Transdifferentiation Mechanisms in Tissue Repair: From Cellular Reprogramming to Clinical Applications
This article provides a comprehensive analysis of transdifferentiation, the direct conversion of one differentiated cell type into another, and its transformative potential in regenerative medicine and tissue repair.
Transdifferentiation Mechanisms in Tissue Repair: From Cellular Reprogramming to Clinical Applications
Abstract
This article provides a comprehensive analysis of transdifferentiation, the direct conversion of one differentiated cell type into another, and its transformative potential in regenerative medicine and tissue repair. It explores foundational biological mechanisms, including the role of master switch genes and transcription factors, while examining both natural and induced transdifferentiation phenomena. The scope encompasses cutting-edge methodological approaches—from transcription factor-mediated reprogramming to chemical induction and mRNA technology—across key therapeutic areas including neurological, cardiac, and pancreatic systems. Critical challenges such as efficiency optimization, safety evaluation, and scalability are addressed, alongside comparative analysis with alternative cell reprogramming technologies. This resource equips researchers and drug development professionals with the current state and future trajectory of transdifferentiation for developing novel therapeutic interventions.
The Biology of Cell Fate Conversion: Uncovering Natural and Pathological Transdifferentiation
Transdifferentiation, also known as direct cell reprogramming, is a process where one mature, differentiated somatic cell type is converted directly into another, without passing through an induced pluripotent stem cell (iPSC) state [1] [2] [3]. This approach offers a more direct, rapid, and potentially safer strategy for cell replacement therapies and regenerative medicine compared to iPSC methods, as it avoids risks of tumorigenesis and uncontrolled proliferation associated with pluripotency [1] [2]. This technical guide synthesizes current advancements in transdifferentiation, detailing its core mechanisms, key methodologies, and therapeutic applications, with a specific focus on its role in tissue repair research.
Regenerative medicine has increasingly turned toward gene-based approaches to repair or replace damaged tissues. Conventional reprogramming to iPSCs involves transforming somatic cells into a pluripotent state, which carries risks of immunogenicity, tumorigenesis, and epigenetic abnormalities [1] [2].
Transdifferentiation circumvents this pluripotent intermediate, offering a paradigm shift in cellular reprogramming. Defined as the irreversible switch of one type of differentiated cell to another, it involves a discrete change in the program of gene expression with a direct ancestor-descendant relationship between the two cell types [4]. The process typically requires dedifferentiation and cell division as essential intermediate steps, though this may not be obligatory in all cases [4]. This direct lineage conversion technology holds great practical promise for in vivo tissue repair without the risks of tumorigenesis, contamination, or cell transplantation [1].
Core Mechanisms of Cell Fate Conversion
Transdifferentiation is presumably caused by a change in the expression of a master switch gene (selector or homeotic gene), whose normal function is to distinguish the two cell types in normal development [4]. This change alters the state of developmental commitment, potentially through somatic mutation or, more commonly, induction by environmental changes [4].
Molecular Drivers and Pathways
The process is orchestrated through several interconnected molecular mechanisms:
- Transcriptional Activation: Master transcription factors (TFs) bind to regulatory regions of genes, initiating widespread changes in gene expression networks that establish a new cellular identity [2].
- Epigenetic Remodeling: Chromatin structure is modified through DNA methylation, histone modifications, and chromatin remodeling complexes, making old identity genes less accessible and new ones more accessible [1].
- Metabolic Shifts: Cells undergo metabolic reprogramming to support energy and biosynthetic requirements of the new cell type [1].
- Signaling Pathway Activation: Key developmental pathways such as Notch, PI3K/AKT, Wnt/β-catenin, and those involved in epithelial-mesenchymal transition (EMT) are often reactivated to guide the differentiation process [5].
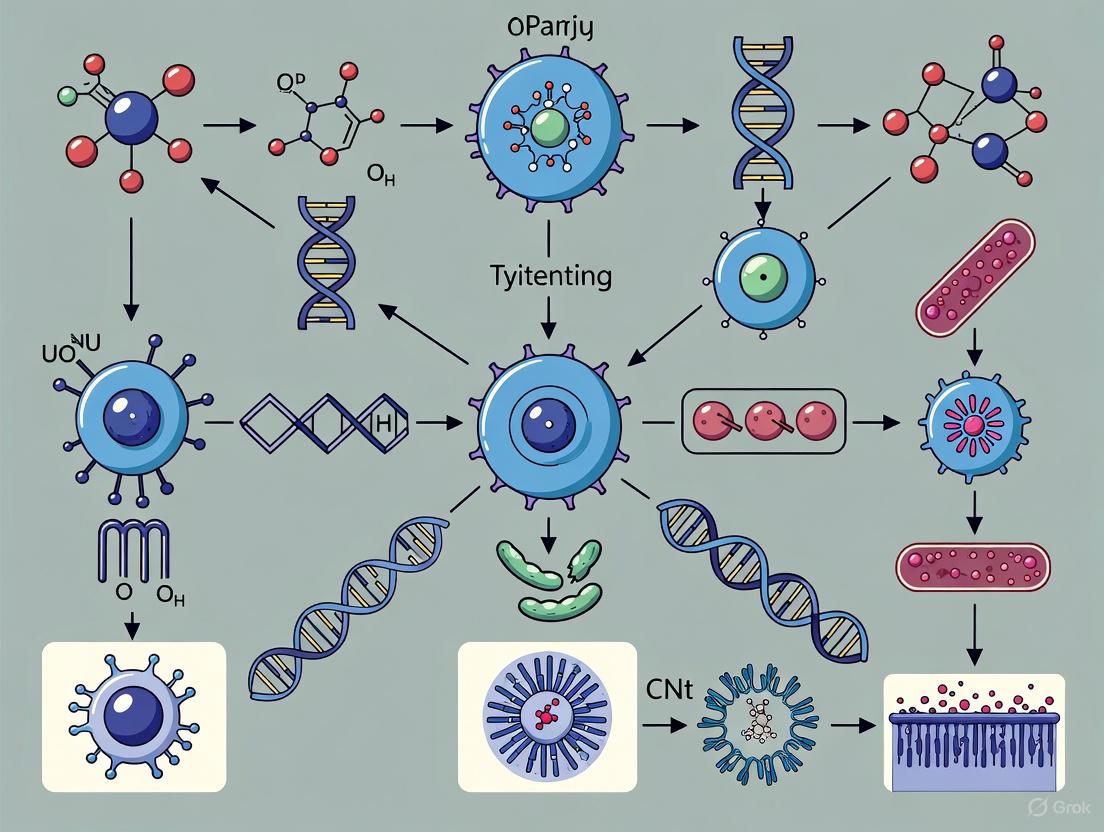
The following diagram illustrates the conceptual framework and major mechanisms driving direct lineage reprogramming.
Methodological Approaches in Direct Reprogramming
Cellular reprogramming can be achieved through multiple methods, each with distinct advantages and challenges. The primary strategies involve introducing or upregulating key reprogramming factors vital for establishing a new cellular identity.
Exogenous Transgene Overexpression
The most prevalent method uses viral vectors to introduce transgenes encoding master transcription factors.
- Lentiviruses/Retroviruses: Effectively integrate DNA into the host genome, leading to stable protein expression. Lentiviruses can infect both non-dividing and dividing cells, while retroviruses only infect dividing cells [2].
- Non-integrating Viruses (Adenoviruses, Sendai viruses): Insert transgenes for transient expression without genomic integration, resulting in lower efficiency but reduced risk of insertional mutagenesis [2].
The typical workflow involves cloning transcription factor coding DNA into viral plasmids, infecting target cells, selecting successfully transfected cells, and inducing TF overexpression to drive lineage conversion [2]. Efficiency can be improved by first overloading factors like Oct4, Sox2, KLF4, and c-Myc (OSKM) to create a "primed" state, enhancing subsequent transdifferentiation efficiency up to 34% in some studies [2].
Endogenous Gene Regulation
- CRISPR/Cas9 Systems: Catalytically inactive dCas9 fused to transcriptional or epigenetic effector domains enables programmable, modular regulation of endogenous genes without altering DNA sequence [1]. This approach offers higher specificity and efficiency compared to viral overexpression [2].
- Physical Delivery Systems: Tissue Nanotransfection (TNT) is a novel non-viral platform that uses localized nanoelectroporation to deliver genetic material (plasmid DNA, mRNA, CRISPR/Cas9 components) directly into tissues in vivo [1]. This method concentrates electric fields through hollow silicon nanochannels, creating transient nanopores in cell membranes for cargo delivery with high specificity and minimal cytotoxicity [1].
Small Molecule and Chemical Approaches
Chemical compounds and pharmacological agents can induce transdifferentiation by targeting transcriptional pathways, triggering immunological responses, or directly altering the epigenetic environment, offering a non-genetic alternative for cellular reprogramming [2].
Table 1: Comparison of Major Transdifferentiation Delivery Methods
| Method | Mechanism | Efficiency | Advantages | Disadvantages |
|---|---|---|---|---|
| Lentiviral Vectors [2] | Genomic integration of transgenes | Variable (e.g., ~7.7% for neurons) [2] | Stable expression; infects dividing & non-dividing cells | Insertional mutagenesis risk; immunogenicity |
| Adenoviral Vectors [2] | Transient episomal expression | Lower (e.g., ~2.7% for neurons) [2] | Reduced integration risk; high transduction efficiency | Transient expression; immunogenicity |
| CRISPR/dCas9 Systems [1] [2] | Epigenetic/transcriptional regulation of endogenous genes | High (improves efficiency) [2] | Programmable, specific; no foreign gene integration | Off-target effects potential; complex delivery |
| Tissue Nanotransfection (TNT) [1] | Nanoelectroporation for physical delivery | High for in vivo applications | Non-viral, minimal cytotoxicity; high specificity | Localized delivery; optimization of parameters needed |
| Small Molecules [2] [3] | Chemical induction of reprogramming | Variable | Non-genetic; controllable timing/dosing | Lower efficiency in some cases; off-target effects |
The following workflow diagram outlines a generalized protocol for conducting a viral vector-mediated transdifferentiation experiment.
Key Experimental Applications in Tissue Repair
Transdifferentiation has demonstrated significant potential across various tissue regeneration contexts, with particular progress in neural and cardiac applications.
Neural System Repair
Neurodegenerative diseases and central nervous system injuries have been a major focus of transdifferentiation research. Proof-of-principle was established in 2013 when resident astrocytes and transplanted fibroblasts in adult mouse brain were successfully converted into functional neurons using Ascl1, Myt1l, and Brn2a transcription factors delivered via viral vector [3]. This approach has since been extended to treat disease models:
- Spinal Cord Injury: Lentiviral delivery of Sox2 to astrocytes in mouse spinal cord induced conversion to neuroblasts (3-6% efficiency), which matured into neurons that synapsed with resident neurons [3].
- Alzheimer's Disease Models: Retroviral delivery of NeuroD1 to astrocytes in mouse brain with stab injury resulted in conversion to neurons with 90% efficiency [3].
Cardiac Tissue Regeneration
Myocardial infarction represents another promising application, where converting cardiac fibroblasts into cardiomyocytes could directly repair damaged heart tissue.
- Initial Studies: Early work demonstrated that adenoviral delivery of MyoD could convert cardiac fibroblasts into skeletal myofibers (2-14% efficiency) in freeze-thaw injured rat hearts [3].
- Cardiomyocyte Generation: The GMT combination (Gata4, Mef2c, Tbx5) delivered via retrovirus converted cardiac fibroblasts into cardiomyocyte-like cells in mouse myocardial infarction models (10-15% efficiency), reducing infarct size and significantly decreasing cardiac dysfunction [3].
- Enhanced Protocols: Adding Hand2 to create GHMT improved conversion efficiency to approximately 7%, while microRNA combinations (miR-1, 133, 208, 499) achieved 12-25% efficiency, both resulting in functional improvement [3].
Table 2: Representative Transdifferentiation Applications in Disease Modeling and Tissue Repair
| Disease/Injury Model | Source Cell | Target Cell | Key Reprogramming Factors | Delivery Method | Efficiency | Functional Outcome |
|---|---|---|---|---|---|---|
| CNS/Brain Repair [3] | Astrocyte, Fibroblast | Induced Neuron (iN) | Myt1l, Ascl1, Brn2a | Lentiviral (in vivo) | 0.4% to 5.9% | iNs integrated in tissue |
| Spinal Cord Injury [3] | Astrocyte | Induced Adult Neuroblast | Sox2 | Lentiviral (stereotactic) | 3-6% | Mature neurons formed synapses |
| Alzheimer's Model [3] | Astrocyte | Induced Neuron (iN) | NeuroD1 | Retroviral (stereotactic) | 90% | Transdifferentiated iNs in tissue |
| Myocardial Infarction [3] | Cardiac Fibroblast | Cardiomyocytes | GMT (Gata4, Mef2c, Tbx5) | Retroviral (intramyocardial) | 10-15% | Reduced infarct size; improved function |
| Myocardial Infarction [3] | Cardiac Fibroblast | Cardiomyocytes | microRNAs 1, 133, 208, 499 | Lentiviral (intramyocardial) | 12-25% | Fibroblast conversion; moderate functional improvement |
| Complete Heart Blockage [3] | Ventricular Cardiomyocyte | Pacemaker Cells | Tbx18 | Adenovirus (percutaneous) | 24.5% | Biological pacemaker; improved bradycardia |
The Scientist's Toolkit: Essential Research Reagents
Successful transdifferentiation experiments require carefully selected reagents and tools. The following table summarizes key materials used in the field.
Table 3: Essential Research Reagents for Transdifferentiation Studies
| Reagent Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Transcription Factors [2] [3] | Ascl1, Brn2, Myt1l (neurons); GMT combo (cardiomyocytes); MyoD (myoblasts) | Master regulators that initiate lineage conversion; often used in combinations | TF choice is critical; developmental regulators are common starting points |
| Viral Vectors [2] | Lentivirus, Retrovirus, Adenovirus | Delivery of genetic cargo into target cells | Lentiviruses preferred for non-dividing cells; integration vs. non-integration strategies |
| Gene Editing Systems [1] [2] | CRISPR/dCas9 with effector domains | Targeted epigenetic and transcriptional regulation | Enables endogenous gene regulation without transgene integration |
| Physical Delivery Systems [1] | Tissue Nanotransfection (TNT) chips | Nanoelectroporation for in vivo gene delivery | Non-viral approach; uses localized electrical pulses for membrane poration |
| Small Molecules [2] [3] | Chemical cocktails for epigenetic modulation | Induce reprogramming without genetic modification | Offers temporal control; lower immunogenicity concern |
| Cell Type Markers [5] | CD133, Nestin, SOX2 (stemness); CD31, CD34 (endothelial); α-SMA (myofibroblasts) | Identification and validation of starting and target cell populations | Multiple markers often needed due to heterogeneity and plasticity |
| Selection Agents [2] | Antibiotics (e.g., puromycin) | Enrichment of successfully transfected/transduced cells | Requires vector incorporation of resistance genes |
| 2-Iodo-1,1'-binaphthalene | 2-Iodo-1,1'-binaphthalene | 2-Iodo-1,1'-binaphthalene is a key synthetic intermediate for chiral ligands. This product is For Research Use Only. Not for diagnostic or personal use. | Bench Chemicals |
| 1-Decyl-4-isocyanobenzene | 1-Decyl-4-isocyanobenzene, CAS:183667-68-7, MF:C17H25N, MW:243.4 g/mol | Chemical Reagent | Bench Chemicals |
Transdifferentiation represents a transformative approach in regenerative medicine, enabling direct lineage conversion for tissue repair without pluripotent intermediates. While significant challenges remain in efficiency, phenotypic stability, and scalable clinical translation, emerging technologies like CRISPR-based regulation and tissue nanotransfection offer promising avenues for advancement. As mechanistic understanding deepens and delivery methods refine, direct reprogramming holds exceptional potential for generating functional cell types to address complex degenerative diseases and tissue injuries, ultimately enabling novel therapeutic strategies in precision regenerative medicine.
This whitepaper explores the phenomenon of transdifferentiation—the direct conversion of one mature, differentiated cell type into another—as a fundamental mechanism in tissue repair and regeneration. By examining two classic paradigms, lens regeneration in newts and pancreatic α-to-β-cell conversion, we dissect the cellular and molecular blueprints that enable such remarkable cellular plasticity. Understanding these evolutionarily conserved mechanisms provides critical insights for developing novel regenerative therapies for human diseases, including diabetes and ocular disorders. The content is framed within a broader thesis on harnessing endogenous repair mechanisms for therapeutic intervention, providing drug development professionals with a technical overview of the field's current state and future directions.
Transdifferentiation represents a powerful mode of tissue regeneration observed across phylogeny, wherein terminally differentiated cells reprogram their transcriptional identity without reverting to a pluripotent state [6]. Unlike stem cell-driven regeneration, this process leverages existing specialized cells within tissues, offering potentially safer and more efficient pathways for therapeutic intervention. The study of natural transdifferentiation models provides invaluable insights into the molecular logic of cell fate control. Among vertebrates, salamanders—particularly newts and axolotls—demonstrate exceptional regenerative capacities, functionally regenerating a wide spectrum of tissues from limbs to cardiac muscle and neural tissues [7]. This review focuses on two exemplary models: the Wolffian lens regeneration in newts, and pancreatic islet cell conversion in mammals, with emphasis on their underlying mechanisms and potential translational applications.
Lens Regeneration in Newts: A Classic Model of Transdifferentiation
Historical Context and Phenomenology
Lens regeneration in adult newts was first documented by Collucci (1891) and independently by Wolff (1895), after whom the process is often termed "Wolfian regeneration" [6]. This remarkable process involves the complete regeneration of a functional lens following surgical removal (lentectomy). The newt remains the only urodele amphibian known to regenerate its lens throughout its adult life, with no diminishment in capacity even after repeated regeneration or with advanced age [6]. Astoundingly, individual Japanese newts (Cynops pyrrhogaster) have been documented to regenerate perfect lenses 18 times over a 16-year period, with the regenerated lenses from the final cycles exhibiting cellular and biochemical properties identical to those of younger animals [6].
Cellular Mechanisms and Source Tissue
The regenerated lens originates not from residual lens tissue but via transdifferentiation of pigment epithelial cells (PECs) from the dorsal iris [6]. This process occurs in two distinct phases:
Dedifferentiation and Proliferation Phase (Days 1-8): The double-layered iris tissue at its dorsal edge disorganizes, PECs lose their pigmentation, re-enter the cell cycle, and upregulate early lens genes including Pax6, Sox2, and MafB [6]. This phase is characterized by increased synthesis of ribosomal RNA through amplification of rRNA genes and elevated transcriptional activity.
Transdifferentiation Phase (Days 8-16): Dedifferentiated cells form a lens vesicle and subsequently differentiate into lens fibers, ultimately restoring a fully functional lens [6].
Molecular Triggers and Signaling Pathways
Fibroblast growth factor 2 (FGF-2) has been identified as a critical initiator of lens regeneration. Key evidence includes:
- Upregulation of FGF-2 in PECs alongside early lens genes post-lentectomy [6].
- High expression of FGFR3 receptor in dorsal iris PECs [6].
- Inhibition of regeneration upon injection of a soluble form of FGFR3 to titrate FGF-2, which blocks all molecular and morphological changes in PECs [6].
- Ectopic lens formation from dorsal iris PECs upon FGF-2 injection into the intact eye, which subsequently replaces the degenerating primary lens [6].
Emerging research is beginning to elucidate the epigenetic and post-transcriptional regulators involved. Studies have revealed the upregulation of cancer-associated genes, apoptosis genes, and chromatin-modifying enzymes during dedifferentiation [6]. Furthermore, microRNAs, particularly miR-124a, appear to play significant roles, with differential regulation of miR-148 and let-7b implicated in controlling proliferation genes [6].
Table 1: Key Molecular Players in Newt Lens Regeneration
| Molecule | Role in Lens Regeneration | Experimental Evidence |
|---|---|---|
| FGF-2 | Master initiator; triggers dedifferentiation and lens gene expression | Injection inhibits regeneration; ectopic expression induces lens formation [6] |
| Pax6 | Master regulatory gene for eye development and regeneration | Upregulated in dedifferentiating PECs [6] |
| Sox2 | Early lens gene; pluripotency factor | Upregulated in dedifferentiating PECs [6] |
| MafB | Transcription factor | Upregulated during dedifferentiation phase [6] |
| miR-124a | Potential regulator of dedifferentiation | Highly expressed in dedifferentiating PECs [6] |
Experimental Protocol: Lentectomy and Lens Regeneration Analysis
Objective: To surgically remove the lens and monitor the process of regeneration from the dorsal iris pigment epithelium.
Procedure:
- Animal Preparation: Adult newts (e.g., Notophthalmus viridescens or Cynops pyrrhogaster) are anesthetized using a 0.1% ethyl 3-aminobenzoate methanesulfonate (MS-222) solution.
- Lentectomy: A corneal incision is made, and the native lens is carefully removed using fine forceps without damaging the dorsal iris.
- Post-operative Care: Animals are maintained in a controlled aquatic environment and allowed to recover. Regeneration is monitored over 2-4 weeks.
- Tissue Collection and Analysis: At designated time points (e.g., 5, 10, 15, 20, 30 days post-lentectomy), eyes are enucleated and processed for:
- Histology: Tissue fixed in 4% paraformaldehyde, embedded in paraffin, sectioned, and stained with Hematoxylin and Eosin to visualize tissue morphology and regenerative stages [6].
- Immunohistochemistry: Staining for markers such as Pax6 to identify early lens cell commitment, and crystallins for terminal lens fiber differentiation [6].
- In situ hybridization: To localize specific mRNA transcripts (e.g., FGF-2, Sox2) in regenerating tissue.
Diagram Title: Newt Lens Regeneration Process
Pancreatic α- to β-Cell Conversion: A Mammalian Paradigm for Diabetes Therapy
Biological Rationale and Therapeutic Potential
The global prevalence of diabetes mellitus underscores the urgent need for therapies that address the fundamental pathophysiological deficit: a reduction in functional pancreatic β-cell mass [8] [9]. Traditional treatments with exogenous insulin or oral hypoglycemic agents often fail to achieve optimal glycemic control, leading to severe complications [8]. Research has consequently focused on replenishing the β-cell population, with transdifferentiation of pancreatic α-cells emerging as a promising therapeutic avenue [8]. α-cells are ideal candidates for conversion due to several factors:
- Developmental Similarity: α-cells and β-cells share a common developmental origin from endocrine progenitors in the pancreatic endoderm, controlled by a network of transcription factors including Pdx1 and Ngn3 [8].
- Close Physical Association: In both mouse and human islets, over 90% of α-cells are in direct contact with β-cells, facilitating potential paracrine interactions and conversion [8].
- Compensatory Proliferation: α-cell proliferation is commonly observed in diabetic animal models and patients, providing a substantial cellular resource for reprogramming [8].
- Functional Redundancy: Significant reduction in α-cell numbers does not adversely affect glucose metabolism, and converting α-cells may mitigate the deleterious effects of glucagon on glycemic control [8].
Molecular Mechanism of Fate Switching
The transdifferentiation of α-cells to β-cells is a tightly regulated process demonstrating the plasticity of pancreatic endocrine cells. It can be divided into three main stages:
- Proliferation of α-cells in response to extensive β-cell loss in diabetic environments [8].
- Reprogramming of α-cell identity, which requires the coordinated suppression of α-cell-maintaining factors and activation of the β-cell transcriptional program.
- Stabilization of the new β-cell identity to prevent reversion or transformation into other cell types.
Table 2: Key Transcription Factors in α- to β-Cell Transdifferentiation
| Transcription Factor | Role in Cell Identity | Effect on Transdifferentiation |
|---|---|---|
| Arx | Maintains α-cell phenotype; suppresses β-cell genes | Deletion induces α-to-β cell conversion, normalizes blood glucose [8] |
| MafB, Brn4, Pax6 | Regulate glucagon production and α-cell stability | Downregulation facilitates transdifferentiation initiation [8] |
| Pdx1 | β-cell identity and function; crucial for insulin production | Upregulation is essential for establishing and maintaining β-cell phenotype [8] |
| MafA | β-cell maturation and function | Upregulation helps stabilize the transdifferentiated state [8] |
| Nkx6.1 | β-cell identity | Upregulation supports the β-cell transcriptional program [8] |
Recent Advances and Human Islet Heterogeneity
Recent single-cell RNA sequencing (scRNA-seq) studies have revealed unprecedented complexity in human pancreatic α-cells, identifying five distinct α-cell subclusters (α1, α2, α3, α4, and AB) with unique transcriptomic profiles [10]. Of particular interest is the AB subcluster, a multihormonal population expressing both GCG (glucagon) and INS (insulin), which may represent a transitional state. Trajectory inference analyses suggest that in non-diabetic islets, cell fate trajectories are bifurcated, while in type 2 diabetic (T2D) islets, trajectories become unidirectional, moving from β-cells to α-cells, indicating β-cell dedifferentiation towards an α-cell-like phenotype [10]. This analysis identified SMOC1 as a key gene in this pathological trajectory. SMOC1, typically an α-cell gene, is expressed in β-cells in T2D. Functional studies demonstrate that enhanced SMOC1 expression in β-cells reduces insulin expression and secretion while increasing dedifferentiation markers, establishing it as an inducer of β-cell dysfunction in diabetes [10].
Experimental Protocol: Assessing β-Cell Mass and Transdifferentiation
Objective: To quantify β-cell mass and identify transdifferentiating cells in pancreatic tissue sections.
Procedure (Automated Quantification using Virtual Slide Technology) [9]:
- Tissue Preparation: Pancreata are weighed, fixed in 4% paraformaldehyde, dehydrated, and embedded in paraffin. Longitudinal sections are cut at 5-μm thickness and collected systematically at 250-μm intervals.
- Immunohistochemistry: Sections are immunolabeled with primary guinea pig anti-insulin antibody, followed by HRP-conjugated secondary antibody. Insulin signal is visualized with DAB chromogen, and sections are counterstained with Eosin-Y.
- High-Resolution Slide Scanning: Entire pancreatic sections are scanned using a high-resolution slide scanner (e.g., ScanScope CS) at 20x magnification.
- Automated Image Analysis (Genie Algorithm Training):
- Class Definition: Three object classes are defined in the image analysis software:
Glass(background),Eosin(exocrine and other tissue), andDAB(insulin-positive β-cells). - Algorithm Training: The algorithm is trained by manually assigning representative regions of the image to each class, encompassing variations in staining intensity and tissue morphology. The training aims for >97% sensitivity and specificity.
- Batch Analysis: The trained macro is run on all pancreatic sections from the study to automatically quantify the total β-cell area (DAB-positive) and pancreatic area.
- Class Definition: Three object classes are defined in the image analysis software:
- Calculation of β-Cell Mass:
β-cell mass = (Total β-cell area / Total pancreatic area) * Pancreas weight - Analysis of Transdifferentiation: Consecutive or double-labeling immunofluorescence for insulin and glucagon is used to identify bihormonal (INS+GCG+) cells, which are quantified manually or via automated analysis to assess the frequency of putative transdifferentiating events [10].
Diagram Title: Molecular Path of α- to β-Cell Conversion
Comparative Analysis and Research Toolkit
Cross-Species Mechanistic Commonalities
Despite the vast phylogenetic distance and differences in the specific tissues involved, newt lens regeneration and pancreatic α-to-β-cell conversion share fundamental mechanistic principles central to the thesis of transdifferentiation in tissue repair:
- Master Regulator Switching: Both processes are governed by the downregulation of fate-defining transcription factors for the starting cell type (e.g., Arx in α-cells, pigment-specific factors in PECs) and concomitant upregulation of master regulators for the target cell type (e.g., Pdx1 in β-cells, Pax6/Sox2 in lens cells) [8] [6].
- Developmental Pathway Reactivation: Key signaling pathways essential during embryonic development, particularly the FGF pathway, are reactivated to drive the reprogramming process [6].
- Cellular Plasticity Precedes Conversion: In both systems, the starting cell must first undergo a degree of dedifferentiation or become more plastic, entering a less stable, progenitor-like state before committing to a new fate [6] [10].
- Role of the Niche: The local microenvironment, or niche, provides critical signals. In newts, the dorsal iris position is crucial, while in the pancreas, close physical contact between α- and β-cells and signals from the diabetic milieu influence the transdifferentiation potential [8] [6].
