein interactions [4] | Maps domains required for association with partners (e.g., Sall4, HDAC1) |
Detailed Protocol: Fluorescence Anisotropy for Nucleic Acid Binding
This method is essential for quantifying SOX2 HMG domain interactions with DNA and RNA, providing key parameters for understanding its binding specificity in dedifferentiation.
Principle: Fluorescently labeled nucleic acids tumble rapidly in solution, emitting depolarized fluorescence when excited by polarized light. Upon protein binding, the complex tumbles more slowly, increasing the proportion of polarized emission (anisotropy) [3].
Procedure:
- Sample Preparation: Purify SOX2 HMG domain (residues 40-123) and label DNA/RNA with fluorophores (e.g., fluorescein).
- Titration Series: Prepare a constant concentration of labeled nucleic acid (0.1-1 nM) with increasing concentrations of SOX2 protein (0.1-1000 nM).
- Measurement: Incubate mixtures for equilibrium binding (15-30 minutes, room temperature) and measure anisotropy using a fluorescence spectrometer with polarizers.
- Data Analysis: Fit anisotropy versus protein concentration data to a binding equation to determine apparent K_D values [3].
Key Applications:
- Determine binding specificity by comparing consensus versus mutant sequences
- Characterize RNA-binding properties using various RNA constructs
- Test the impact of domain mutations on nucleic acid binding
The sophisticated biochemistry of SOX2's functional domains underpins its remarkable capacity to drive cellular dedifferentiation. The structured HMG domain provides sequence-specific DNA recognition while also engaging in high-affinity RNA interactions, and the dynamic transactivation domain serves as a versatile platform for recruiting co-regulatory complexes. The allosteric communication between these domains, particularly the DNA-induced redistribution of the transactivation domain ensemble, enables precise control of transcriptional programs that maintain stemness. Understanding these mechanistic principles provides a foundation for therapeutic strategies targeting SOX2 in cancer and leveraging its reprogramming capabilities in regenerative medicine. Future research should focus on how post-translational modifications of these domains fine-tune SOX2 activity in different dedifferentiation contexts.
The Quintessential Role of SOX2 in Embryonic Development and Tissue Homeostasis
SOX2 (SRY-box 2) represents a master transcriptional regulator integral to embryonic development, cellular pluripotency, and tissue homeostasis. This whitepaper synthesizes current understanding of SOX2's multifaceted functions, emphasizing its emerging role in cellular dedifferentiation processes. We provide a comprehensive analysis of SOX2's mechanistic actions across biological contexts, detailed experimental methodologies for its investigation, and essential research tools for the field. Framed within dedifferentiation research, this review underscores SOX2's dualistic nature—as both a guardian of developmental integrity and a driver of pathological reprogramming—offering critical insights for therapeutic innovation.
SOX2 belongs to the SOX (SRY-related HMG-box) family of transcription factors, characterized by a high-mobility group (HMG) domain that enables sequence-specific DNA binding and chromatin remodeling [10]. Located on chromosome 3q26.3-q27 in humans, the SOX2 gene encodes a 317-amino acid protein that functions as a pivotal regulator of stem cell pluripotency, embryonic patterning, and tissue homeostasis [10] [11]. Its expression must be precisely regulated, as dysregulation has profound implications for both developmental disorders and cancer pathogenesis [10] [12].
Within the context of cellular dedifferentiation research, SOX2 occupies a central position. It is one of the original Yamanaka factors capable of reprogramming somatic cells to induced pluripotent stem cells (iPSCs), effectively reversing cellular differentiation [13]. This reprogramming capability highlights SOX2's powerful role in resetting epigenetic landscapes and transcriptional networks, processes that are harnessed in regenerative medicine but co-opted in pathological states such as cancer stem cell formation [10] [12] [13]. Understanding SOX2's mechanisms therefore provides critical insights for both regenerative biology and oncology drug development.
SOX2 in Embryonic Development: Mechanisms and Pathways
During embryogenesis, SOX2 functions as a cornerstone of the pluripotency network, working in concert with OCT4 and NANOG to maintain embryonic stem cell (ESC) identity and direct lineage specification [10]. Its expression patterns and functional requirements evolve dynamically throughout developmental stages, reflecting its context-dependent functions.
Stage-Specific Roles and Genetic Regulation
Table 1: SOX2 Expression and Function During Embryonic Development
| Developmental Stage | Expression Pattern | Primary Functions | Genetic Interactions |
|---|---|---|---|
| Pre-implantation | High mRNA levels | Epiblast formation, Pluripotency maintenance | Cooperates with OCT4; Prevents trophectoderm differentiation [10] |
| Neural Development | Neural progenitor cells | Neural tube patterning, Neural competence establishment | Regulates NOTCH signaling; Binds VSX2 in retina [14] |
| Foregut Development | Esophageal squamous epithelium | Epithelial differentiation, Homeostasis maintenance | Represses CDX2; Maintains foregut identity [15] |
| Organogenesis | Tissue-specific progenitors | Multiple organ systems development | Context-specific partnerships (e.g., VSX2 in retina) [14] |
Molecular Mechanisms in Specific Developmental Contexts
Neural and Retinal Development: In the developing nervous system, SOX2 functions as a key determinant of neural competence. Recent research demonstrates that SOX2 directly binds and activates enhancers critical for retinal progenitor cell (RPC) function, with conditional knockout resulting in reduced chromatin accessibility at 1,794 genomic regions [14]. SOX2 cooperates with the retinal transcription factor VSX2 to establish a retina-specific transcriptional program, co-occupying enhancers that regulate genes essential for proliferation and lineage specification [14]. This SOX2-VSX2 interaction creates a cooperative transcriptional code that promotes retinal neurogenesis while repressing alternative lineage fates.
Foregut and Esophageal Homeostasis: In the upper gastrointestinal tract, SOX2 maintains foregut squamous epithelial identity by directly activating differentiation-associated genes (e.g., KRT13) and repressing proliferation-associated targets (e.g., MKI67) [15]. Induced Sox2 deletion in murine foregut epithelium leads to increased basal proliferation, reduced squamous differentiation, and expansion of metaplastic glands at the squamocolumnar junction, demonstrating its essential role in maintaining tissue homeostasis and preventing pathological reprogramming [15].
Figure 1: SOX2 Regulatory Networks in Development and Homeostasis. SOX2 coordinates embryonic development through partnerships with key transcription factors and maintains adult tissue homeostasis by balancing differentiation and proliferation programs.
SOX2 in Tissue Homeostasis and Dedifferentiation
In adult tissues, SOX2 continues to play crucial roles in stem cell maintenance, tissue repair, and cellular plasticity. Its expression in adult stem cells (ASCs) contributes to tissue regeneration and immune system regulation, though its specific functions across different tissues remain an active research area [10].
Homeostatic Maintenance and Injury Response
Studies using fate mapping have demonstrated that SOX2+ adult stem cells originate from SOX2+ tissue progenitors during development. Ablation of SOX2+ cells in mice disrupts epithelial tissue homeostasis and leads to lethality, underscoring its non-redundant functions in tissue maintenance [10]. In the esophagus, SOX2 maintains the balance between proliferation and differentiation in squamous epithelium, with its loss triggering a damage response program and initiating metaplastic changes [15].
SOX2 as a Driver of Pathological Dedifferentiation
The dedifferentiation capacity of SOX2 becomes pathogenic in cancer contexts, where it confers stem cell-like properties to malignant cells. In pancreatic ductal adenocarcinoma (PDAC), SOX2 is aberrantly expressed in 19.3% of human tumors and is enriched in the ESA+/CD44+ cancer stem cell (CSC) population [12]. SOX2 promotes dedifferentiation by directly binding to promoters of EMT transcription factors (Snail, Slug, Twist), leading to loss of epithelial markers (E-Cadherin, ZO-1) and acquisition of mesenchymal traits [12].
Table 2: SOX2 in Cellular Dedifferentiation and Cancer Progression
| Cancer Type | Dedifferentiation Mechanisms | Functional Consequences | Therapeutic Implications |
|---|---|---|---|
| Pancreatic Cancer | Binds Snail/Slug/Twist promoters; Induces EMT | Stem cell-like features; Chemoresistance; Invasion | Targeting SOX2+ cells may eliminate CSCs [12] |
| Glioblastoma | Regulates PROM1/CD133 expression | Therapy resistance; Stemness maintenance | CRISPR screening identifies SOX2 as key regulator [16] |
| Esophageal Adenocarcinoma | Loss permits gastric/intestinal reprogramming | Barrett's esophagus progression; Metaplasia | SOX2 decrease initiates pathological reprogramming [15] |
In glioblastoma, SOX2 maintains the CD133+ CSC population that drives therapeutic resistance and tumor aggressiveness. A recent CRISPR-Cas9 functional screen identified SOX2 as a critical regulator of PROM1 (CD133) expression, establishing its essential role in cellular stress response following chemoradiation [16]. This positions SOX2 as a master regulator of the dedifferentiation programs that sustain cancer stemness across multiple malignancies.
Experimental Approaches: Methodologies for SOX2 Research
Key Experimental Protocols
CRISPR-Cas9 Functional Screening in Glioblastoma Stem Cells (GSCs):
- Objective: Identify genetic regulators of CD133 expression in GSCs [16].
- Workflow:
- Transduce 100×10^6 GSCs with TKOv3 lentiviral library (MOI=0.3, >400-fold sgRNA coverage).
- Select with puromycin (1.2 μg/mL) 24h post-transduction.
- Collect 30×10^6 cells for genomic DNA extraction at baseline.
- Culture remaining cells in triplicate, passaging every 7 days (~3 doublings) for 12 doublings.
- Sort top and bottom 5th-percentile CD133-expressing cells by FACS.
- Extract genomic DNA and amplify sgRNA inserts via two-step PCR with Illumina TruSeq adapters.
- Sequence on Illumina HiSeq2500; analyze with Bowtie v.0.12.8 and drugZ (v.1.1.0.2) [16].
Chromatin Accessibility Analysis (ATAC-Seq) in Retinal Progenitor Cells:
- Objective: Profile SOX2-dependent chromatin landscape in developing retina [14].
- Workflow:
- Generate RPC-specific Sox2 conditional knockout (Sox2 cKO) using Chx10-Cre mice.
- Isolate E14.5 retinae from Sox2 cKO and control embryos.
- Perform Assay for Transposase-Accessible Chromatin with Sequencing (ATAC-Seq).
- Identify differentially accessible regions (DARs) using DESeq2 (FDR < 0.05).
- Annotate DARs with ChromHMM enhancer states (H3K27Ac, BRD4, H3K4me1).
- Integrate with RNA-seq data to correlate accessibility with gene expression [14].
SOX2 Functional Characterization in Pancreatic Cancer:
- Objective: Determine SOX2's role in CSC maintenance and EMT [12].
- Workflow:
- Knockdown SOX2 using RNA interference in pancreatic cancer cell lines.
- Assess proliferation via MTT assays; cell cycle by flow cytometry.
- Analyze CSC markers (ALDH1, ESA, CD44) by flow cytometry.
- Perform sphere-formation assays in serum-free medium.
- Conduct chromatin immunoprecipitation (ChIP) for SOX2 binding at Snail, Slug, Twist promoters.
- Evaluate EMT markers (E-Cadherin, ZO-1) by immunoblotting [12].
Figure 2: CRISPR Screening Workflow for SOX2 Functional Genomics. This pipeline identifies SOX2 as a key regulator of CD133 expression in glioblastoma stem cells through genome-wide screening and bioinformatic analysis [16].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX2 Investigation
| Reagent/Tool | Specific Example | Application | Research Context |
|---|---|---|---|
| SOX2 Antibodies | Anti-SOX2 (Abcam ab97959) | Immunofluorescence, Western Blot | Neural stem cell characterization [17] |
| CRISPR Libraries | TKOv3 lentiviral library | Genome-wide functional screens | Identification of CD133 regulators [16] |
| Inducible Mouse Models | Krt5CreER/+ Sox2fl/fl ROSA26tdTomato/+ | Lineage tracing, in vivo deletion | Foregut squamous homeostasis [15] |
| REST Inhibitors | X5050 (REST antagonist) | Proteasomal degradation of REST | REST-SOX2 regulatory axis [17] |
| Organoid Cultures | Patient-derived BE organoids | Disease modeling, heterogeneity | SOX2-CDX2 balance in metaplasia [15] |
| Ppto-OT | Ppto-OT | Ppto-OT is a synthetic oxytocin analog for research. This product is for Research Use Only (RUO) and is not intended for personal use. | Bench Chemicals |
| Gold;thorium | Gold;thorium, CAS:106804-09-5, MF:Au2Th3, MW:1090.046 g/mol | Chemical Reagent | Bench Chemicals |
SOX2-Associated Signaling Pathways in Development and Cancer
SOX2 intersects with multiple key signaling pathways that regulate both developmental processes and cancer progression. These interactions position SOX2 as a nexus integrating extrinsic signals with transcriptional responses.
Key Pathway Interactions
WNT/β-catenin Signaling: SOX2 cooperates with WNT signaling in neural development and is repressed by this pathway in cancer contexts. REST inhibition downregulates β-catenin expression, disrupting this regulatory axis during neurogenesis [17].
Cell Cycle Regulation: In pancreatic cancer, SOX2 directly represses CDK inhibitors p21Cip1 and p27Kip1, promoting S-phase entry and proliferation through cyclin D3 induction [12].
EMT Programming: SOX2 directly activates transcription of EMT master regulators (Snail, Slug, Twist), facilitating cadherin switching and loss of epithelial polarity in dedifferentiation processes [12].
Chromatin Remodeling: SOX2 exhibits pioneer factor activity in retinal development, binding closed chromatin and recruiting remodeling complexes to establish accessible enhancer landscapes [14].
SOX2 emerges as a paradigm of transcriptional regulation with dualistic functions in physiological and pathological contexts. Its non-redundant roles in embryonic development and tissue homeostasis are mirrored by its pathogenic capacity to drive dedifferentiation in cancer. The mechanistic insights into SOX2 function—from chromatin remodeling to pathway integration—provide a foundation for therapeutic targeting in regenerative medicine and oncology.
Future research directions should prioritize understanding context-specific SOX2 interactions, developing targeted delivery systems for SOX2 modulation, and exploiting SOX2-dependent vulnerabilities in cancer stem cells. As technological advances in single-cell genomics, CRISPR screening, and organoid modeling accelerate, SOX2 will undoubtedly remain at the forefront of dedifferentiation research and therapeutic innovation.
SOX2 as a Pioneer Factor in Induced Pluripotency and Cellular Reprogramming
SOX2 stands as a critical pioneer transcription factor in cellular reprogramming, possessing the unique ability to initiate cell fate transitions by binding and opening closed chromatin regions. This whitepaper examines the molecular mechanisms through which SOX2 facilitates induced pluripotency, detailing its role in chromatin remodeling, partnership with other reprogramming factors, and hierarchical organization of the pluripotency network. We present recent advances in SOX2 engineering that have dramatically enhanced reprogramming efficiency, including AI-designed variants achieving over 50-fold improvement in pluripotency marker expression. The document further explores SOX2's clinical implications in cancer stemness and therapeutic development, providing detailed experimental methodologies and resource guidance for researchers pursuing directed cellular reprogramming strategies.
SOX2 represents a fundamental regulator within the SRY-box transcription factor family, playing indispensable roles in maintaining embryonic stem cell pluripotency and orchestrating somatic cell reprogramming. As a bona fide pioneer factor, SOX2 exhibits the distinctive capability to bind nucleosomal DNA in silent chromatin regions and initiate local chromatin opening, thereby enabling transcriptional activation of lineage-specific genes and enhancers [18]. This pioneering activity positions SOX2 as a master regulator of cell fate changes during development and in induced pluripotent stem cell (iPSC) generation.
The functional significance of SOX2 extends beyond developmental biology into therapeutic applications. SOX2 forms part of the classic Yamanaka factor cocktail (OCT4, SOX2, KLF4, MYC/OSKM) that enables reprogramming of differentiated somatic cells into pluripotent stem cells [19]. However, traditional reprogramming methods suffer from poor efficiency, with typically less than 0.1% of cells converting during treatment over three or more weeks [19]. Recent advances in protein engineering and mechanistic understanding of SOX2 function have yielded substantial improvements in reprogramming protocols, highlighting the factor's central role in overcoming epigenetic barriers to pluripotency.
Molecular Mechanisms of SOX2 Pioneer Activity
Chromatin Binding and Remodeling
SOX2 employs distinct molecular strategies to access and remodel closed chromatin configurations. Unlike canonical transcription factors that have weak affinity for nucleosomal DNA, SOX2 possesses intrinsic structural properties enabling nucleosome invasion and stabilization on nucleosomal target sites:
- Chromatin Scanning: SOX2 rapidly diffuses through closed chromatin domains via nonspecific electrostatic interactions with the phosphodiester backbone exposed on the nucleosome surface, facilitating three-dimensional scanning of nucleosomal DNA [18].
- DNA Binding Domain Engagement: The SOX2 DNA-binding domain alone is sufficient for nucleosome binding, preferentially engaging target motifs at nucleosome entry/exit sites where DNA is more accessible [18].
- Nucleosome Surface Interactions: Beyond its DNA-binding domain, SOX2 establishes contacts with histone residues through non-DNA-binding regions, stabilizing its association with nucleosomal targets [18].
Table 1: SOX2 Pioneer Factor Mechanisms and Characteristics
| Mechanism | Molecular Process | Functional Outcome |
|---|---|---|
| Chromatin Scanning | Electrostatic interactions with nucleosome surface | Identification of target binding sites in silent chromatin |
| Nucleosomal DNA Binding | Engagement of DNA motifs at nucleosome entry/exit sites | Initial chromatin engagement and destabilization |
| Local Chromatin Reorganization | Nucleosome structure perturbation without ATP requirement | Increased DNA accessibility for additional factors |
| Collaborative Recruitment | Recruitment of OCT4 and other reprogramming factors | Establishment of pluripotency enhancer networks |
Partnership with OCT4 in Pluripotency Establishment
SOX2 operates in a tightly coordinated partnership with OCT4 to activate the pluripotency network. During mitotic exit in pluripotent stem cells, SOX2 and OCT4 rapidly reoccupy the genome during the anaphase-telophase transition, exhibiting a hierarchical reorganization of their binding landscape that governs transcriptional reactivation after cell division [20]. This partnership follows a specific temporal sequence:
- SOX2 and OCT4 binding occurs predominantly during early mitotic exit
- The factors exhibit sequential changes in chromatin accessibility footprints
- A hierarchical binding pattern emerges with OCT4 and SOX2 governing the reorganization process
- Transcriptional activity progressively ramps up following factor binding
The functional synergy between SOX2 and OCT4 was demonstrated in reprogramming studies where fusing the potent VP16 activation domain to both factors (creating Ov and Sv variants) significantly increased iPSC generation efficiency compared to conventional OSK systems [21]. The OvSvK combination produced approximately 2.5 times more OCT4-GFP+ colonies than the standard OSK system, indicating that enhanced SOX2 and OCT4 activities directly facilitate reprogramming through activation of downstream targets [21].
Signaling Pathway Regulation
SOX2 modulates several critical signaling cascades that support stemness maintenance and reprogramming efficiency. In glioma stem cells, SOX2 directly interacts with the Par6 polarity protein to regulate the EGFR/PI3K/AKT signaling cascade, revealing an unexpected connection between cell polarity pathways and stemness regulation [22]. This SOX2-Par6 interaction:
- Transcriptionally regulates EGFR expression
- Activates PI3K/AKT downstream signaling
- Promotes stemness maintenance in glioma stem cells (GSCs)
- Can be targeted with specific inhibitory peptides (Par6i-P1) to suppress GSC self-renewal
The diagram below illustrates SOX2's role in regulating key signaling pathways:
Experimental Evidence and Quantitative Data
Enhanced Reprogramming Efficiency with Engineered SOX2
Recent protein engineering approaches have demonstrated remarkable improvements in SOX2 reprogramming capability. Through AI-guided design, researchers created RetroSOX variants that differ by more than 100 amino acids on average from wild-type SOX2, with over 30% of these AI-proposed variants outperforming wild-type SOX2 in expressing key pluripotency markers [19]. The combination of top RetroSOX and RetroKLF variants produced dramatic gains:
- 50-fold higher expression of stem cell reprogramming markers compared to wild-type controls
- Earlier appearance of late pluripotency markers (TRA-1-60, NANOG)
- Robust alkaline phosphatase (AP) activity by day 10, indicating pluripotency
- Successful differentiation into all three primary germ layers
- Maintenance of genomic stability across multiple passages
Table 2: Quantitative Assessment of SOX2-Mediated Reprogramming Enhancements
| Parameter | Wild-Type SOX2 | Engineered SOX2 Variants | Experimental Context |
|---|---|---|---|
| Reprogramming Efficiency | <0.1% cell conversion | >30% of cells expressing pluripotency markers by day 7 [19] | Human fibroblasts from middle-aged donors |
| Marker Expression Timing | 3+ weeks for late markers | Late markers appearing several days sooner [19] | Viral vector delivery |
| DNA Damage Repair | Baseline γ-H2AX intensity | Significant reduction in DNA damage markers [19] | DNA damage assay |
| iPSC Colony Formation | Standard efficiency | 2.5x more OCT4-GFP+ colonies with OvSvK [21] | Mouse embryonic fibroblasts |
SOX2 in Cancer Stemness and Prognostic Implications
SOX2 expression demonstrates significant prognostic value across multiple cancer types, reflecting its role in maintaining cancer stem cell populations. A comprehensive pan-cancer analysis revealed:
- SOX2 upregulation in glioblastoma multiforme, lower-grade glioma, lung adenocarcinoma, and lung squamous cell carcinoma [23]
- Poor prognosis association with high SOX2 expression in glioblastoma, glioma, and lung cancers [23]
- Immune checkpoint correlation where tumors with high SOX2 expression showed higher responsiveness to immune checkpoint inhibitors [23]
In glioma specimens, SOX2 co-expression with Par6 predicted poor patient outcomes, with the Par6/SOX2 interaction triggering stemness maintenance through EGFR/PI3K/AKT signaling pathway activation [22]. This partnership represents a promising therapeutic target for improving glioma patient prognosis.
Experimental Protocols and Methodologies
iPSC Generation Using Enhanced SOX2 Variants
The following protocol details the generation of induced pluripotent stem cells using engineered SOX2 factors, adapted from validated experimental approaches [21] [19]:
Cell Culture and Transduction:
- Culture human fibroblasts or mesenchymal stromal cells (MSCs) in appropriate growth medium. For aged donor cells, consider preconditioning with antioxidants to enhance reprogramming efficiency.
- Transduce cells with viral vectors (retroviral or lentiviral) expressing the enhanced Yamanaka factor cocktail (OvSvK or RetroSOX/RetroKLF combinations). For alternative approaches, use mRNA transfection with modified nucleotides to reduce immunogenicity.
- Employ a polycistronic vector system or separate vectors with different selection markers to ensure incorporation of all factors. Optimal multiplicity of infection (MOI) typically ranges from 5-20 depending on cell type and viral titer.
Reprogramming and Colony Selection:
- After 48-72 hours post-transduction, replace viral supernatant with essential 8 (E8) medium or defined iPSC culture medium containing bFGF to support pluripotency [24].
- Monitor daily for morphological changes indicative of reprogramming: emergence of small, compact cells with high nuclear-to-cytoplasmic ratio forming tightly-packed colonies.
- Between days 7-12, stain for alkaline phosphatase activity to identify successfully reprogrammed colonies [19].
- Islate colonies mechanically or through enzymatic digestion using collagenase IV, then transfer onto feeder layers or defined matrices like laminin 521 [24].
Validation and Characterization:
- Confirm pluripotency through immunostaining for key markers (OCT4, NANOG, SOX2, TRA-1-60, SSEA-4) [19].
- Perform karyotype analysis to verify genomic stability after multiple passages [19].
- Demonstrate trilineage differentiation potential through embryoid body formation and germ layer-specific marker expression.
The experimental workflow for SOX2-mediated reprogramming is summarized below:
Assessing SOX2 Chromatin Binding Activity
To evaluate SOX2 pioneer factor activity in experimental systems, researchers can employ the following methodologies:
Chromatin Immunoprecipitation (ChIP) Protocol:
- Crosslink cells with 1% formaldehyde for 10 minutes at room temperature.
- Quench crosslinking with 125mM glycine for 5 minutes.
- Harvest cells and lyse using appropriate buffers (typically containing protease inhibitors).
- Sonicate chromatin to fragment sizes of 200-500 bp.
- Immunoprecipitate with validated SOX2 antibodies overnight at 4°C.
- Capture antibody-chromatin complexes using protein A/G beads.
- Reverse crosslinks and purify DNA for qPCR or sequencing analysis.
ATAC-Seq for Chromatin Accessibility:
- Prepare nuclei from reprogramming intermediates at specific timepoints.
- Treat with Tn5 transposase to tag accessible genomic regions.
- Purify and amplify tagmented DNA for next-generation sequencing.
- Analyze sequencing data to identify SOX2-dependent changes in chromatin landscape.
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX2 Reprogramming Studies
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| SOX2 Expression Vectors | pMXs-Ov (VP16-OCT4), pMXs-Sv (VP16-SOX2), RetroSOX variants [21] [19] | VP16 fusion enhances transcriptional activity; AI-designed variants show superior performance |
| Cell Culture Matrices | Laminin 521, Vitronectin, Matrigel [24] | Defined matrices (laminin 521) reduce batch variability and improve reproducibility |
| Reprogramming Media | Essential 8 (E8) medium, StemPro-34 [24] | Defined, xeno-free media minimize variability and support robust pluripotency maintenance |
| Validation Antibodies | Anti-SOX2 (rabbit polyclonal), Anti-OCT4, Anti-NANOG, Anti-TRA-1-60 [25] [19] | Quality-validated antibodies essential for accurate pluripotency marker assessment |
| Detection Assays | Alkaline Phosphatase Staining Kit, γ-H2AX Immunofluorescence [19] | Functional assessment of reprogramming efficiency and DNA damage response |
SOX2 exemplifies the paradigm of pioneer transcription factors that govern cell fate decisions through chromatin landscape remodeling. Its fundamental role in cellular reprogramming extends from basic developmental processes to therapeutic applications in regenerative medicine. Recent advances in SOX2 protein engineering, particularly through AI-guided design, have demonstrated remarkable improvements in reprogramming efficiency and fidelity, highlighting the potential for optimized factors to overcome current limitations in iPSC generation.
The mechanistic insights into SOX2's partnership with OCT4 and other regulatory factors provide a framework for understanding hierarchical control in pluripotency establishment. Meanwhile, the documented roles of SOX2 in cancer stemness maintenance underscore the importance of regulated SOX2 activity for therapeutic safety. Future research directions should focus on:
- Developing small molecule modulators of SOX2 activity for transient, controlled reprogramming
- Engineering tissue-specific SOX2 variants for directed differentiation applications
- Elucidating the structural basis of SOX2 pioneer activity to inform more precise engineering strategies
- Exploring SOX2's role in in vivo reprogramming for tissue regeneration
As the field advances, the integration of computational design with mechanistic understanding of SOX2 function will likely yield increasingly sophisticated tools for cellular reprogramming and regenerative medicine applications.
Mechanisms of SOX2-Induced Dedifferentiation in Somatic Cells
The transcription factor SOX2 is a master regulator of cellular plasticity, playing indispensable roles in embryonic development, stem cell maintenance, and somatic cell reprogramming. This technical review examines the molecular mechanisms through which SOX2 induces dedifferentiation of somatic cells—a process with profound implications for regenerative medicine, disease modeling, and cancer biology. We synthesize current research demonstrating how SOX2 collaborates with specific partner proteins, regulates critical signaling pathways, and modulates epigenetic landscapes to reverse the epigenetic configuration of differentiated cells back to a less-differentiated, stem-like state. The therapeutic potential and challenges of targeting SOX2-mediated pathways are discussed, with particular emphasis on its context-dependent functions in both physiological reprogramming and pathological dedifferentiation in cancer.
SOX2 (Sex determining region Y-box 2) is a member of the SOX family of transcription factors characterized by a conserved high-mobility group (HMG) DNA-binding domain. As one of the core pluripotency factors, SOX2 is essential for maintaining self-renewal and pluripotency in embryonic stem cells (ESCs) [26]. During early embryonic development, SOX2 expression is initially detected in cells at the morula stage, becoming more specifically located in the inner cell mass (ICM) of the blastocyst and epiblast during later stages [26]. Zygotic deletion of SOX2 is embryonically lethal due to failure to form pluripotent epiblast, unequivocally demonstrating its critical role in establishing pluripotent cells [26].
Beyond its physiological roles, SOX2 exhibits remarkable capacity to reverse the developmental clock of somatic cells. Seminal reprogramming studies identified SOX2 as one of the original Yamanaka factors (OCT4, SOX2, KLF4, and c-MYC) capable of converting terminally differentiated somatic cells into induced pluripotent stem cells (iPSCs) [27]. During reprogramming, activation of endogenous SOX2 represents an early event that initiates a cascade of transcriptional changes leading to pluripotency acquisition [26]. The molecular mechanisms underlying SOX2-mediated dedifferentiation involve complex interactions with signaling pathways, epigenetic modifiers, and cell cycle regulators, which collectively enable the erasure of somatic cell identity and establishment of a stem-like state.
Molecular Mechanisms of SOX2 in Dedifferentiation
Core Transcriptional Networks and Partner Interactions
SOX2 executes its dedifferentiation function through collaborative interactions with specific partner transcription factors that determine its target gene specificity:
Partnership with OCT4: In embryonic stem cells, SOX2 and OCT4 form a specific partnership to coordinately regulate the mechanism that maintains undifferentiated states [28]. Their cooperative interaction between the HMG domain of SOX2 and POU homeodomain of OCT4 is critical for regulating ESC pluripotency [26]. This partnership co-occupies enhancers and promoters of target genes, activating pluripotency genes including NANOG while repressing differentiation genes [26].
