Engineering Hypoimmune Cells for Allogeneic Therapy: Strategies, Applications, and Clinical Frontiers
Allogeneic cell therapies derived from healthy donors or induced pluripotent stem cells (iPSCs) offer transformative potential for treating cancer, diabetes, and autoimmune diseases by providing 'off-the-shelf' availability.
Engineering Hypoimmune Cells for Allogeneic Therapy: Strategies, Applications, and Clinical Frontiers
Abstract
Allogeneic cell therapies derived from healthy donors or induced pluripotent stem cells (iPSCs) offer transformative potential for treating cancer, diabetes, and autoimmune diseases by providing 'off-the-shelf' availability. However, host immune rejection remains a significant barrier. This article synthesizes current strategies for engineering hypoimmune cells, focusing on genetic modifications to evade adaptive and innate immune responses. We explore foundational immune evasion mechanisms, advanced gene-editing methodologies like CRISPR-Cas9 for targeting HLA and incorporating immunomodulatory proteins, and troubleshooting for challenges such as graft-versus-host disease (GvHD) and tumorigenicity. The content also validates these approaches through recent preclinical and clinical trial data, comparing the efficacy and safety of different hypoimmune platforms. This resource is tailored for researchers, scientists, and drug development professionals navigating the evolving landscape of universal cell therapy.
The Immunological Basis for Hypoimmune Engineering: Understanding Rejection and Evasion
The success of allogeneic cell therapies is fundamentally constrained by the host immune system's robust recognition and rejection of foreign tissues. This process, known as the allogeneic barrier, represents a complex immunological challenge for regenerative medicine and cell transplantation [1]. Adaptive immune responses to grafted tissues constitute the primary impediment to successful transplantation, driven by responses to alloantigens—proteins that vary between individuals within a species and are perceived as foreign by recipients [1]. While current approaches often rely on immunosuppressive drugs or autologous cell sources, these strategies face significant limitations in scalability, toxicity, and broad applicability [2] [3]. Consequently, understanding and engineering solutions to overcome this barrier is paramount for developing effective "off-the-shelf" allogeneic cell therapies.
The immunological basis of graft rejection was first systematically elucidated through skin transplantation studies in inbred mice, which established that while autografts (within the same individual) and syngeneic grafts (between genetically identical individuals) are universally accepted, allografts (between genetically different individuals) are consistently rejected [1]. This rejection follows a predictable timeline, with first-set rejection occurring approximately 10-13 days after initial grafting and second-set rejection occurring more rapidly (6-8 days) upon re-grafting from the same donor, demonstrating the specificity and memory of the adaptive immune response [1].
Fundamental Immunological Mechanisms of Graft Rejection
Cellular and Molecular Players in Alloimmunity
The rejection of allogeneic transplants involves a coordinated response from both innate and adaptive immune systems. The key cellular mediators include T lymphocytes, B lymphocytes, natural killer (NK) cells, antigen-presenting cells (APCs), and macrophages [4] [5].
- T Cells: Both CD4+ and CD8+ T cells play central roles. CD8+ cytotoxic T cells directly recognize and kill donor cells, while CD4+ helper T cells orchestrate the broader immune response through cytokine production and help for B cell activation [1] [5].
- B Cells: Produce donor-specific antibodies (DSA) that mediate complement-dependent cytotoxicity and opsonization of donor cells [4].
- NK Cells: Contribute to the "missing-self" response when donor cells lack sufficient MHC class I molecules, and produce pro-inflammatory cytokines including IFN-γ and TNF-α [5].
- Antigen-Presenting Cells: Including dendritic cells and macrophages, these cells initiate immune responses by presenting donor antigens to T cells through various pathways [1] [5].
The molecular recognition events are primarily focused on the major histocompatibility complex (MHC), known in humans as human leukocyte antigens (HLA). These highly polymorphic cell surface proteins present peptide antigens to T cells and are the principal targets of allorecognition [1] [3]. The extraordinary strength of alloreactive T cell responses, engaging up to 10% of the entire peripheral T-cell repertoire (compared to <0.01% for conventional antigens), underscores the potency of this barrier [5].
Pathways of Allorecognition
The immune system recognizes allogeneic grafts through three principal pathways, each with distinct mechanisms and implications for rejection.
Direct Allorecognition
Direct allorecognition occurs when recipient T cells directly recognize intact allogeneic MHC molecules on the surface of donor antigen-presenting cells [1] [5]. This pathway is particularly potent in the early post-transplantation period and is primarily mediated by passenger leukocytes—donor-derived dendritic cells that migrate from the graft to the recipient's secondary lymphoid organs [1] [5]. Following skin transplantation, donor dendritic cells, including both epidermal Langerhans cells and dermal dendritic cells, migrate from the graft via lymphatic vessels to the recipient's draining lymph nodes where they present donor antigens to naive T cells [5]. The critical role of lymphatic drainage was demonstrated in classic studies where skin grafts raised off the recipient bed while preserving blood circulation through a pedicle were not rejected until the pedicle was severed, allowing lymphatic connection [5].
Indirect Allorecognition
Indirect allorecognition involves the uptake and processing of donor alloantigens by recipient antigen-presenting cells, which then present donor-derived peptides on self-MHC molecules to recipient T cells [1]. This pathway resembles conventional T cell recognition of foreign antigens and becomes increasingly important over time as donor passenger leukocytes are replaced by recipient cells [1]. The indirect pathway can activate both CD4+ and CD8+ T cells and is particularly important for generating alloantibody responses and chronic rejection [1].
Semidirect Allorecognition
An additional pathway, the semidirect pathway, has been more recently described, wherein recipient APCs acquire intact donor MHC molecules through membrane transfer and present them to T cells [5]. This hybrid pathway allows a single APC to present both directly and indirectly recognized antigens, potentially amplifying the immune response.
Table 1: Comparison of Allorecognition Pathways
| Feature | Direct Pathway | Indirect Pathway | Semidirect Pathway |
|---|---|---|---|
| Antigen Form | Intact donor MHC molecules | Donor peptides presented by self-MHC | Intact donor MHC acquired by recipient APCs |
| Primary APCs | Donor dendritic cells | Recipient dendritic cells | Recipient dendritic cells |
| T Cell Specificity | Donor MHC | Donor peptides + self-MHC | Donor MHC on recipient APCs |
| Time Course | Dominant early post-transplant | Increases over time | Potential role in both early and late rejection |
| Main Rejection Type | Acute rejection | Chronic rejection, alloantibody response | Not fully characterized |
Classification and Timeline of Rejection Responses
Transplant rejection is classified based on the timing, mechanism, and histopathological features of the immune response. The Banff classification system, developed through international consensus, provides standardized criteria for diagnosing rejection in organ transplantation, particularly kidney grafts [4].
Table 2: Classification of Allograft Rejection Responses
| Rejection Type | Time Course | Primary Mechanisms | Key Histopathological Features |
|---|---|---|---|
| Hyperacute Rejection | Minutes to hours after transplantation | Pre-existing antibodies against HLA or blood group antigens | Diffuse intravascular coagulation, thrombosis, neutrophil infiltration |
| Acute T Cell-Mediated Rejection (aTCMR) | Any time post-op, peak within 3 months | T cell recognition of donor antigens | Interstitial inflammation, tubulitis, intimal arteritis |
| Active Antibody-Mediated Rejection (aABMR) | Any time post-op, peak within 30 days | Donor-specific antibodies binding vascular endothelium | Microvascular inflammation, C4d deposition in capillaries |
| Chronic Active TCMR (caTCMR) | Often >3 months post-transplant | Sustained T cell-mediated injury | Interstitial inflammation in areas of fibrosis, chronic allograft vasculopathy |
| Chronic Active ABMR (caABMR) | Months to years post-transplant | Sustained DSA-mediated microvascular injury | Features of aABMR plus chronic allograft glomerulopathy, capillary basement membrane multilayering |
Engineering Hypoimmunogenic Cells: Strategic Approaches
HLA Editing to Evade Adaptive Immunity
A primary strategy for overcoming the allogeneic barrier involves genetic engineering to eliminate or reduce the expression of polymorphic HLA molecules, thereby minimizing recognition by alloreactive T cells [3] [6] [7].
MHC Class I Disruption: HLA class I molecules, expressed on virtually all nucleated cells, present intracellular peptides to CD8+ cytotoxic T cells. Complete elimination of surface HLA class I expression can be achieved through knockout of β2-microglobulin (B2M), an essential subunit for HLA class I assembly and surface expression [3] [6]. B2M knockout cells show dramatically reduced recognition by CD8+ T cells [3].
MHC Class II Disruption: HLA class II molecules, normally expressed on professional antigen-presenting cells, can be eliminated through knockout of the Class II Major Histocompatibility Complex Transactivator (CIITA), a master regulator of HLA class II expression [6]. This approach prevents CD4+ T cell recognition via the direct pathway [6].
Selective HLA Editing: An alternative approach involves selective knockout of the most polymorphic HLA genes (HLA-A, HLA-B, and HLA-DR) while preserving less polymorphic forms [7]. This strategy aims to reduce the antigenic burden while potentially retaining some immune regulatory functions. Recent research has demonstrated that targeting HLA-DRA (the alpha chain of HLA-DR) can effectively eliminate the entire HLA-DR complex without needing to target multiple DRB genes individually [7].
Overcoming Innate Immune Recognition
Complete elimination of HLA class I expression creates a new challenge: activation of natural killer (NK) cells through "missing-self" recognition [6]. NK cells normally express inhibitory receptors that recognize self-HLA class I molecules; when these are absent, the inhibitory signal is lost, triggering NK cell activation and killing of the target cells [6].
Several strategies have been developed to address this challenge:
CD47 Overexpression: CD47 is a "don't eat me" signal that engages SIRPα on phagocytic cells including macrophages and some NK cells, inhibiting phagocytosis and cell killing [3] [6]. Overexpression of CD47 on engineered cells effectively protects HLA-deficient cells from innate immune attack [6]. In head-to-head comparisons of different immune evasion strategies, CD47 overexpression provided superior protection against NK cell killing compared to other approaches [6].
HLA-E or HLA-G Expression: Non-classical HLA molecules HLA-E and HLA-G can be engineered to engage inhibitory receptors on NK cells (CD94/NKG2A for HLA-E and LILRB1 for HLA-G) [6]. However, these approaches show limitations due to the restricted expression patterns of the corresponding inhibitory receptors on NK cell subsets [6].
PD-L1 Overexpression: Programmed Death-Ligand 1 (PD-L1) engages PD-1 on activated T cells and some NK cells, delivering an inhibitory signal [3]. While useful, PD-L1 overexpression alone provides incomplete protection [3].
The Hypoimmune (HIP) Cell Platform
The most promising results have emerged from combining multiple engineering approaches. The hypoimmune (HIP) platform involves simultaneous disruption of HLA class I and II expression coupled with CD47 overexpression [6]. This integrated approach addresses both adaptive and innate immune recognition:
- B2M knockout eliminates HLA class I, preventing CD8+ T cell recognition
- CIITA knockout eliminates HLA class II, preventing CD4+ T cell recognition
- CD47 overexpression protects against NK cell and macrophage-mediated killing
In rigorous preclinical testing, HIP-engineered cells demonstrated remarkable survival advantages. Rhesus macaque HIP induced pluripotent stem cells (iPSCs) survived for 16 weeks in fully immunocompetent allogeneic recipients, while unmodified control cells were rapidly rejected [6]. Similarly, HIP-edited primary pancreatic islets survived for 40 weeks in an allogeneic rhesus macaque without immunosuppression, whereas unedited islets were quickly rejected [6].
Notably, this approach has now advanced to clinical trials. Allogeneic HIP CD19 CAR-T cells (SC291) demonstrated the ability to evade allorejection in patients with cancer and autoimmune disease, with no de novo immune response against fully edited HIP CAR T cells observed in any patient [8].
Experimental Protocols for Evaluating Alloimmune Responses
In Vitro T Cell Activation Assays
Protocol 4.1.1: Comprehensive Alloreactive T-cell Detection (cATD) Assay
Purpose: To rapidly detect and quantify alloreactive T cells in recipient samples following exposure to donor antigens [9].
Materials:
- Donor and recipient splenocytes or PBMCs
- CD19 MicroBeads (Miltenyi Biotec) for B cell isolation
- Pan T-Cell isolation kit (Miltenyi Biotec)
- Recombinant mouse CD40L multimer (100 ng/mL) and IL-4 (10 ng/mL) for B cell activation
- Anti-CD154 (MR1) and anti-CD137 (17B5) antibodies for flow cytometry
- Complete RPMI 1640 medium with supplements
Procedure:
- Stimulator Preparation: Isolate donor B cells using CD19 MicroBeads. Activate B cells by culturing with CD40L multimer and IL-4 for 24 hours. Irradiate activated B cells with 40 Gy.
- Responder Preparation: Isolate recipient T cells using Pan T-Cell isolation kit.
- Co-culture: Combine responders and stimulators at 1:1 ratio (10^6 cells each) in U-bottom plates with anti-CD154 antibody in culture medium. Incubate for 18 hours. Add monensin for the final 4 hours to inhibit cytokine secretion.
- Analysis: Stain cells with anti-CD3, CD4, CD8, CD154, and CD137 antibodies. Identify alloreactive CD4+ T cells as CD3+CD4+CD154+ and alloreactive CD8+ T cells as CD3+CD8+CD137+ populations by flow cytometry.
Applications: This assay can discriminate between rejection and tolerance states in transplantation models and is useful for monitoring immune status post-transplantation [9].
Protocol 4.1.2: Mixed Lymphocyte Reaction (MLR) Proliferation Assay
Purpose: To measure T cell proliferative responses to allogeneic stimuli [9].
Materials:
- Donor and recipient lymphocytes
- Carboxyfluorescein succinimidyl ester (CFSE)
- Complete RPMI 1640 medium
- Flow cytometry equipment
Procedure:
- Labeling: Label recipient splenocytes with 5 μM CFSE for 5 minutes.
- Stimulator Preparation: Prepare activated donor B cell stimulators as in Protocol 4.1.1.
- Co-culture: Combine CFSE-labeled responders and stimulators at 1:1 ratio in U-bottom plates. Culture for 4 days.
- Analysis: Analyze CFSE dilution by flow cytometry to measure T cell proliferation.
In Vivo Assessment of Hypoimmune Cells
Protocol 4.2.1: Teratoma Formation Assay for Immune Evasion
Purpose: To evaluate the immune evasion capability of engineered hypoimmune pluripotent stem cells in immunocompetent hosts [6].
Materials:
- HIP-engineered iPSCs and wild-type controls
- Firefly luciferase (FLuc)-expressing vectors for in vivo tracking
- Immunocompetent allogeneic recipients (mice or non-human primates)
- In vivo imaging system (IVIS) for bioluminescence imaging
- Matrigel for cell suspension
Procedure:
- Cell Preparation: Engineer iPSCs to express FLuc for tracking. Prepare cell suspensions in appropriate buffer with Matrigel.
- Transplantation: Inject cells intramuscularly or subcutaneously into fully immunocompetent allogeneic recipients. Include wild-type iPSC controls.
- Monitoring: Track cell survival weekly using bioluminescence imaging. Monitor for teratoma formation.
- Endpoint Analysis: Harvest tissues at predetermined endpoints for histological analysis of immune cell infiltration and differentiation potential.
Interpretation: Long-term survival of HIP cells with minimal immune infiltration indicates successful immune evasion, while rejection of wild-type controls validates the model system [6].
Research Reagent Solutions
Table 3: Essential Research Reagents for Hypoimmunogenicity Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Gene Editing Tools | CRISPR-Cas9 (Alt-R Sp Cas9 Nuclease V3), gRNAs targeting B2M, CIITA, HLA-A/B/DRA | Generation of hypoimmune cell lines | Targeted disruption of HLA genes to reduce immunogenicity |
| Immune Modulator Expression Vectors | Lentiviral CD47 constructs, HLA-E/G expression plasmids | Engineering immune checkpoint expression | Protection from innate immune recognition via "don't eat me" signals |
| Cell Isolation Kits | CD19 MicroBeads, Pan T-Cell isolation kit (Miltenyi Biotec) | Preparation of cell populations for functional assays | Rapid isolation of specific immune cell subsets |
| Flow Cytometry Antibodies | Anti-CD154 (MR1), anti-CD137 (17B5), anti-CD3/CD4/CD8, HLA-specific antibodies | Immune cell phenotyping and alloreactive T cell detection | Identification and quantification of immune cell populations and activation states |
| Cytokines & Activation Reagents | Recombinant CD40L multimer, IL-2, IL-4, IFN-γ | Immune cell stimulation and differentiation | Activation of immune cells for functional assays |
| In Vivo Tracking Reagents | Firefly luciferase vectors, CFSE cell proliferation dye | Cell fate tracking in animal models | Non-invasive monitoring of cell survival and proliferation |
Signaling Pathways in Alloimmune Recognition
Direct Allorecognition Pathway
Engineering Hypoimmune Cells
The development of effective strategies to overcome the allogeneic barrier represents a frontier in regenerative medicine and cell therapy. The intricate mechanisms of immune recognition—spanning direct, indirect, and semidirect allorecognition pathways—create a formidable challenge for transplanted cells and tissues. However, recent advances in genetic engineering, particularly the HIP platform that combines HLA disruption with CD47 overexpression, demonstrate that comprehensive immune evasion is achievable [6] [8]. The successful translation of these approaches from preclinical models to clinical trials marks a significant milestone toward the realization of universally compatible "off-the-shelf" cell therapies [8]. As these technologies mature, they hold the potential to transform treatment paradigms for a wide range of conditions requiring cell replacement, from diabetes to degenerative disorders, making regenerative medicine truly scalable and accessible.
Application Note: Engineering Hypo-Immune Cells for Allogeneic Therapy
The development of "off-the-shelf" allogeneic cell therapies represents a paradigm shift in regenerative medicine and cancer treatment, aiming to overcome the limitations of patient-specific autologous products. The core engineering challenge lies in effectively evading host immune rejection while maintaining robust cell function. This is primarily addressed through strategic genetic manipulation of three key target classes: HLA molecules, co-stimulatory signals, and cellular adhesion pathways [2] [10] [11]. Successfully engineering these targets creates hypoimmune cells capable of universal application.
HLA Engineering to Mitigate Adaptive Immune Recognition: The most prominent strategy involves disrupting the Major Histocompatibility Complex (MHC) class I and II molecules, which present foreign antigens to host T cells. Knockout of Beta-2-microglobulin (B2M) ablates surface expression of MHC class I, preventing CD8+ T cell recognition. However, this can trigger missing-self recognition and elimination by natural killer (NK) cells. To counter this, a knock-in strategy is employed, expressing NK-inhibitory ligands like HLA-E or CD47 to cloak the cell from NK-mediated cytotoxicity [10] [11]. This combined edit creates a foundational hypoimmune profile.
Modulating Co-stimulatory Signals for Enhanced Potency: Beyond immune evasion, optimizing intrinsic T cell function is critical for therapeutic efficacy, particularly in CAR-T cell therapies. Second-generation CARs incorporate intracellular co-stimulatory domains, such as CD28 or 4-1BB, alongside the CD3ζ activation domain. The choice of domain dictates the functional phenotype; CD28 promotes potent effector function and rapid expansion, while 4-1BB favors enhanced persistence and memory formation [12] [13]. Fifth-generation CARs further integrate cytokine signaling (e.g., IL-2 receptor β-chain) to activate the JAK/STAT pathway, augmenting CAR-T cell activity and promoting memory formation [12].
Targeting Adhesion Pathways to Regulate Immune Synapse Formation: The innate immune response and initial T cell activation are heavily dependent on cell adhesion molecules. ICAM-1 (Intercellular Adhesion Molecule-1) and its ligand LFA-1 (composed of CD11a and CD18/ITGB2) stabilize the immune synapse between effector and target cells [14] [15]. Knockout of ICAM-1 on allogeneic cells significantly diminishes binding and adhesion of multiple immune cell types, including T cells and neutrophils, thereby reducing T cell proliferation and activation in vitro and improving graft retention in vivo [14]. Conversely, in the context of CAR-T therapy targeting B-cell malignancies, the expression of ITGB2 on tumor cells is a positive predictor of clinical response, as it facilitates the formation of a stable immunological synapse necessary for effective cytotoxicity [15].
Table 1: Core Engineering Targets for Hypo-Immune Cells
| Target Class | Key Molecular Targets | Engineering Strategy | Primary Functional Outcome |
|---|---|---|---|
| HLA Molecules | MHC Class I (B2M), MHC Class II | CRISPR/Cas9 knockout; HLA-E or CD47 knock-in | Prevents CD4+/CD8+ T cell allorecognition; confers NK cell evasion [10] [11] |
| Co-stimulatory Signals | CD28, 4-1BB (CD137), CD3ζ | 2nd-gen CAR design; 5th-gen CAR with cytokine receptor fusion | Enhances T-cell activation, proliferation, in vivo persistence, and antitumor efficacy [12] [13] |
| Adhesion Pathways | ICAM-1, LFA-1 (ITGB2/CD18) | CRISPR/Cas9 knockout (ICAM-1); Pharmacologic upregulation (ITGB2) | Diminishes immune cell adhesion and graft rejection; augments immune synapse and cytotoxicity [14] [15] |
Experimental Protocols
Protocol: Generation of HLA-E-Expressing B2M Knockout Pluripotent Stem Cells
This protocol describes the creation of a first-generation hypoimmune human pluripotent stem cell (hPSC) line via simultaneous knockout of B2M and knock-in of HLA-E.
I. Materials
- Cell Line: Wild-type hPSCs (e.g., H9 line)
- Gene Editing Tool: CRISPR/Cas9 ribonucleoprotein (RNP) complexes
- gRNAs: Designed for B2M locus and a safe-harbor locus (e.g., AAVS1) for knock-in.
- Donor Template: AAVS1 donor vector containing HLA-E single-chain trimer fused to GFP-P2A-puromycin resistance cassette.
- Cell Culture Reagents: hPSC maintenance media (e.g., mTeSR Plus), Matrigel, CloneR supplement, Accutase.
- Validation Reagents: Flow cytometry antibodies for HLA-ABC, HLA-E, B2M; genomic DNA extraction kit, PCR reagents.
II. Procedure
- Design and Preparation: Design and validate gRNAs for B2M knockout and AAVS1-targeted knock-in. Prepare the AAVS1-HLA-E donor vector and CRISPR/Cas9 RNP complexes.
- Transfection: Harvest hPSCs as single cells using Accutase. Transfect 1x10^6 cells with RNP complexes and donor vector via nucleofection using a human stem cell-specific kit.
- Selection and Cloning: 48 hours post-transfection, begin puromycin selection (0.5-1.0 µg/mL) for 7-10 days. Subsequently, pick individual colonies manually or via single-cell sorting into 96-well plates.
- Expansion and Screening: Expand clonal lines. Screen for successful edits by:
- Flow Cytometry: Confirm loss of HLA-ABC/B2M surface expression and presence of HLA-E.
- PCR Genotyping: Validate precise integration at the AAVS1 locus and biallelic disruption of B2M.
- Characterization: Perform karyotyping (e.g., G-banding) to ensure genomic integrity. Differentiate the engineered line into target cell types (e.g., cardiomyocytes, endothelial cells) to confirm retained differentiation potential and stable transgene expression.
Protocol: In Vitro Assessment of Immune Cell Adhesion to ICAM-1 KO Grafts
This protocol quantifies the functional impact of ICAM-1 knockout on immune cell binding, a key metric for innate immune evasion.
I. Materials
- Test Cells: Isogenic pairs of WT and ICAM-1 KO hPSC-derived endothelial cells (ECs) or cardiomyocytes (CMs).
- Immune Cells: Monocytic cell line (U937) or primary human peripheral blood mononuclear cells (PBMCs).
- Reagents: Cell culture media, Matrigel, recombinant human TNF-α and IFN-γ, Calcein-AM fluorescent dye, 4% paraformaldehyde (PFA).
- Equipment: 24-well culture plates, fluorescence microscope or plate reader.
II. Procedure
- Differentiation and Stimulation: Differentiate hPSCs (WT and ICAM-1 KO) into ECs or CMs using standardized protocols. Plate the cells in 24-well plates. Prior to the assay, stimulate the cells for 48 hours with TNF-α (10 ng/mL) and IFN-γ (50 ng/mL) to mimic an inflammatory microenvironment and upregulate ICAM-1 in WT cells [14].
- Immune Cell Labeling: Harvest U937 cells or PBMCs and label with 5 µM Calcein-AM in serum-free media for 30 minutes at 37°C. Wash cells twice to remove excess dye.
- Co-culture and Binding Assay: Add 2x10^5 labeled immune cells to each well containing the differentiated grafts. Co-culture for 1-2 hours at 37°C.
- Washing and Quantification: Gently wash the co-culture wells 3-5 times with PBS to remove non-adherent immune cells. Fix the remaining cells with 4% PFA for 15 minutes.
- Analysis: Quantify adherent immune cells by counting fluorescent cells in multiple microscope fields or by measuring fluorescence intensity using a plate reader. Compare adhesion to WT vs. ICAM-1 KO grafts. A significant reduction in binding to KO grafts demonstrates the efficacy of the edit.
