CRISPR-Cas9 and iPSCs: Precision Gene Correction for Therapeutic Development
This article explores the integrated application of CRISPR-Cas9 gene editing and induced pluripotent stem cell (iPSC) technologies for disease correction and therapeutic development.
CRISPR-Cas9 and iPSCs: Precision Gene Correction for Therapeutic Development
Abstract
This article explores the integrated application of CRISPR-Cas9 gene editing and induced pluripotent stem cell (iPSC) technologies for disease correction and therapeutic development. It covers foundational principles of CRISPR mechanisms and iPSC reprogramming, detailing methodological approaches for correcting mutations in monogenic disorders like Duchenne muscular dystrophy, sickle cell disease, and neurodegenerative conditions. The content addresses critical troubleshooting aspects including editing efficiency optimization, off-target effect mitigation, and delivery challenges in clinically relevant cells. Finally, it examines validation strategies through preclinical models and comparative analysis with traditional therapies, providing researchers and drug development professionals with a comprehensive resource for advancing genetically-corrected, patient-specific cell therapies toward clinical translation.
The Synergy of CRISPR-Cas9 and iPSC Platforms: Mechanisms and Therapeutic Potential
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated protein 9 (Cas9) system represents a transformative genome-editing tool derived from a natural defense mechanism in bacteria [1]. This adaptive immune system protects bacteria from viral infections by capturing and storing fragments of foreign genetic material, which allows for recognition and cleavage of subsequent invasions by the same pathogens [2]. The repurposing of this biological system into a programmable gene-editing technology has revolutionized molecular biology, enabling precise modifications to the DNA of diverse organisms, including humans [1].
The application of CRISPR-Cas9 in induced pluripotent stem cells (iPSCs) has been particularly impactful for disease modeling and therapeutic development [2]. By reprogramming somatic cells into pluripotent stem cells, researchers can obtain an unlimited source of cell resources with a patient's specific genetic background [2]. The combination of iPSC and CRISPR technologies provides a powerful platform for personalized treatment of genetic diseases, overcoming limitations of donor shortages and immune rejection in traditional cell therapy [2] [3].
Core Mechanism: The Molecular Machinery of CRISPR-Cas9
Molecular Components
The CRISPR-Cas9 system requires two fundamental molecular components to function:
Cas9 Nuclease: The effector protein that creates double-strand breaks (DSBs) in DNA. It contains two catalytic domains, HNH and RuvC, each responsible for cleaving one DNA strand [1]. The system requires a short DNA sequence known as the Protospacer Adjacent Motif (PAM) adjacent to the target site for recognition, which for the commonly used Streptococcus pyogenes Cas9 is 5'-NGG-3' [1].
Guide RNA (gRNA): A synthetic chimeric RNA molecule that combines the functions of CRISPR RNA (crRNA) and trans-activating CRISPR RNA (tracrRNA) [1]. The gRNA is designed with a ~20 nucleotide spacer sequence complementary to the target DNA site, which programs Cas9 to recognize and bind specific genomic locations [2] [1].
DNA Recognition and Cleavage Mechanism
The CRISPR-Cas9 mechanism proceeds through several defined steps:
- Complex Formation: Cas9 nuclease forms a ribonucleoprotein (RNP) complex with the gRNA [4].
- Target Recognition: The Cas9-gRNA complex scans DNA, identifying PAM sequences and initiating local DNA melting [1].
- Complementarity Check: If the gRNA sequence demonstrates sufficient complementarity to the target DNA adjacent to the PAM, Cas9 undergoes a conformational change that activates its nuclease domains [1].
- DNA Cleavage: The HNH domain cleaves the complementary strand, while the RuvC domain cleaves the non-complementary strand, resulting in a precise double-strand break 3-4 nucleotides upstream of the PAM site [1].
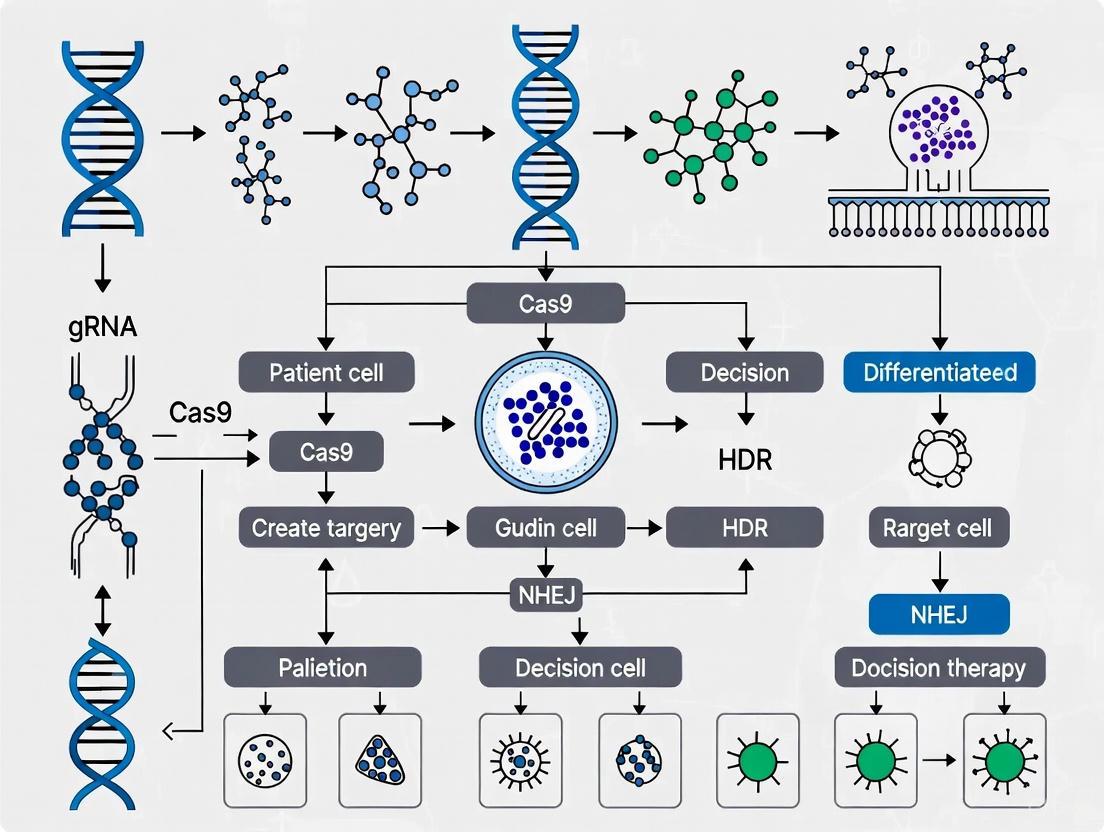
The following diagram illustrates this core mechanism:
DNA Repair Pathways and Editing Outcomes
After Cas9 creates a double-strand break, the cell engages one of two primary DNA repair pathways:
Non-Homologous End Joining (NHEJ): An error-prone repair pathway that directly ligates broken DNA ends, often resulting in small insertions or deletions (indels) that can disrupt gene function, making it suitable for gene knockout strategies [2] [1].
Homology-Directed Repair (HDR): A precise repair mechanism that uses a template DNA molecule (typically supplied by researchers) to incorporate specific genetic modifications at the target site, enabling precise nucleotide changes or gene insertions [2] [1].
Table 1: Comparison of DNA Repair Pathways in CRISPR-Cas9 Genome Editing
| Feature | Non-Homologous End Joining (NHEJ) | Homology-Directed Repair (HDR) |
|---|---|---|
| Template Requirement | No template required | Requires donor DNA template |
| Efficiency | High efficiency in most cells | Inefficient, varies by cell type and cell cycle stage |
| Primary Application | Gene knockouts, gene disruption | Precise gene correction, gene insertion |
| Cell Cycle Preference | Active throughout cell cycle | Preferentially active in S/G2 phases |
| Outcome | Error-prone, creates indels | High-fidelity, precise edits |
| Optimal for iPSCs | Relatively efficient | Challenging, requires optimization [3] |
Advanced CRISPR Systems: Enhancing Precision and Expanding Capabilities
Base Editing
Base editing represents a significant advancement that enables direct chemical conversion of one DNA base to another without creating double-strand breaks [2] [1]. These systems utilize catalytically impaired Cas9 variants (nickases) fused to nucleobase deaminase enzymes:
- Cytosine Base Editors (CBEs): Convert cytosine (C) to thymine (T through a C•G to T•A base pair change [1].
- Adenine Base Editors (ABEs): Convert adenine (A) to guanine (G through an A•T to G•C base pair change [1].
Prime Editing
Prime editing further expands CRISPR capabilities using a Cas9 nickase fused to a reverse transcriptase enzyme and a specialized prime editing guide RNA (pegRNA) [2]. This system can achieve targeted insertions, deletions, and all 12 possible base-to-base conversions without double-strand breaks, offering greater precision and reduced off-target effects [2].
CRISPR-Cas9 Nickases
Paired Cas9 nickases generate single-strand breaks instead of double-strand breaks, reducing off-target effects while maintaining editing efficiency [5]. This approach is particularly valuable for manipulating gene dosage in human iPSCs, enabling simultaneous generation of isogenic cell lines with different gene copy numbers for studying dosage-sensitive diseases like Alzheimer's disease [5].
Application Notes: CRISPR-Cas9 in iPSC Gene Correction
Disease Modeling and Therapeutic Correction
The combination of CRISPR-Cas9 and iPSC technology has enabled groundbreaking advances in modeling and treating genetic diseases:
Monogenic Diseases: CRISPR-corrected iPSCs have been successfully generated for Duchenne muscular dystrophy (DMD), sickle cell disease, β-thalassemia, and cystic fibrosis, with demonstrated functional recovery in differentiated cells [2].
Neurodegenerative Disorders: For Alzheimer's disease, CRISPR-Cas9 has been used in iPSCs to modify pathogenic variants in AD-related genes (APP, PSEN1, PSEN2) and study their effects on amyloid-beta secretion and Tau hyperphosphorylation [6] [5].
Isogenic Controls: A key application involves creating genetically matched control lines by correcting disease-causing mutations in patient-derived iPSCs, providing powerful experimental models for studying disease mechanisms and drug screening [2] [3].
Quantitative Data on Editing Efficiencies in iPSCs
Recent protocol optimizations have significantly improved editing efficiencies in iPSCs, as demonstrated by the following comparative data:
Table 2: Editing Efficiencies in Human iPSCs Using Optimized CRISPR-Cas9 Protocols
| Experimental Condition | Target Gene | Edit Type | Base Protocol Efficiency | Optimized Protocol Efficiency | Fold Improvement |
|---|---|---|---|---|---|
| p53 inhibition + HDR enhancer | EIF2AK3 (rs867529) | Point mutation | 2.8% | 59.5% | 21x [3] |
| p53 shRNA only | EIF2AK3 (rs867529) | Point mutation | 2.8% | 30.8% | 11x [3] |
| Final optimized protocol | EIF2AK3 (rs13045) | Point mutation | 4% | 25% | 6x [3] |
| Final optimized protocol | APOE Christchurch | Knock-in | N/A | 49-99% (bulk), 100% (subclones) | N/A [3] |
| Final optimized protocol | PSEN1 E280A | Reverse mutation | N/A | 97-98% (bulk), 100% (subclones) | N/A [3] |
Experimental Protocols: Genome Editing in Human iPSCs
Optimized Workflow for High-Efficiency Editing
The following comprehensive workflow integrates the most effective strategies for achieving high-efficiency genome editing in human iPSCs:
Critical Protocol Details
gRNA Design and RNP Complex Formation
gRNA Design: Use computational tools (e.g., Invitrogen GeneArt CRISPR Search and Design Tool) to identify optimal target sequences with high on-target and low off-target activity [7] [4]. Prefer targets located less than 10 nucleotides from the intended mutation to maximize HDR efficiency [3].
RNP Complex Formation: Combine 0.6 µM gRNA with 0.85 µg/µL of Alt-R S.p. HiFi Cas9 Nuclease V3 and incubate at room temperature for 20-30 minutes before transfection [3]. RNP delivery significantly reduces off-target effects compared to plasmid-based expression [4].
Enhancement of HDR Efficiency
p53 Suppression: Co-transfect with pCXLE-hOCT3/4-shp53-F plasmid (50 ng/µL) encoding shRNA against p53 to temporarily inhibit the p53-dependent DNA damage response and dramatically improve HDR rates [3].
Pro-survival Supplements: Include 1% Revitacell and 10% CloneR in the cloning media to enhance single-cell survival after editing [3]. ROCK inhibitor (Y-27632) is essential for preventing apoptosis in dissociated iPSCs [4].
HDR Enhancers: Add commercial HDR enhancer compounds (e.g., from IDT) to further boost homologous recombination efficiency [3].
Delivery Methods for iPSCs
Table 3: Comparison of CRISPR-Cas9 Delivery Methods for Human iPSCs
| Method | Components Delivered | Efficiency | Advantages | Disadvantages |
|---|---|---|---|---|
| Lipofectamine CRISPRMAX | RNP complex | >50% cleavage efficiency [4] | Simple protocol, minimal equipment | Lower efficiency than electroporation |
| Neon Transfection System | RNP complex | >80% cleavage efficiency [4] | Highest efficiency, direct delivery | Requires specialized equipment |
| Neon Transfection System | gRNA + Cas9 mRNA | Variable, protocol-dependent [4] | Sustained expression | Increased off-target risk |
| Lipofectamine CRISPRMAX | gRNA + Cas9 plasmid | Lower than RNP delivery [4] | Cost-effective | High off-target risk, cytotoxicity |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for CRISPR-Cas9 Genome Editing in iPSCs
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| Cas9 Enzymes | Alt-R S.p. HiFi Cas9 Nuclease V3, GeneArt Platinum Cas9 Nuclease | Creates double-strand breaks at target sites | HiFi variants reduce off-target effects [3] [4] |
| gRNA Synthesis | GeneArt Precision gRNA Synthesis Kit, custom synthetic gRNAs | Targets Cas9 to specific genomic loci | In vitro transcription or synthetic formats [4] |
| Delivery Reagents | Lipofectamine CRISPRMAX, Neon Transfection System | Introduces editing components into cells | Neon system provides highest efficiency [4] |
| Cell Culture Supplements | RevitaCell Supplement, CloneR, ROCK inhibitor (Y-27632) | Enhances single-cell survival | Critical for clonal expansion after editing [3] [4] |
| HDR Enhancers | IDT HDR Enhancer, p53 shRNA plasmid | Boosts homologous recombination rates | p53 inhibition increases HDR efficiency 11-fold [3] |
| Detection Kits | GeneArt Genomic Cleavage Detection Kit | Assesses editing efficiency | Used 48-72 hours post-transfection [4] |
Quality Control and Safety Considerations
Off-Target Effect Assessment
Comprehensive off-target analysis is essential for clinical applications of CRISPR-edited iPSCs:
- Computational Prediction: Use tools like Cas-OFFinder to identify potential off-target sites based on sequence similarity to the gRNA [3].
- Empirical Methods: Employ GUIDE-seq, Digenome-seq, or CIRCLE-seq to experimentally profile genome-wide off-target activity [2].
- Whole Genome Sequencing: Perform WGS on edited clones to detect unexpected modifications, including large structural variations [3].
Genomic Integrity Monitoring
- Karyotype Analysis: Regular G-banding analysis to detect chromosomal abnormalities that may arise during editing and clonal expansion [3].
- Pluripotency Verification: Confirm that edited iPSCs maintain pluripotency markers and differentiation potential after editing [2].
- Identity Testing: STR profiling to ensure cell line identity throughout the editing process [2].
The integration of CRISPR-Cas9 technology with human iPSCs has created a powerful platform for studying genetic diseases and developing personalized therapies. The core principles of CRISPR-Cas9—from its origin as a bacterial immune mechanism to its current application as a precision genome-editing tool—provide the foundation for ongoing innovations in gene correction strategies. Through continued optimization of editing efficiency, delivery methods, and safety assessment protocols, this combined technological approach promises to accelerate the development of transformative treatments for genetic disorders.
The convergence of induced pluripotent stem cell (iPSC) technology and CRISPR-Cas9 gene editing has revolutionized biomedical research by enabling the creation of physiologically relevant human disease models. iPSCs, generated through the reprogramming of patient somatic cells, provide unlimited access to patient-specific tissues while retaining the complete donor genetic background [8] [9]. When combined with CRISPR-Cas9, researchers can precisely introduce or correct disease-causing mutations in an isogenic background, establishing highly controlled systems for investigating disease mechanisms and developing therapeutic interventions [8] [9]. This powerful integrated platform has become indispensable for modeling neurodegenerative diseases, cardiac disorders, and rare genetic conditions, accelerating the path toward precision medicine [8] [9] [10].
Reprogramming Methodologies: From Somatic Cells to Pluripotency
The generation of iPSCs from somatic cells has evolved significantly since its initial discovery, with modern protocols prioritizing safety, efficiency, and clinical applicability.
Key Reprogramming Protocols
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Mechanism | Advantages | Disadvantages | Reprogramming Efficiency | Genomic Integration |
|---|---|---|---|---|---|
| Retro/Lentiviral | Integrative viral vectors delivering OCT-4, SOX-2, KLF-4, c-MYC | High efficiency | Potential insertional mutagenesis; persistent transgene expression | High | Yes |
| Cre-excisable Lentivirus | Integrative vectors removable via Cre-lox recombination | Eliminates transgene post-reprogramming | Requires lengthy subcloning and validation | High | Temporary |
| Non-integrating Episomal Plasmids | Epstein-Barr virus-derived plasmid vectors | Non-integrating; simple delivery | Lower efficiency compared to viral methods | Moderate | No |
| Sendai Virus (SeV) | Negative-sense RNA virus-based vector | Non-integrating; high efficiency; broad tropism | Difficult to clear residual virus; requires multiple clonal expansions | High | No |
| Self-replicating RNA (Simplicon) | Synthetic RNA mimicking viral RNA | Non-integrating; high efficiency; single transfection; easily eliminated | Requires interferon pathway inhibition | Very High | No |
Detailed Reprogramming Protocol: Simplicon RNA Technology
The Simplicon RNA reprogramming system represents a advanced non-integrating approach that combines high efficiency with enhanced safety profiles [11].
Day 0: Target Cell Seeding
- Determine optimal seeding density for target human fibroblasts to achieve 60-80% confluency after 24 hours. For a 6-well plate, seed between 1×10^5 to 1×10^6 cells per well in fibroblast growth medium.
- Determine optimal puromycin selection concentration by performing a kill curve assay. The working concentration should achieve 50% cell death by days 4-5.
Day 1: Pre-treatment and Transfection
- Pre-treat target cells with 200 ng/mL B18R protein in 1 mL DMEM for 2 hours to inhibit innate interferon response.
- Prepare RNA-transfection complexes by mixing 0.5 μL VEE-OKS-iG RNA (encoding OCT4, KLF4, SOX2) and 0.5 μL B18R RNA in 250 μL Opti-MEM with 4.0 μL RiboJuice transfection reagent.
- Add RNA-transfection complexes dropwise to cells, incubate for 4 hours at 37°C, 5% CO2.
- After incubation, supplement with DMEM containing 10% FBS, 1X glutamine, and 200 ng/mL B18R protein.
Days 2-11: Selection and Colony Expansion
- Replace medium daily with fresh medium containing 200 ng/mL B18R protein and the predetermined optimal puromycin concentration.
- Monitor cell death daily, adjusting puromycin concentration to maintain 30-60% cell death until day 11.
- When puromycin-resistant cells reach 70-90% confluency (typically between days 9-18), passage onto Matrigel-coated plates or inactivated MEF feeder layers.
Days 18-30: Colony Picking and Expansion
- Monitor for emergence of compact iPSC colonies with defined borders.
- Pick colonies reaching approximately 200 cells using manual selection or automated picking systems.
- Expand selected colonies in PluriSTEM Human ES/iPSC medium or similar defined culture system for further characterization and banking [11].
Alternative Protocol: PBMC Reprogramming Using STEMCCA Lentivirus
Day 0: PBMC Isolation and Expansion
- Isolate peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation with CPT tubes.
- Centrifuge at 1,800 × g for 30 minutes at room temperature, collect buffy coat layer.
- Wash cells with PBS, centrifuge at 300 × g for 15 minutes.
- Resuspend 1-2×10^6 cells in 2 mL expansion medium containing QBSF-60 stem cell medium supplemented with 50 μg/mL ascorbic acid, 50 ng/mL SCF, 10 ng/mL IL-3, 2 U/mL EPO, 40 ng/mL IGF-1, 1 μM dexamethasone, and 1% Pen/Strep.
- Culture at 37°C, 5% CO2.
Days 3 and 6: Medium Refresh
- Transfer cells to conical tubes, wash to collect adherent cells, centrifuge at 300 × g for 10 minutes.
- Resuspend in fresh expansion medium, return to culture.
Day 9: STEMCCA Lentiviral Transduction
- Harvest cells, wash, and centrifuge as above.
- Resuspend in 1 mL fresh expansion medium containing 5 μg/mL polybrene and STEMCCA lentivirus at MOI 1-10.
- Transfer to 12-well plate, spinoculate at 2,250 rpm for 90 minutes at 25°C.
- After spinoculation, add additional 1 mL expansion medium with polybrene, culture at 37°C, 5% CO2.
Day 10: Post-transduction Processing
- Harvest transduced cells, wash with QBSF-60 medium, centrifuge at 300 × g for 10 minutes.
Day 11: Plating on Feeder Layers
- Seed transduced cells on 0.1% gelatin-coated plates containing inactivated mouse embryonic fibroblasts (MEFs) in appropriate iPSC culture medium [11].
Quality Control and Characterization of iPSCs
Rigorous quality control is essential for ensuring the integrity, safety, and functionality of iPSC lines, particularly for clinical applications and disease modeling research.
Comprehensive QC Assay Panel
Table 2: iPSC Quality Control and Characterization Methods
| Test Category | Specific Assay | Purpose | Key Outcome Measures |
|---|---|---|---|
| Genetic Integrity | Karyotyping (G-banding) | Detect chromosomal abnormalities | Chromosome number, structural variations |
| High-throughput sequencing | Identify point mutations, off-target effects | Mutation load, specific variants | |
| Pluripotency Status | Alkaline Phosphatase staining | Detect undifferentiated cells | Enzyme activity, colony staining intensity |
| PluriTest (microarray/RNA-seq) | Transcriptomic pluripotency assessment | Pluripotency score, novelty score | |
| Teratoma formation | In vivo differentiation potential | Three germ layer formation | |
| Differentiation Potential | ScoreCard (qPCR-based) | Quantitative differentiation capacity | Expression of germ layer markers |
| Flow cytometry | Surface marker quantification | TRA-1-60, SSEA-4, OCT4 positivity | |
| In vitro trilineage differentiation | Directed differentiation capability | Morphology, lineage-specific markers | |
| Functional Characterization | Telomere length analysis (Q-FISH) | Replicative capacity assessment | Telomere length, telomerase activity |
| Microfluidic chip detection | Rare undifferentiated cell detection | Sensitivity to 0.001% residual iPSCs |
Advanced Pluripotency Assessment
The PluriTest platform provides a bioinformatics-based assessment of pluripotency through comparison of transcriptomic data against established reference databases [12]. This assay requires only small cell numbers and can be performed early during iPSC establishment, providing a quantitative pluripotency score and novelty score that indicate similarity to reference pluripotent stem cells [12].
For teratoma formation assays, the TeratoScore algorithm enables quantitative evaluation of differentiation potential by analyzing gene expression patterns in teratomas, moving beyond subjective morphological assessment [12]. This approach establishes differentiation efficiency scores across germ layers, providing standardized metrics for comparison between cell lines.
Telomere analysis has emerged as a critical quality attribute, with telomere length maintenance and telomerase activation serving as indicators of successful reprogramming and differentiation potential [12]. Techniques such as quantitative fluorescence in situ hybridization (Q-FISH) and telomeric repeat amplification protocol (TRAP) assess telomere length and telomerase activity respectively, providing functional readouts of iPSC quality [12].
CRISPR-Cas9 Mediated Genome Editing in iPSCs
The integration of CRISPR-Cas9 technology with iPSCs enables precise genetic manipulation for disease modeling, creating isogenic cell lines that differ only at specific pathogenic loci.
CRISPR-Cas9 Systems for iPSC Engineering
The most widely used CRISPR system derives from Streptococcus pyogenes (SpCas9) and requires an NGG protospacer adjacent motif (PAM) for target recognition [8]. Recent advancements have expanded the CRISPR toolbox to include:
- CRISPR-Cpf1: Recognizes broader PAM sequences, generates 5' overhangs instead of blunt ends, and requires only a single RNA guide [8]
- Base editors: Enable precise single-nucleotide changes without creating double-strand breaks [9]
- CRISPR interference/activation (CRISPRi/CRISPRa): Utilize catalytically dead Cas9 (dCas9) fused to repressor (KRAB) or activator (VP64) domains to modulate gene expression without altering DNA sequence [8]
Isogenic iPSC Line Generation Protocol
Step 1: gRNA Design and Vector Construction
- Design 2-3 single guide RNAs (sgRNAs) targeting the genomic region of interest using validated design tools
- Clone sgRNAs into appropriate Cas9 expression vectors (e.g., all-in-one or separate expression systems)
- For knock-in approaches, design donor templates with 500-800 bp homology arms flanking the desired modification
Step 2: iPSC Transfection and Editing
- Culture iPSCs in defined media such as Essential 8 or B8 on Matrigel-coated plates [10]
- At 60-70% confluency, dissociate to single cells using EDTA or TrypLE
- Transfect using electroporation (Amaxa Nucleofector) or lipofection methods
- For homology-directed repair, include ssODN or plasmid donor templates
- Include ROCK inhibitor (Y27632, 10 μM) for 24 hours post-transfection to enhance viability [10]
Step 3: Single-Cell Cloning and Expansion
- 48-72 hours post-transfection, dissociate and seed at clonal density (500-1000 cells/10 cm plate)
- Isolate individual colonies using manual picking or automated systems
- Expand clones in 96-well plates for screening
Step 4: Genotypic Validation
- Screen clones using PCR amplification of targeted locus
- Confirm edits by Sanger sequencing or next-generation sequencing
- Perform off-target analysis by examining top predicted off-target sites
- Validate pluripotency maintenance post-editing through flow cytometry and differentiation potential assays
Step 5: Banking and Characterization
- Expand validated clones, cryopreserve multiple vials
- Perform full quality control including karyotyping, mycoplasma testing, and identity confirmation [9] [13]
Disease Modeling Applications and Protocols
The CRISPR-iPSC platform has enabled unprecedented precision in modeling human diseases, particularly for neurological disorders and cardiac conditions.
Neurodegenerative Disease Modeling: Epilepsy Case Study
A compelling application of this technology involves investigating SCN1A loss-of-function mutations associated with Dravet syndrome and other epileptic disorders [13]. The experimental approach included:
Step 1: Isogenic Line Generation
- Derived iPSCs from a patient with SCN1A mutation (Q1923R)
- Corrected the mutation using TALEN-mediated gene editing to create an isogenic control
- Introduced tdTomato fluorescent reporter into the GAD1 locus to label GABAergic neurons
Step 2: Neural Differentiation
- Differentiated iPSCs into mixed neuronal cultures containing both GABAergic and glutamatergic neurons
- Used specific patterning factors to enhance GABAergic neuronal production
Step 3: Electrophysiological Analysis
- Performed whole-cell patch clamp recordings on tdTomato-positive GABAergic neurons
- Measured sodium current properties, action potential parameters, and synaptic activity
- Recorded spontaneous inhibitory and excitatory postsynaptic currents (sIPSCs/sEPSCs)
Key Findings:
- Patient-derived GABAergic neurons showed reduced sodium current density and altered activation properties
- Action potential amplitudes were reduced and thresholds increased in mutant neurons
- sIPSC frequencies were significantly decreased in patient-derived neuronal networks
- The balance of synaptic activity shifted from inhibition-dominated to excitation-dominated, explaining the epileptogenesis mechanism [13]
High-Content Analysis for Neurodegenerative Disease Phenotyping
High-content imaging (HCI) approaches enable quantitative analysis of complex neurodegenerative disease phenotypes in iPSC-derived neurons [14]. Standardized protocols include:
Neurite Outgrowth and Morphology Analysis
- Plate iPSC-derived neurons in 96-well imaging plates
- Fix at specific timepoints and immunostain for neuronal markers (βIII-tubulin, MAP2)
- Acquire images using automated microscopes (Operetta CLS, Opera Phenix)
- Analyze using CellProfiler or ImageJ with NeuriteTracer plugin
- Quantify: total neurite length, branching points, soma size, process complexity
Mitochondrial Function Assessment
- Label mitochondria with MitoTracker or immunostaining for TOM20
- Measure mitochondrial membrane potential using TMRE or JC-1 dyes
- Quantify mitochondrial morphology (network connectivity, area, aspect ratio)
- Assess mitochondrial distribution along neurites
Synaptic Density and Protein Aggregation Analysis
- Co-stain for pre- and post-synaptic markers (synapsin, PSD95)
- Quantify synaptic puncta density and colocalization
- Measure intracellular protein aggregation (tau, α-synuclein) using conformation-specific antibodies
- Employ super-resolution microscopy (STED, SIM) for nanoscale analysis of synaptic structures [14]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Reagents for iPSC Generation, Culture, and Differentiation
| Category | Specific Reagent | Function | Example Products |
|---|---|---|---|
| Reprogramming | VEE-OKS-iG RNA | Synthetic self-replicating RNA encoding OCT4, KLF4, SOX2 | Simplicon RNA Reprogramming Kit |
| B18R Protein | Interferon inhibitor, enhances RNA reprogramming efficiency | Recombinant B18R | |
| Culture Media | Essential 8 / B8 | Chemically defined, xeno-free maintenance media | Thermo Fisher, Stemcell Technologies |
| mTeSR1 | Defined maintenance medium for pluripotent stem cells | Stemcell Technologies | |
| Culture Matrices | Matrigel | Basement membrane extract for attachment and signaling | Corning Matrigel |
| Vitronectin | Recombinant attachment substrate for defined culture | Synthemax, VTN-N | |
| Differentiation | RPMI/B27 | Standard medium for cardiac differentiation | Thermo Fisher |
| Y-27632 | ROCK inhibitor, enhances single-cell survival | STEMCELL Technologies | |
| Genome Editing | SpCas9 | CRISPR endonuclease for DNA cleavage | Various suppliers |
| Alt-R CRISPR-Cas9 | Synthetic CRISPR system with high efficiency | Integrated DNA Technologies | |
| Characterization | PluriTest | Bioinformatics assay for pluripotency assessment | PluriTest |
| ScoreCard | qPCR-based differentiation potential assay | TaqMan Scorecard Panel |
The integration of iPSC technology with CRISPR-Cas9 genome editing has created a powerful paradigm for human disease modeling and therapeutic development. The protocols and applications detailed in this technical review provide researchers with comprehensive frameworks for generating patient-specific disease models, conducting precise genetic manipulations, and performing quantitative phenotypic analyses. As these technologies continue to evolve through improvements in reprogramming efficiency, editing precision, and analytical capabilities, they will increasingly enable the deconstruction of complex disease mechanisms and accelerate the development of targeted interventions for personalized medicine applications.
The efficacy of CRISPR-Cas9 gene editing is fundamentally governed by the cellular DNA repair machinery that responds to Cas9-induced double-strand breaks (DSBs). Three primary pathways—Non-Homologous End Joining (NHEJ), Homology-Directed Repair (HDR), and Microhomology-Mediated End Joining (MMEJ)—compete to determine editing outcomes, presenting a critical challenge for researchers seeking precise genetic modifications in induced pluripotent stem cells (iPSCs) for disease modeling and correction [15] [16]. Understanding the distinct mechanisms, kinetics, and factors influencing these pathways is essential for developing strategies that favor desired editing outcomes over error-prone repair.
NHEJ operates throughout the cell cycle and functions without a repair template, directly ligating broken DNA ends in an error-prone manner that often introduces small insertions or deletions (indels) [16]. This makes NHEJ the dominant and most efficient pathway for generating gene knockouts. In contrast, HDR requires a donor DNA template with homology arms and is restricted primarily to the S and G2 phases of the cell cycle, enabling precise edits including nucleotide substitutions or gene insertions [15] [16]. MMEJ represents a third pathway that utilizes 5-25 base pair microhomology regions flanking the DSB for repair, resulting in predictable deletions and serving as an intermediate option between the randomness of NHEJ and the precision of HDR [15].
The competitive balance between these pathways varies significantly across cell types, with iPSCs and primary cells presenting particular challenges due to their preference for NHEJ over HDR and frequently residing in quiescent states [17] [16]. Recent advances have revealed that editing kinetics further differentiate these pathways, with short indels from NHEJ occurring faster than longer deletions, while HDR kinetics fall between NHEJ and MMEJ [17]. This complex interplay necessitates sophisticated experimental approaches to steer editing outcomes toward precise genome modifications required for therapeutic applications.
Comparative Analysis of DNA Repair Pathways
Mechanism and Kinetics
Table 1: Characteristics of Major DNA Repair Pathways in CRISPR Editing
| Feature | NHEJ | HDR | MMEJ |
|---|---|---|---|
| Repair Template | Not required | Homologous donor DNA required | Uses microhomology (5-25 bp) |
| Cell Cycle Phase | All phases | S and G2 phases | M and early S phases |
| Repair Fidelity | Error-prone (indels common) | High-fidelity, precise | Predictable deletions |
| Kinetics (T50) | Fastest (especially +A/T indels) | Intermediate | Slower than NHEJ |
| Key Enzymes | Ku70/80, DNA-PKcs, XLF, XRCC4 | Rad51, BRCA2, Rad52 | POLQ (DNA polymerase theta), PARP1 |
| Primary Outcome | Gene knockouts | Precise edits, knock-ins | Defined deletions, alternative knock-in |
| Advantages | Highly efficient, works in non-dividing cells | Precise, versatile for various edits | Easier donor design than HDR, more predictable than NHEJ |
| Disadvantages | Unpredictable indels, low precision | Low efficiency, cell cycle dependent | Still introduces deletions, less characterized |
The kinetic competition between repair pathways significantly influences editing outcomes. Research quantifying T50 (time to reach half of the maximum editing frequency) has demonstrated that short indels, particularly +A/T events, occur more rapidly than longer (>2 bp) deletions, with HDR kinetics positioned between NHEJ and MMEJ [17]. This temporal hierarchy means that AAV6-mediated HDR effectively competes with longer MMEJ-mediated deletions but cannot outcompete faster NHEJ-mediated indels [17]. These kinetic properties underscore the importance of timing when introducing donor templates and implementing interventions to modulate pathway activity.
