Designing Next-Generation Clinical Trials for Advanced Therapy Medicinal Products: Strategies, Challenges, and Regulatory Considerations
This comprehensive review examines the evolving landscape of clinical trial design for Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies.
Designing Next-Generation Clinical Trials for Advanced Therapy Medicinal Products: Strategies, Challenges, and Regulatory Considerations
Abstract
This comprehensive review examines the evolving landscape of clinical trial design for Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies. Targeting researchers, scientists, and drug development professionals, it explores foundational regulatory requirements, innovative methodological approaches, optimization strategies for common challenges, and validation frameworks. The article synthesizes recent regulatory developments from EMA and FDA, analyzes adaptive trial designs for small populations, and provides practical guidance for navigating the unique complexities of ATMP clinical development, from early-stage exploration to comparative effectiveness assessment.
Understanding the ATMP Landscape: Regulatory Frameworks and Fundamental Design Principles
The development of Advanced Therapy Medicinal Products (ATMPs), encompassing gene therapies, cell-based therapies, and tissue-engineered products, represents one of the most innovative yet regulatory-complex frontiers in modern medicine. The European Medicines Agency (EMA) has introduced a significant regulatory milestone with its "Guideline on quality, non-clinical and clinical requirements for investigational advanced therapy medicinal products in clinical trials," which comes into effect July 1, 2025 [1] [2]. This comprehensive document, adopted by EMA's Committee for Medicinal Products for Human Use (CHMP) on January 20, 2025, consolidates guidance from over 40 separate guidelines and reflection papers into a single multidisciplinary reference [1]. Simultaneously, global regulatory bodies including the U.S. Food and Drug Administration (FDA) and China's Center for Drug Evaluation (CDE) are advancing their own frameworks for these transformative therapies [3] [4]. This evolving landscape creates both challenges and opportunities for researchers and drug development professionals navigating clinical trial design for ATMPs, particularly as efforts toward global regulatory convergence accelerate while respecting regional requirements.
Comparative Analysis of EMA and FDA Regulatory Frameworks
EMA's New Clinical-Stage ATMP Guideline: Key Provisions
The EMA's new guideline provides a comprehensive framework for clinical trial applications involving investigational ATMPs in both early-phase exploratory and late-stage confirmatory trials [1]. Spanning approximately 60 pages, the document addresses quality (CMC) documentation, non-clinical studies, and clinical development requirements with special attention to first-in-human trials, confirmatory studies, and emerging technologies like genome editing [1] [2]. The guideline emphasizes that immature quality development could potentially compromise the use of clinical trial data to support marketing authorization, highlighting the critical importance of robust CMC systems from the earliest development stages [1].
The guideline intentionally mirrors the Common Technical Document (CTD) structure for Module 3, providing a roadmap for organizing CMC information in investigational or marketing applications [1]. This alignment facilitates a more standardized approach to regulatory submissions across the European Union. Notably, the guideline encourages sponsors to adopt a risk-based approach when evaluating quality, non-clinical, and clinical data generated for ATMPs and emphasizes seeking early regulatory guidance at either national member state or European level to inform development strategy [1].
FDA-EMA Convergence and Divergence in ATMP Regulation
Significant regulatory convergence has transpired between EMA and FDA regarding CMC requirements for ATMPs, though important distinctions remain that developers must navigate [1] [4]. The table below summarizes key areas of alignment and divergence between the two regulatory frameworks:
Table 1: Comparative Analysis of EMA and FDA Regulatory Approaches to ATMPs
| Regulatory Aspect | EMA Approach | FDA Approach | Convergence Status |
|---|---|---|---|
| GMP Compliance | Mandatory self-inspections with documented results providing evidence of effective quality system [1] | Phase-appropriate attestation with verification during pre-license inspection [1] | Partial Convergence |
| Donor Eligibility | Compliance with EU and member state-specific legal requirements; limited specific guidance [1] | Prescriptive requirements for screening, testing, laboratory qualifications, and pooling restrictions [1] | Divergence |
| Terminology | "Active substance" and "Investigational medicinal product" [1] | "Drug substance" and "Drug product" [1] | Terminological Divergence |
| Clinical Evidence | Acceptance of small, open-label, non-randomized studies for orphan indications [5] | Similar flexibility for orphan diseases with post-marketing requirements [5] | Substantial Convergence |
| Trial Application Review | Centralized through Clinical Trial Regulation with one EU-based opinion [6] | Traditional IND review process through CBER [1] | Procedural Divergence |
The regulatory convergence between EMA and FDA is particularly evident in the CMC domain, where the overwhelming majority of content in the EMA's quality documentation section would be familiar to FDA CMC reviewers [1]. This alignment reflects a conscious effort by regulatory authorities to address the global nature of ATMP development, though differences in implementation and specific requirements continue to present challenges for sponsors pursuing simultaneous development in multiple regions [1] [6].
Global Regulatory Expansion: China's Emerging ATMP Framework
Concurrent with developments in Western regulatory systems, China has taken significant steps toward establishing a comprehensive ATMP framework. In June 2025, China's Center for Drug Evaluation (CDE) released the "Scope, Classification, and Interpretation of Advanced Therapy Medicinal Products (Draft for Public Comments)" – the country's first systematic regulation of ATMPs [3]. This draft defines ATMPs as medicinal products developed, produced, and regulated through the pharmaceutical pathway that are "produced through ex vivo manipulation to function within the human body" [3]. The initiative aims to clarify the regulatory framework for cutting-edge biopharmaceutical fields including cell therapy and gene therapy, representing China's effort to align with global standards while optimizing review and approval processes to enhance industry competitiveness [3].
Experimental Design and Methodological Considerations
Clinical Development Strategies for ATMPs
The clinical development of ATMPs presents unique challenges that require methodologically sound approaches and sometimes departure from traditional clinical trial designs. Current regulatory approvals for ATMPs have primarily been based on small, open-label, non-randomized, single-arm studies using intermediate endpoints and historical controls [5]. This approach has been justified by the nature of target diseases (often orphan indications with high unmet medical needs) and ethical considerations regarding randomization when investigational therapies show dramatic efficacy signals [5].
Table 2: Clinical Trial Design Characteristics for Approved ATMPs
| ATMP Category | Common Trial Design Features | Typical Endpoints | Patient Population Size |
|---|---|---|---|
| Gene Therapy Products | Single-arm, historical controls, intermediate variables [5] | Biomarker response, disease-specific metrics [5] | Small (12-147 patients) [5] |
| Somatic Cell Therapies | Mixed designs (some controlled Phase III) [5] | Survival, response rates [5] | Variable (71-512 patients) [5] |
| Tissue-Engineered Products | Randomized and non-randomized designs [5] | Structural/functional improvement [5] | Moderate (138-177 patients) [5] |
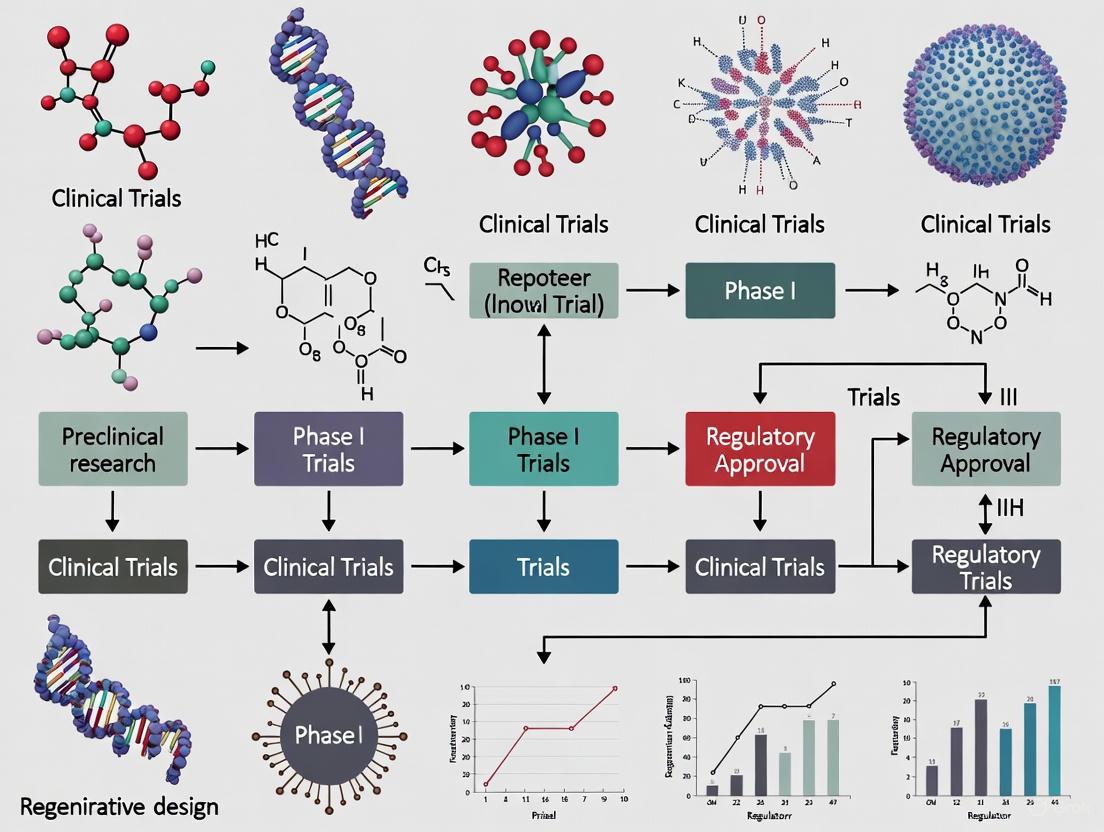
The following workflow diagram illustrates the key decision points in designing ATMP clinical development programs that meet regulatory requirements across multiple jurisdictions:
Quality and Manufacturing Considerations
The EMA guideline dedicates approximately 70% of its content to quality documentation requirements, underscoring the critical importance of CMC considerations in ATMP development [1]. The guideline emphasizes that a weak quality system could prevent authorization of a clinical trial if deficiencies pose risks to participant safety or data robustness [1]. Concurrently, the EMA has proposed revisions to Part IV of the EU Guidelines on Good Manufacturing Practice (GMP) specific to ATMPs, which focus on alignment with the revised Annex 1, integration of ICH Q9 and Q10 principles, and adaptation to technological advancements in manufacturing [7].
Key areas of focus in ATMP manufacturing and quality control include:
- Starting Materials: Proper characterization and testing of human cell-based starting materials, with compliance to regional requirements for donor screening and testing for infectious diseases [1]
- Manufacturing Process Controls: Implementation of closed single-use systems, automated technologies, and appropriate cleanroom classifications with barrier systems [7]
- Quality Control Testing: Development of validated assays for potency, identity, purity, and safety, considering the often limited shelf-life of cellular products [6]
- Comparability Protocols: Establishment of strategies for managing manufacturing changes while maintaining product consistency [1]
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and quality control of ATMPs requires specialized reagents and materials to ensure product safety, identity, purity, and potency. The following table outlines key research reagent solutions essential for ATMP development:
Table 3: Essential Research Reagent Solutions for ATMP Development
| Reagent Category | Specific Examples | Function in ATMP Development |
|---|---|---|
| Cell Separation Media | Ficoll-Paque, Magnetic bead-based separation kits | Isolation of specific cell populations from starting materials [5] |
| Cell Culture Supplements | Serum-free media, Cytokines (IL-2, IL-7, IL-15), Growth factors | Ex vivo expansion and maintenance of cellular products [5] |
| Gene Delivery Vectors | Lentiviral vectors, Retroviral vectors, AAV vectors, Transposon systems | Genetic modification of cells for gene and engineered cell therapies [1] [5] |
| Characterization Antibodies | Flow cytometry antibodies, Immunofluorescence reagents | Phenotypic characterization of cell products and assessment of identity [5] |
| Potency Assay Reagents | Cytokine detection kits, Target cells, Cytotoxicity reagents | Measurement of biological activity and potency [1] |
| Safety Testing Materials | Mycoplasma detection kits, Endotoxin testing reagents, Sterility testing media | Assessment of product safety and freedom from contaminants [1] [7] |
Regulatory Convergence Initiatives and Future Directions
The global development of ATMPs has stimulated increased attention to regulatory convergence initiatives aimed at aligning requirements across jurisdictions while respecting regional legal frameworks and public health needs [1] [4]. The FDA's Center for Biologics Evaluation and Research (CBER) defines regulatory convergence as the alignment of requirements across countries or regions that results in incremental adoption of "internationally recognized technical guidance documents, standards and scientific principles, common or similar practices and procedures" [1]. This concept has become a recurring topic at international conferences focused on cell and gene therapy, with sessions dedicated to opportunities for harmonization in CMC requirements, building global standards, and balancing convergence efficiencies against unique regional requirements [1].
Current initiatives promoting regulatory convergence include:
- Public-Private Consortia: Organizations like the Bespoke Gene Therapy Consortium (BGTC), which includes FDA participation, aim to build platforms and standards to accelerate gene therapy development [6]
- International Collaboration: Efforts between regulatory authorities, industry, non-profit, and academic organizations to develop harmonized approaches to ATMP evaluation [6]
- Mutual Recognition: While current mutual recognition agreements for GMP do not extend to ATMPs, there have been exceptions based on product limitations (e.g., Luxturna, Zolgensma), suggesting potential evolution in this area [6]
The following diagram illustrates the key components and stakeholders in the global regulatory convergence ecosystem for ATMPs:
The introduction of EMA's new clinical-stage ATMP guideline effective July 2025, coupled with ongoing global regulatory developments, presents both challenges and opportunities for researchers and drug development professionals. Successful navigation of this evolving landscape requires a strategic approach to clinical trial design and regulatory planning that incorporates several key considerations:
First, sponsors should engage early with regulatory authorities through scientific advice procedures at both national and European levels to align development plans with evolving expectations [1]. Second, implementing a risk-based approach to quality, non-clinical, and clinical development can help prioritize resources while maintaining regulatory compliance [1]. Third, developers should consider global regulatory strategies from the outset, acknowledging both convergent and divergent requirements across regions to enable efficient multi-jurisdictional development [4] [6].
As the ATMP field continues to evolve, regulatory frameworks will undoubtedly undergo further refinement. The EMA has indicated that the current guideline will be updated to include additional information on gene-editing products as experience accumulates [1]. Similarly, ongoing initiatives to modernize ICH guidelines to better accommodate ATMP-specific challenges may further facilitate global harmonization [6]. By maintaining awareness of these developments and adopting proactive, strategic approaches to ATMP development, researchers and drug development professionals can navigate this complex regulatory environment while advancing transformative therapies for patients with serious unmet medical needs.
Advanced Therapy Medicinal Products (ATMPs) represent a innovative class of biopharmaceuticals that encompass gene therapy medicines, somatic cell therapy medicines, and tissue-engineered medicines [8]. These therapies are highly research-driven and characterized by complex, innovative manufacturing processes [9]. According to European regulations, ATMPs are biological medicinal products that contain or consist of engineered cells or tissues and are used with a view to treating, preventing, or diagnosing diseases through pharmacological, immunological, or metabolic actions, or to regenerating, repairing, or replacing human tissue [10]. The European Medicines Agency (EMA) plays a central role in the scientific assessment of these therapies through its Committee for Advanced Therapies (CAT), which provides expertise needed to evaluate their quality, safety, and efficacy [8] [11].
The development of ATMPs has grown significantly in recent years, with clinical trials investigating these innovative therapies spanning various disease areas including cancer, cardiovascular diseases, musculoskeletal disorders, and immune system diseases [12]. These products differ fundamentally from traditional chemical medicines—they often comprise viable cells or genetically modified materials, work through complex mechanisms of action, and may integrate into or be rejected by the recipient's body [9]. This complexity demands specialized regulatory frameworks and development approaches, which have been established in the European Union through Regulation (EC) No 1394/2007 and supporting guidelines [11] [9].
Classification and Definitions of ATMP Categories
Gene Therapy Medicinal Products (GTMPs)
Gene therapy medicinal products contain genes that lead to a therapeutic, prophylactic, or diagnostic effect [8]. These products work by inserting 'recombinant' genes into the body, typically to treat a variety of diseases including genetic disorders, cancer, or long-term diseases [8]. A recombinant gene is a stretch of DNA created in the laboratory that brings together DNA from different sources [8]. The classification of a product as a GTMP depends on the addition of a recombinant nucleic acid sequence [9]. In the European regulatory framework, GTMPs are defined according to Part IV of Annex I to Directive 2001/83/EC [11].
Somatic Cell Therapy Medicinal Products (sCTMPs)
Somatic cell therapy medicinal products contain cells or tissues that have been manipulated to change their biological characteristics or cells or tissues not intended to be used for the same essential functions in the body [10] [8]. These products are intended for the prevention, diagnosis, and/or treatment of diseases through pharmacological, immunological, or metabolic actions [10]. The European definition specifies that sCTMPs must contain or consist of cells or tissues that have been subject to substantial manipulation so that biological characteristics, physiological functions, or structural properties relevant for the intended clinical use have been altered, or consist of cells or tissues that are not intended to be used for the same essential function in the recipient and the donor [10]. The full legal definition is provided in Directive 2009/120/EC, Directive 2003/63/EC part IV, and Directive 2001/83/EC Annex I part IV [10].
Tissue-Engineered Products (TEPs)
Tissue-engineered products contain cells or tissues that have been modified so they can be used to repair, regenerate, or replace human tissue [10] [8]. According to the European guidelines, TEPs contain or consist of engineered cells or tissues, and cells or tissues are considered 'engineered' if they fulfill at least one of two conditions: (1) the cells or tissues have been subject to substantial manipulation, so that biological characteristics, physiological functions, or structural properties relevant for the intended regeneration, repair, or replacement are achieved, or (2) the cells or tissues are not intended to be used for the same essential function in the recipient as in the donor [10]. These products are presented as having properties for, or are used in or administered to human beings with a view to regenerating, repairing, or replacing a human tissue [10]. The regulatory definition is provided in article 2(1)(b) of the Clinical Trial Regulation (1394/2007/EG) [10].
Combined ATMPs
Some ATMPs may contain one or more medical devices as an integral part of the medicine, which are referred to as combined ATMPs [8]. An example includes cells embedded in a biodegradable matrix or scaffold [8]. These combination products are not only regulated under the guidelines for medicinal products but also for medical devices [13]. The regulatory framework for these combined products involves interaction between the CAT and notified bodies to prepare draft opinions [13].
Table 1: Comparative Analysis of ATMP Categories
| Category | Key Components | Substantial Manipulation Required | Primary Intended Use | Regulatory Definition Source |
|---|---|---|---|---|
| Gene Therapy Medicinal Products (GTMPs) | Recombinant nucleic acids | Not necessarily (based on nucleic acid content) | Treatment, prevention, or diagnosis of disease through gene expression | Directive 2001/83/EC Annex I part IV [11] |
| Somatic Cell Therapy Medicinal Products (sCTMPs) | Cells or tissues | Yes (unless non-homologous use) | Treatment, prevention, or diagnosis of disease through pharmacological, immunological, or metabolic actions | Directive 2009/120/EC [10] |
| Tissue-Engineered Products (TEPs) | Engineered cells or tissues | Yes (unless non-homologous use) | Regeneration, repair, or replacement of human tissue | Regulation (EC) No 1394/2007 [10] [11] |
| Combined ATMPs | ATMP combined with medical device | Dependent on cellular component | Dependent on primary mode of action | Regulation (EC) No 1394/2007 [8] |
Regulatory Framework and Classification Procedures
The European Regulatory Landscape
The regulatory framework for ATMPs in the European Union is established by Regulation (EC) No 1394/2007, which came into force on December 30, 2008 [11] [9]. This regulation provides the overall framework for ATMPs and amended previous legislation including Directive 2001/83/EC and Regulation (EC) No 726/2004 [11]. The framework is further supported by Commission Directive 2009/120/EC, which updated the definitions and detailed scientific and technical requirements for gene therapy medicinal products and somatic cell therapy medicinal products [11]. This directive also established detailed requirements for tissue-engineered products and for ATMPs containing devices and combined ATMPs [11].
A key feature of the European regulatory system is the mandatory centralized procedure for marketing authorization applications (MAAs) for ATMPs [13] [9]. This ensures that these innovative products benefit from a single evaluation and authorization procedure applicable across the EU member states [8]. The centralized procedure may grant marketing authorization through three pathways: standard marketing authorization, conditional marketing authorization (for innovative medicines addressing unmet medical needs), and marketing authorization under exceptional circumstances (for rare diseases or difficult-to-measure clinical endpoints) [13].
The Committee for Advanced Therapies (CAT)
The Regulation (EC) No 1394/2007 established the Committee for Advanced Therapies (CAT) as a multidisciplinary committee within the European Medicines Agency [11]. The CAT is composed of members with specific expertise in ATMPs, including gene therapy, cell therapy, tissue engineering, medical devices, pharmacovigilance, and ethics, with representatives of patient associations and clinicians also included [9]. The primary responsibility of the CAT is to assess the quality, safety, and efficacy of ATMPs [11]. During the assessment procedure, the CAT prepares a draft opinion on the advanced therapy medicine, which it sends to the Committee for Medicinal Products for Human Use (CHMP) [8]. The CHMP then adopts an opinion recommending or not recommending the authorization of the medicine by the European Commission [8].
Beyond product evaluation, the CAT has several other important responsibilities: providing recommendations on the classification of advanced therapy medicines, evaluating applications for certification of quality and non-clinical data for small and medium-sized enterprises (SMEs), contributing to scientific advice on advanced therapy medicines, and assisting in the elaboration of documents related to the objectives of the ATMP Regulation [8]. The CAT also works to encourage the development of advanced therapy medicines and provides scientific expertise for initiatives related to innovative medicines and therapies [8].
ATMP Classification Procedure
The CAT provides scientific recommendations on ATMP classification in accordance with Article 17 of the ATMP Regulation [11]. This classification procedure helps developers determine whether their product falls within the definition of an ATMP based on scientific grounds [9]. The recommendations are based on definitions laid down in EU legislative texts, particularly Regulation (EC) No 1394/2007 for tissue-engineered products and combined ATMPs, and Part IV of Annex I to Directive 2001/83/EC for gene therapy and somatic cell therapy medicinal products [11].
The classification as a tissue-engineered product or somatic cell therapy product depends on whether the cells are 'engineered,' which requires fulfillment of one of two conditions: (1) the cells have been subject to substantial manipulation, or (2) the cells are not intended to be used for the same essential function in the recipient and the donor (non-homologous use) [9]. Substantial manipulation is defined as processing that alters biological characteristics, physiological functions, or structural properties relevant for the intended regeneration, repair, or replacement [9]. The CAT has published a Reflection Paper on Classification of Advanced Therapy Medicinal Products to provide further guidance on classification, including discussion of borderline cases [9].
Table 2: ATMP Clinical Trial Landscape (Based on 939 Registered Trials)
| Trial Characteristic | Category | Number/Percentage of Trials | Phase Distribution |
|---|---|---|---|
| ATMP Category | Somatic Cell Therapies | 53.6% | Phase I, I/II: 64.3% [12] |
| Tissue-Engineered Products | 22.8% | Phase II, II/III: 27.9% [12] | |
| Gene Therapies | 22.4% | Phase III: 6.9% [12] | |
| Combined ATMPs | 1.2% | ||
| Therapeutic Area | Cancer | 24.8% | |
| Cardiovascular Diseases | 19.4% | ||
| Musculoskeletal | 10.5% | ||
| Immune System and Inflammation | 11.5% | ||
| Neurology | 9.1% | ||
| Trial Size | Small trials (<25 patients) | 47.2% |
The ATMP classification procedure is a non-mandatory, free-of-charge service that provides legally non-binding recommendations [9]. Despite being non-binding, it serves as an important tool for developers to clarify the applicable regulatory framework and development path [9]. It also offers an opportunity to initiate dialogue with regulatory bodies early in the development process [9]. Between 2011 and 2013, the CAT classified 71 medicinal products, with the majority (87%) classified as ATMPs distributed nearly equally between the three product categories [9].
Experimental Protocols for ATMP Development
Quality Control and Characterization Protocols
Quality control of ATMPs requires sophisticated testing strategies that differ significantly from those used for conventional chemical compounds [14]. The complexity of these products, particularly those containing genetically modified cells, necessitates comprehensive characterization to address potential risks such as malignant transformation and off-target effects [14]. The following protocols outline key quality assessment methodologies for ATMPs.
Protocol 1: Potency Assay Development for Cell-Based ATMPs Potency assays must be developed prior to first-in-human studies and should quantitatively measure the biological activity linked to the product's mechanism of action [15]. For cell-based ATMPs, this typically involves:
- Identify Critical Quality Attributes (CQAs): Determine specific phenotypic markers, secretory profiles, or functional activities that correlate with biological activity
- Select Appropriate Assay Format: Implement flow cytometry for surface marker quantification, ELISA for secretory factor measurement, or co-culture systems for functional assessment
- Establish Reference Standards: Create well-characterized reference materials for assay calibration and normalization
- Validate Assay Performance: Determine accuracy, precision, specificity, and linearity across the anticipated potency range
- Implement Quality Control Procedures: Include appropriate controls for each assay run to ensure reliability
Protocol 2: Genetic Modification Characterization for GTMPs For gene therapy products and genetically modified cell therapies, comprehensive characterization of the genetic modification is essential [14]:
- Vector Copy Number Determination: Use digital droplet PCR to quantify vector copies per cell
- Integration Site Analysis: Employ next-generation sequencing methods to identify genomic integration sites
- Off-Target Editing Assessment: For gene-edited products, conduct whole-genome sequencing or in silico prediction tools to identify potential off-target effects
- Expression Analysis: Quantify transgene expression using RT-qPCR, RNA-seq, or Western blot
- Vector Integrity Verification: Perform restriction mapping or full vector sequencing to confirm construct integrity
Manufacturing and Process Development Protocols
ATMP manufacturing must comply with Good Manufacturing Practice (GMP) guidelines, though these products present unique challenges due to their biological complexity and frequently small-scale, personalized production [14]. The EMA's guideline on clinical-stage ATMPs emphasizes that immature quality development may compromise the use of clinical trial data to support marketing authorization [16].
Protocol 3: Process Comparability Studies When manufacturing process changes occur during development, comparability must be demonstrated through rigorous assessment [15]:
- Define Analytical Similarity Margins: Establish pre-defined acceptance criteria for critical quality attributes
- Conduct Side-by-Side Testing: Manufacture multiple lots using both old and new processes for direct comparison
- Perform Extended Characterization: Go beyond routine quality control testing to include comprehensive molecular and functional analyses
- Assess Impact on Biological Function: Evaluate potency, differentiation potential, and other functional endpoints
- Document Justification for Changes: Provide scientific rationale supporting the manufacturing modification
Protocol 4: Allogeneic Donor Screening and Testing For allogeneic cell-based ATMPs, comprehensive donor screening is essential to prevent transmission of communicable diseases [16]:
- Donor Medical History Review: Assess donor health history and risk factors for communicable diseases
- Infectious Disease Marker Testing: Screen for relevant communicable disease agents using serological and molecular methods
- Quality Assurance of Testing Laboratories: Ensure testing is performed in qualified laboratories with appropriate certifications
- Donor Eligibility Determination Documentation: Maintain complete records of donor eligibility determination
- Quarantine Procedures: Implement appropriate quarantine of cellular materials pending completion of testing
Diagram 1: ATMP Classification Decision Pathway. This workflow outlines the key decision points for classifying products as Advanced Therapy Medicinal Products according to European regulatory criteria.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for ATMP Development
| Reagent/Material | Category | Function in ATMP Development | Application Examples |
|---|---|---|---|
| GMP-grade Cytokines and Growth Factors | Cell Culture Supplements | Direct cell differentiation, expansion, and maintenance | TEP manufacturing, sCTMP process development |
| Vector Packaging Systems | Gene Delivery | Facilitate genetic modification of target cells | Lentiviral/retroviral packaging for GTMPs |
| Cell Separation Media and Reagents | Cell Processing | Isulate specific cell populations from heterogeneous mixtures | Density gradient media, magnetic bead separation |
| Flow Cytometry Antibody Panels | Characterization | Identify and quantify cell surface and intracellular markers | Phenotypic characterization, potency assessment |
| PCR and qPCR Reagents | Molecular Biology | Detect and quantify genetic elements, vector copies | Vector copy number analysis, mycoplasma testing |
| Extracellular Matrix Components | Tissue Engineering | Provide structural support for tissue development | Scaffolds for TEPs, 3D culture systems |
| Cell Counting and Viability Assays | Quality Control | Determine cell number, viability, and metabolic activity | Trypan blue exclusion, MTT assays |
| Mycoplasma Detection Kits | Safety Testing | Screen for mycoplasma contamination in cell cultures | Required safety testing for all cell-based ATMPs |
| Endotoxin Testing Reagents | Safety Testing | Detect and quantify bacterial endotoxins | Product release testing for parenteral administration |
| Cryopreservation Media | Cell Banking | Maintain cell viability during frozen storage | Master/working cell bank creation, product storage |
Recent Regulatory Developments and Future Perspectives
The regulatory landscape for ATMPs continues to evolve rapidly, with significant new guidelines recently adopted. Effective July 1, 2025, the EMA's new Guideline on quality, non-clinical, and clinical requirements for investigational advanced therapy medicinal products in clinical trials comes into effect [16]. This comprehensive document consolidates information from over 40 separate guidelines and reflection papers, providing a unified framework for gene therapy, somatic cell therapy, and tissue-engineered products [16]. The guideline emphasizes a risk-based approach to ATMP development and addresses several critical areas including potency assay requirements, genome editing products, continuous manufacturing, and ATMP-device combinations [15].
Another significant development is the implementation of the new SoHO (Substances of Human Origin) regulation (2024/1938), which affects traceability requirements for ATMPs containing human cells or tissues [15]. This regulation aims to harmonize standards for donation, procurement, testing, processing, preservation, storage, and distribution of human tissues and cells across the European Union [15]. Additionally, the guideline explicitly addresses continuous manufacturing for the first time and provides clarified expectations for comparability studies aligned with ICH Q5E [15].
The field of ATMPs continues to face challenges related to manufacturing complexity, characterization difficulties, and the need for specialized regulatory expertise [14]. However, ongoing regulatory science initiatives aim to address these challenges through the development of new tools, standards, and approaches to assess the safety, efficacy, quality, and performance of these innovative products [14]. As the field advances, regulatory convergence between major regions like the European Union and United States is becoming increasingly important to facilitate global development of these promising therapies [13] [16].
Diagram 2: ATMP Regulatory Pathway in the European Union. This diagram illustrates the key regulatory procedures and interactions between sponsors and regulatory bodies throughout the ATMP development lifecycle.
First-in-human (FIH) trials represent a milestone step in translational science, transforming basic scientific discoveries into therapeutic applications by advancing drug candidates from preclinical studies to initial human testing [17]. These trials serve as the crucial link to advance new promising drug candidates and are conducted primarily to determine the safe dose range for further clinical development [17]. For Advanced Therapy Medicinal Products (ATMPs), including gene therapies, somatic cell therapies, and tissue-engineered products, FIH trials present unique challenges due to their groundbreaking nature in treating previously untreatable diseases [18]. The European Medicines Agency (EMA) emphasizes that establishing appropriate strategies to minimise risk in early phase clinical trials is necessary and should be a priority for the safety and wellness of clinical trial participants, whether patients or healthy volunteers [19].