Table 2: Key Reagent Solutions for Hypo-Immune Cell Engineering
| Research Reagent | Function / Application | Example Use Case |
|---|---|---|
| CRISPR/Cas9 System | Precise genomic editing (knockout, knock-in) | Disruption of B2M, TRAC, or ICAM-1 loci [14] [10] |
| TALENs/mRNA | Alternative nuclease for gene editing | TCR disruption in UCART19 [10] |
| Anti-ICAM-1 Blocking Antibody | Functional validation of adhesion target | In vitro blockade to confirm reduced leukocyte binding [14] |
| Pro-inflammatory Cytokines (TNF-α, IFN-γ) | Mimic inflammatory TME in vitro | Upregulation of MHC and ICAM-1 on target cells for functional assays [14] |
| Flow Cytometry Antibodies | Phenotypic validation of surface protein expression | Confirmation of MHC-I/II loss, HLA-E, or ICAM-1 expression [14] [10] |
| Venetoclax | BCL-2 inhibitor that upregulates ITGB2 | Pharmacological enhancement of immune synapse in B-cell malignancies for improved CAR-T efficacy [15] |
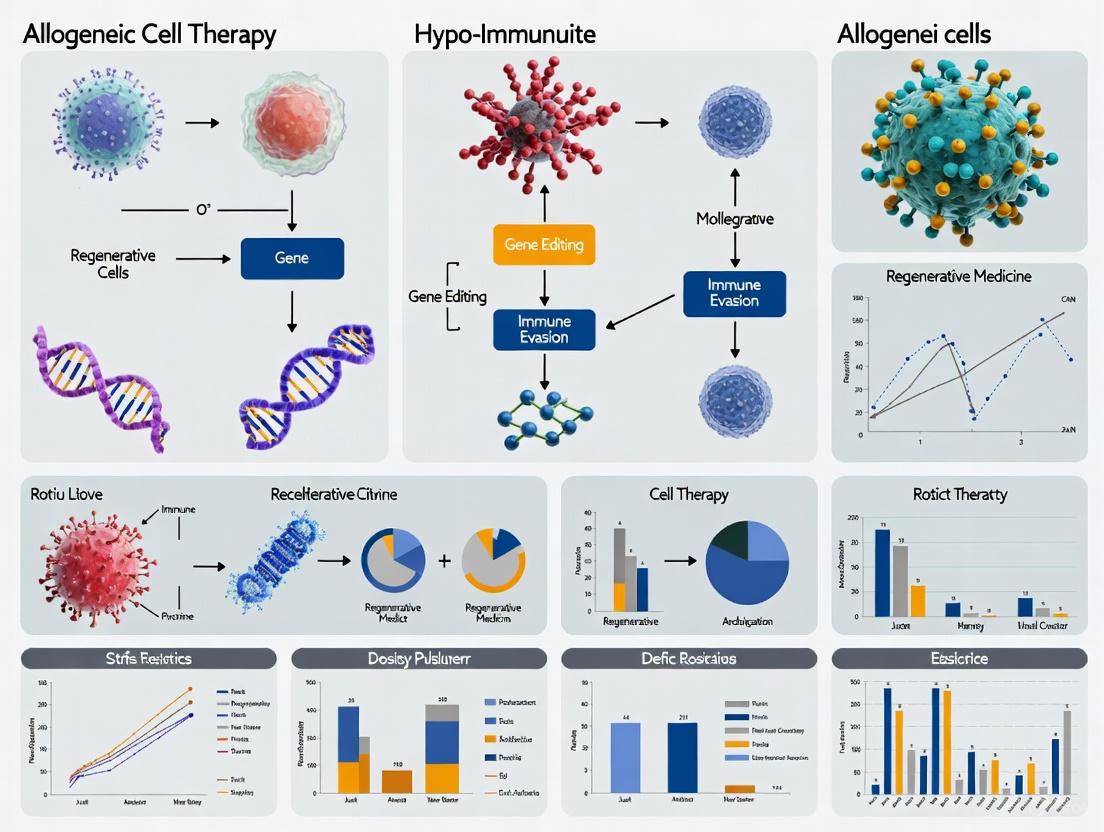
Signaling Pathway and Workflow Visualizations
Diagram 1: Hypoimmune Cell Engineering Workflow
Diagram 2: CAR-T Cell Co-stimulatory Signaling Pathways
Diagram 3: ICAM-1/LFA-1 Mediated Immune Synapse
Immune privilege refers to the remarkable ability of certain tissues and organs to tolerate the introduction of foreign antigens without mounting a destructive immune response. This biological phenomenon represents nature's solution to preventing inflammatory damage to vital tissues, and it offers invaluable lessons for advancing allogeneic cell therapies. Two particularly instructive examples of naturally immune-privileged tissues are the cornea and placenta. The cornea maintains transparency for vision by avoiding inflammatory reactions to environmental antigens, while the placenta enables fetal development by preventing maternal immune rejection of paternal antigens. Both tissues employ sophisticated, multi-layered strategies to modulate immune responses—strategies that researchers are now harnessing to engineer "hypo-immune" therapeutic cells that can evade rejection without systemic immunosuppression.
Understanding these natural mechanisms of immune regulation provides a blueprint for overcoming the fundamental challenge in allogeneic cell therapy: how to protect transplanted cells from host immune rejection while maintaining their therapeutic function. This application note examines the key mechanisms of immune privilege in cornea and placenta, translates these biological principles into engineered strategies for cell therapies, and provides detailed protocols for implementing these approaches in research settings.
Mechanisms of Natural Immune Privilege
Corneal Immune Privilege
The cornea enjoys one of the most robust forms of immune privilege in the human body, with first-time corneal transplants achieving >90% success rates without HLA matching or systemic immunosuppression [16] [17]. This privileged status stems from multiple integrated mechanisms:
Table 1: Mechanisms of Corneal Immune Privilege
| Mechanism Category | Specific Components | Function in Immune Privilege |
|---|---|---|
| Anatomical Barriers | Avascularity, Lack of lymphatic drainage | Prevents immune cell infiltration and antigen presentation to immune system |
| Molecular Factors | Soluble VEGFR-2, Endostatin | Inhibits hemangiogenesis and lymphangiogenesis |
| Immunomodulatory Molecules | TGF-β, PD-L1, CD86 | Induces T-cell anergy and generates regulatory T cells |
| Cellular Mechanisms | Anterior chamber-associated immune deviation (ACAID) | Generates systemic immune tolerance to ocular antigens |
The avascular nature of the normal cornea represents a cornerstone of its immune privilege, creating a physical barrier that limits both the afferent (recognition) and efferent (effector) arms of the immune response [17]. This avascular state is actively maintained by multiple anti-angiogenic factors, including endostatin and soluble VEGFR-2, which inhibit both blood (hemangiogenesis) and lymphatic (lymphangiogenesis) vessel formation [17]. When corneal avascularity is compromised—such as in chemical burns, infection, or inflammatory conditions—the risk of corneal graft rejection increases dramatically from <10% to 50-70% [18] [16]. The critical importance of lymphatics in corneal graft rejection was demonstrated in experiments showing that selective blockade of lymphangiogenesis (while preserving hemangiogenesis) dramatically improved corneal allograft survival [17].
The cornea also employs numerous immunomodulatory factors that actively suppress immune responses. The aqueous humor contains multiple immunomodulatory factors including TGF-β, which inhibits T-cell activation and promotes the generation of regulatory T cells (Tregs) [17]. The phenomenon of anterior chamber-associated immune deviation (ACAID) represents a sophisticated systemic component of corneal immune privilege, inducing antigen-specific suppression of delayed-type hypersensitivity and promoting the production of non-complement-fixing antibodies [17].
Placental Immune Privilege
The human placenta, particularly the amniotic membrane and its derived cells, has evolved sophisticated mechanisms to prevent maternal immune rejection of the semi-allogeneic fetus. Human amniotic mesenchymal stromal cells (hAMSCs) exhibit potent immunomodulatory properties that make them particularly valuable for regenerative medicine applications [19]:
Table 2: Immune Modulatory Properties of Human Amniotic Mesenchymal Stromal Cells (hAMSCs)
| Property | Mechanism | Therapeutic Application |
|---|---|---|
| Low Immunogenicity | Low MHC-I expression, absence of MHC-II and co-stimulatory molecules (CD40, CD80, CD86) | Evades T-cell recognition and activation |
| Immunosuppressive Secretome | Releases cytokines (FGF-2, IGF-1, HGF, VEGF, EGF) with proliferative and anti-apoptotic effects | Modulates local immune environment and promotes tissue repair |
| T-cell Modulation | Suppresses T-cell proliferation and activation through both direct contact and soluble factors | Reduces adaptive immune responses against allografts |
| Angiogenic Regulation | Expresses pro-angiogenic (VEGF-A, angiopoietin-1) and anti-angiogenic factors depending on microenvironment | Supports vascularization while preventing pathological neovascularization |
hAMSCs possess a unique immune-privileged status essential for maternal-fetal tolerance. They exhibit low expression of MHC-I and lack expression of MHC-II as well as co-stimulatory molecules (CD40, CD80, CD86), thereby evading immune recognition [19]. This low immunogenicity profile makes them ideal candidates for allogeneic transplantation. Beyond their inherent low immunogenicity, hAMSCs actively modulate immune responses through their secretome, releasing cytokines (FGF-2, IGF-1, HGF, VEGF, EGF) that exert proliferative and anti-apoptotic effects while creating an immunosuppressive local environment [19]. These properties have been leveraged in various preclinical models, including intracameral injection of hAMSCs in a corneal injury model, which reduced neovascularization, opacity, and inflammatory infiltration [19].
Engineering Hypo-Immune Cells: From Biological Principles to Therapeutic Applications
The natural immune evasion strategies of cornea and placenta provide a roadmap for engineering hypo-immune therapeutic cells. Several key approaches have emerged, focusing on modifying critical immune recognition and activation pathways.
HLA Engineering Strategies
Major Histocompatibility Complex (MHC) molecules, known as Human Leukocyte Antigens (HLA) in humans, represent the primary barrier to allogeneic cell transplantation. HLA class I molecules (HLA-A, -B, and -C) are expressed on nearly all nucleated cells and present intracellular antigens to CD8+ T cells, initiating cytotoxic killing [20]. Current HLA engineering strategies aim to disrupt this recognition while avoiding natural killer (NK) cell activation:
Diagram: HLA Engineering Strategies and Challenges. Disruption of HLA class I (e.g., via B2M knockout) prevents T-cell recognition but risks NK cell activation via "missing self" signals. Co-expression of non-classical HLA molecules (HLA-E, HLA-G), retention of HLA-C, or expression of CD47 can mitigate NK cell activation.
Complete elimination of HLA class I expression, typically achieved through β2-microglobulin (B2M) knockout, prevents CD8+ T cell recognition but creates a "missing self" signal that activates NK cells [20]. To address this, researchers have developed complementary strategies including:
- Expression of non-classical HLA molecules: HLA-E and HLA-G serve as ligands for NK cell inhibitory receptors (NKG2A and KIR2DL4, respectively) [20]. One successful approach uses B2M−/− pluripotent stem cells with co-expression of the minimally polymorphic HLA-E [20].
- Retention of HLA-C: Unlike HLA-A and -B, HLA-C interacts with killer immunoglobulin-like receptors (KIRs) on NK cells to deliver inhibitory signals [20].
- Combinatorial approaches: CIITA knockout (eliminating HLA class II) with expression of PD-L1, HLA-G, and CD47 has shown promise in protecting allografts [20].
Expression of Immunomodulatory Molecules
Beyond HLA modification, engineering cells to express natural immunomodulatory molecules represents a powerful strategy to actively suppress immune responses:
Diagram: Engineered Immunomodulatory Pathways for Hypo-Immune Cells. Surface expression of PD-L1, CD47, HLA-G, and CTLA-4-Ig on engineered cells engages inhibitory receptors on immune cells (T cells, macrophages, NK cells), suppressing effector functions through multiple mechanisms.
Key immunomodulatory molecules for engineering include:
- PD-L1 (Programmed Death-Ligand 1): Engagement of PD-1 on T cells delivers inhibitory signals that suppress T-cell activation and promotes T-cell exhaustion [20]. Expression of PD-L1 on graft cells provides localized immunosuppression without systemic effects.
- CD47: This "don't eat me" signal binds to SIRPα on macrophages and dendritic cells, inhibiting phagocytosis [20]. CD47 expression protects cells from innate immune clearance and complements HLA engineering strategies.
- HLA-G: A non-classical HLA class I molecule with potent immunosuppressive properties, HLA-G inhibits NK cell cytotoxicity, T-cell proliferation, and dendritic cell maturation [20].
- CTLA-4-Ig: A fusion protein that blocks CD28-B7 co-stimulation, preventing T-cell activation. Expression of CTLA-4-Ig on graft cells provides localized co-stimulation blockade [20].
Experimental Protocols
Protocol: Generation of HLA-Engineered Hypo-Immune Pluripotent Stem Cells
This protocol describes the creation of hypo-immune pluripotent stem cells (PSCs) through CRISPR/Cas9-mediated gene editing and transgene expression.
Materials:
- Human PSCs (hESCs or hiPSCs)
- CRISPR/Cas9 reagents (ribonucleoprotein complexes for B2M and CIITA)
- Donor template for HLA-E/GFP knock-in to B2M locus
- Electroporation system (e.g., Neon Transfection System)
- mTeSR1 or equivalent PSC maintenance medium
- Rock inhibitor (Y-27632)
- Flow cytometry antibodies: HLA-ABC, HLA-DR, HLA-E, B2M
- PCR reagents for genotyping
Procedure:
Design and Preparation of Editing Reagents:
- Design guide RNAs targeting B2M exon 1 and CIITA exon 2
- Design donor template containing HLA-E with B2M signal sequence followed by T2A-GFP
- Form ribonucleoprotein (RNP) complexes by incubating sgRNAs with Cas9 protein
Cell Preparation and Electroporation:
- Culture PSCs to 70-80% confluence in 6-well plates
- Harvest cells with Accutase and resuspend in electroporation buffer
- Mix 1×10^5 cells with RNP complexes (10 μg each) and donor template (2 μg)
- Electroporate using appropriate settings (e.g., 1400V, 10ms, 3 pulses for Neon system)
- Plate transfected cells in mTeSR1 with Rock inhibitor on Matrigel-coated plates
Selection and Screening:
- After 48 hours, analyze GFP expression by flow cytometry to assess knock-in efficiency
- Single-cell sort GFP+ cells into 96-well plates
- Expand clones for 2-3 weeks, then harvest for genotyping
- Confirm B2M and CIITA knockout by sequencing and flow cytometry
- Verify HLA-E expression by flow cytometry using HLA-E specific antibodies
Functional Validation:
- Differentiate edited PSCs into target cell type (e.g., β-cells, cardiomyocytes)
- Perform mixed lymphocyte reaction assays to assess T-cell activation
- Conduct NK cell cytotoxicity assays using primary NK cells
- Validate in vivo survival in humanized mouse models
Protocol: Assessment of Immune Evasion Properties
This protocol describes comprehensive in vitro assessment of the immune evasion capacity of engineered hypo-immune cells.
Materials:
- Engineered hypo-immune cells and unmodified controls
- Peripheral blood mononuclear cells (PBMCs) from multiple donors
- NK cell isolation kit
- Anti-CD3/CD28 activation beads
- CFSE cell proliferation dye
- Flow cytometry antibodies: CD3, CD4, CD8, CD56, CD107a, IFN-γ, Granzyme B
- ELISA kits for IFN-γ, TNF-α, IL-2
- Incucyte Live-Cell Analysis System (optional)
Procedure:
T-cell Activation Assay:
- Label PBMCs with CFSE and activate with anti-CD3/CD28 beads
- Co-culture activated PBMCs with engineered cells at 10:1 and 5:1 ratios
- After 5 days, analyze T-cell proliferation by CFSE dilution
- Collect supernatants for cytokine analysis by ELISA
- Perform intracellular staining for IFN-γ and Granzyme B
NK Cell Cytotoxicity Assay:
- Isolate NK cells from PBMCs using negative selection
- Culture NK cells with IL-15 (10 ng/mL) for 24 hours to enhance cytotoxicity
- Label target cells with Calcein-AM and co-culture with NK cells at various E:T ratios
- After 4 hours, measure Calcein release in supernatants
- Analyze CD107a expression on NK cells as a degranulation marker
Macrophage Phagocytosis Assay:
- Differentiate monocytes to macrophages with M-CSF (50 ng/mL) for 7 days
- Label target cells with pHrodo Red (fluorescence increases in acidic phagosomes)
- Co-culture macrophages with labeled target cells at 5:1 ratio
- Monitor phagocytosis by flow cytometry or live-cell imaging over 24 hours
- Quantify phagocytic index: (percentage of pHrodo+ macrophages) × (mean fluorescence intensity)
Statistical Analysis:
- Perform experiments with at least 3 different PBMC donors
- Use one-way ANOVA with post-hoc Tukey test for multiple comparisons
- Express data as mean ± SEM, with p < 0.05 considered significant
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Hypo-Immune Cell Engineering
| Reagent Category | Specific Examples | Application/Function |
|---|---|---|
| Gene Editing Tools | CRISPR/Cas9 (B2M, CIITA gRNAs), TALENs | Targeted disruption of HLA and related genes |
| Vector Systems | Lentiviral vectors (PD-L1, CD47, HLA-G), AAVS1 safe harbor targeting | Stable expression of immunomodulatory transgenes |
| Cell Culture Reagents | mTeSR1, StemFlex, Recombinant Laminin-521 | Maintenance of pluripotent stem cells during engineering |
| Differentiation Kits | STEMdiff Pancreatic Progenitor Kit, Cardiomyocyte Differentiation Kit | Generation of target cell types from engineered PSCs |
| Flow Cytometry Antibodies | Anti-HLA-ABC, HLA-DR, CD47, PD-L1, B2M, CD3, CD56 | Characterization of engineered cells and immune responses |
| Functional Assay Kits | CFSE Cell Division Tracker, LDH Cytotoxicity Assay, Cytokine ELISA Kits | Assessment of immune evasion properties in vitro |
The natural immune privilege mechanisms of cornea and placenta provide powerful paradigms for engineering hypo-immune cells for allogeneic therapy. The cornea teaches us the importance of physical barriers (avascularity), local immunomodulation, and systemic tolerance induction, while the placenta demonstrates the efficacy of low immunogenicity combined with active immunosuppression. By translating these principles through genetic engineering—particularly through HLA modification and expression of immunomodulatory molecules like PD-L1 and CD47—researchers are making significant progress toward creating universally compatible allogeneic cell products.
The emerging clinical success of hypo-immune engineered cells, particularly in the diabetes field where genetically modified allogeneic islets have shown positive six-month clinical results [20], validates this bioinspired approach. As the field advances, key challenges remain, including ensuring long-term safety of engineered cells, preventing potential off-target effects of gene editing, and addressing regulatory considerations. Nevertheless, learning from nature's solutions to immune tolerance continues to provide the most promising roadmap for overcoming the immune barriers to allogeneic cell therapy, potentially enabling off-the-shelf cellular therapeutics that can benefit broad patient populations without the need for lifelong immunosuppression.
The advancement of allogeneic cell therapies is fundamentally constrained by the host immune response to transplanted cells. Successfully engineering hypo-immune cells requires a deep understanding of the inherent immunogenic profiles of different cellular source materials. The two principal sources for these therapies are primary donor cells, obtained directly from healthy donors, and induced pluripotent stem cells (iPSCs), which are master cell lines capable of unlimited expansion and differentiation. Each source presents a distinct set of immunological challenges and advantages that dictate the engineering strategy required to achieve a "stealth" therapeutic product. This application note provides a comparative analysis of the immunogenic profiles of iPSCs and primary donor cells, summarizes key quantitative data for informed decision-making, and outlines essential experimental protocols for profiling and mitigating immune responses in the context of developing hypo-immune cell therapies for research.
The choice between primary donor cells and iPSCs has profound implications for the immunogenicity of the final therapeutic product. Key factors include the expression of Human Leukocyte Antigen (HLA) molecules, which are the primary triggers of adaptive immune rejection, and the susceptibility to innate immune effector cells like Natural Killer (NK) cells.
Table 1: Immunogenic Profile of Primary Donor Cells vs. iPSCs
| Feature | Primary Donor Cells (T/NK Cells) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| HLA Class I Expression | High and constitutive [21] [22] | Low in undifferentiated state; can increase upon differentiation or IFN-γ exposure [22] |
| HLA Class II Expression | Can be present and upregulated by IFN-γ (e.g., on antigen-presenting cells) [22] | Typically negative, and not robustly upregulated by IFN-γ [22] |
| Susceptibility to T-Cell Alloreactivity | High, due to full HLA expression and presence of endogenous TCR (for T cells) [10] [23] [11] | Variable; can be low in undifferentiated state but increases with differentiation [21] [24] |
| Risk of Graft-versus-Host Disease (GvHD) | High for αβ T cells without TCR disruption [23] [11] | Negligible for differentiated non-immune cells; relevant for iPSC-derived T/iT cells unless TCR is disrupted [25] |
| Susceptibility to NK Cell "Missing-Self" Killing | Lower, due to high HLA class I expression engaging NK inhibitory receptors [21] | Higher, particularly for HLA-engineered (e.g., β2M KO) or HLA-homozygous cells, which may lack ligands for all NK inhibitory receptors [21] [24] |
| Batch-to-Batch Variability | High, due to donor-to-donor genetic and physiological differences [10] | Low, as a single, well-characterized master iPSC clone can be used for all products [10] [26] |
A critical consideration for allogeneic therapies is the "missing-self" response mediated by recipient NK cells. NK cells are equipped with inhibitory receptors that recognize "self" HLA class I molecules. When they encounter a cell with absent or insufficient expression of these self-ligands, as is the case with HLA-downregulated or HLA-homozygous cells, they become activated and kill the target cell [21] [24]. Therefore, while knocking out HLA class I protects from T cell rejection, it can simultaneously render the cell vulnerable to NK cell-mediated killing.
Experimental Protocols for Immunogenicity Assessment
Robust preclinical assessment of immune responses is essential for developing successful hypo-immune cell therapies. The following protocols outline key in vitro and in vivo experiments to evaluate and benchmark the immunogenic profile of your candidate cell products.
Protocol: In Vitro Mixed Lymphocyte Reaction (MLR) to Assess T Cell Alloreactivity
Purpose: To quantitatively measure the ability of candidate therapeutic cells (stimulators) to provoke proliferation of allogeneic T cells (responders), thereby assessing their potential to cause T cell-mediated immune rejection [22].
Materials:
- Responder Cells: Peripheral blood mononuclear cells (PBMCs) isolated from healthy donors.
- Stimulator Cells: Candidate therapeutic cells (e.g., differentiated iPSC-derived cells or primary donor cells).
- Culture Medium: RPMI-1640 supplemented with 10% human AB serum, L-glutamine, and penicillin/streptomycin.
- Mitomycin C or irradiation source for stimulator cell arrest.
- Flow Cytometer with antibodies for T cell markers (CD3, CD4, CD8) and proliferation dyes (e.g., CFSE).
Method:
- Stimulator Cell Preparation: Treat candidate therapeutic cells with Mitomycin C (e.g., 25 µg/mL for 30 minutes at 37°C) or irradiate (e.g., 30-100 Gy) to arrest proliferation. Wash cells thoroughly.
- Responder Cell Preparation: Islect PBMCs from fresh blood or a cryopreserved vial of a healthy donor using Ficoll density gradient centrifugation.
- Co-culture Setup: Plate stimulator cells (e.g., 1x10^5 per well) with responder PBMCs (e.g., 1x10^5 to 1x10^6 per well) in a 96-well U-bottom plate in culture medium. Include controls: responders alone (negative control) and responders with a potent stimulator like anti-CD3/CD28 beads (positive control).
- Culture and Analysis: Culture cells for 5-7 days. To track proliferation, label responder PBMCs with CFSE prior to co-culture. Analyze T cell proliferation by flow cytometry, gating on CD3+ T cells and measuring CFSE dilution.
Data Interpretation: High proliferation in test wells compared to the negative control indicates strong alloreactivity. Hypo-immune engineered cells should show significantly reduced T cell proliferation.
Protocol: In Vitro NK Cell Cytotoxicity Assay to Assess "Missing-Self" Response
Purpose: To evaluate the susceptibility of HLA-engineered candidate cells to lysis by allogeneic NK cells, a key risk for hypo-immune cells with low HLA class I expression [21] [24].
Materials:
- Target Cells: Candidate therapeutic cells (e.g., HLA-engineered iPSC-derived cells).
- Effector Cells: NK cells isolated from healthy donor PBMCs (e.g., using negative selection kit).
- Culture Medium: As above, supplemented with 100-200 U/mL of recombinant human IL-2 for NK cell pre-activation (optional, for enhanced activity).
- Lactate Dehydrogenase (LDH) Release Detection Kit or flow cytometry-based cytotoxicity assay (e.g., using Annexin V/Propidium Iodide).
Method:
- Effector Cell Preparation: Isolate and if desired, pre-activate NK cells by culturing with IL-2 for 16-24 hours.
- Target Cell Preparation: Harvest candidate cells and label with a fluorescent marker if using flow cytometry-based readout.
- Co-culture Setup: Plate target cells in a 96-well plate. Add effector NK cells at varying Effector:Target (E:T) ratios (e.g., 5:1, 10:1, 20:1). Include controls for spontaneous release (targets alone) and maximum release (targets with lysis solution).
- Incubation and Measurement: Incubate for 4-6 hours at 37°C. Measure specific lysis using the LDH kit according to the manufacturer's instructions. Alternatively, for flow cytometry, analyze the percentage of dead/dying target cells using viability dyes.
Data Interpretation: High specific lysis at low E:T ratios indicates high susceptibility to NK cell killing. Successful hypo-immune strategies may require additional engineering (e.g., HLA-E or CD47 overexpression) to inhibit NK cell activity.
Protocol: Utilizing Humanized Immune System (HIS) Mouse Models for In Vivo Rejection Studies
Purpose: To assess the survival, engraftment, and immune rejection of candidate hypo-immune cells in a more physiologically relevant in vivo context that includes both human T and NK cell compartments [21].
Materials:
- HIS Mice: Immunodeficient mice (e.g., NSG) reconstituted with a human immune system via engraftment of human CD34+ hematopoietic stem cells.
- Candidate Cells: Luciferase-expressing therapeutic cells for in vivo tracking.
- In Vivo Imaging System (IVIS) to monitor cell persistence.
