Engineering MSC Exosomes for Targeted Drug Delivery in Chronic Wounds: Mechanisms, Methods, and Clinical Translation
Chronic wounds represent a significant clinical challenge due to their complex pathophysiology and failure to progress through normal healing stages.
Engineering MSC Exosomes for Targeted Drug Delivery in Chronic Wounds: Mechanisms, Methods, and Clinical Translation
Abstract
Chronic wounds represent a significant clinical challenge due to their complex pathophysiology and failure to progress through normal healing stages. This article explores the burgeoning field of mesenchymal stem cell (MSC)-derived exosomes as engineered, cell-free therapeutic platforms for targeted drug delivery in wound management. We examine the foundational biology of exosomes and their native roles in wound healing phases, detail advanced methodologies for cargo loading and surface modification to enhance targeting and efficacy, and address key challenges in manufacturing and standardization. Furthermore, we synthesize current preclinical and clinical validation data, comparing engineered exosomes with conventional therapies and natural vesicles. By integrating recent advances from 2024-2025, this review provides a comprehensive resource for researchers and drug development professionals aiming to translate exosome-based nanomedicines from bench to bedside.
The Biology of MSC Exosomes and Their Native Role in Wound Healing
Exosomes are nanosized, lipid bilayer-delimited extracellular vesicles (EVs), typically 30–150 nm in diameter, that are naturally secreted by all cell types, including Mesenchymal Stem Cells (MSCs) [1] [2]. They originate from the endosomal pathway and are released into the extracellular space upon fusion of Multivesicular Bodies (MVBs) with the plasma membrane [3] [4]. Once considered mere cellular waste bags, exosomes are now recognized as potent mediators of intercellular communication due to their capacity to transport a diverse array of bioactive molecules, including proteins, lipids, nucleic acids (DNA, mRNA, miRNA, circRNA), and metabolites [5] [2]. Their innate biocompatibility, low immunogenicity, stability in circulation, and ability to penetrate biological barriers make them promising natural vehicles for targeted drug delivery [5] [6] [1]. In the context of chronic wounds, engineered MSC-derived exosomes hold particular promise for delivering therapeutic cargo to precisely modulate the dysfunctional wound healing process [7].
Molecular Machinery of Exosome Biogenesis
Exosome biogenesis is a complex, multi-step process meticulously regulated by cellular machinery. It can be divided into four key stages: (1) cargo sorting, (2) MVB formation and maturation, (3) intracellular transport of MVBs, and (4) fusion of MVBs with the plasma membrane [4].
Key Biogenesis Pathways
The formation of intraluminal vesicles (ILVs) within MVBs is driven by several distinct but potentially overlapping molecular pathways.
2.1.1. The ESCRT-Dependent Pathway The Endosomal Sorting Complex Required for Transport (ESCRT) machinery is a well-studied mechanism comprising four complexes (ESCRT-0, -I, -II, -III) and associated proteins like VPS4 and ALIX [4] [8].
- ESCRT-0 (including Hrs and STAM) recognizes and sequesters ubiquitinated cargo proteins on the endosomal membrane [4] [8].
- ESCRT-I and -II are recruited to drive membrane deformation and initiate budding.
- ESCRT-III forms filaments that constrict the neck of the budding vesicle.
- The VPS4 ATPase complex provides energy for membrane scission and the recycling of ESCRT components [4]. This pathway is crucial for sorting ubiquitinated proteins and various other cargoes into nascent ILVs [5].
2.1.2. ESCRT-Independent Pathways Several mechanisms can generate ILVs without the full ESCRT apparatus.
- The nSMase2-Ceramide Pathway: Neutral sphingomyelinase 2 (nSMase2) converts sphingomyelin to ceramide on the endosomal membrane. Ceramide's conical structure promotes membrane curvature and inward budding, facilitating the sorting of cargoes like the prion protein and specific RNAs [4].
- Tetraspanin-Enriched Microdomains: Tetraspanins (e.g., CD9, CD63, CD81) are abundant on exosome membranes and can form specialized microdomains that recruit specific client proteins and promote membrane budding and fission in an ESCRT-independent manner [8]. For instance, CD63 knockdown has been shown to reduce exosome production [8].
- The Syndecan-Syntenin-ALIX Pathway: Transmembrane proteoglycans (syndecans) bind the adaptor protein syntenin, which then recruits ALIX. ALIX, in turn, engages ESCRT-III and VPS4 to facilitate ILV formation, serving as a bridge between specific cargo and the ESCRT machinery [4].
The following diagram illustrates the coordination of these primary pathways during exosome biogenesis:
Figure 1: Key Pathways of Exosome Biogenesis. This diagram illustrates the primary ESCRT-dependent and ESCRT-independent pathways (nSMase2-ceramide and tetraspanin microdomains) that drive the formation of intraluminal vesicles (ILVs) within multivesicular bodies (MVBs), culminating in exosome release.
Fate of MVBs and Exosome Release
Once formed, MVBs face one of two fates: degradation or exocytosis. MVBs destined for degradation fuse with lysosomes, leading to the breakdown of their contents. In contrast, MVBs programmed for exosome release are trafficked along microtubules to the cell periphery. This transport involves Rab GTPases (e.g., Rab27a/b, Rab11, Rab35) [8]. At the plasma membrane, SNARE complexes facilitate the docking and fusion of the MVB with the plasma membrane, releasing the ILVs into the extracellular space as exosomes [4].
Composition and Selective Cargo Sorting
The molecular composition of exosomes is not random; it is a highly regulated process that determines the exosome's functional destiny upon delivery to a recipient cell.
Major Cargo Components
Exosomes encapsulate a diverse repertoire of biomolecules that mirror their cell of origin but are often enriched through active sorting mechanisms.
Table 1: Major Cargo Components of Exosomes
| Cargo Category | Specific Examples | Functional Roles / Notes |
|---|---|---|
| Proteins | Tetraspanins (CD9, CD63, CD81), ESCRT-related proteins (ALIX, TSG101), Heat shock proteins (HSP70, HSP90), Integrins, MHC molecules [5] [8] | Often used as exosome marker proteins; involved in biogenesis, targeting, and signaling. |
| Lipids | Cholesterol, Sphingomyelin, Ceramide, Phosphatidylserine, Bisphosphatidic acid (LBPA) [5] [4] | Contribute to membrane stability, curvature, and budding during biogenesis. |
| Nucleic Acids | miRNA, mRNA, lncRNA, circRNA, mitochondrial DNA (mtDNA), genomic DNA [5] [2] | Can alter gene expression and function in recipient cells. miRNA is extensively studied for therapeutic regulation. |
Mechanisms of Cargo Sorting
Cargo is selectively packaged into ILVs through specific interactions with the biogenesis machinery.
- Ubiquitin-Dependent Sorting: Ubiquitinated proteins are recognized by ESCRT-0 for incorporation into ILVs via the canonical ESCRT pathway [4] [8].
- Ubiquitin-Independent Sorting: The Syndecan-Syntenin-ALIX axis sorts cargo like fibroblast growth factor receptor (FGFR) without requiring ubiquitination [4].
- RNA Sorting: RNA-binding proteins (RBPs) such as SAFB and hnRNPK are involved in sorting specific RNAs into exosomes, sometimes through interactions with components like LC3 on the MVB membrane [4].
The following experimental workflow outlines key protocols for isolating and analyzing this exosomal cargo:
Figure 2: Experimental Workflow for Exosome Isolation and Analysis. This diagram outlines the standard protocol from cell culture to exosome characterization and cargo analysis, highlighting key techniques like nanoparticle tracking analysis (NTA), transmission electron microscopy (TEM), and Western blot.
Application Notes: Engineering MSC Exosomes for Chronic Wounds
Chronic wounds are characterized by a failure to proceed through an orderly healing process, marked by persistent inflammation, impaired angiogenesis, and inadequate tissue remodeling [7]. Engineered MSC exosomes offer a novel, cell-free therapeutic strategy to overcome these challenges.
Rationale for Using MSC Exosomes
MSC-derived exosomes inherently possess pro-regenerative properties, including anti-inflammatory, pro-angiogenic, and pro-migratory effects on skin cells [7]. Their lipid bilayer protects therapeutic cargo from degradation, and their surface can be modified to enhance targeting to specific cell types in the wound bed (e.g., fibroblasts, keratinocytes, endothelial cells) [6] [1]. This makes them superior to synthetic nanoparticles for drug delivery in wound healing contexts.
Strategies for Engineering Therapeutic Exosomes
4.2.1. Cargo Loading Techniques Two primary approaches are used to load therapeutic molecules into exosomes.
Table 2: Methods for Loading Cargo into Exosomes
| Method Category | Specific Technique | Principle | Example Cargo | Considerations |
|---|---|---|---|---|
| Cell-Based (Endogenous) | Incubation / Transfection | Donor cells (e.g., MSCs) are treated with small molecules or transfected to overexpress nucleic acids, which are then packaged into secreted exosomes [9]. | Doxorubicin, Curcumin, miRNA (e.g., miR-21, miR-146a), siRNA, mRNA [9] [7] | Simple but offers limited control over loading efficiency. |
| Non-Cell-Based (Exogenous) | Electroporation | A short electrical pulse creates temporary pores in the exosome membrane, allowing cargo diffusion into the lumen [6] [9]. | siRNA, miRNA, small molecules | Can cause cargo aggregation and exosome aggregation. |
| Sonication | Exosomes are subjected to ultrasound waves to disrupt the membrane, enabling cargo entry before membrane reassembly [6] [9]. | Proteins, small molecules | May compromise exosome membrane integrity. | |
| Incubation | Simple co-incubation of cargo with pre-isolated exosomes, relying on passive diffusion and membrane permeability [6] [9]. | Hydrophobic small molecules (e.g., Curcumin) | Simple but often has low efficiency. |
4.2.2. Targeting and Functionalization For precise delivery in chronic wounds, exosome surfaces can be engineered.
- Ligand Display: Expression of targeting peptides, antibodies, or receptor ligands on the exosome surface (e.g., via genetic fusion to abundant exosomal membrane proteins like CD63 or Lamp2b) can direct exosomes to specific cell types or the wound ECM [6] [2].
- Hybrid Systems: Combining exosomes with functional biomaterials, such as injectable hyaluronic acid hydrogels, can create a sustained-release depot at the wound site, protecting exosomes and enhancing their local retention and efficacy [10] [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Exosome Research
| Reagent / Tool | Function / Application | Specific Examples / Notes |
|---|---|---|
| Isolation Kits | Commercial kits for rapid exosome precipitation or immunoaffinity capture from cell media or biofluids. | Total Exosome Isolation kits, kits with anti-CD63/CD81 magnetic beads. |
| ESCRT Inhibitors | Chemical inhibitors to dissect the role of the ESCRT pathway in biogenesis and cargo sorting. | GW4869 (inhibits nSMase2/ceramide pathway) [4], VPS4 inhibitors. |
| Tetraspanin Antibodies | Essential for exosome characterization via Western Blot, Flow Cytometry, and Immunofluorescence. | Anti-CD9, Anti-CD63, Anti-CD81 [2] [8]. |
| Characterization Instruments | For determining the size, concentration, and morphology of isolated exosomes. | Nanoparticle Tracking Analysis (NTA) for size/concentration, Transmission Electron Microscopy (TEM) for morphology [2]. |
| Loading Equipment | Instruments for exogenous cargo loading into pre-isolated exosomes. | Electroporator (for electroporation), Sonicator (for sonication) [6] [9]. |
| Engineered Cell Lines | Donor cells (e.g., HEK293T, MSCs) genetically modified to stably produce exosomes with desired cargo or surface proteins. | Cells overexpressing miRNA, targeting ligands (e.g., RGD peptide), or reporter proteins (e.g., GFP) [9]. |
Exosomes represent a sophisticated natural nanocarrier system whose biogenesis and cargo loading are governed by precise molecular mechanisms. A deep understanding of the ESCRT machinery, tetraspanin networks, and lipid-mediated sorting is fundamental to leveraging these vesicles for therapeutic purposes. In chronic wound research, the ability to engineer MSC exosomes—by loading them with specific regenerative cargoes like anti-inflammatory miRNAs and functionalizing their surface for targeted delivery—offers a powerful and promising strategy. This approach holds the potential to shift the paradigm from conventional wound management to precise, effective, and cell-free nanomedicine, ultimately promoting functional tissue regeneration.
The Four Phases of Wound Healing and Exosome Participation
Chronic wounds represent a significant clinical challenge, failing to progress through the normal, orderly sequence of wound healing phases. Within the broader thesis of engineering mesenchymal stem cell (MSC) exosomes for targeted drug delivery in chronic wound research, understanding the fundamental biology of wound healing is paramount. Exosomes, nanosized extracellular vesicles secreted by cells, have emerged as promising therapeutic agents and drug delivery vehicles due to their role in intercellular communication and regenerative processes [11] [12]. These vesicles, typically 30-150 nm in diameter, carry bioactive molecules including proteins, lipids, mRNAs, and microRNAs that can modulate recipient cell behavior [13] [14]. This application note details the four phases of wound healing, examines exosome participation in each phase, and provides structured experimental data and protocols to support research into engineered MSC exosomes for chronic wound therapy.
The Four Phases of Wound Healing
Normal wound healing progresses through four highly integrated and overlapping phases: hemostasis, inflammation, proliferation, and remodeling [12] [14]. Chronic wounds are characterized by disruptions in this progression, often remaining arrested in the inflammatory phase [12]. The following sections analyze each phase and the participative role of exosomes, with supporting quantitative data.
Hemostasis Phase
Immediately following injury, the hemostasis phase initiates to stop bleeding and establish a provisional wound matrix. Platelets adhere to exposed subendothelial matrix, activate, and form a platelet plug [14]. The coagulation cascade converts fibrinogen to fibrin, stabilizing the clot [14]. Activated platelets release chemokines including platelet-derived growth factor (PDGF) and transforming growth factor-β (TGF-β), initiating recruitment of inflammatory cells and fibroblasts [14].
Exosome Participation: While platelets themselves release extracellular vesicles, MSC-derived exosomes can influence this phase by modulating initial inflammatory signals and cellular recruitment. Their surface proteins facilitate binding to extracellular matrix components, potentially enhancing localization to wound sites.
Inflammatory Phase
Following hemostasis, neutrophils infiltrate to phagocytose pathogens and damaged tissue, followed by monocyte-derived macrophages which initially exhibit a pro-inflammatory (M1) phenotype before transitioning to an anti-inflammatory, pro-repair (M2) phenotype [14]. This transition is crucial for progression to subsequent healing phases. Chronic wounds often display persistent inflammation with sustained M1 polarization and elevated pro-inflammatory cytokines [12].
Exosome Participation: MSC-derived exosomes contain immunomodulatory molecules that facilitate macrophage polarization from M1 to M2 phenotype [14]. Specific exosomal miRNAs, including miR-146a and miR-223, inhibit NF-κB signaling and suppress NLRP3 inflammasome activation, resolving excessive inflammation [14]. Preconditioned MSC-derived exosomes further enhance anti-inflammatory polarization via let-7b signaling [14].
Proliferative Phase
This phase features re-epithelialization, angiogenesis, and fibroblast activation. Keratinocytes migrate across the wound bed to restore epidermis, while endothelial cells form new capillaries under guidance of vascular endothelial growth factor (VEGF) and fibroblast growth factor 2 (FGF-2) [14]. Fibroblasts infiltrate and secrete type III collagen and fibronectin, forming granulation tissue [12]. TGF-β1 activates fibroblasts to synthesize extracellular matrix (ECM) [14].
Exosome Participation: MSC and adipose-derived stem cell (ADSC) exosomes enhance fibroblast proliferation and migration via miRNAs including miR-21, miR-29a, and others [14]. They promote angiogenesis by transferring pro-angiogenic factors and miRNAs to endothelial cells [11]. Evidence indicates stem cell-derived exosomes accelerate collagen synthesis and epithelialization [11].
Remodeling Phase
The final phase can extend for months to years after wound closure, involving neovasculature regression, ECM reorganization, and collagen maturation from type III to type I [12] [14]. This process restores tissue strength and functionality. Aberrant remodeling leads to pathological scarring, characterized by excessive fibroblast proliferation and ECM deposition [12].
Exosome Participation: Exosomes modulate scar formation by regulating fibroblast differentiation and collagen deposition. Engineered exosomes (eExo) can be designed with specific "anti-scarring" properties to prevent hypertrophic scarring and keloid formation [12]. They influence TGF-β signaling pathways that control myofibroblast differentiation and activity.
Quantitative Analysis of Exosome Therapeutic Effects
Recent clinical and preclinical studies demonstrate the therapeutic potential of exosomes in wound healing. The following tables summarize key quantitative findings.
Table 1: Clinical Outcomes of Exosome Therapy in Chronic Wound Management
| Case Profile | Wound Characteristics | Exosome Treatment Protocol | Key Clinical Outcomes | Doppler Ultrasound Findings |
|---|---|---|---|---|
| 58-year-old female with diabetes and venous insufficiency [15] [16] | Chronic ulcer >6 months duration [15] [16] | Monthly applications of ADSC-derived exosomes (Exo-HL) for 3 months [15] [16] | Wound size reduction with healthy granulation tissue within 15 days [15] [16] | Arterial resistive index: 0.89→0.72; Venous reflux time: 2.8→1.2 seconds [15] [16] |
| 62-year-old female with recurrent ulcers [15] [16] | Ulcers persistent >2 years despite conventional therapy [15] [16] | Monthly applications of ADSC-derived exosomes (Exo-HL) [15] [16] | Complete granulation and re-epithelialization with no inflammation/necrosis [15] [16] | Peak systolic velocity: 28→42 cm/s; Resistive index: 0.92→0.78 [15] [16] |
| 42-year-old male with chronic venous insufficiency [15] [16] | 6-year history of recurrent ulcers refractory to treatment [15] [16] | Monthly applications of ADSC-derived exosomes (Exo-HL) over 7 months [15] [16] | Near-complete resolution with restored skin integrity by month 7 [15] [16] | Resistive index: 0.95→0.75; Venous reflux time: 3.2→1.6 seconds [15] [16] |
| 44-year-old female with post-cellulitis ulcer [16] | Chronic ulcer with recommended amputation [16] | Monthly applications of ADSC-derived exosomes (Exo-HL) [16] | Complete ulcer closure with restored skin integrity [16] | Peak systolic velocity: 15→38 cm/s; Resistive index: 0.97→0.82 [16] |
Table 2: Molecular Cargo of MSC-Derived Exosomes in Wound Healing
| Exosome Cargo Category | Specific Components | Biological Functions in Wound Healing | Target Cells/Pathways |
|---|---|---|---|
| Growth Factors [15] | VEGF, FGF, TGF-β, EGF, PDGF [15] | Stimulate angiogenesis, promote cell proliferation, enhance ECM synthesis, modulate immune response [15] | Endothelial cells, fibroblasts, keratinocytes [15] |
| MicroRNAs (miRNAs) [15] [14] | miR-21, miR-29a, miR-146a, miR-223, let-7b [14] | Regulate gene expression related to inflammation, angiogenesis, fibroblast proliferation [15] [14] | NF-κB signaling, NLRP3 inflammasome, TGF-β pathways [14] |
| Proteins [13] | Tetraspanins (CD9, CD63, CD81), ESCRT-related proteins (Tsg101, Alix), heat shock proteins (Hsp90, Hsp70) [13] [2] | Structural components, cargo sorting, cell targeting, stress response [13] [2] | Recipient cell membranes, endosomal pathways [13] |
Experimental Protocols for Evaluating Exosome Effects in Wound Healing
Protocol: Isolation and Characterization of MSC-Derived Exosomes
Principle: Exosomes are isolated from MSC conditioned media via differential ultracentrifugation and characterized for size, concentration, and marker expression [15] [2].
Reagents and Equipment:
- MSC culture medium (e.g., DMEM with 10% exosome-depleted FBS)
- Phosphate-buffered saline (PBS)
- Ultracentrifuge with fixed-angle and swinging-bucket rotors
- Nanoparticle Tracking Analysis (NTA) instrument
- Transmission Electron Microscope (TEM)
- Western blot equipment
- Antibodies against exosomal markers (CD9, CD63, CD81, Tsg101)
Procedure:
- Cell Culture: Culture MSCs to 70-80% confluence in complete medium. Replace with serum-free medium or medium containing exosome-depleted FBS for 48 hours [2].
- Conditioned Media Collection: Collect conditioned media and perform sequential centrifugation: 300 × g for 10 min (remove cells), 2,000 × g for 20 min (remove dead cells), 10,000 × g for 30 min (remove cell debris) [2].
- Ultracentrifugation: Transfer supernatant to ultracentrifuge tubes. Centrifuge at 100,000 × g for 70 minutes at 4°C. Discard supernatant, resuspend pellet in PBS, and repeat ultracentrifugation [15] [2].
- Resuspension: Resuspend final exosome pellet in PBS and store at -80°C [15].
- Characterization:
- NTA: Dilute exosomes in PBS and analyze using NTA to determine size distribution and concentration [15] [2].
- TEM: Apply exosomes to formvar/carbon-coated grids, negative stain with uranyl acetate, and image via TEM to assess morphology [2].
- Western Blot: Confirm presence of exosomal markers (CD9, CD63, CD81, Tsg101) and absence of negative markers (e.g., calnexin) [2].
Protocol: In Vitro Wound Healing Assay (Scratch Assay) with Exosome Treatment
Principle: This assay evaluates the effect of exosomes on fibroblast and keratinocyte migration, critical processes in the proliferative phase of wound healing.
Reagents and Equipment:
- Human dermal fibroblasts or keratinocytes
- Cell culture plates (6-well or 24-well)
- Exosome preparations (20-100 μg/mL)
- Mitomycin C (optional, to inhibit proliferation)
- Time-lapse microscope or standard inverted microscope
- ImageJ software with wound healing plugin
Procedure:
- Cell Seeding: Seed fibroblasts or keratinocytes in 6-well plates at high density (2-5×10^5 cells/well) and culture until 90-100% confluent.
