Direct Lineage Conversion Using Modified mRNA: A Non-Integrative Strategy for Cell Reprogramming and Regenerative Medicine
This article explores the transformative potential of modified mRNA (modRNA) technology in direct lineage conversion, a process that directly reprograms one specialized cell type into another without reverting to a...
Direct Lineage Conversion Using Modified mRNA: A Non-Integrative Strategy for Cell Reprogramming and Regenerative Medicine
Abstract
This article explores the transformative potential of modified mRNA (modRNA) technology in direct lineage conversion, a process that directly reprograms one specialized cell type into another without reverting to a pluripotent state. Tailored for researchers, scientists, and drug development professionals, we examine the foundational principles that enable modRNA to overcome the instability and immunogenicity of conventional mRNA. The scope encompasses the methodology of synthetic mRNA design and delivery, its application in generating induced pluripotent stem cells (iPSCs) and transdifferentiated therapeutic cells (such as myoblasts and neurons), and the critical optimization of factors like nucleoside modifications and lipid nanoparticles (LNPs) for efficient transfection. Finally, we provide a comparative analysis against other reprogramming methods, validating the utility of modRNA-derived cells in disease modeling, drug screening, and the future of cell-based therapies.
The Foundations of Direct Lineage Conversion: From MyoD to Modified mRNA
Defining Direct Lineage Reprogramming and its Distinction from Pluripotency
Direct lineage reprogramming, also known as transdifferentiation, represents a groundbreaking technology in regenerative medicine that enables the direct conversion of one specialized somatic cell type into another without passing through an intermediate pluripotent state [1]. This approach fundamentally challenges traditional concepts of epigenetic stability and linear cell differentiation, offering researchers a powerful tool for generating patient-specific cells for disease modeling, drug screening, and potential cell-based therapies [2]. Unlike strategies involving induced pluripotent stem cells (iPSCs), direct reprogramming avoids the ethical concerns associated with embryonic stem cells and eliminates the tumorigenic risks posed by residual pluripotent cells in therapeutic applications [3] [1].
The conceptual foundation of direct lineage reprogramming rests on the understanding that cellular identity is maintained primarily through epigenetic mechanisms rather than irreversible genetic alterations [3]. Although all nucleated somatic cells in an organism contain essentially the same genomic information, their diverse phenotypes emerge from specific patterns of gene expression governed by transcription factors, chromatin modifications, and non-coding RNAs [1]. The breakthrough discovery that somatic cells could be reprogrammed to pluripotency using defined factors (iPSC technology) demonstrated that differentiated cell states are reversible [4]. This pivotal finding paved the way for more direct conversion approaches that bypass the pluripotent intermediate altogether [2].
Key Mechanistic Distinctions: Direct Reprogramming vs. Pluripotency Reprogramming
Fundamental Differences in Process and Methodology
Table 1: Core Differences Between Direct Lineage Reprogramming and Pluripotency Reprogramming
| Feature | Direct Lineage Reprogramming | Pluripotency Reprogramming |
|---|---|---|
| Intermediate State | Bypasses pluripotent state [1] | Requires transition through pluripotent state [4] |
| Theoretical Basis | Transdifferentiation; direct conversion [1] | Dedifferentiation to pluripotency followed by differentiation [4] |
| Key Transcription Factors | Cell type-specific factors (e.g., Bmi1+FGFR2 for keratinocytes; SAPG for hair cells) [3] [5] | Pluripotency factors (OSKM: Oct4, Sox2, Klf4, c-Myc) [4] |
| Tumorigenic Risk | Lower risk, no teratoma formation [1] | Higher risk due to potential residual pluripotent cells [1] |
| Time Required | Typically faster (days to weeks) [5] | Generally slower (weeks to months) [4] |
| Efficiency | Variable, often low but improving with new methods [6] | Variable, can be enhanced with small molecules [6] |
| Epigenetic Remodeling | Targeted, lineage-specific changes [2] | Global reorganization to pluripotent state [4] |
| Therapeutic Applications | In vivo and in vitro direct conversion [3] [7] | Primarily in vitro differentiation followed by transplantation [4] |
Molecular Mechanisms and Signaling Pathways
The molecular events governing direct lineage reprogramming differ significantly from pluripotency reprogramming. While pluripotency reprogramming involves global epigenetic remodeling and activation of core pluripotency networks, direct reprogramming employs lineage-specific transcription factors that redirect the existing transcriptional machinery toward a new somatic cell fate [2]. During pluripotency reprogramming, the process follows a biphasic pattern: an early stochastic phase where somatic genes are silenced and early pluripotency genes activated, followed by a deterministic phase where late pluripotency genes are established [4]. This process involves profound metabolic alterations, mesenchymal-to-epithelial transition (MET), and global chromatin restructuring [4].
In contrast, direct reprogramming utilizes master regulator transcription factors specific to the target cell type to orchestrate a more focused epigenetic reorganization. For example, in fibroblast-to-keratinocyte reprogramming, the combination of Bmi1 and FGFR2 (B2 factors) activates the keratinocyte genetic program while suppressing the fibroblastic identity [3]. Similarly, reprogramming fibroblasts to induced hair cell-like cells employs SIX1, ATOH1, POU4F3, and GFI1 (SAPG factors) to directly activate the hair cell differentiation program [5]. The emerging understanding of epigenetic modifiers including RNA modifications such as m5C mediated by NSUN family methyltransferases further reveals additional layers of regulation in cell fate determination [8].
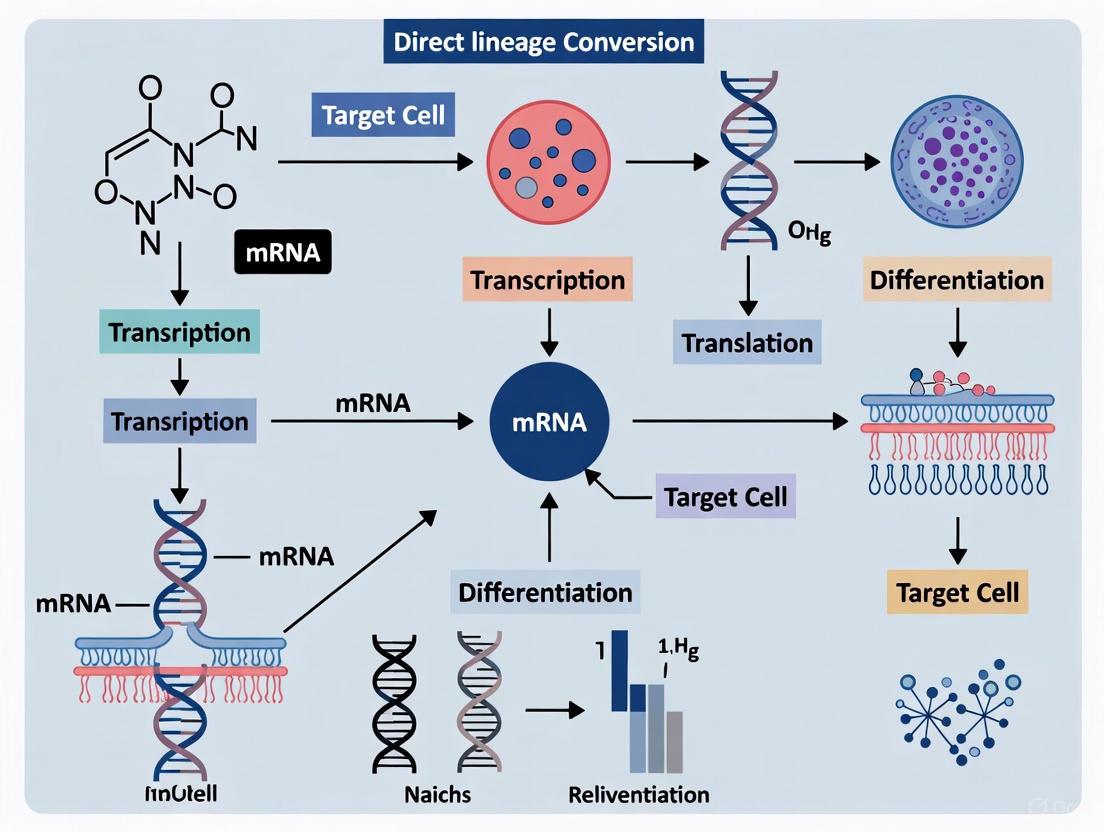
Diagram Title: Direct vs. Pluripotency Reprogramming Pathways
Experimental Protocols for Direct Lineage Reprogramming
Protocol 1: Direct Reprogramming of Fibroblasts to Keratinocyte-like Cells (iKCs) Using B2 Factors
This protocol describes the conversion of mouse fibroblasts into functional keratinocyte-like cells using BMI1 and FGFR2 (B2 combination), representing a promising approach for skin regeneration and wound healing applications [3].
Materials and Reagents:
- Source cells: Mouse fibroblasts (L929 cell line or primary mouse dermal fibroblasts)
- Reprogramming factors: BMI1 and FGFR2 genes
- Delivery vector: Adeno-associated virus serotype 9 (AAV9) vectors
- Culture media: Serum-free medium supplemented with growth factors
- Analysis tools: qRT-PCR reagents, Western blot equipment, immunofluorescence supplies
Procedure:
- Cell Preparation: Plate mouse fibroblasts at appropriate density in culture vessels and maintain in standard fibroblast growth medium until 70-80% confluent.
- Factor Delivery: Transduce cells with AAV9 vectors carrying BMI1 and FGFR2 at the following concentrations:
- AAV9-BMI1: 5.28 × 10^13 vg/mL
- AAV9-FGFR2: 1.80 × 10^13 vg/mL
- Total viral concentration: 6.64 × 10^13 vg/mL
- Culture Conditions: Maintain transduced cells in serum-free medium supplemented with specific growth factors to support keratinocyte differentiation.
- Morphological Monitoring: Observe daily for morphological changes from fibroblastic to epithelial-like appearance, typically occurring within 7-14 days.
- Functional Validation: After 2-3 weeks, analyze resulting induced keratinocyte-like cells (iKCs) for:
- Gene expression: Keratinocyte markers (keratins, involucrin) by qRT-PCR
- Protein expression: Immunofluorescence for keratinocyte-specific proteins
- Functional capacity: Barrier function assays, stratification potential
Applications: This methodology shows particular promise for treating diabetic foot ulcers, with in vivo studies demonstrating significantly promoted wound closure, reconstructed stratified epithelium, and restored barrier function in diabetic mouse models [3].
Protocol 2: Virus-Free Direct Reprogramming to Hair Cell-like Cells Using Inducible SAPG Factors
This advanced protocol generates human inner ear hair cell-like cells using a virus-free, inducible system, providing a scalable platform for hearing loss research and drug screening [5].
Materials and Reagents:
- Source cells: Human induced pluripotent stem cells (iPSCs)
- Reprogramming construct: Doxycycline-inducible cassette expressing SIX1, ATOH1, POU4F3, and GFI1 (SAPG)
- Culture media: Appropriate iPSC maintenance and differentiation media
- Induction agent: Doxycycline
- Analysis tools: Single-cell RNA sequencing reagents, electrophysiology equipment, immunostaining supplies
Procedure:
- Cell Line Engineering: Generate a stable human iPSC line carrying doxycycline-inducible SAPG reprogramming factors targeted to the CLYBL safe harbor locus using CRISPR/Cas9-mediated knock-in.
- Factor Induction: Treat engineered iPSCs with doxycycline (typically 1-2 μg/mL) to activate simultaneous expression of all four reprogramming factors.
- Temporal Control: Maintain doxycycline induction for optimized duration (approximately 7-14 days based on target maturity).
- Efficiency Assessment: Monitor reprogramming efficiency through expression of hair cell markers such as MYO7A, ESPIN, and POU4F3.
- Functional Characterization: Perform comprehensive analysis of resulting hair cell-like cells including:
- Immunostaining for hair cell-specific proteins
- Single-cell RNA sequencing to evaluate transcriptional similarity to native hair cells
- Electrophysiological analysis to detect characteristic ion currents
Key Advantages: This virus-free system demonstrates a 19-fold increase in conversion efficiency compared to retroviral methods and achieves reprogramming in half the time. The resulting cells closely resemble developing fetal hair cells and exhibit diverse voltage-dependent ion currents, including robust, quick-activating, slowly inactivating currents characteristic of primary hair cells [5].
Protocol 3: Direct Reprogramming of Fibroblasts to Alveolar Epithelial-like Cells (iPULs)
This protocol describes the generation of induced pulmonary alveolar epithelial-like cells (iPULs) through direct reprogramming, offering potential for lung regeneration and disease modeling [9].
Materials and Reagents:
- Source cells: Mouse tail-tip fibroblasts (TTFs) or embryonic fibroblasts (MEFs)
- Reprogramming factors: Nkx2-1, Foxa1, Foxa2, and Gata6
- Delivery system: Retroviral vectors
- Culture system: 3D organoid culture conditions
- Supplements: Wnt pathway activators, growth factors, Smad inhibitors
- Sorting markers: Thy1.2 (negative selection), EpCAM (positive selection)
Procedure:
- Factor Screening: Identify optimal transcription factor combination through systematic screening. The quartet of Nkx2-1, Foxa1, Foxa2, and Gata6 demonstrates strongest induction of surfactant protein-C (Sftpc) expression.
- 3D Culture Setup: Transduce fibroblasts with retroviral vectors carrying the four factors and culture in 3D organoid system instead of traditional 2D conditions.
- Media Optimization: Supplement serum-free medium with Wnt pathway activators, specific growth factors, and Smad inhibitors to enhance reprogramming efficiency.
- Cell Sorting: After 7 days, isolate reprogrammed cells using fluorescence-activated cell sorting (FACS) for Sftpc-GFP+ (in reporter systems), Thy1.2-, and EpCAM+ populations.
- Characterization: Validate resulting iPULs through:
- Transcriptomic analysis comparing to primary alveolar epithelial cells
- Functional assessment of lamellar body formation
- In vivo integration potential following transplantation
Efficiency and Applications: This approach achieves approximately 2-3% reprogramming efficiency of starting fibroblasts. The resulting iPULs integrate into alveolar surfaces when administered intratracheally in bleomycin-induced pulmonary fibrosis models and form both alveolar epithelial type 1 and type 2-like cells, demonstrating therapeutic potential for lung diseases [9].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Direct Lineage Reprogramming
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Reprogramming Factors | B2 (BMI1+FGFR2), SAPG (SIX1+ATOH1+POU4F3+GFI1), NKX2-1+FOXA1+FOXA2+GATA6 | Master regulators that initiate cell fate conversion [3] [5] [9] |
| Delivery Systems | AAV9 vectors, Retroviral vectors, Doxycycline-inducible systems, Non-integrating methods | Introduce reprogramming factors into target cells [3] [5] |
| Culture Systems | 3D organoid platforms, Serum-free media, Defined growth factor cocktails | Provide appropriate microenvironment for reprogramming and maturation [9] |
| Enhancement Molecules | Wnt pathway activators, Smad inhibitors, Specific growth factors | Improve reprogramming efficiency and kinetics [6] [9] |
| Characterization Tools | scRNA-seq, Immunofluorescence, Electrophysiology, Functional assays | Validate successful reprogramming and functionality [5] |
| Cell Sorting Markers | Thy1.2 (fibroblast negative), EpCAM (epithelial positive), Lineage-specific reporters | Isate successfully reprogrammed cells from starting population [9] |
Direct lineage reprogramming represents a transformative approach in regenerative medicine that distinguishes itself from pluripotency-based strategies through its direct conversion methodology, reduced tumorigenic risk, and potential for in vivo applications. The experimental protocols outlined demonstrate the remarkable versatility of this technology across different tissue types, from skin and sensory cells to pulmonary epithelium. As the molecular mechanisms underlying cell fate determination become increasingly elucidated, particularly through advanced understanding of epigenetic regulators like RNA modifications [8], the efficiency and specificity of direct reprogramming continue to improve.
The future of direct lineage reprogramming lies in refining factor combinations, delivery methods, and microenvironmental conditions to enhance efficiency and functionality. Particularly promising are the advances in virus-free, RNA-based reprogramming techniques that align with the modified mRNA research context [10], offering improved safety profiles for potential therapeutic applications. As these technologies mature, direct lineage reprogramming stands to revolutionize personalized medicine by enabling the generation of patient-specific functional cells for disease modeling, drug screening, and regenerative therapies across a broad spectrum of degenerative conditions.
{The Pioneering Role of Transcription Factors like MyoD}
The discovery of the skeletal muscle-specific transcription factor MyoD represents a milestone in the field of transcriptional regulation during differentiation and cell-fate reprogramming [11]. MyoD was the first tissue-specific factor found capable of converting non-muscle somatic cells into skeletal muscle cells, establishing a powerful paradigm for direct lineage conversion [11]. A unique feature of MyoD, with respect to other lineage-specific factors, is its ability to dramatically change cell fate even when expressed alone, without requiring the coordinated expression of multiple transcription factors that many other reprogramming processes necessitate [11].
Within the context of modern modified mRNA research, MyoD has emerged as a particularly promising candidate for therapeutic reprogramming strategies. The transient nature of modified mRNA expression makes it ideally suited for directing cellular conversions without genomic integration, thereby enhancing safety profiles for potential clinical applications [12]. This application note details the molecular mechanisms, experimental protocols, and practical implementation strategies for leveraging MyoD in direct lineage conversion research, with particular emphasis on modified mRNA delivery systems.
Molecular Mechanisms of MyoD-Mediated Reprogramming
Transcriptional Activation and Myogenic Programming
MyoD belongs to the basic helix-loop-helix (bHLH) class of transcription factors and recognizes short DNA sequences (CANNTG), termed E-box motifs, in the regulatory regions of muscle-specific target genes [11]. MyoD binding to E-boxes and subsequent transactivation require heterodimerization with ubiquitous bHLH E-proteins, such as E12 and E47 [11]. The specificity of DNA binding and target activation by MyoD is determined by several cooperating mechanisms:
- Sequence Preference: MyoD exhibits preference for internal and flanking sequences of E-boxes [11]
- Co-factor Cooperation: Transcription factors including MEF2 family members, Sp1, Pbx, and Six proteins cooperate with MyoD by directly binding to adjacent sites [11]
- Epigenetic Engagement: MyoD interacts with the epigenetic machinery to remodel chromatin and activate silent loci [11]
MyoD-induced trans-differentiation involves activation of a complex program of gene expression, beginning with direct targets such as the bHLH muscle-specific transcription factor myogenin and the co-activator MEF2 [11]. MyoD also induces its own transcription and the expression of other transcription factors, creating positive feedback loops and amplifying cascades that reinforce the myogenic commitment [11].
Signaling Pathway Integration and Regulation
MyoD-dependent transcription integrates extracellular cues through several signaling cascades. The table below summarizes key pathways that regulate or enhance MyoD-mediated reprogramming:
Table 1: Signaling Pathways Regulating MyoD Activity in Cellular Reprogramming
| Pathway | Effect on MyoD | Key Modulators | Experimental Utility |
|---|---|---|---|
| p38 MAPK | Promotes MyoD activity | Targets co-factors (MEF2, E proteins) and chromatin complexes [11] | Enhances terminal differentiation |
| JNK | Inhibition enhances reprogramming | SP600125 (JNK inhibitor) [12] | Increases Pax7+ iMPC formation (~55-60% vs ~30% with F/R/C alone) [12] |
| JAK/STAT | Inhibition enhances reprogramming | CP690550 (JAK inhibitor) [12] | Increases Pax7+ iMPC formation [12] |
| Notch | Inhibits MyoD function | Hes1/Hey1 (bHLH repressors competing for E-box binding) [11] | Modulates proliferation vs differentiation balance |
| Mitogenic Signals | Inhibit MyoD function | Id proteins, cyclin/cdk complexes [11] | Serum withdrawal promotes terminal differentiation |
The following diagram illustrates the core molecular interactions and signaling pathways involved in MyoD-mediated reprogramming:
Figure 1: Core Molecular Mechanisms of MyoD-Mediated Reprogramming. MyoD heterodimerizes with E-proteins, binds E-box motifs, and activates a myogenic transcriptional program while engaging chromatin remodeling machinery. Key signaling pathways modulate this process.
Experimental Protocols for MyoD-Mediated Reprogramming
Transgene-Free Direct Conversion Using Modified mRNA
Recent advances have enabled highly efficient transgene-free approaches to directly convert mouse fibroblasts into induced myogenic progenitor cells (iMPCs) by overexpression of synthetic MyoD-mRNA in concert with enhanced small molecule cocktails [12]. The optimized protocol achieves robust and rapid reprogramming in as little as 10 days, with resulting iMPCs expressing characteristic myogenic stem cell markers, extensive proliferative capacity in vitro, and the ability to differentiate into multinucleated, contractile myotubes [12].
Table 2: Modified mRNA Reprogramming Protocol for Fibroblast to iMPC Conversion
| Step | Procedure | Duration | Key Components | Purpose |
|---|---|---|---|---|
| 1. Cell Preparation | Plate Rep-MEFs or primary fibroblasts | 24 hours | DMEM + 10% FCS [13] | Establish subconfluent culture |
| 2. Mesendoderm Priming | Treat with mesendoderm-inducing factors | 3 days | CHIR99021, BMP4 [14] | Enhance chromatin accessibility for myogenic programming |
| 3. MyoD-mRNA Transfection | Daily transfection with synthetic MyoD-mRNA | 7 days | Modified MyoD-mRNA (pseudouridine, 5-methylcytidine) [12] | Activate myogenic transcriptional program |
| 4. Small Molecule Cocktail | Continuous treatment with pathway modulators | Entire reprogramming period | F/R/C + SP600125 + CP690550 [12] | Enhance conversion efficiency and Pax7+ stem cell population |
| 5. Colony Selection | Manual picking or FACS of Pax7+ cells | Day 10-14 | Pax7-nGFP reporter or immunostaining [12] | Isolate pure iMPC population |
The following workflow diagram visualizes the complete reprogramming protocol:
Figure 2: Workflow for Transgene-Free iMPC Generation. This optimized protocol converts fibroblasts into functional induced myogenic progenitor cells using modified MyoD-mRNA and small molecule cocktails.
Critical Parameters for Successful Reprogramming
Several parameters critically influence the success and efficiency of MyoD-mediated reprogramming:
- MRNA Modifications: Incorporation of pseudouridine and 5-methylcytidine is essential to mitigate cellular immune reactions against exogenous mRNA molecules [12]
- Transfection Frequency: Daily transfections for 7 days are required to sustain MyoD protein expression due to the transient nature of mRNA [14]
- Cell Density: Initial plating at appropriate density (30-50% confluence) is crucial for successful reprogramming [13]
- Small Molecule Timing: Continuous presence of pathway modulators throughout the reprogramming process enhances conversion efficiency [12]
Research Reagent Solutions for MyoD Reprogramming
The table below summarizes essential research reagents and their applications in MyoD-mediated direct lineage conversion studies:
Table 3: Essential Research Reagents for MyoD Reprogramming Studies
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| MyoD Delivery Systems | Modified MyoD-mRNA (pseudouridine) [12], Lentiviral vectors (Tet-On) [13] | Ectopic MyoD expression | Modified mRNA avoids genomic integration; viral methods offer higher efficiency [12] |
| Small Molecule Enhancers | Forskolin (F), RepSox (R), CHIR99210 (C) [12], SP600125 (JNK inhibitor), CP690550 (JAK inhibitor) [12] | Enhance reprogramming efficiency | JNK and JAK/STAT inhibition increases Pax7+ population (~2-fold) [12] |
| Cell Culture Media | DMEM + 10% FCS (proliferation) [13], Serum-free media (differentiation) [11] | Support cell growth and differentiation | Serum withdrawal promotes terminal differentiation [11] |
| Reporter Systems | Pax7-CreERT2; R26-LSL-ntdTomato [12], Pax7-nuclear GFP [12] | Track reprogramming efficiency | Enable FACS-based isolation of iMPCs |
| Analysis Tools | Anti-MyoD, anti-Desmin, anti-α-actin antibodies [13] | Validate reprogramming success | Immunofluorescence and Western blot analysis |
Applications and Therapeutic Translation
In Vivo Engraftment and Regeneration
Transgene-free iMPCs generated via MyoD-mRNA reprogramming demonstrate significant therapeutic potential. Upon transplantation into skeletal muscles of Duchenne muscular dystrophy (DMD) mouse models, these cells robustly engraft and restore dystrophin expression in hundreds of myofibers [12]. This demonstrates the functional capacity of the reprogrammed cells and their potential for regenerative medicine applications.
Technology Integration and Advanced Delivery Systems
Emerging technologies are further enhancing the potential of MyoD-based reprogramming strategies:
- Tissue Nanotransfection (TNT): A novel non-viral nanotechnology platform that enables in vivo gene delivery and direct cellular reprogramming through localized nanoelectroporation [15]
- Optimized mRNA Design: Algorithms like LinearDesign can optimize mRNA sequences for improved stability and immunogenicity, potentially enhancing MyoD expression and reprogramming efficiency [16]
- Organ-on-Chip Models: Microfluidic platforms enable direct on-chip programming of human pluripotent stem cells into skeletal myocytes using MYOD modified mRNA [14]
MyoD continues to serve as a paradigm for transcription factor-mediated direct lineage conversion, with modern modified mRNA technologies addressing critical safety concerns associated with viral delivery methods. The optimized protocols and reagent systems detailed in this application note provide researchers with robust methodologies for generating functional myogenic cells through transgene-free reprogramming. As mRNA design algorithms and delivery technologies continue to advance, MyoD-based cellular reprogramming holds increasing promise for regenerative medicine, disease modeling, and therapeutic development for muscular disorders.
The therapeutic application of messenger RNA (mRNA) represents a revolutionary platform for a wide range of biomedical applications, from infectious disease vaccines to protein replacement therapies and direct lineage conversion. The core principle involves introducing in vitro transcribed (IVT) mRNA into target cells to direct the synthesis of specific proteins that can elicit immune responses, replace deficient proteins, or even reprogram cell identity. However, the clinical translation of mRNA-based therapeutics faces two interconnected fundamental challenges: mRNA instability and innate immunogenicity [17] [18]. These properties are intrinsically linked to mRNA's biological function as a transient information carrier in cells.
Naked, unmodified mRNA is inherently unstable and rapidly degraded by extracellular and intracellular nucleases, leading to insufficient protein expression for therapeutic efficacy [18] [19]. Compounding this instability, foreign mRNA is recognized by the host's innate immune system through pattern recognition receptors (PRRs), triggering potent antiviral responses and inflammatory cytokine production that can severely limit protein expression and potentially cause adverse effects [17] [20]. For researchers pursuing direct lineage conversion—the process of transforming one somatic cell type directly into another without reverting to a pluripotent state—these challenges are particularly pronounced. Successful reprogramming requires sustained expression of key transcription factors at appropriate levels, which is difficult to achieve when the mRNA instructions are rapidly degraded or when immune responses alter the cellular environment in ways that might inhibit reprogramming efficiency.
This Application Note provides a structured framework for overcoming these challenges through optimized mRNA design, chemical modifications, and delivery strategies, with particular emphasis on protocols suitable for lineage conversion research.
