Engineering Complexity: How 3D Bioprinting is Building the Future of Tissues and Therapeutics
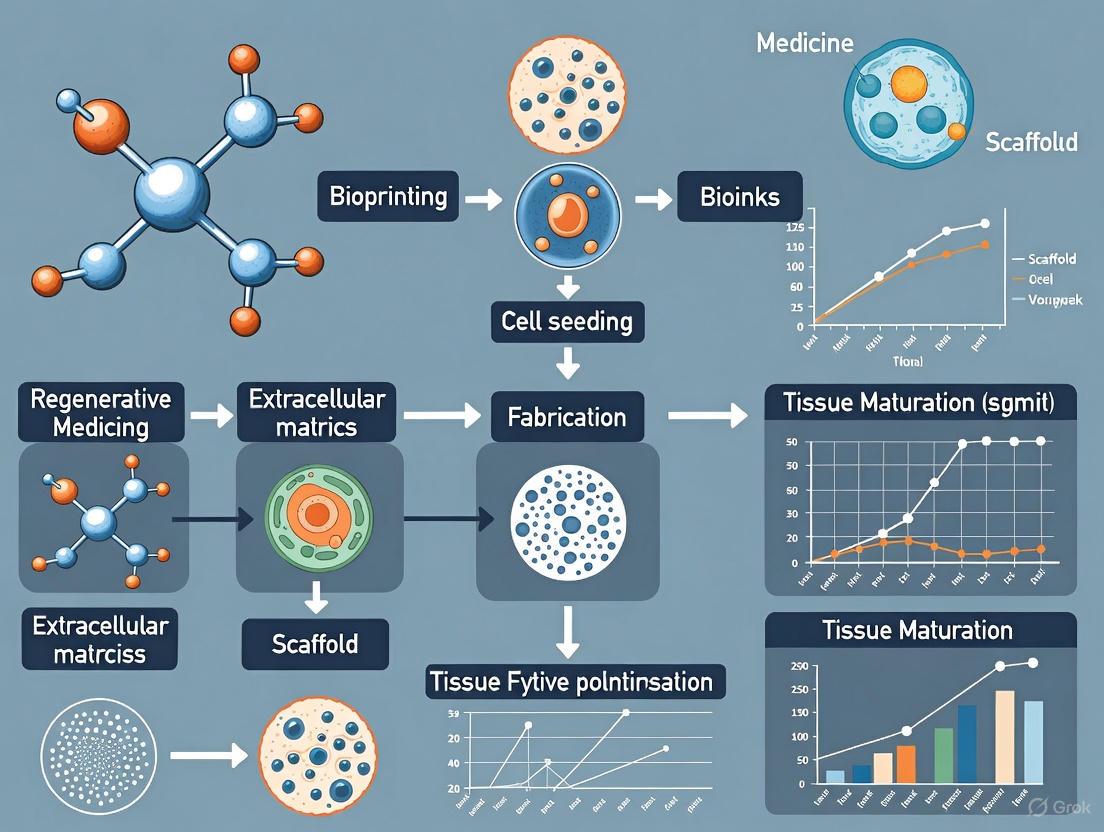
This article explores the transformative role of 3D bioprinting in fabricating complex, biomimetic tissue architectures for advanced biomedical applications.
Engineering Complexity: How 3D Bioprinting is Building the Future of Tissues and Therapeutics
Abstract
This article explores the transformative role of 3D bioprinting in fabricating complex, biomimetic tissue architectures for advanced biomedical applications. It provides a comprehensive overview for researchers and drug development professionals, covering the foundational principles of bioprinting, from bioink design to process mechanics. The scope extends to cutting-edge methodological advances, including high-throughput systems and vascularization strategies, alongside critical troubleshooting for defect minimization and process optimization. Finally, the article examines the application and validation of these engineered tissues in drug screening and disease modeling, highlighting their superior predictive power over traditional 2D models and their growing impact on precision medicine and the drug development pipeline.
The Blueprint of Life: Core Principles of 3D Bioprinting for Tissue Architecture
The field of tissue engineering is undergoing a revolutionary transformation through the integration of digital design tools and advanced biomanufacturing. Three-dimensional (3D) bioprinting represents an innovative technology that combines engineering, manufacturing, and medicine to create biologically relevant tissue architectures [1]. This digital workflow enables researchers to move beyond traditional two-dimensional cell culture toward constructing complex, patient-specific tissue models with precise spatial control over cellular organization and extracellular matrix composition. The process involves incorporating living cells with biocompatible materials to design required tissue or organ models in situ for various in vivo and in vitro applications, fundamentally changing approaches to disease modeling, drug discovery, and regenerative medicine [1] [2].
The significance of this digital transition extends throughout the research pipeline. For drug development professionals, 3D bioprinted tissues offer more physiologically relevant models for compound screening, potentially identifying efficacy and toxicity issues earlier in the development process [2]. For translational scientists, the technology enables creation of patient-specific tissue constructs that mirror native tissue complexity more accurately than conventional models [3]. The global market size of 3D bioprinting, valued at $1.7 billion USD in 2021 and expected to reach $1.94 billion by 2025, reflects the growing investment and confidence in these technologies [1].
The Digital Workflow: From Virtual Design to Biological Construct
The complete digital workflow for tissue design integrates multiple stages, each requiring specialized tools and protocols. The process transforms virtual designs into living biological constructs through a coordinated sequence of pre-bioprinting, bioprinting, and post-bioprinting stages.
Pre-Bioprinting Phase: Digital Design and Preparation
The foundation of successful bioprinting lies in meticulous pre-bioprinting preparation, where digital design meets biological preparation.
Imaging and 3D Model Generation: The process begins with acquiring high-resolution 3D images of the target tissue or organ architecture using diagnostic tools like MRI, CT, or micro-CT [1]. These images in DICOM format are processed through segmentation algorithms to create 3D virtual models of the defect or tissue structure. For bone regeneration applications, Cone Beam Computed Tomography (CBCT) provides the necessary resolution for creating accurate 3D bone defect models (3DBM) [4]. The segmented models are exported as Standard Tessellation Language (STL) files, which serve as the universal format for 3D printing platforms [4].
Bioink Preparation and Cell Culture: Parallel to model generation, researchers prepare bioinks—the printable materials containing living cells and biomaterials that form the tissue construct. Bioinks typically consist of a combination of natural or synthetic polymers (such as alginate, gelatin, chitosan, collagen, or hyaluronic acid) mixed with specific cell populations [1] [3]. Cells are expanded through conventional 2D culture or as 3D spheroids, which exhibit improved biological function due to their native-like tissue microenvironment that enables direct cell-cell signaling and cell-matrix interactions [3]. For applications requiring high cell density, spheroids offer a promising alternative with cell density similar to human tissue [5].
Design Principles for Bioprinting: Three main approaches guide the design process in bioprinting:
- Biomimicry: Seeking to replicate the identical biological components and configuration of native tissues, including their specific cellular organization and extracellular matrix composition [1].
- Autonomous self-assembly: Utilizing the innate mechanisms of tissue formation in embryonic development, where cells organize themselves into functional structures [1].
- Mini-tissue building blocks: Combining both approaches by creating the smallest structural and functional tissue components (spheroids, rods) and assembling them into larger constructs [1].
Table 1: Key Software Tools in the Digital Bioprinting Workflow
| Software Type | Examples | Primary Function | Compatibility/Format |
|---|---|---|---|
| Medical Imaging | CoDiagnostiX, Dental Wings | Convert DICOM images to 3D models | STL file export [4] |
| CAD Design | Meshmixer, DNA Studio | 3D modeling and mesh design | Open-source/proprietary [4] [2] |
| Printer Control | Manufacturer-specific | Printer operation and parameter control | G-code generation |
Bioprinting Phase: Fabrication Strategies and Modalities
The bioprinting phase translates digital designs into physical biological constructs through additive manufacturing approaches. The core principle involves layer-by-layer deposition of bioinks following a predetermined path generated from the digital model [2]. Different bioprinting technologies offer distinct advantages for specific tissue types and applications.
Extrusion-Based Bioprinting: This most common approach uses mechanical (piston or screw-driven) or pneumatic pressure to force bioink through a nozzle, depositing continuous filaments in a controlled pattern [1]. Researchers load cell-laden bioink into cartridges and set printing parameters including pressure, speed, and nozzle height to optimize structural integrity and cell viability [2]. A novel advancement in this category is the High-throughput Integrated Tissue Fabrication System for Bioprinting (HITS-Bio), which uses a digitally controlled nozzle array (e.g., 4×4 configuration) to manipulate multiple spheroids simultaneously, increasing printing speed by 10-fold while maintaining >90% cell viability [5].
Light-Based Bioprinting: This modality uses projected light patterns to selectively polymerize photosensitive bioinks in a vat, forming complex structures with high resolution [2]. Digital Light Processing (DLP) stereolithography offers advantages for creating constructs with fine features and smooth surfaces.
Emerging Hybrid Approaches: Recent advances include 3D hybrid bioprinting platforms that integrate multiple printing modules under optimized conditions for continuous bioprinting with both soft and hard biomaterials [6]. These systems can create multi-hydrogel hybrid constructs with over 1000-fold increase in mechanical strength compared to hydrogel-only constructs, making them suitable for load-bearing musculoskeletal and orthopedic tissue engineering [6].
Table 2: Quantitative Comparison of Bioprinting Technologies
| Bioprinting Technology | Resolution Range | Speed | Cell Viability | Suitable Bioinks |
|---|---|---|---|---|
| Extrusion-Based | 100-500 μm [5] | Moderate (conventional) to High (HITS-Bio: 10x faster) [5] | 80-95% [5] | High-viscosity hydrogels, cell spheroids |
| Light-Based | 10-100 μm | Fast | 75-90% | Photocrosslinkable hydrogels |
| Hybrid Systems | 50-200 μm [6] | Variable | >90% [6] | Multiple material classes |
Post-Bioprinting Phase: Maturation and Validation
The post-bioprinting phase transitions the printed construct into a functional tissue through maturation and stabilization processes.
Crosslinking and Stabilization: Most 3D bioprinted structures require crosslinking to achieve structural stability and mechanical integrity. This is typically achieved through chemical (ionic solutions) or physical (UV light) methods that create covalent bonds between polymer chains [2]. The specific crosslinking method depends on the bioink composition, with alginate-based inks often using calcium chloride solutions while gelatin methacryloyl (GelMA) requires photoinitiators and UV exposure.
Quality Control and Process Monitoring: Advanced monitoring techniques are essential for ensuring reproducible tissue fabrication. A novel approach developed at MIT integrates a modular, low-cost (<$500) monitoring system with a digital microscope that captures high-resolution images of tissues during printing [7]. An AI-based image analysis pipeline rapidly compares these images to the intended design, identifying defects such as over- or under-deposition of bioink. This system enables real-time inspection and adaptive correction, serving as a foundation for intelligent process control in embedded bioprinting [7].
Maturation and Functional Assessment: Following crosslinking, constructs are transferred to bioreactors that provide appropriate physiological stimulation (flow, compression, stretch) and nutrient delivery to promote tissue development and functionality [1]. The maturation period varies from days to weeks depending on the tissue complexity. During this phase, constructs are regularly assessed for metabolic activity, gene expression, protein secretion, and structural organization to validate their biological relevance.
Advanced Applications in Complex Tissue Architecture
The digital workflow enables fabrication of increasingly complex tissue architectures that better replicate native tissue organization and function.
Vascularized Tissue Constructs
A significant challenge in tissue engineering has been creating vascular networks that support nutrient and oxygen transport in thick constructs. Advanced bioprinting approaches now enable fabrication of hierarchical vascular structures through multi-material printing. By combining different bioinks in core-shell configurations or printing sacrificial materials that can be subsequently removed, researchers create perfusable channel networks within tissue constructs [6]. These vascularized tissues better sustain high cell densities and can be integrated with host vasculature upon implantation.
Bone and Cartilage Regeneration
Digital workflows have shown particular promise in orthopedic applications. In one approach, researchers used CAD-CAM technology to design custom titanium meshes for guided bone regeneration (GBR) [4]. The process involved creating a 3D bone defect model from CBCT scans, designing a patient-specific mesh with controlled porosity (0.3 mm pore width) and thickness (0.5 mm) using open-source software, and 3D laser printing the final titanium mesh [4]. This digital approach provided superior fit and mechanical support compared to manually shaped meshes.
For cartilage repair, the HITS-Bio platform demonstrated fabrication of one-cubic centimeter cartilage constructs containing approximately 600 spheroids in less than 40 minutes [5]. The high cell density and organization achieved through this rapid printing process facilitated formation of functional cartilage tissue with appropriate biochemical and mechanical properties.
Multi-Tissue Interfaces and Organ-on-Chip Models
Hybrid bioprinting platforms enable creation of complex multi-tissue interfaces, such as bone-cartilage or tendon-muscle junctions, by seamlessly integrating different biomaterials and cell types within a single construct [6]. These models are particularly valuable for studying tissue development, disease progression, and drug responses at tissue interfaces. Similarly, bioprinting facilitates development of sophisticated microphysiological systems (MPS) and organ-on-chip models that incorporate multiple cell types in physiologically relevant geometries [7]. These systems offer more predictive platforms for drug screening and disease modeling compared to conventional 2D cultures.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the digital tissue design workflow requires careful selection of materials, reagents, and equipment. The following table details key components of the research toolkit for bioprinting applications.
Table 3: Essential Research Reagents and Materials for Digital Tissue Design
| Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| Natural Polymer Bioinks | Alginate, Gelatin, Chitosan, Collagen, Hyaluronic Acid, Fibrinogen [3] | Provide extracellular matrix-like environment for cell encapsulation and growth | Biocompatibility, biodegradability, cell adhesion motifs |
| Synthetic Polymer Bioinks | PEG-based hydrogels, Pluronics, Polycaprolactone (PCL) | Structural support, tunable mechanical properties | Controlled polymerization, consistent batch-to-batch properties |
| Crosslinking Agents | Calcium chloride (for alginate), Photoinitiators (Irgacure 2959), Genipin | Stabilize printed structures through chemical or physical crosslinking | Cytocompatible concentrations, rapid gelation kinetics |
| Cell Sources | Primary cells, stem cells (MSCs, iPSCs), cell lines (e.g., HEK293, HepG2) | Provide biological functionality to printed constructs | Expansion capacity, differentiation potential, functional markers |
| Software Platforms | Meshmixer, DNA Studio, CoDiagnostiX, manufacturer-specific printer software | Design, simulation, and printer control | STL compatibility, user-friendly interface, parameter adjustment capability |
| Process Monitoring Tools | Digital microscope systems, AI-based image analysis pipelines [7] | Real-time quality control during printing | High-resolution imaging, rapid comparison to design specifications |
Quality Control and Process Optimization
Implementing robust quality control measures throughout the digital workflow is essential for generating reproducible, reliable tissue constructs.
AI-Enhanced Process Monitoring
A cutting-edge approach developed by MIT researchers addresses the critical need for process control in bioprinting. This system integrates a compact digital microscope that captures high-resolution images of tissues during the printing process [7]. An AI-based image analysis pipeline then rapidly compares these images to the intended digital design, identifying defects such as over- or under-deposition of bioink. This method enables researchers to quickly identify optimal print parameters for a variety of different materials, improving inter-tissue reproducibility and enhancing resource efficiency by limiting material waste [7]. The system serves as a foundation for intelligent process control in embedded bioprinting, with potential for real-time adaptive correction and automated parameter tuning.
Characterization and Validation Methods
Comprehensive characterization of bioprinted tissues involves multiple analytical approaches:
- Structural analysis: Micro-CT, scanning electron microscopy (SEM), and histology assess architectural features and porosity.
- Mechanical testing: Compression, tension, and indentation tests evaluate mechanical properties relevant to native tissues.
- Biological validation: Cell viability assays (live/dead staining), immunostaining, gene expression analysis (qPCR, RNA-seq), and functional assays confirm tissue maturation and functionality.
Future Perspectives and Concluding Remarks
The field of digital tissue design is rapidly evolving, with several emerging trends poised to expand capabilities further. Machine learning integration is optimizing printing parameters and predicting tissue maturation outcomes, while 4D bioprinting introduces dynamic materials that change shape or functionality post-printing in response to environmental stimuli [1]. The development of novel bioinks with supramolecular functionality, reversible crosslinking polymers, and stimuli-responsive hydrogels continues to advance the complexity of printable tissues [3]. As resolution and speed improve simultaneously through technologies like HITS-Bio, the field moves closer to clinical application of bioprinted tissues for transplantation [5].
The digital workflow from CAD to cell represents a fundamental shift in how researchers approach tissue engineering and regenerative medicine. By integrating advanced imaging, computational design, and precision manufacturing with biology, this approach enables creation of tissue architectures with unprecedented control and complexity. For drug development professionals, these technologies offer more predictive models for compound screening. For translational scientists, they provide pathways to patient-specific tissue repairs. As the field continues to mature, the synergy between digital design and biological fabrication will undoubtedly yield increasingly sophisticated tissue constructs, ultimately blurring the boundaries between artificial fabrication and natural tissue formation.
In the rapidly advancing field of 3D bioprinting for complex tissue architecture research, the development of sophisticated bioinks represents a critical frontier. Bioinks—the cell-laden materials used in 3D bioprinting—serve as temporary, supportive scaffolds that mimic the native extracellular matrix (ECM), providing not only structural integrity but also essential biological cues for cellular adhesion, proliferation, and differentiation. Among the plethora of biomaterials investigated, three components have emerged as particularly promising: alginate, a seaweed-derived polysaccharide prized for its excellent printability and gentle crosslinking; gelatin, a collagen derivative that provides natural cell-adhesive motifs; and decellularized extracellular matrix (dECM), which offers tissue-specific biological signaling. When strategically combined, these materials create composite bioinks that overcome the limitations of individual components, enabling the fabrication of complex, functional tissue constructs for research and therapeutic applications.
The quest to replicate native tissue microenvironments in vitro demands bioinks that satisfy two often conflicting requirements: printability (the ability to form and maintain complex 3D structures during and after printing) and biofunctionality (the capacity to support cell viability and direct cellular behavior). Alginate-gelatin-dECM composites represent a sophisticated approach to balancing these demands, offering researchers a versatile platform for creating physiologically relevant tissue models for drug screening, disease modeling, and fundamental biological investigation. This technical guide decodes the formulation strategies, characterization methods, and practical applications of these advanced bioink systems, providing researchers with the foundational knowledge needed to design and optimize scaffolds for specific tissue engineering applications.
Component Fundamentals: Properties and Functions
Understanding the individual properties of each bioink component is essential for rational design of composite formulations. The table below summarizes the key characteristics, advantages, and limitations of alginate, gelatin, and dECM.
Table 1: Fundamental Properties of Core Bioink Components
| Component | Source/Origin | Key Properties | Advantages | Limitations |
|---|---|---|---|---|
| Alginate | Seaweed | Ionic crosslinking (via Ca²⁺), shear-thinning, biocompatible | Excellent printability, mild crosslinking, tunable mechanical properties | Lack of cell-adhesive motifs, limited biodegradability |
| Gelatin | Denatured collagen | Thermo-reversible gelation, RGD sequences, enzymatically degradable | Enhanced cell adhesion, biocompatibility, promotes cell proliferation | Low mechanical strength, unstable at physiological temperatures |
| dECM | Decellularized tissues | Tissue-specific biochemical composition, native ultrastructure, biomechanical cues | Recapitulates native microenvironment, contains growth factors, superior bioactivity | Poor printability, low viscosity, batch-to-batch variability |
Alginate: The Structural Backbone
Alginate, a natural polysaccharide derived from brown seaweed, serves as the structural workhorse in many composite bioinks. Its capacity for rapid ionic crosslinking in the presence of divalent cations (particularly calcium chloride) makes it exceptionally valuable for maintaining structural fidelity during and after the printing process. Alginate exhibits pseudoplastic (shear-thinning) behavior, meaning its viscosity decreases under shear stress during extrusion through printing nozzles and rapidly recovers once deposited, enabling precise deposition of filamentous structures [8]. This property is crucial for achieving high-resolution printing of complex architectures.
The mechanical properties of alginate hydrogels can be precisely tuned by adjusting parameters such as molecular weight, concentration, and crosslinking density, allowing researchers to match the stiffness of various native tissues [9]. However, a significant limitation of pure alginate is its lack of inherent cell-adhesive motifs, which can limit cell-matrix interactions crucial for tissue development. Additionally, alginate degrades primarily through slow, unpredictable dissolution rather than controlled enzymatic breakdown, which may not ideally match the timeline of new tissue formation [8].
Gelatin: The Biofunctional Enhancer
Gelatin, produced through partial hydrolysis of collagen, introduces critical biological functionality to composite bioinks. Its most valuable attribute is the presence of arginine-glycine-aspartic acid (RGD) sequences, which are recognized by integrin receptors on cell surfaces, facilitating cell adhesion, spreading, and migration [10]. Gelatin exhibits thermoresponsive behavior, transitioning from a liquid state at elevated temperatures (above ~30°C) to a gel state at lower temperatures, which can be harnessed to achieve temporary stabilization immediately after printing before permanent crosslinking of other components.
The main challenges with gelatin include its relatively low mechanical strength and thermal instability at physiological temperatures (37°C), where it tends to dissolve, compromising long-term structural integrity [10]. Consequently, gelatin is typically combined with materials that provide structural reinforcement or is chemically modified (e.g., gelatin methacryloyl or GelMA) to create stable covalent networks through photo-crosslinking. In alginate-gelatin composites, gelatin enhances cellular interactions while alginate provides the mechanical framework.
Decellularized Extracellular Matrix (dECM): The Biological Gold Standard
dECM bioinks are created by decellularizing native tissues or organs, followed by processing the remaining ECM into a printable form. The resulting material preserves tissue-specific biochemical composition and architectural cues, including collagens, glycosaminoglycans (GAGs), glycoproteins, and growth factors that regulate cellular behavior [11]. This complex biochemical microenvironment provides instructional signals that can enhance stem cell differentiation, promote tissue-specific functionality, and support the formation of sophisticated tissue structures that more closely mimic their in vivo counterparts.
The primary challenge with dECM bioinks is their poor printability and low mechanical properties when used alone. dECM solutions typically exhibit low viscosity and slow gelation, resulting in limited shape fidelity after printing [11]. Consequently, dECM is most often used as a bioactive component within composite bioinks, where it contributes biological signaling while other components (particularly alginate) provide structural integrity. The decellularization process itself is critical—overly aggressive methods can damage ECM components, while insufficient decellularization may leave immunogenic cellular material [12].
Formulation Strategies and Optimization
Creating optimal alginate-gelatin-dECM composites requires careful balancing of component ratios and crosslinking strategies to achieve the desired printability and bioactivity. The table below summarizes key formulation parameters and their effects on bioink properties.
Table 2: Bioink Formulation Optimization Parameters
| Parameter | Effects on Printability | Effects on Bioactivity | Optimal Range |
|---|---|---|---|
| Alginate Concentration | Higher concentration improves viscosity and shape fidelity | Very high concentrations may limit nutrient diffusion | 2-4% (w/v) |
| Gelatin Concentration | Moderate concentrations aid extrusion; too high causes nozzle clogging | Higher concentrations improve cell adhesion via RGD sequences | 5-15% (w/v) |
| dECM Content | High content reduces printability and structural stability | Higher content enhances tissue-specific bioactivity | 1-5 mg/mL |
| Crosslinker (CaCl₂) Concentration | Higher concentration increases stiffness and stability | Excessive crosslinking may reduce porosity and cell mobility | 100-200 mM |
Composite Design Principles
Successful bioink formulations leverage the complementary properties of each component. A typical approach uses alginate as the structural backbone that provides immediate shape fidelity through rapid ionic crosslinking, gelatin as a bioadhesive component that enhances cellular interactions and provides temporary thermal gelling, and dECM as a bioactive supplement that confers tissue-specific signaling [12] [13]. The specific ratios depend on the target tissue and printing methodology, but generally fall within the ranges indicated in Table 2.
Research demonstrates that the addition of gelatin to alginate significantly improves hydrophilicity and viscoelasticity, while alginate enhances mechanical properties and porosity [12]. One study reported that optimal formulations containing 15% gelatin achieved swelling ratios of 835.43 ± 130.61%, compression modulus of 9.64 ± 0.41 kPa, and porosity of 76.62 ± 4.43%—properties conducive to nutrient diffusion and cell infiltration [12]. The incorporation of dECM further enhances the biological performance without substantially altering mechanical properties when added at appropriate concentrations.
Crosslinking Strategies
Effective crosslinking is essential for maintaining structural stability in bioprinted constructs. Dual-crosslinking approaches have proven particularly effective for alginate-gelatin-dECM composites [13]. A typical strategy involves:
- Thermal gelation: Immediate stabilization after printing through gelatin gelation when the bioink cools below its gelation temperature (approximately 25°C).
- Ionic crosslinking: Subsequent immersion in calcium chloride solution to permanently crosslink the alginate network.
This combination allows for adequate time for precise printing while ensuring long-term stability under physiological conditions. In some cases, additional crosslinking methods may be employed, such as enzymatic crosslinking for gelatin or photo-crosslinking for modified polymers, providing further control over the mechanical and degradation properties of the final construct [10].
Experimental Protocols and Characterization
Bioink Preparation and Sterilization
Protocol: dECM-Enriched Alginate-Gelatin Bioink Formulation
- Materials: Porcine liver dECM powder, gelatin (Type A, 300 bloom), sodium alginate, Dulbecco's Phosphate Buffered Saline (DPBS), calcium chloride, pepsin.
- Procedure:
- dECM Solution Preparation: Digest dECM powder at 10 mg/mL in 0.1 M acetic acid containing 1 mg/mL pepsin. Stir for 48-72 hours at 4°C until fully dissolved. Neutralize to pH 7.4 using NaOH and dilute with DPBS to desired concentration [11].
