Herbal Medicine Standardization: Advanced Methods for Quality Control and Evidence-Based Research
This article provides a comprehensive overview of contemporary standardization methods for herbal medicine preparations, tailored for researchers, scientists, and drug development professionals.
Herbal Medicine Standardization: Advanced Methods for Quality Control and Evidence-Based Research
Abstract
This article provides a comprehensive overview of contemporary standardization methods for herbal medicine preparations, tailored for researchers, scientists, and drug development professionals. It explores the foundational necessity of quality control for ensuring safety and efficacy, details advanced methodological approaches from pharmacognosy to modern analytics, addresses key challenges in research and regulation, and evaluates validation frameworks and comparative regulatory landscapes. By synthesizing traditional knowledge with cutting-edge scientific rigor, this review aims to bridge the gap between herbal medicine and mainstream pharmaceutical development, promoting reproducible, high-quality, and evidence-based herbal products.
The Critical Need for Standardization in Modern Herbal Medicine
Troubleshooting Guides
Inconsistent Bioactive Compound Levels Between Batches
Problem: High batch-to-batch variability in the concentration of key active compounds or markers, leading to unreliable therapeutic outcomes [1].
Solution:
- Root Cause: Lack of robust standardization protocols for raw materials and extraction processes.
- Corrective Action: Implement a comprehensive standardization workflow for herbal materials.
- Step 1: Authentication: Use macroscopic, microscopic, and DNA barcoding to verify the correct botanical species and plant part [1] [2].
- Step 2: Quantitative Analysis: Employ chromatographic techniques (HPLC, TLC, GC) to quantify levels of active compounds or marker compounds [1] [3].
- Step 3: Establish Reference Standards: Use certified reference materials as benchmarks for quality control testing to ensure consistency across production batches [1].
- Step 4: Process Validation: Standardize and validate the extraction methodology to ensure reliable and reproducible extraction of bioactive constituents [2].
Contamination and Adulteration
Problem: Herbal products test positive for contaminants such as heavy metals, pesticides, or microbial organisms, or are adulterated with undeclared, potentially harmful substances [1].
Solution:
- Root Cause: Inadequate quality control testing and insufficient supply chain traceability.
- Corrective Action: Enforce stringent quality assurance testing and documentation.
- Step 1: Implement Testing Protocols: Conduct rigorous physicochemical and microbiological testing on all incoming raw materials and final products [2].
- Step 2: Detect Contaminants: Use modern analytical techniques like ICP-MS for heavy metal testing and chromatography for pesticide residue analysis [2].
- Step 3: Adulteration Screening: Apply spectroscopic methods and chemical marker analysis to detect and prevent the presence of non-declared substances or synthetic dyes [2].
- Step 4: Ensure Traceability: Maintain detailed Batch Manufacturing Records (BMRs) that document the source and movement of all material inputs within the supply chain [2].
Lack of Reproducible Efficacy in Preclinical/Clinical Studies
Problem: Herbal preparations demonstrate variable therapeutic effects in research settings, making it difficult to obtain reproducible and reliable data [1].
Solution:
- Root Cause: Failure to account for multiple sources of variation, including herb quality, patient/disease factors, and preparation methods.
- Corrective Action: Adopt a multivariable optimization framework in study design [4].
- Step 1: Control Herb Variation: Through quality optimization and rigorous herbal drug development protocols as detailed in sections 1.1 and 1.2 [4].
- Step 2: Account for Disease Variation: Integrate traditional diagnostic criteria and ensure research practitioners are thoroughly trained in the specific traditional context of the herbal medicine [4].
- Step 3: Address Patient Variation: Incorporate personalized medicine principles by considering factors such as genetics, metabolism, and individual health status when designing trials and interpreting results [4].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental definition of "standardization" in the context of herbal medicine research?
Standardization is a systematic process of defining and maintaining consistent levels of active compounds or marker compounds in herbal medication products [1]. It involves establishing and adhering to predetermined quality specifications to minimize batch-to-batch variability, ensuring the product is reproducible, safe, and possesses consistent pharmacological activity [1] [3]. This is distinct from merely identifying plants; it focuses on chemical and biological consistency.
Q2: Which analytical techniques are considered essential for the standardization of herbal drugs?
A combination of techniques is required to comprehensively assess the quality of an herbal drug. The following table summarizes the key methods and their primary applications in standardization.
| Technique | Primary Application in Standardization | Brief Description |
|---|---|---|
| Chromatographic Fingerprinting (HPLC, TLC) [1] [2] | Identity confirmation & quantification of active/marker compounds. | Creates a unique chemical "profile" of the herb for identification and quantitation. |
| DNA Barcoding [1] [2] | Authentication of botanical species. | Uses a short genetic marker to identify the plant species and detect adulteration. |
| Spectroscopy (UV-Vis, IR, NMR) [1] | Quantitative analysis and structural elucidation. | Measures the interaction of light with matter to determine concentration or identify compounds. |
| ICP-MS / AAS [2] | Heavy metal testing. | Precisely detects and quantifies toxic heavy metal residues (e.g., arsenic, lead). |
Q3: What are the critical quality control parameters for herbal manufacturers, and how are they tested?
According to WHO and good manufacturing practices (GMP), critical parameters ensure safety, purity, and consistency. The tests must be performed on raw materials, in-process materials, and the final product [2].
| Quality Parameter | Purpose | Common Tests/Techniques |
|---|---|---|
| Physicochemical Testing [2] | Assess product consistency and chemical properties. | pH, viscosity, solubility, HPLC, TLC. |
| Microbiological Testing [2] | Ensure absence of harmful microorganisms. | Total viable aerobic count, tests for yeast/mold, E. coli, Salmonella. |
| Heavy Metal & Pesticide Limits [2] | Verify compliance with safety limits for toxic residues. | ICP-MS, AAS, chromatography for pesticide residue. |
| Adulteration & Contaminants [2] | Detect and prevent presence of non-declared or harmful substances. | Visual inspection, spectroscopy, chemical marker analysis. |
Q4: How do regulatory frameworks for herbal medicines differ from those for conventional pharmaceutical drugs?
The regulatory framework for herbal products differs starkly from that of prescription drugs. In many regions, including the U.S. under the DSHEA Act of 1994, herbal products do not require prior regulatory approval (e.g., from the FDA) for safety or effectiveness before being marketed [5]. Unlike conventional drugs, which undergo stringent pre-market testing for potency and safety, herbal supplements are often regulated as dietary supplements, placing more emphasis on post-market surveillance and adherence to Good Manufacturing Practices (cGMP) [5] [3]. This fundamental difference underscores the critical need for rigorous self-regulation and quality control within the herbal research and manufacturing industries.
Q5: What is a multivariable optimization framework in herbal medicine research?
A multivariable optimization framework is a modern approach designed to overcome the limitations of traditional single-variable standardization. It simultaneously controls for the three main sources of variability that compromise herbal therapy outcomes:
- Herb Variation: Addressed through quality optimization (e.g., GAP, GMP) and advanced analytical methods [4].
- Disease Variation: Managed by integrating traditional knowledge and training practitioners in specific diagnostic criteria [4].
- Patient Variation: Addressed by tailoring treatments using personalized medicine principles, potentially leveraging multi-omics tools [4]. This framework aims to enhance treatment reliability and safety over conventional methods and facilitate the integration of herbal medicine into modern evidence-based healthcare [4].
Experimental Protocols & Workflows
Protocol: Standardization of Raw Herbal Material
Objective: To authenticate the plant material and establish a chemical fingerprint for quality control.
Materials:
- Herbal raw material (e.g., dried root, leaf)
- Solvents (e.g., methanol, ethanol, water)
- Reference standards for marker compounds
- TLC plates or HPLC columns
- DNA extraction and amplification kits
Methodology:
- Authentication:
- Chromatographic Fingerprinting:
- Sample Preparation: Prepare a representative extract of the herbal material using a standardized solvent and method [1].
- Analysis: Inject the sample into an HPLC or apply to a TLC plate alongside reference standards.
- Data Interpretation: Generate a chromatogram or TLC profile. Identify the marker compounds by comparing retention times/Rf values with standards. Use this fingerprint as a benchmark for future batches [1] [2].
Workflow: Quality Control for Herbal Drug Development
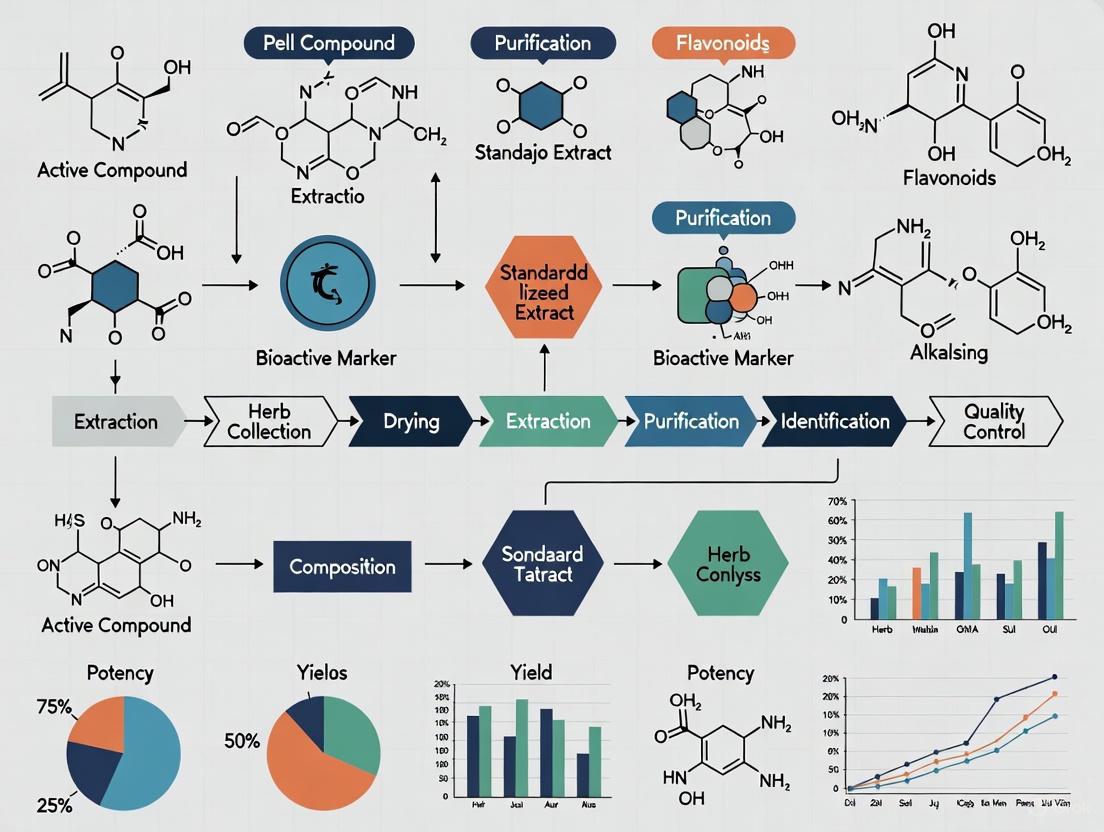
The following diagram illustrates the logical workflow for ensuring quality throughout the herbal drug development process, integrating key steps from authentication to final product release.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the standardization and quality control of herbal preparations.
| Item | Function/Explanation |
|---|---|
| Certified Reference Standards [1] | Pure, well-characterized chemical compounds used as benchmarks in analytical methods (e.g., HPLC, TLC) to identify and quantify active or marker compounds in herbal samples. |
| DNA Barcoding Kits [1] [2] | Kits containing reagents for DNA extraction, purification, PCR amplification, and sequencing of standard barcode regions (e.g., ITS, rbcL) to authenticate botanical species and detect adulteration. |
| Chromatography Consumables [1] [3] | Includes specific HPLC columns (e.g., C18), TLC plates, solvents, and mobile phases tailored for the separation and analysis of complex phytochemical mixtures in herbal extracts. |
| Stable Isotope-Labeled Internal Standards | Used in advanced mass spectrometry (e.g., LC-MS) for highly accurate and precise quantification of compounds, correcting for analyte loss during sample preparation and matrix effects. |
| Microbiological Culture Media [2] | Selective and non-selective media used in pharmacopoeial tests to determine the total viable aerobic microbial count and test for the absence of specified pathogens (e.g., E. coli, Salmonella). |
The Global Reliance on Herbal Medicine and Implications for Public Health
Herbal medicine represents a cornerstone of healthcare for a significant portion of the global population. The World Health Organization (WHO) reports that approximately 80% of the world's population relies on traditional medicine, a category predominantly comprised of herbal remedies, for primary healthcare needs [2]. This reliance is reflected in the market's robust growth, with the global medicinal herbs sector projected to increase from an estimated USD 227.65 billion in 2025 to USD 478.93 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 11.21% [6]. This surge is largely driven by rising consumer preference for natural and organic healthcare solutions, particularly for chronic and lifestyle-related conditions [6].
The recent WHO Global Traditional Medicine Strategy (2025–2034), adopted at the 78th World Health Assembly, marks a pivotal milestone. This strategy aims to accelerate the integration of evidence-based Traditional, Complementary and Integrative Medicine (TCIM) into health systems worldwide, emphasizing the establishment of a robust evidence base, regulatory mechanisms for quality and safety, and the protection of Indigenous knowledge and rights [7] [8]. For researchers and drug development professionals, this global momentum underscores an urgent need for standardized, reproducible, and high-quality research methodologies to validate herbal medicine practices and products, ensuring their safety and efficacy for public health.
Technical Support & Troubleshooting Hub
This section addresses common experimental challenges in herbal medicine research, providing targeted solutions and methodologies to enhance the reliability and reproducibility of your findings.
Frequently Asked Questions (FAQs)
1. How can I resolve batch-to-batch variability in my herbal test material? Batch-to-batch inconsistency is a major challenge that can invalidate research outcomes. To address this:
- Standardize the Source: Begin with rigorous botanical authentication of raw materials using macroscopic, microscopic, and DNA barcoding techniques to ensure species and plant part correctness [1] [2].
- Establish Quality Parameters: Define and monitor key physicochemical parameters such as the content of active compounds or marker substances using HPLC or TLC. Implement chromatographic fingerprinting to create a unique chemical profile for consistency checks [1] [9].
- Control the Process: Adhere to standardized, validated extraction and manufacturing processes. Utilize Good Manufacturing Practices (GMP) to ensure every production step is controlled and documented, from raw material sourcing to final product packaging [2].
2. What are the best practices for authenticating herbal ingredients and detecting adulterants? Authentication and adulteration detection require a multi-faceted analytical approach:
- Hierarchical Analysis: Start with simple methods like macroscopic and microscopic examination, then progress to more complex techniques.
- Chromatographic Profiling: Techniques like Thin-Layer Chromatography (TLC) and High-Performance Liquid Chromatography (HPLC) are essential for comparing the chemical profile of your sample against a verified reference standard [1].
- Advanced Techniques: For high specificity, employ DNA barcoding for species-level genetic authentication. Use Mass Spectrometry (e.g., LC-MS) to detect and identify unexpected chemical compounds, such as synthetic drug adulterants or contaminants [1] [9].
3. My experimental results are inconsistent with historical or traditional use data. Why? Discrepancies between laboratory results and traditional knowledge can arise from several factors:
- Preparation Disparity: The laboratory extraction method (e.g., using a single solvent like methanol) may differ significantly from traditional preparation methods (e.g., decoctions in water), leading to different phytochemical profiles and bioactivity [9].
- Holistic vs. Reductionist Approach: Traditional medicine often uses polyherbal formulations where the therapeutic effect is synergistic. Isolating a single compound may not capture the full effect [10].
- Insufficient Quality Control: The test material used in your study may be adulterated, contaminated, or degraded, leading to results that do not reflect the authentic traditional medicine practice [1]. Re-evaluate the quality of your research material against the specifications of the traditional system you are studying.
4. How do I design a placebo for a clinical trial involving a distinctive-smelling or tasting herbal product? Creating a convincing placebo for herbal products is critical for maintaining blinding.
- Placebo Matching: Develop a placebo that matches the active product in every physical aspect—size, shape, color, and weight.
- Taste and Smell Masking: For distinctive organoleptic properties, use food-grade flavorings and odorants that mimic the herbal product. Inactive herb powders with similar characteristics can also be blended.
- Encapsulation: The most effective method is often to encapsulate both the active product and the placebo in opaque, size-matched capsules to minimize sensory differences [10]. A successful placebo should be indistinguishable from the verum in a blind test.
Experimental Protocols for Key Analyses
Protocol 1: Chromatographic Fingerprinting for Standardization
- Objective: To create a unique chemical profile for quality control and batch consistency of an herbal extract.
- Materials: Herbal test sample, reference standard (e.g., from a pharmacopoeia), HPLC system with UV/VIS or DAD detector, analytical column (C18), solvents (HPLC-grade water, acetonitrile, methanol), and filtration apparatus.
- Method:
- Sample Preparation: Accurately weigh a specified amount of herbal extract. Dissolve and dilute in an appropriate solvent. Filter through a 0.45 µm or 0.22 µm membrane filter.
- HPLC Conditions:
- Column: C18 (e.g., 250 mm x 4.6 mm, 5 µm)
- Mobile Phase: Gradient of solvent A (0.1% formic acid in water) and solvent B (acetonitrile).
- Flow Rate: 1.0 mL/min
- Detection: UV-Vis/DAD, typically at 254-280 nm (or a wavelength specific to the target compounds).
- Injection Volume: 10-20 µL
- Analysis: Inject the reference standard and the test sample. The fingerprint of the test sample should match the profile and relative retention times of the peaks in the reference standard fingerprint [1] [2].
Protocol 2: DNA Barcoding for Botanical Authentication
- Objective: To genetically identify the plant species in an herbal material to prevent misidentification and adulteration.
- Materials: Plant sample, DNA extraction kit, PCR thermal cycler, primers for standard barcode regions (e.g., matK, rbcL, ITS2), gel electrophoresis equipment, and sequencing facility access.
- Method:
- DNA Extraction: Isolate genomic DNA from the herbal material (fresh, dried, or powdered) using a commercial kit optimized for plants.
- PCR Amplification: Amplify the selected barcode region(s) using universal primers in a PCR reaction.
- Gel Electrophoresis: Confirm successful amplification by running the PCR product on an agarose gel.
- Sequencing and Analysis: Purify the PCR product and send it for Sanger sequencing. Compare the resulting DNA sequence to a curated reference database (e.g., GenBank, BOLD) for species identification [1] [2].
Table 1: Global Medicinal Herbs Market Overview (2025-2032 Projection)
| Metric | Value / Forecast | Notes / Source |
|---|---|---|
| Market Size (2025) | USD 227.65 Billion | [6] |
| Projected Market Size (2032) | USD 478.93 Billion | [6] |
| Compound Annual Growth Rate (CAGR) | 11.21% | Projected for 2025-2032 [6] |
| Top-Selling Herb Type (2025) | Ginseng | 16.6% market revenue share [6] |
| Dominant Application (2025) | Pharmaceuticals | Revenue ~USD 95.8 Billion [6] |
| Leading Regional Market (2025) | Asia-Pacific | >40% global revenue share [6] |
Table 2: Key Quality Control Parameters for Herbal Materials [1] [2]
| Parameter | Purpose | Common Analytical Methods |
|---|---|---|
| Physicochemical Testing | Assess product consistency and chemical properties | pH, viscosity, solubility, HPLC, TLC |
| Microbiological Testing | Ensure absence of harmful microorganisms | Total viable aerobic count, tests for yeast/mold, E. coli, Salmonella |
| Heavy Metal & Pesticide Limits | Verify compliance with safety limits for toxic residues | ICP-MS, AAS, Chromatography (GC-MS/LC-MS) |
| Adulteration & Contaminants | Detect non-declared or harmful substances | Visual inspection, spectroscopy, chemical marker analysis |
| Chromatographic Fingerprinting | Confirm identity and quantify active compounds | TLC, HPLC, HPTLC with reference marker compounds |
Research Workflow Visualization
Quality Control Workflow for Herbal Medicine Research
Herbal Ingredient Authentication Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Herbal Medicine Standardization
| Item | Function / Application |
|---|---|
| Reference Standards | Certified chemical compounds used to identify and quantify active markers or impurities in herbal samples via HPLC, GC, or TLC. Critical for method validation and standardization [1]. |
| DNA Extraction Kits | Optimized reagents for isolating high-quality genomic DNA from complex plant tissues, which is the first critical step for DNA barcoding and genetic authentication [1]. |
| PCR Primers (e.g., matK, rbcL) | Short, specific DNA sequences designed to amplify standard barcode regions for plant species identification and phylogenetic analysis [1]. |
| Chromatography Columns (C18) | The stationary phase in Reverse-Phase HPLC systems for separating complex mixtures of phytochemicals based on their hydrophobicity [1] [9]. |
| Mobile Phase Solvents | High-purity solvents (e.g., Acetonitrile, Methanol) and modifiers used as the liquid medium in HPLC to elute compounds from the column [1]. |
| Microbiological Culture Media | Used in microbial limit tests to detect and enumerate total viable aerobic count, yeast, and mold in herbal products to ensure safety [2]. |
Core Concepts: Understanding Quality Control Failures
What are the primary consequences of inadequate quality control in herbal medicine research?