Molecular Mechanisms Underlying mRNA Instability and Immunogenicity
Pathways of mRNA Recognition and Degradation
Understanding the molecular mechanisms that govern mRNA stability and immunogenicity is essential for developing effective therapeutic mRNA constructs. The cellular machinery that normally regulates endogenous mRNA half-life and quality control represents the same barriers that exogenous therapeutic mRNA must overcome.
Immunogenicity Mechanisms: The innate immune system detects foreign RNA primarily through Toll-like receptors (TLRs) located in endosomal membranes and retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs) in the cytoplasm [17]. Specifically, TLR3, TLR7, and TLR8 recognize single-stranded and double-stranded RNA motifs, while RIG-I and MDA-5 detect cytoplasmic RNA. These recognition events trigger signaling cascades that result in type I interferon (IFN) production and subsequent upregulation of interferon-stimulated genes (ISGs), creating an antiviral state that strongly inhibits translation of the exogenous mRNA [17] [18]. This immune activation not only reduces protein expression but may also alter the cellular phenotype in ways that could interfere with directed differentiation or lineage conversion protocols.
Instability Mechanisms: Endogenous mRNA degradation occurs through multiple pathways, including deadenylation (removal of the 3' poly(A) tail), decapping (removal of the 5' cap structure), and nuclease-mediated cleavage [19]. Exogenous IVT mRNA is particularly susceptible to these degradation pathways. The half-life of IVT mRNA in cells is typically limited to hours, while many therapeutic applications—especially those involving cell reprogramming—require sustained protein expression over several days to effectively alter cell identity and function [19] [20].
The following diagram illustrates the key cellular pathways that detect and degrade conventional mRNA, highlighting potential intervention points for engineered solutions:
Quantitative Impact on Protein Expression
The combined effects of immunogenicity and instability significantly limit both the magnitude and duration of protein expression from conventional mRNA. The following table summarizes key quantitative findings from preclinical studies:
Table 1: Quantitative Impact of mRNA Instability and Immunogenicity on Protein Expression
| Parameter | Conventional mRNA | Modified/Optimized mRNA | Experimental Evidence |
|---|---|---|---|
| Protein expression duration | <24-48 hours | Extended to several days | VEGF mRNA expression declined within 24 hours after intradermal administration in clinical trials [19] |
| Antibody response | Baseline (reference) | Up to 128-fold increase | LinearDesign-optimized COVID-19 vaccines in mice [16] |
| mRNA half-life | Minutes to hours | Significantly prolonged | circRNA half-life "significantly exceeds" linear mRNA [20] |
| Immunogenicity | High IFN and cytokine production | Greatly reduced | Ψ and m1Ψ modifications reduce PRR activation [17] |
Research Reagent Solutions for mRNA Engineering
Overcoming the challenges of immunogenicity and instability requires a multifaceted approach combining specialized reagents, optimized sequences, and delivery systems. The following table catalogs key reagents and their functions for developing enhanced mRNA constructs:
Table 2: Essential Research Reagents for mRNA Engineering
| Reagent Category | Specific Examples | Function & Mechanism | Application Notes |
|---|---|---|---|
| Nucleotide Analogs | Pseudouridine (Ψ), N1-methylpseudouridine (m1Ψ), 5-methylcytidine (m5C) | Reduce immunogenicity by evading pattern recognition receptors | m1Ψ used in COVID-19 vaccines; note potential for ribosomal frameshifting [17] |
| Capping Reagents | CleanCap analogs, anti-reverse cap analogs (ARCA) | Enhance translation initiation and protect from 5' decay | Critical for protein expression yield; affects capping efficiency [21] [20] |
| Stabilizing Sequences | Optimized 5' and 3' UTRs, structured elements | Increase half-life by impeding nuclease access | Algorithmic design (e.g., LinearDesign) improves stability [16] |
| Poly(A) Tail Enzymes | Poly(A) polymerases, defined-length tails | Control tail length for stability and translation | Optimal length typically 100-150 nucleotides [21] [20] |
| Purification Kits | HPLC, FPLC systems, dsRNA removal | Remove immunogenic impurities (e.g., dsRNA) | Essential for reducing innate immune activation [21] |
Experimental Protocols for mRNA Evaluation
Protocol 1: Assessment of mRNA Immunogenicity in Vitro
Purpose: To quantitatively evaluate the innate immune response activation by novel mRNA constructs in mammalian cells.
Materials:
- HEK293T or THP-1 cell lines
- Test mRNA constructs (including unmodified control)
- Transfection reagent (e.g., Lipofectamine MessengerMAX)
- RNA extraction kit
- qRT-PCR reagents for IFN-β, IL-6, and other cytokines
- ELISA kits for IFN-α, IFN-β, TNF-α
- Cell culture media and standard lab equipment
Procedure:
- Cell Seeding: Seed 2×10^5 cells per well in 24-well plates 24 hours before transfection to achieve 70-80% confluency.
- mRNA Transfection: Prepare complexes of test mRNA (100 ng/well) with transfection reagent according to manufacturer's instructions. Include an unmodified mRNA control and a mock transfection control.
- Incubation: Incubate cells with mRNA complexes for 6-24 hours at 37°C, 5% CO₂.
- RNA Extraction and qRT-PCR:
- Extract total RNA using appropriate kits
- Synthesize cDNA using reverse transcriptase
- Perform qPCR with primers for IFN-β, IL-6, and RIG-I
- Normalize to housekeeping genes (GAPDH, β-actin)
- Protein Analysis:
- Collect cell culture supernatants at 24 hours
- Measure secreted cytokine levels using ELISA
- Data Analysis: Calculate fold changes relative to mock-transfected controls. Statistical analysis should include at least three independent experiments.
Troubleshooting: High baseline immunity in control cells may indicate endotoxin contamination. Use nuclease-free techniques and endotoxin-free reagents throughout.
Protocol 2: Determination of mRNA Stability and Half-Life
Purpose: To quantitatively measure the intracellular stability and decay kinetics of mRNA constructs.
Materials:
- Appropriate cell line for application (e.g., fibroblasts for lineage conversion)
- Test mRNA constructs
- Actinomycin D (5 μg/mL) or other transcription inhibitors
- RNA extraction kit
- qRT-PCR reagents
- Capillary electrophoresis system (e.g., Fragment Analyzer)
Procedure:
- Cell Seeding and Transfection: Seed cells as described in Protocol 1 and transfert with test mRNA constructs.
- Transcription Inhibition: At 4 hours post-transfection, add actinomycin D to inhibit new RNA synthesis.
- Time-Course Sampling: Collect cell samples at 0, 2, 4, 8, 12, and 24 hours after actinomycin D addition.
- RNA Quantification:
- Extract total RNA from each time point
- Analyze mRNA integrity using capillary electrophoresis
- Perform qRT-PCR with assays targeting the encoded transgene
- Half-Life Calculation:
- Normalize mRNA levels to internal controls
- Plot remaining mRNA (%) versus time
- Calculate decay constant (k) from logarithmic plot
- Determine half-life using t½ = ln(2)/k
Alternative Approach: For applications requiring longer observation, use tet-inducible systems or photoactivatable nucleotides to monitor decay without global transcription inhibition.
The following workflow diagram illustrates the key steps in designing, producing, and evaluating enhanced mRNA constructs for research applications:
Analytical Methods for mRNA Characterization
Rigorous characterization of mRNA constructs is essential for understanding structure-function relationships and ensuring reproducible results. The following analytical approaches are recommended:
Integrity and Purity Assessment:
- Capillary Gel Electrophoresis (CGE): Provides high-resolution analysis of mRNA size distribution and identifies truncated species [21]. Critical for quantifying full-length product percentage.
- Agarose Gel Electrophoresis: Useful for initial quality assessment but less quantitative than CGE.
- Ion-Pair Reversed-Phase Liquid Chromatography (IP-RP LC): Separates mRNA based on hydrophobic interactions, resolving impurities and degradation products [21].
Structural Characterization:
- Mass Spectrometry: LC-MS/MS enables precise identification of chemical modifications and sequence verification [21].
- Direct RNA Sequencing: Confirms sequence identity and can detect nucleotide modifications [21].
Functional Characterization:
- In Vitro Translation Assays: Cell-free systems to assess translation efficiency without delivery complications.
- Western Blotting: Quantifies protein production levels and confirms protein identity.
- Cell-Based Assays: Measures biological activity in relevant cellular models.
For lineage conversion applications specifically, additional functional assays should include immunocytochemistry for cell-type-specific markers and RNA sequencing to evaluate transcriptional programs indicative of successful reprogramming.
Emerging Platforms and Future Perspectives
Beyond conventional linear mRNA, several innovative platforms show promise for applications requiring sustained protein expression such as lineage conversion:
Self-Amplifying RNA (saRNA): Derived from alphavirus genomes, saRNA contains replicase genes that enable intracellular amplification of the original RNA dose, dramatically extending duration of expression and reducing the required dose [17] [20]. However, the larger size (approximately 9-12 kb) presents delivery challenges, and the prolonged expression may increase safety concerns for some applications.
Circular RNA (circRNA): These covalently closed RNAs lack free ends, conferring exceptional resistance to exonuclease-mediated degradation [17] [22] [20]. The extended half-life makes circRNA particularly attractive for lineage conversion protocols that require sustained transcription factor expression. Recent studies have also revealed that circRNAs can directly interact with linear mRNAs to regulate their stability and translation [22], adding another layer of regulatory complexity to consider in experimental design.
The field of mRNA therapeutics continues to evolve rapidly, with ongoing research addressing remaining challenges in targeted delivery, precise temporal control of expression, and reducing unwanted immunogenicity while maintaining effective immune responses for vaccine applications. For lineage conversion research, these advances will enable more efficient and reproducible reprogramming protocols with potential applications in disease modeling, drug discovery, and regenerative medicine.
The application of synthetic messenger RNA (mRNA) as a therapeutic agent represents a paradigm shift in modern medicine, particularly for precise interventions like direct lineage conversion. Historically, its path was hindered by two major biological hurdles: innate instability leading to rapid degradation, and inherent immunogenicity triggering undesirable inflammatory responses [23] [24]. Overcoming these challenges was a prerequisite for the clinical success of mRNA technologies. Through strategic chemical modifications and sophisticated design, researchers have engineered modified mRNA (modRNA) that is both highly stable and minimally immunogenic [25] [26]. These advancements are foundational to its use in direct lineage conversion, where controlled, transient, and efficient protein expression is required to safely reprogram cell fate. This Application Note details the core mechanisms, key quantitative data, and essential protocols that underpin the development of effective modRNA for research in regenerative medicine and drug development.
Core Mechanisms: How Modifications Confer Stability and Reduce Immunogenicity
The historical limitations of unmodified mRNA have been systematically addressed through targeted engineering of its structure. The following diagrams and sections outline the key mechanisms and logical workflow for developing optimized modRNA.
Enhanced mRNA Stability
The stability of mRNA is critical for achieving sufficient therapeutic protein expression. Three primary structural elements are engineered to resist degradation:
- 5' Cap Analogues: The 5' cap protects mRNA from exonuclease degradation and recruits translation initiation factors. Anti-Reverse Cap Analogue (ARCA) ensures proper cap orientation, significantly enhancing translation [25]. Advanced Cap 1 structures (e.g., via CleanCap technology), which include a 2'-O-methylation on the first transcribed nucleotide, further increase stability and protein yield by reducing immune recognition compared to Cap 0 [24].
- Nucleotide Modifications: The strategic substitution of natural nucleotides with modified analogues is a cornerstone of stability enhancement. Recent research indicates that position-specific introduction of ribose modifications, such as 2'-fluoro (2'-F) at the first nucleoside of a codon, can significantly bolster mRNA stability without compromising translational efficiency [27].
- Optimized UTRs and Poly(A) Tail: The 5' and 3' Untranslated Regions (UTRs) are engineered using sequences from highly expressed genes (e.g., α-globin or β-globin) to enhance mRNA stability and regulate translational efficiency [23] [24]. A poly(A) tail of optimal length (typically 120-150 nucleotides) is also crucial for protecting the mRNA from rapid decay [23].
Reduced Immunogenicity
Unmodified mRNA is recognized by pattern recognition receptors (e.g., TLR7, TLR8), triggering the production of type I interferons and other inflammatory cytokines, which can inhibit translation and cause cell death [23].
- Nucleotide Substitution: Incorporating modified nucleotides such as N1-methylpseudouridine (N1mΨ) or pseudouridine (Ψ) and 5-methylcytidine (5mC) is the primary strategy to evade immune detection. These modifications cloak the mRNA, preventing its recognition by innate immune sensors and thereby drastically reducing interferon responses [25] [23] [27].
- Purification and Delivery: Following in vitro transcription (IVT), rigorous purification is necessary to remove double-stranded RNA (dsRNA) contaminants, which are potent inducers of innate immunity [25]. Furthermore, delivery systems like Lipid Nanoparticles (LNPs) protect the mRNA from extracellular RNases and facilitate efficient cellular uptake, further minimizing immune activation [28] [24].
Key Experimental Data and Comparative Analysis
The impact of specific modifications can be quantified through protein expression and immunogenicity assays. The table below summarizes key findings from optimization studies.
Table 1: Quantitative Impact of modRNA Optimization Strategies
| Optimization Strategy | Experimental System | Key Outcome Metric | Result vs. Control | Citation |
|---|---|---|---|---|
| ARCA 10 Protocol (High ARCA, lower N1mΨ) | In vitro transfection (HeLa, HUVEC, primary cardiac cells) | Luciferase & GFP protein expression | Significantly increased expression vs. standard ARCA 5 protocol | [25] |
| Nucleotide Modification (N1mΨ substitution) | In vitro transfection; in vivo delivery | Interferon-α/β levels; Protein expression | Reduced immunogenicity; Increased protein expression vs. unmodified mRNA | [25] [23] |
| Position-specific 2'-F modification (1st nucleoside in codon) | Cell-free translation system (HeLa lysate) | Peptide expression (ELISA) | Enhanced stability & high translational activity vs. unmodified and other modification patterns | [27] |
| Terminal Modifications (2'-O-MOE with phosphorothioate) | Cell-free translation system | Peptide expression (ELISA) | Increased peptide production vs. non-terminally modified mRNA | [27] |
Detailed Experimental Protocols
Protocol: modRNA Synthesis via In Vitro Transcription (IVT) and Purification
This protocol is adapted from optimized procedures for cost-effective production of high-yield, low-immunogenicity modRNA [25].
I. Reagent Setup (Nucleotide Composition for ARCA 10 Protocol):
- Template DNA: Linearized plasmid DNA template with T7 promoter and poly(A) region (85% reduction from traditional amounts).
- Nucleotide Master Mix:
- ARCA (Cap Analog): 10 mM
- GTP: 2.7 mM
- ATP: 8.1 mM
- CTP: 8.1 mM
- N1-methylpseudouridine-5'-triphosphate (N1mΨTP): 2.7 mM
- 10X T7 Reaction Buffer
- T7 RNA Polymerase
II. Step-by-Step Procedure:
- IVT Reaction: Combine the nucleotide master mix, template DNA, and T7 RNA Polymerase. Incubate at 37°C for 2-4 hours.
- DNase I Treatment: Add DNase I to the reaction and incubate for 15 minutes at 37°C to digest the DNA template.
- Primary Purification (Desalting): Use Amicon centrifugal filters (e.g., 100K MWCO) to remove unincorporated nucleotides and salts. This step is as effective as more expensive kit-based purification for this purpose [25].
- Poly(A) Tailing (If not encoded in template): If the poly(A) tail is not encoded, use Poly(A) Polymerase to add a tail of ~150 nucleotides to the 3' end.
- Final Purification: Purify the modRNA using a commercial RNA cleanup kit (e.g., MEGAclear) to remove enzymes, salts, and any residual dsRNA contaminants. This step is critical for reducing immunogenicity.
- Quality Control: Quantify modRNA by spectrophotometry (A260/A280). Assess integrity and purity using a bioanalyzer (e.g., Agilent Bioanalyzer).
Protocol: Assessing modRNA Immunogenicity and Expression In Vitro
I. Reagent Setup:
- Test modRNA: Prepared using the protocol above.
- Control RNA: Unmodified mRNA.
- Cell Line: HEK293 cells or primary human fibroblasts.
- Delivery Vehicle: Cationic lipid transfection reagent.
- Assay Kits: ELISA kits for Human IFN-α and IFN-β.
II. Step-by-Step Procedure:
- Cell Seeding: Seed cells in a 24-well plate to reach 70-80% confluence at transfection.
- Transfection Complex Formation: For each well, dilute 0.5 µg of modRNA (test or control) in opti-MEM. In a separate tube, dilute lipid transfection reagent in opti-MEM. Combine the diluted RNA and lipid reagent, incubate for 15-20 minutes.
- Transfection: Add the complexes to the cells.
- Incubation: Incubate cells for 24 hours.
- Harvest and Analysis:
- Immunogenicity: Collect cell culture supernatant at 24 hours post-transfection. Measure IFN-α and IFN-β levels using ELISA kits. modRNA with successful modification should show significantly reduced cytokine levels compared to unmodified mRNA controls [25].
- Expression Analysis: For encoded reporter genes (e.g., GFP, Luciferase), assay directly at 24-48 hours. For other proteins, lysate cells and perform Western blot or other functional assays to confirm high-level protein production.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for modRNA Research and Their Functions
| Reagent / Material | Function / Application | Key Notes |
|---|---|---|
| N1-methylpseudouridine (N1mΨ) | Modified nucleotide | Reduces immunogenicity, enhances translational efficiency. A key replacement for uridine. |
| Anti-Reverse Cap Analogue (ARCA) | 5' capping | Ensures proper cap orientation for high translation initiation efficiency. |
| CleanCap AG | Co-transcriptional capping | Enables one-step synthesis of the superior Cap 1 structure with high efficiency (>94%) [24]. |
| Lipid Nanoparticles (LNPs) | Delivery system | Protects modRNA, facilitates cellular uptake and endosomal escape; the gold standard for in vivo delivery. |
| T7 RNA Polymerase | In vitro transcription | High-yield enzyme for synthesizing mRNA from a DNA template. |
| β-globin UTRs | mRNA structural elements | Engineered into the construct to enhance mRNA stability and translational efficiency. |
Application in Direct Lineage Conversion: A Pathway View
In direct lineage conversion, modRNA encodes transcription factors that reprogram cell identity. The stability and low immunogenicity of modRNA are crucial for the repeated transfections required without triggering an antiviral state that would block reprogramming. The following diagram illustrates this application pathway.
The direct conversion of one somatic cell type into another, known as direct lineage conversion, represents a transformative approach in regenerative medicine for generating therapeutic cell types without passing through a pluripotent intermediate state. Within this field, modified mRNA (modRNA) technology has emerged as a superior non-integrative and controllable strategy for driving cell fate decisions. Unlike DNA-based methods that pose a risk of genomic integration and insertional mutagenesis, modRNA-based reprogramming delivers genetic instructions transiently through synthetic, chemically modified mRNA molecules. This approach provides a safe, efficient, and precise means of expressing transcription factors and other reprogramming molecules to orchestrate lineage conversion, offering significant potential for future clinical applications [29] [10].
Core Technological Advantages of Modified mRNA
The superiority of modRNA for cell fate manipulation is rooted in its distinct biological mechanism and safety profile compared to traditional vector-based systems. The table below summarizes its key advantages.
Table 1: Key Advantages of Modified mRNA for Cell Fate Manipulation
| Feature | Mechanistic Basis | Functional Outcome |
|---|---|---|
| Non-Integrative | Remains in the cytoplasm and does not enter the nucleus; degraded by normal cellular processes [28] [10]. | Eliminates risk of insertional mutagenesis and permanent genomic alteration; favorable safety profile for clinical use. |
| Controllable/Transient | Protein expression is transient, typically lasting from hours to a few days, dependent on mRNA half-life [29]. | Allows for precise, pulsed expression of reprogramming factors; avoids sustained transgene expression that can cause tumorigenesis. |
| High Reprogramming Efficiency | Efficient transfection and direct translation in the cytoplasm bypasses the nuclear barrier; modified nucleotides enhance protein yield [10]. | Achieves high-efficiency lineage conversion; suitable for hard-to-transfect primary cells. |
| Rapid and Scalable Production | Manufactured via in vitro transcription (IVT), a cell-free process [28]. | Enables rapid production of research and therapeutic batches; platform can be quickly adapted to encode different proteins. |
The following diagram illustrates the workflow for direct lineage conversion using modified mRNA, from design to functional cell analysis.
Diagram 1: modRNA Lineage Conversion Workflow.
Quantitative Comparison of Reprogramming Technologies
Selecting an appropriate delivery method is a critical determinant of success and safety in lineage conversion experiments. The table below provides a comparative analysis of the most common technologies.
Table 2: Comparative Analysis of Cell Reprogramming and Lineage Conversion Technologies
| Technology | Reprogramming Efficiency | Genomic Integration? | Key Advantages | Key Limitations & Risks |
|---|---|---|---|---|
| Modified mRNA (modRNA) | High (superior to non-integrative DNA methods) [10] | No [28] [10] | Non-integrative, controllable, high protein yield, rapid production. | Requires repeated transfections; can trigger innate immune response without modification. |
| Sendai Virus (SeV) | High [10] | No (RNA virus, replicates in cytoplasm) [10] | Highly efficient transduction, works in hard-to-transfect cells. | Requires diligent clearance; potential for cytopathogenicity. |
| Episomal Plasmads | Low [10] | No (but foreign DNA is present) [10] | Simple to use, no viral components. | Very low efficiency; potential risk of random integration. |
| Integrating Lenthviruses | High [10] | Yes [10] | Highly efficient, stable long-term expression. | High risk of insertional mutagenesis and oncogenesis; unsuitable for clinical use. |
| Protein Transduction | Very Low [10] | No [10] | Completely DNA-free; minimal safety concerns. | Extremely low efficiency; costly and technically challenging. |
Application Notes & Protocol: Direct Lineage Conversion Using modRNA
This protocol outlines a standardized procedure for converting human fibroblasts into induced neurons (iNs) using modified mRNA, based on established reprogramming methodologies.
Background and Principle
Direct lineage conversion allows for the trans-differentiation of a somatic cell into another somatic cell type by forced expression of specific transcription factors, bypassing the pluripotent state [10]. Using modRNA to deliver these factors combines the high efficiency of viral methods with the enhanced safety profile of a non-integrative, transient system. This is particularly critical for generating neuronal cells for disease modeling and regenerative therapies.
Experimental Protocol
Part I: Preparation of Modified mRNA
- Template Design: Clone the open reading frames (ORFs) of key pro-neural transcription factors (e.g., Brn2/Pou3f2, Ascl1, Myt1l) into an in vitro transcription (IVT) plasmid vector containing 5' and 3' untranslated regions (UTRs) known to enhance stability and translation (e.g., alpha-globin UTRs) [28].
- Template Linearization: Linearize the plasmid template downstream of the poly-A tail sequence using a restriction enzyme. Purify the linearized DNA.
- In Vitro Transcription (IVT): Synthesize mRNA using an IVT kit. To reduce immunogenicity and enhance stability, replace standard nucleotides with a modified nucleotide cocktail (e.g., pseudouridine-5'-triphosphate and 5-methylcytidine-5'-triphosphate) [10].
- Capping and Polyadenylation: Co-transcriptionally add a Cap 1 structure to the 5' end. Enzymatically add a poly-A tail to the 3' end if not encoded in the template, aiming for a tail of ~150 adenosine residues to maximize translational efficiency [28].
- Purification and Quality Control: Purify the modRNA product using LiCl precipitation or column-based methods. Analyze integrity via agarose gel electrophoresis and quantify concentration via spectrophotometry. Aliquot and store at -80°C.
Part II: Cell Culture and Transfection
- Cell Culture: Maintain human dermal fibroblasts in standard culture medium. One day before transfection, plate cells at a density of 5 x 10^4 cells per well in a 24-well plate coated with poly-L-ornithine/laminin.
- Transfection Complex Formation: For each well, prepare two solutions.
- Solution A (modRNA): Dilute a total of 1-2 µg of modRNA (a cocktail of the pro-neural factors) in 100 µL of serum-free medium.
- Solution B (Transfection Reagent): Dilute a commercial lipid-based transfection reagent in 100 µL of serum-free medium.
- Combine Solutions A and B, mix gently, and incubate for 10-20 minutes at room temperature to allow complex formation.
- Transfection: Add the entire 200 µL of complexes dropwise to the cells in fresh culture medium. Incubate cells at 37°C, 5% CO2.
- Transfection Regimen: Repeat the transfection process every 24 hours for a period of 10-14 days. The repetitive delivery is crucial for maintaining sufficient levels of the transient reprogramming factors to drive the conversion process [10].
Part III: Post-Transfection and Analysis
- Culture Maintenance: 4-6 hours after each transfection, perform a complete medium change. This is critical to minimize cellular toxicity and innate immune responses triggered by RNA and transfection reagents.
- Immunostaining: After 10-14 days, fix cells and perform immunocytochemistry for neuronal markers such as Tuj1 (neuron-specific class III β-tubulin) and Map2 (microtubule-associated protein 2) to confirm neuronal identity.
- Functional Analysis: Assess the electrophysiological properties of the induced neurons using patch-clamp recording to validate the presence of active sodium and potassium channels and the ability to fire action potentials.
The following diagram visualizes the molecular mechanism of how the delivered modRNA leads to protein expression and subsequent cell fate change.
Diagram 2: modRNA Mechanism of Action.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of modRNA-based lineage conversion requires a suite of specialized reagents and tools.
Table 3: Essential Research Reagent Solutions for modRNA Lineage Conversion
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| IVT Plasmid Vectors | pIVT2, pGEM series | Backbone for template DNA; contains bacteriophage promoter (T7, SP6) for high-yield mRNA synthesis. |
| Modified Nucleotides | Pseudouridine-5'-Triphosphate, 5-Methylcytidine-5'-Triphosphate | Replaces UTP and CTP; critical for reducing innate immune recognition and enhancing translational efficiency [10]. |
| Capping Reagents | Trivalent Cap 1 Analog (CleanCap) | Enables co-transcriptional capping for superior translation initiation and mRNA stability. |
| Transfection Reagents | Lipid-based (e.g., Lipofectamine RNAiMAX, Messenger Max) | Forms protective complexes with modRNA for efficient cellular uptake and endosomal escape. |
| Immune Suppressors | B18R protein, IFN-γ receptor blocking antibodies | Optional supplements to further suppress PKR pathway activation and interferon response, boosting protein yield. |
| Cell Culture Matrix | Poly-L-ornithine/Laminin, Geltrex | Provides a supportive surface for sensitive cell types like neurons during and after conversion. |
Engineering Cell Fate: Methodology and Therapeutic Applications of modRNA
Modified messenger RNA (modRNA) has emerged as a powerful tool for direct lineage conversion, enabling the reprogramming of somatic cells into specific target cell types without genomic integration. The structural components of synthetic mRNA—the 5' cap, 5' and 3' untranslated regions (UTRs), nucleoside modifications, and codon-optimized open reading frame (ORF)—collectively determine its translational efficiency, stability, and immunogenicity [17] [23]. For lineage conversion protocols, where precise temporal control and high levels of protein expression are critical for efficient reprogramming, optimizing each of these elements is paramount. This application note provides detailed methodologies and current optimization strategies for constructing high-performance modRNAs, with particular emphasis on their application in direct lineage conversion research.
