Comparative Analysis of ADSC, BMSC, and UC-MSC Exosomes for Angiogenesis: Sources, Efficacy, and Clinical Translation
Exosomes derived from mesenchymal stem cells (MSCs) are emerging as potent acellular therapeutic agents for promoting angiogenesis in regenerative medicine and drug development.
Comparative Analysis of ADSC, BMSC, and UC-MSC Exosomes for Angiogenesis: Sources, Efficacy, and Clinical Translation
Abstract
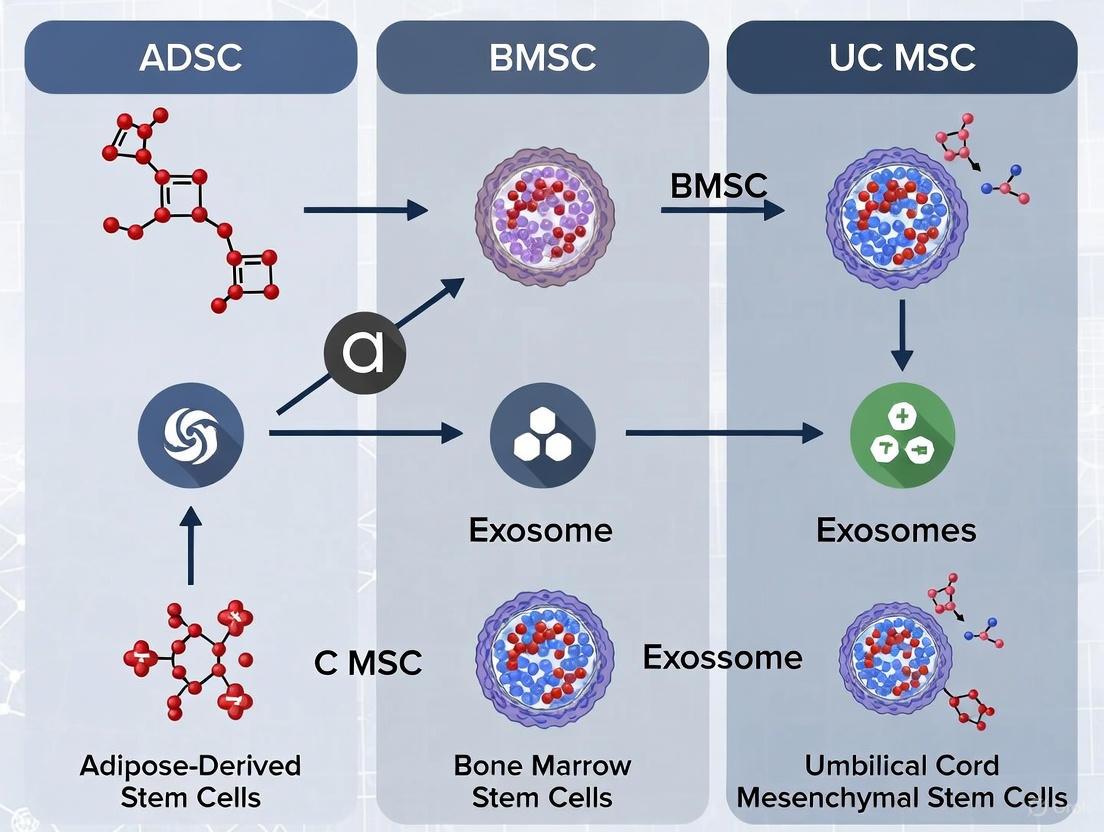
Exosomes derived from mesenchymal stem cells (MSCs) are emerging as potent acellular therapeutic agents for promoting angiogenesis in regenerative medicine and drug development. This review provides a comprehensive comparative analysis of exosomes from three key sources: Adipose-Derived Stem Cells (ADSCs), Bone Marrow-Mesenchymal Stem Cells (BMSCs), and Umbilical Cord-Mesenchymal Stem Cells (UC-MSCs). We systematically evaluate their inherent angiogenic potential, the impact of cell culture and isolation methodologies on exosome bioactivity, and strategies for optimizing their therapeutic efficacy. By synthesizing findings from foundational, methodological, and validation-focused studies, this article serves as a strategic guide for researchers and scientists in selecting and engineering the most appropriate exosome source for specific vascular regeneration applications, thereby accelerating the path to clinical translation.
Understanding the Native Angiogenic Potential of MSC Exosomes
Biogenesis and Core Composition of Pro-Angiogenic Exosomes
Exosomes, nanoscale extracellular vesicles (30-150 nm in diameter), have emerged as critical mediators of intercellular communication and promising therapeutic agents in regenerative medicine, particularly for their pro-angiogenic capabilities. These vesicles are secreted by various cell types, with mesenchymal stem cells (MSCs) representing a particularly rich and therapeutically valuable source. This review provides a comprehensive comparison of exosomes derived from three prominent MSC sources: adipose-derived stem cells (ADSCs), bone marrow mesenchymal stem cells (BMSCs), and umbilical cord mesenchymal stem cells (UCMSCs). We systematically analyze their biogenesis pathways, core molecular compositions, and relative efficacies in promoting angiogenesis, supported by experimental data and detailed methodologies. The objective comparison presented herein aims to guide researchers and drug development professionals in selecting optimal exosome sources for specific angiogenic applications.
Exosomes are formed via a highly conserved biogenetic pathway originating from the endosomal system. The process begins with the inward budding of the limiting membrane of early endosomes, leading to the creation of intraluminal vesicles (ILVs) within large multivesicular bodies (MVBs). These MVBs subsequently fuse with the plasma membrane, releasing ILVs into the extracellular space as exosomes [1] [2]. This biogenesis occurs through both endosomal sorting complex required for transport (ESCRT)-dependent and ESCRT-independent mechanisms, the latter involving tetraspanin microdomains and lipids such as ceramide [1].
The pro-angiogenic potency of exosomes is largely dictated by their molecular cargo, which includes proteins, lipids, and various nucleic acid species. This cargo is selectively packaged from the parent cell, reflecting its physiological state and environmental conditions [1]. MSC-derived exosomes contain growth factors, cytokines, and a diverse profile of microRNAs (miRNAs) that collectively target pathways critical for endothelial cell proliferation, migration, and tube formation—the fundamental processes underpinning angiogenesis [3] [2]. The composition of this cargo, and thus the exosome's functional capacity, varies significantly depending on the cellular source of the exosomes, necessitating a systematic comparison for research and therapeutic development.
The selection of parent cell type is a primary determinant of exosome function. ADSCs, BMSCs, and UCMSCs are among the most extensively studied MSC sources, each offering distinct advantages and characteristic cargo profiles that influence their angiogenic potential.
Source-Specific Advantages and Limitations
- Adipose-Derived Stem Cells (ADSCs): ADSCs are isolated from lipoaspirated subcutaneous adipose tissue. This source is characterized by its high accessibility and abundance, with colony-forming units significantly surpassing those of BMSCs [4]. ADSCs exhibit robust proliferative capacity in vitro and possess low immunogenicity, making them suitable for allogeneic applications [5] [6]. The autologous nature of adipose tissue minimizes immune rejection risks compared to allogeneic sources [4].
- Bone Marrow Mesenchymal Stem Cells (BMSCs): As the first discovered and most historically studied MSC source, BMSCs are considered a gold standard in many contexts. However, their isolation from bone marrow aspirates is more invasive and traumatic for donors compared to adipose tissue harvesting. Furthermore, the yield of stem cells from bone marrow is generally lower, often necessitating extensive in vitro expansion to obtain clinically relevant numbers [5].
- Umbilical Cord Mesenchymal Stem Cells (UCMSCs): UCMSCs are obtained from Wharton's jelly and other cord tissues, which are medical waste after birth. This makes them a source with minimal ethical concerns [5]. They are considered immunologically naive and possess a strong proliferative potential. However, their use is limited to allogeneic settings, and scalability can be challenged by donor variability [4].
Quantitative Comparison of Pro-Angiogenic Cargo
The therapeutic efficacy of MSC-derived exosomes in angiogenesis is largely mediated by their cargo of specific proteins and miRNAs. The table below summarizes key pro-angiogenic molecules identified in exosomes from different MSC sources.
Table 1: Key Pro-Angiogenic Cargo in MSC-Derived Exosomes
| Molecule Type | Specific Molecule | ADSC-Exos | BMSC-Exos | UCMSC-Exos | Function in Angiogenesis |
|---|---|---|---|---|---|
| Proteins | VEGF | Present [6] | Present [2] | Information Missing | Stimulates endothelial cell proliferation and permeability |
| FGF2 | Present [6] | Information Missing | Information Missing | Promotes endothelial cell proliferation and migration | |
| Ang-1 | Present [6] | Present [7] | Information Missing | Stabilizes newly formed blood vessels | |
| HGF | Present [6] | Information Missing | Information Missing | Enhances endothelial cell migration and tubulogenesis | |
| MicroRNAs | miR-21-5p | Information Missing | Promoted angiogenesis in stroke [7] | Information Missing | Targets PTEN, activating AKT pathway; enhances HUVEC migration/proliferation |
| miR-126 | Promoted angiogenesis via PI3K/Akt [6] | Information Missing | Information Missing | Enhances VEGF signaling; promotes endothelial cell proliferation/migration | |
| miR-31a | Information Missing | Information Missing | Information Missing | Promotes endothelial cell proliferation and tube formation | |
| let-7f | Information Missing | Information Missing | Information Missing | Suppresses TGF-β signaling; enhances endothelial cell migration | |
| miR-146a | Present [6] | Information Missing | Information Missing | Inhibits NF-κB signaling, reducing inflammation in vascular repair |
Experimental Data on Angiogenic Potency
Direct comparisons and individual studies demonstrate the functional consequences of these cargo differences.
- BMSC-Exos in Cerebral Ischemia: In a mouse model of ischemic stroke, administration of BMSC-Exos significantly improved neurological function, reduced infarct volume, and upregulated microvessel density. This pro-angiogenic effect was mechanistically linked to the transfer of miR-21-5p, which enhanced the proliferation, migration, and tube formation of human umbilical vein endothelial cells (HUVECs) in vitro by increasing the expression of VEGF, VEGFR2, Ang-1, and Tie-2 [7].
- ADSC-Exos in Wound Healing: ADSC-Exos have shown remarkable efficacy in promoting wound healing, a process dependent on robust angiogenesis. They enhanced wound closure rates, collagen deposition, and neovascularization in preclinical models. Their potency can be further amplified through preconditioning strategies; for example, hypoxia-exposed ADSCs produce exosomes with higher concentrations of angiogenic proteins like VEGF, FGF2, and PDGF [8] [4] [6].
- Comparative Performance: A review of studies suggests that ADSC-Exos may hold an advantage in terms of accessibility and yield. ADSCs are more abundant and easier to obtain than BMSCs, and they exhibit greater genetic stability and proliferative capacity in prolonged culture [6]. This makes ADSC-Exos a highly practical and efficient source for large-scale production required for clinical applications.
Table 2: Functional Comparison of MSC-Exos in Angiogenesis Models
| Exosome Source | Experimental Model | Key Findings | Proposed Mechanism | Reference |
|---|---|---|---|---|
| BMSC-Exos | Mouse MCAO (Stroke) | Improved neurological function, reduced infarct volume, increased microvessel density | miR-21-5p transfer; upregulation of VEGF/VEGFR2/Ang-1/Tie-2 | [7] |
| ADSC-Exos | Wound Healing (in vivo) | Accelerated wound closure, enhanced collagen remodeling, increased capillary density | Activation of PI3K/Akt pathway via miR-126; delivery of VEGF and FGF2 | [4] [6] |
| ADSC-Exos | HUVEC Tube Formation (in vitro) | Enhanced endothelial cell proliferation, migration, and tube formation capacity | Contained pro-angiogenic miRNAs (e.g., miR-126, miR-146a) and proteins | [6] |
Experimental Protocols for Pro-Angiogenic Exosome Research
Standardized Isolation and Characterization of Exosomes
To ensure reproducibility and reliability in angiogenesis research, adhering to standardized protocols for exosome isolation and characterization is paramount, in line with MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [8].
- Isolation via Ultracentrifugation: The most widely used method involves a series of differential centrifugations. Cell culture supernatant is sequentially centrifuged at:
- 300 × g for 10 min to remove live cells.
- 2,000 × g for 10 min to remove dead cells.
- 10,000 × g for 30 min to remove cell debris.
- 100,000 × g for 70 min to pellet exosomes, followed by a wash in PBS and a final ultracentrifugation at 100,000 × g for 70 min [7].
- Characterization: Isolated exosomes must be characterized by:
- Nanoparticle Tracking Analysis (NTA): To determine particle size distribution and concentration [7].
- Transmission Electron Microscopy (TEM): To confirm classic cup-shaped morphology [7].
- Western Blot: To detect positive markers (e.g., CD9, CD63, CD81, TSG101, Alix) and absence of negative markers (e.g., calnexin) [7] [1].
Key Methodologies for Assessing Angiogenic Potential
The following in vitro and in vivo assays are fundamental for evaluating the pro-angiogenic capacity of MSC-derived exosomes.
- In Vitro HUVEC Functional Assays:
- Proliferation Assay: HUVECs are treated with exosomes, and proliferation is measured via CCK-8 or EdA assay after 24-48 hours [7].
- Migration Assay: A scratch ("wound") is created in a confluent HUVEC monolayer. The rate of gap closure over 12-24 hours, with and without exosome treatment, is quantified to assess migration [7].
- Tube Formation Assay: HUVECs are seeded on a Matrigel matrix and treated with exosomes. The formation of capillary-like structures is imaged after 4-8 hours, and parameters like mesh number, tube length, and junction number are quantified [7].
- In Vivo Models:
- Ischemic Stroke Model (MCAO): Mice/rats undergo middle cerebral artery occlusion to induce cerebral ischemia. Exosomes are administered intravenously post-injury. Outcomes include neurological scoring, infarct volume measurement, and immunohistochemical analysis of microvessel density (e.g., using BrdU/vWF staining) [7].
- Wound Healing Model: Full-thickness skin wounds are created on rodents. Exosomes are applied topically, often via a biomaterial scaffold (e.g., hydrogel). Wound closure rate and histological analysis of granulation tissue thickness and CD31+ blood vessels are performed [4].
Visualization of Key Signaling Pathways
The pro-angiogenic effects of MSC-exosomes are mediated through the activation of several key signaling pathways in recipient endothelial cells. The following diagram illustrates the primary molecular mechanisms facilitated by the transfer of exosomal cargo.
Pro-Angiogenic Signaling Pathways Activated by MSC-Exosomes
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Exosome Angiogenesis Research
| Reagent / Kit | Specific Example | Function in Workflow |
|---|---|---|
| Cell Culture Medium | DMEM/F12 or RPMI-1640 with Exosome-Free FBS | To culture parent cells (MSCs) and ensure that isolated exosomes originate from the cells of interest and not serum. |
| Isolation Kits | Size-Exclusion Chromatography (SEC) columns; Polymer-based precipitation kits | Alternative methods to ultracentrifugation for isolating exosomes from conditioned medium or biofluids. |
| Characterization Instruments | Nanoparticle Tracking Analyzer (e.g., Malvern NanoSight); Transmission Electron Microscope | For determining exosome size, concentration, and morphological confirmation. |
| Endothelial Cell Line | Human Umbilical Vein Endothelial Cells (HUVECs) | The standard in vitro model for conducting proliferation, migration, and tube formation assays. |
| Extracellular Matrix | Growth Factor-Reduced Matrigel | A basement membrane matrix used for the in vitro tube formation assay to support the development of capillary-like structures. |
| Antibodies for Western Blot | Anti-CD63, Anti-CD81, Anti-CD9, Anti-TSG101, Anti-Alix | For confirming the presence of exosome-specific marker proteins after isolation. |
| Antibodies for Immunofluorescence | Anti-CD31 (PECAM-1), Anti-vWF | For staining and identifying endothelial cells and newly formed blood vessels in in vivo tissue sections. |
Pro-angiogenic exosomes from ADSCs, BMSCs, and UCMSCs all demonstrate significant potential for advancing therapeutic angiogenesis in conditions like ischemic diseases and wound healing. While they share a common biogenesis pathway, their core composition and functional efficacy are distinctly shaped by their cellular origin. ADSC-Exos present a compelling profile due to their source abundance, practical isolability, and potent cargo rich in angiogenic factors and miRNAs. BMSC-Exos remain a well-characterized option with proven efficacy, notably through mechanisms like miR-21-5p transfer. UCMSC-Exos offer an ethically favorable alternative. The choice of exosome source should be guided by the specific requirements of the research or therapeutic application, considering factors such as cargo profile, required yield, and functional potency as validated through standardized in vitro and in vivo assays. Future research will benefit from enhanced isolation standardization and engineering strategies to further optimize the angiogenic potential of these remarkable natural nanotherapeutics.
Mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as pivotal acellular therapeutic agents in regenerative medicine, primarily functioning through sophisticated paracrine communication [9] [10]. These nano-sized vesicles (30-150 nm) transfer bioactive cargo—including proteins, lipids, and nucleic acids—to recipient cells, orchestrating crucial biological processes such as angiogenesis, immunomodulation, and tissue repair [6] [11]. Among the various MSC sources, adipose-derived stem cells (ADSCs), bone marrow mesenchymal stem cells (BMSCs), and umbilical cord mesenchymal stem cells (UC-MSCs) represent the most extensively investigated and therapeutically relevant populations [9]. The angiogenic potential of their exosomal cargo varies significantly based on parental cell origin, creating a compelling landscape for comparative analysis. This guide systematically evaluates the inherent angiogenic profiles of ADSC, BMSC, and UC-MSC exosomes, providing researchers and drug development professionals with objective, data-driven insights for selecting optimal exosome sources for specific vascular regeneration applications.
Comparative Angiogenic Potential of MSC Exosomes
Quantitative Comparison of Angiogenic Cargo and Efficacy
The therapeutic efficacy of MSC exosomes in promoting angiogenesis is intrinsically linked to their biomolecular composition, which varies significantly across source tissues. The table below summarizes key comparative data on angiogenic cargo and functional outcomes.
Table 1: Comparative Angiogenic Profiles of MSC Exosomes from Different Sources
| Exosome Source | Key Angiogenic Cargo | Target Pathways/Mechanisms | Documented Functional Outcomes | Relative Efficacy Notes |
|---|---|---|---|---|
| ADSC-Exos | miR-205, miR-126, VEGF, FGF2, IL-10, HGF, Ang-1 [6] | miR-205 suppresses cardiomyocyte apoptosis; miR-126 activates PI3K/Akt in endothelium; FGF2 & VEGF promote angiogenesis [6]. | Enhanced capillary density in myocardial infarction models; reduced pulmonary edema; improved cardiac function post-MI [6]. | Potent immunomodulatory properties; effective across multiple organ systems; high proliferation rate of parent cells [6] [5]. |
| BMSC-Exos | VEGF, miR-21, miR-196a, BMPs, various growth factors [12] [11] | Promotes angiogenesis and osteogenesis via Wnt/β-catenin pathway; key in bone regeneration [12] [13]. | Improved functional scores in neurological and musculoskeletal disorders; promotes bone regeneration and vascularization [9] [12]. | Considered one of the most effective sources per umbrella review; high efficacy in neurological and renal models [9]. |
| UC-MSC-Exos | Specific cargo less documented; generally rich in growth factors and cytokines [11] | Regulates AMPK/NR4A1, TGF-β1/Smad3, Wnt/β-catenin, and Hippo signaling pathways [11]. | Significant improvement in functional recovery; effective in treating premature ovarian failure via angiogenesis [11]. | Highly effective alongside BMSC and ADSC exosomes; modified UC-MSC exosomes show enhanced outcomes [9]. |
A 2025 umbrella review analyzing 47 meta-analyses across 27 diseases established that exosomes derived from bone marrow, adipose tissue, and umbilical cord are the most effective sources, with modified EVs consistently showing enhanced therapeutic outcomes [9]. The choice of source often involves a trade-off between angiogenic potency, tissue-specificity, and practical considerations like cell harvest yield and expansion potential.
ADSCs offer the significant advantage of being easily obtained from autologous adipose tissue in large quantities with minimal ethical concerns, and they exhibit a high proliferation rate [5]. BMSCs, while more invasive to harvest, are often considered a "gold standard" and demonstrate high efficacy, particularly in neurological and renal applications [9] [14]. UC-MSCs represent a potent allogeneic source with robust paracrine activity [11].
Experimental Protocols for Angiogenic Assessment
Standard Workflow for Exosome Isolation and Characterization
To ensure the reliability and reproducibility of comparative data, standardized protocols for exosome production and validation are critical. The following workflow is commonly employed, with variations depending on the required scale and purity.
Figure 1: Standard workflow for MSC exosome isolation and characterization. Key steps include cell culture, conditioned media collection, isolation (choosing between Ultracentrifugation for lab scale or Tangential Flow Filtration for GMP scale), and multi-method characterization [14] [15].
Key Methodological Details:
- Cell Culture: BMSCs cultured in α-MEM show a higher expansion ratio and particle yield compared to those cultured in DMEM, though not always statistically significant [14].
- Isolation Methods: Tangential Flow Filtration (TFF) provides a statistically higher particle yield compared to traditional Ultracentrifugation (UC) and is more suitable for large-scale, GMP-compliant production [14] [15].
- Characterization: Isolated particles must be confirmed as exosomes through multiple techniques:
- Nanoparticle Tracking Analysis (NTA): Determines particle size (~100-150 nm) and concentration [14].
- Transmission Electron Microscopy (TEM): Confirms classic cup-shaped morphology [14].
- Western Blotting: Verifies the presence of exosomal surface markers (CD9, CD63, CD81, TSG101) and the absence of negative markers like calnexin [14] [15].