- Recombinant Human IL-15 cytokine or engineered vectors for enhancing human NK cell reconstitution in HIS mice [21].
Method:
- Model Validation: Confirm robust reconstitution of human T and NK cells in HIS mice by flow cytometry prior to study initiation. Administer IL-15 or other cytokines if needed to boost NK cell numbers [21].
- Cell Administration: Inject luciferase-expressing candidate cells (test group) and appropriate control cells (e.g., non-engineered, immunogenic cells) into HIS mice.
- Longitudinal Monitoring: Track the bioluminescent signal from the injected cells weekly using IVIS imaging.
- Endpoint Analysis: At the end of the study, harvest tissues (e.g., blood, spleen, liver) to analyze human cell persistence and immune cell infiltration by flow cytometry and histology.
Data Interpretation: A stable or increasing bioluminescent signal over time indicates successful evasion of immune rejection. A rapidly declining signal suggests rejection by human T or NK cells in the HIS model.
The Scientist's Toolkit: Key Reagents for Hypo-Immune Cell Research
Table 2: Essential Research Reagents for Hypo-Immune Cell Engineering and Profiling
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| CRISPR-Cas9 Gene Editing System | Disruption of immunogenicity genes (e.g., B2M for HLA-I, CIITA for HLA-II, TRAC for TCR) [10] [11]. | High efficiency but requires careful off-target analysis. Newer systems (e.g., base editing) may offer improved safety. |
| AAV or Lentiviral Vectors | Delivery of transgenes for "stealth" molecules (e.g., HLA-G, HLA-E, CD47) [23] [11]. | AAV has a larger payload capacity; lentivirus integrates into the genome for stable expression. |
| Recombinant Human Cytokines (IL-2, IL-15) | Expansion and activation of NK cells for in vitro cytotoxicity assays [21]. | IL-15 is critical for NK cell development and survival. |
| HIS Mouse Models (e.g., NSG with human CD34+ cells) | In vivo assessment of immune rejection in a model with a functional human immune system [21]. | Reconstitution levels of different immune lineages (T, NK, myeloid) can be variable and must be quantified. |
| Flow Cytometry Antibodies | Characterization of HLA expression, immune cell markers, and detection of cell death in co-culture assays. | Panels should include antibodies against HLA-A,B,C, HLA-II, CD3, CD56, and viability dyes. |
Visualizing the Hypo-Immune Cell Engineering Workflow
The development of a hypo-immune cell therapy from iPSCs involves a multi-step process of differentiation, genetic engineering, and rigorous immunogenicity testing. The following diagram outlines a generalized workflow for creating and validating an iPSC-derived, hypo-immune cell product.
Diagram 1: A generalized workflow for developing an iPSC-derived hypo-immune cell therapy, involving key steps of genetic engineering, differentiation, and multi-layered immunogenicity validation.
The core challenge in hypo-immune engineering is balancing the evasion of the adaptive immune system (T cells) with the risk of triggering the innate immune system (NK cells). The following diagram illustrates this "Immunogenicity Balancing Act" and common engineering strategies to address it.
Diagram 2: The core challenge in hypo-immune cell engineering. Ablating HLA to avoid T cell recognition can paradoxically activate NK cell killing via the 'missing-self' response, necessitating complementary engineering strategies to inhibit NK cells.
Genetic Engineering Toolkit: Designing and Building Hypoimmune Cell Products
The development of "off-the-shelf" or allogeneic cell therapies represents a transformative advancement in biomedical science, aiming to overcome the limitations of patient-specific (autologous) treatments. A central challenge in this field is preventing immune-mediated rejection of donor cells by the recipient's immune system. The engineering of hypo-immune cells—donor cells with reduced immunogenicity—is therefore a critical research focus. This process strategically involves the knockout of key immune genes to minimize graft-versus-host disease (GvHD) and host-versus-graft rejection [27] [11]. Three powerful gene-editing technologies—CRISPR-Cas9, TALENs, and ZFNs—serve as the primary workhorses for creating these engineered cells. This application note provides a detailed comparison of these platforms and standard protocols for their use in knocking out immunogenic genes, specifically targeting the T-cell receptor (TCR) and Major Histocompatibility Complex (MHC) molecules, to generate universal allogeneic cell therapies.
The following table summarizes the core characteristics of the three major gene-editing platforms.
Table 1: Comparison of Major Gene-Editing Technologies
| Feature | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| DNA Recognition Mechanism | Protein-DNA (Zinc Finger domains) | Protein-DNA (TALE repeats) | RNA-DNA (guide RNA) |
| Target Sequence Length | 9-18 bp [28] | 14-20 bp [28] | 20 bp + PAM sequence [29] |
| Nuclease | FokI dimer [28] | FokI dimer [28] | Cas9 [30] |
| Efficiency | Moderate [29] | Moderate [29] | High [29] |
| Specificity | Lower [29] | Moderate [29] | High, though off-target effects remain a concern [29] |
| Multiplexing Capability | Single | Single | Multiple (via co-delivery of multiple gRNAs) [31] |
| Design & Cloning | Complicated; requires protein engineering [28] | Complicated; repetitive TALE array cloning [28] | Simple; requires only sgRNA synthesis [29] |
| Clinical Trial Prevalence | Moderate [29] | Low [29] | High [29] |
Mechanism of Action for Gene Knockout
All three technologies function by inducing a double-strand break (DSB) at a specific genomic locus. The cell's primary repair pathway, Non-Homologous End Joining (NHEJ), is error-prone and often results in small insertions or deletions (indels) at the break site. When these indels occur within a protein-coding exon, they can cause a frameshift mutation, leading to a premature stop codon and effectively knocking out the gene [32] [28]. This principle is harnessed to disrupt genes responsible for immune recognition.
Application: Engineering Allogeneic CAR-T Cells
Chimeric Antigen Receptor (CAR)-T cell therapy has revolutionized cancer treatment, but its autologous nature presents challenges of high cost, manufacturing delays, and variable cell quality [27] [11]. Creating universal allogeneic CAR-T cells from healthy donors requires specific gene knockouts to ensure safety and efficacy, as illustrated in the workflow below.
Key Knockout Targets for Hypo-immune CAR-T Cells
Table 2: Essential Immune Gene Knockouts for Allogeneic CAR-T Cells
| Target Gene | Function | Purpose of Knockout | Result of Knockout |
|---|---|---|---|
| TRAC (T-cell receptor α constant) | Encodes a constant region of the T-cell receptor α chain [27] | Prevent Graft-versus-Host Disease (GvHD) [33] | Eliminates TCR surface expression, preventing donor T cells from attacking host tissues [27] [11] |
| B2M (β-2-microglobulin) | Essential component of the MHC Class I complex [33] | Prevent Host-versus-Graft Rejection [33] | Abolishes surface MHC I expression, evading recognition and elimination by host CD8+ T cells [33] |
| Regnase-1 | RNA-binding protein that degrades inflammatory mRNAs [33] | Enhance CAR-T cell persistence and potency [33] | Increases cytokine secretion and effector function, improving anti-tumor efficacy [33] |
| TGFBR2 (Transforming growth factor beta receptor 2) | Mediates immunosuppressive TGF-β signaling [33] | Confer resistance to tumor microenvironment [33] | Maintains CAR-T cell activity even in high TGF-β environments [33] |
Experimental Protocols
Protocol 1: Multiplexed Knockout of TRAC and B2M in Human T Cells Using CRISPR-Cas9
This protocol is designed for the simultaneous knockout of two key immunogenic genes to generate a universal CAR-T cell base.
4.1.1 Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Knockout in T Cells
| Reagent | Function | Example/Note |
|---|---|---|
| CRISPR-Cas9 System | Ribonucleoprotein (RNP) complex for DNA cleavage. | Recombinant SpCas9 protein and synthetic sgRNAs targeting TRAC and B2M. |
| sgRNAs | Guides the Cas9 nuclease to the specific DNA target. | Design sgRNAs with high on-target and low off-target scores. Target sequences: TRAC exon 1; B2M exon 1. |
| T Cell Activation Kit | Stimulates T cell proliferation and enhances editing efficiency. | Anti-CD3/CD28 magnetic beads. |
| Electroporation System | Enables efficient delivery of RNP complexes into T cells. | Lonza 4D-Nucleofector. |
| Cell Culture Media | Supports the growth and expansion of edited T cells. | OpTmizer T Cell Expansion SFM, supplemented with IL-2 and IL-7. |
4.1.2 Step-by-Step Workflow
sgRNA Design and Preparation:
- Design sgRNAs targeting the first exons of the TRAC (e.g., within the leader or variable domain) and B2M genes.
- Ensure the target sequence is followed by a 5'-NGG-3' Protospacer Adjacent Motif (PAM).
- Synthesize sgRNAs commercially or in vitro.
T Cell Isolation and Activation:
- Isolate peripheral blood mononuclear cells (PBMCs) from a leukapheresis product of a healthy donor.
- Isolate T cells using a negative selection kit.
- Activate T cells using anti-CD3/CD28 beads at a 1:1 bead-to-cell ratio in culture media supplemented with IL-2 (100 U/mL) for 24-48 hours.
Ribonucleoprotein (RNP) Complex Formation:
- For each knockout, combine 10 µg of SpCas9 protein with a 1.5x molar ratio of each sgRNA (e.g., TRAC sgRNA and B2M sgRNA for multiplexing).
- Incubate at room temperature for 10-20 minutes to form the RNP complex.
Electroporation:
- Harvest activated T cells and wash with PBS.
- Resuspend 1-2 million T cells in 100 µL of proprietary electroporation buffer.
- Add the pre-formed RNP complex to the cell suspension.
- Electroporate using a pre-optimized program for human T cells (e.g., DS-130 on the 4D-Nucleofector).
Post-Electroporation Culture and Expansion:
- Immediately transfer electroporated cells to pre-warmed culture media with cytokines (IL-2 and IL-7).
- Remove activation beads 3-5 days post-electroporation.
- Expand cells for 7-14 days, maintaining a cell concentration between 0.5-2 x 10^6 cells/mL.
Validation and Analysis:
- Flow Cytometry: At day 7-10, stain cells with antibodies against TCRα/β and MHC I to confirm knockout efficiency at the protein level.
- T7 Endonuclease I Assay or Sanger Sequencing: Genomically DNA extract and assess the frequency of indels at the target loci.
Protocol 2: Knockout of TRAC using TALENs or ZFNs
While CRISPR-Cas9 is more common, TALENs and ZFNs are still effectively used, especially in clinical settings.
4.2.1 Key Considerations:
- Design Complexity: Both TALENs and ZFNs require the design of two proteins that bind flanking sequences on opposite DNA strands, with the FokI nuclease domain dimerizing to create the DSB [28].
- Delivery: Unlike CRISPR's RNA-based targeting, TALENs and ZFNs are typically delivered as mRNA encoding the engineered proteins.
4.2.2 Workflow for TALEN-mediated TRAC Knockout:
- TALEN Design: Design a TALEN pair targeting the TRAC gene's constant region. The binding sites should be 14-20 bp in length and separated by a 12-20 bp spacer [28].
- mRNA Synthesis: Clone the TALEN sequences into an appropriate plasmid vector and perform in vitro transcription to produce capped and polyadenylated mRNA.
- T Cell Activation: (Same as Protocol 1, Step 2).
- Electroporation: Electroporate activated T cells with 2-5 µg of each TALEN mRNA.
- Culture and Expansion: (Same as Protocol 1, Step 5).
- Validation: (Same as Protocol 1, Step 6).
CRISPR-Cas9, TALENs, and ZFNs are powerful technologies enabling the precise knockout of immune genes to create hypo-immune cells for allogeneic therapy. CRISPR-Cas9 currently leads in popularity due to its simplicity, high efficiency, and ease of multiplexing. The choice of platform depends on the specific application, regulatory considerations, and required precision. The protocols outlined here provide a foundational methodology for researchers to engineer the next generation of universal, off-the-shelf cell therapies, paving the way for more accessible and cost-effective treatments for cancer and other diseases.
The development of allogeneic cell therapies represents a paradigm shift in regenerative medicine and cancer treatment, offering the potential for "off-the-shelf" cellular products that can be manufactured at scale and made readily available to patients. However, a significant biological barrier impedes this vision: host versus graft immune rejection. When cells from a donor are introduced into a recipient, the recipient's immune system recognizes foreign human leukocyte antigen (HLA) molecules on the donor cells, triggering their elimination through adaptive immune responses [34]. This immunogenic recognition is primarily mediated by T cells responding to HLA class I and II complexes, necessitating strategies to engineer cells that can evade this detection [35] [20].
The molecular basis of this immune recognition lies in the HLA complex, where HLA class I molecules (HLA-A, -B, and -C) are expressed on nearly all nucleated cells and present intracellular peptides to CD8+ cytotoxic T cells. These molecules require β2-microglobulin (B2M) for stable cell surface expression. Conversely, HLA class II molecules (HLA-DP, -DQ, and -DR) are typically expressed on antigen-presenting cells and present exogenous antigens to CD4+ helper T cells, with their expression critically dependent on the class II transactivator (CIITA) [34] [36]. The strategic knockout of B2M and CIITA thus disrupts the assembly and surface expression of both HLA classes, forming the cornerstone of hypoimmune cell engineering [35] [37].
This application note provides a comprehensive framework for implementing B2M and CIITA targeting strategies to create hypoimmune cells, detailing experimental protocols, validation methodologies, and reagent solutions to support researchers in advancing allogeneic cell therapies.
Molecular Strategies for HLA Ablation
Core Gene Editing Approaches
Multiple gene editing platforms can be employed to disrupt B2M and CIITA genes, each with distinct advantages for hypoimmune cell engineering.
CRISPR-Cas9 Systems: The most widely utilized approach employs the Cas9 nuclease complexed with sequence-specific guide RNAs (gRNAs) to create double-strand breaks in target genes. The cell's subsequent repair via error-prone non-homologous end joining (NHEJ) introduces insertion/deletion (indel) mutations that disrupt the reading frame, effectively knocking out the gene. This method has been successfully demonstrated in induced pluripotent stem cells (iPSCs) to generate clones with biallelic B2M and CIITA knockouts [37]. For enhanced specificity, nickase variants (Cas9n) can be used, which require two adjacent gRNAs to generate a double-strand break, significantly reducing off-target effects [37].
RNA Interference (shRNA): For applications where transient or partial knockdown is preferred over complete knockout, or to circumvent potential challenges with CRISPR editing efficiency, short hairpin RNA (shRNA) constructs provide an alternative. Lentiviral vectors can deliver shRNAs that specifically target transcripts of the HLA-ABC heavy chain or B2M. A key advantage is the ability to design shRNAs that selectively knock down classical HLA-A, -B, and -C without affecting the non-classical HLA-E, which is crucial for evading Natural Killer (NK) cell responses [38].
Other Nuclease Platforms: Transcription activator-like effector nucleases (TALENs) and zinc-finger nucleases (ZFNs) represent earlier generation editing tools that can also be applied for B2M and CIITA disruption. While these are less commonly used today due to the ease of CRISPR, they may still be valuable in specific contexts where CRISPR off-target concerns are paramount.
Addressing the "Missing Self" Response
A critical consequence of ablating HLA class I expression (e.g., via B2M knockout) is the creation of a "missing self" signal, which can trigger lysis by NK cells [35] [20] [36]. NK cells possess inhibitory receptors (e.g., NKG2A) that normally engage with HLA class I molecules, transmitting a "self" signal that prevents activation. The absence of this interaction, coupled with activating signals, leads to NK cell-mediated killing of the HLA-deficient cells [36]. Therefore, a complete hypoimmune strategy must incorporate mechanisms to mitigate this innate immune response. The most prominent solutions include:
Overexpression of "Don't Eat Me" Signals: Engineering cells to overexpress CD47, a ligand for the inhibitory receptor SIRPα on macrophages and some NK cells, can provide a potent "don't eat me" signal that inhibits phagocytosis [35] [34]. CD24 has also been identified as a key ligand that engages Siglec-10 on macrophages to suppress phagocytosis, and its overexpression has been successfully combined with B2M/CIITA knockout in iPSCs [35].
Expression of Non-Classical HLA Molecules: Retaining or introducing ligands for NK cell inhibitory receptors is another validated strategy. This includes the expression of non-polymorphic HLA-E, which can be engineered as a single-chain trimer (fusion of HLA-E heavy chain, B2M, and a peptide) to ensure surface expression even in a B2M-knockout background. HLA-E effectively engages NKG2A on NK cells and a subset of T cells, delivering a strong inhibitory signal [38] [36].
Overexpression of Immune Checkpoints: Engineering cells to express PD-L1, the ligand for the PD-1 receptor on activated T cells, can directly suppress T cell activity. This not only helps counter residual T cell recognition but has also been shown to enhance the persistence and function of allogeneic cell products like CAR-NK cells [38].
The following diagram illustrates the logical workflow for designing a comprehensive hypoimmune engineering strategy, integrating both HLA ablation and innate immune evasion components.
Experimental Protocols and Methodologies
Protocol 1: CRISPR-Cas9-Mediated B2M/CIITA Knockout in iPSCs
This protocol outlines the key steps for generating clonal B2M/CIITA knockout iPSC lines using CRISPR-Cas9.
- gRNA Design and Cloning: Design gRNAs targeting critical early exons of the B2M and CIITA genes to ensure frameshift mutations result in non-functional proteins. The B2M gRNA sequence
CACCGAAGTTGACTTACTGAAGAAand CIITA gRNA sequenceCACCGCCTGGCTCCACGCCCTGCThave been successfully used [37]. Clone annealed oligonucleotides into a Cas9-plasmid (e.g., pX462, which allows for puromycin selection). - Cell Culture and Transfection: Culture human iPSCs in feeder-free conditions (e.g., on Matrigel-coated plates with mTeSR1 medium). For electroporation, harvest 1×10^5 cells and resuspend in an appropriate buffer. Mix with 6 µg of the guide plasmid DNA and electroporate using a system like the Neon Transfection System (1100 V, one 10 ms pulse) [37].
- Selection and Clonal Isolation: After transfection, apply puromycin selection for 48-72 hours to eliminate non-transfected cells. Subsequently, dissociate cells into single cells and seed at a very low density for clonal expansion. Isolate individual colonies using cloning discs or by serial dilution in 100-mm dishes.
- Genotype Validation: Extract genomic DNA from expanded clones. Perform PCR amplification of the targeted regions and subject the products to Sanger sequencing. Analyze chromatograms for the presence of indels. Confirm the absence of B2M and HLA class I protein expression by flow cytometry and Western blotting [37].
Protocol 2: In Vitro Immune Cell Activation Assay
This assay quantitatively measures the ability of engineered hypoimmune cells to mitigate the activation of allogeneic immune cells.
- Co-culture Setup: Isolate peripheral blood mononuclear cells (PBMCs) from healthy human donors by density gradient centrifugation. Seed engineered hypoimmune cells (e.g., B2M−/−CIITA−/− iPSCs or their differentiated derivatives) as adherent monolayers. Add allogeneic PBMCs at a standardized effector-to-target ratio (e.g., 10:1) in complete RPMI medium. Include control wells with wild-type cells and PBMCs alone.
- Activation Readout: After 3-5 days of co-culture, harvest the PBMCs and stain with fluorescent antibodies for activation markers. Key markers include CD69 (early activation) and CD25 (IL-2 receptor alpha chain) on T cells (CD3+). Analyze by flow cytometry.
- Data Analysis: Quantify the percentage of CD3+ T cells that are CD69+ or CD25+ in each condition. Successful engineering is indicated by a significantly lower percentage of activated T cells in co-cultures with B2M/CIITA knockout cells compared to wild-type controls. This reduced T cell activation has been demonstrated in multiple studies [35] [37].
Protocol 3: In Vivo Assessment in Humanized Mouse Models
This protocol describes the use of humanized mouse models for pre-clinical validation of hypoimmune cell survival and function.
- Model Generation: Utilize immunodeficient mice such as NOD-scid IL2Rγnull (NSG). Humanize the mice by intravenously injecting CD34+ hematopoietic stem cells isolated from human umbilical cord blood. Allow 12-16 weeks for full reconstitution of a human immune system [35].
- Cell Transplantation and Disease Modeling: For disease modeling, such as peripheral arterial disease (PAD), induce hindlimb ischemia in the humanized mice by ligating and excising the femoral artery. Subsequently, transplant the therapeutic hypoimmune cells (e.g., universal iPSC-derived endothelial cells, U-ECs) into the ischemic muscle [35].
- Outcome Assessment:
- Cell Survival: After a set period (e.g., 4 weeks), harvest the tissue and quantify the persistence of human cells (e.g., by human-specific antigen staining or luciferase imaging) [35].
- Immune Infiltration: Analyze tissue sections by immunohistochemistry for infiltration of human T cells (CD3+), B cells (CD20+), and NK cells (CD56+) [37].
- Functional Efficacy: Assess the functional recovery, such as restoration of blood flow in the PAD model measured by laser Doppler perfusion imaging [35].
Table 1: Key In Vivo Findings from Pre-clinical Studies of Hypoimmune Cells
| Cell Type | Model | Genetic Modifications | Key Outcome | Reference |
|---|---|---|---|---|
| Human iPSCs | Monkey wound model | B2M−/− CIITA−/− | Reduced T & B cell infiltration; enhanced survival & wound healing vs. single KO or WT. | [37] |
| iPSC-derived Endothelial Cells (U-ECs) | Humanized PAD mouse (hindlimb ischemia) | B2M−/− CIITA−/− CD24OE | Significant blood flow restoration; greater cell survival & weaker immune response vs. WT-ECs. | [35] |
| CAR-NK Cells | Xenograft mouse model | shRNA-HLA-ABC + PD-L1 or SCE OE | Evaded host CD8+ T & NK cell rejection; enhanced tumor control & improved safety profile. | [38] |
The Scientist's Toolkit: Research Reagent Solutions
A successful hypoimmune cell engineering project relies on a suite of specialized reagents and tools. The table below catalogs essential solutions for key experimental stages.
Table 2: Essential Research Reagents for Hypoimmune Cell Engineering
| Product Category | Specific Example | Application/Function | Considerations |
|---|---|---|---|
| Gene Editing Platform | CRISPR-Cas9 plasmids (e.g., pX462); Cas9 protein + synthetic gRNA | Creates targeted double-strand breaks in B2M and CIITA genes. | Optimize delivery method (electroporation, lipofection); validate gRNA efficiency and specificity. |
| Cell Culture Systems | Feeder-free iPSC culture (mTeSR1 medium; GFR Matrigel) | Maintains pluripotency of iPSCs during and after gene editing. | Essential for preserving differentiation potential post-knockout. |
| Validation Antibodies | Anti-B2M (flow cytometry/WB); Anti-HLA-ABC (flow); Anti-CIITA (WB) | Confirms loss of target protein expression in engineered clones. | Use isotype controls; confirm antibody specificity for the target. |
| Immune Assay Reagents | Anti-human CD3, CD4, CD8, CD69, CD25; Mixed Lymphocyte Reaction (MLR) kits | Measures T cell activation and proliferation in response to engineered cells. | Use fresh or properly thawed PBMCs from multiple donors for robust allogeneic response. |
| Innate Evasion Modalities | Lentiviral vectors for CD47, CD24, PD-L1, or single-chain HLA-E (SCE) | Provides "don't eat me" signals and inhibits NK cell and T cell activity. | Monitor transduction efficiency; consider multi-cistronic vectors for co-expression. |
| Animal Models | Immunodeficient mice (e.g., NSG); CD34+ HSCs from human cord blood | Creates in vivo humanized model for testing cell survival and immune evasion. | Long lead time (12+ weeks) for immune system reconstitution; confirm engraftment level. |
Data Presentation and Analysis
Quantitative data from immune activation assays and in vivo studies are crucial for validating the success of hypoimmune engineering. The following table summarizes typical experimental outcomes that demonstrate reduced immunogenicity.
Table 3: Representative Quantitative Data from Hypoimmune Cell Studies
| Experimental Readout | Wild-Type (WT) Control Cells | B2M/CIITA Knockout Cells | Notes / Context |
|---|---|---|---|
| T Cell Activation (% CD3+CD69+) | 45.2% ± 5.1% | 12.8% ± 2.9% | Measured after 5-day co-culture with allogeneic PBMCs [35]. |
| Proliferation of Allogeneic T cells | High (Reference = 1.0) | Reduced by ~70% | Compared to stimulation index of WT-iPSCs [37]. |
| In Vivo Cell Survival (Day 28) | 5.2% ± 1.8% of initial graft | 35.5% ± 6.2% of initial graft | Quantification of human cells in humanized mouse model [35]. |
| Lymphocyte Infiltration (in vivo) | Extensive CD3+ and CD20+ infiltration | Significantly reduced infiltration | Histological scoring of graft site in monkey model [37]. |
| NK Cell Lysis (in vitro) | 15% ± 3% (B2M−/− only) | <5% (with HLA-E/CD47) | % specific lysis, showing necessity of innate evasion strategies [38] [36]. |
The experimental workflow for generating and validating hypoimmune cells involves a multi-stage process, from initial gene editing to final in vivo functional assessment, as visualized below.
The strategic knockout of B2M and CIITA, coupled with innovative solutions to counter the ensuing "missing self" response, provides a robust foundation for creating hypoimmune cells capable of evading adaptive immunity. The protocols and data outlined in this application note demonstrate the technical feasibility of this approach across multiple cell types, including iPSCs, iPSC-derived endothelial cells, and CAR-NK cells [35] [37] [38]. The ability to generate such "universal" cell products holds immense promise for making off-the-shelf allogeneic therapies a widespread clinical reality, potentially transforming treatment paradigms for conditions ranging from peripheral arterial disease and diabetes to cancer [35] [20] [36].