- Scratch Creation: Create a straight scratch in the cell monolayer using a sterile 200 μL pipette tip. Wash gently with PBS to remove detached cells.
- Exosome Treatment: Add exosomes suspended in serum-free medium at desired concentration (typically 20-100 μg/mL). Include controls (vehicle alone).
- Image Acquisition: Capture images at the beginning (0 hour) and at regular intervals (e.g., 6, 12, 24 hours) at the same location using a microscope.
- Quantitative Analysis: Measure scratch area using ImageJ software. Calculate percentage wound closure: [(Initial area - Area at time t)/Initial area] × 100.
- Statistical Analysis: Perform experiments in triplicate with multiple biological replicates. Analyze using Student's t-test or ANOVA with post-hoc tests.
Protocol: In Vivo Evaluation of Engineered Exosomes in Diabetic Wound Healing
Principle: This protocol assesses the efficacy of engineered MSC exosomes in a diabetic mouse wound healing model, monitoring wound closure, histology, and vascularization.
Reagents and Equipment:
- Diabetic mice (e.g., db/db mice or STZ-induced diabetic C57BL/6 mice)
- Engineered MSC exosomes
- Hydrogel delivery system (e.g., hyaluronic acid hydrogel) [10]
- Digital calipers or photographic wound measurement system
- Histology equipment
- CD31 antibodies for immunohistochemistry
Procedure:
- Wound Creation: Anesthetize mice and create full-thickness excisional wounds on dorsal skin (typically 6-8 mm diameter).
- Exosome Administration:
- Wound Monitoring: Photograph wounds daily with scale reference. Calculate wound area using image analysis software.
- Tissue Collection: Euthanize mice at predetermined time points (e.g., days 7, 14, 21). Harvest wound tissue with surrounding normal skin.
- Histological Analysis:
- Process tissue for paraffin embedding and sectioning.
- Perform H&E staining to assess re-epithelialization and granulation tissue formation.
- Use Masson's trichrome staining to evaluate collagen deposition and organization.
- Conduct immunohistochemistry for CD31 to quantify angiogenesis (microvessel density).
- Data Analysis: Compare wound closure rates, complete healing time, and histological parameters between treatment groups.
Research Reagent Solutions
Table 3: Essential Research Reagents for Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Exosome Isolation Kits | Total Exosome Isolation Kit, miRCURY Exosome Kit | Isolation of exosomes from cell culture media or biological fluids | Rapid extraction of exosomes using polymer-based precipitation or immunoaffinity methods |
| Characterization Instruments | Nanoparticle Tracking Analyzer (NTA), qNano | Size distribution and concentration analysis of exosome preparations | Quantitative analysis of exosome size and concentration through light scattering and Brownian motion tracking |
| Surface Marker Antibodies | Anti-CD9, Anti-CD63, Anti-CD81, Anti-Tsg101 | Identification and validation of exosomes via Western blot, flow cytometry | Confirmation of exosomal identity through detection of characteristic surface and internal proteins |
| Engineered Exosome Systems | HEK293T-derived engineered exosomes, MSC-derived exosomes with modified surface proteins | Targeted drug delivery to specific wound cell types | Enhanced specificity and therapeutic efficacy through surface engineering with targeting ligands (peptides, antibodies) |
| Hydrogel Delivery Systems | Hyaluronic acid hydrogel, Chitosan hydrogel | Sustained release of exosomes at wound site | Provision of moist wound environment with controlled release kinetics for prolonged exosome activity [10] |
| Cell Culture Models | Human dermal fibroblasts, Keratinocytes (HaCaT), Human umbilical vein endothelial cells (HUVECs) | In vitro assessment of exosome effects on cellular processes | Modeling cellular responses including migration, proliferation, and tube formation relevant to wound healing phases |
Signaling Pathways and Experimental Workflows
Diagram 1: The Four Phases of Wound Healing and Exosome Participation. This workflow illustrates the sequential progression through hemostasis, inflammation, proliferation, and remodeling phases, with specific exosome-mediated mechanisms participating in each phase [12] [14].
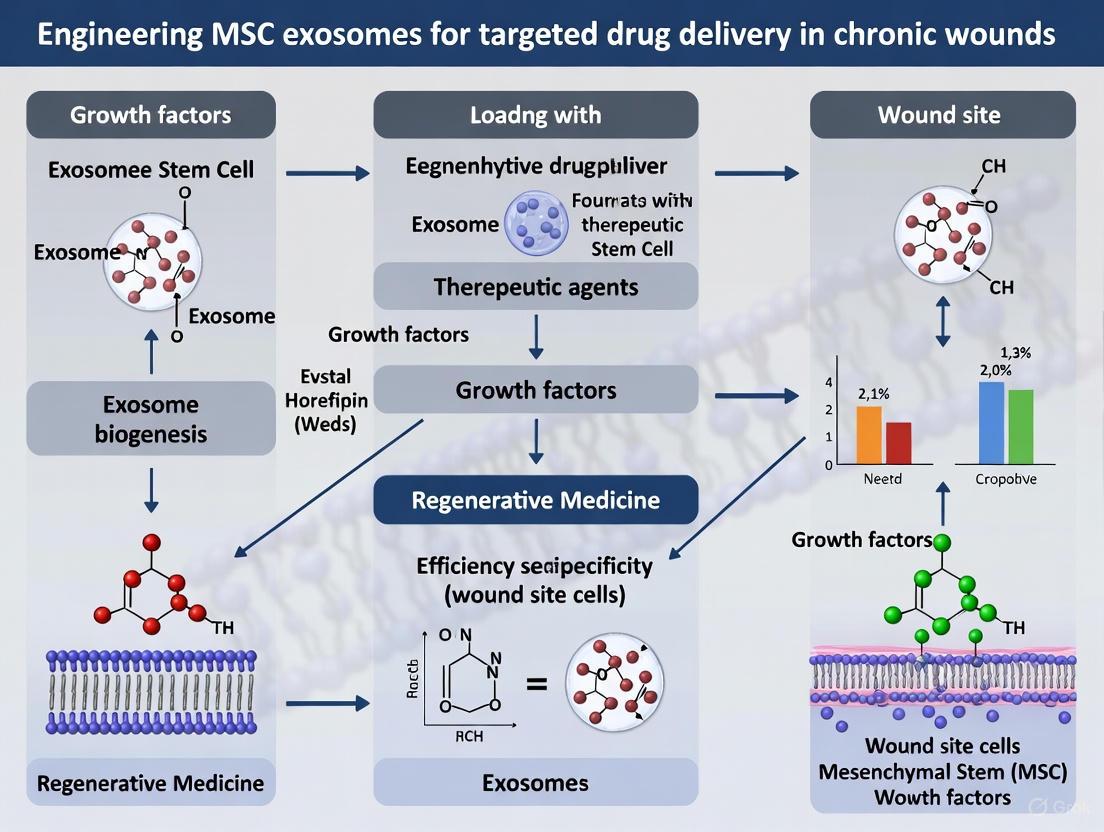
Diagram 2: Engineered Exosome Workflow for Chronic Wound Therapy. This diagram outlines the process from MSC source selection through exosome isolation, engineering, delivery, and therapeutic mechanisms leading to improved healing outcomes [11] [10] [12].
The participation of exosomes across all four phases of wound healing underscores their therapeutic potential for chronic wound management. Engineered MSC exosomes represent a promising platform for targeted drug delivery, addressing multiple pathological aspects of chronic wounds simultaneously. The structured data, experimental protocols, and reagent solutions provided in this application note offer researchers a foundation for advancing this innovative therapeutic approach. As the field progresses, standardization of isolation methods, optimization of engineering strategies, and comprehensive safety profiling will be essential for clinical translation. Future research should focus on personalized exosome therapeutics tailored to specific wound etiologies and patient profiles.
The therapeutic potential of mesenchymal stem cell (MSC)-derived exosomes in chronic wound healing stems from their diverse cargo of biologically active molecules. These nano-sized extracellular vesicles (30-150 nm) function as sophisticated intercellular communication systems, delivering specific miRNAs, proteins, and lipids that collectively modulate the wound microenvironment [14] [17]. By transferring these bioactive components to recipient cells, MSC exosomes promote anti-inflammatory responses, enhance angiogenesis, stimulate cellular proliferation and migration, and facilitate extracellular matrix remodeling—addressing multiple pathological aspects of chronic wounds simultaneously [18] [19] [12]. The inherent biocompatibility, low immunogenicity, and targetability of exosomes present significant advantages over whole-cell therapies, positioning them as promising next-generation therapeutics for recalcitrant wounds [14] [19] [20].
Recent advances in exosome engineering have further enhanced their therapeutic potential by enabling precise cargo loading and surface modifications for improved targeting and efficacy [12]. This Application Note provides a comprehensive overview of key therapeutic cargos in MSC exosomes, detailed experimental protocols for their analysis and engineering, and advanced delivery strategies optimized for chronic wound applications. The integration of engineered exosomes into biomaterial scaffolds represents a particularly promising approach for creating pro-regenerative wound dressings that provide sustained release of therapeutic factors at the wound site [12] [21].
Quantitative Analysis of Key Exosomal Cargos
Therapeutic miRNAs in MSC Exosomes for Skin Regeneration
Table 1: Key Exosomal miRNAs and Their Functions in Wound Healing
| miRNA | Biological Target/Pathway | Primary Functions | Therapeutic Effects | Reference |
|---|---|---|---|---|
| miR-21 | PTEN/PDCD4 | Anti-apoptotic, promotes fibroblast migration | Regulates apoptosis, enhances cell survival | [18] [22] |
| miR-126 | PI3K/Akt, SPRED1 | Angiogenesis promotion | Increases tube formation, accelerates wound closure | [18] [23] |
| miR-124 | p250GAP, anti-inflammatory pathways | Neuroprotection, anti-inflammatory | Reduces neural tissue inflammation, promotes neuronal growth | [22] |
| miR-133b | RhoA, PI3K/Akt pathways | Neural regeneration | Improves nerve cell survival, promotes nerve regeneration | [22] |
| miR-146a | NF-κB signaling | Anti-inflammatory | Inhibits NF-κB, reduces inflammatory response | [14] |
| miR-29a | ECM proteins | Fibrosis regulation | Promotes fibroblast migration, reduces scarring | [14] |
| miR-135a | LATS2 (Hippo pathway) | Promotes epithelialization | Enhances keratinocyte and fibroblast migration | [23] |
| miR-210 | HIF-1 signaling, DNA repair | Angiogenesis, cellular survival | Enhances DNA repair in hypoxic conditions | [23] |
| miR-17-92 | PTEN/Akt/FOXO1 | Angiogenesis, cell survival | Promotes neural regeneration | [22] |
| let-7b | Inflammatory signaling | Macrophage polarization | Enhances anti-inflammatory polarization | [14] |
The miRNA cargo within MSC-derived exosomes represents a master regulatory network that coordinates multiple aspects of wound repair. These small non-coding RNAs (typically 19-24 nucleotides in length) function through partial complementarity to target mRNAs, leading to mRNA degradation or translational repression [18]. The selective sorting of specific miRNAs into exosomes ensures their protected delivery to recipient cells in the wound microenvironment, where they simultaneously modulate clusters of genes involved in inflammation, angiogenesis, and tissue remodeling [18] [24].
Mechanistically, miR-126 exemplifies the pro-angiogenic capacity of exosomal miRNAs by targeting SPRED1 and enhancing VEGF signaling through the PI3K/Akt and MAPK pathways, directly addressing the impaired angiogenesis characteristic of chronic wounds [18] [23]. Similarly, miR-21 modulates apoptosis through FasL/PTEN/PDCD4 pathways, promoting fibroblast survival in the hostile wound environment [18] [22]. The anti-inflammatory miRNA-146a suppresses NF-κB signaling, thereby reducing persistent inflammation that impedes chronic wound healing [14]. These miRNAs operate in concert, creating a coordinated regenerative program that makes exosomes uniquely suited for addressing the multifactorial pathology of chronic wounds.
Protein and Lipid Cargos in MSC Exosomes
Table 2: Functional Protein and Lipid Cargos in MSC Exosomes
| Cargo Type | Specific Components | Biological Functions | Therapeutic Effects | |
|---|---|---|---|---|
| Tetraspanins | CD63, CD9, CD81 | Exosome biogenesis, cellular uptake | Facilitates target cell recognition and fusion | [18] [19] |
| Heat Shock Proteins | HSP70, HSP90 | Protein folding, membrane fusion | Enhances cellular stress response, promotes vesicle fusion | [19] |
| Annexins | Annexin I, II, V | Membrane fusion, anti-inflammatory | Mediates exosome-cell membrane fusion | [19] |
| Growth Factors | VEGF, FGF, TGF-β1 | Angiogenesis, cell proliferation | Stimulates new blood vessel formation, tissue regeneration | [14] [17] |
| ECM Proteins | Fibronectin, Collagens | Matrix organization, cell adhesion | Supports granulation tissue formation | [17] |
| Lipids | Cholesterol, Sphingolipids, Phosphatidylserine | Membrane stability, signaling | Maintains structural integrity, enables cell recognition | [18] [17] |
| Rab GTPases | Rab27a/b | Exosome secretion, trafficking | Regulates exosome release and intracellular trafficking | [19] |
The protein and lipid components of MSC exosomes contribute significantly to their therapeutic efficacy through both structural and functional roles. Tetraspanins (CD63, CD9, CD81) not only serve as characteristic exosome markers but also facilitate cellular uptake and target cell recognition [18] [19]. Heat shock proteins, particularly HSP70 and HSP90, contribute to protein folding and enhance cellular stress response in recipient cells, while also participating in membrane fusion processes [19]. Growth factors including VEGF, FGF, and TGF-β1 are frequently identified in MSC exosomes and work synergistically with miRNA cargo to promote angiogenesis and tissue repair [14] [17].
The lipid bilayer of exosomes contains cholesterol, sphingolipids, and phosphatidylserine, which not only provide structural integrity but also participate in signaling and cellular recognition [18] [17]. The lipid composition contributes to the stability of exosomes in biological fluids and influences their fusion capabilities with target cell membranes. This complex integration of proteins and lipids with nucleic acid cargo creates a multifaceted therapeutic system that surpasses single-factor approaches for chronic wound management.
Experimental Protocols
Protocol 1: Isolation and Characterization of MSC-Derived Exosomes
Principle: Isolate and characterize exosomes from MSC-conditioned media using ultracentrifugation and validate through size, concentration, and marker expression analysis.
Materials:
- Human MSCs (bone marrow or adipose-derived)
- Serum-free MSC culture medium
- Differential ultracentrifugation equipment
- PBS (phosphate-buffered saline)
- Transmission Electron Microscope (TEM)
- Nanoparticle Tracking Analysis (NTA) system
- BCA protein assay kit
- Antibodies for CD63, CD81, CD9, TSG101, Calnexin
Procedure:
- Cell Culture and Conditioning: Culture MSCs to 70-80% confluence in complete medium. Replace with serum-free medium and culture for 48 hours. Collect conditioned medium and remove cells and debris by centrifugation at 2,000 × g for 30 minutes [17] [20].
Exosome Isolation: Ultracentrifuge the supernatant at 10,000 × g for 30 minutes to remove larger vesicles. Filter through a 0.22 μm membrane. Ultracentrifuge at 100,000 × g for 70 minutes. Wash pellet in PBS and repeat ultracentrifugation. Resuspend final exosome pellet in PBS [17] [12].
Characterization:
- NTA: Dilute exosomes 1:1000 in PBS and analyze using Nanoparticle Tracking Analysis to determine size distribution and concentration [17].
- TEM: Fix exosomes in 2% paraformaldehyde, deposit on Formvar-carbon coated grids, negative stain with 2% uranyl acetate, and image by transmission electron microscopy to confirm cup-shaped morphology [18] [17].
- Western Blotting: Confirm presence of exosomal markers (CD63, CD81, CD9, TSG101) and absence of negative marker (Calnexin) [17] [12].
- Protein Quantification: Determine protein concentration using BCA assay [17].
Quality Control: Ensure particle size distribution of 30-150 nm with peak around 100 nm. Confirm presence of at least three positive markers and absence of negative markers. Maintain sterility throughout the process for therapeutic applications.
Protocol 2: miRNA Cargo Analysis by qRT-PCR
Principle: Isolate and quantify specific miRNAs from exosomes to characterize their cargo profile and potential therapeutic activity.
Materials:
- Isolated exosomes (from Protocol 1)
- miRNeasy Mini Kit or equivalent
- miScript II RT Kit
- miScript SYBR Green PCR Kit
- miRNA-specific primers
- Real-time PCR system
Procedure:
- RNA Extraction: Add Qiazol to exosome sample (max 200 μL). Add chloroform and centrifuge at 12,000 × g for 15 minutes. Transfer aqueous phase to new tube and add 1.5 volumes ethanol. Pass through RNeasy column, wash, and elute in RNase-free water [18] [22].
cDNA Synthesis: Use miScript HiFlex Buffer to reverse transcribe all RNAs including miRNAs. Use 1 μg total RNA in 20 μL reaction. Incubate at 37°C for 60 minutes, then 95°C for 5 minutes [18].
qPCR Amplification: Prepare reactions with 2× QuantiTect SYBR Green PCR Master Mix, 10× miScript Primer Assay (specific for target miRNAs), template cDNA, and RNase-free water. Run with activation at 95°C for 15 minutes, followed by 40 cycles of 94°C for 15 seconds, 55°C for 30 seconds, and 70°C for 30 seconds [18] [22].
Data Analysis: Use the 2^(-ΔΔCt) method to calculate relative expression levels. Normalize to spiked-in cel-miR-39 or endogenous controls (e.g., RNU6B, SNORDs) [22].
Troubleshooting: Low RNA yield may indicate inefficient exosome isolation. Include positive controls for RNA extraction and RT steps. Ensure primer specificity for mature miRNAs, not precursors.
Protocol 3: Engineering MSC Exosomes for Enhanced miRNA Loading
Principle: Modify MSC exosomes to enrich specific therapeutic miRNAs using electroporation-based loading methods.
Materials:
- Isolated exosomes (from Protocol 1)
- Synthetic miRNA mimics or inhibitors
- Electroporation system with cuvettes (2-4 mm gap)
- Opti-MEM reduced serum medium
- Heparin (to prevent aggregation)
- RNase inhibitor
Procedure:
- Preparation: Isolate exosomes as in Protocol 1. Resuspend in sterile PBS. Synthesize or purchase synthetic miRNA mimics with modified sequences for enhanced stability [12].
Electroporation: Mix exosomes (100-500 μg protein) with miRNA (10-100 pmol) in electroporation buffer. Transfer to pre-chilled electroporation cuvette. Apply optimized electroporation parameters (typically 400-700 V, 125-150 μF, ∞ resistance) [12].
Post-treatment: Immediately after electroporation, incubate on ice for 30 minutes. Add RNase inhibitor to final concentration of 0.5 U/μL to degrade unencapsulated miRNA. Add heparin (10 U/mL) to prevent aggregation [12].
Purification: Remove unencapsulated miRNAs using size-exclusion chromatography (e.g., qEV columns) or ultracentrifugation. Validate loading efficiency using qRT-PCR (Protocol 2) [12].
Validation: Compare miRNA levels before and after loading. Assess exosome integrity by TEM and NTA. Confirm functional delivery to recipient cells using reporter assays.
Signaling Pathway Diagrams
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Exosome Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations | |
|---|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, qEV size exclusion columns | Rapid exosome purification from conditioned media | Balance between purity, yield, and cost for specific applications | [17] |
| Characterization Instruments | Nanoparticle Tracking Analyzer, TEM, Western Blot apparatus | Size distribution analysis, morphological confirmation, marker validation | NTA provides size/concentration; TEM confirms morphology; WB validates markers | [17] [12] |
| miRNA Analysis Kits | miRNeasy kits, miScript PCR kits, TaqMan MicroRNA assays | RNA extraction, cDNA synthesis, miRNA quantification | Select appropriate normalization controls (spiked-in synthetic miRNAs recommended) | [18] [22] |
| Engineering Tools | Electroporation systems, Lipofectamine, Click Chemistry reagents | Loading therapeutic cargo into exosomes, surface modifications | Electroporation optimizes miRNA loading; surface modifications enhance targeting | [12] |
| Cell Culture reagents | Serum-free MSC media, characterization antibodies (CD73, CD90, CD105) | MSC expansion, phenotype confirmation | Use serum-free conditions for therapeutic exosome production | [17] [20] |
| Functional Assay Kits | Tube formation assay kits, migration assay kits, apoptosis detection kits | In vitro validation of exosome bioactivity | Test relevant functions: angiogenesis, migration, anti-apoptotic effects | [14] [23] |
Advanced Delivery Systems for Chronic Wounds
The translation of exosome therapeutics into clinical applications for chronic wounds requires advanced delivery systems that protect exosomes and provide controlled release at the wound site. Biomaterial-based scaffolds have emerged as particularly promising delivery platforms that can maintain exosome viability and extend their retention in the dynamic wound environment [12] [21].
Hydrogel systems, including hyaluronic acid, chitosan, and alginate-based formulations, offer tunable physical properties that can be customized to match specific wound characteristics. These hydrophilic networks protect exosomes from degradation while allowing controlled diffusion to the wound bed. Recent advances include the development of thermosensitive hydrogels that transition from liquid to gel at body temperature, facilitating conformal application to irregular wound surfaces [12]. Additionally, scaffold systems incorporating exosomes within nanofibrous matrices mimic the native extracellular architecture, providing both structural support and sustained release of therapeutic factors.