Functional Assays for Angiogenic Potential
The pro-angiogenic capacity of isolated MSC exosomes is typically validated using a combination of in vitro and in vivo models.
Table 2: Standard Functional Assays for Angiogenic Validation
| Assay Type | Specific Model/Test | Measured Parameters | Interpretation of Angiogenic Potential |
|---|---|---|---|
| In Vitro | Human Umbilical Vein Endothelial Cell (HUVEC) Assay [6] | Tube formation (number, length, junctions); Cell proliferation & migration; Gene expression (VEGFR2, Ang-1) [6]. | Enhanced tube formation and cell migration indicate strong pro-angiogenic activity. |
| In Vivo | Myocardial Infarction (MI) Rodent Model [6] | Capillary density in border zone; Infarct size reduction; Cardiac function (ejection fraction) [6]. | Increased capillary density and improved cardiac function demonstrate therapeutic angiogenesis. |
| In Vivo | Hindlimb Ischemia Model | Blood perfusion (Laser Doppler); New vessel formation (histology) | Improved perfusion and visible new vessels confirm functional vessel growth. |
| Molecular Analysis | RNA Sequencing / PCR [13] | miRNA and mRNA expression profiles (e.g., miR-206, miR-126) [6] [13]. | Identifies specific pro-angiogenic cargo and upstream molecular mechanisms. |
Key Angiogenic Signaling Pathways
The therapeutic effects of MSC exosomes are mediated through the activation or inhibition of specific signaling pathways in recipient cells. The following diagram illustrates the central mechanisms by which ADSC exosomes, in particular, promote angiogenesis, drawing from detailed cargo analyses [6].
Figure 2: Key angiogenic signaling pathways activated by ADSC-exosome cargo. Exosomal miRNAs and proteins coordinate to promote endothelial cell survival, proliferation, and new vessel formation through parallel pathways [6].
The Scientist's Toolkit: Essential Research Reagents
Successful research into MSC exosomes requires a suite of specialized reagents and equipment. The following table details key solutions essential for isolation, characterization, and functional analysis.
Table 3: Essential Research Reagents and Tools for MSC Exosome Studies
| Reagent / Solution | Function / Application | Example Use Case |
|---|---|---|
| Alpha Minimum Essential Medium (α-MEM) | Cell culture medium for MSC expansion. | Found to yield higher BMSC proliferation and exosome yield compared to DMEM [14]. |
| Human Platelet Lysate (hPL) | Xeno-free supplement for cell culture media. | Used as a serum alternative in GMP-compliant MSC culture systems [14]. |
| Trypsin-EDTA | Enzymatic detachment of adherent cells. | Standard procedure for passaging and harvesting MSCs. |
| Phosphate Buffered Saline (PBS) | Washing buffer and exosome resuspension. | Used for washing cells and as a vehicle for exosome storage and injection. |
| CD9, CD63, CD81 Antibodies | Exosome surface marker detection. | Critical for Western Blot characterization of isolated vesicles [14] [15]. |
| TSG101, ALIX Antibodies | Luminal exosome marker detection. | Further confirmation of exosomal identity via Western Blot [15]. |
| Calnexin Antibody | Negative marker for exosome purity. | Detection of this endoplasmic reticulum protein indicates contamination with cell debris [14]. |
| Paraformaldehyde (PFA) | Fixation agent for cell and tissue samples. | Used in preparing samples for imaging techniques like TEM and immunofluorescence. |
| Triton X-100 | Permeabilization detergent. | Permeabilizes cell membranes for intracellular staining in immunoassays. |
| DAPI Staining Solution | Nuclear counterstain. | Labels cell nuclei in fluorescence microscopy. |
| Alexa Fluor-conjugated Antibodies | Fluorescent labeling for detection. | Used in flow cytometry and immunofluorescence to detect specific antigens. |
| Matrigel | Basement membrane matrix. | Used for in vitro tube formation assays with HUVECs to assess angiogenic potential. |
This comparative analysis elucidates that ADSC, BMSC, and UC-MSC exosomes possess distinct inherent angiogenic profiles, driven by their unique biomolecular cargo. ADSC exosomes are particularly notable for their rich miRNA content targeting endothelial survival and vascular stability. BMSC exosomes demonstrate robust efficacy in integrating angiogenesis with osteogenesis. UC-MSC exosomes present a potent, less invasive option with strong regenerative signaling. The ongoing standardization of isolation protocols and a deeper mechanistic understanding of their cargo will further empower researchers to select and potentially engineer the most optimal exosome source for targeted angiogenic therapies.
Key Signaling Pathways (VEGF, PI3K/Akt, Wnt) and Cargo (miRNAs, Proteins)
The selection of an optimal exosome source is a critical determinant of success in angiogenesis research and therapeutic development. Exosomes derived from Mesenchymal Stem Cells (MSCs) have emerged as potent mediators of intercellular communication, capable of transferring bioactive cargo such as microRNAs (miRNAs) and proteins to recipient cells, thereby influencing key signaling pathways central to blood vessel formation [8] [4]. This guide provides a comparative analysis of exosomes from three prominent sources—Adipose-Derived Stem Cells (ADSCs), Bone Marrow-Mesenchymal Stem Cells (BMSCs), and Umbilical Cord-Mesenchymal Stem Cells (UCMSCs)—focusing on their distinct impacts on VEGF, PI3K/Akt, and Wnt signaling pathways. We synthesize experimental data and methodologies to equip researchers with evidence-based insights for selecting the most appropriate exosome source for specific angiogenic applications.
Exosome Biogenesis and Cargo Selection
Exosomes are nano-sized extracellular vesicles (30-150 nm in diameter) that originate from the endosomal system [16]. Their biogenesis begins with the inward budding of the endosomal membrane, leading to the formation of intraluminal vesicles (ILVs) within multivesicular bodies (MVBs) [17] [16]. These MVBs subsequently fuse with the plasma membrane, releasing ILVs as exosomes into the extracellular space [17].
The molecular cargo of exosomes—including proteins, lipids, and nucleic acids—is not packaged randomly but through highly regulated mechanisms [16]. The Endosomal Sorting Complex Required for Transport (ESCRT) machinery plays a pivotal role in sorting ubiquitinated proteins into ILVs [17] [16]. Additionally, ESCRT-independent pathways exist, involving tetraspanins (e.g., CD63, CD81, CD9) and lipids such as ceramide [4] [16]. The selective sorting of miRNAs is governed by RNA-binding proteins (RBPs) like hnRNPA2B1, which recognize specific nucleotide sequences in miRNAs known as EXOmotifs, ensuring their enrichment in exosomes [17].
Table: Key Machinery in Exosome Biogenesis and Cargo Sorting
| Component | Function | Key Examples |
|---|---|---|
| ESCRT Complex | Recognizes ubiquitinated cargo and mediates inward budding of endosomal membrane [16] | ESCRT-0, -I, -II, -III, VPS4, ALIX, TSG101 [17] |
| Tetraspanins | Organize membrane microdomains for cargo clustering; serve as common exosome markers [4] | CD63, CD81, CD9 [4] |
| RNA-Binding Proteins (RBPs) | Recognize specific motifs (e.g., EXOmotifs) to selectively load miRNAs into exosomes [17] | hnRNPA2B1, AUF1 [17] |
| Lipids | Promote membrane curvature and ILV formation in ESCRT-independent pathways [4] | Ceramide [4] |
Diagram 1: Exosome Biogenesis, Cargo Sorting, and Angiogenic Function. This diagram illustrates the pathway from exosome formation through endocytosis to the activation of key signaling pathways in a recipient cell, highlighting major cargo sorting mechanisms.
The therapeutic potential of MSC-derived exosomes in angiogenesis is significantly influenced by the tissue of origin, which dictates their molecular cargo and functional properties [8] [18].
ADSC-Exosomes (Adipose-Derived Stem Cell Exosomes)
ADSC-Exos are noted for their accessibility and high yield, as adipose tissue is abundant and easily obtainable via liposuction [4]. They demonstrate potent pro-angiogenic capabilities, largely through the delivery of specific miRNAs that enhance endothelial cell function and vessel stability [4]. Studies highlight their efficacy in wound healing models, where they promote cellular proliferation, migration, and new blood vessel formation [4].
UCMSC-Exosomes (Umbilical Cord Mesenchymal Stem Cell Exosomes)
UCMSC-Exos are often characterized by their strong pro-angiogenic potential. Direct comparative studies have shown that UCMSCs exhibit greater pro-angiogenesis activity than ADMSCs in vitro and in vivo, as evidenced by enhanced tube formation in assays [18]. This makes them a highly promising candidate for applications requiring robust blood vessel growth, such as in myocardial infarction repair [18].
BMSC-Exosomes (Bone Marrow Mesenchymal Stem Cell Exosomes)
While BMSCs were one of the first MSC types to be studied, their exosomes can be influenced by donor age. For instance, exosomes derived from older BMSCs exhibit diminished effects in osteogenic and lipogenic abilities compared to those from younger BMSCs [8]. This suggests that donor-related factors are a critical consideration when using BMSC-Exos.
Table: Comparative Profile of MSC-Exosome Sources for Angiogenesis
| Feature | ADSC-Exosomes | UCMSC-Exosomes | BMSC-Exosomes |
|---|---|---|---|
| Key Advantages | Easily accessible source, high yield, low immunogenicity [4] | Strong pro-angiogenic potential, young donor source [18] | Extensive historical data and characterization [19] |
| Documented Pro-Angiogenic Cargo | miR-125a, miR-31, miR-21-5p, miR-424 [4] | Not specified in results | Not specified in results |
| Reported Functional Efficacy | Promotes wound healing, endothelial cell proliferation & migration [4] | Superior tube formation in vitro compared to ADMSCs [18] | Efficacy can be donor-age dependent [8] |
| Considerations | Varies with donor site and collection method [8] | Direct comparative data vs. ADMSCs shows superior angiogenesis [18] | Functional heterogeneity and potential for age-related decline [8] |
Key Signaling Pathways in Angiogenesis
Exosomes mediate their angiogenic effects primarily by modulating three core signaling pathways.
VEGF Signaling Pathway
The Vascular Endothelial Growth Factor (VEGF) pathway is a master regulator of angiogenesis. When VEGF ligands bind to their receptors (e.g., VEGFR2) on endothelial cells, it triggers receptor dimerization and autophosphorylation, initiating a downstream signaling cascade [18]. This cascade promotes endothelial cell survival, proliferation, migration, and ultimately the formation of new blood vessels. MSC-exosomes can carry VEGF protein itself or miRNAs that modulate the expression of VEGF and its receptors [18] [4].
PI3K/Akt Signaling Pathway
The PI3K/Akt pathway is a crucial downstream effector of VEGF signaling and a key promoter of endothelial cell survival. Activation of receptor tyrosine kinases (like VEGFR) recruits and activates PI3K, which converts PIP2 to PIP3. This leads to the phosphorylation and activation of Akt [20]. Activated Akt then phosphorylates several substrates, including endothelial nitric oxide synthase (eNOS), which promotes vasodilation and angiogenesis, and Bad, which inhibits apoptosis [20]. The pathway is negatively regulated by the phosphatase PTEN [20].
Wnt Signaling Pathway
The Wnt/β-catenin (canonical) pathway is highly conserved and involved in development and tissue homeostasis [21] [22]. In the "off" state (without Wnt ligand), a destruction complex (containing APC, Axin, CK1α, GSK3β) phosphorylates β-catenin, targeting it for ubiquitination and proteasomal degradation [21] [22]. When a Wnt ligand binds to its Frizzled receptor and LRP5/6 co-receptor, it disrupts the destruction complex. This allows β-catenin to accumulate in the cytoplasm and translocate to the nucleus, where it partners with TCF/LEF transcription factors to activate target genes like c-MYC and VEGF, which can promote angiogenesis and cell proliferation [21] [22] [20].
Diagram 2: Core Angiogenic Signaling Pathways. This diagram outlines the key components and sequence of events in the VEGF, PI3K/Akt, and Wnt/β-catenin pathways, highlighting their role in promoting angiogenesis.
Experimental Data and Protocols for Angiogenesis Assessment
Key Experimental Models and Data
Robust in vitro and in vivo models are essential for evaluating the pro-angiogenic capacity of different MSC-exosomes.
Table: Summary of Key Experimental Findings
| Exosome Source | Experimental Model | Key Quantitative Findings | Reference |
|---|---|---|---|
| UCMSC | Mouse Myocardial Infarction (MI) | Improved cardiac function, decreased infarction area, promoted angiogenesis post-MI [18] | [18] |
| UCMSC vs ADMSC | In Vitro Tube Formation Assay | UCMSCs presented greater pro-angiogenesis activity than ADMSCs [18] | [18] |
| ADSC | In Vivo Wound Healing | 200 μg/mL exosome concentration showed efficacy in promoting wound healing [8] | [8] |
| BMSC | Sciatic Nerve Crush Injury | Effective at a concentration of 0.9 × 10^10 particles/mL in vitro [8] | [8] |
Detailed Methodologies for Key Assays
Endothelial Cell Tube Formation Assay
This in vitro assay is a fundamental test for assessing the ability of exosomes to stimulate blood vessel-like structure formation.
- Procedure [18]:
- Matrigel Coating: Coat a 96-well plate with 50 μL of growth factor-reduced Matrigel per well. Allow the Matrigel to polymerize for 1 hour at 37°C.
- Cell Seeding: Harvest Human Umbilical Vein Endothelial Cells (HUVECs) and seed them onto the solidified Matrigel at a density of 20,000 cells per well. The cells should be suspended in the conditioned medium collected from the MSC cultures (containing the exosomes to be tested) or in a control medium.
- Incubation: Incubate the plate at 37°C with 5% CO2 for 6-8 hours.
- Imaging and Analysis: After incubation, randomly photograph the formed capillary-like networks using a microscope. Analyze the images with software such as ImageJ to quantify key parameters, including:
- Total Tube Length: The combined length of all tubular structures.
- Number of Nodes: The branching points within the network.
- Number of Junctions: The connection points between tubes.
Matrigel Plug Assay
This in vivo assay evaluates the ability of exosomes to stimulate new blood vessel growth in a living organism.
- Procedure [18]:
- Plug Preparation: Mix the test MSCs (e.g., 5 x 10^5 cells) or their exosomes with liquid Matrigel (stored on ice). Matrigel alone serves as a negative control.
- Implantation: Anesthetize mice (e.g., female BALB/C nude mice) with isoflurane. Subcutaneously inject the Matrigel mixture (e.g., 200 μL per site) into the left and right groin of each mouse.
- Harvesting: After a set period (e.g., 14 days), euthanize the mice and surgically retrieve the Matrigel plugs.
- Analysis: The plugs can be analyzed by:
- Visual Inspection: Assessing the degree of vascularization (visible blood vessels) on the plug surface.
- Histology: Fixing, sectioning, and staining the plugs with antibodies against endothelial cell markers like CD31 to identify and quantify the newly formed blood vessels within the plug.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Kits for Exosome and Angiogenesis Research
| Reagent/Kits | Function/Application | Key Characteristics |
|---|---|---|
| Growth Factor-Reduced Matrigel | Provides a basement membrane matrix for in vitro tube formation assays and in vivo Matrigel plug assays [18] | Mimics the complex extracellular environment; essential for HUVEC tube formation [18] |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Standard primary cell model for studying endothelial cell biology and angiogenesis in vitro [18] | Responsive to pro-angiogenic factors; form capillary-like tubes on Matrigel [18] |
| CD31 (PECAM-1) Antibody | Histological marker for identifying and quantifying endothelial cells in tissue sections (e.g., from Matrigel plugs) [18] | Well-established immunohistochemical marker for vascularization [18] |
| CD63, CD81, CD9 Antibodies | Detection of exosome-specific tetraspanins by western blot, flow cytometry, or immuno-EM for exosome characterization [4] [16] | Common surface markers used to identify and validate exosome isolates [4] |
| Ultracentrifugation & SEC Kits | Standardized methods for isolating and purifying exosomes from cell culture conditioned medium or biological fluids [8] | Ultracentrifugation is widely used but time-consuming; SEC can preserve exosome integrity and bioactivity [8] |
Production, Isolation, and Functional Characterization for Angiogenesis
The isolation of high-purity exosomes is a critical prerequisite for advancing angiogenesis research and therapeutic development. Exosomes derived from Mesenchymal Stem Cells (MSCs)—including those from adipose tissue (ADSC), bone marrow (BMSC), and umbilical cord (UC-MSC)—carry distinct pro-angiogenic cargo that holds great potential for treating ischemic diseases and supporting tissue regeneration [8] [23]. The recovery of these bioactive molecules is highly dependent on the isolation technique employed. Ultracentrifugation (UC) remains the most commonly used method, but emerging techniques like Size-Exclusion Chromatography (SEC) and combined approaches claim improvements in yield, purity, and functionality [24] [25]. This guide provides an objective, data-driven comparison of these core isolation methodologies to inform protocol selection for angiogenesis research.
Comparative Analysis of Isolation Techniques
Principles and Trade-offs of Major Methods
The choice of isolation method directly impacts exosome yield, purity, and biological activity, which are critical parameters for downstream angiogenesis applications.
- Ultracentrifugation (UC): This method relies on applying high centrifugal forces over extended periods to pellet exosomes based on their size and density. While it is considered the "gold standard" and is cost-effective for consumables, it is often criticized for being time-consuming, requiring specialized equipment, and potentially compromising exosome integrity through high shear forces. A significant drawback is its moderate purity, as it frequently co-precipitates non-exosomal proteins and lipoproteins [24] [26] [25].
- Size-Exclusion Chromatography (SEC): SEC separates exosomes from smaller soluble proteins by passing the sample through a porous gel matrix. Smaller molecules enter the pores and are delayed, while larger exosomes pass through more quickly. This method is praised for its speed, excellent preservation of exosome integrity and biological activity, and superior purity in removing contaminating proteins. However, its primary limitations are a lower yield and a relatively small sample processing volume [24] [8] [27].
- Combined Methods (UC-SEC): Hybrid protocols, such as an initial UC step to concentrate exosomes followed by SEC for final polishing, aim to balance the benefits of both parent methods. This approach typically results in higher purity than UC or SEC alone and maintains good exosome integrity. The trade-off is increased protocol complexity and total processing time [24].
Quantitative Performance Comparison
The following table summarizes key performance metrics for these methods, drawing from direct comparative studies.
Table 1: Quantitative Comparison of Exosome Isolation Method Performance
| Method | Purity (Protein Contamination) | Yield (Particle Recovery) | Exosome Integrity | Processing Time | Scalability |
|---|---|---|---|---|---|
| Ultracentrifugation (UC) | Moderate (High contaminant protein) [24] | Moderate (Potential particle loss/aggregation) [25] | Variable (Potential damage from shear forces) [26] [25] | Long (>4 hours) [26] | Low to Moderate [25] |
| Size-Exclusion Chromatography (SEC) | High (Effectively removes >95% of soluble proteins) [24] | Lower (Diluted samples, limited load volume) [24] [8] | High (Preserves structure and function) [8] [25] | Short (~1-2 hours) [27] | Low [25] |
| Combined UC-SEC | Very High (Significantly higher than SEC alone) [24] | High (Concentration via UC step) [24] | High (Final gentle SEC step) [24] | Long (Combined time of both methods) [24] | Moderate [25] |
| Tangential Flow Filtration-SEC (TFF-SEC)* | High [25] | Very High (Superior to UC) [25] | High (Gentle filtration) [25] | Moderate [25] | High (Suitable for large volumes) [25] |
Note: TFF-SEC is an advanced, scalable method included for context. It uses cross-flow filtration to concentrate exosomes from large volumes before a polishing SEC step [25].
Impact on Angiogenesis Research
The isolation method can directly influence the outcomes of angiogenesis studies by determining the quality and composition of the exosome preparation.
- Preservation of Pro-Angiogenic Cargo: Gentle methods like SEC and TFF-SEC are superior at maintaining the integrity of key pro-angiogenic molecules, such as miRNAs and proteins, which are crucial for stimulating endothelial cell migration and tube formation [8] [25].
- Purity and Specificity: High-purity isolates from SEC or combined methods minimize the co-isolation of contaminating proteins that could confound experimental results or trigger unintended immune responses in therapeutic applications [24] [19]. For instance, one study noted that UC-isolated exosomes from serum had several times higher serum protein contamination than those purified with an optimized UC-SEC method [24].
- Functional Yield: While UC may provide a high particle count, the presence of aggregates or damaged vesicles can overestimate the functional yield. Methods that ensure integrity, like SEC, provide a more accurate count of bioactive exosomes capable of inducing angiogenesis [28] [25].
Experimental Protocols for Isolation
Optimized Ultracentrifugation Protocol for Serum/Plasma
This protocol is adapted from a study comparing isolation methods for human serum exosomes [24].
- Sample Pre-processing: Dilute serum or plasma with an equal volume of phosphate-buffered saline (PBS) to reduce viscosity. Centrifuge at 2,000 × g for 10 minutes at 4°C to remove cells and debris. Transfer the supernatant to a new tube.
- High-Speed Centrifugation: Centrifuge the supernatant at 10,000 × g for 30 minutes at 4°C to pellet larger extracellular vesicles and organelles. Carefully collect the resulting supernatant.
- Ultracentrifugation (First Cycle): Transfer the supernatant to ultracentrifuge tubes. Centrifuge at 100,000 × g for 120 minutes at 4°C using a fixed-angle rotor.
- Wash Cycles: Carefully discard the supernatant, leaving a small volume to avoid disturbing the pellet. Resuspend the pellet in a large volume of PBS (e.g., 4 mL). Repeat ultracentrifugation at 100,000 × g for 70 minutes at 4°C. This wash cycle is typically repeated 3-4 more times to adequately reduce protein contamination [24].