Context-Dependent Partner Switching: SOX2 demonstrates remarkable partner flexibility across different cellular contexts. In neural stem cells (NSCs), SOX2 interacts with POU factors such as Pax6, Brn1, and Brn2 to regulate self-renewal and differentiation [28]. SOX2 can also bind to Prx1 (MHox1/Prrx1) in certain NSC populations, potentially regulating target genes involved in maintaining undifferentiated states [28].
Complementary Factor Interactions: Recent research has identified novel SOX2 partnerships in pathological contexts. In glioma stem cells (GSCs), SOX2 directly binds to Par6 to maintain stemness through regulation of the EGFR/PI3K/AKT signaling cascade [22]. Disruption of this interaction with a specific inhibitory peptide (Par6i-P1) significantly suppresses stemness maintenance, suggesting therapeutic potential [22].
Table 1: SOX2 Partner Proteins and Their Cellular Contexts
| Partner Protein | Cellular Context | Functional Outcome |
|---|---|---|
| OCT4 | Embryonic Stem Cells | Maintenance of pluripotency; activation of NANOG |
| Par6 | Glioma Stem Cells | Stemness maintenance via EGFR/PI3K/AKT signaling |
| Pax6 | Neural Stem Cells | Regulation of NSC self-renewal and differentiation |
| Brn1/Brn2 | Neural Stem Cells | Nestin gene expression regulation |
| Prx1 | Neural Stem Cells | Maintenance of undifferentiated state (proposed) |
Signaling Pathway Regulation
SOX2-mediated dedifferentiation involves intricate crosstalk with multiple signaling pathways that create permissive conditions for cellular reprogramming:
PI3K/AKT Signaling: The AKT pathway plays a crucial role in stabilizing SOX2 protein levels in multiple cellular contexts. AKT binds to and phosphorylates SOX2 at T116, preventing SOX2 ubiquitination and proteasome-dependent degradation by ubiquitin E3 ligases UBR5 and STUB1 [29]. This phosphorylation significantly enhances SOX2 protein stability, creating a positive feedback loop that maintains the dedifferentiated state.
Wnt/β-catenin Signaling: SOX2 exhibits complex interactions with Wnt signaling that are highly context-dependent. In human ESCs, SOX2 suppresses non-neural lineages by inhibiting canonical Wnt signaling through direct transcriptional regulation of important Wnt signaling modulators WLS and SFRP2 [30]. Conversely, during neural differentiation, SOX2 and Tcf act as molecular switches that regulate NeuroD1 expression, illustrating how SOX2-Wnt interactions vary across developmental stages [28].
EGFR Signaling Pathway: In neural stem cells, a positive feedback mechanism exists between SOX2 and EGFR signaling. EGFR stimulation increases SOX2 expression, while SOX2 enhances EGFR expression, creating a self-reinforcing loop that maintains stem cell properties [28]. In glioma stem cells, the Par6/SOX2 interaction triggers stemness maintenance through activation of the EGFR/PI3K/AKT signaling pathway [22].
TGF-β Signaling: SOX2 has been functionally linked to epithelial-to-mesenchymal transition (EMT) in various cancer contexts. In pancreatic cancer cells, SOX2 directly binds to the Snail, Slug and Twist promoters, leading to loss of E-Cadherin and ZO-1 expression [12]. This SOX2-mediated EMT induction facilitates acquisition of stem cell-like features and promotes dedifferentiation.
The diagram below illustrates the core signaling network through which SOX2 promotes dedifferentiation:
Epigenetic Modulation
SOX2-mediated dedifferentiation involves significant reorganization of the epigenetic landscape through several mechanisms:
Polycomb Recruitment: SOX2 ensures pluripotent epigenetic landscapes via recruiting polycomb repressor complex 2 (PRC2) to poise developmental genes in hESCs [30]. This maintains key developmental genes in a transcriptionally silent but primed state, ready for activation upon differentiation cues.
Histone Variant Interaction: SOX2 interacts with histone variant H2A.Z to establish permissive chromatin states in embryonic stem cells [30]. H2A.Z facilitates access of both active and repressive complexes to chromatin, contributing to the dynamic gene regulation required for pluripotency.
DNA Methylation Dynamics: SOX2 is subject to epigenetic regulation itself, with its expression controlled by DNA methylation status in specific cellular contexts [10]. During dedifferentiation, SOX2 in turn influences global DNA methylation patterns, contributing to the erasure of somatic memory.
Enhancer-Promoter Architecture: SOX2 participates in reshaping higher-order chromatin structure during dedifferentiation. Spatiotemporal analysis of the Sox2 locus has revealed that enhancer-promoter interactions within topologically associating domains (TADs) are critical for proper SOX2 regulation during cell fate transitions [10].
Experimental Approaches for Studying SOX2-Mediated Dedifferentiation
Key Methodologies and Workflows
Research into SOX2-mediated dedifferentiation employs sophisticated experimental approaches to unravel the complex molecular mechanisms involved:
Table 2: Key Experimental Methods for SOX2 Dedifferentiation Research
| Method Category | Specific Techniques | Key Applications |
|---|---|---|
| Gene Manipulation | Lentiviral knockdown/overexpression, CRISPR-Cas9, siRNA | Establishing causal relationships between SOX2 and dedifferentiation phenotypes |
| Omics Profiling | RNA-seq, ChIP-seq, ATAC-seq, Proteomics | Genome-wide identification of SOX2 targets and epigenetic modifications |
| Functional Assays | Sphere formation, Colony formation, Chemoresistance tests | Quantifying stemness properties and therapeutic resistance |
| Protein Analysis | Western blot, Co-immunoprecipitation, Phosphoproteomics | Studying SOX2 protein stability, modifications, and interactions |
| Imaging Approaches | Immunofluorescence, Immunohistochemistry, Live-cell imaging | Spatial localization and expression patterns of SOX2 |
The experimental workflow for investigating SOX2 in cellular reprogramming typically follows a multi-stage process as illustrated below:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX2 Dedifferentiation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| SOX2 Modulators | SOX2 shRNA, SOX2 overexpression vectors, SOX2 CRISPR/Cas9 constructs | Direct manipulation of SOX2 expression levels |
| Signaling Inhibitors | MK2206 (AKT inhibitor), Wnt pathway modulators, EGFR inhibitors | Dissecting specific pathway contributions to SOX2 function |
| Protein Degradation Tools | MG132 (proteasome inhibitor), UBR5/STUB1 modulators | Studying SOX2 protein stability and turnover |
| Stemness Assay Reagents | Ultra-low attachment plates, defined growth factors | Assessing functional outcomes of dedifferentiation |
| Detection Reagents | SOX2 antibodies, pluripotency marker detection kits | Quantifying dedifferentiation efficiency and markers |
| Pyrene, 1-(4-nitrophenyl)- | Pyrene, 1-(4-nitrophenyl)-, CAS:95069-74-2, MF:C22H13NO2, MW:323.3 g/mol | Chemical Reagent |
| 7-Methyloct-7-EN-1-YN-4-OL | 7-Methyloct-7-en-1-yn-4-ol|C9H14O | High-purity 7-Methyloct-7-en-1-yn-4-ol for research applications. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Functional Consequences of SOX2-Mediated Dedifferentiation
Cell Cycle and Proliferation Alterations
SOX2-mediated dedifferentiation significantly impacts cell cycle regulation and proliferation dynamics:
Cell Cycle Progression: SOX2 expression promotes S-phase entry and cell proliferation associated with cyclin D3 induction [12]. Conversely, SOX2 knockdown in pancreatic cancer cells results in cell growth inhibition via cell cycle arrest associated with p21Cip1 and p27Kip1 induction [12].
CDK Inhibitor Regulation: SOX2 can directly bind to the p21Cip1 and p27Kip1 promoters, leading to repression of these cell cycle inhibitors and facilitating cell cycle progression [12]. This direct transcriptional regulation represents a key mechanism through which SOX2 promotes the proliferative capacity characteristic of dedifferentiated cells.
Therapeutic Implications: The impact of SOX2 on cell cycle regulation has significant implications for cancer therapy, as SOX2-high cells often demonstrate enhanced chemoresistance. In osteosarcoma, the AKT-SOX2 axis represents a significant modulator of cancer stemness and chemoresistance [29].
Stemness and Therapy Resistance
SOX2-induced dedifferentiation confers hallmark stemness properties and therapeutic resistance across multiple cancer types:
Cancer Stem Cell Enrichment: SOX2 expression is associated with increased levels of cancer stem cell markers. In pancreatic cancer, SOX2 expression correlates with elevated ALDH1, ESA and CD44, and is enriched in the ESA+/CD44+ CSC population [12]. Similarly, in urothelial carcinoma, SOX2 expression is suggested to be a marker for a subpopulation of cancer stem cells that co-express keratin 14 (KRT14) and CD44v6 [27].
Therapy Resistance Mechanisms: SOX2 contributes significantly to chemoresistance through multiple mechanisms. In osteosarcoma, SOX2 overexpression is associated with more aggressiveness, increased metastasis, chemotherapy resistance and poorer prognosis [29]. Combination treatment with SOX2 pathway inhibitors and conventional chemotherapy has shown synergistic effects in preclinical models [22] [29].
Sphere-Forming Capacity: SOX2 enhances the self-renewal capacity of cancer stem cells as measured by sphere formation assays. In osteosarcoma, SOX2 knockdown significantly reduced tumor sphere formation, while SOX2 overexpression not only increased the number of tumor spheres but also markedly enlarged their sizes [29].
Therapeutic Targeting of SOX2-Mediated Dedifferentiation
Challenges in Direct SOX2 Targeting
Direct targeting of SOX2 has proven challenging due to its nature as a transcription factor, making it traditionally considered "undruggable" [29]. Several innovative approaches have been developed to overcome this limitation:
Kinase Targeting: Identification of upstream kinases that regulate SOX2 stability offers promising indirect targeting strategies. AKT has been identified as a kinase essential for robust SOX2 expression in osteosarcoma cells, and AKT inhibition effectively reduces SOX2 protein levels [29].
Protein-Protein Interaction Disruption: Developing inhibitory peptides that disrupt critical SOX2 interactions represents another viable strategy. In glioma, the Par6/SOX2 interaction can be effectively blocked with a specific inhibitory peptide (Par6i-P1), which significantly suppresses stemness maintenance [22].
Epigenetic Modulators: Targeting the epigenetic regulators that control SOX2 expression or activity offers additional therapeutic avenues. DNA methylation inhibitors and histone modification-targeting compounds can indirectly modulate SOX2 function.
Preclinical Evidence for Combination Therapies
Accumulating preclinical evidence supports the potential of targeting SOX2 pathways in combination with conventional therapies:
AKT Inhibition in Osteosarcoma: The combination of AKT inhibitor MK2206 and cisplatin resulted in synergistic and potent inhibition of OS tumor growth in PDX models [29]. This approach effectively targets the AKT-SOX2 axis that promotes cancer stemness and chemoresistance.
Par6/SOX2 Disruption in Glioma: Targeting the Par6/SOX2 interaction with specific inhibitory peptides effectively mitigated GSC-mediated chemotherapy resistance in temozolomide (TMZ) treatment, improving malignancy and prognosis in orthotopically transplanted mice [22].
SOX2 Knockdown in Urothelial Carcinoma: SOX2 knockdown in UC cells of the basal/squamous subtype decreased the expression of stem-associated proteins, oncoproteins, and basal keratins, while inducing several luminal markers and enhancing cisplatin sensitivity [27].
SOX2-mediated dedifferentiation represents a fundamental biological process with profound implications for development, regeneration, and disease. The molecular mechanisms through which SOX2 orchestrates cellular reprogramming involve complex interactions with specific partner proteins, precise modulation of multiple signaling pathways, and extensive reorganization of the epigenetic landscape. While significant progress has been made in understanding these mechanisms, several challenges remain.
Future research directions should focus on elucidating the context-dependent functions of SOX2 across different tissue types and disease states, developing more specific strategies for targeting SOX2-related pathways in cancer, and harnessing SOX2-mediated dedifferentiation for regenerative medicine applications. The continued refinement of experimental approaches, including single-cell technologies and advanced genome editing tools, will undoubtedly provide deeper insights into how this master transcription factor controls cellular identity.
As our understanding of SOX2 biology advances, so too will our ability to manipulate cellular plasticity for therapeutic benefit, potentially unlocking new treatments for degenerative diseases, injuries, and cancer. The dual nature of SOX2 in both physiological reprogramming and pathological dedifferentiation underscores the importance of context-specific approaches when considering therapeutic interventions targeting this pivotal regulator of cell fate.
Epigenetic Regulation of the SOX2 Gene and its Overlapping Transcript (SOX2OT)
The SRY-related HMG-box 2 (SOX2) gene encodes a transcription factor essential for maintaining pluripotency in embryonic stem cells (ESCs), cellular reprogramming, and tissue homeostasis. Its genomic architecture is particularly notable because it resides within an intron of the SOX2 overlapping transcript (SOX2OT), a long non-coding RNA (lncRNA) gene. This unique arrangement suggests a potential regulatory relationship that has significant implications for cellular identity and dedifferentiation processes. Both SOX2 and SOX2OT are located on chromosome 3q26.33, a region frequently amplified in various cancers. In the context of cellular dedifferentiation—a hallmark of cancer stem cells (CSCs) and induced pluripotent stem cell (iPSC) generation—understanding the epigenetic interplay between this protein-coding gene and its non-coding host is paramount. This review synthesizes current evidence on the epigenetic mechanisms governing SOX2 and SOX2OT, framing their regulation within the broader thesis of cellular dedifferentiation in development, disease, and regenerative medicine.
Molecular Mechanisms of Epigenetic Regulation
DNA Methylation and CpG Island Dynamics
The SOX2 locus features a critical intragenic CpG island (iCpGI) that spans its entire single-exon coding sequence [31]. This iCpGI is a key platform for dynamic DNA methylation, which directly influences transcriptional activity.
- Pluripotent State: In ESCs and induced pluripotent stem cells (iPSCs), the SOX2 iCpGI is maintained in a hypomethylated state, facilitating an open chromatin configuration and permitting active transcription [31].
- Differentiated State: As cells differentiate, de novo DNA methylation occurs at this iCpGI, leading to stable transcriptional repression and silencing of the SOX2 gene. This methylation-dependent silencing is a crucial step in exiting the pluripotent state [31].
- Evolutionary Conservation: Phylo-epigenetic comparisons across primate species reveal strong conservation of these CpG-rich regions, underscoring their fundamental regulatory importance. These regions are subject to methylation-dependent deamination, leading to characteristic CpG→TpG and CpG→CpA transitions over evolutionary time, highlighting them as constrained yet plastic elements in mammalian developmental evolution [31].
Histone Modifications and Chromatin State
The chromatin state of the SOX2 locus is precisely regulated through post-translational modifications of histones.
- Bivalent Domains: In embryonic stem cells, the SOX2 promoter can be marked by bivalent chromatin domains, which simultaneously harbor the activating mark H3K4me3 and the repressive mark H3K27me3 [31]. This poised state allows for rapid transcriptional activation or repression during lineage commitment.
- Resolution upon Differentiation: During differentiation, these bivalent domains resolve into consistently active (H3K4me3-only) or repressive (H3K27me3-only) states, locking the SOX2 gene into a silenced configuration in most somatic cells [31].
The Role of the Long Non-Coding RNA SOX2OT
SOX2OT is a multi-exon lncRNA that transcriptionally overlaps the SOX2 gene. Evidence suggests it functions as a positive regulator of SOX2 expression, particularly in dedifferentiated cell states.
- Concordant Expression: SOX2OT and SOX2 expression are often concordantly upregulated in cancer cells and under stem cell culture conditions (e.g., suspension mammosphere culture) that favor a dedifferentiated, stem-like phenotype [32].
- Enhancer-like Function: Ectopic overexpression of SOX2OT in breast cancer cells (MDA-MB-231) led to an almost 20-fold increase in SOX2 mRNA levels, suggesting a role in promoting SOX2 transcription, potentially through an enhancer-like mechanism [32]. This upregulation was associated with reduced cellular proliferation but increased anchorage-independent growth, a feature of transformed cells [32].
- Transcriptional Interference via YY1 Interaction: In contrast, a study in mouse cortical neural progenitors revealed a repressive mechanism. In this context, Sox2ot was shown to physically interact with the transcription factor YY1 [33]. This Sox2ot-YY1 complex bound to CpG islands within the Sox2 locus, facilitating the repression of Sox2 and promoting neuronal differentiation [33]. This indicates that the functional outcome of the SOX2OT-SOX2 relationship may be highly context-dependent.
Table 1: Key Epigenetic Regulators of the SOX2 Locus and Their Functions
| Regulatory Mechanism | Molecular Effect | Functional Outcome in Pluripotency/Dedifferentiation |
|---|---|---|
| SOX2 iCpGI Hypomethylation | Open chromatin; permits transcription factor binding | Maintains SOX2 expression; sustains pluripotency and self-renewal [31] |
| SOX2 iCpGI Hypermethylation | Closed chromatin; gene silencing | Promotes differentiation; silences SOX2 in somatic cells [31] |
| Bivalent Histone Marks (H3K4me3/H3K27me3) | Poised chromatin state | Allows rapid lineage-specific activation or repression of SOX2 [31] |
| SOX2OT Overexpression | Upregulation of SOX2 transcription | Promotes stem-like phenotypes in cancer; enhances reprogramming efficiency [32] |
| SOX2OT-YY1 Interaction | Recruitment of repressive complexes to Sox2 locus | Represses Sox2; promotes differentiation (neural progenitors) [33] |
Functional Consequences in Development and Cancer
Role in Cellular Dedifferentiation and Reprogramming
SOX2 is a core pioneer transcription factor in the reprogramming of somatic cells to iPSCs. Its precise expression level is critical, as minor deviations can tip the balance between pluripotency and differentiation [21]. Recent research demonstrates that enhancing the activity of SOX2, in conjunction with OCT4, dramatically improves reprogramming efficiency. Fusing the potent VP16 activation domain to both OCT4 and SOX2 (a combination termed OvSvK) generated iPSCs approximately 2.5 times more efficiently than the standard set of factors (OSK) [21]. This enhanced activity directly activated downstream targets involved in cell cycle regulation, leading to a shortened G1 phase and a shift in epigenetic markers like reduced H3K27me3 levels on specific genes, thereby facilitating reprogramming [21].
Implications in Cancer Stemness and Therapy Resistance
The SOX2-SOX2OT axis is a potent driver of tumorigenesis in numerous cancers, primarily by promoting a dedifferentiated, stem-like state.
- Amplification in Cancers: The 3q26.33 locus, containing both SOX2 and SOX2OT, is frequently amplified in cancers such as small-cell lung cancer (SCLC), lung squamous cell carcinoma (LSCC), glioblastoma, and esophageal squamous cell carcinoma [34].
- Maintenance of Cancer Stem Cells (CSCs): SOX2 is a critical regulator of CSCs. A 2025 CRISPR-Cas9 screen in glioblastoma stem cells (GSCs) identified SOX2 as a key upstream regulator of PROM1 (the CD133 gene), a well-established marker of GSCs associated with therapy resistance and tumor aggressiveness [16]. This places SOX2 at the apex of a regulatory hierarchy controlling stemness and stress response in tumors.
- Promotion of Oncogenic Phenotypes: SOX2 amplification and overexpression drive sustained proliferative signaling, evasion of apoptosis, activation of invasion and metastasis, and self-renewal of CSCs across cancer types [34]. It achieves this by modulating key oncogenic pathways, including WNT/β-catenin, PI3K/AKT, and Hedgehog signaling [34].
Table 2: SOX2/SOX2OT Alterations and Functional Roles in Select Cancers
| Cancer Type | Genetic/Alteration | Documented Oncogenic Roles |
|---|---|---|
| Glioblastoma | SOX2 amplification; SOX2OT upregulation | Regulates CD133+ cancer stem cells; promotes self-renewal, therapy resistance, and aggressive tumor phenotypes [34] [16] |
| Lung Squamous Cell Carcinoma | Co-amplification of SOX2 and PRKCI | Drives cancer stem cell phenotype and tumorigenesis [34] |
| Breast Cancer | SOX2 and SOX2OT concordant expression | Upregulated in estrogen receptor-negative tumors; promotes mammosphere formation, anchorage-independent growth, and metastatic potential [34] [32] |
| Testicular Germ Cell Tumors | Epigenetic dysregulation | Part of a core pluripotency gene network (OCT4/POU5F1, SOX2, LIN28, NANOG) driving embryonal carcinoma [35] |
Experimental Analysis and Methodologies
Key Experimental Protocols
Investigating the SOX2-SOX2OT axis requires a combination of molecular, cellular, and functional assays.
Protocol 1: Assessing Functional Regulation via SOX2OT Ectopic Expression
- Vector Construction: Clone the full-length human SOX2OT transcript (e.g., RefSeq NR_004053) into an expression vector under a strong promoter (e.g., CMV), preferably with a selectable marker like puromycin and a reporter like GFP [32].
- Cell Transfection: Transfect target cells (e.g., MDA-MB-231 breast cancer cells) using a lipid-based transfection reagent (e.g., Lipofectamine Plus). Include an empty vector as a control [32].
- Selection and Enrichment: After 24-48 hours, select transfected cells using puromycin. Further enrich for transfected populations by Fluorescence-Activated Cell Sorting (FACS) based on GFP expression [32].
- Downstream Analysis:
- qRT-PCR: Quantify changes in SOX2 and SOX2OT mRNA levels in sorted cells using SYBR Green-based qRT-PCR. Normalize to housekeeping genes (GAPDH, HPRT) [32].
- Functional Assays: Perform assays like sulforhodamine B (SRB) for cell proliferation and soft agar colony formation for anchorage-independent growth to assess phenotypic consequences [32].
Protocol 2: In vivo Functional Studies in Neural Progenitors via In Utero Electroporation
- Construct Preparation: Prepare plasmids for Sox2ot overexpression (cDNA) or knockdown (shRNA) alongside a GFP reporter plasmid to visualize transfected cells [33].
- Surgical Procedure: At a specific embryonic stage (e.g., E13.5 in mice), inject plasmid DNA into the lateral ventricle of the developing brain. Apply precise electrical pulses to facilitate DNA uptake by neural progenitor cells in the ventricular zone [33].
- BrdU Labeling: Administer a pulse of bromodeoxyuridine (BrdU) to label cells in S-phase before tissue collection [33].
- Tissue Analysis: Harvest brains at desired timepoints (e.g., E14.5). Process for immunohistochemistry to analyze markers of proliferation (BrdU), neural progenitors (SOX2, PAX6, TBR2), and differentiation (neuronal markers). Quantification is performed by calculating the ratio of marker-positive cells within the GFP-positive transfected population [33].
Protocol 3: Identifying Regulators via CRISPR-Cas9 Screening
- Library Transduction: Transduce CD133+ glioblastoma stem cells (GSCs) with a genome-wide CRISPR knockout (e.g., TKOv3) lentiviral library at a low Multiplicity of Infection (MOI ~0.3) to ensure single guide RNA (sgRNA) integration. Use puromycin selection to eliminate non-transduced cells [16].
- Population Passaging and Sorting: Culture the transduced cell pool for multiple doublings (e.g., 12 doublings). Harvest a final sample and use Flow-Activated Cell Sorting (FACS) to isolate the top and bottom 5% of cells based on CD133 surface expression [16].
- Genomic DNA Extraction and Sequencing: Extract genomic DNA from the starting population, final unsorted population, and sorted populations. Amplify the integrated sgRNA sequences via PCR and subject them to high-throughput sequencing [16].
- Bioinformatic Analysis: Align sequences to the sgRNA library. Compare sgRNA abundance in the CD133-high and CD133-low populations to the reference population using analysis tools like drugZ to identify genes whose knockout significantly alters CD133 expression. SOX2 is a key hit in such screens [16].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying SOX2/SOX2OT Biology
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| SOX2OT Expression Plasmid | Ectopic overexpression of the lncRNA | Functional gain-of-study to assess impact on SOX2 expression and cell phenotype [32] |
| SOX2OT shRNAs | Knockdown of endogenous lncRNA | Loss-of-function studies to determine necessity in maintaining SOX2 levels and stemness [33] |
| Anti-SOX2 Antibody | Immunodetection of SOX2 protein | Western blotting, immunohistochemistry, and flow cytometry for protein-level analysis [32] |
| TKOv3 CRISPR Library | Genome-wide knockout screening | Unbiased identification of genetic regulators of SOX2/CD133 in cancer stem cells [16] |
| CD133/2-PE Antibody | Detection of CD133 cell surface protein | Flow cytometry analysis and sorting of cancer stem cell populations [16] |
| NeuroCult Basal Medium | Serum-free culture of neural and glioma stem cells | Maintenance of GSCs in an undifferentiated state for in vitro assays [16] |
| 6-(Propan-2-yl)azulene | 6-(Propan-2-yl)azulene|High-Purity Azulene Research | |
| N-(2-Sulfanylpropyl)glycine | N-(2-Sulfanylpropyl)glycine|High-Purity Reference Standard | [Briefly state core research value, e.g., 'A thiol-functionalized glycine derivative for biochemical research']. N-(2-Sulfanylpropyl)glycine is for Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Visualization of Key Mechanisms and Workflows
SOX2OT Regulatory Mechanisms
The following diagram summarizes the dual regulatory mechanisms of SOX2OT, which can either activate or repress SOX2 depending on cellular context.
Diagram Title: Context-Dependent SOX2OT Regulation of SOX2
SOX2-CD133 Regulatory Axis in Glioblastoma
This diagram illustrates the regulatory network centered on SOX2 in glioblastoma stem cells, as revealed by CRISPR screening.
Diagram Title: SOX2 Regulates CD133 in Glioblastoma Stem Cells
Future Directions and Therapeutic Implications
The intricate epigenetic regulation of SOX2 and SOX2OT presents both challenges and opportunities. Future research should focus on:
- Decoding Context-Specificity: A primary goal is to determine the precise molecular signals and co-factors that dictate whether SOX2OT acts as an activator or repressor of SOX2 in different cellular and disease contexts.
- Targeting LncRNAs Therapeutically: The upregulation of SOX2OT in multiple cancers makes it an attractive therapeutic target. Developing strategies to specifically inhibit oncogenic lncRNAs (e.g., using antisense oligonucleotides or small molecules) could disrupt the SOX2-SOX2OT axis and deplete the cancer stem cell population.
- Harnessing for Regenerative Medicine: Insights from the OvSvK reprogramming system [21] could be refined to improve the efficiency and safety of generating patient-specific iPSCs for regenerative applications, by precisely modulating the epigenetic landscape.
- Liquid Biopsy Biomarkers: Detecting methylated SOX2 DNA or specific SOX2OT isoforms in liquid biopsies holds promise as a non-invasive biomarker for cancer diagnosis, prognosis, and monitoring of minimal residual disease.
In conclusion, the SOX2-SOX2OT locus represents a paradigm of complex epigenetic regulation central to the control of cellular differentiation states. Its study not only advances our fundamental understanding of cell identity but also opens avenues for novel therapeutic interventions in cancer and regenerative medicine.
Research Tools and Translational Applications: Harnessing SOX2 for Cell Engineering and Disease Modeling
The transcription factor SOX2 is a master regulator of pluripotency and self-renewal in embryonic and adult stem cells. Its precise expression is critical for maintaining cellular identity during division and for guiding differentiation, and its dysregulation is a hallmark of cancer stem cells. This whitepaper provides a technical guide on the development and application of SOX2 reporter cell lines as indispensable in vitro tools for visualizing and quantifying these dynamic processes. We detail the molecular engineering of these reporter systems, present standardized protocols for their use in tracking cell fate, and synthesize quantitative data on their performance. Framed within the context of SOX2's function in cellular dedifferentiation, this resource is designed to equip researchers with the methodologies needed to leverage these models for advanced stem cell research and therapeutic development.
SOX2, a member of the SOXB1 group of transcription factors, is a cornerstone of the core pluripotency network, operating in a tight partnership with OCT4 and NANOG [36] [10]. Its function extends beyond embryonic stem cells (ESCs) to adult tissue homeostasis and is aberrantly reactivated in numerous cancers, facilitating a dedifferentiated, stem-cell-like state [12] [10]. A key mechanism for maintaining cellular identity through successive divisions is mitotic bookmarking, where SOX2 remains bound to specific genomic loci on mitotic chromosomes. This bookmarking is mediated by its High Mobility Group (HMG) DNA-binding domain and is crucial for the rapid re-establishment of transcriptional programs after mitosis, thereby ensuring phenotypic maintenance in stem and progenitor cells [37]. The forced expression of SOX2, in combination with other factors like OCT4 and KLF4, is sufficient to reprogram somatic cells into induced pluripotent stem cells (iPSCs), directly demonstrating its powerful role in driving dedifferentiation [27] [36]. Given its central role, the ability to track SOX2 expression in living cells in real-time provides a critical window into the molecular underpinnings of stemness, lineage commitment, and oncogenic transformation.
Generation of SOX2 Reporter Cell Lines
The creation of robust SOX2 reporter lines relies on precise genomic engineering to ensure the reporter gene faithfully reflects the expression dynamics of the endogenous SOX2 locus.
Molecular Design and Targeting Strategies
The most reliable method involves using CRISPR-Cas9 to knock-in a reporter construct directly into the 3' untranslated region (3' UTR) of the SOX2 gene. This approach preserves all endogenous regulatory elements, ensuring that the reporter is subject to the same transcriptional and post-transcriptional controls as the native SOX2 [38].
A common design uses a T2A "self-cleaving" peptide sequence to enable bicistronic expression from a single mRNA transcript. The construct follows the schema: SOX2 genomic sequence - T2A peptide - Reporter Gene - Selection Cassette - 3' Homology Arm. The T2A peptide ensures efficient co-translational separation of the SOX2 protein and the reporter protein, such as eGFP or firefly luciferase (Luc) [37] [38]. For dual-reporter lines, a second reporter (e.g., mCherry) can be targeted to a gene of a differentiated lineage (e.g., GCG for alpha cells) or a maturation marker (e.g., MAFA for beta cells), allowing for the simultaneous monitoring of pluripotency exit and lineage specification [38].