Innovative delivery formats such as lyophilized exosome powders, dissolvable microneedle arrays, and sprayable formulations address the practical challenges of clinical wound care. Lyophilization preserves exosome stability during storage while allowing reconstitution at the point of care, with trehalose-based cryoprotectants demonstrating particular efficacy in maintaining vesicle integrity [19]. These advanced delivery strategies significantly enhance the translational potential of MSC exosome therapies by improving handling, stability, and application efficiency.
MSC-derived exosomes represent a sophisticated natural delivery system for multiple therapeutic cargos that collectively address the complex pathophysiology of chronic wounds. The coordinated action of miRNAs, proteins, and lipids within these nanovesicles enables simultaneous modulation of inflammation, angiogenesis, cellular migration, and extracellular matrix remodeling—key processes that are dysregulated in non-healing wounds. The experimental protocols outlined in this Application Note provide a foundation for the isolation, characterization, and engineering of MSC exosomes to enhance their therapeutic potential.
Future developments in exosome therapeutics will likely focus on precision engineering approaches to create customized vesicles with optimized cargo loading and cell-specific targeting capabilities. The integration of multi-omics technologies will enable more comprehensive characterization of exosome cargo profiles and their functional correlates. Additionally, standardized manufacturing protocols and rigorous quality control measures will be essential for clinical translation. As the field advances, combination therapies integrating engineered exosomes with advanced biomaterials and conventional wound care approaches offer promising strategies for addressing the significant clinical challenge of chronic wounds.
Mesenchymal stem cell-derived exosomes (MSC-Exos) represent a transformative advancement in regenerative medicine, particularly for chronic wound treatment, by addressing critical safety concerns associated with whole-cell therapies. While mesenchymal stem cells (MSCs) themselves have demonstrated therapeutic potential, their clinical application is hampered by significant risks, including immunogenicity, tumorigenicity, and embolism formation from cell entrapment in pulmonary capillaries [25] [26]. MSC-derived exosomes, as natural, nanoscale extracellular vesicles (30-150 nm in diameter), encapsulate the therapeutic components of MSCs—such as proteins, lipids, and nucleic acids—while exhibiting markedly reduced risks [25] [27]. Their inherent biological properties make them particularly suitable for the complex, dysregulated microenvironment of chronic wounds, offering a sophisticated, cell-free system for targeted drug delivery and tissue regeneration.
Key Advantages of MSC Exosomes Over Cell-Based Approaches
Reduced Immunogenicity
The low immunogenic potential of MSC-Exos is a cornerstone of their therapeutic safety profile, stemming from several intrinsic characteristics:
- Absence of Major Histocompatibility Complex (MHC) Molecules: Unlike their parent MSCs, MSC-Exos lack major histocompatibility complex class I (MHC-I) molecules and do not express MHC-II molecules under normal conditions [25] [26]. This fundamental difference significantly lowers the risk of immune recognition and rejection upon administration [25].
- Surface Marker Profile: MSC-Exos carry surface markers common to all exosomes (CD63, CD81, CD9) as well as markers from the original stem cell (CD44, CD73, CD90) [27]. This profile contributes to their biocompatibility and minimizes nonspecific immune activation.
The practical consequence of these properties is that MSC-Exos can be administered allogeneically (from a donor to a non-identical recipient) without triggering a significant immune response, thereby eliminating the need for patient-specific, autologous cell harvesting and expansion [25]. This advantage is particularly valuable in chronic wound management, where repeated applications may be necessary over extended periods.
Minimal Tumorigenicity Risk
The tumorigenicity risk of MSC-Exos is substantially lower compared to whole-cell therapies due to their non-replicative nature:
- Lack of Replicative Capacity: As acellular vesicles, exosomes cannot replicate or divide, eliminating the risk of uncontrolled growth or formation of ectopic tissue [25] [28]. This intrinsic safety feature addresses one of the most significant concerns surrounding stem cell-based interventions.
- Controlled Biological Activity: While MSC-Exos actively modulate recipient cell behavior through cargo delivery (e.g., microRNAs, proteins), they do not integrate into the host genome or possess transformative potential, further minimizing theoretical oncogenic risks [17].
This safety profile is especially relevant for chronic wound patients, who may have underlying conditions that predispose them to neoplastic transformations, and for whom long-term therapeutic safety is paramount.
Table 1: Quantitative Comparison of Key Safety Parameters Between MSCs and MSC-Exos
| Safety Parameter | MSC-Based Therapy | MSC-Exosome Therapy | References |
|---|---|---|---|
| Immunogenicity Profile | Expresses MHC-I; potential for immune recognition | Lacks MHC complexes; minimal immune activation | [25] [26] |
| Tumorigenic Potential | Theoretical risk of uncontrolled differentiation/growth | Non-replicative; no risk of uncontrolled growth | [25] [28] |
| Administration Risks | Risk of pulmonary embolism from cell entrapment | Nanoscale size prevents vascular occlusion | [25] [26] |
| Therapeutic Precision | Broad paracrine signaling with variable effects | Targeted delivery of specific bioactive cargo | [12] [28] |
Experimental Protocols for Evaluating Immunogenicity and Tumorigenicity
Robust assessment of immunogenicity and tumorigenicity is essential for validating the safety profile of MSC-Exos in chronic wound applications. The following protocols provide standardized methodologies for these critical evaluations.
Protocol 1: In Vitro Immunogenicity Assessment
This protocol evaluates the potential of MSC-Exos to stimulate immune cell proliferation and activation, key indicators of immunogenicity.
Materials and Reagents:
- Isolation: Ficoll-Paque PLUS density gradient medium
- Culture: RPMI-1640 medium supplemented with 10% exosome-depleted FBS, 1% penicillin-streptomycin, 2 mM L-glutamine
- Stimulation: Phytohemagglutinin (PHA)
- Detection: CFSE cell proliferation dye, anti-human CD3/CD28 activation antibodies, flow cytometry antibodies for CD4, CD8, CD25, CD69
Procedure:
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Isolate PBMCs from healthy human donors using density gradient centrifugation with Ficoll-Paque PLUS.
- CFSE Labeling: Resuspend PBMCs at 1×10^7 cells/mL in PBS containing 1 μM CFSE and incubate for 10 minutes at 37°C. Quench staining with 5 volumes of ice-cold complete media.
- Co-culture Setup: Seed CFSE-labeled PBMCs (1×10^5 cells/well) in 96-well U-bottom plates with:
- Negative control: Media alone
- Positive control: PHA (5 μg/mL)
- Experimental groups: MSC-Exos (1×10^10 particles/mL) or whole MSCs (1:10 MSC:PBMC ratio)
- Incubation and Analysis: Culture for 5 days at 37°C with 5% CO2. Harvest cells and stain with anti-CD3, CD4, CD8, CD25, and CD69 antibodies. Analyze T cell proliferation (CFSE dilution) and activation (CD25/CD69 expression) using flow cytometry.
Expected Outcomes: MSC-Exos should demonstrate significantly reduced T cell proliferation and activation marker expression compared to PHA-positive controls and whole MSCs, confirming their low immunogenicity.
Protocol 2: In Vivo Tumorigenicity Assay
This protocol assesses the potential for in vivo tumor formation following MSC-Exo administration, using an immunodeficient mouse model that permits the growth of human cells.
Materials and Reagents:
- Animals: NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice, 6-8 weeks old
- Test Articles: MSC-Exos (1×10^11 particles), whole MSCs (1×10^6 cells)
- Injection: Sterile PBS, 27-gauge needles
- Monitoring: Calipers, in vivo imaging system (if using luciferase-labeled MSCs)
Procedure:
- Preparation: Resuspend MSC-Exos in 100 μL sterile PBS for injection. Prepare whole MSCs similarly as a positive control group.
- Administration: Divide NSG mice into three groups (n=10/group):
- Group 1: Subcutaneous injection of MSC-Exos into the right flank
- Group 2: Subcutaneous injection of whole MSCs into the right flank
- Group 3: Subcutaneous injection of PBS (vehicle control)
- Observation Period: Monitor mice twice weekly for 16 weeks for:
- Palpable mass formation at injection site
- Body weight and general health status
- Any signs of distress or morbidity
- Terminal Analysis: At 16 weeks, euthanize all remaining animals and conduct complete necropsy. Weigh and preserve any masses for histological analysis (H&E staining).
Expected Outcomes: The MSC group may develop palpable masses confirming the model's sensitivity, while the MSC-Exos group should show no evidence of tumor formation, comparable to the PBS control group.
Research Reagent Solutions for MSC Exosome Studies
Table 2: Essential Research Reagents for MSC Exosome Characterization and Functional Analysis
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Isolation Kits | ExoQuick-TC, Total Exosome Isolation Kit | Exosome purification from cell culture media | Polymer-based precipitation for high-yield recovery |
| Characterization Antibodies | Anti-CD63, CD81, CD9, Alix, TSG101 | Western blot, flow cytometry, immunoelectron microscopy | Confirmation of exosomal identity and purity |
| MSC Marker Antibodies | Anti-CD73, CD90, CD105, CD44 | Flow cytometry of parent cells and exosomes | Verification of MSC origin |
| Nanoparticle Tracking | NanoSight NS300, ZetaView | Size distribution and concentration analysis | Quantitative measurement of exosome preparation |
| miRNA Analysis | miRNeasy Mini Kit, TaqMan MicroRNA Assays | Cargo analysis and functional studies | Identification of therapeutic miRNAs in exosomes |
Signaling Pathways in MSC Exosome-mediated Wound Healing
The therapeutic effects of MSC-Exos in chronic wounds are mediated through precise modulation of key signaling pathways. The following diagram illustrates the primary molecular mechanisms through which MSC-Exos promote healing while avoiding excessive immune activation or fibrotic responses.
The demonstrated safety advantages of MSC-derived exosomes—specifically their low immunogenicity and minimal tumorigenicity risk—position them as superior therapeutic agents compared to whole-cell therapies for chronic wound management. These intrinsic safety characteristics, combined with their robust regenerative capabilities, facilitate their transition from research tools to clinical therapeutics. The standardized protocols and analytical frameworks presented herein provide researchers with validated methodologies for rigorously assessing these critical safety parameters, ensuring that future MSC-Exo applications in wound healing continue to meet the highest standards of efficacy and safety. As the field advances, engineered exosomes with enhanced targeting specificity and controlled cargo release will further amplify these inherent advantages, ultimately offering personalized, precise therapeutic interventions for patients suffering from chronic wounds.
Engineering Strategies for Enhanced Targeting and Cargo Delivery
The therapeutic potential of mesenchymal stem cell (MSC)-derived exosomes in chronic wound healing is increasingly recognized, with their ability to modulate inflammation, promote angiogenesis, and enhance tissue regeneration [14] [12]. A critical step in engineering these exosomes for targeted drug delivery involves the efficient loading of therapeutic cargoes, such as nucleic acids, proteins, or small molecule drugs. This application note provides a detailed comparison and standardized protocols for three fundamental loading techniques: transfection, electroporation, and sonication, specifically framed within the context of chronic wound research.
Comparative Analysis of Loading Techniques
The choice of loading method significantly impacts the loading efficiency, exosome integrity, and subsequent biological activity. The table below summarizes the key characteristics of each technique for loading MSC exosomes.
Table 1: Quantitative Comparison of Exosome Cargo Loading Techniques
| Parameter | Transfection | Electroporation | Sonication |
|---|---|---|---|
| Primary Mechanism | Chemical-based complex formation and endocytosis [29] | Electrical field-induced membrane pores [29] | Ultrasonic cavitation and mechanical disruption [30] |
| Typical Loading Efficiency | Variable; highly cargo-dependent | ~10-20% for miRNAs/siRNAs; can be lower for plasmids [29] | High for small molecules and proteins |
| Cargo Type | Nucleic acids (DNA, RNA), proteins [29] | Primarily nucleic acids (siRNA, miRNA, plasmid DNA) [29] | Proteins, small molecule drugs, nucleic acids |
| Exosome Integrity Risk | Low to Moderate | High (can cause cargo aggregation & membrane damage) | Moderate to High (over-sonication causes irreversible damage) |
| Throughput | High (easily scalable) | Medium | Medium |
| Key Advantage | Compatibility with diverse cargo types; ease of use | Direct, physical method for nucleic acid loading | Efficient for a broad range of cargo sizes and types |
| Key Limitation | Potential cytotoxicity; need for optimization of reagent:cargo ratio | Risk of exosome aggregation and cargo precipitation [29] | Requires precise parameter control to avoid destruction |
Detailed Experimental Protocols
Transfection of Parent MSCs
This protocol involves loading the desired cargo into parent MSCs, leading to the secretion of naturally packaged exosomes.
Workflow: Transfection of Parent MSCs
Materials:
- MSCs: Human adipose-derived or bone marrow MSCs (Passage 3-5) [14] [15].
- Therapeutic Cargo: e.g., plasmid DNA encoding an anti-inflammatory cytokine (e.g., IL-10) or miRNA mimic/inhibitor.
- Transfection Reagent: A commercial cationic polymer or lipid-based reagent (e.g., polyethyleneimine (PEI) [29]).
- Opti-MEM Reduced Serum Medium.
Procedure:
- Cell Seeding: Seed 5 x 10^5 MSCs into a T-75 culture flask and incubate overnight until 60-80% confluent.
- Complex Formation:
- Dilute 5 µg of plasmid DNA in 250 µL of Opti-MEM. Mix gently.
- Dilulate the transfection reagent (volume according to manufacturer's instructions, e.g., a 2:1 reagent:DNA ratio for PEI) in 250 µL of Opti-MEM. Incubate for 5 minutes at room temperature.
- Combine the diluted DNA and diluted transfection reagent. Mix gently and incubate for 20 minutes at room temperature to allow complex formation.
- Transfection:
- Aspirate the growth medium from the MSCs and wash once with PBS.
- Add 5 mL of fresh, pre-warmed complete growth medium to the flask.
- Add the DNA-transfection reagent complex dropwise onto the cells. Gently swirl the flask to distribute evenly.
- Incubation and Exosome Harvest:
- Incubate cells at 37°C for 6 hours.
- Carefully aspirate the medium containing the complexes, wash cells with PBS, and add 15 mL of exosome-depleted complete medium.
- Incubate for 48 hours to allow exosome secretion.
- Exosome Isolation:
Electroporation of Isolated Exosomes
This protocol describes the direct loading of cargo into pre-isolated MSC exosomes.
Workflow: Direct Exosome Electroporation
Materials:
- Purified MSC Exosomes: 1 x 10^10 particles in PBS.
- Cargo: e.g., 2 nmol of siRNA targeting a pro-fibrotic gene (e.g., TGF-β1) for scar revision [12].
- Electroporation Buffer: Low-conductivity buffer, such as 250 mM sucrose or specialized commercial buffers.
- Electroporator and corresponding 2- or 4-mm gap cuvettes.
Procedure:
- Sample Preparation: Mix the purified exosomes with the siRNA cargo in a final volume of 100-200 µL of electroporation buffer. Gently pipette to mix.
- Electroporation:
- Transfer the mixture to a pre-chilled electroporation cuvette.
- Apply a single electrical pulse. Optimization Note: For siRNA loading, parameters in the range of 150-500 V and a 5-10 ms pulse length are a common starting point. Excessive voltage can cause exosome aggregation [29].
- Post-Pulse Recovery: Immediately after electroporation, incubate the cuvette on ice for 30-60 minutes to allow pore resealing.
- Purification: To remove unencapsulated siRNA, use a centrifugal ultrafiltration device (e.g., 100 kDa MWCO) or size-exclusion chromatography. Resuspend the final loaded exosomes in PBS for downstream applications.
Sonication of Isolated Exosomes
This protocol uses ultrasound to transiently disrupt the exosome membrane for cargo loading.
Workflow: Sonication for Exosome Loading
Materials:
- Purified MSC Exosomes: 1 x 10^10 particles in PBS.
- Cargo: e.g., 50 µM of an anti-inflammatory small molecule drug (e.g., Curcumin) or a fluorescent dye for tracking.
- Probe Sonicator with a micro-tip.
Procedure:
- Sample Preparation: Mix the purified exosomes with the cargo in a total volume of 100-200 µL in a microcentrifuge tube. Keep the tube on ice throughout the procedure.
- Sonication:
- Insert the sterilized micro-tip of the sonicator into the sample. Ensure the tip is fully immersed but not touching the tube walls.
- Sonicate the mixture on ice. A typical protocol uses a pulse sequence of 5 seconds ON and 10 seconds OFF, for a total ON time of 60-120 seconds, at a power output of 20-40 W [30]. Critical Note: Power and time must be optimized to balance loading efficiency with exosome integrity. Over-sonication leads to irreversible damage.
- Recovery and Purification: After sonication, incubate the sample on ice for 30-60 minutes to allow membrane recovery. Remove unincorporated cargo using a centrifugal ultrafiltration device (e.g., 100 kDa MWCO).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Exosome Engineering
| Item | Function/Description | Example & Notes |
|---|---|---|
| Cationic Polymers | Complex with nucleic acids for transfection; facilitate cellular uptake and endosomal escape [29]. | Polyethyleneimine (PEI): High efficiency but can be cytotoxic; requires ratio optimization. |
| Electroporation Buffer | Low-conductivity medium for electroporation; minimizes heat generation and preserves exosome viability. | 250 mM Sucrose solution: A common, non-ionic buffer that provides a suitable environment for pulse delivery. |
| Ultrafiltration Devices | Concentrate and purify exosomes; remove unincorporated cargo and small contaminants post-loading. | 100 kDa MWCO centrifugal filters: Effectively retain exosomes while allowing free small molecules and salts to pass through. |
| Exosome-Depleted FBS | Used in cell culture during exosome production; ensures that isolated exosomes are host cell-derived, not serum-derived. | Commercial FBS, ultracentrifuged or filtered: Critical for controlled experiments and therapeutic applications. |
| Probe Sonicator | Applies high-frequency sound waves to disrupt exosome membranes for sonication-based loading. | Micro-tip sonicator: Essential for small sample volumes (100-500 µL); must be used on ice to prevent overheating. |
Concluding Remarks
The selection of an optimal cargo loading technique is a critical determinant for the success of engineered MSC exosome therapies in chronic wound healing. Transfection is ideal for pre-loading nucleic acids via parent cells, while direct electroporation offers a rapid method for nucleic acid encapsulation into pre-formed exosomes, albeit with aggregation risks. Sonication provides versatility for various cargo types but requires careful parameter control. The protocols outlined herein provide a foundation for researchers to standardize and optimize the engineering of MSC exosomes, paving the way for advanced, cell-free therapeutics for complex wound management.
Within the broader thesis focus on engineering mesenchymal stem cell (MSC) exosomes for targeted drug delivery in chronic wound therapy, precise surface functionalization is paramount. Chronic wounds are characterized by a complex microenvironment featuring persistent inflammation, impaired angiogenesis, and excessive proteolytic activity [31] [12]. Surface engineering enables the decoration of exosomes with specific targeting ligands, such as peptides, to direct these natural nanocarriers to particular cell types within the wound bed—such as endothelial cells, keratinocytes, or macrophages—thereby enhancing therapeutic efficacy and reducing off-target effects [32] [33]. This Application Note details the core ligand conjugation strategies and provides standardized protocols for achieving robust and reproducible exosome targeting.
Ligand Conjugation Strategies: A Comparative Analysis
Multiple post-production strategies exist for conjugating targeting ligands to extracellular vesicles (EVs), including MSC-derived exosomes. The choice of strategy significantly impacts the conjugation efficiency, ligand orientation, and ultimately, the targeting specificity. The following table summarizes the primary technical approaches.
Table 1: Comparison of Post-Production Ligand Conjugation Strategies for MSC Exosomes
| Strategy | Mechanism | Key Advantages | Key Limitations | Typical Ligand Density (Per 100 nm²) |
|---|---|---|---|---|
| Hydrophobic Insertion | Ligand-lipid conjugates (e.g., DSPE-PEG-MAL) insert into the exosome membrane via hydrophobic interactions [34] [32]. | Simple procedure; high conjugation efficiency (>90%); high ligand density [32]. | Potential ligand leakage; possible formation of micelle contaminants [32]. | Several to tens of ligands [32]. |
| Enzyme-Mediated Conjugation | Phospholipase D (e.g., sPLD) catalyzes the transfer of functional groups (e.g., maleimide) onto surface phospholipids for subsequent ligand coupling [32]. | Uniform ligand distribution; minimal disruption to endogenous surface proteins; superior targeting performance in some systems [32]. | Requires optimized enzyme activity and concentration [32]. | High, can be tuned by enzyme dose [32]. |
| Chemical Coupling (Protein) | Disulfide bonds on exosome surface proteins are reduced to thiols, allowing covalent conjugation to maleimide-functionalized ligands [32]. | Covalent bond ensures stability; high conjugation efficiency (>90%) [32]. | Can alter native structure/function of surface proteins; may affect inherent exosome tropism [32]. | Varies, can decrease at high reductant concentrations [32]. |
The following workflow diagram illustrates the decision-making process for selecting and implementing a conjugation strategy.
Conjugation Strategy Workflow
Experimental Protocols
This section provides detailed, step-by-step methodologies for two prominent surface engineering techniques: enzyme-mediated conjugation and hydrophobic insertion.
Protocol: Enzyme-Mediated Conjugation via sPLD
This protocol describes the use of Streptomyces phospholipase D (sPLD) to introduce maleimide groups onto exosome surfaces for precise, covalent ligand attachment [32].
Principle: The sPLD enzyme catalyzes the transphosphatidylation of phosphatidylcholine (PC) on the exosome membrane, replacing the choline headgroup with a maleimide-functionalized alcohol (e.g., HEMI). This introduces a bio-orthogonal handle for site-specific conjugation of thiol-containing ligands [32].