- Final Resuspension: After the final wash, resuspend the purified exosome pellet in a small volume of PBS (50-200 µL) and store at 4°C for short-term use or -80°C for long-term storage.
Size-Exclusion Chromatography Protocol
This protocol outlines the use of commercial SEC columns (e.g., qEV columns from Izon Science) for plasma exosome isolation [24] [27].
- Sample Preparation and Column Equilibration: Pre-process the plasma or serum sample as described in Steps 1 and 2 of the UC protocol. Meanwhile, equilibrate the SEC column by rinsing with 15 mL of PBS.
- Sample Loading and Elution: Load the pre-processed sample onto the column (typically 0.5 mL per column). Continuously add PBS to the column to prevent it from running dry. Discard the first 3.5 mL of eluent (void volume), which contains larger proteins and vesicles.
- Fraction Collection: Collect the next 0.5-1.0 mL of eluent. This fraction is enriched with exosomes.
- Column Regeneration: After collection, flush the column with 30 mL of PBS, followed by 10 mL of 0.5 M NaOH for cleaning. Re-equilibrate with 50 mL of PBS before the next use.
- Exosome Concentration (Optional): If a more concentrated sample is required, the collected fraction can be concentrated using a final ultracentrifugation step (100,000 × g for 70 minutes) [24].
Combined UC-SEC Workflow Protocol
The combined method leverages the concentration power of UC and the high purity of SEC [24].
- Initial Concentration via UC: Follow Steps 1 through 3 of the Ultracentrifugation protocol to obtain a crude exosome pellet.
- Pellet Resuspension: Resuspend the pellet in a small, defined volume of PBS (e.g., 0.5 mL).
- Final Purification via SEC: Load the entire resuspended sample onto a pre-equilibrated SEC column and follow Steps 2 through 4 of the SEC protocol to obtain the purified exosome fraction.
Diagram Title: Experimental Workflow for Exosome Isolation
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents and Materials for Exosome Isolation
| Item | Function/Application | Example Specifications |
|---|---|---|
| Ultracentrifuge | High-speed centrifugation for pelleting exosomes. | Beckman Coulter Optima series with fixed-angle rotors (e.g., 50.2 Ti) [24]. |
| SEC Columns | Gel filtration for separating exosomes from soluble proteins. | qEV columns (Izon Science) or lab-packed Sepharose CL-2B columns [24] [27]. |
| Ultracentrifuge Tubes | Tubes capable of withstanding high G-forces. | Beckman Ultra-Clear tubes or equivalent [24]. |
| PBS Buffer | Universal suspension and dilution buffer. | 0.22 µm filtered, pH 7.4 [24] [27]. |
| Exosome-Depleted FBS | For cell culture to prevent bovine exosome contamination. | FBS ultracentrifuged at 100,000g overnight or commercially available [25]. |
| Filtration Units | Sterile filtration of buffers and sample pre-clearing. | 0.22 µm pore size PVDF or PES membranes [27] [25]. |
| Protein Assay Kits | Quantifying total protein to assess purity. | BCA or Bradford Assay kits [24]. |
| Antibodies for Characterization | Confirming exosome identity via Western Blot. | Anti-CD9, CD63, CD81, TSG101, Alix [8] [27] [23]. |
The selection of an exosome isolation technique is a fundamental decision that directly shapes research outcomes in angiogenesis. Ultracentrifugation offers a established, low-cost method but suffers from variable purity and potential vesicle damage. SEC provides superior purity and preserves bioactivity at the cost of lower yield. For the most demanding applications where both high purity and functional integrity are paramount, such as profiling the subtle angiogenic differences between ADSC-, BMSC-, and UC-MSC-derived exosomes, combined UC-SEC methods or advanced alternatives like TFF-SEC present the most robust and reliable choice. Researchers should align their selection with the specific priorities of their experimental or therapeutic goals.
In the field of angiogenesis research, exosomes derived from Mesenchymal Stem Cells (MSCs) have emerged as powerful cell-free therapeutic agents. These nanoscale vesicles transfer bioactive molecules that can promote new blood vessel formation, a critical process in tissue regeneration and repair. The three most common MSC sources are Adipose-Derived Stem Cells (ADSCs), Bone Marrow-derived MSCs (BMSCs), and Umbilical Cord-derived MSCs (UCSCs). However, the angiogenic potency of their exosomes is not solely defined by the cellular source; it is profoundly influenced by the culture environment in which the parent cells are grown. The choice between serum-contained media, traditionally supplemented with Fetal Bovine Serum (FBS), and chemically defined serum-free media (SFM) is a critical decision that impacts exosome yield, purity, bioactivity, and ultimately, their therapeutic potential. This guide provides an objective comparison of these two culture systems, underpinned by experimental data, to inform research and development strategies.
Direct Comparison: Key Parameters at a Glance
The following tables summarize the comparative impact of serum-free and serum-contained media on MSC exosomes, based on aggregated experimental findings.
Table 1: Impact on Exosome Characteristics and Production
| Parameter | Serum-Contained Media (FBS) | Serum-Free Media (SFM) | Supporting Evidence |
|---|---|---|---|
| Exosome Purity | Lower; high risk of contamination with bovine serum-derived EVs and proteins [29] [30]. | Higher; eliminates contaminating animal-derived vesicles and undefined serum components [29] [31]. | |
| Production Yield | Variable; can be high but requires a starvation period that stresses cells and reduces yield [29]. | Higher; specialized SFM can support continuous production without starvation, enhancing total output [29] [32]. | |
| Immunogenicity Risk | Higher; MSCs can internalize and present bovine antigens (e.g., Neu5Gc), risking immune reactions [31]. | Lower; absence of xeno-antigens reduces the potential for immune responses, favoring allogeneic therapy [31]. | |
| Batch-to-Batch Consistency | Lower; undefined serum composition leads to variability between production runs [31]. | Higher; chemically defined composition ensures superior reproducibility [31]. | |
| Therapeutic Angiogenesis | Potent pro-angiogenic effects demonstrated in various models. | Enhanced or Comparable; studies show SFM-cultured exosomes can have superior or equal wound healing and angiogenic capacity [29] [33]. |
Table 2: Impact on Parent MSC Characteristics
| Parameter | Serum-Contained Media (FBS) | Serum-Free Media (SFM) | Supporting Evidence |
|---|---|---|---|
| Proliferation Rate | Generally robust but can lead to increased senescence at later passages [31]. | More Stable; can provide a more consistent population doubling time into later passages [31]. | |
| Cellular Senescence | Higher levels observed in ADSCs cultivated long-term in FBS-media [31]. | Reduced; ADSCs in SFM showed lower levels of cellular senescence [31]. | |
| Genetic Stability | Lower compared to SFM-cultured cells [31]. | Higher; ADSCs cultivated in SFM demonstrated superior genetic stability [31]. | |
| Chondrogenic Differentiation | Maintains chondrogenic potential, supporting cartilage repair in vivo [34]. | Variable; SFM-expanded MSCs may show poor in vivo cartilage repair despite high proliferation, indicating differentiation potential is media-dependent [34]. |
Experimental Data and Detailed Methodologies
Enhancing Exosome Bioactivity for Angiogenesis
Objective: To compare the angiogenic and wound-healing efficacy of exosomes derived from human Umbilical Cord MSCs (UCMSCs) cultured under serum-free versus serum-contained conditions [29].
Experimental Protocol:
- Cell Culture: UCMSCs were cultured in two different media:
- Normal Media (NM): 10% FBS-supplemented DMEM.
- Chemically Defined Media (CDM): CellCor CD MSC SFM.
- Exosome Isolation:
- For the NM group, the medium was replaced with serum-free DMEM for 48 hours (starvation) to isolate UCMSC-derived exosomes without FBS contamination.
- For the CDM group, the same serum-free medium was used continuously for culture and exosome isolation.
- Exosomes were isolated from the conditioned media using Tangential Flow Filtration (TFF) with a 500 kDa molecular weight cut-off filter.
- Analysis:
- Characterization: Particle size and concentration were determined via Nanoparticle Tracking Analysis (NTA). Morphology was confirmed by Transmission Electron Microscopy (TEM). Purity was verified by Western blotting for exosome markers (CD63, CD81).
- Cytokine Analysis: The expression levels of angiogenic and pro-inflammatory cytokines in the exosomes were compared.
- Functional Assays:
- In Vitro Wound Healing: A scratch assay was performed to measure cell migration.
- In Vitro Angiogenesis: A tube formation assay on Matrigel using Human Umbital Vein Endothelial Cells (HUVECs) was conducted.
Key Findings:
- Exosomes from the SFM (CDM) group showed higher expression of regeneration-related cytokines and lower levels of pro-inflammatory cytokines.
- These exosomes demonstrated enhanced wound healing and significantly improved angiogenic activity in the tube formation assay compared to exosomes derived from starved cells in the NM group [29].
Ensuring Safety and Genetic Stability
Objective: To comprehensively compare the safety and characteristics of Adipose-Derived Stem Cells (ADSCs) cultivated in SFM versus FBS-containing media [31].
Experimental Protocol:
- Cell Culture: Human ADSCs from multiple donors were expanded in parallel using commercial SFM (CellCor, StemPro, MesenCult) and traditional FBS-containing media.
- Long-Term Analysis: Cells were passaged repeatedly to assess:
- Population Doubling Time (PDT) and Accumulated Cell Number (ACN).
- Surface Markers: Flow cytometry for standard MSC markers (CD73, CD90, CD105) and immunogenicity markers (HLA-DR, Neu5Gc).
- Cellular Senescence: Senescence-associated β-galactosidase staining.
- Genetic Stability: Karyotype analysis.
- Multi-Omics Profiling: Differential expression analysis of mRNAs and proteins.
Key Findings:
- ADSCs in SFM showed a more stable PDT to later passages and could produce more cells in a shorter time.
- SFM-cultured ADSCs exhibited lower cellular senescence, lower immunogenicity (minimal Neu5Gc expression), and higher genetic stability than FBS-cultured cells.
- mRNA and protein analysis revealed that genes related to apoptosis, immune response, and inflammation were significantly up-regulated in FBS-cultured ADSCs [31].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Exosome Production and Angiogenesis Research
| Reagent / Solution | Function / Application | Considerations for Use |
|---|---|---|
| Chemically Defined SFM (e.g., CellCor CD MSC, StemPro MSC SFM) | Supports the expansion of MSCs and production of exosomes in a serum-free, xeno-free environment. | Requires validation for specific MSC sources and therapeutic applications (e.g., chondrogenesis may be impaired [34]). |
| Tangential Flow Filtration (TFF) System | Scalable and efficient method for isolating and concentrating exosomes from large volumes of conditioned media. | Superior for reducing albumin contamination compared to ultracentrifugation; allows for high recovery rates [29] [30]. |
| Human Platelet Lysate (hPL) | Human-derived supplement alternative to FBS for clinical-grade MSC manufacturing. | Must be processed to deplete endogenous EVs and fibrinogen to ensure exosome purity [30]. |
| Annexin V / Propidium Iodide | Staining kits to assess cell viability and apoptosis during culture, crucial for monitoring cell health in SFM. | |
| Angiogenesis Antibody Array | Multiplexed protein detection tool to profile a panel of pro- and anti-angiogenic factors in exosomes or conditioned media [33]. | Provides a more comprehensive functional profile than single-analyte ELISAs. |
Visualizing the Workflow and Signaling Impact
The following diagrams illustrate the core experimental workflow for comparing culture media and how the resulting exosomes functionally influence angiogenesis.
Diagram 1: Experimental comparison workflow for MSC exosomes from different culture systems.
Diagram 2: Functional impact of exosome cargo on angiogenesis pathways.
The collective evidence indicates that serum-free media offer significant advantages for manufacturing MSC-derived exosomes intended for angiogenesis research and therapeutic development. The benefits of SFM—including superior exosome purity, reduced immunogenicity, enhanced genetic stability of parent cells, and potentially greater bioactivity—are compelling reasons to transition away from traditional FBS-contained systems. While the choice of SFM must be validated for specific MSC sources and targeted applications, the move towards defined, xeno-free culture conditions is essential for achieving reproducible, safe, and potent exosome-based regenerative therapies.
Angiogenesis, the process of new blood vessel formation from pre-existing vasculature, is a critical phenomenon in physiological processes like embryonic development and tissue repair, as well as in pathological conditions such as cancer and cardiovascular diseases [35]. In vitro angiogenesis assays serve as essential tools for evaluating the pro- or anti-angiogenic effects of various stimuli, including potential therapeutic compounds [35]. These assays primarily focus on key stages of the angiogenic process: endothelial cell proliferation, migration, and the formation of tubular structures that mimic capillary networks [35].
The choice between in vitro and ex vivo models represents a critical methodological consideration. While in vitro models involve cultivating isolated tissue components in controlled environments, ex vivo models utilize tissues or organs extracted from living organisms, thereby retaining more natural architecture and metabolic processes [35]. Recent advances have introduced more physiologically relevant human-centric models, including organ-on-a-chip technologies and 3D bioprinting, which better represent human physiology than conventional animal models [35].
This guide focuses on the foundational in vitro methods—tube formation, migration, and proliferation assays—within the specific context of evaluating the angiogenic potential of exosomes derived from different mesenchymal stem cell (MSC) sources: adipose-derived (ADSC), bone marrow-derived (BMSC), and umbilical cord-derived (UC MSC).
MSCs are multipotent stromal cells capable of self-renewal and differentiation into various mesodermal lineages [36]. They have emerged as a promising source of therapeutic exosomes for angiogenesis research due to their paracrine signaling capabilities. The tissue origin of MSCs significantly influences their biological properties, secretory profile, and consequently, their therapeutic potential [18] [37] [36].
Table 1: Comparison of MSC Sources for Angiogenesis Research
| MSC Source | Key Angiogenic Properties | Advantages for Research | Limitations |
|---|---|---|---|
| Adipose-Derived (ADSC) | Strong anti-apoptotic effects; promotes cardiomyocyte survival post-MI [18] | Easily harvested with high yield; minimal invasiveness [36] | Weaker chondrogenic differentiation potential [38] |
| Bone Marrow-Derived (BMSC) | High differentiation potential; strong immunomodulatory effects [36] | Most extensively studied; well-characterized [36] | Invasive extraction procedure; donor-age-related functional decline [37] [38] |
| Umbilical Cord-Derived (UC MSC) | Superior pro-angiogenic activity; high levels of pro-angiogenic factors [18] | Non-invasive harvest; high proliferative capacity; low immunogenicity [37] [36] | Immunomodulatory effects may diminish with in vivo aging [38] |
The paradigm in MSC research has shifted from cell replacement therapy to recognizing their secreted factors as primary therapeutic effectors [37]. The MSC secretome—comprising soluble proteins, cytokines, growth factors, and extracellular vesicles (including exosomes)—mediates beneficial effects through paracrine signaling [37]. Key functional components include proangiogenic factors like vascular endothelial growth factor (VEGF), insulin-like growth factor-1 (IGF-1), and hepatocyte growth factor (HGF), which collectively promote new blood vessel formation [37].
Comparative studies reveal that UCMSCs present greater pro-angiogenesis activity than ADMSCs in both in vitro and in vivo settings, while ADMSCs exert stronger anti-apoptotic effects on residual cardiomyocytes [18]. This functional specialization suggests that optimal MSC source selection depends on the specific therapeutic goal—whether promoting new vessel growth or protecting existing tissues is paramount.
Core Angiogenesis Assay Methodologies
Tube Formation Assay
The tube formation assay represents the most commonly used in vitro method for evaluating angiogenic properties by measuring the formation of tubular structures from vascular endothelial cells (ECs) [39] [40]. This assay models the final stage of angiogenesis where ECs differentiate and form capillary-like structures.
Standard Protocol:
- Matrix Preparation: Coat 24-well plates with ice-cold, phenol red-free Matrigel (approximately 50-300 μL/well depending on desired thickness) and incubate at 37°C for 30-60 minutes to allow polymerization [39] [40].
- Cell Seeding: Harvest endothelial cells (HUVECs or ECFCs) and seed them onto the polymerized Matrigel at a density of 15×10⁴ cells/well in 1 mL of reduced serum medium (2% FBS) [40].
- Treatment Application: Add experimental treatments (MSC-derived exosomes, growth factors, or inhibitors) to appropriate wells. Include positive controls (VEGF 30-50 ng/mL or FGF-2) and negative controls (untreated or vehicle-treated) [40].
- Incubation and Imaging: Incubate cells at 37°C with 5% CO₂ for 6-12 hours. Image tubular structures using phase contrast microscopy at regular intervals (e.g., every 1-4 hours) [40].
- Image Analysis: Quantify parameters including total tube length, number of nodes, number of junctions, and number of meshes using image analysis software such as ImageJ with the Angiogenesis Analyzer plugin [39].
Advanced Modifications:
- Real-time Monitoring: Use a real-time cell recorder to track tube formation every hour for up to 48 hours, capturing the dynamic progression of tube formation, elongation, and regression [40].
- Image Stitching: Employ image-stitching software to create larger observation areas (e.g., 2×2 stitched images from 4× objective lens), minimizing analysis error due to limited observation fields [40].
- Alternative Cell Sources: Utilize endothelial colony-forming cells (ECFCs) instead of HUVECs. ECFCs, as endothelial precursors, demonstrate robust proliferative capacity and more defined angiogenic characteristics compared to mature ECs [40].
The tube formation assay is particularly valuable for its simplicity, rapidity, and cost-efficiency, providing initial evidence of angiogenic properties before moving to more complex in vivo studies [40].
Migration Assay
Endothelial cell migration is a critical early step in angiogenesis, enabling cells to move toward angiogenic stimuli. The scratch wound (wound healing) assay is a common method to evaluate this process.
Standard Protocol:
- Cell Culture: Seed endothelial cells in well plates and incubate until 90% confluency is reached [35].
- Wound Creation: Scrape the cell monolayer using a 200 μL pipette tip or cell scraper to create a linear "wound" [35].
- Washing and Treatment: Wash the plate with PBS to remove floating cells and debris. Add fresh medium containing experimental treatments (MSC-derived exosomes, controls) [35].
- Imaging and Analysis: Observe the wound area immediately after scratching (0 hour) and at regular intervals (e.g., 6, 12, 24 hours) using an inverted microscope. Measure the remaining wound area and calculate migration rate [35].
This approach enables assessment of fundamental cell migration properties including speed, persistence, and polarity [35]. For example, in studies evaluating the α7-nAChR agonist ISO-1, the scratch assay demonstrated significant pro-migratory effects at concentrations of 10⁻⁶ and 10⁻⁴ M, similar to responses observed with nicotine and choline [41].
Proliferation Assay
Endothelial cell proliferation provides the necessary cellular expansion to support new vessel growth. The MTS assay offers a colorimetric method for quantifying this process.
Standard Protocol:
- Cell Seeding: Seed endothelial cells in 96-well plates at optimal density (e.g., 3×10⁴ cells/well) and incubate for 24 hours [35] [41].
- Treatment Application: Replace medium with treatment-containing medium (MSC-derived exosomes, controls) and incubate for desired duration (typically 24-72 hours) [41].
- MTS Reagent Addition: Add 10 μL of MTS reagent to each well and incubate plates for 3-5 hours at 37°C [35].
- Absorbance Measurement: Remove media and add 100 μL of DMSO to solubilize the formazan product. Measure absorbance at 570 nm using a spectrophotometer [35].
The MTS assay measures mitochondrial activity as a surrogate for cell viability and proliferation. The yellow tetrazole compound is converted to purple formazan in metabolically active cells, with color intensity correlating with cell number [35]. Alternative methods include the sulforhodamine B (SRB) assay, which measures cellular protein content, and DNA synthesis assays using BrdU incorporation [35] [41].
Table 2: Key Parameters for Core Angiogenesis Assays
| Assay Type | Primary Readout | Incubation Duration | Key Endpoints |
|---|---|---|---|
| Tube Formation | Capillary-like structure formation | 6-12 hours (up to 48h for real-time) | Total tube length, number of nodes, number of junctions, number of meshes [39] [40] |
| Migration (Scratch) | Wound closure | 6-24 hours | Migration rate, wound closure percentage [35] |
| Proliferation (MTS) | Metabolic activity | 24-72 hours | Absorbance at 570nm, cell viability percentage [35] |
Comparative Experimental Data
Direct comparisons of MSC sources reveal distinct angiogenic profiles that inform exosome research. A 2025 study comparing UCMSCs and ADMSCs in a mouse myocardial infarction model demonstrated that while both MSC types improved cardiac function and decreased infarction area, they exhibited different mechanistic strengths [18].
Transcriptomic profiling through RNA sequencing revealed differences in gene expression related to angiogenesis and apoptosis pathways between UCMSCs and ADMSCs [18]. Functional assessments demonstrated that UCMSCs presented greater pro-angiogenesis activity in both in vitro and in vivo settings, while ADMSCs exerted stronger cardioprotective functions and more potent anti-apoptotic effects on residual cardiomyocytes [18].
The Fibrin Bead Assay (FBA), an alternative 3D model, provides complementary information to the traditional tube formation assay. In this assay, Cytodex beads are coated with HUVECs and embedded in a fibrin gel matrix with fibroblasts seeded on top, promoting the growth of 3D capillary-like patterns [39] [42]. When analyzed using the Angiogenesis Analyzer for ImageJ, this method allows quantification of sprouting initiation capacities and pseudo-vascular tree length, parameters that correlate with different biological stages of angiogenesis compared to traditional tube formation metrics [39].
Advanced transcriptomic approaches like TRAP sequencing (Translating Ribosome Affinity Purification) have been applied to 3D angiogenesis models, revealing distinct gene expression changes during morphogenesis [42]. This technology enables enrichment of endothelial RNA in co-culture systems, overcoming limitations of bulk RNA sequencing when studying minority cell types [42]. These studies have identified dynamic changes in the endothelial translatome, particularly in genes involved in mitogenesis, blood vessel development, and NOTCH signaling pathway during 3D morphogenesis [42].