Future developments in this field will likely focus on enhancing the safety and precision of these engineering strategies. This includes the development of transient mRNA-based editing to minimize off-target risks, the refinement of gene-editing without double-strand breaks (e.g., base editing, prime editing), and the exploration of inducible safety switches to allow controlled elimination of transplanted cells if necessary. As these technologies mature, the path to clinical application will be paved, ultimately enabling the broad deployment of effective, scalable, and accessible allogeneic cell therapies.
The development of "off-the-shelf" allogeneic cell therapies represents a paradigm shift in regenerative medicine and cancer treatment. A central hurdle to this approach is host-mediated rejection, which involves not only the adaptive immune system (T cells) but also potent innate immune effectors, particularly natural killer (NK) cells. Hypoimmune engineering aims to create universally compatible cells by genetically masking their "foreign" identity. While β2-microglobulin (B2M) knockout is a common strategy to eliminate surface expression of polymorphic HLA class I molecules (HLA-A, -B, -C) and evade T cells, this creates a "missing-self" phenotype, triggering activation and cytolysis by host NK cells [39] [40]. This application note details protocols for countering this innate immune response through the coordinated overexpression of NK-inhibitory ligands (HLA-E, HLA-G) and the macrophage checkpoint molecule CD47.
Immunological Rationale and Key Signaling Pathways
NK cell activity is governed by a delicate balance of activating and inhibitory signals. Inhibitory receptors, such as NKG2A and KIRs, recognize self-HLA molecules and transmit signals that prevent the killing of healthy host cells. The strategic overexpression of non-polymorphic HLA molecules like HLA-E and HLA-G provides a conserved inhibitory signal that effectively tricks NK cells into tolerating the graft.
- HLA-E functions as a high-affinity ligand for the inhibitory CD94/NKG2A receptor complex expressed on a large subset of NK cells and a portion of CD8+ T cells [38] [41]. Its expression can be engineered to replace the lost inhibitory signal following B2M knockout.
- HLA-G is a potent immunosuppressive molecule that binds to multiple inhibitory receptors, including LILRB1 (ILT2) and KIR2DL4, directly dampening the cytolytic activity of NK cells and other immune effectors [41] [40].
- CD47 is a ubiquitously expressed "don't eat me" signal that engages SIRPα on macrophages and other myeloid cells, thereby inhibiting phagocytic clearance [39] [42]. Overexpression on therapeutic cells is critical for preventing macrophage-mediated destruction in the reticuloendothelial system.
The following diagram illustrates the core signaling pathways involved in this engineered immune evasion.
The efficacy of individual and combined immune-evasion strategies has been quantitatively assessed in various in vitro and in vivo models. The data below summarize key findings on the performance of HLA-E, HLA-G, and CD47 in enhancing cell survival.
Table 1: Summary of Quantitative Data for Immune Evasion Strategies
| Engineering Strategy | Experimental Model | Key Quantitative Outcome | Citation |
|---|---|---|---|
| B2M KO + HLA-E OE | iPSC-derived endothelial cells in NK cytotoxicity assay | Significant reduction in NK cell-mediated lysis compared to wild-type controls. | [43] |
| B2M KO + CD47 OE | iPSC-derived endothelial cells in humanized NSG mice | Enhanced survival of edited cells in vivo compared to wild-type controls. | [43] |
| shRNA HLA-ABC + PD-L1/SCE | Allogeneic CAR-NK cells in xenograft mouse model | Dramatic reduction of host vs. graft rejection; superior tumor control and persistence. | [38] |
| CD47 OE (on target cells) In vitro phagocytosis assay | Impaired antibody-dependent cellular phagocytosis (ADCP) by macrophages. | [42] | |
| Anti-CD47 Treatment | GVHD mouse model | Elevated phagocytosis of alloreactive T cells in the GIT; induced immunosuppressive responses and improved survival. | [42] |
Detailed Experimental Protocols
Protocol 1: Generation of Hypoimmune iPSCs with B2M KO and HLA-E/CD47 OE
This protocol outlines the creation of a master hypoimmune iPSC line suitable for differentiation into various therapeutic cell types [43].
- Starting Material: Begin with a clinically relevant human iPSC line (e.g., derived from PBMCs).
- B2M Knockout:
- Method: CRISPR-Cpf1 or CRISPR-Cas9-mediated knockout.
- Guide RNA Design: Design gRNAs targeting early exons of the B2M gene to ensure a complete null allele.
- Delivery: Electroporation of ribonucleoprotein (RNP) complexes.
- Validation: Select clonal populations and validate knockout via Sanger sequencing and flow cytometry confirming loss of surface HLA-ABC.
- Overexpression of HLA-E and CD47:
- Method: Lentiviral transduction.
- Vector Design: Use a constitutive promoter (e.g., EF1α) to drive simultaneous expression of HLA-E (or a single-chain trimer, SCT) and CD47 from a bicistronic vector. A puromycin resistance gene can be included for selection.
- Transduction: Transduce the B2M-KO iPSCs at an appropriate MOI.
- Selection: Apply puromycin for 5-7 days to select stable integrants.
- Validation: Confirm >99% co-expression of HLA-E and CD47 via flow cytometry. Assess pluripotency (e.g., teratoma formation, pluripotency marker staining) and karyotypic stability.
- Application: This engineered iPSC line can subsequently be differentiated into the desired therapeutic cell type (e.g., endothelial cells, cardiomyocytes, neural progenitors) using established protocols, with the immune-evasive properties retained post-differentiation.
Protocol 2: In Vitro Validation via NK Cell Cytotoxicity Assay
This protocol is used to functionally validate the resistance of engineered cells to NK cell attack [43].
- Target Cell Preparation:
- Differentiate hypoimmune and control (unmodified) iPSCs into the target cell type.
- Label the cells with a fluorescent dye (e.g., Calcein-AM) according to manufacturer's instructions.
- Effector Cell Preparation:
- Isolate NK cells from healthy donor PBMCs using a negative selection kit.
- Alternatively, use an activated NK cell line (e.g., NK-92).
- Co-culture and Measurement:
- Co-culture target and effector cells in a U-bottom 96-well plate at various Effector:Target (E:T) ratios (e.g., 5:1, 10:1, 20:1). Include replicates.
- Include controls for spontaneous release (target cells alone) and maximum release (target cells with lysis buffer).
- Incubate for 4-6 hours at 37°C.
- Centrifuge the plates and measure the fluorescence (F) of the supernatant.
- Data Analysis:
- Calculate the percentage of specific lysis using the formula:
% Specific Lysis = (F_Experimental - F_Spontaneous) / (F_Maximum - F_Spontaneous) * 100 - Expected Outcome: Hypoimmune cells (B2M KO + HLA-E/CD47 OE) should show a significant reduction in % specific lysis across all E:T ratios compared to control cells.
- Calculate the percentage of specific lysis using the formula:
The workflow for generating and validating hypoimmune cells is summarized below.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Hypoimmune Engineering
| Reagent / Tool | Function / Application | Example & Notes |
|---|---|---|
| CRISPR Systems (Cas9/Cpf1) | Precise knockout of immune-related genes (e.g., B2M, CIITA). | CRISPR-Cas9 RNPs for high-efficiency, footprint-free editing. |
| Lentiviral Vectors | Stable integration of transgenes (e.g., HLA-E, CD47, HLA-G). | Bicistronic vectors (e.g., P2A-linked) for co-expression. |
| Single-Chain HLA-E (SCE) | A engineered molecule combining HLA-E heavy chain, B2M, and peptide; ensures surface expression independent of endogenous B2M. | Critical for use in B2M-KO backgrounds [38]. |
| Flow Cytometry Antibodies | Validation of surface protein expression/knockout. | Anti-HLA-ABC (clone W6/32), Anti-HLA-E (clone 3D12), Anti-CD47. |
| Humanized Mouse Models | In vivo assessment of cell persistence and immunogenicity. | NSG mice engrafted with human PBMCs or a human immune system. |
| In Vitro NK Assay Kits | Functional validation of NK cell evasion. | Kits using Calcein-AM or LDH release to quantify cytotoxicity. |
The combinatorial strategy of ablating polymorphic HLA molecules while enforcing expression of conserved inhibitory checkpoints like HLA-E, HLA-G, and CD47 presents a robust framework for engineering hypoimmune cells. These protocols provide a foundational roadmap for researchers developing allogeneic therapies. Future directions will involve refining these edits further—for example, by incorporating TIGIT deletion to enhance NK cell cytotoxicity against tumors [39] or ICAM-1 knockout to impair immune cell adhesion and extravasation [14]. The integration of artificial intelligence and computational design will also play a pivotal role in predicting optimal, patient-specific editing strategies, ultimately accelerating the clinical translation of universal, off-the-shelf cell therapies [39].
Within the field of allogeneic cell therapy, the overarching goal of engineering hypoimmune cells is to create "off-the-shelf" therapeutic products that evade host immune rejection without requiring broad immunosuppression. A promising strategy to achieve this involves the co-expression of key immunomodulatory molecules—Programmed Death-Ligand 1 (PD-L1), Interleukin-10 (IL-10), and Fas Ligand (FasL). This triple-armoring approach simultaneously targets multiple facets of the immune response, from T-cell activation and cytokine polarization to direct immune cell deletion. This Application Note details the mechanistic rationale, quantitative expression profiles, and standardized protocols for implementing this strategy in engineered cell products, providing a framework for researchers developing advanced hypoimmune therapies.
Scientific Rationale and Mechanistic Insights
The co-expression strategy is designed to disrupt the immune rejection cascade at critical checkpoints. Individually, each molecule employs a distinct mechanism; together, they create a synergistic shield against alloreactivity.
- PD-L1 functions as a critical checkpoint regulator. By engaging the PD-1 receptor on activated T cells, it inhibits T-cell receptor-mediated proliferation and cytokine secretion, effectively delivering a co-inhibitory signal that dampens the cytotoxic T-cell response [44] [45]. Its expression is highly regulated by cytokines such as IFN-γ and IL-6 via the JAK/STAT signaling pathway [44].
- IL-10 is a potent anti-inflammatory cytokine that acts broadly on antigen-presenting cells (APCs), such as dendritic cells. It inhibits their maturation and the subsequent priming of naïve T-helper cells, shifting the immune balance away from a pro-inflammatory Th1 response [46]. Furthermore, IL-10 can upregulate PD-L1 expression on certain cell types, creating a self-reinforcing immunosuppressive loop [46].
- FasL (CD95L) mediates contact-dependent immune privilege. Upon interaction with its receptor, Fas (CD95), on the surface of activated immune cells, it triggers the Fas/FasL apoptosis pathway, leading to the direct elimination of infiltrating cytotoxic T lymphocytes and other inflammatory cells [47] [36]. This mechanism is employed by immune-privileged sites like the testis and cornea to maintain local tolerance [36].
The signaling interactions between these molecules and the host immune system are illustrated below.
Quantitative Data and Expression Profiles
A critical step in engineering is understanding the native regulation and expression levels of these immunomodulators to inform synthetic expression system design. The following table summarizes key quantitative data and regulatory mechanisms for each molecule.
Table 1: Quantitative Data and Regulatory Profiles of Key Immunomodulators
| Immunomodulator | Key Regulatory Factors & Pathways | Expression Impact & Kinetics | Noteworthy Quantitative Findings |
|---|---|---|---|
| PD-L1 (CD274) | - IFN-γ: JAK/STAT/IRF1 pathway [44]- IL-6: JAK/STAT3 pathway [44]- TNF-α: NF-κB pathway [44]- EGFR/MAPK signaling [44] | Rapid upregulation post-cytokine exposure (e.g., within 24h of IFN-γ stimulation) [44]. Post-translational modifications (glycosylation, ubiquitination) significantly affect protein stability and half-life [44]. | Co-expression with CD47 and HLA-G enhances hypoimmune phenotype in stem cell-derived islets [36]. |
| IL-10 | Produced by Tregs, macrophages, B cells, and some tumors [46]. Its expression can be feedback-regulated by the inflammatory milieu. | Secreted cytokine acting in a paracrine manner. Serum levels >3.6 pg/mL correlated with lower complete remission rates in peripheral T-cell lymphoma [46]. | Conflicting roles in cancer: High serum IL-10 generally correlates with worse prognosis, but retained expression in stage I NSCLC associated with better survival [46]. |
| FasL (CD178) | Constitutively expressed in immune-privileged tissues [36]. Expression can be induced by pro-inflammatory cytokines. | Membrane-bound or cleaved soluble form. Membrane-bound form is more effective at inducing apoptosis [47]. | Constitutive expression in placental trophoblasts, testis, and cornea contributes to immune privilege [36]. |
The regulatory network controlling PD-L1 expression is particularly complex, spanning multiple levels from the genome to the cell membrane, as detailed below.
Table 2: Multi-Level Regulatory Mechanisms of PD-L1 Expression [44]
| Regulatory Stage | Key Regulators / Mechanisms | Effect on PD-L1 |
|---|---|---|
| Genomic & Epigenetic | - Chromosome 9p24.1 rearrangements [44]- Histone modifications (H3K4me3, H3K27me3) [44]- DNA methylation of CpG islands [44] | ↑ / ↓ |
| Transcriptional | - IFN-γ (JAK/STAT/IRF1) [44]- IL-6 (JAK/STAT3) [44]- TNF-α (NF-κB) [44]- MAPK signaling [44] | ↑ |
| Post-Transcriptional | - miRNAs (e.g., miR-34a, miR-200, miR-142-5p) [44]- mRNA stability mechanisms (e.g., m6A methylation) [44] | ↓ / ↑ |
| Post-Translational | - Glycosylation (stabilizes) [44]- Ubiquitination (destabilizes) [44]- Palmitoylation (inhibits ubiquitination) [44] | ↑ / ↓ |
Experimental Protocols
Protocol 1: In Vitro Evaluation of Alloreactive T-Cell Suppression via Mixed Lymphocyte Reaction (MLR)
This protocol assesses the functional efficacy of armored cells in suppressing allogeneic T-cell responses in vitro [47].
Workflow Overview:
Materials:
- Research Reagent Solutions:
- Ficoll-Paque PLUS: For density gradient centrifugation to isolate peripheral blood mononuclear cells (PBMCs).
- Irradiator: Source (e.g., X-ray or gamma) to halt stimulator cell proliferation.
- Cell Culture Media: RPMI-1640 supplemented with 10% FBS, 1% L-Glutamine, 1% Penicillin-Streptomycin.
- Anti-human CD3, CD28 antibodies: For T-cell restimulation prior to cytokine measurement.
- ELISA Kits: For human IFN-γ, IL-2, TNF-α.
Procedure:
- Stimulator Cell Preparation: Isolate PBMCs from a healthy donor using Ficoll density gradient centrifugation. Irradiate the PBMCs (typically 30-50 Gy) to prevent blast transformation.
- Effector Cell Preparation: Harvest and count your engineered hypoimmune cells (e.g., mesenchymal stem cells, hypoimmune stem cell-derived derivatives, or armored CAR-T cells).
- Co-culture Setup: Plate the irradiated stimulator PBMCs and the armored effector cells in a U-bottom 96-well plate. A typical responder (armored cell): stimulator (PBMC) ratio can range from 1:1 to 1:10. Include controls: stimulators alone and effector cells alone.
- Incubation: Incubate the co-culture for 5-7 days at 37°C with 5% CO₂.
- Analysis:
- Flow Cytometry: Harvest cells and stain for T-cell activation markers (e.g., CD69, CD25) on CD3+ T cells.
- Cytokine Measurement: Collect supernatant. Analyze levels of pro-inflammatory cytokines like IFN-γ using ELISA, following manufacturer instructions.
Protocol 2: Functional Validation of FasL-Mediated Apoptosis
This protocol specifically tests the cytotoxic capability of membrane-bound FasL on armored cells.
Workflow Overview:
Materials:
- Jurkat T-cell line: A human T-lymphocyte cell line.
- Recombinant Human Fas-Fc Chimera: Serves as a blocking agent for the negative control.
- Annexin V Apoptosis Detection Kit: With FITC/PI or equivalent fluorophores.
- Caspase-Glo 3/7 Assay: A luminescent assay for caspase activity.
Procedure:
- T-cell Activation: Culture Jurkat cells and activate them using PMA (e.g., 10 ng/mL) and Ionomycin (e.g., 1 µM) for 16-24 hours to upregulate Fas receptor expression.
- Co-culture Setup: Plate your armored cells. Pre-treat one set of wells with Fas-Fc chimera (e.g., 5 µg/mL) for 1 hour to block FasL functionality as a control. Add the activated Jurkat cells to the armored cells at a defined effector:target ratio (e.g., 1:5).
- Incubation: Co-culture for 6-16 hours.
- Apoptosis Analysis:
- Annexin V/PI Staining: Harvest co-cultured cells, stain with Annexin V and Propidium Iodide (PI) according to kit instructions. Analyze by flow cytometry. Annexin V+/PI- cells are in early apoptosis; Annexin V+/PI+ are in late apoptosis/necrosis.
- Caspase Activity: Alternatively, transfer a portion of the co-culture to a white-walled plate and add Caspase-Glo 3/7 reagent. Measure luminescence after incubation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Hypoimmune Cell Engineering and Validation
| Reagent / Tool | Function & Application | Example Use-Case |
|---|---|---|
| Lentiviral/Viral Vectors | Stable gene delivery for co-expressing PD-L1, IL-10, and FasL transgenes. | Generating constitutively or inductibly armored cell lines. |
| CRISPR-Cas9 Systems | Knock-in of transgenes into safe-harbor loci (e.g., AAVS1) or knockout of endogenous HLA genes [20]. | Creating B2M-/- parental lines to eliminate HLA Class I expression [20] [36]. |
| Recombinant Cytokines (IFN-γ, IL-6) | Induce and validate endogenous PD-L1 upregulation pathways [44]. | Pre-treatment of cells to enhance PD-L1 expression prior to functional assays. |
| Anti-PD-L1 Blocking Antibodies | Function-blocking antibodies to confirm PD-L1/PD-1 pathway dependency in assays. | Adding to MLR co-cultures to reverse T-cell suppression. |
| Recombinant Fas-Fc Chimera | Soluble decoy receptor that binds and neutralizes FasL; critical negative control. | Validating FasL-specific apoptosis in co-culture assays (Protocol 4.2). |
| ELISA & Multiplex Assay Kits | Quantify secreted IL-10 and other cytokines (IFN-γ, IL-2) from co-cultures. | Measuring immunosuppressive potency in MLR supernatant. |
Concluding Remarks
The coordinated co-expression of PD-L1, IL-10, and FasL represents a sophisticated, multi-pronged bioengineering strategy to confer durable hypoimmune status to allogeneic cell products. The structured data and standardized protocols provided herein serve as a foundational toolkit for researchers aiming to validate and deploy this advanced armoring strategy. Successfully implemented, this approach has the potential to overcome the significant hurdle of immune rejection, accelerating the development of universally compatible "off-the-shelf" cellular therapies for a wide range of diseases.
Application Note: Engineering Hypoimmune Cells for Allogeneic Therapy
The development of hypoimmune cells represents a paradigm shift in regenerative medicine and cell therapy, aiming to create universal "off-the-shelf" cell products that evade host immune rejection without requiring immunosuppression. This approach leverages genetic engineering to modify critical immune signaling pathways, enabling long-term engraftment and function of allogeneic cells. The core strategy involves disrupting antigen presentation while simultaneously reinforcing "don't-eat-me" signals, creating cells that are invisible to the adaptive immune system yet protected from innate immune clearance. This application note outlines the current landscape, key engineering strategies, and translational progress across three major therapeutic modalities: CAR immune cells, stem cell-derived islets, and mesenchymal stem cells (MSCs), framing them within the broader context of hypoimmune engineering for allogeneic therapy research.
Clinical Trial and Regulatory Landscape
The translational pathway for advanced cell therapies is marked by key regulatory milestones and an expanding clinical trial footprint, particularly for allogeneic and hypoimmune-engineered products.
Table 1: Recent Regulatory Milestones for Cell Therapies (2023-2025)
| Product Name | Therapeutic Type | Indication | Regulatory Status & Date | Key Significance |
|---|---|---|---|---|
| Ryoncil | Allogeneic Bone Marrow-derived MSCs | Pediatric Steroid-Refractory acute GvHD | FDA Approved (Dec 2024) | First FDA-approved MSC therapy [48] |
| Lyfgenia | Autologous Gene-modified HSCs | Sickle Cell Disease | FDA Approved (Dec 2023) | Cell-based gene therapy [48] |
| Omisirge | Nicotinamide-modified Cord Blood HSCs | Hematologic Malignancies | FDA Approved (Apr 2023) | Accelerates neutrophil recovery [48] |
| Fertilo | iPSC-derived Ovarian Support Cells | In vitro oocyte maturation | FDA IND Cleared (Feb 2025) | First iPSC-based therapy in US Phase III trials [48] |
| FT819 | iPSC-derived CAR-T Cell | Systemic Lupus Erythematosus | FDA RMAT Designation (Apr 2025) | Off-the-shelf CAR-T for autoimmune disease [48] |
| Zimislecel | Allogeneic Stem Cell-Derived Islets | Type 1 Diabetes | Phase 1/2 Results (2025) | 83% insulin independence at 1 year (with immunosuppression) [49] |
| HIP Islets | Gene-edited Hypoimmune Islets | Type 1 Diabetes | Proof-of-Concept (2025) | Engraftment without immunosuppression [49] |
Table 2: Global Pluripotent Stem Cell (PSC) Clinical Trial Landscape (as of Dec 2024) [48]
| Parameter | Statistics |
|---|---|
| Total Global Clinical Trials | 115 |
| Distinct PSC-Derived Products | 83 |
| Total Patients Dosed | > 1,200 |
| Total Cells Administered | > 10¹¹ |
| Leading Therapeutic Areas | Ophthalmology, Neurology, Oncology |
| Reported Safety Profile | No significant class-wide safety concerns |
Hypoimmune Engineering Strategies and Protocols
Core Engineering Strategies for Immune Evasion
The foundation of hypoimmune cell generation lies in the coordinated disruption of adaptive immune recognition and protection from innate immune cytotoxicity.
Protocol: Generating Hypoimmune Induced Pluripotent Stem Cells (iPSCs)
This protocol details the creation of a hypoimmune iPSC line suitable for deriving universally compatible therapeutic cells [20] [41].
Title: Multiplex Gene Editing of Human iPSCs for Hypoimmune Phenotype
Key Principles: The protocol aims to eliminate polymorphic HLA molecules to prevent T-cell recognition while introducing non-polymorphic inhibitory ligands to protect against Natural Killer (NK) cell-mediated lysis.
Materials:
- Starting Cells: A clinically certified human iPSC line.
- Nucleofection System: For high-efficiency delivery of editing reagents.
- CRISPR Reagents: Ribonucleoprotein (RNP) complexes for:
- B2M gene knockout
- CIITA gene knockout
- Donor Template: A double-stranded DNA template for the B2M locus, encoding a fused HLA-E/β2M single-chain trimer.
- Cell Culture Reagents: Defined, xeno-free iPSC culture medium, Rock inhibitor (Y-27632).
- Analysis Reagents: Antibodies for flow cytometry (anti-HLA-ABC, anti-HLA-DR, anti-CD47, anti-HLA-G), genomic DNA extraction kit, PCR reagents for genotyping.
Procedure:
- iPSC Preparation: Culture iPSCs to ~80% confluency in a state of optimal growth. Harvest cells using a gentle cell dissociation reagent. Treat cells with Rock inhibitor to enhance survival after editing.
- RNP Complex Formation: Complex purified Cas9 protein with synthetic guide RNAs (gRNAs) targeting the B2M and CIITA genes to form RNP complexes.
- Nucleofection: Combine the iPSCs with the RNP complexes and the HLA-E trimer donor DNA template. Electroporate using a pre-optimized nucleofection program.
- Recovery and Expansion: Plate the transfected cells at low density in medium containing Rock inhibitor. Allow recovery for 48-72 hours.
- Single-Cell Cloning: Using fluorescence-activated cell sorting (FACS) or limited dilution, isolate single cells into 96-well plates to establish clonal lines.
- Genotypic Validation:
- PCR & Sequencing: Confirm B2M and CIITA knockout and precise knock-in of the HLA-E transgene via PCR and Sanger sequencing.
- Off-Target Analysis: Perform whole-genome sequencing or targeted deep sequencing of predicted off-target sites to select a clone with a clean editing profile.
- Phenotypic Validation:
- Flow Cytometry: Confirm loss of surface HLA-ABC and HLA-DR expression. Validate surface expression of the engineered HLA-E and CD47.
- Functional Assays: Co-culture edited iPSCs with allogeneic peripheral blood mononuclear cells (PBMCs) to demonstrate reduced T-cell activation and proliferation. Co-culture with activated NK cells to confirm protection from cytotoxicity.
Application: Stem Cell-Derived and Hypoimmune Islets for Type 1 Diabetes
Beta cell replacement via islet transplantation is a promising curative strategy for Type 1 Diabetes (T1D), limited by donor scarcity and lifelong immunosuppression. Hypoimmune engineering of stem cell-derived islets directly addresses these barriers [50] [49] [20].
Protocol: In Vivo Assessment of Hypoimmune Islet Function
Title: Transplantation of Hypoimmune Stem Cell-Derived Islets into a Mouse Model of Diabetes
Objective: To evaluate the capacity of engineered hypoimmune islets to achieve normoglycemia in allogeneic, immunocompetent diabetic mice without immunosuppression.
Materials:
- Animals: Immunocompetent mice (e.g., C57BL/6) rendered diabetic via Streptozotocin (STZ) injection.
- Test Articles: Hypoimmune stem cell-derived islets (SC-islets); Wild-type (WT) allogeneic SC-islets as a control.
- Supplies: Insulin syringe, surgical tools, blood glucose meter, ELISA kit for mouse C-peptide.
Procedure:
- Diabetic Model Induction: Administer STZ to mice to ablate endogenous beta cells. Confirm stable hyperglycemia (blood glucose >350 mg/dL) for one week prior to transplantation.