Inadequate quality control in herbal medicine research leads to three primary consequences: variability in product composition, contamination with harmful substances, and adulteration with undeclared ingredients. These failures compromise experimental reproducibility, product safety, and therapeutic efficacy, ultimately undermining the validity and reliability of research findings [1] [9].
- Variability: Inconsistent levels of active compounds between batches creates significant challenges for reproducing experimental results and establishing reliable dose-response relationships [1]. This inconsistency stems from insufficient standardization of raw materials and manufacturing processes.
- Contaminants: Herbal products may contain biological (microbes, molds), chemical (pesticides, heavy metals), or physical (glass, metal) contaminants introduced during cultivation, processing, or storage [1] [11]. These pose direct safety risks to research subjects and consumers.
- Adulteration: The deliberate substitution or addition of undeclared substances, including synthetic drugs or inferior herbal species, constitutes adulteration [12]. This practice misrepresents the true nature of the test material and invalidates experimental conclusions.
How do these quality failures impact drug development timelines and costs?
Quality failures significantly increase drug development timelines and costs through multiple mechanisms:
- Preclinical Delays: Variable composition necessitates repeated experiments to verify biological activity, increasing animal studies and in vitro testing requirements.
- Clinical Setbacks: Contaminant discoveries during clinical trials can halt studies entirely, requiring investigation, protocol revisions, and regulatory resubmissions.
- Regulatory Rejection: Insufficient quality control data results in regulatory authority requests for additional information or complete rejection of marketing applications [2].
- Product Recalls: Marketed products requiring recall due to quality issues generate substantial financial losses and reputational damage [12].
Troubleshooting Guides
Problem: Inconsistent Bioactivity Between Batches
Problem Identification: Researchers observe significant variation in pharmacological activity between different batches of the same herbal extract despite using identical experimental protocols.
Root Cause Analysis:
- Source Variation: Differences in growing conditions, harvest time, or plant genetics affecting phytochemical profiles [1]
- Processing Inconsistency: Variable extraction parameters (temperature, solvent, time) or post-extraction handling
- Authentication Issues: Misidentification of plant species or use of incorrect plant parts
Resolution Protocol:
- Implement Chromatographic Fingerprinting: Develop HPLC or HPTLC fingerprints to establish a baseline chemical profile for reference batches [2] [9]
- Quantify Marker Compounds: Identify and quantify key active compounds or chemical markers to establish minimum potency thresholds [1]
- Standardize Extraction Procedures: Document and strictly control all extraction parameters including solvent composition, temperature, time, and particle size
- Validate Analytical Methods: Establish method precision, accuracy, and reproducibility following ICH guidelines [2]
Preventive Measures:
- Develop standardized operating procedures (SOPs) for all processing steps
- Establish quality specifications for raw materials including botanical identity and chemical composition
- Implement reference standard comparison for each new batch
Problem: Suspected Adulteration with Synthetic Compounds
Problem Identification: Unexpected pharmacological effects or analytical results suggest potential adulteration with synthetic pharmaceutical compounds.
Root Cause Analysis:
- Economic Motive: Deliberate adulteration to enhance perceived efficacy at lower cost [12]
- Supply Chain Complexity: Lack of transparency in multi-tier supplier networks
- Insufficient Screening: Inadequate analytical methods to detect non-botanical substances
Resolution Protocol:
- Comprehensive Screening: Employ LC-MS/MS to screen for common synthetic adulterants based on product claims
- Comparative Analysis: Compare chromatographic profiles with authenticated reference samples
- Forensic Investigation: Trace supply chain documentation to identify potential points of adulteration
- Bioactivity Assessment: Evaluate whether observed pharmacological effects align with expected herbal activity
Preventive Measures:
- Implement supplier verification programs with rigorous qualification criteria
- Conduct random testing of incoming raw materials using targeted and untargeted methods
- Establish chemical fingerprints for authenticated reference materials
Problem: Contamination with Heavy Metals or Pesticides
Problem Identification: Routine testing detects heavy metals or pesticide residues above acceptable thresholds in herbal test materials.
Root Cause Analysis:
- Environmental Factors: Contaminated soil or water from cultivation sites [1]
- Agricultural Practices: Use of banned or excessive pesticides during cultivation
- Processing Equipment: Leaching of metals from processing machinery or containers
Resolution Protocol:
- Source Identification: Use ICP-MS for heavy metal profiling and GC-MS for pesticide analysis to identify contaminants [2]
- Supplier Assessment: Audit cultivation practices and environmental conditions at source farms
- Purification Evaluation: Assess whether processing methods can reduce contaminants to acceptable levels
- Material Rejection: Establish rejection criteria for contaminated materials exceeding safety thresholds
Preventive Measures:
- Implement rigorous supplier qualification including environmental testing
- Establish certificate of analysis requirements with specific contaminant limits
- Conduct regular audits of cultivation and collection practices
Frequently Asked Questions (FAQs)
What are the minimum quality control parameters for herbal material in preclinical research?
For credible preclinical research, herbal materials should be characterized against these minimum parameters:
Table: Essential Quality Control Parameters for Herbal Research Materials
| Parameter | Purpose | Recommended Methods | Acceptance Criteria |
|---|---|---|---|
| Botanical Authentication | Verify correct species and plant part | Macroscopic/microscopy examination, DNA barcoding [1] | Match to authenticated voucher specimen |
| Chemical Fingerprinting | Establish chemical profile consistency | HPTLC, HPLC, GC [9] | Minimum 80% similarity to reference fingerprint |
| Marker Compound Quantification | Standardize potency | HPLC-UV, LC-MS [1] | ±15% of reference batch concentration |
| Contaminant Screening | Ensure material safety | ICP-MS (heavy metals), GC-MS (pesticides) [2] | Below ICH/USP regulatory limits |
| Microbial Limits | Prevent biological contamination | Total viable count, pathogen testing [2] | Meet pharmacopeial standards |
How can researchers authenticate herbal species when reference standards are unavailable?
When certified reference standards are unavailable, researchers can employ these authentication strategies:
- Comparative Morphology: Conduct macroscopic and microscopic examination against authoritative botanical descriptions [1]
- DNA Barcoding: Sequence specific genomic regions (e.g., ITS, rbcL) and compare to genomic databases [1] [2]
- Voucher Specimens: Deposit authenticated specimens in herbarium for future reference
- Chemical Profiling: Develop characteristic fingerprints using multiple analytical techniques
- Expert Verification: Consult botanical taxonomists for species identification
What analytical techniques are most suitable for detecting different types of adulteration?
Adulteration detection requires technique selection based on the nature of suspected adulterants:
Table: Analytical Techniques for Adulterant Detection
| Adulteration Type | Primary Techniques | Secondary Techniques | Detection Capability |
|---|---|---|---|
| Species Substitution | DNA barcoding [1], HPTLC [9] | Microscopy, HPLC fingerprinting | Genetic differences, chemical profile variances |
| Addition of Synthetic Drugs | LC-MS/MS, HPLC-DAD | GC-MS, NMR | Nanogram-level detection of pharmaceuticals |
| Undisclosed Fillers | FT-IR, NIR spectroscopy | Microscopy, chemical tests | Identification of starch, sugars, other diluents |
| Heavy Metal Contamination | ICP-MS, AAS [2] | XRF, ICP-OES | Parts-per-billion detection of toxic elements |
| Pesticide Residues | GC-MS/MS, LC-MS/MS | HPLC, ELISA | Multiple residue screening at regulatory limits |
Experimental Protocols
Protocol: Development of Chromatographic Fingerprints for Batch Standardization
Principle: Chromatographic fingerprinting provides a comprehensive profile of multiple constituents to ensure consistent chemical composition across research batches [9].
Materials and Equipment:
- Herbal test material (minimum 3 batches from different sources)
- Reference standard compounds (if available)
- HPLC/HPTLC system with photodiode array detector
- Analytical balance (±0.0001 g precision)
- Ultrasonic bath for extraction
- HPLC-grade solvents (methanol, acetonitrile, water)
- Chromatography columns/cellulose plates
Procedure:
- Sample Preparation: Precisely weigh 1.0 g powdered herb, extract with 10 mL methanol-water (70:30) via ultrasonication (30 min, 25°C)
- Centrifugation: Centrifuge at 10,000 rpm for 10 minutes, filter through 0.45 μm membrane
- Instrument Conditions:
- Column: C18 (250 × 4.6 mm, 5 μm)
- Mobile phase: Gradient of 0.1% formic acid (A) and acetonitrile (B)
- Flow rate: 1.0 mL/min
- Detection: 190-400 nm scanning
- Injection volume: 10 μL
- Analysis: Inject samples in triplicate, record chromatograms at multiple wavelengths
- Data Processing: Calculate relative retention times and peak areas of characteristic peaks
Validation Parameters:
- Precision (RSD < 2% for retention times)
- Stability (RSD < 3% over 24 hours)
- Reproducibility (RSD < 5% between instruments)
Interpretation: Fingerprints from test batches should show minimum 80% similarity to reference fingerprint when evaluated using chemometric software.
Protocol: Heavy Metal Analysis via ICP-MS
Principle: Inductively coupled plasma mass spectrometry provides sensitive multi-element detection for toxic heavy metals in herbal materials [2].
Materials and Equipment:
- ICP-MS instrument with collision/reaction cell
- Certified reference material (CRM) for quality control
- High-purity nitric acid (trace metal grade)
- Microwave digestion system
- Ultra-pure water (18.2 MΩ·cm)
- Single-element standard solutions (As, Cd, Pb, Hg)
Procedure:
- Sample Digestion: Accurately weigh 0.5 g powdered sample into digestion vessel, add 5 mL nitric acid
- Microwave Program:
- Step 1: Ramp to 100°C in 10 min, hold 5 min
- Step 2: Ramp to 180°C in 10 min, hold 15 min
- Cooling: 30 min to room temperature
- Dilution: Transfer digestate to 50 mL volumetric flask, dilute to volume with ultra-pure water
- Calibration: Prepare standard curve (0, 0.5, 1, 5, 10, 50 μg/L) for each element
- ICP-MS Analysis:
- RF power: 1550 W
- Carrier gas: 0.8 L/min argon
- Integration time: 0.5-1.0 s per mass
- Measured isotopes: 75As, 111Cd, 208Pb, 202Hg
Quality Control:
- Analyze method blank with each batch
- Include CRM every 10 samples (recovery 85-115%)
- Internal standard (e.g., 115In, 209Bi) for drift correction
Calculation: Element concentration (mg/kg) = (C × V × D) / W Where: C = concentration from calibration (μg/L), V = final volume (mL), D = dilution factor, W = sample weight (g)
Visualizations
Quality Control Failure Investigation Pathway
Herbal Material Authentication Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Essential Materials for Herbal Medicine Quality Control Research
| Category | Specific Items | Research Application | Quality Specifications |
|---|---|---|---|
| Reference Standards | Certified chemical markers, authenticated botanical specimens [1] | Method validation, compound identification | ≥95% purity, documented provenance |
| Chromatography Supplies | HPLC columns (C18, HILIC), HPTLC plates, GC capillaries [9] | Compound separation, fingerprint development | LC-MS grade solvents, certified columns |
| Molecular Biology Kits | DNA extraction kits, PCR master mixes, sequencing primers [1] | Genetic authentication, species identification | DNA-free components, high fidelity enzymes |
| Sample Preparation | Solid-phase extraction cartridges, filtration units, microwave digestion vessels | Sample clean-up, contaminant removal | Low extractable backgrounds, high recovery |
| Spectroscopy Supplies | ICP-MS calibration standards, AAS lamps, NMR solvents [2] | Elemental analysis, structural elucidation | Traceable standards, deuterated solvents |
| Microbiology Materials | Culture media, membrane filters, incubation equipment | Microbial limit testing, sterility verification | Sterility-certified, growth-promoting tested |
Bridging Traditional Knowledge and Modern Scientific Validation
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What constitutes a scientifically valid approach for documenting traditional herbal knowledge? A1: Valid documentation requires a structured ethnobotanical framework combining:
- Scientific Authentication: Proper botanical identification using macroscopic, microscopic, and molecular methods (e.g., DNA barcoding) to verify species and plant parts used [13] [2].
- Traditional Context Recording: Detailed documentation of traditional preparation methods, dosage forms, administration routes, and cultural protocols through interviews with knowledge holders [13] [14].
- Chemical Profiling: Initial phytochemical screening using chromatographic fingerprinting (TLC, HPLC) to identify marker compounds and potential bioactive constituents [4] [13].
Q2: How can researchers address batch-to-batch variability in herbal material? A2: Implement a multivariable optimization framework controlling three key domains [4]:
- Herb Variation: Standardize cultivation (Good Agricultural Practices), harvesting timing, and processing methods to minimize phytochemical fluctuations.
- Disease Variation: Develop clear diagnostic criteria and practitioner training for consistent application.
- Patient Variation: Incorporate personalized medicine principles considering individual patient factors and constitutions.
Q3: What are the essential quality control parameters for herbal medicine research? A3: The WHO outlines critical quality parameters that should be standardized [2]:
Table: Essential Quality Control Parameters for Herbal Research
| Parameter | Purpose | Standard Methods | Acceptance Criteria |
|---|---|---|---|
| Botanical Authentication | Verify plant species & part | Macroscopic/microscopic examination, DNA barcoding | Match reference standards |
| Physicochemical Properties | Assess consistency | pH, viscosity, solubility, HPLC, TLC | Meet predefined specifications |
| Microbiological Quality | Ensure safety | Total viable count, pathogen testing | Comply with pharmacopeial limits |
| Contaminant Testing | Detect harmful residues | Heavy metals, pesticides, mycotoxins analysis | Below regulatory thresholds |
| Marker Compound Quantification | Standardize potency | HPLC-MS, LC-MS, reference standards | Consistent across batches |
Q4: How can traditional preparation methods be reconciled with modern extraction protocols? A4: Research should:
- Document Traditional Methods: Precisely record traditional preparation techniques (infusion times, solvent types, temperature controls) used by knowledge holders [15] [16].
- Compare Extraction Efficiency: Systematically evaluate traditional methods against modern techniques for biomarker yield and biological activity.
- Validate Traditional Knowledge: Identify scientific rationale behind traditional methods (e.g., why specific solvents or preparation times are used) [13] [17].
Troubleshooting Common Experimental Challenges
Problem: Inconsistent biological activity between batches of the same herbal material.
Possible Causes & Solutions:
- Cause 1: Improper plant identification or seasonal variation
- Cause 2: Suboptimal extraction method for target compounds
- Solution: Match extraction method to compound chemistry: hydroalcoholic extraction for resins, low-alcohol for mucilaginous herbs, and validate extraction efficiency [18].
- Cause 3: Degradation of active constituents during processing or storage
- Solution: Conduct stability studies under various conditions (temperature, light, humidity) to establish shelf-life and optimal storage parameters [2].
Problem: Lack of correlation between traditional use and laboratory bioassay results.
Possible Causes & Solutions:
- Cause 1: Testing isolated compounds instead of whole preparations
- Solution: Investigate both single compounds and traditional combination formulas to identify synergistic effects [19].
- Cause 2: Using inappropriate disease models or endpoints
- Cause 3: Ignoring traditional preparation methods in extraction protocols
- Solution: Faithfully replicate traditional preparation methods before proceeding to standardized extracts [16].
Experimental Protocols for Validation Research
Protocol 1: Comprehensive Herbal Material Standardization
Objective: Establish consistent, quality-controlled herbal research material.
Methodology:
- Botanical Verification: Collect voucher specimens with expert identification; deposit in herbarium [13].
- Standardized Processing: Implement consistent drying conditions (temperature, duration, airflow) based on traditional knowledge where applicable.
- Chemical Fingerprinting: Develop HPLC or TLC fingerprints using reference standards; quantify marker compounds.
- Stability Testing: Monitor chemical and physical stability under controlled storage conditions over time.
Table: Research Reagent Solutions for Herbal Standardization
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Reference Standards | Quantify marker compounds | Source from certified suppliers; verify purity |
| Chromatography Solvents | Extract and separate compounds | HPLC-grade for analysis; food-grade for preparations |
| Authentication Kits | Verify species identity | DNA barcoding reagents; microscopic staining solutions |
| Culture Media | Microbial quality testing | TSA, SCD agar for aerobic counts; selective media for pathogens |
Protocol 2: Ethnobotanical Data Collection and Validation
Objective: Systematically document and validate traditional knowledge.
Methodology:
- Community Engagement: Obtain free, prior, and informed consent following ethical guidelines for working with Indigenous communities [14] [17].
- Structured Interviews: Use standardized questionnaires to record plant uses, preparation methods, dosage, and administration routes.
- Cross-Verification: Interview multiple knowledge holders to verify information.
- Scientific Correlation: Analyze documented uses against phytochemical and pharmacological data.
Methodological Workflows
Research Reagent Solutions
Table: Essential Materials for Herbal Medicine Research
| Category | Specific Items | Research Function |
|---|---|---|
| Authentication | DNA barcoding kits, Microscopy stains, Herbarium supplies | Verify plant species and prevent adulteration |
| Extraction | Food-grade solvents, Standardized reference compounds | Reproduce traditional preparations and ensure consistency |
| Analysis | HPLC columns, TLC plates, Mass spectrometry standards | Quantify active constituents and create chemical fingerprints |
| Quality Control | Microbial testing media, Heavy metal analysis kits | Ensure safety and compliance with regulatory standards |
| Bioactivity Testing | Cell culture reagents, Enzyme assay kits, Animal model supplies | Evaluate pharmacological effects and mechanisms of action |
This technical support framework provides researchers with practical methodologies for bridging traditional herbal knowledge and modern scientific validation, emphasizing standardized approaches, troubleshooting guidance, and ethical collaboration with traditional knowledge holders.
A Methodological Toolkit: From Classical Pharmacognosy to Advanced Analytics
What is the primary goal of applying these classical techniques in modern herbal research? The primary goal is to ensure the quality, safety, and efficacy of herbal medicines by confirming the correct identity of raw materials, detecting adulteration, and guaranteeing batch-to-batch consistency. This standardization is a fundamental prerequisite for integrating herbal products into modern evidence-based healthcare and is emphasized in guidelines from bodies like the WHO [2] [4].
How do morphological, microscopic, and physicochemical analyses work together? These techniques form a hierarchical quality assessment chain. Morphological evaluation provides the first line of identification through gross physical inspection. Microscopic analysis offers a more detailed, structural verification that can detect adulteration even in powdered materials. Physicochemical profiling then quantifies material properties and ensures purity, creating a comprehensive quality control protocol [20] [21].
Within a thesis on standardization, what is the significance of establishing a "reference standard"? The entire standardization process depends on a well-characterized reference standard. This refers to a validated sample of the plant material against which all future batches are compared. It is typically characterized using all three classical techniques—morphology, microscopy, and physicochemical parameters—to create a definitive fingerprint that ensures consistency and reliability in research and production [20] [2].
Morphological Evaluation: Troubleshooting Guide
Issue: Observed high morphological variation between plant samples, causing identification uncertainty.
- Potential Cause: Natural phenotypic plasticity due to growing conditions (soil, climate) or misidentification of a closely related species.
- Solution:
- Standardize Assessment: Create a standardized checklist of diagnostic characters (e.g., leaf shape, margin, venation, surface texture, flower color and structure) based on an authoritative pharmacopoeia or botanical reference.
- Use Reference Samples: Always compare unknown samples directly against a verified voucher specimen.
- Document Thoroughly: Use high-resolution photography with a scale under consistent lighting. Capture details of both sides of the leaf, the stem, and flowers/fruits if available [22] [21].
Issue: Reliably distinguishing between dried plant parts that look superficially similar.
- Potential Cause: Key diagnostic features like color or smell can fade or change upon drying.
- Solution:
- Focus on Stable Characters: Prioritize structural characteristics that are less variable, such as the arrangement of flowers (inflorescence type), fruit type, and seed morphology.
- Rehydrate if Necessary: Briefly soak dried leaves or stems to restore texture and make features like venation patterns more visible.