Table 3: The Scientist's Toolkit: Essential Reagents for Transdifferentiation Research
| Research Reagent / Tool | Function/Application | Example Use Case |
|---|---|---|
| Anti-Insulin Antibody | Immunohistochemical identification of β-cells and insulin-producing cells | Quantifying β-cell area/mass in pancreatic sections; identifying transdifferentiated cells [9] |
| Anti-Glucagon Antibody | Immunohistochemical identification of α-cells | Co-staining with insulin to identify bihormonal (transitional) cells [10] |
| Anti-Pax6 Antibody | Marker for early lens cell commitment and eye development | Staining newt iris sections during early lens regeneration [6] |
| FGF-2 (Recombinant Protein) | Soluble signaling factor to trigger dedifferentiation and proliferation | Testing sufficiency to induce lens transdifferentiation in newt iris culture [6] |
| Soluble FGFR3 | Decoy receptor to sequester and inhibit FGF signaling | Testing necessity of FGF signaling in lens regeneration [6] |
| scRNA-seq/snRNA-seq | Unbiased profiling of cell populations and trajectory inference | Identifying α-cell subclusters and β-to-α cell trajectories in human diabetic islets [10] |
| Aperio ScanScope & Genie Algorithm | High-resolution slide scanning and automated image analysis | High-throughput, accurate quantification of β-cell mass in whole pancreatic sections [9] |
| 2-Oxetanone, 4-cyclohexyl- | 2-Oxetanone, 4-cyclohexyl-, CAS:132835-55-3, MF:C9H14O2, MW:154.21 g/mol | Chemical Reagent |
| Propyl perfluoroheptanoate | Propyl Perfluoroheptanoate|C10H7F13O2 | High-purity Propyl perfluoroheptanoate for research on PFAS. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
The natural paradigms of lens regeneration in newts and pancreatic α-to-β-cell conversion provide a powerful conceptual framework for understanding transdifferentiation. They reveal that the potential for significant cellular reprogramming is retained in specific contexts even in adult vertebrates. For drug development professionals, these models highlight key molecular targets (e.g., Arx, SMOC1, FGF-signaling) and strategic considerations, such as the need to manage the stability of the newly acquired cell fate. Future research must focus on refining the efficiency and safety of targeted transdifferentiation in human tissues, potentially by combining transcriptional manipulation with modulation of the local microenvironment. Leveraging these endogenous blueprints for repair holds the promise of developing next-generation regenerative therapies that restore tissue function by harnessing the body's own cellular plasticity.
Within the field of regenerative medicine, a paradigm shift is underway, moving beyond the use of pluripotent stem cells toward the direct conversion of one mature cell type into another. This process, known as transdifferentiation, is fundamentally governed by a class of proteins called "master switch" transcription factors (TFs). These TFs, such as MyoD and Pax6, commandeer cellular identity by reprogramming gene expression networks. This whitepaper provides an in-depth technical examination of how these factors operate, detailing their mechanisms, key experimental methodologies, and their profound implications for directing cell fate in therapeutic contexts, particularly tissue repair. By elucidating the control logic of cell identity, we unlock novel strategies for regenerative medicine and drug development.
Transdifferentiation is defined as the irreversible conversion of one differentiated cell type into another, without proceeding through a pluripotent intermediate state [4] [11]. This phenomenon represents a powerful tool for regenerative medicine, as it offers the potential to directly replace lost or damaged cells from a patient's own resident tissues, thereby circumventing the risks of tumorigenesis and ethical concerns associated with pluripotent stem cells [11].
At the heart of transdifferentiation are master switch genes. These genes encode transcription factors that, when expressed, can initiate and enforce an entire genetic program sufficient to define a specific cell lineage. The seminal discovery of MyoD demonstrated that a single TF could convert fibroblasts into striated muscle cells, establishing the conceptual foundation for this field [11]. Similarly, the TF Pax6 is essential for the development of the eye, pancreas, and central nervous system, and its dysfunction is linked to human diseases [12] [13]. These factors function as nodal points in gene regulatory networks (GRNs), activating batteries of genes characteristic of the target cell type while simultaneously repressing genes associated with alternative fates [12] [13]. The growing understanding of these mechanisms provides a rational basis for designing transdifferentiation protocols for tissue repair, positioning master switch genes as high-value targets for therapeutic intervention.
Core Mechanisms of Action
Master switch TFs exert control over cell identity through coordinated and multi-layered regulatory mechanisms.
2.1 Transcriptional Activation and Repression: These TFs bind to specific DNA sequences in the regulatory regions (promoters and enhancers) of their target genes. For instance, Pax6 directly binds to and activates genes required for neuronal development, such as Ift74, which is critical for neuronal migration [13]. Concurrently, Pax6 represses genes of alternative lineages; in pancreatic β-cells, it directly represses genes encoding hormones like glucagon and somatostatin, which are hallmarks of α- and δ-cells, respectively [12]. This dual function ensures the stability of the desired cellular phenotype.
2.2 Cooperation with Other Factors: The activity of a master TF is not executed in isolation. It often depends on synergistic interactions with the cellular environment and other TFs. A prime example is the cooperation between Pax6 and Sox2 in neural progenitor cells. These factors co-occupy a large number of promoters, where they functionally cooperate to regulate genes underlying neuronal specification [13]. This cooperativity allows for a more robust and specific control of the transcriptional program.
2.3 Epigenetic Remodeling: Large-scale changes in chromatin architecture are a prerequisite for cell fate conversion. The process of transdifferentiation involves genome-wide chromatin reorganization, which is closely linked to cellular plasticity [14]. Master TFs can pioneer these changes by binding to closed chromatin and initiating the opening of new regulatory regions, thereby making genes accessible for transcription.
The following diagram illustrates the core mechanisms by which a master switch transcription factor, such as Pax6, governs cell identity.
Key Master Switch Genes: MyoD and Pax6
3.1 MyoD: The Master Regulator of Myogenesis MyoD is the prototypical master regulator. Its forced expression is sufficient to induce a skeletal muscle program in a variety of cell types, including fibroblasts. It operates by activating the expression of muscle-specific genes, such as those for myosin and creatine kinase, while concurrently halting the cell cycle.
3.2 Pax6: A Multifunctional Regulator in Development and Disease Pax6 is a paired box and homeodomain-containing TF with pleiotropic roles. Its function is highly context-dependent, and it acts as a master regulator in several tissues.
Table 1: Key Functions of the Pax6 Master Regulator
| Tissue/Cell Type | Primary Function of Pax6 | Consequence of Loss-of-Function | Key Target Genes/Pathways |
|---|---|---|---|
| Pancreatic β-cells | Maintains β-cell identity and function by repressing alternative islet cell genes (ghrelin, glucagon, somatostatin) [12]. | Lethal hyperglycemia and ketosis; loss of β-cell function and expansion of α-cells [12]. | Direct activator of β-cell genes; repressor of ARX, GCG, SST [12]. |
| Neural Progenitors | Activates neuronal (ectodermal) genes while repressing mesodermal and endodermal genes, ensuring unidirectional neurogenesis [13]. | Reduced neurons in cerebral cortex; misspecified neurons that undergo cell death [13]. | Sox2 (cooperation), Ift74 (neuronal migration), Neurog2, components of Notch signaling [13]. |
| Corneal Epithelium | Transcriptional activator of CXCL14 post-injury, enhancing stemness, proliferation, and migration of central corneal epithelial cells [15]. | Impaired repair of corneal injury and disrupted homeostasis [15]. | CXCL14 (activator), which engages SDC1 receptor and NF-κB pathway [15]. |
| Lens Development | Regulates expression of crystallin genes and other factors essential for lens development and homeostasis [16]. | Abnormal lens fiber cells and persistent corneal-lenticular stalk (in heterozygotes) [16]. | c-Maf, Foxe3, Mab21l2, Tgfb2, crystallin genes [16]. |
Experimental Approaches and Methodologies
Studying master switch genes requires a suite of advanced molecular and cellular techniques to validate their function and mechanisms.
4.1 In Vitro Transdifferentiation Protocols A common approach involves the forced expression of TFs in a somatic cell to induce transdifferentiation.
- Starting Cells: Fibroblasts remain the most commonly used starting population [11].
- TF Delivery: Transient forced expression is achieved via viral vectors (e.g., lentiviruses, adenoviruses) or non-viral methods like transfection. For example, a combination of Brn2, Ascl1, and Myt1l (BAM) can convert fibroblasts into induced neurons (iNs) [11].
- Enhancing Efficiency: Culture conditions are critical. Hypoxia (which activates HIFs) can enhance conversion efficiency, as shown in the transdifferentiation of human fibroblasts to dopaminergic neurons [11]. Suppression of p53 or inducing cell cycle arrest also increases efficiency [11].
4.2 Key Analytical Techniques
- Chromatin Immunoprecipitation (ChIP): This is the definitive method to identify direct genomic targets of a TF. ChIP, followed by sequencing (ChIP-seq), revealed that Pax6 binds thousands of promoters in neural progenitors, many of which are co-occupied by Sox2 and marked by active histone marks like H3K4me2 [13].
- Lineage Tracing: This in vivo technique uses genetic labeling to trace the fate of specific cell populations and their progeny, confirming that one cell type has converted into another.
- Functional Assays: The ultimate validation of transdifferentiated cells involves functional tests. For neurons, this includes patch-clamp electrophysiology to demonstrate action potentials and synaptic activity. For other cell types, it may involve measuring secreted hormones or demonstrating regenerative capacity in injury models.
The workflow for a typical experiment investigating a master switch gene is outlined below.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Investigating Master Switch Genes and Transdifferentiation
| Reagent / Tool | Function and Application | Example Use Case |
|---|---|---|
| Specific TF Antibodies | Used for Chromatin Immunoprecipitation (ChIP), immunofluorescence, and Western blot to localize and quantify TF expression. | Affinity-purified Pax6 antibody for ChIP to map its genomic targets in neural progenitors [13]. |
| Lentiviral/Adenoviral Vectors | For efficient and stable (lentivirus) or transient (adenovirus) delivery of TF genes into target somatic cells. | Overexpressing CXCL14 via lentivirus in corneal epithelial cells to study its role in wound healing [15]. |
| Lineage Tracing Systems | Genetically labels a specific cell population and all its descendants in vivo to track cell fate changes. | Confirming the conversion of supporting cells into hair cells in the cochlea after manipulating Notch signaling [17]. |
| Organoid Cultures | 3D in vitro models that recapitulate tissue architecture, used to study TF function in a near-physiological context. | Using intrahepatic cholangiocyte organoids to study transdifferentiation into hepatocytes [14]. |
| scRNA-seq / snATAC-seq | Single-cell/nucleus assays to profile gene expression (RNA-seq) and chromatin accessibility (ATAC-seq) simultaneously. | Uncovering transcriptomic and epigenetic mechanisms in cholangiocyte transdifferentiation [14]. |
| Dodeca-4,11-dien-1-ol | High-purity Dodeca-4,11-dien-1-ol for research (RUO). A key intermediate in synthetic chemistry and aroma composition. Not for human or household use. | |
| 3-Cyclopropyl-1H-indene | 3-Cyclopropyl-1H-indene |
Implications for Tissue Repair and Therapeutic Outlook
The manipulation of master switch genes holds immense promise for regenerative medicine, offering novel strategies for treating a wide array of degenerative diseases and injuries.
- Neurodegenerative Diseases: Direct transdifferentiation of a patient's glial cells into functional neurons in situ represents a potential therapeutic avenue for conditions like Parkinson's and Alzheimer's disease. Protocols have been established to generate dopaminergic iNs and motor iNs from fibroblasts, which can be used for disease modeling and cell therapy [11].
- Metabolic Disorders: In diabetes, the transdifferentiation of pancreatic α-cells or other cell types into functional, glucose-responsive β-cells could restore insulin production. The role of Pax6 in maintaining β-cell identity makes it a critical target for such approaches [12].
- Organ Repair and Regeneration: The liver exhibits remarkable plasticity. Recent human studies show that cholangiocytes (bile duct cells) can transdifferentiate into hepatocytes in chronic liver disease, a process driven by TFs like HNF4G and involving extensive epigenetic remodeling [14]. Similarly, the PAX6/CXCL14 axis has been identified as a critical driver of corneal epithelial repair, with recombinant CXCL14 protein showing therapeutic potential for corneal injuries [15].
The future of the field lies in refining the specificity and safety of these interventions. This includes developing non-integrating delivery methods for TF genes, using small molecules to induce or enhance transdifferentiation [11], and achieving precise spatial and temporal control over the process to ensure the generation of fully functional, region-specific cell types for effective tissue repair.
Metaplasia is defined as the conversion of one differentiated cell type into another and represents a critical adaptive response in pathology, often serving as a precursor state to both cancer and fibrosis. This phenomenon belongs to a wider class of cell type transformations that includes transdifferentiation, which is more specifically defined as the irreversible switch of one type of differentiated cell to another, typically involving dedifferentiation and cell division as intermediate processes [4]. In pathological contexts, metaplasia occurs as a tissue healing response to chronic injury, inflammation, or environmental stressors. However, when these insults persist, the metaplastic state can be co-opted toward pathological outcomes, serving as a critical crossroads in disease progression toward carcinogenesis or fibrotic remodeling [18] [4].
The clinical significance of metaplastic transitions is twofold. First, metaplasia predisposes to certain forms of neoplasia, with one of the best-studied examples being Barrett's esophagus, where stratified squamous epithelium undergoes metaplastic transformation to intestinal-type epithelium, creating a precursor to esophageal adenocarcinoma [4]. Second, metaplastic changes are increasingly recognized as fundamental drivers of fibrotic processes across multiple organ systems, including pulmonary, hepatic, and cardiac tissues [19] [20]. Understanding the molecular mechanisms governing these cellular plasticity events provides crucial insights for developing early detection strategies and targeted interventions for these debilitating conditions [4] [21].
Metaplasia as a Precursor to Gastric Cancer
The Correa Cascade and Gastric Intestinal Metaplasia
Gastric cancer represents the fifth most commonly diagnosed cancer and the fourth leading cause of cancer-related mortality worldwide, with approximately 26,780 new U.S. cases annually and a poor 5-year survival of 36% [22] [23]. The majority of gastric cancers follow the established Correa cascade, a stepwise progression from chronic gastritis through a series of precursor lesions—atrophic gastritis, intestinal metaplasia, and dysplasia—before developing into invasive cancer [23]. Within this sequence, gastric intestinal metaplasia (GIM) represents a potentially irreversible state with increased cancer risk, particularly when extending into the corpus [22].
Global prevalence estimates highlight the significance of GIM, with a worldwide prevalence of 17.5%, though with considerable geographic variation ranging from 8.3% in Africa to 18.6% in the Americas [23]. The progression rates of these precursor lesions to gastric cancer provide critical data for surveillance strategies, with global pooled estimates indicating that the annual progression rate per 1,000 person-years is 2.09 for atrophic gastritis, 2.89 for intestinal metaplasia, and 10.09 for dysplasia [23]. These findings underscore the importance of metaplastic transitions as key intervention points for gastric cancer prevention.
Table 1: Progression Rates of Gastric Precancerous Lesions to Gastric Cancer
| Precursor Lesion | Annual Progression Rate (per 1,000 person-years) | 95% Confidence Interval |
|---|---|---|
| Atrophic Gastritis | 2.09 | 1.46–2.99 |
| Intestinal Metaplasia | 2.89 | 2.03–4.11 |
| Dysplasia | 10.09 | 5.23–19.49 |
Molecular Mechanisms and Microenvironment
Recent single-cell transcriptomic analyses have revealed that diverse injury stimuli, including Helicobacter pylori infection and autoimmune gastritis, induce cancer-associated metaplasia through both convergent and divergent pathways [18]. These studies have identified a transcriptionally diverse array of metaplastic lineages, with spasmolytic polypeptide-expressing metaplasia (SPEM) representing a particularly consequential program. Although SPEM was initially considered a reparative lineage, persistent injury leads to the emergence of mature chief cells as cryptic progenitors for metaplasia, creating a cellular context susceptible to malignant transformation [18] [23].
The tissue microenvironment plays a crucial role in metaplastic progression. Apposition of fibroblasts with metaplastic gastric cells promotes dysplastic transition, indicating that stromal-epithelial crosstalk establishes a permissive niche for malignant transformation [18]. Specific biomarkers have emerged as promising indicators of progression risk, including ANPEP/CD13, which shows elevated expression in gastric metaplasia with higher potential for malignant progression [18]. Additionally, gastrokine 3 and cadherin-17 (CDH17) have been identified as molecular markers associated with metaplastic development and early-stage gastric cancer prognosis [18].
Figure 1: Molecular Pathways of Gastric Metaplasia and Cancer Progression. The diagram illustrates the key steps in the Correa cascade, highlighting the role of transdifferentiation and microenvironmental signaling in driving progression from metaplasia to gastric cancer.
Metaplasia in Fibrotic Diseases
The Global Burden of Fibrosis and Metaplastic Involvement
Fibrotic diseases contribute to nearly half of all deaths in industrialized countries, with a steadily increasing global burden. Recent analyses of Global Burden of Disease (GBD) 2021 data across 204 countries and territories revealed that from 1990 to 2021, fibrosis-related disability-adjusted life years (DALYs) and mortality increased by 16.71% and 4.83%, respectively [19]. This growing burden is disproportionately concentrated in regions with low socio-demographic index (SDI), where limited diagnostic capabilities prevent early detection and intervention [19].
Metaplastic changes are increasingly recognized as fundamental components of fibrotic processes across multiple organ systems. In pulmonary fibrosis, a fatal disease characterized by progressive scarring of lung tissue with a median post-diagnosis survival of only 2-6 years, "proximalized epithelial metaplasia" represents a hallmark finding [24] [25]. This process involves the appearance of conducting airway cell types in the distal lung epithelium, disrupting normal alveolar structure and function [25]. Similarly, in cardiogenic liver disease, biliary metaplasia defines the cellular landscape, with hepatocytes undergoing phenotypic conversion to biliary-like epithelium in response to congestive hepatopathy [20].
Molecular Drivers of Fibrosis-Associated Metaplasia
The molecular pathways driving metaplasia in fibrotic contexts share common features across organs, centered on aberrant activation of developmental programs and response to mechanical stress. In pulmonary fibrosis, spatial transcriptomic analyses of 1.6 million cells from 35 unique lungs have identified a VGLL3-mediated pathway as central to fibrotic remodeling [19] [25]. VGLL3 is a transcriptional co-regulator rich in intrinsically disordered regions that is consistently upregulated in multi-organ fibrosis and mediates early activation of fibroblasts in response to matrix stiffness [19].
Single-cell RNA sequencing has revealed that in the remodeling lung, a spectrum of activated "fibrotic" fibroblasts expressing varying levels of CTHRC1, FAP, and POSTN concentrate in subepithelial regions underlying areas of extensive epithelial metaplasia [25]. These fibroblasts create a pro-fibrotic niche that perpetuates metaplastic changes and extracellular matrix deposition. Similarly, metabolic reprogramming, particularly disorders of lipid metabolism, has been identified as a significant characteristic of idiopathic pulmonary fibrosis (IPF), with specific metabolites like palmitoyl ethanolamide (PEA) and 2-amino-1,3,4-octadecanetriol serving as potential biomarkers for diagnosis and prognosis evaluation [26].
Table 2: Key Biomarkers in Fibrosis-Associated Metaplasia
| Biomarker | Role in Metaplasia and Fibrosis | Pathological Context |
|---|---|---|
| VGLL3 | Transcriptional co-regulator mediating early fibroblast activation in response to matrix stiffness | Multi-organ fibrosis [19] |
| CTHRC1 | Expressed by activated fibrotic fibroblasts in subepithelial regions underlying metaplastic epithelium | Pulmonary fibrosis [25] |
| KRT5-/KRT17+ | Aberrant basaloid cells located in proximity to activated fibroblasts in remodeling lung | Pulmonary fibrosis [25] |
| PEA | Lipid metabolite significantly increased in IPF patients; potential diagnostic and prognostic biomarker | Idiopathic pulmonary fibrosis [26] |
| LCN2 | Lipocalin 2 associated with macrophage activation in biliary metaplasia | Cardiogenic liver disease [20] |
Experimental Models and Methodologies
Animal Models of Metaplasia
Animal models have been instrumental in elucidating the pathogenesis of metaplasia and its progression to cancer and fibrosis. For gastric cancer, the mouse model represents the most commonly utilized system, with several established approaches [23]:
Helicobacter infection models: C57BL/6 mice infected with Helicobacter felis closely mirror the progression from chronic gastritis through metaplasia to dysplasia, though these models primarily produce SPEM rather than true intestinal metaplasia.
Chemical carcinogen models: Utilizing compounds like N-methyl-N′-nitro-N-nitrosoguanidine (MNNG) or N-methyl-N-nitrosourea (MNU) reliably produces tumors but often bypasses intermediate precancerous stages.
Genetically engineered mouse models: Stomach-specific inducible Cre recombinase systems targeting gastric progenitor cells have yielded models that faithfully reproduce the spectrum of human gastric cancer subtypes with metastatic features.
Standardized evaluation of these models is crucial, with the internationally recognized "Histologic Scoring of Gastritis and Gastric Cancer in Mouse Models" system providing a comprehensive framework for assessing active inflammation, chronic inflammation, atrophy, SPEM, intestinal metaplasia, and dysplasia through semi-quantitative scoring [23].
Spatial Transcriptomics in Fibrosis Research
Cutting-edge spatial transcriptomic approaches have revolutionized our understanding of metaplasia in fibrotic diseases. Recent investigations utilizing image-based spatial transcriptomics have analyzed the gene expression of 1.6 million cells from 35 unique lungs, enabling unprecedented resolution of the spatial contexts driving disease pathogenesis [25]. The experimental workflow typically involves:
Tissue Preparation and Imaging:
- Fresh frozen tissue sections (typically 10μm thickness) mounted on specialized slides
- Permeabilization to release RNA for capture
- Hybridization with gene-specific probes with barcodes corresponding to spatial location
Data Acquisition and Analysis:
- Automated cell segmentation using nuclear boundaries
- Quality filtering to retain high-confidence cellular transcriptomes
- Complementary cell-based and cell-agnostic computational approaches to identify spatial niches
- Graph neural network models to aggregate local neighborhood information and define embedding spaces
This approach has enabled researchers to characterize the localization of disease-emergent cell types, establish the cellular and molecular basis of classical histopathologic features, and identify distinct molecularly defined spatial niches in control and fibrotic lungs [25].
Biomarker Detection Methodologies
Advanced detection methodologies are crucial for identifying and validating biomarkers associated with metaplastic progression:
VGLL3-Targeted Immunoassay Protocol [19]:
- Antigen Design: Five truncated VGLL3 variants (residues 1–168, 1–194, 1–237, 1–251, and 1–297) designed based on domain prediction
- Protein Expression: Recombinant plasmids transformed into E. coli HST08 cells, grown in LB medium with kanamycin
- Antibody Generation: Laying hens immunized with purified VGLL3 (1–237) antigen, initial dose of 250μg emulsified in Freund's complete adjuvant
- Assay Performance: Detection range of 27.01–2512.36 nM with limit of detection of 12.55 nM
Serum Metabolomics for IPF Biomarkers [26]:
- Metabolite Extraction: 100μL liquid sample mixed with 400μL prechilled methanol, incubated on ice, centrifuged
- LC-MS/MS Analysis: Vanquish UHPLC system coupled with Orbitrap Q Exactive HF mass spectrometer
- Chromatographic Conditions: Hyperil Gold column (C18), 40°C column temperature, 0.2 mL/min flow rate
- Multivariate regression analysis and correlation network modeling to analyze relationships between metabolites and clinical parameters
Figure 2: Spatial Transcriptomics Workflow for Metaplasia Research. The diagram outlines key methodological steps from tissue preparation through computational analysis to identify spatially-resolved biomarkers in metaplastic and fibrotic tissues.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Metaplasia and Transdifferentiation Studies
| Reagent/Material | Application | Function |
|---|---|---|
| Recombinant VGLL3 antigens (residues 1-237) | Fibrosis biomarker studies | Immunogen for generating specific antibodies; detects early fibrotic remodeling [19] |
| Anti-VGLL3 avian antibodies | VGLL3 detection assays | Cost-effective alternative to mammalian IgG with superior stability and specificity for immunoassays [19] |
| CK7 antibody | Hepatic metaplasia studies | Marker for biliary differentiation in cardiogenic liver disease [20] |
| ANPEP/CD13 antibody | Gastric cancer progression studies | Identifies metaplastic cells with higher potential for malignant progression [18] |
| pET-28a(+) vector with N-terminal SUMO tag | Recombinant protein expression | Enhances solubility of difficult-to-express proteins like VGLL3 for antibody production [19] |
| Liquid chromatography-mass spectrometry (LC-MS/MS) | Metabolomic profiling | Identifies lipid metabolites (PEA, 2-amino-1,3,4-octadecanetriol) as potential IPF biomarkers [26] |
| Xenium spatial transcriptomics platform | Spatial gene expression analysis | Enables subcellular resolution mapping of 343 genes across tissue sections to identify metaplastic niches [25] |
| Stomach-specific inducible Cre recombinase systems | Genetic mouse models | Targets gastric progenitor cells to recapitulate human gastric cancer progression from metaplasia [23] |
| 2,2'-Diethyl-3,3'-bioxolane | 2,2'-Diethyl-3,3'-bioxolane | 2,2'-Diethyl-3,3'-bioxolane is for research use only (RUO). It is a high-purity chemical for applications in organic synthesis and as a specialty solvent. Not for human consumption. |
| 1-Iodonona-1,3-diene | 1-Iodonona-1,3-diene, CAS:169339-71-3, MF:C9H15I, MW:250.12 g/mol | Chemical Reagent |
Therapeutic Implications and Future Directions
The investigation of metaplasia as a precursor to cancer and fibrosis holds significant implications for therapeutic development. In gastric cancer prevention, surveillance strategies for patients with gastric intestinal metaplasia are being refined through standardized coding practices, with the 2021 introduction of specific ICD-10-CM codes (K31.A) for GIM allowing precise classification of anatomical specificity and dysplasia status, providing a novel opportunity to improve risk stratification and endoscopic surveillance [22]. Studies have demonstrated a 3-4 fold increase in documented GIM cases following implementation of these standardized codes, suggesting previous systematic underdiagnosis that potentially affected surveillance strategies and risk assessment for gastric cancer prevention [22].
In fibrosis treatment, the identification of VGLL3 as a key transcriptional regulator opens promising avenues for therapeutic intervention. VGLL3 responds to changes in matrix stiffness, binds to TEAD, and directly mediates fibroblast collagen production, playing a key role in liver, cardiac, and skin fibrosis [19]. In VGLL3 knockout studies, mice showed significantly reduced fibrosis after myocardial infarction and improved cardiac function, highlighting its potential as a therapeutic target [19]. Similarly, in keloids, VGLL3 promotes fibroblast proliferation by activating the Wnt pathway, suggesting that pathway inhibition could mitigate fibrotic progression [19].
Future research directions will likely focus on integrating advanced technologies such as single-cell RNA sequencing with existing animal models, developing more sophisticated organoid models of metaplasia, and investigating the complex interactions among genetic predisposition, microbial infection, and environmental factors in driving metaplastic progression [23]. The convergence of multi-omics technologies is fostering the development of multidimensional biomarker frameworks encompassing molecular, histological, imaging, and functional parameters that hold promise for enhancing precision in early screening, target identification, dynamic monitoring, and prognostic evaluation of both cancerous and fibrotic conditions [24] [26].
As these fields advance, the concept of targeting metaplastic transitions themselves—rather than waiting for established cancer or fibrosis—represents a paradigm shift in therapeutic strategy. By intercepting the molecular drivers of pathological metaplasia, particularly through modulation of master switch genes and microenvironmental signaling, future therapies may potentially reverse or stabilize these precursor states before they progress to irreversible endpoint diseases.
Within the context of regenerative medicine, the concept of transdifferentiation—the direct conversion of one differentiated cell type into another—presents a promising therapeutic avenue. A significant hurdle in this field is the developmental boundary imposed by embryonic germ layers. This whitepaper assesses the current understanding of the limits of cross-conversion between the ectoderm, mesoderm, and endoderm. We synthesize contemporary evidence from developmental biology, single-cell transcriptomics, and mechanical reprogramming, framing the discussion within the broader thesis of harnessing transdifferentiation mechanisms for tissue repair. The document provides a technical guide for researchers and drug development professionals, incorporating structured quantitative data, detailed experimental protocols, and essential visualization tools to advance the field.
The three primary germ layers—ectoderm, mesoderm, and endoderm—are fundamental to embryonic development, giving rise to all tissues and organs in a multicellular organism. The ectoderm forms the epidermis and the entire nervous system; the mesoderm generates connective tissues, the circulatory system, and muscles; and the endoderm differentiates into the linings of the gastrointestinal and respiratory tracts and associated organs [27]. The classical view posits that once cells are committed to a specific germ layer lineage, their developmental potential is severely restricted.
However, the field of regenerative medicine has challenged this dogma through the study of transdifferentiation, a direct cell fate conversion that bypasses a pluripotent intermediate state. The core thesis of this whitepaper is that a detailed understanding of the molecular and biophysical determinants of germ layer boundaries will unlock novel strategies for tissue repair. Successful cross-conversion across these boundaries could enable the regeneration of tissues lost to disease or injury, such as creating pancreatic beta cells (endodermal) from a patient's skin fibroblasts (ectodermal). This guide will explore the limits of such conversions, evaluating both the barriers and the emerging methodologies to overcome them.
Molecular Specification of Germ Layers
The establishment of the three germ layers during gastrulation is governed by a highly conserved Gene Regulatory Network (GRN) involving key signaling pathways. Seminal work in amphibian embryos established the "three-signal model" for mesoderm and endoderm formation [28].
- Initial Induction: The process begins with the induction of mesendoderm, a bipotent precursor, from naive ectoderm. This is primarily driven by signals from the vegetal endoderm, with key secreted factors including members of the Nodal/Activin and Wnt families [28].
- Patterning and Segregation: The mesendoderm is subsequently patterned into definitive mesoderm and endoderm. This involves a combination of signaling gradients; for instance, high levels of Nodal/Activin signaling promote endodermal fate, while intermediate levels direct mesodermal fates. Fibroblast Growth Factors (FGFs) play a critical role in this stage, often acting as competence factors that enable cells to respond to TGF-β signals like Activin [28].
- Ectoderm Specification: The default state of the embryo is often considered to be ectodermal. The formation of neuroectoderm versus epidermal ectoderm is then determined by signals from the underlying mesoderm, particularly from the Spemann-Mangold organizer, which secretes inhibitors of BMP signaling to induce neural tissue [28].