- Gelatin Solution Preparation: Dissolve gelatin in DPBS at 37°C for 1 hour on a rotational shaker to achieve final concentration of 5-15% (w/v).
- Composite Bioink Preparation: Add sodium alginate (2-4% w/v final concentration) to the gelatin solution and mix at 37°C for 3 hours. Slowly incorporate the dECM solution into the alginate-gelatin mixture while stirring. Maintain at 37°C until printing to prevent gelation [12].
- Sterilization: Filter sterilize through 0.22 μm filters under aseptic conditions. Validate sterility by inoculating aliquots into bacterial culture media and monitoring turbidity [10].
Rheological and Printability Assessment
Characterizing the flow behavior and printing performance is essential for bioink optimization. Key assessments include:
- Rheological Testing: Using a rotational rheometer, measure viscosity versus shear rate to confirm shear-thinning behavior. Perform time sweeps to monitor storage (G') and loss (G") moduli during gelation. Bioinks should exhibit G' > G" after crosslinking, indicating solid-like behavior [9].
- Printability Tests:
- Filament Collapse Test: Print filaments across gaps of 1-16 mm and measure deflection angles. Smaller angles indicate better structural integrity [10].
- Fusion Test: Print grid structures with varying spacing between filaments to determine minimum printable feature size without pore closure [9].
- Shape Fidelity Assessment: Print multi-layered structures and compare actual dimensions to digital models using quantitative metrics like printability (Pr) value [9].
The following workflow diagram illustrates the key stages in bioink development and characterization:
Diagram 1: Bioink Development and Characterization Workflow. This diagram outlines the key stages in formulating, characterizing, and validating alginate-gelatin-dECM bioinks, from initial component selection through functional assessment of bioprinted constructs.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Bioink Development and Evaluation
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Base Biomaterials | Sodium alginate, Gelatin (Type A), dECM powders | Structural and bioactive components of bioink formulation |
| Crosslinking Agents | Calcium chloride (CaCl₂), Glutaraldehyde | Induce hydrogel formation and stabilize printed structures |
| Cell Culture Reagents | DMEM/F12, Fetal Bovine Serum, Penicillin-Streptomycin | Maintain cell viability during and after bioprinting process |
| Cell Viability Assays | Calcein-AM, Propidium Iodide, CCK-8 kit | Assess live/dead cell distribution and metabolic activity |
| Decellularization Agents | Triton X-100, Sodium dodecyl sulfate (SDS), DNase/RNase | Remove cellular material from native tissues to produce dECM |
| Characterization Tools | Rotational rheometer, Compression tester, Micro-CT | Evaluate mechanical properties, printability, and scaffold architecture |
Advanced Applications and Future Perspectives
Current Research Applications
Alginate-gelatin-dECM bioinks have demonstrated success across multiple tissue engineering applications. In vascular tissue engineering, researchers have developed self-supporting, multi-layered constructs using aorta-derived dECM combined with alginate-gelatin, achieving structural stability comparable to native blood vessels [13]. For skin tissue engineering, optimized formulations containing 15% gelatin crosslinked with 150 mM CaCl₂ supported the formation of bilayer skin models with homogeneous cell distribution and sustained viability over 14 days [10]. In cancer research, 3D breast tumor models fabricated with liver-derived dECM, gelatin, and alginate more accurately replicated the tumor microenvironment, enabling improved drug screening and study of metastasis mechanisms [12].
Emerging Trends and Future Directions
The field of bioink development is rapidly evolving, with several emerging trends poised to advance capabilities:
- Intelligent Process Control: Integration of AI-driven monitoring systems that use real-time imaging to detect print defects and automatically adjust parameters, improving reproducibility and reducing material waste [7].
- 4D Bioprinting: Development of bioinks that change shape or functionality over time in response to environmental stimuli, enabling creation of dynamic tissue models that better mimic physiological processes [8].
- Advanced Vascularization Strategies: Incorporation of sacrificial bioinks and angiogenic factors to create perfusable vascular networks within thick tissue constructs, addressing the critical challenge of nutrient and oxygen diffusion [8] [14].
- Multi-Material Bioprinting: Development of printing systems capable of depositing multiple bioinks with spatially controlled composition, enabling recreation of tissue interfaces and gradients found in native organs [14].
The following diagram illustrates the advanced crosslinking mechanisms that enhance bioink performance:
Diagram 2: Advanced Crosslinking Mechanisms for Bioinks. This diagram categorizes the primary crosslinking strategies used to stabilize alginate-gelatin-dECM bioinks, from physical methods to sophisticated dual-crosslinking approaches that combine multiple mechanisms.
As these technologies mature, alginate-gelatin-dECM bioinks are poised to become increasingly sophisticated, ultimately enabling the fabrication of complex tissue architectures that more faithfully replicate native tissue structure and function. This progress will accelerate drug development through more physiologically relevant in vitro models and advance the field toward clinically applicable tissue replacements.
The advancement of complex tissue architecture research is intrinsically linked to the development and refinement of 3D bioprinting technologies. Among the plethora of available methods, extrusion, inkjet, and laser-assisted bioprinting have emerged as the three cornerstone technologies, each offering a unique balance of strengths and limitations. This whitepaper provides an in-depth technical comparison of these core bioprinting modalities, detailing their working principles, operational parameters, and suitability for specific biomedical applications. For researchers and drug development professionals, understanding this "bioprinting trinity" is crucial for selecting the appropriate technology to fabricate physiologically relevant tissue models, thereby accelerating progress in regenerative medicine, drug screening, and disease modeling.
Three-dimensional (3D) bioprinting is an innovative additive manufacturing technology that revolutionizes the field of biomedical applications by combining engineering, manufacturing, and medicine [1]. This process involves the layer-by-layer deposition of bioinks—a combination of living cells, biomaterials, and bioactive molecules—to design and fabricate 3D tissue and organ models in situ for various in vivo and in vitro applications [1]. The transition from conventional 3D printing to bioprinting incorporates additional biological complexities, including material choice, cell types, and their growth and differentiation factors [1].
The global 3D bioprinting market, valued at approximately USD 1.3 billion in 2024 and projected to reach USD 2.8 billion by 2030, reflects the growing importance and adoption of this technology across research and clinical domains [15]. The field is driven by critical medical needs, including the severe global shortage of donor organs—with over 103,000 individuals on the national transplant waiting list in the U.S. alone—and the increasing demand for more predictive models in pharmaceutical development [16] [15]. For complex tissue architecture research, the fundamental challenge lies in replicating the intricate microenvironments, cell densities, and vascular networks of native tissues, a challenge that demands precise understanding and selection of available bioprinting technologies.
Core Bioprinting Technologies: A Technical Deep Dive
Extrusion-Based Bioprinting
Working Principle: Extrusion-based bioprinting (EBB) utilizes mechanical (piston or screw) or pneumatic pressure to force continuous filaments of bioink through a nozzle, depositing them layer-by-layer according to a digital design [17]. It is characterized by its ability to handle a wide range of material viscosities.
Key Characteristics:
- Bioink Viscosity: Handles high-viscosity materials (30-6×10⁷ mPa·s) [17].
- Cell Density: Supports higher cell densities, crucial for achieving physiologically relevant tissue constructs [17].
- Resolution: Typically ranges from 5 μm to hundreds of microns, influenced by nozzle diameter, pressure, and print speed [17].
- Speed: Generally has a lower printing speed compared to other methods, which can be a limitation for large-scale tissue fabrication [17].
Impact on Cells: The process subjects cells to substantial shear stress, which can compromise cell viability and affect cell adhesion, proliferation, morphology, and metabolic activity [18] [19]. In cancer research, shear stress has been shown to induce epithelial-to-mesenchymal transition, a hallmark of cancer metastasis, and alter gene expression [19].
Inkjet-Based Bioprinting
Working Principle: Inkjet bioprinting operates on a drop-on-demand principle, using thermal or acoustic forces to generate precisely controlled picoliter-sized droplets of bioink [20] [21]. The technology is known for its non-contact nature, which reduces risks of cross-contamination [21].
Key Characteristics:
- Bioink Viscosity: Limited to low-viscosity bioinks (3-12 mPa·s) to facilitate droplet formation [17].
- Cell Density: Constrained by the requirement for low-viscosity bioinks, limiting achievable cell concentrations [17].
- Resolution: Offers high printing accuracy, generating identical small droplets with high positional precision [21].
- Speed: Provides high printing speeds, making it suitable for applications requiring rapid patterning [20].
- Cost: Recognized as a low-cost bioprinting approach [21].
Impact on Cells: While shear stress is less pronounced than in extrusion-based methods, it can still occur during droplet formation and impact cell viability and function.
Laser-Assisted Bioprinting
Working Principle: Laser-assisted bioprinting (LAB) uses laser-induced forward transfer (LIFT) or related techniques, where a laser pulse is focused on a donor layer (often called a "ribbon") coated with bioink, generating a high-pressure bubble that propels a droplet of the bioink onto a substrate [16]. This is a nozzle-free approach.
Key Characteristics:
- Bioink Viscosity: Can handle a broad range of viscosities (1-300 mPa·s) [16].
- Cell Density: Enables high cell densities without compromising printability, as it is not limited by nozzle clogging.
- Resolution: Provides exceptional, sub-micron precision and high resolution, allowing for the fabrication of complex microarchitectures [16].
- Speed: Generally has a slower printing speed compared to other methods, particularly for larger constructs [16].
- Viability: Maintains high cell viability and function due to its gentle, nozzle-free process [16].
Impact on Cells: The primary cellular stressor in LAB is phototoxicity from the UV or near-UV laser, which can cause DNA damage and potentially lead to carcinogenesis [18] [19]. However, modern systems are optimized to minimize this risk.
Quantitative Technology Comparison
Table 1: Comparative Analysis of Core Bioprinting Technologies
| Parameter | Extrusion-Based | Inkjet-Based | Laser-Assisted |
|---|---|---|---|
| Working Principle | Pneumatic or mechanical extrusion | Thermal or acoustic droplet generation | Laser-induced forward transfer |
| Max Resolution | 5 - 500 μm [17] | < 1 picoliter droplet volume [20] | Sub-micron precision [16] |
| Bioink Viscosity | Very High (30 - 60,000,000 mPa·s) [17] | Low (3 - 12 mPa·s) [17] | Medium (1 - 300 mPa·s) [16] |
| Cell Density | High [17] | Low [17] | High [16] |
| Cell Viability | Lower (subject to high shear stress) [17] | >90% (with optimized parameters) [20] | High (>95%) [16] |
| Relative Speed | Medium | High (ten times faster than some techniques) [17] | Low [16] |
| Relative Cost | Medium | Low [21] | Very High [16] |
| Key Advantage | High structural integrity, multi-material printing | High speed, low cost, contactless printing [21] | Excellent resolution, high cell viability, no nozzle clogging [16] |
| Primary Limitation | Shear stress on cells, limited resolution | Low bioink viscosity constraints, potential nozzle clogging [17] | Phototoxicity risk, low throughput, high equipment cost [16] |
Table 2: Application Suitability for Tissue Engineering
| Application | Recommended Technology | Rationale |
|---|---|---|
| Vascular Grafts | Laser-Assisted or Inkjet | High resolution is critical for mimicking fine capillary networks [16]. |
| Dense Connective Tissues (Bone, Cartilage) | Extrusion-Based | Ability to handle high-viscosity, mechanically robust bioinks [17]. |
| High-Throughput Drug Screening | Inkjet-Based | Speed and low cost are advantageous for printing large numbers of uniform tissue models [20] [21]. |
| Volumetric Tissue Constructs | Advanced Extrusion (e.g., HITS-Bio) | High-throughput integrated systems can achieve physiologically relevant cell densities at scale [17]. |
| Multi-Cellular Co-cultures | Laser-Assisted | High precision allows for precise spatial arrangement of different cell types [16]. |
| Skin & Epithelial Tissues | Inkjet or Extrusion | Balances speed, resolution, and the ability to create stratified layers [15]. |
Advanced Experimental Protocol: High-Throughput Spheroid Bioprinting for Bone Regeneration
The following protocol details a cutting-edge application of extrusion bioprinting, HITS-Bio (High-throughput Integrated Tissue Fabrication System for Bioprinting), which addresses the critical challenge of achieving physiologically relevant cell densities in engineered tissues [17].
The diagram below illustrates the HITS-Bio workflow for calvarial bone regeneration, from spheroid preparation to in vivo implantation.
Detailed Methodology
Step 1: Spheroid Formation and Differentiation
- Cell Source: Isolate and expand human adipose-derived stem cells (hASCs) under standard culture conditions.
- Spheroid Generation: Use a low-adhesion U-bottom plate to promote self-assembly of hASCs into spheroids (approximately 500 μm diameter) via the hanging drop method or forced aggregation.
- Osteogenic Commitment: Transfer spheroids to osteogenic differentiation media. Implement combinatorial microRNA (miR) technology—specifically, transfection with osteo-inductive miRNAs (e.g., miR-26a)—to enhance and accelerate osteogenic differentiation prior to printing [17].
Step 2: HITS-Bio Bioprinting Process
- Equipment Setup: The HITS-Bio platform consists of a digitally-controlled nozzle array (DCNA), a high-precision XYZ linear stage, and an extrusion head for depositing a gel substrate. The system is assembled inside a biosafety hood [17].
- Bioink Preparation: Prepare a supportive, printable hydrogel bioink (e.g., a blend of Gelatin Methacryloyl (GelMA) and Hyaluronic Acid) to act as a scaffold for the spheroids. The bioink should be photo-crosslinkable.
- Spheroid Aspiration: Move the DCNA to the spheroid chamber suspended in culture medium. Apply controlled aspiration pressure to selectively open nozzles and pick up multiple spheroids simultaneously. The process is monitored via integrated bottom-view cameras [17].
- Substrate Deposition and Spheroid Placement: Using the extrusion head, deposit a thin layer of the bioink substrate onto the printing bed. Transfer the DCNA loaded with spheroids over the substrate. Gently bring the spheroids into contact with the bioink and cut off the aspiration pressure to deposit them with high positional precision. This multi-spheroid placement process is repeated to form the desired structure [17].
- Encapsulation and Crosslinking: After spheroid placement, deposit a final layer of bioink to envelop the structure. Photo-crosslink the entire construct using a 405 nm light-emitting diode (LED) light source for 60 seconds to stabilize the 3D architecture [17].
Step 3: In Vivo Implantation and Analysis
- Animal Model: Utilize a rat model with a critical-sized calvarial bone defect (e.g., ~5 mm diameter).
- Intraoperative Bioprinting (IOB): For direct in situ repair, the HITS-Bio system can be used intraoperatively to print the miR-transfected spheroids directly into the defect site, significantly reducing surgery time [17].
- Assessment: Monitor bone regeneration over 3-6 weeks using micro-CT imaging for volumetric analysis and histology (e.g., H&E, Masson's Trichrome staining) to evaluate new bone formation, tissue integration, and vascularization. This protocol has demonstrated near-complete defect closure (bone coverage area of ~91% at 3 weeks and ~96% at 6 weeks) [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Advanced 3D Bioprinting Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel bioink; provides a cell-adhesive, tunable 3D matrix. | Serves as the primary scaffold material in extrusion and light-based bioprinting [17] [19]. |
| Live/Dead Viability Kit (e.g., Calcein AM/EthD-1) | Fluorescent staining to quantify live (green) and dead (red) cells within a bioprinted construct. | Standard post-printing quality control to assess cell viability after the printing process [18] [19]. |
| Annexin-V / Propidium Iodide (PI) | Flow cytometry or imaging assays to differentiate between live, apoptotic (Annexin-V+/PI-), and necrotic (Annexin-V+/PI+) cells. | Detailed analysis of cell death pathways triggered by printing-induced stress [19]. |
| Cell Painting Kits (Phenotypic Dyes) | A multiplexed fluorescent staining kit targeting multiple organelles (nuclei, nucleoli, mitochondria, actin, Golgi, ER). | High-content screening to assess subtle printing-induced changes in cell morphology and phenotype in 3D cultures [19]. |
| Fluorescently Tagged Antibodies | Immunofluorescence staining for specific markers (e.g., Ki67 for proliferation, CD31 for endothelial cells). | Validation of cell identity, proliferation status, and functional maturation within bioprinted tissues [18] [19]. |
| hASCs (Human Adipose-Derived Stem Cells) | A multipotent cell source capable of differentiating into osteogenic, chondrogenic, and other lineages. | Ideal cell type for regenerative applications, as used in the HITS-Bio bone regeneration protocol [17]. |
| microRNA Transfection Reagents | Facilitate the introduction of osteo-inductive miRNAs (e.g., miR-26a) into cells to direct differentiation. | Used to pre-condition cells within spheroids before bioprinting to enhance tissue-specific outcomes [17]. |
Technology Selection Workflow for Research Applications
The following decision diagram provides a systematic approach for selecting the optimal bioprinting technology based on key research requirements.
The field of 3D bioprinting is rapidly evolving beyond the core technologies discussed here. Key emerging trends include 4D bioprinting, which incorporates smart materials that change shape or properties over time in response to stimuli, and the integration of artificial intelligence (AI) and machine learning to optimize print parameters, predict cell behavior, and enable real-time process control for enhanced reproducibility [20] [7] [16]. Furthermore, the convergence of bioprinting with organ-on-a-chip technology and the ongoing challenge of vascularizing bioprinted tissues represent critical frontiers for achieving truly functional, clinically relevant tissue constructs [20] [7].
In conclusion, the "bioprinting trinity" of extrusion, inkjet, and laser-assisted technologies provides a versatile toolkit for researchers aiming to engineer complex tissue architectures. The choice of technology is not a matter of identifying a universal best, but rather of strategically matching the unique characteristics of each method—be it the structural robustness of extrusion, the speed and affordability of inkjet, or the superb resolution of laser-assisted systems—to the specific requirements of the intended biological model and research goal. As these technologies continue to mature and converge with advances in materials science, AI, and stem cell biology, their collective impact on disease modeling, drug discovery, and regenerative medicine is poised to be transformative.
In tissue engineering and regenerative medicine, the concept of the native stem cell niche has emerged as a fundamental principle guiding the development of functional biological constructs. The niche represents a dynamic, complex microenvironment where stem cells reside, communicating with their surroundings to maintain homeostasis, respond to injury, and dictate tissue function [22]. Rather than being passive inhabitants, stem cells actively serve as architects of their own niches, generating and modifying their microenvironment to control their own destiny [22]. This intricate bidirectional communication between cells and their environment is essential for proper tissue development, maintenance, and repair.
The pursuit of 3D bioprinting for complex tissue architecture research hinges on recapitulating this sophisticated niche environment. Traditional two-dimensional (2D) cell culture systems fail to replicate the three-dimensional (3D) spatial organization, mechanical cues, and biochemical gradients that define native tissues [23]. As the field advances, the critical challenge lies not merely in arranging cells in three dimensions, but in reconstructing the full complexity of the native tissue niche—a goal that requires integration of multiple cell types, biochemical signaling factors, and precise physical and architectural cues [23] [24].
Deconstructing the Native Tissue Niche
The native tissue niche is a multimolecular engine that drives cellular turnover and tissue regeneration throughout an organism's lifetime. Understanding its components is essential for efforts to mimic it in engineered tissues.
Core Components of the Stem Cell Niche
Native tissues comprise multiple cell types residing within a complex, continuously changing 3D microenvironment consisting of numerous inputs that combine to drive collective tissue function [23]. The stem cell niche encompasses several key elements:
Extracellular Matrix (ECM): The basement membrane rich in ECM and stem cell growth factors provides structural support and biochemical signaling [22]. Cells themselves produce major ECM components, creating a feedback loop that controls their polarity, proliferation, and maintenance [22].
Cellular Constituents: Heterologous niche components include blood vessels, lymphatic capillaries, nerves, stromal, adipose, and various tissue-resident immune cells that function with stem cells to guard against tissue damage and pathogens [22].
Soluble Factors: Cytokines, neurotrophic factors, growth factors, and differentiation cues are constantly synthesized, secreted, transported, and depleted within the niche [24].
Dynamic Niche Communication Networks
Stem cells within their niches follow sophisticated paradigms for transitioning between quiescent and regenerative states [22]. These communication networks break down during aging, often involving deterioration of extrinsic niche components rather than the intrinsic self-renewal capacity of the stem cells themselves [22]. The spatial distribution of individual cells controls structure and function within a tissue, creating microenvironments where factors like oxygen tension vary and influence stem cell maintenance and differentiation [24].
Table 1: Key Components of the Native Tissue Niche and Their Functions
| Niche Component | Key Elements | Primary Functions |
|---|---|---|
| Extracellular Matrix | Collagen, laminin, fibronectin, proteoglycans | Structural support, mechanical signaling, biochemical cue presentation |
| Soluble Factors | Growth factors, cytokines, differentiation cues | Cell fate determination, proliferation control, migration signals |
| Cellular Elements | Immune cells, endothelial cells, stromal cells | Paracrine signaling, immune surveillance, vascular support |
| Physical Cues | Matrix stiffness, topography, interstitial flow | Mechanotransduction, differentiation guidance, migration control |
Technological Approaches to Niche Mimicry
3D Bioprinting Strategies
Three-dimensional bioprinting has emerged as a powerful tool for replicating the structure and function of real biological tissues, with applications in disease modeling, drug discovery, and implantable grafts [7]. The process typically involves:
Digital Model Creation: Tissues are digitized using medical imaging technologies (MRI, ultrasound) to generate a 3D model converted to Standard Triangle Language (STL) format [25].
Bioink Formulation: Living cells are combined with biocompatible materials and growth factors to create bioinks that emulate the target tissue [7] [25].
Layer-by-Layer Deposition: 2D layers of bioinks are deposited into a support bath to build a 3D structure using additive manufacturing techniques [7].
Tissue Maturation: Printed constructs are maintained in specialized bioreactors for maturation before use or study [25].
Recent advances have addressed significant limitations in conventional bioprinting approaches. A major drawback has been the lack of process control methods that limit defects in printed tissues [7]. New techniques incorporate intelligent monitoring systems that capture high-resolution images of tissues during printing and rapidly compare them to intended designs using AI-based image analysis pipelines [7].
Advanced Bioprinting Modalities
High-Throughput Spheroid Bioprinting
A novel technique developed at Penn State uses spheroids (clusters of cells) to create complex tissue with high cell density essential for developing functional tissue for clinical use [5]. The High-throughput Integrated Tissue Fabrication System for Bioprinting (HITS-Bio) employs a digitally controlled nozzle array that manipulates multiple spheroids simultaneously, organizing them in customized patterns to create complex tissue architecture [5]. This approach produces tissue 10-times faster than existing methods while maintaining more than 90% cell viability, enabling the creation of a one-cubic centimeter structure containing approximately 600 spheroids in less than 40 minutes [5].
Hybrid Bioprinting for Multi-Tissue Engineering
Hybrid bioprinting approaches address limitations in integrating soft and rigid multifunctional components for complex multi-tissue applications [6]. These platforms integrate multiple 3D printing modules under optimized conditions for continuous bioprinting with multiple soft and hard biomaterials [6]. Compared with commonly fabricated hydrogel-only constructs, hybrid constructs achieve over a 1000-fold increase in mechanical strength and demonstrate enhanced osteogenic differentiation, underscoring their suitability for load-bearing musculoskeletal and orthopedic tissue engineering [6].
Engineered Biomaterials for Niche Recapitulation
Decellularized ECM (dECM) Biomaterials
dECM biomaterials support specialized cell types and trigger innate regenerative processes by providing a microenvironment close to the native target tissue [23]. During decellularization, cells and immunogenic molecules are removed while structural proteins (collagen, elastin, fibronectin) and macromolecules (proteoglycans, GAGs) are preserved [23]. These biomaterials can be processed into various forms:
- Injectable Hydrogels (53% of dECM-particle biomaterials): Less invasive, adapt to irregular shapes, retain growth factors and bioactive signaling cues [23].
- Bioprinted Scaffolds (20%): Can be designed with layers of differential mechanical properties and tissue-specific cells to replicate varying characteristics of layered ECM structures [23].
- Electrospun Scaffolds (15%): Layered microfibers approximate ECM architecture, with controlled fiber diameter and distribution to induce cell-specific functions [23].
Engineered Peptide and Protein Materials
Engineered peptide and protein materials provide the advantages of a biological matrix with the control of a synthetic polymer [24]. These materials are designed at the molecular level to mimic critical aspects of the stem cell niche, combining predictable amino acid interactions with bioactive sequences. Common amino acid sequences employed to replicate the in vivo niche include cell-adhesive domains derived from:
- Collagen: DGEA, RGD
- Laminin: IKVAV, RGD, YIGSR
- Fibronectin: REDV, RGDS [24]
These designer materials allow researchers to isolate individual variables, such as stiffness, without varying others, such as the density of ligands for integrin binding [24]. This control enables systematic studies of how specific niche parameters influence cell behavior.
Table 2: Quantitative Comparison of Advanced Bioprinting Techniques
| Bioprinting Technique | Throughput/Speed | Cell Viability | Key Advantages | Representative Applications |
|---|---|---|---|---|
| High-Throughput Spheroid Bioprinting (HITS-Bio) | 10x faster than conventional methods | >90% | High cell density, scalable, precise spheroid placement | Cartilage tissue, bone repair |
| Hybrid Bioprinting | Varies by platform | High with optimized conditions | 1000x mechanical strength increase, multi-material integration | Load-bearing tissues, orthopedic engineering |
| Intelligent Bioprinting with AI Monitoring | Enhanced by reduced defects | Improved by defect correction | Real-time defect detection, adaptive parameter tuning | Complex tissue architectures, vascularized constructs |
Experimental Protocols for Niche Mimicry
Protocol: Modular Monitoring for Bioprinting Process Control
This protocol enables real-time quality control during bioprinting processes, addressing the critical need for process optimization in tissue engineering [7].