- Corroborate with Other Techniques: This limitation highlights why morphological evaluation is only the first step and must be followed by microscopic analysis for definitive identification [21].
Microscopic Evaluation: Troubleshooting Guide
Issue: Tissue sections are too thick or fragile, resulting in poor-quality microscopic images.
- Potential Cause: Improper sectioning technique or inadequate sample preparation.
- Solution:
- Softening: For hard or dry materials, soften by soaking in a mixture of water, glycerin, and alcohol before sectioning.
- Support for Fragile Tissues: Embed fragile materials in a supporting matrix like paraffin wax or carboxymethyl cellulose (CMC) to facilitate clean, thin sectioning with a microtome.
- Clearing: Use chloral hydrate solution or lactic acid to clear the section, dissolving cytoplasmic contents and making cell walls and crystals like calcium oxalate more distinct [20] [22].
Issue: Unable to identify key diagnostic microscopic features (e.g., stomata, trichomes) with confidence.
- Potential Cause: Insufficient knowledge of the plant's typical anatomy or incorrect microscope settings.
- Solution:
- Consult Reference Atlases: Use anatomical atlases of medicinal plants or published monographs for the expected microscopic features of your specific plant.
- Utilize Staining Techniques: Employ simple stains to differentiate tissues. For example, iodine solution stains starch grains blue-black, while Sudan Red IV stains cutin and suberin in cell walls.
- Optimize Microscopy: Start with lower magnification to locate areas of interest, then switch to higher magnification (e.g., 400x) for detailed observation of stomata and trichomes. Adjust the condenser and diaphragm for optimal contrast [20].
Issue: Image analysis software provides inconsistent particle shape data.
- Potential Cause: Process variables like inconsistent sample illumination, incorrect greyscale thresholding, or an inappropriate scaling factor (µm/pixel) [23].
- Solution:
- Standardize Illumination: Ensure the light source position and intensity are consistent for all images.
- Calibrate Thresholding: Manually set and validate the greyscale threshold used to distinguish particles from the background.
- Optimize Scaling Factor: Use a scaling factor (optical magnification and pixel size) that is low enough for accurate shape estimation but high enough to maintain a practical field of view. Analyze a statistically sufficient number of particles (often 50-100) for a representative assessment [23].
Experimental Workflow for Microscopic Analysis
The diagram below outlines a standard workflow for the microscopic identification of herbal materials.
Physicochemical Evaluation: Troubleshooting Guide
Issue: Extractive values are consistently lower than the pharmacopoeial requirement.
- Potential Cause: The plant material may be too old or was dried at too high a temperature, degrading active compounds. Alternatively, the particle size of the powder may be too coarse, leading to inefficient extraction.
- Solution:
- Verify Raw Material Quality: Ensure the plant was harvested at the correct time and dried gently (e.g., air-dried in shade).
- Optimize Powder Size: Grind the simplicia to a fine, uniform powder to increase the surface area for extraction, as specified in methods like those in the Materia Medica Indonesia [20].
- Confirm Extraction Protocol: Ensure the maceration time (e.g., 6 hours shaking followed by 18 hours standing) and solvent volume are strictly adhered to [20].
Issue: High ash value, particularly acid-insoluble ash.
- Potential Cause: Contamination with silica-rich earthy materials like sand and soil, or improper cleaning of the raw plant material.
- Solution:
- Improve Raw Material Handling: Implement stricter washing and cleaning procedures for the harvested plant parts.
- Control Source: Audit the cultivation and harvesting practices to minimize soil contamination.
- Interpret Results: The acid-insoluble ash value specifically indicates silicate contamination, and a high value fails quality standards, as seen in requirements where it must not be more than 3% [20].
Issue: Unclear or overlapping spots on TLC plates.
- Potential Cause: Inappropriate mobile phase composition, sample overloading, or an undersaturated TLC chamber.
- Solution:
- Optimize Mobile Phase: Research literature for established mobile phases for your plant's compound class (e.g., hexane-acetone 3:2 v/v for some compounds in Ruta angustifolia) and adjust ratios slightly for better separation [20].
- Dilute Sample: Spot a more dilute sample solution to prevent overloading.
- Saturate Chamber: Ensure the TLC development chamber is properly lined with filter paper and saturated with the mobile phase vapor for at least 20-30 minutes before introducing the plate.
Key Physicochemical Parameters for Quality Control
The following table summarizes standard physicochemical tests and their acceptable criteria, as exemplified by research on Ruta angustifolia leaves, which adhered to the Materia Medica Indonesia [20].
| Parameter | Purpose | Typical Method | Exemplary Result & Requirement |
|---|---|---|---|
| Loss on Drying | Measures moisture content; affects stability & risk of microbial growth. | Drying at 105°C to constant weight. | 10.02% (Requirement: ≤10%) [20] |
| Total Ash | Measures total inorganic residue; indicates mineral content & earthy matter. | Incineration at 600°C. | 10.75% (Requirement: ≥10%) [20] |
| Acid-Insoluble Ash | Measures silicate contaminants like sand and soil. | Ash treated with dilute HCl and reignited. | 0.52% (Requirement: ≤3%) [20] |
| Water-Soluble Extract | Estimates content of water-soluble compounds (e.g., tannins, sugars). | Maceration with water, evaporation, weighing. | 27.14% (Requirement: ≥28%) [20] |
| Ethanol-Soluble Extract | Estimates content of alcohol-soluble compounds (e.g., resins, alkaloids). | Maceration with 95% ethanol, evaporation, weighing. | 20.17% (Requirement: ≥8%) [20] |
| Heavy Metals | Ensures safety by quantifying toxic elements (Pb, Cd, As, Hg). | Atomic Absorption Spectrophotometry (AAS). | e.g., Pb: 0.12 ppm (Requirement: ≤10 ppm) [20] |
Experimental Workflow for Physicochemical Standardization
The diagram below illustrates the logical sequence of key tests in a physicochemical profiling workflow.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key reagents and materials required for performing the classical evaluations discussed.
| Item | Primary Function |
|---|---|
| Chloral Hydrate | A clearing agent used in microscopic slide preparation to dissolve cytoplasm and chlorophyll, making cell walls and crystals clearly visible [20]. |
| Reference Standard (Plant Material) | A botanically verified and fully characterized sample of the plant, serving as the benchmark for all morphological, microscopic, and chemical comparisons [20] [2]. |
| Silica Gel GF254 (TLC Plates) | The stationary phase for Thin Layer Chromatography (TLC); used for the fingerprinting and separation of chemical compounds like flavonoids and alkaloids [20]. |
| Specific Spray Reagents (e.g., Dragendorff's, FeCl₃) | Chemical developers used on TLC plates to visualize specific classes of compounds (e.g., Dragendorff's for alkaloids, FeCl₃ for phenolics) [20]. |
| HPLC-grade Solvents (e.g., Acetonitrile) | High-purity solvents used as the mobile phase in High-Performance Liquid Chromatography (HPLC) to generate precise phytochemical profiles for quantification [20]. |
| Simulated Gastric/Intestinal Fluids | Buffered solutions used in stability testing to determine how an herbal extract or formulation degrades in the gastrointestinal environment [24]. |
Chromatographic Fingerprinting (TLC, HPTLC, HPLC) for Metabolite Profiling
Chromatographic fingerprinting is an analytical methodology that uses an instrumental signal, such as a chromatogram, to obtain non-obvious information about the chemical composition of a complex sample, like an herbal preparation [25]. This fingerprint serves as a unique identity card for the material, enabling both identity and quality testing [25] [26]. Within the critical field of herbal medicine research, this technique is indispensable for standardization, ensuring product consistency, detecting adulteration, and confirming authenticity, thereby directly supporting the efficacy and safety of herbal products [1].
This technical support center provides researchers and scientists with foundational knowledge, detailed protocols, and troubleshooting guides for implementing chromatographic fingerprinting in herbal medicine standardization.
Key Concepts and Methodologies
What is Chromatographic Fingerprinting?
Chromatographic fingerprinting is an analytical methodology that uses a chromatographic signal (the "fingerprint") to obtain information about a material's identity or quality, which is linked to its chemical composition [25]. The information within the fingerprint is implicit and non-specific, meaning it is not obviously tied to individual compounds. Extracting this information requires the application of chemometric data-mining tools on a large set of representative fingerprints [25] [26].
Fingerprinting vs. Profiling:
- Fingerprinting: A high-throughput process aimed at rapidly uncovering compositional differences between samples without necessarily achieving precise quantification or identification of all constituents. The goal is to use the entire chromatographic signal as a differentiating pattern [26].
- Profiling: An approach focused on obtaining detailed qualitative and/or quantitative information on the distribution of a sample's components, either for a pre-defined set of targets (targeted profiling) or for all detected constituents (untargeted profiling) [26].
General Workflow for Chromatographic Fingerprinting
The diagram below illustrates the logical sequence of steps for developing a chromatographic fingerprinting method.
Detailed Experimental Protocols
Protocol for Untargeted Metabolomic Analysis via LC-MS
This protocol is adapted for herbal medicine analysis and is based on a standard untargeted metabolomics workflow [27].
1. Sample Preparation:
- Extraction: Weigh a representative amount of the powdered herbal material. Extract using a solvent system suitable for polar metabolites, such as acetonitrile:methanol:formic acid (74.9:24.9:0.2, v/v/v). Vortex and centrifuge to pellet insoluble debris [27].
- Internal Standards: Incorporate stable isotope-labeled internal standards (e.g., l-Phenylalanine-d8 and l-Valine-d8) into the extraction solvent. This controls for variability during sample preparation and analysis [27].
2. Chromatographic Separation (HILIC for Polar Metabolites):
- Column: Use a hydrophilic interaction liquid chromatography (HILIC) column (e.g., Waters Atlantis HILIC Silica) for separating polar compounds.
- Mobile Phases:
- Mobile Phase A: 10 mM ammonium formate with 0.1% formic acid in LC/MS-grade water.
- Mobile Phase B: 0.1% formic acid in LC/MS-grade acetonitrile.
- Gradient: Employ a gradient elution starting with a high percentage of B (e.g., 85-95%) to retain polar metabolites, gradually increasing A to elute them. The total run time should be optimized for speed while retaining critical information, ideally under 10 minutes where possible [25].
3. Data Acquisition:
- Use a high-resolution mass spectrometer (e.g., Orbitrap or Q-ToF) for accurate mass measurement.
- Acquire data in both positive and negative ionization modes to maximize metabolite coverage.
4. Data Processing:
- Use software (e.g., Thermo Compound Discoverer, open-source tools) for peak picking, alignment, and deconvolution.
- Export a peak intensity table (features × samples) for subsequent chemometric analysis.
Protocol for Herbal Authentication via HPTLC
This protocol supports the authenticity testing required for herbal quality control [1].
1. Sample and Standard Preparation:
- Prepare methanolic or ethanolic extracts of the herbal test samples.
- Prepare a reference standard solution from an authenticated botanical sample of the same species.
2. Application and Development:
- Apply test and reference extracts as bands on an HPTLC plate (e.g., silica gel).
- Develop the plate in a saturated twin-trough chamber with a suitable mobile phase (e.g., ethyl acetate:glacial acetic acid:formic acid:water). Develop until the solvent front has migrated an appropriate distance.
3. Derivatization and Documentation:
- Dry the plate and visualize using appropriate reagents (e.g., anisaldehyde-sulfuric acid for terpenes, natural product reagent for flavonoids).
- Document the plate under UV (254 nm and 366 nm) and white light after derivatization using a digital imaging system.
4. Fingerprint Analysis:
- Compare the banding patterns (Rf values, colors) of the test samples against the reference standard. The pattern serves as the fingerprint for authentication [1].
Troubleshooting Guides and FAQs
HPLC Troubleshooting Guide
Table: Common HPLC Issues and Solutions
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Baseline Noise | Air bubbles in system; Detector cell contaminated; Detector lamp failure [28] | Degas mobile phase; purge system; clean or replace detector cell/flow; replace lamp [28] |
| Baseline Drift | Column temperature fluctuation; Mobile phase composition change; Poor column equilibration [28] | Use a column oven; prepare fresh mobile phase; increase equilibration time with new mobile phase [28] |
| Peak Tailing | Active sites on column; Blocked column; Inappropriate mobile phase pH [28] | Change column; reverse-flush column; adjust mobile phase pH [28] |
| Retention Time Drift | Poor temperature control; Incorrect mobile phase composition; Change in flow rate [28] | Use a thermostat column oven; prepare fresh mobile phase; check and reset flow rate [28] |
| Broad Peaks | Flow rate too low; Column overloading; Column contamination [28] | Increase flow rate; decrease injection volume; replace guard/analytical column [28] |
| High Pressure | Column blockage; Flow rate too high; Mobile phase precipitation [28] | Backflush column; lower flow rate; flush system and prepare fresh mobile phase [28] |
Frequently Asked Questions (FAQs)
Q1: Why is my chromatographic fingerprint for the same herbal batch showing high variability? A1: Inconsistency often stems from inadequate quality control during the initial steps. Ensure standardized sample collection, authentication of herbal ingredients, and strict adherence to the sample preparation protocol (extraction solvent, time, temperature) [1] [4]. Using stable isotope-labeled internal standards can help monitor and correct for this variability [27].
Q2: When should I use a targeted vs. a non-targeted (fingerprinting) approach? A2: Use a targeted approach when you need to accurately quantify a specific, pre-defined set of marker compounds. Use a non-targeted fingerprinting approach when your goal is to compare overall sample patterns, ensure authenticity, detect unknown adulterants, or assess global changes in metabolite profiles without prior knowledge of all constituents [25] [26] [29].
Q3: What are the critical parameters for developing a robust HPLC fingerprint method? A3: The triple decision is critical [25]:
- Sample Preparation: Must be reproducible and extract the relevant compounds.
- Chromatographic Mode/Conditions: Select the appropriate column (e.g., RP-C18, HILIC) and optimize the gradient for reasonable run time and sufficient separation. For fingerprinting, shorter run times (<10 min) can be acceptable even with some resolution sacrifice [25].
- Detection Settings: Wavelength for UV/VIS or parameters for MS detection must be set to capture a wide range of compounds.
Q4: How do I validate a chromatographic fingerprinting method? A4: Validation should demonstrate that the methodology can reliably establish identity and quality [25]. This includes assessing the method's precision (repeatability of fingerprints), stability, and robustness. The developed method should be able to consistently differentiate between authentic and adulterated or low-quality samples through chemometric models [25] [1].
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Materials for Chromatographic Fingerprinting
| Item | Function / Explanation |
|---|---|
| HILIC Column | Separates polar metabolites in untargeted profiling, complementary to reversed-phase chromatography [27]. |
| Stable Isotope-Labeled Internal Standards | Added to samples to monitor and correct for variability during sample preparation and analysis, improving data quality [27]. |
| Reference Standardized Herbal Extracts | Authenticated plant extracts used as a benchmark for comparing TLC/HPTLC banding patterns or HPLC profiles to confirm the identity of test samples [1]. |
| High-Resolution Mass Spectrometer (HR-MS) | Provides accurate mass data for metabolites, enabling confident identification and structural characterization in complex herbal matrices [29]. |
| Chemometric Software | Essential for extracting hidden information from fingerprinting data; used for pattern recognition, classification, and multivariate statistical analysis [25] [26]. |
Logical Workflow for Data Analysis
After data acquisition, processing the fingerprints to extract meaningful information is crucial. The following diagram outlines the standard data analysis pathway.
Spectroscopic Methods (UV-Vis, FTIR, NMR) and DNA Barcoding for Authentication
Troubleshooting Guides
Spectroscopic Analysis: Common Issues and Solutions
Table 1: Troubleshooting UV-Vis, FTIR, and NMR Spectroscopy for Herbal Authentication
| Problem | Possible Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Poor reproducibility of UV-Vis spectra | Inconsistent sample preparation; solvent effects; degradation of active compounds. | Standardize extraction protocol (e.g., solvent, time, temperature); perform analysis immediately after extraction; use degassed solvents. | Use internal standards; validate method robustness [30]. |
| FTIR spectra with low signal-to-noise ratio | Poor sample contact with ATR crystal; insufficient sample concentration; water vapor interference. | Clean ATR crystal thoroughly; ensure uniform powder for solid samples; increase scans; purge instrument with dry air. | Perform background scan immediately before sample; grind sample to fine, uniform particles [31]. |
| Overlapping peaks in NMR spectra | High complexity of herbal extract; low concentration of target analytes; solvent interference. | Use 2D-NMR techniques (e.g., COSY, HSQC) for separation; employ higher magnetic field strength; concentrate sample. | Use deuterated solvents; apply chemometrics (PCA, PLS-DA) for deconvolution [31] [30]. |
| Spectral mismatch with reference database | Natural variability due to geography, season; different processing methods; adulteration. | Develop in-house spectral libraries with authenticated samples; use chemometrics to identify marker peaks. | Apply multivariate analysis to account for acceptable variance; use multiple techniques for confirmation [30]. |
DNA Barcoding: Common Issues and Solutions
Table 2: Troubleshooting DNA Barcoding for Herbal Material Authentication
| Problem | Possible Causes | Solutions | Preventive Measures |
|---|---|---|---|
| PCR amplification failure | DNA degradation in processed herbs; presence of PCR inhibitors (e.g., polysaccharides, polyphenols). | Use mini-barcodes (shorter DNA regions); perform DNA clean-up protocols; add PCR enhancers (e.g., BSA, DMSO). | Optimize DNA extraction for specific material (fresh vs. dried); use silica-based purification columns [32] [33]. |
| Low discriminatory power | The chosen barcode region lacks sufficient sequence variation for closely related species. | Use multi-locus barcodes (e.g., ITS2+psbA-trnH); employ super-barcodes (complete plastid genome). | Select barcodes based on prior validation for the plant family (e.g., ITS2 as a core barcode for plants) [32]. |
| Inability to identify all species in a mixture | Universal primers have amplification bias; some species' DNA dominates the PCR. | Adopt DNA metabarcoding via NGS; use multiple primer sets to cover a wider taxonomic range. | For multi-ingredient products (e.g., CPMs), design the experiment for mixture analysis from the start [32] [33]. |
| Inconclusive or erroneous BLAST results | Reference sequence database lacks the species or contains misidentified sequences. | Use curated databases (e.g., BOLD Systems); cross-verify with morphological/chemical data. | Build a local, validated reference library with voucher specimens [33]. |
Frequently Asked Questions (FAQs)
Q1: Our herbal extract is a complex mixture. How can FTIR be useful when its spectrum has many overlapping peaks?
A1: While FTIR spectra of herbal extracts are complex, the overall profile serves as a chemical fingerprint. The key is not to assign every single peak but to use the entire spectral pattern for comparison. Techniques like chemometrics (e.g., Principal Component Analysis - PCA) can analyze the entire spectrum to differentiate species, detect adulterants, or assess batch-to-batch consistency, even with overlapping peaks [30]. This makes FTIR a rapid and powerful tool for quality control.
Q2: What is the most significant advantage of NMR in herbal medicine standardization compared to other spectroscopic methods?
A2: The primary advantage of NMR is its ability to provide simultaneous qualitative and quantitative information in a single, non-destructive analysis. It can identify multiple compounds and measure their absolute concentrations without requiring specific reference standards for every compound, which is a limitation of chromatographic methods. This makes it exceptionally powerful for profiling the complex, multi-constituent nature of herbal medicines and for detecting unexpected adulterants [31] [30].
Q3: When should we use "mini-barcodes" instead of conventional DNA barcodes?
A3: Use mini-barcodes when working with herbal materials where the DNA is highly degraded, such as in processed products, Chinese patent medicines (CPMs), heat-treated powders, or aged specimens. Conventional barcodes are longer and may not amplify from fragmented DNA, whereas mini-barcodes are short enough to target and sequence from damaged DNA templates, thereby improving identification success [32].
Q4: Our laboratory needs to identify the plant species in a multi-herb formulation. Can DNA barcoding handle this?
A4: Yes, but conventional Sanger sequencing of a single barcode cannot. The solution is DNA metabarcoding, a next-generation sequencing (NGS) approach. It allows for the simultaneous sequencing of DNA barcodes from all species present in a complex mixture, enabling the identification of multiple ingredients from a single sample. This is a major advancement for quality control of multi-herb products [33].
Q5: For quality control, is it better to use chemical fingerprinting (e.g., HPLC, FTIR) or DNA barcoding?
A5: They are complementary, not substitutable, and should be used together for a comprehensive quality assessment.
- DNA barcoding is superior for species authentication—answering "Is this the correct species?" It is highly specific and unaffected by environmental factors or the plant's physiological state.
