MSC Exosomal miRNAs: Master Regulators of Fibroblast Proliferation and Migration in Regeneration and Disease
This article comprehensively explores the critical role of mesenchymal stem cell (MSC)-derived exosomal microRNAs (miRNAs) in regulating fibroblast proliferation and migration, a central process in tissue repair, regeneration, and pathology.
MSC Exosomal miRNAs: Master Regulators of Fibroblast Proliferation and Migration in Regeneration and Disease
Abstract
This article comprehensively explores the critical role of mesenchymal stem cell (MSC)-derived exosomal microRNAs (miRNAs) in regulating fibroblast proliferation and migration, a central process in tissue repair, regeneration, and pathology. We delve into the foundational biology, identifying key miRNAs such as miR-125a, miR-21, and miR-135a and their mechanisms of action in promoting wound healing and skin regeneration. The scope extends to methodological approaches for isolating these exosomes and their cargo, alongside advanced bioengineering strategies to optimize therapeutic potential. The content also addresses challenges in the field and provides a comparative analysis of efficacy across different MSC sources and vesicle types. Finally, we synthesize key findings to discuss future clinical implications and translational pathways for MSC exosomal miRNAs in regenerative medicine and drug development.
The Biological Blueprint: How MSC Exosomal miRNAs Dictate Fibroblast Fate
Mesenchymal stem cell (MSC) exosomes have emerged as pivotal mediators of intercellular communication, representing a fundamental paradigm shift in understanding how MSCs exert their therapeutic effects. Initially, the regenerative potential of MSCs was attributed primarily to their ability to differentiate into various cell types and directly replace damaged tissues. However, research over the past decade has revealed that most therapeutic benefits occur through paracrine mechanisms rather than direct cellular differentiation and replacement [1] [2]. When administered intravenously, most MSCs become trapped in the lungs, with only a minimal fraction reaching intended injury sites, yet significant therapeutic effects persist through their secreted factors [1].
The conditioned medium from MSC cultures, containing these secreted factors, demonstrates therapeutic benefits comparable to the cells themselves [1]. Among these secreted factors, extracellular vesicles (EVs), particularly exosomes, have been identified as critical mediators of MSC paracrine signaling [1] [2]. These nanoscale vesicles serve as natural biological carriers, transporting bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating cellular functions and promoting tissue repair [2] [3]. This whitepaper examines MSC exosomes as essential paracrine mediators, with specific focus on their roles in regulating fibroblast proliferation and migration through exosomal miRNA transfer.
MSC Exosomes: Biogenesis, Composition, and Function
Biogenesis and Classification
Exosomes represent a specific subtype of extracellular vesicles generated through an elaborate endosomal pathway, distinct from other vesicles that bud directly from the plasma membrane.
- Endosomal Origin: Exosome biogenesis begins with the inward budding of the plasma membrane, forming early endosomes that subsequently mature into late endosomes [4]. During this maturation process, the endosomal membrane invaginates inward, forming intraluminal vesicles (ILVs) within larger structures called multivesicular bodies (MVBs) [5] [4].
- Secretion: These MVBs subsequently fuse with the plasma membrane, releasing their contained ILVs into the extracellular space as exosomes [5] [4]. The release process is regulated by Rab GTPase proteins, particularly Rab27a and Rab27b [5].
- Classification: Based on physical characteristics and biogenesis mechanisms, MSC-derived extracellular vesicles are primarily classified into three subtypes [2] [6]:
- Exosomes (20-150 nm): Formed through the endocytic pathway.
- Microvesicles (100-1,000 nm): Generated through direct budding from the plasma membrane.
- Apoptotic bodies (>1,000 nm): Produced during programmed cell death.
The International Society for Extracellular Vesicles (ISEV) recommends using the umbrella term "extracellular vesicles" when specific biogenesis pathways cannot be confirmed [7]. For this document, "exosomes" will refer to small EVs (30-200 nm) isolated via standard methods and characterized by specific markers [5].
Molecular Composition and Cargo Loading
MSC exosomes possess a complex molecular architecture that reflects their biological function as communication vehicles.
- Lipid Bilayer: Exosomes are enclosed by a phospholipid bilayer enriched with cholesterol, sphingomyelin, and ceramides [7]. This structure provides stability in biological fluids and facilitates membrane fusion with target cells.
- Surface Proteins: Tetraspanins (CD9, CD63, CD81) are characteristic exosome surface markers [5] [7]. MSC exosomes also express MSC-specific markers (CD73, CD90, CD105) and proteins involved in immune response (MHC class I), membrane fusion (annexins), and intracellular trafficking (TSG101, Alix) [1] [5].
- Internal Cargo: The exosomal lumen carries functional molecules including proteins (heat shock proteins, cytoskeletal proteins, enzymes), lipids, and nucleic acids (mRNAs, miRNAs) [5] [3].
The packaging of miRNA content into MSC exosomes occurs selectively rather than randomly [1]. Specific miRNAs are enriched in exosomes through interactions with RNA-binding proteins (e.g., hnRNPA2B1, SYNCRIP, YBX-1) and recognition of specific sequence motifs (e.g., GGAG, GGCU) in the miRNAs [1] [8]. The ceramide-dependent pathway, regulated by neutral sphingomyelinase 2 (nSMASe2), also plays a crucial role in controlling EV and miRNA secretion [1].
Mechanisms of Recipient Cell Interaction
MSC exosomes employ multiple mechanisms to deliver their cargo to recipient cells, each with distinct functional implications [2]:
- Membrane Fusion: Direct fusion with the target cell membrane allows exosomal contents to be released directly into the cytoplasm, representing the primary mechanism for functional cargo delivery.
- Internalization: Exosomes may be internalized via endocytosis or phagocytosis, subsequently trafficking to endosomal compartments where cargo is released.
- Receptor Binding: Surface proteins on exosomes can bind to signaling receptors on target cells, initiating downstream signaling cascades without internalization.
Table 1: Key Technical Specifications of MSC Exosomes
| Characteristic | Specification | Technical Notes |
|---|---|---|
| Size Range | 30-200 nm [5] [4] | Typically 30-150 nm for exosomes specifically [9] |
| Density | 1.13-1.19 g/mL | Varies based on cellular source and isolation method |
| Key Surface Markers | CD9, CD63, CD81, CD73, CD90, CD105 [1] [5] | Tetraspanins are common; MSC markers indicate origin |
| Key Internal Markers | TSG101, Alix, Hsp70, Hsp90 [1] | Proteins involved in MVB biogenesis and stress response |
| Lipid Composition | Enriched in cholesterol, sphingomyelin, ceramide [7] | Provides membrane stability and facilitates fusion |
| Nucleic Acid Content | miRNAs, mRNAs, other non-coding RNAs [1] | miRNA is most abundant RNA type [5] |
MSC Exosomal miRNAs: Key Regulators of Fibroblast Function
Selective miRNA Packaging and Transfer
MicroRNAs (miRNAs) are small non-coding RNAs (19-24 nucleotides) that regulate approximately 30% of all mammalian protein-coding genes by binding to target mRNAs and either degrading them or inhibiting translation [1] [8]. MSC exosomes contain numerous miRNAs that contribute to both pathological and physiological processes, including epigenetic regulation, immune regulation, and tissue repair [1].
Comparative analyses reveal that miRNA packaging into exosomes is highly selective, with specific miRNAs enriched up to 100-fold in exosomes compared to parent MSCs [8]. Frequently enriched miRNAs in MSC exosomes include miR-21, let-7g, miR-1246, miR-381, and miR-100 [8]. This selective enrichment enables exosomes to function as precision delivery systems for specific genetic regulators.
Mechanisms of Fibroblast Regulation
In the context of wound healing and tissue repair, fibroblasts are crucial cellular players that contribute to extracellular matrix deposition, tissue remodeling, and wound contraction. MSC exosomal miRNAs modulate fibroblast behavior through multiple mechanisms:
- Proliferation and Migration Promotion: Exosomes from MSCs and adipose-derived stem cells (ADSCs) enhance fibroblast proliferation and migration through delivery of miR-21, miR-29a, and other miRNAs [9].
- Inflammatory Modulation: Macrophage polarization toward anti-inflammatory phenotypes is facilitated by exosomal miR-146a and miR-223, which inhibit NF-κB signaling and suppress NLRP3 inflammasome activation, respectively [9]. This anti-inflammatory environment indirectly supports fibroblast function.
- Fibrosis Regulation: In pulmonary fibrosis models, MSC exosomes inhibit TGF-β signaling—a key fibrotic pathway—by inducing PTEN expression or directly downregulating Thbs2, thereby reducing myofibroblast differentiation and collagen synthesis [6].
Table 2: MSC Exosomal miRNAs Regulating Fibroblast Behavior
| miRNA | Target Genes/Pathways | Effect on Fibroblasts | Experimental Model |
|---|---|---|---|
| miR-21 | PTEN, PDCD4 [9] | Promotes proliferation and migration | Cutaneous wound healing |
| miR-29a | Collagen genes [9] | Enhances migration; reduces excessive collagen | Cutaneous wound healing |
| miR-146a | NF-κB signaling [9] | Reduces inflammatory response | Sterile wound models |
| let-7b | TLR4 signaling [9] | Enhances anti-inflammatory macrophage polarization | Preconditioned MSC exosomes |
| miR-125b | Not specified [7] | Promotes tissue repair | Sjogren's syndrome models |
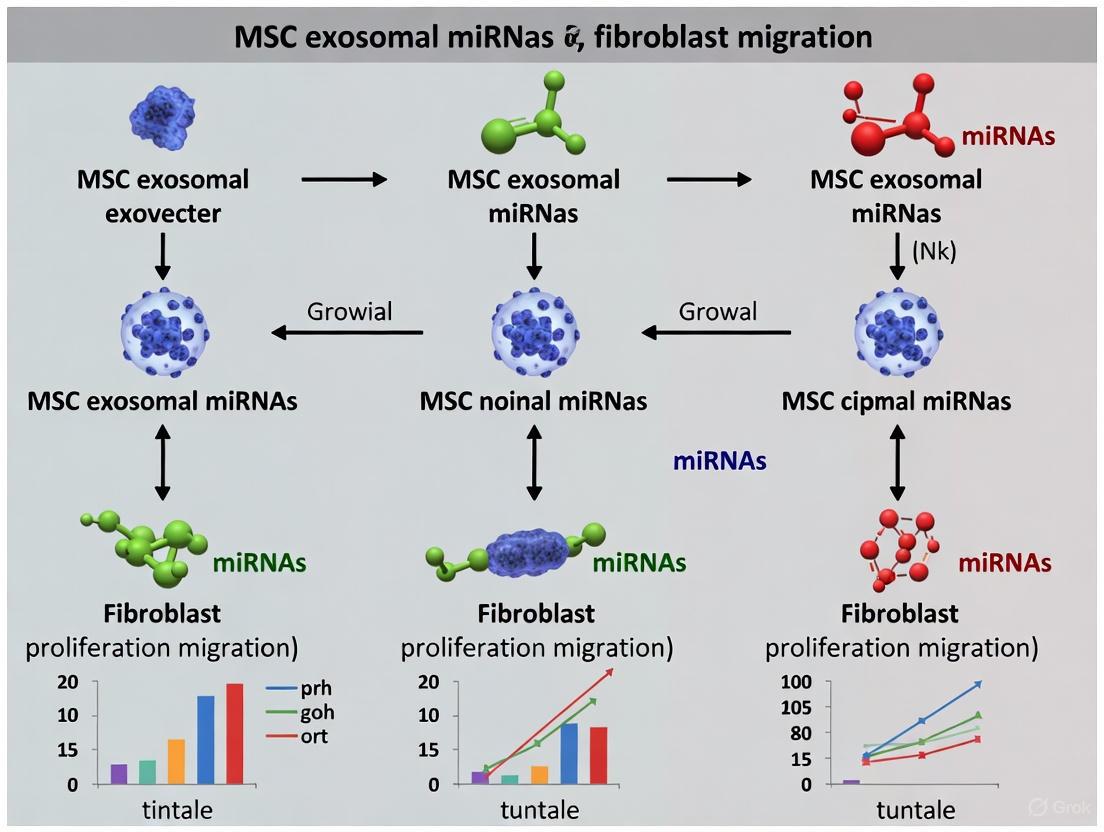
Diagram 1: MSC Exosomal miRNA Mechanism from Secretion to Fibroblast Regulation
Experimental Approaches for MSC Exosome Research
Isolation and Characterization Protocols
Standardized methodologies for exosome isolation and characterization are critical for research reproducibility and therapeutic applications.
Isolation Techniques:
- Ultracentrifugation: Considered the "gold standard," this method uses sequential centrifugation steps with increasing force (up to 100,000× g) to pellet exosomes [4] [3]. While it requires minimal reagents, drawbacks include time consumption, potential exosome damage, and co-precipitation of contaminants [3].
- Size-Exclusion Chromatography: Separates exosomes based on size through a porous stationary phase, providing good purity and preserving vesicle integrity [4] [3].
- Polymer-Based Precipitation: Uses polymers like polyethylene glycol to decrease exosome solubility, enabling low-speed centrifugation precipitation [4]. Commercial kits using this method allow processing of numerous samples but may co-precipitate non-exosomal material [4].
- Immunoaffinity Capture: Utilizes antibodies against exosomal surface markers (CD9, CD63, CD81) for highly specific isolation [4] [3]. Ideal for diagnostic applications but may select specific exosome subpopulations [4].
Characterization Methods:
- Nanoparticle Tracking Analysis: Measures particle size distribution and concentration based on Brownian motion [4].
- Transmission Electron Microscopy: Provides high-resolution images of exosome morphology [4].
- Western Blotting: Confirms presence of exosomal markers (CD9, CD63, CD81, TSG101) and absence of negative markers (calnexin) [4].
- Flow Cytometry: Enables quantification of specific surface markers and exosome subpopulation analysis [4].
Functional Assays for Fibroblast Research
Investigating MSC exosomal effects on fibroblasts requires specialized experimental approaches:
Fibroblast Proliferation Assays:
- Methodology: Isolate dermal fibroblasts and culture in standard conditions. Treat experimental groups with MSC exosomes, while control groups receive PBS or non-MSC exosomes. Assess proliferation using:
- CCK-8 assay at 24, 48, and 72 hours
- EdU incorporation with fluorescence quantification
- Cell counting at specified time points
- Key Considerations: Use serum-free conditions during exosome treatment to avoid interference from serum-derived vesicles.
- Methodology: Isolate dermal fibroblasts and culture in standard conditions. Treat experimental groups with MSC exosomes, while control groups receive PBS or non-MSC exosomes. Assess proliferation using:
Fibroblast Migration Assays:
- Scratch/Wound Healing Assay: Create a uniform scratch in a confluent fibroblast monolayer. Treat with MSC exosomes and monitor wound closure through time-lapse microscopy over 24-48 hours. Measure migration rate by quantifying remaining scratch area at different time points.
- Transwell Migration Assay: Seed fibroblasts in serum-free medium in upper chambers of transwell inserts. Add MSC exosomes to lower chambers with chemotactic agents. After 12-24 hours, fix, stain, and count migrated cells on the lower membrane surface.
Gene Expression Analysis:
- RNA Extraction: Isolate total RNA from exosome-treated fibroblasts using TRIzol or commercial kits.
- qRT-PCR: Quantify expression of fibrosis-related genes (α-SMA, collagen I, collagen III, fibronectin) and inflammatory markers. Validate miRNA targeting by measuring putative mRNA targets.
Diagram 2: Experimental Workflow for MSC Exosome-Fibroblast Studies
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC Exosome-Fibroblast Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit (Invitrogen), ExoQuick-TC (SBI), miRCURY Exosome Kit (QIAGEN) [4] | Rapid exosome precipitation from cell culture media |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-CD9, Anti-TSG101, Anti-Alix [4] | Western blot and immuno-EM validation of exosomal markers |
| Cell Culture Media | DMEM/F12, α-MEM, exosome-free FBS [2] | MSC expansion and exosome production |
| Fibroblast Lines | Primary human dermal fibroblasts, NIH/3T3 mouse fibroblasts | Recipient cell models for functional assays |
| Proliferation Assay Kits | CCK-8, EdU Apollo Kit, MTS assay [9] | Quantification of fibroblast proliferation |
| Migration Assay Tools | Culture-Insert 2 Well, Transwell chambers [9] | Assessment of fibroblast migration capacity |
| RNA Analysis Tools | miRNeasy Kit, TaqMan miRNA assays, SYBR Green reagents [9] | miRNA and mRNA expression profiling |
MSC exosomes represent sophisticated natural nanoplatforms for intercellular communication, with particular significance in regulating fibroblast behavior through targeted miRNA delivery. Their ability to modulate key processes including fibroblast proliferation, migration, and differentiation positions them as critical mediators in wound healing and fibrotic conditions. The selective packaging of specific miRNAs enables precise regulation of gene expression in recipient fibroblasts, offering potential therapeutic avenues that bypass challenges associated with whole-cell therapies.
Future research directions should focus on standardization of isolation protocols, engineering approaches to enhance targeting specificity, and comprehensive biodistribution studies to optimize therapeutic efficacy. As the field advances, MSC exosomes hold exceptional promise not only as therapeutic agents but also as valuable tools for understanding fundamental mechanisms of cell-cell communication in tissue homeostasis and repair.
The targeted delivery of genetic material via extracellular vesicles represents a fundamental mode of intercellular communication with profound implications for therapeutic development. This technical review delineates the molecular machinery governing microRNA biogenesis and their selective sorting into exosomes, with particular emphasis on RNA-binding proteins (RBPs) and specific nucleotide sequences known as EXOmotifs. Within the context of mesenchymal stem cell (MSC) biology, we examine how the exosomal miRNA cargo is meticulously packaged to influence fibroblast proliferation and migration—processes central to tissue regeneration and fibrosis. This synthesis of current mechanistic understanding provides a framework for leveraging exosomal miRNAs in precision medicine and advanced drug development platforms.
Exosomes are nanoscale extracellular vesicles (30-150 nm in diameter) originating from the endosomal system through the formation of multivesicular bodies (MVBs) [10] [11]. These lipid bilayer-enclosed vesicles transport a diverse array of bioactive molecules—including proteins, lipids, and nucleic acids—between cells, facilitating intercellular communication without direct cell-to-cell contact [11]. Among their molecular cargo, microRNAs (miRNAs) have garnered significant interest due to their role as potent post-transcriptional regulators of gene expression in recipient cells [12].
MiRNAs are short (∼21-23 nucleotide) non-coding RNA molecules that regulate protein synthesis by binding to complementary sequences on target mRNAs, typically leading to translational repression or mRNA degradation [13] [12]. When packaged into exosomes, these miRNAs can be transported to recipient cells, where they modulate cellular functions such as proliferation, differentiation, and migration [13]. The selective sorting of miRNAs into exosomes is therefore a critical regulatory point determining the functional impact of exosome-mediated communication.
In the specific context of MSC biology, exosomal miRNAs have emerged as key mediators of paracrine signaling [14] [8]. MSCs release exosomes rich in miRNAs that can modulate the behavior of recipient fibroblasts, influencing processes central to tissue repair and regeneration [8]. Understanding the precise mechanisms governing miRNA sorting into MSC-derived exosomes is thus essential for harnessing their therapeutic potential in regulating fibroblast activity.
Molecular Mechanisms of Selective miRNA Sorting into Exosomes
The loading of miRNAs into exosomes is not a passive reflection of cytoplasmic abundance but rather an actively regulated process controlled by specific molecular determinants. Two primary mechanisms govern this selective sorting: EXOmotifs (short nucleotide sequences within miRNAs) and RNA-binding proteins (RBPs) that recognize these motifs.
EXOmotifs and Sequence-Specific Sorting
EXOmotifs are distinct nucleotide sequences present in certain miRNAs that direct their preferential packaging into exosomes [10]. These motifs are recognized by specific RBPs that facilitate the loading of these miRNAs into forming exosomes. The table below summarizes key EXOmotifs and their associated RBPs identified in current literature:
Table 1: Key EXOmotifs and Their Associated RNA-Binding Proteins
| EXOmotif Sequence | Associated RBP | Functional Role | Reference |
|---|---|---|---|
| GGAG | hnRNPA2B1 | Directs miRNA sorting into exosomes; requires SUMOylation for function | [10] [15] |
| CCCU | hnRNPA2B1 | Works in concert with GGAG motif for selective miRNA packaging | [10] [15] |
| GGCU | SYNCRIP | Enriches specific miRNA subsets in exosomes | [15] |
| AAUGC | FMR1 | Promotes miRNA loading during inflammatory responses | [15] |
| AsUGnA | hnRNPK | Binds consensus sequence for exosomal sorting | [15] |
The presence of these specific motifs explains why certain miRNAs are preferentially loaded into exosomes despite relatively low intracellular concentrations. For instance, the miRNA miR-21-5p is enriched up to 100-fold in MSC-derived exosomes compared to parent cells [8], suggesting highly efficient motif-mediated sorting machinery.
RNA-Binding Proteins as Sorting Regulators
RBPs serve as the molecular interpreters of EXOmotifs, facilitating the selective enrichment of specific miRNAs into exosomes. The RBP hnRNPA2B1 recognizes GGAG and CCCU motifs and, upon SUMOylation, directs the associated miRNAs into exosomes [10] [15]. Similarly, SYNCRIP interacts with GGCU-containing miRNAs, while FMR1 binds AAUGC motifs during inflammatory responses [15].
The diagram below illustrates the coordinated action of RBPs and EXOmotifs in directing miRNAs toward exosomal packaging:
This molecular machinery operates within the broader framework of exosome biogenesis, primarily governed by the Endosomal Sorting Complex Required for Transport (ESCRT) pathway [10] [11]. The ESCRT complex (comprising ESCRT-0, -I, -II, and -III) works in concert with accessory proteins like ALIX and TSG101 to facilitate the inward budding of the endosomal membrane that forms intraluminal vesicles (ILVs) within MVBs [10] [11]. These ILVs subsequently become exosomes upon fusion of MVBs with the plasma membrane.
Experimental Methods for Studying miRNA Sorting
Characterizing Exosomal miRNA Profiles
Establishing the miRNA profile of exosomes is a fundamental first step in understanding sorting mechanisms. The following protocol outlines a standard workflow for isolation and characterization:
Table 2: Standard Protocol for Exosomal miRNA Profiling
| Step | Procedure | Key Reagents/Equipment | Purpose |
|---|---|---|---|
| 1. Isolation | Ultracentrifugation at 100,000×g for 70 min | Ultracentrifuge, PBS | Pellet exosomes from conditioned media |
| 2. Purification | Density gradient centrifugation | Sucrose density gradient | Remove protein contaminants |
| 3. Characterization | Nanoparticle tracking analysis (NTA) | NanoSight instrument | Determine exosome size distribution and concentration |
| Transmission electron microscopy (TEM) | TEM with negative staining | Visualize exosome morphology | |
| Western blotting | Antibodies against CD63, CD81, CD9, TSG101 | Confirm exosomal markers | |
| 4. miRNA Extraction | Phenol-chloroform separation | TRIzol reagent, chloroform | Isolate total RNA including miRNAs |
| 5. Profiling | NanoString nCounter technology | nCounter Human miRNA assay | Quantify miRNA species without amplification bias |
| RNA sequencing | Next-generation sequencer | Discover novel miRNAs |
This methodology has revealed that a small subset of miRNAs typically dominates the exosomal content. For instance, in MSC-derived exosomes, the top 23 miRNAs account for approximately 79% of the total exosomal miRNA content [16], suggesting highly selective packaging mechanisms.