Pathway Competition and Editing Outcomes
Table 2: Quantitative Comparison of Editing Outcomes Across Repair Pathways
| Parameter | NHEJ | HDR | MMEJ |
|---|---|---|---|
| Relative Frequency | Dominant pathway in most cells [18] | Typically <10-30% of edits [16] | Variable by cell type (5-20%) [15] |
| Efficiency with Inhibition | Reduced by NHEJ inhibitors (e.g., Alt-R HDR Enhancer V2) [19] | Enhanced 3-fold with NHEJ inhibition [19] | Reduced by POLQ inhibition (ART558) [19] |
| Indel Pattern | Short insertions/deletions (<50 bp) [19] | Precise integration | Large deletions (≥50 bp) with microhomology [19] |
| HDR/NHEJ Ratio | Highly variable by locus, nuclease, and cell type [18] | Can exceed NHEJ under optimized conditions [18] | Not applicable |
| Perfect HDR Efficiency with NHEJi | Not applicable | 16.8% (Cpf1) to 22.1% (Cas9) [19] | Not applicable |
The distribution of editing outcomes across these pathways exhibits substantial variability depending on experimental conditions. Systematic quantification has revealed that HDR/NHEJ ratios are highly dependent on the target gene locus, nuclease platform, and cell type, with some conditions surprisingly yielding more HDR than NHEJ events [18]. This challenges the conventional wisdom that NHEJ generally dominates editing outcomes and highlights the importance of empirical optimization for specific experimental systems. Even with NHEJ inhibition, perfect HDR events may constitute less than half of all integration events, with the remainder comprising various imprecise repair patterns including asymmetric HDR, blunt integration, and MMEJ-derived outcomes [19].
Experimental Modulation of Repair Pathways
Strategies for Enhancing HDR in iPSCs
Achieving high-efficiency HDR in iPSCs requires multipronged approaches that address both technical and biological barriers. A primary consideration is HDR template design, where optimal homology arm lengths are critical—30-60 nucleotides for single-stranded oligodeoxynucleotide (ssODN) donors and 200-300 base pairs for plasmid-based templates [16]. The positioning of edits relative to the cleavage site further influences strand preference, with PAM-proximal edits favoring the targeting strand while PAM-distal edits benefit from non-targeting strand orientation [16]. For larger insertions such as fluorescent proteins, plasmid donors with 500 base pair homology arms delivered via electroporation typically yield superior results compared to single-stranded templates [16].
Timed intervention with small molecule inhibitors provides powerful control over pathway competition. Combined treatment with M3814 (an NHEJ inhibitor) and Trichostatin A (a histone deacetylase inhibitor) increases HDR efficiency approximately 3-fold by suppressing dominant error-prone repair while potentially opening chromatin structure to enhance donor accessibility [17]. Similarly, Alt-R HDR Enhancer V2 potently inhibits NHEJ, increasing knock-in efficiency from approximately 5.2% to 16.8% for Cpf1-mediated editing and from 6.9% to 22.1% for Cas9-mediated editing in human cells [19]. Additional pathway-specific inhibitors including ART558 for MMEJ (via POLQ inhibition) and D-I03 for single-strand annealing (via Rad52 inhibition) offer further precision for steering repair outcomes, with MMEJ suppression particularly effective at reducing large deletions and complex indels [19].
Diagram 1: DNA Repair Pathway Competition and Outcomes. CRISPR-Cas9 induced double-strand breaks are resolved through competing repair pathways whose balance can be modulated by specific inhibitors to steer outcomes toward precise editing.
The PITCh System: MMEJ for Efficient Knock-in
The Precise Integration into Target Chromosome (PITCh) system represents an innovative approach that leverages MMEJ rather than HDR for gene knock-in, offering particular advantages in cell types with low HDR activity [15]. This method requires only very short microhomology regions (5-25 bp) compared to extensive homology arms needed for HDR, significantly simplifying vector construction while maintaining precision. The system has demonstrated remarkable efficiency, with proper insertion achieved in 80% of clones at the 5' junction and 50% at the 3' junction when integrating a GFP-Puro cassette into the FBL locus of HEK293 cells [15].
The PITCh protocol involves a series of carefully orchestrated steps beginning with the generation of microhomology arms in the donor vector through PCR, followed by co-transfection with vectors expressing Cas9 and both generic PITCh-gRNA and locus-specific gRNA [15]. Selection of puromycin-resistant cells enables enrichment of successfully modified cells, with subsequent PCR amplification and sequencing confirming precise integration. This MMEJ-based strategy has proven particularly valuable in challenging systems such as the pathogenic fungus Aspergillus fumigatus, where traditional HDR approaches are inefficient due to NHEJ dominance [15]. The versatility of the PITCh system makes it a powerful alternative to HDR for knock-in experiments in iPSCs and other therapeutically relevant primary cells.
Research Reagent Solutions
Table 3: Essential Reagents for Modulating DNA Repair Pathways
| Reagent Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| NHEJ Inhibitors | Alt-R HDR Enhancer V2, M3814 | Suppresses dominant NHEJ pathway to enhance HDR efficiency | Increases HDR efficiency 3-fold; treatment for 24h post-electroporation [17] [19] |
| MMEJ Inhibitors | ART558 | Inhibits POLQ to reduce MMEJ-mediated deletions | Reduces large deletions (≥50 bp) and complex indels [19] |
| SSA Inhibitors | D-I03 | Suppresses Rad52 to reduce asymmetric HDR | Decreases imprecise donor integration patterns [19] |
| HDAC Inhibitors | Trichostatin A (TSA) | Chromatin modification to potentially improve donor accessibility | Used in combination with NHEJ inhibitors [17] |
| HDR Donor Templates | AAV6 serotype, ssODNs, dsDNA donors | Provides repair template for precise editing | AAV6 effective for HDR in iPSCs; ssODNs for point mutations [17] [16] |
| Cas Nuclease Systems | Cas9, Cpf1 (Cas12a) | Induces targeted double-strand breaks with different cleavage patterns | Cas9 (blunt ends) vs Cpf1 (staggered ends) affect repair outcomes [19] |
Diagram 2: Optimized Workflow for CRISPR Knock-in Experiments. This streamlined protocol incorporates critical decision points for selecting between HDR and MMEJ systems and includes key steps for enhancing precise editing through pathway modulation.
Advanced Methodologies and Protocol
Comprehensive Protocol for HDR Enhancement
A robust protocol for enhancing HDR efficiency in iPSCs begins with careful experimental design. For the nuclease component, the use of Cas9 ribonucleoprotein (RNP) complexes rather than plasmid-based expression significantly reduces off-target effects and enables more rapid editing [17]. Guide RNA design should position the cut site within 10 base pairs of the intended edit and consider PAM orientation, with the targeting strand preferred for PAM-proximal edits and the non-targeting strand for PAM-distal modifications [16]. For the HDR donor, select appropriate template architecture: ssODNs with 30-60 nucleotide homology arms for small edits (<50 bp) or plasmid donors with 200-500 base pair homology arms for larger insertions [16].
Critical cell culture handling precedes editing. For iPSCs, transient cell cycle synchronization through serum starvation or chemical treatments can increase the proportion of cells in S/G2 phases where HDR is active [16]. Prepare RNP complexes by combining purified Cas9 protein with synthetic guide RNA and incubating for 10-20 minutes at room temperature. For electroporation, combine RNP complexes with donor template at a 1:2 molar ratio and deliver using optimized settings for stem cells [16]. Immediately following delivery, treat cells with pathway modulators—typically NHEJ inhibitors like Alt-R HDR Enhancer V2 or M3814 combined with Trichostatin A for 24 hours, the critical window when most repair occurs [17] [19].
Post-editing processing and validation complete the protocol. Allow 72-96 hours for expression of resistance genes or fluorescent markers before initiating selection. For precise quantification of editing outcomes, employ digital PCR (ddPCR) assays that can simultaneously detect HDR and NHEJ events at endogenous loci [18]. Alternatively, long-read amplicon sequencing with PacBio platforms coupled with computational frameworks like knock-knock enables comprehensive characterization of repair patterns, including perfect HDR, imprecise integration, and various indel outcomes [19]. Screen multiple clones to account for heterogeneity, and validate through Southern blotting or functional assays to ensure intended edits without off-target effects.
Troubleshooting and Optimization
Common challenges in achieving precise editing include low HDR efficiency and high indel background. When facing insufficient HDR rates, consider these evidence-based solutions: First, optimize donor design by testing both single-stranded and double-stranded templates and adjusting homology arm length [16]. Second, titrate nuclease dosage to balance between efficient cutting and minimizing cytotoxicity that can reduce HDR [18]. Third, employ small molecule combinations such as M3814 with Trichostatin A, which synergistically enhance HDR efficiency [17].
When imprecise integration persists despite NHEJ inhibition, investigate contributions from alternative repair pathways. MMEJ inhibition via ART558 specifically reduces large deletions and complex indels [19]. For asymmetric HDR patterns where only one junction is precise, SSA suppression through D-I03 treatment may improve perfect HDR rates [19]. Systematic quantification of all repair outcomes using the ddPCR assay or long-read sequencing provides essential feedback for iterative optimization, revealing how specific pathway manipulations alter the balance between precise and imprecise editing [18] [19].
For challenging cell types like iPSCs where HDR efficiency remains stubbornly low despite optimization, consider alternative approaches such as the PITCh system that leverages MMEJ rather than HDR [15]. This method's requirement for only short microhomology regions simplifies donor design while achieving comparable knock-in efficiency to HDR-based approaches, particularly valuable in translationally relevant primary cells where HDR activity is inherently limited.
The treatment of monogenic disorders, which are caused by mutations in a single gene and affect over 300 million people worldwide, represents a significant challenge for modern medicine due to their low prevalence and consequent limited research investment [20]. CRISPR-Cas9 genome editing has emerged as a transformative therapeutic platform that directly addresses the genetic root cause of these conditions, offering the potential for durable, "one-and-done" treatments that circumvent the limitations of conventional symptom-management approaches [20]. This technology enables precise genetic correction in patient-derived induced pluripotent stem cells (iPSCs), creating a renewable source of autologous, gene-corrected cells for transplantation [21] [22]. The versatility of CRISPR-Cas9 allows researchers to target diverse mutation types—including exonic point mutations, deep intronic variants, and dominant gain-of-function mutations—through tailored editing strategies [21]. When combined with iPSC technology, CRISPR correction facilitates the generation of multilineage therapeutic cell types, providing a comprehensive framework for addressing both systemic and tissue-specific manifestations of monogenic diseases [22].
Quantitative Landscape of CRISPR-Cas9 Applications
Therapeutic Editing Strategies by Mutation Class
Table 1: CRISPR-Cas9 strategies for different genetic mutation types
| Mutation Type | Disease Example | Target Gene | Editing Approach | Efficiency Reported | Key Outcome Measures |
|---|---|---|---|---|---|
| Exonic (homozygous) | Retinitis Pigmentosa | MAK | HDR with ssODN donor | 31.2% cutting efficiency [21] | Restoration of retinal transcript and protein [21] |
| Deep Intronic | Leber Congenital Amaurosis | CEP290 | NHEJ-mediated excision | Not quantified | Correction of transcript splicing and protein expression [21] |
| Dominant Gain-of-Function | Autosomal Dominant RP | RHO | Allele-specific NHEJ | Not quantified | Selective disruption of mutant allele [21] |
| Splice Site | Tuberous Sclerosis Complex | TSC2 | HDR-mediated correction | Successful clone generation [23] | Creation of isogenic lines for disease modeling [23] |
| Small Deletion | Recessive Dystrophic Epidermolysis Bullosa | COL7A1 | HDR with dsDNA donor | 12/17 clones showed HDR [22] | Gene-corrected iPSCs with restored collagen VII [22] |
Advanced CRISPR Tool Selection Guide
Table 2: CRISPR-based editing systems and their applications
| Editing System | Molecular Components | Mechanism of Action | Therapeutic Application | Advantages |
|---|---|---|---|---|
| CRISPR-Cas9 Nuclease | Cas9 nuclease + sgRNA | Creates DSBs, repaired by NHEJ or HDR [24] | Gene disruption, knock-in via HDR [24] | High efficiency for gene knockout [25] |
| Base Editors (CBE, ABE) | Cas9 nickase + deaminase + UGI | Direct chemical conversion of C•G to T•A or A•T to G•C base pairs [20] | Correcting point mutations without DSBs [20] | Avoids DSB-associated risks; theoretically corrects ~95% of pathogenic transition mutations [20] |
| Prime Editors | Cas9 nickase + reverse transcriptase + pegRNA | Uses RT template to copy edited sequence [24] | All 12 possible base-to-base conversions, small insertions/deletions [24] | No DSBs or donor templates needed; highly versatile [24] |
| CRISPRa/i | dCas9 + transcriptional regulators | Activates or represses gene expression without editing DNA sequence [24] | Gene dosage compensation, metabolic pathway regulation [24] | Reversible modulation; no permanent genomic changes [24] |
Experimental Protocol: High-Efficiency Gene Correction in iPSCs
iPSC Culture and Nucleofection
Maintain iPSCs in feeder-free conditions using StemFlex or mTeSR Plus medium on Matrigel-coated plates [26]. For nucleofection, ensure cells are at 80-90% confluency in a 6-well plate and change to cloning media (StemFlex with 1% Revitacell and 10% CloneR) one hour pre-treatment [26]. Dissociate cells with Accutase for 4-5 minutes to create a single-cell suspension. Prepare the ribonucleoprotein (RNP) complex by combining 0.6 µM guide RNA (IDT) and 0.85 µg/µL of Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT #108105559) with incubation at room temperature for 20-30 minutes [26]. For homology-directed repair, add 5 µM single-stranded oligonucleotide (ssODN) repair template to the RNP complex. To significantly enhance HDR efficiency, co-deliver 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid (Addgene #27077) for transient p53 inhibition [26].
Enhanced HDR Protocol with Pro-Survival Factors
Building upon the base protocol, incorporate the following modifications to dramatically improve cell survival and editing efficiency: Include an HDR enhancer (IDT), electrophoresis enhancers (IDT), and CloneR (STEMCELL Technologies) in the nucleofection mixture [26]. These components address the significant cell death associated with CRISPR-induced double-stranded breaks and single-cell cloning. Following nucleofection, plate cells in cloning media and maintain with daily media changes. This optimized approach has demonstrated remarkable improvements in HDR efficiency, achieving rates up to 59.5% in bulk sequencing—a 21-fold increase over the base protocol—and exceeding 90% homologous recombination in some iPSC lines [26]. The combination of p53 inhibition and pro-survival small molecules creates a synergistic effect that allows edited cells to recover and proliferate, reducing the timeline for generating isogenic lines to as little as 8 weeks [26].
Clone Screening and Validation
After puromycin selection (if using a selection cassette), plate cells at low density for clonal isolation and expansion [22]. Screen clones using a combination of PCR-based genotyping and Sanger sequencing to identify precisely edited clones. For comprehensive off-target assessment, employ whole genome sequencing on edited clones using tools like Cas-OFFinder to analyze potential off-target sites [26]. Perform karyotype analysis via G-banding to confirm genomic integrity, as the use of pro-survival factors, while beneficial for efficiency, raises theoretical concerns about promoting chromosomal abnormalities [26]. Validated studies have demonstrated that short-term exposure to these anti-apoptotic compounds does not increase the selection of abnormal karyotypes [26].
Figure 1: High-efficiency CRISPR-Cas9 gene correction workflow in iPSCs, featuring p53 inhibition and pro-survival factors to enhance HDR rates.
Disease-Specific Application Notes
Neurological Disorders: Alzheimer's Disease Modeling
For neurodegenerative conditions like Alzheimer's disease, CRISPR-corrected iPSCs enable precise disease modeling and drug screening platforms. Target early-onset AD genes (APP, PSEN1, PSEN2) in patient-derived iPSCs to create isogenic controls that recapitulate disease pathology in vitro, including Aβ plaque formation and tau tangles [6]. Differentiate corrected iPSCs into neurons, microglia, and astrocytes to study cell-type-specific contributions to disease pathogenesis. Gene-edited iPSCs have demonstrated reduced abnormal Aβ and tau protein accumulation in AD models, with subsequent improvement in cognitive function in animal studies [6]. The integration of stem cell technology with CRISPR editing provides a platform for both disease modeling and developing autologous cell replacement strategies, addressing the limitations of current pharmacological treatments that only manage symptoms without altering disease progression [6].
Metabolic and Hepatic Disorders
The liver has emerged as a particularly amenable target for CRISPR therapies due to the preferential accumulation of lipid nanoparticles (LNPs) in hepatic tissue following systemic administration [27]. Ongoing clinical trials have demonstrated the feasibility of in vivo CRISPR-Cas9 approaches for liver-directed therapies, with Intellia Therapeutics' phase I trial for hereditary transthyretin amyloidosis (hATTR) showing durable ~90% reduction in disease-related protein levels sustained over two years [27]. This systemic LNP delivery approach represents a significant advancement over ex vivo editing strategies, as it eliminates the need for cell transplantation and enables direct in vivo genetic correction. Similar success has been observed with hereditary angioedema (HAE), where LNP-delivered CRISPR therapies reduced kallikrein levels by 86% and dramatically decreased inflammation attacks [27].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents for CRISPR-Cas9 gene editing in iPSCs
| Reagent Category | Specific Product/System | Manufacturer | Function | Application Notes |
|---|---|---|---|---|
| Cas9 Nuclease | Alt-R S.p. HiFi Cas9 Nuclease V3 | IDT | High-fidelity genome editing | Reduces off-target effects [26] |
| iPSC Culture | StemFlex Medium | Gibco | Maintains pluripotency | Feeder-free culture system [26] |
| iPSC Culture | mTeSR Plus | STEMCELL Technologies | Maintains pluripotency | Alternative feeder-free system [26] |
| Transfection | Nucleofection System | Lonza | Efficient RNP delivery | Higher efficiency than lipofection [26] |
| HDR Enhancement | HDR Enhancer | IDT | Improves homology-directed repair | Increases precise editing efficiency [26] |
| Cell Survival | CloneR | STEMCELL Technologies | Enhances single-cell survival | Critical for clonal expansion [26] |
| p53 Inhibition | pCXLE-hOCT3/4-shp53-F | Addgene | Temporary p53 suppression | Boosts HDR efficiency 11-fold [26] |
| Matrix | Matrigel | Corning | iPSC attachment surface | Essential for feeder-free culture [26] |
Mechanism of CRISPR-Cas9 Action and DNA Repair Pathways
Figure 2: CRISPR-Cas9 mechanisms and DNA repair pathways for different genetic outcomes.
The integration of CRISPR-Cas9 technology with iPSC-based disease modeling has created a powerful platform for addressing monogenic disorders through genetic correction. The development of refined editing approaches—including high-efficiency HDR protocols, base editing systems that avoid double-strand breaks, and improved delivery methods like lipid nanoparticles—has accelerated the translation of these technologies toward clinical applications [26] [20] [27]. The recent success of in vivo CRISPR therapies in clinical trials, coupled with the creation of personalized treatments for rare genetic conditions, demonstrates the remarkable potential of this approach to address previously untreatable diseases [27]. As the field advances, key challenges remain in optimizing delivery efficiency, minimizing off-target effects, and establishing international regulatory frameworks [28]. However, the continuous refinement of CRISPR-based therapeutics promises to expand the treatment landscape for monogenic disorders, ultimately enabling personalized, curative approaches that target the fundamental genetic causes of disease rather than merely managing symptoms.
The combination of CRISPR-Cas9 gene editing and human induced pluripotent stem cells (iPSCs) has revolutionized disease modeling by enabling the creation of isogenic cell pairs—genetically identical lines differing only at a specific locus of interest [29]. These meticulously controlled cellular models provide an unprecedented ability to establish causative relationships between genetic variations and disease phenotypes, free from the confounding effects of divergent genetic backgrounds [30] [29]. This application note details the methodologies, applications, and technical considerations for leveraging CRISPR-Cas9 in iPSCs to generate isogenic pairs for functional studies, with particular emphasis on their critical role in advancing disease correction research.
The fundamental power of isogenic pairs lies in their capacity to isolate the functional impact of a single genetic variable. While patient-derived iPSCs retain the complete genetic background of the donor, including all natural genetic variations that can obscure phenotypic analysis, isogenic controls provide a solution to this limitation [9]. Through precise genome editing, researchers can either introduce a specific pathogenic mutation into a healthy iPSC line or correct the disease-causing mutation in a patient-derived line, resulting in genetically matched pairs that differ only at the target locus [29] [9]. This approach has become indispensable for validating disease mechanisms and conducting high-content drug screens with enhanced sensitivity and specificity [30] [9].
Key Methodological Approaches
Strategic Workflow for Isogenic Pair Generation
The generation of isogenic iPSC pairs follows a systematic workflow that can be adapted based on the nature of the genetic modification and the starting cell line. Table 1 outlines the primary strategic approaches for creating these critical research tools.
Table 1: Strategic Approaches for Generating Isogenic iPSC Pairs
| Strategy | Starting Cell Line | Genetic Modification | Research Application |
|---|---|---|---|
| Disease Introduction | Healthy control iPSC line | Introduce pathogenic mutation via HDR [9] | Model disease mechanisms from wild-type baseline |
| Therapeutic Correction | Patient-derived iPSC line | Correct disease-causing mutation via HDR [30] [29] | Study reversal of pathology; autologous therapy development |
| SNP Installation | iPSC line heterozygous at target SNP | Edit to homozygous states using ssODN templates [31] | Functional validation of disease-associated non-coding variants |
The following diagram illustrates the core decision-making workflow for selecting and implementing the appropriate strategy based on research objectives and starting materials:
High-Efficiency CRISPR-Cas9 Editing Protocol
Recent methodological advances have dramatically improved the efficiency of precise genome editing in iPSCs. The protocol below incorporates key enhancements that achieve homologous recombination rates exceeding 90% by addressing the primary challenges of cell death and low HDR efficiency in pluripotent stem cells [3].
Pre-editing Preparation
- gRNA Design: Identify a target site within 10 nucleotides of the intended edit using specialized software (e.g., Benchling) [3] [31]. When possible, design silent mutations in the Protospacer Adjacent Motif (PAM) site in the repair template to prevent re-cutting [3].
- Repair Template Design: For single nucleotide changes, design single-strand oligonucleotides (ssODNs) with approximately 65 bp homology arms flanking the target site [31]. For larger edits, consider using double-stranded DNA templates with longer homology arms.
- Ribonucleoprotein (RNP) Complex Assembly: Combine 0.6 µM guide RNA with 0.85 µg/µL of high-fidelity Cas9 nuclease and incubate at room temperature for 20-30 minutes to form RNP complexes [3]. This approach minimizes off-target effects compared to plasmid-based expression systems.
Cell Preparation and Transfection
- Culture Conditions: Maintain iPSCs in feeder-free conditions using Matrigel-coated plates and defined media (e.g., mTeSR Plus or StemFlex) [3] [31].
- Transfection Enhancements: Change to cloning media supplemented with pro-survival additives 1 hour prior to transfection. The optimized formulation includes:
- Nucleofection: Harvest cells at 80-90% confluency using Accutase. Combine the pre-formed RNP complex with 5 µM ssODN repair template and 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid (for transient p53 suppression) [3]. Use appropriate nucleofection program for your iPSC line.
Post-transfection Recovery and Clonal Isolation
- Recovery Culture: Plate transfected cells at appropriate density in cloning media with pro-survival additives. Maintain cultures for 48-72 hours without disturbance to support recovery.
- Antibiotic Selection: If using a selection strategy, apply appropriate antibiotics 72 hours post-transfection to enrich for successfully edited cells [31].
- Single-Cell Cloning: Using limiting dilution or FACS, isolate single cells into 96-well plates pre-coated with Matrigel and containing conditioned cloning media [3] [31]. Culture for 2-3 weeks with regular media changes until colonies form.
- Screening and Validation: Expand clones and screen using a combination of:
Technical Optimization and Troubleshooting
Enhancing Editing Efficiency
The inherently low efficiency of homology-directed repair in iPSCs represents a significant technical challenge. Table 2 summarizes key optimization strategies that dramatically improve HDR rates while maintaining cell viability.
Table 2: Optimization Strategies for Improving HDR Efficiency in iPSCs
| Challenge | Solution | Mechanism of Action | Reported Improvement |
|---|---|---|---|
| Low HDR efficiency | HDR enhancers (e.g., from IDT) | Modulates DNA repair pathway choice | Up to 21-fold increase [3] |
| Cell death post-transfection | p53 suppression (shRNA) | Reduces apoptosis from DNA damage response | 11-fold increase in HDR [3] |
| Single-cell survival | CloneR supplement | Enhances viability of dissociated cells | Critical for clonal expansion [3] |
| Electroporation stress | ROCK inhibitor (Y-27632) | Prevents anoikis in single cells | Standard in iPSC culture [3] |
Advanced Editing Systems
While CRISPR-Cas9 remains the most widely used platform, emerging CRISPR systems offer additional capabilities:
- CRISPR-Cas12a: This system enables multiplexed genome editing and has demonstrated utility in studying complex genetic interactions in disease models [32] [33]. Cas12a recognizes different PAM sequences than Cas9, expanding the targetable genomic space.
- Base Editing: For precise single-nucleotide changes without double-strand breaks, base editing systems offer an alternative with potentially reduced indel formation [9].
- Prime Editing: This newer technology allows for precise small insertions, deletions, and all possible base-to-base conversions without requiring double-strand breaks or donor templates.
Applications in Disease Modeling and Drug Development
Neurodegenerative Disease Modeling
The CRISPR-iPSC platform has generated significant insights into neurodegenerative disease mechanisms:
- Huntington's Disease: Isogenic iPSC lines with corrected CAG repeats in the Huntingtin gene have demonstrated recovery from phenotypic abnormalities and gene expression changes in derived neural cells [30]. These models have elucidated pathways involving mitochondrial dysfunction, excitotoxicity, and transcriptional dysregulation [30].
- Alzheimer's Disease: Introduction of APP and PSEN1 mutations into isogenic backgrounds has successfully reproduced early pathological features including Aβ deposition and tau phosphorylation in iPSC-derived neurons [9].
- Parkinson's Disease: Isogenic lines with LRRK2 G2019S mutations exhibit mitochondrial dysfunction and enhanced vulnerability in dopaminergic neurons, providing platforms for mechanistic studies and compound screening [9].
High-Throughput Screening Applications
Isogenic iPSC pairs provide exceptional model systems for drug discovery through:
- Target Validation: By comparing compound effects between isogenic pairs, researchers can confidently establish whether therapeutic efficacy is mutation-specific [9].
- Toxicity Assessment: iPSC-derived cardiomyocytes with mutations in KCNQ1 or SCN5A generated via CRISPR editing are widely used for cardiac safety pharmacology [9].
- Personalized Medicine: Creating multiple isogenic lines from different genetic backgrounds allows assessment of how individual genomes influence drug response, advancing precision medicine approaches [9].
The following diagram illustrates the integrated pipeline from isogenic line generation to drug screening applications:
Research Reagent Solutions
Successful generation of isogenic iPSC pairs requires carefully selected reagents and systems. Table 3 catalogizes essential research reagents with their specific functions in the editing workflow.
Table 3: Essential Research Reagents for CRISPR-iPSC Workflows
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| CRISPR Components | Alt-R S.p. HiFi Cas9 Nuclease V3 [3], sgRNAs | Precision DNA cleavage | High-fidelity Cas9 reduces off-target effects |
| Repair Templates | ssODNs [31], dsDNA donors | Homology-directed repair | 65 bp homology arms optimal for ssODNs [31] |
| Cell Culture | mTeSR Plus [3], StemFlex [31], Matrigel | Maintain pluripotency | Feeder-free culture systems preferred |
| Transfection | FuGENE HD [31], Nucleofection systems | Deliver editing components | Liposome-based for simple edits; electroporation for challenging edits |
| Survival Enhancers | CloneR [3], RevitaCell [3], Y-27632 | Enhance single-cell viability | Critical step for clonal expansion post-editing |
| p53 Inhibition | pCXLE-hOCT3/4-shp53-F plasmid [3] | Temporary p53 suppression | Increases HDR efficiency 11-fold [3] |
| Validation Tools | Sanger sequencing, Karyotyping, ICE analysis [3] | Confirm edits and genomic integrity | Essential quality control steps |
The creation of isogenic iPSC pairs through CRISPR-Cas9 genome editing represents a transformative methodology for functional genetic studies. By eliminating confounding genetic variables, these models enable researchers to establish definitive causal relationships between genetic mutations and disease phenotypes. The optimized protocols detailed in this application note—incorporating p53 suppression, pro-survival additives, and refined delivery methods—have dramatically improved editing efficiencies to practically feasible levels.
As the field advances, emerging technologies including CRISPR-Cas12a for multiplexed editing [32] [33], base editing for precision single-nucleotide changes, and organoid differentiation for complex tissue modeling are further expanding the applications of isogenic pairs. When combined with automated screening platforms and computational approaches, these tools are accelerating the pace from disease gene discovery to therapeutic development. The continued refinement of these protocols will undoubtedly enhance our understanding of disease mechanisms and contribute to the development of targeted interventions for genetic disorders.
Implementing CRISPR-iPSC Workflows: From Target Selection to Corrected Cell Lines
Guide RNA Design and Validation Strategies for High-Efficiency Editing
The success of CRISPR-Cas9 genome editing in induced pluripotent stem cells (iPSCs) for disease modeling and correction hinges on the design and validation of highly efficient guide RNAs (gRNAs). The gRNA serves as the molecular GPS, directing the Cas9 nuclease to a specific genomic locus with precision. In the context of therapeutic applications, where the goal is to correct disease-causing mutations in patient-derived iPSCs, achieving high editing efficiency with minimal off-target effects is paramount. This protocol details comprehensive strategies for designing and validating gRNAs to achieve homologous recombination rates exceeding 90% in human iPSCs, a critical benchmark for generating isogenic controls in disease research [26] [34].
Optimized gRNA design must account for multiple factors, including the sequence context of the target site, the choice of Cas9 variant, and the unique biological characteristics of iPSCs. The advent of high-fidelity Cas9 variants and sophisticated deep learning models for gRNA activity prediction has dramatically improved the predictability of editing outcomes. This document integrates these advanced tools with wet-lab validation protocols to provide a complete framework for researchers aiming to develop precise disease models through genome editing [35].
Key Principles of gRNA Design
Sequence Determinants of gRNA Activity
The guide RNA sequence is the primary determinant of both on-target efficiency and off-target specificity. The ideal gRNA spacer sequence is 20 nucleotides long, although some Cas9 orthologs like FrCas9 show optimal activity with 21-22 bp guides [36]. The sequence must be complementary to the target DNA and must be immediately adjacent to a Protospacer Adjacent Motif (PAM). For the most commonly used Cas9 from Streptococcus pyogenes (SpCas9), the PAM sequence is 5'-NGG-3' [37].
Several sequence features influence gRNA activity. A guanine (G) at the first position of the spacer sequence is often beneficial when using the human U6 promoter, though the mouse U6 promoter can initiate transcription with either adenine (A) or G, expanding targetable sites [35]. The melting temperature and local DNA geometry of the target site also contribute to editing efficiency. Furthermore, research has revealed that DNA repair from double-strand breaks is asymmetric, favoring repair in one direction. This property can be exploited by designing gRNAs and repair templates to favor the desired repair outcome [37].
Advanced gRNA Design Tools and Models
Traditional gRNA design rules based on sequence features have been superseded by deep learning models trained on large-scale activity datasets. These models offer superior predictive power for gRNA on-target efficiency.
For instance, the DeepHF tool uses a combination of a recurrent neural network (RNN) and important biological features to predict gRNA activity for wild-type SpCas9 and two high-fidelity variants, eSpCas9(1.1) and SpCas9-HF1 [35]. This tool was developed from a genome-scale screen measuring the indel rates of over 50,000 gRNAs covering approximately 20,000 genes, providing an extensive data foundation for its predictions.
When designing gRNAs for complex genomes, additional considerations apply. For example, in hexaploid wheat, a crop with a large, repetitive genome, researchers must perform exhaustive BLAST analyses to ensure gRNA specificity and avoid off-target editing across highly similar gene homologs [38]. While this example is from plant biology, the principle is equally relevant when targeting gene families with high sequence homology in human iPSCs.
Table 1: Key Design Parameters for High-Efficiency gRNAs
| Design Parameter | Optimal Characteristic | Impact on Editing |
|---|---|---|
| Spacer Length | 20 nt (SpCas9), 21-22 nt (FrCas9) [36] | Ensures proper Cas9 binding and cleavage |
| PAM Sequence | 5'-NGG-3' (SpCas9); 5'-NNTA-3' (FrCas9) [36] | Defines targetable genomic sites |
| 5' Nucleotide | G (hU6 promoter); A or G (mU6 promoter) [35] | Affects gRNA transcription initiation |
| Target Location | <10 bp from desired mutation [26] | Maximizes HDR efficiency for point mutations |
| GC Content | Moderate (40-60%) | Precludes overly stable or unstable binding |
Computational Design and In Silico Validation
gRNA Design Workflow
The initial design phase involves identifying potential gRNA targets within your gene of interest and rigorously filtering them for predicted efficiency and specificity.
Step 1: Target Site Identification. Using a design tool like the one provided by IDT, input the genomic sequence flanking your target site, such as a disease-associated SNP. The tool will output all possible gRNA spacer sequences with their corresponding PAMs [34].
Step 2: Efficiency Scoring. Score the resulting gRNAs using a predictive algorithm like DeepHF, which integrates sequence features and deep learning to rank gRNAs by their predicted on-target activity [35].