Materials:
- Standard 3D bioprinter
- Digital microscope (compact, high-resolution)
- AI-based image analysis pipeline
- Bio-inks (cells in soft gel)
- Support bath
Methodology:
- System Integration: Integrate the digital microscope into the bioprinting setup to capture high-resolution images during the printing process.
- Layer-by-Layer Imaging: Capture images of each deposited layer immediately after printing.
- AI-Pattern Analysis: Utilize the AI-based image analysis pipeline to rapidly compare captured images with the intended digital design.
- Defect Identification: Flag discrepancies such as over-deposition or under-deposition of bio-ink.
- Parameter Optimization: Use identified defects to refine printing parameters for different materials.
This modular, low-cost (less than $500) monitoring technique is printer-agnostic and can be readily implemented on any standard 3D bioprinter [7]. It serves as a foundation for intelligent process control in embedded bioprinting by enabling real-time inspection, adaptive correction, and automated parameter tuning [7].
Protocol: Decellularized ECM (dECM) Hydrogel Preparation
dECM hydrogels provide tissue-specific physical and chemical cues that promote the body's intrinsic capacity for self-repair and regeneration [23].
Materials:
- dECM particles (from target tissue)
- Pepsin solution
- Hydrochloric acid (HCl)
- Sodium hydroxide (NaOH)
- Phosphate-buffered saline (PBS)
- Collagen buffer (for collagen-containing tissues)
Methodology:
- Particle Suspension: Suspend dECM particles in a solution of pepsin and hydrochloric acid.
- Solubilization: Gently mix the suspension at 4°C without generating air bubbles until fully solubilized.
- pH Neutralization: Adjust the pH to physiological level (7.2-7.4) using NaOH and appropriate buffers.
- Gelation: Incubate at physiological temperature (37°C) to induce hydrogel formation.
- Cross-linking (Optional): Apply chemical or physical crosslinking to improve gelation kinetics and mechanical properties.
This methodology retains growth factors and bioactive signaling cues of native ECM while possessing high water content similar to natural tissue [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Tissue Niche Engineering
| Reagent Category | Specific Examples | Function in Niche Engineering |
|---|---|---|
| Structural Hydrogels | GelMA, ColMA, HAMA, Matrigel | Provide 3D scaffold mimicking native ECM, support cell growth and organization |
| Photoinitiators | LAP (lithium phenyl-2,4,6-trimethylbenzoylphosphinate) | Initiate polymerization reactions when exposed to light for structural integrity |
| Thermoplastics | PCL (polycaprolactone) | Provide biodegradable reinforcing structure for tissue-loading constructs |
| Bioink Modifiers | Reconstitution Agents A & P, Collagen Buffer | Adjust pH and isotonicity for cell culture compatibility |
| Engineered Peptides | IKVAV, RGD, YIGSR, DGEA | Reproduce specific cell-adhesive domains from native ECM proteins |
| Support Materials | CELLINK Start | Provide temporary support for complex structures and porous constructions |
Visualizing Experimental Workflows
Intelligent Bioprinting Workflow
Diagram 1: Intelligent bioprinting with AI feedback
Native Niche Component Integration
Diagram 2: Native niche component integration
The field of tissue engineering is progressively bridging the complexity gap between reductionist 2D in vitro cell culture and complex native in vivo tissues [23]. This intermediate complexity allows for producing realistic models and devices while maintaining control and interrogation capabilities not possible in native tissues [23]. Future advances will likely focus on developing materials with multiple layers of bi-directional feedback between cells and matrices, creating more advanced mimics of highly dynamic stem cell niches [24].
The path toward developing improved microsystems and material platforms will involve applying tools from systems biology to the analysis of tissue dynamics and structure—an intersection termed systems tissue engineering [23]. As these technologies mature, they hold the promise of producing truly functional engineered tissues that faithfully recapitulate the architectural and functional complexities of native human tissues, ultimately revolutionizing regenerative medicine, disease modeling, and drug development.
From Print to Function: Advanced Techniques and Real-World Applications
Three-dimensional (3D) bioprinting has made progressive impacts on medical sciences, demonstrating great potential to facilitate the fabrication of functional tissues for transplantation, disease modeling, and drug screening [17]. A significant limitation in the field has been the difficulty in achieving physiologically-relevant cell densities (100-500 million cells/mL) that are essential for effective tissue repair and regeneration [17]. While tissue spheroids—cellular aggregates that exhibit native-like cell density and extracellular matrix secretion—have emerged as promising building blocks for tissue fabrication, most existing bioprinting techniques have been constrained by low throughput, processing only one spheroid at a time and significantly prolonging the bioprinting process (approximately 20 seconds per spheroid) [17]. This review examines a transformative technological advancement known as HITS-Bio (High-throughput Integrated Tissue Fabrication System for Bioprinting), which addresses this long-standing problem through a multi-nozzle array approach that increases fabrication speed by an order of magnitude while maintaining high cell viability (>90%) [17].
Core Technology: The HITS-Bio Platform
System Architecture and Working Mechanism
The HITS-Bio platform represents a significant departure from conventional bioprinting systems through its implementation of a digitally-controlled nozzle array (DCNA) for simultaneous spheroid positioning [17]. The platform features three main components:
- Multi-nozzle DCNA: A digitally-controlled nozzle array that enables selective application of aspiration pressure to multiple nozzles simultaneously [17]
- High-precision XYZ linear stage: Provides 3-axis movement control for the DCNA assembly [17]
- Extrusion head: Deposits gel substrate to support the bioprinted spheroids [17]
The system is operated by custom-made software with a control algorithm and integrates three microscopic cameras for real-time visualization (isometric, bottom, and side views) to verify the precise position of the DCNA in 3D space [17]. This comprehensive visualization system enables quality control throughout the bioprinting process.
The HITS-Bio Bioprinting Process
The HITS-Bio process follows a meticulously optimized workflow:
Spheroid Aspiration: The DCNA moves to a Petri dish containing spheroids suspended in culture medium. Using controlled aspiration pressure through selectively opened nozzles, multiple spheroids are simultaneously lifted from the chamber [17].
Substrate Deposition: A bioink substrate is extruded onto the printing surface to receive the spheroids [17].
Spheroid Placement: The DCNA, loaded with spheroids, transfers over the substrate. When spheroids contact the substrate, aspiration pressure is terminated to deposit them precisely [17].
Encapsulation: After spheroid placement, an additional layer of bioink is deposited to envelop the spheroids, followed by photo-crosslinking using a 405 nm LED light source for 1 minute [17].
This streamlined process eliminates the need for viscous fluid support baths, instead operating within culture medium to simplify handling and avoid challenges associated with increased shear and compression forces [17].
Quantitative Performance Metrics
Comparative Bioprinting Performance
Table 1: Performance comparison of spheroid bioprinting technologies
| Technology | Throughput | Cell Viability | Positioning Precision | Key Limitations |
|---|---|---|---|---|
| HITS-Bio | Ten times faster than existing techniques | >90% | High (visualized by 3 cameras) | Limited by number of nozzles in array |
| Aspiration-Assisted Bioprinting (AAB) | ~20 seconds per spheroid | >90% | ~11% of spheroid size | Processes one spheroid at a time |
| Extrusion Bioprinting | Moderate (random mixing) | Lower due to shear stress | Limited control over placement | Substantial shear stress, limited placement control |
| Kenzan Method | Low | Damage from needle arrays | Fixed by needle arrangement | Low throughput, spheroid damage, restricted versatility |
| Droplet-Based Bioprinting | Moderate | Varies with viscosity | Limited precision | Constrained by bioink viscosity and droplet formation |
Fabrication Scale and Speed Metrics
Table 2: Quantitative output metrics demonstrated in validation studies
| Application | Construct Size | Spheroid Count | Fabrication Time | Outcomes |
|---|---|---|---|---|
| Cartilage Construct | 1 cm³ | ~600 spheroids | <40 minutes | High-throughput efficiency for volumetric defects |
| Calvarial Bone Regeneration | ~30 mm³ | Not specified | Not specified | Near-complete defect closure (91% bone coverage in 3 weeks, 96% in 6 weeks) |
The data demonstrates HITS-Bio's capacity for scalable tissue fabrication, achieving construction of clinically relevant tissue volumes in timeframes compatible with research and potential clinical applications [17].
Enabling Technologies: Spheroid Production and Quality Control
Advanced Spheroid Sorting Platforms
The success of high-throughput bioprinting depends on the availability of homogeneous, high-quality spheroids. Recent advancements in sorting platforms address this critical need:
- Fully Automated Sorting: Integrated systems now provide image acquisition, analysis, and individual spheroid transfer directly from culture plates in a single streamlined process [26]
- Deep Learning Classification: Machine learning algorithms enable label-free characterization of spheroids based on brightfield images, assessing viability and bioprinting compatibility without invasive fluorescent labels [26]
- Transfer Learning Efficacy: Effective model training even with limited spheroid image datasets enhances practicality for diverse research settings [26]
- High-Throughput Capacity: Systems demonstrated sorting of over 12,500 tri-cellular liver spheroids for a single 0.5 cm³ liver construct [26]
Spheroid Sorting Platform Specifications
Table 3: Technical specifications of automated spheroid sorting platforms
| Parameter | Specification | Application Benefit |
|---|---|---|
| Sorting Method | Individual spheroid picking and harvesting | Maintains spheroid integrity and enables selective quality control |
| Imaging Modality | Brightfield microscopy with deep learning analysis | Label-free viability assessment preserves spheroid physiology |
| Handling Precision | Capillary tube (250 μm ID) with automated linear stage | Gentle manipulation of 150 μm-diameter spheroids |
| Throughput | Optimized for thousands of spheroids per session | Supports fabrication of implant-scale tissue constructs |
| Compatibility | Standard biosafety cabinets and culture plates | Integrates with existing laboratory workflows |
Experimental Protocols and Methodologies
HITS-Bio Bioprinting Protocol
Objective: Precise spatial arrangement of multiple spheroids into defined tissue architectures using high-throughput bioprinting.
Materials:
- HITS-Bio platform with DCNA module
- Mature tissue spheroids (150-500 μm diameter)
- Compatible bioink (e.g., gelatin-based hydrogel)
- Cell culture medium
- Photoinitiator (if using light-crosslinkable bioinks)
- 405 nm LED light source
Procedure:
- Spheroid Preparation: Culture spheroids using preferred method (hanging drop, ultra-low attachment plates, or microfluidic devices) until desired maturity and size are achieved.
- System Calibration: Calibrate DCNA height and aspiration pressure settings using test spheroids to optimize pickup and release.
- Bioink Preparation: Prepare bioink according to manufacturer protocols, maintaining sterility throughout.
- Substrate Printing: Deposit a thin base layer of bioink onto the printing surface using the extrusion head.
- Spheroid Bioprinting:
- Program the desired spheroid arrangement pattern into the control software
- Execute simultaneous aspiration of multiple spheroids via DCNA
- Transfer spheroids to target positions and release via pressure cutoff
- Repeat until complete design is deposited
- Encapsulation: Overlay with additional bioink to fully embed spheroids.
- Crosslinking: Initiate hydrogel crosslinking via appropriate method (photo-crosslinking for 1 minute with 405 nm LED for light-sensitive bioinks).
- Culture: Transfer constructs to appropriate culture conditions for maturation.
Technical Notes:
- Optimal spheroid size depends on nozzle diameter; adjust accordingly
- Aspiration pressure must balance reliable pickup with avoidance of spheroid damage
- Bioink rheology should support spheroid suspension without imposing excessive shear stress
Automated Spheroid Sorting Protocol
Objective: Selection of uniform, high-quality spheroids for bioprinting applications using label-free morphological analysis.
Materials:
- SpheroidSorter platform or equivalent
- Spheroid populations in standard culture plates
- Sterile capillary tubes (250 μm ID)
- Collection reservoirs for sorted spheroids
Procedure:
- System Setup: Initialize sorting platform according to manufacturer specifications.
- Dataset Preparation: Acquire representative brightfield images of spheroids for training classification model.
- Model Training: Implement deep learning algorithm to classify spheroids based on size, circularity, and morphological features predictive of viability.
- Sorting Parameters: Define acceptance criteria based on classification output.
- Automated Sorting: Execute sorting process:
- Platform images each spheroid in culture plate
- Classification algorithm assesses each spheroid against criteria
- Acceptable spheroids remain in plate for harvesting
- Unacceptable spheroids are removed via picking system
- Quality Control: Validate sorted population homogeneity through random sampling.
Technical Notes:
- Transfer learning approaches reduce required training dataset size
- Platform compatibility with standard culture plates facilitates workflow integration
- Sorting criteria should be validated against biological outcomes for specific applications
Research Reagent Solutions
Table 4: Essential materials for high-throughput spheroid bioprinting
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Digitally-Controlled Nozzle Array (DCNA) | Simultaneous aspiration and deposition of multiple spheroids | Core component of HITS-Bio; nozzle count determines throughput multiplier |
| Tri-cellular Liver Spheroids | Physiological liver tissue modeling | Demonstrates platform capability with complex multi-cellular systems |
| Photo-crosslinkable Bioinks | Structural support for bioprinted spheroids | Must balance printability with cell compatibility; 405 nm crosslinking typical |
| Deep Learning Classification Software | Label-free spheroid quality assessment | Enables sorting based on viability and morphology without fluorescent markers |
| MicroRNA-Transfected Spheroids | Enhanced osteogenic differentiation capability | Enables intraoperative bioprinting for bone regeneration applications |
| Automated Spheroid Sorting Platform | High-throughput selection of uniform spheroids | Critical for ensuring population homogeneity before bioprinting |
Application Case Studies
Intraoperative Bioprinting for Bone Regeneration
A compelling application of HITS-Bio technology is in intraoperative bioprinting (IOB) for calvarial bone regeneration [17]. The approach combines several advanced technologies:
- Osteogenically-Committed Spheroids: Human adipose-derived stem cell spheroids transfected with combinatorial microRNA technology to enhance osteogenic differentiation [17]
- On-Demand Fabrication: HITS-Bio enables simultaneous or sequential aspiration and bioprinting of miR-transfected spheroins directly at the surgical site [17]
- Rapid Regeneration: In a rat model, this approach achieved near-complete defect closure with approximately 91% bone coverage area in 3 weeks and 96% in 6 weeks, representing approximately 30 mm³ of regenerated bone [17]
This application highlights the clinical potential of high-throughput spheroid bioprinting to reduce surgical time while improving outcomes through precise, biologically-active tissue fabrication.
Scalable Cartilage Construction
The utility of HITS-Bio for fabricating larger tissue volumes was demonstrated through creation of cm³-scale cartilage constructs [17]:
- High-Throughput Efficiency: Each construct containing approximately 600 chondrogenically committed spheroids was assembled in under 40 minutes [17]
- Volumetric Defect Repair: The scale and composition of these constructs indicates potential for addressing clinically relevant cartilage defects [17]
- Architectural Precision: The multi-nozzle array enables precise spatial organization of spheroids, critical for functional tissue outcomes [17]
The development of high-throughput bioprinting systems represents a paradigm shift in tissue engineering, directly addressing the critical bottleneck of fabrication speed that has limited clinical translation. The HITS-Bio platform, with its multi-nozzle DCNA technology, demonstrates that order-of-magnitude improvements in throughput are achievable while maintaining cell viability and positional precision. When integrated with complementary advances in automated spheroid sorting and deep learning quality control, these systems enable fabrication of tissue constructs at scales relevant for clinical application.
Future developments will likely focus on increasing nozzle density in DCNA systems, enhancing bioink formulations to better support spheroid fusion and maturation, and integrating real-time monitoring systems for closed-loop process control. As these technologies mature, high-throughput spheroid bioprinting holds potential not only to accelerate research in drug screening and disease modeling but also to enable clinical applications in intraoperative tissue fabrication and ultimately organ-scale engineering.
Within the field of 3D bioprinting for complex tissue architecture research, the transition from a manual, artisanal process to a reproducible, automated manufacturing discipline hinges on the integration of intelligent process control. The inherent complexity of biological materials, combined with the architectural intricacy required to mimic native tissues, makes traditional open-loop bioprinting susceptible to inconsistencies and structural defects. These flaws, such as over- or under-extrusion, can compromise the structural fidelity and subsequent biological function of the engineered construct [27]. The incorporation of artificial intelligence (AI) and machine learning (ML) for real-time process monitoring and defect detection represents a paradigm shift, enabling the transition to closed-loop control systems. This intelligent integration is critical for ensuring the inter-tissue reproducibility, structural integrity, and ultimately, the clinical translation of bioprinted tissues for applications in disease modeling, drug discovery, and regenerative medicine [7] [28]. This technical guide details the methodologies, algorithms, and experimental protocols that underpin AI-driven quality assurance in advanced bioprinting workflows.
AI-Driven In Situ Monitoring Platforms
The foundation of any intelligent control system is robust data acquisition. In the context of 3D bioprinting, this is achieved through in situ monitoring platforms that capture the printing process as it unfolds.
Modular Sensing Architecture
A primary advancement is the development of modular, low-cost, and printer-agnostic sensing platforms. These systems typically integrate a compact digital microscope or camera system positioned to capture high-resolution images of the print nozzle or the recently deposited layer [27] [7]. The modularity ensures that the system can be readily implemented across a range of existing bioprinting setups without requiring extensive custom engineering. The cost-effectiveness of such platforms (reported at less than $500 [7]) is a significant factor in promoting their widespread adoption within research laboratories.
Data Acquisition and Pre-processing
The sensing architecture captures 2D images in real-time during the bioprinting process. A key finding is that these 2D in situ images provide reliable approximations of 3D filament geometries, allowing for a simplified yet effective analysis of the print outcome [27]. Prior to analysis, images typically undergo pre-processing steps to enhance quality, which may include:
- Noise reduction: Applying filters to minimize visual noise.
- Contrast enhancement: Improving the distinction between the printed filament and the background or support bath.
- Image stabilization: Correcting for minor vibrations or stage movements.
Table 1: Quantitative Performance of an AI-Based Monitoring Platform
| Metric | Reported Performance | Context/Application |
|---|---|---|
| Cost of Monitoring Platform | < $500 | Modular, printer-agnostic system [7] |
| Prediction Accuracy for Vascular Tissue Engineering | > 94% | Using Artificial Neural Networks (ANNs) with >30 variables [28] |
| Key Identified Parameter | Filament Diameter | Sensitive indicator of pressure-related effects [27] |
| Critical Function | Identification of Velocity Thresholds | Determines printing stability for different bioinks [27] |
AI and ML Algorithms for Defect Detection and Image Analysis
The image data acquired from in situ monitoring is processed using sophisticated AI and ML models to identify defects and quantify print quality.
Vision Transformer Model for Image Segmentation
A leading approach for defect detection utilizes a vision transformer model for image segmentation [27]. This deep learning architecture is particularly adept at understanding global contexts within an image, making it highly effective for precisely delineating the boundaries of printed filaments. The segmentation process converts the raw image into a structured map where each pixel is classified as either part of the filament or the background, enabling precise, layer-by-layer evaluation of the printed construct.
Unsupervised Deep Learning for Tissue Architecture Mapping
For more complex analyses that go beyond simple geometry, unsupervised deep learning methods like UTAG (Unsupervised discovery of tissue architecture with graphs) can be employed. UTAG converts cellular phenotypes from images into a numeric feature matrix and constructs a graph of physical cellular interactions based on spatial location [29]. This combined data structure allows clustering algorithms to group phenotypically and spatially related cells into tissue domains without prior knowledge, providing a powerful tool for assessing the micro-architectural fidelity of bioprinted tissues.
The following diagram illustrates the workflow for AI-driven defect detection in bioprinting.
Experimental Protocols for AI Integration in Bioprinting
The successful implementation of an AI-driven monitoring and control system requires a structured experimental protocol. The following provides a detailed methodology for establishing and validating such a system.
Protocol: Establishing a Closed-Loop AI Monitoring System for Embedded Bioprinting
Objective: To integrate a modular AI-based monitoring platform for real-time defect detection and print quality assessment of acellular and cellular bioinks in an embedded bioprinting workflow.
Materials and Equipment:
- 3D Bioprinter (extrusion-based)
- Modular digital microscope/camera system
- Computing unit with GPU for model inference
- Bioinks (e.g., alginate, gelatin methacryloyl (GelMA), cellular bioinks)
- Support bath (if using embedded printing)
Methodology:
- System Integration and Calibration:
- Mount the digital microscope to the bioprinter gantry or a fixed position with a clear view of the print zone.
- Establish a communication link between the camera and the computing unit.
- Calibrate the image scale (pixels to micrometers) using a reference object printed under identical conditions.
Reference Data Collection and Model Training:
- Print a series of calibration structures (e.g., simple grids, lines) while systematically varying key process parameters (e.g., pressure, print velocity, nozzle diameter).
- For each print, capture in situ images and perform post-print metrology to measure actual filament diameters and identify defects. This creates a labeled dataset.
- Train the vision transformer or other chosen segmentation model on this dataset to learn the relationship between image features and print quality metrics.
Validation and Threshold Determination:
- Use the trained model to analyze new prints of complex structures.
- Quantify the relationship between input parameters and output quality. For instance, establish the correlation between pressure and filament diameter and identify the critical velocity thresholds beyond which printing stability is lost for each bioink [27].
- Define acceptance criteria for print quality based on the divergence between the printed image and the intended digital design.
Closed-Loop Integration (Forward-Looking):
- Develop a control algorithm that can adjust print parameters (e.g., pressure) in response to the real-time quality assessment.
- For example, if the system detects a consistent under-extrusion, the control logic can be programmed to incrementally increase the pressure until the filament diameter returns to the target range.
Expected Outcomes:
- A functional in situ monitoring system capable of layer-by-layer image acquisition.
- A trained AI model that can segment printing images and detect common defects with high accuracy.
- A dataset linking process parameters to print quality, enabling rapid optimization for new bioinks.
Optimization of Process Parameters via AI
The data generated by AI monitoring is not merely for defect detection; it is the fuel for intelligent process optimization. Machine learning algorithms can analyze the vast parameter space of bioprinting to identify optimal printing conditions.
Predictive Modeling for Parameter Selection
Predictive models, particularly Artificial Neural Networks (ANNs) and decision trees, are used to forecast the behavior of cells and bioinks under various stimuli in a virtual environment [28]. For example, ANNs with more than 30 input variables have been used to accurately predict the outcomes of vascular tissue engineering strategies with over 94% accuracy [28]. These models learn from experimental data to predict how changes in parameters like pressure, velocity, and bioink composition will affect the final construct's properties, drastically reducing the number of iterative experiments needed.
AI-Driven Biomaterial and Bioink Optimization
The selection and optimization of biomaterials themselves can be accelerated by AI. ML algorithms can analyze large datasets of polymer properties, synthesis methods, and biological outcomes to predict the performance of new composite biomaterials [28]. This approach helps in refining bioink properties such as viscosity, shear-thinning behavior, and cross-linking density to ensure optimal printability and biological function.
The workflow for this AI-driven optimization is captured in the diagram below.
Table 2: Key AI/ML Models and Their Applications in Intelligent Bioprinting
| AI/ML Model | Primary Application in Bioprinting | Key Advantage |
|---|---|---|
| Vision Transformer | Image segmentation for defect detection [27] | Captures global context for precise filament boundary identification |
| Artificial Neural Networks (ANNs) | Predictive modeling of tissue growth and optimization of process parameters [28] | High accuracy in modeling complex, non-linear relationships from large datasets |
| Decision Trees | Optimization of tissue engineering designs [28] | Provides interpretable, rule-based insights into parameter importance |
| Unsupervised Learning (e.g., UTAG) | Mapping of tissue architecture in printed constructs [29] | Identifies patterns and micro-anatomical domains without pre-labeled data |
The Scientist's Toolkit: Essential Research Reagents and Materials
The implementation of the protocols and systems described above relies on a suite of essential research reagents and hardware solutions.
Table 3: Research Reagent Solutions for AI-Enhanced Bioprinting
| Item | Function | Example Use-Case |
|---|---|---|
| Modular Digital Microscope | Captures high-resolution, in-situ images during the printing process. | Core component of the low-cost, printer-agnostic monitoring platform [27] [7]. |
| GPU-Accelerated Computing Unit | Provides the computational power for training and running deep learning models (e.g., Vision Transformers). | Essential for real-time image analysis and defect detection [27]. |
| Acellular Hydrogel Bioinks | Used for initial system calibration and establishing print parameter-defect relationships. | Alginate or GelMA used to demonstrate pressure-related effects on filament diameter [27]. |
| Cellular Bioinks | Contains living cells to fabricate biological constructs; requires optimized parameters for cell viability. | Used to identify critical velocity thresholds that maintain printing stability and cell health [27]. |
| Support Bath | A hydrogel medium that enables embedded 3D bioprinting of complex, freeform structures. | Provides a suspension medium for the bioink during printing, allowing in situ imaging of the process [27]. |
The integration of AI and ML for process control and defect detection marks a critical evolution in 3D bioprinting, elevating it from a prototyping tool to a reliable manufacturing platform for complex tissue architecture research. The synergy of modular in situ monitoring, robust AI-driven image analysis, and predictive modeling creates a powerful framework for ensuring quality and reproducibility. By providing detailed experimental protocols and highlighting essential tools, this guide aims to empower researchers to implement these intelligent systems in their own laboratories. As these technologies mature, the path will be paved for fully adaptive, closed-loop bioprinting systems capable of self-correction and the robust fabrication of functional, clinically relevant tissues.
Within the field of 3D bioprinting for complex tissue architecture, the inability to create perfusable, hierarchical vascular networks remains a primary barrier to engineering clinically relevant, thick tissues. The diffusion limit of oxygen and nutrients, typically 100–200 micrometers, constrains the survival of cells in the core of engineered constructs, leading to necrotic regions and functional failure [30] [31]. Overcoming this "vascular challenge" is a critical milestone for the advancement of tissue engineering, regenerative medicine, and physiologically relevant drug screening models.
