Breaking the Translational Barrier: A Strategic Roadmap for Advancing Regenerative Pharmacology
Regenerative pharmacology stands at a pivotal crossroads, holding immense promise for curative therapies but facing a persistent translational gap between preclinical discovery and clinical application.
Breaking the Translational Barrier: A Strategic Roadmap for Advancing Regenerative Pharmacology
Abstract
Regenerative pharmacology stands at a pivotal crossroads, holding immense promise for curative therapies but facing a persistent translational gap between preclinical discovery and clinical application. This article provides a comprehensive analysis for researchers and drug development professionals, detailing the multidisciplinary strategies required to overcome these hurdles. We explore the foundational principles of integrative and regenerative pharmacology, examine cutting-edge methodological advances leveraging AI and systems biology, address critical troubleshooting in manufacturing and regulation, and evaluate frameworks for robust clinical validation. By synthesizing insights from recent literature and strategic initiatives, this work serves as a blueprint for accelerating the development of transformative regenerative therapies from bench to bedside.
Defining the Field and Diagnosing the Translational Roadblock
Integrative and Regenerative Pharmacology (IRP) represents a transformative shift in biomedical science, moving beyond the traditional goal of symptom management toward the restoration of biological structure and function of damaged tissues and organs [1]. This field operates at the nexus of pharmacology, regenerative medicine, and systems biology, creating a new therapeutic landscape focused on curative interventions [1]. For researchers and drug development professionals, this paradigm introduces unique experimental challenges and translational barriers. This technical support center provides essential troubleshooting guidance and foundational methodologies to help your research team overcome these hurdles and advance the field of restorative therapeutics.
Core Principles and Definitions
Integrative Pharmacology is defined as the systematic investigation of drug interactions with biological systems across multiple levels—from molecular and cellular to organ and system levels. It combines traditional pharmacology with signaling pathway analysis, bioinformatic tools, and multi-omics approaches (transcriptomics, genomics, proteomics, epigenomics, metabolomics, and microbiomics) to deepen our understanding of disease mechanisms and therapeutic action [1].
Regenerative Pharmacology was formally defined as "the application of pharmacological sciences to accelerate, optimize, and characterize (either in vitro or in vivo) the development, maturation, and function of bioengineered and regenerating tissues" [2]. This approach fuses pharmacological techniques with regenerative medicine principles to develop therapies that actively promote the body's innate healing capabilities [1].
Integrative and Regenerative Pharmacology (IRP) bridges these two fields, merging conventional pharmacology with targeted therapies intended to repair, renew, and regenerate rather than merely block or inhibit disease symptoms. IRP aims to restore physiological structure and function through multi-level, holistic interventions [1].
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: What are the most significant translational barriers facing IRP research, and how can we address them?
Answer: The transition from promising preclinical studies to successful clinical applications remains a significant challenge in IRP. The table below summarizes the primary translational barriers and potential mitigation strategies.
Table 1: Translational Barriers and Mitigation Strategies in IRP Research
| Barrier Category | Specific Challenges | Recommended Mitigation Strategies |
|---|---|---|
| Investigational Hurdles | Unrepresentative preclinical models; unclear mechanisms of action (MoA); long-term safety and efficacy concerns [1]. | Implement more human-relevant models (3D cultures, organ-on-a-chip); employ systems biology approaches to deconstruct MoA; design long-term follow-up studies [1]. |
| Manufacturing Issues | Scalability challenges; lack of automated production; need for Good Manufacturing Practice (GMP) compliance [1]. | Invest in scalable bioreactor technologies; develop standardized, automated bioprocesses; establish GMP-compliant workflows early in development [1]. |
| Regulatory Complexity | Lack of unified guidelines across regions (e.g., EMA vs. FDA); complex pathways for Advanced Therapy Medicinal Products (ATMPs) [1]. | Engage with regulatory agencies early and often; participate in consensus-building initiatives for international standards [1]. |
| Economic & Accessibility | High manufacturing costs; limited reimbursement models; poor accessibility in low- and middle-income countries [1]. | Develop cost-effective biomaterials and manufacturing processes; generate robust health-economic data; explore tiered pricing models [1]. |
FAQ 2: How can we improve the clinical relevance of our preclinical IRP models?
Answer: A common failure point in IRP translation is the use of animal models or simple cell cultures that do not adequately recapitulate human clinical conditions [1]. To enhance clinical relevance:
- Incorporate Human Cells: Utilize patient-derived stem cells (e.g., mesenchymal stem cells) to create more physiologically relevant systems [3].
- Utilize Advanced Model Systems: Employ 3D tissue models, bioreactors, and organ-on-a-chip technologies that better mimic the in vivo microenvironment, including mechanical stresses and cell-cell interactions [1] [2]. Bioreactors, for instance, can apply relevant environmental cues like stretch, flow, and compression that are critical for proper tissue formation and function [2].
- Focus on Clinical Endpoints: Design preclinical studies with clinical endpoints in mind from the outset. Collaboration between basic researchers and clinicians during the study design phase is critical for this [4].
FAQ 3: What are the best practices for combining pharmacological agents with biomaterial scaffolds?
Answer: The development of 'smart' biomaterials that act as reservoirs for bioactive agents is a key strategy in IRP [1] [2]. Effective integration requires:
- Spatiotemporal Control: Design biomaterials that provide controlled release of multiple growth factors (e.g., FGF, VEGF, BMPs) in a sequence that mimics the natural healing process [2].
- Functionalization: Use immobilization techniques to tether bioactive molecules to the scaffold, enhancing local concentration and stability. For example, immobilized hyaluronidase has been shown to improve therapeutic outcomes in some regenerative models [5].
- Stimuli-Responsiveness: Develop biomaterials that alter their drug release profile or mechanical characteristics in response to specific external or internal triggers from the healing environment [1].
FAQ 4: How can we tackle the challenge of high costs and limited accessibility of IRP therapies?
Answer: The high cost of ATMPs is a major barrier to clinical adoption and accessibility [1]. Strategies to address this include:
- Drug Repurposing: Investigate existing drugs for new regenerative applications. This strategy can significantly reduce the time and cost associated with de novo drug development [6]. Computational pharmacology approaches are particularly valuable for identifying repurposing candidates [6].
- Process Optimization: Focus on streamlining and automating cell culture and tissue engineering processes to reduce labor and material costs.
- Open Science and Collaboration: Foster academic-industry-clinical partnerships to share resources, knowledge, and risks associated with IRP therapy development [1].
Essential Experimental Protocols in IRP
Protocol 1: Assessing Drug Efficacy in a 3D In Vitro Wound Healing Model
This protocol is adapted from research on microRNAs and leptin in wound healing [3].
1. Aim: To evaluate the effect of a candidate pharmacological agent (e.g., miRNA mimic/inhibitor, growth factor) on key processes in wound healing using a 3D cell culture model.
2. Materials Required:
Table 2: Research Reagent Solutions for 3D Wound Healing Assay
| Reagent/Material | Function | Example/Notes |
|---|---|---|
| Human Dermal Fibroblasts (HDFs) | Primary cell type for tissue repair and matrix deposition. | Use early passage cells for consistency. |
| 3D Scaffold or Hydrogel | Provides a three-dimensional structure that mimics the extracellular matrix. | Collagen I hydrogel or synthetic polymer scaffolds. |
| Candidate Pharmacological Agent | The therapeutic compound being tested. | e.g., miR-21 mimic, recombinant leptin [3]. |
| Cell Culture Medium | Supports cell growth and viability. | DMEM/F12 supplemented with serum or defined growth factors. |
| Histology Reagents | For fixing, sectioning, and staining the 3D construct. | Formalin, paraffin, antibodies for immunofluorescence. |
3. Methodology: 1. 3D Construct Fabrication: Mix HDFs with a neutralized collagen I solution at a density of 1-2 million cells/mL. Pipet the solution into transwell inserts and allow it to polymerize at 37°C for 1 hour. 2. Equilibration: Add culture medium to the top and bottom of the construct and culture for 24-48 hours to allow cells to equilibrate. 3. Wound Induction: Create a uniform wound in the center of the 3D construct using a sterile biopsy punch (e.g., 3-4mm diameter). 4. Treatment Application: Add the candidate pharmacological agent to the culture medium. Include appropriate vehicle controls and positive controls (e.g., known growth factors). 5. Monitoring and Analysis: * Imaging: Capture brightfield images of the wound area at 0, 24, 48, and 72 hours to monitor closure. * Histological Analysis: At endpoint, fix constructs in formalin, embed in paraffin, section, and stain. Use H&E for general morphology, and immunofluorescence for specific markers (e.g., α-SMA for myofibroblasts, Ki-67 for proliferation, CD31 for endothelial cells if co-cultures are used). * Molecular Analysis: Isolve RNA and protein from the constructs to analyze changes in gene expression (e.g., collagen I, III, fibronectin) and key signaling pathways (e.g., PI3K/AKT, MAPK/ERK) via qPCR and western blot [3].
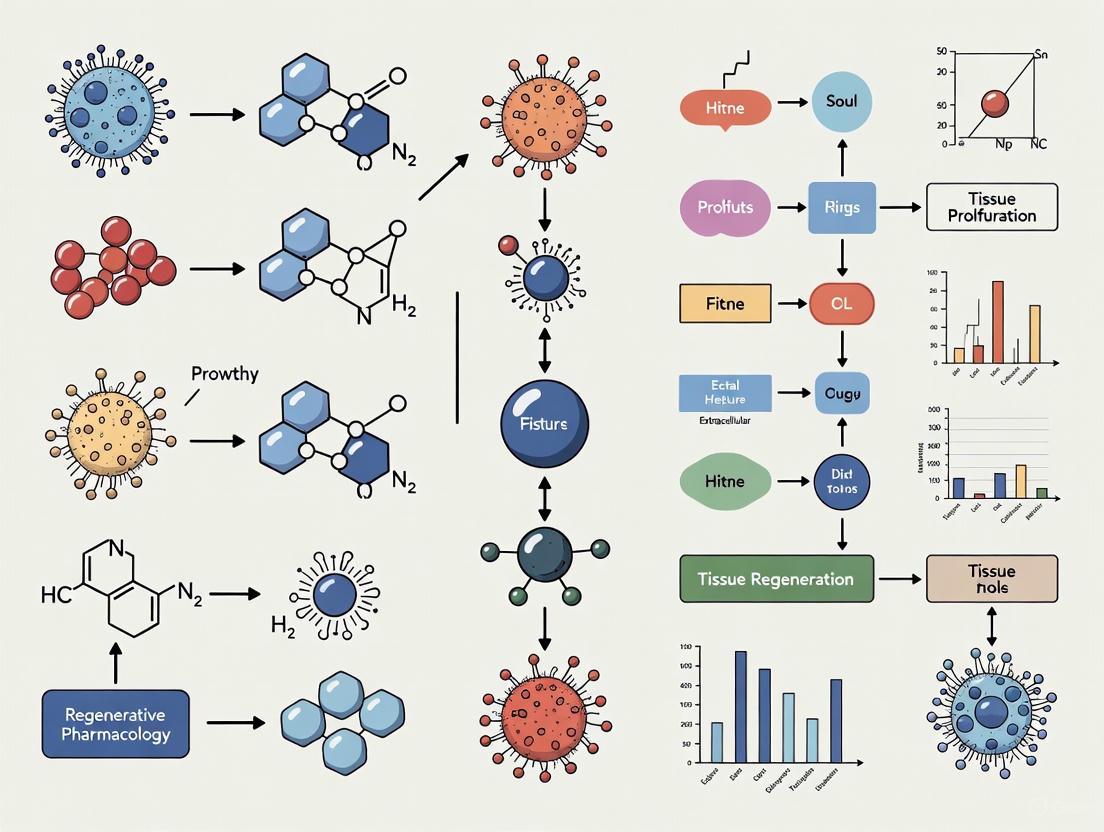
The following diagram illustrates the key signaling pathways involved in wound healing that are often targeted in IRP strategies:
Protocol 2: Evaluating a Pharmacological Agent in a Rat Model of Spinal Cord Injury
This protocol is based on a study investigating the neuroprotective effects of bumetanide [3].
1. Aim: To determine the therapeutic potential of a drug candidate for promoting repair and functional recovery after spinal cord injury (SCI).
2. Materials Required: * Adult Sprague-Dawley rats (250-300g) * Anesthetic cocktail (e.g., Ketamine/Xylazine) * Stereotaxic apparatus * Controlled impactor device for standardized SCI * Candidate drug (e.g., Bumetanide, an NKCC1 inhibitor [3]) * Osmotic minipumps for chronic delivery (optional) * Apparatus for behavioral testing (e.g., Basso, Beattie, Bresnahan (BBB) locomotor rating scale) * Tissue fixation and processing reagents for histology * Antibodies for immunohistochemistry (e.g., against GAP-43, GFAP, NeuN)
3. Methodology: 1. SCI Surgery: Anesthetize the animal and perform a laminectomy to expose the spinal cord at the desired level (e.g., T9-T10). Induce a contusion injury using a controlled impactor with a defined force (e.g., 150 kdyn). 2. Drug Administration: Administer the first dose of the candidate drug (e.g., bumetanide, 10mg/kg, i.p.) or vehicle within a critical window post-injury (e.g., 1-6 hours). Continue administration based on the drug's pharmacokinetic profile (e.g., twice daily for 7 days). 3. Functional Assessment: Evaluate locomotor function weekly for 4-8 weeks using the BBB scale, which scores hindlimb movement, trunk stability, and coordination. 4. Tissue Collection and Analysis: At the study endpoint, transcardially perfuse animals with saline followed by 4% paraformaldehyde. Extract the spinal cord and post-fix. * Histology: Section the tissue and stain with Luxol Fast Blue for myelin or H&E for general morphology. * Immunohistochemistry: Stain sections for markers of axonal regeneration (e.g., GAP-43), astrocytes (GFAP), and neurons (NeuN). Quantify staining intensity and lesion volume using image analysis software. 5. Molecular Analysis: Isolate protein from the injury epicenter to analyze changes in the expression of targets of interest (e.g., NKCC1 and KCC2 transporters) via western blot [3].
The workflow for this in vivo evaluation is summarized below:
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Tools for IRP Research
| Category | Specific Reagent/Technology | Research Function | Application Example |
|---|---|---|---|
| Cell Sources | Mesenchymal Stem Cells (MSCs) | Tunable combinatorial drug manufacture and delivery systems; source for paracrine factors (secretome) [1]. | Injection into degenerated intervertebral discs for treatment of degenerative disc disease [3]. |
| Biomaterials | Stimuli-Responsive "Smart" Biomaterials | Scaffolds that alter drug release or mechanical properties in response to environmental triggers [1]. | Local, temporally controlled delivery of growth factors to orchestrate a complete regenerative response [2]. |
| Drug Delivery Systems | Nanoparticles & Nanofibers | Enhance targeted delivery and bioavailability of regenerative compounds; can be combined with imaging capabilities [1]. | Delivery of microRNAs (e.g., miR-21) to regulate key processes in wound healing [3]. |
| Model Systems | 3D Bioreactors | Devices that recapitulate in vivo physiological cues (stretch, flow, compression) for tissue maturation in vitro [2]. | Creation of advanced 3D tissue constructs (e.g., cartilage, bone) prior to implantation [2]. |
| Analytical Tools | Multi-Omics Technologies (Genomics, Proteomics) | Provide a systems-level view of drug actions and mechanisms; enable identification of novel targets and biomarkers [1]. | Profiling cellular responses to regenerative therapies to fully define the mechanism of action (MoA) [1]. |
| Computational Tools | Artificial Intelligence (AI) & Machine Learning | Predict drug-target interactions, optimize drug delivery systems, and anticipate cellular responses [1]. | Accelerating drug repurposing and predicting pharmacokinetic/pharmacodynamic profiles of regenerative approaches [1] [6]. |
Technical Support Center: Troubleshooting Translational Barriers in Regenerative Pharmacology
Frequently Asked Questions (FAQs)
FAQ 1: Why do our therapeutic candidates consistently show promise in preclinical models but fail in human clinical trials?
This is a primary manifestation of the "Valley of Death," often caused by a "failure to fail" early in the qualification process [7]. The major causes of failure are typically a lack of effectiveness and poor safety profiles not predicted in preclinical studies [8]. Key culprits include:
- Over-reliance on murine models that do not faithfully reproduce human disease pathology or its temporal development [7].
- Poorly specified methods and variable, context-dependent behavior of tools and cell lines, contributing to a widely acknowledged lack of reproducibility in research findings [7].
- Use of "pure" animal models that lack the natural exposures, co-morbidities, and aged physiology of the target human population, which can critically influence therapeutic response [7].
FAQ 2: What are the most significant manufacturing and regulatory hurdles for advanced regenerative therapies?
The transition from small-scale academic production to large-scale, clinically viable manufacturing presents significant hurdles [1].
- Manufacturing Issues: Scalability, automated production methods, and adherence to Good Manufacturing Practice (GMP) are major challenges [1].
- Complex Regulatory Pathways: Different regional requirements from agencies like the EMEA and FDA, with a lack of unified guidelines, complicate the approval process for Advanced Therapy Medicinal Products (ATMPs) [1].
- Characterization Hurdles: A key translational challenge is the need to optimize, characterize, and scale up the manufacturing and maturation of bioengineered and regenerating tissues [1].
FAQ 3: How can we improve the predictive value of our preclinical efficacy and safety studies?
Mitigating this risk requires a multi-faceted strategy:
- Incorporate Human-Relevant Systems: Utilize emerging technologies such as organ/disease-on-a-chip models that can be configured with patient-derived cells of the correct age and exposure history [7].
- Adopt a Holistic Pharmacology Approach: Implement Integrative and Regenerative Pharmacology (IRP) strategies, which include studies ranging from in vitro and ex vivo systems to animal models that better recapitulate human clinical conditions [1].
- Focus on Mechanopharmacology: Consider the effects of drugs on cellular mechanics and, critically, the effects of the mechanical environment on drug actions, as this is often non-physiological in standard assays [7].
Troubleshooting Guides
Guide 1: Troubleshooting Preclinical Translation Failures
| Observed Problem | Potential Causes | Recommended Solutions & Methodologies |
|---|---|---|
| Lack of efficacy in Phase II trials | Poor target validation; unrepresentative animal models; irreproducible data [7] [8]. | - Target Identification: Employ systems biology approaches. Use omics (genomics, proteomics) and bioinformatic tools to identify targets within disease networks [1].- Model System: Develop more physiologically relevant models. Use 3D cell cultures, organoids, and organ-on-a-chip technology to better mimic human pathophysiology [1] [7]. |
| Unexpected toxicity or immune reactions | Poor predictive value of standard toxicological methods; species-specific differences [8] [9]. | - Improved Safety Screening: Utilize human stem cell-derived tissues in organ-on-a-chip systems for more relevant toxicology screening [7].- Biomaterial Testing: For regenerative applications, rigorously test biomaterials (e.g., natural/synthetic polymers) for immune response and degradation profiles in advanced model systems [10]. |
| Inconsistent product quality and function | Lack of standardized, scalable manufacturing processes; insufficient product characterization [1] [11]. | - Process Development: Implement Quality by Design (QbD) principles early in process development.- Characterization Protocols: Develop robust assays to characterize critical quality attributes (CQAs) of the product, such as cell phenotype, secretome, and biomaterial properties [1]. |
Guide 2: Navigating the Translational Pathway - Quantitative Hurdles
The following table summarizes the stark quantitative challenges of crossing the "Valley of Death," based on industry-wide analyses [8].
| Translational Stage | Attrition Rate / Quantitative Challenge | Primary Reasons for Failure |
|---|---|---|
| Basic Research to Human Trials | 80-90% of research projects fail before human testing [8]. | Irrelevance to human disease; lack of funding and technical expertise to advance [8]. |
| Phase III Clinical Trials | ~50% of experimental drugs fail in Phase III [8]. | Lack of effectiveness; poor safety profiles [8]. |
| Overall Process (Discovery to Approval) | Only 0.1% of candidates become approved drugs [8]. | High cumulative attrition across all stages [8]. |
| Development Cost & Time | ~$2.6 billion and >13 years per approved drug [8]. | High failure rates, lengthy timelines, and regulatory costs [8]. |
Experimental Protocols for Overcoming Translational Challenges
Protocol 1: Establishing a Predictive Organ-on-a-Chip Model for Efficacy Screening
This methodology aims to address the limitation of traditional animal models by using a human cell-based system that better mimics the in vivo mechanical and cellular environment [7].
- Chip Design and Fabrication: Select or fabricate a microfluidic device with relevant chamber geometry. The device should incorporate flexible membranes if mechanical strain is a pathophysiological factor.
- Cell Sourcing and Differentiation: Source primary human cells or patient-specific induced pluripotent stem cell (iPSC)-derived cells relevant to the target tissue (e.g., endothelial cells, parenchymal cells).
- Seeding and Culture: Seed cells into the respective chambers of the device under sterile conditions. Allow cells to adhere and form a confluent monolayer or 3D structure.
- Disease Modeling: Induce a disease state in vitro using chemical, mechanical, or genetic stimuli. Validate the model by confirming known disease biomarkers or functional changes.
- Therapeutic Testing: Introduce the therapeutic candidate (small molecule, biologic, or cell therapy) at clinically relevant doses. Include appropriate controls.
- Endpoint Analysis: Assess efficacy using functional readouts (e.g., barrier integrity, contraction force, albumin production), molecular analyses (e.g., qPCR, RNA-seq), and immunohistochemistry.
The workflow for developing and validating such a model is outlined below.
Protocol 2: Implementing a Biomaterial-Based Localized Drug Delivery System
This protocol is for developing localized drug delivery systems (DDSs) to promote healing without systemic side-effects, a key goal in regenerative pharmacology [1] [10].