- Chemical fingerprinting is essential for quality evaluation—answering "Does this sample contain the expected profile of chemical compounds in the right proportions?" It directly assesses the chemical composition, which is linked to efficacy.
A combination of both methods provides the most robust standardization, ensuring both correct identity and desired chemical quality [30].
Experimental Protocols
Detailed Protocol: DNA Metabarcoding for Multi-Ingredient Herbal Products
This protocol is adapted for identifying component species in complex herbal products like tablets or granules [32] [33].
Workflow Overview:
Step-by-Step Methodology:
DNA Extraction:
- Grind the sample to a fine powder using a sterile mortar and pestle or a tissue lyser.
- Use a commercial plant DNA extraction kit (e.g., DNeasy Plant Pro Kit from QIAGEN) designed to remove polysaccharides and polyphenols, which are common PCR inhibitors.
- Quantify the extracted DNA using a fluorometer (e.g., Qubit). Assess quality via agarose gel electrophoresis or Bioanalyzer. Expect fragmented DNA (100-500 bp) in processed products.
PCR Amplification (DNA Metabarcoding):
- Select one or more mini-barcode regions suitable for degraded DNA, such as ITS2, mini-rbcL, or the trnL P6 loop [33].
- Perform PCR in triplicate for each sample to mitigate amplification bias. Use high-fidelity DNA polymerase.
- Primer Example (ITS2): Forward:
5'-GTGAATCATCGAATCTTTGAA-3', Reverse:5'-CGCACATCCGCAACACGAGC-3'(with overhang adapters for NGS).
Library Preparation and Sequencing:
- Purify the pooled PCR products using solid-phase reversible immobilization (SPRI) beads (e.g., Ampure XP).
- Attach dual-indexed sequencing adapters to the amplicons via a limited-cycle PCR.
- Pool the final, uniquely indexed libraries in equimolar ratios. Sequence on an Illumina MiSeq or HiSeq platform (2x250 bp or 2x300 bp chemistry is typical).
Bioinformatics Analysis:
- Demultiplexing: Assign raw reads to each sample based on their unique indexes.
- Quality Filtering & Trimming: Use tools like
TrimmomaticorCutadaptto remove low-quality bases, primers, and adapters. - Clustering: Cluster high-quality reads into Operational Taxonomic Units (OTUs) at 97-100% similarity or denoise into Amplicon Sequence Variants (ASVs) using
DADA2orUNOISE3. - Taxon Assignment: BLAST the representative sequences from each cluster against a curated reference database (e.g., NCBI GenBank, BOLD Systems). Confirm identifications with a high-scoring segment pair (HSP) and a high percentage identity (e.g., >98-99%).
Detailed Protocol: FTIR Fingerprinting with Chemometric Analysis
This protocol outlines the creation of a chemical fingerprint for species differentiation and adulteration detection [31] [30].
Workflow Overview:
Step-by-Step Methodology:
Standardized Sample Preparation:
- Powder authenticated plant material to a consistent particle size (e.g., sieved through a 100-mesh screen).
- For ATR-FTIR, place the powder directly on the crystal and apply consistent pressure using the instrument's anvil.
- For transmission mode, create a KBr pellet by homogenously mixing 1-2 mg of sample with 200 mg of dry KBr and pressing under vacuum.
FTIR Spectral Acquisition:
- Acquire spectra in the mid-IR range (4000-400 cm⁻¹).
- Set resolution to 4 cm⁻¹ and accumulate 32-64 scans per spectrum to ensure a high signal-to-noise ratio.
- Collect a background spectrum before every sample or set of samples.
Spectral Pre-processing:
- Use software (e.g., MATLAB with PLS_Toolbox, R, or Python with SciPy) for pre-processing.
- Apply techniques sequentially:
- Atmospheric Suppression: Remove CO₂ (~2350 cm⁻¹) and H₂O vapor bands.
- Baseline Correction: To correct for scattering effects.
- Vector Normalization or Standard Normal Variate (SNV): To minimize the effects of path length and particle size.
Chemometric Modeling:
- Principal Component Analysis (PCA): An unsupervised method to explore natural clustering of samples and identify outliers.
- Partial Least Squares-Discriminant Analysis (PLS-DA): A supervised method to build a classification model that maximizes the separation between pre-defined groups (e.g., different species). Validate the model using cross-validation and a separate test set of samples.
Research Reagent Solutions
Table 3: Essential Materials for Herbal Authentication Experiments
| Category | Item / Reagent | Function / Application | Example Kits / Vendors |
|---|---|---|---|
| DNA-Based Authentication | Plant DNA Extraction Kit | Isolates high-quality DNA, free of inhibitors, from complex herbal matrices. | DNeasy Plant Pro Kit (QIAGEN), NucleoSpin Plant II (Macherey-Nagel) |
| Universal Barcode Primers | Amplifies standardized genomic regions for species identification. | Pre-designed primers for ITS2, rbcL, matK, psbA-trnH [32] | |
| High-Fidelity DNA Polymerase | Ensures accurate amplification for sequencing and library construction. | Q5 (NEB), Phusion (Thermo Scientific) | |
| SPRI Magnetic Beads | Purifies and size-selects DNA fragments post-amplification for NGS. | Ampure XP Beads (Beckman Coulter) | |
| Spectroscopic Analysis | Deuterated Solvents | Required for NMR spectroscopy to provide a stable lock signal. | DMSO-d6, CDCl₃, CD₃OD (e.g., from Sigma-Aldrich, Cambridge Isotopes) |
| ATR Crystals | Enables direct, non-destructive sampling for FTIR. | Diamond, ZnSe (Standard in FTIR spectrometers like Thermo Nicolet, Bruker) | |
| Internal Standards | Provides a reference for quantitative NMR (qNMR). | Dimethyl sulfone (DMS), Maleic acid [30] | |
| General & Quality Control | Authenticated Reference Plant Material (ARPM) | Provides a verified standard for comparison in all identification methods. | Supplied by botanical gardens, USP, or specialized herbaria [34] [30] |
| Chemical Reference Standards (Markers) | Used as benchmarks for chromatographic and spectroscopic quantification. | Active principles, analytical markers (e.g., curcumin, ginsenosides) [34] |
Implementing WHO GMP and Quality Control Parameters for Herbal Manufacturers
Frequently Asked Questions (FAQs) on WHO GMP & Standardization
FAQ 1: What is the core objective of WHO GMP for herbal medicines? The primary objective is to ensure that herbal products are consistently produced and controlled to the quality standards appropriate to their intended use [35]. It is a part of a quality management system aimed at diminishing the risks inherent in any pharmaceutical production, which can be broadly categorized into cross-contamination, mix-ups, and false labelling [35]. Above all, the goal is to ensure that manufacturers do not place patients at risk due to inadequate safety, quality, or efficacy.
FAQ 2: What are the key WHO quality control parameters for authenticating raw herbal materials? Authentication of raw materials is the critical first step. The key parameters and methods include [2] [1] [36]:
- Macroscopic & Microscopic Examination: Visual and microscopic inspection to identify correct plant species and plant parts.
- DNA Barcoding: A molecular technique used for authenticating species, such as Panax ginseng, to avoid misidentification [2].
- Chromatographic Fingerprinting: Techniques like Thin-Layer Chromatography (TLC) and High-Performance Liquid Chromatography (HPLC) are used to create a unique chemical profile of the herb, confirming identity and quantifying active compounds [2] [1].
FAQ 3: Our herbal extract shows batch-to-batch variation in potency. How can we improve consistency? Batch-to-batch variation is a common challenge addressed through extraction process validation and standardization [2] [1]. You must:
- Validate Extraction Parameters: Standardize and validate the methods for extraction (e.g., solvent, temperature, time) to ensure reliable and consistent extraction of bioactive constituents [2].
- Implement In-Process Controls: Monitor critical steps during manufacturing to detect and address deviations early [2] [37].
- Use Quantitative Analysis: Employ techniques like HPLC with reference standards to quantitatively measure the levels of active compounds or markers in every batch, ensuring they fall within a predefined range [2] [1].
FAQ 4: What are the mandatory labeling requirements for herbal products under WHO guidelines? WHO guidelines specify that labels must provide clear information for safety, traceability, and informed use. The mandatory components are summarized in the table below [2]:
Table 1: Mandatory Labeling Components for Herbal Products per WHO Guidelines
| Component | Details/Requirement | Example |
|---|---|---|
| Product Name | Commercial/trade name | "Herbal Digest-Ease" |
| Botanical Name | Full Latin binomial & plant part used | Curcuma longa L., rhizome |
| Dosage Form & Content | Form and net quantity | 500 mg capsule |
| Manufacturer Info | Name, address, license number, country | XYZ Herbal Ltd., License No. 12345, India |
| Warning Statements | Contraindications or known risks | "Not for use during pregnancy" |
| Dates | Date of Manufacture (DOM) and Expiry (DOE) | MM/YYYY format |
| Batch Number | Unique identifier for full traceability | Lot No: HL2024-03A |
FAQ 5: We've detected microbial contamination in a batch. What is the corrective action process? This triggers a deviation management process [37]:
- Quarantine and Investigate: Immediately quarantine the affected batch. Launch an investigation to determine the root cause, which could involve testing raw materials, reviewing sanitation records, and assessing environmental monitoring data from the production facility [37].
- Implement Corrective Actions: Address the root cause. This may involve deep-cleaning equipment, revising sanitation SOPs, reinforcing personnel hygiene protocols, or qualifying new raw material suppliers [37].
- Implement Preventive Actions (CAPA): Update risk management protocols to prevent recurrence, such as enhancing environmental monitoring frequency or providing additional staff training [37].
Troubleshooting Guides for Common Experimental & Production Issues
Guide 1: Troubleshooting Contaminant Detection
Table 2: Troubleshooting Contaminants in Herbal Products
| Problem | Possible Root Cause | Corrective & Preventive Actions |
|---|---|---|
| High Microbial Count | Contaminated raw materials, inadequate facility sanitation, improper storage conditions. | Test incoming herbs for total viable count, yeast & mold [2]. Validate sanitation procedures and review storage conditions (temperature, humidity) [37]. |
| Heavy Metal Contamination | Contaminated soil or water during cultivation, environmental pollution. | Implement supplier qualification and require Certificate of Analysis (CoA) with testing via ICP-MS or AAS [2]. Source materials from certified suppliers. |
| Pesticide Residue Exceedance | Non-compliant agricultural practices at the farm level. | Enforce stringent sourcing specifications. Test using chromatography methods. Develop long-term partnerships with farms that follow Good Agricultural Practices [2]. |
| Adulteration with Synthetic Drugs | Deliberate adulteration to enhance perceived efficacy. | Employ targeted analytical methods (HPLC-MS/MS) to detect unexpected synthetic compounds [9]. Conduct regular market surveillance on finished products. |
Guide 2: Troubleshooting Chromatographic Fingerprinting for Standardization
Problem: Poor resolution of peaks in HPLC fingerprint.
- Cause 1: Inappropriate mobile phase composition or gradient program.
- Solution: Re-optimize the chromatographic method by systematically varying the pH, buffer concentration, and organic solvent gradient. Reference established pharmacopoeial methods where available [1] [36].
- Cause 2: Column degradation or contamination.
- Solution: Follow the manufacturer's instructions for column cleaning and regeneration. If problems persist, replace the HPLC column.
Problem: Inconsistent fingerprint profiles between batches of the same herb.
- Cause 1: Natural variation due to different geographic origins, harvest times, or post-harvest processing.
- Solution: Establish broader but well-defined acceptance criteria for your fingerprint that account for natural variation, yet ensure bioequivalence. Secure a larger, homogenized reference standard batch for cross-batch comparison [1].
- Cause 2: Inconsistent extraction methodology.
- Solution: Strictly validate and control all extraction parameters, including particle size of the herb, solvent-to-material ratio, extraction time, and temperature [2].
Experimental Protocols for Key Quality Control Parameters
Protocol 1: Chromatographic Fingerprinting for Standardization ofCurcuma longaL. Rhizome Extract
1.0 Objective: To develop a standardized HPLC fingerprint for the authentication and quality control of turmeric extract, quantifying the marker compound curcumin.
2.0 Principle: High-Performance Liquid Chromatography (HPLC) separates complex mixtures based on interaction with stationary and mobile phases, allowing for the identification and quantification of active constituents [2] [1].
3.0 Reagents & Equipment:
- Herbal Material: Powdered Curcuma longa L. rhizome.
- Standard: Curcumin reference standard.
- Solvents: HPLC-grade methanol, water, and acetonitrile.
- Equipment: HPLC system with UV/VIS or DAD detector, C18 reverse-phase column, analytical balance, ultrasonic bath.
4.0 Procedure:
- Standard Solution: Accurately weigh 10 mg of curcumin standard into a 10 mL volumetric flask. Dissolve and make up to volume with methanol to obtain a 1 mg/mL stock solution.
- Test Solution: Weigh 1.0 g of powdered turmeric. Add 20 mL of methanol and sonicate for 30 minutes. Filter the solution through a 0.45 µm membrane filter before injection.
- Chromatographic Conditions:
- Column: C18 (250 mm x 4.6 mm, 5 µm)
- Mobile Phase: Acetonitrile (A) and 2% Acetic acid in water (B), with a gradient elution.
- Flow Rate: 1.0 mL/min
- Detection Wavelength: 425 nm
- Injection Volume: 10 µL
- Analysis: Inject the standard and test solutions. Record the retention time of the curcumin peak in the standard. Identify the corresponding peak in the test solution and quantify its concentration by comparing the peak areas.
5.0 Data Interpretation: The fingerprint of the test sample should match the profile of a reference material in terms of the number, relative retention time, and relative peak area of the key markers [1]. The curcumin content should be calculated as a percentage of the dried weight of the herbal material.
Protocol 2: Determination of Heavy Metal Contamination via ICP-MS
1.0 Objective: To determine the concentration of toxic heavy metals (Arsenic, Cadmium, Lead, Mercury) in an herbal sample using Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
2.0 Principle: ICP-MS atomizes the sample in a high-temperature plasma and then detects atoms based on their mass-to-charge ratio, providing highly sensitive and multi-elemental analysis [2].
3.0 Reagents & Equipment:
- Herbal Material: Powdered herb (e.g., Withania somnifera root).
- Standards: Multi-element calibration standard for As, Cd, Pb, Hg.
- Equipment: ICP-MS instrument, microwave digester, analytical balance.
4.0 Procedure:
- Sample Digestion: Accurately weigh 0.5 g of powdered herb into a digestion vessel. Add 5 mL of concentrated nitric acid. Perform microwave digestion according to the instrument's validated method (e.g., 180°C for 15 minutes).
- Preparation of Calibrants: Prepare a series of calibration standards from the stock solution in dilute nitric acid, covering the expected concentration range.
- Analysis: Introduce the digested sample and calibrants into the ICP-MS. Monitor the specific isotopes (e.g., As75, Cd111, Pb208, Hg202).
5.0 Data Interpretation: The instrument software will calculate the concentration of each metal in the sample solution in µg/L. Compare the results against the permissible limits set by WHO or other relevant regulatory bodies [2].
Workflow and Process Diagrams
Figure 1: Herbal Drug Quality Control Workflow
Figure 2: Contamination Investigation Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Essential Reagents and Materials for Herbal Quality Control
| Item / Solution | Function / Application | Key Considerations |
|---|---|---|
| Reference Standards | Certified compounds used to identify and quantify active markers or contaminants via chromatography. | Must be of high purity and traceable to a recognized standard body. Critical for method validation and quantification [1]. |
| Phytochemical Solvents | HPLC/MS-grade solvents for extraction and analysis. | High purity is essential to prevent interference with analytical results and background noise [9]. |
| DNA Barcoding Kits | Contain reagents for DNA extraction, amplification, and sequencing to authenticate plant species. | Select barcode regions (e.g., ITS2, rbcL) with high discriminatory power for the plant family in question [2]. |
| Microbiological Media | Used in total viable aerobic count and tests for specified microorganisms (E. coli, Salmonella). | Follow pharmacopoeial methods for preparation and incubation. Use positive and negative controls for validity [2]. |
| Chromatography Columns | C18 reverse-phase columns are standard for HPLC analysis of most herbal compounds. | Column longevity depends on proper maintenance, including the use of guard columns and flushing with compatible solvents [1]. |
Navigating Research and Regulatory Hurdles in Herbal Standardization
Addressing Methodological Gaps in Clinical Trial Design and Reporting
Troubleshooting Guides
Incomplete Trial Reporting
Problem: Critical methodological details are missing from the final trial report, making it impossible to assess validity.
Solution: Use the CONSORT 2025 checklist throughout trial design and reporting phases [38] [39] [40].
- Root Cause: Authors omit essential details about randomization, blinding, or statistical methods.
- Verification: Check your manuscript against the 30-item CONSORT 2025 checklist before submission [39].
- Resolution: Ensure your report includes a participant flow diagram and explicitly describes randomization procedures, blinding methods, and any changes to trial outcomes after the study began.
Inadequate Trial Protocol
Problem: The trial protocol lacks sufficient detail for replication or external review.
Solution: Develop the protocol using the SPIRIT 2025 statement [41].
- Root Cause: Protocol writers fail to pre-specify key elements like primary outcomes, statistical methods, or handling of adverse events.
- Verification: Use the SPIRIT 2025 checklist of 34 essential items [41].
- Resolution: The protocol must clearly describe interventions, participant selection, data collection methods, and management, including plans for patient and public involvement.
Poor Clinical Data Management
Problem: Data collected during the trial is error-prone, insecure, or non-compliant with regulations [42].
- Root Cause: Using general-purpose tools like spreadsheets, which lack validation and proper access controls [42].
- Verification: Audit your data collection tools against ISO 14155:2020, which requires systems to be validated for authenticity, accuracy, and reliability [42].
- Resolution: Implement purpose-built, pre-validated Electronic Data Capture (EDC) systems. Ensure the system has APIs for seamless data transfer and established procedures for user access management [42].
Specific Challenge: Standardization in Herbal Medicine Trials
Problem: Significant variation in herb quality, disease factors, and patient responses compromises the reliability of trial results [4].
- Root Cause: Focusing on single-variable standardization is insufficient for complex, multi-component interventions [4].
- Verification: Assess whether your trial design simultaneously controls for source material quality, practitioner training, and personalized treatment principles [4].
- Resolution: Implement a multivariable optimization framework that addresses [4]:
- Herb Variation: Through quality optimization and standardized herbal drug development.
- Disease Variation: Through knowledge management and standardized practitioner training.
- Patient Variation: By tailoring treatments using personalized medicine principles.
Frequently Asked Questions (FAQs)
Q1: What are the most critical updates in the CONSORT 2025 statement that I need to know? The CONSORT 2025 statement introduces several key updates, including the addition of seven new items, a new section on open science practices, and the integration of recommendations from important extensions like Harms, Outcomes, and Non-pharmacological Treatments [39] [40]. This emphasizes greater transparency in trial registration, data sharing, and protocol accessibility.
Q2: How does SPIRIT 2025 help me design a better trial protocol? The SPIRIT 2025 guideline provides a structured 34-item checklist that ensures your protocol addresses all critical elements for planning, conduct, and external review [41]. Key enhancements include a greater emphasis on describing interventions and comparators, assessing harms, and detailing how patients and the public will be involved in the trial [41].
Q3: My clinical trial is on a complex herbal intervention. What is the biggest methodological pitfall and how can I avoid it? The biggest pitfall is addressing variability only through a single factor, such as standardizing a single active compound [4]. A comprehensive approach is needed. You should adopt a multivariable optimization framework that concurrently controls for the three main sources of variability: the herb (quality, composition), the disease (diagnostic criteria), and the patient (individual response) [4]. Future methodologies should leverage multi-omics tools for deeper personalization [4].
Q4: What is the most common data-related mistake in clinical trials, and how can I prevent it? A common mistake is using general-purpose tools like spreadsheets for data collection and management [42]. These tools are difficult to validate for regulatory requirements. To prevent this, use purpose-built, validated clinical data management software and Electronic Data Capture (EDC) systems that are designed for compliance with standards like ISO 14155:2020 [42].
Experimental Protocols
Protocol 1: Implementing CONSORT 2025 for Trial Reporting
Objective: To ensure complete and transparent reporting of a randomized trial's methods and findings.
Methodology:
- Familiarization: Download the CONSORT 2025 checklist and Explanation & Elaboration document from the official website [38].
- Integrated Writing: During manuscript preparation, address each of the 30 checklist items in the relevant sections of your paper [39] [40].
- Flow Diagram: Create a participant flow diagram detailing enrollment, allocation, follow-up, and analysis.
- Open Science: Clearly report trial registration information, where the protocol and statistical analysis plan can be accessed, and your data sharing policy [39].