Signaling Pathways in Angiogenesis
Angiogenesis is regulated by complex signaling pathways that can be modulated by MSC-derived exosomes. The diagram below illustrates key pathways involved in endothelial cell activation during angiogenesis.
Key Signaling Mechanisms:
PI3K/Akt Pathway: Central to angiogenesis regulation, this pathway is activated by various stimuli including VEGF, FGF-2, and calcium influx through α7-nAChR receptors [41]. PI3K signaling orchestrates cytoskeletal remodeling, adherens junction dynamics, and directed cell migration essential for angiogenesis [41].
NOTCH Signaling: Critical for regulating tip cell and stalk cell specification during sprouting angiogenesis [42]. TRAP sequencing studies in 3D cultures show dynamic regulation of NOTCH pathway genes throughout morphogenesis, highlighting its importance in vascular patterning [42].
Calcium-Mediated Signaling: Activation of α7-nicotinic acetylcholine receptors (α7-nAChRs) on endothelial cells increases intracellular Ca²⁺ concentration, promoting kinase activation and subsequent pro-angiogenic responses [41].
MSC-derived exosomes can modulate these pathways through their cargo of miRNAs, cytokines, and growth factors, with variations in exosome composition across different MSC sources contributing to their distinct angiogenic profiles.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Angiogenesis Assays
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Endothelial Cells | HUVECs, HDMECs, ECFCs | Primary cells for angiogenesis assays; ECFCs offer robust proliferation [35] [40] |
| Extracellular Matrices | Matrigel, Collagen, Fibrin Gel | Provide 3D substrate for tube formation and sprouting assays [39] [40] |
| Pro-angiogenic Factors | VEGF (30-50 ng/mL), FGF-2 | Positive controls for assay validation [40] |
| Angiogenesis Inhibitors | Vatalanib, α-bungarotoxin | Negative controls; receptor-specific inhibitors [40] [41] |
| Cell Tracking Reagents | MTS, Neutral Red, SRB | Measure cell viability, proliferation, and cytotoxicity [35] [41] |
| Image Analysis Tools | ImageJ Angiogenesis Analyzer | Quantify network parameters in tube formation assays [39] |
| Specialized Assay Systems | Real-time cell recorder, Microfluidic chips | Dynamic monitoring and advanced modeling of angiogenesis [40] |
In vitro angiogenesis assays—tube formation, migration, and proliferation—provide complementary data for evaluating the angiogenic potential of MSC-derived exosomes. The selection of appropriate assay combinations should align with specific research questions, recognizing that 3D models and real-time monitoring approaches offer enhanced physiological relevance compared to traditional 2D endpoint analyses [40] [43].
The comparative analysis of MSC sources indicates that UCMSCs demonstrate superior pro-angiogenic activity, while ADMSCs exhibit enhanced anti-apoptotic properties, and BMSCs offer well-characterized immunomodulatory effects [18] [36]. This functional specialization suggests that target application should guide MSC source selection for exosome production in angiogenesis research.
Future directions in the field include increased standardization of exosome isolation and characterization methods, integration of more complex 3D and organ-on-a-chip models, and application of advanced transcriptomic technologies like TRAP sequencing to elucidate temporal changes in endothelial cell gene expression during exosome-mediated angiogenesis [42] [43].
In the field of regenerative medicine, the comparative analysis of exosome sources derived from Adipose-Derived Stem Cells (ADSCs), Bone Marrow Mesenchymal Stem Cells (BMSCs), and Umbilical Cord Mesenchymal Stem Cells (UCMSCs) requires robust and standardized in vivo validation models. These models serve as critical platforms for evaluating the pro-angiogenic capacity of therapeutic candidates, providing essential data on their functional performance in complex biological systems. Among the most established and widely utilized systems are wound healing models, myocardial infarction (MI) models, and Matrigel plug assays, each offering unique insights into different aspects of the angiogenic process. Wound healing models replicate the complex cascade of events in tissue repair, including neovascularization; MI models simulate the ischemic conditions that drive therapeutic angiogenesis in cardiac tissue; and Matrigel plug assays provide a quantifiable system for directly assessing new blood vessel formation. For researchers and drug development professionals, understanding the specific applications, experimental protocols, and data interpretation for each model is paramount when comparing the efficacy of different exosome sources. This guide provides a comprehensive comparison of these three fundamental in vivo validation models, with a specific focus on their application in evaluating ADSC, BMSC, and UC-MSC derived exosomes for angiogenesis research.
The therapeutic potential of mesenchymal stem cell-derived exosomes varies significantly based on their tissue of origin. ADSCs, BMSCs, and UCMSCs each possess distinct secretory profiles that influence their angiogenic capabilities [37]. These differences arise from variations in their inherent biological properties, including gene expression patterns, proliferative capacity, and paracrine activity [18] [36]. Understanding these source-dependent characteristics is essential for selecting the most appropriate exosome type for specific angiogenic applications.
Table 1: Comparative Characteristics of MSC Sources for Angiogenesis Research
| Parameter | ADSCs | BMSCs | UCMSCs |
|---|---|---|---|
| Key Angiogenic Factors | VEGF-A, HGF, bFGF, IGF-1 [44] | VEGF, bFGF, Angiopoietin-1 [36] | High levels of VEGF, FGF2, miR-126 [45] |
| Relative Angiogenic Potency | Moderate to high (enhanceable via electrical stimulation) [44] | Moderate (documented decline with donor age) [37] | High intrinsic pro-angiogenic activity [18] [37] |
| Primary Mechanisms | VEGFA-VEGFR2 signaling pathway activation [44] | Paracrine secretion of growth factors and cytokines [36] | Wnt/β-catenin, Notch, and PI3K/Akt pathways [45] |
| Documented Effects in Models | Strong cardioprotective and anti-apoptotic effects in MI; improved blood flow recovery in hindlimb ischemia [18] [44] | Tissue repair and angiogenesis promotion through bioactive molecule release [36] | Superior tube formation and pro-angiogenesis activity in vitro and in vivo [18] |
| Research Advantages | Easier to harvest and higher yields; responsive to potentiation strategies [44] [36] | Most extensively studied; strong immunomodulatory effects [36] | Non-invasive harvest; low immunogenicity; high proliferative capacity [37] [36] |
The selection of MSC source material significantly impacts the angiogenic potential of derived exosomes. UCMSCs consistently demonstrate superior pro-angiogenic activity in direct comparisons, with one study revealing they present "greater pro-angiogenesis activity than ADMSCs in vitro and in vivo" [18]. This enhanced activity is attributed to their rich content of angiogenic factors and activation of key signaling pathways including Wnt/β-catenin, Notch, and PI3K/Akt [45]. ADSCs offer a valuable alternative with the distinct advantage of being relatively easy to harvest in high yields and responsive to potentiation strategies such as electrical stimulation, which can significantly upregulate their secretion of VEGF-A and other angiogenic factors [44]. BMSCs, while historically the most extensively studied, may show functional decline with donor age but remain valuable for their well-characterized immunomodulatory properties [37] [36].
In Vivo Validation Models: Experimental Data and Applications
Matrigel Plug Assay
The Matrigel plug assay serves as a fundamental direct assessment tool for quantifying angiogenesis in vivo. This model involves the subcutaneous injection of Matrigel basement membrane matrix mixed with the test substance into laboratory animals, typically mice. The Matrigel forms a solid plug at body temperature, creating a defined environment where blood vessel infiltration can be measured after a predetermined period, usually 7-14 days [18] [44].
Table 2: Matrigel Plug Assay Protocol and Data Interpretation
| Aspect | Standardized Protocol | Key Measurements | Applications for Exosome Comparison |
|---|---|---|---|
| Plug Preparation | Mix exosomes (50-100 µg) with growth factor-reduced Matrigel (400-500 µL) on ice; optional addition of heparin (10-50 U/mL) and basic FGF (100-500 ng/mL) as positive controls [44] | Hemoglobin content (Drabkin's method), CD31+ endothelial cell infiltration (immunohistochemistry), vessel counting (histology) [44] | Direct comparison of angiogenic potency between ADSC, BMSC, and UC-MSC exosomes |
| Implantation | Subcutaneous injection into ventral region of mice (200-500 µL/site); multiple plugs per animal possible | Visual inspection for color (pale vs. reddish), plug weight, vascular density | Quantification of functional blood vessel formation induced by different exosome sources |
| Harvest & Analysis | Harvest at day 7-14; formalin fixation and paraffin embedding for sectioning; H&E staining and immunostaining | Microscopic analysis of vessel structures, quantification of functional vessels per field | Assessment of specific cell recruitment (endothelial cells, pericytes) mediated by exosome cargo |
In practice, this assay has demonstrated significant differences between MSC sources. Studies with electrically potentiated ADSCs (epMSCs) showed that "plugs from the epMSC group exhibited a reddish color with noticeable blood vessels" compared to controls [44]. Similarly, research comparing UCMSCs and ADMSCs utilized Matrigel plug assays to quantify their relative angiogenic potential [18]. The assay provides particularly valuable data when comparing multiple exosome sources simultaneously, as the plug model allows for high-throughput screening of angiogenic responses in a controlled environment.
Myocardial Infarction Models
Myocardial infarction models represent a critical translational platform for evaluating therapeutic angiogenesis in ischemic tissue, particularly relevant for cardiovascular applications of MSC-derived exosomes. These models typically involve surgical occlusion of coronary arteries in rodents or large animals to simulate the ischemic conditions of human myocardial infarction [18] [46].
Table 3: Myocardial Infarction Model Protocol and Assessment Methods
| Component | Standardized Protocol | Functional Assessment | Histological Analysis |
|---|---|---|---|
| Animal Selection | Mice (C57BL/6) aged 7-8 weeks; pigs for large animal studies [18] [46] | Echocardiography at day 28 post-MI: Left ventricular ejection fraction (LVEF), fractional shortening [18] | Infarction size measurement (TTC staining), capillary density (CD31+ staining), apoptosis (TUNEL assay) [18] |
| MI Induction | LAD coronary artery ligation or transient occlusion; maintenance on ventilator during surgery [18] [46] | Hemodynamic measurements: Left ventricular end-systolic/diastolic dimensions [46] | Assessment of cardiomyocyte apoptosis, fibrosis extent, inflammatory cell infiltration |
| Treatment Administration | Intramyocardial injection of exosomes (10-100 µg in 20-50 µL PBS) or cells (5×10^7) into border zone post-MI [18] [46] | Pressure-volume loop analysis for contractile function | Engraftment survival evaluation, vascular density quantification, tissue remodeling assessment |
The MI model has revealed important source-dependent differences in therapeutic effects. One comprehensive study comparing UCMSCs and ADMSCs in a mouse MI model found that while "both of UCMSCs and ADMSCs improved cardiac function, decreased infarction area and inhibited cardiomyocyte apoptosis while promoting angiogenesis post-MI in mice," notably, "ADMSCs exerted a better cardioprotective function than UCMSCs and stronger anti-apoptotic effect on residual cardiomyocytes" [18]. This suggests that ADSC-derived exosomes may offer superior protection for surviving cardiomyocytes in the infarct border zone, while UC-MSC exosomes might excel at promoting new vessel formation. These nuanced differences highlight the importance of matching exosome source to specific therapeutic objectives in cardiac repair.
Wound Healing Models
Wound healing models provide a comprehensive system for evaluating angiogenic potential within the complex cascade of tissue repair processes. These models typically involve creating full-thickness excisional wounds on the dorsal skin of rodents, with application of test exosomes either directly or via advanced delivery systems such as hydrogels [45] [47].
The wound healing process encompasses multiple overlapping phases—hemostasis, inflammation, proliferation, and remodeling—with angiogenesis playing a crucial role particularly during the proliferation phase [47]. Exosomes derived from different MSC sources contribute to this process through distinct mechanisms. MSC-derived exosomes "promote angiogenesis and improved wound healing outcomes primarily via Vascular Endothelial Growth Factor, FGF2, miR-126, Wnt/β-catenin, Notch and PI3K/Akt pathways" [45]. The choice of delivery vehicle significantly influences exosome efficacy, with hydrogels emerging as a particularly promising platform due to their "high moisture retention, biocompatibility, and ability to mimic the extracellular matrix," thereby supporting controlled release of exosomal cargo throughout the healing process [47].
Key metrics in wound healing studies include wound closure rate measured through serial photography and planimetry, histological assessment of granulation tissue formation, capillary density quantification via CD31 immunohistochemistry, and analysis of re-epithelialization [47]. These parameters allow researchers to compare the efficacy of different exosome sources in stimulating the vascularization necessary for successful tissue repair. The model's strength lies in its ability to evaluate angiogenesis within the context of a complete tissue regeneration program, providing insights that are highly relevant for clinical applications in chronic wounds and tissue engineering.
Experimental Protocols for Key Assays
Matrigel Plug Assay Protocol
The Matrigel plug assay provides a straightforward method for quantifying in vivo angiogenesis. The standard protocol involves the following steps:
- Preparation: Thaw Growth Factor-Reduced (GFR) Matrigel matrix overnight at 4°C. Keep all tubes and syringes on ice throughout the procedure.
- Mixing: Combine test exosomes (50-100 µg) with 400-500 µL of Matrigel. Include positive controls (e.g., 100-500 ng/mL bFGF with 10-50 U/mL heparin) and negative controls (Matrigel alone).
- Injection: Slowly inject the Matrigel mixture subcutaneously into the ventral region of anesthetized mice using pre-chilled syringes. Inject 500 µL per site, with multiple sites possible per animal.
- Incubation: Allow plugs to develop for 7-14 days. Monitor animals regularly for signs of discomfort or infection.
- Harvesting: Euthanize animals and carefully excise plugs. Remove surrounding tissue and document photographic evidence of vascularization.
- Analysis: Weigh plugs, measure hemoglobin content using Drabkin's reagent, and process for histology (fix in formalin, embed in paraffin, section, and stain with H&E or CD31 immunohistochemistry) [18] [44].
Myocardial Infarction Model Protocol
The murine myocardial infarction model requires precise surgical technique:
- Preparation: Anesthetize mice (7-8 weeks old, C57BL/6) with ketamine/xylazine. Intubate and connect to a ventilator.
- Surgical Access: Perform left thoracotomy between the 4th and 5th ribs to expose the heart.
- Infarction Induction: Identify the Left Anterior Descending (LAD) coronary artery and ligate permanently with an 8-0 prolene suture. Successful occlusion is confirmed by blanching of the anterior left ventricular wall.
- Treatment Administration: Immediately post-ligation, inject exosomes (20-50 µL containing 10-100 µg) intramyocardially into the border zone using a 30-gauge needle. Mark injection sites with suture material.
- Closure: Close the thoracic cavity in layers and administer analgesics for post-operative care.
- Functional Assessment: At predetermined endpoints (typically 28 days), perform echocardiography to measure left ventricular function, ejection fraction, and fractional shortening.
- Histological Analysis: Harvest hearts, section, and stain with Triphenyltetrazolium Chloride (TTC) to quantify infarct size, and with CD31 antibodies to assess capillary density [18] [46].
Exosome Isolation and Characterization Protocol
Standardized exosome isolation is crucial for comparative studies:
- Cell Culture: Culture ADSCs, BMSCs, and UCMSCs in serum-free media for 48 hours to collect conditioned media.
- Isolation: Use differential ultracentrifugation: 300 × g for 10 min to remove cells; 2,000 × g for 20 min to remove dead cells; 10,000 × g for 30 min to remove cell debris; and 100,000 × g for 70 min to pellet exosomes.
- Characterization:
Signaling Pathways in Angiogenesis
The pro-angiogenic effects of MSC-derived exosomes are mediated through multiple interconnected signaling pathways. Understanding these mechanisms is essential for elucidating the functional differences between exosomes from ADSCs, BMSCs, and UCMSCs.
Diagram: Signaling Pathways in MSC-Exosome Mediated Angiogenesis. This diagram illustrates the key signaling pathways activated by MSC-derived exosomes to promote angiogenesis, highlighting pathway preferences among different MSC sources.
The diagram above illustrates how exosomes from different MSC sources activate distinct but interconnected pro-angiogenic signaling pathways. UC-MSC exosomes prominently activate Wnt/β-catenin, Notch, and PI3K/Akt pathways, contributing to their superior tube formation capability [45]. ADSC exosomes, particularly from electrically potentiated cells, strongly activate the VEGFA-VEGFR2 signaling axis, enhancing endothelial cell migration and proliferation [44]. These pathway preferences translate to functional differences in angiogenic outcomes, helping researchers select the most appropriate exosome source for specific therapeutic applications.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Angiogenesis Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations for Exosome Studies |
|---|---|---|---|
| Basement Membrane Matrix | Growth Factor-Reduced (GFR) Matrigel (Corning) [18] [44] | Provides 3D substrate for endothelial cell tube formation and in vivo plug assays | GFR formulation essential for isolating exosome-specific effects from endogenous growth factors |
| Angiogenesis Assessment Kits | Drabkin's Reagent Kit (Sigma-Aldrich), CD31 Immunostaining Kits [44] | Quantifies hemoglobin content in Matrigel plugs; identifies endothelial cells | Standardized kits enable cross-study comparisons of angiogenic outcomes |
| MSC Culture Media | DMEM with 10% FBS (Gibco) [18] | Maintains MSC viability and function during exosome production | Use exosome-depleted FBS for pre-conditioning media to avoid contamination |
| Exosome Isolation Kits | Total Exosome Isolation Kits (Thermo Fisher) | Rapid isolation from conditioned media | Enables reproducible exosome yields across MSC sources |
| Characterization Instruments | Nanoparticle Tracking Analyzer (Malvern), Transmission Electron Microscope | Determines exosome size, concentration, and morphology | Critical for quality control before functional studies |
| Endothelial Cell Lines | Human Umbilical Vein Endothelial Cells (HUVECs) [44] | In vitro tube formation and migration assays | Primary cells better reflect physiological responses than immortalized lines |
| Animal Models | BALB/C nude mice, C57BL/6 mice (Gem Pharmatech) [18] | In vivo validation of angiogenic potential | Immunocompromised models prevent rejection of human-derived exosomes |
The comparative analysis of ADSC, BMSC, and UC-MSC derived exosomes for angiogenesis research requires careful selection of appropriate in vivo validation models, each with distinct advantages and applications. Matrigel plug assays offer direct quantification of blood vessel formation, myocardial infarction models provide clinically relevant insights into ischemic tissue revascularization, and wound healing models evaluate angiogenesis within the complex context of tissue repair. The experimental data consistently indicates that UC-MSC exosomes generally demonstrate superior pro-angiogenic activity, while ADSC exosomes exhibit enhanced cardioprotective and anti-apoptotic properties in myocardial infarction models. BMSC exosomes, though potentially less potent than other sources, benefit from extensive characterization and proven immunomodulatory capabilities. The choice of exosome source should align with specific therapeutic objectives, leveraging the unique advantages of each MSC type. As the field advances, standardized protocols across research institutions and improved delivery systems such as advanced hydrogels will enhance the reproducibility and translational potential of findings from these essential validation models.
Strategies to Enhance Exosome Yield, Purity, and Therapeutic Efficacy
Mesenchymal stromal cell (MSC)-derived exosomes have emerged as promising acellular therapeutic agents in regenerative medicine, particularly for promoting angiogenesis and tissue repair [8] [5]. However, the therapeutic efficacy of these exosomes is significantly influenced by both their cellular origin and the specific preconditioning strategies applied to parent cells prior to exosome collection [8] [49]. Preconditioning involves exposing MSCs to sublethal stressors—such as low oxygen, inflammatory cytokines, or pharmacological agents—to enhance their innate biological functions and optimize the cargo of secreted exosomes [49] [50]. This guide provides a comparative analysis of how hypoxia, cytokine exposure, and metformin pretreatment modulate the angiogenic and regenerative potential of exosomes derived from three prominent MSC sources: adipose-derived stem cells (ADSCs), bone marrow-derived MSCs (BMSCs), and umbilical cord-derived MSCs (UCMSCs). By synthesizing experimental data and protocols, we aim to inform researchers and drug development professionals in selecting optimal cell sources and preconditioning methods for specific angiogenic applications.
The tissue origin of MSCs significantly impacts their proliferation capacity, gene expression profiles, and consequent therapeutic potential [51] [52]. Understanding these inherent differences is crucial for selecting the appropriate cell source for specific regenerative applications.
Table 1: Biological Characteristics of MSCs from Different Sources
| Characteristic | ADSCs | BMSCs | UCMSCs |
|---|---|---|---|
| Proliferation Rate | Moderate [51] | Lower [51] | Highest [51] |
| Colony-Forming Ability | High [51] | Not Specified | Lower [51] |
| Key Strengths | Easily accessible, abundant source; strong anti-apoptotic effects [5] [52] | Established model; responsive to pharmacological preconditioning [53] | High proliferation; superior pro-angiogenic activity in vitro [54] [52] |
| Notable Differential Gene Expression | Enriched in anti-apoptotic pathways [52] | N/A | Enriched in angiogenesis-related pathways [52] |
Functional studies in disease models reveal how these biological differences translate to therapeutic outcomes. In a comparative study on radiation-induced lung injury (RILI), all three MSC types mitigated inflammation and oxidative damage, with UCMSCs identified as the most appropriate therapeutic option [54]. Conversely, in an acute myocardial infarction model, ADMSCs demonstrated stronger cardioprotective and anti-apoptotic effects on residual cardiomyocytes than UCMSCs, despite the latter exhibiting greater pro-angiogenic activity in vitro. This suggests that in ischemic conditions, protecting residual cells may be more crucial than promoting new blood vessels [52].
Preconditioning Strategies and Their Functional Outcomes
Preconditioning strategies can significantly enhance the therapeutic profile of MSC-derived exosomes. The following sections and table summarize the effects of three key approaches.