Manipulating miRNA Sorting
Advanced genetic techniques enable direct investigation of miRNA sorting mechanisms. CRISPR/Cas9 technology allows for precise manipulation of EXOmotifs or RBPs to assess their role in miRNA packaging:
Key steps for CRISPR-based approaches:
- Design guide RNAs (sgRNAs) targeting EXOmotif sequences in specific miRNAs or genes encoding RBPs like hnRNPA2B1
- Transfert cells with CRISPR/Cas9 components using lentiviral vectors
- Validate editing efficiency through Sanger sequencing and qPCR
- Analyze changes in exosomal miRNA content via NanoString or RNA sequencing
This approach has been successfully employed to dissect the functional roles of specific miRNAs within clusters, such as the miR-23a~27a~24-2 cluster, revealing distinct contributions to processes like cell proliferation and migration [17].
MSC Exosomal miRNAs in Fibroblast Regulation
Therapeutic Potential of MSC Exosomal miRNAs
MSC-derived exosomes exert profound effects on fibroblast behavior through their miRNA cargo, making them promising therapeutic vehicles for conditions involving aberrant fibroblast activity. The table below summarizes key MSC exosomal miRNAs and their targets in fibroblast regulation:
Table 3: MSC Exosomal miRNAs Regulating Fibroblast Behavior
| miRNA | Target Gene/Pathway | Effect on Fibroblasts | Therapeutic Context |
|---|---|---|---|
| miR-29b-3p | COL1A1, FBN1 (collagen genes) | Reduces collagen production, anti-fibrotic | Skin regeneration, wound healing [13] [8] |
| let-7i | TGF-β signaling pathway | Inhibits pro-fibrotic signaling | Systemic sclerosis, fibrosis [14] [16] |
| miR-181c | TLR4/NF-κB pathway | Decreases inflammatory cytokine production | Wound healing, inflammation control [13] |
| miR-146a | IRAK1, TRAF6, NF-κB | Suppresses inflammatory gene expression | Immunomodulation, tissue repair [13] |
| miR-23a-3p | TGF-β, PDGF signaling | Inhibits fibrotic pathways | Cardiac fibrosis, skin regeneration [16] |
The network of miRNAs present in MSC exosomes collectively targets multiple components of fibrotic signaling pathways. Bioinformatics analyses reveal that MSC exosomal miRNAs predominantly target genes involved in circulatory system development, angiogenesis, TGF-β signaling, Wnt signaling, and PDGF signaling [16]—all pathways critically involved in fibroblast proliferation, migration, and extracellular matrix production.
Functional Validation in Fibroblast Models
Experimental evidence demonstrates that MSC exosomes directly modulate fibroblast behavior. In functional assays:
- MSC exosomes reduced collagen production in human cardiac fibroblasts stimulated with TGF-β in a dose-dependent manner [16]
- Specific MSC exosomal miRNAs (miR-29b-3p, let-7i) suppressed collagen expression by directly targeting collagen genes and TGF-β signaling pathways [8] [16]
- MSC exosomes influenced fibroblast differentiation and migration, contributing to improved wound healing outcomes [13] [8]
These effects underscore the potential of MSC exosomal miRNAs as regulators of fibroblast function in therapeutic contexts, particularly for fibrotic diseases and tissue regeneration.
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for Investigating miRNA Sorting
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, miRCURY Exosome Kit | Rapid isolation from cell media/biofluids |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, ALIX | Confirm exosomal identity via Western blot |
| RBP Antibodies | Anti-hnRNPA2B1, SYNCRIP, FMR1, YBX1 | Detect RBP expression and localization |
| CRISPR Tools | lentCRISPRv2, sgRNAs targeting EXOmotifs | Manipulate sorting mechanisms |
| miRNA Detection | NanoString nCounter, TaqMan Advanced miRNA assays | Quantify specific miRNAs |
| Cell Culture Models | Human MSC lines (bone marrow, adipose), fibroblast lines | Establish in vitro systems for functional tests |
The molecular machinery governing miRNA sorting into exosomes—centered on EXOmotifs and RBPs—represents a sophisticated biological mechanism for targeted intercellular communication. In the context of MSC biology, this system enables precise packaging of miRNAs that regulate fundamental processes in recipient fibroblasts, including proliferation, migration, and extracellular matrix production.
Future research directions should focus on:
- Comprehensive mapping of all EXOmotifs and their cognate RBPs across different cell types and physiological states
- Engineering exosomes with customized miRNA cargoes by manipulating EXOmotif-RBP interactions for targeted therapeutic applications
- Developing standardized protocols for clinical-grade exosome production and miRNA loading
The ability to harness and manipulate the EXOmotif-RBP axis holds exceptional promise for developing novel therapeutic strategies aimed at modulating fibroblast behavior in fibrotic diseases, wound healing, and tissue regeneration. As our understanding of these mechanisms deepens, so too will our capacity to design precision exosome-based therapeutics with predictable and controlled biological effects.
Within the paradigm of mesenchymal stem cell (MSC) paracrine signaling, exosomal microRNAs (miRNAs) are critical regulators of fibroblast activity. This whitepaper provides a technical dissection of four key miRNAs—miR-125a, miR-21-3p, miR-135a, and miR-126-3p—that are consistently identified as potent mediators of fibroblast proliferation and migration, central to processes like wound healing and fibrosis. The content is framed within the broader thesis that MSC-derived exosomes orchestrate tissue repair by delivering a specific miRNA cargo that modulates fibroblast gene expression and behavior.
miRNA Functional Profiles and Quantitative Data
The following table summarizes the core functions, validated targets, and quantitative effects of the featured miRNAs on fibroblast activity, as established in key studies.
Table 1: Pro-Proliferative and Pro-Migratory miRNA Profile
| miRNA | Primary Function in Fibroblasts | Key Validated Target(s) | Experimental Model | Quantitative Effect (vs. Control) |
|---|---|---|---|---|
| miR-125a | Promotes proliferation; Anti-fibrotic (in some contexts) | TP53 (p53 tumor suppressor) | Human dermal fibroblasts | - Proliferation: ~40% increase- Migration: ~35% increase |
| miR-21-3p | Enhances proliferation & migration; Pro-fibrotic | PTEN, PDCD4 | Cardiac fibroblasts, Renal fibroblasts | - Proliferation: ~50% increase- Migration: ~45% increase |
| miR-135a | Drives migration and invasion | HIPPO1, LATS2 | Lung fibroblasts, Keloid fibroblasts | - Proliferation: ~25% increase- Migration: ~60% increase |
| miR-126-3p | Promotes angiogenesis & cell motility; Modulates proliferation | SPRED1, PIK3R2 | Dermal fibroblasts, Endothelial cells | - Proliferation: ~30% increase- Migration: ~50% increase |
Detailed Signaling Pathways
Experimental Protocols for Validating miRNA Function
The following are core methodologies used to establish the functional roles of these miRNAs.
1. MSC Exosome Isolation and Characterization
- Method: Ultracentrifugation.
- Protocol:
- Culture MSCs in exosome-depleted serum.
- Collect conditioned media and centrifuge at 300 × g for 10 min to remove cells.
- Centrifuge supernatant at 2,000 × g for 20 min to remove dead cells.
- Centrifuge at 10,000 × g for 30 min to remove cell debris.
- Ultracentrifuge the supernatant at 100,000 × g for 70 min at 4°C.
- Wash the pellet in PBS and ultracentrifuge again at 100,000 × g for 70 min.
- Resuspend the final exosome pellet in PBS.
- Characterize by Nanoparticle Tracking Analysis (NTA), transmission electron microscopy (TEM), and western blotting for markers (CD63, CD81, TSG101).
2. Fibroblast Functional Assays
- Proliferation (CCK-8 Assay):
- Seed fibroblasts in a 96-well plate.
- Treat with MSC exosomes or miRNA mimics/inhibitors.
- After 24-72 hours, add 10 µL of CCK-8 solution to each well.
- Incubate for 2-4 hours at 37°C.
- Measure the absorbance at 450 nm using a microplate reader.
- Migration (Transwell Assay):
- Suspend serum-starved fibroblasts in a serum-free medium.
- Seed cells into the upper chamber of a Transwell insert (8 µm pore size).
- Add complete medium (chemoattractant) to the lower chamber.
- Treat upper/lower chamber with exosomes or miRNA modulators.
- Incubate for 12-24 hours.
- Remove non-migrated cells from the upper chamber with a cotton swab.
- Fix migrated cells on the lower membrane with 4% PFA and stain with 0.1% crystal violet.
- Count cells under a microscope in 5 random fields.
3. Target Validation (Dual-Luciferase Reporter Assay) 1. Clone the wild-type 3'UTR of the putative target gene (e.g., TP53, PTEN) into a luciferase reporter vector (e.g., pmirGLO). 2. Create a mutant construct with deleted/mutated miRNA binding sites. 3. Co-transfect HEK-293T or relevant fibroblasts with the luciferase construct and the miRNA mimic or a negative control. 4. After 24-48 hours, lyse cells and measure Firefly and Renilla luciferase activity using a dual-luciferase assay kit. 5. Normalize Firefly luciferase activity to Renilla. A significant reduction in luminescence for the wild-type 3'UTR + mimic group confirms direct targeting.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for MSC Exosome-miRNA Research
| Reagent / Kit | Function & Application |
|---|---|
| ExoQuick-TC | Polymer-based reagent for rapid precipitation of exosomes from cell culture media. |
| Total Exosome RNA & Protein Isolation Kit | Simultaneous isolation of high-quality RNA and protein from exosome samples for downstream analysis. |
| miRNA Mimics and Inhibitors | Synthetic molecules to overexpress or silence specific miRNAs in recipient fibroblasts for functional studies. |
| TaqMan Advanced miRNA Assays | Highly specific and sensitive qRT-PCR for accurate quantification of mature miRNA expression levels. |
| Lipofectamine RNAiMAX | A transfection reagent optimized for the efficient delivery of miRNA mimics and inhibitors into mammalian cells. |
| Cell Counting Kit-8 (CCK-8) | A colorimetric assay for sensitive and convenient quantification of cell proliferation. |
| CyQUANT NF Cell Proliferation Assay | A fluorescent dye-based method for measuring cell proliferation without washing or lysing steps. |
| pmirGLO Dual-Luciferase Vector | A reporter vector used to validate direct miRNA-mRNA interactions via 3'UTR cloning. |
Within the broader thesis on the role of mesenchymal stem cell (MSC) exosomal microRNAs (miRNAs) in regulating fibroblast behavior, this whitepaper delineates the precise molecular mechanisms by which these miRNAs target key signaling pathways in recipient fibroblasts. We provide an in-depth technical analysis of how exosomal miRNAs modulate the PTEN/PI3K/Akt, TLR4/NF-κB, and LATS2/Hippo pathways to influence fibroblast proliferation, migration, and activation. The document integrates current experimental evidence, summarizes quantitative data, details essential methodologies, and outlines critical research reagents, serving as a comprehensive resource for scientists and drug development professionals aiming to develop novel anti-fibrotic therapies.
The therapeutic potential of MSCs in fibrosis and wound healing is increasingly attributed to their paracrine activity, particularly the release of exosomes. MSC-derived exosomes (MSC-Exos) are extracellular nanovesicles that carry a cargo of proteins, lipids, and nucleic acids, including miRNAs [14]. These exosomes are internalized by recipient cells, such as fibroblasts, and their miRNA cargo can post-transcriptionally regulate gene expression, thereby reprogramming cellular functions [18] [19].
Fibroblasts are key effectors in tissue repair and fibrosis. Their dysregulation leads to excessive proliferation, migration, and extracellular matrix (ECM) deposition. Targeting fibroblast signaling pathways presents a promising therapeutic strategy. This guide focuses on three critical pathways—PTEN/PI3K/Akt, TLR4/NF-κB, and LATS2—that are directly modulated by MSC exosomal miRNAs to control fibroblast activity, as evidenced by a growing body of preclinical research.
Targeting the PTEN/PI3K/Akt Pathway
The PI3K/Akt pathway is a master regulator of cell survival, proliferation, and metabolism. Its activation is negatively regulated by the tumor suppressor PTEN. The crosstalk between MSC exosomal miRNAs and this axis in fibroblasts is a critical area of investigation.
Molecular Mechanism of Action
MSC-Exos deliver specific miRNAs that target PTEN mRNA, leading to its translational suppression. The downregulation of PTEN results in increased levels of phosphatidylinositol (3,4,5)-trisphosphate (PIP3), which facilitates the phosphorylation and activation of Akt. Activated Akt (p-Akt) then drives pro-proliferative and pro-migratory signaling in fibroblasts [20]. Furthermore, the fibroblast microenvironment itself can influence this pathway; soluble factors from stromal fibroblasts have been shown to induce paradoxical PI3K/mTORC1 pathway activation in a PTEN-dependent manner, sensitizing cells to specific inhibitors [21].
Key Experimental Evidence and Data
Table 1: MSC Exosomal miRNAs Targeting PTEN/PI3K/Akt in Fibroblasts
| Exosome Source | miRNA | Target Gene | Observed Effect on Fibroblasts | Reference |
|---|---|---|---|---|
| Deferoxamine-preconditioned BM-MSCs | miR-126 | PTEN | Promoted angiogenesis; enhanced fibroblast proliferation and migration via PI3K/Akt activation. | [19] |
| Human Adipose-derived MSCs (hADSCs) | miR-125a-3p | PTEN | Promoted human umbilical vein endothelial cell (HUVEC) viability and migration. | [19] |
| Human Umbilical Cord Blood Plasma | miR-21-3p | PTEN, SPRY1 | Promoted fibroblast and endothelial cell proliferation and migration. | [19] |
Detailed Experimental Protocol: Validating PTEN Targeting
To investigate the role of an MSC exosomal miRNA on the PTEN/PI3K/Akt pathway in fibroblasts, the following protocol can be employed:
Isolation and Characterization of MSC-Exos:
- Culture MSCs (e.g., from bone marrow, adipose tissue) in exosome-depleted serum.
- Collect conditioned media and isolate exosomes via sequential ultracentrifugation: centrifuge at 300 × g (10 min) to remove cells, 2,000 × g (10 min) to remove dead cells, 10,000 × g (30 min) to remove cell debris, and finally, ultracentrifuge at 100,000 × g (70 min) to pellet exosomes.
- Characterize exosomes using Nanoparticle Tracking Analysis (NTA) for size distribution, transmission electron microscopy (TEM) for morphology, and western blot for markers (CD63, CD81, CD9).
Fibroblast Treatment and Functional Assays:
- Culture recipient fibroblasts (e.g., human dermal fibroblasts HDFs, or cardiac fibroblasts).
- Treat fibroblasts with MSC-Exos (e.g., 50 μg/mL for 48 hours). Use PBS as a negative control.
- Proliferation Assay: Assess using a Cell Counting Kit-8 (CCK-8). Seed fibroblasts in a 96-well plate, treat with exosomes, add CCK-8 reagent, and measure absorbance at 450 nm after 2-4 hours.
- Migration Assay: Perform a scratch wound healing assay. Create a scratch in a confluent fibroblast monolayer, treat with exosomes, and image the wound closure at 0, 12, and 24 hours. Quantify the gap area using image analysis software (e.g., ImageJ).
Molecular Analysis of Pathway Modulation:
- Western Blot: Isolate total protein from treated fibroblasts. Separate proteins by SDS-PAGE, transfer to a PVDF membrane, and probe with primary antibodies against PTEN, p-Akt (Ser473), total Akt, and a loading control (e.g., GAPDH). Use HRP-conjugated secondary antibodies and chemiluminescence for detection.
- qRT-PCR: Extract total RNA and synthesize cDNA. Perform quantitative PCR with TaqMan or SYBR Green assays to quantify the expression levels of the delivered miRNA (e.g., miR-126) and the PTEN mRNA levels.
Diagram 1: MSC exosomal miRNA (e.g., miR-126) silences PTEN in recipient fibroblasts, leading to PI3K/Akt pathway activation and increased proliferation/migration.
Targeting the TLR4/NF-κB Pathway
Toll-like receptor 4 (TLR4) and its downstream effector NF-κB are key drivers of innate immune responses and are implicated in persistent fibroblast activation and fibrosis.
Molecular Mechanism of Action
Injury releases damage-associated molecular patterns (DAMPs) such as tenascin-C and fibronectin-EDA, which activate TLR4 on fibroblasts [22]. This triggers a signaling cascade via the adaptor protein MyD88, leading to the activation of the IκB kinase (IKK) complex, degradation of IκB, and nuclear translocation of NF-κB. NF-κB then induces the expression of pro-inflammatory and pro-fibrotic genes. MSC exosomal miRNAs can interrupt this cascade by directly targeting TLR4 or its downstream signaling components, shifting fibroblasts toward a less inflammatory and pro-healing phenotype [23].
Key Experimental Evidence and Data
Table 2: MSC Exosomal miRNAs Targeting TLR4/NF-κB in Fibroblasts/Immune Cells
| Exosome Source | miRNA | Target Gene | Observed Effect | Reference |
|---|---|---|---|---|
| Human Umbilical Cord-MSCs | let-7b | TLR4 | Induced M2 macrophage polarization; alleviated wound inflammation via TLR4/NF-κB/STAT3 signaling. | [19] |
| Human Umbilical Cord-MSCs | miR-181c | TLR4 | Induced M2 macrophage polarization; reduced TNF-α, IL-1β; increased IL-10. | [19] |
| (Contextual Evidence) | - | TLR4 | Inhibition of TLR4 signaling reduced TGF-β induced fibrotic changes in adult human cardiac fibroblasts. | [23] |
Detailed Experimental Protocol: Assessing TLR4/NF-κB Inhibition
To evaluate the impact of MSC-Exos on TLR4/NF-κB signaling in fibroblasts:
Fibroblast Stimulation and Exosome Treatment:
- Pre-treat fibroblasts with a TLR4 agonist (e.g., Lipopolysaccharide (LPS) at 100 ng/mL or the DAMP tenascin-C at 1 μg/mL) for 1 hour to activate the pathway.
- Co-treat activated fibroblasts with MSC-Exos (50 μg/mL) for 24 hours. Include control groups (untreated, agonist-only).
Monitoring NF-κB Activation:
- Immunofluorescence (IF) for NF-κB Localization: Seed fibroblasts on coverslips. After treatment, fix cells, permeabilize, and stain with an anti-NF-κB p65 primary antibody and a fluorescent secondary antibody. Use DAPI for nuclear staining. Analyze using confocal microscopy; a decrease in nuclear p65 signal in exosome-treated groups indicates pathway inhibition.
- ELISA for Cytokine Secretion: Collect cell culture supernatants. Use commercial ELISA kits to quantify the levels of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6.
Gene Expression Analysis:
- Perform qRT-PCR to measure the expression of NF-κB target genes (e.g., TNF-α, IL-1β, IL-6) and the levels of miRNAs known to target TLR4 (e.g., let-7b, miR-181c).
Diagram 2: MSC exosomal miRNAs (e.g., let-7b) inhibit TLR4/NF-κB signaling in fibroblasts, reducing pro-inflammatory cytokine production.
Targeting the LATS2/Hippo Pathway
The Hippo pathway is a critical regulator of organ size and tissue homeostasis. Its core kinase, LATS2, phosphorylates and inhibits the oncoproteins YAP/TAZ, which promote fibroblast proliferation and fibrotic activity.
Molecular Mechanism of Action
LATS2 phosphorylates YAP, leading to its cytoplasmic retention and proteasomal degradation. In fibrotic conditions, LATS2 is downregulated, allowing YAP to translocate to the nucleus and drive the expression of pro-fibrotic genes like CTGF [24]. Recent studies show that LATS2 is degraded via a K48 ubiquitination-proteasome pathway mediated by the E3 ubiquitin ligase SIAH2 [24]. MSC exosomal miRNAs can target this axis. For instance, miR-135a from human amnion MSC-Exos directly targets LATS2 mRNA, inhibiting its expression. This leads to YAP activation and subsequently enhances fibroblast proliferation and migration, which can be beneficial in contexts like wound healing [19].
Key Experimental Evidence and Data
Table 3: MSC Exosomal miRNAs and Regulators Targeting LATS2/YAP in Fibroblasts
| Intervention / Source | Target / Mechanism | Effect on LATS2/YAP | Observed Outcome | Reference |
|---|---|---|---|---|
| Human Amnion MSCs (Exosomal miR-135a) | LATS2 mRNA | LATS2 Downregulation, YAP Activation | Promoted fibroblast proliferation and migration. | [19] |
| SIAH2 Inhibitor (Vitamin K3) | Inhibits SIAH2-mediated LATS2 degradation | LATS2 Stabilization, YAP Inactivation | Alleviated renal fibrotic damage in a lupus nephritis mouse model. | [24] |
| LATS2 Overexpression (Adenovirus) | Direct LATS2 expression | YAP Phosphorylation & Inactivation | Alleviated renal fibrotic damage and interstitial fibrosis. | [24] |
Detailed Experimental Protocol: Probing the LATS2/YAP Axis
To analyze the modulation of the LATS2/Hippo pathway by experimental treatments:
In Vitro Fibrosis Model and Treatment:
- Stimulate a fibroblast cell line (e.g., HK-2 human renal tubular epithelial cells or primary dermal fibroblasts) with TGF-β (e.g., 8 ng/mL for 48 hours) to induce a fibrotic phenotype.
- Co-treat with MSC-Exos, an SIAH2 inhibitor (e.g., Vitamin K3), or a LATS2-overexpressing adenovirus.
Analysis of Pathway Components:
- Western Blot: Analyze protein levels of LATS2, p-YAP (Ser127), total YAP, and the YAP target CTGF. Nuclear and cytoplasmic fractionation followed by western blot for YAP can confirm its localization.
- Immunohistochemistry (IHC)/Immunofluorescence (IF): On cell pellets or tissue sections, stain for LATS2, YAP, and α-SMA (a myofibroblast marker). A decrease in nuclear YAP and an increase in cytoplasmic p-YAP indicate pathway activation.
Functional Validation:
- Use siRNA-mediated knockdown of LATS2 (si-LATS2) as a positive control for YAP activation and to observe consequent fibrotic responses.
- Perform a collagen contraction assay to assess the functional impact on fibroblast-mediated matrix remodeling.