5' Cap Analogs: Enhancing Translation Initiation and Stability
The 5' cap is a critical modification that promotes translation initiation, protects the mRNA from exonuclease degradation, and influences immunogenicity. Recent innovations have moved beyond the canonical m7G cap to analogs that confer enhanced properties.
Advanced Cap Analogs and Their Properties
Table 1: Performance Characteristics of Select 5' Cap Analogs
| Core Modification | Notable Structure(s) | eIF4E Affinity (Kd-fold vs. m7GpppG) | Half-life in Cytosolic Extract (t½-fold) | In Vitro Translation Boost (RLU-fold) | Reported Immunogenicity |
|---|---|---|---|---|---|
| Phosphorothioate [30] | m7G-PS-ppG | ~1.1 | 6-8× | ~2.0 | Low (IFIT1 evasion) |
| Tetraphosphate Extension [30] | m7Gppppm7G | ~3.2 | ~2× | ~2.5 | Moderate |
| 7-Benzylguanine [30] | BN7mGpppG | ~2.1 | ~3× | ~3.0 | Very Low |
| Dithiodiphosphate [30] | m7G-S-S-ppG | ~1.3 | ~10× | ~1.8 | Low |
| Trinucleotide (CleanCap AG) [30] | m7GpppAm2′-O-Ψ | ~1.4 | ~4× | ~2.1 | Ultra-Low |
Protocol: In Vitro Transcription with Co-transcriptional Capping
This protocol is optimized for producing high-yield, 5'-capped modRNA using the CleanCap AG analog, which achieves >94% Cap-1 structure incorporation [30].
- Template Preparation: Linearize a plasmid DNA template containing the gene of interest downstream of a bacteriophage promoter (e.g., T7, SP6) or use a PCR-amplified template with an appended promoter. Purify the template via phenol-chloroform extraction and isopropanol precipitation.
- IVT Reaction Setup: Assemble the following reaction on ice:
- Nuclease-free water to 100 μL final volume
- 1x Transcription Buffer (e.g., 200 mM Tris-HCl pH 7.9, 30 mM MgCl₂, 10 mM spermidine)
- DNA template (5–10 μg)
- Nucleoside triphosphates (NTPs, 7.5 mM each of ATP, CTP, UTG, GTP). For modified mRNA, replace UTP with N1-methylpseudouridine-5'-triphosphate (m1Ψ TP).
- 10 mM CleanCap AG trinucleotide cap analog [30].
- Recombinant T7 RNA Polymerase (2000 U).
- Incubation: Incubate the reaction at 37°C for 2–4 hours.
- DNase Treatment: Add 2 U of DNase I (RNase-free) and incubate at 37°C for 15 minutes to digest the DNA template.
- mRNA Purification: Purify the mRNA using magnetic bead-based clean-up kits or lithium chloride precipitation. Assess cap incorporation efficiency by LC-MS or differential enzymatic digestion followed by gel electrophoresis.
Specialized Application: Photocaged "FlashCaps" for Spatiotemporal Control
For lineage conversion studies requiring precise temporal activation, photocaged cap analogs offer a unique solution. These analogs, such as the DMNB- or NPM-caged "FlashCaps," incorporate a photo-cleavable group at the N2 position of the cap guanosine, which prohibits binding to eIF4E and thus inhibits translation [31].
- Workflow: modRNA is synthesized using the FlashCap analog via standard IVT. Upon transfection into cells, the mRNA remains translationally inactive. Irradiation with 365–420 nm light for 60–120 seconds removes the caging group, restoring the native cap structure and triggering robust protein expression [31].
- Application: This system is ideal for dosing transcription factors in a pulsed manner, a critical parameter for enhancing the efficiency and fidelity of direct lineage conversion.
UTR Engineering: Balancing Stability and Translational Efficiency
UTRs are pivotal for mRNA stability and the regulation of translation. While endogenous UTRs from globin genes are commonly used, engineered UTRs can offer superior performance.
Deep Learning-Driven UTR Design
Deep learning models, such as Optimus 5-Prime, can be used to design de novo 5'UTR sequences that maximize the Mean Ribosome Load (MRL), a proxy for translation efficiency [32].
- Protocol: Designing UTRs with Optimus 5-Prime:
- Input: Provide the model with the sequence of your coding region (CDS) and specify the desired UTR length.
- Prediction: The model, trained on MPRAs from multiple cell types (HEK293T, HepG2, T cells), will score a vast number of sequence variants [32].
- Optimization: Use gradient descent (Fast SeqProp) or generative neural networks (DENs) to generate candidate 5'UTR sequences with predicted high MRL [32].
- Validation: Cloning the top candidate UTRs into reporter vectors and testing them in the target cell type for lineage conversion is essential, as the best-performing UTR can be cargo- and cell-type specific [32].
Nucleoside Modifications: Reducing Immunogenicity and Enhancing Expression
Nucleoside modifications are a cornerstone of modern modRNA design, primarily serving to dampen the innate immune response and improve translational efficiency.
Common Modifications and Considerations
The replacement of uridine with pseudouridine (Ψ) or N1-methylpseudouridine (m1Ψ) is a widely adopted strategy to avoid detection by Toll-like receptors (TLRs) and other pattern recognition receptors [17] [23]. This significantly reduces immunogenicity and can increase protein output. However, a recent finding indicates that m1Ψ can cause ribosomal frameshifting during translation, potentially leading to the production of off-target protein variants [17]. Researchers should weigh this potential risk against the benefit of reduced immunogenicity for their specific application.
Protocol: Screening Modified Nucleotides for Lineage Conversion
Different cell types may exhibit varying responses to nucleoside modifications. This protocol outlines a screen for optimal modification profiles.
- mRNA Synthesis: Synthesize a reporter mRNA (e.g., encoding GFP) or a lineage-specifying transcription factor using a panel of different modified NTPs (e.g., Ψ, m1Ψ, 5-methylcytidine (5mC), or combinations thereof).
- Cell Transfection: Transfert the modified mRNAs into your target primary somatic cells (e.g., fibroblasts) using a non-viral method such as cationic lipid nanoparticles (LNPs) or electroporation.
- Assessment:
- Immunogenicity: 24 hours post-transfection, measure the secretion of interferon-beta (IFN-β) and other pro-inflammatory cytokines via ELISA.
- Protein Expression: Quantify the expression level and duration of the encoded protein via flow cytometry (for reporters like GFP) or western blot (for transcription factors).
- Cell Viability: Assess cell health to ensure the modification and delivery method are not overly cytotoxic.
Codon Optimization: Maximizing Protein Yield
Codon optimization is the process of enhancing mRNA translation and stability by selecting synonymous codons without altering the amino acid sequence. Next-generation tools now use deep learning to move beyond simple rule-based approaches.
Advanced Optimization Frameworks
RiboDecode is a deep learning framework that optimizes mRNA sequences by directly learning from large-scale ribosome profiling (Ribo-seq) data. It can optimize for translation efficiency, mRNA stability (via Minimum Free Energy, MFE), or a weighted combination of both [33]. RNop is another deep learning tool that simultaneously optimizes for multiple factors, including species-specific codon adaptation index (CAI), tRNA adaptation index (tAI), and MFE, while employing a specialized loss function (GPLoss) to guarantee 100% amino acid sequence fidelity [34].
Table 2: Comparison of Codon Optimization Tools
| Feature | Traditional Methods (e.g., CAI) | LinearDesign | RiboDecode | RNop |
|---|---|---|---|---|
| Core Approach | Rule-based, codon frequency | Dynamic programming | Deep learning / Ribo-seq | Deep learning / multi-factor |
| Key Optimization Factors | Codon usage bias | CAI, MFE | Translation level, MFE | CAI, tAI, MFE, Fidelity |
| Context Awareness | No | No | Yes (cellular environment) | Yes (target species) |
| Validation | - | In vitro & in vivo | In vitro, in vivo (mouse model) | In vitro, in vivo (functional proteins) |
Protocol: Optimizing a Gene Sequence with RNop
- Input: Provide the wild-type amino acid sequence or cDNA of the transcription factor to be expressed.
- Parameter Selection: Specify the target organism (e.g., H. sapiens) and the relative weights for the different loss functions (e.g., balance between CAILoss for codon usage and MFELoss for secondary structure).
- Sequence Generation: Run the RNop model, which uses a transformer-based architecture to generate high-fidelity optimized codon sequences.
- In Silico Validation: Check the resulting sequences for improved metrics (e.g., higher CAI, lower MFE) compared to the wild-type and sequences optimized by other methods.
- Synthesis and Testing: Proceed with gene synthesis and IVT to produce the modRNA for experimental validation of protein expression.
The Scientist's Toolkit: Essential Reagents for modRNA Workflows
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| CleanCap AG Analog [30] | Co-transcriptional capping for high-efficiency Cap 1 formation. | Standard production of highly translatable, low-immunogenicity modRNA. |
| N1-methylpseudouridine (m1Ψ) [17] | Modified nucleoside to reduce immunogenicity and enhance translation. | Replaces uridine in IVT to create therapeutic-grade modRNA. |
| FlashCap Analogs (e.g., NPM) [31] | Photocaged cap for light-activated translation. | Spatiotemporal control of transcription factor expression in lineage conversion. |
| Lipid Nanoparticles (LNPs) | Non-viral delivery vector for efficient mRNA transfection. | Delivery of modRNA encoding reprogramming factors to primary somatic cells. |
| T7 RNA Polymerase | Bacteriophage RNA polymerase for in vitro transcription. | Enzymatic synthesis of modRNA from a DNA template. |
Integrated Workflow and Pathway Diagram
The following diagram illustrates the logical relationship and workflow for integrating the optimization strategies discussed to create an effective modRNA for direct lineage conversion.
The efficacy of direct lineage conversion using modified mRNA critically depends on the delivery platform that protects the genetic cargo, facilitates its cellular uptake, and ensures its intracellular release. Lipid Nanoparticles (LNPs) represent the most clinically advanced non-viral delivery system, notably enabling the rapid deployment of mRNA COVID-19 vaccines [35]. Their success is attributed to high encapsulation efficiency, robust protection of mRNA, and facilitated endosomal escape [36]. Alternatively, polymer-based systems offer a modular platform with tremendous versatility in structure, composition, and architectural complexity, allowing for tailored parameters including mRNA protection, loading efficacy, and targeted release [37]. This document provides detailed application notes and experimental protocols for these critical delivery platforms, contextualized within the framework of modified mRNA research for direct lineage conversion.
Platform Composition and Rational Design
The functional performance of delivery platforms is dictated by their constituent materials and formulation parameters.
Lipid Nanoparticle (LNP) Components
LNPs are complex, multi-component systems where each lipid plays a distinct functional role. The ionizable lipid is perhaps the most critical, as it is positively charged at acidic pH during formulation, enabling efficient mRNA encapsulation, and neutral at physiological pH, reducing toxicity. It is primarily responsible for facilitating endosomal escape [35]. The table below summarizes the core components of a standard LNP formulation for mRNA delivery.
Table 1: Core Components of mRNA-LNPs and Their Functions
| Component Class | Key Examples | Primary Function | Rationale for Direct Lineage Conversion |
|---|---|---|---|
| Ionizable Lipid | DLin-MC3-DMA, ALC-0315, SM-102 [38] [35] | mRNA encapsulation, endosomal escape | Enables cytosolic delivery of reprogramming mRNA; efficiency is a key determinant of protein expression levels. |
| Phospholipid (Helper Lipid) | DSPC, DOPE [38] [35] | LNP structure, bilayer stability, fusion | DOPE may enhance endosomal escape through its fusogenic properties, critical for mRNA release. |
| Cholesterol | Cholesterol, β-Sitosterol [35] | Membrane integrity, fluidity, stability | Modulates LNP permeability and stability, influencing pharmacokinetics and biodistribution. |
| PEGylated Lipid | DMG-PEG, ALC-0159 [38] [35] | Stability, circulation time, particle size | Shields LNPs, reduces aggregation, and controls particle size; its kinetics can impact cellular uptake. |
Advanced LNP systems are emerging to overcome the natural liver tropism of first-generation LNPs. For instance, the PILOT (Peptide-Ionizable Lipid Nanoparticle) platform uses peptides conjugated to ionizable lipids to achieve organ-specific mRNA delivery to the lungs, spleen, and thymus in mice [39]. Furthermore, the internal structure of LNPs, with mRNA residing at the interface of water clusters and lipids, is crucial for RNA entrapment and release [40].
Polymer-Based System Components
Polymeric architectures for mRNA delivery are categorized based on their charge and responsiveness. Their key advantage is synthetic tunability, which allows for precise manipulation of properties like molecular weight, branching, and the incorporation of functional groups [37].
Table 2: Classes of Polymers for mRNA Delivery
| Polymer Class | Key Examples | Mechanism of Complexation | Advantages and Challenges |
|---|---|---|---|
| Cationic Polymers | Polyethylenimine (PEI), Poly-L-lysine (PLL) [37] [41] | Electrostatic interaction with anionic mRNA | High transfection efficiency but often associated with significant cytotoxicity. |
| Non-Cationic Polymers | Chitosan, PLGA [37] [41] | Entrapment within a biodegradable matrix | Improved biocompatibility but may require optimization for efficient mRNA loading and endosomal escape. |
| Stimuli-Responsive Polymers | pH- or redox-sensitive polymers [37] | Conditional release in specific intracellular environments | Enhances specificity and reduces off-target effects; design complexity can be high. |
Experimental Protocols for Formulation and Characterization
Protocol 1: Microfluidic Formulation of mRNA-LNPs
This protocol describes the preparation of mRNA-LNPs using a microfluidic device, which ensures high reproducibility, controlled mixing, and consistent nanoformulations with high encapsulation efficiency [37].
Materials:
- Lipid Stock Solution: Ionizable lipid, phospholipid (e.g., DSPC), cholesterol, and PEG-lipid dissolved in ethanol (e.g., 90% ethanol with 10% pH 4 citrate buffer) [37]. Typical molar ratios are ~50% ionizable lipid, 10% phospholipid, 38.5% cholesterol, and 1.5% PEG-lipid [35].
- mRNA Solution: Purified, modified mRNA (e.g., N1-methylpseudouridine-modified) in aqueous buffer (e.g., 10 mM citrate, pH 4).
- Dialysis Buffer: PBS or another physiologically relevant buffer (pH 7.4).
- Equipment: Microfluidic mixer (e.g., NanoAssemblr, Staggered Herringbone Micromixer), syringe pumps, dialysis membranes (MWCO 100 kDa).
Procedure:
- Prepare Solutions: Dissolve the lipid mixture in ethanol to a final concentration. Dissolve mRNA in the aqueous buffer to a target concentration. Filter both solutions through a 0.22 µm filter.
- Set Up Microfluidics: Load the lipid and mRNA solutions into separate syringes. Connect them to the microfluidic device with tubing. Set the flow rate ratio (aqueous:organic) typically between 3:1 and 1:1 [37]. The total flow rate is a critical parameter influencing particle size.
- Mixing and Formation: Initiate simultaneous pumping. The rapid mixing in the microfluidic channel leads to a controlled change in polarity, inducing lipid self-assembly and mRNA encapsulation.
- Dialyze: Collect the effluent and immediately transfer it to a dialysis membrane. Dialyze against a large volume of dialysis buffer for 18-24 hours at 4°C to remove ethanol and adjust the external pH to 7.4, trapping the mRNA within the LNP [40].
- Characterize: Measure particle size (e.g., 80-120 nm), polydispersity index (PDI), zeta potential, and mRNA encapsulation efficiency (using a dye exclusion assay like RiboGreen).
The following workflow diagram illustrates the key stages of this LNP formulation process:
Diagram 1: LNP formulation workflow.
Protocol 2: Direct Mixing for Polymer-based Polyplexes
This protocol covers the formation of mRNA-polymer complexes (polyplexes) via direct mixing, a common and relatively simple method.
Materials:
- Polymer Solution: Cationic or ionizable polymer (e.g., PEI, custom biodegradable polymer) dissolved in a water-miscible organic solvent like DMSO or a mild acidic aqueous buffer.
- mRNA Solution: Modified mRNA in nuclease-free water or buffer.
- Equipment: Vortex mixer, pipettes.
Procedure:
- Prepare Stock Solutions: Dilute the polymer and mRNA to working concentrations in the same buffer to ensure compatibility.
- Mixing: Rapidly add the polymer solution to the mRNA solution while vortexing. The order of addition can impact particle size and homogeneity.
- Incubation: Allow the mixture to incubate for 15-30 minutes at room temperature to facilitate complexation.
- Characterize: Determine the N:P ratio (Nitrogen in polymer to Phosphate in RNA), which critically determines complexation, size, stability, and transfection efficiency. Measure particle size, PDI, and zeta potential.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of delivery platforms requires a suite of critical reagents and analytical tools.
Table 3: Essential Research Reagents for Delivery Platform Development
| Reagent / Material | Function / Application | Example Specifications / Notes |
|---|---|---|
| Ionizable Lipids | Core functional lipid for mRNA encapsulation and endosomal escape. | DLin-MC3-DMA (established), novel lipids (e.g., from AI-designed libraries [42]). |
| Cationic Polymers | Electrostatic complexation with mRNA for polyplex formation. | Branched PEI (25 kDa, high transfection, high toxicity), linear PEI, PLL. |
| PEG-Lipids | Stabilize nanoparticles, control size, reduce opsonization. | DMG-PEG2000, DSG-PEG2000, ALC-0159; consider diffusible vs. non-diffusible PEG. |
| Modified mRNA | The therapeutic cargo; modifications enhance stability and reduce immunogenicity. | N1-methylpseudouridine base modification, optimized 5' cap (Cap 1), and poly-A tail length [37]. |
| Microfluidic Device | Reproducible, scalable formulation of LNPs and some polymer systems. | NanoAssemblr, lab-made staggered herringbone mixer (SHM). |
| Analytical Instrumentation | Characterizing Critical Quality Attributes (CQAs) of nanoparticles. | DLS for size/PDI, zeta potential analyzer, Ribogreen assay for encapsulation efficiency, SAXS for internal structure [40]. |
Advanced Applications and Future Perspectives in Lineage Conversion
The application of LNPs and polymer-based systems extends far beyond vaccines into the realm of gene editing and cellular reprogramming.
- Gene Editing In Vivo: The PILOT platform has been used to deliver mRNA encoding prime editors to specific organs in mice, achieving editing rates of 13.1% in the liver and 7.4% in the lungs [39]. This demonstrates the potential for correcting genetic defects underlying lineage-specific diseases.
- Computational Design: The use of transformer-based neural networks like COMET, trained on large LNP datasets (LANCE), can predict LNP efficacy based on lipid components and their ratios. This AI-driven approach can rapidly identify novel LNP formulations optimized for specific tasks, such as delivering reprogramming factors to particular cell types [42].
- Addressing Delivery Barriers: While LNPs have seen immense success, they face challenges like liver tropism, storage stability (cold chain), and PEG-related immunogenicity. Future development focuses on targeted systems (like PILOT), thermostable lyophilized LNPs, and biodegradable lipids and polymers to improve safety and accessibility [43] [35].
The following diagram outlines the critical intracellular pathway and key barriers for mRNA delivery in direct lineage conversion:
Diagram 2: Intracellular mRNA delivery pathway.
Within the context of direct lineage conversion research, the generation of induced pluripotent stem cells (iPSCs) represents a foundational reprogramming methodology. Since the landmark discovery by Takahashi and Yamanaka that somatic cells could be reprogrammed using the transcription factors OCT4, SOX2, KLF4, and c-MYC (OSKM), the field has advanced significantly [44]. These iPSCs, with their unparalleled proliferative capacity and pluripotent differentiation potential, provide an invaluable platform for disease modeling, drug screening, and therapeutic development [44]. Current research focuses on refining reprogramming factors, enhancing the safety of delivery systems, and developing non-integrating methods, including modified mRNA protocols, to generate high-quality iPSCs suitable for precise lineage conversion and clinical applications [44] [29].
Advances in Reprogramming Methods
The core process of somatic cell reprogramming has evolved beyond the original OSKM factors to include various safe and efficient alternatives.
Reprogramming Factor Optimization
The original Yamanaka factors included the oncogene c-Myc, posing significant tumorigenic risks [44]. Subsequent research has identified safer and more efficient alternatives, summarized in the table below.
Table 1: Reprogramming Factors and Their Roles
| Factor Category | Examples | Function in Reprogramming | Notes |
|---|---|---|---|
| Core Factors | OCT4, SOX2 | Master regulators of pluripotency; initiate epigenetic remodeling [44]. | Essential; OCT4 alone can reprogram human neural stem cells [44]. |
| Klf Family | KLF4, KLF2, KLF5 | Facilitates transition to pluripotency; can substitute for one another [44]. | KLF4 is part of the original OSKM combination. |
| Myc Family | c-MYC, L-MYC, N-MYC | Enhances proliferation and reprogramming efficiency; an oncogene [44]. | L-MYC reduces tumorigenic risk compared to c-MYC [44]. |
| Alternative Combinations | NANOG, LIN28 (OSNL) [44] | Sufficient to reprogram human somatic cells without c-MYC. | Addresses tumorigenic concerns of the OSKM set. |
| Small Molecule Replacements | RepSox [44] | Can replace SOX2 in the reprogramming cocktail. | Enhances safety by reducing the number of genetic factors needed. |
Other non-factor additives significantly improve reprogramming. MicroRNAs like miR-302/367 and miR-372 notably enhance the reprogramming of somatic cells to pluripotency [44]. Furthermore, epigenetic modulators such as histone deacetylase inhibitors (e.g., Valproic Acid, VPA) and DNA methyltransferase inhibitors can dramatically increase iPSC generation efficiency. For instance, combining 8-Br-cAMP with VPA increased reprogramming efficiency in human fibroblasts by up to 6.5-fold [44].
Delivery Systems for Reprogramming
The method used to deliver reprogramming factors into a somatic cell is critical, as it impacts the safety, efficiency, and potential clinical applicability of the resulting iPSCs.
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Vector/Platform | Genetic Material | Genomic Integration? | Key Considerations |
|---|---|---|---|
| Retrovirus/Lentivirus | DNA | Yes | High efficiency but risks insertional mutagenesis; silencing can be an issue [44]. |
| Sendai Virus (SeV) | RNA | No | Non-integrating, high efficiency; requires dilution over passages as it is a replicating virus [45]. |
| Episomal Plasmid | DNA | No | Non-integrating; low efficiency; requires repeated transfections [45]. |
| Synthetic RNA | RNA (e.g., modified mRNA) | No | Non-integrating, high efficiency; requires multiple transfections and may trigger innate immune response without proper modification [44] [29]. |
| Recombinant Protein | Protein | No | Safest method; very low efficiency and technically challenging [44]. |
For clinical applications, non-integrating methods like Sendai virus, episomal plasmids, and modified mRNA are preferred due to their superior safety profiles [45]. Modified mRNA technology, in particular, offers a non-integrative and controllable strategy for expressing therapeutic proteins, making it a transformative tool in regenerative medicine [29].
Detailed Experimental Protocols
This section provides a detailed methodology for generating iPSCs using a non-integrating Sendai virus system, a common and reliable method.
Protocol: iPSC Generation Using Sendai Virus
Objective: To reprogram human somatic cells (e.g., fibroblasts) into induced pluripotent stem cells using non-integrating Sendai viral vectors. Principle: The CytoTune-iPS Sendai Virus particles deliver the OSKM or OSKML factors into target cells without integrating into the host genome, initiating the reprogramming process [45].
Materials:
- Somatic Cells: Human fibroblasts (e.g., BJ foreskin fibroblasts or IMR-90 lung fibroblasts) [46] [45].
- Reprogramming Vectors: CytoTune-iPS Sendai Virus Particles (KOS, hc-Myc, hKlf4) or similar.
- Cell Culture Media:
- Fibroblast medium: DMEM supplemented with 10% FBS and 1x GlutaMAX.
- Pluripotent Stem Cell (PSC) medium: Essential 8 or StemFlex medium [45].
- Matrix: Vitronectin (VTN-N) or Geltrex for feeder-free culture.
- Supplements: RevitaCell Supplement for enhanced cell survival.
- Equipment: 6-well culture plates, 37°C CO₂ incubator, inverted microscope.
Procedure:
- Preparation of Somatic Cells:
- Culture human fibroblasts in a 6-well plate until they reach 70-90% confluency. Ensure cells are healthy and actively dividing.
Viral Transduction:
- Calculate the required volume of each virus (KOS, hc-Myc, hKlf4) based on the manufacturer's instructions and the target cell count (typically a Multiplicity of Infection, MOI, of 5-10 for each virus).
- Thaw virus particles on ice and prepare the virus mixture in fibroblast medium containing 4-8 µg/mL polybrene to enhance transduction efficiency.
- Aspirate the medium from the fibroblasts and add the virus-containing medium.
- Incubate cells for 24 hours at 37°C in a CO₂ incubator.
Post-Transduction and Medium Change:
- After 24 hours, carefully remove the virus-containing medium and replace it with fresh, pre-warmed fibroblast medium.
- Culture the transduced cells for an additional 6 days, changing the medium every other day.
Transfer to Feeder-Free Conditions and iPSC Colony Picking:
- On day 7 post-transduction, harvest the cells using dissociation reagents and plate them onto a VTN-N or Geltrex-coated 6-well plate in fibroblast medium supplemented with RevitaCell.
- On the following day, slowly transition the culture medium to Essential 8 or StemFlex medium over several days.
- Over the next 2-4 weeks, monitor the culture for the emergence of compact, embryonic stem cell-like colonies with defined borders.
- Manually pick individual iPSC colonies using a pipette tip or sterile scalpel and transfer them to new coated wells for expansion and characterization.
Protocol: Confirmation of Pluripotency
Objective: To validate the successful reprogramming and pluripotent state of the generated iPSCs. Methods: Characterization involves assessing molecular markers and functional potential [45].
Immunocytochemistry: Fix iPSC colonies and stain for key pluripotency markers.
- Primary Antibodies: Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4.
- Analysis: High-quality iPSC colonies should show strong nuclear staining for OCT4, SOX2, and NANOG, and surface staining for SSEA-4.
In Vitro Differentiation via Embryoid Body (EB) Formation:
- Harvest iPSCs and culture them in low-attachment plates to form EBs in differentiation medium.
- After 7-10 days, plate EBs on gelatin-coated dishes and allow for spontaneous differentiation for another 7-14 days.
- Analyze the resulting cells for markers of all three germ layers:
- Ectoderm: β-III-tubulin (TUJ1)
- Mesoderm: α-smooth muscle actin (α-SMA)
- Endoderm: Alpha-fetoprotein (AFP)
qRT-PCR Analysis:
- Isolve RNA from iPSCs and perform qRT-PCR to detect the expression of endogenous pluripotency genes (OCT4, SOX2, NANOG).