Validation of Reporter Lines
After selection, clones must be rigorously validated:
- Pluripotency Assessment: Confirmed via immunofluorescence and flow cytometry for core pluripotency markers (OCT4, NANOG, SSEA-4) [38].
- Karyotyping: Standard G-banding analysis ensures engineering has not introduced chromosomal abnormalities [38].
- Functional Differentiation: The reporter line must retain the capacity to differentiate into all three germ layers. A definitive test is its efficient differentiation into target cells, such as pancreatic islet-like cells, with the reporter signal diminishing appropriately upon SOX2 downregulation [38].
Table 1: Common Reporter Constructs and Their Applications
| Reporter Gene | Detection Method | Primary Application | Advantages | Disadvantages |
|---|---|---|---|---|
| eGFP/mCherry | Fluorescence Microscopy, FACS | Live-cell imaging, cell sorting and isolation | High spatial resolution, enables purification of live cells | Photobleaching; autofluorescence |
| Firefly Luciferase | Luminescence Imaging | Sensitive tracking in low-expression or 3D cultures | Extremely sensitive, low background, quantitative | No spatial resolution within a single cell |
| GCaMP6 | Fluorescence (Ca²⺠indicator) | Functional assessment of differentiated β-cells [38] | Reports cellular activity in addition to identity | Requires specific functional context |
Experimental Protocols for Key Applications
Protocol: Tracking Pluripotency Exit and Differentiation in Real-Time
This protocol leverages SOX2 reporter lines to monitor the loss of pluripotency during directed differentiation.
- Initial Culture: Maintain the SOX2 reporter human pluripotent stem cells (hPSCs) on Matrigel-coated plates in mTeSR1 medium [38].
- Differentiation Induction: At ~70% confluency, initiate a directed differentiation protocol. For example, to generate pancreatic islet cells, follow a established multi-stage process: definitive endoderm, primitive gut tube, pancreatic progenitors, and endocrine precursors [38].
- Live-Cell Imaging:
- Setup: Use a confocal microscope with an environmental chamber (37°C, 5% CO₂).
- Scheduling: Acquire images of the SOX2 reporter signal (e.g., eGFP) every 12-24 hours over the entire differentiation period (e.g., 14-21 days).
- Analysis: Quantify the mean fluorescence intensity of the reporter over time to generate a kinetic curve of SOX2 downregulation. Co-staining with antibodies for lineage-specific markers (e.g., PDX1 for pancreatic progenitors, INS for β-cells) at endpoint stages confirms correlation between SOX2 loss and acquisition of differentiated fates [38].
Protocol: Quantifying Mitotic Bookmarking via Single-Cell Luminescence Imaging
This protocol assesses the mitotic chromosome-binding (MCB) activity of endogenously tagged SOX2, a key feature of its bookmarking function [37].
- Cell Line: Use a heterozygous knock-in hESC line where the endogenous SOX2 is fused to firefly luciferase (SOX2-Luc) and H2B-Cerulean is constitutively expressed to mark chromatin [37].
- Image Acquisition: Plate cells on glass-bottom dishes. Approximately 15 minutes before cell division, capture luminescence signals using highly sensitive microscopy (e.g., LUMOS microscope [37]).
- Data Analysis:
- The relocalization of the SOX2-Luc signal to the midplane of the cell, colocalizing with H2B-Cerulean-labeled metaphase chromosomes, visually confirms MCB.
- To quantify the strength of MCB, calculate the MCB Index in metaphase cells as the ratio of the fluorescent (or luminescent) signal on mitotic chromosomes to that in the cytoplasm [37].
Diagram 1: Workflow for tracking pluripotency exit during differentiation.
SOX2 in Signaling and Dedifferentiation: A Network View
SOX2 function is inextricably linked to multiple core signaling pathways, and its aberrant expression can drive the dedifferentiation of somatic cells into a stem-like state, a key event in oncogenesis. In cancer, SOX2 promotes dedifferentiation and imparts stem cell-like features by directly binding to and activating promoters of EMT transcription factors like Snail, Slug, and Twist, leading to loss of E-Cadherin and acquisition of invasive properties [12]. It regulates cell cycle progression by repressing CDK inhibitors p21Cip1 and p27Kip1, thereby favoring proliferation, a hallmark of both stem and cancer cells [12]. Furthermore, SOX2 interacts with and modulates critical pathways such as Wnt/β-catenin, SHH, and Notch, which are essential for stem cell maintenance and are often reactivated in cancer [10]. This intricate crosstalk positions SOX2 as a central node in the regulatory network that controls cellular identity, and its dysregulation is sufficient to initiate a dedifferentiation program.
Diagram 2: SOX2 interacts with core pluripotency factors and multiple signaling pathways to regulate EMT and cell cycle, driving dedifferentiation.
Quantitative Data from SOX2 Reporter Studies
Reporter lines provide quantifiable data on SOX2 dynamics. The following table synthesizes key metrics from relevant studies.
Table 2: Quantitative Metrics from SOX2 Reporter and Perturbation Studies
| Cell Line / Model | Intervention / Measurement | Key Quantitative Result | Biological Implication | Source |
|---|---|---|---|---|
| Mouse ESCs (Endogenous SOX2-Luc) | Mitotic Chromosome Binding (MCB) Index | MCB Index for SOX2 > MCB Index for OCT4 | SOX2 has stronger intrinsic mitotic bookmarking activity than OCT4 [37] | |
| Pancreatic Cancer Cells (e.g., L3.6pl) | SOX2 Knockdown (KD) | ~50-75% reduction in colony formation | SOX2 is critical for self-renewal and clonogenic potential of cancer stem cells (CSCs) [12] | |
| Urothelial Carcinoma Cells (As_I, 5637) | SOX2 KD | ~50% reduction in colony formation; Increased doubling time | SOX2 maintains proliferative and self-renewal capacities in basal/squamous subtype cancers [27] | |
| H1 hESCs (SOX2 Reporter) | Differentiation to SC-islets | Increased monohormonal β-cells with N21 supplement | Reporter lines enable optimization of differentiation protocols [38] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for SOX2 Reporter Line Generation and Experimentation
| Reagent / Tool | Function | Example & Notes |
|---|---|---|
| CRISPR-Cas9 System | Precision genome editing for reporter knock-in | Used with homology-directed repair (HDR) donors for targeted integration at the SOX2 locus [38]. |
| T2A Self-Cleaving Peptide | Enables co-expression of SOX2 and reporter from a single transcript | Ensures 1:1 stoichiometry between native SOX2 and reporter protein without fusion protein artifacts [38]. |
| Fluorescent/Luminescent Reporters | Visualizing and quantifying SOX2 expression | eGFP/mCherry for FACS and imaging; Luciferase for sensitive quantification; GCaMP6 for functional Ca²⺠imaging in β-cells [38]. |
| Inducible Expression Systems | Controlled gene expression | Doxycycline-inducible (Tet-On) systems allow controlled expression of SOX2 or mutants for dedifferentiation studies [37]. |
| Specific shRNA/siRNA | Transient knockdown of SOX2 | Validates reporter phenotype by assessing loss-of-function (e.g., reduced self-renewal upon SOX2 KD) [12] [27]. |
| 3-Chloro-1-nitrobut-2-ene | 3-Chloro-1-nitrobut-2-ene | 3-Chloro-1-nitrobut-2-ene is for research use only. It is a versatile reagent for synthesizing bioactive isoxazoline rings and other nitro-functionalized structures. Not for human or veterinary use. |
| N-benzyloctan-4-amine | N-benzyloctan-4-amine | N-benzyloctan-4-amine is a chemical compound for research use only (RUO). Explore its potential applications in medicinal chemistry and organic synthesis. |
SOX2 reporter cell lines are powerful and versatile in vitro models that bridge molecular function with cellular phenotype. They provide a dynamic window into the processes of pluripotency maintenance, lineage commitment, and the dangerous reversion to a stem-like state in cancer. The technical guidelines and experimental frameworks outlined in this whitepaper provide a foundation for researchers to rigorously apply these tools. As the field advances, the combination of these reporters with high-content screening platforms, such as organ-on-a-chip technologies and complex differentiation protocols, will be instrumental in deciphering the nuanced role of SOX2 in development and disease, ultimately accelerating the discovery of novel regenerative and anti-cancer therapies.
The field of cellular reprogramming has been revolutionized by the ability to convert one somatic cell type directly into another, bypassing the pluripotent state. This process, known as direct reprogramming or transdifferentiation, holds immense potential for regenerative medicine, disease modeling, and drug development. Among the key transcription factors driving this cellular fate conversion, SOX2 (SRY-box 2) has emerged as a critical regulator. SOX2 is a transcription factor conserved throughout vertebrate evolution, characterized by a high-mobility-group (HMG) DNA-binding domain that allows it to interact with specific DNA sequences and modulate gene expression programs [39] [26] [1]. While initially recognized for its essential role in maintaining pluripotency in embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), SOX2 is also widely expressed in the early neuroectoderm and neural progenitor cells during development, as well as in neural stem cells in the adult brain [40] [39]. This persistent expression pattern suggests a fundamental function in neural development and maintenance. This technical guide explores the central role of SOX2 in directing the reprogramming of somatic cells into induced neural progenitor cells (iNPCs), framing this capability within the broader context of SOX2's function in cellular dedifferentiation and fate determination. The ability of SOX2 to impart stem cell-like features and promote dedifferentiation is not limited to physiological contexts but also extends to cancer biology, where its aberrant expression contributes to tumorigenesis and stemness [12] [1]. Understanding the molecular mechanisms by which SOX2 drives neural reprogramming is therefore critical for both regenerative medicine and oncology research.
Molecular Mechanisms of SOX2 in Neural Fate Determination
SOX2 as a Lineage Specifier and Epigenetic Modulator
The core pluripotency transcription factors, including SOX2, OCT4, and NANOG, not only maintain pluripotency but also function as lineage specifiers during differentiation [26]. SOX2, in particular, is a critical specifier for the ectodermal lineage, priming cells for neural fate. In ESCs, SOX2, OCT4, and NANOG form a core transcriptional regulatory network that maintains self-renewal by activating pluripotency genes and repressing key genes responsible for differentiation [26]. However, during differentiation, a delicate balance in the expression levels of these factors is crucial. A twofold increase in SOX2 expression is sufficient to alter self-renewal and induce differentiation of ESCs [40]. The protein-biochemical regulation of SOX2 is complex and involves various post-translational modifications—including phosphorylation, ubiquitination, SUMOylation, and acetylation—that critically impact its functionality, often in a tissue and species-specific manner [1]. A key regulatory axis is the PI3K/AKT signaling pathway, which has been shown to phosphorylate SOX2 at specific residues (e.g., T116), thereby stabilizing the SOX2 protein by protecting it from ubiquitin E3 ligase-mediated proteasomal degradation [29] [1]. This stabilization of SOX2 protein levels is a significant mechanism in various cancers, such as osteosarcoma, and is likely also relevant in the context of reprogramming, where sustained SOX2 expression is required for successful fate conversion [29].
Transcriptional Networks and Target Genes
SOX2 exerts its effects by binding to specific enhancer and promoter regions in the genome, often in cooperation with other transcription factors. Recent functional genomics approaches have started to identify SOX2's molecular targets in neural development. In neural stem cells (NSCs), SOX2 directly regulates the expression of genes critical for their maintenance and function. Key among these is Survivin, an inhibitor of cell death, whose regulation by SOX2 helps prevent apoptosis in NSCs [39]. Furthermore, SOX2 deletion in the developing hippocampus leads to downregulation of Sonic Hedgehog (Shh) and Wnt3a signaling, pathways essential for NSC proliferation and maintenance [39]. Reactivation of SHH signaling can rescue the proliferation defects in Sox2 mutant NSCs, pointing to its role as a functional contributor to SOX2-dependent NSC maintenance [39]. The diagram below illustrates the core molecular network through which SOX2 promotes neural progenitor cell identity and prevents differentiation.
Experimental Approaches for SOX2-Mediated Neural Reprogramming
Key Transcription Factor Combinations
Several studies have demonstrated direct reprogramming of mouse and human fibroblasts into immature neural stem or precursor cells using different combinations of transcription factors. A critical observation across these studies is the consistent inclusion of SOX2, either alone or in combination with other factors [40]. The table below summarizes the key transcription factor combinations that have been successfully employed to generate induced neural stem/precursor cells (iNSCs) from somatic cells, primarily fibroblasts.
Table 1: Transcription Factor Combinations for Direct Reprogramming to iNSCs
| Factor Combination | Key Components | Somatic Cell Source | Efficiency & Key Features | Primary Reference |
|---|---|---|---|---|
| Pluripotency Factor-Based | OCT4, SOX2, KLF4, C-MYC (OKSM) | Mouse Embryonic Fibroblasts (MEFs) | Neural stem cell colonies in 4-6 days; no transient pluripotent intermediates; tripotent (neurons, astrocytes, oligodendrocytes) | [40] |
| Neural Factor-Based (Triple) | SOX2, BRN2, FOXG1 | Mouse Embryonic Fibroblasts (MEFs) | SOX2 required for effective reprogramming and neuronal maturation; tripotent | [40] |
| Neural Factor-Based (Five-Factor) | SOX2, BRN2, TLX, C-MYC, BMI1 | Adult Mouse Fibroblasts | Similar to primary NSCs; C-MYC/BMI1 crucial for proliferation/self-renewal; SOX2 indispensable | [40] |
| Single Factor | SOX2 | Mouse & Human Fetal Fibroblasts | Requires specific culture conditions (feeder layer, growth factors); homogeneous, tripotent population after ~6 weeks | [40] |
Detailed Protocol: Direct Reprogramming of Human Adipose Tissue-MSCs to iNP-like Cells
A recent study demonstrated the direct reprogramming of human adipose tissue-derived mesenchymal stem cells (hAT-MSCs) into induced neural progenitor-like cells (iNP-like cells) using a single transcription factor, SOX2 [41]. The following is a detailed methodology based on this report.
1. Preparation of Starting Cells:
- Cell Source: Authenticated human AT-MSCs. Confirm expression of MSC markers (CD90, CD105) and multipotent differentiation potential (osteogenic, chondrogenic, adipogenic) prior to reprogramming.
- Culture Medium: Maintain and amplify hAT-MSCs in Dulbecco's Modified Eagle Medium/Nutrient Mixture F-12 (DMEM/F12) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin.
- Culture Conditions: Incubate at 37°C in a humidified atmosphere with 5% CO₂.
2. Viral Transduction:
- Vector: Use a lentiviral vector with a doxycycline (Dox)-inducible promoter driving the expression of the human SOX2 gene. A puromycin resistance gene should be included for selection.
- Transduction Protocol:
- Seed hAT-MSCs at an appropriate density (e.g., 1x10ⵠcells/cm²).
- Expose cells to viral particles in the presence of a transduction enhancer like Polybrene (e.g., 6-8 µg/mL) for 24-48 hours.
3. Selection and Reprogramming Phase:
- Selection: After transduction, replace the medium with hAT-MSC growth medium containing puromycin (e.g., 1-2 µg/mL) for 72 hours to select successfully transduced cells.
- Induction of SOX2: Following selection, switch to a neural induction medium. This typically consists of DMEM/F12-high glucose supplemented with B27, N2, and doxycycline (e.g., 2 µg/mL) to induce SOX2 expression. The addition of growth factors like FGF2 (bFGF) and EGF is recommended to support neural progenitor survival and proliferation.
- Morphological Changes: The first signs of morphological transformation from a fibroblast-like to a neural-like morphology (smaller, bipolar or multipolar cells forming clusters) can be observed within 14 days.
4. Expansion and Characterization of iNP-like Cells:
- Passaging: Once stable iNP-like cell colonies are established (typically by day 21-28), they can be passaged using enzymatic dissociation (e.g., Accutase).
- Characterization: Validate the successful reprogramming by analyzing the expression of neural progenitor markers using immunocytochemistry and/or RT-qPCR.
- Key Markers: NESTIN (neural stem/progenitor cell marker), SOX2, PAX6, VIMENTIN, and MUSASHI1 [40] [41].
- Functional Validation: Assess the multipotency of the iNP-like cells by subjecting them to differentiation conditions for neurons (β-III-TUBULIN+), astrocytes (GFAP+), and oligodendrocytes (O4+ or GALC+) [41].
The following workflow diagram summarizes this multi-stage protocol.
The Scientist's Toolkit: Essential Reagents for SOX2 Reprogramming
Successful execution of SOX2-mediated reprogramming requires a suite of specific research reagents. The following table details essential materials and their functions.
Table 2: Essential Research Reagents for SOX2-Mediated Neural Reprogramming
| Reagent Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Source Cells | Human Adipose Tissue-MSCs (hAT-MSCs), Human Dermal Fibroblasts, Mouse Embryonic Fibroblasts (MEFs) | Starting somatic cell population for fate conversion; choice influences efficiency and protocol. |
| Gene Delivery Vectors | Doxycycline-Inducible Lentivirus (SOX2), Retrovirus (OKSM) | Safe and efficient delivery and/or regulation of reprogramming factors. |
| Selection Agents | Puromycin, Geneticin (G418) | Selection of successfully transduced cells, enriching for the population that will reprogram. |
| Culture Media & Supplements | DMEM/F12, N2 Supplement, B27 Supplement, KnockOut Serum Replacement (KSR) | Provides a defined, supportive environment that suppresses original cell identity and promotes neural fate. |
| Growth Factors | Recombinant FGF2 (bFGF), Recombinant EGF | Critical for the survival, proliferation, and maintenance of the resulting neural progenitor-like cells. |
| Small Molecule Inducers | Doxycycline Hyclate | Induces expression of SOX2 in inducible vector systems, allowing temporal control. |
| Antibodies for Validation | Anti-SOX2, Anti-NESTIN, Anti-PAX6, Anti-β-III-TUBULIN, Anti-GFAP | Immunocytochemical and functional validation of successful reprogramming and multipotency. |
| Benzoylsulfamic acid | Benzoylsulfamic acid, CAS:89782-96-7, MF:C7H7NO4S, MW:201.20 g/mol | Chemical Reagent |
| Ethyl 2,4-dichlorooctanoate | Ethyl 2,4-dichlorooctanoate, CAS:90284-97-2, MF:C10H18Cl2O2, MW:241.15 g/mol | Chemical Reagent |
SOX2 stands as a powerful molecular tool and a central biological factor in the direct reprogramming of somatic cells to a neural progenitor fate. Its capacity to function as a master regulator, often in conjunction with other transcription factors but sometimes alone under permissive conditions, underscores its pivotal role in orchestrating the epigenetic and transcriptional shifts required for neural lineage commitment [40] [41]. The experimental protocols and mechanistic insights detailed in this guide provide a robust framework for researchers aiming to utilize SOX2 in neural reprogramming applications. Looking forward, several challenges and opportunities remain. A deeper understanding of the post-translational modifications that fine-tune SOX2 activity, such as the AKT-mediated phosphorylation that stabilizes the protein, could lead to improved reprogramming efficiency through small molecule interventions rather than genetic manipulation [29] [1]. Furthermore, translating these methodologies into clinically applicable cell therapies for conditions like multiple sclerosis will require a shift towards non-integrating delivery methods and xenogeneic-free culture systems [41]. Finally, the dual role of SOX2 in promoting stemness in both development and cancer [12] [1] necessitates rigorous safety profiling, including tumorigenicity studies, of any SOX2-derived cellular products. As our knowledge of SOX2's molecular functions continues to expand, so too will our ability to harness its potential for regenerative medicine and therapeutic discovery.
The transcription factor SOX2 (SRY-related HMG-box 2) is a pivotal regulator of embryonic development and stem cell pluripotency. In oncological research, it has emerged as a critical driver of tumorigenesis, therapy resistance, and metastasis through its role in maintaining cancer stem cells (CSCs) [36]. CSCs represent a minor subpopulation within tumors capable of self-renewal, differentiation, and tumor initiation. The study of SOX2 within CSCs is crucial for understanding the molecular basis of tumor recurrence and for developing targeted therapeutic strategies. This technical guide details the core methodologies for investigating SOX2 in CSCs, with a specific focus on the sphere formation assay—a gold-standard technique for CSC enrichment and functional characterization. The content is framed within the broader thesis that SOX2 orchestrates a dedifferentiation program, imparting stem cell-like features to cancer cells and thereby fueling tumor aggressiveness [12] [6].
SOX2 Biology and Oncogenic Signaling Pathways
SOX2 in Stem Cell Maintenance and Dedifferentiation
SOX2 is a core component of the transcriptional network that maintains cellular pluripotency. It operates in a synergistic fashion with other key transcription factors like OCT4 and NANOG to sustain stem cell identity [36]. In cancer, the aberrant expression of SOX2 promotes dedifferentiation, a process where mature cancer cells revert to a stem-like state. This is evidenced by its ability to bind promoters of EMT transcription factors like Snail, Slug, and Twist, leading to loss of epithelial markers (e.g., E-Cadherin) and acquisition of mesenchymal traits, a phenomenon known as epithelial-to-mesenchymal transition (EMT) [12]. SOX2 expression is therefore strongly associated with enhanced tumor cell plasticity, invasiveness, and the emergence of therapeutic resistance.
Key Signaling Pathways Involving SOX2
SOX2's function is intertwined with several critical oncogenic signaling pathways. It is both regulated by and a regulator of pathways such as AKT, NOTCH, WNT, and Hedgehog [42] [29]. A key regulatory mechanism is the post-translational stabilization of SOX2 protein by the AKT kinase. AKT phosphorylates SOX2 at threonine 116, which prevents its recognition and degradation by E3 ubiquitin ligases like UBR5 and STUB1, thereby dramatically increasing SOX2 protein stability and promoting CSC maintenance [29]. This axis represents a critical vulnerability in SOX2-high cancers.
The diagram below illustrates the core signaling pathway that regulates SOX2 protein stability.
AKT-SOX2 Signaling Axis
Core Methodology: The Sphere Formation Assay
The sphere formation assay is a fundamental functional test for CSCs. When cultured under serum-free, non-adherent conditions, only CSCs survive and proliferate, forming three-dimensional structures known as tumorspheres [43] [44]. This assay enriches for the stem cell population and allows for the investigation of self-renewal capacity.
Detailed Experimental Protocol
The following protocol is optimized for SOX2-positive cell lines such as MCF-7 (breast cancer) and 143B (osteosarcoma) [42] [29].
Preparing Complete Serum-Free Medium
- Base Medium: Use PRIME-XV Tumorsphere SFM or DMEM/F12 supplemented with B27 [43] [44].
- Essential Supplements:
- Heparin (2 U/mL): Promoves growth factor binding and signaling.
- Hydrocortisone (0.5 µg/mL): Enhances cell survival and proliferation.
- Growth Factors: Add EGF (20 ng/mL) and FGF (20 ng/mL) to support stem cell self-renewal [44].
- Antibiotics: Penicillin (100 µg/mL) and streptomycin (100 µg/mL) [42].
- Pre-warm the complete medium at 37°C for no more than 30 minutes before use.
Plating Cells for Sphere Formation
- Cell Detachment: Harvest adherent cells using a gentle dissociation enzyme like TrypLE Express to preserve cell viability. Avoid using standard trypsin-EDTA for prolonged periods [43].
- Cell Counting and Seeding: Centrifuge the cell suspension and resuspend the pellet in pre-warmed complete tumorsphere medium. Seed cells into ultra-low attachment plates at a density critical for optimal sphere formation. The optimal density must be determined empirically for each cell line. A recommended starting range is 5 x 10³ to 6 x 10ⵠcells per well of a 6-well plate [43].
- Incubation and Monitoring: Culture cells in a humidified incubator at 37°C with 5% CO₂. Do not disturb the plates for the first 3-5 days to allow for sphere initiation. Sphere formation is typically assessed after 7-10 days [43]. The formation of solid, spherical structures where individual cells are not easily distinguishable indicates successful tumorsphere development [44].
Passaging and Analysis of Tumorspheres
- Harvesting: Collect the sphere-containing medium and let spheres settle by gravity in a conical tube (10-15 minutes).
- Dissociation: Aspirate the supernatant, add a small volume of TrypLE Express, and incubate at 37°C. Gently pipette up and down to dissociate spheres into a single-cell suspension.
- Re-plating or Analysis: Centrifuge the cells, resuspend in fresh tumorsphere medium, and re-plate at the desired density for serial passaging to assess self-renewal. Alternatively, cells can be used for downstream applications like RNA/protein extraction or flow cytometry to analyze SOX2 expression [43].
The overall workflow for a SOX2-focused sphere formation assay is summarized below.
Sphere Assay Workflow
Analytical Methods for SOX2 Expression and Function
Following tumorsphere enrichment, precise analysis of SOX2 is critical. The table below summarizes key quantitative findings from recent studies linking SOX2 to CSC properties.
Table 1: Quantitative Findings on SOX2 in Cancer Stem Cell Models
| Cancer Type | Experimental Model | Key Finding on SOX2 | Functional Impact | Citation |
|---|---|---|---|---|
| Osteosarcoma | 143B & HOS cell lines | SOX2 knockdown reduced tumorsphere formation | Decreased self-renewal capacity | [29] |
| Pancreatic Cancer | L3.6pl cell line | SOX2 binds Snail, Slug, Twist promoters | Induced EMT, loss of E-Cadherin | [12] |
| Breast Cancer | MCF-7 mammospheres | ~60% recovery ratio for SOX2-positive CSCs; SOX2+ cells found exclusively in CTC clusters | Identified as rare event with high metastatic potential | [42] [45] |
| Oral Squamous Cell Carcinoma | 94 patient tumor samples | High SOX2 in recurrence linked to improved survival (p=0.013) | Context-dependent prognostic role | [46] |
Molecular Analysis of SOX2
- RNA Analysis: Reverse Transcription qPCR (RT-qPCR) is used to quantify SOX2 mRNA levels in spheres versus adherent cells. Use GAPDH as a reference gene and TaqMan assays (e.g., Hs04234836_s1 for human SOX2) for high specificity. Data analysis is performed using the ΔΔCt method [42].
- Protein Analysis:
- Western Blotting: Confirm SOX2 protein upregulation in tumorspheres. The AKT-SOX2 axis can be investigated by treating sphere-derived cells with AKT inhibitors (e.g., MK2206) and observing a dose-dependent decrease in SOX2 protein (but not mRNA) levels [29].
- Immunohistochemistry (IHC) / Immunofluorescence (IF): Used to localize SOX2 expression in cells (nuclear staining) and patient tissue samples (e.g., FFPE blocks). This allows for correlation of SOX2 levels with clinical outcomes [46] [47].
Functional Analysis via SOX2 Perturbation
- Knockdown (KD): SOX2 knockdown via shRNA in SOX2-high cells (e.g., 143B osteosarcoma cells) results in cell cycle arrest (increased G0/G1 phase) associated with induction of p21Cip1 and p27Kip1, and significantly impairs proliferation, migration, and sphere-forming capacity [12] [29].
- Overexpression (OE): Ectopic SOX2 expression in SOX2-low cells promotes S-phase entry, cell proliferation, and enhances both the size and number of tumorspheres, demonstrating its role in driving stemness [29].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for SOX2 and CSC Research
| Reagent / Kit | Specific Product Example | Critical Function in Assay |
|---|---|---|
| Tumorsphere Medium | PRIME-XV Tumorsphere SFM (FUJIFILM #91130) | Serum-free base medium for selective CSC growth. |
| Low-Attachment Plates | Corning Costar Ultra-Low Attachment Plates | Prevents cell adhesion, forces 3D sphere growth. |
| Dissociation Reagent | TrypLE Express | Gentle enzyme for dissociating spheres to single cells. |
| SOX2 Antibody (IHC/IF) | Rabbit Polyclonal Anti-SOX2 (Abcam) | Detects and localizes SOX2 protein in cells/tissues. |
| SOX2 qPCR Assay | TaqMan Gene Expression Assay Hs04234836_s1 | Quantifies SOX2 mRNA expression levels with high specificity. |
| AKT Inhibitor | MK2206 | Tool to investigate AKT-mediated regulation of SOX2 protein stability. |
| Carbanide;rhodium(2+) | Carbanide;rhodium(2+) | Carbanide;rhodium(2+) is a dirhodium complex for catalytic research, including C-H functionalization. This product is For Research Use Only. Not for human or veterinary use. |
| 5,5-Dimethoxyhex-1-en-3-ol | 5,5-Dimethoxyhex-1-en-3-ol| | 5,5-Dimethoxyhex-1-en-3-ol is a chemical intermediate for research use only (RUO). Not for human or veterinary use. Explore its applications in organic synthesis. |
The combination of sphere formation assays with robust SOX2 marker analysis provides a powerful, functional approach to interrogate the cancer stem cell population. The evidence confirms that SOX2 is a critical node in the network that governs CSC self-renewal, dedifferentiation, and chemoresistance. Future research should focus on exploiting the identified vulnerabilities, such as the AKT-SOX2 stability axis, for therapeutic intervention. Combining AKT inhibitors with standard chemotherapy has shown promising synergistic effects in preclinical osteosarcoma models, offering a viable strategy to target the SOX2-high CSCs that drive tumor relapse [29]. Mastering these techniques is therefore essential for advancing our understanding of tumor biology and developing the next generation of anti-cancer therapies.
The transcription factor SOX2 (SRY-box 2) is a pivotal regulator of embryonic development, pluripotency, and cellular identity. Within the context of cellular dedifferentiation research, SOX2 demonstrates a powerful capacity to reprogram somatic cells to a pluripotent state and impart stem cell-like features to cancerous cells. This reprogramming capability makes SOX2 a critical factor in understanding the molecular underpinnings of tumor initiation, progression, and therapeutic resistance. In numerous cancers, including glioma, osteosarcoma, and pancreatic ductal adenocarcinoma, aberrant SOX2 expression drives tumorigenesis by promoting cellular dedifferentiation, enabling cancer cells to acquire stemness properties, enhanced self-renewal capacity, and increased resistance to conventional therapies [22] [12]. Consequently, functional assays employing SOX2 knockdown and overexpression have become indispensable tools for delineating the precise mechanisms through which SOX2 governs these processes, offering potential pathways for therapeutic intervention in treatment-resistant cancers.