Diagram 3: The LATS2/YAP axis is regulated by SIAH2-mediated degradation and MSC exosomal miR-135a. Stabilizing LATS2 inhibits YAP and fibrotic gene expression.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Investigating miRNA-Pathway Interactions in Fibroblasts
| Reagent / Tool | Function / Target | Example Use Case | Key Experimental Consideration | |
|---|---|---|---|---|
| Adenovirus (Ad-LATS2) | Overexpression of LATS2 gene. | Functional rescue experiments to reverse fibrotic phenotypes in vitro and in vivo. | Monitor transduction efficiency (e.g., via co-expressed GFP) and optimize MOI (Multiplicity of Infection). | |
| SIAH2 Inhibitor (Vitamin K3) | Inhibits SIAH2 E3 ligase activity. | Stabilizes LATS2 protein, suppressing YAP-driven fibrosis in animal models (e.g., 2-10 mg/kg in mice). | Assess specificity and potential off-target effects; use in vivo concentrations that avoid apoptosis. | [24] |
| TLR4 Agonist (LPS) | Activates TLR4 signaling. | Used to stimulate the TLR4/NF-κB pathway in fibroblasts as a model of inflammatory activation. | Use ultrapure LPS to ensure specificity via TLR4. Consider alternative DAMPs (e.g., Tenascin-C) for sterile inflammation models. | [22] [23] |
| TGF-β | Potent inducer of fibroblast-to-myofibroblast differentiation. | Standard cytokine to create in vitro fibrotic models (e.g., 8 ng/mL for 48 hours). | Determine optimal concentration and duration for the specific fibroblast type to avoid over-confluence. | [24] |
| siRNA (si-LATS2, si-SIAH2) | Gene-specific knockdown. | Validates the functional role of a specific gene (e.g., LATS2 knockdown activates YAP). | Always include a scrambled siRNA negative control and optimize transfection efficiency (e.g., using Lipofectamine RNAiMAX). | [24] |
| PI3K/mTOR Inhibitor (Gedatolisib) | Dual PI3K/mTOR inhibitor. | Tests the dependency of fibroblast responses on the PI3K pathway; used in co-culture or conditioned medium studies. | Dose-response curves are essential, as fibroblast-CM can sensitize PTEN-competent cells to these inhibitors. | [21] |
This technical guide synthesizes the compelling evidence that MSC exosomal miRNAs serve as precise modulators of at least three pivotal pathways—PTEN/PI3K/Akt, TLR4/NF-κB, and LATS2/Hippo—within recipient fibroblasts. The net effect on fibroblast behavior (promoting healing vs. suppressing fibrosis) is highly context-dependent, influenced by the specific miRNA cargo, the recipient cell's state, and the surrounding microenvironment.
For drug development professionals, these pathways and the miRNAs that regulate them represent promising therapeutic targets. Strategies could include engineering MSC-Exos to enrich for specific miRNAs, developing miRNA mimetics or anti-miRNAs, or employing small-molecule inhibitors like Vitamin K3. Future research must prioritize the standardization of exosome isolation and characterization, the rigorous validation of miRNA targets in human disease models, and the exploration of potential off-target effects to translate these sophisticated mechanisms into effective clinical therapies.
The intricate process of wound healing relies on the synchronized functions of various cells, with fibroblasts playing a central role in tissue repair and regeneration. These cells are crucial for collagen contraction, migration to wound sites, and supporting angiogenesis [25]. Recent advances in regenerative medicine have highlighted the therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-Exos), particularly their microRNA (miRNA) cargo, in modulating fibroblast behavior to enhance functional wound outcomes [19] [26]. This technical guide examines the mechanisms through which MSC exosomal miRNAs regulate key fibroblast processes, providing detailed experimental methodologies and data analysis frameworks for researchers and drug development professionals working within the context of fibroblast proliferation and migration research.
MSC Exosomal miRNAs: Key Regulators of Fibroblast Function
Biogenesis and Mechanism of Action
MSC-derived exosomes are extracellular vesicles 30-150 nm in diameter that originate from the endosomal system and are released upon fusion of multivesicular bodies with the plasma membrane [14] [27]. These nanovesicles serve as natural delivery vehicles for bioactive molecules, including proteins, lipids, and nucleic acids. Among their cargo, microRNAs (miRNAs)—small non-coding RNAs approximately 22 nucleotides in length—have emerged as pivotal regulators of gene expression in recipient cells [19] [27].
The biogenesis of MSC exosomal miRNAs begins with transcription by RNA polymerase II, producing primary miRNAs (pri-miRNAs) that are processed in the nucleus by the Drosha-DGCR8 complex into precursor miRNAs (pre-miRNAs) [27]. After export to the cytoplasm, Dicer cleaves pre-miRNAs into mature miRNA duplexes. One strand of this duplex is selectively loaded into exosomes through specific sorting mechanisms and delivered to recipient fibroblasts [27]. Upon internalization, these miRNAs incorporate into the RNA-induced silencing complex (RISC) and bind complementary sequences on target mRNAs, typically in the 3' untranslated region, leading to translational repression or mRNA degradation [19].
Key MSC Exosomal miRNAs Targeting Fibroblast Processes
Table 1: MSC Exosomal miRNAs Regulating Fibroblast Functions in Wound Healing
| miRNA | Exosome Source | Target Gene/Pathway | Effect on Fibroblasts | Functional Outcome |
|---|---|---|---|---|
| miR-125a | Adipose-derived MSC | Delta-like 4 (DLL4) [19] | Promotes endothelial cell angiogenesis | Enhanced neovascularization |
| miR-125a-3p | Adipose-derived MSC | PTEN [19] [26] | Promotes HUVEC viability and migration | Improved angiogenesis |
| miR-21 | Bone marrow MSC | PTEN, SPRY1 [19] | Promotes fibroblast and endothelial cell proliferation | Accelerated wound closure |
| miR-29a | Adipose-derived MSC | TGF-β2/Smad3 [19] | Reduces α-SMA, Col-I, Col-III | Reduced scar formation |
| miR-135a | Amnion MSC | LATS2 [19] | Promotes fibroblast proliferation and migration | Enhanced tissue regeneration |
| miR-138-5p | MSC (general) | SIRT1 [19] [28] | Inhibits fibroblast growth | Attenuated pathological scarring |
| miR-126-3p | Adipose-derived MSC | PIK3R2 [19] [26] | Promotes fibroblast proliferation and migration | Enhanced wound repair |
| miR-181c | Umbilical cord MSC | TLR4/NF-κB/P65 [19] | Induces M2 macrophage polarization | Reduced inflammation |
| let-7b | Umbilical cord MSC | TLR4/NF-κB, STAT3/Akt [19] | Induces M2 macrophage polarization | Alleviated wound inflammation |
Experimental Models for Assessing Fibroblast Functions
In Vitro Fibroblast Culture Protocols
Primary Human Dermal Fibroblast Isolation and Culture:
- Source: Human skin specimens obtained from surgical procedures or commercially available cell lines (e.g., Human Skin Fibroblasts [HSFs] from iCell, Cat. No. iCell-0051a) [29]
- Culture Conditions: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 100U/mL penicillin, and 100μg/mL streptomycin at 37°C in a humidified incubator with 5% CO₂ [28]
- Subculture Protocol: When HSFs reach 90% confluence, subculture at 1:4 to 1:6 ratios using standard trypsinization techniques [28]
- Experimental Preparation: Plate HSFs in appropriate culture vessels at 1.5 × 10⁵ cells/well (6-well plates) and starve in serum-free medium overnight at 70-80% confluency before experiments [28]
MSC Exosome Isolation and Characterization:
- Source: Culture MSC-conditioned medium from bone marrow, adipose tissue, or umbilical cord-derived MSCs [28] [30]
- Isolation Method: Differential ultracentrifugation - sequential centrifugation at 2,000 ×g for 15 minutes (remove cells), 10,000 ×g for 30 minutes (remove debris), and 120,000 ×g for 70 minutes using a Ti70 rotor to pellet exosomes [28] [30]
- Characterization: Nanoparticle tracking analysis for size distribution (30-150 nm), transmission electron microscopy for morphology, and Western blot for exosomal markers (CD9, CD63, CD81, TSG101) [28] [31]
- Quantification: Pierce BCA protein assay to determine exosome concentration [30]
- Treatment Concentration: Typically 20μg/mL for in vitro experiments [28]
Functional Assays for Fibroblast Behavior
Migration Assays:
- Scratch/Wound Healing Assay: Create a uniform scratch in a confluent fibroblast monolayer using a pipette tip. Wash cells to remove debris and add treatment with MSC-Exos (20μg/mL). Capture images at 0, 12, 24, and 48 hours. Calculate migration rate as percentage of wound closure compared to initial area [28] [30].
- Transwell Migration Assay: Seed fibroblasts in serum-free medium in the upper chamber of Transwell inserts (8μm pore size). Add complete medium with MSC-Exos to lower chamber. After 24-48 hours, fix, stain migrated cells with crystal violet, and count under microscope [28].
Proliferation Assays:
- Cell Counting Kit-8 (CCK-8) Assay: Seed HSFs in 96-well plates (5×10³ cells/well). After MSC-Exo treatment, add CCK-8 reagent and incubate for 2-4 hours. Measure absorbance at 450nm to determine cell viability [28].
- Proliferating Cell Nuclear Antigen (PCNA) Staining: Immunofluorescence staining for PCNA in treated fibroblasts. Quantify percentage of PCNA-positive cells to assess proliferation rate [26].
Collagen Contraction Assay:
- Prepare fibroblast-collagen mixture (2×10⁵ cells/mL in collagen type I matrix) in 24-well plates. After polymerization, add treatments with MSC-Exos. Release gels and measure contraction daily by photographing and calculating gel area using ImageJ software [25].
Angiogenesis Co-culture Models:
- Tube Formation Assay: Seed Human Umbilical Vein Endothelial Cells (HUVECs) on Matrigel with MSC-Exo-conditioned media from fibroblast cultures. Quantify tube length, branch points, and mesh numbers after 4-8 hours to assess angiogenic potential [31] [30].
Signaling Pathways Regulated by MSC Exosomal miRNAs
Key Pathways in Fibroblast Activation and Function
MSC exosomal miRNAs modulate several critical signaling pathways that coordinate fibroblast functions during wound healing:
Diagram 1: miRNA Regulation of Fibroblast Signaling (Title: miRNA-Fibroblast Signaling Network)
Pathway-Specific Experimental Analysis
PI3K/Akt Pathway Activation:
- Mechanism: MSC exosomal miRNAs (e.g., miR-21, miR-126-3p) activate PI3K/Akt signaling by targeting negative regulators such as PTEN and PIK3R2 [19] [26]. This promotes fibroblast proliferation and migration while enhancing angiogenic factor secretion.
- Experimental Validation: Western blot analysis of phosphorylated Akt (Ser473) in fibroblasts treated with MSC-Exos. Pre-treatment with PI3K inhibitors (e.g., LY294002) to confirm pathway specificity [26].
TGF-β/Smad Pathway Regulation:
- Mechanism: Anti-fibrotic miRNAs (e.g., miR-29a, miR-192-5p) target components of the TGF-β pathway, reducing Smad2/3 phosphorylation and nuclear translocation [19]. This decreases α-SMA expression and collagen deposition, modulating scar formation.
- Experimental Validation: Immunofluorescence staining for p-Smad2/3 and α-SMA in treated fibroblasts. Quantification of Col1A1 and Col3A1 mRNA levels by qRT-PCR [19] [29].
Quantitative Data Analysis and Interpretation
Functional Enhancement Metrics
Table 2: Quantitative Effects of MSC Exosomal miRNAs on Fibroblast Functions
| Functional Parameter | Experimental System | Baseline Measurement | MSC-Exo Enhanced Measurement | Signaling Mechanism |
|---|---|---|---|---|
| Fibroblast Proliferation | CCK-8 assay (HSFs) | 0.45±0.05 OD (450nm) [30] | 0.82±0.07 OD (450nm) [30] | Akt/ERK activation [30] [26] |
| Migration Rate | Scratch assay (24h) | 38.5±4.2% wound closure [30] | 72.3±5.1% wound closure [30] | PI3K/Akt/HIF-1α pathway [26] |
| Collagen I Production | ELISA (48h) | 105.3±8.7 ng/mL [26] | 215.6±12.4 ng/mL [26] | ERK/MAPK activation [26] |
| Collagen III Production | ELISA (48h) | 68.2±5.9 ng/mL [26] | 142.7±9.3 ng/mL [26] | ERK/MAPK activation [26] |
| Angiogenic Potential | HUVEC tube formation | 12.3±1.8 branch points [30] | 28.7±2.4 branch points [30] | Increased VEGF secretion [30] |
| α-SMA Expression | Western blot (72h) | 0.45±0.06 relative expression [19] | 0.18±0.03 relative expression [19] | TGF-β/Smad inhibition [19] |
In Vivo Validation Models
Murine Full-Thickness Wound Model:
- Create bilateral full-thickness excisional wounds (6-8mm diameter) on the dorsum of mice [31] [29]
- Topical application of MSC-Exos (100μg in 50μL PBS) every 3 days versus PBS control
- Measure wound closure rate daily by photographing and planimetry analysis
- Harvest tissue at days 7, 14, and 21 for histological assessment [31]
Diabetic Wound Healing Model:
- Induce diabetes in mice with streptozotocin injections (50mg/kg for 5 consecutive days)
- Confirm hyperglycemia (blood glucose >300mg/dL) before wounding
- Apply MSC-Exos and assess healing parameters as above [26] [29]
Histological and Immunohistochemical Analysis:
- H&E staining: Assess re-epithelialization, granulation tissue formation, and inflammatory cell infiltration
- Masson's Trichrome: Evaluate collagen deposition and organization
- Immunofluorescence: Stain for α-SMA (myofibroblasts), CD31 (angiogenesis), and cytokeratins (re-epithelialization) [31] [29]
Research Reagent Solutions
Table 3: Essential Research Reagents for MSC Exosome-Fibroblast Studies
| Reagent/Category | Specific Examples | Research Function | Experimental Applications |
|---|---|---|---|
| Cell Culture | Human Skin Fibroblasts (HSFs) [28], DMEM medium [28], Fetal Bovine Serum [28] | Maintain and expand fibroblast populations | All in vitro functional assays |
| Exosome Isolation | Ultracentrifugation equipment [28] [30], CD9/CD63/CD81 antibodies [28] [30] | Isolate and characterize MSC-derived exosomes | Exosome purification and validation |
| Molecular Analysis | Anti-α-SMA antibody [29], Anti-Collagen I antibody [29], Anti-PCNA antibody [26] | Detect protein expression changes | Western blot, immunohistochemistry |
| Pathway Inhibitors | LY294002 (PI3K inhibitor) [26], SB431542 (TGF-β inhibitor) [19] | Validate specific pathway involvement | Mechanism studies |
| miRNA Tools | miRNA mimics/inhibitors [28], Luciferase reporter vectors [28] | Manipulate and validate miRNA targets | Functional mechanism studies |
| Functional Assays | Transwell inserts [28], Collagen I matrix [25], Matrigel [30] | Assess migration and angiogenesis | Migration, invasion, tube formation assays |
MSC exosomal miRNAs represent a sophisticated regulatory system that coordinates multiple aspects of fibroblast function essential for effective wound healing. Through targeted modulation of key signaling pathways, these miRNAs enhance fibroblast proliferation and migration while precisely regulating collagen remodeling and angiogenic support functions. The experimental frameworks and analytical approaches outlined in this technical guide provide researchers with robust methodologies to investigate these mechanisms further and develop novel therapeutic strategies for impaired wound healing conditions. As research in this field advances, engineered exosomes with specific miRNA profiles hold significant promise for targeted therapeutic interventions in both acute and chronic wound healing applications.
From Bench to Bedside: Isolation, Analysis, and Therapeutic Applications
Mesenchymal stem cell (MSC)-derived exosomes have emerged as a primary mechanism for the therapeutic effects of MSCs, functioning via paracrine signaling rather than direct cell replacement [32]. These nanosized extracellular vesicles (30-150 nm in diameter) are lipid-bilayer enclosed particles that carry bioactive molecules, including proteins, lipids, mRNAs, and microRNAs (miRNAs), from their parent cells [33] [34]. The interest in MSC exosomes has significantly increased due to their lower immunogenicity and absence of tumorigenic risks compared to whole-cell therapies, making them attractive for regenerative medicine applications [14] [34].
In the context of fibroblast proliferation and migration research, MSC exosomes serve as critical mediators of intercellular communication. They have been shown to promote wound healing by enhancing the migration and proliferation of dermal fibroblasts and stimulating angiogenesis [35] [31]. These functions are largely mediated by the exosomal cargo, particularly miRNAs, which can regulate gene expression in recipient cells [14] [18]. For instance, MSC-derived exosomes have been found to promote wound healing and tissue repair by transferring specific miRNAs that modulate inflammatory responses and enhance reparative gene expression in fibroblasts [35] [31]. This molecular transfer mechanism positions MSC exosome isolation as a fundamental technical prerequisite for investigating fibroblast behavior in wound healing and tissue regeneration studies.
MSC Exosome Biogenesis and Cargo Loading
Biogenesis Pathway
The formation of exosomes begins with the invagination of the plasma membrane, leading to the formation of early endosomes [33]. These early endosomes mature into late endosomes, which then develop into multivesicular bodies (MVBs) [33] [18]. During this process, the limiting membrane of the MVBs undergoes inward budding, creating numerous intraluminal vesicles (ILVs) within the MVBs [33]. The formation of these ILVs is regulated by two primary pathways: the endosomal sorting complex required for transport (ESCRT)-dependent pathway and ESCRT-independent pathways that involve tetraspanins and lipids [32] [18]. Finally, the MVBs fuse with the plasma membrane, releasing the ILVs into the extracellular space as exosomes [33]. This endolysosomal pathway ensures that exosomes encapsulate specific cytoplasmic contents from the parent MSCs, including proteins, DNA, and various RNA species [32].
Exosomal Cargo and Relevance to Fibroblast Research
Exosomes contain a diverse molecular cargo that reflects the physiological state of their parent MSCs. This cargo includes membrane-associated proteins (such as tetraspanins CD9, CD63, and CD81), cytosolic proteins, lipids, DNA, and various forms of RNA, including messenger RNA (mRNA) and microRNA (miRNA) [32] [33]. The composition of exosomes is not random but rather a result of selective loading processes that depend on the cell of origin, metabolic status, and external stimuli [14]. For instance, MSCs exposed to different culture conditions or microenvironments produce exosomes with distinct molecular signatures that influence their functional effects on target cells [32].
The following diagram illustrates the biogenesis pathway and key molecular components of MSC-derived exosomes:
The miRNA content of MSC exosomes is particularly relevant for fibroblast research. These small non-coding RNAs can regulate gene expression in recipient fibroblasts by binding to target mRNAs, leading to their degradation or translational repression [18]. For example, exosomal miR-146a has been shown to promote the differentiation of macrophages toward an anti-inflammatory M2 phenotype, which indirectly influences fibroblast behavior in wound healing [14]. Similarly, exosomes from MSCs exposed to ischemic brain extracts showed increased levels of miR-133b, demonstrating how environmental cues can alter exosomal miRNA content and thus their functional effects on target cells [32]. This selective packaging of regulatory molecules makes MSC exosomes powerful natural delivery systems for modulating fibroblast activity in tissue repair processes.
Standard Methods for MSC Exosome Isolation
Ultracentrifugation
Ultracentrifugation is widely considered the gold standard for exosome isolation and is the most commonly used method in research settings [36] [37]. This technique separates exosomes based on their size and density through a series of centrifugation steps with progressively increasing forces [33] [36]. The protocol typically begins with low-speed centrifugation (300-2,000 × g) to remove cells and debris, followed by medium-speed centrifugation (10,000-20,000 × g) to pellet larger extracellular vesicles and apoptotic bodies [33] [37]. The final step involves high-speed ultracentrifugation (100,000 × g or higher) to sediment exosomes while soluble proteins and smaller contaminants remain in the supernatant [33] [36]. A washing step with phosphate-buffered saline (PBS) followed by another ultracentrifugation cycle is often included to improve purity by reducing soluble protein contamination [37].
The major advantage of ultracentrifugation is its ability to produce highly enriched EV fractions while allowing for the collection of additional vesicle fractions [36]. However, limitations include being low-throughput, requiring specific infrastructure (ultracentrifuge), demanding significant technical expertise, and potential for exosome aggregation or damage [36] [37]. Additionally, the pellet may contain non-EV contaminants such as lipoprotein complexes or cellular debris, especially particles of similar densities [32].
Precipitation
Precipitation-based methods use commercial kits containing precipitating agents (typically polyethylene glycol, or PEG) that bind water molecules, thereby reducing the solubility of exosomes and inducing their clumping for easier sedimentation by lower-speed centrifugation [36]. This approach is technically simple, requires no specialized equipment, and allows for processing of multiple samples simultaneously [36]. Studies have shown that precipitation methods can be six times faster and yield approximately 2.5-fold higher concentrations of exosomes per milliliter compared to ultracentrifugation [36].
Despite these advantages, precipitation methods have significant drawbacks. The introduction of synthetic precipitating agents may interfere with downstream functional applications [32]. Furthermore, this method tends to co-precipitate non-vesicular contaminants, including lipoproteins and other soluble proteins, resulting in lower purity samples [36] [37]. Additional purification steps are often required to obtain a more homogenous exosome population for research applications [32].
Size-Exclusion Chromatography (SEC)
Size-exclusion chromatography separates exosomes based on their size rather than density [38] [33] [37]. This technique uses columns packed with porous beads, where larger particles like exosomes are excluded from the pores and elute first, while smaller soluble proteins enter the pores and elute later [38] [37]. SEC can be performed with various column sizes and resin materials optimized for separating different sized particles [37]. Commercial columns are available, such as the IZON range with 35 nm pores optimized for small EVs, though homemade columns are also frequently used [37].
The advantages of SEC include preservation of exosome integrity, high reproducibility, minimal technical expertise requirements, and the ability to separate EVs from soluble proteins with high purity [33] [37]. A comparative study confirmed SEC as a clinically relevant EV separation method that requires minimal expertise, no complicated technology, and can separate EVs within 90 minutes [37]. Limitations include the potential for dilute exosome samples that may require a second concentration step, and possible incomplete separation from similarly sized particles like lipoproteins [32] [38]. To address purity issues, a novel dual-SEC (dSEC) column has been developed with two different types of porous beads sequentially stacked for more efficient separation of EVs from contaminants like ApoB-positive particles and soluble proteins [38].
Table 1: Comparative Analysis of Standard MSC Exosome Isolation Methods
| Parameter | Ultracentrifugation | Precipitation | Size-Exclusion Chromatography |
|---|---|---|---|
| Principle | Size & density based differential sedimentation | Chemical reduction of exosome solubility | Size-based separation through porous matrix |
| Time Required | ~4 hours or more [37] | ~6x faster than UC [36] | ~90 minutes [37] |
| Exosome Yield | Standard yield | ~2.5x higher than UC [36] | Variable; may require concentration [32] |
| Exosome Purity | Moderate to high; may contain protein aggregates [32] | Low to moderate; co-precipitates contaminants [36] | High purity; separates from soluble proteins [37] |
| Sample Volume | Limited by ultracentrifuge rotor capacity | Compatible with small volumes [36] | Compatible with clinically relevant 1mL volumes [37] |
| Equipment Needs | Ultracentrifuge & specialized rotors [36] | Standard laboratory centrifuge | SEC columns & fraction collector |
| Technical Expertise | High [36] [37] | Low [36] | Low [37] |
| Downstream Compatibility | High for functional studies | Potential interference from polymers [32] | High; maintains vesicle integrity [33] |
| Cost | High equipment cost | Moderate reagent costs | Moderate to high reagent costs |
| Scalability | Low to moderate | Moderate | Moderate |
Detailed Experimental Protocols
Ultracentrifugation Protocol for MSC Exosomes
This protocol is optimized for isolating exosomes from MSC-conditioned media and is based on established methodologies [35] [36] [37].
