Hypoxic Preconditioning of Stem Cells: Amplifying Paracrine Factor Production for Enhanced Therapeutic Efficacy
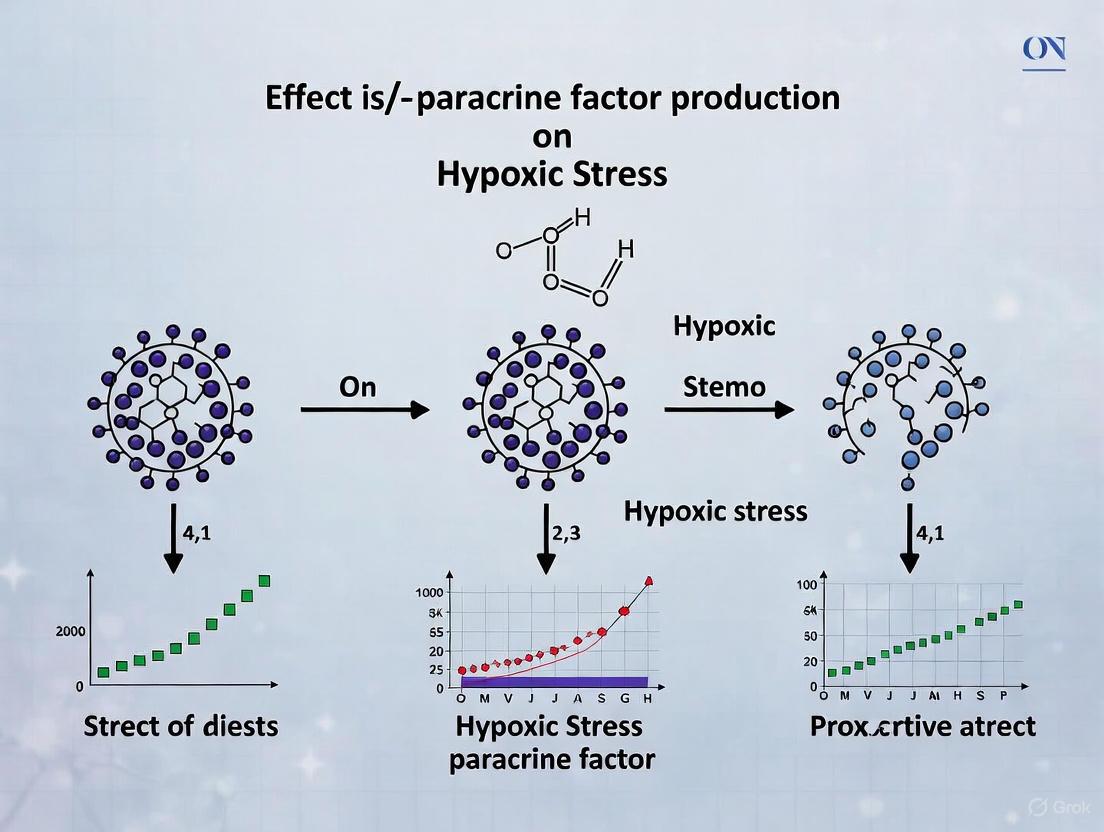
This article synthesizes current research on how hypoxic stress modulates the production of paracrine factors from stem cells, with a focus on mesenchymal stem cells (MSCs).
Hypoxic Preconditioning of Stem Cells: Amplifying Paracrine Factor Production for Enhanced Therapeutic Efficacy
Abstract
This article synthesizes current research on how hypoxic stress modulates the production of paracrine factors from stem cells, with a focus on mesenchymal stem cells (MSCs). It explores the foundational molecular mechanisms, including HIF-1α stabilization and subsequent metabolic reprogramming, that enhance the secretion of therapeutic cytokines, chemokines, and growth factors. We detail methodological approaches for hypoxic conditioning and its application in improving outcomes in preclinical models of cardiovascular, neurological, and musculoskeletal diseases. The content further addresses key challenges in translation, such as optimizing hypoxia protocols and ensuring consistent secretome quality, and provides a comparative analysis of the enhanced efficacy of hypoxia-preconditioned cell therapies and their secretome derivatives against standard counterparts. This resource is tailored for researchers, scientists, and drug development professionals seeking to leverage hypoxic preconditioning to develop more potent, cell-free regenerative therapies.
The Hypoxic Niche: Unraveling the Molecular Triggers of Enhanced Paracrine Signaling
Hypoxia-inducible factor-1α (HIF-1α) serves as the primary transcriptional regulator of cellular adaptation to oxygen deprivation, playing an indispensable role in stem cell biology, particularly within the context of paracrine factor production. As stem cells inhabit and function within physiologically hypoxic niches, HIF-1α-mediated responses become critical for their survival, metabolic adaptation, and secretory functions [1]. The heterodimeric transcription factor, composed of an oxygen-regulated HIF-1α subunit and a constitutively expressed HIF-1β subunit, coordinates the expression of hundreds of target genes containing hypoxia response elements (HREs) [2]. Under normoxic conditions, HIF-1α undergoes rapid proteasomal degradation following prolyl hydroxylation by prolyl-4-hydroxylases (PHDs) and von-Hippel-Lindau (pVHL)-mediated ubiquitination [2] [1]. During hypoxia, hydroxylase activity is oxygen-limited, leading to HIF-1α stabilization, nuclear translocation, dimerization with HIF-1β, and transactivation of target genes [2].
For stem cells, this transcriptional program extends beyond cell-autonomous survival mechanisms to encompass the regulation of paracrine factor secretion that mediates therapeutic effects in regenerative contexts. Research across diverse stem cell types – including dental stem cells, neural stem cells, and intestinal stem cells – consistently demonstrates that HIF-1α activation under hypoxia significantly influences the production of factors that modulate vascularization, immunoregulation, and tissue repair [3] [4] [5]. This whitepaper examines the molecular mechanisms of HIF-1α regulation in stem cells, its role in directing paracrine responses, and provides detailed methodological approaches for investigating HIF-1α-mediated hypoxic signaling in stem cell research.
Molecular Regulation of HIF-1α in Stem Cells
Oxygen-Dependent and Independent Regulation
The canonical regulation of HIF-1α occurs through oxygen-dependent mechanisms, primarily via the PHD-pVHL pathway. Under normoxia, PHDs use oxygen as a cofactor to hydroxylate specific proline residues (Pro402 and Pro564) within the oxygen-dependent degradation (ODD) domain of HIF-1α [2] [1]. This hydroxylation creates a recognition site for the pVHL E3 ubiquitin ligase complex, leading to polyubiquitination and proteasomal degradation of HIF-1α. Concurrently, factor inhibiting HIF-1 (FIH) hydroxylates an asparagine residue (Asn803) within the C-terminal transactivation domain (C-TAD), preventing recruitment of the p300/CBP coactivators and thereby inhibiting transcriptional activity even if HIF-1α escapes degradation [2].
Under hypoxic conditions (typically 0.1%-5% O₂), PHD and FIH activity is limited by oxygen substrate availability, leading to HIF-1α stabilization, nuclear translocation, and functional heterodimerization with HIF-1β [2] [1]. The heterodimer then binds to HREs in promoter/enhancer regions of target genes, recruiting coactivators like p300/CBP to initiate transcription.
Emerging evidence reveals that HIF-1α regulation in stem cells exhibits additional complexity, including oxygen-independent pathways and dynamic binding patterns. In mouse embryonic stem cells (mESCs), HIF-1α displays a "bind–release–bind" pattern during the transition from normoxia to hypoxia, with weakest binding during acute hypoxia and strongest during stable hypoxia, partnering with different transcription factors depending on oxygen levels [6]. This dynamic regulation enables stage-specific control of pluripotency and differentiation pathways.
Metabolic Reprogramming and HIF-1α Targets
HIF-1α orchestrates a metabolic shift from oxidative phosphorylation to glycolysis in stem cells through transcriptional activation of key glycolytic enzymes and glucose transporters, including hexokinase 2 (HK2), pyruvate dehydrogenase kinase 1 (PDK1), and glucose transporter 1 (Glut1) [3] [1]. This adaptation conserves oxygen while maintaining ATP production, which is particularly crucial for stem cell survival in hypoxic niches and post-transplantation environments. PDK1 phosphorylates and inhibits pyruvate dehydrogenase, redirecting pyruvate away from the mitochondrial tricarboxylic acid (TCA) cycle toward lactate production [3]. Additionally, HIF-1α decreases mitochondrial oxygen consumption by inhibiting c-MYC activity, further promoting glycolytic metabolism [1].
Diagram Title: HIF-1α Regulation Under Normoxia and Hypoxia
HIF-1α in Stem Cell Paracrine Function: Mechanisms and Experimental Evidence
Regulation of Angiogenic and Vasculogenic Paracrine Factors
HIF-1α directly regulates the expression of vascular endothelial growth factor (VEGF), a principal mediator of angiogenesis, in multiple stem cell types. In stem cells from human exfoliated deciduous teeth (SHED), HIF-1α stabilization under hypoxia significantly increased VEGF secretion, which subsequently enhanced endothelial cell proliferation and migration in vitro [3]. Genetic silencing of HIF-1α using siRNA or chemical inhibition with YC-1 abrogated this pro-angiogenic paracrine effect, demonstrating the essential role of HIF-1α in mediating this aspect of stem cell secretome.
The functional significance of HIF-1α-mediated paracrine signaling extends beyond in vitro models. In vivo Matrigel plug assays with SHED implanted subcutaneously in immunodeficient mice demonstrated that HIF-1α-silenced cells exhibited significantly reduced vessel formation, evidenced by decreased numbers of both perfused and non-perfused vessels of human or mouse CD31 origin [3]. This finding highlights the role of HIF-1α in enabling stem cells to create a vascular microenvironment conducive to tissue regeneration through paracrine mechanisms.
Extracellular Vesicle-Mediated Paracrine Signaling
Hypoxia and HIF-1α activation significantly influence extracellular vesicle (EV) production and cargo in stem cells, representing a crucial mechanism of paracrine signaling. In neural stem cells (NSCs), hypoxia induces the release of small extracellular vesicles (sEVs) through the HIF-1α/RAB17 pathway [4]. These hypoxic NSC-derived EVs contain enhanced levels of beneficial cytokines and genetic material that promote spinal cord injury repair, even in the absence of significant NSC survival or differentiation at the injury site.
This EV-mediated paracrine mechanism offers substantial therapeutic potential. Modified EVs from hypoxia-preconditioned NSCs, when engineered with CAQK/Angiopep2 targeting peptides, achieved precise delivery to spinal cord injury sites and significantly enhanced functional recovery in mouse models [4]. This approach demonstrates a cell-free, targeted therapeutic strategy that leverages HIF-1α-mediated paracrine responses without the challenges associated with stem cell transplantation survival.
Metabolic Regulation of Paracrine Signaling
HIF-1α influences stem cell paracrine function through metabolic reprogramming that supports survival under stress conditions. In SHED, HIF-1α silencing disrupted redox homeostasis, leading to increased cytoplasmic and mitochondrial reactive oxygen species (ROS) levels under hypoxic, oxidative stress (H₂O₂), and low-glucose conditions [3]. This ROS imbalance impaired cell viability and consequently diminished paracrine function. HIF-1α maintains ROS homeostasis through upregulation of PDK1, which modulates mitochondrial respiration and prevents excessive ROS generation [3].
In intestinal stem cells (ISCs), dietary fiber (inulin) promotes intestinal hypoxia and stabilizes HIF-1α in intestinal epithelial cells through microbiota-dependent mechanisms [5]. HIF-1α then modulates ISC function through metabolic reprogramming, influencing epithelial renewal and barrier function – processes essential for maintaining intestinal homeostasis and mediating paracrine signaling within the crypt niche.
Table 1: HIF-1α-Mediated Paracrine Factors in Stem Cells
| Stem Cell Type | Key Paracrine Factors Regulated by HIF-1α | Functional Outcomes | Experimental Models |
|---|---|---|---|
| SHED [3] | VEGF, PDK1, HK2, GLUT1 | Enhanced endothelial cell proliferation and migration; Improved post-implantation cell survival; Angio-/vasculogenesis | In vitro hypoxia chamber (1% O₂); In vivo Matrigel plug assay in SCID mice |
| Neural Stem Cells [4] | sEVs containing cytokines, genetic material | Spinal cord injury repair; Axonal regeneration; Anti-inflammatory effects | Complete transection and contusion SCI mouse models; Hypoxic preconditioning (1-2% O₂) |
| Intestinal Stem Cells [5] | Metabolic enzymes; Antimicrobial peptides | Epithelial proliferation and differentiation; Barrier maintenance; Microbiome regulation | Inulin-fed mice; Intestinal organoids; Conditional knockout mice (HIF-1αΔIEC) |
| Embryonic Stem Cells [6] | Pluripotency factors; Metabolic enzymes | Maintenance of pluripotency; Metabolic adaptation during hypoxia | Mouse ESCs under acute (4h) and stable (24h) hypoxia; ChIP-Seq analysis |
Research Methodologies: Investigating HIF-1α in Stem Cell Hypoxic Response
Modeling Hypoxic Environments and HIF-1α Manipulation
Controlled Hypoxia Systems: Physiologically relevant hypoxia (0.5%-5% O₂) can be established using specialized hypoxic workstations (e.g., SCI-tiveN hypoxic workstation) that maintain precise oxygen, carbon dioxide, and temperature levels [7]. For HIF-1α stabilization studies, researchers typically expose stem cells to 1% O₂ for 24-48 hours, verifying induction via Western blotting [7] [3].
Chemical Hypoxia Mimetics: Cobalt chloride (CoCl₂, typically 100-200 μM) and dimethyloxalylglycine (DMOG) chemically stabilize HIF-1α by inhibiting PHD activity [7]. While useful, these mimetics may not fully recapitulate the transcriptomic response to physiological hypoxia.
Genetic Manipulation of HIF-1α:
- Stable Knockdown: Lentiviral or retroviral delivery of shRNA/siRNA targeting HIF-1α provides sustained suppression [3] [4]. In SHED, HIF-1α siRNA (Thermo Scientific, #4390824) transfection using Lipofectamine 3000 achieved efficient knockdown [3].
- Inducible Expression Systems: Destabilizing domain technology enables controlled HIF-1α stabilization. Fusion proteins of HIF-1α with a destabilizing domain (e.g., YFP-DD) remain unstable until exposure to stabilizing ligands like trimethoprim (TMP, 10 μM) [7].
- Conditional Knockout Models: Cre-loxP systems (e.g., Villin-cre or Lgr5-CreERT2 crossed with HIF-1αfl/fl mice) enable cell-type-specific HIF-1α deletion in intestinal stem cells or other populations [5].
Pharmacological Inhibition: Small molecule inhibitors like YC-1 (10 mM in vitro; in vivo dosing varies) prevent HIF-1α accumulation under hypoxia [3]. These compounds are valuable for acute HIF-1α inhibition and translational studies.
Assessing HIF-1α Activity and Functional Outcomes
Transcriptional Activity Reporter Assays: HIF-1 reporter mice (e.g., ODD-luciferase) enable in vivo monitoring of HIF-1α stabilization. After luciferin injection (50 mg/kg), bioluminescence imaging quantifies HIF-1 activity in real time [5].
Chromatin Immunoprecipitation Sequencing (ChIP-Seq): Reveals genome-wide HIF-1α binding sites and dynamics under different hypoxic conditions. In mESCs, ChIP-Seq identified a "bind–release–bind" pattern during normoxia-hypoxia transition, with associated changes in transcriptional partners [6].
Metabolic and Survival Assays:
- Cell Viability Under Stress: CCK-8 assays assess stem cell survival under hypoxia, oxidative stress (H₂O₂), and low-glucose conditions [3].
- ROS Detection: CM-H2DCFDA (cellular ROS) and MitoSOX Red (mitochondrial ROS) staining quantify oxidative stress levels in HIF-1α-manipulated stem cells [3].
- Metabolic Analysis: Seahorse XF Analyzers measure oxygen consumption rates (OCR) and extracellular acidification rates (ECAR) to evaluate mitochondrial function and glycolytic flux.
Paracrine Function Assessment:
- Endothelial Cell Proliferation/Migration: Conditioned media from hypoxic stem cells tested on HUVECs using trans-well migration and CCK-8 proliferation assays [3].
- EV Isolation and Characterization: Ultracentrifugation or size-exclusion chromatography isolates EVs from stem cell conditioned media, with characterization by nanoparticle tracking analysis, transmission electron microscopy, and Western blotting for CD9, CD63, CD81, and TSG101 [4].
Diagram Title: Experimental Workflow for HIF-1α Research in Stem Cells
In Vivo Transplantation and Functional Analysis
Matrigel Plug Assay: Assesses in vivo survival and angiogenic potential of stem cells. SHED (3×10⁶ cells/plug) mixed with Matrigel injected subcutaneously into SCID mice, plugs retrieved at day 3 and 7 for histology and immunohistochemistry analysis of cell survival (Ki67, TUNEL), vascularization (CD31), and HIF-1α target expression (PDK1, HK2, Glut1) [3].
Disease Models:
- Spinal Cord Injury: Complete transection or contusion models in mice (e.g., T10 level transection) evaluate therapeutic potential of HIF-1α-modified stem cells or their EVs [4].
- Intestinal Injury: Conditional knockout models (HIF-1αΔIEC) combined with injury paradigms (e.g., radiation, chemical injury) assess ISC function and regeneration [5].
Table 2: Key Research Reagents for HIF-1α and Stem Cell Research
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| HIF-1α Inhibitors | YC-1 (Cayman Chemicals) [7] [3] | Prevents HIF-1α accumulation under hypoxia | In vitro: 10 mM; Effects may be concentration-dependent |
| HIF-1α siRNA | Silencer Select Pre-designed (Thermo Scientific) [3] | Genetic knockdown of HIF-1α | Transfect with Lipofectamine 3000; verify efficiency by WB |
| Chemical Hypoxia Mimetics | CoCl₂ (100 μM) [7] | Stabilizes HIF-1α by inhibiting PHDs | May not fully replicate physiological hypoxia transcriptome |
| HIF-1 Reporters | ODD-luciferase mice [5] | In vivo monitoring of HIF-1α stabilization | Requires luciferin injection (50 mg/kg) and imaging systems |
| Antibodies for Detection | Anti-HIF-1α (BD Biosciences #610959) [7] | Western blot, IHC, and IF detection of HIF-1α | Verify specificity with appropriate controls |
| Metabolic Assay Kits | CCK-8 assay kit [3] | Cell viability under stress conditions | More sensitive than MTT; suitable for high-throughput screening |
| EV Isolation Tools | Ultracentrifugation; Size-exclusion chromatography [4] | Isolation of extracellular vesicles from conditioned media | Characterize by NTA, TEM, and Western for tetraspanins |
| Hypoxia Chambers | SCI-tiveN Hypoxic Workstation [7] | Maintains precise low oxygen environments (1% O₂) | Essential for physiological hypoxia studies |
HIF-1α represents a master regulatory node controlling stem cell responses to hypoxia, with profound implications for their paracrine function and therapeutic efficacy. The multifaceted role of HIF-1α in regulating VEGF secretion, EV production, metabolic reprogramming, and ROS homeostasis underscores its centrality in coordinating stem cell adaptation to oxygen deprivation across diverse tissue contexts. From SHED-mediated angiogenesis to NSC-derived EV repair of spinal cord injury and intestinal stem cell maintenance, HIF-1α activation consistently enhances stem cell secretome potency and functional outcomes.
The experimental methodologies outlined – including sophisticated hypoxia modeling, genetic manipulation techniques, and functional assessment protocols – provide researchers with comprehensive tools for investigating HIF-1α in stem cell biology. As research progresses, therapeutic strategies leveraging HIF-1α modulation, whether through preconditioning approaches, pharmacological activation, or engineering of HIF-1α-enhanced stem cells and EVs, hold significant promise for advancing regenerative medicine. The continued elucidation of HIF-1α's role in stem cell paracrine signaling will undoubtedly yield novel insights and therapeutic approaches for tissue repair and regeneration across diverse pathological conditions.
Metabolic reprogramming, specifically the shift from oxidative phosphorylation to glycolysis, is a fundamental adaptive response in human mesenchymal stem cells (MSCs) exposed to hypoxic environments. This transition, primarily orchestrated by the stabilization of hypoxia-inducible factor 1-alpha (HIF-1α), enhances cell survival, proliferative capacity, and the therapeutic efficacy of the stem cell secretome [8] [9]. Under physiological oxygen tension (typically 1-5% O₂), HIF-1α activation redirects cellular metabolism from mitochondrial oxidative phosphorylation towards aerobic glycolysis, optimizing energy production under oxygen constraints [10] [9]. This metabolic shift is not merely a survival tactic but a functionally essential mechanism that augments the paracrine activity of MSCs. It significantly influences the composition of secreted factors, including extracellular vesicles (exosomes), cytokines, and growth factors, which collectively modulate inflammation, promote angiogenesis, and drive tissue repair processes [8] [11]. The following sections detail the molecular mechanisms, quantitative functional outcomes, experimental methodologies, and essential research tools for investigating this critical phenomenon in regenerative medicine.
In regenerative medicine, the preservation of the native cellular microenvironment is paramount for optimizing mesenchymal stem cell (MSC) function post-transplantation [8] [9]. The physiological niches for MSCs, such as bone marrow and adipose tissue, naturally exist under low oxygen tension (approximately 2-7% O₂), a stark contrast to the standard atmospheric oxygen levels (21% O₂, or normoxia) used in conventional cell culture [8]. This discrepancy can impair MSC survival and therapeutic potential. Hypoxic preconditioning—culturing MSCs under reduced oxygen conditions before therapeutic application—has emerged as a powerful strategy to mimic their natural environment and enhance their regenerative capabilities [8] [10] [9]. Central to this adaptation is metabolic reprogramming, a process where cells shift their primary energy production pathway from mitochondrial oxidative phosphorylation, which requires oxygen, to glycolysis, which can occur in its absence. This whitepaper explores the mechanisms and consequences of this metabolic shift, framing it within the broader context of enhancing stem cell paracrine factor production for therapeutic applications.
Molecular Mechanisms of the Metabolic Shift
The metabolic shift from oxidative phosphorylation to glycolysis under hypoxic conditions is a highly regulated process initiated by the stabilization of the transcription factor HIF-1α. Under normoxia, HIF-1α is continuously synthesized and degraded. However, under hypoxia, this degradation is halted, allowing HIF-1α to accumulate, translocate to the nucleus, and dimerize with HIF-1β. This complex then activates the transcription of a suite of genes that orchestrate the metabolic switch [8] [9].
The following diagram illustrates the core signaling pathway and its downstream metabolic consequences:
Figure 1: HIF-1α-Mediated Metabolic Shift in Hypoxic MSCs. This diagram outlines the central role of HIF-1α stabilization under hypoxic stress in driving a metabolic reprogramming from oxidative phosphorylation (OxPhos) towards glycolysis, resulting in altered paracrine factor secretion.
Key Molecular Events
- HIF-1α Stabilization: The pivotal trigger. Under oxygen concentrations of ≤5%, HIF-1α is stabilized and activates transcriptional programs essential for hypoxic adaptation [10] [9].
- Glycolytic Enzyme Upregulation: HIF-1α directly promotes the expression of key glycolytic enzymes and glucose transporters (e.g., GLUT1), increasing the cell's capacity for glucose uptake and glycolytic flux [9].
- Mitochondrial Modulation: HIF-1α activation suppresses mitochondrial oxidative phosphorylation by inducing factors like pyruvate dehydrogenase kinase 1 (PDK1). PDK1 phosphorylates and inhibits pyruvate dehydrogenase, preventing the conversion of pyruvate to acetyl-CoA for entry into the tricarboxylic acid (TCA) cycle, thereby redirecting pyruvate to lactate [8] [9].
- Paracrine Secretion Enhancement: This metabolic rewiring enhances the production and function of the MSC secretome, including exosomes and other extracellular vesicles loaded with bioactive molecules (e.g., VEGF, SDF-1α, miR-126) that mediate tissue repair [8] [11].
Quantitative Functional Outcomes
The hypoxic-induced metabolic shift leads to measurable changes in MSC biology and secretome composition. The table below summarizes key quantitative findings from investigations into Wharton's Jelly-derived MSCs (WJ-MSCs) and other models.
Table 1: Quantitative Effects of Hypoxic Preconditioning on MSCs
| Parameter | Experimental Finding | Oxygen Concentration & Duration | Implication |
|---|---|---|---|
| Oxidative Stress in CM | Significantly higher Total Oxidant Status (TOS) & Oxidative Stress Index (OSI) in 1% O₂ vs. 5% O₂ after 72h [10]. | 1% vs. 5% O₂; 48h & 72h | Graded hypoxia distinctly modulates redox state of the secretome. |
| Nanoparticle Stability | CM from 5% O₂ cultures showed more stable nanoparticle size profiles and more negative zeta potential, indicating greater colloidal stability [10]. | 1% vs. 5% O₂; 48h & 72h | 5% O₂ may be optimal for producing stable extracellular vesicles. |
| HIF-1α Expression | Markedly increased HIF-1α expression under 1% O₂, confirming hypoxia-induced cellular adaptation [10]. | 1% O₂ | Confirms activation of the primary molecular pathway. |
| Therapeutic Efficacy | Hypoxia-preconditioned MSCs showed superior outcomes in preclinical models (e.g., improved cardiac function, reduced infarct size) [8] [9]. | 1-5% O₂; <48h | Enhanced paracrine activity translates to improved regenerative potential. |
| Extreme Hypoxia Impact | Severe hypoxia (<1% O₂) induces MSC senescence and apoptosis, reducing therapeutic potential [8]. | <1% O₂ | Highlights the need for precise oxygen control in preconditioning protocols. |
Detailed Experimental Protocols
To investigate metabolic reprogramming in MSCs, robust and reproducible experimental protocols are essential. The following section outlines a standard methodology for hypoxic preconditioning and subsequent analysis of its effects on the MSC secretome.
Protocol 1: Hypoxic Preconditioning and Conditioned Media (CM) Collection
This protocol is adapted from studies on Wharton's Jelly-derived MSCs (WJ-MSCs) [10].
Objective: To precondition MSCs under defined hypoxic conditions and collect their conditioned media for analysis.
Materials:
- Cell Source: Human Wharton's Jelly-derived MSCs (e.g., PCS-500-010).
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 1% penicillin-streptomycin, and 1% L-glutamine.
- Hypoxia Chamber: A controlled hypoxia chamber (e.g., from Stemcell Technologies Inc.) capable of maintaining precise O₂ levels (1% and 5%), CO₂ (5%), temperature (37°C), and humidity.
Methodology:
- Cell Expansion: Culture WJ-MSCs under standard normoxic conditions (21% O₂, 5% CO₂, 37°C) until they reach 70-80% confluency. Use cells between passages 2 and 4 for experiments.
- Seeding for Preconditioning: Seed MSCs at a standardized density in culture plates.
- Hypoxic Exposure: Place the seeded plates into the pre-equilibrated hypoxia chamber. Maintain cells under the target oxygen condition (e.g., 1% or 5% O₂) for the desired duration (e.g., 48 or 72 hours).
- Serum Starvation (Optional): To reduce FBS-derived protein contamination in the secretome, replace the growth medium with serum-free medium for the final 48 hours of hypoxic exposure [10].
- CM Collection: After the preconditioning period, collect the culture supernatant (now termed Conditioned Media, or CM).
- CM Processing: Centrifuge the CM at a low speed (e.g., 2,000 × g for 15 min at 4°C) to remove cellular debris. Aliquot the supernatant and store at -80°C for subsequent analysis (e.g., oxidative stress assays, nanoparticle tracking, proteomics).
The workflow for this protocol is visualized below:
Figure 2: Workflow for Hypoxic Preconditioning and CM Collection.
Protocol 2: Analysis of Metabolic and Secretome Parameters
Following CM collection, various analytical techniques can be employed to quantify the effects of hypoxic preconditioning.
Objective: To characterize the metabolic state of MSCs and the physicochemical properties of the derived conditioned media.
Methodology:
- Cell Lysate Preparation:
- Wash preconditioned cells with ice-cold PBS.
- Lyse cells on ice using RIPA buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1% Triton X-100, 0.5% Sodium deoxycholate, 0.1% SDS) for 30 minutes.
- Centrifuge lysate at 2,000 × g for 15 min at 4°C.
- Collect supernatant (soluble protein fraction) and store at -80°C for biochemical analyses [10].
- Oxidative Stress Assays on CM:
- Use commercial kits to assess the Total Oxidant Status (TOS) and Total Antioxidant Status (TAS) of the CM.
- Calculate the Oxidative Stress Index (OSI) as an indicator of redox balance: OSI = (TOS / TAS) × 100 [10].
- Nanoparticle Tracking Analysis:
- Analyze the CM using Dynamic Light Scattering (DLS) to determine the size (hydrodynamic diameter) and zeta potential (surface charge) of secreted nanoparticles, including extracellular vesicles [10].
- HIF-1α Quantification:
- Determine HIF-1α protein levels in cell lysates using a quantitative Enzyme-Linked Immunosorbent Assay (ELISA) to confirm hypoxic activation [10].
- Metabolic Activity Assay:
- Assess cell viability and metabolic activity using an MTT assay, which measures the reduction of a tetrazolium salt by mitochondrial dehydrogenases, providing an indirect measure of metabolic function [10].
The Scientist's Toolkit: Research Reagent Solutions
Successful investigation into metabolic reprogramming requires a suite of reliable research tools and reagents. The following table catalogues essential materials and their functions.
Table 2: Essential Research Reagents and Tools for Investigating Metabolic Reprogramming
| Reagent / Tool | Function / Application | Example / Specification |
|---|---|---|
| Wharton's Jelly MSCs | Primary cell model for studying human MSC biology and therapy. | Commercially sourced (e.g., PCS-500-010); passages 2-4 [10]. |
| Controlled Hypoxia Chamber | Provides a stable, physiologically relevant low-oxygen environment for cell preconditioning. | Chamber with continuous O₂/CO₂/temperature monitoring (e.g., Stemcell Technologies Inc.) [10]. |
| DMEM with Supplements | Standard culture medium for MSC expansion and maintenance. | DMEM + 10% FBS + 1% Penicillin-Streptomycin + 1% L-Glutamine [10]. |
| RIPA Lysis Buffer | For extracting total soluble proteins from cells for downstream biochemical analysis (e.g., ELISA, Western Blot). | Contains Tris-HCl, NaCl, Triton X-100, Sodium Deoxycholate, SDS [10]. |
| Oxidative Stress Assay Kits | For quantifying the redox state of conditioned media (CM). | Kits for Total Oxidant Status (TOS) and Total Antioxidant Status (TAS) [10]. |
| Dynamic Light Scattering (DLS) | Instrumentation for characterizing the size and stability of nanoparticles (e.g., extracellular vesicles) in CM. | Measures hydrodynamic diameter and zeta potential [10]. |
| HIF-1α ELISA Kit | For specific, quantitative measurement of stabilized HIF-1α protein levels in cell lysates. | Commercial sandwich ELISA kit. |
| MTT Assay Kit | A colorimetric assay for assessing cell metabolic activity and viability. | Measures reduction of MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to formazan [10]. |
In regenerative medicine, the therapeutic potential of stem cells, particularly Mesenchymal Stem Cells (MSCs), is largely mediated by their paracrine activity—the secretion of bioactive molecules that modulate the local cellular environment, promote tissue repair, and regulate immune responses [12] [13]. The composition and potency of this secretome are not static but are dynamically regulated by microenvironmental conditions. Among these, hypoxia (low oxygen tension) is a critical physiological and pathological stimulus that profoundly reshapes the paracrine output of stem cells [14] [8].
Hypoxia acts as a powerful instructor, mimicking the conditions of damaged or ischemic tissues and priming stem cells for enhanced regenerative capacity. This response is largely orchestrated by the Hypoxia-Inducible Factor 1-alpha (HIF-1α), a master transcriptional regulator that is stabilized under low oxygen conditions [15] [8]. Upon activation, HIF-1α translocates to the nucleus and binds to Hypoxia-Response Elements (HREs) in the promoter regions of numerous target genes, including key paracrine factors [8]. This molecular cascade enhances the production of factors crucial for angiogenesis, cell survival, homing, and inflammation control [14] [16].
