A Comprehensive Protocol for Autologous Induced Pluripotent Stem Cell Therapy: From Reprogramming to Clinical Translation
This article provides a detailed, state-of-the-art overview of the autologous induced pluripotent stem cell (iPSC) therapy pipeline, tailored for researchers, scientists, and drug development professionals.
A Comprehensive Protocol for Autologous Induced Pluripotent Stem Cell Therapy: From Reprogramming to Clinical Translation
Abstract
This article provides a detailed, state-of-the-art overview of the autologous induced pluripotent stem cell (iPSC) therapy pipeline, tailored for researchers, scientists, and drug development professionals. It systematically covers the foundational principles of somatic cell reprogramming and the unique immunological advantages of using a patient's own cells. The core of the article delves into the step-by-step methodology, from cell sourcing and reprogramming to differentiation, quality control, and clinical administration. It further addresses critical challenges in manufacturing, safety, and scalability, offering troubleshooting and optimization strategies. Finally, the protocol is validated through an analysis of current clinical trial data and a comparative assessment with allogeneic approaches, providing a holistic and practical guide for developing effective and safe autologous iPSC-based treatments.
The Scientific and Clinical Rationale for Autologous iPSC Therapy
The reprogramming of somatic cells to induced pluripotent stem cells (iPSCs) represents a transformative breakthrough in regenerative medicine and biomedical research. Since the landmark discovery by Takahashi and Yamanaka that demonstrated somatic cells could be reprogrammed using defined transcription factors, the field has evolved to encompass diverse methodologies for inducing pluripotency [1]. This protocol outlines the core principles and detailed methodologies for generating iPSCs, with particular emphasis on applications in autologous cell therapy research. The ability to derive patient-specific stem cells bypasses ethical concerns associated with embryonic stem cells and enables development of personalized disease models and regenerative therapies, making mastery of these techniques essential for modern stem cell researchers and therapy developers.
Core Reprogramming Factors and Mechanisms
Fundamental Transcription Factor Combinations
The foundation of somatic cell reprogramming rests on the introduction of specific transcription factors that reactivate the pluripotency network. The original Yamanaka factors (OSKM) consist of:
- OCT4 (Octamer-binding transcription factor 4): A POU-family transcription factor critical for maintaining pluripotent identity
- SOX2 (SRY-box 2): A HMG-box transcription factor that collaborates with OCT4 to regulate pluripotency genes
- KLF4 (Krüppel-like factor 4): A zinc-finger transcription factor that promotes mesenchymal-to-epithelial transition
- c-Myc: A proto-oncogene that enhances global transcription and proliferation [1]
Alternative factor combinations have been developed to address safety concerns, particularly regarding the oncogenic potential of c-Myc. The Thomson group established that OCT4, SOX2, NANOG, and LIN28 (OSNL) can similarly reprogram human somatic cells to pluripotency without c-Myc [1]. Factor substitution studies have revealed that KLF2 and KLF5 can replace KLF4, while SOX1 and SOX3 can substitute for SOX2, though often with reduced efficiency [1].
Enhancing Reprogramming Efficiency
Numerous molecular tools have been identified that significantly enhance reprogramming efficiency:
- Nuclear receptors: NR5A2 can substitute for OCT4 in reprogramming [1]
- Small molecules: The small molecule RepSox can replace SOX2 function [1]
- Epigenetic modifiers: Histone deacetylase inhibitors (VPA, sodium butyrate, trichostatin A) and DNA methyltransferase inhibitors (5-aza-cytidine, RG108) enhance chromatin accessibility [1]
- Signaling pathway regulators: 8-Br-cAMP, when combined with VPA, can increase reprogramming efficiency up to 6.5-fold [1]
- microRNAs: The miR-302/367 cluster and miR-372 significantly improve reprogramming kinetics [1]
Table 1: Key Reprogramming Factor Combinations and Their Applications
| Factor Combination | Components | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| OSKM | OCT4, SOX2, KLF4, c-Myc | High efficiency, well-characterized | Tumorigenic risk from c-Myc | Basic research, disease modeling |
| OSNL | OCT4, SOX2, NANOG, LIN28 | Reduced tumorigenic risk | Lower efficiency for some cell types | Therapeutic applications |
| OSK | OCT4, SOX2, KLF4 | Eliminates c-Myc concerns | Significantly reduced efficiency | Safety-focused applications |
| OSK+L-Myc | OCT4, SOX2, KLF4, L-Myc | Maintains efficiency with reduced risk | Still requires oncogene | Balance of safety and efficiency |
Delivery Systems for Reprogramming Factors
Selecting an appropriate delivery system for reprogramming factors represents a critical decision point in experimental design, balancing efficiency, safety, and clinical applicability.
Viral Delivery Systems
Viral vectors remain the most efficient method for delivering reprogramming factors:
- Retroviruses: Efficient integration and sustained transgene expression but prone to insertional mutagenesis and heterogeneous transgene silencing
- Lentiviruses: Can infect non-dividing cells and offer higher packaging capacity but still present integration risks
- Sendai Virus: RNA virus that remains in cytoplasm without genomic integration, enabling generation of transgene-free iPSCs but requires rigorous clearance verification [1]
Non-Viral and Non-Integrating Methods
For clinical applications, non-integrating methods are preferred:
- Episomal Plasmids: DNA vectors that replicate extrachromosomally and are gradually diluted through cell divisions
- PiggyBac Transposon: Efficient integration with precise excision capability but still involves temporary DNA integration
- Synthetic mRNA: Direct delivery of in vitro transcribed mRNA encoding reprogramming factors; requires multiple transfections but generates transgene-free iPSCs
- Recombinant Protein: Direct delivery of reprogramming factors as proteins; technically challenging with low efficiency but completely DNA-free [1]
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Delivery Method | Genomic Integration | Efficiency | Safety Profile | Clinical Applicability | Technical Difficulty |
|---|---|---|---|---|---|
| Retroviral | Yes | High | Low | Limited | Moderate |
| Lentiviral | Yes | High | Low | Limited | Moderate |
| Sendai Virus | No | High | Moderate | Good | Moderate |
| Episomal Plasmid | No (transient) | Low-Moderate | High | Excellent | Low |
| Synthetic mRNA | No | Moderate | High | Excellent | High |
| Recombinant Protein | No | Low | High | Excellent | Very High |
Detailed Experimental Protocols
Protocol: iPSC Generation Using Non-Integrating Episomal Vectors
This protocol outlines a method suitable for generating clinical-grade iPSCs for autologous therapy applications, utilizing episomal vectors that are gradually lost during cell divisions without genomic integration.
Materials and Reagents
- Source Somatic Cells: Human dermal fibroblasts (HDFs) from punch biopsy or peripheral blood mononuclear cells (PBMCs)
- Culture Medium: DMEM/F12 supplemented with 10% FBS, 1% non-essential amino acids, 1% GlutaMAX, 0.1% β-mercaptoethanol
- Reprogramming Vectors: Epstein-Barr virus (EBV)-based episomal plasmids expressing OCT4, SOX2, KLF4, L-MYC, LIN28, and shRNA for p53 (Addgene plasmids #41813, #41814, #41855)
- Transfection Reagent: Neon Transfection System or similar electroporation system
- Essential Small Molecules: Sodium butyrate (0.25mM), valproic acid (VPA, 0.5-1mM), 8-Br-cAMP (100µM)
- iPSC Culture Medium: Essential 8 (E8) or mTeSR1 medium with daily changes
- Extracellular Matrix: Matrigel or vitronectin-coated plates
Step-by-Step Procedure
Day 1: Somatic Cell Preparation
- Culture human dermal fibroblasts in DMEM/F12 + 10% FBS until 70-80% confluent
- Passage cells at 1:3 ratio and plate in 6-well format at 1×10^5 cells/well
- Incubate at 37°C, 5% CO2 for 24 hours
Day 2: Electroporation
- Prepare episomal plasmid DNA mixture (1μg each of OCT4/SOX2/KLF4/L-MYC/LIN28/shp53, total 6μg DNA)
- Harvest fibroblasts using 0.25% trypsin/EDTA, neutralize with serum-containing medium
- Wash cells with PBS, resuspend in electroporation buffer at 1×10^6 cells/100μL
- Electroporate using Neon Transfection System (1650V, 10ms, 3 pulses)
- Plate transfected cells on Matrigel-coated 6-well plates in fibroblast medium
- Incubate at 37°C, 5% CO2
Day 3-6: Transition Phase
- Continue culture in fibroblast medium with daily changes
- Add sodium butyrate (0.25mM) and VPA (0.5mM) on day 3 post-transfection
- Monitor morphological changes; early reprogramming cells appear more compact with increased nuclear-to-cytoplasmic ratio
Day 7-21: iPSC Emergence and Expansion
- Switch to Essential 8 medium on day 7 when small clusters emerge
- Continue sodium butyrate and VPA until day 14
- Change medium daily, observe for emergence of compact colonies with defined borders
- First iPSC colonies typically appear between days 18-25
- Manually pick and expand individual colonies on Matrigel-coated plates
Day 22+: Characterization and Validation
- Expand clonal lines and validate pluripotency markers (OCT4, NANOG, SSEA-4, TRA-1-60) via immunocytochemistry
- Perform karyotype analysis to confirm genomic integrity
- Verify loss of episomal plasmids via PCR after passage 10
- Conduct in vitro differentiation (embryoid body formation) to confirm trilineage potential
Protocol: Chemical Reprogramming with Small Molecules
Chemical reprogramming represents the safest approach for clinical applications, completely eliminating genetic manipulation.
Materials and Reagents
- 7C Cocktail: CHIR99021 (GSK3β inhibitor), 616452 (TGF-β inhibitor), Forskolin (adenylyl cyclase activator), DZNep (histone methylation inhibitor), VPA (HDAC inhibitor), 2-Methyl-5-hydroxytryptamine (5-HT receptor agonist), Tranylcypromine (LSD1 inhibitor)
- Culture Media: DMEM/F12, FBS, KSR (Knockout Serum Replacement), N2/B27 supplements
- Somatic Cells: Human fibroblasts or PBMCs
Step-by-Step Procedure
- Plate somatic cells at 5×10^4 cells/well in 6-well plates
- Culture in fibroblast medium for 24 hours until 60-70% confluent
- Switch to chemical reprogramming medium (DMEM/F12 + 10% KSR + 7C cocktail)
- Change medium every other day for 2 weeks
- Transfer cells to vitronectin-coated plates in E8 medium + 7C cocktail
- Continue culture until iPSC colonies emerge (typically 4-6 weeks)
- Manually pick and expand colonies in E8 medium without small molecules
The Scientist's Toolkit: Essential Research Reagents
Successful reprogramming requires careful selection of reagents and materials optimized for each step of the process.
Table 3: Essential Research Reagents for Somatic Cell Reprogramming
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| Reprogramming Vectors | Episomal plasmids (Addgene #41813-55), Sendai病毒 (CytoTune), mRNA kits | Delivery of reprogramming factors | Select based on application: research (viral) vs. clinical (non-integrating) |
| Culture Media | DMEM/F12, Essential 8, mTeSR1, ReproTeSR | Support cell growth and reprogramming | E8 for defined conditions; mTeSR for high efficiency |
| Small Molecules | VPA, Sodium butyrate, CHIR99021, RepSox, 8-Br-cAMP | Enhance efficiency, replace transcription factors | Optimize concentration for each cell type; monitor cytotoxicity |
| Extracellular Matrices | Matrigel, Vitronectin, Laminin-521 | Provide structural support and signaling cues | Vitronectin for defined conditions; Matrigel for high attachment |
| Cell Separation | FACS antibodies (SSEA-4, TRA-1-60), MACS sorting | Isolation of fully reprogrammed cells | Use multiple pluripotency markers to ensure complete reprogramming |
| Characterization Tools | Pluripotency antibodies, Karyostat kits, Trilineage differentiation kits | Validate iPSC quality and safety | Essential for confirming authentic pluripotency |
Quality Control and Safety Assessment
Rigorous quality control is essential for iPSCs intended for autologous therapy research:
Pluripotency Validation
- Immunocytochemistry for core pluripotency markers (OCT4, NANOG, SOX2, SSEA-4, TRA-1-60, TRA-1-81)
- RT-PCR analysis of endogenous pluripotency gene expression
- In vitro differentiation via embryoid body formation with assessment of all three germ layers
- Teratoma formation assay in immunocompromised mice (gold standard)
Genomic Integrity
- Karyotype analysis (G-banding) to detect chromosomal abnormalities
- SNP microarray for copy number variations
- Whole genome or exome sequencing to identify point mutations
Clearance Verification
- PCR analysis for vector persistence in episomal or Sendai virus methods
- Southern blot to confirm absence of integration for viral methods
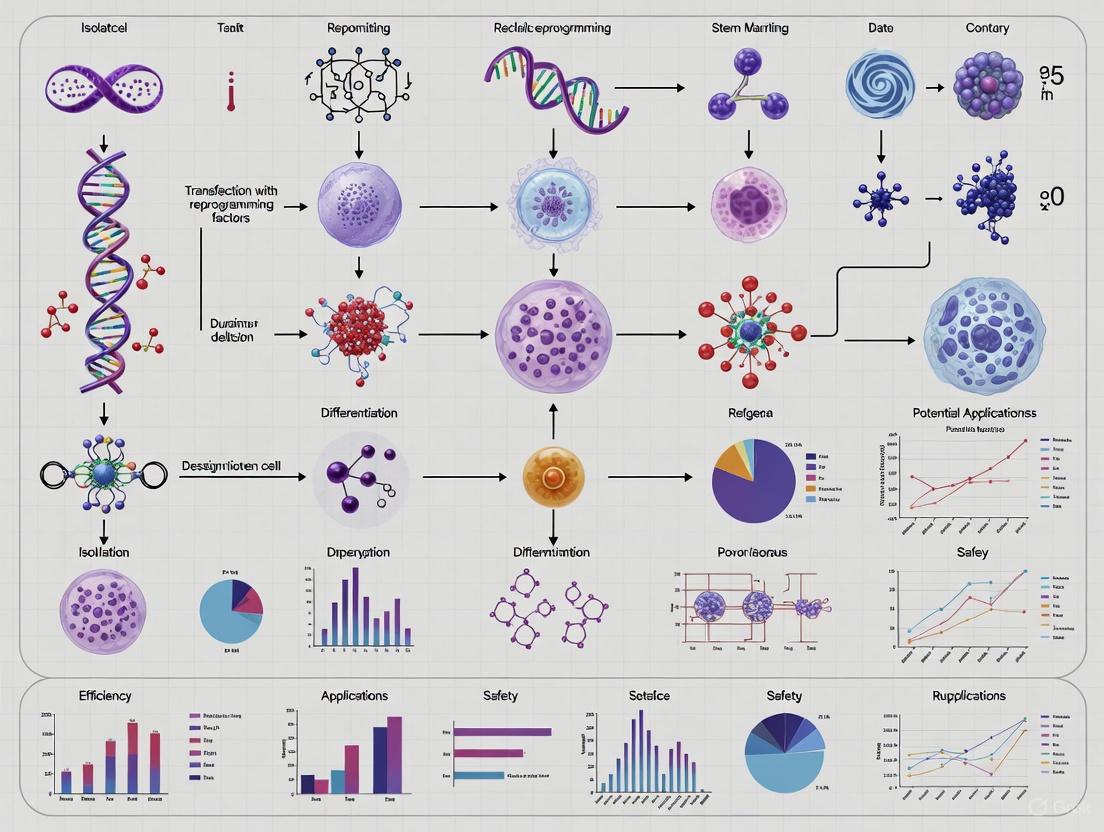
Workflow Visualization
Regulatory and Safety Considerations for Autologous Therapy
When developing iPSCs for autologous therapy within a research framework, several critical regulatory and safety aspects must be addressed:
Ethical Compliance
All research involving human somatic cells and iPSC derivation must comply with international guidelines, including the ISSCR Guidelines for Stem Cell Research and Clinical Translation [2]. Key considerations include:
- Proper informed consent from donors specifically addressing iPSC generation and potential applications
- Oversight by appropriate institutional review boards (IRB) and stem cell research oversight (SCRO) committees
- Adherence to jurisdictional regulations regarding human cell manipulation
Safety Optimization
- Oncogene minimization: Utilize L-Myc or N-Myc instead of c-Myc, or employ chemical reprogramming
- Integration-free methods: Prioritize episomal, mRNA, or protein-based delivery systems
- Rigorous screening: Implement comprehensive genomic and functional assays to ensure iPSC safety
- Documentation: Maintain detailed records of cell lineage, culture conditions, and characterization data
The field continues to evolve with emerging technologies such as chemical reprogramming completely eliminating genetic factors, and improved delivery methods increasing efficiency while reducing risks [1]. These advances promise to enhance the clinical applicability of iPSC technology for autologous therapies in the coming years.
Induced pluripotent stem cell (iPSC) technology has revolutionized regenerative medicine by enabling the generation of patient-specific pluripotent stem cells from somatic cells [3]. In the context of a broader thesis on autologous iPSC therapy protocols, this application note details the distinct immunological advantages of using a patient's own cells. Autologous iPSCs, generated through the reprogramming of a patient's somatic cells (such as fibroblasts), bypass the profound immune compatibility challenges inherent to allogeneic approaches [4]. This intrinsic immune matching fundamentally eliminates the risks of graft-versus-host disease (GvHD) and graft rejection, which remain significant obstacles in allogeneic cell-based therapies [5]. The following sections provide a detailed experimental and quantitative framework for researchers to validate and leverage the autologous advantage.
Table 1: Comparative Analysis of Autologous vs. Allogeneic Cell Therapy Platforms
| Parameter | Autologous iPSC-Derived Therapies | Allogeneic Third-Party Donor Cells | Allogeneic iPSC-Derived Therapies |
|---|---|---|---|
| Risk of GvHD | Negligible [5] | High (requires TCR knockout) [4] [5] | Moderate (requires immune engineering) [4] |
| Host Immune Rejection | Negligible (Self-tolerance maintained) | High (Risk of host-allograft response) [5] | High (Requires HLA camouflage/editing) [4] |
| Batch-to-Batch Variability | Low (Single, patient-specific clone) | High (Donor-dependent heterogeneity) [4] | Low (Clonal master cell line) |
| Typical Manufacturing Time | Prolonged (Patient-specific process) | Short (Off-the-shelf inventory) | Short (Off-the-shelf inventory) |
| Key Safety Modifications | Primarily for underlying disease correction | TCR knockout, HLA editing, safety switches [4] | TCR knockout, HLA editing, "cloaking" [6] |
Table 2: Immune Profiling Data from Xenogeneic MSC/EV Study
| Immune Parameter | Sham + MSC | RAS + MSC | Sham + EV | RAS + EV |
|---|---|---|---|---|
| Intrarenal T-cell Infiltration | Unchanged [7] | Unchanged [7] | Unchanged [7] | Unchanged [7] |
| Circulating Anti-Human Antibodies | Significantly Increased [7] | Significantly Increased [7] | Not Significant | Not Significant |
| Splenic CD19+ B-cells | Not Applicable | Reduced vs. RAS+EV [7] | Not Applicable | Higher vs. RAS+MSC [7] |
| IFN-γ Release (T-cell recall) | Reduced [7] | Reduced [7] | Reduced [7] | Reduced [7] |
Experimental Protocols for Validating Immune Compatibility
Protocol: In Vitro T-cell Recall Assay
Purpose: To assess the immunogenicity of autologous versus allogeneic iPSC-derived cells by measuring T-cell activation.
Methodology:
- Cell Preparation:
- Differentiate autologous and allogeneic iPSCs into the desired target cell type (e.g., neural progenitors, cardiomyocytes).
- Isolate peripheral blood mononuclear cells (PBMCs) from the same donor as the autologous iPSCs and from a genetically mismatched donor.
- Co-culture Setup:
- Irradiate the differentiated cells to arrest proliferation.
- Co-culture irradiated target cells with PBMCs at a standardized ratio (e.g., 1:10) in a 96-well plate for 5-7 days.
- Include positive controls (e.g., PBMCs stimulated with phytohemagglutinin) and negative controls (PBMCs alone).
- Analysis:
- IFN-γ Measurement: Collect supernatant and quantify IFN-γ release using an enzyme-linked immunosorbent assay (ELISA). Reduced IFN-γ levels indicate immunosuppressive properties or low immunogenicity [7].
- Flow Cytometry: Analyze T-cell activation markers (e.g., CD69, CD25) on co-cultured PBMCs using fluorochrome-conjugated antibodies and flow cytometry.
Protocol: Mixed Lymphocyte Reaction (MLR) Assay
Purpose: To evaluate the potential of iPSC-derived cells to elicit or suppress a GvHD-like response.
Methodology:
- Cell Preparation:
- Stimulator Cells: Differentiate allogeneic iPSCs into target cells. Irradiate (e.g., 30-50 Gy) or treat with mitomycin C to prevent proliferation.
- Responder Cells: Isolate PBMCs from a genetically mismatched healthy donor.
- Co-culture:
- Combine stimulator and responder cells in a culture plate. Use responder cells alone and stimulator cells alone as controls.
- Culture for 5-7 days.
- Outcome Measures:
- Proliferation: Measure responder T-cell proliferation using a colorimetric assay (e.g., MTT) or by flow cytometry using cell tracking dyes.
- Cytokine Profiling: Analyze supernatants for pro-inflammatory cytokines (IFN-γ, TNF-α, IL-2) via multiplex ELISA or cytometric bead array [5]. Successful evasion is indicated by minimal proliferation and low cytokine levels.
Protocol: In Vivo GvHD Assessment in Humanized Mouse Models
Purpose: To validate the safety and immune evasion of autologous iPSC-derived grafts in a pre-clinical model.
Methodology:
- Model Generation:
- Utilize immunodeficient mice (e.g., NSG mice).
- Engraft with a functional human immune system by injecting human CD34+ hematopoietic stem cells to create "humanized" mice.
- Graft Transplantation:
- Differentiate autologous (matched to the immune system donor) and allogeneic (mismatched) iPSCs into the desired cell product.
- Transplant the cells into the target organ (e.g., brain for neural grafts) of the humanized mice.
- Post-Mortem Analysis:
- Immune Cell Activation: Monitor blood and cerebrospinal fluid for elevated levels of human inflammatory cytokines.
- Graft Survival: After several weeks, analyze grafts histologically for human T-cell (CD3+) and macrophage (F4/80+) infiltration. Compare autologous and allogeneic groups [6].
- Systemic Immunity: Examine spleen and lymph nodes for enlargement, a sign of systemic immune activation against the graft [6].
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Autologous iPSC Immune Profiling
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Reprogramming Factors | Ectopic expression of OCT4, SOX2, KLF4, MYC to generate iPSCs from somatic cells [3]. | Use integration-free methods (e.g., Sendai virus, mRNA) for clinical compliance. |
| Lymphocyte Separation Medium | Isolation of high-quality PBMCs from patient blood for co-culture assays. | Maintain sterility and cell viability during density gradient centrifugation. |
| Anti-Human Cytokine ELISA Kits | Quantitative measurement of IFN-γ, TNF-α, IL-2, etc., from assay supernatants [7] [5]. | Choose kits with high sensitivity and specificity for human cytokines. |
| Flow Cytometry Antibodies | Detection of immune cell markers (CD3, CD4, CD8, CD69, CD25) and intracellular cytokines. | Utilize multicolor panels with appropriate fluorescence compensation controls. |
| Immunodeficient Mice (e.g., NSG) | Generation of humanized mouse models for in vivo GvHD and rejection studies [6]. | Require specialized animal facility conditions and IACUC protocols. |
| HLA Typing Kit | Confirm genetic match between autologous iPSCs and patient immune cells. | Essential for validating the autologous model and screening allogeneic controls. |
Clinical Trial Outcomes in Parkinson’s Disease and Retinal Diseases
Recent clinical trials demonstrate the progress of iPSC-based therapies for neurodegenerative and retinal diseases. The tables below summarize quantitative safety and efficacy data from key studies.
Table 1: Phase I/II Trial of Allogeneic iPSC-Derived Dopaminergic Progenitors for Parkinson's Disease [8]
| Outcome Measure | Results at 24 Months (n=6 for efficacy) | Notes |
|---|---|---|
| Serious Adverse Events | 0 | No graft overgrowth or tumors on MRI. |
| Other Adverse Events | 73 total events (72 mild, 1 moderate) | Most frequent was application site pruritus (4/7 patients). |
| MDS-UPDRS Part III OFF Score | Average improvement of 9.5 points (20.4%) | 4 of 6 patients showed improvement. |
| MDS-UPDRS Part III ON Score | Average improvement of 4.3 points (35.7%) | 5 of 6 patients showed improvement. |
| Hoehn & Yahr Stage | Improved in 4 patients | Measured during OFF-time. |
Dopamine Production (18F-DOPA Ki) |
Increased by 44.7% in the putamen | Higher increase observed in the high-dose group. |
Table 2: Selected Clinical Trials of Stem Cell Therapies for Retinal Diseases [9] [10] [11]
| Condition | Therapy / Approach | Key Findings |
|---|---|---|
| Age-related Macular Degeneration (AMD) | hESC-derived RPE cells on a scaffold (CPCB-RPE1 implant) [9] | Phase 1/2a showed safety of implant and surgical procedure; immunosuppression required. |
| Wet AMD | Autologous iPSC-derived RPE cell suspension [9] | No rejection or tumor formation at 12 months in a patient; no significant visual acuity improvement. |
| Wet AMD | hESC-derived RPE patch [9] | Improved visual acuity, good host integration, no rejection/tumors at 12 months (Phase 1). |
| Retinitis Pigmentosa (RP) | Allogeneic iPSC-derived retinal organoids [9] | Graft stable at 2 years; progression of vision loss slowed in treated vs. untreated eye. |
| Retinitis Pigmentosa (RP) | Intravitreal injection of autologous CD34+ bone marrow stem cells [9] | Phase 1 showed stabilization or minor improvement in visual acuity at 6 months. |
| Central Retinal Vein Occlusion (CRVO) | Intravitreal autologous CD34+ stem cells (TRUST trial) [10] | Study demonstrated safety and feasibility of the procedure. |
Experimental Protocols
Protocol for the Generation and Transplantation of iPSC-Derived Dopaminergic Progenitors in Parkinson's Disease
This protocol is adapted from the phase I/II clinical trial using allogeneic iPSCs [8].
iPSC Line Generation:
- Establish clinical-grade human iPSCs from a healthy donor's peripheral blood mononuclear cells (PBMCs).
- Select a donor homozygous for high-frequency HLA haplotypes to enable broader immune matching.
Dopaminergic Progenitor Differentiation:
- Induce DA progenitors from iPSCs using a specified cytokine and small molecule protocol.
- On days 11-13 of differentiation, sort for CORIN+ cells to enrich for floor plate-derived DA progenitors.
- Culture the sorted CORIN+ cells in neural differentiation medium to form aggregate spheres.
- Quality Control: Perform single-cell RT-qPCR to confirm the final product composition (approximately 60% DA progenitors and 40% DA neurons). Ensure the absence of TPH2-expressing serotonergic neurons.
Transplantation Surgery:
- Use a neurosurgical navigation system for precise stereotactic transplantation.
- Transplant the fresh cell product bilaterally into the postcommissural putamen.
- Dosing: Administer either a low dose (2.1–2.6 million cells per hemisphere) or a high dose (5.3–5.5 million cells per hemisphere).
Immunosuppression:
- Initiate tacrolimus (0.06 mg/kg twice daily) pre-transplantation, targeting trough levels of 5–10 ng/mL.
- Reduce the tacrolimus dose by half at 12 months and discontinue it at 15 months post-transplantation.
Protocol for iPSC-Derived Retinal Organoid Generation and Modeling of Inherited Retinal Diseases
This protocol outlines the use of patient-specific iPSCs to model IRDs like retinitis pigmentosa (RP) [12].
Somatic Cell Sourcing and Reprogramming:
- Obtain patient somatic cells via a minimally invasive method (e.g., skin biopsy (dermal fibroblasts), peripheral blood draw (PBMCs), or urine cell collection).
- Reprogram somatic cells into iPSCs using non-integrating Sendai virus or episomal vectors delivering reprogramming factors (OCT4, SOX2, KLF4, c-MYC).
Retinal Organoid Differentiation:
- Differentiate iPSCs into 3D retinal organoids using a stepwise protocol mimicking embryonic retinal development.
- Initiate neural induction using dual SMAD inhibition.
- Promote eye field formation by supplementing with IGF1, FGF2, and Nodal.
- Culture aggregates in a 3D matrix to support self-organization into laminated neural retina, containing photoreceptors, bipolar cells, ganglion cells, and retinal pigment epithelium (RPE).
Disease Modeling and Phenotypic Analysis:
- Compare the morphology, gene expression, and protein localization of patient-derived organoids to healthy control organoids.