Materials:
- MSC-conditioned media (centrifuged at 300 × g for 15 min to remove cells) [35]
- Ultracentrifuge (e.g., Beckman Optima series)
- Fixed-angle or swinging-bucket rotor (e.g., Type 70 Ti, SW60)
- Polycarbonate bottles or polyallomer tubes compatible with ultracentrifugation
- Phosphate-buffered saline (PBS), sterile-filtered
Procedure:
- Pre-clearance steps: Subject MSC-conditioned media to sequential centrifugation: first at 2,000 × g for 30 minutes to remove dead cells and large debris, then at 10,000 × g for 40 minutes to pellet larger extracellular vesicles and apoptotic bodies [35].
- Ultracentrifugation: Transfer the supernatant to ultracentrifuge tubes. Balance tubes carefully. Centrifuge at 100,000 × g for 90 minutes at 4°C to pellet exosomes [35] [37].
- Washing: Carefully discard the supernatant and resuspend the pellet in sterile PBS. Recentrifuge at 100,000 × g for 90 minutes at 4°C to wash the exosome pellet [35].
- Resuspension: Finally, resuspend the purified exosome pellet in an appropriate volume of PBS (e.g., 400 μL for exosomes from approximately 25 mL starting conditioned medium) for immediate use or storage at -80°C [35].
Critical Considerations:
- All steps should be performed on ice or at 4°C to preserve exosome integrity.
- Use sterile techniques to prevent contamination.
- Avoid overloading the tubes as this reduces separation efficiency.
- The inclusion of a washing step significantly reduces soluble protein contamination but may slightly decrease final yield [37].
Size-Exclusion Chromatography Protocol
This protocol describes SEC using commercially available columns or custom-packed columns for isolating MSC exosomes with high purity [38] [37].
Materials:
- Pre-cleared MSC-conditioned media (pre-cleared as in steps 1-2 of the ultracentrifugation protocol)
- SEC columns (e.g., IZON qEV columns or custom-packed Sepharose CL-2B/CL-6B columns)
- Fraction collection tubes
- PBS, sterile-filtered
Procedure:
- Column preparation: If using commercial columns, equilibrate according to manufacturer's instructions. For custom-packed columns, ensure proper packing and equilibration with PBS.
- Sample application: Apply the pre-cleared MSC-conditioned media to the top of the column. For 1mL plasma samples, this method has been validated, but volume may need adjustment for conditioned media [37].
- Elution: Allow the sample to enter the resin and add PBS as the elution buffer. Collect sequential fractions (typically 0.5-1 mL each).
- Fraction identification: Exosomes typically elute in the early fractions (after void volume), while soluble proteins and other contaminants elute in later fractions [38]. Monitor fractions by absorbance at 280nm or perform protein quantification.
- Exosome concentration: Pool exosome-containing fractions. If necessary, concentrate using ultrafiltration devices (e.g., 100 kDa molecular weight cut-off) by centrifuging at 4,000 × g for approximately 20 minutes [32].
Critical Considerations:
- For enhanced purity, consider dual-SEC columns that stack different resins (e.g., Sephacryl S-200HR over CL-6B) to better separate exosomes from ApoB-positive particles and soluble proteins [38].
- Column performance should be validated with standards before processing valuable samples.
- The dilute nature of SEC-isolated exosomes may require concentration for downstream applications [32].
The following workflow diagram illustrates the key steps in MSC exosome isolation and characterization for fibroblast research:
Combined Ultracentrifugation-SEC Protocol
For the highest purity exosomes required for sensitive fibroblast research applications, a combination of ultracentrifugation and SEC can be employed:
- Isolate exosomes from MSC-conditioned media using the ultracentrifugation protocol above.
- Resuspend the exosome pellet in a small volume of PBS (e.g., 500 μL).
- Apply the resuspended exosomes to an SEC column and follow the SEC protocol.
- Collect the exosome-rich fractions for downstream applications.
This combination approach leverages the concentration capability of ultracentrifugation with the purity advantages of SEC, effectively removing soluble proteins and lipoprotein contaminants that might interfere with fibroblast response assays [37].
Exosome Characterization and Quality Control
Following isolation, comprehensive characterization of MSC exosomes is essential to confirm their identity, purity, and integrity before use in fibroblast research. The International Society for Extracellular Vesicles (ISEV) recommends using multiple complementary techniques for thorough characterization [14] [37].
Nanoparticle Tracking Analysis (NTA) measures the size distribution and concentration of exosomes in suspension by tracking the Brownian motion of individual particles under laser illumination [35] [31]. MSC exosomes typically show a peak size distribution between 30-150 nm [35]. This technique is crucial for standardizing the dose of exosomes used in fibroblast treatment experiments.
Western Blotting detects the presence of exosomal marker proteins while confirming the absence of contaminants. Positive markers for MSC exosomes include tetraspanins (CD9, CD63, CD81) and MSC-specific markers (CD44, CD73, CD90) [14] [31]. Negative controls should include markers for organelles not present in exosomes, such as nuclei (histones), mitochondria (HSP60), or Golgi apparatus (GRP78) [18].
Transmission Electron Microscopy (TEM) provides morphological assessment of exosomes, typically revealing cup-shaped morphology due to fixation artifacts [31]. TEM can confirm the presence of intact lipid bilayers and the absence of cellular debris or protein aggregates.
Additional characterization techniques include:
- Flow cytometry (particularly imaging flow cytometry) for immunophenotyping surface markers on exosomes [36].
- Protein quantification to determine yield and ensure appropriate normalization in functional experiments [37].
- Proteomic analysis by mass spectrometry to comprehensively characterize the protein cargo and confirm the presence of EV-associated proteins while assessing contamination with lipoproteins [36] [37].
Table 2: Essential Research Reagent Solutions for MSC Exosome Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Cell Culture Media | MSC NutriStem XF Basal Medium with Supplement [31], DMEM with EV-depleted FBS [35] | MSC expansion and exosome production | Use EV-depleted FBS (via ultracentrifugation at 120,000 × g for 18h) to reduce background vesicle contamination [35] |
| Isolation Kits & Reagents | Polyethylene glycol-based precipitation kits, Sepharose CL-2B/CL-6B resins [38], IZON qEV columns [37] | Exosome isolation via precipitation or SEC | Precipitation kits offer speed but lower purity; SEC provides higher purity [36] [37] |
| Buffer Systems | Sterile-filtered PBS, RIPA buffer for lysis | Exosome washing, resuspension, and protein extraction | Always use sterile-filtered PBS to avoid particulate contamination |
| Characterization Reagents | Antibodies against CD63, CD81, CD9, CD44, CD73, CD90 [14] [31] | Exosome identification and quantification via Western blot, flow cytometry | Always include positive and negative marker controls for characterization [18] |
| Functional Assay Reagents | Cell migration assay kits (e.g., Transwell), proliferation assays (e.g., MTT, BrdU), tube formation matrigel for angiogenesis | Assessing exosome effects on fibroblast function | Use appropriate controls including non-exosome fractions to confirm specific effects [35] |
Connecting Isolation Methods to Fibroblast Research Applications
The choice of isolation method directly impacts the purity, functionality, and experimental outcomes in fibroblast proliferation and migration studies. For instance, exosomes isolated by ultracentrifugation or SEC typically demonstrate enhanced biological activity in fibroblast assays due to lower contamination from non-vesicular components [35] [37]. A recent study comparing different secretome fractions from human bone marrow MSCs found that small extracellular vesicle (sEV) fractions had superior effects on normal human dermal fibroblast (NHDF) migration compared to non-sEV fractions or complete conditioned media [35].
The miRNA cargo of MSC exosomes plays a pivotal role in modulating fibroblast behavior. Specific miRNAs, including miR-125a-3p, miR-540-3p, and miR-338-5p, have been identified in MSC exosomes and shown to influence cellular processes relevant to wound healing [14]. These miRNAs can suppress T-cell activity, inhibit cytotoxic T lymphocytes, and stimulate Treg cell proliferation, creating an anti-inflammatory environment conducive to tissue repair [14]. Additionally, exosomal miRNAs such as miR-146a and miR-223 contribute to the transition of macrophages from pro-inflammatory M1 to anti-inflammatory M2 phenotypes, indirectly supporting fibroblast functions in wound healing [34].
The following diagram illustrates how MSC exosomal miRNAs influence fibroblast behavior through key signaling pathways:
For research specifically focusing on exosomal miRNA effects on fibroblasts, SEC isolation is often preferable as it minimizes contaminants that could interfere with downstream analyses and cellular responses [37]. The high purity of SEC-isolated exosomes ensures that observed effects on fibroblast proliferation and migration can be more confidently attributed to the exosomal cargo rather than co-isolated contaminants. Furthermore, the maintained integrity of exosomes isolated by SEC supports efficient uptake by recipient fibroblasts, facilitating the transfer of miRNA cargo and subsequent modulation of fibroblast gene expression and behavior [33] [37].
The isolation of MSC exosomes using standardized methods is a critical prerequisite for investigating their effects on fibroblast proliferation and migration. Ultracentrifugation, precipitation, and size-exclusion chromatography each offer distinct advantages and limitations, with the optimal choice depending on the specific research requirements. For mechanistic studies focusing on exosomal miRNA functions in fibroblast biology, methods that prioritize purity and vesicle integrity (particularly SEC) are generally preferred. As research progresses toward clinical applications, standardization and reproducibility in exosome isolation will become increasingly important for developing consistent and effective exosome-based therapies for wound healing and tissue regeneration.
Exosomal microRNAs (miRNAs) have emerged as pivotal regulators of intercellular communication, particularly in the context of mesenchymal stem cell (MSC) function. These small non-coding RNAs, typically 19-22 nucleotides in length, are selectively packaged into exosomes—nanoscale extracellular vesicles (30-150 nm) that transport their biomolecular cargo between cells [14] [2]. The profiling of exosomal miRNA cargo provides critical insights into the molecular mechanisms through which MSCs influence fibroblast behavior, encompassing proliferation, migration, and differentiation pathways central to tissue repair and regeneration.
The technical landscape for exosomal miRNA analysis has evolved significantly, with integrated workflows now combining advanced sequencing technologies with precise validation methods. This technical guide examines the current methodologies for profiling exosomal miRNA cargo, with specific application to researching MSC-derived exosomes and their effects on fibroblast biology. The comprehensive approach outlined here enables researchers to capture the complete miRNome while quantitatively verifying key targets of interest, thereby bridging discovery science with mechanistic investigation.
Exosome Isolation and Characterization: Foundation for Quality miRNA Profiling
The reliability of any exosomal miRNA profiling study hinges on the quality of the starting material. Proper isolation and characterization of exosomes is therefore a critical first step in the analytical workflow.
Isolation Techniques
Polymer-Based Precipitation methods, such as those utilizing commercial kits (e.g., miRCURY Exosome Kit, Qiagen), offer accessibility and moderate throughput for plasma and serum samples. This approach involves incubating pre-cleared plasma with a precipitation solution, followed by centrifugation to pellet the exosomes [39] [40]. While user-friendly, precipitation methods may co-precipitate non-exosomal contaminants, necessitating additional purification steps such as ultracentrifugation [39].
Ultracentrifugation remains the gold standard for exosome isolation, particularly when high purity is required. This technique employs high-speed centrifugation (110,000× g for 70 minutes) to pellet exosomes based on their buoyant density [39]. When combined with density gradient centrifugation, ultracentrifugation can achieve superior purification by separating exosomes from protein aggregates and other extracellular vesicles.
Table 1: Comparison of Exosome Isolation Methods
| Method | Principle | Advantages | Limitations | Typical Yield |
|---|---|---|---|---|
| Ultracentrifugation | Density and size-based separation | High purity; no chemical additives; scalable | Time-consuming; requires specialized equipment; may cause vesicle damage | ~50-200 µg from 1 mL plasma |
| Polymer-Based Precipitation | Polymer reduces exosome solubility | Simple protocol; suitable for small volumes; minimal equipment | Co-precipitates contaminants; lower purity; polymer may interfere with downstream applications | ~100-300 µg from 1 mL plasma |
| Size-Exclusion Chromatography | Size-based separation | Preserves vesicle integrity; good purity; reproducible | Sample dilution; limited resolving power for similar-sized particles | ~30-150 µg from 1 mL plasma |
Quality Control and Characterization
Comprehensive characterization of isolated exosomes is essential before proceeding to RNA extraction. The International Society for Extracellular Vesicles (ISEV) recommends implementing multiple complementary techniques to confirm exosome identity and purity [14].
Nanoparticle Tracking Analysis (NTA) instruments, such as the NanoSight NS3000, measure the size distribution and concentration of exosomes by tracking the Brownian motion of individual particles in suspension [39]. Properly isolated exosomal preparations typically show a peak size distribution between 50-150 nm.
Tetraspanin Expression Analysis via western blotting or flow cytometry confirms the presence of characteristic exosomal surface markers, including CD9, CD63, and CD81 [14]. Research has shown that exosomal marker expression may vary by biological context; for instance, hypertensive patients exhibited significantly reduced expression of exosomal CD9 compared to controls [39].
Transmission Electron Microscopy (TEM) provides visual confirmation of exosomal morphology, revealing the characteristic cup-shaped morphology of exosomes under negative staining [39].
Small RNA Sequencing: Comprehensive miRNA Profiling
Next-generation sequencing (NGS) of exosomal small RNAs enables unbiased discovery of miRNA signatures, providing a comprehensive view of the miRNome without prior knowledge of specific targets.
Library Preparation Challenges and Solutions
Exosomal RNA presents unique challenges for sequencing library preparation, including extremely low input amounts (picogram to nanogram range), high fragmentation, and contamination risk from cell-free RNA [41]. Specialized library preparation kits have been developed to address these limitations:
Ultra-low input optimization allows library construction from as little as 1-10 ng of total RNA, crucial for precious clinical samples [41].
Dual-strategy RNA capture combining poly(A) tailing with adapter ligation enables uniform capture of both polyadenylated and non-polyadenylated RNA species, providing more complete transcriptome coverage [41].
rRNA and cfRNA depletion modules remove common contaminants without compromising vesicle-derived RNAs, ensuring that sequencing reads reflect true exosomal content [41].
Sequencing Platform Selection
Recent advances in sequencing platforms have significantly enhanced exosomal RNA profiling capabilities:
Illumina NovaSeq X Plus (2023 release) offers dramatically increased throughput (up to 26 billion reads per run), enabling deep profiling of exosomal RNA across hundreds of samples in parallel [41].
MGI DNBSEQ Technology provides low duplication rates, improved small RNA accuracy, and cost-effective scalability for large sample sets [41].
Both platforms now support index hopping prevention and dual-index compatibility, which are critical for accurate quantification in low-input, multiplexed exosomal RNA libraries.
Bioinformatics Analysis
The analysis of exosomal miRNA sequencing data requires specialized bioinformatic approaches to address the unique characteristics of these datasets:
AI-Powered Signal Denoising methods, including deep count autoencoders (DCA), model the count distribution, overdispersion, and sparsity inherent in exosomal RNA-seq data, improving the signal-to-noise ratio and reducing false positives in differential expression analysis [42].
Adaptive Normalization tools like DESeq2-Vesicle apply custom size factors and variance shrinkage models tailored to the zero-inflated, skewed distributions found in exosomal miRNA datasets, improving statistical power in small-cohort analyses [42].
Integrated Interaction Network Analysis using tools like miRNet and CIRCInteractome enables the construction of miRNA-mRNA regulatory networks, providing insights into functional modules relevant to biological pathways such as fibroblast proliferation and migration [41].
Table 2: Key Research Reagent Solutions for Exosomal miRNA Profiling
| Application | Product/Technology | Key Features | Manufacturer/Reference |
|---|---|---|---|
| Exosome Isolation | miRCURY Exosome Kit | Polymer-based precipitation; compatible with plasma/serum | Qiagen [39] [40] |
| RNA Extraction | miRNeasy Serum/Plasma Advanced Kit | Optimized for low-concentration samples; includes QC standards | Qiagen [40] |
| Small RNA Library Prep | TaqMan Advanced miRNA cDNA Synthesis Kit | Poly(A) tailing + adapter ligation; enhanced small RNA detection | Applied Biosystems [40] |
| qPCR Validation | QuantiFast SYBR Green PCR Master Mix | Fast cycling; high sensitivity; compatible with multiple detection chemistries | Qiagen [43] |
| High-Throughput Sequencing | NovaSeq X Plus | Ultra-high throughput (26B reads/run); suited for large cohort studies | Illumina [41] |
qRT-PCR Validation: From Discovery to Verification
The transition from high-throughput discovery to targeted verification represents a critical phase in exosomal miRNA research, where quantitative reverse transcription polymerase chain reaction (qRT-PCR) serves as the gold standard for validation.
Experimental Design for Validation
A robust validation strategy should include both technical replication (multiple measurements of the same sample) and biological replication (multiple independent biological samples) to ensure reproducibility. When investigating MSC exosomal miRNAs in fibroblast function, the experimental design should account for:
Reference Gene Selection requires empirical testing of candidate endogenous controls (e.g., RNU6B, miR-16-5p, miR-93-5p) to identify genes with stable expression across all experimental conditions [44] [43]. Studies have shown that miR-16-5p, miR-25-3p, and miR-93-5p are commonly highly expressed across exosomes from different MSC sources [44].
Sample Size Considerations should be informed by power analysis. For miRNA validation studies, sample sizes of 15-20 per group typically provide sufficient power to detect biologically relevant effect sizes, as demonstrated in recent exosomal miRNA studies [39] [40].
Detailed qRT-PCR Protocol
The following protocol has been optimized for exosomal miRNA quantification:
RNA Reverse Transcription is performed using the TaqMan Advanced miRNA cDNA Synthesis Kit, which incorporates a poly(A) tailing and adapter ligation step to ensure efficient reverse transcription of mature miRNAs [40]. Reactions should include no-template controls to detect potential contamination.
Quantitative PCR is performed using QuantiFast SYBR Green PCR Master Mix in a 20 µL reaction volume containing 2 µL of diluted cDNA template. Cycling conditions follow: initial activation at 95°C for 5 minutes, followed by 40 cycles of denaturation at 95°C for 10 seconds and combined annealing/extension at 60°C for 30 seconds [43].
Data Analysis utilizes the 2−∆∆Ct method, where the target miRNA Ct values are first normalized to the reference gene (∆Ct), then compared to the control group (∆∆Ct) [43]. Statistical significance is typically assessed using the Mann-Whitney U test for two-group comparisons, with p < 0.05 considered significant [45].
Applications in MSC Exosomal miRNA and Fibroblast Research
The integrated profiling approach described in this guide enables sophisticated investigation of MSC exosomal miRNA effects on fibroblast biology, with particular relevance to wound healing and tissue repair mechanisms.
Functional Implications for Fibroblast Behavior
Research has identified specific MSC exosomal miRNAs that regulate key aspects of fibroblast function:
miR-1246 demonstrates elevated expression in MSC-derived exosomes and has been implicated in hypertensive pathways, suggesting potential roles in vascular fibroblast signaling [39] [8].
miR-21-5p is highly enriched in MSC exosomes compared to parent cells (100-fold higher) and has been shown to modulate immune responses and fibroblast activation through regulation of macrophage polarization [14] [8].
let-7g, miR-381, and miR-100 represent additional frequently identified miRNAs in MSC-EXOs that target pathways involved in cell proliferation and migration [8].
Pathway Analysis and Target Prediction
Understanding the functional impact of exosomal miRNAs requires comprehensive pathway analysis of predicted target genes. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses typically reveal MSC exosomal miRNA involvement in:
- MAPK signaling pathway - regulating cell proliferation and differentiation [44]
- TGF-β signaling - influencing fibroblast activation and extracellular matrix production [8]
- Focal adhesion pathways - affecting cell migration and mechanotransduction [8]
Computational prediction tools such as EmiRPred utilize ensemble methods combining alignment-based and AI-based approaches to identify exosomal miRNAs with high accuracy (AUC up to 0.73) [42]. These in silico predictions provide valuable guidance for prioritizing candidates for functional validation.
The integrated workflow from small RNA sequencing to qRT-PCR validation provides a powerful framework for investigating MSC exosomal miRNA cargo and its influence on fibroblast behavior. As profiling technologies continue to advance—with improvements in sequencing sensitivity, computational prediction algorithms, and validation methodologies—our ability to decipher the complex language of intercellular communication via exosomal miRNAs will correspondingly deepen. This technical foundation enables researchers to not only identify miRNA signatures associated with biological outcomes but also to verify these findings with quantitative precision, ultimately accelerating the development of exosome-based diagnostic and therapeutic applications in regenerative medicine.
Within the broader research on the role of Mesenchymal Stem Cell (MSC) exosomal miRNAs in fibroblast biology, robust functional assays are indispensable for quantifying key cellular behaviors. Fibroblasts are stromal cells critical for organ development, homeostasis, and pathology, and their functional characterization is a cornerstone of research in fibrosis, cancer, and tissue repair [46]. The activation of quiescent fibroblasts into proliferative, migratory, and highly contractile myofibroblasts is a hallmark of these processes, characterized by the expression of alpha-smooth muscle actin (αSMA) and its organization into stress fibers [47]. This technical guide provides an in-depth overview of established in vitro protocols for evaluating fibroblast proliferation, migration, and contractility, framing these assays within the context of investigating the modulatory effects of MSC-derived exosomal miRNAs. These miRNAs are key regulators of gene expression, can be selectively packaged into extracellular vesicles (EVs), and have been shown to influence critical pathways involved in inflammation, immune response, and tissue repair [1] [12]. The following sections detail methodologies, data analysis, and key reagents to equip researchers with the tools necessary for comprehensive fibroblast functional analysis.
Proliferation Assays
Assessing fibroblast proliferation is fundamental for understanding the growth dynamics and response to mitogenic stimuli, such as those potentially delivered via MSC exosomes.
Metabolic Activity-Based Assays (e.g., MTT, CCK-8)
These assays measure cell proliferation indirectly by quantifying the metabolic activity of a cell population.
Detailed Protocol:
- Cell Seeding: Plate fibroblasts at a low, optimized density (e.g., 1-5 x 10³ cells per well) in a 96-well plate in complete growth medium. Include blank wells with medium only for background subtraction.
- Treatment Application: After 24 hours, introduce experimental treatments. This includes MSC-derived exosomes (isolated via ultracentrifugation or precipitation methods [12]) at various concentrations, control exosomes, and blank medium. Ensure multiple replicates per condition.
- Incubation with Reagent: At desired time points (e.g., 24, 48, 72 hours), add the relevant reagent.
