Cell Expansion Protocols: A Strategic Guide to Autologous vs. Allogeneic Approaches for Researchers
This article provides a comprehensive analysis of cell expansion protocols for autologous and allogeneic therapies, tailored for researchers, scientists, and drug development professionals.
Cell Expansion Protocols: A Strategic Guide to Autologous vs. Allogeneic Approaches for Researchers
Abstract
This article provides a comprehensive analysis of cell expansion protocols for autologous and allogeneic therapies, tailored for researchers, scientists, and drug development professionals. It covers foundational principles, from defining the core immunological and logistical differences between using a patient's own cells versus a donor's. The scope extends to detailed methodological workflows, critical troubleshooting strategies for manufacturing and scaling, and a direct comparative validation of safety, efficacy, and commercial viability. By synthesizing recent clinical advancements and current industry challenges, this guide aims to inform strategic decision-making in the development of advanced therapy medicinal products (ATMPs).
Core Concepts: Defining Autologous and Allogeneic Cell Sources and Their Fundamental Differences
The field of advanced therapies is fundamentally divided into two distinct manufacturing paradigms: patient-specific therapies and off-the-shelf therapies. This distinction is crucial for researchers and drug development professionals as it dictates every aspect of therapeutic development, from manufacturing strategy and supply chain logistics to clinical implementation and commercial viability. Patient-specific therapies (also referred to as autologous when using the patient's own cells) are customized for each individual patient, where material comes from one patient or donor, is processed, and is returned to the same patient (or a matched patient in the case of a donor source) [1]. In contrast, off-the-shelf therapies (often allogeneic, derived from healthy donors) are manufactured in large batches from a single donor source and can be administered to multiple patients, offering the advantage of immediate availability [1] [2].
The choice between these paradigms carries significant implications for manufacturing scalability, cost structure, and therapeutic application. For patient-specific therapies, scale-out is required to increase manufacturing capacity, where the patient-scale process must be efficiently repeated for each patient. For off-the-shelf therapies, scale-up is the key strategy, where a larger process that yields doses for many patients is developed to achieve economies of scale [1]. Understanding these fundamental differences is essential for designing appropriate expansion protocols and manufacturing systems for advanced therapeutic medicinal products (ATMPs).
Manufacturing Workflows and Economic Considerations
Comparative Manufacturing Processes
The manufacturing workflows for patient-specific versus off-the-shelf therapies differ significantly in their starting materials, production timelines, and quality control approaches. Patient-specific therapies begin with cell collection from an individual patient, typically via leukapheresis or tissue biopsy, followed by cell processing, genetic modification (if applicable), expansion, and final formulation before being returned to the same patient [2]. This process must be repeated for each individual patient, creating substantial logistical challenges including cold-chain maintenance, strict time constraints, and the critical need for end-to-end traceability and chain-of-identity [3].
Off-the-shelf therapies follow a fundamentally different manufacturing model. These therapies begin with cells from a qualified healthy donor, which are used to establish a master cell bank system [4]. Through a scaled-up manufacturing process, potentially using bioreactors and other large-scale culture technologies, a single manufacturing run can produce hundreds or even thousands of therapeutic doses [5] [2]. These doses can be cryopreserved and stored until needed, creating an inventory of available treatments. This approach significantly simplifies supply chain logistics and eliminates the waiting period between patient identification and treatment availability.
Economic and Scalability Analysis
The manufacturing cost structures for these two paradigms differ substantially, with significant implications for commercial viability and patient access. A detailed analysis of manufacturing costs reveals that patient-specific therapies incur considerably higher production expenses due to individualized processing and testing requirements.
Table: Comparative Manufacturing Cost Analysis for Cell Therapies
| Cost Component | Patient-Specific/Autologous Therapy | Off-the-Shelf/Allogeneic Therapy |
|---|---|---|
| Donor Screening & Testing | £990–1320 (US$1590–2110) per patient [4] | £10–20 (US$16–32) per dose (cost spread across many patients) [4] |
| Release Testing | £300–500 (US$480–800) per batch (each patient is a batch) [4] | £3–5 (US$4.8–8) per dose (batch yields ~100 doses) [4] |
| Total Manufacturing Cost per Dose | £2260–3040 (US$3630–4890) [4] | £930–1140 (US$1490–1830) [4] |
| Scalability Approach | Scale-out (repeating process for each patient) [1] | Scale-up (larger batches for multiple patients) [1] |
The economic advantage of off-the-shelf therapies is primarily driven by the ability to amortize donor screening and release testing costs across many treatment doses [4]. For patient-specific therapies, each patient requires their own donor screening and testing, and each patient's product constitutes an individual batch requiring separate release testing. This fundamental difference in manufacturing architecture makes off-the-shelf therapies potentially more economically sustainable for widespread clinical application, particularly for common conditions.
Clinical Applications and Efficacy Data
Therapeutic Performance Across Indications
Both patient-specific and off-the-shelf approaches have demonstrated clinical efficacy across various indications, though with different risk-benefit profiles and implementation challenges. In orthopedic applications, a 2025 study comparing patient-specific versus off-the-shelf unicompartmental knee arthroplasty (UKA) found that while patient-specific implants showed superior patient-reported outcomes (KOOS total score: 89 vs. 76, p=0.020), both groups demonstrated similar biomechanical function during gait analysis [6]. Notably, neither approach fully restored normal knee biomechanics compared to healthy controls, suggesting compensatory mechanisms at adjacent joints [6].
In oncology, autologous CAR-T therapies have demonstrated remarkable efficacy for hematological malignancies, with response rates of 35-40% in difficult-to-treat populations [2]. However, these patient-specific therapies face significant challenges including manufacturing failures in 2-10% of cases, time-consuming production processes (typically three weeks), and T-cell exhaustion in heavily pre-treated patients [2]. These limitations have driven the development of allogeneic, off-the-shelf alternatives that can be manufactured from healthy donor cells and made immediately available to patients.
Table: Clinical Comparison of Autologous vs. Allogeneic CAR-T Therapies
| Parameter | Autologous (Patient-Specific) CAR-T | Allogeneic (Off-the-Shelf) CAR-T |
|---|---|---|
| Source Cells | Patient's own T-cells [2] | Healthy donor PBMCs, umbilical cord blood, or iPSCs [2] |
| Manufacturing Time | ~3 weeks [2] | Pre-manufactured, available immediately [2] |
| Key Challenges | T-cell exhaustion, manufacturing failures (2-10%), time delays [2] | Graft-versus-host disease (GvHD), host-versus-graft rejection, limited persistence [2] |
| Manufacturing Failure Rate | 2-10% of cases [2] | Minimal (uses healthy donor cells) |
| Therapeutic Cost | ~$500,000 per dose [5] | Significantly lower (1% of autologous cost potential) [5] |
Recent clinical data for allogeneic approaches show promising results. In the phase 1 TRAVERSE trial for renal cell carcinoma, an allogeneic CAR-T product (ALLO-316) demonstrated a 25% confirmed objective response rate in heavily pre-treated patients, with no graft-versus-host disease reported [5]. Similarly, advances in CAR-NK cell therapies, which naturally have a lower risk of GvHD, are showing promise as off-the-shelf alternatives [5].
Manufacturing and Scalability Challenges
The manufacturing of both patient-specific and off-the-shelf therapies faces significant technical challenges that impact product quality, consistency, and scalability. For patient-specific therapies, the high variability of starting material from different patients represents a major hurdle. Cells from donors exhibit varying metabolic profiles and capabilities, yet current manufacturing processes often lack the adaptability to normalize these differences [3]. Additionally, maintaining consistent product quality while manufacturing individual batches for each patient requires sophisticated tracking systems and significant quality control resources.
For off-the-shelf therapies, the primary manufacturing challenge lies in scaling up production while maintaining consistent product characteristics and potency. As noted in recent analyses, "the biggest near-term challenge in the cell therapy industry continues to be the high cost of manufacturing doses, particularly with autologous products" [3]. There is a growing recognition that "legacy manufacturing processes, which remain the leading driver of high therapeutic costs" must be replaced with more efficient, automated systems [3]. Both paradigms face challenges related to the need for automated cell culturing to achieve commercial-scale manufacturing, deliver economies of scale, produce more consistent products, and reduce contamination risks [4].
Experimental Protocols
Protocol for Patient-Specific Therapy Manufacturing
Title: Manufacturing Protocol for Autologous CAR-T Cell Therapy
Principle: This protocol outlines the manufacturing process for patient-specific chimeric antigen receptor (CAR) T-cell therapy, which involves genetically modifying a patient's own T-cells to express CARs targeting specific tumor antigens.
Materials:
- Leukapheresis system for cell collection
- Ficoll-Paque PLUS for peripheral blood mononuclear cell (PBMC) separation
- Activation reagents: Anti-CD3/CD28 antibodies
- Viral vector (lentiviral or retroviral) encoding CAR construct
- Cell culture media: X-VIVO 15 or TexMACS with cytokines (IL-2, IL-7, IL-15)
- Bioreactor system for cell expansion (e.g., WAVE, G-Rex)
- Quality control assays: Flow cytometry, qPCR, sterility testing
Procedure:
- Patient Leukapheresis: Perform leukapheresis on the patient to collect peripheral blood mononuclear cells (PBMCs). Process within 24-36 hours of collection.
- PBMC Separation: Isolate PBMCs using density gradient centrifugation with Ficoll-Paque PLUS (400 × g, 30 min, room temperature).
- T-cell Activation: Resuspend PBMCs in complete media supplemented with anti-CD3/CD28 antibodies (1 μg/mL each) and IL-2 (100 IU/mL). Culture at 37°C, 5% CO₂ for 24-48 hours.
- Viral Transduction: Transfer activated T-cells to retronectin-coated plates at 1×10⁶ cells/mL. Add viral vector at multiplicity of infection (MOI) of 5-10. Centrifuge at 2000 × g for 90 min at 32°C (spinoculation).
- Cell Expansion: Transfer transduced cells to bioreactor systems. Culture in complete media with IL-2 (100 IU/mL) for 10-14 days, maintaining cell density between 0.5-2×10⁶ cells/mL.
- Harvest and Formulation: Harvest cells when target expansion is achieved (typically 10-14 days). Wash and formulate in infusion buffer.
- Quality Control: Perform release testing including viability (>70%), sterility, mycoplasma, endotoxin, identity (flow cytometry for CAR expression), and potency.
- Cryopreservation and Shipping: Cryopreserve in 5-10% DMSO at controlled rate freezing. Ship to clinical site in vapor phase liquid nitrogen dry shippers.
Notes: The entire process typically takes 3-4 weeks from leukapheresis to product release. Each patient's product is manufactured as an individual batch, requiring separate quality control testing and documentation.
Protocol for Off-the-Shelf Therapy Manufacturing
Title: Manufacturing Protocol for Allogeneic CAR-NK Cell Therapy
Principle: This protocol describes the manufacturing process for off-the-shelf CAR-natural killer (NK) cell therapy using umbilical cord blood-derived NK cells from healthy donors, enabling large-scale production for multiple patients.
Materials:
- Umbilical cord blood units from screened donors
- Ficoll-Paque PLUS for mononuclear cell separation
- NK cell activation reagents: IL-2, IL-15, IL-21
- NK cell expansion media: StemSpan with FBS and cytokines
- GMP-compliant bioreactor system (e.g., CliniMACS Prodigy)
- CRISPR/Cas9 system for genetic modification (where applicable)
- Cryopreservation solution with DMSO
Procedure:
- Donor Screening and Cell Source Preparation: Screen healthy donors and obtain umbilical cord blood units. Process within 24 hours of collection.
- Mononuclear Cell Separation: Isolate mononuclear cells using density gradient centrifugation with Ficoll-Paque PLUS (400 × g, 30 min, room temperature).
- NK Cell Enrichment: Isolate NK cells using immunomagnetic selection (CD3 depletion followed by CD56 positive selection). Assess purity by flow cytometry (>90% CD56⁺CD3⁻).
- Genetic Modification: Activate NK cells with IL-2 (1000 IU/mL) and IL-15 (10 ng/mL) for 24 hours. Transduce with CAR-encoding viral vector (lentiviral) at MOI 10-20 using spinoculation.
- Large-Scale Expansion: Seed CAR-NK cells in GMP-compliant bioreactor at 0.2×10⁶ cells/mL in NK cell expansion media with IL-2 (1000 IU/mL) and IL-15 (10 ng/mL). Culture for 14-21 days, feeding as needed.
- Harvest and Formulation: Harvest cells when target expansion is achieved (typically 1000-fold expansion). Wash and concentrate cells.
- Quality Control and Batch Release: Perform comprehensive testing including viability, sterility, mycoplasma, endotoxin, CAR expression, cytotoxicity assays, and copy number analysis for viral integration.
- Cryopreservation and Banking: Cryopreserve in multiple aliquots (1-10×10⁷ cells/vial) using controlled-rate freezing. Store in master and working cell banks.
Notes: A single manufacturing run can produce 100-1000 doses for multiple patients. Extensive characterization of master cell banks is required, including identity, purity, potency, and stability studies.
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagents for Cell Therapy Development
| Reagent/Category | Function | Examples/Applications |
|---|---|---|
| Cell Separation Media | Isolation of mononuclear cells from whole blood or tissue samples | Ficoll-Paque PLUS for density gradient centrifugation [2] |
| T-cell Activation Reagents | Activation and stimulation of T-cells prior to genetic modification | Anti-CD3/CD28 antibodies (TransAct, Dynabeads) [2] |
| Gene Delivery Vectors | Introduction of genetic material (CAR constructs) into target cells | Lentiviral vectors, retroviral vectors, CRISPR/Cas9 systems [2] |
| Cytokines and Growth Factors | Promotion of cell expansion, survival, and specific differentiation | IL-2, IL-7, IL-15, IL-21 for T-cell/NK cell expansion [2] |
| Cell Culture Media | Support of cell growth, expansion, and maintenance during manufacturing | X-VIVO 15, TexMACS, StemSpan serum-free media [2] |
| Cell Selection Systems | Isolation and purification of specific cell populations | Immunomagnetic bead systems (CliniMACS, Dynabeads) [2] |
| Analytical Tools | Characterization of cell products and quality control | Flow cytometry, qPCR, ELISA, cytotoxicity assays [2] |
Visualizing Workflows and Decision Pathways
Therapy Manufacturing Workflows
Therapy Selection Decision Pathway
The choice between patient-specific and off-the-shelf therapy paradigms represents a fundamental strategic decision in advanced therapy development, with significant implications for manufacturing, clinical implementation, and commercial viability. Patient-specific therapies offer the advantage of personalized treatments with reduced risk of immune rejection but face challenges in manufacturing scalability and cost control. Off-the-shelf therapies provide immediate availability and potentially lower costs through economies of scale but require sophisticated engineering to address immune compatibility issues.
Future directions in the field will likely focus on overcoming the current limitations of both approaches through technological innovations. For patient-specific therapies, this includes implementing advanced automation to reduce costs and improve consistency [3]. For off-the-shelf therapies, research is focusing on novel engineering strategies to enhance persistence and reduce immunogenicity [5] [2]. The ongoing evolution of both paradigms will continue to expand the therapeutic arsenal available to clinicians and researchers, ultimately enabling more personalized, effective, and accessible treatments for patients across a wide spectrum of diseases.
The development of cell therapies is primarily organized along two distinct pathways: autologous and allogeneic. Each approach leverages fundamentally different biological and manufacturing principles to achieve therapeutic goals. Autologous therapies, which utilize a patient's own cells, capitalize on inherent immune compatibility to avoid rejection, creating a highly personalized but logistically complex treatment [7] [8]. In contrast, allogeneic therapies, derived from healthy donors, pursue scalability through "off-the-shelf" availability, enabling broader patient access but introducing significant immunological challenges [9] [10]. This application note delineates the core advantages, technical requirements, and experimental protocols intrinsic to each modality, providing a framework for researchers to navigate this complex developmental landscape. The critical distinction lies in the cell source, which dictates every subsequent aspect of manufacturing, quality control, and clinical application [7] [11].
Core Advantages and Quantitative Comparison
The Autologous Advantage: Innate Immune Compatibility
The principal strength of autologous cell therapy lies in its biological compatibility. Since the therapeutic product is derived from and reinfused into the same patient, it circumvents the major immunological barriers that plague allogeneic approaches. This eliminates the risk of Graft-versus-Host Disease (GvHD), a potentially life-threatening condition where donor immune cells attack host tissues [7] [8]. Consequently, patients receiving autologous therapies typically do not require concomitant immunosuppressive regimens, sparing them from associated risks of infection, organ toxicity, and other drug-related complications [11]. This inherent self-compatibility also allows for greater in vivo persistence of the therapeutic cells, which is crucial for long-term efficacy, particularly in applications like CAR-T therapy for durable cancer remissions [8] [11].
The Allogeneic Advantage: Manufacturing and Commercial Scalability
Allogeneic cell therapies are defined by their scalability and accessibility. Sourced from healthy donors, these therapies can be manufactured in large, well-characterized batches from a single donor collection, creating an "off-the-shelf" product available for immediate use [9] [12]. This model transforms the treatment timeline, eliminating the weeks-long manufacturing delay associated with autologous processes, which is critical for patients with aggressive diseases [8] [11]. From a development and commercial perspective, the allogeneic approach allows for standardized, centralized manufacturing that leverages economies of scale, potentially reducing the cost per dose and making these therapies more accessible to a wider patient population [7] [12].
Table 1: Quantitative and Qualitative Comparison of Autologous and Allogeneic Cell Therapies
| Characteristic | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [7] [8] | Healthy donor (related or unrelated) [7] [12] |
| Key Advantage | Innate immune compatibility; no GvHD risk [8] [11] | "Off-the-shelf" availability & industrial scalability [9] [12] |
| Primary Challenge | Logistical complexity & high cost of goods [3] [7] | Risk of immune rejection (GvHD) & host-mediated elimination [10] [11] |
| Manufacturing Model | Scale-out (multiple parallel patient-specific batches) [7] | Scale-up (large batches from a single donor) [7] |
| Typical Vein-to-Vein Time | Several weeks [11] | Immediate to a few days [11] |
| Immunosuppression Required | Generally not required [8] | Often required [8] [11] |
| Representative Market Share (2025) | ~84% of cell therapy market [12] | ~16% of cell therapy market [12] |
| Global Market Projection | Projected to grow from USD 10.1B (2025) [13] | Significant growth driven by ~250 products in development [12] |
Experimental Protocols for Cell Expansion
The following protocols outline core expansion workflows for both autologous and allogeneic T-cell therapies, highlighting key process distinctions.
Protocol 1: Autologous CAR-T Cell Expansion from Patient Leukapheresis
Principle: To isolate, activate, genetically modify, and expand a patient's T-cells to create a personalized therapeutic product [8] [14].
Materials:
- Starting Material: Leukapheresis product from the patient.
- Isolation Reagents: Anti-CD3/CD28 magnetic beads or similar for T-cell activation.
- Culture Media: Xeno-free T-cell expansion media, supplemented with IL-2 [14].
- Genetic Modification: Viral vector (e.g., lentivirus) encoding the CAR construct.
- Equipment: Automated cell expansion system (e.g., Terumo BCT's quantum cell expansion system), CO2 incubator, biosafety cabinet [14].
Method:
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Isolate PBMCs from the leukapheresis product via density gradient centrifugation (e.g., Ficoll-Paque).
- T-Cell Activation and Culture: Seed the PBMCs in a pre-coated bioreactor or culture vessel. Activate T-cells using anti-CD3/CD28 beads in xeno-free expansion media. Incubate at 37°C, 5% CO2 [14].
- Genetic Modification (Day 2-3): Transduce activated T-cells with the CAR-encoding viral vector. Optimize the Multiplicity of Infection (MOI) for maximum efficiency and cell viability.
- Cell Expansion (Day 4-12): Continue culture, feeding with fresh media and cytokines as required. Monitor cell density, viability, and phenotype (e.g., CD3+, CD4+/CD8+ ratio) daily.
- Harvest and Formulation: Once target cell numbers are achieved (typically 10-14 days), harvest cells, remove activation beads, and formulate the final drug product in an appropriate infusion solution.
- Quality Control (QC): Perform release tests, including sterility, mycoplasma, endotoxin, vector copy number, CAR expression, and potency.
Protocol 2: Allogeneic CAR-NK Cell Expansion from Master Cell Bank
Principle: To thaw and expand clinically-relevant doses of allogeneic CAR-NK cells from a pre-generated Master Cell Bank derived from cord blood or induced Pluripotent Stem Cells (iPSCs) [9].
Materials:
- Starting Material: Vial from a cGMP-compliant Master Cell Bank of CAR-engineered NK cells.
- Culture Media: Specialized NK cell expansion media (e.g., containing IL-15, IL-21).
- Feeder Cells: Irradiated K562-derived feeder cells expressing membrane-bound cytokines (e.g., 4-1BBL).
- Equipment: Bioreactor (e.g., G-Rex), CO2 incubator, biosafety cabinet.
Method:
- Thaw and Seed: Rapidly thaw a vial of CAR-NK cells from the Master Cell Bank and seed into culture media supplemented with IL-15 in a bioreactor.
- Stimulation and Expansion (Day 1): Add irradiated feeder cells at a specific effector-to-feeder ratio to stimulate robust NK cell proliferation.
- Fed-Batch Culture (Days 2-14): Maintain culture, periodically adding fresh media and cytokines. Monitor cell count, viability, and phenotype (e.g., CD56+, CD3-) closely.
- Harvest and Cryopreservation: Harvest cells when the target yield is reached. Wash and concentrate cells, then cryopreserve in multiple doses using a controlled-rate freezer. This creates the "off-the-shelf" final product inventory [9].
- Quality Control (QC): Perform batch release testing, including sterility, purity, identity, CAR expression, cytotoxicity assays, and checks for residual feeder cells.
