Evaluating Stem Cell Potency: A Comprehensive Guide for Advanced Disease Modeling in 2025
This article provides a comprehensive guide for researchers and drug development professionals on evaluating the potency of stem cell-based disease models.
Evaluating Stem Cell Potency: A Comprehensive Guide for Advanced Disease Modeling in 2025
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on evaluating the potency of stem cell-based disease models. It covers the foundational principles of stem cell biology, from totipotency to unipotency, and explores advanced methodological applications including organoids, assembloids, and gene-edited models. The content addresses key challenges in standardization, maturation, and scalability, while offering frameworks for validation against traditional animal models. By synthesizing current best practices and emerging innovations, this resource aims to enhance the fidelity, reproducibility, and predictive power of stem cell models in translational research and therapeutic development.
Understanding Stem Cell Potency: From Totipotency to Lineage Restriction
Stem cells are foundational units in regenerative medicine and biological research, primarily defined by their potency—the capacity to differentiate into specialized cell types. This article provides a structured comparison of the potency hierarchy, from the broad differentiation potential of totipotent cells to the restricted fate of unipotent cells, framed within the context of their application in stem cell-based disease modeling and research.
The Spectrum of Cell Potency
Cell potency is a continuum that describes a cell's ability to differentiate into other cell types. The hierarchy is traditionally categorized based on the number and types of cells a stem cell can generate.
- Totipotent Stem Cells possess the highest differentiation potential. They can give rise to all the cell types in an organism, including both embryonic and extra-embryonic tissues (such as the placenta) [1] [2]. The only known indisputably totipotent cell is the zygote formed after fertilization, and the early blastomeres resulting from its initial divisions [3] [4].
- Pluripotent Stem Cells can differentiate into all cell types derived from any of the three embryonic germ layers—ectoderm, mesoderm, and endoderm—but they cannot generate extra-embryonic tissues [1] [5] [2]. This category includes Embryonic Stem Cells (ESCs), derived from the inner cell mass of the blastocyst, and Induced Pluripotent Stem Cells (iPSCs), which are adult somatic cells reprogrammed into a pluripotent state [3] [2].
- Multipotent Stem Cells have a more restricted potential, typically limited to differentiating into the cell types of a particular lineage or tissue [1] [4]. Examples include Hematopoietic Stem Cells (HSCs), which generate all blood cell types, and Mesenchymal Stem Cells (MSCs), which can form bone, cartilage, and fat cells [3] [6].
- Unipotent Stem Cells have the most limited developmental potential. They can only produce a single cell type but retain the capacity for self-renewal, which distinguishes them from non-stem cells [5]. An example is a precursor cell that can only differentiate into epidermal cells [5].
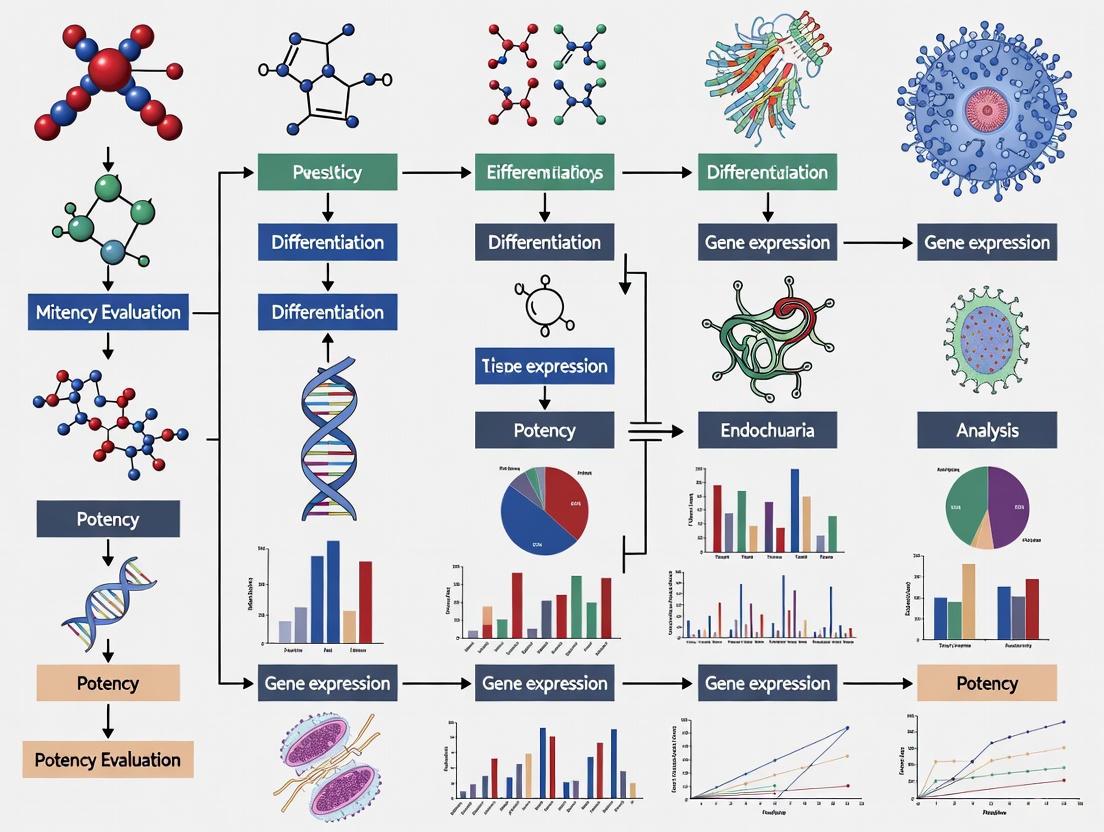
The following diagram illustrates the developmental hierarchy and the narrowing potential from totipotency to unipotency.
Comparative Analysis of Stem Cell Potency
The following table summarizes the key characteristics of the major stem cell types across the potency spectrum, highlighting their origins, differentiation potential, and research applications.
| Feature | Totipotent | Pluripotent | Multipotent |
|---|---|---|---|
| Definition | Can generate all embryonic & extra-embryonic cell types [1] [2] | Can generate all cells from the three germ layers [1] [5] | Can generate a limited range of cell types within a lineage [1] [4] |
| Origin/Source | Zygote, early blastomeres (e.g., up to morula stage) [3] [2] | Inner Cell Mass (ICM) of the blastocyst (ESCs) [3]; Reprogrammed somatic cells (iPSCs) [2] | Various adult tissues (e.g., bone marrow, adipose tissue) [1] [6] |
| Differentiation Potential | Highest; can form a complete organism [3] | High; can form any fetal or adult cell type [5] | Limited; restricted to specific tissue lineages [1] |
| Key Markers/Features | Unique molecular features (e.g., Zscan4, Eomes) [3] | Expression of core pluripotency factors (OCT4, SOX2, NANOG) [5] [3] | Expression of lineage-specific genes [1] |
| Research & Therapeutic Utility | Limited due to ethical considerations and rarity; used to study early development [3] | High; disease modeling, drug screening, developmental biology [3] [6] | High; regenerative medicine (e.g., HSC transplants, MSC therapies), fewer ethical issues [3] [6] |
Experimental Protocols for Assessing Pluripotency
For a stem cell to be classified as pluripotent in a research setting, its functional capacity must be rigorously demonstrated. The gold standard assays for this purpose are in vivo tests.
Teratoma Formation Assay
This is a widely accepted functional test for pluripotency, required for both ESCs and iPSCs [2].
- Objective: To confirm the ability of test cells to differentiate into derivatives of all three germ layers in vivo.
- Methodology:
- Cell Preparation: A suspension of the candidate pluripotent stem cells is prepared.
- Transplantation: The cells are injected into an immunodeficient mouse model. Common injection sites include the kidney capsule, intramuscular, or subcutaneous spaces [2].
- Tumor Monitoring: The injection site is monitored for the formation of a teratoma, a benign tumor.
- Histological Analysis: After several weeks, the teratoma is excised, sectioned, and stained. Proof of pluripotency is the presence of well-differentiated tissues representing:
- Considerations: The assay is costly, operationally burdensome, and requires careful standardization of factors like injection site and cell number. Histological analysis is also subject to interpretation errors [2].
Chimera Formation Assay
This assay, primarily used in mouse models, provides even stronger evidence of developmental potential [5].
- Objective: To test the ability of stem cells to integrate and contribute to all tissues of a developing embryo.
- Methodology:
- Cell Introduction: Pluripotent stem cells are injected into a host mouse blastocyst.
- Embryo Transfer: The injected blastocyst is surgically transferred into a pseudopregnant female mouse.
- Analysis of Offspring: The resulting offspring are chimeras—composed of cells from both the host embryo and the injected stem cells.
- Assessment: Contribution of the test stem cells to various tissues and germlines is assessed, often using fluorescent or genetic markers. The ability to contribute to all three germ layers in a developing organism confirms pluripotency [5].
The Scientist's Toolkit: Key Reagents for Pluripotency Research
Successful stem cell research relies on a suite of specialized reagents and tools to maintain, characterize, and manipulate pluripotent cells.
| Research Reagent/Tool | Function in Pluripotency Research |
|---|---|
| Pluripotency Transcription Factors (OCT4, SOX2, NANOG) | Core markers expressed in pluripotent cells; essential for maintaining the undifferentiated state. Often detected via immunostaining or PCR for cell characterization [5] [3]. |
| Yamanaka Factors (OCT4, SOX2, KLF4, c-MYC) | A set of transcription factors used for the forced expression that reprograms somatic cells into induced Pluripotent Stem Cells (iPSCs) [3] [2]. |
| Basic Fibroblast Growth Factor (bFGF) | A critical cytokine added to culture media to support the self-renewal and maintenance of human pluripotent stem cells [4]. |
| Leukemia Inhibitory Factor (LIF) | A cytokine used to maintain the pluripotency of mouse embryonic stem cells by activating the JAK-STAT3 signaling pathway [4]. |
| Microarray/Gene Expression Profiling | A tool used to assess the global gene expression profile of stem cells. It can distinguish different states of pluripotency and confirm the expression of pluripotency-associated genes while silencing lineage-specific genes [7] [5]. |
Potency in the Context of Cellular Therapies and Disease Modeling
In the translational and regulatory landscape, potency takes on a precise definition: "the specific ability or capacity of the product... to effect a given result" [8]. For cellular therapies, potency is a critical quality attribute that must be measured through potency assays—quantitative tests of a product's biological activity linked to its intended mechanism of action [7] [9].
- Challenges in Potency Testing: Developing these assays for cell therapies is complex due to the living nature of the product, lot-to-lot variability, limited product quantity for testing, and often an incomplete understanding of the product's precise mechanism of action [7] [9].
- Role of Pluripotent Cells: iPSCs, in particular, are powerful for disease modeling. Researchers can generate patient-specific iPSCs, differentiate them into disease-relevant cell types (e.g., dopaminergic neurons for Parkinson's disease), and use these in vitro models to study disease mechanisms and screen potential therapeutics [6]. In these models, the "potency" of the differentiation process to generate the target cell type must be carefully evaluated.
Understanding the fundamental hierarchy of stem cell potency is essential for selecting the appropriate cell type for specific research applications, from basic developmental biology to the development of next-generation regenerative medicines.
The pursuit of physiologically relevant human disease models represents a central challenge in biomedical research. Traditional animal models, while invaluable, often fail to recapitulate key aspects of human pathophysiology due to species-specific differences in genetics, morphology, and molecular pathways [10]. Stem cell-based models have emerged as a transformative platform that overcomes these limitations by providing unrestricted access to authentic human cells and tissues [11]. This comparison guide objectively analyzes the three principal stem cell types—induced pluripotent stem cells (iPSCs), embryonic stem cells (ESCs), and mesenchymal stem cells (MSCs)—for disease modeling applications. Framed within the broader context of potency evaluation in stem cell research, this guide examines the differential capacities of these cells to self-renew and differentiate into disease-relevant cell types, providing researchers with a strategic framework for selecting the optimal cellular system for specific disease modeling objectives.
Comparative Analysis of Key Stem Cell Types
The following section provides a detailed comparison of the defining characteristics, advantages, and limitations of iPSCs, ESCs, and MSCs, with a specific focus on their utility in disease modeling.
Table 1: Fundamental Characteristics of Key Stem Cell Types for Disease Modeling
| Feature | Induced Pluripotent Stem Cells (iPSCs) | Embryonic Stem Cells (ESCs) | Mesenchymal Stem Cells (MSCs) |
|---|---|---|---|
| Origin | Reprogrammed adult somatic cells (e.g., skin fibroblasts, blood cells) [12] | Inner Cell Mass (ICM) of a blastocyst-stage embryo [12] | Various adult tissues (e.g., bone marrow, adipose tissue, umbilical cord) [13] [14] |
| Potency | Pluripotent [12] | Pluripotent [12] | Multipotent (primarily mesodermal lineage) [12] [14] |
| Self-Renewal Capacity | Unlimited in culture [13] | Unlimited in culture [13] | Limited; senesces in prolonged in vitro culture [13] [14] |
| Key Advantages | Patient-specific; avoids embryo destruction; models genetic diseases [15] [10] | Gold standard for pluripotency; genetically normal (when derived from healthy embryos) [15] | Immunomodulatory properties; clinically relevant secretome; lower tumorigenic risk [12] [14] |
| Key Limitations | Epigenetic memory; reprogramming-induced mutations; variable differentiation efficiency [15] | Ethical controversies; limited genetic diversity; immunoincompatibility with patients [15] [12] | Tissue-source and donor-age dependent heterogeneity; limited proliferative capacity [13] [14] |
Table 2: Disease Modeling Applications and Model Fidelity
| Aspect | iPSCs | ESCs | MSCs |
|---|---|---|---|
| Ideal for Modeling | Monogenic diseases, complex polygenic disorders, patient-specific drug responses [15] [11] | Early human development, monogenic diseases (via genetic engineering), "proof-of-concept" models [15] | Connective tissue disorders, immune-mediated diseases, age-related pathologies [13] [14] |
| Representative Diseases Modeled | Amyotrophic Lateral Sclerosis, Spinal Muscular Atrophy, Long QT syndrome [15] | Lesch-Nyhan syndrome, Fragile X syndrome (via PGD-derived ESCs) [15] | Osteoarthritis, Graft-versus-Host Disease, spinocerebellar ataxia [11] [14] |
| Physiological Relevance | High for postnatal and adult-onset diseases; can capture patient's genetic background [15] [10] | High for early developmental processes; may not fully mimic postnatal disease physiology [15] | Context-dependent; influenced by donor age and tissue source, which can be a confounder [13] [14] |
Experimental Protocols for Model Generation and Validation
Protocol 1: Generating an iPSC-Based Neuronal Disease Model
This protocol outlines the key steps for modeling a neurological disorder, such as Amyotrophic Lateral Sclerosis (ALS), using patient-specific iPSCs [15] [11].
- Somatic Cell Reprogramming: Obtain dermal fibroblasts or peripheral blood mononuclear cells from a patient and a genetically matched healthy control. Reprogram the cells using a non-integrating Sendai virus or episomal vectors expressing the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) to generate iPSCs [12] [16].
- iPSC Characterization: Confirm pluripotency by:
- Immunocytochemistry: Detection of pluripotency markers (OCT4, NANOG, SSEA-4) [10].
- In Vitro Differentiation: Formation of embryoid bodies containing cells of all three germ layers.
- Karyotyping: Ensure genomic integrity after reprogramming.
- Neuronal Differentiation: Direct iPSCs toward motor neurons using a standardized, multi-step protocol. This typically involves:
- Dual SMAD inhibition to induce neural induction.
- Treatment with retinoic acid and a Sonic hedgehog (Shh) agonist to pattern the cells toward a spinal motor neuron fate.
- Culture for extended periods (60-100 days) to achieve mature electrophysiological properties [11].
- Phenotypic Analysis: Compare patient and control iPSC-derived motor neurons for disease-specific phenotypes, which may include:
- Protein aggregation (e.g., TDP-43).
- Neurite retraction and reduced survival.
- Electrophysiological deficits.
- Gene Editing for Isogenic Controls (Critical for Potency Evaluation): Use CRISPR-Cas9 to correct the disease-causing mutation in the patient iPSC line. This generates a genetically identical, healthy control line, ensuring that any observed phenotypic differences are solely due to the specific mutation and not background genetic variation [11].
Protocol 2: Establishing an MSC-Based Model for Osteoarthritis
This protocol details the use of primary MSCs to model a connective tissue disease like osteoarthritis [14].
- MSC Isolation and Expansion:
- Source: Isolate MSCs from bone marrow aspirate or adipose tissue (liposuction) from donors with osteoarthritis and healthy controls.
- Isolation Method: Use the explant culture method (minimizes manipulation, yields homogeneous population) or enzymatic digestion (e.g., with collagenase) [12].
- Expansion: Culture cells in Dulbecco's Modified Eagle Medium (DMEM) supplemented with fetal bovine serum (FBS) and fibroblast growth factor (FGF)-2.
- MSC Characterization: Verify identity using the International Society for Cell & Gene Therapy (ISCT) criteria:
- Surface Marker Profiling: Confirm positive expression of CD105, CD73, CD90 (>95%) and negative expression of CD45, CD34, CD14/CD11b, CD79α/CD19 (<2%) via flow cytometry [12] [14].
- Trilineage Differentiation Assay: Differentiate MSCs into osteocytes, adipocytes, and chondrocytes in vitro to confirm multipotency [12].
- Disease Phenotype Induction and Analysis:
- Chondrogenic Differentiation: Pellet the MSCs and culture in a chondrogenic medium containing TGF-β3 to form cartilage-like tissue.
- Phenotypic Analysis: Compare the chondrogenic capacity and cartilage matrix composition (e.g., collagen type II, proteoglycans) between MSCs from osteoarthritic and healthy donors. Assess the production of inflammatory mediators in the culture supernatant.
The Scientist's Toolkit: Essential Research Reagents
Successful disease modeling requires a suite of well-defined reagents and materials. The following table details essential solutions for working with iPSCs, ESCs, and MSCs.
Table 3: Key Research Reagent Solutions for Stem Cell Disease Modeling
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Yamanaka Factor Cocktail | Set of transcription factors (OCT4, SOX2, KLF4, c-MYC) for somatic cell reprogramming to pluripotency [12]. | Use non-integrating delivery methods (e.g., Sendai virus, episomal vectors) for clinical-grade iPSCs. |
| CRISPR-Cas9 System | RNA-guided gene editing tool for generating isogenic control lines or introducing disease-associated mutations [11] [16]. | Critical for establishing causality between genotype and phenotype; requires careful off-target effect analysis. |
| Small Molecule Inhibitors (e.g., SB431542) | Inhibits TGF-β/Activin A signaling; used for efficient neural induction and differentiation of iPSCs/ESCs into MSCs [12]. | Enables directed, monolayer differentiation without embryoid body formation, improving protocol reproducibility. |
| Cytokine & Growth Factor Cocktails | Direct lineage-specific differentiation (e.g., TGF-β3 for chondrogenesis; Retinoic Acid/Shh for motor neuron fate) [12] [14]. | Concentrations and timing are protocol-critical; use GMP-grade factors for preclinical and clinical work. |
| Defined Culture Matrices (e.g., Matrigel, Laminin-521) | Provides a surrogate extracellular matrix for pluripotent stem cell attachment and growth in xeno-free conditions. | Reduces batch-to-batch variability and improves experimental reproducibility compared to mouse feeder layers. |
| Flow Cytometry Antibody Panels | Characterization of surface markers (CD105, CD73, CD90 for MSCs; SSEA-4, TRA-1-60 for PSCs) to assess cell population purity [12] [14]. | Essential for quality control and confirming the identity of both starting populations and differentiated cells. |
The choice between iPSCs, ESCs, and MSCs for disease modeling is not a matter of superiority but of strategic alignment with the specific research question. The following diagram illustrates the decision-making workflow for selecting the optimal stem cell type.
- iPSCs are unparalleled for modeling patient-specific, polygenic diseases and for personalized drug screening, despite challenges related to epigenetic memory and phenotypic variability [15] [10]. Their ability to be gene-edited to create isogenic controls remains a gold standard for establishing genotype-phenotype relationships [11].
- ESCs serve as a critical benchmark for pluripotency and are powerful tools for studying early human development and generating "proof-of-concept" disease models via genetic engineering, though their use is constrained by ethical considerations and limited genetic diversity [15].
- MSCs offer a more direct path for modeling connective tissue and immune-mediated diseases and are already widely used in clinical trials [14]. However, their utility in modeling can be confounded by donor-to-donor heterogeneity and limited expansion potential [13]. The emergence of induced MSCs (iMSCs) generated from iPSCs presents a promising solution, offering a more uniform and scalable source of MSCs with consistent potency [13].
The future of stem cell-based disease modeling lies in leveraging the unique strengths of each cell type, often in combination, and in the continued refinement of differentiation protocols and analytical methods to enhance the physiological relevance and reproducibility of these powerful models.
The Critical Link Between Pluripotency and Disease Model Fidelity
Pluripotency—the capacity of a stem cell to differentiate into any cell type of the body—is the foundational property that enables the creation of sophisticated human disease models in a laboratory setting. The fidelity of these models, meaning how accurately they recapitulate the molecular and phenotypic hallmarks of a human disease, is directly dependent on the quality and stability of the pluripotent stem cell (PSC) starting material. National and international initiatives are now establishing large repositories of human PSCs specifically for modeling disorders, underscoring their critical role in biomedical research [17]. These models, derived from either embryonic stem cells (ESCs) or induced pluripotent stem cells (iPSCs), have been successfully developed for a wide spectrum of conditions, including monogenic, chromosomal, and complex disorders [17]. For researchers and drug development professionals, understanding and controlling the factors that link pluripotency to model fidelity is paramount for producing reliable, reproducible data for mechanistic studies and drug screening campaigns.
Pluripotent Stem Cells as a Platform for Disease Modeling
The utility of PSCs in disease modeling stems from their dual capabilities of self-renewal and multilineage differentiation. This allows for the generation of a virtually unlimited supply of patient-specific cell types that are otherwise inaccessible, such as functional neurons or cardiomyocytes.
- Overcoming Animal Model Limitations: Experimental modeling of human disorders is essential for defining disease mechanisms and developing therapies. PSCs help overcome the significant limitations of animal models for certain human disorders, providing a more direct and often more relevant system for study [17].
- iPSC Technology: The groundbreaking development of iPSC technology, which involves reprogramming adult somatic cells (like fibroblasts or peripheral blood cells) back to a pluripotent state using defined factors, revolutionized the field [17] [18]. This enabled the creation of personalized disease models from virtually any patient.
- Disease-in-a-Dish: The core approach involves deriving patient-specific iPSCs, differentiating them into the cell type(s) affected by the disease (e.g., motor neurons for ALS), and then comparing their characteristics to control cells from healthy individuals. This "disease-in-a-dish" paradigm facilitates the study of cellular and molecular phenotypes and provides a platform for drug screening [17] [18].
Table 1: Applications of PSCs in Disease Modeling and Drug Discovery
| Application Area | Description | Example Disorders Modeled |
|---|---|---|
| Monogenic Disorders | Modeling diseases caused by a mutation in a single gene. | Fragile X syndrome, Lesch-Nyhan disease, sickle cell anemia [17] [18]. |
| Chromosomal Disorders | Studying conditions caused by large-scale chromosomal abnormalities. | Down syndrome, Turner's syndrome [17]. |
| Complex & Psychiatric Disorders | Investigating diseases with multifactorial genetic and environmental causes. | Schizophrenia, Alzheimer's disease, autism spectrum disorder [17]. |
| Drug Discovery & Screening | Using differentiated cells to identify and validate new therapeutic compounds. | Screens for 25+ neurological disorders; drugs identified are progressing to the clinic [17]. |
| Personalized Therapy | Using patient-specific iPSCs for disease modeling and autologous cell transplantation after genome editing. | Fanconi anemia, dyskeratosis congenita, Diamond-Blackfan anemia [18]. |
Methodological Framework: From Pluripotency to Disease Phenotypes
Establishing a high-fidelity disease model requires a rigorous and standardized workflow, from validating the initial pluripotent stem cells to thoroughly characterizing the resulting differentiated cell populations. The following diagram outlines the key stages and critical quality control checkpoints in this process.
Detailed Experimental Protocols
1. Generation and Validation of Patient-Specific iPSCs
- Reprogramming: Patient somatic cells (e.g., dermal fibroblasts or peripheral blood mononuclear cells) are transfected with a set of defined transcription factors (e.g., OCT4, SOX2, KLF4, c-MYC) to induce pluripotency. This can be achieved using integrating methods (lentiviruses) or non-integrating methods (Sendai virus, episomal plasmids) [17] [18].
- Pluripotency Validation: Established iPSC lines must be rigorously tested. The gold standard for human stem cell pluripotency is teratoma formation in immunodeficient mice, where the cells form complex tumors containing tissues from all three germ layers (ectoderm, mesoderm, and endoderm). Additional validation includes demonstrating robust in vitro multilineage differentiation potential and confirming the expression of key pluripotency markers (e.g., NANOG, SSEA-4) via immunostaining or flow cytometry [18].
2. Directed Differentiation and Perturbation
- Protocol Optimization: Differentiating PSCs into a target cell type requires carefully optimized protocols that mimic developmental signaling cues. For example, a mesendoderm-directed differentiation protocol might initiate differentiation using a GSK3β inhibitor (CHIR99021) to activate WNT signaling, followed by specific growth factors to steer cells toward cardiovascular or other mesodermal lineages [19].
- Signaling Perturbation Studies: To understand the role of specific pathways in development and disease, researchers systematically perturb signaling during differentiation. As demonstrated in a recent 2025 atlas, small molecules or recombinant proteins targeting pathways like WNT, BMP4, and VEGF are added at the germ layer stage, and the resulting changes in lineage specification are analyzed using single-cell RNA sequencing [19].
3. Phenotypic Characterization and Potency Assessment
- Molecular & Functional Phenotyping: Disease-relevant phenotypes in differentiated cells are identified through a combination of techniques, including transcriptomics (e.g., scRNA-seq to reveal heterogeneity), electrophysiology (for neurons or cardiomyocytes), and metabolic assays.
- Defining Potency: For cell therapies and models, potency is defined as "the attribute of a product that enables it to achieve its intended mechanism of action" [9]. A potency test is a quantitative bioassay that measures this attribute. For a neuronal disease model, this could be the measured output of a specific electrophysiological function or the secretion of a specific neurotransmitter in response to a stimulus.
Evaluating Model Fidelity: The Role of Potency and Mechanism of Action
A critical challenge in the field is establishing a clear link between the cellular model and the clinical disease it represents. This involves deep understanding of the model's mechanism of action (MOA) and how to measure its functional capacity, or potency.
The following framework illustrates the logical relationship between these key concepts, distinguishing between laboratory-based measurements and clinical outcomes—a common point of confusion during product development [9].
Key Considerations for Potency Assays
- Separating MOA from Potency: It is crucial to distinguish the biological mechanism (MOA) from the measurable attribute (potency). This separation allows for the possibility that a chosen potency assay might not perfectly capture the true MOA, which is often uncertain for complex cell products [9]. For example, a CAR-T cell's MOA is target cell killing, but a common potency test measures IFN-γ secretion upon target engagement—a correlate that may not always predict clinical efficacy [9].
- Correlation with Clinical Outcome: While it is desirable for a laboratory potency test to predict clinical benefit, this correlation is not always required for regulatory approval. The primary roles of the potency test are to ensure manufacturing consistency and product stability [9].
