GMP for Scalable Stem Cell Biomanufacturing: A Guide to Compliance, Automation, and Clinical Translation
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on implementing Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing.
GMP for Scalable Stem Cell Biomanufacturing: A Guide to Compliance, Automation, and Clinical Translation
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on implementing Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing. Covering foundational regulations from the FDA and EMA, it delves into advanced automated platforms like the Quantum® system and CliniMACS Prodigy® for large-scale production. The content addresses critical troubleshooting aspects, including managing knowledge transfer and reducing operational costs, and outlines validation strategies for analytical methods and navigating diverse global regulatory pathways. The synthesis of these elements offers a strategic roadmap for transitioning stem cell therapies from research to robust, compliant, and commercially viable clinical applications.
GMP Fundamentals and Regulatory Frameworks for Stem Cell Therapies
Current Good Manufacturing Practice (CGMP) regulations form the foundation for ensuring pharmaceutical product quality and safety. Established and enforced by the U.S. Food and Drug Administration (FDA), these regulations provide minimum requirements for the methods, facilities, and controls used in manufacturing, processing, and packing of drug products [1] [2]. The fundamental objective is to ensure that drug products have the identity, strength, quality, and purity they claim to possess, ultimately protecting patient safety [3].
The "C" in CGMP stands for "current," requiring manufacturers to employ up-to-date technologies and systems that evolve with modern standards [2]. This dynamic nature distinguishes CGMP from static GMP standards, emphasizing continuous improvement and adoption of advanced manufacturing technologies to achieve higher quality through ongoing enhancement of processes and controls [3] [4]. For stem cell biomanufacturing researchers, understanding these requirements is crucial for developing scalable processes that meet regulatory expectations while maintaining product consistency and quality.
Regulatory Framework and Key Sections
The CGMP regulations are codified in Title 21 of the Code of Federal Regulations (CFR), which interprets the Federal Food, Drug and Cosmetic Act [1]. The pharmaceutical quality-related regulations appear in several parts of Title 21, with specific sections governing different aspects of pharmaceutical manufacturing:
Table: Key CGMP Regulations for Pharmaceutical Products
| CFR Section | Regulatory Focus | Application in Biomanufacturing |
|---|---|---|
| 21 CFR Part 210 | Current Good Manufacturing Practice in Manufacturing, Processing, Packing, or Holding of Drugs | General framework for all drug manufacturing operations |
| 21 CFR Part 211 | Current Good Manufacturing Practice for Finished Pharmaceuticals | Specific requirements for final drug products |
| 21 CFR Part 212 | Current Good Manufacturing Practice for Positron Emission Tomography Drugs | Specialized requirements for radiopharmaceuticals |
| 21 CFR Part 600 | Biological Products: General | Regulations specific to biological products |
| 21 CFR Part 1271 | Human Cells, Tissues, and Cellular and Tissue-Based Products | Directly applicable to stem cell-based products |
For stem cell biomanufacturing, multiple regulatory sections often apply concurrently. While 21 CFR Part 211 establishes requirements for finished pharmaceuticals, Part 1271 provides specific governance for cellular products, creating a comprehensive regulatory framework that researchers must navigate during process development [5].
Core CGMP Requirements: Detailed Analysis
Quality Management Systems
A robust quality management system (QMS) forms the cornerstone of CGMP compliance. The regulations mandate establishing a quality control unit with defined responsibilities and authority to approve or reject all components, drug product containers, closures, in-process materials, packaging materials, labeling, and drug products [5]. This unit must maintain adequate laboratory facilities for testing and approval (or rejection) of materials and products, with all responsibilities and procedures documented in writing [5].
For stem cell biomanufacturing, the QMS must incorporate:
- Quality by Design (QbD): Systematic approach to development that emphasizes product and process understanding based on sound science and quality risk management [6]
- Quality Risk Management: Proactive identification and mitigation of risks throughout the product lifecycle
- Corrective and Preventive Action (CAPA): Processes for investigating and correcting discrepancies while preventing recurrence [3]
- Change Control Management: Formal assessment and documentation of process changes [6]
Facility and Environmental Controls
CGMP regulations specify detailed requirements for manufacturing facilities to prevent contamination and ensure product consistency [5]. For stem cell biomanufacturing, these requirements present unique challenges due to the sensitive nature of living cells.
Table: Facility Requirements for Advanced Therapies
| Facility Element | CGMP Requirement | Stem Cell Application |
|---|---|---|
| Design & Construction | Suitable size, construction and location to facilitate cleaning, maintenance, and proper operations [5] | Segregated areas for different process steps with appropriate environmental controls |
| Air Quality Systems | Adequate ventilation with controls for air pressure, microorganisms, dust, humidity, and temperature [5] | HEPA filtration with appropriate classification for aseptic processing |
| Process Areas | Separate or defined areas to prevent contamination or mixups [5] | Dedicated gowning areas, material airlocks, and classified processing environments |
| Utilities | Potable water meeting EPA standards; proper drainage systems [5] | Water-for-injection systems for critical process steps |
| Sanitation Program | Written procedures for cleaning schedules, methods, equipment, and materials [5] | Validated cleaning procedures with appropriate detergents and sanitizers |
The FDA's guidance emphasizes that facilities must maintain controlled environmental conditions to prevent cross-contamination from adulterants and allergens that may render the product unsafe [7]. For stem cell products, this extends to controlling viable and non-viable particulates, temperature, humidity, and air pressure differentials between process areas.
Equipment Design and Maintenance
Equipment used in manufacturing must be adequately designed, constructed, cleaned, maintained, and calibrated [5]. The January 2025 FDA draft guidance on CGMP further clarifies that equipment adjustments may be made without additional quality unit approval if within preestablished, scientifically justified limits that have been previously approved [8]. This flexibility is particularly relevant for advanced manufacturing technologies where real-time process adjustments may be necessary.
For stem cell biomanufacturing, equipment considerations include:
- Material Compatibility: Equipment surfaces contacting cells or reagents must be non-reactive, non-additive, and non-absorptive [3]
- Calibration Program: Regular calibration according to established schedules and procedures [6]
- Preventive Maintenance: Scheduled maintenance to prevent equipment failure [3]
- Cleaning Validation: Evidence that cleaning procedures effectively remove product and cleaning agent residues [5]
Personnel Qualifications and Training
CGMP regulations emphasize that personnel engaged in manufacturing must have appropriate education, training, and experience to perform their assigned functions [5]. Training must be conducted by qualified individuals on a continuing basis with sufficient frequency to ensure employees remain familiar with CGMP requirements applicable to them [5].
Stem cell biomanufacturing facilities must ensure:
- Technical Competency: Personnel have specific training in aseptic techniques and cell culture methods
- CGMP Training: Regular training on current good manufacturing practice regulations [3]
- Aseptic Technique Qualification: Demonstration of proficiency in aseptic operations
- Health and Hygiene: Practices to prevent product contamination from personnel [5]
Advanced Manufacturing Technologies and CGMP
The FDA's recent draft guidance from January 2025 addresses considerations specific to advanced manufacturing technologies, which include innovative approaches relevant to stem cell biomanufacturing [8]. Advanced manufacturing is defined as a new or innovative manufacturing technology that enhances drug quality, scales up production, and reduces time-to-market [8].
Process Models and Real-Time Monitoring
The draft guidance acknowledges the industry's interest in using process models to monitor in-process materials affecting critical quality attributes and predict uniformity and homogeneity [8]. However, FDA advises against using process models alone and recommends pairing them with in-process material testing or process monitoring to ensure compliance with 21 CFR § 211.110 [8].
For stem cell biomanufacturing, this translates to:
- Process Analytical Technology (PAT): Real-time monitoring of critical process parameters
- Multivariate Analysis: Statistical models correlating process parameters with product quality attributes
- Real-time Release Testing: Ability to evaluate quality attributes during processing rather than through finished product testing alone
Continuous Manufacturing Considerations
The integrated nature of continuous manufacturing presents unique challenges for sampling and testing [8]. FDA recognizes that physical isolation and removal of samples may be less feasible in continuous processes compared to traditional batch manufacturing [8]. The guidance allows for alternative approaches where manufacturers could conduct sampling and testing at appropriate points in the process, with quality unit approval or rejection of in-process material before or after such points [8].
Experimental Protocols for CGMP Compliance
Environmental Monitoring Protocol
Objective: To establish and maintain controlled environmental conditions suitable for aseptic stem cell manufacturing.
Methodology:
- Classification of Cleanrooms: Establish ISO-classified environments based on intended operations (e.g., ISO 5 for critical operations)
- Particulate Monitoring: Continuous monitoring of non-viable particulates in critical areas
- Microbial Monitoring: Routine collection of viable air and surface samples using settle plates, contact plates, and active air samplers
- Personnel Monitoring: Assessment of gowning effectiveness through finger plates and gown contact plates
- Data Analysis: Trend monitoring data and establish alert and action limits
Acceptance Criteria: Environments must maintain classification according to ISO 14644 with no adverse trends in microbial recovery.
Process Validation Protocol
Objective: To establish documented evidence providing high degree of assurance that a specific process consistently produces a product meeting its predetermined specifications and quality attributes.
Methodology:
- Stage 1 - Process Design: Define target product profile, identify critical quality attributes, and establish process parameters
- Stage 2 - Process Qualification: Design facility and equipment qualification followed by process performance qualification
- Stage 3 - Continued Process Verification: Ongoing monitoring to ensure process remains in state of control
Stem Cell Application:
- Focus on critical process parameters affecting cell viability, identity, potency, and purity
- Define in-process controls and testing strategies
- Establish process ranges rather than fixed setpoints where appropriate
In-Process Control Strategy
Following 21 CFR § 211.110, manufacturers must conduct in-process controls, tests, or examinations to prevent contamination and monitor quality attributes of in-process materials [8]. The FDA recommends a scientific and risk-based approach outlining what, where, when, and how in-process controls should be conducted [8].
Implementation Framework:
- Risk Assessment: Identify potential failure modes and their impact on product quality
- Control Point Identification: Determine optimal points in the process for monitoring and control
- Method Selection: Choose appropriate analytical methods capable of detecting variations
- Sampling Plan: Establish statistically justified sampling plans
- Data Management: Implement systems for data collection, analysis, and trend monitoring
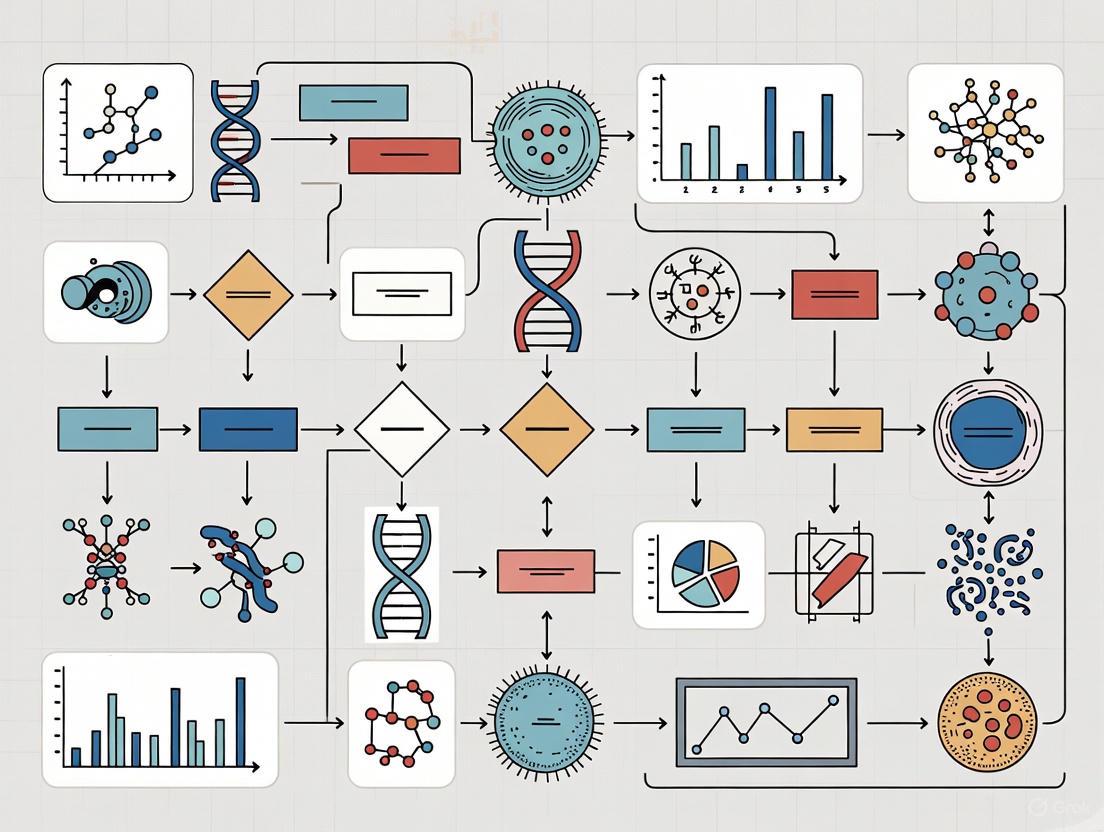
Visualization of CGMP Compliance Framework
CGMP Compliance Framework Diagram
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Critical Materials for Stem Cell Biomanufacturing
| Material/Reagent | Function | CGMP Considerations |
|---|---|---|
| Cell Culture Media | Supports cell growth and maintenance | Qualified components, endotoxin testing, batch-to-batch consistency |
| Growth Factors/Cytokines | Directs cell differentiation and proliferation | Purity documentation, activity verification, supplier qualification |
| Extracellular Matrix Components | Provides structural support for cell attachment | Bioburden control, identity testing, freedom from adventitious agents |
| Dissociation Reagents | Enzymatic or non-enzymatic cell detachment | Purity, specificity, removal validation during process |
| Critical Process Materials | Contact product during manufacturing (filters, tubing, containers) | Extractables and leachables testing, biocompatibility, supplier qualification |
| Cell Sorting Reagents | Isolation of specific cell populations | Purity, specificity, validation of removal if required |
| Cryopreservation Solutions | Long-term storage of cell products | Formulation consistency, sterility, container compatibility |
Implementing CGMP requirements in stem cell biomanufacturing research requires a systematic approach that integrates quality principles from initial process development through scale-up and technology transfer. The flexibility inherent in CGMP regulations allows manufacturers to implement innovative approaches while maintaining compliance, provided they can scientifically justify their methods and demonstrate control [2].
As emphasized in the recent FDA draft guidance, manufacturers should adopt a risk-based approach to in-process controls, leveraging advanced manufacturing technologies where appropriate while maintaining traditional quality systems [8]. For stem cell researchers transitioning from bench to commercial scale, early adoption of CGMP principles facilitates smoother scale-up and regulatory approval, ultimately accelerating the delivery of transformative therapies to patients.
For researchers and scientists pioneering scalable stem cell biomanufacturing, navigating the regulatory landscape is as crucial as the science itself. The U.S. Food and Drug Administration (FDA) establishes current good manufacturing practice (CGMP) requirements to ensure that drugs, including Advanced Therapy Medicinal Products (ATMPs), are consistently produced and controlled to quality standards appropriate for their intended use [9]. These regulations are codified primarily in 21 CFR Parts 210 and 211, which form the foundational regulatory framework for pharmaceutical manufacturing in the United States [10] [5]. For stem cell-based therapies, which are often classified as ATMPs, compliance with these regulations presents unique challenges due to the complex, living nature of the products and the need for aseptic processing throughout manufacturing [11]. This application note provides a detailed analysis of these key regulations within the context of scalable stem cell biomanufacturing research, offering practical guidance and protocols to facilitate regulatory compliance while advancing therapeutic development.
Regulatory Breakdown: 21 CFR Parts 210 & 211
Core Definitions and Interrelationship
21 CFR Part 210, "Current Good Manufacturing Practice in Manufacturing, Processing, Packing, or Holding of Drugs; General," establishes the overarching scope and status of CGMP regulations [10]. It specifies that compliance with these parts constitutes the minimum requirements to assure a drug's safety, identity, strength, quality, and purity [10] [12]. 21 CFR Part 211, "Current Good Manufacturing Practice for Finished Pharmaceuticals," provides the detailed, actionable requirements for implementing these quality standards across all aspects of production [5] [12]. Together, they form a cohesive system where Part 210 defines the "what" and Part 211 prescribes the "how" of drug manufacturing quality [12].
Table 1: Core Scope and Definitions in 21 CFR Part 210 [10] [12]
| Concept | Regulatory Citation | Definition & Significance for Stem Cell Biomanufacturing |
|---|---|---|
| Status of CGMP | §210.1 | Establishes that Parts 210, 211, 225, and 226 contain the minimum CGMP requirements. Non-compliance renders a drug "adulterated." |
| Applicability | §210.2 | Regulations supplement, do not supersede each other. Phase 1 investigational drugs are exempt from Part 211, but this exemption ceases for Phase 2/3 studies. |
| Batch | §210.3(b)(2) | A specific quantity of material intended to be uniform, produced in a single cycle. Critical for defining product lot size and consistency in cell culture. |
| Component | §210.3(b)(3) | Any ingredient used in drug product manufacture. For cell therapies, this includes culture media, growth factors, and cytokines. |
| Quality Control Unit | §210.3(b)(15) | Any person or element designated for quality control duties. Must be independent and have authority to approve/reject materials and products. |
| Representative Sample | §210.3(b)(21) | A sample drawn based on rational criteria to accurately portray the material being sampled. Essential for reliable in-process and final product testing. |
Key Operational Requirements under 21 CFR Part 211
Part 211 provides comprehensive, subpart-specific controls that are critical for establishing a robust manufacturing process for stem cell-based ATMPs.
Organization and Personnel (§211.22-§211.34): Requires a distinct, authoritative quality control unit with responsibility for approving/rejecting all components, containers, closures, in-process materials, and drug products [5]. Personnel must have adequate education, training, and experience, and must adhere to strict hygiene and sanitation practices to prevent product contamination [5] [9].
Buildings and Facilities (§211.42-§211.58): Mandates that facilities be of suitable design to facilitate cleaning, maintenance, and proper operations, with separate or defined areas to prevent contamination and mix-ups [5]. This is particularly critical for aseptic processing of ATMPs, requiring features like HEPA-filtered air under positive pressure and environmental monitoring systems [5] [11].
Production and Process Controls (§211.100-§211.115): Requires written procedures for production and process control, designed to ensure products have the identity, strength, quality, and purity they purport to possess [5]. This includes the critical concept of process validation, confirming that a process consistently produces a result meeting its pre-determined specifications [13].
Table 2: Selected Key Requirements of 21 CFR Part 211 for ATMP Biomanufacturing [5]
| Subpart | Section | Key Focus | Implication for Stem Cell ATMPs |
|---|---|---|---|
| B: Organization & Personnel | 211.22 | Quality Control Unit | Independent oversight and final authority on quality decisions for cell batches. |
| C: Buildings & Facilities | 211.42 | Design & Construction | Defined areas for each operation (e.g., cell processing, packaging) to prevent cross-contamination. |
| D: Equipment | 211.63 | Design & Size | Equipment must be of appropriate design and size for intended use (e.g., bioreactors). |
| E: Component Control | 211.84 | Testing & Approval | Rigorous testing and acceptance of raw materials like cytokines, media, and sera. |
| F: Production & Control | 211.100 | Written Procedures | Strict adherence to and documentation of Standard Operating Procedures (SOPs) for all processes. |
| I: Laboratory Controls | 211.165 | Testing & Release | Establishing scientifically sound specifications and testing for safety, purity, and potency of final cell product. |
| J: Records & Reports | 211.188 | Batch Production Record | Complete and accurate documentation of the production history of each batch of a drug product. |
ATMPs: Classification and Manufacturing Challenges
ATMP Classification and Regulatory Context
Advanced Therapy Medicinal Products (ATMPs) represent a groundbreaking category of medications that utilize biological-based products to treat or replace damaged tissues and organs [11]. Within the regulatory framework, ATMPs are broadly classified into several categories, which can be aligned with specific FDA regulatory pathways. It is important to note that the term "ATMP" itself is derived from European Union/United Kingdom regulatory frameworks, but the FDA regulates analogous products under specific categories for cells, tissues, and gene therapies [11].
Table 3: ATMP Classifications and Corresponding U.S. Regulatory Considerations
| ATMP Category | Core Definition | Examples Relevant to Stem Cells | Key U.S. Regulatory Consideration |
|---|---|---|---|
| Somatic Cell Therapy Medicinal Products (sCTMPs) | Uses autologous or allogeneic cells manipulated ex vivo to change their biological characteristics. | Expanded mesenchymal stem/stromal cells (MSCs), differentiated cardiomyocytes. | Regulated as biologic products under 21 CFR 1271 (HCT/Ps) and 21 CFR 210/211. Often requires BLA. |
| Tissue-Engineered Products (TEPs) | Contains or consists of engineered cells or tissues to repair, regenerate, or replace human tissue. | Stem cell-seeded scaffolds for bone or cartilage repair. | Combination product regulation (device + biologic). CGMP compliance for both components (e.g., 21 CFR 211 & 820). |
| Combined ATMPs | An ATMP that incorporates one or more medical devices as an integral part of the product. | Cell therapy product combined with a biodegradable matrix or delivery device. |
Critical Manufacturing Hurdles in Scalable Stem Cell Biomanufacturing
Transitioning stem cell research from a laboratory discovery to a commercially viable, regulated therapeutic product involves overcoming significant manufacturing challenges under the CGMP framework.
Transitioning from GLP to GMP: A primary barrier is implementing GMP-compliant manufacturing processes that reliably meet the quality specifications defined during product development, including data from Good Laboratory Practice (GLP)-compliant non-clinical studies [11]. While GLP focuses on protecting the integrity of non-clinical safety and efficacy data, GMP is concerned with protecting the final product from contamination and ensuring it consistently meets pre-defined quality standards [11]. This transition requires securing a reliable supply of GMP-grade raw materials, developing standardized cell characterization assays, and implementing robust quality control systems [11].
Safety and Contamination Control: Stem cell products must be free of contamination, but traditional sterilization methods are not feasible as they would compromise cell viability [11]. Consequently, manufacturing must occur under validated aseptic conditions, often requiring closed, automated systems and rigorous environmental monitoring to reduce risk [11]. A paramount safety concern is tumorigenesis, or the potential for stem cells to form tumors, which must be assessed using sensitive in vitro methods and in vivo studies in immunocompromised models [11].
Scalability and Process Validation: Scaling up cell culture from laboratory to clinical and commercial volumes is a multifaceted challenge. The most critical concern is demonstrating product comparability after any manufacturing process change [11]. Regulators require a risk-based comparability assessment, extensive analytical characterization, and staged testing to ensure changes do not impact the safety or efficacy of the final cell product [11]. This often involves moving from planar culture vessels to GMP-compliant bioreactors and developing comprehensive process validation protocols [11].
Practical Application: Protocols for Compliance and Process Validation
Experimental Protocol: Validation of Aseptic Processing (Media Fill)
A "media fill" or process simulation test is a critical validation study that demonstrates the capability of the aseptic manufacturing process to produce a sterile product [11].
1. Objective: To validate the aseptic manufacturing process for a stem cell-based ATMP by simulating all manual aseptic operations using a sterile growth medium, thereby providing sterility assurance.
2. Scope: This protocol applies to the final formulation and filling steps of the ATMP manufacturing process.
3. Materials and Equipment:
- Tryptic Soy Broth (TSB) or other suitable sterile culture media.
- Identical container-closure system used for the final drug product.
- Production-grade biosafety cabinet or isolator.
- All standard production equipment (e.g., tubing, pumps, filters).
- Incubators set at 20-25°C and 30-35°C.
4. Methodology: 1. Preparation: Prepare and sterilize the culture media according to standard procedures. Ensure the processing area is at the operational qualification state and has been cleaned and sanitized per approved SOPs. 2. Simulation Execution: A qualified operator shall perform all routine aseptic manipulations (e.g., connections, transfers, additions) using the sterile media instead of the cell product. The simulation should include the maximum number of interventions and the longest expected run time for a single batch. 3. Filling: Aseptically fill the specified number of units with the sterile media. The number of units filled should be sufficient to detect a potential contamination rate with 95% confidence. 4. Incubation and Observation: Incubate 100% of the filled units at 20-25°C for 7 days, followed by incubation at 30-35°C for 7 days. Observe all units for microbial growth (turbidity) at the end of each incubation period. 5. Positive Control: Inoculate a separate unit of the media with a low level (fewer than 100 CFU) of a suitable microorganism (e.g., Staphylococcus aureus, Bacillus subtilis) to confirm the media's ability to support growth.
5. Acceptance Criteria: The media fill is considered to have passed only if 0 out of the statistically determined number of units (frequently set at a minimum of 4,750-5,000 units for commercial processes) show evidence of microbial growth. Any positive unit constitutes a failure and triggers a thorough investigation and re-validation.
Experimental Protocol: In Vitro Tumorigenicity Assay (Digital Soft Agar)
For pluripotent stem cell (PSC)-derived products, testing for residual undifferentiated cells with tumorigenic potential is a critical safety release criterion [11]. This protocol describes a sensitive digital soft agar method.
1. Objective: To detect and quantify rare transformed cells in a stem cell-based therapeutic product by assessing anchorage-independent growth in a semi-solid medium, a hallmark of neoplastic transformation.
2. Scope: This assay is suitable for final cell products and in-process samples, particularly those derived from PSCs.
3. Materials and Equipment:
- Base Agar (e.g., 1.2% Noble Agar in basal medium).
- Top Agar (e.g., 0.7% Noble Agar in complete growth medium).
- Appropriate positive control cells (e.g., HeLa or other transformed cell line).
- Negative control cells (e.g., primary human fibroblasts).
- 6-well or 12-well cell culture plates.
- Automated cell counter or flow cytometer.
- High-resolution digital scanner or imager.
4. Methodology: 1. Agar Base Layer Preparation: Melt the base agar and maintain at 40-45°C in a water bath. Add a 1-2 mL layer to each well of the culture plate and allow it to solidify at room temperature. 2. Cell Seeding in Top Agar: Trypsinize, count, and resuspend the test article cells and controls. Mix the cell suspension with liquefied top agar (maintained at 37°C) to achieve a final density of 1x10^4 to 5x10^4 cells/mL. Quickly layer 1-2 mL of this cell-top agar mixture over the base layer in each well. Perform this step in triplicate for each sample. 3. Incubation and Feeding: Allow the top agar to solidify, then add a thin layer (0.5-1 mL) of complete growth medium on top to prevent drying. Incubate the plates at 37°C, 5% CO2 for 3-4 weeks, replenishing the top medium weekly. 4. Image Acquisition and Analysis: At the endpoint, digitally scan each well at high resolution. Use image analysis software to automatically identify and count cell colonies larger than a pre-defined threshold (e.g., 50 μm in diameter).
5. Acceptance Criteria: The test article is considered acceptable if the number of colonies formed per 10,000 cells plated is statistically indistinguishable from the negative control and falls below a pre-defined, risk-based specification limit. The positive control must demonstrate robust colony formation for the assay to be valid.
The Scientist's Toolkit: Essential Research Reagent Solutions
The transition from research to GMP-compliant manufacturing necessitates the use of qualified reagents and materials. The following table details key solutions essential for stem cell biomanufacturing research and process development.
Table 4: Key Research Reagent Solutions for Stem Cell Biomanufacturing
| Reagent/Material | Function | GMP-Compliance Consideration |
|---|---|---|
| GMP-Grade Human Serum or Xeno-Free Media Supplements | Provides essential nutrients, growth factors, and hormones for cell growth and maintenance. | Must be sourced from qualified vendors, with certificates of analysis (CoA) and full traceability to ensure absence of adventitious agents. |
| Recombinant Human Growth Factors (e.g., FGF-2, TGF-β) | Directs stem cell proliferation, maintenance of pluripotency, or guides specific differentiation pathways. | Requires GMP-manufactured, animal-origin-free cytokines with documented purity, potency, and stability. |
| Cell Dissociation Enzymes | Passaging and harvesting adherent stem cells from culture surfaces. | Non-animal derived, recombinant enzymes (e.g., recombinant trypsin) are preferred to reduce contamination risk and lot-to-lot variability. |
| Closed-System Bioprocess Containers | Single-use bags and assemblies for media preparation, cell culture, and storage. | Pre-sterilized, USP Class VI certified, and extractables/leachables tested to ensure product compatibility and safety. |
| Annexin V / Viability Assay Kits | Quantifying apoptosis and cell viability for in-process controls and product potency assays. | Assays must be validated for accuracy, precision, and robustness according to ICH guidelines when used for lot release. |
Workflow and Process Diagrams
GMP Transition Workflow for ATMP Development
The following diagram illustrates the logical progression of a stem cell therapy from research to a GMP-compliant clinical product, highlighting key regulatory and development milestones.
Core GMP Control Systems Interrelationship
This diagram depicts the logical relationships between the core control systems required by 21 CFR Part 211 and how they interact to ensure overall product quality.
Successfully navigating the regulatory landscape of 21 CFR Parts 210 and 211 is a fundamental requirement for translating innovative stem cell research into viable, commercially available ATMPs. This journey from a GLP research environment to a GMP-compliant manufacturing operation is complex, requiring meticulous planning, robust process validation, and an unwavering commitment to quality [11]. By understanding the definitions and scope of Part 210, implementing the detailed controls of Part 211, and proactively addressing the unique challenges of ATMP manufacturing—such as aseptic processing, tumorigenicity risk, and scalability—research organizations can build a solid foundation for regulatory success. Embracing these principles not only facilitates compliance but also instills a culture of quality that is essential for developing safe and effective stem cell therapies for patients.
For researchers and scientists engaged in scalable stem cell biomanufacturing, navigating the global regulatory landscape is a critical component of translational success. Current Good Manufacturing Practices (GMP) form the foundation of this landscape, but their interpretation and implementation vary significantly across the European Union (EU), the United States (US), and key Asian markets. Recent and forthcoming regulatory updates, particularly in the EU concerning computerized systems and artificial intelligence, are dramatically reshaping compliance requirements. This application note provides a comparative analysis of these regions, structured tables of quantitative data, detailed experimental protocols for regulatory adherence, and essential workflow visualizations. The aim is to equip drug development professionals with the knowledge and methodologies necessary to align their research and production processes with the most current international standards, thereby facilitating smoother transition from laboratory discovery to clinical application.
The transition from research-scale stem cell culture to GMP-compliant biomanufacturing introduces a complex array of regulatory challenges. The core principle of GMP is to ensure that products are consistently produced and controlled according to quality standards appropriate to their intended use [14]. For stem cell therapies, this involves rigorous control over every aspect of the process, from sourcing of raw materials and characterization of cell lines to the validation of manufacturing processes and quality control testing.
Scalable biomanufacturing presents unique hurdles, such as the adaptation of research protocols to closed, automated systems, the maintenance of cell potency and genetic stability during expansion, and the implementation of real-time quality monitoring. Facilities like the Cedars-Sinai Biomanufacturing Center exemplify the physical and quality system infrastructure required, featuring multiple ISO Class 7 cleanroom suites and dedicated areas for process development to support clinical trials [15]. Similarly, Waisman Biomanufacturing highlights capabilities crucial for the field, including the creation of GMP human embryonic and induced pluripotent stem cell banks, and the development of processes for the expansion and differentiation of these cells [16]. Understanding the regulatory frameworks that govern these operations is the first step in building a compliant and successful biomanufacturing program.
Comparative Analysis of Regional GMP Frameworks
The regulatory philosophies in the EU, US, and Asia, while all founded on the principle of quality and patient safety, differ in their specific requirements, emphasis, and operational details. A comparative analysis reveals distinct regional profiles.
European Union (EU) Regulatory Framework
The EU's regulatory framework, EudraLex Volume 4, is undergoing its most significant transformation in over a decade, with pivotal draft updates released for consultation in July 2025 [17] [18].
- Key Guidelines: The core GMP requirements are detailed in EudraLex Volume 4. The draft Annex 11 (Computerised Systems) has been expanded from 5 to 19 pages, reflecting the modern, digital, and cloud-integrated pharmaceutical environment [17]. Simultaneously, a draft Chapter 4 (Documentation) introduces a stronger focus on the data lifecycle, metadata control, and the management of hybrid systems (paper and electronic) under the Pharmaceutical Quality System (PQS) [18]. A entirely new Annex 22 (Artificial Intelligence) is also proposed, addressing the use of static AI/ML models in GMP environments [17] [18].
- Recent Updates (2025): The draft Annex 11 places a clear emphasis on cybersecurity controls, mandating regular penetration testing for high-risk systems and explicit management responsibility for IT system oversight [17]. It also introduces new requirements for periodic review of system performance and validation status, and expands on data integrity expectations in alignment with ALCOA+ principles [17]. The final versions of these documents are estimated to go live in mid-2026 [17].
- Enforcement Bodies: GMP compliance is overseen by the national competent authorities of member states, coordinated at the EU level by the European Medicines Agency (EMA).
United States (US) Regulatory Framework
The US Food and Drug Administration (FDA) regulates stem cell-based products primarily as biologics, with a strong emphasis on current Good Manufacturing Practices (cGMP).
- Key Guidelines: The foundational regulations for drugs and biologics are enshrined in 21 CFR Parts 210 and 211 [14]. The FDA's guidance documents, such as "Data Integrity and Compliance With Drug CGMP - Questions and Answers," provide further interpretation of these rules [19] [14]. The agency emphasizes a risk-based approach and the use of modern, validated systems, which is encapsulated in the term cGMP (current GMP) [14].
- Recent Updates: While the core regulations are stable, FDA enforcement data reveals trends. For FY2023, the agency intensified action on cGMP gaps and data integrity, issuing over 93 drug-quality-related import alerts [14]. For medical devices, including some combination products, a significant change is the upcoming effectiveness of the Quality Management System Regulation (QMSR) on February 2, 2026, which harmonizes FDA requirements with ISO 13485 [14].
- Enforcement Body: The FDA's Center for Biologics Evaluation and Research (CBER) is primarily responsible for regulating stem cell therapies.
Asian Regulatory Landscape
The Asian regulatory environment is diverse and rapidly evolving, with a growing emphasis on safety assessments and quality systems, though the focus in available literature is often on cosmetics as a proxy for a tightening regulatory environment.