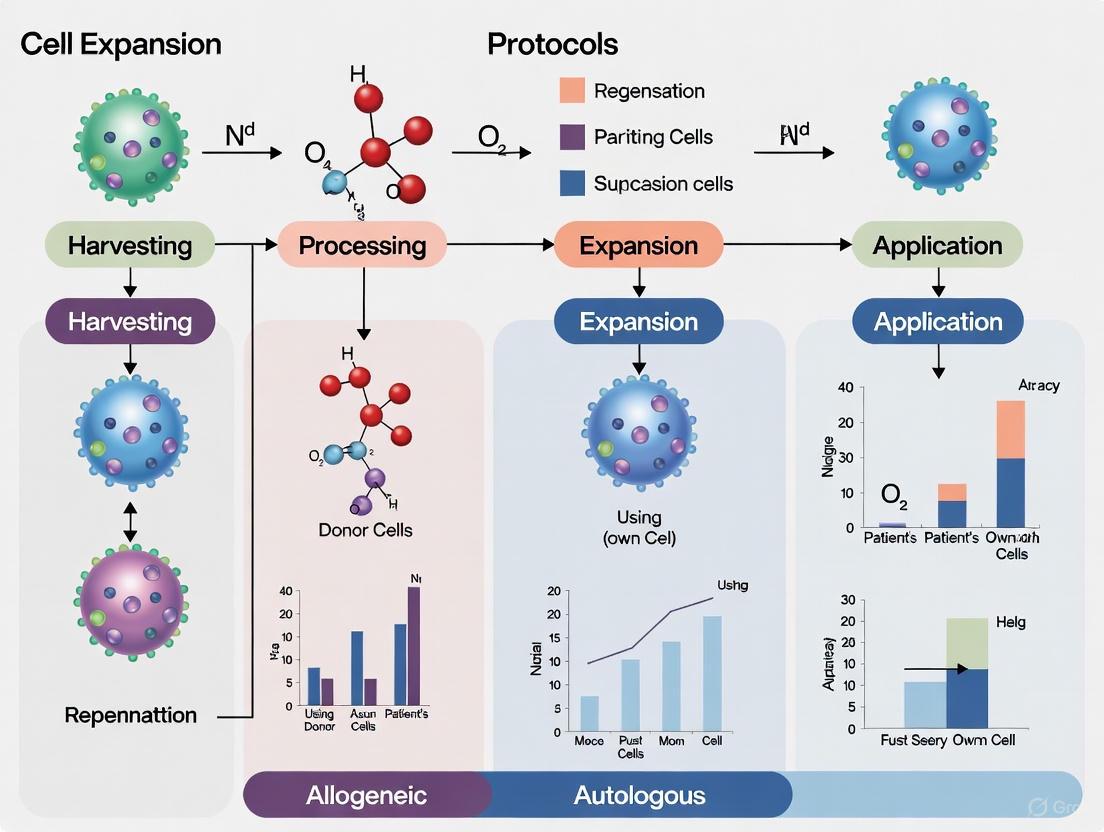
Diagram 1: Cell therapy manufacturing workflows.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of cell expansion protocols requires carefully selected reagents and materials. The following table details key solutions for robust and reproducible results.
Table 2: Key Research Reagent Solutions for Cell Therapy Development
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Xeno-Free Cell Culture Media | Supports growth and maintenance of T-cells and NK cells ex vivo [14]. | Formulations are often cell-type specific (T-cell vs. NK cell); xeno-free status reduces regulatory risk for clinical use. |
| Magnetic Beads (Anti-CD3/CD28) | Provides artificial antigen-independent T-cell receptor stimulation for T-cell activation and proliferation [14]. | Critical first step in T-cell manufacturing; bead removal is required prior to infusion. |
| Recombinant Human Cytokines (e.g., IL-2, IL-15) | Enhances cell expansion, promotes survival, and can influence final cell phenotype (e.g., memory vs. exhausted T-cells) [14]. | Concentration and timing of cytokine addition are crucial parameters for optimization. |
| Viral Vectors (Lentivirus, Retrovirus) | Delivers genetic payload (e.g., CAR) into target cells for stable expression. | High titer and good manufacturing practice (GMP)-compatible production are essential for clinical translation. |
| Cell Separation Reagents (e.g., Ficoll-Paque) | Isolates PBMCs from whole blood or leukapheresis product via density gradient centrifugation. | A standard, foundational step for preparing starting material from patient or donor apheresis. |
| Cryopreservation Medium | Protects cell viability during freeze-thaw cycles for long-term storage of allogeneic "off-the-shelf" doses or cell banks. | Typically contains DMSO and serum/serum substitutes; controlled-rate freezing is recommended. |
The choice between autologous and allogeneic cell therapy is not a simple binary decision but a strategic one, guided by the therapeutic target, patient population, and commercial vision. The field is rapidly evolving to mitigate the inherent limitations of each platform. For autologous therapies, the focus is on automation, process optimization, and point-of-care manufacturing to reduce vein-to-vein time, control costs, and alleviate logistical burdens [3] [15] [14]. For allogeneic therapies, the primary research frontier is immune evasion, employing gene editing tools like CRISPR/Cas9 to disrupt HLA molecules to prevent host rejection and TCR complexes to prevent GvHD, thereby creating more universal products [10] [8]. A promising future direction involves the development of "hypoimmune" cells from iPSCs, which are engineered to avoid immune detection, potentially offering the scalability of allogeneic products with the compatibility of autologous ones [10] [8]. Ultimately, both modalities will coexist, enabling researchers and clinicians to arm themselves with the most appropriate tool for a given disease.
The development of cell therapies is bifurcated into two principal approaches: autologous, using the patient's own cells, and allogeneic, using cells from healthy donors [11]. Each pathway presents a distinct profile of technical challenges. Autologous therapies are predominantly hampered by complex logistical and manufacturing hurdles arising from their patient-specific nature, while allogeneic therapies face significant immunological barriers that threaten graft survival and efficacy [11] [16]. This application note delineates these core challenges and provides detailed experimental protocols to aid researchers in navigating these critical development pathways. The content is structured to support a broader thesis on cell expansion protocols, providing comparative data and methodological details relevant to scientists and drug development professionals.
Autologous Cell Therapies: Conquering Logistical Complexity
Core Logistical and Manufacturing Hurdles
Autologous cell therapies are fundamentally a "service-based" model, where each individual batch is a unique product for a single patient [11]. This paradigm creates a multifaceted logistical challenge summarized in the table below.
Table 1: Key Logistical Challenges in Autologous Cell Therapy Manufacturing
| Challenge Category | Specific Hurdles | Impact on Development & Therapy |
|---|---|---|
| Product Stability & Timing | Short ex vivo half-life (as little as a few hours); extended turnaround time (several weeks) [11]. | Risks product integrity; delays treatment for patients with worsening prognoses [11]. |
| Supply Chain & Coordination | Complex coordination for collection, manufacturing, and delivery; stringent chain-of-identity and custody requirements [11] [7]. | Logistically demanding process requiring robust digital infrastructure for tracking [11]. |
| Manufacturing Complexity | High level of personalization; variability in starting cell quality due to patient age, disease, and prior treatments [11] [7]. | High cost; batch heterogeneity; difficulties in maintaining consistent quality attributes [11]. |
| Scalability | Scale-out strategy requiring multiple parallel production lines; not amenable to traditional scale-up [7]. | Challenging to treat highly prevalent diseases; high per-dose cost [11] [7]. |
Experimental Protocol: Assessing Patient-Derived Cell Viability and Expansion Potential
The quality of patient-derived starting material is highly variable. This protocol outlines a method to evaluate cellular health and expansion capacity prior to major manufacturing investments.
Objective: To determine the viability, phenotypic composition, and ex vivo expansion potential of patient-derived apheresis material or tissue samples.
Materials:
- Research Reagent Solutions:
- Ficoll-Paque PREMIUM: For density gradient centrifugation to isolate peripheral blood mononuclear cells (PBMCs).
- StemSpan SFEM or similar serum-free medium: Base medium for hematopoietic cell culture [17].
- Cytokine Cocktail (e.g., SCF, TPO, Flt3L): Essential growth factors for HSPC expansion [17].
- Flow Antibody Panel (CD34, CD38, CD45RA, CD90, CD133): For phenotyping hematopoietic stem and progenitor cells (HSPCs) via flow cytometry [17].
- 7-AAD or DAPI: Viability dyes for flow cytometry.
- Pre-Gassed Culture Bags/Plates: For cell culture.
Methodology:
- Cell Isolation: Isolate PBMCs from apheresis product via density gradient centrifugation using Ficoll-Paque. Wash cells twice in PBS.
- Baseline Analysis:
- Viability Count: Use an automated cell counter with a viability stain (e.g., Trypan Blue) to determine total nucleated cell count and viability.
- Phenotypic Analysis: Stain a sample of cells (~1x10^6) with antibodies against CD34, CD133, CD38, CD45RA, and CD90. Include a viability dye. Analyze on a flow cytometer to quantify the proportion of primitive HSPCs (e.g., CD34+CD38lo/–CD45RA–CD90+CD49f+) [17].
- Expansion Culture:
- Seed cells in serum-free medium (e.g., StemSpan SFEM) supplemented with a cytokine cocktail (e.g., SCF, TPO, Flt3L) at a density of 1-2 x 10^5 cells/mL [17].
- Maintain cultures in a humidified incubator at 37°C and 5% CO2 for 7-14 days.
- Perform partial medium exchanges or feed cells every 2-3 days.
- Endpoint Analysis:
- On day 7 and/or 14, perform total cell counts and viability assessment.
- Re-stain cells for the same phenotypic markers to track the maintenance or loss of the HSPC population during culture.
- Calculate fold expansion of total cells and, critically, the specific HSPC population.
Data Interpretation: A successful starting material should show high initial viability (>90%) and contain a sufficient baseline proportion of target cells. Effective expansion protocols will demonstrate a significant fold-increase in the total number of phenotypically defined HSPCs, indicating robustness for downstream manufacturing.
Allogeneic Cell Therapies: Navigating the Immunological Landscape
Core Immunological Risks
Allogeneic cell therapies, while logistically attractive, face a formidable barrier: host immune recognition and rejection. The primary immunological challenges are graft rejection and graft-versus-host disease (GvHD) [11].
The immune response to allogeneic cells is orchestrated through multiple pathways of allorecognition [16] [18]. The innate immune system, particularly Natural Killer (NK) cells, targets and kills cells that lack "self" Major Histocompatibility Complex (MHC) class I molecules, a phenomenon known as the "missing-self" hypothesis [16] [18]. The adaptive immune system is activated via T cells through three principal pathways:
- Direct Pathway: Recipient T cells directly recognize intact donor MHC molecules on the surface of the transplanted cells.
- Indirect Pathway: Recipient antigen-presenting cells (APCs) engulf donor cells, process donor proteins, and present them as peptide fragments on self-MHC molecules to recipient T cells.
- Semi-Direct Pathway: Recipient APCs acquire intact donor MHC molecules from donor cells and present them directly to recipient T cells [16] [18].
These pathways can lead to the destruction of the therapeutic cells by CD8+ cytotoxic T cells and provide help for B cell activation, resulting in alloantibody production [16].
Figure 1: Immunological Pathways in Allogeneic Cell Rejection. Allogeneic cells trigger host immune responses via both innate (NK cell) and adaptive (T cell) mechanisms. T cell activation occurs through direct, indirect, and semi-direct allorecognition pathways, leading to graft rejection and alloantibody production [16] [18].
Experimental Protocol: In Vitro Assessment of Allogeneic T Cell-Mediated Rejection
This protocol utilizes a mixed lymphocyte reaction (MLR) to model T cell-dependent immune responses against allogeneic cell therapy products in a controlled setting.
Objective: To evaluate the potential immunogenicity of an allogeneic cell therapy candidate by measuring its ability to provoke T cell activation and proliferation from allogeneic PBMCs.
Materials:
- Research Reagent Solutions:
- Allogeneic Cell Therapy Candidate: The putative "target" cells (e.g., iPSC-derived cells, MSCs).
- Allogeneic PBMCs: From multiple healthy donors, to serve as "effector" cells.
- RPMI-1640 Complete Medium: Supplemented with L-glutamine, HEPES, and 10% human AB serum.
- Carboxyfluorescein Succinimidyl Ester (CFSE): Cell proliferation dye for tracking effector cell division.
- Flow Antibody Panel (CD3, CD4, CD8, CD25, CD69, CD137): For T cell activation markers.
- ELISA Kits (e.g., IFN-γ, Granzyme B): To measure T cell effector function.
Methodology:
- Cell Preparation:
- Irradiate the allogeneic cell therapy candidate (the "stimulator" cells) to prevent their proliferation while maintaining antigen presentation.
- Isolate PBMCs from a healthy donor (the "responder" cells) that is HLA-mismatched with the therapy candidate. Label PBMCs with CFSE according to standard protocols.
- Co-culture Setup:
- Plate irradiated stimulator cells in a 96-well U-bottom plate.
- Add CFSE-labeled responder PBMCs at various stimulator:responder ratios (e.g., 1:1, 1:10).
- Include controls: responder cells alone (negative control) and responder cells with a mitogen like PHA (positive control).
- Culture for 5-7 days in a humidified incubator at 37°C and 5% CO2.
- Endpoint Analysis:
- Proliferation: Analyze CFSE dilution on a flow cytometer within the CD3+ T cell gate to determine the percentage of T cells that have undergone division.
- Activation: Stain cells for early (CD69) and late (CD25, CD137) T cell activation markers.
- Effector Function: Collect supernatant and measure secreted IFN-γ and Granzyme B by ELISA.
Data Interpretation: A potent allogeneic cell therapy candidate engineered for low immunogenicity should show minimal T cell proliferation and low levels of activation markers and inflammatory cytokines compared to a non-engineered control. This assay provides a pre-clinical screen for the likelihood of immune rejection.
Emerging Strategies and Solution Frameworks
Strategic Approaches to Mitigate Challenges
The field is actively developing strategies to overcome the central challenges for both therapeutic modalities.
Table 2: Solution Frameworks for Autologous and Allogeneic Challenges
| Therapy Type | Core Challenge | Proposed Solutions & Technologies |
|---|---|---|
| Autologous | Logistical & Manufacturing Complexity | Automation & Closed Systems: Reduce manual handling, contamination risk, and vein-to-vein time [7] [19]. Point-of-Care Manufacturing: Decentralize production to reduce transport logistics [11]. Advanced Analytics & Digital Tracking: Robust chain-of-identity and custody management [11]. |
| Allogeneic | Immunological Rejection & GvHD | Gene Editing (CRISPR/Cas9, TALENs): Knock-out HLA molecules to create "universal" cells or delete TCR to prevent GvHD [10] [20]. Overexpression of Immunomodulatory Transgenes: Engineered expression of HLA-E, HLA-G, or CD47 to inhibit NK cells and macrophages [16] [18]. Use of Immune-Privileged Cell Types: Mesenchymal Stem/Stromal Cells (MSCs) and some NK cells have inherent low immunogenicity [11]. |
Protocol: CRISPR-Cas9 Mediated Knockout of HLA Class I in iPSCs for Allogeneic Therapy
This protocol outlines a key genetic engineering strategy to evade T cell-mediated rejection.
Objective: To generate HLA class I-deficient induced pluripotent stem cells (iPSCs) using CRISPR-Cas9 gene editing for use as a universal starting material for allogeneic therapies.
Materials:
- Research Reagent Solutions:
- iPSC Line: A well-characterized, clinically relevant iPSC line.
- CRISPR-Cas9 Ribonucleoprotein (RNP) Complex: Cas9 protein pre-complexed with sgRNAs targeting the B2M gene (essential for HLA class I surface expression).
- Electroporation System (e.g., Neon or Amaxa 4D-Nucleofector): For efficient delivery of RNP into iPSCs.
- Flow Antibody against HLA-A,B,C: To confirm knockout efficiency.
- iPSC Culture Reagents: Essential medium (e.g., mTeSR1), Matrigel or Vitronectin, RevitaCell supplement.
Methodology:
- sgRNA Design and RNP Complex Formation: Design and validate sgRNAs targeting the early exons of the B2M gene. Complex purified Cas9 protein with the sgRNAs to form the RNP complex.
- Cell Preparation and Transfection:
- Culture and passage iPSCs to ensure they are in a log-growth phase and >90% viable.
- Harvest a single-cell suspension of iPSCs and resuspend them in the appropriate electroporation buffer.
- Mix the cell suspension with the pre-formed RNP complex and electroporate using an optimized program.
- Post-Transfection Recovery:
- Immediately transfer electroporated cells to a culture plate containing pre-warmed medium supplemented with RevitaCell.
- Allow cells to recover for 48-72 hours before any further manipulation.
- Clonal Isolation and Screening:
- After recovery, dissociate cells into a single-cell suspension and seed at a very low density for clonal expansion.
- Pick individual colonies and expand them in 96-well plates.
- Screen clones for HLA class I knockout by flow cytometry using an antibody against pan-HLA-A,B,C.
- Confirm the genetic modification in HLA-negative clones by Sanger sequencing or next-generation sequencing of the target locus.
Data Interpretation: Successful execution will yield a panel of clonal iPSC lines with complete loss of HLA class I surface expression. These clones can serve as a universal donor source for deriving various differentiated cell types (e.g., neurons, cardiomyocytes) with reduced immunogenicity. It is critical to subsequently evaluate these cells for susceptibility to NK cell-mediated killing due to the "missing-self" response and consider additional engineering steps (e.g., HLA-E expression) to address this [16] [18].
The development of advanced cell therapies, whether autologous (patient-specific) or allogeneic (donor-derived, "off-the-shelf"), relies critically on the selection of appropriate starting cell sources. The choice of source material fundamentally influences manufacturing scalability, product consistency, and therapeutic efficacy [11]. Peripheral Blood Mononuclear Cells (PBMCs), Induced Pluripotent Stem Cells (iPSCs), and Umbilical Cord Blood (UCB) represent three of the most prominent cell sources, each with distinct biological properties and technological applications.
For allogeneic therapies in particular, these sources offer the potential for scalable, off-the-shelf products that can overcome the time, cost, and manufacturing limitations associated with autologous treatments [9] [2]. This document details the characteristic profiles, experimental protocols, and key reagents for working with these critical cell sources within the context of modern cell therapy development.
The table below summarizes the core characteristics, advantages, and challenges of PBMCs, iPSCs, and Umbilical Cord Blood as starting materials for cell therapy.
Table 1: Comparative Analysis of Primary Cell Sources for Cell Therapies
| Feature | PBMCs (Peripheral Blood Mononuclear Cells) | iPSCs (Induced Pluripotent Stem Cells) | Umbilical Cord Blood (UCB) |
|---|---|---|---|
| Source | Peripheral blood of healthy donors or patients [2] | Reprogrammed somatic cells (e.g., fibroblasts, PBMCs) [21] [22] | Umbilical cord and placenta collected at birth [2] |
| Key Cell Types | T cells, B cells, NK cells, monocytes, dendritic cells [2] | Pluripotent stem cells capable of differentiating into any cell type [22] | Hematopoietic stem cells (HSCs), T cells, NK cells [2] |
| Therapeutic Examples | Allogeneic CAR-T cells [2] | iPSC-derived CAR-NK/T cells, tissue-specific cells for regenerative medicine [9] [2] | Allogeneic CAR-NK cells, hematopoietic stem cell transplantation [2] [5] |
| Major Advantages | - Readily accessible from donors- Established isolation protocols- Contains mature immune effector cells [2] | - Unlimited expansion potential- Genetic engineering flexibility- Can generate any cell type [22] [2] | - Immunologically "antigen-naïve"- Lower alloreactivity & GvHD risk- Low exhaustion marker expression [2] |
| Major Challenges | - Donor-to-donor variability- Risk of GvHD in allogeneic settings [2] | - Genomic instability risk during reprogramming/culture- Tumorigenicity risk from residual undifferentiated cells [21] [23] | - Limited cell numbers per donation- Restricted donor pool availability [2] |
Cell Source Specific Protocols
Protocol: Generation of iPSCs from Somatic Cells
The ability to reprogram somatic cells into pluripotent stem cells has opened new avenues for creating allogeneic cell therapies. The following protocol outlines a non-integrating, Sendai viral vector method for iPSC generation, which is favored for clinical applications due to its "zero-footprint" nature [21].
Principle: Somatic cells are reprogrammed into a pluripotent state through the transient expression of key transcription factors (OCT4, SOX2, KLF4, c-MYC) delivered via non-integrating Sendai viral vectors [21] [22].
Materials:
- Source Cells: Fibroblasts (from skin biopsy) or PBMCs [21].
- Reprogramming Vectors: CytoTune-iPS Sendai Reprogramming Kit (or equivalent), containing SeV vectors for KOS (KLF4, OCT4, SOX2), hc-MYC, and hKLF4.
- Culture Vessels: 6-well plates coated with Matrigel or Vitronectin.
- Media: Appropriate somatic cell medium; Essential 8 or mTeSR1 pluripotent stem cell medium.
- Other Reagents: Dulbecco’s Phosphate Buffered Saline (DPBS) with and without calcium and magnesium, TrypLE Select or Accutase.
Procedure:
- Preparation of Somatic Cells: Culture and expand source somatic cells (e.g., fibroblasts) until 70-90% confluent in a 6-well plate. Ensure cells are healthy and proliferating.
- Viral Transduction:
- Calculate the required Multiplicity of Infection (MOI) for each vector. A typical MOI for fibroblasts is KOS=5, hc-MYC=5, hKLF4=3.
- Thaw viral vectors quickly and dilute in the appropriate somatic cell medium.
- Remove the culture medium from the cells and add the virus-containing medium.
- Incubate cells for 24 hours at 37°C, 5% CO₂.
- Post-Transduction Culture:
- After 24 hours, remove the virus-containing medium, wash cells once with DPBS, and add fresh somatic cell medium.
- Culture the transduced cells for an additional 6 days, changing the medium every other day.
- iPSC Colony Expansion:
- On day 7 post-transduction, dissociate the cells into a single-cell suspension using TrypLE Select or Accutase.
- Plate the cells onto Matrigel-coated 6-well plates in somatic cell medium supplemented with a ROCK inhibitor (e.g., Y-27632).
- The following day, switch the medium to Essential 8 or mTeSR1.
- Change the medium daily. Embryonic stem cell-like colonies should become visible within 1-2 weeks.
- Colony Picking and Characterization:
- Manually pick individual, morphologically good colonies and transfer them to new Matrigel-coated 24-well plates.
- Expand clonal lines and characterize established iPSC lines through:
- Pluripotency Marker Analysis: Immunofluorescence for OCT4, SOX2, NANOG.
- Trilineage Differentiation: Via embryoid body formation to confirm differentiation into ectoderm, mesoderm, and endoderm.
- Karyotype Analysis: To ensure genomic integrity.
- Vector Clearance Testing: Perform PCR to confirm the absence of residual Sendai virus after ~10 passages [21].
Protocol: Isolation of Immune Cell Subsets from PBMCs and UCB
This protocol describes the isolation of mononuclear cells and subsequent enrichment of specific immune effector cells, such as T cells or NK cells, from PBMC and UCB sources for use in therapies like CAR-T or CAR-NK.
Principle: Density gradient centrifugation separates mononuclear cells from whole blood or cord blood. Target cell populations are then isolated from PBMCs/UCB-MNCs using positive or negative selection methods based on antibody-bound magnetic beads.
Materials:
- Source Material: Whole blood (for PBMCs) or umbilical cord blood units (for UCB).
- Separation Medium: Ficoll-Paque PREMIUM or Lymphoprep.
- Isolation Kits: CD3 MicroBeads (for T cell isolation) or CD56 MicroBeads (for NK cell isolation) or relevant negative selection kits.
- Buffers: DPBS, pH 7.2, supplemented with 0.5% Bovine Serum Albumin (BSA) or 1% Human Serum Albumin (HSA) and 2 mM EDTA.
- Equipment: Centrifuge, LS Columns, and a MidiMACS or AutoMACS Separator.
Procedure:
- PBMC/UCB-MNC Isolation:
- Dilute blood or cord blood 1:1 with DPBS (with 2 mM EDTA).
- Carefully layer the diluted blood over Ficoll-Paque in a centrifuge tube (e.g., 15 mL of diluted blood over 12 mL of Ficoll).
- Centrifuge at 400 x g for 30-35 minutes at 20°C with the brake turned off.