Table 2: Benchmarking Disease Model Fidelity with Computational Tools
| Tool / Approach | Primary Function | Role in Ensuring Fidelity |
|---|---|---|
| Single-Cell RNA Sequencing (scRNA-seq) | High-throughput analysis of gene expression in individual cells. | Identifies heterogeneity in differentiated cultures and benchmarks the resulting cell states against in vivo reference atlases of human development [19]. |
| CellNet | A network biology-based computational platform. | Assesses the fidelity of cellular engineering more accurately than prior methods by comparing the gene regulatory networks of derived cells to their in vivo counterparts [18]. |
| Kinetic Modeling & Design Space | Model-based determination of optimal cultivation parameters. | Uses prediction intervals to define robust regions (seeding density, harvest time) for consistent cell output, improving process reliability for MSC cultivation [20]. |
Building a robust pluripotent stem cell-based disease model requires a suite of specialized reagents and tools. The following table details key solutions used in the field.
Table 3: Key Research Reagent Solutions for PSC Disease Modeling
| Reagent / Resource | Function | Example Use Case |
|---|---|---|
| Vitronectin XF | A defined, recombinant substrate for coating cell culture plates. | Provides an xeno-free attachment matrix for the maintenance of human PSCs in a undifferentiated state [19]. |
| mTeSR1 Media | A defined, serum-free maintenance medium. | Supports the growth and pluripotency of human ESCs and iPSCs in feeder-free culture conditions [19]. |
| CHIR99021 | A small molecule inhibitor of GSK-3. | Used in differentiation protocols to activate WNT signaling; e.g., to initiate mesendoderm specification [19]. |
| ROCK Inhibitor (Y-27632) | A small molecule inhibitor of Rho-associated coiled-coil kinase. | Significantly improves the survival of PSCs after dissociation into single cells (passaging or thawing) [19]. |
| TotalSeq-A Cell Hashing Antibodies | Antibodies conjugated to oligonucleotide barcodes. | Enables multiplexing of scRNA-seq samples by tagging cells from different conditions with unique barcodes, allowing them to be pooled and sequenced together [19]. |
| BMP4 / VEGF (rh) | Recombinant human growth factors. | Used as signaling perturbations during differentiation to direct lineage specification toward specific mesodermal fates [19]. |
The fidelity of stem cell-based disease models is inextricably linked to the quality of the underlying pluripotent cells and the rigor of the methods used to differentiate and validate them. As the field progresses, the standardization of protocols, coupled with advanced computational tools for benchmarking and a deeper understanding of product potency and MOA, will be critical. By systematically addressing the critical link between pluripotency and model fidelity, researchers can enhance the predictive power of their in vitro systems, thereby accelerating the discovery of novel therapeutic targets and the development of effective new drugs.
Molecular Markers and Functional Assays for Assessing Pluripotent States
Pluripotency, defined as the capacity of a cell to self-renew and differentiate into all derivatives of the three primary germ layers (ectoderm, mesoderm, and endoderm), represents a fundamental property underpinning stem cell-based disease modeling and regenerative medicine [5] [21]. Rigorous assessment of this potential is critical for ensuring the validity of scientific research and the safety of therapeutic applications. The evaluation of pluripotent states relies on two complementary approaches: the analysis of molecular markers that indicate the pluripotent state and functional assays that demonstrate pluripotent function [22]. This guide provides a comparative analysis of the key methodologies, markers, and experimental protocols used to assess pluripotency, offering researchers a framework for selecting appropriate characterization strategies based on their specific project requirements.
Molecular Markers of Pluripotency
Molecular markers serve as essential tools for the initial characterization and routine monitoring of pluripotent stem cells (PSCs). These include transcription factors, surface antigens, and enzymatic activities associated with the pluripotent state.
Traditional and Novel Marker Genes
Conventional pluripotency markers have been widely used for years, but recent research reveals significant limitations and recommends novel, more specific alternatives.
Table 1: Traditional vs. Validated Marker Genes for Pluripotency and Differentiation
| Cell State | Traditional Markers | Validated Novel Markers [23] | Key Considerations |
|---|---|---|---|
| Pluripotency | OCT4, SOX2, NANOG | CNMD, NANOG, SPP1 | SOX2 shows considerable overlap with ectoderm; GDF3 overlaps with endoderm [23]. |
| Endoderm | SOX17, CXCR4 | CER1, EOMES, GATA6 | - |
| Mesoderm | T/BRACHYURY, CD140b | APLNR, HAND1, HOXB7 | NCAM1 shows overlap with ectoderm [23]. |
| Ectoderm | PAX6, SOX1 | HES5, PAMR1, PAX6 | OTX2 shows considerable overlap with endoderm [23]. |
A landmark 2024 study using long-read nanopore transcriptome sequencing identified 172 genes linked to cell states not covered by current guidelines and rigorously validated 12 genes as unique markers for specific cell fates [23]. This work highlighted that many markers recommended for embryoid body (EB) analysis are not directly applicable for evaluating trilineage-differentiated induced pluripotent stem cells (iPSCs), revealing overlapping expression patterns that compromise their specificity [23].
Protein-Level Markers and Quality Control
At the protein level, immunocytochemistry and flow cytometry are routinely employed to detect key pluripotency-associated transcription factors (OCT4, SOX2, NANOG) and extracellular membrane proteins (SSEA-4, TRA-1-60) [22] [21]. However, the expression of these markers in isolation does not confirm functional pluripotency, and some are not fully exclusive to PSCs [22]. Quality control procedures for iPSC lines include short tandem repeat analysis for identity confirmation, residual vector testing to ensure reprogramming vectors are not integrated, karyotyping to detect culture-driven mutations, and viral testing [21]. Single nucleotide polymorphism (SNP) arrays provide approximately 50 times higher resolution than karyotyping for detecting genomic abnormalities [21].
Functional Assays for Assessing Pluripotency
Functional assays remain the gold standard for demonstrating developmental potency, as they provide direct evidence of a cell's capacity to differentiate. These assays range from simple in vitro methods to complex in vivo tests.
Table 2: Comparison of Functional Assays for Assessing Pluripotency
| Technique | Key Principle | Advantages | Disadvantages | Evidence Level |
|---|---|---|---|---|
| Spontaneous Differentiation | Removal of pluripotency maintenance conditions [22] | Inexpensive, accessible, rapid; can reveal lineage biases [22] | Produces immature tissues; stochastic differentiation; culture conditions affect reproducibility [22] | Moderate |
| Directed Differentiation | Addition of exogenous morphogens to induce specific cell fates [22] | Controllable; can generate specific cell types; relatively inexpensive [22] | May not represent full differentiation capacity; mature phenotypes not always achieved [22] | High for specific lineages |
| Embryoid Body (EB) Formation | Cells self-organize into 3D spheres and differentiate [22] | Accessible techniques; presence of three germ layers indicates differentiation capacity [22] | Immature structures with haphazard organization; hypoxia in core may limit studies [22] | Moderate to High |
| Teratoma Assay | PSCs implanted into immunocompromised mice form differentiated tumors [22] | Provides conclusive proof of ability to form complex tissues; gold standard; assesses malignancy [22] | Labour-intensive, expensive, ethical concerns; primarily qualitative; protocol variability [22] | High (Gold Standard) |
| Modern 3D Organoids | Combination of chemical cues and 3D culture to form tissue rudiments [22] [24] | Can generate morphologically identifiable tissues; greater control; avoids animal use [22] | Technically challenging to optimize; requires specialized equipment/reagents [22] | Emerging |
The Teratoma Assay: Protocol and Considerations
The teratoma assay is widely regarded as the most rigorous method for confirming the pluripotency of human PSCs [22]. The standard protocol involves:
- Cell Preparation: Harvest undifferentiated PSCs and prepare a single-cell suspension.
- Implantation: Inject cells (typically 1-5 million) into an immunocompromised murine host, either subcutaneously, intramuscularly, or under the testis capsule.
- Tumor Growth: Allow tumors to develop for 8-16 weeks, monitoring growth periodically.
- Histological Analysis: Harvest tumors, fix, section, and stain with hematoxylin and eosin. Examine for the presence of differentiated tissues representing all three germ layers (e.g., neural rosettes for ectoderm; cartilage, muscle for mesoderm; gut-like epithelium for endoderm).
Despite its status as a gold standard, the teratoma assay has significant limitations, including cost, time requirements, ethical concerns regarding animal use, inter-tumor heterogeneity, and minimal standardization between laboratories [22].
In Vitro Trilineage Differentiation and Analysis
Directed trilineage differentiation provides a standardized alternative to spontaneous differentiation assays. Commercial kits are available for efficient differentiation into the three germ layers. The subsequent analysis of differentiation outcomes typically employs:
- Immunofluorescence/Flow Cytometry: To detect germ layer-specific proteins at single-cell resolution.
- qPCR Analysis: To quantify expression of germ layer-specific marker genes.
A critical advancement in this area is the "hiPSCore" machine learning-based scoring system, trained on 15 iPSC lines and validated on 10 more, which accurately classifies pluripotent and differentiated cells and predicts their potential to become specialized cells [23]. This system reduces the time, subjectivity, and resource use associated with traditional pluripotency assessment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Pluripotency Assessment
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | OSKM (OCT4, SOX2, KLF4, c-MYC); OSNL (OCT4, SOX2, NANOG, LIN28) [24] [25] | Induction of pluripotency in somatic cells; different combinations vary in efficiency and safety profiles. |
| Pluripotency Markers (Antibodies) | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4, Anti-TRA-1-60 [22] [21] | Immunodetection of pluripotency-associated proteins via flow cytometry or immunocytochemistry. |
| Germ Layer Markers (Antibodies) | Anti-SOX17 (endoderm), Anti-PAX6 (ectoderm), Anti-T/Brachyury (mesoderm) [23] [22] | Validation of differentiation potential in functional assays. |
| Validated Novel Marker Panels | CNMD, SPP1 (pluripotency); CER1, EOMES, GATA6 (endoderm); APLNR, HAND1, HOXB7 (mesoderm); HES5, PAMR1 (ectoderm) [23] | Specific, non-overlapping markers for unequivocal identification of differentiation states. |
| Critical Culture Supplements | Leukemia Inhibitory Factor (LIF); FGF2; GDNF; Small molecule inhibitors (2i) [26] | Maintenance of pluripotent state in culture; enhancement of reprogramming efficiency. |
| Directed Differentiation Kits | Commercial trilineage differentiation kits | Standardized protocols for efficient differentiation into the three germ layers. |
Signaling Pathways in Pluripotency and Reprogramming
The molecular mechanisms governing pluripotency maintenance and somatic cell reprogramming involve complex signaling networks. Key pathways include those mediated by Toll-like receptors (TLR), GDNF/RET, interleukins (ILs), FGF/FGFR, and SMAD, alongside activation of NIMA kinases [26]. The process of reprogramming somatic cells to iPSCs involves profound remodeling of chromatin structure and the epigenome, changes in metabolism, cell signaling, intracellular transport, and proteostasis [24] [25]. During the initial phase of reprogramming, c-Myc associates with histone acetyltransferase complexes to induce global histone acetylation, enabling exogenous Oct4 and Sox2 to bind their target loci [25]. The ratio of Sox2 to Oct4 is critical for reprogramming efficiency and iPSC colony quality [25].
Diagram Title: Key Molecular Events in Cellular Reprogramming
The comprehensive assessment of pluripotency requires an integrated approach combining multiple molecular and functional techniques. While traditional markers and the teratoma assay have historically formed the foundation of pluripotency evaluation, recent advances offer more standardized and precise alternatives. The identification of novel, specific marker genes through long-read sequencing and the development of computational tools like hiPSCore represent significant progress toward more objective, efficient quality control [23]. Researchers should select assessment strategies based on their specific application, considering that in vitro models of increasing complexity, such as 3D organoids, may eventually reduce reliance on animal-based assays [22]. As the field advances, continued refinement of pluripotency assessment protocols will enhance the reliability of stem cell-based disease models and accelerate the development of safe, effective regenerative therapies.
Ethical and Regulatory Considerations in Stem Cell Sourcing
The foundation of robust and reproducible stem cell-based disease modeling rests upon the consistent and ethical procurement of starting cellular materials. For researchers, scientists, and drug development professionals, the choice of stem cell source is not merely a technical decision but one fraught with significant ethical and regulatory implications that directly impact experimental validity and clinical translation. Stem cell sourcing refers to the processes of obtaining, characterizing, and banking stem cells for research and therapeutic applications. These processes are governed by an intricate framework of ethical principles and regulatory requirements that vary based on the cellular origin and intended application [27] [28].
The moral weight assigned to different stem cell sources directly influences regulatory scrutiny, funding eligibility, and public perception of research outcomes. Within the context of potency evaluation for disease modeling, understanding these considerations is paramount, as the developmental potential and functional capacity of stem cells are inextricably linked to their origin and the ethical integrity of their procurement [29]. This guide provides a comparative analysis of major stem cell sources, focusing on the ethical and regulatory landscapes that researchers must navigate to ensure their work is both scientifically sound and socially responsible.
The choice of stem cell source carries distinct implications for research applications, particularly in disease modeling and drug development. The table below provides a detailed comparison of the key characteristics of different stem cell sources.
Table 1: Comparative Analysis of Stem Cell Sources for Research and Disease Modeling
| Stem Cell Source | Key Ethical Considerations | Regulatory Classification (U.S. FDA Example) | Key Markers for Potency Evaluation | Primary Research Applications |
|---|---|---|---|---|
| Human Embryonic Stem Cells (hESCs) | Destruction of human embryos; moral status of the embryo [27] [30]. | Typically regulated as biologic drugs; require extensive preclinical data [27]. | OCT4, SOX2, NANOG (Pluripotency TFs) [29]. | Studying early development; disease mechanisms; generating diverse cell types [11]. |
| Induced Pluripotent Stem Cells (iPSCs) | Avoids embryo destruction; donor consent for somatic cell source; potential for germline modification [27] [11] [30]. | Subject to FDA oversight as cell-based products; regulatory pathway depends on manipulation and use [27] [24]. | OCT4, NANOG; Teratoma formation in vivo; Embryoid body formation [29] [24]. | Patient-specific disease modeling; personalized drug screening; autologous cell therapy development [11] [24]. |
| Adult Mesenchymal Stem Cells (MSCs) | Minimal ethical controversy; informed consent for tissue donation (e.g., bone marrow, adipose) [27] [31]. | "Minimally manipulated" products may have different regulatory pathways; more than minimal manipulation triggers stricter oversight [27]. | CD73, CD90, CD105 (surface markers); differentiation into osteocytes, chondrocytes, adipocytes [32] [29]. | Immunomodulation studies; hematopoietic support; regenerative medicine for bone/cartilage [11] [31]. |
| Fetal Stem Cells | Ethical concerns regarding elective abortion; informed consent from donor [27]. | Strictly regulated; sourcing often restricted by law in many jurisdictions. | Varies by tissue source; often tissue-specific progenitors. | Studies of specific developmental stages; certain neurodegenerative diseases. |
Ethical Frameworks and Principles
Stem cell research and sourcing are guided by established ethical frameworks to ensure responsible scientific practice. The following diagram illustrates the application of core bioethical principles to stem cell sourcing.
Figure 1: Ethical principles and their practical applications in stem cell sourcing. The principles of biomedical ethics directly inform specific operational requirements for ethically sound research.
Application of Core Principles in Sourcing
Respect for Autonomy and Informed Consent: The informed consent process is fundamental for all stem cell research involving human donors. This is particularly critical for vulnerable populations and when using biospecimens that might be used to generate iPSC lines, which have the potential for indefinite self-renewal. Consent forms must clearly state the scope of research, including the possibility of future uses, commercial applications, and whether cells will be shared with other researchers [27] [28]. The complexity of stem cell science necessitates that information is delivered in an accessible manner, ensuring true understanding from donors.
Justice and Equitable Access: The benefits of stem cell research must be distributed justly to avoid exacerbating existing health disparities. The high cost of developing stem cell therapies can limit access for disadvantaged populations, creating an ethical imperative for researchers, funders, and policymakers to develop mechanisms that promote broad accessibility [27] [28]. Furthermore, the burdens of research, such as participating in early-phase clinical trials, should not fall disproportionately on populations unlikely to benefit from the resulting therapies.
Regulatory Landscapes and Oversight
A complex global regulatory landscape governs stem cell sourcing and application, ensuring safety and efficacy while fostering innovation. The following diagram outlines a generalized regulatory pathway for stem cell-based products.
Figure 2: A simplified U.S. FDA regulatory pathway for stem cell-based products. The level of regulatory oversight depends heavily on the degree of manipulation and intended use of the cells.
International Standards and Guidelines
The International Society for Stem Cell Research (ISSCR) Guidelines: The ISSCR provides comprehensive, internationally recognized guidelines for stem cell research and clinical translation, which are updated regularly to reflect scientific advances. The 2025 guidelines emphasize rigor, oversight, and transparency. They provide specific recommendations for sensitive areas, including research on human embryos, stem cell-based embryo models (SCBEMs), chimeras, and organoids. A key update in 2025 retired the classification of embryo models as "integrated" or "non-integrated" in favor of the inclusive term SCBEMs, and it prohibits the culture of SCBEMs to the point of potential viability (ectogenesis) [28].
Global Regulatory Variations: Regulatory approaches to stem cell therapies vary significantly worldwide. For example, in Mexico, the regulatory agency COFEPRIS oversees cell therapies, treating them as health inputs requiring sanitary authorization. However, the country has faced challenges with a proliferation of clinics offering unproven stem cell treatments, exploiting regulatory gaps. Mexico is actively working on specific regulations, such as the proposed NOM-260, to provide clearer oversight and curb the marketing of unvalidated "miracle cures" [33]. This highlights the importance for researchers to be aware of not only their local regulations but also international standards, especially when collaborating across borders.
Experimental Protocols for Potency Evaluation
Evaluating the functional potency of sourced stem cells is a critical step in validating their utility for disease modeling. The following section outlines standard experimental workflows.
In Vitro Pluripotency Assessment
Aim: To confirm the differentiation capacity of pluripotent stem cells (PSCs), such as hESCs and iPSCs, into derivatives of the three primary germ layers in a controlled laboratory setting.
Protocol:
- Embryoid Body (EB) Formation: Harvest PSCs and culture them in low-attachment plates in a medium that does not support pluripotency (e.g., without bFGF for hPSCs). This encourages the formation of 3D aggregates known as embryoid bodies [29].
- Spontaneous Differentiation: Maintain EBs in suspension culture for 7-10 days, allowing for spontaneous differentiation.
- Directed Differentiation (Optional): To enhance the yield of a specific germ layer, supplement the culture medium with specific growth factors (e.g., Activin A for endoderm, BMP4 for mesoderm, FGF2 for ectoderm).
- Analysis: After 14-21 days, harvest the EBs. Assess differentiation potential via:
- Immunocytochemistry: Fix EBs, section them, and stain for germ layer-specific markers. Common markers include:
- Ectoderm: β-III-Tubulin (TUJ1) for neurons, Nestin for neural progenitors.
- Mesoderm: Smooth Muscle Actin (SMA) for smooth muscle, Brachyury for early mesoderm.
- Endoderm: Sox17, FoxA2 for definitive endoderm, Alpha-fetoprotein (AFP) for hepatic lineage [29].
- RT-qPCR: Analyze the gene expression of the aforementioned markers relative to undifferentiated PSCs.
- Immunocytochemistry: Fix EBs, section them, and stain for germ layer-specific markers. Common markers include:
In Vivo Teratoma Formation Assay
Aim: To provide definitive evidence of pluripotency by demonstrating the ability of PSCs to form complex, differentiated tissues from all three germ layers in an in vivo environment.
Protocol:
- Cell Preparation: Harvest a concentrated suspension of PSCs (e.g., 1-5 million cells) in a suitable buffer like PBS or Matrigel.
- Transplantation: Immunocompromised mice (e.g., NOD-SCID or NSG strains) are used as hosts to prevent graft rejection. Inject the cell suspension intramuscularly, subcutaneously, or under the testis capsule.
- Monitoring and Tumor Harvest: Monitor the injection site for tumor formation over 8-16 weeks. The growth of a palpable, solid tumor (teratoma) is indicative of successful engraftment and proliferation.
- Histopathological Analysis:
- Surgically remove the teratoma and fix it in formalin.
- Process the tissue for paraffin embedding and sectioning.
- Stain tissue sections with Hematoxylin and Eosin (H&E).
- A qualified pathologist must examine the sections for the presence of well-differentiated tissues derived from all three germ layers, such as:
- Ectoderm: Neural rosettes, pigmented cells (retinal epithelium), keratinocytes.
- Mesoderm: Cartilage, bone, muscle, adipose tissue.
- Endoderm: Gut-like epithelial structures, respiratory tubules [29].
Table 2: Key Assays for Functional Potency Evaluation of Pluripotent Stem Cells
| Assay Type | Key Readouts | Advantages | Disadvantages | Regulatory Relevance |
|---|---|---|---|---|
| In Vitro (Embryoid Body) | Immunostaining for germ layer markers (e.g., TUJ1, SMA, AFP); RT-qPCR analysis. | Relatively quick and inexpensive; avoids animal use. | May not fully replicate in vivo complexity; spontaneous differentiation can be heterogeneous. | Supports initial characterization; required for lot-release in some therapeutic applications. |
| In Vivo (Teratoma) | Histological identification of differentiated tissues from all three germ layers. | Considered the "gold standard" for demonstrating pluripotent capacity. | Time-consuming (8-16 weeks); expensive; requires animal facility; ethical considerations for animal use. | Often required by regulatory bodies as part of the safety package for PSC-based therapies. |
| Flow Cytometry | Quantification of pluripotency surface markers (e.g., SSEA-4, Tra-1-60, Tra-1-81). | High-throughput, quantitative, can be applied to a single-cell suspension. | Does not demonstrate functional differentiation potential; marker expression can be culture-dependent. | Used for routine quality control and stability assessment of cell banks. |
The Scientist's Toolkit: Essential Reagents for Stem Cell Research
Table 3: Key Research Reagent Solutions for Stem Cell Sourcing and Characterization
| Reagent / Material | Function in Research | Example Application in Sourcing/Potency Evaluation |
|---|---|---|
| Pluripotency Transcription Factor Antibodies | Molecular markers for confirming pluripotent state via immunocytochemistry or Western blot. | Detecting OCT4, SOX2, NANOG in newly derived iPSC or hESC lines to confirm successful reprogramming or culture [29]. |
| Germ Layer-Specific Antibodies | Identifying differentiated cell types derived from PSCs. | Staining for β-III-Tubulin (ectoderm), Smooth Muscle Actin (mesoderm), and Sox17 (endoderm) in embryoid bodies to validate multilineage differentiation potential [29]. |
| Reprogramming Factors (OSKM) | Key tools for generating induced pluripotent stem cells (iPSCs) from somatic cells. | Lentiviral or sendai viral vectors expressing OCT4, SOX2, KLF4, and c-MYC used to reprogram patient fibroblasts for disease modeling [30] [24]. |
| Defined Culture Media & Matrices | Providing a consistent, xeno-free environment for the maintenance and differentiation of stem cells. | TeSR-E8 or mTeSR1 media combined with recombinant laminin-521 to support the feeder-free culture of PSCs, reducing variability and enhancing reproducibility [11]. |
| Flow Cytometry Panels | Quantitative analysis of cell surface markers for characterization and purity assessment. | Using antibodies against CD73, CD90, CD105 (positive markers) and CD34, CD45, HLA-DR (negative markers) to characterize mesenchymal stem cell (MSC) populations [32] [29]. |
The ethical and regulatory dimensions of stem cell sourcing are not peripheral concerns but are central to the scientific integrity and translational potential of stem cell-based disease models. As the field progresses with the development of complex organoids and assembloids, these considerations will only increase in complexity. A deep understanding of the ethical principles of autonomy, justice, beneficence, and non-maleficence, combined with a rigorous adherence to evolving international guidelines and regulatory pathways, is indispensable for researchers. By integrating these considerations from the earliest stages of experimental design—including careful source selection, robust informed consent procedures, and comprehensive potency evaluation—scientists can ensure their work on potency evaluation in disease modeling is built upon a responsible, reproducible, and ethically sound foundation.
Building Better Models: Techniques for Potent Stem Cell Differentiation and Application
Advanced Differentiation Protocols for Specific Lineages
The successful derivation of specific, functional cell lineages from pluripotent stem cells is a cornerstone of modern regenerative medicine, disease modeling, and drug development. However, achieving consistent, high-efficiency differentiation remains a significant challenge across multiple tissue types. This comparison guide objectively evaluates advanced differentiation protocols for hematopoietic, myogenic, and renal lineages, framing the analysis within the broader context of potency evaluation for stem cell-based disease models. By examining direct experimental comparisons of efficiency, reproducibility, and functional outcomes, this guide provides researchers with evidence-based recommendations for protocol selection and implementation.
The following analysis reveals substantial variability in the performance of differentiation protocols across key metrics. For hematopoietic differentiation, a modified 2D-multistep approach demonstrates superior efficiency and cost-effectiveness. For myogenic differentiation, monolayer-based protocols with defined signaling pathway modulation outperform embryoid body-based methods. Meanwhile, kidney organoid generation continues to evolve toward more complex assembloid models despite persistent maturation challenges.
Table 1: Overall Differentiation Protocol Performance Ratings
| Lineage | Top-Performing Protocol | Efficiency | Reproducibility | Functional Maturation | Technical Complexity |
|---|---|---|---|---|---|
| Hematopoietic | 2D-Multistep with AhR activation | High | High | Medium | Medium |
| Myogenic | Protocol III (Monolayer) | High | Medium-High | Medium-High | High |
| Renal | Assembled Organoid Models | Medium | Medium | Low-Medium | Very High |
Direct Comparative Analysis of Hematopoietic Differentiation Methods
A rigorous direct comparison of four serum-free, feeder-free hematopoietic differentiation methods revealed striking differences in performance metrics [34]. Researchers improved upon an existing 2D-multistep method incorporating aryl hydrocarbon receptor (AhR) hyperactivation, then compared it against three other established approaches: two utilizing embryoid body (EB) formation (one simple, one multistep) and one additional 2D monolayer method with simpler stages.
Table 2: Quantitative Comparison of Hematopoietic Differentiation Protocols
| Method Type | CD34+ Cell Yield | Functional Progenitors (CFU) | Cost per Well | Hands-on Time | Disease Modeling Sensitivity |
|---|---|---|---|---|---|
| 2D-Multistep (Improved) | 7× original protocol | Highest (Robust multilineage) | 50% of original | 40% reduction | Accurately recapitulated DS and β-thalassemia phenotypes |
| 2D-Simple | Medium | Medium | Low | Low | Not assessed |
| EB-Multistep | Medium | Medium | High | High | Moderate |
| EB-Simple | Low | Low | Medium | Medium | Low |
The optimized 2D-multistep method generated significantly higher numbers of CD34+ progenitor cells (7-fold increase over the original protocol) and functional hematopoietic progenitors capable of forming multilineage colonies, while simultaneously reducing costs by 50% and hands-on time by 40% [34]. This protocol demonstrated superior sensitivity in disease modeling, accurately recapitulating expected hematopoietic defects in Down syndrome and β-thalassemia patient-derived iPSCs.
The methodology involved a staged approach: initial mesoderm induction followed by hematopoietic specification enhanced by AhR activation using 6-formylindolo[3,2-b]carbazole (FICZ). Key modifications included extending Wnt activation, eliminating unnecessary media changes, and adding reagents directly to existing cultures to minimize disturbance [34].
Myogenic Differentiation Protocol Comparison
A side-by-side evaluation of three transgene-free myogenic differentiation protocols revealed clear differences in efficiency based on hierarchical myogenic regulatory factor expression and myotube formation [35].
Table 3: Myogenic Differentiation Protocol Efficiency
| Protocol | Approach | Key Signaling Modulators | MYF5/MYOD Expression | Myotube Formation | CD56 Specificity |
|---|---|---|---|---|---|
| Protocol I | EB-based with selection | ITS, collagen adhesion | Moderate | Low | Not specific |
| Protocol II | EB-based with strong induction | BIO, forskolin, bFGF | Moderate | Medium | Not specific |
| Protocol III | Monolayer with defined media | CHIR99021, DAPT, FGF2 | High | High | Not specific |
Protocol III, employing a monolayer system with defined temporal application of small molecules to precisely manipulate key developmental signaling pathways, demonstrated superior efficiency in generating myogenic cells [35]. The protocol achieved this through sequential media formulations: initial WNT activation using CHIR99021 to induce mesodermal commitment, followed by simultaneous TGF-β and BMP inhibition to promote myotome formation, and finally maturation factors to support terminal differentiation.
