Comparative Efficacy of Biomaterials for Cell Delivery: From Design Principles to Clinical Translation
The efficacy of cell-based therapies is critically dependent on the biomaterial delivery platform, which influences cell viability, retention, and functional integration.
Comparative Efficacy of Biomaterials for Cell Delivery: From Design Principles to Clinical Translation
Abstract
The efficacy of cell-based therapies is critically dependent on the biomaterial delivery platform, which influences cell viability, retention, and functional integration. This review provides a comparative analysis of current biomaterial strategies for therapeutic cell delivery, targeting researchers and drug development professionals. We explore foundational material classes and their properties, evaluate methodological applications across tissue engineering and immunotherapies, address key optimization challenges, and present validation frameworks for comparative efficacy. By synthesizing design principles with preclinical and clinical outcomes, this article establishes a roadmap for selecting and engineering biomaterials to enhance the therapeutic potential of delivered cells in regenerative medicine and drug development.
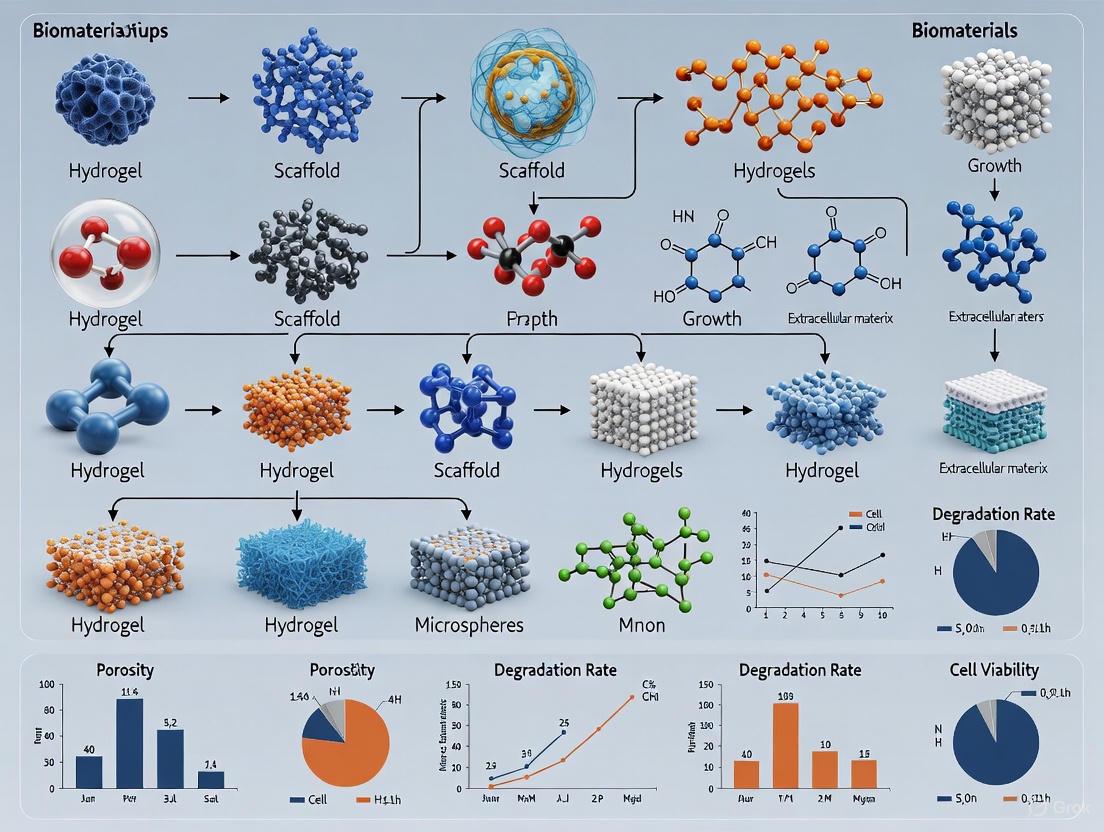
Biomaterial Platforms and Cell Types: Building Blocks for Effective Delivery
The success of advanced cell delivery strategies in regenerative medicine and tissue engineering hinges on the selection of an appropriate biomaterial scaffold. These materials provide the critical three-dimensional (3D) environment that supports cell viability, guides function, and facilitates integration with host tissues. Among the diverse classes of biomaterials available, hydrogels, nanofibers, decellularized extracellular matrix (dECM), and synthetic polymers each offer distinct advantages and limitations. Hydrogels provide highly hydrated environments that mimic native tissues, nanofibers offer topographical cues that guide cell organization, dECM delivers tissue-specific biological signals, and synthetic polymers present tunable mechanical and chemical properties. This guide objectively compares the performance of these major biomaterial classes based on experimental data, focusing on their efficacy in cell delivery applications. Understanding the comparative strengths of each material class enables researchers to make informed decisions for specific cellular delivery applications, from basic research to clinical translation.
Comparative Analysis of Major Biomaterial Classes
Table 1: Comprehensive comparison of major biomaterial classes for cell delivery applications
| Biomaterial Class | Key Composition | Mechanical Properties | Degradation Timeline | Key Advantages | Major Limitations | Primary Cell Delivery Applications |
|---|---|---|---|---|---|---|
| Hydrogels | Natural (collagen, alginate, fibrin) or synthetic (PEG) polymers with high water content [1] | Elastic modulus typically 0.1-20 kPa, highly tunable [2] [1] | Days to months, depending on cross-linking density | High biocompatibility, excellent nutrient diffusion, can mimic tissue elasticity [1] | Often weak mechanical properties, limited structural integrity [1] [3] | Cell encapsulation, 3D bioprinting, soft tissue regeneration |
| Nanofibers | Synthetic (PCL, PLGA) or natural (collagen, chitosan) polymers | High surface area-to-volume ratio, tunable tensile strength | Weeks to years, depending on polymer composition | Mimics native ECM architecture, superior cell adhesion guidance [1] | Limited control over 3D architecture in random scaffolds, potential poor nutrient diffusion to core | Neural guidance, tendon/ligament repair, wound dressing |
| Decellularized ECM (dECM) | Tissue-derived scaffolds preserving native ECM components [4] [5] | Varies by tissue source, often requires reinforcement (e.g., 1.5-6.8 kPa for lung dECM) [2] | Weeks to months, enzyme-mediated | Tissue-specific biochemical cues, innate bioactivity, excellent cellular compatibility [6] [5] | Batch-to-batch variability, potential immunogenicity, poor mechanical integrity [3] [6] | Organoid culture, tissue-specific regeneration, bioactive coatings |
| Synthetic Polymers | PLA, PGA, PLGA, PEG, PCL [7] [8] | Highly tunable (elastic modulus from kPa to GPa) | Days to years, precisely controllable through chemistry | Highly reproducible, tunable mechanical and chemical properties, predictable degradation [8] | Lack of innate bioactivity, may provoke inflammatory response, hydrophobic varieties limit cell adhesion | Controlled release systems, bone fixation devices, structural implants |
Table 2: Experimental performance data for biomaterials in specific applications
| Biomaterial | Experimental Model | Cell Viability/Function | Tissue Regeneration Outcome | Key Measurement | Reference |
|---|---|---|---|---|---|
| Clickable dECM Hybrid-Hydrogel | Primary murine lung fibroblasts | ≈60% increase in Col1a1 and αSMA expression on stiff hydrogels (13.4 kPa) vs. soft (3.6 kPa) [2] | N/A (in vitro model) | Significant increase in myofibroblast transgenes with increased modulus | [2] |
| HA/PLGA/Bleed Scaffold | Critical bone defect in rat calvaria | Enhanced collagen I deposition throughout matrix | Superior bone regeneration at 15, 30, and 60 days vs. HA/PLGA alone | Higher Rank-L immunoexpression indicating increased remodeling | [7] |
| Photocrosslinked dECM Bioink | 3D bioprinting of various tissues | Excellent cell viability and tissue-specific differentiation | Improved structural fidelity and shape retention | Shear-thinning behavior and rapid sol-gel transitions | [6] |
| PEGαMA-dECM Hybrid | Spatial patterning of fibroblast activation | Increased Col1a1 expression on stiff regions of patterned hydrogels | N/A (in vitro model) | Spatiotemporal control over fibroblast activation | [2] |
Detailed Biomaterial Characteristics and Experimental Evidence
Hydrogels
Structural and Functional Properties: Hydrogels are 3D cross-linked insoluble, hydrophilic polymer networks capable of absorbing large amounts of water or biological fluid (up to 99%) due to their interconnected microscopic pores [1]. This high water content creates an environment that physically mimics native tissues, facilitating efficient nutrient and oxygen diffusion to encapsulated cells—a critical advantage for cell viability in 3D constructs. Hydrogels can be fabricated from both natural polymers (including collagen, hyaluronic acid, chitosan, alginate, and fibrin) and synthetic polymers (primarily poly(ethylene glycol) or PEG), with each offering distinct advantages [1] [3]. Their mechanical properties, characterized by elastic modulus typically ranging from 0.1-20 kPa, can be precisely tuned to match target tissues by adjusting polymer concentration, cross-linking density, or fabrication parameters [1].
Key Experimental Evidence: Advanced hydrogel systems have been developed with dynamic capabilities that mirror the evolving nature of living tissues. One innovative approach incorporates clickable decellularized ECM crosslinker into a dynamically responsive poly(ethylene glycol)-α-methacrylate (PEGαMA) hybrid-hydrogel to recreate ECM remodeling in vitro [2]. This system utilizes dual-stage polymerization reactions, beginning with an off-stoichiometry thiol-ene Michael addition between PEGαMA and clickable dECM, resulting in hydrogels with an elastic modulus of 3.6 ± 0.24 kPa, approximating healthy lung tissue. Subsequent reaction of residual αMA groups via photo-initiated homopolymerization increases modulus values to fibrotic levels (13.4 ± 0.82 kPa) in situ [2]. This dynamic system demonstrated that increased elastic moduli, mimicking fibrotic ECM, induced a significant increase (approximately 60%) in the expression of myofibroblast transgenes (collagen 1a1 and alpha-smooth muscle actin) in primary fibroblasts from dual-reporter mouse lungs [2].
Decellularized Extracellular Matrix (dECM)
Structural and Functional Properties: Decellularized ECM represents a sophisticated biomaterial approach that preserves the complex biochemical composition of native tissues while eliminating immunogenic cellular components [5]. The dECM is composed of a complex assembly of structural proteins (primarily collagens, elastin), proteoglycans, glycoproteins, and preserved growth factors that collectively provide tissue-specific biochemical and biophysical cues [4] [5]. These materials can be processed into various forms including solid scaffolds, injectable hydrogels, and bioinks for 3D bioprinting [6] [5]. The primary advantage of dECM over other biomaterials lies in its innate bioactivity and ability to recapitulate tissue-specific microenvironments that guide cell behavior, support differentiation, and enhance functional tissue regeneration [5].
Key Experimental Evidence: Research has demonstrated that dECM hydrogels provide superior microenvironments for specialized tissue development. Studies show that mesenchymal stem cells exhibit distinct gene expression patterns when cultured in various dECM materials, with compositional variations directly influencing stem cell behavior and directing differentiation in a tissue-specific manner [6]. Furthermore, dECM serves as a superior cell culture matrix that significantly enhances the expression of genes associated with cellular maturation and specialized functions compared to traditional biological scaffolds such as Matrigel and collagen [6].
For clinical translation, dECM-based medical devices have shown promise in multiple applications. Patch-type grafts such as Alloderm and GraftJacket have been used for skin and rotator cuff repair, while injectable hydrogel forms like Ventrigel have been applied for cardiac function restoration [6]. In 3D bioprinting applications, dECM bioinks have been developed for adipose, cartilage, and cardiac tissues, providing crucial signals essential for cell implantation, viability, and sustained functionality [6]. These bioinks demonstrate suitable rheological properties including shear-thinning behavior (where viscosity decreases with increasing shear rate) and rapid sol-gel transitions, making them particularly advantageous for extrusion-based printing [6].
Synthetic Polymers
Structural and Functional Properties: Synthetic polymers including polylactic acid (PLA), polyglycolic acid (PGA), poly(lactic-co-glycolic) acid (PLGA), polycaprolactone (PCL), and polyethylene glycol (PEG) offer exceptional tunability and reproducibility as biomaterials [7] [8]. These materials provide precise control over mechanical properties, degradation kinetics, and overall scaffold architecture. Their synthesis can be engineered to achieve specific mechanical characteristics ranging from soft, flexible networks to rigid, load-bearing structures, with degradation timelines that can be programmed from days to years depending on molecular weight, crystallinity, and copolymer ratios [8]. This precise control makes synthetic polymers particularly valuable for applications requiring specific temporal profiles or mechanical support.
Key Experimental Evidence: In bone regeneration studies, composite scaffolds combining hydroxyapatite (HA) with PLGA have demonstrated significant potential as orthopedic implants [7]. In a critical bone defect model in rat calvaria, HA/PLGA scaffolds with added hemostatic polysaccharide (Bleed) showed enhanced collagen I deposition and superior bone regeneration at 15, 30, and 60 days compared to HA/PLGA alone [7]. Histological analysis revealed morphological and structural differences in the neoformed tissue between experimental groups, with the HA/PLGA/Bleed scaffold presenting the highest amount of collagen fibers in its tissue matrix across all evaluated periods [7]. Additionally, receptor activator of nuclear factor kappa-Β ligand (Rank-L) immunoexpression results were higher in the HA/PLGA/Bleed group at 30 and 60 days, indicating increased degradation of the biomaterial and enhanced remodeling activity of the bone [7].
Nanofibers
Structural and Functional Properties: Nanofibrous biomaterials create synthetic extracellular matrices with high surface area-to-volume ratios that closely mimic the topological features of native ECM [1]. These materials can be fabricated through various methods including electrospinning, self-assembly, and phase separation, producing fiber diameters typically ranging from tens to hundreds of nanometers. The high porosity and interconnected pore structure of nanofibrous scaffolds facilitate cell infiltration, nutrient diffusion, and waste removal while providing topographical cues that direct cell alignment, migration, and differentiation. Nanofibers can be composed of both synthetic (PCL, PLGA) and natural (collagen, chitosan) polymers, offering versatility in their biological and mechanical properties [1].
Functional Advantages and Evidence: The primary advantage of nanofibrous architectures lies in their ability to guide cellular organization and tissue formation through physical patterning. The high surface area promotes greater protein adsorption and enhanced cell adhesion compared to flat surfaces or conventional scaffolds [1]. Nanofibers can be aligned to create contact guidance cues that direct cell orientation, a particularly valuable property for engineering anisotropic tissues such as tendons, ligaments, nerves, and cardiac muscle. Furthermore, the mechanical properties of nanofibrous scaffolds can be tuned through material selection, fiber alignment, and processing parameters to match the requirements of target tissues.
Experimental Protocols for Key Evaluations
Protocol: Dual-Stage Polymerization for Dynamic Hydrogel Stiffening
This protocol details the methodology for creating hydrogels with dynamically tunable mechanical properties to study cellular responses to stiffness changes, as described in [2].
Materials:
- 8-arm PEGαMA (10 kg/mol)
- Clickable dECM crosslinker
- Lithium phenyl-2,4,6-trimethylbenzoulphospinate (LAP) photo-initiator
- Buffered solution (pH 7.4)
- UV light source (365 nm, 5-10 mW/cm²)
Procedure:
- Prepare precursor solution: Dissolve PEGαMA at 50-100 mg/mL in buffered solution.
- First-stage crosslinking: Mix PEGαMA solution with clickable dECM at stoichiometric ratio and initiate Michael addition by adding LAP (0.05% w/w). Incubate at 37°C for 30 minutes to form soft hydrogels (≈3-4 kPa).
- Second-stage stiffening: Expose the formed hydrogels to UV light (365 nm, 5-10 mW/cm²) for 3-5 minutes to initiate homopolymerization of residual αMA groups, increasing modulus to fibrotic levels (≈13 kPa).
- Characterization: Confirm modulus values using rheometry or atomic force microscopy.
Applications: This system enables investigation of fibroblast activation, fibrosis progression, and cellular responses to dynamic mechanical changes [2].
Protocol: In Vivo Evaluation of Bone Regeneration in Critical Defects
This protocol outlines the procedure for evaluating biomaterials in critical-sized bone defects, adapted from [7].
Materials:
- HA/PLGA and HA/PLGA/Bleed scaffolds (1.5 mm thickness, 8 mm diameter)
- Male Wistar rats (280 ± 20 g)
- Trephine drill (8-mm diameter)
- Anesthesia (ketamine/xylazine)
- Fixative (10% buffered formalin)
Procedure:
- Surgical procedure: Anesthetize rats and create critical-sized bone defects in the calvaria using an 8-mm trephine drill.
- Implantation: Implant test scaffolds (HA/PLGA or HA/PLGA/Bleed) into defects, with untreated defects as controls.
- Post-operative care: Administer analgesic and allow recovery with free access to food and water.
- Euthanasia and sample collection: Euthanize animals at 15, 30, and 60 days post-implantation and harvest calvaria for analysis.
- Histological processing: Fix samples in formalin, decalcify in EDTA, embed in paraffin, and section at 5 μm thickness.
- Analysis: Perform hematoxylin and eosin staining, collagen I immunohistochemistry, and Rank-L immunoexpression analysis.
Outcome measures: Bone regeneration extent, collagen organization, inflammation presence, and remodeling activity [7].
Biomaterial Selection Workflow
Biomaterial Selection Workflow for Cell Delivery Applications
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for biomaterial experimentation
| Reagent/Material | Function | Example Applications | Key Considerations |
|---|---|---|---|
| Poly(ethylene glycol)-α-methacrylate (PEGαMA) | Synthetic polymer backbone for hybrid hydrogels | Dynamic stiffness hydrogels, 3D cell culture platforms [2] | Molecular weight, degree of functionalization, water solubility |
| Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Photo-initiator for UV-mediated crosslinking | Photopolymerizable hydrogels, bioprinting applications [2] | Cytotoxicity at high concentrations, optimal wavelength 365 nm |
| Decellularized ECM (dECM) | Tissue-specific bioactive scaffold material | Organoid culture, bioinks, regenerative scaffolds [6] [5] | Source tissue, decellularization efficiency, gelation temperature |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable natural polymer | Bioprinting, tissue engineering, drug screening [3] | Degree of methacrylation, viscosity, gelation parameters |
| Hydroxyapatite (HA) | Mineral component for bone regeneration | Bone tissue engineering, orthopedic implants [7] | Particle size, crystallinity, purity |
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable synthetic polymer | Controlled release systems, bone scaffolds [7] [8] | Lactide:glycolide ratio, molecular weight, degradation rate |
| Collagen Type I | Natural polymer hydrogel substrate | 3D cell culture, wound healing, soft tissue models [4] [1] | Source, concentration, fibrillogenesis conditions |
| Alginate | Ionic-crosslinked natural polymer | Cell encapsulation, bioprinting, wound dressings [3] | Molecular weight, guluronate:mannuronate ratio, purity |
The selection of biomaterials for cell delivery applications requires careful consideration of mechanical, biological, and practical parameters. Hydrogels excel in creating hydrous, diffusive environments for 3D culture; dECM provides unmatched bioactivity and tissue-specificity; synthetic polymers offer precision and reproducibility; while nanofibers deliver critical topographical guidance. The experimental data presented enables evidence-based selection, while the provided protocols facilitate standardized evaluation. As the field advances, composite approaches that combine the strengths of multiple material classes will likely yield the most effective solutions for specific cell delivery challenges in regenerative medicine and tissue engineering.
The field of regenerative medicine and immunotherapy is being transformed by advances in therapeutic cell technologies. Among the most prominent of these are Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), Endothelial Colony-Forming Cells (ECFCs), and various immune cells for adoptive cell therapy (ACT). These cells offer unprecedented potential for treating a wide range of diseases, from cancer to degenerative disorders. However, their therapeutic efficacy is often limited by challenges in delivery, engraftment, and controlled functionality within the hostile in vivo environment. The integration of these cells with advanced biomaterials has emerged as a critical strategy to overcome these limitations. Biomaterials can enhance cell survival, provide three-dimensional support, enable localized delivery, and maintain therapeutic phenotypes, thereby significantly improving clinical outcomes. This guide provides a comparative analysis of these key therapeutic cell types, with a specific focus on their interactions with biomaterial-based delivery systems, to inform researchers and drug development professionals in the field.
Comparative Analysis of Therapeutic Cell Types
The table below summarizes the key characteristics, therapeutic mechanisms, and biomaterial interactions of the four major therapeutic cell types.
Table 1: Comparative Analysis of Key Therapeutic Cell Types
| Cell Type | Key Characteristics & Markers | Therapeutic Mechanisms | Primary Clinical Applications | Biomaterial Delivery Advantages |
|---|---|---|---|---|
| MSCs [9] [10] [11] | Plastic-adherent, CD73+, CD90+, CD105+; CD34-, CD45-; Multipotent (osteogenic, chondrogenic, adipogenic) | Paracrine signaling (cytokines, growth factors), immunomodulation, mitochondrial transfer, direct differentiation [12] | Graft-versus-host disease (GVHD), osteoarthritis, spinal cord injury, COVID-19 ARDS [11] [12] | Hydrogels for viability & retention; scaffolds for osteochondral differentiation; controlled cytokine release [9] [13] |
| iPSCs [10] [14] [15] | Pluripotent (differentiate into all germ layers); Express OCT4, SOX2, NANOG; Can be genetically engineered | Source for differentiated cells (e.g., iPSC-MSCs, iPSC-NKs); Avoids embryonic destruction; Potential for autologous therapy | Age-related macular degeneration, Parkinson's disease, heart failure, cancer immunotherapy (as iPSC-NKs) [15] | Biomaterial-assisted 2D/3D differentiation into target cells; Encapsulation for teratoma risk mitigation [9] |
| Immune Cells (for ACT) [13] [16] [17] | Engineered specificity (e.g., CAR-T); Diverse types (T cells, NK cells, DCs); Activated & expanded ex vivo | Direct cytotoxicity (CAR-T, NK), antigen presentation (DCs), immunomodulation | Hematological cancers (B-cell leukemia, lymphoma), solid tumors (trials), autoimmune diseases [16] [17] | Hydrogels for localized tumor delivery; Co-delivery of cytokines (IL-15) to prevent exhaustion; scaffolds for intratumoral retention [13] [16] [17] |
| ECFCs | Highly proliferative endothelial progenitors; CD31+, CD34+, CD146+, VEGFR2+; Form vessel structures | Vasculogenesis and angiogenesis; Direct contribution to vascular lining; Paracrine pro-angiogenic signaling | Ischemic diseases (critical limb ischemia, myocardial infarction), vascularizing engineered tissues | Biofunctionalized scaffolds to guide vascular network formation; Co-delivery with perivascular cells for stability |
Quantitative Efficacy and Manufacturing Data
The following table consolidates key quantitative data from preclinical and clinical studies, highlighting the performance and manufacturing considerations of each cell type.
Table 2: Quantitative Data on Therapeutic Efficacy and Manufacturing
| Cell Type | Key Efficacy Metrics | Manufacturing & Scalability | Stability & Storage | Safety Profile & Key Risks |
|---|---|---|---|---|
| MSCs | >50% reduction in aGVHD symptoms in responders [12]; Significant cartilage regeneration in osteoarthritis trials [11] | Finite expansion in 2D culture; 3D bioreactors can increase yield; Relatively scalable from allogeneic sources | Cryopreservation possible; Phenotype stable for limited passages (e.g., < P10) | Low tumorigenicity; Low immunogenicity allows allogeneic use; Some reports of pro-tumor effects [12] |
| iPSCs | iPSC-NKs: >70% tumor cell killing in vitro models [15]; iPSC-derived grafts: successful engraftment in AMD patients [15] | Virtually unlimited self-renewal; Requires complex, multi-step differentiation protocols; High scalability potential | Master cell banks can be cryopreserved long-term; Differentiated products may have limited shelf-life | Teratoma formation from undifferentiated cells; Genomic instability during reprogramming/culture [10] [15] |
| Immune Cells (for ACT) | >80% remission rates in ALL with CD19 CAR-T [16] [17]; Persistence of CAR-T cells for >10 years in some patients | Autologous: costly, variable; Allogeneic: avoids this but needs HLA editing; Manufacturing time: ~2-3 weeks | Cryopreservation of final product is standard; Limited stability after thawing for infusion | Cytokine Release Syndrome (CRS); Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS); On-target/off-tumor toxicity [16] |
| ECFCs | In vivo: Increased capillary density in murine hindlimb ischemia models; Functional perfusion recovery | Isolated from cord blood or peripheral blood; Moderate expansion capability; Less established large-scale production | Cryopreservation of isolated cells from donors; Limited replicative lifespan in culture | Theoretical risk of aberrant angiogenesis (e.g., in tumors); Generally considered safe in early trials |
Detailed Experimental Protocol: Deriving MSCs from iPSCs Using a Biomaterial-Assisted Approach
This protocol details a method for generating MSCs from human iPSCs using a feeder-free, biomaterial-coated system, adapted from recent research [9] [10] [14]. The derived iPS-MSCs exhibit typical MSC characteristics and offer a solution to the heterogeneity and limited expansion potential of tissue-derived MSCs.
1. Materials and Reagents
- Human iPSCs: Maintained in a pluripotent state on a suitable substrate (e.g., Matrigel, Geltrex).
- MSC Differentiation Medium: Alpha-MEM or DMEM/F12, supplemented with 10% Fetal Bovine Serum (FBS), 1% GlutaMAX, and 1% Non-Essential Amino Acids.
- Small Molecule Inhibitor: SB431542 (a TGF-β pathway inhibitor), reconstituted in DMSO.
- Biomaterial Coatings: Matrigel, Collagen I, or specific synthetic hydrogels (e.g., PEG-based).
- Enzymes: Gentle Cell Dissociation Reagent (for iPSCs) and 0.25% Trypsin-EDTA (for MSCs).
- Characterization Reagents: Antibodies for flow cytometry (CD73, CD90, CD105, CD34, CD45, HLA-DR) and differentiation kits (osteogenic, adipogenic, chondrogenic).
2. Step-by-Step Workflow
Diagram Title: Workflow for iPSC to MSC Differentiation
3. Key Steps Elaboration
- Step 1: Seeding iPSCs: Harvest iPSCs as single cells or small clumps and seed them onto tissue culture plates coated with the chosen biomaterial (e.g., Matrigel at 1:100 dilution). The biomaterial provides critical cues that mimic the native extracellular matrix and support subsequent differentiation.
- Step 2: Differentiation Induction: Culture the cells in MSC Differentiation Medium supplemented with 5-10 µM SB431542. The medium should be changed every other day. SB431542 inhibits SMAD2/3 phosphorylation, directing the cells toward a mesodermal lineage and ultimately to an MSC fate. This step typically takes about 10 days, after which an epithelial-like monolayer should be visible.
- Step 3: Lineage Stabilization: After 10 days, passage the cells using trypsin and re-plate them at a defined density (e.g., 5,000 cells/cm²) in MSC Differentiation Medium without SB431542. The cells should now be maintained and expanded as a standard MSC culture. They will acquire a typical MSC-like fibroblastic morphology over 1-2 passages.
- Step 4: Expansion and Characterization: Expand the iPS-MSCs for several passages. Characterize them according to International Society for Cellular Therapy (ISCT) criteria:
- Surface Markers: Confirm >95% expression of CD73, CD90, and CD105, and <2% expression of CD34, CD45, and HLA-DR via flow cytometry.
- Trilineage Differentiation: Perform in vitro differentiation into osteocytes (mineralization with Alizarin Red staining), adipocytes (lipid droplets with Oil Red O staining), and chondrocytes (cartilage matrix with Alcian Blue staining).
