GMP-Compliant Mesenchymal Stem Cell Isolation: A Feasibility Roadmap for Clinical Translation
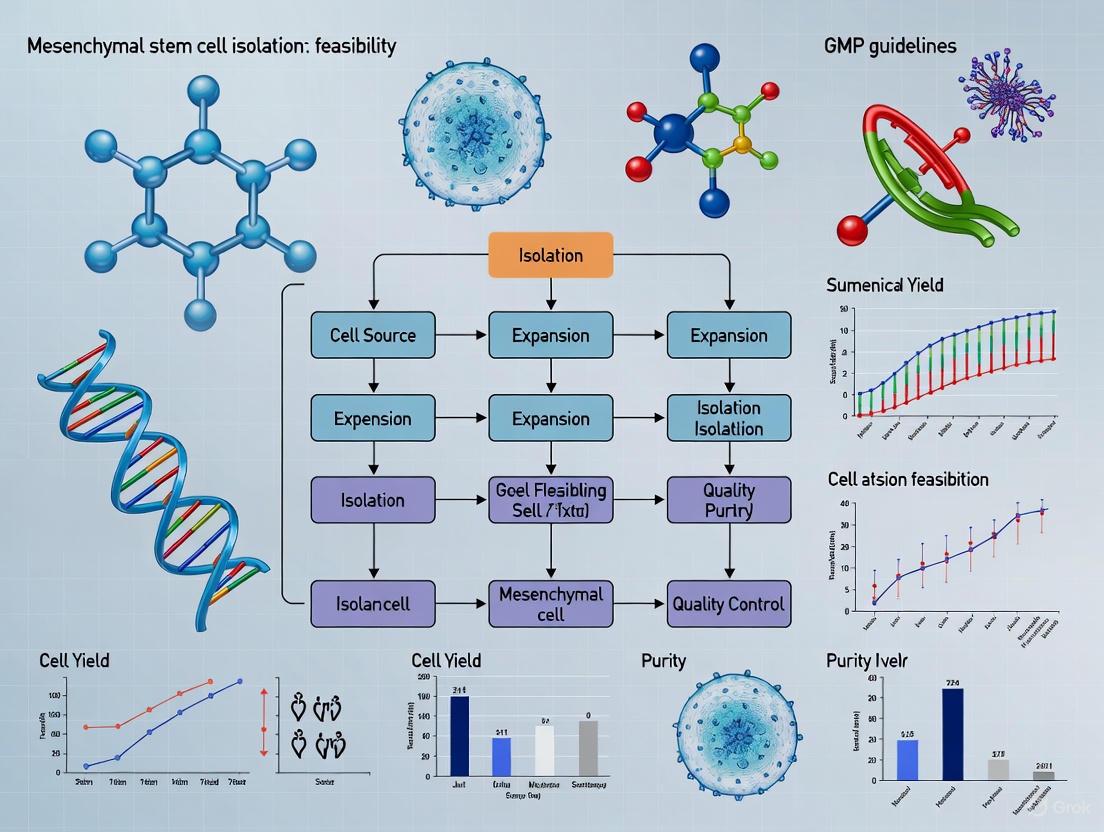
The transition of mesenchymal stem cell (MSC) therapies from research to clinical application hinges on the establishment of robust, reproducible, and standardized Good Manufacturing Practice (GMP)-compliant isolation protocols.
GMP-Compliant Mesenchymal Stem Cell Isolation: A Feasibility Roadmap for Clinical Translation
Abstract
The transition of mesenchymal stem cell (MSC) therapies from research to clinical application hinges on the establishment of robust, reproducible, and standardized Good Manufacturing Practice (GMP)-compliant isolation protocols. This article provides a comprehensive analysis of the feasibility of GMP-grade MSC isolation, addressing the journey from foundational regulatory principles and donor selection to methodological optimization, troubleshooting of manufacturing hurdles, and final product validation. Tailored for researchers, scientists, and drug development professionals, it synthesizes current guidelines, explores advanced culture systems like xenogeneic-free media, and presents comparative data on MSC sources to equip stakeholders with the knowledge to navigate the complex pathway of producing clinical-grade MSCs for regenerative medicine.
Laying the Groundwork: GMP Principles and MSC Biology for Clinical Use
Defining GMP and Regulatory Frameworks for ATMPs (EMA & FDA)
Good Manufacturing Practice (GMP) is a quality assurance system that ensures medicinal products are consistently produced and controlled according to rigorous quality standards appropriate for their intended use [1]. In the context of Advanced Therapy Medicinal Products (ATMPs)—which encompass gene therapies, somatic cell therapies, and tissue-engineered products—GMP compliance is not merely a guideline but a legal requirement in many jurisdictions for products intended for human use [1] [2]. The European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA) classify mesenchymal stem cell (MSC)-based products as ATMPs when they undergo substantial manipulation or are intended for a different essential function, placing them under stringent pharmaceutical legislation [1] [2].
The transition of promising MSC therapies from laboratory research to clinical application hinges on developing and implementing robust, reproducible, and GMP-compliant manufacturing processes [3] [4]. This guide details the core regulatory frameworks of the EMA and FDA, provides a practical breakdown of GMP requirements, and presents a validated experimental case study for the GMP-compliant isolation and expansion of MSCs, serving as a technical roadmap for researchers and drug development professionals.
Regulatory Framework for ATMPs
European Medicines Agency (EMA) Framework
The EMA regulates ATMPs through Regulation (EC) No 1394/2007, with the Committee for Advanced Therapies (CAT) serving as the central expert committee for their scientific assessment [2]. The EMA's centralized authorization procedure results in a single marketing authorization valid across the European Union (EU) and European Economic Area (EEA).
- Classification and Certification: The CAT provides recommendations on whether a product qualifies as an ATMP. For small and medium-sized enterprises (SMEs), the agency offers a certification procedure for quality and non-clinical data [2].
- Comprehensive Guidelines: The EMA has established an extensive set of scientific guidelines relevant to ATMP development. Key overarching guidelines include the "Guideline on human cell-based medicinal products" and the "Reflection paper on stem cell-based medicinal products" [5]. These cover all aspects from quality, non-clinical, and clinical development to environmental risk assessment.
- Support for Developers: The EMA provides various support mechanisms, including scientific advice, an ATMP pilot for academia and non-profit organizations, and fee incentives to encourage innovation and help developers meet regulatory requirements [2].
U.S. Food and Drug Administration (FDA) Framework
The FDA regulates cellular and gene therapy products through the Center for Biologics Evaluation and Research (CBER) under the authority of both the Public Health Service Act and the Federal Food, Drug, and Cosmetic Act [6].
- Risk-Based Approach: The FDA's regulatory framework is risk-based. Products that are minimally manipulated and intended for homologous use may be regulated solely under Section 361 of the PHS Act. In contrast, products that are more than minimally manipulated (like most MSC therapies) are regulated as biological drugs under Section 351 and require an approved Biologics License Application (BLA) [7].
- Detailed Guidance Documents: CBER has issued numerous specific guidance documents to assist sponsors. Recent draft guidances relevant to MSC therapies include "Safety Testing of Human Allogeneic Cells Expanded for Use in Cell-Based Medical Products" (April 2024) and "Considerations for the Use of Human- and Animal-Derived Materials in the Manufacture of Cell and Gene Therapy and Tissue-Engineered Medical Products" (April 2024) [7].
- Expedited Programs: The FDA offers expedited programs, such as the Regenerative Medicine Advanced Therapy (RMAT) designation, for therapies addressing serious conditions, which can accelerate development and review [7].
Table 1: Key Regulatory Bodies and Their Roles for ATMPs
| Agency | Governing Regulation | Key Committee/Office | Primary Authorization Route |
|---|---|---|---|
| European Medicines Agency (EMA) | Regulation (EC) No 1394/2007 | Committee for Advanced Therapies (CAT) | Centralized Marketing Authorization |
| U.S. Food and Drug Administration (FDA) | Public Health Service Act & Federal Food, Drug, and Cosmetic Act | Center for Biologics Evaluation and Research (CBER) | Biologics License Application (BLA) |
Core GMP Principles for ATMP Manufacturing
GMP guidelines are comprehensive, covering all aspects of production to ensure the safety, identity, purity, potency, and quality of the final medicinal product [1]. For ATMPs, which are often comprised of living cells, traditional GMP principles have been adapted to address their unique biological characteristics.
- Quality Management: A comprehensive system must be in place to oversee all aspects of production, from raw materials to final product release. This includes defined responsibilities, change control procedures, and self-inspection regimes.
- Facility and Equipment Control: Manufacturing must occur in controlled environments with defined air quality classifications (cleanrooms) to prevent microbial contamination and cross-contamination. Equipment must be qualified, calibrated, and maintained [1] [8].
- Material and Reagent Control: All starting and raw materials, including human and animal-derived materials (e.g., sera, enzymes), must be qualified and tested for quality and potential adventitious agents. The trend is strongly toward using xeno-free, GMP-grade reagents to mitigate risks [3] [4] [7].
- Process and Documentation Control: All manufacturing processes must be clearly defined, validated, and performed according to standard operating procedures (SOPs). Every step must be accurately and contemporaneously documented to ensure full traceability of the product and its components [1].
- Personnel and Training: All staff must be adequately qualified, trained, and competent in GMP principles and the specific techniques they perform.
- Product Testing and Release: The final product must undergo rigorous testing against predefined specifications. For MSC products, this includes, but is not limited to, viability, sterility (bacteria and fungi), mycoplasma, endotoxin, identity (via surface marker expression), and potency (a quantitative measure of biological activity) [3] [4] [7]. A positive quality control result is mandatory before product release.
Case Study: GMP-Compliant Isolation of Mesenchymal Stem Cells
A 2025 study titled "Optimizing mesenchymal stem cell therapy: from isolation to GMP-compliant expansion for clinical application" provides a practical blueprint for translating MSC research into a GMP-compliant process [3] [4]. The study focused on MSCs derived from the infrapatellar fat pad (FPMSCs), a less invasive source than bone marrow.
Experimental Protocol and Workflow
The methodology was designed with GMP compliance as a core objective, from tissue sourcing to final product cryopreservation.
Tissue Acquisition and Isolation
- Tissue Source: Infrapatellar fat pad (IFP) tissue was obtained as surgical waste from patients undergoing anterior cruciate ligament (ACL) reconstructive surgery, with full ethical approval and informed consent [4].
- Isolation Process: The IFP was minced and digested with 0.1% collagenase in serum-free media for 2 hours at 37°C. The digested tissue was centrifuged, washed, filtered, and the cell pellet was resuspended in culture media [4].
Culture Expansion and Media Comparison
- Media Formulations: The study compared a standard MSC media (with FBS) against two animal component-free, GMP-compliant media: MesenCult-ACF Plus Medium and MSC-Brew GMP Medium [4].
- Cell Culture: Cells were passaged at 80-90% confluency and seeded at a density of 5 × 10³ cells/cm². Critical quality attributes were assessed over multiple passages [4].
Analytical and Quality Control Methods
- Cell Doubling Time: Calculated at each passage to assess proliferation capacity [4].
- Colony Forming Unit (CFU) Assay: Cells were seeded at low densities (20-500 cells/dish) and grown for 10 days before staining with Crystal Violet to assess clonogenic potential, an indicator of stem cell potency [4].
- Flow Cytometry: Used to confirm MSC identity by analyzing the expression of standard positive (CD73, CD90, CD105) and negative (CD45) surface markers [4].
- Viability and Sterility Testing: Trypan Blue exclusion was used for viability counts. Sterility (bacterial/fungal contamination) was checked using the Bact/Alert system, while dedicated assays tested for Mycoplasma and Endotoxin [3] [4].
Key Quantitative Findings and Product Specifications
The study generated robust quantitative data demonstrating the success of the GMP-compliant process. The tables below summarize the key experimental results and the final product release criteria.
Table 2: Performance of FPMSCs in Different Culture Media [4]
| Culture Media | Doubling Time (Hours) | Colony Forming Unit (CFU) Capacity | MSC Marker Expression (CD73+/CD90+/CD105+) |
|---|---|---|---|
| Standard MSC Media (with FBS) | Baseline (Higher) | Baseline | Maintained |
| MesenCult-ACF Plus Medium | Intermediate | Intermediate | Maintained |
| MSC-Brew GMP Medium | Lowest (Enhanced Proliferation) | Highest (Enhanced Potency) | Maintained |
Table 3: GMP-FPMSC Final Product Release Specifications [3]
| Quality Attribute | Test Method | Release Specification | Study Result |
|---|---|---|---|
| Viability | Trypan Blue Exclusion | >70% | >95% |
| Sterility | Bact/Alert System | No Contamination | No Contamination Detected |
| Mycoplasma | Mycoplasma Assay | No Contamination | No Contamination Detected |
| Endotoxin | Endotoxin Assay | Below Specification | Below Specification |
| Identity/Purity | Flow Cytometry | Expression of MSC markers | CD45-, CD73+, CD90+, CD105+ |
| Stability | Post-thaw Viability | Maintains specifications | Stable for up to 180 days |
The data confirmed that MSC-Brew GMP Medium supported superior cell proliferation and potency compared to other media. Furthermore, the GMP-validation across four donors demonstrated that the final FPMSC product consistently met all critical quality attributes, with a viability exceeding 95% and stability maintained for up to 180 days of cryogenic storage, proving the robustness and reproducibility of the protocol [3].
The Scientist's Toolkit: Essential Reagents and Materials
Selecting the correct, GMP-compliant materials is fundamental to successful ATMP development. The following table details key reagents and their functions as utilized in the featured case study and related fields.
Table 4: Essential Research Reagent Solutions for GMP-Compliant MSC Manufacturing
| Reagent / Material | Function / Purpose | GMP-Compliant Example / Consideration |
|---|---|---|
| Animal Component-Free Media | Provides nutrients for cell growth and expansion while eliminating the risk of xenogenic immunogenicity and contamination. | MSC-Brew GMP Medium, MesenCult-ACF Plus Medium [4]. |
| Dissociation Enzymes | Breaks down tissue and dissociates adherent cells for passaging. | Use of GMP-grade, recombinant non-animal-derived collagenase [4] [7]. |
| Cell Separation Systems | Isulates, washes, and concentrates target cell populations in a closed, automated system. | Gibco CTS Rotea Counterflow Centrifugation System [8]. |
| Magnetic Cell Selection Systems | Isolates highly pure cell populations based on surface markers; removes magnetic beads after selection. | Gibco CTS Dynacellect Magnetic Separation System [8]. |
| Cryopreservation Medium | Protects cells from damage during freeze-thaw cycles. | Use of defined, serum-free, GMP-compliant cryomedium containing DMSO [3]. |
| Quality Control Assays | Tests for viability, sterility, mycoplasma, endotoxin, and cell identity to ensure product safety and quality. | Trypan Blue, Bact/Alert, Mycoplasma/Endotoxin kits, Flow Cytometry kits (e.g., BD Stemflow) [3] [4]. |
Navigating the GMP and regulatory landscapes for ATMPs is a complex but essential endeavor for translating MSC therapies from research to clinic. The EMA and FDA provide detailed, albeit distinct, frameworks designed to ensure patient safety and product efficacy. As demonstrated by the recent feasibility study on FPMSCs, success in this field is achievable through a meticulous approach that integrates GMP principles from the very beginning—from sourcing raw materials and optimizing culture conditions to establishing rigorous quality control protocols. By adhering to these frameworks and leveraging advanced, GMP-compliant tools and reagents, researchers and developers can significantly accelerate the development of safe and effective mesenchymal stem cell therapies for patients in need.
Core ISCT Criteria for MSCs and Implications for GMP Characterization
The field of Mesenchymal Stromal Cell (MSC) therapy has witnessed remarkable growth over the past decades, necessitating robust standards to ensure product quality and safety. The International Society for Cell and Gene Therapy (ISCT) established the fundamental criteria for defining MSCs, which have become the cornerstone for both research and clinical applications [9]. These criteria provide the essential foundation upon which Good Manufacturing Practice (GMP) characterization is built, creating a critical pathway for translating laboratory research into clinically viable therapies. The integration of ISCT's core definitions with GMP requirements represents a pivotal strategy for ensuring that MSC-based products are characterized with the rigor, consistency, and quality required for human administration, directly supporting the feasibility of MSC isolation and manufacturing within regulated clinical research frameworks [10].
The Core ISCT Criteria for Defining MSCs
The ISCT criteria, established to standardize the identity of MSCs across the field, are built upon three fundamental pillars that must be conclusively demonstrated for any cell population to be classified as MSCs.
The Three Definitive Pillars of MSC Identity
Adherence to Plastic: Under standard culture conditions, MSCs must demonstrate plastic adherence in vitro. This functional characteristic represents a primary, selective property whereby MSC populations are established and expanded from original tissue digests through their capacity to adhere to tissue culture plastic surfaces [9].
Specific Surface Marker Expression: MSCs must express a defined set of characteristic surface antigens while lacking expression of hematopoietic markers. Specifically, ≥95% of the cell population must express CD105, CD73, and CD90, while ≤2% of the population must lack expression of CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR [9]. This immunophenotypic profile confirms the mesenchymal origin and purity of the cell population.
Multipotent Differentiation Potential: When induced under appropriate in vitro conditions, MSCs must possess the capacity to differentiate into osteoblasts, adipocytes, and chondroblasts. This trilineage differentiation potential provides functional validation of their stromal progenitor functionality [9].
Clarification of MSC Nomenclature
It is crucial to note the official nomenclature clarification by ISCT. While the term "Mesenchymal Stem Cells" remains popular in historical literature, the ISCT has officially defined the term MSC as "Mesenchymal Stromal Cells" for cells isolated from somatic or perinatal tissues based on the above criteria. This reflects the scientific consensus on their biological characteristics and helps distinguish them from truly pluripotent stem cells [9].
GMP Characterization: Translating Criteria into Clinical Grade
The transition from research-grade MSCs to clinically applicable products requires that the core ISCT criteria be evaluated within a GMP framework. This entails implementing rigorous, standardized, and well-documented processes that ensure product safety, purity, potency, and identity throughout manufacturing.
The GMP Imperative for Clinical Translation
The implementation of GMP standards is not merely regulatory compliance but a fundamental requirement for patient safety and therapeutic efficacy. As of 2023, only one MSC product (Ryoncil/Remestemcel-L) had received FDA approval, highlighting the significant challenges in translating MSC therapies to clinical application, largely due to the lack of standardized GMP protocols [10]. GMP compliance eliminates risks associated with animal-derived components, such as potential contamination, immunogenicity, and batch-to-batch variability, which is achieved through the use of animal-component-free media formulations [10]. Furthermore, GMP guidelines require stringent documentation and quality control at every stage, from tissue sourcing to final product release, ensuring process consistency and product reproducibility essential for credible clinical trials [10].
Applying ISCT Criteria Under GMP Standards
Each of the three ISCT pillars must be validated using GMP-compliant methods and specifications:
Plastic Adherence as a Selection Method: Within GMP processes, plastic adherence serves as the primary selection and purification method during initial isolation and expansion. The process must use GMP-grade culture vessels and be conducted in a controlled, aseptic environment [10] [9].
GMP-Compliant Phenotypic Characterization: Flow cytometry analysis for surface markers must utilize GMP-grade antibodies and standardized protocols. The equipment requires regular validation and calibration, and the analysis must include appropriate controls to ensure accuracy. The resulting data provides quantitative, lot-specific release criteria for product identity and purity [10].
Potency Assessment through Differentiation: The trilineage differentiation assay transitions from a qualitative identity test to a quantitative potency assay under GMP. This requires standardized, validated differentiation kits and scoring methods to demonstrate biological activity, with established acceptance criteria for the degree of differentiation achieved [10].
Quantitative GMP Characterization Data and Standards
The implementation of GMP standards establishes specific, quantitative benchmarks for product release. The following table summarizes key characterization data and acceptance criteria derived from GMP validation studies.
Table 1: Quantitative Specifications for GMP-Compliant MSC Characterization
| Characterization Parameter | Test Method | GMP Release Criteria | Experimental Data from GMP Validation [10] |
|---|---|---|---|
| Viability | Trypan Blue Exclusion | >70% minimum requirement | >95% viability post-thaw |
| Sterility | Bact/Alert & Mycoplasma Assay | No contamination detected | Sterility maintained up to 180 days of storage |
| Identity & Purity | Flow Cytometry | ≥95% CD105, CD73, CD90+≤2% CD45, CD34, CD14, CD19, HLA-DR+ | Maintained marker expression post-thaw and across passages |
| Potency | Colony Forming Unit (CFU) Assay | Colony formation capacity | Higher CFU in GMP media (MSC-Brew) vs. standard media |
| Proliferation | Population Doubling Time | Established baseline for cell line | Lower doubling times in MSC-Brew GMP Medium |
| Safety | Endotoxin Assay | Below specified limit | Within acceptable limits for clinical administration |
Advanced GMP Characterization Metrics
Beyond the basic release criteria, comprehensive GMP characterization includes additional critical quality attributes (CQAs) that ensure product consistency and functionality.
Table 2: Advanced Critical Quality Attributes for GMP-Compliant MSCs
| Critical Quality Attribute (CQA) | Analytical Method | Significance for Clinical Feasibility |
|---|---|---|
| Cell Count & Dosage | ISO Cell Counting Standards [11] | Ensures accurate dosing; may shorten regulatory review |
| Karyotype Stability | Karyotyping/G-banding | Confirms genetic stability after extended culture |
| Immunomodulatory Function | Mixed Lymphocyte Reaction (MLR) [9] | Validates mechanistic potency for autoimmune applications |
| Secretome Profile | ELISA/Multiplex Assays | Quantifies trophic factor production (e.g., IDO, IL) |
| Post-Thaw Recovery | Viability & Function Assays | Validates cryopreservation protocol and product shelf-life |
| Morphology & Adherence | Microscopy & Imaging | Confirms typical fibroblast-like morphology and plastic adherence |
Experimental Protocols for GMP-Compliant Characterization
GMP-Compliant Isolation and Culture Protocol
The feasibility of MSC isolation under GMP hinges on rigorously validated protocols. The following workflow outlines a standardized method for deriving clinical-grade MSCs from tissue sources, incorporating data from a 2025 study on infrapatellar fat pad-derived MSCs (FPMSCs) [10].
Key Protocol Details:
- Tissue Source: Infrapatellar fat pad (IFP) tissue acquired as waste tissue from reconstructive surgery, with donor screening and informed consent [10].
- Digestion: 0.1% collagenase in serum-free media for 2 hours at 37°C [10].
- GMP Media Validation: Comparative studies show MSC-Brew GMP Medium (Miltenyi Biotec) supports enhanced proliferation rates and colony formation compared to standard media and other animal-free formulations like MesenCult-ACF Plus Medium [10].
- Culture Conditions: Seeding density of 5 × 10³ cells/cm² and passaging at 80-90% confluency [10].
- Quality Control: Incorporation of sterility testing (Bact/Alert, Mycoplasma assays) and endotoxin testing throughout the process [10].