- Ensure the absence of the Sendai virus genome by performing PCR with primers specific for the Sendai virus RNA.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for iPSC Generation and Culture
| Reagent/Material | Function | Example Products |
|---|---|---|
| Sendai Virus Vectors | Non-integrating delivery of OSKM reprogramming factors. | CytoTune-iPS Sendai Virus Particles [45]. |
| Episomal Plasmids | Non-integrating, DNA-based delivery of reprogramming factors. | Episomal iPSC Reprogramming Vectors [45]. |
| Optimized PSC Media | Supports the growth and maintenance of pluripotent stem cells. | Essential 8, StemFlex, mTeSR1 [45]. |
| Cell Culture Matrices | Provides a defined, feeder-free substrate for PSC attachment and growth. | Vitronectin (VTN-N), Geltrex [45]. |
| Reprogramming Enhancers | Small molecules or compounds that boost reprogramming efficiency. | Sodium Butyrate, Valproic Acid (VPA), RepSox [44]. |
| Transfection Reagents | For delivering plasmid or RNA-based reprogramming factors. | Lipofectamine Stem Transfection Reagent [45]. |
Visualizing the Reprogramming Workflow
The following diagram illustrates the complete experimental workflow for generating and validating iPSCs, from somatic cell preparation to the characterization of fully reprogrammed cells.
Figure 1: iPSC Generation and Validation Workflow.
The molecular pathway of reprogramming involves a cascade of events initiated by the forced expression of the transcription factors, leading to epigenetic remodeling and a metabolic shift.
Figure 2: Key Molecular Events in Cellular Reprogramming.
Direct transdifferentiation, or lineage reprogramming, represents a groundbreaking strategy in regenerative medicine for converting one somatic cell type directly into another without reverting to a pluripotent state. This approach bypasses the ethical concerns and tumorigenic risks associated with induced pluripotent stem cells (iPSCs) and enables more rapid cell fate conversion while preserving age-related epigenetic signatures that are crucial for modeling age-related diseases [47]. Fibroblasts have emerged as a predominant source cell for reprogramming due to their abundance, accessibility, and remarkable plasticity [48] [49].
This Application Note provides detailed methodologies for two prominent case studies in direct transdifferentiation: the conversion of fibroblasts into functional myoblasts and neurons. The protocols are framed within the context of advanced modified mRNA research, offering a non-integrating, efficient alternative to viral vector-based reprogramming that minimizes genomic alteration risks while enabling precise temporal control over transgene expression [12] [17]. These approaches hold significant promise for disease modeling, drug screening, and developing regenerative therapies for conditions including muscular dystrophies, neurodegenerative disorders, and age-related pathologies.
Technical Foundations of Direct Lineage Conversion
Key Advantages of Modified mRNA Platforms
Modified mRNA platforms have emerged as powerful tools for cellular reprogramming due to several distinct advantages over traditional viral methods:
- Non-integrative Nature: Unlike retroviral or lentiviral vectors, modified mRNA does not integrate into the host genome, eliminating the risk of insertional mutagenesis and permanent genetic alterations [12].
- Transient Expression: The transient nature of mRNA expression allows for precise control over the timing and duration of reprogramming factor expression, enabling more refined manipulation of cell fate [17].
- Reduced Immunogenicity: Incorporation of modified nucleosides such as pseudouridine (Ψ) or N1-methyl pseudouridine (m1Ψ) significantly reduces recognition by pattern recognition receptors, minimizing innate immune responses that could compromise cell viability and reprogramming efficiency [17].
- Rapid Protein Production: mRNA translation occurs directly in the cytoplasm, bypassing the need for nuclear entry and accelerating the production of reprogramming factors [50].
Critical Signaling Pathways in Fibroblast Reprogramming
Successful transdifferentiation requires overcoming the robust fibrotic identity maintained by signaling pathways in fibroblasts. Key pathways that must be modulated during reprogramming include:
- TGF-β Signaling: A central pathway sustaining fibroblast identity and promoting fibrosis; its inhibition is frequently necessary for successful reprogramming [48] [12].
- JNK and JAK/STAT Pathways: Inhibition of these pathways has been shown to significantly enhance reprogramming efficiency in fibroblast to myogenic progenitor conversion [12].
- Mechanical Signaling: ECM-derived mechanical cues help maintain fibroblast identity; modulating substrate stiffness can facilitate reprogramming [48].
- Epigenetic Regulators: Chromatin remodeling is essential for accessing new transcriptional programs; epigenetic modifiers can enhance reprogramming efficiency [48].
The following diagram illustrates the core workflow and key molecular interventions in direct fibroblast transdifferentiation:
Case Study 1: Conversion of Fibroblasts to Functional Myoblasts
The direct conversion of fibroblasts to induced myogenic progenitor cells (iMPCs) represents a promising approach for generating therapeutic cells for muscular disorders. The following protocol outlines a highly efficient, transgene-free method utilizing synthetic MyoD-mRNA in combination with a small molecule cocktail to convert mouse fibroblasts into functional iMPCs capable of robust engraftment and dystrophin restoration in vivo [12].
Key advantages of this approach include the generation of a proliferative myogenic stem cell population (unlike direct transdifferentiation which typically produces post-mitotic myotubes), avoidance of genomic integration, and high efficiency with Pax7-positive cells emerging in as little as 10 days [12].
The workflow for fibroblast to myoblast conversion is summarized below:
Detailed Protocol for Myogenic Conversion
Cell Culture and Preparation
Source and Culture Mouse Embryonic Fibroblasts (MEFs):
- Isolate MEFs from E13.5 mouse embryos or utilize commercially available sources.
- Culture in fibroblast growth medium: DMEM supplemented with 10% fetal bovine serum (FBS), 2 mM L-glutamine, 1% non-essential amino acids, and 1% penicillin-streptomycin.
- Maintain at 37°C in a 5% CO₂ humidified incubator.
- Use cells at early passages (P2-P4) for optimal reprogramming efficiency.
Plating for Reprogramming:
- Plate MEFs at a density of 50,000 cells/cm² in 6-well plates coated with Matrigel (1:100 dilution in DMEM).
- Allow cells to adhere for 24 hours prior to initiating reprogramming.
Modified mRNA Synthesis and Transfection
MyoD-mRNA Construct Design:
- Utilize a synthetic MyoD-mRNA sequence codon-optimized for enhanced expression.
- Incorporate modified nucleosides (pseudouridine or N1-methyl pseudouridine) to reduce immunogenicity.
- Include a 5' cap structure (CleanCap or similar) and optimized 5' and 3' UTRs to enhance stability and translation efficiency.
- Incorporate a poly(A) tail of approximately 120 nucleotides.
mRNA Transfection Protocol:
- Prepare transfection complex: Combine 2 µg of synthetic MyoD-mRNA with 4 µL of mRNA transfection reagent in 200 µL of serum-free medium.
- Incubate for 5-10 minutes at room temperature.
- Add complexes dropwise to cells in fresh fibroblast growth medium.
- Perform transfections daily for 5-7 consecutive days.
- Monitor cells for morphological changes indicative of myogenic conversion (appearance of elongated, bipolar cells).
Small Molecule Cocktail Formulation and Application
Preparation of Enhanced Small Molecule Cocktail:
- Prepare stock solutions of the following compounds:
- Forskolin (F): 10 mM in DMSO
- RepSox (R): 10 mM in DMSO
- CHIR99210 (C): 10 mM in DMSO
- SP600125 (SP): 10 mM in DMSO (JNK inhibitor)
- CP690550 (CP): 10 mM in DMSO (JAK/STAT inhibitor)
- Prepare stock solutions of the following compounds:
Treatment Protocol:
- Add small molecules to the culture medium 24 hours after the first mRNA transfection at the following working concentrations:
Table 1: Small Molecule Cocktail for Enhanced Myogenic Conversion
Compound Target Pathway Stock Concentration Working Concentration Function in Reprogramming Forskolin cAMP agonist 10 mM in DMSO 10 µM Enhances reprogramming efficiency RepSox TGF-β receptor inhibitor 10 mM in DMSO 2 µM Suppresses fibrotic signaling CHIR99210 GSK3 inhibitor 10 mM in DMSO 3 µM Promotes myogenic progression SP600125 JNK inhibitor 10 mM in DMSO 10 µM Enhances Pax7+ cell population CP690550 JAK/STAT inhibitor 10 mM in DMSO 1 µM Enhances Pax7+ cell population - Refresh the small molecule cocktail every 48 hours throughout the reprogramming process.
iMPC Culture and Expansion
Transition to Growth Medium:
- After 10-14 days of reprogramming, transition emerging iMPCs to myogenic growth medium: F-10 nutrient mixture supplemented with 20% FBS, 5 ng/mL bFGF, 1% penicillin-streptomycin.
- Passage cells at 70-80% confluence using gentle enzymatic dissociation.
Characterization of iMPCs:
- Assess reprogramming efficiency by immunocytochemistry for Pax7 (muscle stem cell marker) and MyoD (myogenic regulator).
- Perform flow cytometry to quantify the percentage of Pax7-positive cells.
- Evaluate differentiation potential by switching to low-serum medium (2% horse serum) to induce myotube formation.
- Analyze expression of mature muscle markers including myosin heavy chain (MHC) and dystrophin in differentiated myotubes.
In Vivo Functional Validation
Cell Transplantation:
- Harvest iMPCs using standard trypsinization procedures.
- Resuspend 100,000-500,000 cells in 20-30 µL of PBS for intramuscular injection into the tibialis anterior muscle of dystrophic (e.g., mdx) mice.
- Include a dye such as DiI for cell tracking if needed.
Assessment of Engraftment:
- Analyze muscles 4-8 weeks post-transplantation for donor cell engraftment.
- Perform immunohistochemistry for dystrophin and other muscle markers.
- Quantify the number of dystrophin-positive fibers and central nucleated fibers (indicative of regeneration).
Quantitative Outcomes and Efficiency Metrics
Table 2: Representative Efficiency Metrics for Fibroblast to iMPC Conversion
| Parameter | Conventional MyoD Only | MyoD + F/R/C | MyoD + Enhanced Cocktail (F/R/C/SP/CP) |
|---|---|---|---|
| Time to Pax7+ cells | 14-21 days | 12-16 days | 10-14 days |
| Percentage of Pax7+ cells | 5-10% | 25-30% | 55-60% |
| Myogenic marker expression | Low | Moderate | High |
| Proliferation capacity | Limited | Moderate | Extensive |
| In vivo engraftment efficiency | Low | Moderate | High (hundreds of dystrophin+ fibers) |
Case Study 2: Conversion of Fibroblasts to Functional Neurons
The direct conversion of fibroblasts to induced neurons (iNs) offers a valuable model for studying neurological diseases, particularly age-related neurodegenerative disorders like Alzheimer's disease, as iNs retain age-associated epigenetic signatures that are erased during iPSC reprogramming [47]. This protocol describes efficient generation of functional neurons from human fibroblasts using both transcription factor-based and small molecule approaches, with specific application to Alzheimer's disease modeling.
Key advantages include preservation of donor age epigenetic signatures, faster generation compared to iPSC-derived neurons (2-3 weeks versus 2-3 months), and relevance for modeling age-related diseases [47].
The workflow for neuronal conversion is summarized below:
Detailed Protocol for Neuronal Conversion
Fibroblast Culture and Preparation
Source and Culture Human Dermal Fibroblasts (HDFs):
- Obtain fibroblasts from skin biopsies of Alzheimer's disease patients (familial AD with known mutations or sporadic AD) and age-matched healthy controls.
- Culture in fibroblast medium: DMEM supplemented with 10% FBS, 2 mM L-glutamine, 1% non-essential amino acids, and 1% penicillin-streptomycin.
- Use cells between passages 3-8 for consistent reprogramming efficiency.
Plating for Neuronal Reprogramming:
- Plate HDFs at a density of 30,000-50,000 cells/cm² on surface-coated dishes (poly-D-lysine/laminin coating recommended for neuronal culture).
- Allow cells to adhere for 24-48 hours before initiating reprogramming.
Transcription Factor-Mediated Neuronal Conversion
BAM Reprogramming Factors Delivery:
- Utilize lentiviral vectors encoding the BAM factors: Brn2 (Pou3f2), Ascl1, and Myt1L.
- Prepare viral particles with titers of ≥1×10⁸ IU/mL.
- Transduce fibroblasts at a multiplicity of infection (MOI) of 5-10 for each factor in the presence of 6 μg/mL polybrene.
- Replace virus-containing medium with fresh fibroblast medium after 12-16 hours.
Small Molecule-Mediated Neuronal Conversion:
- As a non-integrative alternative, utilize small molecule cocktails to induce neuronal conversion.
- Prepare a combination of molecules including but not limited to:
- CHIR99021 (GSK-3β inhibitor)
- RepSox (TGF-β inhibitor)
- Forskolin (cAMP activator)
- VPA (histone deacetylase inhibitor)
- DAPT (Notch inhibitor)
Neuronal Maturation and Maintenance
Transition to Neuronal Medium:
- 3-5 days post-reprogramming initiation, transition cells to neuronal maturation medium: Neurobasal medium supplemented with B-27, brain-derived neurotrophic factor (BDNF, 20 ng/mL), neurotrophin-3 (NT-3, 20 ng/mL), and laminin (1 μg/mL).
- Include NGF (nerve growth factor) for peripheral neuron specification if desired.
Culture Conditions for Maturation:
- Maintain cultures for 2-4 weeks to allow full neuronal maturation, with half-medium changes every 3-4 days.
- Include mitotic inhibitors (5-fluorodeoxyuridine with uridine) after the first week to prevent proliferation of any non-reprogrammed fibroblasts.
Characterization of Induced Neurons
Immunocytochemical Analysis:
- Fix cells at 2-4 weeks and stain for neuronal markers:
- MAP-2 (mature neuronal marker)
- NeuN (neuronal nuclei marker)
- Synapsin (synaptic marker)
- Tau (axonal marker)
- Assess purity by quantifying the percentage of MAP-2 positive cells.
- Fix cells at 2-4 weeks and stain for neuronal markers:
Functional Characterization:
- Perform patch-clamp electrophysiology to assess action potential generation and synaptic activity.
- Measure calcium transients using Fluo-4 or similar calcium indicators to assess neuronal activity.
AD-Specific Phenotyping:
- For AD patient-derived iNs, analyze disease-relevant phenotypes:
- Amyloid-β metabolism (Aβ40/Aβ42 ratio)
- Phosphorylated tau levels (using phospho-tau specific antibodies)
- Mitochondrial function and oxidative stress markers
- Endosomal abnormalities (common in AD neurons)
- For AD patient-derived iNs, analyze disease-relevant phenotypes:
Quantitative Outcomes and Disease Modeling Applications
Table 3: Efficiency Metrics and AD-Relevant Phenotypes in Fibroblast-to-Neuron Conversion
| Parameter | BAM Factor Method | Small Molecule Method | AD-Specific Phenotypes in iNs |
|---|---|---|---|
| Time to neuronal markers | 7-14 days | 14-21 days | N/A |
| Percentage of MAP-2+ cells | 20-30% | 10-20% | N/A |
| Functional maturity | 3-4 weeks | 4-5 weeks | N/A |
| Amyloid-β pathology | N/A | N/A | Elevated Aβ42/Aβ40 ratio in FAD iNs |
| Tau pathology | N/A | N/A | Increased hyperphosphorylated tau |
| Electrophysiological activity | Action potentials, synaptic currents | Action potentials, synaptic currents | Altered network activity in AD iNs |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Direct Transdifferentiation
| Reagent Category | Specific Examples | Function in Reprogramming | Application Notes |
|---|---|---|---|
| Reprogramming Factors | MyoD (myogenic), BAM factors (neuronal) | Pioneer transcription factors that initiate lineage-specific gene expression programs | Codon-optimized sequences with modified nucleosides enhance expression and reduce immunogenicity [12] [17] |
| Small Molecule Enhancers | Forskolin, RepSox, CHIR99210, SP600125, CP690550 | Modulate key signaling pathways to overcome epigenetic barriers and enhance reprogramming efficiency | JNK and JAK/STAT inhibition specifically increases Pax7+ iMPC population [12] |
| mRNA Modification Tools | Pseudouridine (Ψ), N1-methyl pseudouridine (m1Ψ), 5' cap analogs, optimized UTRs | Enhance mRNA stability, reduce immunogenicity, and improve translation efficiency | Modified nucleosides are critical for reducing innate immune recognition of exogenous mRNA [17] |
| Delivery Systems | Lipid nanoparticles, electroporation, tissue nanotransfection (TNT) | Enable efficient intracellular delivery of reprogramming factors | Nanoelectroporation techniques like TNT allow non-viral, in vivo reprogramming [50] |
| Characterization Tools | Pax7, MyoD, MHC (myogenic); MAP-2, NeuN, Synapsin (neuronal) | Validate successful lineage conversion and functional maturation | Combination of early and late markers needed to assess reprogramming progression |
Technical Considerations and Optimization Strategies
Critical Parameters for Success
Starting Cell Population:
- Fibroblast source and passage number significantly impact reprogramming efficiency.
- Early passage cells (P2-P8) generally reprogram more efficiently than senescent, high-passage cells.
- Consider using defined fibroblast populations to minimize variability.
Temporal Control of Factor Expression:
- For mRNA-based approaches, daily transfections for 5-7 days typically yield optimal results.
- Extended factor expression may promote maturation but can also increase cell stress.
- Small molecule timing should be optimized for each reprogramming protocol.
Metabolic and Epigenetic Priming:
- Pre-treatment with metabolic modulators or epigenetic modifiers can enhance reprogramming efficiency.
- Assessment of mitochondrial function and chromatin accessibility may help predict reprogramming competence.
Troubleshooting Common Challenges
Low Reprogramming Efficiency:
- Optimize transfection parameters and mRNA quality.
- Validate small molecule activity and stability in culture conditions.
- Include pathway-specific enhancers (e.g., JNK inhibitors for myogenic conversion).
Incomplete Maturation:
- Extend culture time in maturation-promoting conditions.
- Include additional maturation factors specific to the target cell type.
- Consider co-culture with primary cells or exposure to target tissue extracts.
Cell Stress and Apoptosis:
- Reduce mRNA dose or increase intervals between transfections.
- Include cytoprotective compounds (e.g., ROCK inhibitors) during critical phases.
- Optimize cell density to prevent overconfluence and nutrient deprivation.
The protocols outlined in this Application Note provide robust frameworks for direct transdifferentiation of fibroblasts into myoblasts and neurons using advanced modified mRNA and small molecule approaches. The myogenic conversion protocol enables generation of functional iMPCs capable of extensive proliferation and in vivo engraftment, offering significant potential for treating muscular disorders. The neuronal conversion methodology facilitates the creation of patient-specific iNs that retain age-related epigenetic signatures, providing clinically relevant models for neurodegenerative disease research and drug screening.
As modified mRNA technologies continue to evolve with innovations in nucleoside chemistry, sequence optimization, and delivery systems, the efficiency and safety of direct lineage conversion will further improve. These approaches represent powerful tools for both basic research investigating cell fate determination and translational applications in regenerative medicine.
Broad Applications in Regenerative Medicine for Cardiac, Liver, and Muscle Repair
Direct lineage conversion, the process of reprogramming one somatic cell type directly into another without reverting to a pluripotent state, represents a paradigm shift in regenerative medicine. The advent of modified messenger RNA (modRNA) technology has significantly advanced this field by enabling transient, high-efficiency expression of reprogramming factors with a superior safety profile compared to viral vectors. Unlike viral methods, modRNA does not integrate into the host genome, eliminating the risk of insertional mutagenesis, and its transient nature allows for precise control over the reprogramming process, making it particularly suitable for clinical applications [12] [51].
This application note details standardized protocols and key experimental data for using modRNA to induce direct lineage conversion in three critical areas: cardiac repair, liver regeneration, and skeletal muscle restoration. The methodologies outlined herein are designed to provide researchers, scientists, and drug development professionals with a robust framework for developing regenerative therapies based on this cutting-edge technology.
Application Note & Protocol: Cardiac Repair after Myocardial Infarction
Background and Rationale
Myocardial infarction (MI) remains a leading cause of death and disability worldwide. The permanent loss of cardiomyocytes and the heart's limited regenerative capacity often lead to chronic heart failure. Current treatments manage symptoms but do not address the underlying loss of cardiac tissue [52]. In vivo reprogramming of cardiac fibroblasts into cardiomyocytes via modRNA offers a promising strategy to replenish lost myocardium, reduce fibrotic scarring, and restore cardiac function [53] [52].
Key Experimental Data and Findings
Recent preclinical studies have demonstrated the efficacy of modRNA-based interventions for cardiac repair. The table below summarizes quantitative data from key studies, highlighting the significant functional improvements achieved.
Table 1: Quantitative Outcomes of modRNA-Based Cardiac Repair in Preclinical Models
| modRNA Construct | Disease Model | Key Functional Outcomes | Cellular/Molecular Outcomes | Source |
|---|---|---|---|---|
| PSAT1-modRNA | Mouse model of heart attack | - Significantly enhanced heart function- Improved survival rate | - Robust increase in cardiomyocyte proliferation- Reduced tissue scarring- Improved blood vessel formation | [52] |
| GHMT Factors* (Gata4, Hand2, Mef2c, Tbx5) | Mouse model of heart failure | - Contribution to ventricular contractility | - Successful conversion of cardiac fibroblasts into induced cardiomyocytes (iCMs)- Integration of iCMs into myocardium | [53] |
Note: The GHMT factors have been delivered via viral vectors in cited literature; their delivery via modRNA represents a promising non-viral approach for this protocol.
Detailed Experimental Protocol
Objective: To directly reprogram cardiac fibroblasts into functional cardiomyocytes in situ using PSAT1-modRNA to repair heart tissue post-myocardial infarction.
Materials:
- Research Reagent Solutions:
- PSAT1-modRNA: Synthetic modified mRNA encoding the PSAT1 gene, optimized for stability and translation (e.g., using N1-methylpseudouridine modifications) [52] [51].
- Lipid Nanoparticles (LNPs): For in vivo delivery. Composed of ionizable lipid, phospholipid, cholesterol, and PEG-lipid [54] [51].
- Phosphate-Buffered Saline (PBS): For vehicle control injections.
Methodology:
- modRNA Formulation: Encapsulate the PSAT1-modRNA in LNPs using a microfluidic mixing device. Purify and concentrate the formulated LNPs using tangential flow filtration. Determine the particle size, polydispersity index, and encapsulation efficiency [54] [51].
- Animal Model and Surgery: Induce myocardial infarction in adult C57BL/6 mice via permanent ligation of the left anterior descending (LAD) coronary artery.
- Therapeutic Administration: Immediately post-MI, perform intramyocardial injections of PSAT1-modRNA-LNPs (e.g., 10 µg modRNA in 30 µL total volume) at multiple sites in the border zone of the infarct. A control group should receive LNPs encapsulating a non-coding modRNA.
- Functional Assessment:
- Echocardiography: At 2 and 4 weeks post-treatment, assess cardiac function parameters, including Left Ventricular Ejection Fraction (LVEF) and Fractional Shortening (FS), under light anesthesia.
- Hemodynamic Measurements: At the study endpoint, perform invasive pressure-volume loop analysis to obtain more precise measures of systolic and diastolic function.
- Tissue Analysis:
- Histology: Harvest hearts at 4 weeks post-treatment. Analyze tissue sections with:
- Masson's Trichrome staining to quantify fibrotic area.
- Immunofluorescence staining for cardiomyocyte markers (α-actinin), proliferation markers (Ki67), and endothelial markers (CD31) to assess cardiomyocyte proliferation and angiogenesis.
- Molecular Analysis: Use RNA sequencing and qPCR on infarct zone tissue to analyze the activation of the serine synthesis pathway (SSP) and expression of pacemaker genes.
- Histology: Harvest hearts at 4 weeks post-treatment. Analyze tissue sections with:
Diagram 1: PSAT1-modRNA Cardiac Repair Workflow
Application Note & Protocol: Liver Repair and Regeneration
Background and Rationale
The liver possesses a remarkable capacity for regeneration. However, in cases of acute liver failure or end-stage chronic disease, this capacity can be overwhelmed. modRNA therapy offers a promising approach to deliver therapeutic proteins, such as growth factors or enzymes, to boost the liver's innate regenerative programs or correct inherited metabolic diseases [54] [55]. The natural tropism of certain lipid nanoparticles (LNPs) for the liver, mediated by ApoE binding to LDL receptors on hepatocytes, makes it an ideal target for modRNA therapies [54].
Key Experimental Data and Findings
Research in liver regeneration has identified key signaling pathways and metabolic reprogramming as critical drivers of repair. The following table summarizes the core molecular mechanisms that can be targeted using modRNA technology.
Table 2: Key Molecular Pathways in Liver Repair and Regeneration
| Target Pathway / Process | Role in Liver Regeneration | Potential modRNA Therapeutic Target |
|---|---|---|
| HGF/c-MET Signaling | Promotes hepatocyte proliferation and inhibits apoptosis. A primary mitogenic pathway. | modRNA encoding HGF variants or engineered c-MET agonists. |
| Wnt/β-catenin Signaling | Critical for zonation and metabolic liver function; activated early during regeneration. | modRNA encoding Wnt ligands or stabilizers of β-catenin. |
| Metabolic Reprogramming | Shift to glycolysis provides biomass and energy for proliferating hepatocytes. | modRNA encoding key metabolic enzymes (e.g., PSAT1, a key enzyme in the serine synthesis pathway). |
| EGF/TGF-α Signaling | Potent stimulators of hepatocyte DNA synthesis and proliferation. | modRNA encoding EGF or TGF-α. |
| JAK/STAT Signaling | Activated by cytokines like IL-6; crucial for the priming phase of hepatocyte proliferation. | modRNA encoding cytokine ligands for specific STAT activation. |
Detailed Experimental Protocol
Objective: To deliver a therapeutic protein via modRNA-LNPs to stimulate hepatocyte proliferation and restore liver function in a model of acute liver injury.
Materials:
- Research Reagent Solutions:
- HGF-modRNA or PSAT1-modRNA: modRNA encoding human Hepatocyte Growth Factor (HGF) or PSAT1.
- Liver-Tropic LNPs: Ionizable lipid nanoparticles known for high hepatocyte transfection efficiency (e.g., containing the lipid SM-102 or ALC-0315) [54].
- Animal Model: Mice with drug-induced (e.g., CCl4) acute liver injury.
Methodology:
- modRNA-LNP Preparation: Formulate modRNA-LNPs as described in Section 2.3, ensuring a particle size of 70-100 nm for optimal hepatocyte uptake.
- Disease Model Induction: Induce acute liver injury in mice via intraperitoneal injection of CCl4 (e.g., 0.5 mL/kg in olive oil).
- Therapeutic Administration: 24 hours post-injury, administer modRNA-LNPs intravenously via the tail vein (e.g., 1-5 mg modRNA per kg body weight). Include control groups receiving saline or empty LNPs.
- Assessment of Regeneration:
- Serum Biochemistry: Collect blood at 24, 48, and 72 hours post-treatment. Measure alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels as markers of liver injury.
- Proliferation Analysis: At 48 hours post-treatment, inject mice with BrdU or EdU. Harvest liver tissue and perform immunofluorescence for BrdU/EdU and the hepatocyte marker HNF4α to quantify proliferating hepatocytes.
- Gene Expression: Analyze liver tissue by qPCR for expression of cell cycle genes (e.g., Cyclin D1, PCNA) and regenerative markers.
- Functional Test: Measure the clearance of a marker dye (e.g., bromosulfophthalein) to assess overall liver metabolic function.