The stability of these germ layer fates in post-embryonic life is maintained by the epigenetic landscape that reinforces the GRN, presenting a significant barrier to transdifferentiation.
Current Research and Quantitative Data on Cross-Conversion
Recent advances in high-resolution spatial transcriptomics and mechanical biology provide new insights into the plasticity of germ layer identity and the potential for cross-conversion. The following table summarizes key quantitative findings from contemporary research.
Table 1: Quantitative Evidence for Germ Layer Cross-Conversion and Associated Mechanisms
| Research Area | Key Finding | Quantitative Data / Outcome | Relevance to Cross-Conversion |
|---|---|---|---|
| Digital Embryo Reconstruction [29] | Identification of a Primordium Determination Zone (PDZ) at the embryonic-extraembryonic interface. | PDZ characterized at E7.75; coordinates signaling for cardiac primordium (mesoderm) formation. | Reveals native signaling hubs where germ layer interactions and potential fate decisions occur. |
| Mechanical Reprogramming [30] | Fibroblasts (mesoderm) on tissue-mimicking hydrogels form aggregates with enhanced multipotency. | Aggregates showed elevated stemness genes and bidirectional (adippo- & osteo-) differentiation potential. | Demonstrates that biophysical cues alone can reverse lineage commitment and enhance plasticity. |
| Germ Layer Origin & Cancer Therapy [31] | Correlation between germ layer origin and cancer therapy response. | Mesoderm-derived hematologic malignancies showed 85.3% ORR to CAR-T; endoderm-derived cancers showed 43.7% ORR to targeted protein inhibition. | Suggests inherent, lineage-based biological properties persist in disease and influence cellular responses. |
| Organoids for Tissue Repair [32] | Use of organoid derivatives in regenerative medicine. | Organoids generated from stem cells of various germ layer origins used for tissue repair. | Provides a platform for in vitro testing of transdifferentiation protocols across germ layers. |
Furthermore, systematic reviews have begun to quantify the relationship between developmental origin and cellular behavior. A meta-analysis of 127 studies (n=487,293 patients) confirmed that germ layer origin is a significant factor in therapeutic response, though it is often superseded by molecular biomarkers like MSI and TMB [31]. This underscores that while germ layer boundaries are influential, they are not absolute and can be modulated.
Experimental Protocols for Assessing Germ Layer Conversion
To empirically assess the limits of germ layer cross-conversion, researchers employ a suite of well-established and novel protocols. Below are detailed methodologies for key experiments in this field.
This protocol generates a high-resolution spatiotemporal transcriptome map to identify transitional cell states during fate conversion.
- Sample Collection: Serial sections are collected from multiple embryos at precise developmental time points (e.g., E7.5-E8.5 for mouse).
- Library Preparation and Sequencing: Single-cell RNA-seq libraries are prepared from dissociated sections using a platform like 10x Genomics. Sequencing is performed to a depth sufficient for robust gene detection.
- Data Integration and 3D Reconstruction: Computational tools (e.g., SEU-3D) are used to integrate the single-cell transcriptomic data with spatial coordinates from the serial sections, reconstructing a full "digital embryo."
- Analysis:
- Cluster Identification: Unsupervised clustering reveals distinct and transitional cell populations.
- Gene-Cell Co-embedding: A space-informed co-embedding approach maps gene expression back into the native spatial context of the embryo.
- Trajectory Inference: Algorithms (e.g., PAGA, Monocle) are used to construct potential differentiation trajectories and infer cells that are transitioning between states.
- Signaling Network Analysis: Ligand-receptor pairing analysis is performed to elucidate signaling networks across germ layers.
This protocol uses a biomimetic mechanical microenvironment to induce reprogramming of mesenchymal cells, testing the role of biophysics in overcoming lineage barriers.
- Hydrogel Fabrication:
- Prepare an interpenetrating network (IPN) hydrogel by combining:
- Viscoelastic component: 10 mg/ml Alginate (shear-thinning).
- Nonlinear elastic component: 1.5 mg/ml Collagen (provides structural nonlinearity).
- Cross-link the alginate by adding Calcium Chloride at varying concentrations (e.g., 5-15 mM) to tune the initial storage modulus.
- Incubate at 37°C for 30 minutes for complete gelation.
- Prepare an interpenetrating network (IPN) hydrogel by combining:
- Cell Seeding and Culture:
- Seed fibroblasts (e.g., 3T3-L1) or other target cells on the surface of the polymerized hydrogel.
- Culture in standard media (e.g., DMEM + 10% FBS) and observe over 24-72 hours.
- Phenotypic Monitoring:
- Use time-lapse microscopy to track cell migration and aggregation behavior.
- Fix cells at specific time points and perform immunofluorescence for cytoskeletal markers (e.g., F-actin with phalloidin) and contractility markers (e.g., phospho-myosin light chain).
- Assessment of Reprogramming:
- Gene Expression: Use qRT-PCR to assess the expression of pluripotency genes (e.g., Oct4, Sox2, Nanog) and lineage-specific markers.
- Differentiation Potential: Challenge the formed aggregates with adipogenic and osteogenic induction media to assess their multipotency.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and their applications in research on germ layer boundaries and transdifferentiation.
Table 2: Research Reagent Solutions for Germ Layer and Transdifferentiation Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Tissue-Mimicking IPN Hydrogel (Alginate-Collagen) [30] | Provides a physiologically relevant mechanical microenvironment (viscoelastic & nonlinear) to study mechanotransduction in cell fate. | Used to demonstrate mechanical reprogramming of fibroblasts into multipotent aggregates. |
| Recombinant Growth Factors (Nodal/Activin, FGF, Wnt) [28] | Key soluble inducers for directed differentiation and transdifferentiation; activate GRNs for specific germ layers. | Used in vitro to direct pluripotent stem cells towards definitive endoderm or mesoderm. |
| Single-Cell RNA Sequencing Kits (e.g., 10x Genomics) [29] | Enables high-resolution profiling of transcriptomes in individual cells to identify novel or transitional states. | Used to construct spatiotemporal atlases of developing embryos and identify signaling interactions. |
| ACT Rule for Contrast Testing [33] | A standardized digital accessibility guideline that ensures sufficient color contrast in visualizations. | Applied to the design of scientific diagrams and software interfaces to guarantee readability for all researchers. |
| N-bromobenzenesulfonamide | N-Bromobenzenesulfonamide|High-Purity|RUO | |
| Methanol;nickel | Methanol;nickel Research Catalyst | Methanol;nickel catalyst for alcohol electro-oxidation and fuel cell research. This product is for Research Use Only (RUO). Not for personal use. |
Signaling Pathways and Experimental Workflows
The following diagrams, generated with Graphviz DOT language, illustrate core concepts and experimental workflows discussed in this whitepaper. The color palette and contrast have been designed for optimal readability according to WCAG guidelines [33] [34].
Germ Layer Specification Network
Title: Key signals in germ layer specification.
Mechanical Reprogramming Workflow
Title: Path from tissue-mimicking hydrogel to multipotency.
Reprogramming Toolkits: Engineering Cell Fate for Neurological, Cardiac, and Metabolic Repair
Transdifferentiation, or direct reprogramming, represents a paradigm shift in regenerative medicine. It refers to the conversion of one somatic cell type directly into another, bypassing the pluripotent state, and is a key mechanism under investigation for in situ tissue repair [35] [36]. In the context of tissue damage—such as myocardial infarction, neuronal loss, or pancreatic dysfunction—the goal is to directly reprogram abundant local cells, like fibroblasts, into the functional cells that have been lost [37] [36]. This approach minimizes risks associated with cell transplantation, such as immune rejection and tumorigenicity, by leveraging the body's own cellular resources [38]. Transcription factor (TF) cocktails are the primary tools for orchestrating this cell fate conversion, as they can reactivate silenced genetic programs and initiate new transcriptional networks, effectively rewriting a cell's identity [39]. This technical guide details the key TF combinations and emerging methodologies for generating neurons, cardiomyocytes, and beta cells, framing them within the practical framework of developing therapies for tissue repair and regeneration.
Transcription Factor Cocktails for Target Cell Types
The core of direct reprogramming lies in identifying the minimal set of key transcription factors that can act as master regulators to define a target cell's identity. The tables below summarize the established and optimized TF combinations for generating neurons, cardiomyocytes, and the investigational cocktails for beta cells, incorporating critical data on efficiency and maturation.
Table 1: Transcription Factor Cocktails for Neuronal and Cardiomyocyte Generation
| Target Cell Type | Key Transcription Factor Cocktail | Reprogramming Factors (Abbreviations) | Reprogramming Efficiency | Notable Characteristics | Primary Source Cell |
|---|---|---|---|---|---|
| Induced Motor Neurons (iMNs) | Neurogenin 2, Islet-1, LIM Homeobox 3 | Ngn2, Isl1, Lhx3 | ~21% (with DDRR* cocktail) [39] | Optimized minimal 3-factor cocktail; high purity and functional maturity [39]. | Mouse Embryonic Fibroblasts (MEFs) [39] |
| Induced Cardiomyocytes (iCMs) | GATA Binding Protein 4, Myocyte Enhancer Factor 2C, T-Box Transcription Factor 5 | Gata4, Mef2c, Tbx5 (GMT) | Low efficiency in early studies [37] [40] | Foundational cocktail; functional but relatively immature state [37]. | Cardiac Fibroblasts [37] [36] |
| Induced Cardiomyocytes (iCMs) | Gata4, Mef2c, Tbx5, Hand2 | GHMT | Improved efficiency over GMT [37] | Enhanced reprogramming for a more robust cardiac phenotype. | Cardiac Fibroblasts [37] |
| Ethyl benzoylphosphonate | Diethyl Benzoylphosphonate | Research-grade Diethyl Benzoylphosphonate for synthesis and C-C bond formation. This product is for laboratory research use only; not for human consumption. | Bench Chemicals | ||
| 14-Sulfanyltetradecan-1-OL | 14-Sulfanyltetradecan-1-OL, CAS:131215-94-6, MF:C14H30OS, MW:246.45 g/mol | Chemical Reagent | Bench Chemicals |
Table 2: Investigational and Alternative Reprogramming Approaches
| Target Cell Type | Key Transcription Factor Cocktail | Reprogramming Factors (Abbreviations) | Reprogramming Efficiency | Notable Characteristics | Primary Source Cell |
|---|---|---|---|---|---|
| Beta Cells | Information Not Specified in Search Results | N/A | N/A | Direct TF combinations for beta cells not detailed in available sources. | N/A |
| Chemically Induced Cardiomyocytes (hCiCMs) | Small Molecule Cocktail (15 compounds) | N/A (Non-genetic) | 15.08% (Day 30), ~96.67% purity (Day 60) [40] | Xeno-free, chemically defined method; avoids genetic integration [40]. | Human Urine-Derived Cells (hUCs) [40] |
| Partial Reprogramming | Oct4, Sox2, Klf4, c-Myc (OSKM) | OSKM | N/A | Transient activation reverses aging markers without changing cell identity for rejuvenation [35]. | Senescent cells [35] |
Note: DDRR cocktail consists of p53DD, HRASG12V, and the TGF-β inhibitor RepSox [39].
Experimental Protocols for Direct Reprogramming
High-Efficiency Direct Conversion to Motor Neurons
This protocol is adapted from a 2025 study that achieved a high yield of induced motor neurons (iMNs) by minimizing extrinsic variation and leveraging a hyperproliferative cell state [39].
- 1. Cell Source and Culture: Use Mouse Embryonic Fibroblasts (MEFs) from transgenic reporter mice (e.g., Hb9::GFP) for easy visualization of motor neurons. Culture cells in standard fibroblast medium.
- 2. Viral Transduction:
- Vector: Use a single polycistronic lentiviral vector encoding the minimal TF cocktail (Ngn2, Isl1, Lhx3).
- Infection: Transduce MEFs with the viral supernatant. The use of a single vector ensures consistent stoichiometric delivery of all TFs into each cell.
- 3. Hyperproliferation Induction (DDRR Cocktail): Following transduction, treat cells with the DDRR chemo-genetic cocktail to induce a transient state of hyperproliferation:
- p53DD: A dominant-negative p53 mutant.
- HRASG12V: An oncogenic form of HRAS.
- RepSox: A small molecule inhibitor of the TGF-β pathway.
- Cells with this hyperproliferative (hyperP) history convert to iMNs at a 4-fold higher rate.
- 4. Media Switch and Maturation: 48-72 hours post-transduction, replace the fibroblast medium with motor neuron maturation medium, typically containing neurotrophic factors like BDNF, CNTF, and GDNF.
- 5. Functional Validation: After 2-3 weeks, validate iMNs using:
- Immunostaining: for TUBB3 (neuronal marker) and ISL1/2 (motor neuron markers).
- Patch-Clamp Electrophysiology: to confirm the ability to generate action potentials.
- Calcium Imaging: to demonstrate electrical activity.
Chemical Reprogramming of Human Urine-derived Cells to Cardiomyocytes
This 2025 protocol outlines a non-integrating, xeno-free method for generating human cardiac-induced cardiomyocytes (hCiCMs) [40].
- 1. Cell Source and Isolation: Collect fresh human urine samples (approx. 50 ml). Centrifuge at 500 × g for 5 minutes to pellet cells. Resuspend the pellet in a specific medium (1:1 DMEM/F12 and Keratinocyte SFM, supplemented with 5% FBS and antibiotics) and seed onto culture plates.
- 2. Expansion of Human Urine-derived Cells (hUCs): Culture the isolated cells in hUC medium, changing the medium every two days until colonies form. Passage cells at 70-80% confluency.
- 3. Chemical Induction:
- Initiation: Seed hUCs at a density of 1x10â´ cells per well in a 6-well plate.
- Cocktail: Treat the cells with a defined cocktail of 15 small molecules. The specific molecules were not listed, but such cocktails typically include inhibitors of key signaling pathways (e.g., TGF-β, GSK3β) and activators of cardiac development.
- Duration: Maintain the cells in the induction cocktail with regular medium changes. Significant morphological changes towards a cardiomyocyte-like phenotype can be observed within 30 days.
- 4. Maturation and Purity: Continue the culture for up to 60 days to achieve high purity (over 96%) and functional maturation.
- 5. Characterization:
- Immunofluorescence: Confirm expression of cardiac proteins like cardiac Troponin T (cTnT) and α-Actinin, showing organized sarcomeric structures.
- Electrophysiology: Use patch-clamp recording to validate ventricular-like action potentials.
- Transcriptomics: Perform single-cell RNA sequencing to confirm a gene expression profile resembling human embryonic cardiomyocytes.
Signaling Pathways and Molecular Mechanisms
The process of transdifferentiation is driven by the forced expression of TFs that initiate a cascade of transcriptional and epigenetic changes. The diagram below illustrates the core mechanistic pathway from cellular reprogramming to functional integration in tissue repair.
Diagram 1: Core pathway of transdifferentiation from reprogramming to tissue repair.
The molecular mechanisms underpinning the pathways in Diagram 1 involve profound changes within the cell:
- Transcriptional Activation and Silencing: Pioneer TFs, such as Ngn2 in neuronal reprogramming, are capable of binding to closed chromatin and initiating the opening of cell-type-specific enhancers and promoters [35]. This activates the transcriptional network of the target cell (e.g., neurons) while silencing the program of the original cell (e.g., fibroblast).
- Epigenetic Remodeling: The reprogramming factors recruit chromatin-modifying enzymes to establish new, stable epigenetic landscapes, including DNA methylation and histone modification patterns characteristic of the target cell [35]. This "epigenetic memory" erasure is crucial for stable cell fate conversion.
- Metabolic Shifts: Successful reprogramming involves a metabolic rewiring from a glycolytic phenotype often associated with proliferation to an oxidative metabolic state supportive of the target cell's function, such as the high energy demand of contracting cardiomyocytes [35].
- In Vivo Tissue Repair: In animal models of myocardial infarction, transplantation of reprogrammed cardiomyocytes has been shown to improve heart function by reducing fibrosis and scar size, and improving contractile measures like ejection fraction [37] [40]. The ultimate goal is the electrical and mechanical integration of new cells with the host tissue.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Direct Reprogramming Experiments
| Reagent / Technology | Function / Application | Technical Notes |
|---|---|---|
| Lentiviral / Retroviral Vectors | Stable delivery of transcription factor genes into target cells. | Allows for sustained TF expression; potential insertional mutagenesis risk [36] [40]. |
| Tissue Nanotransfection (TNT) | Non-viral, in vivo gene delivery via nanoelectroporation [35]. | Silicon chip with hollow needles for localized, non-viral transfection; high specificity and minimal cytotoxicity. |
| Small Molecule Cocktails | Chemical induction of reprogramming; modulate signaling pathways. | Non-integrative, offer temporal control; used for cardiac reprogramming from urine cells [40]. |
| DDRR Cocktail (p53DD, HRASG12V, RepSox) | Enhances reprogramming efficiency by inducing a transient hyperproliferative state [39]. | Critical for high-yield motor neuron conversion; proliferation history impacts TF responsiveness. |
| MOA-seq (MNase-defined Cistrome Occupancy Analysis) | Genome-wide mapping of TF binding sites (cis-elements) with high resolution [41]. | Identifies functional non-coding variants (bQTL) crucial for understanding TF binding and trait heritability. |
| Patch-Clamp Electrophysiology | Gold-standard for functional validation of excitable cells (neurons, cardiomyocytes). | Measures action potentials and ion channel activity confirming functional maturity [40]. |
| Single-Cell RNA Sequencing (scRNA-seq) | Characterization of transcriptional identity and heterogeneity in reprogrammed cell populations. | Identifies cardiomyocyte subpopulations and assesses maturation by comparing to developmental stages [40]. |
| n-Acetyl-d-alanyl-d-serine | n-Acetyl-d-alanyl-d-serine, CAS:159957-07-0, MF:C8H14N2O5, MW:218.21 g/mol | Chemical Reagent |
| Iforrestine | Iforrestine, CAS:125287-08-3, MF:C14H12N4O3, MW:284.27 g/mol | Chemical Reagent |
Chemical reprogramming represents a paradigm shift in cellular manipulation, utilizing defined small molecules to override somatic cell identity and induce a pluripotent state. This approach offers a novel alternative to transcription-factor-driven reprogramming, enabling precise control over cell fate transitions through temporal modulation of signaling pathways and epigenetic landscapes without genetic modification [42]. The breakthrough achievement of generating human chemically induced pluripotent stem cells (hCiPSCs) in 2022 demonstrated that specific chemical combinations can overcome the stable epigenome of human somatic cells, establishing a viable platform for regenerative medicine applications [43]. This methodology provides distinct advantages for therapeutic development, including reduced tumorigenicity risks, non-immunogenicity, and the ability to precisely control compound concentrations and treatment durations for optimized outcomes [44].
Within the broader context of transdifferentiation mechanisms in tissue repair, chemical reprogramming shares fundamental principles with natural regeneration processes observed in model organisms like axolotls, where differentiated cells revert to plastic states capable of reconstructing complex structures [42]. The chemical induction of an intermediate plastic state during reprogramming mirrors this dedifferentiation phase, activating similar regenerative genetic programs that enable cellular identity switching [43]. This parallel provides valuable insights for developing therapeutic strategies that leverage endogenous repair mechanisms through well-defined pharmacological interventions.
Fundamental Mechanisms of Chemical Reprogramming
Molecular Principles and Key Events
Chemical reprogramming employs small molecules that target specific cellular signaling pathways, epigenetic modifiers, and metabolic processes to orchestrate a stepwise transformation of somatic cells into pluripotent stem cells. Unlike transcription factor-based approaches that forcibly impose new gene expression programs, chemical reprogramming manipulates the cell's inherent regulatory networks to guide natural progression toward pluripotency [42]. The process involves three critical molecular events that must occur sequentially: erasure of the original somatic cell identity, induction of a transient intermediate plastic state, and establishment of a stable pluripotency network [42].
The complete chemical reprogramming trajectory can be visualized as a phased process with distinct regulatory checkpoints:
Figure 1. The three-stage molecular trajectory of chemical reprogramming from somatic cells to pluripotent stem cells through an intermediate plastic state.
Signaling Pathways and Molecular Targets
Small molecules employed in chemical reprogramming function through targeted modulation of specific signaling cascades that regulate cell identity. The JNK pathway has been identified as a major barrier to chemical reprogramming in human cells, with its inhibition being indispensable for inducing cellular plasticity by suppressing pro-inflammatory pathways [43]. Additional critical pathways include Wnt signaling, which controls self-renewal and pluripotency through TCF3-mediated regulation of pluripotency genes; TGF-β signaling, whose inhibition promotes mesenchymal-epithelial transition (MET); and MEK/ERK signaling, whose blockade prevents differentiation and supports pluripotency maintenance [44].
The coordinated regulation of these pathways creates a permissive environment for identity switching:
Figure 2. Key signaling pathways modulated by small molecules to induce cellular plasticity during chemical reprogramming.
Experimental Protocols and Methodologies
Human Chemical Reprogramming Workflow
The establishment of hCiPSCs requires a meticulously optimized protocol with specific chemical combinations administered in a temporal sequence. The following workflow delineates the core methodology based on successful human fibroblast reprogramming [43]:
Stage 1: Initiation (Days 1-12)
- Culture human dermal fibroblasts in essential medium supplemented with CHIR99021 (GSK-3β inhibitor), A83-01 (TGF-β inhibitor), BIX01294 (G9a inhibitor), and AS8351 (KDM5 inhibitor)
- Refresh medium every 48 hours while monitoring morphological changes indicating identity erosion
- Assess emergence of plastic state markers (SALL4, LIN28A) via immunostaining or RT-qPCR
Stage 2: Stabilization (Days 13-24)
- Transition to medium containing CHIR99021, A83-01, VPA (HDAC inhibitor), and EPZ004777 (DOT1L inhibitor)
- Observe formation of compact cell colonies with epithelial morphology
- Verify suppression of inflammatory pathways and activation of regeneration-associated genes
Stage 3: Pluripotency Establishment (Days 25-36)
- Apply final maturation medium with CHIR99021, A83-01, VPA, and DZNep (EZH2 inhibitor)
- Monitor emergence of embryonic stem cell-like colonies with defined borders
- Iscrete and expand hCiPSC colonies using standard pluripotent stem cell culture conditions
Key Small Molecules and Their Functions
Table 1. Essential small molecules for human chemical reprogramming and their mechanisms of action
| Small Molecule | Primary Target | Molecular Function | Reprogramming Phase | Concentration Range |
|---|---|---|---|---|
| CHIR99021 | GSK-3β inhibitor | Activates Wnt signaling by stabilizing β-catenin; promotes self-renewal | Throughout | 3-6 μM |
| A83-01 | TGF-β receptor inhibitor | Blocks EMT; facilitates MET transition | Throughout | 0.5-2 μM |
| BIX01294 | G9a histone methyltransferase inhibitor | Reduces H3K9me2/3 repressive marks; opens chromatin | Early stage | 2-5 μM |
| AS8351 | KDM5 histone demethylase agonist | Promotes H3K4 methylation; activates pluripotency genes | Early stage | 0.5-1 μM |
| Valproic acid (VPA) | HDAC inhibitor | Increases global histone acetylation; enhances chromatin accessibility | Middle/Late stage | 0.5-2 mM |
| EPZ004777 | DOT1L histone methyltransferase inhibitor | Reduces H3K79 methylation; diminishes differentiation barriers | Middle stage | 1-5 μM |
| DZNep | EZH2 inhibitor | Decreases H3K27me3 repressive marks; facilitates pluripotency | Late stage | 0.1-0.5 μM |
Quality Control and Validation
Following chemical reprogramming, rigorous validation of resulting hCiPSCs is essential through multiple analytical approaches:
- Pluripotency marker expression: Immunofluorescence and flow cytometry analysis for OCT4, SOX2, NANOG, SSEA-4, TRA-1-60, and TRA-1-81
- Trilineage differentiation capacity: In vitro embryoid body formation followed by immunostaining for ectodermal (β-III-tubulin), mesodermal (α-SMA), and endodermal (AFP) markers
- Gene expression profiling: RNA sequencing to confirm transcriptional similarity to reference embryonic stem cell lines
- Epigenetic status: Bisulfite sequencing to assess demethylation of pluripotency promoter regions (OCT4, NANOG)
- Functional assessment: Teratoma formation assays in immunodeficient mice to validate in vivo differentiation potential
The Scientist's Toolkit: Essential Research Reagents
Table 2. Key research reagent solutions for chemical reprogramming experiments
| Reagent Category | Specific Examples | Function in Reprogramming | Considerations for Use |
|---|---|---|---|
| Signaling Pathway Modulators | CHIR99021 (Wnt activator), A83-01 (TGF-β inhibitor), DMH1 (BMP inhibitor) | Regulate core signaling pathways that maintain or alter cell identity | Concentration optimization critical; temporal specificity important |
| Epigenetic Modifiers | VPA (HDAC inhibitor), BIX01294 (G9a inhibitor), EPZ004777 (DOT1L inhibitor) | Alter chromatin accessibility and DNA methylation patterns | Combinatorial effects significant; monitor cellular toxicity |
| Metabolic Regulators | PS48 (PDK1 activator), Sodium butyrate (HDAC inhibitor) | Shift energy metabolism from oxidative phosphorylation to glycolysis | Culture conditions affect efficacy; requires precise timing |
| Cell Identity Markers | Antibodies against SALL4, LIN28A, OCT4, NANOG, SSEA-4 | Track progression through reprogramming stages | Essential for quality control; multiple markers recommended |
| Culture System Components | Vitronectin, Laminin-521, Essential 8 Medium | Support pluripotent stem cell survival and expansion | Xeno-free systems preferred for clinical applications |
| 12-Aminododecane-1-thiol | 12-Aminododecane-1-thiol, CAS:158399-18-9, MF:C12H27NS, MW:217.42 g/mol | Chemical Reagent | Bench Chemicals |
Applications in Regenerative Medicine and Disease Modeling
Therapeutic Applications
Chemical reprogramming technologies have demonstrated significant potential across multiple therapeutic domains. Recent clinical applications include the transplantation of chemically induced pluripotent stem cell-derived islets under the abdominal anterior rectus sheath in a type 1 diabetes patient, establishing a promising regenerative therapy for metabolic disease [42]. Additionally, hCiPSCs have been successfully differentiated into eosinophils that demonstrate potent cytotoxicity against solid tumors, opening novel cancer immunotherapy avenues [42]. The generation of dual-attribute iTNK cells from hPSCs for cancer immunotherapy further expands the potential oncological applications of chemically reprogrammed cells [42].
In neurodegenerative disease research, chemical reprogramming offers particular promise, as demonstrated by the direct conversion of normal and Alzheimer's disease human fibroblasts into neuronal cells using small molecule cocktails [11]. This approach enables the generation of patient-specific neuronal cells that retain age-related epigenetic signatures, providing superior models for studying late-onset neurodegenerative pathologies compared to embryo-like iPSC-derived neurons [11].
Comparative Analysis with Other Reprogramming Approaches
Table 3. Comparison of chemical reprogramming with alternative cell fate manipulation strategies
| Parameter | Chemical Reprogramming | Transcription Factor-Based iPSCs | Direct Lineage Conversion |
|---|---|---|---|
| Genetic Modification | None required | Permanent integration of exogenous genes | Often requires transcription factors |
| Efficiency | Moderate (0.1-1%) | Variable (0.01-1%) | Generally low (0.001-0.1%) |
| Tumorigenic Risk | Low | Moderate (insertional mutagenesis) | Low (no pluripotent intermediate) |
| Kinetics | Slow (4-6 weeks) | Moderate (3-4 weeks) | Fast (1-2 weeks) |
| Mechanistic Control | High (temporal precision) | Moderate (constitutive expression) | Variable |
| Epigenetic Memory | Minimal | Often present | Retains some donor cell characteristics |
| Clinical Translation Potential | High | Limited | Moderate |
Current Challenges and Future Perspectives
Despite significant advances, chemical reprogramming faces several technical hurdles requiring resolution before widespread clinical application. The efficiency of human chemical reprogramming remains suboptimal, with recent protocols achieving successful conversion in only a fraction of treated somatic cells [42]. The extended duration required for complete reprogramming (approximately 36 days in current protocols) presents challenges for practical implementation and increases risks of cultural artifacts [43]. Additionally, the complex mechanistic basis of many small molecule cocktails remains incompletely characterized, necessitating further investigation into the precise molecular events driving fate conversion [42].
Future development directions include the identification of novel small molecule combinations that accelerate reprogramming kinetics while improving efficiency, potentially through high-throughput compound screening approaches [44]. The application of chemical reprogramming to diverse human somatic cell types beyond fibroblasts represents another critical research frontier [42]. Emerging evidence suggests that partial reprogramming strategies using abbreviated chemical treatment may enable epigenetic rejuvenation without complete identity erasure, potentially offering novel therapeutic approaches for age-related diseases [45].
The remarkable parallel between chemically induced intermediate plastic states and natural regeneration programs in model organisms like axolotls provides a rich framework for future discovery [42] [43]. By elucidating the conserved molecular principles underlying these processes, researchers may identify novel targets for manipulating cell fate in therapeutic contexts, ultimately bridging the gap between regenerative biology and clinical medicine through well-defined chemical approaches.