- Islet Preparation: Harvest and count 100-200 SC-islet equivalents per mouse for both hypoimmune and WT groups.
- Transplantation: Under anesthesia, transplant islets under the kidney capsule of each mouse. Include a sham-operated control group.
- Monitoring:
- Glycemia: Measure non-fasting blood glucose levels 3 times per week. Graft function is defined as a return to and maintenance of blood glucose <200 mg/dL.
- Body Weight: Record twice weekly.
- Functional Testing:
- Intraperitoneal Glucose Tolerance Test (IPGTT): Perform at 4, 8, and 12 weeks post-transplant. Measure blood glucose at 0, 15, 30, 60, and 120 minutes after glucose injection.
- Stimulated C-peptide: Collect plasma samples during IPGTT to measure C-peptide secretion as a marker of insulin production.
- Endpoint Analysis:
- Graft Retrieval: Remove the graft-bearing kidney for histological analysis (e.g., insulin/glucagon staining).
- Immune Profiling: Analyze the graft site by immunohistochemistry for the presence of T cells (CD3+) and macrophages (F4/80+).
Expected Outcomes: Mice receiving WT allogeneic islets will rapidly reject the graft, with blood glucose returning to diabetic levels within days. Mice transplanted with hypoimmune islets are expected to maintain normoglycemia for the study's duration, with minimal immune cell infiltration into the graft, demonstrating successful immune evasion.
Application: Allogeneic CAR-T and CAR-NK Cell Therapies
Allogeneic CAR-T and CAR-NK cell therapies are engineered from healthy donors to create "off-the-shelf" products, overcoming the manufacturing and cost limitations of autologous therapies [51] [52] [12].
Protocol: Producing Allogeneic CAR-NK Cells from iPSCs
Title: Manufacturing Off-the-Shelf CAR-NK Cells from a Clonal Master iPSC Line
Rationale: Using a single, engineered master iPSC line ensures a consistent, scalable, and quality-controlled cell product [48].
Materials:
- Starter Cells: A clonal master iPSC line, potentially hypoimmune-engineered.
- Differentiation Reagents: Cytokines and small molecules for definitive hemogenic endothelium and NK cell lineage specification (e.g., BMP4, VEGF, SCF, IL-3, IL-15).
- CAR Transgene: A lentiviral vector or a piggyBac transposon system containing the CAR construct (e.g., anti-BCMA for multiple myeloma).
- Cell Culture Equipment: Feeder-free cultureware for iPSCs, gas-permeable culture bags for NK cell expansion.
- Analytical Tools: Flow cytometers with antibodies against CD45, CD56, NKG2D for NK cell phenotyping.
Procedure:
- iPSC Maintenance: Culture the master iPSC line in a pluripotent state.
- NK Cell Differentiation: Initiate a multi-stage differentiation protocol over ~30 days to direct iPSCs towards the hematopoietic lineage and subsequently into functional NK cells.
- CAR Engineering: Transduce differentiating progenitor cells with the CAR vector at the hematopoietic progenitor stage. Alternatively, the CAR can be introduced into the master iPSC line itself.
- NK Cell Expansion: Culture CAR-positive NK cells with irradiated feeder cells and IL-2/IL-15 to achieve a clinically relevant cell number.
- Quality Control and Release Testing:
- Phenotype: Confirm >90% expression of NK cell markers (CD45+, CD56+) and CAR.
- Potency: Perform a co-culture cytotoxicity assay against target antigen-positive tumor cells. Measure IFN-γ release.
- Safety: Test for sterility, mycoplasma, and endotoxin.
Application: Mesenchymal Stem Cells (MSCs) in Regenerative Medicine
MSCs exert therapeutic effects primarily through paracrine signaling and immunomodulation. Allogeneic MSCs have low intrinsic immunogenicity but can still be rejected upon repeated administration, making them a candidate for hypoimmune engineering [53] [54].
Protocol: Testing MSCs in a Venous Leg Ulcer Model
Title: Phase I/II Randomized Controlled Trial of Allogeneic MSCs for Venous Ulcers [53]
Study Design: A multicenter, randomized, controlled, open-label clinical trial.
Materials:
- Biological Product: Bioengineered Artificial Mesenchymal Sheet (BAMS) containing allogeneic adult MSCs.
- Control: Conventional wound therapy.
- Participants: 20 patients with venous leg ulcers, randomized 1:1.
Intervention:
- Treatment Group: Local application of 4 doses of BAMS, administered once per week.
- Control Group: Receives conventional therapy.
Primary Endpoints:
- Feasibility: Ability to complete 4-dose administration in ≥80% of patients.
- Safety: Incidence of adverse and serious adverse effects.
- Efficacy:
- Percentage of wound closure (wound area reduction).
- Macroscopic assessment (RESVECH 2.0 scale).
- Analysis of growth factors and inflammatory cytokines (ELISA).
- Pain levels (VAS scale) and quality of life (CIVIQ-20).
Table 3: Essential Research Reagents for Hypoimmune Cell Engineering
| Reagent / Resource | Function / Description | Example Application |
|---|---|---|
| CRISPR-Cas9 RNP Complexes | Enables precise, footprint-free gene knockout (e.g., B2M, CIITA). | Generation of HLA-deficient base lines [20] [41]. |
| HLA-E Single-Chain Trimer Donor Template | DNA template for knock-in to replace B2M, provides NK cell inhibition. | Protecting HLA class I-negative cells from NK cell killing [41]. |
| Anti-HLA-ABC Antibody (Flow Cytometry) | Validates surface loss of HLA class I after B2M knockout. | Phenotypic screening of edited clones [41]. |
| REPROCELL StemRNA Clinical Seed iPSCs | GMP-compliant, DMF-filed master iPSC lines. | Consistent, scalable starting material for therapy development [48]. |
| Lentiviral CAR Vector | Stable integration of CAR construct into host cell genome. | Engineering CAR-T or CAR-NK cells from iPSCs [52]. |
| PiggyBac Transposon System | Non-viral method for stable genomic integration of large transgenes. | CAR gene delivery as an alternative to viral vectors [52]. |
| IL-2/IL-15 Cytokines | Critical for the expansion and functional maturation of NK cells. | In vitro production of CAR-NK cells from progenitors [51]. |
Navigating Development Challenges: Safety, Efficacy, and Manufacturing Hurdles
The advancement of allogeneic cell-based immunotherapies represents a paradigm shift in regenerative medicine and cancer treatment, offering scalable "off-the-shelf" alternatives to patient-specific autologous therapies. Unlike autologous approaches, allogeneic therapies utilize cells derived from healthy donors, enabling standardized manufacturing processes and immediate product availability [47]. However, this therapeutic class faces three interconnected critical safety barriers: Graft-versus-Host Disease (GvHD), host-mediated allorejection, and tumorigenicity. GvHD occurs when donor-derived immune cells recognize and attack recipient tissues, potentially causing severe multi-organ damage [47]. Simultaneously, the host immune system can recognize transplanted cells as foreign, leading to their rejection and limiting therapeutic persistence [36]. Furthermore, stem cell-based products carry inherent tumorigenic risks due to their self-renewal capacity and potential for uncontrolled proliferation [55] [56]. This application note delineates comprehensive risk assessment and mitigation protocols within the context of engineering hypoimmune cells for allogeneic therapy research.
Quantitative Risk Profiling: Clinical and Preclinical Data
A systematic analysis of recent clinical outcomes and preclinical studies provides a quantitative foundation for risk assessment and benchmarking of mitigation strategies.
Table 1: Clinical Outcomes of Allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT)
| Parameter | Standard allo-HSCT | Novel Therapy (Orca-T) | Notes |
|---|---|---|---|
| 1-Yr Survival without Moderate/Severe chronic GvHD | 38% | 78% | Phase 3 Precision-T trial (n=187) [57] |
| One-Year Overall Survival | 83% | 94% | Phase 3 Precision-T trial [57] |
| Cumulative Incidence of Moderate-to-Severe GvHD | 44% | 13% | At one year [57] |
| Grade 3/4 Acute GvHD | 17% | 6% | [57] |
| Three-Year Overall Survival (Aged ≥70) | 34.9% | N/A | Pooled data from meta-analysis (n=2519) [58] |
| Pooled Median Overall Survival (Aged ≥70) | 14.84 months | N/A | Follow-up: 23.2 months [58] |
Table 2: Tumorigenicity Risk Profile of Stem Cell-Based Therapeutic Products
| Cell Type | Primary Tumorigenicity Risk | Reported Incidence | Key Risk Factors |
|---|---|---|---|
| Pluripotent Stem Cells (PSCs: hESCs, iPSCs) | Teratoma formation from residual undifferentiated cells [56] | Observed in animal models and clinical case reports [56] | High proportion of undifferentiated cells; insufficient differentiation [59] |
| Mesenchymal Stem Cells (MSCs) | Glioproliferative lesions (rare) [56] | Case reports (e.g., intrathecal infusion) [56] | Unreliable cell sources; lack of proper oversight [56] |
| General Risk Threshold | >100 - 10,000 undifferentiated cells per million [56] | 0% tumorigenicity with 10 spiked ESCs in mice (n=30) [56] | Cell number and viability post-transplantation |
Graft-versus-Host Disease (GvHD): Mechanisms and Mitigation
Pathophysiological Basis and Signaling Pathways
GvHD progresses through a well-characterized sequence of immunological events. The process initiates in a pro-inflammatory environment, often pre-existing in patients with advanced disease, characterized by elevated levels of TNF-α, IL-1, and various chemokines [47]. This milieu enhances host antigen-presenting cell (APC) activation, upregulating Major Histocompatibility Complex (MHC/HLA) molecules. Donor T cells subsequently recognize these mismatched host HLA antigens, triggering their activation through T-cell receptor (TCR) signaling and co-stimulatory pathways [47]. Fully activated donor T cells mediate tissue damage via direct cytotoxicity (perforin/granzyme and Fas/FasL pathways) and prolific cytokine release (e.g., IFN-γ, IL-2, TNF-α), which further amplifies the inflammatory cascade and leads to the characteristic damage to the skin, gastrointestinal tract, and liver [47].
Experimental Protocol: In Vitro GvHD Assessment via Mixed Lymphocyte Reaction (MLR)
Principle: The MLR assay evaluates the potential of donor-derived cells to mount a proliferative and cytotoxic response against recipient immune cells, simulating the initial phase of GvHD in vitro [47].
Procedure:
- Cell Preparation:
- Stimulator Cells: Isolate Peripheral Blood Mononuclear Cells (PBMCs) from a healthy donor representing the recipient's immune profile. Render these cells incapable of proliferation by treatment with gamma irradiation (e.g., 25-50 Gy) or mitomycin C.
- Effector Cells: Prepare the investigational allogeneic cell product (e.g., TCR-engineered T-cells, NK cells, NKT cells) representing the donor's cells.
- Co-culture:
- Combine stimulator and effector cells in a defined ratio (e.g., 1:1) in a suitable culture medium. Include control wells containing only stimulators or only effectors to account for background activation and proliferation.
- Incubate for 3-7 days in a humidified incubator at 37°C with 5% CO₂.
- Readout and Analysis:
- Flow Cytometry: Analyze T-cell activation markers (e.g., CD69, CD25) and differentiation profiles (e.g., CD45RA, CD45RO) on effector cells post-co-culture [47].
- Cytokine ELISA: Quantify the concentration of pro-inflammatory cytokines (e.g., IFN-γ, TNF-α) in the culture supernatant [47].
- Proliferation Assays: Use CFSE dilution or ³H-thymidine incorporation to measure the proliferation of effector cells in response to allogeneic stimulators.
Interpretation: A significant increase in activation markers, cytokine secretion, and proliferation in the co-culture compared to controls indicates a high potential for alloreactivity and GvHD risk.
Allorejection: Engineering Hypoimmune Cells
Molecular Basis of Immune Recognition and Evasion Strategies
Allorejection is primarily mediated by host T cells and natural killer (NK) cells recognizing non-self antigens on donor cells. The core of this recognition involves HLA molecules. CD8⁺ cytotoxic T cells recognize foreign HLA class I molecules (HLA-A, -B, -C), leading to donor cell killing [36]. NK cells, conversely, attack cells with absent or low expression of HLA class I ("missing-self" hypothesis) [36]. Strategies to create hypoimmunogenic cells therefore focus on disrupting this recognition.
Key genetic engineering approaches to mitigate allorejection include:
- HLA Ablation: Knockout of Beta-2-Microglobulin (B2M) eliminates surface expression of all HLA class I molecules, effectively preventing CD8⁺ T cell recognition [36] [47].
- TCR Disruption: Knocking out the T-cell receptor alpha constant (TRAC) gene in allogeneic T-cell products prevents graft-versus-host responses [47].
- "Don't Eat Me" Signals: Overexpression of CD47, a "self" marker, inhibits phagocytosis by host macrophages [36].
- NK Cell Inhibition: Ectopic expression of non-classical HLA molecules (HLA-E, HLA-G) engages inhibitory receptors (e.g., NKG2A) on NK cells, suppressing their cytotoxic activity [36].
- Immunomodulatory Factors: Overexpression of PD-L1 induces local immune tolerance by engaging the PD-1 receptor on activated T cells, leading to their exhaustion or apoptosis [36].
The Scientist's Toolkit: Key Reagents for Hypoimmunogenic Engineering
Table 3: Essential Research Reagents for Engineering Hypoimmune Cells
| Research Reagent / Tool | Function / Target | Application in Hypoimmune Engineering |
|---|---|---|
| CRISPR/Cas9 System | Gene knockout (e.g., B2M, TCR, CIITA) | Disrupts genes responsible for immune recognition (HLA, TCR) [47]. |
| TALENs | Gene knockout | Alternative nuclease for precise gene editing [47]. |
| CD47 Expression Vector | "Don't eat me" signal | Protects donor cells from macrophage/monocyte phagocytosis [36]. |
| PD-L1 Expression Vector | Immune checkpoint | Suppresses activated T-cells in the local microenvironment [36]. |
| HLA-G/HLA-E Expression Vector | NK cell inhibitory ligands | Engages inhibitory receptors on NK cells to prevent "missing-self" attack [36]. |
Tumorigenicity: Assessment and Control Strategies
Tumorigenicity is a critical safety concern, particularly for therapies derived from Pluripotent Stem Cells (PSCs). The primary risk stems from residual undifferentiated PSCs in the final product, which can form teratomas—benign tumors containing multiple tissue types—in vivo [56]. Although the risk is lower for somatic stem cells like MSCs, cases of glioproliferative lesions have been reported following the administration of poorly characterized cells from unreliable sources [56]. Global regulatory agencies require a thorough tumorigenicity risk evaluation based on the product's cell source, phenotype, differentiation status, and manufacturing process, though standardized technical guidelines are still evolving [59].
Experimental Protocol: Comprehensive Tumorigenicity Assessment Workflow
A tiered approach is recommended for a robust tumorigenicity assessment, combining in vitro and in vivo methods.
1. In Vitro Quality Control and Screening:
- Flow Cytometry: Quantify the percentage of residual undifferentiated cells using cell surface markers specific to PSCs (e.g., SSEA-4, TRA-1-60). This provides a rapid, quantitative readout for batch-to-batch quality control [56].
- qPCR: Measure the expression levels of pluripotency-associated genes (e.g., OCT3/4, SOX2, NANOG). This highly sensitive method can detect low levels of residual undifferentiated cells [56].
- Soft Agar Colony Formation Assay: Assess anchorage-independent growth, a hallmark of cellular transformation. The inability of non-tumorigenic, differentiated cells to form colonies in soft agar provides evidence of safety [56].
2. In Vivo Confirmation (Gold Standard):
- Animal Model: Utilize immunocompromised mice (e.g., NOD-scid, NSG) to avoid rejection of human cells, allowing for the assessment of intrinsic tumorigenic potential.
- Procedure:
- Divide mice into test groups receiving the final differentiated cell product and control groups receiving a known number of undifferentiated PSCs (positive control).
- Administer cells via the clinically relevant route (e.g., subcutaneous, intramuscular) at a dose significantly higher than the intended human dose.
- Monitor animals for 4 to 7 months, as per FDA recommendations, for any signs of tumor formation [56].
- Perform detailed histopathological analysis on recovered masses to confirm tumor type (e.g., teratoma).
Interpretation: A product is considered to have a low tumorigenic risk if it passes in vitro specifications (e.g., <100 undifferentiated cells per million) and shows no tumor formation in vivo at the tested sensitivity, while positive controls do form tumors.
The future of allogeneic cell therapies hinges on a multi-pronged strategy that integrates advanced engineering with rigorous safety testing. Promising clinical results, such as those from the Orca-T trial (a cell therapy comprising purified regulatory T-cells and conventional T-cells), demonstrate that sophisticated cell processing can drastically reduce GvHD while maintaining high efficacy [57]. Simultaneously, the field is moving towards generating standardized, "off-the-shelf" hypoimmunogenic cells through precise genetic edits that abolish immune recognition without compromising therapeutic function [2] [36]. Finally, implementing a robust, multi-tiered tumorigenicity assessment protocol from product development through batch release is non-negotiable for ensuring patient safety [59] [56]. By systematically addressing the triad of GvHD, allorejection, and tumorigenicity through the engineering and validation strategies outlined herein, researchers can accelerate the development of safer and more effective allogeneic cell therapies.
The development of universal, off-the-shelf allogeneic cell therapies represents a transformative goal in regenerative medicine and cancer treatment. A significant barrier to this goal is immune rejection, particularly by natural killer (NK) cells triggered by the 'missing-self' response [3]. This response occurs when transplanted cells lack surface expression of major histocompatibility complex (MHC) class I molecules (human leukocyte antigen [HLA] class I in humans), which normally engage with inhibitory receptors on NK cells to signal 'self' [6] [3]. Without this inhibitory signal, NK cells perceive the cells as dangerous or damaged and initiate cytotoxic killing [60].
This application note details the mechanistic basis of the 'missing-self' response and provides validated, practical strategies—including genetic engineering approaches and experimental protocols—to prevent NK cell-mediated cytotoxicity. These methods are essential for advancing the development of durable hypoimmune cell therapies.
Background: NK Cell Biology and Cytotoxicity Mechanisms
Effector Mechanisms of NK Cell-Mediated Killing
NK cells eliminate target cells through several coordinated mechanisms [60]:
- Lytic Granule Exocytosis: Release of perforin and granzymes that induce apoptosis in target cells.
- Death Receptor-Mediated Apoptosis: Expression of Fas ligand (FasL) or TNF-related apoptosis-inducing ligand (TRAIL) to engage death receptors.
- Cytokine Production: Secretion of IFN-γ and TNF that modulate the immune environment.
The biogenesis of perforin and granzymes is highly regulated to prevent damage during synthesis, and NK cells possess self-protective mechanisms to avoid their own cytotoxic activity during degranulation [60].
The Concept of NK Cell Education
NK cell function is governed by a balance of signals from activating and inhibitory receptors [61] [62]. The education process, often termed licensing, occurs during NK cell development. NK cells become fully functional ("licensed") when their inhibitory receptors, such as Killer cell Immunoglobulin-like Receptors (KIRs) and CD94/NKG2A, engage with self-MHC class I molecules [62]. Conversely, NK cells that lack inhibitory receptors for self-MHC remain hyporesponsive ("uneducated") [61]. This process is recapitulated after allogeneic hematopoietic stem cell transplantation, providing a unique window to study human NK cell education [61].
Table: Key NK Cell Receptors and Ligands
| Receptor | Ligand | Function | Signaling Effect |
|---|---|---|---|
| KIR (e.g., KIR2DL1) | HLA-C (group C2) | Inhibitory | Prevents killing upon recognition of self-HLA [61] |
| CD94/NKG2A | HLA-E | Inhibitory | Inhibits NK cell activity [6] |
| NKG2D | MICA/B, ULBPs | Activating | Recognizes stress-induced ligands [60] |
| Natural Cytotoxicity Receptors (NCRs) | Viral/bacterial ligands,? | Activating | Triggers killing of infected/cancer cells [63] |
| CD16 (FcγRIIIA) | Antibody Fc region | Activating | Mediates Antibody-Dependent Cellular Cytotoxicity (ADCC) [64] |
| SIRPα | CD47 | Inhibitory | Delivers "don't eat me" signal to macrophages; also inhibits NK cells [6] |
Engineering Strategies to Evade the 'Missing-Self' Response
A common strategy to avoid T cell-mediated rejection is knocking out HLA class I molecules, typically by disrupting the β2-microglobulin (B2M) gene. However, this renders cells vulnerable to the NK cell 'missing-self' response [6] [3]. The following engineering strategies address this vulnerability.
CD47 Overexpression
Rationale: CD47 is a "don't eat me" signal that binds to Signal Regulatory Protein Alpha (SIRPα) on macrophages and NK cells, delivering a potent inhibitory signal [6] [3].
Experimental Evidence:
- A head-to-head comparison of immune evasion strategies showed that K562 cells overexpressing CD47 were comprehensively protected from killing by IL-2-stimulated human NK cells, whereas strategies using HLA-E or HLA-G were only effective against NK subsets expressing the specific inhibitory receptor [6].
- In a rigorous in vivo model, rhesus macaque hypoimmune induced pluripotent stem cells (HIP iPSCs) engineered with B2M and CIITA knockout and macaque CD47 overexpression survived for 16 weeks in fully immunocompetent allogeneic recipients, whereas wild-type cells were vigorously rejected [6].
Protocol: Engineering CD47 Overexpression
- Knockout B2M and CIITA: Use CRISPR-Cas9 to disrupt the B2M and CIITA genes in your parent cell line (e.g., iPSCs).
- Introduce CD47 Transgene: Transduce the cells with a lentiviral vector carrying the species-matched CD47 gene. A strong, universal promoter (e.g., EF1α) is recommended.
- Validate Expression: Use flow cytometry to confirm the loss of HLA class I/II and high surface expression of CD47.
- Functional Validation: Co-culture engineered cells with activated allogeneic NK cells and assess cell death (see Section 5.2 for detailed protocol).
Expression of Non-Polymorphic HLA Molecules
Rationale: Introducing minimally polymorphic HLA molecules like HLA-E or HLA-G can provide a conserved inhibitory signal to NK cells without presenting a broad range of foreign antigens to T cells [6] [20].
Considerations and Limitations:
- HLA-E binds to the CD94/NKG2A inhibitory receptor on NK cells [6].
- HLA-E and HLA-G require association with B2M for surface expression. In a B2M−/− background, this necessitates creating a fusion construct linking the HLA heavy chain to a transgenic B2M [6].
- This approach is not universally protective. The protective effect is limited to the subset of NK cells that express the specific inhibitory receptor (CD94/NKG2A for HLA-E; ILT2 for HLA-G). One study showed only 31.4% of IL-2-stimulated human NK cells expressed CD94, and CD94⁻ NK cells efficiently killed HLA-E-expressing targets [6].
Combinatorial Approaches and Future Directions
The most robust protection is likely achieved by combining multiple strategies. For instance, a hypoimmune (HIP) cell profile can be created by knocking out B2M and CIITA (to evade T cells) and overexpressing CD47 (to broadly inhibit innate immunity) [6]. Other promising molecules under investigation include:
- PD-L1: Overexpression can inhibit PD-1⁺ NK cells and macrophages [3].
- CD24: Shown to inhibit macrophagic phagocytosis via Siglec-10, though its application in iPSC engineering is not yet reported [3].
Diagram: NK cell activation is determined by the balance of signals received from activating and inhibitory receptors on the target cell. 'Missing-self' due to B2M knockout removes a key inhibitory signal (red dashed line), but engineered expression of inhibitors like CD47 and HLA-E can restore protection.
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Studying NK Cell 'Missing-Self' Responses
| Reagent / Tool | Function/Application | Key Examples / Notes |
|---|---|---|
| K562 Cell Line | Target Cell Model: An HLA class I- and II-negative human erythroleukemia cell line; used to stimulate NK cells and test 'missing-self' killing [61] [6]. | Can be engineered to express transgenes (e.g., CD47, HLA-E) for head-to-head comparison of strategies [6]. |
| IL-2 | NK Cell Activator: Cytokine used to pre-activate and expand NK cells in vitro, enhancing their cytotoxic potential [6]. | Used at varying concentrations (e.g., 100-1000 U/mL) to modulate NK cell activity. |
| Anti-CD107a Antibody | Degranulation Assay: Marker for lytic granule exocytosis. Added to NK-target co-culture to measure NK cell activation by flow cytometry [61]. | Clone H4A3; used with protein transport inhibitors (Brefeldin A/Monensin) [61]. |
| CRISPR-Cas9 System | Gene Editing: Used to knock out genes like B2M and CIITA in pluripotent stem cells or primary cells to reduce immunogenicity [6] [3]. | Enables creation of hypoimmune base lines for further engineering. |
| Lentiviral Vectors | Gene Delivery: For stable overexpression of transgenes (e.g., CD47, HLA-E, PD-L1) in target cell lines [6]. | Allows for strong, constitutive expression of immune-modulatory genes. |
| Recombinant IL-15 | NK Cell Priming: Cytokine that can rapidly increase target-inducible IFN-γ production in reconstituting NK cells [61]. | Potential therapeutic tool to enhance NK cell function post-transplant [61]. |
Experimental Protocols for Validation
Protocol: In Vitro NK Cell Cytotoxicity and Degranulation Assay
This protocol measures the ability of engineered hypoimmune cells to resist killing by allogeneic NK cells [61].
Materials:
- Effector Cells: IL-2-activated human peripheral blood NK cells (isolated, e.g., by negative selection)
- Target Cells: Engineered hypoimmune cells and wild-type control cells
- Culture medium (e.g., RPMI-1640 with 10% FBS)
- Anti-CD107a antibody (e.g., PerCP-Cy5.5 anti-human CD107a, clone H4A3)
- Protein transport inhibitors: Brefeldin A (GolgiPlug) and Monensin (GolgiStop)
- Flow cytometry antibodies: anti-CD45, anti-CD3, anti-CD56, anti-IFN-γ
Procedure:
- NK Cell Activation: Isolate NK cells from healthy donor PBMCs and culture with 100-500 U/mL recombinant human IL-2 for 16-24 hours prior to the assay.