Table 2: Research Reagent Solutions for sPLD Conjugation
| Item | Function/Description | Exemplary Supplier/Type |
|---|---|---|
| MSC-Exosomes | The therapeutic nanocarrier to be functionalized. | Isolated from MSC conditioned media via ultracentrifugation or SEC [31]. |
| sPLD Enzyme | Catalyzes the headgroup exchange on surface phospholipids. | Recombinant Streptomyces phospholipase D [32]. |
| N-(2-Hydroxyethyl)maleimide (HEMI) | Substrate providing maleimide handle for conjugation. | Chemical synthesis supplier [32]. |
| Thiolated Targeting Ligand | The peptide or other molecule conferring target specificity. | Synthesized peptide with C-terminal cysteine [33]. |
Procedure:
- Exosome Preparation: Isolate and purify MSC-derived exosomes using size-exclusion chromatography (SEC) or ultracentrifugation. Resuspend the exosome pellet in reaction buffer (e.g., 25 mM HEPES, 150 mM NaCl, pH 7.4) to a concentration of 1-5 × 10¹¹ particles/mL.
- Maleimide Functionalization: To the exosome solution, add HEMI to a final concentration of 1 mM and sPLD at an optimized concentration (e.g., 1-10 U/mL). Incubate the reaction mixture for 2 hours at 37°C with gentle agitation [32].
- Purification: Remove excess HEMI and enzyme by passing the mixture through a SEC column (e.g., qEVoriginal) equilibrated with conjugation buffer (e.g., PBS, pH 7.0).
- Ligand Conjugation: Immediately incubate the maleimide-functionalized exosomes with the thiolated targeting peptide (e.g., at a 50:1 molar ratio of peptide to exosomes) for 4-16 hours at 4°C, protected from light.
- Purification of Final Product: Separate conjugated exosomes from unreacted peptide using a SEC column. Collect the exosome-rich fractions and characterize the ligand density and size (e.g., via nFCM, NTA) [32].
Protocol: Hydrophobic Insertion of Peptide-Lipid Conjugates
This protocol outlines a method to modify exosomes by incorporating synthesized peptide-PEG-lipid conjugates directly into the lipid bilayer [32] [35].
Principle: Amphiphathic molecules, such as DSPE-PEG-MAL (1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[maleimide(polyethylene glycol)]), spontaneously insert their hydrophobic lipid tails into the exosome membrane via hydrophobic interactions. The PEG spacer improves solubility and ligand presentation, while the terminal maleimide group allows for covalent conjugation to thiolated peptides [32] [35].
Procedure:
- Peptide-Lipid Conjugate Preparation: Synthesize or obtain the DSPE-PEG-MAL conjugate. Alternatively, first incorporate DSPE-PEG-MAL into exosomes, then conjugate the peptide. For the latter, incubate purified exosomes with DSPE-PEG-MAL (e.g., at a 1:5000 molar ratio of lipid to exosomes) for 1-2 hours at room temperature [35].
- Purification of Intermediate: Remove unincorporated DSPE-PEG-MAL by SEC.
- Peptide Coupling: Incubate the DSPE-PEG-MAL-bearing exosomes with a thiolated homing peptide (e.g., CRPPR, which targets SDF-1 expressing sites in wounds) [34] at a predetermined optimal ratio. React for 4-16 hours at 4°C with gentle mixing, protected from light.
- Purification of Final Product: Separate peptide-conjugated exosomes from free peptide using SEC.
- Quality Control: Analyze the final product for particle concentration, size distribution, and conjugation efficiency. Techniques like nano-flow cytometry (nFCM) are highly suitable for quantifying ligand density on individual particles [32].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key materials required for the surface engineering of exosomes as discussed in this note.
Table 3: Essential Research Reagents for Exosome Surface Engineering
| Category | Reagent | Specific Function |
|---|---|---|
| Isolation & Purification | Size-Exclusion Chromatography (SEC) Columns | Isolate exosomes from contaminants and free labels based on size [32]. |
| Targeting Ligands | CRPPR Peptide | A homing peptide that targets sites expressing the chemokine SDF-1, relevant in wound healing [34]. |
| RGD Motif Peptides | Target integrins overexpressed on endothelial cells during angiogenesis [33] [35]. | |
| Chemical Linkers | DSPE-PEG-MAL | Amphiphilic polymer for membrane insertion and providing a maleimide group for peptide coupling [32] [35]. |
| Enzymatic Tools | Streptomyces Phospholipase D (sPLD) | Engineered phospholipase D for precise functionalization of surface phosphatidylcholine [32]. |
| Characterization | Nano-Flow Cytometry (nFCM) | Single-particle analysis for quantifying ligand density, size, and heterogeneity [32]. |
| Transmission Electron Microscopy (TEM) | Validates structural integrity of exosomes post-modification [32]. |
Concluding Remarks
The strategic application of surface engineering is a critical component in advancing MSC exosome-based therapies for chronic wounds. The protocols outlined herein for enzyme-mediated conjugation and hydrophobic insertion provide robust, quantifiable methods to equip exosomes with targeting ligands. The choice of method depends on the specific requirements for stability, ligand density, and preservation of native exosome function. As the field progresses, the standardization of these protocols and rigorous characterization using techniques like nFCM will be essential for translating engineered exosomes from a research tool to a clinically viable therapeutic for targeted drug delivery in chronic wound repair.
The therapeutic potential of mesenchymal stem cells (MSCs) in regenerative medicine, particularly for complex conditions such as chronic wounds, is primarily mediated through their potent paracrine activity. A significant component of this activity is attributed to MSC-derived exosomes (MSC-Exos), which are nano-sized extracellular vesicles that facilitate intercellular communication by transferring proteins, lipids, and nucleic acids to recipient cells [36] [37]. However, the inherent variability and often subdued potency of naïve MSCs and their exosomes following in vivo administration present significant clinical challenges. To overcome these limitations, preconditioning has emerged as a critical strategy. This process involves the deliberate exposure of MSCs to sub-lethal physiological or pathological stimuli ex vivo, thereby enhancing their subsequent therapeutic efficacy [38] [39].
Preconditioning operates on the principle of hormesis, where a moderate stressor triggers an adaptive cellular response, leading to improved function and resilience. In the context of a thesis focused on engineering MSC exosomes for targeted drug delivery in chronic wounds, preconditioning is a pivotal first step. It is a form of primary engineering that optimizes the "raw material"—the exosomes themselves—by enriching their cargo with beneficial miRNAs, proteins, and growth factors, thereby boosting their innate regenerative, anti-inflammatory, and angiogenic capabilities [39] [12]. This document provides detailed application notes and standardized protocols for three cornerstone preconditioning strategies: hypoxia, inflammatory cytokines, and lipopolysaccharide (LPS).
Preconditioning Strategies: Mechanisms and Quantitative Effects
Preconditioning enhances the immunomodulatory and regenerative functions of MSCs and their exosomes by mimicking the hostile environments of injury sites, such as chronic wounds. The table below summarizes the key effects and optimal conditions for each strategy.
Table 1: Summary of Preconditioning Strategies for MSCs
| Preconditioning Stimulus | Key Mediators/Pathways Upregulated | Primary Functional Outcomes | Optimal Protocol Parameters |
|---|---|---|---|
| Hypoxia | HIF-1α, AKT, VEGF, ANG, FGF, BDNF [38] | Enhanced cell survival, angiogenesis, & migration [38] | 1-5% O₂ for 24-72 hours [38] |
| Cytokines (IFN-γ & TNF-α) | IDO, PGE2, COX-2, Factor H [40] [38] | Potent immunomodulation; shifts macrophages to M2 anti-inflammatory phenotype [38] | IFN-γ: 10-50 ng/mL; TNF-α: 10-20 ng/mL; Duration: 24-48 hours [38] [39] |
| Lipopolysaccharide (LPS) | let-7 microRNA, TLR/NF-κB/STAT3/AKT pathway, miR-146a, miR-181a-5p [38] [39] | Enhanced anti-microbial & anti-inflammatory priming; promotes M2 macrophage polarization [38] [39] | Low-dose: 0.1 - 1 µg/mL; Duration: 24-48 hours [39] |
The quantitative enhancement of MSC secretome through preconditioning is particularly evident in the increased secretion of critical growth factors. The following table compiles experimental data demonstrating this effect.
Table 2: Quantitative Enhancement of Growth Factor Secretion in Preconditioned MSCs (Sample Data)
| Growth Factor | Naïve MSCs-S (pg/mL) | AA + IFN-γ Preconditioned MSCs-S (pg/mL) | Fold Change | Function |
|---|---|---|---|---|
| HGF | ~1250 | ~3500 | ~2.8x | Mitogenesis, Angiogenesis [40] |
| NGF | ~7.5 | ~25 | ~3.3x | Neurite outgrowth, Cell survival [40] |
| VEGF | ~40 | ~125 | ~3.1x | Angiogenesis, Vascular permeability [40] |
| FGF2 | ~7 | ~20 | ~2.9x | Angiogenesis, Wound repair [40] |
Detailed Experimental Protocols
Protocol 1: Hypoxic Preconditioning
Principle: Culturing MSCs in a low-oxygen environment (1-5% O₂) to mimic the ischemic nature of chronic wounds and stabilize Hypoxia-Inducible Factor-1α (HIF-1α), activating a pro-survival and angiogenic genetic program [38].
Materials:
- Confluent (70-80%) flask of human MSCs (e.g., BM-MSCs or UC-MSCs).
- Standard MSC growth medium.
- Hypoxia chamber or multi-gas CO₂ incubator.
- Pre-mixed gas mixture (1% O₂, 5% CO₂, balanced N₂).
- Phosphate Buffered Saline (PBS) and trypsin/EDTA.
Procedure:
- Cell Preparation: Harvest MSCs using standard trypsin/EDTA protocol. Count and seed cells at a density of 5,000-8,000 cells/cm² in standard growth medium. Allow cells to adhere for 24 hours under normal culture conditions (37°C, 5% CO₂, 21% O₂).
- Preconditioning: After 24 hours, replace the medium with fresh, pre-warmed growth medium.
- Hypoxia Induction: Quickly transfer the culture flasks/plates to the pre-equilibrated hypoxia chamber or incubator set to 1% O₂ and 5% CO₂ at 37°C.
- Incubation: Incubate the cells under hypoxic conditions for 48 hours. Ensure the chamber maintains a tight seal to prevent oxygen leakage.
- Collection of Conditioned Media (for Exosome Isolation): After 48 hours, carefully collect the conditioned media from the hypoxic cultures.
- Cell/Exosome Processing: Proceed to isolate exosomes immediately from the conditioned media using your method of choice (e.g., ultracentrifugation, tangential flow filtration). Alternatively, pre-conditioned MSCs can be harvested for direct therapy or analyzed for efficacy.
Notes: A combination of hypoxia followed by reoxygenation can further enhance the expression of trophic factors [38].
Protocol 2: Cytokine Preconditioning (IFN-γ and TNF-α)
Principle: Priming MSCs with key inflammatory cytokines to boost the expression of critical immunomodulatory enzymes like IDO and PGE2, thereby pre-activating their anti-inflammatory capacity for a more robust response in the wound microenvironment [40] [38].
Materials:
- Confluent (70-80%) flask of human MSCs.
- Standard MSC growth medium (e.g., DMEM/F12 with 10% FBS).
- Recombinant Human IFN-γ and TNF-α proteins.
- Sterile, PBS for cytokine reconstitution.
Procedure:
- Cytokine Solution Preparation: Reconstitute IFN-γ and TNF-α cytokines according to the manufacturer's instructions to create a concentrated stock solution. Prepare the working preconditioning medium by diluting the cytokines in fresh, serum-free or standard growth medium to a final concentration of 20-50 ng/mL for IFN-γ and 10-20 ng/mL for TNF-α [40] [38] [39].
- Cell Preparation: Harvest and seed MSCs as described in Protocol 1, allowing them to adhere for 24 hours.
- Medium Exchange: Aspirate the standard growth medium and gently wash the cell layer with pre-warmed PBS to remove residual serum.
- Preconditioning: Add the freshly prepared cytokine-containing medium to the cells.
- Incubation: Incubate the cells with the cytokine medium for 24-48 hours at 37°C in a standard 5% CO₂ incubator.
- Collection and Processing: After the incubation period, collect the conditioned media for exosome isolation. The pre-conditioned MSCs can also be harvested for downstream applications.
Notes: Efficacy of preconditioning should be validated by measuring the upregulation of IDO activity (e.g., via kynurenine assay) or PGE2 secretion using ELISA [38].
Protocol 3: LPS Preconditioning
Principle: Using low-dose bacterial endotoxin to safely "prime" MSCs via Toll-like receptor 4 (TLR4) activation, enhancing the anti-inflammatory miRNA content of their exosomes (e.g., miR-146a, miR-181a-5p) without inducing a pro-inflammatory cascade, which is beneficial for managing infected or highly inflammatory wounds [38] [39].
Materials:
- Confluent (70-80%) flask of human MSCs.
- Standard MSC growth medium.
- Ultrapure Lipopolysaccharide (LPS) from E. coli (e.g., Serotype O55:B5).
- Sterile PBS.
Procedure:
- LPS Solution Preparation: Reconstitute LPS in sterile PBS to create a 1 mg/mL stock solution. Aliquot and store at -20°C. Avoid repeated freeze-thaw cycles.
- Cell Preparation: Harvest and seed MSCs as described in previous protocols.
- Medium Exchange: Aspirate the old medium and wash cells with PBS.
- Preconditioning: Add fresh growth medium containing a low dose of LPS (0.1 - 1 µg/mL) to the cells [39]. A dose of 0.5 µg/mL is effective for enriching specific miRNAs like miR-181a-5p [39].
- Incubation: Incubate the cells for 24 hours at 37°C, 5% CO₂.
- Collection and Processing: Collect the conditioned media for exosome isolation. Analyze the exosomal miRNA cargo (e.g., via qRT-PCR for miR-146a or miR-181a-5p) to confirm preconditioning efficacy.
Notes: The response to LPS is highly dose-dependent. High doses may trigger a pro-inflammatory response, so adherence to low-dose protocols is critical for the desired immunomodulatory outcome [39].
Signaling Pathways and Workflows
Signaling Pathways in MSC Preconditioning
The following diagram illustrates the core molecular pathways activated by the three preconditioning strategies, culminating in enhanced exosome biogenesis and cargo loading.
Integrated Preconditioning Workflow
This flowchart outlines the complete experimental workflow from cell culture to the final application of engineered exosomes in chronic wound research.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential reagents and their critical functions for implementing the described preconditioning protocols.
Table 3: Essential Research Reagents for MSC Preconditioning
| Reagent / Material | Function / Application in Preconditioning | Example Specifications / Notes |
|---|---|---|
| Recombinant Human IFN-γ | Cytokine preconditioning; induces IDO and PGE2 expression for immunomodulation [38]. | Purity: >98%. Carrier-free is recommended for accurate dosing. Store at -20°C. |
| Recombinant Human TNF-α | Cytokine preconditioning; synergizes with IFN-γ to enhance immunomodulatory factor production [38] [39]. | Purity: >97%. Bioactivity should be verified. Store at -20°C. |
| Ultrapure LPS | LPS preconditioning; TLR4 agonist for priming anti-inflammatory exosomal miRNA profiles [38] [39]. | Source: E. coli O55:B5. Use low-endotoxin solvents for reconstitution. |
| Hypoxia Chamber/Incubator | Provides a controlled low-oxygen environment (1-5% O₂) for hypoxic preconditioning [38]. | Must reliably maintain set O₂ and CO₂ levels. Multi-gas incubators are ideal. |
| Fetal Bovine Serum (FBS) for MSC Culture | Critical for MSC growth and expansion prior to preconditioning. | Use exosome-depleted FBS during the preconditioning phase to avoid contaminating vesicles. |
| Ultracentrifugation System | Gold-standard method for isolating exosomes from conditioned media post-preconditioning [41]. | Requires fixed-angle or swinging-bucket rotors capable of >100,000 × g. |
| Tangential Flow Filtration (TFF) System | Scalable alternative to ultracentrifugation for exosome isolation, suitable for larger volumes [41]. | Enables gentle concentration and buffer exchange. |
| Antibodies for Characterization | Validation of exosome identity (CD63, CD81, TSG101) and MSC surface markers (CD73, CD90, CD105) [40] [41]. | Use for Western Blot, Flow Cytometry, or Nanoparticle Tracking Analysis. |
Biomaterial-assisted delivery systems, particularly hydrogels and scaffolds, are engineered to provide controlled, sustained release of therapeutic agents, directly addressing the challenge of frequent dosing in conventional treatments. Within the context of engineering mesenchymal stem cell (MSC) exosomes for targeted drug delivery in chronic wounds, these biomaterials act as protective reservoirs and delivery matrices. They enhance the stability and retention of therapeutically active exosomes at the wound site, facilitating localized and prolonged modulation of the wound microenvironment to promote healing. This document outlines key characterization data, detailed protocols, and essential reagents for developing such advanced drug delivery systems.
Quantitative Characterization of Hydrogel Systems
The performance of hydrogel-based delivery systems is quantified through key physicochemical and release properties. The data below, synthesized from recent literature, provides benchmarks for system design.
Table 1: Key Characterization Parameters for Sustained Release Hydrogel Scaffolds
| Parameter | Typical Values/Results | Experimental Context | Significance for Drug Delivery |
|---|---|---|---|
| Swelling Ratio (SR %) | 362% - 412% after 24 h [42] | Chitosan/Gelatin/Iota-Carrageenan hydrogels in PBS (pH 7.2) at 37°C [42]. | High water uptake indicates hydrogel hydrophilicity and capacity to create a diffusional environment for drug release. |
| Porosity | 72.4% - 78% [42] | Porous, interconnected microstructure observed via SEM; porosity increases with iota-carrageenan concentration [42]. | Facilitates nutrient transport, cell migration, and influences the diffusion rate of encapsulated therapeutics. |
| Mechanical Strength (Fracture Stress) | 0.0358 - 0.1665 Kgf/mm² [42] | Measured for different formulations of Chitosan/Gelatin/Iota-Carrageenan hydrogels [42]. | Determines the scaffold's ability to withstand mechanical forces at the implantation site and maintain structural integrity. |
| Drug Release Duration | ~10 hours (sustained release) [42] | Release profile of ciprofloxacin hydrochloride from a loaded hydrogel scaffold [42]. | Demonstrates the system's ability to extend drug release, reducing dosing frequency. |
| Release Kinetics (Best Fit) | First-Order Model (R² = 0.9814) [42] | Kinetic modeling of ciprofloxacin hydrochloride release data [42]. | Informs the underlying release mechanism (e.g., diffusion-dominated). |
| Triphasic Release from Stimuli-Responsive Systems | 1. Slow, linear pre-stimulus2. Fast, logistic post-stimulus (0-10 h)3. Steady, linear sustained release (Day 2-10) [43] | Acoustically responsive scaffold (ARS) releasing dextran (10 kDa) upon ultrasound-triggered phase transition [43]. | Enables complex, on-demand release profiles; the sustained phase is critical for long-term therapeutic efficacy. |
Experimental Protocols
Protocol: Fabrication of a Drug-Loaded Polysaccharide Hydrogel Scaffold
This protocol details the synthesis of a biocompatible, sustained-release hydrogel scaffold based on natural polymers, adapted from a study loading ciprofloxacin hydrochloride [42].
Objective: To prepare a crosslinked chitosan/gelatin/iota-carrageenan hydrogel scaffold for the sustained release of a model drug.
Materials:
- Polymers: Chitosan (medium molecular weight), Gelatin (Type B, from bovine skin), Iota-Carrageenan (IC).
- Solvents: Acetic acid (1% v/v aqueous), Distilled water.
- Crosslinker: Glutaraldehyde (50% w/w).
- Drug Model: Ciprofloxacin hydrochloride.
- Equipment: Magnetic stirrer with hotplate, freeze-dryer, desiccator.
Procedure:
- Polymer Solution Preparation:
- Chitosan Solution (1% w/v): Dissolve chitosan in 1% acetic acid solution with continuous stirring at room temperature until fully dissolved.
- Gelatin Solution (10% w/v): Dissolve gelatin in distilled water at 50°C with continuous stirring until clear.
- Iota-Carrageenan Solution (1% w/v): Dissolve iota-carrageenan in distilled water at 70°C with continuous stirring until fully dissolved.
Hydrogel Formulation and Drug Loading:
- Combine the polymer solutions in the desired volume ratios (e.g., as per Table 1 of the source material [42]) in a beaker.
- To load the drug, add the therapeutic agent (e.g., 2.5 mg ciprofloxacin hydrochloride) to the mixed polymer solution. Stir thoroughly at ambient conditions to ensure homogeneous dispersion.
- Add the crosslinker, glutaraldehyde (1 mL of 50% w/w), to the mixture. Stir using a magnetic stirrer for 1 hour at room temperature to initiate and complete the crosslinking reaction.
Post-Processing and Storage:
- Wash the formed hydrogel repeatedly with distilled water to remove any unreacted crosslinker.
- Freeze the hydrogel and lyophilize using a freeze-dryer to obtain the final dried, porous scaffold.
- Store the dried hydrogel in a desiccator until further use and characterization.
Protocol: Integrating MSC Exosomes into a Hydrogel Delivery System
This protocol describes a strategy for creating a hybrid therapeutic system by incorporating MSC-derived exosomes into a hydrogel matrix for wound healing applications [44] [14] [12].
Objective: To encapsulate MSC-derived exosomes within a hydrogel to create a cell-free, sustained-release system for chronic wound therapy.
Materials:
- MSC Exosomes: Isolated and purified from MSC culture supernatant via differential ultracentrifugation or other validated methods [44] [45].
- Hydrogel Precursor: A biocompatible hydrogel system (e.g., Fibrin-based [43], Chitosan-based [42], or Pluronic F-127 hydrogel [44]).
- Buffer: Sterile phosphate-buffered saline (PBS) or culture medium.