- Biomaterial Selection: Choose a biomaterial based on application needs. Common options include:
- Natural Polymers: Alginate, collagen, hyaluronic acid (good biocompatibility).
- Synthetic Polymers: PLGA, PCL (tunable degradation and mechanical properties).
- Drug/Bioactive Molecule Incorporation: Incorporate the therapeutic agent (e.g., growth factor, small molecule, siRNA) into the biomaterial matrix. Methods include physical adsorption, covalent bonding, or encapsulation within nanoparticles.
- System Fabrication: Fabricate the final DDS. This could involve electrospinning to create nanofibrous scaffolds, 3D bioprinting to create structured constructs, or crosslinking to form hydrogels.
- In Vitro Release Kinetics and Bioactivity Testing: Immerse the DDS in a buffer solution (PBS) at 37°C. Sample the release medium at predetermined time points and quantify the released drug via HPLC or ELISA. Test the bioactivity of the released compound on target cells.
- In Vivo Efficacy and Safety Testing: Implant the drug-loaded DDS in a relevant animal model of disease/injury. Assess functional recovery over time and upon endpoint, analyze the tissue for regeneration, integration, and immune response (histology).
The following diagram illustrates the decision-making process for developing such a system.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and platforms used in advanced translational research for regenerative pharmacology.
| Research Reagent / Platform | Function in Translational Research |
|---|---|
| Organ-on-a-Chip Microfluidic Devices | Micro-engineered systems that recapitulate organ-level physiology and disease pathology for more predictive drug efficacy and toxicity testing than conventional models [7]. |
| Natural & Synthetic Biomaterials | Polymers (e.g., alginate, collagen, PLGA) used as scaffolds or drug delivery vehicles to provide mechanical support and sustained, local release of bioactive molecules in tissue engineering [1] [10]. |
| Stimuli-Responsive "Smart" Biomaterials | Biomaterials engineered to alter their properties (e.g., shape, drug release profile) in response to internal or external triggers (e.g., pH, enzyme activity), enabling targeted and controlled therapy [1]. |
| Patient-Derived Induced Pluripotent Stem Cells (iPSCs) | A source of patient-specific cells for creating disease models, screening drugs, and developing personalized cell therapies, directly supporting precision medicine goals [1] [11]. |
| Advanced Omics Profiling Tools | Platforms for genomics, proteomics, and metabolomics that help deconstruct mechanisms of action, identify biomarkers, and map disease networks for better target identification [1]. |
Troubleshooting Guide: Navigating Common Translational Roadblocks
This guide provides targeted solutions for frequent challenges encountered in translational regenerative pharmacology, helping you advance your research from the bench to the bedside.
FAQ: My cell-based therapy shows inconsistent efficacy in animal models. How can I troubleshoot this?
Problem: Variable therapeutic outcomes in preclinical testing of regenerative therapies.
Solution: Implement a systematic troubleshooting protocol to identify the root cause [12] [13].
Step 1: Verify Cellular Material Quality Check for genetic and epigenetic variants that emerge during in vitro culture, as these can create aberrant subpopulations with reduced regenerative potency [14]. Use fluorescence-activated cell sorting to isolate subpopulations with validated markers of therapeutic efficacy [14].
Step 2: Assess Biomaterial-Tissue Interaction Confirm your delivery system (e.g., hydrogel) interacts appropriately with the host environment. Inconsistent cell-material interactions due to improper protein adsorption or interfacial geometry can drastically alter therapeutic outcomes [14].
Step 3: Analyze the Host Immune Response The host immune system significantly impacts therapy integration and performance [14]. Evaluate innate and adaptive immune responses to your therapeutic construct, as uncontrolled inflammation can destroy regenerative potential.
Preventive Measures:
- Implement rigorous pre-screening of cell subpopulations before transplantation [14].
- Use biomaterials with tissue-matched mechanical properties that provide appropriate spatial and temporal cues [14].
Table: Troubleshooting Inconsistent Preclinical Efficacy
| Problem Area | Diagnostic Tests | Potential Solutions |
|---|---|---|
| Cellular Variability | Genetic screening, potency assays, FACS analysis | Isolate therapeutic subpopulations; optimize culture conditions [14] |
| Biomaterial Integration | Histology, mechanical testing, protein adsorption assays | Modify material hydrophilicity; incorporate cell-binding domains [14] |
| Host Immune Rejection | Cytokine profiling, immune cell infiltration analysis | Use immunosuppressants; employ immune-modulating biomaterials [14] |
FAQ: How can I navigate the complex regulatory pathways for Advanced Therapy Medicinal Products (ATMPs)?
Problem: Regulatory approval processes for regenerative therapies are complex, vary by region, and contribute significantly to development timelines [15] [1].
Solution: Develop a proactive regulatory strategy that begins early in development.
Engage Regulatory Agencies Early: Seek input from the FDA, EMA, and other relevant bodies during early development stages to clarify expectations and study design requirements [15]. Pre-IND meetings can prevent costly delays later.
Understand Regional Differences: Regulatory frameworks differ significantly across regions [15] [1]. While the FDA emphasizes randomized controlled trials, the EMA often requires additional real-world evidence for certain drug classes [15].
Utilize Accelerated Pathways: For therapies addressing unmet medical needs, explore designated pathways like the FDA's Breakthrough Therapy Designation or the EMA's PRIME initiative, which can expedite reviews [15].
Implement Robust Quality Systems: Adhere to Good Manufacturing Practices (GMP) and establish a comprehensive Quality Management System (QMS). Non-compliance can result in approval delays or post-market recalls, even for effective therapies [15] [16].
Critical Documentation:
- Maintain meticulous records of preclinical and clinical trial data, pharmacokinetics, toxicology reports, and manufacturing protocols [15].
- Ensure all regulatory submissions are complete and properly formatted to avoid rejection or requests for additional data [15].
FAQ: My regenerative therapy faces manufacturing scalability challenges. What should I consider?
Problem: Transitioning from laboratory-scale production to commercially viable manufacturing while maintaining quality and consistency.
Solution: Address key manufacturing hurdles through strategic planning and technology adoption.
Automate Production Processes: Invest in automated production methods and technologies to ensure consistency and reduce contamination risks [1] [17].
Implement Digital Quality Systems: Leverage AI-driven analytics to monitor environmental conditions and predict equipment failures, mitigating risks that can halt production [17].
Adopt Modular Manufacturing Platforms: Consider portable, scalable bioreactors that reduce cross-contamination risks and offer production flexibility [17].
Plan for Economic Sustainability: High manufacturing costs limit accessibility, particularly in low and middle-income countries [1]. Develop cost-effective manufacturing strategies early in development.
Table: Comparative Analysis of Regulatory Pathways for ATMPs
| Regulatory Aspect | U.S. (FDA) | European Union (EMA) | Accelerated Pathways |
|---|---|---|---|
| Primary Authority | Center for Biologics Evaluation and Research (CBER) | Committee for Advanced Therapies (CAT) | Breakthrough Therapy, Fast Track (FDA); PRIME (EMA) [15] |
| Clinical Evidence | Emphasizes randomized controlled trials [15] | May require additional real-world evidence [15] | Substantial improvement over existing therapies [15] |
| Manufacturing Standards | Good Manufacturing Practice (GMP) [15] | Good Manufacturing Practice (GMP) [1] | Same rigorous standards but with more agency collaboration [15] |
| Post-Market Surveillance | Required long-term safety monitoring [15] | Required long-term safety monitoring [1] | Often enhanced monitoring requirements [15] |
Experimental Protocols for Translational Research
Protocol: Standardized Procedure for Evaluating MSC-Hydrogel System Efficacy
Purpose: To systematically assess the therapeutic potential of mesenchymal stem cell (MSC)-hydrogel systems for burn wound regeneration [18].
Materials:
- Research Reagent Solutions:
- Mesenchymal Stem Cells (MSCs): Primary therapeutic agents; promote angiogenesis, modulate inflammation [18] [14].
- Hydrogel Scaffold: 3D biomaterial network; provides structural support, controls cell delivery [18] [14].
- Chondrogenic Lineage Markers: Antibodies for CD44, CD73, CD90; verify MSC phenotype and differentiation potential [14].
- Angiogenesis Assay Kit: Quantifies vascular endothelial growth factor (VEGF) secretion; measures pro-angiogenic activity [18].
- TNF-α & IL-6 ELISA Kits: Measures inflammatory cytokine levels; assesses immunomodulatory capacity [18].
Methodology:
- Cell Preparation: Isolate and expand MSCs using fluorescence-activated cell sorting to isolate highly chondrogenic subpopulations [14].
- Hydrogel Encapsulation: Seed MSCs into hydrogel system at optimized density. For advanced systems, use 3D-bioprinted scaffolds or exosome-enriched hydrogels [18].
- In Vivo Implantation: Apply MSC-hydrogel construct to burn wound model. Include appropriate controls (hydrogel only, untreated wound) [18].
- Efficacy Assessment:
- Monitor wound closure rates weekly
- Collect tissue biopsies for histology at predetermined endpoints
- Assess angiogenesis (CD31 staining), inflammation (CD45 staining), and ECM deposition (Masson's trichrome)
- Quantify regenerative biomarkers via ELISA or qPCR [18]
- Statistical Analysis: Perform appropriate statistical tests with significance set at P<0.05 [19].
Troubleshooting Notes:
- If wound healing is impaired, check MSC viability post-encapsulation and inflammatory status of wound bed [14].
- For excessive inflammation, consider modifying hydrogel properties or adding anti-inflammatory factors [18].
Protocol: Systematic Troubleshooting of Experimental Failures
Purpose: To provide a structured approach for identifying and resolving research problems [12] [13].
Methodology:
- Identify the Problem: Clearly define what went wrong without speculating on causes [13]. Example: "No PCR product detected" rather than "Taq polymerase was bad" [13].
- List All Possible Explanations: Brainstorm both obvious and non-obvious potential causes [13]. For molecular biology experiments, consider reagents, equipment, and procedural variations [12].
- Collect Data: Systematically investigate each potential cause, starting with the easiest to check [13].
- Verify equipment function
- Review control results
- Check reagent storage conditions and expiration dates
- Compare your procedure with established protocols [12]
- Eliminate Explanations: Based on collected data, rule out factors that are not contributing to the problem [13].
- Check with Experimentation: Design targeted experiments to test remaining hypotheses. Change only one variable at a time to isolate the true cause [12] [19].
- Identify the Cause: Once determined, implement corrective actions and document the solution thoroughly [13].
Key Principles:
- Always repeat experiments unless cost or time prohibitive [12].
- Maintain meticulous documentation in a lab notebook [12] [13].
- Consult with experienced colleagues who may have encountered similar issues [12].
Visualizing Translational Workflows
Regenerative Therapy Translation Path
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents for Regenerative Pharmacology Research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary therapeutic agents; promote angiogenesis, modulate inflammation, differentiate into multiple lineages [18] [14] | Source carefully (autologous vs. allogeneic); screen for genetic variants; isolate subpopulations with enhanced potency [14] |
| 3D-Bioprinted Scaffolds | Provide structural support for tissue formation; enable spatial control of cell delivery [18] | Use stimuli-responsive systems that alter properties in response to environmental triggers [18] [1] |
| Exosome-Enriched Hydrogels | Enhanced regenerative capacity; cell-free alternative to whole-cell therapies [18] | Isolate from conditioned media of therapeutic cells; characterize cargo before use [18] |
| Stimuli-Responsive Biomaterials | "Smart" materials that release bioactive compounds in response to specific triggers [1] | Design to respond to physiological cues (pH, enzymes) for localized, controlled drug delivery [1] |
| Quality Control Assays | Ensure safety, potency, and consistency of regenerative products [15] [14] | Include genetic stability tests, potency assays, sterility testing, and characterization of critical quality attributes [14] |
Integrative and Regenerative Pharmacology (IRP) represents a paradigm shift in biomedical science, merging pharmacology, systems biology, and regenerative medicine to develop therapies that restore physiological structure and function rather than merely managing symptoms [1]. This approach faces significant translational barriers that delay the movement of promising therapies from bench to bedside. Interestingly, researchers in neurodegenerative diseases and rare diseases confront strikingly similar challenges, particularly regarding biological barriers, manufacturing complexity, and regulatory hurdles. This technical support center synthesizes troubleshooting guidance and methodological approaches from these analogous fields, providing regenerative pharmacology researchers with practical strategies to overcome critical translational roadblocks.
Technical Troubleshooting Guides
Challenge 1: Overcoming Biological Barriers for Targeted Delivery
Core Issue: The blood-brain barrier (BBB) prevents more than 98% of small molecules and all biologics from entering the central nervous system, while similar biological barriers impede delivery to target tissues in regenerative therapies [20] [21].
| Solution Approach | Underlying Principle | Key Limitations | Translational Readiness |
|---|---|---|---|
| Receptor-mediated transcytosis | Utilizes endogenous transport systems (TfR, IR, LRP1) for brain delivery [20] | Limited receptor capacity, immunogenicity concerns | Clinical stage (bispecific antibodies) |
| Ligand-decorated nanoparticles | Surface-functionalized carriers for active targeting [20] | Scalability, batch-to-batch variability | Preclinical/early clinical |
| Focused ultrasound + microbubbles | Temporarily disrupts BBB under image guidance [20] [21] | Precision required, safety concerns for repeated use | Mid-stage clinical trials |
| Cell-based "Trojan horse" | Uses cells (e.g., stem cells, macrophages) as carriers [20] | Cell viability, limited payload capacity | Preclinical development |
| Intranasal delivery | Bypasses BBB via olfactory and trigeminal pathways [20] | Limited dosage, mucosal clearance | Early clinical evaluation |
Recommended Experimental Protocol: Screening for BBB Permeability
- In silico prediction: Utilize machine learning models (e.g., SwissSimilarity, Pharmit) to screen compound libraries based on physicochemical properties and structural similarity to known CNS-active drugs [22].
- Pharmacophore modeling: Develop ligand-based pharmacophore models using approved CNS drugs as templates for virtual screening [22].
- BBB permeability classification: Apply BBB prediction models to classify compounds as permeable (CNS+) or non-permeable (CNS-) based on brain-to-blood ratio calculations [22].
- ADME and toxicity profiling: Evaluate pharmacokinetics, toxicophores, and drug-likeness properties to prioritize lead compounds [22].
- In vitro validation: Use human brain microvascular endothelial cell models to confirm BBB permeation predicted in silico.
Challenge 2: Manufacturing and Scalability Constraints
Core Issue: The complex, personalized nature of regenerative therapies and cell/gene therapies presents significant challenges for scaled production, particularly with the limited number of production facilities and high costs associated with small-batch production [23].
Troubleshooting Strategies:
- Implement advanced automation: Streamline manufacturing processes to improve efficiency and scalability while reducing contamination risks [23].
- Establish decentralized production hubs: Create regional manufacturing centers to facilitate quicker, localized access to therapies [23].
- Develop "off-the-shelf" approaches: Where possible, engineer universal donor cell lines or standardized biomaterial platforms to reduce personalization requirements [1].
- Optimize cryopreservation protocols: Enhance cell viability and functionality post-thaw to improve logistics and extend shelf-life.
- Adopt quality-by-design (QbD) principles: Implement systematic approaches to process development that ensure product quality through design rather than through end-product testing alone.
Challenge 3: Clinical Translation and Regulatory Navigation
Core Issue: Complex regulatory pathways, challenges in patient recruitment for rare diseases, and lack of historical precedent for novel therapeutic modalities create significant delays in approval and clinical adoption [23] [1].
Troubleshooting Strategies:
- Engage regulatory agencies early: Pursue pre-IND meetings with FDA/EMA to align on development plans, endpoints, and CMC requirements [23].
- Incorporate real-world evidence (RWE): Collect and standardize RWE alongside traditional clinical trial data to provide additional insights into effectiveness and safety [23].
- Leverage expedited regulatory programs: Pursue appropriate designations (RMAT, Breakthrough Therapy, Priority Review) that can shorten development timelines [23] [24].
- Implement decentralized trial designs: Utilize remote monitoring and telemedicine to enhance patient accessibility and recruitment [23].
- Collaborate with patient advocacy groups (PAGs): Partner with PAGs for patient education, support, and enrollment, while gaining actionable insights into real-world needs [23].
Experimental Workflow: From Target Identification to Translation
The following diagram illustrates an integrative workflow that incorporates lessons from neurodegenerative and rare disease research to overcome translational barriers in regenerative pharmacology.
The Scientist's Toolkit: Key Research Reagent Solutions
| Research Reagent / Tool | Primary Function | Application Context | Translational Consideration |
|---|---|---|---|
| Machine learning prediction models | In silico BBB permeability and CNS activity screening [22] | Early compound prioritization | Reduces late-stage attrition; requires experimental validation |
| Ligand-decorated nanoparticles | Targeted drug delivery across biological barriers [20] | Preclinical proof-of-concept studies | Surface chemistry critical for targeting efficacy; scalability challenges |
| Stimuli-responsive biomaterials | Spatiotemporally controlled drug release [1] | Tissue engineering and regenerative applications | Responsiveness to physiological triggers must match disease environment |
| Human brain microvascular endothelial cells | In vitro BBB model development [22] | Permeability and transport mechanism studies | Limited complexity compared to in vivo neurovascular unit |
| Real-world evidence (RWE) frameworks | Post-marketing safety and effectiveness monitoring [23] | Clinical development and regulatory submissions | Requires standardized data collection and validation methodologies |
| Patient-derived cellular models | Disease modeling and personalized therapy screening [1] | Preclinical efficacy assessment | Better predicts human response than animal models; genetic stability concerns |
Frequently Asked Questions (FAQs)
Q1: What computational approaches are most effective for early prediction of blood-brain barrier permeability in regenerative therapy candidates?
A: Machine learning models that incorporate physicochemical properties and structure-activity relationships have demonstrated high predictability for BBB permeability [22]. Implement a tiered approach beginning with ligand-based virtual screening using tools like Pharmit and SwissSimilarity, followed by BBB-specific classification models, and finally ADME/toxicity profiling. This sequential filtering can identify CNS-active molecules with appropriate barrier penetration properties while reducing late-stage attrition [22].
Q2: How can we address the manufacturing scalability challenges for personalized regenerative therapies?
A: Advanced automation and data analytics can streamline complex manufacturing processes [23]. Consider establishing decentralized production hubs to facilitate localized access [23]. For cell-based approaches, invest in "off-the-shelf" technologies such as universal donor cell lines that reduce personalization requirements. Early collaboration with regulatory agencies on Chemistry, Manufacturing, and Controls (CMC) strategies is essential to avoid scalability-related delays.
Q3: What regulatory strategies can accelerate the development of regenerative pharmacology products?
A: Pursue expedited regulatory programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation, which provides intensive FDA guidance throughout development [24]. Incorporate real-world evidence (RWE) collection into development plans to support effectiveness claims [23]. Engage patient advocacy groups early for insights on meaningful endpoints and to support recruitment, as their involvement is increasingly valued by regulators.
Q4: How can we improve patient recruitment for clinical trials of rare disease treatments?
A: Implement artificial intelligence-driven patient matching to efficiently identify eligible participants [23]. Adopt decentralized trial designs with remote monitoring to reduce geographic and mobility barriers [23]. Collaborate closely with patient advocacy groups (PAGs) for patient education and outreach, as they are instrumental in building trust and awareness within rare disease communities.
Q5: What targeted delivery approaches show most promise for overcoming the blood-brain barrier?
A: Ligand-decorated nanoparticles functionalized with transferrin receptor or insulin receptor antibodies show significant promise by leveraging receptor-mediated transcytosis [20]. Bispecific antibody shuttles that engage endogenous transport systems while targeting disease-specific pathways are advancing clinically [20]. Focused ultrasound-mediated BBB disruption offers temporary, image-guided barrier opening for localized delivery, though it requires specialized equipment and expertise [20] [21].
Key Signaling Pathways in Neuroregeneration
The following diagram illustrates major signaling pathways involved in neuroregeneration and their modulation by pharmacological interventions, integrating knowledge from neurodegenerative disease research.
Bridging the Gap: Technological Innovations and Disruptive Tools
FAQs: Foundational AI Concepts for Drug Discovery
Q1: What are the core AI technologies used in modern drug discovery troubleshooting? Modern AI-driven drug discovery primarily leverages Machine Learning (ML), Deep Learning (DL), and Natural Language Processing (NLP) to identify, diagnose, and resolve technical issues. ML models analyze vast datasets to predict equipment failures and diagnose root causes. DL, including architectures like Convolutional Neural Networks (CNNs) and Recurrent Neural Networks (RNNs), is used for complex tasks such as predicting drug-target interactions and drug sensitivity. NLP systems power intelligent chatbots and analyze scientific literature to provide context-aware support and extract hidden biological connections [25] [26].
Q2: Why is data quality often cited as the most critical factor for AI success? The principle of "garbage in, garbage out" is paramount. AI models are only as reliable as their input data. Poor quality data—such as inconsistent formats, unreproducible results, or outdated information—can lead to incorrectly chosen drug targets, biased models, and ultimately, failed experiments. High-quality, structured data is the non-negotiable foundation for generating accurate, trustworthy AI insights [27] [28].
Q3: What are the FAIR data principles and why are they important for AI? FAIR stands for Findable, Accessible, Interoperable, and Reusable. Adhering to these principles ensures that data is:
- Findable: Richly described with metadata for easy discovery.
- Accessible: Available through standard protocols.
- Interoperable: Structured and integrated for use across different projects and platforms.
- Reusable: Well-described and governed to support replication and further research. Implementing FAIR principles prevents data silos, facilitates seamless data integration for AI models, and creates a scalable foundation for innovation [27].
Q4: How does AI-powered technical support enhance the research workflow? AI-powered support systems transform research efficiency by providing:
- 24/7 Availability: Continuous assistance without human intervention.
- Predictive Analytics: Identifying potential issues before they cause downtime.