- Analyze disease-specific phenotypes, such as:
Therapeutic Intervention Testing:
- Gene Correction: Use CRISPR/Cas9 to correct the pathogenic mutation in patient iPSCs prior to differentiation. Use the isogenic, corrected cell line as a critical control to confirm rescue of the disease phenotype in subsequent organoids [12].
- Drug Screening: Utilize the patient-derived organoids to test the efficacy of small molecules or neuroprotective factors aimed at slowing photoreceptor degeneration.
iPSC Therapy Workflow
The end-to-end process for developing an autologous iPSC therapy, from patient cell collection to transplantation and monitoring, is shown below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for iPSC-Based Therapy Development
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Reprogramming Factors | Induction of pluripotency in somatic cells. | Yamanaka Factors (OSKM): Oct4, Sox2, Klf4, c-Myc. Delivered via non-integrating methods (e.g., Sendai virus, mRNA) [12]. |
| Differentiation Media Components | Directing iPSC fate toward specific lineages. | Neural Induction: SMAD inhibitors (e.g., LDN-193189, SB-431542) [12]. Dopaminergic Induction: Specific cytokine cocktails [8]. Retinal Induction: IGF1, FGF2, Nodal [12]. |
| Cell Sorting Reagents | Isolation of target progenitor cells. | Antibodies against surface markers (e.g., anti-CORIN for dopaminergic progenitors [8]). |
| Culture Matrices & Scaffolds | 3D support for organoid development or transplantation. | Synthetic membranes (e.g., parylene scaffold for RPE sheets [9]). Basement membrane extracts (e.g., Matrigel) for organoid culture. |
| Gene Editing Tools | Correction of disease-causing mutations in patient iPSCs. | CRISPR/Cas9 system for precise genome editing [12]. |
| Immunosuppressants | Prevention of allogeneic graft rejection in clinical trials. | Tacrolimus [8] [13]. Autologous therapies aim to eliminate this requirement [14]. |
Ethical and Regulatory Landscape for Patient-Specific Therapies
This document provides a detailed framework of the ethical and regulatory considerations essential for conducting research on autologous induced pluripotent stem cell (iPSC) therapies. The convergence of personalized medicine and advanced cellular technologies necessitates rigorous protocols to ensure patient safety, data integrity, and regulatory compliance. These application notes are designed to guide researchers, scientists, and drug development professionals in navigating the complex landscape of patient-specific therapy development, with a specific focus on iPSCs, which are generated by reprogramming a patient's own somatic cells to a pluripotent state, thereby avoiding the ethical concerns associated with embryonic stem cells [15].
The development of autologous iPSC-based therapies operates within a dynamic regulatory environment and is subject to a suite of ethical requirements. Key among these are the principles of autonomy, beneficence, non-maleficence, and justice [15]. These principles directly inform protocols for informed consent, patient privacy, and the equitable distribution of emerging treatments. Furthermore, regulatory bodies like the U.S. Food and Drug Administration (FDA) provide specific pathways for the oversight of such therapies, classifying them as drugs or biologics when they undergo more than minimal manipulation [15]. Adherence to these guidelines is not optional but is fundamental to the responsible translation of research from the laboratory to the clinic.
Ethical Framework and Considerations
The ethical foundation of patient-specific therapy research is built upon widely shared principles that call for rigor, oversight, and transparency in all areas of practice [2]. Adherence to these principles provides assurance that research is conducted with scientific and ethical integrity.
Core Ethical Principles
The four ethical principles of autonomy, beneficence, non-maleficence, and justice provide a robust framework for evaluating research and clinical applications of stem cell-based therapies [15].
- Autonomy underscores an individual’s right to make informed decisions about their own body and health. This is operationalized through the process of informed consent, where patients are given accurate, complete, and understandable information to facilitate a decision [15] [16].
- Beneficence entails the obligation to act in the best interests of the patient or research participant, maximizing potential benefits while minimizing harm. For example, in developing stem cell therapies for spinal cord injury, researchers must weigh the potential benefits of neurological improvement against the risks of invasive procedures and potential adverse events [15].
- Non-maleficence refers to the clinician's and researcher's obligation to "do no harm." This includes thorough preclinical testing to evaluate risks and establishing follow-up protocols to detect and manage complications [15].
- Justice ensures the fair, equitable, and appropriate use of stem cell therapies, without discrimination or exploitation of vulnerable populations. This includes addressing challenges due to structural injustices and ensuring that the risks and benefits of research are distributed justly [2].
Table 1: Application of Core Ethical Principles in Autologous iPSC Research
| Ethical Principle | Practical Application in iPSC Protocol | Key Considerations |
|---|---|---|
| Autonomy | Obtaining informed consent for somatic cell donation, genetic reprogramming, and long-term data use. | Explain complex information simply; document consent for primary and secondary research uses; ensure right to withdraw [17] [15]. |
| Beneficence | Conducting rigorous preclinical in vitro and in vivo studies to establish a positive risk-benefit profile. | Maximize potential therapeutic benefit while minimizing risks of tumorigenicity or incorrect differentiation [15]. |
| Non-maleficence | Implementing stringent quality control and safety testing for the final cellular product. | Test for genomic instability, contamination, and teratoma formation; plan long-term patient follow-up [15]. |
| Justice | Designing clinical trials and access programs to include diverse populations. | Address socioeconomic barriers that may limit access to expensive, personalized treatments [2] [15]. |
Informed Consent Protocol
Informed consent is a process, not a single event, and is critical for respecting patient autonomy. The following protocol outlines the key steps for obtaining valid informed consent in autologous iPSC research.
Protocol 2.2: Informed Consent for Autologous iPSC Donation and Use
Objective: To ensure the donor participant fully understands the purpose, procedures, risks, benefits, and alternatives of the research before providing voluntary consent for the derivation and use of iPSCs from their somatic cells.
Materials:
- IRB-approved informed consent document
- Consent form written in plain language at an 8th-grade reading level
- Visual aids (e.g., diagrams, flowcharts) explaining cell reprogramming and differentiation
- Private consultation room
- Documentation system (electronic or paper-based)
Methodology:
- Pre-Consent Preparation: The research team must ensure the consent form is reviewed and approved by an Institutional Review Board (IRB) or Ethics Committee. The form must clearly distinguish between standard of care and investigational procedures.
- Participant Engagement: A trained member of the research team meets with the potential participant in a private setting. The researcher must assess the participant's capacity to understand the information and make a decision.
- Information Disclosure: The researcher presents all material information verbally and in writing, including:
- The primary research purpose and that the therapy is investigational.
- The complete procedure for somatic cell collection (e.g., skin biopsy, blood draw).
- The scientific process of reprogramming somatic cells into iPSCs and subsequent differentiation into the target cell type.
- Potential risks, including those from cell collection, unforeseen risks from the cellular product (e.g., tumor formation, immune reactions), and privacy risks associated with genetic data.
- Potential benefits to the participant and to society.
- Alternatives to participation in the research.
- Procedures for protecting the confidentiality of genetic and health information.
- The possibility of long-term storage and future use (secondary research) of cells and data, with a clear option to consent or decline this use [17].
- The right to refuse or withdraw at any time without penalty.
- Assessment of Understanding: The researcher assesses the participant's understanding by asking open-ended questions (e.g., "Can you tell me in your own words what the main goal of this study is?" or "What are the potential risks that concern you the most?").
- Documentation of Consent: After all questions are answered and understanding is confirmed, the participant is invited to sign and date the consent form. The researcher also signs the form. A copy is provided to the participant.
- Ongoing Consent: The consent process is ongoing. Participants must be re-contacted to provide additional consent if significant new information arises or if their cells/data are to be used for a new research purpose not covered in the original consent [17] [15].
Privacy and Data Security
Genetic and cellular data generated in iPSC research are uniquely identifiable and sensitive. A 2024 National Health Database report documented 1,247 incidents of genetic data misuse in healthcare settings, highlighting the critical need for robust protections [17]. By 2025, between 100 million and 1 billion genomes are expected to be sequenced globally, increasing privacy risks.
Best practices for protecting patient information include:
- Encryption: Using cutting-edge cryptographic protocols to encode all patient data, allowing only authorized access [17].
- Anonymization and Pseudonymization: Stripping personal identifiers from data and using a code that can be reversed only by an authorized holder. Techniques include adding random noise or limiting data release, though these must be balanced against data utility [17].
- Secure Systems: Implementing systems with rigorous security audits and updates to shield data from breaches.
Regulatory Landscape and Compliance
Navigating the regulatory pathway is critical for the clinical translation of autologous iPSC therapies. The regulatory environment is evolving rapidly, with a focus on ensuring safety and efficacy while facilitating innovation.
FDA Regulatory Pathways
In the United States, the FDA regulates regenerative medicine products, including iPSC-based therapies. The regulatory status of a product depends on the nature of its manipulation and use.
- Minimally Manipulated HCT/Ps: Human cells, tissues, and cellular and tissue-based products (HCT/Ps) that are minimally manipulated, intended for homologous use, and not combined with another article are regulated under Section 361 of the Public Health Service Act. This pathway focuses on preventing the transmission of infectious disease [15].
- More than Minimal Manipulation: Autologous iPSCs are subject to more than minimal manipulation due to the reprogramming process. Consequently, they do not qualify for the Section 361 exemption and are regulated as drugs or biologics [15]. This requires an Investigational New Drug (IND) application before initiating clinical trials, followed by a New Drug Application (NDA) or Biologics License Application (BLA) for market approval.
The FDA has established initiatives like the Regenerative Medicine Advanced Therapy (RMAT) designation to expedite the development and review of promising regenerative medicine therapies [15].
Table 2: Key Regulatory and Ethical Changes Impacting Clinical Trials (2025)
| Change Area | Description | Impact on Autologous iPSC Trials |
|---|---|---|
| ICH E6(R3) Guidelines | New international standards emphasizing data integrity and traceability [18]. | Requires detailed documentation for every stage of the cellular product lifecycle, from cell sourcing to final product administration and long-term storage. |
| Single IRB Review | FDA harmonization on using a single IRB for multicenter studies [18]. | Streamlines the ethical review process, reducing duplication and accelerating trial start-up times across different clinical sites. |
| AI and Real-World Data | FDA draft guidance on using AI and real-world data in regulatory decision-making [18]. | Potential to use AI for analyzing complex iPSC differentiation data and to incorporate RWD for long-term safety and effectiveness monitoring. |
| Diverse Participant Enrollment | Increased regulatory focus on enrolling diverse populations in clinical trials [18]. | Requires proactive trial design to ensure participant diversity in age, sex, gender identity, and ethnicity to improve generalizability of results [2]. |
International Guidelines and Oversight
Internationally, guidelines such as those from the International Society for Stem Cell Research (ISSCR) provide critical guidance. The ISSCR guidelines promote "an ethical, practical, and sustainable approach to stem cell research and the development of cell therapies" [2]. They emphasize fundamental principles such as the integrity of the research enterprise, primacy of patient welfare, respect for research subjects, transparency, and social justice [2]. While these guidelines do not supersede local laws, they complement legal frameworks and inform the development of national regulations. Key recommendations relevant to iPSC research include stringent oversight for stem cell-based embryo models (SCBEMs) and a clear prohibition on transferring these models into a uterus [2].
Experimental and Clinical Workflow Protocol
This section outlines a comprehensive workflow from cell sourcing to clinical application, integrating the ethical and regulatory checkpoints detailed in previous sections.
Protocol 4.0: Preclinical Development of Autologous iPSC-Derived Cardiomyocytes
Objective: To generate and characterize functional cardiomyocytes from a patient's somatic cells for potential therapeutic use, following good laboratory practices (GLP) and preparing for regulatory submission.
Materials:
- Research Reagent Solutions: See Table 3.
- Sterile tissue culture equipment (hood, incubator, centrifuge)
- Inverted phase-contrast microscope
- Flow cytometer
- PCR machine and supplies for qRT-PCR
- Immunocytochemistry supplies (primary and secondary antibodies, mounting medium with DAPI)
- Animal model for in vivo safety testing (e.g., immunodeficient mouse)
Table 3: Research Reagent Solutions for iPSC-Cardiomyocyte Differentiation
| Reagent/Material | Function | Example |
|---|---|---|
| Dermal Fibroblast Media | Maintenance of somatic cells prior to reprogramming. | Dulbecco's Modified Eagle Medium (DMEM) with 10% Fetal Bovine Serum (FBS). |
| Reprogramming Vector | Delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC). | Non-integrating Sendai virus or episomal plasmids. |
| iPSC Maintenance Media | Culture of established iPSC lines in an undifferentiated state. | mTeSR1 or StemFlex media containing FGF2 and TGF-β. |
| Cardiac Differentiation Media | Directed differentiation of iPSCs toward the cardiac lineage. | RPMI 1640 media with B-27 supplement, sequentially using activin A, BMP4, and Wnt inhibitors. |
| Flow Cytometry Antibodies | Characterization of cell surface and intracellular markers. | Antibodies against TRA-1-60 (pluripotency), cTnT (cardiomyocytes). |
| LIVE/DEAD Viability/Cytotoxicity Kit | Assessment of cell viability and cytotoxicity in the final product. | -- |
Methodology:
- Cell Sourcing and Consent: Obtain a skin punch biopsy or peripheral blood sample from the donor after full informed consent (as per Protocol 2.2) and IRB approval.
- Reprogramming to iPSCs: Isolate dermal fibroblasts or peripheral blood mononuclear cells (PBMCs). Transduce cells with a non-integrating reprogramming vector. Culture cells on feeder layers or defined matrices until iPSC colonies appear (typically 2-3 weeks). Pick and expand individual colonies.
- iPSC Characterization: Validate the pluripotent state of established lines through:
- Immunocytochemistry: Stain for pluripotency markers (OCT4, SOX2, NANOG, TRA-1-60).
- qRT-PCR: Analyze expression of endogenous pluripotency genes.
- Embryoid Body Formation: Demonstrate spontaneous differentiation into cell types of all three germ layers in vitro.
- Directed Differentiation to Cardiomyocytes: Differentiate iPSCs using a standardized small molecule-directed protocol. Initiate differentiation with activin A and BMP4 to induce mesoderm formation, followed by Wnt inhibition to promote cardiac specification. Spontaneously beating clusters should appear after 7-10 days.
- Functional and Safety Testing:
- Purity: Analyze the percentage of cells expressing cardiac troponin T (cTnT) via flow cytometry (target >90%).
- Function: Assess electrophysiological activity via patch clamp or multi-electrode array (MEA).
- Safety: Perform in vivo teratoma assay by injecting undifferentiated iPSCs into immunodeficient mice to confirm the absence of tumorigenic cells in the final differentiated product. Test for mycoplasma and endotoxin contamination.
- Data Compilation for Regulatory Submission: Compile all data from characterization, differentiation, and safety testing into a comprehensive report to support an IND application to the FDA.
A Step-by-Step Protocol: From Patient Cell to Clinical Product
The initial phase of any autologous induced pluripotent stem cell (iPSC) therapy program is critical, establishing the foundation for all subsequent manufacturing and clinical outcomes. This stage encompasses the identification of suitable patients and the selection and acquisition of a somatic cell source that will be reprogrammed. The chosen somatic cell type must not only be accessible and feasible to collect but also possess molecular characteristics conducive to efficient reprogramming, ensuring the generation of high-quality iPSCs. This document details standardized protocols for patient screening and the evaluation of various somatic cell sources, with a particular focus on peripheral blood, for use in autologous iPSC therapy research and development.
Patient Screening and Eligibility
The first operational step involves creating a trial-ready cohort of potential patient candidates through a comprehensive screening study [19]. The objective is to identify individuals who meet specific clinical and molecular criteria before proceeding to cell harvest.
Key Screening Considerations
- Clinical Phenotype and Diagnosis: Precise and confirmed diagnosis of the target disease (e.g., idiopathic Parkinson's disease) is essential, as the derived iPSCs will model the patient's specific condition [19] [20].
- Genetic Background: Understanding the patient's genetic landscape is crucial, particularly for genetically defined diseases. This includes screening for known pathogenic variants and assessing the potential impact of clonal hematopoiesis (CH) when using blood-derived cells [21].
- General Health and Comorbidities: Patients should be evaluated for conditions that could complicate cell collection, reprogramming, or future re-implantation, such as active infections, uncontrolled immune disorders, or bleeding diatheses.
- Informed Consent: A rigorous informed consent process, overseen by an Institutional Review Board (IRB) or Ethics Committee, is mandatory. Patients must be clearly informed about the investigational nature of the therapy, the multi-step process, long-term follow-up requirements, and potential risks, including tumorigenicity [2].
Screening for Clonal Hematopoiesis
When considering peripheral blood as a cell source, it is imperative to screen for clonal hematopoiesis (CH). CH is an age-related condition where hematopoietic stem cells acquire mutations that confer a fitness advantage, leading to clonal expansion [21]. Using blood cells harboring such driver mutations for reprogramming could result in iPSCs with compromised genomic integrity or biased differentiation potential.
Recommendation: For patients over 40, consider using exome or genome sequencing of blood-derived DNA to screen for somatic mutations in classical CH driver genes (e.g., DNMT3A, TET2, ASXL1, PPM1D, JAK2) and novel fitness-inferred drivers (e.g., CHEK2, SH2B3, SRCAP) [21]. The presence of a large CH clone (VAF > 0.1) may necessitate the selection of an alternative somatic cell source.
Table 1: Comparison of Common Somatic Cell Sources for iPSC Generation
| Cell Source | Collection Method | Invasiveness | Reprogramming Efficiency | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Venipuncture | Minimally invasive | Moderate to High [22] | Readily available, large donor pool, established transport protocols. | Requires stimulation for proliferation; risk of pre-existing somatic mutations (CH) [21]. |
| Skin Fibroblasts | Punch biopsy | Invasive | Moderate [22] | Robust culture, well-established reprogramming protocols. | Slower expansion, requires tissue dissection, visible scar. |
| Keratinocytes (Plucked Hair) | Plucking hair follicles | Non-invasive | High [22] | High reprogramming efficiency, easy and inexpensive collection/transport. | Limited cell number per plucking, potential for microbial contamination. |
| Urinary Epithelial Cells | Urine sample | Non-invasive | Moderate [22] | Completely non-invasive, suitable for repeated sampling. | Lower cell yield, heterogeneity of cell types, potential contaminants. |
Protocols for Somatic Cell Collection and Initial Culture
Below are detailed protocols for the collection and initial processing of two commonly used somatic cell sources: peripheral blood and keratinocytes from plucked hair.
Protocol: Isolation and Culture of Peripheral Blood Mononuclear Cells (PBMCs)
Principle: PBMCs, primarily lymphocytes and monocytes, are isolated from whole blood via density gradient centrifugation and can be reprogrammed directly or after expansion.
Materials:
- Sodium Heparin or EDTA blood collection tubes
- Ficoll-Paque PLUS or equivalent density gradient medium
- Phosphate-Buffered Saline (PBS), without Ca2+/Mg2+
- PBMC culture medium: RPMI-1640 supplemented with 10% Fetal Bovine Serum (FBS), 1% Glutamax, 1% Non-Essential Amino Acids (NEAA), 1% Sodium Pyruvate, 0.1% β-Mercaptoethanol, and 1% Penicillin-Streptomycin.
- T-cell expansion stimulants (e.g., IL-2, CD3/CD28 activator) if expansion is required.
Method:
- Blood Collection: Collect 20-40 mL of venous blood into heparin or EDTA tubes. Invert gently to mix.
- Dilution: Dilute the blood 1:1 with PBS.
- Density Gradient Centrifugation:
- Carefully layer the diluted blood over half its volume of Ficoll-Paque in a centrifuge tube.
- Centrifuge at 400 × g for 30-40 minutes at room temperature with the brake off.
- After centrifugation, four layers will form. The PBMCs are located at the interface between the plasma (top) and Ficoll (middle) layers.
- PBMC Harvesting:
- Gently aspirate the upper plasma layer.
- Carefully transfer the cloudy PBMC interface layer to a new 50 mL tube using a sterile pipette.
- Washing:
- Fill the tube with PBS and centrifuge at 300 × g for 10 minutes.
- Aspirate the supernatant. Resuspend the cell pellet in PBS and repeat the wash step.
- Cell Counting and Cryopreservation:
- Resuspend the final cell pellet in a suitable cryopreservation medium (e.g., 90% FBS, 10% DMSO).
- Count cells using a hemocytometer. Aliquot and freeze cells at a concentration of 5-10 million cells/mL using a controlled-rate freezer, then transfer to liquid nitrogen for long-term storage.
- Optional T-cell Expansion: For enhanced reprogramming efficiency, thawed PBMCs can be stimulated with human IL-2 (50-100 U/mL) and CD3/CD28 activators for 3-5 days in PBMC culture medium before reprogramming.
Protocol: Harvesting and Culture of Keratinocytes from Plucked Hair
Principle: Plucked hair follicles contain actively proliferating keratinocyte stem cells and transit-amplifying cells in the bulge and bulb regions, which are highly amenable to reprogramming [22].
Materials:
- Sterile forceps
- Disinfectant (e.g., 70% ethanol)
- Coated culture vessels (e.g., Collagen I, Fibronectin)
- Keratinocyte Serum-Free Medium (K-SFM) with supplements (Bovine Pituitary Extract, recombinant EGF)
- Antibiotic-Antimycotic solution
Method:
- Hair Plucking: Identify an area for plucking (typically scalp or beard). Clean the skin with 70% ethanol. Using sterile forceps, firmly grasp 10-20 hair shafts and pluck rapidly in the direction of growth to ensure the root (bulb) is extracted.
- Transport: Place plucked hairs immediately into a sterile tube containing K-SFM with 2x Antibiotic-Antimycotic. Store at 4°C for short-term transport (up to 24h).
- Primary Explant Culture:
- In a biosafety cabinet, transfer each hair follicle to a well of a 24-well plate pre-coated with collagen.
- Gently place the follicle in the center of the well and add a minimal volume of K-SFM (just enough to cover the follicle but not allow it to float).
- Incubate the plate at 37°C, 5% CO2 for 2-3 days to allow for attachment.
- Outgrowth and Expansion:
- After attachment, carefully add more K-SFM to fully cover the well.
- Change the medium every 2-3 days.
- Keratinocyte outgrowth from the follicle is typically visible within 5-7 days.
- Once outgrowths are substantial, dissociate and passage cells using trypsin/EDTA onto larger coated vessels for expansion before reprogramming or cryopreservation.
Workflow Visualization
The following diagram summarizes the key decision points and pathways in the initial patient screening and somatic cell selection process.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Somatic Cell Isolation and Culture
| Research Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Density Gradient Medium | Isolation of PBMCs from whole blood based on buoyancy. | Ficoll-Paque PLUS, Lymphoprep. Must be at room temperature for optimal separation. |
| Keratinocyte Serum-Free Medium (K-SFM) | Selective medium for the culture and expansion of human keratinocytes. | Gibco K-SFM, defined formulation with EGF and BPE supplements; inhibits fibroblast overgrowth. |
| Cryopreservation Medium | Long-term storage of somatic cells prior to reprogramming. | Typically contains 90% FBS/10% DMSO or commercial serum-free alternatives; controlled-rate freezing is critical. |
| Cell Culture Coatings | Provides a substrate for adhesion and growth of adherent somatic cells like keratinocytes and fibroblasts. | Collagen I, Collagen IV, Fibronectin, Vitronectin. |
| T-Cell Activation Reagents | Stimulates proliferation of T-lymphocytes from PBMCs, enhancing reprogramming efficiency. | Recombinant human IL-2, anti-CD3/CD28 antibodies or beads. |
| Antibiotic-Antimycotic | Prevents bacterial and fungal contamination in primary cell cultures, especially from non-sterile sources like hair and urine. | Penicillin-Streptomycin-Amphotericin B solutions. Use at higher concentrations for initial explant culture. |
The choice of reprogramming strategy is a critical first step in establishing a protocol for autologous induced pluripotent stem cell (iPSC) therapy research. Reprogramming methods are broadly categorized based on whether the genetic material carrying the reprogramming factors integrates into the host cell's genome. This decision fundamentally impacts the safety profile, efficiency, and subsequent applicability of the resulting iPSCs for clinical use [23] [24]. Selecting an appropriate method requires balancing these factors against the specific needs of the research, with a general trajectory favoring non-integrating methods for clinical translation to minimize the risks of insertional mutagenesis and tumorigenicity [25] [24]. This document provides a detailed comparison of these strategies and standardized protocols for their implementation.
Method Comparison & Selection Guide
The table below summarizes the key characteristics of major reprogramming vector systems, providing a basis for informed experimental selection.
Table 1: Comparative Analysis of iPSC Reprogramming Methods
| Method Type | Specific Vector/Platform | Genomic Integration | Reprogramming Efficiency | Key Advantages | Key Disadvantages & Clinical Concerns |
|---|---|---|---|---|---|
| Integrating | Retrovirus [23] [26] | Yes | Moderate to High | Robust protocol; high efficiency in dividing cells. | Random integration; insertional mutagenesis; transgene reactivation risk (e.g., c-Myc) [23]. |
| Integrating | Lentivirus [25] | Yes | Moderate to High | Can transduce non-dividing cells; consistent expression. | Random integration; complex clearance; potential for residual vector expression [25]. |
| Non-Integrating | Sendai Virus (SeV) [23] [24] | No | High | High efficiency; robust reprogramming; does not require transfection. | Viral immunogenicity; lengthy process to dilute/clear viral components [23]. |
| Non-Integrating | Episomal Vectors [23] [25] | No (Low) | Low | Non-viral; simple structure; transgene clearance is rapid [23]. | Low efficiency often requires oncogenes (c-Myc/Lin28) or p53 suppression to be effective [23]. |
| Non-Integrating | Synthetic mRNA [23] [24] | No | Moderate | Non-viral; highly defined; precise control. | Labor-intensive (daily transfections); can trigger innate immune response [23]. |
| Non-Integrating | Recombinant Protein [24] | No | Very Low | Genetically unmodified end product; high safety potential. | Extremely low efficiency; technically challenging; requires protein purification [24]. |
To guide the selection process, the following workflow diagram outlines the key decision points when choosing a reprogramming strategy for autologous therapy research.
Detailed Experimental Protocols
Protocol A: Reprogramming with Non-Integrating Episomal Vectors
This protocol is optimized for generating clinical-grade iPSCs from human dermal fibroblasts (HDFs) or peripheral blood mononuclear cells (PBMCs) using episomal plasmids, as described in [23].
Key Research Reagent Solutions:
- Reprogramming Vector Kit: Commercially available episomal plasmid kit (e.g., Invitrogen CytoTune-iPS 2.1 Sendai Free Episomal Kit).
- Cell Culture Medium: Fibroblast growth medium (DMEM + 10% FBS) or PBMC medium (RPMI-1640 + 10% FBS).
- Nucleofector System & Kit: (e.g., Lonza Nucleofector 2b Device and appropriate Cell Line Nucleofector Kit).
- iPSC Culture Medium: Essential 8 or mTeSR1 medium.
- Matrix: Vitronectin (VTN-N) or Matrigel-coated plates.
Procedure:
- Cell Preparation: Expand and passage target somatic cells (HDFs or PBMCs). One day before nucleofection, harvest and count cells. Ensure >90% viability.
- DNA Preparation: Prepare a sterile mixture of episomal plasmids (e.g., expressing OCT3/4, SOX2, KLF4, L-MYC, LIN28, and shRNA for p53). Use 1-2 µg of total DNA per nucleofection.
- Nucleofection: For 1x10^6 cells, resuspend the cell pellet in 100 µL of Nucleofector Solution. Add the DNA mixture and transfer to a certified cuvette. Run the appropriate nucleofection program (e.g., U-023 for PBMCs). Immediately add pre-warmed culture medium post-nucleofection.
- Plating & Recovery: Plate the transfected cells onto a vitronectin-coated 6-well plate at a density of 1-3x10^5 cells per well. Culture under standard conditions (37°C, 5% CO2). Change medium after 48 hours.
- Transition to iPSC Culture: Between days 5-7, gently transition the culture to iPSC culture medium. Continue feeding daily.
- Colony Picking: iPSC colonies with compact, hESC-like morphology will appear between days 18-28. Manually pick individual colonies using a stereomicroscope and transfer them to a 24-well plate pre-coated with matrix for expansion.
- Quality Control: Confirm the absence of episomal plasmids via PCR after passage 5-7. Perform standard pluripotency characterization (e.g., immunocytochemistry for OCT4, SOX2, NANOG; flow cytometry for TRA-1-60, SSEA4).
Protocol B: Reprogramming with Non-Integrating Sendai Virus (SeV)
This protocol uses the CytoTune-iPS Sendai Virus Kit, offering high efficiency for difficult-to-transfect cells [23] [24].
Key Research Reagent Solutions:
- Sendai Virus Vectors: CytoTune 2.1 Sendai Virus particles (SeV-OS, SeV-K, SeV-M).