Application Note & Protocol: Skeletal Muscle Repair
Background and Rationale
Duchenne Muscular Dystrophy (DMD) and volumetric muscle loss are conditions with high unmet medical needs. Direct reprogramming of fibroblasts into induced myogenic progenitor cells (iMPCs) offers a strategy to generate new muscle stem cells that can engraft, proliferate, and regenerate functional muscle tissue [12]. Using modRNA to deliver key myogenic transcription factors like MyoD provides a transgene-free, clinically safer alternative to viral vectors.
Key Experimental Data and Findings
A landmark study demonstrated the efficient conversion of fibroblasts into functional muscle stem cells using synthetic MyoD-mRNA combined with a small molecule cocktail. The key findings and optimized reagent conditions are summarized below.
Table 3: Key Outcomes from Transgene-Free iMPC Reprogramming
| Parameter | Result with MyoD-mRNA + F/R/C | Enhanced Result with MyoD-mRNA + F/R/C/SP/CP |
|---|---|---|
| Reprogramming Efficiency (Pax7+ cells) | ~30% | ~55-60% |
| Reprogramming Timeline | Robust reprogramming achieved in 10 days. | Similar rapid timeline maintained. |
| Cell Phenotype | Pax7+ iMPCs resembling satellite cells; capable of proliferation and differentiation into multinucleated, contractile myotubes. | Heterogeneous culture containing a higher stem cell (Pax7+) subpopulation. |
| In Vivo Engraftment | Robust engraftment in DMD mouse model, restoring dystrophin expression in hundreds of myofibers. | Data supports efficient engraftment and contribution to muscle regeneration. |
Detailed Experimental Protocol
Objective: To generate transgene-free induced myogenic progenitor cells (iMPCs) from murine fibroblasts using synthetic MyoD-mRNA and a defined small molecule cocktail.
Materials:
- Research Reagent Solutions:
- Synthetic MyoD-mRNA: Codon-optimized mRNA encoding the MyoD gene, modified with pseudouridine or N1-methylpseudouridine.
- Small Molecule Cocktail:
- Forskolin (F): Cyclic AMP agonist.
- RepSox (R): TGF-β receptor inhibitor.
- CHIR99210 (C): GSK3 inhibitor.
- SP600125 (SP): JNK inhibitor.
- CP690550 (CP): JAK inhibitor.
- Transfection Reagent: A commercial mRNA transfection reagent suitable for fibroblasts.
- Cell Culture Media: Growth media (e.g., DMEM with 15% FBS) and myogenic differentiation media (e.g., DMEM with 2% horse serum).
Methodology:
- Fibroblast Culture: Plate mouse embryonic fibroblasts (MEFs) or dermal fibroblasts at a density of 20,000 cells/cm² in growth media.
- Transfection and Reprogramming:
- Day 0: Transfert cells with synthetic MyoD-mRNA using the optimized protocol. This typically involves complexing 1 µg mRNA per 24-well with the transfection reagent.
- Day 1: Replace the transfection medium with fresh growth media supplemented with the small molecule cocktail F/R/C/SP/CP.
- Repeat the mRNA transfection every other day for a total of 5-7 transfections, refreshing the small molecule cocktail with each medium change.
- iMPC Expansion and Analysis:
- After 10-14 days, dissociate the emerging iMPC clusters and re-plate them on collagen-coated dishes for expansion.
- Immunofluorescence: Stain for the myogenic stem cell marker Pax7, the early myogenic marker MyoD, and the differentiation marker myosin heavy chain (MHC).
- Flow Cytometry: Quantify the percentage of Pax7-positive cells.
- In Vitro Differentiation: Induce differentiation by switching to low-serum media. Assess the formation of multinucleated myotubes via MHC staining.
- In Vivo Functional Assay:
- Transplant 100,000 - 500,000 iMPCs into the tibialis anterior muscles of immunodeficient DMD (mdx) mice.
- After 4-8 weeks, analyze muscles for engraftment (e.g., human spectrin or dystrophin staining) and quantify the number of dystrophin-positive myofibers.
Diagram 2: MyoD-mRNA Skeletal Muscle Reprogramming Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key reagents essential for implementing the modRNA-based reprogramming protocols described in this document.
Table 4: Essential Research Reagents for modRNA-Based Lineage Conversion
| Reagent Category | Specific Example | Function in Reprogramming |
|---|---|---|
| Modified mRNA | PSAT1-modRNA; MyoD-mRNA; HGF-modRNA | The core reprogramming factor; encodes the protein that drives cell fate conversion. Modified nucleotides reduce immunogenicity and increase stability. |
| Delivery Vector | Lipid Nanoparticles (LNPs); Tissue Nanotransfection (TNT) | Protects modRNA and enables efficient cellular uptake. LNPs can be tuned for specific organ tropism (e.g., liver). TNT uses nanoelectroporation for localized delivery. |
| Small Molecule Enhancers | Forskolin (F), RepSox (R), CHIR99210 (C), SP600125, CP690550 | Enhance reprogramming efficiency by modulating key signaling pathways (e.g., cAMP, TGF-β, WNT, JNK, JAK/STAT). |
| Cell Culture Matrix | Collagen-coated plates, Matrigel | Provides a supportive physical and chemical microenvironment for the growth and maintenance of target cells (e.g., iMPCs, hepatocytes). |
| In Vivo Model | Mouse MI (LAD Ligation), Mouse Liver Injury (CCl4), DMD model (mdx mouse) | Provides a physiologically relevant system to test the safety and efficacy of the modRNA-based therapeutic intervention. |
| Analysis Tools | Antibodies (Pax7, α-actinin, Ki67), LNP characterization (DLS), RNA-seq | Used to validate the success of reprogramming at the molecular, cellular, and functional levels. |
Optimizing modRNA Reprogramming: Tackling Efficiency, Delivery, and Maturity
Addressing Innate Immune Recognition and Interferon Response
The application of modified mRNA for direct lineage conversion represents a transformative approach in regenerative medicine. However, the efficacy of this technology is significantly influenced by the host's innate immune system. The RNA molecule itself can be a potent trigger for Pattern Recognition Receptors (PRRs), leading to the production of type I interferons (IFN-I) [56]. This IFN-I response, while a fundamental aspect of antiviral defense, can inhibit translation and reduce the efficiency of target protein production—a critical challenge when the goal is to express lineage-defining transcription factors [57] [56]. This application note details protocols for assessing and mitigating these immune responses to optimize modified mRNA-based direct lineage conversion strategies.
Background and Mechanisms
The innate immune system detects exogenous RNA through various PRRs. Key among these are the RIG-I-like receptors (RLRs), such as RIG-I and MDA5, located in the cytoplasm, and Toll-like receptors (TLRs), specifically TLR3, TLR7, and TLR8, within endosomal compartments [56]. RIG-I is activated by short double-stranded RNA (dsRNA) with 5'-triphosphate ends, while MDA5 senses longer dsRNA structures [56]. Upon recognition, these receptors initiate signaling cascades—often through the adaptor mitochondrial antiviral-signaling protein (MAVS)—that culminate in the activation of transcription factors like IRF3 and NF-κB [56]. This drives the expression of IFN-I and pro-inflammatory cytokines [56].
The subsequent binding of IFN-I to the interferon-α/β receptor (IFNAR) activates the JAK-STAT signaling pathway, leading to the expression of hundreds of interferon-stimulated genes (ISGs). These ISGs establish an anti-viral state in the cell, which can strongly suppress translation [57]. This is particularly problematic for direct lineage conversion, where sustained, high-level expression of reprogramming factors is essential. Studies on Lipid Nanoparticle (LNP)-encapsulated mRNA (LNP-mRNA) vaccines have demonstrated that the mRNA component itself is a primary trigger for this IFNAR-dependent immune activation, which can paradoxically attenuate the desired adaptive immune response [57] [58]. In the context of cell reprogramming, a similar attenuation of protein expression and conversion efficiency can occur.
The following diagram illustrates this core signaling pathway that is triggered by exogenous mRNA.
Application Notes and Experimental Protocols
Protocol 1: Quantifying Innate Immune Activation After mRNA Transfection
This protocol is designed to measure key markers of innate immune activation in cells following transfection with modified mRNA.
3.1.1. Materials and Reagents
- Cells for Reprogramming: Primary human dermal fibroblasts (HDFs) or other target somatic cells.
- Modified mRNA: Purified, nucleoside-modified mRNA (e.g., m1Ψ-modified) encoding lineage-specific transcription factors, and a non-coding control mRNA [57] [58].
- Transfection Reagent: A standard reagent suitable for mRNA delivery (e.g., Lipofectamine MessengerMAX).
- RNA Extraction Kit: A commercial kit for high-quality total RNA isolation.
- qRT-PCR Supplies: Reverse transcription kit, SYBR Green or TaqMan qPCR master mix, primers for IFN-β, ISG15, RIG-I, MX1, and a housekeeping gene (e.g., GAPDH).
- ELISA Kits: For quantifying secreted IFN-β and IP-10/CXCL10.
- Cell Culture Equipment: Standard tissue culture hood, incubator, plates.
3.1.2. Procedure
- Cell Seeding: Seed HDFs in 12-well plates at a density of 1-2 x 10^5 cells/well and culture overnight to reach 70-80% confluency.
- mRNA Transfection: Transfect cells with a range of concentrations (e.g., 0.1 µg/mL to 1.0 µg/mL) of the modified mRNA or non-coding mRNA control per manufacturer's instructions. Include a mock-transfected control.
- Sample Collection:
- For mRNA Analysis: At 6, 24, and 48 hours post-transfection, lyse cells and extract total RNA. Synthesize cDNA.
- For Protein Analysis: At 24 and 48 hours post-transfection, collect cell culture supernatants and centrifuge to remove debris.
- qRT-PCR Analysis: Perform qPCR using immune gene-specific primers. Calculate fold-change in gene expression using the 2^(-ΔΔCt) method relative to mock-transfected controls.
- Cytokine Measurement: Analyze supernatants using IFN-β and IP-10 ELISA kits according to the manufacturer's protocols.
3.1.3. Anticipated Results and Data Presentation Data can be summarized in a table for clear comparison across experimental conditions.
Table 1: Example Data for Innate Immune Marker Expression 24 Hours Post-mRNA Transfection
| mRNA Construct | Concentration (µg/mL) | IFN-β mRNA (Fold Change) | ISG15 mRNA (Fold Change) | Secreted IFN-β (pg/mL) |
|---|---|---|---|---|
| Mock Transfection | - | 1.0 ± 0.2 | 1.0 ± 0.3 | 5.1 ± 1.5 |
| Non-coding mRNA | 0.5 | 25.5 ± 4.2 | 18.7 ± 3.1 | 155.3 ± 22.4 |
| Lineage mRNA (m1Ψ) | 0.5 | 5.3 ± 1.1 | 4.2 ± 0.9 | 35.7 ± 8.9 |
Protocol 2: Transient Blockade of IFNAR Signaling to Enhance Protein Output
This protocol uses a blocking antibody to temporarily inhibit IFNAR signaling, thereby potentially increasing the yield of the target protein encoded by the modified mRNA.
3.2.1. Materials and Reagents
- Anti-IFNAR1 Monoclonal Antibody: Purified neutralizing antibody (e.g., Leinco Technologies, I-401) [57] [58].
- Isotype Control Antibody: A matched IgG isotype control.
- Modified mRNA and Transfection Reagent as in Protocol 1.
- Flow Cytometry Antibodies: For detecting the expressed target protein (e.g., a transcription factor with a tag).
3.2.2. Procedure
- Antibody Pre-treatment: 24 hours prior to mRNA transfection, add anti-IFNAR1 antibody or isotype control (e.g., 25 µg/mL) to the cell culture medium of HDFs [57] [58].
- mRNA Transfection: Transfect cells with modified mRNA encoding the lineage-specific factor as described in Protocol 1.
- Antibody Post-treatment: Approximately 24 hours post-transfection, refresh the medium containing the same concentration of anti-IFNAR1 or isotype control antibody [57] [58].
- Analysis: 48-72 hours post-transfection, harvest cells.
- Analyze the percentage of cells expressing the target protein and the mean fluorescence intensity (MFI) via flow cytometry.
- Assess differentiation markers specific to the target lineage (e.g., immunocytochemistry, RT-qPCR).
3.2.3. Anticipated Results Transient IFNAR blockade is expected to enhance the efficiency of protein production. This can be quantified as shown in the example table below.
Table 2: Effect of IFNAR Blockade on Target Protein Expression
| Experimental Condition | Target Protein Positive Cells (%) | Mean Fluorescence Intensity (MFI) | Lineage Marker Expression (Fold Change) |
|---|---|---|---|
| Isotype Control + mRNA | 45 ± 6 | 10,250 ± 1,450 | 5.5 ± 1.2 |
| α-IFNAR + mRNA | 78 ± 8 | 28,500 ± 3,100 | 15.8 ± 2.7 |
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential reagents for investigating innate immune responses in modified mRNA studies.
Table 3: Essential Reagents for Investigating Immune Responses to mRNA
| Reagent / Tool | Function / Application | Example Product / Citation |
|---|---|---|
| Nucleoside-modified mRNA | Reduces immunogenicity and enhances translation of mRNA by evading certain PRRs [56]. | m1Ψ-modified mRNA [57] [58]. |
| Non-coding mRNA control | Serves as a critical control to distinguish immune activation triggered by the mRNA molecule itself from that of the encoded antigen [57] [58]. | Cellulose-purified, non-coding sequence [57] [58]. |
| Anti-IFNAR1 Blocking Antibody | Temporarily inhibits the IFN-I signaling pathway to assess its impact on mRNA translation and protein output [57] [58]. | MAR1-5A3 clone or equivalent (Leinco I-401) [57] [58]. |
| IFN-β & IP-10 ELISA Kits | Quantify secreted cytokines/chemokines as a direct measure of innate immune activation post-transfection. | Commercial kits from R&D Systems, Thermo Fisher, etc. |
| PRR-Specific Inhibitors | Small molecules to dissect the contribution of specific PRR pathways (e.g., RIG-I, MDA5, TLRs). | e.g., Deucravacitinib (inhibits TLR7/8/9 signaling) [58]. |
Integrated Workflow for Assessing and Mitigating Immune Responses
The following diagram outlines a complete experimental workflow, integrating the protocols and concepts described above to optimize modified mRNA-based direct lineage conversion.
Sustained protein expression is a critical requirement in direct lineage conversion research, where the transient nature of conventional modified mRNA transfection often falls short. This application note details the rationale and methodologies for implementing repeated transfection strategies to achieve the persistent, high-level protein expression necessary for successful cellular reprogramming.
Direct lineage conversion using modified mRNA requires sustained expression of reprogramming transcription factors to guide cells through epigenetic remodeling and identity changes. Unlike applications in vaccination, where short-term protein expression is sufficient, lineage conversion is a protracted process. Conventional transient transfection results in protein expression that typically peaks within 24 hours and diminishes rapidly due to the innate degradation of mRNA and dilution during cell division [59]. This transient expression window is often inadequate for complete cellular reprogramming. Repeated transfection, or Extended Gene Expression (EGE), addresses this limitation by periodically reintroducing mRNA into the culture, thereby maintaining therapeutic protein levels throughout the critical reprogramming period. This strategy is particularly vital for modified mRNA-based approaches, which offer the advantages of non-integrating gene expression and enhanced safety profiles, making them ideal for therapeutic applications [29] [17].
Molecular Strategies for Enhanced and Sustained Expression
mRNA Engineering for Stability and Translational Efficiency
The foundation of effective repeated transfection lies in the design of the mRNA molecule itself. Several key modifications synergistically enhance stability, reduce immunogenicity, and increase protein yield per microgram of transfected mRNA.
- Nucleoside Modifications: Replacing uridine with N1-methyl-pseudouridine (m1Ψ) significantly reduces the activation of innate immune sensors like Toll-like receptors (TLRs) and retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs). This suppression of the immune response prevents mRNA degradation and interferon signaling, leading to enhanced translation efficiency and prolonged protein production [17].
- 5' Capping and 3' Tail Engineering: A 5' cap structure (e.g., CleanCap) is essential for stability and efficient translation initiation by recruiting initiation factors [60] [61]. Furthermore, optimizing the poly(A) tail length and incorporating stabilized sequences in the 5' and 3' untranslated regions (UTRs) protect the mRNA from exonucleolytic degradation, thereby extending its functional half-life in the cytoplasm [17] [62].
- Advanced mRNA Constructs: For applications requiring extremely durable expression, novel formats such as self-amplifying RNA (saRNA) and circular RNA (circRNA) are being explored. These RNAs can maintain protein expression for weeks from a single transfection by either replicating the mRNA strand or evading linear RNA decay pathways [17].
The EGE Strategy: Rationale and Workflow
The Extended Gene Expression (EGE) strategy systematically combines medium exchange with repeated transfection to overcome the limitations of a single transfection. The logical workflow and key decision points for implementing this strategy are outlined below.
Figure 1: Logic Flow of a Repeated Transfection Strategy for Sustained Protein Expression.
The rationale for this approach is multi-faceted. First, it counteracts the natural degradation and dilution of mRNA. Second, medium exchange removes metabolic waste products and replenishes nutrients, maintaining a healthy cellular environment conducive to high translational output [63]. Research demonstrates that this EGE strategy can prolong the production period to between 192 and 240 hours, resulting in a 4 to 12-fold increase in the yield of various recombinant products, including intracellular proteins, secreted proteins, and complex virus-like particles (VLPs) compared to a single transfection [63].
Experimental Protocols
Protocol for High-Quality Modified mRNA Production
A robust, open-source protocol for producing research-grade mRNA is essential for implementing repeated transfection strategies [60] [64]. The following workflow is equipment-agnostic and designed for standard molecular biology laboratories.
Workflow Overview: From DNA Template to mRNA
mRNA Primary Sequence Design
- Utilize software like
mRNArchitectto design constructs featuring a 5' cap, optimized coding sequence (CDS) with codon optimization and uridine depletion, stabilizing 5' and 3' UTRs, and a poly(A) tail [60]. - Incorporate m1Ψ in place of uridine triphosphate during synthesis to reduce immunogenicity [60] [17].
- Utilize software like
DNA Template Preparation via PCR
- Use PCR amplification with forward primers that introduce a T7 promoter and reverse primers that encode the poly(A) tail. This method is faster and cleaner than using plasmid DNA, as it eliminates bacterial endotoxin contamination [60] [64].
- Quality Control (QC): Assess DNA yield and purity using UV spectrophotometry. Confirm specificity and integrity via capillary gel electrophoresis (CGE) [60].
mRNA Synthesis via In Vitro Transcription (IVT)
- Perform IVT using T7 RNA polymerase with a nucleotide mix containing m1Ψ.
- Use co-transcriptional capping (e.g., CleanCap) to ensure a high percentage of properly capped transcripts.
- Typical yields are achieved within 2–3 hours [60].
mRNA Quality Control
- Concentration and Purity: Measure via UV spectrophotometry.
- Integrity: Assess via CGE.
- Purity: Use an ELISA-based assay to detect and quantify double-stranded RNA (dsRNA) contaminants, which are potent inducers of the innate immune response [60].
Protocol for Lipid Nanoparticle (LNP) Formulation and Repeated Transfection
For delivery to target cells, mRNA must be encapsulated in LNPs to protect it from degradation and facilitate cellular uptake.
LNP Formulation via Microfluidic Mixing
- Utilize a microfluidic mixer (e.g., NanoAssemblr Ignite).
- Standard lipid composition:
- SM-102 (or equivalent ionizable lipid)
- Cholesterol (for structural stability)
- DSPC (for membrane integrity)
- DMG-PEG2000 (to confer stealth properties and prevent aggregation) [60].
- LNP QC: Measure particle size and PDI via dynamic light scattering (DLS). Quantify mRNA encapsulation efficiency (>90%) using a Ribogreen assay [60].
Repeated Transfection (EGE) Protocol for Cell Culture This protocol is adapted for adherent or suspension cells, such as HEK293, used in recombinant protein production and lineage conversion studies [63].
Day 0: Plate Cells
- Seed cells at an appropriate density in a multi-well plate or culture flask to reach 70-90% confluency at the time of transfection.
Day 1: First Transfection
- Transfect cells using a suitable reagent (e.g., MessengerMax, polyethylenimine (PEI)) or by adding pre-formed mRNA-LNPs to the culture medium.
- Dose: A starting dose of eGFP mRNA (0.5 µg/well) in a 24-well plate can be used for optimization [60].
Day 2-3: Monitor Expression and Initiate EGE
- By 48 hours post-transfection, protein expression will typically peak and begin to decline.
- First Medium Exchange: Carefully remove the spent transfection medium, replace it with fresh, pre-warmed complete medium. This step removes transfection by-products and replenishes nutrients.
Day 3-4: Second Transfection
- Perform a second transfection with the same mRNA construct and dose, following the same protocol as the first transfection.
Monitoring and Further Cycles
- Continue monitoring protein expression (e.g., via fluorescence for eGFP or ELISA for secreted proteins).
- The cycle of medium exchange and transfection can be repeated every 48-96 hours as needed, with studies demonstrating sustained production for up to 240 hours [63].
Table 1: Key Parameters for Repeated Transfection in HEK293 Cells
| Parameter | Experimental Condition | Impact on Sustained Expression |
|---|---|---|
| Production Period | 192 - 240 hours | Prolongs expression window 2-3x versus conventional TGE [63]. |
| Product Yield Increase | 4-fold to 12-fold | Varies with product type (intracellular, secreted, VLP) [63]. |
| Transfection Interval | 48 - 96 hours | Balances protein level maintenance with cellular stress [63]. |
| Model Products | Intracellular GFP, Secreted GFP, Gag-GFP VLPs | Validates strategy for diverse protein types [63]. |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these strategies requires a suite of reliable reagents and tools. The following table details key components for mRNA production and transfection.
Table 2: Research Reagent Solutions for mRNA Production and Transfection
| Item | Function | Example/Note |
|---|---|---|
| mRNArchitect Software | mRNA sequence design, including UTR optimization and codon usage. | Enables rational design of constructs for enhanced stability and translation [60]. |
| T7 RNA Polymerase | Drives in vitro transcription from a DNA template. | Core enzyme for mRNA synthesis [60]. |
| N1-methyl-pseudouridine | Modified nucleotide replacing uridine. | Reduces immunogenicity and increases translational efficiency [60] [17]. |
| CleanCap AG | Co-transcriptional capping reagent. | Ensures high-fidelity 5' cap addition for improved translation initiation [60] [61]. |
| SM-102 / DLin-MC3-DMA | Ionizable lipid for LNP formulation. | Enables endosomal escape and mRNA release into the cytoplasm [60]. |
| DMG-PEG2000 | PEGylated lipid in LNP formulation. | Stabilizes nanoparticles and reduces non-specific binding [60]. |
| NanoAssemblr Ignite | Microfluidic mixer. | Allows for reproducible, scalable LNP formation with high encapsulation efficiency [60]. |
| Polyethylenimine (PEI) | A cationic polymer transfection reagent. | A cost-effective and efficient method for transient transfection in cell culture [63]. |
The strategy of repeated transfection is indispensable for direct lineage conversion research using modified mRNA. By systematically addressing the transient nature of mRNA through molecular engineering of the transcript itself and implementing a disciplined EGE protocol in cell culture, researchers can achieve the sustained, high-level protein expression required to drive complex cellular reprogramming. The integrated use of modified nucleotides, advanced LNP delivery systems, and optimized transfection schedules provides a powerful framework for advancing therapeutic applications in regenerative medicine.
Direct lineage conversion using modified mRNA (cmRNA) represents a transformative approach for regenerative medicine, offering a non-integrative method for cell reprogramming and transdifferentiation [23] [29]. The clinical success of lipid nanoparticles (LNPs) in mRNA vaccine delivery has established them as the leading non-viral platform for nucleic acid delivery [65] [66]. However, a formidable biological barrier limits their broader application: the inefficient release of mRNA cargo from endosomes into the cytosol [67] [66]. It is estimated that only 1-2% of internalized mRNA successfully escapes endosomal compartments to reach the cytoplasm and be translated into functional protein [66]. This bottleneck is particularly critical for cell fate conversion protocols, which require robust and sustained expression of reprogramming factors. This Application Note details the mechanistic insights into these cellular barriers and provides validated experimental protocols to quantify and enhance endosomal escape for more effective cmRNA-based therapies.
Cellular Journey of mRNA-LNPs and Key Bottlenecks
Understanding the intracellular fate of mRNA-loaded LNPs is essential for devising strategies to improve their functional delivery. The pathway involves a series of distinct, inefficient steps [67] [66].
- Cellular Uptake: LNPs are internalized primarily via endocytosis, with the specific pathway (e.g., clathrin-mediated, caveolae-mediated) influencing subsequent trafficking.
- Endosomal Trafficking: Internalized LNPs are trafficked through the endosomal-lysosomal system, where the environment acidifies (pH drops to ~6.0–6.5 in early endosomes).
- Endosomal Escape: The protonation of the ionizable lipid within LNPs is theorized to promote interaction with the endosomal membrane. This can cause membrane destabilization, potentially leading to the formation of pores or inverted hexagonal phases that allow mRNA release.
- Cytosolic Release and Translation: Successfully escaped mRNA is translated by ribosomes, while the remainder is degraded within lysosomes.
Recent live-cell and super-resolution microscopy studies have revealed multiple, distinct inefficiencies in this process using MC3-based LNPs [67]. Key quantitative findings include:
- Only a fraction of internalized LNPs trigger endosomal damage. Many LNPs are trafficked for degradation without ever attempting cargo release.
- Membrane damage, marked by galectin-9 recruitment, is conducive to cytosolic release. However, not all galectin-9-positive damaged endosomes contain detectable RNA cargo. The "hit rate" (damaged vesicles with detectable cargo) is approximately 70% for siRNA-LNPs but only about 20% for mRNA-LNPs [67].
- Inefficient Cargo Release: Even in damaged, galectin-9-positive endosomes that do contain RNA, only a small fraction of the total nucleic acid cargo is released to the cytosol [67].
- Component Segregation: During endosomal sorting, the ionizable lipid and RNA payload can segregate from each other, both within single endosomes and across different compartments, further reducing delivery efficiency [67].
Table 1: Key Quantitative Barriers to Cytosolic Delivery Identified by Microscopy
| Barrier Description | Experimental Readout | Quantitative Finding | Implication for Delivery |
|---|---|---|---|
| Failure to Damage Endosome | Galectin-9 Recruitment vs. LNP Uptake | Only a subset of internalized LNPs recruit galectin-9. | Majority of LNPs are degraded without attempting release. |
| Empty Damaged Endosomes | RNA Cargo Detection in Galectin-9+ Vesicles | ~20% hit rate for mRNA-LNPs; ~70% for siRNA-LNPs. | Many membrane damage events are non-productive for the specific cargo. |
| Inefficient Release from Damaged Vesicles | RNA Signal Loss per Vesicle Post-Damage | Only a small fraction of the total endosomal RNA content is released. | Cargo release is partial, even under conducive conditions. |
| Lipid-RNA Segregation | Co-localization of Fluorescent Lipid & RNA | Segregation occurs during endosomal sorting. | The LNP can disassemble before the RNA is in a position to escape. |
Visualizing the Intracellular Fate of mRNA-LNPs
The following diagram illustrates the critical bottlenecks in the intracellular journey of mRNA-LNPs, as revealed by recent mechanistic studies.