This technical guide delineates the core strategies being deployed to engineer perfusable vascular networks, with a focus on bioprinting methodologies. We delve into the specific technical details of sacrificial and direct printing techniques, provide quantitative data on material properties and performance, and outline detailed experimental protocols. The objective is to provide researchers and drug development professionals with a foundational toolkit for integrating functional vasculature into their 3D bioprinted tissues.
Core Bioprinting Strategies for Vascularization
Two overarching paradigms have emerged for creating vascular networks: those that use a temporary, sacrificial template to define channel geometry, and those that directly fabricate tubular structures.
Sacrificial Bioprinting
Sacrificial bioprinting involves the deposition of a "fugitive" or sacrificial ink into a surrounding cell-laden hydrogel matrix. After the matrix is solidified, the sacrificial ink is removed via liquefaction or dissolution, leaving behind a hollow, perfusable channel. These channels can subsequently be lined with endothelial cells to create a biomimetic vessel lining [32] [30].
- Materials: A common sacrificial ink is Pluronic F-127, a thermoreversible block copolymer that is liquid when cold and solid at room temperature. Its concentration can be optimized (e.g., 40% w/v) for printability and structural stability [33]. Gelatin is another popular choice, which can be liquefied by raising the temperature above its melting point [34].
- Process: The fugitive ink is printed into a support bath or a cast hydrogel. For instance, a suspension bath of GelMA microspheres can be used, which is later crosslinked with UV light. The printed Pluronic F-127 structure is then liquefied and evacuated by cooling, leaving a patent microchannel network [33] [30].
- Advantages: This method offers high design flexibility, allowing for the creation of complex, branching, and hierarchical networks that closely mimic in vivo vasculature [32].
Direct Bioprinting
Direct bioprinting techniques aim to fabricate hollow, tubular structures in a single, continuous process, eliminating the need for sacrificial material removal.
- Coaxial Extrusion: This technique employs concentric nozzles to extrude a tubular filament directly. Typically, a crosslinking agent (e.g., CaCl₂ solution) flows through the inner core, while a cell-laden bioink (e.g., a blend of GelMA, alginate, and PEGTA) flows through the outer shell. The bioink undergoes immediate ionic crosslinking upon contact with the core fluid, forming a stable hollow tube upon deposition [32] [35].
- Embedded Printing: In this approach, a bioink is extruded directly into a support bath that possesses yield-stress properties. The bath provides temporary mechanical support, preventing the collapse of the printed structure during the fabrication process. This enables the creation of complex and fragile vascular architectures that would not be possible in air [32] [36].
The following diagram illustrates the logical workflow and key decision points for selecting and implementing these core vascularization strategies.
Quantitative Analysis of Materials and Methods
The success of vascularization strategies is highly dependent on the properties of the biomaterials, or bioinks, used. The tables below summarize key quantitative data from recent research.
Table 1: Comparison of Bioink Formulations for Vascular Bioprinting
| Bioink Composition | Crosslinking Mechanism | Key Functional Properties | Reported Cell Viability/Response | Reference |
|---|---|---|---|---|
| GelMA (8% w/v) | UV Photocrosslinking | Porosity: High; Diffusion Coefficient (FITC-dextran): Tunable based on MW | Supported co-culture of Neuroblastoma cells, hMSCs, and HUVECs; Endothelial layer formation in 14 days | [33] |
| GelMA-Alginate-PEGTA Blend | Ionic (Ca²⁺) + UV Photocrosslinking | Mechanical strength: Tunable with PEGTA concentration (1-3%) | Supported spreading and proliferation of encapsulated endothelial and stem cells | [35] |
| Pluronic F-127 (40% w/v) | Sacrificial (Thermoreversible) | Printability: Stable pillar formation; suitable for fugitive ink | N/A (Sacrificial material, removed post-printing) | [33] |
Table 2: Performance Metrics of Vascularized Constructs
| Construct Description | Vascular Channel Diameter | Perfusion Capability | Culture Duration & Key Outcome | Reference |
|---|---|---|---|---|
| Vascularized Neuroblastoma Model | Not Specified | Yes, with customized perfusion system | Up to 3 weeks; Proof of endothelial layer formation and cancer cell migration | [33] |
| Directly Printed Perfusable Hollow Tube | Tunable via coaxial nozzle geometry | Yes, immediately after printing | Sustained cell viability and biological function post-printing | [35] |
| SINP Construct (GelMA Microspheres) | Created by sacrificial writing | Yes, promotes nutrient diffusion | Enhanced cell infiltration and viability in vivo; Improved vascularized adipose tissue formation | [30] |
Detailed Experimental Protocols
Protocol: Sacrificial Bioprinting with Pluronic F-127
This protocol is adapted from studies on creating vascularized cancer niche models [33].
Materials:
- Bioink (Cell-laden matrix): 8% (w/v) Gelatin Methacryloyl (GelMA) with 0.5% (w/v) photoinitiator (Irgacure 2959) in 1x PBS.
- Sacrificial Ink: 40% (w/v) Pluronic F-127 in cold (4°C) 1x PBS.
- Cells: Relevant cell types (e.g., HUVECs, mesenchymal stem cells, tissue-specific cells).
- Bioprinter: Extrusion-based bioprinter capable of multi-material printing and temperature control.
Method:
- Bioink Preparation: Synthesize GelMA and dissolve in PBS with photoinitiator. Sterilize and mix with cells at the desired density. Keep at 37°C until printing.
- Sacrificial Ink Preparation: Dissolve Pluronic F-127 powder in cold PBS (4°C) to achieve a 40% w/v solution. Intermittent vortexing may be necessary.
- Printing Process: Load the bioink and sacrificial ink into separate printing cartridges.
- Use a multi-material printing approach, depositing the Pluronic F-127 ink in the desired vascular network pattern.
- Simultaneously or subsequently, encapsulate the sacrificial pattern within the cell-laden GelMA bioink.
- Post-Printing Crosslinking: Expose the entire construct to UV light (e.g., 365 nm) to photocrosslink the GelMA matrix.
- Sacrificial Ink Removal: Culture the construct in a perfusion system at a temperature below the gelation point of Pluronic F-127 (e.g., 4°C) to liquefy and flush out the sacrificial ink, leaving behind hollow, perfusable channels.
- Endothelialization: Perfuse endothelial cells (e.g., HUVECs) through the channels and culture under flow to facilitate their adhesion and formation of a confluent endothelium.
Protocol: Direct Bioprinting via Coaxial Extrusion
This protocol is based on methods for directly printing perfusable vascular constructs [35].
Materials:
- Blend Bioink: 7% (w/v) GelMA, 3% (w/v) Sodium Alginate, and 2% (w/v) 4-arm PEGTA, dissolved in de-ionized water with 0.25% (w/v) photoinitiator and 10% (v/v) FBS.
- Crosslinking Core Solution: 0.3 M Calcium Chloride (CaCl₂) in 10% (v/v) FBS solution.
- Cells: Endothelial cells and/or mesenchymal stem cells.
- Bioprinter: Extrusion system equipped with a custom multilayered coaxial nozzle.
Method:
- Bioink Preparation: Prepare the sterile blend bioink and encapsulate cells at the desired density. Maintain at 37°C.
- Printer Setup: Configure the coaxial nozzle. The core solution (CaCl₂) is fed through the innermost channel, and the cell-laden blend bioink is fed through the outer channel.
- Printing Process: Extrude the bioink and core solution simultaneously.
- Upon contact, the alginate in the bioink undergoes immediate ionic crosslinking with calcium ions, forming a stable hollow filament at the point of deposition.
- Precisely control the deposition to create 3D tubular structures.
- Secondary Crosslinking: After printing, expose the construct to UV light to covalently photocrosslink the GelMA and PEGTA components, permanently fixing the structure and enhancing its mechanical strength.
- Perfusion Culture: Transfer the bioprinted tubular construct to a bioreactor for perfusion culture, applying physiological flow rates to mature the endothelium and promote tissue development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Vascularization Experiments
| Reagent / Material | Function | Example Application |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel providing cell-adhesive motifs and tunable mechanical properties. | Primary matrix for encapsulating parenchymal and stromal cells. [33] [35] |
| Pluronic F-127 | Thermoreversible sacrificial polymer used to create hollow channel templates. | Fugitive ink for defining the architecture of perfusable networks. [33] |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary endothelial cells used to form the inner lining of blood vessels. | Seeding into channels to create a biomimetic, non-thrombogenic endothelium. [33] [30] |
| Sodium Alginate | Polysaccharide used for rapid ionic crosslinking, providing initial structural integrity. | Component of blend bioinks for direct coaxial bioprinting. [35] |
| Vascular Endothelial Growth Factor (VEGF) | Key signaling protein that stimulates angiogenesis and endothelial cell survival. | Supplementation in culture media to promote vascular network formation and stability. [37] [31] |
| Poly(ethylene glycol)-tetra-acrylate (PEGTA) | Synthetic polymer used to enhance the mechanical strength and crosslinking density of bioinks. | Modifying the mechanical properties of natural polymer-based bioinks (e.g., GelMA). [35] |
The strategies outlined herein—sacrificial and direct bioprinting—represent the forefront of efforts to solve the vascularization challenge in 3D bioprinting. The quantitative data and detailed protocols provide a roadmap for researchers to implement these techniques. The choice of strategy and materials must be guided by the specific requirements of the target tissue, including its architectural complexity, mechanical environment, and biological function.
Future progress will hinge on the development of more advanced bioinks that seamlessly combine printability, mechanical robustness, and full biological functionality. Furthermore, the integration of these engineered vascular networks with host circulation upon implantation remains a critical area of investigation. By systematically applying and refining these strategies, the goal of creating complex, fully functional, and clinically viable tissues draws closer to reality.
The field of 3D bioprinting has rapidly evolved from a novel fabrication technique to a disruptive technology capable of constructing complex, living tissue architectures. This advancement is pivotal for research on complex tissue architectures, as it enables the creation of in vitro models that closely mimic the in vivo microenvironment. Unlike traditional 2D cell cultures, 3D-bioprinted constructs incorporate cells, extracellular matrix (ECM), and biomolecules in a spatially controlled manner, offering a more physiologically relevant platform for biomedical applications [38] [39]. Within the context of a broader thesis on complex tissue architecture, this whitepaper details the transformative impact of 3D bioprinting across three critical domains: drug screening, disease modeling, and surgical repair. By providing precise control over the mechanical properties, composition, and spatial arrangement of tissues, 3D bioprinting is bridging the long-standing gap between animal models and human clinical trials, leading to more predictive, ethical, and personalized solutions in healthcare [14] [40].
3D Bioprinting in Drug Screening and Development
The pharmaceutical industry faces significant challenges, with over 90% of drug candidates failing during clinical trials, often due to insufficient efficacy or safety concerns that were not predicted by existing preclinical models [38] [39]. A primary reason for this high failure rate is the heavy reliance on traditional 2D cell cultures and animal models, which poorly recapitulate human physiology and suffer from interspecies differences [38]. 3D bioprinting addresses this translational gap by enabling the fabrication of biomimetic human tissue models that are one step closer to native human tissues, thereby producing more reliable and clinically relevant data [38].
Engineered Tissues for Toxicity and Efficacy Testing
Bioprinted tissue constructs are increasingly being used for toxicology and drug efficacy studies, providing pharmacokinetic, pharmacodynamic, and toxicity information in a human-specific context [40]. These models allow researchers to study the biochemical, genetic, and histological consequences of specific drugs.
Cardiac Tissue Models: A prominent example is the bioprinting of 3D contractile cardiac tissues. In one approach, rat primary cardiomyocytes encapsulated in a fibrin-based bioink were bioprinted to create constructs that exhibited spontaneous and synchronous contractions [40]. These tissues were used to test physiological responses to known cardiotoxic drugs; exposure to 200 nM epinephrine increased the beating frequency from 80 to 110 beats per minute, while 10 μM carbachol decreased it to 40 beats per minute [40]. More advanced endothelialized myocardial tissues have also been developed by co-printing human umbilical vein endothelial cells (HUVECs) with cardiomyocytes in an alginate/GelMA blend bioink. When this model was integrated into a microfluidic bioreactor and exposed to the anti-cancer drug doxorubicin, it showed a time- and dose-dependent decrease in the beating rate of cardiomyocytes and a simultaneous reduction in the secretion of von Willebrand factor (vWF) by the HUVECs, demonstrating its utility in evaluating complex drug-induced toxicity [40].
Other Tissue Models: Similar efforts are underway for other organs. For instance, renal constructs bioprinted using kidney-derived decellularized extracellular matrix (dECM) bioinks have been shown to exhibit physiologically relevant features of native renal tissue, making them promising for nephrotoxicity screening [40].
High-Throughput Capabilities
A significant advantage of 3D bioprinting for pharmaceutical research is its scalability. By incorporating 3D-bioprinted entities within multi-well plates, it becomes feasible to conduct medium- and even high-throughput drug screening, allowing for the rapid testing of compound libraries on highly biomimetic tissue models [38].
Table 1: Quantitative Impact of 3D Bioprinting in Drug Discovery
| Metric | Traditional Model Performance | Impact of 3D Bioprinted Models |
|---|---|---|
| Clinical Trial Failure Rate | >90% for drugs entering clinical phases [38] | Aims to reduce failure by improving preclinical prediction [38] |
| Preclinical Testing Cost | Contributes to high R&D investment (e.g., $133B invested by top pharma in 2021) [38] | Reduces cost of preclinical trials by half by potentially eliminating animal testing [15] |
| Model Predictive Value | Low, due to interspecies differences and lack of human physiology in 2D models [38] | High, due to ability to closely mimic human in vivo microenvironment [38] [39] |
Advancing Disease Modeling with 3D Architectures
3D bioprinting enables the reconstruction of not just healthy tissues but also diseased states, providing powerful platforms for studying disease mechanisms and progression. The technology allows for the incorporation of patient-specific cells, the precise design of pathological tissue architectures, and the inclusion of key elements like vasculature, which are often hallmarks of disease [40] [41].
Fabricating Biomimetic Tissue and Disease Models
The process of creating a 3D-bioprinted disease model is multi-staged and requires careful optimization at each step to ensure biological relevance.
Pre-bioprinting Stage: This critical first step involves designing the digital 3D model of the desired tissue structure, typically using Computer-Aided Design (CAD) software or data from medical imaging like CT or MRI scans [14]. The selection of bioink is equally crucial, as it must provide structural support and the necessary biological cues for cell survival and function [14] [40].
Bioprinting Stage: Different bioprinting modalities are selected based on the requirements of the model. Common technologies include:
- Extrusion-based Bioprinting: Uses mechanical or pneumatic forces to dispense continuous filaments of bioink. It is the most common method, suitable for high-viscosity bioinks, but has lower resolution and printing speed [40] [41].
- Inkjet Bioprinting: Employs thermal, piezo, or acoustic forces to deposit bioink droplets. It offers faster fabrication speeds but requires low-viscosity bioinks and achieves lower cell densities [40].
- Laser-assisted Bioprinting: A nozzle-free technique that uses laser pulses to transfer bioink. It allows for the deposition of highly viscous bioinks but can have lower cell survival rates [40].
- Stereolithographic (SLA) Bioprinting: Utilizes patterns of light to photopolymerize photosensitive polymers layer-by-layer. It offers high resolution, rapid fabrication, and high cell viability [40].
Post-bioprinting Stage: The printed structures are often matured in bioreactors that provide biochemical and mechanical stimuli to promote tissue development and functionality. This stage includes incubation to provide stability and promote tissue growth, alongside mechanical testing to assess the construct's integrity [14].
Experimental Workflow for a Bioprinted Tissue Model
The following diagram visualizes the comprehensive workflow involved in creating and validating a 3D-bioprinted tissue model for disease modeling or drug testing.
3D Bioprinting for Surgical Repair and Regenerative Medicine
Beyond the laboratory, 3D bioprinting holds immense promise for creating functional grafts and implants for surgical repair, moving the field towards personalized regenerative medicine. The global market for 3D bioprinting in tissue and organ regeneration is projected to grow at a CAGR of 15.0% from 2025 to 2034, underscoring the significant clinical and commercial interest in this application [42].
Clinical Applications in Tissue Regeneration
The primary driver for this market is the critical shortage of organ donors and the growing need for solutions for congenital diseases, trauma, and tissue damage [15] [42]. 3D bioprinting addresses this by enabling the fabrication of patient-specific tissue constructs.
- Skin and Cartilage: Bioprinting has shown considerable success in producing skin grafts for burn victims and cartilage for reconstructive and corrective surgeries. The demand is high, with over 15 million surgical cosmetic procedures performed globally in 2022, highlighting the vast potential for bioprinted solutions [15]. Bioprinted skin offers better restoration than conventional grafts for severe burn accidents [15].
- Vascularized Tissues: A major focus of research is the integration of vascular networks into bioprinted tissues. This is crucial for ensuring the survival of larger, more complex engineered tissues after implantation, as it facilitates the delivery of nutrients and oxygen and the removal of waste products [14] [43]. Recent advances have enabled the formation of vascularised tissues nearly ten times thicker than previously possible [14].
- Ophthalmic Applications: In ophthalmology, 3D bioprinting is being explored for corneal and retinal repair. The technology allows for the creation of micro-precision, layered tissues and patient-specific grafts with minimal immune rejection, which is particularly important for the delicate structures of the eye [41]. Strategies include printing hydrogel-based bioinks containing corneal cells to replicate the corneal microstructure and developing encapsulated cell-delivery systems for sustained therapeutic protein delivery to treat degenerative retinal diseases [41].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful development of 3D-bioprinted models and tissues relies on a suite of specialized reagents and materials. The following table details key components of the 3D bioprinting workflow.
Table 2: Essential Research Reagents and Materials for 3D Bioprinting
| Category | Specific Examples | Function and Rationale |
|---|---|---|
| Bioink Biomaterials | Natural: Collagen, Gelatin (GelMA), Alginate, Hyaluronic Acid, Fibrin, dECM [14] [40] | Mimics the native extracellular matrix (ECM); provides biocompatibility, cell adhesion sites, and tunable degradation. dECM is particularly advanced as it preserves tissue-specific biochemical cues [40]. |
| Synthetic: PEG (e.g., PEGTA), PVA [40] | Offers high definability, reproducibility, and tunable mechanical properties. Often combined with natural materials to improve cell adhesion and bioactivity [40]. | |
| Cells | Stem Cells: iPSCs, MSCs, ESCs [15] [41] | Pluripotent or multipotent cells used for their ability to differentiate into various cell types, crucial for complex tissue formation. Used in ~70% of global research projects [15]. |
| Differentiated Cells: Chondrocytes, Keratinocytes, Cardiomyocytes, RPE cells [40] [41] | Primary or immortalized cells used to create specific, functional tissues. Patient-derived (autologous) cells are ideal for personalized grafts to avoid immune rejection [41]. | |
| Analysis & Validation Reagents | Viability Stains: Calcein AM (live), EthD-1 (dead) [19] | Standard live/dead assay to determine cell viability within the 3D construct post-printing. |
| Immunofluorescence (IF) Antibodies: Ki67 (proliferation), Caspases (apoptosis), Cell-specific markers (e.g., CD31 for endothelium) [19] | Used to verify cell identity, proliferation status, and the formation of specific tissue structures (e.g., cell junctions). | |
| Cell Painting Dyes: e.g., Phalloidin (F-actin), Concanavalin A (ER/membranes) [19] | A suite of fluorescent dyes staining multiple organelles to visualize cellular morphology and response to perturbations in a high-content manner. |
Current Challenges and Future Directions
Despite rapid progress, the clinical translation of 3D-bioprinted tissues faces several hurdles. Key challenges include the high cost of bioprinting equipment, which can range from USD 100,000 to USD 200,000 for advanced systems, and bioinks that can cost USD 100 to 500 per milliliter [15]. Scalability for producing large, functional tissues and navigating stringent regulatory pathways for approval also remain significant obstacles [15] [43].
Future growth is being catalyzed by the integration of Artificial Intelligence (AI) and machine learning to automate design and optimize printing processes, thereby improving precision and reducing errors [15] [7]. For instance, researchers at MIT have developed a low-cost monitoring technique that uses a digital microscope and an AI-based image analysis pipeline to identify print defects in real-time, enhancing reproducibility and reducing material waste [7]. Furthermore, the development of more sophisticated bioinks with enhanced biomimetic properties and a focus on vascularization and innervation will be critical for creating fully functional, implantable tissues [43]. As these technologies mature, 3D bioprinting is poised to move beyond the lab bench and into the clinic, fundamentally transforming approaches to drug development, disease research, and regenerative surgery.
Table 3: Global Market and Growth Projections for 3D Bioprinting
| Market Segment | 2024/2025 Value | Projected 2030/2034 Value | CAGR (Compound Annual Growth Rate) | Key Drivers |
|---|---|---|---|---|
| Overall 3D Bioprinting Market | ~USD 1.3 billion (2024) [15] | USD 2.8 billion (2030) [15] | 13.6% (2025-2030) [15] | Drug testing applications, R&D investments, personalized medicine [15]. |
| Tissue Structure 3D Bioprinters | ~USD 250 million (2025) [43] | ~USD 1.2 billion (2033) [43] | 20% (2025-2033) [43] | Advancements in bioinks, demand for regenerative therapies for chronic diseases [43]. |
| Tissue & Organ Regeneration | N/A | N/A | 15.0% (2025-2034) [42] | Aging population, rising trauma cases, high organ transplant costs [42]. |
Overcoming Bottlenecks: Strategies for Enhancing Fidelity and Viability
In the rapidly advancing field of 3D bioprinting for complex tissue architecture research, maintaining high cell viability during the printing process remains a fundamental challenge. The very nature of bioprinting—extruding living cells through fine nozzles, subjecting them to shear forces, and exposing them to potential chemical and environmental stressors—creates a hostile environment that can compromise cellular integrity and function. For researchers and drug development professionals, understanding and mitigating these stresses is not merely a technical obstacle but a prerequisite for creating physiologically relevant tissue models that accurately mimic native tissue environments. The success of bioprinted constructs, from pancreatic islets for diabetes research to cardiac patches for regenerative medicine, hinges on the ability to navigate these pressures effectively [44] [45] [36].
This technical guide examines the primary sources of cell stress during the bioprinting process and details evidence-based strategies to enhance cell survival. By integrating recent advancements in bioink formulation, printing technology, and process optimization, researchers can significantly improve the physiological functionality of their resulting constructs, thereby accelerating progress in tissue engineering and drug development.
Principal Stressors and Their Impact on Cell Viability
Cells encounter multiple stressors throughout the bioprinting workflow, each capable of inducing mechano-physiological damage, reducing viability, and impairing post-printing function. The major stress categories are mechanical, chemical, and environmental.
Mechanical Stress: Shear and Extensional Forces
During extrusion-based bioprinting—the most common method for depositing high-cell-density bioinks—cells experience significant shear stress within the printer nozzle and upon exit. These forces can damage cell membranes, disrupt cytoskeletal organization, and trigger apoptotic pathways [46]. The degree of shear stress is governed by bioink viscosity, printing pressure, nozzle geometry, and printing speed. Excessive pressure, while sometimes necessary to extrude high-viscosity materials, dramatically increases this risk. Conversely, a recent breakthrough in printing functional human islets demonstrated that fine-tuned parameters—specifically low pressure (30 kPa) and a slow print speed (20 mm per minute)—successfully reduced physical stress on delicate primary cells, resulting in over 90% cell survival and maintained strong insulin responsiveness [45].
Chemical Stress: Crosslinking and Bioink Composition
The chemical microenvironment surrounding cells during and immediately after printing constitutes another critical stressor. This includes the biocompatibility of the bioink polymers themselves, the kinetics of the crosslinking process (whether chemical, ionic, or photo-crosslinking), and the potential cytotoxicity of crosslinking agents or initiators [3] [47]. For instance, while UV light is often used to crosslink materials like GelMA, prolonged exposure can be harmful to cells. One study addressed this by using a LAP photoinitiator and safe blue light crosslinking for formulations containing nanoparticles to maintain cell compatibility [47]. Furthermore, the degradation byproducts of biomaterials must be non-toxic to ensure long-term cell survival and function [3].
Environmental Stress: Hydration and Temperature Fluctuations
Maintaining a sterile, hydrated, and physiologically temperature-controlled environment is crucial throughout the printing process. Even brief periods of desiccation can be fatal to cells. Similarly, deviations from 37°C can disrupt cellular metabolism. While not always explicitly detailed in reports, advanced bioprinting systems incorporate humidity chambers and temperature-controlled print beds and bioink reservoirs as standard features to mitigate these environmental risks.
Table 1: Major Cell Stressors in the Bioprinting Process
| Stress Category | Source | Impact on Cells | Key Influencing Factors |
|---|---|---|---|
| Mechanical Stress | Shear forces in print nozzle, extensional flow at nozzle exit | Membrane deformation, necrosis, apoptosis, reduced post-print function | Nozzle diameter/length, printing pressure/ppeed, bioink viscosity |
| Chemical Stress | Bioink polymer chemistry, crosslinking agents (e.g., UV light, ionic solutions) | Cytotoxicity, DNA damage, altered metabolism | Crosslinking duration/intensity, initiator concentration, material cytocompatibility |
| Environmental Stress | Ambient temperature, humidity, sterility | Metabolic shutdown, desiccation, contamination | Chamber humidity, temperature control, aseptic technique |
Quantitative Analysis of Printing Parameters and Cell Outcomes
Optimizing the printing process requires a quantitative understanding of how adjustable parameters directly influence cell viability and function. The table below synthesizes data from recent studies, providing a reference for researchers to benchmark their protocols.