Analytical Methods for ISCT Criterion Verification
The following workflow details the specific analytical methods required to verify that the isolated cells meet all three ISCT criteria within a GMP-compliant framework.
Key Analytical Details:
- Flow Cytometry: Utilization of standardized kits such as the BD Stemflow Human MSC Analysis Kit with gating strategies established for consistency across batches [10].
- Potency Assays: Differentiation kits must be GMP-grade, and staining protocols must be standardized with established scoring criteria to quantitatively assess differentiation potential.
- Additional Testing: The GMP framework also requires karyotype analysis to rule out genetic abnormalities and sterility testing to ensure the product is free from microbial contamination [10].
Essential Research Reagent Solutions for GMP Characterization
The feasibility of GMP-compliant MSC characterization depends on the use of specific, quality-controlled reagents. The following table catalogues essential materials and their functions based on cited protocols.
Table 3: Research Reagent Solutions for GMP-Compliant MSC Workflows
| Reagent Category | Specific Product Examples | GMP-Compliant Function |
|---|---|---|
| Animal-Free Media | MSC-Brew GMP Medium (Miltenyi Biotec) [10]MesenCult-ACF Plus Medium (StemCell Technologies) [10] | Supports expansion & maintenance; eliminates xeno-contamination risks |
| Dissociation Enzymes | Collagenase (0.1%) [10] | Tissue dissociation for primary cell isolation |
| Characterization Kits | BD Stemflow Human MSC Analysis Kit (BD Biosciences) [10] | Standardized immunophenotyping for ISCT surface markers |
| Differentiation Kits | Trilineage Differentiation Kits (Various GMP Suppliers) | Validated induction of osteogenic, adipogenic, and chondrogenic lineages |
| Cryopreservation Media | FBS with 10% DMSO [10] | Long-term storage while maintaining post-thaw viability and function |
| Quality Control Assays | Bact/Alert, Mycoplasma Assay, Endotoxin Test [10] | Ensures product sterility and safety for clinical use |
The integration of core ISCT criteria with rigorous GMP characterization protocols provides a essential roadmap for the feasible development of clinically relevant MSC-based therapies. The ISCT standards establish the fundamental biological identity of MSCs, while GMP requirements translate these definitions into a framework of quality, safety, and consistency. As the field advances, with emerging sources such as infrapatellar fat pad-derived MSCs [10] and induced pluripotent stem cell-derived MSCs [9] demonstrating promise, adherence to this combined standard will remain paramount. The continued refinement of these characterization protocols, guided by both ISCT and regulatory bodies, will undoubtedly enhance the feasibility, reproducibility, and ultimate success of MSC isolation and manufacturing for clinical research and therapeutic application.
Mesenchymal stromal cells (MSCs) represent a cornerstone of regenerative medicine and immunotherapeutic research due to their multipotent differentiation capabilities, immunomodulatory properties, and paracrine activity [12]. The International Society for Cell & Gene Therapy (ISCT) has established critical criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD45-, CD34-, CD14- or CD11b-, CD79α- or CD19-, HLA-DR-), and trilineage differentiation potential (osteogenic, adipogenic, chondrogenic) [13] [12]. For clinical applications, particularly in the European Union and Germany, MSC-based products are classified as Advanced Therapy Medicinal Products (ATMPs) and must be manufactured under strict Good Manufacturing Practice (GMP) standards to ensure quality, safety, and efficacy [13]. This manufacturing process requires a formal license and adherence to comprehensive quality control measures, making the choice of MSC source a critical determinant in the feasibility and scalability of GMP-compliant production [13] [14].
MSCs can be isolated from multiple tissue sources, with bone marrow (BM), adipose tissue (AT), and umbilical cord (UC), specifically Wharton's Jelly (WJ), being the most extensively studied. Each source presents distinct advantages and limitations in the context of GMP-compliant manufacturing for clinical applications.
Table 1: Comparative Characteristics of MSC Sources for GMP-Compliant Manufacturing
| Feature | Bone Marrow (BM) | Adipose Tissue (AT) | Umbilical Cord (WJ) |
|---|---|---|---|
| Tissue Availability | Invasive harvest; limited donor supply [4] | Minimally invasive harvest (e.g., liposuction); relatively abundant [4] [12] | Medical waste; non-invasive collection; easily accessible [15] |
| Cell Yield & Proliferation | Lower yield; slower proliferation (e.g., DT: ~99 hrs) [16] | High yield; moderate proliferation (e.g., DT: ~40 hrs) [16] | High yield; rapid proliferation (e.g., DT: ~21 hrs) [15] [16] |
| Immunomodulatory Potency | High immunomodulatory activity [16] | Moderate immunomodulatory activity [16] | Moderate immunomodulatory activity [16] |
| Therapeutic Secretome | Lower secretion of some neurotrophic factors [16] | Favorable secretome profile for neuroregeneration [16] | Favorable secretome profile for neuroregeneration [16] |
| Risk of Contamination | Risk from hematopoietic cells [13] | - | Low immunogenicity; reduced ethical concerns [15] |
Table 2: Functional and Therapeutic Potential of Different MSC Sources
| Parameter | Bone Marrow (BM-MSCs) | Adipose Tissue (AT-MSCs) | Umbilical Cord (WJ-MSCs) |
|---|---|---|---|
| Immunosuppression (Contact) | Strong inhibition up to PBMC:MSC ratio 40:1 [16] | Inhibition at lower ratios only (e.g., 10:1) [16] | Inhibition at lower ratios only (e.g., 10:1) [16] |
| Immunosuppression (Non-Contact) | Strong inhibition up to PBMC:MSC ratio 5:1 [16] | Limited non-contact inhibition [16] | Limited non-contact inhibition [16] |
| Neurotrophic Potential | Moderate | High | High |
| Clinical-Grade Expansion | Challenging due to slower growth [16] | Feasible with optimized protocols [4] | Highly feasible; excellent scalability [15] |
| Donor Variability | Subject to age-related decline [17] | - | Consistent "younger" cell phenotype [15] |
GMP-Compliant Isolation and Culture Methodologies
Transitioning from research-grade to clinical-grade MSC manufacturing necessitates stringent protocols that eliminate animal-derived components and ensure batch-to-batch consistency.
Donor Selection and Tissue Sourcing
For BM-MSCs, a minimum of 10–20 mL of bone marrow aspirate is typically required for successful isolation [13]. Donors must be thoroughly screened for transmissible diseases, and the resulting cell population is inherently heterogeneous [13]. For WJ-MSCs, umbilical cords are collected post-cesarean section from mothers aged 20–35 who are free from infectious diseases and have provided written informed consent [15]. The cord is transported at 2–10°C and processed within 24 hours, followed by decontamination and vessel removal to isolate Wharton's jelly [15].
Isolation Techniques
Two primary isolation methods are employed:
- Enzymatic Digestion: For WJ-MSCs, optimal isolation parameters include using 0.4 PZ U/mL of GMP-grade collagenase (e.g., Collagenase NB6) with a digestion time of 3 hours at 37°C [15]. This method yields a high number of primary (P0) cells and is generally faster than the explant method [15].
- Explant Method: This technique involves mincing the tissue into small fragments (1–4 mm³) and culturing them directly. It is simpler and minimizes exposure to enzymes but can be more challenging to standardize and may have a slower initial outgrowth [15].
Culture Medium and Supplements
A critical step in GMP compliance is moving away from fetal bovine serum (FBS) due to risks of immunogenicity and pathogen transmission [13] [14]. Current GMP-compliant strategies include:
- Human Platelet Lysate (hPL): Serves as a effective xeno-free supplement. Studies show that concentrations of 2% to 5% hPL can effectively support MSC expansion [4] [15]. However, hPL is a crude derivative that can exhibit batch-to-batch variation and must be sourced from pathogen-screened donors, sometimes requiring pooling to minimize variability [14].
- Defined Serum-Free/Xeno-Free Media: Commercially available formulations like MSC-Brew GMP Medium and MesenCult-ACF Plus Medium provide a fully defined environment [4]. Research demonstrates that MSCs cultured in MSC-Brew GMP Medium exhibit enhanced proliferation rates and colony-forming capacity compared to standard media [4].
Diagram 1: GMP-Compliant MSC Manufacturing Workflow
Expansion and Scalability
For large-scale clinical applications, traditional flask-based culture is insufficient. Bioprocess engineering using bioreactors for 3D culture provides a controlled microenvironment that can improve stem cell yield, function, and safety under cGMP [18]. Studies show that passages 2 to 5 (P2-P5) are optimal for WJ-MSCs, exhibiting high viability and proliferation ability, while extended passaging should be avoided to prevent senescence [4] [15]. The population doubling time of WJ-MSCs (approximately 21 hours) is significantly lower than that of BM-MSCs (approximately 99 hours), facilitating more efficient scale-up [16].
Quality Control and Functional Validation
Robust quality control is indispensable for GMP-compliant MSC manufacturing. This extends beyond basic characterization to include functional potency assays.
Release Criteria and Testing
- Viability and Sterility: Post-thaw cell viability should exceed 95% [4]. Products must undergo sterility testing (e.g., using Bact/Alert systems) and mycoplasma and endotoxin assays [4].
- Immunophenotyping: Flow cytometry must confirm expression of CD73, CD90, and CD105 on >90% of cells, and lack of expression of CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR on >98% of cells, as per ISCT guidelines [13] [12]. The 2025 ISCT standards emphasize quantitative reporting of these markers [19].
- Karyotyping and Tumorigenicity Testing: Genetic stability must be verified to ensure safety, particularly after extensive in vitro expansion [13].
- Potency Assays: These are critical quality attributes (CQAs) that should reflect the intended clinical mechanism of action. For immunomodulatory applications, this could involve measuring the suppression of peripheral blood mononuclear cell (PBMC) proliferation [13] [16]. The new 2025 ISCT standards specifically require the assessment of efficacy and functional properties as CQAs [19].
Emerging Biomarkers: Cellular Deformability
Recent research highlights cellular deformability—a cell's ability to change shape under force—as a novel, integrative biomarker for MSC quality [17]. It correlates with therapeutic attributes such as stemness, homing efficiency, and differentiation status [17]. MSCs with higher deformability show greater migration and secretory potential, while stiffer cells are often associated with aging and differentiation [17]. Techniques like real-time deformability cytometry (RT-DC) offer high-throughput analysis for quality control, potentially enabling the enrichment of therapeutically potent MSC subpopulations and reducing product heterogeneity [17].
Essential Research Reagent Solutions for GMP-Compliant MSC Culture
Table 3: Key Reagents for GMP-Compliant MSC Manufacturing
| Reagent Category | Example Products | Function & Importance |
|---|---|---|
| Basal Media | MEM-α, DMEM | Provides essential nutrients and salts for cell growth and maintenance. |
| Xeno-Free Supplements | Human Platelet Lysate (hPL), MSC-Brew GMP Medium | Replaces FBS to eliminate xenogenic risks; promotes expansion under defined conditions [4] [14]. |
| GMP-Grade Enzymes | Collagenase NB6 | Used for tissue dissociation during isolation; critical for yield and viability [15]. |
| Cell Dissociation Agents | Trypsin-EDTA, TrypLE | Detaches adherent cells for passaging and subculture. |
| Cryopreservation Media | DMSO-containing formulations with serum-free base | Preserves cell viability and functionality during long-term storage. |
The feasibility of GMP-compliant isolation and expansion of MSCs is highly dependent on the selected tissue source. Bone marrow-derived MSCs, while functionally potent, present challenges in scalability due to invasive harvesting and slower proliferation. Adipose tissue offers a viable alternative with higher cell yields and less invasive collection. Wharton's jelly-derived MSCs from the umbilical cord emerge as a highly promising source, characterized by rapid proliferation, ease of access without ethical concerns, and robust performance in scalable, GMP-compliant manufacturing processes [15] [16].
Future advancements in MSC therapy will be driven by the implementation of revised ISCT standards [19], the adoption of advanced functional biomarkers like cellular deformability [17], and the continued refinement of bioprocessing techniques in bioreactors [18]. The integration of these elements will ensure the consistent production of high-quality, safe, and potent MSC-based therapeutics, ultimately fulfilling their potential in regenerative medicine.
The feasibility of isolating and manufacturing mesenchymal stem cells (MSCs) under Good Manufacturing Practice (GMP) standards is critically dependent on rigorous donor selection criteria. Donor characteristics significantly impact the functional properties, therapeutic potency, and overall quality of the final MSC product [20] [21]. This technical guide examines the core considerations for donor eligibility—specifically age, health status, and ethical compliance—framed within the context of GMP-compliant MSC isolation for clinical applications. As MSC therapies transition from research to clinical use, establishing standardized, evidence-based donor selection protocols becomes paramount for ensuring product safety, efficacy, and reproducibility [21] [22].
The inherent heterogeneity of MSC populations, substantially influenced by donor-specific factors, presents a major challenge in producing standardized cell therapy products [20] [23]. Selecting the appropriate MSC donor is particularly crucial when developing allogeneic "off-the-shelf" therapies, where cells from a single donor are expanded for multiple recipients [21] [24]. This guide synthesizes current research and regulatory expectations to provide a comprehensive framework for donor evaluation in GMP-compliant MSC manufacturing.
Impact of Donor Age on MSC Characteristics
Donor age is a primary consideration in donor selection, with substantial evidence indicating its influence on MSC proliferation, differentiation potential, and senescence. However, the relationship is complex and varies across tissue sources and species.
Proliferation and Senescence
Table 1: Impact of Donor Age on MSC Proliferation Capacity
| Age Group | Species/Breed | Proliferation Capacity | Research Findings |
|---|---|---|---|
| Fetal | Bovine (Holstein Friesian) | High | 6 of 7 donors surpassed 30 population doublings [20] |
| Calf | Bovine (Holstein Friesian) | High | 4 of 7 donors surpassed 30 population doublings [20] |
| Adult | Bovine (Holstein Friesian) | Reduced | Lower proliferation capacity compared to fetal and calf [20] |
| Aged (≥60 years) | Human | Significantly Reduced | Decreased proliferative potential and increased senescence [24] |
MSCs from younger donors generally demonstrate enhanced proliferative capacity and delayed senescence. In bovine models, fetal and calf MSCs from Holstein Friesian breeds showed superior population doubling capacity, with most donors exceeding 30 population doublings [20]. Similarly, human bone marrow-derived MSCs (BM-MSCs) from older donors (60-80 years) exhibit reduced proliferative potential and increased morphological changes associated with senescence compared to those from younger donors (30-40 years) [24]. This decline is attributed to accumulated oxidative stress and reduced antioxidant defense mechanisms in aged cells [24].
Differentiation Potential
Table 2: Age-Related Changes in MSC Differentiation Potential
| Lineage | Age Effect | Research Evidence |
|---|---|---|
| Osteogenic | Variable (Decreased in Aged) | Slight negative correlation of alkaline phosphatase (ALP) expression with donor age in human BM-MSCs; breed effect more prominent than age in bovine MSCs [20] [25] |
| Adipogenic | Variable | Higher potential in fetal and adult bovine MSCs (Holstein Friesian); decreased potential in aged human BM-MSCs and gingival MSCs [20] |
| Chondrogenic | Generally Decreased | Significantly reduced potential with increasing age in human studies [20] |
The effect of donor age on differentiation potential is lineage-dependent and shows considerable variation. While some studies report a slight negative correlation between donor age and osteogenic differentiation in human BM-MSCs, evidenced by reduced alkaline phosphatase expression [25], other research suggests that breed or species differences may outweigh age effects [20]. Chondrogenic differentiation appears to consistently decline with increasing donor age across multiple studies [20].
Molecular Signature of Aging
Genome-wide expression analyses of human BM-MSCs from donors aged 17-84 have identified specific genetic markers correlated with aging, despite considerable donor-to-donor variation in clinical parameters and in vitro performance [25]. These molecular signatures provide potential tools for assessing MSC quality and "biological age" beyond chronological age, which could be valuable for standardizing donor selection in GMP manufacturing.
Figure 1: Relationship between donor age and MSC functional characteristics. Aging negatively impacts proliferation and increases senescence, while differentiation effects vary. Molecular changes include increased oxidative stress and specific genetic markers.
Health Status and Biological Factors
Beyond chronological age, the overall health status and biological characteristics of donors significantly influence MSC quality and must be carefully evaluated for GMP-compliant manufacturing.
Donor Health and Medical History
Comprehensive donor screening is essential to exclude individuals with conditions that might compromise MSC quality or pose safety risks to recipients. Key considerations include:
- Infectious Disease Screening: Donors must be screened for transmissible diseases following standard blood and tissue banking protocols [22].
- Comorbidities and Medications: Underlying health conditions and pharmacological treatments may alter MSC functionality, though specific criteria remain poorly defined [21].
- Genetic Stability: The risk of karyotypic abnormalities may be higher in older or diseased donors, though it is unclear whether this is intrinsic or results from ex vivo expansion [21].
Sex and Gender Effects
Emerging evidence indicates that donor sex influences MSC properties, including differentiation potential, proliferation capacity, secretome profile, and therapeutic efficacy [21] [24]. While not yet standardized in all protocols, sex-matching between donor and recipient may optimize outcomes for specific applications, particularly in autoimmune disease treatment [24].
Tissue Source Considerations
The tissue origin of MSCs introduces another variable in donor selection, as biological source significantly impacts MSC characteristics:
- Bone Marrow: Traditionally considered the "gold standard" but requires invasive extraction with risk of patient morbidity [4] [22].
- Adipose Tissue: Abundant MSC yield with less invasive collection procedures; cells may express CD34 in early passages [20] [22].
- Infrapatellar Fat Pad: Less characterized source with practical advantages for orthopedic applications; can be harvested with minimal invasiveness during knee surgery [4].
- Neonatal Tissues (placenta, umbilical cord, Wharton's jelly): Considered more primitive MSCs but with practical challenges in consistent collection [22].
Ethical Framework and Regulatory Compliance
Ethical donor selection and adherence to regulatory guidelines are fundamental to GMP-compliant MSC manufacturing, ensuring patient safety and maintaining public trust.
Core Ethical Principles
The International Society for Stem Cell Research (ISSCR) outlines fundamental principles for stem cell research and clinical translation, emphasizing integrity, patient welfare, respect for research subjects, transparency, and social justice [26]. These principles provide an ethical foundation for donor selection protocols.
Informed Consent Process
Valid informed consent represents a cornerstone of ethical MSC donation, particularly for personalized medicine approaches using autologous cells [27]. Key elements include:
- Voluntary Participation: Donors must provide consent without coercion, based on comprehensive understanding of the donation process and intended use [27] [26].
- Altruistic Donation: European standards emphasize altruism and solidarity between donor and recipient, encouraging voluntary unpaid donations to enhance safety standards [27].
- Anonymity: Maintenance of donor and recipient anonymity is typically required, except in autologous applications [27].
Regulatory Landscape
Table 3: Regulatory Framework for MSC-Based Therapies
| Region | Regulatory Classification | Governing Documents | Key Requirements |
|---|---|---|---|
| European Union | Advanced Therapy Medicinal Product (ATMP) | Regulation 1394/2007/EC; Directive 2009/120/EC; EudraLex Volume 4 [21] [22] | GMP compliance; centralized marketing authorization; specific technical requirements |
| United States | Human Cells, Tissues, and Cellular/Tissue-Based Products (HCT/Ps) | Code of Federal Regulations (CFR) Title 21, Parts 1271 [22] | Current Good Tissue Practice (cGTP); establishment registration; donor eligibility determination |
MSCs are classified as Advanced Therapy Medicinal Products (ATMPs) in Europe and subject to specific FDA regulations in the United States [21] [22]. Both regulatory frameworks require rigorous donor eligibility determination, screening, and testing to prevent transmission of communicable diseases [22]. The complex regulatory environment represents a significant challenge for academic institutions and small-to-medium enterprises (SMEs) developing MSC therapies [21].
Figure 2: Ethical and regulatory framework for donor selection in MSC manufacturing. Core ethical principles, informed consent requirements, and regional regulations govern donor eligibility.
GMP-Compliant Donor Selection Workflow
Implementing a standardized, documented workflow for donor selection is essential for GMP-compliant MSC manufacturing. This systematic approach ensures consistency, traceability, and quality of the final cell product.
Donor Screening Protocol
A comprehensive donor screening protocol should integrate multiple criteria to assess donor suitability:
- Age Evaluation: Documented verification of donor age with consideration for the intended therapeutic application (e.g., preference for younger donors for allogeneic banking) [20] [24].
- Medical History Review: Comprehensive assessment of current and past medical conditions, medications, and potential risk factors [21].
- Infectious Disease Testing: Required serological and molecular testing for relevant blood-borne pathogens [22].
- Lifestyle Risk Assessment: Evaluation of behavioral factors that might increase transmission risk [22].
Documentation and Traceability
GMP requirements mandate complete documentation of all donor selection decisions, including:
- Donor eligibility determination records
- Informed consent documentation
- Testing results and interpretation
- Deviation documentation and justification
This documentation ensures full traceability from original donor to final MSC product, a fundamental requirement for ATMPs [21] [22].
Experimental Protocols for Donor Evaluation
Rigorous experimental assessment of donor-derived MSCs provides critical data for evaluating donor suitability and establishing release criteria for clinical-grade cell banks.
proliferation and Senescence Assays
Protocol: Population Doubling Time Calculation
- Objective: Quantify in vitro proliferation capacity of donor MSCs [20] [4].
- Methodology:
- Seed MSCs at standardized density (e.g., 5,000 cells/cm²) [4].
- Culture until 70-90% confluency in defined media.
- Harvest and count cells using validated method (e.g., hemocytometer, automated cell counter).
- Repeat for multiple passages to establish growth kinetics.
- Calculate doubling time using the formula:
( Doubling\ Time = \frac{duration \times \ln{2}}{\ln{(final\ concentration / initial\ concentration)} } ) [4].
- GMP Considerations: Use defined, xenogeneic-free media (e.g., MSC-Brew GMP Medium, MesenCult-ACF Plus Medium) to ensure clinical compatibility [4].
Protocol: Senescence-Associated β-Galactosidase Staining
- Objective: Detect senescent cells in donor MSC populations [20].
- Methodology:
- Culture MSCs on chamber slides until subconfluent.
- Fix cells with formaldehyde/glutaraldehyde solution.
- Incubate with X-gal solution at pH 6.0 overnight at 37°C (non-CO₂ incubator).
- Counterstain and quantify percentage of blue-stained senescent cells.
- Interpretation: Higher percentage of SA-β-gal positive cells indicates increased senescence, typically associated with older donors or extended in vitro culture [20].
Potency and Differentiation Assays
Protocol: Trilineage Differentiation Potential
- Objective: Verify multipotency of donor MSCs per ISCT criteria [20] [22].
- Osteogenic Differentiation:
- Adipogenic Differentiation:
- Culture MSCs in adipogenic induction media with dexamethasone, indomethacin, and IBMX.
- Visualize lipid vacuoles with Oil Red O staining after 2-3 weeks [20].
- Chondrogenic Differentiation:
- Pellet culture in chondrogenic media with TGF-β for 3-4 weeks.
- Analyze proteoglycan deposition with Safranin O or Alcian Blue staining [20].