The critical methodological insight was that CD56, often used as a myogenic marker, demonstrated poor specificity across all protocols, suggesting researchers should rely instead on the hierarchical expression of myogenic regulatory factors (MYF5, MYOD, MYOG) and structural proteins like embryonic and adult myosin heavy chains (MYH3, MYH2) [35].
Advanced Technology Integration in Differentiation Optimization
Machine Learning for Early Efficiency Prediction
The extended timeframes required for many differentiation protocols (often 80+ days) present significant bottlenecks in optimization and quality control. Researchers have developed a non-destructive prediction system using phase-contrast imaging and machine learning to forecast muscle stem cell differentiation efficiency approximately 50 days before protocol completion [36].
This approach employs Fast Fourier Transform (FFT) feature extraction from cellular images taken between days 14-38, followed by random forest classification to predict final MYF5+ cell percentage on day 82. The system achieved accurate classification of high and low-efficiency samples, enabling early quality assessment without destructive sampling [36]. This methodology is particularly valuable for optimizing protocols and selecting high-quality cultures early in lengthy differentiation processes.
Design of Experiments for Systematic Optimization
Traditional "one-factor-at-a-time" optimization approaches are inefficient for complex differentiation protocols with multiple interacting variables. Design of Experiments (DOE) methodologies enable researchers to strategically screen numerous culture conditions through reduced experimental runs while capturing interaction effects between factors [37].
Fractional factorial designs, orthogonal arrays, and response surface methodology have been successfully applied to optimize pluripotent stem cell differentiation processes, offering more efficient condition screening and quantitative modeling of differentiation outcomes. These approaches are increasingly recommended by regulatory authorities for cell production process development [37].
Systems Biology and Artificial Intelligence
The integration of systems biology and artificial intelligence (SysBioAI) is transforming stem cell differentiation protocol development by enabling holistic analysis of large-scale multi-omics datasets [38]. This approach helps address persistent challenges in stem cell therapy development, including product heterogeneity, incomplete mechanistic understanding, and limited predictive power of traditional trial designs.
SysBioAI tools can analyze molecular-level data (transcriptomics, proteomics), cellular and tissue-level characteristics (3D spatial features), and complex system behaviors to identify critical quality attributes and optimize differentiation protocols through iterative refinement cycles [38].
Signaling Pathways Governing Lineage Specification
The differentiation protocols examined share common principles of developmental biology, manipulating conserved signaling pathways to direct cell fate decisions. The diagram below illustrates the key pathways targeted in the most effective protocols.
Kidney Organoid Differentiation: Advances and Challenges
Recent advances in kidney differentiation have progressed from simple nephron-containing organoids to more complex models incorporating ureteric epithelium and stromal components [39]. The latest protocols generate ureteric organoids that can be combined with nephron-forming organoids to create integrated assembloid models, better recapitulating native kidney architecture.
However, significant challenges remain in evaluating the transcriptional complexity of these models, eliminating off-target cell types, achieving postnatal maturation levels, and ensuring quality control for potential therapeutic applications [39]. Current kidney differentiation protocols primarily model embryonic development, limiting their utility for studying adult-onset kidney diseases.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Advanced Differentiation Protocols
| Reagent Category | Specific Examples | Function in Differentiation | Protocol Applications |
|---|---|---|---|
| Wnt Pathway Modulators | CHIR99021 (agonist) | Mesoderm induction, hematopoietic specification | Myogenic (Protocol III), Hematopoietic |
| TGF-β/BMP Inhibitors | SB431542, LDN193189 | Promote myogenesis, inhibit alternative fates | Myogenic (Protocol III) |
| AhR Activators | FICZ (6-formylindolo[3,2-b]carbazole) | Expand hematopoietic progenitors | Hematopoietic (2D-Multistep) |
| Growth Factors | bFGF, VEGF, SCF, TPO, IGF-1, HGF | Support proliferation and lineage specification | Hematopoietic, Myogenic |
| Extracellular Matrices | Matrigel, Collagen I | Provide structural support and biochemical cues | Myogenic, General iPSC culture |
| Metabolic Regulators | ITS (Insulin-Transferrin-Selenium) | Support cell growth and differentiation | Myogenic (Protocol I) |
The direct comparison of differentiation protocols reveals that methods incorporating precise temporal control of developmental signaling pathways, whether through small molecules or growth factors, consistently outperform less targeted approaches. The optimal 2D-multistep hematopoietic protocol and monolayer myogenic method both demonstrate the importance of staged, chemically-defined conditions that mirror embryonic development.
Future protocol development will increasingly leverage computational approaches, including DOE for systematic optimization, machine learning for non-destructive quality prediction, and systems biology for mechanistic understanding. As the field progresses toward clinical applications, standardization, scalability, and rigorous potency assessment will become increasingly critical for translating stem cell technologies into reliable research tools and ultimately transformative therapies.
Organoid and Assembloid Technology for Complex Tissue Modeling
The pursuit of physiologically relevant models that accurately recapitulate human biology has long been a challenge in biomedical research. Traditional two-dimensional (2D) cell cultures, while valuable for many applications, lack the three-dimensional architecture, cellular diversity, and cell-cell interactions characteristic of native tissues [40]. Similarly, animal models, despite their contributions to scientific discovery, present significant species differences that limit their translational potential for human disease [41]. The advent of three-dimensional (3D) organoid technology has revolutionized our approach to modeling human tissues in vitro. Organoids are self-organizing 3D structures derived from pluripotent stem cells (PSCs) or adult stem cells (AdSCs) that mimic the cellular composition, structure, and function of organs [42] [40]. These miniature organ-like structures can be generated from either human pluripotent stem cells (hPSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), or tissue-specific resident stem cells [42] [43].
Building upon organoid technology, assembloids represent a more recent advancement that enables the modeling of complex interactions between different tissue types or brain regions. Assembloids are 3D preparations formed by the integration of multiple organoids or their combination with other specialized cell types, creating systems that recapitulate inter-regional communication and cellular migration [44]. This modular approach allows researchers to reconstruct specific biological pathways and investigate emergent properties that arise from cellular crosstalk, providing unprecedented opportunities for studying human development, disease mechanisms, and therapeutic interventions [45] [44]. The progression from organoids to assembloids marks a significant evolution in stem cell technology, offering increasingly sophisticated tools for modeling the intricate complexity of human tissues and their interactions in health and disease.
Technological Foundations: From Organoids to Assembloids
The foundation of both organoid and assembloid technologies lies in the stem cells from which they are derived. The most commonly used stem cells for generating brain organoids and assembloids are embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) [43]. Human ESCs (hESCs) are pluripotent cells isolated from the inner cell mass of blastocysts and were first established in 1998 [40]. These cells can self-renew indefinitely while maintaining the potential to differentiate into derivatives of all three germ layers. However, the use of hESCs raises ethical concerns regarding embryo destruction, prompting the search for alternative approaches [43].
The development of induced pluripotent stem cells (iPSCs) addressed these ethical limitations and opened new avenues for personalized disease modeling. iPSCs are generated by reprogramming adult somatic cells through the introduction of specific pluripotency factors, initially demonstrated using the OSKM factors (Oct3/4, Sox2, Klf4, and c-Myc) [43] [40]. These "embryonic stem cell-like" cells share the pluripotency and self-renewal capabilities of ESCs while maintaining the genetic background of the donor, making them particularly valuable for modeling genetic disorders and developing patient-specific therapies [43]. Significant advancements have been made to improve reprogramming efficiency and safety, including the use of non-integrating delivery methods and small molecules that enhance the reprogramming process [43].
Table 1: Comparison of Stem Cell Sources for Organoid and Assembloid Generation
| Stem Cell Type | Origin | Pluripotency | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocysts | Pluripotent | Well-established differentiation protocols; Genetically stable | Ethical concerns; Immunological rejection upon transplantation | Early human development studies; Disease modeling (non-patient specific) |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells | Pluripotent | Patient-specific modeling; No ethical concerns; Broadly applicable | Potential genetic instability during reprogramming; Variable reprogramming efficiency | Personalized disease modeling; Drug screening; Regenerative medicine |
| Adult Stem Cells (AdSCs) | Specific adult tissues | Multipotent or unipotent | Tissue-specific maturity; Faster protocol; Maintain age-related characteristics | Limited expansion potential; Restricted to certain tissues | Modeling adult tissues; Infectious diseases; Cancer research |
Beyond PSCs, neural progenitor cells (NPCs) represent another important cell source for neural-specific models. NPCs are multipotent neural stem cells capable of self-renewal and differentiation into neurons and glial cells, though they do not give rise to non-neuronal cells of the central nervous system [43]. These cells can be found throughout the CNS during development and in adult brains, and can also be generated in vitro through the differentiation of ESCs or iPSCs using specific neural induction growth factors [43].
The choice between PSC-derived and AdSC-derived organoids depends on the research objectives. PSC-derived organoids typically undergo a stepwise differentiation process that mimics embryonic development, resulting in complex cellular compositions that may include multiple lineage descendants [40]. These models are particularly valuable for studying early organogenesis and developmental disorders. In contrast, AdSC-derived organoids are directly generated from tissue-specific stem cells and generally exhibit greater maturity and similarity to adult tissues, making them suitable for studying tissue homeostasis, adult-onset diseases, and infectious processes [40].
Organoid Generation and Regional Specification
Organoid generation typically involves a series of carefully orchestrated steps that guide stem cells through processes resembling in vivo development. The methodology generally revolves around three main steps: (1) induction or inhibition of key signaling pathways to establish appropriate regional identity during stem cell differentiation; (2) implementation of media formulations that support terminal differentiation of required cell types; and (3) propagation of cells in three-dimensional environments using extracellular matrix scaffolds to support complex tissue architecture [42].
Regional specification of organoids is achieved through the timed administration of specific patterning factors that mimic embryonic signaling centers. For brain organoids, these patterning cues establish positional identities along the dorsal-ventral (D-V) and anterior-posterior (A-P) axes, leading to the formation of distinct brain regions [40]. For example, the generation of dorsal spinal cord organoids involves modifying protocols for ventral spinal cord organoids by excluding ventralizing cues [45], while cerebral cortical organoids are generated through inhibition of both WNT and transforming growth factor-β (TGF-β) signaling [40]. The continuous refinement of differentiation protocols has resulted in organoids with increasingly complex architectures and cellular diversity, better recapitulating the complexity of native tissues [42].
Assembloid Integration Strategies
Assembloids represent a significant advancement beyond single organoids by enabling the study of interactions between different tissue types or brain regions. These integrated systems are typically created by combining pre-differentiated organoids in a way that promotes their functional integration [44]. The assembly process must be carefully timed to match the developmental maturity of the components and provide appropriate environmental cues to support the formation of functional connections.
Current assembloid strategies can be categorized into four main types: multi-region assembloids that combine different brain areas; multi-lineage assembloids that incorporate cells from different germ layers; multi-gradient assembloids that establish positional signaling cues; and multi-layer assembloids that stack different tissue types [46]. For example, in the nervous system, forebrain assembloids have been created by combining pallial (dorsal forebrain) organoids containing primarily glutamatergic neurons with subpallial organoids rich in GABAergic neurons, enabling the study of interneuron migration and integration [44]. More complex four-part assembloids have recently been developed to model the entire ascending somatosensory pathway, incorporating somatosensory, spinal, thalamic, and cortical organoids [45].
The successful integration of assembloids requires not only physical proximity but also the establishment of functional connections. This process is supported by the inherent migratory and axon guidance mechanisms of the component cells, which, when provided with the appropriate environmental cues, can recapitulate aspects of natural circuit formation [44]. The resulting models enable researchers to study processes that were previously inaccessible in vitro, such as neural circuit assembly, long-distance cell migration, and complex inter-tissue signaling.
Comparative Analysis: Organoids vs. Assembloids
Structural and Functional Complexity
The fundamental distinction between organoids and assembloids lies in their architectural complexity and functional capabilities. Organoids typically model single tissue units or specific organ regions, exhibiting remarkable internal organization but limited capacity to represent interactions between different tissues. For instance, cerebral organoids can recapitulate aspects of human cortical development, including the formation of progenitor zones and layered neuronal organization [40], while intestinal organoids contain functional enterocytes, goblet cells, Paneth cells, and neuroendocrine cells [42]. However, these models often lack the supporting stroma and tissue-tissue interfaces characteristic of intact organs.
Assembloids address this limitation by enabling the integration of multiple discrete units into a coordinated system. This approach allows for the reconstruction of specific biological pathways that span different anatomical regions. A notable example is the human ascending somatosensory assembloid (hASA), which integrates four distinct components—somatosensory organoids, dorsal spinal cord organoids, thalamic organoids, and cortical organoids—to model the complete spinothalamic pathway responsible for pain, touch, and body movement sensation [45]. This multi-part integration enables researchers to study information flow across a complete neural circuit, from sensory detection to cortical processing, in a way that single organoids cannot achieve.
Table 2: Structural and Functional Comparison of Organoids and Assembloids
| Feature | Organoids | Assembloids |
|---|---|---|
| Architectural Complexity | Single tissue unit or brain region | Multiple integrated tissue units or regions |
| Cellular Diversity | Limited to derivatives of a specific lineage or region | Combines multiple lineages or regional identities |
| Modeling Capabilities | Organ development, tissue-specific diseases | Inter-regional communication, neural circuits, multi-organ interactions |
| Key Applications | Disease modeling of single tissues, developmental biology, drug screening | Circuit-level dysfunction, cell migration, axon guidance, systemic diseases |
| Technical Challenges | Reproducibility, maturation, vascularization | Integration timing, functional connectivity, increased complexity |
| Examples | Cerebral organoids, intestinal organoids, hepatic organoids | Forebrain assembloids, cortico-spino-muscular assembloids, sensory pathway assembloids |
Applications in Disease Modeling
Both organoids and assembloids have demonstrated significant utility in modeling human diseases, though their applications differ in scope and biological complexity. Organoids have been particularly valuable for studying monolithic disorders affecting specific tissues or organs. For example, brain organoids have been used to model neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), and Huntington's disease (HD) [47]. These models recapitulate key pathological features, including amyloid-beta deposition and tau pathology in AD, α-synuclein accumulation in PD, and mutant huntingtin protein aggregation in HD [47]. Similarly, gastric organoids have been employed to study Helicobacter pylori infection, while intestinal organoids have been used to model cystic fibrosis and study drug responses [42].
Assembloids extend these capabilities to circuit-level and multi-tissue disorders that involve interactions between different cell types or anatomical regions. The forebrain assembloid platform has been instrumental in studying Timothy syndrome, a neurodevelopmental disorder associated with autism spectrum disorder, intellectual disability, and epilepsy [44]. Research using patient-derived assembloids revealed abnormal migration patterns of cortical interneurons and identified two distinct phenotypic mechanisms: decreased saltation length regulated by increased calcium influx through L-type calcium channels, and increased saltation frequency downstream of upregulated GABAergic receptors [44]. Similarly, the hASA platform has been used to study pain disorders associated with mutations in the SCN9A gene encoding the NaV1.7 sodium channel, demonstrating that loss-of-function mutations disrupt synchronized activity while gain-of-function mutations induce hypersynchrony throughout the sensory pathway [45].
Experimental Throughput and Data Generation
In terms of experimental throughput, organoids generally offer advantages for high-content screening applications due to their relative simplicity and standardization. Cerebral organoids have been used for drug screening against various neurological conditions, leveraging their reproducible cellular composition and disease-related phenotypes [43]. The scalability of organoid systems enables medium- to high-throughput compound testing, particularly when combined with automated imaging and analysis platforms.
Assembloids, while more complex to generate and maintain, provide unique opportunities for circuit-level functional analysis that cannot be achieved with simpler systems. The integration of multiple components creates emergent properties that enable more comprehensive functional assessment. For instance, in the hASA model, researchers can trace neuronal connectivity across the four components using modified rabies virus and monitor coordinated responses to stimuli using calcium imaging [45]. Extracellular recordings can detect synchronized activity across the entire assembloid, providing measures of functional integration [45]. These capabilities make assembloids particularly valuable for studying network-level dysfunction in neurological disorders and for evaluating therapeutic interventions that target circuit-level properties.
Experimental Approaches and Methodologies
Key Experimental Protocols
The experimental utility of organoid and assembloid systems relies on a range of methodological approaches that enable the characterization of their structural and functional properties. For lineage validation and cellular characterization, single-cell RNA sequencing (scRNA-seq) has become an indispensable tool. This approach allows researchers to identify distinct cell types within organoids and verify their similarity to in vivo counterparts. In the hASA model, scRNA-seq confirmed the presence of key neuronal populations, including cortical glutamatergic neurons (FOXG1+, SLC17A7+), thalamic excitatory neurons (TCF7L2+, SLC17A6+), dorsal spinal cord projection neurons (HOXB4+), and primary afferent somatosensory neurons (POU4F1+) [45]. Immunostaining provides complementary protein-level validation of region-specific markers and cellular organization.
For connectivity analysis, modified rabies virus tracing has proven particularly valuable in assembloid systems. This technique allows for the precise mapping of synaptic connections between different components. In the hASA model, rabies tracing demonstrated that sensory neurons connect to dorsal spinal cord neurons, which in turn form connections with thalamic neurons, recapitulating the polysynaptic pathway of the native sensory system [45]. This approach provides anatomical evidence of functional integration between assembloid components.
Functional assessment of organoids and assembloids typically employs live imaging and electrophysiological approaches. Calcium imaging using genetically encoded indicators enables the monitoring of neuronal activity in response to various stimuli. For example, in sensory organoids, bath application of agonists for specific receptors (e.g., α,β-methyleneATP for P2RX3 and capsaicin for TRPV1) induces characteristic calcium transients, demonstrating the functional properties of sensory neurons [45]. Similarly, electrophysiological recordings using multi-electrode arrays or patch clamping can assess synaptic activity and network properties. In assembloids, these techniques can detect synchronized activity across multiple components, providing evidence of functional integration [45].
Signaling Pathways in Regional Patterning
The generation of region-specific organoids requires precise manipulation of key developmental signaling pathways. These pathways are typically modulated through the timed addition of small molecules or growth factors that either activate or inhibit specific signaling cascades.
Diagram 1: Key Signaling Pathways in Neural Organoid Patterning. The differentiation of human pluripotent stem cells (hPSCs) into specific neural lineages is guided by modulation of key developmental signaling pathways, including WNT, TGF-β/BMP, and SHH.
The schematic above illustrates how strategic manipulation of these signaling pathways directs the differentiation of hPSCs toward specific neural fates. For example, WNT inhibition promotes anterior fates (forebrain), while WNT activation drives posterior identities (spinal cord) [40]. Within the anterior neural domain, sonic hedgehog (SHH) activation induces ventral patterns, while its inhibition allows dorsal identities to emerge. Similarly, in posterior regions, bone morphogenetic protein (BMP) signaling helps establish dorsal spinal cord identities, while its inhibition promotes ventral fates [45]. Understanding and manipulating these pathways is essential for generating the specific organoid components needed for assembloid integration.
The Scientist's Toolkit: Essential Research Reagents
The generation and analysis of organoids and assembloids rely on a specific set of research reagents and tools that enable the precise control of differentiation, integration, and functional assessment.
Table 3: Essential Research Reagents for Organoid and Assembloid Research
| Reagent Category | Specific Examples | Function | Application Examples |
|---|---|---|---|
| Stem Cell Sources | Human ESCs, iPSCs, tissue-derived adult stem cells | Self-renewal and differentiation potential | Patient-specific modeling (iPSCs), developmental studies (ESCs) |
| Patterning Factors | Small molecules (CHIR99021, DMH1), growth factors (FGF, EGF, BMP, WNT, SHH) | Regional specification and differentiation | Dorsal-ventral patterning, anterior-posterior axis formation |
| Extracellular Matrices | Matrigel, synthetic hydrogels | 3D structural support, biomechanical cues | Organoid embedding, assembloid integration |
| Cell Type Markers | Antibodies for FOXG1, HOXB4, POU4F1, SLC17A7 | Lineage validation and characterization | Immunostaining, flow cytometry |
| Functional Assay Tools | Genetically encoded calcium indicators (GCaMP), modified rabies virus, channel agonists/antagonists | Connectivity mapping and functional assessment | Calcium imaging, synaptic tracing, pharmacological testing |
| Gene Editing Tools | CRISPR/Cas9 systems, antisense nucleotides | Genetic manipulation, disease modeling, gene correction | Introducing disease mutations, gene knockout, therapeutic screening |
Applications in Disease Modeling and Drug Development
Neurodevelopmental and Neuropsychiatric Disorders
Organoid and assembloid technologies have particularly transformed the study of neurodevelopmental disorders, providing unprecedented access to previously inaccessible stages of human brain development. Forebrain assembloids have been instrumental in elucidating the mechanisms underlying Timothy syndrome, a genetic disorder caused by mutations in the CACNA1C gene encoding an L-type calcium channel [44]. Patient-derived assembloids revealed defects in the migration of cortical interneurons from ventral to dorsal regions, characterized by abnormal saltatory migration with decreased saltation length but increased frequency [44]. These findings identified two distinct mechanisms: calcium-dependent regulation of nucleokinesis and enhanced GABA sensitivity, providing new insights into how channelopathies can disrupt human brain development.
The assembloid platform has also enabled large-scale CRISPR-based genetic screens to identify genes critical for human interneuron development. One such screen conducted in approximately 1,000 assembloids identified LNPK, which encodes an endoplasmic reticulum-related protein, as essential for proper interneuron migration [44]. Further investigation revealed that during migration, the endoplasmic reticulum is displaced along the leading neuronal branch prior to nuclear translocation, and LNPK deletion disrupts this process, leading to abnormal migration. This discovery links endoplasmic reticulum dynamics to interneuron migration and provides mechanistic insights into how its disruption may contribute to epileptic encephalopathy in patients with LNPK mutations [44].
Neurodegenerative Diseases
Brain organoids have become valuable tools for modeling age-related neurodegenerative disorders, despite challenges in replicating late-onset phenotypes in developing systems. Alzheimer's disease (AD) models have been generated by introducing familial AD mutations (in APP, PSEN1, or PSEN2) into iPSCs prior to cerebral organoid differentiation [47]. These models recapitulate key pathological features, including amyloid-beta accumulation and tau hyperphosphorylation, providing platforms for investigating disease mechanisms and screening potential therapeutics. Similarly, Parkinson's disease (PD) organoids modeling mutations in genes such as LRRK2 and SNCA exhibit characteristics such as α-synuclein accumulation and selective vulnerability of dopaminergic neurons [47].
To better model the complexity of neurodegenerative processes, researchers are developing more sophisticated assembloid approaches that incorporate multiple cell types relevant to disease pathogenesis. This includes not only neurons but also glial cells, which play crucial roles in neuroinflammation and disease progression. The integration of microglia into brain assembloids enables the study of neuroimmune interactions, while the incorporation of vascular components may help address limitations in nutrient and oxygen exchange, potentially supporting greater organoid maturation and longevity needed to model late-onset phenotypes [47].
Cancer and Tumor Microenvironment
Organoid technology has been extensively applied to cancer modeling through the development of tumor organoids derived from patient samples. Glioblastoma organoids, for example, have been established to model the hypoxic gradients and cellular heterogeneity of this aggressive brain tumor [42]. These models have been used for both diagnostic purposes and therapeutic testing, including the assessment of personalized treatment responses [42]. Prostate organoids derived from primary tissue specimens have demonstrated differential drug responses between patients, highlighting their potential for personalized medicine approaches [42].
Assembloid approaches further advance cancer modeling by enabling the reconstruction of the tumor microenvironment, including interactions between cancer cells and immune components. Glioblastoma organoids have been combined with CAR-T cells in assembloid platforms to study tumor-immune interactions and evaluate antigen-specific CAR-T cell treatments [44]. This application has significant implications for immunotherapy development and personalized treatment strategies. Similarly, assembloids containing metastatic cancer cells and neural organoids have been used to study patterns of tumor infiltration and migration within the nervous system, providing insights into the mechanisms of cancer metastasis [44].
Sensory Biology and Pain Research
Recent advances in assembloid technology have enabled the modeling of complete sensory pathways, opening new avenues for studying sensory biology and pain mechanisms. The human ascending somatosensory assembloid (hASA) represents a particularly sophisticated model that integrates four distinct components: somatosensory organoids (containing sensory neurons), dorsal spinal cord organoids, thalamic organoids, and cortical organoids [45]. This system recapitulates the polysynaptic pathway responsible for transmitting pain, touch, and body movement sensations from the periphery to the brain.
The hASA platform has demonstrated remarkable functional capabilities, including coordinated responses to noxious chemical stimulation and synchronized activity across components [45]. Notably, this model has been used to investigate the circuit-level effects of sodium channel NaV1.7 mutations associated with congenital insensitivity to pain and extreme pain disorders [45]. Experiments revealed that loss-of-function SCN9A mutations (causing pain insensitivity) disrupt synchronized activity throughout the assembloid, while gain-of-function mutations (associated with extreme pain) induce hypersynchrony [45]. These findings illustrate how assembloids can capture circuit-level pathophysiology underlying sensory disorders, providing a powerful platform for both basic research and therapeutic development.
Current Challenges and Future Perspectives
Technical Limitations and Optimization Strategies
Despite their considerable promise, organoid and assembloid technologies face several significant challenges that must be addressed to fully realize their potential. Reproducibility and standardization remain considerable hurdles, with batch-to-batch variability in organoid generation potentially confounding experimental results [42] [46]. This variability stems from multiple factors, including differences in stem cell lines, extracellular matrix compositions, and differentiation protocols. Addressing these challenges will require the development of standardized protocols, quality control metrics, and improved characterization standards.
Vascularization and maturation represent another major challenge, particularly for modeling later developmental stages and adult-onset diseases. Current organoid systems generally lack functional vascular networks, limiting their size and maturation potential due to inadequate nutrient and oxygen diffusion [46]. Several strategies are being explored to address this limitation, including the incorporation of endothelial cells and perfusion using microfluidic organ-on-a-chip platforms [48]. These approaches aim to create vascularized organoids that better recapitulate tissue physiology and enable the study of neurovascular interactions.
Cell type completeness and proportional representation also present challenges, as current organoid protocols may not generate all relevant cell types in appropriate ratios. For example, many brain organoid systems contain relatively few microglia, the resident immune cells of the brain, limiting their utility for studying neuroinflammation [47]. Similarly, the proportions of different neuronal subtypes may not accurately reflect in vivo conditions. Emerging approaches to address these limitations include co-culture strategies, improved patterning protocols, and the generation of multi-lineage organoids that better capture the cellular diversity of native tissues.
Integration with Advanced Technologies
The future development of organoid and assembloid technologies will likely involve increased integration with other advanced platforms to enhance their functionality and experimental utility. Organ-on-a-chip systems, which incorporate microfluidic perfusion, offer solutions to vascularization challenges and enable the study of inter-organ communication through linked tissue compartments [48]. These platforms provide greater control over the cellular microenvironment and can incorporate mechanical cues such as fluid flow and stretch, which are important for proper tissue maturation and function.
Advanced imaging and analysis techniques are also being integrated with organoid and assembloid research to extract more comprehensive information from these complex systems. Light-sheet microscopy enables long-term, high-resolution imaging of organoid development and function, while spatial transcriptomics provides detailed information about gene expression patterns within their architectural context [48]. These approaches, combined with computational modeling and artificial intelligence-based analysis, will enhance our ability to interpret the complex data generated from organoid and assembloid experiments.