This review provides an in-depth technical analysis of five core paracrine factors—VEGF, FGF-2, IGF-1, Angiogenin, and SDF-1α—whose expression is significantly upregulated by hypoxic preconditioning in stem cells. It details their functions, quantitative upregulation, underlying molecular mechanisms, and standard experimental protocols for their study, serving as a comprehensive resource for researchers and drug development professionals in the field.
Factor Profiles and Quantitative Upregulation
The following table summarizes the core functions and documented quantitative upregulation of these key factors in response to hypoxic conditioning of stem cells.
Table 1: Key Hypoxia-Upregulated Paracrine Factors: Functions and Quantitative Expression
| Factor | Primary Functions | Reported Upregulation | Cell Model | Hypoxic Conditions |
|---|---|---|---|---|
| VEGF-A (Vascular Endothelial Growth Factor A) | Promotes angiogenesis, endothelial cell proliferation, survival, and permeability [15] [16]. | Significant increase at protein and transcriptional level [16]. | Human Adipose-Derived Stem Cells (ASCs) | <0.1% O₂ for 24 hours |
| FGF-2 (Fibroblast Growth Factor-2, bFGF) | Stimulates proliferation of MSCs and endothelial cells, supports tissue repair and angiogenesis [8]. | Upregulated transcriptional expression [16]. | Human Adipose-Derived Stem Cells (ASCs) | <0.1% O₂ for 24 hours |
| IGF-1 (Insulin-like Growth Factor-1) | Enhances cell survival and proliferation, inhibits apoptosis, promotes tissue regeneration [16]. | Upregulated transcriptional expression [16]. | Human Adipose-Derived Stem Cells (ASCs) | <0.1% O₂ for 24 hours |
| Angiogenin (ANG) | Induces blood vessel formation, has ribonucleolytic activity, promotes cell adhesion and migration [16]. | Significant increase at protein and transcriptional level [16]. | Human Adipose-Derived Stem Cells (ASCs) | <0.1% O₂ for 24 hours |
| SDF-1α (Stromal Cell-Derived Factor-1α, CXCL12) | Critical for stem cell homing and migration via CXCR4 receptor interaction; supports angiogenesis [8]. | Upregulated transcriptional expression [16]. | Human Adipose-Derived Stem Cells (ASCs) | <0.1% O₂ for 24 hours |
Molecular Mechanisms and Experimental Analysis
Core Hypoxia Signaling Pathway
The cellular response to hypoxia is primarily mediated by the HIF-1α pathway. Under normoxic conditions, HIF-1α is continuously synthesized but rapidly degraded by the proteasome following prolyl hydroxylation and von Hippel-Lindau (pVHL) protein binding. In hypoxia, this degradation is halted, allowing HIF-1α to accumulate, dimerize with HIF-1β, and activate the transcription of key paracrine factors.
Standard Experimental Protocol for Hypoxic Preconditioning and Analysis
A typical workflow for investigating hypoxia-induced paracrine factor secretion involves cell culture under controlled oxygen tension, followed by quantitative analysis of the resulting secretome.
Table 2: Essential Research Reagents for Hypoxic Paracrine Factor Studies
| Reagent / Material | Typical Specification / Example | Primary Function in Protocol |
|---|---|---|
| Stem Cells | Human Adipose-Derived Stem Cells (ASCs), Bone Marrow MSCs (BM-MSCs) | Primary cellular model for hypoxic preconditioning and secretome analysis [16]. |
| Tri-Gas Incubator | HERAcell 150 or equivalent | Provides precise, controlled low-oxygen environment (e.g., 1% O₂) for cell culture [16]. |
| Hypoxia Chamber | GENbox Jar (bioMérieux) or equivalent | Creates severe hypoxia (<0.1% O₂) within a standard incubator [16]. |
| Serum-Free Medium | DMEM-low glucose, without FBS | Used during hypoxic exposure to condition medium, preventing interference from serum proteins [16]. |
| Centrifugal Filters | Amicon Ultra-15, 3 kDa MWCO | Concentrates conditioned medium to enable detection of low-abundance factors [16]. |
| TaqMan Probes | Assay-On-Demand for VEGF-A, FGF-2, ANG, etc. | Enables precise quantification of gene expression changes via qRT-PCR [16]. |
| ELISA Kits | Quantikine ELISA for VEGF, Angiogenin, etc. | Gold-standard method for absolute quantification of specific secreted proteins in conditioned medium [16]. |
Detailed Methodological Protocols
Hypoxic Preconditioning and Conditioned Medium Collection
This protocol is adapted from established methodologies for conditioning human Adipose-Derived Stem Cells (ASCs) [16].
- Cell Culture: Culture ASCs (passages 3-6) in complete growth medium (e.g., DMEM-low glucose with 10% FBS) until 80% confluent.
- Serum Starvation: Replace complete medium with serum-free DMEM to prevent interference from serum proteins in subsequent analyses.
- Hypoxic Exposure: Place culture flasks into a sealed hypoxia chamber (e.g., GENbox Jar) that is then incubated at 37°C to achieve severe hypoxia (<0.1% O₂). Alternatively, use a tri-gas incubator set to 1% O₂, 5% CO₂. A control group should be maintained under standard normoxic conditions (20% O₂).
- Incubation Period: Expose cells to hypoxia for a defined period, typically 24 hours. Exposure times beyond 48 hours may induce senescence and reduce efficacy [8].
- Collection: Collect the conditioned medium (CM) and centrifuge at 875g for 10 minutes to remove cell debris.
- Concentration: Filter the supernatant through a 0.2-μm filter and concentrate using centrifugal filter units (e.g., Amicon Ultra-15 with 3 kDa molecular weight cut-off) by a factor of 50x. The concentrated CM can be aliquoted and stored at -80°C.
Quantitative Gene Expression Analysis (qRT-PCR)
This protocol details the steps to quantify the transcriptional upregulation of target factors [16].
- RNA Extraction: Following hypoxic exposure, lyse cells directly in the culture flask using TriReagent or a similar reagent to extract total RNA. Precipitate RNA using chloroform and isopropanol.
- cDNA Synthesis: Synthesize complementary DNA (cDNA) from 1 μg of total RNA using a high-capacity cDNA reverse transcription kit with random primers.
- Quantitative PCR: Perform real-time PCR using TaqMan probe-based chemistry. Use Assay-On-Demand primers and probes for target genes (VEGF-A: Hs00900054m1; FGF-2: Hs00266645m1; ANG: Hs02379000s1; SDF-1: Hs00930455m1). Amplify 18S ribosomal RNA (Hs99999901_s1) as an endogenous control.
- Data Analysis: Run reactions in duplicate. Calculate the relative fold change in gene expression in hypoxic samples compared to normoxic controls using the 2^(-ΔΔCt) method.
Protein Quantification (ELISA)
This protocol describes the quantification of secreted proteins in the conditioned medium [16].
- Standard Preparation: Reconstitute the standard provided in the commercial ELISA kit (e.g., Quantikine for VEGF-A) and prepare a serial dilution series.
- Sample Preparation: Use the concentrated conditioned medium. A 50-fold concentration factor is often necessary to detect secreted factors above the assay's limit of detection.
- Assay Procedure: Follow the manufacturer's instructions. Briefly, add standards and samples to the antibody-coated wells. After incubation and washing, add a detection antibody conjugated to an enzyme (e.g., horseradish peroxidase).
- Detection and Quantification: Develop the assay with a substrate solution that produces a colorimetric signal. Stop the reaction and measure the optical density at the specified wavelength (e.g., 450 nm with a correction at 550 nm). Interpolate the protein concentration of samples from the standard curve.
The strategic application of hypoxic preconditioning to stem cells represents a powerful, non-genetic approach to enhance their therapeutic secretome. The coordinated upregulation of VEGF, FGF-2, IGF-1, Angiogenin, and SDF-1α, driven by the HIF-1α signaling axis, creates a potent regenerative cocktail that promotes angiogenesis, cell survival, and tissue repair. The standardized experimental protocols outlined here provide a robust framework for researchers to quantify these effects and further explore the potential of hypoxia-primed MSC therapies. As the field progresses, optimizing preconditioning parameters and leveraging the "hypoxia-lactate-lactylation" axis [14] will be crucial for developing more effective, consistent, and clinically relevant cell-based or cell-free regenerative treatments.
Macrophages, central players of the innate immune system, exhibit remarkable functional plasticity in response to environmental signals. Their polarization state exists on a spectrum, predominantly classified into the pro-inflammatory, classically activated M1 phenotype and the anti-inflammatory, alternatively activated M2 phenotype [17]. Within the context of stem cell research, particularly under hypoxic stress, the paracrine factors secreted by stem cells are potent modulators of this polarization process. Hypoxic stress, a common feature in pathological conditions and stem cell niches, significantly alters the secretory profile of mesenchymal stem cells (MSCs), enhancing their immunomodulatory capacity [18] [19]. This whitepaper provides an in-depth technical guide on the mechanisms and methodologies for driving the M1-to-M2 shift, framed within contemporary research on hypoxic preconditioning of stem cells. Understanding and controlling this shift is critical for developing novel therapeutic strategies for inflammatory diseases, wound healing, and regenerative medicine.
Biology of M1 and M2 Macrophage Polarization
Stimuli and Signaling Pathways
The polarization of macrophages is directed by specific cytokines, pathogen-associated molecular patterns (PAMPs), and damage-associated molecular patterns (DAMPs) that activate distinct signaling cascades and transcriptional programs.
- M1 Polarization (Classical Activation): Triggered by interferon-gamma (IFN-γ) alone or in synergy with microbial products like lipopolysaccharide (LPS) [17]. IFN-γ binding to its receptor activates the JAK-STAT1 signaling pathway. Concurrently, LPS engagement of TLR4 activates downstream signaling primarily through the MyD88-dependent pathway, leading to the activation of the transcription factor NF-κB and the production of pro-inflammatory cytokines such as TNF, IL-1β, and IL-12 [17].
- M2 Polarization (Alternative Activation): Primarily induced by the Th2 cytokines IL-4 and IL-13 [17]. These cytokines bind to receptors that activate the JAK-STAT6 signaling pathway. The transcription factors STAT6, IRF4, and PPARγ are instrumental in driving the expression of characteristic M2 markers. Other stimuli, including IL-10 and glucocorticoids, can also promote an M2-like, immunoregulatory phenotype through STAT3 activation and glucocorticoid receptor signaling, respectively [17].
Table 1: Key Inducers, Signaling Pathways, and Functional Outputs of Macrophage Polarization
| Polarization State | Primary Inducers | Key Signaling Pathways | Characteristic Markers | Principal Functions |
|---|---|---|---|---|
| M1 | IFN-γ, LPS, TNF [17] | JAK-STAT1, TLR-MyD88-NF-κB [17] | CD86, HLA-DR, iNOS, IL-1β, TNF-α [20] [17] | Pro-inflammatory response, pathogen killing, tissue destruction [17] |
| M2 | IL-4, IL-13, IL-10, Glucocorticoids [17] | JAK-STAT6, STAT3, Glucocorticoid Receptor [17] | CD206, CD163, Arg1, CCL17, IL-10 [20] [17] | Anti-inflammatory response, tissue repair, angiogenesis, immunoregulation [17] |
The Impact of Hypoxia on Macrophage Polarization
Hypoxia is a potent environmental modifier of macrophage function. Research indicates that hypoxic conditions can directly promote macrophage polarization towards the M2 phenotype [20]. A study exposing human macrophages to 1% oxygen found that hypoxia favored the M2 phenotype and modified the inflammatory microenvironment by decreasing pro-inflammatory cytokine release [20]. This process was identified to be regulated by p38 MAPK signaling, rather than HIF-1α, in this specific context [20]. This direct effect of hypoxia on macrophages is a crucial consideration when studying the tumor microenvironment or chronic inflammatory conditions where low oxygen tension is prevalent.
Stem Cell Paracrine Factors as Polarization Modulators
The Role of Hypoxic Preconditioning
The therapeutic efficacy of mesenchymal stem cells (MSCs) is largely attributed to their paracrine activity. Hypoxic preconditioning of MSCs—culturing them under low oxygen tension (typically 1-5% O₂)—significantly enhances their secretome, particularly the yield and bioactivity of extracellular vesicles (EVs) [18] [19]. This is physiologically relevant as MSCs naturally reside in hypoxic niches in the body, such as bone marrow and adipose tissue [19]. Hypoxia increases the secretion of EVs and enriches them with specific miRNAs and proteins that modulate immune responses and promote tissue repair [18] [19].
Mechanisms of MSC-Induced M2 Polarization
Hypoxia-induced MSCs and their derived EVs (hy-EVs) drive the M1-to-M2 shift through several interconnected mechanisms:
- Modulation of Macrophage Signaling: hy-EVs from human umbilical cord MSCs (HUCMSCs) have been shown to promote the expression of CD206 (an M2 marker) while decreasing the expression of CD86 (an M1 marker) [19]. This shift is mediated by the transfer of bioactive molecules.
- Delivery of Regulatory miRNAs: hy-EVs are enriched with specific microRNAs. For instance, miR-146a transferred from MSCs to macrophages can promote M2 polarization [18]. Hypoxic conditions can also upregulate miR-126 in MSC-EVs, further enhancing tissue repair capabilities [18].
- Activation of HIF-1α in Target Cells: hy-EVs derived from HUCMSCs can enhance the expression of HIF-1α and its downstream target VEGFA in human umbilical vein endothelial cells (HUVECs) [19]. While this study focused on angiogenesis, the HIF-1α pathway is also intimately involved in immune cell metabolism and function.
- Attenuation of Oxidative Stress: hy-EVs can inhibit the production of reactive oxygen species (ROS) in target cells, reducing oxidative stress and creating an environment more conducive to the M2 anti-inflammatory phenotype [19].
Table 2: Effects of Hypoxia-Preconditioned MSC Secretome on Macrophages and Microenvironment
| Secretome Component | Effect on Macrophages | Impact on Microenvironment | Key Molecular Players |
|---|---|---|---|
| Hypoxia-Induced Extracellular Vesicles (hy-EVs) | Promotes shift from M1 to M2 phenotype [19] | Enhances angiogenesis, reduces oxidative stress [19] | miR-146a, HIF-1α, VEGFA, CD206, CD86 [18] [19] |
| Cytokines & Growth Factors | Modulates activation state and function [18] | Regulates inflammation, promotes tissue repair [18] | IL-10, TGF-β, VEGF [18] |
| Exosomes (from miR-486-modified DPSCs) | Enhances anti-inflammatory regulation [18] | Particularly effective in high-altitude pulmonary edema models [18] | miR-486 [18] |
Experimental Protocols for Investigating Polarization
In Vitro Model of Macrophage Polarization
This protocol outlines a standard method for generating and polarizing human macrophages from a monocytic cell line.
Protocol: Generating and Polarizing Human Macrophages
Monocyte-to-Macrophage Differentiation:
- Use the human myeloid leukemia THP-1 cell line.
- Culture THP-1 cells in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin.
- To differentiate monocytes into macrophages (M0 phenotype), treat the cells with 10 ng/mL Phorbol 12-myristate 13-acetate (PMA) for 24 hours [20].
M1 Polarization:
- Following differentiation, polarize M0 macrophages towards the M1 phenotype by culturing them in fresh medium containing 100 ng/mL Lipopolysaccharide (LPS) and 20 ng/mL Interferon-γ (IFN-γ) for 48 hours [20].
M2 Polarization:
- Polarize M0 macrophages towards the M2 phenotype by culturing them in fresh medium containing 20 ng/mL Interleukin-4 (IL-4) for 48 hours [20].
Hypoxic Stimulation:
Protocol for Isolating and Applying Hypoxia-Induced EVs
This protocol describes the production of hy-EVs from HUCMSCs and their application to macrophage cultures.
Protocol: Production and Application of hy-EVs
Cell Culture and Hypoxic Preconditioning:
- Isolate and culture HUCMSCs. Use early passage cells (e.g., 5th generation) [19].
- At ~80% confluence, replace the medium with serum-free medium.
- For hy-EV production, culture HUCMSCs in a hypoxic incubator with 3% O₂, 5% CO₂, and 92% N₂ for 48 hours. For normoxia-EV (n-EV) controls, use standard conditions (21% O₂) [19].
EV Isolation and Characterization:
- Collect the conditioned medium and subject it to differential ultracentrifugation.
- First, centrifuge at 300 × g for 10 min, then at 2,000 × g for 20 min to remove cells and debris.
- Filter the supernatant through a 0.22 µm filter.
- Perform ultracentrifugation at 120,000 × g for 70 min at 4°C. Repeat this step twice with PBS washing [19].
- Resuspend the final EV pellet in PBS.
- Characterize EVs using:
Treatment of Macrophages:
- Differentiate and polarize macrophages as described in Section 4.1.
- To test the effect of hy-EVs, add a quantified amount of hy-EVs (e.g., 10-100 µg/mL) to the macrophage culture medium during or after polarization.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Macrophage Polarization and Analysis
| Reagent / Tool | Function / Specificity | Example Application |
|---|---|---|
| Phorbol 12-myristate 13-acetate (PMA) | Differentiates monocytic cell lines into macrophages [20] | Generating M0 macrophages from THP-1 cells [20] |
| Lipopolysaccharide (LPS) & Interferon-γ (IFN-γ) | Potent inducers of classical M1 macrophage activation [20] [17] | Polarizing M0 macrophages to the M1 phenotype in vitro [20] |
| Interleukin-4 (IL-4) | Primary inducer of alternative M2 macrophage activation [20] [17] | Polarizing M0 macrophages to the M2a phenotype in vitro [20] |
| SB203580 | Inhibitor of p38 MAPK signaling [20] | Investigating the role of p38 in hypoxia-mediated polarization [20] |
| Anti-CD86 (PE-conjugated) | Surface marker for M1 macrophage identification [20] [19] | Flow cytometry analysis of M1 macrophage populations [20] |
| Anti-CD206 (PE-conjugated) | Surface marker for M2 macrophage identification [20] [19] | Flow cytometry analysis of M2 macrophage populations [20] |
| Hypoxia Inducor | Creates a controlled, low-oxygen cell culture environment [19] | Preconditioning MSCs to generate hy-EVs; studying direct hypoxia effects on macrophages [20] [19] |
Signaling Pathway Visualizations
Diagram 1: Signaling pathways in macrophage polarization under hypoxia.
Diagram 2: Experimental workflow for hy-EV production and M2 polarization assay.
The paradigm of stem cell-mediated tissue repair is shifting from a direct cell-replacement model to a paracrine-focused mechanism, where secreted factors orchestrate regenerative processes. Within this framework, hypoxic stress has been identified as a powerful physiological stimulus that profoundly enhances the therapeutic efficacy of the stem cell secretome. This whitepaper details how hypoxia preconditioning transforms the molecular cargo of extracellular vesicles (EVs) and exosomes, turning them into potent vectors of intercellular communication that influence angiogenesis, immunomodulation, and cell survival. The targeted application of these hypoxia-induced EVs presents a novel, cell-free therapeutic strategy with significant implications for regenerative medicine and drug development, offering solutions to challenges in complex disease environments such as chronic wounds and cancer.
The traditional view of stem cell function, centered on differentiation and engraftment, has been substantially augmented by the understanding of their potent paracrine activity [21]. Mesenchymal stem cells (MSCs), in particular, secrete a complex mixture of cytokines, growth factors, and signaling molecules that can induce cytoprotection, promote neovascularization, and modulate immune responses [21]. Crucially, the composition and potency of this secretome are not static; they are dynamically regulated by the cellular microenvironment.
Hypoxia, often perceived as a pathological state, is in fact a key physiological component of stem cell niches. The partial pressure of oxygen in the bone marrow is typically 1–9%, in adipose tissue 5–9%, and in the umbilical cord 1–6% [19]. When MSCs are cultured under hypoxic conditions in vitro, it mimics their native environment, enhancing their survival and activating adaptive responses primarily mediated by the master regulator Hypoxia-Inducible Factor (HIF-1α). This activation leads to a significant shift in the cells' secretory profile, most notably altering the biogenesis, yield, and bioactivity of EVs and exosomes [19] [22]. These hypoxia-induced EVs (hy-EVs) are emerging as superior therapeutic agents compared to those derived under normoxic conditions (n-EVs), offering a promising avenue for treating conditions with impaired healing and complex pathophysiologies.
Molecular Composition and Cargo Loading in Hypoxia-Induced EVs
Hypoxia preconditioning fundamentally reprogrammes the molecular payload of EVs, enriching them with specific proteins, lipids, and nucleic acids that mediate their enhanced therapeutic effects. The table below summarizes the key alterations in EV cargo induced by hypoxia.
Table 1: Key Cargo Components of Hypoxia-Induced Extracellular Vesicles
| Cargo Type | Specific Components | Functional Role | Experimental Evidence |
|---|---|---|---|
| Proteins | HIF-1α, TGF-β1, VEGF | Angiogenesis activation, M2 macrophage polarization, cytoprotection | [19] [23] [24] |
| MicroRNAs | miR-21-5p, miR-146a, miR-144-3p | Suppression of pro-apoptotic genes (PTEN, PDCD4), promotion of M2 polarization | [22] [23] |
| Lipids | Glycerolipids, Sphingolipids, Sterol lipids | Structural integrity, recipient cell modulation, immune regulation | [25] |
| Other Factors | Matrix Metalloproteinases (MMPs), Collagen | Tissue remodeling, extracellular matrix synthesis | [24] |
The biogenesis of EVs is a regulated process. Exosomes, for instance, are formed within the cell through the endocytic pathway, where early endosomes mature into multivesicular bodies (MVBs) that contain intraluminal vesicles. These MVBs can then fuse with the plasma membrane to release exosomes into the extracellular space [25]. Hypoxia influences this process, often increasing the secretion of EVs and altering their size distribution [24]. The molecular cargo is loaded into EVs during this biogenesis, a process that can be influenced by hypoxia-driven changes in gene expression, such as the upregulation of miR-21-5p, which is selectively packaged into EVs from hypoxia-preconditioned MSCs [22].
Detailed Experimental Protocols for hy-EV Research
To ensure reproducibility and support the translation of hy-EV research, this section outlines standardized protocols for key experimental procedures.
Hypoxic Preconditioning and EV Isolation
Cell Culture and Hypoxic Induction:
- Isolate and culture primary human MSCs (e.g., from umbilical cord [19] or bone marrow [22]) until passage 5.
- At approximately 80-85% confluency, replace the medium with a serum-free formulation.
- For the hypoxic group (hy-EVs), transfer cells to a modular hypoxia incubator set to 1-3% O₂, 5% CO₂, and balance N₂ for 24-48 hours [19] [22]. Precise control is achieved using a modular oxygen monitor [19].
- For the control group (n-EVs), maintain cells under standard normoxic conditions (21% O₂).
EV Isolation via Ultracentrifugation:
- Collect conditioned medium and subject it to sequential centrifugation to remove cells and debris:
- Filter the supernatant through a 0.22 µm membrane to remove larger particles.
- Perform ultracentrifugation of the filtrate at 100,000 × g for 70 minutes at 4°C [19].
- Wash the EV pellet by resuspending in a large volume of phosphate-buffered saline (PBS) and repeat the ultracentrifugation step.
- Resuspend the final EV pellet in 100-200 µL of PBS and aliquot for immediate use or storage at -80°C.
EV Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the particle size distribution and concentration. hy-EVs typically show a mode size of 100-110 nm [19] [23].
- Transmission Electron Microscopy (TEM): Confirm the cup-shaped or spherical morphology of the vesicles [19] [24].
- Western Blot Analysis: Verify the presence of positive EV markers (e.g., CD9, CD63, CD81, Alix, Tsg101) and the absence of negative markers (e.g., calnexin) [19] [23].
- Protein Quantification: Use the Bradford assay to standardize EV preparations by protein content for functional experiments [24].
Functional Assays for hy-EV Efficacy
In Vitro Angiogenesis Assay (Tube Formation):
- Culture human umbilical vein endothelial cells (HUVECs) in high-glucose medium.
- Seed HUVECs on a layer of growth factor-reduced Matrigel.
- Treat cells with hy-EVs, n-EVs, or PBS control.
- Incubate for 4-18 hours and image the cellular networks.
- Quantify the total tube length, number of branches, and number of master junctions using image analysis software to demonstrate the pro-angiogenic capacity of hy-EVs [19] [23].
Macrophage Polarization Assay:
- Differentiate human primary monocytes into macrophages using phorbol ester.
- Induce M1 polarization with lipopolysaccharide (LPS) for 48 hours.
- Treat macrophages with hy-EVs or controls.
- Analyze polarization by flow cytometry, measuring the expression of M2 markers (e.g., CD206) versus M1 markers (e.g., CD86).
- Confirm functional polarization by ELISA for associated cytokines (e.g., IL-10 for M2) [19] [22].
In Vivo Diabetic Wound Healing Model:
- Establish a type I diabetic mouse model (e.g., using streptozotocin).
- Create full-thickness excisional wounds on the dorsum.
- Topically apply hy-EVs, n-EVs, or vehicle control to the wound bed via injection or a hydrogel delivery system at multiple time points post-wounding.
- Monitor wound closure rates over time through digital planimetry.
- Harvest wound tissue at endpoint for histological analysis (e.g., H&E staining for re-epithelialization, Masson's trichrome for collagen deposition, immunohistochemistry for CD31 to assess angiogenesis) [19].
Signaling Pathways and Mechanisms of Action
The therapeutic benefits of hy-EVs are mediated through the activation of specific signaling pathways in recipient cells. The following diagrams, generated using Graphviz DOT language, illustrate the key mechanistic pathways.
HIF-1α Angiogenic Signaling Pathway
Diagram Title: hy-EV Activation of Angiogenesis via HIF-1α
This diagram outlines the central pathway through which hy-EVs promote blood vessel formation. Upon uptake by endothelial cells (e.g., HUVECs), hy-EVs deliver cargo that leads to the stabilization and activation of the transcription factor HIF-1α [19]. This, in turn, upregulates the expression of key angiogenic factors like Vascular Endothelial Growth Factor A (VEGFA) and the adhesion molecule CD31 (PECAM-1). The culmination of this signaling cascade is a significant enhancement of endothelial cell proliferation, migration, and the formation of capillary-like tubes, which are critical steps in angiogenesis [19].
Immunomodulation via Macrophage Polarization
Diagram Title: hy-EV Driven Macrophage M2 Polarization
This diagram illustrates the immunomodulatory capacity of hy-EVs. A key mechanism is the promotion of a switch in macrophage phenotype from the pro-inflammatory M1-state to the anti-inflammatory, pro-repair M2-state [19] [22]. hy-EVs achieve this through multiple cargo molecules. For instance, miR-21-5p delivered by hy-EVs suppresses the expression of target genes like PTEN and PDCD4 in macrophages, creating a milieu conducive to M2 polarization [22]. Simultaneously, hy-EVs enriched in Transforming Growth Factor-beta 1 (TGF-β1) can directly activate the TGF-β/Smad2/3 pathway, further driving the expression of M2 markers like CD206 and establishing an anti-inflammatory, tissue-reparative environment [23].
The enhanced therapeutic profile of hy-EVs is substantiated by robust quantitative data from in vitro and in vivo studies. The tables below consolidate key findings for direct comparison.
Table 2: In Vitro Functional Enhancement by hy-EVs
| Cell Type | Assay | hy-EV Effect vs. n-EV | Key Molecular Changes |
|---|---|---|---|
| HUVECs | Proliferation/Migration | Markedly enhanced [19] | Upregulation of HIF-1α, VEGFA, CD31 [19] |
| HUVECs | Tube Formation | Greatly enhanced angiogenic ability [19] | Activation of HIF-1α pathway [19] |
| Macrophages | Polarization (M1→M2) | Increased CD206+; Decreased CD86+ [19] | miR-21-5p mediated PTEN downregulation [22] |
| Human Dermal Fibroblasts (HSFs) | Wound Repair | Markedly improved functional activities [19] | Inhibition of ROS production [19] |
| bEnd.3 Cells (OGD Model) | Cell Viability / Angiogenesis | Promoted via TGF-β/Smad2/3 [23] | Increased p-Smad2/3 [23] |
Table 3: In Vivo Therapeutic Outcomes of hy-EV Treatment
| Disease Model | Treatment | Key Results | Reference |
|---|---|---|---|
| Diabetic Wound | hy-EVs vs. n-EVs | Enhanced collagen deposition, angiogenesis, modulated macrophage polarization, faster healing [19] | [19] |
| Photoaging (Mouse) | hypADSC-Exo | Reduced wrinkles & skin thickness, improved hydration & elasticity, increased collagen density, decreased MMPs [24] | [24] |
| Stroke (Mouse) | Microglia hy-EVs | Promoted angiogenesis, repressed apoptosis, better functional recovery via TGF-β/Smad2/3 [23] | [23] |
| Lung Cancer (Mouse) | MSC H-EV (miR-21-5p) | Increased tumor growth, angiogenesis, intra-tumoral M2 polarization [22] | [22] |
The Scientist's Toolkit: Essential Research Reagents
A successful hy-EV research program relies on a standardized set of reagents and tools. The following table catalogs the essential components of the research toolkit.
Table 4: Essential Research Reagents for hy-EV Studies
| Reagent / Tool | Function / Purpose | Example Specification / Catalog Number |
|---|---|---|
| Human Umbilical Cord MSCs | Primary cell source for EV production | Isolated from full-term donors, used at passage 5 [19] |
| Hypoxia Incubator | Precise low-oxygen culture | Capable of maintaining 1-3% O₂ with modular monitor (e.g., MOM5003) [19] |
| Ultracentrifuge | Isolation of EVs from conditioned media | Fixed-angle rotor for 100,000 × g spins [19] [24] |
| Nanoparticle Tracker | EV size and concentration analysis | ZetaView PMX 110 or Nanotrac Flex system [19] [24] |
| Transmission Electron Microscope | EV morphology validation | HITACHI H7650 [19] |
| Antibody Panel (Flow Cytometry) | EV characterization & phenotyping | Anti-CD9-PE, Anti-CD63-PE, Anti-CD81-APC [24] |
| HUVECs / bEnd.3 Cells | In vitro angiogenesis models | AW-CH0165; bEnd.3 cell line [19] [23] |
| Matrigel | Substrate for tube formation assay | Growth factor-reduced [19] |
| siRNA for miR-21-5p / TGF-β1 | Functional validation of cargo | miR-21-5p inhibitor, TGF-β1 siRNA (50 nM) [22] [23] |
| Streptozotocin | Induction of diabetic mouse model | For in vivo wound healing studies [19] |
The strategic application of hypoxic preconditioning represents a significant leap forward in harnessing the paracrine power of stem cells. By packaging a therapeutically enhanced molecular cargo into extracellular vesicles, hypoxia creates a targeted, efficient, and cell-free system that regulates core regenerative processes. The evidence is clear: hy-EVs outperform their normoxic counterparts in promoting angiogenesis, modulating the immune response, and facilitating repair in complex disease models.
Future research must focus on standardizing hypoxic protocols and EV isolation methods to ensure clinical-grade reproducibility. Furthermore, a deeper mechanistic understanding of cargo loading and recipient cell targeting will pave the way for engineering even more potent and specific hy-EV therapeutics. As the field progresses, hypoxia-induced EVs are poised to become a cornerstone of next-generation regenerative and immunomodulatory strategies, transforming the therapeutic landscape for conditions ranging from chronic wounds to ischemic diseases and beyond.
From Lab to Therapy: Protocols and Preclinical Applications of Hypoxia-Conditioned Secretomes
Hypoxic conditioning has emerged as a pivotal strategy in regenerative medicine, enhancing the therapeutic potential of mesenchymal stem cells (MSCs) by mimicking their native physiological microenvironment. Unlike the hyperoxic conditions (21% O₂) of conventional cell culture, physiological oxygen levels in stem cell niches such as bone marrow and adipose tissue typically range from 1% to 7% O₂ [8]. Controlled exposure to mild hypoxia (1%-5% O₂) for defined periods (<48 hours) represents a critical window for activating cellular adaptive responses without inducing damage, ultimately optimizing the production of paracrine factors that mediate tissue repair [8] [26]. This technical guide synthesizes current evidence and methodologies for standardizing hypoxic preconditioning protocols to maximize the secretory profile and regenerative capacity of MSCs for therapeutic applications.