Step 3: Specificity Analysis. Perform a BLAST search or use dedicated off-target prediction tools to identify genomic loci with high sequence similarity to your candidate gRNA. A high-quality gRNA should have minimal (≤3) off-target sites with 1-3 mismatches, especially in seed regions near the PAM [38].
Step 4: Secondary Structure Check. Analyze the candidate gRNA sequence for potential secondary structures or self-complementarity that could impede its binding to the Cas9 protein or the target DNA. Tools like RNAfold can predict secondary structures and calculate Gibbs free energy, where a less negative ΔG indicates a more stable and functional gRNA [38].
The following diagram illustrates the core decision-making workflow for selecting a candidate gRNA:
Designing the Repair Template
For precise gene correction via Homology-Directed Repair (HDR), a single-stranded oligodeoxynucleotide (ssODN) repair template must be co-designed with the gRNA. The repair template should contain the desired corrective mutation flanked by homology arms.
To prevent re-cleavage of the edited locus by Cas9, introduce silent mutations in the PAM sequence or in the seed region of the protospacer within the repair template. This is a critical step for enriching HDR-edited cells [26]. The repair template should be designed so the mutation is located close to the Cas9 cut site (ideally within 10 bp) to maximize HDR efficiency [26].
Experimental Validation of gRNA Efficiency
A High-Efficiency Workflow for iPSCs
Achieving high editing efficiency in iPSCs requires not only a well-designed gRNA but also optimized delivery and cell culture conditions to enhance cell survival post-editing. The following protocol, which can be completed in approximately 8 weeks, has been shown to achieve homologous recombination rates over 90% in human iPSCs [34].
Key Reagents and Materials:
- Biological Material: Human iPSC line (e.g., NDC1)
- Culture Medium: mTeSR Plus or Stemflex medium, supplemented with CloneR and RevitaCell to support single-cell survival.
- Nucleofection System: Lonza 4D Nucleofector with P3 Primary Cell Solution.
- CRISPR Components:
- Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT)
- Synthetic sgRNA (IDT, custom)
- ssODN repair template (IDT, 4 nmol Ultramer scale)
- Pro-Survival Supplements:
- Alt-R Cas9 HDR enhancer (IDT)
- p53 shRNA plasmid (e.g., pCXLE-hOCT3/4-shp53-F from Addgene)
Table 2: Research Reagent Solutions for iPSC Editing
| Reagent / Solution | Function / Purpose | Example Source / Catalog |
|---|---|---|
| Alt-R S.p. HiFi Cas9 V3 | High-fidelity nuclease for targeted DNA cleavage | IDT #10810559 |
| Synthetic sgRNA | Guides Cas9 to the specific genomic target; increases efficiency and reproducibility | IDT (custom) |
| ssODN Repair Template | Single-stranded DNA donor for introducing precise edits via HDR | IDT Ultramer |
| P3 Primary Cell Solution | Buffer optimized for nucleofection of sensitive cells like iPSCs | Lonza |
| CloneR & RevitaCell | Supplements that inhibit ROCK and improve single-cell survival post-editing | STEMCELL Technologies |
| Alt-R HDR Enhancer | Small molecule that improves the frequency of homology-directed repair | IDT #1081062 |
| p53 shRNA Plasmid | Knocking down p53 reduces CRISPR-induced apoptosis, improving cell survival | Addgene #27077 |
Step-by-Step Protocol:
- In Silico Design: Design sgRNA and ssODN using the IDT online tool. The ssODN should contain your desired edit and silent mutations to disrupt the PAM [34].
- RNP Complex Formation: For each nucleofection reaction, combine 0.85 µg/µL HiFi Cas9 V3 and 100 µM sgRNA in Duplex Buffer. Incubate at room temperature for 20-30 minutes to form the Ribonucleoprotein (RNP) complex [34].
- Cell Preparation: Culture iPSCs to 80-90% confluency in a 6-well plate. Pre-treat cells by changing to cloning media (Stemflex with 1% RevitaCell and 10% CloneR) 1 hour before nucleofection. Dissociate cells into a single-cell suspension using Accutase and count them [34].
- Nucleofection Reaction: For each test reaction, combine:
- 1 µL shp53-f2 plasmid (50 ng/µL)
- 1 µL Alt-R Electroporation Enhancer
- 1 µL ssODN (100 µM)
- 5 µL prepared RNP complex
- ~1 million cells in 11 µL
- Complete to 20 µL with P3 nucleofector solution mix. Include controls: a GFP-only control for transfection efficiency and a no-pulse control for viability [34].
- Nucleofection and Recovery: Transfer the reaction to a 16-well Nucleocuvette Strip and nucleofect using the appropriate program (e.g., CA-137 for iPSCs). Immediately after nucleofection, add pre-warmed Nucleofection Media (CloneR media with HDR enhancer) and transfer the cells to a Matrigel-coated plate [34].
- Culture and Analysis: Change the media to cloning media the next day. After 48-72 hours, extract genomic DNA using a kit like Zymo quick DNA MicroPrep. Analyze editing efficiency using TIDE decomposition or ICE analysis (Synthego) on PCR-amplified target sites [26] [34].
The entire experimental journey, from design to validation, is summarized below:
Validation and Analysis
Following editing, precise validation is crucial.
- Initial Efficiency Check: Use TIDE (Tracking of Indels by Decomposition) or ICE (Inference of CRISPR Edits) analysis on bulk PCR products from the edited cell population. This provides a quantitative estimate of the indel frequency or HDR efficiency without the need for single-cell cloning [26].
- Clone Isolation and Screening: If a clonal population is required, single-cell sort the edited iPSCs and expand them into individual clones. Screen these clones by Sanger sequencing to identify those carrying the precise genetic correction.
- Off-Target Assessment: Use tools like Cas-OFFinder to predict potential off-target sites based on the gRNA sequence [26]. Amplify and sequence the top candidate off-target loci from your final edited clonal line to confirm editing specificity. Whole-genome sequencing provides the most comprehensive safety profile [26].
The integration of sophisticated computational design with optimized wet-lab protocols has transformed the landscape of genome editing in iPSCs. By adhering to the detailed strategies outlined in this document—selecting gRNAs with high predicted activity using deep learning models, designing repair templates with PAM-disrupting mutations, and employing a cell-friendly workflow featuring RNP delivery and p53 inhibition—researchers can consistently achieve high-efficiency precision editing. This robust framework enables the reliable generation of isogenic iPSC lines, accelerating the study of disease mechanisms and the development of future regenerative therapies.
The application of CRISPR-Cas9 gene editing in induced pluripotent stem cells (iPSCs) represents a paradigm-shifting approach for modeling genetic diseases and developing autologous cell replacement therapies [39] [8]. However, a significant technical challenge in this field remains the efficient and safe delivery of CRISPR components into these hard-to-transfect cells [39]. The delivery platform chosen directly impacts editing efficiency, specificity, cell viability, and ultimately the translational potential of the research. This application note provides a systematic comparison of three prominent delivery platforms—electroporation, viral vectors, and virus-like particles (VLPs)—within the specific context of CRISPR-Cas9 genome editing in iPSCs for disease correction research. We include structured quantitative comparisons, detailed experimental protocols, and essential workflow diagrams to guide researchers in selecting and implementing the optimal delivery strategy for their experimental goals.
Comparative Analysis of Delivery Platforms
The choice of delivery method is governed by multiple interrelated factors, including the desired editing outcome, the format of the CRISPR cargo, and the requirements for downstream applications. Table 1 provides a quantitative comparison of the three platforms across key performance metrics.
Table 1: Platform Comparison for CRISPR Delivery in iPSCs
| Parameter | Electroporation | Viral Vectors (AAV) | VLP Platforms |
|---|---|---|---|
| Typical Cargo Format | RNP (preferred), mRNA, plasmid DNA [40] [41] | Plasmid DNA (size-limited) [40] | Pre-assembled RNP complexes [42] |
| Editing Efficiency in iPSCs | High (with optimized protocols) [43] | Moderate to High [41] | High (demonstrated in HEK293 for VLP production) [42] |
| Time to Max Editing Activity | Very rapid (hours for RNP) [41] | Delayed (days, requires transcription) [39] | Rapid (immediate activity upon delivery) [40] |
| Off-Target Risk | Low (transient activity of RNP) [40] [41] | Moderate (prolonged expression) [42] [40] | Very Low (highly transient delivery) [42] [40] |
| Cargo Capacity | Virtually unlimited [41] | Very Limited (~4.7 kb for AAV) [40] [41] | Limited by VLP packaging [40] |
| Cell Viability Impact | Moderate to High (requires optimization) [39] | High (low cytotoxicity) [40] | High (low cytotoxicity) [40] |
| Immunogenicity Concern | Low | Moderate (host immune response) [40] | Low (no viral genome) [40] |
| Ideal Application | High-efficiency knockout/knock-in (ex vivo) | In vivo delivery, stable expression [41] | Transient, safe editing (ex vivo & in vivo potential) [42] [40] |
| Relative Cost | Moderate | High | High [40] |
Platform-Specific Protocols
Electroporation for RNP Delivery in iPSCs
Electroporation is a physical method that uses electrical pulses to create transient pores in the cell membrane, allowing for the direct cytosolic delivery of macromolecules like CRISPR RNP complexes [39]. It is currently the gold standard for achieving high editing efficiencies in iPSCs with minimal off-target effects due to the transient nature of RNP activity [40] [41].
Detailed Protocol: CRISPR-Cas9 RNP Nucleofection in hiPSCs
Key Reagent Solutions:
- Cells: High-quality, healthy human iPSCs grown in clonal densities or as a monolayer with >90% viability.
- CRISPR RNP Complex: Synthesize by combining purified Cas9 protein (e.g., 30-60 pmol) with synthetic sgRNA (at a 1:2 molar ratio) in nuclease-free buffer. Incubate at 25°C for 10-20 minutes to form the RNP complex.
- Nucleofector Device & Kit: Use a system specifically optimized for stem cells (e.g., Lonza Nucleofector 2b Device with the P3 Primary Cell 96-Well Nucleofector Kit).
Procedure:
- Harvesting Cells: Gently dissociate iPSCs into a single-cell suspension using a non-enzymatic cell dissociation reagent. Accurate cell counting and determination of viability (>90%) are critical.
- Preparation: For each nucleofection, centrifuge 1 x 10^5 to 2 x 10^5 cells. Aspirate the supernatant completely.
- Resuspension: Resuspend the cell pellet in 20 µL of pre-warmed Nucleofector Solution supplemented with 4 µL of Supplement.
- RNP Delivery: Add the pre-complexed RNP (up to 5 µL) to the cell suspension. Mix gently by pipetting. Avoid introducing bubbles.
- Electroporation: Transfer the entire cell-RNP mixture into a single well of a 96-well Nucleofector cuvette. Execute the appropriate pre-optimized electrical program (e.g., CA-137 for hiPSCs on the Lonza system).
- Recovery: Immediately after pulsing, add 80 µL of pre-warmed, antibiotic-free culture medium to the cuvette. Gently transfer the cell suspension (total ~100 µL) onto a Matrigel-coated well containing pre-warmed complete medium with a ROCK inhibitor (e.g., Y-27632).
- Post-Transfection Culture: Change the medium 24 hours post-nucleofection to remove the ROCK inhibitor and any dead cells. Allow cells to recover for 48-72 hours before assaying for editing efficiency or proceeding with clonal expansion.
Troubleshooting Notes:
- Low Viability: Optimize cell number, ensure the health of the starting culture, and avoid over-trypsinization.
- Low Editing Efficiency: Titrate the RNP concentration, verify sgRNA activity, and ensure the RNP complex is properly formed.
- Procedure: A generalized workflow for this protocol is illustrated in Figure 1.
- Figure 1: Electroporation Workflow for iPSCs. This diagram outlines the key steps for delivering CRISPR-Cas9 via RNP nucleofection into human iPSCs.
Viral Vector-Mediated Delivery (AAV)
Adeno-associated virus (AAV) is a popular viral vector for gene delivery due to its low immunogenicity and ability to infect non-dividing cells [40] [41]. Its primary limitation for CRISPR delivery is a constrained cargo capacity of ~4.7 kb, which is insufficient for the standard SpCas9 (∼4.2 kb) plus sgRNA expression cassettes [40]. Strategies to overcome this include using smaller Cas9 orthologs (e.g., SaCas9) or splitting the Cas9 and sgRNA across two separate AAV vectors [41].
Detailed Protocol: AAV Transduction of iPSCs for CRISPR Delivery
Key Reagent Solutions:
- AAV Vectors: Purified AAV vectors (e.g., AAV-DJ or AAV6 serotypes with good tropism for stem cells) containing either a SaCas9 expression construct and sgRNA, or a split-intein SpCas9 system.
- Cells: iPSCs seeded as small clusters or a confluent monolayer.
- Polybrene: Used to enhance viral transduction efficiency.
Procedure:
- Cell Seeding: Plate healthy iPSCs at an appropriate density (e.g., 1x10^5 cells/well in a 24-well plate) 24 hours before transduction.
- Virus Preparation: Thaw AAV vectors on ice. Prepare the viral inoculum in cold culture medium supplemented with 4-8 µg/mL polybrane.
- Transduction: Aspirate the medium from the cells and carefully add the virus-containing medium.
- Incubation: Incubate the cells with the virus for 24 hours at 37°C. Gently rock the plate every few hours to ensure even distribution.
- Medium Change: After 24 hours, carefully remove the virus-containing medium and replace it with fresh, complete stem cell medium.
- Expression & Analysis: Allow 48-72 hours for transgene expression and genome editing to occur before analyzing editing efficiency.
Troubleshooting Notes:
- Low Transduction Efficiency: Titrate the multiplicity of infection (MOI), test different AAV serotypes, and optimize polybrane concentration.
- Cytotoxicity: Reduce the MOI or polybrane concentration if toxicity is observed.
- Procedure: The general process for viral vector production and transduction is summarized in Figure 2.
- Figure 2: AAV Transduction Workflow. This diagram illustrates the primary steps for transducing iPSCs with CRISPR-loaded AAV vectors.
Virus-Like Particle (VLP) Platforms
VLPs are engineered particles that mimic the structure of viruses but lack the viral genome, making them non-replicative and non-integrating [42] [40]. They are emerging as a promising platform for the transient and safe delivery of CRISPR RNP complexes, combining the high efficiency of viral transduction with the favorable safety profile of non-viral methods [42].
Detailed Protocol: Using Pre-packaged VLPs for iPSC Transduction
Key Reagent Solutions:
- CRISPR VLPs: Pre-manufactured, purified VLPs loaded with Cas9 RNPs. These are often produced by transfecting packaging cells (e.g., HEK293) with plasmids encoding structural viral proteins and the CRISPR cargo, typically via scalable electroporation [42].
- Cells: iPSCs seeded as small clusters.
Procedure:
- Cell Seeding: Plate iPSCs one day prior to transduction.
- VLP Preparation: Thaw VLPs on ice. Dilute to the desired working concentration in cold culture medium.
- Transduction: Aspirate the medium from the cells and add the VLP-containing medium.
- Incubation & Harvest: Incubate cells with VLPs for 24-48 hours. VLP-mediated editing can be very rapid, with functional harvests possible as early as 24 hours post-transduction [42].
- Analysis: Harvest cells to assess editing efficiency. No need to remove the VLP-containing medium if the analysis is performed within 48 hours.
Troubleshooting Notes:
- Low Editing Activity: Titrate the volume or concentration of VLP stock used. Ensure VLPs have been stored and handled correctly to maintain stability.
- Procedure: The manufacturing and application process for CRISPR VLPs is shown in Figure 3.
- Figure 3: VLP-Mediated Delivery Workflow. This diagram outlines the process from VLP production in packaging cells to the transduction of target iPSCs.
The Scientist's Toolkit: Essential Research Reagents
Successful genome editing in iPSCs relies on a suite of specialized reagents. Table 2 catalogs the key materials required for the experiments described in this note.
Table 2: Essential Reagents for CRISPR Delivery in iPSCs
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| CRISPR Cargo | Purified Cas9 Protein [41] | Core nuclease for RNP assembly; ensures rapid, transient activity. |
| Synthetic sgRNA [41] | Guides Cas9 to specific genomic locus; chemical synthesis ensures high purity. | |
| HDR Donor Template [21] [43] | Single-stranded oligodeoxynucleotide (ssODN) or double-stranded DNA vector for precise gene correction. | |
| Delivery-Specific Reagents | Nucleofector Kit for Stem Cells [43] | Optimized buffers and reagents for high-efficiency electroporation of sensitive iPSCs. |
| AAV Vectors (e.g., AAV-DJ/6) [41] | For viral delivery; serotype choice affects tropism and efficiency in iPSCs. | |
| Pre-packaged CRISPR VLPs [42] | For transient RNP delivery with viral-like efficiency but enhanced safety. | |
| Cell Culture & Support | ROCK Inhibitor (Y-27632) [43] | Critical for enhancing survival of iPSCs post-dissociation and electroporation. |
| Matrigel or Recombinant Laminin-521 [43] | Defined substrates for coating culture vessels to support iPSC attachment and growth. | |
| Analysis & Validation | T7 Endonuclease I or Surveyor Assay | Detects induced mutations at the target site via mismatch cleavage. |
| Sanger Sequencing & ICE Analysis [42] | Confirms editing and quantifies the percentage of insertions/deletions (indels). |
Electroporation, viral vectors, and VLP platforms each offer distinct advantages and limitations for delivering CRISPR-Cas9 to iPSCs. Electroporation of RNP complexes remains the preferred method for most ex vivo applications requiring high efficiency and minimal off-target effects. AAV vectors are invaluable for specific in vivo applications and when stable expression is needed, despite cargo constraints. VLPs represent a cutting-edge alternative that merges the high efficiency of viral transduction with the favorable safety profile of non-viral RNP delivery. The choice of platform should be guided by the specific experimental objectives, whether for high-throughput disease modeling, precise gene correction for therapeutic development, or in vivo investigation. The protocols and data summarized herein provide a foundational guide for researchers to navigate these critical methodological decisions.
Duchenne Muscular Dystrophy (DMD) is a severe X-linked neuromuscular disorder affecting approximately 1 in 3,800-6,300 male births, characterized by progressive muscle degeneration due to mutations in the dystrophin gene [44] [45]. The emergence of CRISPR-Cas9 genome editing technology, particularly when integrated with human induced pluripotent stem cells (iPSCs), has revolutionized therapeutic approaches for monogenic disorders like DMD [2]. This case study examines the application of CRISPR-mediated exon skipping strategies to correct DMD mutations, with a focus on methodology, efficiency quantification, and translational potential. We present detailed protocols for creating DMD models and implementing corrective editing, providing researchers with practical frameworks for therapeutic development.
The dystrophin gene encompasses 79 exons spanning approximately 2.3 megabases, encoding a critical protein that stabilizes the sarcolemma and mediates force transmission in muscle cells [44] [45]. Mutations disrupting the open reading frame—primarily large deletions (68% of cases), nonsense mutations, or duplications—prevent production of functional dystrophin, leading to progressive muscle weakness, respiratory insufficiency, and cardiomyopathy [44] [46]. Most DMD mutations cluster within two primary hotspots: exons 2-20 and exons 45-55 [44].
Exon skipping therapy aims to convert severe DMD phenotypes to the milder Becker muscular dystrophy (BMD) by restoring the dystrophin reading frame. While antisense oligonucleotides (AONs) can induce transient exon skipping, CRISPR-based approaches enable permanent genomic correction [46] [47]. By targeting splice acceptor or donor sites, CRISPR systems induce selective exon exclusion during RNA processing, producing truncated but functional dystrophin proteins [44] [45].
The integration of iPSC technology provides an ideal platform for developing and testing these strategies. Patient-specific iPSCs can be genetically corrected, differentiated into affected cell types (especially cardiomyocytes and skeletal myoblasts), and analyzed for functional recovery [44] [2].
Quantitative Analysis of CRISPR Exon Skipping Efficiency
Editing Efficiency Across Multiple Exon Targets
Research demonstrates that CRISPR systems can target numerous exons within the DMD mutational hotspots. The table below summarizes efficiency data for various exon targets in iPSC-derived cardiomyocytes (iCMs):
Table 1: Editing Efficiency for DMD Exon Targets in iPSC-Derived Cardiomyocytes
| Target Exon | Editing System | Efficiency (%) | Dystrophin Restoration | Reference |
|---|---|---|---|---|
| Exon 55 | ABE8eV106W-SpCas9 | 35.9% ± 5.7% | 42.5% ± 11% of WT | [44] |
| Exon 45-55 region | Dual CRISPR-Cas3 | High deletion efficiency | Confirmed protein restoration | [48] |
| Exons 6, 7, 8, 43, 44, 46, 53 | ABE with gRNAs | Efficient skipping demonstrated | Functional protein expected | [44] |
| Exon 45 | NanoMEDIC EV delivery | >90% | Confirmed in patient iPSCs | [49] |
Multi-Exon Deletion Strategies for Broader Applicability
To address the diverse mutational landscape of DMD, researchers have developed strategies targeting larger genomic regions applicable to multiple patient genotypes:
Table 2: Multi-Exon Skipping Approaches for DMD Correction
| Target Region | Approach | Deletion Size | Patient Coverage | Key Findings | |
|---|---|---|---|---|---|
| Exons 45-55 | Dual CRISPR-Cas3 | ~340 kb | Applicable to various DMD mutations | Restored dystrophin in iPSCs with three distinct mutations | [48] |
| Exons 48-54 | CRISPR-Cas9 deletion | Variable | Model for exon 55 skipping | Established isogenic DMD model hiPSC line | [44] |
| Exon 45 | NanoMEDIC RNP delivery | Single exon | Specific for Δ44 mutations | Optimized for hard-to-transfect cells | [49] |
Experimental Protocols
Protocol 1: Generation of DMD Model iPSC Line Using CRISPR-Cas9
Purpose: Create an isogenic DMD iPSC line with specific exon deletions for disease modeling and therapeutic testing [44] [50].
Materials:
- Control hiPSC line (wild-type)
- Plasmid vectors: DMD-specific gRNA_Cas9 (e.g., targeting introns 47 and 54 for ΔE48-54), GFP reporter
- Electroporation system
- FACS sorter for GFP+ cells
- Genomic DNA extraction kit
- PCR reagents for genotyping
- Immunofluorescence staining materials (OCT4, NANOG antibodies)
- Trilineage differentiation reagents
Procedure:
- Design and Validation: Design gRNA pairs targeting intronic regions flanking exons of interest (e.g., introns 47 and 54 for ΔE48-54 deletion). Validate gRNA efficiency in preliminary tests [44].
- Cell Transfection: Co-transfect hiPSCs with DMDgRNA_Cas9 plasmids and GFP plasmid via electroporation [44].
- Clone Selection: Sort single GFP+ cells into 96-well plates using FACS at 48-72 hours post-transfection [44].
- Clone Expansion: Culture sorted cells with feeder-conditioned media or defined essential media until colonies form [44].
- Genotypic Validation:
- Extract genomic DNA from expanded clones
- Perform PCR with primers flanking target deletion region
- Confirm precise deletion by Sanger sequencing of PCR products [44]
- Pluripotency Verification:
- Perform immunofluorescence staining for pluripotency markers (OCT4, NANOG)
- Conduct trilineage differentiation assay assessing ectoderm (PAX6), endoderm (SOX17), and mesoderm (CXCR4) markers [44]
Troubleshooting:
- Low transfection efficiency: Optimize electroporation parameters or use alternative delivery methods
- Low deletion rate: Test multiple gRNA pairs with high on-target activity
- Pluripotency loss: Use lower passage hiPSCs and optimize culture conditions
Protocol 2: ABE-Mediated Exon Skipping in DMD iPSC-Derived Cardiomyocytes
Purpose: Restore dystrophin expression in DMD patient iPSC-derived cardiomyocytes through adenine base editing of splice acceptor sites [44].
Materials:
- DMD iPSC line (e.g., ΔE48-54)
- ABE8eV106W-SpCas9 plasmid (engineered for reduced off-target effects)
- gRNA targeting splice acceptor site (e.g., intron 54 for exon 55 skipping)
- Cardiomyocyte differentiation reagents
- RT-PCR reagents
- Western blot equipment and dystrophin antibodies
- Immunofluorescence staining materials
Procedure:
- gRNA Design: Design gRNA with nucleotide A of splice acceptor (AG) at position 5 of spacer sequence to enable ABE conversion to GG [44].
- Cell Transfection: Transfect DMD hiPSCs with ABE8eV106W-SpCas9 and gRNA plasmid via electroporation [44].
- Editing Efficiency Assessment:
- Extract genomic DNA from pool population
- Perform Sanger sequencing of target region
- Calculate editing efficiency using BEAT analysis or similar tools [44]
- Cardiomyocyte Differentiation: Differentiate transfected iPSCs into cardiomyocytes using established serum-free protocols with small molecules [44].
- Exon Skipping Validation:
- Perform RT-PCR with primers flanking skipped exon
- Confirm exon skipping by reduced amplicon size and Sanger sequencing [44]
- Dystrophin Restoration Assessment:
- Analyze protein expression by western blotting
- Quantify dystrophin levels compared to wild-type controls
- Perform immunofluorescence staining for dystrophin and cardiac markers (e.g., cTnT) [44]
Troubleshooting:
- Low editing efficiency: Optimize gRNA design and transfection parameters
- Incomplete exon skipping: Test multiple gRNAs targeting same splice site
- Variable differentiation: Standardize cardiomyocyte differentiation protocol
Protocol 3: NanoMEDIC Extracellular Nanovesicle Delivery for In Vivo Application
Purpose: Achieve efficient in vivo genome editing using transient RNP delivery via engineered extracellular vesicles to minimize immunogenicity and off-target effects [49].
Materials:
- HEK293T producer cells
- Plasmid constructs: FKBP12-Gag, FRB-SpCas9 (N-terminal fusion)
- sgRNA expression vector with Ψ+ packaging signal and ribozymes
- AP21967 dimerizer ligand
- Ultracentrifuge for EV isolation
- Target cells (DMD iPSCs, myoblasts, or in vivo models)
- T7E1 assay or next-generation sequencing for indel analysis
Procedure:
- EV Producer Cell Preparation:
- Transfect HEK293T cells with FKBP12-Gag, FRB-SpCas9, and sgRNA vectors
- Add AP21967 ligand to culture media to induce dimerization and Cas9 packaging [49]
- NanoMEDIC Isolation:
- Collect conditioned media at 48-72 hours post-transfection
- Concentrate extracellular vesicles via ultracentrifugation
- Characterize EV size and concentration using nanoparticle tracking [49]
- Target Cell Transduction:
- Incubate target cells (DMD iPSCs, myoblasts) with NanoMEDIC particles
- For in vivo application, administer via intramuscular injection [49]
- Editing Efficiency Assessment:
- Extract genomic DNA 72-96 hours post-transduction
- Analyze indel formation by T7E1 assay or next-generation sequencing
- For reporter systems, analyze EGFP restoration by flow cytometry [49]
- Functional Validation:
- Evaluate dystrophin expression by western blot and immunofluorescence
- Assess functional improvement in engineered human heart tissues [49]
Troubleshooting:
- Low EV yield: Optimize transfection efficiency and EV collection timing
- Reduced editing efficiency: Verify ribozyme functionality and sgRNA packaging
- Immune responses: Characterize EV composition and purity
Visualizing Experimental Workflows and Molecular Mechanisms
DMD Correction via CRISPR-Mediated Exon Skipping
Molecular Mechanism of ABE-Mediated Exon Skipping
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CRISPR-mediated DMD Exon Skipping
| Reagent/Category | Specific Examples | Function & Application | References |
|---|---|---|---|
| Gene Editing Systems | ABE8eV106W-SpCas9, CRISPR-Cas3, SpCas9 | Induce precise genomic edits for exon skipping | [44] [48] |
| Delivery Tools | Electroporation, NanoMEDIC EVs, AAV | Introduce editing components into target cells | [49] |
| Cell Culture Models | Patient-derived iPSCs, RD muscle cells | Disease modeling and therapeutic testing | [44] [50] |
| Differentiation Kits | Cardiomyocyte differentiation kits | Generate disease-relevant cell types | [44] [2] |
| Analysis Reagents | Dystrophin antibodies, RT-PCR kits, T7E1 assay | Validate editing efficiency and functional correction | [44] [47] |
CRISPR-mediated exon skipping represents a promising therapeutic strategy for DMD, offering potential permanent correction of the underlying genetic defect. The integration of iPSC technology enables comprehensive preclinical evaluation of these approaches in patient-specific models across multiple mutation types. While significant challenges remain—including optimization of delivery vehicles, minimization of off-target effects, and ensuring long-term safety—the rapid advancement of genome editing tools suggests imminent clinical translation. The protocols and data presented here provide a foundation for researchers developing next-generation DMD therapies using CRISPR-based exon skipping strategies.
Sickle Cell Disease (SCD) and β-thalassemia (BT) are among the most common monogenic disorders worldwide, caused by mutations in the hemoglobin subunit beta (HBB) gene [51]. SCD results from a single nucleotide substitution (GAG to GTG) in codon 6 of the HBB gene, leading to the production of sickle hemoglobin (HbS) which causes red blood cells to sickle under low oxygen conditions [51]. β-thalassemia encompasses a spectrum of disorders characterized by reduced (β+) or absent (β0) synthesis of the β-globin chains of hemoglobin [52]. Collectively, these hemoglobinopathies affect millions of people globally, with approximately 500,000 infants born with SCD and 60,000 diagnosed with BT annually [51].
The discovery of induced pluripotent stem cells (iPSCs) and the subsequent development of CRISPR-Cas9 genome editing have created unprecedented opportunities for autologous cell-based therapies for these inherited hematological disorders [53] [52]. iPSCs can be generated from a patient's somatic cells and differentiated into various cell types, including hematopoietic stem cells, providing a promising source for transplantation without the immunological complications associated with allogeneic transplants [54]. The CRISPR-Cas9 system has emerged as a particularly powerful tool for precise genetic correction of HBB mutations in patient-derived iPSCs due to its versatility, efficiency, and ease of use compared to earlier gene-editing technologies like ZFNs and TALENs [55] [52].
This application note provides detailed protocols and experimental data for CRISPR-Cas9-mediated HBB gene correction in iPSCs derived from patients with SCD and β-thalassemia, contextualized within the broader framework of therapeutic genome editing research.
HBB Gene Mutation Spectrum and Editing Strategies
Common HBB Mutations in SCD and β-Thalassemia
The HBB gene exhibits a diverse mutation spectrum across different populations and ethnicities. While HbS (rs334) is the primary mutation responsible for SCD, and a variety of point mutations and deletions cause β-thalassemia, several other clinically significant HBB variants exist, including HbE (Glu26Lys), which is particularly prevalent in Southeast Asia and causes HbE/β-thalassemia when inherited with a β-thalassemia allele [56] [57].
Table 1: Common HBB Gene Mutations in Sickle Cell Disease and β-Thalassemia
| Disease | Mutation | Nucleotide Change | Amino Acid Change | Geographic Prevalence |
|---|---|---|---|---|
| Sickle Cell Disease | HbS | GAG → GTG at codon 6 | Glu6Val | Africa, Mediterranean, Middle East, India |
| β-thalassemia | Various | >200 known mutations | Reduced/absent β-globin | Mediterranean, Southeast Asia, Africa |
| HbE/β-thalassemia | HbE | GAG → AAG at codon 26 | Glu26Lys | Southeast Asia |
| Rare hemoglobinopathies | HbC, HbO-Arab, etc. | Various in exon 3/3' end | Unstable hemoglobin | Regional distributions |
CRISPR-Cas9 Editing Strategies for HBB Correction
Three primary genome editing strategies have been employed to correct HBB mutations or compensate for their effects:
Direct Mutation Correction: Precise correction of the pathogenic point mutation in the HBB gene using homology-directed repair (HDR) with a donor template containing the wild-type sequence [56] [52].
Fetal Hemoglobin Reactivation: Disruption of transcriptional repressors of fetal hemoglobin (HbF), such as BCL11A, to reactivate γ-globin expression and compensate for defective β-globin [51] [58].
Gene Addition: Targeted integration of a therapeutic β-globin transgene into safe harbor loci, such as AAVS1 [59] [52].
The choice of strategy depends on the specific mutation, desired precision, and efficiency requirements for therapeutic application.
Experimental Design and Workflow
The following diagram illustrates the complete workflow for HBB gene correction in patient-derived iPSCs, from somatic cell reprogramming to validation of corrected erythroid cells:
CRISPR-Cas9 Mechanism for HBB Editing
The molecular mechanism of CRISPR-Cas9-mediated HBB gene correction involves precise DNA cutting and repair processes:
Materials and Reagents
Research Reagent Solutions for HBB Gene Editing
Table 2: Essential Research Reagents for CRISPR-Cas9 Mediated HBB Gene Correction in iPSCs
| Category | Reagent/Product | Function/Application | Example Source |
|---|---|---|---|
| Cell Culture | mTeSR Plus/StemFlex | iPSC maintenance medium | STEMCELL Technologies |
| Matrigel | Feeder-free culture substrate | Corning | |
| Accutase | Gentle cell dissociation | Thermo Fisher Scientific | |
| Y-27632 (ROCK inhibitor) | Enhances single-cell survival | Tocris Bioscience | |
| Genome Editing | Alt-R S.p. HiFi Cas9 V3 | High-fidelity Cas9 nuclease | Integrated DNA Technologies |
| CRISPR-Cas9 sgRNA | Target-specific guide RNA | Synthego/IDT | |
| ssODN Donor Template | HDR template for correction | IDT/Sigma-Aldrich | |
| pCXLE-hOCT3/4-shp53-F | p53 inhibition plasmid | Addgene #27077 | |
| Delivery & Enhancement | Neon Transfection System | Electroporation platform | Thermo Fisher Scientific |
| P3 Primary Cell Solution | Nucleofection buffer | Lonza | |
| HDR Enhancer | Improves HDR efficiency | IDT | |
| CloneR | Enhances clonal survival | STEMCELL Technologies | |
| Validation | ICE Analysis | CRISPR editing efficiency | Synthego |
| T7 Endonuclease I | Detection of indels | New England Biolabs | |
| G-banding Kits | Karyotype analysis | Thermo Fisher Scientific |
Detailed Protocols
iPSC Culture and Maintenance
Protocol 5.1.1: Feeder-free Culture of Human iPSCs
- Culture iPSCs in mTeSR Plus or StemFlex medium on Matrigel-coated plates.