- Automated Ticketing: Categorizing and prioritizing support requests based on urgency.
- Continuous Learning: Improving diagnostic accuracy over time by learning from new data and user interactions [25]. This allows research teams to focus on complex, high-value problems while routine troubleshooting is automated.
Troubleshooting Guides: Common Experimental Scenarios
Guide 1: Troubleshooting Poor AI Model Performance
Problem: Your AI model for predicting drug-target interactions is producing inaccurate or unreliable results.
Solution:
- Step 1: Audit Your Data Quality and Quantity
- Verify data provenance and ensure rigorous quality control procedures are in place. Every data point should be overseen by a human expert where possible [28].
- Assess if you have enough high-quality data. AI-first methods can be limited by the extremely small fraction of the drug-like chemical universe for which experimental data exists [29].
- Check for a lack of "negative data" (e.g., failed experiments), which is as crucial as positive findings for training a robust model [29].
- Step 2: Validate Against a Benchmark Dataset
- Test your model on established, public benchmark datasets to determine if the problem is with your model or your proprietary data. Commonly used datasets include those for Drug-Target Interactions (DTIs) and Drug-Drug Interactions (DDIs) [26].
- Step 3: Increase Model Transparency
- For instilling confidence, document and communicate the model's constraints, inherent assumptions, and validation processes. Use tools that provide visibility into which features (e.g., mechanism of action, clinical trial history) are positively or negatively affecting a prediction [28].
- Step 4: Foster Cross-Disciplinary Collaboration
- Ensure close collaboration between data scientists and therapeutic area experts. Generalist platforms relying solely on data scientists often lack the granular life science insights needed for meaningful outputs [28].
Guide 2: Troubleshooting Assay Integration with AI Predictions
Problem: There is a significant discrepancy between AI-predicted compound activity and experimental assay results.
Solution:
- Step 1: Verify Instrumentation and Reagents
- A complete lack of an assay window often points to an instrument setup problem. Consult instrument setup guides for specific assay types (e.g., TR-FRET) [30].
- For TR-FRET assays, the single most common failure point is the use of incorrect emission filters. Ensure you are using the exact filters recommended for your instrument [30].
- Test your microplate reader’s setup using control reagents before running your main experiment [30].
- Step 2: Analyze Compound and Stock Solutions
- Differences in EC50/IC50 values between labs are frequently traced back to differences in stock solution preparation [30].
- In cell-based assays, consider if the compound is unable to cross the cell membrane, is being pumped out, or is targeting an inactive form of the kinase, which would not be active in a biochemical assay [30].
- Step 3: Implement Robust Data Analysis
- For TR-FRET, always use ratiometric data analysis (acceptor signal / donor signal). This accounts for pipetting variances and lot-to-lot reagent variability [30].
- Use the Z'-factor to assess assay robustness. An assay with a large window but high noise (low Z'-factor) is less reliable than one with a smaller window and low noise. A Z'-factor > 0.5 is generally considered suitable for screening [30].
Guide 3: Troubleshooting ADMET Prediction Errors
Problem: AI models accurately predict a compound's potency, but it fails due to poor Absorption, Distribution, Metabolism, Excretion, or Toxicity (ADMET) properties.
Solution:
- Step 1: Integrate Specialized ADMET Tools
- Use AI platforms specifically tailored for ADMET optimization, which use custom deep-learning architectures to predict complex assay outcomes in real-time during the compound design phase [31].
- Step 2: Leverage Consortium Data
- Participate in or utilize models trained on pre-competitive, shared ADMET data from multiple pharma partners. This "flywheel effect" expands the training dataset with high-quality, experimental ADMET data, improving model accuracy for challenges like metabolic stability and permeability [31].
- Step 3: Prioritize Explainable Predictions
- Choose platforms that provide probability estimates and highlight which specific parts of a molecule are likely causing the ADMET issue, allowing chemists to make informed design adjustments before synthesis [31].
Data Presentation: AI Platforms & Data Management
Comparison of Leading AI Drug Discovery Platforms
Table 1: Top AI Platforms for Drug Discovery in 2025: Features, Pros, and Cons
| Platform Name | Best For | Standout Feature | Key Pros | Key Cons/Limitations |
|---|---|---|---|---|
| Exscientia [32] | Large pharma, Oncology | Centaur AI for rapid drug design | Reduces early-stage development time by up to 70%; High Phase I success rate. | Complex setup for teams without AI expertise; Focus primarily on small molecules. |
| BenevolentAI [32] | Rare diseases, Drug repurposing | Massive knowledge graph for uncovering hidden biological connections | Cuts development costs by up to 70%; Strong focus on rare diseases. | High dependency on input data quality; Requires robust computational infrastructure. |
| Insilico Medicine [32] | End-to-end drug discovery | Pharma.AI suite (target discovery to clinical prediction) | Comprehensive, validated suite; High success rate in identifying actionable targets. | Steep learning curve; Pricing can be prohibitive for small startups. |
| Atomwise [32] | Biotech startups, Rare diseases | AtomNet for structure-based drug design & binding affinity prediction | Fast screening reduces early-stage timelines; Accessible for academic teams. | Requires high-quality structural data; Limited focus on clinical trial prediction. |
| Inductive Bio [31] | ADMET optimization | Custom deep learning for real-time, molecular-level ADMET insights | Solves a key bottleneck; Real-time, explainable predictions for chemists. | Focused exclusively on ADMET, not a full pipeline solution. |
Essential Data Management Practices for AI-Ready Research
Table 2: Key Practices to Overcome Data Pitfalls in AI-Driven Discovery
| Practice Category | Specific Action | Function & Benefit |
|---|---|---|
| Data Structuring [27] | Organize data into standardized, machine-readable formats with consistent naming conventions. | Lays the groundwork for AI; enables models to extract meaningful insights efficiently. |
| Centralized Management [27] | Implement a specialized Laboratory Information Management System (LIMS). | Prevents data fragmentation; ensures all teams access the same structured, consistent data. |
| FAIR Principles [27] | Make data Findable, Accessible, Interoperable, and Reusable. | Creates a robust, scalable foundation for AI; prevents data silos and enables data reuse. |
| Governance & Curation [28] | Establish data provenance and implement continuous quality checks for new data. | Ensures output reliability; helps avoid decisions based on outdated or biased information. |
| Cross-Disciplinary Collaboration [28] | Foster collaboration between data scientists and domain experts. | Combines technical know-how with therapeutic insight to develop effective, reliable models. |
Experimental Protocols & Workflows
Protocol: AI-Human Partnership for Drug Repurposing
This protocol outlines a hybrid workflow for identifying new drug targets for existing compounds, leveraging the strengths of both AI and human expertise [28].
- AI-Powered Knowledge Extraction: Use algorithms to extract and analyze knowledge from integrated drug discovery databases (e.g., Cortellis Drug Discovery Intelligence) and public sources.
- Machine Learning Prioritization: Apply ML models to the extracted data to generate an initial list of prioritized drug targets for a given disease indication.
- Expert Review and Refinement: Subject matter experts review the AI-generated list. This involves manual mechanism reconstruction and applying deep domain knowledge to refine the target list.
- Report Generation: Produce a final report for each prioritized target, detailing supporting evidence, mechanism of action, relevant pathways, and clinical status of modulating drugs.
The following workflow diagram illustrates this collaborative, multi-stage process:
Protocol: Troubleshooting a Failed TR-FRET Assay
This guide provides a step-by-step methodology for diagnosing a TR-FRET assay that shows no signal or a poor assay window [30].
Reader Setup Verification:
- Consult the instrument compatibility portal for your specific microplate reader model.
- Confirm that the exact recommended emission and excitation filters for TR-FRET are correctly installed. This is the most common point of failure.
- Use control reagents from your assay kit to test the reader's TR-FRET functionality before using precious experimental samples.
Reagent and Compound Check:
- Verify the preparation of all stock solutions and dilutions. Inconsistent compound stocks are a primary reason for EC50/IC50 discrepancies between labs.
- Confirm the activity and specificity of enzymes (e.g., kinases) and other biological reagents.
Ratiometric Data Analysis:
- Calculate the emission ratio (Acceptor Signal / Donor Signal, e.g., 520nm/495nm for Tb). Do not rely on raw RFU values from a single channel.
- The donor signal acts as an internal reference, normalizing for pipetting variance and lot-to-lot reagent variability.
Assay Robustness Calculation:
- Calculate the Z'-factor using the formula:
Z' = 1 - [3*(σ_positive_control + σ_negative_control) / |μ_positive_control - μ_negative_control|]. - A Z'-factor > 0.5 indicates a robust assay suitable for screening. A large assay window with high noise (low Z'-factor) is not reliable.
- Calculate the Z'-factor using the formula:
The logical troubleshooting path for this scenario is as follows:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Their Functions in AI-Integrated Discovery
| Reagent / Tool Category | Specific Example(s) | Primary Function in Experimentation |
|---|---|---|
| TR-FRET Assay Kits [30] | LanthaScreen Eu/Tb Kinase Binding Assays | Enable homogeneous, high-throughput screening and profiling of compound-target interactions by measuring resonance energy transfer. |
| Validation Controls [30] | 100% Phosphopeptide Control, 0% Phosphorylation Control (Substrate) | Provide reference points for assay window (Z'-factor) calculation and verify proper functioning of the assay development reaction. |
| Specialized LIMS [27] | Biologics LIMS | Centralizes and structures complex biologics data (samples, assays, entities); ensures data is AI-ready and FAIR-compliant. |
| AI for ADMET Optimization [31] | Inductive Bio's Compass Platform | Provides real-time, explainable predictions on absorption, distribution, metabolism, excretion, and toxicity during compound design. |
| Multi-Omics Data Sources [28] [26] | Genomic, Proteomic, Patient-Centric Data | Provides the high-quality, diverse biological data required to train AI models for target identification and patient stratification. |
Technical Support Center: Troubleshooting Guides and FAQs
This section addresses common experimental challenges in the development of advanced biomaterials and smart scaffolds for regenerative pharmacology, providing targeted solutions to help overcome key translational barriers.
Frequently Asked Questions (FAQs)
FAQ 1: Our 3D-bioprinted construct lacks sufficient vascularization for larger tissue models. What strategies can improve this?
- Challenge: A primary translational barrier for engineered tissues is the inability to create perfusable, complex vascular networks that supply nutrients and oxygen to core regions, leading to necrotic centers [33] [34].
- Solutions:
- Co-printing with Bio-inks: Utilize bio-inks laden with endothelial cells and supporting cells (like pericytes) in a defined architecture alongside your primary tissue bio-ink [33].
- Incorporation of Angiogenic Factors: Design your scaffold material to controllably release angiogenic growth factors, such as VEGF (Vascular Endothelial Growth Factor) or SDF-1 (Stromal Cell-Derived Factor-1), to promote host-derived vasculature infiltration and network formation [35].
- Sacrificial Printing: Employ a fugitive bio-ink (e.g., Pluronic F127 or gelatin) that is printed into a network pattern and then liquefied and removed, leaving behind patent, perfusable channels that can be seeded with endothelial cells [33].
FAQ 2: The immune response to our scaffold is causing excessive fibrosis and encapsulation, hindering integration. How can this be modulated?
- Challenge: The foreign body response can lead to fibrotic encapsulation, isolating the scaffold from the host tissue and impairing its function [36] [34].
- Solutions:
- Use Immune-Modulatory Biomaterials: Select or functionalize materials with known anti-inflammatory or pro-regenerative macrophage polarization properties. Examples include certain types of chitosan, decellularized extracellular matrix (ECM), or polymers incorporating IL-10 or TGF-β [37] [35].
- Modify Surface Physicochemical Properties: Tune surface topography (e.g., using micro- and nano-patterning), stiffness, and wettability to create a surface that minimizes the pro-fibrotic immune response and promotes a healing environment [34].
- Controlled Release of Immunomodulators: Load the scaffold with controlled-release systems (e.g., PLGA nanoparticles) containing immune-modulating cytokines or small molecules to actively direct the local immune response toward a regenerative, anti-fibrotic phenotype [38] [37].
FAQ 3: How can I achieve a sustained, multi-stage release of multiple growth factors (e.g., for proliferation followed by differentiation) from a single scaffold?
- Challenge: Native tissue repair occurs in distinct phases, each requiring different biochemical cues. A major translational challenge is replicating this dynamic signaling in vivo [35].
- Solutions:
- Multi-Material Scaffolds: Fabricate a composite scaffold with distinct compartments (e.g., core-shell fibers or multi-layered hydrogels). Each compartment can be tailored with different material properties (e.g., degradation rate) to release its specific payload sequentially [33] [38].
- Layered Incorporation: Incorporate growth factors into the scaffold using different methods for each factor. For instance, one factor can be physically adsorbed for a quick release, while another is encapsulated within slower-degrading microspheres embedded in the scaffold matrix for delayed release [35].
- Stimuli-Responsive Systems: Develop "smart" scaffolds using biomaterials that release their cargo in response to specific physiological stimuli (e.g., matrix metalloproteinases (MMPs) present during remodeling, or a shift in pH) that coincide with different stages of healing [33] [38].
FAQ 4: Our nanoparticle-based delivery system for genes/ drugs shows low encapsulation efficiency and rapid burst release. What are the key parameters to optimize?
- Challenge: Low encapsulation efficiency wastes expensive therapeutic cargo (e.g., DNA, RNA, growth factors), and an initial burst release prevents sustained, long-term delivery, potentially causing off-target effects [38] [37].
- Solutions:
- Optimize Formulation Parameters: Systematically vary the polymer-to-drug ratio, surfactant concentration (e.g., PEGylation for PLGA NPs), and solvent selection during the emulsion process to improve drug loading and control release kinetics [37].
- Explore Alternative Materials: Consider cationic polymers like Polyethyleneimine (PEI), which strongly complex nucleic acids through electrostatic interactions, offering high encapsulation and protection from degradation, though its cytotoxicity must be managed [37].
- Post-Formulation Modifications: After nanoparticle formation, surface modification with targeting ligands (e.g., peptides, antibodies) can enhance specificity, while cross-linking the surface can slow down the initial diffusion-based release and provide a more sustained profile [38].
Troubleshooting Common Experimental Workflows
Issue: Poor Cell Viability and Infiltration in 3D-Bioprinted Constructs
| Observation | Potential Cause | Solution |
|---|---|---|
| Low cell viability immediately after printing. | Shear stress during extrusion. Nozzle clogging. | Optimize printing pressure and nozzle diameter. Use bio-inks with higher cell viability, such as peptide-based hydrogels or thermo-responsive polymers. Increase bio-ink concentration to reduce shear. |
| Cells fail to proliferate and migrate into the scaffold core. | Scaffold porosity is too low. Pore size is too small. Material is too stiff. | Adjust fabrication parameters (e.g., print temperature, crosslinking density) to create larger, interconnected pores. Select a softer hydrogel material that mimics the native tissue modulus to facilitate cell migration. |
| Viability decreases over time in culture. | Lack of vascularization leading to nutrient/waste diffusion limits. Inadequate degradation creating a physical barrier. | Incorporate angiogenic factors as in FAQ 1. Design the scaffold with a degradation rate that matches tissue ingrowth, using hydrogels sensitive to cell-secreted enzymes (e.g., MMP-sensitive peptides) [33]. |
Issue: Inconsistent or Uncontrolled Drug Release from Smart Scaffolds
| Observation | Potential Cause | Solution |
|---|---|---|
| High initial "burst release" of therapeutic agent. | Drug is adsorbed on or near the surface of the scaffold/microparticles. | Increase the density of the polymer matrix or cross-linking. Use a core-shell structure where the shell acts as a diffusion barrier. Switch from physical adsorption to encapsulation methods. |
| Release kinetics do not respond to the intended stimulus (e.g., enzyme, pH). | The stimuli-responsive linker is inaccessible or inefficiently cleaved. The material's responsiveness is not tuned to the physiological range. | Ensure the responsive elements are located in the main degradation pathway of the scaffold. Validate the sensitivity of the material in vitro using relevant concentrations of the stimulus (e.g., specific MMPs at physiological levels). |
| Incomplete release of the encapsulated payload. | The therapeutic agent becomes denatured or trapped within the non-degraded polymer matrix. | Screen for compatibility between the drug and polymer. Consider using a more readily degradable polymer or a polymer blend. Incorporate porogens to create additional release pathways. |
Experimental Protocols & Data Presentation
Detailed Protocol: Fabrication and Characterization of a Dual-Growth Factor Releasing, Core-Shell Fibrous Scaffold
This protocol provides a methodology for creating a scaffold that sequentially releases multiple growth factors, addressing the challenge of replicating the dynamic signaling of natural healing processes [35].
1. Materials Synthesis
- Core Solution: Prepare a 10% w/v solution of slow-degrading polymer (e.g., PLGA 75:25) in an organic solvent (e.g., Dichloromethane, DCM). Encapsulate the differentiation factor (e.g., BMP-2) into this solution.
- Shell Solution: Prepare a 5% w/v solution of fast-degrading polymer (e.g., PLGA 50:50) or a natural polymer like gelatin in a compatible solvent/water. Encapsulate the proliferation factor (e.g., FGF-2) into this solution.
2. Scaffold Fabrication via Coaxial Electrospinning
- Set up a coaxial electrospinning apparatus with two separate syringes pumping the core and shell solutions through a coaxial spinneret.
- Key Parameters:
- Flow Rates: Optimize core and shell flow rates (e.g., 0.5 mL/h and 1.0 mL/h, respectively).
- Voltage: Apply a high voltage (e.g., 15-20 kV) to the spinneret.
- Collector Distance: Maintain a fixed distance (e.g., 15 cm) between the spinneret and the grounded collector drum.
- Collect the core-shell fibers on the drum to form a non-woven mat.
3. Scaffold Sterilization and Hydration
- Sterilize the fibrous mats by exposure to UV light on each side for 30 minutes.
- Hydrate the scaffolds by immersing in 70% ethanol followed by serial washes in phosphate-buffered saline (PBS).
4. In Vitro Release Kinetics Assay
- Cut scaffold samples to a standardized size and mass (e.g., 1 cm² discs, 10 mg).
- Immerse each sample in 1 mL of release medium (PBS with 0.1% BSA) in a microcentrifuge tube.
- Incubate at 37°C under gentle agitation.
- At predetermined time points (e.g., 1, 3, 6, 12, 24 hours, then daily), completely remove the release medium and replace it with fresh pre-warmed medium.
- Analyze the collected medium using an ELISA to quantify the concentration of each growth factor released over time.
Table 1: Characteristic Properties of Common Biomaterials Used in Drug Delivery and Scaffolding
| Material | Type | Key Properties | Common Applications | Key Translational Challenges |
|---|---|---|---|---|
| PLGA [37] | Synthetic Polymer | Biocompatible, biodegradable, tunable degradation rate, FDA-approved for some uses. | Sustained release microparticles/nanoparticles, 3D scaffolds. | Acidic degradation products can cause local inflammation; burst release can be an issue. |
| Chitosan (CS) [37] | Natural Polymer | Bioadhesive, mucoadhesive, inherent hemostatic and antimicrobial properties. | Nasal/vaccine delivery, wound healing dressings, hydrogel matrices. | Poor solubility at neutral/basic pH; batch-to-batch variability. |
| Polyethyleneimine (PEI) [37] | Synthetic Polymer | High cationic charge density, "proton-sponge" effect for high transfection efficiency. | Gene/drug delivery, nucleic acid complexation. | Dose-dependent cytotoxicity; limited biodegradability. |
| Fibrin | Natural Polymer (Biologically Derived) | Naturally derived from clotting cascade, excellent cell adhesion and biocompatibility. | Hydrogel for cell encapsulation, nerve guide conduits, cardiac patch. | Rapid, uncontrolled degradation; low mechanical strength. |
Table 2: Example In Vitro Release Kinetics Data from a Hypothetical Core-Shell Scaffold
This table summarizes expected data from the protocol in Section 2.1, demonstrating sequential release.
| Time Point (Days) | Cumulative FGF-2 Release from Shell (%) | Cumulative BMP-2 Release from Core (%) |
|---|---|---|
| 1 | 45.2 ± 5.1 | 8.5 ± 2.1 |
| 3 | 78.6 ± 4.3 | 15.3 ± 3.0 |
| 7 | 92.1 ± 2.8 | 25.7 ± 4.2 |
| 14 | 95.5 ± 1.5 | 48.9 ± 5.6 |
| 21 | 96.8 ± 1.2 | 72.4 ± 6.1 |
| 28 | 97.5 ± 1.0 | 89.7 ± 4.8 |
Signaling Pathways and Experimental Workflows
Key Signaling Pathways in Osteogenic Differentiation
This diagram illustrates the primary signaling pathways targeted for bone regeneration, a common goal in regenerative pharmacology. The release of growth factors like BMP-2 and FGF-2 from scaffolds activates these pathways to direct stem cell fate.