Protocol: Colony-Forming Unit (CFU) Assay
- Objective: Assess clonogenic potential of donor MSCs [4] [23].
- Methodology:
- Interpretation: Higher CFU efficiency indicates greater clonogenic potential, characteristic of more potent MSCs from optimal donors [23].
Immunophenotyping
Protocol: Flow Cytometry Analysis
- Objective: Verify MSC surface marker expression profile [20] [4].
- Methodology:
- Harvest and wash MSC populations.
- Incubate with fluorochrome-conjugated antibodies against positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) markers.
- Analyze using flow cytometry with appropriate isotype controls.
- Define population purity as percentage of CD45-/CD73+/CD90+/CD105+ cells [4].
- GMP Considerations: Use validated antibody panels and standardized operating procedures to ensure reproducibility [4] [22].
Research Reagent Solutions for Donor Evaluation
Table 4: Essential Reagents for GMP-Compliant MSC Donor Characterization
| Reagent Category | Specific Examples | Function | GMP Compliance |
|---|---|---|---|
| Cell Culture Media | MSC-Brew GMP Medium; MesenCult-ACF Plus Medium | Supports MSC expansion and maintenance | Xenogeneic-free, chemically defined [4] |
| Dissociation Reagents | Liberase; 0.1% Collagenase | Tissue digestion and cell harvesting | GMP-grade enzymes with certificate of analysis [20] [4] |
| Characterization Antibodies | BD Stemflow Human MSC Analysis Kit | Immunophenotyping by flow cytometry | Validated for clinical use [4] |
| Differentiation Kits | Osteogenic/Adipogenic/Chondrogenic Differentiation Media | Functional potency assessment | Defined compositions, lot-to-lot consistency [20] |
| Cryopreservation Media | DMSO-free cryoprotectants | Long-term cell storage | Xenogeneic-free, chemically defined [21] |
Donor selection represents a critical determinant in the feasibility of isolating clinically relevant MSCs under GMP standards. Chronological age significantly impacts proliferation capacity and differentiation potential, with younger donors generally providing more robust cells, though the relationship is complex and influenced by additional factors including biological source, sex, and genetic background. Comprehensive health status evaluation and rigorous infectious disease screening are essential for ensuring product safety. These biological considerations must be integrated within a robust ethical and regulatory framework that prioritizes informed consent, donor welfare, and transparency.
As the field advances, developing more predictive biomarkers of MSC potency and functionality will enhance donor selection protocols beyond chronological age and standard markers. The implementation of standardized, GMP-compliant workflows for donor evaluation—incorporating the experimental protocols and reagent systems outlined in this guide—will be essential for producing consistent, high-quality MSC therapies that fulfill their promising clinical potential while maintaining the highest ethical standards.
From Tissue to Vial: Step-by-Step GMP Isolation and Expansion Protocols
The translation of Mesenchymal Stem Cell (MSC) therapies from research to clinical application hinges on the development of robust, reproducible, and standardized isolation protocols that comply with Good Manufacturing Practice (GMP). The isolation method serves as the foundational step in manufacturing, directly influencing cell yield, purity, potency, and ultimately, the safety and efficacy of the final therapeutic product [3] [28]. Within this framework, two primary techniques—enzymatic digestion and explant culture—have emerged as the standard approaches for isolating MSCs from various tissues. The choice between these methods is critical for GMP-compliant production, as it affects process scalability, consistency, and the defined Critical Quality Attributes (CQAs) of the cell product [15] [28]. This technical guide provides an in-depth analysis of both techniques, comparing their parameters, outcomes, and applications within a GMP feasibility context to inform researchers and drug development professionals.
Core Technique Principles and Comparative Analysis
Enzymatic Digestion Method
The enzymatic digestion method utilizes specific enzymes, most commonly collagenases, to chemically degrade the extracellular matrix of tissue samples, thereby liberating individual cells for culture [15] [9]. This process involves tissue mincing, enzymatic dissociation, neutralization of the enzyme, and subsequent centrifugation to collect the cell pellet for seeding.
Optimized parameters for GMP-compliant enzymatic digestion, particularly for Wharton's jelly-derived MSCs (WJ-MSCs), have been established. Key findings indicate that a concentration of 0.4 PZ U/mL of a GMP-grade collagenase (e.g., Collagenase NB6) with a digestion time of 3 hours at 37°C yields the highest number of viable P0 cells [15]. The process must use enzymes that are GMP-compliant to mitigate risks associated with animal-derived components.
Explant Method
The explant method is a mechanical approach that relies on the migratory capacity of MSCs from tissue fragments. The process involves mincing the source tissue into small fragments (typically 1–4 mm^3), placing them directly onto culture vessel surfaces, and allowing cells to migrate out from the tissue explant to adhere to the plastic substrate [15] [9]. This method is generally considered simpler and minimizes exposure to external factors like enzymes, potentially better preserving cell viability and functionality [15].
Quantitative Comparison of Method Outcomes
The choice between isolation methods significantly impacts initial cell yield, outgrowth timing, and subsequent cell characteristics. The following table summarizes a direct comparative analysis based on validation studies.
Table 1: Quantitative Comparison of Enzymatic Digestion vs. Explant Isolation Methods
| Parameter | Enzymatic Digestion | Explant Method | GMP Feasibility Implications |
|---|---|---|---|
| Initial Cell Yield (P0) | Higher yield at optimal concentration (0.4 PZ U/mL) [15] | Lower initial yield [15] | Digestion supports larger batch sizes; critical for allogeneic therapies. |
| Time to Primary Culture | Faster outgrowth of first cells [15] | Slower initial outgrowth [15] | Digestion can reduce production timeline for P0. |
| Process Complexity | Higher complexity; requires enzyme optimization, inactivation, and removal [15] | Lower complexity; fewer steps and variables [15] | Explant may offer simpler validation but requires control of fragment size/distribution. |
| Risk of Cell Damage | Potential risk if enzymatic parameters are sub-optimal [15] | Minimizes enzymatic stress on cells [15] | Explant may enhance initial viability; digestion requires rigorous parameter control. |
| Post-Passage Characteristics | No significant differences in viability, morphology, proliferation, surface marker expression, or differentiation capacity after passaging [15] | No significant differences in viability, morphology, proliferation, surface marker expression, or differentiation capacity after passaging [15] | Choice of method for P0 may not affect the final cell product characteristics post-expansion. |
Detailed Experimental Protocols for GMP-Compliant Isolation
GMP-Compliant Enzymatic Digestion Protocol for Umbilical Cord
This protocol is adapted from a 2024 study establishing a GMP-compliant manufacturing method for Wharton's jelly-derived MSCs [15].
Tissue Pre-processing:
- Collection & Transport: Obtain umbilical cord tissue following ethical guidelines and informed consent. Transport in a sterile container at 2-10°C within 24 hours of collection [15].
- Decontamination & Dissection: Rinse the cord with DPBS without Ca2+/Mg2+. Decontaminate using a 0.5% povidone-iodine solution for 3 minutes, followed by three thorough rinses in DPBS to remove residual disinfectant and blood [15].
- Vessel Removal & Mincing: Dissect the cord to expose Wharton's jelly. Carefully remove two arteries and one vein. Mince the remaining Wharton's jelly tissue into fragments of 1–4 mm^3 [15].
Enzymatic Digestion:
- Digestion Reaction: Incubate the minced tissue fragments with a GMP-grade collagenase solution at a concentration of 0.4 PZ U/mL in a shaking incubator at 37°C for 3 hours [15].
- Reaction Termination & Filtration: Neutralize the enzyme by adding a volume of culture medium containing serum or human platelet lysate (hPL). Filter the resulting cell suspension through a 100 µm cell strainer to remove undigested tissue fragments and debris [3].
- Cell Pellet Collection: Centrifuge the filtrate at 300–400 × g for 10 minutes. Carefully aspirate the supernatant and resuspend the cell pellet in an appropriate animal component-free expansion medium, such as MSC-Brew GMP Medium or NutriStem supplemented with 2-5% hPL [3] [15].
Standardized Explant Culture Protocol
Tissue Pre-processing:
- Steps 1-3: Follow the identical tissue collection, decontamination, dissection, and mincing steps as described in the enzymatic digestion protocol [15] [9].
Explant Seeding and Culture:
- Fragment Seeding: Evenly distribute the pre-weighed, minced tissue fragments directly onto the surface of a culture-treated flask (e.g., 1 g of tissue per 75 cm² flask). Allow fragments to adhere to the plastic for a brief period (e.g., 15-30 minutes) in a small volume of medium to prevent them from floating [15] [9].
- Initial Culture: Carefully add a sufficient volume of pre-warmed, animal component-free culture medium to the flask without dislodging the fragments. Incubate the culture at 37°C, 5% CO2 [15].
- Medium Exchange and Monitoring: Perform a partial medium exchange every 2-3 days, taking care not to disturb the adherent explants. Monitor the cultures microscopically for the outgrowth of fibroblast-like, adherent MSCs, which typically begins within 5-14 days [15] [9].
- First Passage (P0): Once the outgrown cells reach 70–80% confluence, remove the original tissue fragments and detach the cells using a GMP-compliant dissociation reagent for subsequent expansion and passage [9].
Workflow Visualization of GMP Isolation Pathways
The following diagram illustrates the key decision points and parallel workflows for the two isolation methods within a GMP-compliant framework.
The Scientist's Toolkit: Essential Reagents for GMP-Compliant Isolation
The transition to clinical-grade manufacturing necessitates using GMP-compliant, xeno-free reagents. The following table details key solutions for MSC isolation and initial culture.
Table 2: Research Reagent Solutions for GMP-Compliant MSC Isolation
| Reagent / Material | Function / Purpose | GMP-Compliant Examples / Specifications |
|---|---|---|
| Collagenase NB6 GMP | Enzymatic digestion of collagen in the extracellular matrix to release cells. | GMP-grade enzyme with defined PZ U/mL activity; recommended concentration: 0.4 PZ U/mL [15]. |
| Animal Component-Free Media | Supports cell growth and expansion without animal-derived components, reducing contamination risk. | MSC-Brew GMP Medium, NutriStem, MesenCult-ACF Plus Medium [3] [15] [10]. |
| Human Platelet Lysate (hPL) | Serum substitute providing growth factors and attachment factors; enhances proliferation. | GMP-compliant, pathogen-inactivated. Effective at 2% or 5% concentration [15]. |
| DPBS (without Ca2+, Mg2+) | Washing and dilution buffer; absence of divalent cations is crucial for enzymatic digestion. | Must be sterile and endotoxin-free [15]. |
| Povidone-Iodine Solution (0.5%) | Tissue decontamination to minimize microbial load from the source tissue. | Used for a defined contact time (e.g., 3 minutes) followed by thorough rinsing [15]. |
| Cell Strainers (100 µm) | Removal of undigested tissue clumps and debris post-digestion to obtain a single-cell suspension. | Sterile, non-pyrogenic [3]. |
The feasibility of mesenchymal stem cell isolation under GMP research is critically dependent on a scientifically justified and well-controlled isolation process. Both enzymatic digestion and explant methods can yield MSCs that meet the ISCT's minimal criteria for identity, provided they are followed by standardized expansion and quality control procedures [15] [9]. The decision matrix for selecting a method should be based on the specific requirements of the therapeutic development program:
- Select Enzymatic Digestion when: The primary objective is to maximize the initial yield (P0) from a valuable tissue sample, the production process can accommodate higher complexity and tighter parameter control, and the timeline for generating P0 cells is a critical factor [15].
- Select Explant Culture when: The priority is to minimize process complexity and potential stressors on cells during initial isolation, the available infrastructure favors simpler, more contained processes, and a slightly longer time to primary culture is acceptable [15].
Ultimately, the chosen protocol must be thoroughly optimized, validated, and documented within a Quality Management System. This ensures process robustness, lot-to-lot consistency, and the production of a safe, high-quality MSC-based investigational medicinal product for clinical trials [3] [28].
The Shift to GMP-Compliant, Xenogeneic-Free Culture Media
The field of regenerative medicine is undergoing a critical transformation, moving from research-grade tools toward standardized, clinically compliant production systems. This shift is particularly evident in the culture of Mesenchymal Stem Cells (MSCs), which are a cornerstone of cell-based therapies for their immunomodulatory and regenerative properties [10]. The traditional use of fetal bovine serum (FBS) in cell culture media presents significant barriers to clinical translation, including risks of xenogeneic immune responses, batch-to-batch variability, and potential contamination with adventitious agents [10] [29]. These challenges have catalyzed the move toward xenogeneic-free media formulations manufactured under Good Manufacturing Practice (GMP) guidelines. This transition is not merely a technical improvement but a fundamental requirement for ensuring the safety, efficacy, and consistent quality of MSC-based therapies destined for human clinical applications [30]. This guide examines the feasibility of isolating and expanding MSCs under these stringent new conditions, providing researchers with the technical insights needed to navigate this essential shift.
GMP and Xenogeneic-Free Media: Definitions and Significance
What Constitutes GMP-Compliant Cell Culture Media?
For cell culture media to be classified as "GMP-grade," it must be manufactured and controlled according to a comprehensive set of quality assurance principles. These guidelines ensure consistent production of high-quality pharmaceutical products and excipients while minimizing risks associated with contamination, errors, and deviations [30]. Key aspects of GMP compliance for cell culture media include:
- Quality Control and Testing: Rigorous testing for microbial contamination, endotoxin levels, pH, osmolality, and nutritional content, often following standards described in the European Pharmacopoeia [30].
- Documentation and Traceability: Comprehensive documentation of manufacturing processes, quality control procedures, and testing results, along with full traceability of all ingredients to their original sources [30].
- Validation and Qualification: Manufacturing processes must be validated, and equipment must be qualified to ensure they consistently produce media that meet predetermined specifications [30].
- Personnel and Training: Employees involved in production must be adequately trained in GMP principles and practices, forming the backbone of a compliant manufacturing environment [30].
The Critical Importance of Xenogeneic-Free Formulations
Xenogeneic-free media are specifically designed to eliminate animal-derived components, replacing them with fully defined human-derived or synthetic alternatives. This elimination addresses several critical challenges:
- Reduced Immunogenicity: Animal-derived components can introduce immunogenic non-human epitopes, such as N-glycolylneuraminic acid, which risk triggering immune responses in human recipients [31].
- Enhanced Safety Profile: Removing animal-derived components minimizes the risk of transmitting zoonotic pathogens or introducing unknown contaminants [10].
- Improved Batch-to-Batch Consistency: Chemically defined formulations offer greater reproducibility compared to biologically derived sera, which naturally vary between batches [10] [31].
Experimental Evidence: Comparing Media Performance in MSC Culture
Quantitative Assessment of MSC Growth and Functionality
Recent studies have provided compelling quantitative data demonstrating the efficacy of GMP-compliant, xenogeneic-free media for MSC culture. The following table summarizes key findings from a 2025 study investigating infrapatellar fat pad-derived MSCs (FPMSCs):
Table 1: Performance Comparison of FPMSCs Cultured in Different Media Formulations [10]
| Parameter Assessed | Standard MSC Media (with FBS) | MesenCult-ACF Plus Medium | MSC-Brew GMP Medium |
|---|---|---|---|
| Doubling Time | Baseline (reference) | Lower than standard media | Lowest across passages |
| Colony Forming Unit (CFU) Capacity | Baseline (reference) | Higher than standard media | Highest observed |
| Post-Thaw Viability | Not specified | Not specified | >95% (up to 180 days of storage) |
| Sterility and Endotoxin | Not specified | Not specified | Meets all release specifications |
This study demonstrated that FPMSCs exhibited enhanced proliferation rates when cultured in MSC-Brew GMP Medium, as evidenced by lower doubling times across passages. Furthermore, a higher colony formation capacity indicated enhanced potency, a critical attribute for therapeutic efficacy [10].
Successful GMP-Validation and Long-Term Stability
The transition to GMP-compliance extends beyond media formulation to encompass the entire cell manufacturing process. Validation studies involving MSCs from four different donors confirmed that GMP-compliant protocols yielded cells that maintained stem cell marker expression and met all product release specifications [10]. Notably, these GMP-FPMSCs maintained viability exceeding 95% even after extended cryostorage (up to 180 days), demonstrating both the robustness of the isolation protocol and the stability of the final cell product [10]. This long-term stability is essential for creating off-the-shelf allogeneic MSC therapies.
Detailed Methodologies: Isolation and Culture Under GMP Conditions
Protocol: GMP-Compliant Isolation and Expansion of FPMSCs
The following workflow details a validated method for isolating and expanding MSCs in a GMP-compliant, xenogeneic-free system [10]:
Protocol: Assessment of Critical Quality Attributes
To ensure cells manufactured under GMP conditions meet release criteria, the following quality control assessments must be performed:
- Cell Doubling Time Calculation: Cells are seeded at a density of 5 × 10³ cells/cm² and grown to 80-90% confluency over multiple passages. Doubling time is calculated using the formula: Doubling Time = (Duration of Culture × Log2) / (Log Final Cell Count - Log Initial Cell Count) [10].
- Colony Forming Unit (CFU) Assay: Cells are seeded at low densities (20, 50, 100, and 500 cells per dish) and cultured for 10 days. Colonies are then fixed with formalin, stained with Crystal Violet, and counted to assess clonogenic potential, a key indicator of stem cell potency [10].
- Immunophenotyping by Flow Cytometry: Cells are harvested and stained using a validated panel of antibodies against MSC surface markers (e.g., CD73, CD90, CD105, with absence of hematopoietic markers). Analysis is performed using a flow cytometer with appropriate gating strategies to confirm MSC identity and purity [10] [9].
Essential Reagents for GMP-Compliant MSC Research
Transitioning to GMP-compliant workflows requires careful selection of every reagent. The table below catalogues key solutions for establishing a xenogeneic-free MSC research platform.
Table 2: Research Reagent Solutions for GMP-Compliant, Xenogeneic-Free MSC Culture
| Reagent / Material | Function / Purpose | Example Product / Alternative |
|---|---|---|
| GMP-Compliant Basal Media | Provides essential nutrients and buffer system for cell growth. | MSC-Brew GMP Medium [10], MesenCult-ACF Plus Medium [10], PromoExQ Media [30] [32] |
| Xenogeneic-Free Supplement | Supplements basal media with growth factors and adhesion proteins. | Human Platelet Lysate (hPL) [33], Human AB Serum [29] [34] |
| GMP-Grade Enzymes | For tissue dissociation and cell passaging; non-animal derived. | Recombinant Trypsin, Collagenase (GMP-grade) [10] |
| Cell Culture Substrates | Functionalized surface to support cell attachment and growth. | XF-DISC (functional polymer-coated substrates) [31] |
| Characterization Kits | Validated kits for immunophenotyping per ISCT guidelines. | BD Stemflow Human MSC Analysis Kit [10] |
The collective evidence confirms that the isolation and expansion of MSCs under GMP-compliant, xenogeneic-free conditions is not only feasible but also advantageous for clinical translation. Studies consistently show that MSCs cultured in advanced GMP media can demonstrate superior proliferative capacity, enhanced potency, and excellent post-preservation viability compared to those maintained in traditional FBS-containing systems [10] [33]. The availability of rigorously tested, GMP-grade reagents and standardized protocols provides researchers with the necessary toolkit to overcome the historical challenges of batch variability and safety concerns. As the field advances, the adoption of these standardized systems will be paramount for generating reproducible, safe, and effective MSC-based therapies, ultimately fulfilling their promise in regenerative medicine.
The transition of Mesenchymal Stem Cell (MSC) therapies from research to clinical application hinges on the establishment of robust, reproducible, and standardized manufacturing processes compliant with Good Manufacturing Practice (GMP). Central to this endeavor is the optimization of critical process parameters, primarily seeding density and population doubling time, which fundamentally determine the quality, efficacy, and safety of the final cell product [21]. These parameters are not merely indicators of growth; they are pivotal determinants of MSC stemness, functionality, and therapeutic potency [35]. The inherent heterogeneity of MSC cultures, influenced by donor variability and tissue source, necessitates a rigorously controlled manufacturing process to ensure a consistent and reliable product [21]. This guide details the experimental approaches and technical considerations for optimizing these parameters within a GMP framework, providing a foundation for the feasible isolation and expansion of MSCs for translational research.
Seeding Density: A Critical Determinant of MSC Quality and Homogeneity
The Impact of Seeding Density on Colony Formation and Cell Fitness
Seeding density, defined as the number of cells initially plated per unit area of culture surface, directly influences the clonogenic potential, proliferative capacity, and ultimate purity of the MSC population. Optimizing this parameter is essential for selecting for specific subpopulations with enhanced therapeutic potential.
A seminal study investigating the seeding density of bone marrow mononuclear cells (MNCs) revealed that lower densities (e.g., (1.25 \times 10^5) cells/cm²) foster the development of distinct colonies from single progenitor cells [36]. This low-density culture allows for the proportional expansion of highly proliferative MSCs over time, while faster-enlarging, less proliferative cells can be selectively removed through adjusted detachment protocols, thereby increasing the purity of the final product [36]. In contrast, high seeding densities ((1.25 \times 10^6) cells/cm²) lead to rapid confluence and do not favor this selective enrichment, resulting in MSCs with inferior proliferative and differentiation potential [36].
For the expansion of already-isolated MSCs, a seeding density of approximately 5,000 cells/cm² is widely recommended to balance efficient proliferation with the maintenance of stemness characteristics [37]. This density provides adequate space and resources for cell division while preventing the negative effects of overcrowding, such as nutrient depletion and accelerated differentiation.
Table 1: Impact of Mononuclear Cell (MNC) Seeding Density on MSC Isolation Outcomes
| Seeding Density (cells/cm²) | Colony Formation Characteristics | Proliferative Potential of Resulting MSCs | Differentiation Potential |
|---|---|---|---|
| Low ((1.25 \times 10^5)) | Distinct, well-separated colonies [36] | Significantly higher [36] | Enhanced adipogenic and chondrogenic potential [36] |
| High ((1.25 \times 10^6)) | Rapid, confluent growth; no distinct colonies [36] | Lower [36] | Reduced (except possibly osteogenic) [36] |
Experimental Protocol: Optimizing and Assessing Seeding Density
Objective: To determine the optimal seeding density of MNCs or passage MSCs for maximizing the yield and quality of MSCs.
Materials:
- Source of MSCs (e.g., bone marrow aspirate, infrapatellar fat pad tissue)
- GMP-compliant, animal component-free culture medium (e.g., MSC-Brew GMP Medium [10])
- Culture vessels (tissue-culture treated)
- Phosphate-Buffered Saline (PBS)
- GMP-compliant detachment agent (e.g., TrypLE Select [36])
- Hemacytometer or automated cell counter
- Crystal Violet stain (for colony-forming assays)
Method:
- Cell Isolation: Isolate MNCs from tissue using a GMP-compliant protocol, such as collagenase digestion followed by centrifugation and filtration [10].