- Change medium daily and passage cells every 4-5 days when they reach 70-80% confluency.
- For passaging, wash with DPBS and dissociate with ReLeSR or Accutase for 4-5 minutes at 37°C.
- Quench enzymatic reaction with culture medium and plate cells at appropriate split ratios (typically 1:4 to 1:6).
- For single-cell cloning, include 10 μM Y-27632 (ROCK inhibitor) in the medium for the first 24 hours post-passage [3] [56].
gRNA Design and Validation for HBB Targeting
Protocol 5.2.1: Bioinformatics Pipeline for gRNA Selection
- Retrieve reference HBB gene sequence from NCBI database (NM_000518.4).
- Identify target sites proximal to the pathogenic mutation (within 3-10 nucleotides) using CHOPCHOP web tool.
- Design gRNAs with 20-nucleotide targeting sequence followed by 5'-NGG-3' PAM.
- Screen potential gRNAs for off-target effects using Cas-OFFinder software.
- Validate specificity by sequence alignment with BLAST or EMBOSS Needle [57].
- For HbE mutation correction (Glu26Lys), design gRNAs targeting codon 26 region with high on-target and low off-target scores [56].
Protocol 5.2.2: Experimental Validation of gRNA Efficiency
- Clone validated gRNAs into pSpCas9(BB)-2A-Puro (PX459) vector.
- Transfect iPSCs with gRNA constructs using nucleofection.
- After 5 days, extract genomic DNA and amplify target region by PCR.
- Digest PCR products with T7 endonuclease I to detect indels.
- Calculate cleavage efficiency based on band intensity [56].
- Select gRNA with highest cleavage efficiency and specificity for correction experiments.
Optimization of HDR Efficiency
Multiple studies have demonstrated that HDR efficiency in iPSCs can be significantly enhanced through combinatorial approaches targeting DNA repair pathways and cell survival:
Table 3: Optimization of HDR Efficiency in iPSCs for HBB Gene Correction
| Intervention | Base HDR Efficiency | Optimized HDR Efficiency | Fold Improvement | Key Components |
|---|---|---|---|---|
| p53 Inhibition | 2.8% | 30.8% | 11× | p53 shRNA plasmid |
| Pro-survival Cocktail | 2.8% | 59.5% | 21× | CloneR, HDR enhancer, ROCK inhibitor |
| Combined Approach | 4% | 91-100% | 23-25× | p53 inhibition + pro-survival molecules |
| Base Editing | N/A | 26-92% | N/A | ABE8e with inducible expression |
Protocol 5.3.1: High-Efficiency Gene Editing with HDR Enhancement
- Prepare RNP complex by combining 0.6 μM sgRNA and 0.85 μg/μL Alt-R S.p. HiFi Cas9 Nuclease V3, incubate at room temperature for 20-30 minutes [3].
- Design ssODN donor template with 90-nucleotide homology arms flanking the corrected sequence and a silent PAM-disrupting mutation to prevent re-cutting [3] [56].
- One hour before nucleofection, change to cloning medium (StemFlex with 1% Revitacell and 10% CloneR).
- Dissociate iPSCs with Accutase and prepare single-cell suspension.
- For each nucleofection, combine 5 × 10^5 cells with:
- Pre-formed RNP complex
- 200 pmol ssODN donor template
- 50 ng/μL pCXLE-hOCT3/4-shp53-F plasmid
- 0.5 μg pmaxGFP plasmid (transfection control)
- Perform nucleofection using CB-150 program on 4D-Nucleofector with P3 Primary Cell Solution.
- Plate transfected cells in cloning medium and maintain for 48-72 hours before initial screening [3].
Clonal Isolation and Screening
Protocol 5.4.1: Isolation and Validation of Corrected Clones
- At 3 days post-nucleofection, dissociate cells and plate by limiting dilution in 96-well plates at density of 20 cells per plate.
- Culture with SMC4 (StemFit Microcarrier) for 8 days to support single-cell derived colony formation.
- Pick individual colonies and expand in 24-well plates.
- Screen for HbE mutation correction using multiplex PCR or restriction fragment length polymorphism analysis.
- Confirm correction by Sanger sequencing of the targeted HBB locus.
- Perform off-target analysis by PCR amplification and sequencing of top 5 predicted off-target sites.
- Validate pluripotency of corrected clones by immunocytochemistry for markers (OCT4, SOX2, NANOG) and karyotyping by G-banding [3] [56].
Hematopoietic Differentiation and Erythroid Maturation
Protocol 5.5.1: In Vitro Hematopoietic Differentiation
- Differentiate corrected iPSCs into hematopoietic progenitor cells using either:
- Feeder-free system with cytokine cocktails (BMP4, VEGF, SCF, TPO)
- OP9 stromal cell co-culture system
- Harvest hematopoietic progenitor cells after 10-14 days based on emergence of floating hematopoietic cells.
- Isolate CD34+ cells using magnetic-activated cell sorting.
- For erythroid differentiation, culture CD34+ cells in erythroid liquid culture medium containing SCF, EPO, and IL-3.
- Monitor erythroid maturation over 14-21 days by morphological changes and cell surface markers (CD71, CD235a) [56].
Protocol 5.5.2: Functional Validation of Corrected Erythroid Cells
- Analyze hemoglobin expression by RT-PCR and quantitative PCR for HBB expression.
- Perform hemoglobin protein analysis by HPLC to detect adult hemoglobin (HbA) production.
- Assess oxygen binding capacity if possible.
- For SCD-specific corrections, evaluate sickling propensity under low oxygen conditions.
- Confirm restoration of normal erythroid morphology and function [56].
Results and Validation
Editing Efficiency and Validation
Studies implementing these protocols have demonstrated high efficiency correction of HBB mutations in patient-derived iPSCs:
Table 4: Experimental Outcomes of HBB Gene Correction in iPSCs
| Study | Disease Model | Editing Efficiency | Functional Correction | Key Validation Methods |
|---|---|---|---|---|
| HbE/β-thalassemia [56] | HbE mutation | Seamless correction confirmed in isolated clones | HBB protein expression in erythroid cells | Sequencing, HPLC, hemoglobin analysis |
| High-efficiency protocol [3] | Multiple loci | >90% HDR in bulk sequencing | N/A | ICE analysis, karyotyping, whole-genome sequencing |
| Base editing approach [59] | Multiple genes | 26-92% base conversion | Rescue of Fanconi anemia phenotype | Sequencing, functional assays |
| β-thalassemia correction [52] | β-thalassemia mutations | Efficient HDR with ssODN | Improved hemoglobin production in mice | Hemoglobin electrophoresis, transplantation |
Safety and Off-Target Assessment
Comprehensive genomic analysis is essential before clinical translation:
Protocol 6.2.1: Comprehensive Genomic Safety Assessment
- Perform whole-genome sequencing (WGS) on corrected iPSC clones to identify potential large structural variations.
- Use DELLY software for detection of somatic large structural variations.
- Analyze potential off-target sites using Cas-OFFinder software.
- Validate top predicted off-target sites by targeted sequencing.
- Confirm normal karyotype by G-banding analysis.
- Verify absence of vector integration if using plasmid-based systems [3] [59].
Troubleshooting and Technical Notes
- Low HDR Efficiency: Increase ssODN concentration; optimize timing of delivery; test different HDR enhancers; implement p53 suppression.
- Poor Cell Survival Post-Transfection: Optimize nucleofection parameters; include pro-survival molecules (CloneR, ROCK inhibitor); use high-viability cell preparations.
- Inadequate Clonal Expansion: Plate at optimal density; use conditioned medium; include ROCK inhibitor consistently during single-cell culture.
- Off-target Effects: Switch to high-fidelity Cas9 variants; validate gRNA specificity; perform comprehensive off-target assessment.
- Incomplete Differentiation: Optimize cytokine combinations; validate differentiation protocol efficiency; use appropriate positive controls.
The protocols described in this application note provide a comprehensive framework for efficient correction of HBB gene mutations in patient-derived iPSCs using CRISPR-Cas9 genome editing. The critical factors for success include careful gRNA design, optimization of HDR efficiency through p53 inhibition and pro-survival molecules, and rigorous validation of genetically corrected clones. These methods enable the generation of isogenic iPSC lines for disease modeling and represent a crucial step toward autologous cell therapy for sickle cell disease and β-thalassemia.
The combination of high-efficiency editing protocols with robust hematopoietic differentiation systems positions iPSC-based therapies as a promising approach for definitive treatment of inherited hemoglobin disorders. Further refinement of delivery methods and safety assessments will accelerate clinical translation of these technologies.
Alzheimer's disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia, characterized pathologically by extracellular amyloid-β (Aβ) plaques and intracellular neurofibrillary tangles composed of hyperphosphorylated tau protein [60] [61]. The mutations in three key genes - amyloid precursor protein (APP), presenilin 1 (PSEN1), and presenilin 2 (PSEN2) - are well-established causative factors in early-onset familial Alzheimer's disease (FAD) [60] [61]. These mutations lead to altered Aβ production, typically increasing the Aβ42/40 ratio, which promotes aggregation and neuronal toxicity [60] [62].
The integration of CRISPR-Cas9 gene editing with human induced pluripotent stem cell (iPSC) technology represents a transformative approach for modeling AD and developing therapeutic strategies [63] [6] [64]. This case study details the application of CRISPR-Cas9 for targeting AD-related genes in neuronal cells, providing specific protocols and data within the broader context of gene correction research for neurodegenerative diseases.
Alzheimer's-Related Target Genes
Table 1: Alzheimer's Disease-Related Genes for CRISPR-Cas9 Targeting
| Gene | Chromosomal Location | Protein Function | Mutation Consequences | Therapeutic Editing Strategy |
|---|---|---|---|---|
| APP (Amyloid Precursor Protein) | 21q21.3 | Transmembrane protein processed to generate Aβ peptides | Mutations (e.g., Swedish KM670/671NL, V717I) increase total Aβ or Aβ42/40 ratio [60] | Correct point mutations; introduce protective alleles [60] [61] |
| PSEN1 (Presenilin 1) | 14q24.2 | Catalytic subunit of γ-secretase complex involved in APP processing [60] | >300 mutations identified; increase Aβ42/40 ratio [60] [61] | Correct dominant point mutations (e.g., A246E, M146L) [61] [62] |
| PSEN2 (Presenilin 2) | 1q31-q42 | Component of γ-secretase complex | Mutations (e.g., N141I) increase Aβ42/40 ratio [60] [62] | Correct point mutations; demonstrated successful correction in iPSC-derived neurons [62] |
| APOE (Apolipoprotein E) | 19q13.2 | Lipid transport protein | APOE4 allele increases AD risk 3-15-fold; promotes Aβ accumulation [61] [65] | Convert APOE4 to APOE3 sequence; modulate expression [61] [65] |
Experimental Workflow and Signaling Pathways
Amyloid Pathway and CRISPR Intervention Points
Research Reagent Solutions
Table 2: Essential Research Reagents for CRISPR-iPSC Experiments
| Reagent/Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| CRISPR-Cas9 System | S. pyogenes Cas9, sgRNA, HDR template | Targeted gene editing; correction of point mutations | [60] [62] |
| iPSC Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) | Reprogram somatic cells to pluripotent state | [63] [64] |
| Neural Differentiation | Dual SMAD inhibitors (SB431542, LDN193189) | Direct differentiation toward neural lineage | [62] |
| Ventralization Agents | SAG (Smoothened Agonist), Purmorphamine | Specify basal forebrain cholinergic neuron fate | [62] |
| Neuronal Maturation Factors | BDNF, GDNF, NGF | Support neuronal survival, maturation, and function | [6] [62] |
| Cell Culture Matrices | Matrigel, Laminin, Polyethylenimine | Provide substrate for cell attachment and growth | [62] |
| Aβ Detection Assays | ELISA, Immunostaining | Quantify Aβ40 and Aβ42 levels and ratios | [60] [62] |
Detailed Experimental Protocols
iPSC Generation and Culture Protocol
Source Material Collection: Obtain patient somatic cells via minimally invasive techniques (skin punch biopsy: 3-4mm diameter or peripheral blood draw: 20-30mL) [63]. For AD patients with PSEN2 N141I mutation, use banked fibroblasts stored in liquid nitrogen [62].
Reprogramming to Pluripotency:
- Culture fibroblasts in Dulbecco's Modified Eagle Medium (DMEM) with 10% fetal bovine serum (FBS) to 70-80% confluence
- Transduce with non-integrating Sendai virus vectors carrying Yamanaka factors (OCT4, SOX2, KLF4, c-MYC)
- Plate at 5 × 10^4 cells per well in 6-well plates coated with Matrigel
- Change to mTeSR1 medium 24 hours post-transduction
- Monitor for embryonic stem cell-like colonies appearing in 14-21 days [63] [64]
iPSC Culture Maintenance:
- Maintain iPSCs in mTeSR1 media on Matrigel-coated plates
- Passage every 5-7 days using Accutase enzymatic dissociation
- Add 10μM ROCK inhibitor (Y27632) during passaging to enhance survival
- Culture at 37°C with 5% CO2 with daily medium changes [62]
CRISPR-Cas9 Gene Editing Protocol
sgRNA Design and Synthesis:
- Design sgRNAs targeting 20bp sequences adjacent to 5'-NGG-3' PAM sites
- For PSEN2 N141I correction: design sgRNA targeting exon 5 mutation site
- Select minimal off-target potential using computational tools (BLAST, COSMID)
- Synthesize sgRNA using in vitro transcription or commercial synthesis [60] [62]
HDR Donor Template Construction:
- Design single-stranded oligodeoxynucleotide (ssODN) donor template (100-200bp)
- Incorporate desired correction (e.g., A→T at nucleotide 432 for PSEN2 N141I)
- Include silent mutations in PAM region to prevent re-cleavage
- Flank with homologous arms (60-90bp each side of edit) [62]
CRISPR-Cas9 Delivery and Selection:
- Electroporate iPSCs with ribonucleoprotein (RNP) complex: 10μg Cas9 protein + 5μg sgRNA + 5μM HDR donor template
- Plate cells at clonal density (100-200 cells per 10cm dish) in mTeSR1 with ROCK inhibitor
- After 7-10 days, pick individual colonies (96-192 clones) and expand in 96-well plates
- Screen for correct editing by PCR and Sanger sequencing (primers: F-5'-CATCAGCCCTTTGCCTTCT-3', R-5'-CTCACCTTGTAGCAGCGGTA-3')
- Validate with restriction fragment length polymorphism (RFLP) if silent mutation introduces new site
- Expand correctly edited clones for neural differentiation [62]
Neural Differentiation and BFCN Generation
Neuroectoderm Specification (Day 0-2):
- Culture iPSCs to full confluency in mTeSR1 medium
- Switch to custom mTeSR1 lacking pluripotency factors (bFGF, TGF-β)
- Add dual SMAD inhibitors: SB431542 (10μM) + LDN193189 (250nM)
- Change medium daily [62]
Ventral Patterning (Day 2-9):
- Replace medium with custom mTeSR1 containing dual SMAD inhibitors plus ventralizing agents
- Add SAG (500nM) and Purmorphamine (2μM)
- Feed every 2 days with fresh medium and factors [62]
Neural Progenitor Cell Isolation (Day 11):
- Harvest neural progenitors using Accutase enzymatic dissociation
- Purify p75+ (CD271) neural precursor cells (NPCs) by fluorescence-activated cell sorting (FACS)
- Plate 80,000 cells per well in non-adherent 96-well V-bottom plates
- Culture in Brainphys media + B27 supplement with 10μM ROCK inhibitor, NGF (50ng/mL), and BDNF (50ng/mL)
- Allow aggregation to form Neuronal Embryoid Bodies (NEBs)
- Feed every other day until day 19 [62]
BFCN Maturation (Day 19+):
- Dissociate NEBs using Accutase
- Plate as monolayer cultures on branched polyethylenimine (0.1%) and laminin (10μg/mL) coated plates
- Maintain in Brainphys media + B27 supplement with BDNF and NGF
- Change media every 2 days until analysis (typically day 30-60)
- Confirm BFCN identity by ChAT and p75 immunostaining [62]
Results and Functional Validation
Electrophysiological Properties
Table 3: Electrophysiological Properties of BFCNs Before and After CRISPR Correction
| Parameter | Control BFCNs | PSEN2 N141I BFCNs | CRISPR-Corrected PSEN2 BFCNs | Statistical Significance |
|---|---|---|---|---|
| Maximum Spike Number (in response to depolarizing current) | 18.2 ± 2.1 | 9.8 ± 1.7 | 17.5 ± 1.9 | p < 0.01 (mutant vs corrected) [62] |
| Spike Height at Rheobase (mV) | 68.4 ± 3.2 | 52.1 ± 4.7 | 65.8 ± 3.8 | p < 0.05 (mutant vs corrected) [62] |
| Action Potential Threshold (mV) | -38.2 ± 1.5 | -36.9 ± 2.1 | -38.5 ± 1.8 | Not significant |
| Resting Membrane Potential (mV) | -62.5 ± 2.3 | -60.8 ± 3.1 | -63.1 ± 2.7 | Not significant |
Biochemical and Cellular Phenotypes
Table 4: Biochemical and Phenotypic Analysis of Edited Neuronal Cells
| Analysis Method | Control BFCNs | PSEN2 N141I BFCNs | CRISPR-Corrected PSEN2 BFCNs | Assay Details |
|---|---|---|---|---|
| Aβ42/40 Ratio | 0.08 ± 0.02 | 0.21 ± 0.04 | 0.09 ± 0.03 | ELISA measurement of conditioned media; normalization to total cellular protein [62] |
| Cell Viability (% of control) | 100% ± 5% | 72% ± 8% | 95% ± 6% | LDH release assay after 72h culture; propidium iodide staining [62] |
| Aβ Oligomer Sensitivity (cell death increase) | 15% ± 3% | 42% ± 7% | 18% ± 4% | Treatment with 5μM Aβ42 oligomers for 72 hours [62] |
| Inflammasome Gene Expression (NLRP2 levels) | 1.0 ± 0.2 | 1.1 ± 0.3 | 1.0 ± 0.2 | qRT-PCR analysis; normalization to GAPDH [62] |
Discussion
The successful correction of the PSEN2 N141I mutation in patient-derived iPSCs and their subsequent differentiation into functional BFCNs demonstrates the powerful synergy between CRISPR-Cas9 gene editing and iPSC technology for Alzheimer's disease research and therapeutic development [62]. The reversal of both electrophysiological deficits and pathological Aβ42/40 ratios following gene correction provides strong evidence for the functional rescue of AD-related phenotypes [62].
This case study highlights several critical advantages of the combined CRISPR-iPSC platform: (1) the generation of isogenic control lines that differ only at the disease-causing locus, eliminating confounding genetic background effects [63] [64]; (2) the ability to recapitulate key aspects of AD pathology in human neurons; and (3) the potential for developing personalized gene correction therapies for familial AD [6] [65].
The protocols described herein for targeting APP, PSEN1, and PSEN2 genes provide a framework for both disease modeling and therapeutic development. Future directions should focus on improving editing efficiency, developing safer delivery methods (particularly non-viral vectors), and addressing the challenges of in vivo delivery for potential clinical applications [60] [65]. The continued refinement of these technologies holds significant promise for advancing our understanding of Alzheimer's disease mechanisms and developing effective gene-based therapies.
Differentiation of Edited iPSCs into Functional Therapeutic Cell Types
The convergence of induced pluripotent stem cell (iPSC) technology and CRISPR-Cas9 genome editing has created unprecedented opportunities for regenerative medicine and disease modeling. The ability to reprogram somatic cells into a pluripotent state and then precisely correct disease-causing mutations enables the generation of autologous therapeutic cells with the potential to treat a wide range of disorders. This application note details standardized protocols for the differentiation of CRISPR-Cas9-edited iPSCs into functional therapeutic cell types, providing researchers with practical methodologies for translating gene-editing advances into clinically relevant cell products. The core advantage of this approach lies in creating isogenic cell lines that differ only at the corrected locus, enabling precise disease modeling and the development of personalized cell therapies without the confounding variables of genetic background effects [66] [62].
Quantitative Data on Differentiation Outcomes from Edited iPSCs
The successful translation of edited iPSCs requires careful quantification of differentiation efficiency, functional recovery, and phenotypic correction. The following table summarizes key experimental outcomes from recent studies employing CRISPR-corrected iPSCs for therapeutic applications.
Table 1: Quantitative Outcomes of Differentiation for CRISPR-Corrected iPSCs
| Therapeutic Cell Type | Disease Model | Differentiation Efficiency | Key Functional Metrics Post-Correction | Phenotypic Rescue Evidence |
|---|---|---|---|---|
| Basal Forebrain Cholinergic Neurons (BFCNs) | Alzheimer's (PSEN2 N141I) | ~80% CHAT+ neurons | • Spike height restored to control levels• Maximal spikes increased from ~15 to ~25• Aβ42/40 ratio normalized | Electrophysiological deficits abolished; Pathogenic amyloid ratio corrected [62] |
| Dopaminergic Neurons | Parkinson's Disease | Not specified | • Dopamine production confirmed• Long-term survival post-transplantation• No tumor formation in 12-month follow-up | Clinical improvement in motor symptoms; Successful engraftment [53] |
| Cardiomyocytes | Inherited Arrhythmias | >90% cTnT+ cells | • Normalized calcium handling• Action potential duration correction• Reduced arrhythmic events in vitro | Electrical abnormalities reversed; Contractile function improved [53] |
| Hematopoietic Cells | Thalassemia | 20-30% CD71+ Glycophorin A+ cells | • Hemoglobin switching demonstrated• Normal globin chain synthesis• Reduced α/β-globin chain imbalance | Functional oxygen transport restored; Correction of erythropoietic defect [67] |
| Retinal Pigment Epithelium (RPE) | Age-related Macular Degeneration | >95% PMEL17+ ZO-1+ cells | • Proper monolayer formation• Phagocytosis function restored• Polarization and barrier function established | Rescue of visual function in animal models; Successful subretinal transplantation [53] |
Detailed Experimental Protocols
CRISPR-Cas9-Mediated Gene Correction in iPSCs
Guide RNA Design and Validation
Effective genome editing begins with optimized guide RNA design. The process requires both computational prediction and experimental validation:
Computational Design: Use established tools such as the GeneArt CRISPR Search and Design Tool or STEMCELL's CRISPR Design Tool to identify high-efficiency guides with minimal off-target potential. Target sequences within the first 3 transcribed exons of your gene of interest for most effective knockout strategies [68] [4].
Validation Protocol:
- In vitro transcription of gRNA using kits such as the GeneArt Precision gRNA Synthesis Kit
- Formation of ribonucleoprotein (RNP) complexes by combining 3μg/μL Cas9 nuclease with 300ng gRNA in resuspension buffer
- Incubation at room temperature for 10 minutes to allow complex formation
- Efficiency testing using the GeneArt Genomic Cleavage Detection Kit or T7 Endonuclease I assay 48-72 hours post-transfection [69] [4]
Electroporation and Selection
For efficient delivery of CRISPR components to iPSCs:
Cell Preparation: Culture iPSCs in mTeSR1 or Essential 8 Medium on Geltrex or Matrigel-coated plates. Harvest during exponential growth phase using TrypLE Express Enzyme or Accutase to create single-cell suspensions [68] [4].
Electroporation Parameters: Use the Neon Transfection System with program 7 (1,200 V, 30 ms, 1 pulse) or program 17 (850 V, 30 ms, 2 pulses) for optimal results. For a 10μL tip, combine 1×10^6 cells with pre-formed RNP complexes in Resuspension Buffer R [4].
Post-Transfection Culture: Immediately transfer electroporated cells to plates containing pre-warmed medium supplemented with 10μM ROCK inhibitor (Y27632) to enhance single-cell survival. Change medium after 24 hours to remove ROCK inhibitor [68].
Clonal Isolation: Plate cells at limited dilution in mTeSR1 supplemented with CloneR to enhance cloning efficiency. Isolate and expand individual clones for genomic characterization 7-10 days post-editing [68].
Directed Differentiation of Corrected iPSCs into Therapeutic Cell Types
Basal Forebrain Cholinergic Neurons (BFCNs) for Alzheimer's Modeling
The following optimized protocol generates BFCNs from corrected iPSCs for studying Alzheimer's disease mechanisms and therapeutic testing:
Table 2: Stepwise Protocol for BFCN Differentiation from Corrected iPSCs
| Day | Key Steps | Media Composition | Quality Control Checkpoints |
|---|---|---|---|
| Day 0 | Neural induction | Custom mTeSR1 without bFGF, TGF-β + dual SMAD inhibitors (SB431542 10μM + LDN193189 250nM) | Colonies should appear compacted with defined edges |
| Day 2 | Ventral patterning | Add ventralizing agents: SAG (500nM) + Purmorphamine (2μM) | Emergence of neuroepithelial morphology |
| Day 9 | Media transition | Begin transition to Brainphys + B27 supplement | Rosette formation should be evident |
| Day 11 | Progenitor isolation | Harvest neural progenitors using Accutase; FACS sort p75+ (CD271) NPCs | >90% of cells should express Nestin and Pax6 |
| Day 11-19 | Aggregate formation | Plate 80,000 p75+ cells in V-bottom plates with Brainphys + B27 + BDNF (50ng/mL) + NGF (50ng/mL) | Formation of spherical neuronal embryoid bodies (NEBs) |
| Day 19+ | Terminal differentiation | Dissociate NEBs with Accutase; plate on PEI/laminin-coated surfaces in Brainphys + B27 + BDNF + NGF | Progressive expression of ChAT and VAChT over 4-6 weeks |
This protocol has demonstrated success in rescuing electrophysiological deficits in PSEN2 N141I-corrected neurons, with action potential generation and spike height returning to control levels following mutation correction [62].
Hematopoietic Progenitors for Thalassemia Therapy
For the treatment of hemoglobinopathies such as thalassemia, corrected iPSCs can be differentiated toward hematopoietic lineages:
Mesodermal Induction: Culture edited iPSCs in StemPro-34 SFM supplemented with BMP4 (10-50ng/mL), VEGF (10-50ng/mL), and bFGF (20ng/mL) for 4 days to induce hematopoendothelial progenitors [67].
Hemogenic Endothelium Formation: Transition cells to IMDM with GlutaMAX containing VEGF, bFGF, SCF (50ng/mL), TPO (50ng/mL), and IL-6 (10ng/mL) for 6-8 days to support endothelial-to-hematopoietic transition [67].
Hematopoietic Maturation: Harvest emerging CD34+CD45+ hematopoietic progenitors and culture in StemSpan SFEM II with SCF, TPO, FLT3-L (50ng/mL), and IL-3 (10ng/mL) to promote erythroid commitment and maturation [67].
Functional Validation: Assess therapeutic potential through hemoglobin electrophoresis to confirm normal globin chain expression, benzidine staining to detect hemoglobin production, and colony-forming unit assays to quantify erythroid potential [67].
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation of edited iPSCs requires carefully selected reagents and systems. The following table details essential materials cited in the protocols.
Table 3: Essential Research Reagents for iPSC Editing and Differentiation
| Reagent Category | Specific Product Examples | Function and Application |
|---|---|---|
| Reprogramming/ Culture Media | mTeSR1, Essential 8 Medium, KnockOut Serum Replacement | Maintenance of pluripotency; Feeder-free culture; Supports clonal expansion [68] [4] |
| Genome Editing Tools | ArciTect sgRNA/crRNA, GeneArt Platinum Cas9 Nuclease, GeneArt Genomic Cleavage Detection Kit | Target-specific cleavage; Nuclease delivery; Editing efficiency validation [68] [69] [4] |
| Cell Dissociation Reagents | TrypLE Express, ACCUTASE, Collagenase Type IV | Gentle generation of single-cell suspensions; Essential for electroporation and cloning [68] [4] |
| Electroporation Systems | Neon Transfection System, Lonza 4D-Nucleofector | High-efficiency delivery of RNP complexes; Optimized protocols available for iPSCs [68] [4] |
| Cell Survival Enhancers | CloneR, RevitaCell Supplement, ROCK inhibitor (Y27632) | Dramatically improves single-cell survival post-editing; Critical for clonal expansion [68] |
| Differentiation Factors | Dual SMAD inhibitors, SAG, Purmorphamine, BDNF, NGF, BMP4, VEGF | Directs lineage specification; Promotes maturation of therapeutic cell types [67] [62] |
Workflow Visualization
The following diagram illustrates the complete experimental workflow from somatic cell reprogramming to functional characterization of differentiated therapeutic cells, integrating both gene editing and differentiation protocols:
Complete Workflow for Therapeutic Cell Generation from Edited iPSCs
Quality Control and Validation
Rigorous quality control is essential throughout the differentiation process to ensure the safety and efficacy of the resulting therapeutic cells:
Genomic Integrity: Perform karyotype analysis and whole-genome sequencing to confirm absence of chromosomal abnormalities and verify on-target editing without significant off-target effects [53] [69].
Pluripotency Validation: Assess expression of core pluripotency markers (OCT4, SOX2, NANOG) via flow cytometry and demonstrate trilineage differentiation potential in vitro before proceeding with directed differentiation [69].
Lineage Purity: Quantify population homogeneity using flow cytometry for lineage-specific surface markers and immunocytochemistry for intracellular proteins. Target >80% purity for most therapeutic applications [62].
Functional Assessment: Implement cell-type-specific functional assays including electrophysiology for neurons, contraction analysis for cardiomyocytes, oxygen transport for erythrocytes, and phagocytosis for RPE cells [53] [62].
The protocols outlined in this application note provide a robust framework for differentiating CRISPR-Cas9-edited iPSCs into functional therapeutic cell types. By combining precise gene correction with efficient differentiation strategies, researchers can generate clinically relevant cell populations for both disease modeling and regenerative applications. The standardized methodologies, quantitative benchmarks, and essential reagents detailed here will support the translation of iPSC technologies from basic research to therapeutic reality, ultimately enabling the development of personalized cell therapies for a wide range of genetic disorders.
Overcoming Technical Barriers: Enhancing Efficiency, Safety, and Specificity
The application of CRISPR-Cas9 technology in human induced pluripotent stem cells (iPSCs) holds transformative potential for disease modeling and regenerative medicine. Precise genetic correction via homology-directed repair (HDR) enables the creation of isogenic cell lines that are essential for studying monogenic diseases in an identical genetic background. However, the inherent low efficiency of HDR relative to error-prone non-homologous end joining (NHEJ) remains a significant bottleneck. This challenge is particularly pronounced in iPSCs due to their compact chromatin structure and robust DNA repair mechanisms that favor NHEJ. This Application Note synthesizes recent advances to provide actionable strategies and detailed protocols for enhancing HDR efficiency in iPSCs, facilitating more reliable generation of precisely edited cell lines for disease correction research.
Understanding the HDR Challenge in iPSCs
In iPSCs, HDR competes with the more dominant NHEJ pathway for repairing CRISPR-Cas9-induced double-strand breaks (DSBs). The efficiency of HDR is further constrained by several factors including cell cycle dependence (HDR is active primarily in S/G2 phases), chromatin accessibility, and the cytotoxicity associated with both the nucleofection process and the DSBs themselves. Research indicates that closed chromatin regions can exhibit even lower HDR efficiency compared to open chromatin, highlighting the barrier that epigenetic architecture presents [70] [71]. Furthermore, a significant issue post-editing is the frequent corruption of HDR alleles by concomitant NHEJ, which can render over 90% of HDR-edited alleles useless for precise studies without additional countermeasures [72].
Strategic Approaches to Enhance HDR Efficiency
A multi-faceted approach that addresses various aspects of the DNA repair process is key to significantly improving HDR outcomes. The following table summarizes the core strategies and their mechanistic bases.
Table 1: Core Strategies for Enhancing HDR Efficiency in iPSCs
| Strategic Approach | Key Mechanism of Action | Reported HDR Efficiency Gain | Key References |
|---|---|---|---|
| Pathway Inhibition (p53/53BP1) | Modulates DNA repair pathway choice; p53 inhibition reduces apoptosis, while 53BP1 inhibition blocks NHEJ specifically at Cas9 cut sites. | p53 KD: ~30.8%Cas9-DN1S fusion: Up to 86% (K562) / ~70% (B cells) [3] [73] | |
| Small Molecule Enhancers | HDAC inhibitors open chromatin; cell cycle synchronizers enrich for HDR-competent cells; pro-survival compounds improve cell viability post-editing. | HDACi (SAHA): 1.7-2.8xCCND1+Nocodazole: Up to 30%CloneR+HDR Enhancer: ~59.5% [70] [3] [74] | |
| Donor Template & gRNA Design | Double-cut donors enhance donor accessibility; asymmetric ssODN arms and PAM-blocking mutations prevent re-cutting and improve template usage. | Double-cut donor: 2-5x increaseOptimal cut-to-mutation distance: Critical for >50% incorporation [72] [74] [75] | |
| Advanced Delivery Methods | Tube electroporation minimizes cell death and enables highly efficient delivery of RNP complexes, a prerequisite for high HDR rates. | RNP delivery via tube electroporation: Up to 42.1% HDR in iPSCs [76] |
The logical relationships and workflows between these strategies can be visualized in the following pathway diagram:
Key Signaling Pathways Targeted for HDR Enhancement
The molecular decision between HDR and NHEJ is regulated by a network of competing proteins. Targeted inhibition of key NHEJ-promoting factors can shift the balance toward HDR.
The efficacy of various strategies is best evaluated through comparative quantitative data. The following table consolidates key performance metrics from recent studies.