Protocol 2: Applying a Multivariable Framework for a Herbal Medicine Trial
Objective: To design a robust clinical trial for a herbal intervention that controls for multiple sources of variability.
Methodology:
- Herb Standardization:
- Use Good Agricultural and Collection Practices (GACP) for raw materials.
- Employ analytical techniques (e.g., HPLC, LC-MS) to create a chemical fingerprint of the final product [4].
- Practitioner Standardization:
- Develop precise clinical practice guidelines (CPGs) or decision-making guidelines (DMGs) based on the traditional medicine system (e.g., TCM).
- Provide standardized training and certification for all practitioners involved in the trial [4].
- Patient Personalization:
- Within the randomized trial design, pre-define stratification variables or subgroup analyses based on traditional diagnostic criteria (e.g., "present Dhatu Chao Ruean" in Thai medicine) [4].
- Collect biospecimens for potential future multi-omics analysis (genomics, metabolomics) to understand differential patient responses [4].
Key Reporting Standards: CONSORT 2025 vs. SPIRIT 2025
The following table summarizes the core components of the two main guidelines for clinical trials.
| Feature | CONSORT 2025 Statement | SPIRIT 2025 Statement |
|---|---|---|
| Purpose | Reporting results of a completed randomized trial [39]. | Designing a protocol for a randomized trial [41]. |
| Core Content | 30-item checklist [39] [40]. | 34-item checklist [41]. |
| Key Diagram | Participant flow diagram [39]. | Schedule of enrolment, interventions, and assessments [41]. |
| Primary Focus | Transparency and completeness of results and methods as executed. | Transparency and completeness of planned methods and procedures. |
| New in 2025 | 7 new items; new Open Science section; integration of Harms, Outcomes, and NPT recommendations [39]. | New Open Science section; emphasis on harms, intervention description, and patient involvement [41]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function / Application |
|---|---|
| Validated Electronic Data Capture (EDC) System | A purpose-built software platform for clinical data management that is validated for regulatory compliance (e.g., ISO 14155:2020), ensuring data authenticity, accuracy, and security [42]. |
| High-Performance Liquid Chromatography (HPLC) | An analytical technique used in herbal drug development to separate, identify, and quantify the chemical components of a complex herbal mixture, essential for quality control and standardization [4]. |
| Liquid Chromatography–Mass Spectrometry (LC-MS) | A highly sensitive and specific analytical method used to provide a detailed chemical fingerprint of an herbal preparation, enabling precise standardization and quality optimization [4]. |
| CONSORT 2025 Checklist | A reporting guideline providing a minimum set of 30 essential items that should be included in any report of a randomized trial to ensure its publication is complete and transparent [38] [39]. |
| SPIRIT 2013/2025 Checklist | A guideline for protocol development that outlines the minimum content to be addressed in a clinical trial protocol, facilitating proper trial planning, conduct, and external review [41]. |
Workflow Diagrams
Trial Reporting Workflow
Multivariable Herbal Trial Design
Overcoming Challenges in Feasibility Assessment and Sample Size Justification
This technical support center provides targeted guidance for researchers navigating the critical planning phases of studies on herbal medicine preparations. The following FAQs and troubleshooting guides address common methodological challenges.
Frequently Asked Questions (FAQs)
1. What is the primary purpose of a pilot or feasibility study in herbal drug development?
The main purpose is to test the feasibility of methods and procedures for a future large-scale study, not to test efficacy. The focus is on assessing practical aspects like recruitment rates, data collection protocols, intervention fidelity, and the acceptability of the herbal preparation in your target population. This step is crucial for identifying and rectifying logistical problems before committing to a full-scale trial [43].
2. Why is it problematic to use a pilot study to estimate effect sizes for a power calculation?
Pilot studies typically have small sample sizes. Effect sizes estimated from these small samples are often inaccurate and unstable, with very large confidence intervals. Basing the sample size of a subsequent main trial on these unreliable estimates can lead to a severely underpowered study. The current recommended approach is to use feasibility outcomes (like recruitment or adherence rates) and confidence intervals for planning, or to use a predefined smallest effect size of interest for powering the main study [43] [44].
3. My study has multiple feasibility outcomes (recruitment, adherence, acceptability). How do I justify the sample size?
When a study has multiple objectives, the sample size should be justified based on the most demanding one. A common mistake is to use a "rule of thumb" (e.g., 12 per group) that is only suitable for estimating a single parameter, like a standard deviation. You should [44]:
- Identify all primary feasibility parameters (e.g., recruitment rate, adherence proportion).
- Determine the sample size required to estimate each key parameter with a desired level of precision (i.e., a sufficiently narrow confidence interval).
- Choose the largest sample size from these calculations to ensure all objectives are met. For example, a sample that is adequate for estimating the standard deviation might be far too small for estimating a recruitment rate with useful precision [44].
4. How can I assess the acceptability of a herbal intervention in a feasibility study?
Acceptability is a key feasibility indicator and is best assessed using a mixed-methods approach [43]:
- Quantitatively: Use structured surveys to measure participant satisfaction, perceived burden, and willingness to recommend the intervention. Track adherence rates (e.g., consumption of the herbal product, attendance at sessions).
- Qualitatively: Conduct semi-structured interviews or focus groups to gather in-depth feedback on the intervention's content, format, and any perceived benefits or drawbacks. This is especially important when adapting an intervention for a new cultural group [43].
5. What are the key feasibility indicators to monitor during a pilot study on herbal medicine standardization?
You should systematically evaluate several areas of feasibility. The table below summarizes the key indicators and assessment methods.
Table: Key Feasibility Indicators for Herbal Medicine Research
| Area of Feasibility | Key Indicators | Assessment Methods |
|---|---|---|
| Participant Recruitment & Retention | Recruitment rate, consent rate, dropout rate, reasons for refusal/dropout [43] | Administrative tracking logs, brief interviews [43] |
| Assessment Procedures | Completion rates for questionnaires/biospecimens, time to complete, perceived burden, score distributions [43] | Compliance logs, timing of tasks, participant feedback surveys [43] |
| Intervention Fidelity & Acceptability | Adherence to protocol, participant engagement, attendance, satisfaction scores [43] | Interventionist checklists, adherence rates (e.g., pill counts), satisfaction surveys, qualitative interviews [43] |
| Data Collection Methods | Missing data patterns, feasibility of remote assessments (e.g., telehealth), inter-rater reliability [43] | Data audit, equipment testing, reliability statistics (e.g., intra-class correlation) [43] |
Troubleshooting Guides
Challenge: Low Recruitment Rate
Problem: You are failing to recruit enough participants into your study on the pharmacokinetics of a novel herbal formulation.
Potential Solutions & Methodology:
- Review Inclusion/Exclusion Criteria: Are they too restrictive? Consider if any criteria can be relaxed without compromising safety or the research question.
- Enhance Recruitment Strategies:
- Procedure: Use multiple recruitment channels (clinics, community centers, online platforms). Develop culturally and linguistically appropriate recruitment materials.
- Feasibility Assessment: Track the yield from each channel to identify the most effective ones [43].
- Address Participant Burden:
- Procedure: Simplify study procedures where possible. Offer flexible scheduling for visits and consider compensating participants for their time and travel.
- Feasibility Assessment: Use qualitative interviews to understand potential participants' perceived barriers to joining the study [43].
Challenge: High Dropout Rate
Problem: A significant number of participants are discontinuing the herbal product intervention in your stability study.
Potential Solutions & Methodology:
- Investigate Tolerability:
- Procedure: Systematically record all adverse events and suspected side effects. Conduct brief interviews with participants who drop out to understand their specific reasons.
- Feasibility Assessment: Closely monitor adherence rates and product quality (e.g., through chemical analysis) to rule out issues like contamination or incorrect formulation that could cause adverse effects [1].
- Improve Participant Engagement:
- Procedure: Implement regular check-in calls or messages. Provide educational materials about the study's importance. Ensure the intervention schedule is not overly demanding.
- Feasibility Assessment: Quantify engagement through contact logs and track its correlation with dropout rates [43].
Challenge: Unclear Sample Size Justification
Problem: Your protocol requires a sample size justification for a feasibility study aiming to optimize a herbal drug extraction process, but you are unsure how to proceed.
Potential Solutions & Methodology:
- Precision-Based Approach:
- Procedure: Define your primary feasibility parameters (e.g., the rate of achieving target compound purity). Specify the desired width of the confidence interval for this estimate. Use statistical software to calculate the sample size needed to achieve that precision [45].
- Example: To estimate an adherence rate with a margin of error of ±10%, a larger sample is needed than if you were only estimating the standard deviation of a chemical yield [44].
- Formal Feasibility Criteria Approach:
- Procedure: Pre-specify "stop/go" progression criteria for your main study (e.g., "≥70% of participants must achieve adequate bioavailability"). Use a sample size calculation that provides sufficient operating characteristics to make a reliable decision, such as a high probability of correctly stopping a non-viable project [44].
- Resource-Led Justification:
- Procedure: Acknowledge that the sample size is determined by practical constraints (e.g., time, budget, or available cases of a rare herb). The key is to then transparently report the precision or "information value" this sample provides. For instance, state: "Given our resources, we can include N=30 participants. This will allow us to estimate the recruitment rate with a 95% CI of approximately ±18%." This honestly communicates the study's limitations [45].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Herbal Medicine Feasibility Research
| Item | Function in Feasibility Research |
|---|---|
| Standardized Herbal Extract | Provides a consistent, chemically-defined material for intervention, crucial for testing fidelity and reproducibility [1]. |
| High-Performance Liquid Chromatography (HPLC) | Authenticates herbs, quantifies key bioactive compounds, and monitors batch-to-batch variation, directly assessing the "herb variation" domain [1] [4]. |
| Validated Participant Questionnaires | Measures feasibility indicators like acceptability, adherence, and perceived burden quantitatively [43]. |
| Cognitive Interview Guide | Used qualitatively to ensure participants from diverse backgrounds understand questions and concepts as intended, testing conceptual adequacy [43]. |
| Electronic Data Capture (EDC) System | Tests the feasibility of data collection protocols, allows for remote assessments, and helps track data completeness and missingness patterns [43]. |
Experimental Workflow & Logical Diagrams
Feasibility Assessment Workflow
Sample Size Justification Pathways
For researchers and drug development professionals, navigating the global landscape of herbal medicine regulation presents a significant challenge. The absence of a unified, international regulatory framework leads to divergent requirements for safety, efficacy, and quality between countries. These disparities create substantial barriers to the development, evaluation, and global trade of standardized herbal products. This technical support center addresses the most pressing issues encountered in this complex environment, providing troubleshooting guidance and methodological support for research on herbal medicine preparations.
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: Why is there no universal regulatory classification for herbal medicines?
- Problem: A single herbal product can be classified as a drug in one country, a dietary supplement in another, and a traditional medicine in a third, complicating multi-jurisdictional research and development.
- Explanation: Regulatory classification varies because it is deeply rooted in a country's unique historical, cultural, and legal recognition of herbal products. For instance, some nations integrate traditional knowledge into their regulatory systems, while others apply a strictly pharmacological model [46] [47]. This results in fundamentally different pathways to market.
- Solution: Before initiating research intended for a global context, conduct a thorough regulatory landscape analysis for all target countries. Categorize your herbal product according to the specific definitions of each jurisdiction to determine the applicable regulatory requirements.
FAQ 2: How do regulatory classification variances impact the design of clinical trials?
- Problem: Clinical trials designed for one regulatory framework may be invalid or insufficient for approval in another country.
- Explanation: Different classifications demand different levels of evidence. A jurisdiction classifying an herb as a drug will require rigorous, randomized controlled trials (RCTs) with modern diagnostic criteria. In contrast, a traditional medicine pathway might accept historical use and evidence based on traditional diagnosis [46] [48]. This affects everything from inclusion criteria to outcome measures.
- Solution: Adopt a strategic trial design. For global applicability, consider a "double classification method" where subjects are diagnosed using both modern biomedical and relevant traditional medicine criteria, and outcomes are evaluated for both systems [48].
FAQ 3: What are the common methodological pitfalls in pilot trials for herbal medicines?
- Problem: Pilot trials for herbal medicines often fail to adequately inform the design of subsequent full-scale studies.
- Explanation: Common pitfalls include inadequate assessment of feasibility, lack of justification for sample size, and poor reporting of randomization methods [49]. Critically, many trials omit herb-specific details such as ingredient processing, quality control procedures, and safety assessments, which are essential for reproducibility and regulatory evaluation.
- Solution: Implement a comprehensive pilot trial protocol that explicitly addresses:
- Feasibility: Test recruitment strategies, adherence to complex herbal regimens, and practitioner variability.
- Sample Size: Justify pilot sample size using statistical methods for pilot studies, not for definitive trials.
- Reporting: Adhere to CONSORT guidelines and fully document all quality control measures for the herbal intervention [49].
FAQ 4: How can we ensure the quality and authenticity of herbal research materials?
- Problem: Batch-to-batch variability, adulteration, and misidentification of herbal materials undermine research validity and reproducibility.
- Explanation: Herbal products are complex mixtures with chemical composition that can vary due to species, growing conditions, and processing methods. Inadequate quality control can lead to inconsistent levels of active compounds, contaminants, or the wrong plant species being used [1] [50].
- Solution: Establish a robust "Chain of Authentication" for all research materials. This includes botanical verification, chemical standardization, and contamination screening, as detailed in the experimental protocols below.
Data Summaries
Table 1: Global Disparities in Herbal Product Classification
This table summarizes how major regions categorize and regulate herbal products, impacting the type of evidence required.
| Region/Country | Primary Regulatory Classification(s) | Key Regulatory Body | Typical Evidence Requirements |
|---|---|---|---|
| United States | Dietary Supplement | Food and Drug Administration (FDA) | Pre-market approval not required for safety/efficacy; post-market surveillance [46] [5]. |
| European Union | Herbal Medicinal Product | European Medicines Agency (EMA) | Requires proof of quality, safety, and efficacy; traditional use registration available for products >30 years [46]. |
| China | Traditional Chinese Medicine (TCM) | National Medical Products Administration (NMPA) | Integration of historical traditional knowledge with modern pharmaceutical data [46] [51]. |
| India | Ayurvedic, Unani, Siddha Drugs | Ministry of AYUSH | Governed by Drugs and Cosmetics Act; relies on traditional texts and growing modern research requirements [48] [50]. |
| Canada | Natural Health Product (NHP) | Health Canada | Pre-market licensing requiring evidence of safety, efficacy, and quality [46]. |
Table 2: Key Methodological Gaps in Herbal Medicine Pilot Trials
An analysis of 123 HM pilot trials revealed critical reporting and design deficiencies that hinder their utility [49].
| Methodological Element | Frequency of Adequate Reporting | Consequence of Poor Reporting |
|---|---|---|
| Assessment of Feasibility | 13.1% | Inability to judge if a full-scale trial is practical or how to design it. |
| Sample Size Justification | 47.2% | Unclear if the pilot was sufficiently powered to meet its objectives. |
| Randomization Method | 35.8% | Raises concerns about selection bias and reduces result credibility. |
| Quality Control of Herbals | Inconsistent | Undermines reproducibility and makes it impossible to attribute effects to a defined intervention. |
| Progression to Full-Scale Trial | 3.3% | Suggests pilot trials are often not fulfilling their purpose as a stepping stone. |
Experimental Protocols
Protocol 1: Standardized Workflow for Herbal Material Authentication & Quality Control
This protocol provides a detailed methodology for ensuring the quality and authenticity of herbal research materials, a foundational step for reproducible research.
1.0 Objective: To authenticate the plant material and ensure its chemical and biological consistency throughout the research study.
2.0 Materials:
- Research Material: Dried plant material or herbal extract.
- Key Reagents: Reference standards for key marker compounds, DNA extraction kits, solvents for chromatography (HPLC grade).
- Equipment: Microscope, Thin-Layer Chromatography (TLC) or High-Performance Liquid Chromatography (HPLC) system, DNA sequencer.
3.0 Methodology:
Step 3.1: Macroscopic and Microscopic Examination
- Visually inspect the raw plant material for correct organoleptic characteristics (shape, color, odor, taste).
- Prepare histological sections and examine under a microscope to identify characteristic anatomical features (e.g., trichomes, stomata, calcium oxalate crystals) that confirm botanical identity [1] [50].
Step 3.2: Chemical Profiling
- Extract the herbal material using a standardized solvent system.
- Perform TLC or HPLC analysis alongside authentic reference standards of known marker compounds.
- Develop a chemical fingerprint (chromatogram) for the batch. This fingerprint must be consistent for all material used in the study [1].
Step 3.3: DNA Barcoding (for definitive authentication)
- Extract genomic DNA from a sample of the plant material.
- Amplify and sequence a standard DNA barcode region (e.g., ITS2, rbcL).
- Compare the sequence against a curated reference database (e.g., GenBank, BOLD) to confirm species identity at the genetic level [1].
Step 3.4: Contaminant Screening
- Test the material for potential contaminants, including:
4.0 Documentation:
- Maintain a detailed Certificate of Analysis (CoA) for every batch of material used, containing all data from steps 3.1 to 3.4.
Protocol 2: Guidance for Designing a Clinically Relevant Herbal Medicine Trial
1.0 Objective: To design a clinical trial for an herbal medicine that meets regulatory standards for safety and efficacy across multiple potential jurisdictions.
2.0 Pre-Trial Considerations:
Step 2.1: Define the Regulatory Context
- Determine the target regulatory pathway(s) (e.g., drug, traditional medicine) for the product, as this will dictate the trial design [46].
Step 2.2: Standardize the Investigational Product
- Follow Protocol 1 to ensure a characterized, quality-controlled product. The dosage form and regimen should be clearly defined and justifiable [51].
3.0 Trial Design Methodology:
Step 3.1: Selection of Control
- Placebo Control: Use a placebo that is matched in appearance, smell, and taste to the greatest extent possible. This is critical for blinding, though challenging for herbs with strong odors [48] [49].
- Active Control: If comparing to a conventional therapy, use an established, effective treatment.
Step 3.2: Blinding and Randomization
- Strive for double-blinding (participant and outcome assessor). If the herbal intervention involves non-blinded practitioner interaction (e.g., traditional diagnosis), use a partial blinding model where the outcome assessor is blinded [48].
- Use a computer-generated randomization sequence with allocation concealment. Clearly report the method used [49].
Step 3.3: Patient Diagnosis and Outcomes
- For global relevance, use the "double classification method": enroll patients using modern, internationally recognized diagnostic criteria, but also classify them according to the relevant traditional medicine system if applicable. Measure outcomes using validated instruments for both systems [48].
Step 3.4: Safety and Pharmacovigilance
- Actively monitor and record all adverse events.
- Report herb-drug interactions, especially if participants are permitted to continue concomitant medications. Use standardized grading systems (e.g., CTCAE) [52] [5].
Visualizations
Diagram 1: Barriers to Global Regulatory Harmonization
Diagram 2: Herbal Research Material Authentication Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and their functions for ensuring quality in herbal medicine research.
| Research Reagent / Material | Function & Application in Herbal Research |
|---|---|
| Authentic Reference Standards | Pure chemical compounds used to identify and quantify marker compounds in herbal extracts via HPLC or TLC; critical for standardization [1]. |
| DNA Barcoding Kits | Kits for extracting, amplifying, and sequencing plant DNA to provide definitive species-level authentication and detect adulteration [1]. |
| Chromatography Solvents & Columns | High-purity solvents and HPLC/TLC columns for separating and analyzing the complex chemical constituents of an herbal extract [1] [50]. |
| Validated Herbal Placebo | A matched placebo that mimics the taste, smell, and appearance of the active herbal intervention, which is essential for robust blinding in clinical trials [48] [49]. |
| Certified Reference Plant Material | Voucher specimens or commercially sourced plant material with authenticated species identity, used as a benchmark for all analyses [1] [50]. |
Leveraging AI, Metabolomics, and Nanotechnology for Enhanced Quality Assurance
This technical support center is designed for researchers and drug development professionals working on the standardization of herbal medicine preparations. It provides targeted troubleshooting guides and FAQs to address common experimental challenges encountered at the intersection of artificial intelligence (AI), metabolomics, and nanotechnology. The integration of these advanced technologies is revolutionizing herbal medicine quality assurance by enabling more precise compound identification, standardized nano-formulations, and data-driven validation of traditional knowledge, ultimately contributing to more reliable and efficacious herbal products [53] [54] [55].
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: AI and Machine Learning for Herbal Image Identification
- Q: Our AI model for identifying medicinal plant species from leaf images performs well on training data but poorly on new, unseen images. What could be the issue?