Core Principles and Molecular Mechanisms
The Oxygen Paradox: Hormesis in Hypoxic Conditioning
The beneficial effects of hypoxic conditioning operate on the principle of hormesis, a biphasic dose-response relationship where low-dose exposures elicit stimulatory or adaptive effects, while high-dose exposures produce inhibitory or damaging outcomes [27]. In practice, mild to moderate hypoxia (1%-5% O₂) activates cytoprotective and pro-regenerative pathways, whereas severe hypoxia (<1% O₂) or prolonged exposure can trigger cellular senescence, apoptosis, and diminished therapeutic function [8] [27]. This delicate balance underscores the necessity for precise protocol optimization, where the "hypoxic dose"—defined by oxygen concentration, exposure duration, and number of cycles—must be carefully calibrated to achieve desired therapeutic outcomes [27].
Key Signaling Pathways and Metabolic Reprogramming
The cellular response to hypoxia is predominantly orchestrated by the hypoxia-inducible factor 1-alpha (HIF-1α). Under normoxic conditions, HIF-1α is continuously degraded. However, oxygen deprivation stabilizes HIF-1α, allowing it to translocate to the nucleus and activate the transcription of hundreds of genes governing angiogenesis, cell survival, and metabolism [8].
The following diagram illustrates the core signaling pathway activated by hypoxic conditioning:
Figure 1: Core HIF-1α Signaling Pathway in Hypoxic Conditioning. The stabilization of HIF-1α under low oxygen conditions initiates a transcriptional program that enhances angiogenesis, metabolic reprogramming, and cell survival.
Metabolically, HIF-1α activation shifts MSC energy production from oxidative phosphorylation toward glycolysis, a more efficient pathway under low oxygen conditions [8]. This reprogramming reduces reactive oxygen species (ROS) generation during preconditioning, enhancing cellular resilience to subsequent oxidative stress encountered after transplantation into damaged tissues [26]. Furthermore, hypoxia induces significant changes in the MSC secretome, increasing the production and release of extracellular vesicles (EVs), particularly exosomes, which are enriched with pro-regenerative microRNAs and proteins that modulate inflammation, promote angiogenesis, and stimulate tissue repair [8].
Optimizing Protocol Parameters
Oxygen Concentration Guidelines
The optimal oxygen concentration for hypoxic conditioning is application-dependent, but evidence consistently identifies the 1%-5% O₂ range as most beneficial for enhancing MSC paracrine function while maintaining cell viability.
Table 1: Effects of Different Oxygen Concentrations on MSC Properties
| O₂ Concentration | Effects on MSCs | Key Implications for Therapy |
|---|---|---|
| 1% - 5% (Mild/Moderate) | Enhanced proliferation, HIF-1α stabilization, increased secretion of angiogenic factors (VEGF, FGF), improved resistance to oxidative stress, enhanced immunomodulation [8]. | Optimal for preconditioning. Maximizes paracrine output and survival post-transplantation. |
| <1% (Severe) | Induction of senescence and apoptosis, reduced viability, compromised therapeutic function [8]. | Generally detrimental; should be avoided in preconditioning protocols. |
| ~7% (Near-Physiological) | Represents the average O₂ level in some stem cell niches (e.g., bone marrow) [8]. | Suitable for maintaining MSCs in a more native state during culture. |
| 21% (Atmospheric Normoxia) | Hyperoxia relative to physiology; can promote oxidative stress, accelerated aging, and suboptimal function [8]. | Not recommended for preconditioning; represents a poor mimic of the in vivo environment. |
Exposure Duration and Timing
Controlling the duration of hypoxic exposure is critical for triggering adaptive responses without overwhelming the cells. The <48-hour window is consistently supported by experimental data as both effective and safe.
Table 2: Optimizing Hypoxic Exposure Duration for MSCs
| Exposure Duration | Reported Outcomes | Protocol Recommendations |
|---|---|---|
| < 48 hours | Significantly enhanced cell viability, proliferation, and secretion of angiogenic factors; upregulation of pro-survival and anti-apoptotic genes; peak activation of protective mechanisms [8] [26]. | The recommended optimal window for preconditioning. A duration of 24 hours is frequently used and effective [26]. |
| > 48 hours | Can trigger accelerated cellular aging, senescence, and reduced therapeutic efficacy; increased risk of transitioning from adaptive to detrimental responses [8]. | Should be avoided in standard preconditioning protocols. |
| Short Cycles (Minutes-Hours) | Used in intermittent hypoxia models, cycling between hypoxic and normoxic conditions [27]. | More common in clinical/athletic applications; less standard for in vitro MSC preconditioning than sustained exposure. |
Experimental Protocols and Workflows
This section provides a detailed, actionable methodology for implementing hypoxic preconditioning in a research setting.
Standardized Preconditioning Workflow
The following diagram outlines a generalized experimental workflow for preconditioning MSCs, from culture to post-conditioning analysis:
Figure 2: Experimental Workflow for MSC Hypoxic Preconditioning. A step-by-step guide from cell expansion through post-conditioning analysis.
Detailed Methodology: A Representative Protocol
The following protocol is based on studies that successfully enhanced MSC paracrine factor production and stress resilience [8] [26].
Step 1: Cell Culture and Seeding
- Isolate and expand MSCs from a chosen source (e.g., bone marrow, Wharton's jelly, adipose tissue) under standard culture conditions (37°C, 5% CO₂, 21% O₂) [26].
- At passage 3-4, once cells reach 70-80% confluence, harvest them using a standard trypsin-EDTA solution.
- Seed the MSCs at an appropriate density (e.g., 3 x 10⁴ cells/mL for a 96-well plate for viability assays; higher densities for flasks for secretome collection) and allow them to attach for 24 hours under normoxic conditions [26].
Step 2: Hypoxic Conditioning
- Place the culture vessels into a pre-equilibrated hypoxia workstation or incubator capable of maintaining a precise O₂ level.
- Set and maintain the environmental parameters: 1-5% O₂, 5% CO₂, 37°C, and high humidity.
- Initiate the hypoxic exposure. A 24-hour period is a common and effective starting point within the <48-hour window.
- For chemical induction of hypoxia (an alternative to physical hypoxia chambers), add 100 µM Cobalt Chloride (CoCl₂) to the culture medium for 24 hours [26].
Step 3: Post-Conditioning Cell Processing and Analysis
- For analysis of the secretome, collect conditioned media. Centrifuge to remove cells and debris, then aliquot and store at -80°C for subsequent analysis (e.g., ELISA for VEGF, FGF, SDF-1α) [8].
- To assess cell viability and proliferation, perform assays like CCK-8 or trypan blue exclusion immediately after the conditioning period [26].
- For gene expression analysis, extract RNA and perform qRT-PCR to quantify transcripts of interest (e.g., HIF-1α, VEGF, SOD1, CAT) [26].
- To test functional resilience, challenge preconditioned MSCs with 100 µM H₂O₂ for 1-24 hours and measure viability relative to non-preconditioned controls [26].
The Scientist's Toolkit: Essential Reagents and Equipment
Successful implementation of hypoxic conditioning relies on specific laboratory tools and reagents.
Table 3: Key Research Reagent Solutions for Hypoxic Conditioning
| Tool/Reagent | Specification/Function | Application in Hypoxic Conditioning |
|---|---|---|
| Hypoxia Workstation | Sealed chamber with active O₂ and CO₂ control (e.g., HypoxyLab) [28]. | Provides a stable, controllable, and reproducible hypoxic environment for cell culture. Essential for precise physical hypoxia. |
| O₂ Probe / Monitor | Real-time optical sensor (e.g., OxyLite) [28]. | Directly measures pericellular dissolved O₂ (pO₂) in culture media, critical for validating the actual conditions cells experience. |
| Chemical Hypoxia Mimetics | Cobalt Chloride (CoCl₂), Deferoxamine [27]. | Stabilizes HIF-1α by inhibiting prolyl hydroxylases (PHDs). A convenient, low-cost alternative to physical hypoxia workstations. |
| HIF-1α Antibodies | Validated for Western Blot, Immunofluorescence, ELISA. | Essential for confirming the activation of the hypoxic response pathway at the protein level. |
| ELISA Kits | For VEGF, FGF, SDF-1α, other cytokines. | Quantifies the enhanced production of paracrine factors in conditioned media following hypoxic preconditioning. |
| Cell Viability Assays | CCK-8, MTT, Trypan Blue Exclusion. | Assesses the impact of the hypoxic protocol on cell health and proliferation capacity. |
| Oxidative Stress Inducers | Hydrogen Peroxide (H₂O₂) [26]. | Used to challenge preconditioned MSCs and test their acquired resilience to stress in functional assays. |
Advanced Concepts and Synergistic Strategies
Intermittent Hypoxia and Combined Conditioning
Beyond sustained exposure, intermittent hypoxia conditioning (IHC)—cycling between hypoxic and normoxic periods—is a recognized model that may further amplify adaptive responses through a process of reoxygenation-triggered signaling [27]. Furthermore, synergistic preconditioning combines hypoxia with other stimuli. A prominent example is co-treatment with low-dose Lipopolysaccharide (LPS; 10 ng/mL), which mimics an inflammatory environment and has been shown to further enhance MSC viability, reduce population doubling time, and increase resistance to oxidative stress beyond hypoxia alone [26].
Engineering the Microenvironment
Advanced biomaterial strategies are being developed to maintain a beneficial hypoxic microenvironment after cell transplantation. One innovative approach involves encapsulating MSCs in cell-tethering colloidal hydrogels that incorporate oxygenating microparticles. This system creates a controlled, mild hypoxic niche around the cells, prevents their egression, and has been shown to significantly boost the local and sustained secretion of angiogenic cytokines, leading to improved outcomes in models of hindlimb ischemia [29].
The therapeutic paradigm in regenerative medicine is undergoing a significant shift from whole-cell transplantation to the utilization of cell-free therapies based on stem cell secretions. This transition is fueled by growing recognition that the therapeutic benefits of stem cells originate largely from their paracrine activity rather than direct differentiation and engraftment [30]. The complete set of bioactive molecules secreted by cells, known as the secretome, represents a promising new frontier in therapeutic development. These secretions include both soluble factors and membrane-bound extracellular vesicles (EVs) that play crucial roles in intercellular communication by activating tissue repair-associated signaling pathways such as cell proliferation, angiogenesis, apoptosis, and inflammation modulation [31].
Within this paradigm, hypoxic conditioning has emerged as a powerful strategy to enhance the therapeutic potential of stem cell secretions. When stem cells are exposed to low oxygen conditions mimicking their physiological niche, they respond by significantly altering their secretory profile, particularly increasing production of factors that promote angiogenesis and cell survival [16]. This technical guide provides researchers with comprehensive methodologies for harnessing the secretome—from fundamental concepts of hypoxic preconditioning through advanced purification and characterization of extracellular vesicles, with a specific focus on establishing robust, GMP-compliant processes for therapeutic development.
Hypoxic Conditioning: Principles and Implementation
Biological Rationale for Hypoxic Preconditioning
Hypoxic conditioning exploits an evolutionary conserved adaptive response where brief exposure to sublethal low oxygen conditions enhances cellular resilience to subsequent lethal insults—a phenomenon known as preconditioning [16]. This approach originated from observations in ischemic myocardium and has since been adapted for enhancing stem cell secretome potency. The hypoxia-inducible factor-1 (HIF-1) serves as the master regulator of this response, activating transcription of numerous genes involved in angiogenesis, cell survival, and metabolism.
Molecularly, hypoxia triggers a comprehensive reprogramming of stem cell secretory activity. Research using adipose-derived stem cells (ASCs) demonstrates that a single exposure to severe hypoxia (<0.1% O₂) significantly increases both transcriptional and translational levels of key angiogenic factors including vascular endothelial growth factor-A (VEGF-A) and angiogenin (ANG) [16]. This enhanced paracrine production translates directly to improved biological function, with hypoxic-conditioned media demonstrating significantly increased angiogenic potential in vivo compared to normoxic controls.
Technical Implementation of Hypoxic Conditioning
Table 1: Methods for Implementing Hypoxic Conditioning of Stem Cells
| Parameter | Specification | Experimental Notes |
|---|---|---|
| Oxygen Levels | 1% O₂ or <0.1% O₂ | <0.1% O₂ induces stronger HIF-1 activation |
| Equipment | Tri-gas incubators or specialized hypoxia chambers (e.g., GENbox Jar) | GENbox Jar provides more severe hypoxia (<0.1% O₂) |
| Exposure Duration | 12-72 hours | 24 hours optimal for ASC angiogenic response [16] |
| Cell Density | 5×10³ cells/cm² at 80% confluence | Avoid over-confluence which alters secretory profile |
| Culture Medium | Serum-free basal medium during conditioning | Prevents serum protein contamination of secretome |
The workflow for hypoxic conditioning begins with establishing optimal baseline culture conditions. For adipose-derived stem cells, researchers should seed cells at a density of 5×10³ cells per cm² and culture until 80% confluence in complete growth medium [16]. For the conditioning phase itself, cells should be switched to serum-free medium and placed in either a tri-gas incubator (for 1% O₂) or a specialized hypoxia system like the GENbox Jar (for <0.1% O₂) for the designated period. The specific oxygen concentration and duration should be optimized for each cell type and intended therapeutic application.
Diagram 1: Hypoxic conditioning triggers a defined molecular cascade that enhances secretion of therapeutic factors through HIF-1α activation.
From Conditioned Media to Purified Extracellular Vesicles
Secretome Collection and Primary Processing
The initial collection and processing phases are critical for maintaining secretome integrity and functionality. For adipose-derived stem cells, conditioned medium should be collected following the hypoxic conditioning period and subjected to sequential clarification steps [16]:
- Centrifugation at 875×g for 10 minutes to remove cellular debris
- Filtration through 0.2-μm filters to eliminate remaining particulates
- Concentration using centrifugal filter columns with 3-kDa molecular weight cutoff (50× concentration)
During this phase, maintenance of biochemical stability is paramount. Processing should be performed at 4°C whenever possible to minimize protein degradation, and protease inhibitors may be added to preserve secretome integrity, particularly for subsequent proteomic analyses.
Extracellular Vesicle Purification and Characterization
EV purification represents a crucial technical challenge in secretome processing. Tangential flow filtration (TFF) has emerged as a robust, scalable method suitable for GMP-compliant manufacturing [31]. TFF allows for processing of large volumes of conditioned media while maintaining EV integrity and biological activity through a continuous flow system that minimizes membrane fouling.
Table 2: Extracellular Vesicle Purification and Characterization Methods
| Method | Principle | Application | Considerations |
|---|---|---|---|
| Tangential Flow Filtration (TFF) | Size-based separation in continuous flow | Large-scale GMP production [31] | Closed-system, scalable, maintains EV integrity |
| Ultracentrifugation | High-speed pelleting of EVs | Research-scale isolation | Gold standard but difficult to scale |
| Size-Exclusion Chromatography | Size-based separation in columns | High-purity research applications | Excellent purity but limited scalability |
| Polymer-Based Precipitation | Polymer-induced EV precipitation | Simple research applications | Co-precipitation of contaminants |
| hiSPECS Method | Click chemistry-based glycoprotein capture | Proteomic secretome analysis [32] | Miniaturized for primary cells |
For comprehensive EV characterization, researchers should employ a multi-parametric approach following MISEV2018 guidelines [31]:
- Nanoparticle Tracking Analysis for size distribution and concentration
- Transmission Electron Microscopy for morphological assessment
- Western Blot for EV marker detection (CD9, CD63, CD81, TSG101)
- Proteomic Analysis for comprehensive cargo profiling
The recently developed hiSPECS (high-performance secretome protein enrichment with click sugars) method provides a advanced approach for miniaturized secretome analysis, enabling characterization from limited primary cell samples [32]. This method utilizes metabolic labeling with N-azido-mannosamine (ManNAz) followed by lectin-based precipitation and copper-free click chemistry to capture glycoproteins for mass spectrometry analysis, dramatically improving sensitivity over conventional methods.
Diagram 2: The complete workflow from conditioned media collection to purified extracellular vesicles involves sequential clarification, concentration, and purification steps followed by comprehensive characterization.
Quality Control and Analytical Techniques
Comprehensive QC Strategy for Secretome-Based Products
Developing a robust quality control strategy is essential for clinical translation of secretome-based products. A GMP-compliant approach should include in-process testing, release testing, and stability monitoring [31]. Key quality attributes to assess include:
- Identity: Confirmation of EV markers (CD9, CD63, CD81) and absence of cellular contaminants
- Safety: Sterility, endotoxin testing, and mycoplasma screening
- Purity: Residual host cell DNA and protein contaminants
- Potency: Functional assays relevant to intended mechanism of action
For EV-enriched secretomes, regulatory approval for clinical trials requires demonstration of manufacturing process consistency and comprehensive safety profiling including in vitro immunogenicity assessment and in vivo toxicology studies [31].
Advanced Proteomic Analysis of Secretome
Mass spectrometry-based proteomics has become indispensable for secretome characterization. The hiSPECS method enables high-sensitivity analysis from small cell numbers (as few as one million primary cells) by incorporating four major improvements over previous techniques [32]:
- Lectin-based precipitation using concanavalin A to reduce albumin contamination
- Covalent binding to magnetic DBCO-alkyne beads using copper-free click chemistry
- On-bead digestion to release tryptic peptides for mass spectrometry
- Data-independent acquisition (DIA) mass spectrometry to extend dynamic range
This approach identifies not only soluble secreted proteins but also proteolytically cleaved membrane protein ectodomains that contribute significantly to total secretome composition, providing a more comprehensive picture of cellular communication.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Secretome Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Culture Media | DMEM-low glucose, serum-free formulations | Base medium for hypoxic conditioning and secretome collection [16] |
| Hypoxia Systems | Tri-gas incubators, GENbox Jar | Precise oxygen control for preconditioning experiments [16] |
| Concentration Devices | Amicon Ultra-15 centrifugal filters, TFF systems | Volume reduction and secretome concentration [16] |
| EV Characterization | Antibodies against CD9, CD63, CD81 | EV identity confirmation by Western blot [31] |
| Proteomic Tools | ManNAz, DBCO-alkyne beads, ConA | Metabolic labeling and glycoprotein capture for hiSPECS [32] |
| Analytical Instruments | Nanoparticle tracker, TEM, MS with DIA | Comprehensive physical and molecular characterization [32] |
The methodology for harnessing the secretome has evolved from simple conditioned media collection to sophisticated purification and characterization of extracellular vesicles. Hypoxic conditioning stands as a powerful, non-genetic approach to enhance the therapeutic potency of stem cell secretions, particularly for applications in angiogenesis and tissue repair. The continuing development of advanced analytical techniques like hiSPECS proteomics will enable increasingly comprehensive profiling of secretome composition and function.
For clinical translation, future work must focus on standardizing protocols and establishing quality control metrics that ensure batch-to-batch consistency [30]. The successful regulatory approval of an EV-enriched secretome for a Phase I cardiac clinical trial demonstrates the feasibility of this approach and provides a roadmap for other therapeutic applications [31]. As the field progresses, integration of hypoxic preconditioning with GMP-compliant manufacturing processes will unlock the full potential of secretome-based therapies for regenerative medicine.
Myocardial infarction (MI) remains a leading cause of global mortality and morbidity, often progressing to congestive heart failure despite advances in interventional therapies [33] [34]. The establishment of coronary collateral circulation in the infarct border zone can effectively relieve myocardial ischemia and impede cell death, making therapeutic angiogenesis a promising strategy for salvaging ischemic myocardium [35]. Within this paradigm, stem cell therapy has generated significant interest, with growing evidence suggesting that its benefits are mediated primarily through paracrine mechanisms rather than direct tissue replacement [33] [34]. This technical guide examines how hypoxic stress enhances the production of key paracrine factors from various stem cell populations, exploring their roles in promoting angiogenesis and cardioprotection within myocardial infarction models.
Paracrine Mechanisms of Stem Cell-Mediated Repair
The Paracrine Hypothesis
The traditional view that stem cells mediate repair through direct differentiation and engraftment has been challenged by observations that these events occur too infrequently to account for the significant functional improvements observed in preclinical models [33]. Instead, a growing body of evidence supports the paracrine hypothesis, which posits that stem cells secrete bioactive factors that orchestrate multiple restorative processes in the damaged myocardium [33] [34]. These factors act in a dynamic spatial-temporal manner to direct myocardial protection, neovascularization, cardiac remodeling, and endogenous regeneration [34].
Stem Cell Populations and Their Paracrine Signatures
Various adult stem cell populations have demonstrated therapeutic potential through paracrine activities, each with distinct factor secretion profiles:
Table: Stem Cell Types and Their Key Paracrine Factors in Cardiac Repair
| Stem Cell Type | Key Paracrine Factors | Primary Repair Mechanisms |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Sfrp2, HASF, STC-1, VEGF, bFGF, HGF, Angiopoietins [33] | Myocardial protection, Neovascularization, Attenuation of fibrosis [33] |
| Bone Marrow Mononuclear Cells (BM-MNCs) | IL-10, bFGF, VEGF, IL-1β, TNF-α [33] | Neovascularization, T-cell recruitment modulation, Collagen deposition regulation [33] |
| Endothelial Progenitor Cells (EPCs) | VEGF, HGF, G-CSF [33] | Endothelial regeneration, Angiogenesis [33] |
| Resident Cardiac Progenitor Cells (CPCs) | VEGF, HGF, IGF-1 [33] | Cardiomyocyte survival, Endothelial cell tube formation [33] |
Hypoxic Conditioning and Enhanced Paracrine Factor Production
Hypoxic Stress as a Regulatory Signal
Hypoxic stress serves as a powerful natural inducer of paracrine factor production in stem cells. When exposed to ischemic or hypoxic conditions similar to the infarcted myocardial microenvironment, stem cells significantly upregulate their secretion of cytoprotective and angiogenic factors [33]. This adaptive response forms the mechanistic basis for the beneficial effects observed in stem cell therapy for cardiac repair. The hypoxia-inducible factor-1α (HIF-1α) pathway serves as the master regulator of this response, coordinating the expression of numerous downstream genes involved in angiogenesis and cell survival [36] [37].
Experimental Evidence of Hypoxic Enhancement
Several studies demonstrate the enhancement of paracrine factor production under hypoxic conditions:
- Akt-MSCs under hypoxia: Show significant upregulation of secreted frizzled-related protein 2 (Sfrp2) and Hypoxic induced Akt regulated Stem cell Factor (HASF), mediating survival effects in isolated hypoxic cardiomyocytes via PKC-ε signaling [33].
- Genetic modification: MSCs overexpressing Akt gene (Akt-MSCs) release paracrine factors that inhibit apoptosis of cardiomyocytes exposed to hypoxia, demonstrated by reduced morphologic evidence of necrotic/apoptotic cell death and attenuated Caspase 3 release [33].
- Preconditioning strategies: Preconditioning of MSCs enhances their survival and paracrine activity, leading to improved attenuation of left ventricular remodeling [33].
Key Signaling Pathways in Angiogenesis and Cardioprotection
The HIF-1α/VEGF Axis
The HIF-1α/VEGF signaling pathway represents the central regulatory axis for angiogenesis following myocardial infarction [37]. Under normoxic conditions, HIF-1α undergoes rapid degradation, but under hypoxic conditions, it accumulates and translocates to the nucleus, where it dimerizes with HIF-1β and activates transcription of target genes including VEGF [36] [37].
HIF-1α activation can be enhanced through prolyl hydroxylase domain (PHD) protein inhibition. Oral administration of a non-isoform-specific PHD inhibitor in rats improved microvascular density in the peri-infarct area, preventing deterioration of cardiac function and left ventricular dilation after MI [36]. Combined shRNA-induced knockdown of PHD-2 and Factor Inhibiting HIF (FIH) in mice similarly improved left ventricular function and enhanced neovascularization [36].
Additional Signaling Pathways
Beyond the HIF-1α/VEGF axis, several other signaling pathways contribute to paracrine-mediated repair:
- Sfrp2/Wnt Pathway: Secreted frizzled-related protein 2 (Sfrp2), significantly upregulated in Akt-MSCs, mediates cytoprotective effects that can be abrogated by siRNA silencing [33].
- TNF Receptor Signaling: Ablation of TNF receptor 1 (TNFR1) from mouse MSCs increases growth factor production and enhances cardioprotective effects, whereas TNFR2 appears to mediate beneficial effects [33].
- Toll-like Receptor Signaling: TLR2 has been shown to control VEGF production increase following cytokine or ischemic treatment in MSCs [33].
Experimental Models and Methodologies
Myocardial Infarction Modeling
Table: Key Experimental Model Parameters for Myocardial Infarction Research
| Parameter | Specifications | Applications |
|---|---|---|
| Animal Model | Adult male C57BL/6J mice (20-30g) [37] | Genetic consistency, reproducible infarct size |
| Anesthesia | Isoflurane inhalation throughout operation [37] | Maintained normal breathing via ventilator |
| MI Induction | LAD ligation with 6-0 silk thread 2mm below left atrial appendage [37] | Visual confirmation by left ventricular whitening |
| Post-op Analgesia | Buprenorphine (0.5mg/kg) SC every 6h for two days [37] | Welfare scoring system for additional dosing |
| Functional Assessment | Vivid 9 high-frequency color Doppler ultrasound [37] | LVEF, LVFS, LVIDs, LVIDd measurements |
Assessment of Angiogenic and Functional Outcomes
Comprehensive evaluation of therapeutic efficacy requires multimodal assessment:
Infarct Size Measurement:
- Heart removal and sectioning into 2mm slices
- Incubation with 1% 2,3,5-triphenyltetrazolium chloride (TTC) solution at 37°C for 15-20 minutes [37]
- Fixation with 4% paraformaldehyde for 48 hours
- Image analysis with ImageJ software to calculate white infarct area [37]
Histopathological and Immunofluorescence Analysis:
- Heart fixation in 4% paraformaldehyde for 24 hours
- Paraffin embedding and 4μm sectioning
- Masson trichrome staining for collagen fibrosis (blue staining) [37]
- Immunofluorescence with anti-CD31 antibody for endothelial cell marking [37]
- DAPI counterstaining for nuclear visualization
- Capillary density quantification via red CD31+ dots [37]
In Vitro Angiogenesis Assays
Tube Formation Assay:
- HUVEC culture in RPMI 1640 with 10% FBS [37]
- Treatment with experimental factors (e.g., gastrin at 10⁻⁹ mol/L) for 3-72 hours [37]
- Inoculation of growth factor-reduced Matrigel in 96-well plates (50μL/well) [37]
- 30-minute incubation at 37°C for gel polymerization
- HUVEC seeding (1×10⁶ cells/injection) and 6-hour incubation [37]
- Image capture and analysis of tube structures using ImageJ software
Research Reagent Solutions
Table: Essential Research Reagents for Cardiac Repair Studies
| Reagent/Cell Line | Specifications | Application/Function |
|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | Purchased from ATCC [37] | In vitro angiogenesis models (tube formation) |
| Gastrin | 30μg/kg/d in vivo; 10⁻⁹ mol/L in vitro [37] | HIF-1α/VEGF pathway activation |
| CI-988 | 300μg/kg/d in vivo; 10⁻⁸ mol/L in vitro [37] | CCKBR antagonist (gastrin effect blockade) |
| Anti-CD31 Antibody | Commercial source (e.g., Abcam) [37] | Endothelial cell marker for immunofluorescence |
| Growth Factor-Reduced Matrigel | BD Biosciences [37] | Extracellular matrix for tube formation assay |
| Akt-MSCs | Genetically modified mesenchymal stem cells [33] | Enhanced paracrine factor production |
Experimental Workflow Integration
The comprehensive experimental approach from hypothesis testing to therapeutic assessment can be visualized as an integrated workflow:
The strategic enhancement of angiogenesis and cardioprotection through hypoxia-primed stem cell paracrine mechanisms represents a promising therapeutic approach for myocardial infarction. The HIF-1α/VEGF pathway serves as the central regulatory axis, with multiple additional signaling cascades contributing to the comprehensive repair process. Future research directions should focus on optimizing hypoxic preconditioning protocols, developing combination therapies that target multiple aspects of the paracrine response, and translating these findings into clinical applications that can improve outcomes for patients suffering from myocardial infarction. As our understanding of stem cell paracrine biology deepens, the potential for developing novel, effective therapies for cardiovascular repair continues to expand.
Hypoxic-ischemic brain injury, a consequence of interrupted cerebral blood flow and oxygen supply, represents a significant cause of neurological morbidity and mortality. Conditions such as hypoxic-ischemic encephalopathy (HIE) in newborns and high-altitude cerebral edema (HACE) in adults trigger complex pathological cascades involving excitotoxicity, oxidative stress, and neuroinflammation, ultimately leading to neuronal death and blood-brain barrier (BBB) disruption [38] [39]. Within the context of a broader thesis on hypoxic stress effects on stem cell biology, this review explores how the hypoxic microenvironment not only causes brain damage but also strategically enhances the therapeutic potential of stem cells. Emerging evidence demonstrates that preconditioning stem cells under hypoxic conditions profoundly influences their paracrine signature, amplifying the production of bioactive factors that mediate tissue repair, immunomodulation, and vascular stabilization [18] [8]. This in-depth technical guide examines the mechanisms, experimental protocols, and reagent solutions underpinning stem cell-based therapies for mitigating hypoxic-ischemic brain injury and resolving cerebral edema, providing a resource for researchers and drug development professionals.
Stem Cell Types and Their Therapeutic Mechanisms
Various stem cell types have been investigated for their reparative potential in neurological injuries, each with distinct advantages and mechanistic pathways.
- Mesenchymal Stem Cells (MSCs): Sourced from bone marrow, adipose tissue, or umbilical cord, MSCs are widely utilized due to their potent paracrine activity, immunomodulation, and lack of significant immunogenicity [18] [13]. Their therapeutic effects are primarily mediated through the secretion of growth factors, cytokines, and extracellular vesicles (EVs) that promote angiogenesis, reduce inflammation, and enhance cell survival, rather than through direct differentiation and replacement of neural cells [13] [40]. The International Society for Cellular Therapy (ISCT) defines MSCs by plastic adherence, specific surface marker expression (CD105+, CD73+, CD90+; CD45-, CD34-, CD14-/CD11b-, CD79α-/CD19-, HLA-DR-), and tri-lineage differentiation potential [18] [13].
- Neural Stem Cells (NSCs): These cells, derived from embryonic brain tissue or induced pluripotent stem cells (iPSCs), possess the innate capacity to differentiate into neurons, astrocytes, and oligodendrocytes [38] [18]. Studies in rat HIE models demonstrate that transplanted human NSCs (hNSCs) can migrate to injured brain regions, differentiate into mature neural lineages (approximately 30.68% into neurons, 23.50% into oligodendrocytes, and 14.00% into astrocytes), and restore cognitive and motor function [38].
- Induced Pluripotent Stem Cells (iPSCs): iPSCs, generated by reprogramming adult somatic cells, offer a patient-specific, unlimited cell source with pluripotent differentiation capability [18] [40]. While they present a significant promise for personalized therapy, challenges related to genetic stability and tumorigenicity require further resolution before widespread clinical application [18].