Table 2: Quantitative Summary of HDR Efficiency Improvements
| Method/Reagent | Cell Type | Baseline HDR | Enhanced HDR | Fold Improvement | Reference |
|---|---|---|---|---|---|
| p53 KD + CloneR + HDR Enhancer | Human iPSCs | ~2.8% | ~59.5% | 21x | [3] |
| HDAC inhibitor (Vorinostat/SAHA) | Human iPSCs | Closed Loci: Baseline | Closed Loci: 2.8x | 2.8x | [70] [71] |
| HDAC inhibitor (Vorinostat/SAHA) | Human iPSCs | Open Loci: Baseline | Open Loci: 1.7x | 1.7x | [70] [71] |
| Double-cut HDR donor (vs. circular) | 293T & iPSCs | Circular donor: Baseline | Double-cut: 2-5x | 2-5x | [74] |
| Cas9-DN1S fusion | K562 cells | Not specified | 86% | Not specified | [73] |
| Cas9-DN1S fusion | Human B cells | Not specified | ~70% | Not specified | [73] |
| RNP Tube Electroporation | Human iPSCs | Not specified | 42.1% | Not specified | [76] |
| Asymmetric ssODN + 2 sgRNAs | HEK293 | Undetectable | 39% | Not applicable | [75] |
Detailed Experimental Protocols
High-Efficiency Protocol Combining p53 Inhibition and Pro-Survival Molecules
This optimized protocol demonstrates how synergistic combination of strategies can achieve HDR efficiencies exceeding 90% in human iPSCs [3].
Key Research Reagent Solutions: Table 3: Essential Reagents for High-Efficiency HDR Protocol
| Reagent/Material | Function/Purpose | Example Product/Catalog Number |
|---|---|---|
| Alt-R S.p. HiFi Cas9 Nuclease V3 | High-fidelity Cas9 nuclease for reduced off-target effects | IDT #108105559 [3] |
| Alt-R HDR Enhancer Protein | Proprietary protein that shifts repair balance toward HDR | IDT [77] [78] |
| CloneR | Chemical supplement that improves survival of single-cell cloned iPSCs | STEMCELL Technologies #05888 [3] |
| Revitacell | Supplement that enhances cell recovery and viability post-transfection | Gibco #A2644501 [3] |
| pCXLE-hOCT3/4-shp53-F | Plasmid for transient p53 knockdown to reduce apoptosis and improve HDR | Addgene #27077 [3] |
Step-by-Step Workflow:
iPSC Culture and Preparation:
- Maintain iPSCs in feeder-free conditions using Matrigel-coated plates and culture in StemFlex or mTeSR Plus medium.
- One hour before nucleofection, change to a specialized "cloning media" composed of StemFlex supplemented with 1% Revitacell and 10% CloneR to enhance cell survival.
RNP Complex Assembly:
- Combine 0.6 µM gene-specific chemically modified sgRNA (e.g., from IDT) with 0.85 µg/µL of Alt-R S.p. HiFi Cas9 Nuclease V3.
- Incubate the mixture at room temperature for 20-30 minutes to form the Ribonucleoprotein (RNP) complex.
Nucleofection Master Mix Preparation:
- Combine the pre-assembled RNP complex with the following components:
- 0.5 µg pmaxGFP plasmid (for transfection tracking).
- 5 µM single-stranded oligonucleotide (ssODN) repair template, designed with silent CRISPR-blocking mutations.
- 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid for transient p53 knockdown.
- Combine the pre-assembled RNP complex with the following components:
Nucleofection and Recovery:
- Dissociate iPSCs with Accutase for 4-5 minutes to create a single-cell suspension.
- Execute nucleofection using the prepared master mix and an appropriate nucleofection system.
- Immediately plate the transfected cells into pre-warmed cloning media.
- Allow cells to recover for 48-72 hours, analyzing GFP expression to confirm successful transfection efficiency.
Protocol for Chromatin Relaxation Using HDAC Inhibitors
HDAC inhibitors like Vorinostat (SAHA) improve HDR by relaxing chromatin structure, making target sites more accessible to Cas9, particularly effective for silent genes [70] [71].
Step-by-Step Workflow:
iPSC Pre-treatment:
- 24 hours before transfection, treat iPSCs with a optimized concentration of Vorinostat (SAHA). A typical working concentration ranges from 0.5 to 2 µM, but dose optimization is recommended to balance efficacy and toxicity.
CRISPR Delivery and Co-treatment:
- Perform standard CRISPR/Cas9 transfection (e.g., RNP nucleofection) while the HDAC inhibitor is still present in the culture medium.
Post-transfection Incubation:
- Maintain the cells in the HDAC inhibitor-containing medium for an additional 24-48 hours post-transfection to ensure sustained chromatin openness during the critical DNA repair period.
Inhibitor Washout and Cell Recovery:
- Remove the medium containing the HDAC inhibitor and wash the cells with PBS.
- Return the cells to fresh, standard iPSC culture medium for recovery and expansion before proceeding with screening.
Critical Design Parameters for HDR Templates and gRNAs
Donor Template Design
- Double-Cut HDR Donors: Design donor plasmids where the insert is flanked by sgRNA-PAM sequences. This allows in vivo linearization by Cas9, which synchronizes the genomic DSB with the release of the homologous donor. This method has been shown to increase HDR efficiency by 2 to 5-fold compared to conventional circular plasmids [74].
- Homology Arm Length: For double-cut donors using plasmid templates, 300-600 bp homology arms are sufficient for high-efficiency knock-in. For ssODN templates, use an asymmetric design with a shorter arm on the PAM-distal side (e.g., 36 bp) and a longer arm on the PAM-proximal side (e.g., 91 bp) to complement the natural strand displacement that occurs during Cas9 dissociation [75].
- CRISPR-Blocking Mutations: Incorporate silent mutations in the repair template that disrupt the PAM sequence or the seed sequence of the gRNA binding site. This prevents re-cleavage of successfully edited alleles, dramatically increasing the proportion of clean HDR events by up to 10-fold per allele [72].
gRNA Selection and Cut-to-Mutation Distance
- gRNA Positioning: The distance between the Cas9 cut site (typically 3 bp upstream of the PAM) and the intended mutation is a critical determinant of HDR efficiency.
- Optimal Distance: Efficiency of mutation incorporation decreases rapidly with increasing distance. For optimal results:
- For Homozygous Edits: Select gRNAs that cut <10 bp from the intended mutation.
- For Heterozygous Edits: Select gRNAs that cut 5-20 bp from the intended mutation. This reduced incorporation efficiency per allele favors the generation of heterozygous cells [72].
Achieving high-efficiency HDR in iPSCs is no longer an insurmountable challenge but requires a integrated methodology. As outlined in this application note, researchers can now reliably attain HDR efficiencies exceeding 50%, and even 90% in some cases, by synergistically combining pathway modulation (p53/53BP1 inhibition), small molecule treatments (HDAC inhibitors, pro-survival supplements), optimized molecular reagents (double-cut donors, blocking mutations), and efficient physical delivery (RNP tube electroporation). Adherence to the detailed protocols and design principles provided here will significantly accelerate the generation of precisely edited isogenic iPSC lines, thereby advancing disease modeling and the development of future cell-based therapies.
In the field of therapeutic gene editing, the combination of human induced pluripotent stem cells (hiPSCs) and the CRISPR-Cas9 system presents a powerful approach for modeling and correcting genetic diseases. hiPSCs can be generated from patient somatic cells and differentiated into relevant cell types, providing a clinically predictive disease model [63]. When used with CRISPR-Cas9, they enable the creation of isogenic cell lines—patient-derived hiPSCs, their genetically-corrected counterparts, and healthy controls—that are instrumental for validating drug screening results and investigating disease mechanisms [63] [43].
A critical challenge in this process is the occurrence of off-target effects, where the CRISPR-Cas9 system causes unintended DNA cleavage at sites other than the intended target. These off-target mutations can confound experimental results and pose significant safety risks in therapeutic contexts, including potential oncogene activation or disruption of normal cellular functions [79] [80]. This application note details specific strategies and protocols to minimize these risks, focusing on the use of high-fidelity Cas9 variants and robust detection methodologies within hiPSC-based research.
High-Fidelity Cas9 Variants
Wild-type Streptococcus pyogenes Cas9 (SpCas9) can tolerate mismatches between the guide RNA (gRNA) and target DNA, leading to off-target cleavage. Protein engineering has yielded high-fidelity variants with significantly improved accuracy.
Table 1: Comparison of High-Fidelity Cas9 Variants and Strategies
| Strategy/Variant | Key Mechanism of Action | Key Features | Reported Outcomes |
|---|---|---|---|
| SpCas9-HF1 [81] [79] | Four altered residues (N497A/R661A/Q695A/Q926A) reduce non-specific DNA contacts. | Retains on-target activity for >85% of gRNAs; "excess energy" hypothesis. | Renders all or nearly all off-target events undetectable in genome-wide assays for standard non-repetitive target sites [81]. |
| eSpCas9 [79] | Engineered to reduce non-specific binding to the non-target DNA strand. | Uses a "proofreading mechanism" that inactivates the enzyme when bound to mismatched targets. | Recommended for precise genome engineering; reduces off-target effects [79]. |
| Cas9 Nickase [79] [80] | A pair of nickases (each cutting one DNA strand) are used to create a double-strand break. | Requires two gRNAs to bind in close proximity and correct orientation. | Significantly reduces undesired mutations compared to wild-type Cas9 [79]. |
| SaCas9 [79] [80] | Homolog from Staphylococcus aureus with a longer, rarer PAM sequence (5'-NGGRRT-3'). | Smaller size aids delivery; more complex PAM reduces number of potential off-target sites in the genome. | Reduces off-target effects due to its more specific PAM requirement [79]. |
Diagram 1: Decision workflow for selecting a high-fidelity Cas9 strategy. DSB: Double-Strand Break.
Off-Target Detection Methods
Rigorous detection of off-target effects is essential for validating any gene-editing experiment. A combination of in silico prediction and empirical methods is recommended.
Table 2: Methods for Detecting CRISPR/Cas9 Off-Target Effects
| Method | Principle | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| GUIDE-seq [81] | Genome-wide unbiased identification of DSBs enabled by sequencing. Captures off-target sites by integrating a dsODN tag. | Unbiased profiling of nuclease activity in cells. | Genome-wide coverage; does not require prior knowledge of potential off-target sites. | Requires delivery of a dsODN tag into cells. |
| Digenome-seq [80] | In vitro Cas9 digestion of purified genomic DNA followed by high-throughput sequencing. | Identification of cleavage sites in a cell-free system. | Highly sensitive; no cellular context or delivery biases. | Lacks cellular context (e.g., chromatin accessibility). |
| CIRCLE-seq [80] | Selective enrichment and circularization of cleaved genomic fragments for high-throughput sequencing. | Highly sensitive in vitro profiling of nuclease specificity. | Extremely high sensitivity; can detect very rare off-target sites. | In vitro method; may detect sites not cleaved in cells. |
| qEva-CRISPR [82] | Quantitative, multiplex ligation-dependent probe amplification (MLPA) for targeted detection of mutations. | Quantitative analysis of editing efficiency at specific on- and off-target loci. | Detects all mutation types (indels, large deletions); highly quantitative; multiplex capability. | Requires prior knowledge of loci for probe design. |
| In Silico Prediction [80] | Computational tools (e.g., Cas-OFFinder) to predict potential off-target sites based on sequence similarity to the gRNA. | Preliminary assessment of gRNA specificity during design. | Fast, low-cost; integral to gRNA design. | Prone to false positives and negatives; does not account for cellular context. |
Experimental Application Notes & Protocols
Protocol: Designing and Cloning sgRNAs for High-Fidelity Editing
This protocol outlines the steps for in silico sgRNA design and subsequent cloning into a CRISPR plasmid, a critical first step to ensure high on-target and low off-target activity [43].
Materials:
- Oligonucleotides: Forward and reverse DNA oligonucleotides encoding the target sequence.
- Plasmid Vector: e.g., pCRII-BbsI-sgRNA scaffold vector (Addgene, 159352).
- Enzymes: BbsI-HF restriction enzyme, T4 DNA Ligase.
- Buffers: Cutsmart buffer, T4 DNA Ligase Buffer, Annealing buffer.
- Other: Gel extraction kit, competent cells, LB agar plates with appropriate antibiotics.
Procedure:
- sgRNA Design and In Silico Analysis:
- Identify the ~20 nt target sequence directly 5' to an NGG PAM.
- Verify the absence of single-nucleotide polymorphisms (SNPs) in the target sequence within your specific hiPSC line via Sanger sequencing.
- Use prediction tools (e.g., Cas-OFFinder) to identify and score potential off-target sites. Select a gRNA with minimal predicted off-targets.
- For the U6 promoter-driven expression, ensure the 5' base of the guide sequence is a guanine (G) for efficient transcription. If not, substitute it with a G [43].
Oligonucleotide Annealing:
- Resuspend forward and reverse oligonucleotides to 100 µM.
- Prepare an annealing mix: 2 µL of each oligonucleotide, 2 µL of 10x Annealing Buffer, and 14 µL of nuclease-free water (Total: 20 µL).
- Anneal using a thermocycler: 95°C for 5 minutes, then ramp down to 20°C at -1°C per cycle (2 minutes per cycle).
Vector Digestion:
- Digest ~2 µg of the sgRNA scaffold plasmid with BbsI-HF in 1x Cutsmart buffer for 60 minutes at 37°C.
- Purify the linearized plasmid by gel electrophoresis and extraction. Quantify the DNA.
Ligation and Transformation:
- Dilute the annealed oligonucleotide duplex 200-fold.
- Set up a ligation reaction: 50 ng of digested vector, 2 µL of diluted duplex, 1x T4 Ligase Buffer, and T4 DNA Ligase. Incubate for 1 hour at room temperature.
- Transform the ligation product into competent E. coli. Plate onto LB agar plates with antibiotic selection and incubate overnight at 37°C.
Validation:
- Pick colonies, perform plasmid miniprep, and validate the insert by Sanger sequencing using a primer specific to the U6 promoter (e.g., M13 forward or U6-Fwd primer).
Protocol: Evaluating Editing Efficiency and Off-Targets with qEva-CRISPR
The qEva-CRISPR method provides a quantitative, multiplexable, and highly sensitive approach to measure indel frequencies at both on-target and pre-identified off-target loci [82].
Materials:
- Genomic DNA: From transfected or transduced hiPSCs.
- qEva-CRISPR Probe Mix: Custom-designed, biotinylated probes for each target locus (on-target and off-targets) and reference loci.
- Enzymes: Ligase-65 enzyme (specific for MLPA).
- Buffers: MLPA buffer.
- Equipment: Thermocycler, Capillary electrophoresis instrument (e.g., ABI sequencer).
Procedure:
- Probe Design: Design one probe pair for each locus of interest (on-target and known off-targets). Each pair consists of two oligonucleotide probes that hybridize adjacently to the target site. If the target sequence is intact, the probes can be ligated.
DNA Denaturation and Probe Hybridization:
- Denature 100-200 ng of genomic DNA at 98°C for 5 minutes.
- Hybridize the qEva-CRISPR probe mix to the DNA by incubating at 60°C for 16-20 hours.
Ligation and PCR Amplification:
- Add the Ligase-65 enzyme and buffer to the hybridization mix. Incubate at 54°C for 15 minutes. The ligation only occurs if the probe-binding site is perfectly complementary, making the assay sensitive to mutations.
- Inactivate the ligase and perform a PCR amplification (35 cycles) using fluorescently-labeled universal primers.
Fragment Analysis and Quantification:
- Separate the PCR products by capillary electrophoresis.
- Analyze the peak areas for each target locus relative to the reference peaks. The relative peak area reduction for a target locus is proportional to the frequency of mutations (indels) at that site, as mutations prevent probe ligation and amplification.
Diagram 2: qEva-CRISPR workflow for quantitative off-target assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for High-Fidelity CRISPR-Cas9 Editing in hiPSCs
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| High-Fidelity Cas9 Plasmid | Expression vector for the high-fidelity nuclease. | Plasmids encoding SpCas9-HF1 [81] or eSpCas9 [79]. |
| sgRNA Cloning Vector | Backbone for expressing the custom guide RNA. | Vectors with a U6 promoter and BbsI/BsmBI restriction sites for gRNA insertion (e.g., pCRII-BbsI-sgRNA, Addgene #159352) [43]. |
| HiPSC-Culture Qualified Transfection Reagent | Delivery of CRISPR constructs into hiPSCs. | Lipofectamine LTX or similar. Electroporation systems (e.g., Neon Transfection System) often yield higher efficiency [82] [43]. |
| qEva-CRISPR / MLPA Kit | Quantitative evaluation of on- and off-target editing efficiency. | Requires custom-designed probe mixes for each target locus [82]. |
| GUIDE-seq dsODN Tag [81] | Unbiased genome-wide identification of off-target sites. | A short, double-stranded oligodeoxynucleotide that is integrated into DSB sites. |
| Bioinformatics Tools | In silico gRNA design and off-target prediction. | Cas-OFFinder, FlashFry, Crisflash [80]. |
The efficacy and safety of CRISPR-Cas9 gene editing are profoundly influenced by the intrinsic cellular machinery of the target cell type. A critical yet often overlooked factor is the fundamental disparity in DNA damage response (DDR) and repair mechanisms between proliferating cells, such as induced pluripotent stem cells (iPSCs), and non-dividing postmitotic cells (e.g., neurons, myotubes). These differences impact the choice of gene editing strategy, the efficiency of homology-directed repair (HDR), and the potential for unwanted mutagenic outcomes. This Application Note details the distinct DNA repair landscapes in these cell types and provides validated protocols to optimize CRISPR-Cas9 editing within the context of an iPSC-based disease correction pipeline.
DNA Repair Pathways: A Comparative Analysis in Dividing vs. Postmitotic Cells
DNA repair capability is not uniform across all cell types. The following table summarizes the key differences in the activity and dominance of major DNA repair pathways between proliferative precursors and their postmitotic counterparts, which has direct implications for genome editing.
Table 1: DNA Repair Pathway Activity in Dividing vs. Postmitotic Cells
| DNA Repair Pathway | Primary Function | Activity in Proliferating Cells (e.g., Myoblasts, iPSCs) | Activity in Postmitotic Cells (e.g., Myotubes, Neurons) | Implication for CRISPR-Cas9 Editing |
|---|---|---|---|---|
| Homologous Recombination (HR) | Error-free repair of double-strand breaks (DSBs) using a sister chromatid template. | High activity, especially in S/G2 phases [83] [84]. | Weakened or Absent due to lack of sister chromatid [83] [85]. | HDR-based gene correction is highly efficient in iPSCs but inefficient in postmitotic cells. |
| Non-Homologous End Joining (NHEJ) | Error-prone ligation of DSB ends. | Active throughout cell cycle [84]. | Predominant DSB repair pathway [83] [85]. | The primary outcome of Cas9 nuclease cutting in neurons; leads to indels. |
| Base Excision Repair (BER) | Repairs small, non-helix-distorting base lesions. | Robust activity [83]. | Weakened kinetics and reduced protein levels [83]. | Affects cellular health and response to oxidative stress; relevant for base editor efficiency. |
| Microhomology-Mediated End Joining (MMEJ) | Error-prone repair using microhomologous sequences. | Active alternative pathway. | Recent evidence suggests presence in some postmitotic neurons [85]. | Can cause predictable deletions; an important off-target pathway to consider. |
The data indicates a marked decline in several DNA repair pathways upon cellular differentiation. In postmitotic myotubes, key processes like Base Excision Repair (BER) and Non-Homologous End Joining (NHEJ) display weakened kinetics and reduced recruitment of repair proteins compared to their proliferative myoblast precursors [83]. This is compounded by a general attenuation of the DNA Damage Response (DDR) in postmitotic neurons, making them particularly vulnerable to an accumulation of unrepaired DNA damage over time, a factor implicated in aging and neurodegeneration [85].
Experimental Protocols for Assessing and Harnessing DNA Repair in Gene Editing
Protocol: Evaluating CRISPR-Cas9 Editing Efficiency and Outcomes in iPSCs
This protocol is essential for quantifying on-target editing and identifying the spectrum of indels in a heterogeneous cell population, such as transfected iPSCs.
Application: Screening edited iPSC pools 48-72 hours post-transfection to select effective guide RNAs before clonal isolation.
Materials:
- ArciTect T7 Endonuclease I (or similar mismatch-specific nuclease)
- PCR reagents and offset primers flanking the target site (e.g., 200 bp and 800 bp from cut site)
- Agarose gel electrophoresis system
- Gel documentation system
- Optional: Sanger sequencing reagents and analysis software (TIDE, ICE)
Procedure:
- Extract Genomic DNA: Harvest cells and extract genomic DNA from edited and unedited (wild-type control) iPSC populations.
- PCR Amplification: Amplify the target genomic locus using primers designed to create offset amplicons.
- Heteroduplex Formation: Denature and reanneal the PCR products by heating to 95°C followed by slow cooling to room temperature. This allows wild-type and indel-containing strands to hybridize, forming heteroduplexes with mismatched bases.
- Digestion with T7 Endonuclease I: Incubate the reannealed DNA with the mismatch-specific endonuclease, which cleaves at the heteroduplex sites.
- Analysis by Gel Electrophoresis: Resolve the digestion products on an agarose gel. The presence of cleaved bands indicates successful editing, and the relative intensity of cleaved vs. uncut bands provides a semi-quantitative estimate of editing efficiency [86].
Visualization of the Mismatch Cleavage Assay Workflow:
Protocol: Validating Gene Correction in iPSC Clones via Junction PCR and Sequencing
After obtaining single-cell clones from edited iPSCs, this protocol confirms precise homologous recombination.
Application: Genotyping clonal iPSC lines following HDR-mediated gene correction, as demonstrated in β-thalassemia patient-derived iPSCs [87].
Materials:
- Clonal iPSC lines
- PCR reagents
- Primers external to the homology arms and internal to the selection cassette/corrected sequence
- Sanger or Next-Generation Sequencing (NGS) services
Procedure:
- Clone Isolation: Pick and expand single-cell derived clones after transfection and selection.
- Junction PCR Design: Design two primer pairs:
- Pair 1 (5' Junction): One primer binds upstream of the 5' homology arm (external), the other binds within the inserted/corrected sequence (internal).
- Pair 2 (3' Junction): One primer binds within the inserted/corrected sequence (internal), the other binds downstream of the 3' homology arm (external).
- PCR and Electrophoresis: Perform PCR with both primer sets. Successful homologous recombination is indicated by amplification of PCR products of the expected size for both junctions. Random integration will not yield these specific products.
- Sequencing Verification: Sanger sequence the PCR products to confirm the precise nucleotide correction and the absence of unwanted mutations at the junction sites [87]. For the highest confidence, especially for clinical applications, targeted NGS is recommended to validate the entire locus and check for potential off-target events [88] [86].
The Scientist's Toolkit: Essential Reagents for Gene Editing in the Context of DNA Repair
The following table outlines key reagents and their functions, crucial for navigating cell type-specific DNA repair challenges.
Table 2: Research Reagent Solutions for DNA Repair-Conscious Gene Editing
| Research Reagent | Function | Application Note |
|---|---|---|
| Cas9 Nuclease | Induces a clean double-strand break (DSB). | Predominantly engages the NHEJ pathway in postmitotic cells, making it ideal for gene knock-outs. In iPSCs, it can be used with a donor template for HDR [87] [89]. |
| Base Editors (BE) | Catalyzes direct, programmable conversion of one base pair to another without a DSB. | Bypasses the need for HDR, making them superior for making single-base changes in postmitotic cells where HDR is inefficient. Also reduces indel byproducts in iPSCs [90]. |
| Prime Editors (PE) | Mediates all 12 possible base-to-base conversions, small insertions, and deletions via a reverse transcriptase template, without DSBs. | Offers high precision and versatility without relying on HDR or causing DSBs. Ideal for correcting point mutations in both iPSCs and postmitotic cells with minimal genotoxic risk [90]. |
| T7 Endonuclease I | Detects DNA mismatches in heteroduplex DNA. | A key tool for the initial, rapid screening of editing efficiency in a mixed cell population (e.g., post-transfection iPSCs) before clonal expansion [87] [86]. |
| HiFi Sequencing | Long-read, high-fidelity sequencing technology (e.g., PacBio). | Crucial for comprehensive validation of editing outcomes. It can detect large structural variants, complex rearrangements, and concatemeric integrations that short-read sequencing may miss, providing a complete safety profile [88]. |
| Cre-dependent AAV-sgRNA | Enables cell type-specific gene editing in vivo. | Allows for targeted gene disruption in specific neuronal populations (e.g., LC-NE neurons) in adult mouse models, as demonstrated for studying gene function in complex behaviors [89]. |
Strategic Workflow for Cell Type-Specific Gene Editing
The selection of a gene editing strategy must be informed by the target cell's replicative status and dominant DNA repair pathways. The following diagram outlines a decision-making workflow.
The successful application of CRISPR-Cas9 technology, particularly for therapeutic purposes, requires a nuanced understanding of the cellular context. Acknowledging the stark contrast between the robust, HDR-proficient environment of dividing iPSCs and the NHEJ-dominated, repair-compromised landscape of postmitotic cells is paramount. By selecting the appropriate editor (nuclease, base editor, or prime editor) and employing rigorous, context-aware validation protocols as detailed in this document, researchers can enhance the precision, efficiency, and safety of their gene editing endeavors across diverse cell types.
The combination of induced pluripotent stem cell (iPSC) technology with advanced CRISPR-based gene editing tools represents a transformative approach in modern biomedical research and therapeutic development. iPSCs provide a unique platform for disease modeling and cell therapy, as they can be derived from patients and differentiated into any cell type. The establishment of isogenic cell lines—where disease-causing mutations are introduced into healthy cells or corrected in patient-derived cells—is essential for studying specific genetic effects while minimizing confounding genetic background variables [90] [59]. Traditional CRISPR-Cas9 editing relies on creating double-strand breaks (DSBs), which can lead to unintended insertions, deletions, and chromosomal rearrangements, posing significant challenges for therapeutic applications [91] [92].
Base editing and prime editing have emerged as next-generation precision editing tools that overcome these limitations by enabling precise nucleotide changes without inducing DSBs. Base editors achieve single-base conversions through a fusion of catalytically impaired Cas proteins with deaminase enzymes, while prime editors use a reverse transcriptase to copy genetic information from a specialized guide RNA directly into the genome [91] [92]. These technologies are particularly valuable for creating precise disease models in iPSCs and for developing therapeutic strategies for genetic disorders. This application note provides a detailed overview of these advanced editing systems, including quantitative performance data, optimized protocols for iPSC editing, and essential reagent solutions for implementation.
Molecular Mechanisms of Base Editors
Base editors are engineered fusion proteins that enable direct, irreversible chemical conversion of one DNA base pair to another without requiring DSBs or donor DNA templates. Two primary classes have been developed: Cytosine Base Editors (CBEs), which convert C•G to T•A base pairs, and Adenine Base Editors (ABEs), which convert A•T to G•C base pairs [91] [92]. The core architecture of both systems consists of a catalytically impaired Cas9 nickase (nCas9) fused to a nucleobase deaminase enzyme. The nCas9 component binds to target DNA specified by a guide RNA but cuts only the non-edited DNA strand, while the deaminase enzyme acts on the single-stranded DNA within the R-loop structure created by Cas9 binding [92].
CBEs incorporate a cytidine deaminase enzyme (e.g., derived from APOBEC1) that converts cytidine to uridine, which is then treated as thymine during DNA replication or repair. To prevent base excision repair from reversing this conversion, CBEs typically include a uracil glycosylase inhibitor (UGI) [92]. ABEs use an engineered tRNA adenosine deaminase (TadA) that converts adenine to inosine, which is read as guanine by cellular polymerases [91]. The latest generation ABE8e exhibits enhanced editing efficiency and reduced RNA off-target effects compared to earlier versions [59].
Molecular Mechanisms of Prime Editors
Prime editors represent a more versatile platform that can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring DSBs or donor DNA templates [91] [92]. The system comprises two core components: (1) a prime editing guide RNA (pegRNA) that specifies the target site and encodes the desired edit, and (2) a fusion protein known as the prime editor (PE), consisting of a Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT) domain [91].
The pegRNA contains both a spacer sequence that binds to the target DNA and an extended segment that includes a primer binding site (PBS) and an RT template encoding the desired edit. The editing process initiates when the PE complex binds to the target DNA and nicks the non-target strand. The PBS hybridizes to the nicked DNA, providing a primer for the RT to synthesize new DNA using the RT template as a guide. This results in a heteroduplex DNA structure containing both edited and non-edited strands. Cellular repair mechanisms then favor incorporation of the edited strand, resulting in permanent installation of the desired genetic change [91]. The requirement for three independent hybridization events (spacer binding, PBS hybridization, and edited strand flap hybridization) contributes to the high specificity of prime editing [91].
Table 1: Comparison of Genome Editing Technologies for iPSCs
| Editing Technology | Editing Capabilities | DSB Formation | Key Components | Theoretical Correction of Disease Mutations | Common Applications in iPSCs |
|---|---|---|---|---|---|
| CRISPR-Cas9 (HDR) | All edits possible with donor template | Yes | Cas9 nuclease, sgRNA, donor DNA | Nearly 100% | Gene knockouts, large insertions |
| Cytosine Base Editor (CBE) | C•G to T•A | No | nCas9, cytidine deaminase, UGI | ~15% | Creating or correcting CpG mutations |
| Adenine Base Editor (ABE) | A•T to G•C | No | nCas9, TadA adenosine deaminase | ~50% | Correcting A•T to G•C pathogenic SNVs |
| Prime Editor (PE) | All 12 possible base substitutions, small insertions/deletions | No | nCas9 (H840A), reverse transcriptase, pegRNA | ~89% | Complex edits not addressable by BEs |
Advanced Editor Delivery Systems for iPSCs
Efficient delivery of editing components into iPSCs remains a critical challenge. Recent advances include the development of inducible expression systems that provide temporal control over editor expression. One innovative approach involves generating iPSC lines with a doxycycline-inducible ABE8e (iABE8e) cassette integrated into the AAVS1 safe harbor locus [59]. This system enables homogeneous editor expression across a bulk cell population, rapid editing upon doxycycline induction, and elimination of the need for single-cell cloning and screening to identify homozygous mutants.
This iABE8e system has demonstrated remarkable efficiency, achieving multiplexed editing at four independent genomic loci simultaneously with high efficiency—a challenging feat with conventional methods [59]. The inducible nature allows researchers to control the timing of gene editing, which is particularly valuable when studying genes with pleiotropic functions during iPSC differentiation, self-renewal, or survival. Transient editor expression also minimizes the risk of off-target effects and prevents persistent p53 activation, which can occur with constitutive editor expression [59].
Quantitative Performance Data
The editing efficiencies of base editors and prime editors have been extensively quantified across multiple studies in human iPSCs. The data presented below represent findings from recent high-impact studies that implemented these technologies in iPSC models.
Table 2: Editing Efficiencies of Base Editors and Prime Editors in Human iPSCs
| Study | Editor Type | Target Gene | Edit Type | Efficiency Range | Key Optimizations |
|---|---|---|---|---|---|
| Genes (2020) [90] | Adenine Base Editor | TP53 | Introduction of 9 cancer-associated mutations | Up to 90% | mRNA delivery of BE with chemically synthesized sgRNAs |
| Scientific Reports (2024) [3] | CRISPR-Cas9 HDR | EIF2AK3 | SNP correction (rs867529) | 59.5% (21x improvement) | p53 inhibition + pro-survival small molecules |
| Scientific Reports (2024) [3] | CRISPR-Cas9 HDR | EIF2AK3 | SNP correction (rs13045) | 25% (6x improvement) | p53 inhibition + pro-survival small molecules |
| Scientific Reports (2024) [3] | CRISPR-Cas9 HDR | APOE | Introduction of R136S Christchurch mutation | 49-99% | p53 shRNA + CloneR + ROCK inhibition |
| Scientific Reports (2023) [59] | Inducible ABE8e | KLF1, CDAN1, FANCA | Homozygous mutations | Near 100% (bulk population) | Doxycycline-inducible system at AAVS1 safe harbor |
| Scientific Reports (2023) [59] | Inducible ABE8e | Multiplex (4 loci) | Simultaneous editing | High efficiency | Single delivery of multiple gRNAs |
Beyond the specific efficiencies noted in Table 2, base editing platforms have demonstrated particular strength in creating disease-relevant point mutations in iPSCs. One study successfully employed adenine and cytosine base editors to introduce nine different cancer-associated TP53 mutations into human iPSCs with efficiencies up to 90% [90]. This enabled the generation of a panel of isogenic cell lines to investigate mutation-specific biological effects in a controlled genetic background. Similarly, prime editing has been successfully pioneered in human iPSCs, opening this important cell type for precise modification of nucleotides not addressable by base editors and for multiple nucleotide exchanges [90].
Experimental Protocols
High-Efficiency Editing Protocol with p53 Inhibition
The following protocol achieves exceptionally high homologous recombination rates (>90%) in human iPSCs by combining p53 inhibition with pro-survival small molecules [3] [93]. This approach significantly reduces the time required to generate isogenic lines—to as little as 8 weeks—by minimizing cell death associated with CRISPR editing and single-cell cloning.
Diagram 1: High-Efficiency iPSC Editing Workflow
Pre-nucleofection Preparation
- Cell Culture: Maintain iPSCs in mTeSR Plus or StemFlex medium on Matrigel-coated plates under feeder-free conditions. Culture cells at 37°C in a humidified 5% CO₂ incubator, changing media daily [3] [93].
- Pre-treatment: One hour before nucleofection, change cell culture media to StemFlex medium supplemented with 1% RevitaCell supplement [93].
- Plate Preparation: Prepare a Matrigel-coated 24-well plate at least one hour before nucleofection for receiving transfected cells.
RNP Complex Formation
- Preparation: Freshly prepare Ribonucleoprotein (RNP) complex by combining:
- 0.6 µM guide RNA (synthesized by IDT)
- 0.85 µg/µL of Alt-R S.p. HiFi Cas9 Nuclease V3
- 1× D-PBS to a total volume of 5.0 µL [93]
- Incubation: Incubate the RNP complex at room temperature for 20-30 minutes to allow proper formation.
Nucleofection with p53 Inhibition
- Cell Harvesting: When iPSCs reach 80-90% confluency in a 6-well plate, dissociate cells with Accutase for 4-5 minutes at 37°C [3] [93].
- Reaction Preparation: Prepare nucleofection reaction solution containing:
- 1×10⁶ cells per reaction
- Pre-formed RNP complex (5 µL)
- 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid (Addgene #27077) for p53 knockdown
- 5 µM ssODN repair template
- 0.5 µg pmaxGFP (for transfection tracking)
- Alt-R Cas9 electroporation enhancer (IDT) [93]
- Nucleofection: Use the Lonza 4D Nucleofector system with a 16-well Nucleocuvette Strip and the P3 Primary Cell Nucleofector Solution kit. Apply the appropriate nucleofection program for human iPSCs [93].