Experimental Protocol: Quantifying Endosomal Escape and Membrane Damage
This protocol outlines how to use live-cell imaging to visualize LNP-induced endosomal membrane damage and correlate it with RNA cargo release, a key methodology for screening next-generation LNP formulations [67].
Materials and Reagents
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Description | Example / Notes |
|---|---|---|
| Galectin-9 Sensor | Marker for endosomal membrane damage. | Recombinant fluorescently tagged protein (e.g., Galectin-9-GFP). |
| Fluorescently Labeled RNA | Enables tracking of RNA cargo. | AlexaFluor 647- or Cy5-labeled mRNA/siRNA. |
| Fluorescently Labeled Ionizable Lipid | Enables tracking of LNP lipid component. | e.g., BODIPY-MC3. |
| Live-Cell Imaging Chamber | Maintains cell viability during microscopy. | Chamber with controlled temperature and CO₂. |
| Confocal or Super-Resolution Microscope | High-resolution imaging of intracellular events. | Enables tracking of single vesicles. |
| LNP Formulations | Test particles for delivery efficiency. | LNPs with varying ionizable lipids, helper lipids, etc. |
Step-by-Step Procedure
- Cell Preparation:
- Plate appropriate cells (e.g., primary fibroblasts or HeLa cells) on glass-bottom imaging dishes 24-48 hours before the experiment to achieve 50-70% confluency.
- Sensor Expression/Loading:
- Transfect cells with a plasmid encoding Galectin-9-GFP 24 hours prior to LNP addition to express the membrane damage sensor. Alternatively, recombinant Galectin-9 protein can be added to the medium.
- LNP Treatment and Live-Cell Imaging:
- Replace the medium with a live-cell imaging-compatible buffer.
- Add LNPs containing both Cy5-mRNA and a BODIPY-labeled ionizable lipid to the cells. A typical working concentration is 0.5-1.0 µg/mL mRNA [67].
- Immediately transfer the dish to a pre-warmed microscope stage.
- Acquire time-lapse images (e.g., every 5-10 minutes for 2-4 hours) using high-resolution confocal microscopy. Capture Z-stacks if possible to fully capture vesicles.
- Image and Data Analysis:
- Vesicle Tracking: Use tracking software to identify individual endosomes and track their fluorescence over time.
- Event Identification: Identify de novo recruitment of Galectin-9-GFP to a vesicle as a membrane damage event.
- Quantification:
- Hit Rate Calculation: For each Galectin-9-positive vesicle, determine if it contains detectable Cy5-mRNA signal. Calculate the percentage of damaged vesicles that contain cargo.
Hit Rate = (Number of Galectin-9+ vesicles with Cy5 signal / Total Number of Galectin-9+ vesicles) * 100 - Cargo Release Efficiency: Measure the fluorescence intensity of the Cy5-mRNA signal in the vesicle before and after Galectin-9 recruitment. A decrease indicates release.
- Lipid-RNA Co-localization: Quantify the Pearson's correlation coefficient between the BODIPY-lipid and Cy5-mRNA signals in individual endosomes over time. A decrease indicates segregation.
- Hit Rate Calculation: For each Galectin-9-positive vesicle, determine if it contains detectable Cy5-mRNA signal. Calculate the percentage of damaged vesicles that contain cargo.
Optimization Strategies: Enhancing Endosomal Escape for Cell Reprogramming
Improving the efficiency of endosomal escape is a multi-faceted challenge requiring optimization of the mRNA molecule, the LNP vector, and the understanding of cellular pathways.
mRNA Molecular Engineering
For cell reprogramming, where prolonged expression of transcription factors is often desired, optimizing the mRNA transcript is crucial [23] [29].
- Nucleoside Modifications: Use of modified nucleosides like 5-methylcytidine (5mC) and pseudouridine (Ψ) reduces immunogenicity and enhances translational efficiency, which is critical for repeated transfections in reprogramming protocols [23].
- Cap and Tail Optimization: A synthetic 5'-Cap (e.g., CleanCap) and optimized poly(A) tail length of 120-150 nucleotides significantly increase mRNA stability and protein expression [23] [65].
- UTR Engineering: Incorporating stable 5' and 3' Untranslated Regions (UTRs), such as from α/β-globin genes, can enhance both the stability and translation efficiency of reprogramming factor mRNAs [23].
LNP Formulation and Lipid Design
The composition of the LNP is the primary determinant of its endosomal escape capability [66]. Rational design focuses on the ionizable lipid, which is protonated in the acidic endosome.
- Ionizable Lipid Optimization: The pKa of the ionizable lipid should be in the range of early endosomal pH (6.0-6.5) for optimal protonation. Novel lipids are being designed to promote more efficient membrane disruption via the formation of inverted hexagonal (HII) phases [67] [66].
- Helper Lipid and PEG Modulation: The choice of helper phospholipid (e.g., DOPE, which favors non-bilayer structures) and the molar percentage of PEG-lipid can be tuned to balance stability, cellular uptake, and endosomal escape [65] [66].
- Selective Organ Targeting (SORT) Molecules: Adding supplemental lipids to the standard LNP formulation can enable specific targeting to extrahepatic tissues, a major goal for in vivo cell fate conversion therapies [65] [66].
Table 3: Strategies to Overcome Specific Barriers in LNP Delivery
| Identified Barrier | Proposed Solution | Mechanistic Rationale |
|---|---|---|
| Low "Hit Rate" for mRNA | Optimize LNP disintegration kinetics; ensure RNA is in proximity to site of membrane damage. | Prevents scenarios where the membrane is damaged but the RNA cargo is not positioned for release. |
| Inefficient Release from Damaged Vesicles | Engineer ionizable lipids with stronger membrane-destabilizing capacity. | Promotes larger or more sustained disruptions, allowing more cargo to exit. |
| Lipid-RNA Segregation | Reformulate LNP core structure and stability to maintain integrity in the endosome. | Keeps the RNA associated with the protonated lipids that drive the escape process. |
| Activation of ESCRT Repair | Design LNPs that cause membrane perturbations resistant to ESCRT-mediated repair. | Increases the time window available for RNA release before the damage is sealed. |
Visualizing the Optimization Strategy Workflow
The following diagram outlines a rational, iterative workflow for developing enhanced LNPs, from formulation to mechanistic evaluation.
The Scientist's Toolkit: Essential Reagents and Methods
Beyond the core protocol, several advanced techniques are critical for comprehensive characterization.
- AF4-SAXS for LNP Characterization: Coupling Asymmetrical-Flow Field-Flow Fractionation (AF4) with Small-Angle X-ray Scattering (SAXS) provides a quantitative, size-resolved analysis of LNP critical quality attributes, including absolute size distribution, drug loading, and internal structure [68]. This is vital for correlating LNP physical properties with biological performance.
- Proximity-Labeling for mRNA Trafficking: Adapted APEXseq approaches use proximity biotinylation and RT-qPCR to directly and quantitatively measure mRNA delivery to specific subcellular locations like the cytoplasm and endoplasmic reticulum, providing a direct readout of functional delivery [69].
- Computational and AI-Guided Design: Computational frameworks using synthetic transcriptomics and AI (e.g., Random Forest models) can predict immune activation and optimize LNP design parameters (size, charge, PEG content) in silico, dramatically accelerating the development timeline [70].
Enhancing the endosomal escape and cytosolic delivery of mRNA is the pivotal challenge for realizing the full potential of direct lineage conversion therapies. The application of advanced imaging techniques has moved the field beyond black-box optimization, revealing a multi-step process with several distinct points of failure. By adopting the detailed protocols and rational design strategies outlined here—including the quantification of membrane damage and cargo release, the engineering of novel ionizable lipids, and the use of sophisticated characterization tools—researchers can systematically develop next-generation LNP platforms. These advanced delivery systems will underpin more efficient, reliable, and safe cmRNA-based cell reprogramming and regenerative medicine applications.
Pre-patterning represents a critical preparatory phase in direct lineage conversion, wherein somatic cells are primed through specific molecular cues to acquire enhanced responsiveness to reprogramming factors. This process establishes a permissive epigenetic and transcriptional landscape that mirrors the target cell state, significantly improving the efficiency and fidelity of cell fate conversion. Within modified mRNA research, where transient expression kinetics demand precise temporal control, pre-patterming provides the necessary foundation for synchronized and coordinated reprogramming events. The strategic implementation of pre-patterming addresses fundamental challenges in the field, including low conversion yields, incomplete reprogramming, and the emergence of transient cell populations that fail to stabilize into mature functional phenotypes [71] [50].
The biological significance of pre-patterning extends beyond technical optimization, reflecting fundamental developmental principles. During embryogenesis, coordinated morphogen gradients and signaling pathways establish patterned territories that precede and guide the emergence of distinct cell lineages. Similarly, in direct reprogramming, pre-patterming recapitulates these developmental cues to guide cells toward target fates. Research across multiple systems demonstrates that manipulating key signaling pathways—including TGF-β, WNT, and BMP—during the pre-patterning phase can profoundly influence reprogramming outcomes by reshaping the epigenetic landscape and modulating transcriptional networks [72] [50]. This approach aligns with the broader thesis on modified mRNA research by creating a cellular context optimally positioned to respond to the transient, pulsatile expression patterns characteristic of this delivery method.
Key Signaling Pathways in Pre-Patterning
Pre-patterming strategies strategically modulate conserved signaling pathways to establish a permissive environment for lineage conversion. The following table summarizes the core pathways, their functions, and targeted interventions:
Table 1: Key Signaling Pathways in Pre-Patterming for Lineage Conversion
| Pathway | Primary Role in Pre-Patterming | Representative Modulators | Experimental Outcomes |
|---|---|---|---|
| TGF-β/SMAD | Regulates mesendodermal patterning; inhibition promotes epithelialization and certain lineage specifications | ALK5 inhibitors (e.g., RepSox); SB431542 | Inhibition in fibroblasts upregulated MSC markers (CD73, CD90, CD105) and enabled tri-lineage differentiation [71] |
| WNT/β-catenin | Directs anterior-posterior patterning; critical for cardiac mesoderm specification | CHIR99021 (GSK3β inhibitor); IWP-2 (WNT inhibitor) | Modulation rescued cardiac progenitor defects in GATA6 mutants; precise timing essential for mesendoderm induction [72] |
| BMP | Patterns mesoderm and promotes epithelial-to-mesenchymal transition; concentration-dependent effects | BMP4; NOGGIN (BMP inhibitor) | Cooperates with WNT; required for lateral mesoderm formation preceding cardiogenesis [72] |
| Rho/ROCK | Modulates cytoskeletal dynamics and cell adhesion; inhibition enhances survival and reprogramming efficiency | Fasudil; Y-27632 | Combined with TGF-β and ATM inhibition to support morphological changes during conversion to MSC-like cells [71] |
The coordinated manipulation of these pathways enables researchers to establish a transcriptional and epigenetic foundation that predisposes cells to acquire new identities in response to reprogramming factors.
Experimental Protocols for Pre-Patterming
Chemical Pre-Patterming of Fibroblasts to MSC-like States
This protocol describes the direct conversion of human dermal fibroblasts (HDFs) into mesenchymal stem cell-like cells (cdMSCs) using a chemical pre-patterming approach, adapted from published research [71].
- Primary Cells: Normal human dermal fibroblasts (HDFs)
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 100 mM non-essential amino acids, 100 U/mL penicillin, 100 μg/mL streptomycin, and 10% fetal bovine serum (FBS) - referred to as Complete Medium (CM)
- Pre-Patterming Cocktail:
- ALK5 inhibitor II (RepSox): 32 μM in CM. (TGF-β pathway inhibitor)
- Fasudil: 1 μM in CM. (ROCK inhibitor)
- KU-60019: 1 μM in CM. (ATM inhibitor)
- Equipment: Standard cell culture equipment (CO₂ incubator, biosafety cabinet, centrifuge), 6-well and 24-well tissue culture plates, flow cytometer for analysis
Procedure:
- Day -1: Cell Seeding
- Culture HDFs in CM until 70-80% confluent.
- Resuspend cells in CM and seed onto 6-well plates at a density of 1 × 10⁵ cells per well.
- Day 0: Pre-Patterming Induction
- Replace the culture medium with fresh CM containing the triple chemical cocktail (32 μM ALK5i, 1 μM Fasudil, and 1 μM KU-60019).
- Ensure the reagents are thoroughly mixed in the medium before application.
- Days 1-7: Maintenance
- Culture the cells for 7 days, replacing the pre-patterming medium every 3-4 days.
- Monitor morphological changes daily using phase-contrast microscopy. Expect a shift from a elongated, fibroblastic morphology to a more spindle-shaped, MSC-like appearance.
- Day 7: Characterization of cdMSCs
- Harvest cells using a standard detachment method (e.g., trypsin-EDTA).
- Flow Cytometry: Analyze the expression of MSC surface markers (CD73, CD90, CD105) using fluorescence-labeled antibodies. Compare to untreated HDFs and positive control MSCs.
- Tri-Lineage Differentiation Assessment:
- Osteogenic Differentiation: Culture cdMSCs in Osteogenic Medium (OGM: CM with 50 μg/mL ascorbic acid, 10 mM β-glycerol phosphate, 100 nM dexamethasone) for 14-21 days. Confirm differentiation by Alizarin Red S staining for calcium deposits.
- Adipogenic Differentiation: Culture cdMSCs in Adipogenic Medium (AGM: CM with 10 μg/mL insulin, 1 μM dexamethasone, 1 mM IBMX) for 14-21 days. Confirm differentiation by Oil Red O staining for lipid droplets.
- Chondrogenic Differentiation: Use a micro-mass culture method in Chondrogenic Medium (CGM: DMEM with 1% FBS, 1% ITS, 50 μg/mL ascorbic acid, 10 ng/mL each of BMP-2, b-FGF, TGF-β, GDF5) for 21 days. Confirm differentiation by Alcian Blue staining for sulfated proteoglycans.
Pre-Patterming hPSCs for Cardiac Lineage Specification
This protocol outlines a pre-patterming strategy to direct human pluripotent stem cells (hPSCs) through mesoderm specification for efficient cardiac differentiation, incorporating insights from GATA6 studies [72].
- Cell Line: GATA6 wild-type (WT), heterozygous (GATA6⁺/⁻), and homozygous mutant (GATA6⁻/⁻) H1 human embryonic stem cells (hESCs)
- Base Medium: Chemically defined medium appropriate for hPSC maintenance (e.g., mTeSR¹)
- Cardiac Differentiation Medium: RPMI 1640 medium supplemented with B-27 supplement (minus insulin)
- Pre-Patterming / Differentiation Factors:
- CHIR99021: 6-8 μM in cardiac differentiation medium. (WNT pathway activator)
- BMP4: 10-20 ng/mL in cardiac differentiation medium.
- IWP-2: 5 μM in cardiac differentiation medium. (WNT pathway inhibitor)
- Equipment: Matrigel-coated tissue culture plates, CO₂ incubator, flow cytometer with anti-cardiac Troponin T (cTnT) antibodies
Procedure:
- Day -2: hPSC Maintenance
- Culture hPSCs on Matrigel-coated plates in mTeSR¹ medium until they reach 80-90% confluence. Ensure cells are in a state of active, undifferentiated growth.
- Day 0: Mesendoderm Priming
- Begin differentiation by switching to Cardiac Differentiation Medium supplemented with a high dose of CHIR99021 (e.g., 6-8 μM) and BMP4 (e.g., 20 ng/mL).
- Incubate for 24 hours. This critical pre-patterming step induces primitive streak/mesendoderm formation.
- Day 1: Medium Refresh
- Replace the medium with fresh Cardiac Differentiation Medium without any factors.
- Day 3: Cardiac Mesoderm Specification
- Add Cardiac Differentiation Medium containing IWP-2 (5 μM) to inhibit WNT signaling and promote cardiac mesoderm specification.
- Incubate for 48 hours.
- Day 5 onwards: Maturation
- From day 5, feed cells every 2-3 days with fresh Cardiac Differentiation Medium.
- Spontaneously contracting cardiomyocytes should emerge from approximately day 8 onwards.
- Days 13-18: Efficiency Analysis
- Harvest the cells and analyze the percentage of cardiomyocytes by flow cytometry using antibodies against cardiac Troponin T (cTnT).
- Troubleshooting: If efficiency is low, particularly in GATA6 mutant lines, optimize the concentration and timing of CHIR99021 and BMP4 during the initial 48-hour pre-patterming window [72].
Signaling Pathways and Experimental Workflow Visualization
Diagram 1: Pre-patterming enables lineage conversion. The pre-patterming phase modulates key signaling pathways to prime the cell. The conversion phase uses modified mRNA to express fate-determining transcription factors (TFs), yielding the target cell type [71] [72] [50].
Diagram 2: Pre-patterming directs cardiac differentiation. A monolayer cytokine-based protocol shows key pre-patterming decisions. Critical WNT/BMP activation on Day 0 patterns mesendoderm, preceding cardiac specification [72].
Research Reagent Solutions for Pre-Patterming
Table 2: Essential Research Reagents for Pre-Patterming and Conversion Experiments
| Reagent / Tool | Category | Primary Function in Pre-Patterming | Example Application |
|---|---|---|---|
| RepSox (ALK5i II) | Small Molecule Inhibitor | Inhibits TGF-β/Activin A signaling to disrupt native fibroblast identity and promote epithelial/MSC fates. | Chemical reprogramming of HDFs to cdMSCs; used at 32 μM [71]. |
| CHIR99021 | Small Molecule Agonist | Activates WNT/β-catenin signaling by inhibiting GSK-3β; critical for mesendoderm priming. | Cardiac differentiation of hPSCs; concentration titrated between 6-8 μM for initial patterning [72]. |
| BMP4 | Recombinant Protein | Activates BMP/SMAD signaling; patterns mesoderm and supports epithelial-to-mesenchymal transition. | Combined with CHIR99021 for anterior primitive streak induction in cardiogenesis [72]. |
| Fasudil (HA-1077) | Small Molecule Inhibitor | Inhibits ROCK kinase to reduce cytoskeletal tension, enhance cell survival, and improve reprogramming efficiency. | Component of chemical cocktail for cdMSC generation; used at 1 μM [71]. |
| Modified mRNA | Nucleic Acid Tool | Delivers transient, non-integrating expression of reprogramming factors; ideal for directing final conversion from pre-patterned state. | Expression of lineage-specific transcription factors (e.g., GATA, MEF2, TBX families) post-patterming [50]. |
| Tissue Nanotransfection (TNT) | Physical Delivery System | Nanoelectroporation platform for highly efficient, localized delivery of genetic cargo (pDNA, mRNA) in vivo. | Enables in vivo reprogramming by delivering patterning and conversion factors directly to tissue [50]. |
Ensuring Functional Maturity of Derived Cells for Translational Utility
The successful application of directly reprogrammed cells in regenerative medicine, disease modeling, and drug development is critically dependent on their functional maturity. Cells derived via modified mRNA-mediated lineage conversion often exhibit an immature phenotype, limiting their translational utility. This protocol details a standardized, multifactorial approach to assess and promote functional maturity, ensuring that derived cells closely mirror their in vivo counterparts in both form and function. The framework is built upon the principle that maturity is a multi-parameter construct, requiring validation across morphological, electrophysiological, calcium-handling, and gene-expression domains.
Quantitative Metrics for Functional Maturity Assessment
A cornerstone of this protocol is the quantitative assessment of maturity. The following metrics, derived from established studies on neurons and cardiomyocytes, provide a benchmark for evaluation. Data should be collected at multiple time points to track maturation progression.
Table 1: Quantitative Maturity Metrics for Human iPSC-Derived Neurons (h-iPSC-Ns)
| Maturity Parameter | Immature State (Week 1-3) | Mature State (Week 6+) | Measurement Technique |
|---|---|---|---|
| Membrane Resistance | High (>1 GΩ) | Lower (<500 MΩ) | Whole-cell patch clamp [73] |
| Firing Profile | Immature, irregular | Mature, regular firing | Whole-cell patch clamp [73] |
| Synaptic Activity | Sparse or absent | Abundant, fast glutamatergic & GABAergic | Spontaneous post-synaptic current recording [73] |
| Network Activity | Unsynchronized | Synchronized bursts | Calcium imaging [73] |
| Neurite Complexity | Low number of intersections | High number of intersections, increased branching | Sholl analysis [73] |
Table 2: Quantitative Maturity Metrics for Human iPSC-Derived Cardiomyocytes (hPSC-CMs)
| Maturity Parameter | Immature State | Mature State | Measurement Technique |
|---|---|---|---|
| Cell Morphology | Rounded, mononucleated | Rod-shaped, multinucleated | Microscopy & image analysis [74] |
| Sarcomere Organization | Disorganized, shorter | Highly organized, aligned | Immunostaining (e.g., α-actinin) [74] |
| Presence of T-Tubules | Absent | Present | Electron microscopy, dye staining [74] |
| Calcium Transient | Slow, unsynchronized | Fast, synchronous | Calcium imaging [74] |
| Key Gene Expression | Low CASQ2 |
High CASQ2 |
RNA sequencing, qPCR [74] |
Experimental Protocols for Maturation and Validation
Protocol A: Maturation and Functional Validation of mRNA-Reprogrammed Neurons
This protocol is adapted from studies on the multifactorial maturation of human iPSC-derived neurons [73].
1. Cell Culture and Differentiation:
- Starting Material: Use human Neural Precursor Cells (NPCs) generated via mRNA reprogramming [75] [76].
- Coating: Coat culture surfaces with Poly-L-Ornithine (0.01%) for 1 hour at 37°C, followed by laminin (3 µg/cm²) overnight.
- Differentiation Medium: Use BrainPhys Neuronal Medium supplemented with:
- 1% N2 Supplement
- 2% B27 Supplement
- 1 µg/mL laminin
- Key Maturation Factors: 10 ng/mL BDNF (Brain-Derived Neurotrophic Factor) and 10 ng/mL GDNF (Glial Cell Line-Derived Neurotrophic Factor) [73].
- Additional components: 1 mM dibutyryl cyclic-AMP and 200 µM ascorbic acid.
- Culture Duration: Maintain differentiation for a minimum of 6-10 weeks, with half-medium changes performed twice weekly.
2. Functional Validation via Patch Clamp Electrophysiology:
- Equipment: Standard whole-cell patch clamp setup on an inverted microscope.
- Procedure:
- At designated time points (e.g., bi-weekly), transfer a coverslip with neurons to a recording chamber.
- Obtain whole-cell access using appropriate pipette and bath solutions.
- To test excitability, inject a series of depolarizing current steps (e.g., 10-50 pA increments). Mature neurons (from week 5+) will fire repetitive, regular action potentials without adaptation [73].
- To record synaptic activity, hold the cell at -70 mV and monitor for spontaneous postsynaptic currents. Mature cultures (from week 6+) will show frequent, fast glutamatergic currents [73].
3. Network-Level Analysis via Calcium Imaging:
- Dye Loading: Incubate neurons with a calcium-sensitive dye (e.g., Cal-520 AM, 2 µM) for 30 minutes at 37°C.
- Imaging: Use a high-speed, wide-field or confocal microscope to record fluorescence changes over time (e.g., 10-30 frames per second).
- Analysis: Process recordings to detect calcium transients in individual cells. The emergence of synchronized network bursts across the population is a hallmark of functional maturity, typically observed from week 6 of differentiation [73].
Protocol B: Promoting and Assessing Cardiomyocyte Maturity
This protocol leverages data-driven insights to guide hPSC-CM maturation [74].
1. Long-Term Culture and Stimulation:
- Culture Duration: Extend the culture time of hPSC-CMs up to 120 days to promote maturation. Culture time is a feasible proxy for maturity level [74].
- Maturation Cues: Implement combinatorial stimulation:
- Electrical Stimulation: Apply field stimulation with a defined frequency and duration.
- Biochemical Cues: Optimize media to support metabolic maturation (e.g., fatty acid supplementation).
- 3D Tissue Modeling: Embed cells in engineered scaffolds or form 3D cardiac microtissues to enhance structural maturity.
2. Data-Driven Maturity Evaluation:
- Gene Expression Profiling: At multiple time points, extract RNA and perform transcriptomic analysis (e.g., RNA-seq, microarrays).
- Machine Learning Analysis:
- Use culture time as the primary outcome variable.
- Apply machine learning algorithms (e.g., regression models) to identify genes whose expression most strongly correlates with culture duration.
- The gene CASQ2 (Calsequestrin 2) has been identified as a critical biomarker for hPSC-CM maturation, playing a key role in calcium ion storage [74]. Its upregulation is a strong indicator of progressing maturity.
- Morphological Analysis: Use image analysis software to quantify parameters such as cell aspect ratio, sarcomere length, and percentage of multinucleation [74].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for mRNA Reprogramming and Maturation
| Reagent / Solution | Function | Example / Note |
|---|---|---|
| Synthetic mRNA Constructs | Non-integrating delivery of reprogramming (e.g., OCT4, SOX2, KLF4, c-MYC) or lineage-specific transcription factors. | Use modified nucleotides to evade innate immune response [76]. |
| BDNF & GDNF | Critical neurotrophic factors that promote neuronal survival, maturation, and synaptic connectivity. | Used in neuronal differentiation medium [73]. |
| BrainPhys Neuronal Medium | A defined medium formulated to support synaptic activity and long-term neuronal health. | Superior to standard media for functional maturation [73]. |
| CASQ2 as a Biomarker | A key protein for calcium buffering in the sarcoplasmic reticulum; its gene expression is a top correlate of cardiomyocyte maturity. | Monitor via qPCR or RNA-seq for maturity assessment [74]. |
| Tissue Nanotransfection (TNT) Device | A nanoelectroporation platform for the highly efficient, localized delivery of mRNA payloads in vivo. | Enables potential in situ reprogramming and maturation [50]. |
Supporting Visualizations
Maturity Assessment Workflow
The following diagram outlines the core workflow for ensuring the functional maturity of derived cells, from reprogramming to final validation.
Key Maturation Signaling Pathways
This diagram illustrates the primary signaling pathways targeted by key maturation factors to drive functional development in derived cells.
Validating modRNA-Derived Cells: A Comparative Analysis with Other Technologies
This application note provides a structured framework for the transcriptomic and epigenomic validation of cell types generated via modified mRNA (modRNA)-based direct lineage conversion. It outlines specific experimental protocols and quality control metrics to quantitatively assess how faithfully these in vitro-generated cells recapitulate their native in vivo counterparts, a critical consideration for drug development and cell therapy research.
Direct lineage conversion using non-integrating modified mRNA (modRNA) represents a promising strategy for generating target cell types for research and therapeutic applications, including the production of hepatocyte-like cells [77]. A central challenge, however, lies in conclusively demonstrating that the resulting cells (modRNA-cells) authentically mimic the molecular and functional profiles of native cells. This requires a multi-faceted approach that moves beyond the confirmation of a few marker genes to a comprehensive, genome-wide assessment of the cell's molecular state. Profiling both the epigenome, which governs cellular identity by regulating gene accessibility, and the transcriptome, which reflects the active gene expression program, is essential for this validation [78]. This document details standardized protocols and analytical workflows to ensure rigorous and reproducible characterization.