The irreversible loss of neurons following injury or in progressive neurodegenerative diseases represents a fundamental challenge in contemporary neuroscience. Unlike other tissues, the adult mammalian central nervous system (CNS) has limited capacity for self-repair, leading to permanent functional deficits [46]. Within this context, in vivo glia-to-neuron (GtN) transdifferentiation has emerged as a paradigm-shifting regenerative strategy. This approach aims to reprogram abundant, resident glial cells directly into functional neurons to replace those lost to pathology, thereby rebuilding neural circuits [46] [11]. Glial cells, including astrocytes, oligodendrocyte precursor cells (OPCs), and Müller glia in the retina, are ideally suited for this role due to their proximity to neuronal circuits, shared lineage, and abundance in the CNS [47] [48]. This whitepaper examines the mechanistic foundations, key experimental models, and methodological considerations of in vivo glial transdifferentiation, framing it within the broader thesis of harnessing endogenous cell plasticity for tissue repair.
Core Mechanisms and Signaling Pathways
The molecular machinery driving glial transdifferentiation involves a complex interplay of transcription factors, epigenetic regulators, and signaling pathways that collectively override the established glial identity and instigate a neuronal gene expression program.
Transcriptional and Epigenetic Control
The forced expression of lineage-determining transcription factors is the most widely employed strategy to initiate transdifferentiation. Key factors include NEUROD1, ASCL1, SOX2, and Brn2 (Pou3f2), which can directly activate neurogenic programs [3] [11]. For instance, NEUROD1 expression in astrocytes has been reported to convert them into neurons with functional properties [46]. A critical insight from comparative biology is that the epigenetic landscape of glial cells can pose a barrier to reprogramming. In zebrafish, which possess a remarkable capacity for CNS regeneration, retinal injury triggers chromatin remodelling mediated by histone deacetylases (HDACs) and other modifiers, making pro-neurogenic genes accessible to factors like Ascl1a [48]. In contrast, mammalian Müller glia exhibit a more restrictive chromatin state, explaining their limited spontaneous regenerative response. Combining transcription factor expression with HDAC inhibitors can enhance reprogramming efficiency in mammals by overcoming this epigenetic barrier [48].
Key Signaling Pathways
Extracellular cues and their corresponding intracellular signaling pathways play a pivotal role in creating a permissive microenvironment for transdifferentiation. These pathways are often activated by injury and can be harnessed for therapeutic strategies.
The following diagram illustrates the core signaling pathways that regulate glial transdifferentiation, integrating extracellular cues with intracellular transcriptional and epigenetic machinery:
Figure 1: Core Signaling Pathways in Glial Transdifferentiation. This diagram integrates injury-induced extracellular cues with the intracellular signaling and nuclear reprogramming events that drive glia-to-neuron conversion. Key pathways include JAK/STAT, MAPK, and PI3K/Akt, which converge on transcriptional regulators like STAT3 and ASCL1, ultimately leading to epigenetic remodeling and fate conversion [49] [48].
Model Systems and Evidence for Glial Transdifferentiation
Evidence supporting the feasibility of glial transdifferentiation comes from a diverse array of model organisms, each offering unique insights into the physiological and molecular requirements for successful cell fate conversion.
Physiological Transdifferentiation in Invertebrates and Lower Vertebrates
Recent work in Drosophila melanogaster has provided the first evidence of physiological transdifferentiation in the adult CNS following injury. Using a ventral nerve cord crush model, researchers demonstrated that astrocyte-like glia (ALG) and ensheathing glia (EG) can exchange identities, and more importantly, that neuropil-associated glia directly transdifferentiate into neurons. This conversion was shown to increase under injury conditions, revealing a native, evolutionarily conserved mechanism for CNS repair [50] [51] [52]. In C. elegans, a programmed, sex-specific transdifferentiation event occurs during male sexual maturation, where the PHso1 socket glial cell directly converts into a cholinergic, peptidergic neuron (PHD). This process is controlled cell-autonomously by the sex-determination pathway and does not involve cell division, providing a powerful genetic model to dissect the mechanisms of direct lineage conversion [53].
The zebrafish retina represents a gold standard for studying spontaneous glia-mediated regeneration. Upon injury, Müller glia (MG) undergo reprogramming, re-enter the cell cycle, and generate multipotent progenitors that differentiate into all retinal neuronal types, restoring vision. This process is driven by a well-orchestrated cascade of extracellular signals (e.g., HB-EGF, TNF-α), activation of the JAK/STAT and MAPK pathways, and crucial transcriptional regulators like Stat3 and Ascl1a [48].
Engineered Transdifferentiation in Mammalian Models
In mammals, where spontaneous transdifferentiation is limited, the strategy relies on artificial genetic interventions. Key studies have focused on converting astrocytes and Müller glia into various neuronal subtypes in mouse models of injury and disease.
Table 1: Key In Vivo Glia-to-Neuron Transdifferentiation Studies in Mammalian Models
| Target Glia | Desired Neuron | Reprogramming Factor(s) | Model System | Reported Efficiency | Functional Outcome | Citation |
|---|---|---|---|---|---|---|
| Astrocyte | Cortical Neuron | NEUROD1 | Mouse ischemic stroke | High (reporter-based) | Improved motor function | [46] |
| Astrocyte | Dopaminergic Neuron | NEUROD1 | Mouse Parkinson's disease | High (reporter-based) | Improved motor function | [46] |
| Astrocyte | Neuron (Various) | PTBP1 knockdown | Mouse Parkinson's disease, retinal injury | High (reporter-based) | Improved behavior & vision | [46] |
| Retinal Müller Glia | Photoreceptor / Interneuron | ASCL1 + HDAC inhibitor | Mouse retinal degeneration | Limited | N/D | [48] |
| NG2 Glia / Astrocyte | Induced Neuroblast | SOX2 | Mouse spinal cord injury | 3-6% | Synapse formation | [3] |
Critical Methodological Considerations and Experimental Protocols
The promise of glial transdifferentiation is tempered by significant technical challenges and controversies, necessitating rigorous experimental design and validation.
The Critical Importance of Lineage Tracing
A major controversy in the field involves the misinterpretation of viral reporter expression. Several high-profile studies that used AAV vectors with glial promoters (e.g., GFAP) to express NEUROD1 or shPTBP1 reported extraordinarily efficient conversion and functional recovery [46]. However, subsequent independent studies using genetic lineage tracing—the gold standard for establishing cell origin—demonstrated that the virus-labeled "new" neurons were largely preexisting endogenous neurons that had taken up the virus, rather than astrocytes that had undergone conversion [46]. This highlights a critical pitfall: certain transcription factors and viral constructs can lead to cis-regulation of the reporter gene, causing its expression in neurons independent of the original promoter's activity [46]. Therefore, definitive proof of transdifferentiation requires inducible, Cre-based lineage tracing systems that permanently label the glial population of interest and all its progeny before the reprogramming intervention.
A Standard Workflow for Validated In Vivo Transdifferentiation
The following protocol outlines a robust experimental workflow designed to conclusively demonstrate glia-to-neuron transdifferentiation.
Figure 2: Validated Workflow for In Vivo Transdifferentiation. A rigorous protocol emphasizing the necessity of genetic lineage tracing (Step 1) to unambiguously determine the glial origin of newly generated neurons, followed by multi-parametric validation of neuronal identity and function [46] [3] [48].
The Scientist's Toolkit: Essential Research Reagents
Advancing this field requires a specific set of research tools for lineage tracing, genetic manipulation, and functional validation.
Table 2: Essential Research Reagent Solutions for Glial Transdifferentiation Studies
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Genetic Lineage Tracing Models | Aldh1l1-CreERT2; GFAP-CreERT2; hGFAP-Cre | Critical function: Inducible, permanent labeling of astrocytes and their progeny to definitively track cell origin. |
| Viral Delivery Vectors | AAV (Serotypes 2, 5, 9); Lentivirus; Retrovirus | Delivery of transgenes (e.g., NEUROD1, ASCL1) or shRNAs (e.g., against PTBP1) to specific glial populations. |
| Reprogramming Factors | NEUROD1, ASCL1, SOX2, Brn2, Neurog2, miR-124 | Ectopic expression of these transcription factors and microRNAs drives the glial-to-neuronal fate switch. |
| Cell Cycle Indicators | EdU/BrdU; FLY-FUCCI (in Drosophila) | Label proliferating cells to monitor glial division and the expansion of progenitor pools during reprogramming. |
| Neuronal Subtype Inducers | Lmx1a, FoxA2 (dopaminergic); Fezf2 (corticofugal); Tbx18 (pacemaker) | Co-factors to specify target neuronal subtype identity during conversion. |
In vivo glial transdifferentiation stands as a compelling therapeutic target with the potential to revolutionize the treatment of CNS injuries and neurodegenerative diseases. The convergence of evidence from diverse model organisms confirms that glial cell fate is plastic and can be harnessed for regeneration. However, the path to clinical translation is fraught with challenges. Future research must prioritize the development of safer, more controllable delivery systems for reprogramming factors, such as small molecules or modified mRNAs, to avoid the pitfalls of viral vectorology. A deeper understanding of the epigenetic roadblocks that inhibit transdifferentiation in mammals, informed by studies in zebrafish, will be crucial. Furthermore, generating specific, functionally integrated neuronal subtypes remains a significant hurdle. Overcoming these challenges will require a multidisciplinary effort, solidly grounded in rigorous lineage tracing and functional validation, to realize the promise of turning the brain's abundant support cells into a source of new neurons for repair.
The field of regenerative medicine is increasingly focused on transdifferentiation—the direct conversion of one differentiated cell type into another—as a fundamental mechanism for tissue repair. This whitepaper examines organ-specific applications of this principle through three advanced case studies: heart repair, diabetes therapy, and neural regeneration. Unlike approaches using pluripotent stem cells, transdifferentiation strategies aim to directly reprogram resident cells at injury sites, offering potentially faster functional recovery with reduced risks of tumorigenesis. The following sections provide technical analysis of experimental protocols, quantitative outcomes, and molecular pathways currently demonstrating efficacy in preclinical and clinical settings, providing drug development professionals with actionable insights for therapeutic development.
Cardiac Repair Through Macrophage Reprogramming
Molecular Mechanism of Circular RNA-Mediated Repair
Following cardiac injury, the balance between inflammatory and reparative immune responses critically determines functional recovery. Recent research has identified circular RNAs (circRNAs) as key regulators of macrophage polarization toward a reparative phenotype. Specifically, circ-cdr1as modulates post-infarct healing by maintaining macrophages in an anti-inflammatory, pro-reparative state [54].
The molecular mechanism involves a sponge function where circ-cdr1as sequesters microRNAs that would otherwise suppress reparative pathways. When circ-cdr1as levels decrease after myocardial infarction, this suppression is lifted, shifting macrophages toward a pro-inflammatory phenotype that exacerbates tissue damage [54].
Table: Key Experimental Findings in Cardiac circRNA Research
| Experimental Model | Intervention | Functional Outcome | Tissue Damage Assessment |
|---|---|---|---|
| In vivo mouse myocardial infarction | Macrophage overexpression of circ-cdr1as | Improved cardiac function | Significant reduction in scar size |
| In vitro macrophage culture | circ-cdr1as knockdown via siRNA | Increased inflammatory markers | N/A |
| In vivo delivery via viral vector | Systemic circ-cdr1as supplementation | Enhanced contractility on echocardiography | Improved tissue preservation |
Experimental Protocol for circRNA Research
The foundational protocol for establishing circ-cdr1as efficacy involves:
- Myocardial Infarction Induction: Permanent ligation of the left anterior descending coronary artery in C57BL/6 mice
- Cell Isolation and Manipulation:
- Harvest bone marrow-derived macrophages
- Transduce with lentivirus containing circ-cdr1as sequence
- Confirm overexpression via qPCR with divergent primers
- Cell Transplantation: Direct intramyocardial injection of 5×10^5 circ-cdr1as-overexpressing macrophages into peri-infarct border zone
- Functional Assessment:
- Echocardiography at days 7, 14, and 28 post-infarction
- Measurement of left ventricular ejection fraction and end-systolic diameter
- Histological Analysis:
- Masson's trichrome staining for collagen deposition
- Immunofluorescence for macrophage markers (CD68, CD206)
- TUNEL assay for apoptotic cells [54]
Research Reagent Solutions for Cardiac Repair Studies
Table: Essential Research Reagents for circRNA Cardiac Studies
| Reagent/Cell Type | Specific Function | Application in Protocol |
|---|---|---|
| Bone marrow-derived macrophages (C57BL/6) | Primary cells for manipulation | circRNA overexpression and transplantation |
| Lentiviral vector system | circ-cdr1as delivery | Stable gene expression in primary cells |
| Divergent primers | circRNA-specific amplification | Differentiates circRNA from linear mRNA |
| CD68/CD206 antibodies | Macrophage phenotype identification | Immunofluorescence staining |
| Masson's trichrome stain | Collagen visualization | Quantification of fibrosis |
Diabetes Therapy via β-Cell Replacement and Immune Reset
Transdifferentiation Approaches in Diabetes Management
Diabetes therapy has advanced beyond conventional insulin replacement to strategies focused on β-cell transdifferentiation and immune system resetting. Two complementary approaches show particular promise: stem cell-derived islet replacement and combined blood stem cell-islet transplantation that creates a hybrid immune system to prevent autoimmune destruction [55].
The Vertex FORWARD trial of zimislecel (VX-880) represents the most advanced stem cell-derived islet replacement approach, demonstrating remarkable outcomes: at one-year post-infusion, patients achieved insulin independence (0 units versus 36 units baseline), with time-in-range improving from 56% to 95% and HbA1c decreasing from 7.4% to 5.9% [56].
Table: Comparative Outcomes in Beta Cell Replacement Therapies
| Therapy | Study Phase | Insulin Independence Rate | Mechanism of Action |
|---|---|---|---|
| Lantidra (donislecel) | FDA-approved | 70% at 1 year; 34% at 5 years | Allogeneic islet cell infusion [57] |
| Vertex zimislecel | Phase 1/2/3 | 100% in initial cohort (n=12) | Stem cell-derived islets [56] |
| Stanford hybrid immune approach | Preclinical (murine) | 100% in prevented (19/19) and cured (9/9) mice | Blood stem cell + islet co-transplantation [55] |
Experimental Protocol for Hybrid Immune System Approach
The Stanford protocol for resetting autoimmunity in Type 1 diabetes involves:
- Pre-conditioning Regimen (initiated 7 days pre-transplant):
- Administration of immune-targeting antibodies (anti-CD117, anti-CD47)
- Low-dose radiation (1-3 Gy total body irradiation)
- Addition of autoimmune disease drug (exact compound proprietary)
- Donor Cell Preparation:
- Isolation of blood stem cells (CD34+ selection) from immunologically mismatched donor
- Harvest of pancreatic islets from same donor
- Transplantation Procedure:
- Sequential intravenous infusion of blood stem cells
- Intraportal infusion of islet cells (500-1000 islet equivalents/kg)
- Monitoring Protocol:
- Daily blood glucose measurements
- Intraperitoneal glucose tolerance testing weekly
- Flow cytometry for immune chimerism (donor vs. host cells)
- Monitoring for graft-versus-host disease [55]
Research Reagent Solutions for Diabetes Studies
Table: Essential Research Reagents for Diabetes Cell Therapy
| Reagent/Cell Type | Specific Function | Application in Protocol |
|---|---|---|
| CD34+ magnetic beads | Blood stem cell isolation | Positive selection from donor tissue |
| Anti-CD117/anti-CD47 antibodies | Immune cell depletion | Pre-conditioning regimen |
| Glucose tolerance test reagents | Metabolic function assessment | Post-transplant efficacy monitoring |
| Flow cytometry antibodies (CD3, CD4, CD8, CD19) | Immune phenotyping | Chimerism analysis |
| Immunosuppressants (tacrolimus, sirolimus) | Graft protection | Clinical translation (Lantidra) [57] |
Neural Regeneration via BDNF-Enhanced Stem Cell Strategies
BDNF-Mediated Axonal Guidance in Neural Repair
Neural regeneration faces the fundamental challenge of not just replacing lost neurons but establishing functional connections. A novel strategy combining stem cell therapy with brain-derived neurotrophic factor (BDNF) overexpression demonstrates enhanced neuronal maturation, activity, and targeted axonal growth [58].
The mechanism involves BDNF creating a concentration gradient that acts as a chemoattractant for growing axons, directing them toward appropriate targets. When neural progenitor cells (NPCs) derived from human induced pluripotent stem cells (iPSCs) are engineered to overexpress BDNF, they generate more mature neuronal cultures with higher spontaneous activity and improved network formation without altering synaptic organization [58].
Experimental Protocol for BDNF-Enhanced Neural Regeneration
The University of Barcelona protocol for BDNF-enhanced neuronal regeneration:
- iPSC Generation and Neural Differentiation:
- Obtain human dermal fibroblasts via punch biopsy
- Reprogram to iPSCs using Sendai virus expressing Yamanaka factors
- Differentiate into neural progenitor cells using dual-SMAD inhibition
- BDNF Gene Engineering:
- Lentiviral transduction of BDNF gene under constitutive promoter
- Antibiotic selection (puromycin 1μg/mL for 7 days)
- Clone selection and expansion
- Microfluidic Chamber Assay:
- Plate BDNF-overexpressing NPCs in one chamber
- Plate wild-type NPCs in adjacent chamber
- Allow axon extension through microgrooves (450μm length)
- Quantify axon attraction toward BDNF source
- Functional Assessment:
- Multi-electrode array recording of neuronal activity
- Calcium imaging for network synchronization analysis
- Immunostaining for synaptic markers (PSD95, synapsin) [58]
Research Reagent Solutions for Neural Regeneration
Table: Essential Research Reagents for BDNF Neural Studies
| Reagent/Cell Type | Specific Function | Application in Protocol |
|---|---|---|
| Sendai virus (CytoTune kit) | iPSC reprogramming | Fibroblast to pluripotent state conversion |
| - SMAD inhibitors (dorsomorphin, SB431542) | Neural induction | Directs differentiation toward neural lineage |
| - Microfluidic chambers (e.g., XonaChips) | Compartmentalized culture | Axon guidance and chemotaxis assays |
| - Multi-electrode arrays | Network activity recording | Functional integration assessment |
| - Anti-BDNF antibodies | Protein expression validation | ELISA and immunocytochemistry |
Cross-Disciplinary Implications for Transdifferentiation Research
The case studies presented demonstrate how organ-specific regeneration strategies converge on shared principles of transdifferentiation mechanisms. Several cross-cutting themes emerge:
First, the microenvironmental niche proves critical across all three systems. In cardiac repair, circ-cdr1as modulates the inflammatory niche to favor regeneration. In diabetes, the hybrid immune system creates a tolerant niche for donor islets. In neural repair, BDNF creates a permissive niche for axonal growth [54] [55] [58].
Second, signaling gradient establishment represents a shared mechanism for guiding cellular responses. While BDNF forms spatial gradients for axonal guidance, pancreatic islet transplantation relies on vascular-derived signals for endocrine cell function, highlighting how engineered morphogen gradients could enhance future transdifferentiation approaches [59].
Third, the nervous system integration emerges as an underappreciated regulator of organ regeneration beyond the brain. Pancreatic islets require autonomic innervation for proper development and function, suggesting that future diabetes therapies may need to incorporate neural components for optimal outcomes [59].
These common principles suggest that advances in one organ system will increasingly inform strategies across other tissues, accelerating the entire field of regenerative medicine and highlighting the fundamental role of transdifferentiation mechanisms in tissue repair research.
Overcoming Technical Hurdles: Strategies for Enhancing Efficiency, Safety, and Specificity
Cell reprogramming, the process of converting one cell type into another, has fundamentally changed the landscape of developmental biology and regenerative medicine [60]. Within this field, transdifferentiation—the direct conversion of one differentiated somatic cell type to another without reverting to a pluripotent intermediate—represents a promising strategy for tissue repair mechanisms [4]. However, a significant efficiency gap persists between mouse and human cell reprogramming, presenting a substantial barrier to clinical translation. Mouse cells typically reprogram within 1-2 weeks with relatively higher efficiency, whereas human cells may require 3-4 weeks with markedly lower efficiency [61]. This discrepancy is not merely an inconvenience but points to fundamental biological differences between species that must be understood and bridged for effective therapeutic applications in drug development and cell-based therapies [60] [62].
Quantitative Analysis of the Reprogramming Efficiency Gap
The disparities between mouse and human reprogramming efficiencies are evident across multiple studies and reprogramming approaches. The table below summarizes key quantitative differences documented in the literature.
Table 1: Comparative Efficiency of Mouse and Human Fibroblast Reprogramming to iPSCs
| Reprogramming Factor Combination | Starting Cell Type | Reprogramming Efficiency | Key Observations | Reference |
|---|---|---|---|---|
| OSKM (retroviral) | Mouse Embryonic Fibroblasts (MEFs) | ~0.1% | Baseline efficiency established in foundational research | [60] |
| OSKM (retroviral) | Human Dermal Fibroblasts (HDFs) | ~0.02% | Efficiency approximately 5-fold lower than in mouse | [60] |
| OSKM + VPA (retroviral) | Human Foreskin Fibroblasts (HFF) | 0.73%-1.1% | Chemical enhancement significantly improves human efficiency | [60] |
| OSKM + Vc, VPA (retroviral) | Human Skin Fibroblasts | 7.05% | Combined chemical treatment dramatically boosts efficiency | [60] |
| OSKM (chemical cocktails) | HEFs, hADSCs, hASFs | ~0.016% - 31% | Wide efficiency range depending on specific cocktail composition | [60] |
Beyond efficiency metrics, the temporal dynamics of reprogramming differ substantially between species. The prolonged reprogramming timeline in human cells increases opportunities for the accumulation of DNA damage and other epigenetic barriers, potentially explaining both the reduced efficiency and increased genomic instability observed in human induced pluripotent stem cells (iPSCs) [63].
Fundamental Biological Differences Underlying the Disparity
Chromatin Accessibility and Factor Binding Dynamics
Comparative analyses of reprogramming factor binding reveal that OSK factors in human fibroblasts initially target significantly more closed chromatin sites compared to mouse [61]. This suggests that human chromatin presents a more substantial barrier to reprogramming factors, requiring more extensive chromatin remodeling. While the general features of OSKM binding—including intra- and intergenic distribution, target genes, primary binding motifs, and combinatorial binding patterns—are largely similar between species, the specific genomic locations of binding events show limited conservation [61].
Table 2: Species-Specific Differences in Early Reprogramming Events
| Molecular Feature | Mouse System | Human System | Functional Significance | |
|---|---|---|---|---|
| c-Myc binding distribution | Preferentially proximal to TSS | Primarily distal to TSS | Suggests different regulatory mechanisms for this critical factor | [61] |
| Conserved binding in syntenic regions | Limited conservation | Limited conservation | Indicates extensive evolutionary divergence in regulatory networks | [61] |
| Pluripotency state achieved | Naïve state | Primed state | Fundamental differences in the endpoint pluripotency state | [64] |
Distinct Pluripotency States and Regulatory Networks
The pluripotent states readily attainable in mouse and human cells differ fundamentally. Mouse reprogramming typically generates naïve pluripotent stem cells resembling the pre-implantation inner cell mass, while human reprogramming yields primed pluripotent stem cells similar to the post-implantation epiblast [64]. This distinction reflects deeper biological differences beyond technical approaches, as human cells resist adopting the naïve state without additional genetic or chemical manipulation.
Computational analyses comparing transcriptomics data from different pluripotency states reveal that reprogrammed human cells in a supposedly "naïve-like" state still share mechanisms with primed mouse cells, particularly those related to cellular response and differentiation-related mechanisms [64]. This incomplete transition to a true naïve state may contribute to the reduced stability and efficiency of human reprogramming.
DNA Damage Response and Repair Pathways
Reprogramming to pluripotency is intrinsically linked to DNA damage, with reprogramming factors inducing replication stress and double-strand breaks [63]. The BRCA1 tumor suppressor and its role in homology-directed repair (HDR) have been identified as crucial for efficient reprogramming in both species [63] [65]. Cells deficient in HDR reprogram with significantly reduced efficiency, while manipulation of DNA repair pathway choice through 53BP1 inactivation can enhance reprogramming efficiency [63] [65]. The prolonged timeline of human reprogramming may exacerbate replication-associated DNA damage, creating an additional barrier absent in the faster mouse system.
Figure 1: DNA Repair Pathway Choices Influence Reprogramming Outcomes. The balance between homology-directed repair and error-prone non-homologous end joining, regulated by BRCA1/BRCA2 and 53BP1, significantly impacts reprogramming efficiency [63] [65].
Experimental Strategies to Enhance Human Reprogramming
Chemical Enhancement Approaches
The efficiency gap between mouse and human reprogramming can be partially bridged through chemical interventions. The addition of valproic acid (VPA), a histone deacetylase inhibitor, to OSKM factors significantly enhances human reprogramming efficiency from approximately 0.02% to over 1% [60]. More sophisticated chemical cocktails have demonstrated even more dramatic improvements, with some combinations achieving up to 31% efficiency in specific human cell types [60]. These chemical approaches primarily target the epigenetic barriers that are more pronounced in human cells.
Advanced Genetic Tools
Novel genetic approaches are also being developed to address human reprogramming limitations. CRISPR activation (CRISPRa) systems enable high-fidelity reprogramming into human pluripotent stem cells through targeted epigenetic activation rather than transgenic overexpression [66]. This approach potentially reduces the genomic stress associated with conventional factor expression and may provide more precise control over the reprogramming process.
Modulation of DNA Repair Pathways
Given the crucial role of DNA damage response in reprogramming, strategies to manipulate repair pathways show promise for enhancing human efficiency. Inactivation of 53BP1, a factor that competes with BRCA1 and promotes error-prone non-homologous end joining, can rescue reprogramming efficiency in BRCA1-deficient cells [63] [65]. This suggests that tilting the balance toward high-fidelity homology-directed repair may represent a productive strategy for improving human reprogramming outcomes.
Table 3: Research Reagent Solutions for Enhancing Reprogramming Efficiency
| Reagent Category | Specific Examples | Function in Reprogramming | Species Specificity | |
|---|---|---|---|---|
| Epigenetic Modulators | VPA, Tranylcypromine, DZNep | Open closed chromatin, facilitate epigenetic remodeling | Particularly important for human cells | [60] |
| Signaling Pathway Modulators | CHIR99021 (GSK3β inhibitor), 616452 (TGF-β inhibitor) | Modulate signaling pathways to support pluripotency acquisition | Effective in both, with different optimal concentrations | [60] |
| Metabolic Regulators | Vitamin C, Forskolin | Reduce oxidative stress, promote epigenetic changes | Beneficial across species | [60] |
| Novel Genetic Tools | CRISPRa systems, miRNA clusters (e.g., mir-302/367) | Provide precise activation of endogenous pluripotency factors | Particularly promising for human cell applications | [66] |
Figure 2: Strategic Approaches to Enhance Human Reprogramming Efficiency. Multiple intervention points can be targeted to overcome the specific barriers that limit human reprogramming compared to mouse systems.
Best Practices and Standardization in Reprogramming Research
The inherent variability in human reprogramming necessitates rigorous standards and best practices, particularly for neuropsychiatric research and drug discovery applications [62]. Key recommendations include:
- Comprehensive donor characterization: Collecting detailed demographic, clinical, medical, and genetic data from donors provides essential context for interpreting variability between cell lines [62].
- Appropriate control selection: Using sex-matched family members or carefully matched controls from similar geographical locations improves experimental rigor [62].
- Focus on biological replicates: Prioritizing increased donor numbers over multiple clones per donor enhances statistical power and experimental relevance [62].
- Standardized quality control: Implementing consistent quality metrics for resulting iPSCs ensures reproducible outcomes across experiments [62].
These practices are particularly crucial for human reprogramming studies where genetic heterogeneity and epigenetic variability present greater challenges than in inbred mouse models.
The efficiency gap between mouse and human cell reprogramming stems from fundamental biological differences including chromatin accessibility, pluripotency network architecture, and DNA damage response mechanisms. While significant challenges remain, integrated approaches combining chemical enhancement, advanced genetic tools, and DNA repair pathway modulation show promise for bridging this disparity.
Future research directions should focus on better understanding the unique epigenetic landscape of human cells, developing more precise methods to manipulate human pluripotency networks, and creating standardized protocols that account for human-specific reprogramming barriers. Success in these areas will accelerate the translation of transdifferentiation approaches into viable regenerative therapies for human applications, ultimately fulfilling the promise of personalized medicine through patient-specific cellular reprogramming.
Transdifferentiation, the direct conversion of one somatic cell type into another, represents a paradigm shift in regenerative medicine and tissue repair research. This process bypasses the pluripotent state, potentially offering a safer and more efficient path for cell-based therapies by generating desired cell types in situ. A central challenge in this field has been the rational identification of the specific transcription factors (TFs) required to force a cell to switch its identity. Historically, this discovery process has been slow and largely empirical, relying on trial-and-error based on known developmental biology. The Mogrify algorithm emerges as a powerful computational solution to this problem, providing a systematic, data-driven method for predicting the optimal combination of factors for direct cellular reprogramming. By leveraging large-scale genomic and gene regulatory network data, Mogrify enables researchers to move beyond educated guesses to targeted, rational transcription factor selection, thereby accelerating the development of transdifferentiation-based therapies for tissue repair [67].
The Mogrify Algorithm: A Computational Framework for Prediction
Mogrify is a predictive computational framework specifically designed to identify the transcription factors necessary to induce transdifferentiation between human cell types. Its core innovation lies in its integrated approach, which moves beyond simple expression analysis to model the underlying gene regulatory networks (GRNs) that define cellular identity.