Workflow for Developing a Smart Scaffold
This flowchart outlines a generalized experimental workflow for the design, fabrication, and validation of a smart, responsive scaffold, from initial concept to pre-clinical testing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Smart Scaffold Development
| Item | Function / Rationale | Example & Notes |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) [37] | A versatile, FDA-approved biodegradable polymer for creating sustained-release microparticles and 3D scaffolds. | Available in various LA:GA ratios (e.g., 50:50, 75:25) to control degradation rate from weeks to months. |
| MMP-Sensitive Peptide Crosslinker | Enables creation of "smart" hydrogels that degrade specifically in response to cell-secreted enzymes during tissue remodeling. | Sequence: GGPQGIWGQGK (cleavable by MMP-2 and MMP-9). Used in PEG-based or other hydrogels. |
| Chitosan [37] | A natural, bioadhesive polymer with intrinsic antimicrobial properties, ideal for wound healing and mucosal delivery applications. | Often chemically modified (e.g., trimethyl chitosan) to improve solubility and enhance penetration. |
| Recombinant Growth Factors (BMP-2, FGF-2, VEGF) [35] | Key signaling molecules to direct cell proliferation, differentiation, and angiogenesis within the engineered construct. | Highly sensitive to denaturation. Requires careful incorporation and release kinetics testing to ensure bioactivity. |
| Polyethyleneimine (PEI) [37] | A cationic polymer for efficient complexation and delivery of nucleic acids (DNA, siRNA) to cells within the scaffold. | Branched PEI (25 kDa) is common but cytotoxic. Linear PEI or lower molecular weight versions are often better tolerated. |
| RGD Peptide | A common cell-adhesive ligand (Arg-Gly-Asp) grafted onto biomaterial surfaces to promote integrin-mediated cell attachment and spreading. | Crucial for synthetic materials like PEG that lack inherent cell-binding domains. |
| Dual-Syringe Coaxial Electrospinning Setup | Apparatus for fabricating core-shell fibrous scaffolds that allow for sequential or dual delivery of therapeutics. | Allows for spatial control over the location of different drugs/growth factors within a single fiber. |
Harnessing Multi-Omics and Systems Biology for Patient Stratification and Mechanism Deconvolution
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of a multi-omics approach over single-omics studies in translational research? A multi-omics approach provides a more comprehensive molecular profile by integrating data from various biological layers (e.g., genome, transcriptome, proteome, metabolome). This integration is crucial for understanding complex diseases, as a single omics layer cannot fully capture the causal relationships and regulatory mechanisms underlying disease pathogenesis. Multi-omics enables the identification of robust biomarkers, patient subtypes, and dysregulated pathways that would be missed in single-omics studies, thereby enhancing the potential for successful clinical translation [39] [40].
FAQ 2: How can multi-omics data integration help in identifying novel drug targets? Multi-omics integration can uncover key molecular players and signaling pathways involved in disease pathology. By combining genomics, transcriptomics, and proteomics, researchers can move beyond mere associations to understand causal mechanisms. This allows for the identification of "actionable" targets, particularly at the proteome level which is closer to the phenotype. Furthermore, this approach can facilitate drug repurposing by revealing new disease contexts for existing drugs [40] [41].
FAQ 3: What are the key computational challenges in multi-omics data integration, and how can they be addressed? Key challenges include data heterogeneity (different technologies/platforms), data wrangling (ID mapping, normalization, imputation), and dimensionality. To address these:
- Data Wrangling: Implement careful sample registration and robust metadata recording. Use transformation (scaling, normalization) and mapping (harmonizing IDs across omics) processes [41].
- Data Heterogeneity & Dimensionality: Employ tools designed for integration, such as those using matrix factorization, network fusion, or factor analysis (e.g., MOFA, mixOmics, SNF) for dimension reduction and feature extraction [41].
FAQ 4: What is cellular deconvolution, and why is it important for analyzing bulk tissue samples? Cellular deconvolution is a computational technique used to estimate the proportion of different cell types within a bulk tissue sample based on omics data (e.g., gene expression). This is critical because bulk samples are a mixture of cell types, and variations in cell type composition can confound analyses like differential gene expression. Deconvolution helps dissect this cellular heterogeneity, leading to more accurate interpretation of results and reducing confounding effects in functional analyses [42] [43].
FAQ 5: How can multi-omics profiling be applied to patients who are currently healthy? Multi-omics can stratify healthy individuals into subgroups with distinct molecular profiles, uncovering subclinical risk factors. For example, one study identified a subgroup of healthy individuals with molecular patterns associated with dyslipoproteinemia, suggesting a predisposition to future cardiovascular issues. This enables a framework for precision medicine aimed at early prevention and targeted monitoring strategies [44].
Troubleshooting Guides
Guide 1: Troubleshooting Patient Stratification and Subtype Identification
Problem: Unstable or biologically irrelevant patient clusters derived from multi-omics data.
| Problem Cause | Diagnostic Checks | Corrective Actions |
|---|---|---|
| High Technical Variation | Check for batch effects using PCA colored by batch. | Apply batch effect correction methods (e.g., ComBat). Include batch as a covariate in models. |
| Inappropriate Data Preprocessing | Verify each omic layer is properly normalized and scaled. | Normalize data per platform-specific best practices. Use variance-stabilizing transformations. |
| Noisy or Irrelevant Features | Assess if clustering is driven by a small number of features. | Perform feature selection (e.g., select most variable features) prior to integration and clustering. |
| Poor Choice of Integration Method | Evaluate if the method can handle your data types and sample size. | Select a method suited for your goal (see Table 2). Consider benchmark studies (e.g., from [40]). |
Recommended Workflow:
- Preprocessing: Normalize and scale each omics dataset individually.
- Batch Correction: Identify and correct for technical batch effects.
- Integration: Use a dedicated multi-omics clustering tool (see Table 2).
- Validation: Validate clusters using survival analysis (if clinical data exists) or known biological markers.
Guide 2: Troubleshooting Cellular Deconvolution
Problem: Inaccurate estimation of cell type proportions from bulk transcriptomic data.
| Problem Cause | Diagnostic Checks | Corrective Actions |
|---|---|---|
| Mismatched Reference | Compare the cell types in your reference to expected types in your tissue. | Use a reference profile generated from a similar tissue, disease state, and demographic. |
| Poor Quality Reference Matrix | Check if marker genes are highly expressed and specific to one cell type. | Use a reference built from single-cell RNA-seq data or purified cell populations. |
| Presence of Uncharacterized Cell Types | See if deconvolution residuals are high, indicating missing cell types. | Use a reference-free or partial-reference method that can identify unknown cell types [43]. |
| Low Sequencing Depth | Check the total read count per sample. Low counts increase noise. | Use deconvolution methods robust to low counts. If possible, sequence samples deeper. |
Recommended Workflow:
- Reference Selection: Choose a context-appropriate reference matrix (e.g., from single-cell data of a similar cohort).
- Method Selection: Select a deconvolution algorithm (see Table 2).
- Quality Control: Examine the sum of estimated proportions and the model's goodness-of-fit.
- Downstream Analysis: Correlate cell proportions with clinical phenotypes or use proportions as covariates in differential expression analysis.
Guide 3: Troubleshooting Multi-Omics Data Integration for Regulatory Mechanism
Problem: Difficulty in identifying causal regulatory relationships (e.g., how a genetic variant influences a disease via gene expression and protein levels).
| Problem Cause | Diagnostic Checks | Corrective Actions |
|---|---|---|
| Temporal Misalignment | Data omics layers are collected from the same sample but represent different snapshots in time. | If possible, collect longitudinal samples. Use computational methods that infer temporal causality (e.g., dynamic Bayesian networks). |
| Lack of Paired Samples | Omics data are not generated from the exact same patient samples. | Design studies where all omics assays are performed on the same sample aliquot. |
| Complex, Non-Linear Relationships | Simple correlation analyses fail to find strong associations. | Employ machine learning models (e.g., Random Forests, Neural Networks) that can capture non-linear interactions [39]. |
| Insufficient Functional Validation | Computational predictions remain as correlations without experimental proof. | Plan for functional follow-up experiments (e.g., CRISPR knockouts, reporter assays) to validate key predicted regulators. |
Recommended Workflow:
- Study Design: Ensure multi-omics data is generated from the same patient samples.
- DI Method Selection: Choose an integration method designed for mechanistic insight (see Table 2).
- Network Analysis: Build molecular interaction networks from integrated data.
- Prioritization: Prioritize key driver molecules (e.g., master regulators, central nodes in the network).
- Experimental Validation: Validate top candidates using targeted in vitro or in vivo experiments.
Research Reagent Solutions and Computational Tools
Table 1: Essential Multi-Omics Data Resources
| Resource Name | Omics Content | Species | Primary Application |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) [40] | Genomics, Epigenomics, Transcriptomics, Proteomics | Human | Pan-cancer molecular profiling; biomarker discovery & patient stratification. |
| Answer ALS [40] | Whole-genome sequencing, RNA transcriptomics, ATAC-sequencing, Proteomics | Human | Neurodegenerative disease research; integrating deep clinical data with multi-omics. |
| jMorp [40] | Genomics, Methylomics, Transcriptomics, Metabolomics | Human | Multi-omics population data; reference for normal variation and disease association. |
| Fibromine [40] | Transcriptomics, Proteomics | Human, Mouse | Fibrosis-specific research; curated data on fibrotic pathways and targets. |
Table 2: Key Computational Tools for Multi-Omics and Deconvolution
| Tool Name | Category | Primary Function | Key Application |
|---|---|---|---|
| MOFA+ [41] | Multi-omics Integration | Factor analysis to identify latent factors across omics. | Unsupervised discovery of sources of variation; patient stratification. |
| mixOmics [41] | Multi-omics Integration | Projection-based methods (e.g., PCA, PLS) for DI. | Dimension reduction, visualization, and identification of multi-omics biomarkers. |
| CIBERSORTx [43] | Cellular Deconvolution | Reference-based deconvolution of bulk gene expression. | Estimating immune cell infiltration; correcting for cell type heterogeneity in bulk data. |
| MuSiC [43] | Cellular Deconvolution | Reference-based deconvolution using single-cell RNA-seq data. | Leveraging scRNA-seq to accurately deconvolve bulk data from similar tissues. |
| TOAST [43] | Cellular Deconvolution | Reference-free & reference-based deconvolution. | Deconvolution when reference is unavailable or incomplete. |
FAQs: Core Concepts and Strategic Choices
Q1: What are the primary strategic advantages of allogeneic cell therapies over autologous ones?
Allogeneic therapies, derived from healthy donors, are manufactured in large, standardized batches. This contrasts with autologous therapies, which are created on a per-patient basis using a patient's own cells. The primary advantage of allogeneic products is their potential for "off-the-shelf" availability, which can significantly reduce costs, increase treatment accessibility, and eliminate the vein-to-vein time that can be critical for patients with aggressive diseases [45] [46]. However, allogeneic cells face major immune system barriers, as the recipient's body will likely recognize them as foreign and reject them [45].
Q2: What are the main biological challenges associated with allogeneic cell therapies?
The central challenge is preventing immune rejection without relying on long-term, systemic immunosuppression, which has serious side effects [45]. Two key strategies are being developed to overcome this:
- Inducing Immune Tolerance: This involves "retraining" the recipient's immune system to accept the donor cells. Approaches include creating mixed chimerism in the hematopoietic system or using modified thymic epithelial cells [45].
- Immune Evasion: This involves engineering the donor tissue to be "invisible" to the immune system or physically sequestering it within an immune-protective barrier [45].
Q3: How does cellular plasticity influence regenerative medicine, and how can it be controlled?
Cellular plasticity—the ability of a differentiated cell to alter its identity—is a fundamental mechanism for tissue repair. In response to injury, some cells can undergo adaptive cellular reprogramming to become transient repair cells or directly replace lost cells [47]. Key genes like Msx1 and signaling pathways like BMP and Notch are critical regulators of this plasticity [48]. Controlling this process, potentially through pharmacology rather than genetic manipulation, is a major focus for harnessing the body's own regenerative capabilities [47].
Q4: What are the critical safety concerns regarding viral vectors used in cell engineering?
Viral vectors, such as γ-retroviruses and lentiviruses, are highly efficient at delivering genetic material like chimeric antigen receptors (CARs) but carry inherent risks. The primary concern is insertional mutagenesis, where the semi-random integration of the viral genome into the host cell's DNA can disrupt key cellular genes, potentially leading to oncogenesis [46]. While modern self-inactivating (SIN) vector designs and rigorous testing have mitigated the risk of generating replication-competent viruses, cases of secondary cancers following CAR T-cell therapy have highlighted that this remains a vital safety consideration [46].
Troubleshooting Guides for Common Experimental Challenges
Table 1: Troubleshooting Cell Source and Viability Issues
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low viability of primary cells after thawing | Improper thawing technique or rough handling. | Thaw cells rapidly (<2 mins at 37°C). Use wide-bore pipette tips, mix slowly, and plate cells immediately after counting [49]. |
| Poor attachment of primary cells | Lack of attachment factors; dried coating matrix; incorrect seeding density. | Use an appropriate coating matrix (e.g., Collagen I). Ensure the matrix does not dry before cell seeding. Verify the optimal seeding density for your cell type [49]. |
| Senescent cells in culture (e.g., large, non-proliferating cells) | Normal for primary cell cultures; population has undergone many doublings. | This is expected in adult primary cultures. Ensure proper care and use cells within the recommended number of population doublings. Younger, proliferating cells will be smaller [49]. |
| Failure of neural induction from human pluripotent stem cells (hPSCs) | Low hPSC quality; incorrect cell density at induction. | Remove differentiated hPSCs before induction. Plate hPSCs as cell clumps (not single cells) at the recommended density (e.g., 2–2.5 x 10^4 cells/cm²) [49]. |
Table 2: Troubleshooting Genetic Engineering and Transgene Expression
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low transduction efficiency in sensitive primary cells (e.g., T-cells) | Cell sensitivity; suboptimal transduction conditions. | Use specialized transfection/transduction reagents designed for sensitive primary cells. Optimize the multiplicity of infection (MOI) and consider the use of transduction enhancers [49] [46]. |
| Unintended genomic alterations | Use of viral vectors or gene-editing tools (e.g., CRISPR/Cas9). | Consider non-integrating vector systems (e.g., mRNA, adenovirus) for transient expression. For stable expression, utilize safer gene-editing platforms like base editing or prime editing that minimize double-strand DNA breaks [46]. |
| Low or transient transgene expression | Use of non-integrating delivery systems; promoter silencing. | For long-term expression, use integrating systems (lentivirus, retrovirus, transposons). Verify the activity and stability of the promoter in your specific cell type [46]. |
| Poor functional persistence of engineered cells (e.g., CAR T-cells) | T-cell exhaustion; chronic antigen stimulation; immunosuppressive microenvironment. | Engineer cells to overcome exhaustion, e.g., by knocking out genes for inhibitory receptors (e.g., PD-1) or introducing cytokine switches to enhance persistence [46]. |
Signaling Pathways and Experimental Workflows in Cellular Reprogramming
The following diagram illustrates a simplified, consolidated signaling pathway based on key genes known to be active in regenerative models, which can be targeted to control cellular plasticity.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Cell Engineering and Culture
| Reagent / Material | Function | Example Application |
|---|---|---|
| Coating Matrix (e.g., Collagen I, Geltrex) | Provides a surface for cell attachment and spreading. | Essential for culturing sensitive primary cells like hepatocytes and keratinocytes [49]. |
| B-27 Supplement | A serum-free supplement optimized for the survival and growth of neurons and other neural cells. | Critical for maintaining primary neuron cultures; requires careful handling and storage to maintain efficacy [49]. |
| ROCK Inhibitor (Y-27632) | Inhibits Rho-associated kinase, reducing apoptosis in dissociated stem cells. | Used to improve cell survival after passaging of human pluripotent stem cells (hPSCs) [49]. |
| Viral Vectors (Lentivirus, Retrovirus) | Efficient delivery of transgenes for stable, long-term expression. | Generation of CAR T-cells; requires safety controls like self-inactivating (SIN) designs [46]. |
| CRISPR/Cas9 System | Precise genome editing for gene knockout, knock-in, or regulation. | Engineering allogeneic CAR T-cells by knocking out the TCR and HLA genes to avoid graft-versus-host disease [46]. |
| Williams Medium E | A complex medium formulation designed for hepatocyte culture. | Used with specific plating and incubation supplements to maintain primary hepatocyte function in vitro [49]. |
Solving the Core Challenges: Manufacturing, Safety, and Regulation
Technical Support Center: Troubleshooting GMP Compliance in ATMP Manufacturing
Core Concepts: ATMPs and GMP
What are the main categories of Advanced Therapy Medicinal Products (ATMPs)?
ATMPs represent a new generation of medicines in regenerative medicine, primarily categorized as follows [50]:
- Cell-based Therapy Medicinal Products (CTMPs): Living cells are collected via apheresis, then modified, expanded, and administered to the patient to treat diseases at the cellular level.
- Gene Therapy Medicinal Products (GTMPs): Consist of recombinant nucleic acids intended to regulate genetic sequences in the patient (in-vivo) or in their cells after collection (ex-vivo).
- Tissue-Engineered Products (TEPs): Use immature or differentiated stem cell populations to repair structurally compromised tissues.
What is the fundamental purpose of Good Manufacturing Practice (GMP) in ATMP production?
GMP is a system for ensuring that products are consistently produced and controlled according to established quality standards [51]. The main purpose is to prevent harm to the end user by safeguarding product safety, identity, strength, quality, and purity [52]. This involves maintaining clean and hygienic manufacturing areas, controlled environmental conditions, clearly defined and validated processes, and comprehensive documentation [52].
How does a risk-based approach (RBA) aid in ATMP GMP compliance?
Given the unique and evolving nature of ATMPs, a rigid application of traditional GMP is often not feasible. A risk-based approach is therefore critical [53]. It allows manufacturers to:
- Scientifically identify the specific risks inherent to their unique ATMP process.
- Justify control measures based on a deep understanding of the product, materials, and process.
- Demonstrate to regulators that the principles of quality and safety are met, even when specific written rules do not yet exist for a novel technology or approach [53].
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: Our autologous ATMP has a very short shelf life, but traditional sterility testing takes 14 days. How can we release products safely and in a timely manner?
- The Challenge: Traditional growth-based sterility testing creates an impossible situation where the product must be administered to the patient before test results are available, posing a significant safety risk [54].
- The Solution: Implement rapid microbiological methods, such as real-time polymerase chain reaction (PCR) sterility testing.
- Troubleshooting Guide:
- Problem: Inability to perform final product sterility testing before patient administration.
- Root Cause: The brief viability window of living cell therapies does not align with lengthy, traditional quality control (QC) methods.
- Solution & Protocol: Adopt a real-time PCR sterility test kit.
- Methodology: This method detects microbial DNA contaminants, providing results in hours instead of weeks [54].
- Key Benefit: It offers a time saving of more than 90% over growth-based QC release, allowing for results within the product's shelf life [54].
- Actionable Step: Validate the rapid PCR method against your specific product to demonstrate its equivalence or superiority to the pharmacopoeial method for your QC release strategy.
FAQ 2: How do we manage the high degree of variability in patient-derived starting materials?
- The Challenge: The intrinsic variability of starting material (due to the patient's age, health, and illness) threatens batch consistency and quality [50].
- The Solution: Strengthen in-process controls (IPCs) and implement a robust tracking system.
- Troubleshooting Guide:
- Problem: Unacceptable variability in the quality of the final product due to inconsistent starting materials.
- Root Cause: Patient-specific factors lead to heterogeneous raw materials.
- Solution & Protocol: Enhance process control and documentation.
- IPC Implementation: Use in-process controls as an essential tool to monitor the safety and quality of the production process in real-time, allowing for adjustments as needed [50].
- Batch Tracking: Implement a system that ensures impeccable batch identity and tracking from the patient through all manufacturing steps and back to the patient [50]. This is non-negotiable for tracing any deviations.
- Actionable Step: Define Critical Process Parameters (CPPs) and establish IPC checkpoints to ensure the process remains controlled despite input variability.
FAQ 3: The regulatory guidelines from different agencies (e.g., EMA and PIC/S) seem to conflict on GMP boundaries. How should we design our facility?
- The Challenge: Regulatory documents like the EU's EudraLex Part IV and PIC/S Annex 2A may have differing philosophies on aspects like environmental classification for closed systems [53].
- The Solution: Focus on the intent behind the regulations using a risk-based approach rather than a word-for-word comparison.
- Troubleshooting Guide:
- Problem: Conflicting interpretation of GMP requirements for facility design, leading to uncertainty and potential non-compliance.
- Root Cause: The rapid pace of ATMP innovation has led to a lag in fully harmonized international regulations [53].
- Solution & Protocol: Conduct a facility-specific risk assessment.
- Understand Intent: The core intention of all guidelines is to ensure product sterility, safety, and quality. Your design should be justified by this principle.
- Risk-Based Justification: For example, if using a closed system, you may scientifically justify a lower environmental classification (e.g., Grade C or D) by demonstrating the system's integrity through pressure hold tests and continuous monitoring, rather than defaulting to a Grade A environment [53].
- Actionable Step: Document a comprehensive risk assessment that evaluates your product, process closure, and technologies to justify your facility design choices to any regulatory agency.
FAQ 4: We need to update an analytical tool for an already approved ATMP process. What are the key considerations for a successful change?
- The Challenge: Embracing improved technologies while ensuring continued regulatory compliance for an approved product [55].
- The Solution: A structured, data-driven approach to process and analytical method changes.
- Troubleshooting Guide:
- Problem: The need to implement a new, improved analytical technology without jeopardizing the marketing authorization.
- Root Cause: The continuous innovation in process and analytical tools in the cell and gene therapy field [55].
- Solution & Protocol: Follow a strict change management and validation protocol.
- Comparability Exercise: Plan and execute a study to demonstrate that the new method provides equivalent or superior results compared to the established method. The data must show the change does not adversely impact the critical quality attributes of the product.
- Regulatory Notification: Understand the regulatory filing requirements for the level of change you are implementing. Some changes require prior approval, while others can be managed through your Pharmaceutical Quality System (PQS).
- Actionable Step: Before implementation, generate a full validation package for the new analytical method that includes precision, accuracy, specificity, and a direct comparison to the old method using archived samples.