Gene editing technologies, particularly CRISPR-Cas9 systems, continue to expand the experimental capabilities of organoid and assembloid platforms [42]. These tools enable the introduction of disease-associated mutations, creation of reporter lines for specific cell types, and functional screening through genetic perturbation. When combined with assembloids, CRISPR-based approaches enable large-scale genetic screens in systems that recapitulate intercellular interactions, as demonstrated by the identification of LNPK's role in interneuron migration [44].
Ethical Considerations and Future Directions
As organoid and assembloid technologies become more sophisticated, they raise important ethical considerations that warrant careful discussion. The increasing complexity of brain organoids, including the emergence of organized neural activity, prompts questions about the potential for consciousness or sentience in these systems [41]. While current evidence suggests that brain organoids do not possess the circuitry necessary for conscious experience, the field would benefit from ongoing ethical analysis and the development of guidelines for this rapidly advancing technology.
Looking forward, organoid and assembloid technologies are poised to transform drug discovery and development by providing more physiologically relevant human models for target validation, efficacy testing, and toxicity assessment [42] [43]. The ability to model patient-specific diseases using iPSC-derived systems offers particular promise for personalized medicine approaches, potentially enabling the identification of optimal treatments for individual patients based on their specific genetic background and disease characteristics [40].
As these technologies continue to evolve, they will likely become increasingly integrated into the drug development pipeline, potentially reducing the current heavy reliance on animal models and improving the translational success of therapeutic candidates. With ongoing advancements in standardization, vascularization, and cellular complexity, organoid and assembloid platforms represent powerful tools that will continue to enhance our understanding of human biology and disease.
CRISPR and Prime Editing for Creating Isogenic Disease Models
The development of isogenic disease models—where the genetic background is identical except for a specific, engineered mutation—has revolutionized the study of human diseases. These models provide a controlled system for dissecting disease mechanisms and evaluating therapeutic potency, particularly in stem cell-based research. For decades, scientists relied on homologous recombination in mouse embryonic stem cells to generate such models, but this approach was time-consuming, inefficient, and not easily translatable to human cells. The emergence of programmable genome-editing technologies, particularly CRISPR-Cas systems and the more recent prime editing, has dramatically accelerated and refined this process. These tools enable precise genetic modifications in human pluripotent stem cells (iPSCs), allowing researchers to create genetically matched pairs of healthy and diseased cells that are ideal for probing gene function and screening drug candidates.
This guide provides a comparative analysis of CRISPR-Cas9 and prime editing platforms for generating isogenic disease models, focusing on their applications in stem cell research. We will examine their underlying mechanisms, editing efficiencies, and practical considerations through experimental data and protocols, providing a framework for selecting the appropriate technology for specific research goals in disease modeling and drug development.
Technology Comparison: Mechanisms and Capabilities
Core Architectures and Editing Mechanisms
CRISPR-Cas9 operates as a versatile DNA-cleaving system. The core machinery consists of the Cas9 nuclease and a guide RNA (gRNA) that directs Cas9 to a specific genomic locus complementary to its sequence. Upon binding, Cas9 induces a double-strand break (DSB) in the DNA. The cell then repairs this break using its endogenous DNA repair pathways, primarily the error-prone non-homologous end joining (NHEJ), which often results in insertions or deletions (indels) that disrupt the gene, or the more precise homology-directed repair (HDR), which can incorporate a co-delivered donor DNA template to introduce specific sequence changes [49] [50].
Prime editing represents a "search-and-replace" technology that offers greater precision without requiring DSBs. The system uses a prime editor protein, a fusion of a Cas9 nickase (H840A) and an engineered reverse transcriptase (RT), programmed by a specialized prime editing guide RNA (pegRNA) [51]. The pegRNA not only specifies the target site but also contains a template for the new genetic sequence. The Cas9 nickase makes a single-strand cut in the DNA, and the reverse transcriptase uses the pegRNA's template to directly "write" the new genetic information into the genome. This process is resolved by cellular machinery that incorporates the edit, enabling precise point mutations, small insertions, and deletions without DSBs [51] [52].
Comparative Analysis of Editing Profiles
The table below summarizes the key characteristics of each platform relevant to creating isogenic models.
Table 1: Platform Comparison for Isogenic Model Generation
| Feature | CRISPR-Cas9 (with HDR) | Prime Editing |
|---|---|---|
| Primary Editing Mechanism | Creates double-strand breaks (DSBs) [49] | Uses a "nick" and reverse transcription; no DSBs [51] |
| Key Components | Cas9 nuclease, sgRNA, donor DNA template [50] | Cas9 nickase-Reverse Transcriptase fusion, pegRNA [51] |
| Types of Edits Possible | Gene knockouts (via NHEJ), precise knock-ins (via HDR) [50] | All 12 possible base-to-base conversions, small insertions, deletions [51] |
| Typical Efficiency in iPSCs | Variable; HDR is typically low (often <10%) and requires active cell division [49] | Highly variable (10%-50%) depending on locus and editor version; improving with new systems [51] |
| Key Advantage | Well-established, effective for gene knockouts, can insert large sequences | High precision, avoids DSBs and their associated risks [51] |
| Primary Limitation | Relies on HDR for precise edits, which is inefficient in non-dividing cells; prone to off-target indels [53] [49] | Limited by pegRNA design and efficiency; cargo size constraints for insertions [51] |
| Impact on DNA Repair | Triggers complex DNA damage response; repair outcomes differ in dividing vs. non-dividing cells [53] | Engages flap-based resolution; avoids activation of DSB repair pathways [49] |
Experimental Data and Workflow for Stem Cell Editing
Quantitative Editing Outcomes
Efficiency and precision are critical metrics when editing precious stem cell lines. The following table collates experimental data from key studies demonstrating the performance of both platforms.
Table 2: Experimental Editing Outcomes in Disease Modeling
| Study Context | Editing Platform | Target / Disease Model | Key Quantitative Outcome |
|---|---|---|---|
| In vivo stem cell editing (Mouse SCD Model) [54] | Prime Editing (PE5max) | HBB gene / Sickle Cell Anemia | 43.6% gene correction in hematopoietic stem cells (HSCs); 43% normal hemoglobin (HbA) replacement. |
| DNA Repair Study (iPSC-derived neurons) [53] | CRISPR-Cas9 | B2Mg1 and other loci | Neurons show prolonged, weeks-long indel accumulation with a bias toward small NHEJ-like indels, unlike dividing cells. |
| Preclinical Therapy (hATTR) [55] | CRISPR-Cas9 (LNP delivery) | TTR gene / Hereditary Transthyretin Amyloidosis | Sustained ~90% reduction in disease-causing TTR protein levels over 2 years post-single dose. |
| Phenylketonuria (PKU) Mouse Model [56] | Prime Editing (PE7 via mRNA-LNP) | Pahenu2 mutation / Phenylketonuria | 20.7% correction of pathogenic mutation; blood phenylalanine reduced below therapeutic threshold. |
Detailed Experimental Protocol
Creating an isogenic model via prime editing in iPSCs involves a structured workflow to ensure high efficiency and clonal purity.
Protocol: Generating an Isogenic iPSC Line with a Point Mutation Using Prime Editing
- pegRNA and nicking sgRNA Design: Design the pegRNA to hybridize to the target strand and encode the desired edit within its reverse transcriptase template (RTT) sequence. For improved efficiency, a second nicking sgRNA targeting the non-edited strand (PE3b system) is often designed [51].
- Delivery into iPSCs: Transfect cultured iPSCs with plasmids or ribonucleoprotein (RNP) complexes containing the prime editor (e.g., PE2, PEmax) along with the pegRNA and nicking sgRNA. Common delivery methods include electroporation or lipid nanoparticles (LNPs) [56].
- Editing and Enrichment: Allow editing to occur for 48-72 hours. To enrich for edited cells, you may use a co-delivered fluorescent marker for FACS sorting or a drug resistance gene for antibiotic selection.
- Single-Cell Cloning: Dissociate the transfected cell population and seed them at a very low density to allow for the growth of single-cell-derived clones. Manually pick individual clones and expand them in 96-well plates.
- Genotypic Validation:
- Initial Screening: Use a mismatch-specific detection assay (e.g., T7E1 or TIDE) on PCR-amplified genomic DNA from mini-preps to identify positively edited clones.
- Deep Sequencing: Perform next-generation sequencing (NGS) of the target locus on candidate clones to confirm the precise edit and quantify the percentage of edited alleles. This is crucial to rule out mosaic clones.
- Off-Target Analysis: Use computational tools to predict potential off-target sites based on the pegRNA sequence. Amplify these loci from the final cloned line and sequence them to ensure no unintended edits have occurred [51] [52].
- Isogenic Line Expansion: Expand a validated, clonally pure, and edited line for downstream differentiation and functional assays.
Diagram 1: Prime editing workflow for isogenic iPSC line generation.
The Scientist's Toolkit: Essential Reagents and Solutions
Successful genome editing requires a suite of specialized reagents. The table below lists key solutions for implementing CRISPR and prime editing in a research setting.
Table 3: Essential Research Reagent Solutions for Genome Editing
| Reagent / Solution | Function | Example & Notes |
|---|---|---|
| Editor Expression Plasmid | Encodes the editor protein (e.g., Cas9, Base Editor, Prime Editor). | PEmax plasmid: A high-performance prime editor backbone for mammalian expression [51]. |
| Guide RNA Expression System | Produces the sgRNA or pegRNA inside the cell. | U6-promoter driven vectors for high-level gRNA expression; modified scaffolds (epegRNA) enhance pegRNA stability [51]. |
| Delivery Vehicle | Facilitates intracellular delivery of editing components. | Lipid Nanoparticles (LNPs): For in vivo delivery or sensitive cells [55]. Electroporation: Standard for iPSCs and immune cells [53]. Virus-Like Particles (VLPs): For protein delivery with reduced off-target persistence [53]. |
| HDR Enhancer | Boosts HDR efficiency for CRISPR-Cas9 edits. | Alt-R HDR Enhancer: A chemical compound that transiently inhibits NHEJ to favor HDR [57]. |
| Stem Cell Culture Media | Maintains pluripotency and viability of iPSCs during and after editing. | Essential for ensuring high cell fitness, which is critical for achieving high editing efficiency and successful clonal expansion. |
| Genomic DNA Extraction Kit | Isolates high-quality DNA from cell clones for genotyping. | A critical first step for all downstream validation assays. |
| NGS Library Prep Kit | Prepares amplicons of the target locus for deep sequencing. | Allows for precise quantification of editing efficiency and detection of unwanted indels or byproducts. |
Pathway and Mechanism Visualization
Understanding the molecular mechanisms of each editor is key to anticipating outcomes and troubleshooting experiments. The diagram below illustrates the core biochemical pathways each system engages.
Diagram 2: Core editing mechanisms of CRISPR-Cas9 and Prime Editing.
The choice between CRISPR-Cas9 and prime editing for creating isogenic disease models is not a matter of one being universally superior, but rather of selecting the right tool for the specific genetic perturbation and cellular context. CRISPR-Cas9 remains a powerful and robust method for generating gene knockouts and, with careful optimization, for inserting larger DNA fragments via HDR. However, its reliance on DSB repair can be a significant drawback in stem cells and non-dividing cells, where HDR efficiency is low and genotoxic stress is a concern.
Prime editing offers a paradigm shift toward greater precision and safety by avoiding DSBs, making it ideally suited for introducing or correcting point mutations and small indels—the types of variants that underlie a vast number of human genetic diseases. Its evolving efficiency, especially with systems like PE5max and PE7, positions it as the emerging technology of choice for creating precise, genomically clean isogenic models in human iPSCs. As delivery methods and editor versions continue to improve, prime editing is poised to become an indispensable tool in the functional genomics and drug discovery pipeline, enabling more accurate modeling of disease and evaluation of therapeutic potency.
Stem cell-based disease models have become cornerstone tools in biomedical research, providing unprecedented insights into human pathology and therapeutic development. This guide objectively compares the experimental applications, performance, and supporting data of these models across three critical areas: neurological, cardiovascular, and renal diseases, within the broader context of potency evaluation in stem cell research.
Neurological Disease Models
Stem cell models are revolutionizing the study of complex neurodegenerative diseases (NDs) by providing human-relevant systems for mechanistic studies and drug screening.
Clinical Trial Landscape and Experimental Data
An analysis of 94 clinical trials reveals the current state of stem cell therapy for major NDs, illustrating the transition from preclinical models to clinical application. The data below summarizes trial phases and participant enrollment across key diseases [58].
Table 1: Analysis of Stem Cell Clinical Trials for Neurodegenerative Diseases (n=94) [58]
| Disease | Total Trials | Phase 3 Trials | Phase 2 Trials | Participants (Cumulative) | Earliest Trial Year |
|---|---|---|---|---|---|
| Alzheimer's Disease (AD) | ~44% of 94 | 0 | 2 ongoing | ~70% of 8000+ | 2011 |
| Parkinson's Disease (PD) | - | 0 | 2 completed, 1 ongoing | - | 2011 |
| Amyotrophic Lateral Sclerosis (ALS) | - | 1 completed, 1 ongoing | 2 completed, 2 ongoing, 1 Phase 2/3 completed | - | 2007 |
| Huntington's Disease (HD) | - | 1 ongoing | 1 completed | - | 2014 |
Note: "-" indicates specific counts not detailed in the source, though proportions and statuses are verifiable.
Key Experimental Protocols and Model Potency
Protocol: Differentiation of Dopaminergic Neurons for Parkinson's Disease Modeling
- Cell Source: Induced Pluripotent Stem Cells (iPSCs) from patients or healthy controls; Ovarian cortical-derived progenitors present an alternative autologous source [11].
- Reprogramming: Using non-integrating Sendai virus or episomal vectors for patient-specific iPSC generation [11].
- Differentiation Method: Sequential application of small molecules to mimic embryonic midbrain development (e.g., SMAD inhibitors, SHH pathway activation) [11] [59].
- Characterization: Immunocytochemistry for tyrosine hydroxylase (TH) and Nurr1; Patch-clamp electrophysiology to confirm electrophysiological activity [11].
- Potency Assessment: Quantification of the percentage of TH-positive neurons; Measurement of dopamine release via HPLC; Functional assessment through electrophysiological activity [11] [58].
Emerging Protocol: Stem Cell-Derived Exosomes for Neurodegenerative Therapy
- Source: Mesenchymal Stem Cell (MSC)-conditioned media [58].
- Isolation: Ultracentrifugation or size-exclusion chromatography [58].
- Engineering: Surface modification with neuron-targeting ligands (e.g., RVG peptide); Loaded with therapeutic miRNAs or anti-inflammatory compounds [58].
- Experimental Application: Intravenous injection in rodent ND models; Tracking biodistribution and assessing reduction in neuroinflammation and oxidative stress markers [58].
Diagram 1: Workflow for generating and validating iPSC-derived dopaminergic neurons for Parkinson's disease modeling.
Cardiovascular Disease Models
Cardiovascular regenerative medicine (CaVaReM) leverages stem cells to model cardiac diseases, screen for cardiotoxicity, and develop regenerative therapies [60].
Model Performance and Therapeutic Efficacy Data
Stem cell-derived cardiovascular organoids and specific cell therapies have shown promising results in both modeling and treating heart disease.
Table 2: Performance Data of Cardiovascular Stem Cell Models and Therapies
| Model / Therapy Type | Key Application | Performance Metrics / Experimental Outcomes | Key Challenges |
|---|---|---|---|
| Pluripotent Stem Cell-Derived Cardiovascular Organoids [11] | Disease modeling, drug-induced cardiotoxicity screening | Recapitulate aspects of cardiac tissue-level electrophysiology and development. | Limited vascularization and structural maturation; Fetal-like gene expression profiles [11] [60]. |
| MSC Therapy for Low Ejection Fraction [61] | Treatment of heart failure | Meta-analysis (52 large animal studies): 7.5% improvement in LVEF [61]. Clinical trials: Improved LVEF, reduced scar size, and reduced rehospitalization rates [61]. | Inconsistent efficacy in trials; Optimal dose, timing, and delivery route not fully standardized [60] [61]. |
| Wharton's Jelly MSC (WJ-MSC) Therapy [61] | Treatment of ischemic heart disease | Clinical trial (n=60): Significant improvement in LVEF [61]. |
Key Experimental Protocols
Protocol: Generating Cardiovascular Organoids from Pluripotent Stem Cells
- Cell Source: Human iPSCs or Embryonic Stem Cells (ESCs) [11] [60].
- Differentiation Induction: Aggregation in 3D culture via forced aggregation or microwell plates.
- Key Signaling Manipulation: Sequential modulation of WNT and BMP signaling pathways to direct mesodermal and cardiac progenitor fate [11].
- Maturation Strategies: Prolonged culture; Application of mechanical stress; Electrical stimulation; Co-culture with endothelial cells [11] [60].
- Functional Assays: Calcium imaging to assess electrophysiology; Contraction analysis; Measurement of secreted kidney hormones for organoid function [11] [62].
Protocol: MSC Therapy for Ischemic Cardiomyopathy
- Cell Source: Bone marrow, adipose tissue, or umbilical cord (e.g., Wharton's Jelly) [60] [61].
- Cell Preparation: In vitro expansion under cGMP conditions; Quality control for surface markers (CD73+, CD90+, CD105+, CD34-, CD45-) [61].
- Delivery Method: Intracoronary infusion, transendocardial injection, or intravenous injection [61].
- Potency and Efficacy Assessment:
- Primary Endpoint: Change in Left Ventricular Ejection Fraction (LVEF) measured by echocardiography or MRI.
- Secondary Endpoints: Reduction in infarct scar size (via MRI); Incidence of Major Adverse Cardiovascular Events (MACE); Functional status (e.g., 6-minute walk test) [61].
Diagram 2: Key pathways and outcomes in MSC-based therapy for cardiovascular disease.
Renal Disease Models
Stem cell-based kidney models have advanced significantly, progressing from simple organoids to complex, functional assembloids that better mimic native kidney physiology and disease.
Research Trends and Model Fidelity
A bibliometric analysis of 1,874 publications from 2015-2024 shows China (31.6%) and the United States (26.5%) as the leading contributors, with a sharp increase in publications in recent years, indicating a rapidly growing field [63] [64]. Mesenchymal stem cells and acute kidney injury models are current focal points [63].
Table 3: Evolution and Application of Stem Cell-Derived Kidney Models
| Model Type | Key Features | Experimental Applications and Performance | Limitations |
|---|---|---|---|
| Kidney Organoids [11] | Self-organizing 3D structures containing nephron components. | Modeling ADPKD: Organoids with PKD1/PKD2 mutations form cysts [11]. | Embryonic stage maturity; Lack of functional collecting duct system [11] [62]. |
| Kidney Assembloids [62] | Combined nephron and collecting duct organoids. | Most advanced model: Demonstrates blood filtration, albumin uptake, hormone secretion, and early urine production in mice. Mouse assembloids achieved newborn-level maturity [62]. | Human assembloid maturity level relative to postnatal development is uncertain [62]. |
| MSC Therapy for Kidney Disease [63] | Focus on paracrine effects, immunomodulation. | Preclinical studies show promise for Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD). Extracellular Vesicles (EVs) are emerging as a key mechanism [63]. | Challenges in safety, efficacy, and patient response variability [63]. |
Key Experimental Protocols
Protocol: Generating Kidney Assembloids for Disease Modeling
- Cell Source: Human iPSCs [62].
- Protocol Workflow:
- Separate Differentiation: Generate nephron progenitor organoids and collecting duct progenitor organoids separately in 3D culture.
- Combination: Physically combine the two organoid types to form assembloids.
- Maturation: Transplant assembloids into immunodeficient mouse kidney capsule for in vivo maturation and vascularization [62].
- Disease Modeling (e.g., for ADPKD): Use iPSCs with CRISPR-Cas9-edited PKD1 or PKD2 mutations [11] [62].
- Functional and Potency Assessment:
- Quantitative Morphometry: Measure cyst number and size.
- Functional Assays: Assess albumin uptake; Measure secretion of kidney-specific hormones.
- Histopathological Analysis: Assess advanced disease features like inflammation and fibrosis [62].
Protocol: MSC-Derived Extracellular Vesicle (EV) Therapy for AKI
- EV Source: MSCs from bone marrow or umbilical cord [63].
- EV Isolation: Tangential flow filtration or size-exclusion chromatography for high-purity EV yield.
- Characterization: Nanoparticle tracking analysis (NTA) for size/concentration; Western blot for EV markers (CD63, CD81, TSG101) [63].
- Experimental Application: Intravenous injection in rodent AKI models (e.g., ischemia-reperfusion injury).
- Efficacy Assessment: Reductions in serum creatinine and blood urea nitrogen (BUN); Histological scoring of tubular injury [63].
Diagram 3: Workflow for generating kidney assembloids and their application in disease modeling.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagent Solutions for Stem Cell Disease Modeling
| Reagent / Solution | Function in Experimental Protocol | Example Application |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) [11] | Patient-specific starting material for generating disease-relevant cell types. | Isogenic cell line generation for disease modeling (e.g., ADPKD, PD). |
| CRISPR-Cas9 Gene Editing Systems [11] | Introduces or corrects disease-associated mutations; creates isogenic control lines. | Knocking out PKD1 in iPSCs to model polycystic kidney disease in assembloids [11] [62]. |
| Small Molecule Inhibitors/Activators [11] | Directs stem cell differentiation by modulating key signaling pathways (e.g., WNT, BMP, SHH). | Generating dopaminergic neurons or cardiomyocytes from pluripotent stem cells. |
| Matrigel / Synthetic Hydrogels [62] | Provides a 3D extracellular matrix environment for organoid and assembloid culture. | Supporting the self-organization and structural integrity of kidney assembloids. |
| cGMP-compliant Cell Culture Media [11] [61] | Supports the expansion and maintenance of cells under standardized, quality-controlled conditions. | Manufacturing MSCs for clinical trials in heart failure or kidney disease. |
| Mesenchymal Stem Cells (MSCs) [11] [60] [61] | Used directly in therapy or as a source of therapeutic exosomes/paracrine factors. | Clinical trials for heart failure, spinocerebellar ataxia, and acute kidney injury. |
| Exosome Isolation Kits [58] | Purifies extracellular vesicles from stem cell-conditioned media for therapeutic or mechanistic studies. | Investigating MSC-derived exosomes as a therapy for neurodegenerative diseases. |
High-Content Screening in Stem Cell-Based Drug Discovery
High-content screening (HCS) represents a transformative technological paradigm in stem cell-based drug discovery. By integrating automated microscopy, sophisticated image processing, and quantitative data analysis, HCS enables the detailed investigation of complex biological processes within stem cells and their derivatives at a previously unattainable scale [65]. This approach is revolutionizing how researchers evaluate drug efficacy, safety, and mechanisms of action using physiologically relevant human stem cell models.
The adoption of HCS is particularly valuable in the context of potency evaluation for stem cell-based disease models. As regulatory agencies emphasize the need for quantitative measures of biological function, HCS provides multidimensional data that can establish correlation between in vitro observations and clinical outcomes [66]. The global HCS market, projected to grow from $3.1 billion in 2023 to $5.1 billion by 2029, reflects the increasing importance of this technology in pharmaceutical research and development [65].
When combined with stem cell-based platforms—including induced pluripotent stem cells (iPSCs) and 3D organoids—HCS enables unprecedented analysis of disease mechanisms, drug responses, and therapeutic potential while reducing reliance on traditional animal models [67]. The convergence of these technologies represents a significant advancement toward more human-relevant, predictive, and individualized approaches to drug discovery.
HCS Technology Platforms and System Comparisons
High-content screening systems vary significantly in their capabilities, configurations, and optimal application scenarios. Understanding these differences is crucial for selecting the appropriate platform for specific research needs in stem cell-based drug discovery.
Core HCS Technologies and Applications
Modern HCS platforms incorporate multiple advanced technologies that enhance their utility for stem cell research:
- High-resolution fluorescence microscopy enables visualization of cellular structures, protein interactions, and disease markers with remarkable clarity, which is vital for early disease detection and monitoring cellular responses to drugs [65].
- Live-cell imaging allows continuous observation of cell behavior over extended periods, enabling researchers to track stem cell differentiation, disease progression, and drug interactions in real-time [65].
- 3D cell culture & organoid screening provides a more accurate representation of human tissue architecture and function, significantly enhancing the physiological relevance of stem cell-based assays [65].
- CRISPR-based functional screening enables researchers to modify genes and analyze their effects in stem cell models, helping identify mechanisms of drug resistance and advance precision medicine applications [65].
Comparative Analysis of Major HCS Systems
Table 1: Comparison of High-Content Screening Systems Relevant to Stem Cell Research
| Vendor/System | Key Technology | Stem Cell Application Strengths | Throughput Capacity |
|---|---|---|---|
| Molecular Devices ImageXpress Micro Confocal | Confocal high-content imaging | Cancer research, regenerative medicine, neurobiology | High-throughput, automated high-speed imaging |
| Sartorius Incucyte Live-Cell Analysis | Live-cell imaging | Long-term monitoring of stem cell behavior, cancer and stem cell research | Continuous monitoring over days or weeks |
| Yokogawa Electric CellVoyager CQ1 | High-speed confocal imaging | Cancer research, infectious disease studies | Automated, high-speed image acquisition |
| PerkinElmer Harmony Software | Advanced image processing | Biomarker detection, drug screening analysis | Automated image analysis for large-scale projects |
| Thermo Fisher Scientific Nunclon Sphera Plates | 3D cell culture support | Spheroid and organoid formation, preclinical testing | Enhanced physiological relevance for screening |
The selection of an appropriate HCS system depends heavily on specific research requirements. Systems with confocal capabilities, such as the ImageXpress Micro Confocal and CellVoyager CQ1, provide superior imaging quality for 3D stem cell models like organoids and spheroids [65]. For longitudinal studies of stem cell differentiation or drug response, live-cell imaging systems like the Incucyte offer significant advantages by enabling continuous observation without disrupting culture conditions [65].
Advanced image processing software, exemplified by PerkinElmer's Harmony platform, is particularly valuable for analyzing complex stem cell phenotypes and minimizing analytical errors in high-throughput applications [65]. The integration of these systems with laboratory automation and robotics further enhances efficiency, reduces human error, and ensures reproducible results across experiments—critical considerations for drug discovery pipelines [65].
Experimental Design and Methodologies for Potency Evaluation
Robust experimental design is fundamental to generating meaningful potency data from stem cell-based HCS assays. The following sections detail key methodologies and analytical approaches specifically tailored for evaluating therapeutic potential.
3D Surface Integrative Spheroid Profiling (3D-SiSP) for Tumorigenesis Assessment
The 3D-SiSP methodology represents a significant advancement over traditional approaches for analyzing stem cell-derived cancer models, particularly for assessing tumorigenic potential and drug response [68].
Table 2: Key Steps in 3D-SiSP Protocol for Cancer Stem Cell Analysis
| Step | Procedure | Purpose | Technical Considerations |
|---|---|---|---|
| 1. Spheroid Culture | Seed cells in 0.7% methyl cellulose in ULA flat-bottom plates | Promote formation of distinct spheroids with minimal aggregation | Methyl cellulose reduces cell-cell adhesion, maintaining individual spheroid integrity |
| 2. Live Cell Staining | Label with Hoechst 33342 nuclear stain | Enable fluorescent visualization of spheroid architecture | Non-toxic staining allows subsequent functional assays |
| 3. Image Acquisition | Capture 3-6 z-stack planes per spheroid | Comprehensive coverage of entire 3D structure | Maximum projection images preserve highest fluorescent intensities |
| 4. Area-Based Analysis | Quantify spheroid area using 3D-SiSP algorithm | Accurate size measurement regardless of morphology | Overcomes overestimation limitations of length-based methods |
This methodology has demonstrated particular utility in cancer stem cell (CSC) research, where it enables simultaneous quantification of spheroid growth and CSC content using live-cell biosensors [68]. When applied to cholangiocarcinoma models, 3D-SiSP revealed that larger spheroids contained more undifferentiated cells, providing insights into the relationship between tumorigenic potential and stemness [68]. Furthermore, the technology facilitates real-time monitoring of CSC dynamics during anti-cancer drug testing, offering valuable information for therapeutic development [68].