- China: The National Medical Products Administration (NMPA) continues to enhance its regulatory framework. As of May 1, 2025, cosmetic companies are required to submit a full safety assessment report for product notification/registration, a move indicative of a broader trend towards greater scrutiny of product safety and documentation [20].
- South Korea: The Ministry of Food and Drug Safety (MFDS) is preparing to implement new cosmetic safety regulations from 2028, following a grace period. A forthcoming draft is expected to introduce new responsibilities for the Responsible Person (RP) and establish a new role of "safety assessor" [20].
- Taiwan: The Taiwan FDA (TFDA) has been aligning its Cosmetic Hygiene and Safety Act with international standards. The agency has rolled out a phased implementation schedule for Product Information Files (PIFs) and GMP compliance for manufacturing sites. Baby, lip, and eye products must establish PIFs and comply with GMP by July 1, 2025, with general cosmetics following a year later [20].
Table 1: Comparative Analysis of Key Regional GMP Frameworks for Biomanufacturing
| Aspect | European Union (EU) | United States (US) | Asia (Representative Examples) |
|---|---|---|---|
| Core Regulation | EudraLex Volume 4 (GMP) [21] | 21 CFR Parts 210, 211 (cGMP) [14] | Variable (e.g., Taiwan: Cosmetic Hygiene & Safety Act) [20] |
| Computerized Systems | Annex 11 (Under major revision) [17] | 21 CFR Part 11 (Electronic Records/Signatures) & CSA [17] | Often references or aligns with EU/US principles |
| Key 2025 Update | Draft Annex 11 (Cybersecurity, AI, Cloud) [17] [18] | QMSR harmonization with ISO 13485 (Effective 2026) [14] | China: Full safety assessment reports for cosmetics [20] |
| Data Integrity Focus | ALCOA+, embedded in PQS, audit trail review [18] | ALCOA, data integrity CGMP guidance [19] [14] | Increasingly emphasized (e.g., PIF requirements) [20] |
| Quality System Emphasis | Pharmaceutical Quality System (PQS) [18] | Quality System (cGMP) & QMSR for devices [14] | Good Manufacturing Practice (GMP) adoption [20] |
Essential Reagents and Materials for GMP-Compliant Stem Cell Research
Transitioning from research-grade to GMP-compliant materials is a critical step in clinical translation. The following table details key reagent solutions and their functions in a stem cell biomanufacturing context.
Table 2: The Scientist's Toolkit: Essential Reagents for GMP Stem Cell Biomanufacturing
| Reagent/Material Solution | Function in Stem Cell Biomanufacturing | GMP Compliance Consideration |
|---|---|---|
| GMP-Grade Human Pluripotent Stem Cells (hPSCs) | Starting material for differentiation into therapeutic cell types; requires rigorous characterization. | Must be sourced from a qualified supplier, accompanied by a comprehensive Certificate of Analysis (CoA) and tested for adventitious agents [16]. |
| Xeno-Free Culture Media | Provides nutrients and signaling molecules for cell growth and maintenance; excludes animal-derived components. | Raw materials must be qualified, and the final media formulation must be produced under a quality system. Full traceability and lot-to-lot consistency are critical. |
| GMP-Grade Growth Factors & Cytokines | Directs stem cell differentiation towards specific lineages (e.g., neural, cardiac). | Requires vendor qualification, CoA with data on purity, potency, and sterility. The definition of "GMP-grade" should be clearly understood and documented. |
| Cell Dissociation Reagents | Used for passaging adherent stem cells and harvesting cell products. | Must be compliant for human clinical use. The reagent's mechanism and any residual components must be shown to not impact cell safety or function. |
| GMP Plasmid DNA | Critical for the generation of induced Pluripotent Stem Cells (iPSCs) and gene-editing processes. | Sourced from a GMP plasmid service provider that ensures quality controls, documentation, and traceability throughout manufacturing [22] [23]. |
| Final Formulation Solutions (Cryopreservation Media) | Protects cell viability during freeze-thaw cycles for storage and transport. | Composition must be defined and validated. The cryopreservation and thawing process must be optimized and controlled to ensure consistent post-thaw cell recovery and function. |
Experimental Protocol for Establishing a GMP-Compliant Stem Cell Workflow
This protocol outlines the key methodological steps for establishing a scalable and GMP-compliant process for human pluripotent stem cell (hPSC) expansion, a foundational stage in stem cell biomanufacturing.
Protocol: Scalable Expansion of GMP-Compliant Human Pluripotent Stem Cells
Objective: To establish a validated, closed-system workflow for the expansion of GMP-grade hPSCs, ensuring maintenance of pluripotency and genetic stability for use in clinical trials.
Materials:
- GMP-grade hPSC Master Cell Bank (MCB) [16]
- Qualified, xeno-free hPSC culture medium and GMP-grade recombinant growth factors
- Closed-system bioreactor (e.g., suspension bioreactor) or multi-layer cell factories [16] [15]
- GMP-grade cell dissociation agent
- QC equipment for in-process monitoring (e.g., cell counter, flow cytometer, metabolyzer)
Methodology:
- System Preparation: Assemble the closed-system bioreactor or cell stack according to validated procedures. Prime the system with pre-warmed, GMP-grade culture medium. Ensure all environmental parameters (temperature, CO₂, humidity) are monitored and within specified ranges.
- Cell Seeding: Aseptically thaw a vial from the GMP-grade hPSC Working Cell Bank (WCB) following a validated protocol. Seed the cells into the prepared system at a pre-determined and optimized cell density.
- Controlled Expansion: Maintain the culture with periodic, automated medium exchange. Continuously monitor and record key process parameters (KPPs) such as pH, dissolved oxygen, and metabolite levels (e.g., glucose, lactate). The process should be designed to minimize manual intervention and open manipulations.
- In-process Monitoring: Take representative samples using aseptic, closed sampling systems.
- Perform daily cell counts and viability assessments.
- At specified intermediate stages, analyze samples for pluripotency markers (e.g., Oct4, TRA-1-60) via flow cytometry to ensure phenotypic stability.
- Harvest: Once the culture reaches the target cell density or confluence, terminate the expansion phase. Detach cells using a GMP-grade dissociation reagent and harvest using continuous centrifugation technologies (e.g., kSep, LOVO) [16].
- Formulation and Cryopreservation: Wash and resuspend the cell pellet in a defined, GMP-grade cryopreservation medium. Fill the final cell product into cryobags or vials using an automated filling system. Cryopreserve using a controlled-rate freezer and transfer to a validated, monitored liquid nitrogen storage system [16].
- Quality Control Testing: The final cell product must undergo rigorous QC testing, which typically includes, but is not limited to:
- Sterility testing (e.g., BacT/ALERT)
- Mycoplasma testing
- Identity testing (STR DNA profiling)
- Purity/Pluripotency analysis (Flow Cytometry)
- Potency assay (e.g., trilineage differentiation potential)
- Karyotype analysis to confirm genetic stability
The entire process, from cell thaw to final cryopreservation, must be conducted under the facility's quality system, with all activities documented in batch records and all data, including metadata and audit trails, retained in compliance with regional data integrity requirements [17] [18] [14].
Workflow Visualization: GMP-Compliant Stem Cell Biomanufacturing
The following diagram illustrates the logical workflow and the critical quality control checkpoints in a GMP-compliant stem cell biomanufacturing process.
Diagram 1: GMP stem cell manufacturing workflow with quality controls.
Workflow Visualization: Regulatory Strategy Across Regions
Developing a regulatory strategy requires understanding how regional frameworks interact with the product lifecycle. The following diagram outlines a logical approach for global regulatory alignment.
Diagram 2: Strategy for multi-regional GMP compliance.
The global regulatory landscape for GMP in stem cell biomanufacturing is dynamic and regionally distinct, yet converging on core principles of data integrity, risk management, and robust quality systems. The most significant changes are on the horizon in the EU, with a comprehensive modernization of Annex 11 that explicitly brings cloud, AI, and advanced cybersecurity under the GMP umbrella. For researchers and drug development professionals, proactive engagement is key. This involves conducting thorough gap analyses of current systems against these evolving standards, updating validation protocols and quality agreements, and investing in training for personnel. By integrating regulatory compliance as a foundational element of the research and development process, scientists can accelerate the translation of promising stem cell therapies from the laboratory bench to the patient bedside, navigating the complexities of the global market with confidence.
This document provides detailed application notes and protocols for establishing and maintaining controlled environments for aseptic processing, with a specific focus on applications in scalable stem cell biomanufacturing. Adherence to these principles is critical for ensuring the quality, safety, and efficacy of sterile cell-based therapies.
Regulatory Landscape and the Contamination Control Strategy (CCS)
The regulatory framework for sterile manufacturing has evolved to emphasize "built-in" quality over reliance on end-product testing. Key guidelines from the US FDA, WHO, and Health Canada now centralize the requirement for a holistic, living Contamination Control Strategy (CCS) [24]. A CCS is not a single document but a comprehensive plan that proactively links all contamination control measures—from raw materials to final product release [25] [24].
Table 1: Key Regulatory Pillars for Aseptic Processing in 2025
| Regulatory Authority | Guidance Document | Core Emphasis |
|---|---|---|
| US FDA | Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing | Sterility is assured by process validation, not testing. Requires robust facility design, validated sterilization cycles, and rigorous personnel training [24]. |
| World Health Organization (WHO) | Annex 6: GMP for Sterile Pharmaceutical Products | Harmonized with global standards; mandates specific cleanroom grades (A-D) and details expectations for barrier technologies and the CCS [24]. |
| Health Canada | GUI-0119 (Annex to GMP Guide) | Provides granular expectations for environmental and process monitoring, stressing risk-based program design to detect process drift [24]. |
The CCS operates on a continuous cycle: Identify contamination risks, Assess the sufficiency of existing controls, Monitor performance with data, and Review & Improve the strategy periodically [24].
Facility Design and Critical Utilities
Modern facility design focuses on segregation and aerodynamic protection to minimize contamination risk.
Zoning, Airflow, and Pressure Cascades
Cleanrooms are classified into grades (A/B/C/D) that act as successive buffers. A robust pressure differential cascade (a minimum of 10-15 Pascals between adjacent zones) must be maintained to prevent lower-quality air from flowing into higher-grade areas [24].
Table 2: Cleanroom Classification and Environmental Limits
| Grade | ISO Equivalent | Airflow Principle | Maximum Permitted Particles (≥0.5μm/m³) | Microbial Action Limits (Settle Plates, Ø90mm, CFU/4 hours) |
|---|---|---|---|---|
| A | ISO 5 | Unidirectional (Laminar) | 3,520 | <1 [25] |
| B | ISO 7 | Turbulent (but filtered) | 352,000 | 5 [25] |
| C | ISO 8 | Turbulent | 3,520,000 | 50 [25] |
| D | ISO 9 | Turbulent | Not specified | 100 [25] |
Barrier Technologies: RABS vs. Isolators
Advanced barrier systems are increasingly favored to separate personnel from the process [24].
- Isolators: Provide complete physical separation. They allow for automated bio-decontamination (e.g., with Vaporized Hydrogen Peroxide) and can often operate in a less rigorous background environment (Grade C or D) [26] [24].
- RABS (Restricted Access Barrier Systems): Provide a rigid wall enclosure with glove ports but are not fully sealed. They rely on dynamic airflow and must be operated in a Grade B background [24].
Selection Guide: Isolators are preferred for high-potency drugs and maximum sterility assurance, while RABS offer more flexibility for faster product changeovers [24].
Personnel and Aseptic Behavior Control
The operator is the single greatest contamination risk. Controlling personnel is therefore paramount [24].
- Gowning: Sterile, non-shedding gowns that cover all skin are mandatory for Grade A/B entry. A formal gowning qualification program is required, with typical requalification occurring annually or more frequently following an excursion [25] [24].
- Aseptic Technique: Personnel must be rigorously trained in:
- Slow, deliberate movement to minimize turbulence.
- The "First Air" principle: Never obstruct the path of sterile HEPA air before it reaches the critical product surface.
- Minimal intervention: Processes should be designed to reduce or eliminate manual interventions [24].
Environmental and Process Monitoring
Monitoring verifies that the process is in a state of control but does not itself assure sterility [24].
Table 3: Elements of an Environmental Monitoring Program
| Monitoring Type | Method | Frequency (Example) | Key Parameter |
|---|---|---|---|
| Viable Air | Active Air Sampler (Volumetric) | Each operating shift | Colony Forming Units (CFU)/m³ |
| Viable Surface | Contact Plates (e.g., 55cm²) | Each operating session | CFU/plate |
| Viable Personnel | Finger Dabs, Gown Plates | Each exit from Grade A/B | CFU/plate |
| Non-Viable Particles | Real-time, continuous monitor | Continuously in Grade A | Particles (≥0.5μm and ≥5.0μm)/m³ |
Trend Analysis: Modern expectations require analyzing data trends over time to detect slow drifts in facility performance before they become major failures [27] [24].
Aseptic Process Simulation (Media Fill)
An Aseptic Process Simulation (APS), or media fill, is the ultimate validation of the aseptic process, using a sterile microbial growth medium in place of the actual product [25] [24].
Protocol 1: Aseptic Process Simulation (Media Fill) for a Stem Cell Suspension
- Objective: To demonstrate that the aseptic processing operations can produce sterile product.
- Frequency: Typically required semi-annually for each processing line and shift [24].
- Media: Tryptic Soy Broth (TSB) or another suitable sterile liquid growth medium.
- Procedure:
- The medium is subjected to the entire aseptic process, including thawing, dilution, transfer through closed systems or open manipulations under laminar airflow, and filling into final containers.
- The process must simulate "worst-case" conditions, including the maximum number of personnel, all permitted interventions, and the longest run duration.
- All containers are then incubated at 20-25°C for 7 days, followed by 30-35°C for 7 days.
- Acceptance Criteria: The target is zero growth-positive units. Any positive unit indicates a potential breach in sterility assurance and warrants a thorough investigation. The process typically requires three consecutive successful media fills to be requalified [24].
Protocol: GMP-Compliant Aseptic Thaw and Dilution of Cryopreserved Cells
This protocol outlines a standardized method for the aseptic preparation of cell therapy products, a common critical operation in stem cell biomanufacturing.
Stability Consideration: Studies on Wharton's Jelly-derived MSCs show that multiple freeze-thaw cycles and post-thaw storage at room temperature (20-27°C) lead to a significant decrease in cell viability and viable cell concentration. Thawed products should be processed as quickly as possible [28].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key GMP-Compliant Reagents for Cell Biomanufacturing
| Reagent / Material | Function | GMP-Compliant Example / Specification |
|---|---|---|
| Human Platelet Lysate (hPL) | Serum-free, xeno-free cell culture supplement providing growth factors and attachment proteins. | GMP-grade, pathogen-inactivated [28]. Concentrations of 2% and 5% have shown similar efficacy for WJ-MSC expansion [28]. |
| GMP-Grade Enzymes | Isolation of cells from tissue matrices (e.g., umbilical cord Wharton's Jelly). | Collagenase NB6 GMP (Nordmark Biochemicals) at optimized concentrations (e.g., 0.4 PZ U/mL) [28]. |
| Defined, Xeno-Free Basal Medium | Base nutrient medium for cell culture and expansion. | Commercially available MSC Serum- and Xeno-Free Medium (e.g., NutriStem) [28]. |
| Sterile Disinfectants & Sporicides | For cleanroom and equipment decontamination. | A validated two-tier rotation system, including a sporicidal agent, is a regulatory expectation. Efficacy must be validated against environmental isolates [25] [24]. |
| Pre-Validated Aseptic Garments | To minimize particulate and microbial shedding from personnel. | Fabric selection and qualification are critical. A User Requirement Specification (URS) should be prepared for gowning systems [25]. |
Data Analytics and Continuous Improvement
Data analytics is crucial for optimizing GMP processes and enabling continuous improvement. It helps identify root causes of quality issues, monitor improvement outcomes, and foster a data-driven culture [27].
- Identifying Trends: Use real-time dashboards to track Key Performance Indicators (KPIs) like environmental monitoring data and media fill success rates to spot patterns and anomalies [27].
- Trend Analysis: Move beyond reacting to excursions. Analyze data trends over time to detect slow drifts in facility performance before they become failures [24].
The global stem cell market is experiencing robust growth, propelled by their expanding therapeutic applications in regenerative medicine, oncology, and drug discovery. The market size, valued at USD 16.74 billion in 2024, is projected to grow at a CAGR of 11.30% from 2025 to 2034, reaching approximately USD 48.83 billion by 2034 [29]. Concurrently, the stem cell manufacturing market is growing even faster, with an expected CAGR of 13.1%, aiming to reach USD 44.2 billion by 2034 from USD 12.9 billion in 2024 [30]. This growth is underpinned by rising demand for scalable, high-quality production of clinical-grade stem cells that comply with Good Manufacturing Practice (GMP) standards—a critical prerequisite for translating laboratory research into clinically applicable therapies [31] [32].
The transition from research-scale to industrial and clinical-scale stem cell production presents significant scientific and regulatory challenges. These include maintaining cell potency and genetic stability, controlling differentiation, ensuring reproducibility, and implementing rigorous quality control throughout the manufacturing process [33] [32]. This document outlines key market dynamics, provides detailed experimental protocols for GMP-compliant stem cell manufacturing, and explores the automated platforms and reagent solutions essential for scalable production.
Table: Global Stem Cell and Manufacturing Market Outlook
| Market Segment | 2024/2025 Base Value | Projected Value (2034) | CAGR | Primary Growth Driver |
|---|---|---|---|---|
| Overall Stem Cell Market [29] | USD 16.74 Billion (2024) | USD 48.83 Billion | 11.30% | Rising demand for regenerative medicines & expansion of clinical trials. |
| Stem Cell Manufacturing Market [30] | USD 12.9 Billion (2024) | USD 44.2 Billion | 13.1% | Advancements in biomanufacturing tech and rising chronic disease prevalence. |
| U.S. Stem Cell Market [29] | USD 5.75 Billion (2025) | USD 15.79 Billion | 11.90% | High R&D investment and concentration of biopharma companies. |
| Asia Pacific Manufacturing Market [30] | - | - | Fastest Growing | Strong product pipelines, government initiatives, and large patient pool. |
Market Dynamics and Regional Analysis
Key Market Drivers and Segmentation
The expansion of the stem cell market is fueled by several interconnected factors:
- Rising Therapeutic Applications: Stem cells hold significant promise for treating chronic and degenerative diseases, with the oncology segment exhibiting the highest growth rate due to various pipeline products [29]. The increasing prevalence of conditions like heart failure and diabetes is driving demand for regenerative therapies [30] [34].
- Technological Integration: The infusion of automation, artificial intelligence (AI), and advanced bioreactors is streamlining workflows, enhancing product consistency, and unlocking new revenue channels [35] [36]. AI is being utilized for predictive modeling, cell characterization, and quality control [37].
- Substantial Investments: Growing venture capital investment and favorable government initiatives are stimulating market growth, enabling cutting-edge research and the development of advanced manufacturing techniques [34].
Market segmentation reveals distinct trends. By product, adult stem cells, particularly Mesenchymal Stem Cells (MSCs), dominate due to lower contamination risks and better compatibility with the human body [29] [32]. By application, drug discovery and development is the largest segment, accounting for 53.8% of the manufacturing market in 2024, as stem cells enable more accurate, human-relevant biological assessments for pharmaceutical R&D [30].
Regional Landscape
The global stem cell market exhibits varied regional dynamics, influencing strategic expansion and collaboration opportunities.
Table: Regional Market Dynamics and Opportunities
| Region | Market Highlights & Drivers | Key Opportunities |
|---|---|---|
| North America [29] [30] | Leader with 44% market share (2024); strong R&D infrastructure; supportive regulatory framework; high concentration of pharma & biotech companies. | Enhancing scalable manufacturing platforms; leading innovation in automated bioprocessing and AI integration. |
| Asia-Pacific [29] [30] [37] | Fastest-growing market; driven by government support (e.g., China, Japan, South Korea), large patient pool, and rising healthcare investment. | Becoming a cost-effective manufacturing hub; expanding clinical trial activities; developing scalable production platforms for regional demand. |
| Europe [35] [37] | Mature market with strong focus on regulatory compliance and sustainability; advanced engineering and manufacturing bases in Germany, UK, and France. | Leading in green manufacturing technologies; fostering academia-industry collaborations for innovation. |
| Latin America [29] | Emerging market with promising growth in urban centers like São Paulo and Mexico City; challenges include regulatory heterogeneity and limited GMP capacity. | Establishing regional CDMO hubs; implementing tiered pricing strategies and local cryobanks to improve patient access. |
GMP-Compliant Protocol: Isolation and Expansion of Mesenchymal Stem Cells
The following section provides a detailed protocol for the GMP-compliant isolation and expansion of Mesenchymal Stem Cells (MSCs) from the infrapatellar fat pad (IFP), adapted from recent research [31]. The workflow below outlines the complete process from tissue acquisition to product release.
GMP-Compliant MSC Manufacturing Workflow
Reagents and Equipment
Source Tissue: Infrapatellar fat pad (IFP) tissue (10-20 g) obtained as surgical waste from patients undergoing anterior cruciate ligament (ACL) reconstructive surgery, following informed consent and ethical approval [31].
Critical Reagents:
- Collagenase (0.1% in serum-free media)
- GMP-compliant Culture Media: MSC-Brew GMP Medium (Miltenyi Biotec) or MesenCult-ACF Plus Medium (StemCell Technologies). These are animal component-free [31].
- Supplements: Human Platelet Lysate (hPL) where applicable, to replace Fetal Bovine Serum [32].
- Phosphate-Buffered Saline (PBS)
- Cryopreservation Solution: FBS containing 10% dimethyl sulfoxide [31].
Equipment:
- Class A/B cleanroom facility with laminar flow hoods [32]
- CO₂ Incubator
- Centrifuge
- Automated cell counter or Bright-Line Hemacytometer
- Flow Cytometer (for quality control)
- Automated Bioreactor Systems (e.g., Quantum, CliniMACS Prodigy) for large-scale expansion [32]
Step-by-Step Procedure
Tissue Digestion and Primary Cell Isolation
- Processing: Mince the acquired IFP tissue into approximately 1 mm³ pieces using sterile surgical instruments [31].
- Digestion: Incubate the minced tissue with 0.1% collagenase in serum-free media for 2 hours at 37°C with constant agitation [31].
- Cell Harvesting:
- Centrifuge the digested tissue at 300 × g for 10 minutes.
- Carefully remove the supernatant and surfactant layer.
- Resuspend the cell pellet in PBS and filter the suspension through a 100 μm filter to remove debris.
- Centrifuge again at 300 × g for 10 minutes and resuspend the final cell pellet in standard MSC media or the chosen GMP-compliant medium [31].
- Initial Seeding (Passage 0): Seed the isolated cells in culture flasks and incubate at 37°C with 5% CO₂.
- Medium Change: Replace the culture medium every 2-3 days to remove non-adherent cells.
Subculture and Expansion
- Passaging: Once cells reach 80-90% confluency, passage them using a standard trypsinization protocol.
- Expansion: Seed cells at a density of 5 × 10³ cells/cm² in the selected GMP-compliant medium for subsequent expansions [31].
- Large-Scale Culture: For clinical-scale production, transfer the process to an automated, closed-system bioreactor such as the Quantum or CliniMACS Prodigy system to enhance yield and maintain consistency while minimizing open manipulations [32].
Quality Control and Product Release Specifications
Rigorous quality control is fundamental to GMP. The final cell product must meet predefined release criteria before clinical application [31] [32].
Table: Quality Control Assays and Release Criteria for MSCs
| Test Category | Specific Assay / Marker | GMP Release Criteria | Purpose |
|---|---|---|---|
| Viability & Sterility | Trypan Blue Exclusion | > 95% Viability (Minimum >70%) [31] | Ensures metabolic competence of the final product. |
| Bact/Alert, Endotoxin, Mycoplasma | Sterile, No microbial contamination [31] | Confirms product safety, free from adventitious agents. | |
| Purity & Identity (Flow Cytometry) | Positive: CD73, CD90, CD105 | > 95% Positive Expression [31] [32] | Verifies MSC identity as per ISCT standards. |
| Negative: CD45, CD34, HLA-DR | < 5% Positive Expression [32] | Confirms absence of hematopoietic cells. | |
| Potency & Functionality | Colony Forming Unit (CFU) Assay | High colony formation capacity [31] | Demonstrates clonogenic and self-renewal potential. |
| Trilineage Differentiation (in vitro) | Differentiation into osteocytes, chondrocytes, adipocytes [32] | Confirms multilineage differentiation potential. | |
| Immunomodulatory Assay | Suppression of T-cell activation [32] | Validates therapeutic functionality for specific applications. |
Scaling Up: Automated Manufacturing Platforms
Automated closed-system bioreactors are pivotal for scaling up MSC production while adhering to GMP standards. They reduce labor intensity, minimize contamination risks, and improve process reproducibility [32]. The diagram below compares the core functions of two major automated platforms.
Automated Platform Comparison: Quantum vs. CliniMACS Prodigy
Table: Comparison of Automated Stem Cell Manufacturing Platforms
| Platform | Technology | Key Features | Process & Yield | GMP Compliance |
|---|---|---|---|---|
| Quantum (Terumo BCT) [32] | Hollow Fiber Bioreactor | Provides 21,000 cm² area; enables continuous medium exchange and hypoxia culture. | 7-day expansion yields 100-276 million BM-MSCs from a 20-million cell seed. | Closed, automated system reduces open manipulations from ~54,400 to 133 steps. |
| CliniMACS Prodigy (Miltenyi Biotec) [31] [32] | Integrated Tubing Set (TS730) with Adherent Cell Culture (ACC) | Fully automated from isolation and inoculation to harvest; uses MSC-Brew GMP medium. | 10-day procedure generates ~29-50 million MSCs at Passage 0 from primary tissue. | Integrated closed system ensures aseptic processing from start to finish. |
| Other Platforms (e.g., Xuri, Cocoon) [32] | Stirred-tank or fixed-bed bioreactors | Scalable wave-induced agitation or modular personalized therapy production. | Varies with system scale and cell type. | Designed as closed systems to meet GMP requirements for clinical production. |
The Scientist's Toolkit: Essential Reagent Solutions
The shift to GMP-compliant, scalable manufacturing requires a critical set of reagent solutions that ensure safety, consistency, and efficacy.
Table: Essential Research Reagent Solutions for GMP-Compliant Stem Cell Manufacturing
| Reagent Category | Specific Example | Function & Importance | GMP / Scalability Benefit |
|---|---|---|---|
| Culture Media | MSC-Brew GMP Medium [31] | Animal component-free medium formulated for MSC expansion. | Eliminates xeno-risks; ensures batch-to-batch consistency; compliant with regulatory standards. |
| Growth Supplements | Human Platelet Lysate (hPL) [32] | Replacement for Fetal Bovine Serum (FBS) as a growth supplement. | Animal-free; enhances cell proliferation; reduces immunogenicity risk in clinical applications. |
| Dissociation Enzymes | GMP-grade Collagenase [31] | Enzymatic digestion of tissues for primary cell isolation. | Traceable, non-animal origin versions available to ensure safety and quality of the cell product. |
| Critical Reagents | GM-grade DLL4 Protein [34] | Recombinant protein used in directing stem cell differentiation. | High-purity, well-characterized reagent crucial for consistent and controlled differentiation protocols. |
| Cryopreservation Media | Defined, Serum-Free Cryomedium | Protects cell viability and functionality during frozen storage. | Xeno-free formulation prevents contamination and maintains cell integrity post-thaw, critical for biobanking. |
The stem cell market's rapid growth is intrinsically linked to the successful development of robust, scalable, and GMP-compliant manufacturing processes. As documented herein, the market's double-digit growth trajectory is a powerful incentive for industry and academia to collaborate on standardizing protocols, optimizing culture conditions with animal-free reagents like MSC-Brew GMP Medium and hPL, and integrating automated platforms such as the Quantum and CliniMACS Prodigy systems. The detailed protocol and quality control framework provided serve as a foundational guide for researchers and drug development professionals aiming to translate stem cell innovations from the laboratory bench to the clinic, ultimately fulfilling the promise of regenerative medicine for a wider patient population.
Scalable Technologies and Automated Platforms for GMP-Compliant Production
The transition to Good Manufacturing Practice (GMP)-compliant biomanufacturing necessitates a shift from manual, open processes to automated, closed-system technologies [38] [9]. Automated bioreactor systems are central to this transition, enabling the standardization, scalability, and control required for the production of stem cell and T cell-based therapeutics [39] [40]. These systems minimize operator-dependent variability and reduce the risk of contamination, which is critical for meeting the stringent requirements of clinical-grade manufacturing [9] [41]. This document provides detailed application notes and experimental protocols for three prominent automated systems: the Quantum, CliniMACS Prodigy, and Cocoon platforms, framing their use within a scalable GMP biomanufacturing workflow.
System Profiles
- Quantum System (Cytiva): The Quantum is a hollow-fiber bioreactor designed for the rapid expansion of various cell types, including T cells. It is a functionally closed system that supports high-density cell culture, making it suitable for processes where cells are in the exponential growth phase [39].
- CliniMACS Prodigy (Miltenyi Biotec): The CliniMACS Prodigy is an integrated, automated platform that performs end-to-end manufacturing of cell therapies, from cell isolation and purification to transduction and expansion, within a single device [39] [40]. Its core technology includes magnetic separation for cell selection and an integrated culture chamber with pre-programmed process steps [39].
- Cocoon Platform (Lonza): The Cocoon Platform is a fully automated, closed-system designed for point-of-care (POC) or decentralized manufacturing of cell therapies [40]. It utilizes single-use, standardized "cassettes" or disposables to automate the entire manufacturing process, aiming to simplify production and ensure consistency in hospital or clinical settings [40].
System Comparison and Selection Guide
The table below summarizes the key operational characteristics of the three systems to aid in selection based on research and production goals.
Table 1: Quantitative Comparison of Automated Bioreactor Systems
| Feature | Quantum | CliniMACS Prodigy | Cocoon Platform |
|---|---|---|---|
| Primary Application | Rapid cell expansion once cells are in exponential growth [39] | End-to-end manufacturing from selection to final harvest [39] [40] | End-to-end automated manufacturing at the point of care [40] |
| Process Integration | Expansion only; requires upstream activation [39] | Fully integrated process (selection, activation, culture, harvest) [39] | Fully integrated process within single-use cassettes [40] |
| Target Cell Capacity | Information not available in search results | Up to (3 \times 10^9) target cells [39] | Information not available in search results |
| Manufacturing Model | Centralized | Centralized or Decentralized [39] [40] | Decentralized / Point-of-Care [40] |
| Key Automation Feature | Hollow-fiber technology for high-density culture [39] | Integrated magnetic selection and culture chamber [39] | Single-use, standardized cassette for closed processing [40] |
Experimental Protocols for GMP-Compliant Manufacturing
Protocol 1: T Cell Expansion using the Quantum System
This protocol assumes T cells have been previously isolated and activated.
- System Setup and Priming: Aseptically install the Quantum disposable cartridge and tubing set. Prime the system with pre-warmed cell culture medium according to the manufacturer's instructions to remove air bubbles and condition the circuit.
- Cell Inoculation: Harvest activated T cells and resuspend them in complete medium. Connect the cell bag to the system and initiate the inoculation sequence to load cells into the bioreactor cartridge. The recommended seeding density is highly process-dependent and should be optimized.
- Expansion Phase: The system continuously perfuses fresh medium through the hollow fibers while removing waste products. Monitor key parameters daily, including glucose consumption, lactate production, and gas exchange rates. Monitor cell growth through daily sampling and cell counting.
- Harvest: Once the target cell count or expansion fold is reached (typically after several days), initiate the harvest sequence. The system will wash and concentrate the cells into a final collection bag.
- Quality Control: Sample the final product for critical quality attributes (CQAs), including viability (target > 95%), cell count, sterility, and phenotype (e.g., CD3+, CD4+/CD8+ ratio) [39].
Protocol 2: CAR-T Cell Manufacturing on the CliniMACS Prodigy
This protocol describes an automated process for generating chimeric antigen receptor (CAR)-T cells from a starting apheresis product.
- Load Starting Materials: Aseptically load the leukapheresis product, appropriate GMP-grade buffers, and all required single-use sets (e.g., tubing set, culture bag) onto the CliniMACS Prodigy device [39].
- Cell Selection (Automated): Select the "CD4+/CD8+ Cell Selection" program. The system automatically performs density gradient centrifugation (if needed) and magnetic-activated cell sorting (MACS) using anti-CD4 and anti-CD8 microbeads, typically yielding a T cell population of >90% purity [39].
- Activation and Transduction (Automated): The system transfers the selected T cells to the integrated culture chamber. It then automatically adds T cell activation reagents (e.g., TransAct) and the viral vector for CAR gene transduction. The culture is maintained under controlled conditions with gentle agitation [39].
- Expansion (Automated): The system continues the culture, monitoring and maintaining parameters like temperature and gas exchange. The expansion typically continues for 7-10 days, with the system potentially performing media exchanges or feeds as programmed.
- Final Harvest and Formulation (Automated): Upon process completion, the system automatically washes and concentrates the CAR-T cells into a final bag, ready for fill-finish and cryopreservation. The entire process requires minimal hands-on time [39] [40].
Protocol 3: Point-of-Care Cell Therapy Production on the Cocoon Platform
This protocol outlines the use of the Cocoon for automated, decentralized manufacturing.
- Cassette Loading: In a GMP-compliant environment (potentially as low as Grade D), load the patient's starting material (e.g., purified T cells or PBMCs) and all required reagents into the single-use, pre-sterilized cassette [40] [42].
- System Initiation: Load the cassette into the Cocoon Platform. The system's software will automatically recognize the cassette and initiate the pre-validated manufacturing protocol.
- Hands-Off Processing: The platform is a functionally closed system, automating all subsequent unit operations. This includes cell activation, viral transduction, medium exchanges, and cell expansion within the bioreactor module. The system can incorporate in-process monitoring and controls to ensure product quality [40].
- Product Harvesting: After the prescribed culture period, the system automatically terminates the culture, washes the cells, and formulates the final therapeutic product into an infusion bag.