- A: This is a classic case of overfitting, often due to limited or non-diverse training datasets.
- Troubleshooting Guide:
- Data Augmentation: Artificially expand your dataset by applying rotations, flips, brightness adjustments, and scaling to your existing images.
- Increase Data Diversity: Ensure your training set includes images of the same species from different geographical regions, growth stages, and under varying lighting conditions [56].
- Model Simplification: If using a deep learning model, reduce the number of layers or parameters to prevent the model from memorizing the training data.
- Employ Transfer Learning: Utilize a pre-trained model (e.g., ResNet, Inception) on a large dataset like ImageNet and fine-tune it on your specific herbal image dataset. This leverages general feature knowledge and can improve generalization [57].
FAQ 2: Metabolomics for Quality Control and Standardization
- Q: Our metabolomic profiling (e.g., via LC-MS) of a herbal extract shows high batch-to-batch variation in metabolite levels, hindering standardization. How can we address this?
- A: Variation can stem from genetic, environmental, post-harvest, and processing factors.
- Troubleshooting Guide:
- Source Control: Implement genomic tools like DNA barcoding for precise species authentication to ensure starting material consistency [58].
- Standardized Processing: Establish and strictly adhere to Standard Operating Procedures (SOPs) for drying, storage, and extraction to minimize processing-induced variations [59].
- Chemometric Analysis: Use multivariate statistical analysis (e.g., PCA, PLS-DA) on your metabolomics data to identify the key marker compounds responsible for the variation. Focus standardization efforts on controlling these critical quality attributes (CQAs) [55].
- Data Integration: Integrate metabolomics with other omics data (transcriptomics, proteomics) to understand the biological basis of variation and guide cultivation practices for more consistent yields of active compounds [58].
FAQ 3: Nanotechnology for Herbal Formulations
- Q: The encapsulation efficiency of a bioactive herbal compound in our nano-liposomes is consistently low. What factors should we investigate?
- A: Low encapsulation efficiency is often related to the properties of the compound and the formulation process.
- Troubleshooting Guide:
- Compatibility Check: Analyze the lipophilicity/hydrophilicity (log P) of the bioactive compound. Highly water-soluble compounds are difficult to encapsulate in lipid bilayers. Consider using nanoemulsions or polymeric nanoparticles instead [54].
- Process Optimization: Key parameters to optimize include:
- Phase Volume Ratio: The ratio of aqueous to lipid phases.
- Solvent Selection: Use solvents that efficiently dissolve both the lipid and the herbal compound.
- Energy Input: Ensure sufficient homogenization or sonication energy is applied to form uniform, small-sized vesicles [54].
- Formulation Re-design: Explore different lipid compositions or the use of edge activators (for transferosomes) to improve loading capacity.
FAQ 4: Integrating Multi-Omics Data with AI
- Q: We have generated genomic, transcriptomic, and metabolomic data for a medicinal plant but are struggling to integrate it to elucidate a biosynthetic pathway. What AI approaches can help?
- A: The challenge is to correlate gene expression with metabolite abundance.
- Troubleshooting Guide:
- Correlation Analysis: Use weighted gene co-expression network analysis (WGCNA) or similar methods to identify clusters of highly correlated genes. Then, link these gene modules to the accumulation of specific metabolites [58].
- Pathway Mining Tools: Employ bioinformatics tools and databases (e.g., KEGG, PlantCyc) to map your differentially expressed genes onto known biosynthetic pathways.
- Machine Learning Models: Train regression models (e.g., Random Forest) to predict metabolite levels based on gene expression patterns. The most important features (genes) in the model are strong candidates for involvement in the pathway [53] [58].
FAQ 5: Ethical and Data Governance in AI for Traditional Medicine
- Q: Our project involves using AI to analyze traditional knowledge associated with medicinal plants. How can we ensure ethical compliance and respect data sovereignty?
- A: This is a critical concern for safeguarding cultural heritage.
- Troubleshooting Guide:
- Adhere to FPIC: Always obtain Free, Prior, and Informed Consent (FPIC) from indigenous communities and traditional knowledge holders before data collection and use [60].
- Implement IDSov Principles: Uphold Indigenous Data Sovereignty (IDSov), which asserts the rights of Indigenous peoples to govern the collection, ownership, and application of their data [60].
- Use Digital Repositories: Consider using AI-powered digital libraries, like India's Traditional Knowledge Digital Library (TKDL), which help protect against biopiracy by documenting knowledge in a defensive prior-art repository [60].
- Establish Benefit-Sharing Agreements: Develop clear, equitable frameworks for sharing any commercial or research benefits that arise from the use of traditional knowledge [60].
Experimental Protocols for Key Standardization Methods
Protocol 1: AI-Assisted Quality Evaluation of Herbal Medicine Using Spectroscopic Data
- Objective: To develop a machine learning model for rapid quality grading and detection of adulterants in herbal powders using Fourier-Transform Infrared (FTIR) spectroscopy.
- Materials: FTIR spectrometer, certified reference herbal materials, test samples (including potential adulterants), computing software (e.g., Python with scikit-learn, R).
- Methodology:
- Sample Preparation & Spectral Acquisition: Grind all samples to a uniform particle size. Acquire FTIR spectra for all reference and test samples under consistent parameters (e.g., 4 cm⁻¹ resolution, 16 scans).
- Data Pre-processing: Pre-process spectra to remove artifacts: perform baseline correction, normalization (e.g., Standard Normal Variate), and smoothing [61] [56].
- Dataset Construction: Label spectra according to their known class (e.g., "high-quality," "low-quality," "adulterant X"). Split data into training (70%), validation (15%), and test (15%) sets.
- Model Training: Train a Support Vector Machine (SVM) or a Convolutional Neural Network (CNN) on the training set. Use the validation set for hyperparameter tuning.
- Model Evaluation: Assess the final model on the held-out test set using metrics: accuracy, precision, recall, and F1-score [56].
- Troubleshooting: If model accuracy is low, ensure your reference materials are unequivocally authenticated and increase the diversity of adulterants in your training set.
Protocol 2: Development and Characterization of a Nano-Herbal Formulation (Phytosomes)
- Objective: To enhance the bioavailability of a poorly water-soluble herbal extract (e.g., Ginkgo biloba flavonoid extract) by forming a phytosomal complex.
- Materials: Herbal extract, phosphatidylcholine (soy or egg), anhydrous solvent (e.g., dioxane), rotary evaporator, dynamic light scattering (DLS) instrument, dialysis tubing.
- Methodology:
- Complex Formation: Dissolve the herbal extract and phosphatidylcholine in a 1:1-1:3 molar ratio in the solvent. Stir the reaction mixture at 40-60°C for 1-3 hours under an inert atmosphere [54].
- Solvent Removal: Remove the solvent using a rotary evaporator until a thin film is formed. Hydrate the film with buffer (pH 7.4) to obtain the phytosomal suspension.
- Characterization:
- Particle Size & Polydispersity Index (PDI): Measure by DLS. PDI < 0.3 indicates a monodisperse population.
- Entrapment Efficiency: Separate unentrapped extract by ultracentrifugation or dialysis. Analyze the supernatant/filtrate using HPLC to calculate the percentage of compound entrapped [54].
- Morphology: Confirm spherical, vesicular structure using Transmission Electron Microscopy (TEM).
- Troubleshooting: If particle size is too large, probe-sonicate the suspension or pass it through a microfluidizer. Low entrapment efficiency may require optimization of the drug-to-lipid ratio or solvent system.
Data Presentation Tables
Table 1: Common AI/ML Models in Herbal Medicine Research and Their Applications
| AI Model | Primary Application in Herbal Research | Key Advantage | Example Use-Case from Literature |
|---|---|---|---|
| Support Vector Machine (SVM) | Spectral data analysis, Origin identification [56] | Effective in high-dimensional spaces | Classification of herbal samples based on FTIR or NIR spectra [57] [56] |
| Convolutional Neural Network (CNN) | Image-based species identification, Quality grading | Automatically learns relevant features from images | Automated identification of medicinal plants from leaf/root images [53] [61] |
| Random Forest | Linking omics data, Predicting bioactivity | Handles mixed data types, provides feature importance | Identifying key genes in a metabolic pathway from transcriptomic data [58] |
| Large Language Models (LLMs) | Mining scientific literature, Knowledge graph construction | Natural language processing of vast text corpora | Extracting structured knowledge on herb-drug interactions from publications [53] |
Table 2: Key Characterization Parameters for Nano-Herbal Formulations
| Parameter | Analytical Technique | Purpose in Quality Assurance | Target Range (Example) | |||
|---|---|---|---|---|---|---|
| Particle Size & PDI | Dynamic Light Scattering (DLS) | Determines uniformity, stability, and biological fate | Size: 50-200 nm; PDI: <0.3 [54] | |||
| Zeta Potential | Electrophoretic Light Scattering | Predicts colloidal stability; high value prevents aggregation | > | ±30 | mV [54] | |
| Entrapment Efficiency | HPLC, UV-Vis Spectrometry | Measures successful loading of active compound | >80% [54] | |||
| Drug Release Profile | Dialysis in dissolution media | Simulates in-vivo release kinetics for bioavailability | Sustained release over 12-24 hours [54] |
Signaling Pathways and Workflow Diagrams
Diagram 1: AI-Driven Quality Assurance Workflow
AI-Driven Quality Assurance Workflow: This diagram outlines the sequential process from raw material to quality assessment using AI.
Diagram 2: Multi-Omics Integration for Pathway Elucidation
Multi-Omics Integration for Pathway Elucidation: This diagram shows how data from different omics layers are integrated using AI to discover biosynthetic pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Advanced Herbal Medicine Research
| Item / Technology | Function / Application | Key Consideration |
|---|---|---|
| DNA Barcoding Kits | Molecular authentication of plant species to ensure starting material integrity [58]. | Select barcode regions (e.g., ITS2, rbcL) with high discriminatory power for your plant family. |
| LC-HRMS Systems | Untargeted metabolomics for comprehensive profiling of herbal extracts and biomarker discovery [55]. | High mass accuracy and resolution are critical for confident compound identification. |
| Lipids for Nano-Formulations (e.g., Phosphatidylcholine, PLGA, Glycerol monostearate) | Creating nanocarriers (liposomes, phytosomes, SLNs, polymeric NPs) for enhanced bioavailability and targeted delivery [54]. | Purity, source (natural/synthetic), and compatibility with the herbal API are key selection factors. |
| CRISPR-Cas9 Systems | Functional genomics and precision breeding in medicinal plants to enhance yield of bioactive compounds [58]. | Requires established plant transformation and tissue culture protocols for the target species. |
| Reference Standard Compounds | Quantitative analysis and method validation in chromatography for quality control [59] [55]. | Source certified reference materials (CRMs) from reputable suppliers for accurate quantification. |
| AI/ML Software Platforms (e.g., Python/R libraries, Cloud AI services) | Data analysis, model building, and prediction for complex datasets from omics, imaging, and spectroscopy [53] [56]. | Requires computational skills or collaboration; start with user-friendly platforms like Orange or Knime. |
Validation Frameworks and Comparative Global Regulatory Analysis
Troubleshooting Guides
Guide 1: Addressing Inconsistent Herbal Preparation Efficacy
Problem: Experimental results show high batch-to-batch variability and inconsistent therapeutic effects.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Raw Material Variation | - Perform macroscopic/microscopic examination of herbs [1]- Conduct chemical fingerprinting via HPLC or TLC [1] | - Implement stringent herb authentication protocols [1]- Establish reference standards for key active compounds [1] |
| Inadequate Standardization | - Quantify marker compounds via HPLC/LC-MS [1] [4]- Compare bioactivity between batches | - Adopt multivariable standardization controlling for herb quality, disease, and patient factors [4]- Establish quantitative levels for active compounds/markers [1] |
| Improper Extraction Methods | - Analyze extraction efficiency for different solvents- Compare pharmacokinetic parameters | - Optimize extraction methodology (menstruum, time, temperature) [62]- Validate extraction consistency across multiple batches |
Guide 2: Managing Contamination and Adulteration
Problem: Herbal preparations test positive for contaminants or show evidence of adulteration.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Environmental Contaminants | - Test for heavy metals, pesticides, microbes [1]- Verify compliance with safety limits | - Source herbs from certified organic, sustainably harvested suppliers [62]- Implement Good Agricultural Practices (GAP) [4] |
| Deliberate Adulteration | - Use DNA barcoding for species authentication [1]- Analyze for unexpected chemical markers | - Establish robust supply chain verification- Conduct identity confirmation on all incoming materials |
| Manufacturing Contaminants | - Audit manufacturing processes- Test for cross-contamination | - Adhere to Good Manufacturing Practices (GMP) [63] [5]- Implement quality assurance protocols throughout production [1] |
Frequently Asked Questions (FAQs)
Preclinical Validation
Q: What are the critical steps for preclinical validation of an herbal medicine?
A: A robust preclinical validation program includes four key phases [63]:
- Basic Research & Target Identification: Understand disease biology and identify potential therapeutic targets [63] [64].
- Drug Discovery & Candidate Nomination: Screen compounds for interaction with targets and narrow down to promising candidates [63].
- Lead Optimization: Chemically modify leads to improve performance and establish dosing strategy [63].
- IND-Enabling Studies: Conduct advanced safety assessments (toxicology, pharmacokinetics) and manufacturing documentation required for regulatory approval to proceed to clinical trials [63].
Q: How can we improve confidence in our molecular target for an herbal preparation?
A: Use a multi-validation approach to increase confidence [65] [64]:
- Genetic Techniques: Use siRNA, antisense oligonucleotides, or transgenic animals (knockout/knock-in) to modulate the target and observe phenotypic effects [64].
- Tool Compounds: Employ monoclonal antibodies or small molecule inhibitors that selectively interact with the target [64].
- Human Evidence: Leverage clinical observations and "experiments of nature" (e.g., natural human mutations) to validate the target's role in disease [65].
- Expression Analysis: Examine target expression in diseased versus healthy human tissues [65].
Clinical Validation
Q: What framework can address variability in herbal clinical trials?
A: Implement a multivariable optimization framework that simultaneously controls for three key domains of variability [4]:
- Herb Variation: Through quality optimization and standardized herbal drug development.
- Disease Variation: By knowledge management and training practitioners on consistent diagnostic criteria.
- Patient Variation: By tailoring treatments using personalized medicine principles.
Q: How should a clinical research protocol for herbal medicine be structured?
A: A comprehensive protocol should include [66] [67]:
- Administrative Details: Main investigator, involved centers, and contacts.
- Study Specifics: Title, acronym, keywords, and rationale with literature review.
- Study Design: Type (e.g., randomized, controlled, blinded), primary objectives, and endpoints.
- Methodology: Detailed population, inclusion/exclusion criteria, sample size justification, treatment plan, and statistical analysis plan.
- Safety & Compliance: Informed consent, safety advisories, and regulatory compliance.
Pharmacological Validation
Q: What key pharmacological properties must be assessed for herbal medicines?
A: Essential properties and assessment methods are summarized below:
| Property | Assessment Method | Importance |
|---|---|---|
| Pharmacokinetics (ADME) | In vivo/In vitro studies on Absorption, Distribution, Metabolism, Excretion [63] | Determines bioavailability, dosing regimen, and potential interactions. |
| Pharmacodynamics | Dose-response studies, receptor binding assays [63] | Measures biological effect and relationship to drug concentration. |
| Toxicology | Acute and chronic toxicity studies, genetic toxicology [63] | Identifies safe starting dose for clinical trials and potential adverse effects. |
| Drug Interaction Potential | CYP enzyme inhibition/induction studies, plasma protein binding assays [5] | Predicts herb-drug interactions that can compromise safety/efficacy. |
Q: How do we demonstrate a clinically relevant mechanism of action for a complex herbal product?
A: Combine multiple techniques to build a compelling case [65] [64]:
- In Vitro Models: Use cellular assays to show functional pharmacological activity at the target [65] [64].
- Preclinical Disease Models: Utilize animal models that mimic human disease pathophysiology to demonstrate efficacy [65]. Use translational biomarkers to bridge results from models to humans [65].
- Chemical Genomics: Apply diverse chemical tools to probe the function of potential targets within the complex herbal mixture [64].
- Human Tissue Studies: Investigate target pathway activity in relevant diseased human tissues to confirm relevance [65].
Experimental Protocols & Methodologies
Protocol 1: Standardization of Herbal Material via HPLC Fingerprinting
Objective: To establish a reproducible chemical profile for quality control of an herbal preparation.
Materials:
- Herbal test material (multiple batches)
- Reference compounds (e.g., marker compounds)
- HPLC system with DAD/UV detector
- Reference standards for calibration [1]
Procedure:
- Sample Preparation: Precisely weigh powdered herbal material. Extract using a standardized method (specify solvent, volume, time, temperature). Filter the extract [1].
- HPLC Conditions: Develop and validate the method. Specify column, mobile phase (gradient or isocratic), flow rate, injection volume, and detection wavelengths [1].
- System Suitability: Inject reference standard solution to ensure resolution, peak shape, and reproducibility meet pre-set criteria before running samples.
- Analysis: Inject sample solutions. Record the chromatographic fingerprint and quantify marker compounds against the calibration curve of reference standards [1].
- Data Analysis: Compare fingerprints of different batches using chemometric software if necessary. Ensure concentrations of marker compounds fall within specified ranges [1].
Protocol 2: In Vivo Target Validation Using a Genetic Approach
Objective: To validate the role of a specific molecular target in the therapeutic effect of an herbal extract using a knockdown model.
Materials:
- Target-specific siRNA or antisense oligonucleotides [64]
- Appropriate control (scrambled siRNA/sense oligonucleotide)
- Animal model of the disease
- Herbal test extract
- Relevant behavioral, biochemical, or histological endpoints
Procedure:
- Model Development: Administer the target-specific siRNA (or control) to animals in the disease model via an appropriate route (e.g., intrathecal, intravenous) to reduce target protein expression [64].
- Treatment: Divide animals into groups: (1) Disease model + control oligonucleotide, (2) Disease model + target knockdown, (3) Disease model + target knockdown + herbal extract, (4) Healthy controls.
- Dosing: Administer the herbal extract at a pre-determined dose and schedule.
- Assessment: Measure pre-defined efficacy endpoints (e.g., pain threshold, tumor size, biochemical markers) and confirm target knockdown (e.g., via Western blot or qPCR) [64].
- Interpretation: A significantly reduced effect of the herbal extract in the target knockdown group compared to the control group provides evidence that the extract's efficacy is mediated through that specific target [64].
Research Reagent Solutions
Essential materials and tools for herbal medicine validation research:
| Reagent/Tool | Function | Application in Herbal Medicine |
|---|---|---|
| Chemical Reference Standards | Benchmark for identity, purity, and quantitative analysis [1] | Standardizing HPLC/LC-MS methods; quantifying active compounds or markers. |
| DNA Barcoding Kits | Authenticate botanical species using genetic markers [1] | Verifying the correct species of herbal material to prevent adulteration. |
| siRNA/shRNA Tools | Knock down gene expression of a putative molecular target [64] | Functionally validating the therapeutic target of an herbal extract in cellular or animal models. |
| Tool Antibodies | Selectively bind to and inhibit specific protein targets [64] | A highly specific method for target validation, especially for cell surface proteins. |
| Metabolomics Kits (NMR, LC-MS) | Comprehensively profile small molecule metabolites [4] | Creating a comprehensive chemical fingerprint of a complex herbal product. |
| Transgenic Animal Models | Study target function in a whole-organism context [65] [64] | Investigating the role of a specific target in disease and the effect of herbal treatment. |
Validation Pathways & Workflows
Multivariable Optimization Framework
Preclinical Target Validation Workflow
Adherence to CONSORT Guidelines and Best Practices for Herbal Medicine Research
Troubleshooting Guides
Guide 1: Addressing Incomplete Reporting in Herbal Pilot Trials
Problem: Pilot trials for herbal interventions frequently fail to progress to full-scale studies, often due to inadequate reporting that does not adequately inform definitive trial design [49].
| Reported Issue | Frequency in Herbal Pilot Trials (n=123) | Recommended CONSORT Action |
|---|---|---|
| Feasibility Assessments | 13.1% | Explicitly state pilot objectives and report all feasibility outcomes (e.g., recruitment rates, adherence) [49]. |
| Sample Size Rationale | 47.2% | Justify pilot sample size; do not power for effectiveness. Use feasibility objectives like confidence interval width [49]. |
| Randomization Methods | 35.8% | Detail the random sequence generation, allocation concealment, and implementation method [49]. |
| Herbal-Specific Details | Inconsistent | Use extensions like CONSORT-CHM Formulas to detail processing, quality control, and formulation [38] [68]. |
Experimental Protocol for Feasibility Assessment:
- Primary Feasibility Objectives: Pre-define clear criteria for success. Examples include:
- Recruitment Rate: Target ≥80% of the projected monthly recruitment figure.