Table 2: Quantitative Impact of Printing Parameters on Cell Viability and Function
| Printing Parameter | Typical Range | Observed Effect on Cell Survival/Function | Reference Case |
|---|---|---|---|
| Printing Pressure | 15 - 80 kPa | >90% viability achieved at 30 kPa for human islets; viability decreases with increasing pressure | Human pancreatic islets in alginate-based bioink [45] |
| Print Speed | 10 - 30 mm/s | Slower speeds (e.g., 20 mm/min) reduce shear and preserve 3D islet structure and function | Functional human islet printing [45] |
| Nozzle Diameter | 80 - 400 μm | Larger diameters reduce shear but limit printing resolution; a balance must be struck based on cell cluster size | General extrusion bioprinting [46] |
| Bioink Concentration | 5 - 20% (w/v) for GelMA | Higher polymer concentration increases viscosity and shear stress but improves structural integrity | GelMA-based bioinks with contrast agents [47] |
| UV Crosslinking Duration | 15 - 60 seconds | Longer exposure risks DNA damage; LAP initiator with blue light (4 min) showed good compatibility | DLP bioprinting with nanoparticle-laden bioinks [47] |
Experimental Protocols for Assessing Cell Viability and Function
To systematically evaluate and optimize printing conditions, researchers must employ a suite of characterization protocols. The following methodologies are standard in the field for quantifying the effects of printing-induced stress.
Protocol for Assessing Post-Printing Cell Viability
Objective: To quantify the percentage of living cells immediately after the bioprinting process and at subsequent time points. Reagents: Phosphate Buffered Saline (PBS), Calcein-AM, Ethidium homodimer-1 (or propidium iodide), culture medium. Equipment: Fluorescence microscope, cell culture incubator. Procedure:
- After printing, incubate the construct in a solution of Calcein-AM (2 µM) and Ethidium homodimer-1 (4 µM) in PBS for 30-45 minutes at 37°C.
- Rinse the construct gently with PBS to remove excess dye.
- Image the construct using a fluorescence microscope with appropriate filter sets. Calcein-AM (green fluorescence) stains live cells, while Ethidium homodimer-1 (red fluorescence) stains dead cells.
- Quantify the number of live and dead cells from multiple images using image analysis software (e.g., ImageJ). Calculate viability as: % Viability = (Number of Live Cells / Total Number of Cells) × 100. Application Note: This method was used to confirm over 90% cell survival in 3D-bioprinted human islets [45]. Longitudinal tracking over days or weeks is crucial to assess long-term health and function.
Protocol for Evaluating Metabolic Function
Objective: To ensure that cells not only survive but also maintain their specialized biological functions after the stress of printing. Reagents: Glucose-containing buffer, specific agonists/antagonists, ELISA kits for relevant secreted proteins (e.g., insulin). Equipment: Multi-well plate reader, cell culture incubator. Procedure (Example for Pancreatic Islets):
- Culture the bioprinted islet constructs for a defined period (e.g., 1-21 days).
- Challenge the constructs with a low-glucose (2.8 mM) solution for 1 hour, then switch to a high-glucose (16.7 mM) solution for another hour.
- Collect the supernatant from each incubation period.
- Quantify the amount of insulin secreted into the supernatant using a standardized ELISA or radioimmunoassay.
- A functional response is indicated by a significant increase in insulin secretion in the high-glucose supernatant compared to the low-glucose control. Application Note: This glucose-stimulated insulin secretion (GSIS) assay demonstrated that bioprinted human islets maintained a stronger insulin response over three weeks compared to standard preparations [45].
Workflow: From Printing to Functional Analysis
The following diagram illustrates the integrated workflow from printer setup to functional validation of bioprinted constructs, highlighting key decision points for ensuring cell survival.
The Scientist's Toolkit: Essential Reagents and Materials
Success in bioprinting complex tissues relies on a carefully selected suite of reagents and materials. The table below details key components referenced in recent literature, explaining their function in the context of ensuring cell survival.
Table 3: Research Reagent Solutions for Stress Mitigation in Bioprinting
| Reagent/Material | Function/Role | Example in Context | Reference |
|---|---|---|---|
| Alginate-Decellularized Matrix Bioink | Provides a biocompatible, biomimetic 3D microenvironment that supports cell adhesion and protects cells during printing. | Used to successfully print functional human pancreatic islets, enhancing oxygen/nutrient diffusion and supporting 90%+ viability. | [45] |
| Gelatin Methacryloyl (GelMA) | A versatile, photocrosslinkable hydrogel that mimics the extracellular matrix (ECM). Its mechanical properties are tunable to reduce shear stress. | A common base for bioinks; used at 12-20% concentration, often modified with nanoparticles for traceability or enhanced properties. | [47] [46] |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | A photoinitiator that enables rapid crosslinking with cytocompatible visible blue light, reducing the DNA damage risk associated with UV light. | Employed in DLP printing of GelMA with gold nanoparticles to ensure cell compatibility during crosslinking. | [47] |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | A photoinitiator that enables rapid crosslinking with cytocompatible visible blue light, reducing the DNA damage risk associated with UV light. | Employed in DLP printing of GelMA with gold nanoparticles to ensure cell compatibility during crosslinking. | [47] |
| Support Bath (e.g., FRESH) | A thermoreversible gel that supports the printed structure during fabrication, allowing the use of softer bioinks and lower printing pressures. | Enables fabrication of complex, delicate structures like collagen-based vascular networks that would collapse under their own weight. | [36] |
| Oxygen-Releasing Biomaterials | Mitigates post-printing hypoxia, a major cause of cell death in the core of thick constructs. | Incorporated into scaffolds to increase the survival and function of oxygen-sensitive cells like pancreatic β-cells. | [44] |
Integrated Stress Mitigation Strategy Diagram
A comprehensive approach to ensuring cell survival integrates material science, engineering controls, and biological design. The following diagram maps the interconnected strategies for navigating bioprinting stresses.
Navigating the pressures and stresses of the bioprinting process is a multifaceted challenge that requires a synergistic approach. As detailed in this guide, there is no single solution; instead, success is achieved through the careful optimization of bioink properties (rheology, biocompatibility), printing parameters (pressure, speed), and post-printing culture conditions. The evidence is clear that gentle printing processes, such as low-pressure extrusion, are not just feasible but essential for fabricating complex, functional tissues like pancreatic islets that exhibit robust post-printing viability and function [45]. The continued development of advanced biomaterials and precision bioprinting technologies, guided by quantitative viability and functional assessment, will be paramount in advancing 3D bioprinting from a research tool to a reliable platform for generating complex tissue architectures for therapeutic and drug development applications.
The field of 3D bioprinting aims to replicate the structure and function of real biological tissues for applications in disease modeling, drug discovery, and implantable grafts [7]. This layer-by-layer additive manufacturing approach uses living cells, biocompatible materials, and growth factors to build three-dimensional tissue and organ structures [7] [48]. However, a significant barrier hindering the clinical translation and widespread adoption of this technology is the critical challenge of reproducibility. Current 3D bioprinting approaches often lack integrated process control methods that limit defects in printed tissues, leading to inconsistencies that compromise structural fidelity and biological function [7] [49].
The reproduction of complex tissue architectures demands exceptional precision. A major drawback of current systems is their inability to ensure inter-tissue reproducibility and resource efficiency, often resulting in material waste [7]. This challenge was starkly highlighted in a recent round robin study on extrusion-based bioprinting standardization across 12 different academic laboratories, which concluded that current standardization conditions still leave room for operator intervention due to missing equipment automation, significantly affecting the reproducibility and comparability of experiments [49]. As the field advances toward more automated and scalable tissue fabrication, real-time process monitoring becomes indispensable for improving reproducibility, minimizing structural defects, and ultimately enabling adaptive closed-loop control systems that can reliably produce bioidentical tissues for research and clinical applications [27].
Core Technologies and Monitoring Solutions
Emerging Monitoring Platforms
Recent technological innovations are addressing the reproducibility challenge through modular monitoring systems that provide real-time quality assessment. Researchers have developed a printer-agnostic monitoring platform that combines a compact sensing architecture with an AI-based image-analysis pipeline to enable in situ process monitoring and defect detection [7] [27]. This system represents a significant advancement in the quest for reproducibility through several key features:
- Modular and Low-Cost Design: The platform is implemented for less than $500, making it an accessible solution for research laboratories [7].
- Layer-by-Layer Imaging: A digital microscope captures high-resolution images of tissues during printing, allowing for precise tracking of fabrication progress [7].
- AI-Driven Image Analysis: An automated segmentation strategy using a vision transformer model enables rapid comparison between printed layers and the intended design [27].
This approach enables researchers to quickly identify print defects, such as over- or under-extrusion of bio-ink, thus facilitating the identification of optimal print parameters for a variety of different materials [7]. The platform has demonstrated that 2D in situ images provide reliable approximations of 3D filament geometries, reveal pressure-related effects on filament diameters, and identify critical velocity thresholds for printing stability across different acellular and cellular bioinks [27].
Experimental Protocol: Implementation of In-Situ Monitoring
Implementing an effective in-situ monitoring system requires a methodical approach to ensure accurate defect detection and process optimization:
System Setup: Integrate a digital microscope into the bioprinter setup, ensuring it is positioned to capture high-resolution images of each layer during the deposition process. The system should be calibrated to maintain consistent focus and lighting across all captured images [7].
Image Acquisition Protocol: Capture images after the deposition of each complete layer. Maintain consistent imaging parameters (resolution, lighting, orientation) throughout the printing process to enable reliable comparison across layers [7].
AI-Analysis Pipeline: Process acquired images through a pre-trained vision transformer model specialized for bioprinting applications. The model segments the image to isolate the printed structure and compares its geometrical features against the intended digital design [27].
Defect Identification: The analysis pipeline automatically flags discrepancies between the printed structure and design specifications, classifying defects by type (dimensional inaccuracies, material inconsistencies, structural flaws) and magnitude [7] [27].
Parameter Optimization: Use defect data to iteratively refine printing parameters, including deposition pressure, printhead velocity, and material viscosity. The system can identify optimal parameters for specific bioink formulations by correlating parameter settings with defect occurrence [27].
This protocol enables researchers to establish quantitative quality control metrics and create customized printing parameter profiles for different bioink formulations and target tissue architectures.
Quantitative Analysis of Bioprinting Processes
Performance Metrics and Defect Classification
Table 1: Key Performance Metrics for Bioprinting Process Control
| Metric Category | Specific Parameter | Target Value/Range | Impact on Print Quality |
|---|---|---|---|
| Geometrical Accuracy | Filament Diameter Consistency | <5% deviation from target | Affects structural integrity and pore architecture |
| Layer Alignment Precision | <10μm layer-to-layer registration | Determines overall construct fidelity | |
| Structural Properties | Porosity Percentage | 70-90% for most tissues | Influences nutrient diffusion and cell migration |
| Pore Interconnectivity | >95% connected pores | Critical for vascularization and tissue integration | |
| Biological Parameters | Cell Viability Post-Printing | >90% for most applications | Determines functional performance |
| Cell Distribution Homogeneity | <15% coefficient of variation | Affects uniform tissue maturation |
Table 2: Common Bioprinting Defects and Their Root Causes
| Defect Type | Visual Identification | Primary Causes | Corrective Actions |
|---|---|---|---|
| Under-Extrusion | Gaps in deposited filaments; inconsistent structure | Insufficient pressure; nozzle clogging; improper viscosity | Increase pressure; filter bioink; optimize cross-linking |
| Over-Extrusion | Excess material spreading; loss of defined features | Excessive pressure; slow printhead velocity | Reduce pressure; increase print speed; adjust viscosity |
| Layer Misalignment | Structural shifting; dimensional inaccuracies | Incorrect Z-axis calibration; stage vibration | Recalibrate motion system; stabilize platform |
| Void Formation | Random empty spaces within constructs | Air bubbles in bioink; inconsistent flow | Degas bioink; optimize priming procedure |
The quantitative assessment of bioprinting processes relies on measuring specific parameters that correlate with final construct quality. The in-situ monitoring platform enables tracking of these metrics throughout the fabrication process, allowing for real-time quality assessment and intervention [7]. Research has demonstrated that this approach can identify critical velocity thresholds for printing stability and reveal pressure-related effects on filament diameters across different bioink formulations [27]. By establishing baseline performance metrics for each material and printer configuration, researchers can create standardized quality control protocols that significantly enhance inter-laboratory reproducibility [49].
Research Reagent Solutions for Enhanced Reproducibility
Table 3: Essential Research Reagents for Reproducible Bioprinting
| Material Category | Specific Examples | Function in Bioprinting | Considerations for Reproducibility |
|---|---|---|---|
| Structural Polymers | Alginate, GelMA, Hyaluronic Acid, PEGDA | Provides mechanical integrity; influences cell behavior | Batch-to-batch consistency critical; source certification recommended |
| Natural Matrices | Collagen, Fibrin, Decellularized ECM | Enhances bioactivity; improves cell-matrix interactions | Complex purification needed; biological variability concerns |
| Support Materials | Carbopol, Pluronic F-127, PU nanoparticles | Enables suspended printing; temporary scaffolding | Viscosity stability paramount; cross-contamination prevention |
| Cross-linking Agents | Calcium Chloride, UV initiators (LAP) | Stabilizes printed structure; controls gelation kinetics | Concentration precision essential; fresh preparation advised |
The selection and consistent use of high-quality research reagents is fundamental to achieving reproducible bioprinting outcomes. Bioinks must balance multiple requirements including printability, mechanical properties, and bioactivity [48] [50]. For instance, alginate-based bioinks offer excellent printability but may require blending with other materials like collagen or hyaluronic acid to enhance cellular interaction [48]. Similarly, synthetic polymers like PEG (polyethylene glycol) provide highly reproducible mechanical properties but often need functionalization with adhesive peptides to support cell attachment [50]. Establishing standardized formulation protocols and rigorous quality control measures for all research reagents is essential for minimizing batch-to-batch variability and ensuring consistent performance across experiments [49].
Visualization of Monitoring Workflows
In-Situ Monitoring Process
In-Situ Monitoring and Correction Workflow
This workflow illustrates the continuous monitoring and correction cycle enabled by modern in-situ monitoring platforms. The process begins with the printing of a single layer using specific parameters including deposition pressure, printhead velocity, and nozzle size [7]. After each layer is deposited, a digital microscope captures a high-resolution image, which is then processed through an AI-based image analysis pipeline utilizing a vision transformer model [27]. The system compares the geometrical features of the printed layer with the intended digital design to identify any deviations or defects [7]. If defects are detected, the system either alerts the operator or automatically adjusts printing parameters before proceeding to the next layer, creating a closed-loop control system that significantly enhances reproducibility and reduces material waste [7] [27].
Defect Classification System
Bioprinting Defect Classification System
The defect classification system categorizes bioprinting anomalies into three primary classes: geometric defects, material defects, and structural defects [7] [27]. Geometric defects include issues such as under-extrusion (characterized by gaps in deposited filaments), over-extrusion (identified by excess material spreading beyond intended boundaries), and layer misalignment (manifesting as structural shifting between layers) [7]. Material defects encompass inconsistencies in bioink properties, nozzle contamination leading to partial clogging, and bioink degradation due to improper handling or storage conditions [49]. Structural defects include layer delamination resulting from poor interlayer adhesion, structural deformation due to inadequate mechanical support, and void formation caused by air bubbles or inconsistent material flow [7] [27]. This classification system enables systematic identification and remediation of specific failure modes in the bioprinting process.
The integration of in-situ monitoring and process control systems represents a transformative advancement in the quest for reproducibility in 3D bioprinting. The development of modular, low-cost monitoring platforms that combine real-time imaging with AI-driven analysis addresses a critical gap in current bioprinting workflows [7] [27]. These technologies enable researchers to move beyond post-print quality assessment to active process control, where defects are identified and corrected during the fabrication process rather than after completion.
As the field progresses, the implementation of standardized monitoring protocols and quality metrics will be essential for enabling technology transfers between laboratories and facilitating meaningful comparisons of research findings [49]. The round robin study demonstrating variability across 12 laboratories highlights both the urgent need for standardization and the potential of automated image analysis as a methodology for quality assurance [49]. Future developments in closed-loop control systems that automatically adjust printing parameters based on real-time feedback will further enhance reproducibility and reduce the dependency on operator expertise [7] [27].
Ultimately, these advancements in process control and in-situ monitoring will accelerate the translation of 3D bioprinting from research laboratories to clinical applications, enabling the reliable production of complex tissue architectures for disease modeling, drug development, and regenerative medicine. By addressing the fundamental challenge of reproducibility, these technologies pave the way for the widespread adoption of bioprinting as a robust and standardized platform for tissue engineering.
The transition of 3D bioprinting from research laboratories to clinically impactful technologies hinges on overcoming a critical bottleneck: the effective scaling of fabrication processes from small-scale prototypes to high-throughput platforms. While traditional tissue engineering methods often depend on labor-intensive manual processes that are difficult to reproduce, 3D bioprinting offers a promising pathway toward standardized, automated production [51]. The scalability challenge extends beyond merely printing larger constructs; it encompasses the entire workflow—from digital design and bioink formulation to printing automation, quality control, and post-printing maturation. Current limitations range from sub-optimal bioink properties and lack of standardized processes to insufficient biomimicry of bioprintable architectures [52]. This technical guide examines the core principles and methodologies essential for scaling 3D bioprinting processes, with a specific focus on addressing the needs of researchers and drug development professionals working with complex tissue architectures.
Foundational Technologies and Scaling Limitations
The selection of appropriate bioprinting technologies forms the foundation for any scalable workflow. Each primary bioprinting method presents distinct advantages and limitations for high-throughput applications.
Table 1: Comparison of Primary 3D Bioprinting Technologies for Scaling Applications
| Bioprinting Method | Key Advantages | Scaling Limitations | Optimal Use Cases for Scaling |
|---|---|---|---|
| Extrusion-Based | High cell density printing; wide bioink viscosity range; multi-material capability [53] | Lower resolution (≥100 μm); shear stress on cells; slower printing speeds [53] | Large tissue constructs; vascularized tissues; high-strength scaffolds |
| Droplet-Based (Inkjet) | Higher resolution (20-100 μm); faster deposition for small areas [53] | Limited bioink viscosity; nozzle clogging; poor structural integrity [53] | High-resolution patterning; small tissue models; drug screening platforms |
| Laser-Assisted | Highest cell viability (>95%); single-cell resolution [53] | Very low throughput; complex setup; limited bioink options [53] | High-precision cellular patterning; niche research applications |
| Light-Based (DLP) | Fast fabrication speeds; high resolution (<20 μm) [53] | Limited material selection; potential cytotoxicity of resins [53] | High-resolution acellular scaffolds; organ-on-chip components |
The scalability of these technologies is further constrained by bioink performance requirements. Bioinks must satisfy often conflicting rheological and biological demands, exhibiting optimal viscosity, shear-thinning behavior, and rapid gelation kinetics while maintaining cell viability and function [54]. This trade-off becomes increasingly pronounced at larger scales, where structural integrity and nutrient diffusion limitations impose significant constraints on construct design.
Strategic Framework for Scaling Bioprinting Processes
Integrated Automation and Process Control
Achieving reproducible, high-throughput bioprinting requires integrating automation throughout the entire fabrication pipeline. The bioprinting process chain can be systematically divided into three phases: print preparation, printing procedure, and post-printing tissue maturation [51]. Each phase offers distinct automation potentials:
Print Preparation: Automated 3D model generation using parametric design and AI-assisted approaches can significantly accelerate the digital design phase [55]. Implementation of automated bioink synthesis and cell cultivation systems standardizes the crucial first step in the production pipeline.
Printing Procedure: Robotic systems for automated substrate loading and unloading, coupled with sensor-integrated print heads, enable continuous operation [51]. Real-time monitoring systems provide immediate feedback for process adjustment.
Post-Printing Handling: Automated transfer of printed constructs to bioreactor systems for maturation reduces manual handling and potential contamination [51].
A recent innovation demonstrating this approach comes from MIT researchers, who developed a modular, low-cost monitoring technique that integrates layer-by-layer imaging with an AI-based image analysis pipeline [7]. This system captures high-resolution images of tissues during printing and rapidly compares them to the intended design, enabling quick identification of print defects such as over- or under-deposition of bioink [7]. Such process control technologies are essential for maintaining inter-tissue reproducibility and enhancing resource efficiency in scaled operations.
Quality Assurance and In-Process Monitoring
Implementing robust quality assurance (QA) mechanisms is fundamental to scaling bioprinting processes. Sensor integration and online quality assessment pave the way for standardized manufacturing platforms capable of meeting regulatory requirements [51]. Effective QA frameworks for scaled bioprinting incorporate multiple monitoring modalities:
Optical Monitoring: Camera systems with computer vision algorithms detect structural anomalies and deviations from design specifications [7] [51].
Rheological Sensing: In-line viscosity and pressure sensors monitor bioink behavior throughout the printing process, ensuring consistent deposition [51].
Biological Status Assessment: Spectroscopy and microscopy integrated into the bioprinting environment can assess cell viability and distribution [51].
The integration of Artificial Intelligence (AI) for data analysis from these diverse sensors represents a transformative advancement for scalable bioprinting. AI systems can identify subtle patterns indicative of process drift or impending failures that might escape human detection, enabling predictive adjustments and maintaining quality across extended production runs [51].
Table 2: Key Automation Components for Scaled Bioprinting Systems
| Process Step | Automation Component | Function | Impact on Scaling |
|---|---|---|---|
| Material Handling | Robotic grippers | Substrate and construct transportation | Enables continuous operation |
| Bioink Delivery | Microfluidic bioink supply | Precise material delivery to print heads | Reduces waste; maintains material consistency |
| Process Control | Integrated sensor systems | Real-time monitoring of printing parameters | Ensures quality and reproducibility |
| Defect Correction | AI-based image analysis | Layer-by-layer comparison to design [7] | Identifies optimal parameters; reduces failures |
Experimental Protocol: Automated Quality Control for High-Throughput Bioprinting
Objective: Implement a real-time quality control system to detect printing defects and ensure dimensional accuracy across multiple bioprinted constructs.
Materials and Equipment:
- Extrusion-based bioprinter with open architecture for hardware integration
- Digital microscope (compatible with automated positioning)
- Computational unit for image analysis
- Custom software for image acquisition and processing
Methodology:
- System Integration: Mount the digital microscope to the bioprinter gantry system to enable coordinated movement with the print head. Calibrate the microscope focus and lighting for consistent image capture.
- Reference Image Generation: For each design, generate reference images from the sliced G-code file, representing the ideal deposition pattern for each layer.
- Image Acquisition Protocol: Program the system to capture high-resolution images of each completed layer using the integrated microscope. Standardize imaging parameters (lighting, exposure) across all samples.
- Defect Detection Analysis: Employ a machine learning algorithm trained to compare captured layer images with reference images. Key detection parameters include:
- Filament width deviation (>±15% from target)
- Layer alignment errors (>50 μm displacement)
- Porosity or gap detection (>100 μm gaps)
- Extrusion inconsistencies (over-/under-deposition)
- Corrective Action Protocol: Program automated responses to detected defects:
- For minor deviations (<20% from specification): Adjust subsequent layer parameters to compensate.
- For major deviations (>20% from specification): Pause printing and alert operator for intervention.
- Data Logging: Record all quality metrics, images, and corrective actions for each construct to establish a manufacturing history.
This protocol, adapted from recent research [7], provides a framework for maintaining quality across extended print runs, which is essential for producing clinically relevant tissue equivalents at scale.
Enabling Technologies for Scaled Production
Advanced Bioink Design for Scalable Formulations
Bioink development represents one of the most significant challenges in scaling 3D bioprinting processes. Next-generation bioinks must balance often contradictory requirements: demonstrating optimal rheology for printability while maintaining biological functionality [54]. Key considerations for scalable bioink design include:
Shear-Thinning Behavior: Bioinks must exhibit decreased viscosity under shear stress during extrusion, followed by rapid recovery to maintain structural integrity post-deposition [54]. This property is particularly crucial for continuous printing operations.
Tunable Gelation Kinetics: Controlled crosslinking mechanisms (thermal, ionic, photoinitiated) must be engineered for rapid stabilization without compromising cell viability [54].
Biomimetic Composition: Incorporation of decellularized extracellular matrix (dECM) components and exosomes has shown promise in enhancing tissue formation and cell viability in scaled constructs [14].
The development of composite bioinks that combine natural polymers like collagen or alginate with synthetic polymers such as PEG or PCL offers a promising pathway to achieving the necessary balance between biocompatibility and mechanical stability required for large-scale tissue constructs [54].
Integrated Workflow for Scaled Bioprinting
The transition from small-scale to high-throughput bioprinting requires a seamlessly integrated digital-physical workflow. The diagram below illustrates the core processes and decision points in a scalable bioprinting system.
This integrated workflow highlights the critical feedback loops and quality control checkpoints necessary for maintaining consistency across scaled production. The implementation of such systems enables the transition from manual craftsmanship to standardized manufacturing in tissue engineering.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Scaled Bioprinting Applications
| Reagent/Material | Function | Considerations for Scaling |
|---|---|---|
| Collagen-Based Bioinks | Structural scaffold providing native ECM environment [56] | Batch-to-batch consistency; concentration optimization for print fidelity |
| Hybrid Polymer Systems | Combining natural (gelatin, alginate) and synthetic (PEG, PCL) polymers [54] | Balancing printability with biocompatibility; sterilization requirements |
| Vascularization Factors | Promoting formation of blood vessel networks [14] | Spatial patterning; controlled release kinetics |
| Support Bath Materials | Thermo-reversible gelatin microparticles for FRESH printing [56] | Reusability potential; compatibility with different bioinks |
| Crosslinking Agents | Ionic (CaCl₂) or photo-initiators for structural integrity [54] | Cytotoxicity profiling; uniform application in large constructs |
| Decellularized ECM (dECM) | Tissue-specific biochemical cues [14] | Source variability; standardization challenges |
Case Study: Scaling Vascularized Tissue Production
The production of vascularized tissues represents both a critical goal and significant challenge in scaling 3D bioprinting processes. Recent research demonstrates a promising approach through the development of collagen-based high-resolution internally perfusable scaffolds (CHIPS) fabricated using freeform reversible embedding of suspended hydrogels (FRESH) technology [56]. This methodology enables the direct 3D bioprinting of collagen-based hydrogels, ECM, and cells into fully biologic perfusable scaffolds with high-fidelity control of structure and composition.