Table 1: Core Stem Cell Types for Neurological Applications
| Cell Type | Main Sources | Key Therapeutic Mechanisms | Advantages | Key Limitations |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone Marrow, Umbilical Cord, Adipose Tissue [13] | Paracrine factor secretion (VEGF, BDNF), Immunomodulation, Extracellular Vesicle release [18] [13] | Low immunogenicity, Ease of isolation, Strong paracrine activity [18] | Limited neuronal differentiation, Mechanisms not fully elucidated [18] |
| Neural Stem Cells (NSCs) | Embryonic Brain Tissue, iPSCs [18] | Direct differentiation into neurons and glia, Neurotrophic factor secretion, Cell replacement [38] [18] | Direct lineage commitment, Robust integration potential [18] | Limited availability, Ethical considerations, Tumorigenicity risk [18] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed Somatic Cells [18] | Unlimited proliferation, Patient-specific derivation, Differentiation into any cell type [18] [40] | Personalized therapy, No ethical concerns regarding source [18] | Technically complex, Genetic/epigenetic instability, Tumorigenicity [18] |
The Impact of Hypoxic Preconditioning on Stem Cell Paracrine Function
A key advancement in the field involves "hypoxic preconditioning"—exposing stem cells to low oxygen tension before transplantation—to mimic their native niche and enhance their therapeutic efficacy. This process induces metabolic reprogramming that fundamentally alters the cells' paracrine output [8].
Molecular Mediators of Hypoxic Response
The cellular response to hypoxia is predominantly orchestrated by Hypoxia-Inducible Factor 1-alpha (HIF-1α). Under normoxia, HIF-1α is degraded, but under hypoxia, it stabilizes and translocates to the nucleus, dimerizing with HIF-1β to activate transcription of genes involved in angiogenesis, cell survival, and metabolism [8]. This includes upregulation of:
- Vascular Endothelial Growth Factor (VEGF): A critical angiogenic factor.
- Stromal Cell-Derived Factor-1α (SDF-1α) and its receptor CXCR4: Enhancing homing and migration to injury sites [8].
- Brain-Derived Neurotrophic Factor (BDNF): Supporting neuronal survival and plasticity [38].
Enhanced Paracrine Secretion and Extracellular Vesicles
Hypoxic preconditioning boosts the secretion of bioactive factors and alters the cargo of extracellular vesicles (EVs), particularly exosomes. These EVs act as key paracrine mediators, transferring proteins, lipids, and nucleic acids to recipient cells [18] [41]. For instance, hypoxia-preconditioned MSC exosomes (H-EXO) are enriched with specific microRNAs like miR-125a-5p, which targets RTEF-1 to inhibit hypoxia-induced aberrant angiogenesis and protect BBB integrity—a crucial mechanism in mitigating HACE [41]. Similarly, H-EXO loaded with miR-126 and miR-146a enhance tissue repair and promote anti-inflammatory M2 macrophage polarization [18].
Diagram 1: Hypoxia-Induced Molecular Pathways in Stem Cells. This diagram illustrates the key molecular mechanisms activated in stem cells by hypoxic preconditioning, leading to enhanced therapeutic potential. HIF-1α stabilization drives the expression of factors critical for angiogenesis, homing, and blood-brain barrier protection.
Experimental Models and Quantitative Outcomes
Robust preclinical models are essential for validating the efficacy of stem cell therapies. The quantitative data below demonstrates the significant impact of these interventions, particularly when stem cells are preconditioned.
Table 2: Quantitative Outcomes of Stem Cell Therapy in Preclinical Models of Brain Injury
| Experimental Model | Intervention | Key Quantitative Outcomes | Proposed Mechanism | Source |
|---|---|---|---|---|
| Rat HIE Model | Human Neural Stem Cells (hNSCs) | - ↑ VEGF & BDNF expression (P < 0.05)- ↓ M1 microglia (P < 0.001), ↑ M2 microglia (P < 0.01)- ↓ Apoptosis (P < 0.001)- 30.68% ± 4.30% differentiated into neurons | Paracrine action, Microglial polarization, Cell differentiation | [38] |
| Mouse HACE Model | Hypoxia-preconditioned MSC Exosomes (H-EXO) | - Attenuated pathological angiogenesis- Maintained blood-brain barrier integrity- Protected neurovascular function | miR-125a-5p/RTEF-1 axis inhibition | [41] |
| Rat Massive Hepatectomy Model | Hypoxia-preconditioned Bone Marrow MSCs | - Enhanced liver regeneration- Upregulated VEGF levels | Enhanced paracrine activity | [8] |
| Nonhuman Primate Myocardial Infarction | Hypoxia-preconditioned MSCs | - Improved cardiac function- Reduced infarct size- No increased arrhythmogenic risk | Enhanced paracrine activity | [8] |
Detailed Experimental Protocols
To facilitate replication and further research, below are detailed methodologies for key experiments cited in this review.
Protocol: Hypoxic Preconditioning of Mesenchymal Stem Cells
This protocol is adapted from methods used to generate hypoxia-preconditioned MSCs and their exosomes for treating HACE [41] [8].
- Cell Culture: Culture human MSCs (e.g., from bone marrow or umbilical cord) in standard growth medium (e.g., DMEM with 10% FBS and 1% penicillin/streptomycin) at 37°C in a 21% O₂, 5% CO₂ incubator until 70-80% confluent.
- Hypoxia Induction: Place culture flasks/plates in a modular hypoxic chamber. Flush the chamber with a gas mixture of 1-5% O₂, 5% CO₂, and balance N₂ for 10-15 minutes to achieve stable low oxygen tension. Seal the chamber and incubate at 37°C for 24-48 hours [8]. Critical Note: Exposure beyond 48 hours may induce senescence [8].
- Exosome Isolation (Optional): For H-EXO collection, after hypoxia, culture cells in exosome-depleted FBS medium for another 48 hours. Collect conditioned medium and centrifuge at 2,000 × g for 30 minutes to remove cells and debris. Ultracentrifuge the supernatant at 100,000 × g for 70 minutes at 4°C to pellet exosomes. Resuspend the exosome pellet in PBS and characterize by nanoparticle tracking analysis (NTA) and western blot for markers (CD63, CD81, TSG101) [41].
- Cell Harvesting for Transplantation: After hypoxia exposure, wash cells with PBS, trypsinize, and resuspend in sterile PBS or serum-free medium at the desired concentration for in vivo administration.
Protocol: Assessing Therapeutic Efficacy in a Rat HIE Model
This protocol summarizes the procedures used to evaluate hNSC therapy, as referenced in [38].
- HIE Model Induction: Use postnatal day 7-10 rat pups. Anesthetize and surgically expose the left common carotid artery. Ligate the artery permanently. After recovery, place pups in a hypoxic chamber with 8% O₂ for 90 minutes at 37°C to induce hypoxia-ischemia.
- Cell Transplantation: Within 24 hours post-HIE, randomly assign pups to treatment (hNSCs) or control (vehicle) groups. Anesthetize pups and stereotactically inject ~100,000 - 500,000 cells in 2-3 µL of vehicle into the ipsilateral ventricle or parenchyma. Sham-operated rats undergo anesthesia and skin incision only.
- Tissue Analysis at 10 Days:
- Immunohistochemistry: Perfuse and fix brains. Section brains and immunostain for M1 (e.g., iNOS) and M2 (e.g., ARG1) microglial markers, apoptotic markers (e.g., TUNEL assay, Caspase-3), and human-specific markers to track transplanted cells.
- ELISA: Homogenize brain tissue from the injured hemisphere and quantify VEGF and BDNF levels using commercial ELISA kits.
- Long-term Functional Assessment (12 weeks):
- Morris Water Maze: Test spatial learning and memory over 5-7 days. Record escape latency and time spent in the target quadrant.
- Cylinder Test: Assess forelimb use asymmetry by counting the number of times the rat places its left vs. right forelimb on the cylinder wall during rearing.
- CatWalk Gait Analysis: Evaluate motor coordination and gait by having the rat walk across a glass plate and analyzing parameters like stride length and regularity index.
- Histology: Perform Hematoxylin-eosin (H&E) staining to quantify overall brain tissue damage and immunohistochemistry for neuronal (NeuN), oligodendrocyte (O4), and astrocyte (GFAP) markers to assess hNSC differentiation.
Diagram 2: Workflow for Evaluating hNSCs in a Rat HIE Model. This experimental workflow outlines the key steps from the induction of hypoxic-ischemic injury to long-term functional and histological assessment of therapeutic outcomes.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Stem Cell Studies in Neurological Injury
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Hypoxic Chamber | Creates a controlled, low-oxygen environment for cell preconditioning. | Preconditioning MSCs at 1-5% O₂ to enhance their paracrine function prior to transplantation [8]. |
| CD105, CD73, CD90 Antibodies | Positive surface markers for identifying and characterizing MSCs via flow cytometry. | Verifying MSC phenotype according to ISCT criteria before experimental use [18] [13]. |
| CD45, CD34, HLA-DR Antibodies | Negative surface markers for MSC characterization. | Confirming the absence of hematopoietic and endothelial cell contamination in MSC cultures [13]. |
| Anti-iNOS and Anti-ARG1 Antibodies | Immunohistochemistry markers for identifying pro-inflammatory M1 and anti-inflammatory M2 microglia, respectively. | Quantifying shifts in microglial polarization in brain tissue sections following stem cell therapy [38]. |
| Human VEGF & BDNF ELISA Kits | Quantify protein levels of critical paracrine factors in tissue homogenates or conditioned media. | Measuring the upregulation of neurotrophic and angiogenic factors in the brains of treated animals [38]. |
| Exosome Depletion Kit | Removes bovine exosomes from fetal bovine serum (FBS) used in cell culture. | Preparing "exosome-depleted" media for production of clean, research-grade MSC-derived exosomes [41]. |
| Neurobehavioral Testing Equipment (e.g., Water Maze, CatWalk) | Assess cognitive and motor function recovery in rodent models. | Evaluating the functional efficacy of stem cell treatments in models of HIE or TBI [38] [42]. |
Stem cell therapy, particularly when enhanced through hypoxic preconditioning, represents a transformative frontier in combating hypoxic-ischemic brain injury and cerebral edema. The evidence demonstrates that the strategic application of hypoxic stress to stem cells like MSCs and NSCs potently modulates their paracrine secretome, amplifying the release of factors and EVs that orchestrate neuroprotection, immunomodulation, angiogenesis, and BBB repair. While clinical translation is underway, as evidenced by early-phase trials combining MSCs with hypothermia for neonatal HIE [43], the future lies in refining these approaches. Further research must focus on standardizing preconditioning protocols, elucidating the precise roles of specific EV cargos, and developing off-the-shelf, cell-free therapies based on the critical paracrine factors identified. Integrating these advanced regenerative strategies holds the promise of significantly improving outcomes for patients suffering from these devastating neurological conditions.
Accelerated Wound Healing and Tissue Regeneration in Musculoskeletal and Cutaneous Models
The pursuit of advanced therapeutic strategies for accelerated wound healing and tissue regeneration represents a cornerstone of modern regenerative medicine. Chronic wounds, affecting over 6.5 million people in the U.S. alone with economic costs exceeding $25 billion annually, pose a significant clinical challenge that demands innovative solutions [44]. Within this landscape, the role of stem cells, particularly under hypoxic stress conditions, has emerged as a critical area of investigation. Hypoxic preconditioning of mesenchymal stem cells (MSCs) has been shown to significantly enhance their therapeutic potential by modulating their paracrine factor production, creating a more potent secretome that drives tissue repair processes [8]. This technical guide explores the sophisticated mechanisms through which hypoxic stress influences stem cell biology and its implications for advancing wound healing and tissue regeneration in musculoskeletal and cutaneous models, providing researchers and drug development professionals with a comprehensive framework for leveraging these mechanisms in therapeutic development.
Molecular Mechanisms of Hypoxic Stress on Stem Cell Paracrine Function
HIF-1α Signaling Pathway and Metabolic Reprogramming
The cellular response to hypoxia is centrally orchestrated by the hypoxia-inducible factor 1-alpha (HIF-1α), which serves as a master regulator of oxygen homeostasis. Under normoxic conditions, HIF-1α undergoes rapid proteasomal degradation following prolyl hydroxylation. However, under hypoxic conditions, HIF-1α stabilization occurs, leading to its translocation to the nucleus where it heterodimerizes with HIF-1β and activates transcription of numerous target genes [8]. This fundamental molecular switch drives the adaptive responses of stem cells to low oxygen tension.
Hypoxic preconditioning induces a significant metabolic reprogramming in MSCs, shifting their energy production from oxidative phosphorylation to glycolysis. This metabolic adaptation enhances cell survival under low oxygen conditions while simultaneously influencing their paracrine signature. The upregulation of glycolytic enzymes under HIF-1α control enables MSCs to maintain ATP production despite mitochondrial respiration limitations, ensuring their functionality in the typically hypoxic wound microenvironment [8]. This metabolic shift is not merely about energy conservation but represents a strategic reprogramming that enhances the stem cells' regenerative capabilities.
Enhanced Paracrine Secretion and Angiogenic Factor Production
The hypoxic secretome of MSCs demonstrates remarkable therapeutic potency, characterized by increased production of growth factors, cytokines, and extracellular vesicles (EVs). Hypoxia preconditioning significantly upregulates the expression of key angiogenic factors including vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), stromal cell-derived factor-1α (SDF-1α), and C-X-C chemokine receptor type 4 (CXCR4) [8]. These factors collectively promote angiogenesis—a critical process in wound healing that ensures adequate oxygen and nutrient supply to regenerating tissues.
Hypoxia also enhances the immunomodulatory properties of MSCs by suppressing pro-inflammatory cytokines (IL-6, IL-8) while increasing anti-inflammatory factors (IL-1ra, GM-CSF) [8]. This immunomodulatory shift creates a more favorable environment for tissue repair by reducing destructive inflammation while preserving the necessary immune signaling for regeneration. Furthermore, hypoxic conditions reduce senescence and apoptosis in MSCs by downregulating pro-apoptotic genes (BCL-2, CASP3), thereby extending their therapeutic window [8]. The combination of these effects results in a potentiated stem cell population capable of significantly enhancing the wound healing process through multiple synergistic mechanisms.
Figure 1: Hypoxic Stress Activation of Stem Cell Paracrine Signaling. This diagram illustrates the molecular pathway through which hypoxic stress enhances stem cell paracrine function, leading to improved tissue repair outcomes.
Quantitative Analysis of Hypoxia-Enhanced Therapeutic Effects
Comparative Efficacy of Hypoxic Preconditioning Strategies
Table 1: Quantitative Effects of Hypoxic Preconditioning on MSC Therapeutic Properties
| Therapeutic Parameter | Hypoxic Condition | Fold Change vs Normoxia | Functional Significance |
|---|---|---|---|
| VEGF Secretion | 1-5% O₂ for 24-48h | 2.5-3.5x increase | Enhanced angiogenesis and vascularization [8] |
| Exosome Production | 1-5% O₂ for 24-48h | 2.0-3.0x increase | Increased delivery of miRNA and bioactive factors [8] |
| Cell Proliferation Rate | 1-5% O₂ for 24-48h | 1.8-2.5x increase | Improved expansion and engraftment potential [8] |
| SDF-1α Expression | 1-5% O₂ for 24-48h | 2.0-2.8x increase | Enhanced homing to injury sites [8] |
| Anti-inflammatory Factor Production | 1-5% O₂ for 24-48h | 1.5-2.2x increase | Improved immunomodulation and reduced inflammation [8] |
| Cell Survival Post-Transplantation | 1-5% O₂ for 24-48h | 2.0-3.0x increase | Extended therapeutic window and durability [8] |
The data presented in Table 1 demonstrates the significant enhancement of key therapeutic properties of MSCs following hypoxic preconditioning. The optimal oxygen concentration for these effects ranges from 1-5% O₂, with exposure times typically less than 48 hours to avoid inducing cellular senescence and apoptosis [8]. The consistency in fold-changes across multiple studies indicates the robustness of hypoxic preconditioning as a method for potentiating MSC therapeutic efficacy. These quantitative improvements translate directly to enhanced functional outcomes in wound healing models, including accelerated re-epithelialization, improved granulation tissue formation, and enhanced neovascularization.
In Vivo Performance Metrics in Preclinical Models
Table 2: Wound Healing Outcomes with Hypoxia-Preconditioned Stem Cells in Preclinical Models
| Model System | Cell Type | Key Outcome Metrics | Significance vs Control |
|---|---|---|---|
| Porcine Burn Model | iPSC-derived MSCs | Accelerated wound closure; Enhanced epithelialization; Reduced contracture [45] | p<0.05 for 10K-iMSC group vs acellular Integra [45] |
| Murine Cutaneous Wound | Fetal Skin-derived Stem Cells (FSSCs) | Increased collagen secretion; Enhanced angiogenesis (CD31, VEGF); Regulated inflammatory mediators (TNF-α, IL-6) [46] | Superior to ADSCs in wound closure rate and protein expression [46] |
| Rat Hepatectomy Model | Hypoxia-preconditioned BM-MSCs | Enhanced liver regeneration; Upregulated VEGF levels [8] | Significant functional improvement vs normoxic MSCs [8] |
| Nonhuman Primate Myocardial Infarction | Hypoxia-preconditioned MSCs | Improved cardiac function; Reduced infarct size; No increased arrhythmogenic risks [8] | Superior outcomes attributed to enhanced paracrine activity [8] |
The in vivo data summarized in Table 2 demonstrates consistent and significant improvements in wound healing and tissue regeneration across multiple preclinical models and tissue types when using hypoxia-preconditioned stem cells. The porcine burn model results are particularly noteworthy, as porcine skin closely resembles human skin, providing strong translational evidence for the efficacy of this approach [45]. The performance of FSSCs over ADSCs in murine models highlights the importance of cell source selection, with fetal-derived cells demonstrating superior proliferation, migration, and collagen secretion capabilities [46]. The cardiac and liver regeneration models further support the broad applicability of hypoxia preconditioning across different regenerative contexts, underscoring the universal nature of the hypoxic response mechanism in enhancing stem cell efficacy.
Experimental Protocols for Hypoxic Preconditioning and Evaluation
Standardized Hypoxic Preconditioning Methodology
The following protocol details the optimal procedure for hypoxic preconditioning of MSCs for enhanced wound healing applications:
Cell Culture and Expansion:
- Isolate MSCs from desired tissue source (bone marrow, adipose tissue, umbilical cord, or iPSC-derived) and culture under standard conditions (37°C, 5% CO₂, 21% O₂) until 70-80% confluence [13] [45].
- Use validated MSC markers (CD105, CD73, CD90 ≥95%; CD34, CD45, CD14, CD19, HLA-DR ≤2%) to confirm cell identity prior to preconditioning [13].
- Culture cells in appropriate basal medium supplemented with 15% fetal bovine serum, 1% penicillin/streptomycin, and 1% L-glutamine [46].
Hypoxic Preconditioning Phase:
- At passage 3-5, transfer cells to a hypoxic chamber or multi-gas incubator capable of maintaining precise oxygen control.
- Set oxygen concentration to 1-5% O₂, with 5% CO₂, and balance N₂ for optimal preconditioning [8].
- Maintain cells under hypoxic conditions for 24-48 hours. Exposure beyond 48 hours may induce senescence and reduce therapeutic efficacy [8].
- During preconditioning, monitor cell morphology and confluence. Hypoxic MSCs typically maintain spindle-shaped morphology but may exhibit enhanced proliferation rates [8].
Post-Preconditioning Processing:
- For direct cell therapy: Harvest cells using standard trypsinization procedures and resuspend in appropriate delivery vehicle at desired concentration for in vivo administration.
- For conditioned medium collection: Replace medium 24 hours before harvest, collect supernatant, and centrifuge (2,000 × g for 10 minutes) to remove cellular debris.
- For exosome isolation: Ultracentrifuge conditioned medium at 100,000 × g for 70 minutes to pellet exosomes, then resuspend in PBS or appropriate buffer [8].
- Validate preconditioning efficacy through HIF-1α immunostaining or Western blot analysis, and quantify VEGF secretion via ELISA to confirm enhanced paracrine function.
In Vivo Evaluation in Porcine Burn Model
The porcine thermal injury model represents a clinically relevant system for evaluating the efficacy of hypoxia-preconditioned stem cells for wound healing applications:
Burn Creation and Cell Application:
- Create full-thickness excisional wounds (5 × 5 cm) on porcine skin following appropriate ethical approvals and anesthetic protocols [45].
- Incorporate hypoxia-preconditioned MSCs into Integra Dermal Regeneration Template at densities ranging from 5,000-20,000 cells/cm² [45].
- Apply cell-seeded scaffolds to wound beds and secure with appropriate surgical dressing.
- Include control groups: burn alone, acellular Integra, and normoxic MSC-seeded Integra for comparative analysis.
Assessment Timeline and Outcome Measures:
- Monitor wound closure daily through photographic documentation and planimetric analysis.
- Assess re-epithelialization between days 10-14 post-application after removal of the silicone layer [45].
- Evaluate healing outcomes at day 40 through histopathological analysis of tissue samples collected at sacrifice.
- Quantify granulation tissue formation, neovascularization (CD31 immunohistochemistry), collagen deposition (Masson's trichrome), and fibrosis markers (α-SMA, TGF-β) [45].
- Assess scar quality using Vancouver Scar Scale (VSS) scoring and measure wound contracture rates [45].
This comprehensive protocol enables rigorous evaluation of hypoxia-preconditioned stem cells in a translational model system, providing critical preclinical data for therapeutic development.
Figure 2: Experimental Workflow for Hypoxic Preconditioning and Evaluation. This diagram outlines the standardized methodology for hypoxic preconditioning of MSCs and their subsequent evaluation in preclinical models.
Advanced Therapeutic Applications and Engineering Approaches
Innovative Delivery Systems and Engineered Constructs
The translation of hypoxia-preconditioned stem cells into clinical applications requires sophisticated delivery systems that maintain cell viability and function while facilitating integration into the wound environment. Several advanced approaches have demonstrated significant promise:
Nanogenerator-Driven Electrostimulation Bandages:
- This cutting-edge technology utilizes wearable nanogenerators that convert motion-generated energy into therapeutic electrical currents [44].
- The self-powered electrostimulation promotes wound healing through enhanced tissue regeneration and accelerated healing processes without requiring external power sources or bulky batteries [44].
- These disposable, over-the-counter bandage designs represent a low-cost, sustainable approach suitable for worldwide use, including resource-limited settings [44].
Scaffold-Based Delivery Systems:
- Integra Dermal Regeneration Template serves as an effective scaffold for stem cell delivery, providing a bovine collagen I matrix cross-linked with shark cartilage that supports cellular growth and tissue synthesis [45].
- Alternative biomaterials include polynucleotide-hyaluronic acid (PN-HA) mixtures that demonstrate superior mechanical stability and enhance fibroblast and keratinocyte migration, proliferation, and VEGF expression [47].
- Three-dimensional bioprinting approaches enable precise spatial arrangement of multiple cell types within biomaterial scaffolds, creating complex tissue architectures that more closely mimic native skin [48].
Engineered Cell Constructs:
- Induced pluripotent stem cell-derived MSCs (iMSCs) offer significant advantages over primary MSCs, including unlimited expansion capacity and consistent therapeutic properties [45].
- Genetic modification of MSCs to overexpress specific factors such as miR-146a or miR-126 further enhances their immunomodulatory and angiogenic capabilities, particularly when combined with hypoxic preconditioning [18].
- Fetal skin-derived stem cells (FSSCs) demonstrate superior therapeutic potential compared to adult stem cells, with enhanced proliferation, migration, collagen secretion, and angiogenic promotion capabilities [46].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Hypoxia and Wound Healing Research
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Stem Cell Sources | BM-MSCs, AD-MSCs, UC-MSCs, FSSCs, iMSCs [46] [13] [45] | Comparative efficacy studies | Provide cellular platforms with varying proliferation, differentiation, and paracrine activity |
| Hypoxia Culture Systems | Multi-gas incubators, hypoxia chambers, hypoxia mimetics (CoCl₂, DFO) [8] | Hypoxic preconditioning protocols | Enable precise control of oxygen tension to mimic physiological niches |
| Characterization Antibodies | CD105, CD73, CD90, CD34, CD45, CD14, HLA-DR [46] [13] | MSC identification and validation | Verify MSC identity and purity according to ISCT standards |
| Scaffold Materials | Integra Dermal Template, PN-HA hydrogels, collagen matrices [47] [45] | 3D culture and in vivo delivery | Provide structural support for cell attachment, proliferation, and tissue integration |
| Angiogenesis Assays | HUVEC tube formation, CD31 IHC, VEGF ELISA [46] [47] | Assessment of neovascularization | Quantify blood vessel formation and angiogenic factor secretion |
| Molecular Analysis Tools | HIF-1α antibodies, miRNA assays, extracellular vesicle isolation kits [18] [8] | Mechanism investigation | Elucidate molecular pathways underlying hypoxic preconditioning effects |
This comprehensive toolkit enables researchers to rigorously investigate the effects of hypoxic stress on stem cell function and develop advanced therapeutic strategies for wound healing and tissue regeneration. The selection of appropriate reagents and systems should be guided by specific research questions and intended applications, with particular attention to validation and quality control measures.
The strategic application of hypoxic stress to enhance stem cell paracrine function represents a paradigm shift in regenerative medicine approaches to accelerated wound healing and tissue regeneration. The molecular mechanisms centered on HIF-1α stabilization and metabolic reprogramming create a potentiated cellular therapeutic with enhanced angiogenic, immunomodulatory, and regenerative capabilities. The consistent quantitative improvements observed across multiple preclinical models, combined with advanced delivery platforms and engineering approaches, provide a robust foundation for clinical translation. As research continues to refine hypoxic preconditioning protocols and elucidate the complex mechanisms underlying its benefits, the potential for developing highly effective, standardized therapies for complex wounds and tissue defects continues to expand. The integration of these approaches with emerging technologies in biomaterials, genetic engineering, and monitoring systems promises to further accelerate the development of next-generation regenerative therapies with significant clinical impact.
Navigating Translational Hurdles: Safety, Standardization, and Scalability
The therapeutic potential of stem cells, particularly mesenchymal stem cells (MSCs), is significantly influenced by their microenvironment, with oxygen tension being a critical determinant. Hypoxic preconditioning has emerged as a powerful strategy to enhance the therapeutic efficacy of MSCs by mimicking their physiological niche, which typically ranges from 1% to 7% O₂, significantly lower than the 21% O₂ found in standard atmospheric culture conditions [9]. This approach leverages the cells' innate adaptive mechanisms to enhance their survival, paracrine activity, and regenerative properties post-transplantation. However, the implementation of hypoxia is a delicate balancing act. While moderate hypoxia can enhance stem cell function, severe hypoxia (<1% O₂) acts as a potent stressor, triggering cascades that lead to cellular senescence and apoptosis, ultimately compromising therapeutic outcomes [9] [49]. This technical guide explores the mechanisms underlying this dichotomy and provides a detailed framework for researchers to optimize hypoxic protocols, thereby avoiding these critical pitfalls while maximizing the beneficial paracrine functions of stem cells.
The core of this balance lies in the cellular response to oxygen sensing. The hypoxia-inducible factor 1-alpha (HIF-1α) is the master regulator of this response. Under normoxic conditions, HIF-1α is continuously synthesized and degraded. In hypoxia, HIF-1α stabilization initiates a transcriptional program promoting cell survival, metabolic adaptation, and pro-angiogenic factor secretion [9] [3]. Yet, under severe or prolonged oxygen deprivation, the same signaling axes can devolve, activating DNA damage responses, disrupting redox homeostasis, and inducing irreversible cell cycle arrest or programmed cell death [50] [49]. For research focused on the modulation of paracrine factor production, understanding and controlling these thresholds is indispensable, as the secretory profile of stem cells—the very mediator of their therapeutic effect—is exquisitely sensitive to these stress pathways.
Molecular Mechanisms: The Fine Line Between Adaptation and Damage
HIF-1α: Master Regulator at the Crossroads
The cellular response to hypoxia is predominantly orchestrated by the transcription factor HIF-1α. Its role is pivotal in determining whether a cell adapts and thrives or enters senescence and apoptosis.
Stabilization and Adaptive Signaling: Under hypoxic conditions, HIF-1α protein is stabilized, dimerizes with HIF-1β, and translocates to the nucleus. Here, it binds to Hypoxia Response Elements (HREs), activating a battery of genes crucial for adaptation. Key targets include genes involved in glycolytic metabolism (e.g., PDK1, HK2, Glut1), angiogenesis (e.g., VEGF), and cell survival [9] [3]. This metabolic shift from oxidative phosphorylation to glycolysis reduces mitochondrial reactive oxygen species (ROS) generation, thereby mitigating oxidative stress and promoting survival in a low-oxygen environment [3].
Transition to Pathological Signaling: However, in severe hypoxia, the sustained and intense activation of HIF-1α can paradoxically contribute to negative outcomes. It can engage in complex cross-talk with other stress-responsive pathways, such as the DNA damage response (DDR) and ROS signaling networks, which can promote the expression of cyclin-dependent kinase inhibitors like p21CIP1, leading to cell cycle arrest and the initiation of senescence [49]. The precise molecular context, including cell type, hypoxia severity, and exposure duration, dictates this shift from pro-survival to pro-senescence signaling.
Oxidative Stress and Metabolic Crisis
A central mechanism underpinning hypoxia-induced senescence and apoptosis is the disruption of redox homeostasis.
ROS Generation and Consequences: While moderate hypoxia may initially reduce ROS, severe hypoxia can lead to a paradoxical burst of ROS, particularly from dysfunctional mitochondria [50] [3]. Excessive ROS causes oxidative stress, damaging lipids, proteins, and DNA. This macromolecular damage acts as a potent trigger for both senescence, via the p53-p21 axis, and intrinsic apoptosis [50].
Antioxidant Defense Failure: The transition to a senescent or apoptotic state often coincides with the failure of cellular antioxidant systems, such as the Nrf2/Keap1/ARE pathway [50]. When this critical defense system is overwhelmed, the cell becomes vulnerable to oxidative damage.
Activation of Senescence and Apoptotic Programs
The culmination of the aforementioned stresses is the activation of definitive executers of cell fate.
Cellular Senescence: This is a state of stable, irreversible cell cycle arrest. Hypoxia-induced senescence is characterized by the upregulation of senescence-associated β-galactosidase (SA-β-gal) activity, formation of senescence-associated heterochromatin foci (SAHFs), and a distinct senescence-associated secretory phenotype (SASP) [49]. The SASP involves the secretion of pro-inflammatory cytokines, growth factors, and proteases, which can have deleterious paracrine effects on the surrounding tissue microenvironment [49].
Apoptosis Activation: When damage is too severe to be compatible with a viable senescent state, apoptosis is initiated. Severe hypoxia can trigger the mitochondrial (intrinsic) apoptotic pathway, characterized by increased mitochondrial membrane permeability and the release of cytochrome c, leading to caspase activation and programmed cell death [9] [50]. The balance between pro-survival (e.g., BCL-2, BCL-xL) and pro-apoptotic (e.g., BAX) BCL-2 family proteins is crucial in determining the threshold for apoptosis, and this balance is disrupted under severe hypoxic stress [49].
Table 1: Key Molecular Players in Hypoxia-Induced Adaptation vs. Damage
| Molecular Component | Function | Role in Adaptation (Moderate Hypoxia) | Role in Damage (Severe Hypoxia) |
|---|---|---|---|
| HIF-1α | Master transcription factor | Stabilized, promotes glycolysis, angiogenesis, & survival [9] [3] | Sustained activation can promote senescence via p21 and disrupt redox balance [49] |
| Mitochondrial ROS | Signaling molecules & damaging agents | Levels may be controlled; signal for adaptation [3] | Paradoxical burst causes oxidative damage, triggers DDR & apoptosis [50] [3] |
| p53/p21 | Tumor suppressor / CDK inhibitor | Minimally activated | Strongly induced, leading to cell cycle arrest and senescence [49] |
| BCL-2 Family | Apoptosis regulators | Pro-survival members (BCL-2, BCL-xL) dominate [49] | Pro-apoptotic members (BAX) activated, triggering caspase-mediated apoptosis [50] |
| SASP | Secretory phenotype | Not typically induced | Secretion of pro-inflammatory factors (IL-6, IL-8), altering tissue microenvironment [49] |
Critical Experimental Parameters for Controlling Cell Fate
The fate of stem cells under hypoxia is not random but is determined by specific, controllable experimental variables. Meticulous optimization of these parameters is essential to steer cells toward a therapeutic phenotype and away from senescence or apoptosis.