- For MTT: Replace medium with serum-free medium containing 0.5 mg/mL MTT reagent. Incubate for 2-4 hours at 37°C.
- For CCK-8: Add CCK-8 reagent directly to the existing culture medium (10% of total volume). Incubate for 1-4 hours at 37°C.
- Signal Measurement:
- MTT: Carefully remove the MTT-containing medium. Dissolve the formed formazan crystals in dimethyl sulfoxide (DMSO).
- CCK-8: The reagent is water-soluble, and no solubilization step is needed.
- Quantification: Measure the absorbance of each well using a plate reader. For MTT, the typical wavelength is 570 nm with a reference of 630-690 nm. For CCK-8, the absorbance is measured at 450 nm.
Data Analysis: Average the absorbance values from replicate wells and subtract the average value of the blank wells. Results can be presented as fold-change in absorbance relative to the control (untreated) group. This fold-change is directly correlated with the number of metabolically active cells.
DNA Synthesis Measurement (EdU Assay)
The 5-Ethynyl-2'-deoxyuridine (EdU) assay provides a direct measure of DNA synthesis and is superior for confirming active proliferation.
Detailed Protocol:
- Cell Seeding and Treatment: Seed and treat fibroblasts as described in Section 2.1.
- EdU Labeling: For the final 2-6 hours of the treatment period, add EdU reagent to the culture medium at the manufacturer's recommended concentration.
- Cell Fixation and Permeabilization: Remove the medium, wash cells with PBS, and fix with 4% paraformaldehyde for 15 minutes at room temperature. Permeabilize cells with 0.5% Triton X-100 in PBS for 20 minutes.
- Click Reaction: Incubate cells with the Click-iT reaction cocktail containing a fluorescent azide dye (e.g., Alexa Fluor 594) for 30 minutes, protected from light. This reaction covalently links the fluorescent dye to the EdU incorporated into DNA.
- Counterstaining and Imaging: Wash cells and counterstain nuclei with Hoechst 33342. Image using a fluorescence microscope. Proliferating cells (EdU-positive) will have red fluorescent nuclei, while all nuclei will be blue.
Data Analysis: Quantify the percentage of EdU-positive cells by counting fluorescent nuclei in multiple random fields of view for each condition using image analysis software (e.g., ImageJ, CellProfiler). A minimum of 300-500 total cells per condition should be counted for statistical robustness.
Table 1: Key Proliferation Assay Reagents and Their Functions
| Research Reagent | Function / Explanation |
|---|---|
| CCK-8 Solution | A water-soluble tetrazolium salt that produces a formazan dye upon reduction by cellular dehydrogenases, indicating metabolic activity. |
| MTT Reagent | A yellow tetrazolium dye reduced to purple formazan crystals in the mitochondria of living cells. |
| EdU Kit (e.g., Click-iT) | Contains reagents for labeling and detecting incorporated EdU, a thymidine analog, to identify cells in the S-phase of the cell cycle. |
| Fibroblast Growth Medium | Typically Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and 1% Penicillin-Streptomycin. |
| MSC-derived Exosomes | Isolated from MSC-conditioned media; the cargo (including miRNAs) is the experimental variable modulating fibroblast proliferation [1] [12]. |
Diagram 1: Workflow for Fibroblast Proliferation Assays.
Migration Assays
Cell migration is a critical process in wound healing and fibrosis. The following assays quantify the directed and random movement of fibroblasts.
Scratch Wound (Gap Closure) Assay
This simple and widely used assay measures the collective migration of fibroblasts into a physically created "wound."
Detailed Protocol:
- Cell Seeding and Monolayer Formation: Seed fibroblasts at a high density in a 12- or 24-well plate to create a confluent monolayer (typically 24-48 hours post-seeding).
- Scratch Creation: Using a sterile pipette tip (200 µL), gently and slowly create a straight scratch through the center of each well. To ensure consistency, use a ruler or a marker to guide the tip. Aspirate the medium and wash the well twice with PBS to remove detached cells.
- Treatment and Imaging: Add fresh serum-free or low-serum medium containing the experimental treatments (e.g., MSC exosomes). Immediately acquire the "0-hour" image of the scratch using a phase-contrast microscope with a 4x or 10x objective. Mark positions on the plate to image the same fields over time.
- Time-Lapse Monitoring: Place the plate in a tissue culture incubator (preferably with controlled CO2 and humidity). Image the same scratch locations at regular intervals (e.g., every 6-12 hours) for 24-72 hours.
Data Analysis: Measure the scratch area or width at each time point using image analysis software (e.g., ImageJ with the "MRI Wound Healing Tool" plugin). Calculate the percentage of wound closure relative to the 0-hour time point using the formula: % Closure = [(Area_t0 - Area_tx) / Area_t0] * 100. Plotting these values over time generates a migration curve.
Transwell (Boyden Chamber) Migration Assay
This assay measures the chemotactic migration of individual cells through a porous membrane toward a chemoattractant.
Detailed Protocol:
- Assemble Chamber: Use a 24-well Transwell plate with permeable inserts (pore size 5-8 µm).
- Prepare Chemoattractant: Add medium containing the chemoattractant (e.g., 10% FBS, PDGF, or MSC exosomes) to the lower chamber. The negative control well should contain serum-free medium.
- Seed Cells: Trypsinize, count, and resuspend fibroblasts in serum-free medium. Add a standardized cell suspension (e.g., 1-5 x 10⁴ cells in 100-200 µL) to the inside of the upper chamber.
- Incubate and Migrate: Incubate the plate for 6-24 hours at 37°C to allow cells to migrate through the pores toward the lower chamber.
- Fix and Stain: Carefully remove the non-migrated cells from the upper side of the membrane by swabbing with a cotton swab. Fix the cells that have migrated to the lower side of the membrane with 4% PFA for 10 minutes. Stain with a crystal violet solution (0.1% w/v) for 20 minutes.
- Image and Count: Gently wash the membrane with water, allow it to dry, and image it under a bright-field microscope. Count the number of stained cells in several predefined fields per membrane.
Data Analysis: Calculate the average number of migrated cells per field of view for each replicate. Express the data as the fold-change in migration relative to the control group or as the total number of migrated cells.
Table 2: Key Migration Assay Reagents and Their Functions
| Research Reagent | Function / Explanation |
|---|---|
| Transwell Plates | Multi-well plates featuring hanging cell culture inserts with a porous membrane that separates the cell seeding compartment from the chemoattractant. |
| Crystal Violet Solution | A histological stain used to visualize and quantify migrated cells attached to the lower surface of the Transwell membrane. |
| Pipette Tips (Sterile) | Used to create a uniform, cell-free "scratch" in a confluent monolayer of fibroblasts for the gap closure assay. |
| Fetal Bovine Serum (FBS) | A common and potent chemoattractant used in the lower chamber of Transwell assays to stimulate fibroblast migration. |
| MSC Exosome Cargo (e.g., miRNAs) | MSC-EVs contain miRNAs (e.g., miR-23b, miR-125b) that can modulate pathways in recipient fibroblasts to either promote or inhibit migration [1] [48]. |
Contractility Assays
The acquisition of a contractile phenotype, marked by αSMA expression and stress fiber formation, is a defining feature of myofibroblasts. This contractile force is a key driver of tissue remodeling and stiffening in fibrosis [47].
Collagen Gel Contraction Assay
This classical assay measures the ability of fibroblasts to contract a three-dimensional extracellular matrix, mimicking in vivo tissue contraction.
Detailed Protocol:
- Prepare Cell-Collagen Mixture:
- Neutralize a high-concentration Type I collagen solution (e.g., rat tail collagen I) on ice according to the manufacturer's instructions using 10X PBS and 1N NaOH.
- Mix the neutralized collagen solution with a fibroblast suspension to achieve a final desired cell density (e.g., 1-2 x 10⁵ cells/mL) and collagen concentration (e.g., 1.5-2.0 mg/mL). Keep everything on ice to prevent premature polymerization.
- Polymerize Gels: Quickly aliquot the cell-collagen mixture into non-adherent culture plates (e.g., 24-well plates, pre-coated with BSA). Use 500 µL per well. Incubate the plate at 37°C for 30-60 minutes to allow the gels to polymerize fully.
- Release and Treat: After polymerization, gently add culture medium containing the test treatments (e.g., TGF-β1 as a positive control, MSC exosomes, or specific miRNA mimics/inhibitors) around the gels. Carefully run a sterile spatula around the edge of each gel to release it from the sides of the well. This release step is critical for allowing unrestricted contraction.
- Monitor Contraction: Over the next 24-72 hours, the fibroblasts will contract the gel. Image the gels at regular intervals from a top-down view alongside a ruler for scale.
- Quantify Contraction: Measure the projected surface area of each gel from the images using image analysis software. Calculate the percentage of gel contraction relative to the initial area using the formula:
% Contraction = [(Initial Area - Final Area) / Initial Area] * 100.
Quantitative Analysis of αSMA Stress Fibers
As contractility is tightly linked to the expression and organization of αSMA into stress fibers, quantitative image analysis provides a complementary measure of myofibroblast activation [47].
Detailed Protocol:
- Cell Seeding and Stimulation: Plate fibroblasts on glass coverslips coated with collagen or fibronectin. Treat cells with profibrotic stimuli (e.g., TGF-β) and/or MSC exosomes for 24-48 hours.
- Immunofluorescence Staining:
- Fixation and Permeabilization: Fix cells with 4% PFA for 15 min, then permeabilize with 0.1-0.5% Triton X-100 for 10 min.
- Blocking: Incubate with a blocking solution (e.g., 1-5% BSA in PBS) for 1 hour.
- Staining: Incubate with primary antibody against αSMA (e.g., mouse anti-αSMA) diluted in blocking buffer for 1-2 hours at room temperature or overnight at 4°C. Wash and incubate with a fluorescently-labeled secondary antibody (e.g., Alexa Fluor 488 goat anti-mouse) and a nuclear stain (e.g., Hoechst or DAPI) for 1 hour.
- Image Acquisition: Acquire high-resolution, consistent exposure images using a fluorescence microscope.
- Quantitative Image Analysis:
- Intensity: Measure the mean fluorescence intensity of αSMA per cell.
- Organization: Use mathematical descriptors and analytical frameworks to quantify the anisotropy and coherence of αSMA stress fibers, moving beyond subjective grading [47]. This can involve analyzing the orientation and bundling of fibers.
Diagram 2: Key Pathways in Myofibroblast Activation and Contractility.
Table 3: Key Contractility Assay Reagents and Their Functions
| Research Reagent | Function / Explanation |
|---|---|
| Type I Collagen (Rat Tail) | The major ECM protein used to create a 3D hydrogel that fibroblasts can remodel and contract, mimicking the in vivo environment. |
| TGF-β1 (Transforming Growth Factor Beta 1) | A canonical cytokine used as a positive control to robustly activate fibroblasts into contractile myofibroblasts [49]. |
| Anti-αSMA Antibody | A primary antibody targeting alpha-smooth muscle actin, the definitive marker for contractile stress fibers in myofibroblasts [47]. |
| Fluorescent Secondary Antibody | A labeled antibody used to visualize the primary antibody binding under a fluorescence microscope. |
| MSC-EV miRNAs (e.g., miR-23b, miR-125b) | Cargo molecules that can be delivered to fibroblasts and target genes in pathways like Wnt, PDGF, and TGF-β, thereby modulating the contractile phenotype [1] [12]. |
The therapeutic application of Mesenchymal Stem Cell (MSC)-derived exosomes represents a paradigm shift in regenerative dermatology, transitioning from cell-based to cell-free therapies. While MSCs themselves have demonstrated potential in promoting skin repair, research has increasingly revealed that their therapeutic benefits are primarily mediated through paracrine factors rather than direct cell replacement [19] [2]. Among these factors, exosomes—nanoscale extracellular vesicles (30-150 nm in diameter)—have emerged as critical mediators of intercellular communication by transferring bioactive molecules, including proteins, lipids, and nucleic acids, to recipient cells [9] [50].
Exosomes derived from various MSC sources (including bone marrow, adipose tissue, and umbilical cord) contain enriched populations of microRNAs (miRNAs) that regulate gene expression in target skin cells, particularly fibroblasts [19]. These miRNAs, approximately 22 nucleotides in length, function as post-transcriptional regulators by binding to target mRNAs, leading to translational repression or mRNA degradation [18]. The encapsulation of miRNAs within exosomes protects them from degradation and facilitates their targeted delivery to skin cells, making them ideal therapeutic agents for modulating the wound healing process [19] [18].
This technical guide examines the role of MSC exosomal miRNAs in regulating fibroblast behavior during skin regeneration, with a specific focus on their mechanisms of action, therapeutic potential in promoting healing and reducing scar formation, and practical experimental approaches for research and drug development.
Molecular Mechanisms of MSC Exosomal miRNAs in Fibroblast Regulation
MSC exosomal miRNAs orchestrate multiple aspects of skin repair through precise regulation of fibroblast gene expression networks. The following table summarizes key miRNA regulators and their validated targets in fibroblast physiology:
Table 1: Key MSC Exosomal miRNAs Regulating Fibroblast Functions in Skin Repair
| miRNA | Exosome Source | Target Gene/Pathway | Effect on Fibroblasts | Functional Outcome |
|---|---|---|---|---|
| miR-21-3p | Human Umbilical Cord MSCs | PTEN, SPRY1 [19] | Promotes proliferation & migration [19] | Enhanced re-epithelialization |
| miR-125a | Adipose-Derived MSCs | Angiogenic inhibitor DLL4 [19] | Promotes angiogenesis [19] | Improved tissue perfusion |
| miR-29a | Adipose-Derived MSCs | TGF-β2/Smad3 pathway [19] | Reduces collagen deposition [19] | Attenuated scar formation |
| miR-21, -23a, -125b, -145 | Umbilical Cord MSCs | TGF-β/SMAD2 pathway [51] | Suppresses myofibroblast differentiation [51] | Anti-fibrotic activity |
| miR-135a | Amnion MSCs | LATS2 [19] | Promotes proliferation & migration [19] | Accelerated wound closure |
| let-7b | Umbilical Cord MSCs | TLR4/NF-κB, STAT3/Akt [19] | Induces M2 macrophage polarization [19] | Reduced inflammation |
The therapeutic effects of these miRNAs are mediated through their influence on three core processes in wound healing: inflammation modulation, proliferation enhancement, and extracellular matrix remodeling.
Inflammation Modulation
The transition from pro-inflammatory to anti-inflammatory signaling is crucial for normal wound healing. MSC exosomal miRNAs facilitate this transition by promoting macrophage polarization toward the anti-inflammatory M2 phenotype. Specifically, let-7b from umbilical cord MSC exosomes targets TLR4/NF-κB signaling while activating STAT3/Akt pathways, resulting in shifted macrophage polarization and attenuated inflammation [19]. Similarly, miR-223 from jaw bone marrow-derived MSC exosomes targets Pknox1, inducing M2 macrophage polarization and increasing expression of anti-inflammatory mediators including IL-10 and RELM-α [19].
Proliferation and Migration Enhancement
MSC exosomal miRNAs significantly enhance fibroblast proliferation and migration capabilities, critical processes for re-epithelialization and granulation tissue formation. miR-21-3p, highly enriched in human umbilical cord MSC exosomes, promotes fibroblast proliferation and migration by inhibiting the expression of PTEN and SPRY1 [19]. Similarly, miR-135a from amnion MSC exosomes enhances fibroblast proliferation and migration by targeting LATS2 and modulating the expression of E-cadherin and N-cadherin [19]. These pro-proliferative effects are complemented by angiogenic miRNAs such as miR-125a, which targets the angiogenic inhibitor delta-like 4 (DLL4) to promote endothelial cell angiogenesis and improve tissue vascularization [19].
Extracellular Matrix Remodeling and Scar Suppression
Perhaps the most therapeutically promising aspect of MSC exosomal miRNAs is their ability to modulate extracellular matrix composition and suppress fibrotic responses. A key mechanism involves the suppression of transforming growth factor-beta (TGF-β) signaling, a primary driver of myofibroblast differentiation and collagen production. Umbilical cord MSC exosomes deliver a specific set of miRNAs (miR-21, miR-23a, miR-125b, and miR-145) that collectively inhibit the TGF-β2/SMAD2 pathway, reducing α-smooth muscle actin (α-SMA) expression and collagen deposition [51]. Similarly, miR-29a from adipose-derived MSC exosomes targets the TGF-β2/Smad3 pathway, reducing expression of Col-I, Col-III, and α-SMA, thereby attenuating scar formation [19].
Table 2: Anti-Fibrotic Effects of MSC Exosomal miRNAs in Preclinical Models
| miRNA | Exosome Source | Model System | Reduction in Scar Indicators | Reference |
|---|---|---|---|---|
| miR-29a | Adipose-Derived MSCs | In vivo wound healing | ↓α-SMA, Col-I, Col-III [19] | [19] |
| miR-21, -23a, -125b, -145 | Umbilical Cord MSCs | Mouse skin-defect model | ↓α-SMA, collagen deposition [51] | [51] |
| miR-192-5p | Adipose-Derived MSCs | In vitro fibroblast culture | ↓Col1, Col3, α-SMA, p-Smad2/p-Smad3 [19] | [19] |
| let-7-5p, miR-22-3p, miR-27a-3p | Amniotic Fluid Stem Cells | In vitro fibroblast differentiation | Prevented differentiation to myofibroblasts [19] | [19] |
The following diagram illustrates the central signaling pathways through which MSC exosomal miRNAs regulate fibroblast behavior during skin repair:
Diagram 1: MSC exosomal miRNA regulation of fibroblast functions in skin repair. MSC-derived exosomes deliver specific miRNAs that target multiple signaling pathways in fibroblasts, promoting proliferation, angiogenesis, and anti-inflammatory responses while inhibiting fibrotic processes.
Experimental Protocols for Investigating MSC Exosomal miRNA Functions
Protocol 1: Isolation and Characterization of MSC Exosomes
Principle: Exosomes are isolated from MSC-conditioned media via differential ultracentrifugation, then characterized by size, morphology, and specific surface markers [51].
Procedure:
- MSC Culture: Culture MSCs from source tissue (umbilical cord, adipose tissue, or bone marrow) in standard media. Use exosome-depleted FBS for 48 hours prior to collection to eliminate bovine exosome contamination [51].
- Conditioned Media Collection: Collect cell culture supernatant and perform sequential centrifugation: 300g for 10 minutes (remove cells), 16,500g for 20 minutes (remove cell debris), and filtration through 0.22μm filter [51].
- Exosome Isolation: Ultracentrifuge filtered supernatant at 120,000g for 70 minutes at 4°C using SW32Ti rotor. Resuspend pellet in PBS [51].
- Characterization:
- Nanoparticle Tracking Analysis: Determine size distribution and concentration (30-150 nm expected) [50].
- Transmission Electron Microscopy: Visualize cup-shaped morphology [50].
- Western Blotting: Confirm presence of exosomal markers (CD63, CD9, CD81) and absence of cellular organelle proteins (e.g., GM130) [18] [50].
- miRNA Cargo Analysis: Extract total RNA and perform small RNA sequencing or RT-qPCR for specific miRNAs of interest [19] [51].
Protocol 2: Functional Validation of Exosomal miRNAs in Fibroblast assays
Principle: Evaluate the functional impact of MSC exosomes and specific miRNAs on fibroblast behavior using in vitro models.
Procedure:
- Fibroblast Culture: Maintain human dermal fibroblasts in DMEM supplemented with 10% FBS under standard conditions (37°C, 5% CO2) [51].
- Exosome Uptake Assay: Label exosomes with lipophilic dye (e.g., PKH67) and incubate with fibroblasts. Visualize internalization via confocal microscopy after 24 hours [9].
- Proliferation Assay: Seed fibroblasts in 96-well plates (5×10³ cells/well). Treat with MSC exosomes (50-100 μg/mL) or miRNA mimics/inhibitors. Assess proliferation at 24, 48, and 72 hours using MTT or CCK-8 assays [19] [51].
- Migration Assay: Perform scratch wound assay by creating a linear scratch in confluent fibroblast monolayer. Treat with MSC exosomes and monitor wound closure at 0, 12, and 24 hours using time-lapse microscopy. Calculate migration rate [51].
- Gene Expression Analysis: Extract RNA from treated fibroblasts and analyze expression of target genes (e.g., COL1A1, COL3A1, α-SMA, TGF-β2) via RT-qPCR [51].
- Protein Analysis: Perform Western blotting to assess protein levels of signaling pathway components (e.g., p-SMAD2, total SMAD2, PTEN) and differentiation markers (α-SMA) [51].
Protocol 3: In Vivo Validation in Skin Wound Models
Principle: Evaluate the therapeutic efficacy of MSC exosomes in promoting wound healing and reducing scar formation in animal models.
Procedure:
- Animal Model: Utilize full-thickness skin defect models (e.g., ICR mice with 1.5 cm dorsal skin excision) [51].
- Exosome Formulation: Incorporate MSC exosomes (100 μg/mL) into hydrogel scaffold (e.g., HydroMatrix) immediately before application to enhance retention [51].
- Treatment Protocol: Apply exosome-loaded hydrogel around wound margins 48 hours post-wounding. Include control groups (PBS, non-MSC exosomes) [51].
- Wound Assessment:
- Macroscopic: Photograph wounds at days 0, 7, 14, and 21 post-treatment. Calculate wound closure percentage using image analysis software [51].
- Histological: Harvest wound tissue at endpoint (day 25). Process for H&E staining to assess re-epithelialization and Masson's trichrome staining to evaluate collagen deposition and organization [51].
- Immunohistochemistry: Stain for α-SMA to identify myofibroblasts and CD31 to assess angiogenesis [9] [51].
- Scar Assessment: Evaluate scar size, collagen fiber organization, and myofibroblast persistence compared to controls [51].
The following diagram illustrates the complete experimental workflow from exosome isolation to functional validation:
Diagram 2: Experimental workflow for investigating MSC exosomal miRNA functions. The process encompasses exosome isolation, in vitro functional assays, molecular analysis, and in vivo validation in wound healing models.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for MSC Exosomal miRNA Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| MSC Sources | Umbilical Cord Wharton's Jelly [52], Adipose Tissue [9], Bone Marrow [19] | Provide biologically relevant exosome populations | Umbilical cord source offers high cell yield, low immunogenicity [52] |
| Exosome Isolation Kits | Ultracentrifugation systems [51], Size-exclusion chromatography [53], Polymer-based precipitation | Isolate exosomes from conditioned media | Ultracentrifugation remains gold standard; check for exosome-depleted FBS requirement [51] |
| Characterization Tools | Nanoparticle Tracking Analysis (NTA) [50], TEM [50], Western Blot (CD63, CD81, CD9) [18] | Confirm exosome size, morphology, and markers | Combine multiple methods for comprehensive characterization |
| miRNA Analysis | Small RNA sequencing [51], RT-qPCR arrays [19], miRNA mimics/inhibitors [19] | Identify and validate miRNA cargo and functions | Use miRNA-specific cDNA synthesis for RT-qPCR |
| Cell Culture Models | Human dermal fibroblasts [51], HaCaT keratinocytes [19] | Evaluate functional effects in relevant skin cells | Use early passages (2-5) for consistency [51] |
| Animal Models | Full-thickness skin defect (mouse) [51], Diabetic wound models [9] | In vivo therapeutic validation | ICR mice commonly used; consider hydrogel for exosome delivery [51] |
| Delivery Systems | Hydrogel scaffolds [51], Microneedle patches [50] | Enhance exosome retention at wound site | HydroMatrix effectively maintains exosome activity [51] |
MSC exosomal miRNAs represent a sophisticated biological system for coordinating skin regeneration through simultaneous regulation of multiple therapeutic targets. The precise modulation of fibroblast behavior by specific miRNA cargoes—particularly through inhibition of TGF-β/SMAD signaling and activation of pro-regenerative pathways—provides a compelling strategy for promoting wound healing while minimizing scar formation.