The algorithm operates on a foundational premise: each cell type is maintained by a stable, cell-specific GRN. To force a conversion from a donor cell (e.g., a fibroblast) to a target cell (e.g., a cardiomyocyte), one must perturb the GRN of the donor cell to dismantle its existing state and simultaneously orchestrate the establishment of the GRN of the target cell. Mogrify tackles this by integrating two primary classes of data:
- Gene Expression Data: Publicly available data from hundreds of human cell and tissue types to define which genes are active or inactive in both the donor and target cell types.
- Gene Regulatory Network Data: Information on protein-DNA interactions to model the regulatory relationships between transcription factors and their target genes.
The algorithm's predictive process can be broken down into several key stages, as illustrated in the diagram below.
Diagram 1: Computational workflow of the Mogrify algorithm for predicting reprogramming factors.
Mogrify first uses gene expression data to infer the cell-specific regulatory subnetworks for both the donor and target cell types. Concurrently, it identifies the suite of genes that are differentially expressed between the two cell types. The algorithm then ranks all transcription factors based on their potential "influence" over these differentially expressed genes within the reconstructed regulatory networks. The final, critical step is the selection of a minimal set of transcription factors that collectively exert the highest possible influence over the target cell's gene expression profile. This systematic, network-based approach correctly predicted known human conversion factors and successfully proposed new combinations for previously unachieved transdifferentiation events, such as the conversion of fibroblasts to keratinocyte-like cells and keratinocytes to endothelial-like cells [67].
Case Study: Cardiac Direct Reprogramming with Mogrify
The power of Mogrify is best illustrated by its application to a critical challenge in regenerative medicine: the repair of damaged heart tissue. While the combination of Gata4, Mef2c, and Tbx5 (GMT) had proven successful in reprogramming mouse fibroblasts into cardiomyocyte-like cells, this protocol was notoriously inefficient in human cells, limiting its clinical potential [68]. This inefficiency suggested significant inter-species differences in gene regulatory networks and indicated that GMT might not be the optimal starting point for human reprogramming.
To address this, researchers employed Mogrify in an unbiased search for more effective transcription factor combinations for human cardiac direct reprogramming. This computational prediction was then validated using a novel, automated high-throughput screening platform. The platform utilized acoustic liquid handling to test 4,960 unique transcription factor combinations on low-passage primary human cardiac fibroblasts from 24 patients. Reprogramming success was assessed via high-content kinetic imaging cytometry, tracking the expression of cardiomyocyte-specific reporters (TNNT2 and MYH6) and functional characteristics like calcium cycling [68].
This large-scale screen revealed that the most successful combination was MYOCD, SMAD6, and TBX20 (MST)—a cocktail distinct from the traditional GMT-based formulas. The quantitative outcomes of this Mogrify-inspired combination are summarized in the table below.
Table 1: Quantitative Outcomes of MST-Mediated Cardiac Direct Reprogramming
| Metric | Result | Details |
|---|---|---|
| Reprogramming Efficiency | Up to 40% TNNT2+ cells in 25 days | Consistently high efficiency across patient samples [68] |
| Early Myogenic Markers | 33% MYH6+ and 17% TNNT2+ cells on average by day 6 | Indicates rapid initiation of the reprogramming process [68] |
| Functional Maturation | Spontaneous contraction and cardiomyocyte-like calcium transients | Observed upon addition of FGF2 and XAV939 to the MST cocktail [68] |
The MST combination demonstrated a dramatic improvement over previous methods, achieving efficiencies that began to rival those seen in mouse models. The addition of small molecules (FGF2 and XAV939) was crucial for driving the reprogrammed cells toward full functional maturity, evidenced by spontaneous contraction—a gold-standard characteristic of cardiomyocytes that had been difficult to achieve conclusively in human cells without co-culture [68]. This case study underscores how Mogrify can identify non-intuitive, highly effective transcription factor combinations that bypass the limitations of traditional, incremental approaches.
Experimental Protocol: Validating Cardiac Reprogramming In Vitro
The following detailed methodology was used to validate the Mogrify-predicted MST combination in human primary cells.
- Cell Source: Primary cardiac fibroblasts were isolated from de-identified human heart samples obtained from 24 patients (aged 4 days to 21 years) undergoing cardiac surgery. Tissues were minced and explants were cultured in IMDM medium supplemented with 20% FBS on growth factor-reduced Matrigel-coated plates. Fibroblasts that migrated out were passaged upon reaching 90% confluence [68].
- Reprogramming Factor Delivery: The transcription factors MYOCD, SMAD6, and TBX20 were delivered using a lentiviral system. VSV-G pseudotyped, doxycycline-inducible lentiviruses were produced in HEK293T cells. This system was chosen for its stability through freeze-thaw cycles and consistent factor expression [68].
- Reporter System: A dual fluorescent reporter system was utilized to track reprogramming kinetics: TNNT2-mScarlet for cardiac troponin T expression and MYH6-mNeonGreen for myosin heavy chain 6 expression [68].
- Culture Conditions: Transduced fibroblasts were maintained in defined reprogramming media. The small molecule XAV939 (a Wnt/β-catenin signaling inhibitor) and the growth factor FGF2 (Fibroblast Growth Factor 2) were added to the culture medium to enhance maturation and functionality [68].
- Phenotypic Assessment:
- High-Content Imaging: Automated microscopy was used to monitor reporter activation and cell morphology over time.
- Kinetic Imaging Cytometry: This technology was employed to assess functional maturity by measuring spontaneous calcium transients in the reprogrammed cells.
- Gene Expression Analysis: End-point RT-qPCR or RNA-seq was performed to confirm the upregulation of a broad panel of cardiomyocyte-associated genes and the downregulation of fibroblast markers [68].
Essential Research Reagents and Solutions
The successful application of Mogrify-predicted factors relies on a suite of key research reagents. The table below details the essential materials used in the featured cardiac reprogramming study and their critical functions.
Table 2: Research Reagent Solutions for Direct Reprogramming Experiments
| Reagent/Solution | Function in the Experimental Protocol |
|---|---|
| Primary Human Cardiac Fibroblasts | Biologically relevant starting cell type for modeling cardiac repair; sourced from patient tissues [68]. |
| Doxycycline-Inducible Lentiviruses | Enables stable, controllable, and high-efficiency delivery of predicted transcription factors (e.g., MYOCD, SMAD6, TBX20) [68]. |
| Dual Fluorescent Reporter (TNNT2-mScarlet, MYH6-mNeonGreen) | Allows for high-throughput, kinetic tracking of reprogramming efficiency without cell fixation [68]. |
| Growth Factor-Reduced Matrigel | Provides a defined, biocompatible substrate for culturing primary fibroblasts and supporting reprogrammed cell structures [68]. |
| FGF2 (Growth Factor) | Promotes cell survival and maturation, contributing to the functional development of reprogrammed cardiomyocytes [68]. |
| XAV939 (Small Molecule Inhibitor) | Enhances reprogramming efficiency and functional maturation by inhibiting Wnt/β-catenin signaling [68]. |
| High-Content Kinetic Imaging Cytometer | Key instrument for automated, quantitative assessment of reporter expression, cell morphology, and functional calcium cycling [68]. |
Mogrify in a Broader Transdifferentiation Context
The utility of Mogrify and the principles of transdifferentiation extend far beyond cardiac repair, impacting diverse fields of biological research and therapeutic development.
Cancer Biology: Transdifferentiation is recognized as a key mechanism of cellular plasticity that drives drug resistance in certain cancers. For instance, in castration-resistant prostate cancer, adenocarcinoma cells can transdifferentiate into neuroendocrine cells (CRPC-NE) in a process facilitated by the inactivation of tumor suppressors like TP53 and PTEN [69]. Similarly, in pancreatic cancer, the transdifferentiation of acinar cells into ductal-like cells (acinar-to-ductal metaplasia, ADM) is a critical early step in tumor development. Research shows that the kinase TAK1 acts as a decision point, suppressing programmed cell death to empower the survival and proliferation of these transdifferentiated cells [70]. Understanding these natural, pathological reprogramming events provides insights into the regulatory networks that tools like Mogrify are designed to manipulate.
Bioscience and Cultured Meat: Transdifferentiation strategies are being harnessed for sustainable production of animal products. Chicken fibroblasts have been successfully transdifferentiated into muscle cells to produce cultured meat. By forcing the expression of the key myogenic transcription factor MyoD, researchers can convert fibroblasts into multinucleated myotubes that express mature muscle proteins. This process can be further manipulated in 3D hydrogel scaffolds to create structured meat products and even induce intramuscular fat deposition, tailoring the nutritional and sensory properties of the final product [71].
The following diagram illustrates the common logic of a transdifferentiation experiment, from computational prediction to in vitro validation, showcasing its wide applicability.
Diagram 2: Generalized workflow for a transdifferentiation experiment, from prediction to validation.
Mogrify represents a transformative tool in the field of cellular reprogramming, moving the discipline from a state of empirical guesswork to one of rational, algorithm-guided design. Its successful application in predicting the MST combination for cardiac reprogramming demonstrates its power to overcome longstanding biological challenges, such as inter-species inefficiency. As a predictive framework, it is poised to accelerate the discovery of reprogramming cocktails for a wider array of clinically relevant cell types, advancing strategies for tissue repair and disease modeling.
Future developments will likely focus on refining Mogrify's predictions by incorporating more complex layers of regulatory information, such as epigenetic marks and non-coding RNAs. Furthermore, the integration of high-throughput functional validation platforms, as demonstrated in the cardiac case study, will be essential for rapidly testing and iterating upon computational predictions. As our understanding of pathological transdifferentiation in cancer and other diseases deepens, Mogrify may also be inverted to identify factors that can reverse undesirable cell fates, opening new avenues for drug discovery. Ultimately, the synergy between computational prediction and experimental validation is paving the way for a new era in regenerative medicine, where customizing cell identity for therapeutic purposes becomes a routine and precise practice.
Cell fate transitions are fundamental to developmental biology and regenerative medicine, yet efficient transdifferentiation is often hindered by robust epigenetic barriers. This whitepaper examines the dynamic chromatin modifications that govern cell identity and the experimental approaches to manipulate these landscapes for therapeutic applications in tissue repair. We explore how specific histone modifications, including H3K4me3, H3K27me3, and H3K27ac, create molecular roadblocks that maintain cellular differentiation states while also serving as potential targets for reprogramming. Through comprehensive analysis of quantitative datasets and experimental methodologies, we provide a technical framework for researchers aiming to overcome epigenetic constraints to facilitate directed cell fate switching. The integration of mechanical cues with epigenetic modulation represents a promising frontier in enhancing transdifferentiation efficiency for regenerative applications.
Epigenetic modifications serve as fundamental regulators of cellular identity by establishing and maintaining gene expression patterns without altering the underlying DNA sequence. These heritable changes encompass DNA methylation, histone modifications, chromatin remodeling, and non-coding RNA regulation, which collectively determine cellular phenotype by controlling access to genetic information [72] [73]. In the context of tissue repair and regeneration, understanding how to manipulate these epigenetic barriers is crucial for developing effective transdifferentiation strategies that can convert readily available cell types into therapeutically valuable ones.
The concept of epigenetic plasticity is particularly relevant during early embryonic development, where rapid and dramatic cell fate transitions occur. Studies of mouse preimplantation development have revealed that the epigenetic landscape undergoes profound reprogramming upon fertilization to establish totipotency, with extensive remodeling of epigenetic marks continuing throughout subsequent cell fate commitments [72]. This developmental window offers valuable insights into the natural mechanisms of epigenetic reprogramming that might be harnessed for therapeutic purposes. Similarly, somatic cell nuclear transfer (SCNT) and induced pluripotent stem cell (iPSC) generation demonstrate that epigenetic constraints can be overcome to revert differentiated cells to more primitive states, though efficiency remains a significant challenge.
Within the framework of tissue repair research, the targeted modification of epigenetic barriers represents a promising approach for direct lineage conversion, bypassing the pluripotent intermediate stage and its associated risks. The potential applications span various degenerative conditions, including neurodegenerative diseases, cardiac damage, and musculoskeletal disorders, where restoring functional cell populations could reverse pathological processes. This technical guide examines the specific chromatin modifications that constitute barriers to cell fate switching and details experimental methodologies for their manipulation to facilitate transdifferentiation in regenerative contexts.
Chromatin Landscapes as Gatekeepers of Cell Fate
Histone Modification Dynamics
Histone modifications serve as critical components of the epigenetic code that either facilitate or restrict cellular plasticity. Among these modifications, the balance between activating and repressive marks at gene regulatory elements creates a molecular environment that either permits or inhibits transcription factor binding and gene expression. Key histone modifications include:
H3K4me3: An activating mark associated with transcription start sites that exhibits both canonical sharp domains and noncanonical broad domains during development [72]. The transition from noncanonical to canonical H3K4me3 at the two-cell stage in mouse embryos requires zygotic genome activation and is essential for proper development [72]. Precise regulation of H3K4me3 breadth is critical, as artificial widening through knockdown of demethylases like Kdm5b disrupts lineage differentiation at the blastocyst stage [72].
H3K27me3: A repressive mark deposited by Polycomb Repressive Complex 2 (PRC2) that silences developmental genes. During early embryonic development, global H3K27me3 levels decrease significantly, with extensive loss observed at Hox and other developmental genes upon fertilization [72]. In neural organoid systems, H3K27me3-mediated repression of region-specific transcription factors outside their expression domains helps maintain fate restriction [74].
H3K27ac: An activating mark associated with active enhancers and promoters that defines cell-type-specific regulatory elements. During neural differentiation, H3K27ac dynamics reveal transitions from pluripotency through neuroepithelium to region-specific neuronal fates [74].
Table 1: Key Histone Modifications and Their Roles in Cell Fate Regulation
| Modification | Type | Genomic Location | Function in Fate Transitions | Enzymes |
|---|---|---|---|---|
| H3K4me3 | Activating | Promoters | Estishes transcription-permissive environment; breadth must be regulated | KMT2 family, KDM5 family |
| H3K27me3 | Repressive | Promoters & distal regions | Silences developmental genes; maintains fate restriction | EZH2, KDM6 family |
| H3K27ac | Activating | Enhancers & promoters | Marks active regulatory elements; defines cell identity | p300/CBP |
| H3K9me3 | Repressive | Heterochromatin | Maintains constitutive heterochromatin; barrier to reprogramming | SUV39H, SETDB1 |
Chromatin State Transitions During Development
Single-cell epigenomic analyses of human neural organoids have revealed that repressive and activating epigenetic modifications can precede and predict cell fate decisions at each developmental stage [74]. The switching between these modifications provides a temporal census of gene regulatory elements and transcription factors that guide identity acquisition. For example, removal of H3K27me3 at the neuroectoderm stage disrupts fate restriction, leading to aberrant cell identity acquisition [74].
During the maternal-to-zygotic transition (MZT) in mouse embryos, which is mostly completed by the two-cell stage, the chromatin state is significantly reprogrammed after zygotic genome activation (ZGA) [72]. This reprogramming involves the erasure of broad H3K4me3 domains inherited from oocytes, which is required for ZGA and full developmental potential [72]. The existence of H3K4me3 and H3K27me3 tends to be exclusive in early cleavage stages, though this nonoverlapping distribution weakens at later developmental timepoints [72].
Quantitative Mapping of Epigenetic Transitions
Multi-Omics Approaches to Cell Fate Transitions
Advanced sequencing technologies have enabled comprehensive mapping of epigenetic dynamics during cell fate transitions. Low-input chromatin immunoprecipitation followed by sequencing (ChIP-seq) methods have been particularly valuable for profiling global dynamics of histone modifications in preimplantation embryos [72]. These approaches have revealed that:
- Noncanonical H3K4me3 domains exist as broad regions on promoters and distal loci in full-grown and mature oocytes, which are negatively correlated with DNA methylation [72].
- The global gain of H3K27me3 is relatively mild after fertilization, with the number of H3K27me3-marked promoters significantly decreasing at the two-cell stage compared with MII oocytes [72].
- Extensive loss of promoter H3K27me3 at Hox and other developmental genes occurs upon fertilization, while non-promoter H3K27me3 domains persist in maternal alleles [72].
Single-cell CUT&Tag technologies applied to human brain organoids have enabled the reconstruction of epigenomic trajectories from pluripotency to differentiated neural fates [74]. This approach has captured transitions from pluripotency through neuroepithelium to retinal and brain region specification, providing unprecedented resolution of epigenetic changes during lineage commitment.
Table 2: Quantitative Epigenetic Dynamics During Mouse Preimplantation Development
| Developmental Stage | H3K4me3 State | H3K27me3 State | DNA Methylation | Key Transitions |
|---|---|---|---|---|
| Oocyte (GV) | Broad domains | Moderate levels | High | Metabolism-related proteins enriched |
| Oocyte (MII) | Broad domains | High at specific loci | High | Cell-cycle regulators, epigenetic modifiers enriched |
| Zygote | Broad domains inherited | Paternal erasure | Active demethylation | Ubiquitination-related proteins enriched |
| 2-Cell | Transition to canonical | Global decrease | Low | Zygotic genome activation |
| Morula | Canonical sharp domains | Begin reestablishment | Remethylation begins | Cell polarity establishment |
| Blastocyst | Canonical sharp domains | Patterned repression | Tissue-specific patterns | Lineage specification |
Proteomic and Transcriptomic Correlations
Quantitative mass spectrometry strategies have revealed regulation gaps between transcript expression levels and protein abundance during the maternal-to-zygotic transition [72]. This disconnect highlights the importance of posttranscriptional regulation and the necessity for proteomic profiling to fully understand molecular mechanisms driving developmental events. Protein co-expression modules in early embryos have identified highly correlated core factors including Rrp9, Cript, and Zcchc8, which are proposed to be indispensable during early development [72].
Experimental Methodologies for Epigenetic Manipulation
Chromatin Profiling Techniques
scCUT&Tag for Single-Cell Epigenomic Mapping
Single-cell Cleavage Under Targets and Tagmentation (scCUT&Tag) enables genome-wide profiling of histone modifications in individual cells. The methodology involves:
- Cell Permeabilization: Cells are permeabilized with digitonin to allow antibody entry while maintaining nuclear structure.
- Antibody Binding: Specific primary antibodies against histone modifications (e.g., H3K27me3, H3K27ac, H3K4me3) are incubated with permeabilized cells.
- pA-Tn5 Adapter Binding: Protein A-Tn5 transposase preloaded with sequencing adapters binds to the primary antibody.
- Tagmentation: Magnesium chloride activation induces tagmentation by Tn5, inserting adapters into chromatin regions adjacent to antibody-bound sites.
- Library Preparation and Sequencing: DNA is extracted, amplified, and prepared for high-throughput sequencing.
This approach has been successfully applied to human brain organoids, capturing 33,533 cells for H3K27ac, 34,357 cells for H3K27me3, and 42,053 cells for H3K4me3 [74]. The method yields high-quality data as reflected by the fraction of reads in peaks, nucleosome pattern, and fragment counts (median: H3K4me3, 722; H3K27ac, 641; H3K27me3, 302) [74].
Multi-Omics Integration Approaches
Integration of scCUT&Tag with single-cell RNA sequencing from the same cell suspensions enables direct correlation of epigenetic states with transcriptional outputs. Computational integration involves:
- High-resolution Louvain clustering for each modality separately to enhance robustness through increased fragment counts.
- Comparison of epigenomic clusters with annotated scRNA-seq clusters using minimum-cost, maximum-flow (MCMF) bipartite matching based on correlation for activating marks and anti-correlation for repressive marks.
- Label transfer from RNA to chromatin modalities to annotate cell states in epigenomic datasets.
This integrated approach has revealed that cell state proportions remain similar across modalities, with even rare populations recoverable in histone modification datasets [74].
Diagram 1: scCUT&Tag Workflow - This diagram illustrates the key steps in the scCUT&Tag protocol for single-cell epigenomic profiling.
Epigenetic Perturbation Strategies
Pharmacological Inhibition
Small molecule inhibitors targeting epigenetic modifiers provide reversible manipulation of chromatin states:
- DNA methyltransferase inhibitors (DNMTis): Azacitidine and decitabine promote DNA hypomethylation, potentially reactivating silenced genes.
- Histone deacetylase inhibitors (HDACis): Vorinostat and romidepsin increase histone acetylation, creating a more open chromatin state.
- Histone methyltransferase inhibitors (HMTis): Target specific histone methyltransferases like EZH2 (H3K27me3 writer).
- BET inhibitors: Disrupt bromodomain recognition of acetylated histones, affecting transcription of growth and proliferation genes.
Epidrugs have shown promise in cancer treatment by reversing aberrant epigenetic states, with Azacitidine being the first FDA-approved epigenetic drug in 2004 for myelodysplastic syndrome [75] [73].
Genetic Manipulation
CRISPR-based approaches enable precise targeting of epigenetic modifiers:
- CRISPR-dCas9 fusions with catalytic domains of epigenetic enzymes allow locus-specific epigenetic editing.
- shRNA-mediated knockdown of epigenetic regulators demonstrates the requirement for specific factors in fate transitions (e.g., Kdm5b knockdown widens H3K4me3 domains and blocks differentiation) [72].
- Conditional knockout systems enable stage-specific ablation of epigenetic regulators, such as EED removal at neuroectoderm stage disrupting fate restriction [74].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Epigenetic Reprogramming Research
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Histone Modification Antibodies | Anti-H3K4me3, Anti-H3K27me3, Anti-H3K27ac | Chromatin immunoprecipitation, immunofluorescence, CUT&Tag | Validate specificity; lot-to-lot variability |
| Epigenetic Inhibitors | DNMT inhibitors (Azacitidine), HDAC inhibitors (Vorinostat), EZH2 inhibitors (Tazemetostat) | Pharmacological manipulation of epigenetic states | Off-target effects; concentration optimization |
| CRISPR Epigenetic Editors | dCas9-DNMT3A, dCas9-TET1, dCas9-p300, dCas9-KRAB | Locus-specific epigenetic modification | Efficiency; delivery method; persistence |
| Low-Input Sequencing Kits | SMART-Seq, Nextera XT | Transcriptomic and epigenomic profiling of rare cell populations | Sensitivity; amplification bias |
| Tissue-Mimicking Hydrogels | Collagen-alginate IPN, PEG-based systems | Mechanical reprogramming studies | Stiffness tuning; functionalization options |
| scCUT&Tag Reagents | Hyperactive Tn5, Protein A-Tn5 conjugates, digitonin | Single-cell epigenomic profiling | Permeabilization optimization; antibody validation |
Mechanical Reprogramming as an Epigenetic Modulator
Emerging evidence indicates that biophysical cues from the extracellular environment can influence epigenetic states and cellular identity. Tissue-mimicking hydrogels that combine both viscoelastic and nonlinear elastic components can reprogram cellular behavior without genetic manipulation [30]. These hydrogels, typically composed of collagen-alginate interpenetrated networks, mimic the mechanical properties of native tissues and have been shown to:
- Promote mesenchymal aggregation of fibroblasts, leading to elevated expression of stemness genes and enhanced bidirectional differentiation potentials [30].
- Require cell contraction for aggregate formation, as compromising contractility prevents aggregation and eliminates reprogramming [30].
- Enable adipogenic transdifferentiation of non-small-lung cancer cells, reversing epithelial-to-mesenchymal transition genes and suppressing oncogene expression [30].
The mechanism underlying mechanical reprogramming involves enhanced cell contractility on stiffer tissue-mimicking hydrogels, which promotes cells to crowd together and form aggregates [30]. This process contrasts with behavior on purely elastic substrates, where increased stiffness typically promotes cell spreading and prevents aggregation [30].
Diagram 2: Mechanical Reprogramming Pathway - This diagram illustrates how tissue-mimicking hydrogels promote cell fate reprogramming through mechanical cues.
Therapeutic Applications in Tissue Repair and Regeneration
Epigenetic Approaches to Transdifferentiation
The manipulation of epigenetic barriers holds significant promise for regenerative medicine by enabling direct lineage conversion for tissue repair. Key applications include:
Neuroregeneration: Single-cell epigenomic analyses of neural organoids have identified critical transitions in histone modification states that precede neuronal fate decisions [74]. Targeted manipulation of these epigenetic checkpoints could enhance the generation of specific neuronal subtypes for treating neurodegenerative conditions like Parkinson's and Alzheimer's disease.
Cardiac Repair: Direct reprogramming of cardiac fibroblasts to cardiomyocytes through epigenetic modulation represents a promising approach for restoring function after myocardial infarction. The dynamic changes in H3K27me3 at key developmental regulators appear to be particularly important for this transition.
Cancer Transdifferentiation: Mechanical reprogramming using tissue-mimicking hydrogels has been shown to promote adipogenic transdifferentiation of non-small-cell lung carcinoma cells, suppressing oncogene expression and reversing epithelial-to-mesenchymal transition [30]. This approach, termed transdifferentiation therapy, could potentially convert malignant cells into less harmful or more treatable cell types.
Combination Strategies with Biomaterials
The integration of epigenetic manipulation with advanced biomaterials creates synergistic approaches for enhanced tissue regeneration:
- Hydrogel-mediated delivery of epidrugs enables localized and sustained epigenetic modulation at injury sites, potentially improving efficacy while reducing systemic toxicity.
- Matrix stiffness tuning can prime cells for epigenetic reprogramming by altering nuclear morphology and chromatin organization, potentially lowering barriers to fate switching.
- Spatiotemporally controlled release of epigenetic modifiers from biomaterial scaffolds could guide sequential fate transitions mirroring developmental processes.
The strategic modification of chromatin landscapes represents a powerful approach for overcoming epigenetic barriers to cell fate switching in tissue repair contexts. The dynamic nature of epigenetic modifications, particularly the balance between activating marks like H3K4me3 and H3K27ac and repressive marks like H3K27me3, creates a malleable system that can be therapeutically manipulated. Advances in single-cell epigenomic technologies have provided unprecedented resolution of these transitions during development and reprogramming, offering new insights into the molecular roadblocks that maintain cellular identity.
Future directions in this field will likely focus on the temporal precision of epigenetic manipulations, as the sequence of chromatin modifications appears critical for proper fate transitions. Additionally, the integration of mechanical cues with biochemical and genetic approaches represents a promising frontier for enhancing reprogramming efficiency. The development of more specific epigenetic tools, including next-generation epidrugs with reduced off-target effects and improved delivery systems, will be essential for clinical translation.
As our understanding of epigenetic regulation in cell fate decisions continues to expand, so too will our ability to harness these mechanisms for regenerative purposes. The combination of epigenetic manipulation with emerging technologies in biomaterials, gene editing, and single-cell analysis holds particular promise for developing novel therapeutic strategies that overcome the inherent limitations of current regenerative approaches.
In vivo reprogramming represents a transformative approach in regenerative medicine, enabling direct conversion of cell identities within living organisms to repair damaged tissues. Built upon the foundational discovery of induced pluripotent stem cells (iPSCs), this paradigm leverages transient expression of reprogramming factors—most commonly the Yamanaka factors (OCT4, SOX2, KLF4, and c-MYC, collectively termed OSKM)—to restore regenerative capacity across diverse tissues including heart, brain, liver, and skeletal muscle [76] [77]. Unlike traditional cell transplantation strategies, in vivo reprogramming offers the distinct advantage of generating new cell types from existing cells within the body, eliminating the need for complex laboratory steps and potentially yielding more mature, functional tissues [78].
However, the tremendous therapeutic potential of in vivo reprogramming is counterbalanced by significant safety concerns, with tumorigenic risk standing as the primary barrier to clinical translation. The fundamental challenge lies in the precarious balance between achieving sufficient reprogramming for therapeutic effect and avoiding over-reprogramming that can lead to teratoma formation or oncogenic transformation [78]. When reprogramming factors are delivered in vivo, even minor inconsistencies in factor expression levels, duration, or cellular context can push cells toward a pluripotent state rather than the intended partially reprogrammed or transdifferentiated state, creating populations of cells with uncontrolled proliferative potential [76] [77]. This review examines the current mechanistic understanding of tumorigenic risks in in vivo reprogramming and details the sophisticated strategies being developed to mitigate these dangers within the context of transdifferentiation mechanisms for tissue repair.
Molecular Mechanisms of Tumorigenesis in Reprogramming
Pathways to Pluripotency and Oncogenic Transformation
The tumorigenic risks associated with in vivo reprogramming primarily manifest through two distinct but interrelated mechanisms: teratoma formation from partially reprogrammed pluripotent cells and oncogenic transformation driven by the reprogramming factors themselves, particularly c-MYC [78] [77]. Teratomas, benign tumors containing multiple tissue types, arise when reprogrammed cells escape differentiation protocols and maintain pluripotent characteristics. During the reprogramming process, incomplete epigenetic remodeling can create unstable intermediate states that harbor tumorigenic potential, even without achieving full pluripotency [76].
The molecular pathways governed by the Yamanaka factors create inherent oncogenic risks. OCT4 and SOX2, while essential for establishing pluripotency, can activate downstream targets that promote uncontrolled proliferation when expressed persistently or at supraphysiological levels [35]. c-MYC, a well-established proto-oncogene, amplifies this risk by driving global changes in gene expression that favor cell cycle progression and metabolic reprogramming. The epigenetic instability during reprogramming—characterized by widespread DNA demethylation and histone modification—can inadvertently activate silenced oncogenes or repress tumor suppressor genes [76] [35]. Additionally, the oxidative stress and DNA damage response triggered by the reprogramming process may introduce mutations that further increase transformation risk, particularly in aged tissues with diminished DNA repair capacity [76].