- Product Release and Administration: The final product is removed from the system and can undergo rapid, local quality control testing before being released for patient administration at the same site, significantly reducing vein-to-vein time [40].
The Scientist's Toolkit: Essential Reagents and Materials
The table below lists key reagents and materials critical for successful bioprocess development and manufacturing using these automated systems.
Table 2: Key Research Reagent Solutions for Automated Biomanufacturing
| Reagent/Material | Function | GMP Consideration |
|---|---|---|
| Cell Culture Media | Provides nutrients for cell growth and expansion. | Use serum-free, xeno-free, GMP-grade formulations to reduce variability and contamination risk [42]. |
| Cell Activation Reagents | Stimulates T cells (e.g., via CD3/CD28) to initiate proliferation. | GMP-grade soluble antibodies or complexes (e.g., TransAct) are required for clinical production [39]. |
| Viral Vectors | Delivers genetic material (e.g., CAR transgene) to target cells. | Must be produced under GMP conditions; titer and purity are Critical Quality Attributes [39]. |
| Cell Selection Beads | Isolates target cell populations (e.g., CD4+/CD8+ T cells) via magnetic separation. | GMP-compliant, clinical-grade beads (e.g., CliniMACS) are essential for integrated systems [39]. |
| Single-Use Bioprocess Containers | Closed-system bags and tubing sets for fluid handling and cell culture. | Must be sterilized and validated for extractables and leachables to ensure product safety [41]. |
Workflow and System Integration Diagrams
GMP Biomanufacturing Workflow Integration
Closed-System Automation for GMP Compliance
In the field of scalable stem cell biomanufacturing, achieving high-efficiency genetic modification without compromising cell health or compliance is a significant challenge. Lentiviral vectors (LVs) are powerful tools for delivering genetic material into cells but often require high multiplicities of infection (MOI) to achieve therapeutic transduction levels in difficult-to-transfect primary cells, substantially driving up manufacturing costs [43]. Transduction enhancers (TEs) have emerged as critical reagents to overcome these barriers.
Framed within Good Manufacturing Practice (GMP) for clinical-scale production, this application note details the use of LentiBOOST, a poloxamer-based, non-cytotoxic transduction enhancer [44] [45]. We provide structured quantitative data and detailed protocols to enable researchers to effectively integrate this technology into robust, scalable, and cost-effective stem cell manufacturing processes.
LentiBOOST Mechanism and Key Advantages
LentiBOOST functions as a universal, receptor-independent manufacturing aid that facilitates the fusion of the lentivirus with the cell membrane [44] [45]. This mechanism leads to an increased vector copy number and significantly improved lentiviral transduction efficiency, allowing for the same therapeutic effect at a lower MOI [44].
This action translates into three key advantages for GMP biomanufacturing:
- Reduced Cost of Goods (COGs): Decreasing the required vector quantity directly lowers one of the most significant cost drivers in cell and gene therapy production [44] [43].
- Enhanced Therapeutic Response Rates: By improving transduction efficiency, particularly in challenging cell populations like exhausted T-cells or those available in limited numbers, LentiBOOST can increase the likelihood of a successful therapeutic outcome [44].
- GMP-Ready Formulations: The reagent is available in both pharma grade for research/process development and GMP grade for clinical trials and commercial therapy, complete with the required documentation (e.g., Certificate of Analysis) for regulatory submissions [44].
Quantitative Performance Data
The following tables summarize key performance data for LentiBOOST across various cell types, as demonstrated in research and clinical settings.
Table 1: Transduction Efficiency Enhancement Across Clinically Relevant Cell Types
| Cell Type | Baseline Transduction (without LentiBOOST) | Enhanced Transduction (with LentiBOOST) | Fold Increase | Key Findings |
|---|---|---|---|---|
| Human CD34+ PBSCs [44] | ~20% (GFP+ at MOI=10) | Up to 80% (GFP+ at MOI=10) | ~4-fold | Dose-dependent improvement; no cytotoxicity observed. |
| Primary Human T-cells [44] | ~20% (at high MOI) | Up to ~100% (at high MOI) | ~5-fold | Strongest enhancing effect compared to other enhancers. |
| Human Dendritic Cells (iDCs) [46] | 22% | >80% | ~3.6-fold | Efficient transduction maintained cell phenotype and function. |
| Human Hematopoietic Stem Cells (HSCs) [44] | Not Specified | Significant improvement | ~5-fold (vector reduction) | Enabled ~5-fold reduction in vector use while maintaining efficacy. |
Table 2: Impact on Process Economics and Cell Health
| Parameter | Impact of LentiBOOST | Implication for GMP Biomanufacturing |
|---|---|---|
| Vector Consumption [44] | Up to 5-fold reduction | Major reduction in Cost of Goods (COGs), alleviates a key production bottleneck. |
| Cell Viability [44] [46] | No cytotoxicity observed in HSCs, T-cells, DCs. | Maintains compliance with critical quality attributes (CQAs) for cell health. |
| Cell Functionality [44] | No impact on HSC differentiation potential. | Ensures the final cell product retains its intended therapeutic mechanism of action. |
| Vector Copy Number [44] | Controllable and adjustable. | Allows optimization in accordance with EMA/FDA safety guidelines. |
Experimental Protocol for Transduction Enhancement
This standardized protocol for enhancing lentiviral transduction of human T-cells and CD34+ hematopoietic stem cells can be adapted for other cell types with optimization.
Materials and Reagents
Table 3: The Scientist's Toolkit - Essential Research Reagent Solutions
| Item | Function / Description | Example / Note |
|---|---|---|
| LentiBOOST | Pharma or GMP-grade transduction enhancer. | Supplied at 100 mg/mL; use at 1:100 to 1:400 dilution [44]. |
| Lentiviral Vector | Vehicle for gene of interest delivery. | Titer must be pre-determined for accurate MOI calculation. |
| Cell Culture Medium | Supports cell growth and health during transduction. | Use serum-free or appropriate formulation for target cell type. |
| Target Cells | Primary cells for genetic modification. | e.g., Activated T-cells, CD34+ HSCs. Ensure high viability. |
| Centrifuge | For spinoculation. | Enhances virus-cell contact. |
| Cell Culture Vessels | For cell culture and transduction. | Multi-well plates, flasks, or closed-system bioreactor bags. |
Step-by-Step Workflow
Critical Process Parameters and Optimization
- LentiBOOST Concentration: Performance is dose-dependent. A final dilution between 1:100 and 1:400 (from a 100 mg/mL stock) is typically effective, but titration is recommended for each new cell type or process [44].
- Multiplicity of Infection (MOI): A key advantage of LentiBOOST is the ability to significantly reduce the MOI. Begin process development with an MOI 3-5 times lower than your standard protocol [44].
- Cell Health and Quality: The starting cell population must be healthy and have high viability. Using "exhausted" cells from severely ill patients can result in weaker responses and less effective transduction [47].
- Control and Monitoring: Always include a non-transduced control and a transduction-only (no LentiBOOST) control to accurately quantify the enhancement effect and monitor for any potential cytotoxicity.
GMP Manufacturing Integration
Integrating LentiBOOST into a GMP-compliant process requires careful planning beyond the bench-scale protocol.
Regulatory and Supply Chain Considerations
- Grade Selection: For clinical trials and commercial production, LentiBOOST GMP grade must be used. This material is manufactured under GMP conditions and comes with a full regulatory support package, including a Certificate of Analysis (CoA) and drug master file (DMF) references for regulatory submissions to agencies like the FDA and EMA [44].
- Licensing: Commercial and academic clinical trials require a license from Revvity. The company offers different licensing models tailored to the developer's stage and needs [44].
- Supply Chain Security: A reliable and secure supply chain is critical for commercial therapies. The manufacturer uses an automated fill-and-finish process under GMP to ensure batch-to-batch consistency and reliable supply [44].
Integration with Scalable Production Processes
To achieve true scalability, the transduction process must be integrated with advanced manufacturing platforms.
- Suspension Cell Culture: Transitioning from adherent cultures to suspension-based systems in bioreactors is crucial for scalability. Processes using suspension cell lines (e.g., HEK293SF) can be scaled up to 2000L if needed, unlike adherent systems which are limited by surface area [43].
- Advanced Bioprocessing: Moving from simple batch culture to perfusion or fed-batch processes in bioreactors can significantly increase LV titers and product quality. Perfusion, where fresh media is continuously added and harvest is collected, supports higher cell viability and decreases the residence time of labile LV particles in the bioreactor, leading to a reported 10-fold increase in cumulative titer compared to batch mode [43] [48].
- Automation and Closed Systems: Implementing automation in cell therapy manufacturing reduces human-induced variability and contamination risk, enhancing process reliability and reproducibility. This is a key strategy for scaling up while maintaining GMP compliance [47].
LentiBOOST is a robust and well-characterized transduction enhancer that directly addresses key challenges in GMP biomanufacturing of genetically modified stem cell therapies. The data and protocols provided here demonstrate its ability to significantly improve transduction efficiency, reduce vector-associated costs, and maintain cell viability and function—all within a regulatory framework designed for clinical application. By integrating this technology with scalable suspension bioreactor processes and automated systems, developers can create more robust, cost-effective, and commercially viable manufacturing processes for advanced cell and gene therapies.
The transition to xeno-free and GMP-grade supplements represents a critical advancement in stem cell biomanufacturing, addressing fundamental challenges in therapeutic development. Traditional culture systems relying on fetal bovine serum (FBS) present significant limitations for clinical translation, including ill-defined composition, batch-to-batch variability, and risks of transmitting zoonotic infections or provoking immune reactions [49]. Within the framework of Good Manufacturing Practice (GMP), these concerns necessitate a paradigm shift toward defined, clinically compliant alternatives that ensure product safety, consistency, and scalability.
This evolution is particularly crucial for human mesenchymal stromal cells (hMSCs), which are being investigated in over 900 clinical trials for regenerative and immunomodulatory applications [50]. The culture environment directly influences critical quality attributes (CQAs) of these cells, including their proliferation capacity, differentiation potential, genetic stability, and ultimate therapeutic efficacy. Therefore, implementing robust, standardized, and xeno-free protocols is not merely a technical improvement but a foundational requirement for the successful clinical translation and commercialization of stem cell-based therapies [31] [51].
The Rationale for Transitioning from FBS
FBS has been a cornerstone of cell culture for decades, valued for its rich mixture of growth factors and adhesion proteins. However, its suitability for clinical-grade biomanufacturing is severely limited by several critical factors.
Scientific and Safety Concerns: FBS is an ill-defined supplement with high inconsistency in the quality and quantity of its bioactive compounds [49]. Different commercial lots vary significantly in their concentrations of growth-stimulatory and inhibitory factors, directly impacting cell growth rates and introducing unacceptable variability into manufacturing processes [49]. More gravely, FBS carries risks of microbiological contamination, including viruses, prions, mycoplasma, and endotoxins. Bovine viral diarrhea (BVD) virus genetic material and bovine mycoplasma species have been detected in serum batches, posing a risk of zoonotic transmission to patients [49].
Regulatory and Ethical Pressures: Regulatory guidelines, such as Directive 2004/23/EC in Europe, emphasize stringent safety measures for tissues and cells intended for human applications [49]. The use of animal-derived materials like FBS is increasingly scrutinized, with agencies recommending a move to non-animal, non-ruminant materials wherever possible [50] [51]. Ethically, FBS production involves the painful harvest of blood from bovine fetuses without anesthesia, raising significant humanitarian concerns [49].
Table 1: Key Challenges Associated with the Use of Fetal Bovine Serum (FBS)
| Challenge Category | Specific Limitations |
|---|---|
| Definition & Composition | Ill-defined supplement with unknown components; high lot-to-lot variability [49]. |
| Safety Profile | Risk of transmitting adventitious agents (viruses, prions, mycoplasma); potential for immune reactions in patients [49]. |
| Manufacturing Impact | Introduces process variability; requires extensive and costly pre-qualification of lots [50] [49]. |
| Regulatory & Ethical | Increasingly discouraged by regulatory bodies; involves inhumane harvesting practices [49]. |
Xeno-Free Supplement Alternatives: A Comparative Analysis
Several xeno-free supplements have been developed as alternatives to FBS, primarily falling into two categories: human blood derivatives and completely defined, serum-free formulations.
Human Blood-Derived Supplements
Human Serum (HS): Derived from human blood, HS serves as a direct xeno-free replacement for FBS. Studies demonstrate that HS can outperform FBS in supporting cell culture. For instance, research on fetal pancreas-derived MSCs (FPMSCs) showed that cells expanded in HS exhibited a higher proliferative effect and reached senescence later than those cultured in FBS [51]. This makes HS a powerful alternative for clinical-grade manufacturing, particularly for sensitive cell types.
Human Platelet Lysate (hPL): Produced from platelet-rich plasma via freeze-thaw cycles, hPL releases a high concentration of growth factors that stimulate mitogenesis and cell adherence [50]. A survey of European bone marrow transplantation centers indicated that 77% of centers use hPL-supplemented media for clinical trials involving hMSCs, underscoring its broad acceptance [50]. While effective, its limited availability and potential for donor variability can be bottlenecks for large-scale production.
Defined, Serum-Free Formulations
Chemically defined, serum-free media (SFM) represent the ideal for GMP manufacturing, offering a fully controlled environment free of human or animal components. These formulations are typically supplemented with recombinant proteins, growth factors, lipids, and hormones.
Commercial media like MSC-Brew GMP Medium (Miltenyi Biotec) and StemPro MSC SFM XenoFree (Thermo Fisher Scientific) are specifically designed for this purpose. A study comparing media for infrapatellar fat pad-derived MSCs (FPMSCs) found that MSC-Brew GMP Medium significantly enhanced cell proliferation and colony-forming potential compared to standard media [31]. Similarly, StemPro MSC SFM XenoFree supports the expansion of MSCs while maintaining their multipotent differentiation potential, providing a performance comparable to FBS-containing systems but with superior clinical safety [52].
Table 2: Performance Comparison of Xeno-Free Culture Supplements
| Supplement Type | Proliferation Rate | Key Advantages | Reported Outcomes in MSC Culture |
|---|---|---|---|
| Human Serum (HS) | High | Xeno-free, reduces senescence | Lower doubling time, delayed senescence compared to FBS [51] |
| Human Platelet Lysate (hPL) | High | Rich in human growth factors, widely adopted in clinics | Supported large-scale expansion; used in 77% of surveyed EU centers [50] |
| Defined Serum-Free/Xeno-Free Media | Medium to High | Fully defined composition, minimal risk profile, highly scalable | Maintained differentiation potential and proliferation; enabled clinical-grade expansion [31] [52] |
The following workflow diagram illustrates the decision-making process for selecting and implementing a GMP-compliant, xeno-free culture system, from raw material qualification to final product release.
GMP-Compliant Protocols for Xeno-Free MSC Expansion
Implementing a xeno-free protocol requires careful attention to every aspect of the manufacturing process, from cell isolation and thawing to expansion and passaging. The following section outlines detailed, actionable protocols.
Protocol 1: Isolation and Initial Expansion of MSCs in Xeno-Free Conditions
This protocol is adapted from established methods for isolating MSCs from bone marrow under xeno-free conditions [52].
Materials Required:
- StemPro MSC SFM XenoFree (Basal Medium & Supplement)
- CELLstart Substrate or equivalent GMP-grade coating material
- TrypLE Express or other animal-free dissociation enzyme
- Human bone marrow aspirate
- HBSS, calcium, magnesium, no phenol red
- Heat-inactivated and pooled AB-Human Serum
- Gradient density media (e.g., Ficoll-Paque PREMIUM 1.073)
Step-by-Step Procedure:
- Prepare Primary Isolation Medium: Aseptically combine 477.5 mL MSC SFM Basal Medium, 5 mL MSC SFM XenoFree Supplement, 12.5 mL (2.5%) filtered AB-Human Serum, 5 mL GlutaMAX, and optional gentamicin (50 µL). Warm to room temperature before use [52].
- Coating Culture Vessels: Dilute CELLstart substrate 1:100 in DPBS. Add to culture flasks to ensure complete surface coverage. Incubate at 37°C for 60-120 minutes. Remove coating solution immediately before use; do not rinse [52].
- Isolate Mononuclear Cells (MNCs):
- Mix bone marrow aspirate 1:2 with HBSS.
- Carefully layer 20 mL of diluted aspirate over 15 mL of gradient density media in a 50 mL tube.
- Centrifuge at 400 × g for 35 minutes at 20°C with the brake off.
- Carefully collect the mononuclear cell (MNC) layer using a sterile pipette.
- Wash and Plate Cells:
- Add 30 mL HBSS to the harvested MNCs and centrifuge at 400-500 × g for 10 minutes. Remove supernatant. Repeat this wash step.
- Resuspend the final cell pellet in primary isolation medium.
- Seed the cells into the pre-coated culture vessels.
- Incubate at 37°C in a humidified atmosphere of 4-6% CO₂.
- Initial Culture and Medium Change: After 72 hours, perform a full medium change to remove non-adherent cells. Continue culturing, refreshing the medium every 2-3 days until cells reach ~90% confluency.
Protocol 2: Adaptation of Cryopreserved MSCs to Xeno-Free Media
Transitioning existing MSC lines from research-grade (FBS-containing) to xeno-free media requires a careful adaptation phase to maintain cell health and phenotype.
Materials Required:
- Cryopreserved MSCs (originally grown in FBS)
- StemPro MSC SFM XenoFree complete medium
- CELLstart coated vessels
- TrypLE Express
Step-by-Step Procedure:
- Thaw and Initial Plate: Rapidly thaw a vial of MSCs in a 37°C water bath. Transfer the contents to a conical tube and slowly dilute with pre-warmed xeno-free complete medium. Centrifuge at 100-200 × g for 5 minutes, resuspend the pellet in fresh medium, and seed at a density of ≥5 × 10³ cells/cm² onto a CELLstart-coated flask [52].
- Sequential Adaptation: Upon the first passage, begin transitioning the cells.
- Passage 1 (P1): Culture the cells in a 1:1 mixture of their original FBS-based medium and the new xeno-free complete medium.
- Passage 2 (P2): Transition to culture in 100% xeno-free complete medium.
- Monitor Cell Health: Closely observe morphology, doubling time, and confluence. A slight adjustment period is normal. By P3, cells should be fully adapted.
- Routine Passaging: Once adapted, passage cells at 80-90% confluency using TrypLE Express. A recommended seeding density for continued expansion is 5 × 10³ cells/cm² [52]. Refresh the medium every 2-3 days.
Quality Control and Safety Testing in GMP-Compliant Manufacturing
Ensuring the final cell product's safety, purity, potency, and identity is paramount. This requires a rigorous QC regimen aligned with global regulatory expectations [50].
Critical Quality Attributes (CQAs) and Release Criteria: A defined set of CQAs must be established and tested for final product release. These typically include:
- Viability: Post-thaw viability should exceed a specified threshold, often >70% or, as demonstrated in some GMP protocols, >95% [31].
- Identity and Purity: Confirmation via flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) MSC surface markers, as per ISCT criteria [31] [51].
- Potency: Functional assays demonstrating differentiation potential (osteogenic, adipogenic, chondrogenic) and/or immunomodulatory capacity [31] [50].
- Safety: Comprehensive testing for sterility (bacteria, fungi), mycoplasma, and endotoxin levels [31].
The Role of AI in Advanced Quality Monitoring: Artificial intelligence (AI) is emerging as a transformative tool for real-time, non-invasive quality control. Convolutional Neural Networks (CNNs) can analyze high-resolution images to track cell morphology and predict colony formation with over 90% accuracy, replacing labor-intensive manual microscopy [53]. Predictive models can also analyze sensor data from bioreactors (e.g., dissolved oxygen, pH) to forecast environmental deviations hours in advance, allowing for proactive process control [53]. These AI-driven techniques enhance scalability, reproducibility, and process automation in stem cell biomanufacturing.
The following diagram maps the key quality control checkpoints and the modern AI-driven tools that can be deployed throughout the manufacturing workflow to ensure product consistency and safety.
The Scientist's Toolkit: Essential Reagents for Xeno-Free GMP Manufacturing
Successfully implementing a xeno-free protocol depends on the selection of qualified, GMP-grade reagents. The table below details essential components of a clinical-grade toolkit.
Table 3: Essential Reagents for Xeno-Free, GMP-Compliant MSC Manufacturing
| Reagent Category | Example Products | Function & GMP Rationale |
|---|---|---|
| Basal Medium | StemPro MSC SFM Basal Medium, MSC-Brew GMP Basal Medium | Provides essential nutrients and salts; GMP-grade ensures traceability and consistent performance for scalable production [31] [52]. |
| Xeno-Free Supplement | StemPro MSC SFM XenoFree Supplement, MSC-Brew GMP Medium | Replaces FBS; formulated with defined, human-derived or recombinant factors to support growth and maintain phenotype under clinical-grade conditions [31] [52]. |
| Cell Dissociation Enzyme | TrypLE Express | Animal-origin-free recombinant protease for cell passaging; eliminates risk of animal pathogen contamination present in trypsin [52]. |
| Culture Surface Coating | CELLstart CTS Substrate, Recombinant Laminin-521 | Functionalized, xeno-free surface to support cell attachment and proliferation; critical for replacing gelatin or other animal-derived matrices [52]. |
| Critical Raw Materials | Human Platelet Lysate (hPL), Pooled AB Human Serum | Xeno-free supplements for isolation or enhancing growth; must be sourced from certified donors and tested for pathogens to ensure safety [50] [51]. |
The strategic transition to xeno-free and GMP-grade culture supplements is an indispensable component of modern, scalable stem cell biomanufacturing. Moving away from ill-defined and high-risk materials like FBS to well-characterized alternatives such as human platelet lysate, human serum, and defined serum-free media directly addresses critical challenges in product safety, consistency, and regulatory compliance. The integration of advanced technologies, including automated bioreactors and AI-driven quality monitoring, further enhances the robustness and scalability of these processes. By adopting the detailed protocols and quality frameworks outlined in this document, researchers and drug development professionals can significantly accelerate the translation of promising stem cell research into safe and effective clinical therapies.
Hematopoietic stem cell gene therapy (HSCGT) represents a transformative therapeutic strategy for treating various neurodegenerative and metabolic disorders [54]. This approach involves the ex vivo genetic modification of a patient's own CD34+ hematopoietic stem cells, followed by reinfusion to establish a long-lasting source of the functional protein throughout the body, including the central nervous system via cross-correction mechanisms [54] [55]. The successful clinical translation of HSCGT critically depends on robust, optimized, and validated Good Manufacturing Practice (GMP) protocols that ensure the safety, efficacy, and consistency of the final investigational medicinal product [54]. This case study details the development of a GMP manufacturing process for HSCGT targeting Mucopolysaccharidosis type II (MPSII or Hunter syndrome), providing a framework for scalable stem cell biomanufacturing within a broader research thesis on advanced therapy medicinal products (ATMPs).
Experimental Design and Workflow
The GMP manufacturing process for HSCGT was designed with scalability and regulatory compliance as core principles, focusing on optimizing critical parameters such as transduction efficiency (TD) while maintaining cell viability and function.
The diagram below illustrates the complete HSCGT workflow from cell collection to patient infusion, with the core GMP manufacturing process highlighted.
Critical Process Parameters and Quality Attributes
A systematic approach was employed to identify and control Critical Process Parameters (CPPs) that influence Critical Quality Attributes (CQAs) of the final HSCGT product.
Materials and Methods
Research Reagent Solutions
The table below details the essential reagents, materials, and equipment used in the GMP manufacturing process, with their specific functions and applications.
| Category | Product/Reagent | Function/Application | GMP Grade |
|---|---|---|---|
| Starting Material | Mobilized CD34+ Cells | Source of HSCs for genetic modification | Clinical Grade |
| Gene Delivery | IDS.ApoEII Lentiviral Vector | Delivery of functional IDS gene fused to ApoEII brain-targeting peptide | GMP [54] |
| Transduction Enhancers | LentiBOOST and Protamine Sulfate | Increase transduction efficiency, reduce vector requirements | GMP [54] |
| Cell Culture Media | X-VIVO-15 with 1% Human Albumin Serum | Serum-free basal medium for HSC culture | GMP [54] |
| Cytokines | Flt3-L, SCF, TPO, IL-3 | HSC pre-stimulation and maintenance of stemness during culture | GMP [54] |
| Cell Processing | Gibco CTS Rotea System | Closed system for cell processing, washing, and concentration | GMP-compliant [56] |
| Cell Separation | Gibco CTS Dynaclect System | Automated magnetic cell separation and bead removal | GMP-compliant [56] |
| Quality Control | Colony-Forming Unit (CFU) Assay | Assessment of hematopoietic progenitor potency and differentiation potential | Research Use [54] |
Detailed Manufacturing Protocol
Cell Collection and Preparation
- Cell Source: Hematopoietic stem cells were collected via leukapheresis from patients following mobilization with granulocyte-colony stimulating factor (G-CSF) and plerixafor [54].
- CD34+ Isolation: CD34+ cells were isolated using clinical-grade magnetic bead separation systems (e.g., CliniMACSplus instrument) under aseptic conditions [54].
- Pre-stimulation: Isolated CD34+ cells were cultured in serum-free X-VIVO-15 medium supplemented with 1% human albumin serum and cytokines (Flt3-L, SCF, TPO, IL-3) for pre-stimulation [54].
Lentiviral Transduction Optimization
- Vector Preparation: GMP-grade IDS.ApoEII lentiviral vector was used at varying multiplicities of infection (MOI: 12.5, 25, 50, 100) [54].
- Transduction Enhancers: LentiBOOST and protamine sulfate were added to the transduction medium to enhance efficiency [54].
- Transduction Protocol: Cells underwent two rounds of transduction with the lentiviral vector in the presence of transduction enhancers [54].
Cell Expansion and Harvest
- Culture Conditions: Transduced cells were maintained in optimized cytokine-containing medium in appropriate culture vessels selected during scale-up validation studies [54].
- Expansion Duration: Cells were cultured for sufficient duration to achieve target cell numbers while maintaining stem cell properties [54].
- Harvest: Genetically modified cells were harvested and prepared for cryopreservation or fresh infusion [54].
Quality Control and Release Testing
- Vector Copy Number (VCN): Genomic DNA was analyzed by qPCR to determine the average number of vector integrations per cell [54].
- Transduction Efficiency: Flow cytometry and colony-forming unit (CFU) assays were used to assess the percentage of genetically modified cells [54].
- Product Potency: Intracellular IDS enzyme activity was measured using specific enzymatic assays [54].
- Safety Testing: Tests for sterility, mycoplasma, endotoxin, and adventitious agents were performed according to pharmacopeial standards [54].
Results and Data Analysis
Transduction Efficiency and Cell Function Analysis
Comprehensive analysis of transduction parameters and functional outcomes provided critical data for process optimization.
Table 1: Effect of Transduction Enhancers on Colony Formation and Transduction Efficiency
| Culture Condition | BFU-E Colonies | CFU-GM Colonies | CFU-GEMM Colonies | BFU-E TD Efficiency (%) | CFU-GM TD Efficiency (%) |
|---|---|---|---|---|---|
| Non-transduced (no TEs) | 140 | 127 | 21 | - | - |
| Non-transduced (with TEs) | 73 | 73 | 12 | - | - |
| MOI 12.5 (no TEs) | 95 | 98 | N/D | 33.3 | 55.6 |
| MOI 12.5 (with TEs) | 99 | 105 | N/D | 94.1 | 94.1 |
| MOI 25 (no TEs) | N/D | N/D | N/D | 72.2 | 61.1 |
| MOI 25 (with TEs) | N/D | N/D | N/D | 82.4 | 94.1 |
| MOI 50 (no TEs) | 124 | 118 | N/D | N/D | N/D |
| MOI 50 (with TEs) | 134 | 105 | N/D | N/D | N/D |
| MOI 100 (with TEs) | <10 | <10 | 0 | N/D | N/D |
N/D: Not specifically documented in the source material
Table 2: Vector Copy Number and IDS Enzyme Activity After Transduction
| Culture Condition | Vector Copy Number (VCN) | Fold Increase in VCN with TEs | Intracellular IDS Activity Fold-Increase with TEs |
|---|---|---|---|
| MOI 12.5 (no TEs) | Baseline | 2.5-2.9x | ~4.8x |
| MOI 12.5 (with TEs) | Increased | - | - |
| MOI 25 (no TEs) | Baseline | 2.5-2.9x | ~4.8x |
| MOI 25 (with TEs) | Increased | - | - |
| MOI 50 (no TEs) | Baseline | 2.5-2.9x | ~4.8x |
| MOI 50 (with TEs) | Increased | - | - |
Process Optimization Outcomes
The optimization studies demonstrated that inclusion of transduction enhancers (LentiBOOST and protamine sulfate) significantly improved transduction efficiency by at least 3-fold while reducing the required vector quantity [54]. This enhancement was particularly pronounced at lower MOIs, with TD efficiency increasing from 33.3% to 94.1% for BFU-E colonies and from 55.6% to 94.1% for CFU-GM colonies at MOI 12.5 [54]. The vector copy number increased between 2.5- and 2.9-fold across all vector concentrations when transduction enhancers were used [54]. Most notably, intracellular IDS enzyme activity increased on average by 4.8-fold in pooled CFU colonies when transduction enhancers were incorporated into the protocol [54].
GMP Compliance and Scalability
Quality Control Systems
Implementation of robust quality control systems was essential for ensuring product consistency and compliance with regulatory standards.
Regulatory Framework
The manufacturing process was developed in compliance with EU GMP guidelines, specifically following Annex 2 for "Manufacture of Biological active substances and Medicinal Products for Human Use" and the dedicated "Guideline on Good Manufacturing Practice for Advanced Therapy Medicinal Products" published in Part IV of Eudralex Volume 4 [57]. Additionally, the process adhered to FDA requirements outlined in 21 CFR Parts 210 and 211 [58]. Critical documentation included Standard Operating Procedures (SOPs) for all manufacturing and quality control processes, comprehensive batch records, and validation protocols for equipment and processes [58] [57].
This case study demonstrates a successfully optimized and validated GMP manufacturing protocol for hematopoietic stem cell gene therapy targeting MPSII. The strategic inclusion of transduction enhancers (LentiBOOST and protamine sulfate) significantly improved transduction efficiency while reducing vector requirements, addressing both efficacy and cost considerations in ATMP manufacturing [54]. The comprehensive dataset presented, including colony formation, vector copy number, and IDS enzyme activity, provides critical quality attributes for process control and validation. This protocol represents a scalable and transferable model for GMP-compliant stem cell biomanufacturing that can be adapted for other HSCGT applications, contributing valuable insights to the broader field of regenerative medicine and advanced therapy development. The integration of automation technologies, closed processing systems, and robust quality control frameworks establishes a foundation for scalable production of personalized gene therapies that can meet growing clinical demands [56].
The convergence of artificial intelligence (AI), machine learning (ML), and single-use systems (SUS) is establishing a new paradigm for scalable and compliant stem cell biomanufacturing. This integrated approach directly addresses critical challenges in Good Manufacturing Practice (GMP) environments, including process variability, contamination risks, and the need for real-time quality control. AI-driven analytics enable dynamic process optimization and predictive monitoring of critical quality attributes, while SUS provide the flexible, closed-system architecture essential for automating these advanced workflows. The quantitative benefits of this technological integration are summarized in the table below.
Table 1: Quantitative Impact of Integrated Technologies on Stem Cell Biomanufacturing
| Metric | Impact of AI/ML & SUS |
|---|---|
| Market Growth (Stem Cell Manufacturing) | Projected to reach USD 44.2 Billion by 2034, with a CAGR of 13.1% from 2024 [59]. |
| Process Efficiency | AI-guided environmental control can improve culture expansion efficiency by ≥15% [53]. |
| Quality Monitoring Accuracy | Convolutional Neural Networks (CNNs) can predict iPSC colony formation with >90% accuracy non-invasively [53]. |
| Contamination Risk | Closed, automated SUS significantly reduce contamination risks compared to open manual processes [56]. |
| Data Integrity | Automated platforms with integrated software ensure data traceability and support CFR 21 Part 11 compliance [56]. |
The transition of stem cell therapies from laboratory research to commercialized medicines is contingent on the development of robust, scalable, and reproducible manufacturing processes. Adherence to GMP is not merely a regulatory hurdle but a fundamental requirement to ensure the safety, identity, purity, and potency of cell-based products [60] [41]. Traditional biomanufacturing approaches, which often rely on manual, open processes and endpoint quality testing, are inherently ill-suited to meet these demands. They are labor-intensive, prone to human error and contamination, and lack the real-time data required for proactive process control [53] [61].
The integration of AI/ML and SUS creates a synergistic technological stack that directly addresses these limitations. SUS provide the foundational physical infrastructure: scalable, closed, and standardized components that minimize cross-contamination and allow for rapid process changeover [61] [56]. AI and ML act as the intelligent control layer, analyzing high-volume, multi-parameter data from the bioprocess in real-time to predict outcomes, detect anomalies, and automate decision-making [53] [62]. This combination enables a shift from a static, batch-based production model to a dynamic, adaptive, and continuous manufacturing paradigm, which is essential for the economic viability and clinical success of advanced stem cell therapies.
AI and Machine Learning for Predictive Process Control and Quality Monitoring
AI and ML algorithms are transformative in their ability to convert raw process data into actionable intelligence. By continuously analyzing data from in-line sensors and imaging systems, these models facilitate an unprecedented level of oversight and control over the delicate process of stem cell cultivation.
Monitoring Critical Quality Attributes (CQAs) with AI
Maintaining CQAs is paramount for stem cell product quality. AI technologies offer non-invasive, real-time monitoring solutions that surpass the capabilities of traditional destructive assays [53].
- Cell Morphology and Viability: Convolutional Neural Networks (CNNs) can analyze high-resolution microscopy images to track cell confluence, morphology, and predict viability with over 90% accuracy, as demonstrated in iPSC colony formation [53].
- Differentiation Potential: Support Vector Machines (SVMs) and other classifiers can be trained on time-series imaging data to identify early markers of lineage commitment, achieving high sensitivity in distinguishing differentiation stages [53].