Table 2: Impact of Preconditioning Strategies on MSC Exosomes for Angiogenesis
| Preconditioning Strategy | MSC Source | Key Experimental Findings | Proposed Mechanism(s) | Reference |
|---|---|---|---|---|
| Hypoxia | ADSCs | Enhanced wound closure in diabetic mice; promoted HDF proliferation, migration, and tube formation; upregulated wound-healing-related miRNAs [55]. | Activation of USP22/HIF-1α axis; delivery of pro-angiogenic circRNAs (e.g., circ-snhg11) and miRNAs [55]. | |
| Hypoxia | BMSCs | Improved engraftment and lung repair in pulmonary fibrosis model; increased survival of engrafted cells; attenuated apoptosis and ECM production [50]. | Upregulation of cytoprotective genes and HGF; modulation of TGF-β1-mediated Akt signaling [50]. | |
| Inflammatory Cytokines (IFN-γ, TNF-α) + Hypoxia | MSCs (Unspecified Source) | The soluble secretome fraction lost its pro-angiogenic capacity, while the EV/exosome fraction retained its angiogenic potential [49]. | Inflammation redirected soluble protein secretion toward immune modulation; EV miRNA cargo was stable and protected from environmental stimuli [49]. | |
| Metformin (Pharmacological) | BMSCs | Accelerated diabetic wound repair; promoted endothelial cell migration, tube formation, and angiogenesis in vivo [53]. | LINC-PINT in exosomes acts as a competitive endogenous RNA for miR-139-3p, leading to upregulation of FOXC2 [53]. |
Hypoxic Preconditioning
Hypoxic preconditioning typically involves culturing MSCs in low oxygen tension (1-5% O₂) to mimic a niche-like environment, which has been shown to reduce cellular senescence and enhance the stem cells' paracrine activity [55] [50]. For ADSCs, hypoxia increases the secretion of exosomes and enriches their cargo with pro-angiogenic factors. Studies demonstrate that hypoxic ADSC-derived exosomes (hypADSC-Exo) are more effective than their normoxic counterparts in promoting the proliferation, migration, and tube formation of human dermal fibroblasts (HDFs) and human umbilical vein endothelial cells (HUVECs) [55]. This enhanced functionality is linked to the activation of specific signaling axes, such as USP22/HIF-1α, and the transfer of circular RNAs like circ-snhg11 [55]. Similarly, hypoxia-preconditioned BMSCs (HP-MSCs) exhibit improved survival and engraftment after transplantation in a murine model of bleomycin-induced pulmonary fibrosis. These HP-MSCs demonstrated superior therapeutic effects, including reduced lung edema and decreased levels of pro-inflammatory and fibrotic factors, which were attributed to the upregulation of hepatocyte growth factor (HGF) [50].
Cytokine Preconditioning
Preconditioning with inflammatory cytokines such as interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α) aims to prime MSCs for the harsh inflammatory environment of injury sites. A critical study dissecting the effects of combined cytokine and hypoxia preconditioning revealed a divergent impact on the MSC secretome [49]. While the soluble protein fraction of the secretome lost its pro-angiogenic capacity upon inflammatory stimulation, the extracellular vesicle (EV) or exosome fraction retained its angiogenic potential. This finding underscores that the angiogenic capability of MSC-derived exosomes is remarkably resilient to inflammatory environments. Furthermore, the study highlighted that inflammation-activated MSCs release proteins involved in tissue remodeling and repair, whereas MSCs in non-inflamed conditions modulate the expression of angiogenic proteins in response to oxygen levels [49].
Pharmacological Preconditioning
Pharmacological preconditioning involves treating MSCs with bioactive compounds to enhance their therapeutic properties. A prominent example is the use of metformin, an anti-diabetic drug. Exosomes derived from metformin-pretreated BMSCs (MET-Exos) significantly accelerated wound healing in diabetic mice by promoting angiogenesis [53]. Mechanistic studies identified a novel axis wherein a long non-coding RNA, LINC-PINT, packaged within the MET-Exos, functioned as a molecular sponge for miR-139-3p. This sequestration led to the upregulation of FOXC2, a key transcription factor governing angiogenesis, thereby stimulating new blood vessel formation [53].
Experimental Protocols for Key Studies
Protocol: Hypoxic Preconditioning of ADSCs for Wound Healing
This protocol is adapted from studies investigating the effects of hypoxic ADSC-Exos on diabetic wound healing [55].
- Cell Culture and Preconditioning: Isolate and characterize ADSCs from infant (e.g., polydactyly surgery waste) or adult (e.g., lipoaspirate) donors. Culture ADSCs in Dulbecco's Modified Eagle Media (DMEM) supplemented with 10% fetal bovine serum (FBS). For hypoxic expansion, culture cells at 1% O₂, 5% CO₂, and 94% N₂. Maintain normoxic controls at 20% O₂ and 5% CO₂.
- Exosome Isolation and Characterization: When cells reach 90% confluence, culture them in exosome-depleted FBS medium for 48 hours. Collect conditioned medium and sequentially centrifuge at 300 × g (5 min), 2,000 × g (30 min), and 10,000 × g (30 min) to remove cells and debris. Filter the supernatant through a 0.22 µm membrane and concentrate using 100-kDa molecular weight cutoff (MWCO) centrifugal filters. Further purify exosomes via ultracentrifugation at 100,000 × g for 70 minutes. Characterize exosomes using Nanoparticle Tracking Analysis (NTA) for size/concentration, Transmission Electron Microscopy (TEM) for morphology, and Western Blot or flow cytometry for surface markers (CD9, CD63, CD81) [55] [56].
- In Vivo Efficacy Testing: Utilize db/db diabetic mice as a model of impaired wound healing. Create full-thickness excisional wounds on the dorsum. Topically apply exosomes (e.g., 50-100 µg in a suitable hydrogel or PBS) periodically. Monitor wound closure biweekly using digital photography and planimetry. At endpoint, harvest tissue for histological analysis (H&E for re-epithelialization, Masson's trichrome for collagen density, CD31 immunohistochemistry for angiogenesis) [55].
Protocol: Metformin Preconditioning of BMSCs for Angiogenesis
This protocol is based on the study demonstrating the efficacy of MET-Exos in diabetic wound repair [53].
- Preconditioning and Exosome Isolation: Culture BMSCs in standard medium. Treat cells with a defined concentration of metformin (e.g., 0.1-1 mM) for a specified period to generate MET-Exos. Isolate exosomes from the conditioned medium using standard ultracentrifugation or SEC methods, as described in section 4.1.
- In Vitro Angiogenic Assays:
- Tube Formation Assay: Seed HUVECs (20,000 cells/well) on a layer of solidified Matrigel in a 96-well plate. Culture the cells in conditioned medium from MET-Exos or controls. After 4-8 hours, image the formed capillary-like structures and quantify parameters like total tube length, number of nodes, and number of junctions using image analysis software (e.g., ImageJ).
- Cell Migration Assay: Perform a scratch wound assay on a confluent monolayer of HUVECs or use a transwell system. Treat cells with MET-Exos. Monitor and quantify the migration of cells into the scratch area over 24-48 hours, or count the cells that migrate through the transwell membrane.
- Mechanistic Investigation: To probe the LINC-PINT/miR-139-3p/FOXC2 axis, employ techniques such as quantitative PCR (qPCR) to measure gene expression levels, RNA immunoprecipitation to validate molecular binding, and siRNA-mediated knockdown to confirm the functional role of specific molecules [53].
Signaling Pathways in Preconditioned Exosome Function
The therapeutic effects of preconditioned MSC-derived exosomes are mediated through specific molecular cargo that modulates key signaling pathways in recipient cells. The following diagram illustrates two key mechanisms identified in the cited research: the mechanism of metformin-preconditioned BMSC exosomes (MET-Exos) in promoting angiogenesis, and the general role of hypoxic exosomes in combating skin photoaging.
Diagram Title: Key Molecular Mechanisms of Preconditioned Exosomes
Diagram A illustrates the mechanism by which exosomes from metformin-preconditioned BMSCs (MET-Exos) promote angiogenesis. These exosomes deliver high levels of the long non-coding RNA LINC-PINT, which acts as a molecular sponge to sequester miR-139-3p. This inhibition prevents miR-139-3p from suppressing its target, the transcription factor FOXC2. The subsequent upregulation of FOXC2 drives the expression of genes involved in endothelial cell migration and tube formation, thereby accelerating wound repair [53].
Diagram B summarizes the multi-faceted approach of hypoxic ADSC-derived exosomes (hypADSC-Exo) in combating skin photoaging. These exosomes simultaneously reduce senescence in dermal fibroblasts, increase the production of structural collagens (I and III), and decrease the expression of matrix metalloproteinases (MMPs) that degrade the extracellular matrix. The concerted action of these effects leads to overall skin rejuvenation, characterized by improved hydration, elasticity, and reduced wrinkles [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents and Kits for Exosome and Preconditioning Research
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Exosome-Depleted FBS | Serum for cell culture that has been processed to remove bovine exosomes, preventing contamination of isolated MSC-exosomes. | Used during the exosome production phase when collecting conditioned medium from MSCs [55]. |
| Ultracentrifugation System | Standard method for isolating and purifying exosomes from conditioned cell culture media or biological fluids via high-speed centrifugation. | Used to pellet exosomes after differential centrifugation steps to remove cells and debris [55] [56]. |
| Nanoparticle Tracking Analysis (NTA) | Instrumentation to characterize the size distribution and concentration of particles in an exosome preparation. | Used to confirm the isolated vesicles are within the expected size range for exosomes (e.g., 30-200 nm) and to quantify yield [55] [56]. |
| Transmission Electron Microscopy (TEM) | High-resolution imaging technique to visualize the cup-shaped morphology characteristic of exosomes. | Used for morphological validation of isolated exosomes [55] [56]. |
| Matrigel Basement Membrane Matrix | A solubilized basement membrane preparation used for in vitro tube formation assays to assess angiogenic potential. | HUVECs are seeded on Matrigel and treated with exosomes; tube formation is quantified to measure angiogenesis [52]. |
| Hypoxic Chamber/Bag | A sealed chamber or bag system that can maintain a controlled, low-oxygen atmosphere (e.g., 1-5% O₂) for cell culture. | Used for the hypoxic preconditioning of MSCs prior to exosome collection [55] [50]. |
The strategic selection of MSC source and preconditioning protocol is paramount for optimizing the efficacy of exosome-based therapies in angiogenesis and regenerative medicine. UCMSCs demonstrate inherent strengths in proliferation and pro-angiogenic gene expression, ADSCs excel in anti-apoptotic pathways and are highly accessible, while BMSCs remain a well-characterized model responsive to pharmacological priming. Hypoxic preconditioning consistently enhances the pro-regenerative functions of exosomes across different MSC sources, primarily through the activation of HIF-1α and related pathways. Cytokine priming appears to uniquely preserve the angiogenic potential of the exosome fraction even under inflammatory stress. Pharmacological agents like metformin open new avenues for engineering exosome cargo via specific RNA networks. Future research should focus on standardizing preconditioning protocols, exploring combination strategies, and conducting direct, head-to-head comparisons of exosomes from different preconditioned sources within the same disease model to identify the most potent and clinically translatable candidates.
Exosomes have emerged as a pivotal therapeutic paradigm in regenerative medicine, offering a cell-free alternative to whole-cell therapies. These nano-sized extracellular vesicles facilitate intercellular communication by shuttling bioactive cargo—including proteins, lipids, and nucleic acids—between cells [48]. Their inherent stability, low immunogenicity, and capacity to be engineered make them exceptionally suitable for therapeutic applications [57]. The efficacy of exosome-based therapies is profoundly influenced by their cellular origin. This guide provides a comparative analysis of exosomes derived from three principal mesenchymal stem cell (MSC) sources: Adipose-Derived Stem Cells (ADSCs), Bone Marrow-Mesenchymal Stem Cells (BMSCs), and Umbilical Cord-Mesenchymal Stem Cells (UC-MSCs). We objectively compare their performance in angiogenesis research, supported by experimental data, and detail the methodologies for their engineering through surface functionalization and cargo loading.
The therapeutic potential of MSC-derived exosomes (MSC-Exos) varies significantly based on the tissue source of the parent cells. Key characteristics, advantages, and limitations of ADSC-Exos, BMSC-Exos, and UC-MSC-Exos are summarized below.
Table 1: Comparison of MSC-Derived Exosome Sources
| Feature | ADSC-Exos | BMSC-Exos | UC-MSC-Exos |
|---|---|---|---|
| Source Tissue | Adipose Tissue | Bone Marrow | Umbilical Cord (Wharton's Jelly) |
| Isolation Yield | High [57] | Moderate (Constrained by donor availability and invasive extraction) [57] | High proliferation capacity [58] |
| Key Advantages | Minimally invasive harvesting; abundant tissue source; strong chondrogenic and osteogenic potential [57] | Extensive research history; strong immunomodulatory and chondroprotective effects [58] | Non-invasive collection; no ethical concerns; superior immunomodulatory and anti-inflammatory properties [58] [57] |
| Primary Limitations | Inferior anti-inflammatory efficacy in direct comparisons [58] | Invasive extraction procedure; limited donor availability [57] | Less established research history compared to BMSCs [57] |
| Angiogenesis Potential | Promotes angiogenesis via VEGF and other factors [57] [45] | Promotes angiogenesis and modulates immune homeostasis [57] | Promotes angiogenesis; induces macrophage polarization to anti-inflammatory phenotype [58] |
Quantitative data from a 2025 study directly comparing the therapeutic efficacy of these exosomes in an osteoarthritis model provides critical insights for angiogenesis research, as inflammation and repair processes are often intertwined [58].
Table 2: Quantitative Comparison of Anti-inflammatory and Regenerative Efficacy (In Vitro/Ex Vivo Models)
| Therapeutic Effect | ADSC-Exos | BMSC-Exos | UC-MSC-Exos |
|---|---|---|---|
| Cell Viability (Cytotoxicity) | Minimal to no cytotoxicity at concentrations up to 1000 μg/mL [58] | Minimal to no cytotoxicity at concentrations up to 1000 μg/mL [58] | Minimal to no cytotoxicity at concentrations up to 1000 μg/mL [58] |
| Inhibition of NF-κB Pathway | Moderate reduction in phosphorylated p65 levels [58] | Strong and superior reduction in phosphorylated p65 levels [58] | Strong and superior reduction in phosphorylated p65 levels [58] |
| Inhibition of MAPK Pathway | Moderate reduction in pp38, pJNK, pERK [58] | Strong and superior reduction in pp38, pJNK, pERK [58] | Strong and superior reduction in pp38, pJNK, pERK [58] |
| Enhancement of Chondrocyte Migration | Marked enhancement [58] | Marked enhancement [58] | Marked enhancement [58] |
| Overall Efficacy Ranking in OA Models | Less effective [58] | Superior [58] | Superior [58] |
Experimental Protocols for Evaluating Exosome Efficacy
To ensure the reliability and reproducibility of comparative studies, standardized experimental protocols are essential. The following methodologies are commonly employed to isolate, characterize, and evaluate the therapeutic potential of MSC-Exos.
Exosome Isolation and Characterization
- Isolation via Aqueous Two-Phase System (ATPS): Exosomes can be isolated from conditioned cell culture media using the ATPS method, which separates particles based on their affinity for two immiscible aqueous phases (e.g., PEG/Dextran) [58].
- Nanoparticle Tracking Analysis (NTA): This technique determines the size distribution and particle concentration of the isolated exosome suspension. Typical yields are in the range of 6.9 × 10^7 particles/mL for BMSC-Exos, 8.0 × 10^7 particles/mL for ADSC-Exos, and up to 1.2 × 10^8 particles/mL for UC-MSC-Exos, with a size range of 30-150 nm [58].
- Transmission Electron Microscopy (TEM): Used to confirm the classic cup-shaped morphology and structural integrity of the isolated vesicles [58].
- Western Blot Analysis: Confirms the presence of exosomal marker proteins (e.g., CD63, CD81, CD9, ALIX, TSG101) to verify exosomal identity and purity [58] [48].
In Vitro Efficacy and Cytotoxicity Assays
- Cell Cytotoxicity (CCK-8 Assay): To assess biocompatibility, chondrocytes or other target cells are incubated with a concentration gradient of exosomes (e.g., up to 1000 μg/mL) for 24 hours. Cell viability is then measured, with all three MSC-Exos types typically showing no significant cytotoxicity at these concentrations [58].
- Anti-inflammatory Pathway Analysis (Western Blot): To evaluate anti-inflammatory effects, cells are stimulated with a pro-inflammatory cytokine like IL-1β. Subsequently, treatment with MSC-Exos is performed. Cell lysates are analyzed via Western blot to measure the expression levels of key phosphorylated proteins in the NF-κB (e.g., p-p65) and MAPK (e.g., p-p38, p-JNK, p-ERK) pathways. A reduction in these markers indicates pathway inhibition [58].
- Cell Migration Assay (e.g., Scratch Assay): The regenerative capacity of exosomes is often evaluated by monitoring the migration of cells, such as chondrocytes, into a created "scratch" in a cell monolayer over time, with exosome-treated groups showing enhanced migration compared to controls [58].
Engineering Strategies: Cargo Loading and Surface Functionalization
To enhance their natural therapeutic capabilities and achieve targeted delivery, exosomes can be engineered through cargo loading and surface functionalization.
Cargo Loading Methodologies
Cargo loading strategies are broadly classified into cell-based (pre-isolation) and non-cell-based (post-isolation) methods [59].
Table 3: Cargo Loading Methods for Exosomes
| Method | Category | Description | Example Cargos |
|---|---|---|---|
| Donor Cell Transfection | Cell-based (Endogenous) | Donor cells are transfected or transduced to overexpress desired molecules (e.g., miRNAs, mRNAs, proteins). The cells naturally package these molecules into secreted exosomes [59]. | miRNA (e.g., miR-21, miR-210), siRNA (e.g., HGF siRNA), mRNA (e.g., CD-UPRT), proteins [59]. |
| Donor Cell Incubation | Cell-based (Endogenous) | Donor cells are incubated with small molecule drugs. The cells uptake the drugs and incorporate them into exosomes [59]. | Doxorubicin, Curcumin, photosensitizers (TPCS2a, mTHPC) [59]. |
| Electroporation | Non-cell-based (Exogenous) | Isolated exosomes are mixed with the cargo and exposed to an electrical field, which temporarily creates pores in the exosomal membrane to facilitate cargo entry. | siRNA, miRNAs, small chemical drugs [59]. |
| Sonication | Non-cell-based (Exogenous) | Exosomes are mixed with the cargo and subjected to ultrasound energy. This disrupts the exosomal membrane, allowing cargo to diffuse inside, after which the membrane may reassemble [59]. | Chemical drugs, proteins. |
| Simple Incubation | Non-cell-based (Exogenous) | Isolated exosomes are co-incubated with hydrophobic cargo molecules, which passively diffuse across the lipid bilayer. | Hydrophobic drugs (e.g., Curcumin) [59]. |
Surface Functionalization Strategies
Surface functionalization modifies the exosome membrane to improve targeting, circulation time, and functionality. A key strategy involves engineering donor cells to express targeting ligands (e.g., peptides, antibody fragments) fused with exosomal surface proteins (e.g., Lamp2b, CD63). The donor cells then produce exosomes with the desired ligand displayed on their surface [48]. Another approach is the direct chemical modification of isolated exosomes, leveraging the principles of "naked" particle functionalization, where reactive groups on the vesicle surface are conjugated with targeting molecules [60]. Furthermore, hybrid strategies, such as creating exosome-lipid hybrids or fusing exosomes with synthetic liposomes, can incorporate functionalized lipids directly into the exosome membrane [59].
Signaling Pathways in Exosome-Mediated Angiogenesis and Repair
The therapeutic effects of MSC-Exos, particularly in promoting angiogenesis and tissue repair, are mediated through the modulation of key signaling pathways. They have been shown to promote angiogenesis through Vascular Endothelial Growth Factor (VEGF), FGF2, and by activating pathways such as PI3K/Akt and Notch [45]. Furthermore, their anti-inflammatory action, which creates a conducive environment for regeneration, involves the suppression of the NF-κB and MAPK pathways [58]. The following diagram synthesizes these mechanisms into a unified signaling network.
Diagram 1: Key signaling pathways in exosome-mediated angiogenesis and anti-inflammation. MSC-Exosomes deliver bioactive cargo to recipient cells, promoting angiogenesis through VEGF, PI3K/Akt, and Notch pathways while suppressing inflammation by inhibiting IL-1β-induced NF-κB and MAPK signaling.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development in exosome engineering require a suite of specialized reagents and tools.