Key Design Considerations for FIH Trials
Core Objectives and Regulatory Alignment
FIH trials for both traditional therapeutics and ATMPs share common objectives but require different emphases based on product characteristics. The primary goals include determining human pharmacology, tolerability, and safety profiles, while gaining early evidence of effectiveness [19] [20]. For ATMPs specifically, additional objectives include feasibility assessment of complex manufacturing and administration processes [20].
Table 1: Key Objective Comparisons Across Therapeutic Modalities
| Objective Component | Small Molecules & Biologicals [20] | Cellular & Gene Therapies [20] |
|---|---|---|
| Safety Evaluation | Determine side effects associated with increasing doses | Evaluate specific risks (e.g., delayed infusion reactions, autoimmunity, graft failure, GVHD) |
| Pharmacology | Determine metabolism and pharmacologic actions | Assess biodistribution, persistence, and functional activity |
| Effectiveness | Gain early evidence of effectiveness | Gather preliminary evidence of effectiveness and activity |
| Dosing | Estimate relationship of effects to dose | Explore dose regimen and define therapeutic window |
| Feasibility | Assess feasibility of administration | Evaluate complex manufacturing and administration processes |
Population Selection and Dose Strategy
The choice between healthy volunteers and patients requires careful consideration of toxicities, PK variability, lifestyle conditions, benefits to patients, and special populations [19]. Studies with healthy volunteers must have inclusion/exclusion criteria that require vital signs, ECGs, and clinical laboratory assessments to be normal [19].
Dose selection protocols need to outline and explain the estimated initial drug dose, maximum dose exposure, and subsequent dose escalation steps [19]. All available non-clinical information, such as toxicology profiles, should be considered for starting doses, dose escalation, and maximum exposure in early phase clinical trials [17].
Table 2: Quantitative Dose Escalation Considerations
| Design Element | Traditional FIH Trials [19] | ATMP-Specific Adaptations [18] |
|---|---|---|
| Starting Dose | Based on non-clinical toxicology profiles | May consider minimal anticipated biological effect level (MABEL) |
| Dose Escalation | Defined steps with clear criteria | May require longer intervals between cohorts for immunogenicity monitoring |
| Sentinel Dosing | Required for first SAD and MAD cohorts (one active, one placebo) | Particularly critical for novel mechanisms with unknown safety profiles |
| Maximum Dose | Based on exposure margins from toxicology studies | May be limited by manufacturing capabilities or vector-related toxicities |
| Stopping Rules | Defined for individuals, cohorts, and entire study | Must account for delayed effects common with cellular and gene therapies |
Experimental Protocols and Methodologies
FIH Trial Protocol Development Workflow
ATMP-Specific Safety Assessment Protocol
For Advanced Therapy Medicinal Products, safety evaluation requires specialized methodologies that account for their unique mechanisms of action and potential delayed effects. The protocol must include comprehensive plans for long-term follow-up, immunogenicity assessment, and product-specific safety concerns [18] [20].
Methodology:
- Baseline Assessment: Comprehensive clinical laboratory tests, imaging studies, and functional assessments specific to the product mechanism
- Acute Monitoring: Continuous monitoring for immediate adverse events (e.g., cytokine release syndrome, infusion reactions) with predefined management algorithms
- Long-Term Follow-Up: Minimum 15-year follow-up for gene therapies to monitor for delayed adverse effects, including secondary malignancies [18]
- Immunogenicity Testing: Regular assessment of immune responses against the therapeutic product (e.g., neutralizing antibodies against AAV vectors)
- Product-Specific Endpoints: Monitoring for ectopic tissue formation, graft failure, viral reactivation, or autoimmunity [20]
Research Reagent Solutions for ATMP Development
Table 3: Essential Research Reagents for ATMP Characterization
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Viral Vector Quantification | Measures genome titer of viral vectors | GelGreen dye, GelRed dye, picoGreen, qPCR, ddPCR assays [21] |
| Cell Characterization | Identifies and quantifies cell populations | Flow cytometry antibodies, cell viability assays, functional potency assays |
| Process-Related Impurities | Detects residuals from manufacturing | ELISA kits for host cell proteins, DNA quantification assays, endotoxin tests |
| Product Potency | Measures biological activity | Cell-based bioassays, enzymatic activity tests, functional response assays |
| Vector Genome Integrity | Assesses vector quality and stability | Alkaline agarose gel electrophoresis, southern blotting, sequencing assays [21] |
Integrated Protocol Design for Efficient Development
Modern FIH trials increasingly utilize integrated protocols that combine different study parts to optimize knowledge gain while ensuring participant safety [19]. These complex protocols require meticulous planning and clear criteria for transitioning between study components.
Integration Principles and Decision Criteria
Integrated protocols combine single ascending dose (SAD), multiple ascending dose (MAD), and sometimes food effect or drug-drug interaction (DDI) components within a single trial [19]. The criteria to move from one part of a study, such as SAD to MAD, must be explicitly defined in the protocol [19]. While it is acceptable to overlap SAD and MAD portions of a trial, it is necessary for the expected exposure to already have been evaluated in a SAD cohort prior to being evaluated in a MAD cohort [19]. Food effect studies can be conducted in parallel with the SAD, provided the dose level in the food effect trial has been evaluated in a prior SAD cohort [19]. However, drug-drug interaction studies should not be integrated into FIH and dose escalation protocols unless there is a need that requires a specific concomitant medication in the initial patient studies [19].
Risk Mitigation and Safety Monitoring Framework
Effective risk mitigation strategies are essential for protecting participant safety while advancing innovative therapies. The EMA guideline emphasizes improved strategies to identify and mitigate risks for trial participants [19].
Safety Monitoring Protocol
Methodology:
- Sentinel Dosing: At minimum, sentinel dosing of two subjects (one active, one placebo) is required for the first SAD and MAD cohorts [19]
- Stopping Rules Definition: Protocols must define stopping rules for individuals, cohorts, dose escalation, and the entire study, specifying whether the rule is temporary or final [19]
- Safety Review Process: Independent data monitoring committees with predefined review timelines and decision-making criteria
- Dose-Limiting Toxicity Criteria: Explicit definition of DLTs, including grading scales, relationship assessment, and duration criteria
- Emergency Management: Site preparedness for medical emergencies with access to emergency supplies and specialized equipment [19]
Site Selection and Monitoring Considerations
FIH clinical trials should be conducted at facilities with investigators and staff possessing necessary training and experience in early phase clinical trials [19]. These studies must occur under controlled conditions with close supervision of trial participants during and after dosing [19]. While FIH studies should ideally be conducted at a single site, if multiple sites are required for enrolment, protocols should include a description of measures to reduce risks that might occur from the use of multiple sites [19].
Well-designed FIH trials balance the need for efficient drug development with comprehensive safety assessment, particularly crucial for novel therapeutic modalities like ATMPs. By implementing robust protocols, clear decision criteria, and appropriate risk mitigation strategies, researchers can advance promising therapies while safeguarding participant welfare. The integration of adaptive designs and strategic early-phase planning ultimately accelerates the delivery of innovative treatments to patients in need.
For developers of Advanced Therapy Medicinal Products (ATMPs), the chemistry, manufacturing, and controls (CMC) section is a critical strategic element that directly shapes clinical trial design and execution. The inherent complexity and sensitivity of cell and gene therapies (CGT) mean that manufacturing variability can directly impact patient safety and the assessment of treatment efficacy in clinical studies [22]. Consequently, CMC considerations are not merely regulatory checkpoints but fundamental components that influence trial feasibility, endpoint selection, and data interpretation. This article details the specific CMC requirements that clinical researchers must integrate into trial designs for ATMPs, providing actionable protocols and analytical frameworks to navigate this complex landscape.
CMC-Driven Design Considerations for Clinical Trials
Regional Regulatory Nuances in CMC Requirements
Global development of ATMPs requires careful navigation of regional CMC differences. The requirements of major regulatory agencies, while aligned on many ICH principles, contain critical distinctions in key areas that impact clinical trial planning and product characterization [22]. The following table summarizes these pivotal differences.
Table 1: Key Regional CMC Regulatory Nuances Impacting Clinical Trial Design for ATMPs
| CMC Consideration | FDA (US) Position | EMA (EU) Position |
|---|---|---|
| Starting/Raw Materials | Uses 'critical raw materials'; expects enhanced material control based on risk and development stage [22]. | Has a regulatory definition for 'starting materials' (materials that become part of the drug substance); requires GMP principles for their preparation [22]. |
| Viral Vector Classification | Classifies in vitro viral vectors used to modify cell therapy products as a drug substance [22]. | Considers in vitro viral vectors to be starting materials [22]. |
| Potency Testing for Viral Vectors | A validated functional potency assay is essential for assessing the efficacy of the drug product used in pivotal studies [22]. | Infectivity and transgene expression are often sufficient in early phases, with less functional assays sometimes acceptable later [22]. |
| Replication Competent Virus (RCV) Testing | Requires testing on the final cell-based drug product [22]. | If absence of RCV is demonstrated on the in vitro vector, further testing on the resulting genetically modified cells is typically not required [22]. |
| Demonstrating Comparability | Detailed in FDA CGT-specific draft guidance (July 2023). Extent of testing increases with development stage [22]. | Guided by EMA Q&A documents and multidisciplinary guidelines. Extent of testing increases with development stage [22]. |
| Use of Historical Data for Comparability | Inclusion of historical data is recommended [22]. | Comparison to historical data is not required or recommended [22]. |
The Impact of Manufacturing Controls on Trial Integrity
Manufacturing process controls and their verification are paramount for ATMPs. The complexity of manufacturing and the living nature of these products mean that process changes during a clinical program are likely. A well-defined comparability protocol is therefore not just a regulatory requirement but a crucial tool for maintaining the integrity of an ongoing clinical trial [23]. If a manufacturing change occurs mid-trial without a pre-defined and agreed-upon strategy, the entire clinical dataset may be compromised, as it becomes difficult to attribute clinical outcomes to a single, well-defined product.
Furthermore, the analytical control strategy must be robust enough to detect subtle changes in product quality that could impact efficacy or safety. This is particularly important for trial designs that rely on long-term follow-up or are targeted at chronic conditions. The inability to demonstrate product consistency throughout the clinical program introduces significant variability and risk.
Diagram: The logical workflow integrating CMC strategy directly into clinical trial design to ensure robust outcomes.
Application Note: A Proactive CMC Strategy for Phase I-III ATMP Trials
Objective
To outline a phase-appropriate, integrated CMC and clinical development strategy that ensures the continuous supply of a consistent, high-quality ATMP for clinical trials while meeting evolving regulatory requirements from first-in-human to pivotal studies.
Detailed Protocol and Experimental Workflow
A successful clinical program for an ATMP depends on a CMC strategy that is both rigorous and adaptable. The following workflow and detailed steps ensure that manufacturing and quality considerations are embedded in the clinical development plan from the outset.
Diagram: The parallel and iterative development of CMC and clinical strategies across trial phases.
Phase I - Proof-of-Concept and Initial Safety
- CMC Objectives: The primary goal is to ensure patient safety. Generate materials under GMP-like conditions with a focus on sterility, identity, and safety-potency.
- Clinical Trial Design Impact:
- Dosing Strategy: Trial design must account for limited initial product stability. Dosing schedules and patient recruitment are contingent on real-time release data.
- Site Selection: Trials are typically limited to a small number of sites in close proximity to the manufacturing facility to simplify logistics and minimize product hold times.
- Endpoint Selection: Primary endpoints focus on safety and feasibility, which are directly dependent on the CMC-controlled product attributes.
Phase II - Dose Optimization and Process Refinement
- CMC Objectives: Demonstrate process consistency across multiple manufacturing runs. Refine and validate analytical methods. Formalize the control strategy for raw materials, especially critical ones like viral vectors or cell sources [22].
- Clinical Trial Design Impact:
- Multi-Center Trials: With improved process consistency and longer preliminary stability data, trials can expand to multiple centers.
- Dosing and Efficacy: This phase often explores different dosing regimens. The CMC team must be prepared to manufacture and characterize different product presentations (e.g., different doses) and establish comparability between them if needed.
- Blinding: The product's physical characteristics (e.g., appearance, packaging) must be considered to enable effective blinding, which is often managed under CMC's container closure system design.
Phase III - Pivotal Trial and Commercial Readiness
- CMC Objectives: The process must be locked, validated, and commercially viable. All analytical methods must be fully validated. Generate comprehensive long-term stability data to support the proposed shelf life for marketing approval.
- Clinical Trial Design Impact:
- Global Trial Supply: The CMC strategy must support a complex global supply chain, which may involve technology transfer to additional GMP facilities, shipping validation across different climatic zones, and managing a multi-national comparability protocol [24].
- Definitive Endpoints: The product used must be representative of the to-be-marketed product. Any critical quality attributes (e.g., potency, purity) must be tightly controlled and monitored, as they will be linked to the clinical outcomes in the marketing application.
The Scientist's Toolkit: Essential Research Reagent Solutions
The characterization of ATMPs relies on a suite of sophisticated analytical tools. The following table details key reagents and their functions in ensuring product quality and supporting the link between CMC data and clinical outcomes.
Table 2: Key Research Reagent Solutions for ATMP Characterization and Testing
| Research Reagent / Material | Function & Rationale |
|---|---|
| Reference Standards | Qualified materials used as benchmarks in analytical assays (e.g., potency, identity). Essential for ensuring data consistency and demonstrating comparability throughout clinical development [23]. |
| Cell-Based Potency Assays | Functional assays that measure the biological activity of the product relative to its mechanism of action. Critical for linking a specific CQA (potency) to the clinical effect and is a major focus for both FDA and EMA [22]. |
| Vector Copy Number (VCN) Assays | qPCR or ddPCR-based assays to quantify the number of viral vector integrations per cell in genetically modified therapies. A key safety and consistency attribute [22]. |
| Replication Competent Virus (RCV) Assays | Biosafety assays to detect the presence of replication-competent virus in viral vector-based products. Required for patient safety, with regional differences in testing requirements [22]. |
| Characterized Cell Banks | Master and Working Cell Banks used in production. Their thorough characterization (identity, sterility, freedom from adventitious agents) forms the foundation of product quality and safety [23]. |
The integration of a robust, forward-looking CMC strategy is not ancillary but central to the successful design and execution of clinical trials for ATMPs. From the classification of starting materials and the implementation of comparability protocols to the development of phase-appropriate analytical methods, CMC considerations directly dictate critical trial parameters including site selection, patient dosing, endpoint reliability, and global supply chain logistics. Sponsors who embed CMC planning into the earliest stages of clinical development, and who proactively engage with regulators to align on region-specific requirements, will be best positioned to generate interpretable clinical data, maintain trial integrity, and ultimately advance these complex therapies to patients efficiently and safely.
Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies, represent a groundbreaking class of biologics that treat diseases by altering, augmenting, or replacing pathological organs, tissues, cells, and genes [25]. The conventional centralized manufacturing model poses significant challenges for autologous ATMPs, where patient-specific starting materials undergo complex logistics and face time constraints due to short product shelf lives [26]. This has catalyzed the development of decentralized manufacturing and point-of-care (POC) production frameworks, which relocate manufacturing to facilities near the patient's bedside [27] [26].
Regulatory agencies worldwide are establishing novel frameworks to govern these innovative approaches. The United Kingdom's Medicines and Healthcare products Regulatory Agency (MHRA) has pioneered this effort by implementing the first comprehensive regulatory framework for point-of-care manufacture of ATMPs, effective July 23, 2025 [28] [27]. This article examines these emerging regulatory frameworks, provides implementation protocols, and discusses their implications for clinical trial design in ATMP research.
Regulatory Frameworks for Decentralized Manufacturing
The MHRA Regulatory Framework
The MHRA has established a tailored regulatory framework under The Human Medicines (Amendment) (Modular Manufacture and Point of Care) Regulations 2025 (U.K. Statutory Instruments 2025 No. 87), which amends the Human Medicines Regulations 2012 [28] [27]. This framework introduces two distinct manufacturing pathways:
- Point of Care (POC) Manufacturing: Medicinal products that, for reasons relating to method of manufacture, shelf life, constituents, or administration, can only be manufactured at or near the place of use [28].
- Modular Manufacture (MM) Manufacturing: Medicinal products that, for deployment reasons, must be manufactured or assembled in a relocatable modular unit [28].
The framework creates corresponding license types: "manufacturer's licence (POC)" and "manufacturer's licence (MM)", each requiring a designated Control Site that maintains supervision over manufacturing activities [27]. The Control Site holds responsibility for creating and maintaining Master Files (POC master file or MM master file) that detail arrangements for manufacturing or assembly [28].
Table 1: Key Definitions in the MHRA Regulatory Framework
| Term | Definition |
|---|---|
| POC Medicinal Product | A product that can only be manufactured at or near its place of use due to shelf life, constituents, or administration method [28] |
| Manufacturer's Licence (POC) | A license for manufacturing or assembling specified POC medicinal products [28] |
| POC Control Site | Premises where the license holder supervises and controls POC manufacturing [28] |
| POC Master File | Detailed description of arrangements for manufacturing or assembling a POC product [28] |
| Modular Unit | A relocatable manufacturing unit [28] |
Control Site Model and Responsibilities
The Control Site serves as the regulatory nexus in decentralized manufacturing models, maintaining ultimate responsibility for product quality and regulatory compliance [26]. Its key functions include:
- Serving as the primary point of interaction with regulatory agencies
- Maintaining and controlling the POC Master File
- Providing quality assurance oversight and Qualified Person (QP) services
- Ensuring consistency across all decentralized manufacturing sites
- Implementing and maintaining the overarching Quality Management System (QMS) [26]
This model enables product release at the centralized manufacturing facility rather than at the bedside, significantly simplifying the release process while maintaining quality assurance [27].
International Regulatory Landscape
Other regulatory agencies are also advancing frameworks for decentralized manufacturing:
- FDA: Through the Emerging Technology Program and Framework for Regulatory Advanced Manufacturing Evaluation (FRAME), the FDA is exploring distributed manufacturing platforms that can be deployed to multiple locations [26]. The agency emphasizes demonstrating product comparability across different manufacturing locations [26].
- EMA: Has acknowledged decentralized manufacturing potential in its Network Strategy 2025 and provides guidelines for batch release processes in decentralized manufacturing settings [26].
Table 2: Global Regulatory Approaches to Decentralized Manufacturing
| Regulatory Agency | Approach to Decentralized Manufacturing | Key Features |
|---|---|---|
| MHRA (UK) | Comprehensive regulatory framework effective July 2025 | Specific POC and MM licenses, Control Site model, Master Files [28] [27] |
| FDA (US) | Emerging framework through FRAME initiative | Emphasis on product comparability across sites, distributed manufacturing platforms [26] |
| EMA (EU) | Acknowledgment in strategic documents | Guidelines for batch release in decentralized settings, GMP specific to ATMPs [26] |
Implementation Framework for POC Manufacturing
Quality Management System for Decentralized Manufacturing
Implementing a robust Quality Management System (QMS) is paramount for successful decentralized manufacturing. The proposed QMS framework integrates current Good Manufacturing Practice (cGMP) principles with regulatory oversight through the Control Site model [26]. Key components include:
- Centralized QMS Administration: The Control Site establishes and maintains standardized procedures, quality control measures, and documentation systems across all manufacturing sites [26].
- Automated Closed-System Technologies: Implementing closed-system automated manufacturing platforms minimizes process variability and hardware deviations, enhancing product quality consistency [26].
- Standardized Training Platforms: Comprehensive training programs ensure consistent operations across all manufacturing sites, covering technical procedures, quality standards, and emergency protocols [26].
- Documentation Control: The POC Master File, maintained by the Control Site, provides detailed manufacturing instructions and must be followed by all satellite sites [27].
Technology Platform Selection
Decentralized manufacturing requires specialized technology platforms that support consistency and compliance across multiple sites:
- Closed-System Automated Bioreactors: Enable standardized cell expansion with minimal operator intervention, reducing contamination risk and variability [26] [29].
- Deployable Prefabricated Units: Modular GMP-compliant units allow rapid expansion of manufacturing capacity and can be installed at treatment centers [26].
- Digital Monitoring Systems: Real-time data capture and monitoring platforms enable the Control Site to oversee operations across all manufacturing locations [30] [26].
Diagram 1: POC Control Site Regulatory Model
Clinical Trial Design Considerations
Pre-Trial Planning (6-12 Months Before Trial Start)
Early phase advanced therapy trials require meticulous planning across regulatory, operational, and scientific domains [30]. Critical steps include:
- Engage Key Opinion Leaders (KOLs): Consult experienced KOLs early to shape trial design, endpoints, and patient selection criteria, ensuring alignment with scientific and regulatory nuances of ATMPs [30].
- Involve Patient Advocacy Groups (PAGs): Especially for rare diseases, work with advocacy groups to improve protocol feasibility and patient engagement [30].
- Request Scientific Advice: Seek early regulatory feedback from EMA or MHRA to align expectations on nonclinical and clinical data requirements [30].
- Classify Your Product: Submit a formal ATMP classification request to appropriate regulatory agencies, which can unlock access to specific incentives [30].
- Assess Competitive Landscape: Study comparable ATMP pipelines, focusing on their safety, efficacy, target population, and trial designs to anticipate regulatory hurdles [30].
Manufacturing and Logistics Strategy
Developing a robust manufacturing and logistics strategy is essential for decentralized trials:
- Confirm Intellectual Property & Manufacturing Strategy: Protect critical elements such as vectors, cell lines, or gene editing tools. Select GMP-certified manufacturers with ATMP experience [30].
- Scale-Out Planning: While early trial batch sizes may be small, consider how manufacturing will be scaled across multiple sites for late-stage trials and commercialization [30] [26].
- Cold-Chain Logistics: Implement specialized logistics for cell-based therapies, including EU-specific customs processes and UK-specific regulations where applicable [30].
Table 3: Clinical Trial Timeline for ATMPs with POC Manufacturing
| Time Before Trial Start | Critical Activities | Key Considerations |
|---|---|---|
| 6-12 Months | Pre-Trial Planning | KOL engagement, regulatory advice, product classification, competitive assessment [30] |
| 6-12 Months | Manufacturing Strategy | IP protection, GMP manufacturer selection, scale-out planning [30] |
| 6-9 Months | Vendor Selection | Choose CROs with ATMP expertise, specialized assay development, cold-chain logistics [30] |
| 4-6 Months | Protocol Development | Prepare CTA and IMPD, incorporate risk-based approach, long-term follow-up plans [30] |
| 1-3 Months | Pre-Trial Execution | GMO clearance (if applicable), site training, system validation [30] |
Regulatory Submissions and Documentation
For clinical trials involving POC manufacturing, specific regulatory submissions are required:
- Clinical Trial Application (CTA): Unlike the IND process in the US, the EU and UK require a CTA, including the Investigational Medicinal Product Dossier (IMPD) [30].
- Investigational Medicinal Product Dossier (IMPD): Must outline product composition, manufacturing process, preclinical data, and proposed trial design with safety monitoring [30].
- Risk-Based Approach: For ATMPs, include detailed risk assessment addressing product-specific risks such as immunogenicity and off-target effects [30].
- Long-Term Follow-Up (LTFU): Build LTFU requirements upfront into trial design due to durable therapeutic effects of ATMPs [30].
Experimental Protocols for POC Manufacturing
Protocol: Technology Transfer to POC Sites
Objective: Establish comparable manufacturing processes across multiple POC sites to ensure consistent product quality.
Materials:
- Master cell bank
- GMP-grade culture media and supplements
- Closed-system automated bioreactors
- Quality control testing reagents
- Standard operating procedures (SOPs)
Methodology:
- Process Definition: Document and validate the entire manufacturing process at the Control Site, establishing critical process parameters (CPPs) and critical quality attributes (CQAs) [26] [29].
- Equipment Qualification: Ensure identical equipment configurations across all POC sites, performing installation qualification (IQ), operational qualification (OQ), and performance qualification (PQ) [26].
- Personnel Training: Implement standardized training programs for operators at all POC sites, including theoretical and hands-on components [26].
- Process Performance Qualification: Execute three consecutive successful manufacturing runs at each POC site, demonstrating process consistency and product comparability [26] [29].
- Comparative Analysis: Conduct extensive analytical comparability assessment between products manufactured at Control Site and POC sites, including potency assays, identity tests, and purity assessments [26].
Acceptance Criteria: All POC sites must demonstrate manufacturing success rates ≥95% and product characteristics falling within predefined specifications established at the Control Site.
Protocol: Environmental Monitoring for POC Sites
Objective: Ensure aseptic manufacturing conditions at POC sites with equivalent quality standards to centralized facilities.
Materials:
- Active air samplers
- Settle plates
- Surface contact plates
- Particulate counters
- Microbial identification systems
Methodology:
- Baseline Assessment: Perform comprehensive environmental monitoring before initiating manufacturing, including viable and non-viable particle counts in critical areas [29].
- Continuous Monitoring: Implement real-time particulate monitoring in Grade A and B areas during manufacturing operations [29].
- Microbial Monitoring: Place settle plates for airborne viable contamination and use contact plates for surface monitoring at predetermined locations [29].
- Personnel Monitoring: Perform gowning qualification and regular monitoring of operators through finger plates and garment contact plates [29].
- Data Integration: Incorporate environmental monitoring data into batch records and establish alert and action limits based on historical data [26] [29].
Acceptance Criteria: Meet ISO Class 5 (Grade A) conditions in critical processing areas with no recoverable microbial contamination during manufacturing operations.
Diagram 2: POC Manufacturing Quality Assurance Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for POC ATMP Manufacturing
| Research Reagent | Function | Application Notes |
|---|---|---|
| GMP-grade Cell Culture Media | Supports cell growth and maintenance | Formulated without animal components; quality testing includes sterility, endotoxin, and mycoplasma assessments [29] |
| Cell Separation Reagents | Isolates specific cell populations | Magnetic-activated cell sorting (MACS) or fluorescence-activated cell sorting (FACS) reagents with defined purity specifications [29] |
| Viral Vector Systems | Delivers genetic material to cells | GMP-produced lentiviral or retroviral vectors with certificates of analysis including titer, sterility, and identity [25] [29] |
| Cryopreservation Media | Preserves cellular products for storage | Formulated with defined DMSO concentrations; undergoes container compatibility and stability testing [29] |
| Quality Control Assay Kits | Characterizes final product attributes | Includes flow cytometry panels, potency assays, sterility tests, and mycoplasma detection kits [26] [29] |
| Closed-System Bioreactors | Scalable cell expansion platforms | Automated, functionally closed systems with predefined protocols and parameter controls [26] [29] |
The emergence of regulatory frameworks for point-of-care manufacturing and decentralized trials represents a transformative development for ATMPs. The MHRA's pioneering regulations provide a structured pathway for implementing these innovative manufacturing approaches while maintaining rigorous quality standards. The Control Site model with Master File documentation offers a practical solution for overseeing decentralized manufacturing networks.
Successful implementation requires robust Quality Management Systems, standardized technology platforms, and meticulous clinical trial planning. As regulatory agencies worldwide continue to refine their approaches to decentralized manufacturing, researchers and developers must maintain flexibility and engage early with regulators. These evolving frameworks promise to enhance the accessibility, scalability, and cost-effectiveness of ATMPs, ultimately benefiting patients through accelerated access to groundbreaking therapies.
Innovative Trial Methodologies for ATMPs: Adaptive Designs, Endpoints, and Statistical Approaches
Single-arm trials (SATs) represent a specialized clinical study design in which all enrolled subjects receive the same investigational treatment, conducted without a parallel control group. These trials serve as a vital alternative to randomized controlled trials (RCTs) in specific scenarios where traditional trial designs are impractical or unethical [31]. In the context of advanced therapy medicinal products (ATMPs) research—which often targets rare diseases, complex malignancies, and conditions with high unmet medical need—SATs enable expedited evaluation of therapeutic interventions and can form the foundation for regulatory approvals [31] [32].
The fundamental characteristic of SATs is their single-treatment-group structure, which eliminates randomization processes and control or placebo groups that are hallmark features of RCTs [33]. Instead, researchers utilize treatment effects observed in comparable patient populations as a reference standard, either through predetermined efficacy thresholds or external controls for comparative analysis [33]. This design obviates the need for concurrent controls, resulting in simpler implementation, shorter timelines, and smaller sample size requirements compared to traditional RCTs [31] [33].
For ATMP developers facing challenges with patient recruitment, ethical constraints, or urgent medical needs, SATs offer a potentially accelerated pathway for drug development and approval [33]. However, this design presents significantly greater interpretation complexity compared to RCTs, requiring sophisticated analytical approaches and careful consideration of multiple assumptions that are inherently controlled for in randomized designs [33]. The growing accessibility of historical data and real-world evidence has further motivated interest in leveraging external controls to enhance the scientific validity of SATs in ATMP research [34].
Applications and Appropriate Use Cases
Single-arm trials are strategically employed in specialized clinical contexts where randomized controlled trials face significant practical or ethical challenges. Understanding the appropriate applications of SATs is crucial for their effective implementation in ATMP research.
Established Applications
SATs find their strongest justification in several well-defined scenarios frequently encountered in advanced therapy development. Rare diseases and orphan drug development represent a primary application, where constrained patient recruitment pools make large-scale randomized trials impractical [31] [33]. In these contexts, SATs become a viable alternative for generating pivotal efficacy evidence. Similarly, advanced malignancies with no effective treatment options often warrant SAT designs, particularly for oncology drugs targeting life-threatening conditions where SATs may provide early evidence of efficacy in urgent situations [33].
The evaluation of novel treatment modalities, including many ATMPs such as gene therapies and cellular products, represents another key application area [31]. When these therapies demonstrate dramatic effects in early studies, SATs can serve as confirmatory evidence. Furthermore, SATs are applicable in contexts involving life-threatening conditions where ethical concerns prevent the use of placebo or standard-of-care control groups [31] [32]. In such scenarios, the ethical feasibility of SATs includes preventing the assignment of unsuitable patients to a control group receiving potentially ineffective treatment [33].
Regulatory Context and Acceptance
Regulatory agencies including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have established specific contexts where SATs may be acceptable for supporting efficacy claims. Historically, both agencies have accepted SATs in exceptional cases, typically when a condition has a highly predictable and dire natural history, treatment effects are dramatic and unprecedented, or randomization is deemed unethical or impractical [35]. However, recent regulatory guidance reflects increasingly stringent expectations.
The 2024 EMA Reflection Paper marks a pivotal shift, stating unequivocally that "Single-arm trials lack the internal validity to support stand-alone conclusions on efficacy and safety unless exceptional justifications apply" [35]. Similarly, the FDA has warned sponsors not to expect approval based solely on single-arm data, with recent market withdrawals exposing the fragility of SAT-based strategies [35]. Both regulators now emphasize that SATs may only be justified if all feasible alternatives have been ruled out, and even then, often must be followed by well-powered confirmatory trials [35].
Advantages in ATMP Research
For ATMP developers, SATs offer several compelling advantages that align with the unique challenges of advanced therapy development. Smaller sample size requirements address the practical constraints of studying therapies for rare diseases [31] [32]. Faster implementation timelines enable more rapid evaluation of promising therapies for conditions with urgent unmet needs [31]. Reduced operational complexity simplifies trial execution in specialized medical centers with limited research infrastructure [32]. Ethical acceptability in contexts where randomization to control may be problematic [32]. These advantages make SATs particularly relevant for ATMPs targeting rare genetic disorders, ultra-orphan indications, and conditions with predictable natural history and high mortality.