Core Principles of SOX2 Functional Manipulation
SOX2 in Stemness and Dedifferentiation
SOX2 operates as a core component of the transcriptional network that maintains pluripotency in embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). It forms a critical autoregulatory circuit with OCT4 and NANOG to activate genes responsible for self-renewal while simultaneously repressing differentiation pathways [26]. In the context of cancer, this inherent capacity to maintain stemness is hijacked, with SOX2 overexpression driving dedifferentiation—the process by which mature, specialized cells revert to a more primitive, stem-like state. This dedifferentiation confers cellular plasticity, enabling tumor cells to acquire characteristics of cancer stem cells (CSCs), a subpopulation responsible for tumor maintenance, metastasis, and chemoresistance [12]. Research in pancreatic cancer has demonstrated that SOX2 imparts stem cell-like features to cancer cells and is enriched in CSC populations marked by ALDH1, ESA, and CD44 [12]. Similarly, in glioma, the interaction between SOX2 and the polarity protein Par6 is a significant modulator of stemness maintenance in glioma stem cells (GSCs) [22]. Therefore, investigating SOX2 function is not merely about understanding a transcription factor but about decoding a fundamental mechanism of cellular reprogramming and tumor plasticity.
Rationale for Knockdown and Overexpression Studies
Given that SOX2 is often an "undruggable" transcription factor directly, functional assays that modulate its expression levels provide the most direct means to elucidate its mechanistic roles. Knockdown (KD) or knockout (KO) experiments, typically using RNA interference (shRNA/siRNA) or CRISPR-Cas9 systems, allow researchers to determine the phenotypic consequences of SOX2 loss-of-function. These experiments can reveal whether SOX2 is necessary for maintaining specific cancer hallmarks, such as proliferation, self-renewal, or chemoresistance. Conversely, overexpression (OE) studies, often achieved through lentiviral transduction, establish the sufficiency of SOX2 to drive these same processes in cells that normally express it at low levels. By comparing isogenic cell lines with modulated SOX2 expression to their control counterparts, researchers can directly attribute observed phenotypic changes to SOX2 and use transcriptomic and proteomic analyses to map the resulting alterations in signaling pathways and gene expression networks.
Experimental Methodologies for SOX2 Manipulation
SOX2 Knockdown Protocols
1. shRNA-Mediated Knockdown:
- Vector Design: Utilize lentiviral or retroviral vectors expressing short hairpin RNAs (shRNAs) targeting specific exons of the SOX2 mRNA. Multiple distinct shRNA sequences should be used to control for off-target effects.
- Cell Transduction: Plate target cells (e.g., 143B osteosarcoma, HOS, or L3.6 pancreatic cancer cells) at 50-60% confluency. Incubate with viral supernatant containing polybrene (8 µg/mL) for 24 hours.
- Selection and Validation: Replace media with selection media containing puromycin (1-2 µg/mL, concentration to be determined by kill curve) for 5-7 days. Validate knockdown efficiency via Western blot (e.g., using anti-SOX2 antibody) and quantitative RT-PCR (qRT-PCR) [48] [12].
2. Phenotypic Analysis Post-Knockdown:
- Proliferation Assays: Perform MTT or CellTiter-Glo assays at 24, 48, 72, and 96 hours post-selection. SOX2 knockdown in pancreatic cancer cells has been shown to significantly reduce cell proliferation [12].
- Cell Cycle Analysis: Fix cells with 70% ethanol, stain with propidium iodide, and analyze via flow cytometry. SOX2 knockdown consistently results in a decrease of cells in S-phase and an accumulation in G0/G1 phase [12].
- Sphere-Formation Assay: Plate 5,000-10,000 single cells in low-attachment plates with serum-free medium supplemented with B27, EGF (20 ng/mL), and FGF (20 ng/mL). Count spheres (>50 µm) after 7-10 days. SOX2 knockdown in 143B and HOS osteosarcoma cells significantly reduces tumor sphere formation, indicating impaired self-renewal capacity [48].
SOX2 Overexpression Protocols
1. Lentiviral Overexpression:
- Vector Construction: Clone the full-length human SOX2 cDNA into a lentiviral expression plasmid (e.g., pLX304). Use an empty vector as a negative control (LVCtrl).
- Virus Production and Transduction: Co-transfect the transfer plasmid with packaging plasmids (psPAX2) and envelope plasmid (pMD2.G) into HEK-293T cells using a transfection reagent. Harvest viral supernatant at 48 and 72 hours. Transduce target cells (e.g., U2OS, MG63) with the supernatant and polybrene.
- Validation: Select transduced cells with blasticidin (5 µg/mL) or another appropriate antibiotic. Confirm SOX2 overexpression via Western blot and qRT-PCR. In U2OS and MG63 osteosarcoma cells, which normally express low SOX2 levels, this leads to increased tumor sphere formation and enlargement [48].
2. Phenotypic Analysis Post-Overexpression:
- Colony Formation Assay: Plate 500-1,000 cells in 6-well plates and culture for 10-14 days. Fix with methanol, stain with crystal violet (0.5%), and count colonies >50 cells.
- Migration and Invasion Assays:
- Wound Healing/Scratch Assay: Create a scratch in a confluent cell monolayer with a pipette tip. Measure wound closure at 0, 12, and 24 hours. SOX2 knockdown severely impairs migration ability [48].
- Transwell Assay: Seed serum-starved cells in the upper chamber of a transwell insert (with Matrigel for invasion, without for migration). After 24-48 hours, fix, stain, and count cells that migrated to the lower chamber.
- Chemoresistance Assays: Treat SOX2-modulated cells with chemotherapeutic agents (e.g., Cisplatin for osteosarcoma, Temozolomide for glioma) for 48-72 hours. Assess cell viability using MTT assays and calculate IC50 values. SOX2 overexpression is strongly linked to chemoresistance, which can be overcome by targeting its regulatory pathways [48] [22].
Quantitative Data from Key SOX2 Functional Studies
The following tables summarize key quantitative findings from seminal studies employing SOX2 knockdown and overexpression across different cancer types.
Table 1: Phenotypic Consequences of SOX2 Knockdown in Cancer Models
| Cancer Type | Proliferation Impact | Cell Cycle Changes | Sphere Formation | Migration/Invasion | Key Molecular Changes |
|---|---|---|---|---|---|
| Osteosarcoma [48] | Significant decrease in cell viability | Information Missing | Severe reduction in 143B & HOS cells | Severely impaired migration (wound healing & transwell) | Reduced SOX2 protein stability; increased degradation |
| Pancreatic Cancer [12] | Significant growth inhibition | G0/G1 arrest; Reduced S-phase | Only forms in SOX2-high lines (L3.6, CFPAC) | Information Missing | Induction of p21Cip1 and p27Kip1 CDK inhibitors |
| Glioma [22] | Information Missing | Information Missing | Disrupted stemness maintenance | Information Missing | Attenuated EGFR/PI3K/AKT signaling; reduced chemoresistance |
Table 2: Phenotypic Consequences of SOX2 Overexpression in Cancer Models
| Cancer Type | Proliferation Impact | Cell Cycle Changes | Sphere Formation | Stemness Markers | Key Molecular Changes |
|---|---|---|---|---|---|
| Osteosarcoma [48] | Information Missing | Information Missing | Increased number and size in U2OS & MG63 | Information Missing | Information Missing |
| Pancreatic Cancer [12] | Promotes S-phase entry & proliferation | Information Missing | Enables sphere formation in permissive lines | Increased ALDH1, ESA, CD44 | Induction of Cyclin D3; repression of E-Cadherin, ZO-1 |
| Glioma [22] | Promotes tumor growth in vivo | Information Missing | Promotes self-renewal | Information Missing | Activates EGFR/PI3K/AKT signaling pathway |
Table 3: Correlation of SOX2 Expression with Clinical Outcomes
| Cancer Type | Expression in Tumor vs. Normal | Correlation with Survival | Association with Clinical Features |
|---|---|---|---|
| Osteosarcoma [48] | Significantly higher in tumor tissues | SOX2-high linked to poor overall survival | Correlated with lung metastasis, ALP levels, chemoresistance |
| Pancreatic Cancer [12] | Ectopic expression in 19.3% of tumors | Information Missing | Observed in high-grade cancer, adenosquamous, anaplastic tumors |
| Glioma [22] | Information Missing | Co-expression with Par6 predicts poor outcomes | Information Missing |
Elucidating Molecular Mechanisms: Signaling Pathways and Interactions
Functional manipulation of SOX2 has been instrumental in mapping its position within critical oncogenic signaling networks. Two key mechanisms are highlighted below: the post-translational regulation of SOX2 stability and its role in a transcriptional complex regulating stemness.
AKT-Mediated Stabilization of SOX2
In osteosarcoma, a kinase inhibitor screen identified AKT as a critical kinase essential for robust SOX2 expression [48]. Subsequent mechanistic studies revealed that AKT does not affect SOX2 transcription but instead promotes its protein stability. AKT binds to and phosphorylates SOX2 at the threonine 116 (T116) residue. This phosphorylation event prevents the association of SOX2 with the E3 ubiquitin ligases UBR5 and STUB1, thereby blocking SOX2 ubiquitination and subsequent proteasome-dependent degradation [48]. This AKT-SOX2 axis was shown to be a significant modulator of cancer stemness and chemoresistance. The functional validation for this mechanism came from knockdown experiments, where AKT knockdown dramatically reduced the half-life of the SOX2 protein from ~9 hours to less than 6 hours, an effect that could be blocked by the proteasome inhibitor MG132 [48].
Diagram 1: AKT phosphorylation stabilizes SOX2 to promote stemness.
Par6/SOX2 Interaction in Glioma Stemness
In glioma, the polarity protein Par6 was found to interact directly with SOX2 to modulate stemness maintenance in GSCs [22]. The physical interaction between Par6 and SOX2 promotes stemness in a complementary manner. Mechanistically, this complex transcriptionally regulates the EGFR gene, leading to the activation of the downstream PI3K/AKT signaling cascade. This pathway was identified as a key downstream target through RNA-seq analysis of U87MG glioma cells overexpressing Par6. The functional significance was demonstrated by using a specific inhibitory peptide (Par6i-P1) to disrupt the Par6/SOX2 interaction. This disruption significantly suppressed GSC stemness, and, in combination with Temozolomide (TMZ), it enhanced the inhibition of glioma xenograft growth, indicating a reversal of chemotherapy resistance [22].
Diagram 2: Par6/SOX2 interaction drives stemness via EGFR/PI3K/AKT.
The Scientist's Toolkit: Essential Reagents for SOX2 Functional Studies
Table 4: Key Research Reagent Solutions for SOX2 Functional Assays
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| SOX2 shRNA Lentiviral Particles | Stable knockdown of SOX2 expression | Validating necessity of SOX2 for proliferation and sphere formation in osteosarcoma and pancreatic cancer cells [48] [12]. |
| SOX2 Overexpression Lentivirus | Ectopic expression of SOX2 cDNA | Testing sufficiency of SOX2 to drive stemness in low-SOX2 expressers like U2OS cells [48]. |
| Anti-SOX2 Antibody | Detection of SOX2 protein via Western Blot, IHC, IF | Validating knockdown/overexpression efficiency; assessing SOX2 protein levels in clinical samples [48] [12]. |
| AKT Inhibitor (e.g., MK2206) | Pharmacological inhibition of AKT kinase | probing the AKT-SOX2 stability axis; demonstrating downregulation of SOX2 protein in a dose-dependent manner [48]. |
| Par6/SOX2 Inhibitory Peptide (Par6i-P1) | Disruption of protein-protein interaction | Targeting the Par6/SOX2 complex to mitigate glioma stemness and TMZ resistance [22]. |
| Proteasome Inhibitor (e.g., MG132) | Blocks proteasomal degradation | Confirming that SOX2 downregulation upon AKT inhibition occurs via the proteasome pathway [48]. |
| Temozolomide (TMZ) / Cisplatin | Chemotherapeutic agents for in vitro and in vivo studies | Assessing the role of SOX2 in mediating chemoresistance in glioma and osteosarcoma models [48] [22]. |
| 2,2-Dimethyl-5-oxooctanal | 2,2-Dimethyl-5-oxooctanal|C8H14O2|RUO | 2,2-Dimethyl-5-oxooctanal is a high-purity keto-aldehyde for research, like organic synthesis. For Research Use Only. Not for human use. |
| Bicyclo[4.3.1]decan-7-one | Bicyclo[4.3.1]decan-7-one|C10H16O | Bicyclo[4.3.1]decan-7-one (C10H16O) is a bridged bicyclic ketone for research applications. This product is For Research Use Only. Not for human or veterinary use. |
The transcription factor SOX2 (SRY-box 2) is a master regulator of embryonic development and stem cell pluripotency essential for maintaining cellular identity. Beyond its physiological roles, SOX2 is a critical driver of tumorigenesis through its ability to promote cellular dedifferentiation and impart stem cell-like features to cancer cells. It facilitates epithelial-to-mesenchymal transition (EMT), enhances tumor initiation, and drives therapy resistance across diverse cancer types, including pancreatic cancer, osteosarcoma, and small cell lung cancer [12] [49] [29]. SOX2 is recognized as a "super pioneer factor" capable of accessing compacted chromatin and modulating the DNA methylation landscape at its binding sites, thereby exerting profound influence on cellular transcription programs [50]. However, its function as a transcription factor makes it notoriously "undruggable," creating an urgent need for innovative therapeutic strategies targeting its regulatory network [49]. This whitepaper examines how high-throughput screening approaches are uncovering vulnerable nodes in the SOX2 pathway, providing new avenues for therapeutic discovery aimed at disrupting SOX2-driven oncogenesis.
High-Throughput Screening Approaches for SOX2 Pathway Discovery
Functional Genetic and Chemical Screens
High-throughput screening technologies enable systematic identification of regulators and potential therapeutic targets within the SOX2 network. Key approaches include:
Kinase Inhibitor Library Screening: Screening of small-molecule kinase inhibitor libraries identifies upstream regulators of SOX2 protein stability. This approach successfully identified AKT as a critical kinase maintaining robust SOX2 expression in osteosarcoma cells [29]. The screening methodology involves treating SOX2-positive cancer cells with a library of kinase inhibitors targeting major cellular kinases, followed by quantification of SOX2 protein levels via western blotting or immunofluorescence.
Highly Parallelized PF Activity Screening: Advanced screening platforms investigate pioneer transcription factor ability to bind methylated DNA and induce DNA demethylation. This approach has categorized SOX2 as a "super pioneer factor" based on its unique capacity to induce passive DNA demethylation at its binding sites, an activity enhanced by co-binding of OCT4 [50].
CRISPR-Based Functional Genomics: Genome-wide CRISPR screens help identify genetic dependencies and synthetic lethal interactions in SOX2-high cancers, though specific protocols were not detailed in the available search results.
Table 1: Key High-Throughput Screening Platforms for SOX2 Pathway Discovery
| Screening Platform | Key Discovery | Experimental Readout | Biological Significance |
|---|---|---|---|
| Kinase inhibitor library | AKT stabilizes SOX2 protein | SOX2 protein levels via western blot | Identified druggable kinase regulating SOX2 stability |
| Pioneer factor activity screening | SOX2 induces passive DNA demethylation | DNA methylation status at binding sites | Revealed epigenetic mechanism of SOX2 pioneering activity |
| Chemical library screening | HDAC inhibitors target drug-tolerant state | Viable cell count with EGFR inhibition | Uncovered strategy to overcome SOX2-mediated drug tolerance |
Genomic Mapping of SOX2 Regulatory Networks
Comprehensive mapping of SOX2 binding sites and transcriptional targets provides critical insights into its oncogenic functions:
Chromatin Immunoprecipitation Sequencing (ChIP-Seq): This powerful technique combines chromatin immunoprecipitation with next-generation sequencing to investigate SOX2-DNA interactions genome-wide. In small cell lung cancer (SCLC), ChIP-Seq analysis has revealed SOX2 binding to critical regulatory regions influencing oncogenic pathways, including genes such as ESR1, CPE, BASP1, and tubulin genes [51].
Experimental Workflow: The standard ChIP-Seq protocol involves: (1) cross-linking proteins to DNA in living cells; (2) chromatin fragmentation by sonication; (3) immunoprecipitation with SOX2-specific antibodies; (4) library preparation and high-throughput sequencing; (5) bioinformatic analysis to identify enriched binding regions.
Diagram 1: ChIP-Seq Workflow for SOX2 Binding Site Identification
SOX2 in Cellular Dedifferentiation and Stemness
Mechanisms of Dedifferentiation
Within the context of cellular dedifferentiation research, SOX2 functions as a master regulator that reprograms differentiated cells toward stem-like states through multiple mechanisms:
Direct Transcriptional Control of EMT Regulators: SOX2 directly binds to promoters of key EMT transcription factors including Snail, Slug, and Twist, leading to loss of epithelial markers (E-cadherin, ZO-1) and acquisition of mesenchymal characteristics [12]. This EMT program is intimately linked with dedifferentiation and stemness acquisition.
Cell Cycle Regulation: SOX2 promotes S-phase entry and cell proliferation through cyclin D3 induction while suppressing cell cycle inhibitors p21Cip1 and p27Kip1, establishing a proliferative foundation for dedifferentiated cell states [12].
Cancer Stem Cell Population Maintenance: SOX2 is enriched in and essential for pancreatic cancer stem cell (CSC) populations characterized by markers ALDH1, ESA, and CD44. SOX2 knockdown significantly inhibits self-renewal capabilities in epithelial PDAC cell variants [12] [52].
SOX2-Mediated Signaling in Dedifferentiation
The molecular pathways through which SOX2 promotes dedifferentiation represent potential intervention points for therapeutic targeting:
Diagram 2: SOX2-Associated Signaling in Dedifferentiation
Key Signaling Pathways and Regulatory Networks
AKT-SOX2 Axis
The AKT-SOX2 signaling axis represents one of the most promising therapeutic targets emerging from high-throughput screens:
AKT-Mediated SOX2 Stabilization: AKT binds and phosphorylates SOX2 at threonine 116, preventing SOX2 ubiquitination and subsequent proteasome-dependent degradation by E3 ligases UBR5 and STUB1 [29]. This post-translational regulation represents a key mechanism maintaining high SOX2 levels in cancers.
Therapeutic Implications: Combined inhibition of AKT (using MK2206) with conventional chemotherapy (cisplatin) demonstrates synergistic inhibition of osteosarcoma tumor growth in patient-derived xenograft (PDX) models, providing preclinical validation for this combinatorial approach [29].
SOX2 in Drug Tolerance and Resistance
High-throughput transcriptional analyses have revealed SOX2 induction as an adaptive survival mechanism in multiple cancer contexts:
EGFR-Mutant Lung Cancer: SOX2 is rapidly induced following erlotinib treatment in EGFR-mutant non-small cell lung cancers through relief of EGFR-dependent suppression of FOXO6. SOX2 in turn represses pro-apoptotic BH3-only genes BIM and BMF, attenuating oncogene addiction-mediated cell death [53].
Experimental Evidence: siRNA-mediated SOX2 knockdown sensitizes cells to erlotinib-induced apoptosis and decreases acquired resistance, while SOX2 overexpression reduces drug-induced cell death, functionally validating its role in drug tolerance [53].
Table 2: Experimentally Validated SOX2-Regulated Processes in Cancer
| Cellular Process | SOX2 Function | Experimental Model | Key Regulated Genes |
|---|---|---|---|
| Cell cycle progression | Promotes G1/S transition | Pancreatic cancer cells | Cyclin D3 induction; p21Cip1/p27Kip1 repression |
| EMT and invasion | Induces mesenchymal transition | Pancreatic cancer, colorectal cancer | Snail, Slug, Twist; E-cadherin loss |
| Apoptosis evasion | Suppresses pro-apoptotic signals | EGFR-mutant lung cancer | BIM, BMF repression |
| Stemness maintenance | Enriches CSC populations | Osteosarcoma, pancreatic cancer | ALDH1, CD44, ESA upregulation |
| Drug tolerance | Promotes survival during treatment | Multiple cancer types | FOXO6-mediated survival pathways |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX2 Pathway Investigation
| Reagent Category | Specific Examples | Research Application | Functional Outcome |
|---|---|---|---|
| SOX2 knockdown reagents | siRNA, shRNA against SOX2 | Loss-of-function studies | Reduced proliferation, sphere formation, and tumorigenicity |
| Kinase inhibitors | MK2206 (AKT inhibitor) | Target validation | Decreased SOX2 protein stability and stemness |
| Proteasome inhibitors | MG132 | Protein turnover studies | Blocks AKT inhibition-mediated SOX2 degradation |
| Chromatin IP reagents | SOX2 antibodies | Genomic binding studies | Mapping SOX2 target genes and binding sites |
| Cell culture models | H29, H82 (SCLC); Panc1, Panc89 (PDAC) | Disease modeling | Study SOX2 in different cancer contexts |
High-throughput screening approaches have fundamentally advanced our understanding of the SOX2 pathway, revealing its central role in cellular dedifferentiation and identifying promising therapeutic targets. The AKT-SOX2 axis represents a particularly compelling target given the clinical availability of AKT inhibitors and compelling preclinical evidence supporting their combination with conventional chemotherapy. Future efforts should focus on developing more sophisticated screening platforms that better model the tumor microenvironment and cancer stem cell niches where SOX2 functions. Additionally, advancing technologies to directly target transcription factors, such as proteolysis-targeting chimeras (PROTACs) or protein-protein interaction inhibitors, may eventually overcome the "undruggable" nature of SOX2 itself. As screening technologies continue to evolve, they will undoubtedly uncover additional vulnerable nodes in the SOX2 network, providing new therapeutic opportunities for targeting SOX2-driven cancers.
Overcoming Research and Therapeutic Hurdles in SOX2 Biology
Challenges in Achieving Stable and Controlled SOX2 Expression for Reprogramming
The transcription factor SOX2 is a cornerstone of cellular reprogramming, essential for inducing pluripotency and driving dedifferentiation. However, its therapeutic application is fraught with a fundamental challenge: its function is exquisitely dosage-dependent [54] [55]. Achieving stable and controlled SOX2 expression is not merely a technical hurdle but a critical determinant between successful reprogramming and unintended consequences like differentiation, senescence, or tumorigenesis [54] [9] [56]. Within the context of cellular dedifferentiation research, mastering SOX2 expression is paramount for harnessing its potential in regenerative medicine while mitigating the risks associated with its dysregulation. This guide delves into the molecular basis of these challenges and outlines experimental strategies for overcoming them, providing a framework for researchers and drug development professionals working at the forefront of reprogramming technologies.
The Fundamental Challenge: SOX2 Dosage Sensitivity
The core challenge in manipulating SOX2 for reprogramming is its narrow therapeutic window. SOX2 does not operate as a simple on-off switch; instead, its effects are governed by precise concentration thresholds that dictate cellular fate.
Consequences of Dosage Imbalance
- Elevated SOX2 Expression: Even a modest increase in SOX2 levels (approximately 2-fold or less) can induce differentiation of embryonic stem cells (ESCs) into multiple cell lineages, including neuroendoderm, mesoderm, and trophectoderm [54]. In the context of reprogramming somatic cells into induced pluripotent stem cells (iPSCs), elevated SOX2 expression paradoxically reduces reprogramming efficiency and increases the generation of partially reprogrammed cells [54].
- Reduced SOX2 Expression: Knocking down SOX2 in ESCs disrupts self-renewal and promotes differentiation [54] [9]. In somatic cells, insufficient SOX2 levels fail to initiate or complete the reprogramming process, underscoring its non-negotiable role in establishing pluripotency.
Table 1: Consequences of SOX2 Dosage Imbalance in Cellular Models
| Cellular System | SOX2 Level | Observed Outcome | Reference |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Increased (~2-fold) | Differentiation into multiple cell types | [54] |
| Somatic Cell Reprogramming | Increased | Reduced reprogramming efficiency; more partially reprogrammed cells | [54] |
| ESCs / Osteoblasts | Decreased | Induction of differentiation; senescence-like phenotype | [54] [9] |
| Pancreatic Cancer Cells | Knockdown | Cell growth inhibition & G0/G1 cell cycle arrest | [12] |
This dosage sensitivity extends beyond in vitro models into development and disease. During mammalian development, Sox2 levels influence major cell fate decisions in organs including the eye, brain, esophagus, stomach, and lung [54] [55]. In cancer, tumor cells appear to optimize SOX2 levels to maximize growth, as both too little and too much SOX2 can suppress tumor cell proliferation [56].
Molecular Mechanisms Governing SOX2 Protein Homeostasis
The cellular levels of SOX2 are regulated by a multi-layered network of controls at the transcriptional, post-transcriptional, and post-translational levels. Understanding these mechanisms is a prerequisite for developing strategies to achieve controlled expression.
Post-Translational Regulation and Protein Turnover
The stability of the SOX2 protein is dynamically regulated by a balance of ubiquitin ligases and deubiquitylating enzymes (DUBs). This represents a critical fast-acting control mechanism for SOX2 dosage.
- Key E3 Ubiquitin Ligases Promoting SOX2 Degradation:
- CUL4ADET1-COP1 Complex: This Cullin-RING ligase (CRL) complex is a major regulator of SOX2 stability in neural progenitor cells (NPCs). The substrate receptor COP1 (RFWD2) directly interacts with and ubiquitylates SOX2, targeting it for proteasomal degradation. The expression of CUL4A and COP1 increases during NPC differentiation, correlating with declining SOX2 protein levels [57].
- WWP2: A HECT-type E3 ligase identified as a genuine SOX2-targeting ligase in glioblastoma stem cells (GSCs) and ESCs. It promotes SOX2 polyubiquitylation and degradation [58] [57].
- Key Deubiquitylating Enzyme Stabilizing SOX2:
- OTUD7B (Cezanne-1): This DUB removes polyUb chains from SOX2, thereby increasing its stability. Its expression declines alongside SOX2 during NPC differentiation, and its knockdown destabilizes SOX2 and induces differentiation [57].
- Competitive Stabilization Mechanism:
- TRIM26: An E3 ligase that, in GSCs, stabilizes SOX2 via a non-canonical mechanism. TRIM26 competes with WWP2 for binding to SOX2. By occupying the interaction site, TRIM26 acts as a competitive inhibitor of WWP2-mediated ubiquitylation, thereby protecting SOX2 from degradation [58].
The following diagram illustrates this dynamic regulatory network:
Experimental Strategies for Controlled SOX2 Expression
To navigate SOX2's dosage sensitivity, researchers must employ precise experimental strategies. The following table summarizes key reagents and their applications in studying SOX2.
Table 2: Research Reagent Solutions for SOX2 Regulation Studies
| Reagent / Tool | Function / Mechanism | Experimental Application |
|---|---|---|
| Doxycycline-Inducible Promoter Systems | Enables precise temporal control over SOX2 transgene expression [54]. | Titrating SOX2 expression levels to determine optimal dosage for reprogramming without inducing differentiation [54]. |
| Lentiviral shRNA (e.g., targeting CUL4A, COP1) | Knocks down specific E3 ubiquitin ligases [57]. | Stabilizing endogenous SOX2 protein to study its effects on stem cell maintenance and delay differentiation [57]. |
| Lentiviral shRNA (e.g., targeting OTUD7B) | Knocks down the stabilizing deubiquitylase [57]. | Destabilizing endogenous SOX2 to probe its necessity in stemness and to induce differentiation in NPCs [57]. |
| COP1 Overexpression Vector | Increases expression of the SOX2-targeting ubiquitin ligase complex component [57]. | Accelerating SOX2 protein turnover to study exit from pluripotency and initiation of differentiation. |
| SOX2 Deletion Mutants (e.g., ΔC-terminal TA) | Lacks transactivation domains or β-catenin binding regions [9]. | Dissecting the structural domains of SOX2 required for self-renewal vs. inhibition of differentiation pathways like Wnt [9]. |
| Proteasome Inhibitor (e.g., MG132) | Blocks the proteasome-mediated degradation of ubiquitylated proteins [57]. | Confirming SOX2 degradation via the ubiquitin-proteasome system and detecting endogenous ubiquitylated SOX2. |
Detailed Methodologies for Key Experiments
Quantifying SOX2 Protein Turnover During Cell State Transitions
This protocol is critical for understanding how SOX2 stability changes during processes like differentiation, which is fundamental to overcoming instability in reprogramming.
- Induction of Differentiation: Culture neural progenitor cells (NPCs) in neural induction medium. Plate neurospheres on Matrigel-coated plates to initiate neuronal differentiation. A successful differentiation is marked by an increase in neuronal marker TUJ1 (β-tubulin III) over a time course (e.g., 9 days) [57].
- Cycloheximide (CHX) Chase Assay: At various time points during differentiation, treat cells with the protein synthesis inhibitor CHX (e.g., 100 µg/mL).
- Sample Collection and Analysis: Harvest cell lysates at defined intervals after CHX treatment (e.g., 0, 30, 60, 90 minutes). Perform Western Blot analysis using anti-SOX2 antibodies. Use housekeeping proteins (e.g., Actin) for normalization.
- Data Interpretation: Quantify band intensities to determine the half-life of SOX2. As differentiation proceeds, the half-life of SOX2 is significantly shortened, indicating increased protein turnover [57].
Manipulating SOX2 Stability via the Ubiquitin-Proteasome System (UPS)
This methodology allows direct interrogation of the specific enzymes controlling SOX2 proteostasis.
- Genetic Perturbation of E3 Ligases/DUBs:
- Functional Validation:
- Western Blotting: Confirm changes in SOX2 protein levels 72-96 hours post-transduction.
- Immunoprecipitation (IP): To detect SOX2 ubiquitylation, lyse cells treated with MG132 (10 µM, 4-6 hours) in a mild lysis buffer (e.g., 0.5% Triton X-100). Immunoprecipitate SOX2 and probe the blot with an anti-Ubiquitin antibody [57].