- After centrifugation, aspirate the upper plasma layer. Carefully collect the mononuclear cell layer at the interface and transfer it to a new tube.
- Wash cells with DPBS/BSA/EDTA buffer by centrifuging at 300 x g for 10 minutes. Repeat wash twice.
- Magnetic-Activated Cell Sorting (MACS):
- Resuspend the cell pellet in MACS buffer (DPBS, 0.5% BSA, 2mM EDTA) at a concentration of 10⁷ cells per 80 µL.
- Add 20 µL of the appropriate MACS MicroBeads per 10⁷ cells. Mix well and incubate for 15 minutes in the refrigerator (2-8°C).
- Wash cells by adding 10-20x the labeling volume of buffer and centrifuge at 300 x g for 10 minutes.
- Place an LS Column in the magnetic field of the MACS Separator. Prepare the column by applying 3 mL of buffer.
- Resuspend the cell pellet in 500 µL of buffer and apply the cell suspension to the column.
- Collect the unlabeled, flow-through fraction (for negative selection). Wash the column 3 times with 3 mL of buffer.
- Remove the column from the magnet and place it on a collection tube. Pipette 5 mL of buffer onto the column and firmly flush out the magnetically labeled cells using the plunger.
- Cell Analysis and Cryopreservation:
- Count the isolated cells and assess viability using Trypan Blue exclusion.
- Analyze purity by flow cytometry (e.g., check CD3+ percentage for T cells or CD56+ for NK cells).
- For long-term storage, cryopreserve cells in a controlled-rate freezer using cryoprotectant medium (e.g., 90% FBS/10% DMSO) and store in liquid nitrogen vapor phase.
Workflow Visualization
The following diagram illustrates the parallel development pathways for creating allogeneic cell therapies from PBMCs, iPSCs, and Umbilical Cord Blood, highlighting key steps from source material to final product.
Diagram 1: Parallel workflows for developing allogeneic cell therapies from PBMCs, iPSCs, and Umbilical Cord Blood.
The Scientist's Toolkit: Essential Reagents and Materials
Successful cell therapy development depends on a suite of specialized reagents and tools. The table below lists key solutions for critical experimental procedures.
Table 2: Essential Research Reagent Solutions for Cell Therapy Development
| Reagent/Material | Primary Function | Example Protocols & Notes |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolation of PBMCs and UCB-MNCs from whole blood [2] | PBMC/UCB-MNC Isolation Protocol; critical for obtaining a pure mononuclear cell population. |
| MACS MicroBeads | Magnetic bead-based cell separation for positive or negative selection of specific cell types (e.g., CD3+ T cells, CD56+ NK cells) [2] | Immune Cell Subset Isolation; enables high-purity isolation of target effector cells for engineering. |
| Sendai Virus Vectors | Non-integrating viral vectors for efficient delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC) to somatic cells [21] | iPSC Generation Protocol; preferred for clinical-grade iPSC generation due to non-integrating nature. |
| CRISPR/Cas9 System | Precision gene-editing tool for knocking out genes (e.g., TCR, HLA) to reduce allorejection and GvHD in allogeneic products [10] [2] | Genetic Engineering of Allogeneic Cells; used to create universal, hypoimmunogenic cell therapies. |
| Lentiviral Vectors | Integrating viral vectors for stable delivery of transgenes, such as Chimeric Antigen Receptors (CARs), into target cells [2] | CAR Transduction; commonly used for engineering CAR-T and CAR-NK cells from various cell sources. |
| Essential 8 / mTeSR1 | Xeno-free, defined cell culture media optimized for the maintenance and expansion of human pluripotent stem cells, including iPSCs [21] | iPSC Culture; supports feeder-free culture of iPSCs, maintaining pluripotency and genomic stability. |
| Recombinant Human Cytokines (e.g., IL-2, IL-7, IL-15, SCF, FLT-3L) | Proteins that promote the survival, proliferation, and differentiation of hematopoietic and immune cells during culture [2] | Cell Expansion; essential for ex vivo expansion of T cells, NK cells, and hematopoietic progenitors. |
| Matrigel / Vitronectin | Extracellular matrix proteins used as a substrate for coating culture vessels to support adherent cell growth, particularly for iPSCs [22] | iPSC Culture; provides a defined attachment surface for robust pluripotent stem cell growth. |
From Lab to Clinic: Methodological Workflows and Clinical Translation of Expansion Protocols
Autologous cell therapy represents a highly personalized treatment modality where a patient's own cells are harvested, processed, and subsequently re-infused back into the same individual. This approach stands in contrast to allogeneic therapies, which utilize cells from healthy donors. The fundamental advantage of autologous therapy lies in its inherent immunological compatibility; since the cells originate from the patient, the risks of immune rejection and graft-versus-host disease (GvHD) are significantly minimized, eliminating the need for immunosuppressive therapy to support graft survival [8]. This personalized approach is particularly valuable for patients with compromised immune systems and has demonstrated remarkable success in treating hematological malignancies, autoimmune diseases, and degenerative disorders [8] [24].
However, the autologous process presents substantial challenges in manufacturing and logistics. Each patient's treatment constitutes a unique product batch, requiring complex coordination from collection to re-infusion. The entire process is time-sensitive, often taking several weeks, which can be problematic for patients with aggressive diseases [8] [11]. Furthermore, the quality and potency of autologous cells can be highly variable due to factors such as the patient's age, underlying disease, and prior treatments, potentially affecting therapeutic efficacy [8]. Despite these challenges, the autologous cell therapy market is experiencing significant growth, with projections indicating expansion from US$11.41 billion in 2025 to US$54.21 billion by 2034, driven by advances in regenerative medicine and increasing adoption of personalized healthcare [25].
This application note provides a detailed technical protocol for the autologous cell therapy process, from initial leukapheresis through final re-infusion, with particular emphasis on optimization strategies for cell expansion and activation.
Technical Protocol: The Autologous Workflow
The autologous cell therapy manufacturing process comprises multiple interconnected stages, each requiring precise execution and quality control. The following workflow outlines the critical path from patient mobilization to product administration.
Patient Mobilization and Leukapheresis
The initial phase focuses on mobilizing hematopoietic stem cells from the bone marrow into the peripheral blood, followed by collection via leukapheresis.
Mobilization Strategies:
- Granulocyte Colony-Stimulating Factor (G-CSF): Administration of filgrastim (G-CSF) at 5-10 μg/kg/day for 4-5 days is the standard protocol for mobilizing CD34+ cells into peripheral blood [26]. This approach is typically well-tolerated, with side effects including bone pain, headache, and low-grade fever that rarely interfere with collection [26].
- Chemotherapy plus G-CSF: For patients with certain malignancies, mobilization using cyclophosphamide-based chemotherapy followed by G-CSF administration may yield higher CD34+ cell counts, though this approach carries greater toxicity and requires careful monitoring [26].
Leukapheresis and CD34+ Monitoring: Leukapheresis is typically initiated when the peripheral blood CD34+ count reaches ≥10-20×10³/mL, which generally occurs 4-5 days after starting G-CSF mobilization or approximately 11 days following cyclophosphamide-based regimens [26]. The quantification of CD34+ progenitor cells by flow cytometry using the International Society of Hemotherapy and Graft Engineering (ISHAGE) protocol serves as a critical predictor of collection success [26]. Studies demonstrate a moderate positive correlation between peripheral blood CD34+ cell count and total CD34+ cell count/kg collected during apheresis (r=0.596; p<0.001), with every increase of 5 CD34+ cells/μL in peripheral blood predicting a mean increase of 0.38×10⁶ CD34+ cells/kg in the apheresis product [26].
Table 1: Key Parameters for Leukapheresis Monitoring and Collection
| Parameter | Target Value | Analytical Method | Clinical Significance |
|---|---|---|---|
| Peripheral Blood CD34+ Count | ≥10-20×10³/μL | Flow cytometry (ISHAGE protocol) | Predicts successful collection; minimum threshold for initiating apheresis [26] |
| Pre-apheresis White Blood Cell Count | 35,000-40,000/μL | Automated hematology analyzer | Indicates adequate mobilization response [26] |
| CD34+ Cell Percentage in PB | 0.03% (median) | Flow cytometry | Quality indicator of mobilization efficacy [26] |
| Minimum CD34+ Collection | 2-5×10⁶ cells/kg | Flow cytometry | Required for consistent engraftment [26] |
Cell Processing, Activation, and Expansion
Following collection, cells undergo processing, activation, and expansion to generate therapeutic quantities. For T-cell therapies like CAR-T, this represents the most technically complex phase.
Cell Processing and Selection:
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Density gradient centrifugation (Ficoll-Paque) separates mononuclear cells from other blood components.
- T-cell Selection: Negative or positive selection methods isolate T-cells using immunomagnetic techniques. Negative selection typically yields higher purity and preserves native functionality by avoiding antibody binding to critical surface receptors [27].
T-cell Activation and Expansion Protocol: The expansion protocol must balance achieving sufficient cell numbers while maintaining therapeutic potency and preventing terminal differentiation.
Table 2: Optimized T-cell Expansion Protocol Parameters
| Parameter | Optimal Condition | Alternative Options | Impact on Expansion |
|---|---|---|---|
| Initial Seeding Density | 1×10⁶ cells/mL | 0.5-2×10⁶ cells/mL | Higher densities can limit expansion potential [28] |
| Activation Method | ImmunoCult CD3/CD28/CD2 T-cell Activator at 25 μL/mL | CD3/CD28 beads alone | Triple activation enhances expansion (405±174-fold vs 240±90-fold) [28] |
| Cytokine Supplementation | 10 ng/mL IL-2 | IL-7, IL-15 for memory phenotypes | IL-2 supports robust expansion but may drive differentiation [28] |
| Day 3 Dilution | 8-fold volume increase | 4-16 fold increases | Critical optimization point; 8-fold increase maximizes expansion [28] |
| Subsequent Dilutions | 4-fold increases on days 5 & 7 | Variable based on cell density | Maintains cells at optimal density (1-2.5×10⁵ cells/mL) [28] |
| Total Expansion Period | 10-14 days | 7-21 days depending on application | Longer cultures risk differentiation and exhaustion [28] |
Detailed Expansion Methodology:
- Day 0 - Activation: Resuspend isolated T-cells at 1×10⁶ cells/mL in ImmunoCult-XF T Cell Expansion Medium supplemented with 10 ng/mL recombinant human IL-2. Add ImmunoCult Human CD3/CD28/CD2 T Cell Activator at 25 μL/mL [28].
- Day 3 - First Dilution: Increase total culture volume 8-fold with fresh medium containing IL-2. This critical step reduces cell density to approximately 1.25×10⁵ cells/mL, preventing contact-mediated inhibition and replenishing nutrients [28].
- Days 5 & 7 - Subsequent Dilutions: Perform 4-fold volume increases with fresh medium to maintain cells within the optimal density range of 1-2.5×10⁵ cells/mL [28].
- Days 10-14 - Harvest: When expansion plateaus (typically 800-fold expansion achievable), harvest cells for genetic modification or formulation. Monitor viability throughout, aiming for >85% [28].
This optimized protocol emphasizes the importance of early cell dilution, with day 3 identified as a critical intervention point for maximizing expansion potential. Research indicates that maintaining T-cells at lower densities during early expansion phases significantly improves both cell growth and viability, potentially by increasing nutrient availability per cell after activation signals have been received [28].
Genetic Modification (CAR Transduction)
For chimeric antigen receptor (CAR) T-cell therapies, genetic modification typically occurs following activation and prior to the main expansion phase.
Transduction Protocol:
- Timing: Transduce activated T-cells 24-48 hours post-activation, when cells are actively proliferating and most receptive to genetic modification.
- Viral Vector Application: Add lentiviral or retroviral vectors containing the CAR construct at appropriate multiplicity of infection (MOI), typically ranging from 1-10, depending on vector potency and cell type.
- Enhancement Strategies: Consider incorporating transduction enhancers such as retronectin or protamine sulfate to improve transduction efficiency.
- Expansion: Continue culture expansion post-transduction according to the established protocol, typically for 7-10 additional days to achieve therapeutic cell numbers.
The critical manufacturing challenge for autologous CAR-T therapies lies in maintaining consistent transduction efficiency and CAR expression across patient-specific batches with variable starting T-cell quality [8] [3].
Product Formulation, Cryopreservation, and Re-infusion
The final manufacturing stages focus on product formulation, quality control, and administration.
Formulation and Cryopreservation:
- Formulation: Wash and resuspend expanded cells in appropriate cryopreservation medium containing protein stabilizer (e.g., human serum albumin) and cryoprotectant (e.g., DMSO).
- Cryopreservation: Controlled-rate freezing followed by storage in vapor-phase liquid nitrogen ensures product stability during storage and transport.
Quality Control Testing: Each autologous product must undergo rigorous release testing including:
- Identity: Confirmation of cell type and CAR expression (if applicable)
- Potency: Cytotoxic activity against target cells
- Purity: Percentage of desired cell population
- Safety: Sterility, mycoplasma, endotoxin, and replication-competent virus testing
Patient Conditioning and Re-infusion:
- Lymphodepleting Chemotherapy: Patients typically receive conditioning chemotherapy (commonly fludarabine and cyclophosphamide) 2-7 days before infusion to enhance engraftment and persistence of therapeutic cells.
- Product Administration: Thaw cryopreserved product at bedside and administer via intravenous infusion according to established protocols, with appropriate premedication and monitoring for acute reactions.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Autologous Cell Therapy
| Reagent/Material | Function | Example Products | Application Notes |
|---|---|---|---|
| Cell Separation Media | Density gradient isolation of PBMCs | Ficoll-Paque Premium | Maintain sterile technique; process samples promptly after collection [27] |
| Immunomagnetic Cell Separation Kits | Negative or positive selection of target cells | EasySep Human T-cell Isolation Kit | Negative selection preserves native receptor function [27] |
| T-cell Activation Reagents | Polyclonal T-cell activation via CD3/CD28 signaling | ImmunoCult CD3/CD28/CD2 T Cell Activator | Triple activation enhances expansion compared to CD3/CD28 alone [28] |
| Cell Expansion Medium | Optimized nutrient formulation for T-cell growth | ImmunoCult-XF T Cell Expansion Medium | Xeno-free formulation suitable for clinical applications [28] |
| Recombinant Cytokines | Support T-cell proliferation and survival | Human Recombinant IL-2 | Concentration optimization critical (typically 10-100 IU/mL) [28] |
| Viral Vectors | Delivery of genetic material for modification | Lentiviral, retroviral vectors | Quality critical for consistent transduction efficiency [8] |
| Flow Cytometry Antibodies | Cell phenotyping and quantification | CD34, CD3, CD45, CD4, CD8 antibodies | ISHAGE protocol standard for CD34+ enumeration [26] |
Comparative Analysis: Autologous vs. Allogeneic Approaches
The autologous process described above differs fundamentally from allogeneic approaches in several key aspects that impact manufacturing strategy and clinical application.
Table 4: Autologous vs. Allogeneic Manufacturing Considerations
| Characteristic | Autologous Process | Allogeneic Process |
|---|---|---|
| Starting Material | Patient-derived cells (variable quality) | Healthy donor cells (consistent quality) [8] |
| Manufacturing Model | Patient-specific batch | Large-scale, off-the-shelf batches [8] [11] |
| Production Timeline | Several weeks | Immediate availability from cryostock [8] |
| Immune Compatibility | Perfect match; no rejection risk | Requires HLA matching or immunosuppression [8] |
| Manufacturing Cost | High per batch (service model) | Lower per dose (mass production model) [25] [11] |
| Scalability | Limited by patient-specific logistics | Highly scalable for broad distribution [8] [11] |
| Product Consistency | High variability between batches | Highly consistent across doses [11] |
| Regulatory Challenges | Complex chain of identity management | Standardized manufacturing controls [11] |
Technical Challenges and Innovative Solutions
The autologous cell therapy process faces several persistent challenges that drive ongoing research and development:
Manufacturing Efficiency: The high cost of autologous therapies (ranging from $300,000-$500,000 per patient) stems from complex, labor-intensive manufacturing processes [25]. Emerging solutions include:
- Automation and AI Integration: AI-powered systems are being implemented to optimize manufacturing, reduce costs, and improve scalability. Platforms utilizing predictive analytics, digital twins, and reinforcement learning algorithms enable adaptive manufacturing of CAR-T and iPSC-based autologous therapies [25].
- Process Intensification: Research focuses on shortening production timelines through rapid expansion protocols and reducing manual operations through closed automated systems [3].
Supply Chain Complexity: The patient-specific supply chain for autologous therapies introduces unique challenges in cold-chain maintenance, strict time constraints, and end-to-end traceability [3]. Innovative approaches include:
- Decentralized Manufacturing: Movement toward patient-adjacent, regionalized manufacturing facilities to reduce logistics complexity [3].
- Advanced Tracking Systems: Robust digital infrastructure to maintain chain-of-identity and chain-of-custody across the entire process [11].
Product Quality and Variability: The inherent variability of patient-derived starting material necessitates adaptive manufacturing approaches. Strategies include:
- Process Analytical Technologies: Implementation of real-time monitoring systems to adjust processes based on incoming cell quality [3].
- Alternative Cell Sources: Investigation of rejuvenation strategies for cells from heavily pretreated patients [8].
The autologous cell therapy process, from leukapheresis to re-infusion, represents a remarkable convergence of medical science and precision manufacturing. While technically demanding and resource-intensive, this patient-specific approach offers unparalleled immunological compatibility and has demonstrated transformative potential for conditions with limited treatment options. The continued refinement of activation protocols, expansion methodologies, and manufacturing technologies will be crucial for enhancing the efficiency, consistency, and accessibility of autologous therapies. As the field advances, integration of automation, artificial intelligence, and innovative supply chain solutions promises to address current limitations while maintaining the fundamental personalized nature of autologous treatment. The optimized protocols and technical insights provided in this application note serve as a foundation for researchers and clinicians working to advance this rapidly evolving field and bring the benefits of autologous cell therapy to broader patient populations.
Within the rapidly advancing field of regenerative medicine, the therapeutic paradigm is shifting from personalized, patient-specific (autologous) treatments toward scalable, donor-derived (allogeneic) "off-the-shelf" products [11]. This transition is fundamentally enabled by the creation of Master Cell Banks (MCBs)—highly characterized, uniform cell populations that serve as the perpetual starting material for producing thousands of therapeutic doses [4]. The establishment of robust MCBs is critical for ensuring the long-term consistency, safety, and commercial viability of allogeneic therapies, which are poised for significant market growth with a projected CAGR of 15.0% to 27.41% [29] [30].
Framed within a broader thesis comparing allogeneic and autologous expansion protocols, this document details the application notes and experimental protocols for generating and qualifying MCBs. The allogeneic approach offers a substantial manufacturing cost advantage, with estimated production costs of £930–1140 per dose compared to £2260–3040 for autologous therapies, largely due to standardized donor testing and batch release processes [4]. The following sections provide a detailed methodology for creating these foundational MCBs, a cornerstone for scaling up allogeneic cell therapies.
Application Notes: The Role and Importance of Master Cell Banks
Fundamental Principles of Master Cell Banks
An MCB is a collection of cells of uniform composition derived from a single tissue source, processed, cultured, and preserved under defined conditions. It serves as the primary source for all future production runs, ensuring a consistent and reproducible starting material for many years [4]. The key advantage of an MCB-based system is its ability to supply a virtually limitless number of doses for thousands of patients from a single, thoroughly qualified donor source [11] [8].
Strategic Advantages in Allogeneic Scale-Up
The use of an MCB system directly addresses several critical challenges in cell therapy manufacturing:
- Scalability and Cost-Effectiveness: Once established, an MCB enables the production of therapies on a commercial scale, dramatically reducing the per-dose cost of goods. This creates a more financially sustainable model compared to the complex, patient-specific "service-based" logistics of autologous therapies [11] [4].
- Product Consistency and Quality Control: By originating from a single, well-characterized donor, the MCB ensures unprecedented batch-to-batch consistency. This minimizes the product heterogeneity often encountered in autologous systems, where the patient's age, disease state, and prior treatments can compromise cell quality and potency [8] [4].
- Regulatory Path and "Off-the-Shelf" Availability: A fully qualified MCB is a key regulatory requirement. It underpins the "off-the-shelf" business model, allowing therapies to be produced, quality-tested, and made readily available for acute medical conditions, eliminating the weeks-long manufacturing wait associated with autologous treatments [11] [31].
Table 1: Quantitative Impact of Master Cell Bank Implementation on Manufacturing
| Manufacturing Aspect | Autologous Model (Per Patient) | Allogeneic Model (with MCB) |
|---|---|---|
| Donor Screening Cost (per dose) | £990–1320 [4] | £10–20 [4] |
| Release Testing Cost (per dose) | £300–500 (per batch of one) [4] | £3–5 (per batch of 100 doses) [4] |
| Total Manufacturing Cost (per dose) | £2260–3040 [4] | £930–1140 [4] |
| Product Availability | Weeks of turnaround time [11] [8] | Immediate, "off-the-shelf" [11] [8] |
| Batch Consistency | High variability between patients [8] | High consistency from a single source [4] |
Experimental Protocols
This protocol outlines the complete workflow for establishing a GMP-compliant Master Cell Bank, from donor selection to the cryopreservation of the MCB vials.
The following diagram illustrates the multi-stage workflow for creating a Master Cell Bank, from donor selection to the generation of a Working Cell Bank for production.
Diagram 1: Master Cell Bank Establishment Workflow.
Detailed Protocol Steps
Step 1: Donor Screening and Tissue Acquisition
- Objective: To identify a suitable healthy donor and acquire starting material free of adventitious agents and genetic abnormalities.
- Procedure:
- Donor Recruitment: Recruit a healthy donor following informed consent and ethical approval per ISSCR guidelines and local regulations [32].
- Comprehensive Donor Testing: Perform extensive screening on the donor. This includes:
- Infectious Disease Testing: Serological and molecular testing for HIV-1/2, HBV, HCV, HTLV, Syphilis, and other relevant pathogens.
- Genetic Screening: Karyotyping and genetic analysis to rule out predispositions to pertinent diseases (e.g., cancer) [4].
- Tissue Harvesting: Under aseptic conditions, collect the source tissue (e.g., peripheral blood, bone marrow, cord blood). For induced pluripotent stem cells (iPSCs), collect fibroblasts or peripheral blood mononuclear cells (PBMCs) as the starting material [31].
- Critical Reagents: Donor history questionnaire, sterile collection kits, pathogen test kits, cell culture medium.
Step 2: Cell Isolation, Reprogramming, and Expansion
- Objective: To establish a pure, undifferentiated, and expandable cell population from the donor tissue.
- Procedure:
- Cell Isolation: Isolate the target cell population using density gradient centrifugation (for MNCs) or enzymatic digestion (for tissues). For mesenchymal stem cells (MSCs), use plastic adherence selection [8].
- Reprogramming (for iPSC lines): If generating an iPSC-MCB, transfer the isolated somatic cells with non-integrating reprogramming vectors (e.g., Sendai virus, episomal plasmids) to create clonal induced pluripotent stem cell lines [31]. This step is bypassed for primary cell lines (e.g., primary MSCs).