Procedure:
- Exosome Isolation and Characterization:
- Isolate exosomes from the conditioned medium of cultured MSCs using differential ultracentrifugation (e.g., 100,000 × g for 70 minutes) [44] [45].
- Characterize the isolated exosomes for size, concentration (via Nanoparticle Tracking Analysis, NTA), and identity (via Western blot for markers CD63, CD81, TSG101) [45].
Hydrogel-Exosome Composite Formation:
- Direct Incorporation: Resuspend the purified exosome pellet in the liquid hydrogel precursor solution (e.g., fibrinogen solution for fibrin hydrogels). Gently mix to achieve a uniform suspension without forming bubbles [43].
- Gelation: Induce gelation according to the specific hydrogel's protocol. For fibrin hydrogels, this involves adding thrombin to the fibrinogen-exosome mixture [43]. For thermosensitive hydrogels like Pluronic F-127, gelation occurs upon warming to physiological temperature [44].
Release and Efficacy Assessment:
- In Vitro Release Study: Immerse the exosome-loaded hydrogel in a release buffer (e.g., PBS at 37°C). Collect release media at predetermined time points and quantify exosome or cargo release using NTA, protein assays (BCA), or miRNA-specific assays [14].
- Functional Assays: Evaluate the biological activity of the released exosomes using cell-based assays, such as:
Signaling Pathways and Workflow Visualization
MSC Exosome Mechanisms in Wound Healing
The following diagram summarizes the key mechanisms by which engineered MSC exosomes, delivered via hydrogels, promote healing in chronic wounds.
Experimental Workflow for Hybrid System Development
This workflow outlines the key steps for researchers to develop and characterize an exosome-loaded hydrogel system.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Hydrogel-Exosome Hybrid System Development
| Reagent/Category | Function & Rationale | Specific Examples |
|---|---|---|
| Natural Polymer Hydrogels | Form the bulk 3D scaffold; provide biocompatibility, biodegradability, and ECM-mimetic properties. | Chitosan [42], Gelatin [42], Alginate [46], Fibrin [43], Hyaluronic Acid, Iota-Carrageenan [42] |
| Synthetic Polymer Hydrogels | Offer precisely tunable mechanical properties and controlled chemical functionality. | Poly(ethylene glycol) (PEG) [47], Pluronic F-127 [44] |
| Crosslinking Agents | Create the 3D network structure of the hydrogel, determining its mechanical strength and stability. | Glutaraldehyde [42], Thrombin (for Fibrin) [43], Enzymatic crosslinkers (e.g., Factor XIII) [43] |
| MSC Exosome Source | The therapeutic cargo; provides paracrine effects (anti-inflammatory, pro-angiogenic, pro-regenerative) without cell-based risks. | Exosomes from Bone Marrow-MSCs [44], Adipose-derived MSCs [14], Umbilical Cord-MSCs [44] |
| Characterization Tools | Essential for validating the system's physical structure, drug release profile, and biological activity. | FTIR/ATR-IR [42], Scanning Electron Microscope (SEM) [42], Nanoparticle Tracking Analysis (NTA) [45], ELISA/Western Blot [45] |
Overcoming Technical and Manufacturing Hurdles in Clinical Translation
The therapeutic application of mesenchymal stem cell (MSC)-derived exosomes for chronic wound treatment represents a paradigm shift in regenerative medicine. These nanoscale extracellular vesicles (30-150 nm) transfer bioactive molecules—proteins, lipids, and nucleic acids—to recipient cells, promoting angiogenesis, modulating inflammation, and stimulating tissue regeneration [31] [48]. However, the translational pathway from laboratory discovery to clinical application is obstructed by a critical bottleneck: the isolation and purification of exosomes at sufficient quantity, quality, and purity. Ultracentrifugation, long considered the gold standard, faces significant limitations for clinical-scale production [49] [50].
The pursuit of engineered MSC exosomes for targeted drug delivery in chronic wound management demands isolation methods that not only preserve exosome integrity and biological activity but also accommodate scalability and reproducibility. Chronic wounds, such as diabetic foot ulcers and pressure ulcers, are characterized by prolonged inflammation, impaired angiogenesis, and failure to re-epithelialize [12]. MSC exosomes can reverse these pathologies, but their efficacy is contingent upon isolation techniques that yield functionally intact vesicles. This Application Note examines the limitations of traditional ultracentrifugation, evaluates advanced alternative isolation methodologies, and provides detailed protocols for researchers navigating the transition toward scalable, GMP-compliant exosome production.
Limitations of Ultracentrifugation for Clinical Translation
Despite its longstanding status as the most common isolation technique, ultracentrifugation presents considerable drawbacks for therapeutic exosome production, particularly for the sensitive vesicles derived from MSCs.
Table 1: Key Limitations of Ultracentrifugation for Therapeutic MSC Exosome Isolation
| Limitation Category | Specific Challenges | Impact on Therapeutic Potential |
|---|---|---|
| Process-Related | Time-consuming (up to 10 hours) and low-throughput [50] [51] | Hinders scalable production for clinical trials and treatment |
| Requires expensive, specialized equipment [51] | Increases production costs and limits accessibility | |
| Product Quality | High centrifugal forces can damage exosome structure [51] | Compromises vesicle integrity and biological activity |
| Co-precipitation of non-exosomal contaminants (e.g., protein aggregates, lipoproteins) [50] [52] | Reduces purity, risks unwanted immune reactions, confuses efficacy data | |
| Yield and Reproducibility | Low exosome recovery rates (~30%) during repeated washing steps [52] | Inefficient use of valuable MSC culture supernatant |
| Sensitivity to operator technique and parameters leads to batch-to-batch variability [53] | Challenges in ensuring reproducible, standardized therapeutic doses |
The fundamental issue is that the excessive gravitational forces and prolonged run times inherent to ultracentrifugation can compromise the very properties that make MSC exosomes therapeutically valuable for wound healing [31]. Furthermore, the demonstrated contamination with apolipoproteins underscores the purity limitations, which is a major concern for regulatory approval of injectable therapeutics [50].
Advanced Isolation Techniques: A Comparative Analysis
Moving beyond ultracentrifugation necessitates the adoption of alternative and complementary technologies designed to address its shortcomings. The ideal method balances yield, purity, scalability, and preservation of biological function.
Table 2: Quantitative Comparison of Exosome Isolation Methods
| Isolation Method | Principle | Processing Time | Relative Yield | Key Advantages | Major Drawbacks |
|---|---|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation based on size/density [52] | 5-10 hours [50] | Baseline | Considered gold standard; no reagent cost [50] | Long runtime, low yield, potential vesicle damage, lipoprotein contamination [50] [51] |
| Precipitation | Polymer-based (e.g., PEG) vesicle aggregation [50] | ~2 hours [50] | ~2.5x higher than UC [50] | Fast, simple, high yield, requires no special equipment [50] | Co-precipitates contaminants (e.g., lipoproteins), requires additional purification [50] |
| Size-Based Chromatography | Size-exclusion using porous polymer matrix [52] | 1-2 hours | High (sample dependent) | Preserves vesicle integrity, good purity | Sample viscosity can affect resolution, may require pre-filtration |
| Tangential Flow Filtration | Size-based separation via continuous flow [52] [54] | 2-4 hours | High | Highly scalable, suitable for large volumes, closed system | Membrane fouling, initial setup cost |
| Immunoaffinity Capture | Antibody-binding to surface markers (e.g., CD63, CD81) [53] [54] | 3-5 hours (including incubation) | Low (highly specific) | Exceptional purity, isolates specific subpopulations | High cost, limited to known markers, may not capture all MSC exosomes |
| Microfluidic Devices | Lab-on-a-chip using immunoaffinity, size, or acoustic waves [49] [54] | Minutes to <1 hour | Varies with design | Rapid, minimal sample volume, high purity potential, automatable | Currently low throughput, not yet suited for large-scale production |
For engineered MSC exosomes intended for chronic wound therapy, a combination of methods often yields the best results. For instance, Tangential Flow Filtration (TFF) is exceptionally suited for the initial concentration of large-volume MSC conditioned media, as it is gentle, scalable, and maintains exosome function [54]. This can be followed by a polishing step using Size-Exclusion Chromatography (SEC) to remove residual soluble proteins and contaminants, resulting in a pure, functional exosome preparation ready for downstream engineering or direct application [52].
Workflow Diagram: Integrated Isolation for Therapeutic MSC Exosomes
The following diagram illustrates a recommended integrated workflow for isolating high-purity MSC exosomes for therapeutic use in chronic wound research, combining the scalability of TFF with the purity of SEC.
Detailed Experimental Protocols
Protocol 1: Isolation via Precipitation (for Rapid Screening)
Precipitation methods offer a rapid, accessible alternative for initial proof-concept studies in wound healing models.
Protocol: Exosome Isolation from MSC Conditioned Media Using Precipitation
Materials & Reagents:
- Commercially available exosome precipitation solution (e.g., PEG-based)
- Centrifuge capable of 10,000 × g
- MSC-conditioned media, cell-free (centrifuged at 2,000 × g for 30 min)
- Phosphate-buffered saline (PBS)
Procedure:
- Pre-analytical Processing: Clarify MSC-conditioned media by centrifugation at 2,000 × g for 30 minutes to remove cells and large debris. Transfer the supernatant to a new tube.
- Precipitation: Mix the clarified supernatant with the precipitation solution at a predetermined ratio (e.g., 1:2 to 1:5 volume/volume). Vortex thoroughly to ensure complete mixing.
- Incubation: Incubate the mixture overnight (for at least 12 hours) at 4°C to allow for exosome precipitation.
- Recovery: Centrifuge the sample at 10,000 × g for 1 hour at 4°C. A beige or white pellet should be visible at the bottom of the tube.
- Resuspension: Carefully decant the supernatant. Resuspend the exosome pellet in a suitable volume of PBS (e.g., 50-200 µL) for immediate use or storage at -80°C.
- Post-isolation Purification (Optional but Recommended): To reduce co-precipitated contaminant, pass the resuspended exosomes through a size-exclusion chromatography column [50].
Protocol 2: Isolation via Integrated TFF-SEC (for Scalable GMP-Compliant Production)
This integrated protocol is designed for higher purity and scalability, which is critical for preclinical and clinical development.
Protocol: Integrated TFF-SEC for Scalable MSC Exosome Isolation
Materials & Reagents:
- Tangential Flow Filtration system with a 100-500 kDa molecular weight cut-off (MWCO) membrane
- Size-exclusion chromatography columns (e.g., qEVoriginal)
- Peristaltic pump
- Sterile phosphate-buffered saline (PBS), pH 7.4
Procedure: Part A: Tangential Flow Filtration
- System Setup: Flush and equilibrate the TFF system with PBS according to the manufacturer's instructions.
- Clarification: Clarify the MSC-conditioned media as in Protocol 1, Step 1.
- Concentration and Diafiltration: Pump the clarified supernatant through the TFF system. The system will continuously concentrate the exosomes while simultaneously exchanging the buffer into PBS. This process continues until the initial volume is reduced 50- to 100-fold.
- Final Recovery: Flush the system with a small volume of PBS to recover any exosomes retained in the filter assembly. The resulting retentate is a concentrated exosome suspension.
Part B: Size-Exclusion Chromatography
- Column Equilibration: Equilibrate the SEC column with at least 2 column volumes of PBS.
- Sample Application: Carefully load the concentrated exosome retentate from Part A onto the column. Do not exceed the recommended loading volume.
- Fraction Collection: Elute the column with PBS and collect sequential fractions. The exosomes will elute in the early, void-volume fractions, which appear slightly opaque. Later fractions containing contaminants like proteins can be discarded.
- Concentration (Optional): If a higher concentration is required, the purified exosome fractions can be concentrated using a centrifugal concentrator with an appropriate MWCO.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Exosome Isolation and Analysis
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Polyethylene Glycol (PEG)-based Solution | Induces exosome precipitation by volume exclusion [50] | Rapid isolation from small-volume MSC cultures for initial functional screens in fibroblast assays. |
| TFF Cassette (100-500 kDa MWCO) | Scalable concentration and buffer exchange of exosomes from large volumes [52] [54] | Processing liters of MSC bioreactor supernatant for a pre-clinical animal study on diabetic ulcers. |
| Size-Exclusion Chromatography Columns | High-resolution separation of exosomes from soluble proteins based on hydrodynamic radius [52] | Final polishing step after TFF to remove contaminating albumin and other proteins for pure therapeutic preparation. |
| Anti-Tetraspanin Antibodies (CD63, CD81, CD9) | Immunoaffinity capture and characterization of exosomes via flow cytometry or immuno-EM [53] | Confirming the presence of exosomes in an isolate and quantifying specific subpopulations. |
| NTA Instrument (e.g., NanoSight) | Measures particle size distribution and concentration in liquid suspension [50] [53] | Standard quality control to determine exosome yield and confirm size profile (30-150 nm) post-isolation. |
The journey toward effective MSC exosome-based therapies for chronic wounds is inextricably linked to overcoming isolation and purification challenges. While ultracentrifugation remains a useful research tool, its limitations in scalability, reproducibility, and product quality render it inadequate for clinical translation. Embracing advanced integrated strategies, particularly those combining gentle concentration methods like Tangential Flow Filtration with high-resolution purification like Size-Exclusion Chromatography, provides a viable path forward. These protocols enable the production of high-quality, functionally intact MSC exosomes that are essential for meaningful therapeutic outcomes and successful engineering into targeted drug delivery systems for complex wound healing applications.
Standardization and Scalability for Industrial Production
The clinical translation of Mesenchymal Stem Cell (MSC)-derived exosomes for chronic wound therapy hinges on overcoming critical bottlenecks in industrial-scale production. While laboratory-scale methods yield exosomes with demonstrated therapeutic potential—promoting angiogenesis, modulating inflammation, and enhancing tissue regeneration—their transition to commercially viable therapeutics requires standardized, scalable, and reproducible manufacturing processes [14] [17]. Current challenges include donor variability in primary MSCs, finite expansion capacity, phenotypic drift during in vitro passaging, and batch-to-batch heterogeneity [55] [17]. This document outlines standardized protocols and scalability strategies for industrial production of MSC-derived exosomes, contextualized within a framework of engineered exosomes for targeted drug delivery in chronic wound research.
Quantitative Landscape of Industrial Production
The table below summarizes key quantitative data and scalability parameters for different production systems, highlighting the advantages of bioreactor-based platforms.
Table 1: Comparative Analysis of Scalability and Production Yields
| Production System | Scale/Culture Format | Reported Cell Expansion | Reported EV Yield | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Traditional 2D Flasks [56] | T-flasks, Cell Factories | Limited by surface area | Laboratory scale (varies) | Simplicity, low initial cost | Low scalability, high labor, inconsistency |
| Microcarrier Suspension Bioreactor [55] | 3D Suspension Culture | High-density culture | Not specified in source | Scalable iMSC generation from EPSCs | Requires downstream transfer for EV production |
| Fixed-Bed Bioreactor [55] | Integrated fixed-bed system | > 5 × 10⁸ cells/batch | ~1.2 × 10¹³ particles/day | Integrated, continuous EV harvesting; GMP-compatible | Higher complexity and capital investment |
| Tangential Flow Filtration (TFF) [56] [57] | Downstream Processing | N/A | High recovery rate | Scalable purification, maintains exosome integrity | Requires optimization to avoid membrane clogging |
Standardized Protocols for Scalable Production
Advanced Cell Source Generation (iMSCs from Pluripotent Stem Cells)
To address donor variability, a robust protocol for generating induced MSCs (iMSCs) from extended pluripotent stem cells (EPSCs) is recommended [55].
Protocol: Directed Differentiation of EPSCs to iMSCs
EPSC Induction:
- Culture iPSCs to 70-80% confluency.
- Dissociate cells using TrypLE and seed on Matrigel-coated plates at 1 × 10^5 cells/well in EPSC induction medium.
- Refresh the medium every 2 days. By Day 6, EPSCs are ready for characterization [55].
Trophoblast-like Cell (TLC) Differentiation:
- On Day 6, dissociate EPSCs and seed on Matrigel at 1 × 10^5 cells/well.
- Transition cells to TLC differentiation medium with full medium replacement every 2 days until Day 6 [55].
MSC Induction and Expansion:
- Dissociate differentiated TLCs and seed onto Matrigel-coated flasks at 8 × 10^4 cells/cm² in MSC complete medium (α-MEM + 5% Human Platelet Lysate).
- Passage cells upon confluence, sequentially reducing density to 1 × 10^4/cm² by Passage 4.
- Validate iMSCs via flow cytometry for positive markers (CD44, CD73, CD90, CD105, CD166) and negative markers (HLA-DR, CD34, CD45) [55].
Scalable Bioreactor Expansion and EV Harvesting
Protocol: Integrated Bioreactor Production of iMSC-Exosomes
Upstream Processing - Large-Scale iMSC Culture:
- Utilize a microcarrier suspension bioreactor system for the initial expansion of iMSCs, achieving high cell densities as a master cell bank [55].
Continuous EV Production:
- Transfer iMSCs to a fixed-bed bioreactor system. This system provides uniform nutrient perfusion and minimal shear stress, supporting high-density adherent culture and continuous conditioning of the culture medium [55].
- Maintain culture parameters (pH, dissolved oxygen, temperature) under strict control to ensure consistent exosome quality.
Downstream Processing - Harvest and Initial Clarification:
- Continuously or semi-continuously harvest conditioned medium from the bioreactor.
- Perform initial clarification via centrifugation at low speed (e.g., 2,000 × g for 30 min) followed by depth filtration (0.22 µm) to remove cells, large debris, and microvesicles [57].
Industrial-Scale Exosome Isolation and Purification
Protocol: Tangential Flow Filtration (TFF) with Size-Exclusion Chromatography (SEC)
Concentration and Initial Purification:
- Process the clarified medium using a TFF system with a 500 kDa molecular weight cut-off (MWCO) membrane [57]. This step concentrates the exosomes and removes smaller contaminants like proteins.
High-Resolution Purification:
- Further purify the TFF-retentate using Size-Exclusion Chromatography (SEC). This step separates exosomes from co-purified proteins and lipoproteins based on size, resulting in a high-purity preparation with preserved vesicle integrity [56].
- The eluted exosome fractions are pooled and concentrated if necessary.
Formulation and Storage:
- Diafilter the purified exosome preparation into the final formulation buffer (e.g., PBS). For stability, include stabilizers like trehalose or human serum albumin [58].
- For long-term storage, aliquot and freeze at -80°C, minimizing freeze-thaw cycles. Use protein-low binding tubes to prevent surface adsorption and loss [58].
Diagram 1: GMP-compliant production workflow for clinical-grade MSC exosomes.
Critical Quality Control (QC) and Analytical Techniques
A robust QC strategy is paramount for standardizing exosome products. The following table outlines the essential "Research Reagent Solutions" and analytical methods required for comprehensive characterization.
Table 2: Research Reagent Solutions for Exosome Characterization
| Analysis Category | Essential Reagents / Kit | Key Target / Function | Purpose in Standardization |
|---|---|---|---|
| Identity & Purity | Antibodies against CD63, CD81, CD9, ALIX, TSG101 [59] [58] [56] | Confirm exosomal surface and intraluminal markers | Identity testing via Western Blot or flow cytometry. |
| Antibodies against HLA-DR, CD34, CD45 [55] | Negative markers for MSC origin | Ensure purity and absence of cellular contaminants. | |
| Particle & Size Analysis | Phosphate-Buffered Saline (PBS), filter sterilized [57] | Diluent for sample preparation | For accurate NTA and DLS measurements. |
| Uranyl Acetate solution [57] | Negative stain for electron microscopy | Visualize cup-shaped morphology and integrity via TEM. | |
| Potency & Bioactivity | IL-1β cytokine [59] | Pro-inflammatory stimulant | In vitro potency assay to test anti-inflammatory efficacy (e.g., NF-κB pathway inhibition). |
| CCK-8 Assay kit [59] | Cell viability and proliferation | Assess pro-regenerative and cytotoxic effects on recipient cells (e.g., chondrocytes, fibroblasts). | |
| Safety & Impurities | Limulus Amebocyte Lysate (LAL) assay | Endotoxin detection | Critical safety test for parenteral administration. |
| Sterility testing kits (e.g., BacT/ALERT) | Microbial contamination | Ensures product sterility according to pharmacopeial standards. |
Protocol: Standardized Characterization of MSC-Exosomes
Particle Concentration and Size Distribution:
- Dilute purified exosomes in filtered PBS.
- Analyze using Nanoparticle Tracking Analysis (NTA). Settings should be standardized: sensitivity ~75, shutter ~300, minimum trace length ~15, cell temperature 25°C [57]. This provides concentration (particles/mL) and size distribution (expect 70-150 nm) [55].
Morphological Analysis:
- Adsorb exosomes onto a carbon-film copper grid.
- Negative stain with 2% uranyl acetate for 1-2 minutes.
- Image using Transmission Electron Microscopy (TEM) at 80 kV to confirm the characteristic cup-shaped morphology [57].
Western Blot for Marker Profiling:
Potency Assay (Anti-inflammatory Activity):
- Pre-treat human chondrocytes or dermal fibroblasts with IL-1β (e.g., 10 ng/mL) to induce inflammation.
- Co-incubate with MSC-derived exosomes for 24 hours.
- Lyse cells and perform Western Blot analysis for phosphorylated p65 (pp65) and phosphorylated p38 (pp38) to quantify inhibition of NF-κB and MAPK signaling pathways, respectively [59].
Concluding Perspective
The path to successful industrial production of engineered MSC exosomes for chronic wounds requires a closed, automated, and well-controlled platform from cell bank to final product. The integration of iPSC-derived iMSCs with bioreactor technology and TFF-SEC purification represents a transformative strategy to achieve the requisite scalability, quality, and consistency. Adherence to the evolving MISEV guidelines and forthcoming regulatory frameworks will be critical for clinical translation [58] [17]. By implementing these standardized protocols and quality control strategies, researchers and manufacturers can accelerate the development of effective exosome-based therapies for chronic wound healing.