- Environmental Conditions: Predictive models can use historical sensor data (e.g., dissolved oxygen, lactate, pH) to forecast future process deviations hours in advance, allowing for preemptive corrections [53]. Reinforcement Learning (RL) algorithms have been used to dynamically adjust gas composition, improving expansion efficiency by 15% [53].
- Genetic Stability and Contamination: Deep learning models can fuse multi-omics data (genomics, transcriptomics) to identify patterns of genetic instability [53]. Furthermore, random forest classifiers and CNNs can detect subtle anomalies in sensor or imaging data that signal microbial contamination [53].
Table 2: AI/ML Models for Monitoring Critical Quality Attributes
| Critical Quality Attribute (CQA) | AI-Based Monitoring Strategy | Reported Performance / Benefit |
|---|---|---|
| Cell Morphology | CNN-based image analysis [53] | >90% accuracy in predicting iPSC colony formation [53] |
| Differentiation Potential | SVM for lineage classification [53] | 88% accuracy in forecasting differentiation outcomes [53] |
| Environmental Conditions | Predictive modeling & Reinforcement Learning [53] | 15% improvement in expansion efficiency [53] |
| Genetic Stability | Multi-omics data fusion using deep learning [53] | Detects latent instability trajectories [53] |
| Contamination Risk | Anomaly detection via random forest/CNNs [53] | Enables early, non-invasive detection [53] |
Experimental Protocol: Real-Time Differentiation Tracking via CNN
Objective: To non-invasively monitor and classify the differentiation stage of human Mesenchymal Stem Cells (MSCs) into osteogenic lineage using live-cell imaging and a pre-trained CNN model.
Materials:
- Cell Culture: Human MSCs, GMP-grade MSC media [63], osteogenic induction supplements.
- Equipment: Automated live-cell imaging microscope (e.g., Incucyte), humidified CO2 incubator maintained at 37°C.
- AI/ML Tools: TensorFlow or PyTorch framework; pre-trained CNN model (e.g., ResNet-50) [62].
- Software: Python environment with OpenCV and scikit-learn libraries.
Methodology:
- Cell Seeding and Differentiation: Seed MSCs at a defined density in multi-well plates. Initiate osteogenic differentiation in test wells, maintaining control wells in expansion media.
- Image Acquisition: Program the live-cell imager to capture brightfield and/or phase-contrast images of the cultures at regular intervals (e.g., every 6 hours) for the duration of the differentiation protocol (14-21 days).
- Data Preprocessing and Labeling: Manually assign a limited set of images from various time points to differentiation stages (e.g., "Proliferating," "Early Osteoblast," "Mature Osteoblast") based on established morphological criteria. This serves as the ground-truth dataset.
- Model Training and Validation:
- Split the labeled dataset into training (70%), validation (15%), and test (15%) sets.
- Fine-tune the pre-trained CNN on the training set, using the validation set to prevent overfitting.
- Assess the final model's performance on the held-out test set by calculating accuracy, precision, and recall.
- Real-Time Prediction: Deploy the validated model to analyze new, unlabeled images as they are acquired. The model will output a probability score for each differentiation stage.
- Data Integration and Feedback: Integrate the model's classification data with the process monitoring software. Set thresholds to trigger alerts for off-target differentiation, enabling potential process intervention.
Single-Use Systems as an Enabling Platform for Automation and Flexibility
Single-use systems provide the physical substrate for implementing flexible and automated AI-driven processes. Composed of pre-sterilized, disposable components like bioreactors, bags, tubing, and connectors, SUS offer distinct advantages over traditional stainless-steel infrastructure [61] [56].
Advantages and Implementation Challenges of SUS
The primary advantages of SUS include a significant reduction in cross-contamination risk, the elimination of costly and time-consuming cleaning validation, and greater operational flexibility for multi-product facilities [61] [56]. However, successful implementation requires careful management of several challenges:
- Extractables and Leachables (E&L): Comprehensive testing is required to identify and quantify compounds that may migrate from the plastic into the cell culture media, potentially affecting product safety and efficacy [61].
- Supply Chain and Scalability: Reliance on customized components necessitates a resilient supply chain to prevent production delays. Scalability can be challenging if SUS for larger production volumes are not readily available [61].
- Waste Management: The significant plastic waste generated requires dedicated and often costly disposal or recycling strategies [61].
- Integration and Standardization: Connecting SUS components from different suppliers can lead to compatibility issues, highlighting the need for standardized connectors and better interoperability [61].
cGMP Compliance in SUS and Automated Workflows
Current Good Manufacturing Practice (cGMP) emphasizes the use of modern, effective systems and technologies [41]. For SUS and automation, this translates to specific requirements:
- Documentation and Data Integrity: Automated systems must electronically record batch production records and process data in compliance with 21 CFR Part 11, ensuring data authenticity and traceability [56] [41].
- Process Validation: SUS and automated equipment must be rigorously validated to demonstrate consistent performance. This includes installation qualification (IQ), operational qualification (OQ), and performance qualification (PQ) [60].
- Standard Operating Procedures (SOPs): Robust SOPs are critical for the handling, assembly, and operation of SUS and automated platforms to minimize operator-dependent variability and errors [41].
- Quality of Raw Materials: All SUS components and contact materials must be certified for cGMP use, with supporting E&L data where applicable [61] [63].
Integrated Experimental Protocol: Automated, AI-Optimized MSC Expansion
This protocol outlines a complete workflow for the automated expansion of MSCs using an integrated single-use and AI-powered bioprocessing platform.
Objective: To automate the expansion of human MSCs in a SUS bioreactor with AI-driven, real-time optimization of culture parameters to maximize cell yield and maintain quality.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for Automated MSC Expansion
| Item | Function | GMP Considerations |
|---|---|---|
| GMP-grade MSC Media [63] | Provides nutrients and signals for cell growth and maintenance. | Serum-free, xeno-free formulations ensure consistency and reduce contamination risk. |
| Single-Use Bioreactor (e.g., 2L scale) | Scalable, closed vessel for cell culture. | Pre-sterilized; supplied with E&L data; compatible with control systems. |
| Gibco CTS Rotea System [56] | Closed system for cell washing, concentration, and volume reduction. | Enables intermediate processing steps within a closed, automated workflow. |
| pH and DO Sensors | Real-time monitoring of critical process parameters. | Pre-calibrated, single-use sensors that integrate with bioreactor control software. |
| AI/ML Platform (e.g., Azure ML, TensorFlow) [62] | Hosts predictive models for process optimization and anomaly detection. | Software must be validated for intended use; supports data integrity (21 CFR Part 11). |
Methodology:
- System Setup and Integration:
- Assemble the single-use bioreactor and flow path within a qualified biosafety cabinet.
- Integrate all components (bioreactor, CTS Rotea system, media hold bags) using sterile tube welders or aseptic connectors.
- Calibrate in-line single-use sensors for pH and dissolved oxygen (DO). Connect the system to the automated control and data acquisition software (e.g., CTS Cellmation software [56]).
Bioreactor Inoculation and Process Initiation:
- Pre-condition the bioreactor with GMP-grade MSC media.
- Inoculate with cryopreserved MSC working cell bank at a defined seeding density.
- Initiate the pre-defined base process protocol, setting initial parameters (e.g., pH 7.4, DO 40%, temperature 37°C, agitation).
AI-Driven Process Control:
- The AI platform continuously ingests real-time data (pH, DO, metabolite levels, off-gas analysis).
- A pre-trained reinforcement learning model dynamically adjusts gas flow rates (O2, N2, CO2) and agitation speed to maintain the setpoints for CQAs, moving beyond simple PID control [53] [62].
- A separate CNN model analyzes periodic images from an in-line microscope to monitor confluence and morphology, predicting the optimal harvest time.
Automated Cell Processing:
- Upon reaching target confluence (as predicted by the AI), the culture is automatically transferred to the CTS Rotea system for volume reduction and buffer exchange into the final formulation buffer [56].
- The final cell suspension is automatically filled into single-use cryobags using a system like RoSS.FILL [41].
Data Recording and Batch Release:
- The automated software documents all process parameters, interventions, and AI-driven setpoint changes in the electronic batch record.
- This data, combined with QC analytics (e.g., viability, identity, potency), is used for final product release.
Visualizing the Integrated Workflow
The following diagram illustrates the data and material flow within the integrated AI and SUS-based biomanufacturing system.
Integrated AI and SUS Biomanufacturing Workflow
The strategic integration of AI, machine learning, and single-use systems is not a distant future for stem cell biomanufacturing but an actionable present-day framework. This synergy creates a powerful ecosystem for GMP-compliant production, where the flexibility and closed nature of SUS provide an ideal platform for the data-driven, adaptive control enabled by AI. This results in enhanced process robustness, improved product quality, and a faster path to clinical translation. As these technologies continue to co-evolve, they will undoubtedly unlock new levels of automation and intelligence, paving the way for the widespread availability of safe and effective stem cell therapies.
Allogeneic cell therapies represent a transformative shift in regenerative medicine, offering “off-the-shelf” options to treat multiple patients from a single cell source [64]. Unlike autologous therapies, which are individualized, allogeneic therapies are inherently more scalable, making them a promising pathway to more accessible treatments at a sustainable price [65]. The global allogeneic cell therapy market, valued at $0.98 billion in 2024, is projected to grow to $2.74 billion by 2035, reflecting a compound annual growth rate (CAGR) of 5.9% [65]. This growth is driven by the increasing need for novel therapies, a growing development pipeline, and encouraging clinical trial results. Establishing robust, GMP-compliant manufacturing frameworks is crucial to support this commercial scale production, ensuring consistent quality, safety, and efficacy of these advanced therapeutic products [66].
Key Manufacturing Challenges and Strategic Frameworks
Scaling allogeneic cell therapy production presents several complex challenges that require strategic frameworks to overcome.
Table 1: Key Challenges and Strategic Frameworks in Allogeneic Therapy Manufacturing
| Challenge | Impact on Production | Strategic Framework / Solution |
|---|---|---|
| Donor Variability [64] | Inconsistent starting material quality affects batch standardization and therapeutic efficacy. | Rigorous donor screening and quality control; use of well-characterized master cell banks [67]. |
| Scalability & Batch Consistency [66] [64] | Traditional 2D culture is labor-intensive and lacks scalability; difficult to maintain cell quality at large scale. | Transition to suspension culture in bioreactors; implementation of automation and closed systems [66]. |
| Immunogenicity [64] | Risk of immune rejection in recipients, limiting therapeutic application. | Employ gene-editing technologies (e.g., CRISPR/Cas9) to engineer immune-evasive cells [68] [65]. |
| Cryopreservation & Storage [69] [64] | Post-thaw viability and functionality loss during long-term storage for "off-the-shelf" availability. | Optimize cryopreservation protocols using defined, GMP-compliant media; validate post-thaw recovery [67]. |
| Regulatory Compliance [67] | Complex and stringent guidelines for GMP production can delay timelines and increase costs. | Early engagement with regulatory experts; use of GMP-grade reagents and documented processes from development [67]. |
Quantitative Production Data and Scaling Models
Commercial scale manufacturing for allogeneic therapies, particularly those derived from pluripotent stem cells (PSCs), must accommodate massive cell numbers. It is expected that commercial scale batch sizes will need to be between 200 and 2,000 liters to meet annual production demands for a single product ranging from 10^11 to 10^14 cells [66]. Scaling to these volumes requires careful planning of the seed train and selection of appropriate bioreactor hardware.
Table 2: Single-Use Bioreactor Platforms for Large-Scale Allogeneic Production
| Bioreactor Platform | Vendor | Volume Range (L) | Key Characteristics |
|---|---|---|---|
| Xcellerex XDR-10 | GE Healthcare | 10 - 2000 | Low volumetric barrier to entry (4.5L min working volume); aspect ratio (h/d) >1:1 [66]. |
| BIOSTAT | Sartorius | 50 - 2000 | Traditional vessel geometry (h/d >1:1); requires 12.5L minimum working volume [66]. |
| Allegro | Pall | 200 - 2000 | Unique 1:1 aspect ratio for operational access; larger manufacturing footprint; 60L min working volume [66]. |
The choice of culture system is critical. A shift from 2D adherent cultures to 3D suspension cultures in stirred-tank reactors (STRs) is essential for scalability [66]. Suspension culture, preferably without microcarriers, provides a cost-efficient and scalable manufacturing strategy with downstream purification advantages [66].
Detailed Experimental Protocols
Protocol: GMP-Compliant Cryopreservation of Allogeneic Cell Therapies
Cryopreservation is a critical unit operation enabling batch production, stockpiling, and global distribution of "off-the-shelf" allogeneic therapies [67]. This protocol ensures the preservation of cell viability, identity, and potency.
- Objective: To freeze allogeneic cell products (e.g., MSCs, NK cells, PSC-derived progenitors) in a GMP-compliant manner for long-term storage while maintaining critical quality attributes (CQAs) post-thaw.
- Materials:
- Cell Suspension: Final formulated cell product, typically in the range of 10-150 x 10^6 cells/mL.
- Cryopreservation Medium: A defined, animal component-free medium manufactured under GMP standards. The medium should contain a cryoprotectant like DMSO (e.g., 10% final concentration) and may be combined with other agents such as hydroxyethyl starch (HES) [69].
- Controlled-Rate Freezer: Validated for the required freezing curve.
- Cryogenic Storage Vessels: GMP-grade cryobags or vials.
- Labeled Metal Cassettes: For housing cryobags during freezing and storage [69].
- Procedure:
- Formulation: Gently mix the concentrated cell suspension with an equal volume of pre-chilled (2-8°C) 2X cryopreservation medium to achieve the final desired cell concentration and cryoprotectant concentration. Maintain samples on a chilled block or in an ice bath.
- Aseptic Filling: Under a Grade A environment (e.g., laminar flow hood), aseptically dispense the formulated product into pre-labeled sterile cryobags. Seal the bags according to the manufacturer's instructions.
- Loading: Place the filled cryobags into designated, labeled metal cassettes to ensure efficient heat transfer and physical protection [69].
- Controlled-Rate Freezing: Place the cassettes into the controlled-rate freezer. Initiate a validated freezing curve. A standard curve may begin with a hold at 4°C, followed by a slow cooling rate of -1°C/min to a temperature between -40°C and -60°C, then a faster ramp to below -100°C before transfer to vapor phase liquid nitrogen.
- Long-Term Storage: Transfer the frozen product to a GMP-compliant cryostorage unit (vapor phase liquid nitrogen, typically ≤ -150°C) with continuous temperature monitoring and alarm systems.
- Quality Control:
- Post-Thaw Assessment: Perform viability testing (e.g., flow cytometry with 7-AAD or trypan blue exclusion), cell count recovery, and potency assays (e.g., differentiation capacity, cytokine secretion) on stability and release samples. One study reported post-thaw viability of 98.8 ± 0.5% for mononuclear cells using a DMSO/HES protocol [69].
- Sterility: Test for mycoplasma, bacteria, and fungi in accordance with pharmacopeial standards.
Protocol: Scaling Production in a Stirred-Tank Bioreactor
This protocol outlines the expansion of allogeneic cells, such as PSCs grown as aggregates, in a single-use stirred-tank reactor (STR).
- Objective: To achieve a high-density expansion of therapeutic cells in a controlled, scalable suspension culture system.
- Materials:
- Bioreactor System: Single-use STR (e.g., Xcellerex XDR series, BIOSTAT) with integrated pH, dissolved oxygen (DO), and temperature probes.
- Base Medium and Supplements: Serum-free, xeno-free medium formulated for the specific cell type.
- Inoculum: A log-phase growth culture of cells, prepared as a single-cell suspension or small aggregates.
- Procedure:
- Bioreactor Setup and Calibration: Install the single-use bioreactor vessel and aseptically connect all tubing. Calibrate the pH and DO probes according to the manufacturer's instructions.
- Basal Medium Addition: Add the pre-warmed basal medium to the bioreactor, typically at 50-70% of the final working volume.
- Parameter Set-Up: Set the initial process parameters. Agitation is set to maintain homogeneity and prevent aggregate sedimentation without causing damaging shear forces (e.g., 60-100 rpm, depending on scale and impeller). Temperature is set to 37°C. pH is typically controlled at 7.2-7.4 using CO₂ and base (e.g., Na₂CO₃), and DO is maintained at 20-50% through sparging with air, O₂, and N₂.
- Inoculation: Transfer the prepared inoculum into the bioreactor to achieve the target seeding density (e.g., 0.5 - 2.0 x 10^6 cells/mL for many PSC lines).
- Fed-Batch Process: Once the cells are inoculated, initiate a fed-batch strategy. This involves periodic addition of concentrated nutrient feeds or continuous perfusion to maintain nutrient levels and remove waste products. The feed rate is determined based on the cell growth rate and metabolite consumption.
- Process Monitoring: Monitor key parameters online (pH, DO, temperature) and offline (cell count, viability, glucose/lactate levels, aggregate size distribution) daily.
- Harvest: Once the target cell density is reached (or during late exponential phase), harvest the culture. For aggregate cultures, this may involve settling or using a low-shear separation system to concentrate the cells and remove spent medium.
- Process Control Considerations: Implementing advanced process analytical technology (PAT) for real-time monitoring of critical quality attributes (CQAs) is recommended for robust commercial manufacturing [66].
Diagram 1: Allogeneic cell therapy manufacturing workflow from cell bank to final product.
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the right reagents is fundamental to developing a robust and scalable manufacturing process. Early adoption of GMP-grade materials facilitates a smoother transition from research to clinical production.
Table 3: Essential Reagent Solutions for Allogeneic Therapy Production
| Reagent / Material | Function | Critical Considerations for Scalability & GMP |
|---|---|---|
| Excipient GMP-Grade Cell Culture Media [67] | Supports cell growth, expansion, and maintains phenotype and potency. | Defined, serum-free, xeno-free formulations reduce batch-to-batch variability. Early selection locks in consistency for scale-up. |
| GMP-Grade Cryopreservation Medium [67] | Preserves cell viability and functionality during frozen storage. | Defined, animal component-free, manufactured under GMP standards with traceable raw materials. |
| Cell Dissociation Reagents | Passages adherent cultures or dissociates aggregates for sub-culture or harvest. | Enzymatic (e.g., trypsin replacements) or non-enzymatic solutions that are defined and qualified for the specific cell type. |
| Growth Factors & Cytokines | Directs differentiation, maintains pluripotency, or enhances specific cell functions. | Recombinant human proteins with high purity and consistency. Sourcing with vendor audit trails is critical for regulatory filings. |
| Single-Use Bioreactors [66] | Provides a controlled, scalable environment for suspension-based cell culture. | Single-use technology eliminates cleaning validation, reduces cross-contamination risk, and improves operational efficiency. |
Process Workflow and Critical Control Points
A well-defined workflow from cell bank to final product, integrated with a tiered cell banking system, is the backbone of scalable allogeneic therapy production. This framework ensures a consistent and unlimited starting source for manufacturing [67].
The process begins with a well-characterized Master Cell Bank (MCB), which serves as the single source of truth for all production batches. A Working Cell Bank (WCB) is generated from the MCB to supply the manufacturing process without repeatedly drawing down the master bank [67]. The manufacturing process itself is segmented into Upstream Processing (USP) and Downstream Processing (DSP). USP involves all steps from thawing a vial from the WCB through to the expansion of cells in a production bioreactor. A key strategic decision here is the shift from planar culture to 3D suspension culture in bioreactors, which is necessary to achieve the required commercial scale [66]. DSP encompasses harvesting the cells from the bioreactor, followed by formulation and cryopreservation using a GMP-compliant protocol [67]. Finally, the product undergoes rigorous Quality Control (QC) testing, including assessments of viability, identity, purity, potency, and sterility, before final release as a cryopreserved "off-the-shelf" product [69] [67].
Diagram 2: Four-tiered GMP cell banking system for consistent allogeneic production.
Overcoming Critical Challenges in Scale-Up and Cost Management
The successful translation of stem cell research into clinically viable therapies hinges on a critical, yet often challenging, process: the transfer of technology (tech transfer) from a research and development (R&D) environment to a Good Manufacturing Practice (GMP)-compliant facility. This transition is fraught with operational complexities, particularly for first-in-human, early-phase clinical trials, which set the groundwork for safety and efficacy [70]. A haphazard transfer can introduce risks to product quality and patient safety, ultimately derailing the development of promising therapies. This document outlines structured strategies and provides a practical protocol to bridge the knowledge gap between R&D and GMP, specifically within the context of scalable stem cell biomanufacturing. By adopting a phase-appropriate, risk-based framework, researchers and drug development professionals can enhance the reproducibility, quality, and regulatory compliance of their cell-based products.
The Strategic Framework for Tech Transfer
A successful tech transfer is more than a simple hand-off of a protocol; it is a managed, collaborative project. A proactive risk management framework serves as the cornerstone of operations, strategically evaluating each unit operation throughout the product development life cycle [70].
Quality Risk Management and Regulatory Foundations
A risk-based approach to Phase-I GMP compliance, as advocated by the U.S. FDA, allows for some procedural flexibility but insists on stringent controls over sterility, cell viability, safety assays, and batch consistency [70]. Furthermore, guidelines such as the WHO's draft document on technology transfer emphasize integrating Quality Risk Management principles throughout the process [71]. This involves identifying potential failure points in the R&D process early on and defining controls to mitigate them before scaling up.
The Four Phases of a Tech Transfer Project
The World Health Organization (WHO) outlines a structured approach to tech transfer, dividing it into four distinct phases [71]. This model ensures thorough planning and execution:
- Phase 1: Project Initiation: This initial phase includes feasibility assessment and due diligence. The transferring and receiving units, along with their Quality units, conduct a gap analysis to review documentation and facility capabilities [71].
- Phase 2: Project Planning: A comprehensive technology transfer protocol is developed jointly by the sending (R&D) and receiving (GMP) units. This document outlines responsibilities, raw material specifications, the process flowchart, analytical methods, and acceptance criteria [71] [72].
- Phase 3: Project Transfer Execution: This phase involves the active transfer of knowledge, materials, and analytical methods. It typically includes training, equipment qualification (IQ/OQ/PQ), and the execution of trial or engineering batches to demonstrate process control at the receiving site [72].
- Phase 4: Project Review and Closeout: A summary report is prepared, documenting the conclusion of the transfer. This report should list any discrepancies and the corrective actions taken, formally closing the project [71] [72].
The following diagram illustrates the logical flow and key activities within this four-phase project life cycle.
Diagram: The Four Phases of a Technology Transfer Project, adapted from WHO guidelines [71].
Application Note: GMP-Compliant Expansion of Mesenchymal Stem Cells (MSCs)
Background and Challenge
Mesenchymal stem cells (MSCs) are a key component in cell-based therapies for their immunomodulatory and regenerative properties. However, many research-grade protocols for isolating and expanding human MSCs rely on animal-derived supplements, which pose risks of contamination, immunogenicity, and batch-to-batch variability, making them unsuitable for clinical use [73]. This application note summarizes a study that developed a GMP-compliant protocol for the isolation and expansion of Infrapatellar Fat Pad-derived MSCs (FPMSCs), translating the process from research to clinical-grade manufacturing.
The study optimized culture conditions by evaluating two animal component-free media against a standard MSC media. The key performance metrics—cell proliferation (doubling time) and potency (colony-forming unit capacity)—were significantly enhanced in one of the GMP-compliant media [73].
Table 1: Quantitative Comparison of MSC Performance in Different Culture Media [73]
| Performance Metric | Standard MSC Media | MesenCult-ACF Plus Medium | MSC-Brew GMP Medium |
|---|---|---|---|
| Cell Doubling Time | Baseline (Higher) | Intermediate | Lowest (Indicating enhanced proliferation) |
| Colony Forming Unit (CFU) Capacity | Baseline (Lower) | Intermediate | Highest (Indicating enhanced potency) |
| Compliance Status | Research-grade | GMP-compliant, Animal component-free | GMP-compliant, Animal component-free |
| Key Implication for Manufacturing | Not suitable for clinical use | Reduced risk, suitable for clinical use | Reduced risk, enhanced proliferation & potency for clinical use |
Furthermore, the GMP-validation from four different donors demonstrated that the final cell product maintained >95% viability (well exceeding the >70% requirement) and sterility after extended storage (up to 180 days), confirming the protocol's robustness and reproducibility for clinical application [73].
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the right raw materials is critical for a successful tech transfer. Their properties must be well-defined and consistent between the R&D and GMP units [72]. The following table details key reagents used in the featured MSC study and their critical functions.
Table 2: Key Research Reagent Solutions for GMP-Compliant MSC Manufacturing
| Reagent / Material | Function in the Process | GMP-Compliant Consideration |
|---|---|---|
| MSC-Brew GMP Medium (Miltenyi Biotec) | Animal component-free culture medium for cell expansion. | Eliminates risk of xenogenic contaminants; supports enhanced proliferation and potency [73]. |
| MesenCult-ACF Plus Medium (StemCell Technologies) | Animal component-free culture medium for cell expansion. | Provides a GMP-compliant alternative for cell culture, reducing immunogenicity risks [73]. |
| Collagenase | Enzyme for digesting tissue to isolate primary cells. | Should be sourced as a GMP-grade material with defined activity and purity to ensure consistent isolation efficiency [73]. |
| Dimethyl Sulfoxide (DMSO) | Cryoprotectant for the final cell product. | Must be high-purity, GMP-grade to ensure cell viability and patient safety during cryopreservation and storage [73]. |
Detailed Experimental Protocol: GMP-Compliant MSC Isolation, Expansion, and Release Testing
This protocol provides a step-by-step methodology for the isolation and expansion of MSCs under GMP-compliant conditions, as validated in the cited study [73]. It serves as a template for the kind of detailed documentation required for a successful tech transfer.
Materials and Equipment
- Source Tissue: Infrapatellar fat pad (IFP) waste tissue from arthroscopic surgery, obtained with informed consent and IRB approval.
- Reagents: GMP-grade, animal component-free culture medium (e.g., MSC-Brew GMP Medium), GMP-grade collagenase, Phosphate-Buffered Saline (PBS), DMSO.
- Labware: Sterile tissue culture flasks/plates, 100 µm cell strainers, sterile collection tubes.
- Equipment: Class II Biological Safety Cabinet, CO₂ incubator, centrifuge, inverted microscope, hemacytometer, flow cytometer.
Step-by-Step Workflow Procedure
Diagram: GMP-Compliant Workflow for MSC Isolation and Expansion.
Tissue Digestion and Primary Cell Isolation:
- Mince the IFP tissue into approximately 1mm³ pieces.
- Digest the tissue with 0.1% GMP-grade collagenase in serum-free media for 2 hours at 37°C with gentle agitation.
- Centrifuge the digested mixture at 300 × g for 10 minutes. Carefully remove the supernatant and surfactant.
- Wash the cell pellet with PBS and filter the suspension through a 100 µm sterile filter to remove debris.
- Centrifuge again at 300 × g for 10 minutes and resuspend the cell pellet in the chosen GMP-compliant culture medium.
GMP-Compliant Cell Expansion:
- Seed the isolated cells into culture flasks at a density of 5 × 10³ cells/cm².
- Maintain the cultures in a humidified incubator at 37°C with 5% CO₂.
- Refresh the GMP-compliant medium every 2-3 days.
- Passage cells at 80-90% confluency. To calculate population doubling time, count cells at each passage using a hemacytometer and the formula:
Doubling Time = (Duration of Culture × log(2)) / (log(Final Cell Concentration) - log(Initial Cell Concentration)). - For colony-forming unit (CFU) assays, seed cells at low densities (20, 50, 100, 500 cells per dish) and culture for 10 days. Stain with Crystal Violet to visualize and count colonies.
Harvest, Cryopreservation, and Storage:
- Upon reaching the desired expansion, harvest cells using a GMP-compliant dissociation reagent.
- Resuspend the cell pellet in a cryopreservation solution (e.g., containing 10% DMSO) at the required final concentration.
- Use a controlled-rate freezer to cool the cells before transferring them to long-term storage in the vapor phase of liquid nitrogen.
Analytical Methods and Release Specifications
The final cell product must be tested against pre-defined specifications to ensure safety, purity, potency, and identity before release.
Table 3: Example of Product Release Tests and Specifications for GMP-FPMSCs [73]
| Quality Attribute | Test Method | Release Specification | Purpose |
|---|---|---|---|
| Viability | Trypan Blue Exclusion | >95% | Ensure metabolic competence and product fitness. |
| Sterility | Bact/Alert | No growth (Sterile) | Ensure freedom from microbial contamination. |
| Mycoplasma | Mycoplasma Assay | Negative | Ensure freedom from mycoplasma contamination. |
| Endotoxin | Endotoxin Assay | Below specified limit | Ensure safety, absence of pyrogens. |
| Identity/Purity | Flow Cytometry | Positive for CD73, CD90, CD105; Negative for CD34, CD45, HLA-DR | Confirm MSC phenotype and absence of contaminating cell types. |
| Potency | Colony Forming Unit (CFU) Assay | Meets pre-set criteria for colony formation | Demonstrate functional capacity. |
The path from research to clinic is a meticulously structured journey, not a simple leap. Effective tech transfer is the essential bridge on this path, transforming an innovative laboratory protocol into a robust, reliable, and regulated manufacturing process. As demonstrated in the MSC application note, success is achieved through a forward-looking, risk-based approach, phase-appropriate compliance, and meticulous attention to detail—from raw material selection to final product release testing. By adopting the structured strategies and detailed protocols outlined herein, researchers and manufacturers can mitigate the inherent risks in scaling cell therapies, ensure patient safety, and accelerate the delivery of transformative stem cell treatments to the clinic.
Mitigating High Operational Costs in Cell Isolation, Purification, and Storage
For researchers and drug development professionals advancing stem cell therapies, transitioning from laboratory research to Good Manufacturing Practice (GMP)-compliant processes presents significant financial challenges. High operational costs, particularly in cell isolation, purification, and storage, remain critical barriers to scalable biomanufacturing. The global market for GMP cell therapy consumables is projected to grow at a CAGR of 28.9% from 2025 to 2035, driven by rising demand for advanced therapies, yet this growth is constrained by cost inefficiencies throughout the production workflow [74]. This application note provides detailed, data-backed protocols and strategic frameworks to optimize these essential processes, enabling more economically viable and scalable pathways for clinical translation.
Strategic Framework for Cost Mitigation
A multi-faceted approach is essential for significant cost reduction without compromising quality. The following strategies form the core of an effective cost-mitigation plan:
- Process Automation: Implementing closed, automated systems reduces manual errors and contamination risks, enhancing consistency while reducing labor costs and cleanroom requirements [56].
- Media Optimization: Selecting high-performance, animal component-free media improves cell proliferation and potency, reducing expansion time and overall production costs [75] [31].
- Method Selection: Choosing isolation methods based on target cell yield, regulatory status, and application scope significantly impacts initial processing costs and downstream regulatory burden [76].
- Cryopreservation Strategy: Implementing robust, standardized cryopreservation protocols with defined shelf-life extends product viability and enables banking, maximizing value from each manufacturing run [75] [76].
Protocols for Cost-Effective Cell Isolation & Purification
Comparative Analysis of Isolation Method Efficiencies
Cell isolation represents the first major cost center in the biomanufacturing workflow. The choice of isolation method directly impacts cell yield, viability, regulatory classification, and subsequent processing requirements.
Table 1: Performance and Cost Metrics of Primary Cell Isolation Methods
| Isolation Method | Typical Cell Yield (cells/mL) | Typical Viability (%) | Regulatory Classification | Relative Cost Factor |
|---|---|---|---|---|
| Enzymatic Digestion | 2.3×10⁵ – 1.8×10⁶ | 70–99 | Advanced Therapy Medicinal Product (ATMP) | High |
| Mechanical Isolation | 0.3×10⁴ – 2.67×10⁶ | 46–97.5 | Minimally Manipulated | Low |
| Hybrid Systems | Data Incomplete | Data Incomplete | Case-by-Case Basis | Moderate |
Data synthesized from adipose-derived Stromal Vascular Fraction (SVF) isolation studies demonstrate that enzymatic digestion, while yielding the highest cell numbers, carries a higher regulatory burden and cost due to its classification as an Advanced Therapy Medicinal Product (ATMP) [76]. Mechanical isolation offers a lower-cost alternative with an easier regulatory path but produces more variable yields. Emerging hybrid systems that combine ultrasonic energy or mild enzymes with mechanical disruption present a promising middle ground for balancing cost and efficiency [76].
Detailed Protocol: GMP-Compliant Mesenchymal Stem Cell Isolation from Infrapatellar Fat Pad
The following protocol, validated under GMP conditions, outlines a standardized process for isolating mesenchymal stem cells (MSCs) from the infrapatellar fat pad (IFP), a promising and less invasive tissue source [31].
Materials and Reagents:
- Tissue Source: Infrapatellar fat pad (IFP) tissue (10-20g) obtained as surgical waste during reconstructive surgery.
- Digestion Enzyme: 0.1% collagenase in serum-free media.
- Wash Buffer: Phosphate-Buffered Saline (PBS).
- Basal Medium: MEM α.
- Supplement: 10% fetal bovine serum (FBS) or animal component-free alternatives, 20 µg/mL gentamicin.
- Equipment: Sterile collection chamber, 100 μm filter, centrifuges maintained under GMP-grade calibration.
Procedure:
- Tissue Collection and Transport: Collect IFP tissue using an arthroscopic shaver into a sterile in-line collection chamber. Transport to the processing facility at a controlled 4°C within 24 hours of collection to preserve cell viability [31] [76].
- Tissue Preparation: Aseptically transfer tissue to a sterile biosafety cabinet. Mince the tissue into approximately 1mm³ pieces using surgical scalpels.
- Enzymatic Digestion: Transfer the minced tissue to a digestion vessel. Add 0.1% collagenase solution. Incubate for 2 hours at 37°C with continuous agitation.
- Digestion Termination and Washing: Centrifuge the digested suspension at 300 × g for 10 minutes. Carefully aspirate the supernatant containing adipocytes, oil, and enzyme solution. Resuspend the cell pellet (the stromal vascular fraction) in PBS and filter through a 100 μm filter to remove debris.
- Primary Culture: Centrifuge the filtered suspension again at 300 × g for 10 minutes. Resuspend the final cell pellet in standard MSC media (MEM α + 10% FBS + gentamicin). Seed cells in culture vessels at a density of 5 × 10³ cells/cm² [31].
