Functional Outcomes of Reprogramming Strategies: From In Vivo Rejuvenation to Targeted Transdifferentiation
This article provides a comprehensive analysis of the functional outcomes achieved by diverse cellular reprogramming strategies, tailored for researchers and drug development professionals.
Functional Outcomes of Reprogramming Strategies: From In Vivo Rejuvenation to Targeted Transdifferentiation
Abstract
This article provides a comprehensive analysis of the functional outcomes achieved by diverse cellular reprogramming strategies, tailored for researchers and drug development professionals. It explores the foundational principles of in vivo reprogramming and its potential for tissue regeneration and age reversal. The review details methodological advances in direct fibroblast reprogramming for specific cell types, such as cardiomyocytes and alveolar epithelial cells, and investigates the critical challenges of safety, efficiency, and controllability. Finally, it offers a comparative analysis of reprogramming outcomes across different model systems and delivery methods, synthesizing the current state of the field and its implications for future clinical translation.
Cellular Reprogramming Foundations: Mechanisms and Therapeutic Potential for Regeneration and Rejuvenation
The field of cellular reprogramming has revolutionized regenerative medicine by enabling the conversion of one cell type into another, bypassing developmental barriers. Two primary paradigms have emerged: induced pluripotency, which reverts somatic cells to a pluripotent state, and direct lineage conversion, which directly transforms somatic cells into other specific cell types without passing through pluripotency. These approaches offer complementary advantages for disease modeling, drug screening, and cell-based therapies, each with distinct functional outcomes that researchers must consider when designing experimental and therapeutic strategies.
Induced pluripotent stem cells (iPSCs) were first established in 2006 when Takahashi and Yamanaka demonstrated that somatic cells could be reprogrammed to a pluripotent state using defined factors [1]. Since this landmark discovery, the technology has rapidly advanced, with clinical applications now emerging. As of December 2024, regulatory approvals have been granted for 115 clinical trials testing 83 human pluripotent stem cell products, primarily targeting eye, central nervous system, and cancer conditions, with over 1,200 patients already treated with no generalizable safety concerns [2]. Meanwhile, direct reprogramming has developed as a powerful alternative, enabling more rapid generation of specific cell types with potentially lower tumorigenicity risks.
Induced Pluripotency: Mechanisms and Methodologies
Fundamental Principles and Transcription Factors
Induced pluripotency involves reprogramming differentiated somatic cells back to an embryonic-like pluripotent state, enabling them to differentiate into virtually any cell type. The original reprogramming factors—Oct4, Sox2, Klf4, and c-Myc (OSKM)—function through coordinated mechanisms to erase epigenetic memory and establish pluripotency [1]. During early reprogramming, c-Myc associates with histone acetyltransferase complexes to induce global histone acetylation, facilitating binding of exogenous Oct4 and Sox2 to target loci. The specific expression levels and ratios of Sox2 and Oct4 significantly impact reprogramming efficiency and iPSC colony quality, while Klf4 suppresses somatic cell genes while activating pluripotency networks [1].
Alternative factor combinations have also been identified, including Oct4, Sox2, Nanog, and Lin28 (OSNL), where Nanog functions as an essential pluripotency maintenance factor alongside Oct4 and Sox2, and Lin28 accelerates cell proliferation during early reprogramming phases [1]. Some studies have even combined six factors (OSKMNL) to achieve a 10-fold increase in reprogramming efficiency, particularly for fibroblasts from aged donors [1].
Reprogramming Delivery Methods
The method of delivering reprogramming factors significantly impacts efficiency, safety, and clinical applicability. Early methods used integrating retroviral and lentiviral vectors, raising concerns about insertional mutagenesis and residual transgene expression. Non-integrating methods have since been developed to enhance safety profiles:
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Mechanism | Efficiency | Advantages | Limitations | Best For |
|---|---|---|---|---|---|
| Sendai Virus (SeV) | Non-integrating RNA virus | High (~fold higher than episomal) [3] | Non-integrating, high efficiency, broad tropism | Viral clearance needed, potential immunogenicity | Clinical applications requiring high efficiency |
| Episomal Vectors | OriP/EBNA1 plasmids | Moderate [3] | Non-integrating, simple production | Lower efficiency, requires nucleofection | Research with stringent safety requirements |
| mRNA Transfection | Modified mRNA molecules | Moderate-High [4] | Non-integrating, controlled expression | Requires multiple transfections, potential immune response | Clinical-grade iPSC generation |
| Chemical Reprogramming | Small molecule cocktails | Improving [5] | Non-integrating, standardized production | Still optimizing efficiency across cell types | Future clinical applications |
Comparative studies evaluating these methods have found that while source material (fibroblasts, LCLs, PBMCs) does not significantly impact success rates, the Sendai virus method yields significantly higher reprogramming success rates compared to episomal methods [3]. This makes SeV particularly valuable for biobanking applications where long-term reliability and reproducibility are crucial.
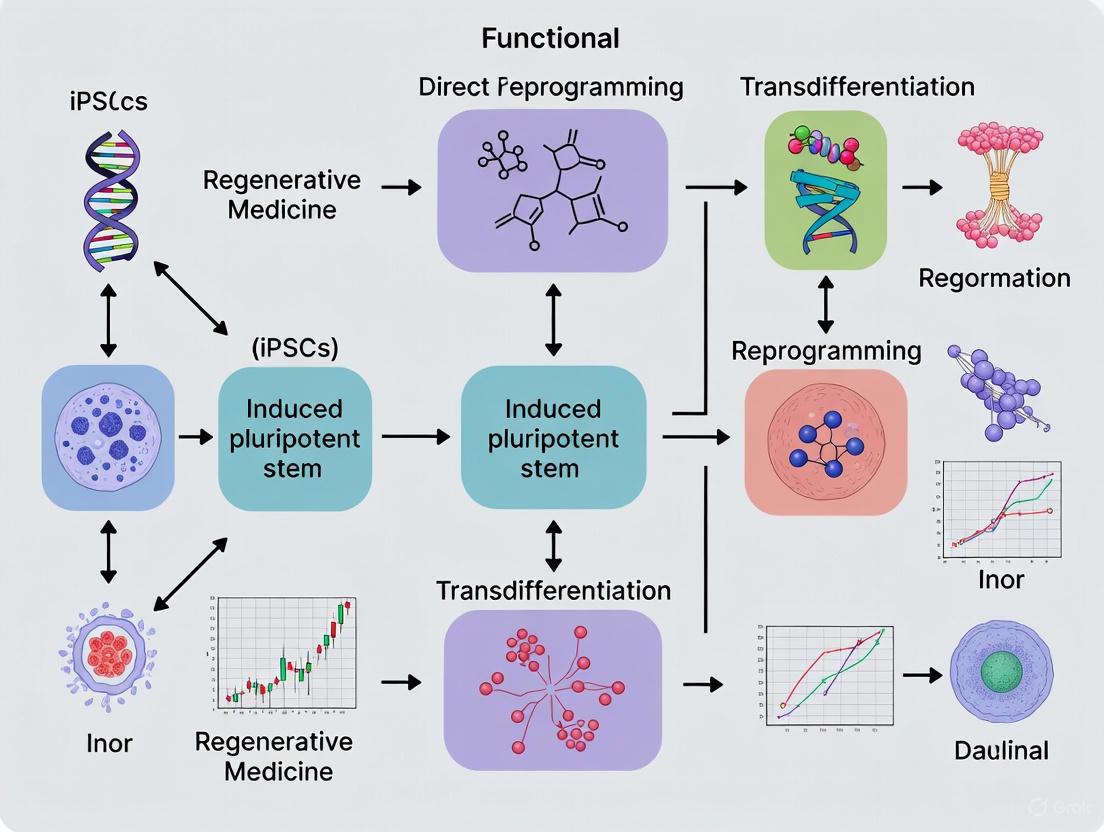
Figure 1: Induced Pluripotency Workflow: Somatic cells are reprogrammed using various methods to generate iPSCs, which can then be differentiated into target cell types.
Key Signaling Pathways in Pluripotency Induction
The molecular mechanisms governing pluripotency induction involve complex signaling networks. The canonical Wnt signaling pathway plays a particularly important role, as activation increases reprogramming efficiency by inducing chromatin remodeling and gene expression changes [6]. Endogenous Wnt activation, primarily mediated by WNT2B, is required for initiating direct reprogramming in some systems [6]. Other crucial pathways include BMP, TGF-β, and various growth factor signaling cascades that maintain pluripotency and self-renewal.
The process involves extensive epigenetic remodeling, where somatic cell identity genes are silenced through histone modification and DNA methylation, while pluripotency networks are activated. This epigenetic resetting creates cells with differentiation potential nearly equivalent to embryonic stem cells, enabling derivation of diverse cell types including neurons, cardiomyocytes, hepatocytes, and pancreatic β-cells [4].
Direct Lineage Conversion: Principles and Applications
Fundamental Concepts
Direct lineage conversion (also called transdifferentiation) enables direct reprogramming of somatic cells into other specific cell types without passing through a pluripotent intermediate. This approach offers several advantages, including faster conversion times (days rather than weeks), reduced tumorigenicity risk by avoiding pluripotent states, and preservation of epigenetic age that may be important for certain applications [7].
The fundamental principle involves identifying key transcription factors that function as "pioneer factors" to access closed chromatin regions and initiate transcriptional cascades that override existing cellular identity. Successful direct reprogramming typically requires combinations of factors that simultaneously suppress original cell identity while activating target cell genetic programs. This process often involves intermediate states that may represent plastic or partially reprogrammed cells before full conversion is achieved [7].
Representative Direct Reprogramming Systems
Several well-established direct reprogramming systems demonstrate the versatility and therapeutic potential of this approach:
Hair Cell-like Cells: A virus-free, inducible system using SIX1, ATOH1, POU4F3, and GFI1 (SAPG) transcription factors can reprogram human iPSCs into induced hair cell-like cells with 19-fold greater conversion efficiency compared to retroviral methods in half the time [8]. These cells express hair cell-specific markers, exhibit appropriate electrophysiological properties, and closely resemble developing fetal hair cells, offering significant potential for hearing loss treatments.
Alveolar Epithelial-like Cells: Mouse fibroblasts can be directly reprogrammed into induced pulmonary alveolar epithelial-like cells (iPULs) using Nkx2-1, Foxa1, Foxa2, and Gata6 transcription factors combined with 3D organoid culture [7]. The reprogramming efficiency significantly improved from 0.002% in 2D culture to approximately 2-3% of sorted cells in 3D culture conditions. These iPULs showed lamellar body-like structures and key properties of pulmonary alveolar epithelial cells, demonstrating potential for treating lung diseases.
Hepatic Progenitor Cells: Human umbilical vein endothelial cells (HUVECs) can be reprogrammed into human induced hepatic progenitor cells (hiHepPCs) using FOXA3, HNF1A, and HNF6 transcription factors [6]. Activation of canonical Wnt signaling increases reprogramming efficiency by rapidly inducing chromatin remodeling and gene expression changes, with endogenous Wnt activation mediated primarily by WNT2B.
Table 2: Direct Lineage Conversion Systems and Efficiencies
| Target Cell Type | Source Cell | Key Transcription Factors | Reprogramming Efficiency | Functional Assessment |
|---|---|---|---|---|
| Hair Cell-like Cells | Human iPSCs | SIX1, ATOH1, POU4F3, GFI1 | 19-fold improvement vs. retroviral method [8] | Electrophysiology, marker expression, single-cell RNA-seq |
| Alveolar Epithelial-like Cells (iPULs) | Mouse fibroblasts | Nkx2-1, Foxa1, Foxa2, Gata6 | ~2-3% of sorted cells (from 0.002% in 2D) [7] | Lamellar body structures, organoid formation, in vivo integration |
| Hepatic Progenitor Cells | HUVECs | FOXA3, HNF1A, HNF6 + Wnt activation | Increased efficiency with Wnt [6] | Hepatic marker expression, functional analysis |
| Neurons | Fibroblasts | Various combinations (e.g., Ascl1, Brn2, Myt1l) | Varies by protocol | Electrophysiology, synaptic activity |
Figure 2: Direct Lineage Conversion Pathway: Somatic cells are directly converted to target cell types using specific transcription factor combinations, bypassing the pluripotent state entirely.
Comparative Functional Outcomes
Efficiency and Kinetics
The two reprogramming paradigms show marked differences in efficiency and timing. Induced pluripotency typically requires 3-4 weeks to generate established iPSC lines, followed by additional time for differentiation into specific cell types. In contrast, direct lineage conversion can produce functional target cells within 1-2 weeks [8] [7]. However, direct conversion generally yields lower percentages of fully reprogrammed cells compared to the robust efficiency of iPSC differentiation protocols once stable lines are established.
Direct reprogramming efficiency can be significantly enhanced through various strategies. Three-dimensional culture systems have shown remarkable improvements, increasing efficiency from 0.002% in 2D to 2-3% in 3D for alveolar epithelial-like cells [7]. Similarly, signaling pathway activation through Wnt stimulation boosted hepatic progenitor cell reprogramming efficiency [6]. For hair cell reprogramming, switching from retroviral methods to a virus-free inducible system increased efficiency by 19-fold while reducing the required time [8].
Safety Profiles and Genomic Integrity
Safety considerations differ substantially between the approaches. iPSC technologies carry inherent risks of teratoma formation if undifferentiated cells remain after differentiation, necessitating rigorous purification protocols. Additionally, the extensive proliferation capacity of iPSCs increases opportunities for acquiring genetic and epigenetic abnormalities during culture [1]. However, current non-integrating reprogramming methods have significantly improved the safety profile of iPSCs, with clinical trials demonstrating no generalizable safety concerns across more than 1,200 treated patients [2].
Direct lineage conversion minimizes cancer risk by avoiding pluripotent intermediates, though the potential for incomplete reprogramming or aberrant cell states remains. The use of integrating vectors in some direct reprogramming protocols raises similar insertional mutagenesis concerns as early iPSC methods, prompting development of non-integrating approaches including mRNA, protein transduction, and small molecules [8] [5].
Functional Maturation and Therapeutic Potential
Both strategies can generate cells with functional characteristics of their native counterparts, though maturation level varies. iPSC-derived cells often exhibit fetal-like properties, which may be advantageous for certain applications but limiting for others. Directly reprogrammed cells may maintain some epigenetic memory of their original identity, potentially influencing functionality [7].
Therapeutic applications are advancing for both approaches. iPSC-derived products have entered clinical trials for eye diseases, neurodegenerative disorders, and cardiovascular conditions [2] [9]. Directly reprogrammed cells show promise in disease modeling and may advance to clinical applications, particularly for tissues like lung alveoli and inner ear hair cells where access is challenging [8] [7].
Experimental Protocols and Methodologies
Detailed iPSC Generation Protocol Using Sendai Virus
The following protocol has been optimized for high-efficiency reprogramming of fibroblasts and PBMCs using the CytoTune Sendai Reprogramming Kit [3]:
Day 0: Seeding Source Cells
- Plate 5×10^4 fibroblasts or 1×10^5 PBMCs per well in a 6-well plate with appropriate medium
- Incubate at 37°C, 5% CO₂ for 24 hours
Day 1: Viral Transduction
- Replace medium with fresh medium containing SeV vectors expressing hOCT4, hSOX2, hKLF4, hC-MYC, and EmGFP
- Incubate for 24 hours
Day 2: Medium Refresh
- Replace with fresh medium without vectors
- Culture for approximately 6 additional days with medium exchange every other day
- Monitor transduction efficiency via GFP-positive cells
Day 7-8: Replating
- Harvest transduced cells and replate onto feeder layers or Matrigel-coated plates
- Culture in essential 8 medium or similar defined medium
Day 21-28: Colony Picking
- Manually pick at least 24 colonies exhibiting typical iPSC morphology
- Expand individual clones in 12-well plates
Quality Control:
- Validate pluripotency markers (Nanog, Oct4, SSEA-4, TRA-1-60) via immunostaining
- Perform karyotyping analysis
- Test for mycoplasma contamination
- Confirm Sendai virus clearance by PCR after passage 10-12
Direct Reprogramming to Alveolar Epithelial-like Cells
This protocol details the direct conversion of mouse fibroblasts to iPULs using 4 transcription factors and 3D culture [7]:
Initial Transduction:
- Isolate mouse embryonic fibroblasts (MEFs) or tail-tip fibroblasts (TTFs)
- Transduce with retroviral vectors carrying Nkx2-1, Foxa1, Foxa2, and Gata6
- Culture in 2D for 7 days in DMEM with 10% FBS
3D Organoid Culture:
- Transfer transduced cells to low-attachment plates in serum-free medium
- Supplement with Wnt pathway activators (CHIR99021), growth factors (KGF, FGF10, FGF7), and BMP inhibitors (Noggin)
- Culture for 7-14 days, monitoring organoid formation
Cell Sorting and Purification:
- Dissociate organoids to single cells
- Sort for Sftpc-GFP⁺, Thy1.2⁻, EpCAM⁺ population using FACS
- Replate sorted cells in 3D Matrigel culture with alveolar epithelial cell medium
Functional Validation:
- Assess lamellar body formation via electron microscopy
- Measure surfactant protein expression (SP-A, SP-B, SP-C, SP-D) by qPCR and immunostaining
- Evaluate transcriptome similarity to primary AT2 cells by RNA-seq
- Test in vivo integration capability using bleomycin-induced lung injury model
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Reprogramming Studies
| Reagent Category | Specific Examples | Function | Applications |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc (OSKM); SIX1, ATOH1, POU4F3, GFI1 (SAPG); Nkx2-1, Foxa1, Foxa2, Gata6 | Master regulators of cell identity and fate | Both iPSC and direct reprogramming |
| Delivery Systems | Sendai virus vectors, episomal plasmids, mRNA transfection kits | Introduce reprogramming factors into cells | Method-dependent efficiency optimization |
| Signaling Modulators | CHIR99021 (Wnt activator), Y-27632 (ROCK inhibitor), A83-01 (TGF-β inhibitor) | Enhance reprogramming efficiency and cell survival | Both paradigms; culture condition optimization |
| Culture Matrices | Matrigel, laminin-521, vitronectin | Provide structural support and signaling cues | Maintenance of pluripotency or differentiated states |
| Characterization Tools | Flow cytometry antibodies (SSEA-4, TRA-1-60), single-cell RNA-seq kits | Assess reprogramming success and purity | Quality control and mechanistic studies |
The choice between induced pluripotency and direct lineage conversion depends on specific research or therapeutic objectives. Induced pluripotency offers unparalleled versatility for generating multiple cell types from a single source and enables extensive expansion for large-scale applications. The established safety profile of iPSCs in clinical trials supports their use for therapeutic development [2]. However, the extended timeline and potential tumorigenicity risks remain important considerations.
Direct lineage conversion provides faster generation of specific cell types with potentially superior safety profiles by avoiding pluripotent intermediates. The preservation of epigenetic age in directly converted cells may better model age-related diseases. However, lower efficiencies and limited expansion capacity present challenges for some applications.
Future directions will likely focus on hybrid approaches that combine strengths of both paradigms, enhanced safety through non-integrating methods, and improved maturation protocols. The continued development of chemical reprogramming using entirely small-molecule approaches promises to further transform the field by offering completely non-genetic methods for cell fate manipulation [5]. As both technologies evolve, they will increasingly enable personalized disease modeling, drug screening, and regenerative therapies across diverse medical specialties.
In vivo reprogramming represents a revolutionary approach in regenerative medicine that involves directly changing cell identity within a living organism. This strategy builds upon the foundational discovery by Shinya Yamanaka that forced expression of four transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as OSKM)—can reprogram specialized adult cells into induced pluripotent stem cells (iPSCs) [10]. While initial applications focused on generating patient-specific stem cells in laboratory settings, recent advances have demonstrated that transient, controlled expression of these same factors directly in living organisms can promote tissue regeneration and reverse age-related physiological decline without requiring cell transplantation [11] [12].
The fundamental premise of in vivo reprogramming hinges on the concept of epigenetic remodeling—the ability to reset age-associated changes in gene regulation and chromatin organization [11] [13]. When applied in a partial or cyclical manner, OSKM expression appears to rejuvenate cells by restoring youthful epigenetic patterns and transcriptional profiles while avoiding complete dedifferentiation to a pluripotent state [14] [13]. This approach has demonstrated remarkable potential across diverse tissue types and disease models, though significant challenges remain in achieving precise spatiotemporal control to maximize therapeutic benefits while minimizing risks such as teratoma formation [11] [15]. The growing body of evidence supporting OSKM-mediated rejuvenation has generated substantial interest in both academic and biotechnology sectors, positioning in vivo reprogramming as a promising frontier for addressing age-related diseases and degenerative conditions [16] [14].
Mechanisms of Action: From Epigenetic Remodeling to Functional Restoration
Key Molecular Mechanisms of OSKM-Mediated Reprogramming
The OSKM factors function as powerful regulators of cellular identity by orchestrating widespread changes in gene expression patterns and chromatin architecture. At the molecular level, OCT4 and SOX2 act as pioneer factors that bind to closed chromatin regions and initiate the opening of pluripotency-associated loci, while KLF4 and c-MYC further facilitate epigenetic remodeling and cell cycle re-entry [10] [17]. During in vivo reprogramming, these factors collaboratively target thousands of genomic sites, with significant conservation of target genes between human and mouse systems despite differences in specific binding locations [17]. This initial binding triggers a cascade of epigenetic changes, including modifications to histone marks such as H3K9me3 and DNA methylation patterns, which progressively erase age-associated epigenetic signatures and restore a more youthful regulatory landscape [11] [13].
The mechanistic parallels between injury-induced dedifferentiation and OSKM-mediated reprogramming provide valuable insights into how partial reprogramming promotes regeneration. In tissues with innate regenerative capacity, such as the liver and intestine, OSKM expression appears to amplify endogenous plasticity programs rather than introducing regeneration de novo [11]. Conversely, in tissues with limited regenerative potential like the heart and retina, OSKM reprogramming functions as an exogenous driver that overcomes epigenetic barriers to induce repair [11] [18]. The process generates transient regenerative progenitors that can subsequently redifferentiate into functional tissue-specific cells, thereby restoring organ function without forming teratomas when properly controlled [11].
Signaling Pathways and Molecular Trajectories
The following diagram illustrates the core molecular pathway through which OSKM factors mediate cellular reprogramming and rejuvenation in vivo:
Figure 1: OSKM-Mediated Reprogramming Pathway. This diagram illustrates the molecular cascade initiated by OSKM factors, from epigenetic remodeling to functional tissue outcomes.
Comparative Performance Analysis Across Tissue Types
Regenerative Outcomes in Various Organs
In vivo reprogramming with OSKM factors has demonstrated remarkable potential for promoting tissue regeneration across diverse organ systems. The therapeutic effects and underlying mechanisms vary significantly depending on the intrinsic regenerative capacity of each tissue type. The following table summarizes key experimental findings from recent studies investigating OSKM-mediated regeneration in different tissues:
Table 1: Tissue-Specific Outcomes of OSKM-Mediated In Vivo Reprogramming
| Tissue/Organ | Experimental Model | Key Findings | Functional Outcomes | Proposed Mechanisms |
|---|---|---|---|---|
| Heart | Mouse myocardial infarction model [18] | Reprogramming of cardiac fibroblasts to cardiomyocytes | Improved ventricular contractility; Reduced fibrosis | Direct lineage conversion; Modulation of fibroblast heterogeneity |
| Skeletal Muscle | Aged mice [11] | Enhanced muscle regeneration after injury | Improved muscle function; Reduced fibrosis | Epigenetic remodeling; Enhanced satellite cell activity |
| Retina | Mouse glaucoma model [11] | Restoration of visual function | Improved visual responses; Neuronal regeneration | Dedifferentiation and redifferentiation of retinal cells |
| Liver | Mouse partial hepatectomy [11] | Accelerated tissue regeneration | Improved liver function; Enhanced regenerative capacity | Amplification of endogenous dedifferentiation programs |
| Skin | Mouse wound healing model [11] [13] | Reduced fibrotic responses; Improved repair | Accelerated wound closure; Reduced scarring | Inhibition of fibroblast-to-myofibroblast transition |
| Pancreas | Aged mice [11] | Improved β-cell function | Enhanced glucose regulation; Tissue rejuvenation | Epigenetic reset of age-related changes |
| Brain | Aged mouse model [11] | Reversal of age-related transcriptional changes | Cognitive improvements; Neuronal function restoration | Epigenetic remodeling; Reduced inflammation |
The data reveals two distinct paradigms for OSKM-mediated regeneration based on the innate regenerative capacity of the target tissue. In organs with limited regenerative potential, such as the heart, retina, and skeletal muscle, OSKM reprogramming functions as an exogenous driver that actively induces repair by overcoming epigenetic barriers [11] [18]. Conversely, in organs with inherent regenerative capacity like the liver and intestine, OSKM expression appears to amplify endogenous plasticity programs rather than introducing regeneration de novo [11]. This distinction has important implications for therapeutic development, as optimal reprogramming protocols may need to be tailored to specific tissue contexts.
Rejuvenation Effects in Aging Models
Perhaps the most striking application of in vivo reprogramming has been in the context of age reversal. Landmark studies using progeria mouse models have demonstrated that cyclic induction of OSKM factors can significantly extend lifespan and ameliorate multiple aging-related pathological features [11] [13]. In one pivotal study, progeria mice subjected to a cyclic OSKM induction regimen (2 days ON, 5 days OFF) exhibited a 33% extension in median lifespan alongside improvements in cardiovascular function, skin integrity, and spinal curvature [11] [13]. Subsequent research in naturally aged wild-type mice has confirmed that similar approaches can restore youthful DNA methylation patterns, transcriptomic profiles, and metabolic function across multiple tissues including the spleen, liver, skin, kidney, lung, and skeletal muscle [11] [14].
The rejuvenating effects of partial reprogramming appear to operate through both cell-autonomous and systemic mechanisms. At the cellular level, OSKM exposure reverses age-associated epigenetic marks, enhances mitochondrial function, reduces DNA damage accumulation, and ameliorates cellular senescence [14] [13]. These changes collectively contribute to improved tissue homeostasis and regenerative capacity in aged animals. Importantly, the rejuvenation observed following partial reprogramming is distinct from complete dedifferentiation, as treated cells maintain their tissue identity while resetting age-related molecular signatures [13]. This distinction is crucial for therapeutic applications, as it suggests that age reversal can be achieved without compromising tissue organization or function.
Experimental Protocols and Methodological Approaches
Key Experimental Systems for In Vivo Reprogramming
Research on OSKM-mediated in vivo reprogramming has employed several sophisticated genetic systems to achieve precise temporal control over factor expression. The most widely utilized approach involves transgenic mouse models with doxycycline (Dox)-inducible OSKM cassettes, enabling researchers to initiate reprogramming through simple administration of Dox in drinking water or food [11]. The most common models include:
- 4Fj and 4Fk mice: Feature OSKM or OKSM cassettes inserted at the Col1a1 locus using Tet-On systems [11]
- 4F-A (4FsA) and 4F-B (4FsB) models: Contain OSKM cassettes integrated at the Neto2 and Pparg loci, respectively [11]
- Progeria mouse models: Express mutant lamin A to mimic human Hutchinson-Gilford progeria syndrome (HGPS), allowing assessment of rejuvenation effects [11] [10]
These systems demonstrate striking tissue specificity in OSKM activation, with robust induction typically observed in the intestine, liver, and skin, and comparatively lower activation in the brain, heart, and skeletal muscle [11]. This variability reflects inherent differences in chromatin accessibility and promoter activity across tissues, highlighting the importance of considering tissue-specific responses when designing reprogramming protocols.
Beyond transgenic models, recent studies have explored viral delivery methods for OSKM factors, particularly adeno-associated viruses (AAVs) with tissue-specific tropism [18] [13]. For example, AAV9 vectors have been used to deliver OSK factors (excluding c-MYC to reduce tumorigenic risk) to multiple tissues in wild-type mice, resulting in significant extension of remaining lifespan in aged animals [13]. This gene therapy approach offers potential translational advantages over transgenic models, as it could theoretically be applied to human patients without requiring germline genetic modifications.
Induction Protocols and Regimen Optimization
The specific parameters of OSKM induction critically determine the balance between therapeutic efficacy and safety concerns. Research has identified several key variables that influence reprogramming outcomes:
- Induction duration: Short-term induction (typically 1-7 days) favors partial reprogramming and rejuvenation, while prolonged continuous induction (weeks) frequently leads to teratoma formation [11]
- Cyclical regimens: Protocols such as "2 days ON, 5 days OFF" or "1 day ON, 6 days OFF" have demonstrated efficacy in promoting rejuvenation while minimizing tumorigenic risks [11] [13]
- Factor composition: Some studies omit c-MYC from the cocktail (using only OSK) to reduce oncogenic potential while retaining significant rejuvenation capacity [13]
- Tissue-specific optimization: Delivery methods and induction parameters may require customization based on the target tissue's accessibility, cellular composition, and intrinsic plasticity [18]
The timing of intervention also appears to influence reprogramming efficiency, with aged cells generally exhibiting reduced transdifferentiation capacity compared to their younger counterparts [18]. This age-dependent decline in reprogramming efficiency presents a particular challenge for clinical translation, as the patients most likely to benefit from rejuvenation therapies are typically older. Overcoming this limitation may require complementary approaches such as metabolic interventions or modulation of age-related signaling pathways [18].