Diagram 2: Multi-attribute quality control framework for exosome products.
Biodistribution and Pharmacokinetic Profiling
Within the development of engineered Mesenchymal Stem Cell (MSC) exosomes for targeted drug delivery in chronic wound therapy, understanding their in vivo journey is paramount. Biodistribution—where exosomes travel in the body—and pharmacokinetics (PK)—how the body handles exosomes over time—are critical for evaluating therapeutic efficacy and safety. For chronic wounds, characterized by a complex and hostile microenvironment, the targeted delivery and sustained retention of exosome-based therapeutics are essential for successful regeneration. This document provides detailed application notes and protocols for profiling these parameters, specifically framed within preclinical studies for chronic wound applications.
Quantitative Biodistribution Data
Systemically administered exosomes exhibit a characteristic biodistribution pattern, predominantly accumulating in the organs of the mononuclear phagocyte system. The table below summarizes quantitative data from a rodent study using radiolabeled exosomes [60].
Table 1: Quantitative Biodistribution of Intravenously Administered 89Zr-Labeled Exosomes in Rodents
| Organ/Tissue | Distribution in Mice (% Injected Dose) | Distribution in Rats (% Injected Dose) | Notes |
|---|---|---|---|
| Liver | High (Primary site) | High (Primary site) | Sustained retention >24 hours [61] [60]. |
| Spleen | High | Moderate to High | Secondary major organ of accumulation [61] [60]. |
| Kidney | Moderate | Moderate | |
| Lung | Moderate | Moderate | Initial pulmonary entrapment can occur post-IV injection [62]. |
| Gastrointestinal Tract | Moderate | Moderate | Includes stomach and intestine [60]. |
| Heart | Low | Low | |
| Brain | Low | Low | Targeted engineering can enhance delivery [61]. |
| Blood Circulation | Very Low (Rapid clearance) | Very Low (Rapid clearance) | Half-life (t1/2) of only a few minutes [61] [60]. |
Key Experimental Protocols
Protocol: Radiolabeling of MSC Exosomes with Zirconium-89 for PET/CT Imaging
This protocol details the surface radiolabeling of GMP-grade MSC exosomes for sensitive and quantitative biodistribution and PK studies using Positron Emission Tomography/Computed Tomography (PET/CT) [60].
Table 2: Research Reagent Solutions for 89Zr Radiolabeling
| Reagent/Material | Function in the Protocol |
|---|---|
| GMP-grade MSC Exosomes (e.g., ILB-202) | The therapeutic nanoparticle whose biodistribution is being studied. |
| Amine-reactive Desferrioxamine (DFO; p-NCS-Bn-DFO) | Chelator that covalently binds to surface amines on exosomes to capture the radioisotope. |
| Zirconium-89 (89Zr) Oxalate | Positron-emitting radioisotope for sensitive detection and quantification via PET. |
| Size-Exclusion Chromatography (SEC) Columns | For purifying labeled exosomes from free, unincorporated 89Zr and DFO. |
| Phosphate-Buffered Saline (PBS) | Buffer for exosome resuspension and column equilibration/washing. |
Procedure:
- DFO Conjugation: Resuspend purified MSC exosomes (100-500 µg protein) in PBS. Add amine-reactive DFO (dissolved in DMSO) to the exosome suspension at a molar ratio optimized for your exosome preparation (e.g., 50-200 µM final DFO concentration). Incubate the mixture for 1 hour at 37°C with gentle agitation.
- Purification: Remove unreacted DFO by passing the mixture through a size-exclusion chromatography column (e.g., PD-10 desalting column) pre-equilibrated with PBS. Collect the exosome-containing fractions.
- 89Zr Labeling: Add the purified DFO-exosomes directly to neutralized 89Zr oxalate (37-74 MBq). Incubate the reaction for 1 hour at room temperature with gentle mixing.
- Final Purification: Pass the labeling reaction mixture through a fresh SEC column to separate 89Zr-labeled exosomes (89Zr-Exo) from free 89Zr. Collect the purified 89Zr-Exo fraction in PBS.
- Quality Control: Determine radiochemical purity and stability using instant thin-layer chromatography (iTLC). Measure exosome concentration (e.g., via BCA protein assay) and radioactivity using a gamma counter. Confirm that labeling does not alter exosome size or integrity using Nanoparticle Tracking Analysis (NTA).
Protocol: Quantitative Biodistribution and PK Analysis in Rodent Models
This protocol describes the in vivo and ex vivo assessment of 89Zr-Exo in mouse and rat models to simulate systemic delivery for chronic wound therapy [60].
Procedure:
- Animal Dosing: Administer the purified 89Zr-Exo (e.g., 100 µL containing 1-5 MBq) via intravenous injection (e.g., tail vein) into mice or rats. Ensure all animal procedures are approved by the relevant Institutional Animal Care and Use Committee (IACUC).
- In Vivo PET/CT Imaging: At predetermined time points post-injection (e.g., 5 minutes, 1, 4, 24, 48, and 72 hours), anesthetize the animals. Acquire PET scans followed by CT scans for anatomical co-registration. Quantify the radioactivity signal in regions of interest (ROIs) drawn over major organs and the wound site (if present) using imaging analysis software. Standardize uptake values as Percentage of Injected Dose per Gram of tissue (%ID/g).
- Ex Vivo Gamma Counting: At the terminal time point (e.g., 7 days post-injection), euthanize the animals. Collect blood, major organs (liver, spleen, kidneys, lungs, heart, brain), and wound tissue. Weigh each sample and measure radioactivity using a gamma counter. Calculate the %ID/g for each tissue, providing highly accurate quantitative data to complement the imaging results.
- PK Analysis: Plot blood radioactivity levels over time. Use non-compartmental analysis in PK software to calculate key PK parameters, including elimination half-life (t1/2), clearance (CL), and volume of distribution (Vd).
Visualization of Experimental Workflow
The following diagram illustrates the complete experimental workflow for the radiolabeling and biodistribution study of engineered MSC exosomes.
Diagram 1: Experimental workflow for exosome biodistribution study.
Factors Influencing Biodistribution and Targeting Strategies
The inherent biodistribution of exosomes can be modulated by several factors. Understanding these is key to engineering exosomes for improved targeting to chronic wounds.
The following diagram summarizes the major factors affecting exosome biodistribution and how they inform engineering strategies for targeted delivery to chronic wounds.
Diagram 2: Factors affecting biodistribution and engineering strategies.
Key Factors and Engineering Implications:
- Cellular Origin: Exosomes from different cellular sources show distinct biodistribution patterns. Neural stem cell-derived EVs show preferential brain targeting compared to MSC-EVs, while tumor-derived exosomes may home to their parental tumors [61]. Implication: Selecting MSCs from specific tissues (e.g., umbilical cord, adipose) or preconditioning them to mimic wound-homing phenotypes can influence the inherent targeting of their exosomes [31] [14].
- Membrane Composition: Proteins (e.g., integrins, tetraspanins), lipids, and glycans on the exosomal surface dictate organotropism and cellular uptake by interacting with receptors on target cells [61]. Implication: Genetically engineering parent MSCs to express targeting ligands (e.g., RGD peptides for angiogenesis, anti-ICAM-1 for inflamed endothelium) or chemically conjugating these ligands directly to the exosome surface can actively redirect exosomes to specific cells within the chronic wound microenvironment [31] [61] [63].
- Administration Route: Intravenous administration leads to initial pulmonary entrapment and widespread systemic distribution [62]. Implication: For chronic wounds, local administration (e.g., topical, intradermal) or the use of biomaterial-based scaffolds (e.g., hydrogels) can dramatically enhance local retention at the wound site, providing sustained release and overcoming rapid systemic clearance [31] [21] [64].
Strategies to Minimize Off-Target Effects and Maximize Wound Site Retention
The therapeutic potential of mesenchymal stem cell (MSC)-derived exosomes in chronic wound healing is significantly hampered by two major challenges: rapid clearance from the wound site and insufficiently specific targeting, leading to potential off-target effects and reduced therapeutic efficacy [65] [37]. The hostile, protease-rich wound environment further degrades exosomes before they can exert their full regenerative influence [66] [67]. This application note details a suite of engineered strategies designed to overcome these biological barriers. By systematically modifying the exosome surface, controlling their release kinetics, and leveraging active targeting mechanisms, these protocols aim to enhance local retention and precision, thereby maximizing therapeutic outcomes while minimizing systemic exposure in chronic wound treatment.
Core Engineering Strategies
The following table summarizes the primary engineering approaches to optimize exosome pharmacokinetics and biodistribution.
Table 1: Core Engineering Strategies for MSC Exosomes in Wound Healing
| Strategy Category | Specific Method | Key Mechanism of Action | Primary Outcome |
|---|---|---|---|
| Surface Modification | Genetic engineering of parent MSCs to express RGD peptide on exosome surface [65] | Binds to αvβ3 integrins highly expressed on endothelial cells in angiogenic wound vasculature [65] | Enhanced active targeting to wound neovasculature; Increased cellular uptake |
| Surface Modification | CP05 peptide conjugation to exosome surface [65] | Binds to heparan sulfate proteoglycans on target cell membranes [65] | Improved specificity for cellular entry at the wound site |
| Biomaterial Integration | Encapsulation within injectable hyaluronic acid (HA) hydrogel [10] | Forms a biodegradable, in-situ crosslinked matrix that acts as a sustained-release reservoir [10] | Prolonged exosome residence time in the wound bed; Protection from degradation |
| Biomaterial Integration | Incorporation into PEGylated poly(glycerol sebacate) acrylate hydrogel [65] | Provides a scaffold for localized delivery and controlled release [65] | Increased localization and bioavailability at the target site |
| Preconditioning & Cargo Loading | Hypoxic preconditioning of parent MSCs [68] | Upregulates pro-angiogenic miRNAs (e.g., miR-524-5p) and lncRNAs via HIF-1α stabilization [68] | Enhances intrinsic angiogenic activity; Modulates inflammatory response |
| Preconditioning & Cargo Loading | TM-nanoEP system for loading specific mRNAs (e.g., VEGF-A, BMP-2) [65] | Enables mass production of exosomes pre-loaded with specific therapeutic genetic cargo [65] | Targeted multi-factor therapy promoting synergistic angiogenic-osteogenic pathways |
Diagram: Integrated Engineering Strategies for Targeted Exosome Delivery. This map illustrates how surface modification, biomaterial integration, and preconditioning synergize to enhance wound site retention and minimize off-target effects.
Quantitative Assessment of Engineered Exosomes
Rigorous in vitro and in vivo characterization is essential to validate the efficacy of engineered exosomes. The following table outlines key quantitative metrics and the methods used to assess them.
Table 2: Key Metrics and Methods for Assessing Engineered Exosome Performance
| Performance Metric | Analytical Method | Description & Target Outcome |
|---|---|---|
| Size & Concentration | Nanoparticle Tracking Analysis (NTA) [65] [2] | Confirms exosome size (30-150 nm) and quantifies yield post-engineering. |
| Cellular Uptake & Targeting | Confocal Laser Scanning Microscopy (CLSM) [69] | Visualizes fluorescently-labeled (e.g., PKH67, DiD) exosome uptake by target cells (e.g., keratinocytes, fibroblasts). |
| Wound Retention & Biodistribution | In Vivo Imaging System (IVIS) [65] | Tracks near-infrared (NIR) dye-labeled (e.g., DiR) exosomes over time in animal wound models to quantify retention. |
| In Vivo Therapeutic Efficacy | Histological Analysis [67] | Measures enhanced re-epithelialization, granulation tissue thickness, and angiogenesis in wound tissues. |
| Surface Marker Purity | Western Blotting [65] [2] | Detects presence of exosomal markers (CD63, CD81, CD9, TSG101) and absence of contaminants. |
Detailed Experimental Protocols
Protocol: Functionalization of MSC Exosomes with RGD Peptide
Objective: To genetically engineer MSC-derived exosomes to display RGD peptides on their surface for enhanced targeting of integrins in the wound bed [65].
Materials:
- Parent MSCs (e.g., human adipose-derived MSCs)
- Lentiviral vector encoding a fusion protein: Lamp2b-RGD
- Polybrene (8 µg/mL)
- Polycarbonate membranes (100 nm)
- Exosome-depleted FBS
- Ultracentrifugation equipment
Procedure:
- Genetic Modification: Transduce parent MSCs with the Lentiviral-Lamp2b-RGD construct in the presence of 8 µg/mL Polybrene for 24 hours [65].
- Selection & Expansion: Select successfully transduced cells using an appropriate antibiotic (e.g., puromycin) for 1-2 weeks. Expand the stable cell line.
- Exosome Production: Culture engineered MSCs in media supplemented with exosome-depleted FBS for 48 hours.
- Isolation & Purification: Collect conditioned media. Isolate exosomes via differential ultracentrifugation: 300 × g for 10 min (remove cells), 2,000 × g for 20 min (remove debris), 10,000 × g for 30 min (remove large vesicles), and finally 100,000 × g for 70 min (pellet exosomes) [2]. Resuspend the pellet in PBS.
- Validation: Confirm RGD presence on the exosome surface via western blot for the Lamp2b fusion protein and demonstrate enhanced binding to αvβ3 integrin in a solid-phase binding assay [65].
Protocol: Incorporation of Engineered Exosomes into an Injectable Hydrogel
Objective: To encapsulate RGD-functionalized exosomes within a hyaluronic acid-based hydrogel for sustained release at the wound site [10].
Materials:
- Methacrylated hyaluronic acid (Me-HA)
- Photoinitiator (e.g., LAP - Lithium phenyl-2,4,6-trimethylbenzoylphosphinate)
- RGD-functionalized MSC exosomes (from Protocol 4.1)
- UV light source (365 nm, 5-10 mW/cm²)
Procedure:
- Hydrogel Precursor Preparation: Dissolve Me-HA in PBS to a final concentration of 2% (w/v). Add the LAP photoinitiator to a final concentration of 0.05% (w/v) [10].
- Exosome Encapsulation: Mix the engineered exosomes uniformly into the Me-HA/LAP solution on a rotator at 4°C to prevent premature gelling.
- In Situ Crosslinking: Apply the exosome-loaded Me-HA solution directly onto the wound bed in an animal model. Illuminate with UV light (365 nm) for 2-5 minutes to initiate crosslinking and form a stable hydrogel in situ [10].
- Release Kinetics: To quantify release, immerse the formed hydrogel in PBS at 37°C under gentle agitation. Collect release medium at predetermined time points and use NTA or ELISA to measure exosome concentration.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Engineering and Evaluating Targeted Exosomes
| Reagent / Material | Function | Justification |
|---|---|---|
| Lentiviral-Lamp2b-RGD Vector [65] | Genetically engineers parent MSCs to display targeting peptides on exosome surface. | Provides a stable and heritable method for consistent exosome surface engineering. |
| Methacrylated Hyaluronic Acid [10] | Forms the backbone of an in-situ crosslinkable, bioactive hydrogel delivery system. | Biocompatible, biodegradable, and mimics the native extracellular matrix, supporting wound healing. |
| Photoinitiator (LAP) [10] | Initiates crosslinking of the hydrogel upon UV exposure, entrapping exosomes. | Enables rapid, controllable gelation directly in the wound bed, forming a localized depot. |
| Near-Infrared Dye (DiR) [65] | Labels exosomes for non-invasive in vivo tracking and biodistribution studies. | Allows longitudinal quantification of wound retention and off-target distribution using IVIS. |
| CD63 / CD81 Antibodies [2] | Identifies and validates isolated exosomes via Western Blot or flow cytometry. | Standard markers for confirming exosome identity and purity post-isolation. |
| Track-Etched Membrane-Based Nanoelectroporation System [65] | Actively loads therapeutic nucleic acids (mRNA, miRNA) into pre-formed exosomes. | Enables high-efficiency loading of specific cargo without damaging exosome integrity. |
The synergistic application of surface engineering, biomaterial-assisted delivery, and cargo optimization represents a paradigm shift in the use of MSC exosomes for chronic wound therapy. The protocols detailed herein provide a robust framework for researchers to create next-generation exosome therapies that remain active at the wound site with greater specificity. By systematically addressing the key challenges of retention and targeting, these strategies unlock the full potential of exosomes as programmable nanomedicines, paving the way for enhanced precision and efficacy in regenerative wound care.
Preclinical and Clinical Evidence: Efficacy, Safety, and Competitive Positioning
Within the framework of a thesis on engineering mesenchymal stem cell (MSC) exosomes for targeted drug delivery, the selection and application of biologically relevant animal models is a critical prerequisite for generating translatable data. Chronic wounds, including diabetic, venous, and pressure ulcers, represent a major challenge in clinical practice, characterized by complex, impaired healing processes. The path to clinical translation for novel therapies like engineered exosomes is paved by rigorous preclinical testing in animal models that faithfully recapitulate key aspects of human disease pathophysiology. This document provides a detailed overview of the efficacy, application notes, and standardized protocols for the most clinically relevant animal models of diabetic, venous, and pressure ulcers, with a specific focus on their utility in evaluating MSC-exosome based therapeutics.
Comparative Efficacy of Animal Models for Chronic Wounds
The tables below summarize the key characteristics and quantitative efficacy data of prominent animal models for diabetic, pressure, and ischemic wounds, providing a basis for model selection.
Table 1: Efficacy and Characteristics of Major Diabetic Ulcer Models
| Model Type | Wound Healing Delay (vs. Control) | Key Advantages | Key Limitations | Best Use for Exosome Therapy Testing |
|---|---|---|---|---|
| db/db Mouse | Largest consistent delay; Significant at days 3, 7, 11, 15 [70] | Robust, consistent healing impairment; Genetic type 2 diabetes background [70] [71] | Obesity as confounding factor; Requires careful monitoring | Evaluating pro-proliferative and re-epithelialization effects |
| STZ-Induced Diabetic Mouse | Significantly decreased healing at all time points [70] | Inducible model; Allows use of various mouse strains and genetic backgrounds [70] [71] | Chemical toxicity; Variable diabetes induction | Testing anti-inflammatory and immunomodulatory exosome functions |
| STZ + High-Fat Diet Mouse | Significantly delayed healing [70] | Models metabolic syndrome; More human-like pathophysiology [70] | Complex and time-consuming to establish | Assessing exosome function in complex metabolic dysfunction |
| ob/ob Mouse | Delayed healing, but based on fewer studies [70] | Genetic model of leptin deficiency leading to type 2 diabetes [71] | Severe obesity; Leptin pathway not primary in humans | Investigating mechanisms in leptin-related pathways |
Table 2: Models for Pressure and Ischemic Ulcers
| Model Type | Animal Species | Induction Method | Wound Healing Delay & Key Findings | Relevance to Human Condition |
|---|---|---|---|---|
| Pressure Ulcer | Mouse | Magnet-induced Ischemia-Reperfusion (IR) | Persistent wound infection with S. aureus; Controlled, reproducible injury [72] | Highly relevant; mimics human ischemia-reperfusion injury [73] [72] |
| Pressure Ulcer | Mouse | Compression Device (IR) | Full-thickness skin breakdown [73] | Models deep tissue injury [73] |
| Ischemic Limb Ulcer | Rat, Mouse, Rabbit | Femoral/iliac artery ligation | Day 7 SMD: 5.36; Day 14 SMD: 4.50; Day 21 SMD: 2.53 [74] | Directly models critical limb ischemia [74] |
Detailed Experimental Protocols
Protocol for db/db Mouse Diabetic Ulcer Model
This protocol is designed to test the efficacy of engineered MSC exosomes in a robust model of impaired wound healing.
- Animal Model: db/db mice (C57BL/KsJ background), 8-12 weeks old, gender as required by study design. Note: Age influences wound healing in this model [70].
- Control: db/+ or wild-type littermates.
- Materials:
- Anesthesia apparatus (Isoflurane recommended)
- Depilatory cream
- Surgical clippers
- Ethanol (70%) and betadine swabs
- Biopsy punch (4-6 mm diameter)
- Silicone splints (e.g., from 0.5 mm thick sheet)
- Cyanocrylate tissue adhesive (e.g., Vetbond) or sutures
- Non-adhesive dressing (e.g., Tegaderm)
- Test Article: Engineered MSC exosomes in suitable vehicle (e.g., hydrogel)
- Control: Vehicle alone
- Pre-operative Procedure:
- Acclimate mice for at least 7 days.
- Confirm hyperglycemia (blood glucose >300 mg/dL).
- Anesthetize the mouse.
- Remove hair from the dorsal surface using clippers and depilatory cream.
- Disinfect the skin with alternating betadine and 70% ethanol swabs.
- Wound Creation & Splinting:
- Place the mouse in a lateral recumbent position.
- Critical Step: Center a silicone splint over the dorsal skin and secure it firmly to the skin using cyanocrylate adhesive. The splint prevents wound contraction, forcing healing primarily by re-epithelialization, which more closely mimics human healing [70].
- Using a sterile biopsy punch, create a full-thickness excisional wound within the splint's center.
- Apply direct pressure with a sterile swab to ensure complete hemostasis.
- Treatment & Post-operative Care:
- Randomize animals into treatment and control groups.
- Apply the first dose of engineered exosomes in vehicle (or vehicle alone) topically to the wound bed.
- Cover the wound and splint with a non-adhesive dressing.
- House mice individually post-operation.
- Administer treatments according to the study schedule (e.g., daily, every other day).
- Change dressings and re-apply treatment at each time point.
- Outcome Measures:
- Macroscopic: Daily wound photography with a scale reference. Calculate wound area using image analysis software (e.g., ImageJ). Plot wound closure percentage over time.