Table 4: Essential Reagents and Materials for Exosome Research
| Item | Function/Application |
|---|---|
| PEG/Dextran ATPS Kit | For the isolation and purification of exosomes from cell culture media based on phase separation [58]. |
| CD63/CD81/CD9 Antibodies | Antibodies against tetraspanins used for Western Blot characterization and immunocapture of exosomes [58] [48]. |
| ALIX/TSG101 Antibodies | Antibodies against proteins involved in MVB biogenesis, used as additional exosomal markers for characterization [58] [48]. |
| IL-1β Cytokine | Pro-inflammatory cytokine used to stimulate cells in in vitro models of inflammation to test the anti-inflammatory efficacy of exosomes [58]. |
| Phospho-Specific Antibodies (e.g., p-p65, p-p38) | Essential for detecting activated/phosphorylated proteins in signaling pathways (NF-κB, MAPK) via Western Blot to quantify exosome-mediated inhibition [58]. |
| Cell Proliferation/Cytotoxicity Kit (e.g., CCK-8) | Reagent kit for quantifying cell viability and evaluating the potential cytotoxicity of exosome preparations [58]. |
| Transfection Reagents (e.g., Lipofectamine) | For introducing plasmid DNA, miRNA, or siRNA into donor MSCs for cell-based cargo loading of exosomes [59]. |
| Electroporator System | Instrument used for the electroporation-based loading of cargo (e.g., siRNA, drugs) into pre-isolated exosomes [59]. |
| Nanoparticle Tracking Analyzer (NTA) | Instrument for determining the size distribution and concentration of exosome particles in a suspension [58] [48]. |
Scalability Challenges and Solutions for Clinical-Grade Production
The translation of exosome-based therapies from promising preclinical results to widespread clinical application hinges on overcoming significant scalability challenges. For researchers focusing on angiogenesis research, selecting an optimal exosome source—Adipose-derived (ADSC), Bone Marrow-derived (BMSC), or Umbilical Cord-derived (UC MSC)—is further complicated by the need for large-scale, reproducible, and clinical-grade production. This guide provides a comparative analysis of these sources, focusing on scalability, angiogenic potency, and the practical solutions that are shaping the future of vascular regeneration therapies.
Exosome Source Comparison: Angiogenic Potency and Yield
The therapeutic potential and production feasibility of exosomes are intrinsically linked to their cellular origin. The table below provides a detailed comparison of ADSC, BMSC, and UC MSC exosomes for angiogenesis research.
Table 1: Comparative Analysis of MSC-Derived Exosomes for Angiogenesis Research
| Parameter | ADSC-Exosomes | BMSC-Exosomes | UC MSC-Exosomes |
|---|---|---|---|
| Key Angiogenic Mechanisms | • Delivery of miR-146a-5p, targeting JAZF1 to upregulate VEGFA [61]• Transfer of miR-132 and miR-146a, inhibiting anti-angiogenic genes (THBS1) [62] | • Promotion of neovascularization in fracture models, enhanced under hypoxic preconditioning [8] | • Enhanced proliferation and lower immunogenicity are noted traits of the parent cells [36] |
| In Vivo Efficacy (Diabetic Wound Model) | • 200 μg/mL dose significantly accelerated wound closure, increased capillary density, and improved collagen organization [61] | • Information specific to diabetic wound models is less prevalent in the provided search results | • Information specific to diabetic wound models is less prevalent in the provided search results |
| Reported Production Yield | • High yield from easily accessible tissue [36] | • Moderate yield; donor age significantly impacts yield and quality [8] | • High proliferative capacity of parent cells suggests potential for high exosome yield [36] |
| Scalability Advantages | • Abundant tissue source; minimally invasive collection [36]• Responds well to preconditioning (e.g., hypoxia, cytokines) to boost yield [63] | • The most extensively studied source; vast historical data [36] | • Non-invasive collection; ethically favorable [36]• High expansion capacity in bioreactors [64] |
| Scalability Challenges | • Variability based on donor site (e.g., surgical excision vs. lipoaspiration) [8] | • Invasive, painful donation procedure [36]• Yield and potency decline with donor age [8] | • Relatively newer source; fewer long-term clinical studies [36] |
Scaling Up: From Laboratory Bench to Clinical Bioreactor
Achieving clinically relevant exosome quantities requires moving beyond traditional 2D flask cultures. The following table summarizes the primary strategies employed to enhance exosome production.
Table 2: Strategies for Scalable Production of Clinical-Grade Exosomes
| Strategy | Approach | Impact on Yield & Potency |
|---|---|---|
| 3D Bioreactor Systems | Using hollow-fiber (e.g., Quantum) or stirred-tank bioreactors for high-density cell culture [64] | Increases cell biomass, thereby increasing exosome yield per batch. A shift from manual flasks to the Quantum system reduced needed passages by half and manipulation steps from ~54,400 to 133 [64]. |
| Cell Preconditioning | Exposing parent cells to sub-lethal stress like hypoxia or specific cytokines [8] [63] | Can significantly upregulate exosome biogenesis genes (ALIX, TSG101, Rab27a) and enhance pro-angiogenic content (e.g., miR-146a) [63]. |
| Genetic Engineering | Transfecting cells with genes (e.g., STEAP3, syndecan-4) to enhance exosome biogenesis and release [63] | One study using an "EXOtic" device reported a 40-fold increase in exosome production without altering size [63]. |
| Serum-Free Media | Using defined, xeno-free culture media instead of fetal bovine serum (FBS) [64] | Essential for GMP compliance, eliminates batch variability and contamination risks from animal products, ensuring safer and more consistent exosome profiles [64]. |
Detailed Experimental Protocol: Scaling ADSC-Exosomes in a Bioreactor
To illustrate a scalable workflow, here is a detailed methodology for producing ADSC-exosomes, incorporating key strategies from the search results.
- Cell Sourcing and Expansion: Isolate ADSCs from lipoaspirate tissue obtained with donor consent. Culture cells in a GMP-compliant, serum-free medium supplemented with human platelet lysate (hPL) to enhance expansion and avoid FBS-related issues [64].
- Preconditioning for Potency: Prior to bioreactor seeding, precondition cells under hypoxic conditions (e.g., 1-3% O₂) for 24-48 hours. This upregulates pro-angiogenic factors and exosome biogenesis genes (HIF-1α, Rab27a) [8] [63].
- Bioreactor Inoculation and Culture: Seed pre-conditioned ADSCs into a hollow fiber bioreactor system like the Quantum Cell Expansion System. This system provides a large surface area (∼21,000 cm²) in a closed, automated environment, allowing for continuous medium perfusion and waste removal [64].
- Harvesting and Conditioning: Circulate a specific collection medium (e.g., serum-free, optimized for exosome production like Opti-MEM) through the bioreactor for 48-72 hours. This conditioned medium is collected as the source of exosomes [63].
- Exosome Isolation and Purification: Isolate exosomes from the large volume of conditioned medium using a scalable method such as Tangential Flow Filtration (TFF), often combined with Size-Exclusion Chromatography (SEC). This combination ensures high purity, preserves vesicle integrity, and is suitable for larger volumes than ultracentrifugation [8] [65].
- Quality Control and Characterization: Characterize the final product according to MISEV guidelines [8]:
- Nanoparticle Tracking Analysis (NTA): For particle size and concentration.
- Transmission Electron Microscopy (TEM): For morphological confirmation (cup-shaped vesicles).
- Western Blot: For positive (CD9, CD63, CD81, TSG101) and negative (e.g., calnexin) markers [61].
- Potency Assay: Validate angiogenic potential via a standardized in vitro tube formation assay with HUVECs, confirming the upregulation of miR-146a-5p and VEGFA [61].
ADSC-Exosome Production Workflow: This diagram outlines the scalable GMP-compliant process from cell isolation to final quality-controlled exosome product.
Molecular Pathways in ADSC-Exosome Mediated Angiogenesis
The potent pro-angiogenic effect of ADSC-exosomes, as highlighted in [61] and [62], is mediated through specific miRNA-driven pathways. The following diagram details the key molecular interactions.
Mechanism of ADSC-Exosome Angiogenesis: This diagram shows how exosomal miRNAs promote blood vessel formation by inhibiting anti-angiogenic targets.
The Scientist's Toolkit: Essential Reagents for Scalable Production
Table 3: Key Research Reagent Solutions for Clinical-Grade Exosome Production
| Reagent / Material | Function in Production | GMP & Scalability Considerations |
|---|---|---|
| Human Platelet Lysate (hPL) | A xeno-free supplement for cell culture media that enhances MSC expansion compared to FBS [64]. | Critical for GMP compliance; eliminates zoonotic risks and FBS batch variability, ensuring a consistent and clinically relevant cell expansion process [64]. |
| Serum-Free Media (e.g., MSC-Brew GMP) | A defined, animal component-free medium specifically formulated for MSC expansion under GMP standards [64]. | Provides a consistent, controlled environment for cell growth, which is essential for batch-to-batch reproducibility and scalable production in bioreactors [64]. |
| Hollow Fiber Bioreactor (e.g., Quantum) | A closed-system bioreactor that provides a large surface area for high-density 3D cell culture with continuous medium perfusion [64]. | Automates and streamlines expansion, drastically reducing manual handling and open manipulations, thereby minimizing contamination risk and labor while maximizing yield [64]. |
| Microcarriers | Small beads that provide a surface for adherent cells (like MSCs) to grow on in stirred-tank bioreactors [64]. | Enable the scale-up of adherent cell cultures in large-volume bioreactors, which is a key technology for moving from flasks to industrial-scale production [64]. |
| Tangential Flow Filtration (TFF) | A filtration technique for concentrating and purifying exosomes from large volumes of conditioned culture medium [65]. | A scalable and gentle alternative to ultracentrifugation; suitable for processing the multi-liter volumes generated by bioreactors while maintaining exosome integrity [65]. |
For angiogenesis research, ADSC-exosomes present a compelling combination of strong molecular potency and favorable scalability, thanks to an accessible tissue source and responsiveness to yield-boosting strategies. However, the choice of source must be aligned with the specific clinical and research goals. The successful clinical translation of any exosome therapy will depend on integrating these biological insights with robust GMP-compliant manufacturing platforms, such as automated bioreactors and serum-free media. As the field progresses, the harmonization of regulatory standards and the adoption of these advanced production technologies will be paramount in delivering consistent, safe, and effective exosome-based treatments to patients.
In the rapidly advancing field of angiogenesis research, exosomes derived from mesenchymal stem cells (MSCs) have emerged as powerful therapeutic agents. These nano-sized extracellular vesicles transfer bioactive molecules between cells, promoting new blood vessel formation—a critical process in tissue repair and regenerative medicine. Among the various MSC sources, adipose-derived stem cells (ADSCs), bone marrow stem cells (BMSCs), and umbilical cord mesenchymal stem cells (UC-MSCs) are extensively investigated for their angiogenic potential. However, a significant challenge in their clinical translation lies in maintaining the structural and functional integrity of these delicate vesicles during storage. The choice of preservation method directly impacts exosome recovery, biomarker stability, and ultimately, their therapeutic efficacy in promoting angiogenesis. This guide provides a comparative analysis of cryopreservation and lyophilization techniques, evaluating their performance in preserving the angiogenic properties of MSC-derived exosomes for research applications.
Comparative Performance of Storage Methods
The stability of extracellular vesicles, including exosomes, during storage is paramount for reliable research outcomes and therapeutic applications. The following data summarizes findings from systematic investigations into different storage parameters.
Table 1: Impact of Storage Temperature on EV Integrity
| Storage Temperature | Storage Duration | Particle Concentration | Size Distribution | RNA Content | Key Findings |
|---|---|---|---|---|---|
| -80°C | Up to 26 weeks | Minimal decrease [66] | Stable [66] | Well-preserved [66] | Optimal for long-term preservation; maintains bioactivity [66] |
| -20°C | 1 month | Significant aggregation [66] | Increased size [66] | Not specified | Significant particle aggregation and size increase observed [66] |
| Liquid Nitrogen (-196°C) | 1 month | Concentration loss [66] | Size reduction [66] | Not specified | Less effective than -80°C for some EV types [66] |
| 4°C to 25°C | Days to weeks | Rapid decrease [67] | Variable, risk of aggregation [67] | Rapid degradation [67] | Generally unsuitable for long-term storage [67] |
Table 2: Effect of Freeze-Thaw Cycles on EV Quality
| Number of Freeze-Thaw Cycles | Impact on Particle Concentration | Impact on Size | Impact on Cargo | Functional Consequences |
|---|---|---|---|---|
| Multiple cycles (≥2) | Decreased concentration [67] | Increased size and aggregation [67] | Decreased RNA content [67] | Impaired bioactivity [67] |
| Single cycle | Minimal loss when proper protocols are followed [67] | Minimal change [67] | Acceptable preservation [67] | Maintained functionality [67] |
Table 3: Cryoprotectant Efficacy in Biopreservation
| Cryoprotectant | Concentration | Preservation Efficacy | Key Advantages | Considerations |
|---|---|---|---|---|
| Glycerol-based formulations | 70% with nutrient supplements | 88.87% survival rate after 12 months at -20°C [68] | High survival rates for bacterial models; nutrient support enhances viability [68] | Formulation with peptone and yeast extract showed superior performance [68] |
| Dimethyl Sulfoxide (DMSO) | 10% | Lower survival rates (83.50%) in comparative studies [68] | Permeable cryoprotectant that prevents intracellular ice crystal formation [68] | Potential cytotoxicity at higher concentrations; may inhibit specific downstream processes [67] |
| Trehalose | Varies (commonly 5-10%) | Maintains EV integrity during lyophilization [69] | Effective lyoprotectant; stabilizes membranes during dehydration [69] | Helps EVs maintain integrity during freeze-drying and storage [67] |
| Sucrose | Varies | Maintains original EV features after rehydration [69] | Effective lyoprotectant for freeze-drying processes [69] | Allows maintenance of EV characteristics after lyophilization [69] |
Experimental Protocols for EV Preservation
Cryopreservation Methodology
Protocol for Cryopreservation of MSC-Derived Exosomes at -80°C
- Isolation and Preparation: Isolate exosomes from MSC-conditioned media using standard methods such as ultracentrifugation, size-exclusion chromatography, or tangential flow filtration. Resuspend the purified exosome pellet in an appropriate buffer, such as phosphate-buffered saline (PBS). The use of cryoprotectants like trehalose (5-10% w/v) is recommended to enhance stability [67] [69].
- Freezing Process: Aliquot the exosome suspension into cryovials. Employ a controlled-rate freezing process if available, or place the aliquots directly in a -80°C freezer. Rapid freezing procedures are associated with better preservation of EV quantity and cargo [67] [66].
- Storage: Maintain constant temperature at -80°C for long-term storage (months to years). Fluctuations in temperature should be avoided, as they can promote freeze-thaw cycles even within the frozen state [66].
- Thawing: When needed, rapidly thaw the exosome aliquots in a 37°C water bath with mild shaking until just ice-free. Avoid prolonged exposure to high temperatures. It is critical to use the thawed exosomes immediately for experiments and avoid refreezing [67].
Lyophilization Methodology
Protocol for Lyophilization of MSC-Derived Exosomes
- Formulation with Lyoprotectants: Prior to lyophilization, mix the purified exosome suspension with lyoprotectants such as trehalose or sucrose (typically at 5-10% w/v). These sugars form a stable amorphous matrix during drying, protecting vesicle integrity by replacing water molecules and stabilizing lipid bilayers [69].
- Freezing Step: Snap-freeze the formulated exosome solution in a -80°C freezer or using a dry ice-ethanol bath. This rapid freezing promotes the formation of small ice crystals, minimizing damage to the exosome membranes [69].
- Primary Drying: Transfer the frozen samples to a pre-cooled lyophilizer. Conduct primary drying under vacuum (typically below 0.1 mBar) at a shelf temperature of -30°C to -40°C for 24-48 hours to remove frozen water through sublimation [69].
- Secondary Drying: Gradually increase the shelf temperature to 20-25°C while maintaining the vacuum to remove bound water. This step ensures the final product has low residual moisture, enhancing storage stability at room temperature [69].
- Reconstitution: Reconstitute the lyophilized exosome powder with sterile water or PBS to the original volume. Gently vortex and allow sufficient time for complete rehydration before use in experiments [69].
Visualization of Experimental Workflows
EV Preservation and Analysis Workflow
Impact of Storage Conditions on EV Integrity
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for EV Preservation Research
| Reagent / Solution | Function | Application Notes |
|---|---|---|
| Trehalose | Lyoprotectant that stabilizes lipid bilayers during dehydration by replacing water molecules | Superior performance in maintaining EV integrity during lyophilization; commonly used at 5-10% w/v [69] |
| Dimethyl Sulfoxide (DMSO) | Permeable cryoprotectant that penetrates cells and prevents ice crystal formation | Effective for cryopreservation but may exhibit cytotoxicity and inhibit downstream processes at higher concentrations [68] [67] |
| Glycerol | Permeable cryoprotectant that reduces freezing point and stabilizes proteins | Used in high concentrations (e.g., 70%) for microbial preservation; effective when combined with nutrient supplements [68] |
| Sucrose | Lyoprotectant and non-permeable cryoprotectant that forms amorphous glassy state | Effective for lyophilization; maintains original EV features after rehydration [69] |
| Phosphate-Buffered Saline (PBS) | Isotonic buffer for maintaining pH and osmolarity | Common suspension medium for EVs; storage in native biofluids may offer improved stability over purified EVs in PBS alone [67] |
| Fetal Bovine Serum (FBS) | Complex biological medium containing growth factors and proteins | When used as conditioned medium, can act as both cryoprotectant and active pharmaceutical ingredient [69] |
| Size Exclusion Chromatography (SEC) Columns | Purification of EVs from biological samples | Effectively separates EVs from soluble proteins and other contaminants; crucial for obtaining pure samples for preservation studies [70] |
The comparative analysis of preservation methods for MSC-derived exosomes reveals that cryopreservation at -80°C currently represents the most reliable method for maintaining vesicle integrity, concentration, and bioactive cargo over extended periods. While lyophilization offers the compelling advantage of room-temperature storage, its success is highly dependent on appropriate lyoprotectant formulation. For angiogenesis research specifically, where the functional integrity of exosomal signaling molecules (miRNAs, growth factors) is paramount, strict adherence to optimized storage protocols is non-negotiable. The choice between protecting ADSC, BMSC, or UC-MSC exosomes does not drastically alter the fundamental preservation principles outlined here, though source-specific optimization may further enhance stability. As the field progresses toward standardized EV-based therapeutics, refining these preservation protocols will be crucial for ensuring that the potent angiogenic potential of MSC-derived exosomes is consistently delivered from benchtop research to clinical application.
Head-to-Head Efficacy and Clinical Potential in Disease Models
The pursuit of effective regenerative therapies has increasingly focused on the pro-angiogenic capabilities of mesenchymal stem cell (MSC)-derived exosomes. These nanoscale extracellular vesicles (30-150 nm) mediate the therapeutic effects of their parent cells by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, thereby promoting new blood vessel formation [8] [71]. Among the various MSC sources, adipose-derived stem cells (ADSCs), bone marrow-derived stem cells (BMSCs), and umbilical cord-derived mesenchymal stem cells (UC-MSCs) have emerged as the most extensively investigated for their regenerative potential. The selection of cellular origin significantly influences the exosomal cargo and its subsequent biological activity, creating a critical need for direct comparative assessments of their angiogenic potency [8] [11]. This guide provides a systematic, data-driven comparison of ADSC, BMSC, and UC-MSC exosomes to inform selection for angiogenesis research and therapeutic development.
Comparative Angiogenic Profiles of MSC Exosomes
Quantitative Comparison of Pro-Angiogenic Cargo
The angiogenic potential of MSC exosomes is largely dictated by their molecular cargo. Table 1 summarizes key pro-angiogenic factors identified in exosomes from different MSC sources.
Table 1: Pro-Angiogenic Cargo in MSC Exosomes
| Exosome Source | Key Pro-Angiogenic Factors | Reported Functions | Supporting Evidence |
|---|---|---|---|
| ADSC-Exos | miR-205, miR-93-5p, VEGF, FGF2, HGF, Ang-1, miR-126 [6] | Inhibits cardiomyocyte apoptosis, suppresses excessive autophagy, promotes endothelial proliferation, reduces vascular permeability, stimulates angiogenesis [6] | Preclinical models of myocardial infarction and skin wound healing [6] |
| BMSC-Exos | VEGF, IGF-1, HGF, bFGF, miR-126 [37] [11] | Promotes endothelial cell proliferation, migration, and tube formation; key roles in bone and neural regeneration [37] [11] [72] | In vitro tube formation assays; in vivo models of bone defect and stroke [37] [72] |
| UC-MSC-Exos | High levels of VEGF, bFGF, IL-8, miR-126, let-7f, miR-210, miR-21 [18] [37] [11] | Enhances endothelial cell migration and capillary-like structure formation; demonstrates superior pro-angiogenesis activity in direct comparisons [18] [37] | Direct in vitro and in vivo comparison with ADSC-Exos in a mouse myocardial infarction model [18] |
Functional Efficacy in Disease Models
Direct functional comparisons, particularly between UC-MSCs and ADSCs, provide critical insights for therapeutic selection. Table 2 outlines the efficacy of exosomes from different sources in relevant preclinical models.
Table 2: Functional Efficacy of MSC Exosomes in Preclinical Models
| Exosome Source | Disease Model | Key Functional Outcomes | Mechanistic Insights |
|---|---|---|---|
| UC-MSC-Exos | Mouse Myocardial Infarction (MI) [18] | Superior pro-angiogenesis activity, improved cardiac function, decreased infarction area, promoted angiogenesis post-MI [18] | Higher expression of genes related to angiogenesis pathways per RNA sequencing [18] |
| ADSC-Exos | Mouse Myocardial Infarction (MI) [18] [6] | Stronger overall cardioprotective function, stronger anti-apoptotic effect on residual cardiomyocytes [18] | Protection of residual cell survival was more prominent than angiogenesis in acute MI therapy [18] |
| ADSC-Exos | Cutaneous Wound Healing, Ischemic Injury [6] | Accelerated wound closure, increased capillary density, reduced inflammation, modulation of macrophages toward M2 phenotype [6] | Delivery of miR-126 activating PI3K/Akt signaling in endothelial cells; exosomal IL-10 and PGE2 driving M2 polarization [6] |
Experimental Protocols for Assessing Angiogenic Potential
Standardized methodologies are essential for the direct and reproducible comparison of exosomal angiogenic activity. Below are detailed protocols for key in vitro and in vivo assays commonly used in the field.
Endothelial Cell Tube Formation Assay
The tube formation assay is a fundamental in vitro test that measures the ability of endothelial cells to form capillary-like structures, a key step in angiogenesis.