- Clonal Selection & Expansion: Plate cells at clonal density. Manually pick and expand morphologically superior colonies to establish a clonal cell line. Culture and expand the cells over multiple passages in a GMP-compliant, xeno-free medium to achieve the target cell number for banking [33].
- Critical Reagents: GMP-grade enzymes (e.g., Collagenase), xeno-free cell culture media and growth factors, recombinant trypsin/EDTA, non-integrating reprogramming vectors.
Step 3: Master Cell Bank Creation and Cryopreservation
- Objective: To create a large inventory of characterized, cryopreserved cells at a low passage number.
- Procedure:
- Harvesting: When the culture reaches the desired cell density and population doublings, detach the cells using a gentle enzyme.
- Formulation: Wash and resuspend the cell pellet in a GMP-grade cryopreservation medium (e.g., containing 10% DMSO and a protein source like human serum albumin).
- Vialing & Controlled-Rate Freezing: Aseptically aliquot the cell suspension into several hundred cryovials (e.g., 1-5 x 10^6 cells/vial). Place the vials in a controlled-rate freezer, cooling at -1°C/min to -80°C to minimize ice crystal formation.
- Long-Term Storage: Transfer the vials to the vapor phase of a liquid nitrogen storage tank (-135°C to -196°C) for long-term preservation. Maintain a detailed inventory and chain-of-custody log.
- Critical Reagents: GMP-grade cryoprotectant (e.g., DMSO), formulation buffer, controlled-rate freezer, validated liquid nitrogen storage system.
Step 4: Quality Control and Characterization of the MCB
- Objective: To ensure the MCB's safety, identity, purity, and potency before its use in production.
- Procedure: Perform the following tests on representative vials thawed from the MCB.
Table 2: Master Cell Bank Quality Control Tests and Specifications
| Test Category | Specific Assay | Acceptance Criteria |
|---|---|---|
| Safety | Sterility (USP <71>) | No microbial growth [33] |
| Mycoplasma (e.g., PCR) | Negative | |
| Endotoxin (LAL) | < 0.5 EU/mL | |
| In vitro Adventitious Virus Assay | Negative | |
| Identity | Short Tandem Repeat (STR) Profiling | Matches donor sample [33] |
| Flow Cytometry for Cell Surface Markers | ≥ 95% positive for expected markers (e.g., CD73, CD90, CD105 for MSCs; Tra-1-60, SSEA-4 for iPSCs) [8] | |
| Purity | Viability (e.g., Trypan Blue Exclusion) | ≥ 90% post-thaw |
| Flow Cytometry for Contaminating Markers | ≤ 2% positive for lineage-specific markers not expected | |
| Potency | In vitro Differentiation Assay (e.g., to osteo-, adipo-, chondro-lineages) | Demonstration of multi-lineage potential [33] |
| Functional Assay (e.g., immunomodulation) | Meets established product-specific benchmarks | |
| Genetic Stability | Karyotyping (G-banding) | Normal diploid karyotype |
| Copy Number Variant (CNV) Analysis | No major aberrations |
Step 5: Working Cell Bank (WCB) Generation
- Objective: To create an intermediate bank from the MCB to supply the manufacturing process without exhausting the master bank.
- Procedure: Thaw one vial of the qualified MCB. Expand the cells for a limited number of population doublings (typically 2-4 passages) under the same conditions used for the MCB. Harvest, cryopreserve, and quality-control the WCB vials using a subset of the tests performed on the MCB (e.g., viability, sterility, mycoplasma, identity). A single WCB is used to generate one batch of the final product [4].
The Scientist's Toolkit: Essential Reagent Solutions
The following table lists key reagents and materials critical for the successful execution of the MCB establishment protocol.
Table 3: Essential Research Reagent Solutions for MCB Generation
| Reagent/Material | Function & Role in MCB Protocol | Key Considerations |
|---|---|---|
| GMP-Grade Culture Media | Supports cell growth, expansion, and maintenance of cell phenotype. | Must be xeno-free and chemically defined to ensure consistency and reduce risk of contamination [33]. |
| Pathogen Test Kits | Detects infectious agents in donor samples and final MCB to ensure product safety. | Kits must be validated for high sensitivity and specificity per regulatory standards (e.g., FDA, EMA) [4]. |
| Non-Integrating Reprogramming Vectors | For iPSC-MCB generation; safely reverts somatic cells to pluripotency without genomic integration. | Use of Sendai virus or episomal plasmids minimizes risk of insertional mutagenesis, a key safety concern [31]. |
| GMP-Grade Cryopreservation Medium | Protects cells from ice crystal damage during freezing and long-term storage. | Contains DMSO and a protein stabilizer (e.g., HSA). Must be pre-qualified for cell viability and recovery post-thaw. |
| Characterization Antibodies | Used in flow cytometry to confirm cell identity (e.g., MSC or pluripotency markers) and purity. | Antibody panels must be validated for specificity to ensure accurate characterization of the cell product [33]. |
The creation of a rigorously characterized Master Cell Bank is a foundational and non-negotiable step in the development of safe, effective, and commercially viable allogeneic cell therapies. The protocols outlined here provide a roadmap for establishing an MCB that meets regulatory standards and supports the scalable production of "off-the-shelf" treatments. By implementing this structured approach, researchers and drug development professionals can overcome the key limitations of autologous therapies, paving the way for broader patient access to the transformative promise of regenerative medicine.
The development of allogeneic ("off-the-shelf") cell therapies represents a paradigm shift in the treatment of cancer and autoimmune diseases, aiming to overcome critical limitations of autologous therapies, including high costs, labor-intensive manufacturing, and lengthy production timelines [9] [34]. A central challenge in this field is balancing the dual objectives of enhancing therapeutic potency while simultaneously overcoming host immune rejection. Allogeneic cells, derived from healthy donors, face elimination by the recipient's immune system through two primary mechanisms: allorejection by host T cells recognizing foreign human leukocyte antigen (HLA) molecules, and graft-versus-host disease (GvHD) wherein donor T cells attack recipient tissues [34] [35]. This application note details cutting-edge genetic engineering strategies and provides standardized protocols to address these challenges, providing a framework for researchers developing next-generation allogeneic cell therapies.
Strategic Approaches to Overcome Allorejection
HLA Engineering for Immune Evasion
A cornerstone of allogeneic cell therapy is engineering donor cells to evade host immune detection. Strategies focus on modifying the HLA complex to reduce its immunogenicity while retaining protective functions.
Table 1: HLA Engineering Strategies for Immune Evasion
| Strategy | Genetic Approach | Key Molecular Targets | Functional Outcome | Reported Editing Efficiency |
|---|---|---|---|---|
| HLA Class I/II Knockout | CRISPR-Cas9 nuclease editing [36] | HLA-A, HLA-B, CIITA (Class II regulator) [36] | Prevents CD8+ and CD4+ T cell allorecognition | High (>80% KO) [36] |
| HLA-C Retention | Base editing (Nme2Cas9) [36] | Selective KO of HLA-A/B while retaining HLA-C | Protects from NK cell-mediated killing via KIR interaction [36] | High, with precise allele retention [36] |
| HLA Camouflage | Overexpression of non-classical HLA molecules [34] | HLA-E, HLA-G | Engages NK inhibitory receptors (NKG2A/CD94) to suppress NK cell activity [34] | N/A |
Protocol: Multiplex Base Editing for HLA Engineering
This protocol details the generation of HLA-engineered T cells or iPSCs using cytosine base editors to knockout HLA-A and HLA-B while preserving HLA-C.
Materials:
- Nme2Cas9 Cytosine Base Editor: For precise C-to-T conversion without double-strand breaks [36].
- sgRNAs: Designed against PAM sites in the HLA-A and HLA-B gene sequences.
- Lipid Nanoparticles (LNPs): For delivery of base editor mRNA and sgRNAs [36].
- Activated Human T Cells or iPSCs: From a homozygous HLA-C donor.
- Flow Cytometry Antibodies: For HLA-A, HLA-B, and HLA-C surface staining to validate editing.
Procedure:
- Cell Preparation: Activate and expand T cells from a donor homozygous for a common HLA-C allele using anti-CD3/CD28 beads. Alternatively, culture and passage iPSCs from a similar donor.
- RNP Complex Formation: Complex the Nme2Cas9 base editor mRNA and sgRNA targeting HLA-A and HLA-B.
- Electroporation/Delivery: Deliver the ribonucleoprotein (RNP) complexes into the target cells via electroporation. Alternatively, use LNPs for delivery [36].
- Recovery and Expansion: Culture cells in appropriate medium (e.g., X-VIVO 15 for T cells, mTeSR for iPSCs). Allow 4-7 days for expression and editing.
- Validation: Analyze edited cells by flow cytometry to confirm loss of HLA-A/B expression and retention of HLA-C. Perform Sanger sequencing or next-generation sequencing (NGS) on target loci to confirm base conversions and assess off-target effects.
Strategies to Enhance Therapeutic Potency and Persistence
Genetic Modifications to Boost Anti-Tumor Function
Overcoming the hostile tumor microenvironment and preventing T cell exhaustion are critical for sustained efficacy. "Armoring" CAR cells with additional genes can significantly enhance their potency.
Table 2: Genetic Modifications for Enhanced CAR Cell Potency
| Modification Type | Example Transgene/Action | Mechanism of Action | Observed Outcome in Preclinical/Clinical Studies |
|---|---|---|---|
| Cytokine Armoring | Membrane-bound IL-15 (mbIL-15) [34] | Provides constitutive pro-survival and proliferative signals | Improves in vivo persistence and antitumor activity [34] |
| Cytokine Armoring | IL-21 signaling at culture initiation [37] | Directs T cells toward favorable memory phenotypes | Long-lasting effects on expansion and function [37] |
| Inhibitory Receptor KO | CRISPR knockout of intracellular checkpoints (e.g., ARIH2, CCNC) [5] | Removes intrinsic barriers to NK/T cell activation | Enhances tumor killing and cytokine production; identified via CRISPR screens [5] |
| "Dagger" Technology | CD70-targeting CAR alongside tumor-targeting CAR [38] | Depletes host CD70+ alloreactive T cells, reducing rejection | Enables expansion and persistence in mismatched hosts; may reduce need for lymphodepletion [38] |
| CAR Design Innovation | Single ITAM CAR signaling [34] | Alters intracellular signaling kinetics | Balances effector function and memory formation, improving persistence [34] |
Protocol: CRISPR Screening to Identify Potency-Enhancing Targets
Genome-wide CRISPR knockout screens in primary human NK cells (e.g., the PreCiSE tool) can systematically identify genes whose disruption enhances function [5].
Materials:
- Genome-Wide CRISPR Library: A lentiviral library containing sgRNAs targeting thousands of human genes.
- Primary Human NK Cells: Isolated from healthy donor PBMCs.
- Activation Cytokines: IL-2, IL-15, IL-21.
- Tumor Cell Co-culture System: To model the immunosuppressive tumor microenvironment.
- Next-Generation Sequencing (NGS) Platform.
Procedure:
- Virus Production: Package the genome-wide CRISPR sgRNA library into lentiviral particles.
- NK Cell Transduction: Activate primary NK cells with cytokines and transduce with the lentiviral CRISPR library at a low MOI to ensure one sgRNA per cell.
- Selection and Expansion: Select transduced cells with puromycin and expand the population.
- Functional Pressure: Co-culture the sgRNA-expressing NK cell pool with target tumor cells for multiple days. A control group is cultured without tumor pressure.
- Genomic DNA Extraction and NGS: After the selection period, extract genomic DNA from both the pressure-treated and control cells. Amplify the integrated sgRNA sequences by PCR and subject them to NGS.
- Data Analysis: sgRNAs that are enriched in the surviving NK cell population after tumor co-culture represent knockouts that confer a survival or functional advantage. These are considered hits for enhancing NK cell potency [5].
Integrated Workflow and Reagent Solutions
The following diagram illustrates a consolidated workflow for creating a potent, immune-evasive allogeneic cell therapy product, integrating the strategies described above.
Diagram Title: Allogeneic CAR Cell Engineering Workflow
Table 3: Research Reagent Solutions for Allogeneic Cell Engineering
| Reagent/Category | Specific Example | Function in Protocol |
|---|---|---|
| Gene Editing Tools | Nme2Cas9 Cytosine Base Editor [36] | Enables precise single-nucleotide editing without double-strand breaks for HLA engineering. |
| CRISPR-Cas9 Nuclease (SpyCas9) [34] [36] | Knocks out TCR and endogenous genes; integrates CAR transgene. | |
| Delivery Systems | Lipid Nanoparticles (LNPs) [36] | Delivers editing machinery (mRNA, sgRNA) into cells. |
| Adeno-associated Virus (AAV) [36] | Serves as a template for homology-directed repair (HDR) during site-specific CAR integration. | |
| Activation/Expansion | Anti-CD3/CD28 Antibodies [37] | Activates and expands T cells ex vivo. |
| Cytokine Combinations (IL-2, IL-15, IL-21) [37] | Promotes NK cell expansion and survival in feeder-free cultures. | |
| Engineering Targets | sgRNAs targeting TRAC, HLA-A/B, CIITA [34] [36] | Guides nucleases to specific genomic loci for knockout. |
| CAR Constructs (CD19, BCMA, CD70) [34] [38] | Confers antigen-specific tumor recognition. | |
| Safety Switches | RQR8 "suicide gene" [34] | Allows for ablation of engineered cells via clinical-grade antibody (Rituximab) in case of adverse events. |
The future of allogeneic cell therapy hinges on sophisticated genetic engineering that concurrently tackles immune rejection and enhances anti-disease potency. The protocols and data summarized here provide a roadmap for developing robust, "off-the-shelf" cellular products. As the field progresses, the integration of multiplexed base editing, innovative CAR designs, and insights from functional genomic screens will be crucial for advancing these transformative therapies from the bench to the clinic, potentially offering broader access to patients with cancer and autoimmune diseases.
Cell-based therapies represent a paradigm shift in treating conditions ranging from hematologic malignancies to degenerative diseases. These therapies primarily fall into two categories: autologous (using the patient's own cells) and allogeneic (using cells from a healthy donor) [11]. The choice between these approaches involves critical trade-offs in manufacturing complexity, immunological compatibility, scalability, and cost [11] [4] [39]. This article provides detailed application notes and protocols for researchers, framing the discussion within a broader thesis on cell expansion protocols. We present structured data, experimental methodologies, and visualization tools to inform preclinical and clinical development.
Clinical Applications and Case Studies
Oncology
Chimeric Antigen Receptor (CAR)-T Cell Therapy has demonstrated exceptional efficacy in hematologic malignancies such as acute lymphoblastic leukemia and lymphoma [40]. However, its application to solid tumors faces significant hurdles, including antigen heterogeneity, an immunosuppressive tumor microenvironment (TME), and limited trafficking and infiltration into tumor sites [40].
- Case Study: Dual-Targeting CAR-T for Glioblastoma
- Challenge: Antigen escape in solid tumors, where tumor cells stop expressing the single target antigen [40].
- Protocol: CAR-T cells are engineered to target both HER2 and IL13Rα2 to reduce antigen escape [40].
- Outcome: This dual-targeting strategy has shown improved efficacy in preclinical glioblastoma models by addressing tumor heterogeneity [40].
Allogeneic "Off-the-Shelf" CAR-NK Cell Therapy is emerging as a promising alternative [9]. Derived from cord blood or induced pluripotent stem cells (iPSCs), allogeneic CAR-Natural Killer (NK) cells offer a lower risk of graft-versus-host disease (GvHD) and can be produced as a ready-to-use therapeutic [40] [9].
- Case Study: CAR-NK for Breast Cancer
- Challenge: Improving potency and specificity in solid tumors.
- Protocol: Engineering CAR-NK cells to target both HER2 and EGFR in breast cancer models [40].
- Outcome: These dual-targeting CAR-NK cells demonstrated enhanced tumor cell killing compared to single-target cells, showcasing a viable strategy for allogeneic therapy in solid tumors [40].
Autoimmunity
Allogeneic cell therapies are being explored for modulating aberrant immune responses in autoimmune diseases [9].
- Mechanism of Action: These therapies aim to restore immune tolerance by leveraging the immunomodulatory properties of certain cell types, such as mesenchymal stromal cells (MSCs) or regulatory T-cells (Tregs). Allogeneic approaches are particularly attractive here due to the potential for immediate "off-the-shelf" availability, which is critical during acute disease flares [9].
Regenerative Medicine
This field aims to repair or replace damaged tissues and organs. The choice between autologous and allogeneic sources depends on the clinical context.
Autologous Case Study: Orthopedic Repair
- Application: Treatment of knee osteoarthritis, rotator cuff tendonitis, and cartilage defects [41] [42].
- Protocol: A patient's bone marrow or adipose tissue is harvested. Mesenchymal stem cells (MSCs) are isolated, minimally manipulated, and reinjected into the damaged joint [41].
- Advantage: Minimal risk of immune rejection [11] [39].
Allogeneic Case Study: iPSC-Derived Dopamine Neurons for Parkinson's Disease
- Application: Cell replacement therapy [11].
- Protocol: iPSCs from a healthy donor are differentiated into midbrain dopamine neurons in a controlled, GMP-compliant environment before transplantation [11] [23].
- Advantage: Standardized, quality-controlled "off-the-shelf" product that is readily available, unlike a patient's own cells which may be affected by age or disease [11].
Quantitative Data Comparison
Table 1: Comparative Analysis of Autologous vs. Allogeneic Cell Therapies
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [11] [39] | Healthy donor (e.g., PBMCs, cord blood, iPSCs) [11] [9] |
| Key Advantage | Perfect HLA match; no GvHD risk [11] [39] | "Off-the-shelf" availability; scalable batch production [11] [9] |
| Key Challenge | Logistically complex, patient-specific production; high cost [11] [43] | Risk of immune rejection (GvHD & host rejection) [11] [40] |
| Manufacturing Model | Personalized, service-based [11] [43] | Batch production, scalable [11] [4] |
| Production Timeline | Several weeks [11] [39] | Pre-manufactured; immediate availability [11] [39] |
| Immunosuppression | Generally not required [11] | Often required to prevent rejection [11] |
| Estimated Manufacturing Cost/Dose | £2,260 - £3,040 (~$3,630 - $4,890) [4] | £930 - £1,140 (~$1,490 - $1,830) [4] |
| Therapeutic Persistence | Long-term (months/years) potential [11] | May be limited by host immune response [11] |
Table 2: Representative Therapy Costs by Indication (Patient Out-of-Pocket)
| Condition / Therapy Type | Cost Range (USD) | Notes |
|---|---|---|
| Orthopedic (Knee Injury) | $5,000 - $10,000 | Typically autologous, minimally manipulated procedures [41] [42] |
| Spinal Conditions | $10,000 - $20,000 | --- [42] |
| Multiple Sclerosis / ALS | $20,000 - $50,000+ | Often requires systemic approach; complex protocols [41] [42] |
| Autologous (General) | $5,000 - $15,000 | --- [42] |
| Allogeneic (General) | $20,000+ | Higher cost due to donor screening & processing [42] |
Experimental Protocols
Protocol 1: Manufacturing Autologous CAR-T Cells for B-Cell Malignancies
Objective: To manufacture genetically modified autologous T cells expressing a CD19-specific CAR for patient reinfusion.
Workflow Overview:
Materials:
- Starting Material: Patient leukapheresis product.
- Reagents: T-cell activation beads (e.g., TransACT), IL-2 cytokine, specialized cell culture media.
- Vector: Lentiviral vector encoding the anti-CD19 CAR construct.
- Equipment: Closed-system bioreactor (e.g., G-Rex), CO2 incubator, flow cytometer.
Detailed Steps:
- Cell Isolation & Activation: Isolate mononuclear cells (PBMCs) from the leukapheresis product via density gradient centrifugation. Activate T-cells using anti-CD3/CD28 beads and recombinant IL-2 (typically 100 IU/mL) for 24-48 hours [40].
- Genetic Modification: Transduce activated T-cells with the lentiviral CAR vector at a pre-optimized Multiplicity of Infection (MOI) in the presence of a transduction enhancer (e.g., protamine sulfate). Centrifuge plates to enhance viral contact (spinoculation) [40].
- Ex Vivo Expansion: Culture transduced cells in a closed-system bioreactor with IL-2-supplemented media for 7-10 days. Monitor cell density and viability daily, splitting cultures as needed to maintain optimal cell concentration [40] [43].
- Harvest & Formulation: Harvest cells when target cell numbers are met. Wash cells to remove media components and resuspend in cryopreservation medium containing DMSO. Fill final product into infusion bags [43].
- Quality Control (QC): Perform rigorous in-process and lot-release testing. This includes:
Protocol 2: Generating Allogeneic iPSC-Derived Dopamine Neurons
Objective: To differentiate allogeneic iPSCs into midbrain dopamine neurons for Parkinson's disease therapy.
Workflow Overview:
Materials:
- Starting Material: GMP-grade iPSC Master Cell Bank from a healthy donor [23].
- Small Molecules & Growth Factors: Recombinant SHH, FGF8b, CHIR99021 (GSK3 inhibitor), LDN-193189 (BMP inhibitor), BDNF, GDNF, Ascorbic Acid.
- Cell Culture: Defined neural induction medium, laminin-coated culture plates.
Detailed Steps:
- Midbrain Patterning: Dissociate iPSCs into single cells and seed them at high density. Initiate neural induction using dual-SMAD inhibition (e.g., SB431542 and LDN-193189). Simultaneously, pattern the cells toward a midbrain fate by adding SHH (100-500 ng/mL) and FGF8b (100 ng/mL) for 7-10 days [23].
- Floor Plate Induction: Continue culture with SHH and FGF8b, adding CHIR99021 (3 µM) to activate Wnt signaling. This promotes the formation of FOXA2+/LMX1A+ midbrain floor plate progenitor cells over ~7 days.
- Dopaminergic Differentiation: Withdraw patterning factors and transition cells to a differentiation medium containing BDNF (20 ng/mL), GDNF (20 ng/mL), Ascorbic Acid (0.2 mM), and db-cAMP (0.5 mM) to promote terminal differentiation into tyrosine hydroxylase (TH)-positive neurons over 2-3 weeks.
- Neuronal Maturation: Maintain cells in maturation media for an additional 2-4 weeks, allowing for the development of neuronal morphology and electrophysiological properties.
- Purification and QC: Harvest the cell population. Purity can be enhanced using fluorescence-activated cell sorting (FACS) for specific surface markers. Perform QC including:
- Identity: Immunostaining for TH, FOXA2, and Nurr1.
- Potency: HPLC measurement of dopamine secretion.