- Cell Culture Medium & Matrix: As in Protocol A.
- Anti-Sendai Antibody: For confirming viral clearance.
Procedure:
- Cell Preparation: Plate somatic cells (e.g., HDFs) 24 hours before transduction at a density of 5x10^4 cells per well of a 12-well plate. Ensure cells are 30-50% confluent at transduction.
- Virus Transduction: Calculate the required Multiplicity of Infection (MOI) for each virus. Thaw virus particles on ice. Dilute in cell culture medium and add the virus mixture directly to the cells. Add 1-2 µL of TPro reagent to enhance transduction.
- Incubation: Incubate cells with the virus mixture for 24 hours at 37°C, 5% CO2.
- Medium Change: After 24 hours, carefully remove the virus-containing medium and replace it with fresh pre-warmed cell culture medium.
- Passaging & Medium Transition: At day 7 post-transduction, harvest the cells using Accutase and re-plate them onto a vitronectin-coated 6-well plate at a density of 1x10^5 to 5x10^5 cells per well in iPSC culture medium. Feed daily.
- Colony Picking & Expansion: Colonies will emerge from day 14 onwards. Pick and expand colonies as described in Protocol A, Step 6.
- Viral Clearance QC: Monitor for the presence of Sendai virus RNA by RT-PCR over multiple passages (typically >10). Only virus-free clones should be selected for master cell banking.
Genomic Integrity and Safety Assessment
A primary rationale for using non-integrating methods is the preservation of genomic integrity. The data below, derived from high-resolution Cytoscan HD array analysis, quantitatively demonstrates the superior genomic safety profile of non-integrating methods compared to integrating methods like lentivirus [25].
Table 2: Genomic Aberration Profile of iPSCs from Different Reprogramming Methods
| Genomic Aberration Metric | hESC Lines | Non-Integrating iPSC Lines (Episomal) | Integrating iPSC Lines (Lentiviral) |
|---|---|---|---|
| Maximum CNV Size | Baseline | Comparable to hESC baseline | 20x larger than non-integrating lines [25] |
| Total Number of CNVs | Low | Low | Significantly higher [25] |
| Number of Novel CNVs | Low | Low | Highest [25] |
| Single Nucleotide Variations (SNVs) | Baseline | Low, similar to parental somatic cells | Increased compared to parental cells and non-integrating lines [25] |
| Presence of Mosaicism | Low | Low | Higher than in non-integrating lines [25] |
This data strongly supports the use of non-integrating methods for clinical-grade iPSC generation to minimize the risk of oncogenic transformation and ensure the long-term safety of derived cell products.
The Scientist's Toolkit
Table 3: Essential Research Reagents for iPSC Reprogramming
| Reagent Category | Specific Example | Function in Reprogramming |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC/L-MYC (OSKM) [23] [1] | Core transcription factors that initiate the epigenetic remodeling to induce pluripotency. |
| Small Molecules | Valproic Acid (VPA), Sodium Butyrate, 8-Br-cAMP [1] | Epigenetic modulators that enhance reprogramming efficiency by modulating chromatin structure. |
| Delivery Vectors | Episomal Plasmids, Sendai Virus, Synthetic mRNA [23] [24] | Vehicles for introducing reprogramming factors into somatic cells. |
| Culture Matrix | Vitronectin (VTN-N), Matrigel, Laminin-521 [25] | Provides a defined, xeno-free substrate that supports pluripotent stem cell attachment and growth. |
| Culture Medium | Essential 8, mTeSR1 [25] | A chemically defined, nutrient-rich medium that maintains iPSCs in a pluripotent state. |
| Transfection System | Nucleofector Technology [27] | Enables high-efficiency delivery of nucleic acids (e.g., plasmids, mRNA) directly into the cell nucleus. |
| Characterization Antibodies | Anti-OCT4, Anti-SSEA4, Anti-TRA-1-60 [27] | Critical reagents for confirming the pluripotent state of derived iPSC lines via immunostaining or flow cytometry. |
This application note details a standardized protocol for the critical stage of selecting, expanding, and banking clonal induced pluripotent stem cell (iPSC) lines, specifically tailored for autologous cell therapy research. The creation of a well-characterized Master Cell Bank (MCB) is a foundational step in the therapeutic development pipeline, ensuring a consistent and high-quality starting material for the generation of differentiated cell products [28] [29]. Adherence to robust banking practices is essential for maintaining cell line integrity, genetic stability, and pluripotency, thereby supporting the validity and reproducibility of preclinical and clinical data [29]. This document provides researchers with detailed methodologies and quality control checkpoints to establish a clinical-grade iPSC MCB.
Single-Cell Cloning of iPSCs
Following reprogramming and initial picking of candidate colonies, the derived polyclonal iPSC lines must be subjected to single-cell cloning. This process isolates genetically homogeneous clones, which is critical for minimizing phenotypic variability in downstream experiments and therapies. The protocol below describes a high-efficiency method for single-cell cloning using Fluorescent-Assisted Cell Sorting (FACS).
High-Efficiency Single-Cell Cloning Protocol
This protocol, adapted from Front. Cell Dev. Biol., enables the generation of single-cell clones with efficiencies approaching 40% within 7–10 days [30].
Materials and Reagents:
- hPSC Defined Medium (DM): mTeSR1, StemPRO hESC SFM, or E8 medium.
- Single-Cell Cloning (SCC) Medium: DM supplemented with 10% KnockOut Serum Replacement (KSR) and a ROCK inhibitor (e.g., Y27632 or RevitaCell Supplement).
- Feeder Cells: Irradiated Mouse Embryonic Fibroblasts (MEFs).
- Dissociation Reagent: Accutase.
- Basement Membrane Matrix: Geltrex, Cultrex, or Matrigel.
- Equipment: Fluorescent-assisted cell sorter, 96-well cell culture plates.
Procedure:
Stage 1: Adaptation to Single-Cell Passaging
- Culture the polyclonal iPSC line on a Geltrex-coated plate in Defined Medium.
- When colonies are large (~500 µm diameter) but not touching, passage the cells using Accutase to create a single-cell suspension.
- Re-seed the cells at an appropriate density and continue this passaging method for at least two cycles to adapt the cells to single-cell survival.
Stage 2: Seeding Single Cells via FACS
- Prepare 96-well plates pre-coated with a feeder layer of MEFs.
- Harvest the adapted iPSCs using Accutase to create a single-cell suspension.
- Resuspend the cell pellet in SCC Medium.
- Use a FACS sorter to deposit one single cell per well into the prepared 96-well plates containing SCC Medium. The use of a ROCK inhibitor in the medium is crucial for enhancing single-cell survival.
Stage 3: Clonal Expansion and Passaging
- Change the medium every day, transitioning from SCC Medium to standard Defined Medium after 3-5 days, once small colonies are visible.
- Allow colonies to expand until they are large enough for passaging (typically 7-10 days post-sorting).
- Manually pick or enzymatically passage the established clonal colonies into larger vessels for further expansion and characterization.
Table 1: Key Reagent Solutions for Single-Cell Cloning
| Research Reagent | Function/Benefit |
|---|---|
| ROCK Inhibitor (Y27632) | Significantly improves survival of dissociated single iPSCs by inhibiting apoptosis. |
| KnockOut Serum Replacement (KSR) | A defined, serum-free formulation that supports pluripotency and growth in SCC medium. |
| Accutase | A gentle enzymatic blend of proteases and collagenases that generates a high-viability single-cell suspension. |
| Mouse Embryonic Fibroblasts (MEFs) | Provides a supportive feeder layer that secretes essential growth factors for single-cell cloning. |
Workflow Visualization
The following diagram illustrates the sequential workflow for the single-cell cloning of iPSCs.
Expansion and Quality Control of Clonal Lines
Selected clones must be expanded and rigorously characterized before MCB creation. Key quality attributes must be verified to ensure the clones are suitable for therapeutic development.
Expansion Protocol:
- Expand clonal lines using standardized culture conditions, preferably in a defined, xeno-free medium on a suitable substrate (e.g., Geltrex).
- Maintain cells in a state of active proliferation, passaging as clumps or as single cells with ROCK inhibitor support before reaching confluence to prevent spontaneous differentiation and maintain genomic stability.
- Scale up the culture to obtain a sufficient number of cells for the MCB. For a typical MCB, this involves expanding cells to create a pooled, homogeneous population from which 10-15 vials (or more, depending on scale) will be cryopreserved [29].
Pre-MCB Quality Control: The following table summarizes the critical quality control tests to be performed on the expanded clonal population prior to banking.
Table 2: Essential Pre-MCB Quality Control Tests for iPSC Clones
| Quality Attribute | Test Method | Acceptance Criteria |
|---|---|---|
| Pluripotency Marker Expression | Immunocytochemistry (OCT4, SOX2, NANOG) and Flow Cytometry | >95% positive for key pluripotency markers. |
| Trilineage Differentiation Potential | Directed differentiation or Embryoid Body (EB) formation followed by immunostaining for ectoderm, mesoderm, and endoderm markers. | Successful differentiation into derivatives of all three germ layers. |
| Karyotype / Genomic Stability | G-banding karyotype analysis or high-resolution array CGH. | Normal, stable karyotype (46, XX or 46, XY) with no major aberrations. |
| Identity / Authentication | Short Tandem Repeat (STR) profiling. | Match to the original donor somatic cell sample. |
| Sterility | Mycoplasma testing (e.g., by PCR). | Negative. |
| Vector Clearance | qPCR for reprogramming factors (if using integrating vectors). | Silencing of exogenous reprogramming factors. |
Master Cell Bank (MCB) Creation
The MCB represents the primary stock of cells from which all future work will be derived. Its creation must follow a rigorous and standardized procedure.
Banking Strategy and Protocol
A two-tiered banking system—consisting of a Master Cell Bank (MCB) and a Working Cell Bank (WCB)—is recommended by the International Society for Stem Cell Research (ISSCR) [29].
Procedure for MCB Creation:
- Cell Pooling and Harvest: From the expanded and quality-controlled clonal culture, create a single, homogeneous cell suspension. Pool all cells from multiple culture vessels to ensure consistency across all vials in the bank [29].
- Cryopreservation: Centrifuge the pooled cell suspension and resuspend in a chilled, appropriate cryopreservation medium (e.g., containing DMSO). Aliquot the cell suspension into cryovials at a consistent cell density per vial.
- Controlled-Rate Freezing: Place the cryovials in an isopropanol-based freezing chamber or a controlled-rate freezer and cool at a rate of approximately -1°C per minute to -80°C before transferring to long-term storage in the vapor phase of liquid nitrogen (-140°C to -196°C) [31] [29].
- Quality Control of the MCB: Thaw one representative vial from the MCB and perform a full panel of characterization tests, as Artificially Extended in Table 3. The results from this vial are considered representative of the entire bank [29].
- WCB Generation: The Working Cell Bank is created by thawing one vial from the qualified MCB, expanding the cells, and creating a second, larger bank of vials for day-to-day experimental use. The WCB should also undergo a subset of quality control tests (viability, sterility, identity) [29].
Table 3: Characterization Testing for Master and Working Cell Banks (per ISSCR Standards)
| Characteristic | Master Cell Bank (MCB) | Working Cell Bank (WCB) |
|---|---|---|
| Post-thaw Viability | ||
| Authentication (STR Profiling) | ||
| Sterility (Mycoplasma, Adventitious Agents) | ||
| Genomic Stability (Karyotyping) | ||
| Gene & Marker Expression (Pluripotency) | (Optional) | |
| Functional Pluripotency | (Not required) |
Banking Workflow and Regulatory Context
The following diagram summarizes the complete workflow from single-cell clone to the two-tiered banking system, highlighting the critical quality gates.
For autologous therapies, the regulatory landscape governing MCB creation is defined by agencies like the U.S. FDA and the European EMA [28]. Key considerations include:
- Characterization: Extensive testing for identity, purity (freedom from adventitious agents), potency (pluripotency), and genomic stability is required [28] [29].
- Harmonization: There is a recognized need for further guidance on minimum requirements for identity and purity testing, stability testing, and the types of expression vectors authorized for clinical-grade iPSC generation [28].
- Ethical Compliance: All banking and research activities must adhere to international ethical guidelines, such as the ISSCR Guidelines for Stem Cell Research and Clinical Translation, which emphasize rigor, oversight, and transparency [2].
The establishment of a thoroughly characterized MCB is a non-negotiable prerequisite for advancing autologous iPSC therapies into clinical development. The protocols Artificially Extended here for single-cell cloning, expansion, and banking provide a framework for generating a high-quality, consistent, and reliable source of iPSCs. By implementing these standardized practices and adhering to evolving regulatory guidelines, researchers can ensure the integrity of their cell lines, thereby strengthening the foundation of their therapeutic development programs and accelerating the translation of iPSC technology from the laboratory to the clinic.
This application note details a small molecule-directed protocol for the differentiation of human induced pluripotent stem cells (hiPSCs) into functionally mature dopaminergic (DA) neurons [32]. Within the framework of autologous iPSC therapy research, this process is critical for generating the specific cell types needed to replace those lost in neurodegenerative disorders such as Parkinson's disease (PD) [32] [33]. The ability to derive authentic midbrain DA neurons from a patient's own cells provides a renewable, genetically matched cell source for transplantation, circumventing issues of immune rejection and ethical concerns associated with alternative cell sources [2] [33]. The following sections provide a detailed methodology, relevant quantitative data, and essential resources for implementing this protocol in a research setting.
Experimental Workflow and Key Signaling Pathways
The differentiation process involves a carefully orchestrated sequence of signaling cues that mimic embryonic development, guiding hiPSCs through key intermediate stages to a mature dopaminergic fate.
Directed Differentiation Workflow
The following diagram illustrates the multi-stage process of differentiating hiPSCs into dopaminergic neurons, highlighting key patterning factors and timeline:
Key Patterning Pathways and Factors
The successful specification of midbrain DA neurons relies on the precise temporal activation of specific signaling pathways, summarized in the table below.
Table 1: Key Signaling Pathways and Factors in DA Differentiation
| Stage | Signaling Pathway | Key Factors/Modulators | Primary Function |
|---|---|---|---|
| Neural Induction (Days 0-5) | SMAD Inhibition | Small molecule inhibitors (e.g., SB431542, LDN193189) [32] | Promotes neural ectoderm formation by inhibiting BMP and TGF-β signaling. |
| Patterning (Days 5-11) | Sonic Hedgehog (SHH) | Purmorphamine or SAG (SMAD agonist) [32] | Specifies ventral midline identity, critical for floor plate induction. |
| Patterning (Days 5-11) | WNT Signaling | CHIR99021 (GSK-3β inhibitor) [32] | Promotes posteriorization toward a midbrain fate. |
| Maturation (Days 11-25+) | Neurotrophic Support | BDNF, GDNF, Ascorbic Acid, TGF-β3 [32] [33] | Supports terminal differentiation, survival, and functional maturation of DA neurons. |
Research Reagent Solutions
The following table catalogs essential reagents and materials required for the successful execution of this dopaminergic neuron differentiation protocol.
Table 2: Essential Research Reagents for DA Neuron Differentiation
| Reagent/Material | Function/Application | Example/Category |
|---|---|---|
| hiPSC Line | Autologous cell source; self-renewing starting material. | Patient-derived fibroblast or blood cell reprogrammed line [32]. |
| Small Molecules | Directs cell fate through precise modulation of signaling pathways. | SMAD inhibitors, SHH agonist, WNT activator [32]. |
| Growth Factors | Supports neuronal survival, maturation, and phenotype maintenance. | BDNF, GDNF, Ascorbic Acid [32] [33]. |
| Basal Medium | Base nutrient medium for cell survival and growth. | DMEM/F-12 or other specialized neural induction/ differentiation media [32]. |
| Cell Dissociation Agent | Passaging and harvesting of cells at different stages. | Enzymatic reagents like Accutase or Trypsin. |
| Extracellular Matrix | Coating substrate to support cell adhesion and growth. | Matrigel, Laminin, or Poly-L-Ornithine/Laminin [32]. |
Validation and Functional Maturation
The endpoint of the differentiation protocol is the generation of functionally mature dopaminergic neurons. Rigorous validation is required to confirm cellular identity and function before any downstream application.
Characterization Methods and Key Metrics
The quality and success of the differentiation process are assessed through a combination of molecular, biochemical, and functional assays.
Table 3: Key Metrics for Validation of Dopaminergic Neurons
| Validation Method | Target/Analyte | Expected Outcome |
|---|---|---|
| Immunocytochemistry | Transcription factors: FOXA2, LMX1A; Enzymes: Tyrosine Hydroxylase (TH) [32] [33] | Co-expression of FOXA2/LMX1A and TH, confirming midbrain DA identity. |
| qPCR / RNA-Seq | mRNA expression of TH, NURR1 (NR4A2), PITX3, DAT [32] | Significant upregulation of midbrain DA gene markers compared to undifferentiated hiPSCs. |
| HPLC / ELISA | Dopamine secretion in cell culture supernatant [32] | Measurable dopamine release, often enhanced upon potassium depolarization. |
| Electrophysiology | Whole-cell patch clamp [32] | Display of action potentials and spontaneous post-synaptic currents, indicating functional neuronal maturity. |
| In vivo Validation | Graft survival & function in PD animal models [33] | Graft survival, striatal re-innervation, and amelioration of motor deficits (e.g., in rotational behavior). |
Clinical Context and Preclinical Validation
The translational relevance of this differentiation approach is supported by clinical data. A recent Phase I trial for Parkinson's disease utilized DA neurons derived from human embryonic stem cells (hESCs) via a similar floor-plate-based protocol [33]. The cryopreserved cell product, bemdaneprocel, was transplanted into the putamen of 12 patients. The trial successfully met its primary safety endpoints and, at 18 months post-transplantation, showed increased putaminal 18F-DOPA PET uptake (indicating graft survival) and improved motor scores (MDS-UPDRS Part III OFF scores improved by an average of 23 points in the high-dose cohort) without graft-induced dyskinesias [33]. These results underscore the potential of stem cell-derived DA neurons and validate the core biological principles of the differentiation strategy outlined in this protocol.
The successful translation of autologous induced pluripotent stem cell (iPSC) therapies into clinical applications is contingent upon the rigorous purification and comprehensive characterization of the final differentiated cell product. This step is critical for ensuring patient safety, confirming the absence of residual undifferentiated cells that could form teratomas, and validating the functional identity of the therapeutic population. This protocol outlines detailed methodologies for the purification and quality assessment of differentiated cells, framed within the context of current good practice principles for stem cell-based interventions [2].
Purification Strategies
Following the differentiation of iPSCs into a target lineage, the cell population is often heterogeneous, containing undesired cell types and potentially residual undifferentiated iPSCs. Purification is essential to isolate the specific functional cell population for therapeutic use.
Magnetic-Activated Cell Sorting (MACS)
MACS is a high-throughput, gentle method suitable for the separation of large cell numbers under sterile conditions, making it ideal for clinical-grade purification.
- Experimental Protocol:
- Harvesting: Gently dissociate the differentiated cell culture into a single-cell suspension using a non-enzymatic cell dissociation buffer or a gentle enzyme (e.g., Accutase). Preserve cell surface antigens by avoiding harsh proteases.
- Antibody Labeling: Resuspend the cell pellet in a cold, sterile sorting buffer (e.g., PBS pH 7.2, 0.5% BSA, 2 mM EDTA). Add a biotinylated or microbead-conjugated primary antibody specific for a surface antigen on the target cells (e.g., CD34 for hematopoietic progenitors). Incubate for 15-30 minutes at 4°C.
- Washing: Add excess buffer to the cell suspension and centrifuge at 300 x g for 5 minutes to remove unbound antibodies. Decant the supernatant completely.
- Magnetic Separation: For biotinylated antibodies, resuspend the cell pellet in sorting buffer and add magnetic microbeads conjugated to an anti-biotin antibody. Incubate for 15 minutes at 4°C. Wash again to remove unbound beads.
- Column Preparation: Place a sterile LS or MS MACS Column in the magnetic field of a suitable separator. Rinse the column with 3-5 mL of sorting buffer.
- Cell Sorting: Apply the cell suspension to the column. The magnetically labeled target cells will be retained, while unlabeled cells pass through. Wash the column with 5-10 mL of buffer.
- Elution: Remove the column from the magnetic field and immediately flush out the magnetically retained cells (the positive fraction) using the provided plunger and a collection tube filled with culture medium.
- Analysis: Determine the purity and viability of the positive fraction via flow cytometry and trypan blue exclusion, respectively.
Fluorescence-Activated Cell Sorting (FACS)
FACS offers high specificity based on multiple surface and intracellular markers simultaneously, providing the highest purity for critical applications.
- Experimental Protocol:
- Cell Preparation: Create a single-cell suspension as described for MACS.
- Staining: Aliquot cells into FACS tubes. Add fluorochrome-conjugated antibodies targeting specific surface markers (e.g., CD73, CD90, CD105 for mesenchymal stromal cells) [34]. Include a viability dye (e.g., DAPI or Propidium Iodide) to exclude dead cells. For intracellular markers, cells must be fixed and permeabilized prior to antibody staining.
- Incubation and Washing: Incubate cells with antibodies for 20-30 minutes at 4°C in the dark. Wash twice with FACS buffer to remove unbound antibody.
- Filtering: Filter the cell suspension through a 35-70 μm cell strainer cap to remove clumps and ensure a single-cell stream.
- Sorting: Resuspend cells in a sterile sorting medium. Use a sterile, high-speed cell sorter to isolate the target population based on pre-defined gating strategies. Collect sorted cells directly into a tube containing collection medium.
- Post-Sort Analysis: Re-analyze a small aliquot of the sorted population to confirm purity, which should typically exceed 95% for clinical applications.
The following workflow summarizes the key decision points and processes in the purification and characterization pipeline:
Characterization Assays
A multi-parametric characterization strategy is required to confirm the identity, purity, potency, and safety of the purified cell product, aligning with guidelines from the International Society for Cell and Gene Therapy (ISCT) [34].
Immunophenotyping by Flow Cytometry
This assay quantitatively assesses the expression of defining cell surface markers to confirm cellular identity and purity [34].
- Experimental Protocol:
- Sample Preparation: Aliquot 1-5 x 10^5 purified cells per FACS tube. Include unstained and single-color compensation controls.
- Staining: Add predetermined optimal concentrations of fluorochrome-conjugated antibodies to the cell pellets. Vortex gently and incubate for 20-30 minutes at 4°C in the dark.
- Washing: Add 2 mL of FACS buffer (PBS + 1% FBS) to each tube. Centrifuge at 300 x g for 5 minutes. Decant the supernatant carefully.
- Fixation: Resuspend cells in 200-500 μL of FACS buffer, optionally adding 1% paraformaldehyde for fixation if analysis is not immediate.
- Acquisition: Analyze the samples on a flow cytometer. Collect a minimum of 10,000 events per sample.
- Analysis: Use flow cytometry analysis software to gate on the viable cell population based on forward/side scatter and viability dye exclusion. Report the percentage of cells positive for target markers.
The table below summarizes the key markers used for characterizing different cell types derived from iPSCs, based on established criteria [34].
Table 1: Marker Profiles for Characterizing Differentiated Cell Types
| Cell Type | Positive Markers (≥95%) | Negative Markers (≤2%) | Key Functional Assay |
|---|---|---|---|
| Mesenchymal Stromal Cells (MSCs) | CD73, CD90, CD105 [34] | CD34, CD45, CD11b, CD19, HLA-DR [34] | Trilineage differentiation (osteogenic, adipogenic, chondrogenic) |
| Hematopoietic Progenitors | CD34, CD45 | CD3, CD19, CD33 | Colony-forming unit (CFU) assay |
| Cardiomyocytes | cTnT, NKX2-5, α-Actinin | CD90, CD31 | Spontaneous contraction, Calcium imaging |
| Neural Progenitors | SOX1, SOX2, PAX6, Nestin | SOX17, Brachyury | Differentiation into neurons/glia |
Functional Potency Assays
Functional validation is necessary to confirm that the purified cells possess the intended biological activity.
- Trilineage Differentiation Assay (for MSCs):
- Seeding: Seed the purified MSC population at a defined density (e.g., 2.1 x 10^4 cells/cm²) in 24-well plates.
- Induction:
- Osteogenic: Culture cells in basal medium supplemented with 0.1 μM dexamethasone, 10 mM β-glycerophosphate, and 50 μM ascorbate-2-phosphate for 21 days. Differentiated osteocytes can be confirmed by fixing with 70% ethanol and staining with 2% Alizarin Red S to detect calcium deposits [34].
- Adipogenic: Culture cells in basal medium with 1 μM dexamethasone, 0.5 mM IBMX, 10 μg/mL insulin, and 100 μM indomethacin for 21 days. Differentiated adipocytes can be confirmed by fixing with 4% PFA and staining with Oil Red O to detect lipid vacuoles [34].
- Chondrogenic: Pellet 2.5 x 10^5 cells and culture in a defined chondrogenic medium with 10 ng/mL TGF-β3 for 28 days. Differentiated chondrocytes can be confirmed by fixing with 4% PFA, embedding in paraffin, sectioning, and staining with Alcian Blue for sulfated proteoglycans [34].
- Analysis: Document staining with bright-field microscopy and quantify dye elution if required.
Safety and Purity Assessment
Ensuring the final product is free from contaminants and has a low risk of tumorigenicity is paramount [2].
Residual Undifferentiated iPSC Detection:
- Flow Cytometry: Analyze the purified cell product for the presence of markers highly expressed on pluripotent cells, such as TRA-1-60, TRA-1-81, or SSEA4. The acceptable limit should be strictly defined (e.g., <0.1%).
- qRT-PCR: Isolve total RNA from a sample of the cell product. Perform qRT-PCR for pluripotency genes (e.g., NANOG, OCT4, SOX2). Compare the cycle threshold (Ct) values to a standard curve generated from known numbers of iPSCs to estimate the level of contamination.
Karyotype Analysis:
- Cell Culture: Culture an aliquot of the purified cells and arrest them in metaphase using colcemid.
- Processing: Harvest cells, subject them to hypotonic treatment, and fix with Carnoy's fixative (3:1 methanol:glacial acetic acid).
- Staining and Imaging: Drop the cell suspension onto slides, stain with Giemsa (G-banding), and analyze at least 20 metaphase spreads under a microscope for chromosomal abnormalities.
The Scientist's Toolkit
Table 2: Essential Research Reagents for Purification and Characterization
| Item | Function & Application |
|---|---|
| MACS Cell Separation Kit | Immunomagnetic labeling and separation of cell populations; used for high-throughput, gentle purification. |
| Fluorochrome-Conjugated Antibodies | Tagging specific cell surface and intracellular antigens for detection and isolation by flow cytometry/FACS. |
| Viability Dye (e.g., DAPI, 7-AAD) | Distinguishing live cells from dead cells during flow analysis to ensure accurate gating and results. |
| Cell Dissociation Reagent (e.g., Accutase) | Generating a single-cell suspension from adherent cultures while preserving surface antigen integrity. |
| Trilineage Differentiation Media Kits | Inducing and assessing the multipotent differentiation capacity of MSCs into osteocytes, adipocytes, and chondrocytes. |
| qRT-PCR Assays for Pluripotency Factors | Sensitive detection and quantification of residual undifferentiated iPSCs in the final cell product. |
| Flow Cytometry Compensation Beads | Setting up the flow cytometer for accurate fluorescence compensation in multicolor experiments. |
Formulation and Cryopreservation Medium Composition
The formulation of a robust cryopreservation medium is critical for maintaining induced pluripotent stem cell (iPSC) viability and pluripotency post-thaw. The table below summarizes a standard composition for a xeno-free cryopreservation medium.
Table 1: Essential components of a defined, xeno-free cryopreservation medium for iPSCs.
| Component Category | Specific Example | Final Concentration | Primary Function |
|---|---|---|---|
| Base Medium | DMEM/F-12 | 80-85% (v/v) | Osmotically balanced nutrient foundation |
| Membrane Permeant Cryoprotectant | DMSO | 10% (v/v) | Penetrates cells, suppresses ice crystal formation |
| Membrane Impermeant Cryoprotectant | Sucrose | 0.2 M | Creates osmotic gradient, dehydrates cells to limit intracellular ice |
| Macromolecular Additive | Hydroxyethyl starch (HES) | 5-6% (w/v) | Stabilizes cell membranes, reduces solution effects |
| Recombinant Protein | Recombinant Human Albumin | 1-2% (w/v) | Provides protein stabilizer, replaces animal-sourced albumin |
Detailed Cryopreservation Protocol
Pre-Freeze Formulation and Cell Preparation
- Cell Culture: Culture iPSCs to 70-80% confluency in a defined, feeder-free system to ensure a homogeneous, undifferentiated population.
- Dissociation: Gently dissociate cells into a single-cell suspension using a non-enzymatic, EDTA-based dissociation reagent or a gentle enzyme like Accutase to minimize clumping and preserve surface markers.