- Safety: Perform karyotyping to ensure genomic stability and consider a teratoma assay in immunodeficient mice to confirm the absence of residual pluripotent cells.
Biomaterial Strategies for Enhanced Cell Delivery
Rational Design of Biomaterial Carriers
Biomaterials are engineered to address the specific limitations of each cell type, with design criteria focusing on cytocompatibility, bioactivity, and mass transfer [16] [17]. The following table outlines key material classes and their functions in cell delivery.
Table 3: The Scientist's Toolkit: Biomaterials and Reagents for Cell Delivery
| Material/Reagent Category | Specific Examples | Primary Function in Cell Therapy |
|---|---|---|
| Natural Polymer Hydrogels | Alginate, Chitosan, Collagen, Hyaluronic Acid, Fibrin | Provide a soft, hydrated 3D microenvironment that supports cell viability and can be modified with adhesion motifs (e.g., RGD). |
| Synthetic Polymer Hydrogels | Poly(ethylene glycol) (PEG), Poly(lactic-co-glycolic acid) (PLGA) | Offer highly tunable mechanical properties, degradation rates, and minimal batch-to-batch variation. |
| Cytokines & Growth Factors | IL-15, IL-2, GM-CSF, TGF-β, VEGF | Co-delivered to maintain cell viability, promote activation (e.g., prevent T-cell exhaustion), or steer differentiation. |
| Engineered Scaffolds & Microparticles | 3D-printed polymer scaffolds, Degradable microspheres | Act as a physical reservoir for localized cell delivery and sustained release of bioactive factors. |
| Small Molecule Inhibitors/Inducers | SB431542, CHIR99021, Dorsomorphin | Used in differentiation protocols (e.g., iPSC to MSC) to precisely control signaling pathways. |
Biomaterial Applications by Cell Type
- Enhancing MSC Therapies: Biomaterials are used to overcome the limited persistence of systemically infused MSCs. Hydrogels based on alginate or PEG can encapsulate MSCs, providing mechanical protection and tethering them to the target site, thereby increasing engraftment [9]. For bone regeneration, MSCs are often loaded onto rigid, osteoconductive scaffolds (e.g., hydroxyapatite or tricalcium phosphate) that provide the structural and chemical cues necessary for osteogenic differentiation [11].
- Boosting Adoptive Immune Cell Therapy: A major challenge for CAR-T cells in solid tumors is poor infiltration and rapid exhaustion. Biomaterial solutions include injectable hydrogels that can be deposited locally in the tumor resection cavity, creating a "factory" for the sustained release of functional CAR-T cells and supportive cytokines like IL-15 [13] [16] [17]. This local delivery maintains an activated T-cell phenotype and improves tumor cell killing while reducing systemic toxicity.
- Supporting iPSC-Derived Cell Products: Biomaterials play a dual role for iPSCs. First, they are crucial for directing the efficient and scalable differentiation of iPSCs into target cells like MSCs or cardiomyocytes in 3D culture systems [9]. Second, they can be used to encapsulate and deliver the final differentiated product, potentially containing any residual undifferentiated cells and mitigating the risk of teratoma formation.
The diagram below illustrates how a biomaterial scaffold can be designed to create a supportive microenvironment for delivered therapeutic cells.
Diagram Title: Multifunctional Biomaterial Scaffold for Cell Delivery
The therapeutic landscape for MSCs, iPSCs, ECFCs, and adoptive immune cells is rapidly evolving, with biomaterials playing an increasingly critical role in translating their potential into clinical reality. As this guide illustrates, the choice of cell type is dictated by the specific clinical target, whether it is immunomodulation, tissue regeneration, or targeted cytotoxicity. However, the efficacy of these cells is no longer solely dependent on their inherent biology; it is profoundly enhanced by the smart design of biomaterial delivery systems. These systems provide a protective, instructive, and localized microenvironment that overcomes common barriers such as poor cell survival, inadequate retention, and loss of function. Future progress in the field will hinge on the development of even more sophisticated "smart" biomaterials that can actively respond to the physiological environment and the continued refinement of manufacturing protocols to ensure the consistent, safe, and scalable production of these combined cell-biomaterial therapies.
The efficacy of any biomaterial in cell delivery and regenerative medicine is fundamentally governed by its interactions with the biological environment. These interactions—dictated by biocompatibility, mechanical properties, and degradation behavior—determine host response, cell viability, and ultimate therapeutic success. A comparative analysis of biomaterial performance is therefore critical for selecting optimal platforms for specific clinical applications. This guide objectively compares the performance of major biomaterial classes used in cell delivery, supported by experimental data, to inform research and development strategies.
Comparative Performance of Biomaterial Delivery Vehicles
The choice of biomaterial vehicle significantly impacts the acute retention and survival of delivered cells, which is a critical performance metric in therapies such as cardiac regeneration after myocardial infarction. The following data summarizes key experimental findings from a controlled comparative study.
Table 1: Comparison of Biomaterial Vehicles for Acute Stem Cell Retention in the Infarcted Heart [18]
| Biomaterial Delivery Vehicle | Type | Cell Retention at 24 Hours (Fold Increase vs. Saline Control) | Approximate Percentage of Initially Transplanted Cells Retained |
|---|---|---|---|
| Saline (Clinical Standard) | Injectable | (Baseline = 1x) | ~10% |
| Alginate Hydrogel | Injectable | ~8x | ~50% |
| Chitosan/β-GP Hydrogel | Injectable | ~14x | ~50% |
| Collagen Patch | Epicardial Patch | ~47x | 50-60% |
| Alginate Patch | Epicardial Patch | ~59x | 50-60% |
Key Findings: All biomaterial carriers dramatically outperformed the saline control, with epicardial patches demonstrating superior cell retention. The alginate patch achieved the highest retention, showing a 59-fold increase over saline. Notably, all four biomaterials retained 50-60% of the cells initially present after transplantation, a five to six-fold improvement over the 10% retention with saline. [18] This highlights that the physical encapsulation and protection provided by biomaterials are crucial for overcoming the harsh in vivo environment that leads to rapid cell loss.
Experimental Protocols for Evaluating Biomaterial-Cell Interactions
Robust and standardized experimental methodologies are essential for generating reliable, comparable data on biomaterial efficacy. The following protocols detail key procedures for evaluating cell retention and host response.
Protocol: In Vivo Quantification of Cell Retention
This protocol is adapted from a comparative study of biomaterials for stem cell delivery to the heart. [18]
- Objective: To quantify and compare the acute retention of delivered cells using different biomaterial carriers in a disease model.
- Materials:
- Experimental animal model (e.g., rat myocardial infarct model).
- Cells for delivery (e.g., Human Mesenchymal Stem Cells - hMSCs).
- Test biomaterials (e.g., alginate hydrogel, chitosan/β-GP hydrogel, collagen patch, alginate patch).
- Saline control.
- Fluorescent cell tracker (e.g., CM-Dil or similar for fluorescence quantification).
- Methods:
- Induction of Myocardial Infarction: Surgically induce myocardial infarction in the animal model to create the target pathology.
- Cell Labeling: Label hMSCs with a fluorescent cell tracker according to manufacturer protocols.
- Cell-Biomaterial Preparation:
- For injectable hydrogels: Mix the fluorescently labeled cells with the pre-gel solution (e.g., alginate or chitosan/β-GP).
- For epicardial patches: Seed the labeled cells onto the pre-formed patches (e.g., collagen or alginate).
- Delivery: Implant the cell-biomaterial constructs into the target site (e.g., infarct border zone). For injectables, use direct injection; for patches, use surgical attachment.
- Quantification: After 24 hours, harvest the target tissue.
- Quantify the retained fluorescence intensity using a pre-calibrated imaging or spectrophotometric system.
- Calculate retained cell numbers based on the fluorescence signal relative to a standard curve.
- Perform immunohistochemical analysis on tissue sections to qualitatively confirm cell presence and distribution.
- Analysis: Compare the fluorescence (cell retention) across different biomaterial groups and the saline control, typically expressed as a fold-increase relative to the control.
Protocol: Assessing the Host Immune Response
- Objective: To evaluate the biocompatibility and inflammatory response elicited by a biomaterial.
- Materials:
- Biomaterial samples.
- In vitro cell culture (e.g., macrophages) or in vivo implantation model.
- ELISA kits or PCR reagents for cytokine analysis.
- Histological staining supplies.
- Methods:
- Implantation: Implant the biomaterial subcutaneously or in the target organ.
- Tissue Collection: Harvest the surrounding tissue and the implant site at predetermined time points (e.g., 3, 7, 14 days).
- Analysis:
- Histology: Process tissue for sectioning and stain with Hematoxylin and Eosin (H&E) to visualize general tissue architecture and immune cell infiltration. Use specific stains (e.g., for macrophages) to identify immune cell types.
- Cytokine Profiling: Homogenize tissue and analyze the supernatant for pro-inflammatory (e.g., TNF-α, IL-6) and anti-inflammatory (e.g., IL-10) cytokines using ELISA.
- Analysis: A more biocompatible material will typically show a resolved, mild inflammatory response over time, while a poor material will trigger a sustained, severe inflammatory reaction.
Signaling Pathways in Material-Cell Interactions
The interaction between a biomaterial and a cell is not passive; it initiates a cascade of intracellular signals that dictate cell fate. The extracellular matrix (ECM) is a natural scaffold that provides critical biochemical and mechanical cues. [19] Synthetic biomaterials are engineered to mimic these functions. The following diagram illustrates the core signaling pathway activated when a cell engages with a biomaterial via integrin receptors.
Biomaterial Induced Cell Signaling [19] [20]
This pathway highlights how biomaterials directly influence cell behavior by activating specific genetic programs.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful research into material-cell interactions relies on a suite of specialized reagents and materials. The following table details essential tools and their functions in this field.
Table 2: Essential Research Reagents for Biomaterial-Cell Interaction Studies
| Research Reagent / Material | Function and Role in Biomaterial Studies |
|---|---|
| Alginate | A natural polymer used to form gentle, injectable hydrogels or patches; ideal for cell encapsulation and delivery due to its biocompatibility and tunable properties. [18] |
| Chitosan/β-Glycerophosphate (β-GP) | A temperature-sensitive hydrogel that is liquid at room temperature and gels at body temperature; enables minimally invasive injection of cells. [18] |
| Collagen | A major component of the natural ECM; used as patches or hydrogels to provide a bioactive and highly biocompatible scaffold that promotes cell adhesion and integration. [18] |
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable synthetic polymer and a cornerstone of controlled-release drug delivery systems; its degradation rate and drug release profile can be finely tuned. [21] |
| Human Mesenchymal Stem Cells (hMSCs) | A primary cell type frequently used in regenerative medicine research due to their multipotent differentiation potential, immunomodulatory properties, and relevance for cell therapy. [18] |
| Fluorescent Cell Trackers (e.g., CM-Dil) | Vital dyes used to label living cells prior to transplantation, allowing for their quantification and tracking within the host tissue over time using fluorescence imaging or spectrometry. [18] |
| ECM Proteins (Fibronectin, Laminin) | Proteins used to coat biomaterial surfaces to enhance cell adhesion and activity by mimicking the natural cellular environment and presenting specific integrin-binding motifs. [19] |
The efficacy of stem cell therapies is governed not solely by the intrinsic potential of the cells themselves but by the highly specialized microenvironments, or niches, in which they reside. A stem cell niche is an anatomical unit that integrates structural, biochemical, and mechanical cues to regulate stem cell self-renewal, quiescence, and differentiation [22] [23]. The core premise of modern regenerative medicine is that successful therapeutic outcomes depend on treating stem cells and their microenvironment as an inseparable unit [24] [23]. This represents a significant paradigm shift from a cell-centric to a niche-centric model, rationalizing the design of biomaterial delivery systems that recapitulate key aspects of the native stem cell niche to enhance cell survival, retention, and functional integration post-transplantation [25] [26].
The following sections provide a comparative analysis of biomaterial strategies for stem cell delivery, presenting quantitative data on their performance, detailing key experimental methodologies, and dissecting the molecular mechanisms through which they exert their effects.
Quantitative Comparison of Biomaterial Delivery Vehicles
A critical challenge in cell therapy is the acute loss of transplanted cells. Comparative studies have systematically evaluated various biomaterial carriers against the saline injection control, which represents the current clinical standard. The table below summarizes the acute cell retention performance of different biomaterial vehicles in a rat myocardial infarct model, a common testbed for regenerative therapies [27].
Table 1: Acute Cell Retention of Biomaterial Delivery Vehicles in a Rat Myocardial Infarct Model
| Delivery Vehicle | Vehicle Type | Fold Increase in Retention (vs. Saline Control) | Approximate Retained Cells at 24 Hours |
|---|---|---|---|
| Saline (Control) | Injectable | (Baseline) | ~10% of immediately transplanted cells |
| Alginate Hydrogel | Injectable | 8-fold | ~50-60% of immediately transplanted cells |
| Chitosan/β-GP Hydrogel | Injectable | 14-fold | ~50-60% of immediately transplanted cells |
| Collagen Patch | Epicardial Patch | 47-fold | ~50-60% of immediately transplanted cells |
| Alginate Patch | Epicardial Patch | 59-fold | ~50-60% of immediately transplanted cells |
The data reveals two key findings: first, all biomaterials significantly outperformed the saline control, with epicardial patches demonstrating superior retention; and second, all four biomaterials retained over half of the cells present immediately after transplantation, a five to six-fold improvement over the saline control [27]. This highlights the profound impact of a supportive microenvironment on cell survival.
Beyond simple retention, mimicking niche properties can enhance the functional potency of the cells themselves. Research on cardiac-derived cells demonstrates that culturing them as three-dimensional cardiospheres recapitulates a niche-like microenvironment, leading to enhanced therapeutic efficacy [25].
Table 2: Functional Benefits of Niches in Stem Cell Culture and Delivery
| Culture/Delivery Method | Key Niche-Mimicking Features | Impact on Cell Properties & Therapeutic Outcome |
|---|---|---|
| Traditional Monolayer Culture | Two-dimensional, lacks complex cell-cell/cell-ECM interactions | Standard for expansion but does not fully emulate native niche conditions. |
| Cardiosphere Culture | 3D suspension culture; rich in stemness and cell-matrix interactions; upregulated ECM and adhesion molecules (e.g., integrin-α2, laminin-β1) [25] | Higher proportion of c-kit+ cells; upregulated stemness factors (SOX2, Nanog); enhanced resistance to oxidative stress; improved engraftment and myocardial function in infarcted hearts [25]. |
| Dissociated Cardiospheres | Loss of 3D structure and cell-matrix interactions | Decreased expression of ECM and adhesion molecules; undermined stress resistance; negated functional benefit in vivo [25]. |
Experimental Protocols for Evaluating Biomaterial Efficacy
To ensure the reliability and reproducibility of comparative data, researchers employ standardized experimental protocols. The following outlines key methodologies used to generate the performance data presented in this guide.
Protocol for Quantifying Acute Cell Retention
This protocol is designed to objectively compare the efficiency of different biomaterials in delivering and retaining cells at the target site [27].
- Step 1: Cell Preparation and Labeling. Human Mesenchymal Stem Cells (hMSCs) are expanded in culture. Before implantation, cells are labeled with a fluorescent marker, such as a lipophilic membrane dye (e.g., DiI, CM-Dil) or a fluorescent reporter gene (e.g., GFP, Luciferase), to enable tracking.
- Step 2: Biomaterial Cell Encapsulation. For injectable hydrogels (e.g., alginate, chitosan/β-GP), the labeled cells are gently mixed with the polymer solution under sterile conditions. The mixture is kept on ice to prevent premature gelling. For epicardial patches, cells are seeded onto pre-formed collagen or alginate scaffolds and allowed to adhere.
- Step 3: In Vivo Delivery to Infarcted Heart. A rodent model (typically rat or mouse) of myocardial infarction is used. The infarction is induced surgically, often by permanent ligation of the left anterior descending coronary artery. After a set period, the animal is re-anesthetized, and the cell-biomaterial construct is delivered to the infarct border zone. Saline-injected animals serve as the control group.
- Step 4: Quantification at Endpoint. At a predetermined time point (e.g., 24 hours post-implantation), the heart is explanted and processed. Quantification is performed using fluorescence imaging. The total fluorescence signal from the heart is measured and compared to a standard curve created from a known number of labeled cells to calculate the absolute number of retained cells. This data is confirmed qualitatively by immunohistochemistry, where tissue sections are stained with fluorescent antibodies against the human cells [27].
Protocol for Assessing Functional Potency via Cardiosphere Formation
This method evaluates how a 3D niche-like culture system enhances stem cell function [25].
- Step 1: Isolation of Cardiac-Derived Cells. Human cardiac stem and supporting cells are obtained from endomyocardial biopsies.
- Step 2: Cardiosphere Culture. The cardiac-derived cells are plated on a low-attachment surface in a serum-free, growth factor-supplemented medium. This non-adherent condition promotes the self-assembly of cells into three-dimensional spherical structures, the cardiospheres, over several days.
- Step 3: In Vitro Functional Assays.
- Gene Expression Analysis: RNA is extracted from cardiospheres and compared to monolayer-cultured cells via quantitative real-time PCR (qRT-PCR) and PCR arrays to assess the upregulation of stemness factors (e.g., SOX2, Nanog), ECM molecules, and pro-survival genes (e.g., IGF-1) [25].
- Stress Resistance Assay: Cardiospheres and dissociated single cells from cardiospheres are exposed to oxidative stress (e.g., hydrogen peroxide). Cell viability is measured after a set period to compare resistance.
- Step 4: In Vivo Functional Assessment. Cardiospheres or dissociated cardiosphere-derived cells are implanted into the infarcted hearts of immunodeficient (e.g., SCID) mice. Control groups receive monolayer-cultured cells.
- Engraftment: After several weeks, heart sections are analyzed to quantify the number of persisting human cells.
- Functional Improvement: Global heart function is assessed using echocardiography to measure parameters like Left Ventricular Ejection Fraction (LVEF) and fractional shortening, comparing pre- and post-implantation values [25].
Molecular Mechanisms: Signaling Pathways Animating the Niche
The enhanced functional potency observed in niche-mimicking environments is mediated by conserved signaling pathways that are activated by specific microenvironmental cues. The following diagram illustrates the core signaling axes that are critical for maintaining stem cell behavior and how biomaterials can be designed to modulate these pathways.
The diagram shows how engineered biomaterials are designed to replicate the signaling functions of the native niche. Key pathways include [24] [23]:
- Wnt/β-catenin: Promotes stem cell self-renewal and proliferation. Its activation in cardiospheres and through biomaterial-bound ligands enhances "stemness" [25].
- Notch: Maintains stem cell quiescence and regulates cell-fate decisions. This is crucial for preventing premature differentiation and preserving the stem cell pool.
- Bone Morphogenetic Protein (BMP): Often functions in a balance with Wnt signaling to regulate the switch between proliferation and differentiation.
- Integrin-mediated signaling: Activated by interactions between cell surface integrins and the extracellular matrix (ECM) of the niche or biomaterial. This signaling enhances cell survival, resistance to stress, and is a key reason for the superior performance of 3D cultures like cardiospheres and ECM-mimicking hydrogels [25] [27].
The Scientist's Toolkit: Essential Research Reagents and Materials
Translating niche biology into therapeutic applications requires a specific set of research tools. The table below details key reagents and materials essential for developing and testing niche-mimicking biomaterials for stem cell delivery.
Table 3: Essential Reagents for Niche-Mimicking Biomaterial Research
| Research Reagent / Material | Function and Application in Niche Research |
|---|---|
| Alginate | A natural polysaccharide used to form injectable hydrogels or patches; its stiffness and degradation can be tuned to mimic mechanical properties of the native ECM [27]. |
| Chitosan/β-Glycerophosphate (β-GP) | A thermo-responsive polymer system that is liquid at low temperatures and forms a gel at body temperature, enabling minimally invasive injection and cell encapsulation [27]. |
| Collagen Type I | A major component of the native ECM; used as a base for epicardial patches and 3D scaffolds to provide natural cell-adhesion motifs and biological cues [27]. |
| Laminin & Fibronectin | Core ECM proteins often incorporated into biomaterials to promote specific integrin-mediated cell adhesion and activation of pro-survival signaling pathways [25] [23]. |
| Recombinant Growth Factors (e.g., IGF-1, VEGF, FGF) | Soluble signaling molecules used to supplement culture media or to be bound within biomaterials to replicate the biochemical signaling of the niche (e.g., IGF-1 upregulation in cardiospheres) [25] [24]. |
| Fluorescent Cell Labeling Dyes (e.g., CM-Dil, DiI) | Lipophilic membrane dyes for labeling cells before transplantation, allowing for quantitative tracking and retention studies using fluorescence imaging [27]. |
| Antibodies for Flow Cytometry (e.g., CD44, CD133, c-Kit) | Used for the identification and isolation of specific stem cell populations based on surface markers, a critical step in purifying cells for therapy [28]. |
| qRT-PCR Assays for Stemness Markers | Primer-probe sets for genes like SOX2 and Nanog to quantitatively assess the "stemness" state of cells cultured under different niche-mimicking conditions [25]. |
The comparative data and methodologies presented in this guide underscore a fundamental principle: the therapeutic efficacy of stem cells is inextricably linked to their microenvironment. Biomaterial strategies that move beyond passive cell delivery to actively mimic the structural, mechanical, and biochemical properties of the native stem cell niche—from injectable hydrogels and patches to 3D cardiospheres—consistently demonstrate superior outcomes in terms of cell retention, survival, and functional potency. The future of regenerative medicine lies in a nuanced, niche-centric approach, where engineered microenvironments are tailored to specific tissues and clinical indications to unlock the full potential of stem cell therapy.
Application-Specific Delivery Strategies Across Therapeutic Areas
3D Bioprinting and Scaffold-Based Approaches for Tissue Engineering
The field of regenerative medicine is fundamentally centered on the challenge of effectively delivering functional cells to repair or replace damaged tissues and organs. Within this context, two dominant yet philosophically distinct paradigms have emerged: scaffold-based tissue engineering and scaffold-free cell-based therapies [29]. The core thesis of this comparison is that while scaffold-based strategies, particularly those employing 3D bioprinting, offer superior structural control and the ability to create complex, anatomically-shaped constructs, scaffold-free strategies excel in biomimicry by leveraging native cell-to-cell interactions and often face fewer regulatory hurdles due to the absence of exogenous materials [29]. The choice between these approaches is not a matter of superiority but of strategic alignment with the target clinical application, balancing the need for mechanical support, biological complexity, and translational feasibility.
The critical need for advanced cell delivery systems is underscored by the profound limitations of direct cell suspension injections. Conventional delivery methods, such as intravenous infusion or direct intra-tissue injection, result in exceptionally low cell retention and survival, with studies showing that less than 5% of injected cells persist at the site of injury within the first days post-transplantation [29]. This failure to engraft significantly undermines therapeutic efficacy and has driven the development of engineered strategies that protect cells, enhance localization, and support their long-term survival and function.
Comparative Analysis of Scaffold-Based and Scaffold-Free Approaches
The following table provides a high-level comparison of the core characteristics, advantages, and challenges associated with scaffold-based and scaffold-free tissue engineering strategies.
Table 1: Core Characteristics of Scaffold-Based and Scaffold-Free Approaches
| Aspect | Scaffold-Based Approaches | Scaffold-Free Approaches |
|---|---|---|
| Core Principle | Cells are seeded onto or encapsulated within a biodegradable, porous 3D matrix [30] [31] | Cells autonomously self-assemble and secrete their own extracellular matrix to form tissue-like surrogates [29] [32] |
| Key Advantages | High mechanical integrity; design control over architecture (porosity, interconnectivity); wide range of tunable materials [30] [33] | Superior biocompatibility; dense cell packing; strong cell-cell interactions; minimal risk of foreign body response [29] |
| Primary Challenges | Potential for inflammatory response to degradation products; difficulty in replicating native ECM complexity [30] [34] | Limited initial structural strength; lengthy culture times to develop ECM; scalability issues for large tissues [29] [32] |
| Ideal Applications | Large bone defects, load-bearing cartilage, and tissues requiring immediate mechanical function [33] [31] | Tubular structures (vessels, nerves), cell sheets for surface repair, and miniature tissue models for drug screening [29] |
Quantitative Performance Data
To move beyond theoretical comparison, the table below summarizes key quantitative findings from experimental studies, highlighting the performance metrics of specific implementations within both paradigms.
Table 2: Experimental Data from Representative Studies
| Construct / Strategy | Key Quantitative Findings | Experimental Context | Source |
|---|---|---|---|
| Tissue Strands (Scaffold-Free) | Ultimate tensile strength increased from 283.1 kPa (Week 1) to 3,371 kPa (Week 3); Young's Modulus reached 5,316 kPa by Week 3 [32] | In vitro culture of chondrocyte-based tissue strands for articular cartilage engineering [32] | Scientific Reports (2016) |
| Cell Sheet (Scaffold-Free) | A single cell sheet from human endometrial gland-derived MSCs had a thickness of ~50 µm [29] | In vitro formation of cell sheets using temperature-responsive culture surfaces [29] | npj Regenerative Medicine (2021) |
| Direct Cell Injection | <5% cell retention at the site of injury post-transplantation; survival rates as low as 1% [29] | Preclinical and clinical trials of cell therapy via intravenous/intra-arterial infusion or direct injection [29] | npj Regenerative Medicine (2021) |
| 3D Bioprinted Scaffold | Enables creation of complex structures with pore size, porosity, and mechanical properties controlled via computer-aided design [33] | Fabrication of tissue engineering scaffolds for nerve, skin, bone, and vascular repair [33] | Frontiers in Materials (2022) |
Experimental Protocols for Key Methodologies
Protocol 1: Fabrication and Bioprinting of Scaffold-Free Tissue Strands
The development of scalable, scaffold-free "tissue strands" represents an advanced biofabrication method that combines high cell density with printability [32].
- Coaxial Extrusion of Tubular Capsules: A coaxial nozzle system is used to directly print long, semi-permeable, tubular alginate capsules. The average luminal and outer diameters are precisely controlled, typically around 709 µm and 1,248 µm, respectively [32].
- Cell Microinjection: A high-density cell pellet (e.g., chondrocytes) is microinjected into the lumen of the tubular alginate capsule using a gas-tight microsyringe. This process can accommodate large cell numbers (e.g., ~200 million cells) [32].
- Tissue Strand Maturation: The injected capsules are cultured in vitro. Cells within the non-adhesive capsule aggregate and self-assemble, forming a cohesive, cylindrical tissue strand. Over 10-14 days, the strand undergoes radial contraction, stabilizing at a diameter of approximately 500 µm while maintaining high cell viability (>85%) [32].
- Bioink Preparation & Bioprinting: The alginate capsule is dissolved to release the mature tissue strand. This strand, now a "bioink," is loaded into a bioprinter and robotically deposited in a predefined 3D architecture without the need for a support mold or liquid delivery medium [32].
- Post-Printing Fusion & Maturation: The bioprinted strands are cultured further, where they rapidly fuse with neighboring strands (fusion initiation within 12 hours, near completion by 7 days) and continue to mature, depositing tissue-specific ECM [32].
Protocol 2: 3D Bioprinting of a Cell-Laden Hydrogel Scaffold
Bioprinting of scaffold-based constructs is a multi-step process that integrates living cells with scaffold materials to create structured tissue analogues [33] [35].
- Pre-Bioprinting:
- Digital Design: A 3D model of the target tissue or organ is created using computer-aided design (CAD) software, often derived from medical imaging data (e.g., CT or MRI scans) [33] [35].