- Cryopreservation of Passage 1 Cells: At 80-90% confluency, harvest cells. Cryopreserve in FBS containing 10% dimethyl sulfoxide for long-term storage in a validated liquid nitrogen storage system [31].
Workflow Diagram: Cell Isolation & Purification
The following diagram illustrates the logical workflow and decision points for selecting and implementing a cost-effective cell isolation strategy.
Protocols for Cost-Effective Cell Culture and Expansion
Quantitative Media Performance for Enhanced Proliferation
Cell culture media and supplements constitute a recurring and substantial cost, accounting for 41.40% of the GMP cell therapy consumables market [74]. Optimizing media formulation is therefore critical for cost-effective expansion. A 2025 study directly compared animal component-free media for culturing infrapatellar fat pad-derived MSCs (FPMSCs), providing robust quantitative data for informed decision-making [75] [31].
Table 2: Performance Comparison of GMP-Compliant, Animal Component-Free Culture Media
| Media Formulation | Impact on Cell Doubling Time | Impact on Colony Forming Units (CFU) | Post-Thaw Viability (after 180 days) | Key Characteristics |
|---|---|---|---|---|
| MSC-Brew GMP Medium | Lower doubling times across passages, indicating increased proliferation | Higher colony formation, indicating enhanced potency | > 95% | Optimized for MSC expansion under GMP compliance |
| MesenCult-ACF Plus Medium | Evaluated but outperformed by MSC-Brew in the cited study [31] | Evaluated but outperformed by MSC-Brew in the cited study [31] | Data not specified in results | Animal component-free formulation |
The data demonstrate that MSC-Brew GMP Medium significantly enhanced proliferation rates and potency of FPMSCs compared to standard MSC media, as evidenced by lower doubling times and higher colony formation [75] [31]. Investing in such high-performance media can reduce the time and resources required to achieve target cell numbers, thereby lowering overall production costs.
Detailed Protocol: GMP-Compliant Cell Expansion and Media Evaluation
This protocol provides a methodology for evaluating and implementing optimized media in a scalable expansion process.
Materials and Reagents:
- Test Media: MSC-Brew GMP Medium (Miltenyi Biotec, Cat# 170-076-325) and other candidate media.
- Cells: FPMSCs or other MSC types at passage 2-4.
- Equipment: Standard cell culture plasticware, bright-line hemacytometer or automated cell counter, materials for Colony Forming Unit (CFU) assay (Crystal Violet, neutral buffered formalin).
Procedure:
- Cell Seeding: Thaw and pre-culture cells in a standard medium. Seed cells at a density of 5 × 10³ cells/cm² in parallel culture vessels for each media formulation to be tested [31].
- Cell Passage and Doubling Time Calculation: Culture cells to 80-90% confluency. Detach and count cells using a hemacytometer. Repeat for at least 3 passages. Calculate the doubling time (DT) at each passage using the formula: [ Doubling\;Time = \frac{duration \times ln2}{ln(final\;concentration/initial\;concentration)} ] [31].
- Potency Assay (CFU Assay): Seed cells at low densities (e.g., 20, 50, 100, and 500 cells) in large culture dishes containing the test media. Culture for 10 days. Fix cells with 10% neutral buffered formalin for 30 minutes, wash with PBS, and stain with 10% Crystal Violet. Count the number of formed colonies (>50 cells) to assess clonogenic potential [31].
- Cell Characterization: Analyze MSC surface marker expression (CD73+, CD90+, CD105+, CD45-) using flow cytometry to ensure phenotype maintenance in the optimized media [31].
Workflow Diagram: Media Selection & Expansion
This diagram outlines the experimental workflow for systematically evaluating and selecting a cost-effective culture media for expansion.
Protocols for Cost-Effective Cell Storage and Quality Control
Cryopreservation Parameters for Long-Term Stability
Effective cryopreservation prevents product loss and allows for the creation of cell banks, which is fundamental for scalable production and quality control. A validated GMP protocol demonstrated that FPMSCs maintained >95% viability and sterility even after 180 days of cryopreservation, far exceeding the minimum requirement of >70% viability [75] [31].
Table 3: Standardized Cryopreservation Protocols and Outcomes
| Cryopreservation Component | Standardized Parameters | Validated Outcome | Emerging Alternatives |
|---|---|---|---|
| Cryoprotectant | 10% DMSO in FBS | Standard, reliable protection | Defined, animal-free cryoprotectant mixes |
| Freezing Method | Slow freezing at 1°C per minute using a controlled-rate freezer | >95% post-thaw viability after 180 days | Nano-vitrification |
| Storage Temperature | Liquid nitrogen vapor phase | Maintains long-term stability and sterility | N/A |
| Quality Control Release | >70% viability (validated to >95%), sterility (Bact/Alert), mycoplasma, endotoxin testing | Ensures product safety and efficacy | Recombinant endotoxin tests (e.g., PyroSense) |
The slow-freezing method using DMSO combined with human serum albumin (HSA) is the current standard, effectively protecting cell membranes during freezing [76]. Emerging techniques like nano-vitrification, which uses nanoparticles for even thermal distribution, are being explored to further improve post-thaw viability for delicate cell populations [76].
Detailed Protocol: GMP-Compliant Cryopreservation and Product Release
Materials and Reagents:
- Cryoprotectant Medium: 10% DMSO in FBS or, for defined conditions, in a solution containing HSA.
- Cryovials: GMP-compliant, sterile, leak-proof vials.
- Equipment: Controlled-rate freezer, liquid nitrogen storage tank, -80°C freezer.
- QC Assays: Trypan Blue or automated fluorescence-based viability counter, Bact/Alert system for sterility, LAL-based endotoxin detection kit, Mycoplasma assay kit.
Procedure:
- Cell Preparation: Harvest cells at the desired passage (e.g., 80-90% confluency). Perform a cell count and viability assessment.
- Cryosolution Addition: Resuspend the cell pellet in pre-chilled cryoprotectant medium to the target concentration (e.g., 1-5 x 10^6 cells/mL). Aliquot into cryovials.
- Controlled-Rate Freezing: Place cryovials in a controlled-rate freezer programmed to cool at -1°C per minute until reaching at least -80°C. Alternatively, use a passive freezing container pre-cooled at -80°C.
- Long-Term Storage: After 24 hours, promptly transfer vials to the vapor phase of a liquid nitrogen storage system for long-term preservation.
- Quality Control (Product Release Tests): For each batch, perform release tests:
- Viability: Use Trypan Blue exclusion or a fluorescence-based automated counter on a post-thaw sample. Must meet predefined criteria (e.g., >70%, validated to >95%) [75] [76].
- Sterility: Incubate samples in a Bact/Alert system to detect microbial contamination.
- Endotoxin and Mycoplasma: Perform LAL-based endotoxin assay and a validated Mycoplasma test.
- Potency and Phenotype: Depending on the product specifications, perform CFU assays and flow cytometry for marker expression [31] [76].
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the right reagents is fundamental to establishing a robust, cost-effective, and GMP-compliant process.
Table 4: Key Reagents for GMP Cell Processing
| Reagent / Kit | Manufacturer / Example | Function in the Workflow | GMP Compliance & Impact |
|---|---|---|---|
| Animal Component-Free Media | MSC-Brew GMP Medium [31] | Supports expansion & maintenance of MSCs | Defined, xeno-free formulation eliminates contamination risks and batch variability. |
| Collagenase | Type I, II, or V [76] | Enzymatic digestion of tissue for initial cell isolation | Critical for cell yield; requires GMP-grade for clinical use. |
| Cell Separation Consumables | Magnetic beads, columns [74] | Isolation and purification of specific cell types | Single-use systems minimize cross-contamination; a major cost driver. |
| Cryopreservation Media | DMSO with HSA [76] | Protects cells during freezing and long-term storage | Standardized formulation ensures high post-thaw viability and batch consistency. |
| QC Testing Kits | Bact/Alert, LAL Endotoxin kits [75] [76] | Ensures product sterility and safety | Mandatory for product release; automated systems (e.g., Bact/Alert) reduce false positives. |
| Flow Cytometry Kit | BD Stemflow Human MSC Analysis Kit [31] | Confirms cell identity and purity (e.g., CD73+/90+/105+) | Standardized for phenotypic characterization, a key release criterion. |
Mitigating the high operational costs of cell therapy biomanufacturing is achievable through a strategic combination of process optimization, strategic reagent selection, and automation. By implementing the detailed protocols and frameworks provided—including the validated isolation and expansion methods, data-driven media selection, and robust cryopreservation strategies—research scientists and drug developers can significantly enhance the economic viability of their GMP workflows. This approach directly supports the broader thesis of scalable stem cell biomanufacturing, paving the way for more accessible and commercially sustainable advanced therapies.
Maintaining Cell Quality and Potency During Large-Scale Expansion
In the field of regenerative medicine, the transition of stem cell therapies from research to clinical application hinges on the ability to perform large-scale expansion without compromising the critical quality attributes of the cells. Within the framework of Good Manufacturing Practice (GMP) for scalable biomanufacturing, maintaining cell quality, identity, and functional potency during scale-up presents a formidable challenge [50] [32]. The inherent complexity of stem cell biology, combined with the stringent requirements for clinical-grade production, necessitates an integrated approach combining advanced bioreactor systems, defined culture environments, and rigorous quality control. This application note details practical methodologies and protocols to address the central challenge of preserving cell quality and potency during large-scale expansion of mesenchymal stromal cells (MSCs) and induced pluripotent stem cells (iPSCs), aligning with quality-by-design (QbD) principles to ensure regulatory compliance and therapeutic efficacy [77] [78].
Critical Quality Attributes (CQAs) and Risk Assessment
Implementing a risk-based framework begins with identifying Critical Quality Attributes (CQAs)—physical, chemical, biological, or microbiological properties that must be controlled within appropriate limits to ensure product quality [78]. The International Society for Cell & Gene Therapy (ISCT) has established minimal criteria for defining MSCs, which include plastic adherence, specific surface marker expression (CD105+, CD73+, CD90+; CD45-, CD34-, CD14-/CD11b-, CD79α-, HLA-DR-), and tri-lineage differentiation potential (adiopogenic, chondrogenic, osteogenic) [32]. For iPSCs, key CQAs include pluripotency marker expression, genomic stability, and differentiation capacity [77] [79]. The table below summarizes core CQAs and associated risks during large-scale expansion.
Table 1: Critical Quality Attributes and Associated Risks in Large-Scale Expansion
| Cell Type | Critical Quality Attribute (CQA) | Potential Impact of Scale-Up | Recommended Control Strategy |
|---|---|---|---|
| MSCs | Immunomodulatory Potency | Functional attenuation due to culture-induced senescence [50] | Standardized functional assays (e.g., T-cell suppression); monitor secretion of bioactive molecules [50] [32] |
| MSCs | Surface Marker Phenotype | Drift in marker expression profile [32] | Flow cytometry at multiple passages; adherence to ISCT criteria [32] |
| MSCs/iPSCs | Genomic Stability | Increased risk of karyotypic abnormalities [77] [50] | Regular karyotyping and genetic stability assays (e.g., qPCR) [77] |
| iPSCs | Pluripotency | Spontaneous differentiation in suboptimal 3D environments [79] | Immunocytochemistry for markers (OCT4, SOX2, NANOG); pluripotency tests [77] [79] |
| iPSCs | Differentiation Capacity | Limited functional integrity in non-physiological 3D suspension [79] | Directed differentiation protocols followed by functional and marker analysis [79] |
| All Cells | Sterility (Bacteria, Fungi, Mycoplasma) | Contamination risk in bioreactor systems [32] | Closed processing; aseptic sampling; rigorous sterility testing per pharmacopoeia standards [50] [32] |
Protocols for Scalable Expansion with Quality Control
Protocol: Large-Scale Expansion of MSCs in a Hollow Fiber Bioreactor
This protocol outlines the expansion of bone marrow-derived MSCs (BM-MSCs) using the Quantum Cell Expansion System, a closed, automated hollow fiber bioreactor, which significantly reduces manual handling steps compared to traditional flasks [32].
Key Materials:
- Bioreactor: Quantum Cell Expansion System (Terumo BCT) [32]
- Culture Medium: Xeno-free, serum-free medium (e.g., MSC-Brew GMP) or base medium supplemented with 5-10% Human Platelet Lysate (hPL) [50] [32]
- Bioreactor Coating: Fibronectin, vimentin, or cryoprecipitate [32]
- Cells: BM-MSCs at Passage 2 (P2)
Methodology:
- Bioreactor Setup and Coating: Aseptically install the hollow fiber bioreactor and coating solution according to the manufacturer's instructions.
- Cell Seeding: Load a minimum of ( 20 \times 10^6 ) cells into the bioreactor [32].
- Expansion Process: Initiate the automated expansion process. The system provides continuous medium perfusion.
- Harvesting: After approximately 7-10 days, initiate the automated harvest procedure. Typical yields range from ( 100 \times 10^6 ) to ( 276 \times 10^6 ) cells [32].
Quality Control Checks:
- Pre-harvest: Monitor cell morphology and confluency via integrated imaging or sample analysis.
- Post-harvest: Determine Cell Viability (should be >90% via Trypan Blue exclusion), Cell Count, and Phenotype (flow cytometry for ISCT markers) [32].
- Potency Assay: Perform a functional assay, such as an in vitro T-cell suppression assay, to confirm immunomodulatory capacity [50] [32].
Protocol: Expansion of hiPSCs as Aggregates in a Vertical-Wheel Bioreactor
This protocol describes the generation and expansion of hiPSC aggregates in a PBS-MINI bioreactor with a vertical-wheel impeller, which offers gentle mixing to minimize shear stress [77] [79].
Key Materials:
- Bioreactor: PBS-MINI Bioreactor (PBS Biotech) with a Vertical-Wheel impeller [80] [77]
- Culture Medium: Defined, xeno-free medium such as mTeSR 3D or TeSR-AOF 3D [80]
- Cells: High-quality, undifferentiated hiPSCs.
Methodology:
- Inoculum Preparation: Harvest hiPSCs from 2D culture to create a single-cell suspension. Use a reagent such as ReLeSR or Accutase to ensure high viability.
- Bioreactor Inoculation: Seed the hiPSCs into the bioreactor at a density of ( 2 \times 10^5 ) cells/mL in a working volume of 60-300 mL [77].
- Expansion Process: Culture for 6-9 days with continuous agitation.
- Medium Exchange: Perform periodic medium exchanges (e.g., 50-80% daily) via perfusion or batch-fed modes to maintain nutrient levels and remove waste.
Quality Control Checks:
- Daily Monitoring: Assess aggregate size and morphology. Ideal aggregates are 100-300 µm in diameter [79].
- Post-expansion Analysis:
- Viability and Cell Yield: Final cell concentrations can reach ( 2.3 \times 10^6 ) cells/mL [77]. Assess viability, which in suspension can range from 81% to 93% [79].
- Pluripotency: Analyze expression of pluripotency markers (OCT4, SOX2, NANOG) via flow cytometry or immunocytochemistry.
- Genomic Stability: Perform karyotype analysis or SNP analysis to detect chromosomal abnormalities [77].
Manufacturing Platforms and Monitoring Technologies
Advanced manufacturing platforms are essential for standardizing production. The table below compares several automated GMP-compliant systems.
Table 2: Comparison of Automated GMP-Compliant Cell Expansion Systems
| System Name | Technology | Scale / Culture Area | Reported Output (Cell Type) | Key Feature |
|---|---|---|---|---|
| Quantum Cell Expansion System [32] | Hollow Fiber Bioreactor | 21,000 cm² | ( 100 - 276 \times 10^6 ) BM-MSCs in 7-10 days [32] | Closed, automated processing; continuous perfusion |
| CliniMACS Prodigy [32] | Integrated Automation with Adherent Cell Culture | 1-layer CellSTACK | ( 29 - 50 \times 10^6 ) MSCs (P0) from equine blood [32] | End-to-end automation from isolation to harvest |
| PBS-MINI Bioreactor [80] [77] | Vertical-Wheel Stirred-Tank | 80-300 mL working volume | ( 2.3 \times 10^6 ) hiPSCs/mL [77] | Low-shear mixing; suitable for shear-sensitive cells |
| Fixed-Bed Bioreactor [81] | Fixed-Bed for Adherent Culture | N/A | ~ ( 1.2 \times 10^{13} ) EV particles/day from iMSCs [81] | Enables continuous harvesting of cells or secretome |
Advanced Process Monitoring
Integrating smart sensor technology and Process Analytical Technology (PAT) is a core QbD principle for maintaining CQAs [82] [78].
- Smart Sensors: These use data-driven models (e.g., artificial neural networks, fuzzy logic) to predict key variables like viable cell density and metabolite concentrations (glucose, lactate) from real-time sensor data (pH, DO). In the AIDPATH platform, such sensors demonstrated an 86-88% consensus in event detection, providing reliable early warnings for process deviations [82].
- In-line Spectroscopy: Raman or NIR spectroscopy can be used for real-time monitoring of culture components, providing a fingerprint of the biochemical environment [82].
The following diagram illustrates the operational workflow of an automated, smart-sensor-controlled bioreactor system.
Diagram: Workflow of an Automated, Smart-Sensor Controlled Bioreactor
The Scientist's Toolkit: Essential Research Reagent Solutions
The selection of raw materials is critical for GMP compliance and process consistency. The following table details key reagents and their functions.
Table 3: Essential Reagents for GMP-Compliant Stem Cell Manufacturing
| Reagent Category | Example Product | Function & GMP Relevance | Reference |
|---|---|---|---|
| Xeno-Free Medium | MSC-Brew GMP | Defined, serum-free medium for MSC expansion; eliminates lot-to-lot variability and xeno-contamination risk. | [32] |
| Human Platelet Lysate (hPL) | Commercial GMP-grade hPL | Xeno-free supplement for MSC culture; superior to FBS in promoting expansion while maintaining functionality. | [50] [32] |
| 3D hiPSC Medium | mTeSR 3D / TeSR-AOF 3D | Defined, animal-origin free medium formulated for suspension culture of hiPSC aggregates. | [80] |
| Synthetic Hydrogel | PGmatrix (PepGel) | Synthetic peptide hydrogel for 3D hiPSC culture; provides a physiologically relevant, defined microenvironment, superior to animal-derived Matrigel. | [79] |
| Cell Dissociation Reagents | TrypLE Select, Accutase | Recombinant, animal-origin free enzymes for gentle cell passaging; crucial for maintaining high viability and genetic stability. | [80] |
| GMP-Grade Cytokines | GMP-grade FGF-2, TGF-β | Defined growth factors for maintaining pluripotency or directing differentiation; essential for process standardization and potency. | [50] |
The path to successful commercial and clinical translation of stem cell therapies is paved with robust, scalable, and well-controlled manufacturing processes. Adherence to QbD principles, leveraging advanced bioreactor platforms with integrated monitoring, and utilizing defined, GMP-compliant reagents are no longer optional but essential to ensure that expanded cells meet the stringent requirements for identity, purity, potency, and safety. The protocols and strategies outlined herein provide a actionable framework for researchers and process development scientists to overcome the critical challenge of maintaining cell quality and potency during large-scale expansion, thereby accelerating the delivery of transformative stem cell-based therapies to patients.
Optimizing Cryopreservation for Batch Production and Global Logistics
Within Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing, cryopreservation is not merely a storage step but a critical process parameter that directly impacts product quality, regulatory compliance, and commercial viability. The transition from laboratory-scale research to industrial-scale production necessitates cryopreservation protocols that ensure consistent post-thaw viability and functionality across manufacturing batches and throughout complex global supply chains [83]. This application note details optimized, GMP-aligned methodologies for cryopreserving stem cell products, with a specific focus on achieving robustness for batch production and logistical handling.
The foundational challenge in cryopreservation lies in mitigating damage from intracellular ice formation and osmotic stress during freeze-thaw cycles [84]. For stem cell biomanufacturing, this is compounded by the need for process reproducibility and product stability during transport between manufacturing facilities, testing laboratories, and clinical sites. Advanced controlled rate freeze-thaw (CRFT) systems and optimized cryoprotectant formulations have become essential tools to de-risk this scale-up process [83].
Key Optimization Parameters and Quantitative Data
Successful optimization requires careful balancing of multiple interdependent variables. The table below summarizes the core parameters and their optimized ranges for mesenchymal stromal cells (MSCs), a common therapeutic cell type.
Table 1: Key Optimization Parameters for Stem Cell Cryopreservation
| Parameter | Optimal Range or Condition | Impact on Viability & Function |
|---|---|---|
| Cooling Rate | -1°C/min [85] | Minimizes intracellular ice formation; critical for controlled-rate freezing. |
| Thawing Rate | Rapid (e.g., 37°C water bath) [86] [85] | Reduces damaging ice recrystallization during warming. |
| Cell Concentration | 1x10^3 - 1x10^6 cells/mL [85] | Prevents low viability from over-dilution or toxic metabolite accumulation from over-concentration. |
| Cryoprotectant (CPA) | 10% DMSO (standard) or DMSO-free alternatives (e.g., polyampholytes) [84] [85] | DMSO offers proven efficacy but has toxicity concerns; new agents aim to reduce toxicity. |
| Post-Thaw Recovery | Allow 24-hour incubation before analysis [86] | Enables cellular repair and recovery of membrane integrity and metabolic function. |
The global market for cell cryopreservation reflects its critical importance, projected to grow from USD 12.85 billion in 2025 to USD 96.99 billion by 2035, driven largely by the expansion of cell-based therapies [87]. This underscores the economic imperative for robust, scalable cryopreservation strategies.
Experimental Protocols
Core GMP Cryopreservation Protocol for MSCs
This protocol is designed for the cryopreservation of human mesenchymal stromal cells (e.g., Bone Marrow-MSCs, Adipose-derived MSCs) in a GMP-compliant, serum-free system.
Materials:
- Cells: Harvested MSC culture (>80% confluent, in maximum growth phase) [85].
- Cryopreservation Medium: Pre-formulated, serum-free, GMP-manufactured medium (e.g., CryoStor CS10) [85].
- Consumables: Sterile cryogenic vials (internal-threaded recommended) [85].
- Equipment: Controlled-rate freezer (CRF) or isopropanol freezing container (e.g., CoolCell) [83] [85], -80°C freezer, liquid nitrogen storage tank.
Procedure:
- Harvesting: Detach cells using a GMP-grade enzyme (e.g., collagenase NB6 for tissue-derived cells or TrypLE for monolayer culture) [28] [88]. Quench the enzyme with an appropriate complete medium.
- Centrifugation & Counting: Centrifuge the cell suspension. Carefully aspirate the supernatant. Resuspend the cell pellet in a small volume of baseline medium and perform a viable cell count.
- Formulation: Dilute the cell concentrate with cold (2-8°C) cryopreservation medium to the target final concentration (e.g., 1-5 x 10^6 cells/mL). Gently mix to ensure homogeneity. Note: Working quickly and keeping the cell suspension cold at this stage helps maintain viability.
- Aliquoting: Aseptically aliquot the cell suspension into cryogenic vials (e.g., 1.0 mL/vial). Label vials with a unique identifier resistant to liquid nitrogen.
- Controlled-Rate Freezing:
- Option A (Controlled-Rate Freezer): Place vials in the CRF and initiate a freeze cycle of -1°C/min from +4°C to at least -40°C, followed by a faster ramp down to -100°C or lower [83].
- Option B (Freezing Container): Transfer vials to an isopropanol-free freezing container (e.g., CoolCell) and immediately place in a -80°C freezer for a minimum of 4 hours (or overnight). The container ensures an approximate cooling rate of -1°C/min [85].
- Long-Term Storage: Promptly transfer the frozen vials to the vapor phase of a liquid nitrogen storage system (<-135°C) for long-term stability [85]. Avoid storage at -80°C for more than one month.
Protocol for Optimizing Cryoprotectant Formulation
This Design of Experiment (DoE) aims to identify the optimal CPA type and concentration for a novel cell type or to transition to a DMSO-reduced formulation.
Materials:
- CPAs: Permeating (e.g., DMSO, glycerol) and non-permeating (e.g., trehalose, sucrose, hydroxyethyl starch) agents [84] [89].
- Basal Medium: Cell-specific, serum-free basal medium.
- CRFT System: A system capable of programming and testing multiple freeze-thaw profiles in parallel [83].
Procedure:
- DoE Setup: Define variables: CPA type (e.g., 10% DMSO vs. 5% DMSO + 150mM trehalose), cooling rate (e.g., -1°C/min vs. -3°C/min), and cell concentration [83].
- Formulation: Prepare small batches (e.g., 10 mL) of each candidate freezing medium.
- CRFT Screening: Use the CRFT system to freeze cell aliquots in each medium according to the defined matrix of cooling rates. Log the exact thermal profile for each run [83].
- Post-Thaw Analysis: Thaw samples rapidly in a 37°C water bath. Assess key performance indicators:
- Viability: Use trypan blue exclusion or flow-based methods (e.g., NucleoCounter) [88].
- Recovery: Calculate the percentage of viable cells recovered relative to the pre-freeze count.
- Potency/Function: Conduct a cell-specific functional assay (e.g., differentiation potential for MSCs, metabolic activity, or phenotype retention via flow cytometry) [83] [28].
- Data-Driven Optimization: Use statistical analysis to identify the formulation and parameters that maximize all critical quality attributes.
The experimental workflow for this optimization process is illustrated below.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials and their GMP-critical functions for establishing a robust cryopreservation workflow.
Table 2: Essential Reagents and Materials for GMP Cryopreservation
| Item | GMP-Compliant Function | Example Use-Case |
|---|---|---|
| Defined Cryomedium | Provides a serum-free, xeno-free, chemically defined environment with cryoprotectants; ensures lot-to-lot consistency and reduces regulatory risk [85]. | CryoStor CS10; mFreSR for pluripotent stem cells. |
| Controlled-Rate Freezer (CRF) | Ensures precise, reproducible, and documented cooling rates (e.g., -1°C/min), directly translating bench-scale results to production [83]. | Grant Instruments CRFT system. |
| Internal-Threaded Cryovials | Prevents contamination during filling and storage in liquid nitrogen; single-use and sterile [85]. | Corning Cryogenic Vials. |
| Liquid Nitrogen Storage | Provides long-term storage at <-135°C (vapor phase) to maintain cell viability and genetic stability for years [85]. | Chart Industries storage tanks. |
| Human Platelet Lysate (hPL) | A GMP-suitable, xeno-free growth supplement for cell culture and freezing media, replacing fetal bovine serum [28] [88]. | Sexton Biotechnologies Stemulate. |
| GMP-Grade Enzymes | Ensure safe and effective cell harvesting; critical for cell isolation and passaging pre-cryopreservation [28] [88]. | Nordmark Collagenase NB6. |
Advanced Engineering Strategies: Overcoming Scale-Up Challenges
Advanced bioengineering strategies are being developed to overcome the fundamental physical challenges of ice formation and rewarming at scale.
Synergistic Ice Inhibition
This strategy combines multiple approaches to mitigate cryoinjury more effectively than any single method. A key advancement is the use of Ice Recrystallization Inhibitors (IRIs), such as antifreeze proteins (AFPs) or synthetic mimics like polyampholytes and polyvinyl alcohol (PVA) [84]. These materials adsorb to ice crystal surfaces, preventing small crystals from fusing into larger, more damaging ones during the thawing process. When added to standard cryomedium, PVA has been shown to increase MSC viability from 71.2% to 95.4% [84]. Combining IRIs with controlled-rate freezing and cell-specific CPA formulations represents the cutting edge of cryopreservation protocol design.
Advanced Rewarming Technologies
Devitrification (ice recrystallization during warming) is a major cause of cell death. While rapid thawing in a water bath is standard, it becomes inconsistent at larger volumes. Emerging technologies aim to overcome this:
- Electromagnetic Rewarming: Uses radiofrequency or microwave energy to heat the sample volumetrically and rapidly, avoiding the slow thermal conduction that allows ice recrystallization [84].
- Photothermal Rewarming: Incorporates nanoparticles (e.g., graphene, silicon) into the cryopreservation solution. When irradiated with laser light, these nanoparticles generate heat uniformly and instantly throughout the sample [84].
These "nanowarming" techniques show great promise for scaling up cryopreservation to larger volumes, such as organs and tissue constructs, by ensuring a rapid and uniform thawing process.
The relationship between these advanced strategies and their cellular protective mechanisms is summarized in the following diagram.
Optimizing cryopreservation is a critical enabler for the transition of stem cell therapies from research to clinical and commercial reality. By implementing GMP-compliant protocols that leverage controlled-rate freezing, defined cryomedia, and rapid thawing, biomanufacturers can ensure high post-thaw viability and batch-to-batch consistency. The integration of advanced strategies—such as ice-recrystallization inhibitors and novel rewarming technologies—will further de-risk scale-up and facilitate robust global logistics. As the cell therapy market continues its rapid growth, standardized, data-driven, and scalable cryopreservation will remain a cornerstone of successful GMP biomanufacturing.
Addressing Scalability Hurdles in Viral Vector and Consumable Production
The successful clinical and commercial translation of stem cell and gene therapies is critically dependent on overcoming a fundamental manufacturing bottleneck: the scalable production of viral vectors and the GMP-compliant consumables required for their manufacture. For therapies targeting more common diseases, manufacturing bottlenecks become particularly pronounced during late-stage clinical trials and commercial launch [90]. While current methods can satisfy demands for early-phase clinical trials, they face significant challenges in yielding sufficient product for Phase 3 trials and beyond [90]. This application note details the specific scalability hurdles in viral vector manufacturing and presents integrated strategies and robust protocols designed to enhance production scalability within a stringent GMP framework for stem cell biomanufacturing research.
Quantitative Analysis of Scalability Parameters
A systematic, data-driven approach is essential for evaluating and improving process scalability. The following tables summarize key quantitative parameters critical for assessing viral vector production and associated consumables.
Table 1: Key Process Input Variables (PIVs) and Process Output Variables (POVs) for Scalable Bioprocessing [91]
| Process Input Variables (PIVs) | Process Output Variables (POVs) |
|---|---|
| Bioreactor design & agitation rate | Cell growth rate & fold expansion |
| Cell culture media formulation | Aggregate size & morphology |
| Feeding regime | Harvest recovery efficiency |
| Inoculation density | Genomic stability |
| Harvest-related parameters | Pluripotency marker expression |
Table 2: Comparative Analysis of Viral Vector Production Platforms [92] [90]
| Production Platform Attribute | Traditional Adherent (e.g., HEK293) | Novel Suspension (e.g., CAP-GT) |
|---|---|---|
| Scalability Method | Scale-out (multiplying cell factories) | Scale-up (increasing bioreactor capacity) |
| Process Efficiency | Tedious, manual process | High-density growth, adaptable to standard bioreactors |
| Transfection Method | Transient transfection | Stable transfection packaging cells |
| Relative Vector Titer | Baseline | 2 to 10-fold higher titers reported |
| Risk of Replication Competent Virus (RCA) | Higher risk for Adenovirus | Reduced risk via engineered cell lines |
Experimental Protocols for Robust Bioprocess Design
Protocol: Serial Expansion and Evaluation of hiPSCs in Bioreactors for Process Robustness
This protocol assesses the robustness of hiPSC expansion processes in Vertical-Wheel bioreactors, a critical evaluation for scalable upstream operations [91].
- Objective: To evaluate key process attributes through long-term serial passage suspension culture for determining overall process robustness with different commercially available media and cell lines.
- Materials:
- Cell Lines: Human induced pluripotent stem cells (hiPSCs), e.g., 4YA, TC1133, or PLX1 lines.
- Equipment: Vertical-Wheel (VW) bioreactors, static culture T-flasks, biosafety cabinet, incubator (37°C, 5% CO2).
- Reagents: Five commercial media for evaluation (e.g., mTeSR1), Matrigel, Y-27632, Accutase, Ca− and Mg− PBS.
- Methodology:
- Static Seed Train: Perform two serial passages of hiPSCs post-thaw in T-75 flasks coated with Matrigel using a control medium like mTeSR1, supplemented with 10 µM Y-27632 at seeding.
- Bioreactor Inoculation: Seed hiPSC aggregates or single cells into the VW bioreactor.
- Serial Bioreactor Culture: Culture cells in the bioreactor over multiple passages (e.g., 3 to 10 passages), maintaining a consistent feeding regime and agitation rate.
- In-Vessel Dissociation: At harvest, perform dissociation operations within the bioreactor vessel to generate a single-cell suspension for re-inoculation.
- Process Monitoring: At each passage, track key POVs:
- Growth Kinetics: Calculate fold expansion and growth rate.
- Aggregate Morphology: Monitor size and shape visually and microscopically.
- Harvest Efficiency: Quantify cell recovery post-dissociation.
- Product Quality: Assess genomic stability and functional pluripotency via appropriate assays.
- Data Analysis: Compare the performance of different media formulations. Profound differences in cell growth and quality are often revealed only through long-term serial expansion, highlighting the insufficiency of short-term (e.g., one-passage) data for process validation [91].
Protocol: Transitioning from Transient to Stable Viral Vector Production
This protocol outlines a strategy for moving from a scalable transient transfection system to a highly robust and efficient stable production process for viral vectors, addressing a major industry bottleneck [90].
- Objective: To establish a stable viral vector production process that eliminates the variability and DNA supply challenges of transient transfection, thereby improving reproducibility and yield.
- Materials:
- Cell Line: Proprietary suspension cell line (e.g., CAP-GT technology).
- Reagents: Plasmid DNA containing the gene-of-interest, chemical induction agents, GMP-grade culture media.
- Equipment: Bioreactors of appropriate scale.
- Methodology:
- Stable Transfection: Stably transfect the gene-of-interest into the viral packaging cells.
- Clone Selection: Screen and select a high-producing, stable clone.
- Cell Bank Creation: Create a Master Cell Bank from the selected clone under defined conditions.
- Production Scale-Up: Expand the chosen clone to the desired production volume in a bioreactor.
- Induction: Chemically induce viral vector production in the scaled-up culture. Note that for AAV production, some stable systems do not require infection with helper viruses.
- Harvest and Purification: Harvest the culture medium and purify the viral vectors using chromatographic and filtration methods [92].
- Quality Control: A critical quality requirement is the demonstration of the absence of replication-competent virus particles, achieved through strategic genetic design of the producer cell line and vector genome [90].