- Wash and Concentration: Centrifuge the cell suspension and resuspend the pellet in a cold, serum-free base medium to remove residual enzymes and conditioned medium.
- Formulation with Cryomedium: Slowly and dropwise, mix the concentrated cell pellet with the pre-chilled (2-8°C) cryopreservation medium to achieve a final concentration of 1-5 x 10^6 cells/mL. Gently mix to ensure homogeneity without introducing shear stress.
Controlled-Rate Freezing
A critical element for success is a controlled, slow cooling rate to facilitate cellular dehydration before the solution vitrifies. The protocol below uses a "freezing container" method, which provides an approximate cooling rate of -1°C per minute.
Table 2: Step-by-step controlled-rate freezing protocol.
| Step | Temperature Range | Rate | Duration / Endpoint | Key Process |
|---|---|---|---|---|
| 1. Equilibration | +4°C to -5°C | N/A | 30 minutes | Cells equilibrate with cryoprotectants on ice or in a refrigerator. |
| 2. Initiation of Ice Formation (Seeding) | ~ -5°C to -7°C | N/A | Momentary | Manually induce ice crystallization in the extracellular solution to prevent supercooling. |
| 3. Primary Cooling Phase | -7°C to -40°C | -1°C / minute | ~33 minutes | Slow cooling promotes osmotic dehydration; critical for survival. |
| 4. Secondary Cooling Phase | -40°C to -80°C | -2°C to -5°C / minute | ~10-20 minutes | Further cooling to a temperature below the glass transition. |
| 5. Transfer to Long-Term Storage | -80°C to -196°C | Rapid transfer | N/A | Promptly transfer vials to the vapor phase of a liquid nitrogen storage Dewar for long-term stability [35]. |
Transportation to Clinic (Cryoshipping)
The secure transport of cryopreserved iPSCs to a clinical site is a highly regulated process requiring meticulous planning and specialized equipment [36].
Pre-Transport Coordination and Documentation
- Order Placement and Scheduling: Initiate a formal request with the specialized cryoshipping provider, detailing material type (autologous iPSCs), origin/destination clinics, and timeframe.
- Documentation Verification: Ensure all necessary documentation is prepared and verified. This includes [36]:
- Import/Export Permits: For international transport.
- Customs Declarations: To comply with border control regulations.
- Material Transfer Agreements (MTAs) and Certificates of Analysis (CoA): Legitimizing the cell line and transfer.
- Patient Consent Forms and Medical Records: Confirming ethical and regulatory compliance.
- Payment and Final Review: Secure payment processing and conduct a final review confirming all documentation, clinic contacts, and handling protocols are in place.
Specialized Transport Equipment and Conditions
- Advanced Cryogenic Dewars: Use validated, dry vapor shippers certified to maintain a stable temperature of -150°C to -196°C for the entire duration of the shipment [36].
- Integrity Monitoring: Equip containers with continuous temperature data loggers to provide a verifiable record of thermal stability throughout transit [36].
- X-Ray Mitigation: Adhere to IATA regulations for X-ray-free shipping. Arrange for physical inspection or non-ionizing scanning techniques at security checkpoints to prevent radiation damage to cellular material [36].
Receipt and Post-Delivery Verification
- Unpacking and Inspection: Upon arrival, the receiving clinic's personnel should immediately inspect the shipment. Verify the integrity of the cryogenic Dewar.
- Data Log Review: Download and review the temperature log to confirm that cryogenic conditions were maintained without deviation.
- Inventory and Storage: Transfer the cryovials to the clinic's designated long-term liquid nitrogen storage system and update the cell bank inventory. The shipping provider should supply a delivery confirmation and compliance certificate for the patient's record [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key reagents and materials for iPSC cryopreservation and handling.
| Item | Function / Application | Notes for Clinical Compliance |
|---|---|---|
| Defined, Xeno-Free Base Medium | Serves as the foundation for cryopreservation medium; free of animal components. | Essential for clinical-grade applications to prevent xenogeneic immune responses. |
| Clinical-Grade DMSO | Membrane-permeant cryoprotectant. | Must be certified for clinical use; associated with potential patient toxicity, hence post-thaw washing is critical. |
| Non-Enzymatic Dissociation Reagent | Generates a single-cell suspension from iPSC cultures with high viability. | Prevents residual enzymatic activity from affecting cell integrity; preferred over trypsin for minimal surface protein damage. |
| Programmable Controlled-Rate Freezer | Provides precise, reproducible cooling profiles for optimal vitrification. | Gold standard for clinical production; superior to passive cooling devices. |
| Cryogenic Vials (Internally Threaded) | Secure, leak-proof containment of cell suspension. | Internally threaded design is preferred for biobanking to prevent contamination upon immersion in liquid nitrogen. |
| Validated Dry Vapor Shipper | Maintains cryogenic temperatures during transport without liquid nitrogen spillage. | Must be pre-qualified for hold time; IATA-compliant for safe air transport [36]. |
| Temperature Data Logger | Provides a continuous, verifiable record of thermal conditions during storage and transport. | Critical for chain of custody and quality assurance; data is part of the product release documentation [36]. |
Application Notes: Patient Administration
This protocol outlines the procedures for the administration of autologous induced pluripotent stem cell (iPSC)-derived products and subsequent long-term monitoring of recipients. The primary goals are to ensure patient safety, monitor for potential adverse events, and collect robust efficacy data in a research setting. Adherence to these procedures is critical for assessing the therapeutic outcome and long-term stability of the intervention.
Key considerations include:
- Patient Preparation: Patients must meet all predefined inclusion criteria and provide informed consent. Pre-admission conditioning regimens, if applicable, should be administered as per the study protocol.
- Product Handling: The iPSC-derived product is to be handled as a viable cellular entity. Thawing and preparation must occur immediately prior to administration to maximize cell viability.
- Administration Procedure: The route of administration (e.g., intravenous infusion, localized injection) must be performed by qualified clinical personnel in a controlled environment equipped to manage acute adverse events.
- Documentation: All procedures, including product details (e.g., batch number, viability, dose) and patient status, must be meticulously documented in the case report form (CRF).
Experimental Protocols
Protocol: Intravenous Infusion of iPSC-Derived Cellular Product
I. Purpose To standardize the aseptic thawing, preparation, and intravenous infusion of a cryopreserved autologous iPSC-derived cellular product.
II. Materials and Reagents
- Cryopreserved vial(s) of iPSC-derived cells
- Personal Protective Equipment (PPE): lab coat, gloves, eye protection
- Water bath or bead bath (set to 37°C)
- 70% alcohol wipes
- Pre-warmed complete infusion medium (See Reagent Solutions, Table 1)
- Sterile syringes and needles
- IV infusion set (with in-line filter, if specified)
- Normal Saline (0.9% Sodium Chloride Injection, USP)
- Vital signs monitor
- Crash cart with emergency medications
III. Methodology
- Pre-infusion Patient Assessment: Confirm patient identity. Record baseline vital signs. Pre-medicate the patient as required by the study protocol (e.g., antipyretics, antihistamines).
- Product Thawing and Preparation: a. Retrieve the cryopreserved vial from liquid nitrogen storage using appropriate PPE. b. Gently agitate the vial in the 37°C water bath until only a small ice crystal remains (approximately 1-2 minutes). c. Decontaminate the vial's septum with 70% alcohol and allow it to dry. d. Using a sterile syringe, immediately aspirate the cell suspension from the vial. e. Transfer the cell suspension into a bag containing the pre-warmed infusion medium. Gently mix to homogenize.
- Line Priming: Prime the IV infusion set with the cell suspension, ensuring no air bubbles are present.
- Infusion: a. Administer the product via a peripheral or central venous line. b. Infuse at the rate specified in the study protocol (e.g., over 15-30 minutes). c. Monitor the patient closely for any signs of adverse reactions (e.g., fever, chills, rash, dyspnea) throughout the infusion.
- Post-infusion Flush: Upon completion, flush the line with a small volume of Normal Saline to ensure the entire dose is administered.
- Waste Disposal: Dispose of all used vials, syringes, and lines as biohazardous waste.
Protocol: Serial Monitoring for Teratoma Formation
I. Purpose To systematically monitor patients for the potential formation of teratomas, a known risk associated with iPSC-derived therapies, using a combination of imaging and biomarker analysis.
II. Materials and Reagents
- MRI or CT imaging system
- Blood collection tubes (e.g., serum separator tubes)
- ELISA kits for pluripotency markers (e.g., TRA-1-60, SSEA-4)
- PCR instrumentation and reagents
III. Methodology
- Imaging Schedule: Conduct MRI or CT scans of the administration/target site at baseline, and post-administration at intervals defined in Table 2 (e.g., 3, 6, 12 months, and annually thereafter).
- Biomarker Analysis: a. Collect peripheral blood samples at each monitoring timepoint. b. Iserate serum and analyze for the presence of secreted pluripotency markers using validated ELISA kits. c. Isolate circulating DNA and perform ddPCR assays for transgene or specific genomic sequences unique to the iPSC line to detect the presence of undifferentiated cells.
- Data Analysis: Correlate imaging findings with biomarker levels. Any suspicious mass on imaging with concomitant elevation in pluripotency markers should be investigated further, potentially with a biopsy.
Data Presentation
Table 1: Research Reagent Solutions for iPSC Administration
| Reagent / Solution Name | Composition / Specification | Function in Protocol |
|---|---|---|
| Complete Infusion Medium | Base medium (e.g., PlasmaLyte A) + 1-5% Human Serum Albumin | Serves as the carrier solution for the cellular product, providing osmotic stability and reducing cell clumping during infusion. |
| Pluripotency Marker ELISA Kit | Pre-coated plates with capture antibodies, detection antibodies, and standards for TRA-1-60 or SSEA-4 | A highly sensitive immunoassay to detect and quantify serum biomarkers indicative of the presence of undifferentiated pluripotent cells. |
| Cell Viability Stain | Trypan Blue (0.4%) or Fluorescent viability dyes (e.g., Propidium Iodide) | Used to determine the percentage of live cells in the final product prior to administration, a critical quality release criterion. |
| ddPCR Assay Mix | Primers and probes specific to the reprogramming transgene or a unique genomic locus in the iPSC line; ddPCR Supermix | A digital PCR technique used for ultra-sensitive detection of trace amounts of DNA from potentially undifferentiated cells in patient blood. |
Table 2: Post-Transplantation Monitoring Schedule and Key Assessments
| Timepoint | Clinical & Vital Signs | Imaging Studies | Biomarker Analysis | Immune Monitoring | Biobanking |
|---|---|---|---|---|---|
| Baseline (Pre-dose) | X | X (MRI/CT) | X (ELISA, ddPCR) | Immunophenotyping | PBMCs, Serum |
| Day 1-14 (Daily) | X (Frequent) | - | - | - | Serum (select days) |
| Week 2, 4, 8 | X | - | X (ELISA, ddPCR) | Immunophenotyping | PBMCs, Serum |
| Month 3, 6 | X | X (MRI/CT) | X (ELISA, ddPCR) | Immunophenotyping | PBMCs, Serum |
| Annually (Years 1-15) | X | X (MRI/CT) | X (ELISA, ddPCR) | Immunophenotyping | PBMCs, Serum |
Mandatory Visualizations
iPSC Therapy Monitoring Workflow
Teratoma Surveillance Pathway
Overcoming Critical Challenges in Manufacturing and Safety
The development of autologous induced pluripotent stem cell (iPSC)-based therapies represents a frontier in regenerative medicine and personalized treatment. However, a significant challenge in their clinical translation is the inherent variability introduced by donor-specific factors. Donor age, health status, and genetic background collectively influence the reprogramming efficiency, genomic stability, and functional characteristics of derived iPSCs and their differentiated progeny [37] [38]. This application note details standardized protocols designed to characterize and mitigate this variability, ensuring the generation of robust, high-quality, and therapeutically relevant iPSC lines for research and drug development.
Quantitative Impact of Donor Factors on iPSC Characteristics
The following tables summarize the quantitative and qualitative impacts of key donor factors, as established in the scientific literature.
Table 1: Impact of Donor Age on iPSC Properties
| Donor Age Parameter | Impact on Reprogramming | Impact on iPSC & Differentiated Cell Functionality | Key References |
|---|---|---|---|
| Advanced Age (e.g., Centenarians) | Reduced efficiency reported; requires optimized culture conditions and/or reprogramming factors (e.g., +Nanog, LIN28). Successfully achieved. [39] [40] | No diminished differentiation potential; no functional impairments or early senescence in derived cells; longer telomeres and improved mitochondrial function than parent somatic cells. [37] [40] | [37] [39] [40] |
| Cellular Senescence (e.g., p21 upregulation) | Decreased efficiency; can be improved by knockdown of p21 or targeting senescence effectors. [39] [40] | Reversion of typical cellular ageing signs during reprogramming (telomerase reactivation, epigenetic resetting). [37] [39] | [37] [39] [40] |
| Somatic Cell Culture Time | Prolonged passaging before reprogramming decreases efficiency. [39] [40] | Increases risk of pre-existing mutations; older somatic cells (e.g., skin fibroblasts) may harbor more UV-related damage. [38] | [38] [39] [40] |
Table 2: Impact of Donor Health Status and Genetic Background
| Donor Factor | Impact on iPSC Properties | Implications for Therapy | Key References |
|---|---|---|---|
| Genetic Background | Strain differences in reprogramming efficiency, pluripotent stability, and culture requirements (e.g., LIF concentration). [41] | Critical for allogeneic therapy donor selection; affects standardization of manufacturing processes. [38] [41] | [38] [41] |
| Somatic Cell Type | Varying reprogramming efficiency and time; source-specific mutation load (e.g., skin fibroblasts vs. blood cells). [38] | Influences choice of starter cells; balance between accessibility, quality, and scalability. [38] | [38] |
| Disease Status | Healthy donor cells may not accurately model disease or respond therapeutically as diseased cells. [42] | Essential to use diseased donor material for relevant preclinical models and autologous therapy development. [42] [43] | [42] [43] |
Experimental Protocols for Characterizing Donor Variability
Protocol: Assessment of Reprogramming Efficiency Across Donor Demographics
Objective: To quantitatively evaluate the impact of donor age and genetic background on the efficiency of iPSC generation.
Materials:
- Donor somatic cells (e.g., fibroblasts, PBMCs) from cohorts of varying age, health status, and genetic background.
- Non-integrative reprogramming kit (e.g., Sendai virus or episomal vectors containing OSKM factors).
- Feeder-free culture ware and defined iPSC culture medium.
- Alkaline Phosphatase (AP) Live Stain or fixing kit and AP stain.
- Flow cytometer with antibodies against pluripotency markers (e.g., TRA-1-60, SSEA-4).
Method:
- Cell Preparation: Expand and passage all donor somatic cells a standardized number of times (e.g., P2-P4) to minimize the impact of ex vivo culture. [39] [40]
- Reprogramming: Transduce/transfect a defined number of cells (e.g., 1x10^5) from each donor using a consistent reprogramming method and virus/pDNA batch.
- iPSC Culture: Plate cells under identical conditions and refresh medium daily.
- Colony Quantification (Day 21-28):
- Data Analysis: Normalize the colony count or percentage of positive cells to the initial number of cells plated. Compare efficiencies across donor groups using statistical analysis (e.g., ANOVA).
Protocol: Genomic and Epigenomic Analysis of Donor-Matched iPSCs
Objective: To identify age- and genotype-associated mutations and epigenetic signatures in established iPSC lines.
Materials:
- Donor genomic DNA (from primary somatic cells).
- iPSC genomic DNA (from early passage clones).
- Whole-genome or whole-exome sequencing service/platform.
- Epigenetic analysis kit (e.g., Illumina EPIC array for DNA methylation).
- Bioinformatics software for variant calling (e.g., GATK) and epigenetic clock analysis.
Method:
- DNA Extraction: Isolate high-quality DNA from donor somatic cells and a minimum of three derived iPSC clones per donor.
- Sequencing & Analysis: Perform whole-exome sequencing on all samples.
- Variant Calling: Identify single-nucleotide variants (SNVs) and small indels.
- Mutation Burden: Compare the number of exomic mutations in iPSC lines to the donor's baseline. Note that mutations can increase linearly with donor age. [44]
- Clonal Analysis: Identify mutations present in individual iPSC clones that were missed by bulk sequencing of the donor, revealing somatic mutations in the donor's cell population. [44]
- DNA Methylation Profiling:
- Analysis: Process the data to calculate an "epigenetic age" for each sample using established clocks (e.g., Horvath's clock).
- Interpretation: Compare the epigenetic age of iPSCs to the chronological age of the donor. Note that iPSCs from older donors may retain an epigenetic signature of age, which can be reduced through passaging. [44]
Diagram 1: Genomic and Epigenomic Analysis Workflow for Donor-Matched iPSCs.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for iPSC Generation and Characterization
| Reagent Category | Specific Example(s) | Function & Rationale |
|---|---|---|
| Reprogramming Vectors | Sendai Virus (RNA virus), Episomal Vectors, mRNA | Non-integrative methods for factor delivery; critical for clinical-grade iPSCs to avoid insertional mutagenesis. [38] [39] |
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc (OSKM); Oct4, Sox2, Nanog, LIN28 | Core transcription factors to induce pluripotency. Alternative cocktails may improve efficiency, especially for recalcitrant cells. [3] [39] |
| Culture Supplements | LIF (Leukemia Inhibitory Factor), CHIR99021 (GSK3β inhibitor) | Supports pluripotency maintenance in mouse iPSCs. Small molecule that can enhance reprogramming efficiency and replace certain factors. [41] |
| Pluripotency Validation | Antibodies: TRA-1-60, SSEA-4; Alkaline Phosphatase Staining | Detection of key pluripotency-associated surface markers and enzymes. Functional assay for pluripotency, demonstrating differentiation into all three germ layers. [41] |
Strategic Workflow for Donor Selection and iPSC Line Validation
The following diagram outlines a logical pathway for making informed decisions regarding donor material and for validating the resulting iPSC lines in the context of autologous therapy development.
Diagram 2: Strategic Workflow for Donor Selection and iPSC Line Validation.
Ensuring Genomic Stability and Mitigating Tumorigenicity Risks
The clinical implementation of autologous induced pluripotent stem cell (iPSC) therapies represents a frontier in regenerative medicine, offering potential treatments for conditions previously considered untreatable. However, a formidable obstacle to their clinical translation is the inherent risk of tumorigenicity, which can arise from two primary sources: (1) the presence of residual undifferentiated pluripotent stem cells in the final product and (2) the acquisition of genomic instability in iPSCs during in vitro culture. Residual undifferentiated iPSCs can form teratomas upon transplantation, while genomically unstable cells may undergo malignant transformation. A rigorous, multi-parameter biosafety assessment is therefore essential to ensure the safe translation of these therapies from preclinical research to clinical application [45] [46]. This application note details a comprehensive protocol for assessing and mitigating these risks within the context of autologous iPSC therapy development.
Risk Assessment: Key Parameters and Their Evaluation
A thorough biosafety assessment must evaluate multiple critical parameters related to genomic stability and tumorigenic potential. The following framework translates key risks into operational principles [45].
Table 1: Key Risk Parameters in iPSC Therapy Biosafety Assessment
| Risk Parameter | Description | Primary Preclinical Assessment Methods |
|---|---|---|
| Oncogenicity/Tumorigenicity | Risk of malignant transformation and tumor formation. | In vitro transformation assays; In vivo tumorigenicity studies in immunocompromised animals; Teratoma formation assays [45]. |
| Genomic Stability | Maintenance of chromosomal integrity and number during culture. | Karyotyping (G-banding); Multiplex FISH (M-FISH); Targeted qPCR for common abnormalities; DNA sequencing [47] [48]. |
| Biodistribution | Migration, persistence, and localization of administered cells. | Quantitative PCR (qPCR) of human-specific sequences; In vivo imaging (PET, MRI) with labeled cells [45]. |
| Immunogenicity | Potential to provoke undesirable immune responses in the host. | HLA typing; Assessment of innate (complement, NK-cell) and adaptive (T-cell) immune responses [45]. |
| Cell Product Quality | Consistent production of a sterile, authentic, and potent cell product. | Sterility, mycoplasma, and endotoxin testing; Flow cytometry for identity markers; Functional potency assays [45]. |
Monitoring Genomic Stability in iPSC Cultures
Chromosomal instability is a common feature of pluripotent stem cells (PSCs) in culture. A key gene, Retinol Saturase (RetSat), has been identified as a specific stabilizer of mitotic chromosome segregation in PSCs. RetSat protein localizes to mitotic chromosomes specifically in stemness-positive cells, and its deletion leads to dramatic chromosome instability, including bridging, lagging, and micronuclei formation. RetSat-deficient PSCs upregulate cancer-associated gene pathways and display higher tumorigenic capacity, highlighting its value as a biomarker for PSC quality [47].
Protocol: Genomic Stability Assessment via Targeted RT-qPCR
Routine monitoring of karyotypic abnormalities is a practical strategy to reduce variability in differentiation outcomes and mitigate tumorigenic risk [48].
1. Principle: This bulk RT-qPCR assay screens for the nine most common karyotypic abnormalities in human iPSCs, providing a rapid and accessible quality control tool compared to full karyotyping.
2. Reagents and Equipment:
- RNA Extraction Kit: RNeasy Mini Kit (or equivalent).
- Reverse Transcription Kit: Includes Reverse Transcriptase, dNTPs, and buffer.
- qPCR Master Mix: SYBR Green or TaqMan-based.
- Primer Sets: Designed to target genomic loci on chromosomes commonly gained (e.g., 1, 12, 17, 20) or lost in iPSCs.
- Real-time PCR Instrument.
3. Procedure:
- Step 1: RNA Isolation. Extract total RNA from a sample of the iPSC culture following the manufacturer's instructions, including a DNase I treatment step to remove genomic DNA contamination.
- Step 2: cDNA Synthesis. Convert equal amounts of RNA (e.g., 1 µg) into cDNA using a Reverse Transcription kit.
- Step 3: Quantitative PCR. Perform qPCR reactions with the cDNA template and each primer set targeting specific chromosomes and a reference control gene (e.g., on a stable chromosome).
- Step 4: Data Analysis. Calculate the relative chromosomal copy number using the ΔΔCq method. Normalize the Cq values of target loci to the reference gene.
4. Interpretation: Cell lines with chromosomal copy numbers significantly deviating from 2 (e.g., < 1.5 or > 2.5 for autosomes; < 0.7 or > 1.3 for chromosome X in male lines) are considered "abnormal" and should be flagged. Cultures derived from genomically stable iPSCs exhibit reduced variance in differentiation and improved marker expression profiles [48].
The Impact of Developmental Signaling on Chromosome Segregation
External developmental signals directly influence chromosome segregation fidelity in pluripotent stem cells. Research shows that signaling pathways including WNT, BMP, and FGF converge to modulate DNA replication stress, which in turn controls the rate of chromosome missegregation [49].
Diagram: Signaling pathways converge on GSK3 to modulate DNA replication stress and chromosome segregation fidelity. WNT and BMP signaling suppress replication stress, while FGF signaling can promote it [49].
Key Findings:
- Protective Signals: Inhibition of endogenous WNT (by DKK1) or BMP (by Noggin) signaling increases chromosome missegregation in hiPSCs.
- Inductive Signal: Activation of FGF signaling (by FGF2) also promotes chromosome segregation errors.
- Epistatic Rescue: Activation of WNT signaling downstream (via GSK3 inhibition) can rescue the chromosome missegregation caused by both DKK1 and FGF2, placing GSK3 as a central integrator. This suggests that maintaining appropriate WNT/GSK3 signaling is crucial for genomic stability in pluripotency [49].
Strategies for the Elimination of Tumorigenic Pluripotent Stem Cells
A critical step in the manufacturing of iPSC-derived products is the removal of residual undifferentiated cells. Current strategies primarily target hPSC-specific surface markers or physiological vulnerabilities [46].
Table 2: Strategies for Eliminating Tumorigenic Pluripotent Stem Cells
| Strategy Category | Mechanism of Action | Key Features / Targets |
|---|---|---|
| Physical Methods | Separation based on physical properties (size, density) or antibody binding. | Density gradient centrifugation; Magnetic-activated cell sorting (MACS); Fluorescence-activated cell sorting (FACS). |
| Antibody-Based Methods | Utilizes cytotoxic agents conjugated to antibodies against PSC-specific surface markers. | Targets include SSEA-5, CD30, CD50, and anti-glycan antibodies. |
| Pharmacological Methods | Exploits the unique metabolic and signaling dependencies of PSCs. | Small molecule inhibitors targeting pro-survival pathways (e.g., LSD1, TRPV1, A3 adenosine receptor). |
| Metabolic/Physiological Methods | Leverages the heightened sensitivity of PSCs to certain stressors. | Induces selective PSC death via disruption of global DNA methylation; Inhibition of antiapoptotic signals; Treatment with cardiac glycosides. |
Experimental Protocol: Integrated Biosafety Assessment Workflow
The following protocol outlines a comprehensive workflow for assessing the biosafety of an autologous iPSC-derived product, from the starting cell line to the final product release.
Diagram: A sequential workflow for the integrated biosafety assessment of an autologous iPSC-derived therapy.
Part A: Tumorigenicity Testing via Teratoma Formation Assay
1. Principle: The gold-standard assay for assessing the functional tumorigenic potential of an iPSC population or a final cell product is the teratoma formation assay in immunocompromised mice. This test evaluates the ability of residual undifferentiated cells to form complex tissues from all three germ layers, confirming pluripotency, and monitors for malignant transformation.
2. Reagents and Materials:
- Animals: Immunocompromised mice (e.g., NOD/SCID, NSG).
- Matrigel: Growth factor-reduced, kept on ice.
- Cell Culture Reagents: Trypsin/EDTA, culture medium.
- Equipment: Sterile surgical tools, insulin syringes (e.g., 0.5 mL), ice bucket.
3. Procedure:
- Step 1: Cell Preparation. Harvest the iPSCs or final cell product using standard methods. Prepare a single-cell suspension and mix the required cell number (e.g., 1x10^6 to 5x10^6 cells) with an equal volume of cold Matrigel. Keep the cell-Matrigel mixture on ice to prevent polymerization.
- Step 2: Injection. Using an insulin syringe, inject the cell-Matrigel mixture (e.g., 100-200 µL total volume) subcutaneously into the flank or intramuscularly into the hind leg of the anesthetized mouse. Multiple test sites can be used per animal.
- Step 3: Monitoring. Palpate the injection sites weekly to monitor for tumor formation. The study duration is typically 12-20 weeks.
- Step 4: Necropsy and Analysis. Euthanize the animal at the study endpoint or if the tumor volume exceeds ethical limits. Excise the tumor, measure its weight and dimensions, and fix it in formalin for histological processing. Section and stain with Hematoxylin and Eosin (H&E).
4. Interpretation: A positive teratoma will show well-differentiated tissues derived from ectoderm (e.g., neural rosettes, pigmented epithelium), mesoderm (e.g., cartilage, bone, muscle), and endoderm (e.g., gut-like epithelial structures). The absence of teratoma formation is a strong indicator of successful tumorigenic cell elimination. Furthermore, the histology should be scrutinized for any undifferentiated components or malignant features, which would indicate a failed product [45] [46].
Part B: Biodistribution Assessment via Quantitative PCR (qPCR)
1. Principle: This method tracks the presence and persistence of administered human cells in various mouse tissues over time by quantifying a human-specific DNA sequence.
2. Reagents and Materials:
- Tissue Samples: Organs collected at necropsy (e.g., injection site, liver, lungs, spleen, brain, gonads).
- DNA Extraction Kit: Suitable for animal tissues.
- qPCR Master Mix: SYBR Green or TaqMan-based.
- Primers/Probes: Designed to target a human-specific multi-copy gene (e.g., Alu sequences, hTERT) and a mouse-specific reference gene for normalization.
3. Procedure:
- Step 1: DNA Isolation. Extract genomic DNA from homogenized mouse tissue samples following the kit protocol.
- Step 2: Standard Curve Preparation. Extract DNA from a known number of the human cells used for injection. Serially dilute this DNA in mouse genomic DNA to create a standard curve (e.g., from 10^6 to 10 human cell equivalents).
- Step 3: Quantitative PCR. Perform qPCR on all standard curve points and experimental tissue DNA samples using the human-specific and mouse-specific primer sets.
- Step 4: Data Analysis. Use the standard curve to interpolate the number of human cell equivalents in each tissue sample. Normalize the data to the input mass of DNA or the mouse reference gene.