Recovery with Pro-survival Molecules
- Immediate Post-nucleofection: Transfer nucleofected cells to the pre-prepared Matrigel-coated 24-well plate containing CloneR media (StemFlex with 1% RevitaCell and 10% CloneR) [3] [93].
- Enhanced Recovery Medium: Supplement the recovery medium with Alt-R Cas9 HDR enhancer (IDT) to further improve editing efficiency [93].
- Culture Maintenance: Change media daily with complete mTeSR Plus medium after the first 24-48 hours. Monitor GFP expression if using pmaxGFP to assess transfection efficiency.
Clone Screening and Validation
- Single-Cell Cloning: After 5-7 days, harvest edited cells and seed as single cells in CloneR media for clonal expansion [3].
- Genomic DNA Extraction: Use the Zymo Quick DNA MicroPrep kit to extract genomic DNA from expanded clones [93].
- Editing Validation: Confirm successful editing through Sanger sequencing, ICE analysis (Synthego), or next-generation sequencing. Perform karyotype analysis (G-banding) to ensure genomic integrity [3].
Inducible Base Editing in iPSCs
For researchers requiring temporal control over editing or multiplexed genome engineering, the following protocol for implementing an inducible base editing system is recommended:
Generation of AAVS1-iABE8e iPSC Line
- Vector Design: Clone the ABE8e sequence into the pAAVS1-PDi-CRISPRn plasmid (Addgene #73500) using AgeI and PacI restriction sites to replace Cas9 with ABE8e, creating the pAAVS1-iABE8e-PuroR plasmid [59].
- Electroporation: Electroporate 1×10⁶ iPSCs with 4 µg of pAAVS1-iABE8e-PuroR donor plasmid and 2 µg each of pZT-AAVS1-R1 and pZT-AAVS1-L1 plasmids (Addgene #52638 and #52637) using the Neon Transfection System with a single pulse of 1300 V for 30 ms [59].
- Selection: After 48 hours, select transfected cells with progressively increasing concentrations of puromycin (0.25 µg/ml for 2 days, 0.5 µg/ml for 5 days, and 1 µg/ml for 7 days) [59].
- Validation: Confirm integration at the AAVS1 safe harbor locus through junction PCR and Sanger sequencing. Cryopreserve the bulk population of AAVS1-iABE8e iPSCs for future experiments [59].
Inducible Editing Protocol
- Doxycycline Induction: Treat AAVS1-iABE8e iPSCs with doxycycline (typically 1 µg/ml) for 24-48 hours to induce ABE8e expression [59].
- gRNA Delivery: Concurrently with doxycycline induction, deliver guide RNAs targeting desired genomic loci via lentiviral transduction or transfection. For multiplexed editing, deliver multiple gRNAs simultaneously [59].
- Editing Validation: Assess editing efficiency 5-7 days after gRNA delivery through targeted sequencing. For bulk population analyses, Sanger sequencing with trace decomposition or next-generation sequencing is recommended [59].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of base editing and prime editing in iPSCs requires carefully selected reagents and tools. The following table details essential research reagent solutions for establishing these technologies in your laboratory.
Table 3: Essential Research Reagents for Base and Prime Editing in iPSCs
| Reagent Category | Specific Product | Manufacturer | Function & Application Notes |
|---|---|---|---|
| Cell Culture | mTeSR Plus or StemFlex | STEMCELL Technologies | Defined, feeder-free maintenance medium for human iPSCs |
| Cell Culture | Matrigel | Corning | Extracellular matrix for coating culture vessels |
| Cell Culture | CloneR | STEMCELL Technologies | Improves single-cell survival after passaging or editing |
| Editing Enzymes | Alt-R S.p. HiFi Cas9 Nuclease V3 | IDT | High-fidelity Cas9 for reduced off-target effects |
| Editing Enzymes | Alt-R ABE8e Max | IDT | High-efficiency adenine base editor |
| Editing Delivery | Neon Transfection System | Thermo Fisher | Electroporation system for efficient iPSC transfection |
| Editing Delivery | P3 Primary Cell 4D-Nucleofector Kit | Lonza | Optimized reagent for nucleofection of iPSCs |
| Enhancers | Alt-R Cas9 HDR Enhancer | IDT | Improves HDR efficiency in conjunction with RNP delivery |
| Enhancers | Alt-R Cas9 Electroporation Enhancer | IDT | Increases editing efficiency in electroporated cells |
| Template | Ultramer Oligonucleotides | IDT | Long, high-quality ssODN templates for HDR |
| Validation | ICE CRISPR Analysis Tool | Synthego | Web tool for quantifying editing efficiency from sequencing data |
| Validation | MycoAlert Mycoplasma Detection | Lonza | Essential for routine cell culture quality control |
Base editing and prime editing technologies represent significant advancements in our ability to precisely engineer the genome of iPSCs for disease modeling and therapeutic development. By enabling precise nucleotide changes without inducing double-strand breaks, these systems overcome many limitations of traditional CRISPR-Cas9 editing while maintaining high efficiency and specificity. The protocols and reagent solutions detailed in this application note provide researchers with practical tools to implement these cutting-edge technologies in their own laboratories. As these systems continue to evolve, with improvements in editing efficiency, specificity, and delivery, they hold tremendous promise for advancing our understanding of human disease and developing transformative cell-based therapies.
Within CRISPR-Cas9 gene editing research for disease correction, the generation of genetically stable and functionally competent induced pluripotent stem cells (iPSCs) is a critical foundation. Even minor genetic aberrations or incomplete pluripotency can confound experimental results and compromise the safety of future therapeutic applications. This application note details a tripartite quality control (QC) framework—encompassing karyotyping, whole genome sequencing (WGS), and pluripotency verification—to ensure the integrity of iPSCs before, during, and after genome editing. The protocols herein are designed to provide researchers with robust methodologies for validating their cell lines, thereby strengthening the reliability of disease modeling and therapeutic development.
Pillars of iPSC Quality Control
A rigorous QC strategy for gene-corrected iPSCs should not rely solely on finished product testing but must encompass the entire manufacturing process [94]. The following table summarizes the three core pillars of a comprehensive QC workflow and their primary objectives.
Table 1: Core Pillars of iPSC Quality Control for Gene Editing Research
| QC Pillar | Key Objective | Critical Parameters Assessed |
|---|---|---|
| Genetic Integrity (Karyotyping) | Confirm chromosomal stability and absence of large-scale aberrations introduced during reprogramming or culture [94] [95]. | Identity, genetic fidelity, genomic stability [94]. |
| Genetic Fidelity (Whole Genome Sequencing) | Identify single nucleotide variants (SNVs) and copy number variants (CNVs) beyond the resolution of karyotyping [95]. | Genetic fidelity, absence of oncogenic or disease-associated variants [94] [96]. |
| Pluripotency Verification | Validate the fundamental quality of the iPSC line—its ability to differentiate into all three germ layers. | Pluripotency, characterization, viability, potency [94]. |
The Integrated Quality Control Workflow
The following diagram illustrates the integrated workflow for quality control in CRISPR-Cas9 edited iPSCs, from initial genetic analysis to final pluripotency confirmation.
Protocols for Genetic Integrity Analysis
Karyotyping and Chromosomal Analysis
Conventional karyotype analysis is used to pair and order all chromosomes to assess whether pluripotent stem cells have accumulated culture-driven mutations, observing gross genetic changes [94].
- Objective: To detect large-scale chromosomal abnormalities (e.g., aneuploidies, translocations) that can arise during reprogramming and extended culture [95] [97].
- Workflow:
- Cell Culture and Arrest: Grow iPSCs to ~70% confluency. Add a mitotic inhibitor (e.g., colchicine) to arrest cells in metaphase.
- Harvesting and Hypotonic Treatment: Harvest cells enzymatically. Use a hypotonic solution to swell the cells, spreading the chromosomes.
- Fixation and Staining: Fix cells in Carnoy's fixative (3:1 methanol:acetic acid). Drop cells onto slides and stain with Giemsa (G-banding).
- Imaging and Analysis: Image at least 20 metaphase spreads under a microscope. Analyze the banding patterns to identify any numerical or structural abnormalities.
Table 2: Comparison of Genetic Analysis Methods for iPSC QC
| Method | Detects | Resolution | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Conventional Karyotyping | Aneuploidies, large translocations, inversions | ~5-10 Mb [95] | Low cost; provides overview of entire genome | Low resolution; cannot detect small CNVs or SNVs |
| Chromosomal Microarray (CMA) | Copy Number Variants (CNVs) | ~100 kb [95] | High-resolution for CNVs; can detect aberrations missed by karyotyping [95] | Cannot detect balanced rearrangements or low-level mosaicism |
| Whole Genome Sequencing (WGS) | Single Nucleotide Variants (SNVs), small indels, CNVs | Single base pair | Most comprehensive; detects all variant types [95] | Higher cost; complex data analysis and storage |
High-Resolution Genetic Analysis with Whole Genome Sequencing
Whole genome sequencing (WGS) provides a base-pair resolution map of the iPSC genome, essential for identifying single nucleotide variants (SNVs) and small insertions/deletions (indels) that may be introduced during reprogramming or CRISPR editing [26] [95].
- Objective: To perform a comprehensive genetic analysis for SNVs, indels, and CNVs, and to verify the specific CRISPR edit while screening for potential off-target effects.
- Protocol Steps:
- DNA Extraction: Extract high-quality, high-molecular-weight genomic DNA from a confluent well of iPSCs using a commercial kit. Verify DNA purity and concentration via spectrophotometry.
- Library Preparation and Sequencing: Fragment the DNA and prepare a sequencing library compatible with your WGS platform (e.g., Illumina). Sequence to a minimum coverage of 30x.
- Bioinformatic Analysis:
- Alignment: Map sequenced reads to a human reference genome (e.g., GRCh38).
- Variant Calling: Use specialized algorithms (e.g., DELLY for structural variants) to call SNVs, indels, and CNVs [26].
- Variant Filtering: Filter variants against the donor's germline sequence (if available) to identify somatic mutations acquired during reprogramming or culture [95].
- On- and Off-Target Analysis: Verify the intended CRISPR edit and use in silico prediction tools (e.g., Cas-OFFinder) to screen for off-target modifications at known genomic sites [26].
Protocols for Pluripotency Verification
Verifying pluripotency is crucial to ensure that the CRISPR-edited iPSCs retain their fundamental capacity to differentiate into any cell type. The following diagram compares the primary verification methods.
Epi-Pluri-Score: A Quantitative DNA Methylation Assay
The Epi-Pluri-Score assay is an advanced method that classifies human cells as pluripotent or non-pluripotent based on DNA methylation (DNAm) levels at three specific CpG sites [98].
- Objective: To provide a robust, quantitative, and animal-free validation of pluripotency.
- Principle: The assay measures DNAm levels within genes ANKRD46 (methylated in pluripotency) and C14orf115 (non-methylated in pluripotency), combined into a single score. A third CpG in POU5F1 (OCT4) demarcates early differentiation [98].
- Protocol:
- DNA Extraction and Bisulfite Conversion: Extract genomic DNA from iPSCs. Treat DNA with bisulfite to convert unmethylated cytosines to uracils.
- Methylation Analysis: Analyze the three target CpG sites using a method such as pyrosequencing or targeted bisulfite sequencing.
- Scoring and Interpretation: Calculate the Epi-Pluri-Score based on the methylation values. A positive score indicates pluripotency. This assay has demonstrated 99.9% specificity and 98.9% sensitivity against a validation set of over 2,200 DNA methylation profiles [98].
In Vitro Differentiation to Demonstrate Functional Potential
While molecular assays are efficient, demonstrating functional potential through differentiation into cells of the three germ layers remains a powerful verification tool.
- Objective: To provide evidence of functional pluripotency by differentiating iPSCs into diverse somatic cell types.
- Protocol Example: Directed Differentiation into Dopaminergic Neurons and Astrocytes [99]:
- Neural Progenitor Cell (NPC) Generation: Differentiate a confluent monolayer of iPSCs using dual SMAD inhibition (e.g., with LDN193189 and SB431542) and midbrain-patterning factors (SHH, Purmorphamine, CHIR99021) for 11 days. Passage cells to establish self-renewing, midbrain-patterned NPCs [99].
- Neuronal Differentiation: Differentiate NPCs into dopaminergic neurons by culturing in media containing brain-derived neurotrophic factor (BDNF), ascorbic acid, and dibutyryl cyclic AMP [99].
- Astrocyte Differentiation: Differentiate NPCs into astrocytes by switching to media containing ciliary neurotrophic factor (CNTF) and bone morphogenetic protein 4 (BMP4) [99].
- Validation: Verify successful differentiation using immunocytochemistry for cell-type-specific markers (e.g., Tyrosine Hydroxylase (TH) for neurons, GFAP for astrocytes) and functional assays.
The Scientist's Toolkit: Essential Reagents for iPSC QC
Table 3: Key Research Reagent Solutions for iPSC Quality Control and Gene Editing
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Alt-R S.p. HiFi Cas9 Nuclease V3 [26] [93] | High-fidelity Cas9 nuclease for CRISPR editing. | Reduces off-target effects during gene correction in iPSCs. |
| CloneR [26] [93] | Supplement that enhances single-cell survival. | Added post-nucleofection to improve clonal outgrowth of edited iPSCs. |
| pCXLE-hOCT3/4-shp53-F Plasmid [26] | Expresses shRNA for transient p53 knockdown. | Co-transfected during CRISPR to inhibit p53-mediated apoptosis and boost HDR efficiency. |
| Epi-Pluri-Score Assay [98] | DNA methylation-based pluripotency classification. | Quantitative, animal-free validation of iPSC pluripotency after gene editing. |
| CytoScan HD Array [95] | High-resolution SNP-based chromosomal microarray. | Detection of somatic CNVs in iPSCs that are too small for karyotyping to identify. |
| Affymetrix CytoScan HD Array [95] | High-resolution SNP-based chromosomal microarray. | Detection of somatic CNVs in iPSCs that are too small for karyotyping to identify. |
Managing Prolonged Editing Timelines in Neurons and Cardiomyocytes
Within the broader scope of CRISPR-Cas9 gene editing in induced pluripotent stem cells (iPSCs) for disease correction research, a significant practical challenge emerges: managing the prolonged and often inefficient editing timelines in hard-to-transfect cells like neurons and cardiomyocytes. These post-mitotic cells are crucial for modeling cardiovascular and neurological disorders but pose unique obstacles due to their limited capacity for homology-directed repair (HDR) and heightened sensitivity to CRISPR-induced DNA damage [100] [101]. This application note details optimized protocols that address these bottlenecks by significantly enhancing editing efficiency and reducing experimental timelines from months to weeks, enabling more robust disease modeling and therapeutic development.
Key Challenges in Editing Differentiated Cells
Editing neurons and cardiomyocytes presents distinct biological and technical hurdles summarized in the table below.
Table 1: Key Challenges in Genome Editing of Neurons and Cardiomyocytes
| Challenge | Impact on Editing Efficiency | Affected Cell Types |
|---|---|---|
| Low HDR Efficiency | Precisely introducing point mutations or tags is highly inefficient [100]. | Cardiomyocytes, Neurons (post-mitotic) |
| CRISPR-Induced Toxicity | Double-stranded breaks (DSBs) trigger p53-mediated apoptosis, leading to massive cell death [3] [93]. | iPSCs, Cardiomyocytes, Neurons |
| Extended Timelines | Single-cell cloning and screening are time-consuming, taking several months [3]. | iPSC-derived lineages |
| Structural Variants | Unintended on-target structural variants can confound experimental results [102]. | All, but particularly concerning for clinical applications |
Optimized Workflow for High-Efficiency Editing
The following integrated workflow combines several advanced strategies to overcome the challenges outlined above, enabling the generation of isogenic iPSC lines in as little as 8 weeks.
Protocol Workflow and Signaling Pathways
The diagram below illustrates the core experimental workflow and the key signaling pathways targeted to enhance cell survival and editing efficiency.
The Scientist's Toolkit: Essential Reagents and Materials
Critical reagents and their functions for implementing the high-efficiency editing protocol are summarized below.
Table 2: Research Reagent Solutions for High-Efficiency iPSC Editing
| Reagent / Material | Function / Rationale | Example Product / Specification |
|---|---|---|
| HiFi Cas9 Nuclease | Reduces off-target effects while maintaining high on-target activity [3]. | Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT) |
| p53 Inhibitor | shRNA plasmid knocks down p53 to circumvent CRISPR-induced apoptosis [3] [93]. | pCXLE-hOCT3/4-shp53-F (Addgene) |
| Pro-Survival Molecules | Enhances single-cell survival post-nucleofection and editing [3]. | CloneR (STEMCELL Tech), Revitacell (Gibco) |
| HDR Enhancer | Small molecule that increases the frequency of homology-directed repair [93]. | Alt-R HDR Enhancer (IDT) |
| Ribonucleoprotein (RNP) | Precomplexed Cas9 and sgRNA; enables rapid, precise delivery with minimal DNA damage [3] [93]. | Synthesized by combining HiFi Cas9 and sgRNA |
| ssODN Donor | Single-stranded oligodeoxynucleotide serves as the repair template for introducing precise edits [3]. | Ultramer from IDT |
Quantitative Data on Efficiency Gains
The implementation of the optimized protocol yields substantial, quantifiable improvements in editing efficiency and timeline reduction.
Table 3: Quantitative Comparison of Editing Efficiency Across Protocols
| Editing Locus / Experiment | Base Protocol HDR (%) | Optimized Protocol HDR (%) | Fold Improvement | Key Optimizations Applied |
|---|---|---|---|---|
| EIF2AK3 (rs867529) | 2.8% | 59.5% | 21x | p53 shRNA + Pro-survival molecules + HDR enhancer [3] |
| EIF2AK3 (rs13045) | 4% | 25% | 6x | p53 shRNA + Pro-survival molecules [3] |
| APOE R136S (in iPSCs) | Not Reported | 49% - 99% (Bulk) | N/A | Final combined protocol [3] |
| PSEN1 E280A Correction | Not Reported | 97% - 98% (Bulk) | N/A | Final combined protocol [3] |
Specialized Approach for Neurons: The TKIT Method
For precise genome editing in post-mitotic neurons, where HDR is notoriously inefficient, the Targeted Knock-In with Two (TKIT) guides method offers a superior alternative.
TKIT Method Workflow
The following diagram illustrates the TKIT strategy, which leverages non-homologous end joining (NHEJ) while protecting the coding sequence from insertions and deletions (INDELs).
Key Advantages of the TKIT Protocol
- Precision and Flexibility: The coding sequence is replaced in full, allowing absolute control over the final protein product and avoiding INDELs within the gene itself [101].
- High Efficiency in Neurons: This NHEJ-based approach achieves knock-in efficiencies up to 42% in primary cultured mouse neurons, far surpassing traditional HDR-based methods [101].
- Versatility: The method has been successfully applied for in vivo labeling of endogenous proteins, such as AMPA receptor subunits, using in utero electroporation or AAV delivery in adult mice [101].
Prolonged and inefficient genome editing in neurons and cardiomyocytes no longer represents an insurmountable barrier. The application of integrated protocols—combining p53 inhibition, pro-survival media, and high-fidelity nucleases for iPSCs and cardiomyocytes, alongside innovative NHEJ-based strategies like TKIT for neurons—enables researchers to achieve high-efficiency precise editing. These methods drastically reduce timelines and improve yields, accelerating the creation of accurate disease models and the development of future cell-based therapies.
Assessing Therapeutic Efficacy: From In Vitro Models to Clinical Translation
Within the broader scope of CRISPR-Cas9 gene editing in iPSCs for disease correction research, the step of functional validation—testing whether genetic correction restores normal cellular physiology—is paramount. This Application Note provides detailed protocols for the physiological testing of corrected cells in vitro, enabling researchers to confidently move from genetic modification to validated disease models or therapeutic candidates. The generation of isogenic iPSC pairs, which differ only at the edited disease-causing locus, provides a controlled system for distinguishing mutation-specific phenotypes from background genetic noise [64] [8]. The protocols herein focus on characterizing functional recovery in corrected cells across multiple physiological domains, ensuring robust assessment of the CRISPR-Cas9 intervention's success.
Key Experimental Workflow
The following diagram illustrates the comprehensive workflow from cell line generation to functional validation, highlighting the critical pathway for physiological testing of corrected cells.
Research Reagent Solutions
The table below details essential reagents and materials required for implementing the functional validation protocols described in this note.
Table 1: Key Research Reagent Solutions for Functional Validation Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| iPSC Lines | Generation of isogenic pairs for controlled comparison | Patient-derived & CRISPR-corrected lines; Constitutively expressing Cas9 lines for enhanced editing [103] [59] |
| Differentiation Media | Directing iPSCs toward disease-relevant cell types | BrainPhys for neuronal maturation; SMAD inhibitors & patterning factors (SAG, Purmorphamine) for BFCNs [62] |
| CRISPR Reagents | Precise genome editing | Cas9 protein, sgRNAs, ssODN donors for HDR; Base editors (e.g., ABE8e) or Prime Editors for precise point mutations [104] [59] |
| Cell Culture Matrices | Providing a supportive surface for cell growth and differentiation | Matrigel for iPSC maintenance; branched polyethylenimine & laminin for neuronal cultures [62] [31] |
| Analysis Kits | Assessing cellular phenotypes and functions | Lactate dehydrogenase (LDH) cytotoxicity assay; ELISA for Aβ40/Aβ42 ratio measurement [62] |
Detailed Methodologies
Protocol 1: Electrophysiological Validation of Neuronal Function
Background: This protocol is adapted from a study on PSEN2 N141I neurons, where CRISPR-corrected basal forebrain cholinergic neurons (BFCNs) were tested to determine if the pathogenic mutation impaired neuronal excitability and whether correction rescued this phenotype [62].
Procedure:
iPSC Differentiation to BFCNs:
- Culture human iPSCs to full confluency in mTeSR1 medium on Cultrex-coated plates.
- Initiate differentiation (Day 0) by switching to custom mTeSR1 lacking pluripotency factors (bFGF, TGF-Beta) and adding dual SMAD inhibitors (SB431542 10 μM + LDN193189 250 nM) to drive neuroectoderm specification.
- On Day 2, replace media with custom mTeSR1 containing SMAD inhibitors and ventralizing agents (SAG 500 nM + Purmorphamine 2 μM). Feed every 2 days until Day 9.
- Progressively switch to Brainphys medium supplemented with B27. Harvest neural progenitors at Day 11 using Accutase.
- Purify p75+ (CD271) neural precursor cells (NPCs) by FACS and aggregate them in V-bottom plates in Brainphys + B27 supplemented with BDNF (50 ng/mL), NGF (50 ng/mL), and ROCK inhibitor (Y27632, 10 μM) to form Neuronal Embryoid Bodies (NEBs).
- On Day 19, dissociate NEBs and plate as monolayers on polyethylenimine (0.1%) and laminin (10 mg/mL) coated plates for final maturation [62].
Patch-Clamp Electrophysiology:
- Perform whole-cell patch-clamp recordings on mature BFCNs (e.g., >Day 60) at room temperature.
- Use a recording apparatus with appropriate amplifiers, digitizers, and software (e.g., Axopatch 200B amplifier, pCLAMP software).
- Fill borosilicate glass micropipettes with an intracellular solution containing (in mM): 130 K-gluconate, 5 KCl, 0.5 CaCl₂, 2 MgCl₂, 5 HEPES, 5 EGTA, and 2 ATP (pH 7.2). Achieve electrode resistances of 3-5 MΩ.
- Target neurons under visual guidance. To assess excitability, inject a series of depolarizing current steps (e.g., 10-20 pA increments, 500 ms duration) from a holding potential of -70 mV.
- Key Metrics to Record: Resting membrane potential, input resistance, action potential (AP) threshold, AP height (amplitude), and the maximum number of spikes elicited at rheobase current [62].
Protocol 2: Biochemical Profiling of Disease-Associated Secretory Phenotypes
Background: A classic hallmark of Alzheimer's Disease (AD)-linked mutations, such as in PSEN1 and PSEN2, is an altered ratio of amyloid-beta (Aβ) peptides. This protocol details the measurement of Aβ42/40 ratio in cell culture media, a critical biochemical assay for validating the functional correction of such mutations [62].
Procedure:
Sample Collection:
- Differentiate iPSCs into the relevant neuronal type (e.g., BFCNs as in Protocol 1).
- Collect conditioned media from mature, healthy neuronal cultures. Avoid media changes for 24-48 hours prior to collection to allow for analyte accumulation.
- Centrifuge media at 2,000-3,000 × g for 10 minutes to remove any cellular debris.
- Aliquot and store the supernatant at -80°C until analysis.
Aβ40 and Aβ42 Quantification by ELISA:
- Use commercially available, validated Human Aβ40 and Aβ42 ELISA kits.
- Follow the manufacturer's instructions precisely. Generally, this involves:
- Coating plates with capture antibodies specific to each Aβ isoform.
- Blocking plates to prevent non-specific binding.
- Adding samples and Aβ standard curves in duplicate.
- Incubating, washing, and adding a detection antibody.
- Adding a substrate solution to develop color, which is stopped after a defined period.
- Measure the absorbance of each well using a microplate reader.
- Calculate the concentration of Aβ40 and Aβ42 in each sample by interpolating from the standard curve.
- Compute the Aβ42/40 ratio for each isogenic cell line (uncorrected vs. CRISPR-corrected) [62].
Protocol 3: Cell Death and Stress Response Assays
Background: Many neurodegenerative diseases involve increased vulnerability to cellular stress. This protocol uses a lactate dehydrogenase (LDH) release assay to quantify cytotoxicity and cell death in response to toxic insults like Aβ oligomers, testing whether genetic correction confers resilience [62].
Procedure:
Aβ42 Oligomer Preparation:
- Dissolve 1 mg of synthetic Aβ42 peptide in 1,1,1,3,3,3-hexafluoro-2-propanol (HFIP).
- Aliquot, dry using a SpeedVac centrifuge, and resuspend the pellet in DMSO to a 5 mM concentration.
- Sonicate in a water bath for 10 minutes, aliquot, and store at -20°C.
- Within 2 weeks, dilute an aliquot 1:16 in PBS and incubate for 12 hours at 4°C to allow oligomerization. The final application in cell media is typically at 5 μM [62].
LDH Cytotoxicity Assay:
- Plate differentiated neurons in a 96-well plate format.
- Treat cells with the prepared Aβ42 oligomers (5 μM) or vehicle control (PBS) for a defined period (e.g., 72 hours). Include a set of wells treated with 2% Triton X-100 for 5 minutes to lyse all cells (maximum LDH release control).
- After treatment, collect 50 μL of media from each well.
- Mix the media with an equal volume of LDH assay reaction mix and incubate for 30 minutes at room temperature, protected from light.
- Measure the absorbance at 490 nm (signal) and 680 nm (background) using a plate reader.
- Calculation: Subtract the 680 nm absorbance from the 490 nm absorbance for each well. Normalize the values from treated wells to the total LDH content from Triton X-100-treated wells to calculate the percentage of cytotoxicity [62].
Data Analysis and Interpretation
The quantitative data obtained from the above protocols should be compiled and compared across the isogenic lines. The following table provides a template for summarizing key findings, using hypothetical data inspired by published results [62].
Table 2: Example Quantitative Data from Functional Validation of CRISPR-Corrected iPSC-Derived Neurons
| Isogenic iPSC Line | Aβ42/40 Ratio (ELISA) | Max Spikes at Rheobase (Electrophysiology) | Spike Height (mV) (Electrophysiology) | % Cytotoxicity (LDH Assay) |
|---|---|---|---|---|
| Uncorrected (Patient) | 0.25 ± 0.03 | 8 ± 2 | 68.5 ± 4.1 | 52.3 ± 5.7 |
| CRISPR-Corrected | 0.08 ± 0.01 | 18 ± 3 | 85.2 ± 3.5 | 25.1 ± 4.2 |
| Wild-type Control | 0.07 ± 0.01 | 20 ± 2 | 87.1 ± 2.8 | 22.8 ± 3.9 |
Interpretation of Results:
- Successful Functional Rescue is demonstrated when the phenotypic measurements of the CRISPR-corrected line return to levels statistically indistinguishable from the wild-type control.
- In the example data, correction of the PSEN2 N141I mutation normalized the elevated Aβ42/40 ratio, restored the ability of neurons to fire multiple action potentials, increased action potential height, and reduced vulnerability to Aβ-induced cytotoxicity [62].
- The use of multiple, orthogonal assays strengthens the conclusion that the genetic correction was functionally effective, moving beyond genotyping to a comprehensive physiological validation.
The integration of CRISPR-Cas9 gene editing with human induced pluripotent stem cells (iPSCs) represents a transformative approach for correcting disease-causing mutations and creating novel therapeutic interventions. Preclinical animal models serve as the critical bridge between in vitro research and clinical applications, providing indispensable platforms for evaluating the efficacy and safety of these edited cells in a complex living system [63] [105]. These models enable researchers to assess functional recovery, long-term engraftment, tumorigenicity, and potential off-target effects within a physiological context that approximates human conditions [106]. The selection of appropriate animal models, coupled with rigorous experimental design, is therefore paramount for generating meaningful data that can support translational progress and regulatory approval for CRISPR-iPSC-based therapies.
The fundamental purpose of preclinical testing is to demonstrate proof-of-concept that gene-corrected iPSCs can safely differentiate into target cell types, integrate into host tissues, and restore physiological function without causing adverse effects [105]. Different model systems offer distinct advantages: mouse models provide genetic tractability and well-characterized phenotypes; larger animal models such as dogs and pigs better recapitulate human physiology and disease progression; and humanized models incorporating human cells or tissues create a more relevant microenvironment for testing human iPSC-derived therapies [106]. The evolving regulatory landscape, including recent FDA guidelines that no longer mandate animal testing for all new drugs, underscores the importance of selecting the most predictive models rather than simply checking a box for regulatory requirements [105].
CRISPR-iPSC Workflow for Disease Correction
The following diagram illustrates the comprehensive workflow from iPSC collection to preclinical assessment in animal models:
CRISPR-iPSC Therapeutic Development Pipeline This workflow outlines the key stages from patient sample collection to preclinical assessment, highlighting critical decision points for animal model selection.
Disease-Specific Preclinical Models and Outcomes
Preclinical studies utilizing CRISPR-edited iPSCs have demonstrated promising results across multiple disease domains. The table below summarizes key findings from recent investigations:
Table 1: Preclinical Applications of CRISPR-Edited iPSCs in Animal Models
| Disease Category | Specific Disease | Animal Model | Key Genetic Target | Outcome Measures | Results | Reference |
|---|---|---|---|---|---|---|
| Neuromuscular | Duchenne Muscular Dystrophy (DMD) | mdx mouse | Dystrophin exon | Dystrophin expression, muscle function | Partial dystrophin restoration, improved muscle function | [106] |
| Neuromuscular | Duchenne Muscular Dystrophy (DMD) | Canine (deltaE50-MD) | Dystrophin exon 50 | Dystrophin expression in cardiac & skeletal muscle | Systemic dystrophin restoration across multiple muscles | [106] |
| Hematological | β-Thalassemia | Mouse xenograft | β-globin gene | Hemoglobin production, red blood cell morphology | Correction of hemoglobin imbalance, improved RBC function | [67] |
| Hematological | Sickle Cell Disease | Mouse xenograft | β-globin gene | Fetal hemoglobin production, sickling reduction | Increased HbF, reduced sickling in patient-derived cells | [107] |
| Metabolic | Hereditary Tyrosinemia | Mouse model | Fah gene | Liver function, survival | Metabolic correction, improved survival | [107] |
| Cardiovascular | Atherosclerosis | Mouse model | PCSK9 gene | Cholesterol levels, plaque formation | Reduced cholesterol, attenuated atherosclerosis | [107] |
The selection of appropriate animal models depends heavily on the disease pathophysiology and target tissue. For Duchenne Muscular Dystrophy, the mdx mouse model has been extensively utilized due to its well-characterized mutation in exon 23 of the dystrophin gene, although its relatively mild phenotype compared to human DMD has prompted the development of larger animal models such as the deltaE50-MD canine model, which better recapitulates the progressive muscle weakness and cardiac complications seen in patients [106]. For hematological disorders like β-thalassemia and sickle cell disease, humanized mouse models (e.g., NSG mice) that can engraft with human iPSC-derived hematopoietic stem cells provide critical platforms for evaluating the production of functional hemoglobin from corrected cells [67].
Experimental Protocols for Preclinical Assessment
Protocol: CRISPR-Cas9 Editing of iPSCs for Disease Correction
Objective: To precisely correct disease-causing mutations in patient-derived iPSCs using CRISPR-Cas9 genome editing technology.
Materials:
- Patient-derived iPSCs (maintained in feeder-free or feeder-dependent culture)
- CRISPR-Cas9 components (sgRNA, Cas9 protein or expression plasmid, donor DNA template if using HDR)
- Transfection reagents (electroporation system or chemical transfection kit)
- Culture media (essential 8 medium for iPSC maintenance, appropriate differentiation media)
- Validation primers and sequencing reagents
Procedure:
- Design and Preparation of CRISPR Components:
- Design sgRNAs targeting the genomic region of interest using established design tools
- Synthesize sgRNA as synthetic RNA or clone into appropriate expression vector
- Prepare Cas9 as protein, mRNA, or expression plasmid based on delivery method
- Design and prepare donor DNA template for HDR-mediated correction if applicable
Delivery of CRISPR Components:
- Dissociate iPSCs into single-cell suspension using appropriate enzyme
- For electroporation: Mix 1-5 million cells with sgRNA (50-100 pmol) and Cas9 (30-50 pmol protein or 10-20 μg plasmid) in electroporation buffer
- Apply optimized electrical pulses (e.g., Neon Transfection System: 1400V, 10ms, 3 pulses)
- Plate transfected cells on matrix-coated plates with recovery medium containing ROCK inhibitor
Isolation and Validation of Edited Clones:
- Allow recovery for 48-72 hours, then passage cells at low density for single-cell cloning
- Expand individual clones for 10-14 days, then split for genomic DNA extraction and cryopreservation
- Screen clones by PCR amplification of target region and Sanger sequencing
- Validate top candidates by off-target assessment at predicted sites and karyotyping
Differentiation of Corrected iPSCs:
- Direct validated clones toward disease-relevant cell lineages using established protocols
- Characterize differentiated cells by flow cytometry, immunocytochemistry, and functional assays
Troubleshooting Tips:
- Low editing efficiency: Optimize sgRNA design, test different Cas9 formats, adjust delivery parameters
- Poor cell survival: Reduce electrical pulse parameters, ensure high cell viability before transfection, optimize ROCK inhibitor concentration
- Low HDR efficiency: Use single-stranded DNA donors, synchronize cells in S-phase, consider NHEJ inhibitors
Protocol: Transplantation and Assessment in Murine Models
Objective: To evaluate the functional efficacy and safety of CRISPR-corrected iPSC-derived cells in appropriate mouse models.