- Phenotypic Assays:
- Sphere-Formation Assay: Seed transduced cells at low density in non-adherent plates with serum-free medium. Count the number and size of spheres formed after 7-10 days. This assesses self-renewal capacity, which is maintained by stable SOX2 [9] [57] [12].
- Differentiation Markers: Analyze the expression of differentiation markers (e.g., TUJ1 for neurons) via immunofluorescence or qRT-PCR following manipulation of UPS components.
The experimental workflow for investigating SOX2 stability is summarized below:
Therapeutic Implications and Future Perspectives
The challenges of controlling SOX2 expression are not confined to basic research but directly impact its potential as a therapeutic target, particularly in oncology and regenerative medicine.
SOX2 in Cancer and Drug Resistance
In many cancers, SOX2 is overexpressed or amplified and is associated with poor patient prognosis [55] [56]. It confers cancer stem cell (CSC)-like properties, including self-renewal, tumor initiation, and drug resistance [12] [56]. SOX2 promotes resistance to therapies like EGFR-TKIs in non-small cell lung cancer by facilitating epithelial-to-mesenchymal transition (EMT) and metabolic reprogramming [59]. Therefore, strategies to destabilize SOX2 or inhibit its function are actively pursued. Targeting its stabilizing regulators, such as TRIM26, or enhancing the activity of degradative complexes, could sensitize tumors to treatment [58] [57] [55].
The Future of SOX2 Control in Reprogramming
For safe and effective reprogramming, future strategies must move beyond simple overexpression. These include:
- Inducible Systems with Fine Control: Utilizing advanced, titratable gene expression systems that allow for precise adjustment of SOX2 levels during different stages of reprogramming and differentiation.
- Exploiting Endogenous Regulation: Using small molecules or genetic tools to transiently modulate the activity of endogenous SOX2 regulators (e.g., OTUD7B, COP1) to boost reprogramming efficiency without genomic integration of transgenes.
- Synthetic Biology Approaches: Designing engineered SOX2 variants with altered stability or activity that can be controlled by exogenous small molecules, providing a safety switch for therapeutic applications.
In conclusion, the path to harnessing SOX2's power in dedifferentiation research is through a deep understanding and meticulous control of its expression. By respecting its dosage sensitivity and leveraging the growing knowledge of its complex regulation, researchers can overcome these challenges to unlock new frontiers in regenerative medicine and cancer therapy.
Addressing Tumorigenic Risk and Safety in SOX2-Based Cell Therapies
The transcription factor SOX2 is a master regulator of cellular pluripotency and self-renewal, playing an indispensable role during embryonic development and in maintaining stem cell fate [26] [55]. Its ability to promote cellular dedifferentiation and reprogram somatic cells into induced pluripotent stem cells (iPSCs) has positioned SOX2 as a pivotal factor in regenerative medicine [60]. However, this very capability confers significant tumorigenic risk, as aberrant SOX2 expression is a well-documented driver in numerous cancers [34] [61]. The oncogenic potential of SOX2 stems from its capacity to promote sustained proliferation, inhibit apoptosis, induce epithelial-mesenchymal transition (EMT), and maintain cancer stem cell (CSC) populations that drive tumor initiation, progression, and therapy resistance [62] [12]. This technical guide comprehensively addresses the tumorigenic risks associated with SOX2-based cell therapies and provides a framework for safety assessment and risk mitigation strategies essential for therapeutic development.
Molecular Mechanisms of SOX2-Mediated Tumorigenesis
SOX2 Amplification and Overexpression in Human Cancers
SOX2 is located on chromosome 3q26.3, a region frequently amplified in various carcinomas [34]. Gene amplification and subsequent protein overexpression are established mechanisms of SOX2 dysregulation in human cancers. Elevated SOX2 levels are associated with poor prognosis across multiple cancer types due to its role in maintaining stemness and driving aggressive tumor phenotypes [55].
Table 1: SOX2 Amplification and Overexpression in Human Cancers
| Cancer Type | SOX2 Genetic Alteration | Key Tumorigenic Effects | Clinical Association |
|---|---|---|---|
| Small Cell Lung Cancer | Frequent amplification [34] | Cell proliferation, survival, migration [34] | Poor prognosis [55] |
| Lung Squamous Cell Carcinoma | Co-amplification with PRKCI, FGFR1 [34] | Cancer stem cell phenotype [34] | Increased aggressiveness |
| Esophageal SCC | Amplification [34] | Cell proliferation, tumor growth [34] | Advanced disease |
| Glioblastoma | Amplification and promoter hypomethylation [34] | Invasion, migration, self-renewal [34] | Therapy resistance |
| Head and Neck SCC | Amplification at 3q26 [63] | Tumor initiation, progression [63] | Early predictor of cancer risk [63] |
| Prostate Cancer | Overexpression (not amplification) [62] | Therapy resistance, neuroendocrine differentiation [62] | Castration resistance, poor outcome [62] |
Signaling Pathways Regulated by SOX2
SOX2 operates within an extensive regulatory network, interacting with key transcription factors, non-coding RNAs, and epigenetic modifications to control numerous oncogenic signaling pathways [62]. The diagram below illustrates the major signaling pathways through which SOX2 exerts its tumorigenic effects.
SOX2 in Cancer Stem Cells and Cellular Dedifferentiation
SOX2 is a critical regulator of cancer stem cells (CSCs), a subpopulation within tumors responsible for self-renewal, tumor propagation, and therapeutic resistance [12]. In pancreatic cancer, SOX2 imparts stem cell-like features and promotes dedifferentiation through direct binding to promoters of EMT transcription factors Snail, Slug, and Twist, resulting in loss of epithelial markers E-Cadherin and ZO-1 [12]. This dedifferentiation capacity, while valuable for cellular reprogramming in regenerative applications, represents a significant safety concern in therapeutic contexts, as it can potentially initiate malignant transformation in previously differentiated cells.
Assessing Tumorigenic Risk in SOX2-Based Therapies
Quantitative SOX2 Detection Methodologies
Accurate measurement of SOX2 expression is crucial for risk assessment. The following experimental protocols outline standardized methods for SOX2 detection and quantification.
Protocol 1: Quantitative Real-Time PCR (qRT-PCR) for SOX2 mRNA Detection
- Principle: Quantifies SOX2 transcript levels using sequence-specific amplification.
- Sample Requirements: 500 ng total RNA from test cells or tissue.
- Primer Sequences:
- Forward: 5′-CTCCGGGACATGATCAGC-3′
- Reverse: 5′-CTGGGACATGTGAAGTCTGC-3′ [63]
- Reference Gene: COL7A1 or GAPDH [63] [64]
- Reaction Setup: Use SYBR Green Master Mix on a standardized real-time PCR system.
- Data Analysis: Calculate relative expression using the 2^(-ΔΔCt) method [64].
- Quality Control: Include no-template controls, assess RNA integrity (A260/A280 ratio 1.8-2.0), and perform reactions in technical duplicates [64].
Protocol 2: Immunohistochemistry (IHC) for SOX2 Protein Localization
- Principle: Visualizes nuclear SOX2 protein expression in tissue sections.
- Antibody: Anti-SOX2 rabbit polyclonal antibody (e.g., Merck Millipore #AB5603) at 1:1000 dilution [63].
- Staining Platform: Automated staining workstation with EnVision Flex+ Visualization System.
- Antigen Retrieval: High-pH target retrieval solution.
- Quantification: Score as percentage of cells with definitive nuclear staining. A validated cut-off of >12.5% positive cells is associated with increased cancer risk [63].
Protocol 3: Chromatin Immunoprecipitation (ChIP) for SOX2 Target Gene Analysis
- Principle: Identifies direct genomic binding sites of SOX2 protein.
- Cell Fixation: Crosslink proteins to DNA with 1% formaldehyde for 10 minutes.
- Immunoprecipitation: Use anti-SOX2 antibody to pull down bound DNA fragments.
- Analysis: Quantify specific target gene promoters (e.g., p21Cip1, p27Kip1, Snail, Slug, Twist) by qPCR [12].
- Application: Determines if SOX2 is appropriately regulating its target genes or driving oncogenic programs.
Functional Assays for Tumorigenic Potential
Table 2: Functional Assays for Assessing SOX2-Mediated Tumorigenicity
| Assay Type | Experimental Readout | Tumorigenic Indication | Key Methodological Considerations |
|---|---|---|---|
| Soft Agar Colony Formation | Number and size of colonies growing in anchorage-independent conditions [60] [34] | Increased transformation potential | Count colonies >50μm after 3-4 weeks; compare to control cells |
| Sphere Formation Assay | Number and size of spheres in non-adherent culture [12] | Enhanced self-renewal and cancer stem cell activity | Use serum-free medium with growth factors; assess serial passaging capability |
| Xenograft Tumorigenicity | Tumor incidence, volume, and growth rate in immunodeficient mice [60] | In vivo tumor formation capacity | Monitor for 8-12 weeks; histologically analyze resulting tumors |
| Invasion/Migration Assay | Cell penetration through Matrigel-coated membranes [34] | Metastatic potential | Quantify cells that invade versus migrate through uncoated membranes |
| Drug Resistance Profiling | Viability after chemotherapeutic or targeted agent exposure [62] [55] | Therapy-resistant phenotype | Test multiple drug classes; compare IC50 values to control cells |
Risk Mitigation Strategies for SOX2-Based Therapies
Controlling SOX2 Expression and Delivery
Several technological approaches can minimize oncogenic risk while preserving SOX2's therapeutic potential:
- Transient Expression Systems: Use non-integrating episomal vectors, synthetic mRNA, or protein delivery to achieve temporary SOX2 expression sufficient for reprogramming without genomic integration [55].
- Precise Expression Control: Implement inducible promoter systems (tet-on/off) or lineage-specific promoters that restrict SOX2 expression to specific cell types or time windows.
- Small Molecule Replacements: Identify and use small molecules that can transiently activate endogenous SOX2 or mimic its functional role in reprogramming, eliminating the need for genetic manipulation.
- Combinatorial Factor Balancing: Maintain optimal SOX2 expression levels, as both insufficient and excessive SOX2 can disrupt the pluripotency network and promote differentiation or transformation [26].
Monitoring and Quality Control
Rigorous pre-clinical safety assessment is essential before clinical application of SOX2-based therapies:
- Comprehensive Genomic Analysis: Perform whole-genome sequencing to rule out insertional mutagenesis and off-target effects in genetically modified cells.
- Transcriptomic Profiling: Use RNA-seq to verify that SOX2-expressing cells maintain appropriate gene expression patterns without activation of oncogenic signatures.
- Long-Term Observation: Monitor cell populations in vitro and in animal models for extended periods (≥3 months) to detect delayed transformation events.
- Elimination Strategies: Incorporate suicide genes (e.g., herpes simplex virus thymidine kinase) or cell surface markers that enable selective ablation of transplanted cells if tumor formation occurs.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for SOX2 Tumorigenicity Research
| Reagent Category | Specific Examples | Research Application | Safety Assessment Utility |
|---|---|---|---|
| SOX2 Detection Antibodies | Anti-SOX2 rabbit polyclonal (Merck Millipore #AB5603) [63] | IHC, Western blot, immunofluorescence | Quantify SOX2 protein expression in target cells |
| SOX2 Modulators | LSD1 inhibitor (CBB1007) [60], Neddylation inhibitor (MLN4924/Pevonedistat) [60] | Pathway manipulation, SOX2 inhibition | Test dependency on SOX2 signaling; potential safety switch |
| qPCR Assays | Validated primer sets [63], SYBR Green Master Mix | SOX2 mRNA quantification | Monitor SOX2 expression levels during therapy development |
| Cell Line Models | SOX2-amplified cancer lines (lung, esophageal SCC) [34], Inducible SOX2 overexpression systems [12] | Mechanism studies, control experiments | Compare oncogenic versus therapeutic SOX2 expression |
| Pathway Reporters | Wnt/β-catenin, STAT3, or EMT responsive luciferase constructs [10] | Signaling pathway activation | Monitor oncogenic pathway activity in SOX2-expressing cells |
| In Vivo Models | Immunodeficient mice (NSG, nude) [60] | Tumorigenicity testing | Assess in vivo tumor formation potential of SOX2-modified cells |
The therapeutic application of SOX2 represents a double-edged sword, balancing its remarkable capacity for cellular reprogramming against its well-established oncogenic potential. Ensuring the safety of SOX2-based cell therapies requires a multi-faceted approach that includes precise control of SOX2 expression levels, comprehensive pre-clinical tumorigenicity assessment using the methodologies outlined herein, and implementation of fail-safe mechanisms to eliminate potentially dangerous cell populations. As research advances, developing strategies to temporally and spatially restrict SOX2 activity, or to identify small molecule substitutes that can transiently mimic its reprogramming functions, will be crucial for harnessing SOX2's regenerative potential while minimizing the risk of iatrogenic tumorigenesis. The experimental frameworks and safety assessment protocols provided in this technical guide establish a foundation for the responsible development of SOX2-based cellular therapies.
The transcription factor SOX2 is a pivotal regulator of embryonic development and stem cell pluripotency. In cancer, however, SOX2 displays a remarkable functional duality, acting as either an oncogene or a tumor suppressor in a context-dependent manner. This whitepaper synthesizes current research on the mechanisms underlying SOX2's dual roles in cancer biology, focusing on its regulation of stemness, cell cycle progression, epithelial-to-mesenchymal transition (EMT), and epigenetic plasticity. We provide comprehensive experimental protocols for investigating SOX2 function, detailed signaling pathway diagrams, and essential research reagent solutions to support drug development efforts targeting SOX2 in human malignancies.
SOX2 (SRY-box transcription factor 2) is a member of the SOX family of transcription factors characterized by a high-mobility group (HMG) DNA-binding domain. Located on chromosome 3q26.3-q27, SOX2 encodes a 317-amino acid protein that functions as a key pluripotency regulator during embryonic development [65] [26]. While SOX2 is essential for maintaining embryonic stem cell identity and tissue homeostasis, its dysregulation has been increasingly implicated in tumorigenesis. The oncogenic versus tumor suppressor functions of SOX2 depend on multiple factors, including cellular context, genetic background, tumor type, and microenvironmental influences. Understanding this duality is critical for developing targeted therapeutic strategies.
SOX2 as an Oncogene: Mechanisms and Evidence
Stemness Maintenance and Cellular Reprogramming
SOX2 contributes to cancer stem cell (CSC) maintenance across multiple malignancies. In pancreatic ductal adenocarcinoma (PDAC), SOX2 is aberrantly expressed in 19.3% of human tumors and is enriched in the ESA+/CD44+ CSC population [5]. SOX2 knockdown experiments demonstrate its critical role in maintaining stemness properties through direct regulation of core stemness factors.
Table 1: SOX2 Expression in Human Cancers with Oncogenic Functions
| Cancer Type | Expression Pattern | Functional Consequences | Clinical Correlation |
|---|---|---|---|
| Pancreatic Cancer | Ectopic expression in 19.3% of tumors [5] | Enhanced proliferation, stemness, EMT | Associated with high-grade disease [5] |
| Lung Cancer | Upregulated in lung adenocarcinoma and squamous cell carcinoma [23] | Promotion of tumor growth and survival | Poor prognosis [23] |
| Glioblastoma | Upregulated [23] | Maintenance of glioma stem cells | Poor prognosis [23] |
| Prostate Cancer | Overexpressed [65] | Enhanced invasion, metastasis, treatment resistance | Marker for lymph node metastasis [65] |
| Bladder Cancer | High SOX2 in stem cell subpopulation [66] | Self-renewal, lineage plasticity, invasion | Correlates with tumor progression [66] |
Cell Cycle Regulation and Proliferation
SOX2 promotes cell cycle progression by directly repressing cyclin-dependent kinase inhibitors. In pancreatic cancer cells, SOX2 knockdown induces cell cycle arrest at G0/G1 phase associated with increased p21Cip1 and p27Kip1 expression [5]. Chromatin immunoprecipitation experiments confirm SOX2 binding at both p21Cip1 and p27Kip1 promoters, demonstrating direct transcriptional repression [5]. Conversely, SOX2 overexpression promotes S-phase entry and cell proliferation through cyclin D3 induction [5].
Epithelial-to-Mesenchymal Transition and Metastasis
SOX2 promotes metastatic progression by regulating EMT regulators. In pancreatic cancer models, SOX2 directly binds to Snail, Slug, and Twist promoters, leading to E-cadherin and ZO-1 loss [5]. Recent research demonstrates that SOX2 overexpression induces morphological changes associated with EMT and increases cancer cell migration [67]. Analysis of human breast cancer samples confirms the correlation between SOX2 overexpression and metastatic phenotypes [67].
SOX2 as a Tumor Suppressor: Contextual Evidence
Despite extensive evidence supporting SOX2's oncogenic functions, certain contexts reveal tumor-suppressive activities. A pan-cancer analysis identified significant SOX2 downregulation in several malignancies, including colorectal adenocarcinoma, esophageal carcinoma, rectum adenocarcinoma, stomach adenocarcinoma, and testicular germ cell tumors [23]. In these contexts, low SOX2 expression correlates with worse prognosis, suggesting tumor-suppressive functions.
Molecular Mechanisms Governing SOX2 Dualism
Regulatory Networks and Signaling Pathways
SOX2 interacts with multiple signaling pathways that determine its functional output:
Wnt Signaling Pathway: SOX2 inhibits canonical Wnt signaling in human embryonic stem cells (hESCs) by directly transcriptionally regulating important Wnt signaling modulators WLS and SFRP2 [30]. This regulation maintains pluripotency and suppresses differentiation. Conversely, in hepatocellular carcinoma, DNMT1-mediated regulation activates WNT/β-catenin signaling to sustain CSC maintenance [68].
p53 Regulatory Axis: TP53 transcriptionally represses SOX2 through direct binding to its promoter and SRR2 enhancer regions [67]. TP53 deficiency alleviates SOX2 repression, leading to increased SOX2 expression that promotes EMT and migration [67]. This mechanism explains SOX2 dysregulation in p53-deficient tumors.
Epigenetic Regulation: SOX2 expression is controlled by epigenetic mechanisms including DNA methylation and histone modifications. In acute myeloid leukemia (AML), DNMT1 promotes leukemogenesis by repressing tumor suppressor and differentiation genes through hypermethylation [68]. SOX2 also contributes to epigenetic regulation by interacting with histone variant H2A.Z and recruiting polycomb repressor complex 2 to poise developmental genes in hESCs [30].
Post-Transcriptional Regulation
The m6A reader protein YTHDC2 suppresses SOX2 expression in bladder cancer by recognizing m6A-modified SOX2 mRNA and inhibiting its translation [66]. YTHDC2 depletion increases bladder cancer stem cells, promoting a phenotypic shift toward more invasive subtypes [66]. This pathway represents a crucial post-transcriptional mechanism controlling SOX2-mediated tumor plasticity.
Experimental Approaches for Investigating SOX2 Function
Protocol: Assessing SOX2 Function in Cell Proliferation
Purpose: To evaluate SOX2's role in cancer cell proliferation and cell cycle regulation.
Materials:
- Pancreatic cancer cell lines (e.g., L3.6, CFPAC, BxPC3)
- SOX2 shRNA constructs and scrambled control
- MTT assay kit
- Propidium iodide solution
- Flow cytometer
- qRT-PCR reagents
- Western blot equipment
Methodology:
- SOX2 Knockdown: Transfect cells with SOX2-specific shRNA using appropriate transfection reagent. Include scrambled shRNA as negative control.
- Efficiency Validation: Confirm SOX2 knockdown at 72 hours post-transfection using qRT-PCR and immunoblotting.
- Proliferation Assay: Seed transfected cells in 96-well plates (2,000 cells/well). Perform MTT assay daily for 5 days according to manufacturer's protocol.
- Cell Cycle Analysis: At 48 hours post-transfection, harvest cells, fix in 70% ethanol, and stain with propidium iodide solution. Analyze DNA content by flow cytometry.
- Target Analysis: Evaluate expression of cell cycle regulators p21Cip1 and p27Kip1 by qRT-PCR and western blot.
Expected Results: SOX2 knockdown should reduce cell proliferation, increase G0/G1 phase population, and elevate p21Cip1 and p27Kip1 expression [5].
Protocol: Investigating SOX2-Mediated EMT
Purpose: To determine SOX2's role in epithelial-to-mesenchymal transition.
Materials:
- Appropriate cancer cell lines (e.g., breast cancer, pancreatic cancer)
- SOX2 expression plasmid and empty vector control
- Transwell migration and invasion chambers
- Matrigel matrix
- Antibodies for E-cadherin, N-cadherin, Snail, Slug, Twist
Methodology:
- SOX2 Overexpression: Transfect cells with SOX2 expression plasmid or empty vector.
- Migration/Invasion Assay: Seed transfected cells in serum-free medium into upper chambers (with Matrigel for invasion, without for migration). Add complete medium to lower chamber. Incubate 24-48 hours, then fix and stain migrated cells.
- EMT Marker Analysis: Evaluate EMT markers by western blot and immunofluorescence 72 hours post-transfection.
- Chromatin Immunoprecipitation: Crosslink proteins to DNA, immunoprecipitate with SOX2 antibody, and analyze Snail, Slug, and Twist promoters by qPCR.
Expected Results: SOX2 overexpression should increase migration/invasion, decrease E-cadherin, increase N-cadherin, and enhance SOX2 binding to EMT transcription factor promoters [5] [67].
Signaling Pathway Visualization
Figure 1: SOX2 Regulatory Network. SOX2 is regulated at multiple levels, including translational inhibition by YTHDC2 [66], transcriptional repression by p53 [67], and epigenetic control through DNA methylation [68]. SOX2 protein promotes oncogenic processes including cell cycle progression, EMT, and stemness maintenance [5] [67].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SOX2 Research
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| SOX2 Modulators | pMXs-Sox2-IP (Addgene #15919) [67] | SOX2 overexpression studies | Enforced SOX2 expression |
| LT3GEPIR-shSOX2 [67] | SOX2 knockdown experiments | RNAi-mediated SOX2 suppression | |
| SOX2 Detection | Anti-SOX2 antibodies | Immunoblotting, IHC, ChIP | SOX2 protein detection and localization |
| SOX2-specific primers | qRT-PCR, ChIP-analysis | SOX2 expression and binding assessment | |
| Cell Models | Patient-derived SOX2+ cells [5] | Cancer stem cell studies | Modeling tumor-initiating cells |
| PL-SIN-EOS-C(3+)-EiP [67] | SOX2-high cell enrichment | Isolation of SOX2-expressing populations | |
| Pathway Reporters | Wnt/β-catenin signaling reporters | Pathway activity assessment | Monitoring SOX2-regulated signaling |
| EMT marker antibodies (E-cadherin, N-cadherin) [5] | EMT characterization | Detecting mesenchymal transition |
The dual nature of SOX2 as both oncogene and tumor suppressor presents both challenges and opportunities for therapeutic development. Context-dependent factors including cellular environment, genetic background, and regulatory networks determine SOX2's functional output. Promising therapeutic strategies include targeting SOX2-positive cancer stem cells, exploiting synthetic lethal interactions in SOX2-high tumors, and modulating upstream regulators like YTHDC2 and TP53. Future research should focus on comprehensive mapping of SOX2 interaction networks across different cellular contexts to enable precise targeting of SOX2-driven malignancies. The experimental frameworks and reagent solutions provided herein offer foundational resources for these ongoing investigations.
Strategies to Overcome SOX2-Mediated Therapy Resistance in Cancers
The transcription factor SOX2 is a critical regulator of embryonic development and stem cell maintenance, and its aberrant re-expression in cancers drives tumorigenesis, metastasis, and therapeutic resistance. Its role is particularly pronounced in maintaining cancer stem cell (CSC) populations—a subpopulation of cells with self-renewal capacity, enhanced survival mechanisms, and intrinsic resistance to conventional therapies, leading to tumor relapse and progression [69]. SOX2 contributes to a highly plastic state in cancer cells, enabling them to adapt, evade treatment, and survive therapeutic pressure [70] [71]. This adaptability facilitates lineage plasticity, such as the transformation of prostate adenocarcinomas into aggressive, treatment-resistant neuroendocrine prostate cancer (NEPC) [70] [71]. Overcoming SOX2-mediated resistance is therefore a critical frontier in oncology, requiring strategies that target SOX2 itself, its regulatory pathways, or the vulnerabilities it creates. This guide synthesizes current research to provide a strategic framework for targeting SOX2-mediated resistance, aimed at researchers and drug development professionals.
Mechanisms of SOX2-Mediated Therapy Resistance
Understanding the multifaceted mechanisms by which SOX2 promotes resistance is foundational to developing counter-strategies. SOX2 operates within a complex regulatory network, influencing key oncogenic processes.
Core Functional Roles of SOX2 in Cancer
- Stemness and Self-Renewal: SOX2 is a master regulator of stem cell properties. It enhances tumor sphere formation and maintains the self-renewal capacity of CSCs, as demonstrated in osteosarcoma, glioblastoma, and pancreatic cancer models [29] [16] [52].
- Cell Proliferation and Survival: SOX2 enhances cell viability and proliferation while inhibiting apoptosis [70] [29].
- Invasion and Metastasis: Through regulating epithelial-mesenchymal transition (EMT) and other processes, SOX2 drives invasion and metastatic spread [70] [29].
- Lineage Plasticity: In prostate cancer, SOX2 expression is significantly up-regulated in NEPC and some metastatic castration-resistant prostate cancer (mCRPC) patients, facilitating a cell fate switch that bypasses androgen receptor-targeted therapies [70] [71].
Molecular Drivers of SOX2 Overexpression and Stability
A key mechanism for SOX2 dysregulation in cancer occurs at the post-translational level. The PI3K/AKT signaling pathway is a pivotal regulator of SOX2 protein stability. Research across multiple cancers, including osteosarcoma and ovarian cancer, has established that AKT binds to and phosphorylates SOX2 at threonine 116 (T116). This phosphorylation event prevents SOX2 from being recognized by E3 ubiquitin ligases like UBR5 and STUB1, thereby protecting it from proteasome-dependent degradation and leading to its accumulation in cancer cells [29] [72].
Table 1: Key Mechanisms of SOX2-Mediated Therapy Resistance
| Resistance Mechanism | Molecular/Pathway Involvement | Functional Outcome in Cancer Cells |
|---|---|---|
| Chemoresistance (e.g., Cisplatin) | Upregulated via PI3K/AKT, WNT, Hippo, and TGF-β pathways [73] | Enhanced DNA repair, survival pathway activation, reduced apoptosis |
| Stemness Maintenance | Regulation of PROM1 (CD133), OCT4, NANOG [16] [72] | Self-renewal, tumor initiation, generation of cellular heterogeneity |
| Lineage Plasticity | Interaction with BRN2, ASCL1; loss of RB1 and TP53 [70] [71] | Transdifferentiation to therapy-resistant states (e.g., NEPC) |
| Protein Stabilization | AKT-mediated phosphorylation at T116 [29] [72] | Increased SOX2 protein half-life, sustained oncogenic activity |
| Metabolic Reprogramming | Reprogramming lipid metabolism, enhancing histone acetylation [74] | Epigenetic modulation, creation of super-enhancers |
Strategic Approaches to Overcome SOX2-Mediated Resistance
Given that SOX2 itself is a transcription factor and considered "undruggable," current strategies focus on targeting its regulators, downstream effectors, and associated pathways.
Targeting Upstream Regulators: The AKT-SOX2 Axis
Inhibiting the AKT pathway has emerged as a promising strategy to indirectly target SOX2. Preclinical studies show that AKT inhibitors (e.g., MK2206) or AKT1-specific shRNAs drastically reduce SOX2 protein levels without affecting its mRNA, thereby impairing the growth and stemness of SOX2-positive cancer cells [29] [72]. This approach sensitizes tumor cells to chemotherapy; for instance, combining MK2206 with cisplatin resulted in synergistic and potent inhibition of osteosarcoma tumor growth in a patient-derived xenograft (PDX) model [29].
Disrupting SOX2-Driven Stemness and Signaling
Targeting the downstream functional outputs of SOX2 is another viable approach. This includes:
- Dual Metabolic Inhibition: SOX2 reprograms lipid metabolism to support global histone acetylation and super-enhancer function [74]. Targeting these metabolic dependencies could disrupt SOX2-driven oncogenic programs.
- Immunotherapy-Based Approaches: For cancers with defined CSC surface markers, chimeric antigen receptor (CAR)-T cell therapy has shown preclinical promise. For example, CAR-T cells targeting EpCAM, a CSC marker in prostate cancer, can eliminate CSCs and improve outcomes [69].
- Combination Therapies: An integrative approach combining metabolic reprogramming, immunomodulation, and targeted inhibition is considered essential for developing effective CSC-directed therapies [69].
The following diagram illustrates the core signaling pathway that stabilizes SOX2 and the primary strategic points for therapeutic intervention.
Experimental Protocols for Investigating SOX2 Function and Inhibition
To advance research in this field, standardized and robust experimental methodologies are required. Below are detailed protocols for key assays cited in the literature.
Protocol: CRISPR-Cas9 Screen for SOX2 Regulators
This protocol is adapted from a study identifying SOX2 as a critical regulator of CD133 in glioblastoma stem cells (GSCs) [16].
- Cell Line Preparation: Use primary GSCs or other SOX2-positive cancer stem cells cultured in defined, serum-free neural stem cell medium supplemented with EGF and FGF.
- Library Transduction: Transduce cells with a genome-wide CRISPR knockout library (e.g., TKOv3) at a low Multiplicity of Infection (MOI ~0.3) to ensure single-copy integration. Use a cell number that provides >400-fold coverage per sgRNA.
- Selection and Passaging: 24 hours post-transduction, select transduced cells with puromycin (e.g., 1.2 µg/mL) for 72 hours. Collect an initial sample (e.g., 30 million cells) for genomic DNA extraction as the T0 baseline. Continue to passage the remaining cells in triplicate for approximately 12 population doublings.