Tissue-Specific Vulnerability Factors
The tumorigenic potential of reprogramming factors varies significantly across tissue contexts, influenced by cellular microenvironment, pre-existing mutations, and tissue-specific susceptibility to transformation. For example, in cardiac reprogramming studies, the use of alternative factor combinations (such as GMT: GATA4, Mef2C, and Tbx5) that bypass the pluripotent state entirely has demonstrated reduced tumorigenic risk compared to OSKM-based approaches [37]. The presence of senescent cells in aged or injured tissues may further complicate risk profiles, as senescent secretomes can create a pro-inflammatory microenvironment that favors malignant progression of partially reprogrammed cells [76].
Table 1: Tumorigenic Risks Associated with Reprogramming Factors
| Reprogramming Factor | Primary Function | Tumorigenic Mechanism | Risk Level |
|---|---|---|---|
| OCT4 (POU5F1) | Establishment of pluripotency | Reactivation of embryonic programs; suppression of differentiation | High |
| SOX2 | Maintenance of stemness | Uncontrolled self-renewal signaling; genomic instability | Medium-High |
| KLF4 | Cell cycle regulation | Context-dependent oncogene/tumor suppressor | Medium |
| c-MYC | Metabolic reprogramming | Global transcriptional amplification; DNA replication stress | Very High |
Strategic Paradigms for Risk Mitigation
Partial Reprogramming Approaches
Partial reprogramming has emerged as a leading strategy to mitigate tumorigenic risk while preserving therapeutic benefits. This approach involves transient, cyclic induction of reprogramming factors, allowing cells to reset aging-related epigenetic markers without fully reverting to a pluripotent state [77] [79]. By carefully controlling the duration and intensity of factor expression, researchers can guide cells to a "younger" epigenetic state that maintains lineage identity and specialized function while reversing age-associated dysfunction [76]. Notably, studies have demonstrated that cyclic OSKM expression can reverse cellular aging hallmarks—including telomere attrition, epigenetic alterations, and mitochondrial dysfunction—without inducing teratoma formation or premature death in animal models [77] [79].
The therapeutic window for partial reprogramming appears remarkably narrow; insufficient exposure yields minimal rejuvenation effect, while excessive exposure drives cells toward pluripotency with associated tumorigenic risk [76]. Successful protocols typically employ short-cycle induction (e.g., 2 days on/5 days off for multiple cycles) that permits gradual epigenetic resetting while allowing cells to maintain differentiation status [77]. The molecular basis for this safety profile lies in the sequential nature of epigenetic remodeling during reprogramming, where aging-related epigenetic marks are reversed early in the process, while lineage-defining epigenetic architecture remains intact through transient factor expression [76].
Direct Lineage Conversion (Transdifferentiation)
Direct lineage conversion, or transdifferentiation, represents the most targeted approach for avoiding tumorigenic risk by completely bypassing the pluripotent intermediate state [35] [37]. This method utilizes tissue-specific transcription factors rather than pluripotency-associated factors to directly convert one somatic cell type into another within the same developmental lineage. For example, cardiac fibroblasts can be directly reprogrammed into induced cardiomyocyte-like cells (iCMs) using combinations of cardiac transcription factors such as GATA4, Mef2C, Tbx5 (GMT), or with additional factors like Hand2 (GHMT) [37].
The fundamental safety advantage of transdifferentiation lies in its avoidance of the epigenetic instability and proliferation potential associated with pluripotent states [35]. Since cells never dedifferentiate to a pluripotent stage, the risk of teratoma formation is virtually eliminated. Additionally, the resulting iCMs exhibit molecular and functional characteristics that more closely resemble adult cardiomyocytes rather than the neonatal-like cardiomyocytes typically derived from iPSC protocols, potentially reducing arrhythmogenic risk [37]. However, transdifferentiation approaches face their own challenges, including typically low conversion efficiencies (<10%) and incomplete maturation of converted cells, which may limit therapeutic efficacy despite improved safety profiles [37].
Enabling Technologies for Safe Reprogramming
Advanced Delivery Systems
The method of delivering reprogramming factors profoundly influences both efficacy and safety outcomes. Non-viral delivery systems have gained prominence for their favorable safety profiles, including reduced immunogenicity, minimal risk of insertional mutagenesis, and capacity for transient expression [35]. Among these, Tissue Nanotransfection (TNT) has emerged as a particularly promising platform for safe in vivo reprogramming. TNT utilizes a nanoelectroporation-based approach to deliver genetic cargo (plasmid DNA, mRNA, or CRISPR/Cas9 components) directly to target tissues through hollow microneedle arrays [35]. This technology enables highly localized reprogramming with minimal off-target effects, as the electric field is concentrated at needle tips, creating transient pores in cell membranes for precise genetic material transfer without significant tissue damage [35].
The transient nature of non-viral systems is particularly advantageous for safety, as it automatically limits the duration of reprogramming factor expression. Plasmid DNA and mRNA-based approaches provide especially short-term expression windows that naturally prevent sustained factor expression associated with tumorigenic progression [35]. For applications requiring more precise transcriptional control, CRISPR/Cas9-based synthetic transcription factors offer programmable, multiplexable regulation of endogenous genes without permanent genomic alteration [35]. These systems can be further refined with safety switches such as chemically inducible systems or miRNA-based regulatory circuits that trigger factor degradation in response to specific cellular signals [35].
Table 2: Comparison of Delivery Systems for In Vivo Reprogramming
| Delivery System | Therapeutic Cargo | Integration Risk | Expression Duration | Tumorigenic Risk Profile |
|---|---|---|---|---|
| Retroviral Vectors | DNA | High | Long-lasting | High (insertional mutagenesis) |
| Lentiviral Vectors | DNA | Medium | Long-lasting | Medium-High |
| Adenoviral Vectors | DNA | None | Medium (weeks) | Medium (immune response) |
| Plasmid DNA | DNA | Very Low | Short (days) | Low |
| mRNA | RNA | None | Very Short (hours-days) | Very Low |
| Tissue Nanotransfection | DNA/RNA | None | Configurable | Low (localized delivery) |
Microenvironmental Control Strategies
Beyond genetic approaches, biophysical and biochemical cues from the cellular microenvironment provide powerful levers for enhancing reprogramming safety. The extracellular matrix (ECM) composition and mechanical properties significantly influence cell fate decisions during reprogramming, with specific tissue-mimicking substrates demonstrating capacity to guide cells toward desired lineages while suppressing aberrant differentiation [30]. Engineered hydrogels that replicate the viscoelastic and nonlinear elastic properties of native tissues have shown remarkable ability to promote formation of mesenchymal aggregates with enhanced differentiation potential while maintaining lineage appropriateness [30].
These tissue-mimicking hydrogels, typically composed of interpenetrating networks of collagen (providing nonlinear elasticity) and alginate (providing viscoelasticity), create a mechanical microenvironment that supports controlled reprogramming [30]. Fibroblasts cultured on such substrates spontaneously form aggregates that upregulate stemness genes but demonstrate restricted, appropriate differentiation potential—suggesting the mechanical context helps maintain boundary conditions that limit tumorigenic progression [30]. This mechanical reprogramming approach has even been applied to non-small-cell lung cancer cells, promoting adipogenic transdifferentiation that suppresses oncogenic gene expression [30]. The mechanism appears to involve enhanced cell contractility and matrix remodeling that initiates signaling cascades favoring lineage-stabilized outcomes over pluripotent dedifferentiation [30].
Research Reagent Solutions for Safety-Optimized Reprogramming
Table 3: Essential Research Reagents for Safe In Vivo Reprogramming Studies
| Reagent Category | Specific Examples | Safety Function | Implementation Considerations |
|---|---|---|---|
| Factor Delivery | Plasmid DNA (OSKM, GMT) | Transient expression; no genomic integration | Optimal purity and supercoiling enhance efficiency [35] |
| Modified mRNA (OSKM variants) | Ultra-short expression; no nuclear entry | Chemical modifications reduce immunogenicity [35] | |
| CRISPR/dCas9 systems | Epigenetic editing without DNA cleavage | Enables targeted transcriptional control [35] | |
| Delivery Devices | Tissue Nanotransfection (TNT) chips | Localized delivery; minimal off-target effects | Silicon hollow-needle design critical for efficiency [35] |
| Electroporation systems | Membrane disruption-based delivery | Pulse parameters (voltage, duration) optimize viability [35] | |
| Safety Switches | Doxycycline-inducible systems | Temporal control of factor expression | Leakiness must be minimized in system design |
| miRNA-based regulatory circuits | Cell-type specific factor restriction | Endogenous miRNA profiles determine specificity | |
| Microenvironment | Alginate-collagen IPN hydrogels | Mechanical guidance of cell fate | Stiffness and viscoelasticity must be tissue-matched [30] |
| RGD-functionalized substrates | Enhanced cell adhesion and survival | Concentration optimization prevents excessive spreading [30] |
The path toward clinical implementation of in vivo reprogramming requires meticulous attention to tumorigenic risk mitigation at every stage of therapeutic development. The integrated safety strategy combining partial reprogramming protocols, direct lineage conversion approaches, advanced delivery technologies, and microenvironmental control provides a multi-layered defense against tumorigenic outcomes. As the field progresses, the development of more sophisticated safety switches—including synthetic gene circuits capable of autonomously detecting and eliminating aberrant cells—will further enhance the risk-benefit profile of these transformative therapies.
Current progress toward clinical application is encouraging, with companies like Life Biosciences developing partial epigenetic reprogramming technologies slated for clinical trials in 2026 for liver disease and optic neuropathies [80]. These pioneering efforts will establish critical safety benchmarks for the field. By maintaining rigorous focus on tumorigenic risk mitigation while leveraging the innate regenerative potential of in vivo reprogramming, the vision of safe, effective tissue regeneration and rejuvenation therapies moves steadily toward clinical reality.
Within the paradigm of tissue repair research, transdifferentiation—the direct conversion of one somatic cell type into another—has emerged as a promising strategy for regenerative medicine. [81] The success of this cell fate conversion is not governed solely by intracellular biochemical factors but is profoundly regulated by the extracellular niche. This niche presents a complex milieu of environmental cues, with matrix mechanics and oxygen tension being two dominant, yet often overlooked, physical master regulators. The field of mechanobiology reveals that mechanical forces shape cellular behavior, tissue architecture, and disease progression. [82] Similarly, hypoxia can initiate reprogramming cascades. The convergence of these physical signals within the niche creates a permissive microenvironment that can either facilitate or hinder transdifferentiation. This whitepaper provides an in-depth technical guide on optimizing these parameters to enhance the efficiency and fidelity of direct lineage conversion for therapeutic applications, framing the discussion within the specific context of developing robust protocols for tissue repair.
The Mechanical Landscape of the Niche
The extracellular matrix (ECM) is not a static scaffold but a dynamic, information-rich structure that provides essential mechanical cues to resident cells.
Key Mechanical Properties
Stiffness (Elastic Modulus): Stiffness, often expressed as Young's modulus (kPa), is a central parameter in mechanobiology. It refers to a material's resistance to deformation. Different tissues exhibit characteristic stiffness ranges, and cells are exquisitely tuned to sense these differences. For instance, brain tissue is soft (~0.1-1 kPa), muscle is intermediate (~8-12 kPa), and pre-calcified bone is stiff (>34 kPa). [82] Pathological states, such as fibrosis, are often marked by significant tissue stiffening. [82] The profound influence of stiffness on cell fate was demonstrated in a landmark study where mesenchymal stem cells (MSCs) differentiated into neurocytes on soft matrices (0.1–1 kPa), into skeletal muscle cells on intermediate matrices (8–17 kPa), and into osteoblasts on stiff matrices (>34 kPa). [82]
Viscoelasticity: Unlike purely elastic materials, native tissues are viscoelastic, meaning their mechanical response depends on both the degree and rate of deformation. This property is characterized by stress relaxation—the gradual decrease in stress under a constant strain. [82] In soft tissues, the loss modulus (viscous component) is typically 10-20% of the storage modulus (elastic component). [82] This viscoelasticity enables energy dissipation and is critical for processes like cell migration and differentiation. Engineered materials with tunable stress relaxation have been shown to enhance the development of functional blood vessels and promote healing after heart injury. [82]
Nonlinear Elasticity: Many biological tissues, particularly those with collagen networks, exhibit nonlinear stress-strain relationships, becoming stiffer as they are stretched. [30] This J-shaped curve response is a key characteristic of the native cellular environment.
Table 1: Mechanical Properties of Native Tissues and Synthetic Substrates
| Tissue/Substrate Type | Approximate Stiffness (Elastic Modulus) | Key Mechanical Characteristics | Cell Fate Influence | |||
|---|---|---|---|---|---|---|
| Brain Tissue | 0.1 - 1 kPa | [82] | Soft, viscoelastic | [82] | Promotes neuronal differentiation | [82] |
| Muscle Tissue | ~12 kPa | [82] | Intermediate, viscoelastic | [82] | Promotes myogenic differentiation | [82] |
| Fibrotic Liver | Up to ~20 kPa | [82] | Stiff, altered viscoelasticity | [82] | Drives fibroblast activation | |
| Tendon/Cartilage | MPa range | [82] | Very stiff, viscoelastic | [82] | Promotes chondrogenic/osteogenic differentiation | |
| Tissue Culture Plastic | GPa range | [82] | Linear elastic, non-physiological | [82] | Causes aberrant cell behavior |
Molecular Mechanisms of Mechanosensing
Cells perceive mechanical cues through a process known as mechanotransduction. Transmembrane integrins bind to the ECM and form focal adhesions, which are complex multi-protein structures that link the external matrix to the internal actin cytoskeleton. [82] A key molecular mechanism involves the protein talin, which contains a force-sensitive switch within its R1R2 interface. When stretched by cellular forces, talin undergoes a conformational change that enables it to interact with proteins like ARPC5L, part of the machinery that builds actin fibers. [82] This process directly links matrix mechanics to cytoskeletal organization and downstream signaling, ultimately influencing nuclear architecture and gene expression. [82] The "motor-clutch" model describes the dynamic interactions between actomyosin contractility (motor) and adhesion complexes (clutch) that allow cells to probe and respond to their mechanical environment. [82]
Engineering the Mechanical Niche for Reprogramming
Recent advances in biomaterials have enabled the creation of sophisticated synthetic niches that mimic the mechanical complexity of native tissues.
Tissue-Mimicking Hydrogels
Standard polyacrylamide hydrogels, while tunable in stiffness, behave as linear elastic materials and fail to capture the viscoelastic and nonlinear nature of native ECM. [82] To address this, interpenetrating network (IPN) hydrogels have been developed. One prominent example combines alginate (providing tunable viscoelasticity and stress relaxation) and collagen (providing biological cues and nonlinear elasticity). [30]
- Protocol: Fabrication of Alginate-Collagen IPN Hydrogels for Mechanical Reprogramming [30]
- Preparation: Combine 1.5 mg/ml collagen and 10 mg/ml alginate in a buffer solution.
- Cross-linking: To vary the initial storage modulus ( mimicking tissue age or state), add calcium chloride at different concentrations (e.g., 5-15 mM) to cross-link the alginate polymer chains. Higher calcium concentrations yield a higher initial storage modulus.
- Gelation: Incubate the mixture at 37°C for 30 minutes to allow for collagen fibrillogenesis and the formation of a stable interpenetrating network.
- Cell Seeding: Seed cells, such as fibroblasts (e.g., 3T3-L1), on the surface of the hydrogel.
- Validation: Confirm mechanical properties via rheological analysis, measuring storage modulus (G') and loss modulus (G") across a frequency range.
When fibroblasts are cultured on these tissue-mimicking IPN hydrogels, a unique phenomenon occurs: after initial spreading, the cells migrate toward each other and form 3D mesenchymal aggregates. [30] This behavior is not observed on collagen or alginate-alone substrates and is promoted by a higher initial hydrogel stiffness. [30] These aggregates show elevated expression of stemness genes and enhanced bidirectional (adipto- and osteo-) differentiation potential, a process termed mechanical reprogramming. [30] The formation of these aggregates is dependent on enhanced cell contraction and the reorganization of the collagen network within the IPN. [30]
Diagram 1: Mechanical reprogramming workflow on IPN hydrogels.
Application in Cancer Transdifferentiation
The principles of mechanical reprogramming extend beyond regenerative medicine. Non-small-cell lung cancer cells cultured on the tissue-mimicking IPN hydrogels undergo a mesenchymal-to-epithelial transition (MET)-like process. [30] This makes them more amenable to transdifferentiation into an adipogenic (fat-like) phenotype. Inducing adipogenesis in these cancer cells compromises the expression of oncogenes and pro-oncogenes, suggesting a potential strategy for cancer transdifferentiation therapy. [30]
Integrating Hypoxia into the Reprogramming Niche
While the search results provided a limited direct discussion of hypoxia, its role is critical in the context of a broader thesis on transdifferentiation for tissue repair. Hypoxia (low oxygen tension) is a fundamental characteristic of many stem cell niches and sites of tissue injury. It activates master transcriptional regulators like Hypoxia-Inducible Factors (HIFs), which orchestrate a metabolic shift from oxidative phosphorylation to glycolysis and modulate the expression of hundreds of genes involved in cell survival, proliferation, and differentiation. In reprogramming, hypoxia has been shown to enhance the efficiency of generating induced pluripotent stem cells (iPSCs) and can promote specific lineage conversions. The interaction between hypoxic signaling and mechanotransduction pathways is an area of active investigation, as cells likely integrate these cues to make fate decisions in a three-dimensional, physiologically relevant context.
Experimental Protocols for Niche Analysis
Protocol: Assessing Transdifferentiation in a Defined Mechanical Niche
This protocol outlines the steps to evaluate the effect of matrix mechanics on the transdifferentiation of fibroblasts into a target lineage.
- Substrate Fabrication: Prepare a set of hydrogel substrates with varying mechanical properties. For example, create alginate-collagen IPNs with 5mM, 10mM, and 15mM Ca²⺠to yield a range of stiffnesses. [30] Include control substrates (tissue culture plastic, pure collagen).
- Mechanical Characterization: Use a rheometer to quantify the storage (G') and loss (G") moduli of each hydrogel formulation. Perform stress relaxation tests (applying a constant strain and measuring stress over time) to characterize viscoelasticity. [82]
- Cell Seeding and Culture: Seed primary fibroblasts (e.g., dermal or cardiac fibroblasts) onto the substrates at a defined density. Culture in transdifferentiation media, which may include specific small molecule cocktails or growth factors to induce the target lineage. [81]
- Phenotypic and Functional Assays:
- Immunocytochemistry: Stain for cytoskeletal markers (F-actin), focal adhesion proteins (paxillin, vinculin), and lineage-specific markers (e.g., α-SMA for myofibroblasts, Tuj1 for neurons). [30]
- Gene Expression Analysis: Perform qRT-PCR to measure the mRNA levels of pluripotency genes (e.g., Oct4, Sox2), ECM genes, and lineage-specific genes.
- Functional Assays: Conduct assays relevant to the target cell type, such as calcium imaging for cardiomyocytes or glucose-stimulated insulin secretion for beta cells.
- Inhibition Studies: To validate mechanistic pathways, use specific inhibitors. For example, to probe the role of contractility, use the ROCK inhibitor Y-27632. [30]
Table 2: The Scientist's Toolkit: Key Reagents for Niche Optimization
| Reagent / Tool Category | Specific Example | Function in Niche Optimization | |
|---|---|---|---|
| Tunable Hydrogels | Alginate-Collagen IPN | [30] | Mimics native tissue viscoelasticity and nonlinearity for mechanical reprogramming. |
| Small Molecules | Hecogenin, Laurolitsine | [83] | Inhibits CF transdifferentiation via ADRB2/JNK/c-Jun signaling. |
| ROCK Inhibitor (Y-27632) | [30] | Compromises cell contractility to test mechanism of mechanotransduction. | |
| Gene Delivery Tools | Tissue Nanotransfection (TNT) | [35] | Enables non-viral, in vivo delivery of reprogramming factors (plasmid DNA, mRNA, CRISPR/Cas9). |
| Signaling Pathway Modulators | Propranolol hydrochloride (β-blocker) | [83] | Antagonist of ADRB2; used to validate role of adrenergic signaling in transdifferentiation. |
| Analysis Kits | Hydroxyproline Assay Kit | [83] | Quantifies collagen content as a measure of ECM production and fibrosis. |
The optimization of the cellular niche by integrating matrix mechanics and hypoxia is a transformative approach in the field of transdifferentiation for tissue repair. The development of advanced biomaterials that faithfully recapitulate the viscoelastic and nonlinear properties of native tissues, such as IPN hydrogels, demonstrates that physical cues alone can drive significant reprogramming and alter cellular fate. [82] [30] These strategies, combined with a deeper understanding of hypoxic conditioning and enabled by novel tools like tissue nanotransfection, [35] pave the way for more robust and clinically viable cell therapies. Future research must focus on the intricate crosstalk between hypoxic and mechanotransductive signaling pathways to achieve precise spatiotemporal control over cell fate, ultimately enabling the in situ regeneration of functional tissues for treating a wide array of degenerative diseases and injuries.
Benchmarking Success: Functional Assays and Comparative Analysis with Stem Cell Technologies
Within regenerative medicine and tissue repair research, transdifferentiation—the direct conversion of one differentiated somatic cell type into another—presents a promising strategy for generating patient-specific cells for therapy and disease modeling [11]. However, defining a "successful" conversion requires a multi-faceted analytical approach that moves beyond simple marker expression. For transdifferentiation to be considered truly successful for therapeutic applications, such as repairing a damaged heart, treating neurodegenerative diseases, or restoring pancreatic function, the newly converted cells must demonstrate three key characteristics: (1) correct lineage-specific identity, (2) appropriate physiological function, and (3) long-term stability of their new cellular state [84] [85]. This guide details the critical markers, functional assays, and stability metrics that researchers and drug development professionals must employ to rigorously validate transdifferentiation events, with a particular focus on the context of tissue repair.
A major challenge in the field is that many reprogrammed cells exhibit only partial reprogramming; they may display some correct markers but fail to establish the complete epigenetic blueprint required to maintain their new identity and function over time [85] [86]. Therefore, a comprehensive validation strategy is not merely a technical formality but a fundamental necessity to ensure the safety and efficacy of any transdifferentiation-based therapy.
Confirming Lineage-Specific Differentiation and Identity
The initial step in validating transdifferentiation is to confirm that the starting cell has shed its original identity and has adopted the morphological and molecular characteristics of the target cell type. This requires a multi-pronged approach, as reliance on a single method can lead to false positives or an incomplete understanding of the conversion [84].
Cell Morphology and Lineage-Specific Markers
The converted cells should be examined for distinct morphological changes that are characteristic of the target lineage. For instance, fully mature cardiomyocytes are elongated and rod-shaped with organized sarcomeres, while neurons extend dendrites and axons, and pancreatic β-cells display eccentric nuclei with cytoplasmic granules [84]. While necessary, morphological assessment is insufficient on its own and must be supplemented with analysis of lineage-specific markers.
The tables below summarize key markers used to identify successfully converted cells in the heart, nervous system, and pancreas, which are common targets in tissue repair research.
Table 1: Markers for Cardiac and Neural Lineage Confirmation
| Cardiac Markers | Significance | Neural Markers | Significance |
|---|---|---|---|
| Nkx2.5 | Transcription factor expressed by embroid bodies [84] | CD133 | Cell-surface protein identifying neural stem cells [84] |
| Sarcomeric proteins (e.g., Troponin T) | Protein components of the sarcomere indicating differentiated cardiomyocytes [84] | Glial Fibrillary Acidic Protein (GFAP) | Protein specifically produced by astrocytes [84] |
| Connexin 43 | Gap junction protein expressed by cardiospheres [84] | Microtubule-associated protein-2 (MAP-2) | Dendrite-specific protein found in neuronal branching [84] |
| Atrial Natriuretic Factor (ANF) | A protein hormone expressed by cardiac embroid bodies [84] | Synaptophysin | Neuronal protein located in synapses [84] |
Table 2: Markers for Pancreatic Lineage Confirmation
| Pancreatic Markers | Significance |
|---|---|
| Insulin | Expressed by beta-islet cells; key for diabetes therapy [84] [8] |
| Glucagon | Expressed by alpha-islet cells [84] |
| Pdx1 | Key transcription factor expressed by beta-islet cells [84] [8] |
| MafA | Transcription factor critical for maintaining mature beta-cell identity [8] |
| Nkx6.1 | Transcription factor crucial for beta-cell function and identity stabilization [8] |
These markers are typically detected using techniques such as immunofluorescence, flow cytometry, and Fluorescent Activated Cell Sorting (FACS). A critical consideration is that stem cells may sometimes fuse with host endogenous cells, creating the false appearance of differentiation; therefore, marker analysis should be complemented with other techniques [84].
Gene Expression Analysis
During successful transdifferentiation, the cell's transcriptome is radically reconfigured. There is a downregulation of genes specific to the original cell type and the pluripotency network (e.g., Oct4, Sox2 in intermediate pluripotent stages), coupled with an upregulation of genes specific to the new lineage [84]. For example, the conversion of fibroblasts to cardiomyocytes involves the sequential upregulation of mesodermal regulators (e.g., Twist1, Tbx5), followed by cardiogenic regulators (e.g., GATA4, MEF2C), and finally, mature cardiac structural genes (e.g., cardiac myosins) [84]. Techniques like RNA-Seq and qPCR are essential for quantifying these genome-wide expression changes and confirming that the cells have adopted the correct transcriptional profile [85].
Assessing Functional Capacity
The presence of markers and correct morphology does not guarantee that a cell can perform its intended physiological role. Functional validation is the ultimate test of successful transdifferentiation. The required assays are highly specific to the cell type being generated.
Cell Type-Specific Functional Assays
Table 3: Key Functional Assays for Validated Transdifferentiation
| Target Cell Type | Functional Assay | Protocol Details & Key Metrics |
|---|---|---|
| Cardiomyocytes | Electrophysiology | Using patch-clamp techniques to measure action potentials and the presence of specific ion currents (e.g., L-type calcium channel activity) [84]. |
| Neurons | Electrophysiology & Synaptic Activity | Using patch-clamp to demonstrate the ability to fire action potentials and form functional synapses, evidenced by postsynaptic currents [11]. Calcium imaging can also be used to visualize activity. |
| Pancreatic β-cells | Glucose-Stimulated Insulin Secretion (GSIS) | Exposing cells to low (e.g., 2mM) and high (e.g., 20mM) glucose concentrations and measuring insulin output via ELISA. Functional β-cells will secrete insulin in response to high glucose [84] [8]. |
| Smooth Muscle Cells | Calcium Signaling & Traction Force Microscopy | Measuring intracellular calcium flux in response to agonists like carbachol or potassium chloride. Traction force microscopy assesses the cell's contractile strength [87]. |
| Midbrain Dopaminergic Neurons | Dopamine Release Assay | Using HPLC or ELISA to detect the release of dopamine into the culture medium upon appropriate stimulation [11]. |
For tissue repair, in vivo functional assessment is critical. This involves transplanting the cells into relevant animal models of disease or injury and monitoring for functional recovery, such as improved cardiac function after myocardial infarction, restored glycemic control in diabetic models, or engraftment and electrophysiological integration in the nervous system [84] [11].
Evaluating Long-Term Stability
A defining challenge in transdifferentiation is that many induced cells are unstable and revert to their original identity or acquire an aberrant phenotype after the inducing stimuli are removed [85] [86]. Therefore, assessing stability is a non-negotiable component of defining successful conversion.
The Epigenetic Barrier to Stability
Long-term cellular identity is maintained by epigenetic mechanisms, with DNA methylation being a major determinant. During normal development, cell fate decisions are accompanied by waves of DNA methylation reprogramming that lock in cell identity by methylating regulatory regions of genes not needed for that lineage, while demethylating enhancers and promoters of lineage-specific genes [85].
A pivotal finding is that transdifferentiated cells often fail to complete this essential epigenetic reprogramming. Despite changes in gene expression, these cells frequently retain the DNA methylation signature (methylome) of their cell of origin and fail to establish the correct methylation pattern of the target cell type [85]. For instance:
- Fibroblasts transdifferentiated into myoblasts using MyoD upregulate muscle genes but show no demethylation of key muscle-specific enhancer regions [85].
- Fibroblasts converted into neurons retain a methylome that closely resembles fibroblasts, even after extended culture [85].
- In vivo transdifferentiation of hepatocytes into biliary epithelial cells (BECs) during liver injury shows that, despite transcriptional and chromatin changes, the hepatocyte-specific regulatory loci remain methylated, and BEC-specific regions fail to become demethylated [85].
This inability to reconfigure the epigenome is a primary reason for the partial reprogramming and instability observed in many transdifferentiation protocols.
Stability Metrics and Assays
To evaluate stability, researchers should employ the following:
- Long-term Culture & Withdrawal Studies: Culture the induced cells for extended periods (e.g., 2-3 months) after removing the initial reprogramming factors (e.g., doxycycline in inducible systems). Monitor for the loss of target cell markers and the re-emergence of original cell markers [85] [11].
- In Vivo Engraftment and Function: Transplant cells into immunodeficient or injury-model animals and assess their survival, maintained identity, and function over a prolonged duration (e.g., several months) [84] [11].
- Epigenetic Analysis: Use genome-wide epigenetic profiling techniques to confirm the establishment of the correct cell identity.
- Reduced Representation Bisulfite Sequencing (RRBS) or Whole Genome Bisulfite Sequencing (WGBS) to analyze DNA methylation patterns, specifically focusing on developmentally mandated regulatory regions like enhancers [85].
- ATAC-Seq to assess chromatin accessibility and confirm that the open chromatin regions match those of native target cells [85].