Safety Considerations and Risk Mitigation Strategies
Primary Safety Concerns in OSKM Reprogramming
The tremendous therapeutic potential of in vivo reprogramming is balanced against significant safety considerations that must be addressed before clinical translation. The most serious risks associated with OSKM expression include:
- Teratoma formation: Continuous induction of OSKM over several weeks reliably generates teratomas in multiple organs, while even transient induction (7 days) can initiate dysplastic changes and tumor formation in susceptible tissues like the pancreas, liver, and kidney [11] [15]
- Erosion of cellular identity: Uncontrolled reprogramming can lead to loss of tissue-specific functions through dedifferentiation [11] [12]
- Organ dysfunction: Studies have reported instances of liver failure and intestinal dysfunction following OSKM induction, potentially resulting from disrupted tissue homeostasis [11] [14]
- Cancer promotion: In certain contexts, OSKM expression can accelerate cancer development by driving dedifferentiation of already transformed cells [11]
Interestingly, the relationship between reprogramming and cancer is complex and context-dependent. While OSKM can promote tumorigenesis in some settings, it has also been shown to selectively eradicate leukemia cells bearing the MLL-AF9 fusion gene while sparing normal hematopoietic cells [11]. This paradoxical effect underscores the importance of understanding the specific molecular and cellular contexts in which reprogramming factors operate.
Approaches to Enhance Safety Profiles
Research has identified several promising strategies to mitigate the risks associated with in vivo reprogramming:
Table 2: Safety Challenges and Mitigation Strategies in OSKM Reprogramming
| Safety Challenge | Risk Mitigation Approaches | Experimental Support |
|---|---|---|
| Teratoma formation | Cyclical induction; Factor dosage optimization; Exclusion of c-MYC | [11] [13] |
| Loss of cell identity | Partial reprogramming protocols; Limited induction duration | [11] [12] |
| Inadequate tissue targeting | Tissue-specific promoters; Targeted delivery systems (AAVs, nanoparticles) | [18] [13] |
| Off-target effects | Transient mRNA delivery; Small molecule alternatives | [16] [13] |
| Age-related efficiency reduction | Metabolic interventions; Autophagy enhancement; Mitochondrial optimization | [18] |
The following diagram illustrates the key safety considerations and corresponding mitigation strategies in OSKM-mediated in vivo reprogramming:
Figure 2: Safety Considerations and Mitigation Strategies in OSKM Reprogramming. This diagram outlines major risks associated with in vivo OSKM expression and corresponding approaches to enhance safety profiles.
Research Reagent Solutions and Technical Tools
The investigation of OSKM-mediated reprogramming relies on specialized reagents and technical tools that enable precise control and monitoring of the reprogramming process. The following table outlines key research solutions essential for conducting in vivo reprogramming studies:
Table 3: Essential Research Reagents for In Vivo Reprogramming Studies
| Reagent/Tool | Function/Application | Examples/Specifics | Experimental Utility |
|---|---|---|---|
| Dox-inducible OSKM systems | Controlled factor expression | 4Fj, 4Fk, 4F-A, 4F-B mouse models [11] | Enables temporal regulation via doxycycline administration |
| Lineage tracing models | Fate mapping of reprogrammed cells | Tcf21-iCre, Fsp1-Cre, Postn-lineage tracing [18] | Tracks cellular origins and conversion outcomes |
| AAV delivery vectors | In vivo factor delivery | AAV9-OSK constructs [13] | Facilitates translational gene therapy approaches |
| Epigenetic clocks | Assessment of biological age | DNA methylation patterns; Multi-omics profiles [14] [13] | Quantifies rejuvenation effects at molecular level |
| Pluripotency markers | Monitoring reprogramming status | SSEA-4, TRA-1-60, NANOG, alkaline phosphatase [16] | Identifies intermediate reprogramming states |
| Senescence assays | Detection of age-related changes | β-galactosidase activity; p16/p21 expression [10] | Evaluates rejuvenation efficacy |
| AI-enhanced factors | Improved reprogramming efficiency | RetroSOX, RetroKLF variants [16] | Increases reprogramming efficiency (>50-fold) |
Recent advances in reagent development have substantially enhanced the efficiency and specificity of in vivo reprogramming approaches. Notably, AI-guided protein engineering has yielded novel factor variants such as RetroSOX and RetroKLF that demonstrate dramatically improved reprogramming efficiency compared to wild-type factors [16]. In vitro testing of these engineered variants has shown over 50-fold higher expression of pluripotency markers and enhanced DNA damage repair capabilities, suggesting superior rejuvenation potential [16]. The availability of such optimized tools will accelerate both basic research and therapeutic development in the reprogramming field.
In vivo reprogramming with OSKM factors represents a paradigm-shifting approach with demonstrated potential for promoting tissue regeneration and reversing age-related physiological decline. The accumulating evidence from diverse animal models indicates that partial, cyclical reprogramming can rejuvenate cellular function across multiple tissues without inducing teratoma formation or complete loss of cellular identity [11] [13]. The mechanistic insights gleaned from these studies highlight the crucial role of epigenetic remodeling in restoring regenerative capacity and reversing age-associated molecular signatures.
Despite these promising advances, significant challenges remain in translating OSKM-based therapies to clinical applications. The dualistic nature of reprogramming—balancing therapeutic rejuvenation against risks of tumorigenesis and loss of tissue function—necessitates exquisite control over factor expression, delivery, and duration [11] [15] [14]. Future research directions will likely focus on developing more precise spatiotemporal control systems, optimizing factor combinations and delivery methods for specific tissues, and identifying small molecule alternatives that can mimic or enhance the rejuvenating effects of OSKM factors [16] [13]. As these technical hurdles are addressed, in vivo reprogramming may ultimately transform approaches to treating degenerative diseases and age-related functional decline.
Aging is characterized by a progressive decline in physiological function and an increased susceptibility to chronic diseases, driven by conserved biological processes often termed the "hallmarks of aging" [19]. Among the most promising strategies for intervening in the aging process is partial cellular reprogramming. This technique involves the transient expression of reprogramming factors, such as the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC, collectively OSKM), to reverse age-related epigenetic and transcriptional changes without fully erasing cellular identity [13] [10]. Unlike full reprogramming to induced pluripotent stem cells (iPSCs)—which carries a high risk of teratoma formation—partial reprogramming aims to rejuvenate aged cells and tissues while maintaining their functional specialization and avoiding tumorigenesis [13] [10].
This review objectively compares the functional outcomes of different reprogramming strategies, with a focus on partial reprogramming. We summarize quantitative data from key preclinical studies, provide detailed experimental protocols, and illustrate core signaling pathways. By comparing partial reprogramming against alternative strategies like full reprogramming and transdifferentiation, we aim to provide researchers and drug development professionals with a clear framework for evaluating the therapeutic potential and safety profile of each approach.
Comparative Analysis of Reprogramming Strategies
The field of cellular rejuvenation has developed several distinct strategies to reverse aging hallmarks. Table 1 provides a systematic comparison of three core approaches: partial reprogramming, full reprogramming, and transdifferentiation, highlighting their differential impacts on aging hallmarks and tumorigenic risk.
Table 1: Functional Outcome Comparison of Reprogramming Strategies for Aging Amelioration
| Reprogramming Strategy | Impact on Aging Hallmarks | Effect on Cellular Identity | Tumorigenesis Risk | Key Functional Outcomes in Model Systems |
|---|---|---|---|---|
| Partial Reprogramming | Reverses epigenetic aging clocks, reduces cellular senescence, restores mitochondrial function [13] [14] [20]. | Maintains original cell identity with restored function [13] [10]. | Lower risk; no teratomas in mice with cyclic induction, but requires careful dosing [13] [10]. | Lifespan extension (up to 109% in old wild-type mice), improved wound healing, muscle regeneration, restored visual function in mice [13] [20]. |
| Full Reprogramming (iPSC) | Resets epigenetic age and telomere length to an embryonic state [10] [14]. | Erases somatic identity, creates pluripotent stem cells [10]. | High risk of teratoma formation post-transplantation [10]. | Used for disease modeling; not suitable for direct in vivo rejuvenation due to tumor risk [10]. |
| Transdifferentiation | Impact on hallmarks is variable and less studied; may retain some age-related signatures [14]. | Converts one somatic cell type directly into another [14]. | Context-dependent; risk if pathway involves proliferative intermediates. | Retains senescent phenotype in aged fibroblasts directly converted to neural stem cells [14]. |
Detailed Experimental Protocols for Key Studies
To facilitate replication and further development, this section details the methodologies from seminal studies demonstrating the efficacy and safety of partial reprogramming.
In Vivo Partial Reprogramming in Progeria and Wild-Type Mice
Objective: To assess the potential of cyclic, short-term OSKM expression to reverse aging phenotypes in vivo and extend healthspan and lifespan without inducing tumors [13].
Key Reagents & Models:
- Genetic Model: LAP-MerCreMer transgenic mice (for whole-body, Dox-inducible OSKM expression) or wild-type mice injected with AAV9-OSK vectors.
- Induction Agent: Doxycycline (Dox) in drinking water or chow.
- Key Reagents: AAV9 vectors packaging OSK (OCT4, SOX2, KLF4) and rtTA.
Experimental Workflow:
- Animal Grouping: Progeroid (e.g., LAKI) and wild-type mice are divided into treatment (Dox-induced) and control groups.
- Cyclic Induction: Administration of Dox in cycles (e.g., 2 days on, 5 days off) for multiple cycles (e.g., 35 cycles in progeria models) or long-term (7-10 months) in wild-type mice.
- In Vivo Monitoring: Regular assessment of healthspan parameters (frailty index, skin regeneration, wound healing) and observation for teratoma formation.
- Endpoint Analysis:
- Lifespan: Survival analysis compared to controls.
- Molecular Phenotyping: Multi-omics analysis (transcriptomics, epigenomics, lipidomics) of tissues like liver, skin, and spleen to assess rejuvenation.
- Histopathology: Comprehensive analysis of major organs for teratomas or other abnormalities.
Outcome Summary: This protocol achieved a 33% median lifespan extension in progeroid mice and a 109% remaining lifespan extension in old wild-type mice, with no reported teratoma formation [13].
Partial Chemical Reprogramming of Fibroblasts
Objective: To rejuvenate aged somatic cells using non-integrating, small-molecule cocktails, thereby avoiding genetic manipulation [13].
Key Reagents:
- Cell Source: Mouse or human primary fibroblasts from young and old donors.
- Chemical Cocktail: The "7c" cocktail, consisting of small molecules that modulate key signaling pathways (e.g., TGF-β, GSK3).
- Assay Kits: For measuring mitochondrial function (e.g., ROS, OXPHOS), RNA/DNA sequencing for epigenetic clocks, and senescence-associated beta-galactosidase (SA-β-Gal).
Experimental Workflow:
- Cell Culture: Primary fibroblasts are maintained in standard culture conditions.
- Chemical Treatment: Cells are treated with the 7c cocktail for a defined period (e.g., 10-14 days), with medium changes every few days.
- Assessment of Rejuvenation:
- Cellular Markers: SA-β-Gal staining to quantify senescent cell burden.
- Functional Assays: Measurement of mitochondrial ROS and oxidative phosphorylation (OXPHOS) capacity.
- Molecular Profiling: RNA-seq and DNA methylation analysis (e.g., using epigenetic clocks) to demonstrate a shift to a younger transcriptional and epigenetic profile.
Outcome Summary: Treatment with the 7c cocktail reversed epigenetic and transcriptomic aging clocks and ameliorated age-associated metabolic profiles in human fibroblasts, notably without inducing rapid cell proliferation [13].
Visualization of Core Concepts and Pathways
The following diagrams, generated using DOT language, illustrate the logical relationships and signaling pathways central to partial reprogramming and its contrast with tumorigenic processes.
Partial vs. Full Reprogramming Workflow
Senescence and Reprogramming Signaling Network
The Scientist's Toolkit: Essential Research Reagents
Successful investigation into partial reprogramming relies on a suite of specialized reagents and tools. Table 2 lists key solutions and their applications for researchers in this field.
Table 2: Key Research Reagent Solutions for Partial Reprogramming Studies
| Research Reagent / Tool | Function in Partial Reprogramming Research | Example Application |
|---|---|---|
| Doxycycline (Dox)-Inducible OSKM Systems | Enables precise, transient expression of Yamanaka factors in vitro and in vivo [13]. | Cyclic induction of OSKM in transgenic mouse models (e.g., 2 days on/5 days off) to achieve rejuvenation without teratomas [13]. |
| AAV9 Vectors | Efficient in vivo gene delivery system with broad tissue tropism for OSK(M) factors [13]. | Delivery of OSK factors to aged wild-type mice to extend lifespan and improve healthspan, excluding c-Myc to reduce oncogenic risk [13]. |
| Chemical Reprogramming Cocktails (e.g., 7c) | Non-integrating, small-molecule approach to induce rejuvenation, avoiding genetic manipulation [13]. | Reversal of epigenetic age and restoration of mitochondrial function in aged human fibroblasts in culture [13]. |
| DNA Methylation Clocks | Biomarker tool to quantify biological age pre- and post-reprogramming intervention [13] [21]. | Validation of epigenetic rejuvenation in treated cells (e.g., fibroblasts) and tissues (e.g., liver, spleen) from animal models [13]. |
| Senescence Assays (SA-β-Gal, SASP) | Measures a key aging hallmark—cellular senescence—to assess intervention efficacy [21] [20]. | Quantifying reduction in senescent cell burden following partial reprogramming treatment in tissue sections or cell culture [20]. |
Partial reprogramming represents a frontier in therapeutic rejuvenation, demonstrating a remarkable capacity to ameliorate core aging hallmarks—particularly epigenetic alterations and cellular senescence—while presenting a manageably lower tumorigenic risk compared to full reprogramming [13] [21]. The functional outcomes, including extended healthspan and lifespan in mouse models, underscore its transformative potential [13].
However, the path to clinical translation requires overcoming significant hurdles. Key challenges include optimizing delivery systems for precise spatiotemporal control in humans, fine-tuning dosing to maximize efficacy while eliminating any residual risk of teratoma formation or loss of cellular identity, and developing robust, human-validated biomarkers to track biological age in clinical trials [13] [19] [10]. Future research must prioritize the development of safer, non-genetic delivery methods (e.g., refined chemical cocktails or protein-based approaches) and rigorously assess the long-term functional benefits and safety of these interventions in more complex mammalian models. For researchers and drug developers, the strategic selection of reprogramming factors, delivery vectors, and dosing protocols will be paramount in harnessing the promise of partial reprogramming to transform the treatment of aging and age-related diseases.
Direct reprogramming, or transdifferentiation, represents a paradigm shift in regenerative medicine by enabling the direct conversion of one differentiated somatic cell type into another, bypassing an intermediary pluripotent stem cell state [22] [23]. This groundbreaking approach offers a promising therapeutic strategy for tissue repair and regeneration. A particularly compelling application is the reprogramming of fibroblasts—the primary drivers of pathological fibrosis—into functional tissue-specific cells [22].
Fibrosis, characterized by excessive extracellular matrix (ECM) deposition and tissue scarring, contributes significantly to organ dysfunction across numerous chronic diseases [22]. Activated fibroblasts and myofibroblasts are central players in this process, secreting massive amounts of collagen and other ECM components that disrupt normal tissue architecture and function [22] [23]. Direct reprogramming strategically targets these pathogenic cells, simultaneously reducing the fibrotic cell population while regenerating lost or damaged functional cells [22]. This dual-action mechanism addresses both tissue degeneration and the pathological microenvironment that perpetuates disease progression.
This review comprehensively compares the performance of diverse direct reprogramming strategies across multiple organ systems, evaluating their efficacy in cell fate conversion and anti-fibrotic outcomes within the context of functional recovery. We synthesize experimental data from recent studies to provide researchers and drug development professionals with a rigorous assessment of this rapidly advancing field.
Comparative Analysis of Direct Reprogramming Strategies
Table 1: Cardiac Fibroblast to Induced Cardiomyocyte (iCM) Reprogramming Strategies
| Reprogramming Factor Combination | Delivery Method | Model System | Reprogramming Efficiency | Functional Outcomes | Anti-Fibrotic Effects |
|---|---|---|---|---|---|
| GMT (GATA4, MEF2C, TBX5) [22] | Retroviral | In vivo (Mouse MI) | Not specified | Improved cardiac function; iCMs exhibited action potentials and spontaneous contraction | Reduced scar area |
| GMTH (GMT + HAND2) [22] | Retroviral | In vivo (Mouse MI) | Higher than GMT | Generation of more iCMs; improved cardiac function | Accelerated reduction in fibrotic area |
| MYΔ3A + ASCL1 [22] | Not specified | In vivo (Mouse acute & chronic MI) | Not specified | Improved cardiac function | Alleviated cardiac fibrosis |
| miRNA combo (miR-1, miR-133, miR-208, miR-499) [22] | Lentiviral; Nanoparticle (FNLM) | In vivo (Mouse MI) | Not specified | iCMs with calcium transients and beating capacity; Enhanced conversion with targeted delivery | Significant reduction in cardiac fibrosis |
| Small Molecule Cocktail (CRFVPTM) [22] | Not specified | In vivo | Not specified | Generated iCMs with action potentials | Significantly reduced scar area |
| Small Molecules (SB431542 + Baricitinib) + MT [22] | Not specified | In vitro | Not specified | Selective reprogramming of CFs over other fibroblasts | Not specified |
Table 2: Reprogramming Strategies Across Other Tissues
| Target Cell | Reprogramming Factors | Starting Cell Type | Model System | Key Functional Markers | Therapeutic Outcomes |
|---|---|---|---|---|---|
| Induced Keratinocyte-Like Cells (iKCs) [24] | BMI1 + FGFR2b (B2) | Mouse fibroblasts (L929) | In vitro; In vivo (diabetic mouse wound model) | Expression of keratinocyte markers (KRT10, KRT14) | Promoted wound closure, reconstructed stratified epithelium, restored barrier function, reduced mortality |
| Induced Pulmonary Alveolar Epithelial-like Cells (iPULs) [7] | Nkx2-1, Foxa1, Foxa2, Gata6 | Mouse tail-tip fibroblasts; Mouse embryonic fibroblasts | In vitro (3D organoid culture); In vivo (bleomycin-induced pulmonary fibrosis mouse model) | Surfactant protein-C (Sftpc); Lamellar body-like structures | Integrated into alveolar surface, formed AT1 and AT2-like cells |
| Induced Cardiomyocytes (iCMs) [23] | Gata4, Mef2c, Tbx5 (GMT) | Cardiac fibroblasts | In vitro; In vivo | Cardiomyocyte-like gene expression; Action potentials; Spontaneous beating | Improved heart function; Reduced fibrosis after cardiac injury |
Experimental Protocols and Methodologies
Cardiac Reprogramming Protocol
The foundational protocol for cardiac reprogramming was established by Ieda et al. (2010), demonstrating that a combination of three cardiac transcription factors—Gata4, Mef2c, and Tbx5 (GMT)—could reprogram cardiac fibroblasts into induced cardiomyocytes (iCMs) in vitro [22] [23]. This methodology involves:
Factor Delivery: Transcription factors are typically delivered via retroviral vectors to ensure stable integration and expression in target fibroblasts [22]. For in vivo applications, retroviral GMT is delivered directly to injured hearts in myocardial infarction mouse models [22].
Culture Conditions: Reprogrammed cells are maintained in standard cardiac cell culture media, with spontaneous beating typically observed in a subset of cells within 1-2 weeks post-transduction [22].
Functional Validation: Successful reprogramming is confirmed through multiple assays including patch-clamp electrophysiology to record action potentials, calcium imaging to detect transients, and observation of spontaneous contraction [22].
In Vivo Assessment: In animal models, functional recovery is evaluated through echocardiography to measure cardiac function, while fibrotic area is quantified using histological staining methods (e.g., Masson's trichrome for collagen) [22].
Protocol enhancements have included polycistronic constructs with "self-cleaving" 2A sequences to ensure coordinated expression of multiple factors, with the M-G-T transcriptional order demonstrating highest conversion efficiency [22]. Additional factors like HAND2 have been incorporated to improve reprogramming efficiency and anti-fibrotic effects [22].
Pulmonary Alveolar Epithelial Cell Reprogramming
The generation of induced pulmonary alveolar epithelial-like cells (iPULs) from fibroblasts involves a sophisticated screening and culture approach:
Factor Screening: An initial screen of 14 candidate genes associated with pulmonary alveolar epithelial cell differentiation identified NKX2-1 as essential for inducing surfactant protein-C (Sftpc) expression [7]. Systematic elimination revealed the optimal combination as NKX2-1, FOXA1, FOXA2, and GATA6.
3D Organoid Culture: Transduced mouse embryonic fibroblasts are cultured in three-dimensional organoid systems instead of traditional 2D cultures, significantly improving reprogramming efficacy [7].
Serum-Free Media Supplementation: Culture media is supplemented with Wnt pathway activators, various growth factors, and Smad inhibitors to support alveolar epithelial cell differentiation and maturation [7].
Cell Sorting and Purification: Fluorescence-activated cell sorting (FACS) is employed to isolate successfully reprogrammed cells using the marker combination Sftpc-GFP+ Thy1.2- EpCAM+ [7]. This purification step typically yields 2-3% iPULs from the initial fibroblast population by day 7 post-transduction.
In Vivo Validation: iPULs are administered via intratracheal instillation in bleomycin-induced pulmonary fibrosis mouse models, with subsequent assessment of alveolar integration and differentiation into both AT1 and AT2-like cells [7].
Keratinocyte-Like Cell Reprogramming for Cutaneous Wound Healing
The direct conversion of fibroblasts into induced keratinocyte-like cells (iKCs) for diabetic wound repair utilizes a streamlined two-factor approach:
Factor Combination: The B2 combination (BMI1 + FGFR2b) is delivered via adeno-associated virus 9 (AAV9), which exhibits high epithelial transduction efficiency [24].
In Vivo Delivery: AAV9 vectors encoding BMI1 and FGFR2b are administered directly to wound sites in diabetic (db/db) mouse models through subcutaneous injection or topical application [24].
Molecular Validation: Successful reprogramming is confirmed through qRT-PCR analysis of keratinocyte markers (KRT10, KRT14), Western blot, immunofluorescence, and transcriptomic analysis [24].
Functional Assessment: Wound closure rates are quantified, and histological examination evaluates re-epithelialization, stratification, and restoration of barrier function [24].
Signaling Pathways and Molecular Mechanisms
Direct reprogramming efficiency is critically influenced by the fibrotic microenvironment, with several key signaling pathways acting as barriers to complete cell fate conversion.
The TGF-β signaling pathway represents a major barrier to reprogramming, sustaining fibroblast identity through SMAD-dependent transcription of pro-fibrotic genes [22]. Successful reprogramming strategies often incorporate TGF-β pathway inhibitors (e.g., SB431542, A83-01) to facilitate epigenetic remodeling.
Mechanical signaling from the stiffened extracellular matrix in fibrotic tissues activates YAP/TAZ signaling, reinforcing myofibroblast identity and presenting both physical and biochemical resistance to lineage conversion [22].
Epigenetic modifiers play dual roles in maintaining fibrotic programs and enabling reprogramming. Small molecule inhibitors targeting DNA methyltransferases and histone modifiers can disrupt fibrotic epigenetic memory while opening chromatin at target cell-specific loci [22].
Metabolic reprogramming accompanies successful cell fate conversion, with a shift from glycolysis toward fatty acid oxidation observed during fibroblast-to-cardiomyocyte conversion, mirroring metabolic maturation in native cardiomyocytes [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Direct Reprogramming Studies
| Reagent/Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Transcription Factors | Gata4, Mef2c, Tbx5, HAND2, Nkx2-1, Foxa1, Foxa2, Gata6, BMI1, FGFR2b | Master regulators that initiate gene expression programs of target cell type |
| Viral Delivery Systems | Retrovirus, Lentivirus, Adeno-associated virus (AAV9) | Stable or transient delivery of reprogramming factors to target cells |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK-3 inhibitor), A83-01 (TGF-β inhibitor), SB431542 (TGF-β inhibitor), Valproic acid (HDAC inhibitor), Forskolin (cAMP activator) | Modulate signaling pathways and epigenetic barriers to enhance reprogramming |
| miRNA/siRNA Tools | miR-1, miR-133, miR-208, miR-499 | Non-coding RNA regulators that can alone or in combination induce reprogramming |
| Culture Systems | 3D organoid culture, Serum-free media with specialized supplements | Provide microenvironmental cues that support maturation and maintenance of reprogrammed cells |
| Cell Sorting Markers | Thy1.2 (fibroblast exclusion), EpCAM (epithelial inclusion), Sftpc-GFP (AT2 cell reporter) | Isolation and purification of successfully reprogrammed cells from heterogeneous populations |
| Animal Disease Models | Myocardial infarction (MI) models, Bleomycin-induced pulmonary fibrosis, Diabetic (db/db) wound models | In vivo validation of therapeutic efficacy and anti-fibrotic effects |
Direct reprogramming represents a transformative strategy with dual therapeutic benefits—regenerating functional tissue while simultaneously reducing pathogenic fibrosis. The comparative analysis presented herein demonstrates that while factor combinations and delivery methods must be optimized for specific tissue contexts, the core principle of directly converting fibroblasts into functional parenchymal cells remains consistently viable across organ systems.
The functional outcomes observed in preclinical models, including improved cardiac function, enhanced wound healing, and alveolar regeneration, underscore the therapeutic potential of this approach. The concurrent reduction in fibrotic area across these models highlights how direct reprogramming strategically addresses both tissue loss and the pathological microenvironment.
For researchers and drug development professionals, the ongoing challenges include optimizing reprogramming efficiency, ensuring the functional maturity of converted cells, and developing safe, targeted delivery systems for clinical translation. As understanding of the molecular mechanisms deepens and technologies for precise cellular engineering advance, direct reprogramming continues to emerge as a promising pathway for addressing fibrotic diseases through dual-action regenerative therapy.
In the field of regenerative medicine and cellular engineering, the targeted reprogramming of cellular identity represents a transformative approach for disease modeling, drug discovery, and therapeutic development. Central to this paradigm is the identification of precise transcription factor (TF) cocktails—specific combinations of DNA-binding proteins that can orchestrate the conversion of one cell type to another by activating or repressing critical genetic programs. Within the broader context of functional outcomes in reprogramming strategies research, understanding these key molecular drivers, their target genes, and the experimental evidence supporting their efficacy is fundamental for advancing the field beyond serendipitous discovery toward rational design principles.
This guide systematically compares the performance of established and emerging TF cocktails across different cellular contexts, providing researchers with structured experimental data and methodological frameworks. The convergence of single-cell technologies, computational prediction models, and high-throughput screening methods has dramatically accelerated the identification of effective TF combinations, moving the field from laborious iterative testing to more directed approaches. By examining the quantitative outcomes, target gene networks, and implementation protocols of these reprogramming strategies, scientists can make informed decisions when selecting or developing TF cocktails for specific applications in drug development and cellular therapeutics.
Comparative Analysis of Transcription Factor Cocktails
The following tables provide a structured comparison of transcription factor cocktails, their target cell types, efficiency metrics, and key functional outcomes based on recent experimental studies.
Table 1: Transcription Factor Cocktails for Direct Cell Fate Conversion
| Target Cell Type | Transcription Factor Cocktail | Starting Cell Type | Reprogramming Efficiency | Key Validated Target Genes | Functional Validation |
|---|---|---|---|---|---|
| Microglia-like cells (TFiMGLs) [25] | SPI1, CEBPA, FLI1, MEF2C, CEBPB, IRF8 | Human iPSCs | 4 days; efficient yield across multiple iPSC lines | ITGAM, P2RY12, CX3CR1, TMEM119, TREM2 | Transcriptional similarity to primary microglia; key functional features of human primary microglia |
| Epicardial-like cells [26] | Gata6, Hand2, Tbx5 | Mouse Embryonic Fibroblasts (MEFs) | 36.9% of cells in cluster expressing epicardial markers | Wt1, Bnc1 (endogenous activation) | Morphological and functional similarity to genuine epicardial cells |
| Skeletal muscle cells [26] | MyoD1 | Mouse Embryonic Fibroblasts (MEFs) | Distinct cluster formation; outcompetes 47 other factors | Muscle development genes | Significant enrichment for muscle development gene ontology annotations |
Table 2: Performance Metrics and Experimental Outcomes of Reprogramming Strategies
| TF Cocktail | Screening/Identification Method | Time to Phenotype | Stability Assessment | Key Advantages | Experimental Evidence |
|---|---|---|---|---|---|
| SPI1, CEBPA, FLI1 [25] | Iterative, high-throughput single-cell TF screening | 4 days | Reproducible across distinct iPSC lines | Rapid, efficient; works in standard culture media without additional factors | scRNA-seq confirmation of transcriptional similarity; functional assays |
| Gata6, Hand2 [26] | Reprogram-Seq: scRNA-seq of perturbed cell library | N/A | Derived from reprogramming, not progenitor proliferation | Identified from large combinatorial space without prior bias | Co-expression with endogenous epicardial markers; distinct cluster formation |
| MyoD1 [26] | Reprogram-Seq from 48-factor cardiac library | N/A | Forms distinct, stable cell cluster | Single-factor efficacy; outcompetes numerous other factors | Exclusive cluster formation; enrichment of muscle gene ontology terms |
Experimental Protocols and Methodologies
Iterative Single-Cell Transcription Factor Screening for Microglia
The differentiation of human induced pluripotent stem cells (iPSCs) into microglia-like cells exemplifies a robust, high-throughput methodology for identifying optimal TF combinations. The protocol involves a sequential screening approach to pinpoint factors that drive efficient cell fate conversion [25].