Table: Applications of Single-Arm Trials in ATMP Research
| Application Area | Key Characteristics | Regulatory Considerations |
|---|---|---|
| Rare Diseases | Small patient populations; Limited recruitment pools | Acceptance higher for ultra-rare diseases (<1:50,000) |
| Advanced Malignancies | No effective treatment options; Life-threatening conditions | Often under Accelerated Approval pathways |
| Novel ATMP Modalities | Dramatic treatment effects; Unprecedented mechanisms | Require strong biological plausibility |
| Conditions with Predictable Natural History | Well-characterized disease progression; Consistent endpoints | Historical control data must be high-quality |
| Ethically Constrained Contexts | Randomization to control problematic; Equipoise concerns | Requires strong ethical justification |
Limitations and Methodological Challenges
Despite their operational advantages, single-arm trials face significant methodological limitations that can compromise the validity and reliability of their findings. Understanding these challenges is essential for appropriate design, interpretation, and regulatory acceptance of SATs in ATMP research.
Threats to Validity and Reliability
The fundamental absence of randomization in SAT designs creates an intrinsic limitation in establishing definitive causal attribution of therapeutic effects [33]. In randomized controlled trials, the methodological cornerstone of random allocation ensures approximate equipoise in both measured and latent prognostic factors across treatment arms, establishing a statistically robust framework for causal inference. SATs inherently lack methodological safeguards against confounding from unmeasured prognostic determinants [33]. This inability to account for latent variables systematically compromises internal validity in therapeutic effect estimation.
The same methodological limitation engenders dual threats to external validity, which precludes the direct quantification of treatment effects [33]. The quantification must rely on two critical assumptions: (1) precise characterization of counterfactual outcomes (the hypothetical disease trajectory without intervention), and (2) prognostic equipoise between study participants and external controls across both measured and latent biological determinants [33]. Consequently, SATs-derived efficacy estimates exhibit an inherent context-dependence nature, constrained to narrowly defined patient subgroups under protocol-specified conditions, with limited generalizability beyond the trial's operational parameters [33].
In single-arm trials, the reliability of therapeutic effect estimates may be inherently compromised [33]. Efficacy estimates become particularly susceptible to sampling variability, especially in studies characterized by limited sample sizes and/or high outcome variability. While RCTs rely on statistical properties inherent to randomization that mitigate uncertainty, SATs only directly observe variability within the experimental group, while the variability of a hypothetical control group remains unknown [33].
Specific Biases in SATs
When external controls are employed to contextualize SAT results, multiple sources of bias can systematically impact the validity of treatment effect estimates [33]:
- Selection bias from differences in patient characteristics, inclusion criteria, or participating sites between the SAT and external control populations
- Temporal bias arising from changes in standard care, diagnostic methods, or healthcare systems over time
- Information bias from variations in outcome assessment, follow-up procedures, or data collection methods
- Confounding bias from unmeasured or inadequately adjusted prognostic factors
- Treatment-related bias from differences in concomitant therapies or treatment delivery
- Reporting bias from selective outcome reporting or data availability differences
These biases are particularly problematic in rare disease contexts, where SATs are sometimes seen as a necessity due to small sample sizes [35]. Precisely in this setting, bias matters most—a few misclassified responders or a slightly more severe historical cohort can dramatically distort perceived treatment benefit [35]. In the absence of a randomized comparator, unmeasured confounding—especially selection bias and performance bias—can inflate efficacy signals, with potential consequences including market access refusal, retraction of approval, or product withdrawal [35].
Regulatory and Evidence Limitations
Recent regulatory positions have clarified the limitations of SATs in providing substantial evidence of effectiveness. The EMA's 2024 reflection paper establishes that rarity does not excuse weak methodology, expecting sponsors to explore alternatives before proposing a SAT as pivotal evidence [35]. The FDA has similarly shifted away from SATs as stand-alone evidence, particularly following several high-profile market withdrawals after failed confirmatory trials [35].
The ICH E9(R1) estimand framework, now widely adopted by regulators, demands a clear definition of treatment effects, intercurrent events, and the hypothetical scenario the trial is meant to represent [35]. SATs rarely meet these standards comprehensively, especially when endpoints are subjective or disease progression is variable. This creates challenges in satisfying modern regulatory standards for evidence generation.
Table: Limitations of Single-Arm Trials in ATMP Research
| Limitation Category | Specific Challenges | Impact on Evidence Strength |
|---|---|---|
| Internal Validity | No randomization; Unable to control for unmeasured confounders | Compromised causal inference |
| External Validity | Context-dependent results; Limited generalizability | Restricted to specific patient subgroups |
| Bias Vulnerability | Selection, temporal, information, and confounding biases | Inflated or distorted treatment effects |
| Regulatory Scrutiny | Increasingly stringent standards; Requirement for confirmatory evidence | Limited as stand-alone evidence |
| Statistical Limitations | Uncertainty in effect estimation; Sampling variability | Reduced reliability and precision |
External Control Methodologies
The scientific validity of single-arm trials hinges on the appropriate use of external controls to contextualize observed outcomes. Advanced methodologies for incorporating external data have evolved significantly, offering enhanced approaches for comparative effectiveness assessment in ATMP research.
Types of External Controls
External control arms can be derived from diverse data sources, each with distinct characteristics and applications. Historical controls comprise data from previous clinical trials, natural history studies, or patient registries collected during prior time periods [33]. These represent the most established source of external controls but are susceptible to temporal biases. Concurrent external controls consist of data collected during the same time period as the SAT but in different settings or studies [33]. While potentially reducing temporal bias, these may introduce cross-institutional variability. Real-world data (RWD) sources include electronic health records, claims databases, and disease registries that reflect routine clinical practice [34]. The growing accessibility of high-quality RWD has expanded opportunities for external control construction.
Each control type presents distinct advantages and limitations. Historical controls benefit from established data quality and curation processes but may reflect outdated standards of care. Concurrent external controls minimize temporal shifts in practice patterns but require access to contemporaneous research data. RWD-derived controls offer larger sample sizes and greater generalizability but may exhibit greater heterogeneity in data collection and patient characteristics [34].
Statistical Approaches and Methodological Framework
Statistical methods for incorporating external controls have developed considerably since early approaches. Weighting methods include propensity score techniques, empirical likelihood, entropy balancing, and constrained maximum likelihood, which aim to address selection bias in nonrandomized studies by creating balanced comparisons between SAT participants and external controls [34]. Outcome distribution adjustment methods encompass test-then-pool procedures, matching with bias adjustment, power priors, commensurate priors, and Bayesian hierarchical models, which handle differences in outcome distributions between concurrent and external controls [34].
A promising advancement involves estimators derived from the efficient influence function (EIF), which provide semiparametric efficiency bounds under certain conditions while retaining double robustness properties [34]. These estimators achieve optimal statistical properties while mitigating vulnerabilities to model misspecification. The fundamental premise involves leveraging external control data to reduce the required sample size of the current study while maintaining prespecified type I error and power for hypothesis testing [34].
The prospective incorporation of external controls within trial design represents a methodological shift from traditional post-hoc analyses. A unified experimental design framework encompasses standard RCTs, hybrid trials, and single-arm trials, focusing on sample size determination and power analysis [34]. This framework enables researchers to formally quantify the information contribution of external controls during the design phase, rather than treating them as supplementary analyses.
Hybrid Design Strategies
Hybrid trial designs represent an intermediate approach between traditional RCTs and SATs, incorporating both internal and external control elements. These designs maintain a reduced internal control arm while augmenting with external controls to enhance statistical power and reduce sample size requirements [34]. Hybrid approaches offer a balanced solution that preserves some benefits of randomization while addressing ethical and practical constraints of large control groups.
By borrowing information from external controls, hybrid designs can yield substantial sample size savings, particularly in unbalanced designs with larger treatment allocations in the current study [34]. Simulation studies demonstrate that properly designed hybrid approaches maintain valid type I error and achieve target power across diverse scenarios while requiring substantially fewer subjects in the current study than traditional RCT designs [34].
Diagram 1: External Control Methodology Framework for Single-Arm Trials. This diagram illustrates the integrated process of constructing and analyzing external controls for comparative effectiveness assessment in single-arm trials, incorporating multiple data sources and statistical methodologies.
Experimental Protocols and Implementation
Successful implementation of single-arm trials requires meticulous planning and execution of specific methodological protocols. The following section provides detailed experimental frameworks for key components of SAT design and analysis in ATMP research.
Protocol: Simon's Two-Stage Design for SATs
Simon's two-stage design represents an efficient methodological approach for phase II SATs, minimizing patient exposure to potentially ineffective therapies while providing rigorous efficacy assessment.
Objective: To evaluate preliminary efficacy of an investigational ATMP while controlling statistical error rates and minimizing patient exposure to ineffective treatments.
Methodology:
- Stage 1 Enrollment: Enroll a predetermined number of patients (n1) and administer the investigational therapy.
- Interim Analysis: After completion of Stage 1, assess the primary endpoint. If the number of responses exceeds a predefined threshold (r1), proceed to Stage 2. Otherwise, terminate the trial for futility.
- Stage 2 Enrollment: If Stage 1 criteria are met, enroll additional patients (n2) to achieve total sample size (N = n1 + n2).
- Final Analysis: After completion of Stage 2, compare the total number of responses to a final threshold (r). If exceeded, conclude treatment efficacy.
Statistical Considerations:
- Type I error rate (α) typically set at 0.05-0.10
- Power (1-β) typically set at 0.80-0.90
- Optimal or minimax design selections based on expected response rates
- Pre-specified rules for handling missing data and protocol deviations
Implementation Framework:
- Predefine response criteria according to established standards (e.g., RECIST for oncology)
- Establish independent data monitoring committee for interim analysis
- Pre-specify statistical analysis plan including hypothesis testing framework
- Document decision rules for stage progression and final analysis
This design is particularly valuable for ATMPs with limited preliminary data, as it provides a structured approach for early efficacy assessment while controlling statistical risks.
Protocol: External Control Construction and Validation
The construction of valid external controls requires systematic methodology to ensure comparability with the SAT population and minimize bias.
Objective: To develop a well-characterized external control cohort that approximates the counterfactual experience of the SAT population had they not received the investigational therapy.
Methodology:
- Data Source Evaluation: Assess potential external data sources for completeness, quality, and relevance to the target population.
- Cohort Definition: Apply inclusion/exclusion criteria mirroring the SAT protocol to identify potential external controls.
- Covariate Selection: Identify prognostic factors and potential confounders for adjustment based on clinical knowledge and empirical evidence.
- Propensity Score Development: Estimate propensity scores using logistic regression or machine learning methods to model the probability of being in the SAT versus external control cohort.
- Balance Assessment: Evaluate covariate balance between groups using standardized mean differences (<0.1 indicating adequate balance).
- Weighting or Matching: Apply propensity score weights (IPTW, overlap weights) or matching (1:1, variable ratio) to create balanced comparisons.
- Outcome Model Specification: Develop appropriate outcome models adjusting for residual imbalance and accounting for study design.
Validation Framework:
- Internal Validation: Cross-validation and bootstrap procedures to assess model stability
- Negative Control Outcomes: Test for residual confounding using outcomes known to be unaffected by treatment
- Positive Control Analyses: Compare external control results to known effects from randomized trials when available
- Sensitivity Analyses: Assess robustness to unmeasured confounding using quantitative bias analysis
Quality Assurance Metrics:
- Covariate balance before and after adjustment
- Effective sample size of weighted population
- Consistency of results across multiple analytical approaches
- Transparency in data provenance and methodological choices
This protocol provides a structured approach to external control construction that enhances the scientific validity of comparative effectiveness assessments in SATs.
Protocol: Bayesian Hybrid Control Design
Bayesian approaches offer flexible frameworks for incorporating external controls into SATs while formally quantifying the degree of borrowing based on between-trial heterogeneity.
Objective: To leverage external control data efficiently while controlling type I error inflation and maintaining operational characteristics.
Methodology:
- Prior Specification: Define initial prior distributions for control group parameters based on external data
- Borrowing Mechanism Selection: Choose appropriate dynamic borrowing method (e.g., power prior, commensurate prior, Bayesian hierarchical model)
- Heterogeneity Assessment: Pre-specify criteria for evaluating consistency between current and external data
- Borrowing Degree Determination: Establish rules for the extent of borrowing based on observed heterogeneity
- Decision Criteria Definition: Specify posterior probability thresholds for efficacy conclusions
Implementation Framework:
- Power Prior Approach:
- Specify prior distribution: π(θ|α₀) ∝ [L(θ|D₀)]^α₀ π₀(θ)
- Determine discounting factor α₀ based on prior-data conflict
- Adjust borrowing based on similarity between current and historical data
Commensurate Prior Framework:
- Model relationship between current and historical parameters
- Introduce hyperparameter governing similarity between cohorts
- Estimate borrowing degree from data while maintaining regularization
Bayesian Hierarchical Model:
- Structure: θcurrent ~ N(θhistorical, τ²)
- Place hyperprior on between-trial heterogeneity τ
- Implement full Bayesian estimation or empirical Bayes approaches
Operating Characteristics:
- Simulate type I error rate under null scenarios with varying heterogeneity
- Evaluate power under alternative scenarios with true treatment effects
- Assess robustness to model misspecification and prior choices
- Pre-specify frequentist properties for regulatory acceptance
This protocol enables efficient use of external information while maintaining appropriate statistical properties for regulatory decision-making.
Diagram 2: Single-Arm Trial Implementation Workflow. This diagram outlines the comprehensive workflow for designing, implementing, and analyzing single-arm trials in ATMP research, highlighting key decision points and methodological considerations.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of single-arm trials in ATMP research requires specialized methodological tools and analytical approaches. The following toolkit outlines essential components for designing, implementing, and interpreting SATs.
Table: Research Reagent Solutions for Single-Arm Trial Implementation
| Tool Category | Specific Solutions | Function and Application |
|---|---|---|
| Statistical Design Tools | Simon's Two-Stage Design | Optimizes patient exposure while controlling error rates in phase II trials |
| Bayesian Predictive Power Calculator | Assesses probability of trial success incorporating prior information | |
| Sample Size Determination Framework | Calculates sample requirements for target power using pre-experimental variance estimation | |
| External Control Methodologies | Propensity Score Toolkit | Creates balanced comparisons between SAT and external control populations |
| Efficient Influence Function (EIF) Estimators | Achieves semiparametric efficiency bounds with double robustness properties | |
| Dynamic Borrowing Mechanisms | Controls incorporation of external information based on between-trial heterogeneity | |
| Bias Assessment Tools | Quantitative Bias Analysis | Quantifies potential impact of unmeasured confounding on effect estimates |
| Negative Control Outcome Framework | Tests for residual confounding using known null relationships | |
| E-Value Calculation | Determines minimum strength of unmeasured confounding needed to explain away effects | |
| Regulatory Documentation | ICH E9(R1) Estimand Framework | Defines treatment effects, intercurrent events, and target trial populations |
| External Control Validity Argument | Structured justification for external control comparability and relevance | |
| Sensitivity Analysis Plan | Pre-specified analyses assessing robustness to methodological assumptions | |
| Data Quality Assurance | Source Data Verification Tools | Ensures accuracy and completeness of primary endpoint assessment |
| Independent Endpoint Adjudication | Provides blinded assessment of subjective endpoints to reduce measurement bias | |
| Real-World Data Curations Systems | Transforms raw RWD into analysis-ready datasets for external control construction |
Single-arm trials represent a specialized design option within the methodological arsenal for ATMP development, offering distinct advantages in specific contexts but carrying significant limitations that require careful mitigation. When appropriately designed and implemented with robust external control methodologies, SATs can provide valuable evidence for regulatory decision-making in circumstances where randomized designs are impractical or unethical. However, the evolving regulatory landscape demands increasingly rigorous standards for SATs, with emphasis on comparative effectiveness assessment and robust sensitivity analyses.
The successful application of SATs in ATMP research requires thoughtful integration of advanced statistical methods, transparent reporting of limitations, and strategic planning for evidence generation throughout the product development lifecycle. By adopting the methodologies and protocols outlined in this document, researchers can enhance the scientific validity and regulatory acceptability of single-arm trials while advancing the development of promising advanced therapies for patients with serious unmet medical needs.
Adaptive platform trials represent a transformative approach in clinical research, defined as randomized trial designs that compare at least one intervention to a control with the capacity to add and remove interventions over time according to rules defined in a master protocol [36]. These designs investigate multiple research questions under a shared, ongoing trial infrastructure, leading to significant operational efficiencies and improved resource allocation [36]. For small population studies, such as those involving rare diseases or advanced therapy medicinal products (ATMPs), these efficiencies are particularly valuable where patient numbers are limited and traditional trial designs often prove impractical.
These trials are characterized by their flexible, perpetual nature, allowing them to study multiple interventions for a disease or condition with interventions entering and leaving the platform based on predefined decision algorithms [37]. The "platform" refers to the infrastructure component—a flexible protocol implemented under shared infrastructure—that may incorporate various statistical features including multistage early stopping or factorial design elements [36]. This innovative framework is reshaping clinical trials across diverse therapeutic areas, from oncology to neurology and infectious diseases.
Key Features and Methodological Framework
Core Design Elements
Adaptive platform trials incorporate several distinguishing features that make them particularly suited for research in small populations. The foundational element is the master protocol, which serves as the overarching framework governing multiple sub-studies [37]. This protocol establishes consistent standards for endpoints, data collection, and quality control across all interventions tested within the platform. Through this standardized approach, master protocols eliminate redundant procedures that would otherwise be repeated in standalone trials, creating significant efficiencies.
A critical feature of these designs is the shared control arm, which serves as a common comparator for multiple experimental interventions [36]. This shared control group maximizes the informational value derived from each control patient, a crucial consideration in small population studies where every participant's data is exceptionally valuable. This approach both reduces the total number of patients required and accelerates comparison times between interventions.
Platform trials typically incorporate statistical adaptations guided by accumulating data [36]. These may include early stopping rules for efficacy or futility, response-adaptive randomization that preferentially allocates patients to better-performing treatments, and sample size re-estimation [36] [38]. These adaptive features provide ethical benefits by limiting patient exposure to ineffective therapies and operational benefits by focusing resources on the most promising interventions.
Quantitative Comparison of Design Features
Table 1: Key Adaptive Design Elements and Their Application to Small Populations
| Adaptive Design Element | Application in Small Populations | Key Advantages | Methodological Considerations |
|---|---|---|---|
| Group Sequential Designs [38] | Early stopping for efficacy/futility | Reduces overall sample size; Results disseminated more quickly | May need larger maximum sample size than fixed designs; Early stopping may reduce safety data |
| Sample Size Re-Estimation [38] | Adjusts sample size based on interim effect estimates | Reduces chance of a negative trial with a meaningful effect by increasing sample size to ensure sufficient power | Sample size increase may be infeasible; Unblinded approaches may inflate type I error rate |
| Adaptive Enrichment [38] | Adapts patient population to targeted subgroup | Refines eligibility to enroll subgroups most likely to benefit; Useful for prognostic and predictive enrichment | Subgroups may be very small; Choice of biomarkers may lead to different subgroups |
| Treatment Arm Selection [36] [38] | Adds or terminates study arms based on interim data | Flexible termination of arms for futility/efficacy; Shared control arm increases allocation to experimental interventions | Multiple comparisons may inflate type I error; Complex criteria for arm modifications |
| Response-Adaptive Randomization [36] [38] | Modifies randomization probabilities to favor better-performing arms | Increases probability of allocation to better-performing arms; More participants receive beneficial treatments | Special challenges with temporal trends; Potential for operational unblinding |
Table 2: Operational Characteristics of Platform Trials in Different Disease Areas
| Trial Name | Disease Area | Key Adaptive Features | Operational Efficiency Metrics |
|---|---|---|---|
| HEALEY ALS [39] | Amyotrophic Lateral Sclerosis | Master protocol with multiple regimens; Centralized infrastructure | 54 experienced sites; 4 regimens evaluated; sIRB approval in 120 days; Results within ~2 years of launch |
| REMAP-CAP [36] | Community-Acquired Pneumonia | Response-adaptive randomization; Multiple domains | 66 interventions across 18 domains; ~24,500 randomizations from ~14,000 patients |
| I-SPY2 [40] | Breast Cancer | Adaptive randomization; Bayesian statistical models | "Graduation" of therapies to phase 3; Modular master protocol for adding/removing drugs |
Workflow Visualization of an Adaptive Platform Trial
Platform Trial Adaptive Workflow: This diagram illustrates the cyclical process of evaluation and adaptation in platform trials, highlighting decision points based on interim analyses.
Application Notes for Small Population Studies
Strategic Implementation Considerations
Small population studies present unique challenges that make adaptive platform trials particularly advantageous. These designs are most appropriate when there is considerable clinical equipoise around best practice for a given medical condition that is likely to continue even in the presence of ongoing discoveries [36]. This scenario is common in rare diseases and ATMP development, where limited prior evidence creates significant uncertainty about optimal treatments.
The successful implementation of platform trials in small populations requires strong research collaborations and existing trial networks [36]. These partnerships are essential for achieving adequate patient enrollment across multiple sites. The HEALEY ALS Platform Trial exemplifies this approach, leveraging 54 geographically diverse sites from the Northeast ALS Consortium, all highly experienced in ALS care and research [39]. This collaborative model enables efficient patient recruitment despite the rarity of the condition.
Platform trials require substantial initial investment compared to traditional designs, but this cost is justified when shared across enough research questions [36]. For small populations, the long-term efficiencies outweigh the initial setup costs. Funding bodies are increasingly making targeted calls for such upfront investment to develop platform trials [36]. The operational efficiencies are demonstrated by the HEALEY ALS trial, which completed enrollment for its first three regimens in 15 months and had results available within approximately two years from initial trial launch [39].
Regulatory and Operational Framework
The operational framework for platform trials requires careful planning of governance structures that may include multiple committees beyond those in traditional trials [36]. These typically include a core trial management group, trial steering committee, data monitoring committee, and often additional advisory and operational committees to manage specific interventions, domains, or subgroups. Robust communication firewalls are essential to mitigate operational biases and prevent unblinding [36].
Regulatory coordination is crucial for platform trials evaluating ATMPs. The HEALEY ALS trial utilized a master Investigational New Drug (IND) application, with each regimen added as an amendment [39]. This approach streamlined regulatory oversight while maintaining flexibility. The use of a single Institutional Review Board (sIRB) significantly accelerated startup times, with the master protocol and first three regimens receiving sIRB approval in 120 days, and subsequent regimens in just 21 days [39].
Statistical rigor must be maintained through comprehensive pre-specification and simulation studies [36]. Platform trials often employ Bayesian statistical methods because of their flexibility and principled framework for information borrowing, sequential analysis, and probabilistic interpretation of efficacy [36]. These simulations are essential to ensure the design has satisfactory type I error control and power, and may take many months at the trial design stage.
Experimental Protocols
Interim Analysis Procedures
Interim analyses represent the critical decision points in adaptive platform trials where adaptations are implemented based on accumulating data [41]. The ROBust INterims for adaptive designs (ROBIN) project provides comprehensive guidance for conducting high-quality and rapid interim analyses. The process should not be viewed as a single discrete event but as an integral part of the trial as a whole [41].
The timing and frequency of interim analyses must be carefully planned during the design phase. While adaptive designs are conceptually attractive, they are not always useful, and most benefits may come from relatively straightforward adaptations with fewer interim analyses [41]. Predictable timing of interim analyses, such as basing them on calendar time rather than information time, may help with scheduling, though this introduces variability in sample sizes if recruitment rates are uncertain [41].
Table 3: Essential Research Reagent Solutions for Adaptive Platform Trials
| Research Tool Category | Specific Solutions | Function in Platform Trials |
|---|---|---|
| Statistical Software [36] [38] | Bayesian analytical platforms; Simulation packages | Enable complex adaptive simulations; Interim analysis calculations; Response-adaptive randomization algorithms |
| Data Management Systems [41] | Real-time data capture systems; Centralized monitoring platforms | Ensure timely data delivery for frequent scheduled analyses; Maintain data quality for interim decisions |
| Master Protocol Templates [36] [39] | Modular protocol frameworks; Standardized amendment procedures | Provide flexible yet consistent trial structure; Streamline adding/removing interventions |
| Regulatory Submission Packages [39] [42] | Master IND templates; sIRB application packages | Accelerate regulatory approvals; Facilitate multi-site oversight |
| Randomization Systems [36] [38] | Response-adaptive randomization engines; Centralized allocation services | Implement complex randomization algorithms; Maintain allocation concealment |
Platform Trial Startup Protocol
The startup phase for platform trials requires meticulous planning to establish a flexible yet robust infrastructure. The HEALEY ALS trial provides an exemplary model, beginning with development of platform-level procedures for regulatory oversight, safety, and site management prior to trial launch [39]. The use of central vendors and a single Institutional Review Board creates operational consistency across sites.
The selection of highly experienced sites is particularly crucial for small population studies. Site expertise ensures appropriate patient selection, accurate data collection, and adherence to complex protocol requirements. The HEALEY ALS trial selected 54 geographically diverse sites from the Northeast ALS Consortium, all with specific expertise in ALS care and research [39]. This approach maximizes data quality while facilitating adequate enrollment for rare conditions.
The concurrent launch of multiple investigational products accelerates evidence generation. The HEALEY ALS trial launched with three investigational products as individual regimens, with a fourth product added after the initial launch [39]. This strategy demonstrates the platform's flexibility while maximizing efficiency through parallel evaluation. The modular approach to regimen implementation enables pharmaceutical partners to join the platform at different timepoints while leveraging the existing infrastructure.
Statistical Design and Analysis Protocol
The statistical foundation of adaptive platform trials requires extensive simulation studies to evaluate operating characteristics across numerous scenarios [36]. These simulations ensure the design maintains appropriate type I error control and power under various adaptation rules. The simulation process is typically iterative, with multiple rounds of discussion between statisticians and clinical investigators before arriving at a clinically acceptable design [36].
Bayesian statistical methods are frequently employed in platform trials due to their natural framework for sequential analysis and information borrowing [36] [40]. These methods facilitate probabilistic interpretations of treatment effects and naturally accommodate adaptations based on accumulating data. The I-SPY2 trial pioneered the use of Bayesian models for adaptive randomization, allowing preferential allocation of patients to therapies more likely to benefit their specific disease subtype [40].
The analysis plan must account for multiple features including multiple comparisons, potential time trends, and correlation between treatment effects [36]. Complex platform trials may employ hierarchical models that borrow information across interventions or population subgroups, potentially increasing statistical power in small population settings [36]. These sophisticated approaches require specialized statistical expertise throughout the trial lifecycle.
Interim Analysis Decision Protocol: This diagram outlines the standardized process for conducting interim analyses, maintaining trial integrity while enabling adaptive decisions.
Adaptive platform trials represent a paradigm shift in clinical research methodology, offering efficient strategies for evaluating interventions in small populations. By implementing a master protocol structure with shared infrastructure, these designs maximize the informational value derived from each patient—a critical consideration when patient numbers are limited. The capacity to add and remove interventions based on predefined decision rules creates a responsive research environment that can rapidly identify promising therapies while redirecting resources away from ineffective approaches.
The successful implementation of these designs requires specialized statistical expertise, robust operational planning, and collaborative research networks. Despite their complexity and substantial initial investment, adaptive platform trials offer compelling efficiencies for drug development in rare diseases and advanced therapies. As evidenced by successful implementations in conditions from ALS to community-acquired pneumonia, these innovative designs are transforming clinical research paradigms and accelerating the development of much-needed therapies for patients with limited treatment options.
The development of Advanced Therapy Medicinal Products (ATMPs) demands sophisticated clinical trial designs that accurately capture treatment efficacy and patient-centered benefits. Traditional endpoints often fail to reflect the multifaceted effects of these novel therapies, necessitating a strategic approach to endpoint selection. The integration of biomarkers, patient-reported outcomes (PROs), and robust long-term follow-up creates a comprehensive framework for evaluating ATMPs. This paradigm addresses tumor heterogeneity in oncology, provides unique insights into patients' perceptions of their health, and ensures the capture of meaningful long-term clinical data [43] [44]. This document provides detailed application notes and experimental protocols for implementing these novel endpoints within ATMP clinical trials, framed specifically for the context of advanced therapy research.
Biomarkers as Endpoints: From Prognostic Tools to Surrogate Endpoints
Biomarker Classification and Clinical Utility
Biomarkers are measurable indicators of biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention [45]. Their strategic application enhances the efficiency, accuracy, and ethical integrity of ATMP clinical research. The table below outlines the primary categories of biomarkers and their applications in clinical trial design.
Table 1: Classification and Application of Biomarkers in Clinical Trials
| Biomarker Category | Definition | Clinical Trial Application | Example in ATMP Research |
|---|---|---|---|
| Prognostic | Provides information on the natural history of a disease in an untreated individual [43]. | Identifies patients with different disease outcomes, enabling patient stratification [43]. | Tumor molecular profiling to identify aggressive disease forms. |
| Predictive | Identifies individuals more likely to respond to a specific therapeutic intervention [43] [45]. | Enriches trial population with likely responders, improving trial efficiency and demonstrating targeted efficacy [43] [45]. | HER2 overexpression for trastuzumab trials in breast/gastric cancer [45]. |
| Monitoring | Serial measurement to assess treatment response or disease progression [45]. | Provides real-time data on drug efficacy, enabling early go/no-go decisions [45]. | Circulating tumor DNA (ctDNA) for monitoring minimal residual disease. |
| Safety | Indicates the potential for drug-induced toxicity [45]. | Monitors adverse effects early, ensuring patient safety during trial conduct [45]. | Liver enzymes (ALT, AST) for assessing hepatotoxicity. |
Experimental Protocol: Validating Prognostic and Predictive Biomarkers
Objective: To analytically and clinically validate a biomarker for use in patient selection and stratification within an ATMP clinical trial.
Materials and Reagents:
- Sample Collection System: EDTA vacutainer tubes for plasma, PAXgene tubes for RNA, biopsy kits for tumor tissue [46].
- Processing Equipment: Centrifuge (maintained at 4°C), -80°C freezer, liquid nitrogen storage.
- Analysis Platform: HD-X Analyzer for high-sensitivity immunoassays [46].
- Assay Kits: Quanterix Simoa Assays for neurological markers (e.g., Neurology 3-Plex A, P-tau181 V2, NfL Advantage Kit) [46].
- Image Analysis Software: For quantitative analysis of immunohistochemistry (IHC) results (e.g., HER2, PD-L1) [45].
Methodology:
- Sample Acquisition and Handling: Collect patient biospecimens (blood, tissue, etc.) according to standardized protocols. For plasma biomarkers, centrifuge blood samples at 2000 × g for 10 minutes at 4°C within 30 minutes of collection [46]. Aliquot plasma into polypropylene cryotubes and snap-freeze within two hours. Store at -80°C until analysis.
- Biomarker Quantification: Perform biomarker assays following manufacturer instructions. Include an 8-point calibrator curve, internal kit controls, and plasma controls in each assay run. Analyze samples in duplicate and report the mean value [46]. For novel assays, establish precision (intra- and inter-assay coefficient of variation <15%) and accuracy.
- Data Analysis: Establish a pre-specified cutoff point for a positive/negative biomarker status using Receiver Operating Characteristic (ROC) curve analysis against a clinical gold standard. For predictive biomarkers, test the treatment-by-biomarker interaction in a statistical model to confirm that treatment effect differs by biomarker status [43].
Application Note: The development of drugs with companion diagnostics increases complexity. Engage with regulatory agencies early to align on the biomarker validation strategy and the planned clinical trial design, such as biomarker-stratified or enrichment designs [43].