- Histological: At endpoint, harvest wounds with a margin of unwounded tissue. Process for H&E staining (for re-epithelialization and granulation tissue), Masson's Trichrome (for collagen), and immunohistochemistry (for specific markers like CD31 for angiogenesis, or cell-specific markers to track exosome effects).
- Molecular: Analyze gene expression (qPCR) or protein levels (Western Blot, ELISA) from wound tissue homogenates for cytokines (e.g., TNF-α, IL-10), growth factors (e.g., VEGF, TGF-β), and other relevant targets.
Protocol for Murine Magnet-Induced Pressure Ulcer Model
This model is ideal for testing exosome therapies in the context of ischemia-reperfusion injury and bacterial infection, common in pressure ulcers.
- Animal Model: Balb/c or C57BL/6 mice, 8-12 weeks old.
- Materials:
- Two round ferrite magnets (12 mm diameter, 5 mm thickness, ~0.3 kg pulling force) [72]
- Bioluminescent Staphylococcus aureus strain (e.g., SAP229) for infection studies [72]
- In Vivo Imaging System (IVIS)
- Hydroxyethylcellulose (HEC) gel or similar hydrogel
- Primary dressing (e.g., Mepilex Transfer)
- Secondary dressing (e.g., Tegaderm film)
- Flexible self-adhesive bandage
- Procedure:
- Anesthetize and depilate the dorsal skin of the mouse as in section 3.1.
- Ischemia Induction: Sandwich a fold of the depilated dorsal skin between two magnets, ensuring full contact. Leave a 1 cm space between adjacent magnet pairs if multiple wounds are created [72].
- Return the mouse to its cage. The magnets will stay in place without further restraint.
- After a 16-hour ischemia period, remove the magnets.
- Allow for a 6-hour reperfusion period. A clear, round ischemic area will be visible.
- (Optional) Infection: Inoculate the ischemic wound with 10^4 CFU of bioluminescent S. aureus in a small volume (e.g., 10 μL) [72].
- Treatment & Monitoring:
- Apply the test article (e.g., engineered exosomes in HEC gel) or vehicle control to the wound.
- Cover with a primary dressing, secondary film dressing, and a bandage to secure.
- Change dressings and re-apply treatment under anesthesia as required by the study design.
- Longitudinal Imaging: Monitor infection and wound healing non-invasively using IVIS to quantify bacterial bioluminescence at regular intervals (e.g., days 1, 3, 7, 10, 14) [72].
- Outcome Measures:
- Bioluminescence Imaging: Quantify total flux (photons/sec) to monitor bacterial burden.
- Bacteriology: Swab wounds or homogenize tissue at endpoint for CFU counting.
- Macroscopic: Wound area measurement.
- Histological & Cytokine Analysis: As in section 3.1, with focus on inflammatory markers and bacterial clearance.
Protocol for Ischemic Limb Ulcer Model
This model tests the pro-angiogenic potential of therapies in a context of severe hypoxia.
- Animal Model: Rat (e.g., Sprague-Dawley) or C57BL/6 mouse.
- Materials:
- Microsurgical instruments (fine scissors, forceps, needle holder)
- Silk or nylon sutures (6-0 or 8-0)
- Bipolar coagulator
- Hair clippers and depilatory cream
- Procedure (Femoral Artery Ligation):
- Anesthetize the animal and depilate the groin and inner thigh.
- Make a vertical incision in the skin over the femoral triangle.
- Carefully dissect through the subcutaneous tissue to expose the femoral neurovascular bundle.
- Under high magnification if necessary, meticulously separate the femoral artery from the accompanying femoral vein and nerve.
- Ligate the femoral artery proximally and distally using non-absorbable sutures.
- Critical Step: Excise the artery segment between the two ligatures to prevent spontaneous reperfusion.
- Confirm blanching of the limb as evidence of successful ischemia induction.
- Close the skin incision with sutures or wound clips.
- Wound Creation & Evaluation:
- A full-thickness excisional wound can be created on the dorsal surface of the foot or lateral thigh immediately after ligation [74].
- Apply treatments (exosomes/control) topically as described in previous protocols.
- Monitor wound healing macroscopically and via histology. The primary readout is the significant delay in healing compared to a non-ischemic wound, as quantified in Table 2 [74].
Visualization: Mechanisms and Workflows
The following diagrams illustrate the therapeutic targeting of engineered exosomes and a standardized experimental workflow.
Engineered Exosome Mechanisms in Chronic Wounds
Integrated Workflow for Evaluating Exosome Therapies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Chronic Wound Studies
| Item | Function/Application | Example & Notes |
|---|---|---|
| db/db Mice | Genetic model for Type 2 Diabetic ulcers | C57BL/KsJ background; monitor blood glucose levels [70] [71] |
| Ceramic Magnets | Inducing ischemia-reperfusion injury for pressure ulcers | 12 mm diameter, 5 mm thickness; generates ~50 mmHg pressure [73] [72] |
| Bioluminescent S. aureus | Tracking bacterial load in infected wound models | Strain SAP229; enables non-invasive monitoring via IVIS [72] |
| Silicone Splints | Preventing wound contraction in excisional models | Forces healing by re-epithelialization; improves clinical relevance [70] |
| Hydrogel (e.g., HEC) | Vehicle for topical application of exosomes | Maintains moisture and provides a scaffold for sustained release [72] |
| In Vivo Imaging System (IVIS) | Non-invasive, longitudinal monitoring of infection/wounds | Quantifies bacterial bioluminescence and can use fluorescent probes [72] |
| MSC-Exosome Isolation Kits | Purifying exosomes from conditioned media | Ultracentrifugation or commercial kits (e.g., from System Biosciences) |
| Angiogenesis Antibodies | Histological assessment of vascularization (e.g., CD31/PECAM-1) | Critical for evaluating pro-angiogenic effects of therapies [71] |
| Cytokine ELISA Kits | Quantifying inflammatory markers in wound tissue | Analyze TNF-α, IL-1β, IL-6, IL-10, VEGF, etc. [14] [71] |
Analysis of Ongoing Clinical Trials and Registered Studies
The transition of engineered Mesenchymal Stem Cell (MSC)-derived exosomes from preclinical research to clinical application represents a pivotal frontier in regenerative medicine for chronic wound treatment. As a cell-free therapeutic modality, these exosomes offer a promising alternative to whole-cell therapy by overcoming challenges such as low cell survival, immunogenicity, and tumorigenic risks [75] [76]. This document provides a critical analysis of the current clinical trial landscape, details standardized protocols for exosome engineering and evaluation, and outlines the necessary reagents and methodologies to advance this technology toward clinical validation. The focus is on engineered exosomes (eExo) designed for targeted drug delivery, which demonstrate enhanced stability, specificity, and therapeutic efficacy in the complex microenvironment of chronic wounds [12] [77].
Analysis of Registered Clinical Studies
A systematic search of clinical trial registries, including ClinicalTrials.gov, reveals a nascent but rapidly evolving field. As of the last search, a limited number of interventional clinical trials specifically investigating engineered MSC exosomes for chronic wounds were identified. The majority of registered studies focus on natural, unmodified MSC-derived exosomes or extracellular vesicles (EVs). This gap underscores the translational lag between extensive preclinical validation of eExo and their entry into clinical testing. The available data on relevant clinical registries can be summarized as follows:
- Predominance of Preclinical Data: The vast majority of evidence supporting eExo therapy comes from robust preclinical studies. A recent meta-analysis of 83 preclinical studies confirmed the significant potential of MSC-EVs in promoting wound closure and skin regeneration in both diabetic and non-diabetic animal models [78].
- Therapeutic Advantages Driving Clinical Interest: The registered studies and scientific literature are founded on key therapeutic advantages of MSC exosomes, which are further enhanced through engineering [19] [76]:
- Biocompatibility and Low Immunogenicity: Reduced risk of host immune rejection compared to cell-based therapies.
- Targeted Delivery and Enhanced Penetration: Innate ability to cross biological barriers; this can be improved via surface engineering for precise targeting of wound cell types.
- Stability and Storage: Suitability for long-term storage (e.g., lyophilized forms) and transport without significant loss of bioactivity.
- Multimodal Therapeutic Action: Simultaneous modulation of inflammation, promotion of angiogenesis, and stimulation of cell proliferation.
Detailed Experimental Protocols for eExo Evaluation
This section outlines standardized protocols for the key experiments used to validate engineered exosomes in preclinical models, providing a roadmap for generating data compliant with future clinical trial applications.
Protocol: In Vivo Efficacy Testing in a Diabetic Wound Model
Objective: To evaluate the efficacy of eExo in promoting healing in a genetically diabetic (db/db) mouse model, which mimics human type 2 diabetic foot ulcers [78].
Materials:
- Animals: db/db mice (e.g., BKS.Cg-Dock7m +/+ Leprdb/J).
- eExo Preparation: Engineered exosomes suspended in sterile PBS.
- Control Groups: Natural exosomes, PBS vehicle, and standard-of-care gel (e.g., Puraply).
- Equipment: Punch biopsy tool, digital camera, calipers, histology equipment.
Methodology:
- Wound Creation: Anesthetize mice and create two full-thickness excisional wounds (e.g., 6 mm diameter) on the dorsal skin.
- Randomization and Blinding: Randomly assign animals to treatment groups and code all samples to ensure blinded analysis.
- Treatment Administration:
- Route: Subcutaneous injection around the wound periphery (identified as highly effective [78]) or topical application via a hydrogel dressing [10] [77].
- Dosage: Administer a defined quantity of eExo (e.g., 100 µg in 100 µL PBS) every 3-4 days until wound closure.
- Frequency: Monitor animals and administer treatments according to the predefined schedule.
- Outcome Measures:
- Primary Endpoint: Wound closure rate. Capture digital images daily and calculate wound area using image analysis software (e.g., ImageJ). Present data as percent reduction from original area.
- Secondary Endpoints:
- Histology: Upon sacrifice, harvest wound tissue for H&E staining to assess re-epithelialization and granulation tissue formation. Use Masson's trichrome staining to evaluate collagen deposition and maturity.
- Immunohistochemistry: Stain for CD31 to quantify blood vessel density (angiogenesis) and for specific cell proliferation markers (e.g., Ki67).
- Scar Width Measurement: Measure collagen fiber alignment and scar width in fully healed tissues to assess scar quality [78].
Protocol: Tracking Biodistribution of Engineered Exosomes
Objective: To assess the targeting efficiency and retention of eExo at the wound site following different administration routes.
Materials:
- Labeled eExo: eExo loaded with a lipophilic near-infrared (NIR) dye (e.g., DiR or DIR-BOA [77]).
- Imaging System: In vivo imaging system (IVIS).
Methodology:
- Preparation: Label eExo using a membrane dye according to manufacturer's protocol and remove excess dye via size-exclusion chromatography.
- Administration: Administer the labeled eExo to wounded animals via the routes under investigation (e.g., subcutaneous injection vs. topical hydrogel).
- Imaging: Anesthetize mice and image them at predetermined time points (e.g., 1, 4, 12, 24, 48 hours post-administration) using the IVIS system.
- Analysis: Quantify the fluorescence signal intensity specifically at the wound site and in major organs (liver, spleen, lungs) to evaluate targeting efficiency and systemic clearance.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting research on engineered MSC exosomes for chronic wound therapy.
Table 1: Key Research Reagent Solutions for Engineered MSC Exosome Research
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| MSC Sources | Cellular origin for exosome production. | Adipose tissue (ADSC), Bone Marrow (BMSC), Umbilical Cord (UCMSC). ADSC exosomes show strong effect on wound closure [78] [79]. |
| Isolation Kits | Purification of exosomes from cell culture media. | Ultracentrifugation, size-exclusion chromatography, or commercial kits (e.g., from ThermoFisher, System Biosciences). Combination of methods often yields optimal results [79]. |
| Characterization Antibodies | Confirmation of exosome identity via surface markers. | Anti-CD63, Anti-CD81, Anti-CD9 (Tetraspanins); Anti-TSG101 [79]. |
| Engineering Ligands | Surface functionalization for active targeting. | RVG peptide (neurotropism), Transferrin (BBB crossing), Mannose (macrophage targeting) [80] [12]. |
| Scaffold/ Hydrogel | Sustained release delivery system at the wound site. | Hyaluronic acid hydrogel [10], Chitosan-based scaffolds, Collagen matrices. Critical for maintaining local eExo concentration [77]. |
| Animal Models | Preclinical in vivo efficacy testing. | db/db mouse (Type 2 diabetes), STZ-induced diabetic mouse/rat, full-thickness excisional wound model [78]. |
Visualizing Experimental Workflows and Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate core experimental workflows and the therapeutic mechanisms of eExo.
Workflow for eExo Development and Testing
Diagram Title: Engineered Exosome R&D Workflow
eExo Signaling Mechanisms in Wound Healing
Diagram Title: eExo Mechanisms in Wound Healing
The analysis of the clinical trial landscape confirms that engineered MSC exosomes are poised to revolutionize the treatment of chronic wounds, yet their clinical entry is still in its early stages. The structured protocols and toolkit provided here are designed to standardize preclinical research, bridge the gap between bench and bedside, and accelerate the initiation of robust clinical trials. Future efforts must focus on standardizing manufacturing according to Good Manufacturing Practice (GMP), scaling up production, and conducting rigorous safety and toxicology studies. As engineering strategies become more sophisticated—incorporating features for on-demand drug release or multi-targeting—the transition of eExo from a promising therapeutic concept to a registered clinical product will define the next era of regenerative medicine.
The management of chronic wounds remains a significant clinical challenge, driving the development of advanced therapeutic strategies. This document provides a comparative analysis of emerging exosome-based therapies against conventional treatments, focusing on efficacy, mechanisms of action, and practical application. Engineered exosomes, particularly those derived from mesenchymal stem cells (MSCs), demonstrate enhanced therapeutic potential through targeted drug delivery and precision modulation of the wound microenvironment. We present standardized protocols for the evaluation of these therapies and essential reagent solutions to facilitate translational research in chronic wound healing.
Chronic wounds (CWs), defined as wounds that fail to proceed through an orderly and timely healing process within 3 months, represent a growing global health concern with profound clinical and socioeconomic implications [81] [12]. These wounds, including diabetic foot ulcers, venous leg ulcers, and pressure ulcers, become stalled in the inflammatory phase of healing, preventing normal recovery [81]. Studies indicate that approximately 15% of CWs remain unhealed one year after initial treatment, with an estimated 1-2% of the population in developed countries experiencing CWs during their lifetime [81].
Conventional therapies such as compression bandages, antibiotics, hyperbaric oxygen, and skin grafts face substantial limitations, including toxicity, contraindications, inefficacy in patients with comorbidities like diabetes, and high cost [81]. The inherent complexity of the chronic wound microenvironment—characterized by persistent inflammation, excessive reactive oxygen species (ROS), impaired angiogenesis, and elevated alkaline pH—further complicates treatment efficacy [81] [12]. This therapeutic gap has accelerated research into biologically-driven strategies, particularly extracellular vesicle (EV)-based therapies, which offer innate biocompatibility, targeted biodistribution, and multifunctional regenerative properties [81].
Among EV-based approaches, exosomes have emerged as transformative solutions. These naturally secreted, nanosized particles (30-150 nm) facilitate intercellular communication by transferring bioactive molecules such as proteins, lipids, and nucleic acids to recipient cells [2] [13]. The advent of engineered exosomes represents a significant advancement, enabling enhanced targeting specificity, controlled cargo loading, and improved stability in the challenging wound microenvironment [2] [82]. This Application Note provides a comprehensive framework for comparing the efficacy of natural versus engineered exosomes against conventional therapies, with specific protocols for their evaluation in chronic wound research.
Comparative Analysis of Therapeutic Modalities
Table 1: Comprehensive Comparison of Chronic Wound Therapies
| Therapeutic Characteristic | Conventional Therapies | Natural Exosomes | Engineered Exosomes |
|---|---|---|---|
| Mechanism of Action | Compression, oxygen delivery, antimicrobial activity | Innate immunomodulation, angiogenesis stimulation, cell proliferation | Targeted drug delivery, enhanced immunomodulation, programmed matrix remodeling |
| Key Advantages | Established protocols, widespread availability | High biocompatibility, low immunogenicity, intrinsic regenerative signals | Precision targeting, controlled release, enhanced stability, customizable cargo |
| Primary Limitations | Toxicity, contraindications, inefficacy with comorbidities, high cost [81] | Heterogeneity, limited scalability, rapid clearance, insufficient targeting [81] [82] | Complex manufacturing, standardization challenges, regulatory hurdles [82] |
| Healing Rate Efficacy | Variable: NPWT+HBOT shows 20.15% area reduction by day 12 [83] | Superior to conventional in pre-clinical models | Enhanced over natural exosomes via optimized cargo and targeting |
| Targeting Specificity | Low (systemic effects) | Moderate (passive targeting) | High (active targeting via surface engineering) |
| Manufacturing Complexity | Low to moderate | Moderate (isolation and purification challenges) | High (requires additional engineering steps) |
| Regulatory Status | Established pathways | Emerging frameworks | Complex regulatory pathway |
Analysis of Conventional Therapies
Current conventional therapies for chronic wounds include debridement techniques, negative pressure wound therapy (NPWT), hyperbaric oxygen therapy (HBOT), and skin grafts [81] [84]. The TIME framework (Tissue, Inflammation/Infection, Moisture Imbalance, Epithelial Edge Advancement) provides a systematic approach to wound bed preparation, which is essential for successful integration of any advanced therapy [84]. While these approaches provide foundational care, they face significant limitations: compression therapy is contraindicated in patients with arterial insufficiency, antibiotics struggle with biofilm persistence and microbial resistance, and HBOT is cost-prohibitive and equipment-dependent [81]. Recent clinical evidence demonstrates that combining NPWT with HBOT significantly improves wound healing rates (20.15% vs. 14.9% area reduction by day 12) compared to NPWT alone, highlighting the potential of combination approaches [83].
Natural Exosomes: Mechanisms and Limitations
Natural exosomes, particularly those derived from MSCs, fibroblasts, and keratinocytes, promote wound healing through multiple mechanisms. They facilitate immunomodulation by stimulating macrophage polarization from the pro-inflammatory M1 phenotype to anti-inflammatory M2 phenotype, reducing serum levels of key pro-inflammatory cytokines like TNF-α [81]. Additionally, they promote angiogenesis through delivery of vascular endothelial growth factor (VEGF) and other angiogenic factors, enhance cell proliferation and migration, and facilitate extracellular matrix remodeling [81] [12]. Their innate biocompatibility and low immunogenicity make them attractive therapeutic vehicles. However, natural exosomes face challenges in scalable production, purification complexity, heterogeneity, insufficient targeting capability, and rapid clearance [81] [82]. They primarily accumulate in the liver, spleen, and lung tissue, leading to weak tumor-targeting ability in cancer applications, a limitation that also affects wound targeting efficiency [82].
Engineered Exosomes: Enhanced Therapeutic Potential
Engineered exosomes address the limitations of natural exosomes through advanced bioengineering techniques. Both endogenous and exogenous modification approaches can enhance their functionality [85] [82]. Endogenous strategies involve genetically modifying parent MSCs to modulate EV content or surface proteins, while exogenous techniques include post-isolation loading of therapeutic cargo and membrane modifications [85]. These engineering approaches enable:
- Enhanced Targeting Specificity: Surface modification with targeting ligands (antibodies, peptides) improves precision delivery to wound sites [82].
- Optimized Cargo Loading: Therapeutic molecules including small interfering RNAs (siRNAs), microRNAs (miRNAs), and proteins can be actively loaded for enhanced regenerative effects [85] [13].
- Improved Pharmacokinetics: Surface engineering can extend circulation time and enhance stability in the wound microenvironment [82].
- Combination Therapy Potential: Engineered exosomes can deliver multiple therapeutic agents simultaneously for synergistic effects [13].
Table 2: Engineering Strategies for Enhanced Exosome Functionality
| Engineering Approach | Methodology | Therapeutic Benefit | Application in Chronic Wounds |
|---|---|---|---|
| Surface Modification | Ligand conjugation (peptides, antibodies) | Enhanced targeting to specific cell types | Improved retention in wound bed; targeting of fibroblasts or endothelial cells |
| Cargo Loading | Electroporation, sonication, transfection of parent cells | Delivery of specific therapeutic molecules | Loading of angiogenic miRNAs, anti-fibrotic drugs, or antimicrobial peptides |
| Membrane Engineering | Hybridization with synthetic lipids | Improved stability and circulation time | Enhanced resistance to degradation in proteolytic wound environment |
| Parent Cell Preconditioning | Genetic modification or environmental priming | Modulation of innate exosome composition | Upregulation of pro-regenerative factors via hypoxia or cytokine preconditioning |
Experimental Protocols for Efficacy Evaluation
Protocol: In Vitro Assessment of Exosome-Mediated Macrophage Polarization
Objective: To evaluate the immunomodulatory effects of natural versus engineered exosomes on macrophage polarization in a chronic wound model.
Materials:
- Primary human monocytes or macrophage cell lines (e.g., THP-1)
- Phorbol 12-myristate 13-acetate (PMA) for differentiation
- LPS and IFN-γ for M1 polarization
- IL-4 and IL-13 for M2 polarization
- Natural MSC-derived exosomes
- Engineered exosomes (modified for enhanced immunomodulation)
- Flow cytometry antibodies (CD86 for M1, CD206 for M2)
- ELISA kits for TNF-α, IL-6, IL-10
Methodology:
- Differentiate THP-1 monocytes into macrophages using 100 nM PMA for 48 hours.
- Polarize macrophages toward M1 phenotype with 100 ng/mL LPS and 20 ng/mL IFN-γ for 24 hours.