Oxygen Concentration and Exposure Duration
The intensity and length of hypoxic exposure are the most critical factors.
Physiological vs. Severe Hypoxia: Most MSC niches (bone marrow, adipose tissue) exist at ~2-7% O₂, making this a logical starting point for preconditioning [9]. Exposure to 1-5% O₂ for 24-48 hours has been widely shown to enhance MSC proliferation, colony-forming potential, and pro-angiogenic secretome without inducing significant death or senescence [9]. In contrast, exposure to <1% O₂ (severe hypoxia) consistently leads to negative outcomes, including the onset of senescence and apoptosis [9].
Temporal Dynamics: The duration of exposure is equally crucial. Studies suggest that the optimal exposure time is less than 48 hours, which is sufficient to activate protective mechanisms like HIF-1α and its targets. Longer exposures, even at moderate oxygen levels, can trigger accelerated cellular aging and reduce therapeutic efficacy [9] [49]. Shorter, cyclical hypoxic conditioning (e.g., 12-24 hours) may be a safer and more effective strategy than continuous long-term exposure.
Monitoring Senescence and Apoptosis Markers
Rigorous assessment of cell fate is necessary to validate any hypoxic protocol.
Senescence Assays: Standard assays include:
- Senescence-Associated β-Galactosidase (SA-β-gal) Staining: A hallmark histochemical marker for senescent cells, detectable at pH 6.0 [50] [49].
- Gene Expression Analysis: Quantification of mRNA levels for key senescence effectors like p16INK4a and p21CIP1 [49].
- SASP Factor Detection: Measurement of secreted SASP components such as IL-6 and IL-8 via ELISA or multiplex assays [49].
Apoptosis Assays: Standard methods include:
- Flow Cytometry: Using Annexin V/propidium iodide (PI) staining to distinguish early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) cells.
- Caspase Activity Assays: Fluorometric or colorimetric kits to measure the activation of executioner caspases-3 and -7.
- DNA Fragmentation Analysis: TUNEL (Terminal deoxynucleotidyl transferase dUTP nick end labeling) assay to detect apoptotic DNA breaks [3].
Table 2: Optimizing Hypoxic Preconditioning Parameters to Avoid Senescence and Apoptosis
| Parameter | Recommended Range for Benefit | Risk Range for Senescence/Apoptosis | Key Assays for Monitoring |
|---|---|---|---|
| Oxygen Concentration | 1% - 5% O₂ [9] | <1% O₂ (Severe Hypoxia) [9] | O₂ probe in culture medium, HIF-1α immunoblotting [3] |
| Exposure Duration | 24 - 48 hours [9] | >48 hours (Prolonged exposure) [9] | SA-β-gal staining, Annexin V/PI flow cytometry [50] [49] |
| Cell Confluence | 70-80% (Logarithmic growth) | 100% (Contact inhibition, nutrient depletion) | Microscopy, cell counting [9] |
| Serum Concentration | 2-10% (Serum-reduced may enhance paracrine effects) | 0% (Serum starvation stress) | Viability assays (CCK-8, MTS), LDH release assay [3] |
| Post-Hypoxia Analysis | 24-72 hours after re-oxygenation | Immediate analysis may miss delayed apoptosis | TUNEL assay, caspase-3/7 activity, SASP cytokine array [3] [49] |
Detailed Experimental Protocols for Hypoxic Preconditioning
Standardized Protocol for MSC Hypoxic Preconditioning
This protocol is designed to enhance the paracrine function of MSCs while minimizing the risk of senescence and apoptosis.
Materials:
- Cell Type: Human adipose-derived MSCs (ASCs) or bone marrow-derived MSCs (BM-MSCs), passages 3-6.
- Equipment: Tri-gas incubator (e.g., Heraeus HERAcell 150) or modular hypoxia chamber (e.g., GENbox Jar from bioMérieux) capable of maintaining 1% O₂, 5% CO₂, and balance N₂.
- Culture Media: Serum-free basal medium (e.g., DMEM-low glucose) [16].
Methodology:
- Cell Seeding: Seed MSCs at a density of ~5,000 cells/cm² in standard growth medium and allow them to adhere overnight in a normoxic (21% O₂, 5% CO₂) incubator at 37°C.
- Preconditioning Initiation: Once cells reach 70-80% confluence, replace the growth medium with serum-free medium. Place the culture flasks/plates into the pre-equilibrated hypoxic incubator or chamber set to 1% O₂ and 5% CO₂ at 37°C.
- Hypoxic Exposure: Maintain the cells under hypoxia for 24 hours. This duration has been shown to significantly upregulate pro-angiogenic factors like VEGF and angiogenin without inducing widespread senescence [16].
- Collection of Conditioned Medium (CM): After 24 hours, collect the CM. Centrifuge at 875g for 10 minutes to remove cell debris, and filter through a 0.2-μm filter. The CM can be concentrated using centrifugal filter units (e.g., Amicon Ultra-15, 3 kDa cutoff) and stored at -80°C for later analysis of paracrine factors [16].
- Cell Harvesting and Analysis: To assess the cells themselves, harvest them using standard trypsinization. Perform immediate analyses for viability (Trypan Blue exclusion), apoptosis (Annexin V/PI flow cytometry), and senescence (SA-β-gal staining). For molecular analyses, lyse cells for RNA/protein extraction to quantify HIF-1α, metabolic genes (PDK1, GLUT1), and senescence markers (p16, p21) [3].
Protocol for Assessing HIF-1α Dependency Using siRNA Knockdown
To conclusively link observed effects to HIF-1α signaling, a loss-of-function approach is essential.
Materials:
- Cells: Stem cells from human exfoliated deciduous teeth (SHED) or MSCs.
- Reagents: Pre-made HIF-1α siRNA (e.g., Silencer Select from Thermo Scientific), negative control siRNA, lipofectamine 3000 transfection reagent, Opti-MEM reduced serum medium.
Methodology:
- Transfection: Seed cells in 6-well plates. At 70-90% confluency, transfert with HIF-1α siRNA or control siRNA (e.g., 50-100 nM final concentration) using lipofectamine 3000 in Opti-MEM according to the manufacturer's protocol.
- Hypoxic Exposure: 48 hours post-transfection, replace the medium with serum-free medium and expose the cells to hypoxia (1% O₂) for 24 hours.
- Validation and Analysis: Confirm HIF-1α knockdown efficiency via western blotting or immunofluorescence. Subsequently, analyze the cells for:
- Viability under stress: Use CCK-8 assay under hypoxia, H₂O₂-induced oxidative stress, or low-glucose conditions [3].
- ROS levels: Measure cytoplasmic and mitochondrial ROS using CM-H2DCFDA and MitoSOX Red dyes, respectively [3].
- Paracrine function: Collect CM and measure VEGF secretion by ELISA. Test the functional impact of the CM on endothelial cell (e.g., HUVEC) proliferation and migration [3].
- In vivo survival and angiogenesis: Use an in vivo Matrigel plug assay in immunodeficient mice to compare the survival and angiogenic capacity of siHIF-1α vs. siControl cells [3].
Table 3: Research Reagent Solutions for Hypoxic Stress Studies
| Reagent / Tool | Function & Application | Example & Brief Explanation |
|---|---|---|
| HIF-1α Stabilizer | Mimics hypoxia by inhibiting PHD enzymes, stabilizing HIF-1α. | Dimethyloxalylglycine (DMOG): A cell-permeable competitive inhibitor of HIF prolyl hydroxylases, used to activate HIF-dependent signaling under normoxia. |
| HIF-1α Inhibitor | Chemically inhibits HIF-1α accumulation or function. | YC-1 (3-(5'-Hydroxymethyl-2'-furyl)-1-benzyl indazole): Prevents HIF-1α accumulation in response to hypoxia, used to confirm HIF-1α-specific effects [3]. |
| siRNA/shRNA | Genetically knocks down gene expression to establish functional necessity. | HIF-1α siRNA: Validated siRNA pools for efficient knockdown of HIF-1α, crucial for loss-of-function studies to delineate its role in survival and paracrine signaling [3]. |
| ROS Probes | Detect and quantify intracellular and mitochondrial reactive oxygen species. | CM-H2DCFDA (Cellular ROS) & MitoSOX Red (Mitochondrial ROS): Fluorogenic dyes used in flow cytometry or fluorescence microscopy to measure oxidative stress levels under hypoxia [3]. |
| Hypoxia Chamber | Creates a controlled, low-oxygen environment for cell culture. | GENbox Jar with AnaeroGen sachets: A sealed, modular system that rapidly reduces O₂ to <0.1%, suitable for experiments requiring severe hypoxia without a dedicated incubator [16]. |
| Senescence Detector | Histochemical stain to identify senescent cells. | SA-β-gal Staining Kit: A common kit to detect senescence-associated β-galactosidase activity at pH 6.0, a widely accepted biomarker for cellular senescence [50] [49]. |
| Apoptosis Detector | Flow cytometry assay to quantify apoptotic cell populations. | Annexin V-FITC / PI Apoptosis Detection Kit: Allows discrimination between viable (Annexin-/PI-), early apoptotic (Annexin+/PI-), and late apoptotic/necrotic (Annexin+/PI+) cells. |
Signaling Pathways and Experimental Workflows
HIF-1α Signaling Pathway in Hypoxic Stress
The diagram below illustrates the central role of HIF-1α in mediating the cellular response to hypoxia, highlighting its dual potential to drive both adaptive and detrimental outcomes.
HIF-1α Pathway Fate Decision. This diagram outlines how hypoxic stress, mediated by HIF-1α stabilization, can lead to divergent cellular outcomes. The specific path is determined by key experimental parameters such as oxygen severity and exposure duration [9] [3] [49].
Experimental Workflow for Hypoxic Preconditioning
The following workflow provides a logical roadmap for designing and executing a hypoxic preconditioning study, from initial setup to downstream functional validation.
Hypoxic Preconditioning Workflow. This chart details the sequential steps for a standard hypoxic preconditioning experiment, culminating in the parallel analysis of the secreted paracrine factors and the preconditioned cells themselves, with optional in vivo functional validation [3] [16].
The therapeutic efficacy of mesenchymal stem cells (MSCs) is significantly influenced by their response to hypoxia, a critical component of their native niche and pathological target environments. However, MSCs are not a uniform population; their biological behavior and functional output under low oxygen tension vary considerably depending on their tissue of origin. This technical guide examines the source-dependent variations in hypoxic response among bone marrow-derived MSCs (BM-MSCs), adipose tissue-derived MSCs (AD-MSCs), and amniotic fluid-derived stem cells (AFSCs), with particular emphasis on implications for paracrine factor production. Understanding this heterogeneity is essential for optimizing cell-based therapeutic strategies and manufacturing protocols, especially within the broader context of manipulating hypoxic stress to enhance stem cell secretome production.
Biological Mechanisms of Hypoxic Response in MSCs
The Central Role of HIF-1α Signaling
The cellular response to hypoxia is primarily mediated by the hypoxia-inducible factor (HIF) pathway, with HIF-1α serving as the master regulator. Under normoxic conditions, HIF-1α subunits are continuously synthesized but rapidly degraded by prolyl hydroxylase domain (PHD) enzymes and the ubiquitin-proteasome system. Under hypoxic conditions, this degradation is inhibited, allowing HIF-1α to accumulate, dimerize with HIF-1β, and translocate to the nucleus where it binds to hypoxia-response elements (HREs), activating transcription of numerous target genes [51] [8].
The stabilization of HIF-1α initiates a complex transcriptional program that influences diverse cellular processes including metabolism, angiogenesis, proliferation, and survival. This pathway is conserved across MSC sources, though the magnitude and specific outcomes of its activation demonstrate source-dependent characteristics [51].
Table 1: Key Genes Regulated by HIF-1α Stabilization in MSCs
| Functional Category | Gene Targets | Functional Consequences |
|---|---|---|
| Angiogenesis | VEGF, SDF-1α | Enhanced neovascularization and endothelial cell recruitment [52] [8] |
| Metabolic Reprogramming | GLUT-1, Glycolytic enzymes | Shift from oxidative phosphorylation to glycolysis [51] |
| Cell Survival & Proliferation | TWIST, CXCR4, Survivin | Inhibition of senescence, enhanced proliferation, and improved survival post-transplantation [51] [8] |
| Immunomodulation | IL-6, IL-1ra, GM-CSF | Modulation of macrophage polarization and inflammatory cytokine secretion [18] |
Signaling Pathway Diagram
The following diagram illustrates the core HIF-1α signaling pathway and its downstream effects on MSC biology under hypoxic conditions:
Comparative Analysis of MSC Source-Dependent Variations
Proliferation and Expansion Kinetics
The impact of hypoxia on proliferation capacity demonstrates significant variation across MSC sources, influenced by factors including donor age, tissue origin, and culture conditions.
Table 2: Source-Dependent Proliferation Responses to Hypoxia
| MSC Source | Proliferation Response to Hypoxia | Oxygen Tension | Experimental Context |
|---|---|---|---|
| BM-MSCs | Conflicting reported effects (inhibition to 30-fold increase); long-term culture shows consistent benefits [51] | 1%-7% O₂ | Varies with seeding density, passage number, and culture duration [51] [53] |
| AD-MSCs | Promoted in murine and human models [54] [51] | 2% O₂ | 14-day culture at 3,000 cells/cm² [51] |
| AFSCs | Significantly faster proliferation than normoxic controls [54] | 1% O₂ | Comparative in vitro analysis of multiple MSC sources [54] |
| Umbilical Cord MSCs | Significantly faster proliferation than normoxic controls [54] | 1% O₂ | Comparative in vitro analysis of multiple MSC sources [54] |
A 2014 comparative study provided direct evidence of source-dependent proliferation, demonstrating that only prenatal-derived MSCs (AFSCs and umbilical cord blood MSCs) exhibited significantly faster proliferation under 1% O₂ compared to normoxia. This effect was most robust in AFSCs and correlated with increased HIF-1α expression [54]. For BM-MSCs, long-term hypoxic culture (up to 60 days) inhibits senescence and increases expansion efficiency, despite potential inhibitory effects in short-term culture [51] [53].
Paracrine Factor Production and Secretome Composition
Hypoxia potently modulates the paracrine activity of MSCs, enhancing the secretion of factors that promote angiogenesis, tissue repair, and immunomodulation. These effects also vary by cell source.
Table 3: Source-Specific Paracrine Responses to Hypoxia
| Secreted Factor / Process | BM-MSC Response | AD-MSC Response | AFSC Response |
|---|---|---|---|
| VEGF Upregulation | Documented increase [52] | 5-fold increase documented [52] | Increased HIF1-α expression linked to proliferation [54] |
| Exosome/EV Production | Increased secretion & angiogenic potential via HIF-1α [18] | Altered EV size profile & miRNA content [55] | Information not specified in search results |
| Immunomodulatory Capacity | Enhanced via macrophage polarization to M2 phenotype [18] | Information not specified in search results | Information not specified in search results |
| Key Molecular Findings | miR-146a enrichment in exosomes promotes M2 polarization [18] | Low-dose hypoxic EVs efficient in cartilage repair [55] | Correlation between HIF1-α expression and enhanced proliferation [54] |
Hypoxic preconditioning not only increases the quantity of secreted factors but also alters the quality of the secretome. For AD-MSCs, the beneficial effects of the hypoxic secretome on articular cartilage repair were associated primarily with extracellular vesicles (EVs) rather than soluble factors. These hypoxia-conditioned EVs displayed an altered size profile and enriched miRNA contents, making them more efficacious at promoting chondrocyte migration and matrix deposition while inhibiting inflammation at lower doses [55].
Differentiation Potential
The effect of hypoxia on differentiation capacity is perhaps the most context-dependent, varying by MSC source, oxygen tension, and target lineage.
- Chondrogenesis: Hypoxia (typically 2-5% O₂) generally promotes chondrogenic differentiation across MSC sources, enhancing production of cartilage matrix proteins like collagen II. This is consistent with the avascular, low-oxygen nature of native cartilage (1-8% O₂) [52] [56].
- Osteogenesis: Responses are mixed. Some studies report hypoxia (5% O₂) enhances osteogenic markers in rat BM-MSCs, while others (2% O₂) inhibit osteogenesis in AD-MSCs [52].
- Adipogenesis: Similarly conflicting data exist, with hypoxia inducing an adipose phenotype in BM-MSCs in one study while inhibiting adipogenesis in AD-MSCs in another [52].
Transcriptome analysis of BM-MSCs cultured at 5% O₂ revealed upregulation of genes associated with chondrogenesis and cartilage metabolism, suggesting hypoxia promotes a cartilage-primed phenotype, which is advantageous for orthopedic applications [56].
Experimental Protocols for Assessing Hypoxic Responses
Standardized Hypoxic Culture Methodology
To ensure reproducible and physiologically relevant results, researchers must implement careful control of oxygen tensions throughout culture protocols.
Essential Equipment:
- Hypoxic incubator or modular chamber system capable of maintaining precise O₂ levels (typically 1-5% O₂)
- Oxygen sensor for continuous monitoring
- Pre-equilibrated culture media to prevent transient reoxygenation during feeding
Critical Protocol Considerations:
- Media Pre-equilibration: Culture media must be pre-equilibrated in the hypoxic environment for at least 24 hours before use to achieve proper oxygen tension and pH balance. Transient reoxygenation during medium changes can nullify hypoxic effects [51].
- Seeding Density Optimization: Proliferation responses to hypoxia are density-dependent. Lower seeding densities (e.g., 50-500 cells/cm²) often better demonstrate pro-proliferative effects [51].
- Exposure Duration: For therapeutic preconditioning, studies suggest optimal exposure is less than 48 hours to activate protective mechanisms without causing senescence [8].
Experimental Workflow for Comparative Studies
The following diagram outlines a standardized workflow for comparing hypoxic responses across different MSC sources:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Hypoxic MSC Studies
| Reagent/Category | Specific Examples | Research Application | Considerations |
|---|---|---|---|
| Hypoxia Mimetics | Cobalt Chloride (CoCl₂), Desferrioxamine (DFX) [51] [57] | Chemical induction of HIF-1α stabilization; alternative to chamber hypoxia | May not fully recapitulate all aspects of physiological hypoxia [51] |
| Cell Culture Media | DMEM low glucose, MEM-α [56] | Basal media for MSC expansion | Supplementation with 10% human platelet lysate or FBS required [56] |
| Differentiation Kits | StemPro Adipogenesis/Osteogenesis/Chondrogenesis Kits [56] | Standardized assessment of trilineage potential | Chondrogenesis typically performed in 3D pellet culture [56] |
| Hypoxia Reporters | HIF-1α antibodies, HRE-luciferase constructs | Quantification of HIF pathway activation | Western blot, immunofluorescence, or luciferase assays [51] |
| EV/Exosome Isolation | Ultracentrifugation, Size-exclusion chromatography, Precipitation kits [18] [55] | Isolation of paracrine factors from conditioned media | Characterization of size (NTA) and markers (CD63, CD81) required [18] |
The heterogeneity in hypoxic response among BM-MSCs, AD-MSCs, and AFSCs underscores the necessity of source-specific optimization in both basic research and clinical translation. Key variations in proliferation kinetics, paracrine factor production, and differentiation potential directly impact therapeutic efficacy, particularly for applications targeting ischemic tissues or relying on robust secretome production. AFSCs and other perinatal sources demonstrate enhanced proliferative capacity under hypoxia, while BM-MSCs and AD-MSCs show distinct secretome profiles that can be therapeutically exploited. Future research should prioritize the development of standardized hypoxic culture protocols that account for these source-dependent variations, with particular emphasis on clinical-grade manufacturing for cell-based therapies. The strategic selection of MSC sources based on their inherent hypoxic response profiles will significantly advance the field of regenerative medicine, enabling more predictable and potent therapeutic outcomes.
Within the broader thesis on hypoxic stress effect on stem cell paracrine factor production research, a critical translational challenge emerges: the standardization of quality attributes for hypoxia-preconditioned products. The foundational paradigm in regenerative medicine has shifted from considering mesenchymal stem cells (MSCs) as primarily differentiation-capable units to recognizing them as paracrine powerhouses that secrete bioactive factors to modulate inflammation, promote tissue repair, and support regeneration [9]. This paracrine effect is profoundly enhanced through hypoxic preconditioning—a culture strategy that mimics the physiological oxygen conditions (typically 2%-8% O₂) of their native niches, as opposed to conventional normoxic culture (21% O₂) [9] [58].
However, this advanced preparation technique introduces substantial complexity into manufacturing and quality control. The very adaptability of MSCs to hypoxia—mediated through metabolic reprogramming, transcriptional changes, and altered secretome composition—creates a moving target for standardization [9] [59]. This technical guide examines the critical quality attributes (CQAs) that must be defined to ensure the consistent therapeutic efficacy of hypoxia-preconditioned MSC products, focusing specifically on their paracrine factor production capabilities within the context of modern biomanufacturing requirements.
Metabolic and Functional Changes Induced by Hypoxic Preconditioning
Hypoxic preconditioning triggers a fundamental reprogramming of MSC biology centered around the stabilization of hypoxia-inducible factor-1α (HIF-1α), which acts as a master regulator of cellular response to low oxygen [9] [60]. This metabolic shift enhances what researchers term the "therapeutic potential" of MSCs through multiple interconnected mechanisms:
- Enhanced paracrine activity: Hypoxia preconditioning significantly increases the production of pro-angiogenic factors including vascular endothelial growth factor (VEGF), stromal cell-derived factor-1α (SDF-1α), and other tissue-repair mediators [9].
- Improved survival and engraftment: Preconditioned MSCs demonstrate upregulation of anti-apoptotic proteins and enhanced resistance to the harsh inflammatory environments of damaged tissue post-transplantation [61].
- Modified secretome composition: The production and cargo loading of extracellular vesicles (EVs) and exosomes are substantially altered, with significant changes in their miRNA profiles and protein content [59] [58].
Table 1: Key Functional Enhancements in Hypoxia-Preconditioned MSCs
| Functional Attribute | Hypoxia-Induced Change | Mechanistic Basis | Therapeutic Impact |
|---|---|---|---|
| Angiogenic Potential | Significant increase | HIF-1α-mediated VEGF upregulation | Improved vascularization in ischemic tissues |
| Cell Survival Post-Transplantation | 1.5-2 fold increase | Enhanced anti-apoptotic protein expression (Bcl-xL, Bcl-2) | Better engraftment in hostile microenvironments |
| Immunomodulatory Capacity | Variable enhancement | Increased PGE2, TSG-6, IDO production | Superior inflammation resolution in immune diseases |
| Migratory/Homing Ability | Significantly improved | CXCR4 receptor upregulation | Enhanced targeting to injury sites |
The timing and severity of hypoxia exposure are critical parameters determining therapeutic efficacy. Studies consistently indicate that exposure under 48 hours with oxygen concentrations typically ranging from 2%-5% activates protective mechanisms without triggering significant cellular damage or senescence [9]. However, extreme hypoxia (<1% O₂) or prolonged exposure negatively impacts MSC viability and function, underscoring the delicate balance required in preconditioning protocols [9].
Critical Quality Attributes for Hypoxia-Preconditioned MSC Products
Defining the CQA Landscape
Establishing CQAs for hypoxia-preconditioned MSC products requires monitoring attributes across multiple cellular domains that directly influence product quality and consistency.
Table 2: Essential Critical Quality Attributes for Hypoxia-Preconditioned MSC Products
| CQA Category | Specific Measurable Attributes | Analytical Methods | Impact on Therapeutic Potential |
|---|---|---|---|
| Identity & Viability Markers | Cell viability (>90%), Surface marker expression (CD73, CD90, CD105 >95%), Absence of thrombogenic CD142 | Flow cytometry, CCK-8 assays, Trypan blue exclusion | Ensures product safety and basic functional competence |
| Hypoxic Response Metrics | HIF-1α stabilization and nuclear translocation, VEGF/SDF-1α gene expression, Upregulation of CXCR4 | Western blot, qRT-PCR, Immunofluorescence | Confirms effective preconditioning and predicts in vivo functionality |
| Metabolic & Senescence Indicators | Glycolytic flux, Oxidative phosphorylation rate, Senescence-associated β-galactosidase, Population doubling time | Seahorse analysis, SA-β-gal staining, Growth kinetics | Determines cellular fitness and longevity post-transplantation |
| Secretome & EV Profiles | EV concentration and size distribution, Specific miRNA signatures (miR-210, let-7f-5p), Anti-oxidant proteins (GSTO1) | NTA, Western blot, RNA sequencing, Proteomics | Predicts paracrine efficacy and specific therapeutic mechanisms |
| Functional Potency | T-cell proliferation inhibition, Tubular epithelial cell protection, Endothelial tube formation | Co-culture assays, In vitro injury models | Direct measure of biological activity and therapeutic relevance |
Analytical Methodologies for CQA Assessment
Robust analytical methods are essential for quantifying these CQAs with sufficient precision and accuracy:
Transcriptomic profiling: RNA sequencing of preconditioned MSCs reveals significant alterations, with one study identifying 215 miRNAs upregulated and 369 miRNAs downregulated in hypoxic MSC-derived exosomes compared to normoxic controls [58]. Such comprehensive profiling helps establish molecular signatures for quality control.
Functional potency assays: In vitro co-culture systems demonstrating inhibition of peripheral blood mononuclear cell (PBMC) proliferation or protection of renal tubular epithelial cells from oxidative stress provide critical potency measures [59] [61]. For example, hypoxic MSC-derived EVs showed superior ability to mitigate renal ischemia-reperfusion injury by enhancing proliferation and reducing apoptosis of renal tubular epithelial cells [59].
Metabolic flux analysis: Assessment of glycolytic and oxidative phosphorylation rates provides insight into the metabolic reprogramming essential for hypoxic adaptation [9]. Shifts toward glycolysis represent a fundamental adaptive response that should be monitored as a key quality attribute.
Diagram 1: CQA Development Pathway - This diagram illustrates how hypoxic stimuli trigger molecular responses that ultimately manifest in measurable Critical Quality Attributes.
Standardization Challenges in Preconditioning Protocols
Protocol Variability and Optimization
Substantial heterogeneity in preconditioning methodologies presents significant hurdles to standardization:
Oxygen concentration optimization: Research indicates different optimal oxygen levels for various applications, with studies utilizing 2% O₂ for immunomodulatory enhancement [61], 5% O₂ for EV production [59], and varying concentrations for specific tissue repair applications.
Exposure duration control: The temporal aspect of preconditioning shows a narrow therapeutic window, with most studies employing 24-hour exposure [60] [59] [61], while longer durations (>48 hours) risk inducing senescence and apoptosis [9].
MSC tissue source variability: Response to hypoxic preconditioning differs significantly between MSCs derived from bone marrow, adipose tissue, umbilical cord, and dental pulp, necessitating source-specific protocol optimization [58].
Combination Preconditioning Strategies
Emerging research explores combining hypoxia with other stimuli to further enhance therapeutic properties:
Hypoxia-inflammatory preconditioning: One study demonstrated that combining 2% O₂ with inflammatory factors (IL-1β, TNF-α, IFN-γ) for 24 hours enhanced immunosuppressive properties without damaging fundamental biological characteristics of umbilical cord MSCs [61].
Hypoxia-LPS preconditioning: Research using 100μM CoCl₂ (a chemical hypoxia mimetic) with 10ng/mL LPS showed significantly improved MSC viability, reduced population doubling time, and enhanced oxidative stress resistance compared to hypoxia alone [62].
Table 3: Experimental Preconditioning Protocols and Their Outcomes
| Preconditioning Method | Specific Conditions | Key Functional Outcomes | Reference Model |
|---|---|---|---|
| Hypoxia Alone | 5% O₂ for 24 hours | Increased EV production; Enhanced GSTO1 expression in EVs | Human umbilical cord MSCs [59] |
| Chemical Hypoxia (DFX) | 150μM deferoxamine for 24 hours | Transient HIF-1α activation; Increased BDNF, GDNF, VEGF in secretome | Human umbilical cord MSCs [60] |
| Hypoxia + Inflammatory Factors | 2% O₂ + cytokine mix for 24 hours | Enhanced immunomodulation; Reduced thrombogenic CD142 expression | Human umbilical cord MSCs [61] |
| Chemical Hypoxia + LPS | 100μM CoCl₂ + 10ng/mL LPS for 24 hours | Improved oxidative stress resistance; Shorter population doubling time | Wharton's jelly MSCs [62] |
Experimental Workflows for CQA Assessment
Detailed Methodologies for Key Experiments
Establishing standardized experimental workflows is essential for generating comparable data across research and manufacturing environments:
Protocol 1: Assessment of Hypoxic Response in MSCs
- Cell culture: Human umbilical cord MSCs are cultured in α-MEM supplemented with 5% UltraGRO-Advanced at 37°C in 5% CO₂ [59].
- Hypoxic preconditioning: At 80%-90% confluence, cells are transferred to a humidified multi-gas incubator with 5% CO₂ and 5% O₂ for 24 hours [59].
- HIF-1α verification: Western blot analysis using anti-HIF-1α antibody (CST #14,179) confirms stabilization of the transcription factor [59].
- Functional validation: qRT-PCR analysis of VEGF and SDF-1α expression confirms transcriptional activation of target genes [9].
Protocol 2: EV Characterization from Hypoxic MSCs
- EV isolation: Supernatants from preconditioned MSCs are centrifuged at 2,000 × g for 20 minutes to remove cell debris, followed by ultracentrifugation at 100,000 × g for 1 hour at 4°C [59].
- EV characterization: Isolated EVs are analyzed using nanoparticle tracking analysis (NTA) for size distribution, transmission electron microscopy for morphology, and Western blot for surface markers (CD9, CD63, CD81) [59].
- Functional proteomics: Protein sequencing identifies enriched factors in hypoxic EVs, such as glutathione S-transferase omega 1 (GSTO1), with validation through knockdown experiments [59].
Protocol 3: Functional Potency Assessment
- Immunomodulation assay: MSCs are co-cultured with peripheral blood mononuclear cells (PBMCs) at a 1:3 ratio (MSC:PBMC) with PBMC proliferation measured via CFSE dilution or Ki-67 staining [61].
- Tissue repair models: In vivo efficacy testing in disease models such as rat renal ischemia-reperfusion injury, with functional assessment through serum creatinine and blood urea nitrogen measurements [59].
Diagram 2: CQA Assessment Workflow - This experimental workflow outlines the key steps in characterizing hypoxia-preconditioned MSC products, from initial culture through comprehensive quality attribute assessment.
The Scientist's Toolkit: Essential Research Reagent Solutions
Standardized reagents and materials are fundamental to generating reproducible data in hypoxia preconditioning research. The following table details essential research tools and their applications in CQA development.
Table 4: Essential Research Reagent Solutions for Hypoxia Preconditioning Studies
| Reagent/Material | Specific Examples | Function in Preconditioning Research | Application Notes |
|---|---|---|---|
| Hypoxia Mimetics | Deferoxamine (150μM), Cobalt Chloride (100μM) | Chemical induction of hypoxic response; HIF-1α stabilization | Useful for screening; may not replicate all aspects of physical hypoxia [60] [62] |
| Hypoxia Chambers/Workstations | Multi-gas incubators (2-5% O₂) | Precise physical oxygen control for preconditioning | Essential for clinical translation; enables scale-up [59] [61] |
| HIF-1α Detection Antibodies | CST #14,179 (1:1000 dilution) | Verification of hypoxic response activation through Western blot | Critical quality control checkpoint [59] |
| EV Characterization Tools | CD9/CD63/CD81 antibodies, NTA instruments | Isolation and validation of EV populations from conditioned media | Standardized EV characterization is essential for secretome-based products [59] |
| Oxidative Stress Inducers | H₂O₂ (100μM) | Testing resilience of preconditioned MSCs to transplantation stress | Predictive in vitro potency assay [62] |
| Cytokine/Chemokine Arrays | IFN-γ, TNF-α, IL-1β for combination preconditioning | Enhancing immunomodulatory properties through inflammatory priming | Combination approaches show enhanced efficacy [61] |
| Metabolic Assay Systems | Seahorse extracellular flux analyzers | Monitoring glycolytic and oxidative phosphorylation changes | Confirms metabolic reprogramming [9] |
The transition of hypoxia-preconditioned MSC products from research tools to clinically viable therapeutics hinges on resolving critical standardization challenges. The fundamental plasticity of MSC responses to hypoxic stress—while therapeutically beneficial—creates inherent variability that must be constrained through well-defined CQAs. Current research indicates that the most promising approach involves multi-parameter quality assessment spanning molecular, metabolic, secretome, and functional attributes.