Case Study: Plasma Neurofilament Light (NfL) Chain in Alzheimer's Trial
In a phase 2 trial for mild-to-moderate Alzheimer's disease, plasma NfL was evaluated as a prognostic biomarker. Elevated baseline plasma NfL predicted more rapid clinical decline on the ADAS-Cog11 (Effect Size (ES) = 1.42, 95% CI = [0.43, 2.41]) and CDR-SB (ES = 0.42, 95% CI = [0.10, 0.73]) over 48 weeks [46]. Furthermore, higher baseline NfL predicted increasing ventricular volume (ES = 1.30 cm³) and decreasing mid-temporal cortical volume on MRI [46]. Modeling demonstrated that using high NfL as a trial entry criterion could substantially reduce the requisite sample size, highlighting its utility for enriching trials with patients likely to show progressive decline [46].
Patient-Reported Outcomes (PROs): Capturing the Patient Voice
The Value and Implementation of PROs
PROs are any report of the status of a patient's health condition that comes directly from the patient, without interpretation by a clinician or anyone else [47]. They provide unique information on the impact of a medical condition and its treatment from the patient’s perspective, which is crucial for comprehensively assessing the value of ATMPs [47].
Table 2: Implementing Patient-Reported Outcomes in Clinical Trials
| Aspect | Key Consideration | Recommendation for ATMP Trials |
|---|---|---|
| Endpoint Selection | PROs can be primary, secondary, or exploratory endpoints [44] [47]. | Select PROs based on consensus from patients, caregivers, and HCPs. In kidney transplantation, life participation is the PRO of greatest importance [44]. |
| Measure Selection | Use validated PRO measures (PROMs) to ensure standardized assessment [44] [47]. | Choose PROMs with evidence of psychometric robustness in the target population (e.g., PROMIS for fatigue) [44] [47]. |
| Minimizing Missing Data | High rates of missing data can compromise interpretation [47]. | Implement robust data collection strategies, including training site staff and using electronic data capture where possible. |
| Interpretation | There is no "one-size-fits-all" approach to interpreting PRO data [47]. | Pre-define clinically meaningful differences in the statistical analysis plan. Interpret PROs in conjunction with other clinical outcomes. |
Experimental Protocol: Incorporating PROs in ATMP Trials
Objective: To integrate PROs as secondary endpoints to assess the patient's perspective on treatment benefits and burdens in an ATMP trial.
Materials and Reagents:
- Validated PRO Measures: Condition-specific and generic PROMs (e.g., EQ-5D for health utility, PROMIS item banks, disease-specific measures like the 15-item Glaucoma Quality of Life (GQL-15)) [48] [47].
- Data Capture System: Electronic Clinical Outcome Assessment (eCOA) platforms (e.g., tablets, web-based portals) or paper forms.
- Protocol Document: Detailed PRO section outlining hypotheses, measures, time points, and handling of missing data.
Methodology:
- Identify Relevant PRO Concepts: Conduct qualitative research (e.g., patient interviews, literature review) to identify symptoms and impacts most important to patients. In kidney transplantation, these include life participation, medication adherence, and symptoms/side effects [44].
- Select and Validate PROMs: Select PROMs that measure the identified concepts and are validated in the target population. Avoid developing new tools unless necessary.
- Define PRO Endpoint Strategy: Pre-specify in the protocol the PRO hypotheses, the specific PROMs, the analysis time points, and the statistical methods for analysis. Clearly state whether the PRO is a primary or secondary endpoint.
- Data Collection and Management: Train site personnel on the importance of PROs and standardized administration. Use eCOA systems to improve data quality and completeness. Actively monitor and address missing data.
Application Note: PROMs may not always be sensitive enough to function as primary endpoints, particularly in early-stage disease. For example, in early-stage glaucoma trials, PROMs did not detect differences between treatment and placebo, whereas visual field progression did [48]. PROs remain valuable for assessing side effects, dosing convenience, and other treatment consequences [48].
Long-Term Follow-Up: Capturing Durability of Response
Challenges and Strategic Solutions
ATMPs, such as cell and gene therapies, are often characterized by potentially durable effects, making long-term follow-up (LTFU) critical for assessing sustained efficacy and delayed adverse events. The OAKS study in major gastrointestinal surgery achieved an 82.6% follow-up rate at one year in registered centers, providing key insights into successful LTFU strategies [49].
Table 3: Strategies for Successful Long-Term Follow-Up in Clinical Trials
| Challenge | Impact on LTFU | Evidence-Based Solution |
|---|---|---|
| Investigator Turnover | Common in trainee-led research; disrupts continuity [49]. | Central storage of patient identifiers (72.5% data completeness vs. 48.0% with local storage) [49]. |
| Loss of Patient IDs | Inability to link outcomes to original study data [49]. | Use secure, central electronic databases (e.g., REDCap) for identifier storage, compliant with data protection regulations [49]. |
| Burden of Follow-Up | High patient numbers per center reduce data completeness [49]. | Allocate sufficient resources; centers with <15 patients had 77.4% high completeness vs. 36.8% for >60 patients [49]. |
| Statistical Power | Using the final long-term outcome for interim analyses can be inefficient [50]. | Use repeated short-term measures to improve the efficiency of estimating the long-term treatment difference [50]. |
Experimental Protocol: Establishing a Long-Term Follow-Up System
Objective: To implement a system for collecting one-year clinical outcomes for patients treated with an ATMP.
Materials and Reagents:
- Secure Database: REDCap (Research Electronic Data Capture) or similar HIPAA-compliant system for central storage of patient identifiers and clinical data [49].
- Cohort Management Tool: Tracking system for patient follow-up timepoints.
- Clinical Data Sources: Access to hospital electronic health records (EHR), national death registries, and other relevant databases.
Methodology:
- Pre-Trial Planning: Secure regulatory and institutional approvals for LTFU, including central storage of patient identifiers. Pre-define the LTFU outcomes (e.g., mortality, major events, disease-specific markers) [49].
- Centralized Identifier Management: Store patient hospital identification numbers and linked study-specific identification numbers centrally on a secure, access-controlled platform like REDCap. This mitigates risk from local investigator turnover [49].
- Follow-Up Data Collection: At the pre-specified time point (e.g., one year post-treatment), a follow-up team reviews patient records using the stored identifiers to collect the predefined outcomes. No additional patient visits are required if outcomes are based on routine clinical data [49].
- Data Analysis: Account for missing data in the analysis. Use statistical methods like Mixed-Effects Model Repeated Measures (MMRM) for analyzing continuous longitudinal endpoints, as this is more efficient and reliable than simple imputation methods like Last Observation Carried Forward (LOCF) [51].
Integrated Framework and Visual Workflows
Integrated Endpoint Strategy Diagram
The following diagram illustrates the strategic integration of novel endpoints throughout the clinical trial timeline.
Biomarker Utility and Implementation Diagram
This diagram outlines the decision pathway for biomarker implementation in clinical trials.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Novel Endpoint Implementation
| Item | Function | Example Product/Specification |
|---|---|---|
| Simoa Assay Kits | High-sensitivity measurement of plasma biomarkers (e.g., NfL, GFAP, P-tau) [46]. | Quanterix Neurology 3-Plex A, P-tau181 V2 Advantage Kit, NfL Advantage Kit [46]. |
| HD-X Analyzer | Automated digital immunoassay analyzer for running Simoa assays with single-molecule sensitivity [46]. | Quanterix HD-X Analyzer [46]. |
| REDCap | Secure, web-based platform for building and managing online databases, ideal for central storage of patient identifiers and clinical data [49]. | Research Electronic Data Capture (REDCap) [49]. |
| Validated PROMs | Standardized questionnaires to collect patient-reported data on symptoms, function, and quality of life [44] [47]. | EQ-5D, PROMIS item banks, disease-specific measures (e.g., GQL-15) [48] [47]. |
| eCOA Platforms | Electronic systems (tablets, web portals) for administering PROMs, improving data quality and reducing missing data [44]. | Various commercial and proprietary electronic Clinical Outcome Assessment systems. |
| EDTA Vacutainer Tubes | Standard blood collection tubes for plasma preparation in biomarker analyses [46]. | K2EDTA or K3EDTA Vacutainer tubes. |
| -80°C Freezer | Long-term storage of biospecimens to preserve biomarker integrity until analysis [46]. | Ultra-low temperature freezer. |
The strategic selection of novel endpoints is fundamental to demonstrating the value of Advanced Therapy Medicinal Products. A triad approach—leveraging validated biomarkers for patient stratification and efficacy assessment, incorporating patient-reported outcomes to capture the patient perspective, and implementing robust long-term follow-up systems to document durability—provides a comprehensive and rigorous framework. Adopting the application notes and detailed protocols outlined herein will enable researchers to design more efficient, informative, and patient-centered clinical trials, ultimately accelerating the development of transformative advanced therapies.
Chimeric antigen receptor T-cell (CAR-T) therapy represents a paradigm shift in immunotherapy, employing genetically engineered T-cells to target specific antigens on tumor cells and other pathogenic cells. The clinical trial landscape for CAR-T therapies has expanded dramatically, with 1,580 registered studies on ClinicalTrials.gov as of April 2024, providing an unprecedented dataset for analyzing development trends, methodological approaches, and translational challenges [52]. This comprehensive analysis reveals that CAR-T applications extend beyond their initial success in hematologic malignancies to include solid tumors (24.6% of trials) and autoimmune diseases (2.75%), reflecting the dynamic evolution of this therapeutic modality [52]. The growth trajectory has been remarkable, with trials increasing exponentially since 2017, led predominantly by China and the United States, which together account for approximately 82% of all registered studies [52] [53].
The development of CAR-T therapies faces unique challenges in clinical translation, including complex manufacturing processes, substantial financial burdens exceeding $500,000 per treatment course, and significant safety concerns such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) [52]. Additionally, developmental attrition rates remain concerning, with only 35% of initiated trials progressing beyond Phase 2 [52]. This analysis synthesizes insights from the comprehensive clinical trial registry to identify optimal design strategies, manufacturing innovations, and future directions for advancing CAR-T therapies across diverse disease applications.
Global Distribution and Development Trends
Quantitative Analysis of Registered Clinical Trials
Table 1: Global Distribution and Characteristics of CAR-T Clinical Trials
| Category | Number of Trials | Percentage | Regional Distribution | Primary Focus |
|---|---|---|---|---|
| Total CAR-T Trials | 1,580 | 100% | Global | All indications |
| Hematologic Malignancies | 1,131 | 71.6% | China (636), USA (377) [53] | CD19-targeted (≥50%) [52] |
| Solid Tumors | 389 | 24.6% | Multiple countries | Emerging targets (HER2, MSLN, GPC3) [54] |
| Autoimmune Diseases | 43 | 2.75% | China (48%), USA (34%) [55] | SLE, lupus nephritis [55] |
| Toxicity Management | 51 | 3.2% | Multiple countries | CRS, ICANS mitigation [52] |
| Phase I Trials | 891 | 56.4% | Global | Dose-finding, safety [52] |
| Phase II-IV Trials | 170 | 10.8% | Global | Efficacy confirmation [52] |
Table 2: Trial Design and Reporting Quality in CAR-T Phase I Studies (n=109)
| Design Characteristic | Frequency | Percentage | Implications |
|---|---|---|---|
| 3+3 Dose Escalation Design | 34 | 31.2% | Traditional approach persists despite limitations [56] |
| Unspecified Design Methodology | 66 | 60.6% | Reporting transparency needs improvement [56] |
| Unreported Cohort Size | 65 | 59.6% | Limits reproducibility and interpretation [56] |
| Unspecified Safety Evaluation Timing | 21 | 19.3% | Hinders safety assessment standardization [56] |
| Registered with ClinicalTrials.gov | 96 | 88.1% | Good registration compliance [56] |
| Results Posted on ClinicalTrials.gov | 33 | 33.9% | Results reporting remains suboptimal [56] |
The geographic distribution of CAR-T clinical trials reveals a concentrated effort in specific regions, with China leading in total trial numbers (636 trials), followed by the United States (377 trials), while Europe lags significantly behind (58 trials) [53]. This disparity reflects differences in research investment, regulatory frameworks, and development ecosystems. Analysis of funding sources indicates that the majority of registered studies are funded by non-profit organizations or academic institutions (approximately 50%), with industry-funded studies constituting the second-largest category [52]. Notably, over 30% of trials globally utilize mixed funding sources involving collaborations between industry, government agencies, and academic institutions, with China showing a higher proportion (approximately 40%) of trials with mixed funding compared to other regions (24%) [52].
The distribution of trials across development phases shows a predominance of early-stage investigations, with 891 trials (56.4%) in Phase I or early Phase 1, while only 170 trials (10.8%) have progressed to Phase 2, 3, or 4 [52]. This distribution reflects both the relative novelty of many CAR-T applications and the significant challenges in advancing these therapies through later development stages. The high concentration in early phases is particularly pronounced in emerging applications such as autoimmune diseases, where 64.29% (36/56 trials) are Phase I studies and only 7.14% (4/56 trials) have progressed to Phase II [55].
Methodological Approaches and Trial Designs
Phase I Trial Design Considerations
Phase I trials for CAR-T therapies present unique design challenges due to complex safety profiles, unpredictable pharmacokinetics, and potentially dramatic efficacy signals. Analysis of 109 published CAR-T phase I trials reveals that the traditional 3+3 design remains prevalent (31.2%), despite recognized limitations in efficiency and accuracy for these complex therapies [56]. Concerningly, 60.6% of publications did not specify the dose escalation methodology used, indicating a significant transparency gap in reporting standards [56]. This lack of methodological detail complicates cross-trial comparisons and meta-analyses, potentially slowing the overall development process.
The reporting quality of CAR-T phase I trials shows several areas for improvement. A substantial proportion of manuscripts (59.6%) did not report cohort size, while 19.3% failed to specify the timing of safety evaluation [56]. Furthermore, although 88.1% of trials were registered with ClinicalTrials.gov, only 33.9% had results submitted or posted, limiting the utility of registration databases for comprehensive evidence synthesis [56]. These reporting deficiencies persist even in high-impact factor journals, suggesting systemic challenges in the publication standards for early-phase CAR-T trials.
Advanced Trial Designs and Adaptive Approaches
As the CAR-T field matures, more sophisticated trial designs are emerging to address the unique challenges of these therapies. Model-based and model-assisted designs, which offer improved operating characteristics for dose-finding, were employed in only 5.5% of the reviewed phase I trials [56]. However, their adoption is increasing in more recent studies, particularly for combination therapies and novel constructs. The limited use of these advanced methodologies represents a significant opportunity for efficiency gains in future CAR-T development.
For later-phase trials, there is a trend toward single-arm designs with historical controls, particularly for indications with high unmet medical needs. Analysis of approved advanced therapy medicinal products (ATMPs) reveals that most authorizations were based on small, open-label, non-randomized, single-arm studies using intermediate endpoints for efficacy assessment [5]. While this approach may facilitate accelerated development, it creates greater uncertainty about the benefit-risk profile at the time of marketing authorization and necessitates robust post-marketing studies to confirm clinical benefit.
Disease-Specific Applications and Clinical Progress
Hematologic Malignancies
Hematologic malignancies continue to dominate the CAR-T clinical trial landscape, representing 71.6% of all registered studies [52]. CD19 remains the most frequently targeted antigen, constituting more than 50% of investigational or commercialized cell therapies for B-cell malignancies [52]. The success in acute lymphoblastic leukemia (ALL) and non-Hodgkin lymphoma has established a robust foundation for further innovation, including the development of next-generation constructs with enhanced persistence and reduced exhaustion profiles.
Recent clinical trials have expanded the application of CAR-T therapy in hematologic malignancies to include earlier treatment lines and novel targets. The CARTITUDE-4 trial, evaluating BCMA-targeted CAR-T therapy in multiple myeloma, demonstrates the shift toward earlier intervention in the treatment course, particularly for functionally high-risk patients who relapse within 12-18 months [57]. This trend reflects growing confidence in the therapeutic potential of CAR-T approaches and efforts to maximize their clinical impact by intervening before extensive prior therapy compromises immune system function.
Solid Tumors
The application of CAR-T therapy to solid tumors presents distinct challenges, including tumor heterogeneity, immunosuppressive microenvironments, and limited trafficking to tumor sites. Despite these obstacles, solid tumors represent 24.6% of CAR-T clinical trials [52]. Recent presentations at the 2025 ASCO Annual Meeting highlighted several innovative approaches, including localized delivery methods for glioblastoma and logic-gated constructs to enhance tumor specificity [54].
Promising strategies emerging from recent trials include:
- Bivalent targeting of EGFR and IL13Rα2 in glioblastoma, resulting in tumor shrinkage in 85% of evaluable patients [54]
- Armored CAR-T constructs incorporating dominant-negative TGFβ receptors to resist immunosuppressive signals in the tumor microenvironment [54]
- Localized administration routes including intracerebroventricular delivery for CNS tumors and intrapleural delivery for mesothelioma [54]
- Logic-gated approaches such as A2B694, which targets mesothelin while incorporating an inhibitory signal for HLA-A*02 to minimize on-target, off-tumor toxicity [54]
These innovative approaches demonstrate the field's evolution beyond simple CAR constructs toward sophisticated engineering strategies designed to overcome the unique challenges of solid tumors.
Autoimmune Diseases
The application of CAR-T therapy to autoimmune rheumatic diseases (ARDs) represents a rapidly emerging frontier, with trials increasing notably since 2021 [52]. Currently, 56 clinical trials are investigating CAR-T approaches for conditions including systemic lupus erythematosus (SLE), lupus nephritis, systemic sclerosis, and inflammatory myositis [55]. These approaches aim to achieve a broader reset of the B-cell compartment by targeting surface markers such as CD19 or B-cell maturation antigen (BCMA), offering potential advantages over conventional B-cell-targeted therapies [55].
Early clinical results have demonstrated remarkable efficacy in refractory SLE patients, with CD19-targeted CAR-T therapy inducing significant clinical remission and sustained drug-free remission exceeding 18 months in some cases [55]. The mechanistic advantages of CAR-T therapy in autoimmune diseases include direct cytolytic activity independent of exogenous effector cells and enhanced tissue-homing capacity that facilitates elimination of pathogenic B-cell subsets in antibody-impermeable anatomical sites such as lymphoid follicles [55].
Manufacturing Innovations and Experimental Protocols
Next-Generation Manufacturing Platforms
CAR-T manufacturing processes have evolved significantly from early approaches that required extended ex vivo culture periods. Conventional manufacturing platforms typically require 7-14 days of production time, creating challenges for patients with rapidly progressive diseases [58]. Recent innovations have dramatically shortened these timelines, as demonstrated by the FasT CAR-T (F-CAR-T) next-day manufacturing platform [58]. This approach not only reduces the vein-to-vein time but also produces CAR-T cells with a younger cellular phenotype, less exhaustion, and more potent antitumor activity compared to conventional CAR-T cells in preclinical models [58].
Table 3: Research Reagent Solutions for CAR-T Development
| Reagent/Category | Function | Application Notes |
|---|---|---|
| Dynabeads CD3/CD28 CTS | T-cell isolation and activation | Used in FasT CAR-T platform for rapid T-cell processing [58] |
| Lentiviral Vectors | CAR gene delivery | Standard approach for stable CAR expression; integration safety monitored [58] |
| IL-2 Cytokine | T-cell expansion and viability | Essential component of culture medium; concentration optimization critical [58] |
| X-vivo Culture Medium | Serum-free cell culture | Maintains T-cell fitness during manufacturing process [58] |
| Fludarabine/Cyclophosphamide | Lymphodepleting chemotherapy | Administered prior to CAR-T infusion to enhance engraftment [59] |
| Cryopreservation Media | Cell product storage | Enables quality control testing and transport to clinical sites [58] |
In a first-in-human clinical study of the FasT CAR-T platform for B-cell acute lymphoblastic leukemia, manufacturing was successfully completed for all 25 enrolled patients, with CD19 F-CAR-T cells produced within approximately 30 hours after PBMC harvest [58]. The clinical results demonstrated promising efficacy, with 23 of 25 patients achieving minimal residual disease-negative complete remission by day 14 [58]. This manufacturing innovation addresses two critical challenges in CAR-T development: reducing the risk of clinical deterioration during the manufacturing period and potentially lowering costs through streamlined production processes.
Quality Control and Release Criteria
Robust quality control testing is essential for ensuring the safety and potency of CAR-T products. The FasT CAR-T platform implemented comprehensive release criteria including viability, identity, potency, and safety assessments [58]. CAR expression and positive rates were determined after in vitro culture for 3 days, with products only released after passing all required tests [58]. This rigorous approach to quality control demonstrates the maturation of CAR-T manufacturing protocols and the importance of standardized assessment methods across different production platforms.
Signaling Pathways and Mechanistic Insights
CAR Structure and Signaling Components
The canonical CAR architecture consists of three essential components: an extracellular antigen-binding single-chain variable fragment (scFv), a transmembrane domain, and intracellular activation/co-stimulatory signaling domains [52]. The evolution of CAR designs has progressed through multiple generations, with first-generation constructs containing only the CD3ζ chain, second-generation incorporating one co-stimulatory domain (CD28, 4-1BB, or OX40), and third-generation combining two co-stimulatory domains [53]. More recently, fourth-generation "TRUCKS" (T cells Redirected for antigen-Unrestricted Cytokine-initiated Killing) have been developed, incorporating additional transgenes for cytokines such as IL-12 or IL-15 to enhance antitumor activity [53].
Diagram 1: CAR Structure Components. This diagram illustrates the modular architecture of chimeric antigen receptors, showing extracellular antigen recognition, transmembrane anchoring, and intracellular signaling domains.
Critical Signaling Pathways in CAR-T Activation
Upon antigen engagement, CAR signaling initiates a cascade of phosphorylation events through immunoreceptor tyrosine-based activation motifs (ITAMs) in the CD3ζ chain, leading to T-cell activation, cytokine production, and cytolytic activity. The choice of co-stimulatory domains significantly influences CAR-T performance characteristics, with CD28 domains promoting rapid effector responses and 4-1BB domains enhancing persistence and metabolic fitness [53]. Understanding these signaling nuances enables rational design of CAR constructs tailored to specific disease contexts and therapeutic goals.
Diagram 2: CAR-T Cell Signaling Pathways. This diagram outlines the key signaling events following CAR activation, from initial phosphorylation through downstream pathways to functional outcomes.
Analytical Framework and Future Directions
Translational Challenges and Regulatory Considerations
The development pathway for CAR-T therapies presents unique translational challenges that require specialized regulatory approaches. Analysis of approved advanced therapy medicinal products reveals that most authorizations were based on small, open-label, uncontrolled studies using intermediate endpoints [5]. While this flexible approach facilitates accelerated development for serious conditions, it creates greater uncertainty about benefit-risk profiles at the time of approval. The high failure rate in post-marketing studies (exemplified by Zalmoxis, which was withdrawn after failing to confirm benefit in controlled trials) underscores the importance of robust trial designs even within expedited development pathways [5].
Future progress in CAR-T development will require addressing several critical challenges:
- Optimizing manufacturing processes to reduce costs and improve accessibility
- Enhancing safety profiles through improved toxicity management and potentially incorporating safety switches
- Developing reliable biomarkers for patient selection and response monitoring
- Establishing standardized monitoring networks for long-term safety surveillance
- Expanding global collaborations to accelerate knowledge sharing, with currently only 3.6% of autoimmune disease trials involving both U.S. and Chinese teams [55]
Innovative Trial Designs for Future Development
As the CAR-T field matures, methodological innovations in trial design will be essential for efficiently generating robust evidence. Adaptive trial designs that allow for modification based on accumulating data can accelerate optimization of dosing regimens and patient selection criteria. Platform trials evaluating multiple CAR-T constructs or combination approaches within a unified infrastructure offer efficiencies particularly valuable for rare indications. Additionally, the integration of real-world evidence with clinical trial data can enhance understanding of long-term outcomes and rare adverse events.
The promising clinical results across diverse disease areas, coupled with ongoing technological innovations, suggest that CAR-T therapy will continue to expand its therapeutic reach. However, realizing this potential will require continued methodological rigor, transparent reporting, and collaborative approaches to address the complex challenges inherent in developing these sophisticated therapeutic modalities.
Recombinant adeno-associated viruses (rAAVs) have emerged as one of the most promising platforms for in vivo gene delivery, demonstrating tremendous potential for treating genetic disorders with a "one-and-done" therapeutic approach [60]. The global cell and gene therapy sector is experiencing unprecedented growth, with 1,905 ongoing clinical trials reported in the first half of 2025 and investment reaching $5 billion during this period [61] [62]. AAV vectors constitute a bona fide novel therapeutic drug class, with seven U.S. Food and Drug Administration-approved products and over ten-fold more in clinical development [63].
The AAV capsid, composed of VP1, VP2, and VP3 proteins assembled in an approximate 1:1:10 ratio, forms a non-enveloped icosahedral structure ~25 nm in diameter that encapsulates a single-stranded DNA genome of approximately 4.7 kb [60] [64]. AAV vectors offer several advantageous features for gene therapy, including the ability to transduce both dividing and non-dividing cells, long-term transgene expression, relatively low immunogenicity compared to other viral vectors, and a high affinity for neuronal and glial cells which makes them particularly suitable for central nervous system (CNS) disorders [60]. The AAV genome contains inverted terminal repeats (ITRs) at each end that serve as the origin of DNA replication and packaging signals [60].
Table 1: Global Cell and Gene Therapy Landscape (H1 2025)
| Parameter | Statistics | Data Source |
|---|---|---|
| Ongoing Clinical Trials | 1,905 | ARM/ASGCT Reports |
| North America Trials | 844 | ARM/ASGCT Reports |
| Europe Trials | 453 | ARM/ASGCT Reports |
| Asia-Pacific Trials | 750 | ARM/ASGCT Reports |
| Total CGT Pipeline | 4,469 therapies | ASGCT-Citeline Data |
| Gene Therapies (including CAR-T) | 49% (2,210 assets) | ASGCT-Citeline Data |
| Investment in H1 2025 | $5 billion | ARM Report |
AAV Vector Design and Optimization
Genome Engineering and Regulatory Elements
The rAAV genome controls transgene expression level, cell-type specificity, duration, and other critical aspects of AAV therapeutics. Considerable efforts have been made to optimize components in the genome, including the inverted terminal repeats (ITRs), promoter systems, and other regulatory elements [60].
Inverted Terminal Repeats (ITRs) represent a critical component for AAV replication and packaging. A significant advancement in vector design came with the development of self-complementary AAV (scAAV), which bypasses the requirement for second-strand synthesis in the host cell [60]. This innovation enables five- to 140-fold increased transduction efficiency over single-stranded AAV (ssAAV), though it reduces packaging capacity to approximately 2.4 kb compared to 4.8 kb for ssAAV [60]. A notable consideration with scAAV is heightened innate immune response through enhanced activation of the TLR9/MyD88 signaling pathway, leading to increased production of proinflammatory cytokines such as IL-6 and TNF-α [60]. Research has demonstrated that rational engineering to generate CpG-free ITRs can reduce immunogenicity while maintaining biological potency, though this approach may reduce vector yields approximately threefold [60].
Promoter Selection fundamentally determines expression levels, cell- or tissue-specificity, and spatial and temporal expression characteristics [60]. Analysis of 106 clinical trials reveals that ubiquitous promoters are employed in over 50% of AAV gene therapies, with this percentage rising to 76% for CNS disorders [60]. The most commonly used ubiquitous promoters include the cytomegalovirus immediate early enhancer/chicken β actin/rabbit β-globin (CAG) promoter, chicken beta-acting (CBA) promoter, and cytomegalovirus (CMV) promoter [60]. Conversely, tissue-specific promoters enable precisely localized gene expression to minimize off-target effects and immune-mediated toxicity. For neurological applications, specific promoters such as NSE (neuron-specific enolase) and syn1 (synapsin-1) provide neuron-specific expression, while the hRPE65p promoter targets retinal pigment epithelium [60].
Additional Regulatory Elements can significantly enhance transgene expression:
- Enhancer elements like the CMV enhancer amplify transcriptional signals through physical contact with target promoters [60]. The mouse DLX5/6 enhancer alone can induce specific gene expression in GABAergic interneurons in the forebrain [60].
- Intron elements positioned downstream of promoters enhance gene expression by improving mRNA stability and facilitating nuclear export [60]. The Minute virus of mice (MVM) intron can increase transgene expression by 80-fold in liver cells compared to intron-null AAV [60].
- WPRE element (woodchuck hepatitis post-transcriptional regulatory element) improves viral titer and transduction efficiency by stabilizing mRNA and regulating transcriptional termination [60]. Concerns about potential oncogenic activity have been addressed through WPRE optimization for clinical applications [60].
- miRNA target sequences incorporated into the 3' untranslated region enable detargeting of transgene expression from specific tissues [60]. For example, four tandem copies of the hematopoietic-specific miR-142-3p sequence significantly prevented transgene expression in hematopoietic cells, even with high viral loads [60].
Experimental Protocol: Vector Genome Optimization
Objective: To design and validate an optimized AAV vector genome for enhanced and tissue-specific transgene expression.
Materials:
- Plasmid backbone with AAV2 ITRs
- Candidate promoters (ubiquitous and tissue-specific)
- Regulatory elements (enhancers, introns, WPRE, miRNA target sequences)
- Reporter gene (e.g., GFP, luciferase)
- HEK293 cells for in vitro testing
- Appropriate animal models for in vivo validation
Procedure:
- Construct Assembly: Clone selected promoter, regulatory elements, and transgene into plasmid backbone between ITRs using standard molecular biology techniques.
- In Vitro Screening: Transfect constructs into HEK293 cells and measure reporter gene expression at 24, 48, and 72 hours post-transfection.
- Vector Production: Package selected constructs into appropriate AAV capsids using the triple transfection method in HEK293 cells.
- In Vivo Validation: Administer vectors to animal models via relevant route (intravenous, intracranial, etc.) and assess:
- Transgene expression kinetics (acute and long-term)
- Tissue specificity via immunohistochemistry or other imaging modalities
- Potential immune responses
- Lead Selection: Identify optimal construct based on expression level, specificity, and durability.
Validation Methods:
- qPCR for vector genome biodistribution
- Western blot or ELISA for transgene protein quantification
- Immunohistochemistry for cellular localization
- Clinical chemistry and histopathology for safety assessment
Capsid Engineering Strategies
Natural Serotypes and Engineering Approaches
AAV capsid engineering represents a powerful approach to overcome limitations of natural serotypes, including pre-existing immunity, suboptimal tropism, and manufacturing challenges. Currently, 13 different AAV serotypes and more than 150 variants have been naturally isolated from human, non-human primates, and other animal species [60] [64]. These variants exhibit distinct patterns of transduction and cell tropisms determined by interactions between capsid surface topology and host cell receptors [60].
AAV2 remains the most extensively investigated serotype, with wide tissue tropism particularly efficient for transducing neurons [60]. AAV2's tropism stems from universal distribution of its primary receptor heparan sulfate proteoglycan (HSPG) and multiple co-receptors including FGF receptor, integrins, and CD9 [60]. AAV9 has gained prominence for its ability to cross the blood-brain barrier, making it valuable for CNS applications [61]. According to recent clinical data, AAV2 remains the most utilized capsid in clinical trials (24%), followed by AAV9 (16%) and AAV8 (13%) [61] [62].