- Bioink Formulation: A bioink is prepared by combining a biocompatible hydrogel (e.g., alginate, collagen, hyaluronic acid, or a composite) with cultured patient cells. The bioink must have tailored rheological properties for printability and cell viability [33] [35] [34].
- Bioprinting Process: The bioink is loaded into a printing cartridge and deposited layer-by-layer onto a build platform according to the digital model. The most common method is extrusion-based bioprinting, which uses pneumatic or mechanical pressure to dispense the bioink through a nozzle [33] [35].
- Crosslinking: Immediately after deposition, each layer is stabilized (crosslinked) to solidify the structure. Crosslinking is achieved via methods specific to the bioink chemistry, such as exposure to ultraviolet light, specific ions (e.g., calcium for alginate), or temperature changes [35] [34].
- Post-Bioprinting Maturation: The printed construct is transferred to a bioreactor for incubation. The bioreactor provides dynamic nutrient exchange and mechanical stimulation (e.g., perfusion, compression) to promote cell proliferation, differentiation, and ECM production, leading to a functional tissue-engineered graft [35].
Visualizing Workflows and Biological Principles
The following diagrams illustrate the logical workflows and core biological principles underpinning the two main approaches to tissue engineering.
Scaffold-Based versus Scaffold-Free Bioprinting Workflow
The Cell-Scaffold Biointerface in Tissue Regeneration
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the protocols described above requires a suite of specialized reagents and materials. The following table details key solutions essential for research in both scaffold-based and scaffold-free tissue engineering.
Table 3: Essential Research Reagents and Materials for Tissue Engineering
| Reagent / Material | Core Function | Key Considerations |
|---|---|---|
| Natural Polymer Hydrogels(e.g., Alginate, Chitosan, Collagen, Hyaluronic Acid) [34] | Serve as the primary component of bioinks and scaffolds; provide a hydrous, biocompatible 3D environment that mimics the native extracellular matrix (ECM). | Chosen for biocompatibility, biodegradability, and tunable physical properties (e.g., stiffness, gelation kinetics). Alginate is easily ionically crosslinked, while collagen offers innate cell-adhesion motifs [34]. |
| Temperature-Responsive Polymers(e.g., poly(N-isopropylacrylamide - pNIPAM) [29] | Enable scaffold-free cell sheet engineering. Surfaces are hydrophobic at 37°C for cell culture and become hydrophilic below 32°C, allowing detachment of intact cell sheets with preserved ECM. | Critical for harvesting contiguous cell sheets without enzymatic digestion, preserving cell-cell junctions and deposited ECM proteins for enhanced transplantation efficacy [29]. |
| Crosslinking Agents(e.g., Ca²⁺ for alginate, UV initiators for synthetic hydrogels) [35] [34] | Stabilize and solidify deposited bioinks post-printing, providing the necessary mechanical integrity for 3D constructs. | Must be cytocompatible. Crosslinking density directly influences scaffold stiffness and degradation rate, which in turn affects cell behavior and nutrient diffusion [34]. |
| Growth Factors & Bioactive Molecules(e.g., bFGF, TGF-β) [31] [34] | Direct cell fate (proliferation, differentiation) and promote tissue-specific maturation (e.g., chondrogenesis, osteogenesis). Often incorporated into hydrogel matrices. | Short half-lives in vivo require delivery systems for controlled release. Can be encapsulated within microspheres or covalently bound to the scaffold to prolong activity [31]. |
| Mesenchymal Stem Cells (MSCs) | A primary adult stem cell source for many tissue engineering applications due to their multipotency (ability to differentiate into bone, cartilage, fat) and relative ease of isolation [31]. | Sourced from bone marrow, adipose tissue, or other origins. Their use in clinical strategies requires careful expansion and characterization to ensure safety and potency [29] [31]. |
The comparative analysis reveals that the strategic selection between scaffold-based and scaffold-free approaches hinges on the specific clinical requirement. Scaffold-based bioprinting is indispensable for engineering large, structurally complex tissues where mechanical support from the outset is critical, such as in bone or load-bearing osteochondral defects [33]. The ability to precisely control the scaffold's microarchitecture and composition provides a powerful tool for guiding tissue formation. Conversely, scaffold-free methods, including cell sheets and tissue strands, offer a path to creating biologically dense and authentic tissues that are ideal for repairing thinner or more homogenous tissues, such as in corneal or endothelial repair, and may face a more straightforward regulatory path due to the absence of synthetic materials [29].
The future of the field lies in the convergence of these paradigms. Emerging trends focus on creating hybrid strategies, such as 3D bioprinting scaffold-free tissue strands within a temporary, biodegradable support structure, or fabricating "smart" biomaterial scaffolds that incorporate stimulus-responsive hydrogels and sophisticated growth factor delivery systems to actively guide cellular processes [30] [34]. The ultimate goal remains the consistent and scalable fabrication of clinical-grade, functional human tissues, a mission that will continue to be driven by interdisciplinary collaboration across cell biology, materials science, and biofabrication engineering.
Injectable Hydrogels for Minimally Invasive MSC Delivery in Wound Healing
The field of regenerative medicine increasingly recognizes mesenchymal stromal cells (MSCs) for their significant potential in treating chronic wounds, owing to their multipotent differentiation capacity, secretion of trophic factors, and immunomodulatory properties [36]. However, a critical challenge hindering their clinical translation is the low retention and transient survival of directly injected cells at the wound site [36]. Rapid cell death and washout due to mechanical forces severely compromise therapeutic efficacy [36]. To address these limitations, injectable hydrogels have emerged as a promising strategy for minimally invasive delivery. These biomimetic platforms provide a three-dimensional (3D) microenvironment that recapitulates key features of the native extracellular matrix (ECM), supporting MSC viability, retention, and function upon transplantation [36]. This review provides a comparative analysis of injectable hydrogel systems for MSC delivery in wound healing, evaluating their performance based on recent experimental data to guide researchers and therapy developers.
Comparative Analysis of Hydrogel Systems for MSC Delivery
Injectable hydrogels for MSC delivery can be broadly categorized based on their material origin and design strategy. The table below summarizes the key characteristics and performance metrics of major hydrogel types as demonstrated in preclinical wound healing studies.
Table 1: Performance Comparison of Injectable Hydrogel Systems for MSC Therapy in Wound Healing
| Hydrogel Type | Key Components | Mechanism of Action | Reported Efficacy (Wound Closure) | Key Advantages | Identified Limitations |
|---|---|---|---|---|---|
| Natural Polymer-Based | Hyaluronic Acid, Collagen, Fibrin [36] [37] | Provides ECM-like 3D structure; supports cell adhesion and infiltration [37] | Accelerated closure in diabetic wounds; enhanced re-epithelialization & angiogenesis [38] | High biocompatibility; inherent bioactivity [37] | Rapid degradation; limited mechanical strength [36] |
| Synthetic Polymer-Based | Polyethylene Glycol (PEG), Polyvinyl Alcohol (PVA) [36] | Highly tunable mesh size & mechanical properties; controlled release [36] | Sustained therapeutic activity; prolonged growth factor release [36] | Excellent mechanical tunability & reproducibility [36] | Lack of cell-adhesion motifs (often requires functionalization) [36] |
| Composite/Hybrid | ECM components + Synthetic polymers (e.g., HA-PEG) [36] | Combines bioactivity of natural materials with stability of synthetics [36] | Superior cell retention and regenerative capacity vs. single-component hydrogels [36] | Balanced bioactivity and structural stability [36] | More complex fabrication process; potential batch variability [36] |
| Cell-Free/Secretome-Loaded | HA hydrogel loaded with MSC-derived exosomes [38] | Sustained release of exosomes carrying bioactive molecules (mRNAs, lipids, cytokines) [38] [39] | Significant acceleration of wound closure in diabetic models; enhanced angiogenesis [38] [39] | Off-the-shelf potential; avoids cell viability issues; controls macrophage polarization [39] | Limited duration of action compared to living, secreting MSCs [39] |
Beyond the material origin, the design of "smart" hydrogels that respond to physiological stimuli (e.g., pH, temperature, enzymatic activity) enables controlled release of cells or bioactive molecules in response to local wound cues [36]. Furthermore, the functionalization of these hydrogels with bioactive molecules such as arginine–glycine–aspartic acid (RGD) peptides enhances cell adhesion and activates integrin-mediated signaling pathways [36].
Experimental Data and Methodologies in Preclinical wound Healing
Standardized Protocols for Hydrogel-MSC Construct Evaluation
Robust experimental models are critical for evaluating the efficacy of hydrogel-MSC therapies. The following workflow outlines a standard protocol for fabricating and testing these constructs in a preclinical setting, synthesizing methodologies from key studies.
Diagram 1: Experimental workflow for evaluating hydrogel-MSC constructs.
1. Hydrogel Preparation and MSC Encapsulation: Hydrogels like hyaluronic acid (HA) are often modified to form injectable systems that crosslink in situ [38]. MSCs are typically harvested from bone marrow (BM-MSCs) or adipose tissue (AD-MSCs) and expanded in vitro. For encapsulation, a cell-polymer mixture is prepared, and gelation is triggered by physical (e.g., temperature) or chemical (e.g., crosslinker addition) cues to form a 3D cell-laden network [36].
2. In Vitro Characterization: Critical assays include:
- Cell Viability and Proliferation: Using live/dead staining and metabolic assays (e.g., MTT) to confirm the hydrogel supports MSC survival and growth [36] [38].
- Mechanical and Rheological Testing: Assessing elastic modulus, stress relaxation, and shear-thinning behavior to ensure injectability and appropriate mechanical support [36] [40].
- Bioactivity Assessment: ELISA or multiplex assays to quantify the secretion of pro-regenerative factors (e.g., VEGF, FGF) from encapsulated MSCs [39].
3. In Vivo Wound Healing Models: The most common model is the full-thickness excisional wound in diabetic (e.g., db/db) mice or rats [38] [39]. The hydrogel-MSC construct is injected intradermally around the wound or applied directly into the wound bed. The control groups are crucial and typically include untreated wounds, blank hydrogel-treated wounds, and free MSC-injected wounds.
4. Outcome Assessment: Efficacy is evaluated through:
- Wound Closure Kinetics: Tracking wound area reduction over time (e.g., days 7, 14, 21) [39].
- Histological and Immunohistochemical Analysis: Using stains like H&E and Masson's trichrome to assess tissue architecture, collagen deposition, and re-epithelialization. Key metrics include granulation tissue thickness and scar quality [38].
- Molecular Analysis: Immunostaining for CD31 to quantify neovascularization and for specific cytokines to understand the immunomodulatory effects [38] [39].
Quantitative Efficacy Data from Animal Studies
The table below consolidates quantitative findings from recent preclinical studies, providing a basis for comparing the therapeutic efficacy of different hydrogel-based strategies.
Table 2: Comparative Preclinical Efficacy Data in Animal Wound Models
| Therapeutic Formulation | Animal Model | Wound Closure Rate | Key Histological Outcomes | Source/Study Focus |
|---|---|---|---|---|
| MSC-laden HA Hydrogel | Diabetic rat model | ~95% closure by day 14 | Significant enhancement in re-epithelialization and mature angiogenesis [38] | MSC-derived exosomes injectable hyaluronic acid hydrogel [38] |
| Hydrogel + Cell Conditioned Medium (H-CM) | Full-thickness skin defect | Significant improvement vs. hydrogel alone | Enhanced collagen deposition, tissue remodeling, and macrophage polarization towards M2 phenotype [39] | Advancing wound healing by hydrogel-based dressings loaded with cell-conditioned medium [39] |
| Dynamic Crosslinking Hydrogel | In vivo release model | Reduced initial burst release by ~40% | Sustained long-term delivery of protein cargo over several weeks [40] | Evolving transport properties of dynamic hydrogels [40] |
Mechanisms of Action: How Hydrogel-Enhanced MSCs Accelerate Healing
The therapeutic action of hydrogel-delivered MSCs in wound healing is a multifactorial process, primarily mediated by paracrine signaling rather than direct cell differentiation. The diagram below illustrates the key cellular and molecular pathways involved.
Diagram 2: Signaling pathways in hydrogel-MSC mediated wound repair.
Sustained Paracrine Signaling: The hydrogel acts as a depot, protecting MSCs and facilitating a sustained release of their secretome. This includes growth factors like Vascular Endothelial Growth Factor (VEGF) and Fibroblast Growth Factor (FGF), which are crucial for promoting angiogenesis—the formation of new blood vessels that supply oxygen and nutrients to the healing tissue [36] [39]. Furthermore, MSC-derived exosomes delivered via hydrogel carry miRNAs and other bioactive molecules that facilitate intercellular communication, reducing excessive inflammation and supporting the proliferation of endothelial cells and fibroblasts [38].
Immunomodulation: A key mechanism by which MSCs aid healing is by modulating the hostile inflammatory environment of chronic wounds. The hydrogel-localized MSCs secrete anti-inflammatory cytokines such as IL-10 and IL-1Ra, which help shift the macrophage population from the pro-inflammatory M1 phenotype to the pro-healing M2 phenotype [39]. This transition is critical for resolving inflammation and initiating the proliferation phase of healing.
Direct Cellular Interactions: The 3D hydrogel scaffold not only delivers MSCs but also facilitates the infiltration and activity of host cells like fibroblasts and keratinocytes. By providing an ECM-mimetic structure and presenting adhesion motifs, the hydrogel promotes the migration and proliferation of these cells, leading to improved collagen deposition, re-epithelialization, and tissue remodeling [36] [37].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of injectable hydrogel-MSC systems rely on a specific set of materials and reagents. The following table details key components and their functions for researchers building their experimental toolkit.
Table 3: Essential Research Reagents for Hydrogel-MSC Wound Healing Studies
| Reagent/Material | Function in Research | Common Examples |
|---|---|---|
| Hyaluronic Acid (HA) | Base polymer for hydrogel formation; high biocompatibility and native bioactivity [38] [37] | Methacrylated HA (MeHA) for photo-crosslinking; oxidized HA for Schiff base formation |
| Synthetic Polymers (PEG) | Provides a tunable, reproducible, and mechanically stable network; "blank slate" for functionalization [36] | PEG-diacrylate (PEGDA); multi-armed PEG-NHS or PEG-Maleimide |
| Cell-Adhesion Peptides | Functional motif incorporated into synthetic hydrogels to enable MSC adhesion and survival [36] | RGD (Arginine-Glycine-Aspartic acid) peptide sequences |
| Protease-Degradable Linkers | Allows hydrogel degradation by cell-secreted enzymes, facilitating cell migration and matrix remodeling [36] | Peptide crosslinkers (e.g., VPMS↓MRGG, cleavable by MMP-2) |
| MSC-Specific Media | For the in vitro expansion and maintenance of MSCs prior to encapsulation [41] | Dulbecco's Modified Eagle Medium (DMEM) supplemented with Fetal Bovine Serum (FBS) and growth factors (e.g., FGF-2) |
| Viability/Cytotoxicity Assays | To quantify the survival and metabolic activity of MSCs after encapsulation and delivery [36] | Live/Dead staining (Calcein AM/EthD-1); AlamarBlue; MTT assay |
| Angiogenesis Assay Kits | To evaluate the pro-angiogenic potential of the MSC secretome released from hydrogels in vitro [38] [39] | Tube formation assay using HUVECs; ELISA for quantifying VEGF |
Injectable hydrogels represent a transformative platform for overcoming the delivery challenges of MSC-based wound therapies. Comparative analysis confirms that no single hydrogel type is universally superior; rather, the choice involves a trade-off between the robust bioactivity of natural polymers and the controllable mechanics of synthetic systems. The emerging trend towards composite, "smart," and cell-free secretome-loaded hydrogels holds particular promise for enhancing therapeutic efficacy and simplifying regulatory pathways [36] [38] [39]. For clinical translation, future work must focus on standardizing fabrication using xeno-free, GMP-compliant components and designing larger, controlled clinical studies to firmly establish safety and efficacy in humans [36]. The integration of these advanced biomaterial strategies with the potent biological functions of MSCs is poised to significantly advance the treatment of debilitating chronic wounds.
Biomaterial-Assisted Immune Cell Delivery for Cancer and Inflammatory Diseases
The development of biomaterials for immune cell delivery represents a paradigm shift in managing cancer and inflammatory diseases. These advanced platforms are engineered to overcome fundamental therapeutic challenges: in cancer immunotherapy, they enhance the precision and persistence of antitumor responses while minimizing systemic toxicities [42] [43]; in inflammatory diseases, they provide spatiotemporal control over anti-inflammatory agents, disrupting pathological cycles while preserving protective immunity [44]. The comparative efficacy of these systems hinges on their material properties, targeting mechanisms, and biological interactions, which collectively determine their clinical performance across different disease contexts.
This guide provides a structured comparison of biomaterial platforms based on their intended application, target cells, and experimental outcomes. By examining quantitative data across standardized parameters, researchers can identify optimal material configurations for specific therapeutic objectives, accelerating the rational design of next-generation delivery systems.
Comparative Efficacy of Biomaterial Platforms
Biomaterial Platforms for Cancer Immunotherapy
Table 1: Comparative performance of biomaterial platforms in cancer immunotherapy
| Biomaterial Platform | Target Cell/Process | Key Experimental Findings | Efficacy Metrics | Reference Model | |
|---|---|---|---|---|---|
| Polymeric Nanoparticles (e.g., PLGA) | Dendritic Cells (DCs) | Enhanced antigen cross-presentation and T cell activation; 3.5-fold increase in tumor-infiltrating lymphocytes compared to soluble antigen | 85% antigen loading efficiency; 70% DC uptake in vivo; 60% tumor growth inhibition | Melanoma (B16-OVA) | [42] [43] |
| Microneedle Patches | Skin-resident APCs | Sustained release of anti-PD-1 antibody in tumor microenvironment; improved CD8+ T cell functionality | 90% transdermal delivery efficiency; 2.8-fold higher tumor-specific T cells vs. systemic delivery | Colon carcinoma (MC-38) | [42] |
| Magnetic Nanoparticles | Tumor-associated macrophages | Hyperthermia-induced immunogenic cell death; M1 macrophage polarization; reduced immunosuppressive factors | 45°C local temperature; 40% increase in CD8+ T cell infiltration; 75% reduction in tumor volume at 14 days | Breast cancer (4T1) | [45] |
| Injectable Hydrogels | T cells and APCs | Localized delivery of IL-15 superagonist and anti-PD-L1; promotes stem-like T cell expansion and differentiation | 21-day sustained release; 8-fold increase in antigen-specific T cells; 100% survival at 30 days vs. 40% with free drugs | Lymphoma (EG7) | [42] |
| IMPAC-T Cells (AI-Designed) | Tumor-specific T cells | De novo designed pMHC binders redirect T cells to cancer cells with high specificity; minimal off-target toxicity | 95% cancer cell killing in vitro; 4-6 week development timeline; 80% reduction in cross-reactivity risk | Metastatic melanoma | [46] |
Biomaterial Platforms for Inflammatory Diseases
Table 2: Comparative performance of biomaterial platforms in inflammatory diseases
| Biomaterial Platform | Therapeutic Strategy | Key Experimental Findings | Efficacy Metrics | Disease Model | |
|---|---|---|---|---|---|
| ROS-Scavenging Nanoparticles | Macrophages, Neutrophils | Neutralize reactive oxygen species; reduce oxidative stress and tissue damage | 90% ROS scavenging in vitro; 70% reduction in pro-inflammatory cytokines; 60% improvement in histological scores | Rheumatoid arthritis | [44] |
| Adhesion-Blocking Nanofibers | Endothelial cells, Leukocytes | Inhibit leukocyte-endothelial cell interactions; prevent immune cell extravasation | 80% reduction in leukocyte adhesion; 65% decrease in inflammatory cell infiltration | Atherosclerosis | [44] |
| Targeted SPIONs | Synovial macrophages | MRI-based diagnosis and targeted drug delivery to inflamed synovium; theranostic application | 50% improvement in imaging contrast; 60% reduction in synovitis score | Osteoarthritis | [47] |
| Cationic Ta₂O₅ Nanoparticles | Cartilage (GAG targeting) | Electrostatic targeting of anionic glycosaminoglycans for early OA diagnosis | Preferential absorption in defect regions; correlation with GAG concentration (R²=0.89) | Osteoarthritis | [47] |
| NETs-Inhibiting Gold Nanoparticles | Neutrophils | Prevent formation of neutrophil extracellular traps; reduce inflammation propagation | 75% inhibition of NETosis; 55% reduction in tissue damage markers | Systemic lupus erythematosus | [44] |
Experimental Protocols and Methodologies
Protocol for Evaluating Biomaterial-Based Cancer Vaccines
Objective: Assess the efficacy of nanoparticle-based cancer vaccines in priming antigen-specific T cell responses and inhibiting tumor growth.
Materials:
- PLGA nanoparticles encapsulating ovalbumin (OVA) antigen and CpG adjuvant
- C57BL/6 mice (6-8 weeks old)
- B16-OVA melanoma cells
- Flow cytometry antibodies: CD8, CD4, CD44, CD62L, IFN-γ
- ELISA kits for cytokine detection
Procedure:
- Nanoparticle Characterization: Determine size distribution (110±15 nm expected), zeta potential (-25±5 mV expected), antigen loading efficiency (≥80%), and release kinetics (sustained over 7-10 days) using dynamic light scattering, HPLC, and BCA assay [42].
- Immunization and Challenge:
- Day 0: Subcutaneously immunize mice with PLGA-OVA/CpG (50 µg antigen), empty nanoparticles, or soluble OVA/CpG (n=8/group)
- Day 14: Challenge with 2×10⁵ B16-OVA cells in the right flank
- Immune Monitoring:
- Day 21: Isolate splenocytes and stimulate with OVA257-264 peptide for intracellular IFN-γ staining
- Analyze T cell phenotypes using flow cytometry (central memory: CD44+CD62L+; effector memory: CD44+CD62L-)
- Quantify tumor-infiltrating lymphocytes at day 28
- Tumor Monitoring: Measure tumor dimensions every 2-3 days using calipers; calculate volume as (length × width²)/2
- Statistical Analysis: Compare groups using one-way ANOVA with Tukey's post-hoc test; significance set at p<0.05 [42] [43].
Protocol for Assessing Anti-inflammatory Biomaterials
Objective: Evaluate the capacity of ROS-scavenging nanoparticles to mitigate inflammation in rheumatoid arthritis.
Materials:
- Cerium oxide nanoparticles (nanoceria) with PEG coating
- Collagen-induced arthritis (CIA) model in DBA/1 mice
- Histology reagents: H&E, safranin O, anti-CD68 antibody
- ROS assay kit (DCFDA)
- ELISA kits for TNF-α, IL-6, IL-1β
Procedure:
- Nanoparticle Validation: Confirm ROS-scavenging activity using DCFDA assay (≥90% reduction expected); characterize size (10±2 nm) and surface charge [44].
- Disease Induction and Treatment:
- Day 0: Immunize DBA/1 mice with bovine type II collagen in complete Freund's adjuvant
- Day 21: Boost with collagen in incomplete Freund's adjuvant
- Day 28: Randomize arthritic mice (clinical score ≥2) into treatment groups (n=8)
- Days 28-42: Intra-articular injections of nanoceria (1 mg/kg) or vehicle control every 3 days
- Disease Assessment:
- Clinical scoring (0-4 scale) of each paw every other day
- Ankle diameter measurements daily
- Serum collection for cytokine analysis on days 28, 35, and 42
- Histopathological Analysis:
- Day 42: Harvest joint tissues for H&E staining (inflammation), safranin O (cartilage damage), and immunohistochemistry for macrophages (CD68+)
- Score samples blindly using established grading systems [44].
- Data Analysis: Compare clinical scores, cytokine levels, and histopathology scores using two-way repeated measures ANOVA.
Signaling Pathways in Biomaterial-Immune Cell Interactions
Cancer-Immunity Cycle and Biomaterial Intervention Points
Figure 1: Cancer-Immunity Cycle and Biomaterial Intervention Points. This diagram illustrates the stepwise process of antitumor immunity and key points where biomaterials enhance efficacy through targeted delivery and immunomodulation [42].
Inflammatory Signaling and Biomaterial Modulation Strategies
Figure 2: Inflammatory Signaling and Biomaterial Modulation. This diagram outlines key inflammatory pathways and strategic points where biomaterials intervene to disrupt pathological signaling [44].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents for biomaterial-assisted immune cell delivery
| Reagent Category | Specific Examples | Research Application | Key Function | Commercial Sources/References |
|---|---|---|---|---|
| Biodegradable Polymers | PLGA, PEG, chitosan | Nanoparticle formulation, hydrogel fabrication | Controlled drug release, improved pharmacokinetics, reduced immunogenicity | Sigma-Aldrich, Akina [42] [21] |
| Inorganic Nanoparticles | SPIONs, gold nanoparticles, tantalum oxide | Theranostic applications, hyperthermia, contrast imaging | Magnetic targeting, imaging enhancement, thermal ablation | Nanocomposix, Cytodiagnostics [45] [47] |
| Surface Modification Reagents | NH₂-PEG-COOH, maleimide-PEG-NHS, DSPE-PEG | Stealth coating, ligand conjugation | Reduced protein adsorption, active targeting, prolonged circulation | Creative PEGWorks, Nanocs [42] [48] |
| Immune Cell Isolation Kits | CD8+ T cell isolation, CD11c+ DC isolation | Primary cell culture, ex vivo manipulation | High-purity cell populations for therapy and analysis | Miltenyi Biotec, STEMCELL Technologies [42] [43] |
| Cytokine Detection Assays | LEGENDplex, ELISA kits | Immune monitoring, efficacy assessment | Multiplex quantification of inflammatory mediators | BioLegend, R&D Systems [42] [44] |
| Animal Disease Models | B16 melanoma, MC38 colon cancer, collagen-induced arthritis | Preclinical efficacy testing | Human disease mimicry for therapeutic evaluation | The Jackson Laboratory, Charles River [42] [44] |
| AI/Computational Tools | Protein design algorithms, molecular docking software | De novo biomaterial design, safety screening | Accelerated development, reduced off-target risk | Rosetta, AlphaFold [46] |
The comparative analysis reveals that optimal biomaterial design principles transcend disease boundaries, yet require specific adaptations for clinical context. Size optimization (20-200 nm) proves critical for both tumor accumulation via the EPR effect and inflammatory site targeting through leaky vasculature [44]. Surface functionalization with targeting ligands enhances precision across applications, whether directing materials to specific immune cell populations in cancer or cartilage components in osteoarthritis [42] [47].
Key distinctions emerge in release kinetics requirements: cancer applications often benefit from sustained immunostimulation, while inflammatory diseases may require rapid response to pathological triggers. The integration of AI in biomaterial design, particularly for de novo protein creation as demonstrated in the IMPAC-T cell platform, represents a transformative approach with applications across both therapeutic domains [46]. These comparative insights provide a framework for researchers to strategically adapt biomaterial platforms across the cancer-inflammatory disease spectrum, accelerating the development of precision immunotherapies.
The dependency of organoid technology on Matrigel, a poorly defined, tumor-derived extracellular matrix (ECM), has long been a significant bottleneck for clinical translation and reproducible research. This review provides a comparative analysis of advanced defined hydrogel systems engineered to overcome the limitations of Matrigel. We systematically evaluate the efficacy of natural polymer-based, synthetic, and decellularized ECM hydrogels against the traditional gold standard, supported by summarized experimental data. Furthermore, we detail the methodologies for culturing organoids in these alternative matrices and provide a visual breakdown of hydrogel design and experimental workflows. Finally, we present a curated list of essential research reagents, equipping scientists with the tools to implement these next-generation biomaterials in their own laboratories for disease modeling, drug development, and regenerative medicine.