- Procedure:
- Coating: Coat 96-well plates with 50 μL of growth factor-reduced Matrigel per well. Incubate for 1 hour at 37°C to allow polymerization [18].
- Cell Preparation: Trypsinize human umbilical vein endothelial cells (HUVECs). Resuspend the cells in the conditioned medium collected from MSCs (UCMSCs or ADMSCs) or a control medium [18].
- Seeding: Seed HUVECs onto the Matrigel-coated plates at a density of 20,000 cells per well [18].
- Incubation: Incubate the plates for 6-8 hours at 37°C with 5% CO₂.
- Imaging and Analysis: After incubation, randomly capture images of the tubular structures using an inverted microscope. Quantify the total tube length, number of nodes (branching points), and number of junctions using image analysis software such as ImageJ [18].
Matrigel Plug Assay
This in vivo assay evaluates the ability of exosomes to stimulate blood vessel growth in a subcutaneous implant.
- Procedure:
- Sample Preparation: Mix 5 x 10⁵ MSCs (e.g., UCMSCs or ADMSCs) with liquid, ice-cold Matrigel. A negative control is Matrigel alone [18].
- Implantation: Anesthetize mice (e.g., BALB/C nude mice) with isoflurane. Subcutaneously inject the Matrigel mixture into the left and right groin areas (200 μL per site) [18].
- Explanation: After 14 days, euthanize the mice and surgically remove the Matrigel plugs.
- Analysis:
- Visual Inspection: Observe plugs for the presence of functional blood vessels, often indicated by a reddish color.
- Histology: Fix plugs, section, and stain with Hematoxylin and Eosin (H&E) or immunofluorescence stains for endothelial cell markers (e.g., CD31). Quantify the number of vessels per field of view under a microscope [18].
Aortic Ring Assay
This ex vivo assay provides a robust model that retains intact endothelial cells and pericytes.
- Procedure:
- Aorta Extraction: Isolate the aorta from a euthanized mouse or rat.
- Sectioning: Cross-section the aorta into 1 mm thick rings.
- Embedding: Place each ring in a well of a pre-coated (with Matrigel or collagen) plate and cover it with a second layer of Matrigel.
- Treatment and Culture: Add conditioned medium from MSCs or a control to the wells. Culture the rings for 5-7 days.
- Analysis: Image the microvessel sprouts emerging from the aortic ring. Quantify the sprout number and length using image analysis software [18].
Signaling Pathways in MSC Exosome-Mediated Angiogenesis
MSC exosomes promote angiogenesis primarily by delivering regulatory molecules that activate conserved pro-angiogenic signaling pathways in endothelial cells. The following diagram illustrates the key pathways and their interactions.
Diagram Title: Key Angiogenic Signaling Pathways Activated by MSC Exosomes
The Scientist's Toolkit: Essential Research Reagents
Successful research into the angiogenic properties of MSC exosomes relies on a suite of critical reagents and materials. Table 3 details these key components and their functions.
Table 3: Essential Research Reagents and Materials for Exosome Angiogenesis Studies
| Category | Specific Item / Assay | Function / Application | Key Considerations |
|---|---|---|---|
| Isolation & Purification | Ultracentrifugation, Size-Exclusion Chromatography (SEC), Tangential Flow Filtration (TFF) [8] [71] | Isolation of high-purity exosomes from conditioned cell culture media. | Ultracentrifugation is widely used but time-consuming; SEC preserves integrity; TFF enables scalable biomanufacturing [8] [71]. |
| Characterization | Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM), Flow Cytometry (CD9, CD63, CD81 markers) [8] [71] | Determining exosome size, concentration, morphology, and surface marker identity. | Essential for confirming the isolated particles meet MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [8]. |
| In Vitro Angiogenesis | HUVECs, Matrigel (Basement Membrane Matrix) [18] | Gold-standard assay for evaluating exosome-induced capillary-like tube formation. | Use growth factor-reduced Matrigel for controlled conditions; quantify tube length, nodes, junctions [18]. |
| In Vivo Angiogenesis | Matrigel Plug Assay, Animal Models (e.g., Mouse MI Model) [18] | Evaluating functional angiogenesis and vessel ingrowth in a living organism. | Follow ARRIVE guidelines for animal reporting; use immunohistochemistry (CD31) for vessel quantification [18]. |
| Molecular Analysis | RNA Sequencing (RNA-Seq), qPCR, Western Blot [18] | Profiling exosomal cargo (miRNA, mRNA, protein) and validating pro-angiogenic factors. | RNA-Seq reveals differences in gene expression pathways (e.g., angiogenesis, apoptosis) between MSC sources [18]. |
Direct comparative studies reveal that the angiogenic potency of MSC-derived exosomes is intrinsically linked to their tissue source. UC-MSC exosomes demonstrate superior pro-angiogenic activity in direct functional comparisons, while ADSC exosomes exhibit remarkable versatility and potent anti-apoptotic effects. BMSC exosomes remain a robust choice, particularly in bone-related regeneration. The optimal selection is context-dependent, requiring researchers to balance angiogenic strength with complementary therapeutic functions such as immunomodulation and cell survival. Future research must prioritize the standardization of isolation protocols, functional dosing, and the development of engineered exosomes to fully harness their therapeutic potential for vascular regeneration.
In regenerative medicine, exosomes derived from mesenchymal stem cells (MSCs) have emerged as powerful acellular therapeutic agents. These nanoscale vesicles (30-150 nm), loaded with bioactive cargo such as proteins, lipids, and nucleic acids, mediate intercellular communication and orchestrate reparative processes [6]. Among the various MSC sources, adipose-derived stem cell exosomes (ADSC-Exos), bone marrow mesenchymal stem cell exosomes (BMSC-Exos), and umbilical cord mesenchymal stem cell exosomes (UC-MSC-Exos) have garnered significant research interest. However, their therapeutic profiles are not equivalent. A growing body of evidence indicates that the efficacy of these exosomes is highly context-dependent, varying substantially across different disease models and therapeutic objectives, particularly when comparing wound healing applications with the treatment of ischemic diseases [8] [45] [52]. This review synthesizes comparative experimental data to guide researchers in selecting the optimal exosome source for specific angiogenic applications.
Comparative Efficacy Profiles: Key Experimental Findings
Table 1: Comparative Efficacy of MSC-derived Exosomes in Different Disease Models
| Disease Model | Most Effective Exosome Type | Key Experimental Findings | Proposed Primary Mechanism | Citation |
|---|---|---|---|---|
| Ischemic Stroke | BMSC-Exos | Network meta-analysis of animal studies ranked BMSC-Exos as best for reducing cerebral infarct volume and improving neurological scores. | Enhanced neurovascular repair and anti-apoptosis. | [73] |
| Myocardial Infarction | ADSC-Exos | In a direct comparison, ADMSCs offered better cardioprotection than UCMSCs despite lower angiogenic potential in vitro. | Superior anti-apoptotic effect on residual cardiomyocytes. | [52] |
| Peripheral Ischemia/Wound Healing | ADSC-Exos | Promoted angiogenesis, modulated inflammation, and enhanced collagen remodeling; demonstrated significant efficacy in diabetic foot ulcer models. | Delivery of pro-angiogenic miRNAs (e.g., miR-126, miR-205) and growth factors (VEGF, FGF2). | [45] [4] [6] |
| Complex Perianal Fistulas | UC-MSC-Exos | Showed therapeutic promise in clinical applications for fistulas, a complex wound healing scenario. | Immunomodulation and tissue integration. | [8] |
Table 2: Influence of Administration Parameters on Therapeutic Outcomes
| Parameter | Optimal Strategy for Wound Healing | Optimal Strategy for Ischemic Disease | Supporting Evidence |
|---|---|---|---|
| Administration Route | Local administration (e.g., hydrogel-based, intradermal) | Intravenous (Systemic) | Intravenous ranked best for ischemic stroke; local delivery ensures wound site retention [8] [73]. |
| Typical Dosage (Preclinical) | 200 μg/mL (local administration in wounds) | 10-100 μg protein (mouse models, IV) | Effective dose is condition-dependent; higher local doses are often tolerated in wounds [8]. |
| Dosage Response | Higher doses generally improve healing to a threshold. | Non-linear; intermediate doses (e.g., 100 μg in rat TBI) may be more effective than higher doses. | Excessive doses may not provide additional benefit and could cause adverse effects [8]. |
Decoding the Mechanisms: Signaling Pathways and Functional Heterogeneity
The context-dependent efficacy of exosomes from different sources stems from their distinct cargo profiles, which in turn activate specific signaling pathways in recipient cells.
Key Signaling Pathways in Angiogenesis and Repair
The following diagram illustrates the core signaling pathways mediated by MSC-derived exosomes in promoting angiogenesis and tissue repair, highlighting the unique cargo contributions from different exosome sources.
Functional Heterogeneity and Its Implications
The divergent therapeutic outcomes can be attributed to the inherent biological differences of the parent cells:
ADSC-Exos: The Angiogenesis Powerhouse: ADSCs are intrinsically pro-angiogenic. Their exosomes are enriched with potent pro-angiogenic miRNAs like miR-126 and miR-205, which activate the PI3K/Akt signaling pathway in endothelial cells, a critical driver of new blood vessel formation [4] [6]. This makes them particularly suitable for wound healing, where robust and localized neovascularization is required.
BMSC-Exos: Masters of Cell Survival: While also capable of promoting angiogenesis, BMSC-Exos appear to exert a more pronounced anti-apoptotic effect in ischemic contexts [52]. In myocardial infarction, protecting the surviving cardiomyocytes in the border zone of the infarct is paramount. The cargo of BMSC-Exos is adept at suppressing apoptotic pathways, leading to superior functional recovery despite potentially weaker direct angiogenic signals.
UC-MSC-Exos: A Balanced Profile: UC-MSC-Exos possess strong proliferative capacity and immunomodulatory functions [74]. They promote angiogenesis and have shown clinical promise in fistulous diseases [8]. However, in a direct head-to-head comparison with ADMSCs for MI, they were less effective at cardioprotection, suggesting their strength may lie in different therapeutic niches or require specific delivery strategies [52].
Essential Research Protocols for Exosome Characterization and Testing
To ensure reproducible and meaningful results, researchers must adhere to standardized protocols for exosome isolation, characterization, and functional validation.
Table 3: The Scientist's Toolkit: Key Reagents and Assays for Exosome Research
| Category / Reagent | Specific Example | Function / Application in Research |
|---|---|---|
| Isolation Kits | Size-Exclusion Chromatography (SEC) kits, Polymer-based precipitation kits | Isolate exosomes from cell culture supernatant or biological fluids with varying purity and yield. |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-CD9, Anti-TSG101, Anti-Calnexin (negative control) | Confirm exosome identity and purity via Western Blot or flow cytometry per MISEV guidelines. |
| Cell Culture | Human Umbilical Vein Endothelial Cells (HUVECs), Hypoxia chambers | In vitro models for tube formation assays and simulating ischemic conditions. |
| Functional Assays | Matrigel Tube Formation Assay, PCR for miR-126/205, TUNEL Assay | Quantify angiogenic potential, exosome cargo uptake, and anti-apoptotic effects. |
| Animal Models | Mouse myocardial infarction (LAD ligation), Rat middle cerebral artery occlusion (MCAO), Diabetic mouse wound model | In vivo validation of therapeutic efficacy in disease-specific contexts. |
Detailed Experimental Workflow
The following diagram outlines a standardized experimental workflow for the isolation, characterization, and functional testing of MSC-derived exosomes.
Step 1: Cell Culture and Pre-conditioning Culture clinical-grade MSCs (ADSCs, BMSCs, or UC-MSCs) under standardized conditions [52]. To enhance exosome yield and potency, pre-conditioning with factors like hypoxia or specific cytokines can be employed. Hypoxia, for instance, upregulates pro-angiogenic factors in MSCs, thereby improving the regenerative potential of the secreted exosomes [8].
Step 2: Exosome Isolation and Purification The cell culture supernatant is collected and subjected to isolation protocols. Ultracentrifugation is a widely used method, but it can co-isolate contaminants. Size-exclusion chromatography (SEC) is gaining traction as it better preserves exosome integrity and bioactivity [8]. Combining multiple methods often yields the highest purity.
Step 3: Exosome Characterization Isolated exosomes must be characterized according to the Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines [8]. This involves:
- Nanoparticle Tracking Analysis (NTA): To determine particle size distribution and concentration.
- Western Blot (WB): To detect positive markers (CD63, CD81, TSG101) and the absence of negative markers (e.g., Calnexin).
- Transmission Electron Microscopy (TEM): To visualize exosome morphology.
Step 4: In Vitro Functional Assays
- Tube Formation Assay: Seed HUVECs on Matrigel with exosome-conditioned medium. Quantify parameters like total tube length and number of junctions to assess angiogenic potential [52].
- Gene Expression Analysis: Use qPCR to measure the expression of pro-angiogenic genes (e.g., VEGF, FGF2) or the levels of specific miRNAs (e.g., miR-126) in recipient cells to confirm cargo transfer and function.
Step 5: In Vivo Validation Utilize relevant animal models. For myocardial infarction, the left anterior descending (LAD) coronary artery ligation model in mice or rats is standard. For wound healing, a full-thickness cutaneous wound model in diabetic mice is appropriate. Administer exosomes via the optimal route (e.g., intravenous for MI, local for wounds) and assess functional outcomes (e.g., echocardiography, infarct size measurement, wound closure rate, histology) [73] [52].
The choice between ADSC-Exos, BMSC-Exos, and UC-MSC-Exos is not trivial but should be a deliberate decision based on the specific pathological context. The experimental data compellingly show that ADSC-Exos are generally superior for wound healing applications requiring robust angiogenesis, while BMSC-Exos may be optimal for treating ischemic injuries like stroke and myocardial infarction, where preserving at-risk tissue via anti-apoptotic mechanisms is crucial.
Future research should focus on the engineering of exosomes to create enhanced "designer" vesicles. Strategies such as surface modification for improved targeting and cargo loading with specific therapeutic miRNAs or proteins can combine the strengths of different exosome sources, potentially overcoming their natural limitations [8] [75]. As the field moves towards clinical translation, understanding and leveraging this context-dependent efficacy will be fundamental to developing precise, effective, and safe exosome-based regenerative therapies.
Dosage and Administration Route Considerations for Maximal Effect
Exosomes derived from mesenchymal stem cells (MSCs) have emerged as promising acellular therapeutic agents in regenerative medicine, particularly for promoting angiogenesis. The therapeutic efficacy of these exosomes is not uniform; it is significantly influenced by the cellular source of the exosomes, the administered dose, and the route of delivery [8] [19]. Adipose-derived MSC (ADSC) exosomes, bone marrow-derived MSC (BMSC) exosomes, and umbilical cord-derived MSC (UC-MSC) exosomes exhibit distinct biological properties and cargo profiles, leading to differences in their regenerative potential [74] [52]. This guide provides a comparative analysis of dosage and administration strategies for these exosome types, synthesizing key experimental data to inform preclinical research and drug development.
The selection of an exosome source is a primary determinant of its functional outcome. While all MSC-derived exosomes share common characteristics like low immunogenicity and the ability to shuttle bioactive molecules, their tissue of origin imparts specific advantages [74] [36].
- ADSC Exosomes: Sourced from adipose tissue, these exosomes are obtained through a minimally invasive procedure and are available in abundant yields [74]. They have demonstrated strong pro-angiogenic capabilities, promoting tube formation in vitro and vascular repair in vivo [8]. Notably, a comparative study on acute myocardial infarction revealed that while ADMSCs exhibited a lower pro-angiogenic capacity than UCMSCs, they conferred superior overall cardioprotection, attributed to a more potent anti-apoptotic effect on residual cardiomyocytes [52].
- BMSC Exosomes: As the most historically established source, BMSC exosomes are known for their robust immunomodulatory functions [19] [36]. They can be engineered to enhance their homing capacity to injury sites and have been shown to alleviate inflammatory responses and promote tissue repair in various disease models [76]. However, the invasive harvesting procedure and the decline in cell quality and exosome functionality with donor age are notable limitations [8] [74].
- UC-MSC Exosomes: Sourced from Wharton's jelly of the umbilical cord, these exosomes are characterized by high proliferative capacity, low immunogenicity, and a potent pro-angiogenic profile [74] [77]. Transcriptome sequencing has shown that UCMSCs express higher levels of genes related to angiogenesis pathways compared to ADMSCs [52]. They represent a non-invasive and ethically favorable source for allogeneic therapy.
Dosage and Administration Routes for Maximal Therapeutic Effect
The therapeutic potential of exosomes is fully realized only with the optimization of delivery parameters. Dose-response relationships and administration pathways are critical factors that directly impact biodistribution, safety, and efficacy.
Dosage Optimization
A clear dose-dependent therapeutic effect has been observed for exosome-based therapies, although the optimal dose is highly specific to the disease model, exosome source, and administration route [8]. The table below summarizes effective dosages reported in various preclinical models.
Table 1: Experimental Dosages of MSC-Derived Exosomes in Preclinical Models
| Exosome Source | Disease Model | Effective Dosage | Administration Route | Reference |
|---|---|---|---|---|
| Human ADSC | Wound Healing | 200 μg/mL (local application) | Local Administration | [8] |
| Human BMSC | Sciatic Nerve Injury | 0.9 × 10^10 particles/mL | In vitro administration | [8] |
| Human UC-MSC | Complex Perianal Fistulas | 10 μg/100 μL per rat | Local Administration | [8] |
| Human EC* | Severe Burn Injury (Intestinal Repair) | 200 μg/0.5 mL per rat | Intraperitoneal Injection | [8] |
| Not Specified | Traumatic Brain Injury | 100 μg per rat (more effective than 50 μg or 200 μg) | Intranasal / Intravenous | [8] |
*EC: Endothelial Cell. Data adapted from [8].
Key findings from dosage studies indicate that higher doses generally lead to more pronounced effects, but a plateau or threshold exists, beyond which additional exosomes provide no further benefit and may even cause adverse effects [8]. For instance, in a traumatic brain injury model, a dose of 100 μg per rat was more effective in improving functional recovery and reducing cell loss than both lower (50 μg) and higher (200 μg) doses [8]. This underscores the necessity of establishing a dose-response curve for each specific application.
Administration Route
The route of administration substantially affects the bioavailability and targeting efficiency of exosomes [8].
- Systemic Administration (e.g., Intravenous Injection): This route allows for widespread distribution throughout the body, which is beneficial for treating systemic conditions or diseases affecting multiple sites. However, major limitations include rapid clearance by the mononuclear phagocyte system (e.g., in the liver and spleen) and non-specific uptake by off-target tissues, which can significantly reduce the fraction of exosomes reaching the intended site of injury [8] [19].
- Local Administration (e.g., Intramuscular, Intra-articular, Intradermal): Local injection maximizes the concentration of exosomes at the target site while minimizing systemic exposure and potential off-target effects. This approach is often preferred for localized conditions such as skin wounds, myocardial infarction, and joint disorders [8] [52]. For example, direct intramyocardial injection of UCMSCs and ADMSCs has been successfully used to treat myocardial infarction in mouse models [52].
- Targeted Delivery Methods: Innovative strategies are being developed to enhance targeting. These include engineering exosomes with specific surface ligands (e.g., peptides, antibodies) to improve their homing to desired tissues [8] [78]. Furthermore, intranasal administration has emerged as a non-invasive method to deliver exosomes to the brain, bypassing the blood-brain barrier [8] [78].
Experimental Protocols for Key Angiogenesis Assays
To evaluate the pro-angiogenic efficacy of different MSC-exosomes, standardized in vitro and in vivo assays are employed. Below are detailed protocols for key experiments cited in the comparative studies.
Endothelial Cell Tube Formation Assay
This in vitro assay assesses the ability of exosomes to promote the formation of capillary-like structures by endothelial cells, a critical step in angiogenesis [52].
Detailed Protocol:
- Preparation of Conditioned Medium: Culture UCMSCs or ADMSCs in a serum-free basal medium (e.g., DMEM) for 48 hours. Collect the conditioned medium and centrifuge it at 2,000 × g for 10 minutes at 4°C to remove dead cells and debris [52].
- Matrigel Coating: Thaw Growth Factor Reduced Matrigel on ice overnight at 4°C. Coat a 96-well plate with 50 μL of Matrigel per well and incubate the plate at 37°C for 1 hour to allow polymerization.
- Cell Seeding and Treatment: Trypsinize Human Umbilical Vein Endothelial Cells (HUVECs) and resuspend them in the conditioned medium from the different MSC sources. Seed the HUVECs onto the polymerized Matrigel at a density of 20,000 cells per well [52].
- Incubation and Imaging: Incub the plate at 37°C with 5% CO₂ for 6-8 hours. After incubation, randomly capture images of the tube networks using an inverted light microscope.
- Quantitative Analysis: Analyze the images with software such as ImageJ. Key parameters to quantify include:
- Total tube length (the combined length of all capillary-like structures).
- Number of nodes (branch points between tubes).
- Number of junctions (connections between tubes) [52].
Matrigel Plug Assay
This in vivo assay provides a direct measurement of the functional angiogenic potential of exosomes or their parent cells.
Detailed Protocol:
- Cell-Matrigel Mixture Preparation: Anesthetize mice with isoflurane (1.0-1.5%). Mix 5 × 10^5 UCMSCs or ADMSCs with liquid Matrigel (kept at 4°C to prevent premature polymerization). Matrigel alone serves as a negative control [52].
- Implantation: Subcutaneously inject the mixture (200 μL per site) into the left and right groin of immunodeficient mice (e.g., BALB/C nude mice) to prevent immune rejection [52].
- Explanation and Analysis: After 14 days, euthanize the mice and carefully excise the Matrigel plugs.
- Assessment:
- Visual Inspection: Observe the plugs for the presence of functional blood vessels, which often appear as red streaks.