4. Interpretation: Biodistribution data reveals if cells have migrated from the injection site to non-target organs, which could pose a safety risk. Persistent engraftment in non-target tissues, particularly gonads, requires careful risk-benefit evaluation [45].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Genomic Stability and Tumorigenicity Research
| Reagent / Tool | Function / Target | Application in Protocol |
|---|---|---|
| DKK1 (WNT inhibitor) | Inhibits endogenous WNT signaling. | Used to study the role of WNT in chromosome segregation fidelity [49]. |
| CHIR99021 (GSK3i) | Inhibits GSK3, activating WNT signaling downstream. | Used in rescue experiments to stabilize chromosomes against various stresses [49]. |
| SSEA-5 Antibody | Binds to a PSC-specific cell surface marker. | Used in antibody-based methods for the elimination of tumorigenic PSCs (e.g., FACS, cytotoxic conjugation) [46]. |
| Targeted Karyotyping PCR Primers | Amplify loci on chromosomes prone to aneuploidy (1, 12, 17, 20). | Used in the genomic stability monitoring RT-qPCR assay [48]. |
| RetSat Antibody | Detects the RetSat protein. | Used as a biomarker to assess mitotic chromosome stability in PSCs via immunostaining [47]. |
The successful clinical translation of autologous iPSC therapies is contingent upon a rigorous and multi-faceted approach to biosafety. As outlined in this application note, a robust protocol must integrate continuous genomic stability monitoring using tools like targeted RT-qPCR, an understanding of how extracellular signaling influences chromosome segregation, and the implementation of effective strategies for the elimination of residual undifferentiated cells. The experimental workflows and quality control measures detailed herein provide a foundational framework for researchers and drug development professionals to systematically address the tumorigenicity risks associated with iPSC-based products, thereby paving a safer path toward their application in regenerative medicine.
The clinical translation of autologous induced pluripotent stem cell (iPSC) therapies represents a frontier in regenerative medicine, offering potential treatments for degenerative diseases through patient-specific cell replacement [50]. A significant barrier to commercialization is the inherent scalability challenge of manufacturing a new batch of therapy for each patient, a process burdened by extensive manual labor, high costs, and risks of contamination [50] [51]. This application note details a structured pathway for transitioning from manual, planar culture to automated, closed-system bioreactors, framed within the regulatory context of developing an Investigational New Drug (IND) application [50]. We provide quantitative comparisons and detailed protocols to enable robust, scalable, and economically viable manufacturing processes for autologous iPSC-based therapies.
The Scalability Challenge in Autologous iPSC Therapy
Autologous iPSC therapies require a dedicated manufacturing process for each patient, making scalability fundamentally different from allogeneic approaches. Traditional manual 2D culture systems (e.g., T-flasks and multi-layer stacks) present substantial hurdles for clinical translation [51].
- Labor Intensity and Cost: Manual processes require repetitive tasks for feeding, passaging, and monitoring, leading to high hands-on time. One study noted that automating MSC manufacturing in a hollow fiber bioreactor reduced hands-on time by over 300 hours and decreased the cost per dose by nearly $1,000 [52].
- Process Variability and Contamination Risk: Open-system handling in biosafety cabinets increases the risk of contamination. Operator-dependent techniques also introduce variability, threatening batch-to-batch consistency—a critical attribute for regulatory approval [50] [52].
- Limited Scale-Up Potential: Scaling out by increasing the number of flasks quickly becomes impractical, consuming immense incubator space and manual effort [51]. This model is incompatible with the production demands of clinical trials.
Transitioning to automated 3D bioreactors addresses these challenges by enabling a scalable, closed-system manufacturing platform that enhances reproducibility, reduces contamination risk, and improves economic feasibility [52] [51].
Quantitative Comparison: Manual vs. Automated Systems
The following table summarizes a quantitative comparison between traditional manual culture and advanced automated bioreactor systems, based on published studies and performance data.
Table 1: Quantitative Comparison of Cell Culture Systems for iPSC Manufacturing
| Parameter | Manual 2D Culture (T-Flasks/Cell Stacks) | Automated 3D Bioreactor (Hollow Fiber) |
|---|---|---|
| Scalability | Limited by physical space and labor; scale-out approach [51] | High; single-run production for large cell numbers [52] |
| Hands-on Time | High (e.g., >300 hours per 100 doses) [52] | Significantly reduced (e.g., ~326 hours saved per 100 doses) [52] |
| Cost per Dose | Higher (e.g., base cost + $979.41) [52] | Lower due to reduced labor and improved efficiency [52] |
| Risk of Contamination | Higher due to open-system processing [52] | Lower; closed, automated system [52] |
| Process Control & Monitoring | Limited, manual sampling [51] | Automated, real-time monitoring of pH, DO, temperature [51] |
| Product Homogeneity | Potential heterogeneity across flasks [51] | Improved homogeneity and consistent cell output [52] |
| Cell Yield | Limited by surface area [51] | High yield due to large surface area for growth [52] |
| Physiological Relevance | Low; 2D monolayer [51] | Higher; 3D environment that may improve cell function [52] |
Automated bioreactors offer a paradigm shift from static culture to dynamic, controlled environments. The selection of an appropriate system is critical for process success.
Table 2: Comparison of Automated Bioreactor Technologies for Stem Cell Culture
| Bioreactor Type | Key Pros | Key Cons | Suitability for iPSCs |
|---|---|---|---|
| Stirred-Tank Bioreactor | Industry-standard, scalable, direct monitoring of cell growth [51] | High shear forces can impact cell viability, requires microcarriers for adherent cells [51] | Good, with optimized agitation and microcarriers [51] |
| Vertical-Wheel Bioreactor | Gentle, homogeneous mixing, low power input, single-use [51] | Relatively new technology, fewer detailed engineering studies [51] | Promising; shown for hiPSC expansion on microcarriers [51] |
| Hollow Fiber Bioreactor | Low-shear, high surface area, closed-system, scalable [52] [51] | Cell growth monitoring is challenging, potential for nutrient gradients [52] [51] | Excellent for high-yield expansion; used for MSC manufacturing [52] |
Detailed Protocol: Transitioning to a Hollow Fiber Bioreactor System
This protocol outlines the steps for the expansion of iPSCs using a hollow fiber bioreactor system (e.g., Quantum Cell Expansion System, Terumo BCT), a widely adopted technology for cGMP-compliant cell manufacturing [52].
Pre-culture and Bioreactor Setup
- Objective: Prepare a sufficient cell seed train and assemble the sterile, closed bioreactor system.
- Materials:
- Cell Source: Characterized and banked patient-specific iPSC line.
- Culture Media: Qualified, xeno-free iPSC expansion medium.
- Bioreactor Kit: Single-use, pre-sterilized hollow fiber bioreactor circuit.
- Enzyme: Qualified dissociation reagent (e.g., Accutase).
- Procedure:
- Thaw and Expand iPSCs: Thaw the master cell bank vial and expand iPSCs in a cGMP-compliant, feeder-free 2D culture system (e.g., vitronectin-coated plates) to achieve the required seeding density. Perform medium changes daily.
- Prepare Single-Cell Suspension: Wash cells with DPBS and dissociate using a pre-qualified enzyme. Neutralize the enzyme, count cells, and assess viability (target >90%). Centrifuge and resuspend cells in fresh medium at a predefined concentration.
- Prime the Bioreactor System: Aseptically weld the bioreactor circuit to the culture media bag. Initiate the system's automated priming sequence to remove air from the circuit and equilibrate the fibers with culture medium.
- Seed the Bioreactor: Load the cell suspension into the sample bag. Initiate the automated seeding protocol, which circulates the cell suspension through the extracapillary space (ECS) of the hollow fibers, allowing cells to attach.
Automated Expansion and Monitoring
- Objective: Achieve target cell yield through automated, monitored culture.
- Procedure:
- Initiate Expansion Protocol: The system automatically perfuses fresh medium through the intracapillary (IC) space, allowing nutrients to diffuse to the cells in the ECS and waste products to be removed.
- Monitor Process Parameters: The system controller monitors and logs key parameters in real-time, including gas levels (pO₂, pCO₂) and pH in the effluent medium. These data serve as proxies for cell growth and metabolic activity.
- Feed and Sample: Follow the automated feeding schedule. The closed system allows for aseptic sampling of the conditioned media from the ECS for off-line analysis (e.g., metabolite analysis).
Cell Harvest and Formulation
- Objective: Recover the expanded iPSCs as a single-cell suspension for downstream differentiation or cryopreservation.
- Materials:
- Harvest Solution: cGMP-grade enzyme solution (e.g., TrypLE).
- Wash/Formulation Buffer: Appropriate buffer (e.g., DPBS with human serum albumin).
- Procedure:
- Rinse: The system automatically flushes the ECS with a buffer solution to remove residual medium and metabolites.
- Enzyme Introduction: Aseptically weld the harvest solution bag to the system. The automated protocol introduces the enzyme into the ECS and circulates it for a defined period to dissociate the cells.
- Cell Flush and Collection: The system flushes the ECS with the harvest buffer to recover the detached cells into a sterile collection bag.
- Concentration and Formulation: Concentrate the cell harvest via centrifugation and wash to remove the enzyme. Resuspend the final cell product in the appropriate cryopreservation or formulation medium. Perform final cell count, viability assessment, and release testing.
Diagram Title: Automated Hollow Fiber Bioreactor Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for cGMP-Compliant iPSC Manufacturing
| Item | Function | Considerations for cGMP |
|---|---|---|
| Xeno-Free Culture Medium | Provides nutrients and signals for cell growth and maintenance. | Must be compliant, well-characterized, and free of animal-derived components. Supplier's Quality Agreement is essential. |
| Recombinant Matrix Proteins (e.g., Vitronectin, Laminin) | Provides a defined surface for adherent cell culture. | Human-derived or recombinant sources are preferred over mouse-sourced to ensure safety and consistency. |
| cGMP-Grade Dissociation Enzymes (e.g., TrypLE, Accutase) | Passaging and harvesting cells by breaking cell-matrix and cell-cell adhesions. | Defined, non-animal origin formulations ensure process consistency and reduce contamination risk. |
| Single-Use Bioreactor Kits | Provides a sterile, closed environment for cell expansion. | Pre-sterilized and validated for performance. Eliminates cleaning validation and cross-contamination risk. |
| Process Analytical Technology (PAT) Probes (pH, DO) | In-line monitoring of critical process parameters. | Necessary for real-time quality control and for establishing a Quality by Design (QbD) framework. |
Strategic Implementation and Scaling Roadmap
Successfully integrating automation requires a phased, strategic approach beyond mere technical execution.
Phase 1: Foundation (Months 1-3)
- Activity: Establish a cross-functional team and conduct a thorough process map of the existing manual workflow. Identify key pain points, such as high-error steps and scalability bottlenecks [53].
- Output: A detailed gap analysis and a business case quantifying the true cost of manual processes, including direct labor, error correction, and opportunity costs [53].
Phase 2: Proof of Value (Months 4-6)
- Activity: Execute a pilot study using the chosen bioreactor technology. Use a well-characterized research-grade iPSC line to optimize parameters like seeding density and feeding regimen.
- Output: Parallel comparison data (as in Table 1) demonstrating improved yield, quality, and/or reduced labor. A validated, small-scale prototype of the automated process.
Phase 3: Scale and Tech Transfer (Months 7-12)
- Activity: Transfer the optimized process to a cGMP environment for manufacturing clinical-grade material. Create detailed Standard Operating Procedures (SOPs) and conduct training.
- Output: Engineering and GMP runs generating cells for preclinical safety studies. A robust, locked-down manufacturing process ready for regulatory submission.
Phase 4: Optimize and File (Months 13+)
- Activity: Generate consistency batches to demonstrate process robustness and batch-to-batch comparability. Compile all data into the Chemistry, Manufacturing, and Controls (CMC) section of the IND application [50].
- Output: A complete IND application, enabling the initiation of a Phase I clinical trial.
Diagram Title: Strategic Roadmap for Automation Implementation
The transition from manual processes to automated bioreactors is not merely a technical upgrade but a strategic imperative for the viable commercialization of autologous iPSC therapies. This shift directly addresses the critical challenges of scalability, reproducibility, and cost that have hindered clinical progress. By adopting a structured, data-driven approach—supported by the quantitative comparisons, detailed protocols, and strategic roadmap provided herein—research teams can build robust, regulatory-compliant manufacturing processes. This foundation is essential for successfully navigating the IND pathway and ultimately delivering transformative autologous cell therapies to patients.
The development of autologous induced pluripotent stem cell (iPSC) therapies represents a paradigm shift in regenerative medicine, offering the potential for patient-specific treatments for a range of chronic conditions [23]. Unlike traditional pharmaceuticals, these advanced therapies are living, patient-customized products where each manufacturing run produces a single dose for a specific individual [54]. This "lot of one" nature imposes extraordinary logistical challenges that are as critical to solve as the biological mechanisms themselves [54]. The entire process—from cell collection and reprogramming to differentiation, manufacturing, and reinfusion—requires flawless coordination of complex physical and digital supply chains. This application note provides detailed protocols for managing the two most critical logistical components: maintaining an unbroken chain of identity (CoI) that links patient to product throughout the process, and implementing robust cryogenic logistics to preserve cell viability during transport and storage. Successfully integrating these systems is essential for conducting reproducible, safe, and efficacious autologous iPSC therapy research.
Chain of Identity Management
Definition and Critical Requirements
The chain of identity is a verification system that maintains the unambiguous, non-transferable link between a patient's original cell sample and the final therapeutic product administered to that same patient [54]. In autologous therapies, each product is a "lot of one," making needle-to-needle traceability an absolute requirement for patient safety and regulatory compliance [54]. Unlike traditional biologics with standard tracking systems, autologous cell therapies require identity-linked tracking where the product itself acquires "medicinal status" at the point of infusion [54].
A robust CoI system must prevent the catastrophic consequences of product misidentification, which could include treatment failure or severe adverse events. The system must maintain bidirectional information flow across all stakeholders—patients, providers, collection centers, couriers, and manufacturers—while ensuring comprehensive quality assurance and regulatory compliance throughout the provenance of the cellular therapeutic [55].
Digital Tracking Protocol
Materials:
- Unique patient identifiers (2D barcodes, RFID tags)
- Electronic tracking system (commercial platforms like TrakCel or custom solutions)
- Blockchain or distributed ledger technology (optional for enhanced security)
- Data encryption protocols
Methodology:
Initial Patient Registration and Labeling
- Assign a globally unique identifier to the patient at the initial consultation
- Generate primary collection containers with machine-readable labels containing the patient identifier
- Link identifier to comprehensive patient metadata in secure database
- Verify patient identity using two-factor authentication before sample collection
Sample Collection Documentation
- Scan container label immediately before leukapheresis or biopsy procedure
- Document collection date/time, volume, and initial cell count
- Record personnel identifiers and collection facility information
- Perform initial quality assessment and link results to patient identifier
Chain-of-Custody Transfers
- Scan identifier at each transfer point (collection → shipping → manufacturing → storage → shipping → clinic)
- Record timestamp, location, and responsible party at each transition
- Implement dual-verification system for all critical hand-offs
- Document environmental conditions (temperature, shock) during transfers
Manufacturing Process Integration
- Maintain identifier through all manufacturing processes (reprogramming, expansion, differentiation)
- Scan identifier when transferring between culture vessels or cryogenic containers
- Link manufacturing batch records, quality control data, and potency assays to patient identifier
- Document all reagents and their lot numbers used in manufacturing
Final Product Verification and Administration
- Verify patient identity immediately before product administration
- Scan final product identifier and match to patient identifier using automated system
- Require dual-signoff by independent qualified personnel
- Document administration date, time, and clinical staff involved
The following workflow diagram illustrates the integrated chain of identity management process:
Quality Control and Validation
Regularly validate the CoI system through mock transport exercises and audit trails. Implement automated alerts for any identifier mismatches or protocol deviations. Maintain comprehensive system documentation for regulatory inspections, including data integrity verification protocols and disaster recovery procedures.
Cryogenic Logistics
Fundamental Principles and Challenges
Cryogenic logistics for autologous iPSC therapies require maintaining ultra-low temperatures (typically -150°C to -196°C) throughout transport to preserve cell viability and functionality [54]. Living cells are exceptionally sensitive to temperature fluctuations, pH changes, and mechanical strain induced by vibrations and shear stress during transport [54]. Even brief deviations from required temperature parameters can cause irreversible product degradation, rendering the therapy non-viable [54].
The cryopreservation process itself presents significant challenges. Cells contain >70% water, and freezing without adequate protection causes ice crystal formation that damages cellular structures [54]. Cryoprotectant agents (CPAs) such as DMSO (typically at 5-10% concentration) are essential to mitigate freezing damage, but introduce their own complications including cellular toxicity and patient side effects upon infusion [54]. Maintaining temperatures below the glass transition point (often < -130°C) is critical for long-term stability, requiring specialized equipment and monitoring throughout the supply chain [54].
Cryopreservation and Shipping Protocol
Materials:
- Controlled-rate freezer
- Cryogenic storage containers (cryobags, vials)
- Cryoprotectant agents (DMSO-based freezing media)
- Shipping containers: dry ice (-78.5°C) or liquid nitrogen vapor phase (-150°C to -196°C)
- Temperature data loggers with continuous monitoring
- Qualified cryogenic shipping containers
Methodology:
Pre-shipment Cryopreservation
- Prepare cells in log-phase growth with >90% viability
- Resuspend in appropriate freezing medium containing CPA
- Use controlled-rate freezing protocol: -1°C/minute to -40°C, then -10°C/minute to -100°C
- Transfer to long-term storage vapor phase liquid nitrogen (-150°C or below)
- Document freezing parameters and initial viability assessment
Shipping Container Preparation
- Select shipping container based on transport duration and temperature requirements
- For dry ice shipments: pack with sufficient solid CO₂ to maintain temperature for entire transit plus 24-hour buffer
- For liquid nitrogen dry vapor shippers: verify proper saturation of absorbent material
- Pre-condition shipping container according to manufacturer specifications
- Include temperature data logger with continuous recording capability
Product Packaging and Loading
- Wrap primary container (cryobag/vial) in protective secondary packaging
- Place temperature monitor in direct contact with product container
- Use absorbent material and secondary containment for liquid nitrogen shipments
- Secure product to prevent movement during transport
- Document loading procedures and initial temperature verification
Transport and Monitoring
- Use qualified carriers with specific experience in cell therapy transport
- Implement real-time GPS and temperature monitoring where possible
- Establish emergency response protocols for shipping delays or equipment failure
- Maintain communication chain between shipping, manufacturing, and clinical teams
- Document all transfer points and responsible parties
Receipt and Quality Assessment
- Verify temperature integrity upon receipt before accepting shipment
- Document maximum temperature exposure during transit
- Immediately transfer to secure storage at appropriate temperature
- Perform viability and identity testing before product release
- Document any deviations and corrective actions
Table 1: Comparison of Cryogenic Shipping Methods
| Parameter | Dry Ice | Liquid Nitrogen Dry Vapor |
|---|---|---|
| Temperature Range | -78.5°C | -150°C to -196°C |
| Maximum Duration | 3-5 days | 10-15 days |
| Advantages | Lower cost, widely available | Superior temperature stability, longer duration |
| Limitations | Sublimation requires overpacking, CO₂ buildup risk | Higher cost, specialized equipment required |
| Best Applications | Short-distance transport, backup shipping | International transport, critical cell products |
Thawing and Post-thaw Assessment Protocol
Materials:
- Water bath or dry thawing system (37°C)
- Pre-warmed culture medium
- Dilution medium for CPA removal
- Centrifuge
- Cell counter and viability analyzer
Methodology:
Thawing Procedure
- Prepare water bath or dry thawing system at 37°C
- Remove product from shipping container and immediately thaw using rapid method (60-90 seconds)
- Transfer to pre-warmed container and gradually dilute with culture medium to reduce CPA concentration
- Centrifuge gently to remove CPA and resuspend in appropriate medium
- Document thawing time and procedures
Post-thaw Assessment
- Perform cell count and viability assessment (trypan blue exclusion or automated methods)
- Assess recovery percentage compared to pre-freeze values
- For iPSCs, assess pluripotency markers post-recovery
- Document all quality control parameters
- Proceed to administration or further processing based on acceptance criteria
The following diagram illustrates the complete cryogenic logistics workflow:
Integrated Logistics Management
Orchestration Platform Implementation
Successful autologous iPSC therapy logistics requires integration of CoI and cryogenic systems through a centralized orchestration platform. These digital platforms provide real-time visibility across the entire supply chain, from patient cell collection through final product administration [54]. The platform should integrate temperature monitoring data with chain-of-custody records, providing automated alerts for any deviations in either system.
Implementation should include:
- Real-time dashboard showing status of all products in transit
- Automated alert escalation for temperature deviations or CoI verification failures
- Integration with manufacturing execution systems for seamless data flow
- Secure data exchange between all stakeholders (clinics, manufacturers, couriers)
- Regulatory reporting capabilities for chain-of-identity and chain-of-custody documentation
Contingency Planning and Risk Mitigation
Develop comprehensive contingency plans for potential failure points:
- Backup shipping arrangements for carrier failures
- Emergency product retrieval protocols for temperature excursions
- Redundant communication systems for critical status updates
- Qualification of alternative transport routes and methods
- Emergency product replacement strategies for irretrievable failures
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Autologous iPSC Therapy Logistics
| Category | Specific Items | Function & Application | Critical Parameters |
|---|---|---|---|
| Reprogramming Systems | Episomal vectors (c-Myc free), Sendai vectors, mRNA reprogramming kits | Non-integrating somatic cell reprogramming to pluripotency [23] | Integration-free status, clearance timeline, reprogramming efficiency [23] |
| Cryopreservation Media | DMSO-based cryoprotectant, serum-free freezing media, defined CPA cocktails | Protect cells from ice crystal damage during freezing and thawing [54] | DMSO concentration (5-10%), toxicity profile, post-thaw viability [54] |
| Shipping Medium | Cryostor, HypoThermosol, custom formulated shipping media | Maintain cell viability during transport, reduce temperature stress [54] | Ion balance, energy substrates, pH stability during temperature shifts |
| Temperature Monitoring | Single-use data loggers, wireless IoT sensors, RFID temperature tags | Continuous temperature monitoring during transport and storage [54] | Accuracy (±0.5°C), recording interval, alarm capabilities, battery life |
| Cell Identity Tracking | 2D barcode labels, RFID tags, blockchain verification systems | Maintain chain of identity from patient to final product [54] | Read reliability, data capacity, compatibility with existing systems |
| Quality Assessment | Flow cytometry panels, rapid viability assays, potency assays | Pre- and post-shipment product quality verification [23] | Validation status, turnaround time, correlation with product efficacy |
| Shipping Containers | Dry ice shippers, liquid nitrogen dry vapor shippers, qualified insulated containers | Maintain ultra-low temperatures during transport [54] | Hold time, temperature stability, qualification documentation |
Managing the logistical complexity of autologous iPSC therapy research requires meticulous integration of robust chain of identity systems with reliable cryogenic logistics protocols. The "needle-to-needle" process demands flawless execution at every transition point, with comprehensive documentation and quality control [54]. By implementing the detailed protocols outlined in this application note—including digital tracking systems, validated cryopreservation methods, and integrated orchestration platforms—researchers can establish the foundational infrastructure necessary for successful autologous iPSC therapy development. These logistical frameworks are not merely supportive functions but are essential components that directly impact product viability, patient safety, and ultimately, therapeutic efficacy.
The advancement of autologous induced pluripotent stem cell (iPSC) therapies from research to clinical application hinges on the establishment of robust, standardized quality control (QC) protocols. For patient-specific therapies, where each product constitutes a unique batch, confirming genomic integrity and pluripotency is not merely a regulatory formality but a fundamental prerequisite for ensuring patient safety and therapeutic efficacy [56]. Genomic instability, a recognized concern in iPSCs, can compromise the function of differentiated cells or pose tumorigenic risks, while inadequate pluripotency verification undermines the cells' capacity to generate the desired target tissues [57] [58]. This document outlines detailed application notes and protocols for assessing these critical quality attributes, providing a framework for researchers and drug development professionals to implement rigorous QC within the context of autologous iPSC therapy development.
Assessing Genomic Integrity
The process of reprogramming somatic cells into iPSCs, along with subsequent long-term culture and differentiation, can impose significant stress, potentially leading to genomic alterations. These can range from large-scale karyotypic abnormalities to subtle single-nucleotide variations [57]. A tiered, phase-appropriate analytical strategy is recommended to monitor these changes comprehensively.
Types and Origins of Genomic Abnormalities
Understanding the nature and potential origin of genomic aberrations is crucial for designing effective QC strategies. The table below summarizes the primary types of mutations observed in iPSCs.
Table 1: Common Genomic Abnormalities in Human iPSCs
| Abnormality Type | Description | Common Examples | Primary Detection Methods |
|---|---|---|---|
| Karyotype Aberrations | Gross chromosomal changes visible by microscopy. | Trisomy of chromosomes 12, 17, or X [57]. | G-banding karyotyping. |
| Copy Number Variations (CNVs) | Deletions or amplifications of DNA segments. | Recurrent regions on chr1, 2, 3, 16, and 20, encompassing cancer-associated genes like HCK [59]. | SNP genotyping, CGH-array. |
| Single Point Mutations | Alterations in single nucleotides. | An average of 6-12 protein-coding mutations per iPSC line [57]. | Whole Exome Sequencing (WES). |
| Uniparental Disomy (UPD) | Inheritance of two copies of a chromosome from one parent. | Reported for chromosomes 1 and 17; can lead to loss of heterozygosity [57]. | SNP genotyping. |
These abnormalities can be pre-existing in the somatic cell population and selected during reprogramming, or acquired de novo during the reprogramming process or extended in vitro culture [57]. Furthermore, the choice of somatic cell source impacts genomic stability; for instance, fibroblasts exhibit high genomic stability, while peripheral blood mononuclear cells (PBMCs) offer a less invasive alternative [58].
Recommended QC Assays and Protocols
A combination of techniques is necessary to detect the full spectrum of genomic abnormalities.
Protocol: G-Banding Karyotyping
Purpose: To identify gross chromosomal abnormalities and aneuploidy. Applications: Routine screening at master cell bank (MCB) and end-of-production cell bank (EPCB) stages. Methodology:
- Cell Culture: Culture iPSCs to 70-80% confluence. Add colcemid (final concentration 0.1 µg/mL) to the culture medium for 60-90 minutes to arrest cells in metaphase.
- Harvesting: Detach cells using gentle enzymatic (e.g., Accutase) or mechanical dissociation. Transfer the cell suspension to a centrifuge tube and pellet cells.
- Hypotonic Treatment: Resuspend the cell pellet in a pre-warmed 0.075 M KCl solution and incubate for 20 minutes at 37°C.
- Fixation: Pellet cells and carefully resuspend in freshly prepared Carnoy's fixative (3:1 methanol:glacial acetic acid). Repeat fixation 2-3 times.
- Slide Preparation: Drop the fixed cell suspension onto clean, wet microscope slides and age overnight.
- Staining and Analysis: Stain slides with Giemsa stain. Analyze at least 20 metaphase spreads under a microscope for chromosomal number and structure.
Protocol: SNP Genotyping for CNVs and UPD
Purpose: To detect sub-chromosomal copy number variations (CNVs) and regions of uniparental disomy (UPD). Applications: Essential for characterizing MCB and monitoring genomic stability during long-term culture. Methodology:
- DNA Extraction: Extract high-quality genomic DNA from iPSCs and the donor's somatic cells (e.g., fibroblasts) as an reference, using a commercial kit.
- Genotyping: Use a high-density SNP array (e.g., Illumina Infinium Global Screening Array) according to the manufacturer's instructions.
- Data Analysis: Analyze the data using dedicated software (e.g., GenomeStudio, Nexus CNV) to identify regions of copy number alteration and loss of heterozygosity (LOH) indicative of UPD.
Protocol: Whole Exome Sequencing (WES)
Purpose: To identify single nucleotide variants (SNVs) and small insertions/deletions (indels) in protein-coding regions. Applications: Comprehensive safety assessment of clinical-grade iPSC lines. Methodology:
- Library Preparation: Fragment genomic DNA and prepare a sequencing library with exome capture baits.
- Sequencing: Perform high-throughput sequencing on a platform such as Illumina NovaSeq to achieve >50x coverage.
- Bioinformatic Analysis: Map sequences to a reference genome (e.g., GRCh38) and call variants. Compare variants in the iPSC line to those in the matched somatic cell line to distinguish acquired mutations from pre-existing polymorphisms.
The following workflow diagram summarizes the tiered strategy for genomic integrity assessment:
Figure 1: A tiered workflow for genomic integrity assessment. This multi-faceted approach is recommended for comprehensive screening of iPSC lines, progressing from gross chromosomal analysis to finer-scale genetic variation.
Verification of Pluripotency
Pluripotency defines the foundational capacity of iPSCs to differentiate into derivatives of all three primary germ layers. Rigorous assessment requires a combination of assays that evaluate molecular markers and, crucially, functional capacity.
Key Pluripotency Assays
Pluripotency is not a single attribute but a cellular state characterized by specific markers and functions. The following table outlines the core assays used for its verification.