- Safety: Karyotyping and in vivo tumorigenicity assay in immunodeficient mice to exclude residual undifferentiated iPSCs [23].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Cell Therapy Development
| Reagent / Material | Function | Example Application |
|---|---|---|
| Lentiviral Vectors | Stable integration of genetic material (e.g., CAR) into host cell genome [40]. | CAR-T and CAR-NK cell engineering [40]. |
| Lymphodepleting Chemotherapy | Pre-conditioning regimen to deplete host immune cells, creating a favorable niche for engrafted cells [40]. | Administered prior to CAR-T cell infusion to enhance persistence and efficacy. |
| IL-2 Cytokine | T-cell growth factor that promotes activation and ex vivo expansion [40]. | Added to culture media during CAR-T cell manufacturing [40]. |
| SynNotch Receptors | Synthetic biology platform that allows for precise, user-defined logic-gated control of T-cell activation [40]. | Engineering T-cells that require two tumor antigens for activation, reducing "on-target, off-tumor" toxicity [40]. |
| iPSC Master Cell Bank | A characterized, GMP-compliant repository of pluripotent cells serving as the starting material for consistent, scalable production of differentiated cell types [9] [23]. | Generation of allogeneic dopamine neurons, cardiomyocytes, or immune cells [9] [23]. |
| Closed-System Bioreactors | Automated, scalable equipment for cell expansion in a sterile, controlled environment, minimizing manual handling and contamination risk [3] [43]. | Large-scale expansion of T-cells or iPSC-derived progenitors for allogeneic therapies [3]. |
The development of autologous and allogeneic cell therapies requires navigating a complex landscape of scientific, manufacturing, and clinical trade-offs. Autologous therapies offer a personalized approach with minimal immune risk but face hurdles in scalability, cost, and logistics. Allogeneic therapies promise an "off-the-shelf," scalable solution but must overcome challenges of host rejection and GvHD. The future lies in leveraging advancements in gene editing (e.g., to prevent GvHD), synthetic biology (e.g., logic-gated CARs), and automated, closed-system manufacturing to enhance the safety, efficacy, and accessibility of both modalities across oncology, autoimmunity, and regenerative medicine [11] [40] [9].
Navigating Complexities: Troubleshooting Manufacturing, Scaling, and Safety Hurdles
In the rapidly advancing field of cell therapy, managing variability in cell quality represents a fundamental challenge that directly impacts therapeutic efficacy, manufacturing success, and clinical outcomes. Both autologous (patient-derived) and allogeneic (donor-derived) approaches face distinct yet interconnected challenges in controlling variability, requiring specialized protocols to ensure consistent product quality [8] [12]. For autologous therapies, variability arises from patient-specific factors including disease status, prior treatments, and individual biological characteristics [8]. Allogeneic therapies, while offering the advantage of starting with healthy donor cells, introduce variability through donor-to-donor differences and immune compatibility considerations [12] [10]. This application note provides a structured framework of protocols and analytical methods to systematically address these variability challenges within cell expansion processes, specifically contextualized within the broader comparative analysis of allogeneic versus autologous research.
Table 1: Key Sources and Impacts of Cell Quality Variability
| Variability Source | Autologous Therapies | Allogeneic Therapies | Impact on Manufacturing |
|---|---|---|---|
| Starting Material Quality | Compromised by patient disease, age, prior treatments (chemotherapy/radiotherapy) [8] [3] | "High-grade" healthy donor material possible [12] | Determines expansion potential, success rates, and final cell yield [8] [3] |
| Immune Compatibility | Minimal concern (self-originating) [8] | Requires HLA matching or gene editing to avoid GvHD/rejection [8] [2] | dictates need for immunosuppression or complex engineering [8] |
| Manufacturing Success Rate | High variability; manufacturing failure rate 2-10% [2] | More standardized processes possible [12] | Impacts cost, planning, and patient access [3] [2] |
| Process Scalability | Limited (patient-specific batch) [8] | High (one batch for multiple patients) [8] [12] | Affects production economics and accessibility [12] |
| Product Potency | Variable due to patient T-cell fitness [3] | More consistent from healthy donors [12] | Correlates directly with clinical therapeutic efficacy [3] |
Table 2: Comparative Analysis of Cell Sources for Allogeneic Therapies
| Cell Source | Key Advantages | Key Limitations | Suitability for Scaling |
|---|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Established protocols; ability to create HLA-typed cell banks [2] | Donor-to-donor variability; limited expansion potential [12] | Moderate (dependent on donor availability) [12] |
| Umbilical Cord Blood (UCB) Cells | Antigen-naïve (reduced alloreactivity); lower exhaustion markers [2] | Limited cell numbers per donation [2] | Moderate-High (can use banked units) [2] |
| Induced Pluripotent Stem Cells (iPSCs) | Infinite self-renewal; genetically uniform population [10] [2] | Complex and lengthy differentiation protocols [2] | High (ideal for master cell banks) [10] [2] |
Experimental Protocols for Quality Management
Protocol 1: Pre-Manufacturing Donor and Patient Cell Quality Assessment
This protocol standardizes the evaluation of starting material for both autologous and allogeneic applications.
1.0 Sample Collection and Initial Processing
- 1.1 Collect patient (autologous) or donor (allogeneic) cells via leukapheresis following standard clinical procedures [12] [44].
- 1.2 Isolate Peripheral Blood Mononuclear Cells (PBMCs) using density gradient centrifugation (e.g., Ficoll-Paque PLUS).
- 1.3 Perform cell count and viability assessment using trypan blue exclusion on an automated cell counter.
2.0 Comprehensive Cell Phenotyping
- 2.1 Stain 1x10^6 cells with fluorochrome-conjugated antibodies against key surface markers:
- 2.2 Acquire data on a flow cytometer (e.g., BD Symphony A3) and analyze using FlowJo software.
- 2.3 Acceptance Criteria: For allogeneic donors, require <5% expression of exhaustion markers. For autologous material, document baseline levels.
3.0 Functional Potency Assay
- 3.1 Stimulate 1x10^5 cells with CD3/CD28 Dynabeads at 1:1 bead-to-cell ratio.
- 3.2 After 24 hours, collect supernatant and quantify cytokine production (IFN-γ, IL-2) via ELISA.
- 3.3 Acceptance Criteria: Healthy donor cells should produce >500 pg/mL IFN-γ upon stimulation.
Protocol 2: Rapamycin-Based Treg Expansion for Reduced Variability
This protocol utilizes rapamycin to maintain Treg phenotype and function during expansion, critical for managing variability in therapeutic Treg products [44].
1.0 Treg Isolation and Enrichment
- 1.1 Starting Material: PBMCs from leukapheresis (autologous) or healthy donor (allogeneic).
- 1.2 Enrich CD4+ T cells using negative selection magnetic bead kit (e.g., Miltenyi Biotec).
- 1.3 Further purify Tregs by sorting for CD4+CD25+CD127lo cells using flow cytometry (e.g., Sony sorter) [44].
2.0 Rapamycin-Supplemented Expansion
- 2.1 Culture Media: X-VIVO 15 serum-free media supplemented with 5% human AB serum, IL-2 (300 IU/mL).
- 2.2 Activation: Use CD3/CD28 Dynabeads at 1:1 bead-to-cell ratio.
- 2.3 Rapamycin Addition: Add rapamycin to culture medium at 100 nM final concentration on day 1 [44].
- 2.4 Culture Conditions: Maintain at 37°C, 5% CO2 for 14 days, feeding with fresh media + IL-2 every 2-3 days.
3.0 Quality Control Monitoring
- 3.1 Monitor cell count and viability every 2-3 days.
- 3.2 On day 7, reassess Treg phenotype (CD4+CD25+FOXP3+) via flow cytometry.
- 3.3 On day 14, perform functional suppression assay to confirm maintained potency.
Visualization of Workflows
Autologous vs. Allogeneic Cell Therapy Workflow
Variability Management Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Managing Cell Quality Variability
| Reagent / Material | Specific Function | Application Context |
|---|---|---|
| Rapamycin | mTOR inhibitor; selectively expands Tregs while suppressing effector T cells [44] | Critical for maintaining Treg phenotype during expansion for autoimmunity applications [44] |
| CD3/CD28 Activation Beads | Synthetic T-cell activator; provides primary and co-stimulatory signals [44] | Standardized T-cell activation for both autologous and allogeneic therapies [44] |
| Recombinant Human IL-2 | T-cell growth and survival factor; essential for ex vivo expansion [44] | Maintains T-cell viability and proliferation during culture period |
| Magnetic Cell Separation Beads | Antibody-conjugated beads for cell isolation (e.g., CD4+ T cells, CD25+ Tregs) [44] | Enables isolation of specific cell populations with high purity from heterogeneous mixtures |
| CRISPR/Cas9 Gene Editing System | Gene knockout (e.g., TCR) to reduce GvHD risk in allogeneic products [10] [2] | Creating universal allogeneic cell products with reduced host rejection |
| FOXP3 Staining Kit | Intracellular transcription factor staining for Treg identification [44] | Essential for verifying Treg phenotype maintenance during expansion |
Effectively managing donor and patient cell quality variability requires a multi-faceted approach that addresses both biological and technical sources of heterogeneity. For autologous therapies, this involves robust patient assessment and process adaptations to accommodate variable starting material. For allogeneic therapies, rigorous donor screening, advanced cell banking strategies, and genetic engineering approaches are key to ensuring consistency [10]. The integration of automated platforms, standardized quality control assays, and specialized culture protocols such as rapamycin-based Treg expansion provides a pathway toward more reproducible and potent cell therapy products [15] [44]. As the field progresses, the development of increasingly sophisticated analytical methods and process controls will be essential to overcome variability challenges and fully realize the therapeutic potential of both allogeneic and autologous cell therapies.
The advancement of cell-based therapies, particularly allogeneic treatments, is fundamentally challenged by significant immunological risks. Graft-versus-Host Disease (GvHD) and Host-versus-Graft (HvG) rejection represent two major, opposing immunological barriers that can compromise treatment efficacy and patient safety [45]. Furthermore, immune escape mechanisms, particularly in oncology, allow malignancies to evade immune surveillance, leading to disease relapse [46]. This Application Note details these interconnected risks and provides structured protocols and data analysis frameworks to support the development of robust mitigation strategies, contextualized within the comparative analysis of allogeneic versus autologous cell expansion paradigms.
Comparative Immunological Risk Profiles: Allogeneic vs. Autologous Approaches
The core distinction between autologous (using patient's own cells) and allogeneic (using donor-derived cells) therapies dictates their inherent immunological risk profiles, management requirements, and clinical applications [39].
Table 1: Key Immunological Differentiators Between Autologous and Allogeneic Cell Therapies
| Characteristic | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [39] | Healthy donor cells [39] |
| Immune Compatibility | High; minimal rejection risk [39] | Variable; requires HLA matching [45] |
| Primary Immune Risk | Minimal GvHD or HvG [39] | High risk for both GvHD and HvG rejection [45] |
| GvHD Risk | Negligible [39] | 40-80% (acute, depending on match) [45] |
| Immunosuppression | Generally not required [39] | Essential, often for 6+ months [45] |
| Graft-versus-Tumor Effect | Limited or absent [47] | Potent; can reduce relapse [48] |
| Manufacturing Scale | Patient-specific, complex logistics [39] | Batch production, "off-the-shelf" potential [9] [39] |
Quantitative Data on Clinical Complications and Outcomes
Understanding the incidence and impact of these immunological events is critical for risk-benefit assessment and study design.
Table 2: Incidence and Impact of Key Immunological Complications
| Complication | Incidence Range | Key Contributing Factors | Impact on Mortality |
|---|---|---|---|
| Acute GvHD | 40% (HLA-matched sibling) to 80% (unrelated donor) [45] | HLA mismatch, older age, donor presensitization [45] | High in severe forms; death in 20-40% of chronic GvHD patients [45] |
| Chronic GvHD | 35-50% (HLA-matched sibling) to 60-70% (unrelated donor) [45] | History of acute GvHD, HLA mismatch [45] | Death in 20-40% of affected patients [45] |
| Disease Relapse (Allo-HSCT) | 10-40% [45] | Underlying disease, immune escape [46] | Leading cause of treatment failure [46] |
| HLA Loss Relapse | Up to ~30% in haploidentical transplants [49] | Haploidentical or mismatched donors [49] | Limits efficacy of donor lymphocyte infusions (DLI) [49] |
| Non-Relapse Mortality (Allo-SCT in Myeloma) | Up to 45% in some studies [50] | GvHD, infections, regimen toxicity [50] | Can outweigh therapeutic benefit [50] |
Protocols for Risk Mitigation
Protocol 1: Treg-Based GvHD Prophylaxis
Principle: Infuse regulatory T cells (Tregs) to modulate alloreactive T cell responses and re-establish immune tolerance, thereby reducing GvHD incidence while potentially preserving graft-versus-tumor effects [48].
Materials:
- Starting Material: Leukapheresis product from matched related or unrelated donor.
- Reagents: Anti-CD3/CD28 Dynabeads, IL-2, GMP-grade cell culture media.
- Consumables: CliniMACS Prodigy system with Treg selection kit.
- QC Assays: Flow cytometry (CD4, CD25, CD127, FOXP3), viability staining, endotoxin testing.
Experimental Workflow:
Key Steps:
- Cell Isolation: Isolate CD4+CD25+CD127lo Tregs from a donor leukapheresis product using clinical-grade magnetic-activated cell sorting (CliniMACS) [48].
- Ex Vivo Expansion: Culture isolated Tregs in GMP-grade media supplemented with anti-CD3/CD28 Dynabeads and high-dose IL-2 (1000 IU/mL) for 14-21 days to achieve therapeutic cell numbers [48].
- Harvest and Formulation: Remove activation beads, wash cells, and resuspend in infusion-ready medium. Perform final quality control checks for identity (FOXP3 positivity >80%), viability (>90%), and sterility [48].
- Infusion: Administer Tregs as a prophylactic infusion shortly after the primary stem cell graft, typically at a dose of 1-10 x 10^6 cells/kg [48].
Protocol 2: NGS-Based HLA Loss Detection at Relapse
Principle: Utilize a targeted Next-Generation Sequencing (NGS) assay to detect loss of heterozygosity in the HLA region, a major mechanism of immune escape, to guide post-relapse therapy [49].
Materials:
- Samples: Pre-transplant recipient genomic DNA, post-transplant bone marrow or blood (unsorted or cell-sorted fractions like CD33+).
- Reagents: HLA Loss Assay Kit (e.g., Devyser HLA loss), NGS library preparation reagents, Illumina sequencing reagents.
- Equipment: Illumina MiSeq or MiniSeq, Qubit fluorometer, thermal cycler.
- Software: Vendor-specific analysis suite for chimerism and HLA loss calculation.
Experimental Workflow:
Key Steps:
- Sample Preparation: Extract high-quality DNA from pre-transplant recipient and donor samples, as well as from post-relapse patient samples. Cell sorting of specific populations (e.g., CD33+ myeloid cells) is recommended for sensitivity [49].
- Target Amplification: Perform a single multiplex PCR reaction using primers for the 26 indel markers within the HLA region and 5 flanking markers on chromosome 6 [49].
- Library Preparation & Sequencing: Dilute the initial PCR product and use it as a template for a second PCR to add sequencing adapters and indices. Pool libraries and sequence on an Illumina platform (e.g., 2x75 bp cycles) [49].
- Data Analysis: Calculate allele frequencies for all indel markers. Compare the chimerism level derived from the HLA region markers to the baseline chimerism from other chromosomes (e.g., from a standard chimerism assay). A significant discrepancy (e.g., lower recipient chimerism in the HLA region) indicates HLA loss [49].
- Clinical Action: A positive HLA loss result suggests that Donor Lymphocyte Infusion (DLI) will be ineffective, as donor T cells cannot recognize the HLA-deficient leukemia cells. Alternative therapies should be pursued [49].
Protocol 3: Circadian Timing of Cell Infusion to Reduce GvHD
Principle: Schedule allogeneic stem cell infusions during the recipient's early active phase (before 2 p.m. for humans) to leverage circadian regulation of pro-inflammatory cytokines and reduce the incidence and severity of acute GvHD [51].
Materials:
- Cellular Product: Allogeneic hematopoietic stem cell graft.
- Reagents: Not applicable.
- Equipment: Standard infusion equipment.
- Assays: Clinical pathology for GvHD grading.
Experimental Workflow:
Key Steps:
- Scheduling: Coordinate with the transplant unit and cell processing lab to schedule the start of the stem cell infusion for the morning or early afternoon, ensuring completion before 2 p.m. [51].
- Infusion: Conduct the infusion according to standard clinical protocols, noting the precise start and end times.
- Monitoring: Monitor patients for the development and severity of acute GvHD according to institutional standards (e.g., MAGIC criteria) and compare outcomes between early and late infusion cohorts [51].
- Mechanistic Insight (Preclinical): Murine models indicate that early infusion (ZT5) correlates with lower levels of the pro-inflammatory cytokine IL-1α post-transplantation, resulting in reduced T cell alloreactivity and milder GvHD [51].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Allo-Immune Responses
| Reagent / Solution | Core Function | Application Example |
|---|---|---|
| CliniMACS CD4+CD25+ | Clinical-grade magnetic selection of human Tregs | Isolation of Tregs for expansion protocols in GvHD prophylaxis [48] |
| Anti-CD3/CD28 Dynabeads | Polyclonal activation and expansion of T cells | In vitro stimulation and large-scale expansion of isolated Tregs [48] [52] |
| Recombinant IL-2 | Supports survival and proliferation of activated T cells | Culture supplement for maintaining Treg fitness during expansion [48] |
| HLA Loss NGS Assay | Targeted sequencing of indel markers in HLA region | Detection of genomic HLA loss in relapsed patient samples [49] |
| Anti-IL-1α Neutralizing Antibody | Blocks IL-1α mediated inflammatory signaling | Preclinical tool to investigate cytokine modulation of GvHD [51] |
The successful implementation of allogeneic cell therapies requires a multi-faceted strategy to manage GvHD, HvG rejection, and immune escape. The protocols outlined here—from adoptive Treg transfer and sophisticated genomic monitoring to the simple yet powerful optimization of infusion timing—provide a actionable framework for mitigating these interconnected risks. Integrating these strategies into cell expansion and clinical protocols is paramount for improving the safety and efficacy profile of allogeneic therapies, ultimately widening their therapeutic application.
The transition from Good Laboratory Practice (GLP) to Good Manufacturing Practice (GMP)-compliant manufacturing represents a pivotal challenge in the development of advanced therapy medicinal products (ATMPs). This transition marks the crucial pathway from research and non-clinical safety studies to the production of clinical-grade therapies suitable for human administration [23]. For both allogeneic and autologous cell therapies, scaling manufacturing processes while maintaining product quality, safety, and efficacy presents unique biological, technical, and regulatory hurdles that must be systematically addressed [3] [23].
The fundamental distinction between GLP and GMP frameworks lies in their primary objectives: GLP focuses on protecting scientific data from contamination and ensuring the reliability and accuracy of non-clinical safety data, while GMP protects the final product from contamination and ensures it consistently meets predefined quality standards [23]. Successfully navigating this transition requires implementing robust, validated manufacturing processes that can reliably achieve the critical quality attributes (CQAs) identified during product development [23].
Comparative Analysis of Autologous vs. Allogeneic Scaling Challenges
Fundamental Differences in Scaling Approaches
The scaling challenges differ significantly between autologous and allogeneic cell therapy paradigms, influencing both technological approaches and business models [4]. Autologous therapies follow a patient-specific "service-based" model requiring complex coordination for collection, manufacturing, and delivery, while allogeneic therapies leverage a more traditional "off-the-shelf" model with batch production capabilities [8] [11] [39].
Table 1: Comparative Scaling Challenges for Autologous vs. Allogeneic Cell Therapies
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Production Model | Patient-specific, personalized | Batch production, "off-the-shelf" |
| Manufacturing Scale | Multiple small-scale batches | Large-scale batches from single donor |
| Key Scaling Challenge | Parallel processing of multiple patient-specific batches | Scaling up single batches while maintaining cell quality and function |
| Supply Chain Complexity | High (vein-to-vein logistics) | Lower (centralized manufacturing) |
| Cost Distribution | High per-dose cost (£2260-3040 per dose) [4] | Lower per-dose cost (£930-1140 per dose) [4] |
| Release Testing | Each batch (patient) requires full testing [4] | Single release test covers ~100 doses [4] |
| Donor Screening | Required for every patient [4] | Single screening for master cell bank [4] |
Quantitative Manufacturing Cost Analysis
Detailed cost analysis reveals that autologous therapy manufacturing costs approximately 2-3 times more than allogeneic approaches, primarily due to individualized donor screening and release testing requirements [4]. For autologous therapy, donor screening and testing costs approximately £990-1320 per patient, while release testing adds £300-500 per dose. In contrast, allogeneic therapy distributes these costs across multiple doses, reducing donor screening to £10-20 per dose and release testing to £3-5 per dose [4].
Table 2: Manufacturing Cost Breakdown (per dose) [4]
| Cost Component | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Donor Screening & Testing | £990-1320 | £10-20 |
| Release Testing | £300-500 | £3-5 |
| Cell Banking | Not applicable | £100-200 (amortized) |
| Facility & Equipment | £970-1220 | £817-915 |
| Total Manufacturing Cost | £2260-3040 | £930-1140 |
Core Technical Challenges in GLP to GMP Transition
Raw Material and Supply Chain Management
Securing a reliable supply of GMP-grade raw materials, reagents, and critical components presents a substantial logistical challenge, particularly for novel or specialized products [23]. Strategic partnerships and comprehensive supply chain management strategies are essential to establish reliable sources of GMP-compliant raw materials [23]. The variability in raw material quality can significantly impact final product quality, especially for sensitive cellular products.
Experimental Protocol 3.1: Qualification of GMP-Grade Raw Materials
- Objective: Establish qualification protocols for critical raw materials used in cell expansion processes
- Materials: Basal media, growth factors, cytokines, serum alternatives, dissociation reagents, cytokines, and coating matrices
- Methodology:
- Supplier Qualification: Audit suppliers for GMP compliance and quality management systems
- Incoming Testing: Perform identity, purity, potency, and sterility testing on all critical reagents
- Performance Qualification: Test multiple lots of materials using standardized cell culture assays
- Stability Studies: Establish shelf-life and storage conditions through accelerated and real-time stability testing
- Documentation: Maintain comprehensive traceability records including certificates of analysis
- Acceptance Criteria: Consistent cell growth, viability, phenotype, and functionality across multiple material lots
Process Validation and Comparability
A central challenge in scaling ATMPs is demonstrating product comparability after manufacturing process changes [23]. Regulatory authorities including the FDA, EMA, and MHLW have issued specific guidance emphasizing risk-based comparability assessments, extended analytical characterization, and staged testing to ensure process changes do not impact safety or efficacy [23].
Diagram 1: GLP to GMP Transition Workflow. This workflow outlines the systematic approach for transitioning from non-clinical process definition to validated GMP manufacturing, emphasizing the critical stages of quality attribute identification, process parameter definition, and rigorous qualification.
Cell Variability and Quality Control
Cells derived from patients or donors exhibit significant variability in quality, potency, and stability based on donor age, health status, and genetic background [8] [11]. Ensuring reproducible manufacturing processes that accommodate this variability presents a considerable challenge [23]. Standardized cell characterization and quality control assays are essential to ensure consistent cell product quality [23].