Primary Screening Phase: Researchers first selected 40 candidate TFs based on literature surveys of microglial development, epigenetic patterns, and gene regulatory networks. Each TF was cloned into a PiggyBac transposon vector featuring a doxycycline-inducible expression system and a unique 20-nucleotide barcode inserted between the stop codon and poly-A sequence to distinguish exogenous from endogenous TF transcripts. The plasmid library was transfected into iPSCs at a DNA dose of 5μg, determined to optimally integrate approximately 5-9 TF copies per cell. After puromycin selection for successfully integrated cells, differentiation was induced with doxycycline for four days [25].
Analysis and Validation: Transfected cells were analyzed using fluorescence-activated cell sorting (FACS) for consensus microglial surface proteins (CX3CR1, P2RY12, CD11b). Single-cell RNA sequencing (scRNA-seq) was performed on approximately 10,000 TRA-1-60 negative (differentiated) cells. The barcoding strategy allowed for simultaneous detection of single-cell gene expression and TF integration through amplicon sequencing of co-amplified TF and cell barcodes from cDNAs. Computational analysis comparing TF expression in cells with versus without microglial gene expression identified the most potent inducers—SPI1, FLI1, and CEBPA. These top candidates were then tested in various polycistronic configurations (linked with 2A peptides) to ensure co-expression and optimize relative expression levels, ultimately yielding the final six-factor combination (SPI1, CEBPA, FLI1, MEF2C, CEBPB, IRF8) for efficient microglia production [25].
Reprogram-Seq for Epicardial Cell Reprogramming
The Reprogram-Seq platform provides a generalizable framework for identifying TF cocktails that reprogram fibroblasts to specific cell types by combining single-cell perturbation with computational analysis [26].
Library Construction and Screening: A retroviral library of 48 cardiac-related TFs and genes was packaged and used to infect mouse embryonic fibroblasts (MEFs) at high infectivity, ensuring individual cells expressed multiple exogenous TFs. This created a diverse library of perturbed cells expressing various TF combinations. scRNA-seq was then performed to capture the full transcriptome of each cell, enabling identification of cell clusters where exogenous TFs drove transcriptional reprogramming toward target fates without relying on distal barcoding [26].
Data Analysis and Hit Identification: The single-cell transcriptomes were integrated with a reference atlas of 15,684 primary P0 mouse heart cells. Clusters containing mixtures of in vivo target cells (e.g., epicardial cells) and MEF-derived cells suggested successful reprogramming. The expression of exogenous TFs was examined in these mixed clusters—MEF-derived cells in the epicardial-containing cluster showed significant enrichment for Gata6 (78.6% vs. 22.1% in other MEF-derived cells) and Hand2 (48.8% vs. 9.6%), indicating their reprogramming activity. Functional validation confirmed that the resulting cells not only expressed epicardial markers (Wt1, Bnc1) but also resembled genuine epicardial cells morphologically and functionally [26].
Visualization of Experimental Workflows
The following diagrams illustrate the core methodologies discussed in this review, providing visual representations of the experimental workflows for transcription factor screening and reprogramming.
Figure 1: Iterative TF screening workflow for generating microglia from iPSCs.
Figure 2: Reprogram-Seq workflow for unbiased TF cocktail discovery.
Research Reagent Solutions
The following table details essential reagents and materials used in the transcription factor screening and reprogramming experiments described in this guide.
Table 3: Key Research Reagents for Transcription Factor Reprogramming Studies
| Reagent/Material | Function/Application | Specific Examples from Studies |
|---|---|---|
| PiggyBac Transposon System | Genomic integration of transcription factor genes; enables stable expression | Used for integrating 40 TF library into iPSCs with doxycycline-inducible promoter [25] |
| Barcoded TF Vectors | Distinguishes exogenous from endogenous TF transcripts; enables tracking in pooled screens | 20-nucleotide barcode between stop codon and poly-A sequence [25] |
| Doxycycline-Inducible System | Controls timing of TF expression; allows synchronized differentiation | Used to induce TF expression after puromycin selection [25] |
| Retroviral/Lentiviral Vectors | Efficient delivery and integration of TF genes; suitable for hard-to-transfect cells | Retroviral library for delivering 48 cardiac factors to MEFs [26] |
| Single-Cell RNA Sequencing | Comprehensive transcriptome profiling; identifies cell states and reprogramming efficacy | 10x Genomics platform for analyzing differentiated cells; identifies microglial gene expression [25] |
| Fluorescence-Activated Cell Sorting | Isolation of specific cell populations based on surface markers | Sorting for CX3CR1, P2RY12, CD11B microglial markers or TRA-1-60 negative cells [25] |
| Polycistronic Vectors | Ensures co-expression of multiple TFs from single construct; controls relative expression levels | 2A peptide-linked TF cassettes with different gene orders to optimize expression [25] |
The systematic comparison of transcription factor cocktails presented in this guide highlights significant progress in the rational design of cell fate reprogramming protocols. The emergence of high-throughput screening technologies like iterative single-cell TF screening and Reprogram-Seq has transformed the identification of effective TF combinations from a largely empirical process to a more directed, data-driven endeavor. Quantitative assessments reveal that optimized cocktails can achieve rapid cellular conversion—within just four days for microglia differentiation—with efficiencies sufficient for research and potential therapeutic applications.
Critical examination of the experimental data demonstrates that successful reprogramming strategies share common features: they activate endogenous master regulator genes, establish stable transcriptional networks, and produce functionally competent cells. The methodologies and reagents detailed provide researchers with a toolkit for implementing these approaches across different cellular systems. As the field advances, integrating computational prediction models like GET with experimental screening will likely further accelerate the discovery of TF cocktails for increasingly specific cell subtypes, ultimately enhancing both fundamental understanding of cell fate control and the development of targeted cellular therapies for human diseases.
Reprogramming in Action: Methodologies and Organ-Specific Applications for Functional Recovery
Cardiovascular disease remains a leading cause of mortality worldwide, with myocardial infarction (MI) resulting in the loss of approximately one billion cardiomyocytes [27]. The adult human heart possesses minimal regenerative capacity, and the damaged myocardium is typically replaced by non-contractile fibrotic tissue, ultimately leading to heart failure [18] [28]. Traditional pharmacological interventions and device-based therapies primarily manage symptoms rather than addressing the fundamental loss of contractile cells [18]. While heart transplantation offers a definitive solution, it is constrained by donor scarcity and the necessity for lifelong immunosuppression [18].
Regenerative medicine has emerged as a promising frontier for fundamentally addressing heart failure by restoring lost cardiac tissue [18]. Among various strategies, direct cardiac reprogramming has gained significant traction for its potential to directly convert endogenous cardiac fibroblasts (CFs) into induced cardiomyocytes (iCMs) in situ [18] [28]. This approach leverages the abundant fibroblast population that contributes to pathological scarring post-MI, aiming to simultaneously reduce fibrosis and regenerate functional myocardium [18] [28]. This guide provides a comprehensive comparison of the transcription factor cocktails that drive this cellular transformation, detailing their experimental protocols, efficiencies, and functional outcomes.
Comparative Analysis of Major Reprogramming Cocktails
Direct cardiac reprogramming involves the forced expression of specific transcription factors or microRNAs to directly convert one somatic cell type into another without reverting to a pluripotent state [28]. The following table summarizes the key reprogramming cocktails developed for generating iCMs.
Table 1: Key Transcription Factor Cocktails for Direct Cardiac Reprogramming
| Reprogramming Cocktail | Key Components | Reported Reprogramming Efficiency | Starting Cell Type | Notable Functional Outcomes |
|---|---|---|---|---|
| MGT [28] | Gata4, Mef2c, Tbx5 | Not precisely quantified (initial study) | Neonatal and adult mouse cardiac fibroblasts, tail-tip fibroblasts | Generation of cardiomyocyte-like cells; spontaneous contraction; action potentials; electrical coupling [28] |
| GHMT [28] | Gata4, Hand2, Mef2c, Tbx5 | ~9.2% (αMHC-GFP+ and cTnT+ cells) [28] | Adult tail-tip fibroblasts and cardiac fibroblasts | ~4-fold increase in iCM yield vs. MGT; ventricular-like action potentials [28] |
| microRNA Combo [28] | miR-1, miR-133, miR-208, miR-499 | Not specified | Neonatal mouse cardiac fibroblasts | Generation of cardiomyocyte-like cells; spontaneous contraction; action potentials [28] |
| MGT + miR-133 [28] | Gata4, Mef2c, Tbx5 + miR-133 | ~4-fold increase in cTnT+ cells; ~6-fold more beating cells vs. MGT alone [28] | Mouse embryonic fibroblasts | Sharp increase in functional iCM generation [28] |
| Small Molecule Cocktail [28] | CRFVPTZ (various inhibitors) | Generation of beating cardiomyocyte-like cells | Mouse embryonic fibroblasts | Spontaneous contraction; action potentials; avoids exogenous genetic material [28] |
The field has evolved from the initial MGT cocktail to more complex combinations including additional transcription factors like Hand2 (GHMT) or non-coding RNAs like miR-133 to enhance efficiency and functional maturation [28]. A critical advancement has been the demonstration that these cocktails can successfully reprogram resident cardiac fibroblasts into iCMs within injured mouse hearts, leading to improved vascular perfusion, reduced scar size, and enhanced cardiac function [28] [29].
Experimental Protocols for In Vitro and In Vivo Reprogramming
Standard In Vitro Reprogramming Protocol
The foundational protocol for converting fibroblasts into iCMs in a dish involves several key steps, as standardized across multiple laboratories [28].
- Fibroblast Isolation and Culture: Fibroblasts are typically isolated from neonatal or adult mouse hearts via enzymatic digestion (e.g., collagenase). For lineage tracing, fibroblasts are often harvested from transgenic mice expressing Cre recombinase under fibroblast-specific promoters like Tcf21 or Fsp1 [18].
- Viral Transduction: Isolated fibroblasts are transduced with lentiviral or retroviral vectors carrying the reprogramming factors (e.g., MGT or GHMT). Viruses are added to the culture medium, often in the presence of polybrene to enhance infection efficiency [28].
- Culture and Phenotypic Monitoring: Post-transduction, cells are maintained in standard culture media. The first signs of successful reprogramming, such as spontaneous contraction and sarcomeric organization, can be observed as early as 1-3 weeks [28].
- Validation of Reprogramming:
- Molecular Analysis: Quantitative PCR (qPCR) and immunofluorescence staining are used to detect the upregulation of cardiomyocyte-specific genes and proteins (e.g., cardiac Troponin T, α-actinin) and the downregulation of fibroblast markers (e.g., fibroblast-specific protein-1) [28].
- Functional Analysis: Techniques such as calcium flux imaging, measurement of action potentials, and assessment of response to pharmacological agents are employed to confirm the functional maturity of the newly formed iCMs [28].
In Vivo Reprogramming for Cardiac Repair
Translating this technology to live animals, particularly in models of myocardial infarction, follows a targeted delivery approach.
- Animal Model Creation: Myocardial infarction is induced in mice, commonly through permanent ligation of the left anterior descending (LAD) coronary artery [28].
- Delivery of Reprogramming Factors: Shortly after injury, the reprogramming factors are delivered directly to the infarcted heart and border zone. This is achieved using:
- Viral Vectors: Direct intramyocardial injection of adeno-associated viruses (AAVs) or lentiviruses engineered for cardiac tropism and containing the reprogramming cocktail [18] [28].
- Non-Viral Methods: Alternative strategies include the injection of modified mRNA or extracellular vesicles loaded with reprogramming microRNAs to avoid genomic integration [18] [27].
- Functional and Histological Assessment: Weeks post-injection, hearts are analyzed for functional improvement (e.g., via echocardiography to measure ejection fraction) and histological evidence of reprogramming (e.g., lineage tracing to confirm the fibroblast origin of new iCMs, reduction in scar size, and improved vascularization) [18] [28] [29].
Figure 1: Experimental Workflow for In Vivo Cardiac Reprogramming. This diagram outlines the key steps from myocardial injury to functional repair through fibroblast conversion.
Signaling Pathways and Molecular Mechanisms
The process of direct reprogramming is governed by profound shifts in gene regulatory networks and epigenetic landscapes. Key signaling pathways are modulated to suppress the fibroblast gene program and activate the cardiomyocyte gene program.
- Key Transcriptional Drivers: The core factors Gata4, Mef2c, and Tbx5 (GMT) act synergistically to activate a network of downstream cardiac genes. Gata4 binds to AT-rich sequences, Mef2c is a MADS-box transcription factor that regulates muscle differentiation, and Tbx5 is a T-box factor critical for heart development [28]. The addition of Hand2, a transcription factor involved in ventricular development, further enhances this network, particularly promoting the generation of iCMs with ventricular-like properties [28].
- Epigenetic Remodeling: Successful reprogramming involves extensive chromatin remodeling, leading to a more open conformation at loci of key cardiac developmental genes. This is facilitated by the recruitment of chromatin-modifying enzymes [28].
- Role of MicroRNAs: MicroRNAs such as miR-1, miR-133, miR-208, and miR-499 repress fibroblast-specific genes and non-muscle genes, thereby reducing barriers to reprogramming and reinforcing the cardiac gene program [28]. miR-133, for instance, can sharply increase the yield of functional iCMs when combined with the MGT cocktail [28].
- Impact of the Microenvironment: The tissue environment significantly influences reprogramming efficiency. Extracellular signaling, such as TGF-β and WNT pathways, can pose barriers to reprogramming. Consequently, small molecule inhibitors targeting these pathways (e.g., SB431542 for TGF-β, XAV939 for WNT) are often included in advanced protocols to enhance efficiency [28].
Figure 2: Molecular Mechanisms of Cardiac Reprogramming. This diagram illustrates the key molecular events triggered by reprogramming cocktails that lead to the conversion of a fibroblast into a cardiomyocyte.
Success in cardiac reprogramming research relies on a suite of specialized reagents and tools. The following table details key materials and their applications.
Table 2: Essential Research Reagent Solutions for Cardiac Reprogramming Studies
| Reagent/Tool Category | Specific Examples | Function in Reprogramming Experiments |
|---|---|---|
| Reprogramming Factors | cDNA for Gata4, Mef2c, Tbx5, Hand2; microRNAs (miR-1, -133, -208, -499) [28] | Core inductors of cell fate conversion; provided via viral vectors or synthetic molecules. |
| Delivery Vectors | Retrovirus, Lentivirus, Adeno-associated virus (AAV) [18] [28] | Vehicles for introducing reprogramming factor genes into target fibroblasts. |
| Cell Culture Media | StemMACS CardioDiff Kit [30]; RPMI 1640 + B-27 Supplement [31] | Supports the survival, maintenance, and maturation of reprogrammed iCMs. |
| Lineage Tracing Models | Tcf21-iCre; Fsp1-Cre; αMHC-GFP reporter mice [18] [28] | Genetically labels fibroblasts and/or cardiomyocytes to track cell origin and conversion in vivo. |
| Characterization Antibodies | Anti-cardiac Troponin T (cTnT); Anti-α-actinin; Anti-PECAM1 (for endothelial conversion) [28] [29] | Immunostaining to confirm protein expression and sarcomeric structure in iCMs. |
| Functional Assay Kits | Calcium-sensitive dyes (e.g., Fluo-4); Multi-electrode array (MEA) systems [28] [31] | Measures electrophysiological properties and calcium handling in iCMs. |
Direct cardiac reprogramming represents a paradigm shift in regenerative medicine, offering a promising strategy to remuscularize the injured heart by converting scar-forming fibroblasts into functional cardiomyocytes. While significant progress has been made from the initial MGT cocktail to more efficient multi-factor and small-molecule approaches, challenges remain in achieving high reprogramming efficiency, ensuring the maturation of iCMs to an adult-like state, and developing safe and effective delivery systems for clinical translation [18] [28].
Future research will likely focus on optimizing the specificity and efficacy of in vivo delivery systems, such as engineered viral vectors with cardiac tropism or nanoparticle-based delivery of non-integrating factors [18]. Furthermore, a deeper understanding of fibroblast heterogeneity and the age-related epigenetic barriers to reprogramming will be crucial for applying this therapy to the older patient population most affected by heart failure [18]. As these hurdles are overcome, transcription factor-based cardiac reprogramming holds immense potential to evolve from a powerful laboratory tool into a transformative clinical therapy for heart disease.
Direct Induction of Alveolar Epithelial-like Cells (iPULs) for Lung Regeneration
The field of regenerative medicine for pulmonary diseases is undergoing a significant transformation, moving away from traditional stem cell intermediate stages toward more direct cellular reprogramming approaches. For patients with intractable and irreversible respiratory diseases such as idiopathic pulmonary fibrosis (IPF) and chronic obstructive pulmonary disease (COPD), the therapeutic options remain limited, with lung transplantation constrained by donor scarcity, age restrictions, and postoperative rejection issues [32]. Within this clinical context, alveolar epithelial type 2 (AT2) cells have emerged as a critical therapeutic target due to their dual function as surfactant producers and progenitor cells responsible for alveolar repair and maintenance [32] [33]. The recent development of induced pulmonary alveolar epithelial-like cells (iPULs) via direct reprogramming of fibroblasts represents a technological breakthrough that could potentially overcome the limitations of conventional stem cell-based approaches [32] [33]. This comparison guide objectively analyzes the performance of iPUL technology against established reprogramming strategies, providing researchers and drug development professionals with experimental data and methodological details to inform their therapeutic development decisions.
Comparative Analysis of Reprogramming Strategies
Performance Benchmarking: iPULs Versus Alternative Approaches
Table 1: Comparative Analysis of Pulmonary Cell Reprogramming Strategies
| Parameter | iPULs (Direct Reprogramming) | iPSC-Derived AT2 Cells | Direct Cardiac Reprogramming (iCMs) |
|---|---|---|---|
| Reprogramming Factors | Nkx2-1, Foxa1, Foxa2, Gata6 [32] | OCT4, SOX2, KLF4, c-MYC (OSKM) [34] | GATA4, Mef2C, Tbx5 (GMT) or with Hand2 (GHMT) [27] |
| Starting Cell Type | Mouse tail-tip fibroblasts (TTFs), embryonic fibroblasts (MEFs), dermal fibroblasts (MDFs) [32] | Various somatic cells (e.g., fibroblasts, blood cells) [34] [35] | Cardiac fibroblasts (CFs) [27] |
| Time Required | 7-10 days [32] [33] | Approximately 1 month [33] | Varies; often inefficient (<10% efficiency) [27] |
| Reprogramming Efficiency | ~2-4% of sorted cells became Sftpc-GFP+ Thy1.2– EpCAM+ [32] | Varies with method; requires clone selection [32] | Generally low (<10% efficiency) [27] |
| Key Characteristics | Lamellar body-like structures, AT2-like transcriptome, self-renewal capability [32] | Pluripotency, teratoma risk, requires directed differentiation [32] [35] | Molecular phenotypes resembling adult CMs [27] |
| Tumorigenic Risk | Low (bypasses pluripotent state) [32] [33] | Higher (risk of contaminating undifferentiated iPSCs) [32] [36] | Low (direct conversion) [27] |
| In Vivo Functional Validation | Integrated into alveolar surface, formed both AT1 and AT2-like cells in mouse fibrosis model [32] [33] | Demonstrated in various disease models but with functional limitations [32] | Improves cardiac function in murine MI models [27] |
Key Advantages and Technological Trade-offs
The comparative data reveal distinct advantages of the direct iPULs approach. The most significant benefit is the dramatically reduced timeline of 7-10 days compared to approximately one month for iPSC-derived AT2 cells, potentially accelerating therapeutic applications and research workflows [33]. Furthermore, direct reprogramming eliminates the pluripotent intermediate stage, thereby substantially reducing the risk of teratoma formation associated with contaminating undifferentiated iPSCs [32] [36].
However, the technology presents notable trade-offs. The current reprogramming efficiency of 2-4%, while promising for an emerging technology, remains suboptimal for immediate clinical translation [32]. Additionally, the requirement for four transcription factors (Nkx2-1, Foxa1, Foxa2, and Gata6) complicates delivery mechanisms compared to approaches requiring fewer factors [32]. The field is increasingly exploring small molecule-based reprogramming as an alternative strategy that could potentially offer better control over the reprogramming process and reduced safety concerns associated with genetic manipulation [35].
Experimental Protocols and Methodological Framework
Core Reprogramming Methodology for iPULs Generation
Table 2: Key Research Reagent Solutions for iPULs Generation
| Reagent/Category | Specific Examples | Function in Protocol |
|---|---|---|
| Reprogramming Factors | Nkx2-1, Foxa1, Foxa2, Gata6 [32] | Core transcription factors initiating alveolar epithelial reprogramming |
| Vector System | Retrovirus vectors [32] | Delivery method for transcription factor genes |
| Starting Cells | Mouse tail-tip fibroblasts (TTFs), embryonic fibroblasts (MEFs) from Sftpc-GFP mice [32] | Cellular raw material for reprogramming |
| Culture System | Three-dimensional (3D) organoid culture [32] | Provides appropriate microenvironment for alveolar differentiation |
| Culture Supplements | Serum-free medium with Wnt pathway activators, various growth factors, Smad inhibitors [32] | Enhances reprogramming efficiency and alveolar specification |
| Cell Sorting Markers | Thy1.2 (negative selection), EpCAM (positive selection) [32] | Isolation of successfully reprogrammed epithelial cells |
| Validation Markers | Surfactant protein-C (Sftpc), Lamellar body structures, transcriptomic analysis [32] [33] | Confirmation of AT2-like cell phenotype |
The foundational protocol for iPULs generation involves a meticulously optimized sequence of molecular and cellular manipulations. Researchers begin with mouse embryonic fibroblasts (MEFs) isolated from Sftpc-GFP reporter mice, enabling real-time monitoring of surfactant protein-C expression as a marker of successful reprogramming [32]. The core reprogramming factors—Nkx2-1, Foxa1, Foxa2, and Gata6—are delivered via retroviral transduction, ensuring robust and sustained expression during the critical early reprogramming phase [32].
Following transduction, a critical innovation lies in the implementation of a three-dimensional (3D) organoid culture system rather than conventional two-dimensional substrates. This architectural context proves essential for proper alveolar differentiation, with the culture medium supplemented with Wnt pathway activators, specific growth factors, and Smad inhibitors to enhance reprogramming efficiency [32]. The reprogramming process involves a systematic mesenchymal-to-epithelial transition (MET), characterized by gradual loss of fibroblast marker Vim and concurrent acquisition of epithelial and AT2-specific characteristics [32].
At day 7 post-transduction, researchers employ fluorescence-activated cell sorting (FACS) to isolate successfully reprogrammed cells using a gating strategy that selects for Sftpc-GFP+/Thy12-/EpCAM+ populations, effectively separating the iPULs from partially reprogrammed or non-reprogrammed cells [32]. The purified iPULs population then undergoes rigorous validation through transcriptomic analysis, structural assessment for lamellar body-like organelles, and functional testing in disease models [32] [33].
Factor Screening and Protocol Optimization
The identification of the optimal four-factor combination resulted from an extensive screening process. Researchers initially selected 14 candidate genes (Nkx2-1, Foxa1, Foxa2, Foxj1, Tcf21, Hoxa5, Sox17, Gata6, Tbx4, Gata5, Foxf1, Foxl1, Gli2, and Gli3) associated with pulmonary alveolar epithelial cell differentiation during lung development [32]. Through systematic elimination studies, they determined that removal of Nkx2-1 from the factor pool drastically reduced Sftpc expression, establishing its essential role in the reprogramming process [32]. Subsequent combinatorial testing revealed that Nkx2-1 together with Foxa1, Foxa2, and Gata6 produced the highest Sftpc expression levels, forming the core reprogramming cocktail [32].
Further optimization experiments demonstrated that excluding Gata6 from the protocol significantly reduced both organoid formation and the percentage of AT2-like cells, confirming its importance despite showing the most unstable expression in initial 2D culture screening [32]. The researchers also tested three additional factors (Sox9, Id2, and Etv5) based on literature surveys, but found that the original four factors alone produced the strongest Sftpc expression and organoid formation even in 3D culture conditions [32].
Technological Workflow and Signaling Pathways
iPULs Generation Workflow
Figure 1: Experimental workflow for generating iPULs from mouse embryonic fibroblasts, highlighting key stages from initial factor delivery to functional validation.
Comparative Pathway Analysis
Figure 2: Comparative pathway analysis of reprogramming strategies, highlighting the direct route of iPULs generation versus iPSC intermediary and chemical approaches.
Discussion and Research Applications
Functional Outcomes and Therapeutic Potential
The functional validation of iPULs provides compelling evidence for their therapeutic potential. When transplanted into a bleomycin-induced mouse model of pulmonary fibrosis—a well-established model for human interstitial lung disease—the iPULs demonstrated remarkable engraftment capability and functional plasticity [32] [33]. Specifically, the transplanted cells not only integrated into the damaged alveolar surfaces but also differentiated into both alveolar epithelial type 1 (AT1)-like and AT2-like cells, recapitulating key aspects of alveolar regeneration [32]. This bidirectional differentiation capacity is particularly significant given that the iPULs showed limited spontaneous differentiation into AT1 cells in vitro, suggesting the importance of the in vivo microenvironment for complete functional maturation [32].
From a therapeutic perspective, iPULs technology addresses several critical limitations of current stem cell-based approaches. The use of autologous fibroblasts could potentially eliminate immune rejection concerns without requiring immunosuppressive therapy [33]. Additionally, the significantly shorter production timeline (7-10 days versus approximately one month for iPSC-derived AT2 cells) could facilitate more timely interventions for progressive conditions like IPF [33]. The direct reprogramming approach also demonstrates advantages over emerging alternative technologies such as extracellular vesicle (EV)-based therapies being developed for cardiac repair, as iPULs constitute actual functional tissue cells rather than merely paracrine factor delivery vehicles [27].
Research Implications and Future Directions
The development of iPULs technology creates numerous opportunities for basic and translational research. For disease modeling, this approach enables the generation of patient-specific alveolar epithelial cells from easily accessible fibroblast sources, potentially revolutionizing the study of genetic lung diseases like hereditary surfactant deficiencies [32]. For drug discovery, iPULs provide a more physiologically relevant and scalable platform for compound screening compared to primary AT2 cells, which are challenging to isolate and maintain in culture [32] [33].
Future research directions should prioritize translating this technology to human cells, optimizing reprogramming efficiency, and developing non-integrating delivery methods for the reprogramming factors to enhance clinical safety [33]. The integration of small molecule-based reprogramming approaches—similar to those being developed for pluripotent stem cell generation—could potentially reduce the reliance on transcription factors and improve controllability of the reprogramming process [35]. Additionally, exploring the synergistic potential of iPULs with other regenerative approaches such as biomaterial scaffolds or EV-based signaling modulation could further enhance functional outcomes for patients with end-stage lung diseases [27].
As the field advances, standardization of characterization protocols and functional assessment criteria will be essential for comparing results across studies and accelerating clinical translation. The iPULs technology represents a promising addition to the regenerative medicine toolkit, offering a direct path to functional alveolar epithelial cells that could potentially regenerate damaged lung tissue in patients with currently untreatable respiratory conditions.
The field of therapeutic delivery is undergoing a transformative shift beyond viral vectors, with non-viral systems emerging as versatile platforms for mRNA and small molecule drugs. This transition addresses critical limitations of viral vectors, including immunogenicity, pre-existing immunity, packaging constraints, and manufacturing complexities [37] [38]. The core advantage of non-viral systems lies in their chemical design flexibility, improved safety profiles, and scalable manufacturing potential [38]. The successful deployment of lipid nanoparticle (LNP)-based mRNA vaccines during the COVID-19 pandemic provided definitive clinical validation of non-viral approaches, demonstrating their capacity for rapid development and global scalability [39] [40] [41]. Beyond vaccines, non-viral delivery systems now enable diverse therapeutic strategies, from RNA-targeting small molecules that modulate disease-relevant pathways to mRNA-based protein replacement therapies and gene editing applications [42] [41] [43]. This guide objectively compares the performance of leading non-viral delivery platforms, providing researchers with experimental data and methodologies to inform selection for specific therapeutic applications.