Organoid technology has revolutionized biomedical research by providing in vitro miniature models of human organs that recapitulate complex physiological structures and functions. A cornerstone of this technology is the three-dimensional (3D) scaffold that provides mechanical support and biochemical cues to guide stem cell self-organization and differentiation. For decades, Matrigel, a basement membrane extract derived from Engelbreth-Holm-Swarm mouse sarcoma, has served as the ubiquitous substrate for organoid culture [49] [50]. However, its tumorigenic origin, significant batch-to-batch variability, undefined composition, and presence of xenogenic factors severely limit its utility in reproducible research and clinical applications [51] [52]. The scientific community has therefore prioritized the development of defined hydrogels as alternatives. These engineered matrices aim to replicate crucial aspects of the native extracellular matrix (ECM)—providing tunable mechanical properties, incorporating specific adhesive ligands, and enabling responsiveness to environmental stimuli—all within a controlled and reproducible system [53] [54]. This guide objectively compares the performance of these emerging hydrogel platforms against Matrigel, providing researchers with the data and protocols needed to advance their organoid studies.
Comparative Analysis of Defined Hydrogel Platforms
Researchers have developed several classes of defined hydrogels, each with distinct advantages and limitations. The following sections and comparative tables detail their compositions, properties, and performance in supporting various organoid types.
Natural Polymer-Based Hydrogels
Natural hydrogels, derived from biological sources, offer high biocompatibility and inherent bioactivity. Fibrin-based hydrogels, for instance, have proven highly effective for blood vessel organoid culture. Studies show that vascular organoids cultured in fibrin gels exhibit vascular network formation and endothelial cell sprouting comparable to those in Matrigel, with the added benefit of being a xeno-free, clinically translatable platform [52]. Alginate, a seaweed-derived polysaccharide, supports intestinal and islet organoid viability and structure, though it may yield lower organoid numbers in long-term culture due to its inert nature, which lacks native cell adhesion sites [50]. Collagen I, the most abundant mammalian protein, has been used for intestinal, stomach, and kidney organoids, though it can result in different morphological outcomes, such as promoting smooth, unbudded structures or facilitating the formation of large-scale, fused macroscopic constructs when used in floating cultures [50].
Table 1: Comparison of Natural Polymer-Based Hydrogels for Organoid Culture
| Hydrogel Type | Key Components | Organoids Tested | Performance vs. Matrigel | Key Advantages |
|---|---|---|---|---|
| Fibrin | Fibrinogen, Thrombin | Blood Vessel Organoids [52] | Comparable vascular network formation and sprouting. | Xeno-free, supports angiogenesis, tunable mechanics. |
| Alginate | Alginate polysaccharide | Intestinal [50], Islet [50] | Supports viability & structure; may have lower long-term yield. | Inert, easy gelation, FDA-approved for some uses. |
| Collagen I | Type I Collagen | Intestinal, Stomach, Kidney [50] | Can form unbudded structures or fused macroscopic constructs. | Defined, abundant, allows for macroscopic structure fusion. |
| Multi-Component | Collagen, Laminin, Fibronectin, Hyaluronan | Mammary Organoids [50] | Mimics in vivo environment, supports branched organoids. | Recapitulates complex ECM composition, tunable properties. |
Decellularized Extracellular Matrix (dECM) Hydrogels
dECM hydrogels are produced by decellularizing tissues, preserving the complex, tissue-specific composition of the native ECM. This approach provides a biomimetic microenvironment that closely resembles the in vivo niche. Research on gastrointestinal (GI)-tract derived dECM hydrogels demonstrates their superiority to Matrigel. Proteomic analyses confirm that dECM hydrogels from stomach (SEM) and intestine (IEM) contain a more relevant composition, rich in collagens and proteoglycans, unlike Matrigel, which is predominantly composed of glycoproteins [51]. Functionally, gastric and intestinal organoids grown in these hydrogels show comparable or superior development and function, including enhanced potential for long-term subculture and transplantation [51]. A novel photo-crosslinkable hydrogel combining porcine small intestinal submucosa (SIS), fish collagen (FC), and methacrylate gelatin (GelMA) has also been developed. This FC/SIS/GelMA hydrogel supports the formation of small intestinal organoids with crypt-like structures similar to Matrigel, and its rapid gelation and tunable mechanical properties make it highly attractive for clinical applications, such as intestinal defect repair [55].
Table 2: Performance of Decellularized ECM (dECM) Hydrogels
| Hydrogel Type | Tissue Source | Key ECM Components | Organoids Tested | Experimental Findings vs. Matrigel |
|---|---|---|---|---|
| GI-tract dECM | Stomach (SEM), Intestine (IEM) | Collagens, Proteoglycans [51] | Gastric, Intestinal [51] | ► Proteomics: Higher content of tissue-specific collagens & proteoglycans [51]► Function: Comparable or superior organoid development & function [51]► Biocompatibility: Low immunogenicity, suitable for transplantation [51] |
| FC/SIS/GelMA | Porcine SIS, Fish Collagen, GelMA | dECM, Collagen, Gelatin [55] | Small Intestinal [55] | ► Morphology: Supports crypt-like budding domains [55]► Efficiency: Formation efficiency ~70-80% of Matrigel [55]► Gelation: 65x faster gelation under UV light [55] |
Synthetic and Hybrid Hydrogel Systems
Synthetic hydrogels, such as those based on poly(ethylene glycol) (PEG), offer the highest degree of control over mechanical and biochemical properties. They are inherently inert but can be functionally modified with adhesive peptides (e.g., RGD) and protease-sensitive sequences to make them cell-responsive [51] [50]. PEG-based hydrogels have successfully supported the culture of intestinal, lung, and cardiac organoids [50]. The major advantage of synthetic systems is their high reproducibility and tunability. However, they often require sophisticated functionalization to incorporate the necessary biological cues found in natural ECM. To bridge this gap, hybrid hydrogels that combine synthetic polymers with natural components (e.g., PEG-fibrin for liver organoids) have been developed to leverage the advantages of both worlds [50].
Experimental Protocols for Hydrogel-Based Organoid Culture
Transitioning from Matrigel to defined hydrogels requires specific protocols. Below are detailed methodologies for implementing two promising alternative platforms: fibrin hydrogels for vascular organoids and dECM hydrogels for intestinal organoids.
Protocol: Culturing Blood Vessel Organoids in Fibrin Hydrogel
This protocol adapts the method described by [52] to create a xeno-free environment for human iPSC-derived blood vessel organoid (BVO) culture.
Step 1: hiPSC Pre-Culture on Vitronectin
- Coat tissue culture plates with recombinant human Vitronectin (e.g., Vitronectin XF) according to manufacturer's instructions.
- Maintain and expand hiPSCs under feeder-free and serum-free conditions on the Vitronectin-coated plates. This establishes an animal-free 2D culture foundation.
Step 2: Fibrin Hydrogel Preparation
- Prepare the fibrinogen solution by dissolving fibrinogen in a suitable buffer (e.g., PBS).
- Prepare a working solution of thrombin in a calcium-containing buffer.
- Mix the cell suspension containing differentiated vascular progenitor cells with the fibrinogen solution on ice.
- Quickly add the thrombin solution to the cell-fibrinogen mixture and pipette to ensure homogeneity. A typical final concentration is 5 mg/mL fibrinogen and 2 U/mL thrombin.
- Immediately transfer the mixture to the desired culture vessel (e.g., multi-well plate) and incubate at 37°C for 15-30 minutes to allow complete polymerization.
Step 3: Organoid Culture and Maintenance
- Once polymerized, carefully overlay the fibrin gel with pre-warmed vascular organoid culture medium.
- Change the medium every 2-3 days. The organoids will develop and form vascular networks within the fibrin matrix over 18-21 days.
- For analysis, the fibrin gel can be degraded using fibrinolysis enzymes (e.g., nattokinase) to release the organoids for downstream applications.
Protocol: Culturing Intestinal Organoids in dECM Hydrogel
This protocol is based on the use of gastrointestinal tissue-derived dECM hydrogels, as validated by [51].
Step 1: Preparation of dECM Hydrogel Solution
- Acquire lyophilized dECM powder derived from the desired tissue (e.g., stomach SEM or intestine IEM).
- Dissolve the dECM powder in a weak acid (e.g., 0.5M acetic acid) or a proprietary solubilization buffer on ice, typically at a concentration of 10-20 mg/mL. This may require several hours of gentle mixing or agitation.
- Centrifuge the solution to remove any undissolved particles and keep the supernatant on ice.
Step 2: Encapsulation of Intestinal Crypts
- Isolate intestinal crypts from mouse or human tissue using standard protocols.
- Resuspend the pellet of isolated crypts in the cold, liquid dECM solution. Keep the mixture on ice to prevent premature gelation.
- Pipette the cell-dECM mixture onto a pre-warmed culture dish. For 3D cultures, deposit drops (e.g., 20-30 µL) and avoid disrupting the drops after plating.
- Incubate the culture dish at 37°C for 20-30 minutes to induce thermal gelation, forming a solid hydrogel.
- After gelation, carefully flood the gel with pre-warmed intestinal organoid culture medium.
Step 3: Organoid Maintenance and Passaging
- Change the medium every 2-4 days. Organoid growth and budding should be visible within 3-7 days.
- For passaging, remove the culture medium and mechanically disrupt the hydrogel. Use a digestion enzyme (e.g., collagenase) to dissolve the dECM matrix and recover the organoids for subsequent passages.
Visualization of Hydrogel Design and Workflow
The following diagrams illustrate the core concepts of stimulus-responsive hydrogel design and the typical experimental workflow for establishing organoid cultures in defined matrices.
Diagram 1: Mechanisms of Stimuli-Responsive Hydrogels. External stimuli such as temperature, pH, light, or enzymatic activity trigger changes in the hydrogel's physical and biochemical properties, which in turn precisely control organoid behavior.
Diagram 2: Generic Workflow for Organoid Culture in Defined Hydrogels. The process begins with stem cell expansion on a defined substrate, followed by encapsulation in a liquid hydrogel precursor that is triggered to gel, culminating in long-term 3D culture and analysis.
The Scientist's Toolkit: Essential Research Reagents
Successfully implementing defined hydrogel cultures requires a specific set of reagents and materials. The following table lists key solutions used in the featured experiments.
Table 3: Key Research Reagent Solutions for Defined Organoid Culture
| Reagent Solution | Function & Application | Example Use Case |
|---|---|---|
| Vitronectin XF | A recombinant human protein used as a defined, xeno-free substrate for 2D feeder-free culture of hiPSCs. | Pre-culture coating for hiPSCs before differentiation into vascular organoids [52]. |
| Fibrinogen from Human Plasma | The soluble precursor protein that, upon reaction with thrombin, forms a fibrin hydrogel. | Core component of the 3D fibrin matrix for blood vessel organoid culture [52]. |
| Thrombin from Human Plasma | A serine protease that converts fibrinogen into fibrin, initiating polymerization and gel formation. | Used in combination with fibrinogen to form the fibrin hydrogel for cell encapsulation [52]. |
| Decellularized ECM (dECM) Powder | Lyophilized, solubilized extracellular matrix from specific tissues (e.g., stomach, intestine). | The base material for creating tissue-specific hydrogel scaffolds for GI organoids [51]. |
| Methacrylated Gelatin (GelMA) | A modified gelatin that can form hydrogels via photo-crosslinking when combined with a photoinitiator and UV light. | Component of composite hydrogels (e.g., with SIS and fish collagen) providing tunable mechanical properties [55]. |
| Photo-initiator (e.g., LAP) | A compound that generates free radicals upon exposure to UV or visible light, initiating polymer cross-linking. | Essential for the gelation of light-sensitive hydrogels like GelMA-based systems [55]. |
The move toward defined hydrogel systems represents a paradigm shift in organoid technology, addressing the critical limitations of Matrigel. As this comparison demonstrates, a diverse toolkit of hydrogels—including fibrin for vascular organoids, tissue-specific dECM for GI organoids, and tunable synthetic platforms—now offers robust and often superior alternatives. These materials provide unprecedented control over the biochemical and biophysical microenvironment, leading to enhanced reproducibility, functionality, and clinical relevance of organoid models. By adopting the detailed protocols and reagents outlined in this guide, researchers can confidently integrate these advanced biomaterials into their workflows, thereby accelerating the translation of organoid technology from foundational research into therapeutic and pharmaceutical applications.
Targeting therapeutic agents to hostile microenvironments represents a fundamental challenge in biomedicine. Tissues such as the central nervous system (CNS), bone, and ischemic regions present unique biological barriers and pathological conditions that hinder conventional drug delivery approaches. The blood-brain barrier (BBB) severely restricts access to the CNS, bone tissue possesses a dense, mineralized matrix, and ischemic areas are characterized by inflammation, oxidative stress, and compromised vasculature [56] [57] [58]. Biomaterial-based delivery platforms have emerged as promising solutions to these challenges, offering strategies to enhance targeting, control release kinetics, and protect therapeutic cargo. This review provides a comparative analysis of advanced biomaterial platforms designed for these hostile microenvironments, evaluating their design principles, efficacy data, and experimental validation to guide researchers in selecting appropriate systems for specific applications.
Comparative Analysis of Biomaterial Platforms
Table 1: Comparison of Biomaterial Platforms for Hostile Microenvironments
| Target Tissue | Biomaterial Platform | Therapeutic Cargo | Key Findings/ Efficacy Data | Primary Advantages |
|---|---|---|---|---|
| CNS | Sinomenine-loaded nano-delivery systems [56] | Sinomenine (alkaloid) | Enhanced stability and brain-targeting ability; showed neuroprotective effects in cerebral ischemia models [56] | Overcomes poor pharmacokinetics; leverages bone-brain axis for targeting |
| CNS | Extracellular Vesicles (EVs) [59] | miRNAs, proteins, drugs | In stroke models: increased neurite remodeling, neurofilaments, and synaptic plasticity; functional recovery observed [59] | Innate BBB crossing ability; low immunogenicity; natural cargo delivery |
| CNS | AI-designed biomaterials [57] | Various neuroprotective agents | Accelerated discovery of optimal materials; prediction of brain tissue interactions [57] | Rapid optimization of material properties; personalized design potential |
| Bone | Nanoparticles for bone engineering [60] | Drugs, genes | Regulated bone remodeling based on size, shape, composition, and charge; supported bone regeneration [60] | Tunable physicochemical properties; multi-functional applications |
| Bone | Bone-targeting biomaterial carriers [61] | Bioactive agents for bone repair | Enhanced biodistribution to bone; minimized off-target effects; improved healing in impaired models [61] | Specific affinity for bone mineral components; versatile for local/systemic delivery |
| Ischemic Tissues | Intravascularly injectable biomaterials [62] | Therapeutic cells, proteins | Reduced off-target localization; retention and accumulation within infarct via passive diffusion and targeting [62] | Minimally invasive delivery; stimuli-responsive designs |
| Ischemic Tissues | Biomaterial-based gene delivery systems [58] | Pro-angiogenic genes (ZNF580, VEGF, eNOS) | Promoted vascular regeneration in critical limb ischemia; improved blood perfusion [58] | Enhanced stability and targeting of genes; controlled release profiles |
Experimental Protocols for Key Platforms
Sinomenine Nano-Delivery for Cerebral Ischemia
Objective: To evaluate the neuroprotective efficacy of sinomenine (SIN)-loaded nanotechnology-based delivery systems in experimental cerebral ischemia models, specifically examining their ability to modulate the bone-brain axis [56].
Methodology:
- Animal Model: Establish cerebral ischemia in mice using the bilateral carotid artery stenosis (BCAS) model. Sham-operated controls should be used for comparison.
- Treatment Groups: Divide animals into: (1) Vehicle control, (2) Free SIN, (3) SIN-loaded nanoparticles, (4) SIN-nanoparticles targeting bone-brain axis.
- Administration: Administer treatments via intravenous injection at specified time points post-ischemia.
- Histological Analysis: At sacrifice (e.g., 28 days post-surgery), perfuse animals and collect brain tissue. Perform immunohistochemistry for glial fibrillary acidic protein (GFAP) to assess astrocytic activation. Use Bielschowsky silver and Luxol fast blue double staining to evaluate neurofibrils and myelin integrity respectively.
- Molecular Analysis: Isulate protein from brain tissues and perform Western blotting for tight junction proteins (ZO-1), pro-inflammatory cytokines (IL-1β, TNF-α), and markers of inflammasome activation (NLRP3).
- Behavioral Assessment: Conduct neurological function tests (e.g., modified Neurological Severity Score [mNSS]) at regular intervals to evaluate functional recovery.
- Bone Analysis: Collect bone marrow and analyze CD4+ T cell activation and RANKL expression to investigate bone-brain axis crosstalk.
Key Parameters: Quantify GFAP+ astrocytes, extent of demyelination, axonal injury, tight junction integrity, cytokine levels, and neurological scores across treatment groups [56].
Extracellular Vesicles for CNS Delivery
Objective: To determine the therapeutic potential of mesenchymal stem cell-derived extracellular vesicles (MSC-EVs) in promoting recovery after ischemic stroke by enhancing neurite remodeling and synaptic plasticity [59].
Methodology:
- EV Isolation and Characterization: Isolate EVs from MSC culture supernatants using differential ultracentrifugation. Characterize EVs by nanoparticle tracking analysis (size distribution), transmission electron microscopy (morphology), and Western blotting for exosomal markers (CD63, CD81, TSG101).
- Animal Model and Treatment: Induce focal cerebral ischemia in rats using the middle cerebral artery occlusion (MCAO) model. Randomize animals to receive: (1) Phosphate-buffered saline (PBS) control, (2) MSC-EVs, (3) Liposome control.
- Administration: Administer treatments via tail vein injection at designated time points post-occlusion.
- Histological Analysis: At endpoint, perfuse animals and process brain tissues. Perform the following staining on brain sections containing the ischemic boundary zone (IBZ):
- Bielschowsky silver and Luxol fast blue double staining for neurofibrils.
- Immunofluorescence for SMI-31 (neurofilaments) and synaptophysin (presynaptic vesicles).
- Golgi silver impregnation to visualize neuronal dendritic arborization.
- Image Analysis: Use image analysis software (e.g., ImagePro Plus) to quantify neurite density, branching points, spine density, and synaptophysin-positive areas.
- Functional Assessment: Evaluate motor and sensory function using tests such as the adhesive removal test and corner test at multiple time points.
Key Parameters: Compare neurite remodeling, synaptic density, dendritic complexity, and functional recovery between EV-treated and control groups [59].
Biomaterial-Based Gene Delivery for Ischemic Tissues
Objective: To assess the efficacy of biomaterial-based non-viral gene delivery systems in promoting therapeutic vascularization in a murine model of critical limb ischemia (CLI) [58].
Methodology:
- Vector Preparation: Formulate cationic polymer-based gene vectors (e.g., polyethylenimine derivatives) complexed with plasmid DNA encoding pro-angiogenic genes (e.g., ZNF580, VEGF, eNOS). Ensure optimal N/P ratio for efficient gene complex formation.
- Characterization of Gene Complexes: Determine particle size and zeta potential using dynamic light scattering. Assess gene loading efficiency using gel retardation assay. Test stability against nuclease degradation.
- In Vitro Transfection: Transfect human umbilical vein endothelial cells (HUVECs) with gene complexes. Evaluate transfection efficiency via fluorescence-activated cell sorting (for reporter genes) and quantify target gene expression using RT-qPCR and Western blot.
- Functional Cellular Assays: Perform in vitro tubule formation assay on Matrigel to assess pro-angiogenic potential. Conduct migration (scratch wound) and proliferation (MTT) assays.
- In Vivo Ischemia Model and Treatment: Induce unilateral hindlimb ischemia in mice via femoral artery excision. Randomize animals to receive: (1) Saline control, (2) Naked plasmid DNA, (3) Gene complexes.
- Administration: Inject treatments intramuscularly at multiple sites in the ischemic adductor muscle post-surgery.
- In Vivo Assessment:
- Laser Doppler Perfusion Imaging: Measure hindlimb blood flow weekly for 4-5 weeks. Express results as perfusion ratio (ischemic/non-ischemic limb).
- Histological Analysis: At endpoint, harvest muscle tissues. Process for immunohistochemistry against CD31 (capillary density) and α-smooth muscle actin (arteriole density). Quantify vessel densities.
- Functional Recovery: Assess limb function and tissue necrosis using a standardized scoring system.
Key Parameters: Compare limb perfusion, capillary/arteriolar density, and incidence of auto-amputation between treatment groups [58].
Signaling Pathways in Hostile Microenvironments
Neuroinflammation and Bone-Brain Axis in Cerebral Ischemia
Diagram 1: Signaling Pathways in Cerebral Ischemia and Bone-Brain Axis Crosstalk. This diagram illustrates the key pathophysiological processes in cerebral ischemia, including neuroinflammation and the emerging connection to bone metabolism via the bone-brain axis, highlighting potential therapeutic targets for biomaterial-based interventions [56].
VEGF Signaling in Ischemic Tissue Microenvironment
Diagram 2: VEGF-Mediated Angiogenesis Signaling in Ischemic Tissues. This diagram outlines the cellular response to hypoxia in ischemic tissues, highlighting the central role of HIF-1α and VEGF signaling in attempting to restore perfusion, and the potential points for therapeutic enhancement in conditions like critical limb ischemia [58].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Targeted Delivery Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations for Hostile Microenvironments |
|---|---|---|---|
| Nanoparticle Systems | Polymeric nanoparticles (PLGA, PLLA), Liposomes, Cationic polymers (PEI, PLL) | Drug/gene encapsulation and delivery; enhanced targeting and stability [56] [58] [60] | Size, charge, and surface functionalization must be tailored to overcome specific biological barriers (e.g., BBB, bone matrix) |
| Targeting Ligands | Peptides, Antibodies, Carbohydrates (e.g., RVG peptide for CNS) | Enhance cellular targeting specificity; improve accumulation at desired site [58] [59] | Ligand density and orientation impact binding efficiency; potential immunogenicity requires evaluation |
| Bone-Targeting Moieties | Bisphosphonates, Tetracyclines, Aspartic acid-rich peptides | Confer affinity for bone mineral components (hydroxyapatite) [61] | Binding affinity must be balanced with drug release kinetics; optimal bone-to-soft tissue uptake ratio is crucial |
| Stem Cells & Derived Products | Mesenchymal Stem Cells (MSCs), MSC-derived Extracellular Vesicles (EVs) | Cell-based therapy; paracrine signaling; innate tissue repair and immunomodulation [63] [59] | Source variability (umbilical cord, bone marrow, adipose); EVs offer cell-free alternative with reduced risks |
| Pro-Angiogenic Factors | VEGF, ZNF580, eNOS genes; proteins | Stimulate vascularization in ischemic tissues [58] | Controlled spatiotemporal delivery is essential to avoid aberrant vessel formation; duration of expression is critical |
| Biomaterial Scaffolds | Hydrogels, 3D-bioprinted constructs, Decellularized matrices | Provide structural support for tissue regeneration; localized drug delivery [62] [57] [63] | Degradation rate should match tissue regeneration pace; mechanical properties must mimic native tissue |
| Characterization Tools | Nanoparticle Tracking Analysis, Dynamic Light Scattering, Electron Microscopy | Physicochemical characterization of delivery systems [59] [60] | Standardized protocols are needed for comparative studies between laboratories |
The comparative analysis presented in this review demonstrates significant progress in biomaterial-based delivery strategies for hostile microenvironments. Each target tissue presents distinct challenges that require specialized material design approaches. For CNS applications, sinomenine-loaded nanoparticles and extracellular vesicles show particular promise in overcoming the BBB and providing neuroprotection, with the bone-brain axis emerging as a novel targeting route. In bone regeneration, customizable nanoparticles and bone-targeting carriers enable precise control over bone remodeling processes. For ischemic tissues, intravascularly deliverable biomaterials and sophisticated gene delivery systems offer minimally invasive options for promoting vascularization and repair. The experimental protocols and reagent toolkit provided here serve as a foundation for researchers developing next-generation delivery platforms. Future directions will likely involve greater integration of AI-assisted design to optimize material properties, increased personalization based on patient-specific pathophysiology, and combination approaches that simultaneously address multiple aspects of these complex hostile microenvironments.
Overcoming Delivery Challenges: Engineering Smart Solutions
The clinical success of regenerative medicine and cell-based therapies hinges on the survival and functional integration of transplanted cells. The hostile ischemic microenvironment of injury sites presents a significant bottleneck, where the majority of transplanted cells undergo apoptosis prior to participating in lineage differentiation and cellular integration [64]. This fundamental challenge has driven the development of sophisticated strategies to enhance cell viability and engraftment, primarily through two complementary approaches: cell preconditioning and biomaterial-assisted delivery.
Cell viability, defined as the proportion of healthy, live cells in a population and their ability to maintain physiological functions, is a critical parameter that must be optimized prior to transplantation [65] [66]. Post-transplantation, the ultimate measure of success is engraftment—the process whereby transplanted cells adhere, are retained, survive, and functionally integrate within the host tissue [64]. This guide provides a comparative analysis of the strategies and biomaterials demonstrated to enhance these crucial outcomes, providing researchers with actionable data for therapeutic development.
Cell Preconditioning Strategies: A Comparative Analysis
Cell preconditioning involves exposing cells to sublethal stressors or biochemical cues in vitro to enhance their resilience and therapeutic potential in vivo. These strategies prime cells to withstand the harsh conditions encountered post-transplantation. The table below compares the major preconditioning modalities, their mechanisms of action, and their impact on viability and engraftment.
Table 1: Comparative Analysis of Cell Preconditioning Strategies
| Preconditioning Strategy | Mechanism of Action | Impact on Viability & Engraftment | Key Functional Outcomes |
|---|---|---|---|
| Hypoxic Preconditioning (e.g., 1-5% O₂) [67] | Upregulates HIF-1α, promoting cell survival under low oxygen; alters miRNA cargo in extracellular vesicles (e.g., upregulation of hsa-miR-181c-5p) [67]. | Enhances survival in ischemic tissues; improves anti-inflammatory and pro-regenerative potential of secreted EVs [67]. | Promotes angiogenesis; reduces apoptosis; enhances paracrine signaling [64] [67]. |
| Cytokine Preconditioning (e.g., TNF-α, IL-1β) [67] | Primes cells toward an anti-inflammatory phenotype; enhances immunomodulatory functions. | Increases resistance to inflammatory damage; improves retention in immunologically active environments. | Boosts secretion of anti-inflammatory factors (e.g., IL-4, IL-10, TGF-β); directs macrophage polarization from M1 to M2 [67]. |
| Biomaterial-Based Preconditioning (3D scaffolds) [26] | Replicates native stem cell niche mechanics and biochemistry; provides cell-instructive cues. | Improves differentiation fidelity, functional maturity, and survival of therapeutic cells like MSCs and iPSCs [26]. | Enhances secretory profile (secretome); reduces differentiation variability; prevents post-implantation teratoma from iPSCs [26]. |
| Small Molecule Preconditioning (e.g., growth factors) [65] | Activates specific pro-survival pathways (e.g., PI3K/Akt) to counteract apoptosis. | Directly increases the proportion of viable cells pre-transplantation and their resistance to stress. | Suppresses apoptotic pathways; upregulates expression of key survival genes [65]. |
Biomaterial-Assisted Delivery Platforms for Enhanced Engraftment
Biomaterials can create a protective microenvironment for transplanted cells, mitigating the initial hostile conditions and providing instructional cues that promote retention, survival, and functional integration. The following table compares the major classes of biomaterials used for cell delivery.