Experimental Protocol 3.3: Cell Characterization and Quality Control Panel
- Objective: Establish comprehensive quality control assays for cell therapy products
- Materials: Flow cytometer, PCR equipment, cell culture reagents, sterility testing media, endotoxin testing kit
- Methodology:
- Identity Testing: Flow cytometry for surface markers (≥3 markers), genetic identity testing
- Viability and Potency: Cell viability assays (≥70%), functional potency assays (dose-response)
- Purity and Impurities: Residual component testing, process-related impurity quantification
- Safety Testing: Sterility (14-day culture), mycoplasma (PCR and culture), endotoxin (<5 EU/kg)
- Stability Testing: Real-time and accelerated stability studies
- Acceptance Criteria: Meets all pre-defined specifications for identity, purity, potency, and safety
Scalable Cell Expansion Systems
Transitioning from laboratory-scale culture to large-scale cell expansion required for clinical applications presents significant technical challenges [23]. Extensive cell expansion can alter cellular phenotype and functionality, potentially impacting therapeutic efficacy [3]. Developing scalable, GMP-compliant cell expansion protocols using automated closed-system bioreactors represents a critical solution to this challenge [23].
Diagram 2: Scalable Cell Expansion Workflow. This diagram illustrates the sequential stages of scalable cell expansion from cell banking through harvest, highlighting critical in-process control points that ensure final product quality.
Regulatory Framework and Compliance Strategy
Current Regulatory Landscape
Regulatory bodies including the FDA and EMA have developed specific frameworks to address the unique challenges of ATMPs [23] [53]. The FDA's Regenerative Medicine Advanced Therapy (RMAT) designation and the EMA's PRIME (Priority Medicines) scheme offer expedited development pathways for promising therapies addressing unmet medical needs [53]. Both agencies have updated GMP guidelines specifically for cell therapy manufacturing, focusing on quality control, contamination prevention, and traceability [53].
Experimental Protocol 4.1: Regulatory Submission Preparation
- Objective: Prepare comprehensive Chemistry, Manufacturing, and Controls (CMC) documentation for regulatory submissions
- Materials: Complete manufacturing records, quality control data, analytical method validation reports, stability data
- Methodology:
- Manufacturing Process Description: Detailed, step-wise description of entire manufacturing process
- Control Strategy Documentation: Comprehensive description of in-process and release testing controls
- Analytical Method Validation: Validation reports for all critical analytical methods
- Comparability Data: Data demonstrating comparability between clinical and commercial processes
- Stability Data: Real-time and accelerated stability data supporting proposed shelf-life
- Deliverables: IND/IMPD CMC section, Quality Overall Summary, complete manufacturing documentation
Contamination Control and Aseptic Processing
Traditional sterilization methods are not feasible for cell-based products due to their inherent sensitivity [23]. The manufacturing process must occur under aseptic conditions, validated through media fill simulations [23]. Implementing closed, automated systems significantly reduces contamination risk while enhancing process consistency [4] [23].
Table 3: Contamination Control Strategy Elements
| Control Element | Implementation | Validation Approach |
|---|---|---|
| Environmental Monitoring | Periodic monitoring of production areas | Viable and non-viable particle monitoring, surface and air sampling |
| Personnel Training | Aseptic technique qualification | Media fill performance, ongoing competency assessment |
| Closed Processing | Automated closed-system bioreactors | System integrity testing, prevention of cross-contamination |
| Raw Material Control | GMP-grade materials, in-house testing | Sterility testing, endotoxin testing, bioburden monitoring |
| Process Validation | Aseptic process validation | Media fills simulating entire manufacturing process |
Emerging Technologies and Future Directions
Advanced Manufacturing Platforms
Innovative technologies including automated closed-system bioreactors, artificial intelligence (AI) for process monitoring, and dynamic culture systems are transforming ATMP manufacturing [3] [23]. These technologies address critical challenges in monitoring, automation, and data management while enhancing manufacturing consistency and scalability [23]. The industry is moving toward standardization and scalable manufacturing processes crucial for widespread adoption of allogeneic therapies [53].
Experimental Protocol 5.1: Implementation of Automated Bioreactor System
- Objective: Transition from manual culture to automated bioreactor-based expansion
- Materials: Automated closed-system bioreactor, single-use bioreactor vessels, perfusion systems, process analytical technology (PAT) tools
- Methodology:
- System Qualification: Installation qualification (IQ), operational qualification (OQ), performance qualification (PQ)
- Process Translation: Scale-down model development, parameter translation from manual process
- Process Optimization: DOE studies to optimize critical process parameters (pH, DO, feeding strategies)
- Process Validation: Three consecutive successful batches at target production scale
- Comparability Assessment: Comprehensive comparison of bioreactor vs. manual process products
- Success Criteria: Equivalent or superior product quality, increased consistency, reduced hands-on time
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagent Solutions for GMP Transition
| Reagent Category | Specific Examples | Function in Manufacturing | GMP Considerations |
|---|---|---|---|
| Cell Culture Media | Serum-free, xeno-free media formulations | Supports cell expansion while maintaining phenotype | Defined composition, GMP-grade, vendor qualification |
| Cell Separation Reagents | Magnetic-activated cell sorting (MACS) reagents, density gradient media | Isolation of target cell populations | Closed-system processing, minimal reagent carryover |
| Genetic Modification Tools | CRISPR-Cas9 systems, viral vectors (lentivirus, retrovirus) | Cell engineering for enhanced function | Safety testing, purity, potency, minimal off-target effects |
| Cryopreservation Solutions | DMSO-containing cryoprotectant solutions | Long-term storage of cell products | Formulation consistency, container compatibility |
| Cell Activation Reagents | Anti-CD3/CD28 antibodies, cytokines | T-cell activation for CAR-T manufacturing | Defined concentration, activity validation, endotoxin levels |
The transition from GLP to GMP-compliant manufacturing requires a systematic, phased approach addressing both technical and regulatory challenges. For allogeneic therapies, the focus must be on scalable expansion systems and comprehensive cell banking strategies, while autologous approaches require robust, parallel processing capabilities and patient-specific supply chain management. Implementing advanced technologies such as automated bioreactors, coupled with rigorous quality by design principles, provides a pathway to overcome current scaling limitations and enable broader patient access to these transformative therapies.
The future success of cell therapy manufacturing depends on continued innovation in scalable platforms, harmonized regulatory standards, and strategic partnerships across the development ecosystem. By addressing these scaling challenges systematically, the field can advance from bespoke production toward industrialized manufacturing capable of delivering these breakthrough therapies to growing patient populations worldwide.
The development of cell-based therapies represents a frontier in modern medicine, offering potential cures for previously untreatable conditions. However, their widespread application is severely constrained by high manufacturing costs and complex logistics. The strategic implementation of automation and Point-of-Care (PoC) manufacturing models addresses these challenges directly. For autologous therapies, where cells are harvested from and reintroduced into the same patient, PoC manufacturing simplifies a complex supply chain and reduces turnaround time [11]. For allogeneic therapies, derived from donor cells for "off-the-shelf" use, automation enables the scaled, consistent production necessary for commercial and clinical viability [8] [11]. This document details practical protocols and application notes for integrating these cost-reduction strategies within cell expansion workflows, providing a framework for researchers and drug development professionals to enhance efficiency, reduce operational expenses, and improve patient access.
Core Technologies and Their Economic Impact
Automated Bioprocessing Systems
Automation in bioprocessing is vital for improving quality, consistency, and cost-effectiveness while reducing operational errors in a highly regulated environment [54]. It mitigates risks associated with manual handling, such as microbial contamination and variable product quality, which are leading causes of batch failures [15] [54]. Automated systems are particularly crucial for autologous therapies, where each batch is unique to a patient, and standardization is challenging [11].
Key Automated Platforms:
- CliniMACS Prodigy (Miltenyi Biotec): An integrated system that automates cell separation, expansion, and formulation within a closed, GMP-compliant environment [55].
- Ori Biotech IRO Platform: Automates key stages of cell therapy manufacturing, including cell activation, transduction, expansion, and harvest, facilitating rapid scaling from clinical to commercial production [55].
- Modular Automation: Emerging systems focus on automating specific multi-step processes, such as cell selection, genetic modification, and final formulation, offering flexibility for both allogeneic and autologous production lines [15].
Point-of-Care (PoC) Manufacturing Infrastructure
PoC manufacturing involves producing therapies at or near the clinical setting—such as hospitals, clinics, or specialized units—bypassing traditional centralized bioprocessing facilities [55]. This model is revolutionizing the production of cell and gene therapies, particularly for autologous products, by resolving problems associated with long-distance, cold-chain transport of patient-specific materials [56].
Key PoC Enabling Technologies:
- Closed-System Bioreactors: Single-use bioreactors that eliminate cleaning needs and reduce cross-contamination risks, which is essential for non-classified hospital environments [55] [57].
- Mobile Processing Units: Self-contained or modular units that can be deployed at healthcare facilities, integrating closed-system bioreactors and automated cell expansion for rapid manufacturing of personalized therapies [55].
- Single-Use Systems: Provide flexibility and operational efficiency by eliminating cleaning validation and reducing utility requirements, making them ideal for small-scale, multi-product PoC facilities [57].
Quantitative Economic Analysis of Implementation Strategies
The economic value of automation and PoC models can be quantified through key performance indicators such as cost savings, error reduction, and scalability. The following table summarizes the potential economic impact of these strategies.
Table 1: Economic Impact of Automation and PoC Manufacturing Models
| Strategy | Reported Impact | Primary Source of Savings | Application in Cell Therapy |
|---|---|---|---|
| Automated Cell Processing | Reduces operational errors, a leading cause of batch failures [54]. | Lower labor costs, reduced batch loss, improved consistency [15] [54]. | Suitable for both allogeneic (scale-out) and autologous (standardization) [15]. |
| Point-of-Care (PoC) Models | Logistical simplification for autologous therapies; cited cost as low as \$27,000 per CAR-T treatment in decentralized models [58]. | Eliminates complex cold-chain logistics, reduces turnaround time, cuts shipping costs [56] [58]. | Primarily for autologous therapies (e.g., CAR-T, personalized cell products) [55] [11]. |
| Single-Use Bioreactors | Reduces contamination risk and eliminates cleaning/validation costs [57]. | Lower capital investment, reduced water-for-injection and cleaning agent use [57]. | Universal application in both allogeneic and autologous processes at PoC and centralized sites [57]. |
| Biosimilar Competition & Pricing Models | Potential for ~$80B in savings by 2035 via biosimilars; "cost-plus" models can save >30% on generics [59]. | Increased competition, more transparent pricing models [59]. | Indirectly impacts allogeneic therapy markets as they mature and face competition. |
Application Notes: Strategic Implementation
Selecting an Appropriate Manufacturing Model
The choice between a centralized, PoC, or hybrid model depends on therapy-specific factors. The following workflow diagram outlines the key decision-making criteria for selecting the optimal cost-reduction strategy.
Allogeneic vs. Autologous Therapy Considerations
The core distinction between allogeneic (donor-derived) and autologous (patient-derived) therapies dictates the primary cost-reduction strategy [8] [11].
For Allogeneic Therapies: The primary goal is scalability and consistency. A centralized, highly automated model is most suitable. Here, automation enables the large-scale, standardized production of "off-the-shelf" doses from a single donor source, dramatically reducing the cost per dose [11]. The main challenges are managing the risk of immune rejection (GvHD) and the potential for host-versus-graft responses, which may require additional genetic engineering or immunosuppression [8] [11].
For Autologous Therapies: The primary goal is logistical efficiency and speed. A PoC or decentralized model is ideal. This approach minimizes the complex logistics and time delays of shipping a patient's cells to a central facility and back, which is critical when treating aggressive cancers [11] [58]. A key challenge is managing product variability and ensuring consistent quality across numerous, geographically dispersed manufacturing sites [55] [56].
Experimental Protocols
Protocol: Implementing an Automated Cell Expansion Workflow
This protocol outlines the steps for implementing an automated system, such as the CliniMACS Prodigy or Ori Biotech IRO, for the expansion of human cells, applicable to both allogeneic and autologous processes.
1. Objective: To establish a standardized, automated protocol for the expansion of human-induced pluripotent stem cells (hiPSCs) or T-cells, reducing manual handling and improving batch consistency.
2. Research Reagent Solutions: Table 2: Essential Reagents for Automated Cell Expansion
| Reagent/Material | Function | Example |
|---|---|---|
| Chemically Defined Medium | Provides nutrients and signals for cell growth and maintenance; reduces batch variability. | Commercial stem cell or immune cell media. |
| Single-Use Bioreactor Chamber | Provides a sterile, controlled environment for cell growth within the automated system. | Pre-sterilized, disposable culture cassettes. |
| Recombinant Growth Factors | Directs cell-specific expansion and maintains desired phenotype (e.g., pluripotency, activation). | FGF-2 for hiPSCs; IL-2 for T-cells. |
| Cell Detachment Agent | Enzymatically dissociates adherent cells for passaging or harvest within a closed system. | Recombinant trypsin or enzyme-free alternatives. |
| Quality Control (QC) Assay Kits | Validates critical quality attributes (e.g., viability, identity, potency) post-expansion. | Flow cytometry kits, metabolite analyzers. |
3. Methodology:
- 4.1.1 System Setup and Priming: Within a Grade B/C cleanroom or controlled environment, install the pre-sterilized, single-use bioreactor circuit or chamber according to the manufacturer's instructions. Prime the system with pre-warmed, cell-specific culture medium and calibrate integrated sensors (e.g., pH, dissolved oxygen).
- 4.1.2 Inoculation: For allogeneic processes, inoculate with a master cell bank vial of hiPSCs or donor-derived T-cells. For autologous processes, load the patient's isolated peripheral blood mononuclear cells (PBMCs) or tissue-derived cells. The automated system will typically perform a cell count and viability assessment.
- 4.1.3 Automated Expansion: Initiate the pre-programmed protocol. Key automated steps include:
- Perfusion/Fed-Batch Control: Automated media exchange or feeding based on set parameters (e.g., glucose consumption rate).
- Environmental Control: Continuous monitoring and adjustment of temperature, pH, and dissolved oxygen.
- Cell Passaging (for adherent cells): Automated dissociation using a pre-loaded enzyme, washing, and re-seeding at the optimal density.
- 4.1.4 Harvest and Formulation: Upon reaching the target cell density, the system automatically terminates culture, harvests the cells, and performs washing and concentration into the final formulation buffer.
- 4.1.5 Quality Control and Data Recording: The system exports a batch report with process data. Perform offline QC assays (as per Table 2) to confirm product specifications.
Protocol: Deploying a Point-of-Care Manufacturing Unit for Autologous Therapy
This protocol describes the setup and operation of a mobile or hospital-integrated PoC unit for manufacturing an autologous cell therapy, such as CAR-T cells.
1. Objective: To reliably produce a patient-specific autologous cell therapy product within a clinical setting, minimizing logistics-related delays and costs.
2. Methodology:
- 4.2.1 Unit Configuration and Qualification:
- Deploy a mobile processing unit or establish a dedicated GMP-compliant suite within the hospital [55].
- Install closed-system automated equipment (e.g., CliniMACS Prodigy, closed-system bioreactors). The unit must operate under a unified quality system managed by a central control site [56].
- Qualify the facility and equipment, ensuring compliance with GMP standards for a decentralized model [55] [56].
- 4.2.2 Patient Apheresis and Initiation:
- Perform leukapheresis on the patient at the clinical site.
- Transport the apheresis material to the adjacent PoC manufacturing unit.
- Without cryopreservation, immediately initiate the manufacturing process to maximize cell viability and reduce total vein-to-vein time [58].
- 4.2.3 On-Site Manufacturing Process:
- Isolate target cells (e.g., T-cells) using an integrated, closed-system separation module.
- Perform activation and genetic modification (e.g., viral transduction for CAR insertion) within a closed-system bioreactor.
- Expand the genetically modified cells using automated, pre-defined protocols in a single-use bioreactor.
- Harvest the final product and formulate it in an infusion bag. The entire process must be tracked with a robust chain-of-identity system [11].
- 4.2.4 Product Release and Infusion:
- Perform in-process and release testing using rapid turnaround assays (e.g., rapid sterility tests). The central control site is responsible for the final product release [56].
- Upon release, transport the fresh product to the bedside for patient infusion, typically within hours of harvest, leveraging the biological advantages of fresh cells [58].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the above protocols requires a suite of reliable reagents and materials. The following table details key solutions for automated and PoC cell expansion processes.
Table 3: Essential Research Reagent Solutions for Automated and PoC Workflows
| Category | Specific Product/Kit | Critical Function | Compatibility Note |
|---|---|---|---|
| Cell Separation | Clinical-grade antibody cocktails (e.g., CD3/CD28 beads) | Isolation and activation of target cell populations for therapy. | Must be compatible with closed-system automated platforms [55]. |
| Culture Media | GMP-grade, serum-free expansion media | Supports robust cell growth while ensuring regulatory compliance and lot-to-lot consistency. | Formulated for specific cell types (T-cells, MSCs, hiPSCs). |
| Genetic Mod. Tools | GMP-grade viral vectors (Lentivirus, Retrovirus) | Enables stable genetic modification (e.g., CAR insertion) in target cells. | Titer and purity are critical for efficient transduction and safety. |
| Process Analytics | Automated cell counters, metabolite analyzers (e.g., Nova Bioprofile) | Provides real-time data on critical process parameters (CPPs) for quality control. | Interfaces with automated system software for data tracking. |
| Cryopreservation | Defined, animal origin-free cryoprotectants | Preserves cell viability for allogeneic cell banking or backup autologous doses. | Required for centralized, not necessarily fresh PoC, models [58]. |
The integration of automation and Point-of-Care manufacturing is not a distant future concept but a present-day necessity for the sustainable commercialization of cell therapies. For allogeneic therapies, centralized automation delivers the scale and consistency required for broad patient access. For autologous therapies, PoC models directly attack the logistical and cost barriers that currently limit treatment availability. The protocols and frameworks provided here offer a tangible pathway for researchers and developers to implement these strategies. As regulatory landscapes evolve to support decentralized models [56] and technologies like AI and closed-system processing mature [55] [57], the adoption of these integrated cost-reduction strategies will be paramount in fulfilling the promise of regenerative and personalized medicine for all eligible patients.
Head-to-Head Analysis: Validating Safety, Efficacy, and Commercial Potential
Within the evolving paradigm of cell expansion protocols, the strategic selection between allogeneic and autologous approaches necessitates a rigorous comparative safety assessment. For researchers and drug development professionals, three critical safety endpoints—tumorigenicity, cytokine release syndrome (CRS), and immune effector cell-associated neurotoxicity syndrome (ICANS)—represent significant and distinct risk profiles for each platform. This application note provides a synthesized analysis of current clinical data and outlines standardized experimental protocols for the systematic evaluation of these risks, supporting the broader thesis that safety considerations must be integral to cell therapy development from discovery through clinical application.
Quantitative Safety Profile Comparison
The safety profiles of autologous and allogeneic cell therapies differ substantially, influenced by their fundamental biological mechanisms. Autologous therapies, derived from the patient, circumvent alloimmunity but carry risks of product-mediated toxicity and intrinsic cellular dysfunction. Allogeneic, "off-the-shelf" therapies, derived from healthy donors, offer logistical advantages but introduce risks of graft-versus-host disease (GvHD) and host immune rejection, which can influence both efficacy and safety manifestations like CRS [60] [11]. The aggregated clinical data, particularly from CAR-T and CAR-NK trials, highlight these divergences.
Table 1: Comparative Incidence of CRS and ICANS in Autologous vs. Allogeneic CAR-Based Therapies
| Safety Event | Therapy Platform | Reported Incidence (Grade ≥3) | Key Contributing Factors |
|---|---|---|---|
| Cytokine Release Syndrome (CRS) | Autologous CAR-T | 3% - 71% (varies by product/disease) [61] | High disease burden (e.g., high BM blasts in ALL), CAR-T cell dose, CD28 costimulatory domain [61] |
| Allogeneic CAR-T/CAR-NK | 0.04% (Pooled Grade ≥3) [60] | Cell type (NK vs. T), engineering strategy (e.g., TCR knockout) | |
| Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) | Autologous CAR-T | Up to 67% (any grade); severe cases including cerebral edema reported [61] | Often associated with severe CRS, pre-existing neurological conditions |
| Allogeneic CAR-T/CAR-NK | 0.64% (Pooled Grade ≥3) [60] | Markedly lower incidence compared to autologous CAR-T; mechanism under investigation |
Table 2: Comparative Analysis of Tumorigenicity and Other Key Safety Risks
| Safety Risk | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Tumorigenicity | - Risk from genetically modified autologous cells [62] [63]- Theoretical risk of malignant transformation | - Risk of insertional oncogenesis from gene editing/engineering [62]- Risk from residual undifferentiated pluripotent stem cells in iPSC-derived products [63] |
| Graft-vs-Host Disease (GvHD) | Not applicable | Key risk driver; mitigated via TCR knockout/editing in T-cells or use of innate immune cells (e.g., NK cells) [60] [11] |
| Host vs. Graft Reaction | Not applicable | Host immune system can reject allogeneic cells, limiting persistence and potentially requiring immunosuppression [11] |
| Graft Failure | Rare [64] | A potentially fatal complication [64] |
| Underlying Cell Quality | Can be compromised by patient's disease and prior therapies (e.g., chemotherapy) [11] | Sourced from healthy donors, typically yielding higher quality starting material [11] |
Experimental Protocols for Safety Assessment
A comprehensive preclinical safety assessment is critical for Investigational New Drug (IND) applications and is guided by regulatory documents such as the FDA's "Safety Testing of Human Allogeneic Cells Expanded for Use in Cell-Based Medical Products" [65] [66]. The following protocols provide a framework for evaluating the key safety endpoints.
Protocol for Tumorigenicity Assessment
Objective: To evaluate the potential for uncontrolled cell proliferation, malignant transformation, and teratoma formation in vitro and in vivo.
Methodology:
- In Vitro Studies:
- Soft Agar Colony Formation Assay: Suspend 1x10⁴ cells in 0.4% soft agar layered over 0.8% base agar. Culture for 3-4 weeks, then stain with iodonitrotetrazolium chloride (INT) and count colonies >50μm to assess anchorage-independent growth [63].
- Karyotyping and Genomic Stability: Perform G-band karyotyping on at least 20 metaphase spreads to detect gross chromosomal abnormalities. For higher resolution, utilize Whole Genome Sequencing (WGS) with a minimum of 50x read depth to identify point mutations, small insertions/deletions, and off-target editing events [65] [63].
- In Vivo Studies:
- Animal Model: Use immunodeficient mice (e.g., NOD-scid gamma, NSG) to avoid xenorejection.
- Cell Administration: Implant 1x10⁷ cells (or a clinically relevant dose) via a biologically relevant route (e.g., subcutaneous, intramuscular, or intravenous).
- Study Duration and Endpoints: Monitor animals for 16-24 weeks. Perform regular palpation for mass formation. Terminal endpoints include gross necropsy and detailed histopathological analysis of the administration site and major organs (lungs, liver, kidneys, brain) for tumor formation [63].