Comparative Analysis of Non-Viral Delivery Platforms
Performance Metrics and Functional Outcomes
The selection of an appropriate delivery system hinges on multiple performance parameters that directly impact therapeutic efficacy. The table below provides a structured comparison of major non-viral delivery platforms based on key functional metrics.
Table 1: Performance Comparison of Major Non-Viral Delivery Platforms
| Delivery Platform | Typical Payloads | Targeting Efficiency | Cellular Uptake Mechanism | Transfection Efficiency | Duration of Expression | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | mRNA, siRNA, small molecules [39] [38] | Moderate to High (Liver, immune cells) [44] | Endocytosis [38] | High (in approved drugs) [39] [41] | Transient (days) [38] | Clinical validation, scalable production [39] [41] | Reactogenicity, complex storage requirements [38] |
| Polymeric Nanoparticles | mRNA, siRNA, DNA [39] [38] | Moderate | Endocytosis | Moderate to High | Transient to Sustained | Biodegradability, tunable properties [39] | Potential cytotoxicity [38] |
| GalNAc-Conjugates | siRNA, ASO [39] [41] | Very High (Hepatocytes) | Receptor-mediated endocytosis (ASGPR) [39] | Very High (in hepatocytes) | Long-lasting (weeks-months) [41] | Simple synthesis, high specificity, subcutaneous administration [39] | Restricted to liver targets [39] |
| RNA-Targeting Small Molecules | Binds RNA structures directly [42] | N/A (Depends on biodistribution) | Passive diffusion | N/A | Depends on compound half-life | Oral bioavailability, ability to target specific RNA conformations [42] | Limited target space, identification challenges [42] |
Decision Framework for Platform Selection
Choosing the optimal delivery system requires alignment with therapeutic goals and target biology. For hepatocyte-specific delivery, GalNAc-conjugates are unparalleled due to their exceptional targeting via the asialoglycoprotein receptor (ASGPR) [39] [41]. For broader tissue targeting or vaccination purposes, LNPs currently offer the best combination of efficacy and clinical validation [39] [38]. When sustained intracellular release is desired, biodegradable polymeric nanoparticles provide advantages through controlled release kinetics [39]. For targeting undruggable RNA structures or splicing modulation, RNA-targeting small molecules represent a unique modality that operates through fundamentally different mechanisms [42].
Experimental Protocols and Validation Methodologies
Core Workflow for LNP Development and Evaluation
The development of ionizable lipids for LNPs has been significantly accelerated by integrated computational and experimental approaches. The following workflow visualizes the AGILE platform, a deep learning-powered pipeline for efficient LNP discovery.
Figure 1: The AGILE platform workflow for LNP development, combining deep learning and combinatorial chemistry to accelerate ionizable lipid discovery [44].
Detailed Experimental Protocol for LNP Screening:
- Library Synthesis: Utilize automated robotic liquid handling systems and one-pot multi-component reactions (e.g., Ugi 3-component reaction) to synthesize a diverse library of ionizable lipids (e.g., 1,200 compounds) [44].
- LNP Formulation: Formulate ionizable lipids into LNPs using a standardized microfluidic mixing process with fixed ratios of structural lipids (cholesterol, helper phospholipid, PEG-lipid) [44].
- In Vitro Transfection Screening: Transfect target cells (e.g., HeLa cells, macrophages) with LNP formulations encapsulating reporter mRNA (e.g., encoding fluorescent or luminescent proteins). Quantify transfection efficiency via flow cytometry or luminescence reading 24-48 hours post-transfection to determine mRNA transfection potency (mTP) [44].
- In Vivo Validation: Administer lead LNP formulations via relevant routes (e.g., intramuscular, intravenous) in animal models. Measure protein expression in target tissues over time using immunoassays or imaging techniques to confirm functional delivery [44].
Workflow for Discovering RNA-Targeting Small Molecules
The discovery of small molecules that selectively bind structured RNA elements involves a multidisciplinary approach combining structural biology, computational screening, and functional assays.
Figure 2: Key stages in the discovery of RNA-targeting small molecules, from target identification to lead optimization [42].
Detailed Experimental Protocol for RNA-Small Molecule Screening:
- Target RNA Preparation: Prepare structurally homogeneous RNA samples for screening. Techniques include in vitro transcription with purification, engineering to improve crystal packing (for X-ray crystallography), and selective isotope labeling (for NMR) [42].
- Computational Prescreening: Use molecular docking simulations against high-resolution RNA structures. Apply deep learning models trained on existing RNA-ligand complexes to predict binding affinity and specificity [42].
- Biophysical Binding Validation:
- Surface Plasmon Resonance (SPR): Immobilize RNA target on sensor chip and measure binding kinetics (ka, kd, KD) of small molecule candidates in real-time [42].
- Small-Molecule Microarrays (SMM): Screen thousands of compounds immobilized on slides for binding to fluorescently labeled RNA [42].
- NMR Spectroscopy: Monitor chemical shift perturbations in the RNA or ligand upon binding to confirm interaction and identify binding site [42].
- Functional Activity Assays: Test hit compounds in cell-free or cellular systems for desired functional outcomes:
- Specificity Assessment: Evaluate off-target effects by analyzing transcriptome-wide changes (RNA-Seq) or measuring activity against related RNA structures [42].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the described experimental protocols requires specific reagents and tools. The following table details key solutions for research in non-viral delivery systems.
Table 2: Essential Research Reagent Solutions for Non-Viral Delivery Research
| Reagent / Tool | Function / Application | Key Characteristics | Example Use Cases |
|---|---|---|---|
| Ionizable Lipids | Core functional component of LNPs; enables mRNA encapsulation and endosomal escape [38] [44] | Protonatable amine headgroup; hydrophobic tails; neutral charge at physiological pH, cationic in acidic endosomes [38] [44] | LNP-based mRNA delivery for vaccines and therapeutics [39] [44] |
| In Vitro Transcription (IVT) Kits | Production of research-grade mRNA | Cap analog inclusion; modified nucleotides (e.g., pseudouridine) to reduce immunogenicity [40] [43] | mRNA template for LNP formulation and screening [43] [38] |
| DNA-Encoded Libraries (DELs) | Identification of bioactive small molecules against RNA targets [42] | Millions of small-molecule DNA conjugates; enables ultra-high-throughput screening | Hit discovery for RNA-targeting small molecules [42] |
| Chemical Probing Reagents | RNA structure determination | Selective modification of flexible RNA regions (e.g., DMS, SHAPE reagents) [42] | Mapping RNA secondary structure for small molecule targeting [42] |
| Microfluidic Mixers | Reproducible LNP self-assembly | Precise control of mixing parameters; scalable from micro- to milli-fluidic formats [44] | Formulating LNPs with consistent size and encapsulation efficiency [44] |
| Cationic Polymers | Alternative mRNA delivery vector | High cationic charge density for RNA complexation (e.g., PEI, polyamidoamine) [39] [38] | In vitro mRNA transfection; prototype vaccine development [38] |
The landscape of non-viral delivery has evolved from a fundamental challenge into a strategic enabler of next-generation therapeutics. The comparative data presented in this guide demonstrates that no single platform dominates all applications; rather, researchers now have a toolkit of specialized options from which to select based on target tissue, payload type, and desired duration of effect. The most significant advances are emerging from the integration of complementary technologies—where AI-driven platform discovery, as exemplified by the AGILE approach, accelerates the development of bespoke delivery systems tailored to specific clinical needs [44]. Similarly, combining the programmability of RNA-targeted small molecules [42] with the efficient delivery of LNPs [39] [38] creates powerful synergies for addressing previously intractable diseases. As these fields continue to converge, the functional outcomes of different reprogramming strategies will increasingly depend on selecting not just the right therapeutic payload, but the optimal delivery vehicle to match its biological destination.
Enhancing Efficiency with 3D Organoid Culture Systems and FACS Purification
Three-dimensional (3D) organoid cultures have emerged as a revolutionary tool in biomedical research, providing an invaluable model that bridges the gap between traditional two-dimensional (2D) cell cultures and complex in vivo systems. Organoids are defined as three-dimensional cell cultures derived from human pluripotent stem cells (PSCs) or adult stem cells (ASCs) that recapitulate the cellular heterogeneity, structure, and function of human organs [45]. These microstructures closely mimic the complexity of native tissues while retaining human genetic material, positioning them as powerful assets for advancing our understanding of human biology, enhancing preclinical drug testing, and studying disease mechanisms [45] [46].
The evolution of organoid technology represents a significant milestone in life sciences. Since the first successful cultivation of intestinal organoids from adult stem cells in 2009, the field has witnessed exponential growth with scientists developing protocols for creating organoids from various tissues including liver, pancreas, brain, kidney, and lung [47]. By 2015, patient-derived organoids emerged as powerful tools for personalized medicine, enabling drug screening and disease modeling specific to individual patients [47]. The global market for organoid culture systems is experiencing robust growth, currently projected to reach approximately $3.2 billion by 2025, reflecting a compound annual growth rate of 22.5% from 2020 [47].
This comparison guide objectively evaluates the performance of different 3D organoid culture systems with a specific focus on how fluorescence-activated cell sorting (FACS) purification enhances their efficiency and application in research on functional outcomes of cellular reprogramming strategies.
Comparative Analysis of 3D Organoid Culture Platforms
Stem Cell Source Comparison for Organoid Generation
The choice of stem cell source significantly influences the characteristics, applications, and limitations of the resulting organoids. The three primary cell sources each present distinct advantages and considerations for researchers.
Table 1: Comparison of Stem Cell Sources for Organoid Generation
| Stem Cell Source | Key Characteristics | Differentiation Potential | Primary Applications | Notable Limitations |
|---|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Pluripotent, derived from blastocyst inner cell mass [45] | Broad; can develop into any cell type [45] | Developmental biology, disease modeling [45] | Ethical concerns, limited clinical translation [45] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells (Oct4, Sox2, Klf4, C-Myc) [45] | Broad pluripotency similar to ESCs [45] | Patient-specific disease modeling, drug screening, cell therapy [45] [48] | Potential epigenetic memory, fetal phenotype may limit adult disease modeling [49] |
| Adult Stem Cells (ASCs) | Tissue-resident precursors (e.g., Lgr5+ intestinal stem cells) [45] | Limited to tissue of origin [45] | Tissue-specific modeling, regenerative medicine [45] | Restricted differentiation potential, limited expansion capability [45] |
Technical Performance Metrics of Organoid Culture Systems
Organoid culture systems vary significantly in their technical performance, reproducibility, and scalability. Understanding these metrics is crucial for selecting the appropriate platform for specific research applications.
Table 2: Performance Metrics of 3D Organoid Culture Systems
| Parameter | Conventional Organoid Culture | Advanced/Bioengineered Systems | FACS-Enhanced Workflows |
|---|---|---|---|
| Reproducibility | High batch-to-batch variation [47] | Improved through standardized protocols [47] | Significantly enhanced via precise cell population isolation |
| Scalability | Labor-intensive, limited scale-up capacity [47] | Bioreactor systems enable larger production [47] | Compatible with automated systems for high-throughput processing |
| Vascularization | Typically absent, limits size (<300-400μm) [47] [49] | Emerging co-culture and microfluidic approaches [47] [49] | Enables isolation of endothelial precursors for vascular incorporation |
| Physiological Relevance | Recapitulates basic tissue architecture [45] | Enhanced complexity including immune components [47] | Purified cellular subpopulations improve functional maturation |
| Throughput Capability | Low to medium throughput [49] | Medium throughput with bioreactors [49] | High-throughput cell sorting and analysis possible |
Experimental Protocols for High-Efficiency Organoid Workflows
Optimized Protocol for CRISPR-Edited iPSC-Derived Organoids
Recent advances in gene editing have enabled more precise manipulation of stem cells for organoid generation. The following protocol demonstrates an efficient, virus-free approach for generating knock-in iPSC lines for organoid research, achieving efficiencies above 30% [48].
Day 0: Preparation
- Culture GMP-compliant iPSC lines in a richer alternative medium two days prior to nucleofection to enhance cell viability [48].
- Prepare ribonucleoprotein (RNP) complexes using Alt-R S.p. HiFi Cas9 Nuclease V3 or Cas12a Ultra with target-specific guide RNAs [48].
- Prepare donor plasmid DNA containing the transgene of interest with appropriate homology arms.
Day 1: First Nucleofection (Donor Plasmid Delivery)
- Harvest 3×10^6 iPSCs using gentle dissociation reagent.
- Resuspend cells in P4 Nucleofection Buffer (Lonza) containing donor plasmid DNA.
- Perform nucleofection using Lonza 4D Nucleofector with program CA167 [48].
- Immediately after nucleofection, recover cells in RPMI medium for 10 minutes to significantly enhance cell survival [48].
- Plate cells in iPSC culture medium and incubate at 37°C, 5% CO₂.
Day 2: Second Nucleofection (RNP Delivery)
- Harvest cells from Day 1 using gentle dissociation.
- Resuspend in P4 Nucleofection Buffer containing pre-complexed RNP.
- Perform nucleofection using program CA167.
- Recover cells in RPMI medium for 10 minutes.
- Plate cells and incubate at 32°C ("cold shock") to improve knock-in efficiency [48].
- Return to 37°C after 24 hours.
Days 3-7: Selection and Expansion
- Culture cells in optimized iPSC medium with daily monitoring.
- Around day 7-10, harvest cells for screening via flow cytometry or other selection methods.
- Employ limiting dilution cloning in 96-well plates to isolate homozygous clones [48].
Validation:
- Screen clones for HLA-I expression loss after Interferon γ stimulation to confirm biallelic integration [48].
- Characterize isolated clones for genomic integrity, differentiation capability, and transgene functionality [48].
High-Throughput Organoid Analysis with Cellos Pipeline
The Cellos computational pipeline enables accurate, high-throughput 3D organoid segmentation and nuclear segmentation, allowing for detailed analysis of organoid dynamics at cellular resolution [50].
Sample Preparation and Imaging:
- Generate organoids from target cell sources (e.g., TNBC PDX model cells) [50].
- Label distinct subpopulations with NLS-conjugated EGFP or mCherry for tracking.
- Treat organoids with experimental conditions (e.g., cisplatin concentration range 0-128 μM).
- Fix organoids at appropriate time points.
- Stain nuclei with Hoechst or similar nuclear dye.
- Image using high-content screening system (e.g., PerkinElmer Opera Phenix) with z-stacking capability [50].
Organoid Segmentation:
- Convert fluorescent images to grayscale.
- Preprocess to remove debris and noise using background subtraction algorithms.
- Apply Triangle method for histogram thresholding to create binary images [50].
- Use scikit-image to uniquely label all organoids and remove small objects (<50μm diameter).
- Generate measurements for each organoid (3D bounding box, volume, mean intensity, solidity).
- Stitch fields together and create a comprehensive measurement file for each well.
Nuclear Segmentation with Convolutional Neural Network:
- Use trained Stardist-3D model with ResNet backbone for nuclei segmentation [50].
- Input stitched z-stack images and organoid measurement files.
- Segment individual nuclei within organoids using the trained model (publicly available on Cellos GitHub).
- Generate nuclear measurements (centroid, volume, mean intensity, solidity).
- Analyze cellular composition, nuclear morphologies, and cell-cell spatial relationships.
Data Analysis:
- Quantify treatment effects on organoid growth, morphology, and cellular composition.
- Analyze spatial relationships and ecological affinity between different cell populations.
- Correlate 3D imaging data with traditional viability assays.
Research Reagent Solutions for Organoid Research
Successful organoid culture and analysis requires specific reagents and materials optimized for 3D culture systems. The following table details essential solutions and their functions in organoid workflows.
Table 3: Essential Research Reagents for Advanced Organoid Culture Systems
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| 3D Matrices | Matrigel, Synthetic hydrogels, ECM-based hydrogels [47] [51] | Provides structural support mimicking native extracellular matrix | Matrigel has batch variability; synthetic alternatives address this but may require optimization [47] |
| Specialized Media | Intestinal organoid media, Brain organoid media, Liver organoid media [47] | Tissue-specific formulation containing nutrients, growth factors, signaling molecules | Tailored to specific organoid types; often include Noggin, R-spondin, EGF for intestinal organoids [45] |
| Cell Separation Matrices | Gentle dissociation enzymes, Accutase, Collagenase | Dissociates organoids into single cells while maintaining viability | Critical for creating single-cell suspensions for FACS purification |
| Editing Tools | Cas9 RNP complexes, Cas12a RNP complexes, donor templates [48] | Enables precise genetic modifications in stem cells | RNP complexes offer high editing efficiency with minimal off-target effects [48] |
| Selection Markers | Fluorescent proteins (EGFP, mCherry), antibiotic resistance genes | Identifies and isolates successfully edited cells | Clinical applications prefer non-antibiotic selection methods [48] |
| Vascularization Components | Endothelial cells, pericytes, angiogenic factors | Promotes formation of vascular networks within organoids | Addresses nutrient diffusion limitations and increases organoid size potential [47] [49] |
Signaling Pathways and Workflow Visualization
Organoid Generation and FACS Purification Workflow
Critical Signaling Pathways in Organoid Patterning
The integration of advanced 3D organoid culture systems with FACS purification technologies represents a significant advancement in the field of reprogramming strategy research. Organoids alone provide remarkable physiological relevance, but when combined with precise cell sorting capabilities, researchers can achieve unprecedented control over cellular composition and function. This synergistic approach addresses critical limitations in organoid technology, including heterogeneity, batch-to-batch variability, and incomplete maturation [47] [49].
The experimental data and protocols presented demonstrate that FACS-enhanced organoid workflows improve reproducibility while maintaining the biological complexity essential for meaningful functional outcomes assessment. As the field progresses toward standardized, scalable, and clinically predictive models [47], the integration of purification technologies will play an increasingly vital role in validating the functional consequences of different reprogramming strategies. These technological advances are expected to significantly enhance the predictive power of organoid-based assays for drug discovery and toxicology applications [47], ultimately accelerating the development of safer and more effective therapeutics.
Leveraging MicroRNAs and Nanoparticles for Targeted In Vivo Reprogramming
MicroRNAs (miRNAs) have emerged as powerful regulators of cell identity, offering a promising avenue for targeted in vivo reprogramming. These short non-coding RNAs can modulate complex gene networks by post-transcriptionally regulating hundreds of mRNA targets simultaneously. When combined with advanced nanoparticle delivery systems, miRNAs enable precise manipulation of cell fate for therapeutic purposes without genetic integration. This approach represents a paradigm shift in regenerative medicine and cancer therapy, allowing direct conversion of somatic cells into desired cell types or reprogramming of pathological cells into therapeutic phenotypes.
The fundamental advantage of miRNA-based reprogramming lies in its ability to orchestrate complex transcriptional changes through a single intervention. Unlike transcription factor-mediated reprogramming that often requires multiple viral vectors, specific miRNA combinations can simultaneously activate developmental programs and suppress alternative cell fates. Furthermore, nanoparticle delivery addresses critical challenges in therapeutic miRNA application, including physiological stability, targeted tissue delivery, and cellular uptake efficiency, making in vivo reprogramming clinically feasible.
Comparative Analysis of Reprogramming Strategies
Stem Cell-Derived Exosomes for Tissue Regeneration
Exosomes derived from various stem cell sources contain distinct miRNA profiles that influence their regenerative potential. Recent research has systematically compared exosomes from human induced pluripotent stem cells (hiPSCs), bone marrow mesenchymal stem cells (hBMSCs), and adipose tissue-derived stem cells (hADSCs) for cartilage regeneration [52].
Table 1: miRNA Profiles and Functional Properties of Stem Cell-Derived Exosomes
| Exosome Source | Highly Expressed miRNAs | Unique miRNAs | Functional Effects on Chondrocytes | Therapeutic Efficacy |
|---|---|---|---|---|
| hiPSC-Exos | miR-16-5p, miR-25-3p, miR-93-5p | 17 highly expressed miRNAs | Maintained viability, prevented senescence, promoted glycosaminoglycan and type II collagen formation | Lowest efficacy |
| hBMSC-Exos | miR-16-5p, miR-25-3p, miR-93-5p | 11 highly expressed miRNAs | Enhanced cartilage matrix formation, downregulated fibrocartilage matrix (type I collagen) | Greatest efficacy |
| hADSC-Exos | miR-16-5p, miR-25-3p, miR-93-5p | 13 highly expressed miRNAs | Similar effects to hBMSC-Exos but less potent | Intermediate efficacy |
The overlapping miRNAs (miR-16-5p, miR-25-3p, and miR-93-5p) identified across all three exosome types target genes including MAN2A1, ZNFX1, PHF19, GPR137C, ENPP5, B3GALT2, FNIP1, PKD2, and FBXW7, which are involved in cell growth, bone ossification, and cartilage development via the MAPK signaling pathway [52]. The superior performance of hBMSC-Exos highlights how the cellular origin of exosomes significantly influences their functional properties, despite sharing common miRNA constituents.
Direct Lineage Reprogramming Strategies
Direct lineage reprogramming bypasses pluripotent intermediates, converting somatic cells directly into target cell types. A novel approach for skin regeneration utilizes a two-factor combination (BMI1 + FGFR2b, termed "B2") to convert fibroblasts into induced keratinocyte-like cells (iKCs) [24].
Table 2: Direct Lineage Reprogramming Approaches for Tissue Regeneration
| Reprogramming Approach | Starting Cell Type | Reprogramming Factors | Target Cell Type | In Vivo Delivery | Functional Outcomes |
|---|---|---|---|---|---|
| B2 combination | Mouse fibroblasts | BMI1 + FGFR2b | Induced keratinocyte-like cells (iKCs) | AAV9 vectors | Promoted wound closure, reconstructed stratified epithelium, restored barrier function in diabetic mice |
| Traditional iPSC method | Fibroblasts | Oct4, Sox2, c-Myc, Klf4 | Keratinocytes via differentiation | Not applicable | Low efficiency, risk of tumorigenesis from pluripotent intermediates |
| Four-factor epithelial reprogramming | Wound-resident mesenchymal stromal cells | DNp63α, Grhl2, Tfap2a, c-Myc | Epithelial cells | Viral vectors | Contributed to new epidermal tissue regeneration |
The B2 reprogramming strategy demonstrated significant therapeutic effects in a diabetic mouse wound model, showing enhanced wound closure, stratified epithelium reconstruction, and restored barrier function, while markedly reducing mortality rates from ulcer-associated infections [24]. This approach exemplifies how minimal genetic manipulation can achieve functional tissue regeneration while avoiding the safety concerns associated with pluripotent intermediates.
Immune Cell Reprogramming for Cancer Therapy
Reprogramming tumor-associated macrophages (TAMs) from pro-tumoral M2 to anti-tumoral M1 phenotypes represents a promising cancer immunotherapy strategy. Multiple nanoparticle-based approaches have been developed to deliver reprogramming miRNAs to TAMs [53] [54] [55].
Table 3: Nanoparticle-Mediated Macrophage Reprogramming Strategies
| Reprogramming Strategy | Nanoparticle Platform | miRNA Payload | Targeting Mechanism | Therapeutic Outcomes |
|---|---|---|---|---|
| SIRPα-targeted LNP | Lipid nanoparticle with anti-SIRPα antibody | miR-155 | SIRPα binding on TAMs | Reprogrammed TAMs to pro-inflammatory phenotype, blocked CD47-SIRPα interaction, enhanced phagocytosis |
| miR-10a@H-MNP | RBC membrane-modified liposome with hyaluronic acid | miR-10a | CD44 targeting via hyaluronic acid | Restored mitochondrial respiration, increased histone acetylation, alleviated atherosclerosis in mice |
| Generic miRNA-LNP | Standard lipid nanoparticles | siRNA/miRNA | Passive targeting (EPR effect) | Gene silencing in TAMs, moderate phenotype switching |
The SIRPα-targeted LNP system achieved specific binding to TAMs through SIRPα recognition, while simultaneously blocking the CD47-SIRPα "don't eat me" signal and delivering miR-155 to reprogram macrophages toward an anti-tumoral phenotype [53]. These nanoparticles exhibited uniform size distribution (approximately 200 nm) with zeta potentials varying based on miRNA loading, demonstrating favorable physicochemical characteristics for in vivo delivery.
The miR-10a delivery system employed biomimetic coating with red blood cell membranes to evade immune clearance, coupled with hyaluronic acid for targeting pro-inflammatory macrophages in atherosclerotic plaques [54]. This approach successfully reprogrammed macrophage metabolism by restoring mitochondrial respiration and increasing histone acetylation (H3K9Ac), resulting in reduced atherosclerosis progression in male mice.
Experimental Protocols and Methodologies
Stem Cell Exosome Isolation and Characterization
The comparative analysis of stem cell-derived exosomes followed a standardized protocol [52]:
- Cell Culture: hiPSCs, hBMSCs, and hADSCs were cultured in 10% bovine exosome-depleted fetal bovine serum for 48 hours
- Exosome Collection: Exosomes were isolated from conditioned media using differential ultracentrifugation
- miRNA Profiling: Next-generation sequencing and bioinformatics analysis characterized small RNA profiles
- Functional Assays: Human articular chondrocytes were treated with exosomes for 12 days, assessing viability, senescence, and cartilage matrix formation
This methodology enabled direct comparison of exosomal miRNA cargo and its functional consequences, establishing correlations between miRNA signatures and regenerative potential.
Lipid Nanoparticle Formulation for miRNA Delivery
The preparation of targeted lipid nanoparticles for macrophage reprogramming followed these key steps [53]:
- Lipid Film Formation: 1,2-dioleoyl-sn-glycero-3-ethylphosphocholine, DC-Chol, DPhPE, and DSPE-PEG2000-maleimide were combined using thin-film hydration
- Antibody Conjugation: Anti-SIRPα antibody was conjugated to maleimide-functionalized lipids via thiol-maleimide chemistry
- miRNA Encapsulation: miR-155 was loaded into LNPs through electrostatic interactions
- Characterization: Particle size, zeta potential, and encapsulation efficiency were determined
The resulting miR-155@aSIRPα-LNP formulation achieved efficient TAM reprogramming through dual mechanisms: SIRPα-mediated targeting and miR-155-induced phenotype switching.
In Vivo Reprogramming for Wound Healing
The direct in vivo reprogramming protocol for diabetic wound healing involved [24]:
- Vector Preparation: AAV9 vectors encoding BMI1 and FGFR2b were produced
- Animal Model: Diabetic (db/db) mice with skin wounds received subcutaneous AAV9-B2 injections
- Assessment: Wound closure, epithelial stratification, and barrier function were evaluated over time
- Histological Analysis: Tissue samples were examined for keratinocyte markers and epidermal organization
This approach demonstrated the feasibility of in situ reprogramming without cell transplantation, addressing a major clinical challenge in chronic wound management.
Visualization of Key Mechanisms and Workflows
miRNA Reprogramming Mechanism in Macrophages
Diagram Title: miR-10a Reprogramming Mechanism in Macrophages
Experimental Workflow for Exosome miRNA Analysis
Diagram Title: Stem Cell Exosome miRNA Analysis Workflow
Targeted Nanoparticle Delivery to Macrophages
Diagram Title: Targeted Nanoparticle Delivery to Macrophages
Research Reagent Solutions for miRNA Reprogramming
Table 4: Essential Research Reagents for miRNA Reprogramming Experiments
| Reagent Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Stem Cell Sources | hiPSCs, hBMSCs, hADSCs | Exosome production with distinct miRNA profiles | Differential regenerative efficacy, tissue-specific signatures |
| Nanoparticle Components | EDOPC, DC-Chol, DPhPE, DSPE-PEG2000-maleimide | LNP formulation for miRNA delivery | Biocompatibility, high encapsulation efficiency, targetability |
| Targeting Ligands | Anti-SIRPα antibody, Hyaluronic acid | Cell-specific delivery | SIRPα for TAMs, CD44 for inflammatory macrophages |
| Reprogramming miRNAs | miR-155, miR-10a, miR-16-5p, miR-25-3p, miR-93-5p | Phenotype switching, fate conversion | Multi-target regulation, pathway modulation |
| Delivery Vectors | AAV9, Lentivirus | In vivo gene/miRNA delivery | High transduction efficiency, tissue tropism |
| Characterization Tools | NanoString miRNA Expression Assay, Seahorse Mitochondrial Stress Test | Functional validation | Multiplex miRNA profiling, metabolic analysis |
The strategic combination of specific miRNAs with advanced nanoparticle delivery systems has revolutionized targeted in vivo reprogramming approaches. The comparative data presented herein demonstrates that cellular origin, miRNA cocktail composition, and delivery methodology critically influence functional outcomes. Key findings indicate that hBMSC-derived exosomes outperform other stem cell sources for cartilage regeneration, while SIRPα-targeted LNPs and biomimetic miR-10a nanoparticles effectively reprogram macrophages in cancer and atherosclerosis contexts.