Future standardization efforts should focus on establishing:
- Threshold values for key hypoxic response markers (e.g., minimum HIF-1α stabilization levels, target VEGF expression ranges)
- Reference materials for EV characterization and secretome profiling
- Standardized potency assays that predict in vivo efficacy across different therapeutic applications
- Defined acceptance criteria for combination preconditioning approaches
As the field progresses toward clinical application, the development of universally accepted CQAs will be essential for ensuring that hypoxia-preconditioned MSC products deliver consistent, safe, and effective therapeutic outcomes. The current evidence base, while promising, remains limited by the scarcity of clinical trials specifically evaluating well-characterized hypoxia-preconditioned products, highlighting the need for continued research in this critical area [9].
The therapeutic application of the mesenchymal stem cell (MSC) secretome—a complex mixture of bioactive factors, extracellular vesicles (EVs), and proteins—represents a paradigm shift in regenerative medicine. This cell-free approach leverages the paracrine activity of MSCs while avoiding risks associated with direct cell transplantation [63]. Within this therapeutic framework, hypoxic preconditioning has emerged as a critical strategy to enhance the regenerative potential of the secretome by better mimicking the physiological niche of MSCs, which naturally reside in low oxygen environments ranging from 1% to 7% [8] [64]. Research confirms that hypoxia alters the MSC transcriptional profile and promotes the production of therapeutic factors [8].
However, the transition from laboratory findings to clinically viable therapies depends on addressing a central challenge: scalable manufacturing. Traditional two-dimensional (2D) culture systems are inadequate for producing the required volumes of consistent, high-potency secretome, necessitating advanced bioprocessing solutions [63]. This technical guide explores how integrated bioreactor systems and 3D culture platforms enable the scalable production of hypoxia-conditioned secretome, providing researchers with methodologies to overcome manufacturing bottlenecks in therapeutic development.
Hypoxic Preconditioning: Enhancing Secretome Potency
Molecular Mechanisms of Hypoxic Response
The cellular response to hypoxia is primarily mediated by hypoxia-inducible factor 1-alpha (HIF-1α), which is stabilized under low oxygen conditions and translocates to the nucleus to activate genes involved in angiogenesis, cell survival, and metabolism [8]. In MSCs, this pathway enhances the secretion of therapeutic factors such as VEGF, FGF, SDF-1α, and CXCR4, which are crucial for tissue repair processes [8]. One study demonstrated that hypoxia-conditioned MSC-derived EVs induced significantly increased vascular tube formation in vitro compared to their normoxic counterparts, suggesting enhanced angiogenic potential [65].
Optimizing Hypoxic Conditions
The therapeutic benefits of hypoxic preconditioning are dose-dependent and time-sensitive. Studies indicate that mild hypoxia (1%-5% O₂) enhances MSC proliferation, resistance to oxidative stress, and paracrine function, while extreme hypoxia (<1% O₂) can induce senescence and apoptosis [8]. The optimal exposure time is generally less than 48 hours, which activates protective mechanisms without causing significant cellular damage [8]. Furthermore, environmental factors like glucose concentration can modulate this response, with high-glucose conditions attenuating the production of angiogenic growth factors in hypoxic MSCs through superoxide-induced mechanisms [66].
Figure 1: Hypoxia-Induced Signaling Pathway for Secretome Enhancement. This diagram illustrates the molecular mechanism through which hypoxic preconditioning enhances the therapeutic potential of the MSC secretome. The process is initiated by hypoxia, leading to HIF-1α stabilization and subsequent activation of genes encoding key paracrine factors.
Bioreactor Systems for Scalable Secretome Production
Advanced Bioreactor Configurations
The transition from traditional 2D culture to controlled bioreactor systems is fundamental for scaling secretome production. These systems provide precise regulation of environmental parameters, including oxygen tension, pH, and temperature, while enabling superior process control and monitoring [63] [64].
Stirred-Tank Bioreactors are widely used for large-scale production, as demonstrated by RoosterBio's successful establishment of a 50L cGMP-compatible process for clinical-stage cell therapy manufacturing [67]. These systems can be operated in fed-batch or perfusion modes, allowing for continuous nutrient supply and waste removal, which is crucial for maintaining cell viability during extended hypoxic preconditioning cycles [64].
Microbioreactor Arrays represent an innovative approach for high-throughput process development. These microfluidic platforms enable parallel cultivation under multiple conditions, with short transport distances facilitating rapid environmental control and fast responses to stimuli [68]. This technology is particularly valuable for optimizing hypoxic preconditioning parameters before scaling up to production volumes.
3D Culture Platforms for Enhanced Secretome
Three-dimensional culture systems significantly enhance secretome quality by better replicating the native tissue microenvironment. Multiple 3D platforms have been developed, each with distinct characteristics and applications:
Table 1: Comparison of 3D Culture Systems for Secretome Production
| Culture System | Key Features | Impact on Secretome | Scalability |
|---|---|---|---|
| Suspension Aggregates (Spheroids) | Self-assembled cellular aggregates; Enhanced cell-cell signaling [63] | Increased levels of growth factors and cytokines; Improved angiogenic potential [63] | Moderate; Suitable for stirred systems [63] |
| Hydrogel-Based (Bio-Blocks) | Tunable mechanical properties; Mimics native tissue architecture [69] | Preserves native "stem-like" phenotype; ~44% increase in EV production [69] | High; Modular "puzzle piece" design enables continuous culture [69] |
| Microcarrier-Based | Cells attached to suspended beads; High surface-to-volume ratio [64] | Enables hypoxic preconditioning in dynamic conditions; Modifiable protein profile [64] | High; Established in stirred-tank bioreactors up to 500L [64] |
Comparative studies demonstrate that 3D culture systems significantly outperform 2D cultures in preserving MSC phenotype and secretome quality during extended cultivation. Bio-Block cultures specifically showed approximately 2-fold higher proliferation than spheroid and Matrigel systems, with senescence reduced by 30-37% and apoptosis decreased 2-3-fold over four-week cultures [69].
Experimental Protocols for Secretome Manufacturing
Workflow for Hypoxia-Conditioned Secretome Production
Figure 2: Experimental Workflow for Secretome Production. This diagram outlines the standardized protocol for manufacturing hypoxia-conditioned secretome, from initial cell expansion through final product characterization and storage.
Detailed Methodologies
Hypoxic Preconditioning in Bioreactors
Bioreactor Setup: Utilize a DASGIP Parallel Bioreactor system or equivalent with control capabilities for dissolved oxygen (5% O₂ for hypoxia, 21% O₂ for normoxia), pH (7.4), temperature (37°C), and agitation (52 rpm) [64].
Microcarrier Preparation: Hydrate Cytodex 3 microcarriers in PBS overnight. Autoclave and coat with fetal bovine serum for 6 hours at 37°C to enhance cell attachment. Wash with serum-free medium before inoculating into the bioreactor [64].
Cell Inoculation and Culture: Seed MSCs at an appropriate density (e.g., 3,000 cells/cm²) and culture in serum-free medium such as RoosterCollect EV-Pro to facilitate downstream processing and minimize serum-derived contaminants [69] [65].
Hypoxic Preconditioning: Maintain cultures at 5% O₂ for 24-48 hours. This duration has been shown to activate protective mechanisms without causing significant cellular damage [8]. Monitor cell viability throughout using resazurin-based assays [65].
Secretome Collection and Processing
Conditioned Media Collection: Collect supernatant after 48-72 hours of hypoxic exposure. Centrifuge at 500 × g for 5 minutes followed by 1,500 × g for 15 minutes to remove cells and debris [65].
EV Isolation: Ultracentrifuge the clarified supernatant at 100,000 × g for 90 minutes at 4°C. Resuspend the resulting EV pellet in phosphate-buffered saline for therapeutic applications [65].
Concentration and Buffer Exchange: Use tangential flow filtration or ultrafiltration to concentrate the secretome and exchange into an appropriate formulation buffer for storage.
Characterization and Quality Control
Robust characterization of the hypoxia-conditioned secretome is essential for ensuring batch-to-batch consistency and therapeutic efficacy. The following table outlines key quality control metrics and methods:
Table 2: Secretome Characterization and Functional Assessment
| Parameter | Analytical Method | Target Specifications | Functional Correlates |
|---|---|---|---|
| EV Concentration & Size | Nanoparticle Tracking Analysis (NTA) [65] | Hypoxic vs. normoxic particle count; Size distribution 40-200 nm | Enhanced angiogenic potential of hypoxic EVs [65] |
| Surface Marker Profile | Multiplex bead-based flow cytometry [65] | CD63, CD81, CD73, CD90 expression; Potential CD44 downregulation in hypoxia [65] | Target cell interaction and uptake efficiency |
| Protein Cargo | Proteomic analysis (Mass Spectrometry) [64] | Upregulation of pro-angiogenic factors (VEGF, FGF); Neuroregulatory proteins (GDN, Cys C) [64] | Tissue-specific regenerative capacity [64] |
| Functional Potency | In vitro tube formation assay (HUVEC) [65] | Increased tube length and branching with hypoxic secretome | Angiogenic potential in ischemic disease models |
| Bioactive Factor Quantification | ELISA/Multiplex Immunoassays | 2-3 fold increase in VEGF, FGF, HGF under hypoxia [8] | Correlation with in vivo therapeutic efficacy |
Proteomic analyses reveal that hypoxic preconditioning significantly alters the secretome composition, with proteins such as thymosin-beta, elongation factor 2, and peroxiredoxin-1 being upregulated under hypoxic conditions, while vitronectin and cadherin-2 are predominantly expressed in normoxic conditions [64].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Secretome Production and Characterization
| Reagent / Material | Function | Example Product |
|---|---|---|
| cGMP-grade Cell Culture Medium | Scalable MSC expansion under defined conditions | prcRoosterNourish-MSC-CC [67] |
| Serum-free, EV-production Medium | Secretome collection without serum contaminants | RoosterCollect EV-Pro [69] |
| Microcarriers | 3D substrate for scalable bioreactor culture | Cytodex 3 [64] |
| Hydrogel Scaffolds | Biomimetic 3D culture environment | Bio-Blocks [69] |
| Lactadherin | Flow cytometry detection of EVs exposing phosphatidylserine | Lactadherin-FITC [65] |
| Antibody Panels | EV surface characterization | CD63, CD81, CD73, CD90 antibodies [65] |
The integration of hypoxic preconditioning with advanced bioreactor systems and 3D culture technologies represents a transformative approach for manufacturing consistent, potent MSC secretome products at clinical scale. By carefully optimizing oxygen tension, culture parameters, and purification methods, researchers can enhance the therapeutic profile of the secretome while ensuring scalability and reproducibility. As the field advances, standardized protocols and comprehensive characterization will be crucial for translating promising preclinical findings into effective clinical therapies for a range of degenerative, inflammatory, and ischemic conditions. The methodologies outlined in this technical guide provide a foundation for developing robust manufacturing processes that leverage the synergistic benefits of hypoxic stress and scalable bioprocessing.
Within the broader context of research on hypoxic stress and its effect on stem cell paracrine factor production, a rigorous assessment of the safety and efficacy profiles of cellular therapies is paramount. Mesenchymal stem cells (MSCs), a cornerstone of regenerative medicine, exert their therapeutic effects largely through their secreted paracrine factors, including extracellular vesicles (EVs) and bioactive molecules [8] [13]. Preconditioning MSCs with hypoxia—a state mimicking their physiological niche—has emerged as a powerful strategy to enhance the regenerative and immunomodulatory properties of these cells and their secreted factors [8] [70]. However, the therapeutic augmentation achieved through hypoxia must be carefully balanced against a comprehensive evaluation of critical safety parameters. This whitepaper provides an in-depth technical guide for researchers and drug development professionals, focusing on the assessment of three core safety profiles: tumorigenicity, immunogenicity, and long-term stability, with specific consideration of the impact of hypoxic preconditioning.
Tumorigenicity Assessment
Tumorigenicity refers to the risk of a cell therapy initiating tumor formation due to uncontrolled proliferation or malignant transformation. For hypoxia-preconditioned MSCs, this risk must be thoroughly evaluated, as hypoxia can influence cell proliferation, survival, and genetic stability.
Key Mechanisms and Risk Factors
Hypoxia-inducible factor-1 alpha (HIF-1α), stabilized under low oxygen conditions, is a master regulator of cellular adaptation. While it enhances MSC survival and paracrine function by upregulating pro-survival and angiogenic genes, its signaling pathways can also crosstalk with processes involved in cell cycle control and oncogenesis [8] [71]. Furthermore, the use of viral vectors in some gene-modified stem cell therapies introduces the risk of insertional mutagenesis, where random integration of the viral genome can disrupt tumor suppressor genes or activate oncogenes [72] [73].
Experimental Protocols for Tumorigenicity Evaluation
A combination of in vitro and in vivo studies is required to assess tumorigenic potential.
In Vitro Studies:
- Soft Agar Colony Formation Assay: This test assesses anchorage-independent growth, a hallmark of transformation. Cells are suspended in a semi-solid agar medium and monitored for 3-4 weeks for colony formation. Hypoxia-preconditioned MSCs are compared against normoxic MSCs and positive control cancer cell lines.
- Karyotyping and Genetic Stability Analysis: Chromosomal aberrations are detected using G-banding karyotyping. Cells are arrested in metaphase, harvested, and chromosomes are stained and analyzed for structural and numerical abnormalities. This should be performed after prolonged culture, including after the hypoxic preconditioning process.
- Oncogene/Tumor Suppressor Expression Profiling: The expression levels of key oncogenes (e.g., c-MYC) and tumor suppressor genes (e.g., p53) are quantified via qPCR or Western blotting in hypoxia-preconditioned versus control cells.
In Vivo Studies:
- Ectopic Transplantation in Immunodeficient Mice: A critical in vivo assay. Cells (e.g., 1x10^6 to 5x10^6 per site) are implanted subcutaneously or under the renal capsule of mice such as NOD/SCID or NSG strains. Animals are monitored for at least 12-16 weeks for palpable mass formation. At endpoint, tissues are harvested for histopathological analysis to detect any neoplastic growth [72].
The following diagram illustrates the core signaling pathway and the experimental workflow for tumorigenicity assessment:
Quantitative Data and Standards
Table 1: Key Assays for Tumorigenicity Assessment
| Assessment Method | Experimental Readout | Acceptance Criteria | Relevant Context (Hypoxia) |
|---|---|---|---|
| Soft Agar Assay | Number and size of colonies formed after 3-4 weeks. | No significant colony formation compared to positive control. | Assess if hypoxia alters proliferation in an unanchored state. |
| Karyotyping | Number of metaphase spreads with normal vs. aberrant karyotypes. | ≥90% of cells with normal karyotype after long-term culture. | Confirm genetic stability post-hypoxic preconditioning. |
| In Vivo Tumor Formation | Palpable mass formation, histology confirming neoplastic cells. | No tumor formation at injection site over study duration. | Monitor for ectopic tissue growth from enhanced survival MSCs. |
Immunogenicity Profiling
Immunogenicity encompasses the potential of a cell therapy to provoke an undesirable immune response in the recipient, leading to rejection or adverse inflammatory reactions.
Mechanisms of Immune Recognition
MSCs are generally considered immunoprivileged due to low expression of Major Histocompatibility Complex (MHC) class II and costimulatory molecules (e.g., CD80, CD86) [13]. However, their immunogenicity is not absolute. Hypoxic preconditioning can further modulate the immunogenic profile of MSCs. It has been shown to enhance their immunomodulatory functions, such as by increasing the secretion of anti-inflammatory factors and improving survival post-transplantation, which may reduce rejection risks [8]. Nevertheless, the expression of human leukocyte antigen (HLA) molecules remains a primary concern for allogeneic therapies, as these can be recognized by the host's T cells, triggering cell-mediated rejection [72].
Experimental Protocols for Immunogenicity Evaluation
In Vitro Immune Cell Activation Assays:
- Mixed Lymphocyte Reaction (MLR): This assay tests T-cell activation. Peripheral blood mononuclear cells (PBMCs) from an allogeneic donor (responder) are co-cultured with gamma-irradiated hypoxia-preconditioned MSCs (stimulator) for 5-7 days. T-cell proliferation is measured via ^3^H-thymidine incorporation or CFSE dilution using flow cytometry. Reduced proliferation indicates immunosuppressive capacity.
- HLA Typing and Surface Marker Characterization: The expression of HLA class I and II, as well as costimulatory molecules (CD80, CD86, CD40) on MSCs, is definitively quantified by flow cytometry before and after hypoxic preconditioning. Stimulation with IFN-γ can be used to test inducible HLA class II expression.
- Cytokine Profiling: The secretion profile of immunomodulatory cytokines (e.g., TGF-β, PGE2, IDO) and pro-inflammatory cytokines (e.g., IL-6, IFN-γ) from MSCs cultured under hypoxia vs. normoxia is analyzed using multiplex ELISA or Luminex assays.
In Vivo Studies:
- Allogeneic Transplantation Models: Hypoxia-preconditioned MSCs are administered to immunocompetent allogeneic hosts. Blood and tissue samples are collected at various time points to analyze immune cell infiltration (e.g., CD8+ T cells, NK cells) at the injection site and to measure donor-specific antibodies in the serum.
Long-Term Stability Evaluation
Stability refers to the maintenance of critical quality attributes (CQAs) of the cell product over time, including identity, potency, viability, and purity. This is crucial for ensuring consistent therapeutic efficacy from batch to batch and during shelf-life.
Key Stability Challenges
For cell-based products like MSCs, stability is challenged by their biological complexity and sensitivity to environmental stress during production, cryopreservation, and storage [73]. Maintaining viability and functionality from the end of production to patient administration is a major hurdle. Furthermore, genetic instability during long-term culture can lead to drift in CQAs. Hypoxic preconditioning, while therapeutically beneficial, adds another layer of process complexity that must be controlled and its impact on stability understood.
Experimental Protocols for Stability Testing
A stability study program must be designed to monitor the product under recommended storage conditions.
Real-Time Stability Studies:
- Protocol: Multiple batches of the final product (e.g., cryopreserved in DMSO) are stored at the intended long-term storage temperature (e.g., -150°C or in vapor phase liquid nitrogen). Samples are withdrawn at predefined timepoints (e.g., 0, 3, 6, 9, 12 months) and upon expiry.
- Testing Panel:
- Viability: Measured post-thaw using trypan blue exclusion or flow cytometry with 7-AAD.
- Potency: A defined bioassay relevant to the mechanism of action (MoA). For immunomodulatory MSCs, this could be the ability to suppress T-cell proliferation in an MLR or the quantification of a specific paracrine factor (e.g., VEGF or PGE2) via ELISA.
- Identity: Confirmed via flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) markers, as per ISCT guidelines [13].
- Sterility: Tests for bacterial, fungal, and mycoplasma contamination throughout shelf-life.
Genetic Stability Monitoring:
- Karyotyping, as described in Section 2.2, should be performed on cells at the end of shelf-life to confirm the absence of genetic alterations.
The relationship between stability challenges, testing methods, and the influence of hypoxic manufacturing is summarized below:
Quantitative Data and Standards
Table 2: Critical Quality Attributes for Long-Term Stability
| Critical Quality Attribute (CQA) | Analytical Method | Target Specification | Impact of Hypoxic Preconditioning |
|---|---|---|---|
| Viability | Flow cytometry (7-AAD) or automated cell counter. | Typically ≥70-80% post-thaw viability. | Must be confirmed post-hypoxia and post-thaw. |
| Potency | Bioassay (e.g., T-cell suppression, VEGF ELISA). | Defined per product; e.g., ≥X% suppression or ≥Y pg/mL VEGF. | Hypoxia may enhance potency; requires stability monitoring. |
| Identity | Flow cytometry for CD73+, CD90+, CD105+ (≥95%), CD34-, CD45-, HLA-DR- (≤2%). | Conformance to ISCT minimal criteria [13]. | Must be stable after hypoxic culture. |
| Sterility | BacT/ALERT, mycoplasma PCR, etc. | No growth / Not detected. | Unrelated to hypoxia, but a mandatory release criterion. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials essential for conducting the safety assessments described in this guide.
Table 3: Research Reagent Solutions for Key Experiments
| Reagent / Material | Function / Application | Example in Experimental Context |
|---|---|---|
| Hypoxia Chamber/Workstation | Creates and maintains a controlled low-oxygen environment (e.g., 1-5% O₂) for cell preconditioning. | Preconditioning MSCs prior to harvest for EV isolation or direct transplantation [8] [70]. |
| HIF-1α Stabilizers (e.g., DMOG) | Chemical inhibitor of prolyl hydroxylases (PHDs) that stabilizes HIF-1α, mimicking hypoxia. | Used as a positive control for HIF-1α pathway activation in normoxic cultures [71]. |
| Flow Cytometry Antibodies | Characterization of cell surface markers (identity) and detection of immune cell subsets. | Confirming MSC phenotype (CD73/90/105) and analyzing immune cell infiltration (CD3, CD4, CD8, CD56) [72] [13]. |
| qPCR Assays & Western Blot Reagents | Quantification of gene and protein expression for oncogenes, tumor suppressors, and immunomodulatory factors. | Analyzing HIF-1α, VEGF, p53, and c-MYC expression in hypoxia-preconditioned vs. control MSCs [66]. |
| Immunodeficient Mouse Models (e.g., NSG) | In vivo models for assessing tumorigenicity and biodistribution due to their impaired immune system. | Ectopic transplantation of MSCs to monitor for tumor formation over 12-16 weeks [72]. |
| Cryopreservation Medium (with DMSO) | Protects cells from ice crystal formation during freezing, enabling long-term storage. | Cryopreservation of the final MSC product for stability studies and clinical use [73]. |
Evidence and Efficacy: Comparative Analysis of Hypoxic vs. Normoxic Stem Cell Therapies
Systematic reviews and meta-analyses represent the pinnacle of the evidence hierarchy in medical research, providing empirically supported responses to specific research questions by synthesizing findings from multiple primary studies [74]. In the context of hypoxic stress effects on stem cell paracrine factor production, systematic review methodology enables researchers to consolidate fragmented preclinical evidence into a coherent understanding of molecular mechanisms and therapeutic potential. These reviews use scientific techniques to compile, evaluate, and summarize all pertinent research on a specific subject, reducing the bias present in individual studies and providing more reliable conclusions to guide future clinical research and patient care [74].
The increasing interest in stem cell-derived paracrine factors stems from growing recognition that the therapeutic benefits of mesenchymal stem cells (MSCs) are largely mediated through their secreted factors rather than direct cellular engraftment or differentiation [75]. This "paracrine hypothesis" suggests that MSCs exert their regenerative effects via the secretion of cytokines, chemokines, and growth factors that modulate host cellular responses [75]. When stem cells are exposed to hypoxic preconditioning—a critical mimicry of their natural niche environment—they significantly alter their secretome composition, potentially enhancing its therapeutic efficacy for conditions including ischemic heart disease, skin wounds, and other regenerative applications [76] [77].
Methodological Framework for Preclinical Systematic Reviews
Formulating the Research Question and Search Strategy
The foundation of a robust systematic review lies in establishing a well-defined research question that guides all subsequent stages of the process [74]. For preclinical studies investigating hypoxic stress and stem cell paracrine function, the PICO framework (Population, Intervention, Comparator, Outcome) provides a structured approach, though it requires adaptation to the preclinical context:
- Population: Specific stem cell types (e.g., BM-MSCs, AD-MSCs, CPCs) and species of origin
- Intervention: Hypoxic preconditioning protocols (oxygen concentration, duration, frequency)
- Comparator: Normoxic cultured controls or alternative preconditioning methods
- Outcome: Quantified changes in paracrine factor secretion and functional consequences in vivo
A comprehensive literature search should utilize multiple bibliographic databases including PubMed/MEDLINE, Embase, and Cochrane Library to ensure inclusion of diverse studies [74]. The search strategy should incorporate both published studies and gray literature to reduce publication bias. Reference managers such as EndNote, Zotero, or Mendeley facilitate collection of searched literature and duplicate removal, while specialized tools like Covidence and Rayyan can streamline the screening process through collaborative features and inclusion/exclusion criteria implementation [74].
Study Selection and Quality Assessment
Study selection should follow predefined inclusion and exclusion criteria with multiple investigators independently evaluating titles and abstracts to minimize bias [75]. For preclinical reviews focusing on hypoxic stress and paracrine effects, inclusion criteria typically encompass: (1) clear identification of mesenchymal origin of cell types used; (2) direct demonstration of paracrine factor release; (3) appropriate hypoxic preconditioning protocols; and (4) relevant in vivo functional assessments.
Quality assessment of included studies requires specialized tools adapted to preclinical research. A customized 9-point checklist can evaluate key methodological aspects including: clear statement of aims/objectives, description of main outcomes, characterization of stem cell sources, validation of mesenchymal phenotype using International Society for Cellular Therapy criteria, appropriate experimental controls, and rigorous statistical analysis [75].
Data Extraction and Synthesis
Data extraction should capture essential elements including stem cell origin, hypoxic preconditioning parameters, identified paracrine factors, assessment methodologies, in vivo models, and functional outcomes. Quantitative data synthesis through meta-analysis enhances statistical power and validity of conclusions when sufficient homogeneity exists among included studies [74]. When meta-analysis is not appropriate due to methodological heterogeneity, alternative synthesis methods such as qualitative synthesis or synthesis without meta-analysis (SWiM) provide structured approaches to evidence integration [74].
Experimental Models and Methodologies in Hypoxic Stem Cell Research
Stem Cell Culture and Hypoxic Preconditioning
Human adipose-derived stem cells (hASCs) and other mesenchymal stem cells are typically isolated from tissue sources (lipoaspirate for hASCs) through enzymatic digestion (e.g., collagenase I) and cultured in standard media (DMEM with low glucose supplemented with FBS) [77]. For hypoxic preconditioning, cells are transferred to specialized chambers maintaining precise oxygen tension (typically 1% O₂ for "hypoxic" conditions) for defined periods, often in serum-free media to eliminate confounding factors from serum-borne proteins [77]. Normoxic controls are maintained in standard culture conditions (approximately 21% O₂) with identical media composition to enable valid comparisons.
Proteomic Analysis of Secretomes
Conditioned media collection involves thorough washing of cells followed by incubation with serum-free media during the hypoxic/normoxic exposure period to accumulate secreted factors [77]. Proteomic profiling utilizes techniques such as liquid chromatography-mass spectrometry (LC-MS/MS) to identify and quantify protein components within the secretome. Bioinformatics tools facilitate classification of identified factors into functional categories (angiogenic, immunomodulatory, mitogenic) and pathway analysis to elucidate potential mechanisms of action [77].
In Vivo Validation Models
Full-thickness skin wound models in mice (e.g., C57BL/6) provide a robust system for evaluating the functional effects of hypoxic preconditioned secretomes on tissue repair [77]. Experimental protocols involve creating standardized wounds followed by local injection of concentrated secretome preparations. Outcome measures include wound closure rate, histopathological assessment of re-epithelialization and granulation tissue formation, and immunohistochemical evaluation of vascular density and maturation through analysis of endothelial markers (CD31) and pericyte coverage (NG2, nestin) [77].
Matrigel plug assays enable quantitative assessment of angiogenic potential in vivo [77]. Secretome preparations are mixed with Matrigel基质胶 and injected subcutaneously into mice. After a standardized period (typically 7-14 days), plugs are harvested and analyzed for vascular invasion through hemoglobin content quantification and histological examination of vessel density and structure.
Myocardial infarction models (typically in rodents) investigate cardiac repair potential through induction of ischemia by coronary artery ligation or cryoinjury followed by intramyocardial or systemic administration of secretome preparations [75]. Functional outcomes include echocardiographic assessment of left ventricular ejection fraction, contractility, and compliance; histological evaluation of infarct size, fibrosis, and vessel density; and molecular analysis of apoptotic and hypertrophic markers.
Table 1: In Vivo Models for Assessing Secretome Therapeutic Effects
| Model System | Key Applications | Primary Outcome Measures | Advantages |
|---|---|---|---|
| Full-thickness skin wound [77] | Tissue repair, angiogenesis, re-epithelialization | Wound closure rate, vascular density, pericyte coverage | High clinical relevance, multiple timepoints |
| Matrigel plug assay [77] | Angiogenic potential, vessel formation | Hemoglobin content, vessel invasion, structure analysis | Quantitative, controlled environment |
| Myocardial infarction [75] | Cardiac repair, ischemic injury, vascularization | LV ejection fraction, infarct size, vessel density | Clinically significant, functional assessment |
| Hindlimb ischemia | Peripheral vascular disease, angiogenesis | Blood flow recovery, capillary density, tissue salvage | Reproducible, quantitative perfusion measures |
Key Signaling Pathways in Hypoxic Stem Cell Paracrine Function
Hypoxic Signaling Pathway Activation in Stem Cells
The cellular response to hypoxia centers on hypoxia-inducible factors (HIFs), particularly HIF-1α, which serves as the master regulator of oxygen homeostasis [76]. Under normoxic conditions, HIF-1α undergoes prolyl hydroxylation by prolyl hydroxylases (PHDs), leading to von Hippel-Lindau protein-mediated ubiquitination and proteasomal degradation [76]. Under hypoxic conditions, PHD activity decreases, stabilizing HIF-1α and enabling dimerization with HIF-1β, nuclear translocation, and binding to hypoxia response elements (HREs) in target gene promoters [76].
Epigenetic mechanisms significantly modulate this hypoxic response through chromatin remodeling complexes and histone modifications [76]. The SWI/SNF chromatin remodeling complex recruits to the HIF-1α promoter during hypoxia, facilitating HIF-1α mRNA expression [76]. Additionally, HIF-1α interacts with co-activators including p300/CBP that mediate histone acetylation, further enhancing transcription of target genes involved in angiogenesis, glycolysis, mitochondrial function, and redox homeostasis [76].
Consolidated Findings from Preclinical In Vivo Studies
Effects of Hypoxic Preconditioning on Secretome Composition
Proteomic analyses of hypoxic preconditioned MSC secretomes consistently identify elevated levels of specific paracrine factors across multiple studies and tissue sources. The most consistently upregulated factors include vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), fibroblast growth factor 2 (FGF2), insulin-like growth factor (IGF), and stromal cell-derived factor 1 (SDF-1) [77] [75]. These factors collectively promote angiogenesis, cell survival, proliferation, and migration through coordinated activation of complementary signaling pathways.
Table 2: Key Paracrine Factors Upregulated by Hypoxic Preconditioning
| Paracrine Factor | Primary Functions | Signaling Pathways | Therapeutic Effects |
|---|---|---|---|
| VEGF [77] [75] | Angiogenesis, endothelial cell proliferation and migration | PI3K/Akt, MAPK/ERK | Enhanced neovascularization, improved perfusion |
| HGF [77] [75] | Mitogenesis, motogenesis, morphogenesis | c-Met/PI3K/Akt | Anti-apoptotic, anti-fibrotic, angiogenic |
| FGF2 [75] | Fibroblast proliferation, angiogenesis | FGFR/MAPK | Tissue repair, extracellular matrix remodeling |
| IGF-1/2 [75] | Cell growth, proliferation, differentiation | IGF-1R/PI3K/Akt | Cardiomyocyte protection, hypertrophy regulation |
| SDF-1 [75] | Stem cell homing, angiogenesis | CXCR4/PI3K/Akt | Recruitment of progenitor cells to injury sites |
| MCP-1 [77] | Monocyte recruitment, angiogenesis | CCR2/ERK | Immunomodulation, vascular stabilization |
| Angiogenin [77] | Angiogenesis, rRNA transcription | PI3K/Akt, rRNA stimulation | Endothelial cell invasion, vessel formation |
Functional Outcomes in Preclinical Disease Models
Systematic consolidation of in vivo studies demonstrates consistent therapeutic benefits across multiple disease models. In cutaneous wound healing, hypoxic preconditioned secretomes significantly accelerate wound closure, enhance re-epithelialization, and promote functional angiogenesis characterized by increased vessel density and improved pericyte coverage (NG2+nestin+ pericytes) [77]. These structural improvements correlate with enhanced blood flow recovery and tissue perfusion.