- Cell Sorting and Analysis: At the endpoint (T12), use flow cytometry to sort cell populations based on a SOX2-related phenotype (e.g., high vs. low CD133 expression). Collect the top and bottom 5th percentiles.
- Genomic DNA Extraction and Sequencing: Extract genomic DNA from all samples (T0, T12 bulk, T12 high, T12 low). Amplify the integrated sgRNA sequences via PCR and subject them to high-throughput sequencing (e.g., Illumina HiSeq2500).
- Data Analysis: Process sequencing reads to quantify sgRNA abundance. Compare sgRNA enrichment or depletion in the sorted populations against the T0 baseline using specialized software (e.g., drugZ) to identify genes that critically regulate the SOX2-associated phenotype.
Protocol: Assessing Cancer Stem Cell Function via Tumor Sphere Formation
The tumor sphere assay is a cornerstone for evaluating self-renewal and stemness potential, as used in osteosarcoma and pancreatic cancer research [29] [52].
- Single-Cell Suspension: After trypsinization, dissociate cells into a single-cell suspension and quantify.
- Plating: Seed cells at a low density (e.g., 1,000 cells per well) in a low-attachment 96-well plate. Use serum-free medium supplemented with B27, EGF (20 ng/mL), and FGF (10 ng/mL) to selectively support stem cell growth.
- Incubation and Monitoring: Incubate cells at 37°C with 5% CO2 for 5-10 days. Do not disturb the plates to allow for sphere formation.
- Quantification: After 5 days, manually count the number of spheres under a microscope. A sphere is typically defined as a spherical cluster of three or more cells with a clearly defined, smooth border. The number and size of spheres are indicative of the self-renewal capacity of the cell population. SOX2 knockdown has been shown to significantly reduce sphere number and size, while its overexpression enhances these parameters [29].
Protocol: Evaluating SOX2 Protein Stability and AKT Dependence
This protocol is critical for validating the AKT-SOX2 axis and is widely used [29] [72].
- Treatment and Knockdown: Treat SOX2-positive cancer cells (e.g., HOS, OVCAR3) with an AKT inhibitor (MK2206) or transduce with AKT1-specific shRNAs.
- Protein Stability Assay (Cycloheximide Chase):
- After confirming SOX2 downregulation, treat cells with a protein synthesis inhibitor, cycloheximide (e.g., 100 µg/mL).
- Harvest cell lysates at multiple time points post-treatment (e.g., 0, 2, 4, 6, 8 hours).
- Perform Western blotting to detect SOX2 protein levels at each time point. Use β-actin as a loading control.
- Proteasome Inhibition: To confirm degradation is proteasome-dependent, co-treat cells with the AKT inhibitor and a proteasome inhibitor like MG132. Restoration of SOX2 protein levels upon MG132 treatment confirms proteasome-mediated degradation.
- Quantification: Quantify SOX2 band intensity from Western blots, normalize to the loading control, and plot the values over time to calculate the protein's half-life. AKT inhibition typically reduces the half-life of SOX2 from >9 hours to under 6 hours [29].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents used in the featured studies to investigate and target SOX2.
Table 2: Research Reagent Solutions for SOX2 Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| AKT Inhibitor (MK2206) | Allosteric AKT inhibitor; reduces SOX2 protein stability. | Sensitizes SOX2+ osteosarcoma and ovarian cancer cells to platinum drugs [29] [72]. |
| shRNA against AKT1/SOX2 | Knocks down gene expression to validate target dependency. | AKT1 knockdown decreases SOX2 protein, impairing stemness [29] [72]. |
| TKOv3 CRISPR Library | Genome-wide sgRNA library for functional genetic screens. | Identified SOX2 as a key regulator of CD133 in glioblastoma stem cells [16]. |
| CD133/2-PE Antibody | Fluorescently labels CD133 for flow cytometry and cell sorting. | Isolation of CD133+ glioblastoma stem cell populations for functional analysis [16]. |
| Proteasome Inhibitor (MG132) | Inhibits proteasomal degradation; stabilizes short-lived proteins. | Confirms AKT-mediated SOX2 stabilization is proteasome-dependent [29]. |
| siRNA against NES/SOX2 | Transiently knocks down gene expression in vitro. | Validated Nestin and SOX2 as crucial for self-renewal in pancreatic CSCs [52]. |
| Presto Blue Cell Viability Reagent | Fluorescent indicator of metabolic activity and cell proliferation. | Measured proliferation changes in OS cells upon SOX2 knockdown [29] [16]. |
SOX2-mediated therapy resistance represents a significant barrier to durable cancer treatment. The strategic framework outlined herein—encompassing the direct and indirect targeting of SOX2, disruption of its functional outputs, and exploitation of associated vulnerabilities—provides a roadmap for future research and drug development. The consistent finding across multiple cancers that the AKT-SOX2 axis is a key modulator of stemness and chemoresistance offers a particularly promising near-term therapeutic avenue, especially in combination with standard chemotherapy [29] [73] [72]. Future efforts should focus on translating these preclinical findings into clinical trials, developing more potent and specific inhibitors, and exploring novel modalities like synthetic biology-based interventions and engineered immune cells to finally overcome the challenge of SOX2-driven resistance.
Optimizing Delivery Systems for Targeting SOX2 In Vivo
The transcription factor SOX2 is a well-characterized pluripotency factor essential for stem cell self-renewal, reprogramming, and homeostasis. Its role extends beyond normal physiology into pathology, where it is a key driver of cellular dedifferentiation, imparting stem cell-like features to cancer cells. In many human cancers, SOX2 is dysregulated due to gene amplification and protein overexpression, which is associated with poor patient survival [55]. SOX2 promotes tumorigenesis by driving proliferation, survival, invasion, metastasis, cancer stemness, and drug resistance [55]. Crucially, in pancreatic cancer, SOX2 is not expressed in normal acinar or ductal cells but is ectopically expressed in 19.3% of human tumors, where it contributes to stemness and dedifferentiation by regulating genes that control the G1/S cell cycle transition and the epithelial-to-mesenchymal transition (EMT) phenotype [75] [5]. Given that SOX2 is aberrantly expressed in cancer and enriches for cancer stem cell (CSC) populations, targeting SOX2-positive cells constitutes a promising therapeutic strategy for overcoming therapy resistance and preventing tumor recurrence [75]. However, the intrinsic "undruggable" nature of transcription factors like SOX2 presents a significant challenge, making the development of sophisticated in vivo delivery systems paramount for translating anti-SOX2 therapies into clinical success [76] [55].
SOX2 Function and Regulatory Mechanisms in Dedifferentiation
Molecular Structure and Normal Physiological Function
The SOX2 gene is located on chromosome 3p26.3-q27 and encodes a 317-amino acid protein. As a transcription factor, SOX2 contains three critical functional domains:
- A high mobility group (HMG) domain at the N-terminus, responsible for DNA binding.
- A dimerization (DIM) domain at the center.
- A transactivation (TAD) domain at the C-terminus, which regulates the transcription of target genes [55].
SOX2 is a master regulator of embryonic development and stem cell pluripotency. It is one of the core Yamanaka factors capable of reprogramming somatic cells into induced pluripotent stem cells (iPSCs) [55]. It maintains the stem cell phenotype of embryonic stem cells (ESCs) and is critical for the formation of the inner cell mass in the blastocyst. During development, SOX2 plays a dose-dependent role in the specification of multiple lineages, including the central nervous system, foregut endoderm, and several mesodermal tissues [77] [55].
Role in Cellular Dedifferentiation and Cancer Stemness
In the context of cancer, SOX2 reactivation drives a program of cellular dedifferentiation, whereby differentiated cancer cells revert to a more primitive, stem-like state. This process is a hallmark of CSCs, which are responsible for tumor initiation, therapeutic resistance, and metastasis [75] [5].
Key Mechanisms of SOX2-Driven Dedifferentiation:
- Cell Cycle Regulation: SOX2 knockdown in pancreatic cancer cells induces cell cycle arrest at G0/G1 phase, associated with induction of p21Cip1 and p27Kip1. Conversely, SOX2 overexpression promotes S-phase entry and proliferation via cyclin D3 induction [75] [5].
- Stemness Marker Upregulation: SOX2 expression correlates with increased levels of established pancreatic CSC markers, including ALDH1, ESA, and CD44. SOX2 itself is enriched in the ESA+/CD44+ CSC population from patient samples [5].
- EMT Induction: SOX2 directly binds to the promoters of key EMT transcription factors Snail, Slug, and Twist, resulting in loss of epithelial markers E-Cadherin and ZO-1. This promotes a mesenchymal, invasive phenotype [75].
- Transcriptional Network rewiring: SOX2 drives retinogenesis by shaping the enhancer landscape and cooperating with transcription factors like VSX2. This cooperative binding establishes a shared transcriptional code that promotes neural lineage specification while repressing alternative fates [78].
The following table summarizes the core functions of SOX2 in dedifferentiation and their therapeutic implications:
Table 1: Core Functions of SOX2 in Cellular Dedifferentiation and Therapeutic Implications
| SOX2 Function | Molecular Mechanism | Downstream Effect | Therapeutic Implication |
|---|---|---|---|
| Maintenance of Stemness | Upregulation of ALDH1, ESA, CD44 [5] | Expansion of tumor-propagating Cancer Stem Cell (CSC) populations | Target SOX2 to deplete the therapy-resistant CSC reservoir |
| Cell Cycle Progression | Repression of p21Cip1/p27Kip1; Induction of Cyclin D3 [75] [5] | Uncontrolled proliferation and tumor growth | Inhibit SOX2 to induce cell cycle arrest |
| EMT and Invasion | Direct transactivation of Snail, Slug, Twist promoters [75] | Loss of E-Cadherin, enhanced motility and metastasis | Block SOX2 to suppress metastatic spread |
| Therapy Resistance | Regulation of cellular stress response and survival pathways in CSCs [16] [55] | Resistance to chemo- and radiotherapy | Combine SOX2 targeting with conventional therapies |
Challenges in Targeting SOX2 for Therapeutic Intervention
Targeting SOX2 therapeutically is fraught with challenges, primary among which is its classification as an "undruggable" target. Transcription factors like SOX2 lack deep binding pockets for conventional small-molecule inhibitors, making them refractory to target-based drug discovery approaches [76] [55]. Furthermore, the direct targeting of SOX2 requires intracellular delivery of therapeutic agents, necessitating vehicles that can overcome the plasma and nuclear membrane barriers.
Additional challenges include:
- On-Target Toxicity: Given SOX2's critical role in normal stem cell maintenance and tissue homeostasis (e.g., in neural progenitors, stomach, and trachea), systemic inhibition could cause severe side effects [55]. This underscores the need for delivery systems with high specificity for tumor tissue.
- Compensatory Mechanisms: SOX2 is embedded in a complex regulatory network with other pluripotency factors and signaling pathways. Effective therapy may require combination strategies [55].
- Tumor Heterogeneity: SOX2 expression can be heterogeneous within a tumor, requiring delivery systems that achieve broad distribution or specifically target SOX2-high cell populations [75] [5].
Optimized Delivery Systems for Targeting SOX2In Vivo
Nucleic Acid-Based Artificial Transcription Factors
A powerful approach to silence the SOX2 gene is the use of engineered Zinc-Finger Artificial Transcription Factors (ZF-ATFs). These are modular proteins designed to bind specific DNA sequences in the SOX2 regulatory regions and suppress its transcription.
Experimental Protocol for ZF-ATFs [76]:
- Target Selection: Identify and select 18-bp target sequences within the SOX2 promoter and key enhancer regions (e.g., SRR1, SRR2) using specialized software (e.g., zincfingertools.org).
- ATF Construction:
- Engineer 6-finger ZF arrays, with each finger recognizing a specific 3-base pair DNA sequence.
- Fuse the engineered ZF domain to a potent repressor domain, such as the Kruppel Associated Box (SKD).
- Incorporate a nuclear localization signal (NLS) and an epitope tag (e.g., hemagglutinin, HA) for tracking.
- Clone the final ATF construct into a delivery vector, typically a retroviral vector like pMX-IRES-GFP.
- In Vitro Validation:
- Transduce target cancer cells (e.g., breast cancer cell lines MDA-MB-231, MDA-MB-435s) with the retroviral constructs.
- Measure SOX2 knockdown efficiency at mRNA and protein levels using qRT-PCR and immunoblotting, respectively. Effective ATFs can achieve up to 95% repression.
- Assess functional outcomes: conduct cell proliferation assays (MTT), clonogenic survival assays, and cell cycle analysis (e.g., by flow cytometry) to confirm the anti-tumor effect of SOX2 suppression.
- In Vivo Delivery and Testing:
- Establish xenograft tumors in immunocompromised mice by injecting ATF-expressing cancer cells.
- Monitor tumor growth over time. Induced expression of the ATF in vivo has been shown to inhibit breast cancer cell growth in mouse models.
- Analyze excised tumors to confirm sustained SOX2 repression and long-term therapeutic effect.
The following diagram illustrates the structure and mechanism of a repressive ZF-ATF targeting the SOX2 gene.
In Vitro Transcribed (IVT) mRNA for Reprogramming and Targeting
IVT mRNA offers a transient and genetically safe method for expressing SOX2 (for regenerative purposes) or for delivering SOX2-targeting machinery (e.g., CRISPR components). This method avoids the risk of insertional mutagenesis associated with viral vectors.
Experimental Protocol for SOX2 IVT mRNA Delivery [79]:
- mRNA Synthesis:
- Generate a poly-(A) tailed DNA template for SOX2 (or a SOX2-targeting nuclease like Cas9) by PCR.
- Use an in vitro transcription kit (e.g., MEGAscript T7) with a cap/NTP mixture (e.g., m7G(5')ppp(5')G ARCA) to synthesize the IVT mRNA.
- Cell Transfection and Optimization:
- Optimize transfection conditions (duration, mRNA concentration, transfection reagent) for the target cell type (e.g., human umbilical cord blood-derived mesenchymal stem cells - UCB-MSCs).
- To maintain sustained protein expression and achieve successful cellular reprogramming or editing, perform daily transfections for a defined period.
- To mitigate the innate immune response triggered by exogenous mRNA, consider using media supplements or modified nucleosides.
- Validation of SOX2 Modulation:
- For SOX2 overexpression: confirm the acquisition of neural stem cell (NSC) morphology, expression of NSC markers (e.g., SOX1, Nestin, PAX6), and demonstrated multipotency in vitro.
- For SOX2 knockdown/knockout: verify reduction of SOX2 protein and mRNA, and assess functional consequences on cell proliferation and stemness.
Table 2: Key Research Reagent Solutions for Targeting SOX2
| Reagent / Tool | Function / Description | Key Features / Application |
|---|---|---|
| ZF-ATF Repressor | Engineered protein for targeted SOX2 gene silencing [76] | High specificity (18bp target); Fused to SKD repressor domain; Retroviral delivery |
| SOX2 IVT mRNA | In vitro transcribed mRNA for transient SOX2 expression [79] | Genetically safe; No genome integration; For direct neural reprogramming |
| CRISPR-Cas9 System | Genome editing tool for functional SOX2 knockout screens [16] | Identifies SOX2 genetic networks; Uses lentiviral sgRNA libraries (e.g., TKOv3) |
| SOX2-GFP Reporter Cell Line | hESC line with GFP knocked into the SOX2 locus [77] | Tracks SOX2 expression dynamics; Isolates SOX2+ populations via FACS |
| Anti-CSC Antibodies | Antibodies against CSC markers (CD44, ESA, CD133) [75] [16] [5] | FACS isolation and characterization of SOX2-enriched CSC populations |
Viral and Non-Viral Vector Systems
Different vector systems offer unique advantages and trade-offs for delivering SOX2-targeting therapeutics in vivo.
Viral Vectors:
- Retrovirus/Lentivirus: Provide stable integration and long-term expression of transgenes (e.g., ZF-ATFs, shRNAs against SOX2). Ideal for ex vivo manipulation of cells. Lentivirus can infect non-dividing cells [76].
- Adeno-associated Virus (AAV): Offers efficient in vivo gene delivery with low immunogenicity and long-term episomal persistence. rAAV has been used for highly efficient homologous recombination in hESCs, as demonstrated in the generation of SOX2-GFP reporter lines [77].
Non-Viral Vectors:
- Lipid Nanoparticles (LNPs): The leading platform for in vivo delivery of mRNA and other nucleic acids. They protect the payload from degradation and facilitate cellular uptake. Highly suitable for delivering IVT mRNA or CRISPR-RNPs.
- Polymer-Based Nanoparticles: Alternative biodegradable carriers that can be functionalized with targeting ligands (e.g., antibodies, peptides) to enhance tumor specificity.
The workflow below compares the application of these delivery systems for two primary therapeutic strategies: SOX2 inhibition for cancer therapy and SOX2 expression for regenerative medicine.
Quantitative Analysis of Delivery System Efficacy
The efficacy of any delivery system must be quantitatively evaluated using a standard set of in vitro and in vivo assays. Key parameters include the efficiency of SOX2 modulation, its functional consequences on cancer cells, and the biodistribution and safety of the delivery vehicle itself.
Table 3: Quantitative Metrics for Evaluating SOX2-Targeting Delivery Systems
| Evaluation Parameter | Experimental Method | Exemplary Data from Literature |
|---|---|---|
| SOX2 Knockdown Efficiency | qRT-PCR, Immunoblotting | Up to 95% repression of endogenous SOX2 mRNA with ZF-ATFs in breast cancer cells [76] |
| Effect on Cell Proliferation | MTT assay, Cell counting | Significant reduction in cell proliferation upon SOX2 knockdown in pancreatic cancer cells [5] |
| Effect on Clonogenic Potential | Colony formation assay | Decreased colony formation in breast cancer cells after SOX2 suppression with ZF-ATFs [76] |
| Tumor Growth Inhibition | In vivo xenograft model | Induced ATF expression inhibited breast cancer cell growth in a mouse model [76] |
| CSC Marker Modulation | Flow Cytometry (CD44, ESA, ALDH1) | SOX2 expression associated with increased ALDH1, ESA, CD44 in pancreatic cancer [5] |
| In Vivo Biodistribution | Fluorescence imaging (if payload is labeled) | Not explicitly quantified in results, but critical for system optimization. |
Targeting the oncogenic transcription factor SOX2 in vivo represents a frontier in combating therapy-resistant and metastatic cancers driven by cellular dedifferentiation. While the challenge is significant due to the "undruggable" nature of SOX2, advanced delivery systems such as ZF-ATFs, IVT mRNA, and non-viral nanoparticles offer viable and promising strategies. The future of this field lies in further optimizing these delivery platforms for enhanced in vivo stability, tumor-specific targeting, and safety. Combining SOX2-targeted therapies with conventional chemo- or radiotherapy could be a powerful approach to eradicate CSCs and prevent tumor relapse. As our understanding of SOX2 biology and delivery nanotechnology deepens, the translation of these sophisticated systems into clinical practice holds immense potential for improving outcomes in a wide spectrum of SOX2-driven cancers.
Validating SOX2 Function: Clinical Correlations and Cross-Tissue Analysis
SOX2 (SRY-box 2), a transcription factor pivotal to maintaining pluripotency in embryonic and adult stem cells, has emerged as a critical biomarker in oncology. Its aberrant expression is increasingly implicated in tumor pathogenesis, progression, and clinical outcomes across diverse cancer types. This technical review synthesizes current evidence on SOX2's expression patterns, correlating them with tumor grade, prognostic implications, and recurrence potential. Framed within its broader function in cellular dedifferentiation, we detail how SOX2 imparts stem cell-like features to cancer cells, thereby driving aggressive behavior. The document provides a comprehensive analysis of SOX2's biomarker utility, supported by structured quantitative data, experimental methodologies, and molecular pathways, serving as a resource for researchers and drug development professionals.
SOX2 is a master regulator of embryonic development, maintaining stem cell pluripotency and self-renewal. In the context of cancer, this fundamental role is co-opted to promote cellular dedifferentiation, a process where specialized cells revert to a more primitive, stem-like state. This dedifferentiation is a hallmark of cancer stem cells (CSCs), a subpopulation implicated in tumor initiation, therapeutic resistance, and metastasis [12] [6]. SOX2 contributes to oncogenesis by regulating key processes including cell cycle progression, inhibition of apoptosis, and induction of epithelial-to-mesenchymal transition (EMT), thereby enhancing invasive potential [12] [29]. This whitepaper examines the consequential link between SOX2 expression and clinical tumor parameters, establishing its value as a multi-faceted biomarker.
SOX2 Expression Across Tumor Grades and Types
SOX2 expression is not universal across all cancers; it exhibits distinct patterns of upregulation or downregulation depending on the tissue of origin, reflecting its context-dependent oncogenic or tumor-suppressive roles.
Table 1: SOX2 Expression Patterns Across Human Cancers
| Cancer Type | SOX2 Expression Status | Clinical/Pathological Correlation |
|---|---|---|
| Glioblastoma Multiforme & Lower Grade Glioma | Upregulated [80] [23] | Associated with poor prognosis [80] [23] |
| Lung Adenocarcinoma & Squamous Cell Carcinoma | Upregulated [80] [23] | Associated with poor prognosis [80] [23] |
| Cervical Squamous Cell Carcinoma | Upregulated [80] [23] | |
| Osteosarcoma | Upregulated [29] | Correlates with AKT levels; associated with aggressiveness and chemoresistance [29] |
| Pancreatic Ductal Adenocarcinoma (PDAC) | Ectopically expressed in 19.3% of tumors [12] [6] | Observed in high-grade, poorly differentiated, and invasive cancer [12] |
| Odontogenic Lesions | Strong in Odontogenic Keratocyst (OKC); Moderate in Ameloblastoma; Low in Dentigerous Cyst [25] | Significant correlation with cortical bone perforation and recurrence [25] |
| Colorectal Adenocarcinoma | Downregulated [80] [23] | |
| Esophageal Carcinoma | Downregulated [80] [23] | |
| Stomach Adenocarcinoma | Downregulated [80] [23] | |
| Rectum Adenocarcinoma | Downregulated [80] [23] | |
| Testicular Germ Cell Tumors | Downregulated [80] [23] |
The association of SOX2 with high-grade disease is particularly evident in specific cancers. In pancreatic ductal adenocarcinoma (PDAC), SOX2 is not expressed in normal acinar or ductal cells but is observed in 19.3% of human tumors, specifically in high-grade cancers, including poorly differentiated and invasive PDAC, as well as in premalignant PanIN lesions [12] [6]. Similarly, in benign odontogenic lesions, a marked hierarchy in SOX2 expression aligns with their known aggressiveness; odontogenic keratocysts (OKC) show strong nuclear staining, followed by ameloblastomas, while the less aggressive dentigerous cysts record low positive scores [25].
Correlation with Patient Prognosis and Recurrence
The prognostic value of SOX2 is significant but exhibits a dual nature, dependent on cancer type.
Table 2: SOX2 Correlation with Clinical Outcomes
| Cancer Type | Correlation with Prognosis | Correlation with Recurrence / Other Outcomes |
|---|---|---|
| Lung Adenocarcinoma, Lung Squamous Cell Carcinoma, Glioblastoma, Lower Grade Glioma | High SOX2 associated with poor prognosis [80] [23] | |
| Bladder Cancer, Liver Hepatocellular Carcinoma, Kidney Renal Clear Cell Carcinoma, Sarcoma | Low SOX2 associated with better prognosis [80] [23] | |
| Osteosarcoma | High SOX2 is an adverse prognostic factor, correlated with poor overall survival [29] | Promotes chemoresistance and stemness [29] |
| Recurrent Oral Squamous Cell Carcinoma (re-OSCC) | High SOX2 in the recurrent tumor associated with improved post-recurrence overall and disease-free survival [46] | |
| Odontogenic Lesions (Ameloblastoma, OKC) | Positive SOX2 expression correlates with aggressive biological behavior and poor prognosis [25] | Significant positive correlation with recurrence (P=0.001) [25] |
| Various Cancers (Pan-cancer analysis) | High SOX2 expression correlated with higher responsiveness to immune checkpoint inhibitors [80] [23] |
A key finding in odontogenic lesions is a significant positive correlation between SOX2 expression and both cortical bone perforation and lesion recurrence, underscoring its role in predicting aggressive local behavior and clinical outcome [25]. Conversely, in recurrent oral squamous cell carcinoma (re-OSCC), elevated SOX2 expression was unexpectedly associated with improved post-recurrence survival, suggesting a unique, context-specific biological role distinct from its function in primary tumors [46]. Furthermore, a pan-cancer analysis revealed that despite its association with poor prognosis in some cancers, high SOX2 expression may predict higher responsiveness to immune checkpoint inhibitors, highlighting its potential as a biomarker for immunotherapy [80] [23].
Core Signaling Pathways and Molecular Mechanisms
SOX2 drives tumorigenesis and poor prognosis through several interconnected molecular mechanisms.
Diagram 1: SOX2 Oncogenic Signaling Network. The diagram illustrates key mechanisms by which SOX2 promotes tumorigenesis, including dysregulation of cell cycle, induction of stemness, activation of EMT, and AKT-mediated stabilization that leads to chemoresistance.
AKT-Mediated Stabilization and Chemoresistance
A critical mechanism for SOX2 overexpression in cancers like osteosarcoma is post-transcriptional stabilization. The kinase AKT binds to and phosphorylates SOX2 at threonine 116 (T116). This phosphorylation prevents SOX2 from interacting with the E3 ubiquitin ligases UBR5 and STUB1, thereby blocking its ubiquitination and subsequent proteasome-dependent degradation. This results in SOX2 protein accumulation, which enhances cancer stemness and chemoresistance. Consequently, combining AKT inhibitors with chemotherapy presents a promising therapeutic strategy for SOX2-positive cancers [29].
Essential Experimental Protocols for SOX2 Analysis
Immunohistochemistry (IHC) on Formalin-Fixed Paraffin-Embedded (FFPE) Tissue
IHC is a cornerstone technique for assessing SOX2 protein expression and localization within the tumor architecture [25] [46].
- Tissue Preparation: Surgical specimens are fixed in 10% neutral buffered formalin and embedded in paraffin. For specimens containing bone, gentle decalcification using EDTA is recommended over strong acids to better preserve antigenicity [25].
- Sectioning and Staining: Sections are cut at 4μm thickness. Staining can be performed manually or using automated systems (e.g., Ventana BenchMark). The protocol involves deparaffinization, antigen retrieval, and incubation with a primary antibody against SOX2.
- Antibody: Rabbit polyclonal antibody is commonly used (e.g., from Abcam) [25] [46].
- Visualization and Quantification: SOX2 exhibits nuclear staining [46]. Scoring is typically semi-quantitative, assessing both the intensity of staining (0-3) and the percentage of positive cells. An H-score (ranging from 0-300) may be calculated as (3 × % strong staining) + (2 × % moderate staining) + (1 × % weak staining) to provide a continuous variable for statistical analysis [46].
Detection of Circulating SOX2 as a Liquid Biopsy Biomarker
SOX2 can be detected in blood plasma, offering a non-invasive method for cancer monitoring [64] [81].
- Sample Collection and Processing: Blood is collected in EDTA tubes and processed within 2 hours. Plasma is separated by centrifugation (e.g., 2,000 × g for 10 minutes), aliquoted, and stored at -80°C [64] [81].
- RNA Isolation and qRT-PCR: Total RNA is extracted from plasma. After reverse transcription to cDNA, qRT-PCR is performed using SYBR Green or TaqMan assays with primers specific for SOX2. GAPDH is used as a reference gene for normalization. Relative expression is calculated using the 2^(-ΔΔCt) method [64].
- Enzyme-Linked Immunosorbent Assay (ELISA): Commercial ELISA kits can quantify SOX2 protein levels in plasma. Samples are run in duplicate, and concentrations are determined based on a standard curve [64].
- Circulating Cancer Stem-like Cell (CCSC) Identification: Using systems like CytoTrack, CCSCs can be identified in blood samples based on SOX2 expression. The recovery ratio for such methods has been reported to be approximately 60% [81].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for SOX2 Research
| Reagent / Assay | Specification / Example | Primary Function in SOX2 Research |
|---|---|---|
| Anti-SOX2 Antibody | Rabbit polyclonal (e.g., Abcam) [25] [46] | Detection and localization of SOX2 protein in IHC and immunofluorescence. |
| SOX2 ELISA Kit | Commercial kit (e.g., Fine Biotech) [64] | Quantification of soluble SOX2 protein levels in plasma and other biological fluids. |
| qRT-PCR Assays | TaqMan Gene Expression Assay (Hs04234836_s1) [64] [81] | Quantification of SOX2 mRNA expression levels from tissue, cells, or plasma-derived RNA. |
| Cell Culture Model: Mammosphere | Ultra-Low attachment plates with spheroid medium [81] | Enrichment of cancer stem cells (CSCs) for studying SOX2 function in stemness and self-renewal. |
| Kinase Inhibitor | AKT inhibitor (e.g., MK2206) [29] | Tool for investigating the AKT-SOX2 regulatory axis and its role in SOX2 protein stability. |
| Proteasome Inhibitor | MG132 [29] | Used in protein stability assays to block proteasomal degradation of SOX2. |
SOX2 stands as a robust biomarker with demonstrable correlations to tumor grade, prognosis, and recurrence across a spectrum of malignancies. Its central role in promoting cellular dedifferentiation and maintaining cancer stem cell populations underpins its association with aggressive disease phenotypes, therapy resistance, and poor clinical outcomes. The ongoing delineation of its molecular mechanisms, particularly the AKT-SOX2 axis, opens promising avenues for therapeutic intervention. For the research and drug development community, the consistent methodological frameworks and reagents outlined herein provide a foundation for advancing the clinical translation of SOX2 from a prognostic indicator to a target for novel cancer therapies.