Data & Methodologies
Table 1: Comparison of Sterility Testing Methods for ATMPs
| Feature | Traditional Growth-Based Method | Rapid PCR Method |
|---|---|---|
| Testing Time | 14 days [54] | Approximately 24 hours (90%+ time savings) [54] |
| Methodology | Culture-based growth and enrichment | Detection of microbial DNA |
| Key Advantage | Compendial/standard method | Enables testing within product shelf life |
| Key Disadvantage | Results post-administration | Requires extensive validation |
| Ideal for ATMPs | No | Yes, especially for short-shelf-life products |
Table 2: Key Regulatory Guidelines for ATMP GMP Compliance
| Guideline / Annex | Issuing Body | Key Focus & Applicability |
|---|---|---|
| EudraLex Vol 4, Part IV | European Commission | Stand-alone GMP guidelines specific to ATMPs; emphasizes risk-based approach [53]. |
| PIC/S Annex 2A | PIC/S (Pharmaceutical Inspection Co-operation Scheme) | GMP for ATMPs, frequently references Annex 1 principles for sterile products [53]. |
| Annex 1 (Manufacture of Sterile Medicinal Products) | European Commission & PIC/S | Applies to process streams requiring aseptic handling; critical for ATMPs that cannot be sterile-filtered [53]. |
Detailed Protocol: Implementing a Rapid PCR Sterility Test
This protocol outlines the steps for adopting a rapid microbiological method for quality control release of ATMPs [54].
- Technology Selection: Choose a validated real-time PCR kit designed for sterility testing that covers a broad range of potential microbial contaminants.
- Method Validation: Perform a full validation to demonstrate the method is suitable for your product. This includes:
- Specificity: Test against a panel of relevant microorganisms to ensure detection.
- Accuracy/Spike Recovery: Inoculate your product matrix with a low level of microbes and demonstrate the method can detect them.
- Robustness: Test the method's resilience to small, deliberate variations in protocol parameters.
- Comparison: Run parallel testing with the traditional compendial method to establish correlation.
- Sample Preparation: Adapt the kit's sample processing method for your cellular product. This may involve lysing human cells to release any microbial contaminants while minimizing PCR inhibitors.
- PCR Setup and Run: Follow the kit instructions for preparing the reaction mix, adding the processed sample, and running the real-time PCR instrument.
- Data Analysis: Interpret the results based on the presence or absence of specific fluorescence curves crossing the threshold, indicating microbial contamination.
- QC Release Decision: Based on the validated method's results, make a lot release decision. A negative result allows for release; a positive result triggers a failure and investigation.
Visual Workflows & Diagrams
Generic Autologous ATMP Manufacturing Workflow
Risk-Based Approach to GMP Compliance
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for ATMP Process Development and QC
| Item | Function & Role in GMP Compliance |
|---|---|
| GMP-Grade Cytokines/Growth Factors | Ensure raw materials are free of adventitious agents, supporting product safety and consistent cell growth/differentiation. |
| Cell Separation/Activation Reagents | Critical for the initial processing of patient cells; quality directly impacts yield and viability. Must be validated for human use. |
| Viral Vector (for GTMPs) | Acts as the gene delivery vehicle in gene therapies. Its quality, titer, and purity are Critical Quality Attributes (CQAs). |
| Cell Culture Media & Supplements | Formulates the base nutrient environment for cell growth. Serum-free, xeno-free GMP-grade media reduce contamination risks and variability. |
| Analytical Method Kits (e.g., PCR, Flow Cytometry) | Used for in-process and release testing (e.g., identity, purity, sterility, potency). Must be validated and standardized. |
| Single-Use Bioprocess Containers | Minimizes cross-contamination, reduces cleaning validation, and enhances facility flexibility—key for multi-product ATMP facilities. |
Technical Support Center
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: My pluripotent stem cell (PSC) cultures show excessive differentiation (>20%). How can I reduce this to minimize tumorigenic risk in therapeutic products?
- Problem Explanation: Excessive spontaneous differentiation in culture indicates suboptimal conditions that can lead to heterogeneous cell populations. Upon transplantation, residual undifferentiated cells can form teratomas, while differentiated cells of the wrong lineage can generate unwanted tissues or tumors [56] [57].
- Solution Protocol:
- Quality Control Culture Medium: Ensure your complete cell culture medium (e.g., mTeSR Plus) stored at 2-8°C is used within two weeks of preparation [58].
- Meticulous Passaging:
- Physically remove areas of differentiation from cultures before passaging.
- Passage cultures when colonies are large and compact with dense centers, before they overgrow.
- Ensure cell aggregates created during passaging are evenly sized to promote uniform growth.
- Decrease colony density by plating fewer cell aggregates during passaging.
- Minimize Environmental Stress: Avoid leaving culture plates outside the incubator for extended periods (e.g., >15 minutes) [58].
FAQ 2: What are the most effective strategies to eliminate residual undifferentiated PSCs from a differentiated cell product before transplantation?
- Problem Explanation: Even trace numbers (e.g., 10,000) of undifferentiated human PSCs (hPSCs) can form teratomas in vivo. A 5-log (100,000-fold) depletion is often considered critical for safety when transplanting billions of cells [56] [57].
- Solution Protocol: Genome-Edited Safeguard:
- Engineering a "Kill-Switch": Use Cas9 RNP/AAV6-based genome editing to knock-in an inducible Caspase9 (iCaspase9) cassette and a fluorescent reporter (e.g., YFP) into the NANOG locus. NANOG is a transcription factor highly specific to the pluripotent state [56] [57].
- Mechanism: The engineered NANOG-iCaspase9-YFP construct is only expressed in undifferentiated cells. Treatment with a small molecule (e.g., AP20187/AP20) induces dimerization of the iCaspase9 protein, triggering rapid and irreversible apoptosis specifically in these cells [56] [57].
- Procedure:
- Note: Biallelic knock-in (both gene copies) is recommended to prevent potential escapees [56] [57].
FAQ 3: How can I control the entire PSC-derived cell graft in a patient if an adverse event like tumor formation occurs post-transplantation?
- Problem Explanation: Even after removing undifferentiated cells, the graft itself may malfunction, become tumorigenic due to acquired mutations, or generate unwanted tissues. A "master kill-switch" is needed to address this in vivo risk [56] [57].
- Solution Protocol: Orthogonal Safety Switch:
- Engineering a Pan-Cell Eliminator: Create a second safeguard by inserting a drug-inducible "kill-switch" (e.g., iCaspase9 or a similar system) into a constitutively active, lineage-agnostic gene locus, such as ACTB (Beta-Actin) [56] [57].
- Mechanism: This switch is expressed in all cells derived from the engineered hPSC line, regardless of their differentiation status. Administration of a different small molecule drug activates apoptosis in the entire cell product [56] [57].
- Procedure:
- Establish a cloned hPSC line harboring both the NANOG-iCaspase9 (for in vitro purification) and ACTB-iCaspase9 (for in vivo safety) systems.
- Differentiate this dual-safeguard cell line into your desired therapeutic product.
- Post-transplantation, if adverse events are detected, administer the activating drug for the ACTB-iCaspase9 system to eliminate the entire graft [56] [57].
FAQ 4: I am using CRISPR-Cas9 for engineering. How can I predict, minimize, and detect off-target effects in my PSC lines?
- Problem Explanation: The CRISPR-Cas9 system can cause unintended DNA cleavages at genomic sites with sequence similarity to the target site (off-target effects), potentially disrupting genes and leading to oncogenic transformations [59] [60].
- Solution Protocol:
- In Silico Prediction (Before the Experiment):
- Use online tools like Cas-OFFinder or CCTop to nominate potential off-target sites by searching the genome for sequences similar to your sgRNA, allowing for a few mismatches or bulges [60].
- Minimizing Risk (Experimental Design):
- gRNA Selection: Choose a gRNA with minimal sequence similarity to other genomic sites [59] [60].
- High-Fidelity Cas9: Use engineered, high-fidelity Cas9 variants like HypaCas9, eSpCas9(1.1), or evoCas9 that are less tolerant of gRNA:DNA mismatches [59] [60].
- Dual Nickase Strategy: Use two Cas9 nickases (which create single-strand breaks) with paired gRNAs targeting adjacent sites. A double-strand break only occurs if both nickases act close together, drastically reducing off-target cleavage [59].
- Detection and Validation (After Editing):
- Targeted Sequencing: Perform deep sequencing of the nominated potential off-target sites from the in silico prediction [59] [60].
- Unbiased Methods: For a more comprehensive profile, use methods like GUIDE-seq or Digenome-seq, which experimentally identify off-target cleavage sites in a genome-wide manner [60].
- In Silico Prediction (Before the Experiment):
FAQ 5: Which reprogramming method should I choose for generating clinical-grade iPSCs to minimize tumorigenic risk from the start?
- Problem Explanation: The method used to reprogram somatic cells into induced Pluripotent Stem Cells (iPSCs) can introduce oncogenic risks, either through the use of oncogenes themselves (e.g., c-MYC) or via genomic integration of vectors that might disrupt tumor suppressor genes [61] [62].
- Solution Protocol: Non-Integrating Episomal Vectors:
- Rationale: Episomal vectors are a non-integrating approach that is cleared from cells upon division, eliminating the risk of insertional mutagenesis. They are a common choice for clinical-grade iPSC generation [62].
- Procedure:
- Transfect somatic cells (e.g., fibroblasts, CD34+ cells) with episomal vectors containing reprogramming factors (OCT4, SOX2, KLF4).
- To enhance the typically low reprogramming efficiency without using potent oncogenes, supplement the culture with a cocktail of reprogramming small molecules (e.g., specific inhibitors and activators that modulate signaling pathways conducive to reprogramming) [62].
- This method can yield fully reprogrammed iPSC colonies while lowering the neoplastic risk associated with traditional oncogenes like c-MYC and LIN28 [62].
Data Presentation Tables
Table 1: Quantitative Efficacy of the NANOG-iCaspase9 Safety Switch [56] [57]
| Parameter | Performance Metric | Experimental Context |
|---|---|---|
| Depletion Efficiency | > 1.75 × 10⁶-fold (>> 5-log) | Reduction of undifferentiated hPSCs after AP20 treatment |
| Potency (IC₅₀) | 0.065 nM | Half-maximal inhibitory concentration of AP20 |
| Optimal Treatment Dose | 1 nM | Concentration that effectively kills hPSCs without downregulating NANOG |
| Treatment Duration | 12-24 hours | Sufficient to eliminate undifferentiated hPSCs |
| Specificity | Spares >95% of differentiated cells | Efficacy shown in bone, liver, and forebrain progenitors |
Table 2: Comparison of iPSC Reprogramming Methods and Associated Risks [61] [62]
| Reprogramming Method | Integration Risk | Key Tumorigenicity Concerns | Advantages |
|---|---|---|---|
| Retroviral/Lentiviral | High (Random integration) | Use of oncogenes (c-MYC), potential silencing of tumor suppressors | High efficiency |
| Sendai Virus | None (Cytoplasmic RNA virus) | Requires careful screening to ensure viral clearance, use of oncogenes | Robust efficiency, works on diverse cell types |
| Episomal Vectors | None (Vector is diluted out) | Low efficiency often compensated by using oncogenes; can be mitigated with small molecules | Clinically relevant, non-integrating |
| Self-Replicating RNA | None | Requires immune suppression during transfection, persistent viral RNA components | High efficiency, non-integrating |
| mRNA | None | Laborious (daily transfections), can trigger interferon response | Non-integrating, defined components |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Implementing Genetic Safeguards
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| CRISPR-Cas9 System | Precise genome editing for knock-in of safety switches. | Inserting iCaspase9 cassette into the NANOG or ACTB locus [56] [57]. |
| High-Fidelity Cas9 | Reduces off-target effects during genome editing. | Using eSpCas9(1.1) or HypaCas9 for safer engineering of safeguard lines [59] [60]. |
| Inducible Caspase 9 (iCaspase9) | Genetically encoded "safety switch" that induces apoptosis upon ligand binding. | Core component of both the NANOG-specific and ACTB-wide kill switches [56] [57]. |
| Small Molecule Activator (AP20187) | Dimerizing agent that activates the iCaspase9 protein. | Administered in vitro to purge undifferentiated cells or in vivo to ablate the entire graft [56] [57]. |
| In Silico Prediction Tools (e.g., Cas-OFFinder) | Computational nomination of potential CRISPR off-target sites. | Assessing the risk profile of sgRNAs designed for knock-in experiments [60]. |
| Non-Integrating Reprogramming Vectors | Generate iPSCs without genomic integration. | Creating clinical-grade master iPSC lines with lower inherent tumorigenic risk [62]. |
Experimental Workflow and Pathway Diagrams
Diagram 1: Engineered Safety Switch Mechanism for Tumorigenicity Mitigation
Diagram Title: How engineered safety switches selectively eliminate undifferentiated PSCs.
Diagram 2: Comprehensive Strategy for Safe PSC Therapy Development
Diagram Title: Multi-layered safety strategy from iPSC generation to transplantation.
The field of Advanced Therapy Medicinal Products (ATMPs) represents one of the most innovative yet complex areas of therapeutic development. For researchers and developers navigating this space, understanding the distinct regulatory pathways of the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) is crucial for successful translation from bench to bedside. The global ATMP market is projected to grow from $7.82 billion in 2025 to $29.41 billion by 2033, reflecting an 18% compound annual growth rate [63]. This rapid expansion underscores the critical need for clear regulatory navigation strategies.
The regulatory landscape for ATMPs is characterized by specialized frameworks that go beyond conventional biologic requirements, addressing unique challenges in manufacturing complexity, patient-specific products, and significant safety considerations including tumorigenicity and immunogenicity [64]. This technical support guide provides targeted troubleshooting advice and frequently asked questions to help researchers overcome the most common translational barriers in regenerative pharmacology.
Understanding ATMP Classifications and Regulatory Bodies
What are ATMPs and how are they classified?
FAQ: What constitutes an ATMP and how do classifications differ between regions?
Advanced Therapy Medicinal Products (ATMPs) encompass gene therapies, somatic cell therapies, tissue-engineered products, and combined ATMPs [64]. In the European Union, the term "ATMP" is formally used and regulated under specific legislation, while the United States FDA typically classifies these products under broader categories of "cell and gene therapies" or as "human cells, tissues, and cellular and tissue-based products (HCT/Ps)" [64]. This fundamental terminology difference impacts development strategies from the earliest stages.
Troubleshooting Guide: Classification Challenges
- Problem: Uncertainty about whether a product qualifies as an ATMP and which regulatory framework applies.
- Solution:
- For EU classification, seek formal certification or scientific advice from the Committee for Advanced Therapies (CAT)
- For US determination, consult FDA's CBER regarding whether your product meets the criteria for regulation as a 351 vs 361 HCT/P
- Engage regulatory consultants early for products with ambiguous characteristics
- Problem: Differing classifications for the same product in different regions.
- Solution: Develop a region-specific regulatory strategy that accounts for these differences in your global development plan.
Key Regulatory Bodies and Their Roles
FAQ: Which centers within the FDA and EMA oversee ATMP regulation?
In the European Union, the EMA's Committee for Advanced Therapies (CAT) is specifically responsible for assessing ATMP applications and providing scientific expertise [64]. The CAT works within the broader EMA structure alongside the Committee for Medicinal Products for Human Use (CHMP).
In the United States, the Center for Biologics Evaluation and Research (CBER), a division of the FDA, regulates cell and gene therapy products under the authority of the Public Health Service Act and the Federal Food, Drug, and Cosmetic Act [64].
Regulatory Pathway Comparison: FDA vs. EMA
The journey from preclinical development to market authorization follows distinct yet parallel pathways in the US and EU, as illustrated below:
Comparative Requirements Table
Table 1: Key Regulatory Requirements Comparison Between FDA and EMA
| Requirement | FDA (US) | EMA (EU) |
|---|---|---|
| Preclinical to Clinical Transition | Investigational New Drug (IND) submission [64] | Clinical Trial Application (CTA) submission to national authorities [64] |
| Market Authorization Application | Biologics License Application (BLA) [64] | Marketing Authorization Application (MAA) [64] |
| Advanced Therapy Committee | No specific committee; reviewed within CBER | Committee for Advanced Therapies (CAT) provides expertise [64] |
| Expedited Programs | Fast Track, Breakthrough Therapy, RMAT, Accelerated Approval [64] | PRIME scheme, accelerated assessment [64] |
| GMP Compliance Approach | Phase-appropriate compliance with verification at BLA stage [65] | Mandatory GMP compliance from early clinical trials [65] |
| Donor Eligibility Requirements | Prescriptive requirements for screening and testing [65] | General guidance with reference to EU and member state laws [65] |
| Key Recent Guideline | Multiple disease-specific guidance documents | Guideline on quality, non-clinical and clinical requirements for investigational ATMPs (effective July 2025) [63] [65] |
Troubleshooting Common Regulatory Challenges
Manufacturing and Quality Control Hurdles
FAQ: What are the most common CMC (Chemistry, Manufacturing, and Controls) challenges in ATMP development?
Based on analysis of recent regulatory feedback, approximately 70% of ATMP clinical holds and major objections relate to CMC issues [65]. The new EMA guideline on clinical-stage ATMPs, effective July 2025, emphasizes that "immature quality development may compromise use of clinical trial data to support a marketing authorization" [65].
Troubleshooting Guide: GMP Compliance Differences
- Problem: Differing GMP expectations between the US and EU create resource allocation challenges.
- Solution:
- For US studies: Implement a phase-appropriate GMP compliance strategy with full verification at the BLA stage
- For EU studies: Ensure full GMP compliance from earliest clinical trials, including mandatory self-inspections [65]
- Develop a unified quality system that can accommodate both approaches for global development programs
- Problem: Inconsistent donor eligibility requirements between regions complicate allogeneic product development.
- Solution:
- Implement the more stringent FDA requirements for donor screening and testing as your baseline standard
- For EU studies, additionally comply with relevant member state-specific legal requirements and the upcoming Substances of Human Origin Regulation (SoHO-R) [64]
Clinical Trial Design Considerations
FAQ: How should I design my ATMP clinical trial to meet both FDA and EMA expectations?
The EMA's new clinical-stage ATMP guideline provides a consolidated reference drawn from over 40 separate guidelines and reflection papers, representing a significant effort to harmonize expectations [65]. However, differences remain in specific requirements for early-phase versus late-stage trials.
Troubleshooting Guide: Clinical Development Planning
- Problem: Uncertainty about what data is needed to progress from early-phase to pivotal trials.
- Solution:
- Seek early regulatory advice through FDA pre-IND meetings or EMA ITF briefing meetings
- For EU programs specifically, leverage the new multidisciplinary ATMP guideline as a primary reference for structuring your clinical trial application [65]
- Adopt a risk-based approach when evaluating quality, non-clinical, and clinical data requirements
- Problem: Designing endpoints that will be acceptable for both agencies.
- Solution:
- Include surrogate endpoints that may qualify for accelerated approval pathways (FDA) while collecting longer-term clinical outcomes
- Engage with both agencies early if planning a global development program to identify potential endpoint acceptance differences
Expedited Development Pathways and Special Programs
Available Programs for Accelerated Development
FAQ: What special programs can accelerate ATMP development and approval?
Both the FDA and EMA offer expedited pathways for ATMPs that address unmet medical needs:
FDA Programs:
- Regenerative Medicine Advanced Therapy (RMAT): Specifically for regenerative medicine products addressing unmet needs [64]
- Fast Track: For serious conditions with unmet medical needs [64]
- Breakthrough Therapy: For substantial improvement over available therapies [64]
- Accelerated Approval: Based on surrogate endpoints [64]
EMA Programs:
Expedited Program Comparison Table
Table 2: Expedited Development Program Comparison
| Program Feature | FDA RMAT Designation | EMA PRIME Scheme |
|---|---|---|
| Purpose | Accelerate development/approval of regenerative medicines | Early support for therapies addressing unmet needs |
| Eligibility | Regenerative medicine products for serious conditions with unmet needs | Therapies addressing unmet medical needs |
| Key Benefits | Intensive FDA guidance, rolling BLA review, potential for accelerated approval | Early and enhanced protocol assistance, accelerated assessment |
| Evidence Level | Preliminary clinical evidence | Promising early clinical or non-clinical data |
| Similarities | Both provide early agency interaction, potential for accelerated assessment | Both provide early agency interaction, potential for accelerated assessment |
Essential Research Reagent Solutions for ATMP Development
Table 3: Key Research Reagent Solutions for ATMP Development
| Reagent/Category | Function | Application in ATMP Development |
|---|---|---|
| Allogeneic Cell Sources | Starting material for cell-based ATMPs | Critical for scalable manufacturing; requires compliance with donor screening regulations [64] [65] |
| Gene Editing Tools | Genetic modification of cell products | Enables development of next-generation CAR-T and other genetically modified ATMPs [66] |
| CD19 Targeting Vectors | Engineering CAR-T cells for B-cell targeting | Key component in multiple autoimmune and oncology ATMPs in development [66] |
| GMP-Grade Cytokines/Growth Factors | Cell expansion and differentiation | Essential for manufacturing processes; must meet stringent quality requirements [65] |
| Nanoparticle Tracking Analysis | Characterization of extracellular vesicles and viral vectors | Critical quality control for consistent product manufacturing [67] |
| Exosome Engineering Components | Development of novel delivery systems | Enables targeted delivery approaches as demonstrated in spinal cord injury research [67] |
Strategic Recommendations for Successful Navigation
Early Planning and Regulatory Engagement
FAQ: What is the single most important factor in successfully navigating ATMP regulations?
Early and strategic engagement with regulatory agencies emerges as the most critical success factor. The EMA explicitly encourages ATMP developers "to seek early guidance at either the national member state or European level to inform development" [65]. Similarly, the FDA offers various pre-IND meeting opportunities to align on development plans.
Troubleshooting Guide: Early Regulatory Engagement
- Problem: Uncertainty about when and how to seek regulatory advice.
- Solution:
- For novel technologies, request an EMA ITF briefing meeting during early development
- Schedule FDA pre-IND meetings when sufficient preliminary data exists to support meaningful discussion
- Prepare specific questions focused on areas of greatest uncertainty (e.g., novel endpoints, manufacturing approaches)
- Problem: Managing potentially conflicting advice from different agencies.