- Treat M1-polarized macrophages with:
- Group A: Natural MSC-exosomes (10^10 particles/mL)
- Group B: Engineered MSC-exosomes (modified for enhanced CD206 targeting)
- Group C: Untreated control
- Group D: Conventional therapy control (e.g., 1 μg/mL dexamethasone)
- Incubate for 48 hours and analyze:
- Surface markers via flow cytometry (CD86+ for M1, CD206+ for M2)
- Cytokine secretion via ELISA (TNF-α, IL-6 for M1; IL-10 for M2)
- Gene expression of M1/M2 markers via qRT-PCR
- Statistical analysis: One-way ANOVA with post-hoc Tukey test, n≥3, p<0.05 considered significant.
Expected Outcomes: Engineered exosomes should demonstrate enhanced M2 polarization efficacy compared to natural exosomes and conventional treatments, as evidenced by increased CD206+ cells and IL-10 secretion, with concurrent decrease in M1 markers.
Protocol: In Vivo Evaluation in Diabetic Mouse Wound Model
Objective: To compare the wound healing efficacy of natural exosomes, engineered exosomes, and conventional therapies in a diabetic mouse model.
Materials:
- Lepr db/db mice (8-10 weeks old, male)
- Sterile punch biopsy (6mm)
- Natural MSC-exosomes
- Engineered exosomes (loaded with miR-21-5p and surface-modified with RGD peptide)
- Conventional therapy: NPWT device or topical hydrogel
- Digital camera for wound documentation
- Histology reagents (H&E, Masson's trichrome, CD31 antibody)
Methodology:
- Induce diabetes in mice and confirm hyperglycemia (blood glucose >300 mg/dL).
- Create full-thickness excisional wounds (6mm) on dorsal skin.
- Randomize mice into treatment groups (n=8 per group):
- Group A: Natural exosomes (10^10 particles in 50 μL PBS, topical application every 3 days)
- Group B: Engineered exosomes (same dosage and schedule)
- Group C: NPWT (continuous negative pressure at -125 mmHg)
- Group D: Vehicle control (PBS only)
- Monitor wounds daily and capture digital images on days 0, 3, 7, 10, and 14.
- Calculate wound closure percentage using ImageJ software.
- On day 14, euthanize mice and collect wound tissue for:
- Histological analysis (H&E for re-epithelialization, Masson's trichrome for collagen deposition)
- Immunohistochemistry (CD31 for angiogenesis, α-SMA for myofibroblasts)
- Quantitative analysis of granulation tissue thickness and capillary density
- Statistical analysis: Two-way ANOVA for wound closure kinetics, one-way ANOVA for endpoint measures.
Expected Outcomes: Engineered exosomes should demonstrate accelerated wound closure, enhanced re-epithelialization, superior angiogenesis, and more organized collagen deposition compared to other groups.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Exosome Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Exosome Isolation Kits | Total Exosome Isolation Kit, ExoQuick-TC | Concentration and purification from cell culture media or biological fluids | Evaluate yield and purity; assess for co-isolation of contaminants |
| Characterization Tools | Nanoparticle Tracking Analysis (NTA), CD63/CD81/CD9 antibodies, TEM grids | Size distribution, concentration, and marker confirmation | Combine multiple methods for comprehensive characterization per MISEV guidelines |
| Engineering Reagents | Membrane labeling dyes (PKH67, DiD), sulfo-SANPAH crosslinker, amine-reactive NHS esters | Surface modification and tracking | Optimize labeling to prevent functional alteration; assess targeting efficiency |
| Cell Culture Models | Human umbilical vein endothelial cells (HUVECs), human dermal fibroblasts, THP-1 monocytes | In vitro mechanistic studies | Use primary cells for physiological relevance; consider donor variability |
| Animal Models | Lepr db/db mice, streptozotocin-induced diabetic mice, pressure ulcer models | In vivo efficacy and safety evaluation | Monitor glycemic control in diabetic models; standardize wound creation |
| Analysis Tools | Flow cytometers with <300 nm sensitivity, high-resolution TEM, ELISA kits | Functional assessment and mechanism elucidation | Implement appropriate controls for vesicle analysis; validate antibodies |
Signaling Pathways and Experimental Workflows
Diagram 1: Comparative Mechanisms of Action in Wound Healing. This visualization illustrates the distinct pathways through which natural exosomes, engineered exosomes, and conventional therapies promote wound healing, highlighting the multifaceted approach of engineered exosomes.
Diagram 2: Comprehensive Workflow for Exosome Engineering and Therapeutic Evaluation. This flowchart outlines the sequential process from source selection through engineering strategies to efficacy evaluation, providing a framework for systematic development of exosome-based wound therapies.
The comparative analysis presented in this document demonstrates the significant potential of engineered exosomes to overcome limitations of both conventional therapies and natural exosomes in chronic wound management. Through precise engineering strategies that enhance targeting, cargo delivery, and functional activity, these advanced therapeutics offer a promising approach for addressing the complex pathophysiology of chronic wounds.
Future development in this field should focus on standardizing isolation and engineering protocols, establishing potency assays, addressing manufacturing scalability, and navigating regulatory pathways. The integration of engineered exosomes with advanced delivery systems such as chitosan hydrogels or alginate films may further enhance their stability and functional activity in the challenging wound microenvironment [81]. As research progresses, engineered exosomes are poised to revolutionize personalized wound care, potentially transforming the standard of care for patients with chronic wounds that are unresponsive to existing treatments.
Safety Profile and Immunogenicity Assessment Across Administration Routes
Mesenchymal stem cell-derived exosomes (MSC-Exo) represent a promising acellular therapeutic platform for chronic wound healing, offering a novel strategy for targeted drug delivery. Their inherent biological properties—including low immunogenicity, high biocompatibility, and the ability to traverse biological barriers—make them particularly attractive for regenerative applications [37] [86]. For research and development professionals advancing engineered exosome therapies, comprehensive assessment of safety and immunogenicity across different administration routes is critical for translational success. This document provides detailed application notes and experimental protocols for evaluating these essential parameters within the context of chronic wound research, supporting the broader thesis that engineered MSC exosomes can achieve targeted drug delivery with optimized safety profiles.
MSC Exosomes: inherent Safety and Immunogenicity Profile
MSC-derived exosomes exhibit several intrinsic biological features that contribute to a favorable safety and immunogenicity profile, forming a solid foundation for their therapeutic application in chronic wounds.
Table 1: Inherent Therapeutic Advantages of MSC-Derived Exosomes
| Property | Therapeutic Benefit | Reference |
|---|---|---|
| Small particle size (30-150 nm) | Enables broad and precise tissue distribution; penetrates biological barriers | [87] [13] |
| Low immunogenicity | Reduces probability of immune rejection and associated risks | [87] [37] |
| Lack of nuclear structure | Effectively avoids risk of tumorigenic transformation | [87] [37] |
| High biological stability | Maintains biological activity under diverse environmental conditions | [87] |
| Biocompatible lipid bilayer | Natural origin minimizes immune activation and improves tolerance | [13] [88] |
The low immunogenicity of MSC-Exo is particularly advantageous for chronic wound applications, where the prolonged inflammatory phase is a key pathological feature [87] [37]. Their lack of replication capacity following administration significantly mitigates the risk of carcinogenesis compared to whole-cell therapies [37]. Furthermore, their nanoscale size facilitates not only penetration into wound tissues but also enables versatile administration routes, including topical application, intravenous injection, and potentially oral delivery [37].
Assessment Across Administration Routes
The route of administration directly influences the local and systemic safety profile of engineered exosome therapies. The following table summarizes key considerations for routes relevant to chronic wound management.
Table 2: Safety and Immunogenicity Profile by Administration Route
| Route | Key Safety Considerations | Immunogenicity Risk | Relevance to Chronic Wounds |
|---|---|---|---|
| Topical/Local Injection | Minimal systemic exposure; potential for local inflammatory reaction at application site | Very Low | Direct application to wound bed; high local bioavailability |
| Intravenous (IV) | Risk of infusion reactions; interaction with blood components; biodistribution to off-target organs | Low to Moderate | Potential for systemic effects on comorbid conditions (e.g., diabetes) |
| Intradermal/Perilesional | Local tissue reaction; controlled dispersion within wound microenvironment | Very Low | Precise delivery to wound edge and surrounding tissue |
For chronic wounds, topical application via hydrogels or sprays, combined with local intradermal or perilesional injection, is often the preferred strategy [10] [86]. This approach maximizes target tissue engagement while minimizing systemic exposure and associated risks. Research indicates that IV administration, while effective for systemic conditions, presents a more complex safety profile due to interactions with the immune system and plasma proteins, necessitating more extensive biodistribution and systemic toxicity studies [37] [88].
Experimental Protocols for Safety and Immunogenicity Testing
Protocol: In Vitro Immunogenicity Assessment (Human Peripheral Blood Mononuclear Cells - PBMCs)
Objective: To evaluate the potential of engineered MSC-Exo to activate human immune cells in vitro.
Materials & Reagents:
- Ficoll-Paque PLUS: For density gradient centrifugation to isolate PBMCs from fresh human blood.
- RPMI-1640 Complete Medium: Supplemented with 10% heat-inactivated FBS, 2 mM L-glutamine, 100 U/mL penicillin, and 100 µg/mL streptomycin.
- Lymphocyte Mitogen (e.g., PHA): Serves as a positive control for immune activation.
- Flow Cytometry Antibodies: Anti-CD3 (T-cells), anti-CD19 (B-cells), anti-CD69 (early activation marker), anti-CD25 (activation proliferation marker).
- ELISA Kits: For quantifying pro-inflammatory cytokines (IFN-γ, TNF-α, IL-1β, IL-6).
Procedure:
- PBMC Isolation: Isolate PBMCs from healthy donor buffy coats using standard Ficoll-Paque density gradient centrifugation. Wash cells twice with PBS and resuspend in complete RPMI-1640 medium.
- Experimental Setup: Seed PBMCs (1x10^6 cells/well) in a 24-well plate. Treat with:
- Test Group: Engineered MSC-Exo (escalating doses, e.g., 10^8 - 10^10 particles/mL).
- Negative Control: PBS vehicle.
- Positive Control: PHA (5 µg/mL).
- Incubation: Incubate cells for 72 hours at 37°C in a 5% CO2 humidified incubator.
- Analysis:
- Cell Supernatant: Harvest supernatant at 24h and 72h for cytokine analysis using ELISA kits according to manufacturer protocols.
- Cells: Harvest cells at 72h. Stain with fluorochrome-conjugated antibodies against CD3, CD19, CD69, and CD25. Analyze T-cell and B-cell activation via flow cytometry. Compare activation marker expression in test groups versus controls.
Protocol: In Vivo Repeated Dose Toxicity and Biodistribution
Objective: To assess systemic toxicity and organ distribution of engineered MSC-Exo following repeated administration in a relevant animal model (e.g., diabetic mouse).
Materials & Reagents:
- Animal Model: db/db mice or chemically-induced diabetic mice with impaired wound healing.
- Near-Infrared (NIR) Dye (e.g., DiR): For non-invasive exosome tracking.
- Formalin Solution (10% Neutral Buffered): For tissue fixation.
- Hematoxylin and Eosin (H&E) Stain: For histological examination.
- Clinical Chemistry Analyzer: For assessing serum biochemistry (ALT, AST, BUN, Creatinine).
Procedure:
- Exosome Labeling: Label a batch of engineered MSC-Exo with NIR dye (DiR) according to established protocols. Remove unincorporated dye via size-exclusion chromatography.
- Dosing and Administration: Randomize diabetic mice into groups (n=8-10). Administer engineered MSC-Exo (e.g., 2x10^10 particles/dose) or PBS vehicle control via the intended route (e.g., topical to wound, IV) every 48-72 hours for 28 days.
- In Vivo Imaging: For the NIR-labeled group, image animals at predetermined time points (e.g., 1h, 4h, 24h, 48h post-injection) using an IVIS imaging system. Quantify fluorescence signal intensity at the wound site and major organs (liver, spleen, kidneys, lungs).
- Clinical Observations & Blood Collection: Monitor animals daily for clinical signs (activity, posture, skin/fur condition). At study terminus, collect blood for hematology and clinical chemistry analysis.
- Necropsy and Histopathology: Harvest and weigh key organs (heart, liver, spleen, lungs, kidneys). Fix tissues in 10% formalin, process, embed in paraffin, section, and stain with H&E. Perform blinded histological evaluation for signs of toxicity or inflammation.
Safety Assessment Workflow for MSC-Exo
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Safety and Immunogenicity Assessment
| Research Reagent / Kit | Primary Function in Assessment |
|---|---|
| Human PBMC Isolation Kit | Isulates pure peripheral blood mononuclear cells from donor blood for in vitro immunogenicity assays. |
| Flow Cytometry Antibody Panels | Detects and quantifies immune cell populations (T, B cells) and their activation states (CD69, CD25). |
| Pro-inflammatory Cytokine ELISA Kits | Measures concentrations of key cytokines (e.g., IFN-γ, TNF-α, IL-6) in cell culture supernatants or serum. |
| Near-Infrared (NIR) Lipophilic Dyes (DiR/DiD) | Labels exosome membranes for non-invasive, real-time tracking of biodistribution in live animals. |
| Clinical Chemistry & Hematology Analyzers | Evaluates systemic toxicity by profiling organ function (liver, kidney) and blood cell counts. |
| Histology Staining Reagents (H&E) | Enables microscopic examination of tissue architecture and identification of pathological lesions in organs. |
A rigorous, multi-faceted approach to safety and immunogenicity assessment is non-negotiable for the clinical translation of engineered MSC exosomes for chronic wound therapy. The protocols outlined herein provide a framework for researchers to systematically evaluate these critical parameters. By leveraging the inherent low immunogenicity of MSC-Exo and thoroughly characterizing the impact of engineering modifications and administration routes, drug development professionals can de-risk their programs and accelerate the advancement of safe, effective, and targeted exosome-based therapeutics for complex wound healing applications.
Conclusion
Engineered MSC exosomes represent a paradigm shift in regenerative medicine, offering a targeted, cell-free therapeutic strategy for chronic wounds that surpasses the limitations of conventional treatments and stem cell transplantation. The integration of advanced engineering techniques enables precise control over cargo and targeting, potentially revolutionizing wound care by modulating inflammation, promoting angiogenesis, and enhancing tissue regeneration. Future progress hinges on establishing standardized manufacturing protocols, comprehensive safety and efficacy profiles from robust clinical trials, and innovative solutions for large-scale production. As research advances, these bioinspired nanotherapeutics hold immense promise not only for chronic wound management but also as a versatile platform for broader regenerative and drug delivery applications, ultimately paving the way for a new era of personalized medicine.
References
- 1. Recent advances in extracellular vesicles for therapeutic ... [https://www.nature.com/articles/s12276-024-01201-6]
- 2. Engineered exosomes: a promising drug delivery platform ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1583992/full]
- 3. Current knowledge on exosome biogenesis and release [https://pmc.ncbi.nlm.nih.gov/articles/PMC5756260/]
- 4. Exosome biogenesis: machinery, regulation, and therapeutic ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01671-0]
- 5. Regulation of cargo selection in exosome biogenesis and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11059157/]
- 6. Current Strategies for Exosome Cargo Loading and Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10216928/]
- 7. Precision exosome engineering for enhanced wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12103044/]
- 8. The role of exosomal molecular cargo in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1417758/full]
- 9. Overview and Update on Methods for Cargo Loading into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8096148/]
- 10. MSC-derived exosomes injectable hyaluronic acid ... [https://www.sciencedirect.com/science/article/pii/S0168365925006066]
- 11. as emerging therapeutic platform for Exosome ... wound healing [https://pubmed.ncbi.nlm.nih.gov/41075622/]
- 12. Precision exosome engineering for enhanced wound and... healing [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06578-0]
- 13. Exosome-Based Drug Delivery: A Next-Generation Platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567338/]
- 14. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 15. Exosome Therapy for Chronic Wound Healing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494051/]
- 16. Exosome Therapy for Chronic Wound Healing [https://www.mekostem.com/en/exosome-therapy-for-chronic-wound-healing/]
- 17. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 18. Extracellular vesicle microRNA cargoes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551403/]
- 19. Harnessing Mesenchymal Stem Cell-Derived Exosomes ... [https://www.mdpi.com/2227-9059/12/12/2791]
- 20. Adipose-derived stem cell exosomes: emerging roles and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637342/full]
- 21. Extracellular vesicles in chronic wound therapy [https://www.sciencedirect.com/science/article/pii/S2590006425008683]
- 22. Extracellular vesicle-derived MicroRNAs as potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128652/]
- 23. Advances in stem cell-derived exosome therapy for radiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626575/]
- 24. Therapeutic Potential of Modulating Gene-MicroRNA ... [https://www.mdpi.com/1422-0067/26/20/10060]
- 25. Mesenchymal stem cell-derived exosomes: A paradigm ... [https://www.sciencedirect.com/science/article/abs/pii/S0014482725002125]
- 26. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 27. Mesenchymal Stem-Cell-Derived Exosomes and MicroRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249468/]
- 28. Advancements in engineered exosomes for wound repair [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1301362/full]
- 29. Cell transfection: Methods, emerging applications, and ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/cell-transfection]
- 30. Ultrasound-enhanced gene transfection: vectors, methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547965/]
- 31. Bioengineered MSC-derived exosomes in skin wound repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009159/]
- 32. Unravelling Ligand Conjugation Performance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519427/]
- 33. Peptide-Enabled Targeted Delivery Systems for Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8281044/]
- 34. Cell surface-engineering to embed targeting ligands or ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X16320290]
- 35. Formulation methods for peptide-modified lipid nanoparticles [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006510]
- 36. Mesenchymal Stem Cell-Derived Exosomes as Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11277139/]
- 37. The tiny giants of regeneration: MSC-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310703/]
- 38. Preconditioning of Human Mesenchymal Stem Cells to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5086389/]
- 39. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 40. Ascorbic acid and IFNγ preconditioning enhance the ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576923009682]
- 41. Mesenchymal stem cells-derived exosomes for drug delivery [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02629-7]
- 42. Investigation and kinetics of hydrogel scaffold with ... [https://link.springer.com/article/10.1007/s00289-024-05495-4]
- 43. Unraveling release kinetics and mechanisms for sustained ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592400539X]
- 44. Therapeutic potential of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10907468/]
- 45. Engineered exosomes: a promising drug delivery platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098103/]
- 46. Designing hydrogels for controlled drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5898614/]
- 47. Recent Developments in Nanoparticle‐Hydrogel Hybrid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463025/]
- 48. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 49. Recent advances in scalable exosome production [https://www.sciencedirect.com/science/article/pii/S2096691125000196]
- 50. Exosome Isolation by Ultracentrifugation and Precipitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8088761/]
- 51. What are the cons of ultracentrifugation for exosome ... [https://www.aatbio.com/resources/faq-frequently-asked-questions/what-are-the-cons-of-ultracentrifugation-for-exosome-isolation]
- 52. Efficient methods of isolation and purification of extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463815/]
- 53. Advances in Exosome Quantification Techniques - Halo Labs [https://www.halolabs.com/blog/exosome-quantification-techniques/]
- 54. Optimising exosome isolation techniques for advanced ... [https://immunostep.com/2025/01/28/optimising-exosome-isolation-techniques-for-advanced-therapeutic-applications-whats-working-in-2025/]
- 55. A scalable platform for EPSC-Induced MSC extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04507-y]
- 56. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 57. Comparative Analysis of MSC-Derived Exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169723/]
- 58. Mesenchymal stem cell-derived exosomes as cell-free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632147/]
- 59. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 60. Quantitative Biodistribution and Pharmacokinetics Study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9229812/]
- 61. Biodistribution of Exosomes and Engineering Strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8325750/]
- 62. Pharmacokinetic characteristics of mesenchymal stem cells ... [https://www.nature.com/articles/s41392-024-01936-8]
- 63. Exosome-Based Drug Delivery: A Next-Generation ... [https://www.mdpi.com/1999-4923/17/10/1336]
- 64. Optimizing mesenchymal stem cell extracellular vesicles ... [https://www.sciencedirect.com/science/article/pii/S2352320424001081]
- 65. The Opportunities and Challenges of Mesenchymal Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11640604/]
- 66. Drug Delivery Systems and Materials for Wound Healing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6003879/]
- 67. Growth factors and growth factor gene therapies for treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11135157/]
- 68. Adipose-derived stem cell exosomes - Biomarker Research [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00801-2]
- 69. Vesicular drug delivery systems: A breakthrough in wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0927776525005533]
- 70. Mouse models of diabetes-related ulcers: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10755106/]
- 71. Preclinical study of diabetic foot ulcers: From pathogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10681512/]
- 72. A murine pressure ulcer model for evaluating persistence ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1561732/full]
- 73. Experimental animal modelling for pressure injury [https://pmc.ncbi.nlm.nih.gov/articles/PMC8082114/]
- 74. Animal models of ischemic limb ulcers: a systematic review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7451953/]
- 75. Mesenchymal stem cell-derived extracellular vesicles in skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10433599/]
- 76. Mesenchymal stem cell-derived exosomes: A novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 77. Nanomanaging Chronic Wounds with Targeted Exosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945274/]
- 78. Mesenchymal stem cells-derived small extracellular vesicles ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 79. Therapeutic application of mesenchymal stem cell-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1428793/full]
- 80. Exosome engineering for targeted therapy of brain-infecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528093/]
- 81. Biological Nanoparticles for Enhancing Chronic Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564170/]
- 82. Engineered exosomes: advanced nanocarriers for targeted ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00334-1]
- 83. Efficacy of hyperbaric oxygen therapy combine with ... [https://www.sciencedirect.com/science/article/pii/S2352587825000841]
- 84. What's New in Wound Healing: Treatment Advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436535/]
- 85. Harnessing engineered mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625093/]
- 86. Mesenchymal stem cell-derived exosomes: emerging ... [https://www.sciencedirect.com/science/article/pii/S2773041725000253]
- 87. Mesenchymal stem cell-derived extracellular vesicles [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399395/]
- 88. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]