The scaling protocol involves:
- Design Optimization: Creating centimeter-scale microfluidic devices inspired by organ-on-a-chip designs using CAD software, with internal channel dimensions as small as 500 μm wide by 1000 μm tall [56].
- High-Fidelity Printing: Implementing refined FRESH printing processes to improve filament reproducibility, mechanical accuracy, and layer-by-layer repeatability using collagen-I bioink [56].
- Integrated Perfusion System: Coupling the printed CHIPS with a specialized bioreactor system (vasculature and perfusion organ-on-a-chip reactor - VAPOR) for dynamic culture [56].
- Multi-Material Patterning: Implementing multi-material bioprinting to control 3D spatial patterning, ECM composition, cellularization, and material properties [56].
This integrated approach demonstrates the potential for creating glucose-responsive, insulin-secreting pancreatic-like tissues with vascular endothelial cadherin+ vascular-like networks, highlighting the convergence of engineering and biological strategies necessary for scaling functional tissue production [56].
The continued scaling of 3D bioprinting processes will likely be transformed by several emerging technologies. Artificial intelligence and machine learning are poised to revolutionize both the design optimization and process control aspects of bioprinting, enabling predictive modeling of tissue outcomes and real-time adjustment of printing parameters [51] [52]. The integration of bioprinting with microfluidic organ-on-a-chip technologies creates opportunities for parallelized production of standardized tissue models for drug development [51]. Additionally, the concept of 4D bioprinting, where printed structures evolve their functionality over time, presents intriguing possibilities for creating more biologically relevant tissues that continue to mature post-printing [52].
In conclusion, scaling 3D bioprinting from small-scale designs to high-throughput platforms requires a systematic approach that addresses challenges across the entire workflow—from digital design and bioink formulation to process automation and quality control. By implementing integrated systems that leverage automation, real-time monitoring, and advanced materials, researchers can overcome the current limitations in producing clinically relevant tissue constructs. The continued convergence of engineering principles with biological understanding will ultimately enable the standardized, reproducible production of complex tissue architectures needed to advance regenerative medicine and drug development.
The pursuit of recreating complex tissue architectures in vitro represents a central challenge in regenerative medicine and drug development. Traditional 3D bioprinting approaches have been constrained by the static nature of conventional biomaterials, which fail to replicate the dynamic, responsive nature of native extracellular matrices [3] [57]. Within this context, biomaterials engineered with supramolecular and stimuli-responsive properties are emerging as transformative solutions that bridge the fidelity gap between bioprinted constructs and native tissues.
Supramolecular biomaterials leverage reversible, non-covalent interactions—including hydrogen bonding, π-π interactions, host-guest complexation, and metal-coordination—to create dynamic polymer networks that exhibit unique properties such as self-healing, shear-thinning behavior, and temporal control over structural features [58] [59]. These characteristics are particularly valuable in 3D bioprinting applications, where materials must navigate the competing demands of printability (requiring flow under stress) and structural integrity (requiring stability after deposition) [58] [60].
Complementing these advances, stimuli-responsive biomaterials undergo predictable changes in their physical or chemical properties in response to specific exogenous or endogenous triggers, including light, temperature, magnetic fields, pH, and enzymatic activity [61] [62]. When integrated with 3D bioprinting technologies, these "smart" materials enable the creation of four-dimensional (4D) constructs that evolve over time, dynamically modulating their properties to guide cell behavior, promote vascularization, and facilitate integration with host tissues [60] [62].
This technical guide examines the fundamental design principles, experimental methodologies, and practical applications of these advanced material systems within the framework of 3D bioprinting research for complex tissue architecture.
Supramolecular Biomaterials: Design and Implementation
Fundamental Non-Covalent Interactions
The programmable behavior of supramolecular biomaterials originates from directional interactions between molecular building blocks. The table below summarizes the key non-covalent interactions employed in their design.
Table 1: Fundamental Non-Covalent Interactions in Supramolecular Biomaterials
| Interaction Type | Binding Energy (kJ/mol) | Directionality | Key Functional Groups/Components | Representative Applications in Bioprinting |
|---|---|---|---|---|
| Hydrogen Bonding | 4-60 | High | Ureidopyrimidinone (UPy), Amides, Carboxylic acids | Self-healing bioinks, Reinforced hydrogels [58] [59] |
| π-π Interactions | 0-50 | Moderate | Perylene Bisimides (PBIs), Aromatic rings | Nanofiber formation, Conductive bioinks [58] |
| Host-Guest | 1-60 | High | Cyclodextrin/Adamantane, Cucurbituril | Shear-thinning hydrogels, Modular bioink design [58] [59] |
| Metal-Ligand | 0-400 | Variable | Metal ions (Zn²⁺, Fe³⁺), Polypyridines | Photoluminescent materials, Self-assembling nanostructures [58] [63] |
| Hydrophobic | 0-5 | Low | Alkyl chains, Polymer blocks | Micelle formation, Thermoresponsive hydrogels [58] |
Experimental Protocol: Fabricating Supramolecular Bioinks
Objective: To synthesize and characterize a shear-thinning supramolecular hydrogel bioink based on host-guest interactions between β-cyclodextrin (β-CD) and adamantane (Ad) modified polymers.
Materials Required:
- Hyaluronic acid (MW: 100 kDa)
- β-cyclodextrin
- 1-Adamantane acetic acid
- N-(3-Dimethylaminopropyl)-N'-ethylcarbodiimide hydrochloride (EDC)
- N-Hydroxysuccinimide (NHS)
- Phosphate Buffered Saline (PBS), pH 7.4
- Cell culture media (DMEM/F12)
Synthesis Procedure:
β-CD-modified HA Synthesis:
- Dissolve 1 g of hyaluronic acid in 100 mL of deionized water.
- Activate β-cyclodextrin (2 mmol) using EDC (4 mmol) and NHS (4 mmol) in MES buffer (0.1 M, pH 6.0) for 30 minutes with stirring.
- Add activated β-CD solution to the HA solution and adjust pH to 8.0 using 1M NaOH.
- React for 24 hours at room temperature with continuous stirring.
- Purify via dialysis (MWCO 12-14 kDa) against DI water for 72 hours, followed by lyophilization.
Ad-modified HA Synthesis:
- Follow the same procedure as above, substituting β-CD with 1-adamantane acetic acid (2 mmol).
Hydrogel Formation:
- Prepare separate 2% (w/v) solutions of β-CD-HA and Ad-HA in sterile PBS.
- Filter sterilize using 0.22 μm filters.
- Mix equal volumes of each solution by gentle pipetting or using a dual-barrel syringe.
- Allow crosslinking to proceed for 15-30 minutes at room temperature before characterization.
Characterization Methods:
Rheological Analysis:
- Perform oscillatory rheology to measure storage (G') and loss (G") moduli.
- Conduct shear-thinning tests by monitoring viscosity as a function of shear rate (0.1 to 100 s⁻¹).
- Evaluate recovery kinetics through step-strain tests alternating between 1% and 500% strain.
Printability Assessment:
- Utilize extrusion-based bioprinter to assess filament formation and stacking fidelity.
- Print grid structures (10×10×2 mm) to evaluate structural integrity.
- Quantify strand diameter consistency and pore uniformity.
Diagram Title: Supramolecular Bioink Fabrication Workflow
Stimuli-Responsive Biomaterials for 4D Bioprinting
Classification of Stimuli-Responsive Mechanisms
Stimuli-responsive biomaterials enable dynamic functionality in bioprinted constructs, allowing for temporal control over properties and structure. The table below categorizes the primary stimulus types and their mechanisms of action.
Table 2: Classification of Stimuli-Responsive Biomaterials for 4D Bioprinting
| Stimulus Type | Response Mechanism | Characteristic Response Time | Key Material Systems | Tissue Engineering Applications |
|---|---|---|---|---|
| Thermal | Polymer chain rearrangement, LCST/UCST transition | Seconds to minutes | PNIPAM, Pluronics, PEG-based polymers [62] | Minimally invasive implantation, Shape-memory scaffolds [62] |
| Light | Photochemical reactions, Photothermal effect | Milliseconds to seconds | Azobenzene polymers, Gold nanorods, Spiropyran [60] [62] | Spatiotemporally controlled drug release, Photothermal therapy [61] |
| Magnetic | Magnetic alignment, Hyperthermia | Milliseconds | Fe₃O₄-loaded hydrogels, MREs [62] | Remote actuation, Mechanical stimulation [62] |
| pH | Protonation/deprotonation, Charge density changes | Seconds | Polyacrylic acid, Chitosan, Polylactic acid [61] | Targeted drug delivery to acidic tumor microenvironments [61] |
| Enzymatic | Cleavage of specific peptide sequences | Minutes to hours | MMP-sensitive peptides, Hyaluronic acid-based systems [58] | Cell-responsive matrix remodeling, Disease modeling [58] |
Experimental Protocol: 4D Bioprinting with Temperature-Responsive Hydrogels
Objective: To fabricate and characterize a 4D bioprinted construct using a temperature-responsive shape memory polymer (SMP) that undergoes programmed shape transformation at physiological temperature.
Materials Required:
- Poly(ε-caprolactone) (PCL, MW: 50,000)
- Poly(ethylene glycol) (PEG, MW: 10,000)
- Trimethylene carbonate
- Stannous octoate catalyst
- Dichloromethane
- Phosphate Buffered Saline (PBS)
- Cell culture media
Synthesis of Shape Memory Polymer:
Polymer Synthesis:
- Dry PCL-diol (5 g) and PEG (2 g) under vacuum at 80°C for 2 hours.
- Dissolve in toluene with trimethylene carbonate (3 mol equivalent to OH groups).
- Add stannous octoate (0.1% w/w) as catalyst.
- React at 130°C for 24 hours under nitrogen atmosphere with stirring.
- Precipitate in cold diethyl ether and dry under vacuum.
Construct Fabrication:
- Prepare 15% (w/v) polymer solution in dichloromethane.
- Use extrusion-based bioprinting to fabricate temporary flat mesh structure (20×20×1 mm).
- Program permanent shape by heating to 60°C (above transition temperature), deforming to tubular configuration (Ø8 mm), and fixing while cooling.
Shape Transformation Analysis:
- Immerse programmed flat construct in PBS at 37°C.
- Record shape recovery process using time-lapse photography.
- Quantify recovery rate and final shape fidelity compared to programmed permanent shape.
- For cell-laden constructs, assess viability and morphology during and after shape transformation.
Characterization Methods:
Thermal Analysis:
- Determine transition temperature using Differential Scanning Calorimetry (DSC).
- Perform Thermomechanical Analysis (TMA) to quantify shape fixity and recovery ratios.
Mechanical Testing:
- Conduct tensile tests at both room temperature and 37°C.
- Measure modulus changes during shape transition.
Biological Assessment:
- Seed with human fibroblasts (10⁵ cells/construct) and culture for 7 days.
- Assess viability using Live/Dead staining at days 1, 3, and 7.
- Evaluate cell morphology and alignment using phalloidin/DAPI staining.
Diagram Title: 4D Bioprinting with Stimuli-Responsive Materials
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of supramolecular and stimuli-responsive biomaterials requires specialized reagents and characterization tools. The following table details essential components for research in this domain.
Table 3: Essential Research Reagents for Supramolecular and Stimuli-Responsive Biomaterials
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Supramolecular Motifs | UPy, Cyclodextrin, Cucurbituril, Crown ethers | Directional non-covalent crosslinking, Modular design | Binding affinity, Orthogonality, Cytocompatibility [58] [59] |
| Stimuli-Responsive Polymers | PNIPAM, PLGA, Poly(oxazoline), Elastin-like polypeptides | Temperature, pH, or enzyme-responsive behavior | Transition temperature, Hysteresis, Degradation profile [61] [62] |
| Photoinitiators | LAP, Irgacure 2959, Lithium phenyl-2,4,6-trimethylbenzoylphosphinate | UV and visible light crosslinking | Cytotoxicity, Absorption wavelength, Efficiency [60] |
| Nanoparticles | Gold nanorods, Iron oxide, Quantum dots, Cellulose nanocrystals | Photothermal activation, Reinforcement, Sensing | Size distribution, Surface chemistry, Biocompatibility [63] [62] |
| Dynamic Crosslinkers | Disulfide bonds, Boronic esters, Diels-Alder adducts | Reversible covalent chemistry, Self-healing | Bond stability, Trigger specificity, Reaction kinetics [62] |
| Characterization Tools | Oscillatory rheometer, DSC, SEM, Confocal microscopy | Material characterization, Printability assessment | Resolution, Environmental control, Throughput [58] [57] |
Integrated Application in Complex Tissue Architecture
The convergence of supramolecular and stimuli-responsive material strategies enables unprecedented control over bioprinted tissue complexity. For vascularized tissue constructs, researchers have successfully demonstrated multi-material bioprinting approaches where sacrificial bioinks with temperature-responsive liquefaction are co-printed with supramolecular hydrogels that support endothelial cell proliferation and tubulogenesis [64]. Following printing, temperature reduction triggers sacrificial ink removal, leaving behind perfusable channel networks that can be endothelialized to create functional vasculature.
In neural tissue engineering, supramolecular peptide amphiphiles incorporating IKVAV epitopes self-assemble into nanofibrous scaffolds that promote neurite extension and direct stem cell differentiation toward neuronal lineages [58]. When combined with electroconductive components such as graphene or polypyrrole, these materials can be further enhanced with electrical responsiveness, enabling applied electrical stimulation to enhance neural maturation and network formation [60] [62].
For bone regeneration, 4D printed shape memory scaffolds with programmed porosity changes can be implanted in a compact form through minimally invasive procedures, subsequently expanding to fill complex defect sites and provide immediate mechanical support while releasing osteoinductive factors in response to local inflammatory cues [62]. Metal-organic frameworks (MOFs) incorporated into supramolecular hydrogels further enable sustained delivery of calcium and phosphate ions to promote biomineralization [63].
These integrated approaches demonstrate how dynamic biomaterials are advancing 3D bioprinting from static scaffold fabrication toward the creation of living tissue constructs with architectural complexity, biochemical signaling, and physiological functionality that more closely mimic native tissues.
Proving Efficacy: How 3D Bioprinted Tissues are Revolutionizing Pre-Clinical Models
The drug development pipeline is plagued by a persistent translational gap, where promising results from preclinical models fail to correlate with clinical outcomes in humans. Between 2004 and 2021, 98 unique compounds failed in Phase II and III Alzheimer's clinical trials despite showing promise in preclinical animal studies [65]. This staggering failure rate, driven by inadequate modeling systems, highlights the critical need for more predictive platforms. The emergence of three-dimensional (3D) models, particularly those enabled by advanced 3D bioprinting technologies, represents a paradigm shift in biomedical research. These models capture the complex tissue architectures and cellular interactions that define human physiology with unprecedented fidelity, bridging the critical gap between traditional two-dimensional (2D) cultures, animal testing, and human clinical response. By providing human-relevant, scalable, and ethically advanced platforms, 3D models are positioned to accelerate drug discovery, improve safety profiling, and pave the way for personalized medicine approaches.
The Fundamental Limitations of Traditional Models
The Shortcomings of 2D Cell Culture
Conventional two-dimensional cell culture, while inexpensive and straightforward, modifies fundamental cellular physiology by forcing complex three-dimensional interactions into a simplified monolayer.
- Altered Cell Morphology and Signaling: Cells grown on flat, rigid plastic or glass surfaces experience forced apical-basal polarity and flattened cell shapes that do not reflect their natural morphology in tissues [66]. This distortion alters mechanical and biochemical signaling pathways, leading to aberrant gene expression, protein synthesis, and metabolic activity [66] [65].
- Deficient Microenvironmental Cues: 2D cultures lack the essential three-dimensional extracellular matrix (ECM), cell-cell interactions, and mechanical cues that govern tissue-specific function [65]. For instance, hepatocytes grown in 2D cultures exhibit markedly different cytochrome P450 (CYP) profiles compared to their 3D counterparts, severely compromising their utility for predictive toxicology [65].
- Poor Predictive Value for Drug Responses: The absence of physiological barriers and gradients in 2D cultures leads to uniform drug exposure, failing to replicate the penetration challenges faced by therapeutics in solid tissues. This often results in overestimation of drug efficacy and failure to identify compounds that cannot penetrate beyond surface cell layers [67].
The Challenges of Animal Testing
While animal models provide a whole-organism context, they introduce significant translational obstacles due to interspecies differences.
- Limited Concordance with Human Physiology: The average rate of concordance between animal models and clinical trials barely reaches 8% [66]. Fundamental differences in genetics, metabolism, immune response, and disease pathology between species undermine the predictive validity of animal data. A prominent example is the drug Semagacestat, which worsened symptoms in human Alzheimer's trials despite reducing amyloid beta plaques in animal studies [65].
- Ethical and Regulatory Concerns: Growing ethical considerations regarding animal discomfort in research, coupled with evolving guidance like the FDA Modernization Act 2.0, are promoting the use of human-relevant cell-based assays as alternatives to animals [65].
- High Costs and Time Consumption: Developing and working with animal models is tedious, time-consuming, and costly, significantly constraining the pace of drug discovery [65].
3D Models: A Technologically Superior Paradigm
Fundamental Advantages of 3D Culture Systems
3D models recapitulate critical aspects of native tissue physiology that are absent in 2D systems, providing a more accurate platform for studying disease mechanisms and therapeutic interventions.
- Physiologically Relevant Tissue Architecture: 3D cultures enable cells to assemble into complex microtissues with natural cell-cell and cell-ECM interactions, preserving native cell morphology and polarization [65]. This spatial organization is crucial for modeling organ-level functions, such as the bile canaliculi network in liver tissues and the stratified layers in epithelial barriers.
- Biochemical and Biophysical Gradients: The three-dimensional mass transport dynamics in 3D models create physiological gradients of oxygen, nutrients, pH, and metabolic waste [67]. These gradients are essential for modeling key pathophysiological phenomena, such as hypoxic tumor cores in cancer spheroids, which drive chemoresistance and are absent in 2D cultures [67].
- Enhanced Longevity and Functional Stability: Cells in 3D tissues retain their tissue-specific functions for significantly longer periods (typically 4-6 weeks or longer) compared to their 2D counterparts [65]. Organovo's 3D bioprinted liver tissues, for instance, remain functional for over 40 days, enabling the detection of subtle or longer-term drug effects that would be missed in 2D cultures that typically last only 48 hours [68].
Quantitative Comparison of Model Systems
The table below summarizes key performance differences between 2D cultures, 3D models, and animal testing.
Table 1: Comprehensive Model System Comparison
| Feature | 2D Cell Culture | 3D Models | Animal Testing |
|---|---|---|---|
| Physiological Relevance | Low - Altered cell morphology, no tissue architecture [66] | High - Native tissue architecture, cell-ECM interactions [65] | Moderate - Whole organism but species-specific differences [66] |
| Predictive Value for Drug Efficacy | Poor - Often overestimates efficacy [67] | High - Better predicts clinical response, accounts for penetration [38] | Variable - Low concordance (~8%) with human trials [66] |
| Predictive Value for Toxicity | Limited - Lacks metabolic competence, e.g., declining CYP activity [65] | High - Functional metabolism, e.g., liver tissues show dose-dependent toxicity [68] | Moderate - Affected by species-specific metabolism [38] |
| Experimental Duration | Short-term (days) [68] | Long-term (weeks to months) [65] | Long-term (months to years) |
| Cost | Low | Moderate to High [67] | Very High |
| Throughput | High - Suitable for 384/1536 well plates [65] | Medium - Improving with automation [66] | Low |
| Ethical Considerations | Minimal | Minimal - Human cells only | Significant - Animal welfare concerns [65] |
3D Bioprinting for Complex Tissue Architecture
Core Bioprinting Technologies
3D bioprinting enables the precise, automated fabrication of complex, living tissues by layering cell-laden bioinks according to digital designs. The primary technologies differ in their mechanisms, capabilities, and optimal applications.
Table 2: 3D Bioprinting Technique Comparison
| Technique | Mechanism | Resolution | Speed | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Microextrusion | Pressure-assisted (pneumatic or mechanical) deposition of continuous bioink filaments [69] | ~100 μm [70] | Medium | High cell density printing, structural integrity for large constructs, wide bioink versatility [69] [70] | Shear stress can reduce cell viability [70] |
| Inkjet-Based | Thermal, piezoelectric, or electromagnetic expulsion of bioink droplets [69] | High (droplet-level) [69] | High | High cell viability (>85%), low cost, potential for high-speed multi-nozzle printing [69] [70] | Low viscosity bioinks required (<0.1 Pa·s), risk of nozzle clogging, limited mechanical strength [69] |
| Laser-Assisted | Laser energy to transfer bioink from a donor layer to a substrate [70] | High (pico-liter scale) [70] | Medium | No nozzle clogging, high resolution and cell viability [70] | High equipment cost, complex setup, potential for metal contamination [70] |
| Digital Light Processing (DLP) | Projection of patterned light to photopolymerize an entire layer of bioink simultaneously [69] | ~3-5 μm (XY) [69] | Very High | Fast printing speed (whole layers at once), high resolution [69] | Limited to photopolymerizable bioinks, potential for photo-toxicity [69] |
The Bioprinting Workflow
The process of creating functional, bioprinted tissues involves multiple critical stages from design to maturation.
Pre-Bioprinting Stage: The process begins with imaging (e.g., CT, MRI) to obtain the anatomical structure of the target tissue, which is converted into a digital 3D model using Computer-Aided Design (CAD) software and translated into a printable file (e.g., STL format) [14] [70]. Concurrently, bioink is formulated by combining selected cell sources (e.g., primary cells, iPSCs) with biomaterials (e.g., hydrogels, dECM) that provide structural and biochemical support [14].
Bioprinting Stage: The bioprinter deposits the bioink layer-by-layer according to the digital design using one of the core technologies (e.g., microextrusion, inkjet) to create the initial 3D construct [70].
Post-Bioprinting Stage: The printed construct is transferred to a bioreactor that provides dynamic culture conditions (e.g., nutrient perfusion, mechanical stimulation) to promote tissue maturation, enhance cell viability, and develop functional properties resembling native tissue [70].
Essential Research Reagent Solutions
The following table details key materials and reagents essential for successful 3D bioprinting and complex tissue culture.
Table 3: Essential Research Reagents for 3D Bioprinting
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Bioink Materials | Decellularized ECM (dECM), Alginate, Collagen, Hyaluronic Acid, Fibrin, Polyethylene Glycol (PEG) [14] [70] | Provides a biomimetic scaffold for cell encapsulation; delivers biochemical cues and mechanical support; critical for cell survival and tissue formation. |
| Cell Sources | Induced Pluripotent Stem Cells (iPSCs), Primary Cells, Immortalized Cell Lines [65] | iPSCs enable patient-specific modeling and limitless expansion; primary cells offer high physiological relevance; choice depends on application. |
| Specialized Cultureware | Ultra-Low Attachment (ULA) Plates, Hanging Drop Plates, Microfluidic Organ-on-a-Chip Devices [66] [65] | Promotes spontaneous spheroid formation (ULA); generates uniform spheroids (hanging drop); enables dynamic perfusion and mechanical strain (organ-chip). |
| Maturation Factors | Vascular Endothelial Growth Factor (VEGF), Transforming Growth Factor-β (TGF-β), Fibroblast Growth Factor (FGF) [14] | Directs tissue maturation and specialization; VEGF is crucial for inducing vascularization; other factors guide specific lineage development. |
Experimental Protocols for Model Validation
Protocol 1: Establishing 3D Tumor Spheroids via Ultra-Low Attachment Plates
Purpose: To generate simple, scaffold-free 3D tumor spheroids for drug penetration and efficacy studies.
Methodology:
- Surface Coating: Coat 96-well round-bottom plates with 50 μL of 0.5% poly-HEMA solution in 95% ethanol. Air-dry for 3 days under sterile conditions to create a non-adherent surface [66]. Alternatively, use commercially pre-coated ultra-low attachment plates.
- Cell Seeding: Prepare a single-cell suspension of the target cancer cell line (e.g., SW-480, HCT-116) in complete growth medium. Seed 5,000-10,000 cells in a volume of 100-200 μL per well [66] [67].
- Spheroid Formation: Centrifuge the plate at 300-500 x g for 3-5 minutes to aggregate cells at the well bottom. Incubate at 37°C, 5% CO₂ for 24-72 hours to allow for compact spheroid formation.
- Validation and Monitoring: Confirm spheroid formation and monitor growth daily using brightfield microscopy. Measure spheroid diameter to ensure uniformity (typically 200-500 μm).
- Drug Treatment: After spheroid consolidation (typically day 3-5), add chemotherapeutic agents (e.g., Doxorubicin) in fresh medium. Include vehicle controls.
- Endpoint Analysis:
- Viability: Use the CellTiter 96 AQueous Non-Radioactive Cell Proliferation Assay (MTS) [67].
- Morphology/Apoptosis: Stain with Hoechst 33342 (nuclear) and Propidium Iodide (dead cells) and image via confocal microscopy.
- Data Analysis: Compare IC₅₀ values and penetration gradients to 2D monolayer cultures.
Protocol 2: Bioprinting a Vascularized Liver Model for Toxicity Screening
Purpose: To fabricate a functional, vascularized human liver tissue model for predictive toxicology screening.
Methodology:
- Bioink Formulation:
- Parenchymal Bioink: Combine primary human hepatocytes or iPSC-derived hepatocytes (15-20 million cells/mL) with a sterile blend of 3% (w/v) gelatin methacryloyl (GelMA) and 0.5% (w/v) hyaluronic acid methacrylate [38].