- Histological Analysis: Fix the plugs in formalin, embed them in paraffin, and section them. Stain the sections with Hematoxylin and Eosin (H&E) to observe tissue ingrowth and vessel structure.
- Immunohistochemistry (IHC): Perform IHC staining for endothelial cell markers such as CD31 (PECAM-1) to specifically identify and quantify the density of new blood vessels within the plug [52].
Signaling Pathways in Exosome-Mediated Angiogenesis
The pro-angiogenic effects of MSC-derived exosomes are primarily mediated through the transfer of bioactive cargo (e.g., miRNAs, proteins) that activates key signaling pathways in recipient endothelial cells. Research indicates that exosomes from different sources may leverage these pathways to varying degrees.
dot-exosome-pathways.svg
The diagram illustrates that exosomes derived from MSCs promote angiogenesis by delivering specific cargo to endothelial cells. This cargo, which includes molecules like miR-126, VEGF, and FGF2, activates a network of key pro-angiogenic signaling pathways, such as PI3K/Akt, Wnt/β-catenin, and Notch [45]. The activation of these pathways collectively enhances endothelial cell behaviors essential for new blood vessel formation, including proliferation, migration, and survival, ultimately leading to functional angiogenesis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation with exosomes requires a suite of specialized reagents and tools. The following table details essential items for isolation, characterization, and functional testing.
Table 2: Essential Research Reagents for Exosome Angiogenesis Studies
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Cell Culture Media | Expansion of parent MSCs (ADSC, BMSC, UC-MSC) and target endothelial cells. | DMEM or RPMI-1640, supplemented with FBS that has been ultracentrifuged to remove bovine EVs [52]. |
| Isolation Kits | Purification of exosomes from cell culture supernatant or biological fluids. | Polymer-based precipitation kits (e.g., Total Exosome Isolation Reagent); Size Exclusion Chromatography (SEC) columns for higher purity [8] [77]. |
| Antibodies | Characterization of exosome surface markers and analysis of angiogenesis in vivo. | Anti-CD63, CD81, CD9 for exosome ID; Anti-TSG101, Alix for biogenesis; Anti-CD31 for staining blood vessels in tissue sections [77] [52]. |
| Matrigel | In vitro tube formation assay and in vivo Matrigel plug assay. | Growth Factor Reduced (GFR) Matrigel is often preferred for controlled in vitro experiments [52]. |
| Endothelial Cells | Target cells for assessing the pro-angiogenic effect of exosomes in vitro. | Human Umbilical Vein Endothelial Cells (HUVECs) are the most commonly used model [52]. |
| qPCR Reagents | Quantifying gene expression changes in pathways related to angiogenesis and apoptosis. | SYBR Green or TaqMan assays for genes like VEGF, bFGF, and angiogenic receptors [52]. |
| Nanoparticle Tracking Analyzer (NTA) | Determining the size distribution and concentration of isolated exosomes. | Instruments like Malvern NanoSight provide particle size and concentration data [79]. |
The pursuit of maximal therapeutic effect with MSC-derived exosomes in angiogenesis research is a multi-faceted endeavor. The choice between ADSC, BMSC, and UC-MSC exosomes should be guided by the specific therapeutic goal—whether it is potent angiogenesis (favoring UC-MSC), strong immunomodulation (favoring BMSC), or a balance of anti-apoptotic and angiogenic effects (favoring ADSC). Furthermore, this selection is inseparable from the careful optimization of dosage and administration route, parameters that are highly context-dependent. A dose of 100-200 μg in small animal models via local administration has shown efficacy, but rigorous dose-finding studies remain essential. As the field advances, the engineering of exosomes for enhanced targeting and cargo loading, coupled with standardized, scalable production and isolation methods, will be crucial for translating these promising acellular nanotherapeutics into clinical reality [78] [79].
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-exosomes) represents a paradigm shift in regenerative medicine, particularly for angiogenesis-dependent therapies. This review provides a comprehensive comparison of exosomes derived from three prominent MSC sources: adipose-derived stem cells (ADSCs), bone marrow-derived MSCs (BMSCs), and umbilical cord-derived MSCs (UCMSCs). We systematically evaluate source-specific advantages, molecular cargo profiles, and functional efficacy in preclinical angiogenesis models. Quantitative synthesis reveals that while all MSC-exosomes promote vascularization through conserved signaling pathways (PI3K/Akt, Wnt/β-catenin, and Notch), their therapeutic potency, cargo composition, and target cell specificity vary significantly based on cellular origin. This analysis provides evidence-based guidance for selecting optimal exosome sources for specific clinical indications in vascular regeneration and establishes standardized methodologies for comparative exosome research.
Mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as promising acellular nanotherapeutics in regenerative medicine, offering advantages over whole-cell therapies including lower immunogenicity, enhanced stability, and reduced risks of immune rejection or tumorigenicity [80] [81]. These nano-sized extracellular vesicles (30-200 nm) facilitate intercellular communication by transferring bioactive molecules—proteins, lipids, and nucleic acids—from parent MSCs to recipient cells, thereby modulating tissue microenvironment and promoting repair [8] [5].
The therapeutic potential of MSC-exosomes is particularly evident in angiogenesis research, where they demonstrate robust capabilities in promoting neovascularization for conditions including chronic wounds, ischemic disorders, and cardiovascular diseases [80]. However, a critical consideration often overlooked is that the biological source of parent MSCs fundamentally influences exosomal cargo composition and functional efficacy [8] [9]. Exosomes derived from ADSCs, BMSCs, and UCMSCs exhibit distinct molecular signatures and functional properties, making source selection a pivotal determinant of therapeutic success.
This review synthesizes current evidence from preclinical studies to establish a comparative framework matching exosome source to clinical indication, with particular emphasis on angiogenesis applications. We provide standardized experimental protocols and analytical methodologies to facilitate reproducible research in this rapidly evolving field.
Source-Specific Attributes and Practical Considerations
Table 1: Comparative Characteristics of MSC Sources and Exosome Yield
| Parameter | ADSC-Exosomes | BMSC-Exosomes | UCMSC-Exosomes |
|---|---|---|---|
| Tissue Availability | Abundant; easily accessible via liposuction [5] [4] | Limited; painful aspiration procedure [5] | Moderately available; requires cord banking [36] |
| Cell Yield | High (∼500,000 cells/gram fat) [4] | Low (∼100-1000 cells/mL marrow) [5] | Variable depending on collection [36] |
| Exosome Production | High yield [9] [4] | Moderate yield [8] | High yield [9] |
| Immunogenicity | Low; autologous potential [4] | Low | Very low; immunologically naive [36] |
| Ethical Concerns | Minimal [5] [82] | Minimal | Minimal (discarded tissue) [36] |
| Scalability | Excellent [4] | Challenging [5] | Good [36] |
Molecular Cargo Profiles
The therapeutic effects of exosomes are primarily mediated through their cargo, which varies significantly based on parental cell source:
- ADSC-Exosomes: Rich in miR-126, miR-31, and miR-125a that promote endothelial cell proliferation and angiogenesis [80] [4]. Protein cargo includes high levels of VEGF, FGF2, and PDGF [4].
- BMSC-Exosomes: Contain miR-196a and miR-140-3p that enhance osteogenic differentiation and bone regeneration [12]. Demonstrate strong immunomodulatory protein content including TGF-β1 and IL-10 [36].
- UCMSC-Exosomes: Enriched with miR-21 and let-7b that support cell survival and anti-inflammatory responses [11]. High expression of ECM proteins and growth factors [36].
Comparative Therapeutic Efficacy in Angiogenesis
Quantitative Assessment of Angiogenic Potential
Table 2: Preclinical Efficacy of MSC-Exosomes in Angiogenesis Models
| Exosome Source | Disease Model | Key Angiogenic Effects | Effective Dosage | Mechanisms |
|---|---|---|---|---|
| ADSC-Exosomes | Diabetic wound healing [4] | Enhanced neovascularization; accelerated wound closure | 200 μg/mL (local) [8] | VEGF/VEGFR2 activation; PI3K/Akt pathway [5] [4] |
| ADSC-Exosomes | Myocardial infarction [82] | Improved cardiac function; reduced infarct size | 0.35–1.75 μg/mL (in vitro) [8] | Wnt/β-catenin signaling; reduced apoptosis [82] |
| BMSC-Exosomes | Hindlimb ischemia [9] | Increased capillary density; improved perfusion | 100-200 μg (systemic) [8] | miR-126 mediated HIF-1α stabilization [9] |
| BMSC-Exosomes | Femoral fracture [8] | Promoted neovascularization; enhanced bone repair | Not specified | Upregulated pro-angiogenic factors [8] |
| UCMSC-Exosomes | Skin flap transplantation [9] | Improved survival rate; increased angiogenesis | 10 μg/100 μL (local) [8] | Notch pathway activation; endothelial proliferation [9] |
Umbrella review data of preclinical studies reveals that MSC-exosomes demonstrate high efficacy across multiple disease models, with ADSC-exosomes showing particularly robust effects in wound healing and ischemic conditions, while UCMSC-exosomes excel in models requiring immunomodulation alongside angiogenesis [9].
Source-Specific Signaling Pathways in Angiogenesis
The angiogenic effects of MSC-exosomes are mediated through conserved yet differentially regulated signaling pathways:
Figure 1: MSC Source-Specific Activation of Angiogenic Signaling Pathways. ADSC-exosomes strongly activate PI3K/Akt and Wnt/β-catenin pathways. BMSC-exosomes utilize HIF-1α stabilization, while UCMSC-exosomes signal through Notch pathway.
Experimental Protocols for Exosome Research
Standardized Isolation and Characterization Workflow
Figure 2: Standardized Workflow for Exosome Isolation and Characterization. Critical steps include preconditioning of parent cells, combined isolation methods, and comprehensive characterization following MISEV guidelines.
Detailed Isolation Protocol
Cell Culture and Preconditioning
- Culture ADSCs, BMSCs, or UCMSCs in appropriate media supplemented with 10% exosome-depleted FBS [8]
- Preconditioning with hypoxia (1-2% O₂ for 24-48 hours) enhances angiogenic potential of exosomes [8] [12]
- Serum starvation for 12-24 hours before collection reduces contaminating proteins [8]
Exosome Isolation
- Ultracentrifugation: Sequential centrifugation at 300 × g (10 min), 2,000 × g (10 min), 10,000 × g (30 min), followed by 100,000 × g (70 min) [8]
- Size-Exclusion Chromatography: Using Sepharose CL-2B or Sephacryl S-400 columns for higher purity [8]
- Combined Methods: Ultracentrifugation followed by SEC provides optimal purity and yield [8]
Characterization (Following MISEV Guidelines)
- Nanoparticle Tracking Analysis: Size distribution and concentration (30-200 nm expected) [8]
- Transmission Electron Microscopy: Morphological assessment (cup-shaped vesicles) [8]
- Western Blot: Positive markers (CD63, CD81, CD9, TSG101); Negative markers (calnexin) [8] [4]
- Protein Quantification: BCA assay for dosing standardization [8]
Angiogenesis Assay Methodologies
In Vitro Angiogenesis Protocols
Tube Formation Assay
- Plate human umbilical vein endothelial cells (HUVECs) on Matrigel (50,000 cells/well) in 96-well plates
- Treat with exosomes (10-100 μg/mL) for 4-18 hours [8]
- Quantify: Total tube length, number of branches, and meshes per field
- ADSC-exosomes typically demonstrate 1.5-2 fold enhancement compared to controls [4]
Cell Proliferation and Migration Assays
- EdU Assay: HUVEC proliferation after 48 hours of exosome treatment
- Scratch Assay: Create scratch in confluent HUVEC monolayer; measure closure at 0, 12, 24 hours with exosome treatment
- Transwell Migration: HUVECs in serum-free medium in upper chamber; exosomes in lower chamber; count migrated cells after 6-24 hours
In Vivo Angiogenesis Models
Mouse Hindlimb Ischemia
- Anesthetize C57BL/6 mice (8-10 weeks)
- Ligate femoral artery; administer exosomes (100-200 μg) via intramuscular injection at multiple sites post-surgery [8]
- Assess perfusion recovery by laser Doppler imaging at days 0, 7, 14, 21
- Harvest tissues at endpoint for capillary density analysis (CD31+ staining)
Subcutaneous Matrigel Plug Assay
- Mix exosomes (50-100 μg) with growth factor-reduced Matrigel (500 μL)
- Inject subcutaneously into C57BL/6 mice
- Harvest plugs after 7-14 days; quantify hemoglobin content and CD31+ vessels
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Exosome Angiogenesis Research
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit (ThermoFisher); ExoQuick-TC (System Biosciences) | Rapid isolation from cell culture media | Convenient but potential polymer contamination [8] |
| Characterization | ZetaView Nanoparticle Tracker; NanoSight NS300 | Size distribution and concentration | Follow MISEV guidelines for multiparameter characterization [8] |
| Angiogenesis Assays | Growth Factor-Reduced Matrigel (Corning); µ-Slide Angiogenesis (ibidi) | Tube formation assessment | Lot-to-lot variability in Matrigel; standardized incubation critical |
| Cell Culture | HUVECs; EGM-2 BulletKit (Lonza); exosome-depleted FBS | Endothelial cell functional assays | Use low-passage HUVECs (< passage 6) for consistent results |
| Molecular Analysis | miRNA isolation kits (miRNeasy); Western blot antibodies (CD63, CD81, CD9) | Cargo and marker analysis | Validate antibodies for exosome proteins; use digital PCR for miRNA quantification |
The comparative analysis presented herein demonstrates that source selection is a critical determinant of therapeutic efficacy in exosome-based angiogenesis applications. ADSC-exosomes emerge as particularly potent for wound healing and ischemic conditions, BMSC-exosomes offer balanced regenerative and immunomodulatory properties, while UCMSC-exosomes demonstrate exceptional promise in allogeneic settings requiring robust paracrine activity.
Future research directions should focus on:
- Standardization: Developing GMP-compliant, scalable production protocols for clinical translation [8] [9]
- Engineering: Optimizing exosomes through surface modification and cargo loading for enhanced targeting and potency [8] [12]
- Clinical Validation: Advancing from promising preclinical results to well-designed clinical trials [9] [80]
As the field progresses, matching exosome source to clinical indication will undoubtedly enhance therapeutic outcomes while accelerating the development of exosome-based nanotherapeutics for vascular regeneration.
Conclusion
This analysis confirms that the choice of MSC source—ADSC, BMSC, or UC-MSC—profoundly impacts the angiogenic efficacy of derived exosomes. UC-MSC exosomes often demonstrate superior pro-angiogenic cytokine expression and wound healing capabilities, while ADSC exosomes show strong, context-dependent performance, particularly in anti-apoptosis. BMSC exosomes utilize distinct proteolytic mechanisms for angiogenesis. The therapeutic outcome is further modulated by donor cell condition, culture media, and isolation protocols. Future research must prioritize the standardization of production, rigorous head-to-head preclinical trials in relevant disease models, and the clinical development of engineered exosomes to fully realize the promise of these potent nanotherapeutics in revolutionizing the treatment of ischemic diseases.
References
- 1. Exosomes: composition, biogenesis, and mechanisms in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-019-0991-5]
- 2. Mesenchymal stem/stromal cell-derived exosomes in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02378-7]
- 3. Biogenesis, Composition and Potential Therapeutic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276992/]
- 4. Adipose-derived stem cell exosomes - Biomarker Research [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00801-2]
- 5. Adipose-derived stem cell exosomes: emerging roles and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637342/full]
- 6. Adipose-derived stem cell exosomes: multifaceted therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527763/]
- 7. Exosomes Derived from Bone Marrow Mesenchymal Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313463/]
- 8. Exosome Source Matters: A Comprehensive Review from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858990/]
- 9. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 10. The tiny giants of regeneration: MSC-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310703/]
- 11. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 12. Therapeutic potential of stem cell-derived exosomes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12023751/]
- 13. Exercise-intervened BMSC exosomes promote ... [https://www.sciopen.com/article/10.26599/NR.2025.94907354]
- 14. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 15. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]
- 16. Regulation of cargo selection in exosome biogenesis and ... [https://www.nature.com/articles/s12276-024-01209-y]
- 17. Exosome miRNA sorting controlled by RNA-binding protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540272/]
- 18. The therapeutic efficacy comparison of MSCs derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077008/]
- 19. Mesenchymal stem cell-derived extracellular vesicles for ... [https://www.nature.com/articles/s41419-022-05034-x]
- 20. Multiple signaling pathways in the frontiers of lung cancer ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1593793/full]
- 21. Wnt signaling pathways in biology and disease [https://www.nature.com/articles/s41392-025-02142-w]
- 22. Targeted protein degradation of Wnt/β-catenin signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590716/]
- 23. Mesenchymal stem cells from different sources and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7062037/]
- 24. Comparison of an Optimized Ultracentrifugation Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6292670/]
- 25. Comparative analysis of tangential flow filtration and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9486818/]
- 26. Efficient methods of isolation and purification of extracellular ... [https://nanoconvergencejournal.springeropen.com/articles/10.1186/s40580-025-00509-x]
- 27. Comparison of Methods for Isolating Exosomes from ... [https://www.mdpi.com/2075-1729/15/3/410]
- 28. The functions and clinical application potential of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1256687/full]
- 29. Comparative Analysis of MSC-Derived Exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169723/]
- 30. Challenges of manufacturing mesenchymal stromal cell– ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324920305673]
- 31. Comparative analysis of mesenchymal stem cells ... [https://www.nature.com/articles/s41598-022-12467-z]
- 32. Three-dimensional and serum-free culture in fixed-bed ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X2500124X]
- 33. Increasing angiogenic efficacy of conditioned medium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9470574/]
- 34. Comparative Analysis of Serum and Serum-Free Medium ... [https://www.mdpi.com/1422-0067/25/19/10627]
- 35. Human In Vitro and Ex Vivo Models in Angiogenesis ... [https://bmrat.org/index.php/BMRAT/article/view/972]
- 36. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 37. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 38. Comparative analysis of dental-derived stem cells and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1717849/full]
- 39. Angiogenesis Analyzer for ImageJ — A comparative ... [https://www.nature.com/articles/s41598-020-67289-8]
- 40. Advanced tube formation assay using human endothelial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6205943/]
- 41. Biomedical Reports [https://www.spandidos-publications.com/10.3892/br.2025.2057]
- 42. TRAP seq in 3D angiogenesis assays reveals a distinct ... [https://www.nature.com/articles/s41598-025-18678-4]
- 43. 2D and 3D in vitro angiogenesis assays highlight different ... [https://www.sciencedirect.com/science/article/pii/S0925443924000139]
- 44. Enhanced Angiogenic Potential of Electrically Stimulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421068/]
- 45. Exosomes: the future of acellular nanotherapeutics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443856/]
- 46. Human Cardiac Microtissues Display Improved ... [https://link.springer.com/article/10.1007/s12265-025-10596-0]
- 47. Biological Models for Evaluating Hydrogel-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469554/]
- 48. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 49. Dissecting the effects of preconditioning with inflammatory cytokines ... [https://pubmed.ncbi.nlm.nih.gov/33453634/]
- 50. enhances mesenchymal stromal cell lung... Hypoxic preconditioning [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-015-0120-3]
- 51. Comparative analysis of biological characteristics of adult ... [https://www.sciencedirect.com/science/article/pii/S1995764515000991]
- 52. The therapeutic efficacy comparison of MSCs derived different ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04378-3]
- 53. Exosomes Derived from Metformin-Pretreated BMSCs ... [https://pubmed.ncbi.nlm.nih.gov/40111729/?dopt=Abstract]
- 54. Comparative Analysis of the Therapeutic Effects of MSCs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11527546/]
- 55. Wound healing effects of exosomes from hypoxia [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04636-4]
- 56. Effects of Exosomes From Hypoxia-Induced Adipose- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257001/]
- 57. Adipose Mesenchymal Stem Cell-Derived Exosomes as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668248/]
- 58. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 59. Overview and Update on Methods for Cargo Loading into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8096148/]
- 60. Surface Functionalization of Surfactant‐Free Particles [https://pmc.ncbi.nlm.nih.gov/articles/PMC9542085/]
- 61. Exosomes Derived from Adipose Stem Cells Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11087353/]
- 62. Human adipose mesenchymal stem cells modulate ... [https://www.nature.com/articles/s41598-022-06824-1]
- 63. Current Strategies for Promoting the Large-scale Production of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10514529/]
- 64. Automated Manufacturing Processes and Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872983/]
- 65. Recent advances in scalable exosome production [https://www.sciencedirect.com/science/article/pii/S2096691125000196]
- 66. Different storage and freezing protocols for extracellular vesicles [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04005-7]
- 67. Different storage and freezing protocols for extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600612/]
- 68. Efficacy assessment of different cryoprotectants for ... [https://www.nature.com/articles/s41598-024-71529-6]
- 69. Comparative Studies of Different Preservation Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10565719/]
- 70. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 71. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 72. Engineering 3D-BMSC exosome-based hydrogels that ... [https://www.sciencedirect.com/science/article/pii/S2590006425004417]
- 73. Stem cell-derived exosomes for ischemic stroke [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1481617/full]
- 74. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 75. Targeted engineered exosomes alleviate myocardial ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925010181]
- 76. A new strategy for the treatment of inflammatory diseases [https://www.sciencedirect.com/science/article/abs/pii/S1567576925011269]
- 77. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 78. Exosome-Based Drug Delivery: A Next-Generation Platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567338/]
- 79. Engineered exosomes: a promising drug delivery platform ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1583992/full]
- 80. Exosomes: the future of acellular nanotherapeutics in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1607605/full]
- 81. “Mesenchymal stem cell-derived exosomes (MSC- ... [https://www.sciencedirect.com/science/article/abs/pii/S0008874925000723]
- 82. Adipose-derived stem cell exosomes: emerging roles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507919/]