Table 2: Comparison of Biomaterial Platforms for Cell Delivery and Engraftment
| Biomaterial Class | Key Examples | Mechanisms for Enhancing Engraftment | Advantages & Limitations |
|---|---|---|---|
| ECM-Based Scaffolds [68] | Decellularized tissues; Collagen, Hyaluronic Acid, Fibrin scaffolds. | Provides innate biochemical and structural cues (e.g., RGD sequences) for integrin binding, activating FAK/ERK pathways for cell survival and proliferation [68]. | Advantages: High biocompatibility and bioactivity. Limitations: Potential batch-to-batch variability; complex fabrication [68]. |
| Synthetic Polymers [68] | PLGA, PEG, Self-assembling peptides. | Offers highly tunable mechanical properties and degradation rates; can be functionalized with adhesive peptides to promote integrin clustering and signaling [68] [26]. | Advantages: Reproducible, tunable design. Limitations: Often lacks innate bioactivity [68]. |
| Hydrogels [68] [26] | PEG-based, Alginate, ECM-derived hydrogels. | Creates a hydrated 3D niche that protects cells; enables direct injection; facilitates nutrient/waste exchange; can be designed for stimuli-responsive growth factor release [68]. | Advantages: Can mimic tissue softness; injectable for minimally invasive delivery. Limitations: Mechanical strength can be low [68]. |
| Instructive Biomaterials ("Bottom-Up") [26] | Tailored synthetic niches for iPSCs, MSCs. | "Bottom-up" design prioritizes the biological needs of specific stem cells (e.g., mechanical cues, biochemical gradients) to engineer materials that directly address challenges like differentiation variability and poor survival [26]. | Advantages: Highly specific; addresses root causes of failure. Limitations: Complex, resource-intensive design process [26]. |
Experimental Protocols for Assessing Viability and Engraftment
Robust assessment of cell viability and engraftment is foundational to comparative studies. Below are detailed protocols for key assays cited in the literature.
The MTT assay is a colorimetric method that measures the metabolic activity of viable cells.
- Cell Seeding: Plate cells in a 96-well plate at an optimal density (e.g., 5,000-20,000 cells/well) and culture under experimental conditions.
- MTT Solution Preparation: Dissolve MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) in Dulbecco's Phosphate Buffered Saline (DPBS), pH 7.4, to a concentration of 5 mg/mL. Filter-sterilize and protect from light.
- Incubation: Add the MTT solution to each well to a final concentration of 0.2-0.5 mg/mL. Incubate the plate for 1-4 hours at 37°C. Metabolically active cells will reduce the yellow MTT to purple formazan crystals.
- Solubilization: Carefully remove the medium and add a solubilization solution (e.g., 40% dimethylformamide, 16% SDS, pH 4.7) to dissolve the formazan crystals.
- Spectrophotometric Analysis: Measure the absorbance at 570 nm using a plate-reading spectrophotometer. The amount of formazan produced is proportional to the number of viable cells.
This assay distinguishes live from dead cells based on membrane integrity.
- Cell Harvesting: Gently harvest cells to create a single-cell suspension.
- Staining: Mix 10 µL of the cell suspension with 10 µL of 0.4% Trypan Blue solution.
- Loading: Transfer the mixture to a hemocytometer chamber.
- Counting and Calculation: Count the number of unstained (viable) and blue-stained (non-viable) cells under a microscope. Calculate viability using the formula:
- Cell Viability (%) = (Number of viable cells / Total number of cells) × 100% [65].
Signaling Pathways in Cell Survival and Engraftment
The success of preconditioning and biomaterial strategies is largely mediated through the activation of specific cell survival and adhesion pathways. Integrin-mediated signaling is a key mechanism by which biomaterials engaging the extracellular matrix (ECM) promote cell survival and engraftment [68].
Diagram 1: Integrin-Mediated Survival Signaling. This pathway illustrates how biomaterials mimicking the ECM engage integrin receptors, triggering intracellular signaling cascades that promote cell adhesion, migration, and survival—key processes for successful engraftment [68].
The Scientist's Toolkit: Essential Reagent Solutions
The following table details key reagents and their functions as used in the featured experiments and broader field of cell viability and engraftment research.
Table 3: Key Research Reagent Solutions for Viability and Engraftment Studies
| Reagent / Kit Name | Function / Assay Type | Key Characteristics |
|---|---|---|
| MTT Reagent (e.g., Thiazolyl Blue Tetrazolium Bromide) [69] | Colorimetric cell viability / metabolic activity assay. | Penetrates cells and is reduced to purple formazan by metabolically active cells; requires solubilization step [69]. |
| Trypan Blue Solution (0.4%) [65] [66] | Dye exclusion assay for membrane integrity. | Stains dead cells with compromised membranes blue; viable cells exclude the dye [65]. |
| Resazurin Cell Viability Kit [69] [66] | Fluorometric cell viability / metabolic activity assay. | Reduced by viable cells to fluorescent resorufin; "one-step" protocol with no solubilization [66]. |
| CellTiter 96 Non-Radioactive Assay [69] | Commercial MTT-based cell proliferation/viability assay. | Provides optimized MTT and solubilization solutions in a standardized kit format [69]. |
| TUNEL Assay Kit [66] | Fluorescent detection of apoptotic DNA fragmentation. | Labels 3'-OH ends of fragmented DNA in apoptotic cells; used with flow cytometry or microscopy [66]. |
| CryoShield [70] | Cryoprotectant for cell freezing. | Improves post-thaw cell viability and proliferation during cryopreservation [70]. |
| RGD Peptide Sequences [68] | Functionalization of biomaterials. | Promotes cell adhesion and integrin-mediated signaling by mimicking ECM ligands [68]. |
Enhancing cell viability and engraftment is a multifaceted challenge that requires an integrated approach. As this guide demonstrates, no single strategy is universally superior. The choice between preconditioning methods—such as hypoxia, cytokines, or small molecules—and the selection of a biomaterial platform—from natural ECM scaffolds to synthetically tailored "bottom-up" systems—must be guided by the specific cell type and therapeutic application. The most promising clinical outcomes will likely emerge from combination strategies that leverage both the inherent resilience conferred by preconditioning and the protective, instructive microenvironment provided by advanced biomaterials. By utilizing the standardized assays and comparative data presented here, researchers can make informed decisions to optimize their therapeutic products and accelerate the translation of cell-based therapies from the bench to the bedside.
The "bottom-up" design paradigm represents a fundamental shift in biomaterial engineering for cell delivery. Unlike traditional approaches that adapt cells to pre-existing materials, this strategy involves designing cell-instructive biomaterials from the molecular level upward to meet the specific biological and microenvironmental needs of therapeutic cells [26]. This review systematically compares the efficacy of various bottom-up engineered biomaterial platforms—including nanoparticles, hydrogels, and composite scaffolds—against conventional materials and non-material-assisted cell delivery. Supported by experimental data on key performance metrics such as cell survival, engraftment efficiency, and therapeutic outcome, this analysis provides a structured framework for researchers and drug development professionals to select and optimize biomaterial strategies for enhanced regenerative medicine and cell-based therapies.
The clinical translation of stem cell therapies faces significant challenges, including poor cell survival after transplantation, low retention and engraftment at target sites, incomplete functional maturation, and risks of undesired differentiation or teratoma formation [26] [71]. Conventional cell delivery methods, such as suspension in buffer fluids, offer minimal protection against harsh pathological microenvironments, leading to substantial cell death and diminished therapeutic efficacy [71].
The bottom-up design approach addresses these limitations by prioritizing fundamental stem cell biology. It engineers biomaterials that replicate lineage-specific mechanical, chemical, and spatial cues found in native stem cell niches [26]. This paradigm shifts the role of biomaterials from passive scaffolds to dynamic, cell-instructive platforms that actively direct cell fate, enhance survival, and improve functional integration. By building materials from molecular foundations to mimic natural biological systems, researchers can now create more predictive and effective cell delivery systems for regenerative medicine [26] [72].
Comparative Efficacy of Biomaterial Platforms
The following section provides a comparative analysis of major biomaterial platforms used in bottom-up design for cell delivery, with quantitative data on their performance across critical efficacy parameters.
Table 1: Comparison of Biomaterial Platforms for Cell Delivery
| Biomaterial Platform | Key Advantages for Cell Delivery | Limitations & Challenges | Cell Survival Rate (In Vivo) | Engraftment Efficiency | Therapeutic Payload Capacity |
|---|---|---|---|---|---|
| Nanoparticles (Au, IONPs) | Enhanced imaging capability; Sustainable tracking; High photostability [71] | Potential toxicity concerns; Variable cellular uptake [71] | >90% (in vitro) [71] | N/A (Tracking Focus) | High (Genes, drugs, proteins) [71] |
| Hydrogels (Natural/Synthetic) | Tunable mechanical properties; High water content; Protective microenvironment [26] | Variable degradation rates; Batch-to-batch variability (natural) | Up to 4-fold increase vs. suspension [71] | 2-3 fold improvement [26] | Moderate to High |
| 3D Bioprinted Scaffolds | Precise spatial control; Anatomical mimicry; Structural integrity [26] | Resolution limitations; Material compatibility constraints | ~70-80% (post-printing) [26] | Significantly enhanced [26] | High (Cells, growth factors) |
| Conventional Cell Suspension | Simplicity; Clinical familiarity; Low cost | No protective function; Rapid cell clearance | <10% (at 7 days post-delivery) [71] | Very Low [71] | None |
Table 2: Performance Metrics of Biomaterial-Based Tracking Technologies
| Tracking Technology | Biomaterial Scaffold | Detection Limit (Cell Number) | Imaging Duration | Key Application in Cell Delivery |
|---|---|---|---|---|
| Photoacoustic (PA) Imaging | Silica-coated Gold Nanorods [71] | 9.0×10⁴ cells (in vivo) [71] | Long-term (>14 days) [71] | Intramuscular hMSC tracking [71] |
| Multispectral Optoacoustic Tomography (MSOT) | Silica-coated Gold Nanorods [71] | 2.0×10⁴ cells (in vivo) [71] | Long-term [71] | Subcutaneous hMSC detection [71] |
| Micro-CT Imaging | PLL/RITC-conjugated AuNPs [71] | Low detection threshold [71] | Medium-term | Intracranial hMSC tracking in striatum [71] |
| Magnetic Resonance (MR) Imaging | Tat-functionalized Superparamagnetic NPs [71] | High sensitivity [71] | Long-term | Bone marrow homing of CD34+ cells [71] |
| Near-Infrared Long Persistent Luminescence | PEI-coated LPLNPs [71] | High sensitivity [71] | Long-term, renewable [71] | Glioblastoma tumor retention tracking [71] |
Experimental Protocols: Methodologies for Evaluating Biomaterial Efficacy
To ensure reproducible and comparable results across studies, standardized experimental protocols are essential for evaluating bottom-up engineered biomaterials.
Protocol for Assessing Protective Delivery Function
Objective: Quantify the protective capacity of biomaterial hydrogels on mesenchymal stromal cell (MSC) viability and retention in hostile microenvironments.
Materials:
- Photocrosslinkable methacrylated gelatin (GelMA) or polyethylene glycol (PEG)-based hydrogels
- Human MSCs (passage 3-5)
- Hypoxia chamber (1% O₂)
- Live/Dead assay kit (calcein AM/ethidium homodimer-1)
- In vivo imaging system (IVIS) for luciferase-expressing cells
Methodology:
- Encapsulation: Suspend MSCs in prepolymer solution at 5-20×10⁶ cells/mL. Crosslink using UV light (365 nm, 5-10 mW/cm²) for 60 seconds [26].
- In Vitro Hypoxia Challenge: Culture encapsulated and suspension MSCs in serum-free media under hypoxic conditions (1% O₂) for 72 hours. Assess viability at 24-hour intervals using Live/Dead staining [71].
- In Vivo Retention Test: Subcutaneously implant cell-laden hydrogels (vs. cell suspension injection) in rodent models. Use bioluminescent imaging at days 1, 3, 7, and 14 to quantify cell retention [71].
- Functional Assay: After 14 days, harvest implants and analyze for secretory function (VEGF, IL-10 via ELISA) to confirm therapeutic potency of delivered cells [26].
Protocol for Evaluating Cell Fate Control
Objective: Assess the capacity of engineered biomaterials to direct stem cell differentiation with high fidelity and minimal off-target effects.
Materials:
- Peptide-functionalized hydrogels with controlled stiffness (2-30 kPa)
- Induced pluripotent stem cells (iPSCs)
- Lineage-specific differentiation media
- Immunocytochemistry reagents for marker quantification
- Teratoma formation assay components
Methodology:
- Material Fabrication: Tune hydrogel stiffness to mimic target tissue (neural: ~0.5 kPa, bone: ~25 kPa) via crosslinking density control [26].
- 3D Differentiation Culture: Encapsulate iPSCs in materials with and without covalently attached lineage-specific peptides (e.g., RGD for mesenchymal lineages). Maintain in basal media without exogenous differentiation factors for 14 days [26].
- Fate Analysis: Quantify differentiation efficiency via flow cytometry for lineage-specific markers (e.g., TUJ1 for neural, Runx2 for osteogenic). Compare to soluble factor-induced differentiation.
- Safety Profile: After 30 days, assess for teratoma formation in vivo by implanting differentiated cells in immunocompromised mice and monitoring for 12 weeks [26].
Diagram: The "bottom-up" design approach bridges molecular-scale cues to therapeutic outcomes through hierarchical material design and controlled cell interactions.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of bottom-up biomaterial strategies requires specific reagents and materials designed to mimic native cellular microenvironments.
Table 3: Essential Research Reagents for Bottom-Up Biomaterial Research
| Reagent/Material | Function in Bottom-Up Design | Key Characteristics | Example Applications |
|---|---|---|---|
| Gold Nanorods (Silica-coated) | Stem cell tracking contrast agent | Enhanced cellular uptake; Optimal PA sensitivity [71] | Intramuscular hMSC tracking; MSOT imaging [71] |
| Methacrylated Gelatin (GelMA) | Photocrosslinkable hydrogel base | Tunable stiffness; RGD adhesion motifs [26] | 3D cell encapsulation; Protective delivery [26] |
| Functionalized IONPs | Magnetic cell guidance & MRI tracking | Superparamagnetic; PEI coating for gene binding [71] | Guided homing to bone marrow; Therapeutic gene delivery [71] |
| Peptide-Modified Polymers | Presentation of biochemical cues | Controlled density of bioactive signals [26] | Direction of stem cell differentiation [26] |
| Near-Infrared LPLNPs | Renewable stem cell tracking | Deep tissue penetration; LED-rechargeable [71] | Long-term cell retention monitoring; Glioblastoma therapy [71] |
| Engineered Genetic Circuits | Control of intrinsic cell behavior | Regulatable gene expression; Synthetic biology [72] | Programming therapeutic cell responses [72] |
Bottom-up biomaterial design represents a transformative approach to overcoming the persistent challenges in therapeutic cell delivery. The comparative data presented in this review demonstrates that biomaterial platforms engineered from molecular cues upward significantly outperform conventional delivery methods across critical efficacy parameters including cell survival, retention, and functional integration.
Future developments in this field will likely focus on creating increasingly sophisticated smart biomaterials that respond dynamically to environmental stimuli [73] and integrate more elements of synthetic biology to program cell behavior [72]. As these technologies mature, the convergence of advanced material science with cellular engineering promises to unlock new therapeutic possibilities in regenerative medicine and personalized cell-based treatments. For researchers and drug development professionals, adopting this bottom-up paradigm provides a structured framework for developing more effective, reliable, and clinically translatable cell delivery systems.
Controlling Paracrine Signaling and Secretome Activity via Material Properties
In regenerative medicine and drug development, the therapeutic potential of cells is increasingly attributed not to the cells themselves, but to the bioactive molecules they secrete—their secretome—which includes growth factors, cytokines, and extracellular vesicles. This secretome operates primarily through paracrine signaling, a form of cell-to-cell communication where signaling molecules released by one cell elicit biological responses in neighboring cells [74] [75]. The efficacy of these paracrine signals is profoundly influenced by the extracellular matrix (ECM) and engineered biomaterials that constitute the cellular microenvironment [68]. These materials are not passive scaffolds; they actively modulate secretome composition and signaling activity through their biomechanical and biochemical properties, such as stiffness, ligand presentation, and degradability [68]. This guide provides a comparative analysis of major biomaterial classes—ECM-based scaffolds, synthetic polymers, and lipid-based systems—evaluating their efficacy in controlling paracrine signaling for therapeutic applications. By comparing experimental data and methodologies, we aim to inform the rational selection and design of biomaterials for enhanced cell-free therapies.
Comparative Analysis of Biomaterial Platforms
The following table summarizes the key characteristics and documented effects on paracrine signaling for the primary biomaterial classes used in secretome modulation.
Table 1: Comparative Efficacy of Biomaterial Platforms for Paracrine Signaling Control
| Biomaterial Class | Key Material Properties | Experimental Secretome/Paracrine Outcomes | Quantitative Data from Literature |
|---|---|---|---|
| ECM-Based Scaffolds (e.g., Collagen, Decellularized ECM) | Tissue-specific biochemistry, integrin-binding motifs (e.g., RGD), tunable mechanical stiffness, degradability [68]. | Promotes pro-angiogenic secretome; enhances cell adhesion, migration, and proliferation via integrin-mediated signaling (FAK/ERK pathways) [68]. | • VEGF-A & Angiopoietin-2: Significantly higher in follicles cultured in alginate in groups of 10 (269.77 and 242.82 pg/mL, respectively) vs. groups of 5 [76]. |
| Synthetic Hydrogels (e.g., Alginate, PEG) | Highly tunable stiffness, porosity, and stress relaxation; can be functionalized with adhesive peptides [76] [68]. | Stiffness and cell group size (paracrine source density) synergistically enhance pro-regenerative factor secretion (VEGF, FGF); mechanical properties regulate NF-κB and HIF1α TF activity [76]. | • Cell Spreading Area: ~30% increase in AD-MSCs (from 4007 μm² to 5081 μm²) when treated with WJ-MSC secretome on collagen [77].• Single Cell Modulus: 1.9-fold increase in fibroblast stiffness when treated with thermogenic adipose secretome [78]. |
| Lipid Bicontinuous Cubic Phases (e.g., Monoolein, Phytantriol) | Nanostructured water/lipid channels capable of encapsulating diverse secretome components (proteins, EVs); can fuse with cell membranes [79]. | Enables sustained, protected delivery of the entire MSC secretome; maintains bioactivity of complex mixtures for controlled paracrine stimulation [79]. | • Full incorporation of complex MSC secretome (growth factors, cytokines, extracellular vesicles) confirmed via Small-Angle X-Ray Scattering (SAXS) [79]. |
Experimental Protocols for Key Findings
Protocol: Investigating Paracrine Synergy in Alginate Hydrogels
This methodology, adapted from Stukenborg et al., is used to evaluate how the density of paracrine signal sources and hydrogel encapsulation influences collective cell outcomes [76].
- 1. Cell Isolation & Transduction: Ovaries are retrieved from 10-12-day-old female F1 mice. Individual primary follicles are isolated via enzymatic digestion using Liberase DH. For tracking transcription factor activity, follicles are transduced immediately after isolation using lentiviral reporters (e.g., for NF-κB, HIF1, p53, Gli) at a defined multiplicity of infection (MOI) [76].
- 2. Hydrogel Encapsulation & Culture: Transduced follicles are resuspended in a sodium alginate solution. The cell-polymer mixture is cross-linked using an ionic crosslinker (e.g., calcium chloride) to form hydrogels. Follicles are encapsulated and cultured in groups of 5 (5×) or 10 (10×) to simulate different paracrine source densities in a serum-free medium for 12 days [76].
- 3. Data Collection & Analysis:
- Secretome Profiling: Conditioned media is collected periodically and analyzed via multiplex ELISA or similar assays to quantify cytokines (e.g., VEGF-A, Angiopoietin-2) and steroid hormones [76].
- TF Activity Kinetics: Luciferase activity is measured in lysates from reporter-transduced follicles throughout the culture period using a luminometer to track real-time TF activation [76].
- Phenotypic Endpoints: Follicle survival, growth diameter, and antral cavity formation are assessed microscopically. Data is analyzed using multivariate modeling to correlate TF activity with secretome profiles and phenotypic outcomes [76].
Protocol: Functional Assays for Secretome Bioactivity
This set of protocols is standard for quantifying the functional consequences of paracrine signaling on target cell behavior [80] [77].
- 1. Conditioned Medium (CM) Collection: Mesenchymal Stem Cells (MSCs) or other signal-producing cells are cultured until 70-80% confluent. The medium is replaced with a serum-free formulation, and CM is collected after 24-48 hours. CM is centrifuged and filtered to remove cells and debris before storage or immediate use [80] [77].
- 2. Target Cell Functional Assays:
- Proliferation Assay: Target cells (e.g., AD-MSCs, endothelial cells) are seeded in 96-well plates and treated with CM. Proliferation is measured at 72 hours using metabolic assays like MTT or MTS. Cell cycle profiling via flow cytometry can provide additional mechanistic insight [77].
- Migration/Scratch Assay: A confluent monolayer of target cells is scratched with a pipette tip. Cells are washed and then incubated with CM or control media. Migration into the scratch area is quantified by imaging at 0, 12, and 24 hours, measuring the percentage of wound closure [77].
- Tube Formation Assay (Angiogenesis): Endothelial cells are seeded on a basement membrane matrix (e.g., Matrigel) and treated with CM. The formation of capillary-like tubular structures is imaged after several hours, and total tube length or number of branch points is quantified [80].
- Cell Adhesion & Spreading: Target cells are plated on ECM-coated substrates (e.g., rat tail collagen) in the presence of CM. After 24 hours, cells are fixed, stained (e.g., for actin cytoskeleton), and imaged. Morphometric software is used to quantify cell spreading area and aspect ratio [77].
Signaling Pathways in Material-Guided Paracrine Effects
Biomaterials influence cell behavior by engaging specific receptor systems that activate downstream signaling cascades. These pathways ultimately dictate the composition of the secreted paracrine factors and the cell's response to them. The following diagram synthesizes the key pathways identified in the search results, particularly integrin-mediated signaling and the downstream PI3K/AKT and MAPK/ERK pathways that are central to paracrine-mediated regeneration.
The experimental workflow for investigating these relationships involves a series of coordinated steps, from biomaterial fabrication to functional analysis. The following diagram outlines a generalized protocol that can be adapted to specific research questions.
The Scientist's Toolkit: Essential Research Reagents
Successful experimentation in this field relies on a set of core reagents and tools. The following table details essential solutions for designing studies on paracrine signaling and secretome activity.
Table 2: Key Research Reagent Solutions for Paracrine Signaling Studies
| Research Reagent | Function & Application | Specific Examples from Literature |
|---|---|---|
| Integrin-Binding Peptides | Functionalize synthetic materials to promote cell adhesion and activate integrin-mediated signaling pathways (FAK, MAPK/ERK) [68]. | RGD (Arg-Gly-Asp) peptide sequences grafted onto synthetic hydrogels to enhance cell adhesion and migration [68]. |
| Conditioned Medium (CM) | Cell-free source of paracrine factors used to treat target cells and assess bioactivity of the secretome [80] [77]. | Endothelial Progenitor Cell CM (EPC-CM) to promote brain endothelial cell angiogenesis [80]; WJ-MSC secretome to enhance AD-MSC functionality [77]. |
| Pathway Inhibitors | Pharmacological tools to dissect the contribution of specific signaling pathways to the observed paracrine effects. | LY294002 (PI3K/AKT inhibitor) and PD98059 (MEK/ERK inhibitor) used to block EPC-CM-induced angiogenic responses [80]. |
| TF Activity Reporters | Lentiviral vectors with TF-responsive elements driving luciferase expression to monitor real-time transcription factor activation in response to material cues [76]. | TRanscriptional Activity CEllular aRray (TRACER) with reporters for NF-κB, HIF1, p53, and Gli to track TF activity during follicle development [76]. |
| Lipid Cubic Phases | Nanostructured lipid systems for the encapsulation and sustained delivery of the entire secretome, protecting its components from degradation [79]. | Monoolein or phytantriol-based bicontinuous cubic phases used to fully incorporate the complex MSC secretome, including growth factors and extracellular vesicles [79]. |
The field of drug delivery has undergone a transformative shift with the advent of smart biomaterials, evolving from conventional systems that release therapeutics at a constant rate to sophisticated platforms capable of precise spatiotemporal control. This evolution addresses a fundamental challenge in therapeutics: the need to deliver bioactive agents to the right location, at the right time, and in the right dose, thereby maximizing efficacy while minimizing off-target effects. For researchers and drug development professionals, understanding the comparative efficacy of these systems is paramount for advancing cell delivery and regenerative medicine applications. Smart biomaterials, particularly those with stimuli-responsive characteristics, are defined by their ability to retain payloads until reaching a specific target site, at which point a trigger initiates release due to changes in the carrier's chemistry or structure [81]. This capability is foundational to creating next-generation, precise medicines that actively interface with biological systems, moving beyond passive scaffolds to dynamic, immune-modulating platforms [82].
The "intelligence" of these systems is broadly categorized by their response mechanisms. Endogenous stimuli exploit the physiological or pathological characteristics of the disease microenvironment, such as shifts in pH, enzyme concentration, redox state, or the presence of specific biomolecules [81]. In contrast, exogenous stimuli rely on externally applied triggers like light, magnetic fields, temperature, or ultrasound, which can be controlled with high precision by the clinician or researcher [81]. A third, advanced category comprises multi-responsive systems that integrate several triggers, offering enhanced control and redundancy. The following sections provide a detailed comparative analysis of these smart biomaterial systems, supported by experimental data and standardized protocols, to guide selection for specific research and therapeutic applications.