- Vascular Bioink: Combine human umbilical vein endothelial cells (HUVECs, 10 million cells/mL) and human lung fibroblasts (3 million cells/mL) with 3% (w/v) GelMA.
- Bioprinting Process:
- Utilize a dual-head extrusion bioprinter.
- Load the vascular bioink and print a branching network structure with channel diameters of 150-300 μm.
- Crosslink the structure with brief UV exposure (365 nm, 5-10 seconds).
- Load the parenchymal bioink and print concentric layers around the vascular network to create a parenchymal mass.
- Perform a final crosslinking step (UV, 30-60 seconds).
- Post-Printing Maturation:
- Transfer constructs to a perfusion bioreactor.
- Culture with specialized hepatocyte culture medium, perfusing at a flow rate of 0.1-0.5 mL/min.
- Maintain for 14-28 days, with medium changes every 2-3 days.
- Functional Validation:
- Albumin/Urea Secretion: Quantify in collected supernatant via ELISA and colorimetric assays, respectively, weekly [68].
- Cytochrome P450 Activity: Measure metabolism of specific substrates (e.g., CYP3A4 using Luciferin-IPA) [65].
- Histology: Process tissue for cryosectioning and stain with H&E for morphology, and immunostain for hepatocyte markers (Albumin) and endothelial markers (CD31) to confirm vascular structure.
- Toxicity Testing:
- Dose-Response: Expose mature tissues (day 21) to known hepatotoxicants (e.g., Acetaminophen, Trovafloxacin) for 48 hours [68].
- Endpoint Assessment: Measure lactate dehydrogenase (LDH) release for cytotoxicity, monitor albumin/urea production decline, and analyze tissue viability using live/dead staining.
The transition from traditional 2D cultures and animal models to advanced 3D systems represents a fundamental evolution in biomedical research. 3D bioprinting technologies stand at the forefront of this shift, offering unprecedented control over the fabrication of complex, human-relevant tissues with defined architectures and multicellular compositions. The quantitative and functional superiority of these models—from their ability to maintain physiological gene expression and metabolic profiles to their capacity for modeling drug penetration gradients and long-term toxicity—makes them indispensable for bridging the translational gap. As the field matures with advancements in bioink design, vascularization strategies, and integration with AI-driven analytics, 3D bioprinted models are poised to become the central platform for target validation, lead optimization, and personalized therapy screening, ultimately accelerating the delivery of safer, more effective therapeutics to patients.
The global burden of liver disease represents a significant public health challenge, with more than 2 million deaths annually attributed to hepatic conditions worldwide [71]. In pharmaceutical development, drug-induced liver injury (DILI) remains a primary cause of drug attrition during clinical trials and post-market withdrawal, highlighting the critical limitations of conventional preclinical models [72] [73]. Traditional two-dimensional (2D) hepatocyte cultures and animal models often fail to accurately predict human-specific drug responses due to their inadequate replication of the complex cellular microenvironment, metabolic zonation, and immune interactions characteristic of human liver physiology [71] [74].
This case study examines the convergence of 3D bioprinting technologies and microphysiological systems (MPS) to create advanced liver organoid platforms for toxicity testing. Framed within a broader thesis on 3D bioprinting for complex tissue architecture research, we explore how these technologies address the physiological limitations of previous models through precise spatial control over cellular organization, incorporation of vascular networks, and integration of patient-specific immune components [75] [76]. The resulting platforms demonstrate unprecedented capability in predicting human-relevant toxicological responses, thereby accelerating drug development while reducing reliance on animal testing.
Technical Foundations: Biofabrication Technologies for Liver Organoids
3D Bioprinting Modalities
The fabrication of physiologically relevant liver organoids employs several bioprinting technologies, each offering distinct advantages for specific architectural requirements:
Extrusion-Based Bioprinting: This widely used technique employs continuous deposition of viscous bioinks through a nozzle, enabling the creation of large, complex structures with high cell density. With a resolution range of 100-500 μm, extrusion-based systems can process high-viscosity bioinks (30-60 kPa·s) and are particularly valuable for creating dense tissue constructs with embedded vascular channels [69] [76]. Recent innovations include temperature-controlled printheads and advanced pneumatic dispensing mechanisms that maintain cell viability despite inherent shear stresses [76].
Inkjet-Based Bioprinting: Utilizing thermal or piezoelectric actuators to deposit droplets of low-viscosity bioink, this approach offers high-resolution patterning (100-500 μm) with excellent cell viability. While limited by its constraint to low-viscosity materials and challenges in creating large structures, inkjet bioprinting enables precise cellular positioning and minimal material waste [69].
Light-Based Bioprinting: Including stereolithography (SLA) and digital light processing (DLP), these techniques use projected light patterns to crosslink photopolymerizable bioinks layer-by-layer, achieving high resolutions down to 10 μm. Particularly effective for fabricating intricate vascular networks, SLA/DLP bioprinting produces smooth surface finishes but faces challenges with uniform cell distribution [69] [76]. An emerging technique, volumetric bioprinting (VBP), enables rapid formation of entire 3D structures within seconds through holographic-like light projection, eliminating layer-by-layer fabrication [76].
Laser-Assisted Bioprinting: This nozzle-free approach uses focused laser energy to transfer small bioink volumes onto a substrate, achieving exceptional precision (<10 μm) and high cell viability (>95%). Although slower and more complex than other methods, laser-assisted bioprinting enables single-cell placement control for highly sophisticated tissue architectures [69].
Table 1: Comparison of Bioprinting Technologies for Liver Organoid Fabrication
| Bioprinting Technology | Resolution | Cell Viability | Speed | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Extrusion-Based | 100-500 μm | Moderate (shear stress-dependent) | Medium | High cell density, versatile material compatibility | Nozzle clogging, mechanical stress on cells |
| Inkjet-Based | 100-500 μm | High (>85%) | Fast | Precise droplet control, multi-material capability | Low viscosity bioinks only, limited structural integrity |
| SLA/DLP | 10-50 μm | Moderate-High (70-90%) | Fast (VBP: seconds) | High resolution, smooth surfaces | Limited bioink options, light scattering with high cell density |
| Laser-Assisted | <10 μm | High (>95%) | Slow | Superior precision, nozzle-free | High cost, complex operation |
Advanced Bioink Formulations
Bioinks serve as the foundational matrix for bioprinted liver organoids, providing both structural support and biochemical cues that direct cellular behavior. Advanced bioink formulations have evolved significantly from simple hydrogel systems to sophisticated multi-component blends that better recapitulate the native liver extracellular matrix (ECM) [71] [76].
Key innovations in bioink development include:
Decellularized Liver ECM (dECM): Harvested from porcine or human liver tissues, dECM bioinks preserve native biochemical composition including collagen, glycosaminoglycans, and liver-specific growth factors. These materials provide tissue-specific cues that enhance hepatocyte maturation and function in printed constructs [71].
Hybrid Polymer Systems: Combining natural polymers like gelatin, alginate, or chitosan with synthetic polymers such as Pluronic F127 or polyethylene glycol (PEG) creates bioinks with tunable mechanical properties and improved printability. For instance, a formulation containing 5% gelatin and 2% sodium alginate has successfully supported hepatocyte function and long-term viability in bioprinted liver constructs [71].
Functionalized Hydrogels: Incorporation of liver-specific peptides (e.g., RGD sequences) and growth factors (e.g., HGF, EGF) into hydrogel networks enhances cellular adhesion and maturation. These functionalized bioinks guide hepatic differentiation and promote the formation of bile canaliculi-like structures [77] [76].
Experimental Framework: Protocols for Liver MPS Development
Protocol 1: Fabrication of a Bioprinted Vascularized Liver Organoid
This protocol details the creation of a perfusable liver organoid with embedded vasculature using the SWIFT (Sacrificial Writing into Functional Tissue) technique developed at the Wyss Institute [75].
Materials Required:
- Primary human hepatocytes or iPSC-derived hepatocyte progenitors
- Human umbilical vein endothelial cells (HUVECs) or liver sinusoidal endothelial cells
- Human mesenchymal stem cells (MSCs)
- Gelatin-based sacrificial bioink
- Fibrinogen-thrombin hydrogel matrix
- Organ building blocks (OBBs) from stem-cell-derived aggregates
- Extrusion bioprinter with temperature-controlled printhead
- Perfusion bioreactor system
Methodology:
Preparation of Organ Building Blocks (OBBs):
- Differentiate iPSCs into hepatic progenitors using a defined protocol with Activin A, BMP4, and FGF2 over 7 days.
- Aggregate hepatic progenitors into spheroids (200-300 μm diameter) using forced aggregation plates or hanging drop method.
- Concentrate OBBs into a living matrix at approximately 200 million cells/mL.
Sacrificial Bioprinting:
- Load sacrificial gelatin-based bioink into temperature-controlled printhead (maintained at 20°C).
- Print interconnected vascular network patterns within the OBB matrix.
- Incubate construct at 37°C to liquefy and remove sacrificial ink, creating patent channels.
Endothelial Seeding:
- Introduce HUVEC suspension (5-10×10⁶ cells/mL) into vascular channels via perfusion.
- Culture under continuous perfusion (2-5 μL/min flow rate) for 7-14 days to form confluent endothelium.
Functional Assessment:
- Evaluate albumin secretion via ELISA (target: >40 μg/day/10⁶ cells).
- Assess urea production via colorimetric assay (target: >100 μg/day/10⁶ cells).
- Measure cytochrome P450 activity (CYP3A4) using luciferin-IPA conversion assay.
The following workflow diagram illustrates the key steps in this vascularized liver organoid fabrication process:
Protocol 2: Establishing an Immune-Competent Liver Organoid Platform
This protocol describes the creation of a patient-specific immune-competent liver model for predicting idiosyncratic drug-induced liver injury (iDILI), based on the platform developed by Cincinnati Children's Hospital in collaboration with Roche [72] [73].
Materials Required:
- Patient-derived iPSCs
- Autologous CD8⁺ T cells isolated from peripheral blood
- Matrigel or synthetic ECM substitute
- Hepatocyte differentiation media (sequential formulations)
- T cell activation media (IL-2, IL-7, IL-15)
- Flucloxacillin or other iDILI compounds
- Microarray platform or 96-well format
Methodology:
Hepatocyte Differentiation from iPSCs:
- Culture iPSCs in mTeSR1 medium until 80% confluency.
- Initiate definitive endoderm differentiation using RPMI 1640 with 100 ng/mL Activin A for 3 days.
- Differentiate into hepatic progenitors using 20 ng/mL BMP4 and 10 ng/mL FGF2 for 5 days.
- Mature into hepatocyte-like cells with 20 ng/mL HGF and 10 ng/mL Oncostatin M for 10-14 days.
- Form 3D organoids by embedding in Matrigel droplets.
Autologous T Cell Preparation:
- Isolate PBMCs from patient blood samples via density centrifugation.
- Enrich CD8⁺ T cells using magnetic bead separation.
- Activate T cells with anti-CD3/CD28 antibodies in presence of IL-2 (100 IU/mL) for 3 days.
- Maintain in T cell media with IL-7 and IL-15 (5 ng/mL each).
Co-Culture Establishment:
- Transfer liver organoids to microarray platform or ultra-low attachment 96-well plates.
- Add activated autologous CD8⁺ T cells at 2:1 ratio (T cells:hepatocytes).
- Maintain in hepatocyte-T cell co-culture medium.
iDILI Challenge and Assessment:
- Expose to flucloxacillin (250-500 μM) or vehicle control for 7 days.
- Monitor T cell activation via flow cytometry (CD69, CD25 expression).
- Measure cytokine secretion (IFN-γ, TNF-α) via multiplex ELISA.
- Quantify hepatocyte damage via LDH release and albumin secretion.
Table 2: Key Research Reagents for Immune-Competent Liver Organoid Platform
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Stem Cells | Patient-derived iPSCs | Provide genetically relevant hepatocytes | Screen for HLA-B*57:01 allele for flucloxacillin sensitivity |
| Differentiation Factors | Activin A, BMP4, FGF2, HGF, Oncostatin M | Direct hepatic differentiation from iPSCs | Oncostatin M critical for mature hepatocyte function |
| Immune Cells | Autologous CD8⁺ T cells | Mediate immune-specific drug reactions | Isolate from same donor as iPSCs for genetic matching |
| ECM Substrates | Matrigel, synthetic hydrogels | Provide 3D structural support | Use defined synthetic matrices for enhanced reproducibility |
| iDILI Triggers | Flucloxacillin, Diclofenac, Nevirapine | Model immune-mediated drug toxicity | Dose-response essential; use therapeutic concentrations |
Case Study Analysis: Applications in Predictive Toxicology
Recapitulating Idiosyncratic Drug-Induced Liver Injury
The immune-competent liver organoid platform represents a breakthrough in modeling idiosyncratic drug-induced liver injury (iDILI), which has remained particularly challenging to predict using conventional models [72]. When exposed to flucloxacillin, an antibiotic known to cause iDILI exclusively in carriers of the HLA-B*57:01 genetic variant, the platform demonstrated patient-specific toxicity that closely mirrored clinical observations [72] [73].
Key findings from this application include:
- T Cell Activation: HLA-B*57:01-positive models showed significant CD8⁺ T cell activation (measured by CD69 and CD25 surface expression) following flucloxacillin exposure, while HLA-mismatched controls remained unresponsive.
- Cytokine Release: Activated T cells secreted elevated levels of pro-inflammatory cytokines including IFN-γ and TNF-α, establishing an inflammatory microenvironment characteristic of clinical iDILI.
- Hepatocyte Damage: Markers of hepatocyte injury including LDH release and reduced albumin synthesis were specifically observed in HLA-matched combinations, demonstrating the immune-mediated cytotoxicity [72].
This model successfully addresses a critical gap in pharmaceutical safety testing by incorporating the genetic predisposition and immune components necessary for predicting rare but serious adverse drug reactions.
Modeling Metabolic Zonation and Zone-Specific Toxicity
The liver exhibits remarkable functional heterogeneity along the portocentral axis, with distinct metabolic processes partitioned into different zones. This metabolic zonation critically influences zone-specific susceptibility to hepatotoxicants, a feature that conventional liver models fail to recapture [78].
Recent advances have enabled the generation of multi-zonal human liver organoids (mZ-HLOs) that mimic this physiological organization:
- Zone-Specific Differentiation: By engineering hepatic progenitors with inducible ascorbate synthesis (promoting zone 1 identity) and applying low-dose bilirubin (promoting zone 3 fate), researchers created distinct zonal populations that self-assemble into fused organoids [78].
- Toxicant Sensitivity: The mZ-HLOs demonstrated appropriate zone-specific toxic responses, with allyl alcohol selectively injuring periportal (zone 1) regions and acetaminophen affecting pericentral (zone 3) zones, accurately mirroring known hepatotoxin susceptibility patterns in human liver [78].
- Regulatory Mechanisms: Single-nucleus RNA sequencing confirmed distinct hepatocyte subpopulations with periportal, interzonal, and pericentral identities, while chromatin accessibility mapping identified EP300 as a central regulator of zonal gene expression [78].
The following diagram illustrates the signaling pathways and cellular organization involved in establishing metabolic zonation:
Quantitative Assessment of Organoid Functionality
Rigorous functional characterization is essential for validating liver organoid models. The table below summarizes key functional parameters for assessing physiological relevance in toxicity testing applications:
Table 3: Functional Benchmarking of Advanced Liver Organoid Models
| Functional Category | Specific Assay | Conventional 2D Models | Advanced 3D Organoids | Human Liver Reference |
|---|---|---|---|---|
| Synthetic Function | Albumin Secretion (μg/day/10⁶ cells) | 5-15 | 25-50 | 50-100 |
| Faktor V, VII, VIII, IX Production | Minimal | Detectable | Physiological levels | |
| Metabolic Capacity | CYP3A4 Activity (pmol/min/mg) | 50-200 | 300-800 | 500-2000 |
| Urea Production (μg/day/10⁶ cells) | 50-100 | 150-300 | 200-500 | |
| Ammonia Clearance | Limited | Significant | Complete | |
| Toxicity Prediction | Acetaminophen LD₅₀ (mM) | 5-10 | 2-5 | 2-5 |
| Flucloxacillin iDILI (HLA-B*57:01) | No prediction | Accurate prediction | Clinical correlation | |
| Architectural Features | Bile Canaliculi Formation | Limited | Extensive | Physiological |
| Metabolic Zonation | Absent | Present | Defined zonation | |
| Vascular Network | Absent | Engineered | Extensive |
Integration with Microphysiological Systems
The convergence of 3D bioprinting with microfluidic organ-on-chip technology represents the cutting edge of liver MPS development [76] [74]. This integration addresses critical limitations of standalone organoid systems by introducing dynamic perfusion, mechanical cues, and multi-tissue interactions that better mimic physiological conditions.
Key integration strategies include:
Perfusable Microenvironments: Microfluidic systems enable continuous medium flow through bioprinted constructs, overcoming diffusion limitations and supporting higher cell densities and enhanced functionality. The "Chronotoxici-plate" system developed by Zhou et al. combines microfluidics with 3D printing to maintain circadian rhythms in primary liver organoids, enabling temporal toxicity assessment of compounds like oxaliplatin [71].
Multi-Organ Integration: Bioprinted liver organoids can be fluidically coupled with other tissue models (e.g., intestine, kidney) to simulate systemic drug absorption, metabolism, and excretion. These multi-organ chips provide insights into organ-organ interactions and metabolite-mediated toxicity that cannot be captured in isolated liver models [76].
Sensory Feedback Systems: Advanced MPS platforms incorporate real-time monitoring through embedded biosensors that track oxygen consumption, glucose metabolism, and barrier integrity non-invasively. This enables continuous functional assessment throughout toxicity studies [76].
The integration of 3D bioprinting with microphysiological systems has produced transformative advances in liver organoid technology for toxicity testing. These platforms now demonstrate unprecedented physiological relevance through their structural complexity, metabolic functionality, and patient-specific immune responses. The case studies examined herein highlight the remarkable progress in modeling complex liver phenomena including idiosyncratic drug reactions, metabolic zonation, and vascularized tissue maturation.
Looking forward, several emerging technologies promise to further enhance the capabilities of liver MPS:
- 4D Bioprinting: Incorporating dynamic, time-responsive materials that enable post-printing morphological changes and tissue self-organization [76].
- AI-Driven Design: Utilizing machine learning algorithms to optimize bioink formulations, architectural parameters, and culture conditions based on predictive modeling of tissue function [76].
- High-Throughput Screening: Implementing automated bioprinting and analysis systems like the HITS-Bio technology that can produce tissue constructs 10-times faster than conventional methods, enabling large-scale toxicological screening [5].
As these technologies mature and undergo regulatory validation, bioprinted liver organoid platforms are poised to fundamentally transform pharmaceutical safety assessment, ultimately providing more predictive, human-relevant toxicity models that reduce drug attrition and improve patient safety.
The transition of 3D bioprinting from a promising prototyping technology to a reliable tool for creating complex tissue architectures hinges on the development and implementation of robust, quantitative assessment metrics. While the field has mastered the deposition of cell-laden bioinks in intricate geometries, the true challenge lies in conclusively demonstrating that these constructs mature into functional tissue equivalents. The biological functionality of a printed construct is not guaranteed by printability alone; it depends on a host of geometric, mechanical, and biological factors that collectively create a microenvironment conducive to cell growth, organization, and eventual tissue formation [79]. Without thorough quantitative evaluation, providing desired conditions for cell growth and, therefore, the biological function of the formulated new tissue remains speculative [79].
This guide provides a comprehensive framework for researchers and drug development professionals to quantify the success of bioprinted constructs. It moves beyond qualitative assessments to detail specific, quantifiable metrics and the methodologies required to measure them, thereby ensuring that bioprinted tissues meet the rigorous standards necessary for both complex tissue architecture research and preclinical applications.
Core Quantitative Metrics for Bioprinted Constructs
A multi-faceted approach to assessment is essential, as no single metric can fully capture the complexity of a developing tissue. The following categories of metrics provide a holistic view of construct functionality.
Geometric and Structural Fidelity Metrics
Geometric fidelity ensures the printed construct matches the designed architecture, which is critical for proper nutrient diffusion, cell-cell interaction, and ultimately, physiological function. Evaluations should transition from subjective visual comparisons to objective, quantitative measures.
Table 1: Metrics for Geometric and Structural Fidelity
| Metric | Description | Quantification Method | Target Value/Indicator |
|---|---|---|---|
| Printability (Pr) | Measures the gelation degree and ability to form defined structures [9]. | ( P_r = \frac{L^2}{16A} ) (where L is perimeter and A is area of pores) [9]. | A value of 1 indicates ideal gelation and square pores [9]. |
| Pore Size & Shape Fidelity | Accuracy of interconnected channel geometry versus design [9]. | Image analysis (e.g., ImageJ) of printed construct micrographs [9]. | High similarity to CAD model; absence of filament fusion or collapse [9]. |
| Filament Diameter Uniformity | Consistency of extruded filament diameter [79]. | Online or offline measurement using 3D structured light scanning or high-resolution microscopy [79] [80]. | Low coefficient of variation (<5%) across the construct [79]. |
| Layer Stacking Accuracy | Precision in depositing sequential layers [79]. | 3D reconstruction via structured light camera or OCT, comparing to digital model [79] [80]. | High Z-directional similarity to the designed model [79]. |
Mechanical Property Metrics
The mechanical properties of a construct are not merely structural; they provide critical biomechanical cues that guide cell behavior through mechanotransduction pathways [80]. These properties must be monitored dynamically, as they evolve during and after the printing process.
Table 2: Metrics for Mechanical Properties
| Metric | Description | Quantification Method | Relevance to Function |
|---|---|---|---|
| Storage Modulus (G') | The elastic (solid-like) component of the material's response, indicating stiffness [80] [9]. | Oscillatory rheometry; Ultrasound Shear Wave Elastography with Kelvin-Voigt modeling for in-situ assessment [80] [9]. | Mimics native tissue stiffness; crucial for cell differentiation and maturation [80]. |
| Complex Viscosity ((\eta^*)) | Resistance to flow during extrusion, a key rheological property [9]. | Time-sweep tests via rheometry at printing-relevant temperatures [9]. | Predicts printability and cell viability during extrusion; should be stable during printing [9]. |
| Stress Relaxation | The decrease in stress under a constant strain, indicating viscoelasticity [9]. | Compression-tension or stress relaxation tests on printed mesostructures [9]. | Influences how cells sense and remodel their microenvironment [9]. |
Biological Performance Metrics
Ultimately, the success of a bioprinted construct is determined by its biological performance. This encompasses not only cell survival post-printing but also the ability of cells to proliferate, function, and organize as they would in native tissue.
Table 3: Metrics for Biological Performance
| Metric | Description | Quantification Method | Significance |
|---|---|---|---|
| Cell Viability | Percentage of live cells post-printing. | Live/Dead staining assays conducted at multiple time points (e.g., 1, 7, 21 days) [81]. | High viability (>80-90%) is a baseline requirement for functional success [81]. |
| Cell Proliferation | The rate at which cells divide within the construct. | Metabolic activity assays (e.g., AlamarBlue) and DNA quantification [81]. | Indicates a hospitable microenvironment and potential for tissue growth. |
| Cell Organization & Maturation | The spatial arrangement and development of tissue-specific structures (e.g., aligned myotubes, vascular networks). | Immunohistochemistry for tissue-specific markers and cytoskeletal proteins; confocal microscopy [79] [81]. | Demonstrates progression beyond simple viability toward true tissue-level functionality [79]. |
| Biomolecule Secretion | Production of tissue-specific proteins or factors (e.g., albumin by hepatocytes, ECM proteins). | ELISA, RT-PCR of extracted RNA [81]. | Confirms maintenance of cell phenotype and specialized function. |
Advanced Experimental Protocols for Functional Assessment
Protocol for Real-Time Mechanical Characterization During Bioprinting
The Suspended Bioprinting with In-situ Elasticity Monitoring (SBEM) method allows for nondestructive, quantitative tracking of the storage modulus during the fabrication process [80].
- Setup Integration: Couple a bioprinter with an ultrasound transducer equipped for shear wave elastography. The transducer should be positioned to interrogate the print area within the support bath.
- Bioink Preparation: Prepare a gelatin-based or other photocrosslinkable bioink. For acoustic coupling, incorporate 1% (w/v) psyllium hydrophilic mucilloid fibers (average size 58 ± 15 μm) as acoustic scatterers [80].
- Shear Wave Generation and Data Acquisition: The ultrasound system generates acoustic radiation force to induce micron-scale shear waves within the printed scaffold. Acquire ultrasound In-phase/Quadrature (IQ) data at a high frame rate (e.g., 8000 Hz) to track the shear wave propagation [80].
- Phase Velocity Estimation: Process the IQ data to estimate the shear wave phase velocity at multiple frequencies.
- Elasticity Calculation: Fit the frequency-dependent phase velocity data to a rheological model, such as the Kelvin-Voigt model, to estimate the storage modulus of the scaffold in real-time [80].
- Dynamic Monitoring: Continuously monitor elasticity changes during key process steps, such as photocrosslinking under varying ultraviolet (UV) irradiation durations, to establish a crosslinking-elasticity relationship.
Protocol for High-Resolution Geometric Fidelity Assessment
This protocol uses a 3D visual measurement framework to accurately segment and evaluate the geometric parameters of a bioprinted construct immediately after printing [79].
- System Calibration: Employ a high-accuracy 3D structured light camera (e.g., Zivid Two M70). Calibrate the system for the specific working distance and environmental conditions of the bioprinter.
- Image Acquisition: Immediately after printing, capture a 3D point cloud and a high-resolution 2D image of the construct.
- Data Processing with Computer Vision:
- Apply complementary 2D/3D computer vision algorithms to the acquired data.
- Use the 2D image for initial segmentation of the construct's boundaries.