- Experimental Seeding: Seed the isolated MNCs at a range of densities (e.g., (4.0 \times 10^4), (1.25 \times 10^5), (2.5 \times 10^5), (6.0 \times 10^5), (1.25 \times 10^6) cells/cm²) in culture vessels [36]. For passaging established MSCs, test densities around 5,000 cells/cm².
- Culture Maintenance: Culture cells in a standardized, animal component-free medium. Change the medium every 48-72 hours [37].
- Data Collection and Analysis:
- Colony Formation Unit (CFU) Assay: After ~10-14 days, fix cells with formalin and stain with Crystal Violet. Manually count the number of colonies formed [10] [36]. High-quality isolates are characterized by a high number of CFUs.
- Cell Morphology: Use time-lapse imaging to monitor colony formation and cell morphology daily [36].
- Flow Cytometry: At passage 3, analyze cells for standard MSC positive (CD73, CD90, CD105) and negative (CD34, CD45) surface markers to confirm identity and purity [10] [38].
- Proliferation Assays: Use population doubling time calculations and assays for markers like Ki67 and PCNA to assess growth rates [36].
Population Doubling Time: A Key Metric for MSC Expansion and Stemness
Understanding Doubling Time and Its Implications
Population doubling time (PDT) is a critical measure of the average time required for a cell population to double in number during the exponential growth phase. It serves as a vital indicator of MSC fitness, proliferative capacity, and biological age. A lower, consistent doubling time is indicative of healthy, stemness-retaining cells, while an increasing PDT is a hallmark of cellular senescence and reduced therapeutic potency [35] [39].
The PDT is profoundly influenced by several factors, including the culture medium formulation, donor age, and passage number. For instance, MSCs cultured in optimized, GMP-compliant media like MSC-Brew GMP Medium have demonstrated significantly lower doubling times compared to those in standard media, underscoring the impact of media composition on growth kinetics [10]. Furthermore, PDT tends to increase with successive passages, reflecting the gradual senescence of the culture [38] [39].
Table 2: Impact of Culture Conditions on Mesenchymal Stem Cell Doubling Time
| Culture Condition | Reported Doubling Time | Context and Implications |
|---|---|---|
| MSC-Brew GMP Medium | Lower doubling times across passages [10] | Indicates enhanced proliferation and maintained stemness under GMP conditions [10]. |
| α-MEM vs. DMEM | ~1.85-1.99 days vs. ~1.90-2.25 days [38] | Suggests a potential, though not always significant, advantage for α-MEM in supporting proliferation [38]. |
| High-Passage Cells (P6) | Increased doubling time [38] [39] | Reflects replicative senescence and a gradual loss of proliferative capacity. |
Experimental Protocol: Calculating and Monitoring Population Doubling Time
Objective: To accurately calculate the population doubling time of MSCs across multiple passages to monitor culture health and stability.
Materials:
- Cultured MSCs
- Hemacytometer or automated cell counter
- GMP-compliant culture medium and detachment reagents
Method:
- Seeding and Harvest: Seed MSCs at a known, optimal density (e.g., 5,000 cells/cm²). When cultures reach 80-90% confluency, detach and count the cells using a hemacytometer [10].
- Calculation: The doubling time can be calculated using the standard formula:
( \text{Doubling Time} = \frac{T \times \ln(2)}{\ln(Nf / Ni)} )
Where:
- ( T ) = time in culture (hours or days)
- ( Ni ) = initial number of cells seeded
- ( Nf ) = final number of cells harvested
- Longitudinal Tracking: Repeat this calculation at each passage over at least 3 passages to establish a growth kinetic profile and identify any signs of premature senescence [10].
- Correlative Analysis: Correlate PDT data with other quality metrics, such as CFU capacity, surface marker expression, and differentiation assays, to build a comprehensive picture of cell quality.
An Integrated Workflow for GMP-Compliant MSC Manufacturing
The optimization of seeding density and doubling time is not performed in isolation but is part of an integrated workflow from cell isolation to final product release. The diagram below illustrates this process and the place of these critical parameters within it.
The Scientist's Toolkit: Essential Reagents for GMP-Compliant MSC Process Optimization
The successful translation of MSC manufacturing to the clinic requires a transition from research-grade to GMP-compliant reagents. The following table details key materials essential for experiments optimizing seeding density and doubling time.
Table 3: Essential Reagents for GMP-Compliant MSC Process Development
| Reagent / Material | Function | GMP-Compliant Example / Consideration |
|---|---|---|
| Animal Component-Free Medium | Provides defined nutrients and factors for cell growth, eliminating xenogenic risks. | MSC-Brew GMP Medium [10], MesenCult-ACF Plus Medium [10] |
| Human Platelet Lysate (hPL) | A human-derived serum alternative for cell culture media supplementation. | PLTMax hPL [39]; requires screening for pathogen transmission risk [21]. |
| GMP-Compliant Detachment Reagent | Enzymatically dissociates adherent cells for passaging with minimal damage. | TrypLE Select [36] (a recombinant enzyme solution). |
| Cell Culture Vessels | Surface for cell attachment and expansion. | Tissue-culture treated flasks/plates; material should be validated for compatibility. |
| Flow Cytometry Antibodies | Characterizes MSC surface marker profile for identity and purity. | BD Stemflow Human MSC Analysis Kit [10]; kits must be validated for accuracy. |
The feasibility of manufacturing MSCs under GMP guidelines is inextricably linked to the precise control of critical process parameters. The optimization of seeding density is a powerful tool for selecting a high-fidelity, therapeutically potent MSC population from the outset. Concurrently, the vigilant monitoring of population doubling time provides an essential, real-time readout of culture health and stability throughout expansion. When systematically integrated into a closed, well-defined manufacturing process utilizing GMP-compliant reagents, these parameters form the foundation of a robust and reproducible production system. This rigorous approach ensures that the final MSC product is not only consistent and scalable but also meets the stringent criteria for identity, purity, potency, and safety required for successful clinical translation [10] [21].
The successful translation of Mesenchymal Stem Cell (MSC) therapies from preclinical research to clinical application hinges on the development of robust, scalable manufacturing processes that comply with Good Manufacturing Practice (GMP) standards. For MSC-based products intended for human use, regulatory bodies like the FDA and EMA classify them as Advanced Therapy Medicinal Products (ATMPs), making GMP compliance mandatory [1]. Scalable manufacturing is not merely a production efficiency concern but a fundamental component of feasibility and quality assurance, ensuring that MSC therapies can be produced with consistent purity, potency, and safety profiles across different production scales.
The transition from manual, open processes to automated, bioreactor-based systems represents a critical pathway to overcome the inherent limitations of traditional cell culture. Manual processes, while useful in research and development (R&D), pose significant risks for clinical manufacturing, including potential for contamination and production inconsistencies due to difficulty in implementing stringent process controls [40]. This technical guide examines the core technical, operational, and regulatory considerations for implementing scalable expansion systems within the context of GMP-compliant MSC research and manufacturing.
MSC Isolation and Culture Under GMP-Compliant Conditions
The foundation of any scalable process is a well-defined and reproducible isolation and culture protocol. For GMP-compliance, the entire process, from sourcing to cryopreservation, must be meticulously controlled and documented.
MSCs can be isolated from a variety of sources, each with unique advantages. Common somatic sources include bone marrow (BM), adipose tissue (AT), and dental pulp (DP), while perinatal sources include umbilical cord (UC), placenta, and amniotic fluid (AF) [9]. The International Society for Cell & Gene Therapy (ISCT) has established minimal criteria for defining MSCs: adherence to plastic, specific surface marker expression (e.g., CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-), and tri-lineage differentiation potential (osteogenic, adipogenic, chondrogenic) [9].
Validated isolation methods include:
- Enzymatic Digestion: Tissue is minced and digested with collagenase (e.g., 0.1% collagenase for 2 hours at 37°C for infrapatellar fat pad tissue) to dissociate cells [10] [9].
- Density Gradient Centrifugation: Using media like Ficoll-Paque or Percoll to separate mononuclear cells, including MSCs, from other cellular components [9].
- Explant Culture/Adherence Method: Tissue fragments are placed in culture vessels, allowing MSCs to migrate out and adhere to the plastic surface [9]. This method is particularly common for umbilical cord Wharton's Jelly-derived MSCs (WJ-MSCs) [9].
Transition to Animal Component-Free Media
A critical step in GMP-compliance is the elimination of animal-derived components, such as fetal bovine serum (FBS), to avoid risks of immunogenicity and contamination. Research has demonstrated the efficacy of animal component-free, GMP-compliant media formulations. One study directly compared MesenCult-ACF Plus Medium and MSC-Brew GMP Medium against standard FBS-containing media for culturing infrapatellar fat pad-derived MSCs (FPMSCs) [10]. The results showed that MSC-Brew GMP Medium supported enhanced proliferation, as evidenced by lower population doubling times across passages, and increased colony-forming unit (CFU) capacity, indicating enhanced potency [10].
Table 1: Key Research Reagent Solutions for GMP-Compliant MSC Culture
| Reagent / Material | Function / Purpose | GMP-Compliant Examples / Notes |
|---|---|---|
| Animal-Free Media | Provides nutrients and growth factors without animal-derived components, reducing contamination risk. | MSC-Brew GMP Medium, MesenCult-ACF Plus Medium [10] |
| Collagenase | Enzymatic digestion of tissue to isolate stromal vascular fraction. | Must be GMP-grade; concentration and time vary by tissue source (e.g., 0.1% for 2h for fat pad) [10] |
| Cell Separation Media | Isolates mononuclear cells via density gradient centrifugation. | GMP-grade Ficoll-Paque or Percoll [9] |
| Cryopreservation Medium | Long-term storage of cell banks. | Typically contains a cryoprotectant like DMSO and a protein base (e.g., human albumin), not FBS [10] |
| Characterization Kits | Confirms MSC identity and purity per ISCT criteria. | BD Stemflow Human MSC Analysis Kit (Flow Cytometry) [10] |
Quantitative Comparison: Manual vs. Bioreactor-Based Expansion
The choice between scale-out (multiple manual units) and scale-up (single, larger bioreactors) has profound implications on process outcomes and economic viability.
Table 2: Performance and Economic Comparison of Expansion Systems
| Parameter | Manual Flask / Scale-Out | Bioreactor-Based Scale-Up |
|---|---|---|
| Cell Yield | Limited by surface area/logistics; linear scaling with unit count. | High, concentrated yield; supports 3D culture for higher densities [41]. |
| Viability / Consistency | High risk of inconsistency and heterogeneity between units [40]. | Improved process control enhances consistency and viability [42]. |
| Contamination Risk | Higher risk due to frequent open handling and manual fluid transfers [42]. | Lower risk via functional closed systems and reduced manual intervention [40] [42]. |
| Labor Intensity | Very high; requires skilled technicians for repetitive handling [41]. | Significantly reduced after initial setup; enables automation [42] [43]. |
| Process Control/Monitoring | Limited; relies on offline sampling. | Advanced; allows real-time monitoring and control of parameters like pH, DO, and temperature [44] [45]. |
| GMP Compliance | Challenging due to open processes and documentation burden. | Facilitated by automation, closed systems, and built-in data logging [43]. |
| Cost Drivers | Dominated by labor, facility space, and quality control for multiple batches [42]. | Higher initial capital investment, but lower per-dose cost at scale [42]. |
A pivotal study by Multiply Labs demonstrated that automated robotic systems could achieve cell yields and viability statistically equivalent to manual processes for T-cell expansion, with the added benefit of zero contamination in the automated runs versus contamination in one of the manual replicates [42]. While this data is from T-cells, the principle underscores a key advantage of automation relevant to MSC manufacturing.
Bioreactor Systems: Objectives, Types, and Workflows
Objectives and Benefits for MSC Expansion
Bioreactor systems are designed to tightly control the cellular microenvironment, leading to more efficient and reproducible cell expansion. Their primary objectives include [44] [45]:
- Scale-up and Scale-out: Increasing volume or unit number to achieve clinically relevant cell numbers (often hundreds of millions to billions) [41] [45].
- Process Control and Automation: Automating fluid handling, feeding, and environmental control (temperature, pH, dissolved oxygen) to minimize human error and variability [40] [44].
- GMP Compliance: Enabling functionally closed processing, reducing contamination risks, and facilitating comprehensive data logging for quality assurance [1] [43].
Bioreactor Platforms and Technologies
Various bioreactor designs are employed for MSC expansion, each with distinct mechanisms and advantages.
Stirred-Tank Bioreactors: Used with microcarriers that provide a surface for adherent MSC growth in suspension culture, enabling high-volume scale-up [41]. They require careful optimization to avoid damaging shear forces [41].
Hollow Fiber Bioreactors (HFBs): Such as the Terumo Quantum system, consist of capillary membranes that create a high surface-area-to-volume ratio for cell growth. Medium circulates through the fibers, allowing for efficient nutrient delivery and waste removal in a closed, automated system [43] [45].
Rocking Motion Bioreactors: Systems like the Wave bioreactor use a rocking motion to mix cells and medium in a single-use bag, providing good oxygen transfer and scalability for suspension cultures [45].
New Flexible Platforms: Innovations like the Bioreactor with Expandable Culture Area (BECA) aim to streamline the transition from R&D to manufacturing. The BECA platform uses the same core vessel design for both manual (BECA-S) and automated (BECA-Auto) operation, minimizing process adaptation needs during tech transfer [40].
Implementation and Validation Strategies
Experimental Protocol for Process Comparison
To validate a transition from manual to bioreactor-based expansion, a structured comparative study is essential. The following methodology, adapted from published approaches, provides a framework [10] [42]:
- Cell Source and Inoculum: Use a single, well-characterized GMP-compliant MSC working cell bank (e.g., FPMSCs or BM-MSCs from consented donors) [10]. Use the same pre-culture medium and passage number for both systems.
- Experimental Arms:
- Manual Control: Culture cells in multilayer flasks or culture bags. Perform all medium changes and harvesting manually in a Biosafety Cabinet (BSC).
- Bioreactor System: Culture cells in the selected bioreactor (e.g., BECA-Auto, Quantum, stirred-tank with microcarriers) following the automated protocol.
- Culture Conditions: Maintain both systems at 37°C, 5% CO2, and 90% humidity. Use the same GMP-compliant, animal component-free culture medium (e.g., MSC-Brew GMP Medium) [10].
- Key Performance Indicators (KPIs) and Analytics:
- Cell Yield and Viability: Measure total nucleated cell count and viability (e.g., via Trypan Blue exclusion) at harvest [10] [42].
- Population Doubling Time (PDT): Calculate PDT across passages using the formula: ( PDT = \frac{T \times \ln(2)}{\ln(Nf) - \ln(Ni)} ), where T is culture time, Ni is the initial cell number, and Nf is the final cell number [10].
- Potency and Functionality: Perform CFU assays to assess clonogenic potential [10]. Analyze trilineage differentiation potential post-expansion [9].
- Phenotype Purity: Use flow cytometry (e.g., with a BD Stemflow MSC Analysis Kit) to confirm expression of CD73, CD90, CD105 and lack of hematopoietic markers [10] [9].
- Sterility and Quality: Test for mycoplasma, endotoxin, and microbial contamination per pharmacopoeial methods (e.g., BacT/Alert) [10].
Strategic Considerations for GMP Feasibility
Successfully implementing a scalable system for an MSC therapy requires careful planning.
- Early Integration: Consider scalability and automation during early process development, not as an afterthought. This reduces the need for costly and time-consuming process re-validation later [41] [43].
- Closed-System Processing: Prioritize technologies that enable a functionally closed processing environment from cell isolation through fill-and-finish to minimize contamination risk [43].
- Data and Documentation: Leverage the automated data logging capabilities of bioreactors to build a comprehensive data package for your Chemistry, Manufacturing, and Controls (CMC) section in regulatory submissions [43].
- Partner Selection: For many organizations, partnering with an experienced Contract Development and Manufacturing Organization (CDMO) that offers complete GMP iPSC and MSC platforms can accelerate the path to the clinic [46].
The transition from manual, open-process expansion to automated, bioreactor-based systems is a critical and feasible step for establishing GMP-compliant manufacturing processes for mesenchymal stem cell therapies. While manual scale-out strategies may suffice for early R&D and proof-of-concept studies, they introduce significant risks and economic burdens that hinder clinical translation and commercial viability.
Bioreactor systems address these challenges by providing a path to higher cell yields, superior process control, reduced contamination risk, and enhanced operational efficiency. By adopting a strategic approach that prioritizes scalability and GMP principles from the outset, and by leveraging validated experimental protocols for process comparison and qualification, researchers and drug development professionals can robustly establish the feasibility of their MSC isolation and expansion processes. This ensures that promising regenerative medicines can successfully navigate the path from the laboratory bench to the patient bedside.
Overcoming Manufacturing Hurdles: Ensuring Product Consistency and Potency
Addressing Donor and Source-Related Heterogeneity
The remarkable therapeutic potential of Mesenchymal Stromal Cells (MSCs) in regenerative medicine is tempered by a significant challenge: their inherent heterogeneity. For MSC-based Advanced Therapy Medicinal Products (ATMPs) to be feasible under Good Manufacturing Practice (GMP) standards, this variability must be understood and controlled [47]. Product heterogeneity is suspected to be a major reason for inconsistent outcomes in clinical trials, making interpretation of efficacy difficult and complicating comparisons across studies [47]. This heterogeneity stems broadly from three interconnected categories: the biological source of the cells (tissue origin), the attributes of the donor, and the technical protocols used for manufacturing [47]. Addressing these factors is not merely an academic exercise; it is a prerequisite for developing reproducible, safe, and effective GMP-compliant MSC therapies. This guide provides a technical roadmap for researchers and drug development professionals to systematically identify, characterize, and mitigate donor and source-related heterogeneity.
Origins and Impact of Heterogeneity
The heterogeneity of MSC-based products can be traced to multiple upstream variables, each contributing distinct functional consequences that must be considered for clinical application.
Tissue Source
While MSCs from different sources share fundamental characteristics—adherence to plastic, specific surface marker expression, and trilineage differentiation potential—they exhibit distinct functional profiles. These differences are critical when selecting a cell source for a specific therapeutic indication.
Table 1: Functional Heterogeneity Across Common MSC Sources
| MSC Source | Key Advantages | Proliferative Capacity | Differentiation Potential | Immunomodulatory & Secretory Profile |
|---|---|---|---|---|
| Bone Marrow (BM) | Considered the "gold standard"; well-characterized [10] | Lower proliferative potential compared to AD-MSCs [48] | Higher osteogenic and chondrogenic potential [48] | Advantages in secretion of SDF-1 and HGF; lower immunomodulatory potency than AD-MSCs [48] |
| Adipose Tissue (AT) | Minimally invasive harvest; abundant tissue source [10] [48] | Greater proliferative potential than BM-MSCs [48] | Lower osteogenic and chondrogenic potential [48] | More potent immunomodulatory effects; advantages in secretion of bFGF, IFN-γ, and IGF-1 [48] |
| Infrapatellar Fat Pad (FP) | Harvested as surgical waste; less invasive than BM [10] | Enhanced proliferation in optimized GMP media (e.g., MSC-Brew) [10] | Data less established; requires further characterization | Actively investigated for inflammatory conditions like osteoarthritis [10] |
| Umbilical Cord (Wharton's Jelly) | Perinatal source; considered immunologically naive | Varies with isolation method and culture conditions [9] | Multipotent differentiation capacity confirmed [9] | Fetal phenotype suggests strong paracrine activity; detailed comparisons ongoing |
The following diagram summarizes the primary sources of heterogeneity and their downstream impacts on the final MSC product.
Donor-Specific Factors
Even within the same tissue source, significant variability is introduced by donor-specific biological factors. Donor age, sex, body mass index (BMI), and underlying health conditions can profoundly influence MSC phenotype, morphology, differentiation potential, and overall function [47]. This intrinsic variability presents a major challenge for standardizing allogeneic cell products.
Quantitative Characterization of Heterogeneity
Robust, quantitative assays are essential for mapping the functional landscape of MSCs from different donors and sources. The data below, compiled from comparative studies, highlights the measurable nature of this heterogeneity.
Table 2: Quantitative Comparison of BM-MSCs and AT-MSCs Cultured in Human Platelet Lysate (hPL) Media
| Biological Characteristic | Bone Marrow (BM)-MSCs | Adipose Tissue (AT)-MSCs | Significance & Notes |
|---|---|---|---|
| Proliferation (Cumulative Population Doubling) | Lower | Higher | AT-MSCs exhibit greater expansion potential over serial passages [48] |
| Colony-Forming Unit (CFU) Efficiency | No significant difference reported | No significant difference reported | Similar capacity for self-renewal at the clonal level [48] |
| Osteogenic Differentiation | Higher | Lower | Quantified by alkaline phosphatase activity, calcium deposition, and OCN expression [48] |
| Chondrogenic Differentiation | Higher | Lower | Measured by GAG deposition and ACAN gene expression [48] |
| Adipogenic Differentiation | No significant difference reported | No significant difference reported | Assessed by lipid vacuole formation and FABP4 expression [48] |
| Secretion of bFGF, IFN-γ, IGF-1 | Lower | Higher | Measured via ELISA/multiplex assays; influences tissue repair and immunomodulation [48] |
| Secretion of SDF-1, HGF | Higher | Lower | Key factors for homing and angiogenesis [48] |
| Immunomodulatory Potency | Lower | More potent | Based on inhibition of peripheral blood mononuclear cell (PBMC) proliferation [48] |
Experimental Protocols for Isolation and Characterization
Standardized protocols are the foundation for reliably assessing and comparing MSCs from different origins.
Protocol: Isolation of MSCs from Infrapatellar Fat Pad (FP)
This protocol exemplifies a GMP-compliant isolation process for a specific tissue source [10].
- 1. Tissue Acquisition & Ethics: Obtain infrapatellar fat pad (IFP) tissue as waste tissue from patients undergoing procedures like anterior cruciate ligament (ACL) reconstructive surgery, following informed consent and ethical committee approval [10].
- 2. Tissue Processing: Mince the IFP tissue into small pieces of approximately 1mm³ [10].
- 3. Enzymatic Digestion: Digest the tissue fragments using 0.1% collagenase in serum-free media for 2 hours at 37°C under continuous agitation [10].
- 4. Cell Separation: Centrifuge the digested tissue at 300 × g for 10 minutes. Carefully remove the supernatant and the surfactant layer [10].
- 5. Washing and Filtration: Resuspend the cell pellet in Phosphate-Buffered Saline (PBS) and filter the suspension through a 100 μm filter to remove debris and undigested tissue aggregates [10].
- 6. Initial Plating: Centrifuge the filtrate again, resuspend the pellet in standard MSC media (e.g., MEM α supplemented with 10% FBS), and plate the cells in a culture flask [10].
- 7. Cryopreservation (Optional): Cells can be frozen at the end of the first passage using a cryoprotectant like 10% DMSO in FBS [10].
Protocol: Flow Cytometry for Immunophenotyping
Flow cytometry is critical for confirming MSC identity and purity according to ISCT criteria [10] [47] [9].
- 1. Cell Preparation: Harvest MSCs at the recommended passage (e.g., passage 3) using a standard dissociation reagent. Wash the cells twice with PBS containing 1% bovine serum albumin (BSA) [10] [48].