- Co-culture Setup: Mix effector (NK) and target cells at a standard 2:1 ratio (e.g., 4x10⁶ NK cells with 2x10⁶ target cells) in a V-bottom 96-well plate. Include wells for targets alone (spontaneous release) and targets with lysis buffer (maximum release).
- Degranulation Staining: Add anti-CD107a antibody directly to the co-culture wells.
- Incubate: Incubate plates for 1 hour at 37°C in a 5% CO₂ incubator.
- Inhibit Protein Transport: Add Brefeldin A and Monensin to the wells and incubate for an additional 3-5 hours.
- Harvest and Stain: Centrifuge plates, wash cells, and perform surface staining for CD45, CD3, and CD56 to identify NK cells.
- Intracellular Staining: Fix and permeabilize cells, then stain intracellularly for IFN-γ.
- Acquisition and Analysis: Analyze samples on a flow cytometer. The percentage of CD107a⁺ and/or IFN-γ⁺ cells within the CD3⁻CD56⁺ NK cell population indicates the level of activation and degranulation against the target cells.
Protocol: Validating Hypoimmune Cells In Vivo
This protocol uses a humanized mouse model to assess the survival of engineered cells in a more complex immune environment [6].
Materials:
- Immunodeficient mice (e.g., NSG or NSG-SGM3)
- Human PBMCs or pre-differentiated immune cells for humanization
- Engineered hypoimmune cells and wild-type control cells (e.g., HIP iPSCs and wild-type iPSCs), preferably expressing a luciferase reporter for in vivo imaging
- In vivo imaging system (IVIS) and luciferin substrate
Procedure:
- Humanized Mouse Model: Engraft immunodeficient mice with human PBMCs (to create a "humanized" immune system) several weeks before cell therapy transplantation.
- Cell Transplantation: Inject engineered hypoimmune cells and wild-type control cells into separate sites in the same mouse (e.g., intramuscularly or subcutaneously). A cross-over re-injection design at a later time point can test for immune memory.
- Longitudinal Monitoring: At regular intervals (e.g., weekly), inject mice with luciferin and use IVIS to perform bioluminescence imaging (BLI). Quantify the signal flux from each injection site to track cell survival and proliferation over time (e.g., 4-16 weeks).
- Endpoint Analysis: At the end of the study, harvest the graft sites and analyze by histology and immunofluorescence for immune cell infiltration (e.g., CD3⁺ T cells, CD56⁺ NK cells) and graft cell survival.
- Ex Vivo Immune Assays: Isolate splenocytes or PBMCs from the mice and re-challenge them in vitro with the same cell types used for transplantation in an IFN-γ ELISpot assay to measure T cell memory and activation.
Diagram: A standard workflow for validating NK cell evasion in vitro using a degranulation (CD107a) and cytokine (IFN-γ) assay.
Overcoming the NK cell-mediated 'missing-self' response is a critical milestone for the clinical realization of off-the-shelf allogeneic cell therapies. The strategies outlined here, particularly the engineered overexpression of CD47 in combination with HLA class I and II knockout, have demonstrated robust protection in highly relevant pre-clinical models [6]. The provided experimental protocols offer a framework for researchers to systematically validate these and future strategies, accelerating the development of universally compatible hypoimmune cell products.
Overcoming Batch-to-Batch Variability and Scalability in Manufacturing
In the development of allogeneic cell therapies, manufacturing consistency is a paramount challenge. Batch-to-batch variability poses a significant obstacle to producing reliable, safe, and efficacious "off-the-shelf" therapeutic products [65] [66]. This variability, stemming from differences in donor genetics, starting material quality, and process inconsistencies, can impact critical quality attributes, complicating scale-up and regulatory approval [10] [66]. When framed within the context of engineering hypo-immune cells—designed to evade host immune rejection through genetic modification—the control of manufacturing variability becomes even more critical. Even minor deviations in the manufacturing process can alter the expression of engineered immune-evasive ligands (e.g., HLA, CD47, PD-L1), potentially compromising the entire therapeutic strategy [20] [2]. This Application Note details a structured, data-centric approach and specific experimental protocols to overcome these challenges, ensuring the production of consistent, scalable, and potent hypo-immune cell therapies.
A Data-Centric Framework for Managing Variability
A holistic, data-driven strategy is essential to minimize variability across the development lifecycle, from early research to commercial manufacturing. Key elements of this framework include:
- Holistic Management Approach: Implementing Quality by Design (QbD) principles and Design of Experiments (DoE) allows for systematic exploration of how critical process parameters affect product quality [65]. This is foundational for understanding process robustness.
- Raw Material Control: The quality and consistency of cellular starting material—whether from healthy donors, induced pluripotent stem cells (iPSCs), or umbilical cord blood—significantly impact batch consistency [66] [67]. Rigorous characterization and qualification of raw materials are essential.
- Process Standardization and Automation: Utilizing closed systems and automation enhances efficiency and maintains quality during scale-up by reducing manual interventions and associated risks [66].
- Robust Quality Control: A strong quality control system incorporating advanced analytics and real-time monitoring helps maintain stringent regulatory standards and enables early deviation detection [66].
Quantitative Analysis of Variability and Scalability Solutions
The following quantitative data, compiled from recent studies, illustrates the impact of different manufacturing strategies on batch consistency and scalability.
Table 1: Impact of Donor Pooling on Manufacturing Consistency and Output [68]
| Manufacturing Parameter | Single-Donor Runs (n=155) | Pooled-Donor Runs (6-8 CBU) (n=55) | Implication |
|---|---|---|---|
| Total Cell Fold Expansion | 1193 ± 555 | 1110 ± 232 | Pooling reduces expansion variability by over 50%, enhancing predictability. |
| Total Cell Output | 4.8e9 ± 3.6e9 cells | 2.2e10 ± 7.1e9 cells | Pooling increases total cell yield by approximately 4.5-fold, supporting larger batch sizes. |
| Clinical Doses Generated | Multiple small lots | Large, consistent batches from a single run | Streamlines logistics and enables "off-the-shelf" availability. |
Table 2: Scalability and Market Projections for Allogeneic Cell Therapies [66] [67]
| Metric | Current/Forecasted Value | Notes |
|---|---|---|
| Global Market Value (2024) | ~$0.9 billion | Base year for growth projection. |
| Projected Global Market Value (2035) | ~$2.4 billion | Reflects a Compound Annual Growth Rate (CAGR) of 14-24.1%. |
| Number of Companies in Development | ~195 | Targeting oncology, autoimmune, and other therapeutic areas. |
Detailed Experimental Protocols
Below are standardized protocols for key experiments critical to assessing and mitigating batch-to-batch variability in hypo-immune cell manufacturing.
Protocol: Evaluation of Donor Pooling on Batch Consistency
Objective: To determine the effect of pooling multiple cord blood units (CBUs) on the consistency and yield of expanded CD34+ cells, a common starting material for hypo-immune cell derivatives.
Materials:
- Cryopreserved CBUs from FDA-licensed banks.
- CD34+ cell enrichment kit (e.g., magnetic-activated cell sorting kit).
- Basal expansion medium supplemented with defined cytokines (e.g., SCF, TPO, FLT3-L).
- Bioreactor or cell culture vessels coated with a proprietary Notch ligand (e.g., Delta-1).
Methodology:
- Thawing and Pooling: Thaw multiple (e.g., 6-8) CBUs according to established protocols. Pool the mononuclear cells from all units before CD34+ enrichment to create a homogenous starting population [68].
- CD34+ Enrichment: Isolate CD34+ cells from the pooled cell suspension using a clinical-grade magnetic separation system. Determine cell viability and purity via flow cytometry.
- Cell Expansion: Seed the enriched CD34+ cells at a defined density (e.g., 1x10^4 cells/cm²) in Notch ligand-coated vessels. Culture the cells for 14-16 days in a controlled environment (37°C, 5% CO₂), with medium exchanges or perfusions as per the optimized schedule.
- Harvest and Analysis: Harvest the cells and record total cell count and viability.
- Analytical Measurements: Calculate the fold expansion. Perform flow cytometric analysis for CD34+ purity and other relevant surface markers (e.g., CD45, CD133) to assess phenotype consistency.
- Data Analysis: Compare the mean, standard deviation, and coefficient of variation (CV) for fold expansion and cell output between single-donor and pooled-donor runs.
Protocol: Assessing the Impact of Process Parameters on Hypo-immune Marker Expression
Objective: To utilize Design of Experiments (DoE) to systematically evaluate how critical process parameters influence the expression of key hypo-immune genes (e.g., B2M, CIITA, CD47) in iPSC-derived immune cells.
Materials:
- A well-characterized, master iPSC line engineered with a knockout of B2M and/or CIITA, and potentially a knock-in of CD47 or HLA-E.
- Defined differentiation kits or reagents for directing iPSCs to T cells or NK cells.
- Cell culture reagents and cytokines for differentiation stages.
- Flow cytometry antibodies against HLA-ABC, HLA-II, CD47, HLA-E, and lineage-specific markers (e.g., CD3, CD56).
Methodology:
- DoE Setup: Using a statistical software package, design a multi-factorial experiment. Key process parameters (Input Variables) may include:
- Cell Seeding Density at the start of differentiation.
- Cytokine Concentration (e.g., IL-7, IL-15) at specific differentiation stages.
- Duration of Co-culture with engineered feeder cells.
- Parallel Differentiation: Execute the differentiation runs according to the DoE matrix in a controlled, parallel manner.
- Endpoint Analysis: At the end of the differentiation protocol, harvest the cells and analyze them via flow cytometry.
- Response Variables: Quantify the mean fluorescence intensity (MFI) and percentage of positive cells for each hypo-immune marker (HLA-ABC, CD47, etc.) and the yield of the target cell population.
- Model Building and Analysis: Fit the collected data to a statistical model (e.g., Response Surface Methodology) to identify significant main effects and interaction effects between parameters. Use the model to define the optimal "design space" that maximizes immune-evasive marker expression while maintaining high target cell yield and potency.
Visualizing the Experimental and Analytical Workflow
The following diagram illustrates the integrated workflow for developing and characterizing a hypo-immune cell product, from genetic engineering to batch consistency analysis.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of the aforementioned protocols relies on specific, high-quality reagents and materials.
Table 3: Key Research Reagent Solutions for Hypo-immune Cell Development
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| CRISPR-Cas9 System | Precision gene editing for knockout (e.g., B2M, TCR) or knock-in (e.g., CD47, CAR) of target genes. | Engineering immune-evasive properties and therapeutic transgenes into master iPSC lines [10] [20]. |
| Notch Ligand Coating | Provides critical signals for the differentiation and expansion of hematopoietic progenitors and T cells. | Used in Protocol 4.1 to support the robust expansion of CD34+ cells from cord blood [68]. |
| Defined Differentiation Media | Serum-free, xeno-free media kits containing precise cytokine cocktails for directed differentiation. | Essential for Protocol 4.2 to reproducibly differentiate iPSCs into functional T cells or NK cells. |
| Flow Cytometry Antibody Panels | Multiparametric analysis of cell surface markers for phenotyping, purity, and hypo-immune marker validation. | Used to quantify expression of HLA-ABC, CD47, CD34, CD3, etc., in both protocols [68] [20]. |
| Clinical-Grade Cryopreservation Media | Enables long-term storage of final cell therapy products while maintaining post-thaw viability and function. | Critical for creating an "off-the-shelf" inventory of the final hypo-immune cell product [66]. |
Application Note: Engineering Next-Generation Hypo-Immune Cell Therapies
The development of allogeneic, "off-the-shelf" cell therapies requires innovative engineering strategies to overcome critical biological barriers. Key challenges include host versus graft rejection, graft versus host disease (GvHD), on-target/off-tumor toxicities, and uncontrolled cell proliferation. This application note details three complementary technological pillars—logic-gated chimeric antigen receptors (CARs), synthetic safety switches, and novel target selection—for creating effective hypo-immune cell products suitable for broad patient populations. By integrating these approaches, researchers can design safer, more precise, and universally applicable therapies for cancer and other diseases.
Protocol: Design and Implementation of Key Technologies
Logic-Gated CAR Engineering for Enhanced Specificity
Background: Conventional CAR-T cells can attack healthy tissues expressing low levels of the target antigen, causing severe side effects. Logic-gated CAR systems apply Boolean computing principles to T cell activation, requiring multiple antigen recognition events for cytotoxic activity, thereby enhancing tumor-specific targeting [69].
Principle: These systems engineer T cells with sophisticated recognition circuits that process multiple input signals (antigens) to make context-dependent activation decisions, rather than responding to a single antigen in a binary fashion [69].
Protocol Steps:
- AND-Gate CAR Construction:
- Clone two separate CAR constructs where one provides the primary CD3ζ activation signal and the other supplies a co-stimulatory signal (e.g., CD28 or 4-1BB) [69].
- Use multicistronic viral vectors (e.g., lentiviral or retroviral) with 2A peptide sequences to ensure coordinated expression of both receptors in primary human T cells.
- Validate stoichiometric receptor expression using flow cytometry and confirm functional synergy through co-culture assays with cell lines expressing single or dual antigens.
- SynNotch-Based IF-THEN Gate Implementation:
- Engineer a synthetic Notch (SynNotch) receptor specific for a priming antigen (Antigen A). Upon recognition, its transcription factor domain is cleaved and translocates to the nucleus [69].
- Design a response element within a CAR transgene specific for a different antigen (Antigen B) that is activated by the SynNotch transcription factor.
- Transfer T cells with both constructs. The resulting cells will only express the functional CAR against Antigen B upon encountering Antigen A, restricting cytotoxic activity to tumor sites co-expressing both antigens [69].
Diagram: Logic-Gated CAR T Cell Activation
Incorporating Fail-Safe Safety Switches
Background: Safety switches are critical for mitigating risks associated with allogeneic cell therapies, particularly unforeseen on-target or off-tumor toxicities or uncontrolled cell expansion.
Principle: A genetically encoded "safety switch" can be induced by a small molecule drug to selectively eliminate the engineered cells in vivo [70] [71].
Protocol Steps:
- Selection and Cloning:
- Vector Design and Transduction:
- Incorporate the FailSafe cassette into the same viral vector as your CAR or as a separate construct for co-transduction. Use a high-titer lentivirus for stable integration into human T cells or induced pluripotent stem cells (iPSCs).
- Functional Validation In Vitro:
- After transduction, expand the engineered cells.
- Treat cells with a defined concentration of the activating small molecule drug (e.g., rimiducid). Apoptosis should be detectable within 24 hours.
- Quantify cell death using flow cytometry with Annexin V/propidium iodide staining. A >90% elimination efficiency of switched cells is typically required for clinical advancement.
Targeting Novel Antigens: ICAM-1 in Solid Tumors
Background: Solid tumors present unique challenges, including a lack of truly tumor-specific antigens. ICAM-1 (Intercellular Adhesion Molecule-1) is a promising target as it is frequently overexpressed on aggressive cancers while showing limited expression on healthy tissues [72] [73].
Principle: CAR-T cells targeting ICAM-1 can be affinity-tuned to preferentially bind and kill tumor cells with high ICAM-1 density, sparing healthy cells with basal expression [73].
Protocol Steps:
- CAR Design and Affinity Tuning:
- Generate a scFv library against ICAM-1. Screen for clones with varying affinities to select one that discriminates between high (tumor) and low (healthy) ICAM-1 expression levels.
- Construct a third-generation CAR (e.g., CD28-4-1BB-CD3ζ) using the selected scFv.
- Incorporating a Reporter Gene:
- In Vivo Efficacy and Safety Testing:
- Establish xenograft mouse models using patient-derived anaplastic thyroid cancer (ATC) cells.
- Systemically administer ICAM-1-targeted CAR-T cells.
- Monitor tumor volume and mouse survival. Use DOTATATE PET imaging weekly to visualize CAR-T cell migration to tumor sites.
- Assess on-target/off-tumor toxicity by examining tissues with physiological ICAM-1 expression (e.g., endothelium, lung).
Recent clinical and preclinical studies demonstrate the potential of these innovative strategies. The table below summarizes key quantitative findings.
Table 1: Summary of Clinical and Preclinical Data for Featured Technologies
| Technology / Therapy | Study Phase / Type | Key Efficacy Findings | Key Safety Findings | Source / Context |
|---|---|---|---|---|
| ICAM-1 CAR (AIC100) for Anaplastic Thyroid Cancer | Phase I Clinical Trial | • 50% ORR in ATC patients (dose levels 2/3)• 1 Complete Response, 1 Partial Response• 60% Disease Control Rate in PDTC | • No DLTs at initial dose levels• Grade 1/2 CRS in 10 patients• No ICANS observed• Grade 3 pneumonitis at highest dose | [72] [73] |
| Allogeneic Anti-BCMA CAR-T for Multiple Myeloma | Phase I Clinical Trial | • 86% Overall Response Rate (n=35)• Efficacy in high-risk and EMD patients | • No significant safety issues• No GvHD observed | [74] |
| FailSafe Safety Switch | Platform Technology | • Designed for >90% elimination of engineered cells upon drug induction | • Activated by a safe, globally approved small molecule drug | [70] [71] |
| iACT Immune Cloaking | Platform Technology | • Enables evasion of immune recognition without HLA knockout | • Aims for allogeneic use without chronic immunosuppression | [70] [71] |
The Scientist's Toolkit
Successful implementation of these protocols requires specific, high-quality reagents and tools. The following table details essential components for building and testing hypo-immune cell therapies.
Table 2: Key Research Reagent Solutions for Hypo-Immune Cell Engineering
| Research Tool | Function / Principle | Example Application |
|---|---|---|
| FailSafe Inducible Caspase System | Drug-inducible safety switch for controlled ablation of engineered cells. | Mitigating on-target/off-tumor toxicity or uncontrolled expansion in allogeneic CAR-T or iPSC-derived therapies [70] [71]. |
| iACT Immune Cloaking Technology | Patented "cloaking" that evades immune detection without disrupting HLA expression. | Creating universal "off-the-shelf" cell lines (e.g., iPSCs for islet replacement) that avoid host rejection without immunosuppression [70] [71]. |
| PSXi013 iPSC Line | A proprietary, FDA Drug Master File-registered polyclonal iPSC line. | Serves as a genetically stable, clinically-compliant starting material for complex engineering of differentiated cell products [70] [71]. |
| SynNotch Receptor System | A customizable synthetic receptor that, upon antigen binding, triggers user-defined transcriptional programs. | Building IF-THEN logic gates for spatial control of CAR expression or other therapeutic transgenes [69]. |
| DOTATATE PET Imaging Tracer | A radiopharmaceutical that binds to somatostatin receptor 2 (SSTR2). | Non-invasive in vivo tracking of CAR-T cells engineered to co-express SSTR2, enabling pharmacokinetic and biodistribution studies [72] [73]. |
Diagram: Integrated Workflow for Hypo-Immune CAR-T Cell Generation
The convergence of logic-gated recognition, controllable safety switches, and carefully selected novel targets represents a powerful framework for advancing allogeneic, hypo-immune cell therapies. The detailed protocols and data provided here offer a roadmap for researchers to engineer safer, more precise, and universally applicable therapeutic products. As demonstrated by early clinical results, these technologies hold significant promise for overcoming the core challenges that have limited the scope of cell therapies, potentially unlocking their full potential for a broad range of diseases.
Clinical Translation and Landscape Analysis: Evaluating Hypoimmune Platforms
Application Note: Clinical Efficacy and Safety of Allogeneic CAR Cell Therapies
The development of allogeneic, off-the-shelf chimeric antigen receptor (CAR) cell therapies represents a paradigm shift in cellular immunotherapy, aiming to overcome critical limitations of autologous approaches, including high costs, lengthy manufacturing times, and limited patient access [51]. This application note synthesizes recent clinical trial data for allogeneic CAR-T and CAR-NK cell therapies, framing these advances within the broader thesis of engineering hypoimmune cells for allogeneic therapy research. The strategic elimination of alloreactive immune responses through genetic engineering enables the creation of cell therapeutics that can evade host immunity without requiring immunosuppressive drugs, thereby supporting large-scale manufacturing of universal cell products [2] [6].
Comparative Clinical Outcomes in Hematologic Malignancies
Recent clinical trials demonstrate that allogeneic CAR-T and CAR-NK cell therapies are achieving efficacy and durability profiles that are increasingly comparable to approved autologous CAR-T therapies.
Table 1: Efficacy Outcomes of Allogeneic CAR-T Cell Therapies in B-cell Malignancies
| Therapy / Trial | Target | Population | Patient Number | Overall Response Rate (ORR) | Complete Response (CR) Rate | 12-Month PFS | Durability Notes |
|---|---|---|---|---|---|---|---|
| Vispa-cel (CB-010) ANTLER Phase 1 [75] | CD19 | 2L+ LBCL (Confirmatory Cohort) | N=22 | 82% | 64% | 51% | Median DoR not reached; one ongoing CR at 3 years |
| Vispa-cel (CB-010) ANTLER Phase 1 [75] | CD19 | 2L+ LBCL (Optimized Profile) | N=35 | 86% | 63% | 53% | Median follow-up 11.8 months |
| CT0596 (Exploratory Study) [76] | BCMA | R/R Multiple Myeloma | N=8 (5 evaluable) | Early data: 60% sCR/CR at 4 weeks | 60% (sCR/CR) | NR | 80% MRD-negative; all responses ongoing |
PFS=Progression-free survival; DoR=Duration of response; NR=Not Reported; 2L+=Second-line or later; LBCL=Large B-cell Lymphoma; R/R=Relapsed/Refractory; sCR=Stringent Complete Response; MRD=Minimal Residual Disease
The vispa-cel data are particularly significant, as they demonstrate that an allogeneic CAR-T product can achieve efficacy and durability on par with autologous CAR-T therapies. The "optimized profile" cohort, which utilized young donor-derived T cells and a minimum of 2+ HLA allele matching with the recipient, showed an 86% ORR and 53% PFS at 12 months, with the longest responding patient in complete remission at 3 years post-infusion [75]. This highlights the importance of donor selection and engineering strategies for persistent activity.
Table 2: Efficacy and Safety of Allogeneic CAR-NK Cell Therapies
| Therapy / Trial | Target | Population | Patient Number | ORR (Day 30 & 100) | CR Rate (Day 100) | Key Safety Findings |
|---|---|---|---|---|---|---|
| CAR19/IL-15 NK (Phase 1/2) [77] | CD19 | R/R CD19+ B-cell Malignancies | N=37 | 48.6% | 29.7% | No CRS >G1, no neurotoxicity, no GvHD |
| Allogeneic CD19 CAR-NK [78] | CD19 | Relapsed/Refractory SLE (Autoimmune) | N=18 | 67% DORIS remission* (6/9 with >12mo fu) | N/A | CRS: 6% (G1 only); No neurotoxicity, no DLTs |
SLE=Systemic Lupus Erythematosus; DLTs=Dose-Limiting Toxicities; *DORIS remission is a disease-specific efficacy measure for lupus; fu = follow-up
Cord blood-derived CAR19/IL-15 NK cells exhibited a distinctly favorable safety profile, with no severe cytokine release syndrome (CRS), neurotoxicity, or graft-versus-host disease (GvHD) observed in the 37-patient trial [77]. Furthermore, the application of allogeneic CD19 CAR-NK cells in the autoimmune disease systemic lupus erythematosus (SLE) shows the potential of this platform beyond oncology, with promising efficacy and a high safety margin [78].
Emerging Data in Solid Tumors
The development of allogeneic CAR therapies in solid tumors has been more challenging, but recent data show promising signals. ALLO-316, an allogeneic CAR-T targeting CD70 for advanced or metastatic clear cell renal cell carcinoma (RCC), demonstrated a 31% confirmed objective response rate in patients with high CD70 expression (TPS ≥50%) [79]. Four of the five confirmed responders maintained ongoing responses, with one in remission for over 12 months. The median duration of response had not been reached, indicating potential for durable disease control [79].
Safety Profiles: A Comparative Advantage
A key theme across allogeneic CAR cell trials is a generally improved and manageable safety profile compared to autologous CAR-T cells.
Table 3: Comparative Safety Profiles of Allogeneic CAR Cell Therapies
| Adverse Event | Allo CAR-T (Vispa-cel) [75] (N=84, All Grades) | Allo CAR-NK [77] (N=37, All Grades) | Allo CAR-T (ALLO-316) [79] (N=22, All Grades) |
|---|---|---|---|
| CRS | 55% (<5% ≥G3) | 1 patient (G1 only) | 68% (No ≥G3) |
| ICANS | 14% (5% ≥G3) | 0% | 18% (No ≥G3) |
| GvHD | 0% | 0% | 0% |
| Prolonged Cytopenias | 28% (G3/4) | Reversible hematologic toxicity from LD | 68% (Neutropenia, G3/4) |
| IEC-HS | 2% (G3/4) | Not Reported | 36% (9% G3/4) |
LD=Lymphodepleting Chemotherapy; IEC-HS=Immune Effector Cell-Associated Hemophagocytic Lymphohistiocytosis-like Syndrome
The notably low incidence of severe CRS and ICANS with allogeneic CAR-NK cells and the absence of GvHD across multiple allogeneic platforms underscore their potential as safer, off-the-shelf products that could be administered in outpatient settings [75] [77]. The safety profile of vispa-cel was deemed manageable enough to allow for outpatient administration, which could significantly broaden patient access [75].
Experimental Protocols
Protocol 1: Manufacturing and Administration of Allogeneic CAR-T Cells (Vispa-cel)
Objective: To manufacture and evaluate the safety and efficacy of partially HLA-matched, allogeneic anti-CD19 CAR-T cells (vispa-cel) in patients with relapsed/refractory B-cell non-Hodgkin lymphoma.