- Solution:
- Be transparent with each agency about your global development plans
- Seek to understand the underlying scientific principles behind any divergent recommendations
- Develop a unified strategy that addresses the most stringent requirements from either agency
Embracing Regulatory Convergence Opportunities
While differences persist between FDA and EMA requirements, there is significant movement toward regulatory convergence, particularly in CMC areas. As noted by regulatory experts, "the overwhelming majority of content contained in the quality documentation section of the ATMP guideline is familiar and recognizable as information that is to be included in a clinical trial application" for both agencies [65]. The organizational framework of the new EMA guideline mirrors the Common Technical Document (CTD) structure, further facilitating global development.
By understanding these pathways, anticipating common challenges, and implementing strategic solutions, researchers can more effectively navigate the complex regulatory landscape for ATMPs and advance transformative therapies to patients in need.
Technical Support Center
Troubleshooting Guide: Manufacturing Process Challenges
This guide addresses common manufacturing challenges in regenerative pharmacology, providing step-by-step solutions to ensure economic viability and product quality.
Issue 1: High Variability in Cell Expansion Yields
- Problem: Inconsistent cell numbers or quality during scale-up.
- Solution:
- Audit Raw Materials: Transition to defined, synthetic media to reduce batch-to-buffer variability [68].
- Process Control: Implement in-line sensors to monitor critical parameters like glucose, lactate, and ammonia in real-time [68].
- Equipment Calibration: Ensure bioreactors and environmental control systems (CO₂, temperature) are regularly calibrated.
Issue 2: Contamination in Patient-Specific (Autologous) Production
- Problem: Microbial contamination in small-batch, parallel processes.
- Solution:
- Implement Closed Systems: Utilize closed, automated, and modular manufacturing platforms to minimize open processing steps [69] [68].
- Single-Use Technologies: Adopt single-use bioreactors and disposable fluid paths to eliminate cross-contamination risks [68].
- Environmental Monitoring: Enhance aseptic testing protocols and routine monitoring of the cleanroom environment.
Issue 3: Inefficient Quality Control (QC) Causing Delays
- Problem: QC testing is destructive, slow, and creates a bottleneck.
- Solution:
- Develop Nondestructive QC: Invest in technologies for real-time, in-line monitoring of cell phenotype and density [68].
- Process Analytical Technology (PAT): Define Critical Quality Attributes (CQAs) and use PAT for continuous quality verification instead of end-product testing [69].
- Automated Data Capture: Use software to automatically correlate process data with product release criteria.
Frequently Asked Questions (FAQs)
Q1: What are the most effective strategies to reduce the high costs of growth factors and cell culture media? A1: The most effective strategy is to reduce reliance on high-cost, variable materials. This includes:
- Developing Defined Media: Create or source synthetic, serum-free media formulations. This eliminates variability and high cost associated with fetal bovine serum [68].
- Bulk Purchasing & Supplier Negotiation: For common reagents, negotiate long-term contracts and bulk purchasing discounts to lower per-unit costs [70].
- Value Engineering: Collaborate with suppliers early in the process to identify functionally equivalent, lower-cost alternative materials [70].
Q2: How can we manage the complex logistics and high costs of distributing a living, shelf-stable product globally? A2: Managing distribution requires a platform approach:
- Platform Technologies for Shipping: Develop robust, universal formulations and methods for cryopreservation or lyophilization (freeze-drying) to extend product stability during transit [68].
- Optimized Supply Chain: Use predictive analytics for demand forecasting to plan production and distribution, minimizing delays. Explore localized manufacturing (scale-out) to bring production closer to the patient [69] [71].
Q3: Our automated bioreactor system is failing to achieve target cell densities. What should we check? A3: Follow this systematic troubleshooting protocol:
- Sensor Calibration: Verify the accuracy of pH, dissolved oxygen (DO), and metabolite (e.g., glucose) sensors.
- Process Parameters: Review and adjust feeding schedules, agitation rates, and gas flow parameters against established baselines.
- Cell Line Characterization: Re-assess the growth kinetics and metabolic requirements of your specific cell line, as they may differ from initial models.
- Consult Vendor Protocols: Ensure all procedures align with the bioreactor manufacturer's recommended protocols for your cell type.
Q4: We are facing regulatory hurdles due to a lack of standardized manufacturing protocols. How can we address this? A4: Proactively engage with standardization efforts:
- Adopt Existing Standards: Implement available standards for raw materials, cells, and procedural controls wherever possible [69].
- Develop Platform Procedures: Create standardized, validated protocols for common unit operations (e.g., cell separation, formulation) that can be applied across multiple products [68].
- Engage in Consortia: Participate in pre-competitive industry consortia (e.g., Regenerative Medicine Manufacturing Innovation Consortium) to help develop the needed standards [68].
Data Presentation
Table 1: Quantitative Analysis of Manufacturing Cost Drivers and Mitigation Strategies
| Cost Driver | Potential Financial Impact | Mitigation Strategy | Expected Outcome |
|---|---|---|---|
| Raw Material Variability | High; causes batch failures and delays [69] | Implement defined, synthetic media & reagents [68] | Improved consistency, reduced QC rejections |
| Manual, Open Processes | High labor costs, contamination risk [69] | Adopt closed, automated systems & single-use technologies [68] | Reduced labor, lower contamination rates |
| Inefficient Energy Use | Significant operational expense [70] | Invest in energy-efficient machinery & sustainable practices [72] | 8%+ average energy savings [70] |
| Inventory Holding Costs | Ties up capital, risk of obsolescence [73] | Implement Just-in-Time (JIT) inventory systems [73] [71] | Reduced storage costs, freed-up capital |
Experimental Protocols
Protocol 1: In-Line Monitoring of Bioreactor Metabolites for Process Control
Objective: To enable real-time, nondestructive monitoring of cell culture health and optimize feeding strategies.
Methodology:
- Equipment Setup: Integrate in-line or at-line bioanalyzers (e.g., for glucose, lactate, ammonia) with the bioreactor control system [68].
- Baseline Profiling: For a new cell line, first establish a baseline profile of metabolite consumption/production over time using offline assays.
- Set Control Limits: Define acceptable ranges for each metabolite based on the baseline profile and correlation with cell viability and potency.
- Automate Feedback Loops: Program the bioreactor software to automatically adjust nutrient feed rates in response to real-time metabolite data, maintaining levels within the optimal range.
- Data Correlation: Continuously correlate the real-time metabolite data with critical quality attributes (CQAs) of the final cell product.
Protocol 2: Implementing a Just-in-Time (JIT) Inventory System for Raw Materials
Objective: To minimize inventory holding costs and reduce waste from expired materials.
Methodology:
- Demand Forecasting: Use historical data and production forecasts to accurately predict material needs [70].
- Supplier Collaboration: Establish strong partnerships with reliable suppliers and negotiate agreements for frequent, small-batch deliveries [71] [70].
- Lead Time Analysis: Meticulously track and work to reduce supplier lead-time variability.
- Kanban System Implementation: Use a visual Kanban system (e.g., two-bin system) on the production floor to trigger replenishment orders seamlessly.
- Performance Monitoring: Track key metrics like inventory turnover ratio and stockout frequency to continuously refine the JIT system.
Mandatory Visualization
Diagram 1: Troubleshooting High Cell Variability
Diagram 2: Cost-Effective Manufacturing Strategy Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Cost-Effective Regenerative Medicine Manufacturing
| Item | Function | Rationale for Cost-Effective or Standardized Use |
|---|---|---|
| Defined/Synthetic Media | Provides a consistent, serum-free environment for cell growth. | Reduces batch-to-buffer variability, lowers QC burden, and is more scalable than serum-containing media [68]. |
| Single-Use Bioreactors | Disposable vessels for cell expansion. | Eliminates cleaning validation, reduces cross-contamination risk, and increases facility flexibility [68]. |
| In-line Sensors (pH, DO, Metabolites) | Enables real-time monitoring of culture conditions. | Allows for predictive process control, reduces reliance on destructive offline sampling, and improves yield consistency [68]. |
| Master/Working Cell Banks | Well-characterized, cryopreserved stocks of cells. | Ensures a consistent and reliable starting material for all production runs, which is crucial for product quality and regulatory approval [69]. |
| Platform Purification & Formulation Kits | Standardized kits for downstream processing. | Using platform technologies across multiple products reduces process development time and capital investment [68]. |
Proving Efficacy and Building a Robust Clinical Evidence Base
Frequently Asked Questions (FAQs)
Q1: What are the core regulatory pathways for regenerative medicine advanced therapies, and how do they impact trial design?
A1: Regulatory pathways for Advanced Therapy Medicinal Products (ATMPs), which include many regenerative therapies, vary globally but share common features designed to accelerate development. In the United States, the 21st Century Cures Act established the Regenerative Medicine Advanced Therapy (RMAT) designation, which can expedite the development and review of products for serious conditions [74]. In the European Union, ATMPs—encompassing gene therapy, cell therapy, and tissue-engineered products—are regulated under Regulation (EC) No 1394/2007, with evaluation by the Committee for Advanced Therapies (CAT) [74]. Japan also has specific legislation enacted in 2014 to streamline the regulation of regenerative medicine [74]. These pathways often allow for the use of novel endpoints and adaptive trial designs to address the unique challenges and high unmet medical needs in this field.
Q2: How can a surrogate endpoint be validated for use in a confirmatory clinical trial for a regenerative therapy?
A2: A surrogate endpoint is considered validated when clinical trials have established that it reliably predicts a clinical benefit [75]. The FDA states that a "validated surrogate endpoint" is accepted as evidence of benefit when it has undergone testing to show it can correlate with and predict a clinical outcome, such as how reduced systolic blood pressure predicts a reduced risk of stroke [75]. For contexts where validation is not yet complete, the FDA's Accelerated Approval program allows the use of endpoints that are "reasonably likely" to predict clinical benefit. However, sponsors are then required to conduct post-approval trials to verify the anticipated clinical benefit [75].
Q3: What are the key advantages of using a master protocol framework in regenerative medicine?
A3: Master protocols, which include basket, umbrella, and platform trials, offer several key advantages:
- Efficiency: They allow for the evaluation of multiple therapies or disease subtypes within a single, overarching protocol, optimizing resource use and accelerating the drug development process [76].
- Adaptability: Platform trials, in particular, can allow for the addition of new therapies as they become available and the dropping of ineffective ones based on interim analyses, which is ethically beneficial for patients [77].
- Robust Data: Using a common control arm across multiple investigational arms can increase scientific rigor and reduce the required sample size compared to running multiple independent trials [76].
Q4: What are Synthetic Control Arms (SCAs) and how can they address challenges in trial enrollment for rare diseases?
A4: A Synthetic Control Arm is an innovative approach that uses de-identified patient-level data from prior clinical studies to create a highly contextualized external control group [76]. Instead of enrolling a concurrent control cohort, the outcomes of the investigational therapy are benchmarked against this constructed arm derived from historical data that matches for demographics, covariates, and endpoints. This is especially valuable in areas of high unmet medical need or for rare diseases, where timely patient access to investigational therapies is essential and enrolling a large control cohort is impractical or unethical [76].
Q5: What are the main translational barriers specific to regenerative pharmacology?
A5: Integrative and Regenerative Pharmacology (IRP) faces significant translational barriers that can be systematized as follows [78]:
- Investigational Obstacles: Preclinical animal models are often unrepresentative of human clinical conditions, impacting the clear definition of a therapy's mechanism of action and raising questions about long-term safety and efficacy.
- Manufacturing Issues: Challenges include scalability, the need for automated production methods, and adherence to stringent Good Manufacturing Practice (GMP) standards.
- Complex Regulatory Pathways: Different regional requirements (e.g., from the EMA and FDA) with a lack of unified guidelines create a complex landscape for approval.
- Ethical Issues: Concerns include patient privacy, data security, and the use of certain cell types like embryonic stem cells.
- Economic Factors: High manufacturing costs and uncertain reimbursement strategies limit accessibility, particularly in low- and middle-income countries.
Troubleshooting Guides
Issue 1: High Screen Failure Rate and Slow Patient Enrollment in a Complex Umbrella Trial
Problem: Your master protocol for a complex disease has stringent biomarker criteria, leading to a high rate of screened patients failing to qualify, which slows enrollment to a critical degree.
| Investigation Step | Action Required | Potential Resolution |
|---|---|---|
| Review Inclusion/Exclusion (I/E) Criteria | Analyze screen-fail data to identify the most common reasons for exclusion. | Refine I/E criteria by modeling them against historical clinical trial data to determine which specific subpopulations are most likely to respond, removing unnecessarily restrictive criteria [76]. |
| Assay & Logistics | Audit the turnaround time and accuracy of the biomarker diagnostic test. | Optimize the biomarker assay process or switch to a more rapid, centralized testing service to reduce the window between screening and randomization. |
| Utilize Predictive Tools | Leverage AI-powered analytics and synthetic data on historical trial populations. | Use tools like Simulants, a synthetic data solution, to refine protocols and optimize patient selection by predicting enrollment and identifying high-likelihood responders before trial initiation [76]. |
Issue 2: High-Profile Adverse Events in a Cell Therapy Trial
Problem: A novel CAR-T cell therapy is showing a higher-than-expected incidence of severe Cytokine Release Syndrome (CRS), leading to clinical holds and patient safety concerns.
| Investigation Step | Action Required | Potential Resolution |
|---|---|---|
| Proactive Safety Monitoring | Implement a rigorous safety monitoring plan based on emerging biomarkers. | Benchmark patient data throughout the trial using historical data to proactively determine which patients are most likely to have an adverse event [76]. Research has shown that common lab data can predict severe CRS [76]. |
| Protocol-Specified Intervention | Predefine management guidelines for CRS in the protocol. | Incorporate protocol-specified step-up dosing, prophylactic corticosteroids, or IL-6 receptor antagonists (e.g., tocilizumab) for patients with specific high-risk biomarker profiles identified in Step 1. |
| Dose Optimization | Re-evaluate the cell dosing strategy. | Consider employing a Bayesian optimal interval (BOIN) design or similar model-assisted design to find the optimal biological dose that maximizes efficacy while minimizing toxicity in earlier phase trials [79]. |
Issue 3: Inconsistent Biomarker Readouts for a Surrogate Endpoint
Problem: Measurements for your candidate surrogate endpoint (e.g., a specific growth factor concentration) are highly variable, undermining its reliability for predicting long-term clinical outcomes.
| Investigation Step | Action Required | Potential Resolution |
|---|---|---|
| Standardize Assay Protocol | Audit the entire sample handling and analysis process. | Implement a single, validated assay protocol across all trial sites, including detailed procedures for sample collection, processing, storage, and shipment. |
| Centralize Analysis | Check for inter-site variability in lab techniques and equipment. | Utilize a single, central laboratory for all biomarker analyses to ensure consistency and reduce site-to-site technical variation. |
| Re-evaluate Biomarker Fit | Critically assess the biomarker's link to the pathophysiology. | Revisit the foundational science. The biomarker must be a measurement based on the molecular pharmacology and/or pathophysiology of the disease to reliably assist decision-making [80]. Explore alternative biomarkers or composite scores. |
Data Presentation Tables
Table 1: Global Regulatory Pathways for Advanced Regenerative Therapies
| Region / Agency | Key Legislation / Regulation | Product Designation | Key Expedited Program(s) |
|---|---|---|---|
| USA (FDA) | 21st Century Cures Act; 21 CFR Part 1271 | Regenerative Medicine Therapy | Regenerative Medicine Advanced Therapy (RMAT) [74] |
| European Union (EMA) | Regulation (EC) No 1394/2007 | Advanced Therapy Medicinal Product (ATMP) | Priority Medicines (PRIME) [74] |
| Japan (PMDA) | Act on the Safety of Regenerative Medicine (2014) | Regenerative Medicine Products | Conditional/Time-Limited Approval [74] |
| Canada (Health Canada) | Food & Drugs Act (as Biologics) | Cell Therapy; Gene Therapy | – |
| United Kingdom (MHRA) | Human Medicines Regulations 2012 | Advanced Therapy Medicinal Product (ATMP) | Innovative Licensing and Access Pathway (ILAP) [74] |
Table 2: Classification and Use of Biomarkers and Endpoints in Clinical Development
| Term | Definition | Example in Regenerative Medicine | Regulatory Validation Status |
|---|---|---|---|
| Biomarker | A defined characteristic measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention [75]. | Specific cytokine level (e.g., IL-10); Gene expression signature | Not applicable; used for informed decision-making. |
| Clinical Outcome Endpoint | A direct measurement of how a patient feels, functions, or survives [75]. | Overall survival; Pain score on a validated scale | The gold standard for demonstrating efficacy. |
| Validated Surrogate Endpoint | An endpoint that has been proven to predict clinical benefit based on epidemiological and clinical trial data [75]. | Reduced systolic blood pressure for stroke risk | Accepted by regulators as evidence of benefit for specific contexts of use. |
| Reasonably Likely Surrogate Endpoint | An endpoint that is not yet validated but is considered likely to predict clinical benefit [75]. | Tumor shrinkage for an oncology regenerative therapy | Used in Accelerated Approval, requiring post-market confirmation. |
Experimental Protocol: Implementing a Biomarker-Driven Master Protocol
Objective: To evaluate the efficacy and safety of multiple investigational regenerative therapies in a specific disease (e.g., osteoarthritis) by stratifying patients based on predefined biomarkers within a single, adaptive umbrella trial.
Methodology:
- Trial Design: A multi-arm, biomarker-stratified umbrella protocol with an adaptive design.
- Patient Population: Adults with confirmed moderate to severe disease.
- Biomarker Screening:
- All screened patients provide a tissue (e.g., synovial biopsy) and/or blood sample.
- Samples are analyzed using a predefined multi-omics panel (e.g., transcriptomics, proteomics) at a central laboratory.
- Patients are stratified into biomarker-defined subgroups (e.g., "High Inflammatory," "Cartilage Catabolism High," "Metabolic").
- Randomization & Treatment:
- Patients within each biomarker subgroup are randomly assigned to receive either the investigational therapy deemed most appropriate for their subgroup or a common control therapy (standard of care).
- Adaptive Element: A pre-specified interim analysis is conducted by an independent data monitoring committee. Based on pre-defined rules using Bayesian predictive probability, therapies or biomarker subgroups showing strong evidence of futility may be dropped, and new therapies can be added to the protocol [79] [77].
- Endpoint Assessment:
- Primary Endpoint: A biomarker-driven surrogate endpoint reasonably likely to predict long-term clinical benefit (e.g., quantitative MRI cartilage thickness for osteoarthritis, validated against patient function) [75].
- Secondary Endpoints: Patient-reported outcomes (e.g., pain, quality of life), safety, and overall survival.
- Statistical Analysis: A Bayesian hierarchical model is used to adaptively borrow information across biomarker subgroups when appropriate, improving the precision of treatment effect estimates, especially in small subgroups [79].
The following diagram illustrates the workflow and decision points within this master protocol.
Master Protocol Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item / Technology | Function in Experiment | Specific Example in Regenerative Medicine |
|---|---|---|
| Biomaterial Scaffolds (e.g., Hydrogels) | Provides a 3D structure for cell growth and tissue formation; can be engineered for controlled drug release. | Used in cartilage regeneration to deliver growth factors like BMPs or FGFs with spatiotemporal control [35] [81]. |
| Stimuli-Responsive Nanoparticles | Acts as a targeted delivery vehicle for growth factors/genes; protects therapeutic cargo from degradation. | Used to deliver cytokines like SDF-1 or anti-inflammatory IL-10 to a specific tissue site (e.g., myocardium) in a controlled manner [35] [81]. |
| Synthetic Control Arm (SCA) | Provides a historical control group constructed from prior clinical trial data, reducing enrollment needs. | Used in rare disease trials or oncology (e.g., CAR-T trials) where recruiting a concurrent control arm is unethical or impractical [76]. |
| AI-Powered Synthetic Data (Simulants) | Generates high-fidelity, synthetic patient-level datasets from historical trials for protocol refinement and modeling. | Used to model trial scenarios, optimize inclusion/exclusion criteria, and identify high-risk patient subpopulations before trial start [76]. |
| Bayesian Optimal Interval (BOIN) Design | A statistical software suite for designing efficient early-phase (Phase I/II) dose-finding trials. | Used to find the optimal biological dose (OBD) for novel immunotherapies and targeted agents, balancing efficacy and toxicity [79]. |
Technical Support Center
Troubleshooting Guide: Common Experimental Challenges
This guide addresses frequent issues encountered when working with advanced preclinical models, offering targeted solutions to help overcome critical translational barriers in regenerative pharmacology.
Table 1: Troubleshooting Advanced Preclinical Models
| Challenge Category | Specific Problem | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Organ-on-a-Chip (OOC) Viability & Function | Poor tissue formation and barrier function | Low-quality human cells; Lack of physiological biomechanical cues [82] [83] | Source cells from certified biorepositories; Integrate mechanical actuation (e.g., stretching for lung alveolus, flow for endothelium) [82] [84] |
| High variability between chips | Inconsistent cell seeding; Uncontrolled culture conditions [83] | Automate cell seeding protocols; Implement real-time, continuous monitoring (e.g., Trans-Epithelial Electrical Resistance - TEER) [82] | |
| Humanized Model Predictive Value | Poor translation of drug efficacy/toxicity to humans | Biological discrepancies between animal and human physiology; Incorrect model selection [85] [86] | Use humanized models with full gene replacement (e.g., C3/C5 mice on HUGO-GT platform); Validate with known human-specific therapeutics [85] |
| Inconsistent immune system reconstitution or response | Use of immunodeficient hosts; Lack of human cytokine support [82] | Ensure host strain is appropriate for human cell type; Co-administer relevant human cytokines to support human cell engraftment and function [82] | |
| Platform Integration & Data | Difficulty linking multiple organ systems | Lack of standardized media for multi-OOC platforms; Scaling differences between organ models [84] | Use "body-on-a-chip" systems with shared circulatory flow; Employ physiologically based pharmacokinetic (PBPK) modeling to inform scaling [84] |
| Low reproducibility across labs | Absence of standardized protocols and benchmarks [83] | Adopt and publish detailed Standard Operating Procedures (SOPs); Participate in pre-competitive data-sharing initiatives to establish benchmarks [83] |
Frequently Asked Questions (FAQs)
Q1: Our organ-chip models consistently fail to achieve the tissue maturity levels seen in human organs. What key factors are we likely overlooking?