- 2. Antibody Staining: Resuspend approximately 5x10⁵ cells per tube in a blocking solution (e.g., 3% serum in PBS). Incubate the cells with fluorochrome-conjugated monoclonal antibodies against positive markers (CD105, CD73, CD90) and negative markers (CD45, CD34, CD14/CD11b, CD79a/CD19, HLA-DR) for 30-60 minutes in the dark [10] [48].
- 3. Analysis: Wash the cells to remove unbound antibody and resuspend in an appropriate buffer. Acquire data on a flow cytometer (e.g., BD FACS Fortessa), analyzing at least 10,000 events per sample. The positive expression threshold is typically defined as fluorescence greater than 99% of an unstained control [10] [48].
- 4. Interpretation: A population is considered acceptable for release as MSCs if ≥95% express the positive markers and ≤2% express the negative markers [47].
Strategies to Mitigate Heterogeneity in GMP Production
To ensure product consistency, proactive strategies must be integrated into the GMP workflow to minimize the impact of donor and source variability.
The Scientist's Toolkit: Key Reagents for Standardization
Table 3: Essential Research Reagents for Managing Heterogeneity
| Reagent / Material | Function in Mitigating Heterogeneity | Specific Examples & Notes |
|---|---|---|
| Xeno-Free, GMP Media | Eliminates batch-to-batch variability and immunogenic risks of FBS; supports consistent expansion. | MSC-Brew GMP Medium, MesenCult-ACF Plus Medium. MSC-Brew showed enhanced proliferation and colony formation for FPMSCs [10]. |
| Human Platelet Lysate (hPL) | Human-derived supplement alternative to FBS; promotes growth while enhancing safety profile. | Prepared from pooled platelet-rich plasma; requires heparin anticoagulation in media [48]. |
| GMP-Grade Enzymes | Ensure reproducible and safe dissociation of cells during isolation and passaging. | GMP-grade Collagenase (e.g., Type I) and Trypsin alternatives (e.g., Accutase) [10] [49]. |
| Flow Cytometry Kits | Standardized panels for immunophenotyping ensure consistent quality control and product identity. | BD Stemflow Human MSC Analysis Kit [10]. |
| GMP Cell Separation Kits | Isolate specific cell populations with high purity and viability under closed-system, scalable conditions. | Microbubble-based kits (e.g., Akadeum) for negative selection of T cells; gentle on cells and closed-system compatible [50]. |
A Strategic Workflow for GMP Compliance
The following diagram outlines a comprehensive workflow, from donor screening to final product release, designed to control for heterogeneity.
Implementing this workflow involves several key mitigation strategies:
- Standardized Culture Conditions: Replacing FBS with defined, xeno-free media is paramount. Studies demonstrate that MSCs cultured in serum-free media (SFM) exhibit more stable population doubling times into later passages, lower cellular senescence, reduced immunogenicity, and higher genetic stability compared to those cultured in FBS [49]. Furthermore, specific GMP media like MSC-Brew GMP Medium have been shown to enhance the proliferation and colony-forming potency of FPMSCs [10].
- Rigorous Quality Control & Release Criteria: Adherence to the ISCT's minimal criteria is the baseline [47]. GMP production requires expanded release specifications, which have been validated to include >95% viability (far exceeding the >70% minimum requirement) and confirmation of sterility (e.g., via Bact/Alert and mycoplasma assays), even after extended cryostorage (e.g., 180 days) [10].
- Donor and Cell Pooling: To smooth out individual donor variations, creating pools of MSCs from multiple donors is a proposed strategy to generate a more standardized and reproducible product with an averaged biological activity [47].
Donor and source-related heterogeneity is an inherent and formidable challenge in the development of MSC-based ATMPs. However, as detailed in this guide, it is not insurmountable. By systematically understanding the origins of variability, employing robust quantitative characterization methods, and implementing stringent, standardized GMP protocols—from donor selection and xeno-free culture to comprehensive quality control—researchers and clinicians can significantly mitigate its impact. The feasibility of mesenchymal stem cell isolation and manufacturing under GMP research hinges on this disciplined approach. Embracing these strategies is essential to advance the field from promising preclinical studies to consistent, safe, and effective clinical therapies.
Strategies for Batch-to-Batch Consistency and Scalability
The transition of Mesenchymal Stem Cell (MSC) therapies from research to clinical application represents a pivotal milestone in regenerative medicine. These cells, also referred to as Mesenchymal Stromal Cells or Medicinal Signaling Cells, have demonstrated significant potential for treating a wide range of conditions, from skeletal disorders to inflammatory diseases like graft-versus-host disease (GvHD) [10] [51]. However, this transition necessitates adherence to Good Manufacturing Practice (GMP) guidelines, which ensure that production is consistent and that products are controlled to state-of-the-art quality standards appropriate for human use [1]. Within the regulatory frameworks of both the European Union and the United States, MSC-based products are classified as Advanced Therapy Medicinal Products (ATMPs), placing them under stringent pharmaceutical regulations [1] [52]. The core challenge in this regulatory landscape is achieving batch-to-batch consistency and scalable production without compromising the critical quality attributes of the cells, a challenge that must be overcome to ensure the feasibility and success of clinical applications [10] [51].
The GMP Framework for MSC Manufacturing
Regulatory Foundations
GMP serves as a quality assurance tool intended to ensure that production is consistent and that products are controlled to quality standards appropriate for their intended use [1]. For MSC therapies, this means that the entire manufacturing process—from donor selection to final product fill/finish—must be meticulously controlled and documented.
- Legal Status: In the European Union, the ATMP Regulation (Regulation (EC) No 1394/2007) classifies gene therapy, somatic cell therapy, and tissue-engineered products as pharmaceuticals when intended for human use [1] [52]. Similarly, in the United States, the FDA regulates human cells, tissues, and cellular-based products under Title 21 of the Code of Federal Regulations (21 CFR 1271) [52].
- Core Principles: GMP guidelines cover quality assurance for all manufacturing aspects, including premises, equipment, staff training, operational processes, packaging, storage conditions, and overarching documentation systems [1]. This integrated system aims to protect patient health by ensuring consistent product quality and safety.
Critical Quality Attributes for MSCs
According to the International Society for Cellular Therapy (ISCT), MSCs must meet specific minimal criteria to be defined as such [53]. These criteria form the foundation for quality control testing throughout the manufacturing process:
- Plastic Adherence: MSCs must adhere to plastic surfaces under standard culture conditions.
- Surface Marker Expression: ≥95% of the population must express CD73, CD90, and CD105, while ≤2% must express hematopoietic markers (CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR) [53].
- Multipotent Differentiation Potential: The cells must demonstrate the ability to differentiate into osteoblasts, adipocytes, and chondroblasts in vitro [53] [51].
These criteria provide the fundamental benchmarks for ensuring product identity and purity throughout the scaling process.
Strategic Pillar I: Standardized Cell Sourcing and Donor Selection
The foundation of batch consistency begins with the careful selection of starting materials. Variability in source tissue and donor characteristics significantly impacts the biological properties and functionality of the final MSC product [51] [52].
Tissue Source Considerations
Different tissue sources offer distinct advantages and challenges for GMP-compliant manufacturing:
Table: Comparison of MSC Tissue Sources for GMP Manufacturing
| Tissue Source | Advantages | Disadvantages | Clinical Relevance |
|---|---|---|---|
| Infrapatellar Fat Pad (FP) | Less invasive harvest; often surgical waste; reduced patient morbidity [10] | Less characterized than traditional sources [10] | Promising for osteoarthritis; demonstrated GMP feasibility [10] |
| Adipose Tissue (A-MSCs) | Abundant tissue source; ~500x concentration vs. bone marrow; high proliferative/secretory capacity [51] | Donor health (obesity, diabetes) affects function [51] | Potent immunomodulation; used in numerous clinical trials [51] |
| Bone Marrow (BM-MSCs) | Considered the "gold standard"; well-characterized [10] [51] | Invasive, painful harvest; donor-site morbidity [10] [51] | Historically most used source; strong osteogenic potential [51] |
| Umbilical Cord | Non-invasive collection; young cell source [54] | Limited expansion potential compared to other sources [51] | Increasingly popular for allogeneic banking [54] |
| iPSC-Derived (iMSCs) | Unlimited starting material; high batch-to-batch uniformity [54] | Requires extensive characterization and safety testing [54] | Emerging as scalable, consistent alternative to primary MSCs [54] |
Donor Selection and Screening
Robust donor screening protocols are essential for minimizing initial variability. Directive 2004/23/EC in the EU and 21 CFR 1271 in the US provide frameworks for verifying the quality and safety of human tissues and cells used as starting materials [52]. Key considerations include:
- Donor Health: A-MSCs derived from obese or type 2 diabetic patients showed reduced capacity to suppress lymphocyte proliferation and activate M2 macrophages [51].
- Donor Age: MSCs from aged rats failed to elicit T-cell suppression, while BM-MSC mediated immunosuppression was more effective in young rats [51].
- Screening Protocols: Implementation of detailed inclusion/exclusion criteria, informed consent procedures, and infectious disease testing as mandated by regulatory authorities [10] [52].
Strategic Pillar II: Optimized Culture Platform and Process Control
The transition from research-grade to GMP-compliant culture systems requires eliminating animal-derived components and implementing well-defined, standardized protocols.
Xeno-Free Media Formulations
The use of animal component-free media is crucial for eliminating risks associated with animal-derived components, such as potential contamination, immunogenicity, and batch-to-batch variability [10]. A 2025 study systematically compared media formulations for culturing infrapatellar fat pad-derived MSCs (FPMSCs) and provided quantitative data on performance [10].
Table: Quantitative Comparison of Animal Component-Free Media Performance [10]
| Performance Metric | MSC-Brew GMP Medium | MesenCult-ACF Plus Medium | Standard MSC Media (with FBS) |
|---|---|---|---|
| Doubling Time | Lower across passages | Higher than MSC-Brew | Not specified (used as baseline) |
| Colony Forming Unit (CFU) Capacity | Higher | Lower than MSC-Brew | Not specified (used as baseline) |
| Post-Thaw Viability | >95% (exceeding >70% requirement) | Not specified | Not specified |
| Sterility Maintenance | Maintained up to 180 days | Not specified | Not specified |
| Marker Expression | Maintained | Not specified | Not specified |
Detailed Experimental Protocol: Media Comparison Study
The following methodology from the 2025 study provides a template for evaluating culture media under GMP-like conditions [10]:
- Cell Source: FPMSCs isolated from three different patients (aged 20-24) undergoing ACL reconstructive surgery, with informed consent and ethical approval (Houston Methodist Hospital, Pro00015718) [10].
- Isolation Protocol: Infrapatellar fat pad tissue was cut into ~1mm³ pieces and digested with 0.1% collagenase in serum-free media for 2 hours at 37°C. The digested tissue was centrifuged, filtered through a 100μm filter, and resuspended in standard MSC media [10].
- Culture Conditions: Cells were passaged at 80-90% confluency and seeded at a density of 5 × 10³ cells/cm² in the test media [10].
- Assessment Methods:
- Doubling Time: Calculated over three passages using cell counts from a Bright-Line Hemacytometer.
- Colony Forming Unit (CFU) Assay: Cells seeded at low density (20, 50, 100, and 500 cells/dish) and grown for 10 days before fixing and staining with Crystal Violet.
- Flow Cytometry: Analysis of MSC surface markers using BD Stemflow Human MSC Analysis Kit on a BD FACS Fortessa.
- Statistical Analysis: One-way ANOVA with Tukey's Multiple Comparisons test [10].
Scale-Up Technologies: From Flasks to Bioreactors
Conventional planar tissue culture methods are insufficient for generating the large quantities of MSCs required for clinical applications [51]. Scale-up manufacturing presents both opportunities and challenges for maintaining cell quality.
- Microcarrier-Based Bioreactors: These systems provide high surface-to-volume ratios for cell expansion. Studies have shown that MSCs expanded on microcarriers in chitosan-based systems exhibited spontaneous osteogenesis, indicating that the 3D environment can influence cell differentiation [55].
- Process-Induced Variability: Scaling up production to bioreactors may alter the MSC secretome, a vital component underlying their immunomodulatory properties and clinical effectiveness [51]. This necessitates careful process characterization to ensure critical quality attributes are maintained.
- Automated and Closed Systems: Implementing closed systems like the modular Cytocentric Xvivo system reduces contamination risk while accelerating turnaround times, which is crucial for GMP compliance [54].
Diagram: GMP Manufacturing Workflow for MSCs. This workflow integrates media optimization and quality control at critical stages to ensure batch-to-batch consistency during scale-up.
Strategic Pillar III: Comprehensive Quality Control and Testing
A robust quality control system is the cornerstone of demonstrating batch-to-batch consistency and product safety throughout the manufacturing process.
In-Process and Release Testing
The 2025 FPMSC study established a comprehensive testing panel that aligns with GMP requirements for product release [10]:
- Viability Testing: Using Trypan Blue exclusion, the study demonstrated >95% viability post-thaw, significantly exceeding the >70% minimum requirement [10].
- Sterility Testing: Employing the Bact/Alert system for microbial contamination and additional Endotoxin and Mycoplasma assays [10].
- Identity and Purity: Confirmed through flow cytometry analysis of MSC surface markers (CD73, CD90, CD105) and absence of hematopoietic markers [10] [53].
- Potency Assays: Colony-forming unit (CFU) assays demonstrated the functional potency of the cells, with higher colony formation observed in cells cultured in MSC-Brew GMP Medium [10].
- Stability Assessments: The study confirmed that GMP-FPMSCs maintained specifications, including viability and sterility, even after extended storage (up to 180 days) [10].
Cell Banking Systems
Implementing a cell banking system is essential for ensuring long-term consistency and scalability:
- Master Cell Bank (MCB): This is the primary bank from which all working cell banks (WCBs) are derived. GMP-grade MCBs provide a consistent starting material for multiple production runs [54].
- Working Cell Bank (WCB): Derived from one or more vials of the MCB, WCBs are used directly for production runs [54].
- Stability Monitoring: Ongoing stability testing of cell banks under controlled storage conditions is necessary to define the shelf-life of the cellular product [10] [54].
Diagram: Quality Control Cascade for MSC Banking. A tiered testing approach ensures comprehensive characterization of Master Cell Banks with limited, targeted testing for Working Cell Banks and final products.
The Scientist's Toolkit: Essential Reagents and Materials
Successful GMP-compliant MSC manufacturing requires carefully selected reagents and materials that meet regulatory standards.
Table: Essential Research Reagent Solutions for GMP-Compliant MSC Manufacturing
| Reagent/Material | Function | GMP-Compliant Examples | Key Considerations |
|---|---|---|---|
| Basal Media | Nutrient foundation for cell growth | MEM α [10] | Must be xeno-free; chemically defined |
| Media Supplements | Provide growth factors and hormones | MSC-Brew GMP Medium [10], MesenCult-ACF Plus Medium [10] | Animal component-free; lot-to-lot consistency |
| Dissociation Enzymes | Cell passaging and harvest | 0.1% Collagenase [10] | Recombinant sources preferred; minimal enzyme residue |
| Cell Separation | Initial isolation from tissue | 100μm filters [10] | Closed systems preferred to reduce contamination |
| Cryopreservation | Long-term storage of cells | FBS with 10% DMSO [10] | Transition to xeno-free cryopreservatives needed |
| Quality Control Assays | Identity, purity, potency testing | BD Stemflow Human MSC Analysis Kit [10], Flow Cytometry | Validated methods; standardized protocols |
Achieving batch-to-batch consistency and scalability in MSC manufacturing under GMP standards requires an integrated approach addressing all aspects of production. The 2025 FPMSC study demonstrates that GMP-compliant protocols can yield cells with enhanced proliferation rates, maintained viability >95%, and stable characteristics during storage [10]. Success hinges on several key factors: standardized sourcing materials, optimized xeno-free culture platforms like MSC-Brew GMP Medium, robust quality control systems adhering to ISCT criteria, and appropriate scale-up technologies. As the field advances, emerging approaches such as iPSC-derived MSCs offer promising alternatives for achieving unprecedented levels of batch uniformity [54]. By implementing these comprehensive strategies, researchers and drug development professionals can overcome the critical challenges in MSC manufacturing, paving the way for clinically feasible and reproducible cell therapies that fulfill their therapeutic potential.
The isolation and expansion of Mesenchymal Stem Cells (MSCs) for clinical applications necessitate strict adherence to Good Manufacturing Practice (GMP) standards to ensure product safety, quality, and efficacy. For decades, fetal bovine serum (FBS) has served as the universal supplement in cell culture media, providing essential nutrients, hormones, and growth factors necessary for cell proliferation [56] [57]. However, the translation of MSC therapies from research to clinical applications has revealed significant limitations and risks associated with FBS, prompting a critical shift toward human-derived alternatives and defined media formulations.
The use of FBS in therapeutic cell production raises multiple concerns, including ethical issues regarding animal welfare, potential immunogenic reactions to xenogenic proteins in patients, risks of transmitting zoonotic pathogens, and considerable batch-to-batch variability that challenges manufacturing reproducibility [21] [57]. Regulatory agencies increasingly emphasize minimizing animal-derived components in therapeutic cell products, making FBS-free culture systems essential for advanced clinical trials and licensed therapies [21] [4]. This technical guide examines the feasibility of transitioning from FBS to human platelet lysate (hPL) and defined serum-free media for GMP-compliant MSC isolation and expansion, providing evidence-based protocols and risk mitigation strategies.
Fetal Bovine Serum: Limitations and Regulatory Concerns
Scientific and Safety Limitations of FBS
FBS exhibits several inherent properties that complicate its use in clinical-grade MSC manufacturing. As a biologically complex fluid, FBS contains numerous undefined components that vary significantly between production batches, leading to inconsistencies in cell growth characteristics and functionality [57]. These variations necessitate extensive batch testing before use, increasing costs and creating logistical challenges in manufacturing workflows [57].
From a safety perspective, FBS poses risks of immunogenic reactions in human recipients. Studies indicate that MSCs expanded in FBS can incorporate bovine antigens, potentially provoking immune responses upon transplantation [57]. Documented cases include anaphylaxis and other immune reactions in patients receiving cells cultured with animal-derived products [57]. Furthermore, FBS represents a potential source of microbial contamination, including viruses (particularly bovine viral diarrhea virus), mycoplasma, prions, and other adventitious agents that may cross species barriers [21] [57].
Regulatory and Ethical Considerations
The regulatory landscape for advanced therapy medicinal products (ATMPs) increasingly discourages FBS use in clinical applications. In the European Union, MSCs are classified as somatic cell-based ATMPs and governed by specific regulatory frameworks (Regulation 1394/2007/EC and Directive 2009/120/EC) that emphasize patient safety and product standardization [21]. Similar regulatory trends exist worldwide, with agencies requiring rigorous justification for any animal-derived components in therapeutic cell products.
Ethical concerns regarding FBS production have also gained prominence. The collection process involves cardiac puncture of bovine fetuses from slaughtered pregnant cows, raising animal welfare issues [57]. Additionally, the environmental sustainability of large-scale FBS production has been questioned, with annual worldwide production estimated at approximately 500,000 liters, equating to harvesting from more than one million bovine fetuses [57].
Table 1: Key Limitations of FBS in Clinical-Grade MSC Manufacturing
| Category | Specific limitation | Impact on MSC Manufacturing |
|---|---|---|
| Scientific | Undefined composition with batch-to-batch variability | Compromised reproducibility and quality control |
| Suboptimal for human cell proliferation | Longer doubling times compared to human alternatives | |
| Safety | Risk of xenogenic immunogenicity | Potential immune reactions in patients |
| Potential transmission of zoonotic pathogens | Product safety concerns requiring extensive testing | |
| Regulatory | Non-compliance with evolving ATMP guidelines | Challenges in marketing authorization applications |
| Ethical | Animal welfare concerns in production | Ethical conflicts with patient-centered healthcare values |
| Supply Chain | Limited and fluctuating availability | Manufacturing instability and cost uncertainties |
Human Platelet Lysate: A Viable Alternative for MSC Expansion
Composition and Mechanisms of Action
Human platelet lysate is a hemoderivative obtained through the lysis of human platelet concentrates, typically sourced from expired transfusion units or dedicated donations [56] [58]. hPL contains a complex mixture of growth factors, cytokines, chemokines, and adhesive proteins that collectively support cell proliferation and viability. Key growth factors include platelet-derived growth factor (PDGF-AA, AB, BB), transforming growth factor-β (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin-like growth factor-1 (IGF-1) [56] [58].
These bioactive molecules are naturally sequestered in platelet alpha-granules and released upon activation or lysis, playing crucial roles in wound healing and tissue regeneration processes [58]. The physiological relevance of these factors for human cell proliferation explains the superior performance of hPL compared to FBS in supporting MSC expansion. Research demonstrates that growth factor concentrations in hPL can surpass those in FBS by up to 150-fold, resulting in significantly enhanced MSC proliferation rates [58].
Comparative Performance: hPL versus FBS
Multiple studies have established that hPL outperforms FBS as a culture supplement for MSC expansion. A 2024 comprehensive comparison reported that MSC proliferation rates in media supplemented with 5% hPL equaled or exceeded those in media containing 10% FBS, while maintaining characteristic MSC morphology, surface marker expression, and differentiation potential [56]. The study further demonstrated that hPL-containing media supported successful cryopreservation and post-thaw recovery of MSCs comparable to FBS-containing media [56].
Additional investigations revealed that MSCs expanded in hPL media exhibited enhanced immunomodulatory properties and maintained genomic stability after multiple passages [57]. These findings position hPL as not merely an equivalent alternative but rather a superior supplement for clinical-grade MSC manufacturing.
Table 2: Quantitative Comparison Between FBS and hPL in MSC Culture
| Parameter | FBS (10%) | hPL (5-10%) | Reference |
|---|---|---|---|
| Population doubling time | Baseline | Significantly reduced (up to 50% faster) | [56] [57] |
| Cumulative cell expansion | 24-fold (early passages) | 68-fold (early passages) | [57] |
| Growth factor content | Baseline | 148.7-fold higher | [58] |
| Cell viability post-thaw | >70% | >95% | [4] |
| Colony-forming unit capacity | Baseline | Enhanced | [4] |
| Xenogenic protein carryover | 7-30 mg/10^8 MSCs | None | [57] |
| Batch variability | High | Moderate (reduced by pooling) | [59] |
Standardized Protocol for hPL Preparation and Quality Control
Manufacturing Workflow for GMP-Compliant hPL
The production of hPL for clinical applications must follow standardized protocols to ensure consistency and safety. The following workflow outlines a GMP-compliant process suitable for MSC expansion:
Starting Material Selection: Use human platelet concentrates obtained from approved blood establishments, testing negative for relevant transfusion-transmitted infections (HTLV-1, hepatitis B and C, HIV 1-2, syphilis, Chagas disease) [56]. Preferred sources include expired, leukoreduced apheresis platelet units or buffy-coat-derived pooled platelets.