Protocol for CRS and ICANS Risk Assessment
Objective: To model and quantify the potential for CRS and neurotoxicity induced by cell therapy products.
Methodology:
- In Vitro Cytokine Release Assay:
- Co-culture Setup: Co-culture effector cells (e.g., CAR-T cells) with target antigen-positive tumor cells at various effector-to-target (E:T) ratios. Include controls (effectors alone, targets alone).
- Analysis: Collect supernatant at 24, 48, and 72 hours. Quantify a panel of inflammatory cytokines (e.g., IL-6, IFN-γ, IL-2, TNF-α, GM-CSF) using a multiplex Luminex assay. Elevated levels predict CRS potential [61] [63].
- In Vivo CRS/ICANS Model:
- Animal Model: Utilize humanized mouse models (e.g., NSG mice engrafted with human hematopoietic stem cells) to recapitulate a functional human immune system.
- Cell Administration: Inject a therapeutically active dose of cells intravenously into tumor-bearing humanized mice.
- Monitoring and Endpoints:
- Clinical Scoring: Monitor daily for signs of CRS (weight loss, piloerection, lethargy, hunched posture) and neurotoxicity (grip strength, circling behavior, seizures) using validated scoring systems.
- Cytokine Measurement: Collect serial blood samples for plasma cytokine analysis.
- Histopathology: Perform brain histology post-study to assess vascular leakage, microglial activation, and other neuropathological correlates of ICANS [61].
Signaling Pathways and Experimental Workflows
The pathophysiology of CRS and ICANS involves a cascade of immune cell activation and complex cellular crosstalk. The following diagram outlines the key signaling pathways and cellular effectors involved.
Figure 1: Signaling Pathways in CRS and ICANS. This diagram illustrates the proposed mechanistic pathway from chimeric antigen receptor (CAR) engagement to the clinical manifestations of cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). The process begins with T-cell activation and is amplified by host myeloid cells, leading to endothelial dysfunction and neuroinflammation [61].
The workflow for the comprehensive biosafety assessment of a novel cell therapy product, from initial lot release testing to complex in vivo studies, is outlined below.
Figure 2: Biosafety Assessment Workflow. This workflow delineates the key in vitro and in vivo testing phases required for a comprehensive preclinical safety profile of a cell therapy product, integrating recommendations from regulatory guidance [65] [63].
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and platforms are essential for executing the safety assessment protocols described in this document.
Table 3: Essential Research Reagents for Cell Therapy Safety Assessment
| Reagent/Material | Function in Safety Assessment | Application Example |
|---|---|---|
| Whole Genome Sequencing (WGS) | Detects genomic alterations, off-target editing events, and vector integration sites. Critical for assessing genomic stability and oncogenic risk [65]. | WGS with ≥50x read depth on master cell banks and final products to satisfy regulatory requirements for allogeneic products [65]. |
| Luminex Multiplex Assays | Simultaneously quantifies a broad panel of cytokines (e.g., IL-6, IFN-γ, IL-2, IL-10) from small volume samples. | Profiling cytokine release in supernatant from co-culture assays to model CRS potential in vitro [61] [63]. |
| Immunodeficient Mouse Models (e.g., NSG) | Provides an in vivo model for assessing tumorigenicity, biodistribution, and toxicology in the absence of a functional host immune system. | Evaluating long-term tumorigenic risk by implanting cells and monitoring for mass formation over 16+ weeks [63]. |
| StemRNA Clinical iPSC Seed Clones | Provides a consistent, GMP-compliant, and well-characterized starting material for allogeneic iPSC-derived therapies, referenced in an FDA DMF [31]. | Serves as a standardized, high-quality cell source for developing and scaling up allogeneic therapy manufacturing. |
| qPCR Instruments & Probes | Quantifies the biodistribution and persistence of human cells in murine tissues over time. | Tracking the presence and quantity of administered cells in organs like bone marrow, spleen, and brain in biodistribution studies [63]. |
| Soft Agar | A semi-solid medium used to assess anchorage-independent growth, a hallmark of cellular transformation. | Performing colony formation assays to evaluate the tumorigenic potential of a cell product in vitro [63]. |
The therapeutic landscape for advanced cancers and other intractable diseases has been reshaped by the advent of chimeric antigen receptor (CAR)-engineered cell therapies. Within this domain, a fundamental distinction exists between autologous approaches (using patient's own cells) and allogeneic approaches (using donor-derived cells). Each paradigm presents a unique profile of advantages and challenges pertaining to clinical efficacy, durability of response, and manufacturing logistics [11]. Autologous therapies have demonstrated remarkable efficacy but face limitations in manufacturing scalability and turnaround time [34]. Allogeneic, or "off-the-shelf," therapies aim to overcome these hurdles, offering the promise of immediate treatment availability, though questions regarding their long-term persistence and capacity to elicit durable responses remain active areas of investigation [9]. This Application Note provides a structured analysis of clinical response rates and persistence metrics, alongside detailed protocols for their measurement, framed within the critical comparative context of autologous versus allogeneic cell expansion protocols.
Comparative Clinical Response and Durability
Clinical data reveal that both autologous and allogeneic CAR-T cell therapies can induce profound responses in patients with hematologic malignancies. The tables below summarize key efficacy and durability metrics from recent clinical studies.
Table 1: Comparative Clinical Response Rates of Selected CAR-T Cell Therapies
| Therapy / Trial | Cell Type | Target | Indication | ORR (%) | CR (%) | Key Durability Findings |
|---|---|---|---|---|---|---|
| Axi-cel (ZUMA-1) [67] | Autologous | CD19 | R/R LBCL | 83 | 58 | Median OS 25.8 mo; 5-yr OS 42.6% |
| Tisa-cel (JULIET) [67] | Autologous | CD19 | R/R LBCL | 52 | 40 | Durable response in pts with early CR; median PFS/OS not reached in 3-yr CR pts |
| Liso-cel (TRANSCEND) [67] | Autologous | CD19 | R/R LBCL | 73 | 53 | Estimated 2-yr PFS 40.6%; OS 50.5% |
| Vispa-cel (ANTLER) [68] | Allogeneic | CD19 | R/R B-NHL | 82-86 | 63-64 | 12-mo PFS ~51%; median DOR not reached |
| Eque-cel (BCMA) [69] | Autologous | BCMA | R/R Multiple Myeloma | 96.4 | 80.4 | MRD- rate 96.4%; PFS positively correlated with CAR-T persistence ≥6 mo |
ORR: Overall Response Rate; CR: Complete Response; OS: Overall Survival; PFS: Progression-Free Survival; DOR: Duration of Response; MRD-: Minimal Residual Disease negativity; R/R LBCL: Relapsed/Refractory Large B-Cell Lymphoma; R/R B-NHL: Relapsed/Refractory B-cell Non-Hodgkin Lymphoma.
Table 2: Analysis of Factors Influencing Long-Term Outcomes
| Factor | Impact on Persistence & Durability | Supporting Evidence |
|---|---|---|
| CAR-T Persistence | Sustained presence of functional CAR-T cells correlates with prolonged MRD negativity and improved PFS/OS. | In BCMA CAR-T therapy, persistence ≥6 mo was linked to better outcomes [69]. |
| MRD Negativity | Achieving and sustaining MRD negativity is a strong predictor of long-term remission. | In multiple myeloma, PFS was 58 mo, 64 mo, and not reached for pts with sustained MRD negativity for 12, 24, and 36 mo, respectively [69]. |
| Costimulatory Domain | Influences T-cell expansion, persistence, and metabolic fitness. | CD28 domains associated with robust initial expansion; 4-1BB domains linked to longer persistence [67]. |
| Product Immunogenicity | Host immune response to allogeneic cells can limit persistence (allorejection). | Allogeneic products require genetic edits (e.g., TCR knockout) to prevent GvHD, but this can also affect persistence [34]. |
| Lymphodepletion | Critical for creating a favorable cytokine environment and reducing host immune competition for allogeneic engraftment. | Standard fludarabine/cyclophosphamide regimens support allogeneic cell engraftment and early MRD conversion [70]. |
Experimental Protocols for Measuring Efficacy and Persistence
Accurate measurement of CAR-T cell expansion and persistence is critical for correlating pharmacokinetics with clinical outcomes. The following protocols detail standard methodologies.
Protocol: Measuring CAR-T Cell Persistence via Flow Cytometry
Principle: This method uses fluorophore-conjugated reagents that bind specifically to the CAR protein, allowing for quantification of CAR-positive cells within patient blood samples and assessment of their functional phenotype [67].
Materials:
- Research Reagent Solutions:
- Anti-idiotype Antibody: Fluorophore-conjugated antibody (e.g., anti-FMC63) that binds the scFv of the CAR without cross-reacting with endogenous receptors [67].
- Biotinylated Antigen (e.g., CD19-Fc): Binds the CAR's antigen recognition site; detected via fluorescent streptavidin [67].
- Cell Staining Buffer: PBS containing buffers, proteins, and preservatives to maintain cell viability and minimize non-specific binding.
- Viability Dye: To exclude dead cells from the analysis.
- Antibody Panel for Phenotyping: Antibodies against T-cell markers (e.g., CD3, CD4, CD8, CD45RA, CCR7) for memory subset analysis.
Procedure:
- Sample Collection: Collect peripheral blood samples in EDTA or heparin tubes at predetermined time points (e.g., pre-infusion, days 7, 14, 28, and monthly thereafter).
- PBMC Isolation: Isolate Peripheral Blood Mononuclear Cells (PBMCs) using density gradient centrifugation (e.g., Ficoll-Paque).
- Cell Staining:
- Aliquot 1-5 x 10^5 PBMCs into flow cytometry tubes.
- Add Fc receptor blocking agent to reduce non-specific binding.
- Stain cells with the selected CAR detection reagent (anti-idiotype antibody or biotinylated antigen + streptavidin-fluorophore) and the phenotyping antibody panel for 30 minutes in the dark at 4°C.
- Include fluorescence-minus-one (FMO) and isotype controls for accurate gating.
- Data Acquisition & Analysis:
- Acquire data on a flow cytometer.
- Analyze data by first gating on lymphocytes, then singlets, live cells, and CD3+ T cells.
- The frequency of CAR-positive T cells is determined from the CD3+ population. Results can be reported as percentage of CAR+ cells among total lymphocytes or as absolute counts.
Protocol: Quantifying CAR Transgene Levels via ddPCR
Principle: Digital droplet PCR (ddPCR) provides an absolute quantification of CAR transgene copy numbers in patient DNA samples, offering high sensitivity and reproducibility for tracking persistence [67] [69].
Materials:
- Research Reagent Solutions:
- DNA Extraction Kit: For high-quality genomic DNA from patient PBMCs or whole blood.
- ddPCR Supermix: Reaction mix optimized for droplet formation and PCR.
- CAR-Specific Assay: Hydrolysis (TaqMan) probes and primers designed to uniquely recognize the CAR transgene sequence.
- Reference Gene Assay: Probe/Primer set for a single-copy endogenous reference gene (e.g., RPP30) for normalization and quality control.
- Droplet Generator and Reader: Instrumentation for creating and analyzing droplets.
Procedure:
- DNA Extraction: Extract genomic DNA from patient PBMCs according to the manufacturer's protocol. Quantify DNA concentration and assess purity (A260/A280 ratio).
- Reaction Setup:
- Prepare a 20-22 μL reaction mix containing ddPCR Supermix, CAR-specific assay, reference gene assay, and ~50 ng of genomic DNA.
- Load the reaction mix into a droplet generator cartridge alongside droplet generation oil to create ~20,000 nanodroplets.
- PCR Amplification:
- Transfer the emulsified samples to a 96-well PCR plate.
- Perform PCR amplification on a thermal cycler using optimized cycling conditions.
- Droplet Reading and Analysis:
- Place the plate in a droplet reader, which counts the number of positive and negative droplets for each target (CAR and reference).
- Use the instrument's software to calculate the absolute concentration of the CAR transgene (copies per μL of reaction). The result is often normalized and reported as transgene copies per μg of genomic DNA or copies per 100 ng DNA.
Visualizing Workflows and Signaling
The following diagrams illustrate the core experimental workflow for assessing persistence and a key engineering strategy for allogeneic cells.
CAR-T Persistence Monitoring Workflow
Allogeneic CAR-T Engineering Logic
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for CAR-T Cell Persistence and Efficacy Studies
| Reagent / Tool | Primary Function | Application Context |
|---|---|---|
| Anti-Idiotype Antibodies | Specific detection of unique CAR scFv domain by flow cytometry. | Quantifying CAR+ cell frequency and phenotype in patient samples without background [67]. |
| Biotinylated Antigen (CD19-Fc) | Detection of functional, antigen-binding CARs on the cell surface. | Flow cytometry; useful for staining dual-CAR constructs and verifying CAR functionality [67]. |
| ddPCR/qPCR Assays | Absolute quantification of CAR transgene copy number in genomic DNA. | Highly sensitive tracking of CAR-T cell pharmacokinetics and persistence over time [67] [69]. |
| Cytokine ELISA/MSD Kits | Measurement of cytokine levels (e.g., IFN-γ, IL-6, IL-2) in patient serum. | Monitoring pharmacodynamics, CRS, and overall immune activation post-infusion. |
| CRISPR-Cas9 / TALENs | Gene editing tools for TCR and HLA knockout in allogeneic donor cells. | Engineering allogeneic CAR-T products to mitigate GvHD and host rejection [34]. |
The therapeutic landscape is being transformed by advanced cell therapies, primarily categorized into autologous (patient-derived) and allogeneic (donor-derived) approaches [11]. The choice between these models has profound implications for clinical accessibility, treatment cost, and commercial viability [71]. This analysis provides a comparative evaluation of autologous and allogeneic cell therapies, focusing on critical parameters of cost per dose, vein-to-vein time, and market trajectory. The data and protocols herein are designed to inform researchers, scientists, and drug development professionals in their strategic planning and process development within the broader context of cell expansion protocol research.
Quantitative Economic and Access Comparison
A decisive factor in therapy selection and development strategy is the quantitative performance of each model across key operational and economic metrics. The data below provide a comparative analysis.
Table 1: Comparative Analysis of Autologous vs. Allogeneic Cell Therapy Models
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Definition | Patient-specific; cells harvested from and reintroduced into the same patient [11] | "Off-the-shelf"; cells from a healthy donor administered to multiple patients [11] |
| Typical Cost of Goods (COGS) | $150,000–$300,000 per patient [72] | $25,000–$50,000 per dose [72] |
| Projected Cost at Scale | Limited cost reduction potential due to personalized nature | As low as $7,500–$10,000 per dose [71] |
| Vein-to-Vein Time | Several weeks [11]; can be reduced from 28 to 7 days with decentralized models [72] | Readily available; no wait for manufacturing [71] |
| Manufacturing Scalability | Scale-out model; one batch per patient [71] | Scale-up model; one batch can produce ~100 doses [71] |
| Key Economic Driver | High per-batch quality control and labor [72] | Economies of scale from large-batch production [71] |
| Primary Logistical Challenge | Complex, patient-specific supply chain and cold-chain management [3] [11] | Long-term storage and distribution of frozen doses [11] |
Table 2: Market Metrics and Clinical Dosing (2024-2025)
| Metric | Current Data and Projections |
|---|---|
| 2024 Global Market Share | Autologous: 90.25% [72] |
| Projected CAGR (2025-2034) | Allogeneic CAR-T: 44.35% [73] |
| Cell Therapy Market CAGR | Asia-Pacific: 14.01% [72] |
| Typical Allogeneic Dose Range | 10^5 to 10^9 cells per patient, depending on indication [74] |
| Commercial Lot-Size Need | Up to 10^12 to 10^13 cells per lot [74] |
The following diagram illustrates the core logistical and decision-making pathways differentiating autologous and allogeneic therapy processes, highlighting critical nodes that impact vein-to-vein time and cost.
Experimental Protocols for Cell Expansion
Robust and scalable cell expansion is fundamental to the commercial success of both autologous and allogeneic therapies. The following protocols detail established methodologies.
Protocol: Allogeneic Natural Killer (NK) Cell Generation from Hematopoietic Stem Cells (HSCs)
This protocol, adapted from current industry practice, outlines a scalable, bioreactor-based process for generating allogeneic NK cells from cord blood HSCs [75].
3.1.1 Reagents and Materials
- HSC Source: Cryopreserved cord blood unit (CBU)
- Expansion Molecule: Proprietary HSC expansion agent (e.g., IBR403) [75]
- Cell Culture Media: Commercially available, xeno-free basal media supplemented with cytokine kits
- Bioreactors: Closed-system, stirred-tank bioreactors (e.g., 10 mL screening scale to 1 L production scale)
3.1.2 Step-by-Step Methodology
HSC Expansion:
- Thaw cryopreserved CBU and initiate culture in a small-scale (e.g., 10 mL) stirred-tank bioreactor.
- Supplement media with the HSC expansion molecule (e.g., IBR403) to generate a screening-scale or manufacturing-scale HSC bank.
- Cryopreserve expanded HSCs in single-use vials for future differentiation runs.
Lymphoid Progenitor Differentiation:
- Thaw a vial of expanded HSCs and initiate differentiation in a well-mixed bioreactor.
- Use a stage-specific differentiation medium to drive HSCs toward a lymphoid progenitor cell fate. Process parameter (e.g., dissolved oxygen, pH) should be tightly controlled.
NK Cell Maturation:
- Transfer the lymphoid progenitors to a second bioreactor for terminal maturation into functional NK cells.
- The maturity and yield of the final NK cell product are critical quality attributes.
Product Formulation and Cryopreservation:
- Harvest the NK cells, concentrate via centrifugation, and resuspend in a cryoprotectant solution.
- Fill and cryopreserve final product doses. A single HSC bank can supply multiple NK differentiation runs.
3.1.3 Critical Success Factors
- Scalability: Using well-mixed bioreactors from the initial 10 mL scale ensures a seamless translation to 1 L commercial manufacturing scale [75].
- Donor Selection: Employing scaled-down bioreactor screens to select optimal CBU donors based on HSC expansion potential and NK cell differentiation efficiency is crucial for consistent product quality [75].
Protocol: Autologous CAR-T Cell Manufacturing
This protocol describes a generalized workflow for manufacturing patient-specific CAR-T cells, highlighting areas where integrated platforms can introduce efficiencies [76].
3.2.1 Reagents and Materials
- Starting Material: Patient's leukapheresis product
- Cell Activation Reagents: Anti-CD3/CD28 beads or soluble agonists
- Gene Delivery Vector: Lentiviral vector or non-viral alternatives (e.g., LipidBrick Cell Ready system for mRNA) [76]
- Cell Culture Media: Serum-free T-cell expansion media
- Culture Vessels: Closed, automated bioreactors (e.g., rocking-motion single-use bioreactors)
3.2.2 Step-by-Step Methodology
Cell Isolation and Activation:
- Receive the patient's leukapheresis product and perform density gradient centrifugation or use an integrated selection system to isolate mononuclear cells.
- Activate T-cells using activation reagents for 24-48 hours.
Genetic Modification (Transduction):
- Introduce the CAR transgene using a viral vector or non-viral method.
- For viral transduction, incubate activated T-cells with the lentiviral vector at a specific multiplicity of infection (MOI) in the presence of enhancers like polybrane.
- For non-viral methods, complex the LipidBrick reagent with mRNA payload and simply add it to the cells [76].
Cell Expansion:
- Transfer transduced cells to a bioreactor for ex vivo expansion.
- Culture for 7-14 days, maintaining cell density and supplementing with IL-2 or other cytokines to promote T-cell growth.
Harvest, Formulation, and Cryopreservation:
- Harvest cells when target cell numbers are met.
- Wash cells to remove media components and cytokines.
- Formulate the final drug product in an infusion bag (for fresh shipment) or in cryovials for cryopreservation.
3.2.3 Critical Success Factors
- Vein-to-Vein Time: The entire process must be completed as quickly as possible, ideally under 7 days in optimized, decentralized models [72] [76].
- Process Control: Maintaining consistency is challenging due to the high variability of patient-derived starting material. Automated, closed systems are critical to minimize this variability and reduce labor [76].
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the appropriate reagents and platforms is fundamental to developing robust and scalable cell therapy processes.
Table 3: Essential Reagents and Platforms for Cell Therapy Development
| Item | Function & Application | Key Consideration |
|---|---|---|
| LipidBrick Cell Ready System [76] | Non-viral gene delivery using preformed lipid nanoparticles. Used for transferring mRNA, circRNA, sgRNA, etc., into T cells, NK cells, and HSCs. | Simple reagent-based method; no specialized equipment needed; easily scalable and cost-effective. |
| IBR403 Expansion Molecule [75] | Proprietary molecule for expanding Hematopoietic Stem Cells (HSCs) from cord blood. Critical for creating allogeneic HSC banks. | Enables generation of large HSC numbers for screening and manufacturing, supporting scalable allogeneic processes. |
| Closed-system Automated Bioreactors [74] [76] | Single-use, stirred-tank bioreactors for scalable cell expansion from 10 mL to 1000 L. | Ensures process consistency and facilitates scale-up; reduces contamination risk in GMP manufacturing. |
| Cryopreservation Media | Formulations containing DMSO and other cryoprotectants for long-term storage of cell banks and final drug product. | Vital for creating allogeneic cell banks and managing autologous product inventory; cell viability post-thaw is a CQA. |
| Viral Vectors (Lentivirus) | Classical method for stable genetic modification of cells (e.g., CAR insertion). | Production is complex, expensive, and difficult to scale; a major cost driver and potential supply chain bottleneck [72]. |
Technical and Market Trajectory Analysis
Manufacturing Challenges and Innovations
The core challenges differ significantly between the two therapeutic models.
Autologous Challenges: The primary hurdles are cost, scalability, and vein-to-vein time [3] [76]. The high cost-of-goods (COGS) is driven by labor-intensive processes, batch-specific quality control, and complex logistics [72]. Innovations focus on integrated, closed, and automated platforms that can reduce COGS by >50% and enable decentralized manufacturing at regional centers, cutting vein-to-vein times significantly [76].
Allogeneic Challenges: The major hurdles are immunological rejection (GvHD) and ensuring consistent cell quality at large scales [71] [11]. Scaling production to commercial lot-sizes of 10^11–10^14 cells requires moving from planar technologies to microcarrier-based bioreactors to be cost-effective [74]. Innovations include gene editing (e.g., CRISPR-Cas9) to knock out immune recognition genes and the use of immune-privileged cells like MSCs [71] [11].
Market Trajectory and Future Outlook
The market is poised for a significant shift. While autologous therapies currently dominate the market, the allogeneic segment is growing at a notably faster CAGR (44.35% for allogeneic CAR-T versus the overall cell therapy market growth) [72] [73]. The pressure to reduce costs and increase access is driving this transition. Allogeneic platforms are positioned to eclipse autologous volumes in the future due to their superior scalability and lower costs, which are essential for treating larger patient populations [72]. Geographically, the Asia-Pacific region is expected to be a major growth engine and manufacturing hub, with a CAGR of 14.01% [72]. The future of the field hinges on overcoming manufacturing bottlenecks through automation, process innovation, and strategic partnerships [3] [75].