Comparative Analysis of Stimuli-Responsive Biomaterial Systems
Table 1: Comparison of Endogenous Stimuli-Responsive Biomaterial Systems
| Stimulus Type | Key Mechanism | Common Biomaterials | Therapeutic Applications | Release Kinetics & Experimental Evidence |
|---|---|---|---|---|
| pH-Responsive | Protonation/deprotonation of ionizable groups or cleavage of acid-labile bonds in acidic microenvironments (e.g., tumor sites, inflammatory loci) [82]. | Polymers with pendant catechols (e.g., PAD), polyhistidine, polymers with acetal/orthoester linkages [83] [84]. | Targeted cancer chemotherapy, anti-inflammatory drug delivery [85] [86]. | Catechol-Fe3+ Hydrogel [84]: Rapid color and shape change upon protonation. Transition from mono- to tris-coordinated states with pH increase (pH 3-8), enabling controlled release. Cu-BTC MOF [86]: High drug loading (40.5% for Doxorubicin) with preferential release in acidic pH. |
| Enzyme-Responsive | Specific cleavage of peptide sequences or polymer backbones by disease-overexpressed enzymes (e.g., MMPs in tumors or chronic wounds) [82]. | Peptide-conjugated polymers, hyaluronic acid-based systems, gelatin scaffolds [85] [86]. | Site-specific drug release, modulation of wound healing, cancer therapy [86]. | Gelatin-based HNT Scaffold [86]: Sustained release of Zoledronic Acid (ZA) over days, enhanced human adipose stem cell (hASC) proliferation and osteogenesis in vivo. Hyaluronic Acid Microneedles [82]: Enzyme-triggered release of Zn2+ for bacterial killing and ROS reduction in diabetic wounds. |
| Redox-Responsive | Disulfide bond cleavage in the presence of high glutathione (GSH) concentrations in the cytoplasm or specific cell compartments. | Disulfide-crosslinked polymers, dendrimers, and micelles. | Intracellular delivery of genes and anticancer drugs [81]. | Nanoscaled Niosomal Structures [86]: Enhanced cytotoxic action of Curcumin (Cur-niosome) and miR-34a against cancer cells compared to free forms. Significant tumor growth inhibition in 4T1 xenografted mouse model. |
Table 2: Comparison of Exogenous Stimuli-Responsive Biomaterial Systems
| Stimulus Type | Key Mechanism | Common Biomaterials | Therapeutic Applications | Release Kinetics & Experimental Evidence |
|---|---|---|---|---|
| Thermo-Responsive | Sol-gel transition or structural change upon temperature shift (e.g., to body temperature). | PNIPAM, Chitosan-Silk Fibroin hydrogels, Poloxamers [86] [82]. | Injectable depots for sustained release, cell delivery [85]. | Chitosan-Silk Fibroin Hydrogel [86]: Gelling time and pH tuned via glycerophosphate/sodium hydrogen carbonate. Genipin crosslinking improved mechanical properties (swelling ratio ~6 vs. ~8). Supported HepG2 cell function (increased urea levels). |
| Photo-Responsive | Light-induced isomerization, cleavage, or heating triggers drug release or shape change. | AIEgen-doped hydrogels, gold nanoparticles, spiropyran-containing polymers [83]. | On-demand drug release, information encryption, biomimicry [83]. | BP4VA/PAS Hydrogel [83]: Rapid, high-contrast changes in color, fluorescence, and shape under specific light wavelengths. Applications demonstrated in biomimicry and multi-stage information encryption. |
| Magnetic-Responsive | Heat generation or mechanical force under an alternating magnetic field, triggering drug release. | Fe3O4-embedded polymers, magnetic MOFs [86]. | Hyperthermia-assisted cancer therapy, targeted drug delivery. | Magnetic Cu-BTC MOF [86]: Fe3O4 nanoparticles integrated for imaging and as a drug carrier. Exhibited high loading capacity and pH-responsive drug release, potential for photoactive antibacterial treatment. |
Detailed Experimental Protocols for Key Systems
Protocol: pH-Responsive Catechol-Fe3+ Coordination Hydrogel
This protocol outlines the synthesis and characterization of a poly(acrylamide-co-dopamine acrylamide) glycerol hydrogel (PAD-G-Fe3+), a model system for wide visible color tunability and pH-triggered release [84].
Materials & Reagents:
- Monomers: Acrylamide (AM), Dopamine acrylamide (DAM).
- Crosslinker: N,N'-methylene-bis-acrylamide (MBA).
- Initiator: 2,2'-Azobis(2-methylpropionamidine) dihydrochloride (V50).
- Solvent System: Glycerol/Deionized water mixture (e.g., 20 vol% glycerol).
- Ion Source: Iron(III) chloride hexahydrate (FeCl₃·6H₂O).
Methodology:
- Precursor Solution Preparation: Dissolve AM (1 g), DAM (0.05 g), MBA (0.002 g), and V50 (0.006 g) in a glycerol/water solution (3.2 ml water + 0.8 ml glycerol).
- Oxygen Removal: Transfer the solution to a glass mold and bubble with nitrogen gas for 30 minutes to remove dissolved oxygen, which can inhibit free radical polymerization.
- Polymerization: Seal the mold and place it in a thermostatic chamber at 60°C with 40% relative humidity for several hours to complete the polymerization reaction, forming the PAD-G hydrogel.
- Purification: Immerse the synthesized hydrogel in deionized water for 2 days to remove any unreacted chemicals, changing the water periodically.
- Fe3+ Loading: Immerse the purified PAD-G hydrogel in an aqueous solution of Fe3+ (5 × 10⁻³ M) containing 20 vol% glycerol for 15 minutes to form the final PAD-G-Fe3+ hydrogel via catechol-Fe3+ coordination.
Characterization and Data Analysis:
- Colorimetric pH Response: Monitor the hydrogel's color transition (yellow → green → blue → red) across a pH gradient (from <3 to >8) using digital photography and UV-Vis spectroscopy. The color change corresponds to the dynamic shift between non-coordinated, mono-, bis-, and tris-coordinated catechol-Fe3+ complexes [84].
- Drug Release Profiling: Incorporate a model drug (e.g., an anticancer agent) during the precursor preparation. Immerse the loaded PAD-G-Fe3+ hydrogel in buffers of varying pH (e.g., pH 5.0 to simulate tumors and pH 7.4 for normal tissue). Use high-performance liquid chromatography (HPLC) to quantify the cumulative drug release over time, demonstrating pH-dependent kinetics.
Protocol: Enzyme-Responsive Immunomodulatory Scaffold
This protocol describes the creation of nanofibrous heparin-modified gelatin microspheres (NHG-MS) for the sustained delivery of Interleukin-4 (IL4) to modulate macrophage polarization and promote osteogenesis [87].
Materials & Reagents:
- Base Polymer: Gelatin.
- Modification Agent: Heparin (for cytokine binding).
- Cytokine: Interleukin-4 (IL4).
- Crosslinking Agent: Genipin or similar.
Methodology:
- Microsphere Synthesis: Fabricate gelatin-based microspheres via an emulsion or self-assembly process. Introduce heparin into the structure to create heparin-modified gelatin microspheres (NHG-MS).
- Cytokine Loading: Incorporate IL4 into the NHG-MS by exploiting its specific binding domain with heparin. This binding mimics the natural interaction between cytokines and glycosaminoglycans in the extracellular matrix, stabilizing IL4 and facilitating sustained release.
- Crosslinking: Crosslink the microspheres with genipin to enhance structural stability and control the degradation profile.
Characterization and Data Analysis:
- IL4 Release Kinetics: Incubate IL4-loaded NHG-MS in a physiological buffer at 37°C. Collect supernatant at predetermined time points and use an ELISA kit to measure IL4 concentration, demonstrating a sustained release profile over weeks.
- In Vitro Macrophage Polarization: Culture primary macrophages or a macrophage cell line (e.g., RAW 264.7) with the IL4-releasing microspheres. Use flow cytometry (staining for CD206 for M2 phenotype) and qPCR (measuring Arg1, Ym1/2 expression) to quantify the shift from pro-inflammatory M1 to pro-regenerative M2 macrophages.
- In Vivo Bone Regeneration: Implant the constructs into a critical-sized bone defect model (e.g., a rat calvarial defect or, as referenced, a diabetic rat mandibular defect [87]). After 4-8 weeks, analyze new bone formation using micro-computed tomography (µ-CT) for 3D morphometric analysis (e.g., Bone Volume/Total Volume, BV/TV) and histological staining (e.g., H&E, Masson's Trichrome) to assess bone tissue ingrowth and quality.
Visualization of Mechanisms and Workflows
Catechol-Fe3+ Coordination and pH-Responsive Pathway
The following diagram illustrates the molecular mechanism behind the color and structural changes in pH-responsive hydrogels, which can be harnessed for spatiotemporal release.
Diagram Title: pH-Responsive Hydrogel Mechanism
Experimental Workflow for Smart Biomaterial Evaluation
This workflow outlines a standardized research pipeline for developing and testing a stimuli-responsive drug delivery system, from material synthesis to in vivo validation.
Diagram Title: Smart Biomaterial Testing Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Smart Biomaterial Research
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Dopamine Acrylamide (DAM) | A functional monomer that introduces catechol groups into polymer networks, enabling metal-ion coordination and pH responsiveness. | Synthesis of PAD-G-Fe3+ hydrogels for colorimetric sensing and pH-triggered drug release [84]. |
| Halloysite Nanotubes (HNTs) | Natural aluminosilicate nanotubes with a high surface-to-volume ratio, used as a nanocarrier for sustained drug release. | Fabrication of HNTs-loaded gelatin scaffolds for the controlled release of zoledronic acid in bone tissue engineering [86]. |
| Niosomes (Tween-60/DOTAP) | Non-ionic surfactant-based vesicles for encapsulating hydrophobic and hydrophilic agents, enhancing bioavailability and cellular uptake. | Encapsulation of curcumin and miR-34a for enhanced cytotoxicity and targeted cancer therapy [86]. |
| Genipin | A natural crosslinking agent, less cytotoxic than glutaraldehyde, used to improve the mechanical strength and stability of biopolymer-based scaffolds. | Crosslinking of chitosan-silk fibroin hydrogels and gelatin microspheres to control degradation and sustain drug release [86] [87]. |
| Poly(N-isopropylacrylamide) (PNIPAM) | A classic thermo-responsive polymer exhibiting a Lower Critical Solution Temperature (LCST) near body temperature. | Creating injectable hydrogels that undergo sol-gel transition for cell delivery and drug depots [82]. |
| Mesoporous Silica Nanoparticles (MSNs) | Inorganic nanoparticles with high surface area and tunable pores for high-capacity drug loading and functionalization. | Development of c(RGDfK)-MSN NPs for the co-delivery of siPD-L1 and miR-34a to bladder cancer cells [86]. |
The advancement of biomaterials for cell delivery represents a frontier in regenerative medicine and immunotherapy, offering promising alternatives to conventional treatments. However, the clinical translation of these technologies is contingent upon a thorough comparative evaluation of their ability to mitigate critical risks, including tumorigenicity, immune rejection, and off-target effects [88] [71]. Biomaterials are engineered to enhance the therapeutic efficacy of delivered cells—such as mesenchymal stem cells (MSCs) or immune cells—by improving their survival, retention, and function at the target site [89] [88]. A prime challenge in cell therapies is the poor survival of transplanted cells; biomaterial scaffolds address this by providing a protective, three-dimensional architecture that supports cell viability and function, thereby reducing the number of cells required and the associated risk of aberrant cell growth [89] [71]. Furthermore, the intrinsic properties of biomaterials and their degradation products are critical determinants of the host immune response, influencing outcomes from tolerance to rejection [90] [91]. This guide provides a structured, data-driven comparison of current biomaterial platforms, evaluating their performance against these pivotal safety parameters to inform preclinical development.
Comparative Efficacy of Biomaterial Platforms
The following tables synthesize experimental data from recent studies, comparing the efficacy of various biomaterial platforms in mitigating tumorigenicity, immune rejection, and off-target effects. Performance is quantified using key metrics such as tumor formation incidence, immune cell infiltration, and target tissue accrual.
Table 1: Comparative Efficacy in Mitigating Tumorigenicity
| Biomaterial Platform | Cell Type | Key Performance Metric | Reported Outcome | Reference |
|---|---|---|---|---|
| PLGA Microparticles | Engineered MSCs | Tumor formation incidence | No teratoma formation detected post-implantation | [71] |
| Silica-coated Gold Nanorods | Human MSCs (hMSCs) | In vivo tracking sensitivity (detection limit) | 2.0 x 10^4 cells tracked via MSOT imaging; maintained cell phenotype | [71] |
| Polyelectrolyte Multilayers (iPEMs) | N/A (Cell-free) | Localized immunomodulator delivery | High-density co-assembly without synthetic polymers; reduced off-target inflammation | [92] |
| Peptide-Based Hydrogel | MSCs | Cell survival rate in target tissue | Significant improvement vs. suspension injection; reduced required cell dose | [89] |
Table 2: Comparative Efficacy in Mitigating Immune Rejection and Off-Target Effects
| Biomaterial Platform | Immune Context | Key Performance Metric | Reported Outcome | Reference |
|---|---|---|---|---|
| Hyaluronic Acid Hydrogel | Immune cell delivery | Localization of cytokine release syndrome (CRS) triggers | Reduced systemic toxicity; improved localized tumor infiltration | [88] |
| PLGA-based Scaffold | Adoptive T-cell Therapy | In vivo persistence and function of T cells | Seeded scaffolds enhanced T-cell activity and sustained function vs. systemic transfer | [92] |
| PEI-coated Magnetic Nanocluster | Engineered hMSCs | Control over cell migration in vivo | Magnetic guidance enabled targeted cell accrual; reduced off-target migration | [71] |
| Lipid Nanoparticles | siRNA delivery | Target gene knockdown in immunosuppressive pathways | Knockdown of immunosuppressive cytokines (e.g., TGF-β) reversed T-cell exhaustion | [92] |
Experimental Protocols for Risk Assessment
Assessing Tumorigenicity and Cell Fate Control
Objective: To evaluate the potential of the biomaterial-cell construct to form tumors in vivo, with a focus on tracking cell fate and proliferation. Materials: Biomaterial scaffold (e.g., hydrogel, porous matrix), therapeutic cells (e.g., MSCs, iPSCs), immuno-deficient mouse model (e.g., NOD/SCID), live-animal imaging system (e.g., MSOT, MRI), histological staining reagents (H&E, Ki-67). Methodology:
- Cell Labeling and Construct Fabrication: Cells are pre-labeled with tracking agents, such as silica-coated gold nanorods for photoacoustic imaging or magnetic nanoparticles for MRI [71]. The labeled cells are then incorporated into the biomaterial scaffold (e.g., encapsulation in a hydrogel).
- Implantation and In Vivo Tracking: The cell-biomaterial construct is implanted into the target organ or tissue of the immuno-deficient mouse model. Animal cohorts are monitored over a defined period (e.g., 4-12 weeks). The distribution, retention, and survival of the cells are non-invasively tracked in real-time using appropriate imaging modalities [71].
- Endpoint Analysis: After the study period, animals are euthanized, and the explained tissues are processed for histological analysis. Tissues are sectioned and stained with:
- Hematoxylin and Eosin (H&E) to examine overall tissue morphology and identify any abnormal growths.
- Ki-67 antibody to assess cell proliferation rates within the implant site [71].
- Analysis for specific differentiation markers to confirm the desired cell phenotype and the absence of undifferentiated, pluripotent cells that could lead to teratoma formation [71].
Evaluating Immune Rejection and Host Response
Objective: To characterize the local and systemic immune response elicited by the biomaterial and the delivered cells. Materials: Biomaterial with/without cells, syngeneic and allogeneic mouse models, flow cytometer, multiplex cytokine assay kit, histology equipment. Methodology:
- Study Design and Implantation: The biomaterial, with and without incorporated cells, is implanted into both syngeneic (genetically identical) and allogeneic (genetically different) mouse models. This design allows for the discrimination between the immune response to the biomaterial itself and the response to the foreign cells [90].
- Systemic Immune Profiling: At predetermined time points, blood serum is collected from all animal groups. A multiplex cytokine assay (e.g., Luminex) is performed to quantify the levels of pro-inflammatory (e.g., IL-1β, TNF-α, IFN-γ) and anti-inflammatory (e.g., IL-10) cytokines, providing a measure of systemic immune activation and potential cytokine release syndrome [88].
- Local Immune Phenotyping: Upon study completion, the implant and surrounding tissue are harvested and processed into a single-cell suspension. The cells are stained with fluorescently labeled antibodies for analysis by flow cytometry. Key immune cell populations are quantified, including:
- CD3+CD4+ and CD3+CD8+ T cells: Indicators of adaptive immune activation.
- CD4+FoxP3+ Regulatory T cells (Tregs): Suppressors of immune responses.
- CD11b+Gr-1+ Myeloid-Derived Suppressor Cells (MDSCs): Mediators of immunosuppression.
- F4/80+ Macrophages (with staining for M1/M2 markers like iNOS and CD206) [93]. A higher ratio of immunosuppressive cells (Tregs, MDSCs, M2 macrophages) at the implant site suggests the biomaterial may promote a tolerogenic microenvironment [93].
Signaling Pathways and Risk Mitigation Logic
The strategic application of biomaterials to mitigate risks in cell delivery involves orchestrating specific biological pathways. The following diagram synthesizes these core mechanisms into a unified logical framework.
Diagram: Biomaterial Risk Mitigation Logic
This diagram illustrates how biomaterial strategies directly counter the primary risks associated with cell therapies. The localized delivery and controlled release function is critical for mitigating off-target effects and immune rejection by ensuring immunomodulatory agents (e.g., cytokines, siRNA) act primarily at the disease site, preventing systemic toxicity and promoting local immune activation [88] [92]. Creating an immunomodulatory microenvironment involves designing materials that actively suppress local immunosuppressive cells like Tregs and MDSCs, thereby countering one of the key mechanisms of immune rejection [93]. Furthermore, by significantly enhancing cell viability at the target site, biomaterials reduce the number of cells needed for administration, which directly lowers the risk of tumorigenicity associated with large, uncontrolled cell doses [89] [71].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and their functions essential for conducting rigorous experiments in biomaterial-based cell delivery and risk assessment.
Table 3: Essential Reagents for Biomaterial-Cell Therapy Research
| Research Reagent / Tool | Primary Function in Experimental Protocols | Key Application in Risk Assessment |
|---|---|---|
| Gold Nanorods (Silica-coated) | Contrast agent for photoacoustic imaging | In vivo tracking of cell biodistribution and long-term persistence to assess tumorigenic risk [71]. |
| Magnetic Nanoparticles (e.g., IONPs) | Contrast agent for MRI; cell manipulation | Monitoring cell homing and enabling magnetic guidance to reduce off-target migration [71]. |
| PEI (Polyethylenimine) | Cationic polymer for nucleic acid delivery | Engineering stem cells to express therapeutic or reporter genes; requires careful toxicity evaluation [71]. |
| Fluorescent Antibody Panels | Cell surface and intracellular marker staining | Flow cytometry analysis of immune cell populations (T cells, Tregs, MDSCs) to quantify immune rejection [93]. |
| Multiplex Cytokine Assay Kits | Simultaneous quantification of multiple cytokines | Profiling systemic inflammation (e.g., CRS) and local immune polarization [88] [90]. |
| PLGA (Poly(lactide-co-glycolide)) | Biodegradable polymer for microparticles/scaffolds | Co-delivery and controlled release of antigens, adjuvants, or drugs to localize therapy [92]. |
| siRNA against Immunosuppressive Factors (e.g., TGF-β) | Gene knockdown | Reversing T-cell exhaustion in the tumor microenvironment; often delivered via polymer or lipid carriers [92]. |
Benchmarking Performance: Efficacy Metrics and Clinical Validation
In Vitro and In Vivo Models for Assessing Delivery Efficiency and Therapeutic Outcome
The development of effective cell-based therapies hinges on the precise assessment of two fundamental parameters: the efficiency with which therapeutic cells are delivered to the target site and their subsequent ability to exert a therapeutic effect. The choice between in vitro (conducted in controlled laboratory environments outside living organisms) and in vivo (conducted within living organisms) models represents a critical decision point in preclinical research [94] [95]. These models are not merely alternatives but are complementary tools that, when used in concert, provide a more complete picture of a therapy's potential. For advanced therapies utilizing biomaterials as cell delivery vehicles—such as hydrogels, decellularized matrices, and engineered scaffolds—selecting the appropriate model is paramount [96] [97]. Biomaterials are designed to enhance cell retention, viability, and function, but their performance must be rigorously evaluated in contexts that mimic the intended biological environment as closely as possible [27] [26]. This guide provides a comparative analysis of in vitro and in vivo models, detailing their applications, experimental protocols, and how their integrated use accelerates the development of biomaterial strategies for regenerative medicine and drug development.
Model Comparisons: Scope, Applications, and Limitations
The following section provides a detailed comparison of the core characteristics of in vitro and in vivo models, highlighting their distinct roles in the research workflow.
Table 1: Key Differences Between In Vitro and In Vivo Models
| Aspect | In Vitro Models | In Vivo Models |
|---|---|---|
| Definition | Studies conducted in a controlled lab environment outside a living organism (e.g., petri dishes, test tubes) [94] | Studies conducted within a living organism (e.g., rodents, primates) [94] |
| Primary Applications | Early-stage drug/cell screening, mechanistic studies, toxicity assessments, personalized medicine [94] | Drug discovery and development, toxicology studies, complex disease modelling [94] |
| Key Advantages | Cost-effective, faster results, tightly controlled variables, high-throughput capability, reduced ethical concerns [94] [95] | Provides whole-system physiological response, highly relevant for clinical translation, accounts for complex organism-level interactions [94] [95] |
| Major Limitations | Lack of full organism response (e.g., immune system, metabolic processes), may not predict in vivo efficacy [94] [95] | Ethical concerns regarding animal use, high cost and resource-intensive, time-consuming, interspecies physiological differences [94] [95] |
| Ideal Use Case | Initial screening of biomaterial formulations and mechanistic studies of cell-material interactions [96] | Validation of therapeutic efficacy and safety of lead biomaterial-cell constructs in a complex physiological environment [27] |
Advanced and Integrated Model Systems
Beyond traditional 2D cell cultures, the field has evolved to develop more physiologically relevant models that better bridge the gap between in vitro and in vivo data.
- Complex In Vitro Models (CIVMs): This category includes 3D cell cultures, spheroids, organoids, and organ-on-a-chip (OOC) technologies [96]. These systems aim to mimic the architecture and function of human tissues more closely than 2D cultures. For instance, organoids are self-organizing 3D structures derived from stem cells that can model aspects of organ biology [96], while OOCs use microfluidics to recreate the dynamic mechanical and biochemical microenvironment of human organs [96].
- Ex Vivo Models: This approach involves using tissue explants—portions of tissue cultured outside the organism while attempting to preserve their original structure and function [96]. Explant cultures can serve as an intermediate model that retains some in vivo complexity in a controlled setting.
Quantitative Assessment of Delivery Efficiency and Therapeutic Outcome
Quantitative data from head-to-head comparisons are vital for selecting the optimal biomaterial delivery vehicle. The following table summarizes key experimental findings from seminal studies.
Table 2: Quantitative Comparison of Biomaterial Delivery Vehicles for Cell Therapy
| Delivery Vehicle | Model System | Cell Type | Key Outcome Metric | Result | Reference |
|---|---|---|---|---|---|
| Saline (Control) | Rat myocardial infarct model | Human Mesenchymal Stem Cells (hMSCs) | Cell retention at 24 hours | Baseline (≈10% of immediately transplanted cells) | [27] |
| Alginate Hydrogel (Injectable) | Rat myocardial infarct model | hMSCs | Cell retention at 24 hours | ~8-fold increase vs. saline | [27] |
| Chitosan/β-GP Hydrogel (Injectable) | Rat myocardial infarct model | hMSCs | Cell retention at 24 hours | ~14-fold increase vs. saline | [27] |
| Collagen Patch (Epicardial) | Rat myocardial infarct model | hMSCs | Cell retention at 24 hours | ~47-fold increase vs. saline | [27] |
| Alginate Patch (Epicardial) | Rat myocardial infarct model | hMSCs | Cell retention at 24 hours | ~59-fold increase vs. saline; retained ~50-60% of initial cells | [27] |
| Engineered Virus-Like Particles (eVLPs) | Primary mouse and human cells; Mouse models of disease | Base editor or Cas9 ribonucleoproteins | In vivo base editing efficiency | 78% reduction in serum Pcsk9 (mouse liver); restored visual function in blind mouse model | [98] |
Experimental Protocols for Key Assessments
To ensure reproducibility and robust data generation, standardized protocols are essential. Below are detailed methodologies for critical experiments in both in vitro and in vivo settings.
Protocol: In Vitro Assessment of Biomaterial-Mediated Cell Delivery in 3D Cultures
This protocol is designed to evaluate the effectiveness of a biomaterial scaffold in supporting cell viability and function in a controlled environment [96].
Hydrogel Preparation:
- Material: Select a natural polymer (e.g., collagen, alginate, fibrin) or a synthetic hydrogel [96] [97].
- Cross-linking: Prepare the hydrogel precursor solution according to manufacturer specifications. Induce cross-linking using the appropriate method (e.g., ionic for alginate, enzymatic for fibrin, or photo-initiated for some synthetic polymers) to form a 3D matrix [96].
- Molding: Pipette the hydrogel precursor into a multi-well plate or a specific mold to create scaffolds of uniform size and shape.
Cell Seeding and Culture:
- Cell Type: Use relevant therapeutic cells such as Mesenchymal Stromal Cells (MSCs), induced Pluripotent Stem Cells (iPSCs), or primary cells [26].
- Seeding: Trypsinize, count, and resuspend cells. Mix the cell suspension directly into the hydrogel precursor before cross-linking or seed them onto the surface of pre-formed hydrogels.
- Culture: Maintain the cell-laden constructs in standard cell culture conditions (37°C, 5% CO₂) with regular changes of culture medium.
Efficiency and Outcome Analysis:
- Cell Viability: At predetermined time points (e.g., 24, 72, 168 hours), assess viability using a Live/Dead assay (e.g., Calcein-AM for live cells, Ethidium Homodimer-1 for dead cells) and image with confocal microscopy [96].
- Proliferation: Quantify cell proliferation over time using metabolic assays like AlamarBlue or CCK-8, or by staining for proliferation markers (e.g., Ki67) [96].
- Functionality: Perform functional assays specific to the cell type, such as ELISA to measure secretion of therapeutic proteins (e.g., VEGF for endothelial cells) or qPCR to analyze gene expression of lineage-specific markers [26].
Protocol: In Vivo Assessment of Acute Cell Retention
This protocol quantifies the critical parameter of how many transplanted cells remain at the target site shortly after delivery, a common challenge in cell therapy [27].
Animal Model and Cell Preparation:
- Model: Establish a disease model, such as myocardial infarction in rats induced by coronary artery ligation [27].
- Cell Labeling: Label the therapeutic cells (e.g., hMSCs) with a fluorescent marker, such as a lipophilic membrane dye (e.g., DiI or DiR), or by engineering them to express a reporter gene like luciferase or GFP [27].
- Formulation: Combine the labeled cells with the test biomaterial vehicle (e.g., injectable hydrogel, saline control) according to the optimized in vitro protocol.
Cell Delivery:
- Route: Administer the cell-biomaterial construct to the target tissue. In the myocardial infarction model, this involves injecting the formulation into the infarct border zone [27].
- Control: Include a group where cells are delivered in a standard saline solution as a negative control.
Quantification of Cell Retention:
- Time Point: Euthanize the animals at a standardized acute endpoint, typically 24 hours post-delivery [27].
- Tissue Processing: Harvest the target organ (e.g., the heart) and process it for analysis.
- Quantitative Analysis:
- Fluorescence Measurement: Homogenize the tissue and use a fluorescence plate reader to quantify the total signal, comparing it to a standard curve of known cell numbers to calculate the number of retained cells [27].
- Imaging: Alternatively, use immunohistochemistry on tissue sections to qualitatively confirm cell presence and distribution within the target site [27].
Signaling Pathways in Biomaterial-Cell Interactions
Biomaterials do not merely act as passive carriers; they actively engage with cells through biochemical and mechanical cues. The following diagram illustrates key signaling pathways activated by biomaterial scaffolds that promote vascular regeneration, a key goal in many therapeutic applications.
Diagram Title: Biomaterial-Activated Signaling for Vascular Repair
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described protocols requires a suite of specialized reagents and materials. The following table details these essential components.