Table 2: Core Assays for Pluripotency Verification
| Assay Category | Specific Assay | Measured Parameters | Acceptance Criteria |
|---|---|---|---|
| Molecular Marker Expression | PCR / RT-qPCR | Expression of endogenous pluripotency genes (e.g., OCT4, SOX2, NANOG) [58]. | High expression relative to negative control. |
| Immunocytochemistry / Flow Cytometry | Protein expression of pluripotency markers (e.g., OCT4, SSEA-4, TRA-1-60) [58] [60]. | >95% positive staining for surface/downstream markers. | |
| Functional Capacity | In Vitro Directed Differentiation | Differentiation into representative cell types of ectoderm, mesoderm, and endoderm [58]. | Demonstrated expression of germ layer-specific markers. |
| In Vivo Teratoma Formation | Formation of complex, differentiated tissues from all three germ layers in immunocompromised mice [57]. | Histological evidence of tissues from ectoderm, mesoderm, and endoderm. |
Detailed Experimental Protocols
Protocol: Flow Cytometry for Pluripotency Surface Markers
Purpose: To quantitatively assess the percentage of cells expressing key pluripotency-associated surface markers. Applications: Routine quality check for ongoing culture and pre-differentiation validation. Methodology:
- Cell Preparation: Harvest a single-cell suspension of iPSCs using Accutase. Pass cells through a 40-µm cell strainer to ensure a single-cell suspension.
- Staining: Aliquot cells into tubes. Incubate with fluorochrome-conjugated antibodies against human SSEA-4 and TRA-1-60, alongside appropriate isotype controls, for 30-45 minutes on ice in the dark.
- Analysis: Wash cells to remove unbound antibody and resuspend in buffer containing a viability dye. Analyze on a flow cytometer. A well-characterized iPSC line should demonstrate >95% positivity for these markers.
Protocol:In VitroTrilineage Differentiation
Purpose: To functionally confirm the capacity of iPSCs to differentiate into ectoderm, mesoderm, and endoderm lineages. Applications: Critical demonstration of pluripotency, especially for master cell banks. Methodology: This is a simplified overview; specific, optimized commercial kits are recommended for each lineage.
- Starter Culture: Grow iPSCs to 80-90% confluence in 6-well plates.
- Directed Differentiation:
- Ectoderm: Transition cells to a neural induction medium. Over 7-10 days, cells will adopt a rosette morphology. Confirm by immunostaining for PAX6 (ectoderm progenitor) and later for β-III-Tubulin (neurons).
- Mesoderm: Use a medium containing BMP4, Activin A, and VEGF. After 5-7 days, analyze cells for expression of Brachyury (early mesoderm) and/or α-Smooth Muscle Actin (smooth muscle).
- Endoderm: Differentiate using a protocol involving Activin A and Wnt3a. After 5-7 days, confirm differentiation by immunostaining for SOX17 and FOXA2 (definitive endoderm markers).
- Analysis: Use RT-qPCR or immunocytochemistry to verify the expression of lineage-specific markers for all three germ layers.
The following diagram illustrates the logical sequence of pluripotency verification assays:
Figure 2: A cascading workflow for pluripotency verification. Confirmation typically begins with molecular marker analysis, proceeds to functional in vitro differentiation, and may require in vivo teratoma formation for stringent validation.
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and their critical functions in maintaining iPSC genomic integrity and pluripotency.
Table 3: Essential Research Reagent Solutions for iPQC QC
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Chemically Defined Medium (e.g., mTeSR1, E8) | Supports iPSC self-renewal and inhibits spontaneous differentiation [58]. | Ensures culture standardization; reduces batch-to-batch variability. |
| GMP-Grade Recombinant Laminin-521 | A defined, xeno-free substrate for feeder-free iPSC culture. | Promotes adhesion and proliferation; critical for clinical compliance. |
| Integration-Free Reprogramming Kit (e.g., Sendai virus, mRNA) | Generates iPSCs from somatic cells without genomic integration [58]. | Mitigates risk of insertional mutagenesis; enhances clinical safety. |
| GMP-Grade Growth Factors (FGF2, BMP4, etc.) | Directs iPSC differentiation into specific lineages. | Requires rigorous qualification for identity, purity, and potency [56]. |
| Genomic DNA Extraction Kit | Isolates high-quality DNA for downstream genetic analyses. | Must provide sufficient yield and purity for sequencing and arrays. |
Reducing Costs and Turnaround Time through Platform Process Development
The therapeutic potential of autologous induced pluripotent stem cells (iPSCs) is vast, offering promising avenues for treating a range of conditions from neurodegenerative diseases like Alzheimer's to ischemic stroke [61] [62]. However, their development as a mainstream therapeutic modality is hampered by high costs and prolonged turnaround times. The average cost of stem cell therapies can reach $50,000, with autologous iPSC therapies facing even greater financial and temporal challenges due to their patient-specific nature [63]. A primary driver of these challenges is the reliance on labor-intensive, manual manufacturing processes, which are not only costly but also introduce significant batch-to-batch variation [64]. This application note details a standardized platform process designed to overcome these hurdles by integrating automation, closed-system technologies, and optimized protocols. This approach is essential for making autologous iPSC therapies economically viable and accessible.
Quantitative Analysis of Process Efficiencies
Implementing a platform process fundamentally changes the economic and operational dynamics of autologous iPSC therapy production. The tables below summarize the quantitative impact of key interventions on cost and time.
Table 1: Impact of Automation on Manufacturing Parameters
| Parameter | Manual Process | Automated Platform | Improvement |
|---|---|---|---|
| Hands-on Time per Batch | ~40 hours | ~15 hours | ~62% Reduction [65] |
| Cell Expansion Duration | 4-6 weeks | 3-4 weeks | ~30% Reduction [65] |
| Risk of Contamination | High | Minimal (Closed Systems) | Significant Reduction [64] [65] |
| Batch Failure Rate | 15-20% | <5% | >75% Reduction [65] |
| Process Consistency | High Variability | High Consistency (Automated QC) | Significant Improvement [64] [65] |
Table 2: Cost Distribution Analysis (Pre- and Post-Platform Implementation)
| Cost Component | Traditional Process (% of Total) | Platform Process (% of Total) | Key Driver of Change |
|---|---|---|---|
| Labor | 45-55% | 20-25% | Automation & Reduced Hands-on Time [65] |
| Quality Control & Release | 15-20% | 10-15% | Integrated Real-time Monitoring & AI [65] |
| Raw Materials & Reagents | 15-20% | 25-30% | Standardized Kits & Closed-System Consumables |
| Capital Equipment/Facility | 10-15% | 30-35% | Investment in Automated Bioreactors & Robotic Platforms [64] |
| Estimated Total Cost per Dose | ~$40,000 - $60,000 | ~$15,000 - $25,000 | ~50% Reduction [63] [65] |
Experimental Protocols for Platform Process Development
Protocol: Automated Reprogramming and iPSC Clone Selection
Objective: To consistently generate patient-specific iPSC lines with minimal manual intervention and high efficiency.
Materials:
- Source Cells: Patient-derived fibroblasts or peripheral blood mononuclear cells (PBMCs).
- Reprogramming Method: Non-integrating Sendai viral vectors or mRNA transfection kits.
- Culture Vessel: Automated, closed-system bioreactor or multi-well plates compatible with robotic liquid handling.
- Culture Medium: Commercially available, defined iPSC reprogramming and maintenance medium.
- QC Reagents: Pre-formulated, ready-to-use qPCR assays for pluripotency markers.
Methodology:
- Cell Seeding: Use a robotic liquid handler to dispense a standardized number of source cells (e.g., 50,000 fibroblasts/well) into culture vessels.
- Automated Transduction/Transfection: Program the system to deliver a precise volume and multiplicity of infection (MOI) of the reprogramming vector to the cells.
- Feeding and Monitoring: Employ an automated cell culture system for scheduled medium exchanges. Integrated microscopes capture phase-contrast images for confluence tracking.
- Colony Picking: Utilize an AI-driven image analysis system to identify and select colonies with optimal iPSC morphology. A robotic arm then performs the picking and transfers colonies to expansion plates.
- Quality Control: Automate the extraction of RNA from a representative sample of expanded clones. Use a high-throughput qPCR system with pre-loaded assays for key pluripotency markers (e.g., NANOG, SOX2, OCT4) and a sendai virus clearance assay.
Protocol: Scalable Differentiation in Stirred-Tank Bioreactors
Objective: To differentiate iPSCs into clinically relevant cell types (e.g., neurons, cardiomyocytes) in a controlled, scalable system.
Materials:
- Cell Source: Master cell bank of clonal, characterized iPSCs.
- Bioreactor: Small-scale (e.g., 100-500 mL) single-use stirred-tank bioreactors with integrated sensors for pH, dissolved oxygen (DO), and temperature.
- Differentiation Kits: GMP-grade, defined differentiation kits targeting the desired cell lineage.
- Metabolite Analyzer: Automated, in-line or at-line analyzer for glucose and lactate.
Methodology:
- Inoculum Expansion: Expand iPSCs as aggregates in the bioreactor to achieve a target viable cell concentration for differentiation induction.
- Automated Induction: Initiate differentiation by programming a controlled, linear reduction in DO (for mesodermal lineages) or the addition of specific small molecules via a perfusion system. The system automatically adjusts the gas mix to maintain the DO setpoint.
- Process Control: Maintain pH and temperature within strict ranges. The automated system feeds cells based on real-time glucose consumption rates, switching from batch to fed-batch or perfusion mode as needed.
- Harvesting: At the endpoint, typically determined by a specific marker expression level analyzed by flow cytometry, cool the bioreactor and transfer the cell suspension to an automated filling and cryopreservation system.
Workflow Visualization: Manual vs. Automated iPSC Manufacturing
The following diagram contrasts the workflows, highlighting reductions in complexity and manual intervention points achieved through platform process development.
The Scientist's Toolkit: Essential Research Reagent Solutions
A standardized, off-the-shelf kit-based approach is fundamental to reducing variability and streamlining the platform process.
Table 3: Key Reagent Solutions for an Automated iPSC Platform
| Research Reagent Solution | Function | Impact on Standardization |
|---|---|---|
| GMP-Grade, Defined Medium Kits | Provides a consistent, xeno-free nutrient environment for iPSC expansion and differentiation. | Eliminates batch variability of serum; pre-optimized for specific lineages [66]. |
| Non-Integrating Reprogramming Kits | Efficiently generates footprint-free iPSCs from somatic cells using Sendai virus or mRNA. | Standardizes the critical first step; reduces safety profiling burden [66]. |
| Lineage-Specific Differentiation Kits | Contains pre-mixed, precise concentrations of small molecules and growth factors. | Dramatically reduces protocol optimization time and improves differentiation efficiency reproducibility [61] [66]. |
| Ready-to-Use QC Assay Panels | Multiplexed qPCR or flow cytometry panels for pluripotency, differentiation markers, and sterility. | Enables high-throughput, automated quality control with standardized pass/fail criteria [65]. |
| Closed-System Bioprocess Containers | Single-use, sterile fluid containment bags for media, buffers, and product. | Integrated with automated systems; eliminates cleaning validation and cross-contamination risk [64] [65]. |
The path to clinically and commercially viable autologous iPSC therapies is inextricably linked to the development of robust, cost-effective manufacturing processes. The platform process outlined herein, built on the pillars of automation, closed-system processing, and reagent standardization, demonstrates a clear and quantifiable path to reducing both costs and turnaround times. By adopting this approach, researchers and therapy developers can accelerate the translation of promising iPSC research from the laboratory to the clinic, ultimately fulfilling the promise of personalized regenerative medicine for a broader patient population.
Evaluating Efficacy, Safety, and Strategic Positioning
The development of disease-modifying therapies for Parkinson's disease (PD) has been marked by nearly three decades of clinical trials with limited success [67]. Two fundamental challenges have hindered progress: interventions that may occur too late in the disease course and the considerable biological heterogeneity of PD patient populations [67]. Recent advances in biological staging frameworks and cell-based therapies are now creating new pathways for therapeutic development. This application note examines clinical trial outcomes within the context of a broader thesis on autologous induced pluripotent stem cell (iPSC) therapy research, providing structured data, experimental protocols, and analytical tools for research scientists and drug development professionals.
Clinical Trial Outcomes in Parkinson's Disease
Disease-Modifying Trial Challenges and New Frameworks
Historically, most disease-modifying trials have targeted newly diagnosed PD patients before they begin symptomatic therapy, as it becomes methodologically challenging to dissect experimental drug effects once symptomatic treatments are initiated [67]. The field is now transitioning toward a biological definition of PD based on the presence of synuclein pathology, validated through biomarkers, and dopaminergic dysfunction [67]. This biological staging framework enables researchers to identify candidates for therapeutic interventions earlier in the disease process:
- Stage 1: Biological markers only (no clinical phenotype)
- Stage 2: Clinical phenotype with biomarkers (no functional impairment)
- Stage 3: Biology, clinical phenotype, and slight functional impairment (includes most newly diagnosed patients) [67]
This framework facilitates recruitment of individuals with the appropriate biology before classical PD diagnosis into clinical trials, potentially enabling earlier intervention.
Quantitative Outcomes from Recent Clinical Trials
Recent clinical trials have investigated diverse therapeutic approaches, from small molecules to cell therapies. The tables below summarize key quantitative outcomes from selected studies.
Table 1: Motor Function and Quality of Life Outcomes from Parkinson's Disease Clinical Trials
| Trial/Intervention | Study Details | Primary Outcomes | Secondary Outcomes |
|---|---|---|---|
| A9-DPC Cell Therapy (Phase 1/2a) [68] | - N=12 (low & high dose)- 12-month follow-up | - MDS-UPDRS Part III (Off) Improvement: - Low-dose: -12.7 points - High-dose: -15.5 points- Increased DAT Signal on [18F]FP-CIT PET | - Hoehn & Yahr Stage Improvement: - Low-dose: 3.7 to 2.7 - High-dose: 3.8 to 2.2- NMSS Score Improvement: - Low-dose: -31.7 points - High-dose: -35.8 points |
| Tavapadon (TEMPO-4, Phase 3) [69] | - Open-label- 62-week duration | - Treatment-Emergent AEs: Number of participants- Treatment Discontinuation: Number of participants | - QUIP-RS: Impulse control disorder assessment- MDS-UPDRS Parts I-III: Change from baseline |
| ABBV-951 (Phase 3) [69] | - Advanced PD patients- 96-week treatment | - Adverse Events (AEs): Percentage of participants- AEs of Special Interest: Percentage of participants | - Hauser Diary: Change in "off" time- EQ-5D-5L: Quality of life measure |
Table 2: Safety and Tolerability Outcomes from Parkinson's Disease Clinical Trials
| Trial/Intervention | Safety Profile | Notable Safety Findings | Participant Discontinuation |
|---|---|---|---|
| A9-DPC Cell Therapy [68] | - No tumorigenesis- No cell overgrowth- No ectopic cell migration | - Majority of TEAEs: mild to moderate- One asymptomatic mild hemorrhage case | - No treatment-related discontinuations reported |
| Tavapadon [69] | - Monitoring of TEAEs- Laboratory evaluations | - C-SSRS for suicidal ideation- Epworth Sleepiness Scale | - Tracked for AEs, death, PD worsening, etc. |
| ABBV-951 [69] | - AEs and SAEs monitoring- Specific AESIs tracking | - Focus on infusion-related reactions- Long-term safety over 96 weeks | - Percentage of participants with AEs |
The correlation between increased dopamine transporter (DAT) signals and improved motor function scores in the A9-DPC trial provides evidence supporting the mechanism of action through synaptic restoration via engrafted cells [68].
Experimental Protocols
Autologous iPSC-Derived Dopaminergic Neuron Therapy Protocol
The development of autologous iPSC-based therapies for Parkinson's disease requires rigorous protocols across cell reprogramming, differentiation, and transplantation. The following workflow outlines the key stages:
3.1.1 Somatic Cell Source and iPSC Reprogramming
- Donor Tissue Acquisition: Obtain patient somatic cells (typically dermal fibroblasts or peripheral blood mononuclear cells) under sterile conditions [50].
- Reprogramming Method Selection: Utilize integration-free methods such as Sendai virus, episomal vectors, or mRNA-based reprogramming to generate iPSCs [3] [50].
- Culture Conditions: Maintain cells in defined, xeno-free culture systems with appropriate supplements to ensure reproducible iPSC induction [50].
3.1.2 Dopaminergic Neuron Differentiation
- Neural Induction: Adapt monolayer-based neural induction protocols using dual SMAD inhibition to efficiently generate neural progenitor cells [3] [70].
- Ventral Midbrain Patterning: Apply specific morphogens (SHH, FGF8, GDF5) to pattern neural progenitors toward A9-type dopaminergic neurons with characteristic markers (LMX1A, FOXA2, OTX2) [68].
- Maturation: Culture differentiated cells in the presence of neurotrophic factors (BDNF, GDNF, TGF-β3) for 4-6 weeks to promote terminal differentiation into tyrosine hydroxylase-positive neurons [68].
3.1.3 Quality Control and Safety Testing
- Identity Testing: Verify dopaminergic neuron-specific markers (TH, NURR1, PITX3) via immunocytochemistry and flow cytometry [68] [50].
- Purity Assessment: Ensure >95% purity of dopaminergic precursors and exclusion of undifferentiated pluripotent cells (TRA-1-60, OCT4 negative) [68].
- Safety Testing: Perform sterility testing (bacteria, fungi, mycoplasma), endotoxin testing, and karyotype analysis [50].
- Tumorigenicity Assessment: Conduct in vitro assays and in vivo studies to confirm absence of residual undifferentiated cells with tumor-forming potential [50].
Clinical Transplantation and Assessment Protocol
3.2.1 Pre-transplantation Preparation
- Patient Selection: Enroll participants diagnosed with PD for more than 5 years who exhibit motor complications, using rigorous inclusion/exclusion criteria [68].
- Immunosuppression Regimen: Initiate appropriate immunosuppression prior to transplantation, typically with tacrolimus or similar agents, though autologous therapies may require less immunosuppression [50].
- Cell Product Formulation: Prepare final cell product in appropriate transplantation medium, with careful determination of cell viability (>90%), dose (e.g., 3.15-6.30 million cells), and volume [68].
3.2.2 Stereotactic Transplantation Procedure
- Surgical Planning: Use MRI-guided stereotaxis to identify optimal injection trajectories targeting the putamen [68].
- Transplantation Approach: Employ bilateral putamen transplantation with multiple injection tracks (typically 3 tracks per putamen) and distributed deposition points to maximize distribution of transplanted cells [68].
- Cell Delivery: Utilize specialized cannulas or microinjection systems with controlled infusion rates (e.g., 1-2 μL/min) to minimize backflow and ensure precise cell placement [68].
3.2.3 Post-transplantation Assessment
- Safety Monitoring: Conduct frequent assessments for treatment-emergent adverse events, including neurological exams, vital signs, and laboratory tests [68].
- Motor Function Evaluation: Perform serial MDS-UPDRS Part III assessments in the practically defined "off" state at baseline, 6, 12, and 24 months [68].
- Neuroimaging: Obtain [18F]FP-CIT PET scans at baseline and follow-up intervals to quantify dopamine transporter (DAT) signal changes in the putamen [68].
- Quality of Life Measures: Administer comprehensive assessments including PDQ-39, NMSS, and Schwab and England ADL scales to capture patient-reported outcomes [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Autologous iPSC Parkinson's Therapy Development
| Reagent/Category | Specific Examples | Research Function | Considerations for Autologous Therapy |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, MYC (OSKM); Small molecules | Somatic cell reprogramming to pluripotency | Use integration-free methods; xeno-free components [3] [50] |
| Neural Induction Media | Dual SMAD inhibitors; Defined media components | Direct differentiation toward neural lineage | GMP-grade components; Lot-to-lot consistency [70] |
| Dopaminergic Patterning Factors | SHH, FGF8, GDF5, CHIR99021 | Ventral midbrain specification | Concentration optimization; Temporal control [68] |
| Cell Culture Matrices | Laminin-521, Vitronectin, Synthemax | iPSC attachment and differentiation | Defined, animal-free substrates; Scalability [70] |
| Characterization Antibodies | Anti-TH, FOXA2, LMX1A, OCT4 | Lineage confirmation and purity assessment | Validated for flow cytometry and ICC; GMP-compliant [68] [50] |
Regulatory Pathway for Autologous iPSC Therapies
The development of autologous iPSC-based therapies requires careful navigation of regulatory requirements. The pathway from concept to clinical application involves multiple critical stages as illustrated below:
5.1 Chemistry, Manufacturing, and Controls (CMC)
- Manufacturing Site: Establish GMP-compliant facilities with appropriate equipment, quality control systems, and sterility standard operating procedures [50].
- Process Description: Provide detailed manufacturing workflow including all reagents, testing specifications, and final formulation [50].
- Product Characterization: Implement rigorous characterization of drug substance and drug product, including identity, potency, purity, and viability [50].
5.2 Preclinical Development
- Proof-of-Concept Studies: Demonstrate feasibility and efficacy in relevant preclinical models that recapitulate Parkinsonian features [50].
- GLP Toxicology Studies: Conduct good laboratory practice (GLP)-compliant toxicology studies including single-dose toxicity, repeat-dose toxicity, and tumorigenicity assessments [50].
- Biodistribution Studies: Evaluate cell distribution, persistence, and potential migration to non-target tissues using appropriate animal models [50].
5.3 Clinical Trial Design Considerations
- Phase 1 Objectives: Primary focus on safety evaluation with exploratory efficacy endpoints [68].
- Endpoint Selection: Include standardized measures such as MDS-UPDRS, quality of life scales, and objective neuroimaging biomarkers [69] [68].
- Patient Monitoring Plan: Implement long-term follow-up (up to 5 years post-transplantation) to monitor for delayed adverse events [68] [50].
The regulatory pathway for autologous iPSC therapies presents unique challenges including the need for patient-specific manufacturing runs, comprehensive product characterization for each batch, and demonstration of product comparability across manufacturing cycles [50].
Autologous induced pluripotent stem cell (iPSC) therapy represents a transformative approach for treating chronic ischemic heart disease and other conditions. A critical component of its clinical translation is a rigorous safety profile analysis, which ensures that therapeutic benefits are not outweighed by adverse events. This protocol details comprehensive methodologies for tracking adverse events and assessing long-term engraftment of autologous iPSC-derived cardiomyocytes (iPSC-CMs), providing a framework for researchers and drug development professionals. The guidelines are framed within the context of the International Society for Stem Cell Research (ISSCR) emphasis on rigor, oversight, and transparency in stem cell research and clinical translation [2].
Key Safety Parameters and Quantitative Assessment
A thorough biosafety assessment for autologous iPSC-based therapies must evaluate multiple critical parameters to ensure patient safety. These include tracking the potential for toxicity, tumorigenicity, immunogenicity, and the biodistribution patterns of the administered cells. Furthermore, confirming cellular product quality through assessments of sterility, identity, potency, and viability is essential for therapeutic efficacy and safety [71]. The table below summarizes the core safety parameters, associated risks, and recommended assessment methods.
Table 1: Key Safety Parameters for Autologous iPSC-Based Therapies
| Safety Parameter | Potential Risk | Recommended Assessment Methods |
|---|---|---|
| Long-term Engraftment | Graft failure, loss of therapeutic effect | Longitudinal PET/CT imaging with reporter genes (e.g., NIS), histological analysis [72] |
| Tumorigenicity | Teratoma or other tumor formation | Long-term in vivo modeling in immunocompromised animals, histopathology [72] [71] |
| Immunogenicity | Immune rejection, inflammatory response | Immunohistochemistry for immune cell infiltration, HLA typing, comparison of autologous vs. allogeneic outcomes [72] [71] |
| Biodistribution | Ectopic tissue formation, off-target engraftment | Quantitative PCR (qPCR), PET imaging, MRI [71] |
| Product Quality | Contamination, inconsistent efficacy | Sterility testing, flow cytometry for cell identity, potency assays, viability assays [71] |
| General Toxicity | Systemic or local adverse effects | Clinical pathology (blood/urine tests), histopathological examination of major organs [71] |
Experimental Protocols for Safety and Engraftment Analysis
Protocol for Longitudinal Engraftment Monitoring Using PET/CT Imaging
This protocol utilizes the sodium/iodide symporter (NIS) as a reporter gene to non-invasively track the survival and location of transplanted autologous iPSC-CMs in large animal models, as demonstrated in non-human primates [72].
- Principle: The NIS gene is introduced into iPSCs prior to differentiation. After transplantation, the expression of NIS allows the engrafted cells to be visualized over time using clinical positron emission tomography and computed tomography (PET/CT) imaging following the administration of a radiotracer.
- Materials:
- Autologous iPSCs with stable NIS reporter gene expression.
- Differentiation reagents for generating iPSC-CMs.
- PET/CT imaging system.
- Appropriate radiotracer (e.g., (^{124})I for PET).
- Procedure:
- Cell Preparation: Differentiate NIS-expressing autologous iPSCs into cardiomyocytes (iPSC-CMs) using established protocols.
- Transplantation: Administer iPSC-CMs directly into the target tissue (e.g., myocardium) following the induction of a small, subclinical myocardial infarction.
- Image Acquisition: Perform baseline PET/CT imaging immediately post-transplantation. Schedule subsequent imaging sessions at regular intervals (e.g., monthly) for long-term monitoring (e.g., 6-12 months).
- Image Analysis: Quantify the signal intensity and volume of the radiotracer uptake at the graft site over time. Stable or increasing signal indicates successful long-term engraftment, while a decline suggests graft loss.
- Notes: This method provides quantitative, longitudinal data without the need for terminal procedures, allowing for continuous monitoring in the same subject. The absence of signal in non-target organs confirms the lack of ectopic biodistribution.
Protocol for Histological Assessment of Engraftment and Immune Response
Following the in vivo study endpoint, histological analysis is critical for validating imaging data and providing detailed structural and cellular context.
- Principle: Histological examination of the target tissue confirms the presence, maturation, and integration of transplanted cells and allows for the detection of any immune rejection or tumorigenic events.
- Materials:
- Harvested heart tissue (or other target organ).
- Fixative (e.g., 4% paraformaldehyde).
- Paraffin embedding system and microtome.
- Primary antibodies: Anti-cardiac Troponin (cTnI) for cardiomyocytes, Anti-Ki67 for proliferation, Anti-CD3/CD45 for immune cell infiltration.
- Secondary antibodies and detection system.
- Procedure:
- Tissue Harvesting and Processing: At the study endpoint, perfuse and harvest the target tissue. Fix the tissue, process it, and embed it in paraffin. Section the tissue to 5-10 µm thickness.
- Histological Staining: Perform Hematoxylin and Eosin (H&E) staining for general morphology and Masson's Trichrome staining for collagen deposition and fibrosis assessment.
- Immunohistochemistry (IHC): Deparaffinize and rehydrate sections. Perform antigen retrieval. Incubate with primary antibodies overnight at 4°C, followed by appropriate secondary antibodies. Develop using a chromogenic substrate and counterstain.
- Analysis:
- Engraftment Success: Identify human-specific markers (e.g., human-specific nuclear antigen) to confirm the presence of donor-derived cells.
- Maturation: Assess sarcomeric organization and expression of mature cardiac markers.
- Immune Response: Quantify the presence of CD3+ T-cells or CD45+ leukocytes within and around the graft site. The absence of significant infiltration indicates a lack of rejection, particularly in autologous settings [72].
- Tumorigenicity: Systematically scan all sections for any aberrant tissue structures or teratoma formation.
The experimental workflow for these core protocols is outlined in the diagram below.
Protocol for Assessing Immunological Safety
A key advantage of autologous iPSC therapies is the potential to avoid immune rejection; however, this must be empirically confirmed.
- Principle: This protocol compares the fate of autologous versus allogeneic iPSC-CMs transplanted in a controlled model to directly assess immunogenicity.
- Materials:
- Autologous and allogeneic iPSC-CMs.
- Immunocompetent animal model (e.g., non-human primate).
- Flow cytometry equipment and antibodies for immune phenotyping.
- Procedure:
- Study Design: Transplant autologous iPSC-CMs into one group and allogeneic iPSC-CMs into a control group. A third group can receive allogeneic cells with immunosuppression.
- In Vivo Monitoring: Use the PET/CT imaging protocol described in 3.1 to track graft survival in both groups over time.
- Ex Vivo Analysis: At the study endpoint, analyze graft sites via IHC for T-cell (CD3+) and macrophage (CD68+) infiltration. Compare the extent of infiltration between autologous and allogeneic groups.
- Systemic Immune Analysis: Collect peripheral blood mononuclear cells (PBMCs) at various time points and analyze by flow cytometry for activated T-cell populations.