- Retention Rate: Achieve ≥90% participant completion of the study protocol.
- Adherence: Demonstrate ≥85% participant adherence to the herbal intervention, verified by returned product weight or diary entries.
- Data Collection: Systematically track all feasibility parameters throughout the trial duration.
- Analysis and Reporting: Report raw data for each feasibility outcome (e.g., actual recruitment numbers, dropout rates). Use this data to justify decisions for the main trial, such as the need for protocol modifications or a revised sample size calculation [49].
Guide 2: Managing Herbal Intervention Variability
Problem: Inconsistent quality, composition, and sourcing of herbal products introduce significant variability, compromising trial results and reproducibility [1] [4].
| Problem Source | Consequence | Quality Control Solution |
|---|---|---|
| Botanical Identification | Use of incorrect plant species | Perform authentication via macroscopic/microscopic examination and DNA barcoding [1]. |
| Variable Active Compounds | Inconsistent potency and therapeutic effect | Use chemical fingerprinting (e.g., HPLC, LC-MS) to standardize key markers [1] [4]. |
| Contaminants (heavy metals, microbes) | Patient safety risks and product impurity | Adhere to pharmacopoeial standards (e.g., WHO, USP) for contaminant testing [1] [69]. |
Experimental Protocol for Herbal Standardization:
- Source Authentication: Obtain herbs from certified suppliers following Good Agricultural and Collection Practices (GACP). Document the botanical species, plant part used, geographic origin, and harvest time.
- Chemical Standardization:
- Identify key active compounds or chemical markers through literature review.
- Use High-Performance Liquid Chromatography (HPLC) to create a chemical fingerprint of the batch.
- Establish reference standards and acceptable ranges for the concentration of key markers to ensure batch-to-batch consistency [1].
- Quality Control Testing: Test each batch for contaminants, including pesticides, heavy metals, and microbial loads, following relevant regulatory guidelines (e.g., WHO, ICH, Good Manufacturing Practice) [1] [69].
- Reporting: In the manuscript, detail all the above steps under the "Interventions" section, specifying the botanical name, plant part, extraction method, solvent, standardization markers, and quality control results [38] [68].
Guide 3: Reconciling Personalized Medicine with Standardized RCTs
Problem: The principles of personalized medicine in systems like Traditional Chinese Medicine (TCM) conflict with the standardized protocols required by conventional RCTs [68].
Solution: Employ pragmatic trial designs that incorporate real-world use and patient preferences.
Experimental Protocol for a Pragmatic RCT:
- Patient Preference Design:
- Group A (Randomized): Participants willing to accept any treatment are randomly assigned to the herbal intervention or control group.
- Group B (Preference): Participants with a strong preference are allocated to their chosen group (herbal intervention or control).
- This design allows researchers to assess the effect of randomization versus patient preference on outcomes and adherence [68].
- Outcome Measures: Select clinically relevant, patient-centered primary outcomes (e.g., "time to symptom resolution," "improvement in quality of life") over purely biological markers.
- Flexible Intervention Protocol: While the core herbal formula is fixed, pre-specify allowable modifications based on syndrome differentiation (e.g., adding specific herbs for a documented symptom) and report the frequency and type of these modifications [68].
Frequently Asked Questions (FAQs)
Q1: Which specific CONSORT guideline should I use for my herbal medicine trial? The guideline depends on your trial design. All trials should use the core CONSORT 2010/2025 statement [38] [70]. Additionally, you must consult relevant extensions:
- CONSORT for Chinese Herbal Medicine Formulas (CONSORT-CHM Formulas 2017) for compound formulations [38] [68].
- CONSORT for Non-Pharmacological Treatments for trials involving acupuncture or other manual therapies [38].
- CONSORT for Pilot and Feasibility Trials if you are conducting a preliminary study [38].
- CONSORT-Herbal 2026, which is currently under development and will provide updated, specific guidance for trials of medicinal plant extracts and natural products [71].
Q2: What are the most critical herbal-specific details to report, beyond standard CONSORT items? Under the "Interventions" section, you must provide meticulous detail on [49] [1] [68]:
- Botanical Nomenclature: Full botanical name (genus, species, authority), plant part used (e.g., root, leaf), and type of extract.
- Manufacturing and Quality Control: Details on the manufacturer, dosage form, extraction method and solvent, and chemical standardization (e.g., "standardized to contain X% of marker compound Y"). Report quality control measures and results for contaminants.
- Dosage and Regimen: Precise dosage, frequency, duration of treatment, and any permitted adjustments.
- Practitioner Credentials: If applicable, the training and expertise of the practitioners prescribing or administering the intervention.
Q3: Our pilot trial was successful. How do we justify the sample size for the definitive trial based on pilot data? A pilot trial is not designed to test efficacy, so never use effect size estimates from a pilot to power a main trial. Instead, use the pilot data to inform a Sample Size Justification based on feasibility [49]. Calculate the sample size required for the definitive RCT based on an effect size from existing literature or a clinically meaningful difference. Use the pilot data to validate that this sample size is achievable, for example, by confirming your recruitment rate is sufficient to reach the target within the planned timeline.
Q4: How can we maintain blinding in a trial when the herbal medicine has a distinctive taste or smell? This is a common challenge. Several strategies can be employed:
- Placebo Matching: Invest in sophisticated placebos that match the active intervention in taste, smell, color, and texture. This may involve using taste-masking agents or encapsulation [49].
- Third-Party Blinding: Have an independent pharmacist or staff member who is not involved in outcome assessment prepare and dispense the coded treatments.
- Partial Blinding: Acknowledge if perfect blinding is impossible. In such cases, blind the outcome assessors and statisticians to the fullest extent possible, and discuss this limitation in the manuscript.
The Scientist's Toolkit: Essential Reagents & Materials
This table lists key materials and reagents critical for ensuring quality and reproducibility in herbal medicine research.
| Item | Function & Application | Examples / Standards |
|---|---|---|
| Chemical Reference Standards | Quantitative analysis and quality control; used to calibrate instruments and create chemical fingerprints for batch standardization [1]. | Certified reference materials for marker compounds (e.g., berberine, glycyrrhizin, ginsenosides) from pharmacopoeias (USP, EP). |
| Chromatography Systems | Separation, identification, and quantification of chemical components in a complex herbal mixture [1] [4]. | High-Performance Liquid Chromatography (HPLC), Liquid Chromatography-Mass Spectrometry (LC-MS), Gas Chromatography (GC). |
| DNA Barcoding Kits | Authentication of botanical raw materials to ensure the correct plant species is used, preventing adulteration [1]. | Primers and reagents for amplifying and sequencing standard barcode regions (e.g., ITS2, matK, rbcL). |
| Pharmacopoeial Standards | Provide official testing methods and acceptance criteria for identity, purity, composition, and quality of herbal substances [1] [69]. | WHO Herbal Monographs, US Pharmacopeia (USP), European Pharmacopoeia (EP), Chinese Pharmacopoeia. |
| Good Practice (GxP) Guidelines | A framework of quality standards governing all stages of research and production to ensure safety and consistency [4] [69]. | Good Laboratory Practice (GLP), Good Clinical Practice (GCP), Good Manufacturing Practice (GMP), Good Agricultural Practices (GAP). |
The global herbal medicine market is experiencing significant growth, propelled by rising consumer demand for natural health products. This expansion underscores an urgent need for robust and harmonized regulatory frameworks to ensure the safety, efficacy, and quality of herbal medicinal products (HMPs) worldwide. The World Health Organization (WHO) estimates that 80% of the global population relies on traditional medicine for their primary healthcare needs, highlighting the immense public health significance of this sector [2]. However, the regulatory landscape remains fragmented, with different regions employing distinct approaches to oversight, creating challenges for international trade and scientific cooperation.
This technical guide provides a comparative analysis of the regulatory systems for herbal medicines in the European Union (EU), the United States (US), India, and under WHO guidelines. Designed for researchers, scientists, and drug development professionals, this resource aims to clarify the complex regulatory environment and provide practical, actionable protocols for navigating regional requirements within the context of herbal medicine standardization research. The subsequent sections will dissect specific regulatory pathways, present comparative data, and offer troubleshooting guidance for common challenges encountered during product development and registration.
The regulatory philosophies governing herbal medicines vary significantly across jurisdictions, primarily differing in how they categorize these products and the type of evidence required for market approval. The following table provides a high-level comparison of the core regulatory characteristics in each region.
Table 1: Core Regulatory Characteristics for Herbal Medicines by Region
| Region/Authority | Primary Regulatory Category | Key Governing Legislation/Policy | Core Regulatory Focus |
|---|---|---|---|
| European Union (EU) | Herbal Medicinal Product | Traditional Herbal Medicinal Products Directive (THMPD) 2004/24/EC [72] | Safety, quality, and plausible efficacy based on long-standing use |
| United States (US) | Botanical Drug (as drugs) or Dietary Supplement (as supplements) | Botanical Drug Development Guidance (for drugs); DSHEA (for supplements) [73] | Proof of safety and efficacy for drugs; safety and labeling for supplements |
| India | Ayurvedic, Siddha, Unani (ASU) Drugs | Drugs and Cosmetics Act (Ayurveda, Siddha, Unani Drugs) [74] | Quality, safety, and efficacy based on classical texts and modern parameters |
| WHO | Herbal Medicine | Global Traditional Medicine Strategy 2025-2034 [75] | Evidence generation, safety, regulation, and integration into health systems |
Detailed Regulatory Pathways
European Union (EU): The EU provides a harmonized, yet tiered, approach through the European Medicines Agency (EMA) and its Committee on Herbal Medicinal Products (HMPC). There are three main pathways for market entry [72]:
- Traditional Use Registration: Simplified procedure for products with at least 30 years of medicinal use (including 15 within the EU). Relies on bibliographic data and evidence of traditional use, without requiring clinical trials.
- Well-Established Use Marketing Authorisation: For substances with at least 10 years of well-established use in the EU. Requires detailed scientific literature establishing efficacy and an acceptable safety profile.
- Stand-alone or Mixed Application: For new HMPs, requiring full safety and efficacy data from the company's own pre-clinical and clinical studies.
The HMPC supports these pathways by establishing EU monographs and a list of herbal substances, which provide authoritative information on safe and effective use [72].
United States (US): The US Food and Drug Administration (FDA) operates a dual system for botanicals [73]:
- Dietary Supplements: Regulated under the Dietary Supplement Health and Education Act (DSHEA). Products cannot make disease claims (e.g., "treats cancer") and are not subject to pre-market approval for safety and efficacy. The focus is on post-market surveillance, good manufacturing practices, and ensuring that labeling claims are not misleading.
- Botanical Drugs: Regulated as drugs under the FDA's "Botanical Drug Development Guidance for Industry." This pathway requires rigorous proof of safety and effectiveness through controlled clinical trials, similar to synthetic new chemical entities. To date, only a few botanical products have been approved via this route [73].
India: India regulates herbal medicines primarily under the Ministry of Ayush, which oversees Ayurveda, Yoga & Naturopathy, Unani, Siddha, and Homeopathy. Herbal medicines are regulated as Ayurvedic, Siddha, and Unani (ASU) drugs under the Drugs and Cosmetics Act [74]. They can be marketed with medical claims and are categorized as either prescription or over-the-counter medicines. India leverages its rich historical texts and has established pharmacopoeial standards (Ayurvedic Pharmacopoeia of India) to define quality and manufacturing parameters. The country is actively engaged in shaping global standards, as evidenced by its prominent role in WHO forums [76].
World Health Organization (WHO): The WHO does not regulate products directly but provides global strategic guidance and tools to support member states. Its newly adopted Global Traditional Medicine Strategy 2025-2034 aims to strengthen the evidence base, ensure quality and safety through regulation, and promote the integration of traditional medicine into national health systems [75] [77]. Key initiatives include the forthcoming Traditional Medicine Global Library (TMGL) set to launch in December 2025, which will serve as a comprehensive digital knowledge repository [78]. The WHO also provides detailed technical guidance on Good Manufacturing Practices (GMP), quality control, and labeling to foster international harmonization [2].
Troubleshooting Guide: Common Regulatory and Standardization Challenges
This section addresses specific, high-frequency issues researchers and developers face when preparing HMPs for different regulatory markets.
FAQ 1: How do I resolve species misidentification and adulteration in my herbal raw material?
- Problem: The starting plant material is incorrectly identified or contains other, undeclared plant species, leading to failed quality control tests and potential safety issues.
- Solution: Implement a multi-method authentication protocol.
- Macroscopic & Microscopic Analysis: Use pharmacopoeial methods for initial identification based of botanical features.
- Chemical Profiling: Employ Thin-Layer Chromatography (TLC) or High-Performance Liquid Chromatography (HPLC) to create a chemical fingerprint and quantify marker compounds [2].
- DNA Barcoding: Utilize molecular techniques like DNA barcoding to provide definitive species-level authentication, which is increasingly recommended by WHO and other authorities to combat adulteration [77]. This is critical for differentiating between closely related species, such as various types of Ginseng (Panax species) [2].
- Preventive Measure: Establish a rigorous supplier qualification program and require a Certificate of Analysis (CoA) that includes data from the above methods for every batch of raw material.
FAQ 2: What is the best strategy to prove "Traditional Use" for an EU Traditional Use Registration?
- Problem: Insufficient or poorly documented evidence of long-term use to meet the requirements of Directive 2004/24/EC.
- Solution: Meticulously compile and present bibliographic evidence.
- Demonstrate Duration: Provide evidence from scientific literature, authoritative textbooks, or documented practical experience showing the product has been used for at least 30 years, with at least 15 years within the EU [72].
- Specify Indications: The evidence must clearly describe the traditional use for a specific indication. The route of administration and specified strength must match your product.
- Leverage HMPC Resources: Consult the existing EU herbal monographs and list entries. If your product's composition and use align with these, it significantly simplifies the application process [72].
- Preventive Measure: Conduct a thorough literature review early in the development process to assess the feasibility of this pathway before committing significant resources.
FAQ 3: My HMP is a complex mixture. How can I develop a scientifically valid standardization protocol?
- Problem: The presence of multiple active and synergistic compounds makes it difficult to define a single marker for quality and batch-to-batch consistency, which is a requirement for all major regulatory frameworks.
- Solution: Adopt a multivariable standardization approach as recommended by recent scientific literature [4].
- Move Beyond Single Markers: Instead of relying on a single compound, use chromatographic fingerprinting (e.g., HPTLC, HPLC) to characterize the entire chemical profile [2]. This ensures consistency of the full mixture.
- Identify Key Markers: Select multiple analytical markers, including both active constituents and characteristic compounds, to control throughout the manufacturing process.
- Correlate with Activity: Where possible, use bioassays to link the chemical profile to biological activity, strengthening the evidence for efficacy, which is particularly valuable for the US botanical drug and EU well-established use pathways.
- Experimental Protocol for HPLC Fingerprinting:
- Sample Prep: Extract powdered herb using a validated, reproducible method (e.g., reflux with a specified solvent-to-herb ratio for a set time).
- Standard Preparation: Prepare reference standards of known marker compounds.
- HPLC Analysis: Inject samples and standards into the HPLC system. Use a validated method with a defined column, mobile phase (gradient or isocratic), and detection (e.g., UV/DAD).
- Data Analysis: Compare the chromatograms of test samples against a reference fingerprint for identity. Quantify key marker peaks to ensure they fall within a specified range for batch consistency.
FAQ 4: How do I choose between the US Dietary Supplement and Botanical Drug pathways?
- Problem: Misunderstanding the legal distinction between a supplement and a drug, leading to inappropriate claims and regulatory action.
- Solution: Base the decision entirely on the intended use and claims.
- Choose "Dietary Supplement" if: You intend to make only structure/function claims (e.g., "supports immune health," "promotes relaxation"). You cannot claim to diagnose, mitigate, treat, cure, or prevent a disease [73].
- Choose "Botanical Drug" if: You intend to market the product specifically to treat, prevent, or cure a disease. This requires an Investigational New Drug (IND) application and subsequent New Drug Application (NDA) approval, supported by rigorous clinical trials [73].
- Critical Decision Flowchart: The following diagram illustrates the logical decision-making process for the US market, helping to prevent misbranding.
The Scientist's Toolkit: Essential Reagents and Methods for Standardization
Successful research and development of HMPs require the application of specific analytical techniques and reagents. The table below details key tools for ensuring quality and compliance with regulatory standards.
Table 2: Key Research Reagents and Methods for Herbal Medicine Standardization
| Tool/Reagent | Primary Function in Standardization | Key Application Example | Considerations |
|---|---|---|---|
| DNA Barcoding Kits | Species authentication and detection of adulterants. | Differentiating Panax ginseng from other Panax species [2]. | Requires reliable reference databases; confirms identity but not phytochemical profile. |
| Chemical Reference Standards | Qualitative and quantitative analysis as markers for quality. | Quantifying curcuminoid content in Curcuma longa (turmeric) using HPLC [2]. | Purity and sourcing are critical; should be traceable to a pharmacopoeial standard when available. |
| Chromatography Systems (HPLC, UHPLC, TLC, GC-MS) | Separation, identification, and quantification of chemical constituents; creating chemical fingerprints. | Creating an HPLC fingerprint for Senna leaves to confirm the presence of sennosides [2]. | Method validation is required for regulatory submissions. LC-MS/MS provides superior identification power. |
| Microbiological Culture Media | Ensuring product safety by testing for total viable aerobic count and specified microorganisms. | Testing Echinacea tinctures for absence of E. coli and Salmonella [2]. | Must follow pharmacopoeial methods (e.g., USP, Ph. Eur.) for acceptance criteria. |
| ICP-MS/AAS | Ensuring safety by quantifying toxic element residues. | Testing Ashwagandha root powder for arsenic, lead, cadmium, and mercury levels [2]. | Requires careful calibration and sample digestion to avoid interference. |
Experimental Workflow for Comprehensive Quality Control
A systematic approach to quality control is non-negotiable for regulatory compliance. The following diagram and protocol outline a generalized workflow for ensuring the quality and safety of an herbal material, integrating multiple techniques from the Scientist's Toolkit.
Detailed Protocol for a Integrated Quality Control Assessment:
Sample Authentication:
- Objective: To confirm the correct botanical identity of the raw material.
- Method: Perform DNA barcoding using a standardized kit. Amplify a conserved genomic region (e.g., ITS2, rbcL), sequence it, and compare the sequence against a curated reference database like GenBank or a dedicated plant DNA barcode library.
- Acceptance Criterion: Sequence match must confirm the desired species at a defined confidence threshold (e.g., >99%).
Chemical Standardization via HPLC Fingerprinting:
- Objective: To establish batch-to-batch chemical consistency and quantify key markers.
- Method:
- Extraction: Precisely weigh 1.0 g of powdered herb. Extract with 20 mL of methanol in an ultrasonic bath for 30 minutes. Filter and dilute to volume.
- HPLC Analysis: Use a validated HPLC-DAD method. Example conditions: C18 column; mobile phase of water (A) and acetonitrile (B) with a gradient elution; flow rate 1.0 mL/min; detection at 254 nm. Inject the sample and reference standard solution.
- Data Analysis: Identify peaks in the test sample by comparing retention times and UV spectra with those of the standards. Calculate the concentration of marker compounds. The chromatographic fingerprint of the test sample should be congruent with a reference standard fingerprint.
Safety Profiling:
- Objective: To ensure the material is free from hazardous levels of contaminants.
- Heavy Metals: Using Inductively Coupled Plasma Mass Spectrometry (ICP-MS), test for Arsenic (As), Cadmium (Cd), Lead (Pb), and Mercury (Hg). Results must comply with limits set by the target region's pharmacopoeia (e.g., USP, EP).
- Microbiological Testing: Perform the Total Viable Aerobic Count and test for the absence of specified objectionable microorganisms (E. coli, Salmonella, etc.) according to pharmacopoeial methods.
The comparative analysis reveals that while the EU, US, India, and WHO share common goals of ensuring safety and quality, their regulatory mechanisms and philosophical underpinnings differ substantially. The EU offers a structured, use-based pathway, the US presents a clear dichotomy between supplements and drugs, India integrates traditional knowledge with modern regulation, and the WHO provides the overarching framework for global harmonization.