Materials:
- Immunodeficient mice (e.g., NSG, NOG) for xenograft studies or disease-specific mouse models (e.g., mdx for DMD)
- CRISPR-corrected iPSCs or their differentiated progeny
- Anesthesia equipment, stereotactic injection apparatus (for CNS delivery) or intravenous injection supplies
- In vivo imaging system (if using labeled cells)
- Tissue processing equipment for histology and molecular analysis
Procedure:
- Cell Preparation:
- Differentiate CRISPR-corrected iPSCs into target cell type (e.g., cardiomyocytes, hematopoietic progenitors, neurons)
- Optional: Label cells with luciferase/GFP for tracking or use immunomagnetic selection to purify population
- Prepare single-cell suspension at appropriate concentration in transplantation buffer
Transplantation:
- Anesthetize mice according to approved protocol
- For intramuscular delivery (e.g., DMD models): Inject 10-50μL containing 0.5-1 million cells into tibialis anterior or gastrocnemius muscle
- For intravenous delivery (hematological models): Inject 100-200μL via tail vein
- For CNS delivery: Use stereotactic apparatus to inject 2-5μL into target region
- Monitor animals during recovery and provide analgesic as needed
Functional Assessment:
- Conduct disease-specific functional tests at regular intervals (e.g., grip strength, treadmill for DMD; blood counts for hematological diseases)
- For cell tracking: Perform in vivo imaging at multiple time points if cells are labeled
- Monitor overall health, weight, and behavior for safety assessment
Endpoint Analysis:
- Euthanize animals at predetermined timepoints (e.g., 4, 8, 12 weeks post-transplantation)
- Collect and process target tissues for histology, protein analysis, and genomic assessment
- For efficacy: Quantify engraftment (human-specific markers), expression of corrected protein (e.g., dystrophin, hemoglobin)
- For safety: Assess tumor formation, inflammatory responses, ectopic tissue formation
Troubleshooting Tips:
- Low engraftment: Optimize cell preparation, immunosuppression regimen, delivery technique
- High mortality: Adjust cell dose, improve surgical/transplantation technique, enhance post-procedural care
- Teratoma formation: Implement more rigorous purification of differentiated cells prior to transplantation
Safety Assessment Framework for CRISPR-Edited iPSC Therapies
A comprehensive safety assessment is crucial for clinical translation of CRISPR-edited iPSC therapies. The following diagram outlines key components of this evaluation:
CRISPR-iPSC Safety Assessment Framework This comprehensive safety evaluation covers molecular characterization, functional validation, and in vivo assessment to identify potential risks before clinical application.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for CRISPR-iPSC Preclinical Studies
| Reagent Category | Specific Product | Function in Preclinical Workflow | Considerations for Selection |
|---|---|---|---|
| iPSC Culture | Essential 8 Medium | Feeder-free maintenance of pluripotency | Xeno-free formulation enhances clinical relevance |
| iPSC Culture | Vitronectin or Matrigel | Extracellular matrix for cell attachment | Lot-to-lot variability affects reproducibility |
| CRISPR Delivery | Neon Transfection System | Electroporation for hard-to-transfect iPSCs | Optimized pulse parameters critical for viability |
| CRISPR Format | Cas9-sgRNA RNP complex | Direct delivery minimizes off-target effects | Higher specificity but more costly than plasmid DNA |
| Cell Isolation | FACS or MACS systems | Purification of differentiated cell populations | Purity requirements depend on transplantation safety |
| Animal Models | NSG/NOG mice | Immunodeficient hosts for human cell engraftment | Variable reconstitution across tissue types |
| In Vivo Tracking | Luciferase/GFP reporters | Non-invasive monitoring of cell persistence | Potential immunogenicity with foreign proteins |
| Histology | Human-specific antibodies | Distinguish transplanted from host cells | Species cross-reactivity must be validated |
The selection of appropriate research reagents significantly impacts the success and reproducibility of preclinical studies. For CRISPR editing in iPSCs, the ribonucleoprotein (RNP) complex format has gained prominence due to its transient activity, which reduces off-target effects while maintaining high on-target efficiency [108]. Similarly, the choice of delivery method must balance efficiency with cell viability—electroporation systems like the Neon Transfection System have demonstrated superior performance for hard-to-transfect iPSCs compared to traditional cuvette-based electroporation or chemical methods [108]. For in vivo tracking, lentiviral integration of reporter genes must be carefully evaluated as it can potentially alter cell behavior, while human-specific antibodies enable precise identification of transplanted cells in animal tissues during endpoint analysis.
Preclinical animal models remain indispensable for validating the therapeutic potential and safety profile of CRISPR-corrected iPSCs before clinical translation. The continuous refinement of both disease models and assessment methodologies enhances the predictive value of these preclinical studies. As the field advances, standardized protocols for efficacy and safety assessment will facilitate more direct comparisons across studies and accelerate the development of CRISPR-iPSC-based therapies for a broad range of genetic disorders. The integration of more sophisticated humanized models and sensitive detection methods for off-target effects will further strengthen the preclinical pipeline, ultimately supporting the transition of these promising therapies into clinical trials.
The convergence of induced pluripotent stem cell (iPSC) technology and CRISPR-Cas9 genome editing represents a paradigm shift in therapeutic development [8]. This combination enables the creation of genetically corrected, patient-specific cells for autologous transplantation, moving beyond the limitations of conventional treatments that often manage symptoms rather than address root genetic causes [21] [22]. For researchers and drug development professionals, understanding the comparative advantages, technical protocols, and clinical translation potential of this integrated approach is essential for guiding future therapeutic innovation. This analysis examines the quantitative evidence, detailed methodologies, and practical research tools that position CRISPR-corrected iPSCs as a transformative platform in regenerative medicine.
Quantitative Comparison of Therapeutic Approaches
Therapeutic Outcomes Across Disease Models
Table 1: Comparative analysis of therapeutic outcomes for CRISPR-iPSC, conventional, and other advanced therapies across multiple disease models.
| Disease Model | Therapeutic Approach | Key Efficacy Metrics | Limitations & Challenges | References |
|---|---|---|---|---|
| Inherited Retinal Degeneration | CRISPR-corrected autologous iPSCs | Restoration of retinal transcript and protein expression in patient-derived cells; potential for permanent correction. | Optimization of transplantation efficiency and long-term integration required. | [21] |
| Gene Augmentation (Viral Vector) | Partial functional rescue; clinical trials ongoing. | Risk of overexpression toxicity; limited by viral packaging capacity for large genes. | [21] | |
| Pharmacological Therapy | Manages symptoms only; does not alter disease progression. | Limited efficacy; does not address underlying genetic cause. | - | |
| Recessive Dystrophic Epidermolysis Bullosa (RDEB) | CRISPR-corrected autologous iPSCs | Successful gene correction in primary fibroblasts; derivation of multi-lineage cells (keratinocytes, MSCs, hematopoietic progenitors). | Requires rigorous safety profiling for off-target effects. | [22] |
| Allogeneic Haematopoietic Cell Transplant (HCT) | Can ameliorate some symptoms. | Significant side effects (e.g., graft-versus-host disease); unresponsive blistering persists. | [22] | |
| Palliative Care | Manages pain and bandages wounds. | Non-curative; does not address disease pathophysiology. | [22] | |
| β-Thalassemia | CRISPR-corrected autologous iPSCs | Potential to generate normal hematopoietic cells and red blood cells; autologous source. | In vivo functional validation of derived cells ongoing. | [67] [109] |
| Allogeneic HSCT (Current Standard) | Potentially curative; established protocol. | Scarcity of matched donors; risk of graft rejection and complications. | [67] | |
| Chronic Blood Transfusions & Iron Chelation | Enables patient survival; manages symptoms. | Lifelong treatment required; leads to iron overload and organ damage. | [67] | |
| Sickle Cell Disease (SCD) & Transfusion-Dependent β-Thalassemia (TDT) | CRISPR-Cas9 (ex vivo, non-iPSC, e.g., Casgevy) | FDA-approved; eliminates vaso-occlusive crises (SCD) or transfusion needs (TDT) in majority of patients. | Complex, costly process; myeloablation required; long-term data still being collected. | [27] [1] |
Technical and Economic Considerations
Table 2: Comparison of technical and economic parameters between CRISPR-iPSC therapy and conventional treatments.
| Parameter | CRISPR-Corrected iPSC Therapy | Conventional Therapy (e.g., HSCT, Chronic Management) | CRISPR-based Non-iPSC Therapy (e.g., Casgevy) |
|---|---|---|---|
| Therapeutic Nature | Curative (potential) | Curative (HSCT) / Palliative (Chronic Management) | Curative (potential) |
| Time to Effect | Long (weeks to months for cell manufacturing) | Immediate (Palliative) / Long (HSCT recovery) | Long (months for engraftment) |
| Treatment Duration | Single or limited administration (potential) | Lifelong (Palliative) / Single (HSCT, with lifelong follow-up) | Single administration |
| Immuno-compatibility | Autologous; minimal rejection risk | Allogeneic HSCT requires immunosuppression | Autologous; minimal rejection risk |
| Manufacturing Complexity | High (reprogramming, editing, differentiation) | Low (Palliative) / Medium (Donor matching for HSCT) | High (ex vivo cell editing) |
| Estimated Cost (R&D & Treatment) | Very High (currently) | Low (Palliative) / High (HSCT) | Very High |
| Key Technical Risk Factors | Off-target edits, tumorigenicity (teratomas), genomic instability | Infection, GVHD, iron overload (palliative) | Off-target edits, myeloablation risks |
Experimental Protocols for CRISPR-iPSC Workflow
High-Efficiency Precision Genome Editing in iPSCs
Recent advances have dramatically improved the efficiency of homology-directed repair (HDR) in iPSCs, a previous major bottleneck. The protocol below, adapted from a 2024 study, achieves HDR rates exceeding 90% by enhancing cell survival post-electroporation [3].
Key Reagents:
- Cell Line: Human iPSCs (e.g., maintained in mTeSR Plus or Stemflex medium on Matrigel).
- RNP Complex: Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT) and synthetic sgRNA (IDT).
- Repair Template: Single-stranded oligonucleotide (ssODN) with homologous arms and desired point mutation, incorporating silent mutations in the PAM site to prevent re-cleavage.
- Pro-survival Supplements: CloneR (STEMCELL Technologies), Revitacell (Gibco).
- p53 Suppression: pCXLE-hOCT3/4-shp53-F plasmid (Addgene #27077) or small molecule inhibitors.
Procedure:
- Culture & Preparation: Maintain iPSCs in feeder-free conditions. One day before nucleofection, change to cloning media (Stemflex supplemented with 1% Revitacell and 10% CloneR) [3].
- RNP Complex Formation: Incubate 0.6 µM sgRNA with 0.85 µg/µL HiFi Cas9 protein for 20-30 minutes at room temperature to form the ribonucleoprotein (RNP) complex.
- Nucleofection Mixture: Combine the RNP complex with 5 µM ssODN, 50 ng/µL p53 shRNA plasmid, and 0.5 µg of a GFP reporter plasmid (for transfection tracking).
- Nucleofection: Dissociate iPSCs to single cells using Accutase. Resuspend 1x10^6 cells in the nucleofection solution containing the complete mixture from step 3. Perform nucleofection using an appropriate program (e.g., for a 4D-Nucleofector).
- Post-Nucleofection Recovery: Seed the transfected cells immediately into pre-warmed cloning media. The inclusion of p53 shRNA, CloneR, and ROCK inhibitor is critical for mitigating DNA damage-induced apoptosis and improving the survival of edited cells [3].
- Clonal Isolation & Expansion: After 48-72 hours, begin antibiotic selection if a resistance cassette was co-delivered. Between days 7-14, pick individual colonies and expand them for genotyping.
- Genotyping & Validation: Screen clonal lines by PCR and Sanger sequencing to identify correctly edited clones. Karyotype analysis and whole-genome sequencing are recommended to confirm genomic integrity and check for off-target effects [3].
Multi-Lineage Differentiation of Gene-Corrected iPSCs
A significant advantage of the CRISPR-iPSC platform is the ability to derive multiple therapeutic cell types from a single, genetically corrected clone, as demonstrated for RDEB [22].
Workflow:
- iPSC Derivation: Use a non-integrating reprogramming method (e.g., Sendai virus or episomal vectors) on gene-corrected fibroblasts or directly on CRISPR-edited iPSCs to generate a master cell bank [22] [53].
- Directed Differentiation:
- Keratinocytes: Employ defined differentiation protocols using growth factors like BMP4 and retinoic acid to direct iPSCs toward surface ectoderm and subsequently mature into keratinocytes. Validated by expression of KRT5, KRT14, and KRT10 [22].
- Mesenchymal Stem Cells (MSCs): Differentiate iPSCs into MSCs using protocols that mimic embryonic development of the mesoderm. Resulting cells should express classic MSC surface markers (CD73, CD90, CD105) and possess tri-lineage differentiation potential (adirogenic, chondrogenic, osteogenic) [22] [109].
- Hematopoietic Progenitors: Use a vascular induction strategy or co-culture with stromal cells to generate definitive hematopoietic progenitors. Functionality is confirmed by colony-forming unit (CFU) assays in methylcellulose media [22].
Diagram 1: Experimental workflow for generating autologous cell therapies from CRISPR-corrected iPSCs.
Signaling Pathways and Key Molecular Mechanisms
The CRISPR-Cas9 system induces precise DNA double-strand breaks (DSBs), leveraging the cell's endogenous repair mechanisms. The two primary pathways involved are non-homologous end joining (NHEJ) and homology-directed repair (HDR) [8] [1]. For precise gene correction in iPSCs, HDR is the desired pathway, facilitated by a donor template.
Diagram 2: Core DNA repair pathways activated by CRISPR-Cas9 editing.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and materials for CRISPR-Cas9 gene editing in iPSCs.
| Reagent / Material | Function / Purpose | Example Products & Catalog Numbers |
|---|---|---|
| CRISPR Nuclease | Creates a double-strand break at the target genomic locus. | Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT #108105559) [3] |
| Synthetic sgRNA | Guides the Cas9 nuclease to the specific DNA sequence. | Alt-R CRISPR-Cas9 sgRNA (IDT) [3] [43] |
| HDR Donor Template | Serves as a repair template for precise gene correction. | Single-stranded oligonucleotide (ssODN, Ultramer from IDT) [3] |
| Nucleofector System | Enables efficient delivery of CRISPR components into iPSCs. | 4D-Nucleofector System (Lonza) [3] [43] |
| Pro-Survival Supplement | Enhances single-cell survival post-nucleofection, critical for clonal expansion. | CloneR (STEMCELL Tech #05888) [3] |
| p53 Inhibitor | Transiently suppresses p53-mediated apoptosis to improve HDR efficiency. | pCXLE-hOCT3/4-shp53-F plasmid (Addgene #27077) [3] |
| Stem Cell Culture Media | Maintains iPSC pluripotency and supports growth. | mTeSR Plus (STEMCELL Tech #100-0276), Stemflex (Gibco #A334901) [3] |
| Basement Membrane Matrix | Provides a substrate for feeder-free iPSC culture. | Matrigel (Corning #47743-706) [3] [43] |
| Cell Dissociation Reagent | Dissociates iPSC colonies into single cells for nucleofection. | Accutase (VWR #AT104) [3] |
The therapeutic application of induced pluripotent stem cells (iPSCs) corrected via CRISPR-Cas9 genome editing represents a transformative approach for treating genetic disorders. A critical decision in developing these therapies is the choice between autologous (patient-specific) and allogeneic (donor-derived) cell sources. This application note examines the key immunological factors influencing this choice, providing a structured comparison and detailed protocols to guide researchers and drug development professionals in navigating the complex immune landscape of iPSC-based regenerative medicine. The balance between immune rejection, therapeutic efficacy, and practical manufacturability forms the core challenge in translating these advanced therapies to the clinic [53].
Comparative Analysis: Autologous vs. Allogeneic iPSC Approaches
The table below summarizes the core immunological characteristics, advantages, and challenges associated with autologous and allogeneic approaches to CRISPR-Cas9-edited iPSC therapies.
Table 1: Key Characteristics of Autologous and Allogeneic iPSC-Based Therapeutic Approaches
| Parameter | Autologous Approach (Patient-Specific iPSCs) | Allogeneic Approach (Off-the-Shelf iPSCs) |
|---|---|---|
| Basic Principle | Use of the patient's own cells, which are reprogrammed, genetically corrected, and differentiated. | Use of cells from a healthy donor, creating a master cell bank for multiple patients. |
| Immune Recognition | Theoretically low risk of immune rejection, as the cells are self-derived. [53] | High risk of immune rejection by T-cell-mediated response and NK-cell-mediated cytotoxicity due to HLA mismatch. [110] |
| Key Immune Challenges | Potential immune response due to epigenetic aberrations or neoepitopes formed during reprogramming and differentiation; particularly sensitive to autologous NK-cell killing. [110] | Requires long-term immunosuppression for the recipient or sophisticated immune engineering of the donor cells. [53] |
| Therapeutic Timeline | Lengthy process (several months) for reprogramming, quality control, and differentiation for each individual patient. [110] | Immediate availability of pre-manufactured, quality-controlled cell products for treatment. |
| Scalability & Cost | High cost and complex logistics for personalized manufacturing; difficult to scale. [53] [110] | More favorable cost structure and easier scalability for large patient populations due to standardized, centralized manufacturing. [53] |
| Major Engineering Strategy | CRISPR-Cas9-mediated correction of the disease-causing mutation. [22] | Creation of "hypoimmunogenic" cell lines via CRISPR-Cas9 knockout of B2M (to reduce HLA-I) and CIITA (to reduce HLA-II). [110] |
| Primary Clinical Status | Used in ongoing clinical trials, e.g., autologous iPSC-derived dopamine neurons for Parkinson's disease. [53] | Used in ongoing clinical trials, e.g., allogeneic iPSC-derived dopaminergic progenitors for Parkinson's disease. [53] |
Detailed Experimental Protocol: Assessing Immune Compatibility of iPSC-Derivatives
A critical step in the development of any iPSC-based therapy is the functional assessment of how the derived cells interact with the immune system. The following protocol outlines a robust in vitro method for evaluating the activation of autologous and allogeneic Natural Killer (NK) cells, a key innate immune population, when co-cultured with iPSC-derived target cells [110].
Background and Principle
Despite being derived from a patient's own cells, iPSC-derived somatic cells can remain susceptible to immune attack. This protocol is designed to test the hypothesis that an imbalance in ligands for activating and inhibitory NK-cell receptors on iPSC-derivatives can lead to their recognition and elimination by autologous NK-cells, regardless of their HLA-I status [110].
Materials and Reagents
Table 2: Key Research Reagent Solutions for Immune Co-culture Assay
| Reagent/Solution | Function/Description | Example Supplier/Note |
|---|---|---|
| Isogenic Cell Model | Provides a controlled system for comparison. Includes parental somatic cells (e.g., dermal fibroblasts), CRISPR-edited iPSCs, and their differentiated derivatives. | Generated in-house. Essential for autologous immune response studies. |
| CRISPR-Cas9 System (e.g., PX458 plasmid) | For genetic modification of iPSCs (e.g., B2M knockout to create HLA-I deficient cells). | Addgene #48138; used with transfection reagent like TransIT-LT1. [110] |
| Ficoll-Paque PLUS | Density gradient medium for isolation of Peripheral Blood Mononuclear Cells (PBMCs) from whole blood. | Cytiva |
| NK Cell Isolation Kit (human) | For negative selection of untouched NK cells from PBMCs. | Miltenyi Biotec or STEMCELL Technologies |
| CellTrace CFSE Cell Proliferation Kit | Fluorescent dye for labeling target cells to distinguish them from effector cells in flow cytometry. | Thermo Fisher Scientific |
| Anti-CD107a APC Antibody | Marker for NK-cell degranulation, a key indicator of activation. | BioLegend |
| Recombinant Human IL-2 | Cytokine for maintaining NK-cell viability and activity during culture. | PeproTech |
| Flow Cytometry Assay Buffer | PBS supplemented with 2% FBS for antibody staining and cell resuspension for flow analysis. | N/A |
Step-by-Step Procedure
Establishment of Target Cells:
- Generate an isogenic cell model. This includes:
- Parental fibroblasts from a skin biopsy.
- iPSCs reprogrammed from the fibroblasts (using non-integrating Sendai virus or episomal vectors).
- iPSC-derived fibroblast-like cells (iPS-fibro) via directed differentiation.
- Gene-edited iPS-fibro (e.g., ΔiPS-fibro) with B2M knockout via CRISPR-Cas9 to abolish HLA-I surface expression [110].
- Generate an isogenic cell model. This includes:
Isolation of Effector Immune Cells:
- Collect fresh peripheral blood from the same donor (for autologous assays) or a different donor (for allogeneic assays).
- Isolate PBMCs using density gradient centrifugation with Ficoll-Paque.
- Isolate untouched NK-cells from PBMCs using a negative selection magnetic-activated cell sorting (MACS) kit.
Co-culture and NK-Cell Activation Assay:
- Label the target cells (parental fibroblasts, iPS-fibro, ΔiPS-fibro) with CFSE.
- Seed target cells in a 96-well plate.
- Add NK-cells to the wells at a specific Effector:Target (E:T) ratio (e.g., 5:1).
- Add anti-CD107a antibody directly to the co-culture to capture degranulation events.
- Include controls: NK-cells alone (negative control) and NK-cells stimulated with PMA/Ionomycin (positive control).
- Incubate for 4-6 hours.
Flow Cytometry Analysis:
- Harvest cells from the co-culture.
- Stain with a viability dye and antibodies against NK-cell surface markers (e.g., CD56) and intracellular markers if needed.
- Analyze samples using a flow cytometer.
- Key readouts:
- % of CD107a+ NK-cells: Measures degranulation/activation.
- Cytotoxicity: Calculated by quantifying the loss of CFSE+ target cells.
Data Interpretation
A successful experiment will typically show that iPS-fibro and ΔiPS-fibro elicit significantly higher levels of CD107a expression on autologous NK-cells compared to the parental fibroblasts. This indicates that the process of reprogramming and differentiation alters the cell surface in a way that activates NK-cells. The B2M knockout is expected to further enhance this activation due to the "missing-self" response [110]. This data can be correlated with transcriptomic analysis of ligand expression in the target cells.
Visualizing the Immune Recognition Pathway of iPSC-Derivatives
The following diagram illustrates the molecular mechanism by which iPSC-derived cells are recognized and targeted by autologous NK-cells, a key finding from the referenced research [110].
Diagram: NK-Cell Activation by iPSC-Derivatives Due to Ligand Imbalance.
The choice between autologous and allogeneic approaches for CRISPR-Cas9-corrected iPSC therapies is multifaceted, with immunological safety being a paramount concern. While autologous cells mitigate the risk of T-cell mediated rejection, emerging evidence reveals their vulnerability to the innate immune system, particularly NK-cells [110]. Allogeneic "off-the-shelf" products offer scalability but require extensive immune engineering to evade both adaptive and innate immune responses. A comprehensive in vitro immune profiling, as detailed in this application note, is therefore indispensable for de-risking clinical development. The ultimate selection of a strategy must be guided by the target disease, patient population, manufacturing capabilities, and a thorough understanding of the immune interactions involved.
The clinical application of CRISPR-Cas9 gene editing represents one of the most significant advancements in modern therapeutics, transitioning rapidly from theoretical concept to clinical reality. Since the first regulatory approval of a CRISPR-based medicine, Casgevy (exagamglogene autotemcel) for sickle cell disease and transfusion-dependent beta thalassemia, the field has witnessed exponential growth in clinical investigation [27]. As of February 2025, the global clinical landscape encompasses approximately 250 gene-editing clinical trials, with over 150 trials currently active across multiple therapeutic areas [111]. This expansion is particularly relevant for researchers exploring CRISPR-Cas9 editing in induced pluripotent stem cells (iPSCs) for disease correction, as these investigations form the foundational research that enables subsequent clinical translation. The growing pipeline reflects increasing confidence in gene-editing technologies despite persistent challenges in delivery, efficiency, and safety assessment.
The evolution of genome editing platforms has progressed through several generations, beginning with zinc-finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs), before culminating in the widespread adoption of CRISPR-Cas systems [1]. CRISPR-Cas9 technology has democratized gene editing due to its comparative simplicity, high efficiency, and lower cost compared to previous platforms. For iPSC research specifically, CRISPR has enabled more efficient creation of genetically modified isogenic lines, dramatically enhancing our ability to model human diseases and develop autologous cell replacement therapies [93]. The technology continues to evolve with the recent development of base editing and prime editing systems that offer potentially greater precision without introducing double-strand breaks, addressing some safety concerns associated with traditional CRISPR-Cas9 approaches [1].
Current Clinical Trial Landscape
The clinical trial landscape for gene editing therapies has diversified considerably beyond the initial focus on hematologic disorders. As tracked by CRISPR Medicine News, the field now encompasses a broad array of editing tools including CRISPR-Cas, base editors, prime editors, zinc fingers, TALENs, meganucleases, CAS-CLOVER, RNA editors, and epigenetic-editing technology [111]. The distribution of these trials across disease areas and development phases provides crucial insights for researchers prioritizing therapeutic targets and planning translational pathways.
Table 1: Global Gene Editing Clinical Trials by Therapeutic Area (February 2025)
| Therapeutic Area | Number of Trials | Representative Indications | Noteworthy Phase 3 Trials |
|---|---|---|---|
| Hematological Malignancies | ~70 | B-cell malignancies, AML, Multiple Myeloma | CAR-T trials for B-ALL |
| Hemoglobinopathies | ~25 | Sickle cell disease, Beta thalassemia | Casgevy (approved) |
| Solid Cancers | ~35 | Various solid tumors | CAR-T for solid tumors |
| Metabolic Disorders | ~20 | Hereditary amyloidosis, Hypercholesterolemia | hATTR with cardiomyopathy |
| Autoimmune Diseases | ~15 | SLE, Multiple Sclerosis, Lupus Nephritis | CTX112 for autoimmune indications |
| Cardiovascular Diseases | ~10 | Familial hypercholesterolemia, Elevated Lp(a) | CTX310, CTX320 for cardiovascular risk |
| Infectious Diseases | ~10 | E. coli infections, UTIs | CRISPR-enhanced phage therapies |
| Ophthalmic Diseases | ~5 | Inherited retinal degeneration | CEP290-related LCA |
| Other Rare Diseases | ~40 | Immunodeficiencies, Muscular dystrophy | Various monogenic disorders |
Table 2: CRISPR Clinical Trial Pipeline by Phase and Technology Platform
| Development Phase | Number of Trials | Primary Technologies | Key Objectives |
|---|---|---|---|
| Preclinical/IND-enabling | ~70 | CRISPR-Cas9, Base editing | Safety, efficacy, manufacturing |
| Phase I | ~90 | CRISPR-Cas9, CAR-T editing | Safety, dosage finding |
| Phase II | ~60 | CRISPR-Cas9, Base editing | Efficacy, side effect profile |
| Phase III | ~20 | CRISPR-Cas9, TALENs | Pivotal efficacy, regulatory submission |
| Approved Products | 2+ | CRISPR-Cas9 | Commercial deployment |
Analysis of Key Therapeutic Areas
Hematologic Disorders and Immuno-Oncology
Gene editing for blood disorders continues to lead the field, with the majority of Phase 3 trials targeting sickle cell disease and/or beta thalassemia [111]. The successful approval and commercialization of Casgevy has demonstrated the viability of ex vivo CRISPR-edited cell therapies, with more than 50 authorized treatment centers (ATCs) activated globally and significant progress in securing payer reimbursement [112]. The immuno-oncology segment has also expanded rapidly, with allogeneic and autologous CAR-T therapies dominating the pipeline. Notable advances include CTX112, a next-generation allogeneic CAR-T product candidate targeting CD19, which has demonstrated strong efficacy in relapsed or refractory B-cell malignancies and has received regenerative medicine advanced therapy (RMAT) designation from the FDA [112].
In Vivo Therapeutic Applications
The development of in vivo CRISPR therapies represents a significant technological advancement, eliminating the need for complex ex vivo cell processing. Intellia Therapeutics' phase I trial for hereditary transthyretin amyloidosis (hATTR) was the first clinical trial for a CRISPR-Cas9 therapy delivered systemically via lipid nanoparticle (LNP) [27]. This approach has demonstrated remarkable success, with trial participants showing ~90% reduction in levels of the disease-related TTR protein sustained over two years of follow-up [27]. The success of LNP-mediated delivery to the liver has spurred development of additional programs targeting cardiovascular disease, including CTX310 (targeting ANGPTL3) and CTX320 (targeting LPA), with updates expected in the first half of 2025 [112].
Rare Genetic Diseases and Personalized Approaches
A landmark case reported in 2025 demonstrated the potential for personalized on-demand CRISPR therapies for rare genetic diseases. An infant with CPS1 deficiency received a bespoke in vivo CRISPR therapy developed and delivered in just six months, setting a precedent for a regulatory pathway for rapid approval of platform therapies [27]. This case serves as a proof-of-concept for treating ultra-rare genetic disorders using CRISPR technology and highlights the potential for iPSC-based approaches in creating patient-specific therapies.
Regulatory Framework for CRISPR-Based Therapies
Regulatory Classification and Pathways
CRISPR-based medicinal products are classified as advanced therapy medicinal products (ATMPs) and require rigorous regulatory oversight to ensure safety and efficacy [113]. The regulatory framework for these products has evolved to address the unique challenges posed by gene editing technologies, with agencies like the FDA and EMA developing adaptive pathways that balance innovation with appropriate safeguards. The successful regulatory approval of Casgevy in multiple jurisdictions has established important precedents for future CRISPR-based therapies, particularly in the areas of potency assays, manufacturing quality controls, and long-term safety monitoring [27].
The regulatory pathway for CRISPR therapeutics involves demonstrating comprehensive product characterization, including detailed analysis of on-target editing efficiency, potential off-target effects, and product purity [113]. For ex vivo edited cell products like those derived from iPSCs, regulators require rigorous demonstration of cell viability, identity, potency, and freedom from contaminants throughout the manufacturing process. The regulatory landscape continues to evolve as new editing technologies emerge, with base editors and prime editors presenting additional characterization challenges compared to conventional CRISPR-Cas9 systems [1].
Key Regulatory Considerations for Clinical Trial Applications
Advancing CRISPR-based products into clinical trials requires careful attention to three primary domains: quality (CMC), nonclinical, and clinical development [113]. Each domain presents unique challenges for gene editing therapies, particularly when utilizing iPSC platforms that may involve complex manufacturing processes and extended culture periods.
Table 3: Key Regulatory Requirements for CRISPR-Based Therapies
| Development Area | Key Requirements | iPSC-Specific Considerations |
|---|---|---|
| Quality (CMC) | - Comprehensive product characterization - Editing efficiency validation - Purity and impurity profiling - Stability data | - Genetic stability during culture - Pluripotency confirmation - Differentiation potency - Master cell banking |
| Nonclinical Development | - Proof-of-concept studies - Biodistribution and persistence - Tumorigenicity assessment - Off-target editing analysis | - In vivo teratoma formation assays - Genomic integrity assessment - Differentiation fidelity - Functional integration in animal models |
| Clinical Development | - Appropriate patient population - Risk-benefit assessment - Long-term follow-up plans - Monitoring for off-target effects | - Immunogenicity assessment - Cell survival and engraftment - Functional outcome measures - Appropriate endpoint selection |
CRISPR-Cas9 Genome Editing in iPSCs: Applications and Protocols
iPSC Applications in Disease Modeling and Cell Therapy
The combination of CRISPR-Cas9 and iPSC technology has revolutionized approaches to disease modeling and autologous cell therapy development. iPSCs provide an unlimited source of patient-specific cells that can be differentiated into relevant cell types for studying disease mechanisms and developing regenerative therapies. The application of CRISPR to correct disease-causing mutations in patient-derived iPSCs has been successfully demonstrated for numerous conditions, including Tuberous Sclerosis Complex Type 2 (TSC2) [23], Huntington's disease [30], and inherited retinal degenerations [21].
In Huntington's disease research, HD-iPSCs have been corrected using CRISPR-Cas9 to create isogenic control lines, enabling detailed investigation of disease mechanisms and high-throughput drug screening [30]. Similarly, for inherited retinal diseases, researchers have developed multiple CRISPR strategies to correct different classes of mutations in patient iPSCs, including homology-directed repair for exonic mutations, NHEJ-mediated excision for deep intronic mutations, and allele-specific inactivation for dominant gain-of-function mutations [21]. These approaches demonstrate the versatility of CRISPR-edited iPSCs for addressing diverse genetic disorders.
Enhanced Protocol for High-Efficiency Genome Editing in iPSCs
Recent methodological advances have addressed key challenges in CRISPR editing of iPSCs, particularly low editing efficiency and poor cell survival following nucleofection. The protocol below incorporates p53 inhibition and pro-survival molecules to achieve homologous recombination rates exceeding 90% in human iPSCs, significantly streamlining the generation of isogenic cell lines [93].