- Expected Outcome: As demonstrated in primate studies, autologous grafts should show stable engraftment for over 6-12 months with no significant immune cell infiltration, while allogeneic grafts will be rejected within weeks [72].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the safety and engraftment protocols requires high-quality, well-defined reagents and materials. The following table lists key solutions and their critical functions in the experimental workflow.
Table 2: Essential Research Reagent Solutions for iPSC-CM Safety Analysis
| Research Reagent / Material | Function and Application | Key Considerations |
|---|---|---|
| Reporter Gene Constructs (e.g., NIS) | Enables non-invasive, longitudinal tracking of cell fate and engraftment via PET/CT imaging [72]. | Ensure stable genomic integration and that reporter expression does not impair cell function or differentiation potential. |
| Defined iPSC-CM Differentiation Kits | Generates a consistent and pure population of cardiomyocytes from iPSCs for transplantation. | Use GMP-grade components where possible. Confirm differentiation efficiency via flow cytometry (e.g., cTnT+ cells). |
| Validated Antibody Panels | Critical for IHC analysis of cell identity (cTnI), maturation, proliferation (Ki67), and immune infiltration (CD3, CD45) [72] [71]. | Validate antibodies for specific species and application (e.g., IHC on paraffin-embedded tissue). |
| qPCR Reagents for Biodistribution | Detects and quantifies human-specific DNA sequences in various organs to assess off-target cell migration [71]. | Assays must be highly specific and sensitive to detect low levels of engrafted cells. |
| Laboratory Management Templates | Supports organization and standardization of lab operations, including reagent labeling, cryo-storage, and maintenance schedules [73]. | Promotes reproducibility and compliance with Good Laboratory Practice (GLP). |
The comprehensive safety profile analysis outlined here, incorporating longitudinal imaging, detailed histology, and rigorous immunological assessment, is indispensable for the clinical advancement of autologous iPSC therapies. Adherence to these detailed protocols, supported by the essential research toolkit, will provide the robust, long-term safety data required by regulatory bodies and build the necessary evidence base for transitioning these promising therapies into human clinical trials. As emphasized by the ISSCR, maintaining the highest standards of scientific and ethical integrity is paramount throughout this process [2].
Advanced therapy medicinal products (ATMPs), particularly those based on cells, represent a paradigm shift in treating conditions ranging from cancer to degenerative diseases. The fundamental distinction in this field lies in the source of the therapeutic cells: the patient themselves (autologous) or a healthy donor (allogeneic). For researchers and drug development professionals, the choice between these two pathways has profound implications for therapeutic protocol design, manufacturing logistics, and clinical applicability. This application note provides a detailed, head-to-head comparison of these approaches, framing the analysis within the context of developing a protocol for autologous induced pluripotent stem cell (iPSC) therapy, a rapidly advancing frontier in personalized regenerative medicine [3] [74].
Defining the Therapeutic Approaches
Autologous Cell Therapy
Autologous cell therapy involves the harvest of a patient's own cells (e.g., somatic cells, T cells, or hematopoietic stem cells), which are then manipulated, potentially including genetic modification or differentiation, and subsequently re-administered to the same patient [75] [76]. A prominent example is CAR-T cell therapy for hematological malignancies, where a patient's T cells are engineered to target cancer cells [77]. The autologous iPSC therapy workflow begins with collecting patient somatic cells, such as fibroblasts, which are reprogrammed into pluripotent stem cells. These iPSCs are then expanded, characterized, and differentiated into the desired therapeutic cell type (e.g., midbrain dopaminergic cells for Parkinson's disease) before being transplanted back into the patient [74].
Allogeneic Cell Therapy
Allogeneic cell therapy utilizes cells derived from one or more healthy donors. These cells are processed, often expanded on a large scale, and cryopreserved to create an "off-the-shelf" product that is readily available for infusion into multiple patients [75] [78]. Allogeneic hematopoietic stem cell transplantation (HSCT) for leukemia is a classic example, where donor stem cells replace a patient's diseased bone marrow [76]. The allogeneic process centralizes manufacturing around a master cell bank derived from a single, rigorously screened donor, enabling the production of thousands of doses from a single source [79].
Head-to-Head Comparative Analysis
The following tables provide a quantitative and qualitative comparison of autologous and allogeneic cell therapies across critical parameters for research and development.
Table 1: Comparative Analysis of Core Characteristics
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [77] [76] | Healthy donor(s) [77] [76] |
| Immunological Compatibility | High; minimal risk of immune rejection or GvHD [75] [77] | Lower; requires HLA matching and/or immunosuppression to mitigate GvHD and rejection [75] [80] |
| Treatment Model | Personalized, "service-based" [75] | Standardized, "off-the-shelf" [75] [78] |
| Manufacturing Scale | Scale-out (multiple parallel, patient-specific batches) [76] | Scale-up (large, single batches for multiple patients) [76] |
| Key Advantage | Avoids immune complications [75] | Immediate availability and scalability [75] [78] |
| Primary Challenge | Logistical complexity, high cost, and product variability [75] | Immune rejection, GvHD, and need for immunosuppression [75] [80] |
Table 2: Quantitative Comparison of Manufacturing and Clinical Parameters
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Estimated Manufacturing Cost per Dose | £2,260 - £3,040 (≈ $3,630 - $4,890) [79] | £930 - £1,140 (≈ $1,490 - $1,830) [79] |
| Typical Vein-to-Vein Time | Several weeks [75] | Immediate (from cryostock) [75] |
| Donor Screening & Testing Cost | £990 - £1,320 per patient [79] | £10 - £20 per dose (amortized) [79] |
| Release Testing Cost | £300 - £500 per batch (1 patient) [79] | £3 - £5 per dose (batch = ~100 doses) [79] |
| Non-Relapse Mortality (in multiple myeloma) | 4% - 12% [80] | 15% - 45% [80] |
| 5-Year Overall Survival (in multiple myeloma) | 29% - 54% [80] | 9% - 29% [80] |
Experimental Protocol for Autologous iPSC Therapy
The following workflow diagrams and accompanying protocol detail the critical stages for developing an autologous iPSC-based therapy, from somatic cell reprogramming to preclinical safety and efficacy testing.
Diagram 1: Autologous iPSC Therapy Workflow
Protocol: Generation and Preclinical Validation of Clinical-Grade Autologous iPSCs
4.1.1 Somatic Cell Collection and Reprogramming
- Objective: To establish patient-specific iPSC lines with minimal risk of genomic integration.
- Methodology:
- Biopsy: Obtain a fresh skin punch biopsy (3-4 mm) from a patient under local anesthesia [74].
- Primary Culture: Aseptically dissect and explant the tissue to culture dermal fibroblasts in a GMP-compliant facility. Use xeno-free culture media.
- Reprogramming: Transfect early-passage fibroblasts with non-integrating episomal vectors carrying reprogramming factors (OCT4, SOX2, KLF4, L-MYC, LIN28) [3] [74].
- iPSC Colony Picking: Manually pick and expand clonal iPSC colonies based on embryonic stem cell-like morphology onto a feeder-free substrate.
4.1.2 iPSC Line Characterization and Quality Control
- Objective: To ensure the genomic integrity and pluripotency of established iPSC lines.
- Methodology:
- Genomic Analysis: Perform whole-genome/exome sequencing to rule out deleterious mutations and confirm the absence of integrated reprogramming vectors [74].
- Pluripotency Validation: Conduct RNA sequencing to confirm a gene expression profile consistent with pluripotency. Confirm the expression of key pluripotency markers (OCT4, NANOG, SSEA-4) via immunocytochemistry [3].
- Karyotyping: Perform G-band karyotyping to verify genomic stability at passage 10 and 20.
4.1.3 Directed Differentiation into Therapeutic Cells
- Objective: To efficiently and reproducibly differentiate iPSCs into the target cell type.
- Methodology (for midbrain dopaminergic cells - mDACs):
- Protocol Refinement: Employ a refined, GMP-compatible 21-day protocol [74].
- Dual-SMAD Inhibition: Initiate neural induction using SMAD signaling pathway inhibitors (e.g., LDN-193189, SB-431542) [3].
- Patterning: Add specific morphogens (e.g., SHH, FGF8) to pattern the neural progenitor cells toward a midbrain dopaminergic fate.
- Maturation: Culture the cells in maturation factors (e.g., BDNF, GDNF, ascorbic acid) to promote the final dopaminergic phenotype.
4.1.4 Preclinical Safety and Efficacy Testing
- Objective: To assess the in vivo safety and functional efficacy of the iPSC-derived product.
- Methodology:
- Safety Study: Conduct a 39-week Good Laboratory Practice (GLP)-compliant study in an immunodeficient mouse model. Key endpoints include comprehensive histopathology to search for teratoma formation or ectopic tissue growth [74].
- Efficacy Study: Transplant the mDACs into a rodent model of Parkinson's disease (e.g., 6-hydroxydopamine lesion model). Monitor behavioral recovery (e.g., in amphetamine-induced rotation test) over 6-9 months [74].
- Post-mortem Analysis: Quantify dopaminergic neuron survival and, critically, dopaminergic fiber density in the striatum, which has been identified as a key correlate of functional recovery [74].
Diagram 2: Allogeneic Off-the-Shelf Therapy Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Cell Therapy Research
| Research Reagent / Material | Function in Protocol |
|---|---|
| Non-integrating Reprogramming Vectors (e.g., Episomal vectors, Sendai virus) | Deliver reprogramming factors to somatic cells without genomic integration, a critical safety step for clinical translation [74]. |
| GMP-grade Culture Media & Growth Factors | Support the xeno-free, standardized expansion and maintenance of iPSCs and their derivatives under defined conditions [79] [74]. |
| SMAD Pathway Inhibitors (e.g., LDN-193189, SB-431542) | Key small molecules for efficient neural induction by inhibiting TGF-β and BMP signaling pathways during differentiation [3]. |
| CRISPR/Cas9 System | Enables precise genome editing for creating hypoimmunogenic allogeneic cells (e.g., knockout of B2M and CIITA) or introducing therapeutic transgenes [77]. |
| Flow Cytometry Antibody Panels | Critical for characterizing cell surface markers (e.g., for pluripotency: TRA-1-60, SSEA-4; for mDACs: FOXA2, LMX1A, Tyrosine Hydroxylase) to assess identity and purity [74]. |
| Closed-system Automated Bioreactors | Enable scalable, consistent, and sterile cell expansion, reducing manual handling and contamination risk for both autologous and allogeneic processes [79] [76]. |
The choice between autologous and allogeneic cell therapy is not a simple binary but a strategic decision informed by the target disease, patient population, and commercial considerations. Autologous therapies, exemplified by the iPSC protocol detailed herein, offer a personalized path with a superior immunological safety profile but face significant hurdles in cost, logistics, and product variability [75] [74]. Allogeneic "off-the-shelf" therapies promise greater accessibility and economies of scale but must overcome the persistent challenges of immune rejection and GvHD [75] [80]. For drug development professionals, the future lies in leveraging advanced engineering—such as CRISPR-based gene editing to create universal donor cells—and sophisticated automation to optimize both paradigms, ultimately broadening the availability of these transformative treatments [77].
Analyzing Immunological Response and Long-Term Persistence
Autologous induced pluripotent stem cell (iPSC) therapies represent a frontier in regenerative medicine for treating autoimmune diseases, offering the potential for patient-specific tissue repair and immune modulation. The core therapeutic premise involves reprogramming a patient's somatic cells to pluripotency and differentiating them into desired functional cell types [3]. Since these derived cells are genetically identical to the recipient (isogenic grafts), they are theoretically protected from immune rejection [81]. However, emerging evidence indicates that the process of reprogramming, differentiation, and transplantation can introduce immunogenicity, challenging the assumption of complete immune invisibility [81] [23]. Therefore, a rigorous, standardized protocol for analyzing immunological response and ensuring the long-term persistence of transplanted cells is critical for the advancement of clinical applications. This document provides detailed application notes and experimental protocols for the immunological assessment of autologous iPSC-derived therapies within the broader context of preclinical therapeutic development.
Immunological Assessment Framework for Autologous iPSC Therapies
The immune system's interaction with autologous iPSC-derived cells is complex, involving both innate and adaptive immunity. A comprehensive assessment should evaluate the following key areas:
- Innate Immune Response: This includes monitoring activation of natural killer (NK) cells via "missing-self" recognition and activation of the complement system [81].
- Adaptive Immune Response: Even autologous cells can trigger T-cell and B-cell responses, particularly if they express remnant embryonic antigens or neoantigens acquired during in vitro culture [81].
- Durability and Functional Persistence: Long-term studies are essential to confirm cell survival, integration, and function without tumorigenicity or senescence [23].
A multi-platform approach is recommended for a thorough investigation. The table below summarizes the primary experimental methods for evaluating these responses.
Table 1: Key Methodologies for Immunological Assessment of Autologous iPSC Therapies
| Assessment Goal | In Vitro Platforms | In Vivo Models | Key Readouts |
|---|---|---|---|
| T-Cell Activation | Mixed Lymphocyte Reaction (MLR), Antigen-Specific T-cell assays [81] | Humanized immune system mice [81] | T-cell proliferation, IFN-γ release (e.g., via ELISA) [7], Cytotoxicity |
| NK Cell Activation | NK cell cytotoxicity assays [81] | Not applicable in standard rodent models for human cells | Cytokine release, Direct killing (e.g., LDH assay) |
| Antibody Response | Flow cytometry to detect antibody binding [7] | Serum analysis from treated animals [7] | Circulating anti-donor antibody levels (e.g., IgG, IgM) |
| Long-Term Engraftment | Not applicable | Immunodeficient or humanized mice [81] | Cell survival over time (e.g., bioluminescence), Histology for integration |
| Systemic Immune Status | Multiplex cytokine/chemokine arrays [81] | Blood and serum analysis from host organisms | Profile of inflammatory mediators (e.g., IFN-γ, IL-10, TGF-β) |
Detailed Experimental Protocols
Protocol 1: In Vitro T-Cell Recall Assay
This protocol assesses the potential for iPSC-derived cells to trigger antigen-specific memory T-cell responses, which is crucial for evaluating the risk of rejection.
3.1.1 Materials
- Responder T-cells: Peripheral blood mononuclear cells (PBMCs) isolated from the same donor who provided the somatic cells for iPSC generation.
- Stimulator cells: The differentiated autologous iPSC-derived cell product (e.g., cardiomyocytes, neurons).
- Control cells: Undifferentiated autologous iPSCs, and/or parental somatic cells.
- Culture Medium: RPMI-1640 supplemented with 10% human AB serum, L-glutamine, and penicillin/streptomycin.
- Interferon-gamma (IFN-γ) ELISA Kit: For quantifying T-cell activation.
- Equipment: 96-well U-bottom plates, CO₂ incubator, plate reader.
3.1.2 Procedure
- Cell Preparation: Irradiate (or treat with mitomycin C) the stimulator cells (iPSC-derived product, control cells) to prevent their proliferation.
- Co-culture Setup: Seed irradiated stimulator cells (1-5 x 10⁴ cells/well) with responder PBMCs (1-5 x 10⁵ cells/well) in 96-well plates. Include wells with PBMCs alone (negative control) and PBMCs with a mitogen like phytohemagglutinin (positive control).
- Incubation: Culture cells for 5-7 days at 37°C in a 5% CO₂ incubator.
- Analysis:
- Supernatant Collection: Centrifuge plates and collect supernatants for IFN-γ measurement by ELISA according to the manufacturer's instructions.
- Proliferation Assay (Alternative): After 5 days, pulse wells with ³H-thymidine for 16-18 hours and measure incorporated radioactivity using a beta-counter.
3.1.3 Data Interpretation A significant increase in IFN-γ release or T-cell proliferation in co-cultures with the iPSC-derived product compared to negative controls and parental somatic cells indicates an immunogenic response. This suggests the differentiated cells express antigens recognized by the autologous T-cells [7].
Protocol 2: Assessing Humoral Immune Response In Vivo
This protocol evaluates the generation of antibodies against the autologous cell graft in a pre-clinical model.
3.2.1 Materials
- Experimental Animals: Immunocompetent murine models or, preferably, mice with a humanized immune system.
- Test Article: Differentiated autologous iPSC-derived cells.
- Control Articles: Vehicle control, and potentially allogeneic iPSC-derived cells.
- Reagents: Fluorescently conjugated anti-human IgG and IgM antibodies, Flow cytometry buffer (PBS with 1% BSA).
3.2.2 Procedure
- Cell Administration: Transplant the autologous iPSC-derived cells into the appropriate target tissue (e.g., intramuscular, intrarenal) of the animal model.
- Serum Collection: Collect blood serum from the animals pre-injection and at regular intervals post-injection (e.g., 2, 4, 8 weeks).
- Antibody Detection Assay:
- Harvest a separate batch of the same differentiated cell type used for injection.
- Incubate these cells with serial dilutions of the collected mouse serum.
- Wash cells and stain with a fluorescently labelled antibody against mouse IgG or IgM.
- Analyze cells using flow cytometry to detect bound antibodies.
3.2.3 Data Interpretation An increase in the mean fluorescence intensity (MFI) of antibody-bound cells over time, particularly IgG, indicates a humoral immune response against the graft. This suggests that the transplanted cells express proteins that are recognized as foreign by the host's immune system, even in an autologous setting [7].
Visualization of Key Concepts
Immune Recognition Pathways of iPSC-Derived Grafts
The following diagram illustrates the primary innate and adaptive immune pathways that can be activated by autologous iPSC-derived cellular therapies, informing the design of the above protocols.
The Scientist's Toolkit: Essential Research Reagents
A successful investigation into the immunology of iPSC therapies relies on a suite of key reagents and tools. The following table details essential components for the protocols described in this document.
Table 2: Key Research Reagent Solutions for Immunological Analysis
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Human AB Serum | Supplement for in vitro immune assays (e.g., MLR). Provides human proteins and lipids, reducing non-specific background activation compared to fetal bovine serum. | Batch variability can affect results; recommend screening and using a single batch for a study series. |
| ELISA Kits (e.g., IFN-γ) | Quantification of soluble cytokines and chemokines in cell culture supernatants or animal serum as a measure of immune activation. | Multiplex bead-based arrays (e.g., Luminex) can provide broader cytokine profiles from a single sample. |
| Anti-Human HLA Antibodies | Flow cytometric analysis of HLA Class I and II expression on differentiated iPSC products. Critical for assessing "missing-self" NK cell activation risk. | Include antibodies for classical (HLA-A, B, C) and non-classical (HLA-E, G) molecules. |
| Immunodeficient Mice (e.g., NSG) | In vivo model for studying human cell engraftment and persistence without murine adaptive immunity. | Lacking a full immune system, these models cannot assess adaptive rejection. |
| Humanized Immune System Mice | In vivo model generated by engrafting human hematopoietic stem cells into immunodeficient mice. Allows study of human immune responses to iPSC grafts. | Model variability and incomplete reconstitution of all immune cell types remain challenges. |
| Flow Cytometry Antibodies | Characterization of immune cell populations (T, B, NK cells), activation markers (CD69, CD25), and checkpoint molecules (PD-1, PD-L1). | Complex panel design requires careful consideration of fluorochrome brightness and spillover. |
Concluding Remarks
The path to clinically successful autologous iPSC therapies is paved with a thorough understanding of their interaction with the immune system. By implementing the standardized protocols and analytical frameworks outlined in this document—encompassing detailed in vitro co-culture assays, longitudinal in vivo studies of humoral and cellular immunity, and a deep analysis of graft persistence—researchers can robustly evaluate immunological safety and efficacy. This rigorous approach is indispensable for de-risking translational development, optimizing manufacturing protocols, and ultimately ensuring that autologous iPSC-derived treatments achieve their promise of safe and durable therapeutic benefit for patients with autoimmune and other degenerative diseases.
The emergence of sophisticated cell therapies, particularly those based on induced pluripotent stem cells (iPSCs), presents a paradigm shift in therapeutic development, forcing a critical re-evaluation of traditional economic models. This analysis provides a structured framework for comparing autologous, patient-specific iPSC therapies against allogeneic, off-the-shelf products. The core of this comparison lies at the intersection of therapeutic precision, manufacturing complexity, and economic viability. For researchers and drug development professionals, the decision between these pathways is not merely technical but fundamentally strategic, impacting development timelines, regulatory strategy, and eventual patient access [23] [82].
The global market context underscores the significance of this shift. The hyper-personalized medicine market is experiencing robust growth, projected to expand from $2.77 trillion in 2024 to $5.49 trillion by 2029, driven by advances in genomic technologies and heightened demand for targeted therapies [83]. Within this landscape, iPSC-based cell replacement therapies represent a promising frontier for treating chronic conditions such as macular degeneration, cardiopulmonary disease, and neurodegenerative disorders, areas where traditional small and large molecules have shown limited efficacy [23] [84]. This document outlines detailed protocols and analytical frameworks to guide research and development within this evolving field.
Economic and Clinical Comparative Analysis
A comprehensive cost-benefit analysis must account for direct development costs, long-term economic factors, and distinct clinical profiles. The following tables summarize the critical quantitative and qualitative differentiators.
Table 1: Quantitative Development and Cost Analysis
| Parameter | Autologous iPSC Therapy | Allogeneic Off-the-Shelf Product |
|---|---|---|
| Average Development Cost | Significantly higher (process per patient) | High (bulk process development) |
| Cost of Goods Sold (COGS) | Very High (≥ $20,000 - $50,000+ per dose) [85] [63] [86] | Lower (potential for scale) |
| Therapeutic Price Point | Premium pricing ($25,000 - $50,000+) [63] [87] | Moderate to High (broader reimbursement target) |
| Development Timeline | Protracted (complex logistics, patient-specific batches) | Streamlined (standardized, centralized production) |
| Market Size | Niche populations, rare diseases | Broad patient populations, common indications |
| Insurance Coverage | Typically not covered, considered experimental [85] [86] [87] | Higher likelihood for validated, approved products |
Table 2: Qualitative Clinical and Manufacturing Profile
| Profile | Autologous iPSC Therapy | Allogeneic Off-the-Shelf Product |
|---|---|---|
| Immunogenicity | Lower (self-derived cells) [23] | Higher (requires HLA matching or immunosuppression) |
| Tumorigenicity Risk | Patient-specific; must be managed per batch | Donor-specific; controlled via master cell banks |
| Potency & Reproducibility | Variable (dependent on individual patient cells) [23] [84] | Highly consistent (from a characterized cell bank) |
| Manufacturing Complexity | High (decentralized or complex logistics) | Lower (centralized, scalable bioreactors) |
| Time to Patient | Long (weeks to months for manufacturing) | Short (immediate availability from inventory) |
| Example Applications | Highly personalized regenerative protocols | Cancer immunotherapy, standardized tissue grafts |
Experimental Protocol: iPSC Line Generation and Characterization
The foundation of both autologous and allogeneic therapies is the establishment of a clinically viable iPSC line. This protocol details the key methodology for generating and validating iPSC lines suitable for subsequent differentiation.
Materials and Reagents
Table 3: Essential Research Reagent Solutions
| Reagent/Material | Function | Considerations for cGMP |
|---|---|---|
| Episomal Vectors (e.g., pCXLE-hOCT3/4, pCXLE-hSK, pCXLE-hUL) | Non-integrating reprogramming to deliver pluripotency factors. | Use of GMP-grade plasmids is mandatory for clinical use. |
| Human Dermal Fibroblasts (HDFs) or PBMCs | Somatic cell source for reprogramming. | Must be sourced from a qualified donor (allogeneic) or patient (autologous) under informed consent. |
| Reprogramming Media | Supports reprogramming and initial iPSC colony growth (e.g., containing bFGF). | Formulate with xeno-free, defined components. |
| mTeSR Plus or Equivalent | Feeder-free maintenance culture of established iPSCs. | Use of a defined, cGMP-compliant medium is essential. |
| Rho-associated kinase (ROCK) inhibitor (Y-27632) | Improves survival of single-cell passaged iPSCs. | For use during passaging and cryopreservation. |
| G-band Karyotyping & SNP Microarray | Analyzes genetic integrity and stability. | Required for master cell bank characterization. |
| Flow Cytometry Antibodies | Confirms pluripotency marker expression (e.g., TRA-1-60, SSEA4, OCT4). | Use validated antibody panels for release criteria. |
Step-by-Step Workflow
Somatic Cell Source Preparation:
- Isolate and expand target somatic cells (e.g., HDFs from a 3mm skin biopsy or CD34+ PBMCs from whole blood) under xeno-free culture conditions for a minimum of two passages to obtain sufficient cell numbers (≥ 5 x 10^5 cells).
- Confirm cell viability >95% and absence of microbial contamination via sterility testing.
Non-Integrating Reprogramming:
- Electroporation: Transfect 1 x 10^6 somatic cells with a combination of episomal plasmids (e.g., OCT3/4, SOX2, KLF4, L-MYC, LIN28, p53 shRNA) using a square-wave electroporator (e.g., Neon System, 1650V, 10ms, 3 pulses).
- Alternative Method: For enhanced safety, use a Sendai virus vector, noting that extended culture is required to dilute out viral components [23].
iPSC Colony Picking and Expansion:
- Plate transfected cells on vitronectin-coated plates in reprogramming medium. Refresh medium daily.
- Between days 21-28, manually pick morphologically defined, compact colonies using a stereomicroscope and transfer them to 96-well plates pre-coated with matrix.
- Expand clonal lines in mTeSR Plus medium, passaging as small clusters using EDTA or gentle cell dissociation reagent.
Quality Control and Characterization:
- Pluripotency Validation: Confirm expression of key markers (OCT4, SOX2, NANOG, TRA-1-60, SSEA4) via flow cytometry (>90% positive population) and immunocytochemistry.
- Trilineage Differentiation: Perform in vitro spontaneous differentiation via embryoid body formation and confirm differentiation into endoderm, mesoderm, and ectoderm lineages by RT-PCR and immunostaining.
- Genetic Stability: Perform G-band karyotyping to confirm a normal karyotype. Use SNP microarray to identify copy number variations (CNVs) and other sub-microscopic anomalies.
- Clearance of Reprogramming Vectors: For episomal methods, perform PCR across at least 10 passages to demonstrate the absence of residual plasmids [23].
The logical workflow and key decision points for establishing a clinical-grade iPSC line are summarized in the diagram below.
Experimental Protocol: Directed Differentiation to Cardiomyocytes
As a representative protocol for generating a therapeutic cell product, this section details the differentiation of iPSCs into cardiomyocytes, a target for cardiac repair.
Materials and Reagents
Table 4: Key Reagents for Cardiac Differentiation
| Reagent/Material | Function | Protocol Role |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; Activates Wnt signaling | Mesoderm induction |
| IWPR-1 | Wnt inhibitor; Suppresses Wnt signaling | Cardiac specification |
| RPMI 1640 Medium | Basal differentiation medium | Base for all differentiation stages |
| B-27 Supplement (Insulin-free) | Chemically defined serum-free supplement | Supports cardiac differentiation |
| B-27 Supplement (With Insulin) | Chemically defined serum-free supplement | Supports cardiomyocyte maturation |
| Lactic Acid | Energy source selection agent | Purifies cardiomyocyte population |
| Anti-TNNT2 / cTroponin T Antibody | Cardiomyocyte-specific marker | Flow cytometry validation |
Step-by-Step Workflow
iPSC Preparation for Differentiation:
- Culture iPSCs to 85-90% confluency in a 6-well plate in mTeSR Plus. The cells should be in a state of active, log-phase growth.
- Ensure a uniform monolayer, as patchy or over-confluent cultures impair differentiation efficiency.
Cardiac Mesoderm Induction (Day 0):
- Prepare Induction Medium: RPMI 1640 supplemented with B-27 Supplement (Insulin-free) and 6-8 µM CHIR99021.
- Completely aspirate the mTeSR Plus and add 2 mL of Induction Medium per well of a 6-well plate. This is designated as Day 0 of differentiation.
Wnt Inhibition and Cardiac Specification (Day 3):
- After 72 hours, aspirate the medium. Without washing, add 2 mL of Specification Medium: RPMI 1640 with B-27 Supplement (Insulin-free) and 5 µM IWP-1.
- Incubate the cells for 48 hours.
Basal Culture and Spontaneous Contraction (Day 5 onwards):
- On Day 5, aspirate the medium and replace it with 2 mL of Basal Medium: RPMI 1640 with B-27 Supplement (With Insulin).
- Refresh the Basal Medium every 2-3 days. Observe cultures daily under a microscope for the appearance of spontaneously contracting areas, typically emerging between Days 8-10.
Metabolic Selection and Maturation (Day 12 onwards):
- To enrich for cardiomyocytes, replace the medium with Glucose-Free RPMI 1640 supplemented with B-27 and 4 mM Lactic Acid.
- Culture the cells in this selective medium for 4-7 days, which will eliminate non-cardiac, glucose-dependent cells.
- Return the cells to Basal Medium (RPMI/B-27 With Insulin) for further maturation (≥ 2 weeks).