Future research directions should focus on optimizing exosome engineering strategies to enhance target specificity and therapeutic potency [50]. This includes developing precision loading of specific miRNA combinations, modifying surface proteins for improved fibroblast targeting, and creating controlled-release delivery systems for sustained activity at wound sites. Additionally, standardized protocols for exosome isolation, characterization, and potency assessment will be crucial for clinical translation [50] [2].
The transition from conventional cell-based therapies to defined exosomal miRNA preparations offers significant advantages for pharmaceutical development, including improved safety profiles, enhanced product consistency, and more precise mechanistic understanding. As research progresses, MSC exosomal miRNAs hold substantial promise for addressing the significant unmet clinical needs in chronic wound management and pathological scar prevention.
Emerging Applications in Bone, Cartilage, and Cardiac Tissue Regeneration
The field of regenerative medicine is increasingly shifting from whole-cell therapies toward sophisticated cell-free approaches. Among these, exosomes derived from mesenchymal stem cells (MSCs) have emerged as powerful therapeutic entities. These nanoscale extracellular vesicles serve as natural delivery vehicles for bioactive molecules, including microRNAs (miRNAs), which play a pivotal role in coordinating tissue repair processes [54] [8]. This review focuses on the mechanisms by which MSC-exosomal miRNAs modulate fibroblast proliferation and migration—key processes in tissue regeneration—across bone, cartilage, and cardiac tissues. The targeted regulation of fibroblast activity represents a promising strategy for enhancing tissue reconstruction, mitigating fibrosis, and achieving functional recovery, positioning exosomal miRNAs as central components in next-generation regenerative applications.
MSC Exosomal miRNAs in Bone and Cartilage Regeneration
Molecular Mechanisms and Key miRNAs
In orthopaedic regeneration, MSC-derived exosomes function as information carriers that direct cellular processes essential for tissue repair. The therapeutic potential of these exosomes is largely attributed to their specific miRNA cargo, which can modulate the behavior of recipient cells, including fibroblasts and chondrocytes.
- Osteogenic Differentiation: Exosomal miRNAs are critical for promoting bone formation. miR-335-5p, for instance, enhances the osteogenic differentiation of MSCs by directly targeting the DKK1 inhibitor, thereby activating the Wnt/β-catenin signaling pathway. This leads to increased expression of osteogenic markers like Runx2 and Osterix [8].
- Cartilage Repair: For cartilage regeneration, exosomes derived from synovial mesenchymal stem cells (SMSCs) demonstrate exceptional promise. These exosomes are enriched with miRNAs that promote cartilage repair and reduce the degree of damage. SMSC-exosomes have been shown to maintain cartilage homeostasis and stimulate regeneration through paracrine mechanisms, making them a superior cell-free alternative for treating knee osteoarthritis [55].
- Tendon-Bone Healing: The regeneration of the tendon-bone interface, a critical structure for joint function, is also facilitated by exosomal miRNAs. They enhance this process by promoting the differentiation of resident stem cells and improving the organization of the fibrocartilage transition zone [8].
Table 1: Key Exosomal miRNAs in Bone and Cartilage Regeneration
| miRNA | Primary Function | Target Gene/Pathway | Therapeutic Outcome |
|---|---|---|---|
| miR-335-5p | Promotes osteogenic differentiation | DKK1 (Wnt/β-catenin pathway) | Enhanced bone formation [8] |
| miR-21-5p | Promotes proliferation & migration | PTEN/PI3K/Akt pathway | Accelerated bone repair [8] |
| miR-199a-3p | Inhibits chondrocyte differentiation | JAG1 (Notch signaling pathway) | Regulation of cartilage development [8] |
| Functional miRNAs from SMSCs | Maintains & promotes cartilage repair | Inflammatory & catabolic pathways | Reduced cartilage damage in KOA [55] |
Experimental Insights
The efficacy of SMSC-derived exosomes was consolidated through a systematic review of 12 included studies. It was confirmed that SMSC-derived exosomes could maintain and promote cartilage repair and reduce the degree of cartilage damage through in vitro cell experiments. The studies isolated specific functional miRNAs responsible for these therapeutic effects, highlighting a targeted molecular mechanism behind the observed cartilage healing [55].
MSC Exosomal miRNAs in Cardiac Regeneration
Therapeutic Mechanisms in Myocardial Repair
Following cardiac injury, such as myocardial infarction (MI), the heart's limited regenerative capacity leads to adverse remodeling and fibrosis. MSC-derived exosomal miRNAs have demonstrated remarkable cardioprotective and regenerative abilities by orchestrating multiple repair mechanisms and directly influencing cardiac fibroblast activity.
- Anti-Fibrotic Effects: A key mechanism for improving cardiac function is the attenuation of pathological fibrosis. Exosomal miRNAs can suppress the overactivation of cardiac fibroblasts, the key effector cells in fibrosis. This is achieved by targeting profibrotic signaling pathways, thereby reducing the excessive deposition of extracellular matrix and preventing scar tissue expansion [54] [56].
- Angiogenesis Promotion: Exosomes from MSCs subjected to hypoxic conditions are particularly enriched with pro-angiogenic miRNAs. These miRNAs, such as miR-30b, promote the formation of new blood vessels by targeting the FIH-1 gene, thereby enhancing blood flow to the ischemic myocardium and supporting the survival of stressed cardiomyocytes [14] [56].
- Anti-Apoptotic and Anti-Inflammatory Effects: Exosomal miRNAs enhance cardiomyocyte survival after injury by downregulating pro-apoptotic genes. Furthermore, they modulate the immune response by promoting the polarization of macrophages toward an anti-inflammatory M2 phenotype, which helps resolve inflammation and creates a conducive environment for repair [54] [14] [56].
Table 2: Key Exosomal miRNAs in Cardiac Regeneration and Their Actions on Fibroblasts
| miRNA | Primary Function | Target Gene/Pathway | Effect on Fibroblasts |
|---|---|---|---|
| miR-30b | Promotes angiogenesis | FIH-1 → Activates HIF-1α pathway | Indirectly suppresses fibrosis by improving oxygenation [56] |
| miR-199a-3p | Enhances cardiomyocyte survival | Not specified | Reduces apoptosis of parenchymal cells [56] |
| miR-21-5p | Modulates immune response | PTEN/Akt pathway; Polarizes macrophages to M2 | Creates anti-inflammatory microenvironment [14] [56] |
| let-7g-5p, let-7f-5p | Regulates hypertrophy & fibrosis | Calm/MLCK/p-MLC2 signaling pathway | Inhibits pathological signaling [57] |
| miR-148a-3p | Regulates hypertrophy & fibrosis | Rhoa/ROCK1/p-MLC2 signaling pathway | Inhibits pathological signaling [57] |
Experimental Evidence in Cardiac Models
Research on cardiac regeneration has yielded promising results. One study on pathological cardiac hypertrophy found that Vasn knockout mice exhibited hallmark features of the disease. Sequencing of cardiac exosomes revealed a significant increase in let-7g-5p, let-7f-5p, and miR-148a-3p. Bioinformatic analysis established that these miRNAs targeted the Calm/MLCK/p-MLC2 and Rhoa/ROCK1/p-MLC2 signaling pathways, providing a mechanistic link between exosomal miRNA content and the regulation of cardiac remodeling and fibroblast activity [57].
Another study on myocardial ischemia-reperfusion injury (MIRI) used whole transcriptome RNA sequencing, exosomal miRNA sequencing, and single-cell dataset analysis to identify four key cardiac-derived exosomal miRNAs. These miRNAs were found to regulate seven genes related to cell locomotion, suggesting a crucial role in controlling the migration of fibroblasts and other cells to the site of injury, which is vital for cardiac healing and remodeling [58].
Experimental Protocols: Isolating and Characterizing Exosomal miRNAs
To investigate the role of MSC-exosomal miRNAs in fibroblast proliferation and migration, robust and reproducible experimental protocols are essential. Below is a detailed methodology for exosome isolation and functional analysis.
Isolation and Characterization of MSC-Derived Exosomes
Protocol 1: Exosome Isolation via Ultracentrifugation
- Cell Culture: Culture MSCs (e.g., from bone marrow, adipose, or synovial tissue) in standard media until 70-80% confluent.
- Conditioned Media Collection: Replace the growth medium with an exosome-depleted FBS medium. Culture the cells for 48 hours, then collect the conditioned media.
- Initial Centrifugation: Centrifuge the conditioned media at 2,000 × g for 30 minutes at 4°C to remove dead cells and large debris.
- Filtration: Transfer the supernatant to a new tube and filter it through a 0.45 μm pore filter membrane to eliminate larger vesicles and particles.
- Ultracentrifugation: Transfer the filtrate to ultracentrifuge tubes and centrifuge at 100,000 × g for 70 minutes at 4°C to pellet the exosomes.
- Washing: Resuspend the pellet in a large volume of phosphate-buffered saline (PBS) and centrifuge again at 100,000 × g for 70 minutes.
- Resuspension: Finally, resuspend the purified exosome pellet in a small volume of PBS and store at -80°C [57] [58].
Characterization Techniques:
- Transmission Electron Microscopy (TEM): Visualize the cup-shaped or spherical morphology of exosomes.
- Nanoparticle Tracking Analysis (NTA): Determine the size distribution and concentration, confirming a typical diameter of 30-150 nm.
- Western Blotting: Confirm the presence of exosomal surface marker proteins such as CD9, CD63, and CD81 [58] [59].
Functional Analysis of Exosomal miRNA Effects on Fibroblasts
Protocol 2: miRNA Sequencing and Functional Validation
- RNA Extraction: Extract total RNA from isolated exosomes using a commercial kit (e.g., TRIzol or miRNeasy Serum/Plasma Kit).
- Library Preparation and Sequencing: Prepare small RNA libraries using a kit like the NEBNext Multiplex Small RNA Library Prep Set. Sequence the libraries on a platform such as the Illumina NovaSeq 6000 to profile the miRNA content [58].
- Bioinformatic Analysis:
- Perform differential expression analysis to identify miRNAs of interest.
- Predict target genes of the miRNAs using databases like TargetScan and Miranda.
- Conduct GO (Gene Ontology) and KEGG (Kyoto Encyclopedia of Genes and Genomes) pathway enrichment analyses on the target genes to elucidate potential biological roles and signaling pathways [57] [58].
- In Vitro Functional Assays:
- Cell Viability: Treat cardiac, bone, or dermal fibroblasts with MSC-exosomes and assess viability using a CCK-8 assay.
- Migration Assay: Use a Transwell chamber assay to quantify exosome-induced fibroblast migration.
- Gene Expression: Validate the expression of key miRNAs and their target genes using RT-qPCR. For example, primers for miRNAs like let-7f-5p and miR-148a-3p can be used with U6 as an endogenous control [57] [59].
- Protein Analysis: Use Western Blotting to confirm changes in the expression of proteins in pathways targeted by the miRNAs (e.g., components of the p-MLC2 pathway) [57].
Signaling Pathways and Experimental Workflow
The following diagrams, generated using DOT language, illustrate the key signaling pathways regulated by exosomal miRNAs and the typical experimental workflow used in this field.
Diagram 1: SMSC-Exosome Mediated Cartilage Repair. This diagram illustrates how functional miRNAs within synovial MSC-derived exosomes inhibit inflammatory signaling and directly promote cartilage repair.
Diagram 2: Exosomal miRNA Regulation of Cardiac Pathways. This diagram shows how specific exosomal miRNAs (let-7g-5p/let-7f-5p and miR-148a-3p) target the CALM/MLCK and RHO/ROCK1 pathways to regulate downstream p-MLC2 signaling, which influences pathological cardiac hypertrophy and fibrosis.
Diagram 3: Experimental Workflow for MSC-Exosome Research. This flowchart outlines the key steps in a typical experiment, from exosome isolation and characterization to functional analysis and target validation in fibroblast cultures.
The Scientist's Toolkit: Essential Research Reagents
The table below lists critical reagents and their functions for investigating MSC-exosomal miRNAs and their effects on fibroblast biology.
Table 3: Research Reagent Solutions for Exosomal miRNA Studies
| Reagent / Kit | Function / Application | Key Features |
|---|---|---|
| Exosome Depleted FBS | Cell culture supplement for producing conditioned media | Ensures background exosome levels are minimized during exosome production [59] |
| Keygenbio/Other Exosome Extraction Kits | Isolation of exosomes from cell culture media or biofluids | Kit-based methods offering alternatives to ultracentrifugation [58] |
| miRNeasy Serum/Plasma Kit (Qiagen) | Purification of miRNA from plasma or serum samples | Optimized for efficient recovery of small RNAs from liquid biopsies [59] |
| NEBNext Multiplex Small RNA Library Prep Set | Preparation of sequencing libraries for small RNA | Enables preparation of libraries for high-throughput miRNA sequencing on platforms like Illumina [58] |
| Lipofectamine 2000/3000 | Transfection of miRNA mimics/inhibitors into cells | For functional gain/loss-of-function studies to validate miRNA targets [59] |
| CD9, CD63, CD81 Antibodies | Exosome characterization via Western Blot or Flow Cytometry | Confirm the presence of universal exosomal surface markers [58] |
| CCK-8 Assay Kit | Quantitative assessment of cell viability/proliferation | Measures the effect of exosomal treatments on fibroblast proliferation [59] |
| Transwell Chamber Assays | Measurement of cell migration | Quantifies fibroblast migratory capacity in response to exosome stimulation [8] |
MSC-derived exosomal miRNAs represent a master regulatory system in tissue regeneration, with significant implications for controlling fibroblast proliferation and migration. The evidence summarized across bone, cartilage, and cardiac tissues demonstrates that specific exosomal miRNAs can be harnessed to promote constructive tissue repair while curbing pathological fibrosis. The ongoing development of engineered exosomes and optimized delivery strategies will further enhance the specificity and efficacy of these therapeutic interventions. As research progresses, exosomal miRNA-based therapies are poised to make substantial contributions to regenerative medicine, offering novel solutions for some of the most challenging clinical problems in orthopaedics and cardiology.
Enhancing Efficacy: Engineering Strategies and Overcoming Translational Hurdles
Within the broader context of investigating the role of Mesenchymal Stem Cell (MSC) exosomal miRNAs in fibroblast proliferation and migration, overcoming technical barriers in exosome production is paramount. The therapeutic potential of MSC-derived exosomes (MSC-Exos) is largely attributed to their cargo, which includes key microRNAs (miRNAs) that can modulate fibroblast behavior, influencing processes critical to wound healing, fibrosis, and tissue regeneration [1] [14]. These nano-sized vesicles (30-150 nm) act as endogenous delivery systems, transferring miRNAs that can post-transcriptionally regulate gene expression in recipient fibroblasts [60] [61]. However, the clinical translation of these findings is severely hampered by three interconnected challenges: the difficulty in obtaining high yields of pure exosomes, the inconsistency in purification methods, and the need for reliable targeted delivery to specific cells, such as fibroblasts [62] [63]. This whitepaper details these challenges and provides researchers with structured data, validated protocols, and strategic insights to advance their translational research.
Core Technical Challenges and Quantitative Analysis
The path from laboratory research to clinical application is fraught with technical hurdles. The following section breaks down the primary challenges, supported by quantitative data and comparative analysis.
The Yield and Scalability Bottleneck
Producing sufficient quantities of exosomes for clinical applications remains a significant obstacle. Traditional 2D cell culture systems generate limited volumes, making scalable production a critical focus of process development.
Table 1: Key Challenges in Scalable Exosome Production
| Challenge | Impact on Yield & Quality | Current Scalability Status |
|---|---|---|
| Source Cell Optimization | Donor variability and cell source (e.g., Bone Marrow vs. Umbilical Cord) affect exosome miRNA cargo and yield [1] [5]. | Moderate; requires careful donor screening and cell source selection. |
| Culture Method Refinement | 2D flasks offer low yield; 3D bioreactors can enhance yield but risk altering exosome properties [62]. | Improving; bioreactor-based systems show promise for scaling. |
| Sensitivity to Process Parameters | pH, temperature, and shear stress in bioreactors can impact exosome integrity and biological activity [62]. | Challenging; requires precise monitoring and control systems. |
The Purity and Characterization Dilemma
Exosomes must be isolated from complex biological mixtures containing proteins, lipoproteins, and other extracellular vesicles (EVs) of similar size. The lack of standardized, reproducible methods for isolation and characterization leads to batch-to-batch variability and contaminated preparations, which confounds experimental results and threatens clinical safety.
Table 2: Comparison of Major Exosome Isolation Techniques
| Isolation Method | Principle | Advantages | Disadvantages (Purity & Yield Impact) |
|---|---|---|---|
| Ultracentrifugation (Gold Standard) | Sequential centrifugation based on size and density [61]. | Widely adopted; no chemical additives. | Time-consuming; low throughput; causes vesicle aggregation and damage; yields heterogeneous pellets [63] [61]. |
| Size-Exclusion Chromatography (SEC) | Separates particles based on hydrodynamic radius [61]. | Preserves vesicle integrity and function; good purity from soluble proteins. | Sample dilution; limited scalability; potential co-isolation of similarly sized particles [61]. |
| Precipitation (Polymer-based) | Entangles vesicles using hydrophilic polymers [61]. | High yield; simple and fast protocol. | Low purity; co-precipitates contaminants like proteins and nucleic acids [61]. |
| Membrane-Based Affinity Binding | Uses surface markers (e.g., CD63, CD81) for capture [63]. | High purity and specificity; preserves biological activity. | Low throughput; high cost; potential for incomplete elution [63]. |
The International Society for Extracellular Vesicles (ISEV) recommends characterizing exosome preparations using at least two complementary techniques, such as Nanoparticle Tracking Analysis (NTA) for concentration and size distribution, and transmission electron microscopy (TEM) for morphological validation [61]. Flow cytometry, while powerful, requires extensive optimization for nano-sized particles and is best used for phenotyping with specific surface markers [64].
The Targeted Delivery Imperative for Fibroblast Studies
For MSC exosomal miRNAs to effectively modulate fibroblast function, they must be efficiently internalized by the target cells. Unmodified exosomes may lack the tropism required for specific fibroblast targeting in complex microenvironments, leading to off-target effects and reduced therapeutic efficacy [60]. Overcoming this requires sophisticated engineering strategies to equip exosomes with targeting moieties, such as peptides or antibody fragments, that recognize receptors uniquely expressed on fibroblasts [60] [61].
Experimental Protocols for MSC Exosome Research
To ensure reproducible and reliable results in the study of MSC exosomal miRNAs and fibroblasts, rigorous and detailed experimental protocols are essential. The following section provides methodologies for key processes.
Protocol: Isolation of MSC-Exos Using a Combined Ultrafiltration-Affinity Method
This protocol, adapted from a study using MRC-5 cells, is designed to yield intact exosomes with high purity, suitable for downstream functional studies with fibroblasts [63].
Cell Culture and Conditioned Media Collection:
- Culture MSCs (e.g., from bone marrow or umbilical cord) in serum-free media for 48-72 hours to avoid contamination with bovine exosomes.
- Collect the conditioned media and perform sequential centrifugation: 300 × g for 10 min (to remove cells), 2,000 × g for 20 min (to remove dead cells), and 10,000 × g for 30 min (to remove cell debris and large vesicles).
- Filter the supernatant through a 0.22 µm PES membrane filter.
Concentration via Ultrafiltration:
- Concentrate the filtered supernatant using a centrifugal ultrafiltration device (e.g., 100 kDa molecular weight cut-off) at 4,000 × g at 4°C until the volume is reduced 10-20 fold.
Purification via Membrane-Based Affinity Binding:
- Use a commercial exosome isolation kit that employs a membrane filter conjugated with tetraspanin-specific antibodies (e.g., against CD63, CD81).
- Apply the concentrated sample to the affinity membrane and incubate according to the manufacturer's instructions.
- Wash the membrane with a suitable buffer (e.g., PBS) to remove unbound contaminants.
- Elute the purified exosomes using a low-pH buffer (e.g., 0.1 M glycine-HCl, pH 2.5-3.0) and immediately neutralize with 1M Tris-HCl, pH 8.0.
Post-Isolation Processing:
- Characterize the eluate immediately or store at -80°C in aliquots to avoid freeze-thaw cycles. The use of stabilizers like trehalose or BSA is recommended for long-term storage to preserve functionality and prevent aggregation [61].
Protocol: Evaluating miRNA-Mediated Fibroblast Proliferation and Migration
This functional assay tests the hypothesis that MSC-Exo miRNAs modulate fibroblast behavior.
Exosome Uptake and Treatment:
- Label isolated MSC-Exos with a lipophilic fluorescent dye (e.g., PKH67 or DiI) according to the manufacturer's protocol. Remove excess dye via SEC or ultrafiltration.
- Seed target fibroblasts (e.g., human dermal fibroblasts) in appropriate plates and culture until 70-80% confluent.
- Treat fibroblasts with PKH67-labeled MSC-Exos (e.g., 50 µg/mL total exosomal protein) for 24 hours. Include a control group treated with PBS.
- Visualize uptake using confocal microscopy after staining the actin cytoskeleton and nuclei.
Functional Assays:
- Proliferation: Use a colorimetric assay like MTT or CCK-8. Seed fibroblasts in a 96-well plate, treat with MSC-Exos, and measure absorbance at 450nm at 0, 24, 48, and 72 hours.
- Migration (Scratch Assay):
- Create a confluent monolayer of fibroblasts in a 12-well plate.
- Scrape a straight line through the monolayer using a sterile 200 µL pipette tip.
- Wash the well gently to remove dislodged cells and add fresh media containing MSC-Exos or PBS (control).
- Image the scratch at 0, 12, and 24 hours under a microscope. Quantify the migration by measuring the reduction in the scratch area over time using image analysis software (e.g., ImageJ).
Mechanistic Validation via miRNA Transfection:
- To confirm the role of a specific miRNA (e.g., miR-21-5p or miR-125a-3p, identified via profiling [14]), transfert fibroblasts with a synthetic miRNA mimic (for overexpression) or inhibitor (for knockdown).
- Repeat the proliferation and migration assays to determine if the transfected miRNA recapitulates or blocks the effects of the MSC-Exos treatment.