The future of herbal medicine regulation is moving towards greater integration of advanced technologies. The WHO's 2025-2034 strategy emphasizes digital innovations such as DNA barcoding for authentication and AI for evidence generation [77]. The launch of the Traditional Medicine Global Library (TMGL) in December 2025 will further empower researchers with centralized access to knowledge [78]. For researchers and drug developers, success in this evolving landscape depends on a proactive, science-driven approach: adopting multivariable standardization [4], leveraging digital tools for traceability, and engaging with regulatory agencies early in the development process. By understanding and navigating these complex, multi-jurisdictional requirements, the scientific community can fully unlock the potential of herbal medicines and integrate them effectively into modern, evidence-based healthcare.
Assessing Progression from Pilot to Full-Scale Clinical Studies
Frequently Asked Questions (FAQs)
Q1: What are the most critical barriers preventing herbal medicine pilot studies from progressing to full-scale trials?
The progression from pilot to full-scale clinical trials in herbal medicine faces several significant barriers. A comprehensive review of 123 herbal medicine pilot trials found that only 3.3% (4 studies) progressed to full-scale trials [49]. The primary barriers include inadequate feasibility assessments, insufficient sample size justification, and poor reporting of methodological details. Furthermore, funding constraints and challenges with product standardization consistently hinder progression. Modern herbal medicine trials were 4.7 times more likely to progress than traditional herbal trials, though this result was not statistically significant [49].
Q2: How can researchers improve the methodological rigor of herbal medicine pilot studies?
Improving methodological rigor requires addressing several key areas. Research shows that trial registration and protocol publication significantly improve reporting completeness, with incidence rate ratios of 1.20 and 1.16 respectively [49]. Key strategies include implementing comprehensive feasibility assessments (reported in only 13.1% of trials), providing clear sample size justification (found in 47.2% of trials), and detailing randomization methods (described in 35.8% of trials) [49]. Additionally, reporting herb-specific details like ingredient processing, quality control, and safety assessments is essential for improving methodological quality.
Q3: What specific feasibility criteria should a herbal medicine pilot study address before scaling up?
A robust feasibility assessment for herbal medicine pilot studies should evaluate several critical criteria. These include establishing reliable methods for product standardization across batches, assessing participant recruitment rates and retention strategies, validating outcome measures appropriate for both modern and traditional diagnostic frameworks, evaluating practitioner adherence to protocols, and determining resource requirements for larger-scale production of the standardized herbal product [48] [49]. These criteria ensure that the unique complexities of herbal interventions are adequately addressed before committing to larger trials.
Q4: How should researchers handle standardization and quality control of herbal products across study phases?
Maintaining consistent quality across pilot and full-scale studies requires a multivariable optimization framework addressing three key domains: herb variation (through quality optimization and herbal drug development), disease variation (through knowledge management and practitioner training), and patient variation (through personalized medicine principles) [4]. Quality control parameters should include physicochemical testing (pH, viscosity, HPLC), microbiological testing, heavy metal and pesticide screening, adulteration detection, and chromatographic fingerprinting to ensure batch-to-batch consistency [2]. Implementing Good Agricultural and Collection Practices (GACP) and Good Manufacturing Practices (GMP) throughout the product lifecycle is essential [48].
Q5: What regulatory considerations are unique to herbal medicine clinical development?
Herbal medicines present unique regulatory challenges including classification as either drugs or dietary supplements depending on the region, varying requirements for safety and efficacy evidence, and different standards for quality control [48]. The World Health Organization emphasizes that quality assurance responsibility must be shared between manufacturers and regulatory bodies, with requirements for good agricultural and harvesting practices, good manufacturing practices, and appropriate labeling [48] [2]. Regional variations are significant, with the EU following the Traditional Herbal Medicinal Products Directive, ASEAN having specific GMP guidelines, India regulating through the Ministry of AYUSH, and the US regulating under the Dietary Supplement Health and Education Act (DSHEA) [2].
Troubleshooting Common Experimental Issues
Problem: High participant dropout rates in herbal medicine trials
Solution: Implement the partial randomization approach proposed by Brewin and Bradley, where patients who express strong treatment preferences are allowed their choice, while only those without preferences are randomized [48]. This accommodates the fact that herbal medicine outcomes depend significantly on patient participation, will, and motivation to complete treatment. Additionally, use single blinding where possible, as double blinding is often impossible due to the multidimensional treatment approach involving counseling, lifestyle, and dietary advice alongside herbal prescriptions [48].
Problem: Difficulty matching control preparations to complex herbal interventions
Solution: Develop placebo controls standardized for critical factors including color, odor, taste, duration and frequency of intake, and credibility of treatment to the patient [48]. For herbs with distinctive characteristics like ginger's odor, consider using active controls or different herbal preparations rather than attempting perfect placebo matching. The control should closely match the physical situation in which treatments are administered, and credibility should be tested in preliminary studies to ensure adequate blinding [48].
Problem: Inconsistent results due to variability in herbal product composition
Solution: Implement a comprehensive standardization approach throughout the product lifecycle. Begin with proper botanical identification using macroscopic, microscopic, and molecular methods to avoid misidentification [2]. Standardize extraction methods and validate them for reliable extraction of bioactive constituents. Apply analytical methods such as chromatographic fingerprinting and use reference marker compounds to verify consistency [2]. Maintain detailed batch manufacturing records that document every production stage, and conduct regular stability testing to determine shelf-life and storage recommendations [2].
Problem: Diagnostic mismatch between traditional herbal medicine and modern medical frameworks
Solution: Apply the "double classification method" where subjects are primarily diagnosed using modern diagnostic criteria and then classified according to the traditional system [48]. Treatments are given according to traditional classification, while outcomes are evaluated using criteria for both systems. This approach respects the holistic diagnostic framework of traditional herbal medicine while generating evidence comprehensible within modern scientific paradigms, particularly important when traditional diagnosis doesn't align directly with western medical diagnoses [48].
Key Quantitative Data on Herbal Medicine Pilot Studies
Table 1: Reporting Quality in Herbal Medicine Pilot Trials (n=123)
| Reporting Element | Frequency (%) | Significance for Full-Scale Progression |
|---|---|---|
| Feasibility assessments | 13.1% | Critical for determining study viability |
| Sample size justification | 47.2% | Essential for statistical power planning |
| Randomization methods | 35.8% | Affects result validity and bias control |
| Ingredient processing details | Inconsistent | Crucial for product reproducibility |
| Quality control documentation | Inconsistent | Ensures batch-to-batch consistency |
| Safety assessments | Inconsistent | Required for risk-benefit evaluation |
Source: Adapted from Li et al. comprehensive review of HM pilot trials [49]
Table 2: Progression Rates and Influencing Factors in Herbal Medicine Research
| Factor | Impact Measure | Statistical Significance |
|---|---|---|
| Overall progression to full-scale trials | 3.3% (4/123 studies) | Baseline rate |
| Effect of trial registration | IRR = 1.20 (95% CI: 1.11-1.30) | Positive association with reporting quality |
| Effect of protocol publication | IRR = 1.16 (95% CI: 1.08-1.24) | Positive association with reporting quality |
| Modern vs. traditional HM progression | OR = 4.70 (95% CI: 0.37-252.91) | Not statistically significant (P=.300) |
IRR = Incidence Rate Ratio; OR = Odds Ratio; Source: Li et al. [49]
Experimental Protocols for Critical Assessments
Protocol 1: Comprehensive Feasibility Assessment for Herbal Medicine Trials
Purpose: To systematically evaluate readiness for progression from pilot to full-scale clinical studies.
Methodology:
- Recruitment Feasibility: Track screening, eligibility, and enrollment rates monthly; calculate screen-to-randomization ratio
- Intervention Fidelity: Develop treatment manuals detailing precise procedures; assess practitioner adherence through random audits
- Product Quality Monitoring: Implement batch-by-batch testing using HPLC/TLC fingerprinting; establish acceptable variance thresholds for active constituents
- Participant Retention: Monitor dropout reasons; implement retention strategies tailored to herbal medicine contexts
- Outcome Assessment: Validate patient-reported outcome measures for cultural appropriateness; test inter-rater reliability for practitioner assessments
Success Criteria: ≥80% recruitment target met, ≥90% practitioner protocol adherence, ≤15% dropout rate, consistent product quality across batches [49].
Protocol 2: Herbal Product Standardization and Quality Control
Purpose: To ensure consistent composition and quality of herbal investigational products across study phases.
Methodology:
- Raw Material Authentication: Conduct macroscopic, microscopic, and DNA barcoding identification; reject materials failing any authentication method
- Extraction Standardization: Validate extraction methods for optimal bioactive constituent yield; document solvent, temperature, and duration parameters
- Quality Control Testing: Perform physicochemical (pH, viscosity, HPLC), microbiological (total viable count, pathogens), and contaminant (heavy metals, pesticides) testing
- Stability Studies: Conduct real-time and accelerated stability testing under recommended storage conditions; establish shelf-life based on validated data
- Documentation: Maintain complete batch manufacturing records with full traceability from raw materials to finished product [2]
Acceptance Criteria: All batches must fall within ±10% of reference marker compound levels; meet microbial safety standards; demonstrate stability through proposed study duration [2].
Signaling Pathways and Experimental Workflows
Diagram 1: Herbal Study Progression Pathway
Diagram 2: Multivariable Optimization Framework
Research Reagent Solutions for Herbal Medicine Studies
Table 3: Essential Research Reagents and Materials for Herbal Medicine Clinical Trials
| Reagent/Material | Function | Application Example | Quality Standards |
|---|---|---|---|
| Reference marker compounds | Quantification of active constituents | HPLC quantification of curcumin in turmeric extracts | ≥95% purity, pharmacopeial standards |
| Chromatographic solvents | Herbal fingerprinting and analysis | TLC fingerprinting for sennosides in Senna leaves | HPLC grade, low UV absorbance |
| Microbial testing media | Safety and quality verification | Microbial safety testing for Echinacea tinctures | ISO 11133 compliance |
| DNA barcoding kits | Botanical authentication | Authenticating Panax ginseng species in supplements | High-fidelity polymerase |
| Heavy metal standards | Contaminant testing | ICP-MS detection of arsenic in Ashwagandha | NIST-traceable reference materials |
| Placebo formulation components | Control preparation | Matching color, smell, taste of herbal intervention | GMP-grade excipients |
Conclusion
The standardization of herbal medicines is an indispensable, multidisciplinary endeavor crucial for their integration into evidence-based healthcare. A synergistic approach that combines rigorous classical pharmacognosy with cutting-edge technologies like AI, DNA barcoding, and advanced chromatography is paramount for ensuring product quality, safety, and efficacy. Future progress hinges on overcoming significant challenges, including methodological inconsistencies in clinical research, the high cost of analytical infrastructure, and the lack of globally harmonized regulations. For biomedical and clinical research, the path forward involves strengthening validation frameworks, fostering international regulatory collaboration, and investing in innovative solutions that enhance bioavailability and target specificity. By closing these gaps, the scientific community can fully unlock the therapeutic potential of herbal medicines, paving the way for their standardized and reliable application in modern medicine.
References
- 1. Advancing herbal medicine: enhancing product quality and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10561302/]
- 2. WHO 2025 Guide: Herbal Product Standardization & ... [https://www.foodresearchlab.com/insights/regulation-updates/who-herbal-labeling-2025/]
- 3. Regulation and standardization of herbal drugs [https://www.sciencedirect.com/science/chapter/bookseries/pii/S1871512523000158]
- 4. Optimizing Herbal Drug Use through Multivariable ... [https://www.sciencedirect.com/science/article/pii/S2667031325001782]
- 5. Herbal Remedies 101: Efficacy, Safety, and Best Practices [https://www.indwes.edu/articles/2025/08/herbal-remedies-best-practices]
- 6. Medicinal Herbs Market to Hit US$ 478.93 Billion by 2032, ... [https://www.biospace.com/press-releases/medicinal-herbs-market-to-hit-us-478-93-billion-by-2032-growing-at-11-21-cagr-driven-by-rising-demand-for-natural-remedies-and-product-innovation]
- 7. WHA78: Traditional medicine takes centre stage [https://www.who.int/news/item/02-06-2025-wha78--traditional-medicine-takes-centre-stage]
- 8. Traditional medicine and its contributions to science, health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578528/]
- 9. Quality control of herbal drugs and preparations [https://www.sciencedirect.com/science/article/pii/S2666831921000400]
- 10. Study design of herbal medicine clinical trials: a descriptive ... [https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-024-04697-7]
- 11. Dossier - Physical contamination and food safety [https://www.foodtimes.eu/food-safety/physical-contamination-food-safety-global-regulatory-analysis/]
- 12. Food Adulteration: Risks, Prevention, and Modern Solutions [https://www.linkedin.com/pulse/food-adulteration-risks-prevention-modern-solutions-smartfoodsafe-jusoc]
- 13. Scientific validation of the traditional knowledge of Sikta ... [https://revistas.ucm.es/index.php/MBOT/article/view/60073]
- 14. Integrating Indigenous Knowledge and Western Science in ... [https://indigenousclimatehub.ca/2024/08/bridging-two-worlds-integrating-indigenous-knowledge-and-western-science-in-climate-policy/]
- 15. 5 Common Mistakes Beginning Herbalists Make [https://healingharvesthomestead.com/home/2017/5/10/herbs-dont-work-for-me-reasons-why-herbal-remedies-may-not-work]
- 16. Troubleshooting Fire Cider: Answering Your Questions [https://theherbalacademy.com/blog/troubleshooting-fire-cider/?srsltid=AfmBOorVUE4UBLCSiCVbktklRN9e9hTogvijMw3Zah026n9N51o-GFZh]
- 17. How Can We Bridge the Gap between Traditional ... [https://lifestyle.sustainability-directory.com/question/how-can-we-bridge-the-gap-between-traditional-knowledge-and-modern-science/]
- 18. Reasons Herbs may not be Working [https://www.herbalremediesadvice.org/herbs-not-working.html]
- 19. Bridging Traditional and Modern Medicine: The Role of ... [https://www.frontiersin.org/research-topics/66894/bridging-traditional-and-modern-medicine-the-role-of-botanicals-in-healthcareundefined]
- 20. Microscopic and physicochemical evaluation of Ruta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10365675/]
- 21. Morphological evaluation: Significance and symbolism [https://www.wisdomlib.org/concept/morphological-evaluation]
- 22. A New Era of Morphological Investigations - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10081917/]
- 23. Microscopic image analysis techniques for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354916319438]
- 24. Physicochemical Characterization Assays [https://www.creative-bioarray.com/services/physicochemical-characterization-assays.htm]
- 25. Chromatographic Fingerprinting and Food Identity/Quality [https://pmc.ncbi.nlm.nih.gov/articles/PMC8896688/]
- 26. Chromatographic fingerprinting by comprehensive two ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993620303629]
- 27. A Protocol for Untargeted Metabolomic Analysis: From Sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9284939/]
- 28. HPLC Troubleshooting Guide [https://scioninstruments.com/us/blog/hplc-troubleshooting-guide-2/]
- 29. Metabolite Profiling and Identification (MetID) | Cyprotex [https://www.evotec.com/solutions/drug-discovery-preclinical-development/cyprotex-adme-tox-solutions/adme-pk/drug-metabolism/metabolite-profiling-and-identification]
- 30. Advances in Fingerprint Analysis for Standardization and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.853023/full]
- 31. Modern analytical technology combined with machine ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X2503382X]
- 32. DNA barcoding in herbal medicine: Retrospective and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10257146/]
- 33. Strategies for molecular authentication of herbal products [https://cmjournal.biomedcentral.com/articles/10.1186/s13020-022-00590-y]
- 34. Challenges and scientific issues in the standardization of ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320505012531]
- 35. Guidelines: Production [https://www.who.int/teams/health-product-and-policy-standards/standards-and-specifications/norms-and-standards-for-pharmaceuticals/guidelines/production]
- 36. The use of quality control parameters in the evaluation ... [https://link.springer.com/article/10.1007/s44337-024-00177-6]
- 37. Comprehensive Guide to GMP: Key Elements, Process ... [https://cgmpconsulting.com/comprehensive-guide-to-gmp/]
- 38. CONSORT 2025 Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/consort/]
- 39. CONSORT 2025 statement: Updated guideline for reporting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11996237/]
- 40. CONSORT 2025 statement: updated guideline for reporting ... [https://www.nature.com/articles/s41591-025-03635-5]
- 41. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 42. The 5 most common clinical data pitfalls in 2025 (and how ... [https://www.greenlight.guru/blog/common-clinical-data-pitfalls]
- 43. Guidelines for Designing and Evaluating Feasibility Pilot Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849521/]
- 44. Sample size justification in feasibility studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186404/]
- 45. 8 Sample Size Justification - GitHub Pages [https://lakens.github.io/statistical_inferences/08-samplesizejustification.html]
- 46. Exploration of facilitators and barriers to the regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9442913/]
- 47. Regulatory landscape of dietary supplements and herbal ... [https://www.sciencedirect.com/science/article/pii/S0273230020300738]
- 48. Challenges and guidelines for clinical trial of herbal drugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC4678978/]
- 49. Methodological challenges in pilot trials of herbal medicine [https://www.sciencedirect.com/science/article/abs/pii/S0895435625000873]
- 50. Current demands for standardization of Indian medicinal ... [https://www.sciencedirect.com/science/article/pii/S2590098625000089]
- 51. Herbal Medicine Dosage Standardisation [https://www.sciencedirect.com/science/article/abs/pii/S2210803324000460]
- 52. Herbal Medicine Today: Clinical and Research Issues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2206236/]
- 53. A review of recent artificial intelligence for traditional ... [https://www.sciencedirect.com/science/article/pii/S2225411025000197]
- 54. Nanotechnology-based herbal medicine: Preparation, ... [https://www.sciencedirect.com/science/article/pii/S2666154325000328]
- 55. Metabolomics and Ethnopharmacology in the ... [https://www.frontiersin.org/research-topics/14729/metabolomics-and-ethnopharmacology-in-the-development-of-herbal-and-traditional-medicine/magazine]
- 56. Harnessing the application of artificial intelligence in ... [https://pubmed.ncbi.nlm.nih.gov/41052688/]
- 57. A review based on machine learning and deep learning [https://www.sciencedirect.com/science/article/pii/S2667142525000685]
- 58. Integrating herbgenomics with systems biology ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002685]
- 59. WHO guidelines for quality control of herbal medicines [https://ijpca.org/archive/volume/11/issue/3/article/22100]
- 60. WHO, ITU, WIPO showcase a new report on AI use in ... [https://www.who.int/news/item/11-07-2025-who--itu--wipo-showcase-a-new-report-on-ai-use-in-traditional-medicine]
- 61. Advancing Herbal Quality Assurance: The Role of Artificial ... [https://www.frontiersin.org/research-topics/66074/advancing-herbal-quality-assurance-the-role-of-artificial-intelligence-in-enhancing-quality-control-practicesundefined]
- 62. Top Mistakes You're Making with Herbal Remedies—and ... [https://www.theherbalistspath.com/blog/herbal-remedy-mistakes]
- 63. Preclinical Studies in Drug Development [https://www.ppd.com/what-is-a-cro/preclinical-studies-in-drug-development/]
- 64. Principles of early drug discovery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3058157/]
- 65. Molecular Target Validation in preclinical drug discovery [https://www.drugtargetreview.com/article/821/molecular-target-validation-in-preclinical-drug-discovery/]
- 66. How to Write a Research Protocol: Tips and Tricks - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6172884/]
- 67. Evidence Synthesis & Systematic Review Research [https://guides.library.oregonstate.edu/EvidenceSynthesis/research-protocol]
- 68. Challenges in Traditional Chinese Medicine Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262083/]
- 69. DRUG STANDARDIZATION AND ITS APPLICATIONS TO ... [https://www.jptcp.com/index.php/jptcp/article/view/9701]
- 70. CONSORT 2010 Statement: updated guidelines for reporting ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-8-18]
- 71. Reporting guidelines under development for clinical trials [https://www.equator-network.org/library/reporting-guidelines-under-development/reporting-guidelines-under-development-for-clinical-trials/]
- 72. Herbal medicinal products | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/herbal-medicinal-products]
- 73. What is a Botanical Drug? [https://www.fda.gov/about-fda/cder-offices-and-divisions/what-botanical-drug]
- 74. Traditional herbal medicine legislative and regulatory ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1475297/full]
- 75. Global traditional medicine strategy 2025-2034 [https://www.who.int/publications/i/item/9789240113176]
- 76. India Showcases Traditional Medicine at WHO-IRCH 2025 | [https://theindianpractitioner.com/india-showcases-traditional-medicine-at-who-irch-2025/]
- 77. Policy implications of WHO's Global traditional medicine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578523/]
- 78. WHO Traditional Medicine Global Library to launch in 2025 [https://www.who.int/news/item/25-09-2025-traditional-medicine-global-library-to-launch-in-2025]