In myocardial infarction models, hypoxic preconditioned MSC secretomes improve left ventricular ejection fraction, reduce infarct size, enhance contractility and compliance, and increase vessel density in the peri-infarct region [75]. These functional benefits occur despite limited long-term engraftment of administered cells, supporting the paracrine hypothesis as the primary mechanism of action. The therapeutic effects appear mediated through coordinated activation of pro-survival pathways (particularly PI3K/Akt), inhibition of apoptotic cascades, and modulation of inflammatory responses.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Hypoxic Stem Cell Studies
| Reagent/Material | Specification/Application | Function in Experimental Workflow |
|---|---|---|
| Stem Cell Sources | Human adipose-derived (hASCs), bone marrow (BM-MSCs), cardiac (CPCs) | Primary cellular material for secretome production and mechanistic studies |
| Hypoxia Chamber | 1% O₂, 5% CO₂, balanced N₂ | Precise environmental control for hypoxic preconditioning protocols |
| Serum-free Media | DMEM with low glucose, without FBS | Elimination of serum-derived protein confounding factors in secretome studies |
| Collagenase I | 1 mg/mL concentration for tissue digestion | Isolation of stromal vascular fraction from adipose tissue sources |
| Antibody Panels | CD14, CD34, CD45, CD146, HLA | Immunophenotypic characterization of MSC surface markers |
| Proteomic Tools | LC-MS/MS systems, ELISA kits | Identification and quantification of secreted paracrine factors |
| Matrigel | Growth factor reduced, high concentration | In vivo assessment of angiogenic potential through plug assays |
| HUVECs | Primary human umbilical vein endothelial cells | In vitro validation of angiogenic effects through proliferation, migration, and tube formation assays |
| Animal Models | C57BL/6 mice, Nestin-GFP+/NG2-DsRed+ reporters | In vivo functional assessment in wound healing, ischemia, and disease models |
Experimental Workflow for Hypoxic Preconditioning and Validation
Experimental Workflow for Hypoxic Preconditioning Studies
The standardized experimental workflow begins with stem cell isolation from appropriate tissue sources (e.g., adipose tissue lipoaspirate through collagenase I digestion) followed by expansion in culture and thorough characterization using immunophenotyping and multipotency assays [77]. Hypoxic preconditioning is implemented using serum-free media under precisely controlled oxygen tension (typically 1% O₂) for optimized durations, with parallel normoxic controls [77]. Secretome collection involves concentration and purification of conditioned media followed by comprehensive proteomic analysis to identify and quantify paracrine factors [77].
Functional validation employs in vitro assays including endothelial cell proliferation, migration, and tube formation assessments, followed by in vivo testing in appropriate disease models such as full-thickness skin wounds or myocardial infarction [77] [75]. Systematic data synthesis integrates findings across multiple studies to identify consistent patterns, resolve discrepancies, and guide future research directions toward clinical translation.
Systematic review of preclinical evidence consistently demonstrates that hypoxic preconditioning enhances the therapeutic potential of stem cell secretomes by upregulating key paracrine factors that promote angiogenesis, cell survival, and tissue repair. The consolidated findings provide a robust evidence base supporting the paracrine hypothesis as a primary mechanism underlying MSC therapeutic effects. Future research directions should focus on standardizing hypoxic preconditioning protocols, identifying optimal combinations of paracrine factors for specific clinical applications, and developing manufacturing strategies for clinical-grade secretome products. Through rigorous systematic methodology, the preclinical evidence base can be effectively translated toward transformative therapies for ischemic conditions and tissue regeneration.
Direct comparative studies are fundamental for evaluating the efficacy of therapeutic interventions in ischemic disease models. These studies aim to determine whether differences in treatment protocols, such as the application of stem cells under varying conditions of hypoxic stress, lead to significant differences in important functional outcomes. The design, analysis, and interpretation of these studies require rigorous methodological consideration to yield actionable, evidence-based conclusions for researchers and drug development professionals [78]. This guide frames these methodological principles within a burgeoning area of research: understanding how hypoxic stress modulates the production of paracrine factors by stem cells, and how this, in turn, influences functional recovery in ischemic diseases.
The traditional paradigm for stem cell therapy focused on direct differentiation and cell replacement. However, a significant body of evidence now indicates that the functional benefits observed after stem-cell therapy in cardiac injury models are largely related to the secretion of soluble factors that act in a paracrine fashion [21]. These paracrine factors—which include cytokines, chemokines, and growth factors—protect the heart, attenuate pathological ventricular remodeling, induce neovascularization, and promote regeneration [21]. Crucially, stem cells alter the type and quantity of paracrine factors they secrete in response to external stimuli, with hypoxic stress being a critical modulator [79]. Reactive oxygen species (ROS), which are intrinsically linked to hypoxic conditions, influence stem cell fate and directly modulate the secretion of these paracrine factors [79]. Therefore, direct comparative studies in this context are not merely comparing Cell Type A to Cell Type B, but are often designed to compare the therapeutic outputs of cells conditioned by different hypoxic or ROS-modulating environments.
Core Principles of Direct Comparative Studies
Study Design Types
The quality of a comparative study is dependent on its internal and external validity. Internal validity refers to the extent to which correct conclusions can be drawn from the study, while external validity refers to the generalizability of these conclusions to other settings [78]. The major design types are:
- Randomized Experiments: Participants (which can be animals, cell cultures, or patients) are randomly assigned to intervention or control groups. This is the gold standard for controlling confounding variables.
- Randomized Controlled Trials (RCTs): Individuals are randomly assigned to groups.
- Cluster Randomized Controlled Trials (cRCTs): Naturally occurring groups (e.g., litters of animals, cell culture plates) are randomized as a whole.
- Pragmatic Trials: Designed to test interventions under "real-world" conditions rather than idealistic laboratory settings, with high relevance for translational research [78].
- Non-randomized (Quasi-Experimental) Designs: Used when randomization is not feasible or ethical.
- Intervention group only with pretest and post-test: Measures outcomes in a single group before and after the intervention.
- Intervention and control groups with post-test: Compares an intervention group to a non-randomized control group after the intervention.
- Interrupted Time Series (ITS) Design: Multiple measures are taken before and after the intervention in a single group to establish a trend [78].
Key Methodological Considerations
- Choice of Variables:
- Dependent Variables (Outcomes): The functional outcomes of interest in ischemic disease models (e.g., infarct size, left ventricular ejection fraction, perfusion scores, biomarkers of apoptosis) [78].
- Independent Variables (Explanatory): The conditions being compared (e.g., normoxic vs. hypoxic-preconditioned stem cells, presence or absence of a ROS modulator) [78].
- Sample Size: Adequate sample size is critical for reliability. Its calculation depends on four elements: the significance level (usually 0.05), power (usually 0.8), the minimal clinically relevant effect size, and the estimated variability of the outcome measure [78].
- Bias Control: Common sources of bias must be minimized.
- Selection/Allocation Bias: Controlled through randomization.
- Performance Bias: Reduced by standardizing protocols and blinding caregivers/investigators to the group allocation.
- Detection/Measurement Bias: Mitigated by blinding outcome assessors.
- Attrition Bias: Addressed by implementing intention-to-treat analysis and reporting all dropouts [78].
Quantitative Data Analysis and Presentation
Transforming raw numerical data into meaningful insights is a cornerstone of comparative studies. The two main categories of quantitative analysis are descriptive and inferential statistics [80].
Table 1: Key Quantitative Data Analysis Methods
| Analysis Method | Description | Application in Ischemic Disease Research |
|---|---|---|
| Descriptive Statistics | Summarizes and describes the characteristics of a dataset. | Reporting baseline characteristics of animal models, mean infarct size, standard deviation of ejection fraction measurements. |
| Measures of Central Tendency | Mean (average), median (middle value), mode (most frequent). | Calculating the average improvement in fractional shortening per group. |
| Measures of Dispersion | Range, variance, and standard deviation. | Expressing the variability in capillary density counts after stem cell therapy. |
| Inferential Statistics | Uses sample data to make generalizations or test hypotheses about a larger population. | Determining if the difference in functional outcomes between two treatment groups is statistically significant. |
| T-Tests and ANOVA | Determine significant differences between groups or datasets. | Comparing mean infarct size between control, normoxic stem cell, and hypoxic-preconditioned stem cell groups (e.g., using ANOVA). |
| Regression Analysis | Examines relationships between dependent and independent variables to predict outcomes. | Modeling how the degree of hypoxic preconditioning predicts the level of VEGF release and subsequent improvement in perfusion. |
| Correlation Analysis | Measures the strength and direction of relationships between variables. | Assessing the correlation between the quantity of a specific paracrine factor (e.g., HGF) in serum and the reduction in fibrotic area. |
Data should be presented in clearly structured tables and visualized effectively. Data tables are ideal when specific data points are crucial, and their design should be intentional, using titles and conditional formatting to emphasize key takeaways [81]. For visualizations, tools like ChartExpo can generate Likert scale charts, bar charts, histograms, and scatter plots to make complex datasets and insights more actionable and understandable [80].
Experimental Protocols: Assessing Paracrine Mechanisms in Ischemic Models
The following provides a detailed methodology for a key experiment comparing the therapeutic efficacy of stem cells subjected to different hypoxic preconditioning regimens.
Protocol: Comparative Analysis of Hypoxic-Preconditioned Stem Cells in a Rodent Myocardial Infarction Model
Objective: To directly compare the functional outcomes and paracrine factor expression following transplantation of normoxic stem cells versus hypoxic-preconditioned stem cells in a murine model of acute myocardial infarction.
Materials and Reagents:
- Experimental Animals: Adult C57BL/6 mice (or similar strain).
- Stem Cells: Adipose-derived stem cells (ADSCs) or bone marrow-derived mesenchymal stem cells (MSCs).
- Hypoxia Chamber: A customizable, temperature-controlled, and gas-regulated incubator for in vitro cell culture.
- Reactive Oxygen Species (ROS) Modulator: Chlorin e6 (Ce6) or similar agent for controlled ROS generation [79].
- Antibodies for ELISA/Flow Cytometry: Specific antibodies for paracrine factors (VEGF, HGF, FGF-2, IGF-1, SDF-1) and cell surface markers (CD90, CD44).
- Histology Reagents: Formalin, paraffin, antibodies for immunohistochemistry (e.g., α-actinin, CD31, TUNEL assay kit).
Methodology:
- Stem Cell Culture and Hypoxic Preconditioning:
- Culture ADSCs in standard conditions. At 80% confluence, split into two groups.
- Control Group: Maintain in normoxic conditions (21% O₂, 5% CO₂, 37°C) for 48 hours.
- Hypoxic-Preconditioned Group: Expose to moderate hypoxic conditions (1-3% O₂, 5% CO₂, 37°C) for 48 hours in a hypoxia chamber [79]. For a subgroup, co-treat with a ROS modulator like Ce6 to precisely manipulate the hypoxic response.
- Collect conditioned medium (CM) from both groups for subsequent analysis of paracrine factors via ELISA.
Animal Model and Cell Transplantation:
- Induce myocardial infarction via permanent ligation of the left anterior descending (LAD) coronary artery in mice.
- Immediately post-infarction, randomize animals into three groups:
- Group 1 (Sham Control): Receive intramyocardial injection of saline.
- Group 2 (Normoxic SC): Receive intramyocardial injection of normoxic-conditioned stem cells.
- Group 3 (Hypoxic SC): Receive intramyocardial injection of hypoxic-preconditioned stem cells.
Functional Outcome Assessment (at 4 weeks post-treatment):
- Echocardiography: Perform transthoracic echocardiography under light anesthesia to measure Left Ventricular Ejection Fraction (LVEF), Left Ventricular End-Systolic Diameter (LVESD), and Left Ventricular End-Diastolic Diameter (LVEDD). Compare values to baseline (pre-infarction) measurements.
- Hemodynamics: Perform catheterization of the left ventricle to assess pressure-volume loops, measuring maximal rate of pressure increase (+dP/dt) and decrease (-dP/dt) as indices of contractility and relaxation.
Tissue Harvesting and Analysis:
- Sacrifice animals and harvest hearts.
- Histomorphometry: Section hearts and stain with Masson's Trichrome to quantify fibrotic area and infarct size.
- Immunohistochemistry: Stain for CD31 or von Willebrand Factor to quantify capillary density in the peri-infarct region.
- TUNEL Staining: Quantify cardiomyocyte apoptosis in the border zone.
Table 2: Key Research Reagent Solutions for Paracrine Factor Studies
| Reagent / Tool | Function / Explanation |
|---|---|
| Adipose-Derived Stem Cells (ADSCs) | A type of mesenchymal stem cell advantageous due to ease of isolation, abundant sources, and low immunogenicity. They express surface markers like CD90 and CD44 [79]. |
| Hypoxia Chamber | A controlled environment to subject cells to precise, low-oxygen conditions (e.g., 1-3% O₂) to mimic the ischemic microenvironment and modulate paracrine factor secretion. |
| ROS Modulators (e.g., Chlorin e6) | Chemical tools to accurately control the concentration of reactive oxygen species in the stem cell environment, which is a key factor influencing the type and quantity of secreted paracrine factors [79]. |
| ELISA Kits | Used to quantitatively measure the concentration of specific paracrine factors (e.g., VEGF, HGF, IGF-1) in conditioned medium or blood serum [21]. |
| CD90-Maleimide Conjugate | A targeting agent used to attach probes (e.g., fluorescent markers, ROS generators) specifically to the surface of stem cells via the CD90 antigen for tracking or functional modification [79]. |
Signaling Pathways and Visual Workflows
The experimental workflow and the underlying signaling pathways influenced by hypoxic stress in stem cells can be visualized using the following diagrams, created with Graphviz DOT language. The color palette and contrast are designed for optimal accessibility [82] [83].
Hypoxia & Paracrine Signaling Pathway
Comparative Study Workflow
Direct comparative studies provide the rigorous framework necessary to dissect the complex relationship between hypoxic stress, stem cell paracrine factor production, and functional outcomes in ischemic disease. By applying sound methodological principles—including robust study design, controlled manipulation of the stem cell microenvironment (e.g., via hypoxia and ROS), comprehensive quantitative analysis, and clear data visualization—researchers can generate high-quality, reproducible evidence. This approach is vital for validating the paracrine hypothesis and moving the field toward novel, optimized therapies that harness the power of conditioned stem cells or their secreted factors for treating ischemic cardiovascular disease.
The Cell-Free Advantage: Hypoxic Secretome vs. Whole Cell Transplantation
The field of regenerative medicine is undergoing a fundamental paradigm shift, moving away from the direct transplantation of whole mesenchymal stem cells (MSCs) toward the use of their acellular secretory products, collectively known as the secretome. This transition is driven by growing evidence that the therapeutic benefits of MSCs are primarily mediated by paracrine factors rather than direct cell replacement [84] [85] [86]. This whitepaper examines a critical refinement of this approach: the application of hypoxic preconditioning to enhance the therapeutic profile of the MSC secretome. We provide a detailed, technical comparison between hypoxic secretome-based therapies and traditional whole-cell transplantation, focusing on efficacy, safety, and mechanistic insights. Furthermore, we present standardized protocols for hypoxic preconditioning and secretome production, analyze the underlying molecular pathways, and discuss the essential reagents and quality control measures required for translating this advanced cell-free therapy into clinical and commercial applications.
For decades, regenerative medicine has invested in whole MSC transplantation as a promising strategy for treating a wide array of degenerative and inflammatory diseases. The rationale was rooted in the capacity of MSCs to differentiate and directly replace damaged tissue. However, extensive preclinical and clinical observations have consistently shown that the engraftment rate of administered MSCs is remarkably low, and their persistence in host tissues is transient [84] [85]. Despite this poor engraftment, significant therapeutic effects are still observed, leading to the pivotal conclusion that MSCs act primarily through the secretion of a complex cocktail of bioactive molecules.
This cocktail, the secretome, comprises a diverse array of soluble factors (growth factors, cytokines, chemokines) and extracellular vesicles (EVs) such as exosomes, which carry proteins, lipids, and nucleic acids [84] [87]. These components work in concert to mediate complex therapeutic effects, including immunomodulation, angiogenesis, anti-apoptosis, and anti-fibrosis [13] [86]. The recognition of this paracrine mechanism has paved the way for cell-free therapies, which offer several inherent advantages over cell-based products, including reduced risks of immune rejection, tumorigenicity, and embolization, alongside simpler storage, handling, and standardization [85] [86].
To further amplify the therapeutic potency of the secretome, researchers have developed preconditioning strategies. Among these, hypoxic preconditioning has emerged as a particularly powerful method. By mimicking the physiological oxygen tension of the native MSC niche (typically 1-5% O₂), as opposed to the standard hyperoxic (21% O₂) in vitro culture environment, hypoxia fundamentally reprograms MSC metabolism and enhances the production of key therapeutic factors [8]. This whitepaper delves into the direct comparison between this enhanced, cell-free approach and traditional whole-cell therapy.
Quantitative Comparison: Hypoxic Secretome vs. Whole Cell Transplantation
The theoretical advantages of a cell-free, hypoxic-primed approach are supported by concrete, quantitative data from recent studies. The tables below summarize key comparisons across therapeutic profiles, storage and handling, and manufacturing considerations.
Table 1: Comparison of Therapeutic Profile and Practical Handling
| Parameter | Whole Cell Transplantation | Hypoxic Secretome (Cell-Free) |
|---|---|---|
| Primary Mechanism | Direct differentiation (limited) & Paracrine signaling [84] | Paracrine signaling exclusively; enhanced by hypoxia [8] |
| Therapeutic Potency | Standard; dependent on cell viability and engraftment | Enhanced; hypoxic conditioning increases pro-angiogenic (e.g., VEGF, HGF) and immunomodulatory factors (e.g., IL-10, TSG-6) [8] [86] |
| Safety Profile | Risk of immune reactions, ectopic tissue formation, and pulmonary embolism [84] [85] | Safer; no self-replicating entities, low immunogenicity, can be sterile-filtered [85] |
| Storage & Stability | Requires cryopreservation with DMSO; limited shelf-life; complex logistics | Superior; can be lyophilized. Stable at -80°C for 30 months with >70% growth factor retention; with stabilizers like trehalose, short-term stability at 4°C is possible [88] |
Table 2: Comparison of Manufacturing and Clinical Translation
| Parameter | Whole Cell Transplantation | Hypoxic Secretome (Cell-Free) |
|---|---|---|
| Production Scalability | Challenging; limited by cell expansion capacity and senescence | Highly Scalable; large batches can be produced from a single cell lot and stored [87] [86] |
| Batch-to-Batch Consistency | Variable due to donor-dependent cell potency and passage number | Higher Reproducibility; GMP-compliant production shows small inter-batch differences [85] |
| Quality Control (QC) | Complex; requires tests for viability, differentiation, sterility, and tumorigenicity | Simpler QC; focus on protein/vesicle composition, sterility, and potency assays (e.g., tube formation) [85] |
| Off-the-Shelf Potential | Limited for autologous; allogeneic requires HLA matching | High; low immunogenicity allows for allogeneic, ready-to-use product development [85] [86] |
| Dosing | Based on cell number, which may not correlate with secretory activity | Based on protein concentration or vesicle count, directly linked to active components [87] |
Experimental Protocols for Hypoxic Secretome Production
Standardized protocols are critical for the reproducible manufacturing of a potent hypoxic secretome. The workflow below outlines the key stages from cell culture to final product, with detailed methodologies following.
Diagram 1: Hypoxic Secretome Production Workflow
Detailed Methodologies
1. Cell Culture and Hypoxic Preconditioning
- MSC Source: Human umbilical cord Wharton's jelly (WJ-MSCs) or bone marrow-derived MSCs (BM-MSCs) are commonly used due to their robust growth and secretory profile [88] [86].
- Expansion: Culture MSCs in standard growth medium (e.g., α-MEM supplemented with 10% FBS) under normoxic conditions (21% O₂, 5% CO₂) until 70-80% confluency.
- Serum Deprivation: Prior to preconditioning, wash cells with PBS and replace medium with serum-free medium. This is critical to prevent contamination of the secretome with foreign proteins from FBS [87].
- Hypoxic Stimulation: Place the culture flasks/dish in a dedicated hypoxic chamber or multi-gas incubator. Maintain a atmosphere of 1-5% O₂, 5% CO₂, and balance N₂ at 37°C for 24-48 hours. Exposure beyond 48 hours may induce senescence [8].
2. Secretome Collection and Processing
- Conditioned Medium (CM) Collection: After the hypoxic incubation, carefully collect the CM and centrifuge at 2,000-4,000 × g for 20 minutes to remove cell debris [87] [88].
- Sterile Filtration: Filter the supernatant through a 0.22 µm PES membrane filter to remove any remaining particles and microorganisms, resulting in a sterile, cell-free secretome [85].
- Concentration & Lyophilization:
- Concentrate the filtrate using ultrafiltration units (e.g., 3-10 kDa cutoff) or scalable tangential flow filtration (TFF) systems [86].
- For long-term stability, the concentrated secretome can be lyophilized. The addition of trehalose (e.g., 1-5% w/v) as a cryo-/lyo-protectant significantly stabilizes protein and vesicle integrity during freeze-drying and subsequent storage at elevated temperatures [88].
Molecular Mechanisms of Hypoxia-Induced Enhancement
The enhanced therapeutic profile of the hypoxic secretome is not random; it is the result of a deliberate metabolic reprogramming of the MSCs, orchestrated by key hypoxia-sensitive transcription factors.
Diagram 2: Hypoxia-Induced Molecular Signaling Pathway
Key Mechanistic Insights
- Central Role of HIF-1α: Under normoxia, hypoxia-inducible factor-1 alpha (HIF-1α) is continuously degraded. In a low-oxygen environment, HIF-1α stabilizes and translocates to the nucleus, where it dimerizes with HIF-1β and acts as a master regulator of the cellular adaptive response [8].
- Metabolic Reprogramming: HIF-1α drives a shift in MSC metabolism from oxidative phosphorylation to glycolysis. This "glycolytic switch" ensures energy production in oxygen-limited conditions and provides biosynthetic precursors that support the increased production and secretion of bioactive factors [8].
- Transcriptional Activation of Trophic Factors: HIF-1α binds to hypoxia-response elements (HREs) in the promoter regions of numerous genes encoding for therapeutic proteins. This directly leads to the upregulation of:
- Proangiogenic factors: Vascular Endothelial Growth Factor (VEGF), Angiopoietin-1, which promote new blood vessel formation [8] [86].
- Homing chemokines and receptors: Stromal Cell-Derived Factor-1α (SDF-1α) and its receptor CXCR4, enhancing the recruitment of endogenous repair cells to injury sites [8].
- Immunomodulatory factors: Tumor Necrosis Factor-Stimulated Gene 6 (TSG-6), Interleukin-10 (IL-10), and Prostaglandin E2 (PGE2), which suppress detrimental inflammatory responses and promote M2 macrophage polarization [8] [86].
The Scientist's Toolkit: Essential Reagents and Materials
Successful research and development in hypoxic secretome production require specific, high-quality reagents and equipment. The following table details essential items and their functions.
Table 3: Key Research Reagent Solutions for Hypoxic Secretome Production
| Category | Reagent / Material | Specific Function & Rationale |
|---|---|---|
| Cell Culture | Human WJ-MSCs or BM-MSCs | Preferred cell sources due to high proliferative capacity and potent secretory profile [88] [86]. |
| Serum-Free Medium | Base medium for secretome production; eliminates confounding FBS-derived proteins [87]. | |
| Hypoxic Preconditioning | Multi-Gas Incubator / Hypoxic Chamber | Provides a controlled environment for precise O₂ (1-5%), CO₂ (5%), and temperature (37°C) regulation [8]. |
| Hypoxia Mimetics (e.g., CoCl₂, DFO) | Chemical alternatives to physical hypoxia; stabilize HIF-1α but may not fully replicate the hypoxic response [8]. | |
| Secretome Processing | 0.22 µm PES Syringe Filters | For sterile filtration of conditioned medium, removing microbes and particles without significant protein loss [85]. |
| Ultrafiltration Centrifugal Devices (3-10 kDa) | For concentrating the secretome and exchanging buffers [87]. | |
| Tangential Flow Filtration (TFF) System | Scalable, industrial-grade method for concentrating and purifying large secretome volumes [86]. | |
| Stabilization & Storage | Trehalose | A non-reducing disaccharide that protects proteins and vesicles during lyophilization and storage, improving stability at 4°C and RT [88]. |
| Cryovials & -80°C Freezer | For long-term storage of lyophilized or liquid secretome formulations. |
Discussion and Future Perspectives
The accumulated evidence firmly positions the hypoxic MSC secretome as a superior alternative to whole cell transplantation for many regenerative applications. The "cell-free advantage" encompasses enhanced safety, improved product consistency, and greater therapeutic potency driven by targeted molecular preconditioning.
However, for this field to mature, several challenges must be addressed. Standardization is paramount; protocols for hypoxia (exact O₂ level, duration), secretome collection, and concentration need harmonization to enable direct comparison between studies and ensure batch-to-batch reproducibility [87] [85]. Furthermore, the development of potency assays that reliably predict in vivo therapeutic efficacy is a critical regulatory requirement. These may include quantitative ELISA for key factors (e.g., VEGF, TSG-6), nanoparticle tracking analysis for EVs, and functional assays like endothelial tube formation or macrophage polarization [85].
Future research will likely focus on combinatorial preconditioning strategies, such as coupling hypoxia with inflammatory cytokine priming (e.g., IFN-γ, TNF-α) or 3D culture in advanced hydrogels, to further tailor the secretome for specific clinical indications [29] [89]. The use of lyophilized, trehalose-stabilized secretome formulations will greatly enhance the feasibility of global "off-the-shelf" distribution, making this powerful regenerative therapy accessible worldwide [88].
The move from whole-cell transplantation to cell-free secretome therapies represents a significant evolution in regenerative medicine. By incorporating hypoxic preconditioning, researchers can unlock a more potent, therapeutically optimized product. The hypoxic secretome offers a compelling combination of enhanced biological activity, a superior safety profile, and greater practicality for manufacturing and clinical use. As standardization improves and our understanding of its mechanistic pathways deepens, the hypoxic secretome is poised to become a cornerstone of next-generation, cell-free regenerative therapeutics.
The therapeutic efficacy of stem cells in regenerative medicine is largely mediated by their paracrine activity—the secretion of bioactive factors that promote tissue repair. However, cell survival and function post-transplantation are often limited by the harsh ischemic conditions of the injury microenvironment. This technical guide explores the synergistic combination of hypoxic preconditioning—a strategy that pre-adapts cells to low oxygen—and biomaterial scaffolds that provide structural and biochemical support. Framed within a broader thesis on hypoxic stress, this review details how this combined approach amplifies the production of beneficial paracrine factors, thereby enhancing outcomes in tissue regeneration. We provide a comprehensive breakdown of the underlying molecular mechanisms, detailed experimental protocols, key reagent solutions, and quantitative data to support the implementation of this strategy in research and drug development.
The regenerative potential of mesenchymal stem cells (MSCs) and other adult stem cells is critically influenced by their microenvironment. When transplanted into a damaged tissue, such as an infarcted heart or a chronic wound, cells encounter severe hypoxia and nutrient deprivation, leading to catastrophic cell death and limited therapeutic benefit [90]. The paracrine hypothesis posits that a significant portion of the therapeutic effect of stem cells is not due to their direct differentiation into target tissues, but rather through the secretion of a repertoire of cytokines, chemokines, and growth factors [21] [91]. These factors collectively exert cytoprotective, pro-angiogenic, and immunomodulatory effects.
Hypoxic Preconditioning: This is a controlled cellular stress response where stem cells (e.g., MSCs) are cultured under low oxygen tension (typically 0.5%-3% O₂) for 24-72 hours before transplantation. This process acts as a "stress inoculation," activating key transcriptional programs, most notably via Hypoxia-Inducible Factor-1α (HIF-1α). This activation leads to upregulation of genes responsible for cell survival, metabolism, and the secretion of pro-angiogenic paracrine factors like Vascular Endothelial Growth Factor (VEGF) and Stromal Cell-Derived Factor-1α (SDF-1α) [92] [93]. Preconditioned MSCs demonstrate markedly increased survival and retention in vivo [90].
Biomaterial Scaffolds: Three-dimensional scaffolds provide a physical niche for cells, enhancing engraftment. Beyond mere structural support, advanced biomaterials interact with cells biochemically and mechanically. The topography and composition of a scaffold can independently potentiate the paracrine function of MSCs. For instance, electrospun fibrous scaffolds have been shown to significantly enhance the production of anti-inflammatory and pro-angiogenic cytokines from MSCs compared to conventional two-dimensional plastic culture [94].
The synergy emerges when these two strategies are combined. Hypoxic preconditioning "primes" the cell's secretory machinery, while the scaffold provides a protective microenvironment that maintains this enhanced paracrine state, leading to superior tissue repair and regeneration, as demonstrated in models of bone, skin, and urethral reconstruction [92] [90] [93].
Molecular Mechanisms: How Hypoxia and Scaffolds Modulate Paracrine Signaling
Hypoxic Activation of HIF-1α and Downstream Pathways
The master regulator of the cellular response to hypoxia is HIF-1α. Under normoxic conditions, HIF-1α is continuously degraded. In hypoxia, it stabilizes and translocates to the nucleus, dimerizing with HIF-1β to activate the transcription of over 100 target genes [90]. Key consequences for the paracrine function include:
- Enhanced Angiogenic Factor Secretion: Direct upregulation of VEGF, SDF-1α, and other angiogenic cytokines [93].
- Metabolic Reprogramming: A shift towards glycolysis, which is less oxygen-dependent. Preconditioned MSCs can also induce glycolytic metabolism in neighboring endothelial cells, further promoting vascularization [93].
- Anti-Apoptotic Effects: Upregulation of survival signals such as Akt, which reduces caspase-3/7 activity and increases resistance to apoptosis in the harsh transplant site [90] [21].
Scaffold-Mediated Potentiation of Paracrine Effects
Biomaterials are not passive bystanders. They actively influence cell behavior through:
- Physical Cues: Fiber alignment and stiffness can direct cell morphology, which in turn influences nuclear shape and gene expression.
- Biochemical Cues: The incorporation of specific adhesion peptides (e.g., RGD) enhances cell-matrix interactions, improving overall viability and function [90] [94].
- Sustained Paracrine Signaling: By protecting cells and promoting high-density culture (e.g., in spheroids), scaffolds enable the sustained, localized release of trophic factors into the wound environment [90] [94].
Table 1: Key Paracrine Factors Upregulated by Hypoxic Preconditioning and Their Functions
| Paracrine Factor | Abbreviation | Primary Functions | Documented Change with Hypoxia |
|---|---|---|---|
| Vascular Endothelial Growth Factor | VEGF | Angiogenesis, Cytoprotection, Cell Migration | Significantly increased [92] [93] |
| Stromal Cell-Derived Factor-1α | SDF-1α | Progenitor Cell Homing, Angiogenesis | Significantly increased [92] |
| Hepatocyte Growth Factor | HGF | Cytoprotection, Angiogenesis, Cell Migration | Increased [21] [91] |
| Fibroblast Growth Factor-2 | FGF-2 | Cell Proliferation & Migration, Angiogenesis | Increased [21] [91] |
| Insulin-like Growth Factor-1 | IGF-1 | Cytoprotection, Cell Migration, Contractility | Increased [21] [91] |
| Bone Morphogenetic Protein-2 | BMP2 | Osteogenic Differentiation, Development | Context-dependent increase |
The following diagram illustrates the synergistic signaling pathways and experimental workflow involved in combining these two strategies.
Diagram 1: Synergistic experimental workflow and signaling pathways.