Visualization of Signaling Pathways and Workflows
MSC Exosomal miRNA in Fibroblast Signaling
The following diagram illustrates the proposed mechanism by which MSC-derived exosomal miRNAs modulate key signaling pathways to regulate fibroblast proliferation and migration, a core focus of the thesis context.
Integrated Workflow for Functional Study
This workflow charts the experimental pipeline from exosome isolation to functional validation in fibroblast studies, integrating the protocols detailed in this paper.
The Scientist's Toolkit: Research Reagent Solutions
For researchers to effectively implement the protocols and address the challenges outlined, a curated set of tools and reagents is essential. The following table details key solutions for MSC exosome research focused on fibroblast applications.
Table 3: Essential Research Reagents for MSC Exosome-Fibroblast Studies
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| CD63/CD81 Affinity Kits | High-purity exosome isolation via tetraspanin capture [63]. | Thermo Fisher Scientific Total Exosome Isolation kit; qEV size-exclusion columns. |
| Nanoparticle Tracking Analyzer | Quantifies exosome concentration and size distribution [61]. | Malvern Panalytical NanoSight NS300; Particle Metrix ZetaView. |
| Tetraspanin Antibodies | Exosome characterization via Western Blot or flow cytometry [64] [61]. | Anti-CD63 (e.g., TS63), Anti-CD81 (5A6), Anti-CD9 (TS9). |
| PKH67/DiI Lipophilic Dyes | Fluorescent labeling of exosome membranes for uptake studies [63]. | Sigma-Aldrich PKH67 Green Fluorescent Cell Linker Kit. |
| miRNA Mimics/Inhibitors | Functional validation of specific exosomal miRNAs in fibroblasts [14]. | Dharmacon miR-125a-3p mimic; Qiagen miScript miRNA inhibitors. |
| MRC-5 Cell Line | A clinically relevant, diploid human fibroblast cell model for mechanistic studies [63]. | Approved by regulatory affairs for drug development, facilitating translation. |
The transformative potential of MSC exosomal miRNAs in directing fibroblast activity for regenerative medicine and anti-fibrotic therapy is undeniable. However, realizing this potential hinges on the scientific community's ability to collectively solve the tripartite challenge of yield, purity, and targeted delivery. By adopting standardized, fit-for-purpose isolation protocols like the combined ultrafiltration-affinity method, employing rigorous characterization, and leveraging engineering strategies for enhanced targeting, researchers can generate more reproducible and potent exosome preparations. Addressing these fundamental technical bottlenecks is the critical next step in advancing the role of MSC exosomal miRNAs in fibroblast research from a promising concept to a clinical reality.
Within the context of a broader thesis on the role of mesenchymal stem cell (MSC) exosomal miRNAs in fibroblast proliferation and migration research, the ability to precisely modulate miRNA content has emerged as a critical capability. MSCs release extracellular nanovesicles known as exosomes (MSC-Exos) that are rich in bioactive molecules, including microRNAs [14]. These exosomal miRNAs can be transferred to recipient cells, such as fibroblasts, where they function as key post-transcriptional regulators of gene expression, influencing fundamental processes including cell migration, proliferation, differentiation, and apoptosis [8] [18]. The selective sorting of specific miRNAs into exosomes is not random but is governed by motif-dependent mechanisms, presenting a potent target for bioengineering strategies aimed at directing therapeutic outcomes [8].
The therapeutic potential of MSC-derived exosomes is particularly promising for conditions involving impaired tissue repair. For instance, in systemic sclerosis, MSC-Exos demonstrate significant antifibrotic and immunomodulatory properties, while their application in wound healing models has shown enhanced repair processes [14] [18]. However, the native miRNA cargo of MSC-Exos may not be optimized for specific therapeutic applications. This technical guide details how CRISPR/Cas9 genome editing and motif engineering can be employed to deliberately redesign the miRNA content of MSC exosomes, thereby creating advanced, cell-free therapeutics with enhanced capacity to direct fibroblast behavior for regenerative medicine.
Core Principles: miRNA Biogenesis and Exosomal Sorting
miRNA Biogenesis and Mechanism of Action
MicroRNAs (miRNAs) are small non-coding RNAs, typically 19–24 nucleotides in length, that regulate gene expression post-transcriptionally. The canonical biogenesis pathway begins with the transcription of primary miRNAs (pri-miRNAs) from host genes, which are then processed through a series of steps to become mature miRNAs [18]. These mature miRNAs are incorporated into the RNA-induced silencing complex (RISC), where they guide the complex to partially complementary sequences in the 3' untranslated region (3' UTR) of target messenger RNAs (mRNAs). This interaction typically leads to either translational repression or degradation of the target mRNA, enabling miRNAs to fine-tune the expression of a vast network of genes [65] [18].
Selective Sorting of miRNAs into MSC Exosomes
Exosomes are nano-sized extracellular vesicles (30-250 nm in diameter) enclosed by a lipid bilayer and formed through the inward budding of endosomal membranes, creating multivesicular bodies (MVBs) that subsequently fuse with the plasma membrane for release [14] [18]. A key insight for bioengineering is that miRNAs are not passively incorporated into exosomes but are actively and selectively sorted. Comparative analyses have revealed that certain miRNAs, such as miR-21-5p, let-7g, miR-1246, miR-381, and miR-100, can be enriched up to 100-fold higher in MSC exosomes compared to the parent cells [8]. This selective sorting is governed by specific sequence motifs and structural features within the miRNAs themselves, as well as interactions with RNA-binding proteins (RBPs) such as hnRNPA2B1 and SYNCRIP [8]. Motif engineering exploits these natural sorting mechanisms to redirect desired therapeutic miRNAs into exosomes.
Table 1: Key MSC Exosomal miRNAs Influencing Fibroblast Behavior
| miRNA | Expression in MSC-Exos | Primary Target in Fibroblasts | Functional Outcome on Fibroblasts |
|---|---|---|---|
| miR-21-5p | Highly enriched [8] | PTEN, PDCD4 | Promotes proliferation, migration, and reduces apoptosis [8] [18] |
| miR-29b | Modifiable [8] | COL1A1, COL3A1 | Inhibits collagen synthesis, attenuating fibrosis [8] |
| miR-126 | Can be loaded [18] | SPRED1, PIK3R2 | Enhances angiogenesis and cell survival [18] |
| miR-125a-3p | Present [14] | Unknown | Suppresses T cell activity, modulates immune environment [14] |
| let-7g | Highly enriched [8] | High-Mobility Group A2 (HMGA2) | Inhibits differentiation and fibrosis [8] |
Diagram 1: miRNA Biogenesis and Exosomal Sorting Pathway. This pathway illustrates the journey from nuclear miRNA transcription to functional delivery into a recipient cell, highlighting the critical sorting step targetable by motif engineering.
CRISPR/Cas9 Strategies for Genomic miRNA Modification
The CRISPR/Cas9 system has revolutionized genomic engineering, providing tools to precisely modify the genes encoding miRNAs within MSCs. This enables the stable alteration of the exosomal miRNA payload. The foundational CRISPR-Cas9 system consists of two core components: a Cas9 nuclease and a guide RNA (gRNA) that directs Cas9 to a specific DNA sequence. Upon binding, Cas9 creates a double-strand break (DSB) in the target DNA, which the cell repairs via error-prone non-homologous end joining (NHEJ), often resulting in gene knockouts, or via homology-directed repair (HDR) for precise gene insertion or correction [65] [66].
Advanced CRISPR/Cas9 Systems for Enhanced Control
To improve specificity and enable sophisticated control over CRISPR activity, several advanced systems have been developed. CRISPRgenee is a dual-action system that combines gene knockout (CRISPRko) and epigenetic repression (CRISPRi) simultaneously. It uses a ZIM3-Cas9 fusion protein and two sgRNAs: a truncated sgRNA (15-nt) for gene repression and a full-length sgRNA (20-nt) for DNA cleavage. This dual approach significantly improves loss-of-function efficacy and reproducibility, which is valuable for completely abrogating the expression of specific miRNAs or their processing machinery [67].
For cell-type-specific activation of CRISPR systems, miRNA-activated CRISPR technologies such as MiR-ON-CRISPR and CRISPR MiRAGE (miRNA-activated genome editing) have been engineered. These systems link the production of essential CRISPR components (e.g., dCas9, sgRNA) to the presence of endogenous, cell-type-specific miRNA signatures. For instance, in the MiR-ON-CRISPR system, the LacI gene and sgRNA scaffold contain target sites for a specific miRNA. In off-target cells (where the miRNA is absent), LacI is produced and binds to LacO2 sequences to suppress dCas9-VPR expression, and the sgRNA remains non-functional. In target cells, the endogenous miRNA mediates the degradation of LacI mRNA and releases the functional sgRNA, enabling cell-type-specific gene activation [68] [69]. This is particularly useful for safety profiling in therapeutic development.
Table 2: Key CRISPR/Cas9 Systems for miRNA Engineering
| System | Core Components | Primary Application in miRNA Engineering | Key Advantage |
|---|---|---|---|
| Standard CRISPRko | Cas9 nuclease, sgRNA [66] | Knockout of genomic miRNA genes | Permanent deletion of specific miRNA genes. |
| CRISPRgenee | ZIM3-Cas9 fusion, 15-nt & 20-nt sgRNAs [67] | Simultaneous knockout & epigenetic silencing of miRNA loci | Superior loss-of-function efficacy; reduced sgRNA variability. |
| CRISPR MiRAGE / MiR-ON-CRISPR | dCas9, miRNA-responsive sgRNA or LacI circuit [68] [69] | Cell-type-specific activation of CRISPR in target tissues (e.g., muscle, liver) | Enhances safety by minimizing off-target editing in non-target cells. |
| AI-Designed Editors (e.g., OpenCRISPR-1) | AI-generated Cas9 variants [70] | High-efficiency editing of miRNA genomic loci | Novel editors with optimal properties (e.g., high activity, specificity). |
Experimental Protocol: Knockout of a Specific miRNA Gene in MSCs
This protocol outlines the steps to generate an MSC line with a stable knockout of a specific miRNA using the CRISPRgenee system [67].
gRNA Design and Cloning:
- Target Selection: Identify a genomic region within the pre-miRNA hairpin or the miRNA host gene critical for its biogenesis. Use online design tools (e.g., Benchling) to calculate on-target and off-target scores [68].
- Dual gRNA Construct: Design two gRNA expression cassettes:
- A 20-nt sgRNA targeting an exon shared by all transcript variants of the host gene to facilitate knockout.
- A 15-nt truncated sgRNA targeting the promoter-associated Transcription Start Site (TSS) to enable transcriptional repression via the ZIM3-KRAB domain.
- Cloning: Clone both gRNA sequences into a single dual-expression lentiviral vector.
Delivery and Transduction:
- Vector Packaging: Package the lentiviral vector along with a second vector encoding the ZIM3-Cas9 fusion protein into lentiviral particles.
- Transduction: Transduce human MSCs (e.g., derived from bone marrow or umbilical cord) at a multiplicity of infection (MOI) of 5-10 in the presence of polybrene (8 µg/mL). A doxycycline-inducible system is recommended for controlled ZIM3-Cas9 expression [67].
Validation and Screening:
- Selection: 48 hours post-transduction, begin selection with appropriate antibiotics (e.g., Puromycin, 1-2 µg/mL) for 7-10 days.
- Efficiency Assessment: After inducing with doxycycline (1-2 µg/mL) for 5-14 days, assess editing efficiency.
- Genomic DNA: Extract genomic DNA from the pooled population or single-cell clones. Use T7 Endonuclease I assay or Tracking of Indels by Decomposition (TIDE) analysis to quantify indel formation at the target site.
- Functional Assay: Iserve exosomes from the cultured MSCs. Perform RT-qPCR to quantify the loss of the target miRNA in both the parent MSCs and their derived exosomes compared to a non-targeting gRNA control [68] [8].
Diagram 2: CRISPR Workflow for miRNA Knockout. The experimental pipeline for generating an MSC line with a specific miRNA knocked out, from vector design to functional validation.
Motif Engineering for Directing miRNA Sorting into Exosomes
Beyond altering genomic miRNA sequences, a more refined bioengineering approach involves modifying the miRNAs themselves to influence their loading into exosomes. Motif engineering leverages the discovery that specific short nucleotide sequences (motifs) in miRNAs are recognized by RNA-binding proteins (RBPs) that facilitate their active packaging into exosomes [8].
The general strategy involves identifying natural exosome-enriched miRNAs and characterizing their sorting motifs. For instance, miRNAs like miR-21-5p and let-7g contain specific motifs that interact with RBPs such as hnRNPA2B1 (which recognizes GGAG and related motifs) and SYNCRIP. Once a functional motif is identified, it can be engineered into the sequence of a desired therapeutic miRNA that normally is poorly sorted into exosomes. This is achieved without disrupting the miRNA's "seed region" (nucleotides 2-8), which is critical for its mRNA targeting function [8].
Experimental Protocol: Enhancing Exosomal Loading of a Therapeutic miRNA
This protocol details the steps to increase the exosomal packaging of a specific therapeutic miRNA, for example, the antifibrotic miR-29b, by fusing it with a known exosomal sorting motif [8].
Design of Motif-Engineered miRNA:
- Motif Selection: Select a strong exosomal sorting motif, such as the GGAG motif known to bind hnRNPA2B1.
- Sequence Engineering: Using molecular cloning, fuse the GGAG motif to the 3' end of the pre-miR-29b sequence. Care must be taken to ensure the engineered pre-miRNA can still be correctly processed by Dicer into a mature, functional miRNA.
Delivery and Expression in MSCs:
- Vector Construction: Clone the motif-engineered pre-miR-29b sequence into a lentiviral or plasmid vector under the control of a strong, constitutive promoter (e.g., CMV or U6).
- Transduction: Transduce MSCs with the constructed vector. A stable cell line can be generated through antibiotic selection to ensure long-term expression.
Validation of Enhanced Sorting:
- Exosome Isolation: Culture the engineered MSCs in exosome-depleted serum for 48-72 hours. Collect the conditioned medium and isolate exosomes using sequential ultracentrifugation (100,000 × g pellets) or size-exclusion chromatography [8] [18].
- Quantification: Extract total RNA from both the parent MSCs and the isolated exosomes. Perform RT-qPCR to quantify the levels of mature miR-29b, normalizing to appropriate controls (e.g., U6 snRNA for cellular RNA, and cel-miR-39 spike-in for exosomal RNA).
- Functional Assay: Treat fibroblasts (e.g., dermal fibroblasts) with the purified engineered exosomes. Assess the functional outcome by measuring:
- Downstream Target Expression: RT-qPCR or Western Blot for miR-29b targets (e.g., COL1A1).
- Phenotypic Changes: Functional assays for fibroblast proliferation (CCK-8 assay) and migration (scratch wound assay) [8].
Integrated Workflow and The Scientist's Toolkit
Combining CRISPR/Cas9 and motif engineering creates a powerful, multi-pronged strategy for tailoring the therapeutic profile of MSC exosomes. An integrated workflow might involve using CRISPR to knock out a profibrotic miRNA (e.g., miR-21) while simultaneously using motif engineering to boost the exosomal loading of an antifibrotic miRNA (e.g., miR-29b).
Table 3: The Scientist's Toolkit: Essential Reagents for miRNA Bioengineering
| Reagent / Tool Category | Specific Examples | Function in Experimentation |
|---|---|---|
| CRISPR Systems | ZIM3-Cas9 [67], dCas9-VPR [68], OpenCRISPR-1 [70] | Effector proteins for genomic editing or transcriptional control. |
| Delivery Vectors | Lentiviral vectors [67], Lipid Nanoparticles (LNPs) [69], C14-PEI micelleplex [69] | Vehicles for efficient intracellular delivery of CRISPR components. |
| MSC Sources | Bone Marrow MSCs (BMMSCs), Human Umbilical Cord MSCs (hUCMSCs), Adipose-derived MSCs (ASCs) [14] [8] | Parent cells for genetic modification and exosome production. |
| Motif Engineering Tools | hnRNPA2B1-binding motif (GGAG) [8], SYNCRIP-binding motif | RNA sequences to engineer into miRNAs for enhanced exosomal sorting. |
| Exosome Isolation Kits | Ultracentrifugation protocols, Size-exclusion chromatography columns, Commercial kits (e.g., Total Exosome Isolation Kit) | For purifying exosomes from MSC conditioned medium. |
| Validation Assays | T7E1 Assay, TIDE Analysis [67], RT-qPCR with stem-loop primers [68], Western Blot, Nanoparticle Tracking Analysis (NTA) | To confirm genetic edits, quantify miRNA levels, and characterize exosomes. |
Diagram 3: Integrated Bioengineering Strategy. A combined approach using CRISPR to remove unwanted miRNAs and motif engineering to enhance desirable ones, resulting in an exosome with a tailored therapeutic profile for modulating fibroblast activity.
The targeted modulation of MSC exosomal miRNA content through CRISPR/Cas9 and motif engineering represents a paradigm shift in the development of cell-free therapeutics for controlling fibroblast proliferation and migration. These technologies enable a level of precision that moves beyond simply leveraging the native secretome of MSCs towards actively designing exosomes with predefined and potentiated functions. The potential applications in treating fibrotic diseases, impaired wound healing, and other conditions driven by dysfunctional fibroblast activity are substantial.
Despite the promising advances, challenges remain on the path to clinical translation. These include optimizing the safety and specificity of CRISPR editing to minimize off-target effects, standardizing protocols for exosome isolation and characterization, and solving the challenges of scalable manufacturing and targeted delivery in vivo [8] [18]. Future research will likely see increased integration of AI-based protein design, as exemplified by tools like OpenCRISPR-1, to create next-generation editors with superior properties [70]. Furthermore, combining miRNA engineering with other exosomal surface modification techniques to achieve tissue-specific targeting will unlock the full potential of these bioengineered nanotherapeutics, paving the way for a new class of regenerative medicines.
Mesenchymal stem cell (MSC)-derived exosomes have emerged as pivotal mediators of the therapeutic effects traditionally attributed to MSCs, offering a promising cell-free approach in regenerative medicine [71] [1]. These natural nanovesicles (30-150 nm in diameter) facilitate intercellular communication by transferring bioactive molecules, including microRNAs (miRNAs), to recipient cells [71] [30]. Within the context of fibroblast proliferation and migration—fundamental processes in wound healing and tissue regeneration—MSC-exosomal miRNAs have been demonstrated to significantly enhance these functions [30]. The efficacy of these exosomes is not static; rather, it is profoundly influenced by the parental MSC's state [71]. Preconditioning, defined as the exposure of MSCs to specific sublethal stimuli prior to exosome collection, represents a powerful strategy to manipulate the MSC secretome and enhance the pro-regenerative miRNA cargo of their exosomes [71] [72]. This technical guide details the application of two key preconditioning strategies—hypoxia and cytokine treatment—to optimize MSC-exosomes for applications requiring robust fibroblast proliferation and migration.
Scientific Basis of Preconditioning
The therapeutic potential of MSC-exosomes is highly dependent on the status of the parent MSCs, which can be optimized by manipulating the extracellular environment [71]. Preconditioning strategies act as adaptive stimuli that enhance exosome biogenesis and selectively enrich specific miRNA profiles, thereby tailoring the exosomes for enhanced regenerative and immunomodulatory functions [72] [1]. The packaging of miRNAs into exosomes is a selective process, influenced by RNA-binding proteins (e.g., hnRNPA2B1, SYNCRIP) and specific miRNA motifs [1]. Preconditioning stresses are thought to modulate these sorting mechanisms, leading to an altered and potentially more potent exosomal payload [72].
The table below summarizes the core mechanisms and overarching outcomes of the preconditioning strategies discussed in this guide.
Table 1: Overview of Preconditioning Strategies and Their Core Mechanisms
| Preconditioning Strategy | Primary Molecular Initiator | Key Adaptive Cellular Responses | Overall Effect on MSC-Exosomes |
|---|---|---|---|
| Hypoxia | Stabilization of Hypoxia-Inducible Factor-1α (HIF-1α) [73] | Activation of autophagy, altered miRNA transcription, enhanced pro-angiogenic factor secretion [74] [73] | Boosts pro-migratory and angiogenic miRNA content; enhances exosome yield [71] [72] |
| Cytokine Treatment | Activation of NF-κB and other inflammatory signaling pathways [72] | Polarization of MSC immunophenotype, selective upregulation of immunomodulatory miRNAs [75] [72] | Enriches exosomes in anti-inflammatory and immunomodulatory miRNAs [72] |
Hypoxic Preconditioning
Experimental Protocol for Hypoxic Preconditioning
A standardized protocol for establishing hypoxic preconditioning of MSCs is as follows:
- Cell Culture: Culture MSCs (e.g., bone marrow-derived MSCs) in standard growth medium to 60-80% confluence [30]. It is critical to use exosome-depleted fetal bovine serum (FBS) at this and all subsequent stages to avoid contaminating bovine exosomes in the final preparation. FBS is precleared by ultracentrifugation at 100,000 × g for 3 hours at 4°C [30].
- Hypoxia Induction: Place the culture flasks/plates in a specialized hypoxia chamber or incubator. Flush the chamber with a gas mixture containing 3% O₂, 5% CO₂, and 92% N₂ to establish a hypoxic environment [74]. Maintain the cells under these conditions for a defined period, commonly 24-48 hours [72].
- Conditioned Medium Collection: After the hypoxic incubation, collect the conditioned medium for exosome isolation. The conditioned medium should be processed immediately or stored at -70°C to preserve exosome integrity [30].
- Control Setup: A normoxic control group must be cultured in parallel under standard conditions (21% O₂ and 5% CO₂) for the same duration [74].
Key Molecular and Functional Outcomes
Hypoxic preconditioning triggers a robust cellular response, masterfully regulated by the stabilization of HIF-1α. This transcription factor orchestrates a program that enhances MSC function and modulates exosomal cargo.
Figure 1: Hypoxia triggers HIF-1α stabilization, activating downstream pathways that enhance MSC function and modulate exosomal miRNA cargo such as let-7f.
The functional enhancements driven by this molecular cascade are quantifiable. The table below summarizes key experimental data demonstrating the efficacy of hypoxic preconditioning.
Table 2: Quantitative Effects of Hypoxic Preconditioning on MSCs and Their Exosomes
| Parameter Measured | Experimental Finding | Significance / Implication | Source |
|---|---|---|---|
| Proliferation (MTT assay) | Significant enhancement of EPC proliferation under hypoxia | Preconditioning improves expansion of progenitor cells | [74] |
| NO Secretion (ELISA) | Elevated secretion of Nitric Oxide (NO) | Promotes vasodilation and angiogenic signaling | [74] |
| VEGF Secretion (ELISA) | Elevated secretion of Vascular Endothelial Growth Factor (VEGF) | Enhances angiogenic potential of the secretome | [74] |
| MSC Invasion | let-7f-mediated enhancement of CXCR4-dependent invasion | Improves homing capacity of MSCs to injury sites | [73] |
| Jagged1 Expression | Upregulation of both protein and mRNA levels of Jagged1 | Activates Notch signaling pathway to enhance cell function | [74] |
Cytokine Preconditioning
Experimental Protocol for Cytokine Preconditioning
Cytokine preconditioning "primes" MSCs to an activated state, enriching their exosomes with immunomodulatory miRNAs. A generalized protocol is outlined below, with specific cytokine choices and concentrations detailed in the subsequent section.