Reagent Preparation
Table 4: Essential Reagents for High-Efficiency iPSC Genome Editing
| Reagent Category | Specific Reagents | Function | Notes |
|---|---|---|---|
| CRISPR Components | - Alt-R S.p. HiFi Cas9 Nuclease V3 - Sequence-specific sgRNA - Single-strand oligo donor (ssODN) | - Target recognition and cleavage - Homology-directed repair | - HiFi Cas9 reduces off-target effects - ssODN should contain desired edits with homologous arms |
| Cell Culture | - mTeSR Plus complete media - Matrigel-coated plates - Revitacell supplement - CloneR | - iPSC maintenance - Cell attachment - Enhanced survival post-editing - Clonal expansion | - Quality of extracellular matrix critical for single-cell survival - Revitacell contains ROCK inhibitor |
| Nucleofection | - P3 primary cell nucleofector solution - Alt-R Cas9 HDR enhancer - shp53-f2 plasmid | - Electroporation delivery - Enhances HDR efficiency - Temporary p53 inhibition | - p53 inhibition crucial for preventing apoptosis in edited cells - HDR enhancer improves precise editing |
Step-by-Step Editing Protocol
sgRNA and Donor Design: Design sgRNA using IDT software (https://www.idtdna.com/site/order/designtool/index/HDRDESIGN) targeting the genomic region of interest. Design ssODN with ~100 nt homologous arms flanking the desired edit.
iPSC Culture Preparation: Maintain iPSCs in mTeSR Plus complete media on Matrigel-coated plates. One hour before nucleofection, change to mTeSR Plus with 1% Revitacell supplement.
RNP Complex Assembly: Prepare ribonucleoprotein (RNP) complex by combining:
- 0.8 μL Cas9 nuclease V3 (64 mM)
- 1.2 μL sgRNA (100 μM)
- 3.0 μL D-PBS (1×)
- Total volume: 5.0 μL Incubate at room temperature for 10-20 minutes.
Nucleofection Reaction Preparation: Combine in order:
- 7 μL P3 primary cell nucleofector solution
- 1 μL shp53-f2 plasmid (p53 inhibitor)
- 1 μL Alt-R electroporation enhancer
- 1 μL ssODN (100 μM)
- 5 μL RNP complex
- 11 μL iPSCs (1 million cells)
- Total volume: 20 μL
Nucleofection: Transfer reaction to 16-well Nucleocuvette Strip. Use the 4D-Nucleofector system with program CA-137.
Post-Nucleofection Recovery: Immediately add pre-warmed CloneR media containing Alt-R Cas9 HDR enhancer to nucleofected cells. Plate cells on Matrigel-coated plates at appropriate density.
Culture and Expansion: Culture cells in mTeSR Plus with CloneR for 48 hours, then transition to standard mTeSR Plus media. Allow colonies to form over 7-10 days.
Clone Screening and Validation: Pick individual clones, expand, and screen for desired edits using PCR, restriction fragment length analysis, and Sanger sequencing. Validate clones through karyotyping and pluripotency marker staining.
Diagram 1: High-Efficiency CRISPR Editing Workflow for iPSCs. The protocol integrates key reagent additions at critical steps to enhance cell survival and editing efficiency.
Critical Factors for Successful iPSC Genome Editing
Several factors significantly impact the success of CRISPR genome editing in iPSCs. Cell line variability can profoundly influence editing outcomes, necessitating optimization for specific iPSC lines [93]. The choice of Cas9 variant is also crucial, with High-Fidelity (HiFi) Cas9 offering reduced off-target effects while maintaining high on-target activity. The delivery method represents another critical consideration, with ribonucleoprotein (RNP) complex delivery generally providing higher efficiency and reduced off-target effects compared to plasmid-based approaches.
The timing of p53 inhibition has been shown to dramatically improve homologous recombination rates in human iPSCs by preventing apoptosis triggered by DNA damage response pathways [93]. Similarly, the inclusion of ROCK inhibitors (via Revitacell or CloneR) enhances single-cell survival following nucleofection. For precise editing requiring homology-directed repair, the inclusion of HDR enhancers can significantly improve efficiency by temporarily suppressing the competing NHEJ pathway.
Emerging Trends and Future Perspectives
Technological Advancements
The CRISPR technology landscape continues to evolve rapidly, with several next-generation editing platforms showing promise for clinical applications. Base editing systems enable direct chemical conversion of one DNA base to another without introducing double-strand breaks, potentially offering greater safety profiles for therapeutic applications [1]. Prime editing represents an even more precise approach that can implement all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring donor templates or causing double-strand breaks. These technologies are particularly relevant for iPSC-based therapies where precise genetic correction is required without introducing genomic instability.
Delivery technologies have also advanced significantly, with lipid nanoparticles (LNPs) emerging as a versatile platform for in vivo delivery of CRISPR components [27]. The success of LNP-based delivery to the liver has opened new possibilities for targeting other tissues through modulation of LNP composition and surface properties. Additionally, the demonstration that LNPs don't trigger the immune system like viruses do has enabled the possibility of redosing, as evidenced by multiple patients receiving additional doses of in vivo CRISPR therapies to increase editing efficiency [27].
Challenges and Barriers
Despite significant progress, the field faces several substantial challenges. Delivery remains the primary bottleneck for many therapeutic applications, particularly for tissues beyond the liver and for central nervous system disorders [27] [114]. The high cost of clinical trials and manufacturing has created financial pressures throughout the industry, leading to pipeline narrowing and significant layoffs in some CRISPR-focused companies [27]. Additionally, proposed cuts to US government funding for basic and applied scientific research threaten to slow the pace of innovation, with potential reductions of 40% to the National Institute of Health budget and elimination of graduate STEM education funding [27].
Safety considerations continue to warrant careful attention, particularly off-target effects, long-term persistence of edited cells, and immune responses to editing components. For iPSC-based therapies, additional concerns include tumorigenic potential, genomic instability during culture, and functional integration following transplantation. These challenges highlight the need for continued rigorous preclinical evaluation and comprehensive long-term follow-up in clinical trials.
Diagram 2: Key Challenges in CRISPR Clinical Translation. Multiple interconnected barriers must be addressed to advance CRISPR therapies through clinical development.
Future Directions
The future clinical development of CRISPR-based therapies will likely focus on expanding disease indications beyond the current focus on monogenic disorders to include more common, complex diseases. Cardiovascular disease represents a particularly promising area, with early trials targeting conditions like heterozygous familial hypercholesterolemia showing highly positive results [27]. Neurodegenerative disorders also represent a major opportunity, with research exploring CRISPR approaches for Alzheimer's disease, Parkinson's disease, Huntington's disease, and ALS [114].
The field will also likely see increased emphasis on combination therapies that integrate gene editing with other treatment modalities, such as small molecules or biologics. Additionally, advances in personalized CRISPR treatments for rare genetic disorders, exemplified by the CPS1 deficiency case, may establish new paradigms for treating ultra-rare diseases through rapid, bespoke therapeutic development [27]. For iPSC-based approaches, the convergence of improved editing efficiency, enhanced differentiation protocols, and immune evasion strategies may finally enable the widespread clinical application of autologous cell therapies for a range of degenerative conditions.
The clinical trial landscape for CRISPR-Cas9 gene editing has matured significantly, moving from initial proof-of-concept studies to approved therapeutics and an expanding pipeline of investigational products. The integration of CRISPR with iPSC technology has created powerful platforms for disease modeling and therapeutic development, with protocols now achieving editing efficiencies exceeding 90% [93]. Despite persistent challenges in delivery, safety, and manufacturing, the continued evolution of editing technologies and delivery systems promises to address these limitations. Researchers working at the intersection of CRISPR and iPSCs are well-positioned to contribute to the next wave of genetic medicines, particularly as regulatory pathways become more clearly defined through precedent-setting approvals. The coming years will likely witness continued expansion into new therapeutic areas, increased personalization of treatments, and improved safety profiles through next-generation editing platforms.
Within the broader thesis of utilizing CRISPR-Cas9 for gene correction in induced pluripotent stem cells (iPSCs), comprehensive safety profiling is a critical prerequisite for therapeutic application. The dual risks of intrinsic tumorigenicity associated with undifferentiated iPSCs and genomic instability introduced by gene-editing technologies present significant clinical hurdles [115]. This application note details standardized protocols and analytical frameworks for assessing these risks, providing researchers with methodologies to ensure the long-term genomic stability and safety of CRISPR-edited iPSC lines intended for disease modeling and cell-based therapies.
Tumorigenicity Risk Assessment of iPSCs
The risk of tumor formation from iPSC-derived products stems primarily from two sources: the inherent potential of residual undifferentiated iPSCs to form teratomas and the potential acquisition of oncogenic mutations during reprogramming or culture.
Quantitative Tumorigenicity Testing in Immunodeficient Mice
A sensitive and quantitative in vivo tumorigenicity assay has been established using NOD/Shi-scid IL2Rγnull (NOG) mice. A critical modification involves treating dissociated single-cell hiPSC suspensions with a Rho kinase (ROCK) inhibitor to inhibit apoptosis post-transplantation, significantly enhancing engraftment efficiency [116].
Key Findings from Tumorigenicity Studies: When ten different hiPSC lines were tested using this method, remarkable variation in tumorigenic potential was observed, as summarized in Table 1. These differences highlight that tumorigenicity risk is not only a function of the number of residual undifferentiated cells but also an intrinsic property of the specific iPSC line used [116].
Table 1: Variation in Tumorigenicity Among Human iPSC Lines
| hiPSC Line | Tumor Incidence | Tumor Formation Latency | Final Tumor Volume | Tumor Pathology |
|---|---|---|---|---|
| Line A | High | Short | Large | Immature Teratoma |
| Line B | Medium | Medium | Medium | Immature Teratoma |
| Line C | Low | Long | Small | Immature Teratoma |
| Line D | High | Short | Large | Immature Teratoma |
Quality Attributes and Genetic Analysis
Comprehensive characterization of iPSC lines is essential for risk assessment. Microarray analysis, karyotype examination, and whole exome sequencing of hiPSC lines have revealed that these cells can harbor numerous (61–77) variants in cancer-related genes [116]. Although the analyzed lines did not produce malignant tumors, the presence of these mutations underscores the necessity for rigorous genomic screening of master cell banks used as raw materials for therapeutic products.
High-Efficiency CRISPR Editing and Genomic Safety
Achieving high-efficiency editing is paramount to reducing the time in culture and the number of clones that need to be screened, thereby minimizing the risk of acquiring unwanted mutations. However, the editing process itself must be scrutinized for unintended genomic consequences.
High-Efficiency Genome Editing Protocol
A recently developed protocol for precision genome editing in iPSCs demonstrates homologous recombination rates exceeding 90%, dramatically reducing the resource commitment required to generate isogenic lines [26].
Core Strategy: The protocol centers on improving cell survival post-editing by co-transfecting a plasmid encoding shRNA against p53 to temporarily inhibit the apoptotic response triggered by the double-strand break. This is combined with pro-survival supplements like CloneR and ROCK inhibitors [26].
Detailed Workflow:
- Culture: Maintain iPSCs in feeder-free conditions (e.g., on Matrigel with mTeSR Plus or Stemflex media).
- Nucleofection Preparation: At 80-90% confluency, change media to a "cloning media" containing Stemflex, 1% Revitacell, and 10% CloneR one hour pre-nucleofection.
- Complex Formation: Dissociate cells with Accutase. Form Ribonucleoprotein (RNP) complex by combining 0.6 µM target-specific gRNA (e.g., from IDT) with 0.85 µg/µL Alt-R S.p. HiFi Cas9 Nuclease V3 and incubating for 20-30 minutes.
- Nucleofection: Electroporation of 1 x 10^6 cells with the RNP complex, 5 µM single-stranded oligodeoxynucleotide (ssODN) repair template, and 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid (Addgene #27077) using a system like the Neon Transfection System.
- Recovery & Screening: Plate cells in cloning media and change to standard culture media the next day. Editing efficiency can be analyzed in bulk 48-72 hours post-nucleofection. Single-cell cloning and subsequent karyotyping (e.g., G-banding) are recommended to confirm genomic integrity [26].
Figure 1: Workflow for high-efficiency CRISPR editing in iPSCs, incorporating p53 inhibition and pro-survival factors to enhance HDR rates.
Assessing CRISPR-Editing Genomic Safety
A primary safety concern for CRISPR-based therapies is the generation of unintended structural variants (SVs), which can include large deletions, inversions, insertions, and complex rearrangements [102]. These SVs, if they impact oncogenes or tumor suppressor genes, could potentially drive tumorigenesis.
Preclinical Evidence for Long-Term Safety: A long-term study in SOD1-linked amyotrophic lateral sclerosis (ALS) mouse models provides compelling preclinical safety data. CRISPR-Cas9-mediated editing effectively prevented the development of ALS-like disease and pathology. Crucially, the edited mice were monitored for over 2 years (a significant portion of their natural lifespan) and showed no signs of tumorigenesis or other inflammatory diseases, despite persistent expression of Cas9 and the gRNA from an early embryonic stage [117]. This demonstrates that with high editing efficiency, long-term phenotypic safety is achievable.
Detecting Structural Variants: While the above study reported rare off-target editing, it also identified frequent large DNA deletions (from hundreds to thousands of base pairs) at the on-target site, mediated by proximate identical sequences in Alu elements [117]. This finding, corroborated by other studies, underscores that standard genotyping methods (e.g., PCR and Sanger sequencing) are often insufficient as they can miss these large SVs [102]. Comprehensive SV detection requires more sophisticated methods, as outlined in Table 2.
Table 2: Methods for Detecting Unintended CRISPR Editing Outcomes
| Analysis Type | Standard Method | Limitation | Advanced Method for SV Detection |
|---|---|---|---|
| On-Target Editing | PCR + Sanger Sequencing | Misses large deletions/inversions | Long-range PCR, Southern blotting, WGS |
| Off-Target Editing | In silico prediction + targeted NGS | Misses unpredicted sites | WGS, CIRCLE-seq, DISCOVER-Seq |
| Structural Variants | Karyotyping (G-banding) | Low resolution (>5 Mb) | WGS, FISH, CNV arrays |
Figure 2: Categories of unintended CRISPR editing outcomes, highlighting structural variants that require specialized methods for detection. WGS: Whole Genome Sequencing; FISH: Fluorescence in situ Hybridization.
The Scientist's Toolkit: Essential Reagents for Safe iPSC Gene Editing
The following table lists key reagents and their critical functions in the protocols described for efficient and safe genome editing.
Table 3: Essential Research Reagent Solutions for CRISPR-iPSC Workflows
| Reagent / Tool | Function | Application Note |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Inhibits Rho-associated kinase; dramatically improves survival of single iPSCs. | Use in plating media post-thawing, passaging, and after nucleofection [118]. |
| CloneR Supplement | A defined supplement that enhances clonal survival and recovery of single cells. | Included in cloning media during single-cell subcloning post-editing to improve viability [26]. |
| Alt-R S.p. HiFi Cas9 | High-fidelity variant of Cas9 nuclease; reduces off-target editing. | Used in RNP complex formation to improve specificity while maintaining on-target efficiency [26]. |
| pCXLE-hOCT3/4-shp53-F | Plasmid for transient p53 knockdown. | Co-transfected during nucleofection to transiently inhibit p53-mediated apoptosis and boost HDR efficiency [26]. |
| RevitaCell Supplement | A cocktail of antioxidants and other molecules that support cell health. | Used as a recovery supplement after cryopreservation or stressful processes like electroporation [118]. |
| GeneArt Genomic Cleavage Detection Kit | A simple PCR-based assay for detecting nuclease-induced indels. | For initial, rapid assessment of editing efficiency at the bulk population level [118]. |
Conclusion
The integration of CRISPR-Cas9 with iPSC technology represents a paradigm shift in precision medicine, enabling correction of disease-causing mutations in patient-specific cells for autologous transplantation. While significant progress has been made in optimizing editing efficiency, developing advanced systems like base and prime editing, and demonstrating functional correction in disease models, challenges remain in ensuring complete safety, scaling manufacturing, and achieving reliable engraftment. Future directions will focus on improving delivery methods, particularly for non-dividing cells, enhancing the precision of editing tools to eliminate off-target effects, and advancing through rigorous clinical trials. As these technologies mature, CRISPR-corrected iPSCs are poised to transition from powerful research tools to transformative therapies for genetic disorders within the next 5-10 years, ultimately enabling personalized regenerative medicine approaches that address the root causes of disease rather than just managing symptoms.
References
- 1. Advancing CRISPR genome editing into gene therapy clinical trials: progress and future prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 2. Application Of CRISPR Technology In iPSC Gene Correction [https://www.cellandgene.com/doc/application-of-crispr-technology-in-ipsc-gene-correction-0001]
- 3. A high efficiency precision genome editing method with CRISPR in iPSCs | Scientific Reports [https://www.nature.com/articles/s41598-024-60766-4]
- 4. CRISPR-Cas9 Genome Editing In Human Induced Pluripotent Stem Cells | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/genome-editing/genome-editing-learning-center/genome-editing-resource-library/genome-editing-application-notes/protocol-crispr-cas9-genome-editing-human-induced-pluripotent-stem-cells.html]
- 5. manipulation of gene dosage in human Efficient using... iPSCs [https://pubmed.ncbi.nlm.nih.gov/33580208/]
- 6. Frontiers | Stem cell and CRISPR/Cas9 gene editing technology in Alzheimer’s disease therapy: from basic research to clinical innovation [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1612868/full]
- 7. sgRNA design to maximize activity and minimize Optimized - off ... target [https://pubmed.ncbi.nlm.nih.gov/26780180/]
- 8. and CRISPR : Recent Developments and Future Perspectives in... iPSCs [https://pmc.ncbi.nlm.nih.gov/articles/PMC9428373/]
- 9. And CRISPR And Drug Screening iPSC Disease Modeling [https://www.cellandgene.com/doc/crispr-and-ipsc-disease-modeling-and-drug-screening-0001]
- 10. A review of protocols for human iPSC culture, cardiac differentiation... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405110/]
- 11. Induced Pluripotent Stem Cell Reprogramming Protocols [https://www.sigmaaldrich.com/GN/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/stem-cell-culture/ipsc-reprogramming-protocols]
- 12. Analytical Methods and Testing for iPSC - uBriGene [https://www.ubrigene.com/analytical-methods-and-testing-for-ipsc/]
- 13. / CRISPR facilitates investigation of neural circuit Cas using... 9 disease [https://www.nature.com/articles/tp2015203?error=cookies_not_supported&code=78c73518-653e-43d3-a534-c4b2d7333041]
- 14. Recent Advances in High-Content Imaging and Analysis in iPSC-Based Modelling of Neurodegenerative Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10572296/]
- 15. PITChing MMEJ as an Alternative Route for Gene Editing [https://blog.addgene.org/pitching-mmej-as-an-alternative-route-for-gene-editing]
- 16. Frontiers | Strategies for CRISPR -based knock-ins in primary human... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589729/full]
- 17. and competition of Dynamics -Cas9 ribonucleoproteins and... CRISPR [https://pubmed.ncbi.nlm.nih.gov/33398341/]
- 18. Systematic quantification of HDR and NHEJ reveals effects of locus, nuclease, and cell type on genome-editing | Scientific Reports [https://www.nature.com/articles/srep23549]
- 19. analysis of multiple DNA double-strand break repair... Comparative [https://www.nature.com/articles/s42003-025-08187-5?error=cookies_not_supported&code=89db5eec-1789-475b-a136-06ded1fb848c]
- 20. Frontiers | CRISPR-dependent base editing as a therapeutic strategy for rare monogenic disorders [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1553590/full]
- 21. Using CRISPR-Cas9 to Generate Gene-Corrected Autologous iPSCs for the Treatment of Inherited Retinal Degeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5589061/]
- 22. / CRISPR -based genetic correction for recessive dystrophic... Cas 9 [https://www.nature.com/articles/npjregenmed201614?error=cookies_not_supported&code=f8c9a995-cc53-4e08-80c8-30edd26e73bd]
- 23. CRISPR-Cas9-Mediated Correction of TSC2 Pathogenic Variants in iPSCs from Patients with Tuberous Sclerosis Complex Type 2 - PubMed [https://pubmed.ncbi.nlm.nih.gov/39654514/]
- 24. Advances in CRISPR/Cas-based Gene Therapy in Human Genetic Diseases [https://www.thno.org/v10p4374.htm]
- 25. Frontiers | CRISPR/Cas9 technology in tumor research and drug development application progress and future prospects [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1552741/full]
- 26. A high efficiency precision genome editing method with CRISPR in... [https://www.nature.com/articles/s41598-024-60766-4?error=cookies_not_supported&code=8652b52a-0e73-4ced-9ad2-ad8c5fde7337]
- 27. CRISPR Clinical Trials: A 2025 Update - Innovative Genomics Institute (IGI) [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 28. Frontiers | Mapping the therapeutic of landscape - CRISPR for... Cas 9 [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1558432/full]
- 29. Editing the genome of hiPSC with CRISPR/Cas9: disease models - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569153/]
- 30. / CRISPR Mediated Therapeutic Approach in... Cas 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC9734918/]
- 31. / CRISPR -mediated Precise SNP Editing in Human Cas Lines 9 iPSC [https://bio-protocol.org/en/bpdetail?id=4051&type=0]
- 32. New CRISPR tool enables more seamless gene ... | Yale News editing [https://news.yale.edu/2025/03/20/new-crispr-tool-enables-more-seamless-gene-editing-and-improved-disease-modeling]
- 33. New CRISPR tool enables more seamless gene editing -- and improved disease modeling | ScienceDaily [https://www.sciencedaily.com/releases/2025/03/250320145239.htm]
- 34. / CRISPR -Based Protocol for Precise Genome Editing in Induced... Cas 9 [https://bio-protocol.org/en/bpdetail?id=5141&type=0]
- 35. Optimized CRISPR for two guide -fidelity... RNA design high [https://www.nature.com/articles/s41467-019-12281-8?error=cookies_not_supported&code=3f645726-20d8-4117-b049-4b5b7a3b637c]
- 36. FrCas9 is a CRISPR/Cas9 system with high editing efficiency and fidelity | Nature Communications [https://www.nature.com/articles/s41467-022-29089-8]
- 37. for Strategies Genome Efficient Using Editing - CRISPR - PMC Cas 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC6366907/]
- 38. Frontiers | Comprehensive approaches to design gRNA for... efficient [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1579165/full]
- 39. Recent Advances in CRISPR / Cas Delivery Approaches for... 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10661828/]
- 40. : Cargo, Vehicles, and Challenges CRISPR Delivery Methods [https://www.synthego.com/blog/delivery-crispr-cas9]
- 41. This Way: Choosing Between CRISPR System | VectorBuilder Delivery [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 42. Enables the Efficient, Scalable Packaging of Electroporation VLPs [https://maxcyte.com/resource/maxcyte-electroporation-enables-the-efficient-scalable-packaging-of-crispr-cas9-rnps-in-virus-like-particles/]
- 43. CRISPR-Cas9-Mediated Gene Editing in Human Induced Pluripotent Stem Cells | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-0716-1657-4_16]
- 44. of Correction in human DMD -derived cardiomyocytes by... iPSC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9792405/]
- 45. CRISPR Correction of Duchenne Muscular Dystrophy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6415693/]
- 46. JCI - Correction of muscular dystrophies by CRISPR gene editing [https://www.jci.org/articles/view/136873]
- 47. Restoration of Dystrophin Protein Expression by Exon Skipping Utilizing CRISPR-Cas9 in Myoblasts Derived from DMD Patient iPS Cells | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-4939-8651-4_12]
- 48. Dual CRISPR-Cas3 system for inducing multi-exon skipping in DMD patient-derived iPSCs - PubMed [https://pubmed.ncbi.nlm.nih.gov/37625413/]
- 49. Extracellular nanovesicles for packaging of CRISPR - Cas protein and... 9 [https://www.nature.com/articles/s41467-020-14957-y?error=cookies_not_supported&code=7fe3f89d-7c17-4959-96a1-4aacbc17fe71]
- 50. Creation of DMD Muscle Cell Model Using CRISPR - Cas Genome... 9 [https://pubmed.ncbi.nlm.nih.gov/30171541/]
- 51. Therapeutic promise of CRISPR - Cas in 9 ... gene editing sickle cell [https://pubmed.ncbi.nlm.nih.gov/40252393/]
- 52. editing using Genome / CRISPR to treat hereditary... Cas 9 [https://www.nature.com/articles/s41434-021-00247-9?error=cookies_not_supported&code=473405c9-16a7-4a9d-8e53-11f2188c5d38]
- 53. Frontiers | Clinical translation of human iPSC technologies: advances, safety concerns, and future directions [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 54. Gene correction in patient-specific iPSCs for therapy development and disease modeling - PubMed [https://pubmed.ncbi.nlm.nih.gov/27256364/]
- 55. medicine for blood CRISPR : Progress and challenges in... disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC9853164/]
- 56. One-step genetic correction of hemoglobin E/beta- thalassemia ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0779-3]
- 57. (PDF) Beyond HbS and Thalassemia : CRISPR - Cas Strategies for... 9 [https://www.academia.edu/144300039/Beyond_HbS_and_Thalassemia_CRISPR_Cas9_Strategies_for_Targeting_Rare_Hemoglobin_Gene_Mutations]
- 58. (PDF) Therapeutic gene editing in haematological disorders with... [https://www.academia.edu/129977546/Therapeutic_gene_editing_in_haematological_disorders_with_CRISPR_Cas9]
- 59. Efficient gene editing in induced pluripotent stem cells enabled by an inducible adenine base editor with tunable expression | Scientific Reports [https://www.nature.com/articles/s41598-023-42174-2]
- 60. CRISPR-Cas9: A Promising Genome Therapeutic Tool for... Editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC7606404/]
- 61. The Potential of CRISPR / Cas Gene Editing as a Treatment Strategy... 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC6078432/]
- 62. / CRISPR -Correctable mutation-related molecular and... Cas 9 [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-017-0475-z]
- 63. Application of CRISPR/Cas9 to human-induced pluripotent stem cells: from gene editing to drug discovery | Human Genomics | Full Text [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-020-00276-2]
- 64. Frontiers | Genome Editing in iPSC-Based Neural Systems: From Disease Models to Future Therapeutic Strategies [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2021.630600/full]
- 65. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches in Alzheimer’s Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291668/]
- 66. Genome Editing in Induced Pluripotent Stem Cells using CRISPR / Cas 9 [https://pubmed.ncbi.nlm.nih.gov/29623532/]
- 67. Frontiers | CRISPR/Cas-edited iPSCs and mesenchymal stem cells: a concise review of their potential in thalassemia therapy [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1595897/full]
- 68. Genome Editing of Human Pluripotent Stem Cells Using the ArciTect™ CRISPR-Cas9 System [https://www.stemcell.com/human-pluripotent-stem-cell-genome-editing-using-the-arcitect-crispr-cas9-system.html]
- 69. Efficient Cas9-based Genome Editing Using CRISPR Analysis Webtools in Severe Early-onset-obesity Patient-derived iPSCs - PubMed [https://pubmed.ncbi.nlm.nih.gov/35950852/]
- 70. HDAC inhibitors improve CRISPR-mediated HDR editing efficiency in... [https://pubmed.ncbi.nlm.nih.gov/33420926/]
- 71. HDAC inhibitors improve CRISPR-mediated HDR editing efficiency in iPSCs | Science China Life Sciences [https://link.springer.com/article/10.1007/s11427-020-1855-4]
- 72. 3 Tips to Improve HDR Efficiency for CRISPR Editing in Human Cells [https://blog.addgene.org/3-tips-for-improving-hdr-efficiency-for-editing-human-cells-with-crispr]
- 73. - CRISPR fusion to dominant-negative 53BP1 enhances Cas and... 9 HDR [https://www.nature.com/articles/s41467-019-10735-7?error=cookies_not_supported&code=1772bd5a-1740-49ef-a75c-b921ff8edf0e]
- 74. precise knockin with a double cut Efficient donor after... HDR [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1164-8]
- 75. Systematic analysis of factors that improve homologous direct repair... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7935300/]
- 76. Efficient homology-directed gene editing by CRISPR/Cas9 in human stem and primary cells using tube electroporation | Scientific Reports [https://www.nature.com/articles/s41598-018-30227-w]
- 77. Boost HDR Efficiency with new HDR Enhancer Protein | IDT [https://www.idtdna.com/pages/about/news/2025/09/25/integrated-dna-technologies-launches-new-enhancer-protein-to-accelerate-crispr-based-therapies-from-translational-research-to-clinical-breakthrough]
- 78. Integrated DNA Technologies Launches New Enhancer Protein to Accelerate CRISPR-Based Therapies from Translational Research to Clinical Breakthrough | Nasdaq [https://www.nasdaq.com/press-release/integrated-dna-technologies-launches-new-enhancer-protein-accelerate-crispr-based]
- 79. Recent Advancements in Reducing the Off - Target of... Effect [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802171/]
- 80. - CRISPR - Cas : Challenges and Solutions 9 Off Target Effects [https://www.azolifesciences.com/article/CRISPR-Cas9-Off-Target-Effects-Challenges-and-Solutions.aspx]
- 81. - High - fidelity with undetectable genome-wide... CRISPR Cas 9 variants [https://pmc.ncbi.nlm.nih.gov/articles/PMC4851738/]
- 82. qEva-CRISPR: a method for quantitative evaluation of CRISPR/Cas-mediated genome editing in target and off-target sites - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 83. Decline of DNA damage response along with myogenic differentiation... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10665522/]
- 84. Chromatin structure and DNA damage repair | Epigenetics & Chromatin | Full Text [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/1756-8935-1-9]
- 85. Defective DNA Damage Response – Repair Axis in Post - Mitotic ... [https://www.frontiersin.org/research-topics/20616/defective-dna-damage-response---repair-axis-in-post-mitotic-neurons-in-human-health-and-neurodegenerative-diseases/authors]
- 86. Evaluation of Genome Editing [https://www.stemcell.com/evaluation-of-genome-editing.html]
- 87. Both TALENs and CRISPR / Cas directly target the HBB IVS2–654... 9 [https://www.nature.com/articles/srep12065?error=cookies_not_supported]
- 88. Gene editing - PacBio [https://www.pacb.com/gene-editing/]
- 89. In vivo cell type-specific CRISPR knockdown of dopamine beta hydroxylase reduces locus coeruleus evoked wakefulness | Nature Communications [https://www.nature.com/articles/s41467-018-07566-3]
- 90. Generation and Efficient of Mutations in Human iPS Cells... Correction [https://pubmed.ncbi.nlm.nih.gov/32384610/]
- 91. From bench to bedside: cutting-edge applications of base editing and prime editing in precision medicine | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05957-3]
- 92. CRISPR-Cas9 DNA Base-Editing and Prime-Editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7503568/]
- 93. CRISPR/Cas9-Based Protocol for Precise Genome Editing in Induced Pluripotent Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11669859/]
- 94. Key Techniques in Cell Therapy Quality | Technology Networks Control [https://www.technologynetworks.com/biopharma/lists/key-techniques-in-cell-therapy-quality-control-331890]
- 95. Need for high-resolution Genetic Analysis in iPSC : Results and... [https://www.nature.com/articles/s41598-018-35506-0?error=cookies_not_supported&code=c1380476-3c25-4c7c-b6e2-01e42cc2d172]
- 96. Precision Health Resource of Control Lines for Versatile... iPSC [https://pubmed.ncbi.nlm.nih.gov/31813827/]
- 97. Assessment of human pluripotent stem cells with PluriTest - StemBook - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK133282/]
- 98. Epi-Pluri-Score: Validation of pluripotency of your iPSCs | Cygenia – Innovation for your research [https://www.cygenia.com/our-assays/quality-control-cell-preparations/epi-pluri-score-validation-pluripotency-your-ipscs]
- 99. Preparation and Co‐Culture of iPSC ‐Derived Dopaminergic Neurons... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9285934/]
- 100. Recent advances in CRISPR -based genome editing technology and its... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-023-00447-x]
- 101. An optimized / CRISPR approach for precise genome Cas in... 9 editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC7946428/]
- 102. Unintended CRISPR-Cas9 editing outcomes: a review of the detection and prevalence of structural variants generated by gene-editing in human cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10182114/]
- 103. Improving Physiological Relevance in Functional Genomics Screens [https://www.technologynetworks.com/genomics/posters/overcoming-challenges-in-functional-genomics-screening-387945]
- 104. Gene editing with ‘pencil’ rather than ‘scissors’ in human pluripotent stem cells | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03394-5]
- 105. Advances in CRISPR Disease Modeling : Cells, Organoids, Animals... [https://www.synthego.com/blog/crispr-disease-modeling-trends]
- 106. Thieme E-Journals - Global Medical Genetics / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0044-1791803]
- 107. - CRISPR : A Cas and Clinical Perspective for the... 9 Preclinical [https://pmc.ncbi.nlm.nih.gov/articles/PMC7854284/]
- 108. Recent Advances in CRISPR/Cas9 Delivery Approaches for Therapeutic Gene Editing of Stem Cells | Stem Cell Reviews and Reports [https://link.springer.com/article/10.1007/s12015-023-10585-3]
- 109. CRISPR/Cas-edited iPSCs and mesenchymal stem cells: a concise review of their potential in thalassemia therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441039/]
- 110. -derived cells lack immune tolerance to iPSC NK-cells due... autologous [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03308-5]
- 111. Overview CRISPR Clinical Trials 2025 - Learn | Innovate | Access [https://crisprmedicinenews.com/clinical-trials/]
- 112. CRISPR Therapeutics Highlights Strategic Priorities and Anticipated 2025 Milestones | CRISPR Therapeutics [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and/]
- 113. Regulatory Considerations for Clinical Trial Applications with CRISPR-Based Medicinal Products - PubMed [https://pubmed.ncbi.nlm.nih.gov/35452274/]
- 114. Frontiers | CRISPR - Cas : bridging the gap between aging mechanisms... 9 [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1681891/full]
- 115. Tumorigenicity as a Clinical Hurdle for Pluripotent Stem Cell Therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3967018/]
- 116. Tumorigenicity-associated characteristics of human iPS cell lines | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0205022]
- 117. Efficacy and long-term safety of CRISPR/Cas9 genome editing in the SOD1-linked mouse models of ALS | Communications Biology [https://www.nature.com/articles/s42003-021-01942-4]
- 118. - CRISPR In... | Thermo Fisher Scientific - UK Cas 9 Genome Editing [https://www.thermofisher.com/uk/en/home/life-science/genome-editing/genome-editing-learning-center/genome-editing-resource-library/genome-editing-application-notes/protocol-crispr-cas9-genome-editing-human-induced-pluripotent-stem-cells.html]