The deployment of engineered and novel capsids is accelerating rapidly. As of 2025, 39 clinical trials utilize 15 unique customized capsids, a significant increase from 20 trials with 10 engineered capsids in 2022 [61] [62]. The rationale for engineered capsids includes circumventing pre-existing immunity, enhancing tissue specificity, and improving vector performance [61]. Notably, 32 trials have not publicly disclosed the capsid used, suggesting increased competitive sensitivity around vector design [61] [62].
Table 2: AAV Capsid Engineering Approaches
| Engineering Strategy | Methodology | Key Advantages | Examples/Applications |
|---|---|---|---|
| Natural Discovery | Isolation from human/animal tissues | Naturally evolved functionality | AAVv66 from human clinical sample [65] |
| Rational Design | Site-directed mutagenesis of known capsids | Targeted modification of specific properties | Heparin-binding site modifications [60] |
| Directed Evolution | High-throughput screening of capsid libraries | Discovery of novel tropisms & properties | AAV-PHP series for enhanced CNS targeting [66] |
| In Silico Design | Computational prediction & AI-assisted design | Rapid generation of optimized variants | Machine learning-guided capsid engineering [60] |
Case Study: AAVv66 - A Novel Neurotropic Capsid
The discovery and characterization of AAVv66 illustrates the potential of natural capsid discovery. Identified in a human clinical sample through high-throughput single-molecule real-time (SMRT) sequencing, AAVv66 shares 98% sequence similarity with AAV2 but contains 13 amino acid residue differences [65]. These variations confer several advantageous properties:
- Enhanced Production Yields: AAVv66 demonstrates approximately 2.4-fold higher production of encapsidated, DNase-resistant vector genomes compared to AAV2 [65].
- Improved Thermostability: AAVv66 exhibits superior virion stability compared to AAV2 [65].
- Neurotropic Properties: AAVv66 shows better distribution spread within brain tissue following both intracranial and systemic administration [65].
- Reduced Heparin Binding: Unlike AAV2, AAVv66 transduction is not affected by heparin presence, explaining its improved production efficiency and potentially different tropism [65].
Structural characterization of AAVv66 by cryo-EM at 2.5-Å resolution revealed that critical residues at the three-fold protrusion and at the interface of the five-fold axis of symmetry contribute to these beneficial characteristics [65]. This structural insight facilitates rational design of further improved capsid variants.
Experimental Protocol: Capsid Engineering via Directed Evolution
Objective: To generate novel AAV capsids with enhanced CNS tropism and reduced liver targeting.
Materials:
- AAV capsid library (diversity > 10^6)
- Cre-expressing transgenic mice (e.g., C57BL/6-Tg(CAG-cre))
- Fluorescent reporter construct
- Next-generation sequencing platform
- Cell lines for in vitro validation (HEK293, neuronal cells)
- Animal models for in vivo validation
Procedure:
- Library Design: Create diverse capsid library using DNA shuffling, error-prone PCR, or peptide insertion at surface-exposed loops.
- In Vivo Selection:
- Systemically administer capsid library to Cre-expressing mice
- Allow 2-4 weeks for transduction and expression
- Isolate CNS tissues (brain, spinal cord) and extract genomic DNA
- Capsid Recovery:
- Amplify capsid sequences from CNS tissues using PCR
- Subject to next-generation sequencing
- Identify enriched capsid variants through bioinformatic analysis
- Validation Rounds: Perform 2-3 additional rounds of selection with enriched pools to further refine tropism.
- Clone Isolation: Isolate individual clones and characterize in secondary screens.
Characterization Methods:
- In vitro transduction efficiency across multiple cell types
- In vivo biodistribution following systemic administration
- Neutralization antibody susceptibility assays
- Production yield assessment
- Immunogenicity profiling
Administration Routes and Their Applications
Route Selection for Target Tissues
The administration route significantly influences AAV biodistribution, transduction efficiency, and safety profile. Different routes are selected based on anatomical and biological suitability for target tissues [61] [60]. Current clinical trials employ diverse administration strategies:
- Intravenous (Vascular) Delivery: Remains the dominant administration route, particularly for systemic diseases or when targeting widespread tissues [61]. This approach exposes the vector to the entire circulation but requires higher doses and increases liver exposure [60].
- Ocular-Field Routes: Include subretinal, intravitreal, and suprachoroidal delivery [61]. Ocular tissues represent 26% of AAV clinical trials, reflecting the success of AAV in treating retinal disorders such as RPE65-associated retinal dystrophy (Luxturna) [61] [60].
- Brain-Targeted Methods: Encompass intracerebroventricular, intraparenchymal, and intrathecal delivery [61]. The central nervous system is targeted in 21% of AAV clinical trials [61]. Intrathecal delivery via lumbar puncture has gained traction for broader CNS distribution while being less invasive than direct brain injection [60].
- Novel and Combined Approaches: A small but growing subset of trials utilizes dual routes—such as combining vascular and intracerebroventricular injections—which may necessitate distinct capsids and increased resource investment [61].
Table 3: AAV Administration Routes and Applications
| Administration Route | Target Tissues | Advantages | Limitations | Clinical Applications |
|---|---|---|---|---|
| Intravenous | Liver, skeletal muscle, heart, CNS (with certain capsids) | Broad systemic delivery, less invasive | High liver sequestration, dose-limiting toxicity, pre-existing immunity concerns | Hemophilia, muscular dystrophy, metabolic disorders [61] [63] |
| Intracerebroventricular | Widespread CNS distribution via CSF | Bypasses blood-brain barrier, broader distribution than intraparenchymal | Requires surgical procedure, potential CSF leakage | Neurodegenerative disorders, lysosomal storage diseases [61] [60] |
| Intraparenchymal | Focal brain regions | Direct target engagement, high local concentration | Invasive, limited distribution volume | Parkinson's disease, focal epilepsies [60] |
| Subretinal | Retinal pigment epithelium, photoreceptors | High local concentration, relative immune privilege | Surgical complexity, potential retinal detachment | Retinal dystrophies, AMD [61] [60] |
| Intrathecal | Spinal cord, nerve roots, widespread CNS via CSF | Less invasive than ICV, broader distribution than intraparenchymal | Requires lumbar puncture, potential headache | Spinal muscular atrophy, motor neuron diseases [60] |
Experimental Protocol: Intrathecal Administration for CNS Disorders
Objective: To establish a standardized protocol for intrathecal delivery of AAV vectors for CNS-directed gene therapy.
Materials:
- Purified AAV vector (≥ 1×10^13 vg/mL in sterile formulation buffer)
- Anesthesia equipment and reagents (ketamine/xylazine or isoflurane)
- Sterile surgical instruments
- Microliter syringe with 30-33 gauge needle
- Stereotaxic apparatus (for precise positioning)
- Animal warming pad
- Appropriate animal model (non-human primate or rodent)
Pre-Administration Procedures:
- Vector Preparation: Thaw vector slowly on ice and mix gently by inversion. Avoid vortexing.
- Animal Preparation: Anesthetize animal and confirm surgical plane of anesthesia.
- Positioning: Place animal in prone position with head flexed forward to maximize intervertebral space.
- Aseptic Preparation: Shave and disinfect lumbar area with alternating betadine and alcohol scrubs (3 cycles).
Administration Procedure:
- Needle Insertion: Insert needle between L4-L5 or L5-L6 vertebrae at a 30-degree angle toward the cranial direction.
- CSF Confirmation: Look for clear CSF return to confirm proper needle placement.
- Vector Infusion:
- Infuse vector solution slowly (≤ 5 μL/min for rodents, ≤ 100 μL/min for NHPs)
- Total volume: 10-50 μL for rodents, 1-5 mL for NHPs
- Dose: 1×10^10 - 1×10^14 vg/kg depending on construct and model
- Needle Withdrawal: Wait 60 seconds after completion before slowly withdrawing needle.
- Recovery: Place animal in prone position on warming pad until fully recovered from anesthesia.
Post-Administration Monitoring:
- Assess neurological function daily for first week, then weekly
- Monitor for signs of inflammation or discomfort
- Collect CSF and serum samples at predetermined endpoints for vector genome and protein analysis
- Perform perfusion fixation at study endpoint for tissue analysis
Validation and Analysis:
- qPCR of vector genomes in CNS tissues and peripheral organs
- Immunohistochemistry for transgene expression and cellular localization
- Behavioral assessment for functional improvement
- Clinical pathology for safety assessment
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for AAV Gene Therapy Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| AAV Production Systems | pAAV-RC plasmids, pHelper, pAAV-ITR-transgene | Triple transfection for vector production | Serotype-specific RC plasmids, promoter selection for transgene [64] |
| Cell Lines | HEK293, HEK293T, Sf9 | Vector production, in vitro transduction assays | HEK293 provides adenoviral E1 genes necessary for AAV production [64] |
| Purification Kits/Resins | Iodixanol gradient, AVB Sepharose, Heparin columns | Vector purification and concentration | Different serotypes have varying affinity for heparin [64] [65] |
| Titration Assays | qPCR reagents, ELISA kits for capsid, silver stain | Vector quantification (genome titer, capsid titer) | Critical for dose determination; empty/full capsid ratio important [64] |
| Animal Models | C57BL/6 mice, non-human primates, disease-specific models | In vivo biodistribution, efficacy, and safety studies | Species differences in AAV tropism and immune responses [60] [66] |
| Detection Reagents | Antibodies for transgene product, IHC reagents | Transgene expression analysis | Tissue-specific markers for colocalization studies [60] |
| Sequencing Platforms | SMRT sequencing, NGS systems | Capsid discovery, vector genome integrity | Long-read sequencing enables full capsid sequencing [65] |
The field of AAV gene therapy continues to evolve rapidly, with innovations in vector design, capsid engineering, and administration strategies addressing key challenges in clinical development. The growing clinical pipeline—encompassing 4,469 therapies from preclinical to pre-registration stages—demonstrates the maturing of this therapeutic modality [61] [62]. As of 2025, there are 343 AAV clinical trials registered, representing a 34% increase from mid-2022, with the most pronounced acceleration in early-phase trials [61].
Future directions in AAV optimization will likely focus on several key areas:
- Novel Capsid Development: Continued engineering to enhance tissue specificity, evade pre-existing immunity, and improve blood-brain barrier penetration [60] [66].
- Manufacturing Innovations: Advances in production systems to increase yields, reduce empty capsids, and improve scalability [61] [67].
- Safety Optimization: Strategies to mitigate dose-dependent toxicities, including optimized dosing regimens and vector designs that reduce immunogenicity [61] [64].
- Regulatory Advancements: Evolving regulatory frameworks, such as the FDA's platform technology designations for viral vectors, that may streamline development pathways for validated delivery systems [61].
The integration of computational modeling, artificial intelligence, and high-throughput screening approaches will further accelerate the development of optimized AAV vectors tailored for specific clinical applications [60] [68]. As the field addresses current challenges related to immunogenicity, manufacturing scalability, and targeted delivery, AAV-based gene therapies are poised to transform treatment paradigms for a broad range of genetic disorders.
Addressing ATMP-Specific Challenges: Safety, Manufacturing, and Patient Recruitment Strategies
Overcoming Blood-Brain Barrier Challenges in CNS-Targeted Gene Therapies
The blood-brain barrier (BBB) represents the most significant impediment to the development of effective central nervous system (CNS)-targeted gene therapies [69]. For researchers designing clinical trials for Advanced Therapy Medicinal Products (ATMPs), overcoming this barrier is a critical determinant of success [8]. The BBB is a complex structure composed of endothelial cells connected by tight junctions, pericytes, and astrocyte end-feet, which collectively prevent the passage of over 98% of potential therapeutics, including gene therapy vectors and genetic materials [70]. This application note provides a structured framework and detailed protocols for evaluating BBB-penetrating strategies within the context of ATMP clinical trial design, addressing the key regulatory and scientific challenges in this emerging field.
Strategic Approaches for BBB Penetration in Gene Therapy
Table 1: Classification of BBB Penetration Strategies for CNS-Targeted Gene Therapies
| Strategy Category | Specific Mechanisms | Therapeutic Applications | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Viral Vector Engineering | Receptor-mediated transcytosis (e.g., TfR, LfR), Trojan horse approaches [71] [70] | Alzheimer's disease, Parkinson's disease, Glioblastoma [71] [72] | Long-term gene expression, high transduction efficiency [72] | Immunogenicity, limited packaging capacity, potential off-target effects [69] [72] |
| Non-Viral Nanocarriers | Lipid nanoparticles (LNPs), exosomes, cell-penetrating peptides [70] [73] | Brain tumors, Stroke, Neurodegenerative diseases [71] [73] | Lower immunogenicity, customizable delivery, large payload capacity [73] | Reduced transduction efficiency, potential cytotoxicity [69] |
| Physiological Modulation | Tight junction modulation, efflux transporter inhibition, adsorptive-mediated transcytosis [71] | Enhanced chemotherapy delivery, Antibody delivery | Can enhance delivery of co-administered drugs, uses natural transport pathways [71] | Risk of BBB disruption and neurotoxicity, transient effect [71] |
| Physical Disruption | Focused ultrasound with microbubbles, magnetic field-guided delivery [71] [70] | Glioblastoma, localized neurological disorders | Temporary and localized BBB opening, precise targeting [71] | Invasive, requires specialized equipment, risk of tissue damage [71] |
| Cell-Based Carriers | Engineered hematopoietic stem cells, exosomes, cell membrane coatings [71] [70] | Cancer, neurodegenerative diseases [71] [73] | Natural tropism, biocompatibility, potential for targeted delivery [73] | Complex manufacturing, standardization challenges [8] |
Visualizing Strategic Pathways for BBB Penetration
The following diagram illustrates the primary strategic pathways for overcoming BBB challenges in CNS-targeted gene delivery:
Experimental Protocols for Evaluating BBB Penetration
Protocol: Development of Receptor-Targeted Viral Vectors
Objective: To engineer and evaluate adeno-associated virus (AAV) vectors with enhanced BBB penetration capabilities through receptor-mediated transcytosis.
Materials:
- AAV serotypes (AAV2, AAV9, AAV11) [72]
- Plasmids for capsid modification (e.g., TfR, LfR targeting peptides) [71]
- In vitro BBB model (hCMEC/D3 cell line or primary human brain endothelial cells) [71]
- Animal models (rodents, non-human primates) [69]
- Analytical methods (qPCR, immunohistochemistry, Western blot) [71]
Methodology:
- Vector Design and Production:
- Insert genes encoding targeting ligands (e.g., transferrin, lactoferrin) into AAV capsid proteins via molecular cloning [71]
- Produce recombinant AAV vectors using HEK293 cell transfection system
- Purify vectors using ultracentrifugation or chromatography methods
In Vitro Transcytosis Assay:
- Culture brain endothelial cells on transwell inserts until tight junction formation (TEER > 150 Ω×cm²)
- Apply fluorescently labeled AAV vectors to the apical compartment
- Sample from basolateral compartment at 0, 1, 2, 4, 8, and 24 hours
- Quantify vector transport using qPCR and cell trafficking via confocal microscopy
In Vivo Biodistribution Study:
- Administer 1×10¹¹ vector genomes intravenously to animal models
- Euthanize animals at predetermined timepoints (24h, 7d, 30d)
- Perfuse with PBS to remove intravascular vectors
- Isolate and homogenize brain regions for vector genome quantification
- Perform immunohistochemistry to localize transgene expression
Regulatory Considerations: For ATMP development, document vector characterization, tropism, and biodistribution per EMA CAT guidelines [8] [74].
Protocol: Evaluation of Exosome-Mediated Gene Delivery
Objective: To assess the potential of engineered exosomes as nanocarriers for CNS-targeted gene therapy.
Materials:
- Exosome sources (mesenchymal stem cells, dendritic cells) [73]
- Therapeutic cargo (siRNA, miRNA, CRISPR/Cas components) [73]
- Targeting ligands (RVG peptide, TfR antibodies) [73]
- Characterization equipment (NTA, Western blot, TEM) [73]
Methodology:
- Exosome Engineering and Loading:
- Isolate exosomes from cell culture supernatants via ultracentrifugation or size-exclusion chromatography
- Characterize exosomes by nanoparticle tracking analysis (size distribution) and Western blot (tetraspanin markers)
- Load genetic cargo using electroporation, sonication, or transfection agents
- Conjugate targeting ligands to exosome surface via click chemistry or genetic engineering
BBB Penetration Assessment:
- Use in vitro BBB models to quantify exosome transport
- Inhibit specific pathways (e.g., caveolae-mediated endocytosis) to determine mechanism
- Employ microfluidic BBB-on-chip models for real-time tracking
In Vivo Efficacy Testing:
- Administer fluorescently labeled exosomes via systemic injection
- Image biodistribution using IVIS or similar systems
- Quantify brain delivery via biochemical methods
- Assess therapeutic efficacy in disease models
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for BBB Penetration Studies
| Reagent Category | Specific Examples | Research Application | Key Suppliers |
|---|---|---|---|
| BBB In Vitro Models | hCMEC/D3 cell line, primary brain endothelial cells, BBB-on-chips [71] | Screening BBB penetration in controlled systems | ATCC, Sigma-Aldrich, Emulate |
| Viral Vectors | AAV serotypes (AAV2, AAV9, AAV11), Lentiviral vectors [72] | Gene delivery vehicles with different tropisms | Addgene, Vigene, academic cores |
| Targeting Ligands | Transferrin, Lactoferrin, RVG peptide, TfR antibodies [71] [73] | Enhancing specificity of BBB crossing | Sigma-Aldrich, Abcam, custom synthesis |
| Characterization Tools | Nanoparticle Tracking Analysis, ELISA kits, Tetraspanin antibodies [73] | Quantifying and characterizing delivery systems | Malvern, System Biosciences |
| Animal Models | Wild-type rodents, Disease models (AD, PD), Humanized models [71] [72] | In vivo validation of BBB penetration | Jackson Labs, Charles River |
| Imaging Agents | Fluorescent dyes (DiR, DiD), Luciferase reporters, MRI contrast agents [71] | Tracking biodistribution and penetration | PerkinElmer, Thermo Fisher |
Regulatory Framework and Clinical Trial Design Considerations
The development of CNS-targeted gene therapies must align with the regulatory framework for ATMPs, which in the European Union requires centralized marketing authorization evaluation by the EMA's Committee for Advanced Therapies (CAT) [8] [74]. Clinical trial designs should incorporate:
- Biomarker Strategies: Include validated biomarkers for BBB penetration assessment (e.g., vector genomes in CSF, imaging biomarkers) [71]
- Dose Escalation: Design careful dose escalation protocols based on preclinical biodistribution data [8]
- Immunogenicity Monitoring: Plan for comprehensive immune monitoring due to potential vector-related immune responses [69] [72]
- Long-term Follow-up: Implement extended safety monitoring plans for integrated vectors per regulatory requirements [8]
Overcoming the BBB remains a fundamental challenge in CNS-targeted gene therapy development. The integration of advanced delivery strategies, robust experimental protocols, and regulatory-aware clinical trial design is essential for advancing these promising therapies. Future directions include the application of AI-driven modeling for predicting BBB permeability [71], the development of novel vector systems with enhanced targeting capabilities [70] [72], and the implementation of standardized potency assays for ATMP characterization [8] [74]. As these technologies evolve, they hold the potential to revolutionize the treatment of neurological disorders by enabling precise, effective, and safe gene therapy delivery to the CNS.
Advanced Therapy Medicinal Products (ATMPs), including Chimeric Antigen Receptor (CAR) T-cell therapies and bispecific T-cell engagers (BiTEs), represent a transformative approach to treating cancers and other severe conditions. However, their unique mechanism of action is associated with distinct and potentially severe adverse events, primarily Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS). The clinical development of ATMPs is often based on small, open-label, single-arm trials due to the orphan and unmet medical needs they target, which can create uncertainty about the product's benefit-risk profile at the time of marketing authorization [5] [75]. Consequently, understanding and managing these toxicities is critical for researchers and drug development professionals to ensure patient safety and the successful development of these innovative therapies.
This document provides a structured framework for monitoring and managing CRS and ICANS within clinical trials, presenting quantitative safety data, detailed monitoring protocols, and practical tools to inform trial design and safety planning.
Quantitative Analysis of CRS and ICANS Incidence and Timing
A comprehensive analysis of safety data from both clinical trials and real-world settings is essential for designing appropriate monitoring strategies. The tables below summarize the incidence and timing of CRS and ICANS for specific therapies.
Table 1: Incidence and Timing of CRS and ICANS with Lisocabtagene Maraleucel (liso-cel) [76]
| Parameter | Clinical Trials (n=702) | Real-World Setting (n=877) |
|---|---|---|
| Any-Grade CRS | 54% | 49% |
| Grade ≥3 CRS | 1% | 3% |
| CRS Onset (≤Day 15) | 98% of events | 97% of events |
| Median Time to CRS Resolution | 5 days | 4 days |
| Any-Grade ICANS/NE | 31% | 27% |
| Grade ≥3 ICANS/NE | 5% | 10% |
| ICANS/NE Onset (≤Day 15) | 88% of events | 95% of events (n=150) |
| Median Time to ICANS Resolution | 7 days | 5.5 days |
Table 2: Incidence of CRS and ICANS with Tarlatamab-dlle in SCLC [77]
| Toxicity | Incidence | Median Time to Onset |
|---|---|---|
| CRS | 53% | ~14 hours (after first 2 doses) |
| ICANS | 15% | ~30 days |
The data demonstrate that the vast majority of CRS and ICANS events occur early in the treatment course. For liso-cel, most events happen within the first 15 days post-infusion, supporting the rationale for intensive initial inpatient monitoring [76]. Real-world data also confirm the general safety profile observed in trials but can reveal differences, such as a higher rate of severe ICANS, which must be considered in trial risk assessments [76] [78].
Effective management of CRS and ICANS requires a standardized set of tools and medications. The following table details key components of a safety management toolkit for clinical trials involving ATMPs and BiTEs.
Table 3: Research Reagent Solutions for CRS and ICANS Management
| Reagent / Material | Function / Application |
|---|---|
| Tocilizumab | IL-6 receptor antagonist; first-line intervention for moderate to severe CRS (e.g., Grade ≥2 with cardiac/respiratory symptoms) [77]. |
| Corticosteroids (e.g., Dexamethasone) | Used to manage Grade 2 CRS and as first-line intervention for Grade 2 ICANS [77]. |
| Prophylactic Antibiotics (e.g., Doxycycline, Minocycline) | Part of enhanced dermatologic management to prevent/reduce skin toxicities associated with therapies like amivantamab [77]. |
| Antiepileptics (e.g., Levetiracetam) | Supportive medication for managing neurological symptoms and seizures in ICANS [77]. |
| Chlorhexidine-based Cleansers | Used in prophylactic skin regimens to reduce the risk of dermatologic adverse events and infections [77]. |
| Non-comedogenic Ceramide-based Moisturizer | Mitigates skin toxicity in patients receiving targeted therapies like amivantamab [77]. |
Clinical Monitoring and Management Protocols
Patient Monitoring and Risk Assessment
Robust patient monitoring is the cornerstone of early toxicity detection. Key laboratory parameters for CRS include C-reactive protein (CRP), ferritin, and interleukin-6 (IL-6) levels [79]. The frequency of monitoring should be most intensive during the high-risk period; for CAR T-cell therapies, this is the first two weeks post-infusion [76]. For BiTEs like tarlatamab, admitting patients for approximately 20 hours of observation after the first two doses is recommended due to the early onset of CRS [77]. Critical patient-related risk factors for developing these toxicities should also be identified and incorporated into monitoring plans [78].
CRS Management Protocol
The following diagram outlines a stepwise protocol for the management of CRS based on grading.
ICANS Management Protocol
The management of ICANS is primarily driven by corticosteroid administration, as detailed in the workflow below.
Protocol for Managing Unique Toxicities of Other Advanced Therapies
Therapies like amivantamab require specialized protocols for toxicities beyond CRS and ICANS.
Dermatologic Toxicity Management (e.g., for Amivantamab): The COCOON trial demonstrated that an enhanced prophylactic regimen significantly reduces the incidence of grade ≥2 dermatologic adverse events [77]. This regimen includes:
- Oral doxycycline or minocycline (100 mg twice daily for weeks 1-12).
- Clindamycin 1% lotion applied to the scalp once daily (weeks 13-52).
- Daily hand and foot washing with chlorhexidine 4%.
- Daily application of a non-comedogenic ceramide-based moisturizer to the face and body [77].
Infusion-Related Reaction (IRR) Management: For intravenous amivantamab, which has a 66% IRR incidence, the SKIPPirr trial showed that prophylactic oral dexamethasone (8 mg twice daily on days -2 and -1 prior to infusion) reduced reaction rates to 22% [77]. The subcutaneous formulation is a promising alternative, showing a significantly lower IRR incidence of 13% [77].
Integrating Safety Management into ATMP Clinical Trial Design
The unique safety profiles of ATMPs profoundly influence their clinical development. Regulatory approvals for ATMPs are often based on smaller, single-arm trials, which places greater emphasis on comprehensive safety monitoring and management plans to characterize the benefit-risk balance [5] [75]. The relationship between trial design and safety assessment is illustrated below.
Justifications for deviating from randomized controlled trials (RCTs) include enrollable patient populations that are too small, a lack of effective standard of care where a placebo arm would be unethical, or control group protocols that are excessively burdensome [80]. In such cases, methodologically sound single-arm trials with integrated, proactive safety monitoring protocols are not only acceptable but necessary. These protocols must define clear safety endpoints, standardized grading, and intervention strategies, as detailed in previous sections, to generate the high-quality evidence required by regulators and health technology assessment bodies [5] [80]. Furthermore, post-marketing evidence generation and late-phase controlled studies become unavoidable to confirm long-term safety and address payer expectations [5] [81].
Advanced Therapy Medicinal Products (ATMPs), which include gene therapies, cell-based therapies, and tissue-engineered products, represent a groundbreaking approach to treating severe and chronic diseases [82]. The manufacturing of these complex biological products requires adherence to rigorous quality standards to ensure patient safety and product efficacy. Two critical regulatory frameworks govern this space: Good Manufacturing Practice (GMP) and Good Tissue Practice (GTP). While both aim to ensure product quality and safety, they differ fundamentally in scope and application. GMP provides comprehensive oversight of all aspects of pharmaceutical production, while GTP requirements are specifically focused on preventing the introduction, transmission, and spread of communicable diseases through human cells, tissues, and cellular and tissue-based products (HCT/Ps) [83].
For researchers and drug development professionals working in ATMPs, understanding the distinction and intersection between these frameworks is essential for designing compliant manufacturing processes. The European Medicines Agency has adapted GMP requirements specifically for ATMPs to address their unique characteristics and complex manufacturing scenarios [82]. These adaptations maintain high quality standards while recognizing the novel nature of these therapies. Similarly, the U.S. Food and Drug Administration regulates HCT/Ps under GTP regulations (21 CFR 1270 and 1271), which govern methods used in the manufacturing of these products, including donor screening, product recovery, processing, storage, labeling, and distribution [83].
Regulatory Framework: Distinguishing GMP and GTP Requirements
Core Principles and Scope
Good Manufacturing Practice (GMP) is a national standard for the production of pharmaceuticals that ensures safe and effective drugs [83]. A GMP facility operates under strict environmental controls to assure manufacturing of sterile, potent, and uncontaminated products for human therapies. GMP covers all aspects of production, from raw materials, premises, and equipment to staff training and personal hygiene [84]. It requires detailed written procedures for each process that could affect the quality of the finished product and emphasizes quality management systems, sanitation, facility design, equipment validation, and comprehensive documentation [84].
Good Tissue Practice (GTP), in comparison, has a more focused scope limited to preventing the introduction, transmission, and spread of communicable diseases [83]. These regulations ensure that products do not become contaminated during manufacturing and that product function and integrity are not impaired through improper processing. As noted by UC Davis's stem cell program, "GTP requirements are less extensive in scope than GMP requirements" because they specifically address communicable disease risks rather than comprehensive manufacturing quality [83].
Comparative Analysis of Key Provisions
Table: Key Differences Between GMP and GTP Requirements
| Aspect | Good Manufacturing Practice (GMP) | Good Tissue Practice (GTP) |
|---|---|---|
| Regulatory Scope | Comprehensive pharmaceutical manufacturing standard [83] | Focused on communicable disease prevention [83] |
| Primary Focus | Overall product quality, safety, and efficacy [84] | Prevention of contamination and impairment of HCT/Ps [83] |
| Covered Products | Pharmaceuticals, drugs, biological products [83] | Human cells, tissues, cellular and tissue-based products [83] |
| Facility Requirements | Strict environmental control for sterile manufacturing [83] | Appropriate facilities to prevent contamination [85] |
| Documentation Level | Extensive record-keeping for all processes [84] | Records focused on tissue traceability and processing [85] |
| Quality Systems | Comprehensive Quality Management System required [84] | Quality program focused on GTP objectives [83] |
Quantitative Analysis of GMP and GTP Implementation Parameters
Implementing robust GMP and GTP systems requires careful consideration of critical process parameters and quality controls. The following table summarizes key quantitative aspects based on current regulatory expectations and industry standards for ATMP manufacturing.
Table: Critical Parameters for GMP/GTP Compliance in ATMP Manufacturing
| Parameter Category | GMP Requirements | GTP Requirements | ATMP-Specific Considerations |
|---|---|---|---|
| Environmental Monitoring | Grade A-D cleanrooms with particle counts, pressure differentials, and viable monitoring [83] | Controlled environments to prevent contamination [83] | Often requires aseptic processing throughout due to limited terminal sterilization options [30] |
| Personnel Training | Comprehensive initial and ongoing GMP training [84] | Training specific to tissue handling procedures [85] | Specialized training in aseptic technique and cell culture; regular competency assessments |
| Documentation & Records | Batch records, SOPs, deviation investigations, change controls [84] | Donor eligibility determinations, processing records, storage conditions [85] | Extended record retention (up to 30 years for traceability in EU) [30] |
| Quality Control Testing | Identity, strength, quality, purity tests; process validation [86] | Screening for relevant communicable diseases [83] | Extended characterization including potency assays, identity, purity, viability [30] |
| Supplier Qualification | Rigorous supplier assessment and audit program [84] | Donor screening and testing requirements [83] | Qualified raw material suppliers, especially for critical reagents [30] |
| Data Integrity | Complete audit trails, access controls, data validation [84] | Accurate and complete donor and processing records [85] | Electronic systems compliant with Annex 11; validation for automated processes [30] |
Integrated Protocol: Implementing GMP and GTP Requirements for ATMP Manufacturing
This protocol provides a systematic approach for implementing combined GMP and GTP requirements in ATMP manufacturing facilities. The primary objective is to establish a quality framework that addresses both comprehensive pharmaceutical quality systems (GMP) and specific tissue safety concerns (GTP). The protocol covers facility design, personnel training, process controls, and documentation systems necessary for compliant ATMP production, particularly focusing on early-phase clinical trials where manufacturing consistency is crucial for reliable trial outcomes.