Future development in this field requires addressing several challenges: optimizing cell-specific targeting, enhancing endosomal escape efficiency, and minimizing off-target effects. Furthermore, comprehensive safety evaluations must accompany efficacy studies to ensure clinical translatability. The continued refinement of miRNA-nanoparticle platforms will undoubtedly expand the therapeutic landscape for regenerative medicine, cancer therapy, and treatment of degenerative diseases through precise in vivo reprogramming strategies.
Overcoming Reprogramming Hurdles: Addressing Safety, Efficiency, and Controllability
The application of human pluripotent stem cells (hPSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), in regenerative medicine presents a dual challenge: mitigating the risk of teratoma formation from residual undifferentiated cells and addressing the potential for premature death linked to systemic toxicity. Teratoma formation remains a significant safety hurdle in hPSC-based therapies, as even a small number of contaminating undifferentiated cells (as few as 10,000) can generate these tumors in vivo [56]. Simultaneously, studies on in vivo reprogramming have revealed that continuous induction of reprogramming factors can lead to hepatic and intestinal failure contributing to premature death, highlighting critical safety concerns that must be addressed [57]. This guide provides a comprehensive comparison of current strategies designed to overcome these challenges, presenting objective experimental data to inform researchers and drug development professionals.
Table 1: Comparison of Major Safety Strategies for hPSC-Based Therapies
| Strategy | Mechanism of Action | Reported Efficacy | Advantages | Limitations |
|---|---|---|---|---|
| Genetic Safeguards (NANOG-iCaspase9) | Inducible Caspase9 under NANOG promoter triggers apoptosis in pluripotent cells [56]. | >106-fold depletion of hPSCs; prevented teratoma formation in SCID mice [56]. | High specificity to pluripotent state; rapid activation (12-24 hours) [56]. | Requires genetic modification; potential for silencing or immune response. |
| Suicide Genes (HSV-TK/GCV) | Herpes simplex virus thymidine kinase converts ganciclovir to toxic metabolite in dividing cells [58]. | Effectively eliminated teratoma risk in hESCs; used in FDA-approved drugs [58]. | Clinically validated suicide gene system; scalable approach [58]. | Potential toxicity to differentiated cells; bystander effect [59]. |
| Chemical Inhibitors (LSD1/Survivin) | Small molecules (S2107, YM155) target epigenetic regulators or anti-apoptotic proteins essential for hPSC survival [60] [59]. | YM155 efficiently killed hiPSCs without toxicity to CD34+ cells; fully eradicated teratoma formation [59]. | No genetic modification required; works across multiple hPSC lines [60]. | Potential off-target effects on differentiated progeny; requires optimization of dosing. |
| Antibody-Based Depletion | Surface marker-based removal of undifferentiated hPSCs (e.g., SSEA-5, CD9, CD30) [58]. | Reduced teratoma risk in differentiating cultures [58]. | No genetic manipulation; can be applied to any hPSC line. | Limited by specificity of surface markers; some broadly expressed in differentiated tissues [58]. |
Genetic Safeguard Strategies
NANOG-Promoter Driven Suicide Systems
Experimental Protocol: Researchers have developed a highly specific system to eliminate undifferentiated hPSCs by knocking an inducible Caspase9 (iCaspase9) cassette and a fluorescent reporter (YFP) immediately downstream of the NANOG coding sequence using Cas9 RNP/AAV6-based genome editing. The NANOG, iCaspase9, and YFP genes are transcribed together but separated by T2A self-cleaving peptides, ensuring expression as three separate proteins. The iCaspase9 encodes a Caspase9-FKBPF36V fusion protein that dimerizes with the small molecule AP20187 (AP20) to induce rapid, irreversible apoptosis [56].
Key Experimental Data: This system demonstrated remarkable specificity and efficacy. Treatment with 1 nM AP20 for 24 hours led to a 1.75 × 106-fold depletion of undifferentiated hPSCs across seven independent experiments, exceeding the 5-log reduction considered necessary for clinical safety. The IC50 was determined to be 0.065 nM, and even 12 hours of treatment sufficed to eliminate hESCs. Critically, the system spared >95% of differentiated bone, liver, or forebrain progenitors, demonstrating its specificity for pluripotent cells [56].
HSV-Thymidine Kinase Approach
Experimental Protocol: An alternative genetic approach involves introducing a hyperactive variant of the herpes simplex virus thymidine kinase (HSV-TK) gene into the 3'-untranslated region of the endogenous NANOG gene via homologous recombination. This method leverages the fact that NANOG expression is highly specific to pluripotent cells. When exposed to ganciclovir (GCV), TK-expressing cells convert the prodrug to a toxic metabolite that incorporates into DNA, causing cell death [58].
Key Experimental Data: In SCID mice injected with engineered hESCs, daily intraperitoneal administration of GCV (10 mg/kg/day for 1-2 weeks) completely abolished teratoma formation. The system effectively eliminated the teratoma risk without apparent negative impact on differentiated cell types. This approach is particularly promising for clinical translation as thymidine kinase is already used in human gene therapy trials and is the target of FDA-approved drugs [58].
Diagram Title: Genetic Safeguard Mechanism for Selective Pluripotent Cell Elimination
Chemical and Pharmacological Approaches
Epigenetic Regulator Targeting
Experimental Protocol: Targeting epigenetic regulators represents a promising non-genetic approach to prevent teratoma formation. Research has demonstrated that lysine-specific demethylase 1 (LSD1) expression and function are tightly regulated in hiPSCs, and their deregulation underlies teratoma development. Using gain-of-function and loss-of-function approaches, researchers tested the LSD1 inhibitor S2157 for its ability to prevent teratoma formation [60].
Key Experimental Data: In immunodeficient mice transplanted with hiPSCs, administration of the LSD1 inhibitor S2157 successfully prevented teratoma formation. The study revealed that LSD1 functions at the initial step of tumorigenesis, making it an attractive target for preventing teratoma development from pluripotent cells. This epigenetic approach offers potential for clinical applications without requiring genetic modification of therapeutic cells [60].
Survivin Inhibition Strategy
Experimental Protocol: An alternative chemical approach involves targeting survivin, an anti-apoptotic protein highly expressed in pluripotent cells. Researchers compared the efficiency of hiPSC purge using the survivin inhibitor YM155 versus suicide gene approaches. The study specifically assessed the impact on hematopoietic stem cells (HSCs), which are often the therapeutic product in hematological applications [59].
Key Experimental Data: YM155 demonstrated superior efficiency compared to the iCaspase-9/AP20187 system for killing hiPSCs, without toxicity on CD34+ cells in vitro and in adoptive transfers. Importantly, hiPSC purge by survivin inhibitor fully eradicated teratoma formation in immunodeficient mice. In contrast, the AP20187 prodrug showed nonspecific toxicity on both iCaspase-9-negative hiPSCs and CD34+ cells, strongly impairing CD34+-derived human hematopoiesis in adoptive transfers [59].
Addressing Premature Death from In Vivo Reprogramming
Experimental Protocol: Research on in vivo reprogramming has revealed significant safety concerns. Using complementary genetic approaches, scientists demonstrated that continuous induction of OSKM (Oct4, Sox2, Klf4, c-Myc) factors in vivo leads to hepatic and intestinal dysfunction resulting in decreased body weight and contributing to premature death within one week [57].
Key Experimental Data: By generating a transgenic reprogrammable mouse strain that avoids OSKM expression in both liver and intestine, researchers reduced the early lethality and adverse effects associated with in vivo reprogramming. This modified approach allowed for longer-term continuous induction of OSKM with attenuated toxicity while still inducing a decrease in organismal biological age. This strategy provides a valuable model for understanding both rejuvenation and toxicity during in vivo reprogramming [57].
Diagram Title: In Vivo Reprogramming Toxicity and Mitigation Pathways
Table 2: Experimental Outcomes for Teratoma Prevention Strategies
| Strategy | Model System | Dosage/ Treatment | Efficacy Metrics | Toxicity Observations |
|---|---|---|---|---|
| NANOG-iCaspase9 | SCID mice with hPSC-derived teratomas [56] | 1 nM AP20187 for 24 hours | 1.75 × 106-fold hPSC depletion; >95% differentiated cells spared [56] | No apparent toxicity to differentiated derivatives; higher AP20 concentrations downregulated NANOG [56] |
| HSV-TK/GCV | SCID mice with hESC injection [58] | 10 mg/kg/day GCV for 1-2 weeks | Eliminated teratoma risk; no impact on differentiated cell types [58] | Widely used in human trials; FDA-approved drugs available [58] |
| LSD1 Inhibitor | Immunodeficient mice with hiPSCs [60] | S2157 inhibitor | Prevented teratoma formation from transplanted hiPSCs [60] | Targets epigenetic regulators at initial step of tumorigenesis [60] |
| Survivin Inhibitor | Immunodeficient mice with hiPSCs and CD34+ cells [59] | YM155 treatment | Fully eradicated teratoma formation; no toxicity to CD34+ cells [59] | Superior to suicide gene approaches; no impairment of hematopoiesis [59] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Safety Strategy Implementation
| Reagent / Tool | Function in Research | Example Applications |
|---|---|---|
| Inducible Caspase9 (iCaspase9) | Suicide gene system that induces apoptosis upon dimerization with AP20187 [56] | Selective ablation of undifferentiated hPSCs in NANOG-iCaspase9 systems [56] |
| HSV-Thymidine Kinase (TK) | Suicide gene that converts ganciclovir to toxic DNA-incorporating metabolite [58] | Elimination of TK-expressing hPSCs upon GCV exposure [58] |
| AP20187 | Dimerizing drug for iCaspase9 activation; synthetic ligand for FKBPF36V [56] | Activation of suicide mechanism in iCaspase9-engineered hPSCs; used at 1 nM concentration [56] |
| Ganciclovir (GCV) | Antiviral prodrug activated by HSV-TK phosphorylation [58] | Elimination of TK-expressing cells in suicide gene approaches; used at 10 mg/kg/day in mice [58] |
| YM155 | Chemical survivin inhibitor that targets anti-apoptotic pathway [59] | Selective killing of pluripotent cells without toxicity to CD34+ hematopoietic cells [59] |
| LSD1 Inhibitors (S2157) | Small molecule epigenetic modulators targeting lysine-specific demethylase 1 [60] | Prevention of teratoma formation by targeting epigenetic regulators essential for hiPSC tumorigenicity [60] |
The evolving landscape of safety strategies for stem cell therapies demonstrates significant progress in addressing both teratoma risk and systemic toxicity concerns. Genetic safeguard systems, particularly those leveraging pluripotency-specific promoters like NANOG, offer exquisite specificity and potency, with the NANOG-iCaspase9 system achieving greater than 106-fold depletion of undifferentiated hPSCs. Meanwhile, chemical approaches using LSD1 or survivin inhibitors provide non-genetic alternatives with demonstrated efficacy in preclinical models. The emerging understanding of in vivo reprogramming toxicity mechanisms further highlights the importance of tissue-specific control of reprogramming factors to mitigate systemic adverse effects. As the field advances, the integration of these safety strategies with improved differentiation protocols and delivery systems will be essential for translating the remarkable potential of pluripotent stem cells into safe, effective clinical therapies.
Reprogramming somatic cells to alternative fates represents a cornerstone of modern regenerative medicine and disease modeling. However, the transition from proof-of-concept studies to robust, clinically applicable protocols has been consistently hampered by the challenge of low conversion efficiency. The functional outcomes of different reprogramming strategies—whether for generating induced pluripotent stem cells (iPSCs), neurons, or other specialized cell types—are critically dependent on the precise combination of reprogramming factors and the culture environment that supports this fate transition. This guide systematically compares current reprogramming methodologies, providing researchers with experimentally-validated data on factor combinations and culture conditions to optimize conversion efficiency while maintaining cell quality and functionality.
Comparative Analysis of Reprogramming Methodologies
Non-Integrating Reprogramming Methods for iPSC Generation
The choice of delivery method for reprogramming factors significantly impacts both efficiency and safety profiles. A 2025 comparative analysis of the most prevalent non-integrating reprogramming methods provides crucial insights for method selection [3].
Table 1: Comparison of Non-Integrating iPSC Reprogramming Methods
| Method | Key Factors | Starting Cell Types | Relative Success Rate | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Sendai Virus (SeV) | OSKM (OCT3/4, SOX2, KLF4, c-MYC) | Fibroblasts, PBMCs | Significantly higher than episomal method [3] | High efficiency, minimal genomic damage as single-stranded RNA virus [61] | Requires biosafety level 2, viral clearance confirmation |
| Episomal Vectors | OSKM with sh-p53, hL-MYC, LIN28, EGFP | LCLs, Fibroblasts | Lower than SeV [3] | Non-viral, non-integrating | Lower efficiency, requires nucleofection [3] |
| Chemical Reprogramming | Small molecule cocktails | Blood cells, fibroblasts | Comparable to OSKMP-based approach in PBMCs [62] | Non-genetic, xeno-free conditions possible [63] | Complex multi-step optimization, cell type-specific variations |
Direct Lineage Conversion Approaches
Direct reprogramming bypasses the pluripotent state, converting one somatic cell type directly into another. Recent advances have demonstrated several optimized factor combinations for specific lineage conversions.
Table 2: Factor Combinations for Direct Lineage Reprogramming
| Target Cell Type | Source Cells | Key Transcription Factors | Additional Components | Efficiency | Functional Validation |
|---|---|---|---|---|---|
| Glutamatergic Neurons [61] | Peripheral blood T-cells | NEUROD1 + OSKM (5 factors total) | Sendai virus, Matrigel, MHM+StemFit medium with FBS | ~22.4% of surviving cells (βIII-Tubulin+) [61] | Calcium dynamics, electrophysiology, transcriptomic profiling [61] |
| Alveolar Epithelial-like Cells (iPULs) [7] | Mouse fibroblasts | Nkx2-1, Foxa1, Foxa2, Gata6 (4TFs) | 3D organoid culture, serum-free medium with Wnt activators | 2-3% of sorted cells (Sftpc+ Thy1.2- EpCAM+) [7] | Lamellar body structures, integration into alveolar surface in mouse model [7] |
| Cardiomyocyte-like Cells [63] | Human urine cells | 15 small molecule cocktail | Xeno-free conditions | 15.08% on day 30, 96.67% purity on day 60 [63] | Ventricular-like action potentials, calcium transients, improved cardiac function in MI models [63] |
Experimental Protocols for High-Efficiency Reprogramming
Sendai Virus-Based Neuronal Conversion from Blood Cells
The conversion of human peripheral blood cells into functional neurons represents a minimally invasive approach for patient-specific disease modeling. An optimized protocol demonstrates the critical importance of factor combination and culture conditions [61].
Workflow Overview:
Detailed Methodology:
- Starting Material Preparation: Isolate peripheral blood mononuclear cells (PBMCs) and stimulate T-cells using anti-CD3 antibody for expansion [61].
- Viral Transduction: Transduce stimulated T-cells with Sendai virus vectors expressing NEUROD1 combined with Yamanaka factors (OCT3/4, SOX2, KLF4, c-MYC) at multiplicity of infection (MOI) of 10 [61].
- Culture Conditions: Plate transduced cells on Matrigel-coated surfaces in Media Hormone Mix (MHM) supplemented with StemFit basal medium and 10% fetal bovine serum (FBS). FBS supplementation was found to increase neuron yield by 10-fold [61].
- Medium Optimization: Comparative assessment of basal media revealed that StemFit plus MHM yielded approximately 18-fold higher numbers of βIII-Tubulin-positive cells compared to MHM alone [61].
- Factor Optimization: The 5-factor approach (NEUROD1 + OSKM) demonstrated similar efficiency to the 8-factor approach (NEUROD1, ASCL1, BRN2/POU3F2, ZIC1 + OSKM), simplifying the protocol while maintaining efficacy [61].
Chemical Reprogramming of Human Blood Cells to Pluripotency
Chemical reprogramming offers a non-genetic alternative for generating pluripotent stem cells. A 2025 study established a robust protocol for converting blood cells to chemically induced pluripotent stem (hCiPS) cells [62].
Key Methodology:
- Cell Source Preparation: Isolate mononuclear cells from human cord blood (hCBMCs) or peripheral blood (hPBMCs). For finger-prick samples, collect ~100-200 μL blood into EDTA-containing capillary tubes [62].
- Chemical Cocktail Formulation: Employ a stepwise approach with small molecule combinations targeting epigenetic barriers and signaling pathways. The specific combination was not detailed in the available excerpt, but the method demonstrated higher efficiency compared to OSKMP-based approaches in hPBMCs [62].
- Culture System Optimization: Develop a specialized culture system supporting the transition from suspension blood cells to adherent PSCs, addressing previous challenges with cellular senescence and apoptosis [62].
- Efficiency Assessment: The protocol successfully generated hCiPS cells from fresh, cryopreserved, and minimal finger-prick blood samples, demonstrating reproducibility across donors and sample types [62].
Molecular Mechanisms and Signaling Pathways
The efficiency of cellular reprogramming is governed by the interplay of transcription factors, epigenetic modifiers, and signaling pathways that collectively overcome barriers to cell fate change.
Key Pathway Interactions:
- p53 Pathway Regulation: The p53 pathway serves as a critical barrier to reprogramming. OSKM-mediated reprogramming typically downregulates p53, while chemical reprogramming with the 7c cocktail upregulates this pathway, suggesting distinct mechanistic routes to pluripotency [13].
- Wnt Signaling Activation: 3D organoid culture systems for alveolar epithelial reprogramming utilize Wnt pathway activators to enhance efficiency, reflecting the importance of developmental signaling pathways in fate conversion [7].
- Metabolic Reprogramming: Successful reprogramming involves a shift from oxidative phosphorylation to glycolysis, with partial reprogramming protocols demonstrating reduction in mitochondrial ROS and restoration of younger metabolic patterns [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Optimizing Reprogramming Efficiency
| Reagent Category | Specific Examples | Function in Reprogramming | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT3/4, SOX2, KLF4, c-MYC (OSKM) [3] [61] | Core pluripotency induction | Sendai virus delivery shows highest efficiency [3] |
| Lineage-Specific TFs | NEUROD1 (neuronal) [61], Nkx2-1 (lung) [7] | Direct lineage specification | NEUROD1 with OSKM enables neuronal conversion from blood [61] |
| Small Molecules | 15-molecule cocktail for cardiomyocytes [63], 7c cocktail for partial reprogramming [13] | Epigenetic modulation, signaling pathway regulation | Enable non-genetic, xeno-free reprogramming [63] |
| Culture Matrices | Matrigel, iMatrix-511, laminin, fibronectin [61] | Structural support, signaling cues | Matrigel yielded highest neuron numbers in blood conversion [61] |
| Signaling Modulators | Y-27632 (ROCK inhibitor) [3], Wnt activators [7] | Enhance survival, promote specific differentiation | ROCK inhibitor critical post-thawing [3] |
| Media Formulations | mTeSR1 [3], MHM+StemFit [61], serum-free specialized media | Nutritional support, signaling maintenance | Media optimization crucial for efficiency [61] |
The comparative analysis of reprogramming strategies reveals several key principles for optimizing conversion efficiency:
- Method Selection Balance: Choose delivery methods that balance efficiency with safety considerations. Sendai virus offers highest efficiency for genetic approaches, while chemical reprogramming provides a promising non-genetic alternative [3] [62].
- Factor Combination Optimization: Simplified factor combinations can maintain efficiency while reducing complexity. The 5-factor neuronal conversion (NEUROD1+OSKM) performs equivalently to more complex combinations [61].
- Culture Condition Criticality: Significant efficiency gains are achievable through optimization of culture matrices, media formulations, and signaling pathway modulators. The 10-fold improvement with FBS supplementation in neuronal conversion highlights this potential [61].
- Cell Source Considerations: Minimally invasive sources like blood and urine cells provide viable alternatives to fibroblasts, with optimized protocols now achieving robust efficiencies [61] [63] [62].
These insights provide a framework for researchers to select and optimize reprogramming strategies based on specific application requirements, balancing efficiency, safety, and practicality for both basic research and clinical translation.
The fibrotic microenvironment presents a formidable barrier to drug delivery and efficacy, primarily constituted by two interconnected components: aberrant cytokine signaling and altered biophysical properties. Central to this process is the Transforming Growth Factor-beta (TGF-β) signaling pathway, a critical driver of fibrogenesis across multiple organs [64]. TGF-β activation promotes the transdifferentiation of quiescent cells, such as hepatic stellate cells (HSCs), into activated myofibroblasts that vigorously synthesize extracellular matrix (ECM) components [64]. This leads to the second key barrier component: increased ECM stiffness. The deposited matrix, rich in collagens and cross-linked proteins, creates a biomechanically stiff environment that not only physically impedes drug penetration but also actively promotes disease progression through mechanotransduction signaling [65]. This review comprehensively compares therapeutic strategies targeting these two barrier components, evaluating their functional outcomes in the context of reprogramming fibrotic microenvironments.
TGF-β Signaling Pathway: Mechanisms and Therapeutic Inhibition
The TGF-β signaling cascade encompasses both canonical (Smad-dependent) and non-canonical pathways. In the canonical pathway, TGF-β ligand binding activates receptor complexes that phosphorylate receptor-regulated Smads (R-Smads), primarily Smad2 and Smad3. These then complex with Smad4 and translocate to the nucleus to regulate profibrotic gene expression [64]. Non-canonical pathways include MAPK, PI3K/Akt, and Rho GTPase cascades, which interact with Smad signaling to coordinately regulate fibroblast proliferation and ECM remodeling [64]. In chronic liver diseases, viral hepatitis, fatty liver disease, and other injuries persistently activate TGF-β signaling, driving excessive ECM deposition that can progress to cirrhosis and hepatocellular carcinoma [64].
Comparative Analysis of TGF-β Inhibitory Strategies
Therapeutic inhibition of TGF-β signaling employs diverse approaches with varying mechanisms of action, developmental stages, and limitations. The table below provides a structured comparison of these strategies.
Table 1: Comparison of Therapeutic Strategies Targeting TGF-β Signaling
| Therapeutic Class | Representative Agents | Mechanism of Action | Development Stage | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Neutralizing Antibodies | Fresolimumab, Lerdelimumab | Bind and neutralize circulating TGF-β ligands | Clinical Trials | High specificity for TGF-β isoforms | Potential immune-related adverse events |
| Small Molecule Receptor Antagonists | Galunisertib, LY2157299 | Inhibit TGF-β receptor I kinase activity | Clinical Trials (some agents) | Oral bioavailability; targets intracellular signaling | Off-target effects on other kinases |
| Small Molecule Signaling Inhibitors | SB203580 (p38 inhibitor) | Inhibit non-canonical pathways (e.g., p38 MAPK) | Preclinical/Research | Can bypass resistance to direct receptor inhibition | Complex pathway interactions |
| Natural Compounds/Extracts | Pirfenidone, Hydronidone | Multiple targets including TGF-β pathway modulation | Approved/Clinical Trials (some) | Generally favorable safety profiles | Often pleiotropic mechanisms |
| Oligonucleotide-based Therapies | Antisense oligonucleotides | Target TGF-β mRNA for degradation | Preclinical/Research | High specificity for gene expression | Delivery challenges to target tissues |
Experimental Protocol: Assessing TGF-β Inhibition in 3D Fibrosis Models
Objective: To evaluate the efficacy of TGF-β inhibitors in a physiologically relevant 3D model of liver fibrosis.
Methodology Details:
- Cell Culture: Primary human hepatic stellate cells (HSCs) are cultured in 3D fibrin-based tubular constructs at a density of 500,000 cells/ml [66].
- Activation: HSCs are activated with 1 ng/ml recombinant TGF-β1 for 72 hours to induce myofibroblast transdifferentiation [66].
- Treatment: Test compounds (e.g., small molecule inhibitors, neutralizing antibodies) are applied at varying concentrations alongside TGF-β1 stimulation.
- Mechanical Conditioning: Constructs undergo incremental strain amplitude cyclic stretching (5% to 15% over 5 weeks) using a cyclic distension bioreactor (0.5 Hz frequency, 12.5% duty cycle) to mimic physiological mechanical stress [66].
- Outcome Measures:
- Protein Analysis: Western blotting for α-SMA, p-Smad2/3, total Smad2/3, and ERK phosphorylation at weeks 2, 5, and 7 [66].
- Biochemical Assays: Hydroxyproline assay for collagen content; ELISA for elastin quantification [66].
- Functional Assessment: Uniaxial tensile testing to determine ultimate tensile strength and elastic modulus [66].
ECM Stiffness: Mechanisms and Modulation Strategies
Biomechanical Properties in Fibrosis and Cancer
ECM stiffness is quantitatively measured by the elastic modulus, which characterizes a material's resistance to deformation [65]. In fibrotic progression, significant stiffening occurs: normal liver tissue exhibits stiffness <6 kPa, while fibrotic or cirrhotic liver can exceed 8-12 kPa [65]. This mechanical alteration creates a self-perpetuating cycle where stiffer matrices promote further fibroblast activation and ECM deposition. Key regulators of this process include the lysyl oxidase (LOX) family enzymes that catalyze collagen cross-linking, and Rho-associated protein kinase (ROCK) signaling that enhances matrix production and contractility [65].
Comparative Analysis of ECM Stiffness-Targeting Approaches
Therapeutic strategies aiming to normalize ECM stiffness employ various mechanisms ranging from enzymatic inhibition to mechanical disruption.
Table 2: Comparison of Therapeutic Strategies Targeting ECM Stiffness
| Therapeutic Approach | Representative Agents | Primary Mechanism | Development Stage | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| LOX Family Inhibitors | Simtuzumab, PXS-5156A | Inhibit collagen/elastin cross-linking | Clinical Trials/Preclinical | Reduces fundamental determinant of stiffness | Potential tissue integrity compromise |
| MMP Activators/Inducers | Unknown clinical candidates | Enhance MMP-mediated ECM degradation | Early Research | Promotes degradation of excess matrix | Risk of excessive matrix destruction |
| ROCK Pathway Inhibitors | Fasudil, Y-27632 | Inhibit ROCK signaling, reduce contractility | Preclinical/Research | Targets mechanotransduction signaling | Cardiovascular side effects |
| Hyaluronidase Therapy | PEGPH20 | Degrades hyaluronic acid matrix | Clinical Trials (pancreatic cancer) | Reduces barrier to drug penetration | Limited effect on collagenous matrix |
| Nanomedicine Approaches | Lipid nanoparticles, polymeric NPs | Improve drug penetration through stiff ECM | Preclinical/Clinical | Can be co-loaded with antifibrotics | Complex manufacturing, characterization |
Experimental Protocol: Measuring ECM Stiffness by Atomic Force Microscopy
Objective: To quantitatively assess the stiffness of ECM gels or tissues using atomic force microscopy (AFM).
Methodology Details:
- Sample Preparation: ECM gel is prepared from cultured MDA-MB-231 breast cancer cells or patient-derived fibroblasts to model the fibrotic microenvironment [67].
- AFM Setup: A commercial AFM system is equipped with a sharp tipped probe (nominal spring constant 0.1 N/m) for high-resolution nanomechanical mapping [67].
- Measurement Parameters: The PeakForce Quantitative Nanomechanical Mapping (QNM) mode is employed with the following settings:
- Peak force frequency: 1-2 kHz
- Peak force amplitude: 100-150 nm
- Scan rate: 0.5-1.0 Hz
- Resolution: 128×128 or 256×256 pixels per scan [67]
- Data Acquisition: Multiple regions (minimum 5) per sample are scanned to account for heterogeneity. For each region, at least 10 force-distance curves are collected at different positions.
- Analysis: The elastic (Young's) modulus is derived by fitting the retraction curve of force-distance measurements with the Hertzian contact model. Results are expressed as mean ± standard deviation [67].
Integrated Signaling Pathways in Fibrosis
The following diagram illustrates the core signaling pathways involved in TGF-β-mediated fibrosis and ECM stiffness, highlighting potential therapeutic intervention points:
Diagram Title: Integrated Signaling in Fibrosis and ECM Stiffness
The Scientist's Toolkit: Essential Research Reagents
This section details key reagents and their applications for investigating the fibrotic microenvironment.