The transcription factor SOX2 (SRY-related HMG-box 2) is a master regulator of embryonic development and stem cell pluripotency that has emerged as a critical player in oncogenesis. This nuclear protein, encoded on chromosome 3q26.3-q27, contains a high-mobility group (HMG) domain that facilitates DNA binding, enabling it to regulate diverse transcriptional programs [65] [10]. While SOX2 is essential for maintaining cellular pluripotency and self-renewal in stem cells, its dysregulation contributes significantly to tumorigenesis across multiple cancer types [55]. This whitepaper provides a comprehensive comparative analysis of SOX2's roles in pancreatic ductal adenocarcinoma (PDAC), lung cancer, and prostate cancer, with particular focus on its function in cellular dedifferentiation—a process wherein differentiated cells revert to stem-like states that drive tumor aggressiveness and therapeutic resistance.
SOX2 Expression Patterns Across Cancers
SOX2 demonstrates distinct expression patterns and regulatory mechanisms across different cancer types, as summarized in Table 1.
Table 1: SOX2 Expression Patterns and Clinical Correlations
| Cancer Type | Expression Frequency | Primary Regulation Mechanism | Association with Aggressive Features | Prognostic Significance |
|---|---|---|---|---|
| Pancreatic Cancer | 19.3% of cases [5] | Ectopic expression in high-grade disease [5] | Associated with adenosquamous and anaplastic subtypes [5] | Contributes to chemoresistance [5] |
| Lung Cancer | 20-60% in squamous cell carcinoma [82] | Gene amplification (3q26.3) [82] | Promotes radioresistance and stemness [83] | Poor prognosis in adenocarcinoma [82] |
| Prostate Cancer | Upregulated in advanced disease [65] | Contributes to lineage plasticity [65] | Associated with CRPC and NEPC [65] | Promotes treatment resistance [65] |
Molecular Mechanisms and Signaling Pathways
SOX2 exerts its oncogenic effects through complex, tissue-specific molecular mechanisms and signaling pathway interactions.
Core Signaling Pathway Interactions
Diagram: SOX2 Signaling Network Across Cancers
Pancreatic Cancer Mechanisms
In pancreatic ductal adenocarcinoma, SOX2 is not expressed in normal acinar or ductal cells but becomes ectopically expressed in approximately 19.3% of tumors, particularly in high-grade lesions [5]. SOX2 drives dedifferentiation by directly binding to promoters of EMT transcription factors Snail, Slug, and Twist, resulting in loss of E-cadherin and ZO-1 expression [5] [12]. This promotes acquisition of stem cell-like features and upregulates cancer stem cell (CSC) markers ALDH1, ESA, and CD44 [5]. SOX2 also promotes cell proliferation by repressing cell cycle inhibitors p21Cip1 and p27Kip1 while inducing cyclin D3, facilitating G1/S transition [5]. Interestingly, PDAC cells exhibit rheostat-like sensitivity to SOX2 levels, with both overexpression and knockdown inhibiting growth, suggesting an optimal expression range must be maintained for tumor fitness [84].
Lung Cancer Mechanisms
In lung cancer, SOX2 operates as a lineage-survival oncogene, particularly in squamous cell carcinoma where it is amplified in 20-60% of cases [82]. SOX2 amplification represents the key target within the common 3q amplicon and promotes squamous identity rather than dedifferentiation to a pluripotent state [82]. In small cell lung cancer, SOX2 is overexpressed and cooperates with oncogenes like Wnt1, Wnt2, c-Myc, and Notch to promote tumor occurrence [82]. SOX2 also drives radioresistance in non-small cell lung cancer by regulating tumor cell dedifferentiation and enhancing DNA damage repair capability [83]. Radiation exposure increases SOX2 expression, creating a positive feedback loop that enriches CSC populations following treatment [83].
Prostate Cancer Mechanisms
In prostate cancer, SOX2 enables lineage plasticity and facilitates transition to treatment-resistant states including castration-resistant prostate cancer (CRPC) and neuroendocrine prostate cancer (NEPC) [65]. SOX2 expression is associated with decreased androgen receptor (AR) signaling and promotes emergence of double-negative prostate cancer (DNPC) that lacks both AR and neuroendocrine markers [65]. The LIN28b/let-7/SOX2 axis facilitates neuroendocrine differentiation, while SOX2 collaborates with other pluripotency factors to maintain cancer stem cell populations that drive tumor recurrence and metastasis [65]. SOX2 also promotes epithelial-to-mesenchymal transition (EMT) through regulation of ZEB1, ZEB2, and TGFβ2 genes [65].
Experimental Approaches for SOX2 Research
Key Methodologies
Table 2: Essential Experimental Protocols for SOX2 Research
| Methodology | Key Applications | Technical Considerations | Cancer Context |
|---|---|---|---|
| Inducible SOX2 Expression | Precise control of SOX2 levels using doxycycline-controlled systems [84] | Avoids artifacts from stable overexpression; reveals rheostat function [84] | Pancreatic cancer models [84] |
| Chromatin Immunoprecipitation (ChIP) | Identify direct SOX2 target genes (e.g., p21Cip1, p27Kip1, Snail promoters) [5] | Critical for mapping SOX2 binding to EMT and cell cycle regulators | Pancreatic cancer cell lines [5] |
| Sphere Formation Assays | Evaluate cancer stem cell self-renewal capability [5] [83] | Enriches for CSC populations; serial passage demonstrates stemness | Lung and pancreatic cancer models [5] [83] |
| RNA Interference | Stable or inducible knockdown using shRNA/siRNA [5] [83] | Determines necessity of SOX2 for tumor maintenance | All three cancer types |
| Radiation Resistance Models | Generate radioresistant cells via fractionated irradiation [83] | Mimics clinical radiotherapy; reveals SOX2 role in treatment resistance | Lung cancer models [83] |
The Scientist's Toolkit
Table 3: Essential Research Reagents for SOX2 Investigation
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| SOX2 Modulation Systems | Doxycycline-inducible SOX2 expression lentivectors [84] | Precise control of SOX2 expression levels | Reveals rheostat function in pancreatic cancer [84] |
| CSC Marker Antibodies | Anti-ALDH1, anti-CD44, anti-ESA [5] | Identification and isolation of cancer stem cells | Demonstrates SOX2 association with stemness [5] |
| EMT Marker Antibodies | Anti-E-cadherin, anti-ZO-1, anti-Snail [5] | Evaluation of epithelial-mesenchymal transition | Links SOX2 to metastatic progression [5] |
| Pathway Inhibitors | MEK inhibitors (trametinib), AKT inhibitors (MK-2206) [84] | Testing SOX2-mediated drug resistance | SOX2 expression reduces sensitivity to targeted therapies [84] |
| Radiation Equipment | X-ray irradiator (RS 2000) [83] | Generating radioresistant cell models | SOX2 upregulation following fractionated radiation [83] |
SOX2 in Cellular Dedifferentiation
The process of cellular dedifferentiation represents a fundamental mechanism through which SOX2 contributes to tumor progression across cancer types.
Dedifferentiation Mechanisms
Diagram: SOX2-Mediated Dedifferentiation Process
SOX2 drives dedifferentiation through several interconnected mechanisms. It promotes acquisition of stem cell-like features by directly regulating core stemness factors and activating CSC marker expression [5] [12]. Through induction of EMT via direct binding to Snail, Slug, and Twist promoters, SOX2 facilitates loss of epithelial characteristics and gain of mesenchymal properties associated with stem-like states [5]. SOX2 also modulates cell cycle regulation by repressing p21Cip1 and p27Kip1, creating a proliferation-permissive environment in dedifferentiated cells [5]. Furthermore, SOX2 enhances DNA damage repair capabilities, contributing to radioresistance and chemoresistance in dedifferentiated tumor populations [83].
Functional Consequences
The dedifferentiation process driven by SOX2 has significant clinical implications. It enriches cancer stem cell populations that possess enhanced tumor-initiating capacity and self-renewal potential [5] [12] [83]. SOX2-mediated dedifferentiation promotes therapeutic resistance through multiple mechanisms, including enhanced DNA repair, drug efflux, and survival pathway activation [83] [84]. It also facilitates metastatic progression by enabling EMT and increasing cellular plasticity [5] [65]. Additionally, dedifferentiated SOX2-positive cells demonstrate adaptability to therapeutic pressure, driving tumor evolution and lineage switching in treatment-resistant cancers [65].
Therapeutic Implications and Future Directions
Targeting SOX2 represents a promising but challenging therapeutic avenue. SOX2 contributes to resistance against conventional chemotherapy, radiation, and targeted agents like MEK and AKT inhibitors [83] [84]. The development of SOX2-targeting approaches includes investigation of epigenetic modifiers that influence SOX2 expression, such as LSD1 inhibitors [65], and exploration of synthetic lethality strategies that exploit vulnerabilities in SOX2-high tumors [84]. Immunotherapeutic approaches targeting SOX2-expressing cells are also under investigation, particularly given SOX2's association with immune cell infiltration patterns in certain cancers [85].
Several challenges complicate SOX2-directed therapy development. The transcription factor nature of SOX2 makes it difficult to target with conventional small molecules [55]. Furthermore, the rheostat-like behavior of SOX2, wherein both overexpression and knockdown can inhibit tumor growth in some contexts, necessitates precise therapeutic modulation [84]. Tissue-specific functions of SOX2 also require careful consideration in therapeutic development [10] [55].
Future research directions should prioritize elucidating the context-dependent functions of SOX2 across cancer subtypes, developing clinically viable SOX2 targeting strategies, identifying biomarkers for patient stratification, and understanding SOX2's role in the tumor microenvironment and treatment-induced evolution.
SOX2 serves as a critical regulator of oncogenesis across pancreatic, lung, and prostate cancers through shared and distinct mechanisms. While its roles in promoting stemness, therapeutic resistance, and cellular dedifferentiation represent common themes, the specific pathways, clinical associations, and functional outcomes display significant tissue-specific variation. The rheostat-like properties of SOX2 expression highlight the delicate balance required for its oncogenic functions and present both challenges and opportunities for therapeutic intervention. A comprehensive understanding of SOX2's multifaceted roles across cancer types provides the foundation for developing novel treatment strategies that target this master regulator of cellular plasticity and its associated pathways.
The transcription factor SOX2 (Sex-determining region Y-box 2) is a master regulator of pluripotency essential for embryonic development and stem cell self-renewal. Beyond its physiological roles, SOX2 is aberrantly expressed in numerous cancers, where it drives tumorigenesis, metastasis, and therapy resistance by promoting cellular dedifferentiation and stemness. This technical guide synthesizes current evidence on the functional validation of SOX2's oncogenic functions using in vivo models, providing researchers with methodologies to investigate SOX2-driven mechanisms and therapeutic vulnerabilities. SOX2 contributes to neoplastic progression by accelerating cancer cell proliferation, migration, invasion, and metastasis across at least 25 different human cancers, with its overexpression strongly correlated with poor patient survival [55]. The factor imparts stem cell-like features to cancer cells and promotes epithelial-to-mesenchymal transition (EMT), facilitating metastatic dissemination and therapeutic resistance [5] [86]. This review details the experimental models and methodologies essential for validating these mechanisms in vivo, within the broader context of SOX2's role in cellular dedifferentiation.
In Vivo Model Systems for SOX2 Functional Analysis
Genetically Engineered Mouse Models (GEMMs)
Genetically engineered mouse models have proven invaluable for delineating SOX2's oncogenic potential in autochthonous tumors with intact microenvironments.
The NUT Carcinoma Translocator (NCT) Model: This GEMM employs Cre-lox-mediated interchromosomal recombination to induce a sporadic t(2;17) translocation, generating a Brd4::Nutm1 fusion gene that initiates aggressive tumors resembling human NUT carcinoma. This model demonstrates 100% penetrance and can be directed to specific tissues using lineage-specific Cre drivers (e.g., KRT14-Cre for oral mucosa, Pdx1-Cre for pancreas) [87]. This system was strategically used to investigate SOX2 dependency by crossing with floxed Sox2 alleles, revealing that SOX2 is dispensable for NC initiation and progression—challenging the assumption of its universal requirement in oncogenesis [87].
Sox2-CreERT2-Driven Models: Alternative GEMMs utilize knock-in Brd4::hNUTM1 alleles activated by the FLEx system and Sox2-CreERT2, resulting in consistent tumor formation in the esophagus and gastroesophageal junction. These models confirm that SOX2 overexpression, combined with tumor suppressor inactivation, drives squamous cancer formation [88] [55].
Patient-Derived Xenograft (PDX) and Cell Line-Derived Xenograft Models
Orthotopic and subcutaneous xenografts of human cancer cells in immunocompromised mice provide complementary approaches for studying SOX2-mediated tumor progression and metastasis.
Metastasis Assays: SOX2 overexpression in breast (MCF-7) and prostate (DU145) cancer cells, followed by tail vein or orthotopic implantation, demonstrates enhanced metastatic potential to lungs and other organs. This metastatic promotion is mechanistically linked to SOX2's regulation of the WNT/β-catenin signaling network and induction of EMT [86].
Therapy Response Studies: Xenograft models of non-small cell lung cancer (NSCLC) with elevated SOX2 expression exhibit increased radioresistance. These models are crucial for investigating how SOX2 promotes DNA damage repair and cellular dedifferentiation following radiation treatment [83]. Similarly, PDX models maintain tumor heterogeneity and have been instrumental in linking SOX2 gene dosage to sustained tumor-promoting inflammation via the FOSL2/IL6 axis, which drives disease aggressiveness and genomic instability [89].
Table 1: Key In Vivo Models for SOX2 Functional Validation
| Model Type | Key Features | Applications | References |
|---|---|---|---|
| NCT GEMM | Inducible Brd4::Nutm1 fusion; lineage-specific Cre drivers | SOX2 dependency studies; tumor initiation in native microenvironment | [87] |
| Sox2-CreERT2 GEMM | Brd4::hNUTM1 knock-in; targeted esophageal tumorigenesis | SOX2-driven squamous cell carcinoma; cooperation with tumor suppressors | [88] |
| Orthotopic/Xenograft | Human cancer cells in immunocompromised mice | Metastasis assays; therapy resistance (radioresistance) | [86] [83] |
| Patient-Derived Xenograft (PDX) | Maintains tumor heterogeneity and patient-specific characteristics | SOX2 dosage effects; tumor aggressiveness; inflammatory signaling | [89] |
Quantitative Data from SOX2 Functional Studies
SOX2 Expression and Clinical Correlation
Comprehensive molecular analyses of human tumors have established strong correlations between SOX2 dysregulation and aggressive disease phenotypes.
Pancreatic Cancer: Immunohistochemical analysis of tissue microarrays containing 349 patient samples revealed SOX2 expression in 19.3% (42/217 evaluable cases) of pancreatic tumors, while being absent in normal pancreatic acinar and ductal cells. This expression was exclusively observed in moderate and poorly differentiated tumors, indicating an association with advanced disease [5].
Metastatic Potential: A meta-analysis of 2,643 patients across eight cancer types demonstrated that SOX2 overexpression significantly correlates with both lymph node metastasis (OR = 1.79, 95% CI: 1.20-3.25, P < 0.008) and distant metastasis. This high SOX2 expression was associated with shorter overall survival (HR = 1.65, 95% CI: 1.34-2.04, P < 0.001) and disease-free survival (HR = 1.54, 95% CI: 1.14-2.08, P = 0.005) [90].
Squamous Cancers: Genomic analyses of squamous cancers from diverse tissues (lung, esophagus, head and neck, cervix) show that the SOX2 gene is widely amplified and overexpressed, nominating SOX2 as a lineage-specific oncogene. SOX2 amplification is observed in approximately 9% of squamous cancers and 4% of gliomas from TCGA samples [88].
Table 2: Quantitative Findings from SOX2 Functional Studies
| Parameter | Finding | Model/Data Source | Significance | |
|---|---|---|---|---|
| SOX2+ Pancreatic Tumors | 19.3% (42/217 cases) | Human TMA (349 samples) | Associates with high-grade disease | [5] |
| Metastasis Correlation | OR = 1.79 for distant metastasis | Meta-analysis (2,643 patients) | SOX2 overexpression promotes metastasis | [90] |
| Survival Impact | HR = 1.65 for overall survival | Meta-analysis (multiple cancers) | Poor prognosis with SOX2 overexpression | [90] |
| SOX2 Focal Amplification | 9% of squamous cancers | TCGA SNP-array data | Lineage-specific oncogene amplification | [88] |
| SOX2 Dependency in NC | Tumors form with 100% penetrance without SOX2 | KRT14-Cre; NCT+/−;Sox2fl/fl GEMM | Context-dependent oncogenic function | [87] |
Methodologies for Functional Validation
Lineage Tracing and Conditional Knockout
The NCT GEMM platform enables precise determination of SOX2 requirement in tumor initiation and maintenance. The experimental workflow involves:
- Crossing Strategy: Introduce floxed Sox2 alleles into the NCT model background with specific Cre drivers (e.g., KRT14-Cre for oral mucosa, Nkx2.1-Cre for lung/thyroid, Pdx1-Cre for pancreas).
- Tumor Monitoring: Utilize tdTomato-Luc2 reporters knocked in downstream of the Nutm1 gene for in vivo bioluminescence imaging to track tumor initiation and growth.
- Validation: Confirm SOX2 deletion via immunohistochemistry and assess tumor histology, marker expression (BRD4::NUTM1, MYC, TP63), and transcriptional profiles via RNA sequencing [87].
Metastasis and Therapy Resistance Assays
Experimental Metastasis Assay:
- Cell Preparation: Generate stable SOX2-overexpressing or SOX2-knockdown cells using lentiviral transduction.
- Tail Vein Injection: Inject 1×10^6 viable cells in 100μL PBS into the lateral tail vein of NOD/SCID mice (8-10 weeks old).
- Endpoint Analysis: Sacrifice mice after 6-8 weeks, harvest lungs and other potential metastatic organs, and quantify metastatic nodules through histology and imaging [86].
Radioresistance Studies:
- Model Generation: Establish radioresistant cell lines (e.g., H460-RR for NSCLC) by administering fractional radiation doses (e.g., 6Gy weekly up to 72Gy total) to parent cells.
- Xenograft Implantation: Subcutaneously inject 5×10^6 radioresistant or control cells into mouse flanks.
- Radiation Treatment: Once tumors reach 100-200mm^3, administer localized radiotherapy (e.g., 2-8Gy fractions) using a small-animal irradiator.
- Assessment: Monitor tumor growth kinetics, perform colony formation assays ex vivo, and analyze DNA damage repair markers (γ-H2AX, 53BP1) and stemness markers (CD133, ALDH1) in harvested tumors [83].
Molecular Profiling and Mechanism Investigation
Chromatin Immunoprecipitation (ChIP):
- Crosslink cells with 1% formaldehyde for 10min at room temperature.
- Sonicate chromatin to 200-500bp fragments.
- Immunoprecipitate with validated SOX2 antibodies (e.g., ab75485) and protein A/G beads.
- Analyze enriched DNA by qPCR or sequencing to identify direct SOX2 targets (e.g., Snail, Slug, Twist, β-catenin promoters) [5] [86].
Transcriptional Profiling:
- Perform bulk RNA sequencing on SOX2-proficient versus SOX2-deficient tumors.
- Utilize pathway analysis tools (GSEA, PathfindR) to identify dysregulated pathways (e.g., IL6-JAK-STAT3, TNFA, WNT/β-catenin) [87] [89].
SOX2 in Signaling and Dedifferentiation: Visualizing Key Pathways
SOX2 orchestrates a network of signaling pathways that promote tumor aggressiveness, stemness, and therapy resistance. The following diagram illustrates these core interactions:
Diagram Title: SOX2 Oncogenic Signaling Network
This visualization captures how SOX2 amplification and enhancer activation drive its overexpression, which in turn modulates multiple downstream pathways including WNT/β-catenin, FOSL2-mediated inflammation, and cell cycle regulation, ultimately converging on phenotypes like EMT, stemness, and therapy resistance.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for SOX2 Functional Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| SOX2 Antibodies | Anti-SOX2 (ab75485, Abcam) | IHC, IF, WB; validate SOX2 expression and localization |
| SOX2 Modulators | shSOX2 lentiviral particles; SOX2 overexpression constructs | Gain/loss-of-function studies in vitro and in vivo |
| Cell Line Models | L3.6 (pancreatic); KYSE140 (esophageal); H460-RR (NSCLC radioresistant) | Study SOX2 in proliferation, metastasis, therapy resistance |
| Mouse Models | NCT GEMM; Sox2-CreERT2; Floxed Sox2 | Lineage tracing, conditional knockout, autochthonous tumor studies |
| Signaling Reporters | WNT/β-catenin reporters (TOPflash); EMT reporters | Pathway activity quantification in response to SOX2 modulation |
| ChIP Reagents | SOX2 ChIP-grade antibodies; crosslinking reagents | Identify direct SOX2 target genes and binding sites |
Functional validation of SOX2-driven tumorigenesis and metastasis requires carefully selected in vivo models that capture the complexity of its context-dependent roles in cancer. The integrated use of GEMMs, xenograft systems, and sophisticated molecular profiling techniques has established SOX2 as a critical regulator of dedifferentiation, stemness, and aggressive disease phenotypes. Future research should focus on exploiting the mechanistic insights gained from these models—particularly the SOX2-FOSL2-IL6 axis and SOX2-enhanced DNA damage repair—to develop novel therapeutic strategies that target SOX2-positive cancer cells or overcome SOX2-mediated therapy resistance. As our understanding of SOX2's pleiotropic functions continues to evolve, these experimental approaches will remain fundamental to translating basic research into clinical applications for aggressive cancers.
- SOX2 introduction: Overview of SOX2 as a transcription factor with dual roles in development and cancer, emphasizing its context-dependent functions.
- PI3K/AKT signaling: Detailed mechanism of AKT-mediated SOX2 regulation through protein stabilization and nuclear localization.
- Notch signaling: Complex bidirectional relationship between SOX2 and Notch pathway in neural and cancer contexts.
- Wnt signaling: SOX2-Wnt pathway crosstalk in pluripotency maintenance and cancer progression.
- Experimental methods: Key techniques for studying SOX2-pathway interactions, including loss-of-function approaches and interaction assays.
- Therapeutic targeting: Challenges and emerging strategies for targeting SOX2 in cancer treatment.
The SOX2 Regulatory Axis: Comparing Signaling Pathways (PI3K/AKT, WNT, Notch) Across Contexts
The sex-determining region Y-box 2 (SOX2) transcription factor represents a pivotal regulator of cellular identity with dual significance in embryonic development and cancer progression. As a member of the SOX transcription factor family characterized by a high-mobility group (HMG) DNA-binding domain, SOX2 recognizes specific DNA sequences and regulates gene expression through complex transcriptional networks [91] [10]. SOX2 is located on chromosome 3q26.3-q27 and encodes a 317-amino acid protein containing three critical domains: an N-terminal region, the HMG domain responsible for specific DNA recognition and binding, and a C-terminal transactivation domain [91] [10]. During early embryonic development, SOX2 works in concert with other core pluripotency factors including OCT4 and NANOG to maintain stem cell identity and direct lineage specification [10]. The precise expression level of SOX2 is crucial for proper development, as both deficiency and overexpression can disrupt normal cellular differentiation programs [10].
In cancer biology, SOX2 demonstrates remarkable context-dependent functionality, acting as either an oncogene or tumor suppressor depending on cellular environment and tumor type [10] [92]. Aberrant SOX2 expression has been documented across numerous human malignancies, including lung, ovarian, breast, prostate, bladder, and brain cancers, where it frequently correlates with advanced disease stage, therapy resistance, and poor clinical outcomes [91] [10]. SOX2 contributes to cancer stem cell (CSC) maintenance through its ability to promote self-renewal, cellular plasticity, and therapeutic resistance [91] [69] [10]. The molecular mechanisms underlying SOX2's diverse functions involve complex interactions with multiple signaling pathways that exhibit significant cross-regulation and context-specific outcomes. Understanding these intricate regulatory networks is essential for developing targeted therapeutic approaches aimed at disrupting SOX2-mediated tumorigenesis while preserving its physiological functions in normal tissue homeostasis.
SOX2 and PI3K/AKT Signaling: A Central Regulatory Axis
The PI3K/AKT pathway represents one of the most significant and well-characterized regulatory axes controlling SOX2 protein stability and function in both normal development and cancer contexts. This signaling cascade initiates when extracellular growth factors activate receptor tyrosine kinases (RTKs), leading to phosphorylation of phosphatidylinositol 4,5-bisphosphate (PIP2) to phosphatidylinositol 3,4,5-trisphosphate (PIP3) by phosphoinositide 3-kinase (PI3K) [93]. PIP3 then recruits AKT to the plasma membrane, where it undergoes phosphorylation and activation, subsequently regulating numerous downstream effectors involved in cell survival, growth, and metabolism [93]. In breast carcinoma models, experimental evidence has demonstrated that AKT physically interacts with SOX2 protein to modulate its subcellular distribution, with AKT kinase activity promoting nuclear localization of SOX2 [94]. Inhibition of AKT results in enhanced cytoplasmic retention of SOX2 presumably through impaired nuclear import, followed by proteasomal degradation of the transcription factor [94].
The functional significance of the AKT/SOX2 molecular axis is particularly evident in cancer stem cell populations. In breast cancer stem cells (CSCs), AKT and SOX2 are co-expressed and co-regulated, with depletion of either protein reducing clonogenicity [94]. Importantly, ectopic SOX2 expression can restore clonogenicity and in vivo tumorigenicity in AKT-inhibited cells, positioning SOX2 as a critical functional downstream effector of AKT signaling [94]. Furthermore, AKT inhibitors effectively suppress the growth of SOX2-expressing putative CSCs, whereas conventional chemotherapeutics tend to select for this population, suggesting that targeting the AKT/SOX2 axis may provide therapeutic benefits for SOX2-positive cancers [94]. The PI3K/AKT pathway is frequently dysregulated in human cancers through various mechanisms, including RTK overactivation, PI3K mutations, and PTEN loss-of-function mutations, creating a permissive environment for SOX2 stabilization and CSC maintenance [93].
Table 1: Key Experimental Findings on SOX2-PI3K/AKT Axis
| Experimental System | Key Finding | Functional Consequence | Citation |
|---|---|---|---|
| Breast carcinoma cells | AKT physically interacts with SOX2 | Modulates SOX2 subcellular distribution | [94] |
| Breast CSCs | AKT and SOX2 are co-expressed and co-regulated | Maintains clonogenicity and tumorigenicity | [94] |
| AKT-inhibited BC cells | Ectopic SOX2 restores tumorigenicity | SOX2 acts downstream of AKT | [94] |
| AKT inhibition | SOX2 cytoplasmic retention and degradation | Reduced stemness properties | [94] |
| Various cancers | PI3K mutations/PTEN loss hyperactivate AKT | Creates environment for SOX2 stabilization | [93] |
Diagram 1: AKT-Mediated Regulation of SOX2 Stability and Activity. The PI3K/AKT signaling pathway promotes SOX2 nuclear localization, while AKT inhibition leads to SOX2 cytoplasmic retention and proteasomal degradation. PTEN acts as a negative regulator of this pathway.
SOX2 and Notch Signaling: Developmental Coordination and Oncogenic Collaboration
The Notch signaling pathway represents an evolutionarily conserved system for cell-cell communication that frequently intersects with SOX2 regulatory networks in both developmental and cancer contexts. Canonical Notch signaling is initiated through interactions between Notch receptors (NOTCH1-4 in mammals) and membrane-bound ligands (Jagged-1, Jagged-2, DLL1, DLL3, DLL4) on adjacent cells [95] [96]. This interaction triggers a series of proteolytic cleavages of the Notch receptor, resulting in release of the Notch intracellular domain (NICD) which translocates to the nucleus and forms a complex with the transcription factor CSL/RBP-J, ultimately activating expression of target genes such as the Hes and Hey families [95] [96]. In neural stem cells (NSCs), SOX2 has been demonstrated to regulate Notch signaling through direct transcriptional control of the Jagged1 gene, thereby influencing the stem cell niche and maintaining NSC populations [10]. This regulatory relationship underscores the importance of SOX2-Notch crosstalk in stem cell maintenance during central nervous system development.
In oncogenic contexts, SOX2 and Notch signaling frequently engage in cooperative interactions that drive tumor progression and therapy resistance. In breast cancer models, SOX2 and NOTCH1 exhibit coordinated expression patterns, with SOX2 directly binding to the NOTCH1 promoter to regulate its transcription [10]. This positive feedback loop enhances cancer stem cell properties and contributes to therapeutic resistance. Similarly, in ovarian cancer, SOX2 expression has been linked to regulation of Notch3 receptor levels, further emphasizing the tissue-specific nature of SOX2-Notch interactions [10]. The non-canonical Notch signaling pathway, which operates independently of CSL/RBP-J, may also contribute to SOX2 regulatory networks through interactions with other signaling pathways including NF-κB, PI3K/AKT, Wnt, and HIF-1α [95]. The complex interplay between SOX2 and Notch signaling illustrates how developmental pathways are co-opted in cancer to maintain stem-like cellular states and promote aggressive disease phenotypes.
Table 2: SOX2-Notch Interactions Across Biological Contexts
| Biological Context | Interaction Mechanism | Functional Outcome | Citation |
|---|---|---|---|
| Neural Stem Cells | SOX2 transcriptionally regulates Jagged1 | Maintains NSC population and stem cell niche | [10] |
| Breast Cancer | SOX2 binds NOTCH1 promoter | Enhances CSC properties and therapy resistance | [10] |
| Ovarian Cancer | SOX2 regulates Notch3 receptor levels | Promotes tumor progression | [10] |
| Various Cancers | Non-canonical Notch signaling with SOX2 | Modulates NF-κB, PI3K/AKT, Wnt pathways | [95] |
| Development & Cancer | Bidirectional regulatory loops | Coordinates cell fate decisions | [95] [10] |
SOX2 and Wnt Signaling: Context-Dependent Crosstalk in Pluripotency and Cancer
The Wnt signaling pathway engages in complex, context-dependent interactions with SOX2 that significantly influence both embryonic development and cancer progression. In embryonic stem cells (ESCs), SOX2 and Wnt signaling collaborate to maintain pluripotency through coordinated regulation of shared target genes [10]. SOX2 physically interacts with β-catenin, the central effector of canonical Wnt signaling, and this complex binds to enhancer elements of key pluripotency genes including Sox2 itself, creating a positive feedback loop that reinforces the stem cell state [10]. This synergistic relationship between SOX2 and Wnt/β-catenin signaling represents a fundamental mechanism for maintaining the self-renewal capacity of ESCs while suppressing differentiation programs. The interdependence of these pathways is further demonstrated by the ability of SOX2 to regulate expression of various Wnt pathway components, including Frizzled receptors and Wnt ligands, thereby modulating cellular responsiveness to Wnt signals [10].