Key Materials:
- Source Material: T cells isolated from healthy donor Peripheral Blood Mononuclear Cells (PBMCs).
- Genetic Engineering Platform: CRISPR genome-editing technology.
- Cell Culture Media: Formulations optimized for T-cell expansion and transduction.
- Lymphodepletion (LD) Regimen: Cyclophosphamide (dose range: 350-500 mg/m²) and Fludarabine (dose range: 22.5-30 mg/m²) administered daily for 3 days [75] [76].
- Final Product: Cryopreserved vispa-cel (CB-010) CAR-T cells.
Methodology:
- Donor Selection & Apheresis: T cells are collected from healthy, young donors via apheresis to ensure robust starting material [75].
- T Cell Activation & Engineering: Isolated T cells are activated and genetically modified using CRISPR to disrupt the T-cell receptor (TCR) to prevent GvHD. Cells are transduced with a lentiviral vector encoding the anti-CD19 CAR.
- Ex Vivo Expansion & Formulation: Engineered CAR-T cells are expanded in culture to achieve the target dose. The product is formulated and cryopreserved as an off-the-shelf therapy.
- Patient Lymphodepletion: Patients receive a standard LD regimen of cyclophosphamide and fludarabine for 3 days prior to CAR-T infusion.
- Product Administration: A single dose of vispa-cel is administered intravenously at the Recommended Phase 2 Dose (RP2D) of 80 million CAR-T cells [75].
- Patient Monitoring: Patients are closely monitored for adverse events (CRS, ICANS, infections, cytopenias) and efficacy (tumor response by RECIST criteria, CAR-T cell persistence via qPCR).
Protocol 2: Evaluation of Allogeneic CAR-NK Cells in Autoimmune Disease
Objective: To assess the safety, tolerability, and efficacy of allogeneic CD19 CAR NK-cell therapy in patients with relapsed/refractory Systemic Lupus Erythematosus (SLE).
Key Materials:
- Source Material: Allogeneic Natural Killer (NK) cells.
- Lymphodepletion (LD) Regimen: Fludarabine (25 mg/m²/day) and Cyclophosphamide (300 mg/m²/day) administered daily from days -5 to -3 [78].
- CAR Construct: Anti-CD19 CAR.
- Final Product: Allogeneic CD19 CAR NK cells.
Methodology:
- Patient Selection: Enroll adult patients (aged 18-65 years) with moderate-to-severe SLE who have failed at least two prior standard systemic therapies.
- Lymphodepletion Conditioning: Patients receive the FC-based LD regimen for 3 days.
- Cell Product Administration: Patients receive three infusions of CAR NK-cells within a single treatment cycle at identical dose levels, commencing at 0.75 × 10^9 cells [78].
- Safety Monitoring (Primary Endpoint): Monitor patients for 28 days for dose-limiting toxicities. Record all adverse events graded per NCI CTCAE v5.0, with special attention to CRS, neurotoxicity, and GvHD.
- Efficacy Assessment: Evaluate disease status using the DORIS remission criteria and Lupus Low Disease Activity State (LLDAS). In the initial study, 67% (6/9) of patients with >12 months of follow-up achieved this endpoint [78].
Visualizing Hypoimmune Engineering Strategies
The core strategy for creating hypoimmune cells involves a dual approach: eliminating the primary triggers of adaptive immune rejection and simultaneously inhibiting innate immune attack.
Hypoimmune Cell Engineering Logic - This diagram outlines the core genetic strategy for creating universal allogeneic cell therapies, combining HLA elimination with CD47 overexpression to evade both adaptive and innate immunity [3] [6].
Allogeneic CAR Therapy Workflow - This workflow illustrates the path from donor cell selection to patient administration, highlighting the "off-the-shelf" nature of allogeneic products [75] [77] [51].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for Developing Hypoimmune Allogeneic Cell Therapies
| Reagent / Material | Primary Function in R&D | Research Context from Literature |
|---|---|---|
| CRISPR-Cas9 System | Gene knockout (e.g., B2M, CIITA, TCR) to prevent immune recognition and GvHD. | Used to generate hypoimmune iPSCs by disrupting B2M and CIITA [6]. |
| Lentiviral Vectors | Stable delivery of transgenes (e.g., CAR, CD47, IL-15) into effector cells. | Used to express CAR19/IL-15 in cord blood NK cells [77] and CD47 in HIP cells [6]. |
| Lymphodepletion Regimen (FC) | Fludarabine/Cyclophosphamide conditioning to create a favorable immune environment for engraftment. | Standard pre-conditioning used across multiple clinical trials [78] [79] [75]. |
| Cord Blood Units (CBUs) | Source of allogeneic NK cells with inherent anti-tumor activity and lower risk of GvHD. | Source material for CAR19/IL-15 NK products; selection of optimal CBUs is critical for potency [77]. |
| Inducible Caspase 9 (iC9) | Safety switch to ablate engineered cells in case of severe adverse events. | Incorporated into CAR-NK cells as a safety mechanism to trigger apoptosis upon administration of a small molecule [77]. |
| Cytokine Support (IL-15) | Enhances in vivo expansion and persistence of NK cells. | Engineered into CAR-NK cells to provide autocrine growth signaling [77]. |
The field of cell therapy is undergoing a pivotal shift from patient-specific autologous products towards universally applicable "off-the-shelf" allogeneic treatments. This transition aims to overcome critical limitations of autologous therapies, including lengthy and costly manufacturing, product variability, and inability to treat patients with compromised immune cells [80] [81]. Within this landscape, two primary technological platforms have emerged: hypoimmune induced pluripotent stem cells (iPSCs) and engineered primary cells. Hypoimmune iPSCs are created through genetic engineering of pluripotent stem cells to evade immune recognition, subsequently differentiated into therapeutic cell types [82] [14]. In contrast, engineered primary cells involve direct modification of mature, differentiated cells sourced from donors, such as T-cells or natural killer (NK) cells from peripheral blood or umbilical cord blood [80] [10]. This application note provides a structured, quantitative comparison of these platforms for researchers developing allogeneic therapies, focusing on practical experimental considerations, protocol details, and strategic selection guidance.
Platform Comparison Tables
Table 1: Core Characteristics and Manufacturing Comparison
| Feature | Hypoimmune iPSCs | Engineered Primary Cells |
|---|---|---|
| Starting Cell Source | Reprogrammed somatic cells (e.g., fibroblasts, lymphocytes) [83] | Peripheral blood mononuclear cells (PBMCs), Umbilical Cord Blood (UCB), hematopoietic stem/progenitor cells [80] [10] |
| Scalability & Renewability | Theoretically unlimited self-renewal of master iPSC bank [10] [83] | Limited by donor availability; UCB has low cell numbers per unit [80] [10] |
| Product Homogeneity | High; clonal master cell banks enable uniform genetic background and product [82] [10] | Low to Moderate; subject to donor-to-donor variability in genetics, phenotype, and expansion potential [10] |
| Key Immune Evasion Strategies | Knockout of B2M/CIITA, overexpression of CD47/PD-L1/HLA-G, ICAM-1 knockout [82] [14] | TCR knockout (for T-cells), HLA knockout, overexpression of HLA-E/CD47 [10] [23] |
| Typical Time to Final Product | Longer (weeks to months); requires multi-step differentiation post-editing [82] [83] | Shorter (days to weeks); direct engineering of terminally differentiated cells [80] [81] |
Table 2: Functional and Clinical Attributes
| Attribute | Hypoimmune iPSCs | Engineered Primary Cells |
|---|---|---|
| In Vivo Persistence (Current Data) | Promising in pre-clinical models; long-term human data pending [82] [14] | Often limited (weeks) due to host rejection; a key challenge for allogeneic CAR-T [10] [81] |
| Risk of Graft-versus-Host Disease (GvHD) | Very Low after complete differentiation and TCR knockout [82] [10] | Moderate for T-cells (requires TCR knockout), Low for NK cells (no endogenous TCR) [10] [23] |
| Tumorigenicity Risk | Moderate; risk from residual undifferentiated iPSCs forming teratomas [82] [83] | Low; terminally differentiated cells with limited proliferative capacity [10] |
| Clinical Trial Stage | Primarily pre-clinical and early-phase trials for CNS, cardiac, and islet cell therapies [82] [14] | Phase I/II trials for hematologic cancers (e.g., ALLO-715 for multiple myeloma) [10] [23] |
| Best Suited For | Regenerative medicine (replacing damaged tissues), complex tissue engineering [82] [36] | Immunotherapy (e.g., CAR-T, CAR-NK for cancer), acute interventions [10] [23] |
Experimental Protocols
Protocol 1: Generating a Hypoimmune iPSC Master Cell Line
This protocol details the creation of a clinically relevant hypoimmune iPSC line through multi-locus gene editing to evade both adaptive and innate immune responses [82] [14].
Key Reagent Solutions:
- CRISPR/Cas9 System: For precise knockout of HLA and other target genes. Use high-fidelity Cas9 variants and synthetic sgRNAs to minimize off-target effects.
- Reprogramming Factors: Sendai virus or mRNA-based kits for footprint-free reprogramming of donor somatic cells to iPSCs.
- Electroporation System: For efficient delivery of editing reagents into iPSCs (e.g., Neon Transfection System).
- Karyotyping/G-Banding Analysis: To confirm genomic integrity post-editing [14].
Step-by-Step Workflow:
Reprogramming and Base iPSC Line Establishment:
- Isolate donor somatic cells (e.g., dermal fibroblasts or peripheral blood mononuclear cells).
- Reprogram using a non-integrating method (e.g., Sendai virus vectors or mRNA transfection of OCT4, SOX2, KLF4, MYC) [83].
- Culture emerging colonies on feeder-free substrates (e.g., Vitronectin) with defined mTeSR or equivalent medium. Pick and expand clonal lines.
Sequential Multi-Locus Gene Editing:
- Knockout of HLA Class I: Transfect iPSCs with CRISPR/Cas9 reagents targeting the B2M gene. Isolate clones and validate loss of surface HLA class I by flow cytometry [82] [14].
- Knockout of HLA Class II: Transfer a B2M-/- clone with CRISPR/Cas9 targeting the CIITA gene. Validate loss of HLA class II inducibility after IFN-γ stimulation [82].
- Introduce Innate Immune Evasion: Further edit the B2M-/- CIITA-/- line. Two key strategies exist:
- Strategy A (HLA-E knock-in): Knock a single-chain HLA-E trimer into the B2M locus. This simultaneously eliminates endogenous B2M and expresses HLA-E to inhibit NK cells [82].
- Strategy B (Overexpression): Use a lentiviral vector to stably overexpress immunomodulatory factors CD47 (inhibits phagocytosis) and PD-L1 (inhibits T-cells) in the edited line [82] [36].
Validation and Banking:
- Perform whole-genome sequencing or targeted off-target analysis on candidate clones.
- Confirm pluripotency via teratoma formation assay or in vitro trilineage differentiation.
- Differentiate the final validated hypoimmune clone into the target cell type (e.g., cardiomyocytes, neurons) to confirm the hypoimmune phenotype is retained.
- Create a Master Cell Bank of the hypoimmune iPSC line under GMP-compliant conditions.
Diagram 1: Hypoimmune iPSC line generation workflow.
Protocol 2: Engineering Allogeneic CAR-T Cells from Primary Donor T-cells
This protocol outlines the process for creating "off-the-shelf" CAR-T cells from healthy donor PBMCs, focusing on mitigating GvHD and host rejection [80] [10] [81].
Key Reagent Solutions:
- T-cell Activation Beads: Anti-CD3/CD28 magnetic beads for robust T-cell activation and expansion.
- Gene Editing System: CRISPR-Cas9 (ribonucleoprotein) or TALEN for efficient TCR knockout.
- Lentiviral Vector: Carrying the CAR construct, often targeted to the TRAC locus for uniform expression.
- Cytokines: IL-2 and IL-15 to promote T-cell survival and expansion, potentially favoring stem cell memory phenotypes.
Step-by-Step Workflow:
Donor Selection and Leukapheresis:
- Screen and select a healthy donor. Collect PBMCs via leukapheresis.
T-cell Activation and TCR Knockout:
CAR Integration and Additional Modifications:
- Transduce the cells with a lentiviral vector encoding the CAR. Alternatively, for more controlled expression, knock the CAR construct into the TRAC locus, which simultaneously knocks out the endogenous TCR and places the CAR under its endogenous regulatory control [10].
- For enhanced persistence, co-express a cytokine (e.g., IL-15) or engineer knockout of CD52 to confer resistance to the lymphodepleting agent alemtuzumab [10] [23].
Ex Vivo Expansion and Formulation:
- Expand the engineered T-cells in a bioreactor (e.g., G-Rex) over 9-12 days with appropriate cytokines.
- Harvest the cells, perform a bead-free wash, and formulate into multiple cryopreserved doses.
Quality Control and Release:
- Perform flow cytometry for CAR expression and absence of TCR.
- Conduct sterility, mycoplasma, and endotoxin testing.
- Use a potency assay (e.g., IFN-γ release upon tumor cell co-culture) to confirm functionality.
Diagram 2: Allogeneic CAR-T cell manufacturing workflow.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Hypoimmune Cell Engineering
| Reagent / Solution | Primary Function | Example Applications |
|---|---|---|
| CRISPR-Cas9 Systems | Precise knockout (B2M, CIITA, TRAC) or knock-in (HLA-E) edits [82] [14] | Foundational editing in both iPSC and primary cell platforms. |
| Lentiviral Vectors | Stable integration of transgenes (CARs, CD47, PD-L1) [10] [36] | CAR expression in T-cells; overexpression of immunomodulators in iPSCs. |
| Anti-CD3/CD28 Beads | Robust activation and expansion of primary T-cells [10] | Critical first step in manufacturing allogeneic CAR-T cells. |
| Defined Culture Media | Support pluripotency (mTeSR1) or differentiation (specialized kits) [14] [83] | Maintaining iPSC quality and enabling reproducible differentiation. |
| Recombinant Human Cytokines | Direct cell differentiation, survival, and expansion (IL-2, IL-15, SCF) [10] | Promoting T-cell and NK cell growth; guiding iPSC differentiation. |
| Flow Cytometry Antibodies | Validate protein expression (e.g., HLA-I/II, CAR, TCR, CD47) [82] [14] | Essential for quality control and characterizing the final product. |
The choice between hypoimmune iPSCs and engineered primary cells is not a matter of superiority, but of strategic alignment with the therapeutic application's core requirements.
Select the Hypoimmune iPSC Platform when the goal is long-term engraftment and regeneration of solid tissues (e.g., pancreatic islets for diabetes, dopaminergic neurons for Parkinson's, cardiomyocytes for heart failure) [82] [36]. Its strengths are scalability and product homogeneity, making it ideal for chronic conditions where a permanent cell replacement is needed.
Select the Engineered Primary Cell Platform for immunotherapies, particularly against cancer and infectious diseases [10] [23]. Its key advantage is speed to product, leveraging the innate cytotoxic power of immune cells. This platform is best for acute interventions where immediate effector function is paramount, even if persistence is currently limited.
Future development will focus on combining the strengths of both platforms, such as deriving CAR-engineered immune cells from hypoimmune iPSCs, and on overcoming the remaining hurdle of in vivo persistence for all allogeneic products [10]. This head-to-head analysis provides a framework for researchers to make an informed decision based on the specific demands of their therapeutic target.
{/* The user requires a detailed scientific article with specific visualizations and structured data presentation, targeting research professionals in cell therapy. The content must maintain rigorous scientific accuracy while providing practical experimental protocols. */}
Beyond Oncology: Progress in Hypoimmune Stem Cell-Derived Islets for Type 1 Diabetes
The advent of hypoimmune (HIP) engineering has ushered in a transformative era for allogeneic cell therapies, moving its application beyond oncology to address autoimmune diseases. For Type 1 Diabetes (T1D), this approach aims to generate stem cell-derived islets (SC-islets) that evade immune detection, enabling transplantation without chronic immunosuppression. This application note details the underlying principles, key experimental protocols, and recent preclinical and clinical progress in the field. We summarize quantitative data on the performance of HIP-edited cells, provide detailed methodologies for in vitro and in vivo validation, and visualize critical signaling pathways involved in immune evasion. The emergence of positive clinical data underscores the potential of HIP-edited SC-islets to serve as a scalable, "off-the-shelf" therapy for T1D, fundamentally shifting the paradigm from disease management to a functional cure.
Type 1 Diabetes is an autoimmune disease characterized by the destruction of insulin-producing pancreatic β-cells, resulting in lifelong insulin dependence for over 9 million people globally [84]. Cell replacement therapy via pancreatic islet transplantation can restore physiological insulin secretion; however, its widespread application is hindered by two primary factors: a severe shortage of cadaveric donor islets and the need for chronic immunosuppression to prevent allogeneic graft rejection and recurrent autoimmunity [36] [20]. Immunosuppressive regimens carry significant risks, including infections, malignancy, and drug-specific toxicities, making them unsuitable for the broader T1D population [85].
HIP engineering seeks to overcome these barriers by creating "universal" donor cells that are invisible to the host immune system. Inspired by immune-evasion mechanisms observed in placental trophoblasts and certain cancer cells, this strategy uses genetic engineering to modulate cell-surface proteins that interact with host immune cells [3]. The goal is to produce off-the-shelf SC-islet products that can be transplanted into any recipient without matching for human leukocyte antigen (HLA) and without the need for immunosuppressive drugs, thereby making cell therapy for T1D broadly accessible [36] [84].
Core Engineering Strategies for Hypoimmune Islets
The HIP phenotype is achieved through a multi-pronged genetic engineering approach that disrupts both adaptive and innate immune recognition. The core strategies involve the knockout of immunogenic antigens and the knock-in of immunomodulatory factors.
Table 1: Key Genetic Modifications for Hypoimmune SC-Islets
| Target Gene / Pathway | Type of Modification | Molecular Function | Immune Cell Population Modulated |
|---|---|---|---|
| B2M | Knockout | Required for HLA Class I surface expression [36]. | CD8+ T Cells [20]. |
| CIITA | Knockout | Master regulator of HLA Class II expression [36]. | CD4+ T Cells [20]. |
| CD47 | Overexpression | Binds SIRPα on innate immune cells, delivering a "don't eat me" signal [6] [3]. | Macrophages, NK Cells [6] [3]. |
| PD-L1 | Overexpression | Binds PD-1 on activated T cells, inducing tolerance and exhaustion [36] [20]. | T Cells, NK Cells [36]. |
| HLA-G / HLA-E | Overexpression | Binds inhibitory receptors (LILRB1, NKG2A) on NK and myeloid cells [36] [6]. | NK Cells, Myeloid Cells [36]. |
The most validated strategy to date involves a triple-editing approach: B2M−/−CIITA−/−CD47+ [6]. The knockout of B2M and CIITA ablates HLA class I and class II expression, respectively, effectively preventing direct T-cell recognition. However, the absence of HLA class I creates a "missing self" signal that activates Natural Killer (NK) cells. This innate immune response is counteracted by the overexpression of CD47, which engages SIRPα on NK cells and macrophages to inhibit phagocytosis and cytotoxicity [6] [3].
Recent studies from academic and industry labs have generated robust data on the efficacy of HIP-edited cells in evading immune rejection. The table below consolidates key quantitative findings from preclinical and early clinical investigations.
Table 2: Summary of Experimental Data for HIP-Edited Cells
| Cell Type | Model System | Key Outcome Measure | Result (HIP vs. Control) | Citation |
|---|---|---|---|---|
| Human HIP iPSCs | Allogeneic Rhesus Macaques (Immunocompetent) | Cell Survival Duration | 16 weeks (unrestricted survival) vs. vigorous rejection of wild-type [6]. | |
| Human HIP SC-Islets | Allogeneic Diabetic Humanized Mice | Diabetes Amelioration | Survival for 4 weeks and amelioration of diabetes [6]. | |
| Rhesus Macaque HIP Islets | Allogeneic Rhesus Macaque | Islet Survival without Immunosuppression | Survival for 40 weeks vs. quick rejection of unedited islets [6]. | |
| Human Primary HIP Islets (UP421) | First-in-Human T1D Patient (No Immunosuppression) | C-peptide Production (6 months) | Consistent and responsive C-peptide production, indicating surviving and functioning grafts [86] [87]. | |
| Human HIP iPSCs | In Vitro Co-culture with IL-2 Stimulated NK Cells | Protection from NK Cell Killing | CD47 overexpression provided comprehensive protection; HLA-E/G only protected NK subsets with corresponding receptors [6]. |
Experimental Protocols
This section provides detailed methodologies for key experiments in the development and validation of HIP SC-islets.
Protocol: Generation of HIP Pluripotent Stem Cells
Objective: To create a master HIP pluripotent stem cell (PSC) line through CRISPR-Cas9-mediated gene editing for subsequent differentiation into various therapeutic cell types, including SC-islets.
Materials:
- Parental PSC Line: A well-characterized human induced PSC (iPSC) or embryonic stem cell (ESC) line.
- CRISPR-Cas9 System: Plasmids or ribonucleoproteins (RNPs) for B2M and CIITA knockout.
- Lentiviral Vector: For overexpression of CD47 (and/or PD-L1, HLA-G).
- Cell Culture Reagents: Matrigel, mTeSR Plus medium, Accutase.
- Validation Reagents: Flow cytometry antibodies for B2M, HLA Class II, CD47.
Methodology:
- Knockout of B2M and CIITA:
- Design and synthesize guide RNAs (gRNAs) targeting the B2M and CIITA genes.
- Transfect the PSCs with CRISPR-Cas9 components (e.g., via electroporation).
- Culture transfected cells for 7-10 days, then perform single-cell cloning to isolate pure knockout populations.
- Validate knockout efficiency via Sanger sequencing and flow cytometry for loss of B2M/HLA-Class I and CIITA/HLA-Class II surface expression.
Overexpression of CD47:
- Transduce the B2M−/−CIITA−/− PSCs with a lentiviral vector carrying the CD47 transgene.
- Select transduced cells using an appropriate antibiotic (e.g., Puromycin) for 5-7 days.
- Isulate a polyclonal or monoclonal population with high, stable CD47 expression, as confirmed by flow cytometry.
Quality Control:
- Perform karyotyping to ensure genomic integrity.
- Confirm pluripotency via flow cytometry for markers like OCT4, SOX2, and TRA-1-60.
- Differentiate the master HIP PSC line into SC-islets using a established, multi-step differentiation protocol [20].
Protocol: In Vivo Validation in Immunocompetent Allogeneic Models
Objective: To assess the survival, engraftment, and immune evasion of differentiated HIP SC-islets in a therapeutically relevant animal model.
Materials:
- Animals: Fully immunocompetent, allogeneic non-human primates (e.g., Rhesus Macaques) or humanized mice.
- Test Articles: Differentiated HIP SC-islets and unedited wild-type SC-islets as a control.
- Transplantation Equipment: Catheter for intraportal infusion or surgical tools for intramuscular/omental implantation.
- Monitoring Tools: MRI/PET imaging, Glucose tolerance test kits, C-peptide ELISA kits.
Methodology:
- Cell Preparation: Prepare a single-cell suspension of HIP and wild-type SC-islets. For tracking, cells may be transduced to express a reporter gene like luciferase.
- Transplantation: In a diabetic model, transplant a defined islet mass (e.g., 5,000-10,000 islet equivalents per kg) into a selected site. The forearm muscle is an emerging site that allows for non-invasive monitoring [86] [87]. The liver portal vein is the clinical standard.
- Long-Term Monitoring:
- Graft Function: Measure fasting and stimulated C-peptide levels weekly. Perform glucose tolerance tests periodically.
- Graft Survival: Use non-invasive imaging (e.g., MRI) to visualize the graft site [86].
- Glycemic Control: Track blood glucose levels, HbA1c, and exogenous insulin requirements.
- Immune Response: Collect peripheral blood mononuclear cells (PBMCs) at regular intervals to conduct interferon-γ ELISpot assays against donor antigens and monitor for donor-specific antibodies [6].
- Endpoint Analysis: Upon study completion, explant the graft site for histological analysis (H&E, insulin staining) to directly assess islet survival and immune cell infiltration.
Signaling Pathways and Visual Workflows
The following diagrams illustrate the core logic of HIP engineering and the key signaling pathways involved in evading innate immunity.
Core Logic of HIP Engineering
Innate Immune Evasion Signaling
This diagram details the molecular interactions at the interface between a HIP-edited cell and an innate immune cell (NK cell or Macrophage).
The Scientist's Toolkit: Essential Research Reagents
The table below catalogs key reagents and tools essential for research and development in the HIP SC-islet field.
Table 3: Key Research Reagent Solutions
| Research Reagent / Tool | Function & Application | Example Use Case |
|---|---|---|
| CRISPR-Cas9 Systems | Precision gene editing for knocking out B2M and CIITA genes. | Generation of clonal B2M−/−CIITA−/− PSC lines [6]. |
| Lentiviral Vectors | Stable integration of transgenes (e.g., CD47, PD-L1) into the host cell genome. | Overexpression of immunomodulatory proteins in HIP PSCs [20] [6]. |
| Anti-Human CD47 Antibodies | Flow cytometry validation of CD47 surface expression levels. | Confirming high CD47 expression post-knock-in during quality control. |
| Anti-Human HLA-ABC Antibodies | Flow cytometry detection of HLA Class I surface expression. | Validating successful B2M knockout (loss of HLA-I signal) [6]. |
| Human C-peptide ELISA Kit | Quantification of human C-peptide in serum or culture supernatant. | Measuring in vivo graft function in animal models or clinical trials [86] [87]. |
| IFN-γ ELISpot Kit | Detection of antigen-specific T-cell responses. | Assessing T-cell reactivity against HIP vs. wild-type cells in co-culture assays [6]. |
The field of HIP engineering for T1D therapy has progressed from a compelling concept to tangible clinical validation. The recent first-in-human report of a patient with T1D receiving HIP-engineered primary islets (UP421) without immunosuppression marks a watershed moment. The persistence of C-peptide production and immune evasion at the six-month follow-up provides initial proof that the approach can work in humans [86] [87]. This success with primary islets paves the way for the next generation of therapies: HIP stem cell-derived islets.