Table 3: Essential Research Reagents for Fibrosis Studies
| Reagent/Category | Specific Examples | Primary Research Application | Key Functional Role |
|---|---|---|---|
| TGF-β Signaling Modulators | Recombinant TGF-β1, SB431542, SMAD7 overexpression constructs | TGF-β pathway manipulation | Activate or inhibit canonical TGF-β signaling for mechanistic studies |
| ECM Stiffness Modulators | LOX inhibitors (β-aminopropionitrile), Collagenase, ROCK inhibitors (Y-27632) | ECM biomechanics research | Modulate ECM cross-linking or cellular contractility to study mechanotransduction |
| Cell Culture Systems | Primary hepatic stellate cells, Human dermal fibroblasts, 3D fibrin gel constructs | In vitro fibrosis modeling | Provide physiologically relevant systems for studying fibrotic mechanisms |
| Signaling Antibodies | Phospho-Smad2/3, total Smad2/3, α-SMA, ERK1/2 | Protein expression analysis | Detect activation states of key signaling pathways and cellular phenotypes |
| Stiffness Measurement Tools | Atomic force microscopes, Collagen contraction assays, Traction force microscopy | Biomechanical assessment | Quantify ECM mechanical properties and cellular forces |
| Gene Expression Tools | SMAD3 siRNA, TIMP1 CRISPR/Cas9 constructs, MMP9 reporters | Genetic manipulation | Investigate specific gene function in fibrotic signaling networks |
The comparative analysis of TGF-β signaling inhibitors and ECM stiffness modulators reveals complementary therapeutic profiles. TGF-β inhibitors primarily target the * biochemical drivers* of fibrogenesis, potentially reversing the activation state of profibrotic cells [64]. In contrast, ECM stiffness modulators address the biophysical consequences of fibrosis, potentially improving drug delivery and disrupting mechanotransduction pathways [65]. Emerging approaches include nanomedicine strategies that combine TGF-β pathway inhibitors with ECM-penetrating delivery systems [68], and sequential treatment protocols where mechanical conditioning precedes biochemical modulation to optimize functional outcomes [66]. Future research should focus on personalized profiling of fibrotic microenvironment subtypes to match patients with optimal therapeutic combinations, ultimately overcoming this formidable barrier in chronic disease treatment.
The field of biomedical research has witnessed a paradigm shift in the development of mouse models, moving from conventional genetic approaches to sophisticated systems that offer unprecedented temporal and spatial control. The limitations of traditional methods, including embryonic lethality and compensatory developmental mechanisms, have driven the creation of innovative platforms that enable researchers to bypass these constraints with precision engineering [69]. This evolution has been particularly crucial for studying essential genes and modeling complex diseases, where timing, cell-type specificity, and inducible control are paramount for generating physiologically relevant data.
Current cutting-edge systems now integrate multiple technologies to achieve this precision, with the most advanced platforms combining tissue-specific promoters, inducible gene expression systems, and rapid protein degradation mechanisms. These innovations allow scientists to mimic human diseases with greater accuracy, investigate gene function in specific cell types, and perform target validation studies with reduced off-target effects [69] [70]. The development of these sophisticated tools reflects a broader thesis in reprogramming strategy research: that understanding functional outcomes requires experimental systems with control mechanisms that mirror the dynamic complexity of living organisms.
Comparative Analysis of Mouse Model Technologies
Modern genetically engineered mouse models (GEMMs) employ diverse technologies to achieve spatial and temporal control over gene expression and protein function. The table below compares four prominent approaches used in contemporary research.
Table 1: Comparison of Key Technologies for Advanced Mouse Models
| Technology | Key Mechanism | Temporal Control | Spatial Specificity | Primary Applications |
|---|---|---|---|---|
| Cre-loxP System | Cre recombinase excises DNA sequences between loxP sites [71] | Limited (depends on Cre delivery timing) | High (with tissue-specific promoters) [69] | Gene knockout studies, lineage tracing, target validation [69] |
| CRISPR-Cas9 GEMMs | Cas9 nuclease creates double-strand breaks guided by RNA [71] | Moderate (depends on delivery method) | Moderate to High (with targeted delivery) | Rapid disease modeling, cancer studies, multiplexed gene editing [71] |
| Degron Systems (AID2) | OsTIR1F74G ubiquitin ligase targets AID-tagged proteins with 5-Ph-IAA [70] | High (within hours) [70] | High (with tissue-specific Cre) [70] | Acute protein degradation, signaling pathway analysis, essential gene studies [70] |
| Degron Systems (S4D) | hCRBN ubiquitin ligase targets S4D-tagged proteins with pomalidomide [70] | Very High (within 2 hours) [70] | High (with tissue-specific Cre) [70] | Rapid protein depletion, kinetic studies, drug target validation [70] |
Quantitative Performance Metrics
The functional utility of these technologies can be evaluated through specific performance metrics, including efficiency, kinetics, and operational characteristics as demonstrated in experimental settings.
Table 2: Experimental Performance Metrics of Advanced Mouse Model Technologies
| Technology | Efficiency/ Efficacy | Kinetics | Key Advantages | Limitations/Challenges |
|---|---|---|---|---|
| Cre-loxP System | High (well-established) [71] | Slow (days to weeks for phenotype) | Flexible with large deleter mouse resources [69] | Time-consuming breeding, potential transcriptional deregulation [69] |
| CRISPR-Cas9 GEMMs | 100% tumor formation in KC mice with Ad-P-Cre [71] | Moderate (median 9.6 weeks for sarcoma) [71] | Rapid model generation, complex genetics modeling [71] | Potential off-target effects, clonal heterogeneity [71] |
| OsTIR1-AID2 System | 91% protein degradation in T cells [70] | Degradation within 2-8 hours; full recovery in 72 hours [70] | Low basal degradation, reversible, works for membrane proteins [70] | Requires tag insertion, ligand administration needed |
| hCRBN-S4D System | 94% protein degradation in T cells [70] | Degradation within 2 hours; recovery in 24 hours [70] | Very rapid kinetics, sharp degradation and recovery profile [70] | Solubility challenges with ligands, requires tag insertion [70] |
Experimental Protocols for Advanced Mouse Models
Protocol 1: Combined Cre-loxP and CRISPR-Cas9 System for Sarcoma Modeling
This protocol demonstrates the generation of primary soft tissue sarcomas using a combined approach that leverages the strengths of both Cre-loxP and CRISPR-Cas9 technologies [71].
Method Details:
- Mouse Strain Generation: Cross KrasLSL-G12D/+ (K) mice with Rosa26LSL-Cas9-EGFP/+ (C) mice to generate KrasLSL-G12D/+; Rosa26LSL-Cas9-EGFP/+ (KC) mice that conditionally express oncogenic Kras and Cas9 upon Cre-mediated recombination [71].
- Guide RNA Plasmid Construction: Clone sgRNA targeting Trp53 exon 7 into pX333 plasmid containing Cre recombinase (creating pX333-sgTrp53-Cre) or generate Adeno-sgTrp53-Cre (Ad-P-Cre) adenovirus for in vivo delivery [71].
- Tumor Initiation: Intramuscularly inject Ad-P-Cre adenovirus into KC mice to simultaneously activate KrasG12D expression and target Trp53 for mutagenesis [71].
- Monitoring and Validation: Monitor tumor development (onset typically 7.3-9.6 weeks), then validate through histopathological analysis (undifferentiated pleomorphic sarcoma predominance), Surveyor nuclease assay for indels, and Sanger sequencing to assess clonality [71].
Key Considerations: This approach generates autochthonous tumors that closely mimic human sarcomas in growth kinetics, histology, and mutational profiles compared to traditional Cre-loxP models, while offering significant time savings in model establishment [71].
Protocol 2: Inducible Protein Degradation in Specific Cell Lineages
This protocol utilizes degron systems for acute, inducible protein degradation in targeted cell types, enabling functional studies of essential proteins without developmental compensation [70].
Method Details:
- Degron Tagging: Use CRISPR/Cas9 to introduce S4D (87 bp, 29 aa) or mAID (210 bp, 70 aa) sequences into the gene of interest, creating a fusion protein susceptible to ligand-induced degradation [70].
- E3 Ligase Expression: Cross degron-tagged mice with Rosa26LSL-hCRBN or Rosa26LSL-OsTIR1 mice, then with appropriate tissue-specific Cre drivers (e.g., Cd4Cre for T cells, VavCre for hematopoietic lineages) [70].
- Ligand Administration:
- Kinetic Monitoring: Assess protein degradation and recovery using flow cytometry (for fluorescent tags), western blotting, or functional assays at multiple time points post-induction [70].
Key Considerations: The OsTIR1-AID2 system shows minimal basal degradation and relatively rapid recovery (72 hours), while the hCRBN-S4D system offers extremely sharp kinetics but requires optimized solvent formulations for consistent results [70].
Technological Workflows and System Architecture
The sophisticated mouse models discussed here integrate multiple genetic components in precise configurations. The following diagrams illustrate the key operational workflows for these systems.
Combined Cre-loxP and CRISPR-Cas9 Workflow
Diagram 1: Combined Cre-loxP/CRISPR-Cas9 Sarcoma Model Workflow. This integrated approach enables simultaneous oncogene activation and tumor suppressor mutagenesis for efficient sarcoma modeling.
Inducible Degron System Architecture
Diagram 2: Inducible Degron System Architecture. This system enables rapid, tissue-specific protein degradation through ligand-induced ubiquitination of degron-tagged proteins of interest (POI).
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these advanced mouse models requires specific genetic tools and chemical compounds. The table below catalogues key reagents referenced in the studies discussed.
Table 3: Essential Research Reagents for Advanced Mouse Models
| Reagent/Resource | Type | Function/Application | Example Uses |
|---|---|---|---|
| Cre-loxP System | Genetic Tool | Tissue-specific gene recombination [69] | Bypass embryonic lethality, study cell-type specific gene function [69] |
| CRISPR-Cas9 | Gene Editing | Somatic cell genome editing [71] | Rapid cancer modeling, multiplex gene editing [71] |
| Rosa26LSL-Cas9-EGFP | Mouse Strain | Conditional Cas9 expression [71] | Somatic cell editing in specific tissues [71] |
| Rosa26LSL-hCRBN | Mouse Strain | Conditional human cereblon expression [70] | S4D-tagged protein degradation with pomalidomide [70] |
| Rosa26LSL-OsTIR1 | Mouse Strain | Conditional OsTIR1F74G expression [70] | AID2-tagged protein degradation with 5-Ph-IAA [70] |
| 5-Ph-IAA | Chemical Ligand | Inducer for OsTIR1-AID2 system [70] | Acute protein degradation in AID2-tagged models [70] |
| Pomalidomide (POM) | Chemical Ligand | Inducer for hCRBN-S4D system [70] | Acute protein degradation in S4D-tagged models [70] |
| Adeno-sgTrp53-Cre | Viral Vector | Delivery of sgRNA and Cre recombinase [71] | Simultaneous gene editing and recombination in vivo [71] |
Discussion and Future Perspectives
The development of inducible, tissue-specific mouse models represents a significant advancement in our ability to study gene function and disease mechanisms with physiological relevance. The technologies discussed here each offer distinct advantages: traditional Cre-loxP systems provide well-established, reliable spatial control [69]; CRISPR-Cas9 enabled models facilitate rapid development and complex genetic modeling [71]; while degron systems offer unprecedented temporal precision for studying protein function [70]. The choice among these systems depends on the specific research question, with considerations for the required kinetics, reversibility, and spatial specificity.
These innovative control systems align with the broader thesis in reprogramming strategy research that emphasizes precision and physiological relevance. Just as in vivo reprogramming approaches aim to regenerate tissues by carefully controlling cell identity transitions [15], these mouse model technologies enable precise manipulation of gene expression and protein function to answer fundamental biological questions. The future of this field will likely see increased integration of these technologies, such as combining degron systems with CRISPR-based approaches for multi-level control of gene function. Additionally, further refinement of ligand delivery methods and the development of orthogonal degradation systems will expand the versatility of these platforms for studying complex biological processes and disease mechanisms.
Addressing Cellular Heterogeneity and Senescence in Aged Microenvironments
The aged tissue microenvironment is characterized by the accumulation of senescent cells, which are now recognized as a major driver of age-related functional decline and disease. However, a critical challenge in targeting these cells lies in their profound heterogeneity. Cellular senescence is not a monolithic state but a spectrum of phenotypes that vary dramatically based on cell type, inducing stressor, tissue location, and time [72] [73]. This heterogeneity extends to molecular markers, metabolic profiles, and secretomes, making universal targeting strategies ineffective.
Understanding this complexity is paramount for developing effective therapeutic interventions. While traditional markers like p16 and senescence-associated β-galactosidase (SA-β-gal) activity have been widely used, recent studies demonstrate that they lack universal specificity and sensitivity [72]. Furthermore, the discovery of distinct senescent cell populations marked by p21, uPAR, and GPNMB highlights the existence of multiple senescence phenotypes in vivo, each with potentially different functional impacts on the tissue microenvironment [72]. This guide systematically compares current and emerging strategies for characterizing and targeting heterogeneous senescent cell populations, with a focus on experimental data and methodologies directly applicable to preclinical research.
Comparative Analysis of Senescence Markers and Models
Beyond p16: A Spectrum of Senescence Markers
The reliance on p16 as a primary senescence marker has provided significant insights but has also limited our understanding of senescence heterogeneity. Recent research has identified several new markers that define unique subsets of senescent cells, each with distinct functional properties and responses to senolytics.
Table 1: Comparison of Key Cellular Senescence Markers and Their Heterogeneity
| Marker | Expression Context | Limitations/Specificity | Senolytic Response |
|---|---|---|---|
| p16INK4a | Cell cycle arrest; widely expressed in aged tissues | Not all p16high cells are senescent (e.g., pancreatic β-cells, macrophages); not all senescent cells express p16 [72] | Varies by cell type; targeted by multiple senolytics |
| p21CIP1 | p53-mediated arrest; DNA damage response | Defines a population distinct from p16high cells [72] | Clearance improves function in aged and obese mice [72] |
| uPAR | Identified from bulk RNA-seq of senescent models | Cell surface marker enabling immune targeting [72] | CAR T-cell elimination extends lifespan in cancer models [72] |
| GPNMB | Senescent vascular endothelial cells in atherosclerosis | Glycoprotein cell-surface marker [72] | Genetic elimination and vaccination improve age-related conditions [72] |
| SA-β-gal | Lysosomal enrichment in senescent cells | Can be present in non-senescent cells; activity varies by stressor (e.g., absent in hydroxyurea-induced senescence) [73] | Not a direct target for senolytics |
Stressor-Specific Senescence Phenotypes in Hepatocytes
The inducing stressor creates distinct senescence phenotypes, as demonstrated by a systematic study of primary mouse hepatocytes (PMH) and hepatocyte-derived organoids (HepOrgs) [73]. Different senescence inducers triggered unique combinations of senescence markers, SASP factors, and metabolic alterations, underscoring the necessity of defining senescence by its initiating context.
Table 2: Stressor-Specific Senescence Responses in Primary Mouse Hepatocytes [73]
| Senescence Inducer | SA-β-gal Activity | DNA Damage Response (γH2AX) | p53/p21 Activation | Key SASP Factors | Metabolic Shift |
|---|---|---|---|---|---|
| Doxorubicin (DNA damage) | Strong Increase | Strong Activation | Strong Activation | CCL2, IL-10 | Glycolysis to OxPhos |
| Cisplatin (DNA damage) | Strong Increase | Strong Activation | Strong Activation | CCL2, IL-10 | Glycolysis to OxPhos |
| H2O2 (Oxidative stress) | Strong Increase | Not Activated | p53/p21 Activated | CCL2, IL-10 | Not Reported |
| Etposide (DNA damage) | Not Reported | Not Activated | p53/p21 Activated | CCL2, IL-10 | Not Reported |
| BIBR-1532 (Telomerase inhibitor) | Strong Increase | Activation | Strong Activation | CCL2, IL-10 | Not Reported |
| Nutlin-3a (p53 activator) | Strong Increase | Activation | Strong Activation | CCL2, IL-10 | Not Reported |
| Hydroxyurea (Metabolism inhibitor) | No Effect | Not Activated | p53/p21 Activated | CCL2, IL-10 | Not Reported |
This stressor-specific heterogeneity has profound implications for therapeutic development. For instance, doxorubicin emerged as the most effective inducer of a comprehensive senescence phenotype, while other inducers created partial or atypical senescence states [73]. The SASP also varied, with CCL2 and IL-10 consistently upregulated across most modes of senescence, while Plasminogen Activator Inhibitor-1 was globally downregulated [73].
Spatial Heterogeneity in Aged Liver Microenvironments
The location of cells within a tissue creates another dimension of senescence heterogeneity. Spatial transcriptomics of the aging mouse liver revealed distinct zonation-specific aging patterns [74]. Pericentral areas accumulated large lipid droplets, while periportal hepatocytes exhibited decreased mitochondrial fitness, demonstrating that the same cell type ages differently depending on its spatial microenvironment [74].
These zonation-specific changes were driven by different transcriptional networks: Hnf4a and Foxa3 in periportal areas versus Cebp and Nr4a2 in pericentral zones [74]. This spatial heterogeneity in aging trajectories underscores that the tissue microenvironment exerts a powerful influence on how senescence manifests, which must be considered when designing targeted interventions.
Reprogramming Strategies to Counteract Senescence
Partial Reprogramming to Restore Youthful Epigenetics
Cellular reprogramming using Yamanaka factors (OCT4, SOX2, KLF4, c-MYC - OSKM) represents a promising strategy to reverse age-related cellular decline. Unlike full reprogramming to pluripotency, partial reprogramming applies these factors transiently to reset the epigenetic age of cells without completely altering cell identity [75] [76].
In senescent nucleus pulposus cells (NPCs), delivery of OKS (OCT4, KLF4, SOX2) via engineered exosomes (OKS@M-Exo) successfully ameliorated multiple senescence markers [75]. Treated cells showed:
- Reduced expression of p16INK4a, p21CIP1, and p53
- Decreased DNA damage (γH2A.X foci)
- Restored proliferation capacity (increased EdU incorporation)
- Improved metabolic balance with increased anabolism (Col2, Acan) and decreased catabolism (Mmp13, Adamts5) [75]
This epigenetic rejuvenation approach also demonstrated efficacy in vivo, mitigating intervertebral disc degeneration and associated pain in a rat model [75].
Mitochondrial Reprogramming and Heteroplasmy Shifts
Mitochondrial dysfunction is a key hallmark of aging, and the heteroplasmy (the ratio of mutant to wild-type mitochondrial DNA) significantly influences cellular aging trajectories. Reprogramming of human fibroblasts with heteroplasmic mtDNA mutations to induced pluripotent stem cells (iPSCs) resulted in a bimodal distribution of heteroplasmy - some clones largely cleared the mutations while others showed increased mutation loads [77].
iPSC clones with high levels of mtDNA deletion mutations exhibited:
- Altered growth dynamics
- Transcriptomic and metabolic shifts toward increased investment in neutral lipid synthesis
- Increased epigenetic age compared to isogenic clones without mutations [77]
This demonstrates that mitochondrial heteroplasmy is a critical factor in cellular aging and that reprogramming can either exacerbate or ameliorate this aspect of aging depending on the heteroplasmy outcome.
Figure 1: Partial Reprogramming Reverses Senescence. Transient expression of reprogramming factors (OKS) resets epigenetic aging marks and restores function in senescent cells without altering cellular identity [75].
Experimental Protocols for Senescence Research
Methodologies for Inducing and Analyzing Senescence
Protocol 1: Stressor-Specific Senescence Induction in Primary Cells [73]
- Cell Source: Primary Mouse Hepatocytes (PMH) isolated via collagenase perfusion
- Culture Conditions: William's E-medium with 2% FBS, L-glutamine, hepatocyte growth supplements
- Senescence Inducers and Concentrations:
- Doxorubicin (1 μM, 24h) - DNA damage
- Cisplatin (5 μg/mL, 24h) - DNA damage
- H₂O₂ (200 μM, 24h) - Oxidative stress
- BIBR-1532 (20 μM, 24h) - Telomerase inhibition
- Nutlin-3a (10 μM, 24h) - p53 activation
- Galactosamine (1 mM, 24h) - Metabolic stress
- Validation Assays: SA-β-gal staining, immunoblotting for p53/p21/γH2AX, SASP analysis via ELISA/qPCR, cellular bioenergetics via Seahorse Analyzer
Protocol 2: Partial Reprogramming of Senescent Cells [75]
- Reprogramming Factors: OKS (OCT4, KLF4, SOX2) delivered via Cavin2-modified exosomes (OKS@M-Exo)
- Target Cells: Senescent nucleus pulposus cells (replicative senescence model, passage 6)
- Key Readouts:
- Senescence markers: p16, p21, p53 expression (Western blot)
- DNA damage: γH2A.X foci count (immunofluorescence)
- Epigenetic marks: H4K20me3 and H3K9me3 levels
- Proliferation: EdU incorporation assay
- Metabolic balance: Anabolic (Col2, Acan) vs. catabolic (Mmp13, Adamts5) factors
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Senescence and Reprogramming Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Senescence Inducers | Doxorubicin, Cisplatin, H₂O₂, BIBR-1532, Nutlin-3a [73] | Inducing stressor-specific senescence in vitro | Concentration and exposure time critical for non-toxic senescence induction [73] |
| Senescence Detection | SA-β-gal kit, p16/p21 antibodies, γH2AX antibodies, SASP cytokine arrays [72] [73] | Comprehensive senescence phenotyping | No single marker is sufficient; combination required for reliable identification [72] |
| Reprogramming Tools | OKS/OSKM plasmids, Sendai virus, engineered exosomes [77] [75] | Cellular reprogramming and rejuvenation | Delivery method crucial for efficiency and safety; partial reprogramming requires temporal control [75] |
| Single-Cell Analysis | Single-cell/nucleus RNA-seq, spatial transcriptomics [72] [74] | Resolving senescence heterogeneity | snRNA-seq may better capture fragile senescent cells; spatial context preserves microenvironment [72] [74] |
| Metabolic Analysis | Seahorse Extracellular Flux Analyzer, lipidomics [77] [74] | Assessing metabolic reprogramming | Reveals shifts in glycolysis/OxPhos and lipid remodeling in senescence [74] |
The complex heterogeneity of cellular senescence in aged microenvironments demands a more sophisticated approach to therapeutic development. The research compared in this guide demonstrates that senescence is not a single target but a spectrum of cellular states influenced by origin, inducer, location, and time. Effective strategies must account for this diversity through multidimensional characterization and precision targeting.
The most promising approaches emerging from current research include:
- Marker-guided senolytics that target specific senescent subpopulations (e.g., uPAR- or GPNMB-positive cells)
- Partial reprogramming strategies that reset epigenetic aging without tumorigenic risk
- Metabolic interventions that reverse senescence-associated energetic deficits
- Spatially-informed approaches that account for zonation and microenvironmental influences
Future progress will depend on developing more comprehensive senescence atlases that integrate single-cell transcriptomics, epigenetics, and spatial mapping across tissues and aging timecourses. Such resources will enable the next generation of senotherapeutics that can precisely target the specific senescent cell populations driving pathology while sparing beneficial senescence involved in wound healing and tumor suppression.
Benchmarking Success: Comparative Analysis and Functional Validation of Reprogramming Outcomes
In vivo reprogramming, the process of converting one cell type into another within a living organism, represents a revolutionary frontier in regenerative medicine. The forced expression of key reprogramming factors, most notably Oct4, Sox2, Klf4, and c-Myc (collectively known as OSKM), has demonstrated remarkable potential for reversing age-associated phenotypes and repairing damaged tissues [78]. However, the functional outcomes of these interventions are profoundly influenced by a critical variable: the genetic background of the model organism used in research.
Mounting evidence indicates that strain-specific differences in mice significantly impact nearly all aspects of reprogramming research, from cellular response dynamics to pathological outcomes. These differences present both challenges and opportunities for researchers aiming to translate cellular reprogramming therapies into clinical applications. This comparative guide provides a systematic analysis of reprogrammable mouse models, offering experimental data and methodologies to inform model selection for specific research objectives in drug development and therapeutic innovation.
Comparative Analysis of Key Reprogrammable Mouse Strains
In Vivo Reprogramming Models
Table 1: Strain-Specific Characteristics in Reprogramming Research
| Mouse Strain | Genetic Features | Reprogramming Response | Key Advantages | Major Limitations |
|---|---|---|---|---|
| C57BL/6 | Standard inbred strain; less anxious profile | Standardized response; moderate efficiency | Well-characterized background; preferred for genetic modifications [79] | Less dramatic handling stress differences [79] |
| DBA/2 | Inbred strain; hippocampal dysfunction model [80] | Altered response dynamics; stable performance across tasks [81] | More stable performance in cognitive tasks [81] | Lower hippocampal neurogenesis; reduced LTP [80] |
| 129S1 | Higher susceptibility to infection [82] | Enhanced inflammatory response to challenge | Useful for infection and immune response studies [82] | Distinct basal inflammatory response [82] |
| K18-hACE2 | Transgenic expression of human ACE2 [82] | Protection during viral reinfection | Enables SARS-CoV-2 infection studies [82] | Systemic viral infection risk; high lethality [82] |
| BALB/c | Higher baseline anxiety; Th2 immune bias [79] | Pronounced stress responses | Strong humoral immune response; benefits markedly from tunnel handling [79] | High anxiety confounds behavioral measures |
Strain-Specific Functional Outcomes
Table 2: Quantitative Comparison of Strain Performance in Experimental Paradigms
| Experimental Context | C57BL/6 Performance | DBA/2 Performance | Significance Level |
|---|---|---|---|
| DNMTP Task Accuracy (with increasing delay intervals) | Pronounced accuracy decline [81] | Smaller decline; more stable performance [81] | Strain × delay interaction: P<0.05 [81] |
| Response Requirement Enhancement | Minimal performance improvement [80] | Significant performance improvement [80] | Strain × enhancement interaction: P<0.05 [80] |
| SARS-CoV-2 Reinfection (BA.1 then B.1.351) | Protected against morbidity [82] | Increased morbidity & lung damage [82] | Strain-dependent opposite outcomes [82] |
| Voluntary Interaction (tunnel vs. tail handling) | Moderate improvement with tunnel [79] | Dramatic improvement with tunnel [79] | Strain × method interaction: P<0.01 [79] |
Experimental Protocols for Assessing Strain-Specific Responses
In Vivo Reprogramming Induction Protocol
Objective: To evaluate strain-specific responses to OSKM factor expression in various mouse models.
Materials:
- Reprogrammable mouse strains (C57BL/6, DBA/2, etc.)
- Doxycycline-inducible OSKM expression system
- Control vectors (empty or reporter-only)
- Tissue collection supplies (fixatives, embedding materials)
Methodology:
- Genetic Engineering: Generate mouse strains with doxycycline-inducible OSKM expression cassettes, avoiding expression in specific organs when necessary for safety [78].
- Factor Induction: Administer doxycycline via drinking water (2 mg/mL) or chow (625 mg/kg) for controlled periods (typically 3-7 days for partial reprogramming).
- Cyclic Induction Protocol: Implement short-term induction cycles (e.g., 2 days on/5 days off) to mitigate detrimental effects observed with continuous expression [78].
- Monitoring: Track body weight daily, document survival rates, and observe for teratoma formation or loss of cellular identity.
- Tissue Collection: Harvest target organs (liver, pancreas, brain) at predetermined endpoints for histological and molecular analysis.
- Analysis: Assess reprogramming efficiency via immunohistochemistry (Nanog, SSEA-1) and RNA sequencing of collected tissues.
Key Considerations: Continuous OSKM expression raises safety concerns including teratoma formation, loss of cell identity, decreased body weight, and premature death. Strain-specific tolerance to these effects varies considerably and must be empirically determined [78].
Behavioral Assessment Protocol (DNMTP/DNMTP Tasks)
Objective: To quantify strain differences in spatial working memory, a key functional outcome of reprogramming interventions.
Materials:
- Operant conditioning chambers with nose-poke response keys [80]
- Food pellet reward system (20-mg precision pellets)
- Computer-controlled experimental interface
- Sound-attenuating enclosures
Methodology:
- Habituation: Acclimate mice to handling and testing chambers for 5-7 days.
- Initial Training: Train mice to complete a sequence of four nose-poke responses when keys are illuminated [80].
- DNMTP Training: Implement delayed nonmatching-to-position task where mice must select the opposite location of a previously presented sample stimulus after a delay period [80].
- DMTP Training: Implement delayed matching-to-position task where mice must select the same location as the sample stimulus.
- Variable Delays: Incorporate varying delay intervals (0-30 seconds) to assess memory retention.
- Data Collection: Record accuracy rates, response latencies, and completion rates across 40-trial sessions [80].
Key Analysis: Compare performance stability across strains, particularly the degree of accuracy decline with increasing delay intervals and response to enhanced sample trial requirements [81].
Signaling Pathways and Molecular Mechanisms
The OSKM reprogramming factors function through complex interconnected signaling networks that exhibit strain-specific modulation:
Figure 1: OSKM Reprogramming Pathway With Strain-Specific Modulation Nodes. The diagram illustrates how genetic background influences key reprogramming mechanisms including epigenetic remodeling, signaling pathway activation, and metabolic reprogramming, ultimately affecting functional outcomes.