Pooling and Freezing: Create pools of 5-50 platelet units to minimize donor-to-donor variability. For small-scale production, 50-65 mL units can be individually processed [56]. Freeze pooled platelets at -20°C or lower for a minimum of 24 hours.
Lysis Procedure: Subject frozen platelet pools to 1-3 freeze-thaw cycles (-20°C/37°C or -80°C/37°C) to ensure complete platelet disruption and growth factor release [58]. For enhanced lysis efficiency, combine freeze-thaw cycles with ultrasonication (ultrasonic bath at frequencies around 20 kHz for 30 minutes) [58].
Clarification and Sterilization: Centrifuge the lysate at 3600 × g for 60 minutes at room temperature to remove platelet membranes and debris [56]. Collect the supernatant and filter through 0.2-0.45 μm membranes to ensure sterility.
Quality Control Testing: Assess each hPL batch for key parameters including total protein content (typically 30-50 mg/mL), fibrinogen levels, pH (7.2-7.6), osmolality (280-320 mOsm/kg), and growth factor content (PDGF-BB > 20 ng/mL, TGF-β1 > 30 ng/mL) [59]. Perform sterility testing per pharmacopeial standards.
Storage: Aliquot and store hPL at -20°C or -80°C for long-term preservation, avoiding repeated freeze-thaw cycles.
Diagram 1: hPL Manufacturing Workflow
Standardization Across Multiple Production Sites
Recent efforts have demonstrated the feasibility of standardizing hPL manufacturing across different institutions. A 2025 multicenter study across three European blood establishments implemented a harmonized hPL production protocol using identical production sets and standard operating procedures [59]. Despite differences in local platelet concentrate preparation methods, the resulting hPL batches exhibited comparable total protein levels, pH, ionic strength, lactate content, and growth factor profiles [59].
Notably, international pooling of hPL batches from different sources resulted in lower variability compared to institution-specific ("national") batches, supporting the strategy of large-volume pooling to enhance product consistency [59]. This approach facilitates the creation of standardized hPL stocks suitable for multicentric clinical trials and commercial MSC production.
Defined Serum-Free Media: A Chemically-Defined Alternative
Composition and Benefits
Defined serum-free media represent a fundamentally different approach to cell culture supplementation. Unlike hPL, which still contains a complex mixture of human-derived proteins, serum-free media are chemically defined formulations precisely engineered to support specific cell types without animal or human components [60] [61]. These media typically contain:
- Amino acids (both essential and non-essential)
- Vitamins and cofactors
- Inorganic salts and trace elements
- Energy sources (glucose, lipids)
- Recombinant growth factors and hormones
- Carrier proteins (such as recombinant albumin)
- Attachment factors for cell adhesion
The primary advantages of serum-free media include exceptional batch-to-batch consistency, elimination of pathogen transmission risks, simplified downstream purification of cell products, and alignment with regulatory preferences for fully defined culture systems [60] [61]. These characteristics make serum-free media particularly attractive for large-scale, automated bioprocessing of MSCs.
Limitations and Optimization Requirements
Despite their advantages, serum-free media present challenges that require careful consideration. The high cost of commercial serum-free formulations and recombinant growth factors can significantly impact manufacturing economics [60]. Additionally, serum-free media often require customization for specific cell types and applications, necessitating extensive optimization and validation studies [60].
Some studies report reduced cell growth in serum-free media compared to serum- or hPL-supplemented media, particularly during initial adaptation phases [62]. This limitation underscores the importance of media formulation optimization and potentially the use of transition protocols to gradually adapt cells to serum-free conditions.
Table 3: Commercially Available Serum-Free Media for MSC Culture
| Product Name | Manufacturer | Key Characteristics | Reported Performance |
|---|---|---|---|
| MSC Brew GMP Medium | Miltenyi Biotec | Xeno-free, GMP-grade | Enhanced proliferation and colony formation compared to standard media [4] |
| MesenCult-ACF Plus | StemCell Technologies | Animal component-free | Supports MSC expansion while maintaining differentiation potential [4] |
| StemSpan SFEM | StemCell Technologies | Serum-free expansion medium | Effective for hematopoietic cells but may induce proteostatic stress [62] |
| UltraCulture | Lonza | Low protein, defined formulation | Supports expansion but may compromise stemness in some applications [62] |
Implementation Strategy: Transitioning to FBS-Free Systems
Systematic Approach for Media Conversion
Transitioning from FBS to hPL or serum-free media requires a structured approach to ensure consistent cell quality and process reproducibility:
Comparative Testing: Conduct side-by-side evaluations of new supplements against current FBS-containing media, assessing critical quality attributes including population doubling time, viability, immunophenotype, differentiation potential, and genomic stability.
Adaptation Protocol: Implement a gradual transition using intermediate media mixtures (e.g., 50% FBS/50% hPL) over 1-2 passages before complete conversion to minimize adaptation stress.
Process Re-optimization: Re-evaluate and adjust key process parameters such as seeding density, feeding schedules, and passaging criteria, as these often require modification in new media systems.
Functional Validation: Confirm that MSCs expanded under new conditions maintain critical therapeutic functions, particularly immunomodulatory capacity and secretion of bioactive factors.
Documentation: Meticulously document all process changes and validation data for regulatory submissions.
The Scientist's Toolkit: Essential Reagents for Implementation
Table 4: Key Research Reagent Solutions for FBS Transition
| Reagent/Category | Function in Culture | GMP-Compliant Examples | Considerations for Use |
|---|---|---|---|
| Human Platelet Lysate | Source of growth factors and adhesion proteins | Commercial hPL (e.g., PLTGold, Stemulate) or in-house produced from blood bank platelets | Requires heparin addition to prevent gelation; optimal at 5-10% concentration |
| Serum-Free Media | Defined environment for consistent expansion | MSC Brew GMP Medium, MesenCult-ACF Plus | May require substrate coating for initial cell attachment |
| Recombinant Trypsin | Animal-free cell dissociation | Recombinant trypsin preparations | Eliminates animal-derived enzyme concerns |
| Cell Attachment Matrix | Substitutes for adhesion factors in serum | Recombinant fibronectin, laminin, or synthetic peptides | Essential for serum-free initial isolation |
| Heparin | Prevents fibrin clot formation in hPL | Pharmaceutical-grade heparin | Required in hPL media at 2-4 IU/mL |
| Cryopreservation Media | Maintains cell viability during frozen storage | DMSO-free, protein-free formulations | Enhances post-thaw recovery and eliminates animal components |
Regulatory Considerations and Quality Control
GMP Compliance Framework
The manufacturing of MSCs for clinical use must comply with GMP standards outlined in regulatory guidelines such as EudraLex Volume 4 in the European Union and relevant FDA guidance documents in the United States [21]. Key considerations include:
Donor Eligibility and Testing: For hPL production, platelet donors must meet all applicable blood donor eligibility criteria, and donations must undergo rigorous testing for relevant transfusion-transmitted infections [56] [59].
Traceability and Documentation: Maintain complete traceability from original platelet donors to final hPL batch, documenting all manufacturing steps, quality control results, and storage conditions.
Batch Release Criteria: Establish predefined specifications for hPL batch release, including sterility, mycoplasma, endotoxin levels, growth factor content, and performance in cell culture [59].
Change Control: Implement formal change control procedures for any modifications to hPL manufacturing or MSC culture processes, with appropriate validation studies.
Quality Control Testing Panel
A comprehensive quality control strategy for hPL should include:
- Biochemical Analysis: Total protein, glucose, lactate, calcium, and magnesium levels [56] [59]
- Growth Factor Quantification: PDGF-AB/BB, TGF-β1, VEGF, FGF-2 via multiplex immunoassays [59]
- Safety Testing: Sterility (bacteria, fungi), mycoplasma, endotoxin (<5 EU/mL) [4]
- Functional Assessment: MSC doubling time, colony-forming unit capacity, and differentiation potential [4] [59]
For serum-free media, quality control focuses on consistency of defined components and performance in supporting MSC growth while maintaining critical quality attributes.
The transition from FBS to human platelet lysate and defined serum-free media represents a critical advancement in the evolution of GMP-compliant MSC manufacturing. Both approaches offer distinct advantages in mitigating risks associated with FBS, particularly regarding safety, standardization, and regulatory compliance.
hPL currently presents a robust, immediately implementable solution that supports high proliferation rates while maintaining MSC functionality. The recent demonstration of successful hPL standardization across multiple production sites indicates progress toward addressing batch variability concerns [59]. Meanwhile, serum-free media offer the ultimate in definition and control, albeit with higher costs and potential need for cell line-specific optimization.
Future developments will likely focus on further standardization of hPL production, creation of more advanced serum-free formulations tailored to specific MSC tissue sources and clinical applications, and implementation of integrated bioprocessing systems that leverage these serum alternatives. As regulatory expectations continue to evolve, establishing well-characterized, FBS-free manufacturing processes will be essential for realizing the full clinical potential of MSC-based therapies.
The successful translation of mesenchymal stem cell (MSC)-based therapies from research to clinical application fundamentally depends on robust cryopreservation protocols that maintain cell viability, potency, and functionality post-thaw. Within the framework of Good Manufacturing Practice (GMP) research, cryopreservation is not merely a storage technique but a critical manufacturing step that ensures the reliable production of standardized, quality-controlled cell products [10]. The inherent challenges of MSC-based therapies—including the need for large cell numbers, logistical coordination between manufacturing sites and clinical facilities, and the requirement for repeat dosing—make effective cryopreservation an indispensable component of the therapeutic pipeline [63] [64]. This technical guide examines the fundamental principles, optimized protocols, and viability assessment methods essential for mastering MSC cryopreservation within a GMP-compliant research setting, providing scientists with evidence-based strategies to overcome the primary challenges in maintaining post-thaw viability and function.
Fundamental Principles of Cryopreservation
Mechanisms of Cell Damage and Cryoprotection
The process of freezing and thawing subjects cells to multiple potentially lethal stressors. Understanding these mechanisms is fundamental to developing protective strategies. During freezing, the formation of extracellular ice crystals increases the solute concentration in the remaining liquid, creating an osmotic gradient that draws water out of cells, leading to detrimental cell shrinkage and solute toxicity [63]. If cooling occurs too rapidly, intracellular ice crystals form, causing physical damage to membranes and organelles. Conversely, excessively slow cooling prolongs exposure to hypertonic conditions, resulting in excessive dehydration [65].
Cryoprotective Agents (CPAs) counteract these damaging processes through two primary mechanisms. Penetrating CPAs, such as dimethyl sulfoxide (DMSO) and glycerol, enter the cell and reduce the fraction of water that freezes at any given temperature, thereby minimizing ice crystal formation and stabilizing intracellular proteins [63] [65]. Non-penetrating CPAs, including sugars like sucrose and trehalose, remain extracellular and draw water out of cells in a more controlled manner before freezing, reducing the risk of intracellular ice formation. They also increase the viscosity of the extracellular solution, which can suppress ice crystal growth [63]. The standard slow freezing protocol leverages these protective mechanisms by controlling the cooling rate (typically -1°C/min) to allow sufficient cellular dehydration while minimizing intracellular ice formation, achieving a balance that maximizes post-thaw recovery [65] [66].
Comparison of Primary Cryopreservation Methods
Two primary methodological approaches exist for MSC cryopreservation, each with distinct mechanisms, advantages, and limitations relevant to GMP translation.
Table 1: Comparison of Slow Freezing and Vitrification Methods for MSCs
| Feature | Slow Freezing | Vitrification |
|---|---|---|
| Basic Principle | Controlled, slow cooling induces gradual cellular dehydration, minimizing intracellular ice [65]. | Ultra-rapid cooling solidifies solution into a glassy, non-crystalline state using high CPA concentrations [65]. |
| Cooling Rate | -1°C/min [66] | Exceedingly high (>20,000°C/min) [65] |
| CPA Concentration | Low (e.g., 10% DMSO) [65] | Very High (e.g., 40-50% total CPA mixture) [65] |
| Primary Advantage | Lower CPA toxicity, simpler scalability, widely adopted in GMP settings [10] [65]. | Avoids mechanical damage from ice crystals entirely. |
| Primary Limitation | Risk of extracellular ice formation and solute damage. | High CPA toxicity requires precise handling, challenging for large volumes. |
| Suitability for GMP | High - compatible with standardized, large-scale production [10]. | Low to Moderate - best suited for small samples like tissues or cell clusters. |
For most GMP applications involving large-scale MSC suspensions, slow freezing remains the preferred and most practical method due to its operational simplicity, lower toxicity concerns, and easier integration into controlled manufacturing processes [10] [65] [66].
Quantitative Data on Post-Thaw Viability and Storage
Evaluating the success of a cryopreservation protocol requires a clear understanding of typical viability outcomes and how they are influenced by storage conditions. The following data, compiled from recent studies, provides benchmarks for expectations and optimization efforts.
Table 2: Post-Thaw Viability and Stability Data Under Different Conditions
| Cell Type / Condition | Post-Thaw Viability | Storage Condition & Duration | Key Findings |
|---|---|---|---|
| GMP-FPMSCs [10] | >95% | Liquid nitrogen, up to 180 days | Maintained sterility, viability, and stem cell marker expression, meeting all release specifications. |
| CD34+ Hematopoietic Cells [67] | 94.8% (median) | -80°C, median of 868 days | Viability declined ~1.02% per 100 days; engraftment capability was preserved. |
| MSCs (General Slow Freezing) [65] | 70-80% | Liquid nitrogen (-196°C) | Represents typical recovery range for standard slow-freezing protocols. |
Controlled-rate freezing is strongly associated with superior outcomes. A recent industry survey found that 87% of cell and gene therapy professionals use controlled-rate freezing, with adoption increasing to 100% for late-stage and commercial products [68]. While short-term storage at -80°C is acceptable, long-term storage should be in liquid nitrogen vapor phase (-135°C to -196°C) to ensure optimal stability, as cells kept at -80°C will degrade over time [66].
Optimized GMP Cryopreservation Protocol for MSCs
The following step-by-step protocol synthesizes best practices for the cryopreservation of MSCs under GMP-compliant conditions, emphasizing points of control critical for maintaining viability and function.
Step 1: Cell Harvesting and Pre-Freeze Preparation
- Cell State: Harvest MSCs during their maximum growth phase (log phase) at 80-90% confluency to ensure a healthy, proliferative state before freezing [10] [66].
- Quality Control: Perform pre-freeze mycoplasma testing and ensure cells are free from microbial contamination. Confirm MSC identity via flow cytometry for standard surface markers (CD73, CD90, CD105) and the absence of hematopoietic markers [10] [65].
- Cell Concentration: Resuspend the final cell pellet in a GMP-compliant, animal component-free freezing medium at a concentration between 1x10^6 to 5x10^6 cells/mL [10] [66]. Using a defined, serum-free commercial medium like CryoStor CS10 or MSC-Brew GMP Medium enhances lot-to-lot consistency and safety [10] [66].
Step 2: Cryoprotectant Addition and Aliquotting
- CPA Choice: Use a final concentration of 10% DMSO in a defined, protein-free base medium. For increased biosafety, consider lower DMSO concentrations (e.g., 5-7.5%) supplemented with non-penetrating CPAs like sucrose or trehalose to mitigate toxicity [65].
- Handling: Gently mix the cell suspension with the freezing medium to ensure uniform CPA distribution. Aliquot the suspension into sterile, internally-threaded cryogenic vials to prevent contamination during storage [66].
- Process Speed: Complete the aliquotting process and initiate freezing promptly after CPA addition (typically within 15-20 minutes) to minimize the toxic exposure of cells to liquid DMSO at room temperature [65].
Step 3: Controlled-Rate Freezing
- Cooling Profile: Use a controlled-rate freezer programmed to cool at -1°C/min from room temperature to -40°C, then at -5 to -10°C/min down to -100°C or below [68] [66].
- Alternative Method: If a controlled-rate freezer is unavailable, use an isopropanol-based freezing container (e.g., "Mr. Frosty") or an isopropanol-free alternative (e.g., CoolCell) placed in a -80°C freezer for approximately 18-24 hours. This passive system approximates the -1°C/min cooling rate [66].
- Documentation: In a GMP setting, record and archive the freeze curve data for each batch as part of the manufacturing record [68].
Step 4: Long-Term Storage
- Transfer: After the initial freezing cycle, quickly transfer vials to the long-term storage unit to avoid temperature fluctuations.
- Storage Conditions: Store vials in the vapor phase of liquid nitrogen (-135°C to -190°C) to minimize the risk of cross-contamination, which is higher in the liquid phase [69] [66].
- Inventory Management: Implement a rigorous inventory system with barcoding or RFID tagging to ensure full traceability of all cell bank vials [66].
Step 5: Thawing and Post-Thaw Processing
- Thawing: Rapidly thaw vials by gentle agitation in a 37°C water bath until only a small ice crystal remains (approximately 1-2 minutes) [65] [66]. Using controlled-thawing devices can enhance consistency and reduce contamination risk compared to water baths [68].
- CPA Removal: Immediately after thawing, dilute the cell suspension drop-wise with pre-warmed culture medium (e.g., 5-10 volumes) to gradually reduce the DMSO concentration and prevent osmotic shock. Centrifuge to remove the CPA-containing supernatant [65].
- Initial Culture: Resuspend the cell pellet in fresh, pre-warmed culture medium and seed at a higher density to facilitate recovery. Consider assessing viability after 18-24 hours to allow for the recovery of damaged but viable cells [10].
The workflow below visualizes this optimized GMP cryopreservation process.
Assessment of Viability and Function Post-Thaw
Rigorous post-thaw assessment is critical for validating the success of a cryopreservation protocol, particularly in a GMP environment where product quality is paramount.
Viability and Yield Analysis
- Viability Staining: Use acridine orange (AO)/propidium iodide (PI) or 7-Aminoactinomycin D (7-AAD) flow cytometry for accurate, quantitative viability measurement. AO/PI staining may offer enhanced sensitivity for detecting delayed cellular damage [67].
- Cell Recovery Calculation: Determine the percentage of viable cells recovered relative to the pre-freeze count. A well-optimized protocol should achieve >70% recovery, with advanced protocols exceeding 90% [10] [67].
- Delayed Assessment: Re-assess viability 18-24 hours post-thaw, as some cells incur lethal damage that is not immediately apparent [67].
Potency and Functional Assays
Viability alone is insufficient; confirmation of retained MSC functionality is essential.
- Clonogenic Assay: The Colony-Forming Unit (CFU) assay demonstrates self-renewal capacity. Plate thawed MSCs at low density (e.g., 20-500 cells per dish) and culture for 10-14 days before fixing and staining with crystal violet to count colonies. Cells cultured in optimized GMP media like MSC-Brew GMP Medium show higher colony formation, indicating enhanced potency [10].
- Multilineage Differentiation: Differentiate thawed MSCs toward osteogenic, adipogenic, and chondrogenic lineages in vitro to confirm retained trilineage potential, a defining characteristic of MSCs [10] [65].
- Surface Marker Expression: Use flow cytometry to confirm the retention of characteristic MSC surface markers (CD73, CD90, CD105) and the absence of hematopoietic markers (CD34, CD45, CD11b) after thawing [10] [65].
- Metabolic and Secretory Function: Assess metabolic activity using assays like MTT or Alamar Blue, and evaluate the secretion of key therapeutic paracrine factors (e.g., VEGF, HGF, PGE2) to ensure immunomodulatory capacity is intact [63].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials critical for implementing a successful GMP-compliant MSC cryopreservation protocol.
Table 3: Essential Research Reagent Solutions for MSC Cryopreservation
| Item Category | Specific Examples | Function & Importance |
|---|---|---|
| GMP Cryopreservation Media | MSC-Brew GMP Medium [10], CryoStor CS10 [66] | Provides a defined, animal component-free, and GMP-manufactured environment for freezing, ensuring consistency and safety. |
| Controlled-Rate Freezing Equipment | Controlled-Rate Freezers (CRFs), CoolCell [68] [66] | Enables precise control of cooling rate (-1°C/min), a critical process parameter for maximizing viability and process consistency. |
| Cryogenic Storage Vials | Corning Cryogenic Vials (Internal Thread) [66] | Sterile, secure containers for storage. Internal-threaded vials are preferred to minimize contamination risk in liquid nitrogen storage. |
| Viability Assay Kits | BD Stemflow MSC Analysis Kit [10], AO/PI Staining Solutions [67] | Allows for simultaneous assessment of post-thaw viability and confirmation of MSC immunophenotype for product identity and quality. |
| Animal Component-Free Culture Media | MesenCult-ACF Plus Medium [10] | Used for post-thaw expansion and functional assays, maintaining GMP compliance and reducing variability from animal sera. |
Mastering cryopreservation is a cornerstone in the feasibility of manufacturing GMP-compliant mesenchymal stem cell products. By integrating the fundamental principles of cryobiology with optimized, controlled protocols and rigorous post-thaw assessment, researchers can reliably produce MSC stocks with high viability, robust functionality, and consistent performance. The continued development of animal component-free reagents, advanced controlled-rate freezing equipment, and sensitive analytical techniques will further enhance the standardization and safety profile of cryopreserved MSC products. Adherence to the detailed strategies outlined in this guide provides a solid technical foundation for advancing promising MSC therapies from the research bench toward clinical reality, ensuring that these living medicines retain their therapeutic potential from the cryovial to the patient.
Proving Safety and Efficacy: Quality Control and Comparative Analytics
In the development of Advanced Therapy Medicinal Products (ATMPs) based on mesenchymal stromal cells (MSCs), rigorous quality control (QC) is a non-negotiable requirement for ensuring patient safety and product efficacy. The production of these cell therapies must adhere to Good Manufacturing Practice (GMP) standards, creating a framework where quality is built into every stage of the manufacturing process rather than merely tested at the end [21] [13]. Within this framework, three safety tests—sterility, mycoplasma, and endotoxin testing—form the critical backbone of microbiological control. These tests are essential release criteria, meaning that a batch of MSC-based product cannot be administered to a patient without first demonstrating compliance with stringent specifications for each parameter [70].
The feasibility of isolating and expanding MSCs under GMP-research conditions is heavily dependent on establishing a robust and reliable QC system. Variability inherent in MSC sources and manufacturing processes makes standardized QC testing not just a regulatory hurdle, but a fundamental component of reproducible science [21] [70]. This guide provides an in-depth technical overview of these essential tests, summarizing critical data and providing detailed methodologies to support researchers and drug development professionals in building GMP-compliant MSC manufacturing platforms.
Core Quality Control Specifications for MSC-Based Products
Before delving into individual test methodologies, it is crucial to understand the acceptance criteria that a final MSC-based product must meet. These specifications are derived from pharmacopoeial standards and are applied to the final product before its release for clinical use. The following table summarizes the key safety and quality attributes that must be verified.