The Scientist's Toolkit: Essential Research Reagent Solutions
The selection of GMP-compliant consumables is fundamental to ensuring the safety, purity, and efficacy of the final cell therapy product, directly impacting scalability and regulatory success [93].
Table 3: Key GMP Cell Therapy Consumables for Scalable Biomanufacturing
| Consumable Category | Key Function | Scalability & Quality Considerations |
|---|---|---|
| Cell Culture Media & Supplements | Supports cell growth and differentiation. | Must be serum-free or xeno-free to minimize immunogenicity; produced under ISO standards [93]. |
| Single-Use Bioprocessing Tools | Bioreactor bags, tubing, connectors, and filters for sterile manufacturing. | Reduces contamination risk, supports automation, and facilitates scale-up/scale-out [92] [93]. |
| Cell Separation & Enrichment Reagents | Magnetic beads or reagents for isolating specific cell populations. | GMP versions are validated for low endotoxin levels, sterility, and residual testing [93]. |
| Cryopreservation Materials | Bags and cryoprotectants (e.g., DMSO) for cell storage. | Must maintain cell viability during freeze/thaw and be validated for leachables/extractables [93]. |
Visualizing Scalability Strategies and Workflows
The following diagrams illustrate core concepts and workflows for addressing scalability challenges.
Diagram 1: Strategic Pathways to Overcome Viral Vector Production Scalability Hurdles. This workflow outlines the transition from traditional, limited-scale methods to modern, scalable manufacturing platforms [92] [90].
Diagram 2: Bioprocess Optimization Framework. This diagram shows the logical relationship between key input variables and critical output attributes that must be managed for a robust and scalable bioprocess [91].
Implementing Real-Time Analytics for Rapid Release Testing in Autologous Therapies
Autologous cell therapies represent a transformative advancement in personalized medicine, yet they pose significant manufacturing challenges due to their patient-specific nature and extreme time sensitivity. For these therapies, extended vein-to-vein timelines directly impact clinical outcomes, with data indicating that each additional week in manufacturing can reduce complete response rates by up to 11% [94]. Conventional quality control testing, particularly sterility and mycoplasma methods requiring 7-28 days, creates a critical bottleneck for products with shelf lives as short as 6 days [94] [95]. This application note details the implementation of integrated real-time analytics and rapid microbial methods to accelerate release testing while maintaining compliance with Good Manufacturing Practice (GMP) standards for scalable stem cell biomanufacturing.
The Critical Need for Rapid Analytics
Time Sensitivity of Autologous Therapies
Autologous cell therapies are inherently time-sensitive due to several factors:
- Limited Product Stability: Living cell products have limited viability and potency during ex vivo storage
- Patient Clinical Status: Patients awaiting treatment often have advanced disease states requiring urgent intervention
- Manufacturing Complexity: Patient-specific manufacturing batches prevent traditional inventory stockpiling
Traditional quality control testing has become the primary constraint in minimizing vein-to-vein time. Sterility and mycoplasma testing alone account for the majority of release testing time, typically spanning 7-28 days using compendial methods [94]. This creates an irreconcilable conflict between comprehensive quality assurance and timely patient treatment.
Quantitative Impact of Testing Delays
Table 1: Impact of Manufacturing Delays on Clinical Outcomes in Autologous Therapies
| Manufacturing Delay | Impact on Complete Response Rate | Testing Methods Contributing to Delay |
|---|---|---|
| 1 week | Reduction by up to 11% [94] | Conventional sterility testing (14-28 days) |
| 2 weeks | Reduction by approximately 22% | Traditional mycoplasma testing (28 days) |
| 3 weeks | Reduction by approximately 33% | Method transfer and validation |
Rapid Analytics Implementation Framework
Core Principles
Implementing rapid analytics for autologous therapies requires adherence to several core principles:
- Quality by Design (QbD): Building quality into the process rather than testing it in the final product
- Process Analytical Technology (PAT): Utilizing advanced monitoring for real-time quality assessment
- Risk-Based Approach: Focusing testing efforts on critical quality attributes (CQAs) with greatest patient impact
- Platform Methodologies: Developing standardized approaches adaptable across multiple therapy platforms
Real-Time Mycoplasma Testing Implementation
Mycoplasma contamination presents particular challenges as these organisms are difficult to culture and detect using traditional microbiological methods. Implementing rapid mycoplasma testing requires a structured approach:
Table 2: Comparison of Conventional vs. Rapid Mycoplasma Testing Methods
| Parameter | Conventional Culture Method | Real-Time PCR Method |
|---|---|---|
| Testing Duration | 28 days | 5-6 hours [95] |
| Detection Capability | Viable organisms only | DNA from viable and non-viable organisms |
| Sample Volume Required | High (multiple mL) | Up to 98% reduction [94] |
| Automation Potential | Low | High (full automation possible) |
| Regulatory Status | Compendial method | Approved alternative (EMA, 2013) [95] |
Experimental Protocol: Real-Time PCR Mycoplasma Testing
Principle: This qualitative test detects Mycoplasma DNA through real-time polymerase chain reaction (PCR) amplification with specific primers and fluorescent probes.
Materials and Equipment:
- Real-Time PCR Instrument (calibrated)
- Mycoplasma-specific primer and probe sets
- DNA extraction reagents (including magnetic particle-based purification)
- Positive controls (Mycoplasma DNA)
- Inhibition controls
- Discriminatory Positive/Extraction Control (plasmid with Mycoplasma sequence)
Procedure:
- Sample Preparation: Concentrate any Mycoplasma organisms present via centrifugation
- DNA Extraction:
- Lyse organisms to release nucleic acids
- Digest interfering proteins enzymatically
- Purify DNA using proprietary magnetic particles
- Elute DNA and remove magnetic particles
- PCR Setup:
- Prepare reaction mix with primers, probes, and DNA template
- Include negative control, positive control, extraction control, and inhibition controls
- Amplification and Detection:
- Run thermal cycling protocol with fluorescence monitoring
- Analyze amplification curves and melting temperatures (Tm)
- Results Interpretation:
- Positive samples exhibit a threshold cycle (Ct) inversely proportional to DNA amount
- Confirm positive results with amplicon Tm in specific range
- Validate test with control reactions
Validation Parameters:
- Specificity and Detection Limit (most critical parameters)
- Robustness, Repeatability, and Ruggedness
- Equivalence to compendial method [95]
Advanced Analytics for Identity Testing
Liquid chromatography-mass spectrometry (LC-MS) provides a powerful alternative to conventional identity testing methods such as Enzyme-Linked Immunosorbent Assay (ELISA) and peptide mapping.
Experimental Protocol: LC-MS Identity Testing for Biologics
Principle: This strategy enables reliable identity testing and differentiation of products through mass measurement of subunits or intact proteins.
Materials and Equipment:
- Liquid Chromatography system coupled to Mass Spectrometer
- Reduction buffer (Tris-HCl with dithiothreitol)
- Reverse-phase column
- Mobile phases (water and acetonitrile with trifluoroacetic acid)
Procedure: Workflow 1 - Reduced Analysis for mAbs:
- Reduce mAb inter-chain disulfide bonds using DTT-containing buffer
- Dilute protein sample to 1.0 mg/mL with reducing buffer
- Incubate at 37°C for 30 minutes
- Analyze using LC-MS with reverse-phase chromatography
- Measure light chain (LC) and heavy chain (HC) masses
Workflow 2 - Intact Analysis for Non-mAb Therapies:
- Dilute protein sample to 1.0 mg/mL with compatible buffer
- Directly inject onto LC-MS system
- Perform intact mass measurement under non-denaturing conditions
Advantages Over Conventional Methods:
- Faster Turnaround: Reduced from days to hours [96]
- Higher Specificity: Distinguishes molecules with high sequence homology
- Automated Data Processing: One-click analysis after method setup
- Platform Method Conditions: Minimal molecule-specific development needed
Process Analytical Technology (PAT) Integration
Implementing PAT frameworks enables real-time monitoring of critical process parameters (CPPs) to ensure consistent product quality:
Figure 1: PAT Framework for Real-Time Monitoring and Control in Autologous Therapy Manufacturing. This integrated system enables continuous quality assurance through automated monitoring and adjustment of critical process parameters.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Implementing Rapid Analytics
| Category | Specific Examples | Function |
|---|---|---|
| Molecular Biology | Real-Time PCR reagents [95] | Mycoplasma DNA detection and amplification |
| Mycoplasma-specific primers/probes | Targeted detection of contaminating organisms | |
| DNA extraction kits | Nucleic acid purification from complex samples | |
| Process Sensors | Fluorometric pH/DO sensors [97] | Real-time monitoring of bioreactor conditions |
| Radio-frequency impedance probes [97] | Non-invasive viability and cell density measurement | |
| Chromatography | LC-MS systems [96] | High-resolution identity testing and quality attribute monitoring |
| Reverse-phase columns | Protein separation for mass spectrometric analysis | |
| Cell Culture | Reduced-volume assay kits | Miniaturized testing for limited sample availability |
| Rapid microbial detection media | Accelerated contamination screening |
Implementation Workflow and Regulatory Strategy
Figure 2: Strategic Pathway for Implementing Rapid Analytics in a Regulated Environment. This structured approach ensures regulatory compliance while accelerating testing timelines.
Successful implementation requires careful planning and regulatory engagement:
- Early Regulatory Consultation: Engage with regulatory affairs during method development to support innovative testing plans [94]
- Comprehensive Validation: Demonstrate method equivalence to compendial methods following ICH, USP, and PhEur guidelines [95]
- Risk Management: Implement corrective and preventive action (CAPA) systems to address deviations promptly [98]
- Staff Training: Ensure analysts are proficient in new technologies and methodologies
Implementing real-time analytics for rapid release testing in autologous therapies requires a systematic approach integrating advanced technologies, validated methodologies, and regulatory strategy. The protocols detailed in this application note demonstrate that transitioning from conventional testing to rapid methods can reduce testing timelines from weeks to hours while maintaining GMP compliance. For autologous therapies where time directly impacts clinical outcomes, these advanced analytical approaches are not merely advantageous—they are essential for delivering viable products to patients and advancing the field of scalable stem cell biomanufacturing.
Quality Control, Analytical Validation, and Global Regulatory Strategy
Within the framework of Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing, the accurate determination of viable cell count is a fundamental Critical Quality Attribute (CQA). It serves as a direct measure of product potency and is essential for process control, dose determination, and final product release [99] [100]. Conventional manual cell counting using a hemocytometer, while described in the European Pharmacopoeia, is heavily dependent on operator expertise, time-consuming, and susceptible to variability, making it suboptimal for ensuring the consistency required in GMP environments [99] [101]. This application note details the validation of an automated fluorescence imaging-based cell counting method for human induced pluripotent stem cells (hiPSCs), providing a standardized, precise, and efficient alternative to manual counting for clinical-grade cell therapy manufacturing [99].
Validation Strategy and Regulatory Framework
The validation of analytical procedures for GMP must comply with internationally recognized guidelines. The strategy outlined here is based on the International Council for Harmonisation (ICH) Q2(R1) guidance for analytical method validation and adheres to relevant sections of the European Pharmacopoeia (EP) and EudraLex Volume 4 for Advanced Therapy Medicinal Products (ATMPs) [99] [102] [100]. The objective is to demonstrate that the automated method is fit for its intended purpose—precisely and accurately enumerating viable hiPSCs during expansion and in the final product.
The following workflow illustrates the key stages in the validation of an automated cell counting method:
Comparative Performance Data: Automated vs. Manual Counting
A systematic comparison between an automated cell counting system (NucleoCounter NC-100) and the manual Bürker hemocytometer method reveals significant advantages of automation for GMP compliance [99]. Similar benefits have been observed with other semi-automated systems, such as the Countstar BioTech, when compared to manual hemocytometers [101].
Table 1: Key Validation Parameters for Automated Viable Cell Counting of hiPSCs
| Validation Parameter | Automated Method (NucleoCounter NC-100) | Manual Method (Bürker Hemocytometer) | Regulatory Acceptance Criteria |
|---|---|---|---|
| Accuracy | High agreement with reference method [99] | Reference method | Demonstrated equivalence [99] |
| Precision (Repeatability) | Higher precision; <6% RSD for total cell density [101] | Lower precision; >9% RSD for total cell density [101] | Coefficient of variation (CV) <10% [99] [100] |
| Specificity | Specific for viable cells via fluorescence-based detection [99] | Based on morphology, prone to misinterpretation | No interference from sample matrix [99] |
| Linearity & Range | Linear range demonstrated from 5.0 x 10^3 to 2.0 x 10^6 cells/mL [99] | Linear range typically 5.0 x 10^4 to 5.5 x 10^5 cells/mL [99] | R² > 0.95 within the specified range [99] |
| Analysis Time | Significantly faster; minimal operator hands-on time [99] | Time-consuming and labor-intensive [99] | N/A |
Detailed Experimental Protocol
This section provides a step-by-step protocol for validating and implementing the automated viable cell counting method for hiPSCs, based on the methodology successfully employed in a cGMP facility [99].
Sample Preparation
- Culture hiPSCs: Expand hiPSCs on hESC-qualified Matrigel-coated surfaces in a defined, xeno-free medium such as TeSR-E8. Maintain cultures at 37°C, 5% CO₂ [99].
- Harvest Cells: Wash the cells with DPBS without Ca²⁺ and Mg²⁺. Incubate with a dissociation enzyme like accutase for approximately 5 minutes at 37°C [99].
- Prepare Single-Cell Suspension: Gently detach the cells and collect them in DPBS without Ca²⁺ and Mg²⁺. Pellet the cells via centrifugation at 300 × g for 10 minutes. Resuspend the cell pellet in an appropriate volume of DPBS to achieve a concentration within the linear range of the counting method [99].
- Dilution: If necessary, prepare a dilution of the cell suspension to ensure the final counted concentration falls within the optimal range of the automated instrument (e.g., 5.0 x 10³ to 2.0 x 10⁶ cells/mL for the NucleoCounter NC-100) [99].
Automated Cell Counting Procedure
- Instrument Preparation: Power on the NucleoCounter NC-100 and ensure it has passed all self-checks. Use pre-packaged, single-use Via1-Cassettes which contain the fluorescent dye propidium iodide (PI) [99].
- Load Sample: Pipette 100 µL of the well-mixed cell suspension directly into the cassette chamber [99].
- Analyze Sample: Insert the cassette into the instrument. The system automatically stains the cells, captures fluorescence images, and analyzes them using proprietary software. Non-viable cells with compromised membranes are stained by PI and counted as such; the viable cell count is calculated from the total and non-viable counts [99].
- Record Data: Document the viable cell concentration (cells/mL) and viability percentage provided by the instrument's software.
Validation Experiments
The following workflow outlines the core experimental process for the counting method, from sample preparation to data analysis:
- Accuracy: Compare the results of the automated method (y) against the manual Bürker hemocytometer method (x) for a minimum of three independent hiPSC batches, each analyzed in triplicate. Accuracy is demonstrated by a linear regression line with a slope close to 1 and an intercept close to 0 [99].
- Precision:
- Repeatability (Intra-assay Precision): Have a single analyst perform six replicate counts of the same homogeneous hiPSC sample in one session. The coefficient of variation (CV) for viable cell count should be <10% [99] [100].
- Intermediate Precision (Inter-assay Precision): Have two qualified analysts independently perform cell counts on the same set of hiPSC samples (n=3) on different days. The CV between analysts and between days should be <10% [99].
- Specificity: Analyze the sample matrix (DPBS without Ca²⁺ and Mg²⁺) using the automated method to confirm the absence of interfering particles that could be misidentified as cells [99].
- Linearity and Range: Prepare a series of dilutions from a concentrated hiPSC sample to cover a range from below to above the expected counting range (e.g., 5.0 x 10³ to 2.0 x 10⁶ cells/mL). Analyze each dilution and plot the measured concentration against the expected concentration. The method is linear if the coefficient of determination (R²) is ≥ 0.95 [99].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Automated Cell Counting Validation
| Item | Function / Description | GMP-Grade Consideration |
|---|---|---|
| hiPSC Line | The raw material; patient-derived or master cell bank-derived pluripotent stem cells. | Use of clinical-grade, validated cell banks is essential for cGMP manufacturing [77]. |
| Defined, Xeno-Free Culture Medium | Supports the expansion and maintenance of hiPSCs in an undifferentiated state. | Chemically defined, xeno-free GMP versions are commercially available and required to minimize variability and safety risks [99] [103]. |
| Enzymatic Dissociation Reagent | Generates a single-cell suspension for accurate counting and subculturing. | Use of GMP-grade reagents (e.g., accutase, trypsin) is critical for process consistency and patient safety [99]. |
| Automated Cell Counter & Consumables | Fluorescence-based instrument and single-use cassettes for viable cell enumeration. | Equipment must have installation/operational qualification (IQ/OQ). Software must be compliant with 21 CFR Part 11 for data integrity [99] [100]. |
| Hemocytometer | The reference method for cell counting (e.g., Bürker chamber). | Required for validation and comparator studies. |
| Buffer Solutions | e.g., DPBS without Ca²⁺ and Mg²⁺, for washing and diluting cells. | Must be sterile and of appropriate quality for cell culture and GMP use [99]. |
The validation of automated fluorescence-based cell counting represents a critical step toward robust, scalable, and cGMP-compliant stem cell biomanufacturing. The data and protocols presented herein demonstrate that automated methods meet all regulatory validation requirements while offering superior precision, speed, and standardization compared to traditional manual counting [99] [101]. Adopting such validated analytical methods is indispensable for ensuring the accurate determination of CQAs like viable cell count, ultimately supporting the development of safe and efficacious stem cell therapies.
Within the framework of a thesis on Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing, the establishment of a robust, validated quality control (QC) system is a critical research milestone. The safety, identity, purity, and potency of the final cell-based product are unequivocally dependent on the stringency of in-process and release testing. This document provides detailed Application Notes and Protocols for four fundamental QC tests—cell viability, phenotype, potency, and sterility—integrating quantitative data and actionable methodologies essential for research scientists and drug development professionals navigating the transition from preclinical discovery to clinical application.
Quantitative Quality Control Specifications
The following tables consolidate quantitative acceptance criteria and key performance data from recent GMP-compliant studies for different cell therapy products, providing a benchmark for establishing in-house specifications.
Table 1: General QC Release Criteria for Cell Therapy Products
| Test Parameter | Cell Type | Acceptance Criterion | Reference / Context |
|---|---|---|---|
| Viability | Mesenchymal Stem Cells (MSCs) | >95% (Minimum requirement: >70%) [31] | GMP-expanded infrapatellar fat pad MSCs (GMP-FPMSC) |
| Viability | CAR T-cells (Leukapheresis) | ≥90% (after 73h at 2-8°C) [104] | Stability of starting material for a FiCAR T-cell product |
| Phenotype | Human Induced Pluripotent Stem Cells (hiPSCs) | Expression of ≥3 undifferentiated markers on ≥75% of cells [105] | GMP batch release of an intermediate hiPSC drug product |
| Phenotype | Mesenchymal Stem Cells (MSCs) | Positive for CD73, CD90, CD105; Negative for CD45 [31] | Standard ISCT phenotype criteria for MSCs |
| Potency | hiPSCs (Directed Differentiation) | Detection of ≥2 of 3 lineage-specific markers for each germ layer [105] | Assay to assess trilineage differentiation potential |
| Potency | Bone Marrow Mononuclear Cells (BM-MNC) | Invasion Index of 28.89 ± 16.82% (Mean ± SD) [106] | Migration capacity assay for cells in cardiac regeneration |
| Sterility | General Cell Therapy Product | No microbial contamination in BacT/Alert system [31] | Absence of bacteria and fungi, validated per Ph. Eur. 2.6.1 |
Table 2: hiPSC-Specific Residual Episomal Vector Testing Validation Data
| Validation Parameter | Established Criterion | Rationale |
|---|---|---|
| Minimum Cell Input | 20,000 cells (120 ng genomic DNA) [105] | Ensures accurate determination of REV presence |
| Recommended Passage for Testing | Between passages 8 and 10 [105] | Avoids unnecessary rejection of lines due to passage-dependent vector loss |
| Flow Cytometry Control | Fluorescence Minus One (FMO) control [105] | Ensures control for fluorescent spread in multi-color panels |
Detailed Experimental Protocols
Protocol 1: Cell Viability Assay via Trypan Blue Exclusion
Principle: This method distinguishes between viable cells, which exclude the dye, and non-viable cells, which absorb it, allowing for quantification via manual or automated counting.
Materials:
- Trypan Blue solution (0.4%)
- Phosphate Buffered Saline (PBS)
- Hemacytometer (e.g., Bright-Line) or automated cell counter
- Inverted light microscope
- Centrifuge
Procedure:
- Harvest and Suspend: Harvest cells using a standard method (e.g., enzymatic dissociation, scraping) and create a single-cell suspension. Centrifuge the suspension (e.g., 300 ×g for 10 minutes [31]), aspirate the supernatant, and resuspend the cell pellet in PBS.
- Prepare Stain: Mix 10 µL of the cell suspension with 10 µL of 0.4% Trypan Blue solution. Incubate for 1-3 minutes. Note: Do not exceed 5 minutes, as prolonged exposure can be toxic to live cells.
- Load and Count: Immediately load approximately 10 µL of the mixture onto a hemacytometer. Using an inverted microscope, count the number of unstained (viable) and blue-stained (non-viable) cells in the four corner quadrants.
- Calculate Viability:
- Total Cell Count = (Sum of all cells counted / 4) × Dilution Factor (2) × 10^4
- Percentage Viability = (Number of viable cells / Total number of cells) × 100%
Application Note: This method was used to validate >95% post-thaw viability for GMP-FPMSCs, a key release specification [31]. For processes with short shelf-lives, rapid viability assessment is critical.
Protocol 2: Cell Phenotype Analysis via Multi-Color Flow Cytometry
Principle: Flow cytometry enables simultaneous quantification of multiple cell surface markers, confirming cellular identity and purity, which is critical for lot release.
Materials:
- Fluorescently conjugated antibodies (e.g., against CD73, CD90, CD105, CD45)
- Flow cytometry staining buffer (PBS with 1-2% FBS or BSA)
- Fixation solution (e.g., 1-4% paraformaldehyde, optional)
- BD Stemflow Human MSC Analysis Kit or equivalent
- Flow cytometer (e.g., BD FACS Fortessa) with appropriate lasers
- Fluorescence Minus One (FMO) controls
Procedure:
- Prepare Cells: Harvest and wash cells to obtain a single-cell suspension. Adjust concentration to 1-5 × 10^6 cells/mL in staining buffer.
- Stain Cells: Aliquot 100 µL of cell suspension into flow cytometry tubes. Add pre-titrated antibodies or antibody cocktails. Incubate for 30-60 minutes in the dark at 4°C.
- Wash and Resuspend: Add 2 mL of staining buffer to each tube, centrifuge (e.g., 300 ×g for 5 minutes), and carefully decant the supernatant. Repeat wash step.
- Acquire Data: Resuspend the final cell pellet in an appropriate volume of buffer (e.g., 200-500 µL) and analyze on the flow cytometer. Acquire a minimum of 10,000 events per sample.
- Analyze Data: Use FMO controls to set positive/negative gates accurately [105]. The population of interest (e.g., MSCs) is typically defined as CD45-/CD73+/CD90+/CD105+ [31].
Application Note: For hiPSCs, a cutoff for the undifferentiated state was validated as the expression of at least three individual markers on at least 75% of the cells [105]. Proper validation, including the use of FMO controls, is essential for GMP-compliant assay reproducibility.
Protocol 3: Potency Assay via Directed Differentiation or Functional Capacity
Principle A: Directed Differentiation of hiPSCs This assay evaluates the functional capacity of hiPSCs to differentiate into derivatives of the three germ layers, a key attribute of pluripotency.
Materials:
- Specific differentiation media (e.g., for ectoderm, mesoderm, endoderm)
- Growth factor-reduced Matrigel Matrix or other basement membrane matrix
- Fixative (e.g., 10% Neutral Buffered Formalin)
- Antibodies for immunocytochemistry against lineage-specific markers
Procedure:
- Seed Cells: Seed a defined number of hiPSCs onto Matrigel-coated plates in appropriate maintenance media and allow to attach.
- Induce Differentiation: Once cells reach the desired confluence, switch to specialized differentiation media formulations designed to direct cells toward ectoderm, mesoderm, and endoderm fates. Culture for a defined period (e.g., 10-14 days), with media changes every other day.
- Analyze Differentiation: Fix cells and perform immunocytochemistry or flow cytometry for lineage-specific markers (e.g., β-III-tubulin for ectoderm, α-smooth muscle actin for mesoderm, SOX17 for endoderm).
- Interpret Results: The assay is considered positive for a given germ layer if at least two of three predefined lineage-specific markers are detected. A valid potency assay for hiPSC batch release requires positive results for all three germ layers [105].
Principle B: Migration/Invasion Assay for BM-MNCs For somatic cells like those used in cardiac repair, potency can be linked to a functional attribute like migration capacity, which predicts therapeutic efficacy [106].
Materials:
- Modified Boyden chamber (e.g., Transwell insert)
- Matrigel Matrix (for invasion assays)
- Endocult Basal Medium with supplements (chemoattractant)
- Crystal Violet stain or calcein-AM for quantification
- Fluorescent plate reader or microscope
Procedure:
- Prepare Chambers: For invasion assays, coat the upper side of a porous membrane (e.g., 8 µm pores) with a thin layer of Matrigel and allow it to polymerize.
- Seed Cells: Harvest and count BM-MNCs. Place a defined number of cells in serum-free medium in the upper chamber. Add complete medium with serum or a specific chemoattractant to the lower chamber.
- Incubate and Migrate: Incubate the chambers for 6-24 hours at 37°C to allow cells to migrate through the pores (migration) or degrade the matrix and migrate (invasion) toward the chemoattractant.
- Quantify Cells: Remove non-migrated cells from the upper side of the membrane. Fix, stain migrated cells on the lower side with Crystal Violet, and count manually under a microscope. Alternatively, use calcein-AM to stain migrated cells and measure fluorescence.
- Calculate Invasion Index: Express the result as an invasion index: the ratio between the number of cells invading through the Matrigel-coated membrane relative to cell migration through a control (uncoated) insert membrane [106].
Protocol 4: Sterility Testing by Direct Inoculation
Principle: This compendial method (EU Ph. 2.6.1/USP) ensures the final cell product is free from viable bacteria and fungi by inoculating samples directly into two types of culture media to support aerobic and anaerobic growth.
Materials:
- Fluid Thioglycollate Medium (FTM) - for anaerobic and aerobic bacteria
- Tryptic Soy Broth (TSB) - for aerobic bacteria and fungi
- Biological safety cabinet (Class A/ISO 5)
- Incubators (set at 20-25°C and 30-35°C)
Procedure:
- Sample Preparation: Under aseptic conditions, withdraw a representative sample (e.g., 1-5 mL) from the final cell product suspension.
- Inoculate Media: Aseptically transfer the recommended volume of the sample (e.g., 1-2 mL for 20 mL of media) directly into containers of FTM and TSB. For validation, positive controls (media inoculated with low levels of reference strains like *Staphylococcus aureus and Bacillus subtilis) must be included.*
- Incubate and Observe: Incubate FTM at 30-35°C and TSB at 20-25°C for a minimum of 14 days. Observe the media visually for turbidity (indicating microbial growth) at regular intervals (e.g., days 3, 7, and 14).
- Interpret Results: The product meets sterility requirements if no turbidity is observed in any of the test media after 14 days of incubation. All positive controls must show growth to confirm the validity of the test.
Application Note: This direct inoculation method was successfully validated for a BM-MNC product, where FTM cultures showed positivity for controls after 3 days and TSB for B. subtilis after 3 days and Mycetes after 5 days [106]. For products with short shelf-lives, rapid microbiological methods with shorter read-out times can be used as an alternative [107].
Workflow and Logical Diagrams
GMP Quality Control Testing Workflow
Diagram 1: GMP Quality Control Testing Workflow. This diagram outlines the logical progression of a cell therapy product from starting material to final release, highlighting the critical points for in-process and batch-release quality control testing.
Potency Assay Validation Logic
Diagram 2: Potency Assay Validation Logic. This chart outlines the decision-making process for developing and validating a GMP-compliant potency assay, illustrating how quantitative acceptance criteria are established based on product-specific Critical Quality Attributes (CQAs).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for QC Testing
| Reagent/Kits | Function/Application | Specific Example (from search results) |
|---|---|---|
| Animal Component-Free Media | GMP-compliant cell expansion, maintains stemness and proliferation. | MSC-Brew GMP Medium [31], MesenCult-ACF Plus Medium [31] |
| Flow Cytometry Antibody Panels | Cell phenotype analysis, identity, and purity confirmation. | BD Stemflow Human MSC Analysis Kit (CD73, CD90, CD105, CD45) [31] |
| Limulus Amoebocyte Lysate (LAL) Test | Quantification of bacterial endotoxin levels in final product. | Charles River Endosafe PTS system [106] |
| Matrigel Matrix / Basement Membrane | Potency assay substrate for cell invasion/migration. | Used in modified Boyden chamber for BM-MNC invasion assay [106] |
| Sterility Test Culture Media | Detection of aerobic/anaerobic bacteria and fungi. | Fluid Thioglycollate Medium (FTM), Tryptic Soy Broth (TSB) [106] |
| Automated Cell Processing System | Closed, semi-automated GMP-compliant cell manufacturing. | CliniMACS Prodigy (Miltenyi Biotec) for T-cell/CAR-T manufacturing [104] |
The development and manufacturing of stem cell-based therapies require a rigorous analytical framework to ensure product quality, safety, and efficacy. Adherence to internationally recognized regulatory guidelines is not merely a regulatory obligation but a fundamental component of robust biomanufacturing science. For scalable stem cell biomanufacturing, two regulatory frameworks are particularly critical: the International Council for Harmonisation (ICH) Q2(R1) guideline on the validation of analytical procedures [108] and the EudraLex Volume 4 guidelines on Good Manufacturing Practice (GMP) [57]. The ICH Q2(R1) guideline provides the foundational methodology for validating analytical methods used in assessing the quality attributes of biological products, ensuring that these methods are reliable, reproducible, and suitable for their intended purpose [108] [109]. Concurrently, EudraLex Volume 4 establishes the comprehensive GMP standards that govern the entire manufacturing environment, from facility design and personnel to production and quality control [57]. Together, these frameworks create an integrated ecosystem of quality assurance for advanced therapy medicinal products (ATMPs).
The regulatory landscape is dynamic, with significant updates currently underway. The ICH Q2(R1) guideline has been revised and replaced by ICH Q2(R2) in November 2023 [110] [111] [109]. Similarly, EudraLex Volume 4 is undergoing substantial modernization, with draft revisions for Chapter 4 (Documentation), Annex 11 (Computerised Systems), and a new Annex 22 (Artificial Intelligence) released for public consultation in 2025 [112] [18] [113]. These revisions aim to address technological advancements including digital systems, hybrid documentation, and AI/ML applications in pharmaceutical manufacturing [112] [18]. For stem cell researchers, understanding both the established principles of Q2(R1) and the evolving requirements of Q2(R2) and updated GMP standards is essential for developing future-proof manufacturing platforms.
Analytical Procedure Validation: ICH Q2(R1) & Q2(R2)
Core Principles and Validation Parameters
The ICH Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," establishes harmonized criteria for validating analytical methods used in pharmaceutical development [114] [108]. Its primary purpose is to align regulatory requirements across regions, ensuring that analytical data generated to support drug applications is consistent, reliable, and reproducible [108]. The guideline categorizes analytical tests into three main types: identification tests, testing for impurities (both quantitative and limit tests), and assay procedures for potency or content determination [109]. For each category, it defines specific validation characteristics that must be demonstrated to prove the method is suitable for its intended use [108] [109].
The validation process under ICH Q2(R1) involves demonstrating that the analytical method meets established standards for multiple performance characteristics, the core of which are specificity, accuracy, precision, linearity, range, detection limit, quantitation limit, and robustness [108]. Specificity is the ability to unequivocally assess the analyte in the presence of expected components, while accuracy expresses the closeness of agreement between the measured value and the true value [108]. Precision, encompassing repeatability and intermediate precision, describes the closeness of agreement between a series of measurements [108]. Linearity is the method's ability to obtain test results directly proportional to analyte concentration, and the range defines the interval between upper and lower concentration levels for which suitable precision, accuracy, and linearity have been demonstrated [108]. The detection limit (LOD) and quantitation limit (LOQ) are the lowest amounts of analyte that can be detected or quantified with acceptable accuracy and precision, respectively [108]. Finally, robustness measures the capacity of the method to remain unaffected by small, deliberate variations in method parameters [108].
Transition to ICH Q2(R2): Key Updates
The recently adopted ICH Q2(R2) guideline represents a significant modernization of analytical validation standards, expanding upon Q2(R1) to address emerging technologies and scientific advancements [110] [111] [109]. Officially adopted as a harmonized guideline in November 2023, Q2(R2) introduces several critical updates relevant to sophisticated stem cell analytics [110] [109]. A key advancement is the inclusion of guidance for multivariate analytical procedures and advanced spectroscopic/-metric techniques like Near Infrared (NIR) and Raman spectroscopy, which are increasingly used in Process Analytical Technology (PAT) for real-time monitoring of bioprocesses [111] [109]. The revised guideline also incorporates a lifecycle approach to analytical procedures, aligning with contemporary quality paradigms and encouraging continuous method verification [111] [109].
Other significant enhancements in Q2(R2) include revised requirements for demonstrating stability-indicating properties through specificity/selectivity assessments, updated approaches for establishing the working range, and allowance for combined evaluation of accuracy and precision using statistical tools like tolerance intervals [111] [109]. The guideline also introduces the concept of "reportable range" and provides clearer definitions through an alphabetically sorted glossary [109]. For impurity methods, Q2(R2) explicitly requires that the limit of quantification (LOQ) must be less than or equal to the reporting threshold [109]. These updates collectively provide a more comprehensive framework for validating the complex analytical methods essential for characterizing stem cell products.