Materials and Reagents
Table: Essential Research Reagent Solutions for GMP/GTP-Compliant ATMP Manufacturing
| Reagent/Material | Function | GMP/GTP Considerations |
|---|---|---|
| Cell Culture Media | Supports growth and maintenance of cellular products | Must be USP-grade, qualified for intended use, and tested for sterility and endotoxin [30] |
| Growth Factors/Cytokines | Directs cell differentiation and expansion | Recombinant human proteins preferred; full traceability and qualification data required [30] |
| Vector Systems | Gene delivery for genetically modified ATMPs | GMP-grade viral vectors or plasmid systems with complete characterization [30] |
| Critical Raw Materials | Components contacting product (e.g., cytokines, antibodies) | Supplier qualification, traceability, and testing for adventitious agents [84] |
| Cryopreservation Solutions | Preservation of cellular products | Formulated with USP-grade components; pre-sterilization filtration and sterility testing [30] |
| Quality Control Reagents | Testing for safety, potency, identity | Validated assays; reagents qualified for intended use [84] |
Step-by-Step Methodology
Facility and Equipment Qualification
Initiate with facility qualification by designing manufacturing spaces with proper cleanroom classifications (typically Grade B background with Grade A biosafety cabinets for aseptic operations) [83]. Implement rigorous environmental monitoring programs for particulate matter, viable organisms, pressure differentials, temperature, and humidity. Qualify all equipment through Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ) protocols [84]. For equipment contacting product directly, perform cleaning validation studies to prevent cross-contamination. Establish dedicated areas for specific processing steps with clear material and personnel flows to prevent mix-ups and contamination.
Document Control System Implementation
Develop a comprehensive document control system including Standard Operating Procedures (SOPs), batch records, and forms for all manufacturing and testing activities [84]. Implement electronic document management systems where possible to enhance version control and access management. Create specific SOPs for GTP-related activities including donor eligibility determination, tissue receipt, quarantine, and release procedures [85]. Establish batch records that document all critical processing parameters and allow for complete traceability of all materials, equipment, and personnel involved in each manufacturing run.
Personnel Training and Qualification
Establish a training program covering both technical competencies and regulatory knowledge [84]. Include specific modules on aseptic processing techniques, cellular biology fundamentals, GTP requirements for tissue handling, and GMP requirements for documentation and quality systems. Conduct regular competency assessments through direct observation, knowledge assessments, and media fill simulations for aseptic operations. Maintain complete training records documenting each employee's qualifications for specific tasks.
Process Validation and Quality Control
For late-stage trials and commercial preparation, implement a process validation approach encompassing process design, qualification, and continued verification [84]. For early-phase trials, focus on process characterization and identification of critical process parameters. Establish in-process controls and quality control testing for identity, purity, potency, and safety of the ATMP [86]. Implement a stability program to establish expiration dates based on real-time stability data. For cellular products, include tests for viability, identity, purity, potency, sterility, mycoplasma, and endotoxin.
Supply Chain and Vendor Management
Qualify all critical material suppliers through comprehensive assessment including questionnaires, audits, and testing of supplied materials [84]. Establish specifications for all raw materials and components, particularly those that contact the product directly. Implement a receipt and quarantine process for all incoming materials, including verification against certificates of analysis. For GTP-critical materials, ensure complete traceability back to original donor [83].
Quality Assurance Systems
Establish an independent quality unit responsible for releasing materials, intermediates, and final product [84]. Implement a change control system to evaluate and approve modifications to processes, equipment, or materials. Develop deviation and investigation procedures to address process anomalies. Create a comprehensive Corrective and Preventive Action (CAPA) system to address root causes of quality issues and prevent recurrence. Conduct regular internal audits to verify compliance with established procedures.
Diagram: Integrated GMP-GTP Manufacturing Workflow
Advanced Compliance Strategy: Risk-Based Approaches for ATMPs
The European Medicines Agency encourages a risk-based approach to manufacturing and testing of ATMPs [82]. This approach allows manufacturers to focus resources on the most critical aspects of production based on product-specific characteristics. For cell-based therapies, this might mean enhanced testing for differentiation status and tumorigenicity potential. For gene therapies, emphasis would be placed on vector characterization and testing for replication-competent viruses. A well-defined risk management process includes identification of potential hazards, analysis of their impact, evaluation against risk thresholds, and implementation of appropriate controls.
The implementation of risk-based approaches should be documented in a Quality Risk Management Plan that identifies critical quality attributes (CQAs) and critical process parameters (CPPs). This plan should justify the control strategy based on product and process understanding. For ATMPs with limited shelf lives, such as fresh cellular products, the risk assessment should include contingencies for analytical testing delays and alternative release mechanisms.
Diagram: Risk-Based Approach Integrating GMP and GTP Requirements
Successfully navigating the complementary requirements of GMP and GTP is essential for ensuring manufacturing consistency of ATMPs. While GMP provides the comprehensive quality framework for pharmaceutical manufacturing, GTP adds specific controls for tissue-based products focused on communicable disease prevention. By implementing the integrated protocols and risk-based approaches outlined in this application note, researchers and drug development professionals can establish robust manufacturing systems that comply with regulatory expectations while maintaining the flexibility needed for innovative ATMP development. As the regulatory landscape continues to evolve, maintaining a focus on quality by design and risk management will ensure consistent production of safe and effective advanced therapies for patients with unmet medical needs.
Enhancing Patient Recruitment and Diversity in Rare Disease Trials
The development of Advanced Therapy Medicinal Products (ATMPs), which include gene therapies, somatic cell therapies, and tissue-engineered products, represents a frontier in modern medicine, particularly for rare diseases [12] [8]. However, the clinical development of these therapies faces a formidable challenge: successful patient recruitment while ensuring trial populations are diverse and representative of the eventual treatment demographic. Rare diseases, by definition, affect small populations, which intrinsically complicates trial enrollment [87]. Furthermore, rare disease trials often differ significantly from more common disease trials; they enroll a median of 29 participants versus 62 in non-rare disease trials and are more likely to be single-arm (63.0% vs. 29.6%), non-randomized (64.5% vs. 36.1%), and open-label (78.7% vs. 52.2%) [87] [88]. These design limitations, often necessitated by patient scarcity, heighten the imperative that the patients who are recruited truly represent the affected community. This document outlines application notes and detailed protocols to overcome these hurdles, ensuring that rare disease trials for ATMPs are both efficient and equitable.
Quantitative Analysis of Rare Disease Trial Landscap
A comprehensive analysis of registered trials reveals distinct characteristics and challenges inherent to rare disease studies. The following tables summarize key differences and disparities.
Table 1: Comparative Analysis of Rare vs. Non-Rare Disease Interventional Trial Designs (2006-2012) [87] [88]
| Trial Characteristic | Rare Disease Trials | Non-Rare Disease Trials |
|---|---|---|
| Proportion of Trial Landscape | 11.5% (2,759 of 24,088 trials) | 88.5% (21,329 of 24,088 trials) |
| Median Enrollment | 29 participants | 62 participants |
| Single-Arm Design | 63.0% | 29.6% |
| Non-Randomized | 64.5% | 36.1% |
| Open Label | 78.7% | 52.2% |
| Early Termination Rate | 13.7% | 6.3% |
| Trials Actively Pursuing/Waiting to Enroll | 15.9% | 38.5% |
Table 2: Documented Health Disparities and Representation in Research [89]
| Disease Area | Disparity | Context |
|---|---|---|
| Cardiovascular Health | A Black woman is 22% more likely to die from heart disease than a white woman. | Illustrates broader health inequities. |
| Cancer | A Black woman is 71% more likely to die from cervical cancer than a white woman. | Highlights critical outcome disparities. |
| Respiratory Research | Before COVID, less than 5% of NIH-funded respiratory research reported inclusion of racial or ethnic minorities. | Indicates historical lack of diversity in research participation. |
| Asthma Treatment | Non-responsiveness to albuterol is ~47% in African Americans and ~67% in Puerto Rican children, versus ~20% in Northern European whites. | Demonstrates differential drug response based on ancestry. |
| Funding Equity (Rare Disease Example) | Government funding per person for Cystic Fibrosis (affects primarily white Americans) was nearly $2,000 higher than for Sickle Cell Disease (affects primarily Black Americans) from 2008-2017, despite SCD being 3x more prevalent. | Shows systemic funding inequities for rare diseases affecting different populations. |
Strategic Framework for Enhanced Recruitment and Diversity
A multi-faceted strategy is required to address the dual challenges of recruitment and diversity. The following workflow diagram outlines the key pillars of this approach.
Strategic Workflow for Recruitment and Diversity
Experimental & Operational Protocols
Protocol 4.1: Implementing a Community-Centric Outreach Plan
Objective: To establish trust and increase trial awareness within diverse rare disease communities through authentic partnership.
Materials:
- Research Reagent Solutions:
- Community Advisory Boards (CABs): Comprising patients, caregivers, and community leaders from diverse backgrounds to provide guidance on trial design and materials.
- Culturally & Linguistically Adapted Informed Consent Forms: Translated and simplified documents to ensure true comprehension.
- "Toolkit" of Educational Resources: Brochures, videos, and webinars co-created with patient advocacy groups like RARE-X [90].
Methodology:
- Partnership Formation: Identify and establish formal partnerships with key rare disease patient organizations (e.g., NORD, RARE-X, disease-specific foundations) [90].
- Barrier Assessment: Conduct qualitative research (e.g., focus groups, surveys) with diverse community members to identify specific fears (e.g., historical exploitation, discrimination), and logistical barriers (e.g., transportation, time off work) [89] [90].
- Material Co-Development: Collaborate with the CAB and advocacy groups to develop all patient-facing materials, ensuring cultural competency, appropriate health literacy levels, and transparent messaging.
- Trust-Building Engagement: Host virtual and in-person community engagement events featuring trusted healthcare professionals and community champions to discuss the trial, the disease, and address concerns openly.
Protocol 4.2: Deploying a Decentralized Clinical Trial (DCT) Framework
Objective: To reduce participant burden and geographic barriers to trial access by integrating remote and local care.
Materials:
- Research Reagent Solutions:
- Digital Health Technologies (DHTs): FDA-cleared wearable sensors, electronic Clinical Outcome Assessment (eCOA) apps for symptom tracking.
- Home Health Nursing Networks: Vetted and trained clinical personnel for at-home visits.
- Telemedicine Platform: Secure, HIPAA-compliant video conferencing software for remote study visits.
- Centralized ATMP Logistics: Specialized courier services and tracking systems for handling gene and cell therapy products.
Methodology:
- Feasibility Assessment: Determine which trial procedures (e.g., consenting, routine follow-ups, blood draws, physical therapy) can be safely performed remotely or locally.
- Technology Kit Preparation: Assemble and validate kits for participants containing DHTs and clear instructions for use. Ensure technology is accessible for people with disabilities.
- Hub-and-Spoke Site Model: Establish a central expert site for complex procedures (e.g., ATMP administration) linked with a network of local clinics or home health agencies for routine monitoring. This model was validated during the COVID-19 pandemic, which saw increased diversity in participation as a result of decentralized approaches [89].
- Continuous Support: Provide a 24/7 helpline for participants to troubleshoot technical or clinical issues with the DCT tools and procedures.
Protocol 4.3: Applying AI for Predictive Recruitment and Diversity Optimization
Objective: To use artificial intelligence and real-world data to identify potential trial participants and forecast recruitment rates across diverse demographics accurately.
Materials:
- Research Reagent Solutions:
- De-identified Real-World Data (RWD) Sources: Electronic Health Records (EHRs), insurance claims databases, and patient registry data.
- Natural Language Processing (NLP) Tools: Software to extract unstructured clinical information from physician notes and pathology reports.
- Predictive Analytics Platform: AI-powered software for modeling patient enrollment and identifying under-represented cohorts.
Methodology:
- Algorithm Training: Develop or procure AI algorithms trained on RWD to identify potential rare disease patients based on diagnostic codes, clinical notes, medication use, and genetic testing results, where available. The FDA Modernization Act 2.0 facilitates the use of such non-animal, data-driven methods [89].
- Site Selection Analysis: Use AI to analyze demographic data and healthcare utilization patterns to identify and select clinical trial sites that serve diverse patient populations [89].
- Recruitment Forecasting: Implement models to predict enrollment rates and simulate the impact of different recruitment strategies on achieving diversity targets.
- Patient Matching: Use a secure, privacy-preserving process to flag potentially eligible patients within a healthcare system for outreach by their own providers.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Enhancing Recruitment and Diversity in Rare Disease ATMP Trials
| Tool / Solution | Function | Application Context |
|---|---|---|
| Community Advisory Boards (CABs) | Provides ground-level feedback on trial feasibility, design, and materials from patient and community perspectives. | Essential for pre-trial planning and ongoing oversight to ensure cultural competency and trustworthiness [90]. |
| Decentralized Clinical Trial (DCT) Platforms | Enables remote consent, monitoring, and data collection to reduce geographic and mobility barriers. | Critical for including participants who live far from major academic research centers [89]. |
| AI-Powered Predictive Analytics | Analyzes real-world data to identify potential trial candidates and optimize site selection for diversity. | Used during trial planning and activation to efficiently target enrollment and meet diversity goals [89]. |
| Digital Health Technologies (DHTs) | Captures objective and subjective data directly from patients in their home environment. | Provides continuous efficacy and safety data while reducing clinic visit burden; useful for novel endpoint development [12]. |
| Diversity Action Plan (DAP) Template | A formal document outlining goals, strategies, and enrollment targets for underrepresented racial and ethnic populations. | Required by recent U.S. law (Public Law 117-328) for certain clinical trials; demonstrates regulatory commitment [89]. |
| Culturally Adapted Informed Consent Tools | Utilizes simplified language, translation, and visual aids to ensure true understanding of the trial. | Used during the informed consent process to improve comprehension and autonomy across different literacy and language levels. |
Enhancing patient recruitment and diversity in rare disease ATMP trials is not merely an ethical imperative but a scientific one. The biological differences in treatment response, as starkly illustrated by the variable efficacy of common drugs like albuterol across ancestries, mean that homogenous trials can produce incomplete or even dangerously misleading results [89]. By adopting a structured approach that integrates deep community partnership, innovative decentralized and adaptive trial designs, cutting-edge AI tools, and proactive regulatory planning, researchers can overcome the historical challenges that have plagued this field. The successful implementation of these protocols will lead to more robust, generalizable, and equitable clinical trials, ultimately accelerating the development of advanced therapies for all patients affected by rare diseases.
Troubleshooting Low Transduction Efficiency and Immunogenicity in Gene Therapies
Within the clinical development of Advanced Therapy Medicinal Products (ATMPs), the efficacy and safety of gene therapies are critically dependent on two key biological parameters: transduction efficiency and immunogenicity [91] [92]. Transduction efficiency—the percentage of target cells successfully expressing the therapeutic transgene—directly correlates with therapeutic potency [93]. Concurrently, immunogenicity, the immune response provoked by the viral vector or the transgene product, can compromise both safety and efficacy by eliminating transduced cells and limiting re-dosing potential [91]. The inherent heterogeneity in preclinical methodologies, including vector design, delivery systems, and promoter choices, often impedes the identification of optimal parameters for clinical translation [91]. This application note provides a structured, evidence-based framework for researchers to diagnose and resolve issues related to low transduction efficiency and undesirable immune responses, thereby de-risking the path to clinical trial initiation.
Quantitative Landscape of Transduction Efficiency
A systematic review of preclinical in vivo studies highlights the significant variability in reported transduction outcomes, influenced by factors such as viral serotype, promoter, titer, and route of administration [91]. The table below summarizes key quantitative data from selected studies to establish baseline expectations and illustrate the impact of critical variables.
Table 1: Transduction Efficiencies Achieved in Preclinical In Vivo Studies
| Species/Strain | Age | Vector | Promoter | Route of Administration | Injected Dose | Transduction Efficiency* | Effect on Hearing | Immune Response | |
|---|---|---|---|---|---|---|---|---|---|
| C3Hfe [91] | P15–16 | AAV2/Anc80L65 | CMV | RWM+CF | 1.4 x 109 vg | 89.07% | - | - | |
| C3Hfe [91] | Neonatal | rAAV2/9 | CMV | STVI | 1.64 x 1012 vg | IHC: 96% | OHC: 79.33% | + | - |
| C57BL/6J [91] | P1 | AAV2/1-WPRE | CMV | RWM | 1 x 1010 gc | Moderate to High | - | - | |
| C57BL/6J [91] | P1 | AAV2/Anc80L65-WPRE | CMV | RWM | 1 x 1010 gc | IHC: 100% | OHC: 90% | - | - |
| C3Hfe [91] | P15–16 | AAV2/9 | CMV | RWM | 3.9 x 1010 vg | 30.27% | + | + | |
| Human (Clinical CAR-T) [93] | N/A | Lentiviral | Variable | Ex Vivo | Variable | 30–70% | N/A | Monitor |
Abbreviations: RWM: Round Window Membrane; CF: Canalostomy; STVI: Scala Tympani Viral Injection; IHC: Inner Hair Cells; OHC: Outer Hair Cells; vg: vector genomes; gc: genome copies; N/A: Not Applicable. *Transduction efficiency targets different cell types; IHC, OHC, SGN (Spiral Ganglion Neurons), SC (Supporting Cells).
Diagnostic Framework and Protocol for Root Cause Analysis
A methodical approach is required to identify the fundamental cause of suboptimal transduction or a heightened immune response.
Experimental Protocol: Systemic Analysis of Transduction Failure
Objective: To quantitatively assess key process parameters and identify the limiting factor in the transduction workflow. Materials:
- Target cells (e.g., T cells, NK cells)
- Viral vector (e.g., LV, AAV) of known titer
- Cell culture equipment and transduction enhancers (e.g., polybrene)
- Flow cytometer and qPCR/ddPCR machine
Method:
- Cell Quality & Viability Assessment: Isolate and activate target cells. Confirm >90% viability pre-transduction using trypan blue exclusion or flow cytometry with Annexin V/7-AAD staining [93].
- Vector-Cell Interaction Check: Titrate the Multiplicity of Infection (MOI). Use a standardized MOI (e.g., 5-10 for LVs in T cells) and include a spinoculation step (e.g., 2000 x g, 90 min, 32°C) to enhance cell-vector contact [93].
- Transduction & Analysis: Transduce cells in the presence of a suitable transduction enhancer. After an appropriate incubation period (e.g., 72 hours):
- Analyze Transduction Efficiency: Use flow cytometry to determine the percentage of cells expressing the reporter or therapeutic transgene.
- Quantify Vector Genomes: Use qPCR or droplet digital PCR (ddPCR) to determine the Vector Copy Number (VCN). A clinical standard is to maintain VCN below 5 copies per cell [93].
- Assess Functional Output: For engineered immune cells, perform a functional assay such as an IFN-γ ELISpot or a co-culture cytotoxicity assay to confirm therapeutic activity [93].
The following workflow diagram illustrates the logical decision process for diagnosing the root cause of low efficiency.
Optimization Strategies for Clinical Translation
Based on the root cause analysis, the following targeted strategies are recommended for process improvement.
Strategies to Enhance Transduction Efficiency
Table 2: Optimization Strategies for Critical Process Parameters (CPPs)
| Critical Process Parameter (CPP) | Challenge | Optimization Strategy | Clinical/Preclinical Evidence |
|---|---|---|---|
| Vector Serotype & Tropism | Low affinity of vector for target cell receptors. | Pseudotype LV with VSV-G envelope for broad tropism, or use cell-specific envelopes. For AAV, select novel serotypes (e.g., AAV2/9, AAV2/Anc80L65) [91] [93]. | AAV2/Anc80L65 showed ~90% transduction in inner hair cells, superior to AAV2/9 (30%) via RWM injection [91]. |
| Multiplicity of Infection (MOI) | Low efficiency vs. safety concerns from high VCN. | Titrate MOI to balance efficiency and safety (VCN <5). Use lower MOI ranges to reduce multiple integrations [93]. | In CAR-T manufacturing, careful MOI titration achieves 30-70% efficiency while controlling VCN [93]. |
| Cell Activation State | Quiescent cells are resistant to transduction. | Pre-activate immune cells (e.g., CD3/CD28 for T cells) to upregulate viral receptors and enable cell division for γ-RVs [93]. | T cell activation is a standard step in clinical CAR-T manufacturing protocols [93]. |
| Transduction Method | Insufficient cell-vector contact. | Implement spinoculation (centrifugation during transduction) or use bioreactors to improve co-localization [93]. | Spinoculation is a widely adopted method in both research and clinical manufacturing to enhance efficiency [93]. |
| Transduction Enhancers | Cellular barriers to viral entry. | Incorporate additives like polybrene, protamine sulfate, or poloxamers to neutralize charge repulsion and improve uptake [93]. | The use of enhancers is common in ex vivo manufacturing but requires careful validation for each cell type. |
Strategies to Mitigate Immunogenicity
- Vector Engineering: Utilize modern self-inactivating (SIN) lentiviral and retroviral vector designs. These configurations delete viral enhancer/promoter elements from the LTRs, significantly reducing the risk of insertional mutagenesis and immune activation [93].
- Vector Serotype Selection: Choose low-immunogenicity serotypes. Adeno-associated viruses (AAVs), in particular, are noted for their low immunogenicity, which can allow for repeated administration in some contexts [91] [93].
- Promoter Optimization: Employ tissue-specific or synthetic promoters to restrict transgene expression to the target tissue, thereby minimizing off-target expression and potential immune recognition [91].
- Immunosuppression Regimens: Consider transient peri-transduction immunosuppression with corticosteroids to dampen innate and adaptive immune responses against the vector capsid or transgene product.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Transduction and Immunogenicity Analysis
| Reagent / Solution | Function | Application Example |
|---|---|---|
| Lentiviral Vectors (VSV-G pseudotyped) | Stable integration in dividing & non-dividing cells; broad tropism. | Engineering CAR-T cells and other immune effector cells for long-term persistence [93]. |
| AAV Serotypes (e.g., AAV2/9, AAV2/Anc80L65) | In vivo gene delivery; low immunogenicity; tropism for specific tissues. | Direct in vivo gene transfer to sensory cells (e.g., inner ear, retina) [91]. |
| Polybrene / Protamine Sulfate | Cationic agents that reduce electrostatic repulsion between viral particles and cell membranes. | Enhancing viral transduction efficiency in vitro for a variety of cell lines and primary cells [93]. |
| Recombinant Cytokines (IL-2, IL-7, IL-15) | Support survival, expansion, and function of immune cells during and after transduction. | Culture and maintenance of T cells (IL-2) and NK cells (IL-15) post-transduction [93]. |
| Anti-CD3/CD28 Activator | Robust activation and proliferation of T cells via TCR cross-linking and co-stimulation. | Essential pre-activation step for efficient transduction of primary human T cells [93]. |
| Annexin V / 7-AAD | Flow cytometry-based detection of apoptosis (Annexin V) and cell death (7-AAD). | Assessing post-transduction cell viability and fitness as a Critical Quality Attribute (CQA) [93]. |
| Droplet Digital PCR (ddPCR) | Absolute quantification of Vector Copy Number (VCN) with high precision. | Determining the average number of viral integrations per cell genome for product safety release [93]. |
Analytical Methods for Assessing CQAs and Immunogenicity
Rigorous analytical methods are non-negotiable for characterizing the final product and understanding host immune responses.
Experimental Protocol: Vector Copy Number (VCN) Analysis by ddPCR
Objective: To accurately quantify the average number of viral vector integrations per cell genome. Materials: Genomic DNA (gDNA) from transduced cells, ddPCR supermix, assays for the transgene and a reference single-copy host gene (e.g., RPP30), droplet generator, and droplet reader. Method:
- DNA Isolation & Quantification: Extract high-quality gDNA and quantify using a fluorescence-based method for accuracy.
- Reaction Setup: Prepare a ddPCR reaction mix containing the sample gDNA (~50-100 ng), ddPCR supermix, and primers/probes for both the transgene and the reference gene.
- Droplet Generation & PCR: Generate droplets using a droplet generator. Perform PCR amplification on the droplet emulsion.
- Droplet Reading & Analysis: Run the droplets on a droplet reader to count the positive and negative droplets for each target.
- VCN Calculation:
VCN = (Concentration of transgene target) / (Concentration of reference gene target)Report the average VCN across the cell population, ensuring it aligns with regulatory guidelines (typically below 5 copies/cell) [93].
Immunogenicity Assessment Workflow
The immunogenic potential of a gene therapy product must be evaluated through a multi-faceted approach, assessing both innate and adaptive immune responses.
Troubleshooting transduction efficiency and immunogenicity is not merely a preclinical exercise but a foundational activity that directly informs clinical trial design for ATMPs. The strategies and protocols outlined herein enable the development of a robust Chemistry, Manufacturing, and Controls (CMC) package. Key clinical trial considerations stemming from this work include:
- Dosing Strategy: Justification of the clinical dose based on in vitro and in vivo efficacy data, and the feasibility of achieving the target VCN and transduction efficiency in human products.
- Patient Monitoring Plan: Establishment of a long-term follow-up plan (e.g., 15 years) to monitor for delayed adverse events, including insertional mutagenesis, which is mandated by regulators for integrating vectors [92].
- Immunogenicity Risk Management: Development of patient screening strategies for pre-existing immunity (e.g., NAb assays) and potential protocols for transient immunosuppression to mitigate vector-directed immune responses.
- Potency Assay Definition: Creation of a potency assay that correlates transduction efficiency or VCN with a relevant biological function, which is critical for product release and demonstrating comparability after process changes [93].
By systematically addressing these interconnected challenges, developers can enhance the therapeutic index of gene therapy products, thereby increasing the probability of success in clinical trials and ultimately delivering safe and effective treatments to patients.
Demonstrating Efficacy and Value: Comparative Effectiveness and Real-World Evidence
Single-arm trials (SATs), in which all enrolled participants receive the experimental intervention without concurrent randomization to a control group, represent a crucial design strategy in advanced therapy medicinal products (ATMP) research. While randomized controlled trials (RCTs) remain the gold standard for clinical evidence generation, SATs have emerged as a viable alternative in specific scenarios where RCTs are impractical or unethical [94]. These circumstances include research involving rare diseases, advanced-stage cancers, and conditions with significant unmet medical needs where patient populations are limited and establishing a control group may be ethically problematic [94] [33].
The European Medicines Agency (EMA) has formally acknowledged the potential use of SATs as pivotal evidence in marketing authorization applications, while simultaneously emphasizing that their use requires strong justification and careful addressing of inherent limitations [95]. For drug developers and researchers working with ATMPs, understanding the statistical considerations and bias mitigation strategies specific to SATs is paramount for generating valid, reliable evidence that meets regulatory standards. This application note provides detailed protocols and methodologies for designing, conducting, and interpreting SATs with a focus on validating treatment effects while managing the unique challenges of this trial design.
Regulatory and Methodological Framework for SATs
Key Regulatory Considerations
Regulatory agencies recognize that SATs may be necessary in certain development contexts but have established clear expectations for their appropriate use. The EMA requires robust justification for selecting SATs over RCTs, emphasizing that this design should not be used simply for convenience when RCTs remain feasible [95]. Justification must be grounded in the full clinical context and specific attributes of the investigational treatment, with particular attention to patient population characteristics and ethical considerations.
The primary regulatory concerns regarding SATs center on their heightened susceptibility to various forms of bias and the challenges in establishing definitive causal relationships between intervention and outcome. Without random allocation to treatment groups, SATs cannot automatically ensure comparability between treated patients and what their outcomes would have been without treatment [33]. Consequently, regulators require additional safeguards and methodological rigor to compensate for these inherent limitations when SATs are submitted as pivotal evidence.
Ethical and Practical Advantages in ATMP Research
Despite their methodological limitations, SATs offer distinct ethical and practical advantages in ATMP research, particularly in the context of rare diseases and advanced therapeutic development:
- Equitable Access: All participants receive the potentially beneficial experimental therapy, respecting patient preferences and avoiding randomization to potentially inferior treatments [94]
- Feasibility: Requires fewer participants than RCTs, which is critical when patient populations are limited [94] [33]
- Efficiency: Shorter implementation timelines and reduced costs compared to randomized designs [94] [33]
- Accelerated Development: Provides a pathway for faster drug development and regulatory approval in urgent clinical contexts [33]
These advantages make SATs particularly suitable for ATMPs targeting serious conditions with limited treatment options, where traditional RCTs may be impractical or ethically questionable.
Statistical Considerations for SAT Design and Analysis
Endpoint Selection and Validation
Endpoint selection is critically important in SATs, as the absence of concurrent controls increases reliance on the interpretability of the chosen endpoints. The EMA recommends that primary endpoints in SATs must be objectively measurable, able to isolate treatment effects, and clinically relevant [95]. The suitability of different endpoint types varies considerably in SAT contexts:
Table 1: Endpoint Considerations for Single-Arm Trials
| Endpoint Type | Suitability for SATs | Key Considerations | Regulatory Perspective |
|---|---|---|---|
| Binary Endpoints | High | Must be clearly defined; outcomes should not be achievable without treatment | More suitable if properly defined |
| Continuous Endpoints | Challenging | Subject to natural variability and regression to the mean | Difficult to interpret without concurrent controls |
| Time-to-Event Endpoints | Generally unsuitable | Difficult to attribute outcomes specifically to treatment | Not recommended by EMA and FDA |
For ATMPs, the selection of endpoints should be guided by the mechanism of action and expected treatment effects. Endpoints that demonstrate clear, direct biological activity (e.g., tumor response in oncology, biomarker changes in gene therapies) are generally preferable to composite or subjective endpoints in SAT contexts.
Establishing Efficacy Thresholds and Analytical Approaches
A fundamental challenge in SATs is establishing appropriate benchmarks for evaluating treatment effects without concurrent controls. Two primary approaches are used: threshold-based analyses and direct comparison with external controls [33]. Both methodologies depend on external information to contextualize results, but differ in their implementation:
- Threshold-Based Analysis: A predetermined efficacy threshold is established based on historical data, and the observed effect in the SAT must exceed this threshold to demonstrate efficacy
- External Control Comparison: Direct statistical comparison is made between the SAT cohort and an external control group derived from historical studies or real-world data
Table 2: Methods for Meta-Analysis Combining RCT and Single-Arm Studies
| Method | Framework | Key Assumptions | Performance Characteristics |
|---|---|---|---|
| Begg & Pilote (BP) | Frequentist | Exchangeable baseline effects, common relative treatment effect | Reduced uncertainty but suboptimal coverage unless similar heterogeneity |
| Begg & Pilote with Bias Adjustment (BPbias) | Frequentist | Systematic bias in single-arm data relative to RCT data | Improved handling of known biases between data sources |
| Hierarchical Power Prior (HPP) | Bayesian | Exchangeable treatment effects per arm, correlation between RCT arms | Consistent uncertainty reduction while maintaining coverage |
| Hierarchical Commensurate Prior (HCP) | Bayesian | Exchangeable treatment effects per arm, differences in between-study heterogeneity | Most robust approach when heterogeneity differs between RCT and SAT data |
The statistical analysis plan for SATs must be finalized before trial initiation, as post-hoc modifications are scrutinized by regulatory agencies [95]. The plan should pre-specify methods for handling missing data, sensitivity analyses, and the statistical model for estimating treatment effects with appropriate measures of uncertainty.
Bias Assessment and Mitigation Protocols
Risk of Bias Assessment Tool for SATs
A structured approach to bias assessment is essential for evaluating SAT quality. Recent research has developed specialized risk of bias (ROB) tools for SATs, combining elements from established methodologies like MINORS and modified Cowley's criteria [96]. The tool evaluates studies across multiple domains, with specific emphasis on methodological rigor in patient selection, outcome assessment, and statistical analysis.