A: Achieving high tissue maturity often requires a multi-faceted approach beyond simple 3D culture. Key strategies include:
- Developmental Engineering: Incorporate extended culture times (weeks to months) and provide sequential developmental cues that mimic natural organogenesis [84].
- Biomimetic Cues: Ensure your system replicates critical in vivo environmental factors such as cyclic mechanical strain (for lung, heart, intestine), fluid shear stress (for vasculature, kidney), and electrical stimulation (for nerve, muscle) [82] [84].
- Stromal Co-culture: Do not rely solely on parenchymal cells. Incorporate relevant stromal cells (e.g., fibroblasts, pericytes) as they are crucial for depositing the correct extracellular matrix and providing essential molecular signals for functional maturation [84].
Q2: Why might a therapeutic show excellent efficacy in a humanized mouse model but still fail in human clinical trials due to lack of efficacy?
A: This common translational failure can stem from several issues with the model itself:
- Incomplete Humanization: The model may only express the human target gene in specific cell types or may not fully recapitulate the human immune response. Verify that the human gene is expressed with the correct spatial and temporal patterns and that a functional human immune component is present if relevant [85].
- Model Validation Gap: The model may not have been adequately validated for your specific disease context. Before initiating pivotal studies, confirm that the model replicates key human pathophysiological features and responds predictively to both positive and negative control compounds with known clinical outcomes [85] [86].
- Species-Specific Pathways: Even with a humanized target, surrounding pathways in the mouse may interact differently, altering the net biological effect. Cross-species transcriptomic analysis can help identify these discrepancies early [87].
Q3: What is the most significant regulatory challenge when submitting data from these novel models, and how can we prepare?
A: The primary challenge is the lack of clear, predefined regulatory pathways for accepting data from these emerging technologies [83]. To mitigate this:
- Engage Early: Seek early dialogue with regulators (e.g., FDA) to discuss your proposed use of the model and the data you intend to generate.
- Context of Use: Clearly define the "Context of Use" for your model. Is it for initial screening, target validation, or toxicity prediction? Be precise about what claims the data supports [83].
- Demonstrate Validation: Provide robust data showing that your model is reliable, reproducible, and predictive of human responses for its intended purpose. This includes internal validation and, whenever possible, reference to any available public validation studies [83].
Experimental Protocol: Establishing a Lung Alveolus-on-a-Chip Model
This protocol outlines the key steps for creating a breathing Lung Alveolus Chip to study respiratory infections or inflammatory diseases, based on established methodologies [82].
Objective: To replicate the functional alveolar-capillary interface in vitro for predictive toxicology and drug efficacy testing.
Workflow Overview:
Key Materials and Reagents:
- Microfluidic Device: A commercially available or custom-fabricated chip consisting of two parallel elastomeric (e.g., PDMS) channels separated by a thin, porous, flexible membrane [82] [84].
- Primary Human Cells: Pulmonary microvascular endothelial cells (HMVEC-L) and alveolar epithelial cells (e.g., primary or cell line-derived). The use of patient-specific induced pluripotent stem cell (iPSC)-derived cells is an advanced alternative [82] [83].
- Specialized Culture Media: Use cell-type-specific media, potentially conditioned for the co-culture environment.
- Application-Specific Reagents:
- Analysis Equipment: Confocal microscope, TEER measurement system, ELISA plate reader, equipment for RNA/protein extraction.
Detailed Procedure:
- Chip Preparation: Sterilize the microfluidic device (e.g., via UV light or ethanol). Pre-coat the membrane with appropriate extracellular matrix (ECM) proteins (e.g., collagen IV) to facilitate cell attachment.
- Cell Seeding: Introduce the endothelial cell suspension into the lower ("vascular") channel and the epithelial cell suspension into the upper ("alveolar") channel. Allow cells to attach under static conditions for several hours.
- Flow Initiation and Maturation: After cell attachment, connect the chip to a microfluidic perfusion system. Begin perfusing culture medium through both channels at a low, physiologically relevant shear stress (e.g., ~0.5 - 4 dyn/cm²). Culture for several days to allow a confluent, functional barrier to form.
- Application of Mechanical Strain: Connect the side chambers of the device to a cyclic vacuum source. Apply a vacuum with a frequency and amplitude that mimics normal human breathing (e.g., 10-15% strain, 0.2 Hz). This is a critical step for inducing a mature, in vivo-like phenotype [82].
- Model Validation: Before experiments, validate the model by:
- Measuring TEER regularly until a high, stable value is achieved (>1000 Ω·cm² is often indicative of a strong barrier).
- Confirming the presence of tight junction proteins (e.g., ZO-1) via immunofluorescence.
- Verifying the polarized secretion of biomarkers.
- Dosing and Analysis: Introduce the test agent to the appropriate channel (e.g., pathogens to the alveolar channel, circulating immune cells or drugs to the vascular channel). Monitor the system and harvest for endpoint analyses as required by the experimental design.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Advanced Preclinical Models
| Reagent / Solution | Function / Application | Technical Notes |
|---|---|---|
| Primary Human Cells (iPSCs, Organoids) | Provides human-relevant, patient-specific cellular material for OOCs and humanized models [82] [84] [88]. | Critical to source from high-quality, validated banks. Quality control for viability, identity, and absence of contamination is essential [83]. |
| Tissue-Specific Extracellular Matrix (ECM) | Scaffold for 3D tissue formation; provides biochemical and biophysical cues for cell differentiation and organization (e.g., Matrigel, fibrin, decellularized tissue matrices) [84]. | Different tissues require specific ECM compositions. For muscle, fibrin is often used; for bone, mineralized matrix is preferred [84]. |
| Fab-Oligonucleotide Conjugates (e.g., FORCE Platform) | Enables targeted delivery of oligonucleotide therapeutics to hard-to-transfect tissues like muscle via receptor-mediated uptake (e.g., targeting TfR1) [89]. | Comprises an anti-TfR1 Fab fragment conjugated to an ASO via a cleavable valine-citrulline linker [89]. |
| Human Cytokine Kits | Supports the expansion and function of human immune cells in humanized mouse models or immune-competent OOCs [82]. | Required to maintain human hematopoietic stem cells and progenitors in vivo. |
| Validated Antibody Panels for Flow Cytometry | Characterizes and quantifies human immune cell populations (e.g., CD45+, CD3+, CD19+) in humanized mouse models or perfusate from OOCs. | Cross-reactivity with mouse antigens must be checked for in vivo models. |
| Real-time Metabolic & Barrier Integrity Sensors | Non-invasive, continuous monitoring of tissue health and function in OOCs (e.g., TEER electrodes, metabolite sensors) [82]. | Integrated sensors provide higher-fidelity data than endpoint assays alone. |
Frequently Asked Questions (FAQs)
General PBPK Concepts
What is the fundamental difference between a PBPK model and a classical compartmental PK model?
Classical pharmacokinetic (PK) models use abstract compartments described by rate constants, and their parameters generally lack direct physiological meaning. In contrast, Physiologically Based Pharmacokinetic (PBPK) models consist of compartments that correspond to specific organs and tissues in the body, which are interconnected by the circulating blood system. These models are parameterized using known, species-specific physiological data (e.g., tissue volumes, blood flow rates) and drug-specific properties (e.g., lipophilicity, protein binding). This mechanistic structure allows PBPK models to predict drug concentration-time profiles not only in plasma but also at specific sites of action by simulating the processes of absorption, distribution, metabolism, and excretion (ADME) [90].
When should I consider using a PBPK modeling approach in drug development?
PBPK modeling is particularly valuable in scenarios where clinical trials are challenging, unethical, or impractical. Key application areas include:
- Predicting Drug-Drug Interactions (DDIs): Assessing the risk and magnitude of interactions mediated by metabolizing enzymes or drug transporters [91] [90].
- Extrapolation to Special Populations: Predicting pharmacokinetics in populations like pediatric patients [91] [92] [93], pregnant women [91] [94], or patients with renal or hepatic impairment [91], where physiological parameters differ from healthy adults.
- Formulation and Bioavailability Assessment: Evaluating the impact of different drug formulations on absorption [91] [92].
- Bridging Studies: Translating knowledge from healthy volunteers to patient populations or from adults to children [95].
Model Building & Workflow
What are the essential data requirements for building a new PBPK model?
Building a PBPK model requires two main categories of input parameters, which are often compiled in commercial software platforms [96] [92].
Table 1: Essential Input Parameters for PBPK Model Development
| Parameter Category | Specific Parameters | Source |
|---|---|---|
| System-Dependent (Physiological) | Tissue volumes, blood flow rates, organ composition, expression levels of enzymes/transporters | Literature compilations; built into PBPK software platforms [96] [92] [90] |
| Drug-Dependent | Molecular weight, pKa, lipophilicity (logP), solubility, permeability, plasma protein binding, blood-to-plasma ratio, in vitro metabolism data (e.g., intrinsic clearance) | In vitro assays; in silico predictions [96] [92] |
What is the difference between "bottom-up" and "middle-out" modeling strategies?
The "bottom-up" approach is the initial model construction phase. It relies purely on compound-specific parameters generated from in vitro assays to predict an in vivo PK profile. This approach is common during early drug discovery [96]. The "middle-out" strategy is used to refine and update the initial model once preclinical or clinical in vivo data become available. This hybrid approach uses the experimental data to calibrate the model, improving its predictive performance for prospective simulations of unstudied scenarios [96].
Troubleshooting Common Model Issues
My model simulations do not match the observed clinical data. What could be the reason?
Discrepancies between simulations and observations are key learning opportunities. Potential causes include:
- Incorrect System Parameters: The physiological parameters for the target population (e.g., a specific disease state) may not be accurately represented. Pathophysiological changes in organ function, blood flow, or protein levels might be missing from the model [95].
- Incomplete ADME Processes: The model may be missing key active processes such as transport by specific uptake or efflux transporters, or metabolism by extrahepatic enzymes [92] [90].
- Inaccurate Drug-Specific Parameters: Critical physicochemical or biochemical parameters (e.g., fraction unbound, intrinsic clearance) may be incorrect or derived from unreliable assays [92].
- Structural Model Mis-specification: The assumption of perfusion-rate-limited distribution may be invalid for your drug, requiring a shift to a permeability-rate-limited model that accounts for membrane permeation [96] [90].
How can I improve the predictive power of my model for a specific patient subpopulation?
To enhance predictions for special populations:
- Incorporate Population-Specific Physiology: Integrate quantitative data on physiological changes, such as altered organ sizes, blood flows, or enzyme ontogeny/maturation in pediatrics [93] [94].
- Utilize Bayesian Feedback: Employ Bayesian population PBPK analyses to extract knowledge about physiological and physicochemical parameters from clinical study data. This allows you to quantify interindividual variability and update the model with population-specific parameter distributions [95].
- Extend the Model Structure: For some populations, like pregnant women, a structural extension of the standard model is necessary to include new compartments (e.g., placenta, fetus) [94].
What are the common pitfalls in predicting drug-drug interactions and how can I avoid them?
Common pitfalls include overlooking the contribution of transporters to DDIs and inaccurate estimation of enzyme inhibition/induction parameters. To improve DDI predictions:
- Ensure comprehensive in vitro reaction phenotyping to identify all relevant enzymes and transporters involved in the drug's disposition [96].
- Use robust in vitro data for inhibition constants (Ki, IC50) and induction parameters (Emax, EC50), and apply appropriate scaling factors for in vitro to in vivo extrapolation (IVIVE) [96] [90].
- Validate the model against clinical DDI data for probe substrates and inhibitors whenever possible [91].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Software and Knowledge Resources for PBPK Modeling
| Tool / Resource | Type | Primary Function / Application |
|---|---|---|
| GastroPlus (Simulations Plus) | Software Platform | A comprehensive simulation software for PBPK modeling, absorption, and formulation development [96] [90]. |
| Simcyp Simulator (Certara) | Software Platform | A population-based PBPK simulator widely used for predicting DDIs, and PK in special populations [96] [90]. |
| PK-Sim (Open Systems Pharmacology) | Software Platform | A software tool for whole-body PBPK modeling; often used with MoBi for multiscale and systems pharmacology models [92] [90] [93]. |
| MoBi (Open Systems Pharmacology) | Software Tool | Used to access, manipulate, and extend PK-Sim models, enabling nonparametric extrapolations (e.g., adding a placenta) [92] [94]. |
| Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines | Knowledge Base | Freely available, peer-reviewed guidelines for translating genetic test results into actionable prescribing decisions for specific drug–gene pairs [97]. |
| PharmGKB | Knowledge Base | A curated resource that provides information about the impact of human genetic variation on drug response, including CPIC guidelines [97]. |
Experimental Protocols & Workflows
Protocol 1: Workflow for Building and Qualifying a Base PBPK Model
This protocol outlines the steps for developing a PBPK model using a "middle-out" approach [96] [92].
Objective: To construct a robust PBPK model capable of accurately simulating plasma and tissue concentration-time profiles.
Procedure:
- Data Collection: Gather all necessary system-dependent and drug-dependent parameters as listed in Table 1.
- Model Construction:
- Select an appropriate PBPK software platform and input the collected parameters.
- Define the model structure, typically starting with a perfusion-rate-limited assumption for all tissues unless evidence suggests otherwise.
- Verification in Preclinical Species:
- First, verify the model's prediction of intravenous disposition in a preclinical species (e.g., rat) [96].
- Then, verify the prediction of oral absorption over a range of doses in the same species. This step helps assess the accuracy of distribution and absorption predictions.
- Simulation in Humans: Use the appropriate clearance and distribution methods (selected based on the preclinical verification) to simulate disposition and absorption in humans.
- Model Refinement and Qualification:
- Once clinical data are available, compare the simulations against the observed data.
- Refine the model by adjusting uncertain parameters within physiologically plausible ranges to improve the fit (middle-out approach).
- Qualify the final model by demonstrating its ability to predict data from a different clinical study (e.g., a different dosing regimen) that was not used for model building.
The following diagram illustrates this iterative workflow:
Protocol 2: Protocol for a Bayesian PBPK Analysis to Enable Cross-Population Translation
This protocol is based on a translational systems pharmacology workflow designed to learn and transfer pathophysiological knowledge across patient populations [95].
Objective: To identify pathophysiological alterations in a patient cohort and use this knowledge to predict the pharmacokinetics of a new drug in that population.
Procedure:
- Clinical Study Design: Conduct a clinical study where both a healthy volunteer cohort and the target patient cohort receive a cocktail of probe drugs. The cocktail should include a well-characterized reference probe drug (e.g., midazolam) and the candidate drug of interest (e.g., torsemide) [95].
- Learning Step 1 (Reference in Healthy): Perform a Bayesian PBPK analysis using PK data of the reference drug from a subset of the healthy volunteers. This step acquires knowledge about the baseline physiological parameters.
- Learning Step 2 (Candidate in Healthy): Refine the physiological knowledge and identify the drug-specific parameters for the candidate drug using its PK data from the same subset of healthy volunteers.
- Learning Step 3 (Reference in Patients): Using the known drug parameters for the reference drug, perform a Bayesian PBPK analysis with its PK data from a subset of the patient cohort. This step identifies the specific pathophysiological changes (e.g., in organ function or blood flow) in the patient population.
- Prediction Step (Candidate in Patients): Combine the acquired knowledge of the candidate drug's physicochemistry (from Step 2) with the identified pathophysiology of the patient cohort (from Step 3) to perform a de novo prediction of the candidate drug's population PK in the entire patient cohort.
The logical flow of this knowledge-translation approach is shown below:
Technical Support Center: Regenerative Pharmacology
Frequently Asked Questions (FAQs)
FAQ 1: What is the core mission of a regenerative pharmacology research consortium? The core mission is to bridge the gap between experimental discoveries and clinical applications by fostering interdisciplinary collaboration. These consortia aim to develop curative therapeutic principles that restore the physiological structure and function of damaged tissues, moving beyond merely managing symptoms. This requires integrating diverse fields like pharmacology, biomaterials, stem cell biology, and clinical medicine to accelerate the translation of regenerative therapies [1] [2] [98].
FAQ 2: What are the most significant translational barriers faced by research consortia? Consortia often face multiple, interconnected translational barriers. These can be systematized as:
- Investigational: Unrepresentative preclinical models that fail to recapitulate human clinical conditions, leading to uncertainties about long-term safety and efficacy and poorly defined mechanisms of action (MoA) [1].
- Manufacturing: Challenges in scaling up and automating production under Good Manufacturing Practice (GMP) standards to ensure consistent, high-quality advanced therapy medicinal products (ATMPs) [1].
- Regulatory: Navigating complex and often non-unified regulatory pathways across different regions (e.g., EMA and FDA) [1].
- Economic: High manufacturing costs for ATMPs, which can limit accessibility and complicate reimbursement strategies, especially in low- and middle-income countries [1].
FAQ 3: How can our consortium improve interdisciplinary communication and collaboration? Effective collaboration in large, multidisciplinary teams requires intentional investment in coordination. Key recommendations include:
- Dedicate Time for Team Building: Factor in significantly more time than expected for developing shared understandings and uniting different worldviews [99].
- Invest in Coordination: Employ sophisticated project management and clear, high-quality communications to manage the increasing lines of communication as the team grows [99].
- Foster Psychological Safety: Create an environment that enables open, constructive communication and the constructive resolution of tension, supported by flexibility and senior leadership championing [99].
FAQ 4: What funding strategies are effective for sustaining long-term consortium goals? Seek out and work closely with funders who understand the unique nature of large, mission-oriented, interdisciplinary research. It is crucial to establish shared expectations regarding deliverables, timelines, and resource use, which often differ from traditional, single-discipline research projects. Building contingency and resources for team cohesion into funding applications is also critical [99].
FAQ 5: What role do pharmacological challenge models play in translational research? Pharmacological challenge models are vital for establishing 'proof of pharmacology' in early-phase drug development, especially when testing compounds in healthy volunteers where the disease is absent. These models create temporary, well-controlled physiological or pathophysiological conditions that mimic a disease state, allowing researchers to screen compound activity, determine appropriate dosing, and inform decisions before moving to phase II studies in the target patient population [100].
Troubleshooting Guides for Common Experimental Challenges
Challenge 1: Inconsistent or Poor Functional Outcomes in Bioengineered Tissues
- Problem: Engineered tissues fail to mature or function adequately in vitro or after implantation.
- Solution & Methodology:
- Implement Bioreactor Conditioning: Utilize bioreactor systems that apply physiologically relevant environmental cues (e.g., stretch, flow, compression) to guide tissue development and functional maturation [2].
- Incorporate Pharmacological Cues: Develop "smart" biomaterial scaffolds that act as reservoirs for the sustained and controlled release of multiple bioactive compounds (e.g., growth factors like FGF, VEGF, BMPs) to actively orchestrate the regenerative process [1] [2].
- Preclinical Pharmacological Characterization: Rigorously assess tissue phenotype and function using a combination of in vitro (e.g., contractility, protein secretion), ex vivo (e.g., tissue bath studies), and in vivo models that recapitulate human clinical conditions [2].
Challenge 2: Low Efficiency in Stem/Progenitor Cell Expansion or Differentiation
- Problem: Inability to reliably produce sufficient quantities of the desired, functionally mature cell type.
- Solution & Methodology:
- High-Throughput Screening (HTS): Employ HTS robots to screen large libraries of small molecules and growth factors to identify novel compounds that modulate stem cell expansion and differentiation [2] [101].
- Optimize Culture Systems: Systemically refine cell culture media and protocols. This includes using high-quality recombinant proteins and adjusting media formulations to create a custom environment tailored to specific cell types [102].
- Apply Systems Biology: Use transcriptomic (e.g., RNA-sequencing) and proteomic analyses to monitor global changes during differentiation and identify key pathways and biomarkers for quality control [1].
Challenge 3: Poor Targeted Delivery and Off-Target Effects of Bioactive Compounds
- Problem: Therapeutic molecules do not reach the intended site of action in effective concentrations or cause adverse effects elsewhere.
- Solution & Methodology:
- Develop Advanced Drug Delivery Systems (DDS): Fabricate biomaterial-based DDS such as nanoparticles, hydrogels, and scaffold-based systems using natural (e.g., alginate, chitosan) or synthetic polymers. These systems provide mechanical support and enable sustained, localized release, enhancing therapeutic efficiency and reducing systemic side effects [1] [10].
- Functionalize DDS: Employ strategies to functionalize DDS with targeting moieties (e.g., antibodies, peptides) to improve site-specific delivery [10].
- Incorporate Imaging Capabilities: Combine DDS with imaging agents to allow for real-time, non-invasive monitoring of drug release and the regeneration process [1].
Challenge 4: Difficulty in Defining Mechanism of Action (MoA) for Complex Therapies
- Problem: The MoA for regenerative therapies, such as stem cell-derived products, is poorly understood, hindering regulatory approval.
- Solution & Methodology:
- Leverage Omics Technologies: Apply genomics, proteomics, and metabolomics to create a global picture of cell function and response to therapy. This helps identify candidate genes and pathways relevant to the therapeutic MoA [1] [101].
- Utilize AI and Data-Driven Approaches: Apply artificial intelligence (AI) to analyze complex, multi-omics datasets to predict therapeutic outcomes, DDS effectiveness, and cellular responses, thereby uncovering patterns that define the MoA [1].