Table 1: Comparison of Analytical Validation Parameters in ICH Q2(R1) vs. Q2(R2)
| Validation Parameter | ICH Q2(R1) Requirements | ICH Q2(R2) Enhancements | Relevance to Stem Cell Analytics |
|---|---|---|---|
| Specificity/Selectivity | Ability to assess analyte unequivocally | New requirements for stability-indicating methods; stressed samples; technology-inherent justification | Critical for demonstrating assay specificity in complex cellular matrices |
| Accuracy & Precision | Evaluated separately | Allows combined evaluation using tolerance intervals | Suitable for potency assays with inherent biological variability |
| Linearity | Series of measurements at different concentration levels | Explicit mention of residual plots; removal of residual sum of squares requirement | Applicable to quantitative assays (e.g., metabolite measurements) |
| Range | Interval with suitable precision, accuracy, linearity | Introduction of "reportable range" concept | Essential for defining valid measurement ranges for critical quality attributes |
| LOD/LOQ | Lowest detectable/quantifiable amount | LOQ must be ≤ reporting limit for impurity methods | Important for detecting low levels of process impurities or contaminants |
| Robustness | Not a validation parameter per Q2(R1) | Remains an evaluation parameter during development | Critical for method transfer between facilities in decentralized manufacturing |
| Multivariate Methods | Not specifically addressed | New dedicated section with validation considerations | Enables use of advanced spectroscopy for real-time process monitoring |
| Lifecycle Management | Not explicitly addressed | New section on validation during analytical procedure lifecycle | Supports continuous method verification throughout product development |
Experimental Protocol: Validation of a Flow Cytometry Method for Stem Cell Purity Analysis
Principle: This protocol describes the validation of a flow cytometry method for quantifying the percentage of CD34+ cells in a stem cell product according to ICH Q2(R1)/Q2(R2) guidelines. The method employs fluorescently labeled anti-CD34 antibodies for specific detection and quantification.
Materials and Equipment:
- Flow cytometer with minimum 3-color capability
- CD34-positive control cell line (e.g., KG-1a)
- Isotype-matched negative control antibody
- Fluorescently labeled anti-CD34 antibody
- Phosphate Buffered Saline (PBS) with 1% Bovine Serum Albumin (BSA)
- 7-AAD viability dye
- Procedure for cell counting and viability assessment
- Software for flow cytometry data analysis
Procedure:
- Sample Preparation: Prepare cell suspensions at appropriate concentration (1×10^6 cells/mL) in PBS/1% BSA. Aliquot 100 μL of cell suspension into test tubes.
- Staining: Add predetermined optimal concentration of fluorescent anti-CD34 antibody to test sample. Add isotype control to control tube. Incubate for 30 minutes at 4°C protected from light.
- Washing: Wash cells twice with PBS/1% BSA to remove unbound antibody.
- Viability Staining: Resuspend cell pellet in PBS containing 7-AAD viability dye, incubate for 5-10 minutes at room temperature.
- Acquisition: Acquire a minimum of 10,000 viable cell events per sample on flow cytometer using established instrument settings.
- Analysis: Gate on viable cells (7-AAD negative), then analyze CD34 expression compared to isotype control.
Validation Experiments:
- Specificity: Demonstrate specific binding through parallel analysis with isotype control antibody. Use CD34-positive and negative cell lines as controls.
- Accuracy: Spike recovery experiments using known numbers of CD34+ cells added to a matrix of known CD34- cells. Calculate percentage recovery (target: 80-120%).
- Precision:
- Repeatability: Analyze six replicates of the same sample in one session.
- Intermediate Precision: Analyze the same sample on three different days by two analysts.
- Calculate %RSD for each precision study (acceptance criterion: ≤15%).
- Linearity and Range: Prepare samples with CD34+ cell percentages spanning the expected range (e.g., 5-95%). Establish the range where linearity, accuracy, and precision criteria are met.
- Robustness: Deliberately vary method parameters (antibody incubation time ±10 minutes, staining temperature ±2°C) to evaluate impact on results.
- LOD/LOQ: Serially dilute CD34+ cells in CD34- cells to determine the lowest level that can be reliably detected and quantified.
Acceptance Criteria:
- Specificity: Clear separation between specific antibody and isotype control staining.
- Accuracy: Mean recovery of 80-120% across the validated range.
- Precision: %RSD ≤15% for both repeatability and intermediate precision.
- Linearity: R² value ≥0.95 across the validated range.
GMP Compliance: EudraLex Volume 4 Framework
Structure and Requirements
EudraLex Volume 4, "The Rules Governing Medicinal Products in the European Union: Good Manufacturing Practice (GMP) Guidelines," provides the comprehensive regulatory framework for manufacturing medicinal products in the European Union [57]. This extensive document establishes principles and guidelines to ensure that products are consistently produced and controlled according to quality standards appropriate to their intended use [57]. The structure of Volume 4 is organized into multiple parts and annexes, with Part I covering basic requirements for medicinal products across critical areas including pharmaceutical quality system, personnel, premises and equipment, documentation, production, quality control, and outsourced activities [57]. Part II addresses requirements for active substances used as starting materials, while Part III contains GMP-related documents, and Part IV specifically covers GMP requirements for Advanced Therapy Medicinal Products (ATMPs) [57].
The annexes to EudraLex Volume 4 provide detailed guidance on specific product types and manufacturing aspects particularly relevant to stem cell biomanufacturing [57]. Annex 1 covers the manufacture of sterile medicinal products, fundamental for cell therapies administered parenterally [57]. Annex 2 addresses the manufacture of biological active substances and medicinal products for human use, though it's important to note that Advanced Therapy Medicinal Products are now specifically covered in Part IV [57]. Other critical annexes include Annex 13 on investigational medicinal products, relevant for clinical trial material, and Annex 15 on qualification and validation, which guides the validation of processes, cleaning, and analytical methods [57]. Annex 16 covers certification by a Qualified Person and batch release, a mandatory requirement for commercial stem cell products in the EU [57].
Recent and Proposed Updates to EudraLex Volume 4
The EudraLex Volume 4 guidelines are undergoing significant modernization to address technological advancements and emerging challenges in pharmaceutical manufacturing. In 2025, the European Commission released draft revisions for public consultation on three pivotal components: Chapter 4 (Documentation), Annex 11 (Computerised Systems), and a completely new Annex 22 (Artificial Intelligence) [112] [18] [113]. These updates represent the most substantial revisions in over a decade and have profound implications for digital innovation in stem cell biomanufacturing.
The proposed revision to Chapter 4 (Documentation) marks a fundamental shift from traditional document control toward comprehensive data governance [18] [113]. The draft expands the chapter from 32 to approximately 85 clauses, with a dramatically increased focus on risk-based approaches (mention of "risk" increases from 1 to 54 times), data lifecycle management, and hybrid systems [113]. Key changes include explicit requirements for ALCOA++ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and now Traceable), formalized expectations for metadata control, and strengthened provisions for electronic records and signatures [18] [113]. The revision also introduces a dedicated glossary and examples of GMP documents to support consistent implementation [18].
The updated Annex 11 (Computerised Systems) significantly broadens its scope to encompass modern technologies including cloud services (SaaS, PaaS, IaaS), mobile applications, artificial intelligence and machine learning, blockchain, and Industrial IoT (IIoT) [18]. The draft establishes enhanced requirements for lifecycle management of computerized systems, emphasizing risk-based validation, data integrity controls, tamper-evident audit trails, and cybersecurity measures [18]. It also strengthens expectations for supplier management of external service providers, clarifying that ultimate responsibility cannot be outsourced [18].
The entirely new Annex 22 (Artificial Intelligence) represents a pioneering regulatory framework for AI/ML applications in pharmaceutical manufacturing [112] [18]. It establishes requirements for the selection, training, and validation of AI models, with emphasis on defining intended use, establishing performance metrics, ensuring training data quality, and managing test data [112] [18]. The annex also mandates continuous oversight of AI systems, including change control procedures, performance monitoring, and provisions for human review when necessary [112].
Table 2: Key Updates in EudraLex Volume 4 Draft Revisions (2025)
| Document | Key Focus Areas | Major Changes & Additions | Implications for Stem Cell Biomanufacturing |
|---|---|---|---|
| Chapter 4: Documentation | Data governance, lifecycle management, hybrid systems | - Expanded from 32 to 85 clauses- ALCOA++ principles- Metadata control- Data governance system- Template validation | Ensures data integrity across complex cell culture processes and multimodal data generation |
| Annex 11: Computerised Systems | Modern technologies, data integrity, lifecycle management | - Expanded scope (cloud, AI, IoT, blockchain)- Enhanced validation requirements- Cybersecurity emphasis- Supplier management | Supports implementation of advanced process control and monitoring systems for bioreactors |
| Annex 22: Artificial Intelligence | AI/ML model governance, performance monitoring | - First dedicated AI/ML annex- Model selection/training requirements- Performance metrics- Continuous monitoring | Enables use of AI for predictive analytics, process optimization, and quality prediction |
Experimental Protocol: Environmental Monitoring Program for Aseptic Stem Cell Processing
Principle: This protocol establishes an environmental monitoring program for aseptic processing of stem cell products in a Grade A biosafety cabinet within a Grade B cleanroom, in compliance with EudraLex Volume 4, Annex 1 requirements for sterile medicinal products.
Materials and Equipment:
- Active air sampler with appropriate culture media (e.g., Tryptic Soy Agar)
- Settle plates (90mm diameter, Tryptic Soy Agar)
- Surface contact plates (RODAC plates, 25cm²)
- Particulate counters for Grade A and B areas
- Microbial identification system
- Incubators (20-25°C and 30-35°C)
- Glove fingertip test media plates
- Personnel gowning materials
Procedure:
- Air Viable Monitoring:
- Place active air sampler in Grade A area during processing.
- Sample minimum 1m³ of air per location.
- Incubate plates at 30-35°C for 3-5 days followed by 20-25°C for additional 2-3 days.
- Count colony forming units (CFU) and calculate CFU/m³.
Surface Monitoring:
- Use contact plates to monitor critical surfaces before and after processing.
- Sample locations: inside biosafety cabinet, equipment surfaces, container surfaces.
- Incubate as above and report CFU/plate.
Settle Plates:
- Place settle plates in Grade A area during entire processing operation.
- Expose for maximum 4 hours.
- Incubate as above and report CFU/4 hours.
Personnel Monitoring:
- Perform glove fingertip testing after critical aseptic operations.
- Use appropriate culture media.
- Incubate as above and report CFU/glove.
Non-Viable Particulate Monitoring:
- Continuously monitor ≥0.5μm and ≥5.0μm particles in Grade A area during operations.
- Record results as particles/m³.
Acceptance Criteria:
- Grade A Area:
- Viable air samples: <1 CFU/m³
- Settle plates: <1 CFU/4 hours
- Surface monitoring: <1 CFU/plate
- Glove monitoring: <1 CFU/plate
- Particles ≥0.5μm: <3,520/m³
- Particles ≥5.0μm: <20/m³
- Grade B Area:
- Viable air samples: <10 CFU/m³
- Surface monitoring: <5 CFU/plate
- Particles ≥0.5μm: <3,520,000/m³
- Particles ≥5.0μm: <29,000/m³
Data Documentation: All environmental monitoring data must be recorded in compliance with ALCOA++ principles, including contemporaneous recording, complete metadata, and secure retention [113]. Trends should be reviewed periodically and investigated when alert or action levels are exceeded.
Integrated Application in Stem Cell Biomanufacturing
Quality by Design Framework for Scalable Stem Cell Production
The successful integration of ICH Q2 and EudraLex guidelines enables the implementation of a Quality by Design (QbD) framework for scalable stem cell biomanufacturing. This approach involves systematic development of manufacturing processes based on sound science and quality risk management, where analytical methods validated per ICH Q2(R2) provide the critical data to establish the relationship between critical process parameters (CPPs) and critical quality attributes (CQAs) [111]. The GMP framework of EudraLex Volume 4 ensures that the entire manufacturing environment, from raw material controls to facility design and personnel training, supports consistent production of quality stem cell products [57].
For stem cell therapies, key CQAs typically include identity (specific cell surface markers), purity (percentage of target cells), viability, potency (therapeutic function), and safety (absence of contaminants) [108] [109]. The analytical methods to measure these CQAs must be rigorously validated according to ICH Q2 principles, while the manufacturing process must comply with GMP standards appropriate to the product's development stage [57] [108]. As the process scales from research to commercial production, the analytical methods and quality systems must evolve in parallel, following the lifecycle approach emphasized in both ICH Q2(R2) and the updated EudraLex guidelines [111] [113].
dot code block for workflow diagram:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Stem Cell Biomanufacturing Analytics
| Reagent/Material | Function | Quality/GMP Considerations |
|---|---|---|
| Characterized Cell Banks | Source of consistent, genetically stable cells for manufacturing | Fully characterized for identity, purity, viability; free from adventitious agents; established under GMP conditions |
| GMP-grade Culture Media | Supports cell growth, expansion, and maintains cell function | Defined composition; endotoxin testing; certificate of analysis; manufactured under GMP; absence of animal components |
| Flow Cytometry Antibodies | Characterization of cell identity, purity, and impurities | Validated specificity and reactivity; lot-to-lot consistency; appropriate conjugation; documentation supporting regulatory submissions |
| PCR/qPCR Reagents | Genetic identity testing, mycoplasma detection, residual DNA quantification | High sensitivity and specificity; validated primer/probe sets; minimal batch variability; supplied with comprehensive quality documentation |
| Cell-based Potency Assay Reagents | Measurement of biological activity relevant to therapeutic mechanism | Physiologically relevant; validated performance characteristics; demonstrated stability; qualified reference standards |
| Process-related Impurity Testing Kits | Detection of residuals from manufacturing process (e.g., antibiotics, cytokines) | Appropriate sensitivity (meets LOQ requirements); specific for target analyte; compatible with sample matrix; standardized against reference materials |
Experimental Protocol: Comprehensive Quality Control Testing Strategy for Stem Cell Products
Principle: This protocol outlines a comprehensive quality control testing strategy for final stem cell products, integrating multiple analytical methods validated according to ICH Q2(R2) and performed in compliance with EudraLex Volume 4 GMP requirements.
Test Article: Final formulated stem cell product, cryopreserved in infusion-ready container.
Sampling Plan:
- Representative sampling from filled containers
- Maintain chain of identity and chain of custody throughout
- Document sampling according to ALCOA++ principles
Testing Strategy and Schedule:
dot code block for testing workflow:
Test Methods and Specifications:
- Identity Testing:
- Method: Multicolor flow cytometry for specific cell surface markers
- Acceptance Criteria: ≥90% expression of positive markers; ≤5% expression of negative markers
Viability and Total Nucleated Cell Count:
- Method: Flow cytometry with viability dye
- Acceptance Criteria: ≥70% viability; cell count within specified range
Potency Assay:
- Method: Cell-based functional assay measuring specific biological activity
- Acceptance Criteria: Activity within predefined specification range relative to reference standard
Purity and Impurity Profile:
- Method: Flow cytometry for process-related impurities (e.g., non-target cells)
- Acceptance Criteria: Impurity levels within validated acceptable limits
Safety Testing:
- Sterility: According to Ph. Eur. 2.6.1/USP <71>
- Mycoplasma: According to Ph. Eur. 2.6.7/FDA point-of-origin testing
- Endotoxin: Kinetic chromogenic LAL test
- Acceptance Criteria: Sterile, mycoplasma-free, endotoxin
Data Management and Documentation: All testing must be performed according to validated methods and documented in compliance with EudraLex Chapter 4 requirements [113]. Electronic records must maintain ALCOA++ principles, with particular attention to:
- Attributable: Clear association of data to originating analyst
- Legible: Permanent recording of all raw data and metadata
- Contemporaneous: Real-time recording of activities
- Original: Retention of source data or certified copies
- Accurate: Error-free recording with appropriate corrections
- Complete: Inclusion of all data including repeats/reanalysis
- Consistent: Chronological sequencing maintained
- Enduring: Recorded throughout record retention period
- Traceable: Ability to trace history and modifications of data
The integration of ICH Q2(R1)/Q2(R2) analytical validation principles with the comprehensive GMP framework of EudraLex Volume 4 provides a robust foundation for developing scalable, quality-driven stem cell biomanufacturing processes. As the regulatory landscape evolves with the adoption of ICH Q2(R2) and the ongoing modernization of EudraLex Volume 4, stem cell researchers and manufacturers must maintain vigilance in updating their quality systems and analytical strategies. The experimental protocols and frameworks presented in this document offer practical approaches for implementing these international standards, ultimately supporting the development of safe, efficacious, and consistently manufactured stem cell therapies for patients. By embracing these regulatory guidelines as enabling frameworks rather than compliance obstacles, the field can accelerate the translation of innovative stem cell research into transformative clinical applications.
For researchers and drug development professionals in stem cell therapies, navigating the dual challenges of product development and market access is complex. The journey from a research concept to a commercially viable, reimbursed therapy requires mastering two distinct regulatory paradigms: the accelerated approval pathway for market authorization and the prior authorization (PA) model for coverage and reimbursement. These frameworks, while both critical to a therapy's success, operate on different principles and timelines. This application note delineates these pathways within the context of Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing. We provide structured data and actionable protocols to help scientific teams align their development strategies with the demands of regulators and payers, thereby accelerating the translation of innovative therapies to patients.
Defining the Pathways: Objectives and Stakeholders
The Accelerated Approval and Prior Authorization models serve different primary objectives within the therapeutic lifecycle. Understanding their distinct roles is fundamental for strategic planning.
Accelerated Approval is a regulatory mechanism designed to expedite the availability of promising therapies for serious conditions with unmet medical needs. Driven by regulatory agencies like the U.S. Food and Drug Administration (FDA), its primary objective is to demonstrate safety and efficacy based on surrogate or intermediate endpoints reasonably likely to predict clinical benefit [115]. Subsequent post-approval studies are required to verify the anticipated clinical benefit.
Prior Authorization is a payer-driven utilization management tool. Its primary objective is to verify medical necessity and appropriate use of a treatment after it has been approved for market but before it is delivered to a specific patient. This process, mandated by insurers including Medicare Advantage and commercial plans, ensures that therapies are used in accordance with established clinical criteria and payer-specific policies [116] [117].
The following table summarizes the core differences in their objectives and stakeholder focus.
Table 1: Core Objectives and Stakeholders of Each Pathway
| Feature | Accelerated Approval Pathway | Prior Authorization Model |
|---|---|---|
| Primary Objective | Accelerate patient access to therapies for unmet needs by demonstrating safety and efficacy. | Ensure medical necessity, appropriate use, and cost-effectiveness for a specific patient. |
| Defining Focus | Product-Centric: Focused on the therapy itself. | Patient-Centric: Focused on the individual patient's clinical scenario. |
| Governing Body | Regulatory Agencies (e.g., FDA, EMA) [118] [115] | Payers/Insurers (e.g., CMS, Medicare Advantage, Commercial Plans) [117] [119] |
| Key Stakeholders | Researchers, Sponsors, CMOs, Regulatory Affairs, Patients | Providers, Payer Policy Teams, Patients, RCM (Revenue Cycle Management) Teams |
| Therapeutic Stage | Late-stage development and market entry. | Post-approval, at the point of care. |
Quantitative Analysis of Pathway Attributes
A quantitative comparison of the technical and procedural attributes of each pathway reveals critical differences in timelines, evidence requirements, and success rates that must be factored into project planning.
Timelines and Evidence Requirements
Regulatory approval pathways operate on multi-year timelines contingent upon robust clinical evidence, while prior authorization decisions are measured in days, focusing on immediate clinical justification.
Table 2: Comparative Analysis of Timelines and Evidence Requirements
| Attribute | Accelerated Approval Pathway | Prior Authorization Model |
|---|---|---|
| Typical Timeline | Several years (clinical trials + review) | Urgent: 72 hours; Standard: 7 calendar days (as of 2026) [117] |
| Key Evidence | Clinical trial data (Phases I-III); surrogate endpoint validation; CMC (Chemistry, Manufacturing, and Controls) data [115]. | Clinical notes; physician orders; proof of failure with prior therapies; alignment with payer-specific clinical criteria [119]. |
| Manufacturing Evidence | Extensive CMC dossier requiring rigorous GMP compliance, process validation, and quality control [120] [50]. | Typically not required for individual PA; covered under product's overarching NDA/BLA. |
| Success Metrics | Marketing approval based on surrogate endpoints; confirmed clinical benefit in post-market studies. | Approval rate for treatment requests; first-pass claim acceptance; denial rates [119]. |
Regulatory and Payer Landscape
The regulatory and payer landscape for stem cell therapies is fragmented and varies significantly by region, impacting both development and reimbursement strategy.
Table 3: Regional Regulatory and Payer Variation for Stem Cell Therapies
| Region | Regulatory Approach (Accelerated Approval) | Payer Landscape (Prior Authorization) |
|---|---|---|
| United States | Flexible, risk-based approach; FDA oversees HCT/Ps under 21 CFR Part 1271 [118] [115]. | CMS-mandated electronic PA (ePA) by 2026; varied approval rates by payer (e.g., 33% for CNS vs. 89% for thoracic in Medicare Advantage) [117] [119]. |
| European Union | Rigorous, centralized pathway under EMA; prioritizes safety and ethics [115]. | National payer systems with distinct reimbursement criteria; often requires cost-effectiveness data. |
| Japan & South Korea | Balanced approach with accelerated systems for regenerative medicine products [115]. | Evolving payer systems; often aligned with national health technology assessment. |
Integrated Protocol for Concurrent Pathway Preparation
To minimize delays, preparation for market access and reimbursement should begin during late-stage clinical development. The following protocol outlines a parallel workflow for addressing both Accelerated Approval and Prior Authorization requirements.
Stage 1: Early Payer Engagement and Evidence Planning (Initiate during Phase II)
Objective: Align clinical development with the evidence requirements of both regulators and payers.
- Procedure:
- Payer Policy Analysis: Identify top 5-10 target payers and conduct a systematic analysis of their Medical and Drug Policies for analogous therapies. Document specific coverage criteria, including required patient demographics, prior therapy failures, and contraindications [119].
- Clinical Endpoint Alignment: In parallel with regulatory discussions on surrogate endpoints, assess how these endpoints and the proposed clinical outcomes (e.g., functional improvement, biomarker reduction) align with payer definitions of "medical necessity."
- Gap Analysis: Compare planned Phase III trial endpoints and patient population against identified payer criteria. Identify and document any evidence gaps that could become a source of PA denials.
Stage 2: Payer Communication Package Development (Initiate 12 Months Pre-NDA/BLA Submission)
Objective: Create a comprehensive, evidence-based dossier to facilitate proactive communication with payer medical directors.
- Materials:
- Executive Summary: A two-page document highlighting the unmet need, mechanism of action, and summary of clinical efficacy and safety data.
- Clinical Evidence Compendium: Structured summaries of pivotal trial data, emphasizing patient subgroups most relevant to payer criteria.
- Economic Value Dossier: Early model outlining the potential budget impact and cost-effectiveness of the therapy compared to the standard of care.
- Procedure: Distribute the communication package to payer medical policy teams 6-9 months prior to anticipated FDA approval to inform their internal policy review cycles.
Stage 3: Operational Implementation of Prior Authorization (Initiate 6 Months Pre-Launch)
Objective: Establish internal or partner-supported workflows for efficient, compliant PA request processing.
- Procedure:
- System Configuration: Work with IT and EHR vendors to implement FHIR R4-based Prior Authorization Support (PAS) API systems to enable electronic data exchange, as mandated by the CMS Final Rule for 2026 [117].
- Documentation Toolkit Integration: Embed standardized clinical note templates and checklists into the EHR to ensure that treating physicians consistently document the information required for PA (e.g., prior treatment history, clinical stage, prognostic factors).
- Staff Training: Train a dedicated PA team on the specific clinical attributes of the therapy, the nuances of each major payer's policy, and the use of the new ePA systems. Establish clear Service Level Agreements (SLAs) for internal turnaround times.
The Scientist's Toolkit: Essential GMP-Compliant Reagents for Scalable Manufacturing
The transition from research-scale to GMP-compliant, scalable manufacturing requires careful selection and qualification of raw materials. The following reagents are critical for ensuring product consistency, safety, and regulatory compliance.
Table 4: Key Research Reagent Solutions for Scalable hMSC Biomanufacturing
| Reagent / Material | Function | GMP & Scalability Considerations |
|---|---|---|
| Xeno-Free Culture Medium | Provides nutrients for cell expansion. Replaces fetal bovine serum (FBS) to eliminate xenogenic risks [50]. | Must be fully defined, with qualified vendor and lot-to-lot consistency testing. Scalable to 200L+ bioreactor volumes [120]. |
| Human Platelet Lysate (hPL) | A xeno-free supplement providing growth factors and adhesion proteins for hMSC expansion [50]. | Requires rigorous donor screening and pooling to minimize variability. Must be tested for adventitious agents. |
| Microcarriers | Provide a surface for cell attachment in 3D bioreactor systems, enabling high-volume expansion [121]. | Material composition (e.g., dissolvable polymers) impacts downstream harvesting and cell viability. Must be sterile and non-pyrogenic. |
| Cell Dissociation Reagents | Enzymatically detaches cells from microcarriers or culture vessels for harvesting (e.g., TrypLE Select) [121]. | Animal-component-free, cGMP-grade reagents are essential. Enzyme activity must be consistently high and easily quenched. |
| Cell Separation & Washing Solutions | Used in downstream processing to concentrate cells and remove impurities [9]. | Formulation must be GMP-compatible. Process must be scalable and closed-system to maintain aseptic conditions. |
The path to successful commercialization of a stem cell therapy demands a synchronized strategy that addresses both the Accelerated Approval and Prior Authorization pathways. While the former focuses on establishing the foundational safety and efficacy of the product, the latter is the gatekeeper to widespread patient access and financial viability. By integrating payer evidence requirements into late-stage clinical development and establishing robust, technology-driven PA operations, biotech companies can bridge the gap between regulatory success and commercial sustainability. A proactive, parallel approach to these challenges, grounded in precise GMP manufacturing and clear communication, is paramount for accelerating the delivery of advanced therapies to the patients who need them.
Within the context of Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing, process validation provides the documented evidence that a specific process will consistently produce a product meeting its predetermined specifications and quality attributes [122]. For advanced therapies like stem cell-based products, where the cell is the drug, validation is not a one-time event but a comprehensive lifecycle approach. It ensures that every aspect of the manufacturing environment—from the cleanroom air quality to the specific enzymatic digestion of tissue—is controlled, reliable, and capable of yielding a safe, potent, and pure therapeutic agent. This document outlines the application notes and protocols essential for mastering this process, bridging the gap between foundational cleanroom studies and the intricate manufacturing of Investigational Medicinal Products (IMPs).
Cleanroom Qualification: The Foundation of Aseptic Processing
The cleanroom is the first critical component in preventing contamination during the manufacturing of sterile products. Its qualification is a multi-stage process that verifies the controlled environment is designed, built, and performs to the required standards.
The Qualification Lifecycle
Cleanroom qualification follows a structured lifecycle to ensure the environment is fit for purpose [122]. The stages, along with their key activities, are summarized in the table below.
Table 1: Stages of the Cleanroom Qualification Lifecycle
| Stage | Key Activities & Objectives |
|---|---|
| User Requirements Specification (URS) | Analyzes the need for the cleanroom and defines all requirements, including contamination risks, statutory regulations, and future scalability [122]. |
| Design Qualification (DQ) | Verifies that the proposed design (e.g., surface materials, air handling, door design) is suitable for its intended purpose and meets GMP requirements [122] [123]. |
| Installation Qualification (IQ) | Documents that the cleanroom has been built and installed in accordance with the approved design specifications. This includes verifying HEPA filter installation and instrument calibration [122] [124]. |
| Operational Qualification (OQ) | Demonstrates that the installed cleanroom operates according to specifications across all expected operating ranges under "at-rest" conditions (without personnel activity) [122] [123]. |
| Performance Qualification (PQ) | Provides a high degree of assurance that the cleanroom consistently performs according to specifications under "in-operation" conditions (with typical personnel and process activity) [122] [125]. |
The logical progression and key dependencies between these stages are illustrated in the following workflow.
Key Validation Tests and Parameters
During OQ and PQ, the cleanroom undergoes a series of physical tests to measure its performance against predefined acceptance criteria. These criteria are often aligned with ISO and GMP grades (A-D) [123].
Table 2: Key Cleanroom Performance Tests and Parameters
| Test Parameter | Objective | Standard Method | Typical Acceptance Criteria |
|---|---|---|---|
| Airborne Particle Count | Verify particle concentration meets target ISO class [124]. | Use a calibrated laser particle counter at multiple defined locations [122] [124]. | ISO 5 (Grade A) to ISO 8 (Grade D) per ISO 14644-1 [123]. |
| HEPA/ULPA Filter Integrity | Detect leaks in HEPA/ULPA filters and their seals [122]. | Aerosol challenge upstream with photometer or particle counter scanning downstream [122] [124]. | No leaks exceeding 0.01% of the upstream challenge concentration [122]. |
| Airflow Velocity & Uniformity | Confirm unidirectional or turbulent airflow patterns [124]. | Measure velocity with an anemometer; visualize flow with a smoke test [122] [124]. | Velocity typically 0.45 m/s ±20% for unidirectional flow [122]. |
| Room Pressure Differential | Ensure proper air cascade from cleaner to less clean zones [122]. | Measure using calibrated differential pressure gauges [124]. | Typically +10 to +15 Pa between adjacent rooms of different classifications [124]. |
| Recovery Test | Evaluate the cleanroom's ability to recover from a particle generation event [122]. | Release a controlled particle source, stop it, and measure time to return to baseline [124]. | Time to recover to specified cleanliness level (e.g., ISO 8) is within limits [122]. |
Process Validation Protocol for Stem Cell Manufacturing
Process validation for a stem cell product demonstrates that the manufacturing process, from raw material to final drug product, consistently produces cells with the desired Critical Quality Attributes (CQAs).
Protocol Outline and Responsibilities
A validation protocol is a predefined plan that, when executed, will deliver the documented evidence of process consistency. The following diagram outlines the core workflow for a process validation study, from protocol approval to reporting.
The execution of the protocol is a cross-functional effort [126] [127]:
- Quality Assurance (QA): Responsible for preparing the protocol, monitoring the process, reviewing data, and approving the final report.
- Production: Responsible for executing the manufacturing process strictly according to the approved Batch Manufacturing Record and protocol.
- Quality Control (QC): Responsible for analyzing raw materials, in-process, and finished product samples as per the defined sampling plan.
Sample Protocol for MSC Manufacturing
The following provides a detailed template for a process validation protocol tailored to the manufacturing of Mesenchymal Stromal Cells (MSCs).
1.0 Protocol Approval Signing of this approval page indicates agreement with the validation approach described. Any modifications require a pre-approved addendum [126].
2.0 Objective To validate the manufacturing process for Wharton's Jelly-derived MSCs (WJ-MSCs) and to generate sufficient data to provide assurance that the cells can be manufactured at a commercial scale, meeting all quality attributes consistently. The study shall consist of three consecutive commercial-scale batches [126] [28].
3.0 Scope This protocol is applicable for the first three consecutive commercial-scale batches of WJ-MSCs manufactured with a specific batch size and equipment at [Facility Name].
4.0 Pre-Execution Review Prior to validation execution, the following must be reviewed and found acceptable [126]:
- Qualification status of equipment (e.g., bioreactors, centrifuges) and utilities (e.g., HVAC, WFI).
- Calibration records of critical process instruments.
- Approved Master Formula Records and Batch Manufacturing Records.
- Specifications and analytical methods for raw materials, in-process controls, and the final drug product.
5.0 Product and Process Details
Table 3: WJ-MSC Drug Product Details
| Parameter | Detail |
|---|---|
| Product Name | WJ-MSC, Passage 3 |
| Generic Name | Allogeneic Mesenchymal Stromal Cells |
| Batch Size | 1.0 x 10^8 viable cells per batch |
| Storage Condition | Vapor phase liquid nitrogen ≤ -150°C |
| Shelf Life | To be determined via stability studies |
Table 4: Critical Raw Materials
| Item Code | Ingredient | Grade | Quantity per Batch |
|---|---|---|---|
| COL-NB6 | Collagenase NB6 | GMP | 0.4 PZ U/mL [28] |
| hPL-02 | Human Platelet Lysate | GMP | 2% - 5% [28] |
| NS-XF | Serum-/Xeno-Free Basal Medium | GMP | As per Master Formula |
6.0 Manufacturing Process Flow The manufacturing process shall include the following critical steps, each with defined process parameters and controls [28] [127]:
- Umbilical Cord Tissue Pre-processing: Collection, transport, decontamination, and dissection.
- Isolation: Enzymatic digestion using 0.4 PZ U/mL Collagenase NB6 for 3 hours.
- Primary Culture (P0): Seeding of digested tissue and expansion.
- Cell Passaging: Sequential passaging (P1 to P3) at a predefined seeding density.
- Harvest and Formulation: Detachment, washing, and resuspension in cryopreservation medium.
- Cryopreservation: Controlled-rate freezing and transfer to vapor phase liquid nitrogen storage.
7.0 Critical Process Parameters (CPPs) and Sampling Plan The following CPPs and CQAs must be monitored and tested. Acceptance criteria must be met for successful validation.
Table 5: In-process Controls, Sampling, and Acceptance Criteria
| Process Stage | Critical Process Parameter (CPP) | Critical Quality Attribute (CQA) | Acceptance Criteria |
|---|---|---|---|
| Enzymatic Digestion | Enzyme concentration: 0.4 PZ U/mL; Digestion time: 3 h [28]. | P0 Cell Yield | > [Defined Target] viable cells per gram of tissue [28]. |
| Cell Expansion | Seeding density; Culture duration; Medium composition (e.g., 2% hPL) [28]. | Cell Viability; Population Doubling Time; Morphology. | Viability ≥ 90%; Doubling time within historical range [28]. |
| Harvest | Detachment agent exposure time; Centrifugation speed/time. | Cell Viability Post-Harvest; % of Intact Cells. | Viability ≥ 85%. |
| Final Drug Product | Final formulation and fill. | Identity (Surface marker expression: CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-); Viability; Potency (e.g., immunosuppression assay); Sterility; Freedom from Mycoplasma [28]. | Meets all approved finished product specifications. |
8.0 Stability and Storage Validation batches shall be placed on a stability studies program as per the approved stability protocol to establish and confirm the shelf life of the cryopreserved product [126] [28]. Stability studies should also assess the impact of multiple freeze-thaw cycles and post-thaw hold times on cell viability and function [28].