Table 3: Risk of Bias Assessment Criteria for Single-Arm Trials
| Assessment Domain | Key Criteria | Scoring Guidance |
|---|---|---|
| Patient Selection | Method of selection identified and appropriate; age range and mean stated; type of lesion stated | 0-2 points per item |
| Follow-up and Attrition | Number deceased/lost to follow-up reported; follow-up period, range and mean mentioned; data for deceased individuals | 0-2 points per item |
| Intervention Specification | Scaffold/stent models specified (or interventional strategy); pre-operative diagnosis and percentages given | 0-2 points per item |
| Outcome Assessment | Well-defined criteria for outcomes measurement; quantification of outcomes; clinical outcomes reported at follow-up | 0-2 points per item |
| Analytical Rigor | Valid statistical analysis undertaken; independence of investigators (no conflict of interest) | 0-2 points per item |
Based on this assessment, studies can be categorized as low (24-26/26), moderate (20-23/26), or high risk of bias (<20/26), with high-risk studies generally ineligible for inclusion in systematic reviews or regulatory submissions [96].
Quantitative Bias Analysis for External Control Arms
When using external controls in SATs, quantitative bias analysis (QBA) provides a structured approach to addressing unmeasured confounding. A recent demonstration study evaluating QBA in advanced non-small cell lung cancer found that adjusting for known unmeasured confounders significantly improved the agreement between SAT results and randomized trial findings [97]. The stepwise implementation of QBA involves:
Diagram: Quantitative Bias Analysis Workflow for addressing unmeasured confounding in single-arm trials with external controls.
The Q-BASEL project demonstrated that after adjustment for measured confounders, the mean difference in log hazard ratio estimates between original RCTs and emulated external control analyses was 0.139 (ratio of hazard ratios: 1.22), which further improved to 0.098 (ratio of hazard ratios: 1.17) after QBA adjustment for unmeasured and mismeasured confounders [97]. This suggests that QBA can meaningfully reduce bias in SAT analyses when properly implemented.
Bias Mitigation Strategies Across Trial Phases
Different types of bias require specific mitigation strategies throughout the SAT lifecycle:
- Selection Bias: Precisely predefine and justify inclusion/exclusion criteria; document participant selection process in detail; consider potential prognostic factors [95]
- Assessment Bias: Use objectively measurable endpoints; blind outcome assessors when possible; employ endpoints supported by secondary measures [95]
- Attrition Bias: Minimize missing data through trial design and conduct; implement statistical methods for handling missing data [95]
- Temporal Bias: Account for changes in standard of care; use contemporary external controls when possible; adjust for temporal trends in analysis [33]
Protocols should explicitly address these bias sources with targeted mitigation strategies appropriate for the specific ATMP and disease context.
Experimental Protocols for SAT Validation
Protocol 1: External Control Arm Construction and Validation
Purpose: To construct and validate an external control arm for comparative analysis with SAT data.
Materials and Data Requirements:
- Index SAT data with individual participant-level data
- Potential external data sources (historical clinical trials, disease registries, real-world databases)
- Pre-specified prognostic factors and effect modifiers
- Statistical software capable of propensity score analysis and Bayesian methods
Methodology:
- Cohort Definition: Define index cohort from SAT using the same inclusion/exclusion criteria that would apply to a randomized trial
- Control Source Selection: Identify potential external control sources with similar patient characteristics, era of enrollment, and standard of care
- Covariate Balance Assessment: Evaluate distribution of known prognostic factors between SAT cohort and potential external controls
- Propensity Score Development: Develop propensity score model to estimate probability of being in the SAT based on baseline characteristics
- Matching or Weighting: Implement propensity score matching, weighting, or stratification to achieve balance on measured covariates
- Residual Confounding Assessment: Evaluate the potential impact of unmeasured confounding using quantitative bias analysis
- Sensitivity Analyses: Conduct sensitivity analyses to assess robustness of findings to various assumptions
Validation Metrics:
- Standardized mean differences for covariates (<0.1 indicates adequate balance)
- Empirical coverage probability from simulation studies
- Comparison of known treatment effects with established benchmarks
Protocol 2: Threshold Derivation and Calibration
Purpose: To establish and validate clinically meaningful efficacy thresholds for SAT success criteria.
Materials and Data Requirements:
- Comprehensive collection of historical control data
- Clinical expert input for threshold justification
- Statistical software for meta-analysis and modeling
Methodology:
- Historical Data Collection: Systematically collect data on outcome rates in comparable patient populations from historical studies
- Meta-Analytic Integration: Perform random-effects meta-analysis of historical control data to estimate expected outcome distribution
- Threshold Specification: Establish threshold based on clinical significance and historical benchmarks
- Statistical Power Calculation: Determine sample size needed to demonstrate effect exceeding threshold with adequate power
- Futility Analysis: Implement pre-specified interim analyses for early termination if efficacy threshold unlikely to be met
- Calibration Validation: Validate thresholds against clinical outcomes and expert opinion
Analytical Considerations:
- Account for between-study heterogeneity in historical data
- Consider temporal trends in standard of care and outcomes
- Pre-specify statistical model for threshold comparison (e.g., exact binomial test for response rates)
Research Reagent Solutions for SAT Methodologies
Table 4: Essential Methodological Tools for Single-Arm Trial Research
| Methodological Tool | Primary Function | Application Context | Implementation Considerations |
|---|---|---|---|
| MINORS ROB Tool | Methodological quality assessment | Systematic reviews of SATs | Focuses on methodological rigor and protocol adherence |
| Modified Cowley's Criteria | Risk-of-bias assessment | Cardiovascular and orthopaedic interventions | Emphasizes procedural aspects and clinical outcomes |
| Quantitative Bias Analysis | External adjustment for unmeasured confounding | SATs with external controls | Requires synthesis of external evidence and sensitivity parameters |
| Hierarchical Commensurate Prior Models | Bayesian synthesis of RCT and SAT data | Meta-analysis including both randomized and single-arm studies | Distinguishes between RCT and SAT data, accounts for differences in heterogeneity |
| Propensity Score Methods | Balancing measured covariates | Construction of external control arms | Requires complete data on important prognostic factors |
| Threshold Derivation Algorithms | Establishing clinically meaningful benchmarks | SATs without direct external comparisons | Incorporates historical data and clinical expert input |
Single-arm trials present both opportunities and challenges in ATMP development. When properly designed and analyzed with appropriate attention to statistical considerations and bias mitigation, they can provide valid evidence of treatment efficacy in contexts where randomized trials are not feasible. The key to successful implementation lies in recognizing the inherent limitations of SATs and employing rigorous methodologies to address them.
Researchers should engage early with regulatory agencies to discuss the acceptability of SATs for specific development programs, with particular attention to justification, endpoint selection, and bias mitigation strategies [95]. Investment in thorough statistical planning before trial initiation is essential, as post-hoc modifications are viewed skeptically by regulators. Additionally, gathering robust external data to support assumptions about the natural course of disease and expected outcomes with existing treatments strengthens the interpretability of SAT results.
For ATMPs targeting serious conditions with limited treatment options, SATs represent a valuable design option that can accelerate development while maintaining scientific rigor. By implementing the protocols and methodologies outlined in this application note, researchers can enhance the validity and reliability of SAT evidence, supporting informed regulatory decision-making and ultimately bringing innovative therapies to patients in need.
Advanced Therapy Medicinal Products (ATMPs), encompassing gene therapies, somatic cell therapies, and tissue-engineered products, represent a transformative approach in medicine, holding potential to cure severe chronic conditions rather than merely manage symptoms [81]. The development of these innovative therapies necessitates an evolution in clinical trial design and evidence generation. Unlike conventional pharmaceuticals, ATMPs often target rare disorders, involve complex, living biological systems, and aim for durable, if not curative, effects [81] [98]. This unique profile creates significant challenges for clinical development, including small patient populations, impracticality of blinding, and the need for novel endpoints to capture long-term benefits [98]. Consequently, pivotal trials for ATMPs are typically open-label, single-arm trials with small sample sizes and short follow-up durations [98]. This manuscript, framed within a broader thesis on clinical trial design for ATMP research, provides a detailed protocol for conducting comparative persistence analyses. Such analyses leverage real-world data (RWD) to complement traditional trial data, aiming to quantify the durability of treatment effects and inform value-based reimbursement decisions in an era of high-cost, potentially curative therapies.
Background and Significance
The ATMP development landscape is dynamic and fast-growing. A comprehensive analysis of clinical trials registered up to June 2015 identified 939 clinical trials investigating ATMPs, with the majority (85%) ongoing at the time and 64.3% in early phases (Phase I or I/II) [81]. The distribution of these trials by therapy category and disease area is summarized in Table 1.
Table 1: Distribution of ATMP Clinical Trials (1999-June 2015)
| Category | Number of Trials | Percentage | Primary Disease Areas (with Percentage) |
|---|---|---|---|
| Somatic Cell Therapy | 503 | 53.6% | Cancer (24.8%), Cardiovascular (19.4%) |
| Tissue-Engineered Products | 214 | 22.8% | Musculoskeletal (10.5%) |
| Gene Therapy | 210 | 22.4% | Immune System/Inflammation (11.5%), Neurology (9.1%) |
| Combined ATMPs | 12 | 1.2% | Various |
This promising pipeline, however, faces a critical challenge at the market access stage. Regulatory agencies, acknowledging the high unmet need and novelty of ATMPs, may grant marketing authorization based on limited evidence from single-arm studies using surrogate endpoints [98]. In contrast, Health Technology Assessment (HTA) bodies and payers are more conservative, citing uncertainties surrounding curative potential, magnitude and durability of clinical benefits, and long-term unfavorable effects [98]. This evidence gap between regulators and payers can hinder patient access and challenge the sustainability of healthcare budgets.
For ATMPs, where a primary component of their value proposition is long-term disease modification or cure, persistence of treatment effect is a paramount concern. Traditional clinical trials, with their relatively short follow-up, are ill-equipped to fully characterize this aspect. Comparative Persistence Analysis, using robust methodologies applied to RWD, is therefore not merely supplementary but essential for confirming the long-term value of ATMPs, satisfying payer requirements, and securing sustainable patient access.
Key Methodologies in ATMP Clinical Development
The distinct nature of ATMPs has driven the adoption of novel clinical trial methodologies. Understanding these is crucial for designing complementary real-world studies.
Table 2: Common and Innovative Clinical Trial Designs in ATMP and Immuno-Oncology Research
| Trial Design Category | Key Characteristics | Application in ATMP/IO Research |
|---|---|---|
| Non-Randomized/Single-Arm | Open-label, no concurrent control group; often uses historical controls [99] [98]. | Common for pivotal ATMP trials due to small populations, lack of standard therapy, and ethical concerns with randomization [98]. |
| Adaptive Designs | Pre-planned modifications based on interim data (e.g., sample size re-estimation, arm dropping) [100]. | Improves efficiency and ethics; allows re-allocation of resources to most promising subpopulations or doses [81] [100]. |
| Biomarker-Adapted Designs | Treatment allocation is based on patients' biomarker status [101]. | Informs personalized combination immunotherapy; identifies patients most likely to benefit from specific regimens [101]. |
| Master Protocol Designs | Umbrella, basket, or platform trials that evaluate multiple therapies/diseases under a single protocol [100]. | Efficiently addresses the high development complexity and cost of ATMPs and novel immunotherapies [102]. |
Experimental Protocol: Biomarker-Driven Patient Allocation in Immuno-Oncology
The following protocol, inspired by the ADVISE trial, details a methodology for rapid, biomarker-informed treatment allocation, relevant for ATMP combination therapies [101].
Protocol Title: Rapid Integral Biomarker Program for Patient Allocation in Advanced Therapy Trials.
1. Objective: To enable treatment allocation within 12 business days based on baseline tumor biopsy immunohistochemistry (IHC) analysis of predefined immune markers.
2. Materials and Reagents:
- Tumor Tissue Sample: Fresh or archival FFPE tumor block.
- Antibody Panel: Primary antibodies for CD8, CSF1R, GITR, IDO1, LAG3, NKp46, FOXP3, PD-L1.
- IHC Staining Kit: Automated IHC staining system with detection kit.
- Microscopy & Analysis: Brightfield microscope with image analysis software.
3. Procedure:
- Step 1: Tissue Processing. Section the FFPE tumor block to 4-5 μm thickness and mount on slides.
- Step 2: Immunohistochemistry. Perform IHC staining according to manufacturer's protocols for the predefined antibody panel.
- Step 3: Pathologist Review & Scoring. A certified pathologist reviews and scores each marker for expression level and spatial distribution (e.g., tumor cell, immune cell).
- Step 4: Data Integration & Algorithm Application. Input scored biomarker data into a pre-specified treatment selection algorithm. The algorithm maps biomarker profiles to predefined combination therapy arms.
- Step 5: Treatment Allocation. Assign the patient to the combination therapy regimen indicated by the algorithm output.
4. Quality Control: Include positive and negative control tissues in each IHC run. All steps are performed in a CAP/CLIA-certified laboratory.
Biomarker-Driven Treatment Allocation Workflow
Protocol for Comparative Persistence Analysis
This core protocol outlines a structured approach for comparing the long-term persistence of treatment effects between an ATMP and a standard of care (SoC) using RWD.
Study Design and Data Source
- Design: A retrospective, longitudinal, propensity score-matched cohort study.
- Data Source: Use large, linkable, national or regional registries specific to the disease area (e.g., cancer registries) or comprehensive electronic health record (EHR) databases. Data should include patient demographics, clinical characteristics, treatment history, and long-term outcomes.
Key Definitions and Endpoints
- Persistence of Effect: The maintenance of clinical benefit over time, operationalized through multiple endpoints.
- Primary Endpoint: Treatment-Free Survival (TFS), defined as the time from initial therapy to the need for a subsequent systemic therapy or death. This is a composite endpoint capturing both efficacy and durability.
- Secondary Endpoints:
- Overall Survival (OS): Time from therapy to death from any cause.
- Progression-Free Survival (PFS): Time from therapy to disease progression or death. In metastatic renal cell carcinoma, PFS at 3 and 6 months has been shown to predict OS, suggesting its utility as an intermediate endpoint [103].
- Duration of Response (DoR): Time from initial response to disease progression.
Experimental Protocol: Longitudinal Outcomes Analysis
1. Objective: To compare long-term clinical outcomes, including Treatment-Free Survival and Overall Survival, between patients treated with an ATMP and a matched cohort treated with SoC.
2. Materials and Reagent Solutions:
Table 3: Essential Materials for Analysis
| Item | Function/Description |
|---|---|
| Curated RWD Repository | Database containing structured EHR, claims, and/or registry data with validated outcome fields. |
| Statistical Software (R/Python) | Platform for data management, propensity score matching, and survival analysis. |
| Clinical Data Models (e.g., OMOP CDM) | Standardized data model to harmonize variables across different data sources. |
3. Procedure:
- Step 1: Cohort Identification. Identify all patients in the database who received the ATMP (index cohort) and all eligible patients who received the SoC (potential comparator cohort) within a specified time frame.
- Step 2: Variable Selection & Propensity Score Estimation. Define baseline characteristics for matching (e.g., age, sex, disease stage, comorbidities, prior lines of therapy). Use a logistic regression model to estimate a propensity score for each patient, representing the probability of receiving the ATMP versus SoC.
- Step 3: Matching. Perform 1:1 nearest-neighbor matching without replacement on the logit of the propensity score, using a caliper of 0.2 standard deviations. Assess match quality by checking standardized mean differences (<0.1 indicates good balance).
- Step 4: Outcome Analysis. Compare the matched cohorts using Kaplan-Meier survival analysis for TFS, OS, and PFS. Calculate hazard ratios (HR) and 95% confidence intervals (CI) using a Cox proportional hazards model, with the matched set as a stratification variable.
- Step 5: Sensitivity Analyses. Conduct analyses to assess robustness, including using different matching algorithms, incorporating immortal time bias adjustments, and analyzing pre-specified subgroups.
Comparative Persistence Analysis Workflow
Discussion and Integration into ATMP Development
The proposed Comparative Persistence Analysis protocol provides a structured framework to address critical evidence gaps for ATMPs. By leveraging RWD, this approach can generate comparative evidence on the durability of treatment effects, which is often infeasible to capture in pre-approval pivotal trials due to their limited duration and single-arm nature [98]. The use of Treatment-Free Survival as a primary endpoint is particularly relevant, as it captures both the efficacy and the sustainability of the treatment effect, directly informing the "curative potential" often claimed for ATMPs.
Integrating these real-world analyses into the overall ATMP development plan is crucial. HTA bodies have consistently emphasized the need for post-launch evidence generation to confirm long-term effectiveness and safety [98]. A proactive plan for Comparative Persistence Analysis should be outlined early in dialogues with regulators and payers. Furthermore, the establishment of centralized disease or product registries is highly recommended over sponsor-specific registries, as they streamline data collection, improve quality, and allow for more robust historical comparisons [98].
In conclusion, as the ATMP field evolves towards more complex and personalized therapies, the clinical trial ecosystem must adapt in parallel. This includes embracing innovative pivotal trial designs, such as adaptive and biomarker-driven protocols, and formally integrating robust, pre-planned, comparative RWD analyses to validate the long-term value and persistence of these groundbreaking therapies.
Advanced Therapy Medicinal Products (ATMPs), encompassing gene therapies, somatic cell therapies, and tissue-engineered products, represent a paradigm shift in therapeutic interventions for complex and often untreatable conditions. Their development and regulatory approval pathways frequently utilize accelerated mechanisms to address critical unmet medical needs. Consequently, marketing authorizations (MAs) are often granted based on clinical data from trials that are smaller, shorter in duration, or less controlled than those required for traditional pharmaceuticals [75]. A review of ATMPs approved in the European Union revealed that over half of the pivotal trials supporting initial authorization were single-arm designs, and a significant majority were open-label and non-randomized [75]. This regulatory landscape places a substantial burden on post-approval evidence generation to confirm long-term efficacy, identify rare or delayed adverse events, and fully characterize the product's benefit-risk profile in a broader, real-world patient population.
This Application Note outlines structured frameworks and detailed protocols for designing and implementing robust post-approval studies for ATMPs. It is structured within the broader thesis that clinical trial design for ATMPs must be conceptualized as a continuous lifecycle, where pre-approval investigations are seamlessly connected to post-approval surveillance to ensure patient safety and therapeutic success over the long term.
Methodological Frameworks for Post-Approval Evidence Generation
A multi-faceted approach is essential for comprehensive post-approval monitoring. The following frameworks form the cornerstone of a robust post-approval strategy.
Post-Marketing Surveillance and Pharmacovigilance
Objective: To continuously monitor the safety profile of an approved ATMP within the general treatment population. Description: Unlike pre-approval clinical trials, which involve limited and controlled populations, real-world use exposes drugs to diverse patient demographics, comorbidities, and polypharmacy interactions, often revealing unexpected adverse effects [104]. Post-market surveillance, also known as Phase IV monitoring, ensures continuous assessment of a drug’s safety profile after it reaches a broader patient population [104].
- Spontaneous Reporting Systems: Pharmacovigilance systems collect safety data through spontaneous adverse event reporting databases, including the FDA's Adverse Event Reporting System (FAERS) and the European Medicines Agency’s EudraVigilance [104].
- Risk Evaluation and Mitigation Strategies (REMS): The REMS framework is a critical component in managing known or potential risks associated with high-risk drugs [104]. For ATMPs with specific safety concerns, a REMS program may include elements to ensure safe use.
Registry-Based Studies
Objective: To characterize long-term clinical outcomes in a structured, real-world patient population. Description: Registries provide a mechanism for collecting uniform data on a population defined by a particular disease, condition, or exposure to a specific product. They are particularly valuable for tracking outcomes over extended periods.
- Implementation: As exemplified by an FDA-mandated post-approval study for a transcatheter valve system, this approach leverages existing clinical registries, such as the Society of Thoracic Surgeons (STS)/American College of Cardiology (ACC) Transcatheter Valve Therapy (TVT) Registry [105]. This model can be adapted for ATMPs by establishing or linking to disease-specific registries.
- Data Collection: These studies typically collect data on device/drug success, mortality, major adverse events, and patient-reported outcomes (e.g., quality of life) at predefined intervals for up to 10 years or more [105].
Mandated Post-Authorization Safety and Efficacy Studies
Objective: To address specific residual uncertainties regarding safety or efficacy identified at the time of marketing authorization. Description: Regulatory agencies like the FDA and EMA have the authority to require sponsors to perform post-approval studies as a condition of approval [105] [106]. For ATMPs, these studies are often focused on:
- Long-term safety: Monitoring for delayed adverse events, such as malignancy related to integrating vector gene therapies.
- Durability of response: Confirming that the therapeutic effect, which may have been presented as a "cure," is maintained over many years.
- Additional efficacy endpoints: Gathering further data on clinical outcomes using endpoints that were not feasible in the initial, shorter pivotal trials.
Table 1: Key Methodological Frameworks for ATMP Post-Approval Evidence Generation
| Framework | Primary Objective | Key Data Sources | Typical Study Design |
|---|---|---|---|
| Pharmacovigilance | Detect unknown/rare adverse events | Spontaneous reports (FAERS, EudraVigilance), medical literature | Passive surveillance |
| Registry-Based Study | Long-term effectiveness & safety in routine care | Clinical registries, electronic health records (EHR), claims data | Prospective, observational cohort |
| Mandated Post-Authorization Study | Address specific regulatory questions | Primary data collection, dedicated patient follow-up | Cohort study, randomized trial (if feasible) |
| Active Surveillance | Proactively identify safety signals | Large-scale EHR, insurance claims databases | Longitudinal analysis of longitudinal data |
Detailed Experimental Protocols
The following protocols provide a template for designing specific post-approval studies for ATMPs.
Protocol 1: Long-Term Follow-Up Study for a Gene Therapy Product
1.0 Study Title: A 15-Year Prospective, Long-Term Follow-Up Study of [Product Name] in Patients with [Disease]. 2.0 Objectives:
- Primary: To characterize the long-term safety of [Product Name], with a focus on delayed adverse events.
- Secondary: To assess the persistence of the therapeutic effect and vector presence over 15 years. 3.0 Study Design: A multicenter, prospective, observational cohort study. 4.0 Study Population:
- Inclusion Criteria: All patients who received [Product Name] in any prior clinical trial or through commercial use.
- Sample Size: All available patients (intention-to-treat population). 5.0 Study Procedures and Schedule:
- Visits: Annual visits for clinical assessment, laboratory tests, and imaging as appropriate for the disease and known risks.
- Biomarker Sampling: Annual blood sampling to assess vector persistence and immunogenicity. 6.0 Endpoints:
- Safety Endpoints: Incidence and severity of adverse events, new malignancies, replication-competent virus, and insertional mutagenesis events.
- Efficacy Endpoints: Disease-specific survival, event-free survival, and quality of life metrics.
Protocol 2: Registry-Based Real-World Effectiveness Study
1.0 Study Title: A Registry-Based, Post-Approval Study of the Real-World Use and Effectiveness of [ATMP Name] in the [Disease-Specific] Registry. 2.0 Objectives: To characterize real-world clinical outcomes and utilization patterns. 3.0 Study Design: Retrospective and prospective analysis of data from the [Disease-Specific] Registry. 4.0 Study Population: All patients entered into the registry and treated with the [ATMP Name] for the first 2 years following device approval or a total of 500 consecutively treated patients, whichever is greater [105]. 5.0 Data Collection: Data will be extracted from the registry and supplemented with claims data for long-term endpoint tracking. 6.0 Endpoints:
- Primary Endpoints: Overall survival, disease progression, and major adverse event rates at 30 days, 1 year, and annually up to 10 years [105].
- Secondary Endpoints: Hospitalization rates, quality of life scores, and healthcare resource utilization.
The Scientist's Toolkit: Essential Reagents and Materials
Successful post-approval studies rely on specialized tools and materials for data collection, analysis, and monitoring.
Table 2: Key Research Reagent Solutions for Post-Approval Studies
| Item/Category | Function/Application | Specific Examples / Notes |
|---|---|---|
| Electronic Data Capture (EDC) System | Centralized data collection from multiple study sites; ensures data integrity and quality. | Commercial EDC platforms compliant with 21 CFR Part 11. |
| Biomarker Assay Kits | Monitor vector persistence, immunogenicity, and potential biological events (e.g., malignancy). | qPCR assays for vector sequences, ELISA for anti-transgene antibodies. |
| Patient-Reported Outcome (PRO) Tools | Capture data on quality of life, symptoms, and functional status directly from patients. | Validated disease-specific instruments (e.g., Kansas City Cardiomyopathy Questionnaire - KCCQ) [105]. |
| Clinical Registry Access | Provides a pre-existing infrastructure for patient enrollment and standardized data collection. | Disease-specific registries (e.g., STS/ACC TVT Registry for cardiovascular devices) [105]. |
| Data Visualization & Analytics Software | Perform ongoing quality checks, identify erroneous data, and analyze key endpoints in near real-time. | Interactive platforms for generating Tables, Listings, and Figures (TLFs) [107]. |
Data Management, Analysis, and Visualization
Robust data management and clear visualization are critical for interpreting complex long-term data and meeting regulatory standards.
Data Handling and Quality Control
- Centralized Monitoring: Implementing an interactive erroneous data platform can identify potential outlying study sites, patients, or countries by performing ongoing quality checks on all collected trial data [107].
- Standardized Outputs: The use of standard Tables, Listings, and Figures (TLFs)—covering demographics, medical history, and adverse events—allows project teams to review study progress in near real-time [107].
Visualizing the Post-Approval Strategy Workflow
The following diagram illustrates the integrated strategy for post-approval evidence generation for an ATMP.
Visualizing Long-Term Patient Follow-Up
For individual studies, particularly long-term follow-up protocols, patient journey and data collection points must be clearly defined.
Regulatory and Industry Considerations
Navigating the regulatory environment is a critical component of post-approval evidence generation.
- Regulatory Authority: Agencies like the FDA and EMA can require post-approval studies at the time of approval [105] [106]. A sponsor’s failure to comply with any post-approval requirement may be grounds for withdrawing approval [106].
- Reporting Categories for Changes: Post-approval manufacturing changes (Chemistry, Manufacturing, and Controls - CMC) are categorized by their potential impact. These include Prior Approval Supplement (substantial potential for adverse effect), Changes Being Effected (CBE) Supplement (moderate potential), and Annual Report (minimal potential) [106].
- Emerging Methodologies: The field is evolving with advancements in Real-World Evidence (RWE) and Artificial Intelligence (AI). AI-driven signal detection tools are improving the efficiency of identifying adverse drug reactions in large datasets, while RWE provides more comprehensive safety insights compared to traditional reporting systems [104]. Global collaboration among regulatory agencies also strengthens post-market surveillance through initiatives like the International Council for Harmonisation (ICH) [104].
Advanced Therapy Medicinal Products (ATMPs), encompassing gene therapies, somatic cell therapies, and tissue-engineered products, represent a paradigm shift in treating complex diseases [81]. Their potential to address high-unmet medical needs, particularly in oncology, rare genetic disorders, and musculoskeletal conditions, is counterbalanced by development complexities and premium pricing [108] [5]. Health economic evaluation provides the critical framework to demonstrate the value of these high-cost interventions, ensuring sustainable patient access amidst growing healthcare budget pressures [109]. These evaluations are intrinsically linked to the unique clinical development pathways of ATMPs, which often rely on accelerated approvals based on smaller, single-arm trials, creating significant evidence uncertainty at launch [5] [75]. This application note details protocols for conducting robust economic evaluations within this context, providing methodologies tailored to the evidence constraints of advanced therapies.
Quantitative Landscape of Advanced Therapy Development
The clinical pipeline for ATMPs is expanding rapidly, with a pronounced focus on specific therapeutic areas. Understanding this distribution is essential for anticipating future economic challenges and prioritizing health technology assessment (HTA) resources.
Table 1: Global ATMP Clinical Trial Pipeline by Therapeutic Area (Data synthesized from [81] and [110])
| Therapeutic Area | Percentage of ATMP Trials | Representative Conditions Targeted |
|---|---|---|
| Oncology | 24.8% | Hematological malignancies, solid tumors |
| Cardiovascular Diseases | 19.4% | Heart failure, peripheral artery disease |
| Musculoskeletal | 10.5% | Cartilage defects, osteoarthritis |
| Immune System & Inflammation | 11.5% | Rheumatoid arthritis, graft-versus-host disease |
| Neurology | 9.1% | Spinal muscular atrophy, Parkinson's disease |
| Ophthalmology | Not Specified | Leber congenital amaurosis, corneal burns |
| Other (GI, Diabetes, Pulmonology) | 24.7% | Diabetes, wounds, ulcers, pulmonary diseases |
Table 2: Methodological Characteristics of Pivotal Trials Supporting ATMP Marketing Authorization in the EU (Data from [5] [75])
| Trial Design Characteristic | Gene Therapy Trials (n=14) | Cell & Tissue Therapy Trials (n=9) | Overall ATMP Trials (n=23) |
|---|---|---|---|
| Single-Arm Design | 78.6% | 22.2% | 56.5% |
| Use of Historical Control | 42.9% | 11.1% | 30.4% |
| Active or Placebo Control | 0% | 66.7% | 30.4% |
| Randomized | 14.3% | 75.0% | 39.1% |
| Open-Label | 100.0% | 77.8% | 91.3% |
| Primary Endpoint (Intermediate/Surrogate) | >75% | Not Specified | 78.3% |
| Median Number of Patients | ~22-41 | ~75-212 | 75 (Overall IQR: 22-118) |
Experimental Protocols for Value Assessment
The following protocols provide a structured methodology for generating and synthesizing evidence for the health economic evaluation of ATMPs.
Protocol 1: Building a Partitioned Survival Model for ATMP Cost-Effectiveness Analysis
Objective: To construct a decision-analytic model comparing the long-term costs and health outcomes of an ATMP versus standard of care (SoC).
Materials:
- Modeling Software: Excel with VBA, R (
heemodpackage), or specialized software (TreeAge, DISMOD-II). - Clinical Inputs: Overall survival (OS) and progression-free survival (PFS) Kaplan-Meier curves from the pivotal trial.
- Utility Weights: Health-related quality of life (HRQoL) data, preferably from the trial (e.g., EQ-5D).
- Cost Data: Drug acquisition, administration, monitoring, management of adverse events, and subsequent therapy costs.
Methodology:
- Model Structure: Develop a partitioned survival model with three mutually exclusive health states: Progression-Free, Progressed, and Death. The model cycle length should be chosen to reflect the disease natural history (e.g., 1 month).
- Extrapolation of Survival Curves:
- Digitize Kaplan-Meier curves from the clinical trial report for both the ATMP and SoC arms.
- Fit standard parametric survival distributions (e.g., Weibull, Log-Logistic, Gompertz) to the digitized data.
- Select the best-fitting model based on statistical (Akaike/Bayesian Information Criterion) and clinical plausibility criteria, validating against external data or clinical expert opinion.
- Populating the Model:
- Assign costs and utility values to each health state.
- The ATMP arm should include its one-time cost in the first cycle.
- SoC costs are applied per model cycle based on the treatment regimen.
- Utility weights are multiplied by the time spent in each state to calculate Quality-Adjusted Life Years (QALYs).
- Analysis:
- Run the model over a lifetime horizon (e.g., 50 years) or until all patients have died.
- Calculate total costs and total QALYs for each intervention.
- The primary output is the Incremental Cost-Effectiveness Ratio (ICER): (CostATMP - CostSoC) / (QALYATMP - QALYSoC).
- Conduct deterministic and probabilistic sensitivity analyses to assess parameter uncertainty.
Protocol 2: Implementing a Managed Entry Agreement (MEA)
Objective: To design a risk-sharing agreement between a manufacturer and payer/purchaser to facilitate patient access to an ATMP despite evidence uncertainty or high cost.