Quantitative Functional and Molecular Comparison
A critical first step is to benchmark the functional and molecular outputs of modRNA-cells against primary cells. The following table summarizes key metrics for assessment, using modRNA-generated hepatocyte-like cells (R-iHeps) as an example [77].
Table 1: Benchmarking modRNA-Cells Against Native Counterparts
| Validation Category | Specific Assay | Result in Native Hepatocytes | Result in modRNA-R-iHeps [77] | Key Interpretation |
|---|---|---|---|---|
| Functional Capacity | Albumin Secretion | Secreted | Confirmed via ELISA | Demonstrates synthetic function |
| ICG Uptake | Taken up & cleared | Cells took up dye | Demonstrates transporter activity | |
| Glycogen Storage | Positive PAS Staining | Positive PAS Staining | Demonstrates metabolic storage | |
| Gene Expression (qPCR) | Albumin | High Expression | Expressed | Confirms hepatic gene program |
| Alpha-fetoprotein (AFP) | High Expression | Expressed | Confirms hepatic gene program | |
| HNF4α | High Expression | Expressed | Master regulator of hepatocyte identity | |
| Protein Expression (Immunostaining) | Albumin | Expressed | Expressed | Confirms protein-level expression |
| CK18 | Expressed | Expressed | Confirms cytoskeletal protein | |
| HNF4α | Expressed | Expressed (Nuclear) | Confirms nuclear localization of TF | |
| In Vivo Function | Engraftment in Liver | N/A | Engrafted in mouse liver | Demonstrates functional integration |
Experimental Protocols for Comprehensive Profiling
This protocol describes the generation of hepatocyte-like cells from fibroblasts using modRNA.
- Key Reagents: modRNAs encoding transcription factors (e.g., Foxa3 and HNF4α), Lipofectamine 2000, Mouse Embryonic Fibroblasts (MEFs), DMEM/F-12 culture medium, growth factors (HGF, EGF).
- Procedure:
- modRNA Synthesis: Synthesize modRNAs via in vitro transcription (IVT) from DNA templates for the TFs. Include capping (m7G) and 2′-O-Methylation during synthesis, followed by poly(A) tailing.
- Cell Culture: Seed MEFs in standard culture dishes.
- Transfection: On Day 0 and Day 3, transfect MEFs using a complex of 1.5 µg of each modRNA and 3 µL Lipofectamine 2000 in Opti-MEM. Incubate for 4 hours.
- Hepatic Maturation: After 24 hours, replace medium with hepatic maturation medium. Change the medium every two days.
- Timeline: Hepatocyte-like colonies (R-iHeps) with epithelial morphology typically appear within 10-12 days.
This protocol is adapted for profiling complex cultures or tissues containing modRNA-cells to assess heterogeneity and identity.
- Key Reagents: Fresh or frozen cell pellets/tissue, DAPI stain, lysis buffer, PBS, nuclei suspension buffer, 10x Genomics Chromium controller and Single Cell 3' Reagent Kits.
- Procedure:
- Nuclei Isolation: Gently lyse cells in ice-cold lysis buffer to release nuclei. Centrifuge and wash nuclei pellet with PBS + BSA. Filter through a flow cytometry-compatible strainer.
- Quality Control: Stain an aliquot with DAPI and count using a hemocytometer or automated cell counter. Assess integrity.
- Library Preparation: Follow the 10x Genomics Single Cell 3' Reagent Kit user guide. Aim to load ~10,000 nuclei per sample to capture population heterogeneity.
- Sequencing: Sequence libraries on an Illumina platform to a minimum depth of 50,000 reads per nucleus.
- Bioinformatic Analysis: Process raw data (FASTQ) with Cell Ranger. Use Seurat or Scanpy for downstream analysis: clustering, marker gene identification, and comparison to public reference datasets of primary cells.
ATAC-seq maps open chromatin regions, providing a readout of the epigenomic state and active regulatory elements.
- Key Reagents: Cell culture, ATAC-seq lysis buffer, Transposase (e.g., Illumina Tagmentase TDE1), PBS, Qiagen MinElute PCR Purification Kit, NEBNext High-Fidelity 2X PCR Master Mix.
- Procedure:
- Nuclei Preparation: Wash ~50,000 cells in cold PBS. Lyse cells in ice-cold ATAC-seq lysis buffer. Immediately centrifuge to pellet nuclei.
- Tagmentation: Resuspend nuclei in the transposase reaction mix. Incubate at 37°C for 30 minutes.
- DNA Purification: Purify tagmented DNA using the MinElute kit.
- Library Amplification: Amplify the purified DNA with 10-12 cycles of PCR using barcoded primers.
- Sequencing & Analysis: Sequence on an Illumina platform (minimum 25M reads). Process and align reads, call peaks, and compare accessibility profiles to those of native target cells.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for modRNA Cell Validation
| Item | Function/Role | Example Products/Assays |
|---|---|---|
| modRNA Synthesis Kit | Generation of modified mRNA encoding lineage-specific TFs | MEGAscript T7 kit; ScriptCap capping systems [77] |
| Transfection Reagent | Delivery of modRNA into target somatic cells | Lipofectamine 2000 [77] |
| Single-Cell/ Single-Nuclei RNA-seq Platform | High-resolution transcriptomic profiling of heterogeneous cell populations | 10x Genomics Chromium; snRNA-seq [79] |
| Chromatin Accessibility Assay Kit | Profiling of open chromatin regions to infer regulatory landscape | ATAC-seq [78] |
| DNA Methylation Profiling Array | Genome-wide assessment of 5-methylcytosine (5mC) | Illumina Infinium MethylationEPIC BeadChip [80] [78] |
| Bulk RNA-seq Library Prep Kit | Standard transcriptome sequencing for global gene expression | Various kits (Illumina, NEB) |
| Long-Read Sequencing Platform | Full-length transcript sequencing for isoform resolution | Oxford Nanopore Technologies [81] |
Quality Control and Data Integrity
Rigorous quality control is paramount. The table below outlines critical QC metrics for key assays, based on established guidelines [78]. Failure to meet these thresholds can indicate poor sample quality or technical artifacts, compromising the fidelity assessment.
Table 3: Essential Quality Control Metrics for Profiling Assays [78]
| Assay | Key QC Metric | Passing Threshold | Mitigation for Failed QC |
|---|---|---|---|
| ATAC-seq | Sequencing Depth | ≥ 25 Million Reads | Repeat library preparation |
| Fraction of Reads in Peaks (FRIP) | ≥ 0.1 | Repeat transposition step; check cell viability | |
| TSS Enrichment Score | ≥ 6 | Improve sample preparation; sort viable cells | |
| snRNA-seq | Number of Cells Captured | As per experimental design | Optimize nuclei concentration and viability |
| Median Genes per Cell | Cell-type dependent | Check RNA quality and library preparation | |
| Mitochondrial Read Fraction | < 20% | Improve cell/nuclei viability during prep | |
| MethylationEPIC Array | Percentage of Failed Probes | ≤ 1% | Ensure optimal input DNA for bisulfite conversion |
| Beta Value Distribution | Two clear peaks | Remove unreliable probes; check for contamination |
Faithfully recapitulating native cell identity using modRNA-based direct conversion is a complex but achievable goal. By implementing the integrated multi-omics profiling strategies, detailed protocols, and stringent quality controls outlined in this application note, researchers can move beyond superficial marker checks. This enables a robust, quantitative evaluation of the transcriptional and epigenomic fidelity of modRNA-cells, thereby de-risking their use in downstream drug discovery and cell therapy development.
Within the field of regenerative medicine, the direct lineage conversion of somatic cells into therapeutic cell types represents a transformative strategy for disease modeling, drug screening, and cell transplantation therapy. A pivotal technical consideration in this process is the choice of factor delivery system. This Application Note provides a structured, head-to-head comparison between two leading technologies: modified mRNA (modRNA) and viral vector-based reprogramming. Framed within the context of direct lineage conversion research, this document summarizes key quantitative data and provides detailed protocols to guide researchers and drug development professionals in selecting the optimal platform for their experimental and clinical objectives.
Core Principles
- Modified mRNA (modRNA) Reprogramming: This is a non-integrating, footprint-free method that involves the repeated transfection of somatic cells with synthetic mRNA molecules encoding reprogramming or lineage-specific factors. These transcripts are engineered with nucleoside modifications (e.g., 5-methylcytidine and pseudouridine) to enhance stability and evade innate immune recognition [82] [83]. Protein expression is transient and cytoplasmic, occurring without nuclear entry [15].
- Viral Vector-Based Reprogramming: This approach utilizes engineered viruses to deliver DNA encoding the necessary factors into the target cell's nucleus. The most common systems include:
- Integrating Viruses (Retrovirus/Lentivirus): These vectors permanently integrate a DNA provirus into the host cell's genome, leading to sustained transgene expression [84] [85].
- Non-Integrating Viruses (Sendai Virus, Adenovirus): These vectors persist episomally in the nucleus (Adenovirus) or in the cytoplasm (Sendai virus) for a prolonged but finite duration, offering a non-integrating alternative with high transduction efficiency [86] [85].
Head-to-Head Quantitative Comparison
The following table summarizes the critical performance and safety characteristics of both technologies, based on current literature.
Table 1: Comparative Analysis of modRNA and Viral Vector Reprogramming Technologies
| Parameter | modRNA-Based | Viral Vector-Based (Integrating) | Viral Vector-Based (Non-Integrating, e.g., Sendai) |
|---|---|---|---|
| Genomic Integration | No integration, footprint-free [82] | Yes, permanent integration [84] | No integration; zero-footprint potential [86] |
| Reprogramming Efficiency (iPSC Generation) | Up to ~90.7% of individually plated cells [87] | 0.01% - 0.1% [82] | 0.01% - 1% [82] [86] |
| Oncogenic Risk | Very low (transient expression, no DNA intermediates) [15] | High (insertional mutagenesis, reactivation of oncogenes) [84] | Low, but residual virus may require clearance [82] [86] |
| Immunogenicity | Low (with nucleoside modifications) [82] [83] | Variable, can be immunogenic [84] | Can trigger immune response; requires monitoring [82] |
| Transgene Expression Kinetics | Transient (hours to days), requires repeated transfections [83] | Stable and long-term [84] | Transient but persistent for several passages [86] |
| Primary Cell Reprogramming | Highly efficient (optimized protocols available) [87] | Efficient, but limited by cell division (retrovirus) [84] | Highly efficient for a wide range of cell types [86] |
| Ease of Use and Development Timeline | Complex protocol optimization, repeated transfections [87] | Standardized viral production and transduction | Standardized kits available (e.g., CytoTune) [86] |
| Key Advantage | Safety profile and high efficiency in defined conditions | High transduction efficiency and stable expression | High efficiency with a non-integrating profile |
| Key Limitation | Requires careful optimization to manage cytotoxicity | Risk of genomic mutations and oncogenesis | Requires rigorous clearance of viral vectors [82] |
Experimental Protocols
Detailed Protocol: modRNA-Based Reprogramming of Human Fibroblasts
This protocol, adapted from a high-efficiency study, details the process for generating integration-free induced pluripotent stem cells (iPSCs) from human primary fibroblasts using a combination of modRNA and microRNA mimics [87].
Key Research Reagent Solutions:
- modRNA Cocktail: Synthetic mRNA encoding a 6-factor cocktail (5fM3O: M3O-OCT4, SOX2, KLF4, cMYC, LIN28A, NANOG). Nucleotides are modified with 5-methylcytidine and pseudouridine [82] [87] [83].
- m-miRNA Cocktail: Mature miRNA mimics of the ESC-specific miRNA-367/302s family.
- Transfection Reagent: Lipofectamine RNAiMAX.
- Reprogramming Medium: Knock-out serum replacement (KOSR)-based human iPSC medium.
- Interferon Suppressor: Recombinant B18R protein (optional, but recommended to enhance viability) [83].
Procedure:
- Day 0: Cell Seeding: Seed 500,000 human primary fibroblasts per well of a 6-well plate in fibroblast medium. Ensure cells are in a proliferative state and at a low passage number.
- Day 1: First Transfection:
- Prepare the RNA-lipid complex in Opti-MEM adjusted to pH 8.2, which is critical for high transfection efficiency [87].
- Per well, complex 600 ng of the 5fM3O modRNA cocktail and 20 pmol of the m-miRNA cocktail with RNAiMAX according to the manufacturer's instructions.
- Add the complex dropwise to the cells in fresh KOSR reprogramming medium, supplemented with B18R if used.
- Days 2-13: Repeated Transfection: Replace the medium and repeat the transfection procedure every 48 hours for a total of 7 transfections. Monitor cells daily for morphology changes and cytotoxicity.
- Days 14-21: Colony Expansion: After the final transfection, continue culturing the cells in reprogramming medium without RNA. Dense, ESC-like colonies should become visible. Manually pick and expand TRA-1-60-positive colonies onto feeder layers or feeder-free matrices for further characterization.
The following workflow diagram illustrates the key stages of the modRNA reprogramming protocol.
For comparative purposes, below is an outline of a standard non-integrating viral protocol using the Sendai virus (SeV) system [86].
- Procedure:
- Day 0: Cell Seeding: Seed 50,000 - 500,000 target cells (e.g., fibroblasts) per well of a 6-well plate.
- Day 1: Viral Transduction: Thaw the CytoTune Sendai reprogramming vectors (KOS: Klf4, Oct4, Sox2; hc-Myc) on ice. Add the viral particles to the cells at the recommended multiplicity of infection (MOI). Incubate for 24 hours.
- Day 2: Medium Change: Replace the transduction medium with fresh fibroblast medium.
- Days 3-6: Recovery: Allow cells to recover and proliferate.
- Day 7: Re-plating: Trypsinize and re-plate the transduced cells onto irradiated feeder layers at the recommended density.
- Days 8-30: iPSC Colony Formation: Culture cells in human iPSC medium, with daily changes. iPSC colonies typically appear between 14-30 days post-transduction.
- Clearance (Optional): Due to the cytoplasmic nature of SeV, the virus may be naturally cleared over repeated passages. PCR-based testing for the SeV genome is recommended to confirm clearance [86].
The Scientist's Toolkit
Table 2: Essential Research Reagents for modRNA and Viral Reprogramming
| Reagent / Solution | Function | Example / Key Feature |
|---|---|---|
| modRNA Constructs | Encodes reprogramming factors; modified for stability and low immunogenicity | 5mC and ψU modified bases; anti-reverse cap analog (ARCA) [82] [83] |
| Sendai Virus Vectors | Delivers RNA genome; non-integrating and highly efficient | CytoTune-iPS Sendai Reprogramming Kit (KOSM factors) [86] |
| Lentiviral Vectors | Delivers DNA for stable integration; high transduction efficiency | SIN (self-inactivating) vectors with inducible promoters [84] [85] |
| Lipofectamine RNAiMAX | Transfection reagent for efficient RNA delivery into cells | Cationic lipid formulation optimized for RNA [87] |
| B18R Protein | Interferon suppressor; enhances cell viability during RNA transfection | Vaccinia virus decoy receptor for Type I interferons [83] |
| Opti-MEM (pH 8.2) | Transfection buffer; critical for optimizing modRNA delivery efficiency | pH-adjusted medium significantly boosts transfection rates [87] |
| TRA-1-60 Antibody | Live-cell staining marker for identifying fully reprogrammed human iPSCs | Cell surface glycolipid antigen [87] [86] |
Mechanisms and Pathways in Direct Lineage Conversion
The core objective of direct lineage conversion is to force a change in a cell's transcriptional and epigenetic identity. Both modRNA and viral vectors achieve this by delivering master transcription factors that orchestrate a new gene regulatory network. The diagram below illustrates the distinct intracellular pathways activated by each technology, highlighting the fundamental difference in their mechanism of action: modRNA operates entirely in the cytoplasm, while viral DNA-based methods must enter the nucleus.
The modRNA pathway is notably more direct and avoids the risk of genomic integration, as it bypasses the DNA stage entirely. The persistent expression from viral vectors, especially integrating ones, can interfere with the completion of the reprogramming process and the functional maturation of the target cell type, which is a critical consideration for direct lineage conversion towards terminally differentiated cells [15] [83].
The choice between modRNA and viral vector technologies for direct lineage conversion is not trivial and hinges on the specific research or clinical goals. modRNA-based reprogramming stands out for projects where the highest level of safety (footprint-free) is paramount and where protocol complexity can be managed. Its high efficiency, particularly in optimized protocols, makes it a powerful tool for generating clinical-grade cells. In contrast, viral vector-based systems, particularly non-integrating kits like Sendai virus, offer a robust, user-friendly alternative with high efficiency for basic research and disease modeling where permanent genetic modification is not a primary concern. Researchers must weigh the critical trade-offs between efficiency, safety, and ease of use to select the platform that best aligns with the intended application of the converted cells.
{Application Notes & Protocols}
Comparative Analysis: Lineage-Converted vs. Directed Differentiation-Derived Cells
Within the burgeoning field of regenerative medicine and in vitro disease modeling, two primary strategies have emerged for generating specific, post-mitotic cell types: directed differentiation and direct lineage conversion. The former recapitulates developmental processes by guiding pluripotent stem cells (PSCs) through intermediate germ layers into the target cell. The latter, direct lineage conversion (or transdifferentiation), achieves a fate change through the forced expression of specific transcription factors, bypassing the pluripotent state. This application note provides a structured, quantitative comparison of spinal motor neurons (MNs) generated via these two methods against a primary in vivo benchmark. The data and protocols herein are specifically contextualized for research employing modified mRNA, a transient and non-integrating method for factor delivery, aligning with the latest advancements in RNA-based therapeutics [88] [89].
Quantitative Comparison of Cellular Phenotypes
A rigorous comparative genomic analysis of mouse spinal MNs derived from embryonic sources (EMB MN), directed differentiation of embryonic stem cells (ESC MN), and lineage conversion from fibroblasts (iMN) reveals both remarkable fidelity and critical distinctions. The findings are synthesized in the table below.
Table 1: Quantitative Comparison of Motor Neuron Models
| Feature | Primary Embryonic MNs (EMB MN) | Directed Differentiation MNs (ESC MN) | Lineage-Converted MNs (iMN) |
|---|---|---|---|
| Source Cell | Embryonic spinal cord | Pluripotent Stem Cells (ESCs/iPSCs) | Terminal somatic cells (e.g., fibroblasts) |
| Developmental Path | Native development in vivo | Recapitulation of developmental stages in vitro | Direct, non-developential fate switch |
| Global Transcriptome | Baseline reference profile | Clusters closely with EMB MNs [90] | Clusters closely with EMB MNs [90] |
| Key Differing Pathways | Baseline reference | Fas signaling, Synaptic gene expression [90] [91] | Hox code, Fas signaling [90] [91] |
| Functional Maturity | Fully functional, mature state | Electrophysiologically active; shorter survival in vitro [90] | Electrophysiologically active; longer survival in vitro [90] |
| Phenotypic Stability | N/A | Stable post-differentiation | Stable post-conversion; donor cell epigenetic memory may persist [92] |
| Expansion Potential | None | High (unlimited PSC expansion pre-differentiation) | Low (limited expansion of source cells) |
| Donor Cell Signature | N/A | Silenced | Largely silenced, but small epigenetic memory detectable [92] |
Detailed Experimental Protocols
Protocol 1: Directed Differentiation of Pluripotent Stem Cells into Motor Neurons
This protocol is adapted from established morphogen-based methods to generate spinal MNs from mouse PSCs [90] [93].
Key Research Reagent Solutions:
- Pluripotent Stem Cells: Mouse ESCs or iPSCs maintained on feeder layers or in feeder-free conditions.
- Neural Induction Medium: Comprises DMEM/F12, N2 supplement, non-essential amino acids, and β-mercaptoethanol.
- Morphogens: Recombinant Sonic Hedgehog (SHH) to ventralize the neural tube, and retinoic acid (RA) to caudalize and specify spinal cord identity [93].
- Culture Substrate: Poly-ornithine/laminin-coated plates.
Methodology:
- Embryoid Body (EB) Formation: Harvest PSCs and culture in suspension in bacterial-grade dishes to allow for aggregate formation in medium containing RA.
- Neural Induction: After 4 days, plate EBs onto an adhesive substrate. Change to Neural Induction Medium supplemented with 1 µM RA and 0.5 µM Smoothened Agonist (SAG, a SHH agonist).
- MN Maturation: Culture for an additional 3-7 days in the presence of RA and SAG. Monitor for the emergence of bipolar, neuron-like morphology.
- Purification: At day 7-10 of differentiation, dissociate cultures and purify MNs using FACS for a cell-specific reporter (e.g., Hb9::GFP) [90].
- Validation: Confirm MN identity via immunocytochemistry for markers like Isl1 and Lhx3, and perform functional assays such as patch-clamp electrophysiology.
The following workflow diagram illustrates the key stages of this protocol:
Protocol 2: Direct Lineage Conversion to Induced Motor Neurons (iMNs)
This protocol outlines the transcription factor-mediated conversion of mouse embryonic fibroblasts (MEFs) into functional iMNs, a process amenable to modification using modified mRNA cocktails [90] [2].
Key Research Reagent Solutions:
- Source Cells: Primary Mouse Embryonic Fibroblasts (MEFs).
- Reprogramming Factors: A pool of transcription factors including Ngn2, Isl1, Lhx3, Ascl1, Brn2, Myt1l, and Hb9 [90].
- Delivery Vehicle: For modified mRNA-based protocols, use in vitro transcribed mRNA with nucleoside modifications (e.g., pseudouridine) to enhance stability and reduce immunogenicity [88] [89]. Transfection reagent is required for delivery.
- Culture Medium: Serum-free N3 medium, supplemented with specific neurotrophic factors (BDNF, CNTF, GDNF).
- Co-culture System: Primary mixed glial cells, added at day 3 to support neuronal maturation and survival.
Methodology:
- Factor Delivery: Transduce MEFs with the modified mRNA cocktail encoding the reprogramming factors on day 0. Repeat transfections may be necessary over subsequent days to maintain factor expression.
- Co-culture Initiation: On day 3 post-transduction, detach the converting cells and plate them onto a feeder layer of primary mixed glia.
- Maturation & Purification: Culture cells for a total of 15 days, refreshing medium and factors as needed. Purify iMNs using FACS for Hb9::GFP around day 11-15.
- Validation: Analyze using single-cell qRT-PCR for co-expression of endogenous MN markers (Isl1, Lhx3). Assess functional properties via electrophysiology and synaptic marker expression.
The logical relationship and key steps of this process are summarized below:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Motor Neuron Generation
| Reagent / Solution | Function / Purpose | Example Application |
|---|---|---|
| Modified mRNA Cocktail | Non-integrating, transient delivery of reprogramming transcription factors (e.g., Ngn2, Isl1). | Direct lineage conversion of fibroblasts to iMNs [90] [89]. |
| Small Molecule Agonists (SAG, RA) | Modulate key developmental signaling pathways (SHH, Retinoic Acid) to pattern cells. | Directed differentiation of PSCs into spinal MNs [90] [93]. |
| Serum-Free Media (N3 Supplement) | Provides defined components for survival and maturation of neuronal cells. | Base medium for both lineage conversion and MN differentiation cultures [90]. |
| Primary Mixed Glia | Provides essential trophic support and cues for neuronal maturation and synaptic formation. | Co-culture with iMNs and primary MNs to enhance survival and function [90]. |
| Cell Surface Marker (Hb9::GFP) | Enables fluorescence-activated cell sorting (FACS) for high-purity isolation of target MNs. | Purification of MNs from heterogeneous cultures of both iMNs and ESC-derived MNs [90]. |
Critical Pathway Analysis & Implications
The comparative genomic analysis identified specific signaling pathways and transcriptional programs that differ between the two in vitro MN types, despite their overall similarity to primary MNs. These differences have direct implications for their application in disease modeling and drug screening.
- Hox Code: Lineage-converted iMNs displayed differences in their Hox code, a critical determinant of anterior-posterior positional identity in the nervous system [90]. This suggests that directed differentiation may more faithfully recapitulate the regional identity of MNs, which is crucial for modeling diseases affecting specific neuronal subsets.
- Fas Signaling & Synaptic Gene Expression: Both in vitro MN types showed alterations in Fas-mediated apoptotic signaling and synaptic gene expression profiles compared to their primary counterparts [90] [91]. This is a critical consideration for translational studies, especially for neurodegenerative diseases like ALS where synaptic stability and apoptosis are central to pathology.
The diagram below illustrates the key pathways involved in MN specification and where methodological differences arise.
Directed differentiation and direct lineage conversion are both powerful methods for generating motor neurons that closely approximate the primary in vivo state. The choice of method depends on the specific research or therapeutic application. Directed differentiation offers scalability and recapitulation of regional identity, while lineage conversion provides a more streamlined process that may better preserve age-related markers. The integration of modified mRNA technology for factor delivery enhances the safety profile of lineage conversion by avoiding genomic integration, making it a highly promising approach for both basic research and the future development of personalized cell-based therapies [88] [89]. Researchers should select the method whose strengths align with their experimental needs, whether for high-throughput drug screening, developmental studies, or modeling late-onset diseases.
Assessing Functional Utility in Disease Modeling and Drug Screening Assays
The advent of direct lineage conversion using modified mRNA has opened new avenues for generating patient-specific cell types for disease modeling and drug discovery. However, the true value of these converted cells is determined by rigorous assessment of their functional utility in biologically relevant assays. This application note provides detailed protocols and frameworks for evaluating converted cells, focusing on integration into advanced three-dimensional (3D) disease models and high-throughput drug screening platforms. The convergence of lineage conversion, functional genomics, and precision medicine offers unprecedented opportunities to create next-generation patient-specific disease models that can accurately predict therapeutic response [94]. By employing the methodologies outlined herein, researchers can quantitatively determine the maturity, functionality, and predictive value of converted cells in pharmaceutical and clinical applications.
Comparative Analysis of Preclinical Drug Screening Platforms
Selecting an appropriate screening platform is critical for assessing the functional utility of converted cells. The table below compares the key characteristics of major preclinical models.
Table 1: Comparison of Preclinical Drug Screening Platforms
| Platform | Key Characteristics | Establishment Time | Predictive Accuracy | Advantages | Limitations |
|---|---|---|---|---|---|
| 2D Monolayer Culture | Traditional chemosensitivity assays in flat surfaces [94] | 1-2 weeks | Limited; fails to capture TME | Simple, high-throughput, cost-effective | Lacks 3D architecture, poor drug metabolism representation, significant genetic diversification over time [94] |
| Patient-Derived Organoids (PDOs) | 3D structures from patient tissue embedded in matrix [94] | 4-6 weeks [94] | ~88% (gastrointestinal cancer) [94] | Retains tumor microenvironment features, polyclonality, intratumoral heterogeneity; genetically stable [94] | Limited immune environment; establishment success rate varies (70-90%) [94] |
| Organs-on-a-Chip | Microfluidic devices simulating organ-level physiology | 2-4 weeks | Research ongoing | Dynamic flow conditions, mechanical forces, multi-tissue integration | Technically complex, limited throughput, high cost |
| Patient-Derived Xenografts (PDX) | Human tumor tissue implanted in immunodeficient mice [94] | 3-6 months | High for some cancer types | Preserves tumor stroma and heterogeneity; in vivo context | Expensive, low throughput, requires animal facilities, mouse stroma eventually replaces human |
| 3D Bioprinted Models | Layer-by-layer deposition of cells and biomaterials | 2-3 weeks | Research ongoing | Customizable architecture, controlled patterning, high reproducibility | Requires specialized equipment, optimization challenging for some cell types |
Methodologies for Functional Assessment
Integration of Converted Cells into 3D Disease Models
A Protocol: Generation of Patient-Derived Organoids with Integrated Converted Cells
Purpose: To create physiologically relevant 3D disease models containing directly converted cells for drug screening applications.