The Scientist's Toolkit: Essential Reagents and Experimental Workflows
Below is a table of key research reagent solutions essential for conducting transdifferentiation and validation experiments.
Table 4: Research Reagent Solutions for Transdifferentiation Studies
| Reagent / Tool | Function in Transdifferentiation Research |
|---|---|
| Lentivirus with Inducible Cassette | Allows for controlled, inducible expression of master regulator transcription factors (e.g., MYOCD for smooth muscle, BAM factors for neurons) [87] [11]. |
| MyoD, Ascl1, Brn2, Myt1l (BAM), NeuroD1 | Key transcription factors used to directly reprogram fibroblasts into neurons (iNs) [11]. |
| Pdx1, MafA, Nkx6.1 | Key transcription factors for generating and stabilizing pancreatic β-cell identity [8]. |
| Doxycycline (DOX) | Used in inducible expression systems to "turn on" the transgene of interest, enabling temporal control of the reprogramming process [87]. |
| RRBS or WGBS Kits | Commercial kits for performing genome-wide DNA methylation analysis to assess epigenetic reprogramming and stability [85]. |
| Cell Type-Specific Antibodies | For immunofluorescence and flow cytometry to detect lineage-specific markers (e.g., Insulin, Glucagon, MAP2, Troponin T, α-SMA) [84] [87]. |
| Patch-Clamp Electrophysiology Rig | Setup for performing functional validation of electrically active cells like neurons and cardiomyocytes [84] [11]. |
The following diagram illustrates a core concept and major challenge in the field: the incomplete establishment of epigenetic identity during transdifferentiation.
Diagram 1: The Epigenetic Challenge in Transdifferentiation. Successful conversion requires erasing the original cell's DNA methylation pattern (methylome) and establishing the target cell's methylome. A common failure is the retention of the original methylome, leading to a partially reprogrammed, unstable cell.
The multi-stage workflow for rigorously validating a transdifferentiation event is summarized below.
Diagram 2: A Workflow for Validating Successful Transdifferentiation. A comprehensive approach requires sequential confirmation of lineage identity, physiological function, and long-term stability through integrated in vitro and in vivo assays.
Cellular reprogramming represents a frontier in regenerative medicine, enabling the conversion of a specific lineage of somatic cells into another cell with a different identity. Within this field, two predominant strategies have emerged: Induced Pluripotent Stem Cell (iPSC) technology and Transdifferentiation (also known as direct reprogramming). The fundamental distinction lies in their intermediate states; iPSC technology involves reprogramming somatic cells back into a pluripotent stem cell state, which can then be differentiated into any desired cell type. In contrast, transdifferentiation achieves lineage conversion without passing through a pluripotent intermediate, directly converting one somatic cell type into another [1] [36]. This core difference dictates their respective applications, safety profiles, and technical challenges, making a head-to-head comparison essential for researchers aiming to leverage these tools for tissue repair and drug development.
Fundamental Principles and Mechanisms
Induced Pluripotent Stem Cell (iPSC) Technology
iPSC technology was pioneered by Shinya Yamanaka's lab in 2006, demonstrating that the introduction of four transcription factors—OCT4, SOX2, KLF4, and c-MYC (OSKM)—could reprogram mouse fibroblasts into pluripotent stem cells [88] [89] [90]. This process effectively rewinds the developmental clock, returning somatic cells to an embryonic-like state. The resulting iPSCs exhibit unlimited self-renewal capacity and can differentiate into cells derived from all three germ layers, mirroring the potential of embryonic stem cells but without the associated ethical concerns [89] [90].
The molecular mechanism involves a profound epigenetic remodeling of the somatic cell genome. The exogenous transcription factors activate a network of pluripotency-associated genes while silencing somatic cell-specific genes. This process involves global changes in DNA methylation patterns, histone modifications, and chromatin restructuring to open pluripotency-associated genomic regions [88]. A significant breakthrough has been the development of non-integrating delivery methods—such as Sendai virus vectors, episomal plasmids, and synthetic mRNAs—to enhance the safety profile of clinical-grade iPSCs by avoiding permanent genomic integration [90].
Transdifferentiation (Direct Reprogramming)
Transdifferentiation bypasses the pluripotent state altogether, offering a more direct route for cell fate conversion. This process involves the forced expression of lineage-specific transcription factors, microRNAs, or small molecules that directly suppress the original cell identity while simultaneously activating the gene expression network of the target cell type [1] [36]. For example, the direct conversion of mouse fibroblasts into self-renewing alveolar epithelial-like cells can be achieved using a cocktail of Nkx2-1, Foxa1, Foxa2, and Gata6 [91].
The mechanistic underpinnings involve transcriptional activation of new lineage programs, epigenetic remodeling to establish a new cellular identity, and accompanying metabolic shifts to support the new cell type's function [1]. A key technological advancement enabling efficient in vivo transdifferentiation is Tissue Nanotransfection (TNT), a non-viral nanotechnology that uses localized nanoelectroporation to deliver genetic cargo directly into tissues for cellular reprogramming [1]. Because it avoids a proliferative pluripotent intermediate, transdifferentiation presents a theoretically lower risk of tumorigenesis, making it particularly attractive for in vivo regenerative applications [36].
Comparative Workflow Visualization
The diagram below illustrates the key procedural differences between the iPSC and transdifferentiation pathways.
Comparative Technical Analysis
Key Parameter Comparison
The following table provides a quantitative and qualitative comparison of core parameters between iPSC technology and transdifferentiation.
| Parameter | iPSC Technology | Transdifferentiation |
|---|---|---|
| Reprogramming Factors | Core factors: OCT4, SOX2, KLF4, c-MYC (OSKM) or OSNL (OCT4, SOX2, NANOG, LIN28) [88] | Lineage-specific factors (e.g., Nkx2-1 for lung; Gata4, Tbx5 for heart) [91] [36] |
| Theoretical Risk of Tumorigenesis | Higher (due to potential for residual pluripotent cells and use of oncogenes like c-MYC) [88] [92] | Lower (bypasses pluripotent state) [1] [36] |
| Genetic/Epigenetic Stability | Can harbor genetic and epigenetic abnormalities from reprogramming; requires rigorous quality control [92] [90] | Generally stable, but phenotypic stability can be a challenge [1] |
| Typical Timeline | Weeks to months (Reprogramming: 3-4 weeks; Expansion & Differentiation: several more weeks) [93] [90] | Days to weeks (Direct conversion is generally faster) [1] |
| Reprogramming Efficiency | Variable; can be low, but enhanced with small molecules and optimized protocols [88] | Can be low; improved with optimized factor cocktails and delivery systems like TNT [1] |
| Key Advantages | • Unlimited self-renewal capacity • Can generate any cell type • Ideal for disease modeling, drug screening [89] [94] | • Faster, more direct conversion • Lower tumorigenic risk • Suitable for in vivo repair [1] [36] |
| Major Challenges | • Tumorigenicity risk • Complex, lengthy process • Potential for immature cell phenotype [92] [90] | • Lower efficiency in some cases • Incomplete maturation • Limited expansion capacity of target cells [1] |
Application in Tissue Repair and Disease Modeling
iPSC Applications
iPSCs have become a cornerstone for in vitro disease modeling and drug discovery. Their ability to be derived from patients allows for the creation of "disease-in-a-dish" models. For example, iPSCs from patients with amyotrophic lateral sclerosis (ALS) can be differentiated into motor neurons to study disease-specific pathology and screen potential therapeutics [88]. In the clinical realm, iPSC-derived dopaminergic progenitors are being tested in Phase I/II trials for Parkinson's disease, showing promising results with survived transplantation and dopamine production without tumor formation [90]. Allogeneic "off-the-shelf" iPSC-based therapies are also in development, such as Cynata Therapeutics' CYP-001 for graft-versus-host disease, which has successfully completed a Phase 1 trial [89].
Transdifferentiation Applications
Transdifferentiation excels in applications requiring direct in situ tissue repair. Its primary focus is on regenerating damaged tissues without cell transplantation. A prominent example is cardiac repair after myocardial infarction, where research focuses on directly reprogrambing cardiac fibroblasts into functional cardiomyocytes to replenish lost heart muscle and reduce scar tissue [36]. Advanced delivery technologies like Tissue Nanotransfection (TNT) demonstrate this application's potential, having been used in preclinical models for wound healing, ischemia repair, and neural regeneration by directly reprogramming resident fibroblasts into the required cell types [1].
Experimental Protocols
Detailed Protocol: iPSC Generation and Differentiation into Motor Neurons
This protocol is adapted for modeling neurological diseases like ALS [88] [93].
Step 1: Somatic Cell Source Preparation
- Source: Obtain human dermal fibroblasts via biopsy or use commercially available lines.
- Culture: Maintain in fibroblast medium (DMEM, 10% FBS, 1% GlutaMAX, 1% Non-Essential Amino Acids) at 37°C and 5% CO₂.
- Passaging: Harvest at 80-90% confluency using 0.05% trypsin.
Step 2: Reprogramming into iPSCs using Non-Integrating Methods
- Method Choice: Use Sendai virus vectors (e.g., CytoTune-iPS 2.0 Sendai Kit) for high efficiency and non-integration.
- Procedure: Plate 50,000 fibroblasts in a 6-well plate. The next day, transduce with the Sendai virus particles containing OCT4, SOX2, KLF4, and c-MYC at an appropriate MOI (e.g., 3-5).
- Culture: Change to essential 8 (E8) medium 24 hours post-transduction. Refresh medium daily.
- Observation: Embryonic stem cell-like colonies should appear in 2-3 weeks.
Step 3: iPSC Colony Picking and Expansion
- Picking: Manually pick colonies based on tight, ES-like morphology using a sterile pipette tip.
- Expansion: Transfer to 12-well plates coated with Matrigel and culture in E8 medium. Passage every 5-7 days using EDTA.
Step 4: Differentiation into Motor Neurons (iPSC-MNs)
- Neural Induction: Dissociate iPSCs and form embryoid bodies in low-attachment plates for 4 days in N2B27 medium with dual SMAD inhibition (e.g., Dorsomorphin 1µM, SB431542 10µM).
- Patterning: From day 4-12, pattern towards caudal neural fate using retinoic acid (RA, 0.1µM) and ventralize with a Sonic Hedgehog agonist (SAG, 1µM) to induce motor neuron identity.
- Maturation: Plate cells on poly-ornithine/laminin-coated plates from day 12 onwards in neurobasal medium with BDNF, GDNF, and CNTF to promote maturation.
- Validation: Analyze at day 30-35 for motor neuron markers (e.g., HB9, ISL1, ChAT) via immunocytochemistry and functional electrophysiology.
Detailed Protocol: Direct Reprogramming of Fibroblasts to CardiomyocytesIn Vitro
This protocol outlines direct lineage conversion for cardiac repair applications [36].
Step 1: Fibroblast Culture and Preparation
- Source: Isolate cardiac fibroblasts from mouse heart or use neonatal human dermal fibroblasts.
- Culture: Plate fibroblasts at a density of 20,000 cells/cm² in fibroblast growth medium.
Step 2: Delivery of Cardiogenic Factors
- Factor Cocktail: Use a combination of core cardiac transcription factors: Gata4, Mef2c, and Tbx5 (GMT).
- Delivery Method:
- Lentiviral Delivery: Produce high-titer lentivirus for each factor. Transduce fibroblasts with the GMT cocktail in the presence of polybrene (8µg/mL).
- Alternative Non-Viral Method: Use TNT-based electroporation to deliver plasmid DNA or mRNA encoding the GMT factors.
Step 3: Post-Transduction Culture and Medium Switch
- Timeline: 48-72 hours post-transduction, change the medium to cardiac induction medium (e.g., RPMI 1640 supplemented with B27 minus insulin).
- Observation: Morphological changes from fibroblastic to rod-like or star-shaped may be observed within 1-2 weeks.
Step 4: Validation of Cardiomyocyte Identity
- Timeline: Analyze cells 3-4 weeks post-transduction.
- Structural Markers: Perform immunostaining for α-actinin, cardiac Troponin T (cTnT), and connexin 43.
- Functional Assessment: Use calcium imaging to detect spontaneous calcium transients or patch-clamp recording to identify cardiomyocyte-like action potentials.
Signaling Pathways in Cardiac Direct Reprogramming
The diagram below outlines the key signaling pathways involved in the direct reprogramming of fibroblasts to cardiomyocytes.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and materials essential for implementing the described protocols in cellular reprogramming research.
| Reagent/Material | Function/Purpose | Example Products/Formats |
|---|---|---|
| Reprogramming Factors | Core transcription factors for inducing pluripotency or direct lineage conversion. | • OSKM factors (OCT4, SOX2, KLF4, c-MYC)• GMT factors (Gata4, Mef2c, Tbx5) [88] [36] |
| Delivery Vectors | Vehicles for introducing reprogramming factors into somatic cells. | • Sendai virus vectors (non-integrating)• Lentiviral vectors• Episomal plasmids• Synthetic mRNA [88] [90] |
| Small Molecule Enhancers | Improve reprogramming efficiency and direct conversion; replace transcription factors. | • Valproic acid (VPA, HDAC inhibitor)• CHIR99021 (GSK-3 inhibitor, Wnt activator)• RepSox (TGF-β inhibitor, replaces Sox2) [88] |
| Cell Culture Media | Support cell growth, maintenance, and directed differentiation. | • Fibroblast Medium (DMEM + 10% FBS)• Pluripotency Medium (mTeSR1, Essential 8)• Differentiation Media (N2B27, Cardiomyocyte medium) [88] [93] |
| Extracellular Matrix | Provides a physical scaffold and biochemical cues for cell attachment and growth. | • Matrigel (for iPSC culture)• Geltrex• Poly-ornithine/Laminin (for neurons) [93] |
| Characterization Antibodies | Validate successful reprogramming and differentiation via immunostaining. | • Pluripotency: Anti-OCT4, SOX2, NANOG• Cardiomyocytes: Anti-cTnT, α-actinin• Neurons: Anti-Tuj1, MAP2 [36] [93] |
The choice between iPSC technology and transdifferentiation is not a matter of superiority but of strategic application. iPSC technology offers unparalleled proliferative capacity and differentiation potential, making it the superior tool for large-scale in vitro disease modeling, drug screening, and generating a wide array of cell types for allogeneic cell therapy products. Its main drawbacks—tumorigenicity risk and lengthy protocols—are being actively mitigated through improved non-integrating delivery systems and more precise differentiation protocols [92] [90].
Conversely, transdifferentiation offers a faster, more direct route with a potentially safer profile, positioning it as a promising strategy for in situ tissue regeneration, particularly for conditions like myocardial infarction and neural injury where direct conversion of local fibroblasts could restore function without complex transplantation procedures [1] [36]. Its current limitations in efficiency and maturation are the focus of ongoing research, with technologies like Tissue Nanotransfection (TNT) paving the way for sophisticated in vivo application [1].
The future of cellular reprogramming lies not in the exclusive use of one technology over the other, but in their potential convergence. Insights from iPSC differentiation protocols can inform more efficient transdifferentiation cocktails, while the safety principles of direct reprogramming may guide the development of safer iPSC-derived therapies. As both fields mature, they will continue to provide researchers and drug developers with a powerful and expanding toolkit for regenerative medicine and therapeutic discovery.
This whitepaper explores the critical role of electrophysiology in two seemingly distinct cellular systems: neurons and pancreatic β-cells. Within the broader context of transdifferentiation mechanisms for tissue repair, we examine how electrical activity defines cellular identity and function. For β-cells, we detail the electrophysiological basis of glucose-stimulated insulin secretion (GSIS), a process governed by orchestrated ion channel activity leading to calcium influx and hormone release. For neurons, we consider their intrinsic electrical excitability as a functional benchmark in transdifferentiation research, where somatic cells are directly reprogrammed into neuronal lineages. This guide provides a comparative analysis of these systems, summarizes quantitative electrophysiological data, and presents key experimental protocols, establishing a foundation for leveraging electrophysiological principles in regenerative medicine strategies.
Electrophysiology serves as a fundamental bridge between cellular stimuli and functional responses, both in native tissues and in engineered cellular products for regenerative medicine. In the pancreas, the β-cell's ability to sense blood glucose levels and respond with precisely timed insulin secretion is an electrophysiological process. Similarly, in the nervous system, the generation and propagation of action potentials are the basis of neuronal communication. The growing field of transdifferentiation—the direct conversion of one differentiated cell type into another—aims to create functional cells for tissue repair. A critical measure of success in such endeavors is whether the newly generated cells, such as induced neurons (iNs) or β-cells, possess the correct electrophysiological properties to integrate into existing circuits and perform their intended functions [4] [11]. This whitepaper provides an in-depth technical examination of these processes, offering a guide for researchers and drug development professionals working at the intersection of cellular reprogramming and electrophysiology.
Core Electrophysiological Mechanisms in Pancreatic β-Cells
The Glucose-Triggering Pathway
The canonical triggering pathway of Glucose-Stimulated Insulin Secretion (GSIS) in β-cells is a well-defined cascade linking metabolism to electrical activity and secretion [95]. The process begins with glucose entry into the β-cell via glucose transporters (GLUTs). Subsequently, glucose metabolism increases the intracellular ATP/ADP ratio, leading to the closure of ATP-sensitive K+ (KATP) channels. This closure reduces potassium efflux, causing a depolarization of the membrane potential (Vm). Once this depolarization reaches a threshold, voltage-dependent Ca2+ channels (VDCCs) open, allowing an influx of Ca2+ that triggers the exocytosis of insulin granules [96] [95].
A key feature of β-cell electrical activity is the bursting pattern, observed particularly in rodents, which consists of slow oscillations in membrane potential with superimposed action potentials. These oscillations occur on a timescale of seconds to minutes and are crucial for generating pulsatile insulin secretion [97] [96]. The repolarization phase of action potentials involves the activation of voltage-gated Kv channels and large-conductance Ca2+-activated K+ (BK) channels [98].
Species-Specific Differences and Key Ion Channels
Significant electrophysiological differences exist between species, which is a critical consideration for translational research. The table below summarizes key distinctions between mouse and human β-cells.
Table 1: Key Electrophysiological Differences in Mouse vs. Human β-Cells
| Feature | Mouse β-Cells | Human β-Cells |
|---|---|---|
| Primary Glucose Transporters | GLUT2 (Km ≈17 mM) | GLUT1 & GLUT3 (Km ≈7 mM & 1.8 mM) [95] |
| Dominant Voltage-Gated Ca2+ Channels | CaV1.2 (L-type) >50% [95] | CaV2.1 (P/Q-type) & CaV1.2/1.3 (L-type), ~40-45% each [95] |
| Dominant Voltage-Gated Na+ Channels | NaV1.7 (85% of total current) [95] | NaV1.6 (75% of total current) [95] |
| Pattern of Electrical Activity | Bursts of action potentials (spikes) at intermediate glucose; continuous firing at high glucose [96] [95] | Continuous or irregularly spaced action potentials; bursting is less common [96] [95] |
| Key K+ Channels for Repolarization | Delayed rectifiers (KV2.1), SK4 [95] | BK channels, delayed rectifiers (KV2.2), SK3/SK4 [95] [98] |
Other critical ion channels include Ca2+-dependent K+ channels, which contribute to burst termination, and transient receptor potential (TRP) channels, which are also present and may modulate electrical activity [96].
Experimental Protocols for β-Cell Electrophysiology
Protocol 1: Perforated Patch-Clamp Recording of Glucose-Induced Electrical Activity This configuration is essential for preserving intracellular metabolic pathways while recording electrical activity.
- Cell Preparation: Use primary human islets or validated human β-cell lines like EndoC-βH1/βH2, which conform to primary human β-cell electrophysiology [98].
- Solutions: Extracellular solution: KRB buffer (138 mM NaCl, 3.6 mM KCl, 1.5 mM CaCl2, 0.5 mM MgSO4, 5 mM HEPES, 0.2% BSA) with varying glucose (1-20 mM). Pipette solution: 128 mM K-gluconate, 10 mM KCl, 10 mM NaCl, 1 mM MgCl2, 10 mM HEPES (pH 7.35 with KOH) [98].
- Perforation: Use amphotericin B (0.24 mg/ml) in the pipette to achieve electrical access [98].
- Recording: Maintain temperature at 32-34°C. In current-clamp mode, monitor the membrane potential while perfusing with solutions of increasing glucose concentration. Expect depolarization and onset of electrical activity (action potentials or bursting) as glucose rises from 1 mM to 6-20 mM [98].
Protocol 2: Measuring Exocytosis via Membrane Capacitance This assay directly quantifies insulin granule fusion.
- Configuration: Standard whole-cell patch-clamp.
- Solutions: Extracellular solution to isolate Ca2+ currents: Include 20 mM TEA to block K+ channels. Pipette solution: Cs-based to block K+ currents, with low EGTA (0.05 mM) to minimally buffer Ca2+ [98].
- Stimulation: Apply a train of depolarizing pulses (e.g., from -70 mV to 0 mV) to open VDCCs and trigger vesicle fusion.
- Measurement: Use the "lock-in" amplifier function in the patch-clamp software to monitor changes in membrane capacitance (ΔCm), which directly corresponds to the increase in surface area from granule exocytosis [98].
The following diagram illustrates the core signaling pathway and experimental modulation in β-cell electrophysiology.
Electrophysiology as a Benchmark in Neuronal Transdifferentiation
Functional Validation of Induced Neurons (iNs)
In neuronal transdifferentiation, the ultimate goal is to convert somatic cells (e.g., fibroblasts) directly into functional neurons, termed induced neurons (iNs). The defining characteristic of a mature, functional neuron is its ability to generate and propagate action potentials and form functional synapses. Therefore, electrophysiological analysis is the gold-standard method for validating successful transdifferentiation, moving beyond mere expression of neuronal markers [11].
Key electrophysiological properties measured in iNs include:
- Resting Membrane Potential: A stable, negative resting potential (typically between -50 mV and -70 mV).
- Action Potentials: The ability to generate all-or-nothing, regenerative action potentials in response to depolarizing current injections.
- Voltage-Gated Currents: The presence of tetrodotoxin (TTX)-sensitive Na+ currents and various voltage-gated K+ currents that shape the action potential.
- Synaptic Activity: Evidence of postsynaptic currents (both excitatory and inhibitory) indicating the formation of functional synaptic connections [11].
Protocols for Generating and Validating iNs
Protocol 3: Transcription Factor-Mediated Transdifferentiation to iNs
- Starting Cells: Human fibroblasts are the most commonly used starting cell type [11].
- Key Transcription Factors (TFs): Ectopic expression of combinations of TFs is used. A common combination for generic neurons is Brn2, Ascl1, and Myt1l (BAM). For dopaminergic neurons, factors like Ascl1, Nurr1, and Lmx1a are used [11].
- Delivery Method: Transduction using lentiviral or retroviral vectors.
- Culture Conditions: The process involves a conversion stage and a maturation stage. Culture media is supplemented with growth factors (e.g., BDNF, GDNF, IGF-1). Hypoxia (5% O2) can increase conversion efficiency by 2.4-fold [11].
- Timeline: Human iNs show a slower maturation process compared to mouse cells, often requiring several weeks to develop mature electrophysiological properties [11].
Protocol 4: Whole-Cell Patch-Clamp Characterization of iNs
- Configuration: Standard whole-cell patch-clamp at room temperature or physiological temperature (32-34°C).
- Solutions: Standard artificial cerebrospinal fluid (aCSF) as extracellular solution. K-gluconate-based or KCl-based internal solution for current-clamp and voltage-clamp recordings, respectively.
- Validation Steps:
- Resting Potential: Record immediately after achieving whole-cell configuration.
- Action Potentials: In current-clamp mode, inject steps of depolarizing current to test for action potential generation.
- Voltage-Gated Currents: In voltage-clamp mode, hold the cell at -70 mV and apply step depolarizations to isolate and characterize Na+ and K+ currents. Apply TTX to confirm the Na+ current component.
- Synaptic Currents: Record in voltage-clamp mode while holding the cell at different potentials (e.g., -70 mV for excitatory postsynaptic currents, EPSCs; 0 mV for inhibitory postsynaptic currents, IPSCs) to detect spontaneous synaptic activity.
The Scientist's Toolkit: Essential Research Reagents
The table below catalogs key reagents used in the electrophysiological study and programming of β-cells and neurons.
Table 2: Essential Research Reagents for Electrophysiology and Transdifferentiation
| Reagent | Category/Function | Specific Application |
|---|---|---|
| Tolbutamide | KATP Channel Blocker | Closes KATP channels in β-cells, inducing membrane depolarization and insulin secretion independent of glucose [98]. |
| Diazoxide | KATP Channel Opener | Hyperpolarizes β-cells, suppressing insulin secretion; used to confirm KATP channel role [98]. |
| Tetrodotoxin (TTX) | Na+ Channel Blocker | Blocks voltage-gated Na+ channels; used to isolate Na+ current contribution in β-cells and neurons [98]. |
| Isradipine | L-type Ca2+ Channel Blocker | Inhibits a major class of VDCCs in β-cells and neurons, reducing Ca2+ influx and secretion [98]. |
| Iberiotoxin | BK Channel Blocker | Blocks large-conductance Ca2+-activated K+ channels, prolonging action potential duration in β-cells and neurons [98]. |
| TEA (Tetraethylammonium) | K+ Channel Blocker | Broad-spectrum inhibitor of voltage-gated K+ channels, used to isolate other currents [98]. |
| Brn2, Ascl1, Myt1l | Transcription Factor Cocktail | Core set of TFs for direct reprogramming of fibroblasts into induced neurons (iNs) [11]. |
| CYN154806 | SSTR2 Antagonist | Blocks somatostatin receptor 2, potentially enhancing insulin secretion by inhibiting paracrine somatostatin signaling [98]. |
Integrated Workflow for Transdifferentiation and Validation
The following diagram outlines a comprehensive experimental workflow, from cellular reprogramming to functional electrophysiological validation, integrating the concepts and protocols discussed.
The functional integration of electrophysiological properties is paramount for the success of transdifferentiation strategies in tissue repair. As this whitepaper has detailed, both native β-cells and neurons rely on complex, dynamic electrical activity to perform their essential functions. Generating these properties de novo in reprogrammed cells is a significant challenge. Future research must focus on improving the maturity and stability of the electrophysiological phenotype in transdifferentiated cells. This will involve refining reprogramming protocols to generate specific neuronal subtypes or β-cells with the precise ion channel composition and metabolic coupling of their native counterparts. Furthermore, the development of more sophisticated high-throughput electrophysiological screening platforms will accelerate the discovery of novel reprogramming factors and the validation of resulting cellular therapies. By rigorously applying the principles and protocols outlined herein, researchers can advance the field of regenerative medicine towards generating fully functional cells capable of restoring lost function in diseases like diabetes and neurodegeneration.
The direct reprogramming, or transdifferentiation, of somatic cells presents a transformative strategy for regenerative medicine, aiming to generate desired cell types in situ for tissue repair without traversing a pluripotent state [35] [99]. However, the clinical translation of this technology is critically challenged by immunogenicity—the potential for engineered cells to trigger undesirable immune responses [35]. These responses can lead to the rejection of the reprogrammed cells, failure of tissue engraftment, and potential systemic inflammation, ultimately undermining the therapeutic goal [99].
Immunogenicity in this context arises from multiple factors. The delivery vectors used to introduce reprogramming factors, particularly viral vectors, can themselves provoke immune reactions [35]. Furthermore, the reprogramming process can induce cell stress, leading to the upregulation of ligands that activate immune cells like natural killer (NK) cells [99]. Perhaps most significantly, the profound epigenetic and transcriptional remodeling involved in changing a cell's identity can result in the expression of neoantigens, aberrant self-antigens, or the disruption of major histocompatibility complex (MHC) expression patterns, all of which can flag the reprogrammed cell for immune surveillance and destruction [100] [99]. Understanding and modulating these immune interactions is therefore paramount for developing safe and effective transdifferentiation-based therapies for tissue repair.
Mechanisms of Immune Recognition and Rejection
Reprogrammed somatic cells can be targeted by both the innate and adaptive arms of the immune system through several distinct mechanisms. The rejection process is often initiated by injury signals and the recruitment of immune cells to the site of reprogramming [100] [101].
Innate Immune Activation
The initial inflammatory response to tissue injury, a common precursor to in situ reprogramming therapies, creates a cytokine-rich environment that can attract innate immune cells such as macrophages and neutrophils [100]. These cells recognize damage-associated molecular patterns (DAMPs) released from stressed or dying cells. Reprogramming itself can induce cellular stress, further amplifying this signal. Additionally, changes in the surface protein profile of reprogrammed cells, such as altered MHC class I expression or the presence of stress ligands, can make them targets for Natural Killer (NK) cell-mediated cytotoxicity [99].
Adaptive Immune Responses
The adaptive immune system provides a more specific and potent threat to reprogrammed cells. Antigen-presenting cells (APCs), including dendritic cells, can phagocytose apoptotic reprogrammed cells or their debris, process the novel proteins (neoantigens) expressed during reprogramming, and present these antigens to T lymphocytes [99]. This can lead to the activation and clonal expansion of antigen-specific CD8+ cytotoxic T cells, which are capable of directly lysing the reprogrammed cells. CD4+ T helper cells can also be activated, promoting a pro-inflammatory environment and supporting B-cell activation [100]. The resulting humoral response can generate antibodies that specifically bind to reprogrammed cells, marking them for destruction by complement activation or antibody-dependent cellular cytotoxicity (ADCC) [99].