In transformed cells, the relationship between SOX2 and Wnt signaling becomes more complex and tissue-specific. In certain cancer contexts, particularly colorectal and gastric cancers, SOX2 appears to function as a tumor suppressor that inhibits Wnt/β-catenin signaling activity [10]. This antagonistic relationship contrasts sharply with their collaborative function in ESCs and highlights the context-dependent nature of signaling pathway interactions. However, in other malignancies such as osteosarcoma, SOX2 and Wnt/β-catenin signaling maintain their cooperative relationship, working in concert to promote tumor-initiating potential and metastatic capability [10]. The mechanistic basis for these divergent outcomes likely involves tissue-specific co-factors that modulate the functional consequences of SOX2/Wnt interactions. Additionally, SOX2 has been shown to regulate the expression of specific Frizzled receptors in a tissue-dependent manner, further fine-tuning the cellular response to Wnt ligands and contributing to the pleiotropic effects observed across different cancer types [10].
Diagram 2: SOX2-Wnt/β-catenin Pathway Interactions. SOX2 and β-catenin form a complex that regulates target gene expression, with functional outcomes dependent on cellular context.
Experimental Approaches for Investigating SOX2-Pathway Interactions
Loss-of-Function Methodologies
Elucidating the functional relationships between SOX2 and signaling pathways requires sophisticated genetic and pharmacological approaches. CRISPR/Cas9-mediated knockout provides a complete and permanent elimination of SOX2 expression, allowing assessment of its necessity for pathway regulation and CSC maintenance [92]. The gRNA sequence 5′-GCTCGCCATGCTATTGCCGC-3′ targeting SOX2 has been successfully employed in lung adenocarcinoma models, with knockout validation through Western blot and immunofluorescence staining [92]. Alternatively, doxycycline-inducible shRNA systems enable temporal control of SOX2 knockdown, permitting investigation of acute versus chronic SOX2 depletion effects [92]. The shRNA sequence 5′-CAGCTCGCAGACCTACATGAA-3′ delivered via Tet-pLKO vectors has demonstrated efficacy in SOX2 suppression when combined with 1 μg/mL doxycycline administration every 48 hours [92]. Importantly, recent evidence suggests that complete SOX2 knockout using CRISPR/Cas9 may yield different phenotypic outcomes compared to knockdown approaches, potentially due to adaptive compensation mechanisms in knockout models [92]. This technical consideration highlights the importance of methodological validation in SOX2 functional studies.
Signaling Pathway Modulation and Interaction Assays
Pharmacological inhibition of signaling pathways represents another critical approach for dissecting SOX2 regulatory networks. AKT inhibitors such as MK-2206 (a pan-AKT inhibitor) and Akti1/2 effectively reduce SOX2 protein levels in breast carcinoma cells, with dose-dependent effects observed between 1-10 μM concentrations [94]. Similarly, PI3K inhibitors including wortmannin and GDC-0941 demonstrate SOX2 suppression, while mTOR inhibition with rapamycin does not affect SOX2 protein levels, indicating that SOX2 regulation occurs primarily through AKT rather than downstream mTOR signaling [94]. For investigating protein-protein interactions, co-immunoprecipitation assays have confirmed the physical interaction between AKT and SOX2, with AKT influencing SOX2 subcellular localization through nuclear-cytoplasmic shuttling mechanisms [94]. Additionally, chromatin immunoprecipitation (ChIP) followed by sequencing has revealed genome-wide SOX2 binding sites, with particular enrichment in distal chromatin regions that interact with promoters and carry epigenetic enhancer marks [97] [10]. These SOX2-bound enhancer regions frequently participate in long-range chromatin interactions mediated by RNA polymerase II, as demonstrated by ChIA-PET analysis, highlighting the importance of three-dimensional genome organization in SOX2-mediated transcriptional regulation [97].
Table 3: Essential Research Reagents for SOX2-Pathway Investigations
| Reagent Category | Specific Examples | Application/Function | Experimental Notes | |
|---|---|---|---|---|
| AKT Inhibitors | MK-2206 (pan-AKT), Akti1/2 | Reduces SOX2 protein levels | Dose-dependent effect (1-10 μM); validates AKT-SOX2 regulation | [94] |
| PI3K Inhibitors | Wortmannin, GDC-0941 | Suppresses SOX2 expression | Confirms canonical PI3K/AKT pathway involvement | [94] |
| CRISPR/Cas9 System | lentiCRISPR v2 vector with SOX2 gRNA | Complete SOX2 knockout | gRNA: 5′-GCTCGCCATGCTATTGCCGC-3′; validate by Western blot | [92] |
| Inducible shRNA | Tet-pLKO-puro with SOX2 shRNA | Doxycycline-controlled SOX2 knockdown | shRNA: 5′-CAGCTCGCAGACCTACATGAA-3′; 1 μg/mL doxycycline every 48h | [92] |
| Expression Vectors | pULTRA-SOX2 (wild-type) | SOX2 reconstitution | Rescues phenotype in knockout/knockdown models | [92] |
| ChIP Antibodies | Anti-SOX2, Anti-Pol II | Genome-wide binding site mapping | Identifies SOX2-bound enhancers and promoters | [97] |
Therapeutic Implications and Future Perspectives
The intricate connections between SOX2 and major signaling pathways present both challenges and opportunities for therapeutic intervention in cancer. The context-dependent nature of SOX2 function necessitates careful patient stratification and biomarker development for successful targeting strategies [10] [92]. For instance, in lung adenocarcinoma models, SOX2 knockout does not universally impair cancer stem cell properties across all cell lines, suggesting that SOX2 dependency varies based on genetic background and cellular context [92]. This heterogeneity underscores the importance of comprehensive molecular profiling to identify tumors that rely on SOX2 for maintenance and progression. Several innovative approaches are emerging to target SOX2 and its regulatory networks, including zinc-finger-based artificial transcription factors that can reduce endogenous SOX2 mRNA levels by approximately 95% in glioma models, subsequently inhibiting cell proliferation and inducing apoptosis [10]. Additionally, natural compounds such withaferin A and sulforaphane have demonstrated potential in reducing SOX2 expression in breast and pancreatic cancer models, respectively [10].
Future therapeutic strategies should consider the network-level interactions between SOX2 and multiple signaling pathways rather than targeting individual components in isolation. Combination approaches that simultaneously inhibit SOX2 and its upstream regulators (e.g., AKT) or parallel pathways (e.g., Notch) may prove more effective than monotherapies [94] [10]. The development of SOX2-targeted agents must also account for potential on-target toxicities in normal tissues where SOX2 functions in stem cell maintenance and tissue homeostasis [10]. Advances in delivery systems, including nanoparticle-based approaches and tumor-specific targeting modalities, may enhance the therapeutic window for SOX2-directed therapies. Furthermore, the integration of single-cell sequencing technologies with functional genomics approaches will enable more precise delineation of SOX2 regulatory networks in specific cellular subpopulations within tumors, particularly in cancer stem cell compartments that often drive therapy resistance and disease recurrence [69]. As our understanding of SOX2 biology continues to evolve, so too will opportunities for therapeutic intervention aimed at disrupting the SOX2 regulatory axis in cancer while preserving its physiological functions in normal tissue maintenance and repair.
Benchmarking SOX2 Against Other Pluripotency Factors (OCT4, NANOG) in Dedifferentiation
Abstract The process of cellular dedifferentiation, central to induced pluripotency and cancer pathogenesis, is critically governed by a core set of transcription factors, chiefly SOX2, OCT4, and NANOG. While these factors function in a synergistic network to maintain pluripotency, a growing body of evidence reveals distinct and unique roles for each. This whitepaper provides an in-depth technical benchmark of SOX2 against OCT4 and NANOG, synthesizing current research to delineate the specific and often superior contributions of SOX2 in driving dedifferentiation. We consolidate quantitative data from key studies, detail essential experimental protocols, and map the associated signaling pathways to provide a definitive resource for researchers and drug development professionals targeting dedifferentiation processes.
1. Introduction: The Pluripotency Trinity and the Focus on SOX2 The trinity of transcription factors—SOX2, OCT4, and NANOG—forms a core transcriptional regulatory circuitry that co-operatively controls gene expression to maintain pluripotency in embryonic stem cells (ESCs) [26]. They activate the expression of pluripotent genes, including themselves, while repressing genes responsible for differentiation [26]. The seminal work on induced pluripotent stem cells (iPSCs) cemented their collective role in reprogramming somatic cells to a pluripotent state [12] [5]. However, a nuanced comparison under identical experimental conditions reveals that their functional repertoire is not redundant. SOX2, in particular, demonstrates a potent and multifaceted capacity to impart stem cell-like features and drive dedifferentiation in somatic and cancer contexts, making it a critical focus for both regenerative medicine and oncology research [12] [98].
2. Functional Benchmarking: A Quantitative and Qualitative Comparison Direct comparative studies and pan-cancer analyses provide a foundation for benchmarking SOX2 against OCT4 and NANOG. The data indicate that while all three factors are powerful, SOX2 exhibits distinct and often superior transforming activity.
Table 1: Comparative Analysis of Core Pluripotency Factors in Dedifferentiation and Transformation
| Feature | SOX2 | OCT4 | NANOG |
|---|---|---|---|
| Transforming Activity | Exhibits the strongest transforming activity in immortalized astrocytes (cell proliferation, neurosphere formation, drug resistance, migration/invasion) [98] | Lesser transforming activity compared to SOX2 under the same experimental conditions [98] | Lesser transforming activity compared to SOX2 under the same experimental conditions [98] |
| Role in iPSC Reprogramming | Key factor; activation of endogenous SOX2 is an early event in reprogramming [26]. Can be replaced only by closely related SoxB1 members (Sox1, Sox3) or a modified Sox17 [26] | Essential core factor | Essential core factor |
| Expression in Human Tumors | Aberrantly expressed in 19.3% of pancreatic tumors [12] [5]; upregulated in GBM, LGG, lung cancers [23]; amplification is a hallmark of various cancers [10] | Frequently activated in various cancers [98] | Frequently activated in various cancers [98] |
| Association with Prognosis | High expression associated with poor prognosis in GBM, LGG, lung adenocarcinoma, and lung squamous cell carcinoma [23] | Context-dependent | Context-dependent |
| Mechanism in Cancer Dedifferentiation | Promotes dedifferentiation and imparts CSC features; represses p21Cip1/p27Kip1 [12]; drives EMT via Snail/Slug/Twist [12] [5]; maintains self-renewal in epithelial PDAC CSCs [52] | Sustains CSC populations | Sustains CSC populations |
Table 2: SOX2-Specific Functional Data in Selected Cancers
| Cancer Type | Key Finding on SOX2 Function | Experimental Model |
|---|---|---|
| Pancreatic Ductal Adenocarcinoma (PDAC) | Ectopic expression confers stem cell-like features; enriched in ESA+/CD44+ CSC population; directly binds to Snail, Slug, and Twist promoters to drive EMT [12] [5] | Human tissue microarrays (TMAs), pancreatic cancer cell lines (L3.6, BxPC3) [12] [5] |
| Glioma | Exhibits strongest transforming activity; associated with activation of NF-κB signaling [98] | Human immortalized astrocytes [98] |
| Pan-Cancer Analysis | High SOX2 expression is associated with poor prognosis in specific cancers (e.g., GBM, lung cancers) and correlates with increased immune checkpoint expression and potential response to immunotherapy [23] | Bioinformatic analysis of over 30 cancer types [23] |
3. Detailed Experimental Protocols for Investigating SOX2 in Dedifferentiation To facilitate replication and further research, below are detailed methodologies from key studies benchmarking SOX2.
3.1. Protocol: Assessing Cellular Transforming Activity This protocol is adapted from the comparative study in immortalized astrocytes [98].
- Objective: To quantitatively compare the transforming potential of SOX2, OCT4, and NANOG.
- Cell Line: Human immortalized astrocytes.
- Culture Conditions: Serum-free stem cell culture conditions.
- Transfection: Introduce expression vectors for SOX2, OCT4, or NANOG.
- Functional Assays:
- Cell Proliferation Assay: Use MTT or similar colorimetric assays to measure metabolic activity at 24, 48, 72, and 96 hours post-transfection.
- Neurosphere Formation Assay: Plate single-cell suspensions in ultra-low attachment plates with serum-free medium supplemented with EGF and bFGF. Count the number and measure the diameter of spheres after 7-10 days.
- Drug Resistance Assay: Treat transfected cells with a cytotoxic drug (e.g., Gemcitabine for pancreatic models [12]). Cell viability is assessed via MTT assay after 72 hours. Calculate the IC50 value.
- Migration/Invasion Assay: Use Transwell chambers coated with (invasion) or without (migration) Matrigel. Seed transfected cells in the upper chamber with serum-free medium. Medium with serum as a chemoattractant is placed in the lower chamber. After 24-48 hours, fix, stain, and count cells that migrated/invaded through the membrane.
- Downstream Analysis: Investigate potential signaling pathway activation (e.g., NF-κB) via western blotting or qRT-PCR.
3.2. Protocol: SOX2 Knockdown in Pancreatic Cancer Stem Cells This protocol is adapted from studies on PDAC CSCs [12] [52].
- Objective: To determine the functional necessity of SOX2 in maintaining self-renewal and stemness.
- Cell Lines: Use PDAC cell lines with epithelial phenotypes and high endogenous SOX2 (e.g., Panc89 Holoclone cells) [52].
- SOX2 Knockdown:
- siRNA Design: Use a pool of 3-5 target-specific 19-25 nt siRNAs against SOX2.
- Transfection: Seed 5.0 x 10ⴠcells/well in a 12-well plate. After 24 hours, transfer with 4 µl (0.12 µM) of SOX2-specific siRNA or a non-targeting control siRNA (CTRLsi) complexed with 4 µl HiPerfect transfection reagent in 100 µl OPTI-MEM.
- Incubation: Incubate for 72 hours before analysis.
- Functional Readouts:
- Colony Formation Assay (CFA): After knockdown, re-seed cells at low density and culture for 1-2 weeks. Fix and stain colonies with crystal violet to quantify self-renewal ability.
- qRT-PCR and Immunofluorescence: Confirm knockdown efficiency and analyze expression of stemness (ALDH1, ESA, CD44) and EMT (E-Cadherin, Vimentin) markers.
- Key Consideration: As SOX2 knockdown can induce cell cycle arrest, perform viable cell counts and cell cycle analysis via flow cytometry to distinguish reduced self-renewal from general growth inhibition [12].
4. Signaling Pathways and Molecular Mechanisms SOX2's potent dedifferentiation capability is underpinned by its interaction with multiple signaling pathways. The following diagram maps these key interactions.
Figure 1: SOX2-Centric Network in Dedifferentiation. SOX2 drives dedifferentiation and transformation by regulating key cellular processes through direct gene regulation, pathway activation, and complex feedback loops.
5. The Scientist's Toolkit: Essential Research Reagents The following table catalogs critical reagents used in the featured experiments for studying SOX2-mediated dedifferentiation.
Table 3: Key Research Reagent Solutions for SOX2 Dedifferentiation Studies
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| SOX2-specific siRNAs | siRNA-mediated knockdown to probe SOX2 loss-of-function and its impact on self-renewal, proliferation, and EMT. | A pool of 3-5 target-specific 19-25 nt sequences used in Panc89 PDAC cells [52]. |
| SOX2 Expression Vectors | Forced SOX2 overexpression to assess its gain-of-function in driving dedifferentiation, proliferation, and transformation. | Used in immortalized astrocytes to benchmark transforming activity [98] and in PDAC cells to study stemness [12]. |
| Sphere-Formation Medium | Enriches and assesses cancer stem cell (CSC) populations and their self-renewal capability in vitro. | Serum-free medium supplemented with EGF and bFGF, used for neurosphere assays with astrocytes [98] and pancreatic cancer cells [12]. |
| ALDH1, ESA, CD44 Antibodies | Flow cytometry or immunofluorescence markers for identifying and isolating pancreatic CSCs where SOX2 is enriched. | Used to characterize the CSC population in SOX2-overexpressing pancreatic cancer cells [12]. |
| p21Cip1, p27Kip1, Cyclin D3 Antibodies | Key readouts for SOX2's role in cell cycle regulation via western blotting or qRT-PCR. | SOX2 knockdown induces p21/p27; overexpression induces Cyclin D3 [12] [5]. |
| E-Cadherin, Vimentin, Snail Antibodies | Immunoblotting markers to evaluate SOX2's role in driving Epithelial-to-Mesenchymal Transition (EMT). | SOX2 overexpression leads to loss of E-Cadherin and gain of mesenchymal markers [12]. |
6. Discussion and Future Perspectives The collective evidence firmly positions SOX2 as a preeminent and versatile driver of dedifferentiation. Its benchmarked superiority in cellular transformation, direct regulation of cell cycle and EMT machinery, and context-dependent role in maintaining CSCs underscore its unique position within the pluripotency network. The association of high SOX2 expression with poor prognosis in several cancers and its recently identified link to immune checkpoint expression further elevate its therapeutic profile [23]. Future research should focus on exploiting these findings therapeutically. Strategies including SOX2 inhibition via targeted protein degradation, disruption of its partnership with OCT4, and leveraging its expression to enhance immune checkpoint therapy represent promising frontiers [23] [10]. A deep and nuanced understanding of SOX2's mechanisms, as benchmarked against its coregulators, is paramount for advancing both regenerative medicine and novel oncology treatments.
Conclusion
SOX2 stands as a central orchestrator of cellular dedifferentiation, wielding power over cell fate in both physiological development and pathological states like cancer. Its ability to impart stem cell-like characteristics underscores its dual potential: as a powerful tool for regenerative medicine and a formidable driver of tumor progression and therapy resistance. Future research must focus on unraveling the precise contextual cues that determine SOX2's functional outcomes and developing sophisticated strategies to safely harness or inhibit its activity. Targeting the SOX2 axis presents a promising frontier for overcoming treatment resistance in aggressive cancers and advancing novel cell-based therapies, making it a critical focus for ongoing biomedical and clinical innovation.
References
- 1. SOX2 protein biochemistry in stemness, reprogramming ... [https://www.nature.com/articles/s41388-019-0997-x]
- 2. DNA binding redistributes activation domain ensemble and ... [https://www.nature.com/articles/s41467-024-45847-2]
- 3. The Sox2 transcription factor binds RNA [https://www.nature.com/articles/s41467-020-15571-8]
- 4. Sox2 Uses Multiple Domains to Associate with Proteins ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0015486]
- 5. SOX2 promotes dedifferentiation and imparts stem cell-like ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3759123/]
- 6. SOX2 promotes dedifferentiation and imparts stem cell-like ... [https://mayoclinic.elsevierpure.com/en/publications/sox2-promotes-dedifferentiation-and-imparts-stem-cell-like-featur/]
- 7. Structural mechanism of DNA-mediated Nanog–Sox2 ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9061787/]
- 8. Structural mechanism of DNA-mediated Nanog–Sox2 ... [https://pubs.rsc.org/en/content/articlelanding/2019/ra/c8ra10085c]
- 9. Distinct Functions of Sox2 Control Self-Renewal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3209254/]
- 10. Dissecting SOX2 expression and function reveals an ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X24000672]
- 11. Overview of the roles of Sox2 in stem cell and development [https://www.ovid.com/journals/bioch/abstract/10.1515/hsz-2014-0317~overview-of-the-roles-of-sox2-in-stem-cell-and-development]
- 12. SOX2 promotes dedifferentiation and imparts stem cell-like ... [https://www.nature.com/articles/oncsis201323]
- 13. Organâ€Specific Dedifferentiation and Epigenetic Remodeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610414/]
- 14. SOX2-VSX2 Co-Occupancy Shapes Retinal Neurogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139939/]
- 15. SOX2 regulates foregut squamous epithelial homeostasis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352906/]
- 16. CRISPR screen reveals SOX2 as a critical regulator of ... [https://www.nature.com/articles/s41598-025-20183-7]
- 17. Pharmacological inhibition of RE1 silencing transcription ... [https://link.springer.com/article/10.1007/s11011-025-01744-1]
- 18. Pioneer factors: Roles and their regulation in development [https://pmc.ncbi.nlm.nih.gov/articles/PMC10873006/]
- 19. Accelerating life sciences research [https://openai.com/index/accelerating-life-sciences-research-with-retro-biosciences/]
- 20. Orchestration of pluripotent stem cell genome reactivation ... [https://pubmed.ncbi.nlm.nih.gov/40153434/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1-IhdOtu689NDq4g82S-AMTNWMhAC4cHmIxQs8eYluoRtL_M6z&fc=None&ff=20250329220923&v=2.18.0.post9+e462414]
- 21. Enhanced Activities of OCT4 and SOX2 Promote ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12407333/]
- 22. Par6/SOX2 interact to modulate stemness maintenance in ... [https://www.nature.com/articles/s41388-025-03595-7]
- 23. Pan-cancer analysis of SOX2: Prognostic implications and ... [https://www.sciencedirect.com/science/article/pii/S2405844025005808]
- 24. Defined culture conditions robustly maintain human stem ... [https://www.nature.com/articles/s42003-025-07658-z]
- 25. Evaluation of the prognostic role of SOX2 as a tumor stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579421/]
- 26. Sox2, a key factor in the regulation of pluripotency and neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4131272/]
- 27. SOX2 Regulates Growth, Expression of Basal/Luminal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249187/]
- 28. Sox2 transcription network acts as a molecular switch to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4172677/]
- 29. Targeting AKT as a promising strategy for SOX2-positive, ... [https://www.nature.com/articles/s41413-024-00395-9]
- 30. Comprehensive profiling reveals mechanisms of SOX2 ... [https://www.nature.com/articles/cr201615]
- 31. Phylo- Epigenetic Conservation and CpG Erosion in OCT4, SOX , and... 2 [https://www.mdpi.com/2073-4425/16/9/1102]
- 32. Emerging Role of Long Non-Coding RNA SOX2OT in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4090206/]
- 33. Long noncoding RNA Sox2ot and transcription factor YY1 ... [https://www.nature.com/articles/s41419-018-0840-2]
- 34. SOX2 and cancer: current research and its implications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4126816/]
- 35. of Driver Epigenetic in Testicular Tumorigenesis Regulation Genes [https://pubmed.ncbi.nlm.nih.gov/36835562/]
- 36. SOX2 for Stem Cell Therapy and Medical Use: Pros or Cons? [https://pmc.ncbi.nlm.nih.gov/articles/PMC7444200/]
- 37. A role for mitotic bookmarking of SOX2 in pluripotency and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5159668/]
- 38. Generation and application of novel hES cell reporter lines ... [https://www.nature.com/articles/s41598-024-69645-4]
- 39. Deconstructing Sox2 Function in Brain Development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9139651/]
- 40. The Involvement of SOX2 in Direct Reprogramming of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3726137/]
- 41. Sox2-mediated transdifferentiation of hAT-MSCs into ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816624002544]
- 42. Assessment of SOX2 performance as a marker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413790/]
- 43. Protocol for Tumorsphere Formation of Cancer Stem Cells [https://fujifilmbiosciences.fujifilm.com/protocol-for-tumorsphere-formation-of-cancer-stem-cells]
- 44. Sphere formation assay [https://bio-protocol.org/exchange/minidetail?id=8179309&type=30]
- 45. Assessment of SOX2 performance as a marker for ... [https://pubmed.ncbi.nlm.nih.gov/40918157/]
- 46. Prognostic Value of SOX2 and NANOG Expression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11987986/]
- 47. Evaluation of the prognostic role of SOX2 as a tumor stem cell ... [https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-025-07065-0]
- 48. Targeting AKT as a promising strategy for SOX2-positive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11850766/]
- 49. Functional characterization of SOX2 as an anticancer target [https://pubmed.ncbi.nlm.nih.gov/32728033/]
- 50. identifies High as a super pioneer factor... throughput screening SOX 2 [https://pubmed.ncbi.nlm.nih.gov/34099689/]
- 51. Genome-wide Profiling of SOX Binding Sites in... | Research Square 2 [https://www.researchsquare.com/article/rs-6931497/v1]
- 52. Nestin and SOX2 Maintain self-renewal Abilities of ... [https://link.springer.com/article/10.1007/s12015-025-11006-3]
- 53. Inhibition of mutant EGFR in lung cancer cells triggers... [https://elifesciences.org/articles/06132]
- 54. Sox2 Dosage: A Critical Determinant in the Functions of Sox2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6662612/]
- 55. Functional characterization of SOX2 as an anticancer target [https://www.nature.com/articles/s41392-020-00242-3]
- 56. The dark side of SOX2: cancer - a comprehensive overview [https://www.oncotarget.com/article/16570/text/]
- 57. Dynamic ubiquitylation of Sox2 regulates proteostasis and ... [https://www.nature.com/articles/s41467-018-07025-z]
- 58. E3 连接酶TRIM26 å’ŒWWP2 竞争性结åˆæŽ§åˆ¶èƒ¶è´¨æ¯ç»†èƒžç˜¤ä¸ ... [https://news.bioon.com/article/a5f2e1931428.html]
- 59. Research Progress on the Regulation of Third-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12438653/]
- 60. Targeting oncogenic SOX2 in human cancer cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6954883/]
- 61. : A Regulatory Factor in Tumorigenesis and Metastasis Sox 2 [https://pubmed.ncbi.nlm.nih.gov/30907312/]
- 62. drives progression and therapy resistance in advanced prostate... SOX 2 [https://www.news-medical.net/news/20250822/SOX2-drives-progression-and-therapy-resistance-in-advanced-prostate-cancer.aspx]
- 63. The Novel Role of SOX2 as an Early Predictor of Cancer Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6468607/]
- 64. , PIWI proteins, and MALAT1 – plasma-based... | PLOS One SOX 2 [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328557]
- 65. The molecular pathogenesis of SOX2 in prostate cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11842661/]
- 66. YTHDC2 suppresses bladder cancer by inhibiting SOX2- ... [https://www.nature.com/articles/s41419-025-08079-w]
- 67. Transcriptional repression of SOX2 by p53 in cancer cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232590/]
- 68. Epigenetic regulation of cancer stemness [https://www.nature.com/articles/s41392-025-02340-6]
- 69. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 70. The role of SOX transcription factors in prostate cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357254/]
- 71. Cancer cell plasticity and therapeutic resistance - Hereditas [https://hereditasjournal.biomedcentral.com/articles/10.1186/s41065-025-00564-8]
- 72. AKT1 as a therapeutic target for platinum-resistant SOX2 ... [https://www.nature.com/articles/s41598-025-92036-2]
- 73. Signaling pathways as the pivotal regulators of cisplatin ... [https://pubmed.ncbi.nlm.nih.gov/40844657/]
- 74. SOX2 drives esophageal squamous carcinoma by ... [https://pubmed.ncbi.nlm.nih.gov/40897722/]
- 75. SOX2 promotes dedifferentiation and imparts stem cell-like features to pancreatic cancer cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/23917223/?dopt=Abstract]
- 76. Targeted silencing of the oncogenic transcription factor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3413152/]
- 77. Analysis of SOX2-Expressing Cell Populations Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3841266/]
- 78. SOX2-driven enhancer landscapes define the transcriptional ... [https://pubmed.ncbi.nlm.nih.gov/41159420/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0LYBXPN1kqFLXnwTcYMFJGHudpJ69zhAbt2DTPQBHLI&fc=None&ff=20251109104429&v=2.18.0.post22+67771e2]
- 79. Single-Factor SOX2 Mediates Direct Neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158546/]
- 80. Pan-cancer analysis of SOX2: Prognostic implications and ... [https://pubmed.ncbi.nlm.nih.gov/39944324/]
- 81. Assessment of SOX2 performance as a marker for circulatin... [https://www.degruyterbrill.com/document/doi/10.1515/med-2025-1265/html?srsltid=AfmBOoopGUU_K9IrCSy-IrDh9rpvVEjPUkOPSD9yMkKIcHDzcIXB7tLv]
- 82. The role of SOX2 in small cell lung cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4367598/]
- 83. SOX2 Promotes Radioresistance in Non-small Cell Lung ... [https://www.medsci.org/v20p0781.htm]
- 84. SOX2 functions as a molecular rheostat to control the ... [https://www.oncotarget.com/article/8994/text/]
- 85. Pan-Cancer Analysis Reveals SOX2 as a Promising ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10751676/]
- 86. SOX2 promotes tumor metastasis by stimulating epithelial- ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383513002577]
- 87. SOX2 is a dispensable modulator of NUT carcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634820/]
- 88. A predominant enhancer co-amplified with the SOX2 ... [https://www.nature.com/articles/s41467-021-27055-4]
- 89. SOX2 dosage sustains tumor-promoting inflammation to drive ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01734-w]
- 90. Metastatic potential and prognostic significance of SOX2 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6657218/]
- 91. Impact of SOX2 function and regulation on therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9709205/]
- 92. SOX2 Expression Does Not Guarantee Cancer Stem Cell ... [https://www.mdpi.com/2073-4409/13/3/216]
- 93. PI3K/AKT/mTOR signaling transduction pathway and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01827-6]
- 94. Molecular and functional interactions between AKT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4791249/]
- 95. The Role of Notch, Hedgehog, and Wnt Signaling Pathways in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8100510/]
- 96. Notch signaling pathway: architecture, disease, and ... [https://www.nature.com/articles/s41392-022-00934-y]
- 97. Mapping the Global Chromatin Connectivity Network for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6506828/]
- 98. of Cellular Transforming Activity of Comparison , OCT , and... 4 NANOG [https://pubmed.ncbi.nlm.nih.gov/28933914/]