On-Chip 3D Potency Assay for Clinical Outcome Prediction
A microfluidic on-chip 3D system has emerged as a powerful platform for predicting clinical efficacy of cell therapies, demonstrating superior performance compared to traditional 2D culture systems [66].
Experimental Workflow:
- Sample Preparation: Encapsulate bone marrow aspirate concentrate (BMAC) cells in PEG-4MAL hydrogel functionalized with RGD peptide [66]
- Device Operation: Perfuse cell-laden hydrogel with media at 1.0 μL/min for 24 hours [66]
- Condition Testing: Expose cells to either control media or simulated synovial fluid (simSF) to mimic joint environment [66]
- Secretory Analysis: Quantify 24 immunomodulatory and trophic proteins via multiplexed assays [66]
- Data Modeling: Build linear regression models correlating secretory profiles with patient clinical outcomes [66]
This platform demonstrated significantly elevated levels of immunomodulatory and trophic factors compared to 2D culture, with secreted analyte profiles showing stronger correlation with patient pain scores in osteoarthritis clinical trials [66]. The enhanced predictive validity of this approach addresses a critical bottleneck in cell therapy development by providing more clinically relevant potency metrics.
The following diagram illustrates the integrated workflow of high-content screening within stem cell-based drug discovery:
Essential Research Reagent Solutions
The successful implementation of HCS in stem cell-based drug discovery relies on a carefully selected toolkit of research reagents and materials. These components ensure assay reproducibility, physiological relevance, and analytical robustness.
Table 3: Essential Research Reagent Solutions for HCS in Stem Cell Research
| Reagent/Material | Function | Application Examples | Key Considerations |
|---|---|---|---|
| PEG-4MAL Hydrogel | Synthetic ECM for 3D cell encapsulation | On-chip 3D potency assays [66] | Presents cell-adhesive RGD peptides, tunable mechanical properties |
| Methyl Cellulose | Viscosity modifier for spheroid formation | 3D multi-spheroid models [68] | Reduces cell aggregation, promotes uniform spheroid formation |
| Ultra-Low Attachment (ULA) Plates | Prevent cell adhesion, enable 3D growth | Spheroid and organoid culture [68] | Flat-bottomed design ideal for high-content imaging |
| Simulated Synovial Fluid (simSF) | Physiological mimic for joint environments | Osteoarthritis therapy screening [66] | Contains predominant OA synovial fluid proteins, matched viscosity |
| Live-Cell Biosensors (e.g., SORE6) | Report stem cell status in real-time | Cancer stem cell tracking [68] | Enables monitoring of CSC dynamics during drug treatment |
| Multiplexed Immunoassays | Simultaneous measurement of multiple analytes | Secretory profile characterization [66] | Assesses immunomodulatory and trophic factor secretion |
These reagent solutions address critical challenges in stem cell-based HCS, including the maintenance of physiologically relevant 3D microenvironments, real-time monitoring of cellular phenotypes, and comprehensive characterization of secretory profiles. The selection of appropriate matrices, media supplements, and detection reagents should be guided by specific research objectives and stem cell model requirements.
Data Analysis and Interpretation in Potency Assessment
The transformation of complex HCS data into biologically meaningful insights requires sophisticated analytical approaches specifically tailored for stem cell applications and potency evaluation.
Analytical Methods for 3D Stem Cell Models
Traditional length-based measurements often prove inadequate for irregularly shaped 3D structures, potentially leading to significant overestimation of spheroid size [68]. The 3D-SiSP method addresses this limitation by utilizing area-based quantification derived from maximum projection images of z-stack acquisitions, providing more accurate representation of spheroid size and growth characteristics regardless of morphology [68].
For organoid and complex co-culture systems, high-content analysis must account for cellular heterogeneity and spatial relationships. Advanced segmentation algorithms and machine learning approaches can identify distinct cell populations within these structures, enabling quantitative assessment of differentiation status, cellular organization, and functional responses to therapeutic interventions [67] [65].
Correlation with Clinical Outcomes
The ultimate validation of stem cell-based potency assays lies in their ability to predict clinical efficacy. Recent research demonstrates that secretory profiles from on-chip 3D cultures show stronger correlation with patient outcomes than traditional 2D assays [66]. Linear regression models built from analyte secretion data have successfully predicted clinical responses in osteoarthritis trials, establishing a direct link between in vitro HCS data and therapeutic effectiveness [66].
Multiparametric analysis is particularly valuable in this context, as combinations of biomarkers often provide better predictive power than single endpoints. The integration of HCS data with other omics technologies (transcriptomics, proteomics) further enhances the depth of potency assessment and strengthens the mechanistic understanding of stem cell therapies [67].
High-content screening has emerged as an indispensable technology platform in stem cell-based drug discovery, providing powerful tools for evaluating therapeutic potency and predicting clinical outcomes. The integration of advanced imaging, 3D culture models, and sophisticated data analytics enables researchers to assess stem cell function and drug responses with unprecedented resolution and physiological relevance.
The continuing evolution of HCS technologies—including enhanced automation, AI-driven image analysis, and more complex human stem cell-derived models—promises to further bridge the gap between preclinical testing and clinical efficacy [67] [65]. As the field advances, the standardized implementation of robust HCS methodologies for potency evaluation will be crucial for accelerating the development of effective stem cell-based therapies and advancing personalized medicine approaches.
Overcoming Hurdles: Strategies for Enhancing Model Reproducibility and Maturation
Addressing Protocol Variability and Batch Effects
In stem cell-based disease modeling and drug development, the accurate assessment of cell potency—a cell's inherent ability to differentiate into specialized lineages—is fundamental to research reproducibility and therapeutic efficacy [5]. However, this assessment is critically hampered by protocol variability across laboratories and batch effects introduced during single-cell RNA sequencing (scRNA-seq) workflows [69]. These technical inconsistencies can obscure true biological signals, compromise data integration, and ultimately impede the translation of research findings. This guide objectively compares current computational and experimental methodologies designed to mitigate these challenges, providing researchers with a framework for robust potency evaluation.
Comparative Analysis of Methodologies for Mitigating Variability
The following table summarizes the core approaches for addressing protocol variability and batch effects in potency assessment, highlighting their key functionalities and performance considerations.
| Methodology | Primary Function | Key Advantages | Experimental Validation |
|---|---|---|---|
| CytoTRACE 2 [69] | Deep learning framework for predicting absolute developmental potential from scRNA-seq data. | - Suppresses batch/platform-specific variation- Provides absolute potency scores (0-1) for cross-dataset comparison- Interpretable gene set outputs | Outperformed 8 state-of-the-art methods in developmental hierarchy inference, showing >60% higher correlation with ground truth in 57 developmental systems. |
| Functional Potency Assays [5] [70] | In vitro bioassays measuring specific stem cell functions (e.g., differentiation capacity, immunomodulation). | - Measures biologically relevant, therapeutic mode-of-action- Directly assesses functional potency beyond molecular markers | Macrophage co-culture assay for immunomodulatory capacity validated with guideline-concordant selectivity, accuracy, and precision over 71 MSC batches [70]. |
| Molecular Marker Analysis [5] [71] | Evaluation of transcriptional, epigenetic, and metabolic states via defined molecular markers (e.g., OCT4, NANOG). | - Quick and accessible for initial cell line evaluation- Standardized panels available (e.g., ISCT criteria for MSCs) | Flow cytometry reveals source-dependent variability; BM-/AT-MSCs show >90% MSCA-1 expression vs. none in WJ-MSCs [71]. |
Detailed Experimental Protocols
To ensure reproducibility, below are detailed methodologies for key experiments cited in this guide.
Protocol for In Vitro Immunomodulatory Potency Assay
This protocol measures the anti-inflammatory capacity of Mesenchymal Stromal Cells (MSCs), a key functional potency metric [70].
- Step 1: Macrophage Differentiation and Polarization. Differentiate human THP-1 monocytes into macrophages using phorbol esters (e.g., PMA). Subsequently, polarize the macrophages toward a pro-inflammatory M1 phenotype using interferon-gamma (IFN-γ) and lipopolysaccharide (LPS).
- Step 2: Co-culture System. Establish a co-culture of the ABCB5+ MSCs with the M1-polarized macrophages at a defined cell ratio (optimized ratios between 1:1 and 1:10 MSC/macrophage are typical). Include controls for each cell type cultured alone.
- Step 3: Stimulation and Readout. Maintain the co-culture in an inflammatory environment. The primary readout is the concentration of Interleukin-1 Receptor Antagonist (IL-1RA) secreted by the MSCs into the culture medium, quantified using a validated enzyme-linked immunosorbent assay (ELISA).
- Step 4: Validation and Quality Control. Confirm successful M1 polarization by measuring surface markers (CD36, CD80) via flow cytometry and the release of pro-inflammatory cytokines like Tumor Necrosis Factor-alpha (TNF-α).
Protocol for Computational Potency Prediction with CytoTRACE 2
This protocol outlines the workflow for using CytoTRACE 2 to predict developmental potential from scRNA-seq data, mitigating batch effects [69].
- Step 1: Data Input and Preprocessing. Provide a normalized gene expression matrix (cells x genes) from any standard scRNA-seq platform as input. CytoTRACE 2 is designed to handle diverse datasets without requiring prior batch correction.
- Step 2: Model Application. Run the CytoTRACE 2 algorithm, which utilizes a Gene Set Binary Network (GSBN) architecture. The model intrinsically suppresses technical variation through competing representations of gene expression and training on a diverse atlas of over 400,000 cells.
- Step 3: Output and Interpretation. The primary outputs are: (1) a discrete potency category (e.g., pluripotent, multipotent) for each cell, and (2) a continuous potency score from 1 (highest potency, totipotent) to 0 (lowest potency, differentiated). The model also provides a list of genes driving the predictions for biological interpretation.
Visualizing the Computational Analysis Workflow
The following diagram illustrates the logical workflow of the CytoTRACE 2 analysis protocol.
The Scientist's Toolkit: Essential Reagent Solutions
Successful execution of the described protocols requires specific, high-quality reagents. The table below lists key solutions for standardizing potency evaluation.
| Research Reagent / Solution | Function in Potency Evaluation |
|---|---|
| Human Platelet Lysate (PL) [71] | A xeno-free supplement for clinical-grade MSC culture media, supporting optimal proliferation and preserving differentiation properties. |
| Differentiation Inducers [5] | Chemical cocktails (e.g., for adipogenic, osteogenic, chondrogenic lineages) used in functional assays to validate multipotent differentiation capacity. |
| Validated Antibody Panels [71] | Antibodies against surface markers (e.g., CD73, CD90, CD105 for MSCs; OCT4, NANOG for pluripotency) for immunophenotyping by flow cytometry. |
| M1-Polarization Cytokines [70] | Recombinant proteins (e.g., IFN-γ, LPS) used to differentiate and activate THP-1-derived macrophages into a pro-inflammatory (M1) state for co-culture potency assays. |
| ELISA Kits for Secreted Factors [70] | Ready-to-use kits for quantifying specific proteins (e.g., IL-1RA) in cell culture supernatants, providing a quantitative readout for functional potency. |
Addressing protocol variability and batch effects is not merely a technical exercise but a prerequisite for reliable potency evaluation in stem cell research. As the data demonstrates, a multi-faceted approach is most effective. Computational tools like CytoTRACE 2 offer a powerful, standardized means to derive absolute potency metrics across diverse datasets while inherently suppressing technical noise [69]. Complementing this, well-designed functional bioassays grounded in physiological relevance, such as the macrophage co-culture model, remain the gold standard for quantifying a cell's therapeutic functional capacity [70]. For researchers, the strategic integration of these computational and experimental methodologies—supported by a standardized toolkit of reagents—provides a robust defense against variability, ensuring that assessments of developmental potential are both accurate and reproducible.
Strategies to Overcome Fetal-like Immaturity in Stem Cell Models
The field of stem cell research holds immense promise for regenerative medicine, disease modeling, and drug development. Human pluripotent stem cells (hPSCs), including both embryonic and induced pluripotent stem cells, can theoretically differentiate into any cell type in the body, providing unprecedented opportunities for studying human development and disease [11]. However, a significant challenge persists: stem cell-derived tissues often exhibit fetal-like characteristics that limit their utility for modeling adult-onset diseases and predicting drug responses in adult patients [11] [72]. This immaturity manifests through multiple dimensions, including transcriptional profiles, structural organization, metabolic states, and functional capabilities that more closely resemble fetal rather than adult tissues [11] [72].
The persistence of immature phenotypes presents a substantial barrier to the clinical translation of stem cell technologies. For instance, hiPSC-derived cardiomyocytes (hiPSC-CMs) typically display fetal-like electrophysiological properties, disorganized sarcomeres, and immature metabolic networks, which can lead to inaccurate predictions of drug-induced cardiotoxicity [73]. Similarly, stem cell-derived β-cells (SC-β cells) developed for diabetes treatment frequently fail to achieve the full maturation status of primary adult β-cells, impacting their glucose-responsive insulin secretion capabilities [72]. Overcoming this fetal-like immaturity is therefore essential for realizing the full potential of stem cell-based applications in both therapeutic and pharmaceutical contexts.
This guide systematically compares current strategies to enhance the maturation of stem cell models, providing researchers with experimental data, methodological details, and practical resources to advance their work in stem cell-based disease modeling and drug development.
Characterizing the Immaturity Problem: Insights from Single-Cell Analysis
Advanced transcriptional profiling has revealed crucial insights into the nature of stem cell immaturity. A comprehensive single-cell RNA sequencing (scRNA-seq) analysis comparing SC-β cells with primary human fetal and adult β-cells demonstrated that while SC-β cells share a core β-cell transcriptional identity with their primary counterparts, they persistently express progenitor and neural-biased gene networks characteristic of fetal development stages [72]. This finding indicates that current differentiation protocols do not fully recapitulate the complete developmental trajectory toward adult cellular phenotypes.
The integrated transcriptomic atlas from this study revealed that SC-β cells express significantly lower levels of key maturation markers compared to adult β-cells, including G6PC2, IAPP, HADH, UCN3, CHGB, ADCYAP1 and SIX3 [72]. These molecular deficiencies correlate with functional limitations in glucose-sensing and insulin secretion machinery. Similarly, in other stem cell-derived lineages like cardiomyocytes and neurons, immaturity is evidenced by fetal gene expression patterns, immature electrophysiology, and underdeveloped structural organization [11] [73].
Table 1: Key Transcriptional Differences Between Fetal, SC-β, and Adult β-Cells
| Feature | Fetal β-Cells | SC-β Cells | Adult β-Cells |
|---|---|---|---|
| Core Identity Genes | INS, IAPP, DLK1, PDX1 | INS, IAPP, DLK1, PDX1 | INS, IAPP, DLK1, PDX1 |
| Maturation Markers | Low G6PC2, UCN3 | Low G6PC2, UCN3 | High G6PC2, UCN3 |
| Neural Signature | Present | Present | Absent |
| Progenitor Networks | Active | Persistently Active | Silenced |
| Polyhormonal Cells | Present | Variable | Absent |
Comparative Analysis of Maturation Strategies
Extracellular Matrix (ECM) Engineering
The extracellular microenvironment plays a crucial role in directing cellular maturation. Research demonstrates that human perinatal stem cell-derived ECM (commercially available as Matrix Plus) significantly accelerates structural and functional maturation of hiPSC-CMs compared to conventional mouse-derived ECM (Matrigel) [73]. This human-specific ECM promotes adult-like phenotypes through multiple mechanisms:
- Enhanced Structural Organization: hiPSC-CMs cultured on Matrix Plus developed rod-shaped morphology with highly organized sarcomeres and elevated cardiac troponin I (cTnI) expression within just seven days post-thaw [73].
- Improved Functional Maturity: These cells exhibited mature electrophysiological properties and appropriate responses to hERG channel blockers, including Torsades de Pointes (TdP) reentrant arrhythmia activations in 100% of tested monolayers [73].
- Metabolic Maturation: Matrix Plus promoted mitochondrial distribution and function resembling adult cardiomyocytes, a critical advancement given the metabolic immaturity of conventional hiPSC-CMs [73].
The experimental protocol for implementing this approach involves:
- ECM Coating: Plate preparation using human perinatal stem cell-derived ECM coated plates stored at 4°C, rehydrated in HBSS for 30 minutes at room temperature before cell plating [73].
- Cell Seeding: hiPSC-CMs are thawed and plated onto the rehydrated ECM in serum-containing medium supplemented with blebbistatin to enhance cell survival and attachment [73].
- Maintenance Culture: Cells are maintained in appropriate medium with regular changes, achieving significant maturation within 7 days of culture [73].
Epigenetic Modulation
Cellular differentiation and maturation are fundamentally governed by epigenetic regulation. Research indicates that targeted epigenetic manipulation can overcome the limited lineage differentiation that human stem cells exhibit based on their source and processing [74]. A systematic screen of 84 small molecule epigenetic modifiers identified several compounds that significantly enhance osteogenic differentiation in human mesenchymal stem cells (hMSCs), suggesting similar approaches could be applied to other lineages [74].
Key findings from epigenetic screening include:
- Gemcitabine pre-treatment increased alkaline phosphatase (ALP) activity, an early marker of osteogenic differentiation, by 3.5-fold [74].
- Decitabine and I-CBP112 increased ALP activity by 2.5-fold, while Chidamide and SIRT1/2 Inhibitor IV increased it by 2.3- and 2.2-fold respectively [74].
- These compounds demonstrated specificity for particular lineages, with some enhancing osteogenesis without similarly affecting adipogenesis [74].
The experimental workflow for epigenetic screening encompasses:
- Cell Pre-treatment: hMSCs are pretreated with epigenetic compounds for 24 hours before induction of differentiation.
- Differentiation Induction: Cells are switched to osteogenic medium containing standard differentiation factors.
- Outcome Assessment: Osteogenic differentiation is evaluated at 14 days using ALP activity assays, immunostaining for lineage-specific markers, and cell viability assays [74].
Functional Maturation Through Long-term Culture and Transplantation
Extended culture periods and in vivo transplantation represent additional strategies for promoting stem cell maturation. Studies with SC-β cells have demonstrated that transplantation into mice for 1-6 months drives significant maturation toward adult β-cell phenotypes [72]. Similarly, long-term culture of hiPSC-CMs for 30-100 days has been shown to enhance maturation, though this approach is time-consuming and may be impractical for high-throughput applications [73].
Table 2: Comparison of Maturation Strategies for Stem Cell-Derived Tissues
| Strategy | Mechanism | Timeframe | Key Advantages | Key Limitations |
|---|---|---|---|---|
| ECM Engineering | Provides human-specific maturation signals | 7 days | Rapid, compatible with HTS | Donor variability in ECM composition |
| Epigenetic Modulation | Alters chromatin accessibility and gene expression | 14+ days | Target-specific, potent effects | Potential off-target impacts |
| Long-term Culture | Allows spontaneous maturation over time | 30-100 days | No specialized reagents needed | Time-consuming, variable outcomes |
| In Vivo Transplantation | Provides physiological microenvironment | 1-6 months | Most physiological context | Not applicable for in vitro assays |
| Metabolic Manipulation | Shifts energy metabolism from glycolytic to oxidative | 7-21 days | Addresses core maturity defect | May require combination approaches |
Integration of Advanced Analytics and Machine Learning
The emerging integration of artificial intelligence (AI) and systems biology (SysBio) approaches provides powerful new tools for characterizing and addressing stem cell immaturity [38]. Quantitative phase imaging (QPI) combined with machine learning has enabled non-invasive, label-free monitoring of hematopoietic stem cell (HSC) expansion and functional quality assessment at single-cell resolution [75]. This approach identified previously undetectable diversity in HSC populations that correlated with functional potential, moving beyond snapshot analysis to dynamic, time-resolved prediction of stem cell quality [75].
The application of these technologies includes:
- Temporal Kinetic Analysis: Tracking cellular behavior over time to identify kinetic features predictive of maturation potential [75].
- Image Informatics: Using high-content imaging and machine learning to parse subtle variations in nucleosomal organization and cell states [74] [75].
- Predictive Modeling: Developing algorithms that leverage temporal information to significantly improve prediction accuracy of stem cell functionality [75].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Stem Cell Maturation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Specialized ECM | Matrix Plus (human perinatal stem cell-derived) [73] | Provides human-specific maturational cues for enhanced structural and functional phenotypes |
| Small Molecule Epigenetic Modulators | Gemcitabine, Decitabine, I-CBP112, Chidamide [74] | Alters nucleosomal organization and gene expression to enhance lineage-specific differentiation |
| Metabolic Maturation Reagents | Fatty acids, carnitine, T3 thyroid hormone [11] | Shifts energy metabolism from glycolytic to oxidative phosphorylation dominant states |
| Advanced Imaging Systems | Quantitative Phase Imaging (QPI) [75] | Enables non-invasive, label-free monitoring of live cell dynamics and kinetic analysis |
| Single-Cell Analysis Platforms | scRNA-seq, UMAP clustering [72] [75] | Characterizes transcriptional heterogeneity and identifies immature versus mature subpopulations |
Overcoming the fetal-like immaturity of stem cell models requires multifaceted approaches that address transcriptional, epigenetic, structural, and functional deficiencies. The strategies compared in this guide—from ECM engineering and epigenetic modulation to advanced analytics and functional maturation protocols—provide researchers with a comprehensive toolkit for enhancing the relevance and predictive power of stem cell-based disease models. As these technologies continue to evolve, particularly with the integration of AI and systems biology approaches, the field moves closer to realizing the full potential of stem cells in regenerative medicine, disease modeling, and drug development. The convergence of these innovations promises to bridge the critical gap between stem cell biology and clinically meaningful applications, ultimately enabling more accurate modeling of human diseases and more effective, personalized therapeutic interventions.
Visualizing Key Experimental Workflows and Signaling Pathways
Workflow for ECM-Based Maturation Strategy
Epigenetic Modulation Screening Protocol
Integrated Maturity Assessment Approach
Improving Vascularization and Structural Complexity in 3D Models
The pursuit of physiologically relevant in vitro models is a central goal in modern biomedical research, particularly for stem cell-based disease modeling and drug development. The ability to accurately evaluate the potency of stem cell derivatives hinges on the fidelity of these models to human physiology. A critical limitation of many current three-dimensional (3D) models, including organoids, is their lack of integrated, functional vascular networks. This deficiency impedes nutrient and oxygen delivery, limits growth, and fails to recapitulate crucial tissue-level interactions, ultimately affecting the predictive value of potency assays [11] [76]. This guide provides a comparative analysis of advanced engineering strategies designed to overcome these hurdles by enhancing vascularization and structural complexity.
Comparative Analysis of Vascularization Strategies
The table below compares the core engineering approaches for creating vascularized models, detailing their core principles, applications, and inherent challenges.
| Strategy | Core Principle | Key Applications | Technical Challenges |
|---|---|---|---|
| Organoid Self-Assembly | Spontaneous in vitro morphogenesis and self-organization of stem cells into 3D structures containing vascular cells [11]. | Modeling tissue development (e.g., kidney, brain); creating complex assembloids [11]. | Limited reproducibility; often yields immature, fetal-like networks; low throughput for drug screening [11]. |
| Pre-patterned Microfluidic Systems | Use of lithography or 3D printing to create predefined microchannel architectures within biocompatible materials [76]. | High-throughput drug screening; studying endothelial barrier function and hemodynamics [76]. | Limited biological complexity; requires sophisticated fabrication; can lack native tissue ECM composition [76]. |
| Sacrificial Bioprinting | 3D printing of a temporary "sacrificial" filament (e.g., gelatin) within a cell-laden hydrogel, which is later removed to create patent channels [76]. | Engineering perfusable, patient-specific tissue constructs for implantation; creating multi-scale vascular trees [76]. | Complex multi-step process; can be time-consuming; potential for residual material affecting cell viability [76]. |
| In Vivo Maturation (Host Engraftment) | Implantation of a prevascularized organoid or construct into an animal host, allowing anastomosis with the host circulatory system [11]. | Generation of mature, perfusable human vasculature; study of human-vascular interactions in a living context [11]. | Introduces animal model variability; high cost; raises ethical concerns; not suitable for high-throughput drug screening [11]. |
| AI-Guided 3D Model Generation | Use of deep learning models to generate anatomically realistic and patient-specific 3D vascular geometries from medical images [77] [78] [79]. | Surgical planning; creating physical models for training; generating in silico data for computational fluid dynamics studies [77] [78]. | Dependent on quality and quantity of training data; generated structures may require validation for physiological accuracy [77] [79]. |
Experimental Protocols for Vascularization
To ensure the successful implementation of these strategies, standardized experimental protocols are essential. The following sections detail key methodologies for generating and analyzing vascularized models.
Protocol for Generating Vascularized Organoids from Pluripotent Stem Cells
This protocol is adapted from studies on kidney and cardiovascular organoids, which have been shown to develop endogenous vascular networks [11].
- Step 1: Stem Cell Differentiation: Initiate differentiation of human induced Pluripotent Stem Cells (iPSCs) into the desired lineage (e.g., kidney, liver, brain) using established, stage-specific growth factor cocktails. For example, kidney organoids might require CHIR99021 (a GSK3β inhibitor) and FGF9 to induce mesoderm and metanephric lineages [11].
- Step 2: 3D Aggregation and Culture: Harvest the differentiating progenitor cells and aggregate them in low-attachment U-bottom plates to promote 3D structure formation. Culture the aggregates in a differentiation medium optimized for the target tissue.
- Step 3: Maturation and Support: To enhance vascular network maturity and complexity, transfer the organoids to a 3D matrix, such as Corning Matrigel, which provides a basement membrane-rich environment conducive to endothelial cell invasion and tubulogenesis [11] [80]. Culture the embedded organoids for several weeks, allowing for self-organization and the emergence of CD31-positive vascular networks.
- Step 4: Co-culture for Enhanced Complexity (Optional): For increased physiological relevance, generate assembloids by fusing the primary organoid with a separately generated vascular organoid, or by adding human umbilical vein endothelial cells (HUVECs) and mesenchymal stem cells (MSCs) during the aggregation stage to support the developing vasculature [11].
Protocol for Analyzing 3D Vascular Networks with VESNA
The quantitative analysis of vascular networks is critical for evaluating model quality. The VESNA tool provides an automated, skeleton-based workflow for this purpose [81].
- Step 1: Sample Preparation and Imaging: Fix and immunostain the 3D models using a vasculature-specific marker, such as an antibody against CD31. Acquire high-resolution 3D z-stack images using confocal or light-sheet microscopy.
- Step 2: Image Pre-processing: Load the 3D image into Fiji (ImageJ) and run the VESNA macro. The first step involves pre-processing to reduce noise and enhance vessel signal. This typically involves:
- Brightness Adjustment: Adjusting the minimum and maximum intensity to ensure weakly fluorescing vessels are detected.
- Gaussian Blur: Applying a 3D Gaussian blur (e.g., with a sigma of 1-2 voxels) to reduce heterogeneity in fluorescence and prevent fragmented segmentation [81].
- Step 3: Image Binarization: VESNA automatically converts the pre-processed image into a binary format using the Yen thresholding algorithm. This is followed by post-processing steps:
- "Analyze Particles": Removes small, disconnected artifacts below a defined pixel size.
- 3D Maximum/Minimum Filtering: Connects fragmented vessel structures.
- "Fill Holes": Uses the MorphoLibJ plugin to fill internal holes in the binary objects, which is crucial for generating a clean skeleton [81].
- Step 4: Skeletonization and Quantification: The binary image is skeletonized to a 1-voxel-thick network using the Skeletonize3D plugin. VESNA then uses the AnalyzeSkeleton plugin to extract key quantitative parameters, including:
- Total Vessel Length: The combined length of all vessel segments.