9.0 Revalidation Criteria Revalidation shall be initiated in the event of [126] [127]:
- Any major change in the manufacturing process, batch size, or manufacturing site.
- A change in the source or specification of a critical raw material (e.g., collagenase, hPL).
- A change in critical equipment.
- An observed trend in continuous process monitoring data indicating a drift from a state of control.
Essential Reagents and Materials for GMP-Compliant Cell Manufacturing
The selection of raw materials is a critical aspect of process validation. Using GMP-grade reagents is mandatory for commercial manufacturing.
Table 6: Research Reagent Solutions for GMP Cell Manufacturing
| Reagent/Material | Function in Process | GMP-Grade Example & Key Consideration |
|---|---|---|
| Collagenase Enzyme | Digests the extracellular matrix of umbilical cord tissue to isolate MSCs [28]. | Collagenase NB6 GMP Grade. Critical parameters include enzyme concentration (e.g., 0.4 PZ U/mL) and digestion time (e.g., 3 hours) [28]. |
| Human Platelet Lysate (hPL) | Serum-free supplement for cell culture media that promotes MSC expansion [28]. | Commercially available, pathogen-inactivated hPL. Concentration (e.g., 2% vs. 5%) must be optimized for growth and quality [28]. |
| Serum-/Xeno-Free Basal Medium | Provides nutrients and environment for cell growth without animal-derived components. | NutriStem or equivalent. Eliminates risk of xenogenic immunogens and adventitious agents [28]. |
| Cell Culture Surfaces | Provides a substrate for adherent cell growth (e.g., MSCs). | GMP-compliant, tissue culture-treated multilayered flasks (e.g., Cell Factory, Cell Stack) for scalable expansion [120] [28]. |
| Cryopreservation Medium | Protects cells during freezing and long-term storage. | Formulation containing DMSO and protein stabilizers. Must be validated for post-thaw recovery and viability [28]. |
Mastering process validation is fundamental to the successful translation of stem cell research into commercially viable and compliant therapies. This requires a holistic approach that integrates rigorous cleanroom qualification with a thoroughly documented and scalable manufacturing process. The protocols and guidelines outlined here provide a framework for generating the objective, data-driven evidence required by regulators. By adopting this disciplined, lifecycle-oriented approach from the earliest stages of process development, scientists and manufacturers can ensure the consistent production of high-quality, safe, and effective stem cell-based investigational medicinal products.
Within the framework of Good Manufacturing Practice (GMP) for scalable stem cell biomanufacturing, ensuring product consistency is paramount. Process changes are inevitable during the lifecycle of an Advanced Therapy Medicinal Product (ATMP), occurring during scale-up or technology transfer to new facilities [128] [129]. Comparability studies serve as the critical bridge to demonstrate that such changes do not adversely impact the quality, safety, or efficacy of the biological product [130]. For stem cell-based therapies, where the product is often the cell itself, these studies are complex and require a multi-faceted approach, examining everything from cell identity and potency to purity and genetic stability. This application note outlines a structured protocol for designing and executing comparability studies, providing researchers and drug development professionals with a clear roadmap to navigate process changes while maintaining regulatory compliance.
A Systematic Framework for Comparability
A successful comparability exercise is rooted in science and risk management. The process begins with a thorough Process Risk Assessment to identify potential failure modes and their impact on product quality [128].
Risk Assessment and Planning
The initial step involves a systematic evaluation of the proposed process change. Tools such as Failure Mode and Effects Analysis (FMEA) are employed to identify, evaluate, and control risks that could impact product quality, safety, or efficacy [128]. This assessment provides the foundation for science-based decision-making throughout the product lifecycle and directly informs the scope and depth of the comparability study.
- Risk Identification: Systematically identify potential risks introduced by the process change. Consider equipment variations, raw material differences, human factors, and environmental conditions [128].
- Risk Analysis and Evaluation: Evaluate the likelihood and impact of identified risks. Compare these risks against pre-defined acceptance criteria to determine which require mitigation and extensive comparability testing [128].
- Analytical Quality Attribute Assessment: Categorize product quality attributes (e.g., identity, purity, potency, viability) based on their criticality and risk to the patient. The comparability study should place the greatest emphasis on monitoring critical quality attributes (CQAs) [130].
The output of this stage is a Comparability Study Protocol, which pre-defines the acceptance criteria, study design, analytical methods, and statistical approaches for data analysis.
Experimental Protocols for Stem Cell Comparability
For stem cell-based ATMPs, demonstrating comparability requires a suite of orthogonal analytical methods that probe the product's critical quality attributes. The following protocols provide detailed methodologies for key experiments.
Protocol: Automated Viable Cell Counting and Viability Assessment
Purpose: To provide a rapid, validated, and GMP-compliant method for assessing cell count and viability, a fundamental quality attribute that reflects process robustness [131].
Principle: An automated cell counter based on fluorescence microscopy detects and counts propidium iodide (PI)-stained cells. PI is incorporated by permeable (non-viable) cells and binds to DNA. The viable cell count is calculated as the difference between total and non-viable cells [131].
Materials:
- Instrument: NucleoCounter NC-100 or equivalent automated cell counting system.
- Reagents: Via1-Cassette containing immobilized PI or similar ready-to-use disposable cassettes.
- Sample: Homogeneous cell suspension from the pre- and post-change process.
Procedure:
- Sample Preparation: Ensure a single-cell suspension. Gently mix the sample to avoid clumping.
- Loading: Aspirate 20 µL of the cell suspension and load it into the pre-assembled Via1-Cassette.
- Measurement: Insert the cassette into the NucleoCounter instrument. The analysis is performed automatically.
- Data Collection: Record the total cell concentration (cells/mL) and viability (%) from the instrument display or connected software.
- Validation Parameters: The method should be validated for specificity, linearity, range, accuracy, and precision per ICH Q2(R1) guidelines [131].
Protocol: Process Performance Qualification (PPQ) for a Scale-Up Step
Purpose: To demonstrate that the manufacturing process, after a significant scale-up, consistently produces a stem cell product meeting its pre-defined specifications and quality attributes under routine operating conditions [128].
Principle: A minimum of three consecutive successful batches are manufactured at the new, larger scale. All critical process parameters (CPPs) and critical quality attributes (CQAs) are intensively monitored to establish process consistency and robustness [128].
Materials:
- Cell Source: A consistent and well-characterized cell source (e.g., master cell bank).
- Raw Materials: GMP-grade reagents and culture media, identical between small and large scale.
- Equipment: Qualified large-scale bioreactor or cell culture system.
Procedure:
- PPQ Protocol Development: Create a detailed protocol specifying objectives, sampling plans, test methods, and acceptance criteria [128].
- Facility and Equipment Readiness: Ensure the manufacturing suite and all equipment are properly installed, operational, and qualified.
- Batch Execution: Execute a minimum of three consecutive full-scale batches.
- Enhanced Monitoring: Monitor all CPPs continuously. Implement a comprehensive sampling strategy that provides adequate coverage of batch homogeneity. Test for CQAs such as:
- Data Analysis and Report: Compile all data and perform statistical analysis to demonstrate the process is in a state of control and that the product is comparable to that produced at the smaller scale.
Research Reagent Solutions for Stem Cell Process Development
Table 1: Essential materials used in GMP-compliant stem cell process development and comparability studies.
| Reagent/Material | Function & Importance in Comparability | Example & Notes |
|---|---|---|
| Serum-Free Media | Provides defined, xeno-free nutrients for cell growth; essential for eliminating lot-to-lot variability and ensuring process consistency [132]. | Commercially available GMP-grade MSC media; X-VIVO 15 for hematopoietic cells [54]. |
| Transduction Enhancers (TEs) | Improves gene delivery efficiency in HSCGT; critical for maintaining comparable VCN and potency after process changes [54]. | LentiBOOST and protamine sulfate [54]. |
| Cell Separation Reagents | Enables isolation of specific cell populations (e.g., CD34+ cells) to ensure a consistent starting material [133]. | Reversible Streptamer technology in ATC system allows traceless cell isolation [133]. |
| GMP-Grade Cytokines | Directs stem cell self-renewal and differentiation; using qualified, consistent cytokine lots is vital for maintaining product CQAs [54]. | SCF, TPO, Flt3-L, IL-3 [54]. |
| Validation Kits | For qualifying and validating analytical methods, ensuring that measurements of CQAs (e.g., viability, identity) are accurate and precise [131]. | Kits for automated cell counters following ICH Q2(R1) [131]. |
Data Presentation and Analysis
A core component of the comparability study is the clear and concise presentation of data, allowing for direct comparison between the pre-change and post-change products.
Quantitative Analysis of Critical Quality Attributes
Table 2: Example comparability data table for a hematopoietic stem cell gene therapy product following a process change involving transduction enhancers [54].
| Critical Quality Attribute (CQA) | Pre-Change Process | Post-Change Process | Acceptance Criterion | Conclusion |
|---|---|---|---|---|
| Viability (%) | >95% | >95% | >90% | Comparable |
| Vector Copy Number (VCN) | 2.5 | 5.8 | 1.5 - 6.0 | Comparable, improved |
| CD34+ Purity (%) | >90% | >90% | >85% | Comparable |
| Intracellular IDS Activity (Fold Increase) | 1.0 (Baseline) | 4.8 | >1.5 | Comparable, improved |
| CFU-GM Transduction Efficiency (%) | 55.6 (at MOI 25) | 94.1 (at MOI 25) | >70% | Comparable, improved |
| Sterility | Sterile | Sterile | No growth | Comparable |
Workflow for Comparability Study Execution
The following diagram illustrates the logical workflow and decision-making process for conducting a comparability study, integrating risk assessment and the stage-gate approach.
Adherence to regulatory guidelines is the foundation of a successful comparability study. The ICH Q5E guideline provides the overarching principles for demonstrating comparability of biotechnological/biological products after a process change [130]. The study should provide analytical confirmation that the drug substance or drug product has highly similar quality attributes before and after the change.
For stem cell products, which are classified as ATMPs, production must comply with GMPs [131] [134]. Furthermore, the ISSCR Guidelines for Stem Cell Research and Clinical Translation emphasize the principles of rigor, oversight, and transparency, which are inherent to a well-executed comparability exercise [135]. This includes:
- Transparency: Timely exchange of accurate scientific information and publication of both positive and negative results [135].
- Integrity of the Research Enterprise: Ensuring that information obtained is trustworthy, reliable, and responsive to scientific uncertainties [135].
In conclusion, managing process changes in stem cell biomanufacturing does not have to be a disruptive event. By implementing a structured, risk-based comparability program—as outlined in this application note—organizations can ensure product consistency, maintain regulatory compliance, and confidently advance promising cell therapies to patients. The provided protocols, data presentation templates, and workflow diagrams offer a practical toolkit for researchers and developers to navigate this complex but essential process.
Conclusion
Successful and scalable GMP biomanufacturing of stem cells hinges on the seamless integration of robust regulatory knowledge, advanced automated technologies, proactive troubleshooting, and rigorous validation. The foundational principles of CGMP ensure product safety and identity, while automated bioreactor systems and optimized processes enable the necessary scale-up. Overcoming challenges like high costs and knowledge transfer gaps is critical for commercial viability. Furthermore, a deep understanding of comparative global regulations and a commitment to stringent quality control are indispensable for clinical translation. Future progress will be driven by multi-modal therapies combining gene editing and allogeneic cells, increased use of AI for process control, and collaborative efforts to harmonize international standards, ultimately broadening patient access to these transformative advanced therapies.
References
- 1. ( Current ) Regulations | FDA Good Manufacturing Practice CGMP [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 2. Facts About the Current Good Manufacturing Practice (CGMP) | FDA [https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp]
- 3. What are Current ( Good )? Manufacturing Practices cGMP [https://simplerqms.com/cgmp/]
- 4. GMP vs cGMP : What Are the Key Differences? - Pharmuni [https://pharmuni.com/2025/11/07/gmp-vs-cgmp-key-differences/]
- 5. eCFR :: 21 CFR Part 211 -- Current Good Manufacturing Practice for Finished Pharmaceuticals [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-211]
- 6. Compliance in Pharma: Top 7 FAQs | Scilife cGMP [https://www.scilife.io/blog/complying-with-cgmp-in-pharma]
- 7. Good manufacturing practice - Wikipedia [https://en.wikipedia.org/wiki/Good_manufacturing_practice]
- 8. FDA Issues New Guidance on Current Good Manufacturing Practices for Drugs | Advisories | Arnold & Porter [https://www.arnoldporter.com/en/perspectives/advisories/2025/01/fda-guidance-good-manufacturing-practices-for-drugs]
- 9. Understanding GMP in Biotech Companies [https://www.akadeum.com/blog/gmp-biotech/]
- 10. eCFR :: 21 -- CFR Good Manufacturing Practice in... Part 210 Current [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-210]
- 11. Current challenges and future directions of ATMPs in regenerative medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 12. What you need to know about FDA 21 CFR Part 210 [https://www.qualio.com/blog/21-cfr-210]
- 13. eCFR :: 21 CFR Part 820 -- Quality System Regulation [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-H/part-820]
- 14. ( FDA ): Good Manufacturing Practices GMP 2025 Guide [https://pharmuni.com/2025/11/06/fda-good-manufacturing-practices-complete-year-guide-for-compliance-and-quality/]
- 15. Cedars-Sinai Biomanufacturing Center - CSBIO [https://csbiomfg.com/about-us/]
- 16. GMP Cell Therapeutics | Waisman Biomanufacturing [https://gmpbio.org/clinical-production/cell-bank-and-cell-therapeutics]
- 17. Annex 11 revision EU GMP 2025 [https://jensonr.com/eu-gmp-annex-11-revision-2025/]
- 18. Draft Updates: Chapter 4, Annex 11... | 2025 Insiders EU GMP GMP [https://gmpinsiders.com/2025-eu-gmp-draft-chapter-4-annex-11-annex-22/]
- 19. CMC and GMP Guidances | FDA [https://www.fda.gov/vaccines-blood-biologics/general-biologics-guidances/cmc-and-gmp-guidances]
- 20. APAC regulation 2025: Major cosmetics regulatory issues on the agenda [https://www.cosmeticsdesign-asia.com/Article/2025/01/13/apac-regulation-2025-major-cosmetics-regulatory-issues-on-the-agenda/]
- 21. Guidance on good and good distribution... manufacturing practice [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/compliance-research-development/good-manufacturing-practice/guidance-good-manufacturing-practice-good-distribution-practice-questions-answers]
- 22. GMP Plasmid Service Market: Competitive Dynamics & Global Outlook 2025 [https://www.openpr.com/news/4253963/gmp-plasmid-service-market-competitive-dynamics-global]
- 23. GMP Plasmid Service Market Share, Revenue, Price, Growth Rate Ranking Analysis Report 2025-2031 [https://www.openpr.com/news/4253946/gmp-plasmid-service-market-share-revenue-price-growth-rate]
- 24. and... - Laafon Galaxy Pharmaceuticals Aseptic Processing Control [https://laafon.com/aseptic-processing-control/]
- 25. New EU GMP ( Good ) Annex 1: Compliant Manufacturing Practice [https://www.globenewswire.com/news-release/2025/06/04/3093488/0/en/New-EU-GMP-Good-Manufacturing-Practice-Annex-1-Compliant-Aseptic-Operations-Online-Training-Course-July-1-3-2025-Featuring-Practical-Workshops.html]
- 26. PharmaCongress 2025 - Not only, but also Annex 1 - GMP Journal [https://www.gmp-journal.com/current-articles/details/pharmacongress-2025-not-only-but-also-annex-1.html]
- 27. How can data analytics optimize GMP innovation and continuous improvement? [https://www.linkedin.com/advice/1/how-can-data-analytics-optimize-gmp-innovation]
- 28. A GMP-compliant manufacturing method for Wharton’s jelly-derived mesenchymal stromal cells | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03725-0]
- 29. Size To Surpass USD 48.83 Bn By 2034 Stem Cells Market [https://www.precedenceresearch.com/stem-cells-market]
- 30. Stem Cell Manufacturing Market Growth Analysis | CAGR of 13.1% [https://media.market.us/global-stem-cell-manufacturing-market-news/]
- 31. Optimizing mesenchymal stem cell therapy: from isolation to GMP-compliant expansion for clinical application | BMC Molecular and Cell Biology | Full Text [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-025-00539-7]
- 32. Automated Manufacturing Processes and Platforms for Large-scale... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872983/]
- 33. Bioprocess Solutions | INFORS HT Stem Cell [https://infors-ht.com/en/applications/cell-culture/stem-cell-research]
- 34. Manufacturing Stem Size, Share, Trends Cell -33 Market 2025 [https://www.imarcgroup.com/stem-cell-manufacturing-market]
- 35. Source Stem Outlook Cell : Shifting Through... Market 2025 [https://www.linkedin.com/pulse/stem-cell-source-market-outlook-2025-shifting-qtsde]
- 36. Cell and Gene Therapy Biomanufacturing Industry Outlook 2025-2035: Rising Demand for Personalized Medicine and Regulatory Fast-Tracking Fuel Global Growth [https://www.globenewswire.com/news-release/2025/05/07/3075805/28124/en/Cell-and-Gene-Therapy-Biomanufacturing-Industry-Outlook-2025-2035-Rising-Demand-for-Personalized-Medicine-and-Regulatory-Fast-Tracking-Fuel-Global-Growth.html]
- 37. Manufacturing Stem Trends by Region Cell : Japan Market 2025 [https://www.linkedin.com/pulse/stem-cell-manufacturing-market-trends-region-2025-whwjf]
- 38. design for clinical-grade expansion of Bioreactor stem cells [https://pubmed.ncbi.nlm.nih.gov/23625834/]
- 39. Scaling up and scaling out: Advances and challenges in manufacturing engineered T cell therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815724/]
- 40. Bedside Cell Therapies: Point-of-Care Manufacturing Is Slowly Becoming a Reality [https://www.pharmasalmanac.com/articles/bedside-cell-therapies-point-of-care]
- 41. cGMP - everything you need to know – Single Use Support [https://www.susupport.com/blogs/knowledge/cgmp-everything-need-know]
- 42. -compliant GMP in a closed- manufacturing ... system automated [https://www.insights.bio/cell-and-gene-therapy-insights/webinars/382/GMP-compliant-manufacturing-in-a-closed-system-automated-bioreactor-with-a-novel-cell-culture-media]
- 43. Biomanufacturing- Cost Efficiency of Lentiviral Vectors [https://www.cellandgene.com/doc/cost-effective-biomanufacturing-of-lentiviral-vectors-0001]
- 44. ™: Lentivirus LentiBOOST Enhancer | Revvity Transduction [https://www.revvity.com/category/lentiboost-transduction-enhancer]
- 45. ® – Lentiviral LentiBOOST Enhancer for Transduction ... Clinical [https://www.pharmaceutical-technology.com/downloads/whitepapers/api-biologics/lentiboost-transduction-enhancer/]
- 46. Breaking Entry-and Species Barriers: LentiBOOST ® Plus Polybrene... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8781300/]
- 47. Scale Up Cell & Gene Therapy: Strategies & Challenges [https://www.atlantisbioscience.com/blog/navigating-the-path-to-scalable-cell-and-gene-therapy-production-embracing-process-optimising-automation/]
- 48. Scalable Fed-Batch Bioreactor Process for Lentiviral Vector Production - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/bioprocessing-single-use-equipment-lentiviral-vector-production-scalable]
- 49. Xeno-Free Strategies for Safe Human Mesenchymal Stem/Stromal Cell Expansion: Supplements and Coatings - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5660800/]
- 50. Frontiers | Acceleration of Translational Mesenchymal Stromal Cell Therapy Through Consistent Quality GMP Manufacturing [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.648472/full]
- 51. Xeno- free for protocol -compliant GMP of human fetal... manufacturing [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02946-5]
- 52. Culturing Human Mesenchymal Stem Cells (MSCs) under Serum- Free ... [https://www.thermofisher.com/uk/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols/culturing-human-mesenchymal-stem-cells-mscs-under-serum-free-and-xeno-free-conditions.html]
- 53. AI‐Driven Quality Monitoring and Control in Stem Cultures... Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 54. Design and validation of a GMP for... stem cell manufacturing protocol [https://pmc.ncbi.nlm.nih.gov/articles/PMC11214401/]
- 55. as Targeted Drug Delivery Vehicles | Frontiers Stem ... Cells Research [https://www.frontiersin.org/research-topics/9550/stem-cells-as-targeted-drug-delivery-vehicles/magazine]
- 56. Guide to Cell for Autologous CAR T Therapy GMP Manufacturing [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 57. EudraLex - Volume 4 - Public Health - European Commission [https://health.ec.europa.eu/medicinal-products/eudralex/eudralex-volume-4_en]
- 58. All about GMP labeling: requirements and best practices [https://www.qualio.com/blog/gmp-labeling]
- 59. Market Share Analysis | CAGR of 13.1% Stem Cell Manufacturing [https://media.market.us/stem-cell-manufacturing-market-news/]
- 60. What is GMP and Why Is It Essential in Biomanufacturing? [https://synapse.patsnap.com/article/what-is-gmp-and-why-is-it-essential-in-biomanufacturing]
- 61. in Implementing Challenges - Single Use Systems [https://www.linkedin.com/pulse/challenges-implementing-single-use-systems-chinmaya-ranjan-parida-ontsf]
- 62. Smart Biomanufacturing With AI & Automation - NanoSchool [https://nanoschool.in/biotechnology/btws/smart-biomanufacturing-with-ai-automation/]
- 63. -grade Mesenchymal GMP Media Market Size, Development... Stem Cell [https://www.verifiedmarketreports.com/product/gmp-grade-mesenchymal-stem-cell-media-market/]
- 64. Scaling Allogeneic Cell Therapy Manufacturing - Patheon pharma services [https://www.patheon.com/us/en/insights-resources/blog/scaling-allogeneic-cell-therapy-manufacturing.html]
- 65. Allogeneic Cell Therapy Market Size, Share & Trends 2035 [https://www.rootsanalysis.com/reports/allogeneic-cell-therapy-market.html]
- 66. Frontiers | Commercial Scale Manufacturing of Allogeneic Cell Therapy [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2018.00233/full]
- 67. Establishing GMP -compliant manufacturing for frameworks ... scalable [https://www.regmednet.com/pc_if_act_establishing-gmp-compliant-manufacturing-frameworks-for-scalable-allogeneic-cell-therapies_promocell/]
- 68. Progress and challenges in developing allogeneic cell therapies - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 69. (PDF) An off , the compliant, fully closed... - Academia.edu shelf GMP [https://www.academia.edu/117679283/An_off_the_shelf_GMP_compliant_fully_closed_and_semi_automated_large_scale_production_system_for_allogeneic_NK_cells]
- 70. Navigating Operational Complexities in Phase I GMP Therapy... Cell [https://news.cuanschutz.edu/gates/operational-complexity-in-phase-i-gmp-cell-therapy-manufacturing]
- 71. New Version of WHO Guidelines on Process Transfer Published as a Draft - ECA Academy [https://www.gmp-compliance.org/gmp-news/new-version-of-who-guidelines-on-process-transfer-published-as-a-draft]
- 72. Technology Transfer Guidelines for Pharmaceuticals | Pharmaguideline [https://www.pharmaguideline.com/2015/07/technology-transfer-in-pharmaceuticals.html]
- 73. Optimizing mesenchymal stem cell therapy: from isolation to GMP-compliant expansion for clinical application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054297/]
- 74. Therapy Consumables Market: Solutions, Growth & Trends GMP Cell [https://www.vantagemarketresearch.com/industry-report/gmp-cell-therapy-consumables-market-3965]
- 75. Optimizing mesenchymal stem cell therapy: from isolation to... [https://pubmed.ncbi.nlm.nih.gov/40329219/]
- 76. Adipose-Derived SVF Therapy: Step-by-Step Guide for Isolation ... [https://www.ifaas.co/single-post/adipose-derived-svf-therapy-step-by-step-guide-for-isolation-storage-and-gmp-compliance]
- 77. Critical Analysis of cGMP Large-Scale Expansion Process in Bioreactors of Human Induced Pluripotent Stem Cells in the Framework of Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8561684/]
- 78. Critical Analysis of cGMP Large-Scale Expansion Process in Bioreactors of Human Induced Pluripotent Stem Cells in the Framework of Quality by Design | BioDrugs [https://link.springer.com/article/10.1007/s40259-021-00503-9]
- 79. Physiological Relevant 3D Biomanufacturing of Pluripotent Stem ... [https://link.springer.com/article/10.1007/s40778-025-00250-5]
- 80. ISSCR 2025 : Quality Is Our Common Language [https://www.stemcell.com/virtual-conference-exhibition/isscr]
- 81. A scalable platform for EPSC-Induced MSC extracellular vesicles with... [https://pubmed.ncbi.nlm.nih.gov/40765003/]
- 82. Smart Sensor Control and Monitoring of an Automated Cell Expansion Process - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10748109/]
- 83. Optimizing Cryopreservation Conditions with CRFT: A Scalable... [https://www.grantinstruments.com/posts/optimizing-cryopreservation-conditions-with-crft-a-scalable-approach-from-lab-to-industry]
- 84. Advanced cryopreservation engineering strategies: the critical step to utilize stem cell products | Cell Regeneration | Full Text [https://cellregeneration.springeropen.com/articles/10.1186/s13619-023-00173-8]
- 85. Basics: Cryopreservation and Protocols for Freezing... Best Practices [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 86. in Cryopreservation and Gene Therapy | CGT Cell Global [https://cgt.global/cryopreservation-in-cell-and-gene-therapy-ensuring-high-viability-cells-for-research-manufacturing/]
- 87. Market Size, Share & Trends Forecast 2035 Cell Cryopreservation [https://www.researchnester.com/reports/cell-cryopreservation-market/5636]
- 88. Compliant GMP of a Production Adipose-Derived... Cryopreserved [https://pmc.ncbi.nlm.nih.gov/articles/PMC9236818/]
- 89. Applications and optimization of cryopreservation technologies to cellular therapeutics [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/415/Applications-and-optimization-of-cryopreservation-technologies-to-cellular-therapeutics]
- 90. Addressing the Challenges of Commercial-Scale Viral ... Vector [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/347/addressing-the-challenges-of-commercialscale-viral-vector-production]
- 91. Robust bioprocess design and evaluation of commercial media for the serial expansion of human induced pluripotent stem cell aggregate cultures in vertical-wheel bioreactors | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03819-9]
- 92. : Viral methods & advances vector manufacturing Production [https://www.susupport.com/knowledge/biopharmaceutical-products/drug-delivery/viral-vector-manufacturing-production-methods-future-advances]
- 93. Enabling Safe Innovation: The Role of GMP Cell Therapy... [https://www.insightaceanalytic.com/blogdetails/gmp-cell-therapy-consumables-market]
- 94. Optimizing Analytical Through Reduced Volume And... Release Testing [https://www.cellandgene.com/doc/optimizing-analytical-release-testing-through-reduced-volume-and-turnaround-times-0001]
- 95. Lessons Learned from Validation of a Real - Time PCR Mycoplasma... [https://www.americanpharmaceuticalreview.com/Featured-Articles/148855-Lessons-Learned-from-Validation-of-a-Real-Time-PCR-Mycoplasma-Test-for-Autologous-Cell-Therapy-Products/]
- 96. A comprehensive strategy for the identification of biologics by liquid-chromatography–mass spectrometry for release testing in a regulated environment - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0731708523003497]
- 97. The Potential Application of Real ‑ Time for the... Release Testing [https://www.bioprocessintl.com/cell-therapies/the-potential-application-of-real-time-release-testing-for-the-biomanufacture-of-autologous-cell-based-immunotherapies]
- 98. Biomanufacturing Facility Compliance and GMP Standards | Umbrex [https://umbrex.com/resources/industry-analyses/how-to-analyze-a-biotechnology-company/biomanufacturing-facility-compliance-and-gmp-standards/]
- 99. Validation of an automated method for cGMP... cell counting [https://pmc.ncbi.nlm.nih.gov/articles/PMC8851089/]
- 100. of analytical methods in Validation : the disposable Fast Read... GMP [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-10-112]
- 101. Semi-automated vs. manual: Comparative study of cell culture... | CoLab [https://colab.ws/articles/10.1101%2F2024.05.30.596619]
- 102. of analytical methods in Validation : the disposable Fast Read... GMP [https://pubmed.ncbi.nlm.nih.gov/22650233/]
- 103. Workflow to Produce and Isolate Natural... Scalable Biomanufacturing [https://www.jove.com/t/67227/scalable-biomanufacturing-workflow-to-produce-isolate-natural-killer]
- 104. Establishing a GMP -compliant manufacturing process and... [https://www.nature.com/articles/s41598-025-92736-9?error=cookies_not_supported]
- 105. Validating human induced pluripotent stem -specific cell ... quality [https://pubmed.ncbi.nlm.nih.gov/38703154/]
- 106. A practical approach for the validation of sterility, endotoxin and potency testing of bone marrow mononucleated cells used in cardiac regeneration in compliance with good manufacturing practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2753319/]
- 107. Cell therapy: cGMP facilities and manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3666518/]
- 108. Understanding the ich ( Q ) guideline 2 R 1 [https://www.linkedin.com/pulse/understanding-ich-q2r1-guideline-priyadarshana-asolkar-cipgc]
- 109. What is the ICH ( Q ) guideline? 2 R 1 [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/ich-q2r1]
- 110. Navigating ICH Q2(R2) compliance in analytical method validation: A gap analysis toolkit to streamline risk assessment and change management - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0022354925002072]
- 111. Premier Research | What You Need to Know About ICH Q14 and ICH Q2(R2), Part 2 [https://premier-research.com/perspectives/what-you-need-to-know-about-ich-q14-and-ich-q2r2-part-2/]
- 112. Stakeholders’ Consultation on EudraLex Volume 4 - Good Manufacturing Practice Guidelines: Chapter 4, Annex 11 and New Annex 22 - Public Health [https://health.ec.europa.eu/consultations/stakeholders-consultation-eudralex-volume-4-good-manufacturing-practice-guidelines-chapter-4-annex_en]
- 113. EU-GMP Chapter 4 Revision: Anticipated Changes in Documentation and Data Governance - GxP-CC [https://www.gxp-cc.com/insights/blog/eu-gmp-chapter-4-revision-anticipated-changes-in-documentation-and-data-governance/]
- 114. Volume 3 Validation of Analytical Procedures: Text and... Eudralex [https://www.gmp-compliance.org/guidelines/gmp-guideline/eudralex-volume-3-validation-of-analytical-procedures-text-and-methodology-ich-q2-cpmp-ich-381-95-ich-q2-r1]
- 115. Comparative analysis of regulations and studies on stem ... cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11583560/]
- 116. Insurance Verification Serives vs Guide Prior Authorization 2025 [https://www.sprypt.com/blog/insurance-verification-services-patient-eligibility]
- 117. CMS Prior Auth 2026 (CMS-0057-F) Provider Compliance Guide [https://prombs.com/prior-auth-2026-provider-compliance-guide/]
- 118. Issues in the Therapeutic Use of Regulatory | IntechOpen Stem Cells [https://www.intechopen.com/chapters/44643]
- 119. for Proton Therapy in Prior : What Providers Need... Authorization 2025 [https://proton-therapy.org/prior-authorization-for-proton-therapy-in-2025-what-providers-need-to-know/]
- 120. Design Considerations for Large-Scale Stem Cell Manufacturing | Pharmaceutical Engineering [https://ispe.org/pharmaceutical-engineering/november-december-2023/design-considerations-large-scale-stem-cell]
- 121. Opportunities for BioManufacturing Sciences to Accelerate Upscaled... [https://www.roosterbio.com/blog/opportunities-for-biomanufacturing-sciences-to-accelerate-upscaled-mesenchymal-stem-cell-manufacturing-technologies/]
- 122. Qualification And Cleanroom In Validation | GMP Insiders GMP [https://gmpinsiders.com/cleanroom-qualification-and-validation/]
- 123. Compliance for GMP : A Quick Overview Cleanrooms [https://alliedcleanrooms.com/gmp-compliance-for-cleanrooms/]
- 124. How cleanroom works: Practical advice for an easier... validation [https://standard-tech.it/en/how-cleanroom-validation-works-practical-advice-for-an-easier-process/]
- 125. What Do the GMP Qualification & Validation Look Like? Processes [https://angstromtechnology.com/what-do-the-gmp-qualification-validation-processes-look-like/]
- 126. Sample Process | Pharmaguideline Validation Protocol [https://www.pharmaguideline.com/2013/11/process-validation-sample-protocol.html]
- 127. Sample Process – Pharmaceutical Updates Validation Protocol [https://pharmaceuticalupdates.com/2019/03/15/process-validation-sample-protocol/]
- 128. Comprehensive Guide to Process Scale-up, Validation and... [https://www.linkedin.com/pulse/comprehensive-guide-process-scale-up-validation-technology-singh-l5eme]
- 129. A Unified Approach for Scaling Bioprocess Unit Operations | BioPharm International [https://www.biopharminternational.com/view/a-unified-approach-for-scaling-bioprocess-unit-operations]
- 130. for Proteins and Comparability Studies Biologics [https://www.intertek.com/pharmaceutical/biopharmaceuticals/comparability/]
- 131. Validation of an automated viable cell counting assay for GMP manufacturing of human induced pluripotent stem cells - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1369703X23001481]
- 132. Top GMP -grade Mesenchymal Stem Media Companies & How to... Cell [https://www.linkedin.com/pulse/top-gmp-grade-mesenchymal-stem-cell-media-companies-how-compare-uwkie]
- 133. Next generation automated traceless cell chromatography platform for GMP-compliant cell isolation and activation | Scientific Reports [https://www.nature.com/articles/s41598-022-10320-x]
- 134. Production and validation of a good grade... manufacturing practice [https://stemcellres.biomedcentral.com/articles/10.1186/scrt103]
- 135. — International Society for Guidelines Research Stem Cell [https://www.isscr.org/guidelines]