Experimental Workflow for Comparative Strain Analysis
Figure 2: Workflow for Comparative Analysis of Reprogrammable Mouse Models. The process begins with strategic strain selection and proceeds through model generation, intervention, multi-modal assessment, and data integration to identify strain-specific response patterns.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Reprogramming Studies in Mouse Models
| Reagent/Category | Specific Examples | Function in Research | Strain Considerations |
|---|---|---|---|
| Reprogramming Factor Delivery | Doxycycline-inducible OSKM vectors; Sendai virus-based systems; mRNA reprogramming [83] | Induce pluripotency in somatic cells; enable controlled reprogramming | Strain-specific transduction efficiency; differential immune response to delivery method |
| Cell Culture Media | Pluripotency maintenance media; small molecule cocktails for chemical reprogramming [5] | Support stem cell growth and reprogramming; enhance efficiency | Strain-specific metabolic requirements; optimization needed for different genetic backgrounds |
| Differentiation Inducers | Growth factor combinations; small molecule differentiation inducers | Direct differentiation into specific lineages (neuronal, cardiac, hepatic) | Strain-dependent differentiation biases and efficiencies |
| Analysis Tools | Anti-Nanog, SSEA-1 antibodies; scRNA-seq reagents; epigenetic profiling kits | Assess reprogramming efficiency; characterize molecular changes | Strain-specific antigen recognition; genetic variant considerations in sequencing |
| In Vivo Monitoring | Bioluminescence reporters; in vivo imaging systems | Track reprogramming dynamics and teratoma formation in live animals | Strain-specific background signals; differential reporter expression |
| Metabolic Modulators | Glycolysis promoters; OxPhos inhibitors; hypoxia mimetics | Enhance reprogramming efficiency through metabolic manipulation [84] | Strain-specific metabolic baselines influence response to modulators |
The comparative analysis presented in this guide underscores a fundamental principle: genetic background systematically influences outcomes across all aspects of reprogramming research. The selection of an appropriate mouse strain should be guided by specific research objectives rather than convention or convenience.
For therapeutic reprogramming studies aimed at clinical translation, C57BL/6 models offer the advantage of extensive characterization and standardized responses. For neurological applications, DBA/2 strains provide insights relevant to hippocampal dysfunction, despite their cognitive limitations. For infection and immunity studies, 129S1 and K18-hACE2 models enable exploration of inflammatory responses and viral pathogenesis.
Future research directions should prioritize the development of strain-specific safety protocols, particularly regarding OSKM induction parameters that minimize pathogenic outcomes while maximizing rejuvenation benefits. Additionally, the field would benefit from standardized reporting of genetic backgrounds in publications to enhance reproducibility and meta-analysis capabilities.
Understanding these strain-specific responses enables more precise experimental design, more accurate interpretation of results, and ultimately, more successful translation of reprogramming therapies into clinical applications. The strategic selection of reprogrammable mouse models based on their distinctive characteristics will accelerate progress in regenerative medicine and therapeutic development.
Within the field of regenerative medicine, the functional maturation of induced cells remains a critical benchmark for translating reprogramming technologies into therapies. This guide provides a structured comparison of two pivotal functional outcomes: the electrophysiological maturity of induced cardiomyocytes (iCMs) and the surfactant production capability of induced pulmonary lung cells (iPULs). Research demonstrates that most stem-cell-derived cardiomyocytes structurally and functionally resemble neonatal rather than adult cells, underscoring the necessity of rigorous functional benchmarking [27]. Similarly, the ability of reprogrammed lung cells to produce and secrete functional pulmonary surfactant—a complex mixture of lipids and proteins essential for reducing alveolar surface tension—serves as a key indicator of successful phenotypic conversion for iPULs [85]. This guide objectively compares the experimental frameworks used to quantify these critical outcomes, providing researchers with standardized protocols and benchmarks for evaluating different reprogramming strategies.
Comparative Functional Benchmarking Tables
Benchmarking Table for iCMs
Table 1: Functional Electrophysiology Benchmarks for Induced Cardiomyocytes (iCMs)
| Functional Parameter | Immature iCM / Neonatal Phenotype | Mature Adult iCM Phenotype (Target) | Common Measurement Techniques |
|---|---|---|---|
| Spontaneous Beating Rate | High, irregular (>60 beats per minute) [27] | Low, stable (∼60-100 bpm for humans) [27] | Video recording, patch clamp, multi-electrode arrays (MEA) |
| Action Potential Morphology | Shorter duration, pace-like nodes [27] | Longer duration, ventricular-like morphology | Patch clamp (whole-cell) |
| Excitation-Contraction Coupling | Rudimentary, reliant on transsarcolemmal Ca2+ influx [27] | Mature, reliant on sarcoplasmic reticulum (SR) Ca2+ release | Patch clamp combined with Ca2+ imaging |
| Graft Arrhythmia Incidence | High post-transplantation [27] | Low post-transplantation | Electrocardiogram (ECG) in animal models |
| In Vivo Engraftment & Retention | Poor long-term survival in host tissue [27] | Stable, long-term engraftment | Bioluminescence/fluorescence imaging, histology |
Benchmarking Table for iPULs
Table 2: Functional Surfactant Production Benchmarks for Induced Pulmonary Lung Cells (iPULs)
| Functional Parameter | Low-Functioning iPUL / Progenitor Phenotype | High-Functioning iPUL Phenotype (Target) | Common Measurement Techniques |
|---|---|---|---|
| Phospholipid Composition | Low Phosphatidylcholine (PC), especially Dipalmitoylphosphatidylcholine (DPPC) content | High DPPC content (>50% of total phospholipids) [85] | Mass spectrometry, thin-layer chromatography |
| Surface Tension Reduction | Minimal reduction, fails to reach <10 mN/m | Achieves near-zero minimum surface tension during compression [85] | Pulsating Bubble Surfactometer, Wilhelmy Balance |
| Oxygenation Index (OI) | No significant improvement in animal models [86] | Significant improvement in arterial oxygenation | Blood gas analysis in animal models of ARDS |
| Response to Injury/Inhibitors | Susceptible to surfactant inhibition by blood proteins [85] | Resistant to inactivation by serum proteins | In vitro inhibition assays with albumin/fibrinogen |
| In Vivo Therapeutic Effect | No reduction in mortality in ARDS models [86] | Significant reduction in mortality [86] | Animal models of Acute Respiratory Distress Syndrome (ARDS) |
Experimental Protocols for Functional Assessment
Detailed Protocol for iCM Electrophysiology
The following protocol outlines the key steps for assessing the electrophysiological maturity of iCMs in vitro and in vivo.
- Cell Preparation: Differentiate hiPSCs into cardiomyocytes using established directed differentiation protocols. For patch clamp and MEA, plate cells on appropriate substrates (e.g., glass coverslips or MEA plates) and culture until consistent beating is observed.
- Patch Clamp Electrophysiology:
- Use a patch clamp setup with appropriate amplifiers and software.
- Employ the "whole-cell" configuration to record action potentials (APs) and ionic currents.
- Maintain cells at a physiological temperature (35-37°C).
- Perfuse with a Tyrode's solution containing (in mM): 140 NaCl, 5.4 KCl, 1 MgCl2, 1.8 CaCl2, 10 Glucose, 10 HEPES (pH 7.4 with NaOH).
- Fill borosilicate glass micropipettes (1.5-3 MΩ resistance) with an internal solution, typically containing (in mM): 120 K-Aspartate, 20 KCl, 1 MgCl2, 5 EGTA, 5 Mg-ATP, 10 HEPES (pH 7.2 with KOH).
- Analyze AP parameters: resting membrane potential, AP amplitude, and AP duration at 50% and 90% repolarization (APD50, APD90).
- Multi-Electrode Array (MEA) Analysis:
- Plate iCMs directly on MEA chips and culture until a confluent, synchronously beating monolayer forms.
- Connect the MEA to a recording system and maintain at 37°C with 5% CO2.
- Record extracellular field potentials for several minutes to capture beat rate, beat-rate variability, and field potential duration (a surrogate for APD).
- In Vivo Arrhythmia Assessment:
- Transplant iCMs into an immunodeficient murine model of myocardial infarction [27].
- Continuously monitor animals via telemetric ECG implants for several weeks post-engraftment.
- Quantify the incidence and duration of arrhythmic events, such as ventricular tachycardia, compared to control groups.
Detailed Protocol for iPUL Surfactant Function
The following protocol details the methodology for evaluating surfactant production and function from iPULs.
- Surfactant Isolation:
- Culture iPULs at an air-liquid interface (ALI) to promote mature alveolar type II cell phenotype.
- Harvest surfactant from the apical surface of the cultures by washing with a saline solution.
- Concentrate the lavage fluid via ultracentrifugation at 40,000 x g for 1 hour at 4°C. The resulting pellet contains the surfactant concentrate.
- Biochemical Composition Analysis:
- Extract lipids from the surfactant concentrate using a chloroform-methanol mixture.
- Separate phospholipids via thin-layer chromatography (TLC).
- Quantify the percentage of total phosphatidylcholine and its saturated form, DPPC, using phosphorous assay or mass spectrometry.
- Surface Activity Measurement (Pulsating Bubble Surfactometer):
- Resuspend the isolated surfactant in a saline buffer at a concentration of 2-5 mg phospholipid/mL.
- Load the sample into the chamber of the pulsating bubble surfactometer.
- Create a bubble in the sample and pulsate it at a rate of 20 cycles per minute between maximum (0.55 mm) and minimum radius.
- Measure surface tension at the air-liquid interface.
- Record the minimum surface tension achieved after 5-10 minutes of pulsation. A functionally competent surfactant will achieve a surface tension below 5-10 mN/m.
- In Vivo Therapeutic Efficacy:
- Utilize an animal model (e.g., rodent) of acute respiratory distress syndrome (ARDS) induced by saline lavage or bleomycin injury.
- Administer the isolated iPUL-derived surfactant via intratracheal instillation. The MIST (Minimally Invasive Surfactant Therapy) method, which uses a fine catheter, is a effective and low-risk delivery technique [87].
- Measure the primary outcome of mortality rate. Secondary outcomes include oxygenation index (OI) from blood gas analysis and the number of days without mechanical ventilation [86].
Visualizing Signaling and Workflows
iCM In Vivo Reprogramming Pathway
iPUL Surfactant Adverse Outcome Pathway
Functional Benchmarking Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Functional Benchmarking Studies
| Reagent / Tool | Function in iCM Research | Function in iPUL Research |
|---|---|---|
| Sendai Virus (SeV) Vectors | Efficient, non-integrating delivery of reprogramming factors (e.g., OCT4, SOX2) [3]. | Delivery of transcription factors for pulmonary differentiation. |
| Episomal Vectors | Non-integrating alternative for factor delivery; lower efficiency than SeV [3]. | Non-integrating gene delivery for reprogramming. |
| Y-27632 (ROCK Inhibitor) | Enhances survival of hiPSCs and dissociated hiPSC-CMs post-thawing and during passaging [3]. | Improves viability of primary pulmonary cells in culture. |
| mTeSR1 Medium | Defined, feeder-free maintenance medium for pluripotent stem cells [3]. | Not typically used. |
| Pulsating Bubble Surfactometer | Not applicable. | Gold-standard instrument for measuring surface tension dynamics of surfactant [85]. |
| Air-Liquid Interface (ALI) Culture | Not applicable. | Critical for driving terminal maturation of alveolar epithelial cells, including surfactant production. |
| Patch Clamp Electrophysiology Rig | Gold-standard for measuring action potentials and ionic currents in iCMs [27]. | Not typically used for iPUL functional assessment. |
| Multi-Electrode Array (MEA) System | Non-invasive, long-term recording of extracellular field potentials and beat rate of iCM monolayers. | Not applicable. |
The development of novel reprogramming strategies represents a frontier in regenerative medicine, offering potential treatments for conditions ranging from neurodegenerative diseases to organ failure and fibrotic scarring. However, the transition of these therapies from laboratory research to clinical application hinges on the rigorous and quantitative assessment of their in vivo functional outcomes. For researchers and drug development professionals, evaluating the success of an intervention requires moving beyond simple markers of cell survival to demonstrate meaningful integration into existing tissues, reduction of scar burden, and, ultimately, the recovery of native organ function. This guide provides a comparative analysis of the current methodologies used to measure these critical endpoints, framing them within the broader thesis that functional integration is the key determinant of therapeutic success. We objectively compare the performance of various measurement technologies and experimental protocols, supported by quantitative data, to inform the design of robust preclinical studies.
Measuring Cellular Integration
Cellular integration refers to the ability of newly introduced or reprogrammed cells to structurally and functionally connect with the host's existing tissue architecture. This is a paramount endpoint for therapies targeting the central nervous system (CNS) and other complex organs.
Comparative Analysis of Integration Measurement Techniques
The table below summarizes the primary methods for evaluating cellular integration, highlighting their respective applications, outputs, and limitations.
Table 1: Comparison of Methods for Measuring Cellular Integration
| Method | Primary Application | Key Measurable Outcomes | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Spatial Transcriptomics (e.g., PERTURB-CAST) [88] | Mapping perturbation localization and transcriptomic changes within tissue architecture. | - Spatial distribution of reprogrammed cells.- Co-localization of barcodes/perturbations with phenotypic gene signatures.- Clonal relationships and tumor heterogeneity. | Integrates perturbation mapping with whole-transcriptome data on a standard platform (10X Visium). | Requires specialized barcoded constructs; complex data analysis requiring Bayesian models [88]. |
| Lineage Reprogramming & Circuit Analysis [89] | Assessing the functional incorporation of resident, reprogrammed neurons. | - Location of new neurons within native cytoarchitecture.- Restoration of circuit output (e.g., via electrophysiology).- Behavioral recovery in animal models. | Generates neurons that are already resident in the correct circuitry; autologous source avoids immune rejection [89]. | Limited control over the exact number of recruited cells; efficacy can be influenced by aging and disease milieu [89]. |
| Exogenous Grafting (hESC/iPSC-derived) [89] | Evaluating the integration of transplanted neuronal populations. | - Graft survival, dispersion, and vascularization.- Electrophysiological synaptic activity with host neurons.- Dopamine release (for Parkinson's models). | High control over cell type, purity, and validation pre-grafting; suitable for bulk population replacement [89]. | Risk of immune rejection (unless autologous or HLA-matched); poor dispersion in adult/aged CNS [89]. |
Experimental Protocol: Spatial Mapping of Combinatorial Perturbations
The PERTURB-CAST protocol exemplifies a cutting-edge method for simultaneously tracking multiple interventions and their phenotypic effects in vivo [88].
1. Experimental Design:
- Objective: To spatially link complex genetic alterations to critical disease phenotypes within a tumor ecosystem.
- Model System: Autochthonous mosaic liver cancer model in mice, generated via hydrodynamic-tail-vein (HDTV) injection of a pooled plasmid library [88].
2. In Vivo Intervention:
- Tools: Random Unique Barcode Integration Combinatorics (RUBIX) using a Sleeping Beauty transposon system.
- Procedure: A pool of molecular-barcoded plasmids (e.g., encoding 8 different perturbations: oncogene overexpression or tumor suppressor silencing) is injected via HDTV. This generates a mosaic of genetically diverse tumor clones in a single liver [88].
3. Tissue Processing and Data Acquisition:
- Sample Collection: Tumors are harvested and processed into formalin-fixed paraffin-embedded (FFPE) sections.
- Spatial Transcriptomics: Sections are placed on 10X Visium slides. The key innovation is the use of redeployed, pre-existing RTL probes (normally for chemosensory receptors) to capture the engineered 50-nt barcodes on the perturbation plasmids. This allows for simultaneous mapping of perturbation locations and transcriptome-wide phenotyping on a single, standard platform [88].
4. Data Analysis:
- Barcode Decoding: A variational Bayesian model is used to account for technical variability and assign perturbation identities to each tumor nodule based on the triplet barcode arrays [88].
- Phenotype Correlation: The spatial transcriptomic data is analyzed to correlate specific perturbation combinations with gene expression signatures, tumor microenvironment changes, and other phenotypic readouts.
Figure 1: Workflow for Spatial Mapping of In Vivo Perturbations. HDTV: Hydrodynamic-Tail-Vein Injection; RUBIX: Random Unique Barcode Integration Combinatorics; FFPE: Formalin-Fixed Paraffin-Embedded; RTL: RNA-Templated Ligation.
Quantifying Scar Reduction
Scarring, or fibrosis, is a common endpoint of aberrant tissue repair. Accurate quantification of scar reduction is crucial for evaluating therapies in dermatology, wound healing, and internal organ fibrosis.
Comparative Analysis of Scar Quantification Techniques
The table below compares methods for assessing scar reduction, from clinical scales to advanced hemodynamic measurements.
Table 2: Comparison of Methods for Quantifying Scar Reduction
| Method | Primary Application | Key Measurable Outcomes | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Diffuse Correlation Spectroscopy (DCS) [90] | Non-invasive monitoring of microvascular blood flow (BF) in scars. | - Microvascular blood flow (BF).- Power spectral density (PSD) of blood flow.- Quantitative % change post-therapy. | Provides quantitative, real-time hemodynamic data; sensitive to immediate treatment effects (e.g., BF reduced by 43.27% for vasoconstriction laser therapy) [90]. | Primarily assesses vascularity; does not directly measure collagen architecture. |
| Laser Therapies (Ablative/Non-Ablative) [91] | Treating and monitoring atrophic acne scars. | - Scar volume reduction (e.g., 75% of patients with picosecond laser).- Histological collagen density and organization.- Patient and Observer Scar Assessment Scale (POSAS). | Wide range of validated devices; can be combined with imaging for outcome tracking [91]. | Invasive with risk of side effects (erythema, hyperpigmentation); outcomes are device- and operator-dependent. |
| Clinical Scar Scales (POSAS, VSS) [92] | Subjective clinical assessment of scar quality. | - Pigmentation, vascularity, thickness, relief, pliability.- Patient-rated itch and pain. | Fast, low-cost, and widely used in clinical trials [92]. | Subjective and prone to inter-observer variability; lacks molecular or biomechanical data. |
| Fractional Radiofrequency Microneedling (FRMN) [91] | Treating atrophic scars and assessing remodeling. | - Microchannel-induced neocollagenesis.- HSP70/MMP-3 upregulation for ECM reorganization.- Reduction in scar volume and improved texture. | Combines mechanical and thermal injury; safer for darker skin types (Fitzpatrick IV-VI) [91]. | Invasive procedure; mechanistic outcomes require molecular biology techniques for validation. |
Experimental Protocol: Quantitative Hemodynamic Evaluation of Scars
This protocol utilizes DCS to objectively measure the microvascular response to laser therapy, a key indicator of scar remodeling [90].
1. Pre-Treatment Baseline Measurement:
- Tool: Custom-built or commercial DCS device.
- Procedure: The DCS probe is placed on the target scar tissue. The device emits near-infrared light, and the fluctuating speckle pattern of scattered light is analyzed to calculate a blood flow index (BFI) and its power spectral density (PSD) [90].
2. Therapeutic Intervention:
- Intervention: Application of laser therapy. The protocol can be designed to test different laser types:
- Vasoconstriction Laser: Aimed at reducing scar blood flow.
- Vasodilation Laser: Aimed at promoting blood flow and healing [90].
3. Immediate Post-Treatment Measurement:
- Procedure: The DCS probe is repositioned on the same scar area immediately after laser therapy to record changes in BFI and PSD.
4. Data Analysis and Validation:
- Quantitative Comparison: Calculate the percentage change in BF and PSD from baseline.
- Example Data: One study reported a 43.27% reduction in BF and a 72% reduction in PSD for vasoconstriction treatment, and a 338.73% increase in BF and 917% increase in PSD for vasodilation treatment [90].
- Correlation: These quantitative hemodynamic changes can be correlated with longer-term clinical outcomes, such as improvements in POSAS or VSS scores.
Assessing Organ Function Recovery
The ultimate goal of many regenerative therapies is the restoration of physiological function to a failing organ. This requires sophisticated models and direct functional assays.
Comparative Analysis of Organ Function Assessment Models
The table below contrasts different models used to evaluate the recovery of organ function following therapeutic intervention.
Table 3: Comparison of Models for Assessing Organ Function Recovery
| Model / Method | Primary Application | Key Measurable Outcomes | Key Advantages | Key Limitations |
|---|---|---|---|---|
| In Vivo Reprogramming (e.g., Heart) [15] | Regenerating functional tissue in situ. | - Generation of new, functional heart muscle (contractility).- Improvement in ejection fraction and other hemodynamic parameters.- Integration with host cardiac conduction system. | No cell transplantation needed; avoids lab-associated contamination risks [15]. | High risk of off-target effects and tumorigenesis (teratomas) if reprogramming is imprecise; no way to screen out undesired cells in vivo [15]. |
| Machine Perfusion (MP) of Organs [93] | Ex vivo assessment and repair of donor organ viability. | - Vascular resistance, bile production (liver), urine production (kidney).- Oxygen consumption, lactate levels, ATP synthesis.- Post-transplant outcomes: Primary Non-Function (PNF), Delayed Graft Function (DGF). | Enables viability assessment and therapeutic repair of marginal organs; mitigates ischemia-reperfusion injury [93]. | Technically complex and expensive; risk of organ waste if preservation fails [93]. |
| Lab-Grown Organoid Implants [94] | Functional replacement of damaged tissues. | - Physiological performance (e.g., insulin secretion from pancreatic islets).- Vascularization and integration post-implantation.- Reduction in patient rehabilitation time. | Patient-specific cells possible; addresses donor organ shortage; demonstrates potential for true biological restoration [94]. | Immature organoid structure; challenges with scaling and full vascularization; largely preclinical [94]. |
| Subzero Non-freezing Preservation [93] | Extending viable preservation time for transplantation. | - Organ survival rate post-transplantation.- Recovery of function (e.g., urogenesis in kidneys).- Intracellular ATP levels, endothelial cell damage. | Extends preservation time significantly (e.g., 48+ hours for livers) [93]. | Risk of freezing injury; requires specialized cryoprotectant solutions; delayed functional recovery in some models [93]. |
Experimental Protocol: Ex Vivo Machine Perfusion for Organ Repair and Assessment
Machine perfusion has emerged as a powerful platform not only for organ preservation but also for evaluating and actively improving the function of marginal organs prior to transplantation [93].
1. Organ Procurement and Cannulation:
- Procedure: A donor organ (e.g., liver, kidney) is procured using standard surgical techniques. The main arterial, venous, and ductal structures are cannulated.
2. Connection to Perfusion Device:
- Equipment: A machine perfusion device that controls temperature, flow, pressure, and perfusion solution composition.
- Modalities:
- Hypothermic Machine Perfusion (HMP): Preservation at 4-10°C to slow metabolism.
- Subnormothermic Machine Perfusion (SNMP): Preservation at 20-30°C, allowing for some metabolic activity and potential repair [93].
3. Viability Assessment During Perfusion:
- Key Functional Parameters:
- Vascular Function: Measure vascular resistance. A steady decrease indicates vasodilation and improved microcirculation.
- Metabolic Function: Analyze perfusate for lactate clearance and pH stabilization. Rising glucose consumption and ATP levels indicate active metabolism.
- Organ-Specific Function:
- Liver: Bile production, clearance of transaminases.
- Kidney: Urine production, fractional excretion of sodium [93].
4. Active Repair and Therapeutic Intervention:
- Potential Therapies: The perfusion circuit can be used as a delivery system for therapeutics:
- Drugs: Antibiotics, anti-inflammatory agents.
- Gene Therapies: siRNA or miRNA to knock down pathogenic genes [93].
- Cellular Therapies: Delivery of mesenchymal stem cells.
5. Outcome Correlation:
- Validation: The viability parameters measured during MP are strongly correlated with post-transplant outcomes, such as the incidence of Delayed Graft Function (DGF) and Primary Non-Function (PNF) [93].
Figure 2: Workflow for Ex Vivo Organ Assessment and Repair via Machine Perfusion. ECD: Extended Criteria Donor; HMP: Hypothermic Machine Perfusion; SNMP: Subnormothermic Machine Perfusion.
The Scientist's Toolkit: Essential Reagents and Materials
This section details key reagents and technologies critical for conducting the experiments described in this guide.
Table 4: Essential Research Reagents and Solutions for In Vivo Functional Outcomes
| Tool / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| Barcoded Plasmid Libraries [88] | Enables multiplexed tracking of combinatorial genetic perturbations in vivo. | Used in RUBIX system with Sleeping Beauty transposon; contains triplet barcode arrays for robust detection with PERTURB-CAST [88]. |
| Spatial Transcriptomics Platform [88] | Captures genome-wide gene expression data while retaining spatial location in a tissue section. | 10X Visium platform; PERTURB-CAST redeploys RTL probes to hijack the system for perturbation barcode mapping [88]. |
| Diffuse Correlation Spectroscopy (DCS) Device [90] | Non-invasively quantifies microvascular blood flow in scars and tissues in real-time. | Custom-built or commercial systems; provides quantitative metrics like Blood Flow (BF) and Power Spectral Density (PSD) [90]. |
| Machine Perfusion System [93] | Maintains organs ex vivo in a near-physiological state for preservation, assessment, and repair. | Systems for Hypothermic (HMP) and Subnormothermic (SNMP) perfusion; allows measurement of vascular resistance and metabolic parameters [93]. |
| Cryopreservation & Supercooling Solutions [93] | Enables long-term storage or subzero non-freezing preservation of cells, tissues, and organs. | Contain cryoprotective agents (CPAs) like glycerol, trehalose, PEG; vitrification techniques use high CPA concentrations for ice-free preservation [93]. |
| Lineage Reprogramming Factors [89] | Directly converts resident non-neuronal cells (e.g., astrocytes) into functional neurons in vivo. | Typically delivered via viral vectors (e.g., lentivirus, AAV); a key alternative to exogenous cell grafting for neuronal replacement [89]. |
The efficacy and functional outcomes of cellular reprogramming and therapeutic gene delivery are fundamentally shaped by the choice of delivery strategy. Viral vectors, non-viral vectors, and small-molecule based approaches constitute the primary paradigms for inducing genetic or cellular changes, each with distinct mechanisms and implications for research and therapy. Viral vectors leverage evolved biological machinery for high-efficiency delivery, while non-viral vectors offer synthetic versatility and enhanced safety. Concurrently, small molecules provide a non-genetic alternative for modulating cellular pathways and enhancing endogenous processes. This guide provides a comparative analysis of these strategies, focusing on their efficacy, experimental support, and practical application in reprogramming and drug development. Framed within broader research on functional outcomes, this comparison equips scientists with the data and methodologies necessary for informed platform selection.
Comparative Analysis of Delivery and Reprogramming Approaches
The table below summarizes the core characteristics, advantages, and limitations of viral, non-viral, and small-molecule approaches, providing a high-level overview for initial strategy evaluation.
Table 1: Overall Comparison of Viral, Non-Viral, and Small-Molecule Approaches
| Feature | Viral Vectors | Non-Viral Vectors | Small Molecules |
|---|---|---|---|
| Primary Mechanism | Transduction via viral capsid; genetic material delivery [95] [96] | Electrostatic complexation/cellular delivery of nucleic acids [95] [97] | Pharmacological modulation of endogenous signaling pathways and cellular processes [98] [99] |
| Key Advantage | High transduction efficiency and sustained long-term expression [95] [96] | Superior safety profile (low immunogenicity, no insertional mutagenesis), large cargo capacity [95] [97] | Non-genetic, reversible action; ease of manufacturing and administration; can enhance host cell productivity [99] |
| Key Limitation | Immunogenicity, complex and costly manufacturing, limited cargo capacity [95] [97] | Lower gene transfer efficiency, low target specificity, complex formulation for some types [95] | Potential off-target effects, limited sustained effect without continuous presence, requires well-defined targets [99] |
| Typical Applications | In vivo and ex vivo gene therapy, gene replacement [95] [96] | mRNA vaccines, ex vivo cell modification, siRNA delivery [95] [97] | Inducing pluripotency, modulating immune responses, enhancing productivity of engineered cells [98] [99] |
In-Depth Efficacy and Functional Outcome Comparison
A direct comparison of quantitative performance metrics is critical for evaluating the functional outcomes of these strategies. The following table consolidates key efficacy data from preclinical and clinical studies.
Table 2: Comparative Efficacy and Performance Metrics
| Parameter | Viral Vectors | Non-Viral Vectors | Small Molecules |
|---|---|---|---|
| Transfection/Transfer Efficiency | High (efficient transduction) [95] | Poor to moderate gene transfer efficiency [95] | N/A (Acts via receptor/enzyme binding) |
| Expression Duration | Long-term (months to years), especially with AAVs [96] | Transient (days to weeks) [95] | Transient (hours to days), dependent on half-life [99] |
| Cargo Capacity | Limited (~4.7 kb for AAV; ~8 kb for Lentivirus) [95] [96] | Large cargo capacity (theoretically unlimited) [95] [97] | Small molecular weight (<500-1000 Daltons) |
| Immunogenicity | Moderate to High (can elicit innate/adaptive immune responses) [95] [97] | Low (low immunogenicity and cytotoxicity) [95] [97] | Variable (depends on the molecule and target) |
| Manufacturing Scalability | Complex, costly, challenging to scale [95] [97] | Easier, more cost-effective, highly scalable [95] [97] | Well-established, highly scalable synthesis [100] |
| Therapeutic Efficacy Example | AAV-based gene therapies showing long-term correction in monogenic diseases [95] | siRNA lipid nanoparticles (e.g., Onpattro) achieving clinical gene silencing [95] | Upadacitinib superior in inducing clinical remission (99.6%) and endoscopic improvement (99.2%) in UC [98] |
Experimental Protocols for Efficacy Assessment
To ensure the reproducibility of efficacy studies, detailed methodologies for key experiments are provided below.