- Employ Genetic/ Molecular Techniques: Use techniques like gene expression profiling and genome-wide association studies (GWAS) to link genetic variations and expression changes to treatment efficacy [101].
Table 1: Quantitative Analysis of Translational Barriers in Regenerative Pharmacology
| Barrier Category | Specific Challenge | Impact Level (Reported Frequency) | Potential Mitigation Strategy |
|---|---|---|---|
| Investigational | Unrepresentative preclinical models | High [1] | Use of humanized models & organ-on-a-chip technologies |
| Poorly defined MoA | High [1] | Systems biology & AI-driven target discovery | |
| Manufacturing | Scalability & automation | High [1] | Investment in closed, automated bioprocess systems |
| High cost of ATMPs | High [1] | Development of affordable biomaterials & processes | |
| Regulatory | Lack of unified international guidelines | Medium-High [1] | Early and frequent engagement with regulatory agencies |
| Economic | Reimbursement challenges | Medium-High [1] | Demonstrating long-term cost-effectiveness & value |
| Collaborative | Interdisciplinary communication breakdown | Variable [99] | Dedicated coordination & project management |
Table 2: Key Pharmacological Challenge Models for Translational Research
| Challenge Model | Induced Condition | Mode of Action | Key Readouts & Measurements | Translational Utility |
|---|---|---|---|---|
| Imiquimod | Skin Inflammation (Psoriasis-like) | TLR7/8 agonist, induces IFN and cytokine production [100] | Erythema (colorimetry, visual grading), gene expression (CXCL10, IL-6, TNF-α) [100] | Screening anti-inflammatory drugs for psoriatic diseases |
| UV-B Irradiation | Inflammation, Pain, Erythema | Upregulates PI3K/AKT/mTOR pathway [100] | Skin pigmentation, pain assessment, inflammation biomarkers [100] | Testing photoprotective and anti-inflammatory agents |
| Histamine | Itch | Agonist at H1-H4 receptors, activates CMIA fibers [100] | Itch intensity (VAS), wheal and flare response [100] | Evaluating antipruritic drugs |
| KLH Challenge | Delayed-Type Hypersensitivity | Neo-antigen inducing adaptive immune response [100] | Local inflammation, systemic antibody titers [100] | Assessing immunomodulatory and vaccine candidates |
Detailed Experimental Protocols
Protocol 1: Imiquimod-Induced Skin Inflammation Model for Preclinical Screening
- Objective: To create a controlled, localized skin inflammation for testing the efficacy of topical or systemic anti-inflammatory compounds.
- Materials: Imiquimod cream (e.g., 5% Aldara), occlusion patches, tape-stripping materials, ethanol for cleaning, erythema colorimeter/Laser Speckle Contrast Imaging (LSCI) setup, biopsy punches, RNA extraction kit, qPCR reagents.
- Methodology:
- Subject Selection & Skin Preparation: Healthy volunteers or animal models are recruited with ethical approval. Test sites on the lower back or forearm are cleaned. To enhance response, the skin barrier can be compromised via tape-stripping (e.g., 20-30 strips with adhesive tape until the skin surface appears shiny) [100].
- Application of Imiquimod: A defined dose of imiquimod cream (e.g., 10-100 mg) is applied topically under occlusion. A control site should be treated with a vehicle cream.
- Dosing Regimen: The application is typically repeated once daily for 2 to 7 days, depending on the desired inflammation intensity [100].
- Efficacy Monitoring:
- Clinical Assessment: Erythema is monitored daily using erythema colorimetry, visual grading scales, and LSCI to measure blood perfusion [100].
- Molecular Analysis: After the final application, punch biopsies (e.g., 4mm) are collected from treated and control sites. RNA is extracted and analyzed via qPCR for pro-inflammatory markers (e.g., TNF-α, IL-1β, IL-6, CXCL10) [100].
- Drug Testing: The test compound is applied either prophylactically or therapeutically alongside the imiquimod challenge. Its efficacy is determined by a significant reduction in clinical and molecular readouts compared to the vehicle-treated, imiquimod-challenged control.
Protocol 2: Fabrication of a Drug-Loaded Hydrogel for Sustained Release
- Objective: To create a biomaterial-based drug delivery system for the localized and sustained release of a growth factor (e.g., VEGF) to enhance nerve regeneration.
- Materials: Natural polymers (Chitosan, Alginate) or synthetic polymers (PEG, PLGA), cross-linker (e.g., Calcium Chloride for alginate), recombinant VEGF, dialysis tubing or release apparatus, PBS, ELISA kit for VEGF.
- Methodology:
- Polymer Solution Preparation: Dissolve the chosen polymer (e.g., 2% w/v alginate) in sterile, deionized water under gentle stirring.
- Drug Loading: Add the recombinant VEGF to the polymer solution and mix thoroughly to ensure homogeneous distribution.
- Cross-linking & Hydrogel Formation: For ionic cross-linking, extrude the polymer-drug solution dropwise into a gently stirred calcium chloride solution (e.g., 100mM). Alternatively, use UV light or thermal methods for other polymers. The formed hydrogel beads or constructs are cured for a set time.
- Washing: Rinse the hydrogel constructs with PBS to remove unencapsulated drug and residual cross-linker.
- In Vitro Release Study:
- Place the loaded hydrogel in a tube with a known volume of release medium (PBS, pH 7.4, at 37°C under gentle agitation).
- At predetermined time points (e.g., 1, 3, 6, 24, 48 hours, etc.), collect a sample of the release medium and replace it with fresh pre-warmed medium.
- Analyze the collected samples using an ELISA kit to quantify the released VEGF concentration.
- Plot the cumulative release over time to characterize the release profile (e.g., burst release vs. sustained release) [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Regenerative Pharmacology Experiments
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Recombinant Proteins (e.g., FGF, VEGF, BMPs) | Modulate stem cell expansion, differentiation, and tissue maturation; used in screening and as therapeutic agents in DDS [2]. | Bioactivity, species specificity, carrier protein presence, endotoxin levels. Custom production and labeling services are available [102]. |
| "Smart" Biomaterials (e.g., Alginate, Chitosan, PEG, PLGA) | Serve as scaffolds for 3D tissue growth and as reservoirs for controlled drug delivery in nanoparticles, hydrogels, and other systems [1] [10]. | Biocompatibility, degradation rate, mechanical properties, ease of functionalization. |
| Stem/Progenitor Cells | The "raw material" for cell therapies and for building bioengineered tissues; sources include cord blood, iPSCs, and tissue-specific progenitors [2] [103]. | Purity, potency, viability, ethical sourcing, and GMP-compliant derivation and expansion. |
| High-Throughput Screening (HTS) Platforms | Enable rapid testing of thousands of small molecules or growth factors for their effects on cell behavior (e.g., differentiation) [2] [101]. | Automation, assay miniaturization, robust data analysis pipelines. |
| Pharmacological Challenge Agents (e.g., Imiquimod, KLH) | Used in translational models to induce disease-like states in healthy volunteers or animals for proof-of-pharmacology studies [100]. | Selectivity for the target pathway, reproducibility of the induced phenotype, safety profile. |
Visual Workflows and Pathways
Research Consortia Success Pathway
Imiquimod Skin Inflammation Workflow
Conclusion
Overcoming translational barriers in regenerative pharmacology demands a fundamental shift from isolated innovation to integrated, systems-level collaboration. The path forward is clear: success hinges on the synergistic application of computational intelligence, engineered biomaterials, and standardized, scalable manufacturing. Future progress will be defined by our ability to generate predictive preclinical data, design agile clinical trials, and establish regulatory pathways that encourage innovation while ensuring safety. By embracing this holistic and collaborative approach, the field can finally bridge the translational gap, delivering on the long-held promise of regenerative medicine to provide curative, personalized therapies for a host of debilitating diseases. The call to action is for academia, industry, and regulators to co-create an ecosystem where regeneration is not just possible, but predictably and efficiently delivered to patients.
References
- 1. Frontiers | Unifying pharmacology , systems biology, and ... regenerative [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1729610/full]
- 2. The Pharmacology of Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3698935/]
- 3. Editorial: Methods and application in integrative ... and regenerative [https://pmc.ncbi.nlm.nih.gov/articles/PMC9732651/]
- 4. Clinical translation of neuro- regenerative medicine in India: A study... [https://www.scirp.org/journal/paperinformation?paperid=32109]
- 5. The pharmacological strategy of regenerative medicine | SpringerLink [https://link.springer.com/article/10.1134/S1019331616030151]
- 6. Computational Approaches to Drug Repurposing and Pharmacology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4845762/]
- 7. Translational Pharmacology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5243817/]
- 8. Lost in translation: the valley of death across preclinical and clinical divide – identification of problems and overcoming obstacles | Translational Medicine Communications | Full Text [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 9. Troubleshooting pharmacological and toxicological methods - PubMed [https://pubmed.ncbi.nlm.nih.gov/20184960/]
- 10. Drug-delivery strategies using biomaterials in the field of nerve... [https://pubmed.ncbi.nlm.nih.gov/40536924/]
- 11. strategies and Translational in challenges medicine regenerative [https://www.nature.com/articles/nm.3627?error=cookies_not_supported&code=ec76ef7b-6306-43ed-ada6-ca38c0648bce]
- 12. Troubleshooting Protocols - Biological Sciences: Summer Research Institute (SRI) - CMU LibGuides at Carnegie Mellon University [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 13. How to be a Better Troubleshooter in Your Laboratory | GoldBio [https://goldbio.com/articles/article/how-to-be-a-better-troubleshooter]
- 14. A Blueprint for Translational Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7610850/]
- 15. Navigating Regulatory in Drug Development Hurdles [https://blog.drugbank.com/navigating-regulatory-hurdles-in-drug-development/]
- 16. Overcoming Medical Device Manufacturing Challenges Regulatory [https://tessy.com/news-events/navigating-regulatory-hurdles-in-medical-device-manufacturing/]
- 17. and Opportunities in Biopharma Regulatory Hurdles Manufacturing [https://www.ainvest.com/news/regulatory-hurdles-opportunities-biopharma-manufacturing-2510/]
- 18. Advancing burn wound therapy: Synergistic innovations in... [https://pubmed.ncbi.nlm.nih.gov/40749424/]
- 19. Troubleshooting the Research Process | Office of Undergraduate Research [https://ugradresearch.uconn.edu/2017/09/28/troubleshooting-the-research-process/]
- 20. Overcoming the Blood–Brain Barrier: Advanced Strategies in Targeted Drug Delivery for Neurodegenerative Diseases | MDPI [https://www.mdpi.com/1999-4923/17/8/1041]
- 21. Overcoming the Blood-Brain Barrier: Advanced Strategies in Targeted Drug Delivery for Neurodegenerative Diseases - PubMed [https://pubmed.ncbi.nlm.nih.gov/40871062/]
- 22. Frontiers | Neurotherapeutics across blood–brain barrier : screening of... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1616144/full]
- 23. Breaking Down Barriers : Innovative Approaches for Streamlining... [https://acrpnet.org/2025/04/08/breaking-down-barriers-innovative-approaches-for-streamlining-access-to-rare-disease-therapies]
- 24. Medicine Therapies for Regenerative Rare Diseases [https://pubmed.ncbi.nlm.nih.gov/30613470/]
- 25. AI Troubleshooting Guide [https://www.rapidinnovation.io/post/ai-agents-for-technical-troubleshooting]
- 26. Deep learning in drug : an integrative review and future... discovery [https://link.springer.com/article/10.1007/s10462-022-10306-1]
- 27. Preventing Data Pitfalls in AI | LabKey Drug Discovery [https://www.labkey.com/ai-drug-discovery-pitfalls/]
- 28. Best Practices for AI and ML in Drug and Development Discovery [https://clarivate.com/life-sciences-healthcare/blog/best-practices-for-ai-and-ml-use-across-the-drug-discovery-and-development-lifecycle/]
- 29. Unraveling complexities of AI in drug with Verseon's CEO discovery [https://www.drugdiscoverytrends.com/ai-in-drug-discovery-analysis/]
- 30. Assays Support— Drug Discovery Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 31. Fixing drug ’s most persistent problem with discovery AI [https://www.drugtargetreview.com/article/168391/fixing-drug-discoverys-most-persistent-problem-with-ai/]
- 32. Top 10 AI Platforms in 2025... - DevOpsSchool.com Drug Discovery [https://www.devopsschool.com/blog/top-10-ai-drug-discovery-platforms-in-2025-features-pros-cons-comparison/]
- 33. Frontiers | 3D/4D Bioprinting and Smart for Scaffolds ... Regenerative [https://www.frontiersin.org/research-topics/74686/3d4d-bioprinting-and-smart-scaffolds-for-regenerative-medicine]
- 34. strategies and Translational in challenges medicine regenerative [https://www.nature.com/articles/nm.3627?error=cookies_not_supported&code=11e42278-1a67-4220-9022-2ecd2bb6df07]
- 35. Growth Factors and Cytokines for Regenerative Medicine... [https://link.springer.com/article/10.1007/s40883-025-00458-1]
- 36. Are there specific translational in challenges medicine? regenerative [https://pubmed.ncbi.nlm.nih.gov/26541074/]
- 37. Tailoring biomaterials for vaccine delivery | Journal of... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02758-0]
- 38. Programmable biomaterials for dynamic and responsive drug delivery [https://pubmed.ncbi.nlm.nih.gov/27190245/]
- 39. Applications of multi‐omics analysis in human diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10390758/]
- 40. A guide to multi - omics data collection and integration for translational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9747357/]
- 41. Frontiers | State of the Field in Multi-Omics Research: From Computational Needs to Data Mining and Sharing [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.610798/full]
- 42. Unraveling the complexity: understanding the deconvolutions of RNA-seq data | Translational Medicine Communications | Full Text [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-023-00154-8]
- 43. Cellular deconvolution - Wikipedia [https://en.wikipedia.org/wiki/Cellular_deconvolution]
- 44. - Multi sets the path for early prevention strategies on... omic integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049560/]
- 45. Enabling allogeneic therapies: CIRM-funded strategies for immune... [https://pubmed.ncbi.nlm.nih.gov/32585084/]
- 46. Frontiers | Engineering strategies to safely drive CAR T- cells into the... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1411393/full]
- 47. The Role of Cell Plasticity in Tissue Repair: Adaptive Cellular Reprogramming - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1534580715005857]
- 48. Unraveling the Molecular Basis for Regenerative Cellular Plasticity | PLOS Biology [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.0020232]
- 49. Primary Cell Culture Support—Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/primary-cell-culture-support/primary-cell-culture-support-troubleshooting.html]
- 50. : translating the expertise into a ATMPs process | QbD Group GMP [https://www.qbdgroup.com/en/blog/atmps-translating-the-expertise-into-a-gmp-process]
- 51. What is GMP | Good Manufacturing Practices | SafetyCulture [https://safetyculture.com/topics/gmp]
- 52. Good manufacturing practice - Wikipedia [https://en.wikipedia.org/wiki/Good_manufacturing_practice]
- 53. guidelines for GMP : A practical guide to... ATMP manufacturing [https://www.crbgroup.com/insights/biotechnology/gmp-guidelines-for-atmp-manufacturing]
- 54. Transforming ATMP Safety with Real-Time PCR | Lab Manager [https://www.labmanager.com/a-quicker-way-to-validate-the-quality-of-atmps-31100]
- 55. process and analytical tool changes in an approved... Troubleshooting [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3378/Troubleshooting-process-and-analytical-tool-changes-in-an-approved-ATMP-process]
- 56. Improving the safety of human pluripotent using... stem cell therapies [https://www.nature.com/articles/s41467-020-16455-7?error=cookies_not_supported&code=2143a08f-960b-4fe3-99d5-ba7e70e2c032]
- 57. Improving the safety of human pluripotent using... stem cell therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC7264334/]
- 58. Troubleshooting Guide for Human Pluripotent Stem Cell Culture | STEMCELL Technologies [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 59. CRISPR 101: Off-Target Effects [https://blog.addgene.org/crispr-101-off-target-effects]
- 60. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 61. Possible Strategies to Reduce the Tumorigenic Risk of Reprogrammed... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11120835/]
- 62. The Challenges to Advancing Induced Pluripotent Stem Cell-Dependent Cell Replacement Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 63. ’s New EMA to Reshape the Regulations Market | Global Gr ATMP [https://www.linkedin.com/pulse/emas-new-regulations-reshape-atmp-market-global-18-cagr-md-nasiruddin-w6fdf]
- 64. Navigating the ATMP LandscapeNavigating the... - Evotec Regulatory [https://www.evotec.com/en/sciencepool/navigating-the-atmp-regulatory-landscape?trk=article-ssr-frontend-pulse_little-text-block]
- 65. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect: On The Verge Of Convergence? [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 66. 5 CAR T Cell With Autoimmune Readouts in Therapies - BioSpace 2025 [https://www.biospace.com/drug-development/5-car-t-cell-therapies-with-autoimmune-readouts-in-2025]
- 67. Targeted delivery of the GPX4 activator via HUCMSC-derived exosomes inhibits ferroptosis in spinal cord injury | Journal of Nanobiotechnology | Full Text [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03755-7]
- 68. An Industry‐Driven Roadmap for Manufacturing in Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6090514/]
- 69. Manufacturing Road Map for Tissue Engineering and Regenerative Medicine Technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4303363/]
- 70. How to Lower Manufacturing Costs: A Comprehensive Guide - Prince Manufacturing [https://princemanufacturing.com/how-to-lower-manufacturing-costs-a-comprehensive-guide/]
- 71. 6 Effective -Reduction Cost for Strategies 2025 Manufacturers [https://www.invensis.net/blog/cost-reduction-strategies-for-manufacturing-companies]
- 72. Cost Efficiency in Manufacturing [https://novalinkmx.com/2024/10/24/cost-efficiency-in-manufacturing/]
- 73. 17 Manufacturing Cost Management Best Practices | NetSuite [https://www.netsuite.com/portal/resource/articles/accounting/manufacturing-cost-management.shtml]
- 74. Frontiers | Brief summary of the regulatory frameworks of regenerative medicine therapies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1486812/full]
- 75. FDA Facts: Biomarkers and Surrogate Endpoints | FDA [https://www.fda.gov/about-fda/innovation-fda/fda-facts-biomarkers-and-surrogate-endpoints]
- 76. Clinical Trial Design Software - Create Safer, Effective Trials [https://www.medidata.com/en/clinical-trial-products/medidata-ai/real-world-data/clinical-trial-design-software/]
- 77. Clinical Trial Simulation - DAC Best Practices [https://dac-trials.org/resources/clinical-trial-simulation/]
- 78. Frontiers | Unifying pharmacology, systems biology, and regenerative medicine to advance personalized therapies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1729610/abstract]
- 79. Trial Design [https://www.trialdesign.org/]
- 80. and surrogate Biomarkers : how and when might they... endpoints [https://pubmed.ncbi.nlm.nih.gov/12364814/]
- 81. Advances in Drug Delivery Integrated with Regenerative Medicine: Innovations, Challenges, and Future Frontiers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030587/]
- 82. Human organ for chips - PMC regenerative pharmacology [https://pmc.ncbi.nlm.nih.gov/articles/PMC10751726/]
- 83. Human Organ-On-A-Chip: Technologies Offer Benefits Over Animal Testing but Challenges Limit Wider Adoption | U.S. GAO [https://www.gao.gov/products/gao-25-107335]
- 84. Organs on a chip models for biological research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8417425/]
- 85. Driving Translational Success: A Strategic Analysis of C3 and... [https://www.linkedin.com/pulse/driving-translational-success-strategic-analysis-c3-mlh6c]
- 86. Translational research: Bridging the gap between preclinical and clinical research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10043823/]
- 87. Bridging the Gap: Translating Preclinical Biomarkers to Clinical Success [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 88. Frontiers | Editorial: Latest advancements in organ - on -a- chip technology [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1631320/full]
- 89. FORCE platform overcomes of oligonucleotide delivery to... barriers [https://pmc.ncbi.nlm.nih.gov/articles/PMC11742727/]
- 90. Basic Concepts in Physiologically Based Pharmacokinetic Modeling in Drug Discovery and Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3828005/]
- 91. Applications, Challenges , and Outlook for PBPK and... Modeling [https://pubmed.ncbi.nlm.nih.gov/35552967/]
- 92. Applied Concepts in PBPK Modeling: How to Build a PBPK/PD Model - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5080648/]
- 93. Frontiers | Physiologically Based Pharmacokinetic Modeling of... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00868/full]
- 94. Applied Concepts in PBPK Modeling: How to Extend an Open Systems Pharmacology Model to the Special Population of Pregnant Women - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6063743/]
- 95. learning from clinical studies predicts drug... Translational [https://www.nature.com/articles/s41540-017-0012-5?error=cookies_not_supported]
- 96. modeling and simulation in drug research and development - PMC PBPK [https://pmc.ncbi.nlm.nih.gov/articles/PMC5125732/]
- 97. The Pharmacogenomics Research Network Translational Pharmacogenetics Program: Overcoming Challenges of Real-World Implementation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3720847/]
- 98. – A special interest group | MultiPark Regenerative pharmacology [https://www.multipark.lu.se/article/regenerative-pharmacology-special-interest-group?trk=article-ssr-frontend-pulse_little-text-block]
- 99. Six lessons for newly-forming large research – Integration... consortia [https://i2insights.org/2023/08/15/lessons-for-research-consortia/comment-page-1/]
- 100. Pharmacological Challenge Models in Clinical Drug Developmental Programs | IntechOpen [https://www.intechopen.com/chapters/66350]
- 101. Analytical and Experimental Pharmacology, Challenges Ahead - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3124228/]
- 102. Troubleshooting Guides [https://www.peprotech.com/en/troubleshooting-guides]
- 103. Regenerative Medicine [https://www.aabb.org/blood-biotherapies/biotherapies/facts-about-cellular-therapies/regenerative-medicine]