Table 3: Key Research Reagent Solutions for Cell Delivery Studies
| Item | Function/Application | Specific Examples |
|---|---|---|
| Natural Polymer Hydrogels | Serve as biocompatible, biomimetic scaffolds for 3D cell culture and delivery; provide structural support and biochemical cues. | Collagen, Alginate, Fibrin, Elastin-like polypeptides (ELPs) [97] |
| Decellularized ECM | Provides a biologically relevant scaffold that preserves the complex biochemical and structural composition of native tissues. | Lung-specific ECM, Vascular ECM [97] |
| Synthetic Hydrogels | Offer tunable mechanical properties and controlled degradation rates; can be functionalized with specific bioactive peptides. | Poly(ethylene glycol) (PEG)-based hydrogels, other engineered bio-constructs [96] [97] |
| Therapeutic Cell Types | The core functional unit of the therapy; chosen for their regenerative, immunomodulatory, or tissue-repair capabilities. | Mesenchymal Stromal Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), Endothelial Colony-Forming Cells (ECFCs) [26] |
| Fluorescent Cell Labels | Enable tracking, localization, and quantification of delivered cells in both in vitro and in vivo models. | Lipophilic dyes (DiI, DiR), Lentiviral vectors for GFP/Luciferase expression [27] |
| Virus-Like Particles (VLPs) | Engineered, DNA-free delivery platform for efficient in vivo delivery of macromolecular cargo like gene-editing ribonucleoproteins. | Engineered VLPs (eVLPs) for base editor delivery [98] |
The assessment of delivery efficiency and therapeutic outcome is not a matter of choosing between in vitro and in vivo models, but of strategically integrating them. In vitro models provide a cost-effective, high-throughput platform for the initial screening and mechanistic understanding of biomaterial-cell interactions [96] [94]. Subsequently, in vivo models are indispensable for validating these findings in a physiologically complex environment, providing critical data on safety, biodistribution, and functional efficacy that is directly relevant to clinical translation [94] [27]. The emergence of advanced systems like organoids and organs-on-chip offers a promising bridge, capturing more in vivo-like complexity within an in vitro setting [96]. For researchers developing biomaterials for cell delivery, the most effective pathway involves leveraging the strengths of each model: using in vitro data to intelligently down-select lead formulations for rigorous in vivo testing, thereby de-risking the pipeline and accelerating the development of transformative cell therapies.
The selection between natural and synthetic biomaterials is a fundamental decision in biomedical research, influencing experimental outcomes and therapeutic efficacy. While each class offers distinct advantages, direct comparative studies under standardized conditions are essential to elucidate their performance characteristics objectively. This guide synthesizes data from such comparative research to provide scientists and drug development professionals with a clear, evidence-based framework for biomaterial selection in cell delivery and tissue engineering applications. The analysis is framed within the broader thesis that understanding context-specific performance, rather than identifying a universally superior material, is key to advancing regenerative medicine.
Material Properties at a Glance
The inherent properties of natural and synthetic biomaterials predispose them to different applications and performance outcomes.
Table 1: Fundamental Characteristics of Natural and Synthetic Biomaterials
| Characteristic | Natural Biomaterials | Synthetic Biomaterials |
|---|---|---|
| Origin | Derived from living organisms (e.g., collagen, fibrin, hyaluronic acid) [99] | Artificially created in laboratories (e.g., PLA, PGA, PCL, Dextran Vinyl Sulfone) [99] [100] |
| Biocompatibility | High, due to inherent bioactivity and presence of cell recognition sites [99] | Variable; can be engineered but may elicit adverse immune responses [99] |
| Degradability | Biodegradable via natural enzymatic processes [99] | Tunable and controllable degradation rates [99] |
| Mechanical Properties | Limited and less tunable; can be soft and mechanically weak [99] | Highly controllable strength, elasticity, and stiffness [99] |
| Key Advantages | Promote cell adhesion, proliferation, and tissue-specific behavior; mimic native ECM [99] | High reproducibility, tunable properties, and consistent batch-to-batch performance [99] |
Direct Performance Comparison in Angiogenesis
A pivotal direct comparison of angiogenesis revealed how extracellular matrix (ECM) properties govern vascularization, a critical process for the survival of engineered tissues [100]. This study utilized a multiplexed angiogenesis-on-a-chip platform to standardize conditions for natural (collagen and fibrin) and synthetic (dextran vinyl sulfone, DexVS) hydrogels.
Experimental Protocol for Direct Angiogenesis Comparison
Objective: To quantitatively compare the angiogenic potential (endothelial cell invasion speed, sprout diameter, and perfusability) of natural and synthetic biomaterials in a standardized, side-by-side assay [100].
Methodology:
- Hydrogel Preparation: Collagen, fibrin, and DexVS hydrogels were prepared at varying matrix densities.
- Platform Fabrication: A multiplexed microfluidic device was used to create a standardized 3D environment for endothelial cell (EC) sprouting.
- Cell Seeding and Culture: Human endothelial cells were introduced into the platform and allowed to form sprouts into the different hydrogel matrices.
- Characterization: Hydrogel properties, including Young's modulus (stiffness) and permeability (porosity), were measured.
- Imaging and Analysis: Time-lapse microscopy and image analysis were used to quantify EC invasion depth, sprout diameter, and invasion speed over time.
- In Vivo Validation: Selected hydrogels were implanted into a murine epididymal fat pad model to assess stability and host cell invasion.
Key Quantitative Findings
Table 2: Summary of Key Findings from Direct Angiogenesis Comparison [100]
| Performance Metric | Natural Biomaterials (Collagen/Fibrin) | Synthetic Biomaterials (DexVS) |
|---|---|---|
| EC Invasion Speed | Decreased with increasing matrix density [100] | Not specifically reported, but overall invasion was lower in nanoporous variants [100] |
| Sprout Diameter | Larger, lumenized sprouts formed in vitro [100] | Smaller, non-perfusable sprouts in nanoporous gels [100] |
| Matrix Porosity | Microporous [100] | Nanoporous (unmodified) [100] |
| Correlation | Matrix permeability significantly correlated with EC invasion depth and sprout diameter [100] | Matrix permeability significantly correlated with EC invasion depth and sprout diameter [100] |
| Post-Implantation Stability | Rapidly resorbed in vivo [100] | Comparatively stable in vivo [100] |
| Key Limitation | Rapid in vivo resorption [100] | Poor support for perfusable sprouting due to nanoporosity [100] |
Enhancing Synthetic Biomaterial Performance
The study demonstrated that the performance of synthetic biomaterials could be significantly enhanced by engineering their microstructure. Incorporating sacrificial microgels into DexVS hydrogels created microporosity, which led to the formation of lumenized sprouts in vitro and enhanced cell invasion in vivo [100]. This highlights a key strategy in biomaterial design: modifying synthetic materials to recapitulate the critical physical features of natural matrices.
Molecular Signaling Pathways in Biomaterial-Cell Interactions
Biomaterials influence cellular behavior through orchestrated molecular signaling pathways. Natural biomaterials often engage these pathways via intrinsic ligands, while synthetic materials require biofunctionalization.
Diagram 1: Integrin-mediated signaling pathways activated by biomaterials. Natural biomaterials often contain native ligands for integrin binding, while synthetic biomaterials can be functionalized with peptides (e.g., RGD) to engage these pathways. The YAP/TAZ pathway is particularly sensitive to the mechanical properties of the matrix [68] [97].
The Scientist's Toolkit: Essential Research Reagents
Successful experimentation in biomaterials research relies on a suite of essential reagents and materials.
Table 3: Key Research Reagent Solutions for Biomaterial Studies
| Reagent / Material | Function in Research | Specific Examples & Notes |
|---|---|---|
| Natural Polymer Hydrogels | Serve as biologically active 3D scaffolds that mimic the native extracellular matrix. | Collagen I, Fibrin, Hyaluronic Acid. Promote robust cell adhesion and sprouting [100] [99]. |
| Synthetic Polymer Hydrogels | Provide a tunable, defined scaffold with controllable mechanical and chemical properties. | Poly(lactic acid) (PLA), Polycaprolactone (PCL), Dextran Vinyl Sulfone (DexVS). Offer high reproducibility [99] [100]. |
| Peptide Ligands | Biofunctionalize synthetic materials to induce specific cellular responses. | RGD peptide. Enhances cell adhesion by engaging integrin receptors [68]. |
| Sacrificial Microgels | Create controlled microporosity within synthetic hydrogels to facilitate cell invasion. | Gelatin microspheres. Used to generate pores in DexVS hydrogels, improving angiogenesis [100]. |
| Decellularized ECM | Provides a complex, tissue-specific biological scaffold retaining native structure and signals. | Lung-derived ECM. Supports endothelial cell culture and vascular function [97]. |
| Engineered Cells (iPSCs) | Provide a patient-specific cell source for therapy and disease modeling. | iPSC-derived endothelial cells. Used for high-throughput drug screening and therapeutic applications [97]. |
Direct comparative studies reveal that the choice between natural and synthetic biomaterials is not about superiority but application-specific suitability. Natural biomaterials excel in promoting rapid cellular integration and vascularization but may lack long-term stability. Synthetic biomaterials offer superior control, stability, and reproducibility but require strategic engineering to guide complex biological processes. The future of biomaterial design lies in hybrid and composite systems that merge the bioactivity of natural components with the tunability and robustness of synthetic polymers, enabling next-generation therapies in regenerative medicine and drug delivery.
The therapeutic success of cell-based regenerative medicine hinges on the precise control and quantification of three fundamental functional metrics: cell retention, differentiation, and secretory activity. While stem cells hold immense potential for treating degenerative diseases, their clinical translation faces significant bottlenecks, primarily low retention and survival rates following transplantation into hostile, ischemic environments [101]. Biomaterial-based delivery systems have emerged as crucial enabling technologies to overcome these challenges by providing a supportive microenvironment that enhances cell viability and function.
The comparative efficacy of these biomaterials must be evaluated through standardized quantitative assessments of this critical functional triad. Cell retention measures the percentage of delivered cells that remain at the implantation site, a metric where traditional saline injection performs poorly, retaining only about 10% of cells at 24 hours [27]. Differentiation efficiency quantifies the ability of stem cells to mature into specific, functional cell types, a process heavily influenced by scaffold properties. Secretory activity encompasses the production and release of bioactive factors that mediate therapeutic effects such as immunomodulation and angiogenesis [26]. This guide provides a systematic comparison of biomaterial performance across these metrics, supported by experimental data and methodologies to inform research and development decisions.
Comparative Performance of Biomaterial Delivery Systems
Quantitative Comparison of Cell Retention Across Biomaterial Classes
Cell retention is the most immediately quantifiable metric post-implantation. Comparative animal studies directly measuring retained cell numbers reveal substantial differences between biomaterial classes.
Table 1: Quantitative Comparison of Acute Cell Retention at 24 Hours Post-Implantation
| Biomaterial Category | Specific Material | Retention Fold-Increase vs. Saline | Approximate Retention Percentage | Animal Model |
|---|---|---|---|---|
| Epicardial Patches | Alginate Patch | 59-fold | ~59% | Rat myocardial infarct |
| Collagen Patch | 47-fold | ~47% | Rat myocardial infarct | |
| Injectable Hydrogels | Chitosan/β-GP | 14-fold | ~14% | Rat myocardial infarct |
| Alginate Hydrogel | 8-fold | ~8% | Rat myocardial infarct | |
| Control | Saline Injection | 1-fold (reference) | ~10% | Rat myocardial infarct |
Data derived from a direct comparative study of biomaterial delivery vehicles shows that all biomaterials significantly outperform saline control, with epicardial patches demonstrating superior performance for acute retention [27]. The saline control retained only approximately 10% of delivered cells at 24 hours, whereas biomaterials retained 50-60% of cells present immediately after transplantation [27].
Differentiation Efficiency Across Scaffold Platforms
The three-dimensional microenvironment provided by biomaterial scaffolds significantly influences stem cell differentiation fate and efficiency. Different material properties direct lineage specification through biophysical and biochemical cues.
Table 2: Differentiation Efficiency Across Biomaterial Platforms
| Biomaterial Platform | Stem Cell Type | Differentiation Target | Key Efficiency Metrics | Notable Findings |
|---|---|---|---|---|
| 3D Chitosan Thermosensitive Hydrogel | Mesenchymal Stem Cells (MSCs) | Multiple lineages | Enhanced multi-differentiation potential vs. 2D culture | Superior differentiation outcomes in 3D microenvironment [101] |
| Poly-L-ornithine/Laminin Coating | hiPSC-derived Neural Progenitors | Motor Neurons | Expression of MNX1 and ChAT markers | Direct maturation approach yielded higher efficiency than multi-step protocol [102] |
| Ternary Nanocomposite with MWCNT | Various stem cells | Electrically sensitive tissues | Improved electrical conductivity enhances differentiation | Integration of conductive nanostructures directs fate specification [101] |
| Developmental Engineering Scaffolds | MSCs for bone repair | Osteogenic lineage | Mimics natural healing cascade | Biomimetic process design promotes robust differentiation [101] |
The "bottom-up" biomaterial design approach—creating materials based on fundamental stem cell biological needs—has demonstrated particular promise for enhancing differentiation fidelity and functional maturity of derived cells [26].
Secretory Activity Profiling in Engineered Microenvironments
Secretory activity represents a crucial functional metric for paracrine-mediated therapies, particularly for MSCs whose therapeutic effects are largely attributed to their secretome [26]. Biomaterial environments can significantly modulate the production and release of bioactive factors.
Table 3: Analytical Approaches for Secretory Activity Assessment
| Analytical Method | Key Measured Outputs | Applications in Biomaterial Studies | Technical Considerations |
|---|---|---|---|
| Mass Spectrometry Proteomics | Comprehensive protein identification and quantification | Mapping secretome changes in response to material properties [103] | Requires serum-free conditions; sensitive to intracellular protein contamination |
| iSLET (in situ Secretory protein Labeling) | Selective labeling of ER-transiting proteins in live systems | Tracking tissue-specific secretory proteins in circulation [104] | Enables in vivo kinetic studies; uses Sec61b-TurboID for ER lumen labeling |
| ELISA/Multiplex Immunoassays | Quantitative measurement of specific factors | Validation of key secretory proteins identified via proteomics | Targeted approach; limited to known analytes |
| Conditioned Media Functional Assays | Biological activity of secretome | Testing effects on cell proliferation, differentiation, protection [103] | Assesses functional output rather than individual components |
Proteomic analysis of secretomes has revealed that progenitor and adult cells show approximately 48% overlap in secreted proteins, while significant differences exist between different cell types themselves [103]. Biomaterial scaffolds can be engineered to enhance the production of therapeutic factors; for instance, chitosan has been shown to induce IL-10 secretion and suppress colitis in animal models through modulation of NF-κB signaling [105].
Experimental Protocols for Functional Metric Quantification
Standardized Protocol for Acute Retention Assessment
The quantification of cell retention following implantation employs standardized methodologies to enable cross-study comparisons:
Materials and Reagents:
- Fluorescently labeled cells (e.g., CM-Dil, GFP-transduced)
- Biomaterial vehicles (hydrogels, patches)
- Animal disease model (e.g., rat myocardial infarction)
- Fluorescence imaging system
- Tissue homogenization reagents
- Quantitative standards for calibration
Methodology:
- Cell Labeling and Preparation: Label human Mesenchymal Stem Cells (hMSCs) with fluorescent markers using validated protocols that maintain cell viability and functionality [27].
- Cell-Material Construct Formation: Combine cells with biomaterial vehicles according to optimized ratios. For injectable hydrogels, maintain suspensions in sterile syringes; for patches, seed cells and allow adherence.
- Implantation: Deliver cell-biomaterial constructs to target tissue (e.g., infarct border zone in myocardial infarction models) using appropriate surgical techniques.
- Tissue Collection and Processing: At predetermined endpoints (e.g., 24 hours for acute retention), harvest target tissues and process for fluorescence quantification.
- Quantitative Analysis: Homogenize tissues and quantify fluorescence using standardized curves. Calculate retained cell numbers based on initial delivery fluorescence values.
- Validation: Confirm retention data through immunohistochemical analysis of tissue sections using cell-specific markers [27].
This protocol enabled the direct comparison showing that biomaterials retained 50-60% of initially delivered cells compared to only 10% for saline controls [27].
Protocol for Evaluating Differentiation Efficiency
The assessment of differentiation efficiency requires multimodal characterization across genetic, protein, and functional levels:
Materials and Reagents:
- Stem cell populations (hiPSCs, ESCs, MSCs)
- Lineage-specific differentiation media
- Biomaterial scaffolds or coatings
- Cell fixation and permeabilization reagents
- Primary antibodies for target cell markers
- qRT-PCR reagents for gene expression analysis
- Functional assessment tools (e.g., electrophysiology for neurons)
Methodology for Motor Neuron Differentiation Comparison:
- Neural Induction: Apply dual-SMAD inhibition using defined neural induction media (e.g., STEMDiff SMADi Neural Induction Kit) for 21 days with media changes every other day [102].
- Neural Progenitor Expansion: Culture neural progenitor cells in neural progenitor medium (e.g., STEMDiff Neural Progenitor Medium) for 21 days, passaging with appropriate dissociation reagents [102].
- Differentiation Approaches:
- Efficiency Quantification:
- Gene Expression: Analyze motor neuron markers (HB9, MNX1, ChAT) via qRT-PCR [102].
- Protein Expression: Assess characteristic postmitotic markers (MNX1, ChAT) via immunofluorescence and flow cytometry [102].
- Morphological Analysis: Monitor neuronal network formation using live imaging systems (e.g., IncuCyte) [102].
This methodology revealed that the direct maturation approach (Approach A) generated mature motor neurons more efficiently than the multi-step protocol, providing insights for optimizing differentiation protocols [102].
Protocol for Secretory Activity Profiling
Comprehensive secretome analysis combines multiple analytical approaches to capture the dynamic range of secreted factors:
Materials and Reagents:
- Serum-free cell culture medium
- Protein concentration devices (e.g., centrifugal filters)
- Protease and phosphatase inhibitors
- Biotin for proximity labeling (for iSLET method)
- Streptavidin beads for affinity purification
- Mass spectrometry-grade solvents and reagents
Methodology for In Vivo Secretory Protein Tracking (iSLET):
- System Setup: Express Sec61b-TurboID (ER-anchored TurboID) in target tissue (e.g., mouse liver via tail vein injection of adenovirus) [104].
- Labeling Protocol: Administer biotin to animals to initiate proximity labeling of secretory proteins transiting through the ER lumen.
- Sample Collection: Collect blood plasma at designated time points following biotin administration.
- Affinity Enrichment: Isolate biotinylated proteins from plasma using streptavidin affinity purification [104].
- Proteomic Analysis: Identify labeled secretory proteins via liquid chromatography and tandem mass spectrometry (LC-MS/MS).
- Data Analysis: Process mass spectrometry data through appropriate bioinformatics pipelines to identify tissue-specific secretory proteins and quantify their abundance [104].
The iSLET method enables kinetic studies of secretory protein dynamics, with labeling efficiency observed within 10 minutes of biotin treatment and labeled proteins detectable for up to 8 hours [104].
Signaling Pathways in Biomaterial-Cell Interactions
Biomaterial scaffolds influence cell fate and function through modulation of key signaling pathways. The following diagrams visualize critical pathways implicated in cell retention, differentiation, and secretory activity.
Chitin/Chitosan-Mediated Immunomodulatory Pathways
Chitin and chitosan biomaterials modulate immune responses through specific receptor-mediated signaling pathways, influencing secretory activity and cell survival in inflammatory environments.
Experimental Workflow for Secretory Protein Identification
The iSLET methodology provides a comprehensive approach for in vivo identification of tissue-specific secretory proteins, enabling accurate tracking of secretory activity.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Functional Metric Assessment
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Biomaterial Vehicles | Alginate, Chitosan/β-GP, Collagen patches [27] | Provide 3D microenvironment for cell delivery | Epicardial patches show superior retention; hydrogels suitable for minimally invasive delivery |
| Stem Cell Culture Media | mTeSR1, STEMDiff series [102] | Maintain pluripotency and direct differentiation | Defined, xeno-free media enhance reproducibility for clinical translation |
| Cell Dissociation Reagents | Gentle Cell Dissociation Reagent (GCDR), Accutase [102] | Detach cells while maintaining viability | Gentle enzymes preserve surface markers and cell functionality |
| Reprogramming Factors | Oct4, Sox2, Klf4, L-myc [26] | Generate iPSCs from somatic cells | Non-integrating methods reduce tumorigenic potential |
| Neural Induction Agents | Dual-SMAD inhibitors, Retinoic Acid, SHH [102] | Direct neural lineage specification | Combination treatment mimics developmental cues for motor neuron differentiation |
| Proximity Labeling Enzymes | Sec61b-TurboID [104] | Selective labeling of secretory proteins | Enables in vivo tracking of tissue-specific secretomes |
| Proteomic Analysis Tools | LC-MS/MS, Streptavidin affinity purification [104] | Identify and quantify secreted proteins | Requires specialized instrumentation and bioinformatics support |
| Lineage Tracing Markers | MNX1, ChAT (motor neurons); Osteocalcin (bone); Albumin (hepatocytes) [102] | Assess differentiation efficiency | Multiple markers confirm functional maturity rather than just surface expression |
The comparative analysis of biomaterials for cell delivery reveals a complex landscape where no single material excels across all functional metrics. Epicardial patches demonstrate superior performance for acute cell retention, while 3D hydrogels offer advantages for minimally invasive delivery and creating microenvironments that enhance secretory activity. The selection of appropriate biomaterials must be guided by therapeutic objectives—strategies prioritizing rapid engraftment may favor high-retention patches, while those leveraging paracrine effects might prioritize materials that enhance secretory activity.
Critical gaps remain in understanding long-term functional integration and the dynamic evolution of cell-biomaterial interactions. Future comparative studies should incorporate temporal dimensions, tracking functional metrics beyond acute phases to establish correlations between initial retention and ultimate therapeutic efficacy. As the field progresses toward clinical translation, standardized assessment of this functional triad—retention, differentiation, and secretory activity—will enable more rational biomaterial design and selection, ultimately enhancing the therapeutic efficacy of cell-based regenerative medicine.
The successful clinical translation of cell-based therapies is critically dependent on overcoming the significant challenge of low cell retention and engraftment at the target site following delivery. In the context of the infarcted heart, this challenge is particularly acute, as the harsh microenvironment and mechanical washout lead to massive cell loss, thereby undermining therapeutic efficacy. Biomaterial-based delivery vehicles have emerged as a promising strategy to circumvent this limitation by providing a protective, supportive niche for transplanted cells. This guide provides a objective comparison of the acute retention performance of four biomaterial vehicles—alginate hydrogel, chitosan/β-glycerophosphate (chitosan/ß-GP) hydrogel, alginate patch, and collagen patch—against the saline injection control, the former clinical standard. The data, derived from a seminal comparative preclinical study, offer a quantitative foundation for researchers and drug development professionals to select appropriate delivery systems for early-phase trial development, framed within the broader thesis of optimizing comparative efficacy in biomaterials for cell delivery research [27].
Comparative Performance Analysis of Biomaterial Delivery Vehicles
Quantitative Retention Outcomes
The primary metric for evaluating the efficacy of these delivery systems is the acute retention of human Mesenchymal Stem Cells (hMSCs) in a rat myocardial infarct model at the 24-hour post-implantation mark. The data, summarized in Table 1, reveal profound differences between the biomaterial vehicles and the saline control.
Table 1: Acute Cell Retention of Biomaterial Delivery Vehicles at 24 Hours [27]
| Delivery Vehicle | Category | Fold Increase in Fluorescence vs. Saline | Approximate Retained Cells (% of Initially Transplanted) |
|---|---|---|---|
| Saline (Control) | Injection | (Baseline) | ~10% |
| Alginate Hydrogel | Injection | ~8-fold | ~50-60% |
| Chitosan/ß-GP Hydrogel | Injection | ~14-fold | ~50-60% |
| Alginate Patch | Epicardial Patch | ~59-fold | ~50-60% |
| Collagen Patch | Epicardial Patch | ~47-fold | ~50-60% |
All biomaterial-based delivery systems produced a statistically superior fluorescence signal, corresponding to a higher number of retained cells, compared to the saline control [27]. While both categories of biomaterials drastically outperformed saline, the epicardial patches (alginate and collagen) demonstrated a more substantial fold-increase in acute retention compared to the injectable hydrogels. It is crucial to note that all four biomaterials retained 50-60% of the cells that were present immediately after transplantation, a stark contrast to the mere 10% retained when delivered via saline [27]. This data underscores the universal protective advantage offered by biomaterial carriers during the critical initial post-transplantation period.
Analysis of Key Performance Trends
- Superiority of Epicardial Patches: The data indicates that epicardial patches offer a significant advantage in acute cell retention over injectable hydrogels. This is likely due to their physical nature, which provides a stable, scaffold-based environment that minimizes cell loss to circulation and offers greater mechanical integration with the heart tissue.
- Protective Effect of Hydrogels: While less effective than patches, both alginate and chitosan/ß-GP hydrogels still provided a substantial improvement over saline. These materials function by creating a localized, protective matrix that encapsulates the cells, shielding them from immediate washout and environmental stress.
- Consistent Biomaterial Efficacy: The finding that all four biomaterials retained a similar, high percentage (50-60%) of the initially transplanted cells suggests that the fundamental concept of using a biomaterial carrier is more critical than the specific chemical composition of the materials tested in this study for achieving acute retention.
Experimental Protocol and Methodologies
Detailed Experimental Workflow
The comparative study followed a rigorous and standardized protocol to ensure the validity of the head-to-head comparison. The methodology can be summarized in the following workflow diagram:
Key Methodological Components
- Animal Model and Surgical Procedure: The study utilized a rat model of myocardial infarction. The delivery of cell-biomaterial constructs was performed precisely at the infarct border zone [27].
- Cell Source and Preparation: Human Mesenchymal Stem Cells (hMSCs) were used as the therapeutic cell population. The cells were likely pre-labeled with a fluorescent marker (e.g., for subsequent fluorescence quantification) prior to their incorporation into the delivery vehicles [27].
- Biomaterial Preparation and Cell Incorporation:
- Injectable Hydrogels (Alginate, Chitosan/ß-GP): These materials were prepared as liquid solutions that can gel in vivo upon injection, triggered by specific conditions (e.g., temperature for chitosan/ß-GP, ionic crosslinking for alginate). Cells were mixed homogeneously into the solution before gelling [27].
- Epicardial Patches (Alginate, Collagen): These were pre-formed as solid or gel-like scaffolds. Cells were likely seeded onto the patches and allowed to attach or become embedded within the 3D matrix prior to surgical placement onto the epicardial surface [27].
- Outcome Assessment:
- Primary Quantitative Endpoint: At 24 hours post-delivery, the retained cells were quantified using fluorescence imaging. The intensity of the signal was compared to the baseline signal measured immediately after transplantation to calculate the percentage of cell retention [27].
- Qualitative Confirmatory Analysis: Immunohistochemical analysis was performed on tissue sections to visually confirm the presence and location of the retained cells, providing qualitative support for the quantitative fluorescence data [27].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents for Biomaterial-Cell Delivery Studies
| Reagent / Material | Function in the Experiment |
|---|---|
| Human Mesenchymal Stem Cells (hMSCs) | The therapeutic agent being delivered; a multipotent stromal cell type known for its immunomodulatory and pro-regenerative secretome [27]. |
| Alginate | A naturally derived polysaccharide polymer that can form a gentle hydrogel via ionic crosslinking (e.g., with calcium), used for both injectable and patch-based delivery [27]. |
| Chitosan/β-Glycerophosphate | A temperature-sensitive hydrogel system; liquid at room temperature, it forms a solid gel at body temperature, enabling minimally invasive injection [27]. |
| Collagen | A major component of the native extracellular matrix; used here to form a biocompatible epicardial patch that may promote cell adhesion and integration [27]. |
| Fluorescent Cell Label | A chemical dye or genetic marker used to tag cells, allowing for their tracking and quantification post-delivery via fluorescence imaging [27]. |
| Myocardial Infarction Rat Model | A standardized preclinical animal model used to simulate ischemic heart disease and test the efficacy of therapeutic interventions in a physiologically relevant context [27]. |
Regulatory Pathways and Clinical Translation Benchmarking
The translation of promising preclinical results, such as those detailed above, requires navigation through evolving regulatory landscapes. A structured benchmarking process, as exemplified by the National Cancer Institute's Quantitative Imaging Network (QIN), can be a valuable model for biomaterial-based therapy development. This process defines clear milestones from tool development to clinical validation [106].