Table 1: Essential release criteria and typical specifications for MSC-based ATMPs.
| Quality Attribute | Test Method | Acceptance Criterion | Rationale & Reference |
|---|---|---|---|
| Sterility | Sterility Test (e.g., BacT/Alert) | No growth of aerobic or anaerobic microorganisms [4] | Ensures the product is free from viable contaminating microorganisms. |
| Mycoplasma | PCR and/or Microbial Culture | Absence of mycoplasma contamination [4] [70] | Mycoplasma can alter cell metabolism and proliferation, and poses a significant patient risk. |
| Endotoxin | Limulus Amebocyte Lysate (LAL) Test | ≤ 0.5 Endotoxin Units (EU)/mL [70] | Endotoxins are pyrogenic and can cause severe febrile reactions in patients. |
| Cell Viability | Trypan Blue Exclusion | > 95% (Typical GMP target); >70% (Minimum required) [4] | Ensures a sufficient proportion of living, functional cells are administered. |
| Identity/Purity | Flow Cytometry | Expression of CD73, CD90, CD105 ≥ 95%; Lack of CD45, CD34, CD14, CD19, HLA-DR ≤ 2% [70] [12] | Verifies the product is composed of MSCs and not contaminated with hematopoietic cells. |
Endotoxin Testing
Endotoxins, also known as lipopolysaccharides (LPS), are components of the outer membrane of Gram-negative bacteria. They are potent pyrogens that, if introduced into the bloodstream via an MSC infusion, can trigger severe febrile reactions, septic shock, and organ failure in patients [71]. Because endotoxins can be introduced through raw materials, water, or during the manufacturing process, testing is a mandatory safety requirement for parenteral pharmaceuticals, including MSC-based ATMPs.
Detailed Experimental Protocol: Kinetic Chromogenic LAL Assay
The Limulus Amebocyte Lysate (LAL) test is the standard method for endotoxin detection. The kinetic chromogenic method is widely used for its quantitative precision and ability to detect endotoxin over a broad range.
Workflow Overview:
The following diagram illustrates the key stages of the endotoxin testing protocol, from sample preparation to final release.
Step-by-Step Methodology:
- Sampling: A representative sample of the final MSC product suspension is taken aseptically. The sample must be obtained under defined conditions to ensure it is representative of the entire batch [71].
- Sample Receipt and Storage: The sample is logged upon receipt in the QC laboratory and stored appropriately (often refrigerated or frozen) to preserve its integrity until testing. Improper storage can invalidate the test [71].
- Software Template Setup: The testing software (e.g., on a spectrophotometer) is configured with a standard curve of known endotoxin concentrations. This curve typically has a lower limit (lambda, λ, often 0.005 EU/mL) and an upper limit. Results outside this range will need dilution and retesting [71].
- Standard Preparation: A series of standard solutions are created by diluting a Control Standard Endotoxin (CSE) to generate a calibration curve (e.g., 5.0, 0.5, 0.05, and 0.005 EU/mL) [71].
- Sample Preparation: This is a critical step to overcome assay interference. The MSC product may need to be diluted with LAL reagent water or treated to adjust pH, chelate divalent cations, or disaggregate endotoxin. The official test protocol must be unambiguous to ensure analyst-to-analyst reproducibility [71].
- Testing: Prepared standards and samples are pipetted into a microplate, and LAL reagent is added. The plate is incubated at 37°C, and the absorbance is read kinetically. The software calculates the endotoxin concentration in the samples by extrapolating from the standard curve [71].
- Sample Hold for Retest: The original sample is held under defined storage conditions. This is crucial for investigating any Out-of-Specification (OOS) result, preventing accusations of "testing into compliance" [71].
- Reporting: The final result, including the dilution factor, is calculated and reported in EU/mL. This result is entered into the Laboratory Information Management System (LIMS) and becomes part of the batch record [71].
- Release: The reported value undergoes a second-person verification. If the result meets the specification (e.g., ≤ 0.5 EU/mL), the product is approved for release concerning this quality attribute [71].
Mycoplasma Testing
Mycoplasmas are the smallest self-replicating bacteria that lack a rigid cell wall. They are a major concern in cell culture because they can pass through standard 0.2 µm filters, do not cause turbidity in media, and can chronically infect cultures, altering cell metabolism, proliferation, and causing chromosomal aberrations [72]. For patient safety and product quality, demonstrating the absence of mycoplasma in MSC-based products is mandatory.
Detailed Experimental Protocol: Compendial Culture Method
The most rigorous testing method, often required for market authorization, involves a combination of culture and indicator cell line tests as described in the European Pharmacopoeia (EP 2.6.7) and United States Pharmacopeia (USP <63>).
Workflow Overview:
The compendial method is a multi-week process that involves both liquid broth enrichment and solid agar plating to ensure detection of a wide range of mycoplasma species.
Step-by-Step Methodology:
- Sample Inoculation: The test sample (MSC product supernatant or lysate) is inoculated into liquid broth media. Using at least two different media, such as FREY and FRIIS, is recommended to support the growth of a wide spectrum of mycoplasma species [72].
- Liquid Enrichment Phase: The inoculated broths are incubated for 14-21 days. They are observed every 2-3 days for any color change indicating microbial growth [72].
- Subculture to Solid Agar: On specific days after inoculation (e.g., days 3-4, 6-8, 13-15, and 19-21), a small volume (e.g., 0.2 mL) from each liquid medium is subcultured onto at least one plate of solid agar medium. This step is crucial for detecting slow-growing mycoplasma that might be present in low numbers [72].
- Agar Incubation and Observation: The solid agar plates are incubated under anaerobic conditions for at least 14 days. The plates are then examined microscopically for the presence of characteristic "fried-egg" colonies formed by mycoplasma [72].
- Interpretation and Result: The test is valid if the positive controls show growth and the negative controls remain sterile. The MSC product batch is considered negative for mycoplasma only if no growth is observed in any of the liquid or solid media throughout the test period [72].
Alternative Methods: Nucleic Acid Testing (NAT), such as PCR, is a faster and increasingly common method used for in-process testing and lot release in some regulatory frameworks. However, the culture method is often considered the gold standard for final product release due to its high sensitivity and ability to detect viable organisms.
Sterility Testing
Sterility testing is designed to demonstrate the absence of viable bacteria and fungi in the MSC-based product. Given that these products are typically infused directly into patients, often with compromised immune systems, ensuring sterility is paramount. The test must be conducted using aseptic techniques throughout to avoid false-positive results from environmental contamination.
Detailed Experimental Protocol: Membrane Filtration Method
For cell-based products, the direct inoculation method may not be suitable. The membrane filtration method is often preferred as it allows for the testing of larger volumes and the removal of potential antimicrobial agents present in the cell culture media.
Step-by-Step Methodology:
- Sample Preparation: A sample of the final MSC product is obtained aseptically. The required volume is defined by pharmacopoeial standards and the product's batch size.
- Membrane Filtration: The sample is transferred to a sterile closed-system filtration apparatus containing a membrane with a pore size of 0.45 µm or smaller. The entire volume of the product is passed through this membrane, which traps any potential microorganisms.
- Rinsing: The membrane is rinsed several times with a suitable sterile fluid (e.g., Buffered Sodium Chloride-Peptone Solution) to neutralize or wash away any residual antimicrobial activity from the product or its media.
- Incubation: The membrane is aseptically removed from the apparatus and cut in half. One half is placed into a container of Fluid Thioglycollate Medium (FTM), which primarily supports the growth of anaerobic and aerobic bacteria. The other half is placed into a container of Soybean-Casein Digest Medium (SCDM, also known as Tryptic Soy Broth), which supports the growth of aerobic bacteria and fungi. FTM is incubated at 30-35°C for at least 14 days, and SCDM is incubated at 20-25°C for at least 14 days.
- Observation and Interpretation: The media are examined visually for turbidity indicating microbial growth at regular intervals during the incubation period. The test is considered valid if the positive controls (inoculated with low levels of specific microorganisms) show growth and the negative controls remain clear. The MSC batch meets the sterility requirement only if no growth is observed in any of the test vessels.
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of these QC tests relies on the use of qualified reagents and materials. The following table lists key solutions and their functions in the context of GMP-compliant MSC manufacturing and testing.
Table 2: Key research reagent solutions for quality control testing.
| Reagent/Material | Function & Application | GMP Consideration |
|---|---|---|
| LAL Reagent | The key reactive component derived from horseshoe crab blood used to detect endotoxins via the Limulus Amebocyte Lysate test [71]. | Must be from a qualified supplier and suitable for pharmaceutical testing. |
| Endotoxin Standard (CSE) | Used to create the standard curve for quantifying endotoxin in samples [71]. | Requires traceability and certification to a recognized international standard. |
| Mycoplasma Culture Media (FREY, FRIIS) | Nutrient broths and agars specifically formulated to support the growth of a wide range of mycoplasma species [72]. | Ready-to-use media with extended shelf-life simplify compliance and ensure consistent performance. |
| Sterility Test Culture Media (FTM, SCDM) | Liquid media designed to support the growth of anaerobic/aerobic bacteria (FTM) and fungi/aerobic bacteria (SCDM) [72]. | Must meet compendial specifications (EP, USP) and be qualified for the specific product to demonstrate the absence of antimicrobial activity. |
| Animal Component-Free MSC Media | A basal medium (e.g., MSC-Brew GMP Medium) for expanding MSCs without using animal sera, reducing the risk of contamination [4] [73]. | Xeno-free, chemically defined formulations are GMP-compliant and reduce variability and safety risks associated with FBS. |
| Human Platelet Lysate (hPL) | A human-derived supplement used as a replacement for Fetal Bovine Serum (FBS) in MSC culture media, enhancing safety profile [21]. | Requires rigorous testing for human pathogens; limited availability can be a bottleneck for large-scale production [21]. |
| Flow Cytometry Antibody Panels | Antibodies against CD73, CD90, CD105 (positive) and CD45, CD34, HLA-DR (negative) for MSC identity and purity testing [70] [12]. | Should be sourced as GMP-grade or research-grade with strong validation for consistency and specificity. |
The transition of Mesenchymal Stromal Cell (MSC) therapies from research to clinical application hinges on robust quality control protocols that verify product identity, purity, and potency. These parameters are fundamental to ensuring batch-to-batch consistency, patient safety, and therapeutic efficacy in Good Manufacturing Practice (GMP)-compliant production. As highlighted by the International Society for Stem Cell Research (ISSCR), maintaining the integrity of the research enterprise requires rigorous independent oversight and accountability at each stage [26]. This technical guide details the core methodologies—flow cytometry for identity and purity, and functional bioassays for potency—that researchers must implement to demonstrate the feasibility of MSC isolation and manufacturing under GMP standards.
Establishing Identity and Purity: Flow Cytometry Panels
Flow cytometry serves as the principal analytical technique for confirming MSC identity and purity, in accordance with the criteria established by the International Society for Cell & Gene Therapy (ISCT) [9].
Standard Immunophenotyping Markers
The ISCT defines human MSCs by a specific surface marker profile: positive expression (≥95%) for CD73, CD90, and CD105, and negative expression (≤2%) for hematopoietic markers such as CD45, CD34, CD14 or CD11b, CD79a or CD19, and HLA-DR [9]. This profile confirms the mesenchymal origin and purity of the cell product.
Table 1: Core Flow Cytometry Markers for MSC Characterization
| Marker | Expression | Biological Function | Significance in Characterization |
|---|---|---|---|
| CD73 | Positive | Ecto-5'-nucleotidase | Definitive mesenchymal marker; part of the ISCT minimal criteria [9]. |
| CD90 | Positive | Thy-1 glycoprotein | Definitive mesenchymal marker; part of the ISCT minimal criteria [9]. |
| CD105 | Positive | Endoglin, part of TGF-β receptor | Definitive mesenchymal marker; part of the ISCT minimal criteria [9]. |
| CD45 | Negative | Protein tyrosine phosphatase | Pan-hematopoietic marker; critical for establishing purity and absence of hematopoietic cells [9]. |
| CD34 | Negative | Hematopoietic progenitor cell marker | Absence confirms the cell product is not of hematopoietic origin [9]. |
| HLA-DR | Negative | MHC Class II receptor | Indicates absence of activated immune cells; crucial for assessing immunogenicity [9]. |
GMP-Compliant Flow Cytometry Workflow
Implementing flow cytometry in a GMP environment requires a standardized and qualified method. A recent 2024 study on Natural Killer (NK) cell products outlines a protocol that is directly transferable to MSC analysis [74]. The process involves staining a cell sample with a fluorochrome-labelled antibody mix, incubation, and subsequent acquisition on a flow cytometer. For GMP release, the method's critical parameters—including accuracy, precision, linearity, range, and robustness—must be formally qualified to ensure results are reliable and reproducible [74]. A typical workflow is detailed in the diagram below.
Demonstrating Functional Activity: Potency Assays
A potency assay is a quantitative test that measures the biological activity of a cell product, linking its critical quality attributes to a relevant mechanism of action and, ultimately, clinical efficacy [75] [76]. For MSCs, whose therapeutic effects are primarily immunomodulatory and paracrine, these assays are functionally based [75].
Common Potency Assay Formats for MSCs
Table 2: In Vitro Potency Assays for MSC Immunomodulatory Function
| Assay Format | Measurable Readout | Mechanism of Action Probed | Key Cytokines/Factors |
|---|---|---|---|
| T-cell Suppression Assay [77] | Inhibition of CD4+ T-cell proliferation via CFSE dye dilution. | Immunosuppression, relevant for GvHD and autoimmune diseases. | IFN-γ, IL-10 |
| Macrophage Modulation Assay [78] | Secretion of IL-1RA from MSCs co-cultured with M1 macrophages. | Resolution of inflammation in M1-dominated environments. | IL-1RA, TNF-α |
| PBMC-based Immunopotency Assay [79] | IL-10 release from PBMCs stimulated with LPS and MSC-conditioned medium. | Paracrine immunomodulation and tissue protection. | IL-10 |
| IDO Enzyme Activity Assay | Tryptophan to kynurenine conversion via HPLC or colorimetric methods. | Modulation of local immune microenvironment. | Indoleamine 2,3-dioxygenase (IDO) |
Detailed Experimental Protocol: T-cell Suppression Immunopotency Assay
A well-defined immunopotency assay (IPA) to measure MSC-mediated suppression of T-cell proliferation can be adapted for GMP use [77]. This assay is straightforward, reproducible, and comprehensive in design.
Materials:
- Effector Cells: Clinical-grade MSCs.
- Responder Cells: Peripheral Blood Mononuclear Cells (PBMCs) from a healthy donor.
- Stimulation: Mitogens like PHA or anti-CD3/CD28 beads.
- Detection: CFSE cell proliferation dye and anti-CD4-APC antibody for flow cytometry.
Method:
- Prepare Effector Cells: Seed MSCs in a 96-well plate at varying densities (e.g., 1,000 - 20,000 cells/well) and allow them to adhere overnight.
- Prepare Responder Cells: Isolate PBMCs and label them with CFSE according to manufacturer's instructions.
- Co-culture: Add CFSE-labeled PBMCs to the MSC-seeded wells at a defined ratio (e.g., 10:1 PBMCs:MSCs). Activate T-cell proliferation by adding PHA or anti-CD3/CD28 beads.
- Controls: Include essential controls:
- Positive Control: Activated PBMCs alone (maximum proliferation).
- Negative Control: Unstimulated PBMCs (background proliferation).
- Incubation: Incubate co-cultures for 4-5 days at 37°C, 5% CO₂.
- Harvest and Stain: Harvest non-adherent cells and stain with anti-CD4-APC antibody.
- Flow Cytometry Analysis: Acquire data on a flow cytometer. Using the gating strategy shown below, analyze the CFSE dilution within the CD4+ T-cell population to determine the percentage of proliferated cells.
- Calculate Potency: The immunosuppressive capacity is expressed as the percentage reduction in CD4+ T-cell proliferation compared to the positive control.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these characterization assays requires high-quality, well-defined reagents. The following table lists critical solutions and their functions.
Table 3: Key Research Reagent Solutions for MSC Characterization
| Reagent / Solution | Function in Assay | Example & Notes |
|---|---|---|
| Animal Component-Free Media [10] | GMP-compliant expansion of MSCs, maintaining cell potency and phenotype. | MSC-Brew GMP Medium, MesenCult-ACF Plus Medium. |
| Fluorochrome-Labelled Antibodies [74] | Staining of surface markers (CD73, CD90, CD105, CD45, etc.) for flow cytometry. | Anti-CD45-Krome Orange, 7-AAD viability dye. |
| Enzyme-Linked Immunosorbent Assay (ELISA) [79] [78] | Quantification of secreted cytokines (e.g., IL-10, IL-1RA) in potency assays. | BD OptEIA human ELISA sets. |
| Cell Proliferation Dyes [77] | Tracking and quantifying cell division in potency assays (e.g., T-cell suppression). | CFSE (Carboxyfluorescein succinimidyl ester). |
| Functional Grade Stimulants [77] | Activation of immune cells in co-culture potency assays. | PHA, anti-CD3/CD28 beads, LPS (E. coli 0111:B4). |
Integrating Assays into a GMP Feasibility Framework
Demonstrating the feasibility of MSC isolation under GMP research requires that analytical methods are not only scientifically sound but also compatible with a regulated production environment. This involves:
- Method Qualification and Validation: Prior to GMP manufacturing, methods must be qualified (for early phase) or validated (for pivotal trials) to prove they are "fit-for-purpose." This process assesses specificity, accuracy, precision, linearity, and robustness against pre-defined acceptance criteria [74].
- Stability and Shelf-Life Testing: The final MSC product's stability, including post-thaw viability and potency, must be assessed. A 2025 study on infrapatellar fat pad-derived MSCs (FPMSCs) demonstrated that GMP-grade products could maintain >95% viability and sterility for up to 180 days of cryostorage, a critical finding for clinical logistics [10].
- Defining Product Specifications: Based on data from multiple donors and batches, clear release specifications must be set for identity (>95% positive for MSC markers, <2% for hematopoietic markers), purity (sterility, mycoplasma, endotoxin), viability (e.g., >70% or >95% as demonstrated [10]), and potency (e.g., a minimum percentage of T-cell suppression or cytokine secretion) [10] [77].
In conclusion, the rigorous application of flow cytometry for identity and purity, coupled with mechanism-relevant potency assays, forms the bedrock of quality control for MSC-based advanced therapies. By integrating these validated methods into a GMP-compliant framework, researchers can robustly demonstrate the feasibility of their manufacturing processes, paving the way for safe and efficacious clinical trials.
This case study details the successful development and validation of a Good Manufacturing Practice (GMP)-compliant protocol for the isolation and expansion of mesenchymal stem cells derived from the infrapatellar fat pad (IFP-MSCs). The research demonstrates that IFP-MSCs cultured in a specific GMP-compliant, animal component-free medium exhibited enhanced proliferation and maintained critical quality attributes, meeting all release specifications for clinical use after extended cryostorage. This work provides a robust, reproducible framework that significantly advances the translational potential of IFP-MSCs for regenerative medicine applications by addressing a critical bottleneck in the field: the lack of standardized GMP processes for this promising cell source [10].
The translation of Mesenchymal Stem Cell (MSC) therapies from research to clinical application has been hampered by a lack of standardized protocols compliant with Good Manufacturing Practice (GMP) [10]. GMP standards are essential for ensuring product standardization, reproducibility, quality, and safety throughout the manufacturing process [21]. While MSCs from bone marrow (BM-MSCs) have been considered the gold standard, their harvesting is invasive and can lead to patient morbidity [10].
The infrapatellar fat pad (IFP) of the knee presents a compelling alternative source of MSCs. IFP-derived MSCs (IFP-MSCs) can be harvested with minimal invasiveness, often as surgical waste during knee procedures, thereby reducing patient morbidity and enhancing the practicality of MSC-based therapies [10]. Furthermore, IFP-MSCs have demonstrated potent immunomodulatory and regenerative properties, making them attractive candidates for treating inflammatory conditions like osteoarthritis [80] [12]. However, the feasibility of processing IFP-MSCs under GMP-grade conditions had been less characterized. This case study bridges that critical gap, outlining a validated pathway for producing clinical-grade IFP-MSCs.
Experimental Design and Methodologies
This study was designed with a two-pronged approach: first, to optimize the culture conditions for research-grade IFP-MSCs using animal-free media, and second, to validate the entire isolation, expansion, and storage process under GMP-compliant conditions (GMP-IFP-MSCs) [10]. The GMP validation was conducted using cells from four different donors to ensure robustness and reproducibility. The study placed a strong emphasis on rigorous quality control at each stage, assessing viability, sterility, purity, identity, and stability of the final cell product [10].
Detailed Experimental Protocols
Surgical Harvest and Isolation of IFP-MSCs
The protocol for harvesting and isolating IFP-MSCs is critical for initial cell quality and yield.
- Tissue Source: IFP tissue was obtained as surgical waste from patients undergoing anterior cruciate ligament (ACL) reconstructive surgery or total knee arthroplasty after informed consent [10] [81].
- Harvesting Technique: In arthroscopic procedures, tissue was resected using a standard shaver system, and the minced IFP was collected from the suction stream using a sterile sieve [81]. In open surgeries, the fat pad was mechanically minced with a scalpel under sterile conditions [81].
- Enzymatic Digestion: The minced tissue was digested with 0.1% collagenase (e.g., Collagenase I, Sigma-Aldrich #C0130) in serum-free media for approximately 2 hours at 37°C with continuous agitation [10] [81] [82].
- Isolation and Seeding: The digested solution was centrifuged, the supernatant was removed, and the cell pellet was washed, filtered through a 100 μm strainer, and resuspended in culture media. Cells were typically seeded at a density of 10,000 cells/cm² [10] [81].
Culture Conditions and Media Comparison
A key experiment focused on identifying the optimal GMP-compliant culture medium.
- Media Tested: The study evaluated two animal component-free media against a standard Fetal Bovine Serum (FBS)-containing control:
- MesenCult-ACF Plus Medium (StemCell Technologies)
- MSC-Brew GMP Medium (Miltenyi Biotec)
- Standard MSC Media (MEM α + 10% FBS) as a control [10].
- Cell Culture: Cells from three donors were passaged upon reaching 80-90% confluency and were consistently seeded at a density of 5 × 10³ cells/cm² [10].
Critical Quality Control Assays
The following assays were employed to characterize the IFP-MSCs and validate the final GMP product:
- Cell Doubling Time: Calculated over three passages to assess proliferation kinetics [10].
- Colony-Forming Unit (CFU) Assay: Cells were seeded at low densities (20, 50, 100, 500 cells/dish) and grown for 10 days. Colonies were then fixed and stained with Crystal Violet to assess clonogenicity, an indicator of stem cell potency [10].
- Flow Cytometry: Used to confirm MSC identity based on the International Society for Cell & Gene Therapy (ISCT) criteria. Cells were analyzed for positive expression of CD73, CD90, and CD105 (≥95%) and negative expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR; ≤2%) [10] [12].
- Sterility and Safety Testing: The final GMP-IFP-MSC product was tested for sterility using the Bact/Alert system and for endotoxin and mycoplasma contamination [10].
- Stability and Viability Assessment: Post-thaw viability was assessed using Trypan Blue exclusion, and stability was monitored over 180 days of cryostorage to determine the product's shelf-life [10].