Materials:
- Basement Membrane Matrix: Matrigel or similar basement membrane-mimicking substance [94]
- Organoid Culture Media: Nutrient-rich media specific to cell type
- Directly Converted Cells: Generated via modified mRNA protocol
- Patient-Derived Tissue Samples (optional for co-culture)
- Optical Metabolic Imaging (OMI) Reagents: For single-cell metabolic analysis [94]
Procedure:
- Tissue Processing: Minced patient tissue is plated with nutrient-rich media on basement membrane-mimicking substance [94].
- Cell Integration: Mix directly converted cells with primary tissue fragments at optimized ratios (typically 1:1 to 1:3 converted:primary cells).
- 3D Culture Setup:
- Centrifuge cell mixture at 300 x g for 5 minutes
- Resuspend pellet in 100 μL cold basement membrane matrix
- Plate 20-30 μL droplets in pre-warmed culture plates
- Polymerize for 30 minutes at 37°C
- Overlay with appropriate organoid culture medium
- Culture Maintenance: Replace medium every 2-3 days; passage organoids every 7-21 days based on growth rate.
- Characterization:
- Metabolic Profiling: Employ Optical Metabolic Imaging (OMI) to examine metabolic activity at single-cell level [94]
- Immunofluorescence: Analyze structural markers and cellular organization
- Functional Assays: Perform tissue-specific functional tests
Quality Control Parameters:
- Genetic stability assessment after expansion [94]
- Secondary architecture preservation [94]
- Intratumoral heterogeneity maintenance [94]
- Polyclonality verification [94]
Functional Drug Screening in 3D Models
A Protocol: High-Content Screening of Therapeutic Compounds in 3D Cultures
Purpose: To quantitatively assess drug response in 3D models containing converted cells using high-content imaging and analysis.
Materials:
- Compound Libraries: Small molecules, targeted therapies, chemotherapeutic agents
- Viability Assay Reagents: CellTiter-Glo 3D, calcein-AM/ethidium homodimer, caspase kits
- High-Content Imaging System: Confocal or multiphoton microscope with environmental control
- Image Analysis Software: Custom algorithms for 3D object segmentation and quantification
Procedure:
- Model Standardization:
- Size-select organoids (100-300 μm diameter) using cell strainers
- Plate in 96-well or 384-well ultra-low attachment plates
- Allow 24-hour recovery before treatment
- Compound Treatment:
- Prepare 10-point, 1:3 serial dilutions of test compounds
- Include positive (maximum effect) and negative (no effect) controls
- Treat organoids for 72-120 hours based on doubling time
- Endpoint Assessment:
- Viability Measurement: Add CellTiter-Glo 3D reagent, incubate 30 minutes, record luminescence
- Viability Staining: Incubate with calcein-AM (2 μM) and ethidium homodimer (4 μM) for 45 minutes
- Apoptosis Assessment: Stain with caspase-3/7 reagent per manufacturer protocol
- High-Content Imaging:
- Acquire z-stacks at 10-20 μm intervals using automated microscopy
- Image minimum of 10 organoids per condition
- Capture brightfield and fluorescence channels
- Data Analysis:
- Calculate IC50 values using nonlinear regression
- Determine maximum inhibition (Imax) and minimal inhibition (Imin)
- Quantify morphological changes (size, circularity, texture)
Table 2: Quantitative Assessment Parameters for Drug Screening
| Parameter | Measurement Technique | Typical Range in Responsive Models | Significance |
|---|---|---|---|
| IC50 | Dose-response curve fitting | 0.1-10 μM (therapeutic compounds) | Compound potency |
| Imax | Maximum effect in assay | 70-100% inhibition | Efficacy |
| Therapeutic Index | Ratio of toxic to therapeutic concentration | >10 desired | Selectivity |
| Morphological Changes | High-content image analysis | Organoid-specific | Mechanism-related effects |
| Heterogeneity Index | Coefficient of variation in response | <30% for homogeneous response | Population uniformity |
Genomic and Functional Validation
A Protocol: CRISPR-Cas9-Based Genome Engineering in Converted Cells
Purpose: To introduce disease-relevant mutations or reporter constructs into converted cells for mechanistic studies and reporter assays.
Materials:
- CRISPR Components:
- Delivery Reagents: Electroporation kits or lipid-based transfection reagents
- Selection Markers: Puromycin, GFP, or other selectable markers [96]
Procedure:
- sgRNA Design:
- Complex Formation:
- Combine synthetic sgRNA (60 pmol) with Cas9 protein (40 pmol) [95]
- Incubate 10 minutes at room temperature to form ribonucleoprotein (RNP) complex
- Cell Delivery:
- Harvest converted cells at 70-80% confluence
- Resuspend 1×10^6 cells in 100 μL electroporation buffer with RNP complex
- Electroporate using optimized program (e.g., 1350V, 30ms pulse width)
- Analysis and Validation:
- Extract genomic DNA 48-72 hours post-editing [96]
- Perform T7 endonuclease assay or tracking of indels by decomposition (TIDE) analysis
- Clone edited cells by limiting dilution
- Confirm edits by Sanger sequencing and functional assays
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Functional Assessment
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| 3D Culture Matrices | Matrigel, Basement Membrane Extract, Synthetic hydrogels | Provides physiological 3D environment for cell growth and organization | Matrix composition significantly influences cell morphology, proliferation, differentiation, and drug response [94] |
| CRISPR Components | Synthetic sgRNA, Cas9 nuclease, HDR templates [95] [96] | Precision genome engineering for introducing disease mutations or reporters | Synthetic sgRNA offers advantages over plasmid-expressed or IVT sgRNA including higher purity, reduced immunogenicity, and better editing efficiency [95] |
| Cell Viability Assays | CellTiter-Glo 3D, Calcein-AM/Ethidium homodimer, Caspase-3/7 reagents | Quantification of cell viability, cytotoxicity, and apoptosis | 3D-optimized assays account for diffusion limitations and higher cell densities in organoid models |
| Lineage Tracing Reporters | Fluorescent proteins (GFP, RFP), Luciferase, Surface markers | Tracking cell fate and functionality in real-time | Enables monitoring of converted cell integration, maturation, and persistence in complex models |
| Metabolic Probes | Resazurin, Seahorse probes, OMI reagents | Assessment of metabolic function and heterogeneity | Optical Metabolic Imaging (OMI) can identify treatment-responsive and non-responsive subpopulations at single-cell level [94] |
Workflow Visualization
Experimental Workflow for Functional Assessment
Integrated Drug Screening Platform
Data Integration and Interpretation Framework
Table 4: Multi-Parameter Scoring System for Functional Utility Assessment
| Assessment Category | Parameters Measured | Scoring Metric (0-10) | Weighting Factor | Interpretation Guidelines |
|---|---|---|---|---|
| Structural Maturation | Tissue organization, polarity, marker expression, ultrastructure | 0 (immature) to 10 (fully mature) | 1.2 | Compares to primary tissue standards; requires >7 for high-confidence models |
| Functional Capacity | Electrophysiology, contraction, secretion, metabolic activity, barrier function | 0 (non-functional) to 10 (adult-level function) | 1.5 | Most critical parameter; requires tissue-specific functional benchmarks |
| Drug Response Profile | IC50 values, efficacy maximum, therapeutic index, heterogeneity | 0 (non-predictive) to 10 (highly predictive) | 1.4 | Correlates with clinical response data; weighted by clinical translatability |
| Genetic Stability | Karyotype integrity, mutation load, transcriptome consistency | 0 (unstable) to 10 (highly stable) | 1.0 | Essential for reproducible results across passages |
| Technical Robustness | Success rate, reproducibility across operators, scalability | 0 (variable) to 10 (highly reproducible) | 0.9 | Impacts practical implementation in screening pipelines |
Composite Utility Score Calculation: Composite Score = Σ(Parameter Score × Weighting Factor) / Σ(Weighting Factors)
Interpretation Guidelines:
- ≥8.5: Excellent functional utility; suitable for high-confidence decision making
- 7.0-8.4: Good functional utility; appropriate for mid-tier screening and mechanistic studies
- 5.5-6.9: Moderate functional utility; requires validation in secondary models
- <5.5: Limited functional utility; not recommended for critical applications
The protocols and frameworks presented herein provide a comprehensive approach for assessing the functional utility of directly converted cells in disease modeling and drug screening applications. By implementing these standardized methodologies, researchers can quantitatively evaluate the predictive value of these innovative cellular tools, ultimately enhancing their application in pharmaceutical development and precision medicine. The integration of advanced 3D culture systems with robust functional readouts creates a powerful platform for bridging the gap between in vitro models and clinical response, potentially accelerating the development of more effective therapeutics.
The transition from viral vectors to non-integrative systems represents a pivotal shift in the field of direct lineage conversion using modified mRNA. This paradigm is driven by the critical need to enhance the safety profile of cellular reprogramming for therapeutic applications. Non-integrative methods, including Sendai virus (SeV) vectors, mRNA transfection, and tissue nanotransfection (TNT), eliminate the risk of insertional mutagenesis and minimize genomic instability by avoiding permanent alterations to the host genome [97] [50]. For researchers and drug development professionals, these platforms offer a transformative path toward clinical applications by providing a more controllable, transient expression of reprogramming factors, thereby reducing the potential for tumorigenicity and other long-term safety concerns associated with traditional viral vectors [98] [50].
Quantitative Safety and Efficacy Profile of Non-Integrative Systems
The quantitative advantages of non-integrative systems are demonstrated through their safety profiles, efficiency metrics, and functional outcomes in preclinical models. The table below summarizes key performance data for major non-integrative platforms.
Table 1: Key Performance Data for Major Non-Integrative Platforms
| Platform | Key Safety Feature | Reprogramming Efficiency / Key Outcome | Genomic Integration | Primary Applications |
|---|---|---|---|---|
| Sendai Virus (SeV) | Non-integrating RNA virus | Successful generation of footprint-free feline iPSCs [97] | None detected after passaging [97] | Generation of footprint-free iPSCs [97] |
| Modified mRNA | Transient expression, no nuclear entry | High protein translation efficiency; direct lineage conversion [50] | No | Direct cellular reprogramming, in vivo transfection [50] |
| Tissue Nanotransfection (TNT) | Non-viral, nanoelectroporation | Efficient in vivo gene delivery; direct cellular reprogramming [50] | No | In vivo tissue regeneration, direct lineage conversion [50] |
Beyond these core platforms, other non-viral methods like the Sleeping Beauty (SB) and piggyBac (PB) transposon systems are emerging as versatile alternatives for gene transfer. However, their use requires careful consideration of potential low-level genomic integration events, which can be mitigated through advanced molecular strategies to achieve a "footprint-free" outcome [98].
Experimental Protocols for Non-Integrative Direct Lineage Conversion
Protocol 1: Generation of Footprint-Free iPSCs Using Sendai Virus Vectors
This protocol details the generation of integration-free induced pluripotent stem cells (iPSCs) using the CytoTune-iPS 2.0 Sendai Reprogramming Kit, adapted from a study on feline fetal fibroblasts (FFFs) [97].
- Key Reagents: CytoTune-iPS 2.0 Sendai Reprogramming Kit (Thermo Fisher Scientific); Fetal fibroblasts; KnockOut DMEM; Embryonic Stem (ES) qualified FBS; Feline leukemia inhibitory factor (fLIF); Human basic fibroblast growth factor (bFGF); Inactivated SNL feeder cells.
- Procedure:
- Cell Culture Preparation: Culture source somatic cells (e.g., fetal fibroblasts) in standard medium. Revive and plate mitotically inactivated SNL feeder cells one day before transduction.
- Viral Transduction: Transduce cells at ~70% confluency with CytoTune-iPS 2.0 Sendai Reprogramming vectors at the manufacturer's recommended multiplicity of infection (MOI). Culture for approximately 6 days post-transduction.
- Reprogramming Phase: At day 7 post-transduction, dissociate and replate transduced cells onto inactivated feeder cells. Maintain cultures in iPSC medium with daily changes for 28 days.
- Colony Selection and Expansion: Mechanically pick emerging iPSC colonies exhibiting characteristic morphology (high nuclear-to-cytoplasmic ratio) and transfer to fresh feeder layers. Passage every 6–8 days.
- Quality Control and Validation:
- Alkaline Phosphatase Activity: Assess using a commercial staining kit.
- Pluripotency Marker Expression: Confirm expression of key markers (e.g., OCT4, SOX2, NANOG) via RT-PCR or immunostaining.
- Clearance of SeV Vector: Verify the loss of SeV-derived transgenes through passaging (e.g., by RT-PCR) to confirm footprint-free status [97].
Protocol 2: In Vivo Direct Lineage Conversion via Tissue Nanotransfection (TNT)
This protocol describes the use of the TNT platform for in vivo delivery of modified mRNA to achieve direct lineage conversion, a key application for regenerative medicine [50].
- Key Reagents: TNT device (hollow-needle silicon chip); Genetic cargo (e.g., modified mRNA for reprogramming factors); Pulse generator; Sterilization supplies (e.g., ethylene oxide gas).
- Procedure:
- Device and Cargo Preparation: Sterilize the TNT device using ethylene oxide gas or gamma irradiation. Load the cargo reservoir with the purified modified mRNA solution.
- In Vivo Application: Place the TNT device directly onto the target tissue (e.g., skin). Ensure the dermal electrode is properly positioned and connected to the positive terminal of the pulse generator.
- Nanoelectroporation: Apply a series of optimized electrical pulses. Parameters (voltage, pulse duration, intervals) must be predetermined to maximize delivery efficiency while maintaining cell viability.
- Post-Transfection Monitoring: Remove the device after pulsing. Monitor the tissue for expression of the delivered genetic cargo and evidence of lineage conversion using histological and molecular analyses.
- Critical Considerations: The optimization of electrical pulse parameters is essential for efficient membrane poration and cargo delivery with minimal cytotoxicity [50].
Signaling Pathways and Workflows in Direct Lineage Conversion
The following diagrams, defined using the DOT language and compliant with the specified color and contrast rules, illustrate the core workflows and relationships in non-integrative reprogramming.
Non-Integrative Reprogramming Workflow
Safety Profile Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of non-integrative reprogramming protocols relies on a core set of specialized reagents and tools.
Table 2: Essential Research Reagents for Non-Integrative Reprogramming
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Sendai Reprogramming Vectors | Delivers reprogramming factors (OSKM) without genomic integration. | Generation of footprint-free iPSCs from somatic cells [97]. |
| Modified mRNA | Engineered mRNA for enhanced stability and reduced immunogenicity; enables transient protein expression. | Direct lineage conversion in vivo; cytoplasmic translation without nuclear entry [50]. |
| Tissue Nanotransfection (TNT) Device | A physical nanoelectroporation platform for localized in vivo gene delivery. | Direct reprogramming of tissue at the site of injury for regenerative applications [50]. |
| CRISPR/dCas9 Effectors | Catalytically inactive CRISPR system for targeted transcriptional activation or epigenetic remodeling without DNA cleavage. | Synthetic transcriptional control for precise gene regulation in direct reprogramming [50]. |
| Lineage-Specific Media & Factors | Culture media supplemented with specific growth factors and small molecules to guide differentiation. | Maturation and maintenance of cells after direct lineage conversion. |
Conclusion
Direct lineage conversion using modified mRNA represents a paradigm shift in regenerative medicine, offering a precise, efficient, and safe method for cell fate engineering. The synthesis of insights from foundational science, methodological advances, troubleshooting, and comparative validation confirms that modRNA technology successfully generates functional cells for therapeutic applications while mitigating the risks associated with viral vectors. Future directions must focus on refining delivery systems for specific tissue targeting, enhancing the functional maturation of derived cells, and advancing clinical-grade manufacturing processes. As the field progresses, this technology holds immense promise for developing personalized cell therapies, advancing in vitro disease modeling, and creating a new generation of treatments for degenerative conditions and genetic disorders.
References
- 1. Direct Cell Reprogramming: What Is It & How Does It Work? [https://bioinformant.com/direct-cell-reprogramming/]
- 2. Direct Lineage Reprogramming: Strategies, Mechanisms ... [https://www.sciencedirect.com/science/article/pii/S1934590915000144]
- 3. Direct Lineage Reprogramming of Fibroblasts into Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408679/]
- 4. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 5. Inducible, virus-free direct lineage reprogramming ... [https://elifesciences.org/reviewed-preprints/106550]
- 6. Lineage Reprogramming: Genetic, Chemical, and Physical ... [https://www.mdpi.com/2073-4409/13/8/707]
- 7. To recruit or to graft? Comparing the recruitment of resident ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1589790/full]
- 8. NSUN-Mediated m5C RNA Modification in Stem Cell Regulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564306/]
- 9. Direct reprogramming of mouse fibroblasts into self ... [https://www.nature.com/articles/s41536-025-00411-4]
- 10. RNA-Based Tools for Nuclear Reprogramming and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3838600/]
- 11. MyoD-Induced Trans-Differentiation: A Paradigm for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9654159/]
- 12. Transgene-free direct conversion of murine fibroblasts into ... [https://www.nature.com/articles/s41536-023-00317-z]
- 13. Experimental Studies on the Differentiation of Fibroblasts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3614677/]
- 14. MYOD modified mRNA drives direct on-chip programming ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X21007555]
- 15. Tissue nanotransfection and cellular reprogramming in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213499/]
- 16. Algorithm for optimized mRNA design improves stability ... [https://www.nature.com/articles/s41586-023-06127-z]
- 17. mRNA medicine: Recent progresses in chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311907/]
- 18. Opportunities and Challenges in the Delivery of mRNA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7076378/]
- 19. Unlock the sustained therapeutic efficacy of mRNA [https://www.sciencedirect.com/science/article/abs/pii/S0168365925004572]
- 20. Progress and prospects of mRNA-based drugs in pre- ... [https://www.nature.com/articles/s41392-024-02002-z]
- 21. Current Analytical Strategies for mRNA-Based Therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11990077/]
- 22. Direct circRNA-mRNA Binding Controls mRNA Fate [https://pmc.ncbi.nlm.nih.gov/articles/PMC12285957/]
- 23. Application of Chemically Modified mRNA in Cell Fate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6646692/]
- 24. a comprehensive review of mRNA vaccine technology and ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02645-6]
- 25. Optimizing Modified mRNA In Vitro Synthesis Protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6722299/]
- 26. Modified mRNA: Getting to the Heart of Gene Therapy [https://www.trilinkbiotech.com/modified-mrna-getting-to-the-heart-of-gene-therapy]
- 27. Position-specific ORF nucleoside-ribose modifications ... [https://www.nature.com/articles/s41467-025-65788-8]
- 28. mRNA Vaccines: Current Applications and Future Directions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572956/]
- 29. mRNA-based technology for engineered regenerative ... [https://www.sciencedirect.com/science/article/pii/S305056232500176X]
- 30. mRNA therapeutics: Transforming medicine through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590236/]
- 31. Photocaged 5′ cap analogues for optical control of mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7613264/]
- 32. Optimizing 5'UTRs for mRNA-delivered gene editing using ... [https://www.nature.com/articles/s41467-024-49508-2]
- 33. Deep generative optimization of mRNA codon sequences ... [https://www.nature.com/articles/s41467-025-64894-x]
- 34. A New Deep-learning-Based Approach For mRNA ... [https://arxiv.org/html/2505.23862v1]
- 35. Design Strategies for Novel Lipid Nanoparticle for mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497691/]
- 36. Review Lipid nanoparticles: Composition, formulation, and ... [https://www.sciencedirect.com/science/article/pii/S2329050125000580]
- 37. mRNA Delivery: Challenges and Advances through Polymeric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10855060/]
- 38. Comprehensive analysis of lipid nanoparticle formulation ... [https://www.sciencedirect.com/science/article/pii/S2590156724000550]
- 39. PILOT LNPs take mRNA therapeutics to new destinations [https://www.bioxconomy.com/modalities/pilot-lnps-take-mrna-therapeutics-to-new-destinations]
- 40. Structuring of lipid nanoparticle mRNA formulations at ... [https://pubmed.ncbi.nlm.nih.gov/41127005/]
- 41. Polymers as Efficient Non-Viral Gene Delivery Vectors [https://www.mdpi.com/2073-4360/16/18/2629]
- 42. Designing lipid nanoparticles using a transformer-based ... [https://www.nature.com/articles/s41565-025-01975-4]
- 43. Emerging lipid nanoparticle systems capable of efficient ... [https://pubmed.ncbi.nlm.nih.gov/40901740/]
- 44. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 45. Pluripotent Stem Cell (PSC) Protocols [https://www.thermofisher.com/us/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols.html]
- 46. Unlocking the regulatory code of RNA - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551254/]
- 47. Direct Conversion of Fibroblast into Neurons for Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10578293/]
- 48. Direct fibroblast reprogramming: an emerging strategy for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-06060-3]
- 49. Direct cellular reprogramming and transdifferentiation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10497843/]
- 50. Tissue nanotransfection and cellular reprogramming in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1558735/full]
- 51. Harnessing mRNA for heart health: a new era in ... [https://www.thno.org/v15p7779.htm]
- 52. Researchers Identify New mRNA-Based Therapy that Shows ... [https://medicine.temple.edu/news/2025/07/researchers-identify-new-mrna-based-therapy-shows-promise-heart-regeneration-after-heart-attack]
- 53. In Vivo Targeted Reprogramming of Cardiac Fibroblasts for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466987/]
- 54. Delivering the Message: Translating mRNA Therapy for Liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361847/]
- 55. Molecular mechanisms in liver repair and regeneration [https://www.nature.com/articles/s41392-024-02104-8]
- 56. Decrypting the Immune Symphony for RNA Vaccines [https://www.mdpi.com/2076-393X/13/8/882]
- 57. The mRNA component of LNP-mRNA vaccines triggers ... [https://pubmed.ncbi.nlm.nih.gov/41169401/]
- 58. The mRNA component of LNP-mRNA vaccines triggers ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1670350/full]
- 59. Stable vs. Transient Transfection: Techniques for Gene Expression and Cell Line Development | Sino Biological [https://www.sinobiological.com/resource/protein-review/stable-transient-transfection]
- 60. Step-by-Step Protocol for mRNA & LNP Formulation [https://www.bocsci.com/blog/a-comprehensive-protocol-for-mrna-design-manufacture-and-lnp-formulation/?srsltid=AfmBOopS41KgX1DOAZ7gHllHntW_7JnkTpn5DyQN1cUFAcC6QftSIqgK]
- 61. Enhancing cap-independent translation of linear mRNA [https://www.nature.com/articles/s41467-025-64257-6]
- 62. Considerations for mRNA Product Development, Regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116195/]
- 63. Extended gene expression by medium exchange and repeated transient transfection for recombinant protein production enhancement - PubMed [https://pubmed.ncbi.nlm.nih.gov/25421734/]
- 64. mRNA Synthesis Democratized with Open-source ... [https://www.neb.com/en-us/nebinspired-blog/mrna-synthesis-democratized-with-open-source-approach-by-base-facility-researchers?srsltid=AfmBOorsCiesIlOiW7GkyBeiATQFo9nX2s-386sow2YMX0kqkO47WJHc]
- 65. mRNA-LNP vaccines: rational design, delivery optimization ... [https://pubmed.ncbi.nlm.nih.gov/41251047/]
- 66. Endo/Lysosomal-Escapable Lipid Nanoparticle Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300936/]
- 67. Cellular and biophysical barriers to lipid nanoparticle ... [https://www.nature.com/articles/s41467-025-60959-z]
- 68. Quantitative size-resolved characterization of mRNA ... [https://www.nature.com/articles/s41598-023-42274-z]
- 69. A proximity-labeling-based approach to directly detect ... [https://www.sciencedirect.com/science/article/pii/S2162253125001568]
- 70. A Computational Framework for Optimizing mRNA Vaccine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1628583/full]
- 71. Chemical direct conversion of human fibroblasts to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574161/]
- 72. GATA6 regulates WNT and BMP programs to pattern ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906159/]
- 73. Multifactorial approach is needed to unravel the maturation ... [https://www.nature.com/articles/s41598-024-81140-4]
- 74. Data-Driven Maturity Level Evaluation for Cardiomyocytes ... [https://www.mdpi.com/2079-9292/13/24/4985]
- 75. mRNA Cellular Reprogramming Method [https://pluristyx.com/cellular-reprogramming/]
- 76. HSCI researchers achieve major breakthrough in cell ... [https://www.hsci.harvard.edu/hsci-researchers-achieve-major-breakthrough-cell-reprogramming]
- 77. Nonintegrating Direct Using Conversion into Hepatocyte-Like... mRNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC6171260/]
- 78. Comprehensive guide for epigenetics and transcriptomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11799959/]
- 79. Single-Cell Transcriptomic Profiling Reveals Regional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12112128/]
- 80. A Comparative Overview of Epigenomic Profiling Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC8340004/]
- 81. Real-time transcriptomic profiling in distinct experimental ... [https://elifesciences.org/reviewed-preprints/98768]
- 82. Application of Modified mRNA in Somatic Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8348611/]
- 83. Highly efficient reprogramming to pluripotency and directed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3656821/]
- 84. Vectorology and Factor Delivery in Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4046209/]
- 85. RNA-Based Tools for Nuclear Reprogramming and... [https://link.springer.com/article/10.1007/s12265-013-9494-8]
- 86. Reprogramming Fibroblasts with the CytoTune®-iPS ... [https://www.thermofisher.com/us/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols/reprogramming-fibroblasts-with-cytotune-ips-reprogramming-it.html]
- 87. High-efficiency RNA-based reprogramming of human ... [https://www.nature.com/articles/s41467-018-03190-3]
- 88. The current and future landscape of RNA-based therapies ... [https://www.nature.com/articles/s43856-025-01166-1]
- 89. Advances in RNA-based therapeutics: current ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675209/full]
- 90. Comparative genomic analysis of embryonic, lineage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6262794/]
- 91. Comparative genomic analysis of embryonic, lineage ... [https://pubmed.ncbi.nlm.nih.gov/30337375/]
- 92. Direct Lineage Conversion of Terminally Differentiated ... [https://www.sciencedirect.com/science/article/pii/S1934590911004334]
- 93. Directed differentiation [https://en.wikipedia.org/wiki/Directed_differentiation]
- 94. Functional Drug Screening in the Era of Precision Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC9307928/]
- 95. The Complete Guide to Understanding CRISPR sgRNA [https://www.synthego.com/guide/how-to-use-crispr/sgrna/]
- 96. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 97. Footprint-free induced pluripotent stem cells can be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010622/]
- 98. The Past, Present, and Future of Non-Viral CAR T Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9218214/]