- Number of Branches/Junctions: The number of branch points and endpoints.
- Vessel Volume Fraction: The percentage of the total volume occupied by the vasculature [81].
The workflow for this protocol is summarized in the following diagram:
VESNA Vascular Network Analysis Workflow: This automated pipeline converts 3D fluorescence images into quantitative data on vascular network structure [81].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of vascularization protocols depends on key reagents and tools. The table below lists essential items and their functions in this research.
| Research Reagent / Tool | Function / Application |
|---|---|
| Corning Matrigel | A basement membrane extract used as a 3D culture matrix to support stem cell differentiation, organoid growth, and endothelial cell tubulogenesis [11] [80]. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | A primary cell type used in co-culture systems to introduce a robust vascular component into organoids or microfluidic devices [76]. |
| Mesenchymal Stem Cells (MSCs) | Used to support vascular stability and maturation by differentiating into pericyte-like cells that surround endothelial tubes [11] [82]. |
| CD31/PECAM-1 Antibody | A classic immunohistochemical marker for identifying and visualizing vascular endothelial cells in fixed 3D samples [81]. |
| VESNA (Fiji Macro) | An open-source software tool for automated 3D segmentation, skeletonization, and quantitative analysis of vascular networks from fluorescence images [81]. |
| Liqcreate Flexible-X Resin | A commercial 3D printing resin used with stereolithography (SLA) to create flexible, patient-specific anatomical models that mimic the mechanical properties of blood vessels [83]. |
| Recursive Variational Autoencoder (RVAE) | A deep learning architecture, as used in VesselVAE, designed to generate and analyze the complex hierarchical (tree-like) structure of vascular networks [77] [79]. |
Future Directions and Integration with Potency Evaluation
Emerging technologies are poised to further bridge the gap between in vitro models and in vivo physiology. A key direction is the integration of multiple advanced strategies into a unified workflow, as illustrated below.
Integrated Future Workflow for Vascularized Models: Combining AI, engineering, and biology to create and analyze physiologically relevant models for potency evaluation.
The creation of robust, vascularized 3D models directly enhances the framework for potency evaluation of stem cell-based therapies. A model's "vascularization potential" can serve as a critical quality attribute (CQA) [11]. For instance, the ability of mesenchymal stem cell (MSC) secretions to induce the formation of a complex, stable vascular network in an organoid model is a direct, quantifiable measure of their paracrine function and therapeutic potency [84] [82]. Automated tools like VESNA can standardize this assessment by providing unbiased metrics of network size and architecture, moving beyond traditional, often subjective, potency assays [81]. As these models continue to improve, they will enable more predictive screening of drug efficacy and toxicity, ultimately accelerating the development of safer and more effective regenerative medicines.
Automation and AI-Guided Differentiation for Scalability
The transition of stem cell research from laboratory discovery to clinical application hinges on overcoming a critical bottleneck: scalability. Traditional manual differentiation protocols for stem cells are often plagued by inconsistency, high labor costs, and poor reproducibility, making them unsuitable for the large-scale, clinically relevant production required for drug discovery and regenerative medicine [11]. The inherent variability of biological systems means that achieving standardized, high-quality differentiated cell populations in large quantities has been a persistent challenge for researchers and drug development professionals.
This challenge is central to potency evaluation in stem cell-based disease models. The utility of any disease model in predicting human pathophysiology or therapeutic response depends on the robustness, purity, and functional maturity of the differentiated cell types it comprises. Without scalable and reproducible differentiation methods, the biological relevance and predictive power of these models are compromised, undermining their value in the drug development pipeline [11]. This article objectively compares two technological paradigms—traditional automation and emerging AI-guided differentiation—in addressing this fundamental challenge of scalability while maintaining the quality required for rigorous potency evaluation.
Technology Comparison: Core Principles and Capabilities
Understanding the fundamental differences between automation and AI is crucial for evaluating their respective roles in scaling stem cell differentiation.
Automation in stem cell research involves using hardware and software to perform repetitive, rule-based tasks with minimal human intervention. It is characterized by the execution of predefined protocols and workflows, such as liquid handling, cell passaging, or media changes in a consistent, high-throughput manner. Automation excels at standardizing processes that follow fixed, predictable steps, thereby reducing human error and increasing throughput for established protocols [85] [86].
Artificial Intelligence (AI), particularly machine learning (ML) and deep learning (DL), represents a more adaptive approach. AI systems can analyze complex datasets, recognize patterns, learn from outcomes, and make data-driven decisions to optimize differentiation protocols dynamically. Unlike static automation, AI can handle variability and complexity by adapting to new information, predicting optimal conditions, and improving differentiation efficiency over time [85] [87] [88]. The core functional differences are systematized in Table 1.
Table 1: Fundamental Differences Between Automation and AI in Stem Cell Differentiation
| Aspect | Automation | AI-Guided Systems |
|---|---|---|
| Learning Capability | No inherent learning; follows predefined rules | Learns and improves over time from data [85] |
| Decision-Making Basis | Rule-based and deterministic | Data-driven, predictive, and adaptive [85] [87] |
| Task Complexity | Handles simple, repetitive, structured tasks | Manages complex, variable, and unstructured tasks [85] |
| Protocol Flexibility | Rigid; requires manual reprogramming for changes | Adapts protocols dynamically based on real-time feedback [85] [88] |
| Data Utilization | Limited to pre-programmed parameters | Analyzes large, multi-modal datasets (e.g., omics, images) [87] [88] |
| Primary Value | Increases throughput and reduces labor | Enhances differentiation efficiency, quality, and outcome prediction [88] |
The most powerful applications often emerge from the synergy of both technologies, where AI handles complex decision-making and prediction, while automation executes the resulting protocols at scale. This combination, often termed intelligent automation, is transforming stem cell research by enabling scalable, yet highly optimized differentiation processes [85] [86].
Performance and Experimental Data Comparison
Direct, quantitative comparisons between automation and AI-guided systems reveal significant differences in their impact on differentiation outcomes, efficiency, and scalability. The following experimental data, synthesized from recent studies, provides an objective performance evaluation.
Differentiation Efficiency and Protocol Optimization
A key performance metric is the ability to efficiently produce high-quality, functionally mature target cells. AI-guided systems demonstrate superior performance in optimizing complex, multi-parameter differentiation protocols.
Table 2: Experimental Comparison of Differentiation Efficiency
| Performance Metric | Traditional Automation | AI-Guided Differentiation | Experimental Context |
|---|---|---|---|
| Reprogramming Efficiency | Low and variable (typically <1%) | Predictive modeling increased efficiency by >20% by identifying optimal factor combinations and timing [88]. | Human fibroblast to iPSC reprogramming [88] |
| Cardiomyocyte Differentiation | High throughput but inconsistent purity (60-80%) | AI analysis of time-lapse imaging achieved >90% purity by predicting optimal differentiation windows [88]. | iPSC to cardiomyocyte differentiation [88] |
| Neuronal Differentiation | Standardized but often immature phenotypes | AI-driven multi-omics analysis identified novel cues that enhanced functional maturation, doubling electrophysiological activity [88]. | iPSC to dopaminergic neuron differentiation [87] |
| Process Optimization Speed | Months for manual protocol refinement | AI reduced optimization time from months to weeks by rapidly testing virtual protocol permutations [87] [88]. | Generic protocol development |
Quality Control and Predictive Analytics
Beyond efficiency, ensuring the quality and safety of differentiated cells is paramount for disease modeling and therapeutic applications. AI demonstrates a clear advantage in non-invasive, predictive quality control.
Table 3: Quality Control and Outcome Prediction Capabilities
| Quality Parameter | Traditional Automation | AI-Guided Systems | Methodology |
|---|---|---|---|
| Pluripotency Assessment | Endpoint assays (e.g., flow cytometry, immunostaining) | Real-time prediction of pluripotency from colony morphology with >95% accuracy [88]. | Convolutional Neural Networks (CNNs) on bright-field images [88] |
| Genomic Stability | Periodic karyotyping (low-throughput, costly) | Predictive models flag at-risk cultures using integrated morphological and gene expression data [11] [88]. | ML on integrated omics and image data |
| Cell Line Selection | Manual colony picking based on visual inspection | AI quantifies morphological features to identify high-potency clones, improving differentiation consistency [88]. | Automated image analysis with ML classifiers |
| Differentiation Outcome Prediction | Limited to endpoint analysis | Early prediction of final cell type and function days before molecular markers appear [87] [88]. | Time-series analysis of morphology and -omics data |
The experimental data consistently shows that AI-guided systems not only accelerate and scale the differentiation process but also significantly enhance the quality, purity, and functional maturity of the resulting cells. This leads to more reliable and predictive stem cell-based disease models for drug development.
Experimental Protocols and Methodologies
To ensure reproducibility and provide a clear basis for comparison, this section details the core methodologies underpinning the performance data in the previous section.
Protocol for AI-Guided Optimization of iPSC Cardiomyocyte Differentiation
This representative protocol illustrates how AI is integrated into a standard differentiation workflow to enhance scalability and outcome predictability [88].
- Initial Protocol Setup: A baseline cardiomyocyte differentiation protocol is established using established small molecule-based directed differentiation.
- High-Throughput Data Generation: Automated bioreactors or multi-well plates are used to perform the differentiation protocol under hundreds of slightly varied conditions (e.g., minor timing, concentration, or factor adjustments). This is a prime example of automation enabling AI.
- Multi-Modal Data Capture: Throughout the differentiation process, automated systems collect:
- Time-lapse bright-field microscopy: Capturing morphological changes.
- Transcriptomic samples: For RNA-seq at critical time points.
- Metabolic data: From media sensors.
- Model Training and Validation: The multi-modal data is used to train machine learning models (e.g., CNNs for images, regression models for omics data) to correlate process parameters and intermediate phenotypes with the final output—the purity and functional maturity of cardiomyocytes, as verified by flow cytometry (for cardiac Troponin T) and multi-electrode array (for electrophysiological function).
- AI-Guided Refinement: The trained model identifies the critical parameter windows (e.g., precise timing of Wnt inhibitor addition) that most strongly predict a high-yield, high-purity outcome. The protocol is then dynamically refined based on these insights.
- Scalable Production: The optimized protocol is transferred to large-scale automated bioreactor systems for mass production, with the AI model providing real-time quality control by monitoring cell morphology.
AI-Augmented Differentiation Workflow: This diagram illustrates the iterative cycle where AI analyzes data from automated high-throughput screens to refine and optimize differentiation protocols for scalable production.
Protocol for Automated, Non-Invasive Quality Control Using AI
This protocol highlights the use of AI for a critical scalability task: ensuring quality without disrupting the culture process [88].
- Image Acquisition: Automated microscopes acquire high-resolution, label-free, time-lapse images (e.g., bright-field or phase-contrast) of iPSC colonies or differentiating cultures at regular intervals.
- Data Labeling and Pre-processing: A subset of images is linked to ground-truth quality metrics obtained via endpoint assays (e.g., pluripotency marker immunostaining, karyotyping for genomic integrity, or functional assays for differentiated cells). Images are pre-processed to normalize lighting and contrast.
- Classifier Training: A deep learning model (typically a Convolutional Neural Network, CNN) is trained to predict the ground-truth quality metrics directly from the label-free images.
- Deployment for Real-Time QC: The trained model is integrated into the automated culture system. It analyzes images in real-time to:
- Classify colonies as "high-quality" or "low-quality" for automated picking.
- Predict the differentiation efficiency of a culture days before terminal markers are expressed.
- Flag potential contamination or abnormalities.
- Closed-Loop Feedback (Intelligent Automation): In advanced systems, the AI's prediction can trigger automated actions, such as directing a robotic arm to select only the highest-quality colonies for passage or adjusting media composition in a bioreactor to rescue a suboptimal differentiation.
Signaling Pathways and Molecular Mechanisms
AI's power in optimizing differentiation lies in its ability to infer and model the complex intracellular signaling pathways that dictate cell fate. The following diagram synthesizes the key pathways frequently targeted in AI-guided protocol optimization, particularly for mesodermal and cardiac lineages [88].
Core Differentiation Signaling Network: AI models analyze the activity and outcomes of these core pathways to predict the precise interventions needed to steer stem cells toward a specific fate. The dashed line shows how AI insights directly inform the application of external cues.
The AI's role is to analyze high-dimensional data (e.g., transcriptomics, phosphoproteomics) to predict how manipulations to these pathways—such as the precise timing of WNT activation/inhibition crucial for cardiomyogenesis—will alter the final gene expression profile and functional phenotype of the cells. This moves protocol development from a largely empirical process to a predictive, engineering discipline.
The Scientist's Toolkit: Essential Research Reagents and Materials
The effective implementation of automated and AI-guided differentiation relies on a suite of specialized reagents, tools, and platforms. This table details key solutions for building a scalable workflow for potency evaluation.
Table 4: Essential Research Reagent Solutions for Scalable Differentiation
| Tool Category | Specific Examples / Products | Function in Scalable Workflow |
|---|---|---|
| Stem Cell Lines | Induced Pluripotent Stem Cells (iPSCs), Embryonic Stem Cells (ESCs) [11] [82] | The foundational raw material; patient-specific iPSCs are crucial for creating clinically relevant disease models. |
| Defined Differentiation Kits | Commercially available cardiomyocyte, neuronal, hepatocyte differentiation kits | Provide a standardized, often optimized, baseline protocol that can be further refined by AI, reducing initial development time. |
| Critical Assays | Cell viability & proliferation assays, Differentiation assays [89] | Used for generating the ground-truth data (e.g., flow cytometry for marker expression) required to train and validate AI models. |
| High-Content Screening Instruments | Automated microscopes, flow cytometers, multi-electrode arrays | Generate the high-dimensional, multi-modal data (images, electrophysiology) that serve as the input for AI analysis. |
| Bioinformatics & AI Platforms | Machine Learning (ML) and Deep Learning (DL) software (e.g., TensorFlow, PyTorch), Cloud AI services [87] [88] | The computational engine for analyzing complex datasets, building predictive models of differentiation, and optimizing protocols. |
| Automation Hardware | Liquid handling robots, automated bioreactors, colony pickers | Execute the physical tasks of cell culture and differentiation at scale, with the consistency required for reliable AI model training. |
| Data Management Solutions | Laboratory Information Management Systems (LIMS) | Essential for tracking the vast amounts of metadata, experimental parameters, and results generated in high-throughput scalable workflows. |
The objective comparison presented in this guide demonstrates that while traditional automation is essential for increasing throughput and ensuring procedural consistency, AI-guided differentiation provides a superior, transformative approach for achieving scalability without compromising quality.
For the field of potency evaluation in stem cell-based disease models, the implications are profound. AI's ability to predict differentiation outcomes, ensure functional maturity, and maintain quality control at scale directly addresses the core challenge of generating biologically relevant and reproducible models for drug development [11] [88]. The future of scalable stem cell differentiation lies not in choosing between automation and AI, but in their strategic integration into intelligent, closed-loop systems. In such systems, AI continuously learns from experimental outcomes generated by automated platforms, and in return, provides real-time instructions to refine and optimize the process. This synergy promises to accelerate the delivery of reliable, clinically relevant stem cell models and therapies, ultimately enhancing the efficiency and success rate of the entire drug development pipeline.
Maintaining genomic stability and preventing contamination are fundamental pillars of quality control in stem cell research. For scientists developing stem cell-based disease models, failures in these areas compromise data reproducibility, experimental validity, and ultimately, the translational potential of cell therapies [11] [90]. This guide compares current methodologies for ensuring cellular integrity, providing a practical framework for researchers and drug development professionals.
Methodologies for Genomic Stability Assessment
Genomic instability in stem cells, such as chromosomal aberrations or mutations, can arise during reprogramming, gene editing, or prolonged culture, potentially altering differentiation capacity and functionality [11] [91]. The following table compares key techniques for genetic stability testing.
Table 1: Comparison of Genomic Stability Assessment Methods
| Method | Key Principle | Resolution | Detectable Aberrations | Throughput & Workflow |
|---|---|---|---|---|
| G-Banding Karyotyping | Light microscopy of stained metaphase chromosomes [91]. | 5-10 Mb [91]. | Numerical and large structural abnormalities (aneuploidy, translocations) [91]. | Low-throughput; requires living, dividing cells; high expertise [91]. |
| SNP Array | Hybridization to array probes for SNP loci; analysis of B-allele frequency and Log R ratio [91]. | ~350 kb [91]. | Copy number variations (CNVs), copy-neutral loss of heterozygosity (CN-LOH) [91]. | Medium-to-high throughput; automated analysis possible; cannot detect balanced translocations [91]. |
| Next-Generation Sequencing (NGS) | High-throughput sequencing of the entire genome [92]. | Single-base pair [92]. | Single nucleotide variants (SNVs), insertions/deletions (indels), CNVs, structural variants [92]. | Highest throughput; provides most comprehensive data; requires significant bioinformatics resources [92]. |
Experimental Protocol: SNP Array for hPSC Quality Control
SNP array analysis offers a balanced approach for routine monitoring, combining higher resolution than karyotyping with a more accessible workflow than NGS [91].
Detailed Protocol:
- DNA Extraction: Isolate high-quality genomic DNA from hPSCs using a kit such as the QIAamp DNA Blood Mini Kit [91].
- Array Processing: Process DNA on a platform like Illumina's Global Screening Array. The assay uses Infinium probes for allele-specific primer extension (Type I) or single-base extension (Type II), with fluorescent detection determining the genotype [91].
- Data Analysis in GenomeStudio:
- Quality Control: First, verify the call rate (percentage of successfully genotyped SNPs). A call rate above 95% is recommended for reliable analysis [91].
- CNV Detection: Use the cnvPartition plug-in to analyze the Log R Ratio (LRR, indicating total signal intensity relative to a reference) and B-allele Frequency (BAF, indicating the relative proportion of each allele). Deviations from expected values (e.g., LRR shift, BAF spreading) indicate copy number changes [91].
- Interpretation: This method is highly effective for identifying common hPSC abnormalities such as the gain of chromosome 20q11.21, a known recurrence that can confer a growth advantage [91].
Strategies for Contamination Prevention and Control
Contamination poses a constant threat, with sources ranging from microbial pathogens to cross-contamination with other cell lines [90]. The impact and prevention strategies differ between research and manufacturing settings.
Table 2: Contamination Types, Impacts, and Prevention Strategies
| Contaminant Type | Impact on Research & Development | Key Prevention Strategies |
|---|---|---|
| Microbial (Bacteria, Fungi) | Alters culture pH, causes cell death, compromises experimental data integrity [90]. | Strict aseptic technique, use of pre-sterilized consumables, routine environmental monitoring [90]. |
| Mycoplasma | Changes cellular metabolism and gene expression without visible turbidity, leading to misleading results [90]. | Regular testing via PCR or fluorescence assays; quarantine and validation of new cell lines and reagents [90]. |
| Viral | Can be introduced via raw materials (e.g., serum); risks altering cell biology and poses patient safety concerns [90]. | Use of virus-inactivated/recombinant reagents, rigorous screening of cell banks [90]. |
| Cross-Contamination | Overgrowth by misidentified cell lines (e.g., HeLa) invalidates experimental models and conclusions [90]. | Strict labeling, use of dedicated reagents, regular cell line authentication (e.g., STR profiling) [90]. |
Experimental Insight: Mitigating Culture-Induced Mutations
The choice of culture conditions directly influences genetic stability. A long-term study culturing pluripotent stem cells for over three years found that specific methods can minimize mutation accumulation [93].
Key Experimental Findings:
- Safer Culture Conditions: Stem cells grown on a feeder layer substrate and passaged manually accumulated significantly fewer mutations compared to those grown on feeder-free substrates or passaged with enzymes [93].
- Importance of Monitoring: The study also documented the emergence of deletions in tumor suppressor genes like TP53, underscoring the necessity for ongoing genomic surveillance of stem cell cultures intended for therapeutic use [93].
The Scientist's Toolkit: Essential Reagents & Materials
The following table lists key reagents and their functions for critical quality control experiments in stem cell research.
Table 3: Essential Research Reagent Solutions for Stem Cell QC
| Reagent / Material | Primary Function | Example Application |
|---|---|---|
| Image-iT Cell Painting Kit | Multiplexed fluorescent staining of multiple organelles (nucleus, ER, Golgi, mitochondria, etc.) for high-content morphological profiling [94]. | Detecting subtle phenotypic changes in stem cell-derived neurons after chemical exposure [94]. |
| CellEvent Caspase-3/7 Green Detection Reagent | Fluorescent substrate for activated caspase-3/7, serving as a marker for apoptosis [95]. | Multiplexed assays measuring chemical effects on neural progenitor cell apoptosis [95]. |
| 5-Bromo-2'-deoxyuridine (BrdU) | Synthetic thymidine analog that incorporates into DNA during S-phase, used as a marker for cell proliferation [95]. | Measuring effects on neural progenitor cell proliferation in developmental neurotoxicity screening [95]. |
| QIAamp DNA Blood Mini Kit | Isolation of high-quality genomic DNA from cell samples [91]. | Preparing DNA for downstream genomic stability analysis (e.g., SNP array, NGS) [91]. |
| Illumina Global Screening Array | DNA microarray for genome-wide genotyping of single-nucleotide polymorphisms (SNPs) [91]. | Molecular karyotyping and detection of copy number variations in hPSCs [91]. |
Visualizing Key Workflows
Genomic Stability Analysis via SNP Array
This diagram outlines the core workflow for detecting chromosomal aberrations in human pluripotent stem cells (hPSCs) using SNP array technology.
Multiplexed Profiling for Cell State Assessment
This workflow shows an integrated approach to assessing cell health, proliferation, and death, which are indirect indicators of genomic and cellular integrity.
Benchmarking Success: Validating Stem Cell Models Against Clinical and Preclinical Data
Establishing Validation Frameworks for Predictive Accuracy
In the rapidly advancing field of stem cell research, establishing robust validation frameworks for predictive accuracy represents a fundamental requirement for translating laboratory findings into clinically viable therapies. As stem cell-based disease models and therapeutic products grow increasingly complex, the scientific community faces pressing challenges in standardizing quality assessment, quantifying functional potency, and ensuring reproducible outcomes across diverse experimental and clinical settings [11]. Traditional validation approaches often rely on endpoint assays and surface marker analyses, which provide limited snapshots of cellular behavior and may fail to predict long-term functional efficacy [96]. The emergence of artificial intelligence (AI) and systems biology has introduced transformative opportunities to enhance predictive accuracy through multi-parameter assessment, real-time monitoring, and computational modeling of complex biological systems [38].
This comparative analysis examines traditional and next-generation validation frameworks, focusing specifically on their application to potency evaluation in stem cell-based disease modeling research. For drug development professionals and translational scientists, selecting appropriate validation strategies directly impacts the reliability of preclinical data, regulatory approval timelines, and ultimately, clinical success rates [97]. By objectively comparing the methodological approaches, performance metrics, and experimental requirements of different validation frameworks, this guide provides evidence-based insights to inform research design and implementation across various stages of therapeutic development.
Comparative Analysis of Validation Approaches
The evolution of validation methodologies reflects a paradigm shift from reductionist quality checks toward holistic, predictive systems. The table below summarizes core characteristics of predominant validation frameworks used in stem cell research.
Table 1: Comparison of Validation Frameworks for Stem Cell-Based Models
| Validation Approach | Key Technologies | Primary Applications | Reported Accuracy Metrics | Major Limitations |
|---|---|---|---|---|
| Traditional Functional Assays [98] [99] | Flow cytometry, ELISA, qPCR, Cell viability assays | Lot release testing, Stability studies, Basic potency assessment | Varies by specific assay; Often qualitative or semi-quantitative | Endpoint measurements only, Destructive sampling, Low temporal resolution |
| AI-Enhanced Morphological Classification [96] [100] | Convolutional Neural Networks (CNNs), Deep learning, High-resolution imaging | Stem cell subpopulation identification, Differentiation tracking, Quality monitoring | 90%+ accuracy in HSC/MPP classification [100], >90% colony formation prediction [96] | Requires extensive training datasets, Computational intensity, "Black box" interpretability challenges |
| Systems Biology & Multi-Omics Integration [38] | Machine learning, Multi-omics data fusion, Network analysis | Mechanism of action studies, Biomarker discovery, Clinical trial optimization | 88% accuracy in differentiation outcome forecasting [96] | Data heterogeneity, High computational costs, Complex implementation |
| Real-Time Process Monitoring [96] | Sensor arrays, Predictive modeling, Live-cell imaging | Biomanufacturing, Culture optimization, Adaptive process control | 15% improvement in culture expansion efficiency [96] | Infrastructure requirements, Integration challenges with legacy systems |
Experimental Protocols for Validation Framework Implementation
Deep Learning-Based Stem Cell Classification
The predictive classification of hematopoietic stem cell (HSC) subpopulations using deep learning represents a cutting-edge approach for functional validation without reliance on destructive sampling or extensive antibody panels [100]. The following protocol details the methodology for implementing this validation framework:
Cell Preparation and Image Acquisition
- Isolate bone marrow cells from mouse long bones (tibias, femurs) and ilia using cold DPBS without calcium or magnesium
- Prepare single-cell suspensions following red blood cell lysis
- Sort target cell populations (LT-HSCs, ST-HSCs, MPPs) using fluorescence-activated cell sorting (FACS) with established surface markers (Lineage⁻/ˡᵒʷSca-1⁺c-Kit⁺ with CD150/CD48 or CD34/CD135 staining) [100]
- Plate sorted cells in coverglass-bottomed chambers and maintain in DPBS/2% FBS during imaging
- Acquire Differential Interference Contrast (DIC) images using a confocal microscope (e.g., Olympus FV3000) at 2048×2048 resolution
- Capture simultaneous fluorescence images for ground truth validation when using reporter strains (e.g., α-catulinGFP or Evi1GFP mice)
Image Processing and Model Training
- Detect single cells in DIC images using specialized MATLAB toolboxes with size thresholding and uniqueness checks to remove debris and cell clusters
- Segment cells into cell-centered image crops of 64×64 pixels with appropriate type labeling
- Apply data augmentation techniques to training datasets to enhance model robustness
- Implement a convolutional neural network (CNN) architecture with multiple convolutional layers featuring "learnable" filters whose parameters optimize during training
- Train the three-class classifier (LSM model) to distinguish LT-HSCs, ST-HSCs, and MPPs using extensive image datasets
- Validate model performance with independent datasets not used during training
This protocol demonstrates that deep learning can extract intrinsic morphological features specific to different functional stem cell classes, achieving predictive classification based solely on morphological characteristics observable through light microscopy [100].
AI-Driven Quality Monitoring in Stem Cell Cultures
For ongoing validation during stem cell culture and differentiation processes, AI-driven monitoring systems provide continuous assessment of critical quality attributes (CQAs) [96]:
System Setup and Data Integration
- Implement high-resolution time-lapse microscopy for continuous non-invasive imaging
- Integrate environmental sensors for real-time monitoring of pH, oxygen, nutrient levels, and metabolic byproducts
- Establish data pipelines combining imaging data, sensor readings, and multi-omics profiles where available
- Train convolutional neural networks (CNNs) on reference image sets showing optimal versus suboptimal culture conditions
- Develop predictive algorithms to forecast culture trajectories based on historical sensor data
Quality Attribute Tracking and Analysis
- Track morphological dynamics using CNN-based image analysis with automated time-lapse tracking
- Monitor proliferation rates through AI analysis of confluency progression as a surrogate for direct labeling methods
- Assess differentiation potential using support vector machines (SVM) for lineage classification and regression models for stage prediction
- Detect contamination risks through anomaly detection algorithms applied to sensor data and microscopy images
- Employ reinforcement learning for dynamic adjustment of environmental parameters to maintain optimal culture conditions
This validation framework enables earlier, more accurate, and noninvasive quality assessment compared to traditional endpoint assays, establishing a foundation for dynamic, real-time quality monitoring essential for scalable stem cell biomanufacturing [96].