The primary challenge now lies in scaling manufacturing and ensuring long-term safety and functionality. Ongoing research addresses potential risks such as immune escape, tumorigenicity from residual undifferentiated cells, and the theoretical risk of viral infection due to diminished HLA class I presentation [36]. As the field advances, the integration of HIP technology with scalable stem cell differentiation protocols holds the promise of delivering a universally compatible, one-time curative treatment for T1D, moving beyond the century-old paradigm of insulin replacement.
Emerging Biomarkers and Diagnostic Tools for Monitoring Cell Persistence and Toxicity
The advancement of allogeneic cell therapies hinges on the ability to effectively monitor two critical parameters: long-term cellular persistence and potential toxicities. For hypo-immune engineered cells, which are designed to evade host immune responses through genetic modifications such as MHC knockout and expression of immunomodulatory molecules, traditional monitoring approaches often prove insufficient [14] [20]. This application note provides a comprehensive framework of emerging biomarkers and diagnostic tools essential for characterizing these advanced therapeutic products, with detailed protocols tailored for researchers and drug development professionals.
The complex biology of hypo-immune cells necessitates sophisticated analytical approaches that extend beyond conventional potency assays. These therapies present unique challenges in safety monitoring, particularly regarding delayed toxicities and immune evasion efficacy [88]. Recent advances in multi-omics profiling and functional assays now enable unprecedented resolution in tracking cellular behavior post-administration, providing critical insights for product development and regulatory approval.
Emerging Biomarkers for Persistence and Toxicity Monitoring
Genomic and Epigenomic Biomarkers
Table 1: Genomic Biomarkers for Cell Persistence and Safety Monitoring
| Biomarker Category | Specific Marker/Analysis | Detection Method | Application in Hypo-immune Cells | References |
|---|---|---|---|---|
| Vector Integration | Vector copy number (VCN) | Droplet digital PCR (ddPCR) | Quantification of engineered cell persistence | [89] |
| Integration site analysis | INSPIIRED pipeline, EpiVIA | Monitoring clonal expansion and safety | [89] | |
| TCR Repertoire | TCR sequencing (αβ vs. γδ) | Single-cell RNA-seq with TCR-seq | Assessing impact of TCR knockout on persistence | [89] [90] |
| TCR diversity metrics | Immunogenomic analysis | Correlation with clinical outcomes | [89] | |
| Epigenetic Marks | DNA methylation profiles | Bulk and single-cell epigenomics | Predicting differentiation state and persistence | [89] |
| Chromatin accessibility | ATAC-seq | Understanding long-term functional potential | [89] |
For hypo-immune cells, genomic stability is a paramount concern, particularly with CRISPR/Cas9-engineered products. Vector copy number (VCN) remains a fundamental lot-release criterion for genetically modified cellular products, with ddPCR serving as the gold standard for quantification [89]. Beyond this basic metric, integration site analysis provides critical safety data, especially for therapies utilizing lentiviral or retroviral vectors. The INSPIIRED pipeline enables bulk analysis of integration events, while EpiVIA facilitates single-cell resolution mapping, allowing researchers to monitor for potentially oncogenic integration events that might lead to clonal expansion [89].
The T cell receptor (TCR) repertoire offers valuable insights even in TCR-knockout hypo-immune cells. In autologous settings, TCR diversity within infusion products correlates with clinical outcomes, with oligoclonality and polyclonality influencing treatment efficacy [89]. For allogeneic products, complete TCR knockout is standard practice to prevent graft-versus-host disease, but monitoring the success of this editing is crucial. Furthermore, the presence of γδ T-cells in infusion products may enhance cytotoxicity and correlate with favorable clinical responses, making them a potentially advantageous subset to preserve in certain hypo-immune designs [89] [90].
Epigenomic profiling has emerged as a powerful tool for predicting cellular behavior post-infusion. DNA methylation patterns and chromatin accessibility states can identify differentiation states that correlate with persistence potential [89]. Carlos et al. analyzed DNA methylation profiles in 114 CD19 CAR T-cell products and identified 18 distinct epigenetic loci associated with persistence outcomes, providing a framework that can be adapted for hypo-immune cell monitoring [89].
Protein and Functional Biomarkers
Table 2: Functional Biomarkers for Toxicity and Persistence Monitoring
| Biomarker Category | Specific Marker | Detection Method | Application in Hypo-immune Cells | References |
|---|---|---|---|---|
| Cytokine Release | IFN-γ, TNF-α, IL-2 | Multiplex immunoassays | Potency assessment and CRS monitoring | [89] [91] |
| IL-6, IFN-γ | ELISA, electrochemiluminescence | CRS pathophysiology and intervention | [88] | |
| Cytotoxic Activity | Perforin, Granzyme B | Intracellular staining, functional assays | Effector function quantification | [90] |
| Surface Phenotype | CD16 expression | Flow cytometry | Donor selection for enhanced ADCC | [90] |
| Exhaustion markers (TIM-3, PD-1) | Multicolor flow cytometry | Monitoring functional persistence | [89] [90] | |
| Metabolic Profile | Glycolytic activity, mitochondrial fitness | Metabolic flux analysis | Predicting in vivo fitness | [89] [91] |
Functional biomarkers provide critical insights into the activity and potential toxicities of hypo-immune cells. Cytokine release profiles remain central to potency assessment and toxicity monitoring, with IFN-γ, TNF-α, and IL-2 serving as key indicators of T-cell activation [89] [91]. For safety monitoring, IL-6 and IFN-γ are particularly valuable in predicting and managing cytokine release syndrome (CRS), a known toxicity of cellular therapies [88].
CD16 (FcγRIII) has emerged as a valuable biomarker for donor selection in allogeneic therapies. Research on Vδ2 T-cells has demonstrated that donors with high CD16 expression (CD16Hi) yield products with enhanced cytotoxicity and antibody-dependent cell-mediated cytotoxicity (ADCC) functionality [90]. RNA sequencing analysis supports the augmented effector potential of immune cells derived from CD16Hi donors, making this surface marker a valuable selection criterion for allogeneic cell products [90].
Cellular metabolism serves as a functional biomarker predicting in vivo persistence. Hypo-immune cells with enhanced mitochondrial fitness and balanced glycolytic activity demonstrate improved long-term serial killing capacity and persistence in hostile microenvironments [89] [91]. The AVATAR platform, which cultures cells under hypoxic and hyperbaric conditions mimicking the tumor microenvironment, can identify products with these desirable metabolic characteristics [91].
Diagnostic Tools and Experimental Protocols
Advanced Potency Assay Systems
Figure 1: Integrated workflow for comprehensive potency assessment of hypo-immune cell products, combining multi-omics profiling with functional assays.
Protocol 1: Advanced Potency Assay for Hypo-immune Cell Products
Purpose: To comprehensively evaluate the potency of hypo-immune engineered cells through integrated functional assessments.
Materials:
- AVATAR cell culture system (Xcellbio) or similar physiological mimicry platform
- Target cells expressing relevant antigens
- Hypo-immune cell product
- Multiplex cytokine detection platform
- Metabolic analysis reagents (Seahorse XF reagents recommended)
- Flow cytometer with appropriate antibodies for surface and intracellular markers
Procedure:
- Physiological Culture Conditions: Manufacture hypo-immune cells under hypoxic (1-5% O₂) and hyperbaric conditions using the AVATAR platform to mimic the tumor microenvironment [91].
- Cytotoxic Activity Assessment:
- Co-culture hypo-immune cells with target cells at multiple effector-to-target (E:T) ratios (recommended: 1:1, 5:1, 10:1).
- Measure target cell killing using real-time cell analysis (RTCA) or luciferase-based cytotoxicity assays at 24-hour intervals for 72 hours.
- For serial killing assessment, re-challenge surviving cells with fresh target cells every 24-48 hours.
- Cytokine Profiling:
- Collect supernatant from co-cultures at 6, 24, and 48 hours.
- Analyze IFN-γ, TNF-α, IL-2, IL-6, and other relevant cytokines using multiplex electrochemiluminescence detection.
- Compare secretion profiles to reference standards and historical product data.
- Metabolic Fitness Assessment:
- Perform metabolic flux analysis using Seahorse XF technology.
- Measure basal glycolysis, glycolytic capacity, mitochondrial respiration, and spare respiratory capacity.
- Correlate metabolic parameters with persistence potential.
- Data Integration: Compile all parameters into a potency index that predicts in vivo performance.
Quality Controls:
- Include reference standards with known potency in each assay run.
- Establish acceptance criteria based on clinical correlation data.
- Document assay precision (CV < 20%) and accuracy (80-120% of reference).
Multi-omics Profiling for Comprehensive Characterization
Protocol 2: Integrated Multi-omics Analysis of Hypo-immune Cells
Purpose: To comprehensively characterize hypo-immune cells at genomic, epigenomic, transcriptomic, and proteomic levels for persistence and safety assessment.
Materials:
- Single-cell RNA sequencing platform (10x Genomics recommended)
- Droplet digital PCR system
- ATAC-seq reagents
- Mass cytometer (CyTOF) or high-parameter flow cytometer
- TCR sequencing reagents
- Bioinformatics pipelines for multi-omics integration
Procedure:
- Sample Preparation:
- Collect cells at multiple manufacturing timepoints: pre-editing, post-editing, and final product.
- Preserve aliquots for various analyses using appropriate stabilization methods.
- Genomic Analysis:
- Extract genomic DNA and perform ddPCR for vector copy number determination.
- Conduct integration site analysis using INSPIIRED or EpiVIA pipelines for viral vector-based products.
- Perform off-target analysis using GUIDE-seq or similar methods for CRISPR-edited products.
- Single-cell Multi-omics Profiling:
- Perform paired single-cell RNA sequencing and TCR sequencing to link transcriptional phenotypes with clonality.
- Conduct ATAC-seq to assess chromatin accessibility and epigenetic states.
- Use CITE-seq (cellular indexing of transcriptomes and epitopes) for simultaneous protein and gene expression analysis.
- Bioinformatic Integration:
- Employ clustering algorithms to identify distinct cellular subpopulations.
- Perform trajectory analysis to predict differentiation pathways.
- Correlate omics signatures with functional potency data.
- Persistence Signature Development:
- Identify gene expression modules associated with long-term persistence in vivo.
- Develop persistence scores based on multi-omics signatures.
- Validate signatures using in vivo models and clinical samples.
Quality Controls:
- Ensure sequencing depth >50,000 reads per cell for scRNA-seq.
- Include spike-in controls for quantification accuracy.
- Establish criteria for minimal cell viability (>80%) prior to single-cell analysis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Hypo-immune Cell Monitoring
| Reagent Category | Specific Product/Platform | Application | Key Features |
|---|---|---|---|
| Gene Editing Validation | CRISPOR off-target prediction | Assessing editing specificity | In silico prediction of off-target sites |
| GUIDE-seq reagents | Empirical off-target detection | Genome-wide identification of editing events | |
| Cell Phenotyping | Metal-conjugated antibodies (CyTOF) | High-dimensional immunophenotyping | 40+ parameter single-cell analysis |
| CITE-seq antibodies | Simultaneous protein and RNA measurement | Integrated multi-omics characterization | |
| Functional Assays | AVATAR cell culture system | Physiological potency assessment | Mimics tumor microenvironment conditions |
| Real-time cell analysis (RTCA) | Dynamic cytotoxicity monitoring | Label-free, continuous measurement | |
| Multi-omics Platforms | 10x Genomics Single Cell Immune Profiling | Comprehensive cellular characterization | Linked V(D)J sequencing with gene expression |
| INSPIIRED integration site pipeline | Vector integration safety assessment | Bioinformatics analysis of integration sites |
Data Analysis and Interpretation Framework
Integration of Multi-modal Data
The interpretation of persistence and toxicity biomarkers requires sophisticated data integration approaches. Multi-omics data fusion enables researchers to build predictive models of in vivo behavior by combining genomic, transcriptomic, proteomic, and functional data [89]. Machine learning algorithms can identify signature combinations that correlate with favorable clinical outcomes, enabling product optimization and potency prediction.
For hypo-immune cells specifically, monitoring the efficacy of immune evasion edits is crucial. This includes verifying complete knockout of target genes (MHC classes I and II, TCR) while ensuring that introduced transgenes (CD47, HLA-G, PD-L1) provide the intended immunomodulatory functions without impairing therapeutic efficacy [14] [20]. Functional assays measuring resistance to allogeneic T-cell and NK-cell mediated killing provide critical validation of the hypo-immune phenotype.
Correlation with Clinical Outcomes
Establishing correlations between biomarker data and clinical outcomes represents the ultimate validation of monitoring approaches. Duration of response and progression-free survival serve as key endpoints for persistence correlations, while the incidence and severity of CRS, ICANS, and other toxicities validate safety biomarkers [88] [92].
Recent clinical data from allogeneic CAR T-cell trials provide valuable benchmarks. In the ALPHA and ALPHA2 trials of cema-cel, complete responders demonstrated a median duration of response of 23.1 months, establishing a reference point for persistence expectations in allogeneic products [92]. Safety benchmarks from these trials, including CRS rates of 24% with no severe neurotoxicity, provide context for interpreting toxicity biomarker data [92].
The successful development of hypo-immune cell therapies requires robust biomarkers and diagnostic tools that can accurately predict and monitor persistence and toxicity. The integrated framework presented here, combining multi-omics profiling with advanced functional assays, provides a comprehensive approach to addressing these critical needs. As the field advances, continued refinement of these tools will be essential for realizing the full potential of allogeneic cell therapies and ensuring their safe clinical application.
Researchers should prioritize the validation of biomarker associations with clinical outcomes, as this remains the most significant gap in current monitoring capabilities. Furthermore, standardization of assays across laboratories and products will facilitate comparative analyses and accelerate the development of this promising therapeutic modality.
Conclusion
The engineering of hypoimmune cells marks a paradigm shift in allogeneic therapy, moving the field closer to readily available 'off-the-shelf' treatments. Key takeaways include the critical importance of multi-faceted engineering that addresses both adaptive and innate immunity, the proven clinical feasibility of these approaches in early trials, and the successful application across diverse cell types. Future progress hinges on refining gene-editing precision to enhance safety, developing robust solutions for long-term in vivo persistence, and standardizing manufacturing for clinical-grade products. As these technologies mature, they hold the immense promise of democratizing access to advanced cell therapies for a broad spectrum of diseases, fundamentally changing the treatment landscape for patients worldwide.
References
- 1. Responses to alloantigens and transplant rejection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK27163/]
- 2. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 3. Strategies for Genetically Engineering Hypoimmunogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7270609/]
- 4. Immune Landscape in Kidney Transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581792/]
- 5. Immune recognition and rejection of allogeneic skin grafts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3738014/]
- 6. Hypoimmune induced pluripotent stem cells survive long ... [https://www.nature.com/articles/s41587-023-01784-x]
- 7. Generation of hypoimmunogenic universal iPS cells through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958689/]
- 8. Hypoimmune CD19 CAR T cells evade allorejection in ... [https://www.sciencedirect.com/science/article/pii/S1934590925002668]
- 9. Discrimination of Anti-Donor Response in Allogeneic ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.13879/full]
- 10. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 11. Genome-edited allogeneic CAR-T cells: the next generation of ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01745-8]
- 12. CAR-T cell therapy for cancer: current challenges ... - Nature [https://www.nature.com/articles/s41392-025-02269-w]
- 13. Tracing the development of CAR-T cell design - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326545/]
- 14. Diminished immune cell adhesion in hypoimmune ICAM-1 ... [https://www.nature.com/articles/s41467-025-62568-2]
- 15. Cell adhesion molecule ITGB2 promotes CAR-T ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525005841]
- 16. Corneal Graft Rejection - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK519043/]
- 17. Corneal Transplantation and Immune Privilege - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3885418/]
- 18. Medical and surgical approaches to prevent corneal graft ... [https://www.sciencedirect.com/science/article/abs/pii/S0039625725001821]
- 19. Advances in human amniotic placenta membrane-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1590393/full]
- 20. Engineering hypoimmune stem cell-derived beta cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04745-0]
- 21. Frontiers | Fit-For-All iPSC-Derived Cell Therapies and Their Evaluation in Humanized Mice With NK Cell Immunity [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.662360/full]
- 22. Induced pluripotent stem cells have similar immunogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4352342/]
- 23. Allogeneic CAR-engineered cellular therapy for relapsed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1585556/full]
- 24. Immune reaction and regulation in transplantation based on pluripotent stem cell technology | Inflammation and Regeneration | Full Text [https://inflammregen.biomedcentral.com/articles/10.1186/s41232-020-00125-8]
- 25. Frontiers | Unlocking the potential of iPSC-derived immune cells: engineering iNK and iT cells for cutting-edge immunotherapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1457629/full]
- 26. Shifting Tides: Unleashing the Potential of iPSC-Based ... [https://www.cellistic.com/insights/shifting-tides-unleashing-the-potential-of-ipsc-based-allogeneic-cell-therapy]
- 27. Genome-edited allogeneic CAR-T cells - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553175/]
- 28. Expanding the genetic editing tool kit: ZFNs, TALENs, and CRISPR-Cas9 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4191047/]
- 29. CRISPR/Cas9 system: recent applications in immuno-oncology and cancer immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10647168/]
- 30. CRISPR/Cas9 technology for advancements in cancer immunotherapy: from uncovering regulatory mechanisms to therapeutic applications | Experimental Hematology & Oncology | Full Text [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00570-y]
- 31. Leveraging CRISPR gene editing technology to optimize ... [https://www.nature.com/articles/s41375-024-02444-y]
- 32. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 33. Immuno-Oncology [https://crisprtx.com/focus-areas/immuno-oncology]
- 34. Editing B2M and CIITA to Create Hypoimmune Cell Lines ... [https://www.reprocell.com/blog/editing-b2m-and-ciita-to-create-hypo-immunecell-lines-for-cell-therapy]
- 35. Therapeutic effects of hypoimmunogenic universal human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12330048/]
- 36. Hypoimmune stem cells and islets: hype or a true ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492583/]
- 37. Diminished expression of major histocompatibility complex ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01847-9]
- 38. Selective HLA knockdown and PD-L1 expression prevent ... [https://www.nature.com/articles/s41467-025-63863-8]
- 39. Overcoming Immune Barriers in Allogeneic CAR-NK Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292777/]
- 40. Current status and future perspectives of HLA-edited induced ... [https://inflammregen.biomedcentral.com/articles/10.1186/s41232-020-00132-9]
- 41. Hypoimmunogenic Human iPSCs for Repair and ... [https://www.mdpi.com/2073-4409/14/16/1248]
- 42. Augmented CD47 expression impairs alloreactive T-cell ... [https://www.sciencedirect.com/science/article/pii/S0006497125011267]
- 43. Establishment of Immune-Evasive iPSCs from PBMCs ... [https://pubmed.ncbi.nlm.nih.gov/40682609/]
- 44. The expression mechanism of programmed cell death 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10859298/]
- 45. The Diverse Function of PD-1/PD-L Pathway Beyond Cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.02298/full]
- 46. The Potential Advantage of Targeting Both PD-L1/PD-L2/ ... [https://www.mdpi.com/1424-8247/14/11/1105]
- 47. Addressing graft-versus-host disease in allogeneic cell-based ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00654-3]
- 48. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 49. A New Era in Islet Transplantation: Stem Cell-Derived and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620690/]
- 50. Engineering hypoimmune stem cell-derived beta cells [https://pubmed.ncbi.nlm.nih.gov/41188976/]
- 51. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 52. Emerging CAR immunotherapies: broadening therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321946/]
- 53. Application of allogeneic adult mesenchymal stem cells in ... [https://pubmed.ncbi.nlm.nih.gov/40373055/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1DqqIY7i9Icf9J_BIwh0PRg_lq4ZdpZVa2NCCBt_Z5SBUCUY-a&fc=20220524054013&ff=20250516090919&v=2.18.0.post9+e462414]
- 54. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 55. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 56. Assessing Tumorigenicity in Stem Cell-Derived ... [https://www.mdpi.com/2306-5354/10/7/857]
- 57. Investigational Cell Therapy May Improve Survival Without Chronic GvHD in Patients With Blood Cancer [https://www.aabb.org/news-resources/news/article/2025/03/19/investigational-cell-therapy-may-improve-survival-without-chronic-gvhd-in-patients-with-blood-cancer]
- 58. Outcomes of Allogeneic Hematopoietic Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/39755255/]
- 59. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 60. Mechanisms of natural - killer cellular cell mediated cytotoxicity [https://pubmed.ncbi.nlm.nih.gov/31107565/]
- 61. NK cell education after allogeneic transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC3172795/]
- 62. Functional Reconstitution of Natural Killer Cells in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2016.00144/full]
- 63. Effect of NK cell receptor genetic variation on allogeneic ... [https://www.nature.com/articles/s41598-024-78619-5]
- 64. Frontiers Publishing Partnerships | Cytotoxic Responses Mediated by... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.13867/full]
- 65. Navigating Batch-to-Batch Variability with a Data-Centric ... [https://www.zaether.com/resources/navigating-batch-to-batch-variability-with-a-data-centric-approach/]
- 66. Scaling Allogeneic Cell Therapy Manufacturing [https://www.patheon.com/us/en/insights-resources/blog/scaling-allogeneic-cell-therapy-manufacturing.html]
- 67. Scaling Hope: The Growth of Allogeneic Cell Therapy Sector [https://www.precisionformedicine.com/blog/article-scaling-hope-the-growth-of-allogeneic-cell-therapy-sector/]
- 68. OVERCOMING CURRENT CHALLENGES IN ... [https://www.sciencedirect.com/science/article/pii/S1465324924003335]
- 69. Advancing CAR T Cell Therapy with Logic Gate Engineering [https://www.cellandgene.com/doc/advancing-car-cell-therapy-logic-gate-engineering-0001]
- 70. Pluristyx Collaborates with Breakthrough T1D to Make " ... [https://pluristyx.com/pluristyx-collaborates-with-breakthrough-t1d-to-make-immune-cloaked-and-safety-switch-enabled-allogeneic-cell-line-for-type-1-diabetes-therapies/]
- 71. Pluristyx Collaborates with Breakthrough T1D to Make [https://www.globenewswire.com/news-release/2025/11/17/3189000/0/en/Pluristyx-Collaborates-with-Breakthrough-T1D-to-Make-Immune-Cloaked-and-Safety-Switch-Enabled-Allogeneic-Cell-Line-for-Type-1-Diabetes-Therapies.html]
- 72. AACR: New CAR T cell therapy benefits patients with ... [https://www.mdanderson.org/newsroom/aacr-new-car-t-cell-therapy-benefits-patients-with-advanced-thyroid-cancers.h00-159775656.html]
- 73. ICAM-1 CAR T-Cell Therapy Shows Promise in Aggressive ... [https://www.targetedonc.com/view/icam-1-car-t-cell-therapy-shows-promise-in-aggressive-thyroid-cancers]
- 74. Innovative Allogeneic CAR T Cell Therapy Trial Shows ... [https://www.houstonmethodist.org/leading-medicine-blog/articles/2025/mar/innovative-allogeneic-car-t-cell-therapy-trial-shows-promising-results/]
- 75. Release details [https://investor.cariboubio.com/news-releases/news-release-details/caribou-biosciences-announces-positive-data-antler-phase-1-trial]
- 76. CARsgen Announces Preliminary Clinical Data ... [https://www.carsgen.com/en/news/20150512/]
- 77. Safety, efficacy and determinants of response of allogeneic ... [https://www.nature.com/articles/s41591-023-02785-8]
- 78. Efficacy and safety of allogeneic CD19 CAR NK-cell ... [https://pubmed.ncbi.nlm.nih.gov/41240964/]
- 79. Press Releases [https://ir.allogene.com/news-releases/news-release-details/allogene-therapeutics-provides-updated-phase-1-data-highlighting]
- 80. CAR-T Allogeneic Technologies: Has the Promise Been Met? Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814647/]
- 81. and other innovative chimeric antigen receptor platforms Allogeneic [https://chi.scholasticahq.com/article/121404-allogeneic-and-other-innovative-chimeric-antigen-receptor-platforms]
- 82. Hypoimmunogenic Human iPSCs for Repair and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384217/]
- 83. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 84. Cell therapy for type 1 diabetes: Tracing historical progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12640444/]
- 85. Innovations in bio-engineering and cell-based approaches ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1375177/full]
- 86. Release Details - Investor Relations | Sana Biotechnology, Inc [https://ir.sana.com/news-releases/news-release-details/sana-biotechnology-announces-positive-six-month-clinical-results]
- 87. New data: Hypoimmune islets survive with no ... [https://www.breakthrought1d.org/news-and-updates/new-publication-engineered-islets-making-insulin-and-avoiding-immune-detection-in-first-person-treated/]
- 88. Pharmacovigilance in Cell and Gene Therapy: Evolving Challenges in Risk Management and Long-Term Follow-Up | Drug Safety [https://link.springer.com/article/10.1007/s40264-025-01596-9]
- 89. New insights on potency assays from recent advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 90. Unlocking the potential of allogeneic Vδ2 T cells for ovarian cancer therapy through CD16 biomarker selection and CAR/IL-15 engineering | Nature Communications [https://www.nature.com/articles/s41467-023-42619-2]
- 91. Development of cell-based functional assays to predict ... [https://www.labcorp.com/development-cell-based-functional-assays-predict-car-t-cell-potency-and-persistence]
- 92. Cema-Cel Advances CAR T Therapy for LBCL in ALPHA Trials | Targeted Oncology - Immunotherapy, Biomarkers, and Cancer Pathways [https://www.targetedonc.com/view/cema-cel-advances-car-t-therapy-for-lbcl-in-alpha-trials]