Diagram Title: GMP-IFP-MSC Validation Workflow
Key Findings and Results
Optimized Culture Medium Enhances Proliferation and Potency
The comparison of culture media revealed that MSC-Brew GMP Medium significantly outperformed both MesenCult-ACF Plus and standard FBS-containing media.
Table 1: Quantitative Comparison of Culture Media Performance on IFP-MSCs
| Performance Metric | MSC-Brew GMP Medium | MesenCult-ACF Plus | Standard MSC Media (FBS) |
|---|---|---|---|
| Cell Doubling Time | Lower across passages (indicating faster proliferation) [10] | Not specified | Higher than MSC-Brew [10] |
| Colony Formation (CFU) | Higher number of colonies (indicating enhanced potency) [10] | Not specified | Lower than MSC-Brew [10] |
| GMP Compliance | Yes (Animal component-free, chemically defined) [10] | Yes (Animal component-free) [10] | No (Contains animal-derived FBS) [10] |
Successful GMP Validation and Product Release
The GMP-compliant manufacturing process was successfully validated using cells from four donors, with the final product meeting all pre-defined release specifications.
Table 2: GMP-IFP-MSC Product Release Specifications and Results
| Quality Attribute | Release Specification | Validation Results |
|---|---|---|
| Viability (Post-thaw) | >70% | >95% (Well above requirement) [10] |
| Sterility | Sterile | Pass (Bact/Alert test) [10] |
| Endotoxin/Mycoplasma | Negative | Pass [10] |
| MSC Surface Markers | Expression of CD73, CD90, CD105 (≥95%) | Maintained expression post-thaw [10] |
| Stability (Cryopreserved) | - | Maintained viability & sterility for 180 days [10] |
The data demonstrated that the GMP-IFP-MSCs maintained their defining characteristics and met all quality specifications even after extended cryostorage, proving the robustness of the isolation and cryopreservation protocols [10].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for GMP-Compliant IFP-MSC Research
| Reagent / Material | Function / Purpose | Example Product / Note |
|---|---|---|
| MSC-Brew GMP Medium | GMP-compliant, animal component-free expansion medium | Miltenyi Biotec (#170-076-325); shown to enhance proliferation [10] |
| Collagenase I | Enzymatic digestion of IFP tissue to isolate cells | Sigma-Aldrich (#C0130); 9000 units/10g tissue, 2h digestion [81] [82] |
| Human Platelet Lysate (hPL) | GMP-compliant FBS alternative for culture supplement | Supports regulatory-compliant manufacturing [80] |
| Stem Cell Analysis Kit | Flow cytometry verification of MSC surface markers | BD Stemflow Human MSC Analysis Kit (#562245) [10] |
| Microcarriers & Bioreactors | 3D culture for scalable EV production | Enables large-scale extracellular vesicle production [82] |
Discussion and Future Perspectives
This case study successfully establishes a feasible and reproducible pathway for generating clinical-grade IFP-MSCs. The transition from research-grade reagents, like FBS, to GMP-compliant, animal component-free formulations is a critical step for clinical translation, mitigating risks of immunogenicity and batch-to-batch variability [10] [21]. The superior performance of MSC-Brew GMP Medium in promoting IFP-MSC proliferation and potency underscores the importance of media optimization in therapy development.
A promising future direction lies in transitioning from cell-based therapies to cell-free products utilizing the IFP-MSC secretome, particularly extracellular vesicles (EVs). IFP-MSC-derived exosomes carry a rich cargo of immunomodulatory miRNAs and proteins and present advantages in terms of standardization, safety, and regulatory landscape [80]. Furthermore, for scalable EV production, 3D culture systems using microcarriers in vertical wheel bioreactors have been shown to increase EV yields by roughly 100-fold compared to conventional 2D culture, providing a viable system for pre-clinical and clinical production [82].
This case study provides a comprehensive and validated framework for the GMP-compliant isolation, expansion, and storage of Infrapatellar Fat Pad-derived MSCs. By demonstrating that IFP-MSCs can be reliably manufactured to meet strict quality control specifications, this work significantly advances the feasibility of using this less invasive, potent cell source in regenerative medicine. The protocols and data presented here serve as a foundational resource for researchers and drug development professionals aiming to translate IFP-MSC therapies from the laboratory to the clinic, ultimately contributing to the development of safe and effective treatments for a range of inflammatory and degenerative diseases.
Comparative Analysis of Media Formulations and Their Impact on Proliferation
Within the framework of evaluating the feasibility of mesenchymal stem cell (MSC) isolation under Good Manufacturing Practice (GMP) research, the selection and optimization of culture media formulations emerge as a critical determinant of success. MSCs hold immense promise in regenerative medicine, but their translation from research to clinical application is hampered by a lack of standardized, scalable, and reproducible production protocols [21]. The culture medium is not merely a supportive environment; it directly dictates critical quality attributes of the final cellular product, including proliferation rate, potency, and stability [83]. This whitepaper provides a comparative analysis of different media formulations, focusing on their quantitative impact on MSC proliferation and their compliance with GMP standards. By synthesizing current experimental data and methodologies, this guide aims to equip researchers and drug development professionals with the technical knowledge to select and optimize media for robust, clinically feasible MSC manufacturing.
Media Formulations: From Serum-Containing to Clinically Compliant
The evolution of MSC culture media has been driven by the need to eliminate animal-derived components and ensure defined, consistent composition.
- Serum-Containing Media (SCM): Traditional MSC expansion often relies on basal media, such as α-MEM, supplemented with Fetal Bovine Serum (FBS) [10] [4]. While effective for research, FBS introduces significant risks for clinical applications, including batch-to-batch variability, potential for immunogenic reactions, and risk of transmitting prions or viruses [84] [83]. Its use is therefore not a future viable option for GMP production [21].
- Xenogeneic-Free & Serum-Free Media (SFM): To address the limitations of SCM, GMP-compliant alternatives have been developed.
- Human Platelet Lysate (hPL): As a medium supplement, hPL has been confirmed as a safe and feasible animal-free alternative for large-scale MSC isolation and expansion [84]. It supports robust cell growth, though its limited availability and potential risk of disease transmission can be bottlenecks for large-scale production [21].
- Chemically Defined, Commercial SFM: These ready-to-use formulations, such as MSC-Brew GMP Medium (Miltenyi Biotec) and MesenCult-ACF Plus Medium (StemCell Technologies), are designed to be animal-component-free and chemically defined [10] [4]. They eliminate the risks associated with biological additives and enhance batch-to-batch consistency, making them essential for the clinical translation of MSC therapies [10].
Quantitative Impact of Media Formulations on Proliferation
The choice of media formulation has a direct and measurable impact on MSC proliferation kinetics. The table below summarizes key quantitative findings from recent studies.
Table 1: Comparative Impact of Media Formulations on MSC Proliferation and Potency
| Cell Source | Media Formulation | Key Proliferation/Potency Metrics | Study Findings |
|---|---|---|---|
| Infrapatellar Fat Pad-derived MSCs (FPMSCs) [10] [4] | MSC-Brew GMP Medium | Doubling Time & Colony Formation | Significantly lower doubling times across passages and higher colony formation compared to standard MSC media, indicating enhanced proliferation and potency. |
| Infrapatellar Fat Pad-derived MSCs (FPMSCs) [10] [4] | MesenCult-ACF Plus Medium | Doubling Time & Colony Formation | Showed improved performance over standard media, but was outperformed by MSC-Brew GMP Medium in promoting proliferation. |
| Human Umbilical Cord MSCs (hUC-MSCs) [83] | Customized Serum-Free Media (SFM) | Population Doubling Time (PDT) & Cell Activity | hUC-MSCs exhibited superior proliferative capacity, higher activity, and greater stability over 10 passages compared to those cultured in Serum-Containing Media (SCM). |
| Human Umbilical Cord MSCs (hUC-MSCs) [83] | Various Commercial SFM | Population Doubling Time (PDT) & Senescent Rate | Demonstrated that different SFM formulations can lead to variations in proliferative capacity, senescent rate, and paracrine function. |
| Bone Marrow-derived MSCs [84] | Media supplemented with Platelet Lysate (PL) | Feasibility of Large-Scale Expansion | Established that PL-based protocols support safe, reliable, and efficient large-scale MSC isolation and expansion for clinical application. |
Detailed Experimental Protocols for Media Comparison
To ensure reproducibility and provide a technical toolkit, this section outlines the core methodologies used in the cited studies to generate the comparative data.
- Tissue Acquisition and Digestion: Infrapatellar fat pad (IFP) tissue is acquired as waste tissue from surgeries (e.g., ACL reconstruction). The tissue is minced into ~1 mm³ pieces and digested with 0.1% collagenase in serum-free media for 2 hours at 37°C.
- Cell Seeding and Expansion: The digested tissue is centrifuged, and the cell pellet is resuspended in a standard MSC media (e.g., α-MEM + 10% FBS) for initial plating. After the first passage, cells are transitioned to experimental media (e.g., MSC-Brew GMP Medium, MesenCult-ACF Plus Medium).
- Subculture: Cells are passaged at 80-90% confluency and consistently seeded at a density of 5 × 10³ cells/cm² for experimentation.
Protocol: Assessing Proliferation and Potency
- Cell Doubling Time:
- Method: Cells are seeded at a known density (e.g., 5 × 10³ cells/cm²) and grown to 80-90% confluency over multiple passages. Cells are counted at each passage using a hemacytometer.
- Calculation: Doubling Time is calculated using the formula:
Doubling Time = (duration * ln2) / (ln(final concentration) - ln(initial concentration))[10] [4].
- Colony Forming Unit (CFU) Assay:
- Method: Cells are seeded at very low densities (e.g., 20, 50, 100, and 500 cells) in a large culture dish and grown for 10-14 days.
- Analysis: Cells are fixed with formalin and stained with Crystal Violet. Colonies containing >50 cells are counted. A higher number of colonies indicates greater clonogenic potential and potency [10] [84].
- Post-Thaw Viability and Stability:
- Method: MSCs are cryopreserved in a suitable cryoprotectant (e.g., containing 10% DMSO). After storage (e.g., in liquid nitrogen for up to 180 days), cells are thawed rapidly at 37°C.
- Analysis: Viability is assessed post-thaw using Trypan Blue exclusion. A viability of >95% indicates robust cryopreservation and storage protocols suitable for clinical "off-the-shelf" products [10].
The workflow for these core experiments can be visualized as follows:
The Scientist's Toolkit: Essential Reagents for GMP-Compliant Media Studies
The following table details key reagents and their functions for establishing GMP-compliant MSC media studies.
Table 2: Key Research Reagent Solutions for MSC Media Studies
| Reagent / Material | Function & Role in Media Comparison | Example Product / Component |
|---|---|---|
| Basal Medium | Serves as the foundation, providing salts, vitamins, and energy sources. | α-MEM, UltraCULTURE Serum-free Medium [83] |
| Serum Substitute | Replaces FBS to provide growth factors, hormones, and adhesion proteins in a xenogeneic-free manner. | Human Platelet Lysate (hPL) [84], Commercial Serum-Free Supplements [83] |
| GMP-Compliant Media | Ready-to-use, chemically defined formulations for consistent, clinical-grade cell expansion. | MSC-Brew GMP Medium, MesenCult-ACF Plus Medium [10] [4] |
| Dissociation Enzyme | For detaching adherent MSCs during passaging while maintaining cell health and phenotype. | TRYPZEAN, Trypsin [84] [83] |
| Cryopreservation Medium | For long-term storage of cell banks, ensuring high post-thaw viability and functionality. | Cryoprotectant with DMSO (e.g., 10%) in a defined base medium [10] [83] |
Discussion and Strategic Considerations for GMP Feasibility
The quantitative data unequivocally demonstrates that GMP-compliant, serum-free media can not only match but often surpass the performance of traditional serum-containing media in supporting MSC proliferation. The strategic move towards these formulations is therefore not just a regulatory hurdle, but an opportunity to enhance product quality.
- Batch-to-Batch Consistency: Chemically defined SFM are paramount for ensuring consistency across manufacturing batches, a cornerstone of GMP [85] [86]. Removing undefined components like FBS and hydrolysates directly reduces a significant source of performance variability [85] [83].
- Functional Potency Beyond Proliferation: While proliferation is crucial for achieving therapeutic cell doses, the media formulation also profoundly influences MSC therapeutic potency, including immunomodulatory capacity and secretome profile [83]. A medium that excels in promoting growth for one clinical indication may not be optimal for another, necessitating disease-targeted media optimization [83].
- The "Off-the-Shelf" Product Paradigm: The high post-thaw viability (>95%) demonstrated by MSCs expanded in GMP-compliant media is a critical feasibility factor for allogeneic, "off-the-shelf" MSC products [10]. This ensures that the final cellular therapeutic retains its critical quality attributes after storage and shipment.
In conclusion, the comparative analysis confirms that the evolution of media formulations is a decisive enabler for the GMP-compliant isolation and expansion of MSCs. By adopting standardized, chemically defined, and performance-optimized media, researchers and developers can significantly de-risk the translational pathway and accelerate the delivery of consistent, safe, and efficacious MSC therapies to patients.
Conclusion
The feasibility of isolating MSCs under GMP conditions is unequivocally demonstrated by robust protocols that yield cells meeting stringent release criteria, including high viability, sterility, and defined identity. Success hinges on an integrated approach that combines a deep understanding of regulatory frameworks, meticulous process optimization, and rigorous quality control. The demonstrated success of specific GMP-compliant, animal component-free media in enhancing proliferation and maintaining cell potency underscores the importance of culture conditions. Future directions must focus on harmonizing global regulations, developing more advanced potency assays to predict clinical efficacy, and integrating novel technologies like AI and bioreactors for smarter, scalable manufacturing. This will ultimately accelerate the reliable translation of MSC-based therapies from the bench to the bedside, fulfilling their transformative potential in regenerative medicine.
References
- 1. Regenerative medicine and regulation: what's GMP got to ... [https://www.eurogct.org/regenerative-medicine-and-regulation-whats-gmp-got-do-it]
- 2. Advanced therapy medicinal products: Overview [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview]
- 3. Optimizing mesenchymal therapy: from stem to... cell isolation [https://pubmed.ncbi.nlm.nih.gov/40329219/]
- 4. Optimizing mesenchymal therapy: from stem to... cell isolation [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-025-00539-7]
- 5. Guidelines relevant for advanced therapy medicinal products [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview/guidelines-relevant-advanced-therapy-medicinal-products]
- 6. Cellular & Gene Therapy Products [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products]
- 7. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 8. Guide to Cell Therapy GMP Manufacturing for Autologous ... [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 9. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 10. Optimizing mesenchymal stem cell therapy: from isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054297/]
- 11. All Courses - ISCT Workforce Development [https://www.isctglobal.org/workforce-development/courses]
- 12. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 13. Standardization of Good Manufacturing Practice–compliant ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324914005581]
- 14. Bioprocessing strategies for the large-scale production of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-015-0228-5]
- 15. A GMP-compliant manufacturing method for Wharton's jelly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11069138/]
- 16. A Comparative Analysis of Multipotent Mesenchymal ... [https://www.nature.com/articles/s41598-020-61167-z]
- 17. The Therapeutic Significance of Mesenchymal Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523856/]
- 18. Stem cell bioprocess engineering towards cGMP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4158018/]
- 19. MSC Renamed? From "Stem Cells" to "Stromal Cells" [https://yoconcelltherapy.com/msc-renamed-from-stem-cells-to-stromal-cells-three-major-shifts-to-note/]
- 20. Donor age and breed determine mesenchymal stromal cell characteristics | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04236-2]
- 21. Current good manufacturing practice considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934414/]
- 22. Production of mesenchymal stromal/stem cells according to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3707032/]
- 23. Establishing Criteria for Human Mesenchymal Stem Cell Potency - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5363381/]
- 24. Universal or Personalized Mesenchymal Stem Cell Therapies: Impact of Age, Sex, and Biological Source - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9265811/]
- 25. A Mesenchymal Stromal Cell Gene Signature for Donor Age - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3426516/]
- 26. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 27. Primary MSCs for Personalized Medicine: Ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313419/]
- 28. Processing and Ex Vivo Expansion of Adipose Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8392403/]
- 29. Optimizing monocyte-derived immune cell cultures [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589553/full]
- 30. Biomanufacturing with GMP cell culture media [https://www.regmednet.com/biomanufacturing-with-gmp-cell-culture-media-an-interview-with-maximilian-gert-kleint_promocell/]
- 31. Xenogeneic-free culture of human intestinal stem cells on ... [https://www.nature.com/articles/s41467-024-54653-9]
- 32. PromoCell Adopts GMP Standards with Custom Cell ... [https://www.genengnews.com/topics/bioprocessing/promocell-adopts-gmp-standards-with-custom-cell-culture-media-services/]
- 33. GMP-compatible and xeno-free cultivation of mesenchymal ... [https://pubmed.ncbi.nlm.nih.gov/30635059/]
- 34. Optimizing monocyte-derived immune cell cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540148/]
- 35. Understanding the molecular basis of mesenchymal stem ... [https://www.nature.com/articles/s41419-025-08094-x]
- 36. Optimizing the Seeding Density of Human Mononuclear ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9855129/]
- 37. How to optimize MSC culturing conditions for enhanced growth? [https://yoconcelltherapy.com/how-to-optimize-msc-culturing-conditions-for-enhanced-growth/]
- 38. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 39. Expansion and characterization of bone marrow derived ... [https://www.nature.com/articles/s41598-021-83088-1]
- 40. Transition from manual to automated processes for ... [https://www.nature.com/articles/s41598-025-00015-4]
- 41. Why the scale-up of cell culture is essential for ... [https://greenelephantbiotech.com/blog/why-the-scale-up-of-cell-culture-is-essential-for-manufacturing-cell-and-gene-therapies/]
- 42. Automated and Manual Cell Expansion Analysis Shows ... [https://www.genengnews.com/topics/bioprocessing/automated-manual-cell-expansion-analysis-shows-statistical-equivalence/]
- 43. Automation in cell and gene bioprocessing: challenges, ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/12/Automation-in-cell-and-gene-bioprocessing-challenges-opportunities-and-what-lies-ahead]
- 44. Objectives, benefits and challenges of bioreactor systems ... [https://pubmed.ncbi.nlm.nih.gov/33781889/]
- 45. Objectives, benefits and challenges of bioreactor systems ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975021000410]
- 46. cGMP Cell Therapy Manufacturing Services [https://appliedstemcell.com/ipsc-cgmp-manufacturing/]
- 47. The issue of heterogeneity of MSC-based advanced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1400347/full]
- 48. Comparative analysis of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4453294/]
- 49. Comparative analysis of mesenchymal stem cells ... [https://www.nature.com/articles/s41598-022-12467-z]
- 50. What Makes a GMP Cell Separation Kit? [https://www.akadeum.com/blog/what-makes-a-gmp-cell-separation-kit/?srsltid=AfmBOopz2xBPso2hB6Vzn_ABWPbJBmaFKIidtLirVf-_HhzEbqnIzqxi]
- 51. Biological Considerations in Scaling Up Therapeutic Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7247829/]
- 52. Optimization of Mesenchymal Stromal Cell (MSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9261977/]
- 53. Methods to Validate Mesenchymal Stem Cell Quality [https://www.rndsystems.com/resources/articles/markers-and-methods-verify-mesenchymal-stem-cell-identity-potency-and-quality]
- 54. MCB Generation Services for iMSCs and MSCs: GMP ... [https://www.reprocell.com/clinical-stem-cell-services/gmp-imsc-and-msc-production]
- 55. Scalable and efficient production of mesenchymal stem ... [https://www.sciencedirect.com/science/article/pii/S0024320523001583]
- 56. Comparison between Platelet Lysate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10813006/]
- 57. Evaluation of human platelet lysate versus fetal bovine ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324913007779]
- 58. Human platelet lysate – A potent (and overlooked) orthobiologic [https://pmc.ncbi.nlm.nih.gov/articles/PMC8339333/]
- 59. Human platelet lysate standardization across three ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04445-9]
- 60. Understanding Serum-Free Media: Balancing Benefits and ... [https://yoconcelltherapy.com/serum-free-media-benefits-and-limitations/]
- 61. What Is Serum-Free Media and Why Use It? [https://synapse.patsnap.com/article/what-is-serum-free-media-and-why-use-it]
- 62. Towards the standardization of human platelet lysate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245862/]
- 63. Cryostorage of Mesenchymal Stem Cells and Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9454587/]
- 64. Cryopreservation of Human Stem Cells for Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3088734/]
- 65. Effects, methods and limits of the cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03954-3]
- 66. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 67. Viable and Functional: Long-Term −80 °C Cryopreservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525932/]
- 68. Cryopreservation - Key Survey Findings from the ISCT ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/05/28/cryopreservation-key-survey-findings-from-the-isct]
- 69. Cryopreservation of Stem Cells for Regenerative Medicine ... [https://gmpplastic.com/blogs/news/cryopreservation-of-stem-cells-for-regenerative-medicine-research?srsltid=AfmBOooQ--EjtShz9oMIzVkzoXv1YCqbKiEeAgm3ryWwq7rlfJajFWTd]
- 70. Quality Control Optimization for Minimizing Security Risks ... [https://www.mdpi.com/1422-0067/24/16/12955]
- 71. A Step-by-Step Approach to Effective Endotoxin Testing [https://www.biomerieux.com/corp/en/education/resource-hub/pharma-quality-control/scientific-library/A-Step-by-Step-Approach-to-Effective-Endotoxin-Testing.html]
- 72. Mycoplasma Testing in Pharma [https://www.merckmillipore.com/KE/en/applications/microbiological-testing/mycoplasma-testing]
- 73. GMP-grade Mesenchymal Stem Cell Media in the Real World [https://www.linkedin.com/pulse/gmp-grade-mesenchymal-stem-cell-media-real-gvscc/]
- 74. Qualification of a flow cytometry-based method for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10830575/]
- 75. Potency Assays for Mesenchymal Stromal Cell Secretome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10253866/]
- 76. Potency assays and biomarkers for cell-based advanced ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1186224/full]
- 77. A reproducible immunopotency assay to measure ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324914008020]
- 78. Potency assay to predict the anti-inflammatory capacity of a ... [https://www.sciencedirect.com/science/article/pii/S1465324924000501]
- 79. A Mesenchymal Stem Cell Potency Assay - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3759509/]
- 80. Human infrapatellar fat pad mesenchymal stem cells show ... [https://www.nature.com/articles/s41598-022-07569-7]
- 81. Isolation and Cultivation of Adipose-Derived Mesenchymal ... [https://www.mdpi.com/2409-9279/6/1/3]
- 82. Culture of Hoffa fat pad mesenchymal stem/stromal cells on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03681-9]
- 83. Evaluation of the impact of customized serum-free culture ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03949-0]
- 84. GMP-Compliant Isolation and Large-Scale Expansion of Bone ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0043255]
- 85. Addressing the Complexities of Media Formulation Development | BioPharm International [https://www.biopharminternational.com/view/addressing-the-complexities-of-media-formulation-development]
- 86. Advances in Cell Culture Media Formulation and Development [https://www.genengnews.com/topics/bioprocessing/advances-in-cell-culture-media-formulation-and-development/]