Advanced Therapy Medicinal Products (ATMPs) represent a groundbreaking category of medications that utilize biological-based products to treat or replace damaged organs, offering potential solutions for complex diseases through gene therapy, somatic cell therapy, tissue engineering, and combined therapies [23]. Within the context of cell expansion protocols, the regulatory distinction between allogeneic (from a donor) and autologous (from the patient themselves) approaches is critical, influencing manufacturing complexity, quality control requirements, and ultimately, the regulatory pathway [23]. The regulatory landscape for these innovative therapies remains highly fragmented, with significant differences between the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) [77]. These differences affect clinical trial design, approval timelines, data requirements, and post-marketing surveillance, creating substantial challenges for researchers and drug development professionals seeking approval in both markets [77]. A recent study highlighted these challenges, revealing that only 20% of clinical trial data submitted to both agencies matched, underscoring major inconsistencies in regulatory expectations [77].
The central tension in 2025 lies in balancing scientific innovation with regulatory infrastructure [78]. While therapy approvals are increasing, the industry faces a constrained funding environment and persistent operational inefficiencies [78]. Understanding these divergent regulatory pathways is not merely an administrative requirement but a fundamental component of successful ATMP development, particularly when designing cell expansion protocols for allogeneic versus autologous applications.
Comparative Analysis of FDA and EMA Regulatory Pathways
Key Regulatory Divergences in ATMP Approval
Navigating the regulatory requirements for ATMPs necessitates a clear understanding of the distinct pathways established by the FDA and EMA. The following table summarizes the critical differences across the development and commercialization lifecycle, with particular implications for allogeneic and autologous cell therapy development.
Table 1: Key Regulatory Differences Between FDA and EMA for ATMPs/Cell and Gene Therapies
| Aspect | U.S. Food and Drug Administration (FDA) | European Medicines Agency (EMA) |
|---|---|---|
| Regulatory Classification | Regenerative Medicine Advanced Therapy (RMAT) designation [77] | Advanced Therapy Medicinal Product (ATMP) under Regulation (EC) No 1394/2007 [77] [79] |
| Clinical Trial Approval | Investigational New Drug (IND) Application; 30-day review period [77] | Clinical Trial Application (CTA) via CTIS to National Competent Authorities (NCAs) and Ethics Committees [77] |
| Marketing Application | Biologics License Application (BLA) [77] | Marketing Authorization Application (MAA) [77] |
| Standard Review Timeline | 10 months (Standard); 6 months (Priority Review) [77] | 210 days (Standard); 150 days (Accelerated Assessment) [77] |
| Expedited Pathways | RMAT, Fast Track, Breakthrough Therapy, Accelerated Approval [77] | PRIME Scheme, Conditional Marketing Authorization, Accelerated Assessment [77] |
| GMP Compliance Emphasis | Phase-appropriate attestation, verified via pre-license inspection [79] | Mandatory compliance for clinical trials, verified through self-inspections [79] |
| Allogeneic Donor Eligibility | Prescriptive requirements for donor screening/testing and restrictions on donor pooling [79] | General guidance with compliance to relevant EU and member-state legal requirements [79] |
| Long-Term Follow-Up | 15+ years for gene therapies [77] | Risk-based, generally shorter than FDA [77] |
| Decision-Making Authority | Full approval authority under CBER/OTP [77] | Provides scientific opinion; final decision by European Commission [77] |
Implications for Allogeneic vs. Autologous Cell Expansion
The divergent regulatory requirements have profound implications for the development of cell expansion protocols, particularly when choosing between allogeneic and autologous approaches.
Allogeneic Product Development: For allogeneic therapies, the donor eligibility requirements represent a significant point of regulatory divergence. The FDA maintains more prescriptive requirements for donor screening and testing for infectious diseases, including specifications on qualified testing laboratories and restrictions on pooling cells from multiple donors [79]. Furthermore, the scalability of allogeneic processes introduces challenges in demonstrating product comparability after manufacturing process changes, which are scrutinized differently by the FDA and EMA [23]. The FDA recommends a tiered approach for reporting changes, while the EMA focuses on identifying Critical Quality Attributes (CQAs) susceptible to process variations [23].
Autologous Product Development: Autologous therapies, being patient-specific, face different hurdles, primarily related to manufacturing consistency and logistics. The regulatory challenge lies in validating a process that can accommodate the inherent variability of starting material from different patients [23]. The EMA's GMP guidelines, which are mandatory even for early-stage clinical trials, require robust quality systems for these individualized batches [79]. The complex supply chain, coordinating apheresis, manufacturing, and reinfusion, requires seamless integration and is a key focus for both agencies, though the FDA's phased GMP approach offers more initial flexibility [78] [79].
Essential Protocols for Navigating Regulatory Requirements
Protocol 1: Chemistry, Manufacturing, and Controls (CMC) Development
The CMC section is a cornerstone of any ATMP regulatory submission, encompassing process development, manufacturing, and quality control [80]. For both allogeneic and autologous products, a robust CMC strategy is vital.
Table 2: Research Reagent Solutions for ATMP CMC Development
| Reagent/Material | Function in Development |
|---|---|
| Banked Cell Lines (Allogeneic) / Patient Cells (Autologous) | Starting material for drug substance manufacturing [80] |
| Viral Vectors (e.g., for GTMPs) | Vehicles for delivering recombinant genes [80] |
| Cell Culture Media & Supplements | Supports cell expansion and maintenance during upstream processing [80] |
| Cell Dissociation Agents | Detaches adherent cells for sub-culturing or harvest [80] |
| Cryopreservatives | Protects cell viability during long-term storage of drug substance/product [80] |
| Biodegradable Matrices/Scaffolds | Acts as a structural support in combined ATMPs (tissue-engineered products) [81] |
Experimental Workflow: The CMC workflow for an ATMP, as outlined in the search results, can be visualized through the following logical pathway. This diagram illustrates the journey from starting material to finished drug product, highlighting critical control points.
Methodology:
- Process and Product Characterization: Define Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs) that correlate with product safety and efficacy. For allogeneic products, this includes assessing genetic stability over successive cultures to mitigate tumorigenesis risk [23]. For autologous products, focus on characterizing the variability inherent in patient-derived starting materials [23].
- Analytical Method Validation: Develop and validate analytical methods to assess CQAs. These include assays for potency, identity, viability, purity, sterility, and mycoplasma [80] [23]. The EMA guideline emphasizes that immature quality development can compromise the use of clinical trial data to support a marketing authorization [79].
- Process Validation: Execute a Process Validation Master Plan to demonstrate the manufacturing process consistently produces a drug product meeting its predefined quality attributes [80]. This is crucial for scaling up allogeneic products [23].
- Stability Studies: Conduct real-time stability studies to establish the shelf-life and optimal storage conditions for the drug substance and drug product, ensuring CQAs are maintained [80].
Protocol 2: Implementing a Risk-Based Pharmacovigilance Strategy
Post-market safety monitoring is a critical and stringent requirement for ATMPs, with both agencies mandating long-term follow-up (LTFU) to manage risks such as tumorigenesis [23] [77].
Experimental Workflow: The pharmacovigilance strategies for the FDA and EMA, while sharing common goals, operate through different mechanisms as shown in the workflow below.
Methodology:
- Risk Management Plan (RMP) Development: Develop a comprehensive RMP (required by EMA) or REMS (for high-risk CGTs with the FDA) early in development. This plan should identify known and potential risks, along with pharmacovigilance activities to characterize and minimize them [77].
- Long-Term Follow-Up (LTFU) Protocol Design: Design a robust LTFU study protocol aligned with agency-specific requirements. For gene therapies, the FDA mandates 15+ years of post-market monitoring, while the EMA employs a risk-based approach that may be shorter [77]. The protocol must include endpoints to monitor for delayed adverse events, such as tumorigenicity or unintended gene integration.
- Safety Data Collection and Reporting: Establish systems for collecting and reporting adverse events. For the US, this involves the FDA Adverse Event Reporting System (FAERS), while in the EU, reporting is done via the EudraVigilance database [77]. Prepare for periodic submission of Periodic Safety Update Reports (PSURs) to the EMA [77].
Strategic Regulatory and Manufacturing Considerations
Proactive Regulatory Engagement
A proactive approach to regulatory engagement is essential for navigating the divergent FDA and EMA pathways successfully.
- Early and Parallel Engagement: Engage with both agencies early in the development process through FDA Type B meetings and EMA Scientific Advice [77]. This allows sponsors to understand and anticipate differences in expectations for trial design, endpoints, and CMC data, particularly for novel allogeneic products [79].
- Leverage Expedited Pathways: Identify and strategically leverage expedited pathways such as the FDA's RMAT designation and the EMA's PRIME scheme [77]. These pathways offer opportunities for intensified regulatory guidance and accelerated assessment but require careful planning to meet the specific evidence requirements of each agency.
Addressing Manufacturing and Scalability Challenges
Manufacturing remains one of the most reported challenges for ATMPs, especially when scaling up from clinical to commercial production [23].
- Scalability and Comparability: For allogeneic products, the primary challenge is demonstrating product comparability after scaling-up manufacturing processes [23]. Regulatory authorities in the US and EU have issued tailored guidance emphasizing risk-based comparability assessments and extended analytical characterization [23].
- Contamination Control: Manufacturing under aseptic conditions is paramount, as traditional sterilization methods are not feasible for cell-based products. The use of closed and automated systems, along with rigorous environmental monitoring and process simulation (media fills), is critical to reduce contamination risk [23]. The EMA's proposed revisions to GMP guidelines for ATMPs, released in May 2025, seek to integrate ICH Q9 (Quality Risk Management) and provide clarity on new technologies like these automated systems [82].
- Infrastructure and Partnering: The complex, patient-specific logistics of autologous therapies require highly coordinated supply chains. As noted in the search results, "You’re not just managing logistics, you’re having to synchronize with a patient’s clinic appointment, coordinate apheresis, manufacturing, and then return the therapy in time for reinfusion" [78]. Many developers are turning to strategic supply chain partners to provide end-to-end integration, including GMP biostorage, continuous condition monitoring, and cryopreservation services [78].
Navigating the divergent regulatory pathways of the FDA and EMA for ATMPs is a complex but manageable endeavor that requires strategic planning from the earliest stages of development. The key to success lies in recognizing that a uniform, one-size-fits-all approach is ineffective. Instead, developers must tailor their strategies to meet the distinct expectations of each agency, from clinical trial design and CMC development to post-market surveillance. This is especially critical in the context of cell expansion protocols, where the choice between allogeneic and autologous approaches introduces specific regulatory and manufacturing challenges related to donor eligibility, scalability, and product comparability. By engaging regulators early, leveraging expedited pathways, designing trials with global requirements in mind, and investing in robust, scalable manufacturing and supply chain systems, researchers and drug development professionals can optimize their regulatory strategy. This proactive and informed approach is fundamental to overcoming the current challenges of pressure and scalability, ultimately accelerating the delivery of transformative advanced therapies to patients in need.
Conclusion
The choice between autologous and allogeneic cell expansion is not a matter of one superseding the other, but rather a strategic decision based on the target disease, patient population, and commercial goals. Autologous therapies excel in immune compatibility and long-term persistence for individualized treatment, while allogeneic platforms offer a transformative, scalable model for broader patient access. Future success hinges on overcoming persistent challenges: for allogeneic therapies, this means solving the puzzles of immune rejection and durability; for autologous, it requires streamlining complex logistics and reducing costs. The integration of emerging technologies—such as advanced gene editing (CRISPR, TALEN), AI-driven process optimization, and automated bioreactors—will be pivotal in enhancing the precision, scalability, and safety of both paradigms. The ongoing clinical progress in allogeneic CAR-T and CAR-NK cells signals a promising shift towards more accessible, off-the-shelf cellular medicines, ultimately expanding the reach of these revolutionary treatments.
References
- 1. Why Autologous and Patient-Specific Aren't the Same in Cell ... [https://www.rm.minaris.com/minaris-insights/why-autologous-and-patient-specific-arent-the-same-in-cell-therapy]
- 2. Allogeneic CART progress: platforms, current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198129/]
- 3. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 4. Allogeneic Versus Autologous Stem-Cell Therapy [https://www.biopharminternational.com/view/allogeneic-versus-autologous-stem-cell-therapy]
- 5. Allogeneic cell therapies offer 'transformative potential' [https://www.healio.com/news/hematology-oncology/20251016/allogeneic-cell-therapies-offer-transformative-potential-to-treat-solid-tumors]
- 6. Patient‐specific versus off‐the‐shelf unicompartmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12381529/]
- 7. Differences Between Autologous and Allogeneic Cell ... [https://www.patheon.com/us/en/insights-resources/blog/differences-between-autologous-and-allogeneic-cell-therapies.html]
- 8. Autologous vs allogenic cell therapy: key differences and ... [https://greenelephantbiotech.com/blog/autologous-vs-allogenic-cell-therapy-key-differences-and-applications/]
- 9. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 10. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 11. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 12. Allogeneic Cell Therapies: Opportunities, Challenges & ... [https://www.phacilitate.com/insights-resources/allogeneic-therapies-silver-bullet-future-cell-therapy-developers]
- 13. Autologous Cell Therapy Product Market Forecast [https://www.pharmiweb.com/press-release/2025-11-17/autologous-cell-therapy-product-market-forecast-a-new-era-of-personalized-therapies]
- 14. Optimising T-cell expansion to improve early-stage ... [https://www.drugtargetreview.com/article/169304/optimising-t-cell-expansion-to-improve-early-stage-cell-therapy/]
- 15. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 16. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 17. A Novel High-Throughput Screening Platform Reveals an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5105341/]
- 18. Overcoming immunological barriers in regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC4409427/]
- 19. Challenges to Cell Expansion for Allogenic Cell Therapies [https://www.biopharminternational.com/view/challenges-to-cell-expansion-for-allogenic-cell-therapies]
- 20. Scaling Hope: The Growth of Allogeneic Cell Therapy Sector [https://www.precisionformedicine.com/blog/article-scaling-hope-the-growth-of-allogeneic-cell-therapy-sector/]
- 21. Overcoming the Variability of iPSCs in the Manufacturing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10706975/]
- 22. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 23. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 24. Autologous haematopoietic stem cell transplantation ... [https://www.sciencedirect.com/science/article/pii/S1470211824012338]
- 25. Autologous Cell Therapy Market Expand at 18.9% CAGR ... [https://www.towardshealthcare.com/insights/autologous-cell-therapy-market-sizing]
- 26. Quantification of peripheral blood CD34+ cells prior to stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6098175/]
- 27. Protocol for isolation and expansion of natural killer cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889455/]
- 28. Optimization of Human T Cell Expansion Protocol [https://www.stemcell.com/optimization-of-human-t-cell-expansion-protocol-effects-of-early-cell-dilution.html]
- 29. Allogeneic Cell Therapy Manufacturing Market Current ... [https://www.insightaceanalytic.com/report/allogeneic-cell-therapy-manufacturing-market-size-share--trends-analysis-report-by-product-by-scale-of-operation-preclinical-scale-operations-clinical-scale-operations-commercial-scale-operations-by-region-and-segment-forecasts-2025-2034/1194]
- 30. Allogeneic Cell Therapy Market Size to Hit USD ... [https://www.biospace.com/press-releases/allogeneic-cell-therapy-market-size-to-hit-usd-4-677-38-million-by-203]
- 31. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 32. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 33. Cell and Gene Therapy Spotlights 2025 [https://www.insights.bio/cell-and-gene-therapy-insights/spotlights/year/2025]
- 34. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 35. Progress and challenges in developing allogeneic cell ... [https://pubmed.ncbi.nlm.nih.gov/40185072/]
- 36. A differentiated and durable allogeneic strategy applicable ... [https://pubmed.ncbi.nlm.nih.gov/41201433/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1hm_zfT8jMJsIQ3GbQ-Vn1GNwJy9eMgo-fOSeO7x1x1kVVKkOO&fc=None&ff=20251112121802&v=2.18.0.post22+67771e2]
- 37. Recent advances in feeder-free NK cell expansion as a ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1675353/full]
- 38. Allogene Therapeutics Secures U.S. FDA IND Clearance ... [https://ir.allogene.com/news-releases/news-release-details/allogene-therapeutics-secures-us-fda-ind-clearance-allo-329]
- 39. Autologous Cell Therapy vs Allogeneic: 7 Key Differences ... [https://int.livhospital.com/autologous-cell-therapy-vs-allogeneic-7-key-differences-benefits/]
- 40. Cell-based immunotherapies for solid tumors - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066282/]
- 41. The Cost Of Stem Cell Therapy in 2026 [https://bioinformant.com/cost-of-stem-cell-therapy/]
- 42. How Much Does Stem Cell Therapy Cost in 2025 [https://www.startstemcells.com/stem-cell-therapy-cost.html]
- 43. Manufacturing autologous cell therapies [https://www.patheon.com/us/en/insights-resources/blog/autologous-cell-therapy-manufacturing-challenges-and-best-practices.html]
- 44. Treg cell therapy manufacturability: current state of the art ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12141221/]
- 45. - Immunology; Allergic... Hematopoietic Stem Cell Transplantation [https://www.msdmanuals.com/professional/immunology-allergic-disorders/transplantation/hematopoietic-stem-cell-transplantation]
- 46. (PDF) Immune Escape after Hematopoietic ... Stem Cell [https://www.academia.edu/41430040/Immune_Escape_after_Hematopoietic_Stem_Cell_Transplantation_HSCT_From_Mechanisms_to_Novel_Therapies]
- 47. sciencedirect.com/topics/medicine-and-dentistry/ hematopoietic - stem ... [https://www.sciencedirect.com/topics/medicine-and-dentistry/hematopoietic-stem-cell-transplantation]
- 48. Regulatory T cell approaches for graft-versus-host disease ... [https://pubmed.ncbi.nlm.nih.gov/41172558/]
- 49. Frontiers | Interpreting immune : a novel assay for HLA loss... evasion [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1603188/full]
- 50. Allogeneic versus autologous stem cell transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057802/]
- 51. Optimizing stem cell infusion timing in the prevention of ... [https://www.sciencedirect.com/science/article/abs/pii/S0092867425002958]
- 52. sentinels: empowering survival and Cellular defense in... immune [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03987-2]
- 53. Cell Therapy Trends: Autologous and Allogeneic Perspective [https://www.patheon.com/us/en/insights-resources/blog/emerging-cell-therapy-trends-autologous-and-allogeneic-perspective.html]
- 54. BioPharma By the Numbers: Rise of Bioprocessing ... [https://www.biopharminternational.com/view/biopharma-by-the-numbers-rise-of-bioprocessing-automation]
- 55. Point-of-Care Cell and Gene Therapy Manufacturing ... [https://www.businesswire.com/news/home/20250402936461/en/Point-of-Care-Cell-and-Gene-Therapy-Manufacturing-Market-Report-2025-2035---Closed-System-Bioreactors-and-AI-Bioprocessing-Set-to-Shape-PoC-Manufacturing-by-2035---ResearchAndMarkets.com]
- 56. UK point-of-care production of cell therapies could arrive in ... [https://www.pharmaceutical-technology.com/analyst-comment/uk-point-of-care-production-cell-therapies/]
- 57. Trends in Bioprocessing for 2025 | Innovative Insights [https://www.tecnic.eu/trends-in-bioprocessing-for-2025/]
- 58. Centralized vs. Point-of-Care Manufacturing [https://www.roslinct.com/insights/centralized-vs-point-of-care-manufacturing/]
- 59. Reducing Drug Costs Without Limiting Innovation [https://www.oliverwyman.com/our-expertise/insights/2025/jan/5-innovative-ways-to-reduce-drug-costs.html]
- 60. Frontiers | Allogeneic CAR-engineered cellular therapy for relapsed and refractory large B cell lymphoma: a systematic review and meta-analysis [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1585556/full]
- 61. Taming the Beast: CRS and ICANS after CAR T-cell therapy for ALL - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8592274/]
- 62. Autologous Vs. Allogeneic CAR-T Therapies [https://www.cellandgene.com/doc/autologous-vs-allogeneic-car-t-therapies-time-for-a-second-look-0001]
- 63. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 64. Selection of Autologous or Allogeneic Transplantation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK12844/]
- 65. Safety Testing of Human Allogeneic Cells Expanded for ... [https://www.asgct.org/advocacy/policy-statements/safety-testing-of-human-allogeneic-cells-expanded-for-use-in-cell-based-medical-products]
- 66. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 67. Current Insights of Post-Infusion CAR T Expansion and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523718/]
- 68. Vispa-Cel Shows Comparable Efficacy, Durability to ... [https://www.onclive.com/view/vispa-cel-shows-comparable-efficacy-durability-to-autologous-car-t-cell-therapy-in-r-r-b-cell-nhl]
- 69. Key predictors of long-term outcomes in BCMA-targeted CAR ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06543-x]
- 70. Allogene Therapeutics Reports Second Quarter 2025 ... [https://ir.allogene.com/news-releases/news-release-details/allogene-therapeutics-reports-second-quarter-2025-financial]
- 71. Moving from Autologous to Allogeneic Cell Therapies: Drivers and Hurdles [https://www.pharmasalmanac.com/articles/moving-from-autologous-to-allogeneic-cell-therapies-drivers-and-hurdles]
- 72. Cell Therapy Market Size, Growth, Share & Global Report ... [https://www.mordorintelligence.com/industry-reports/cell-therapy-market]
- 73. CAR T-Cell Therapy Market Size to Surpass USD 146.55 [https://www.globenewswire.com/news-release/2025/10/30/3177604/0/en/CAR-T-Cell-Therapy-Market-Size-to-Surpass-USD-146-55-Billion-by-2034-Fueled-by-Innovations-in-Cancer-Treatment-and-Growing-Demand-for-Personalized-Therapies.html]
- 74. Allogeneic Cell Therapy Bioprocess Economics and Optimization: Single-Use Cell Expansion Technologies - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065358/]
- 75. Building Bridges to Scalable Allogeneic Therapy Cell [https://www.news-medical.net/news/20250527/Building-Bridges-to-Scalable-Allogeneic-Cell-Therapy.aspx]
- 76. Integrated Platforms for Autologous Cell Therapy [https://www.bioprocessintl.com/sponsored-content/autologous-cell-therapy-can-integrated-platforms-break-the-bottlenecks-]
- 77. FDA vs. EMA: Navigating Divergent Regulatory ... [https://cromospharma.com/fda-vs-ema-navigating-divergent-regulatory-expectations-for-cell-and-gene-therapies-what-biopharma-companies-need-to-know/]
- 78. ATMP Development in 2025: Promise, Pressure, and the ... [https://www.cryoport.com/bio-blog-atmp-development-in-2025-promise-pressure-and-the-push-to-scale/]
- 79. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 80. Manufacturing & Controls for Advanced Therapy Medical ... [https://www.eurogct.org/research-pathways/research-and-innovation/fundamental-research/manufacturing-phase/manufacturing]
- 81. Advanced therapy medicinal products: Overview [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview]
- 82. EMA Proposes Revisions to GMP Guideline for ATMPs [https://www.gmp-compliance.org/gmp-news/ema-proposes-revisions-to-gmp-guideline-for-atmps]