Visualization of Validation Frameworks
Traditional Multi-Stage Validation Workflow
Traditional Validation Workflow
AI-Enhanced Integrated Validation System
AI-Enhanced Validation System
Research Reagent Solutions for Validation Experiments
Selecting appropriate reagents and materials is crucial for implementing robust validation frameworks. The following table details essential research solutions for stem cell validation experiments.
Table 2: Essential Research Reagents for Validation Experiments
| Reagent/Material | Specific Function | Application Context | Validation Consideration |
|---|---|---|---|
| Flow Cytometry Antibodies [100] | Surface marker identification (Sca-1, c-Kit, CD150, CD48) | Hematopoietic stem cell isolation and purity assessment | Panel validation required for specific cell types and species |
| Cell Culture Media & Supplements [96] | Maintain stemness or direct differentiation | Stem cell expansion and differentiation protocols | Quality consistency critical for reproducibility |
| qPCR Reagents [98] | Gene expression analysis of pluripotency and lineage markers | Potency assessment, differentiation validation | Reference gene validation required for accurate quantification |
| Reference Standard Materials [97] [99] | Calibrate potency assays and enable relative potency calculations | Assay qualification and validation across batches | Stability profiling required for reliable long-term use |
| Sensor-Integrated Cultureware [96] | Real-time monitoring of dissolved oxygen, pH, metabolites | Process monitoring and quality control | Calibration against reference methods required |
| Live-Cell Imaging Dyes [96] | Non-invasive tracking of cell viability, proliferation | Real-time quality monitoring without destructive sampling | Cytotoxicity validation essential to avoid artifacts |
The comparative analysis presented in this guide demonstrates that validation framework selection significantly impacts the predictive accuracy and translational potential of stem cell-based disease models. Traditional functional assays remain valuable for specific applications, particularly in regulated environments where established methodologies facilitate regulatory approval [98] [99]. However, AI-enhanced approaches offer transformative advantages through multi-parameter integration, real-time capability, and predictive power that surpasses conventional methods [96] [100].
For research and drug development professionals, implementing a phase-appropriate strategy represents the most pragmatic approach to validation [97]. Early-stage discovery research benefits from the rich datasets and predictive capabilities of AI-driven morphological analysis and systems biology approaches. As programs advance toward clinical application, integrating these next-generation methodologies with established quality metrics creates a comprehensive framework that satisfies both scientific and regulatory requirements [38]. This integrated validation strategy ultimately accelerates the development of safer, more effective stem cell-based therapies by establishing robust correlations between product characteristics and clinical performance.
The landscape of preclinical research is undergoing a significant transformation, moving away from traditional animal models toward more human-relevant systems. For decades, animal models have been foundational in biomedical research, contributing substantially to the advancement of vaccines, surgical techniques, and drug discovery [101]. However, growing recognition of their limitations, including interspecies differences, ethical concerns, and poor clinical translation, has accelerated the adoption of human-based alternatives [101] [67].
Stem cell-based models, particularly induced pluripotent stem cells (iPSCs) and three-dimensional organoids, represent a paradigm shift in disease modeling and drug development [102] [67]. These technologies leverage human cells to create patient-specific models that more accurately recapitulate human physiology and disease mechanisms. This comparative analysis examines the relative strengths, limitations, and appropriate applications of stem cell models versus traditional animal models in potency evaluation for disease research.
Fundamental Model Characteristics and Mechanisms
Animal Models: Traditional Mainstay with Inherent Limitations
Animal models, primarily mice, rats, rabbits, and non-human primates, have been the cornerstone of biomedical research. Their use is based on the premise that biological processes are conserved across species, allowing researchers to study complex physiological interactions within a whole living system [101] [103].
Key Applications:
- Drug toxicity and efficacy testing: Required by regulatory agencies for decades
- Disease mechanism studies: Created through genetic modification, surgical intervention, or chemical induction
- Physiological system analysis: Studying interactions between organ systems
- Behavioral studies: Assessing cognitive and motor functions in neurological disorders
Fundamental Limitations: Despite their widespread use, animal models possess inherent limitations. Interspecies differences in genetics, metabolism, immune function, and disease manifestation often render animal data poorly predictive of human responses [101] [103]. For example, a mouse's immune system is adapted for ground-level pathogens, while humans better manage airborne viruses—a crucial difference in respiratory disease and vaccine research [103]. Additionally, ethical concerns surrounding animal use have prompted regulatory changes, with the FDA no longer mandating animal testing for drug safety approval [101] [104].
Stem Cell Models: Human Biology in a Dish
Stem cell-based models leverage human cells to create more physiologically relevant systems for studying human disease. Several stem cell types offer distinct advantages:
Model Types and Characteristics:
- Induced Pluripotent Stem Cells (iPSCs): Adult somatic cells reprogrammed to a pluripotent state, capable of differentiating into any cell type while retaining the donor's genetic background [102] [67]
- Embryonic Stem Cells (ESCs): Derived from early-stage embryos, possessing natural pluripotency but raising ethical considerations [30]
- Organoids: Three-dimensional, self-organizing structures that mimic the architecture and functionality of native organs [101] [67]
- Patient-Derived Organoids (PDOs): Organoids generated from patient samples, preserving individual genetic and phenotypic characteristics [67]
Key Advantages: Stem cell models offer three primary advantages: patient specificity (carrying the donor's genome, including disease-associated mutations), human relevance (recapitulating key functional aspects of human tissue), and scalability (indefinite expansion once protocols are established) [102]. These characteristics make them particularly valuable for modeling rare genetic disorders, predicting individual drug responses, and conducting high-throughput screening [102] [67].
Comparative Analysis: Key Parameters for Research Applications
Table 1: Comprehensive comparison of stem cell models versus animal models across key research parameters
| Evaluation Parameter | Stem Cell Models (iPSCs/Organoids) | Animal Models |
|---|---|---|
| Biological Relevance | Human genetic background; Recapitulates human-specific pathophysiology [102] [67] | Interspecies differences limit predictive value; Often fail to mimic human disease mechanisms [101] [103] |
| Genetic Fidelity | Preserves patient-specific mutations; Enables study of genotype-phenotype relationships [102] [67] | Requires genetic modification; May not capture human genetic complexity [101] |
| Throughput & Scalability | High-throughput screening possible in 384- or 1536-well formats [102] | Low-throughput; Time and resource intensive [101] |
| Cost Considerations | Cost-effective for large-scale screening; Lower long-term costs [101] | High maintenance costs; Complex procedures increase expense [101] |
| Temporal Resolution | Rapid model generation (weeks to months) [102] | Extended timelines for breeding and disease development (months to years) [101] |
| Ethical Compliance | Aligns with 3Rs principles (Replacement, Reduction, Refinement) [101] [67] | Increasing ethical restrictions; Banned for cosmetics in many regions [101] |
| Regulatory Acceptance | Growing acceptance; Used in cardiac safety screening (CiPA initiative) [102] [104] | Traditional gold standard but facing reduced regulatory requirements [101] [104] |
| Complexity Modeling | Recapitulates tissue-level organization but lacks systemic integration [67] [104] | Whole-organism complexity with integrated systemic responses [101] |
| Maturity State | Often exhibit fetal-like characteristics; Limited adult phenotype representation [67] [104] | Adult physiology with age-related processes [101] |
| Standardization | Protocol variability; Batch-to-batch differences [102] [67] | Well-established protocols; Genetic standardization possible [101] |
Disease-Specific Performance and Experimental Evidence
Neurodegenerative Disorders
Table 2: Performance comparison for neurodegenerative disease modeling
| Disease | Animal Model Limitations | Stem Cell Model Advantages |
|---|---|---|
| Parkinson's Disease | Non-human primates, zebrafish, and rodents show species differences in dopamine metabolism; Lack complete human pathophysiology [101] | iPSC-derived dopaminergic neurons from patients model disease phenotypes like mitochondrial dysfunction and α-synuclein aggregation; Enable compound screening [101] [102] |
| Alzheimer's Disease | Transgenic mice (e.g., 5xFAD) cannot completely mimic patient pathophysiology; No complete cure developed in animals [101] | iPSC-derived neurons from patients model tau aggregation and neuronal degeneration; Support phenotypic screens [102] [58] |
| Amyotrophic Lateral Sclerosis (ALS) | Limited representation of human motor neuron vulnerability patterns [58] | iPSC-based neuromuscular models enable study of disease mechanisms and drug discovery [102] [58] |
Experimental Evidence: In Parkinson's disease research, iPSC-derived dopaminergic neurons from patients have successfully modeled disease-specific phenotypes, including mitochondrial dysfunction and protein aggregation. These models have identified compounds capable of rescuing neuronal function in vitro [102]. Similarly, for Alzheimer's disease, iPSC-derived neurons have enabled screening of therapeutics targeting tau pathology, providing human-relevant data not obtainable from animal models [102].
Cardiovascular and Metabolic Diseases
Cardiotoxicity Screening: iPSC-derived cardiomyocytes have become a standard tool for predicting drug-induced arrhythmias, formally integrated into the Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative [102]. These cells express human ion channels and demonstrate higher predictive value for human cardiac responses than animal models [102] [67].
Metabolic Disease Modeling: iPSC-derived hepatocyte-like cells have been used to model familial hypercholesterolemia and test lipid-lowering therapies. In one study, they revealed a drug repurposing opportunity when cardiac glycosides were found to reduce ApoB secretion—a discovery that might not have been possible using conventional animal models [102].
Methodological Framework: Experimental Protocols and Workflows
Stem Cell Model Generation and Quality Control
iPSC Generation Protocol:
- Somatic Cell Isolation: Obtain patient-specific cells (typically dermal fibroblasts or peripheral blood mononuclear cells)
- Reprogramming Factor Delivery: Introduce Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) via viral vectors or non-integrating methods
- Pluripotency Validation: Assess expression of pluripotency markers (NANOG, SSEA-4, TRA-1-60)
- Directed Differentiation: Apply lineage-specific morphogens and signaling molecules
- Functional Maturation: Implement electrical stimulation (cardiomyocytes), mechanical stress (organoids), or co-culture systems
Organoid Generation Protocol:
- Stem Cell Expansion: Culture iPSCs or adult stem cells in defined conditions
- 3D Aggregation: Transfer to low-adhesion plates or microfluidic devices to promote self-organization
- Patterning and Differentiation: Apply region-specific patterning factors
- Long-term Culture: Maintain in specialized media with appropriate biochemical and biomechanical cues
- Quality Assessment: Evaluate morphology, cell-type composition, and functional properties
Quantitative Quality Control: Advanced computational methods like the Web-based Similarity Analytics System (W-SAS) enable quantitative assessment of organoid quality by calculating organ-specific similarity scores based on RNA-seq data [105]. This system uses organ-specific gene expression panels (Organ-GEPs) to provide researchers with similarity percentages compared to human target organs, enabling standardized quality control [105].
Animal Model Generation and Validation
Genetic Engineering Workflow:
- Target Identification: Select gene targets based on human disease genetics
- Vector Construction: Design targeting vectors with appropriate regulatory elements
- Embryonic Stem Cell Modification: Introduce genetic alterations in mouse ES cells
- Blastocyst Injection and Implantation: Generate chimeric animals
- Germline Transmission: Establish stable transgenic lines
- Phenotypic Validation: Characterize disease-relevant phenotypes
Humanized Mouse Generation:
- Immunodeficient Host Selection: Use strains like NSG or NOG mice
- Preconditioning: Administer sublethal irradiation or chemotherapy
- Human Cell Engraftment: Transplant human hematopoietic stem cells or peripheral blood mononuclear cells
- Reconstitution Validation: Assess human immune cell populations in peripheral blood
- Functional Testing: Evaluate immune responses to human-specific pathogens or therapeutics
Research Reagent Solutions for Stem Cell Research
Table 3: Essential research reagents and their applications in stem cell disease modeling
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC | iPSC generation from somatic cells [102] [67] |
| Lineage-Specific Differentiation Kits | Cardiomyocyte, hepatocyte, neuronal differentiation kits | Directed differentiation of pluripotent stem cells [102] [67] |
| Extracellular Matrix Substrates | Matrigel, laminin, collagen-based hydrogels | 3D organoid culture and support [67] [106] |
| Organoid Culture Media | Intestinal, cerebral, hepatic organoid media | Tissue-specific organoid growth and maintenance [67] [106] |
| Cell Characterization Antibodies | Pluripotency markers (NANOG, OCT4); Lineage markers (TUJ1, α-actinin, albumin) | Quality control and differentiation validation [102] [105] |
| CRISPR/Cas9 Gene Editing Systems | Cas9 nucleases, guide RNAs, repair templates | Introduction of disease-associated mutations; Gene correction [102] [67] |
| Cytokines and Growth Factors | BMP, FGF, WNT, EGF pathway modulators | Directed differentiation and pattern formation [67] [105] |
| Functional Assay Kits | Calcium imaging dyes, multi-electrode arrays, metabolic assay kits | Functional assessment of differentiated cells [102] [67] |
Integration of Models: Future Directions and Hybrid Approaches
Organoid-on-Chip Technologies
Microfluidic organ-on-chip platforms represent a convergence technology that addresses certain limitations of both traditional animal models and simple stem cell cultures. By combining the physiological relevance of 3D organoids with precise microenvironmental control, these systems enable more accurate modeling of human pharmacokinetics and pharmacodynamics [67].
Key Advancements:
- Integration of multiple organ systems for systemic toxicity assessment
- Incorporation of fluid flow and mechanical forces to enhance maturation
- Real-time monitoring via embedded biosensors
- Inclusion of immune components to model inflammatory responses [67] [104]
Regulatory Evolution and Standardization
Recent regulatory changes are accelerating the adoption of stem cell-based models. The NIH now requires grant proposals to incorporate New Approach Methodologies (NAMs) alongside animal testing, while the FDA has outlined a roadmap to reduce animal testing to "the exception rather than the norm" in preclinical safety testing within three to five years [104] [106].
Standardization Initiatives:
- International MPS Society: Developing standards for microphysiological systems
- ISO initiatives: Establishing global standards for organoid culture and assay validation
- QC-verified commercial cell providers: Ensuring batch-to-batch consistency [102] [106]
Stem cell models and animal models offer complementary strengths for disease research and drug development. Stem cell-based systems, particularly iPSCs and organoids, provide superior human relevance, genetic fidelity, and scalability for disease modeling and high-throughput screening. However, they currently lack the systemic complexity and adult phenotypes available in animal models.
A strategic integrated approach leverages each system according to its strengths: stem cell models for early discovery, mechanistic studies, and personalized medicine applications, and animal models for systemic safety assessment and complex physiology studies. As stem cell technologies continue to advance—addressing current limitations in maturation, standardization, and complexity—they are poised to increasingly replace animal models, creating more predictive, human-relevant preclinical research pipelines.
Decision Framework for Model Selection
In the field of stem cell research and development, demonstrating functional potency is a critical requirement for both regulatory approval and scientific credibility. Functional validation moves beyond simple marker expression to confirm that stem cell-derived models genuinely replicate the physiological behaviors of their target tissues. For advanced stem cell-based disease models, three critical pillars of functional validation are electrophysiology, metabolism, and secretome profiling. These approaches provide complementary insights into cellular function, from electrical signaling and energy metabolism to paracrine communication. This guide objectively compares experimental methodologies across these three domains, providing researchers with validated protocols and comparative data to inform their potency evaluation strategies.
Comparative Analysis of Validation Methodologies
The table below summarizes the core objectives, key readouts, and applications of the three primary functional validation methodologies.
Table 1: Comparison of Functional Validation Methodologies for Stem Cell-Based Models
| Validation Method | Core Functional Objective | Primary Readouts/Parameters | Primary Applications in Disease Modeling |
|---|---|---|---|
| Electrophysiology | Assess excitability and electrical signaling fidelity | Action potential properties, ion channel currents, synaptic transmission | Neurological disorders, cardiac arrhythmias, channelopathies |
| Metabolism | Quantify energy production and nutrient utilization | Oxygen consumption rate (OCR), extracellular acidification rate (ECAR), metabolite levels | Metabolic syndromes, mitochondrial disorders, cancer metabolism |
| Secretome | Profile paracrine signaling and protein secretion | Cytokine levels, extracellular vesicle (EV) cargo, proteomic/peptidomic profiles | Inflammation, fibrosis, tissue repair, immunomodulation |
Electrophysiology Validation
Experimental Protocols
Patch-Clamp Electrophysiology for Ionic Currents:
- Cell Preparation: Plate cells on glass coverslips coated with appropriate substrate (e.g., poly-D-lysine, laminin). Use within 1-3 days for optimal health.
- Solution Preparation: Prepare an external solution (e.g., Tyrode's solution containing 140 mM NaCl, 5.4 mM KCl, 1.8 mM CaCl2, 1 mM MgCl2, 10 mM HEPES, 10 mM glucose; pH 7.4 with NaOH) and an internal pipette solution (e.g., 120 mM KCl, 1 mM MgCl2, 10 mM HEPES, 10 mM EGTA, 1 mM CaCl2; pH 7.2 with KOH).
- Recording: Pull borosilicate glass capillaries to fabricate recording pipettes with resistances of 2-5 MΩ. Establish a giga-ohm seal (>1 GΩ) on the cell membrane. Apply brief suction to rupture the membrane for whole-cell configuration.
- Stimulation and Data Acquisition: For action potential recording, switch to current-clamp mode and inject depolarizing current. For voltage-gated sodium channel currents, use voltage-clamp mode with a holding potential of -70 mV and apply step depolarizations. Record signals with an amplifier, digitize at a minimum of 50 kHz, and filter at 2-10 kHz.
Microelectrode Array (MEA) for Network Activity:
- Cell Plating: Plate a high density of cells (e.g., neurons, cardiomyocytes) directly onto a commercially available MEA chip pre-coated with adhesion factors.
- Acclimatization and Recording: Allow the cells to recover and form networks for several days. Record spontaneous electrical activity in a cell culture incubator with continuous data acquisition over several minutes.
- Data Analysis: Use vendor software or open-source tools (e.g., Neuroexplorer, MEAtools) to extract parameters like mean firing rate, burst frequency, and inter-spike interval.
Research Reagent Solutions
Table 2: Essential Reagents for Electrophysiology Validation
| Reagent / Solution | Function / Application |
|---|---|
| Borosilicate Glass Capillaries | Fabrication of recording pipettes for patch-clamp. |
| Ion Channel Modulators (e.g., Tetrodotoxin for Na+ channels, E-4031 for hERG K+ channels) | Pharmacological validation of specific ionic currents. |
| Extracellular & Intracellular Solutions | Maintain physiological ionic environment and osmolarity. |
| Adhesion Substrates (e.g., Poly-D-Lysine, Laminin, Matrigel) | Promote cell attachment and maturation on coverslips or MEA chips. |
| MEA Chips & Amplifier Systems | Non-invasive, long-term recording of network-level electrophysiology. |
Figure 1: Electrophysiology validation workflow, covering both detailed patch-clamp and network-level MEA approaches.
Metabolic Validation
Experimental Protocols
Seahorse XF Analyzer for Metabolic Phenotyping:
- Cell Preparation: Seed cells at an optimized density (e.g., 20,000-80,000 cells/well for a XF96 plate) 24-48 hours before the assay. Include background control wells without cells.
- Assay Medium Preparation: On the day of the assay, replace growth medium with XF Base Medium supplemented with 1 mM pyruvate, 2 mM glutamine, and 10 mM glucose (pH 7.4). Incubate the cell culture plate for 45-60 minutes in a non-CO2 incubator at 37°C.
- Port Loading with Modulators: Load the injection ports of the XF assay cartridge with metabolic modulators.
- Port A: 1.5 µM Oligomycin (ATP synthase inhibitor, measures glycolytic capacity and ATP-linked respiration).
- Port B: 1.0 µM FCCP (mitochondrial uncoupler, measures maximal respiratory capacity).
- Port C: 0.5 µM Rotenone/Antimycin A (complex I/III inhibitors, measures non-mitochondrial respiration).
- Run Assay and Analyze Data: Calibrate the cartridge and run the standard Cell Mito Stress Test program. After the run, normalize data to cell count (e.g., via DNA content) using vendor software. Key parameters: Basal Respiration, ATP Production, Maximal Respiration, and Glycolytic Capacity.
Liquid Chromatography-Mass Spectrometry (LC-MS) for Metabolomics:
- Metabolite Extraction: Quickly wash cells with PBS and quench metabolism with cold methanol/acetonitrile (e.g., 80% methanol at -80°C). Scrape cells and perform protein precipitation. Centrifuge and collect the supernatant containing metabolites.
- LC-MS Analysis: Separate metabolites using a reversed-phase or HILIC column. Analyze with a high-resolution mass spectrometer (e.g., Q-TOF, Orbitrap) in both positive and negative ionization modes.
- Data Processing: Use software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and annotation against metabolite databases (e.g., HMDB, METLIN). Perform statistical analysis (e.g., PCA, pathway analysis) to identify differentially abundant metabolites.
Research Reagent Solutions
Table 3: Essential Reagents for Metabolic Validation
| Reagent / Solution | Function / Application |
|---|---|
| XF Assay Kits (e.g., Mito Stress Test, Glycolysis Stress Test) | Standardized reagents for real-time analysis of metabolic fluxes in live cells. |
| Metabolic Modulators (Oligomycin, FCCP, Rotenone, Antimycin A, 2-DG) | Precisely target specific pathways to dissect metabolic function. |
| LC-MS Grade Solvents (Methanol, Acetonitrile, Water) | High-purity solvents for metabolomic sample prep and analysis to minimize background noise. |
| Stable Isotope Tracers (e.g., 13C-Glucose, 15N-Glutamine) | Track nutrient utilization through metabolic pathways for flux analysis. |
| Metabolite Standards & Databases | For accurate identification and quantification of metabolites via LC-MS. |
Figure 2: Key steps in the Seahorse XF Analyzer metabolic flux assay workflow.
Secretome Validation
Experimental Protocols
Conditioned Media Collection for Secretome Analysis:
- Cell Culture and Serum Starvation: Culture cells to 70-80% confluence. To minimize interference from serum proteins, wash cells thoroughly with PBS or serum-free medium [107]. Replace growth medium with a reduced-serum or serum-free medium optimized for cell viability. The starvation period typically lasts 12-48 hours and requires optimization to minimize cell death [107].
- Collection and Processing: Collect the Conditioned Medium (CM) and centrifuge (e.g., 2,000 × g for 10 minutes) to remove cell debris. Concentrate the CM using centrifugal filter units (e.g., 3 kDa cutoff) if necessary. Aliquot and store at -80°C. Always prepare a control of unconditioned medium processed identically.
Mass Spectrometry-Based Proteomic Analysis:
- Protein Digestion: Denature and reduce/alkylate proteins in the CM. Digest proteins into peptides using trypsin.
- Liquid Chromatography and Mass Spectrometry: Separate peptides using a nano-flow liquid chromatography (LC) system. Analyze eluting peptides with a high-resolution mass spectrometer (e.g., Orbitrap) using a data-dependent acquisition (DDA) or data-independent acquisition (DIA) method.
- Data Analysis and Validation: Identify and quantify proteins by searching MS/MS spectra against protein sequence databases (e.g., Swiss-Prot) using search engines like MaxQuant. Use techniques like SILAC (Stable Isotope Labeling by Amino acids in Cell culture) for precise quantification, which involves growing cells in "heavy" vs. "light" amino acid media [107]. Validate key findings using orthogonal methods like ELISA or Western Blot.
Validation via Functional Potency Assay: A robust potency assay measures a secretome's specific biological activity rather than just its composition. For example, to measure anti-inflammatory potency:
- Coculture Setup: Coculture MSCs with THP-1 monocyte-derived M1-polarized macrophages [70].
- Stimulation and Readout: The inflammatory macrophage environment stimulates MSCs to secrete anti-inflammatory factors like the Interleukin-1 Receptor Antagonist (IL-1RA). Quantify IL-1RA in the coculture supernatant using a validated ELISA [70].
- Analysis: The amount of IL-1RA secreted serves as a direct, quantifiable measure of the MSC product's immunomodulatory potency for batch release [70].
Research Reagent Solutions
Table 4: Essential Reagents for Secretome Validation
| Reagent / Solution | Function / Application |
|---|---|
| Serum-Free / Reduced-Serum Media | Allows collection of cell-specific secreted factors without serum protein contamination. |
| Protease Inhibitor Cocktails | Prevent degradation of proteins/peptides in conditioned media post-collection. |
| Ultrafiltration Units (3kDa MWCO) | Concentrate dilute secreted factors from large volumes of conditioned media. |
| SILAC Kits | Enable accurate MS-based quantification by metabolic labeling of newly synthesized proteins [107]. |
| ELISA Kits for Specific Factors (e.g., IL-1RA, VEGF, BDNF) | Target validation and absolute quantification of key paracrine factors. |
| EV Isolation Kits (e.g., based on size-exclusion chromatography) | Isolate extracellular vesicles for separate analysis of their cargo. |
Figure 3: Integrated workflow for secretome analysis, combining comprehensive proteomic profiling with targeted functional potency assays.
Correlating In Vitro Findings with Patient-Derived Data
The transition from preclinical research to clinical success, particularly in complex fields like critical care and oncology, is hampered by a persistent translational gap. Many therapeutic strategies that show promise in traditional laboratory models fail in human trials [108]. This guide objectively compares emerging patient-derived in vitro models against traditional models, framing the comparison within the broader thesis that advanced potency evaluation is key to bridging this gap. For researchers and drug development professionals, the strategic integration of these models could de-risk pipelines and accelerate the development of personalized therapies.
The following table summarizes the core characteristics of various models used in translational research.
Table 1: Comparison of Preclinical Disease Models
| Model Type | Key Characteristics | Advantages | Limitations | Primary Translational Application |
|---|---|---|---|---|
| Traditional 2D Cell Cultures [109] | Immortalized cell lines grown in monolayers. | - Low cost & easy to manipulate- Rapid cell proliferation- Well-established protocols | - Lacks native 3D architecture & cellular diversity- Genetic/ phenotypic drift from original tumor- Absence of physiologic cell-matrix interactions | - Initial high-throughput drug screening- Basic mechanistic studies |
| Animal Models [108] | Typically young, healthy, inbred animals. | - Captures whole-organism & systemic physiology- Allows study of complex organ crosstalk | - Significant interspecies differences- Cannot replicate human immune system in PDX models- Poorly replicates patient heterogeneity | - Evaluation of systemic effects & safety (PK/PD)- Validating findings from human-relevant systems |
| Patient-Derived Cancer Cells (PDCCs) [109] | Cells cultured directly from patient tumor samples. | - Retains genetic & phenotypic traits of original tumor- Can be established via various methods (surgery, biopsy)- Bridges lab research and clinical reality | - Low culture initiation success rates- Difficulty in maintaining tumor heterogeneity ex vivo- Challenges in reproducibility between labs | |
| 3D Tumouroids/Spheroids [109] [110] | 3D aggregates of patient-derived cells. | - Better recapitulates tumor architecture than 2D- Enables non-destructive, continuous imaging for growth tracking- Allows quantification of drug dose-response | - Lacks tumor microenvironment components (e.g., stromal cells) | |
| Patient-Derived Organoids [109] | Self-organizing 3D structures from patient stem/progenitor cells. | - Retains patient-specific heterogeneity & disease endotypes- Useful for personalized drug screening & immunotherapy evaluation- Enables study of rare cancers | - Technically challenging & variable culture success- Scalability for high-throughput screens can be limited | |
| Organ-on-a-Chip Systems [108] | Microfluidic devices with human cells mimicking organ physiology. | - Incorporates biomechanical forces (e.g., fluid flow, stretch)- Enables study of multi-organ crosstalk (e.g., in sepsis)- Can identify functional patient endotypes for stratification | - High technical complexity & cost- Requires interdisciplinary expertise- Standardization and scalability are ongoing challenges |
Experimental Protocols for Potency and Drug Response Evaluation
Deep Learning-Based Prediction of Stem Cell Multipotency
Objective: To non-invasively predict the multipotency and differentiation capacity of human adult stem cells based on cellular morphology, addressing the challenge of donor-dependent variation in cell therapy efficacy [111].