Protocol: Assessing Viral vs. Non-Viral Transduction Efficiency
This protocol is designed to quantitatively compare the transfection/transduction efficiency and transgene expression kinetics of viral and non-viral vectors in vitro.
- Cell Seeding: Seed adherent mammalian cells (e.g., HEK293, HeLa) in 24-well plates at a density of 5 x 10^4 cells per well and culture for 24 hours to reach 70-80% confluence.
- Vector Preparation:
- Viral Vector Group: Prepare serial dilutions of the viral vector (e.g., AAV, LVV) in serum-free medium, calculating the multiplicity of infection (MOI). Include a GFP-reporting construct.
- Non-Viral Vector Group: Formulate complexes of plasmid DNA (pDNA) encoding GFP with different transfection reagents (e.g., Lipofectamine 3000, PEI) per manufacturer's instructions, using a fixed amount of pDNA (e.g., 500 ng per well).
- Control Group: Include untreated cells and cells treated with delivery reagent only.
- Transduction/Transfection: Remove growth medium from cells. Apply the viral vector dilutions or non-viral vector complexes to respective wells. Incubate cells for 4-6 hours, then replace the medium with fresh complete growth medium.
- Analysis and Data Collection:
- Flow Cytometry: At 24, 48, and 72 hours post-transduction/transfection, harvest cells and analyze using a flow cytometer to determine the percentage of GFP-positive cells (transduction efficiency) and mean fluorescence intensity (transgene expression level).
- Microscopy: Use fluorescence microscopy to visually assess transgene expression and cell morphology.
Protocol: Evaluating Small-Molecule Enhancement of Transgene Expression
This protocol tests the ability of small molecules to enhance the productivity of engineered cells, as identified through computational transcriptomic matching [99].
- Cell Seeding and Transfection: Seed H1299 cells (or other relevant cell line) in 96-well plates. After 24 hours, transfect cells with a CMV-driven plasmid encoding a fluorescent reporter (e.g., EGFP or mKate) using a standard method (e.g., lipofection).
- Small Molecule Treatment: At 4 hours post-transfection, treat cells with selected small molecules (e.g., Filgotinib, Ruxolitinib, TWS119) at a range of pre-optimized concentrations. Include a DMSO vehicle control.
- Incubation and Analysis: Incubate cells for 48-72 hours. Harvest cells and analyze fluorescence intensity using flow cytometry or a plate reader. Normalize fluorescence data to the vehicle control to calculate the fold-change in protein expression.
- Viral Transduction Enhancement (Optional): Repeat the treatment with small molecules on cells being transduced with a viral vector (e.g., AAV or LVV) carrying a reporter gene to assess if the molecule boosts viral-mediated expression.
Signaling Pathways and Workflows
The following diagrams illustrate key mechanisms and experimental workflows discussed in this guide.
Small Molecule Enhancement of Transgene Expression
This diagram outlines the mechanism by which computational screening identifies small molecules that enhance transgene expression by mimicking genetic circuits that redistribute cellular resources.
Capsid-Genome Binding as an Antiviral Target
This diagram shows the mechanism of viral capsid-genome binding and how small molecule inhibitors can disrupt this process, a key strategy in antiviral drug development.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of the discussed strategies requires a selection of core reagents and materials. The following table details essential tools for research in this field.
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Examples / Key Characteristics |
|---|---|---|
| Adeno-Associated Virus (AAV) Vectors | In vivo gene delivery with long-term expression; high tropism variety [95] [96] | Serotypes AAV8, AAV9 (muscle tropism); packaging capacity ~4.7 kb [96] |
| Lentiviral Vectors (LVVs) | Stable gene delivery via genome integration; suitable for dividing and non-dividing cells [95] [97] | Third-generation, self-inactivating (SIN) designs for enhanced safety [95] |
| Cationic Lipids / Lipid Nanoparticles (LNPs) | Form complexes with nucleic acids for non-viral delivery; protect cargo and enhance cellular uptake [95] [97] | Component of FDA-approved Onpattro; often multi-component formulations (e.g., ionizable lipid, PEG-lipid, cholesterol) [95] [101] |
| Cationic Polymers | Condense nucleic acids into polyplexes for delivery; can facilitate endosomal escape [95] | Polyethylenimine (PEI), high transfection efficiency but cytotoxicity; biodegradable alternatives (PBAEs, PLAs) [95] |
| Cell-Penetrating Peptides (CPPs) | Short peptides that facilitate cellular uptake of various cargos (proteins, nucleic acids) [97] | TAT peptide (from HIV); used for delivering biomolecules across membranes with low toxicity [97] |
| Productivity-Enhancing Small Molecules | Enhance transgene expression in engineered cells by modulating cellular resource allocation [99] | Filgotinib, Ruxolitinib; identified via DECCODE algorithm to mimic iFFL transcriptomic signature [99] |
| Capsid-Genome Binding Inhibitors | Small molecules that disrupt virus assembly by interfering with capsid-protein/genome interaction [102] | Target capsid proteins of DENV, HBV, SARS-CoV-2; discovered via molecular dynamics and binding assays [102] |
Long-Term Stability and Safety Profiles of Different Reprogramming Strategies
The advent of cell reprogramming technologies has fundamentally altered the landscape of regenerative medicine, disease modeling, and drug discovery. Since the groundbreaking discovery of induced pluripotent stem cells (iPSCs) by Takahashi and Yamanaka in 2006, scientists have developed diverse strategies to reprogram somatic cells into pluripotent stem cells or directly into other somatic cell types [103]. Each reprogramming method presents a unique balance of efficiency, stability, and safety characteristics that directly impacts its suitability for research versus clinical applications. For researchers, scientists, and drug development professionals, selecting an appropriate reprogramming strategy requires careful consideration of these parameters within the specific context of their experimental or therapeutic goals. This guide provides a comprehensive, evidence-based comparison of the long-term stability and safety profiles of major reprogramming methodologies, synthesizing current research findings to inform strategic decision-making in reprogramming-based applications.
Cell reprogramming encompasses several distinct technological approaches, each with characteristic mechanisms and applications. Pluripotent reprogramming involves reverting somatic cells to an embryonic-like pluripotent state, enabling differentiation into virtually any cell type [104] [103]. In contrast, direct reprogramming (or transdifferentiation) converts one somatic cell type directly into another without passing through a pluripotent intermediate [105] [103]. Both approaches can be achieved using different delivery methods for reprogramming factors, including integrating vectors, non-integrating vectors, and chemical induction.
The foundational technology for pluripotent reprogramming relies on delivering key transcription factors. The original method used OCT4, SOX2, KLF4, and c-MYC (OSKM) via retroviral vectors [104] [103]. Subsequent advancements have focused on improving safety by developing non-integrating delivery systems and chemical approaches that eliminate the need for genetic manipulation entirely [5] [103]. Direct reprogramming utilizes lineage-specific transcription factors or chemical cocktails to achieve cell fate conversion, potentially offering safer profiles by avoiding pluripotent states associated with tumorigenic risk [105].
Table 1: Fundamental Reprogramming Approaches
| Approach | Key Factors/Methods | Primary Applications | Key Advantages |
|---|---|---|---|
| Pluripotent Reprogramming | OCT4, SOX2, KLF4, c-MYC (OSKM) via various delivery methods | Disease modeling, drug screening, regenerative medicine | Unlimited expansion potential, broad differentiation capacity |
| Direct Reprogramming | Lineage-specific transcription factors (e.g., Ascl1, Brn2, Myt1l for neurons) | Cell replacement therapy, disease modeling | Bypasses pluripotent stage, potentially faster conversion |
| Chemical Reprogramming | Small molecule cocktails targeting signaling/epigenetic pathways | Regenerative medicine, clinical applications | Non-integrating, potentially more controllable |
Comparative Analysis of Reprogramming Methods
Integration-Based Reprogramming Methods
Initial reprogramming methodologies relied on integrating viral vectors, primarily retroviruses and lentiviruses, to deliver reprogramming factors. These systems provide efficient and stable gene expression, resulting in relatively high reprogramming efficiencies—approximately 0.27% for lentiviral methods according to comparative studies [106]. However, the permanent integration of foreign DNA into the host genome presents significant safety concerns for clinical applications. The integrated transgenes can disrupt essential genes or regulatory regions, potentially leading to oncogenic transformation [104]. Furthermore, persistent expression of reprogramming factors, particularly the oncogene c-MYC, may impede complete reprogramming or promote tumor formation in differentiated cells [103].
Long-term studies of integration-based iPSCs have revealed additional stability concerns. These cell lines demonstrate relatively high rates of aneuploidy (13.5% in retrovirally-derived lines and 4.5% in lentivirally-derived lines), indicating genomic instability potentially exacerbated by viral integration [106]. Despite these limitations, integrating methods remain valuable for basic research applications where long-term genetic stability is less critical than reprogramming efficiency and reliability.
Non-Integrating Reprogramming Methods
To address safety concerns associated with genome integration, researchers have developed several non-integrating reprogramming approaches with distinct safety and stability profiles.
Sendai Virus (SeV) is an RNA virus-based system that remains in the cytoplasm and does not integrate into the host genome. This method offers a strong balance of reliability (94% success rate) and relatively high reprogramming efficiency (0.077%) [106]. SeV-derived iPSCs demonstrate low aneuploidy rates (4.6%), comparable to lentiviral methods but without genomic integration risks [106]. A significant consideration is that SeV RNA is gradually lost during cell passaging, with only 21.2%-34.3% of lines retaining viral RNA by passages 9-11, reducing persistent transgene expression concerns [106]. The method requires minimal hands-on time (3.5 hours until colony picking) but may need additional screening to confirm viral clearance [106].
Episomal (Epi) reprogramming uses plasmid vectors that replicate extrachromosomally. While highly reliable (93% success rate), its reprogramming efficiency is low (0.013%) [106]. A notable stability concern is the persistent retention of episomal plasmids in a substantial subset of lines (33.3% even at passages 9-11), with some lines showing high plasmid copy numbers that might confer growth advantages [106]. These lines also exhibit elevated aneuploidy rates (11.5%), suggesting potential genomic instability possibly linked to prolonged reprogramming factor expression [106].
mRNA Reprogramming involves daily transfections of in vitro transcribed mRNAs encoding reprogramming factors. This method achieves the highest reprogramming efficiency (2.1%) and the lowest aneuploidy rate (2.3%) among all methods [106]. However, its initial success rate was limited (27%) due to extensive cell death from innate immune activation, though supplementing with microRNAs improves this to 73% [106]. The method is particularly labor-intensive (approximately 8 hours hands-on time) but generates colonies quickly (ready for picking around day 14) [106].
Chemical Reprogramming represents the most recent advancement, using small molecules to target signaling and epigenetic pathways without genetic manipulation [5]. This approach offers exceptional safety potential by completely avoiding exogenous genetic material. Recent clinical applications have demonstrated promising results, including transplantation of insulin-producing cells derived from chemically induced pluripotent stem cells (hCiPS cells) for type 1 diabetes treatment [5]. The main challenges include optimizing efficiency across different donor cell types and understanding long-term stability characteristics, though early data suggests this method may overcome many safety barriers associated with biologically-based reprogramming [5].
Table 2: Quantitative Comparison of Reprogramming Method Safety and Efficiency
| Method | Reprogramming Efficiency (%) | Success Rate (%) | Aneuploidy Rate (%) | Genomic Integration | Factor Persistence |
|---|---|---|---|---|---|
| Retroviral | ~0.27 (lentiviral) | 100 | 13.5 | Yes | Persistent |
| Sendai Virus | 0.077 | 94 | 4.6 | No | Lost in 65.7-78.8% by P9-11 |
| Episomal | 0.013 | 93 | 11.5 | No | Retained in 33.3% at P9-11 |
| mRNA | 2.1 | 27 (73 with miRNA) | 2.3 | No | Transient (days) |
| Chemical | Variable by protocol | Under investigation | Limited data | No | None |
Direct Reprogramming Safety and Stability
Direct reprogramming or transdifferentiation offers an alternative approach that bypasses the pluripotent stage altogether, potentially mitigating tumorigenicity risks associated with iPSCs [105]. This method typically uses lineage-specific transcription factors to directly convert one somatic cell type to another. For example, fibroblasts have been successfully reprogrammed into functional neurons using combinations of Ascl1, Brn2, and Myt1l [105], and into oligodendrocyte progenitor cells (iOPCs) using Nkx6.2, Olig2, and Sox10 or Olig2, Sox10, and Zfp536 [107].
The safety advantages include avoided pluripotent intermediates and potentially shorter reprogramming timelines. However, direct reprogramming may yield partially reprogrammed or functionally immature cells that could pose unpredictable risks after transplantation [105]. The long-term stability of directly reprogrammed cells remains less thoroughly characterized than iPSC-derived cells, and the potential for aberrant gene expression resulting from forced transcription factor expression requires careful evaluation [105] [107].
Experimental Protocols for Assessing Safety and Stability
Genomic Stability Assessment
Comprehensive evaluation of genomic integrity is essential for characterizing any reprogrammed cell line. The standard protocol involves:
Karyotype Analysis: Perform G-banding chromosomal analysis of at least 20 metaphase spreads per cell line to detect gross chromosomal abnormalities and aneuploidy [106]. This method identified the significantly higher aneuploidy rates in retroviral (13.5%) and episomal (11.5%) lines compared to mRNA-reprogrammed lines (2.3%) [106].
Copy Number Variation (CNV) Analysis: Utilize array comparative genomic hybridization (aCGH) or whole-genome sequencing to detect submicroscopic structural variations. In one study, aCGH revealed that most CNVs pre-existed in parental somatic cells, with low frequencies of de novo aberrations across all methods [106].
Integration Site Analysis: For vector-based methods, employ techniques such as linear amplification-mediated PCR (LAM-PCR) or sequencing-based integration site analysis to identify genomic integration events and assess potential disruptions to genomic regulatory elements [104].
Tumorigenicity Risk Assessment
Evaluating tumorigenic potential is critical for clinical translation:
Teratoma Formation Assay: The gold standard for assessing pluripotency and tumorigenic risk involves injecting undifferentiated iPSCs (1-5×10^6 cells) into immunodeficient mice and monitoring for teratoma formation over 8-12 weeks. Histological examination should confirm differentiation into all three germ layers without malignant components [104].
In Vitro Transformation assays: Utilize soft agar colony formation assays to detect anchorage-independent growth, and monitor for proliferation control loss in serum-free conditions [104].
Oncogene Expression Profiling: Employ qRT-PCR or RNA sequencing to assess expression of oncogenes and tumor suppressor genes, particularly focusing on the reprogramming factors themselves (especially c-MYC) and genes associated with pluripotency (e.g., NANOG) [106].
Functional Characterization
Ensure reprogrammed cells exhibit functional properties of their target identity:
Lineage-Specific Functional Assays: For neuronal cells, perform patch-clamp electrophysiology to confirm action potential generation and synaptic activity [105]. For cardiomyocytes, assess spontaneous contraction and calcium handling properties [104].
Long-Term Culture Stability: Maintain cells for extended passages (minimum 10-15 passages) while periodically assessing marker expression, genomic stability, and functional characteristics to evaluate phenotypic stability [106].
In Vivo Integration Studies: Transplant differentiated cells into appropriate animal models to assess survival, functional integration, and absence of tumor formation over extended periods (6-12 months) [104] [5].
Visual Summary 1: Safety decision flowchart illustrating how different reprogramming methods influence tumorigenicity risk through specific mechanistic pathways.
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Key Research Reagents for Reprogramming Studies
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Reprogramming Factor Delivery Systems | Cytotune Sendai Virus Kit, Stemgent mRNA Reprogramming Kit, Episomal plasmids | Deliver reprogramming factors to somatic cells via different mechanisms with varying efficiency and safety profiles |
| Reprogramming Media & Supplements | OPC medium for neural differentiation, bFGF, SHH, PDGF-AA, N2/B27 supplements | Support the survival, proliferation, and maturation of reprogrammed cells during and after conversion |
| Quality Control Assays | Karyotype G-banding analysis, aCGH/RNA-seq platforms, Immunostaining antibodies | Assess genomic integrity, gene expression patterns, and lineage-specific marker expression |
| Cell Culture Substrates | Poly-L-ornithine, Laminin, Matrigel, Feeder cells | Provide appropriate extracellular matrix environment supporting reprogramming and pluripotency maintenance |
The optimal reprogramming strategy depends heavily on the specific application and risk-benefit considerations. For basic research where efficiency is prioritized, mRNA reprogramming offers highest efficiency with minimal genomic integration risk, despite being labor-intensive. For clinical applications, Sendai virus and chemical reprogramming provide favorable safety profiles, with chemical methods showing particular promise for completely avoiding exogenous genetic material. Direct reprogramming offers an alternative for specific lineage conversions that bypass pluripotent intermediates entirely.
Future directions will likely focus on combining the best attributes of different approaches—for instance, using small molecules to enhance the efficiency and safety of biological reprogramming methods. As the field progresses toward standardized clinical applications, rigorous long-term stability and tumorigenicity assessment will remain paramount for ensuring the safe implementation of reprogramming technologies in regenerative medicine and drug development.
Visual Summary 2: Decision framework for selecting reprogramming methods based on research objectives and application priorities.
Conclusion
The collective research underscores that distinct reprogramming strategies yield markedly different functional outcomes, each with unique trade-offs between efficacy, safety, and clinical applicability. In vivo partial reprogramming presents a powerful tool for systemic rejuvenation, while direct lineage conversion offers precise tissue repair with inherent anti-fibrotic benefits. The critical path forward hinges on overcoming persistent challenges in efficiency, safety control, and the suppressive fibrotic microenvironment. Future progress will be driven by the development of sophisticated delivery systems, refined factor cocktails, and stringent functional validation in clinically relevant models. Successfully navigating these hurdles will ultimately determine the translation of reprogramming technologies from a promising laboratory phenomenon into transformative regenerative medicines.
References
- 1. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 2. Review Pluripotent stem-cell-derived therapies in clinical trial [https://www.sciencedirect.com/science/article/pii/S1934590924004454]
- 3. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 4. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 5. Improving chemical reprogramming strategies [https://www.nature.com/articles/s41580-025-00836-1]
- 6. Article Activation of canonical Wnt signaling is required for ... [https://www.sciencedirect.com/science/article/pii/S2213671125002929]
- 7. Direct reprogramming of mouse fibroblasts into self ... [https://www.nature.com/articles/s41536-025-00411-4]
- 8. Inducible, virus-free direct lineage reprogramming ... [https://elifesciences.org/reviewed-preprints/106550]
- 9. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 10. Current advances and future prospects of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1546423/full]
- 11. Organ‐Specific Dedifferentiation and Epigenetic Remodeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610414/]
- 12. Review Research of in vivo reprogramming toward clinical ... [https://www.sciencedirect.com/science/article/pii/S2352320424002001]
- 13. The long and winding road of reprogramming-induced ... [https://www.nature.com/articles/s41467-024-46020-5]
- 14. A Review of the Present State of Epigenetic ... [https://www.fightaging.org/archives/2025/10/a-review-of-the-present-state-of-epigenetic-reprogramming-to-treat-aging/]
- 15. What is in vivo reprogramming, its potential pros & cons? [https://ipscell.com/2025/10/what-is-in-vivo-reprogramming-its-potential-pros-cons/]
- 16. Accelerating life sciences research [https://openai.com/index/accelerating-life-sciences-research-with-retro-biosciences/]
- 17. Comparison of reprogramming factor targets reveals both ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6303873/]
- 18. In Vivo Targeted Reprogramming of Cardiac Fibroblasts for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466987/]
- 19. Age reprogramming: Innovations and ethical ... [https://www.spandidos-publications.com/10.3892/br.2025.1974]
- 20. Rejuvenation Roundup September 2025 [https://www.lifespan.io/news/rejuvenation-roundup-september-2025/]
- 21. Reprogramming cellular senescence and aging clocks for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492661/]
- 22. Direct fibroblast reprogramming: an emerging strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11869441/]
- 23. Direct Reprogramming of Resident Non-Myocyte Cells and ... [https://www.mdpi.com/2073-4409/12/8/1166]
- 24. Direct Lineage Reprogramming of Fibroblasts into Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408679/]
- 25. Iterative transcription factor screening enables rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152180/]
- 26. Rational Reprogramming of Cellular States by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6667192/]
- 27. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 28. Fibroblast Reprogramming in Cardiac Repair - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10864899/]
- 29. Direct conversion of cardiac fibroblasts into endothelial-like ... [https://www.nature.com/articles/s41467-024-48354-6]
- 30. Generation and purification of iPSC-derived cardiomyocytes ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04319-0]
- 31. Human induced pluripotent stem cell-cardiomyocytes for ... [https://www.kjpp.net/journal/view.html?doi=10.4196/kjpp.24.413]
- 32. Direct reprogramming of mouse fibroblasts into self-renewable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185750/]
- 33. Lung cells generated from mouse embryonic fibroblasts in ... [https://www.news-medical.net/news/20250703/Lung-cells-generated-from-mouse-embryonic-fibroblasts-in-just-7-to-10-days.aspx]
- 34. Advances in Induced Pluripotent Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/41179113/]
- 35. Role of small molecules as drug candidates for ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482524007467]
- 36. Press Release and Media Coverage [https://www.biolase.com/press-release-and-media/]
- 37. Viral and non-viral vectors in gene therapy: current state ... [https://www.sciencedirect.com/science/article/pii/S2352396425002786]
- 38. Nonviral Delivery Systems of mRNA Vaccines for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8949480/]
- 39. Non-viral vectors for RNA delivery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8743282/]
- 40. The Bright Future of mRNA as a Therapeutic Molecule [https://www.mdpi.com/2073-4425/16/4/376]
- 41. Advances in RNA-based therapeutics: current breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592931/]
- 42. Discovery of RNA‐Targeting Small Molecules - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375692/]
- 43. Progress and prospects of mRNA-based drugs in pre- ... [https://www.nature.com/articles/s41392-024-02002-z]
- 44. AGILE platform: a deep learning powered approach to ... [https://www.nature.com/articles/s41467-024-50619-z]
- 45. Advances in the Development and Application of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11775963/]
- 46. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 47. Examining the Market for Organoid Culture Systems in 2025 [https://eureka.patsnap.com/report-examining-the-market-for-organoid-culture-systems-in-2025]
- 48. Sequential factor delivery enables efficient workflow for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432238/]
- 49. 2025 Trends: Organoids [https://www.genengnews.com/topics/genome-editing/2025-trends-organoids/]
- 50. High-throughput deconvolution of 3D organoid dynamics at ... [https://www.nature.com/articles/s41467-023-44162-6]
- 51. Applications and research trends in organoid based ... [https://www.nature.com/articles/s41598-025-07816-7]
- 52. Comparisons of miRNA profiles of exosomes derived from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359900/]
- 53. MicroRNA-induced reprogramming of tumor-associated ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925002020]
- 54. Reprogramming mitochondrial metabolism and ... [https://www.nature.com/articles/s41467-025-64201-8]
- 55. a game-changer in cancer immunotherapy [https://link.springer.com/article/10.1007/s13346-025-01970-1]
- 56. Improving the safety of human pluripotent stem cell ... [https://www.nature.com/articles/s41467-020-16455-7]
- 57. In vivo reprogramming leads to premature death linked ... [https://pubmed.ncbi.nlm.nih.gov/38012287/]
- 58. A Scalable Approach to Prevent Teratoma Formation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3463330/]
- 59. Preventing Pluripotent Cell Teratoma in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5442801/]
- 60. Lysine-specific demethylase 1 inhibitors prevent teratoma ... [https://pubmed.ncbi.nlm.nih.gov/29464084/]
- 61. NEUROD1 efficiently converts peripheral blood cells into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067290/]
- 62. Chemical reprogramming of human blood cells to ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925002607]
- 63. Reprogramming of human urine cells into cardiomyocytes ... [https://www.nature.com/articles/s43856-025-00963-y]
- 64. TGF-β inhibitors: the future for prevention and treatment of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1583616/full]
- 65. Extracellular matrix stiffness: mechanisms in tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11984264/]
- 66. TGF-β1 diminishes collagen production during long-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3061833/]
- 67. Protocol for evaluating extracellular matrix stiffness post- ... [https://www.sciencedirect.com/science/article/pii/S2666166724006257]
- 68. Nanomedicines in the Treatment of Liver Fibrosis: A Review [https://pubmed.ncbi.nlm.nih.gov/40785947/]
- 69. Tissue-Specific Knockout Mouse | How to focus on one tissue [https://www.genoway.com/product/custom/tissue-specific-ko-mouse]
- 70. Cell-type specific, inducible and acute degradation of ... [https://www.nature.com/articles/s41467-024-54308-9]
- 71. Generation and comparison of CRISPR-Cas9 and Cre ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5508130/]
- 72. The heterogeneity of cellular senescence: insights at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9812642/]
- 73. Delineating the heterogeneity of senescence-induced- ... [https://link.springer.com/article/10.1007/s00018-024-05230-2]
- 74. Spatial and single-cell profiling of the metabolome ... [https://www.nature.com/articles/s43587-023-00513-y]
- 75. Reprogramming to restore youthful epigenetics of ... [https://www.nature.com/articles/s41413-025-00416-1]
- 76. The interplay of cellular senescence and reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066513/]
- 77. Increased mitochondrial mutation heteroplasmy induces aging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11896400/]
- 78. Comparative analysis of mouse strains for in vivo induction ... [https://pubmed.ncbi.nlm.nih.gov/40560729/]
- 79. Strain-Specific Responses to Tunnel Handling vs. Tail ... [https://www.linkedin.com/pulse/strain-specific-responses-tunnel-handling-vs-tail-lab-stefano-ojewf]
- 80. Strain differences between C57Bl/6 and DBA/2 mice (Mus ... [https://peerj.com/articles/19200/]
- 81. Strain differences between C57Bl/6 and DBA/2 mice (Mus ... [https://pubmed.ncbi.nlm.nih.gov/40151453/]
- 82. Outcome of SARS-CoV-2 reinfection depends on genetic ... [https://www.nature.com/articles/s41467-024-54334-7]
- 83. Cell Reprogramming Industry Report 2025-2030: Market ... [https://finance.yahoo.com/news/cell-reprogramming-industry-report-2025-081900361.html]
- 84. Unlocking MSC Potential: Metabolic Reprogramming via ... [https://www.mdpi.com/2674-0583/3/3/13]
- 85. An adverse outcome pathway for lung surfactant function ... [https://www.sciencedirect.com/science/article/pii/S2666027X21000220]
- 86. Safety and efficacy of pulmonary surfactant therapy for ... [https://pubmed.ncbi.nlm.nih.gov/40399976/]
- 87. Comparing the Effects of Two Surfactant Administration ... [https://www.mdpi.com/2543-6031/92/5/36]
- 88. Integrated in vivo combinatorial functional genomics and ... [https://www.nature.com/articles/s41551-025-01437-1]
- 89. To recruit or to graft? Comparing the recruitment of resident ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1589790/full]
- 90. A Novel Quantitative Hemodynamic Evaluation Method ... [https://pubmed.ncbi.nlm.nih.gov/40635207/]
- 91. Advances in the treatment of acne scars [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1643035/full]
- 92. The Future of Scar Management [https://plasticsurgerykey.com/the-future-of-scar-management/]
- 93. Organ preservation: current limitations and optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11980443/]
- 94. Lab-Grown Organs- The Future of Rehabilitation [https://healthcare-bulletin.co.uk/article/lab-grown-organs-the-future-of-rehabilitation-a-systematic-review-4407/]
- 95. Viral vs Non-Viral Vectors in Gene Therapy [https://www.phacilitate.com/insights-resources/gene-therapy-big-debate-viral-vectors-vs-non-viral-vectors]
- 96. Viral and non-viral vectors for gene therapy in the treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0098299725000640]
- 97. The Delivery Dilemma Looking Beyond Viral Vectors for ... [https://www.bioprocessintl.com/gene-therapies/the-delivery-dilemma-looking-beyond-viral-vectors-for-gene-therapy]
- 98. Comparative Efficacy of Biologics and Small Molecule in ... [https://pubmed.ncbi.nlm.nih.gov/39182898/]
- 99. Computational identification of small molecules for ... [https://www.nature.com/articles/s41467-025-62529-9]
- 100. Small Molecule vs Microbiome-Based Clinical Trials [https://www.sgs.com/en-us/news/2025/01/decoding-the-differences-small-molecule-vs-microbiome-based-clinical-trials]
- 101. A general nanoplatform for nucleotide drug delivery [https://pubmed.ncbi.nlm.nih.gov/40975176/]
- 102. New Advances in Small Molecules Targeted at Viral ... [https://www.mdpi.com/1422-0067/26/14/6979]
- 103. Cell reprogramming: methods, mechanisms and applications [https://cellregeneration.springeropen.com/articles/10.1186/s13619-025-00229-x]
- 104. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 105. Potentials of Cellular Reprogramming as a Novel Strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6284065/]
- 106. A comparison of non-integrating reprogramming methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC4329913/]
- 107. Comparison of Reprogramming Methods for Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5499613/]