The 5-Tier Biomaterial Translation Benchmark
The following diagram maps the conceptual pathway for translating a biomaterial delivery system from basic research to clinical use, inspired by the QIN benchmarking framework [106].
Global Regulatory Considerations for 2025
As of 2025, regulatory readiness is paramount for global clinical trials. Key considerations for biomaterial-cell therapies include [107] [108]:
- United States (FDA): The FDA emphasizes a modernized framework with a potential for increased AI oversight and strict compliance. For novel biomaterial-cell combinations, engagement with the FDA through pre-Investigational New Drug (pre-IND) meetings is critical to align on safety and efficacy requirements, including those outlined in 21 CFR 312 [107].
- European Union (EMA): The Clinical Trials Regulation (EU-CTR No 536/2014) provides a streamlined single application model via the CTIS portal. The EU is increasingly integrating real-world data and non-trial evidence into evaluations, which could be relevant for post-marketing surveillance of advanced therapies [107] [108].
- India (CDSCO): India has emerged as a key hub with faster digital reviews and a large patient pool. Submission for clinical trials is done through the SUGAM portal, with standard timelines of 30 days for domestic medicines and 90 days for new foreign-approved therapies. Stricter enforcement of Good Clinical Practice (GCP) is a ongoing focus [107].
- Harmonization: Adherence to ICH-GCP guidelines remains the cornerstone for ensuring the ethical and scientific quality of clinical trials globally, facilitating regulatory acceptance across multiple regions [107].
The comparative data unequivocally demonstrates that biomaterial delivery vehicles significantly enhance the acute retention of stem cells in the infarcted heart compared to saline injection, with epicardial patches showing particular promise. This quantitative head-to-head analysis provides a solid evidence base for researchers to select a delivery system that aligns with their therapeutic strategy, whether it favors a minimally invasive injectable hydrogel or a highly retentive epicardial patch. The translation of such a platform, however, requires careful navigation of regional regulatory pathways and a commitment to a structured, benchmark-driven development process. Future directions in the field will likely involve the development of "bottom-up" designed, cell-instructive biomaterials that not only retain cells but also actively direct their survival, integration, and function through precise mechanical and biochemical cues, ultimately bridging the critical gap between promising preclinical results and successful clinical application [26].
AI and Machine Learning in Predictive Biomaterial Design and Efficacy Modeling
The field of biomaterials science, traditionally guided by resource-intensive trial-and-error methodologies, is undergoing a profound transformation through the integration of artificial intelligence (AI) and machine learning (ML). These technologies are accelerating the design and development of biomaterials for medical applications, from drug delivery systems to regenerative medicine and cell therapy [109]. AI, particularly machine learning and deep learning, enables researchers to analyze complex datasets, identify hidden patterns, and predict material behavior and biological responses with unprecedented accuracy [110]. This paradigm shift is paving the way for predictive biocompatibility modeling and the creation of personalized implant customization, allowing for the design of biomaterials tailored to specific patient needs and therapeutic applications [109]. This guide provides a comparative analysis of AI-driven approaches, their efficacy in predictive modeling, and the experimental frameworks validating their performance in the context of biomaterials for cell delivery.
Fundamental AI Methodologies in Biomaterial Science
The application of AI in biomaterials relies on several core machine-learning paradigms, each suited to different types of data and predictive tasks.
Supervised Learning (SL) is used to predict a specific label or value based on a training dataset with known outcomes. In biomaterials, it is primarily applied to:
- Classification: Categorizing materials, for instance, by their biocompatibility (e.g., biocompatible or not) or by their intended application. Algorithms like support vector machines and decision trees are commonly used, with performance evaluated through metrics like accuracy and F1 score [110].
- Regression: Predicting a continuous value, such as a material's degradation rate or mechanical strength. Techniques include linear regression and random forests, assessed using metrics like mean squared error (MSE) and R-squared (R2) [110].
Unsupervised Learning (UL) is employed to find hidden patterns or intrinsic structures in unlabeled data. Key techniques include:
- Clustering: Grouping similar biomaterials based on their properties without pre-defined categories, using algorithms like K-means [110].
- Dimensionality Reduction: Simplifying high-dimensional data (e.g., from multi-factorial material properties) to principal variables, using methods like Principal Component Analysis (PCA), to enhance model performance and visualization [110].
Deep Learning (DL), a subset of ML using multi-layered neural networks, excels at processing complex and large-scale data. Convolutional Neural Networks (CNNs) are particularly powerful for analyzing medical images to assess material integration, while Recurrent Neural Networks (RNNs) can model time-series data, such as drug release kinetics from a material over time [111].
Multimodal AI represents a frontier in the field, integrating diverse data sources—such as medical imaging, genomic profiles, and clinical records—to build a holistic understanding of biomaterial performance and patient-specific responses [111].
Comparative Efficacy of AI-Enhanced Biomaterials for Cell Delivery
The ultimate test for any biomaterial is its performance in pre-clinical and clinical settings. The table below summarizes quantitative data from a key study comparing the efficacy of different biomaterial vehicles for stem cell delivery in a rat model of myocardial infarction, a critical application in cell delivery research [27].
Table 1: Comparative Acute Retention of Human Mesenchymal Stem Cells (hMSCs) Delivered with Different Biomaterial Vehicles in a Rat Myocardial Infarct Model
| Biomaterial Delivery Vehicle | Delivery Method | Cell Retention at 24 hours (Fold Increase vs. Saline) | Approximate Percentage of Initially Transplanted Cells Retained |
|---|---|---|---|
| Saline (Control) | Injection | (Baseline) | ~10% |
| Alginate Hydrogel | Injection | 8-fold | ~50-60% |
| Chitosan/β-GP Hydrogel | Injection | 14-fold | ~50-60% |
| Collagen Patch | Epicardial Patch | 47-fold | ~50-60% |
| Alginate Patch | Epicardial Patch | 59-fold | ~50-60% |
Key Efficacy Insights: The data demonstrates that all biomaterial carriers significantly outperformed the saline control, which is the conventional clinical standard [27]. Epicardial patches provided a superior scaffold, resulting in dramatically higher cell retention (47 to 59-fold increase) compared to injectable hydrogels. This study underscores that the physical form and delivery method of the biomaterial are critical determinants of efficacy, with patches potentially creating a more protected niche for the delivered cells [27].
Beyond cell retention, AI is also leveraged to design biomaterials that dynamically interact with their environment. For example, smart responsive hydrogels can release their payload in reaction to specific physiological triggers. One developed system uses a thermosensitive chitosan-based hydrogel that gels at body temperature, providing a controlled release of drugs for periodontal tissue regeneration [112]. In a rat model, this system successfully reduced pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) and promoted the expression of bone regeneration markers (Collagen I, Runx2) [112].
Experimental Protocols for Validating AI-Driven Biomaterials
To ensure the reliability of AI-generated predictions, rigorous experimental validation is essential. The following protocols are foundational to evaluating biomaterials designed for cell delivery.
In Vivo Cell Retention and Efficacy Model
Objective: To quantitatively assess the acute retention and engraftment of cells delivered by a biomaterial carrier in a disease model [27].
Methodology:
- Animal and Disease Model: Induce myocardial infarction in rat models to simulate the target pathological environment.
- Cell Preparation and Labeling: Label human Mesenchymal Stem Cells (hMSCs) with a fluorescent marker (e.g., for bioluminescent imaging) to enable tracking.
- Biomaterial-Cell Construct Preparation: Combine the hMSCs with the test biomaterial (e.g., hydrogel or patch).
- Delivery: Implant the biomaterial-cell construct into the infarct border zone of the rat heart. Include a control group receiving cells in saline.
- Quantification: At the endpoint (e.g., 24 hours post-implantation), quantify the retained cells using fluorescence imaging. Compare the signal intensity to the baseline signal measured immediately after transplantation to calculate the percentage of cells retained.
- Histological Validation: Perform immunohistochemical analysis on tissue sections to qualitatively confirm cell presence and distribution within the target tissue [27].
Smart Biomaterial Responsiveness and Drug Release Kinetics
Objective: To evaluate the functionality of an intelligent biomaterial system, specifically its drug release profile and subsequent biological effects [112] [113].
Methodology:
- Drug Loading: Load the therapeutic agent (e.g., Everolimus/Everolimus or bioactive extracts) onto or into the biomaterial (e.g., nanoporous metal, thermosensitive hydrogel) [113] [112].
- In Vitro Release Kinetics:
- Immerse the drug-loaded material in a phosphate-buffered saline (PBS) solution at a controlled physiological pH and temperature.
- Withdraw solution samples at predetermined time intervals.
- Analyze the drug concentration in the samples using ultraviolet-visible (UV-vis) spectrophotometry, comparing against a standard curve.
- Calculate the cumulative drug release over time to establish the release profile [113].
- Functional Biological Assays:
- Cell Migration Assay: Create a scratch in a confluent cell monolayer (e.g., Smooth Muscle Cells). Place the drug-releasing biomaterial in a Transwell insert above the cells. After incubation, measure the reduction in the scratched area to quantify inhibition of cell migration [113].
- Anti-inflammatory Assessment: In an disease model (e.g., rat periodontitis), apply the drug-releasing biomaterial. After a set period, analyze tissue samples to measure the downregulation of inflammatory cytokines (e.g., TNF-α, IL-6) using techniques like ELISA [112].
Workflow Visualization of AI-Driven Biomaterial Development
The following diagram illustrates the integrated, iterative pipeline that combines AI-driven design with experimental validation for developing advanced biomaterials.
AI-Biomaterial Development Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The experimental validation of AI-designed biomaterials relies on a suite of essential reagents and tools. The following table details key materials and their functions in this research domain.
Table 2: Essential Research Reagents and Materials for Biomaterial Cell Delivery Studies
| Research Reagent / Material | Function in Experimental Research |
|---|---|
| Human Mesenchymal Stem Cells (hMSCs) | A primary cell type used in regenerative medicine and cell delivery studies for their multipotent differentiation potential and therapeutic properties [27]. |
| Alginate & Chitosan/β-GP Hydrogels | Injectable biomaterial vehicles that form a protective 3D network to enhance cell retention and survival post-delivery [27]. |
| Collagen & Alginate Patches | Epicardial scaffolds that provide a macro-scale structure for cell sequestration, leading to superior acute cell retention compared to injectables [27]. |
| Fluorescent Cell Labels (e.g., for bioluminescent imaging) | Critical reagents for tagging cells before transplantation, allowing for non-invasive tracking and quantitative measurement of cell retention and distribution over time [27]. |
| Everolimus (EVL) | A model drug used to test the drug-loading capacity and controlled release kinetics of biomaterial systems, such as nanoporous surfaces [113]. |
| Thermosensitive Hydrogels (e.g., Chitosan-based) | "Smart" biomaterial systems that transition from solution to gel at body temperature, enabling in-situ formation and controlled drug/cell release [112]. |
| Electropolishing Setup (for nanoporous metals) | An apparatus used for the surface modification of metallic biomaterials (e.g., stainless steel) to create nanoporous structures that improve biocompatibility and drug-carrying capacity [113]. |
The integration of AI and machine learning into biomaterials science marks a transition from a largely empirical discipline to a predictive and quantitative field. As demonstrated by comparative studies, AI-enhanced biomaterials—particularly structured scaffolds like patches—can significantly improve the efficacy of cell delivery, a cornerstone of regenerative medicine. The future of this convergence lies in the broader adoption of multimodal AI, which synthesizes imaging, genomic, and clinical data to create truly personalized biomaterial solutions [111]. While challenges regarding data quality, model transparency, and ethical considerations remain, the continued refinement of AI tools and experimental protocols promises to unlock a new generation of intelligent, responsive, and highly effective biomaterials for clinical application.
Conclusion
The comparative efficacy of biomaterials for cell delivery is not determined by a single superior material, but by the precise matching of material properties to specific cell types and therapeutic applications. Hydrogels and synthetic scaffolds have demonstrated significant advantages in enhancing cell survival and function, particularly for MSCs in wound healing and tissue regeneration. The emerging 'bottom-up' design paradigm, which prioritizes fundamental cell biology, alongside smart, responsive systems, represents a pivotal shift from passive carriers to dynamic, instructive platforms. Future progress hinges on standardizing efficacy metrics, advancing personalized biomaterial solutions through AI-driven design, and navigating the regulatory landscape for clinical translation. The integration of these strategies will ultimately unlock the full potential of cell-based therapies, enabling safer, more effective, and clinically viable treatments for a wide range of diseases.
References
- 1. Engineering hydrogels as extracellular matrix mimics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2892416/]
- 2. Clickable decellularized extracellular matrix as a new tool for building... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9020195/]
- 3. Nanomaterials-incorporated hydrogels for 3D bioprinting technology | Nano Convergence | Full Text [https://nanoconvergencejournal.springeropen.com/articles/10.1186/s40580-023-00402-5]
- 4. Decellularized ECM-Derived Hydrogels: Modification and Properties | IntechOpen [https://www.intechopen.com/chapters/62030]
- 5. Enhancing organoid culture: harnessing the potential of decellularized ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-01086-7]
- 6. Light-activated decellularized extracellular matrix-based bioinks for enhanced mechanical integrity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12144526/]
- 7. Comparison of two different biomaterials in the bone regeneration (15, 30 and 60 days) of critical defects in rats - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8291905/]
- 8. Biomaterials by design: Harnessing data for future development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8628044/]
- 9. Progress and emerging techniques for biomaterial -based derivation of... [https://pubmed.ncbi.nlm.nih.gov/37072836/]
- 10. . MSCs : Potential in therapeutic applications - PMC vs iPSCs [https://pmc.ncbi.nlm.nih.gov/articles/PMC9666898/]
- 11. Progress and emerging techniques for biomaterial -based derivation of... [https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-023-00371-0]
- 12. Mesenchymal stem/stromal cell -based therapy: mechanism, systemic... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-021-00725-7]
- 13. Recent advances in biomaterial -boosted adoptive therapy cell [https://pubmed.ncbi.nlm.nih.gov/35170589/]
- 14. Frontiers | MSCs vs. iPSCs: Potential in therapeutic applications [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1005926/full]
- 15. Frontiers | Fit-For-All iPSC-Derived Cell Therapies and Their Evaluation in Humanized Mice With NK Cell Immunity [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.662360/full]
- 16. Biomaterial‐Based Therapeutic Delivery of Immune Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11607182/]
- 17. to enhance Biomaterials therapy adoptive cell [https://www.nature.com/articles/s44222-023-00148-z?error=cookies_not_supported&code=8d2d328e-4d78-4d87-940e-7d9855d719c1]
- 18. Comparison of biomaterial delivery vehicles for improving acute retention of stem cells in the infarcted heart - PubMed [https://pubmed.ncbi.nlm.nih.gov/24862441/?dopt=Abstract]
- 19. of protein and Fundamentals in cell interactions biomaterials [https://pubmed.ncbi.nlm.nih.gov/28178627/]
- 20. Biological Basis of Biomaterial - Cell Interactions [https://www.imrpress.com/journal/FBL/special_issues/biomaterial_cell]
- 21. Frontiers | Biomaterial -driven regenerative drug delivery : a vicennial... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1593985/full]
- 22. Stem-cell niche - Latest research and news | Nature [https://www.nature.com/subjects/stem-cell-niche]
- 23. Stem-Cell Niches in Health and Disease: Microenvironmental Determinants of Regeneration and Pathology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249023/]
- 24. Stem-Cell Niches in Health and Disease: Microenvironmental Determinants of Regeneration and Pathology [https://www.mdpi.com/2073-4409/14/13/981]
- 25. Cardiospheres recapitulate a niche -like microenvironment rich in... [https://pubmed.ncbi.nlm.nih.gov/20882531/]
- 26. Frontiers | Bottom-up Biomaterial strategies for creating tailored stem... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 27. of Comparison vehicles for improving acute... biomaterial delivery [https://pubmed.ncbi.nlm.nih.gov/24862441/]
- 28. Frontiers | Cancer stem in personalized therapy: mechanisms... cells [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1619597/full]
- 29. Scaffold-free cell-based tissue engineering therapies: advances, shortfalls and forecast | npj Regenerative Medicine [https://www.nature.com/articles/s41536-021-00133-3]
- 30. for Biomaterial scaffolds tissue engineering [https://pubmed.ncbi.nlm.nih.gov/23276994/]
- 31. Tissue Engineered Scaffolds in Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4236978/]
- 32. Three-dimensional bioprinting using self-assembling scalable... [https://www.nature.com/articles/srep28714?error=cookies_not_supported]
- 33. Frontiers | 3 for D Repair and Regeneration Bioprinted Scaffolds Tissue [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2022.925321/full]
- 34. A Review of the Development of Biopolymer Hydrogel-Based Scaffold Materials for Drug Delivery and Tissue Engineering Applications [https://www.mdpi.com/2310-2861/11/3/178]
- 35. : Definition, History, How it Works, and Types | Xometry 3 D Bioprinting [https://www.xometry.com/resources/3d-printing/3d-printing-in-bioprinting/]
- 36. Frontiers | Mesenchymal stromal cell-laden hydrogels in tissue... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1670649/full]
- 37. Frontiers | Innovative hydrogels in cutaneous wound : current... healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1454903/full]
- 38. -derived exosomes MSC hyaluronic acid injectable for... hydrogel [https://pubmed.ncbi.nlm.nih.gov/40581219/]
- 39. Advancing wound by healing -based dressings loaded with... hydrogel [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03976-x]
- 40. [2503.14915] Evolving transport properties of dynamic hydrogels ... [https://arxiv.org/abs/2503.14915]
- 41. Recent Advances in Hydrogel Technology in Delivering Mesenchymal Stem Cell for Osteoarthritis Therapy [https://www.mdpi.com/2218-273X/14/7/858]
- 42. Advanced Biomaterials for Cell ‐Specific Modulation and Restore of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9165523/]
- 43. - Biomaterial targeted modulation of assisted in immune ... cells cancer [https://www.nature.com/articles/s41563-018-0147-9?error=cookies_not_supported&code=389e3313-d792-4f5d-ac6d-615ed315689b]
- 44. Design of therapeutic biomaterials to control inflammation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8884103/]
- 45. systems for cancer immunotherapy Magnetic [https://pubmed.ncbi.nlm.nih.gov/34522583/]
- 46. AI turns immune cells into precision cancer killers—in just weeks | ScienceDaily [https://www.sciencedaily.com/releases/2025/07/250724232416.htm]
- 47. Intelligent microstructure materials for diagnosis and treatment of osteoarthritis: progress and AI-enpowered future | Bone Research [https://www.nature.com/articles/s41413-025-00458-5]
- 48. Nanomaterials in Immunology: Bridging Innovative Approaches in Immune Modulation, Diagnostics, and Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11355198/]
- 49. Towards organoid culture without Matrigel - PubMed [https://pubmed.ncbi.nlm.nih.gov/34893703/]
- 50. Engineering the Extracellular Matrix for Organoid Culture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8889330/]
- 51. Tissue extracellular matrix hydrogels as alternatives to Matrigel for... [https://www.nature.com/articles/s41467-022-29279-4?error=cookies_not_supported&code=99c6a157-7cfb-48b6-b0af-6b6ad86c66e9]
- 52. Animal-free alternatives for Matrigel in human iPSC-derived blood vessel organoid culture | Scientific Reports [https://www.nature.com/articles/s41598-025-20091-w]
- 53. Frontiers | Organoid scaffold materials: research and application [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1637456/full]
- 54. Harnessing the potential of hydrogels for advanced therapeutic applications: current achievements and future directions | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-024-01852-x]
- 55. Photo-Crosslinking Hydrogel Based on Porcine Small Intestinal... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11766382/]
- 56. Frontiers | Sinomenine in cerebral ischemia : mechanisms, delivery ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1677685/full]
- 57. for Biomaterials disorders: a review of development from... CNS [https://link.springer.com/article/10.1007/s10856-025-06947-7]
- 58. Biomaterial-based vascularization strategies for enhanced treatment of peripheral arterial disease | Journal of Nanobiotechnology | Full Text [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03140-4]
- 59. Extracellular vesicles as drug and gene delivery vehicles in central ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01394h]
- 60. Recent advances of nanoparticles on bone engineering and... tissue [https://pubs.rsc.org/en/content/articlelanding/2024/na/d3na00851g]
- 61. -assisted local and systemic Biomaterial of bioactive agents... delivery [https://pubmed.ncbi.nlm.nih.gov/30711659/]
- 62. Intravascularly Deliverable Biomaterial Platforms for Tissue Repair and Regeneration Post-Myocardial Infarction - PubMed [https://pubmed.ncbi.nlm.nih.gov/36989469/]
- 63. Frontiers | Challenges and future perspectives in using mesenchymal... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1568914/full]
- 64. Insight on stem cell and instructive preconditioning to... biomaterials [https://pubmed.ncbi.nlm.nih.gov/27016619/]
- 65. : Measurement, Assays & Affects | Danaher Life Sciences Cell Viability [https://lifesciences.danaher.com/us/en/library/cell-viability.html]
- 66. What is cell and how is it measured? viability [https://blog.cellsignal.com/cell-process-what-is-cell-viability-and-how-can-it-be-measured]
- 67. Functionalized extracellular vesicles of mesenchymal stem cells for... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03300-6]
- 68. Frontiers | Biomaterials in tissue repair and regeneration: key insights from extracellular matrix biology [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 69. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 70. How to measure and improve cell ? viability [https://www.susupport.com/knowledge/biopharmaceutical-products/cell-gene-therapy/measure-improve-cell-viability]
- 71. Recent advances of biomaterials in stem cell therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10068913/]
- 72. - Bottom approaches in synthetic biology and up for... biomaterials [https://link.springer.com/article/10.1007/s10295-018-2027-3]
- 73. Biomaterials Conferences | Material science Meetings| BIOMATERIALS 2025 | April 14-15, 2025 | Paris, France [https://biomaterials.insightconferences.com/]
- 74. sciencedirect.com/topics/neuroscience/ paracrine - signalling [https://www.sciencedirect.com/topics/neuroscience/paracrine-signalling]
- 75. Types of Signals | Biology for Majors I [https://courses.lumenlearning.com/wm-biology1/chapter/reading-types-of-signals/]
- 76. Synergy of Paracrine Signaling During Early-Stage Mouse Ovarian Follicle Development In Vitro - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6816598/]
- 77. Selective Paracrine Modulation of Stromal Cells... | CoLab [https://colab.ws/articles/10.3390%2Fijms262010095]
- 78. by Distinct Adipose Tissue Depots Regulate... Paracrine Signaling [https://link.springer.com/article/10.1007/s12195-025-00864-z]
- 79. Frontiers | Whole secretome of mesenchymal stem cells is fully... [https://www.frontiersin.org/journals/medical-engineering/articles/10.3389/fmede.2025.1397406/full]
- 80. The secretome of endothelial progenitor cells promotes brain endothelial cell activity through PI3-kinase and MAP-kinase - PubMed [https://pubmed.ncbi.nlm.nih.gov/24755675/]
- 81. Stimuli-responsive Smart for Programmed Drug Biomaterials Delivery [https://www.frontiersin.org/research-topics/30198/smart-stimuli-responsive-biomaterials-for-programmed-drug-delivery/magazine]
- 82. Frontiers | Smart : as active immune modulators to shape... biomaterials [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 83. Nature-Inspired pH-Responsive Hydrogels with Rapid and High Contrast Changes in Color, Fluorescence, and Shape Simultaneously | Chinese Journal of Polymer Science [https://link.springer.com/article/10.1007/s10118-024-3158-9]
- 84. Smart hydrogels with wide visible color tunability | NPG Asia Materials [https://www.nature.com/articles/s41427-022-00379-3]
- 85. Stimuli- Responsive Drug Release from Smart Polymers [https://pubmed.ncbi.nlm.nih.gov/31370252/]
- 86. Editorial: Smart Stimuli-responsive Biomaterials for Programmed Drug... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10240393/]
- 87. Advanced smart and constructs for hard tissue... biomaterials [https://www.nature.com/articles/s41413-018-0032-9?error=cookies_not_supported&code=18f0b17a-2300-45d4-8e06-26d6359f6013]
- 88. -Based Therapeutic Biomaterial of Immune Delivery Cells [https://pubmed.ncbi.nlm.nih.gov/38813869/]
- 89. Frontiers | Application of biomaterials in mesenchymal stem cell ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1518398/full]
- 90. Toxicology of Biomaterials: A Comprehensive Guide [https://www.numberanalytics.com/blog/toxicology-biomaterials-comprehensive-guide]
- 91. Leachables in Biocompatibility: A Comprehensive Guide [https://www.numberanalytics.com/blog/leachables-biocompatibility-toxicology-biomaterials-ultimate-guide]
- 92. Improving the clinical impact of biomaterials in cancer... | Oncotarget [https://www.oncotarget.com/article/7304/text/]
- 93. Immunostimulatory Biomaterials to Boost Tumor Immunogenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7837217/]
- 94. In Vivo vs. In Vitro Models: Key Differences and Applications in Preclinical Research – Home 1 [https://liveonbiolabs.com/in-vivo-vs-in-vitro-models/]
- 95. In vitro vs. In vivo: Is One Better? | UHN Research [https://www.uhnresearch.ca/news/vitro-vs-vivo-one-better]
- 96. for Drug In Systems | SpringerLink Vitro Models Delivery [https://link.springer.com/protocol/10.1007/978-1-0716-4554-3_23]
- 97. Frontiers | Emerging biomaterials and bio-nano interfaces in pulmonary hypertension therapy: transformative strategies for personalized treatment [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1567783/full]
- 98. Engineered virus-like particles for efficient of... in vivo delivery [https://pubmed.ncbi.nlm.nih.gov/35021064/]
- 99. and Natural | Cell and Tissue... | Fiveable Synthetic Biomaterials [https://fiveable.me/cell-and-tissue-engineering/unit-4/natural-synthetic-biomaterials/study-guide/YMRxTUUfuWrajTOj]
- 100. Direct comparison of angiogenesis in natural and synthetic ... [https://pubmed.ncbi.nlm.nih.gov/34469789/]
- 101. Constructing a cell microenvironment with biomaterial scaffolds for... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02650-w]
- 102. The Efficiency of Direct Maturation: the Comparison of Two hiPSC Differentiation Approaches into Motor Neurons - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9757946/]
- 103. Secreted proteins as a fundamental source for biomarker discovery - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3517109/]
- 104. Dynamic tracking and identification of tissue-specific secretory proteins in the circulation of live mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8410947/]
- 105. Bioactive potential of natural biomaterials: identification, retention and assessment of biological properties | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-021-00512-8]
- 106. QIN Benchmarks for Clinical of Translation Imaging... Quantitative [https://pmc.ncbi.nlm.nih.gov/articles/PMC6403038/]
- 107. Global Clinical Trials : 2025 guides in India, US, & EU. Regulatory [https://prorelixresearch.com/global-clinical-trials-2025-regulatory-guides/]
- 108. The Future of Clinical Trials : 2025 Outlook | Signant Health [https://signanthealth.com/resources/blog/the-future-of-clinical-trials-2025-trends]
- 109. Artificial intelligence-Driven Advancements in Biomaterials Science: A Narrative Review - Premier Science [https://premierscience.com/pjs-25-1039/]
- 110. Artificial Intelligence in Biomaterials: A Comprehensive Review [https://www.mdpi.com/2076-3417/14/15/6590]
- 111. Multimodal AI in Biomedicine: Pioneering the Future of Biomaterials, Diagnostics, and Personalized Healthcare [https://www.mdpi.com/2079-4991/15/12/895]
- 112. Frontiers | Editorial: Functional biomaterials for drug delivery [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1550444/full]
- 113. Evaluation of cellular response and drug delivery of... efficacy [https://link.springer.com/article/10.1186/s40824-021-00232-8]