Materials:
- HTA Dossier: Containing the initial economic evaluation with identified evidence gaps.
- Outcome Definitions: Pre-specified, measurable clinical endpoints or utilization criteria.
- Data Infrastructure: Secure system for data collection (e.g., patient registry, electronic health records).
Methodology:
- Evidence Gap Analysis: Identify key uncertainties in the HTA dossier, such as long-term durability of response, effect in subpopulations, or impact on real-world clinical practice.
- Agreement Type Selection:
- Finance-Based: Confidential discounts, price-volume agreements, or expenditure caps.
- Performance-Based (Outcome-Based): Link reimbursement to achievement of pre-defined outcomes. This requires: a. Define Outcomes: Specify measurable endpoints (e.g., survival at 24 months, biomarker response at 12 months). b. Data Collection Plan: Establish a protocol for collecting outcome data from treating centers. c. Payment Terms: Outline financial consequences if outcomes are not met (e.g., partial/full refund).
- Stakeholder Engagement: Establish a governance committee with representatives from the manufacturer, payer, and clinical centers to oversee agreement execution, data verification, and conflict resolution.
- Implementation and Monitoring:
- Execute contracts and train clinical sites on data entry requirements.
- Monitor data completeness and quality periodically.
- At the pre-specified timepoint, analyze collected outcomes and execute financial reconciliation per the agreement terms.
Protocol 3: Generating and Synthesizing Real-World Evidence (RWE)
Objective: To collect and analyze real-world data (RWD) on ATMPs to supplement clinical trial evidence for long-term economic evaluations.
Materials:
- Data Sources: Electronic Health Records (EHRs), claims databases, or purpose-built patient registries.
- Data Dictionary: Standardized definitions for clinical outcomes, resource use, and HRQoL measures.
- Statistical Software: R, Python, or SAS for data analysis.
Methodology:
- Study Design: Define a protocol for an observational cohort study comparing patients receiving the ATMP with a matched historical or concurrent control cohort receiving SoC.
- Data Collection:
- Extract RWD on patient demographics, clinical outcomes (e.g., overall survival, disease progression), healthcare resource utilization (hospitalizations, concomitant medications), and safety events.
- Prospective collection of patient-reported outcomes (PROs) is ideal for HRQoL data.
- Statistical Analysis:
- Use propensity score matching or regression adjustment to control for confounding factors between the ATMP and control cohorts.
- Analyze time-to-event endpoints (e.g., survival) using Kaplan-Meier curves and Cox proportional hazards models.
- Compare healthcare costs between the matched cohorts over a defined follow-up period.
- The synthesized RWE can be used to validate or recalibrate the long-term extrapolations in the partitioned survival model (Protocol 1).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Health Economics and Outcomes Research (HEOR) in ATMPs
| Item / Solution | Function / Application |
|---|---|
R / Python with heemod, survival packages |
Open-source platforms for building and running complex decision-analytic models and survival analyses. |
| Patient Registries | Prospective, structured data collection systems for tracking long-term outcomes of ATMP patients in a real-world setting. |
| EQ-5D Questionnaire | Standardized instrument for measuring health-related quality of life, used to generate utility weights for QALY calculation. |
| Propensity Score Matching Algorithms | Statistical method to reduce selection bias in non-randomized RWE studies by creating comparable treatment and control groups. |
| Digitization Software (e.g., WebPlotDigitizer) | Extracts numerical data from published Kaplan-Meier survival curves for use in model extrapolation. |
Visualizing Value Assessment and Trial Design Workflows
The following diagrams map the logical workflows for value assessment and clinical evidence generation for ATMPs.
Diagram 1: Value Assessment Workflow for ATMPs. This diagram outlines the pathway from identifying evidence gaps in ATMP trials to implementing methodologies that address uncertainty for reimbursement decisions.
Benchmarking against Standard of Care (SoC) is a fundamental yet methodologically challenging aspect of clinical development for Advanced Therapy Medicinal Products (ATMPs). These innovative therapies, which include gene therapies, somatic cell therapies, and tissue-engineered products, often target rare diseases and conditions with high unmet medical needs [5] [12]. This clinical context frequently precludes the use of traditional randomized controlled trial (RCT) designs, making cross-trial comparisons with external controls a necessary alternative for establishing therapeutic value.
The inherent heterogeneity of SoC presents significant interpretive challenges. Usual care can differ substantially for the same condition between patients and practitioners, across clinical sites, and over time [111]. This variability can undermine the validity of comparative assessments if not properly accounted for in trial design and analysis. Furthermore, ATMPs are often approved based on small, open-label, single-arm pivotal trials using intermediate endpoints and historical controls [5], which increases the uncertainty about the product's benefit-risk balance at the time of marketing authorization.
This application note provides structured methodologies and analytical frameworks to enhance the rigor and interpretability of cross-trial comparisons in ATMP research, addressing a critical need for standardized approaches in this evolving field.
Methodological Framework for Defining Standard of Care Comparators
Conceptual Foundation
The term "Standard of Care" implies consistency in practice, but in reality, it encompasses a spectrum of treatments that may vary substantially. When designing a trial, researchers must decide between an "unrestricted" usual care comparator (accepting existing heterogeneity) or a "defined" usual care comparator (specifying treatments at trial onset) [111]. Each approach involves distinct trade-offs between external validity and interpretability.
Decision Drivers for SoC Comparator Design:
- Context Drivers: Understanding the implementation environment, including existing care practices, clinical guidelines, and characteristics of the target population [111]
- Trial Drivers: Addressing trial requirements including ethical obligations, methodological robustness, feasibility constraints, and stakeholder acceptability [111]
A methodology review identified that the content of a SoC comparator should be informed by trial aims, existing care practices, clinical guidelines, and population characteristics, while also fulfilling requirements to protect participants, inform practice, and maintain methodological integrity [111].
Operational Protocol: Defining SoC Comparators
Protocol 1: Systematic SoC Assessment and Definition
Objective: To establish a reproducible methodology for defining appropriate SoC comparators for ATMP trials.
Materials:
- Clinical practice guidelines from relevant professional societies
- Recent systematic reviews of interventions for the target condition
- Treatment pattern studies using healthcare claims data
- Expert consensus panels including clinical specialists
- Patient representatives to assess acceptability of care approaches
Procedure:
- Conduct systematic documentation of current practices
- Perform retrospective chart reviews across multiple centers (minimum 3-5 representative sites)
- Analyze regional and temporal variations in care pathways
- Document concomitant therapies and supportive care standards
Map evidence-based care guidelines
- Identify current clinical practice guidelines from authoritative sources
- Assess strength of evidence supporting guideline recommendations
- Document recommended monitoring and assessment protocols
Constitute multidisciplinary definition panel
- Include clinical specialists, methodologies, and patient representatives
- Review systematic documentation and guideline evidence
- Reach consensus on "defined" SoC elements through modified Delphi process
Establish monitoring framework
- Develop checklist for tracking SoC delivery throughout trial
- Plan interim assessments of protocol adherence
- Document deviations and adaptations in SoC implementation
Output: A clearly defined SoC protocol specifying interventions, monitoring schedules, and modification criteria, with documentation of expected versus actual care delivery.
Analytical Approaches for Cross-Trial Comparisons
Statistical Methods for Comparative Effectiveness
Cross-trial comparisons require careful statistical adjustment to address confounding and bias. The partitioned survival model represents one validated approach for estimating long-term comparative effectiveness when direct randomized comparisons are unavailable [112].
Protocol 2: Partitioned Survival Modeling for Comparative Effectiveness
Objective: To estimate long-term life years (LYs) and quality-adjusted life years (QALYs) for ATMPs compared to SoC using available clinical trial data.
Materials:
- Index trial data for the ATMP (e.g., larotrectinib trial dataset)
- Published survival data for SoC from relevant clinical trials or registries
- Utility weights for health states from published literature or primary data collection
- Statistical software with survival analysis capabilities (R, SAS, or Stata)
Procedure:
- Parametric survival modeling
- Fit multiple survival distributions (Exponential, Weibull, Log-logistic, Lognormal) to progression-free survival (PFS) and overall survival (OS) data
- Select optimal distribution based on goodness-of-fit statistics (AIC, BIC) and clinical plausibility
- Validate model projections against available observed data
Extrapolate long-term outcomes
- Project survival curves beyond trial observation period using selected distributions
- Calculate life-years gained by integrating area under survival curves
- Conduct sensitivity analyses around extrapolation assumptions
Quality-of-life adjustment
- Apply utility weights to time spent in pre-progression and post-progression health states
- Calculate QALYs by summing utility-weighted survival time
- Incorporate uncertainty through probabilistic sensitivity analysis
Comparative analysis
- Calculate differences in LYs and QALYs between ATMP and SoC
- Generate confidence intervals around differences using bootstrapping or Bayesian methods
- Present results in format suitable for health technology assessment submissions
Application Example: In a study comparing larotrectinib to SoC for metastatic TRK fusion cancers, this approach demonstrated that patients receiving larotrectinib gained 7.15-8.26 additional LYs in thyroid cancer, 1.26-1.27 additional LYs in colorectal cancer, and 5.56 additional LYs in soft tissue sarcoma [112].
Handling Heterogeneity in SoC
The variable nature of usual care necessitates specific methodologies to account for heterogeneity in comparator arms.
Table 1: Framework for Addressing SoC Heterogeneity in Cross-Trial Comparisons
| Source of Heterogeneity | Methodological Challenge | Recommended Approach | Interpretation Consideration |
|---|---|---|---|
| Inter-site practice variation | Effect size depends on site-specific care quality | Stratified analysis by site characteristics; meta-analytic approaches | Treatment effects may be contextual to local care standards |
| Temporal trends in care | SoC may evolve during trial period | Time-dependent adjustment; sensitivity analysis excluding early participants | Historical controls may not reflect contemporary outcomes |
| Patient-level customization | SoC differs based on patient characteristics | Propensity score matching; multivariate adjustment | Differential effectiveness may exist across patient subgroups |
| Guideline updates | Standard practices change during trial | Document versioning of SoC definitions; pre-specify analysis accounting for changes | Trial results may have diminishing relevance with practice evolution |
Regulatory and Evidentiary Considerations
Evidence Standards for ATMP Approval
The evidentiary standards for ATMP approval have evolved to accommodate the unique challenges of these therapies while maintaining scientific rigor.
Table 2: Clinical Evidence Characteristics for Approved ATMPs (EU Regulatory Experience)
| Evidence Characteristic | Frequency in Approved ATMPs | Regulatory Implications | Methodological Adaptations |
|---|---|---|---|
| Single-arm trial design | 79% of approved ATMPs [5] | Increased reliance on historical controls | Robust historical control selection; quantitative bias analysis |
| Historical controls | 68% of approved ATMPs [5] | Uncertainty in comparative effectiveness | Synthetic control methods; cross-trial comparison adjustments |
| Intermediate endpoints | 74% of approved ATMPs [5] | Surrogate validation requirements | Establish surrogate relationship with final outcomes |
| Small sample sizes | 47% of trials enrolled <25 patients [12] | Limited precision for subgroup effects | Bayesian methods incorporating external data; adaptive designs |
| Open-label design | 84% of pivotal trials [5] | Potential for assessment bias | Blinded endpoint adjudication; objective outcome measures |
Protocol 3: Bias Assessment in Cross-Trial Comparisons
Objective: To systematically identify and quantify potential biases when comparing ATMP trial results to external controls.
Materials:
- PRECIS-2 tool for assessing pragmatic trial elements
- ROBINS-I tool for assessing non-randomized studies
- Trial protocols for both index and comparator studies
- Patient-level data (if available) or aggregated published results
Procedure:
- Systematic bias assessment
- Evaluate comparability of study populations using design similarity assessment
- Assess measurement consistency for endpoints across trials
- Identify potential confounding factors not adjusted for in analysis
Quantitative bias analysis
- Conduct sensitivity analyses for unmeasured confounding
- Apply quantitative methods like E-values to assess robustness to potential bias
- Evaluate impact of cross-trial differences in entry criteria and outcome assessment
Evidence triangulation
- Compare results across multiple external control sources
- Assess consistency of treatment effects across patient subgroups
- Evaluate mechanistic plausibility of observed effects
Uncertainty characterization
- Distinguish statistical uncertainty from methodological uncertainty
- Quantify confidence in comparative conclusions using structured framework
- Document limitations transparently in evidence summaries
Visualization Frameworks
SoC Definition Workflow
SoC Definition and Implementation Workflow
Cross-Trial Comparison Methodology
Cross-Trial Comparison Methodology
Research Reagent Solutions
Table 3: Essential Methodological Tools for Cross-Trial Comparisons
| Research Tool | Function | Application Context |
|---|---|---|
| Partitioned Survival Models | Extrapolate long-term outcomes from limited trial data | Health technology assessment submissions; value demonstration |
| Propensity Score Methods | Adjust for confounding in non-randomized comparisons | Comparative effectiveness research using external controls |
| Historical Control Databases | Provide context for single-arm trial results | Rare diseases with established natural history or standard care |
| Quantitative Bias Analysis | Assess robustness to unmeasured confounding | Sensitivity analysis for cross-trial comparisons |
| Evidence Triangulation Framework | Integrate multiple sources of comparative evidence | Regulatory decision-making with limited direct evidence |
| PRECIS-2 Tool | Assess pragmatic trial elements in ATMP studies | Design of trials intended to inform practice decisions |
| ROBINS-I Tool | Assess risk of bias in non-randomized studies | Critical appraisal of external comparator studies |
Benchmarking against Standard of Care through cross-trial comparisons presents both necessity and challenge in ATMP development. The methodologies outlined in this application note provide structured approaches to enhance the validity and interpretability of such comparisons. By implementing systematic processes for SoC definition, applying robust statistical methods for comparative analysis, and maintaining transparency about methodological limitations, researchers can generate more reliable evidence for decision-making in this innovative therapeutic area.
As the ATMP landscape evolves, with over 900 clinical trials currently investigating these therapies [12], the standards for evidence generation must similarly advance. Methodologically sound clinical development remains essential not only for initial approval but also for establishing the value proposition of these often high-cost therapies. The frameworks provided here represent practical approaches to address these challenges while maintaining scientific rigor.
Conclusion
The clinical trial landscape for ATMPs requires a paradigm shift from traditional drug development approaches, embracing innovative designs that balance regulatory rigor with practical feasibility. Success hinges on early engagement with evolving regulatory frameworks, strategic application of adaptive methodologies for small populations, proactive management of unique manufacturing and safety challenges, and robust validation strategies that address the limitations of single-arm designs. Future directions will likely see increased regulatory convergence between major agencies, greater integration of real-world evidence, advancement in point-of-care manufacturing models, and continued evolution of statistical methods for demonstrating comparative effectiveness. As the ATMP field matures, developing standardized yet flexible trial frameworks will be crucial for accelerating the delivery of these transformative therapies to patients while maintaining scientific validity and regulatory compliance.
References
- 1. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect On The... [https://www.clinicalsupplyleader.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 2. Releases Final EMA for Guideline Trials ATMP Clinical [https://igmpi.ac.in/news/pharma-gmp/ema-releases-final-guideline-for-atmp-clinical-trials]
- 3. Draft Regulation for Advanced Therapy Medicinal Products- Cisema [https://cisema.com/en/china-atmp-regulation-2025/]
- 4. : EU vs. US & Global ATMP Regulation Convergence [https://www.celegence.com/atmp-regulation-eu-us-global-convergence/]
- 5. Current landscape of clinical development and approval of advanced therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8626628/]
- 6. Why Regulatory Convergence is Key to Global Development of Cell and Gene Therapies - Biopharma Excellence [https://www.biopharma-excellence.com/articles/why-regulatory-convergence-is-key-to-global-development-of-cell-and-gene-therapies/]
- 7. Proposes Revisions to GMP EMA for Guideline - ECA Academy ATMPs [https://www.gmp-compliance.org/gmp-news/ema-proposes-revisions-to-gmp-guideline-for-atmps]
- 8. Advanced therapy medicinal products: Overview | European Medicines... [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview]
- 9. European Regulatory Tools for Advanced Therapy Medicinal Products - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3901598/]
- 10. Somatic cell medicinal products and therapy - tissue ... engineered [https://english.ccmo.nl/investigators/additional-requirements-for-certain-types-of-research/research-on-the-development-of-cell-therapy/scientific-research-aimed-at-the-development-of-cell-therapy/somatic-cell-therapy-medicinal-products-and-tissue-engineered-products-atmps]
- 11. Legal framework: Advanced therapies | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview/legal-framework-advanced-therapies]
- 12. Advanced therapy medicinal products: current and future perspectives [https://pubmed.ncbi.nlm.nih.gov/27123193/]
- 13. Regulatory Framework for Advanced Therapy Medicinal Products in Europe and United States - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6728416/]
- 14. Advanced Therapy Medicinal Products' Translation in Europe: A Developers' Perspective - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8851388/]
- 15. # atmp #gmp # genetherapy #celltherapy #clinicaltrials #ema... [https://www.linkedin.com/posts/biotechnologypr_atmp-gmp-genetherapy-activity-7337463419584843776--fhv]
- 16. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect: On The Verge Of Convergence? [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 17. Design and Conduct Considerations for First - in - Human Trials [https://pubmed.ncbi.nlm.nih.gov/30048046/]
- 18. Key Regulatory and Clinical Strategies for ATMPs [https://www.linkedin.com/pulse/clinical-development-strategies-pragmatic-solutions-advanced-beelke-wdace]
- 19. Five Key Considerations for Writing First - in - Human Protocols Under... [https://www.iconplc.com/insights/blog/2018/08/01/five-key-considerations-f]
- 20. Comparison of international guidelines for early - phase ... clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC8979759/]
- 21. Quantification of Adeno-Associated Virus with Safe Nucleic Acid Dyes... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7588323/]
- 22. Manufacturing and control strategies for Cell and Gene Therapy ... [https://www.parexel.com/insights/blog/manufacturing-and-control-strategies-for-cell-and-gene-therapy-products-navigating-eu-and-us-regulatory-requirements]
- 23. FDA IND CMC Requirements for Biologics: A 2025 Sponsor’s Checklist - scxcmc [https://scxcmc.com/fda-ind-cmc-requirements-for-biologics/]
- 24. Premier Research | CMC Content for Global Clinical Development of Pharmaceuticals [https://premier-research.com/perspectives/cmc-content-for-global-clinical-development-of-pharmaceuticals/]
- 25. 2024 ATMP Review - HiTech Health [https://hitech-health.com/advanced-therapeutic-medicinal-products/]
- 26. Frontiers | Implementation of a quality management system for... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1591751/full]
- 27. MHRA Issues New Regulation On Modular And Point Of Care... [https://www.cellandgene.com/doc/mhra-issues-new-regulation-on-modular-and-point-of-care-manufacture-of-atmps-0001]
- 28. Human medicines Modular Manufacture and Point ... of Care [https://www.gov.uk/government/publications/human-medicines-modular-manufacture-and-point-of-care-regulations-2025-overview/human-medicines-modular-manufacture-and-point-of-care-regulations-2025-overview]
- 29. Current challenges and future directions of ATMPs in regenerative medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 30. Advanced Therapy Trials, Early Phases: A Checklist for Drug Developers [https://pivotalcr.com/advanced-therapy-medicinal-products-atmps-are-transforming-modern-medicine/]
- 31. - Designing Clinical Single : Principles, Arm , and... Trials Applications [https://pubmed.ncbi.nlm.nih.gov/40697795/]
- 32. - Single clinical arm : trials , ethics, principles design [https://pubmed.ncbi.nlm.nih.gov/38834238/]
- 33. Estimating comparative effectiveness using Single - Arm ... trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02660-9]
- 34. Efficient Hybrid and Designing - Single : Arm ... Trials External Control [https://arxiv.org/html/2511.09353v1]
- 35. The Silent Risk of Single - Arm Trials [https://www.linkedin.com/pulse/single-arm-trial-illusion-why-faster-doesnt-mean-beelke--bwjxe]
- 36. : key features, when to use them and Platform ... trials methodological [https://www.mja.com.au/journal/2025/223/3/platform-trials-key-features-when-use-them-and-methodological-challenges]
- 37. Adaptive platform trials: definition, design, conduct and reporting considerations | Nature Reviews Drug Discovery [https://www.nature.com/articles/s41573-019-0034-3]
- 38. Recent innovations in adaptive trial designs: A review of design opportunities in translational research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10260347/]
- 39. Scholars@Duke publication: Operational Development and Launch of... [https://scholars.duke.edu/publication/1678523]
- 40. The Role of Innovative Trial Designs in Transforming Clinical Research [https://www.berryconsultants.com/resource/the-role-of-innovative-trial-designs-in-transforming-clinical-research]
- 41. Practical guidance for conducting high-quality and rapid interim... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04362-x]
- 42. Adaptive Design Clinical Trials for Drugs and Biologics Guidance for Industry | FDA [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/adaptive-design-clinical-trials-drugs-and-biologics-guidance-industry]
- 43. for evaluating the medical utility of Clinical ... trial designs prognostic [https://pubmed.ncbi.nlm.nih.gov/20383292/]
- 44. - Patient as Reported in Outcomes of... Endpoints Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC9163311/]
- 45. : Transforming Biomarkers Research and real-world... Clinical [https://www.linkedin.com/pulse/biomarkers-transforming-clinical-research-real-world-trials-kumar-pc94c]
- 46. value of plasma Prognostic for informing biomarkers ... clinical trial [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01745-3]
- 47. The importance of patient - reported in outcomes and str clinical trials [https://www.dovepress.com/the-importance-of-patient-reported-outcomes-in-clinical-trials-and-str-peer-reviewed-fulltext-article-PROM]
- 48. Can Patient - Reported Serve as Outcomes in Endpoints ? Trials [https://www.aao.org/eyenet/article/patient-reported-outcomes-as-endpoints-in-trials]
- 49. Challenges of one-year longitudinal follow-up of a prospective, observational cohort study using an anonymised database: recommendations for trainee research collaboratives | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-019-0857-y]
- 50. Interim analysis of continuous long-term endpoints in clinical trials with longitudinal outcomes - PubMed [https://pubmed.ncbi.nlm.nih.gov/12754715/]
- 51. Recommendations for the Primary Analysis of Continuous Endpoints in Longitudinal Clinical Trials | Therapeutic Innovation & Regulatory Science [https://link.springer.com/article/10.1177/009286150804200402]
- 52. - CAR cell therapy T : global progress, challenges, and... clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129935/]
- 53. Systematic Review on CAR-T Cell Clinical Trials Up to 2022: Academic Center Input - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9954171/]
- 54. Emerging advances in CAR - T therapy for solid tumors: latest clinical ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01760-9]
- 55. Frontiers | CAR - T cell therapies in autoimmune rheumatic diseases... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1630569/full]
- 56. Phase I CAR-T Clinical Trials Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10132085/]
- 57. EHA 2025 Insights: CARTITUDE-4 Trial Updates On CAR ... | OncLive [https://www.onclive.com/view/eha-2025-insights-cartitude-4-trial-updates-on-car-t-in-early-r-r-mm]
- 58. Next-day manufacture of a novel anti-CD19 CAR - T therapy for B-cell... [https://www.nature.com/articles/s41408-022-00694-6?error=cookies_not_supported&code=26e21934-ebde-4f9e-828b-4e1723ddbace]
- 59. CD19 CAR - T in relapsed t(8;21) AML: a single-center prospective... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01708-z]
- 60. and optimizing Designing -mediated AAV for... gene therapy [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05661-2]
- 61. Advances in Cell and Gene and the Evolving Therapy Landscape... AAV [https://www.linkedin.com/pulse/advances-cell-gene-therapy-evolving-aav-landscape-oxu3e]
- 62. Advances in Cell and Gene Therapy and the Evolving AAV Landscape in 2025 H1 | PackGene Biotech [https://www.packgene.com/learning-center/advances-in-cell-and-gene-therapy-and-the-evolving-aav-landscape-in-2025-h1/]
- 63. Current clinical applications of AAV-mediated gene therapy - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S152500162500365X]
- 64. Frontiers | Human Immune Responses to Adeno-Associated Virus... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00670/full]
- 65. Structural characterization of a novel human... | Nature Communications [https://www.nature.com/articles/s41467-020-17047-1?error=cookies_not_supported&code=4ca71e9d-4aa4-4742-8330-1cd6e769bb74]
- 66. - CLOVER Center AAV Vector Engineering [https://clover.caltech.edu/aav]
- 67. 2025 Forecast For Advanced Therapies [https://www.cellandgene.com/doc/2025-forecast-for-advanced-therapies-0001]
- 68. Prospective approaches to gene therapy computational modeling – spotlight on viral gene therapy | Journal of Pharmacokinetics and Pharmacodynamics [https://link.springer.com/article/10.1007/s10928-023-09889-1]
- 69. Current Status and Challenges Associated with CNS -Targeted Gene ... [https://pubmed.ncbi.nlm.nih.gov/33334049/]
- 70. Frontiers | Skeleton keys and Trojan horses: a review of therapeutic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1674333/full]
- 71. Advances in brain - targeted delivery strategies and natural... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12107825/]
- 72. Frontiers | Significance of gene in neurodegenerative diseases therapy [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1515255/full]
- 73. Exosome-powered neuropharmaceutics: unlocking the blood-brain... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03352-8]
- 74. Regulatory Framework for Advanced Therapy Medicinal Products in Europe and United States - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6728416/]
- 75. Frontiers | Methodological Characteristics of Clinical Trials Supporting the Marketing Authorisation of Advanced Therapies in the European Union [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.773712/full]
- 76. or CRS Are Rare Beyond 2 Weeks After Lisocabtagene... ICANS [https://pubmed.ncbi.nlm.nih.gov/41235976/]
- 77. Reducing the Risks: Managing CRS , ICANS , and... | Pharmacy Times [https://www.pharmacytimes.com/view/reducing-the-risks-managing-crs-icans-and-skin-reactions-in-emerging-lung-cancer-therapies]
- 78. Understanding CRS and ICANS : Real-World Incidence and... | AJMC [https://www.ajmc.com/view/understanding-crs-and-icans-real-world-incidence-and-key-patient-risk-factors]
- 79. Expert Perspectives in Monitoring and Management... | OncLive [https://www.onclive.com/view/expert-perspectives-in-monitoring-and-management-strategies-for-crs-icans-and-other-long-term-toxicities-associated-with-car-t-cell-therapy]
- 80. Considerations driving the choice in clinical trial design of cell and gene therapy products: weighing convenience versus necessity - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1465324925007388]
- 81. Advanced therapy medicinal products: current and future perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846788/]
- 82. New guidelines on good manufacturing practices for advanced therapies | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/news/new-guidelines-good-manufacturing-practices-advanced-therapies]
- 83. Term Definitions — Good Manufacturing Practice Facility [https://health.ucdavis.edu/stemcellresearch/gmp/terms.html]
- 84. Top GMP Guidelines and Best for Practices - JAF Consulting, Inc. 2025 [https://jafconsulting.com/top-gmp-guidelines-and-best-practices-for-2025/]
- 85. PPT - Good ( Manufacturing ), Good Laboratory... Practices GMP [https://www.slideserve.com/mabli/good-manufacturing-practices-gmp-good-laboratory-practices-glp-and-good-tissue-practices-gtp]
- 86. Research Essentials: GCP vs GMP vs GLP Clinical Trials Regulations [https://revivalresearch.org/blogs/gcp-vs-gmp-vs-glp-clinical-trials-regulations/]
- 87. A comparison of interventional clinical trials in rare versus non- rare ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-014-0170-0]
- 88. A comparison of interventional clinical trials in rare versus non- rare ... [https://pubmed.ncbi.nlm.nih.gov/25427578/]
- 89. - The Power of AI in Overcoming CLINICAL ... TRIALS Patient Diversity [https://drug-dev.com/clinical-trials-the-power-of-ai-in-overcoming-patient-diversity-challenges/]
- 90. , equity and inclusion in Diversity : Beyond... rare disease clinical trials [https://www.iconplc.com/insights/therapeutics/rare-and-orphan-diseases/diversity-equity-and-inclusion-in-rare-disease-trials]
- 91. and Transduction of Viral Vectors for... Efficiency Immunogenicity [https://pmc.ncbi.nlm.nih.gov/articles/PMC8435788/]
- 92. and Analysis Strategies for the Development of Clinical ... Design Gene [https://pubmed.ncbi.nlm.nih.gov/33666225/]
- 93. Optimizing viral transduction in immune cell therapy manufacturing... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06524-0]
- 94. Single-arm clinical trials: design, ethics, principles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11874317/]
- 95. - Single as pivotal evidence: Key considerations... :: Parexel arm trials [https://www.parexel.com/insights/blog/single-arm-trials-as-pivotal-evidence-key-considerations-and-implications-for-drug-developers]
- 96. Assessing the risk of bias in single - arm for systematic reviews... trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884709/]
- 97. Quantitative Bias for Analysis - Single With External... Arm Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947839/]
- 98. ISPOR - The Evaluation of Pivotal Trials for Advanced ... Therapies [https://www.ispor.org/publications/journals/value-outcomes-spotlight/vos-archives/issue/view/challenges-in-precision-medicine-aiming-to-align-data-value-and-costs/the-evaluation-of-pivotal-trials-for-advanced-therapies-from-regulatory-and-health-technology-assessment-perspectives-in-europe]
- 99. Clinical trial designs - EUPATI Toolbox [https://toolbox.eupati.eu/resources/clinical-trial-designs/]
- 100. Recent innovations in adaptive trial designs: A review of design opportunities in translational research | Journal of Clinical and Translational Science | Cambridge Core [https://www.cambridge.org/core/journals/journal-of-clinical-and-translational-science/article/recent-innovations-in-adaptive-trial-designs-a-review-of-design-opportunities-in-translational-research/614EAFEA5E89CA035E82E152AF660E5D]
- 101. Rationale and feasibility of a rapid integral biomarker program that informs immune-oncology clinical trials: the ADVISE trial - PubMed [https://pubmed.ncbi.nlm.nih.gov/40389374/]
- 102. A SITC vision: adapting clinical trials to accelerate drug development in cancer immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931932/]
- 103. - Progression as a Predictor of Free in... Survival Overall Survival [https://pmc.ncbi.nlm.nih.gov/articles/PMC3856357/]
- 104. What Happens When Drugs Fail Post - Approval ? [https://www.news-medical.net/life-sciences/What-Happens-When-Drugs-Fail-Post-Approval.aspx]
- 105. - Post (PAS) Database Approval Studies [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma_pas.cfm?t_id=846858&c_id=8462]
- 106. CMC , POST CHANGES.pptx APPROVAL [https://www.slideshare.net/slideshow/cmc-post-approval-changespptx/257153478]
- 107. Clinical Data Visualizations | Tables Listings Figures (TLFs) [https://www.quanticate.com/visualizations]
- 108. Trends: GLP-1 & Rising 2025 Healthcare Costs [https://www.linkedin.com/pulse/2025-health-care-trends-glp-1-drugs-costs-more-rodney-mattos-ec4yc]
- 109. Frontiers | Driving the future of value-based healthcare in the Gulf... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1667846/full]
- 110. Top therapeutic categories by number of R&D products 2025 | Statista [https://www.statista.com/statistics/791346/top-therapies-worldwide-by-number-of-r-and-d-products/]
- 111. Defining usual care comparators when designing pragmatic trials of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10860249/]
- 112. The potential long-term comparative effectiveness of larotrectinib vs... [https://pubmed.ncbi.nlm.nih.gov/35362337/]