Table 1: Key Immune Effectors in the Response to Reprogrammed Somatic Cells
| Immune Effector | Primary Mechanism of Action | Key Triggers on Reprogrammed Cells |
|---|---|---|
| Cytotoxic T Cells | Recognize peptide antigens presented by MHC Class I; induce apoptosis via perforin/granzyme or Fas/FasL pathways. | Expression of neoantigens, viral vector antigens, or disrupted self-antigens [99]. |
| NK Cells | Identify and lyse cells with "missing self" (low MHC Class I) or "induced self" (stress ligand expression). | Altered or downregulated MHC Class I; expression of stress ligands like MICA/B [99]. |
| Macrophages | Phagocytose cells; release pro-inflammatory cytokines (e.g., TNF-α, IL-1β); present antigens to T cells. | Surface exposure of phosphatidylserine ("eat-me" signal); binding of opsonizing antibodies [100]. |
| Dendritic Cells | Phagocytose cell debris; mature and migrate to lymph nodes to prime naive T cells. | Uptake of necrotic/apoptotic reprogrammed cell material containing novel antigens [99]. |
Methodologies for Assessing Immunogenicity
A rigorous assessment of immunogenicity is essential for preclinical development. The following protocols outline key experiments to characterize the immune response to reprogrammed cells.
In Vitro T Cell Activation Assay
This assay measures the ability of reprogrammed cells to activate antigen-specific T cells, a primary mechanism of rejection.
Protocol:
- Cell Preparation: Generate reprogrammed somatic cells (e.g., via TNT with reprogramming factor mRNA [35] [102]) and relevant control cells (unreprogrammed, wild-type target cells). Use irradiated (non-proliferative) reprogrammed cells as antigen-presenting cells.
- T Cell Isolation: Isave CD8+ or CD4+ T cells from a human donor or syngeneic mouse model using magnetic-activated cell sorting (MACS) or fluorescence-activated cell sorting (FACS).
- Co-culture: Co-culture T cells with the irradiated reprogrammed cells at a defined stimulator-to-responder ratio (e.g., 1:10) in a 96-well U-bottom plate for 3-5 days. Include controls with unreprogrammed cells and T cells alone.
- Readout:
- Proliferation: Measure T cell proliferation using a carboxyfluorescein succinimidyl ester (CFSE) dilution assay followed by flow cytometry.
- Activation: Analyze T cell activation markers (e.g., CD69, CD25) via surface staining and flow cytometry after 24-48 hours.
- Cytokine Production: Quantify T cell-derived cytokines (e.g., IFN-γ, IL-2) in the supernatant using enzyme-linked immunosorbent assay (ELISA) or multiplex bead arrays.
In Vivo Engraftment and Immune Profiling
This experiment evaluates the survival and immune rejection of reprogrammed cells in an immunocompetent animal model.
Protocol:
- Cell Engineering and Delivery: Reprogram somatic cells (e.g., fibroblasts) to a target lineage (e.g., neurons, hepatocytes) using a non-viral method like Tissue Nanotransfection (TNT) to deliver plasmid DNA or mRNA [35]. Label the cells with a luciferase reporter for bioluminescent imaging.
- Transplantation: Transplant the labeled, reprogrammed cells into the appropriate tissue (e.g., skin, liver) of an immunocompetent syngeneic host. As a control, transplant cells into an immunodeficient host (e.g., NSG mouse) to establish baseline engraftment without adaptive immunity.
- Longitudinal Monitoring:
- Cell Survival: Monitor the bioluminescent signal weekly to track the survival and expansion of the graft.
- Immune Infiltrate Analysis: At defined endpoints (e.g., day 7, 14, 28), harvest the graft site. Digest the tissue into a single-cell suspension and characterize the immune infiltrate by flow cytometry using a panel for T cells (CD3, CD4, CD8), NK cells (NK1.1/CD49b), macrophages (F4/80, CD11b), and their activation states.
- Histological Examination: Fix the grafted tissue and perform immunohistochemistry staining for immune cell markers (e.g., CD3 for T cells) and a marker for the reprogrammed cell type to visualize the spatial relationship between the graft and the immune infiltrate.
Strategies to Mitigate Immunogenicity
Several innovative strategies are being developed to cloak reprogrammed cells from immune detection, thereby enhancing their persistence and therapeutic function.
Vector and Cargo Engineering
The choice of delivery system for reprogramming factors is critical. Non-viral physical methods, such as Tissue Nanotransfection (TNT), which uses nanoelectroporation to deliver genetic cargo, offer a promising alternative to viral vectors by minimizing immunogenicity and avoiding genomic integration [35]. For genetic payloads, using mRNA (with modified nucleosides like pseudouridine) instead of plasmid DNA directs protein translation in the cytoplasm without nuclear entry, reducing the risk of genomic integration and resulting in only transient expression, which is less likely to provoke a sustained immune response [35] [102]. Furthermore, episomal plasmids or CRISPR/Cas9 systems designed for highly specific gene activation (e.g., dCas9 fused to transcriptional activators) can achieve reprogramming without permanent genetic alteration [35].
Modulation of the Local Microenvironment
The site of reprogramming is not a passive backdrop but an active participant in the immune response. Targeted immunosuppression can be used transiently to allow the reprogrammed cells to establish themselves without immediate rejection. More sophisticated approaches involve local delivery of immunomodulatory factors, such as interleukin-10 (IL-10) or transforming growth factor-beta (TGF-β), to create a tolerogenic niche [100]. This can skew the local immune population towards regulatory phenotypes (Tregs, M2 macrophages) and away from pro-inflammatory, cytotoxic effectors [100] [101]. The extracellular matrix (ECM) also plays a role; engineering the scaffold to present anti-inflammatory signals can further promote immune tolerance of the graft [101].
Cell-Autonomous Stealth Engineering
The most direct strategy is to genetically engineer the reprogrammed cells to evade immune detection. This includes overexpression of immunomodulatory molecules like PD-L1, which engages the PD-1 receptor on T cells to deliver an inhibitory signal, or CD47, a "don't eat me" signal that blocks phagocytosis by macrophages [99]. Another approach is the knockdown of key molecules in the antigen presentation pathway, such as Beta-2-microglobulin (B2M), to reduce surface MHC class I expression and impair CD8+ T cell recognition. A balanced strategy is required, however, as complete loss of MHC class I can trigger NK cell activation [99].
Table 2: Strategies for Mitigating Immunogenicity of Reprogrammed Cells
| Strategy Category | Specific Approach | Mechanism of Action | Key Considerations |
|---|---|---|---|
| Delivery & Cargo | mRNA Reprogramming [35] [102] | Transient, non-integrating expression of factors; reduces risk of mutagenesis and persistent antigen expression. | High efficiency may require multiple doses; nucleoside modifications reduce innate immune sensing. |
| Non-Viral Delivery (TNT) [35] | Localized nanoelectroporation avoids viral vector-associated immunogenicity and pre-existing immunity. | Optimization of electrical parameters is critical for efficiency and cell viability. | |
| Microenvironment | Local Immunomodulation [100] | Co-delivery of tolerogenic cytokines (e.g., IL-10, TGF-β) promotes regulatory T cells and M2 macrophages. | Prevents systemic immunosuppression; requires precise control over factor release kinetics. |
| Cell-Autonomous | PD-L1 Overexpression [99] | Engages PD-1 on T cells to deliver an inhibitory signal, dampening cytotoxic T cell activity. | Potentially reversible effect; may need to be combined with other strategies for long-term graft survival. |
| CD47 Overexpression [99] | Signals via SIRPα on phagocytes to inhibit phagocytosis ("don't eat me" signal). | Effective against innate immune clearance; does not directly affect T cell recognition. |
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Immunogenicity
| Reagent / Tool | Function in Immunogenicity Research |
|---|---|
| Tissue Nanotransfection (TNT) Device [35] | A physical platform for the non-viral, localized delivery of reprogramming cargo (DNA, mRNA) into tissue, minimizing vector-related immunogenicity. |
| Nucleoside-Modified mRNA [35] [102] | Synthetic mRNA encoding reprogramming factors (e.g., OSKM); nucleoside modifications reduce recognition by innate immune sensors, favoring transient expression. |
| CRISPR/dCas9 Epigenetic Editors [35] | Enables targeted transcriptional activation or epigenetic silencing without permanent DNA cleavage, facilitating reprogramming with potentially fewer off-target antigens. |
| Flow Cytometry Panels | Multiplexed antibody panels for characterizing immune infiltrates (T, B, NK, myeloid cells) and their activation states from in vivo grafts or co-cultures. |
| MHC Multimers | Fluorescently labeled peptide-MHC complexes used to identify and isolate T cells with specificity for antigens potentially presented by reprogrammed cells. |
Addressing immunogenicity is not merely a technical hurdle but a fundamental requirement for the successful clinical translation of somatic cell reprogramming therapies. The immune system presents a multi-layered barrier, from innate sensing of delivery vectors to adaptive recognition of neoantigens. A combinatorial approach that integrates stealth delivery systems like TNT and mRNA [35] [102], transient local immunomodulation [100], and cell-autonomous engineering [99] holds the greatest promise for inducing durable immune tolerance.
Future research must focus on high-resolution profiling of the specific antigens presented by reprogrammed cells and the dynamics of the immune response in human contexts. The development of predictive in vitro human immune cell assays and humanized mouse models will be crucial. Furthermore, the emerging concept of in vivo reprogramming, as exemplified by platforms like ImmunoVec's polymeric nanoparticles for immune cell engineering [103], could fundamentally alter the immunogenicity landscape by reprogramming cells within their native tissue microenvironment. As these technologies converge, the goal of achieving safe, effective, and immunologically accepted cell therapies for tissue repair moves closer to reality.
Within the field of regenerative medicine, the direct reprogramming of somatic cells, or transdifferentiation, presents a transformative strategy for tissue repair. This approach enables the conversion of one mature cell type into another, bypassing the pluripotent state and offering a potentially safer and more direct route for cell replacement therapies [35]. The core thesis of this whitepaper is that the therapeutic readiness of a cell conversion strategy is a function of its safety profile, manufacturing scalability, and in vivo efficacy. As such, this guide provides a critical evaluation of three dominant strategies—Induced Pluripotent Stem Cells (iPSCs), Direct Reprogramming (Transdifferentiation), and Mechanical Reprogramming—framed within the context of tissue repair research. It is intended to equip researchers and drug development professionals with the quantitative data, experimental protocols, and analytical frameworks necessary to advance these technologies toward clinical application.
Comparative Analysis of Cell Conversion Strategies
A critical assessment of therapeutic readiness requires a multi-parameter analysis. The following tables summarize the key characteristics, advantages, and limitations of the primary cell conversion strategies.
Table 1: Core Characteristics and Therapeutic Readiness of Cell Conversion Strategies
| Parameter | Induced Pluripotent Stem Cells (iPSCs) | Direct Reprogramming (Transdifferentiation) | Mechanical Reprogramming |
|---|---|---|---|
| Definition | Somatic cells reprogrammed to an embryonic-like pluripotent state [104] | Direct conversion of one somatic cell lineage into another without a pluripotent intermediate [35] | Cell fate reprogramming via biophysical cues in a tissue-mimicking mechanical microenvironment [30] |
| Key Technical Features | Introduction of transcription factors (e.g., Oct3/4, Sox2, Klf4, c-Myc); can be integrated with CRISPR-Cas9 [104] | Overexpression of lineage-specific factors in vivo; uses non-viral methods like Tissue Nanotransfection (TNT) [35] | Culturing cells on hydrogels with specific viscoelastic and nonlinear elastic properties to induce aggregate formation [30] |
| Therapeutic Potential | High; can generate any cell type for disease modeling and therapy [104] | High for specific lineages; ideal for in situ tissue regeneration [35] | Emerging; shows promise in regenerative medicine and cancer transdifferentiation therapy [30] |
| Major Advantages | • Morally acceptable alternative to ESCs [104]• Enables patient-specific therapy [104]• Offers an endless cell supply [104] | • Avoids tumorigenicity risks of pluripotent states [35]• Rapid and potentially safer [35]• Enables in vivo application [35] | • Avoids genetic modification [30]• Uses physiological mechanical cues [30]• Can reverse oncogene expression in cancer cells [30] |
| Key Limitations | • Risk of tumor formation from genetic alterations [104]• Potential for epigenetic memory [104]• Inefficient generation process [104] | • Phenotypic stability can be a challenge [35]• Scalability needs improvement [35]• May require precise control of factor delivery [35] | • Technology is nascent; requires further validation [30]• Mechanisms not fully understood [30]• Standardization of hydrogels is complex [30] |
Table 2: Quantitative and Qualitative Metrics for Strategy Evaluation
| Metric | iPSCs | Direct Reprogramming | Mechanical Reprogramming |
|---|---|---|---|
| Tumorigenicity Risk | High (due to oncogenic factors like c-Myc) [104] | Low (bypasses pluripotent state) [35] | Not reported; presumed low (non-genetic) [30] |
| Immunogenicity Risk | Low (autologous possible) [104] | Low (autologous possible) [35] | Low (autologous possible) [30] |
| Manufacturing Scalability | Challenging and costly [104] | Improving with technologies like TNT [35] | Potential for high scalability with standardized hydrogels [30] |
| In Vivo Application | Primarily ex vivo | Direct in vivo potential via TNT [35] | Primarily in vitro with in vivo potential [30] |
| Regulatory Path | Defined but complex due to safety concerns [104] | Emerging, aided by non-viral delivery [35] | Early stage, regulatory framework under development |
| Therapeutic Readiness Level | Intermediate-High (clinical trials ongoing) [104] | Intermediate (preclinical success) [35] | Low-Intermediate (experimental proof-of-concept) [30] |
Experimental Protocols for Key Methodologies
Protocol: Tissue Nanotransfection (TNT) for Direct In Vivo Reprogramming
TNT is a non-viral, nanoelectroporation platform for delivering reprogramming payloads directly into tissues in vivo [35].
- Device Setup: The TNT device consists of a hollow-needle silicon chip mounted beneath a cargo reservoir for genetic material (e.g., plasmid DNA, mRNA). The device is placed directly on the target tissue, with a dermal electrode serving as the positive terminal [35].
- Genetic Cargo Preparation: Prepare, purify, and optimize the genetic material. Plasmid DNA and mRNA are prioritized for their transient expression and lower risk of genomic integration. For CRISPR/Cas9 applications, plasmids encoding for a catalytically inactive dCas9 fused to transcriptional activators can be used [35].
- Electroporation Procedure: Apply optimized electrical pulses (typical parameters: 10-30 V, 10-100 ms pulse duration, 1-10 pulses). The hollow needles concentrate the electric field, creating transient nanopores in the membranes of underlying cells for cargo entry [35].
- Post-Procedure Monitoring: The nanopores reseal within milliseconds. Monitor the tissue for expression of the reprogramming factors and subsequent phenotypic changes. The transient nature of the expression limits long-term genomic integration risks [35].
Protocol: Mechanical Reprogramming on Tissue-Mimicking Hydrogels
This protocol reprograms cell fate using a synthetic extracellular matrix (ECM) that mimics the biophysical properties of native tissue [30].
- Hydrogel Fabrication: Construct an interpenetrating network (IPN) hydrogel.
- Combine 1.5 mg/ml of collagen (provides nonlinear elasticity) with 10 mg/ml of alginate (provides viscoelasticity).
- Cross-link the alginate component by adding calcium chloride at concentrations between 5-15 mM to achieve the desired initial storage modulus (e.g., 15 mM for a "stiff" hydrogel mimicking aged tissue) [30].
- Cell Seeding and Culture: Seed cells (e.g., 3T3-L1 fibroblasts or non-small-lung cancer cells) onto the surface of the fabricated hydrogel. Culture them in standard media conditions [30].
- Induction of Aggregation: Monitor cells over 8-24 hours. On the tissue-mimicking hydrogel, cells will migrate and crowd together to form 3D mesenchymal aggregates instead of spreading out. This aggregation is driven by enhanced cell contractility and is crucial for the reprogramming event [30].
- Validation of Reprogramming: Assess the success of reprogramming by:
- Gene Expression: Quantifying elevated expression of pluripotency genes (e.g., via qRT-PCR).
- Differentiation Potential: Demonstrating enhanced adipogenic or osteogenic potential after exposure to differentiation cocktails [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Cell Conversion Research
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Reprogramming Transcription Factors | Proteins or genes (e.g., Oct4, Sox2, Klf4, c-Myc) that induce a pluripotent state in somatic cells [104]. | Generation of patient-specific iPSCs for disease modeling [104]. |
| CRISPR/dCas9 Systems | A programmable, non-viral platform for precise gene editing or transcriptional activation/repression without double-strand breaks [35]. | Activating endogenous expression of lineage-specific genes for direct reprogramming [35]. |
| Tissue-Mimicking IPN Hydrogels | A synthetic ECM combining collagen and alginate to provide physiologically relevant mechanical cues for cell fate control [30]. | Studying and inducing mechanical reprogramming of fibroblasts or cancer cells [30]. |
| Nanoelectroporation Devices (TNT) | A physical delivery system for highly efficient, localized, and non-viral transfection of genetic material directly into tissues in vivo [35]. | In vivo direct reprogramming of cells for tissue regeneration and wound healing [35]. |
| Cell Culture Media Supplements | Cytokines (e.g., IL-2, IL-7) and growth factors used to activate, expand, and direct the differentiation of cells during manufacturing [105]. | Expansion of T-cells for CAR-T therapy or directing stem cell differentiation [105]. |
Visualizing Workflows and Signaling Pathways
TNT Workflow for In Vivo Reprogramming
Diagram Title: TNT In Vivo Reprogramming Workflow
Mechanical Reprogramming Experimental Workflow
Diagram Title: Mechanical Reprogramming Experimental Steps
Simplified Signaling in Direct Lineage Conversion
Diagram Title: Signaling in Direct Lineage Conversion
Conclusion
Transdifferentiation represents a paradigm shift in regenerative medicine, offering a direct route to cell replacement that bypasses the technical and safety challenges associated with pluripotent intermediates. The field has progressed from foundational discoveries of natural plasticity to sophisticated reprogramming methodologies capable of generating therapeutically relevant cell types. While significant hurdles in efficiency, maturation, and safety remain, emerging technologies in mRNA delivery, computational prediction, and mechanical reprogramming provide promising paths forward. Future research must focus on achieving robust, scalable, and clinically viable protocols that ensure long-term stability and functional integration of converted cells. As mechanistic understanding deepens, transdifferentiation is poised to transition from a powerful research tool to a cornerstone of next-generation therapies for neurodegenerative diseases, heart failure, diabetes, and other conditions characterized by irreversible cell loss.
References
- 1. Tissue nanotransfection and cellular reprogramming in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213499/]
- 2. Direct cell reprogramming for tissue engineering and ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-019-0144-9]
- 3. Cell Transdifferentiation and Reprogramming in Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8533873/]
- 4. Transdifferentiation, Metaplasia and Tissue Regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC2633984/]
- 5. Endothelial transdifferentiation of glioma stem cells [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-025-02031-x]
- 6. Lens Regeneration - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/lens-regeneration]
- 7. Salamanders: The molecular basis of tissue regeneration and its relevance to human disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8186737/]
- 8. Recent advances in pancreatic α-cell transdifferentiation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1551372/full]
- 9. Automated quantification of pancreatic β-cell mass - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4059986/]
- 10. Human pancreatic α-cell heterogeneity and trajectory ... [https://www.nature.com/articles/s41467-025-62670-5]
- 11. a new promise for neurodegenerative diseases [https://www.nature.com/articles/s41419-018-0891-4]
- 12. PAX6 maintains β cell identity by repressing genes ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/27941241/]
- 13. Mapping gene regulatory circuitry of Pax6 during ... [https://www.nature.com/articles/celldisc201545]
- 14. Transcriptomic and epigenetic mechanisms controlling ... [https://pubmed.ncbi.nlm.nih.gov/41033615/]
- 15. PAX6/CXCL14 regulatory axis promotes the repair of corneal ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05270-z]
- 16. Identification of Pax6-Dependent Gene Regulatory Networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2612750/]
- 17. Transdifferentiation - Latest research and news [https://www.nature.com/subjects/transdifferentiation]
- 18. Unveiling Cancer-Related Metaplastic Cells in Both ... [https://www.sciencedirect.com/science/article/abs/pii/S0016508524054155]
- 19. Global Fibrosis Burden and a Transcriptional Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467191/]
- 20. Biliary Metaplasia and Macrophage Activation Define the ... [https://www.sciencedirect.com/science/article/pii/S2452302X24004510]
- 21. Transdifferentiation: a cell and molecular reprogramming ... [https://pubmed.ncbi.nlm.nih.gov/22526624/]
- 22. Underreporting of Gastric Intestinal Metaplasia Due to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547224/]
- 23. Precancerous pathways to gastric cancer: a review of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1620756/full]
- 24. Trends and hotspots in pulmonary fibrosis biomarker ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1541364/full]
- 25. Spatial transcriptomics identifies molecular niche ... [https://www.nature.com/articles/s41588-025-02080-x]
- 26. Potential biomarkers of idiopathic pulmonary fibrosis [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06975-5]
- 27. Major Structures Arising Out Of Primary Germ Layers [https://jackwestin.com/resources/mcat-content/embryogenesis/major-structures-arising-out-of-primary-germ-layers]
- 28. Molecular specification of germ layers in vertebrate embryos [https://pmc.ncbi.nlm.nih.gov/articles/PMC4744249/]
- 29. Digital reconstruction of full embryos during early mouse ... [https://www.sciencedirect.com/science/article/pii/S0092867425006221]
- 30. Mechanical Cell Reprogramming on Tissue-Mimicking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358751/]
- 31. Embryonic Germ Layer Origin as a Potential Determinant of ... [https://www.medrxiv.org/content/10.1101/2025.06.16.25329631v3]
- 32. Organoids for tissue repair and regeneration [https://www.sciencedirect.com/science/article/pii/S2590006425005836]
- 33. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 34. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 35. Tissue nanotransfection and cellular reprogramming in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1558735/full]
- 36. Cell Reprogramming, Transdifferentiation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988544/]
- 37. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 38. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 39. Proliferation history and transcription factor levels drive ... [https://www.sciencedirect.com/science/article/abs/pii/S2405471225000389]
- 40. Reprogramming of human urine cells into cardiomyocytes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216017/]
- 41. Genetic variation at transcription factor binding sites largely ... [https://www.nature.com/articles/s41588-025-02246-7]
- 42. Decoding human chemical reprogramming: mechanisms ... [https://www.sciencedirect.com/science/article/abs/pii/S0968000425000532]
- 43. Chemical reprogramming of human somatic cells to ... [https://www.nature.com/articles/s41586-022-04593-5]
- 44. Small molecules for reprogramming and transdifferentiation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11107793/]
- 45. Chemical reprogramming for cell fate manipulation [https://www.sciencedirect.com/science/article/pii/S1934590923002849]
- 46. In vivo glia-to-neuron conversion: pitfalls and solutions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9337910/]
- 47. Directed glial differentiation and transdifferentiation for ... [https://www.sciencedirect.com/science/article/abs/pii/S0014488618304011]
- 48. In Vivo Glial Trans-differentiation for Neuronal Replacement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8217397/]
- 49. Human Glial Cells as Innovative Targets for the Therapy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011741/]
- 50. Adult neurogenesis through glial transdifferentiation in a CNS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11888597/]
- 51. Adult neurogenesis through glial transdifferentiation in a ... [https://elifesciences.org/reviewed-preprints/96890]
- 52. Adult neurogenesis through glial transdifferentiation in a ... [https://elifesciences.org/articles/96890]
- 53. Direct glia-to-neuron transdifferentiation gives rise to a pair ... [https://elifesciences.org/articles/48361]
- 54. Temple scientists discover a new way the body repairs itself ... [https://news.temple.edu/news/2025-10-28/temple-scientists-discover-new-way-body-repairs-itself-after-heart-injury]
- 55. Type 1 diabetes cured in mice with gentle blood stem-cell and ... [https://med.stanford.edu/news/all-news/2025/11/type-1-diabetes-cure.html]
- 56. Exciting research updates shared at the 2025 European ... [https://breakthrought1d.ca/exciting-research-updates-shared-at-the-2025-european-association-for-the-study-of-diabetes-easd-meeting/]
- 57. University Hospitals Approved as a US Site [https://news.uhhospitals.org/news-releases/articles/2025/11/uh-approved-as-a-us-site-to-administer-breakthrough-treatment-lantidra-for-type-1-diabetes]
- 58. New stem cell-based strategy could enhance neuronal ... [https://www.news-medical.net/news/20251014/New-stem-cell-based-strategy-could-enhance-neuronal-regeneration-and-neuroplasticity.aspx]
- 59. The nerve center of organ engineering [https://www.nature.com/articles/s41467-025-64801-4]
- 60. Cell reprogramming: methods, mechanisms and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947411/]
- 61. Comparison of reprogramming factor targets reveals both ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6303873/]
- 62. Recommendations, guidelines, and best practice for the use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12244118/]
- 63. BRCA1 and 53BP1 Regulate Reprogramming Efficiency by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11272184/]
- 64. Comparative computational analysis of pluripotency in ... [https://www.nature.com/articles/srep07927]
- 65. BRCA1 and 53BP1 regulate reprogramming efficiency by ... [https://www.sciencedirect.com/science/article/pii/S2211124724003346]
- 66. CRISPR activation enables high-fidelity reprogramming ... [https://www.sciencedirect.com/science/article/pii/S2213671121006561]
- 67. Prediction of reprogramming factors [https://www.nature.com/articles/nrg.2016.6]
- 68. A Novel Transcription Factor Combination for Direct ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10495191/]
- 69. Transdifferentiation as a mechanism of treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5501744/]
- 70. A decision point between transdifferentiation and ... [https://www.nature.com/articles/s41467-025-56493-7]
- 71. Transdifferentiation of fibroblasts into muscle cells to ... [https://elifesciences.org/articles/93220]
- 72. Epigenetic regulation of cell fate transition: learning from early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9310515/]
- 73. Unravelling the epigenetic based mechanism in discovery ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825001561]
- 74. Single-cell epigenomic reconstruction of developmental ... [https://www.nature.com/articles/s41593-024-01652-0]
- 75. Epidrugs in cancer: mechanisms, applications, and future ... [https://pubmed.ncbi.nlm.nih.gov/41062905/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1HoKZG5k4YSGTrpmxwd9h4jUYVua2toCx3K_3oQCgrtW4k5g1d&fc=None&ff=20251011062802&v=2.18.0.post9+e462414]
- 76. Organ-Specific Dedifferentiation and Epigenetic ... [https://pubmed.ncbi.nlm.nih.gov/41114535/]
- 77. Review Research of in vivo reprogramming toward clinical ... [https://www.sciencedirect.com/science/article/pii/S2352320424002001]
- 78. What is in vivo reprogramming, its potential pros & cons? [https://ipscell.com/2025/10/what-is-in-vivo-reprogramming-its-potential-pros-cons/]
- 79. Research of in vivo reprogramming toward clinical ... [https://pubmed.ncbi.nlm.nih.gov/39678397/]
- 80. ARDD 2025: Hitting rewind, not reset, for in vivo rejuvenation [https://www.bioworld.com/articles/723608-ardd-2025-hitting-rewind-not-reset-for-in-vivo-rejuvenation]
- 81. Chemical Transdifferentiation of Somatic Cells - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10669320/]
- 82. Unlocking the therapeutic potential of cellular mechanobiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577691/]
- 83. Cinnamomum migao H.W. Li Ethanol-Water Extract ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563024/]
- 84. Methods to Assess Stem Cell Lineage, Fate and Function [https://pmc.ncbi.nlm.nih.gov/articles/PMC3078641/]
- 85. Transdifferentiation occurs without resetting development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11441492/]
- 86. Perspective: Pathological transdifferentiation—a novel ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2024.1500775/full]
- 87. Transdifferentiation of human endothelial progenitors into ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216000922]
- 88. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 89. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 90. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 91. Recommended reads: direct reprogramming, the road to ... [https://ipscell.com/2025/08/recommended-reads-direct-reprogramming-the-road-to-human-embryos-from-stem-cells-gameto-church-crispr-interview/]
- 92. Induced pluripotent stem cells: The advantages, ... [https://www.clinicaltrialsarena.com/sponsored/induced-pluripotent-stem-cells-the-advantages-challenges-and-advances/]
- 93. Comparing stem cells, transdifferentiation and brain ... [https://www.nature.com/articles/s41398-024-02780-8]
- 94. Trends & Strategies Shaping the $4.6+ Billion Induced ... [https://finance.yahoo.com/news/trends-strategies-shaping-4-6-145400149.html]
- 95. The triggering pathway to insulin secretion - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5710702/]
- 96. Mathematical models of electrical activity of the pancreatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4292577/]
- 97. The Electrophysiology of the β-Cell Based on Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1989707/]
- 98. Electrophysiological properties of human beta-cell lines ... [https://www.nature.com/articles/s41598-018-34743-7]
- 99. Understanding and Modulating Immunity With Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6917620/]
- 100. Epigenetic reprogramming of immune cells in injury, repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6668667/]
- 101. Comparative regenerative mechanisms across different ... [https://www.nature.com/articles/s41536-018-0044-5]
- 102. mRNA-based technology for engineered regenerative ... [https://www.sciencedirect.com/science/article/pii/S305056232500176X]
- 103. New in vivo cell therapy aims to reprogram immune ... [https://www.drugdiscoverynews.com/new-in-vivo-cell-therapy-aims-to-reprogram-immune-cells-to-treat-autoimmune-disease-16749]
- 104. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 105. Process Steps in Cell Therapy Manufacturing [https://www.cellandgene.com/topic/cell-therapy-manufacturing]