Experimental Protocols: A Detailed Methodological Guide
This section provides a step-by-step protocol for implementing the combined strategy, based on established methodologies [92] [90] [93].
Protocol 1: Hypoxic Preconditioning of Human MSCs
Objective: To pre-adapt MSCs to low oxygen, enhancing their survival and paracrine potential.
Materials:
- Human Bone Marrow-derived MSCs (e.g., from Lonza or Allcells) at passage 3-5.
- Standard MSC culture medium: α-MEM or low-glucose DMEM, supplemented with 10% FBS and 1% Penicillin/Streptomycin.
- Hypoxia workstation or multi-gas incubator capable of maintaining 1% O₂, 5% CO₂, and balance N₂.
- Tissue culture flasks/plates.
Procedure:
- Culture Expansion: Expand MSCs under standard culture conditions (37°C, 21% O₂, 5% CO₂) until 70-80% confluent.
- Preconditioning Initiation:
- Wash cells with PBS and add fresh, serum-reduced medium (e.g., 2% FBS) or standard medium.
- Place the culture vessels into the pre-equilibrated hypoxia chamber set to 1% O₂.
- Incubate for 72 hours. (Note: Durations of 24-48 hours are also used; 72 hours shows robust effects on viability [90]).
- Post-Preconditioning Harvest:
- After incubation, remove cells from the hypoxic chamber.
- Wash with PBS, trypsinize, and count cells.
- Proceed immediately to scaffold seeding or spheroid formation.
Quality Control: Validate preconditioning by assaying for HIF-1α protein via Western blot and measuring VEGF concentration in the conditioned medium by ELISA [90].
Protocol 2: Seeding Preconditioned MSCs onto 3D Scaffolds
Objective: To efficiently seed hypoxic-preconditioned MSCs into a 3D biomaterial scaffold.
Materials:
- Scaffold for dermal regeneration (e.g., Integra Matrix) or a porous nanofibrous PLLA/PCL/PLGA scaffold [92] [93].
- Cell culture well plates.
Procedure:
- Scaffold Preparation: Cut the scaffold into appropriate sizes (e.g., 10 mm diameter). Dry with sterile gauze to remove excess moisture and place in a well plate.
- Cell Seeding:
- Resuspend the harvested preconditioned MSCs in a small volume of culture medium (e.g., 2.5 x 10⁵ cells in 300 µL).
- Carefully drop the cell suspension evenly over the scaffold. The dry scaffold will quickly absorb the medium.
- Incubate the plate in the cell culture hood for 30 minutes to allow for initial cell attachment.
- Post-Seeding Culture: After the initial attachment period, gently add additional culture medium to the well until the scaffold is submerged. Culture under standard normoxic conditions for a further 24-48 hours before in vivo implantation or in vitro analysis.
Visualization: Cell distribution and morphology within the scaffold can be confirmed using scanning electron microscopy (SEM) or confocal microscopy after staining actin filaments with phalloidin [92].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of this strategy relies on key reagents. The following table catalogs essential materials and their functions.
Table 2: Key Research Reagent Solutions for Hypoxic Preconditioning and Scaffold-Based Studies
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Mesenchymal Stem Cells | Primary cell source for therapy. | Human Bone Marrow-MSCs (Lonza), Adipose-Derived Stem Cells (ADSCs). Characterize for CD73+, CD90+, CD105+, CD14-, CD34-, CD45- [92]. |
| Hypoxia Chamber/Workstation | Provides a controlled low-oxygen environment for preconditioning. | HERAcell 150i (Thermo Scientific) or similar tri-gas incubator. Precise control of O₂, CO₂, and N₂ is critical [90]. |
| 3D Scaffolds | Provides 3D structural support, enhances paracrine function. | Integra Matrix (Collagen-Chondroitin Sulfate) [92]; PLLA/PCL/PLGA porous nanofibrous scaffolds [93]; RGD-Modified Alginate hydrogels for spheroid encapsulation [90]. |
| Pro-Angiogenic Factor ELISA Kits | Quantitative validation of paracrine factor secretion. | Human VEGF ELISA Kit (R&D Systems) to measure preconditioning efficacy [90] [93]. |
| Cell Viability/Apoptosis Assays | Assessment of preconditioning-enhanced survival. | Caspase-Glo 3/7 Assay (Promega) for apoptosis [90]; MTT Assay for metabolic activity [92]. |
| Antibodies for Western Blot | Mechanistic validation of hypoxic response. | Mouse anti-human HIF-1α monoclonal antibody (BD Biosciences); β-Tubulin as a loading control [90]. |
Quantitative Data: Measuring the Synergistic Effect
The success of the combined strategy is quantifiable through a range of in vitro and in vivo assays. The table below consolidates key quantitative findings from the literature.
Table 3: Quantitative Outcomes of Combined Hypoxic Preconditioning and Scaffold Use
| Assay / Outcome Measure | Experimental Groups | Key Quantitative Findings | Source |
|---|---|---|---|
| In Vitro VEGF Secretion | Normoxia-MSCs vs. Hypoxia-MSCs | Hypoxia-preconditioned ADSCs secreted significantly higher levels of VEGFA (p < 0.05), enhancing HUVEC angiogenesis. | [93] |
| In Vitro Apoptosis (Caspase 3/7 Activity) | Normoxia-MSC Spheroids vs. Hypoxia-MSC Spheroids | Hypoxic preconditioning (1% O₂, 3 days) made MSC spheroids more resistant to apoptosis under serum-deprived, hypoxic culture. | [90] |
| In Vivo Bone Healing | Acellular Gel vs. Individual MSCs vs. MSC Spheroids | Spheroids from hypoxia-preconditioned MSCs in alginate hydrogel induced significantly more bone healing in a rat critical-sized femoral defect. | [90] |
| In Vivo Urethral Reconstruction | Normoxia-ADSCs/Scaffold vs. Hypoxia-ADSCs/Scaffold | The hypoxia-preconditioned group showed a larger urethral lumen diameter, preserved morphology, and enhanced angiogenesis (p < 0.05). | [93] |
| In Vivo Scaffold Vascularization | Normoxia-MSC/SDR vs. Hypoxia-MSC/SDR | MSC-containing scaffolds pre-incubated in hypoxia showed higher infiltration of endothelial cells after implantation in mice. | [92] |
| In Vitro Endothelial Cell Function | HUVECs + Normoxia-CM vs. HUVECs + Hypoxia-CM | Conditioned medium (CM) from hypoxia-preconditioned ADSCs enhanced HUVEC viability, proliferation, migration, and glycolysis (p < 0.05). | [93] |
The strategic combination of hypoxic preconditioning and biomaterial scaffolds represents a powerful paradigm shift in regenerative medicine, moving beyond viewing cells and materials as separate entities toward an integrated, bio-inspired system. This approach directly addresses the central challenge of post-transplantation cell death and inefficient paracrine signaling by pre-adapting cells to stress and providing a supportive microenvironment. The data consistently show that this synergy leads to enhanced secretion of therapeutic factors, improved cell survival, and superior functional outcomes in diverse pre-clinical models.
Future work will focus on further optimizing this combination. This includes developing "smart" biomaterials that can precisely control the release of oxygen [95] [96] or co-deliver specific growth factors to work in concert with the preconditioned cells. Fine-tuning the hypoxic preconditioning protocol—varying oxygen tension, duration, and incorporating cyclic hypoxia—may allow for customizing the paracrine profile for specific clinical applications. As research progresses, this synergistic strategy holds significant promise for bridging the gap between promising pre-clinical results and robust, effective therapies for human patients.
The landscape of clinical trials is a dynamic and critical component of the global biomedical research ecosystem, serving as the primary pathway for translating basic scientific discoveries into new therapies for patients. This overview examines the current state of registered clinical trials, with particular emphasis on emerging trends and the growing field of hypoxic stress research and its effect on stem cell paracrine factor production. Clinical trials provide the essential evidence base for medical product safety and efficacy, making their landscape a key indicator of where therapeutic innovation is heading [97]. Understanding this landscape—including patterns in therapeutic areas, trial designs, sponsorship, and geographical distribution—is crucial for researchers, regulators, and drug development professionals navigating the complex process of clinical translation.
Within this broad context, research into hypoxic preconditioning of stem cells has emerged as a particularly promising area. This approach, which involves exposing cells to low oxygen levels to enhance their therapeutic potential, exemplifies how fundamental mechanistic insights are being translated into clinical applications. The growing understanding that stem cells primarily exert their regenerative effects through paracrine signaling—the release of bioactive factors—rather than direct tissue integration, has opened new avenues for cell-free therapeutic strategies [16] [98]. This review synthesizes the macro-trends in clinical trial registration and activity while providing a technical deep dive into the experimental methodologies driving one of the most innovative areas of translational research.
Global Clinical Trial Activity and Trends
Analysis of ClinicalTrials.gov reveals a consistent increase in clinical trial registrations, with activity peaking in 2021, largely driven by the global response to the COVID-19 pandemic [97]. This surge demonstrates the clinical research enterprise's capacity for rapid mobilization during public health emergencies. The distribution of trials across therapeutic areas reflects the global burden of disease, with oncology representing the most dominant focus [97]. This concentration underscores the substantial unmet medical needs in cancer care and the intensive research efforts to develop more effective treatments.
Between 2019 and 2023, China's pharmaceutical industry demonstrated remarkable growth in innovative drug development, evidenced by a significant rise in both Investigational New Drug (IND) applications and New Drug Applications (NDA) [99]. This expansion reflects China's strategic transition from a generics-dominated market to an increasingly innovation-driven one, positioning the country as a growing force in the global pharmaceutical landscape. Regulatory modernization through the National Medical Products Administration (NMPA) has been instrumental in facilitating this progress, with reforms that have streamlined approval pathways and enhanced clinical trial efficiency [99].
Table 1: Global Clinical Trial Trends and Characteristics (as of March 2025)
| Aspect | Current Trend | Key Details |
|---|---|---|
| Overall Registration | Consistent increase, peak in 2021 | Driven significantly by COVID-19 pandemic research [97] |
| Leading Therapeutic Area | Oncology | Reflects the global disease burden and high unmet need [97] |
| Predominant Trial Design | Randomized Controlled Trials (RCTs) | Considered the gold standard for generating robust efficacy evidence [97] |
| Key Growth Region | China | Rapid rise in IND and NDA applications from 2019-2023 [99] |
| Major Challenge | Participant Demographics | Underrepresentation of pediatric, elderly, and minority populations [97] |
Notable Trials and Readouts in 2025
The clinical trial landscape in 2025 features several pivotal studies with expected readouts that could significantly influence therapeutic areas and market dynamics. These trials represent advanced-stage translation of novel mechanisms and platforms.
Table 2: Selected Key Clinical Trials with Anticipated 2025 Readouts
| Trial/Drug | Sponsor | Therapeutic Area | Mechanism/Type | Key Significance |
|---|---|---|---|---|
| Attain-1 (orforglipron) | Eli Lilly | Obesity/Oral incretin | Chemical-based GLP-1 receptor agonist | Potential first oral incretin for obesity; Phase 3 results in non-diabetics awaited [100] |
| Coast-1, Shore (amlitelimab) | Sanofi | Immunology (Eczema, Asthma) | OX40L inhibitor (anti-inflammatory) | Successor to Dupixent; potential multi-billion euro peak sales [100] |
| Vela-1, Vela-2 (sonelokimab) | Moonlake Immunotherapeutics | Hidradenitis Suppurativa | Anti-IL-17 antibody (binds two cytokines + albumin) | Differentiated profile with less frequent dosing; Phase 3 readout Sept 2025 [100] |
| Harmoni-2 (ivonescimab) | Akeso/Summit Therapeutics | Lung Cancer | Dual PD-1/VEGF inhibitor | Approved in China; final survival analysis in 2025 critical for class validation [100] |
| FENhance 1/2, FENtrepid (fenebrutinib) | Roche | Multiple Sclerosis (Relapsing) | Reversible BTK inhibitor (penetrates brain) | Differentiated mechanism; potential in autoimmune disease despite prior class failures [100] |
The Translational Pathway of Hypoxic Stress and Stem Cell Paracrine Research
From Mechanistic Insight to Therapeutic Application
The translation of basic research on hypoxic stress and stem cell paracrine activity exemplifies the journey from mechanistic discovery to clinical application. Mesenchymal stem cells (MSCs), including those derived from bone marrow (BM-MSCs) and adipose tissue (ASCs), secrete a complex mixture of cytokines, chemokines, and growth factors that collectively promote tissue repair through mechanisms including angiogenesis, immune modulation, and cell survival [16] [98]. The observation that the ischemic myocardium could be protected by brief sublethal ischemia—a phenomenon known as preconditioning—provided the foundational insight for applying hypoxic conditioning to stem cells [16].
Hypoxic conditioning enhances the production of key paracrine factors from stem cells. Research demonstrates that human adipose-derived stem cells (ASCs) subjected to severe hypoxia (<0.1% O₂) significantly increase both the transcriptional and translational levels of pivotal angiogenic factors including vascular endothelial growth factor-A (VEGF-A) and angiogenin (ANG) [16]. This enhanced paracrine profile has demonstrated functional significance in vivo, with hypoxic-conditioned medium from ASCs (ASCCM) stimulating greater angiogenesis in mouse models compared to normoxic-conditioned medium [16]. Similarly, studies of BM-MSCs show they secrete distinctly different and more potent combinations of wound-healing factors—including VEGF-α, IGF-1, EGF, and stromal derived factor-1—compared to dermal fibroblasts [98]. This molecular understanding provides the rationale for using hypoxic-preconditioned stem cells or their conditioned media as a therapeutic tool.
Key Signaling Pathways in Hypoxic Conditioning
The cellular response to hypoxia is centrally coordinated by the hypoxia-inducible factor-1 (HIF-1) transcription factor. The following diagram illustrates the core signaling pathway activated by hypoxic preconditioning in stem cells and its subsequent biological effects.
Diagram Title: Core Pathway of Hypoxic Preconditioning in Stem Cells
This pathway activation results in the secretion of a therapeutically relevant paracrine cocktail. Functional studies confirm that neutralizing antibodies against VEGF-A and ANG significantly diminish the angiogenic response, establishing their critical functional role in the paracrine mechanism [16]. In wound healing models, application of BM-MSC-conditioned medium increases recruitment of CD4/80-positive macrophages and Flk-1-, CD34-, or c-kit-positive endothelial progenitor cells into wounds, accelerating healing compared to controls [98].
Experimental Models and Methodologies for Investigating Paracrine Effects
Standardized Protocol for Hypoxic Conditioning and Analysis
Translating the concept of hypoxic preconditioning into robust, reproducible experimental data requires standardized methodologies. The following workflow outlines a typical protocol for conditioning stem cells and evaluating their paracrine effects in vitro and in vivo.
Diagram Title: Workflow for Hypoxic Paracrine Effect Studies
Detailed Methodology:
Cell Culture and Hypoxic Conditioning: Human adipose-derived stem cells (ASCs) are seeded at a density of 5×10³ cells per cm² and cultured until 80% confluent. For hypoxia induction, cells are placed in a serum-free medium and exposed to either 1% O₂ in a tri-gas incubator or to severe hypoxia (<0.1% O₂) using a sealed GENbox jar system for a period of 12 to 72 hours, typically 24 hours [16].
Conditioned Medium (CM) Collection and Concentration: After hypoxic or normoxic control incubation, the conditioned medium (ASCCM) is collected, centrifuged at 875g to remove cell debris, and filtered through a 0.2-μm filter. The medium is then concentrated 50-fold using centrifugal filter units with a 3-kDa molecular weight cutoff (e.g., Amicon Ultra-15) [16]. For in vivo studies, this concentration step is critical to achieve a therapeutically relevant dose of paracrine factors.
Molecular Analysis of Paracrine Factors:
- Gene Expression: mRNA is extracted from cells post-conditioning using TriReagent. After cDNA synthesis, quantitative real-time PCR (qRT-PCR) is performed using TaqMan probes for key factors such as VEGF-A, ANG, SDF-1, bFGF, HGF, and IL-8 [16].
- Protein Secretion: The concentrated conditioned medium is analyzed via Enzyme-Linked Immunosorbent Assay (ELISA) for specific proteins like VEGF-A, VEGF-C, and VEGF-D using Quantikine kits. Western blotting can be used for additional protein quantification, such as for ANG levels [16].
Functional In Vitro Assays:
- Cell Migration: Assessed using transwell migration assays. Conditioned medium is placed in the lower chamber, and its ability to recruit cells like macrophages (e.g., CD14+ monocytes), keratinocytes, or endothelial cells is measured after a defined incubation period [98].
- Cell Proliferation: Keratinocytes or Human Umbilical Vein Endothelial Cells (HUVECs) are seeded in plates and cultured in conditioned medium. Cell counts are performed over several days to quantify the mitogenic effect of the paracrine factors [98].
- Endothelial Tube Formation: HUVECs are plated on Matrigel and treated with conditioned medium. The formation of capillary-like structures is quantified to assess pro-angiogenic activity [16].
In Vivo Validation Models:
- Subcutaneous Sponge Assay: Sterile polyvinyl alcohol sponges impregnated with conditioned medium are implanted subcutaneously in mice. After 2 weeks, the sponges are harvested, and angiogenesis is quantified morphometrically in anti-CD31-immunolabeled sections by measuring the percentage vascular volume [16].
- Excisional Wound Healing: In mouse models, concentrated conditioned medium is applied to full-thickness skin wounds. The rate of wound closure is tracked over time. Subsequent analysis of wound cell suspensions by flow cytometry can quantify recruited immune and endothelial progenitor cells (e.g., CD4/80+ macrophages, Flk-1+, CD34+ cells) [98].
Essential Research Reagents and Materials
The investigation of hypoxic preconditioning and paracrine effects relies on a specialized toolkit of reagents, assays, and model systems.
Table 3: Research Reagent Solutions for Hypoxic Paracrine Studies
| Reagent/Assay | Specific Example | Function in Experimental Protocol |
|---|---|---|
| Hypoxia System | GENbox Jar, Tri-gas incubator | Creates a controlled, low-oxygen environment (<0.1% to 1% O₂) for cell conditioning [16]. |
| Stem Cell Media | DMEM-low glucose, Serum-free media | Base medium for cell culture and for collecting conditioned secretions without serum interference [16] [98]. |
| Concentration Device | Amicon Ultra-15 Centrifugal Filters (3-kDa cutoff) | Concentrates conditioned medium 50-fold to augment the concentration of secreted paracrine factors [16]. |
| qRT-PCR Assays | TaqMan Gene Expression Assays (VEGF-A, ANG, etc.) | Quantifies transcriptional upregulation of pro-angiogenic and pro-survival genes in response to hypoxia [16]. |
| ELISA Kits | Quantikine ELISA (e.g., for VEGF-A) | Precisely measures the concentration of specific secreted proteins in the conditioned medium [16]. |
| Neutralizing Antibodies | Anti-VEGF-A, Anti-Angiogenin | Functionally validates the contribution of specific factors to the observed biological effects by blocking their activity [16]. |
| In Vivo Model | Mouse subcutaneous sponge implant / Excisional wound | Provides an in vivo system to validate the functional angiogenic or wound-healing capacity of the paracrine factors [16] [98]. |
| Flow Cytometry Antibodies | Anti-CD31, Anti-CD4/80, Anti-CD34, Anti-Flk-1 | Identifies and quantifies specific cell populations (endothelial cells, macrophages, progenitor cells) recruited to sites of treatment in vivo [98]. |
Challenges and Future Directions in Clinical Translation
Persistent Gaps in the Clinical Trial Landscape
Despite overall growth in clinical trial activity, significant challenges persist that limit the generalizability and impact of research findings. A major issue is the underrepresentation of key demographic groups, including pediatric, elderly, and minority populations, in many clinical trials [97]. This disparity can lead to incomplete understanding of how therapies perform across the diverse patient populations that exist in real-world clinical practice. Furthermore, the geographical distribution of clinical trials remains limited, with research activity concentrated in specific regions, potentially overlooking genetic, environmental, and social determinants of health that vary globally [97]. Another critical challenge is the insufficient reporting of trial results, which undermines the scientific knowledge base, contributes to publication bias, and violates ethical obligations to research participants and the broader community.
Advancing Hypoxic and Paracrine Therapies
For the field of hypoxic stem cell research, the primary translational challenge lies in moving from compelling preclinical models to standardized, efficacious human therapies. Future work must focus on optimizing and standardizing the hypoxic preconditioning protocol (O₂ level, exposure duration, cell type) to maximize therapeutic output while ensuring product consistency and safety. The cell-free approach—using concentrated conditioned medium or purified extracellular vesicles—presents a promising strategy that may offer better safety profiles, easier storage, and greater regulatory feasibility than live cell transplantation [16] [98]. Successfully navigating the regulatory pathway for these complex biological products will require robust manufacturing protocols and definitive clinical trials demonstrating safety and efficacy for specific indications, such as chronic wounds or ischemic tissue repair.
The global competitive landscape for such innovative therapies is intensifying. While the United States maintains leadership in first-in-class therapies through advanced regulatory pathways like the FDA's Breakthrough Therapy Designation, China is rapidly emerging as a key player in innovative drug development, particularly in areas like cell and gene therapy [99]. International collaborations, such as Project Orbis for simultaneous oncology drug reviews, are becoming increasingly important, highlighting the need for global coordination in clinical translation [99]. For researchers in the hypoxic stress and stem cell field, engaging with these evolving global frameworks early in the development process will be crucial for successful clinical translation and ultimate patient benefit.
Conclusion
Hypoxic preconditioning emerges as a powerful, non-genetic strategy to profoundly enhance the therapeutic profile of stem cells by amplifying the production of beneficial paracrine factors. The process, orchestrated by HIF-1α, not only boosts the secretion of angiogenic, immunomodulatory, and pro-survival molecules but also refines the cargo of extracellular vesicles. While preclinical data across cardiovascular, neurological, and wound healing models is compelling, the path to clinical translation requires resolving key challenges in protocol standardization, scalable manufacturing, and comprehensive safety profiling. Future research should prioritize the identification of specific potency biomarkers, the development of advanced delivery systems for the secretome, and the execution of rigorous, well-controlled clinical trials. By mastering the hypoxic stimulus, the field can advance toward a new generation of highly effective, cell-free regenerative therapeutics with broad application in human disease.
References
- 1. Hypoxia-Inducible Factor (HIF)-1 Regulatory Pathway and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2140184/]
- 2. Hypoxia Signaling [https://www.cellsignal.com/pathways/hypoxia-signaling-pathway?srsltid=AfmBOopYa1NBYwVPlsjSqw6LmfMDHj82CNQL4N-g5TykYeao8liLRl1G]
- 3. Indispensable Role of HIF-1α Signaling in Post- ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.655073/full]
- 4. Hypoxic Neural Stem Cells Enhance Spinal Cord Repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259395/]
- 5. HIF-1 attenuates high-fiber diet-mediated proliferation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369635/]
- 6. The stage-specific roles of HIF-1α in regulating mESC ... [https://www.sciencedirect.com/science/article/pii/S0021925825021945]
- 7. HIF1-alpha expressing cells induce a hypoxic-like response in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6011406/]
- 8. Frontiers | Hypoxia-induced metabolic reprogramming in mesenchymal stem cells: unlocking the regenerative potential of secreted factors [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1609082/full]
- 9. Hypoxia-induced metabolic reprogramming in mesenchymal stem cells: unlocking the regenerative potential of secreted factors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183037/]
- 10. Impact on Oxidative Stress and Nanoparticle Stability [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113433/]
- 11. Advances in stem cell-based therapeutics for acute high ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1614098/full]
- 12. Effects of microenvironment and biological behavior on the ... [https://www.sciencedirect.com/science/article/pii/S235230422300140X]
- 13. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 14. Functional impacts of lactylation in Hypoxia‒primed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592145/]
- 15. Hypoxia-driven angiogenesis and metabolic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1572909/full]
- 16. Hypoxic Conditioning Enhances the Angiogenic Paracrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3653395/]
- 17. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 18. Advances in stem cell-based therapeutics for acute high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354629/]
- 19. Hypoxia-Induced Extracellular Vesicles Derived from ... [https://www.mdpi.com/2218-273X/15/11/1504]
- 20. Hypoxia modifies the polarization of macrophages and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6865149/]
- 21. Paracrine mechanisms in adult stem cell signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2667788/]
- 22. Extracellular vesicles secreted by hypoxia pre-challenged ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6367822/]
- 23. Extracellular vesicles from hypoxia-preconditioned ... [https://www.nature.com/articles/s41419-021-04363-7]
- 24. Effects of Exosomes From Hypoxia-Induced Adipose- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257001/]
- 25. Extracellular vesicles as biomarkers and drug delivery ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278421/]
- 26. Potential Protection of Mesenchymal Stem Cells Against ... [https://bmrat.biomedpress.org/index.php/BMRAT/article/view/969]
- 27. Intermittent Hypoxia Conditioning: A Potential Multi-Organ ... [https://www.medsci.org/v20p1551.htm]
- 28. Key Considerations for Scientists Venturing into Hypoxia ... [https://www.oxford-optronix.com/resources/key-considerations-for-scientists-venturing-into-hypoxia-or-physoxia-research]
- 29. Synergistic effect of Hypoxic Conditioning and Cell-Tethering ... [https://pubmed.ncbi.nlm.nih.gov/39380372/]
- 30. Method standardization of secretome production, collection ... [https://www.sciencedirect.com/science/article/pii/S2352320425000811]
- 31. GMP‐Compliant Process for the Manufacturing of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365392/]
- 32. An optimized quantitative proteomics method establishes the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7560198/]
- 33. Paracrine mechanisms of stem cell reparative and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021634/]
- 34. Paracrine mechanisms of stem cell reparative and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022282810002920]
- 35. Angiogenesis after acute myocardial infarction: a bibliometric [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1426583/full]
- 36. Angiogenesis in the Infarcted Myocardium - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3567783/]
- 37. Gastrin mediates cardioprotection through angiogenesis ... [https://www.nature.com/articles/s41598-021-95110-7]
- 38. Human Neural Stem Cells Reduce Hypoxia-Ischemic ... [https://pubmed.ncbi.nlm.nih.gov/40519252/]
- 39. Reversing coma by senolytics and stem cells: the future is now [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502250/]
- 40. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 41. Hypoxia preconditioned MSC exosomes attenuate high- ... [https://www.sciencedirect.com/science/article/pii/S2452199X25002464]
- 42. Stem Cell Therapy for TBI: Mechanisms & Effectiveness ... [https://www.dvcstem.com/post/stem-cell-therapy-for-tbi]
- 43. Combined treatment with mesenchymal stem cells and ... [https://www.nature.com/articles/s41598-025-98504-z]
- 44. Surgery and Engineering Researchers Team Up to ... [https://www.surgery.wisc.edu/2025/03/17/surgery-and-engineering-researchers-team-up-to-enhance-wound-healing/]
- 45. Human iPSCs-derived mesenchymal stem cells promote ... [https://www.nature.com/articles/s41536-025-00427-w]
- 46. Rapid cutaneous wound healing in nude mice by fetal skin ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1557973/full]
- 47. Polynucleotide and Hyaluronic Acid Mixture for Skin ... [https://pubmed.ncbi.nlm.nih.gov/40009152/]
- 48. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 49. Cellular senescence or stemness: hypoxia flips the coin [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-02035-0]
- 50. Oxidative Stress in Stem Cell Aging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5680960/]
- 51. Benefits of hypoxic culture on bone marrow multipotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3484415/]
- 52. The Role of Hypoxia in Stem Cell Differentiation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2891942/]
- 53. Effect of low oxygen tension on the biological ... [https://www.sciencedirect.com/science/article/pii/S1355814523005060]
- 54. A comparative analysis of human mesenchymal stem cell ... [https://pubmed.ncbi.nlm.nih.gov/24888834/]
- 55. Secretive derived from hypoxia preconditioned ... [https://www.sciencedirect.com/science/article/pii/S2452199X23001111]
- 56. implication for stem cell therapies targeting intervertebral discs [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-018-1601-9]
- 57. The characterization of the biological effect of hypoxia ... [https://www.sciencedirect.com/science/article/pii/S2667290125000464]
- 58. Advances in application of hypoxia-preconditioned ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1446050/full]
- 59. Enhanced therapeutic effects of hypoxia-preconditioned ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04166-z]
- 60. A comprehensive analysis [https://www.sciencedirect.com/science/article/abs/pii/S0014299925003280]
- 61. Hypoxia and inflammatory factor preconditioning enhances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10696190/]
- 62. Potential Protection of Mesenchymal Stem Cells Against ... [https://bmrat.org/index.php/BMRAT/article/view/969]
- 63. Dynamic Culture of Mesenchymal Stromal/Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9421039/]
- 64. Do hypoxia/normoxia culturing conditions change the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4533943/]
- 65. Hypoxia Conditioned Mesenchymal Stem Cell-Derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2019.00292/full]
- 66. Superoxide induced by a high-glucose concentration attenuates production of angiogenic growth factors in hypoxic mouse mesenchymal stem cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/21068072/]
- 67. RoosterBio & Secretome Therapeutics Announce ... [https://www.roosterbio.com/press_release/roosterbio-secretome-therapeutics-announce-successful-completion-of-large-scale-bioreactor-production-for-clinical-stage-cell-therapy-candidate-stm-01/]
- 68. Microbioreactor arrays for controlling cellular environments [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744042/]
- 69. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562725/]
- 70. Could hypoxic conditioning augment the potential of mesenchymal stromal cell-derived extracellular vesicles as a treatment for type 1 diabetes? | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04153-4]
- 71. Hypoxia-Inducible Factors in Physiology and Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3437543/]
- 72. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 73. A Review on the Stability Challenges of Advanced Biologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114724/]
- 74. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 75. Released by Paracrine of Mesenchymal Origin... Factors Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9622561/]
- 76. Priming adult stem by cells pretreatments for applications in... hypoxic [https://jbiomedsci.biomedcentral.com/articles/10.1186/1423-0127-20-63]
- 77. Secretome from human adipose-derived mesenchymal stem ... cells [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0277863]
- 78. Chapter 10 Methods for Comparative Studies - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK481584/]
- 79. Stem cell-derived paracrine factors by modulated reactive ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365923006612]
- 80. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 81. Data Visualization Toolkit: Data Tables Design Principles [https://dasycenter.org/datavis-toolkit/data-tables/]
- 82. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 83. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 84. the Therapeutic Potential of Stem Comparing and their... Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC8378970/]
- 85. Reproducibility of GMP-compliant production of therapeutic stressed... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1524-2]
- 86. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 87. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 88. Storage conditions affect the composition of the lyophilized secretome ... [https://www.nature.com/articles/s41598-024-60787-z?error=cookies_not_supported&code=a31cb39c-5e42-4083-842f-5be379891f6b]
- 89. Optimizing mesenchymal stromal cells priming strategies ... [https://www.sciencedirect.com/science/article/pii/S0753332225004123]
- 90. Hypoxic Preconditioning of Mesenchymal Stem Cells with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6125201/]
- 91. A Systematic Review of Pre-clinical Studies | Stem Cell ... [https://link.springer.com/article/10.1007/s12015-022-10429-6]
- 92. Hypoxic pre-conditioning increases the infiltration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4626656/]
- 93. Hypoxia-preconditioned adipose-derived stem cells combined ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02052-4]
- 94. Fibrous scaffolds potentiate the paracrine function of ... [https://www.sciencedirect.com/science/article/pii/S0142961217304271]
- 95. Oxygen Releasing Biomaterials for Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC3708668/]
- 96. Breathing life into engineered tissues using oxygen- ... [https://www.nature.com/articles/s41427-019-0166-2]
- 97. The Current Landscape of Clinical Trials [https://pubmed.ncbi.nlm.nih.gov/40217968/]
- 98. Paracrine Factors of Mesenchymal Stem Cells Recruit ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0001886]
- 99. Current landscape of innovative drug development and ... [https://www.nature.com/articles/s41392-025-02267-y]
- 100. 10 clinical trials to watch the rest of 2025 [https://www.biopharmadive.com/news/biotech-pharma-clinical-trials-watch-2025/736120/]