Methodology:
- Cell Sourcing and Preparation: Human Nasal Turbinate Stem Cells (hNTSCs) are obtained from multiple donors and cultured under standardized, clinically relevant conditions (e.g., cGMP) [111].
- Ground Truth Labeling: A subset of cells is immunostained for Stage-Specific Embryonic Antigen-3 (SSEA-3), a known marker of multipotency. Cells are classified as "multipotent" or "non-multipotent" based on staining, creating a labeled dataset [111].
- Image Acquisition: High-resolution bright-field images of the live, unlabeled cell populations are acquired [111].
- Model Training and Validation: A Convolutional Neural Network (CNN), such as DenseNet121 pre-trained on ImageNet, is employed. The model is trained using transfer learning on the dataset of bright-field images and their corresponding multipotency labels [111].
- Performance Metrics: The model's predictive accuracy is validated using metrics such as accuracy, sensitivity, specificity, and Area Under the Curve (AUC). A study achieved a prediction accuracy of 85.98% for multipotency levels using this approach [111].
- Correlation with Functional Outcome: The deep learning prediction is finally correlated with the actual ex vivo differentiation efficacy of the stem cells into the target lineage (e.g., keratocyte progenitors) to confirm its biological relevance [111].
Continuous Imaging Assay for Drug Response in Patient-Derived Tumouroids
Objective: To non-destructively quantify the growth and chemotherapeutic response of colorectal tumouroids within a clinically relevant timeframe, maximizing data extraction from scarce patient material [110].
Methodology:
- Tumouroid Generation: Patient-derived cancer cells are embedded in a 3D matrix (e.g., Matrigel) and cultured to form 3D tumouroids [109] [110].
- Experimental Setup: Tumouroids are exposed to a range of chemotherapeutic drug concentrations (e.g., SN-38, the active metabolite of irinotecan) or a vehicle control [110].
- Continuous Imaging: Plates are placed in an automated imaging system that captures high-content images of the same tumouroids at regular intervals (e.g., every 24 hours) over several days without disrupting the culture [110].
- Image-Based Quantification: Automated image analysis software is used to derive multiple readouts from the images at each time point:
- Dose-Response Modeling: The growth data (e.g., area over time) for each drug concentration is used to fit dose-response models, allowing for the calculation of half-maximal inhibitory concentration (IC50) values and other pharmacodynamic parameters specific to the patient's cancer [110].
Potency Assay for Anti-inflammatory Capacity of Mesenchymal Stromal Cells (MSCs)
Objective: To develop a therapeutically relevant, robust potency assay that measures the immunomodulatory capacity of MSCs in a standardized inflammatory environment, a critical requirement for quality control in cell-based medicinal products [70].
Methodology:
- Inflammation Model Establishment:
- Co-culture and Stimulation: The M1 macrophages are co-cultured with the ABCB5+ MSCs at a range of optimized ratios to identify the condition for near-maximal stimulation of the MSCs [70].
- Readout and Quantification: The cell culture supernatant is collected after a defined period. The concentration of Interleukin-1 Receptor Antagonist (IL-1RA), a key anti-inflammatory mediator secreted by the MSCs, is quantified using a validated enzyme-linked immunosorbent assay (ELISA) [70].
- Assay Validation: The ELISA method is rigorously validated for selectivity, accuracy, and precision over a relevant concentration range. The potency of different MSC batches can be compared based on the absolute maximum levels of IL-1RA secreted per individual MSC [70].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Patient-Derived Model Research
| Item | Function/Application |
|---|---|
| Patient-Derived Cells (from surgery, biopsy, or liquid biopsy) [109] | The foundational biological material that provides patient-specific genetic, immunological, and metabolic characteristics for the model. |
| Specialized 3D Culture Matrices (e.g., Basement Membrane Extract (BME), Matrigel, collagen I) [109] | Provides a scaffold that supports the formation and growth of complex 3D structures like organoids and tumouroids, mimicking the native extracellular matrix. |
| Microfluidic Organ-on-a-Chip Devices [108] | Platforms that emulate the structural, functional, and mechanical microenvironment of human tissues, allowing for real-time analysis and the study of organ crosstalk. |
| IL-1RA ELISA Kit [70] | A critical validated tool for quantifying the secretion of IL-1RA, serving as a key potency readout for the anti-inflammatory capacity of MSCs in co-culture assays. |
| M1 Macrophage Polarization Reagents (e.g., PMA, IFN-γ, LPS) [70] | Used to differentiate and activate THP-1 monocytes into a pro-inflammatory M1 phenotype, creating a standardized inflammatory environment for potency testing. |
| SSEA-3 Antibody [111] | Used for immunofluorescence staining to identify and label multipotent stem cells, establishing the "ground truth" for training deep learning models. |
| Pre-trained Convolutional Neural Network (CNN) Models (e.g., VGG19, DenseNet121) [111] | AI tools adapted via transfer learning to predict stem cell multipotency and other biological features directly from bright-field microscopy images. |
Visualizing the Integrated Translational Pipeline
The following diagram illustrates a proposed integrated research pipeline that synergizes patient-derived in vitro models and animal models to improve clinical translation.
Integrated Translational Research Pipeline
The correlation between in vitro findings and patient-derived data is significantly strengthened by leveraging advanced model systems. While traditional 2D cultures and animal models remain useful for specific applications, patient-derived organoids, tumouroids, and organ-chips offer unparalleled fidelity to human disease biology. When combined with robust, functionally relevant potency assays and AI-driven analytical tools, these models provide a powerful framework for de-risking drug candidates, understanding disease endotypes, and ultimately delivering on the promise of personalized medicine. The integrated pipeline, which uses human-relevant systems for mechanistic insight and initial screening before moving to animal studies for systemic validation, represents a pragmatic and promising strategy for bridging the translational gap [108].
Regulatory Pathways and Standards for Model Acceptance
In stem cell-based disease model research, "model acceptance" refers to the regulatory and scientific endorsement of a cellular system's predictive validity for drug development. The cornerstone of this acceptance is potency evaluation—the quantitative measurement of a product's biological activity—which directly links a model's characteristics to its intended mechanism of action and desired clinical effect [112]. For researchers and drug development professionals, demonstrating potency is not merely a regulatory hurdle; it is a fundamental scientific exercise that validates the model's relevance. Regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require potency assays to reflect the biological mechanism and, ideally, correlate with clinical response [112]. As regulatory pathways evolve, exemplified by the FDA's novel "Plausible Mechanism Pathway" for bespoke therapies, the standards for model acceptance are also shifting, placing greater emphasis on well-characterized biological causes and successful target engagement [113] [114]. This guide provides a comparative analysis of the experimental frameworks and data standards essential for achieving model acceptance in this dynamic landscape.
Comparative Analysis of Regulatory Pathways
The regulatory environment for advanced therapies is adapting to the challenges of personalized and rare disease treatments. The following table compares the established regulatory approach with the newly proposed pathway, highlighting key differences relevant to the development of stem cell-based models.
Table 1: Comparison of Traditional and Novel Regulatory Pathways for Advanced Therapies
| Feature | Traditional Regulatory Pathway | Novel "Plausible Mechanism" Pathway |
|---|---|---|
| Core Principle | Substantial evidence of safety and efficacy, typically from randomized controlled trials (RCTs) [113] | Approval based on a plausible mechanism and confirmed target engagement in successive patients, where RCTs are not feasible [113] [114] |
| Key Evidentiary Standard | One or more adequate and well-controlled investigations, with RCTs as the gold standard [113] | Five core elements, including a known molecular abnormality, successful targeting of the alteration, and a well-characterized natural history [113] |
| Trial Design | Reliance on randomized, controlled studies with larger patient populations [113] | Leverages single-patient expanded access INDs and uses patients as their own controls [113] |
| Role of Animal Models | Often required for non-clinical safety and proof-of-concept studies. | Acknowledges the futility of many animal studies and embraces non-animal models where possible [113] |
| Post-Market Requirements | Standard post-market surveillance; confirmatory trials for accelerated approval [113] | Mandatory real-world evidence (RWE) collection as a postmarketing commitment to preserve efficacy and detect safety signals [113] |
| Applicability to Models | Potency assays must be quantitative, functional, and validated for product release [112] | Provides a framework for accepting models based on strong biological plausibility and in vitro data when clinical trials are impractical. |
The Plausible Mechanism Pathway is particularly significant for stem cell research, as it signals a regulatory willingness to accept compelling biological rationale and in vitro data when clinical trials in rare diseases are not feasible. This pathway requires:
- Identification of a Specific Molecular Abnormality: The disease must have a known biologic cause, not just a constellation of clinical symptoms [113].
- Confirmation of Target Engagement: Researchers must provide data confirming that the therapy successfully targeted the underlying biological alteration, which could be demonstrated using a sophisticated stem cell-based disease model [113] [114].
Standards for Potency Evaluation of Stem Cell-Based Models
Potency is a critical quality attribute that separates biological products from small-molecule drugs. For stem cell-based models, potency testing is expected to be a quantitative, functional assay that reflects the product's Mechanism of Action (MoA) [112]. The following table outlines the key regulatory expectations and the experimental methodologies used to meet them.
Table 2: Standards and Methodologies for Potency Assays in Stem Cell-Based Models
| Aspect | Regulatory Expectation | Common Experimental Methodologies & Protocols |
|---|---|---|
| Assay Type | A quantitative functional potency assay is required for product release [112]. The EMA may allow validated surrogate assays for release if correlated with a functional characterization assay [112]. | Cell-based biological assays: Co-culture systems with target cells.Biochemical assays: ELISA for secreted factors, flow cytometry for surface markers.Genomic assays: qRT-PCR for gene expression, RNA-seq for transcriptional profiling. |
| MoA Linkage | The potency assay must be based on the intended biological effect, which should be linked to the clinical response [112]. | Directed Differentiation: Quantify expression of lineage-specific markers (e.g., via flow cytometry) after differentiation protocol.Trophic Factor Secretion: Use multiplex ELISA (e.g., Luminex) to quantify panel of secreted proteins (e.g., VEGF, IL-6, HGF).Immunomodulation: Measure suppression of T-cell proliferation in a mixed lymphocyte reaction (MLR). |
| Complex MoA | For products with multiple mechanisms, a combination of methods or a matrix approach is needed to fully capture potency [112]. | Matrix Approach: Assign weights to different assays (e.g., 40% differentiation efficiency, 30% secretory profile, 30% immunomodulation) to calculate a composite potency score. |
| Validation | Validated assays are required for commercial production and pivotal clinical trials. Qualified methods are accepted for early-stage development [112]. | Assay validation per ICH guidelines, establishing parameters: accuracy, precision, specificity, linearity, range, and robustness. |
A critical challenge in stem cell model development is addressing products with multiple mechanisms of action. For example, mesenchymal stromal cells (MSCs) may act through immunomodulation, secretion of trophic factors, and direct differentiation [115]. In such cases, regulators expect a "matrix of assays" to capture the complete functional profile, as no single test may be sufficient [112]. Furthermore, the stability-indicating property of the potency assay is crucial; it must be able to detect degradation in the product's biological activity over time, which is a key aspect of model qualification for long-term studies [112].
Experimental Data and Visualization of Workflows
Key Experimental Protocols in Practice
To translate the aforementioned standards into practice, specific experimental protocols are employed. Below is a detailed overview of two common assays used to establish the potency of stem cell-based models.
Table 3: Detailed Experimental Protocols for Key Potency Assays
| Assay Name | In Vitro Immunomodulation Assay (Mixed Lymphocyte Reaction - MLR) | Directed Differentiation & Phenotypic Analysis |
|---|---|---|
| Purpose | To quantify the immunomodulatory capacity of stem cells (e.g., MSCs) by measuring their suppression of immune cell proliferation [115]. | To assess the differentiation efficiency and functional maturity of stem cells directed toward a specific lineage (e.g., cardiac, neural, osteogenic). |
| Mechanism of Action (MoA) Measured | Immunomodulation via paracrine signaling and/or cell-cell contact. | Developmental potential and functional tissue formation. |
| Key Reagents | - Peripheral Blood Mononuclear Cells (PBMCs) from donors- Mitogen (e.g., PHA) or allogeneic PBMCs (for one-way MLR)- CFSE or similar cell proliferation dye- Test stem cells and control cells- Culture medium with/without immunosuppressants | - Lineage-specific differentiation media (e.g., osteogenic: dexamethasone, β-glycerophosphate, ascorbate)- Fixation and permeabilization buffers- Fluorescently conjugated antibodies against lineage markers (e.g., CD90, CD105, CD73 for MSCs; SSEA-4 for pluripotent stem cells)- Live/dead cell stain |
| Step-by-Step Workflow | 1. Isolate and label responder PBMCs with CFSE.2. Stimulate PBMCs with mitogen or allogeneic irradiated PBMCs.3. Co-culture stimulated PBMCs with varying ratios of test stem cells.4. Incubate for 3-5 days.5. Harvest cells and analyze CFSE dilution via flow cytometry.6. Quantify suppression by comparing proliferation in co-culture vs. stimulated PBMCs alone. | 1. Seed stem cells at defined density.2. Induce differentiation by switching to lineage-specific media for 1-4 weeks.3. Harvest cells at defined time points.4. Stain cells for intracellular and surface markers.5. Acquire data using flow cytometry.6. Analyze data to determine the percentage of cells expressing target markers. |
| Data Output & Quantification | Percentage suppression of T-cell proliferation, calculated as: [1 - (Proliferation in Co-culture / Proliferation in Stimulated Control)] × 100%. IC50 values can be derived from dose-response curves. |
Flow cytometry histograms and quantification of the percentage of positively stained cells for specific markers. Alizarin Red S staining (for osteogenesis) or Oil Red O (for adipogenesis) can provide additional quantitative data. |
Visualizing the Potency Assay Workflow
The following diagram illustrates the logical workflow for developing and qualifying a potency assay, from understanding the mechanism of action to final validation, ensuring alignment with regulatory standards.
Diagram: Potency Assay Development Workflow from MoA to Validation.
The Scientist's Toolkit: Essential Research Reagents
Successful potency evaluation relies on a suite of essential reagents and tools. The table below lists key solutions and their functions in establishing robust experimental protocols.
Table 4: Research Reagent Solutions for Potency Evaluation
| Reagent / Solution | Function in Potency Evaluation |
|---|---|
| Lineage-Specific Differentiation Media | Directs stem cell fate toward specific cell types (e.g., cardiomyocytes, neurons); foundational for functional assays [115]. |
| Flow Cytometry Antibody Panels | Quantifies cell surface and intracellular markers to determine purity, identity, and differentiation efficiency [115] [112]. |
| ELISA & Multiplex Immunoassay Kits | Measures concentration of secreted proteins (e.g., trophic factors, cytokines) to assess paracrine activity [112]. |
| Cell Proliferation & Viability Assays | (e.g., CFSE, MTT, ATP assays): Determines cell growth, metabolic activity, and health, which are baseline quality attributes [115]. |
| qPCR/Thermo Fisher Scientific" href="#" target="_blank">RT-qPCR Reagents | Analyzes gene expression changes during differentiation or in response to stimuli, providing molecular-level potency data [112]. |
| CRISPR-Cas9 & Gene Editing Tools | Validates MoA by creating isogenic control lines or introducing disease-specific mutations into stem cell models [112]. |
The regulatory landscape for stem cell-based disease models is strategically evolving, balancing rigorous standards for potency with pragmatic pathways for therapies targeting ultra-rare conditions. The foundational requirement remains the development of a quantitative, mechanism-based potency assay that can reliably predict biological activity. The emergence of the Plausible Mechanism Pathway underscores the growing regulatory acceptance of robust in vitro data and well-characterized biological rationale, especially when clinical trials are impractical. For researchers, this emphasizes the need to deeply understand the mechanism of action of their models and to invest in developing a matrix of functional assays that collectively capture the product's complexity. By systematically employing the detailed experimental protocols, visual workflows, and essential reagents outlined in this guide, scientists can robustly build the evidence needed for model acceptance, thereby accelerating the translation of stem cell research into credible tools for drug development and, ultimately, effective therapies.
Conclusion
The rigorous evaluation of stem cell potency is fundamental to creating disease models that accurately recapitulate human pathology. As the field progresses, the integration of advanced gene editing, 3D culture systems, and AI-driven quality control will be crucial for overcoming current limitations in maturation and reproducibility. The future of stem cell-based disease modeling lies in developing standardized, validated, and clinically predictive platforms that can reliably inform drug discovery and therapeutic development. Collaborative efforts to establish global standards and harmonized validation frameworks will be essential to fully realize the potential of these powerful models in advancing personalized medicine and reducing the translational gap between preclinical research and clinical success.
References
- 1. Cell Potency: Totipotent vs Pluripotent vs Multipotent Stem ... [https://www.technologynetworks.com/cell-science/articles/cell-potency-totipotent-vs-pluripotent-vs-multipotent-stem-cells-303218]
- 2. Cell potency [https://en.wikipedia.org/wiki/Cell_potency]
- 3. Totipotent vs Pluripotent Stem Cells (2025) [https://www.dvcstem.com/post/totipotent-vs-pluripotent]
- 4. Basics of Stem Cell Biology as Applied to the Brain - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK435799/]
- 5. Describing the Stem Cell Potency: The Various Methods of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5118841/]
- 6. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 7. Potency analysis of cellular therapies: the emerging role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1891278/]
- 8. Potency evaluation of tissue engineered and regenerative ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779913001169]
- 9. Mechanism of action, potency and efficacy: considerations for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05179-7]
- 10. Induced Pluripotent (iPSC) and Mesenchymal (MSC) Stem ... [https://www.mdpi.com/1422-0067/26/12/5617]
- 11. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 12. MSCs vs. iPSCs: Potential in therapeutic applications [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1005926/full]
- 13. Induced Mesenchymal Stem Cells: An Emerging Source for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943107/]
- 14. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 15. Comparing ESC and iPSC—Based Models for Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470175/]
- 16. The 2025 Ogawa-Yamanaka Stem Cell Prize Awarded to ... [https://gladstone.org/news/2025-ogawa-yamanaka-stem-cell-prize-awarded-rudolf-jaenisch]
- 17. Pluripotent stem cells in disease modelling and drug discovery | Nature Reviews Molecular Cell Biology [https://www.nature.com/articles/nrm.2015.27]
- 18. Pluripotency | Daley Laboratory [https://daley.hms.harvard.edu/pluripotency]
- 19. A pluripotent stem cell atlas of multilineage differentiation | Scientific Data [https://www.nature.com/articles/s41597-025-05549-w]
- 20. Determination and validation of design space for ... [https://pubmed.ncbi.nlm.nih.gov/40341300/]
- 21. Stem cells: past, present, and future [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1165-5]
- 22. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 23. Reassessment of marker genes in human induced ... [https://www.nature.com/articles/s41467-024-52922-1]
- 24. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 25. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 26. From unipotency to pluripotency: deciphering protein networks ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11612-y]
- 27. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 28. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 29. Describing the Stem Cell Potency: The Various Methods of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2016.00134/full]
- 30. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 31. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 32. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 33. SCA LRA Update - April 2025: Regulatory Landscape of ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/04/09/sca-lra-update-april-2025-regulatory-landscape-of]
- 34. Direct Comparison of Four Hematopoietic Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7486192/]
- 35. Myogenic Differentiation of iPS Cells Shows Different ... [https://www.mdpi.com/2073-4409/10/7/1671]
- 36. Early and non-destructive prediction of the differentiation ... [https://www.nature.com/articles/s41598-025-11108-5]
- 37. Clever Experimental Designs: Shortcuts for Better iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700474/]
- 38. Artificial intelligence and systems biology analysis in stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476622/]
- 39. Advances and continuing challenges in differentiation of ... [https://pubmed.ncbi.nlm.nih.gov/41214197/]
- 40. Human organoids in basic research and clinical applications [https://www.nature.com/articles/s41392-022-01024-9]
- 41. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 42. The Use of Stem Cell-Derived Organoids in Disease Modeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC8303386/]
- 43. Brain Organoids and Assembloids—From Disease Modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155111/]
- 44. Assembloid models of cell-cell interaction to study tissue and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12143640/]
- 45. Human assembloid model of the ascending neural sensory ... [https://www.nature.com/articles/s41586-025-08808-3]
- 46. Evolving from organoid to assembloid with enhanced ... [https://www.sciopen.com/article/10.26599/CO.2025.9410010]
- 47. Brain organoid model systems of neurodegenerative ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1604435/full]
- 48. Advances in humanoid organoid-based research on inter ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06381-x]
- 49. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 50. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 51. Emerging trends in prime editing for precision genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322275/]
- 52. Harnessing artificial intelligence to advance CRISPR ... [https://www.nature.com/articles/s41576-025-00907-1]
- 53. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 54. Prime Editing新突破:体内编辑成功治愈镰状细胞贫血小鼠模型 [https://www.edgene.cn/blog/info/122]
- 55. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 56. CMN Weekly (23 May 2025) - Your ... [https://crisprmedicinenews.com/news/cmn-weekly-23-may-2025-your-weekly-crispr-medicine-news/]
- 57. CMN Weekly (26 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-26-september-2025-your-weekly-crispr-medicine-news/]
- 58. Stem Cell Clinical Trials and Promise of Engineered Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409071/]
- 59. Stem cell models of neurodegeneration 2025 [https://www.ukdri.ac.uk/events/stem-cell-models-neurodegeneration-2025]
- 60. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 61. Stem Cell Therapy for Heart Failure (2025) [https://www.dvcstem.com/post/stem-cells-reverse-heart-disease]
- 62. Lab-grown kidneys show real function in new stem cell study [https://www.drugtargetreview.com/news/188183/lab-grown-kidneys-show-real-function-in-new-stem-cell-study/]
- 63. Worldwide hotspots and trends in stem cell therapy for kidney ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318756/]
- 64. Worldwide Hotspots and Trends in Stem Cell Therapy for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1619291/abstract]
- 65. 10 Key Technologies Driving the High Content Screening ... [https://blog.bccresearch.com/10-key-technologies-driving-the-high-content-screening-hcs-market]
- 66. On-chip 3D potency assay for prediction of clinical ... [https://www.nature.com/articles/s41467-025-60158-w]
- 67. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 68. High-content confocal analysis of tumorigenesis, cancer ... [https://www.nature.com/articles/s41598-025-16144-9]
- 69. Improved reconstruction of single-cell developmental ... [https://www.nature.com/articles/s41592-025-02857-2]
- 70. Potency assay to predict the anti-inflammatory capacity of a ... [https://www.sciencedirect.com/science/article/pii/S1465324924000501]
- 71. A Comparative Analysis of Multipotent Mesenchymal ... [https://www.nature.com/articles/s41598-020-61167-z]
- 72. Comparative and integrative single cell analysis reveals new insights... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10013-x]
- 73. Human perinatal stem derived extracellular matrix enables rapid... cell [https://www.nature.com/articles/s41598-020-76052-y?error=cookies_not_supported&code=a46f0549-7abf-4c15-af13-60827dda7c66]
- 74. Engineering Lineage Potency and Plasticity of Stem Cells ... [https://www.nature.com/articles/s41598-018-34511-7]
- 75. Quantitative phase imaging with temporal kinetics predicts ... [https://www.nature.com/articles/s41467-025-61846-3]
- 76. Engineering in vitro vascular microsystems [https://www.nature.com/articles/s41378-025-00956-w]
- 77. Recursive variational autoencoders for 3D blood vessel ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841525002506]
- 78. Randomized comparison of AI enhanced 3D printing and ... [https://www.nature.com/articles/s41746-025-01571-9]
- 79. Hierarchical Part-based Generative Model for Realistic 3D ... [https://arxiv.org/html/2507.15223v1]
- 80. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 81. VESNA: an open-source tool for automated 3D vessel ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06270-6]
- 82. Stem Cell Therapy: Overview, Benefits & Risks (2025) [https://www.dvcstem.com/post/stem-cell-therapy]
- 83. 3D printed polymers that mimic the mechanical properties ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224845/]
- 84. Stem Cell-Based Therapy, Disease Modeling and Drug ... [https://www.mdpi.com/journal/cells/topical_collections/cell_based_therapy_2021]
- 85. AI and Automation: Understanding the Difference & Impact in 2025 [https://www.codezion.com/blog/ai-and-automation-complete-guide/?srsltid=AfmBOor8vn1bd9Lg8Tv66oQ5LZ9yeOFQjbyTSuQsZNepHFH0gzjgiqL-]
- 86. AI vs Automation: What's Best for Business Growth in 2025? [https://flexlab.io/ai-vs-automation-best-for-business-growth-2025/]
- 87. Applications of artificial intelligence in stem cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427078/]
- 88. Smarter stem cells: how AI is supercharging iPSC technology [https://link.springer.com/article/10.1007/s00441-025-03999-7]
- 89. Stem Cell Assay Market 2025 Rapid Growth with 17.55% ... [https://www.towardshealthcare.com/insights/stem-cell-assay-market]
- 90. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 91. Chromosomal quality control in hPSCs: A practical guide to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259632/]
- 92. Genetic Stability Testing Using NGS and MAM [https://www.genedata.com/resources/learn/details/blog/cho-cell-lines-characterization-with-ngs]
- 93. Study Shows Safer Methods for Stem Cell Culturing [https://www.labmanager.com/study-shows-safer-methods-for-stem-cell-culturing-12238]
- 94. Cell Painting High-Content Image Assay [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-structure/cell-painting-assay.html]
- 95. Development of a Multiplexed, High Content Imaging ... [https://www.sciencedirect.com/science/article/abs/pii/S0300483X25002252]
- 96. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 97. A Phase-Appropriate Approach For Assay Validation In ... [https://www.cellandgene.com/doc/a-phase-appropriate-approach-for-assay-validation-in-cell-gene-therapies-0001]
- 98. Design and Validate a GMP Cell Based Assay [https://www.marinbio.com/design-and-validate-a-gmp-cell-based-assay/]
- 99. Potency Assays for Cell and Gene Therapy [https://insights.forgebiologics.com/how-potency-assays-support-gene-therapy-success]
- 100. Deep learning-based predictive classification of functional ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03682-8]
- 101. Replacing Animal Testing with Stem Cell-Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 102. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 103. Overcoming Challenges with Animal Models in Research [https://cgt.global/overcoming-challenges-with-animal-models-in-research/]
- 104. The end of animals-only testing brings both opportunities and ... [https://hub.jhu.edu/2025/07/16/3-questions-organoids-animal-testing-alternatives-thomas-hartung/]
- 105. Development of a quantitative prediction algorithm for ... [https://www.nature.com/articles/s41467-021-24746-w]
- 106. Beyond animal models: how organoids could transform ... [https://www.nature.com/articles/d42473-025-00219-2]
- 107. Investigating the Secretome: Lessons About the Cells that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3282018/]
- 108. Can patient-derived in vitro models improve clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528567/]
- 109. Advancements and challenges in culturing patient-derived ... [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1663420/full]
- 110. Continuous imaging to evaluate growth and drug ... [https://www.sciencedirect.com/science/article/pii/S2949819825000068]
- 111. Predicting multipotency of human adult stem cells derived ... [https://www.nature.com/articles/s41598-022-25423-8]
- 112. Potency testing of cell and gene therapy products [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1190016/full]
- 113. FDA's New “Plausible Mechanism Pathway” and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 114. FDA unveils new regulatory roadmap for bespoke drug ... [https://www.biopharmadive.com/news/fda-plausible-mechanism-pathway-n-of-1-crispr/805235/]
- 115. Potency assays and biomarkers for cell-based advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288881/]