Characterization of Final Product:
- Purity Analysis: Dissociate cells and analyze by flow cytometry for cardiac Troponin T (TNNT2). A successful differentiation yields >90% TNNT2+ cells.
- Functional Assessment: Perform calcium imaging or patch-clamp electrophysiology to confirm electrophysiological functionality.
The timeline and critical signaling pathway manipulations for the cardiac differentiation protocol are illustrated below.
The Scientist's Toolkit: Critical Reagents and Assays
Successful development of iPSC-based therapies relies on a suite of well-characterized reagents and rigorous quality control assays. The following table expands on the essential tools for researchers in this field.
Table 5: Advanced Research Toolkit for iPSC Therapy Development
| Tool Category | Specific Examples | Research Function & Importance |
|---|---|---|
| Reprogramming Systems | Episomal plasmids, Sendai virus (CytoTune), mRNA kits | Generate integration-free iPSCs. Choice balances efficiency, safety, and cost. |
| cGMP-Grade Media & Matrix | mTeSR Plus, StemFlex, Vitronectin (VTN-N), Laminin-521 | Support xeno-free, feeder-free culture essential for clinical compliance. |
| Gene Editing Tools | CRISPR-Cas9 ribonucleoproteins (RNPs) | Introduce corrective mutations (autologous) or knockout rejection antigens (allogeneic). |
| Cell Sorting & Analysis | Flow Cytometry (e.g., for SSEA4/TRA-1-60), MACS | Purify target cell populations and assess pluripotency/differentiation efficiency. |
| Bioanalytical Assays | G-band Karyotyping, SNP Microarray, NGS (e.g., RNA-Seq), Mycoplasma Testing | Ensure genetic stability, identity, purity, and safety of cell products. |
| Functional Assays | Patch-clamp Electrophysiology (cardiomyocytes), Calcium Imaging, Microelectrode Array (MEA) | Confirm the functional maturity of differentiated cell products in vitro. |
| In Vivo Validation | Teratoma Formation Assay in SCID mice, Disease-specific animal models | Assess pluripotency (teratoma) and therapeutic efficacy of the cell product. |
Regulatory Pathways and Requirements for Market Approval
The development pathway for autologous induced pluripotent stem cell (iPSC) therapies represents one of the most complex challenges in modern regenerative medicine, requiring navigation through evolving regulatory landscapes. Unlike allogeneic (donor-derived) products, autologous therapies utilize a patient's own cells, which are reprogrammed, potentially genetically modified, differentiated, and expanded before being administered back to the same individual. This personalized approach introduces unique manufacturing, characterization, and regulatory hurdles. In 2025, regulatory agencies worldwide have significantly advanced their frameworks to address these challenges, emphasizing risk-based approaches and flexible clinical trial designs while maintaining rigorous safety and efficacy standards [88]. Understanding these pathways is essential for researchers and drug development professionals aiming to translate autologous iPSC therapies from laboratory research to clinically available treatments.
The regulatory ecosystem for these advanced therapies has matured considerably, with the U.S. Food and Drug Administration (FDA) releasing updated guidance documents specifically addressing the unique characteristics of cell and gene therapies. Recent developments include new draft guidances on expedited programs, post-approval monitoring, and innovative trial designs tailored for small populations, all directly relevant to autologous iPSC-based products [88] [89]. Furthermore, international standards such as the International Society for Stem Cell Research (ISSCR) Guidelines provide essential ethical and practical frameworks for clinical translation, emphasizing rigor, oversight, and transparency throughout development [2]. This document synthesizes these evolving requirements into actionable application notes and protocols specifically contextualized within autologous iPSC therapy research.
Current Regulatory Landscape and Expedited Pathways
Recent Regulatory Developments
The regulatory landscape for advanced therapies witnessed significant evolution in 2025, with agencies implementing new mechanisms to balance accelerated access with evidentiary standards. In September 2025, the FDA released three pivotal draft guidance documents that directly impact autologous iPSC therapy development [88] [89]:
- Expedited Programs for Regenerative Medicine Therapies for Serious Conditions: This guidance clarifies how sponsors can leverage the Regenerative Medicine Advanced Therapy (RMAT) designation, Fast Track, and Breakthrough Therapy pathways to accelerate development and review.
- Postapproval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products: This document provides recommendations for using real-world evidence to monitor long-term safety and effectiveness without delaying initial approvals.
- Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations: Recognizing the challenges of rare disease trials, this guidance encourages adaptive, Bayesian, and externally controlled designs to generate robust evidence with fewer patients.
Concurrently, regulatory agencies are increasingly embracing technological advancements to enhance oversight. The FDA has released draft guidance on 'Considerations for the Use of Artificial Intelligence To Support Regulatory Decision-Making for Drug and Biological Products' in January 2025, outlining a risk-based credibility assessment framework for AI models used in drug development [88]. This is particularly relevant for autologous iPSC therapies, where AI may play a role in quality control, manufacturing optimization, and outcome prediction.
Expedited Development Pathways
For autologous iPSC therapies targeting serious or life-threatening conditions, several expedited pathways can significantly reduce development timelines. The RMAT designation, established specifically for regenerative medicine products, offers intensive FDA guidance throughout development and potential priority review [89]. Recent examples include the RMAT designation granted to Fate Therapeutics for FT819, an iPSC-derived CAR T-cell therapy for systemic lupus erythematosus [90]. The designation was supported by early-phase clinical data demonstrating potential to address unmet needs, and it enables the company to work closely with the FDA on an accelerated development strategy.
Table 1: Expedited Regulatory Pathways for Advanced Therapies
| Pathway | Eligibility Criteria | Key Benefits | Relevance to Autologous iPSC |
|---|---|---|---|
| RMAT Designation | Regenerative medicine therapy for serious condition; preliminary clinical evidence indicates potential to address unmet need | Intensive FDA guidance, rolling review, potential for accelerated approval | Ideal for personalized therapies targeting serious diseases with limited options |
| Fast Track | Therapy for serious condition; nonclinical or clinical data demonstrates potential to address unmet medical need | Early and frequent communication with FDA, rolling review | Suitable for autologous iPSC products with compelling preclinical data |
| Breakthrough Therapy | Therapy for serious condition; preliminary clinical evidence shows substantial improvement over available therapies | Intensive guidance on efficient trial design, organizational commitment | Applicable when autologous iPSC therapy shows dramatic early efficacy |
| Accelerated Approval | Therapy for serious condition; effect on surrogate endpoint reasonably likely to predict clinical benefit | Approval based on surrogate endpoint; post-approval confirmation studies required | Valuable for diseases where long-term outcomes are difficult to assess quickly |
Beyond these standardized pathways, the FDA has also launched innovative programs like the Gene Therapies Global Pilot Program (CoGenT), which explores concurrent, collaborative regulatory reviews with international partners such as the European Medicines Agency. This initiative aims to increase regulatory harmonization, improve review efficiency, and ultimately accelerate global patient access to transformative therapies [88].
Preclinical and CMC Requirements
Preclinical Testing Strategies
Preclinical development of autologous iPSC therapies requires comprehensive testing strategies that address the unique characteristics of these living products. The FDA's "Preclinical Assessment of Investigational Cellular and Gene Therapy Products" guidance outlines a science-based, risk-adjusted approach where the extent of preclinical testing should be commensurate with the product's risk profile, considering factors like cell type, differentiation state, route of administration, and persistence in the body [89]. For autologous iPSC-derived products, key preclinical considerations include:
- Tumorigenicity Assessment: Comprehensive evaluation of residual undifferentiated iPSCs and malignant transformation potential through in vitro assays (soft agar colony formation), in vivo studies (teratoma formation in immunodeficient mice), and genomic stability monitoring throughout the manufacturing process.
- Biodistribution and Engraftment Studies: Tracking cell fate, migration, persistence, and functional integration using appropriate animal models. For autologous products, immunocompetent models with analogous human conditions are preferred when available.
- Proof-of-Concept Studies: Demonstration of biological activity and therapeutic effect in clinically relevant disease models, with special consideration for species-specific differences in host microenvironment and disease pathophysiology.
The preclinical package should sufficiently characterize the relationship between product attributes and biological activity to inform initial clinical trial dosing and scheduling, while identifying potential risks for clinical monitoring.
Chemistry, Manufacturing, and Controls
The Chemistry, Manufacturing, and Controls requirements for autologous iPSC therapies represent perhaps the most significant regulatory challenge due to the personalized nature of these products. Unlike traditional pharmaceuticals, each manufacturing lot constitutes a single patient-specific dose, requiring rigorous process controls and comprehensive characterization. Recent FDA guidances, including "Potency Assurance for Cellular and Gene Therapy Products" and "Manufacturing Changes and Comparability for Human Cellular and Gene Therapy Products," provide specific recommendations for these challenges [89].
Table 2: Key CMC Requirements for Autologous iPSC Therapy Products
| CMC Element | Key Requirements | Technical Considerations for Autologous iPSC |
|---|---|---|
| Starting Materials | Donor screening and testing, tissue collection procedures, consent | Patient-specific somatic cells; strict chain of identity and chain of custody |
| Manufacturing Process | Process validation, aseptic processing, in-process controls | Multiple stages: reprogramming, clonal selection, expansion, differentiation, formulation |
| Product Characterization | Identity, purity, viability, potency, genomic stability | Pluripotency markers, lineage-specific markers, functional potency assays, karyotyping |
| Quality Control | Release criteria, sterility, mycoplasma, endotoxin | Batch-specific testing despite single-patient lot; validated rapid microbiology methods |
| Final Product Formulation | Composition, excipients, storage conditions | Cryopreservation optimization; container closure systems compatible with cellular products |
A critical regulatory consideration is whether the autologous iPSC product meets the definition of "minimally manipulated" or constitutes "more than minimal manipulation." Most iPSC-based therapies undergo extensive genetic reprogramming and in vitro differentiation, placing them firmly in the "more than minimal manipulation" category and requiring regulation as drugs or biologics under Section 351 of the Public Health Service Act [15]. This necessitates submission of an Investigational New Drug application prior to clinical trials, followed by a Biologics License Application for market approval.
Clinical Trial Design and Ethical Considerations
Innovative Clinical Trial Designs
The development of autologous iPSC therapies often faces challenges in traditional clinical trial design due to small patient populations, personalized manufacturing, and ethical considerations in placebo controls. The FDA's September 2025 draft guidance on "Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations" specifically addresses these challenges by encouraging adaptive, Bayesian, and externally controlled designs [88]. For autologous iPSC therapies, several design considerations are particularly relevant:
- Adaptive Design Elements: Protocol pre-specified adaptations including sample size re-estimation, dose selection, and population enrichment based on interim analyses. This is especially valuable given the limited preliminary data often available for these novel therapies.
- Bayesian Approaches: Utilization of historical controls and continuous learning from accumulating data to increase trial efficiency, potentially reducing the number of concurrent controls needed.
- Single-Arm Studies with External Controls: Justified when randomization is unethical or impractical, using rigorously selected historical controls from natural history studies or previous trials.
The FDA also encourages discussions about using real-world evidence to supplement clinical trial data, particularly for long-term safety monitoring and for contextualizing outcomes in rare diseases [88]. These flexible approaches are essential for autologous iPSC therapies, where traditional large-scale randomized trials may be impractical.
Ethical Framework and Informed Consent
The ethical development of autologous iPSC therapies extends beyond regulatory compliance to encompass fundamental principles of research ethics. The ISSCR Guidelines emphasize four key ethical principles: autonomy, beneficence, non-maleficence, and justice [2] [15]. For researchers, this translates to specific responsibilities in trial design and participant engagement:
- Comprehensive Informed Consent: The consent process for autologous iPSC therapies must address unique considerations including the complexity of the manufacturing process, theoretical long-term risks (particularly tumorigenicity), privacy of genetic information, and the personalized nature of the therapy. Special attention should be given to communicating uncertainties given the novel nature of these interventions.
- Therapeutic Misconception Management: Researchers must clearly distinguish between research procedures and clinical care, ensuring participants understand the experimental nature of the intervention and do not underestimate risks or overestimate benefits.
- Equitable Access Considerations: While autologous therapies are inherently patient-specific, developers should consider affordability and accessibility in trial design and eventual implementation planning, including strategies to reduce manufacturing costs.
The ISSCR specifically emphasizes that the provision of unproven stem cell-based interventions outside formal research settings constitutes a breach of professional medical ethics and responsible scientific practice [2]. Researchers have an obligation to distinguish their work from direct-to-consumer marketing of unproven therapies, which may utilize "tokens of scientific legitimacy" such as registry listings or institutional affiliations without demonstrating true safety and efficacy [91].
Regulatory Workflow Visualization
Regulatory Pathway for Autologous iPSC Therapy - This diagram illustrates the comprehensive regulatory pathway from preclinical development through post-market surveillance, highlighting key decision points and potential acceleration through expedited programs.
Manufacturing and Quality Control Protocols
Process Development and Characterization
The manufacturing protocol for autologous iPSC therapies requires meticulous attention to process consistency and product characterization, despite the inherent variability of patient-specific starting materials. Recent FDA draft guidance on "Potency Assurance for Cellular and Gene Therapy Products" emphasizes the need for quantitative potency assays that measure biological activity specific to the product's mechanism of action [89]. A standardized manufacturing workflow should incorporate:
- Reprogramming and Clonal Selection: Patient somatic cell reprogramming using integration-free methods, with comprehensive characterization of resulting iPSC clones including pluripotency confirmation and genomic stability assessment.
- Master Cell Bank Establishment: Creation of extensively characterized master cell banks for each patient-specific line, with thorough testing for identity, purity, viability, and sterility.
- Directed Differentiation: Development of robust, scalable differentiation protocols yielding the target cell population with minimal residual undifferentiated cells.
- Final Product Formulation: Optimization of formulation matrices and cryopreservation conditions to maintain cell viability and functionality during storage and transport.
A critical aspect of manufacturing protocol development is implementing process analytical technologies to monitor critical quality attributes throughout production. For autologous products, where traditional batch-release testing may be impractical due to time constraints, quality control strategies should emphasize in-process controls and real-time release testing when justified.
Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Autologous iPSC Therapy Development
| Reagent Category | Specific Examples | Function in Development | Regulatory Considerations |
|---|---|---|---|
| Reprogramming Systems | Non-integrating episomal vectors, Sendai virus, mRNA | Generation of patient-specific iPSCs | Documentation of vector clearance; GMP-grade materials required for clinical use |
| Cell Culture Media | Defined maintenance media, GMP-grade growth factors, small molecules | iPSC expansion and directed differentiation | Chemical definition; absence of animal-derived components; quality documentation |
| Characterization Tools | Pluripotency markers (OCT4, NANOG), flow cytometry panels, karyotyping reagents | Quality assessment throughout manufacturing | Standardized protocols; validated assays; reference materials |
| Gene Editing Reagents | CRISPR-Cas9 systems, nuclease enzymes, donor templates | Genetic modification for therapeutic effect or safety enhancement | Comprehensive off-target analysis; integration site mapping |
| Cell Sorting Reagents | Antibody panels, magnetic beads, viability dyes | Purification of target cell population | GMP-grade separation systems; documentation of reagent removal |
The selection of research reagents during development should anticipate eventual transition to GMP-grade materials for clinical manufacturing. Early engagement with regulatory authorities regarding the qualification of critical reagents is essential, particularly for novel assays or platform technologies. Applied StemCell's submission of a Type II Drug Master File for its GMP-grade hiPSC line represents an emerging strategy to streamline regulatory review by providing established reference materials [90].
Post-Approval Considerations and Global Harmonization
Post-Market Safety Monitoring
The regulatory pathway for autologous iPSC therapies extends beyond initial approval to encompass comprehensive post-market safety monitoring. The FDA's September 2025 draft guidance on "Postapproval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products" emphasizes proactive risk management and real-world evidence collection to identify potential long-term risks that may not be evident in pre-approval clinical trials [88]. Key elements include:
- Long-Term Follow-Up Studies: Implementation of extended monitoring protocols, typically 5-15 years, to detect delayed adverse events such as tumor formation or unexpected tissue integration.
- Registry Development: Establishment of product-specific or disease-specific registries to aggregate safety and effectiveness data across treatment centers, facilitating detection of rare adverse events.
- Risk Evaluation and Mitigation Strategies: Development of targeted strategies to ensure therapy benefits outweigh risks, potentially including restricted distribution, specialized training for providers, or patient monitoring agreements.
For autologous iPSC therapies with genetic modifications, additional monitoring for genomic instability or unintended consequences of editing is essential. The FDA's guidance on "Long Term Follow-up After Administration of Human Gene Therapy Products" provides specific recommendations for these scenarios, even when the primary therapeutic mechanism is cell-based rather than genetic [89].
Global Regulatory Harmonization
The development of autologous iPSC therapies increasingly requires navigation of international regulatory landscapes, particularly as sponsors pursue global development programs. Recent initiatives like the FDA's Gene Therapies Global Pilot Program (CoGenT) aim to explore concurrent, collaborative regulatory reviews with international partners such as the European Medicines Agency [88]. This program, modeled after Project Orbis in oncology, allows foreign regulators to participate in FDA review meetings and share information, potentially reducing duplication and accelerating global access.
Despite these harmonization efforts, significant regional differences persist in regulatory requirements, reimbursement frameworks, and clinical practice standards. The ISSCR Guidelines provide an important international consensus framework for stem cell research and clinical translation, addressing the global diversity of cultural, political, legal, and ethical issues [2]. Developers of autologous iPSC therapies should engage early with regulatory agencies across target markets to understand specific requirements and identify potential harmonization opportunities.
The increasing adoption of decentralized manufacturing models, particularly relevant for autologous therapies, presents both regulatory challenges and opportunities for global access. Some regulatory bodies are showing openness to these models when accompanied by appropriate oversight and quality control systems, potentially improving accessibility in resource-limited settings [88].
Conclusion
Autologous iPSC therapy represents a paradigm shift in personalized regenerative medicine, offering a biologically matched treatment with a superior safety profile regarding immune rejection. While the protocol presents significant challenges in manufacturing scalability, cost, and logistical complexity, recent advances in reprogramming, gene editing, and automated bioprocessing are steadily overcoming these hurdles. The promising results from early-phase clinical trials, particularly in Parkinson's disease, validate its potential clinical benefit and safety. The future of the field lies in optimizing and standardizing these protocols to balance the bespoke nature of autologous treatments with the economic and practical demands of widespread clinical application. Continued research into enhancing differentiation efficiency, ensuring long-term safety, and developing supportive regulatory frameworks will be crucial to fully realizing the transformative potential of autologous iPSC therapies for a broad range of human diseases.
References
- 1. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 2. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 3. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 4. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 5. Addressing graft-versus-host disease in allogeneic cell-based ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00654-3]
- 6. A cloaked human stem-cell-derived neural graft capable of ... [https://www.sciencedirect.com/science/article/pii/S1934590925000980]
- 7. Immune rejection of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079651/]
- 8. Phase I/II trial of iPS-cell-derived dopaminergic cells for ... [https://www.nature.com/articles/s41586-025-08700-0]
- 9. Stem Cell Therapies for Retinal Degenerations [https://www.retinalphysician.com/issues/2025/may/stem-cell-therapies-for-retinal-degenerations/]
- 10. Randomized Study of Intravitreal Autologous CD34+ Stem ... [https://www.sciencedirect.com/science/article/pii/S2666914525002039]
- 11. Applications of Modern Cell Therapies: The Latest Data in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565404/]
- 12. Application of patient-derived induced pluripotent stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03564-5]
- 13. Control of immune response in an iPSC-based allogeneic ... [https://www.sciencedirect.com/science/article/pii/S1934590925002693]
- 14. Aspen Neuroscience Initiates Cohort 3 in ASPIRO Phase 1/ ... [https://aspenneuroscience.com/aspen-neuroscience-initiates-cohort-3-in-aspiro-phase-1-2a-trial-highlighting-commercial-formulation-of-anpd001-and-its-transformative-potential-for-parkinsons-disease/]
- 15. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 16. 2025 Code of Ethics for Nurses Provision 1.4 [https://codeofethics.ana.org/provision-1-4]
- 17. The 2025 Guide to Ethical Standards in Personalized ... [https://www.laboratoriosrubio.com/en/ethical-personalized-medicine/]
- 18. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 19. Aspen Neuroscience Launches First Patient Screening ... [https://aspenneuroscience.com/aspen-neuroscience-launches-first-patient-screening-study-forplanned-clinical-trial-of-personalized-cell-replacement-in-parkinsons-disease/]
- 20. Patient and Disease–Specific Induced Pluripotent Stem Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6934989/]
- 21. Analysis of somatic mutations in whole blood from 200618 ... [https://www.nature.com/articles/s41588-024-01755-1]
- 22. A Comparative View on Human Somatic Cell Sources for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4241335/]
- 23. The Challenges to Advancing Induced Pluripotent Stem Cell-Dependent Cell Replacement Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 24. Frontiers | Clinical translation of human iPSC technologies: advances, safety concerns, and future directions [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 25. Effects of Integrating and Non-Integrating Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4488894/]
- 26. Gene-delivery systems for iPS cell generation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2811526/]
- 27. Site-specific recombinase strategy to create iPS cells efficiently ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC3466168]
- 28. Quality and Regulatory Requirements for the Manufacture ... [https://pubmed.ncbi.nlm.nih.gov/39821060/]
- 29. Human Pluripotent Stem Cell Banking [https://www.stemcell.com/psc-cell-quality/cell-banking]
- 30. An Efficient Protocol for Single-Cell Cloning Human ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6365467/]
- 31. History and Development of Autologous Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8486970/]
- 32. Differentiation of Mature Dopaminergic Neurons from ... [https://pubmed.ncbi.nlm.nih.gov/40220093/]
- 33. Phase I trial of hES cell-derived dopaminergic neurons for ... [https://www.nature.com/articles/s41586-025-08845-y]
- 34. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 35. Cryopreservation Procedures [https://www.alcor.org/cryopreservation-procedures/]
- 36. Cryoshipping Process: From Order to Delivery ... [https://arkcryo.com/blog/cryoshipping-process-from-order-to-delivery-with-ark-cryo.html]
- 37. Age Is Relative-Impact of Donor Age on Induced ... [https://pubmed.ncbi.nlm.nih.gov/29423397/]
- 38. Overcoming the Variability of iPSCs in the Manufacturing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10706975/]
- 39. Age Is Relative—Impact of Donor Age on Induced ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2018.00004/full]
- 40. Age Is Relative—Impact of Donor Age on Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5790033/]
- 41. Genetic background affects induced pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3580468/]
- 42. The hidden risks of over-reliance on healthy donor material [https://www.drugtargetreview.com/article/153651/the-hidden-risks-of-over-reliance-on-healthy-donor-material/]
- 43. New Protocol to Optimize iPS Cells for Genome Analysis of ... [https://pubmed.ncbi.nlm.nih.gov/25773749/]
- 44. Influence of Donor Age on Induced Pluripotent Stem Cells [https://pubmed.ncbi.nlm.nih.gov/27941802/]
- 45. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 46. Elimination of tumorigenic pluripotent stem cells from their ... [https://www.sciencedirect.com/science/article/pii/S221367112500147X]
- 47. RetSat stabilizes mitotic chromosome segregation in ... [https://pubmed.ncbi.nlm.nih.gov/39172275]
- 48. Examining iPSC derived motor neuron variability and ... [https://www.nature.com/articles/s41598-025-23378-0]
- 49. Developmental signals control chromosome segregation ... [https://www.nature.com/articles/s41467-024-51821-9]
- 50. Regulatory considerations for developing a phase I investigational new... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7848308/]
- 51. Next-Generation Stem Cell Expansion Technologies [https://insights.bio/immuno-oncology-insights/journal/article/290/next-generation-stem-cell-expansion-technologies]
- 52. Generation of Current Good Manufacturing Practices-Grade ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940689/]
- 53. How to Scale Process Automation: A Complete Guide - Skan.ai [https://www.skan.ai/blogs/scaling-process-automation]
- 54. Cell & Gene Therapy Logistics: Clinical Trial Supply Chain ... [https://intuitionlabs.ai/articles/cell-gene-therapy-logistics-supply-chain]
- 55. The Importance of Understanding & Designing Cellular ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/368/The-Importance-of-Understanding-Designing-Cellular-Therapy-Supply-Chains]
- 56. From nascent to mainstream: Overcoming barriers in iPSC ... [https://ct.catapult.org.uk/news/from-nascent-to-mainstream-overcoming-barriers-in-ipsc-therapy-development]
- 57. Genomic integrity of human induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6828592/]
- 58. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 59. Genomic integrity of human induced pluripotent stem cells ... [https://www.sciencedirect.com/science/article/pii/S1873506120301057]
- 60. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 61. Advancements in Stem Cell Research for Effective ... [https://pubmed.ncbi.nlm.nih.gov/40327307/]
- 62. Clinical trials and advanced MRI techniques with stem cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07054-5]
- 63. Stem Cell Therapy Cost (2025 Update) [https://www.dvcstem.com/post/stem-cell-therapy-cost-2020]
- 64. Automated Cell Processing System Market Research ... [https://finance.yahoo.com/news/automated-cell-processing-system-market-081800900.html]
- 65. Cell Therapy Manufacturing: Automation Shrinks Time to Market [https://mls.ascentialtech.com/blog/cell-therapy-manufacturing-services-reducing-time-to-market-with-automation/]
- 66. Induced Pluripotent Stem Cell (iPSC) Market Size 2025 [https://www.custommarketinsights.com/report/induced-pluripotent-stem-cell-ipsc-market/]
- 67. modification and Disease ’ Parkinson : s design... disease Clinical trial [https://www.movementdisorders.org/Podcasts/Disease-modification-and-Parkinsons-disease-Clinical-trial-design-and-population-selection--2025-MDS-Congress.htm]
- 68. S.BIOMEDICS Cell Therapy for Parkinson ' s Shows Positive... Disease [https://finance.yahoo.com/news/biomedics-cell-therapy-parkinsons-disease-090200498.html]
- 69. ' Parkinson Guidelines+ s Rundown - Guideline Central Disease Trials [https://www.guidelinecentral.com/insights/prakinsons-disease-trials/]
- 70. Stem Cell Protocols [https://www.rndsystems.com/protocol-types/stem-cell-protocols]
- 71. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 72. Long-term engraftment and maturation of autologous iPSC ... [https://pubmed.ncbi.nlm.nih.gov/38843830/]
- 73. Templates and Spreadsheets to Maximize Your Lab ... [https://www.stemcell.com/forms/lab-templates-and-spreadsheets.html]
- 74. Pre-clinical safety and efficacy of human induced pluripotent ... [https://pubmed.ncbi.nlm.nih.gov/39952239/]
- 75. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 76. Differences Between Autologous and Allogeneic Cell ... [https://www.patheon.com/us/en/insights-resources/blog/differences-between-autologous-and-allogeneic-cell-therapies.html]
- 77. Autologous vs allogenic cell therapy: key differences and ... [https://greenelephantbiotech.com/blog/autologous-vs-allogenic-cell-therapy-key-differences-and-applications/]
- 78. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 79. Allogeneic Versus Autologous Stem-Cell Therapy [https://www.biopharminternational.com/view/allogeneic-versus-autologous-stem-cell-therapy]
- 80. Allogeneic versus autologous stem cell transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057802/]
- 81. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 82. How Clinical Trial Data Supports Accurate Pharma ... [https://www.drugpatentwatch.com/blog/how-clinical-trial-data-supports-accurate-pharma-forecasting/?srsltid=AfmBOoq0lSxyQDq-ASC1yEXIWZF_ubYyDJzHMrDQ7XXRsIOel7yJAfnD]
- 83. Hyper-Personalized Medicine Market Report 2025-2029 ... [https://finance.yahoo.com/news/hyper-personalized-medicine-market-report-150900035.html]
- 84. The Challenges to Advancing Induced Pluripotent Stem ... [https://esmed.org/MRA/mra/article/view/4784]
- 85. Stem cell therapy cost goes up & what to consider looking ahead [https://ipscell.com/2025/10/stem-cell-therapy-cost-goes-up-what-to-consider-looking-ahead/]
- 86. The Cost Of Stem Cell Therapy in 2026 [https://bioinformant.com/cost-of-stem-cell-therapy/]
- 87. How Much Does Stem Cell Therapy Cost in 2025 [https://www.startstemcells.com/stem-cell-therapy-cost.html]
- 88. From the Editors — Cell Therapy Regulation in 2025 [https://www.isctglobal.org/telegrafthub/blogs/isct-head-office1/2025/10/07/from-the-editors-cell-therapy-regulation-in-2025-a]
- 89. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 90. Cell Therapy Weekly: Progress in iPSC-Based Therapies [https://www.regmednet.com/cell-therapy-weekly-progress-in-ipsc-based-therapies/]
- 91. Healthcare Provider Guide [https://www.isctglobal.org/education/ecgt-healthcare-provider-guide]