- Project these boundaries onto the 3D point cloud to achieve an accurate reconstruction of the printed geometry.
- Quantitative Analysis: From the 3D reconstruction, automatically extract key geometric parameters, including:
- Average filament diameter and its standard deviation.
- Pore size and shape fidelity compared to the CAD model.
- Layer height and overall construct thickness.
- Scoring: Utilize novel assessment metrics developed within the evaluation module to generate quantitative scores for uniformity and accuracy, which can then be correlated to printing parameters to find optimal conditions [79].
Visualization of Assessment Workflows
Bioprinted Construct Assessment Workflow
In-Situ Elasticity Monitoring Setup
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Bioprinting Assessment
| Item | Function / Role in Assessment | Example & Notes |
|---|---|---|
| Alginate-Gelatin (AG) Hydrogel | A widely used composite bioink for assessing printability and mechanical effects of mesostructures [9]. | Typical concentration: 2% (w/v) alginate, 5% (w/v) gelatin. Crosslinkable with CaCl₂, allowing study of geometric fidelity in multi-layered structures [9]. |
| Gelatin Methacryloyl (GelMA) | A versatile, photocrosslinkable bioink supporting high cell viability; ideal for studying cell-material interactions [81]. | Allows tuning of mechanical properties via UV crosslinking; contains integrin-binding motifs for cell adhesion [81]. |
| Structured Light 3D Camera | Enables online, accurate 3D reconstruction and measurement of printed constructs for geometric fidelity analysis [79]. | e.g., Zivid Two M70. Used with complementary 2D/3D computer vision algorithms for segmentation [79]. |
| Ultrasound Shear Wave Elastography System | Provides nondestructive, in-situ quantification of the storage modulus of printed scaffolds during fabrication [80]. | Key for the SBEM method; tracks dynamic mechanical changes, crucial for soft tissue constructs [80]. |
| Acoustic Scatterers | Mixed into bioinks to enable effective ultrasound imaging and elastography within homogeneous constructs [80]. | e.g., Psyllium hydrophilic mucilloid fibers (1% w/v, ~58 μm average size) [80]. |
| Live/Dead Viability Assay | The standard fluorescent assay for quantifying cell survival and distribution post-printing. | Conducted at multiple time points to assess not only immediate shear stress effects but also long-term biocompatibility [81]. |
The pathway to reliable and clinically impactful bioprinting is paved with quantitative data. Relying on qualitative assessments or post-printing evaluations alone is insufficient to guarantee the biological functionality of a construct. By integrating the multi-dimensional metrics and advanced protocols outlined in this guide—spanning geometric, mechanical, and biological performance—researchers can move beyond simple shape replication to the engineering of living tissues with defined and predictable function. This rigorous, quantitative framework is indispensable for advancing the field of 3D bioprinting, enabling its full potential in complex tissue architecture research, drug development, and ultimately, regenerative medicine.
The field of 3D bioprinting stands at a pivotal juncture, having demonstrated remarkable feasibility in laboratory settings for creating complex, tissue-like structures. However, its journey from research innovation to mainstream clinical application is fraught with significant challenges. The transition into clinical practice requires navigating a labyrinth of regulatory hurdles, standardization deficits, and technical bottlenecks that must be systematically addressed. This technical guide examines the current landscape of clinical translation for 3D bioprinted tissues, with particular focus on the regulatory pathways and standardization initiatives that will define the future of this transformative technology. As the field evolves from creating simple tissue constructs to engineering complex tissue architectures that mimic native organ structures, understanding these frameworks becomes increasingly critical for researchers, scientists, and drug development professionals working at the forefront of regenerative medicine.
The Current Clinical Landscape of 3D Bioprinting
Quantitative Assessment of Clinical Trial Activity
The clinical translation of 3D bioprinting remains in its nascent stages, with limited but strategically focused trial activity globally. A comprehensive scoping review published in 2025 identified only 11 registered clinical trials that met rigorous criteria for bioprinting applications, with registration dates ranging from 2016 to 2023 [82]. This low number reflects both the technical immaturity of the field and the significant regulatory barriers to clinical entry.
Table 1: Global Distribution and Status of Clinical Trials Involving Bioprinting
| Country | Number of Trials | Primary Applications | Status Overview |
|---|---|---|---|
| China | Most active globally | Implantation and in vitro modeling | Multiple trials ongoing |
| Various (unspecified) | 11 total trials | Regenerative medicine and disease modeling | 4 with published results, 7 ongoing [82] |
The geographical distribution of these trials reveals China as the most active country in clinical bioprinting research, while the limited overall number underscores the global challenge in moving from preclinical validation to human studies.
Primary Clinical Applications in Current Trials
Current clinical applications of bioprinting fall into two distinct categories, each with different regulatory implications:
Implantation Trials: Four interventional trials aim to implant bioprinted tissues created with autologous cells, including blood vessels, trachea, external ear, and wound dressings [82]. These applications represent areas where regulatory pathways are more clearly defined, leveraging existing frameworks for tissue-engineered products.
In Vitro Modeling: Seven interventional and observational trials focus on bioprinting autologous cell-laden in vitro models to study conditions such as cancer [82]. These models serve as platforms for precision medicine, particularly in oncology, where patient-specific tissue models can guide treatment selection without direct implantation challenges.
Technical and Regulatory Hurdles in Clinical Translation
Standardization Deficits in Bioprinting Processes
The absence of well-regulated international standards represents a critical barrier to clinical translation, creating uncertainty among stakeholders regarding reliable and scalable production processes [52]. Standardization needs span multiple aspects of the bioprinting workflow:
Table 2: Key Standardization Gaps in 3D Bioprinting for Clinical Translation
| Standardization Area | Current Challenges | Impact on Clinical Translation |
|---|---|---|
| Bioink Characterization | Sub-optimal properties, lack of defined composition | Variable cell viability, unpredictable tissue formation |
| Process Controls | Undefined printing and post-printing processes | Batch-to-batch variability, poor reproducibility |
| Cell Sourcing | Lack of stem/progenitor cells for massive expansion | Limited scale, functional immaturity of constructs |
| Vocabulary | Inconsistent terminology across field | Impedes regulatory review, collaboration, and benchmarking |
The European Union has recognized these challenges, with standardization initiatives aligning with the EU Industry 5.0 strategy that highlights the importance of innovation and sustainability [83]. Workshops facilitated by organizations such as CEN-CENELEC aim to establish networks for collaboration, knowledge-sharing, and development of standards that meet stakeholder needs [83].
Technical Bottlenecks in Tissue Maturation and Functionality
Beyond standardization, significant technical hurdles impede the development of clinically relevant tissue equivalents:
Vascularization Limitations: Engineering vasculature capable of supporting thick, metabolically active tissues remains a fundamental challenge. While advances have enabled creation of vascularized tissues nearly ten times thicker than previous constructs, these still fall short of supporting complex organ architectures [14].
Functional Immaturity: Current bioprinted tissues often lack the functional maturity of native tissues, with limitations in mechanical properties, biochemical signaling, and long-term stability [52]. The achievement of functionally-mature, clinically-relevant tissue equivalents requires breakthroughs in biomimicry of bioprintable architectures and fundamental knowledge regarding in vitro culturing conditions [52].
Manufacturing Scalability: The transition from laboratory-scale production to industrial manufacturing presents substantial challenges in quality control, sterility assurance, and process validation that must be addressed within regulatory frameworks.
Experimental Protocols for Validating Bioprinted Constructs
Comprehensive Pre-bioprinting Workflow
The pre-bioprinting stage establishes the foundation for successful construct development and requires rigorous protocol implementation:
Digital Design Phase: Create a 3D digital model of the target tissue using Computer-aided design (CAD) software, 3D scanning of existing tissues, or medical imaging data (e.g., CT or MRI scans) [14].
File Conversion: Convert the digital model into a printable file format, typically STL (native to stereolithography CAD software) or G-code that provides layer-by-layer instructions for the bioprinter [14].
Biomaterial Selection: Choose biomaterials based on mechanical properties, biocompatibility, and functional requirements of the target tissue. This selection directly impacts the mechanical properties, biocompatibility, and functionality of the printed structure [14].
Essential Post-bioprinting Validation Procedures
Post-bioprinting processes are critical for assessing construct functionality and safety:
Incubation Protocols: Maintain printed structures in appropriate bioreactor systems to provide stability and promote tissue growth. Parameters must be optimized for specific tissue types, including mechanical stimulation, perfusion rates, and biochemical signaling [14].
Mechanical Testing: Evaluate structural integrity through standardized tests including compression testing, tensile strength measurement, and fatigue resistance assessment under conditions mimicking the physiological environment [14].
Functional Assessment: Employ tissue-specific functional assays such as contractility measurements for cardiac tissue, albumin production for hepatic tissue, or neurotransmitter release for neural tissue.
Biological Safety Testing: Conduct comprehensive evaluations including sterility testing, endotoxin detection, and assessment of biomaterial degradation products to ensure compliance with regulatory safety requirements.
The following workflow diagram illustrates the complete bioprinting validation pipeline from design to functional assessment:
Regulatory Frameworks and Standardization Initiatives
Evolving Regulatory Considerations for Bioprinted Products
The regulatory landscape for 3D bioprinted tissues is evolving alongside the technology itself, with several key considerations emerging:
Classification Challenges: Regulatory agencies struggle with classifying bioprinted products that combine living cells, biomaterials, and manufacturing processes, existing at the intersection of medical devices, biologics, and combination products [52].
Quality Control Requirements: Demonstrating consistent quality across batches requires rigorous control of raw materials (including cell sources and bioinks), manufacturing processes, and final product characterization [83].
Ethical and Legal Dimensions: The ethical and legal aspects of bioprinting, including intellectual property, safety accountability, and the use of stem cells, represent underappreciated challenges that must be addressed within regulatory frameworks [52].
The regulatory pathway is further complicated by the absence of specific guidelines tailored to bioprinted tissues, requiring manufacturers to adapt existing frameworks for tissue-engineered products while advocating for regulatory science development in this emerging field.
International Standardization Efforts
Recognizing these challenges, international standards organizations have initiated efforts to create structured frameworks for bioprinting. The European Union's CEN-CENELEC workshops focus on developing comprehensive standards covering:
- Reliable and well-characterized bioinks and cells
- Defined printing and post-printing processes
- Standardized vocabulary and terminology [83]
These initiatives align with the EU's priority areas for 2024-2029, emphasizing innovation and competitiveness, particularly in the context of the Commission Communication "Building the future with nature: Boosting Biotechnology and Biomanufacturing in the EU" [83].
Future Directions and Transformative Technologies
Emerging Technologies Enhancing Clinical Translation
Several cutting-edge technologies show promise for accelerating the clinical translation of bioprinted tissues:
Advanced Spatial Analysis: New technologies like RAEFISH (Reverse-padlock Amplicon Encoding Fluorescence In Situ Hybridization) enable researchers to view RNA molecules directly inside cells and tissue in minute detail across the entire human genome concurrently [84]. This provides unprecedented insight into gene expression patterns within bioprinted constructs, potentially enhancing quality control and functional validation.
AI-Powered Foundation Models: The development of foundation models like Nicheformer, which integrates single-cell analysis with spatial transcriptomics, offers new capabilities for studying how cells are organized and interact in tissues [85]. Trained on more than 110 million cells, such models can help establish predictive benchmarks for tissue functionality and maturation.
Tissue Code Decryption: Recent research has uncovered a surprisingly simple "tissue code" consisting of five rules that choreograph when, where, and how cells divide, move, and die in tissues [86] [87]. These rules encompass:
- Timing of cell division
- The order in which cells divide
- The direction cells divide and move
- How many times cells divide
- How long a cell lives before it dies [87]
Understanding this code could fundamentally transform tissue engineering approaches by providing a blueprint for achieving self-organization in bioprinted constructs.
Strategic Roadmaps for Clinical Implementation
A research-led workshop focusing on building and rebuilding complex tissues highlighted the need for concerted, long-term studies at the community level to compare regeneration and wound healing in both regenerative and non-regenerative contexts and organisms [88]. Such comparative analyses can identify fundamental principles of tissue organization that inform bioprinting strategies.
Future development should also embrace transformative concepts including:
- 4D Bioprinting: Creating structures that evolve over time in response to environmental cues or programmed signals [52]
- Microgravity Bioprinting: Leveraging space-based environments to create more complex tissue architectures [52]
- AI Integration: Implementing artificial intelligence throughout the bioprinting workflow to enhance precision, predictability, and quality control [52]
Essential Research Reagents and Materials
Successful clinical translation of bioprinted tissues requires carefully selected research reagents and materials that meet regulatory standards for quality and traceability.
Table 3: Research Reagent Solutions for Clinical-Grade Bioprinting
| Reagent Category | Key Functions | Clinical Translation Considerations |
|---|---|---|
| Decellularized ECM (dECM) Bioinks | Provides tissue-specific biochemical cues, enhances cell viability and differentiation [14] | Source traceability, pathogen testing, batch-to-batch consistency |
| Exosome-Enhanced Formulations | Improves intercellular communication, tissue formation [14] | Standardized isolation protocols, characterization, dosing metrics |
| 2D Nanomaterials (e.g., Graphene) | Enhances electrical conductivity, mechanical properties [14] | Biocompatibility profiling, degradation product analysis |
| Autologous Cell Sources | Patient-specific cells eliminating rejection risk [82] | Expansion protocols, quality control, potency assays |
| Vascularization Biofactors | Promotes blood vessel formation in thick tissues [14] | Defined composition, activity validation, stability data |
The path to clinical translation for 3D bioprinted tissues requires a multifaceted approach addressing simultaneous technical optimization and regulatory alignment. While current clinical trial activity remains limited, strategic focus on applications with clearer regulatory pathways—such as in vitro cancer models and implantable structures like blood vessels and trachea—provides valuable stepping stones toward more complex tissues. Success will depend on collaborative efforts between researchers, regulatory bodies, and standards organizations to establish robust frameworks ensuring quality, reliability, and reproducibility. By embracing emerging technologies in spatial analysis, artificial intelligence, and tissue code decryption, while actively participating in standardization initiatives, the research community can systematically overcome existing hurdles. The coming decade will prove critical in determining whether 3D bioprinting can fulfill its potential to bridge the gap between organ demand and availability, ultimately transforming healthcare through engineered functional tissues.
Conclusion
The field of 3D bioprinting for complex tissue architecture is rapidly progressing from a promising technology to a practical tool with profound implications for biomedical research and clinical practice. The synthesis of advanced bioinks, intelligent process control, and high-throughput methodologies is systematically addressing long-standing challenges in reproducibility, scalability, and vascularization. The successful validation of these tissues as predictive models for drug screening and disease study marks a paradigm shift, potentially reducing reliance on inadequate 2D models and ethically contentious animal testing. Future directions must focus on the integration of multi-cellular systems and complex vasculature to create larger, more functional tissue constructs, the continued development of smart biomaterials, and the establishment of clear regulatory pathways. The ongoing convergence of 3D bioprinting with AI, nanotechnology, and precision medicine is poised to unlock a new era of patient-specific therapies, on-demand organ repair, and radically accelerated drug discovery.
References
- 1. 3D bioprinting and its innovative approach for biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790048/]
- 2. Bioprinting, explained simply! [https://www.cellink.com/blog/bioprinting-explained-simply/]
- 3. Current Standing and Future Potential of 3D Bioprinting ... [https://scifiniti.com/3105-0387/2/2025.0015]
- 4. Digital Workflow with Open-Source CAD-CAM Software ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109358/]
- 5. New bioprinting technique creates functional tissue 10x faster [https://www.psu.edu/news/research/story/new-bioprinting-technique-creates-functional-tissue-10x-faster]
- 6. 3D Hybrid Bioprinting for Complex Multi-Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637617/]
- 7. New 3D bioprinting technique may improve production of ... [https://news.mit.edu/2025/new-3d-bioprinting-technique-may-improve-production-engineered-tissue-0917]
- 8. Alginate-based 3D bioprinting strategies for structure–function ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb01489a?page=search]
- 9. Multilayer 3D bioprinting and complex mechanical ... [https://www.nature.com/articles/s41598-023-38323-2]
- 10. Optimization of Gelatin and Crosslinker Concentrations in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11820930/]
- 11. Strategies for improving the 3D printability of decellularized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10196833/]
- 12. A 3D bioprinted tumor model fabricated with gelatin/sodium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9947382/]
- 13. Double-crosslinked dECM bioink to print a self-sustaining ... [https://www.sciencedirect.com/science/article/pii/S240588662400040X]
- 14. 3D Bioprinting in Tissue Engineering: Advancements, ... [https://www.jscimedcentral.com/jounal-article-info/JSM-Regenerative-Medicine-and-Bioengineering/3D-Bioprinting-in-Tissue-Engineering:-Advancements,-Challenges,-and-Pathways-to-Clinical-Translation-12103]
- 15. Global 3D Bioprinting Market Research Report [https://www.marknteladvisors.com/research-library/3d-bioprinting-market.html]
- 16. Laser-Based 3D Bioprinting Market Size to Hit USD 7.11 ... [https://www.precedenceresearch.com/laser-based-3d-bioprinting-market]
- 17. High-throughput bioprinting of spheroids for scalable tissue ... [https://www.nature.com/articles/s41467-024-54504-7]
- 18. advances in imaging and analysis for 3D-bioprinted tissues [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1600077/full]
- 19. advances in imaging and analysis for 3D-bioprinted tissues [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187805/]
- 20. Inkjet-based 3D Bioprinting 2025-2033 Trends [https://www.archivemarketresearch.com/reports/inkjet-based-3d-bioprinting-329173]
- 21. 3D Bioprinting Market Size to Surpass USD 8.57 Billion by ... [https://finance.yahoo.com/news/3d-bioprinting-market-size-surpass-110300791.html]
- 22. Tissue Stem Cells: Architects of Their Niches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7861346/]
- 23. Native Tissue - an overview [https://www.sciencedirect.com/topics/engineering/native-tissue]
- 24. Building stem cell niches from the molecule up through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3691058/]
- 25. Comparison of the potential for bioprinting of different 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10236351/]
- 26. High-throughput platform for label-free sorting of 3D ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1432737/full]
- 27. Modular and AI-driven in situ monitoring platform for real- ... [https://www.sciencedirect.com/science/article/abs/pii/S2666998625002406]
- 28. Recent advances in artificial intelligent strategies for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11348508/]
- 29. A deep learning method to map tissue architecture [https://www.nature.com/articles/s41576-022-00564-8]
- 30. Scaffold internal network bioprinting for vascularized tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S1359836825002938]
- 31. Bioprinting in Vascularization Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6305822/]
- 32. 3D bioprinting strategy for engineering vascularized tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10370342/]
- 33. 3D bioprinting for the production of a perfusable ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1484738/full]
- 34. Recent Advances in 3D Printing: Vascular Network for Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6702061/]
- 35. Direct 3D bioprinting of perfusable vascular constructs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5300870/]
- 36. Three-Dimensional Printing and Bioprinting Strategies for ... [https://www.mdpi.com/2073-4360/17/17/2337]
- 37. 3D Bioprinting for Vascularization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215405/]
- 38. 3D bioprinting for the construction of drug testing models- ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1457872/full]
- 39. 3D bioprinting for the construction of drug testing models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11868281/]
- 40. Three-Dimensional Bioprinting for Tissue and Disease ... [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/materials-science-and-engineering/3d-bioprinting/3d-bioprinting-tissue?srsltid=AfmBOorWU-QTk3YPA-okFnwbqexlBfwmld3e7pd0xSEWC4qFSDODlg3f]
- 41. 3D Bioprinting of Cellular Therapeutic Systems in ... [https://link.springer.com/article/10.1007/s40135-025-00337-6]
- 42. 3D Bioprinting for Tissue and Organ Regeneration Market ... [https://www.insightaceanalytic.com/report/global-3d-bioprinting-for-tissue-and-organ-regeneration-market/1336]
- 43. Tissue Structure 3D Bioprinters 2025-2033 Overview [https://www.datainsightsmarket.com/reports/tissue-structure-3d-bioprinters-1507210]
- 44. Three-dimensional bioprinting of functional β-islet-like constructs [https://pmc.ncbi.nlm.nih.gov/articles/PMC10090816/]
- 45. 3D printing breakthrough: Scientists create functional ... [https://www.eurekalert.org/news-releases/1088201]
- 46. 3D Bioprinted Neural Tissues: Emerging Strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473785/]
- 47. Leveraging 3D Bioprinting and Photon-Counting Computed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842604/]
- 48. An Introduction to 3D Bioprinting: Possibilities, Challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6266989/]
- 49. On the reproducibility of extrusion-based bioprinting: round ... [https://pubmed.ncbi.nlm.nih.gov/37769669/]
- 50. Application of 3D bioprinting in the prevention and ... [https://www.nature.com/articles/s41392-021-00566-8]
- 51. Scalable Biofabrication: A Perspective on the Current State ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9165583/]
- 52. 3D bioprinting in tissue engineering: current state-of-the-art and challenges towards system standardization and clinical translation - PubMed [https://pubmed.ncbi.nlm.nih.gov/40513614/]
- 53. A Review of Bioprinting Techniques, Scaffolds, and Bioinks [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447703/]
- 54. Rheological, Structural, and Biological Trade-Offs in Bioink Design for 3D Bioprinting [https://www.mdpi.com/2310-2861/11/8/659]
- 55. Accelerating 3D Modeling for Bioprinting: A Scalable ... [https://medium.com/@sanvimadan21/accelerating-3d-modeling-for-bioprinting-a-scalable-approach-4ff8a77c6671]
- 56. 3D bioprinting of collagen-based high-resolution internally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12017336/]
- 57. 3D Bioprinting of Human Tissues: Biofabrication, Bioinks, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8069718/]
- 58. Therapeutic Supramolecular Polymers: Designs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10769153/]
- 59. Therapeutic supramolecular polymers: Designs and ... [https://www.sciencedirect.com/science/article/abs/pii/S0079670023001235]
- 60. Three-dimensional printing of smart constructs using ... [https://accscience.com/journal/IJB/9/1/10.18063/ijb.v9i1.638]
- 61. Stimuli-Responsive Materials for Biomedical Applications [https://pubmed.ncbi.nlm.nih.gov/40801175/]
- 62. Stimuli-responsive smart materials for biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/S0927796X25002049]
- 63. 3D-Printed metal organic frameworks-based ... [https://www.sciencedirect.com/science/article/pii/S2667240525000091]
- 64. Tissue Bioprinting: Promise and Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740401/]
- 65. 2D vs 3D Cell Culture: Choosing the Right Model [https://www.tempobioscience.com/2d-vs-3d-cell-culture-choosing-the-right-model-by-tempo-bioscience/]
- 66. Halfway between 2D and Animal Models: Are 3D Cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5796130/]
- 67. 3D vs 2D Cell Culture: Which Model Suits Your Lab in 2025? [https://www.pharmanow.live/knowledge-hub/research/3d-vs-2d-cell-culture-comparison]
- 68. 3D Bioprinting Could Speed Up Drug Development [https://www.lifescienceleader.com/doc/d-bioprinting-could-speed-up-drug-development-0001]
- 69. 3D bioprinting of complex tissues in vitro: state-of-the-art and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8850226/]
- 70. 3D Bioprinting at the Frontier of Regenerative Medicine ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2020.607648/full]
- 71. Innovations in liver organoids: the role of 3D bioprinting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057518/]
- 72. New Human Liver Organoid Platform Predicts Immune ... [https://scienceblog.cincinnatichildrens.org/new-human-liver-organoid-platform-predicts-immune-mediated-drug-toxicity/]
- 73. Stem cell liver model reproduces rare immune drug reactions [https://www.drugtargetreview.com/news/189683/stem-cell-liver-model-reproduces-rare-immune-drug-reactions/]
- 74. 3D organ-on-a-chip: The convergence of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1043117/full]
- 75. 3D Bioprinting of Living Tissues - Wyss Institute [https://wyss.harvard.edu/technology/3d-bioprinting/]
- 76. Advances in 3D Bioprinting and Microfluidics for Organ-on- ... [https://www.mdpi.com/2073-4360/17/22/3078]
- 77. Spatial patterning strategies for liver tissue engineering [https://www.sciencedirect.com/science/article/pii/S0169409X25002224]
- 78. 10 Key Studies on Liver Research with NAMs - 2024/2025 [https://www.cherrybiotech.com/scientific-note/top-10-breakthrough-studies-using-liver-organoids-and-liver-on-chip-for-drug-discovery-2024-2025/]
- 79. Development and Quantitative Evaluation of a Novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520205/]
- 80. Suspended bioprinting with in-situ elasticity monitoring ... [https://www.sciencedirect.com/science/article/abs/pii/S2214860425000314]
- 81. Bioprinting 101: Design, Fabrication, and Evaluation of Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7480731/]
- 82. Assessing the landscape of clinical and observational trials ... [https://threedmedprint.biomedcentral.com/articles/10.1186/s41205-025-00253-2]
- 83. 3D bioprinting: towards standards in biomedicine [https://www.cencenelec.eu/news-events/events/2025/2025-10-21-22-psis/]
- 84. New technique offers bigger and better window into RNA ... [https://news.yale.edu/2025/10/02/new-technique-offers-bigger-and-better-window-rna-activity-complex-tissue]
- 85. New Foundation Model Reveals How Cells Are Organized ... [https://www.helmholtz-munich.de/en/icb/news-detail/new-foundation-model-reveals-how-cells-are-organized-in-tissues]
- 86. New study cracks the “tissue code” — just five rules shape ... [https://www.sciencedaily.com/releases/2025/07/250715043402.htm]
- 87. Scientists Discover a Simple Set of Rules That May Explain ... [https://news.christianacare.org/2025/07/scientists-discover-a-simple-set-of-rules-that-may-explain-how-our-tissues-stay-organized/]
- 88. Building and rebuilding complex tissues: strategic visions ... [https://pubmed.ncbi.nlm.nih.gov/40772789/]