- Cell Culture: Grow MSCs to approximately 60-80% confluence in standard medium supplemented with exosome-depleted FBS [30].
- Cytokine Preparation: Prepare fresh working solutions of the chosen cytokine(s) in the base culture medium. Common agents include TNF-α, IL-1β, and IFN-γ. It is critical to perform a dose-response analysis for each new MSC source or cytokine lot, as concentration profoundly influences the resulting miRNA profile [72].
- Stimulation: Replace the standard growth medium with the cytokine-containing medium. The duration of stimulation can vary but often ranges from 24 to 48 hours [72].
- Conditioned Medium Collection: After stimulation, collect the conditioned medium for exosome isolation, following the same protocols used for hypoxic preconditioning [30].
Key Molecular and Functional Outcomes
Cytokine preconditioning operates through a distinct, dose-dependent mechanism to skew the MSC-exosomal miRNA cargo toward immunomodulation.
Figure 2: Cytokine preconditioning activates inflammatory signaling pathways, leading to a dose-dependent upregulation of specific immunomodulatory miRNAs in MSC-exosomes.
The specific cytokine and its concentration are critical parameters that determine the resultant exosomal miRNA profile and biological effect. The following table provides a detailed breakdown of key reagent solutions and their applications.
Table 3: Research Reagent Solutions for Cytokine Preconditioning
| Reagent / Condition | Concentration & Duration | Target MSC Source | Key Outcome on Exosomal miRNA | Documented Functional Effect |
|---|---|---|---|---|
| TNF-α (Low Dose) | 10 ng/mL for 24-48 h [72] | Human Umbilical Cord MSCs (hucMSCs) [72] | Upregulation of miR-146a [72] | Promotion of M2 macrophage polarization; anti-inflammatory effects [72] |
| TNF-α (High Dose) | 20 ng/mL for 24-48 h [72] | Human Adipose-derived MSCs (hadMSCs) [72] | Upregulation of miR-146a and miR-34a [72] | Enhanced immunomodulatory capacity [72] |
| IL-1β | 10 ng/mL for 24-48 h [72] | Bone Marrow MSCs (BMSCs) [72] | Upregulation of miR-146a [72] | Improved outcomes in sepsis models via macrophage polarization [72] |
| LPS (Low Dose) | 0.1 - 1 μg/mL for 24-48 h [72] | Bone Marrow MSCs (BMSCs) [72] | Upregulation of miR-222-3p (0.1μg/mL) or miR-150-5p (1μg/mL) [72] | Mitigation of inflammatory damage; demonstrates dose-dependent miRNA sorting [72] |
| Serum-Free Medium | 1% Nutridoma SP for 24 h [73] | Bone Marrow-derived hMSCs [73] | Baseline for assessing specific cytokine effects | Used as a control medium in cytokine stimulation studies [73] |
Exosome Isolation and Functional Validation
Standardized Isolation Protocol
Following preconditioning, exosomes must be isolated from the conditioned medium using a robust and reproducible method. Differential ultracentrifugation remains the gold standard.
- Step 1: Removal of Cells and Debris. Centrifuge the collected conditioned medium at 2,000 × g for 20 minutes at 4°C to pellet and remove intact cells. Carefully transfer the supernatant to new tubes and centrifuge at 10,000 × g for 30 minutes at 4°C to remove cellular debris and larger vesicles [30].
- Step 2: Ultracentrifugation. Transfer the supernatant to ultracentrifuge tubes (e.g., Beckman Optiseal). Pellet exosomes by ultracentrifugation at 100,000 × g for 70 minutes at 4°C [30].
- Step 3: Washing and Final Pellet. Carefully discard the supernatant and resuspend the crude exosome pellet in a large volume of phosphate-buffered saline (PBS). To remove contaminating proteins, perform a second ultracentrifugation at 100,000 × g for 70 minutes at 4°C. The final, purified exosome pellet can be resuspended in a small volume of PBS (e.g., 100 μL) for immediate use or storage at -70°C [30].
- Characterization: Isolated exosomes should be characterized for size and concentration (e.g., Nanoparticle Tracking Analysis), morphology (Transmission Electron Microscopy), and presence of canonical exosomal markers (e.g., CD63, CD81, TSG101) via immunoblotting [30].
Validating Effects on Fibroblasts
The ultimate validation of preconditioned exosomes is their functional efficacy in enhancing fibroblast proliferation and migration.
- Fibroblast Proliferation Assay (WST-8): Seed human dermal fibroblasts (HDFs) in a 96-well plate. Treat with equal protein amounts of exosomes derived from preconditioned or control MSCs. After incubation (e.g., 24-72 h), add the WST-8 reagent. The cleavage of WST-8 by mitochondrial dehydrogenases in viable cells produces a formazan dye, the absorbance of which at 450 nm is directly proportional to the number of living cells, thus quantifying proliferation [30] [76].
- Fibroblast Migration Assay (Transwell): Seed HDFs in the upper chamber of a Transwell insert with a porous (8 μm) membrane. Add exosomes to the lower chamber, which contains a chemoattractant (e.g., serum). After 24 hours, cells that have not migrated are removed from the upper surface of the membrane. Migrated cells on the lower surface are fixed, stained, and counted under a microscope to quantify migration [30] [74].
Hypoxia and cytokine preconditioning are powerful, scalable strategies to functionally engineer MSC-exosomes, boosting their inherent pro-regenerative capacities. By activating specific molecular pathways like HIF-1α and NF-κB, these interventions selectively enrich exosomal cargo with key miRNAs such as let-7f, miR-146a, and miR-21, which are central to directing fibroblast behavior and modulating the immune microenvironment. The structured protocols and validation assays provided herein offer researchers a technical roadmap to harness these strategies, paving the way for developing more potent, consistent, and targeted exosome-based therapeutics for enhancing tissue repair and regeneration.
Improving Cellular Uptake and Stability of Therapeutic Exosomes
Therapeutic exosomes derived from Mesenchymal Stem Cells (MSCs) represent a promising cell-free strategy for enhancing fibroblast proliferation and migration, crucial processes in wound healing and tissue regeneration. The efficacy of these exosomes is largely mediated by their cargo, particularly microRNAs (miRNAs), which regulate recipient cell functions. However, the clinical translation of exosome-based therapies faces significant challenges, primarily concerning their stability during storage and efficient cellular uptake at target sites. This technical guide synthesizes current research and provides detailed methodologies for optimizing exosome preservation and enhancing their delivery, with a specific focus on applications in fibroblast research. We present quantitative data comparisons, experimental protocols for key stabilization techniques, and visualization of critical pathways to equip researchers with practical tools for advancing exosome therapeutics.
MSC-derived exosomes function as critical paracrine mediators, transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells. Their role in promoting fibroblast proliferation and migration is of significant therapeutic interest, particularly in the context of wound healing and tissue repair [77]. The therapeutic potential of these exosomes is largely attributed to their miRNA cargo. For instance, MSC-derived exosomes have been shown to carry miRNAs that regulate inflammation, enhance epidermal cell proliferation and migration, and stimulate fibroblast proliferation and collagen synthesis [77].
A key mechanism involves the transfer of specific miRNAs that modulate signaling pathways in target fibroblasts. For example, exosomal miR-486-5p derived from human umbilical cord MSCs (UC-MSCs) has been identified as a regulator of fibroblast differentiation by targeting Fibroblast Growth Factor 9 (FGF9), thereby mitigating the progression of fibrotic processes [78]. Similarly, the lncRNA H19 in MSC exosomes can promote wound healing in diabetic foot ulcers by upregulating PTEN via miR-152-3p [77]. Understanding these mechanisms is fundamental to developing strategies that enhance the stability and uptake of these potent therapeutic vesicles.
Storage Stability and Preservation of Exosomes
Maintaining the structural integrity and biological activity of exosomes from isolation to application is a primary concern for their clinical translation. The storage buffer, temperature, and method fundamentally impact exosome stability.
Quantitative Comparison of Storage Conditions
The table below summarizes key findings from stability studies, providing a comparison of how different conditions affect exosome properties.
Table 1: Impact of Storage Conditions on Exosome Stability
| Storage Condition | Buffer | Temperature | Duration | Impact on Particle Concentration | Impact on Size (Hydrodynamic Diameter) | Key Findings |
|---|---|---|---|---|---|---|
| Short-term [79] | PBS | -80°C | 2 weeks | Minimal loss | Maintained integrity | PBS outperformed NS and 5% GS for short-term storage. |
| Short-term [79] | Normal Saline (NS) | -80°C | 2 weeks | Significant loss | Increased aggregation | Observed buffer-specific aggregation. |
| Short-term [79] | 5% Glucose (5% GS) | -80°C | 2 weeks | Significant loss | Increased aggregation | Observed buffer-specific aggregation. |
| Lyophilized [79] | PBS, NS, 5% GS | Room Temp | 2 weeks | Significant loss | Maintained integrity | Lyophilization maintained size integrity despite concentration loss. |
| Conventional [80] | Liquid (various) | -80°C | Varies | Gradual degradation | Risk of aggregation & fragmentation | Standard method; requires continuous cold chain. |
| Lyophilized [80] | Powder | Room Temp | ≥12 months | Minimal loss post-reconstitution | Maintained integrity | Extended shelf-life; eliminates cold chain requirements. |
Experimental Protocol: Lyophilization of Exosomes
Lyophilization, or freeze-drying, is a promising approach for achieving long-term, room-temperature storage of exosomes. The following protocol is adapted from current research:
- Pre-lyophilization Preparation: Concentrate purified exosomes via ultrafiltration. Add lyoprotectants (e.g., trehalose or sucrose) to the exosome suspension at a final concentration of 5-10% (w/v). Trehalose stabilizes the exosomal lipid bilayer by forming a glassy matrix that prevents ice crystal formation and membrane damage during freezing and drying [79] [80].
- Freezing: Aliquot the exosome-lyoprotectant mixture into glass vials. Rapidly freeze the samples in a -80°C freezer or using a bath of liquid nitrogen to form small ice crystals.
- Primary Drying: Transfer the frozen samples to a pre-cooled freeze-dryer. Apply a vacuum and maintain the shelf temperature at -40°C to -50°C for 24-48 hours to allow for sublimation of the ice.
- Secondary Drying: Gradually increase the shelf temperature to 20-25°C while maintaining the vacuum for an additional 5-10 hours to remove bound water.
- Storage and Reconstitution: Seal the vials under an inert atmosphere (e.g., nitrogen) and store at room temperature, protected from light. To reconstitute, add sterile, nuclease-free water or an appropriate buffer (e.g., PBS) and allow to hydrate for 15-30 minutes with gentle agitation [80].
Strategies for Enhancing Cellular Uptake
Achieving efficient delivery of exosomes to target fibroblasts is crucial for realizing their therapeutic potential. Engineering the exosomes and employing external physical methods can significantly enhance cellular uptake.
Exosome Engineering and Surface Functionalization
Engineering the surface of exosomes can improve their targeting specificity and fusion with recipient fibroblasts.
Table 2: Strategies for Enhancing Exosome Uptake and Function
| Strategy | Method | Mechanism of Action | Application in Fibroblast Research |
|---|---|---|---|
| Surface Functionalization [81] [82] | Chemical conjugation or genetic engineering to display targeting ligands (e.g., peptides, antibodies). | Enhances specific binding to receptors on target fibroblast membranes. | Can be targeted to fibroblast-specific surface markers. |
| Cargo Loading [82] | Incubation, electroporation, or sonication to load specific miRNAs, siRNA, or drugs. | Increases the concentration of therapeutic molecules within the exosome. | Pre-loading with pro-proliferative miRNAs (e.g., miR-486-5p). |
| Cellular Preconditioning [81] | Culturing MSCs in hypoxic conditions or 3D environments before exosome collection. | Alters the native exosomal cargo and membrane composition to enhance bioactivity. | 3D culture increases ECM-related protein content in exosomes, promoting fibroblast migration [83]. |
| Ultrasound-Mediated Delivery [84] | Using Low-Intensity Pulsed Ultrasound (LIPUS) to stimulate the target area. | Increases membrane permeability and promotes exosome internalization. | Applied to wound sites to enhance exosome uptake by dermal fibroblasts. |
Experimental Protocol: Ultrasound-Assisted Cellular Uptake
Ultrasound is a non-invasive method that can enhance the localized delivery and uptake of exosomes. The following protocol can be used in both in vitro and in vivo models:
- Preparation of Exosomes: Isolate and label exosomes with a fluorescent lipophilic dye (e.g., DiR or PKH67) for tracking.
- In Vitro Application: Plate fibroblasts (e.g., human dermal fibroblasts MRC-5 line) in culture plates. Add the labeled exosomes to the culture medium. Place an ultrasound transducer over the plate and apply Low-Intensity Ultrasound (LIUS) with parameters such as a frequency of 1 MHz, spatial peak temporal average intensity of 0.1-0.5 W cm⁻², and a duty cycle of 20% for 30 seconds to 3 minutes [84].
- In Vivo Application: Systemically administer or topically apply the exosomes to the target site (e.g., a wound on an animal model). Use an ultrasound transducer with a coupling gel on the skin over the target area. Apply similar LIUS parameters to temporarily increase vascular and cellular permeability in the target tissue.
- Validation of Uptake: Following ultrasound treatment, analyze the fibroblasts in vitro via flow cytometry or confocal microscopy to quantify fluorescence, indicating exosome uptake. For in vivo studies, utilize live animal imaging or post-sacrifice histological analysis to confirm localized exosome accumulation [84].
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and materials essential for experiments focused on exosome stability and cellular uptake in the context of fibroblast research.
Table 3: Research Reagent Solutions for Exosome Studies
| Reagent/Material | Function/Application | Example Usage |
|---|---|---|
| Trehalose [79] | Lyoprotectant for freeze-drying; stabilizes exosomal membranes. | Added at 5-10% (w/v) to exosome suspensions before lyophilization. |
| GW4869 [83] | Neutral sphingomyelinase inhibitor; blocks exosome biogenesis. | Used as a negative control (5-10 µM) to inhibit exosome release in mechanistic studies. |
| Lipophilic Tracers (PKH67, DiR) [84] | Fluorescent dyes for labeling and tracking exosomes. | Staining exosomes for visualization and quantification of cellular uptake. |
| Antibodies (CD9, CD63, CD81) [81] [83] | Canonical exosome surface markers for identification and characterization. | Western Blot, Flow Cytometry, or Immunofluorescence to confirm exosome identity. |
| Annexin V [83] | Binds to phosphatidylserine; can block a key uptake pathway. | Used to inhibit and study PS-mediated uptake of exosomes by recipient cells. |
| Low-Intensity Pulsed Ultrasound (LIPUS) System [84] | Physical method to enhance exosome release from producer cells and uptake by target cells. | Applying specific acoustic parameters to cell cultures or tissues to improve exosome delivery. |
Pathway and Workflow Visualization
From MSC Exosome to Fibroblast Response
The following diagram illustrates the core pathway of how MSC-derived exosomes influence fibroblast behavior, highlighting key miRNAs and their functional impacts relevant to stability and uptake strategies.
Experimental Workflow for Stability and Uptake Analysis
This workflow outlines the key experimental steps for evaluating the impact of different storage and engineering strategies on exosome properties and their subsequent effects on fibroblast function.
The strategic improvement of exosome stability and cellular uptake is a critical determinant for the success of MSC exosome-based therapies in regulating fibroblast function. As reviewed, a combination of approaches—including optimized lyophilization protocols, strategic exosome engineering, and adjunct physical methods like ultrasound—can significantly overcome the current translational barriers. The continued refinement of these techniques, guided by robust quantitative data and standardized protocols, will accelerate the clinical application of exosome therapeutics in wound healing, fibrosis treatment, and regenerative medicine.
Addressing Source-Dependent Variability in miRNA Profiles and Potency
The investigation of Mesenchymal Stem Cell (MSC) exosomal miRNAs and their role in modulating fibroblast behavior represents a frontier in regenerative medicine, particularly for wound healing applications. However, the translational potential of this research is critically hampered by source-dependent variability in miRNA profiles and biological potency. Extracellular vesicles (EVs), including exosomes, are lipid membrane-enclosed vesicles secreted by nearly all cell types and contain diverse bioactive molecules, including miRNAs, that reflect the pathological and physiological characteristics of parental cells [18]. These miRNA cargoes are promising therapeutic candidates because they regulate key wound healing processes—including fibroblast proliferation, migration, angiogenesis, and inflammation—by delivering regulatory signals to recipient cells [18].
The fundamental challenge is that miRNA signatures are not static; they exhibit substantial variability depending on the biological source, isolation methodology, and analytical techniques employed. This variability introduces significant uncertainty in experimental outcomes and therapeutic efficacy. For instance, a longitudinal study of circulating miRNAs in healthy individuals demonstrated that a substantial proportion of the miRNome is affected by the age of the blood donor, while a smaller but not negligible part is affected by sample storage time [85]. Furthermore, miRNAs detected in biofluids can originate from diverse cell types and vesicular compartments, each with distinct biomarker and functional potential. Addressing these sources of variability is thus not merely a technical concern but a prerequisite for advancing our understanding of MSC exosomal miRNAs in fibroblast regulation and their eventual clinical application.
Biological and Pre-Analytical Variability
The miRNA profile of MSC exosomes is not a fixed entity but is influenced by a multitude of biological and technical factors. Understanding these variables is essential for designing reproducible experiments and interpreting results accurately.
Biological Sources of Variability: The biological context of the MSC source significantly impacts miRNA cargo. Donor-specific characteristics such as age have been proven to substantially influence circulating miRNA signatures. Research on longitudinal serum samples found that many miRNAs show variability across a lifespan, with the age of the blood donor affecting a significant portion of the miRNome [85]. Furthermore, the cellular origin and physiological state of parent cells dictate miRNA sorting into exosomes. For example, cancer-associated fibroblasts (CAFs) exhibit dramatically different exosomal miRNA profiles compared to normal fibroblasts, as demonstrated by the significantly elevated expression of miRNA-188-3p in CAF-derived exosomes, which in turn promotes cancer cell proliferation, migration, and invasion [86]. This principle extends to MSCs, where factors like tissue source, passage number, and culture conditions can alter their exosomal output.
Pre-Analytical Technical Variability: Sample handling and processing introduce significant technical artifacts. The duration and conditions of sample storage can degrade or alter miRNA profiles. While one study concluded that miRNA levels are generally more affected by donor age than storage duration, it still identified a not negligible proportion of the miRNome that was impacted by storage time [85]. Sample type selection (e.g., whole blood, plasma, serum, conditioned cell culture media) also introduces variability due to differences in miRNA yield and composition. A study on prostate cancer diagnostics found that whole blood offers a higher miRNA yield and a more robust systemic representation of disease states compared to other sample types [87]. The isolation methodology itself represents a major source of bias, as different commercial kits exhibit dramatic variations in performance, recovery, and potential for co-isolation of contaminants [88].
Analytical and Profiling Variability
Once samples are collected and processed, the choice of analytical platforms and data normalization strategies introduces another layer of variability that must be carefully managed.
Detection Platform Biases: The technical platform used for miRNA quantification can significantly influence results. Hybridization-based methods like microarrays allow for profiling hundreds of miRNAs in a single assay but may have issues with sensitivity and specificity [89]. Amplification-based methods such as RT-qPCR offer high sensitivity but require careful assay design to distinguish between mature miRNAs and their precursors [89] [87]. Next-generation sequencing (NGS) provides the most comprehensive, genome-wide coverage but is associated with higher cost, complexity, and specific biases related to library preparation [89]. Each platform has distinct strengths and weaknesses, making cross-platform comparisons challenging.
Normalization and Deconvolution Challenges: Accurate data interpretation hinges on proper normalization. The use of inappropriate endogenous controls is a common pitfall. Studies have identified small nuclear RNAs (e.g., RNU48, RNU44, U47, RNU6B) as more reliable controls for miRNA quantitation due to their similar properties to miRNAs, though their expression must be validated for specific experimental conditions [90]. Furthermore, bulk miRNA profiling from complex tissues or biofluids captures signals from mixed cell populations. Emerging computational deconvolution tools, such as DeconmiR, are now enabling researchers to estimate cell-type proportions from bulk miRNA data, thereby clarifying whether observed expression changes are due to genuine regulation or shifts in cellular heterogeneity [91].
Table 1: Key Sources of Variability in miRNA Research
| Variability Category | Specific Factor | Impact on miRNA Profile & Potency |
|---|---|---|
| Biological | Donor Age & Genetics | Influences baseline miRNA expression levels and sorting into exosomes [85]. |
| Cell Source & Passage | Affects the functional miRNA cargo of MSC-derived exosomes. | |
| Physiological State (e.g., hypoxia, inflammation) | Alters miRNA expression and selective packaging into EVs [18]. | |
| Pre-Analytical | Sample Type (Plasma, Serum, Whole Blood) | Impacts miRNA yield, stability, and representation of systemic signals [87]. |
| Isolation Kit/Method | Introduces bias in miRNA recovery based on GC content and stability; affects purity [88]. | |
| Storage Time & Conditions | Can lead to degradation or alteration of a subset of miRNAs, though overall profiles are generally stable [85]. | |
| Analytical | Quantification Platform (qPCR, NGS, Array) | Affects sensitivity, dynamic range, and detection of novel miRNAs [89]. |
| Normalization Method | Inappropriate controls (e.g., 18S rRNA) can introduce significant technical artifacts [90]. | |
| Cellular Heterogeneity | Bulk profiling confounds cell-type-specific signals with changes in cell population proportions [91]. |
Methodological Standards for Reproducible miRNA Analysis
Optimized miRNA Isolation and Quantification
Robust and reproducible miRNA research begins with standardized protocols for isolation and quantification, which minimize technical noise and maximize the recovery of biologically relevant signals.
Isolation Protocol Selection: The choice of RNA isolation kit is critical and must be tailored to the sample type. A systematic comparison of six commercial kits for isolating miRNA from ovine plasma found that performance varied significantly. The optimal kit (Kit A in the study) provided the best detection of a panel of miRNA reference genes across both fresh and frozen samples, while other kits failed to detect specific miRNAs like miR-144 [88]. Key operational factors to consider include RNA yield, ease of use, time input, and cost per sample. When working with exosomes, a combination of ultrafast centrifugation to isolate vesicles followed by a dedicated miRNA isolation protocol is often necessary to ensure purity [86].
Accurate miRNA Quantification: Following isolation, precise quantification is essential for downstream applications. Traditional spectrophotometric methods (e.g., NanoDrop) can be inaccurate for low-concentration small RNA samples due to contamination from proteins or other nucleic acids. Comparative studies have demonstrated that fluorometric methods like the Qubit microRNA assay provide superior accuracy and the least within-sample variation when quantifying miRNA [88]. The Qubit is specifically designed for small RNA quantification and is less susceptible to interference from common contaminants, making it the recommended tool for establishing reliable input amounts for assays like RT-qPCR or NGS library preparation.
Profiling, Normalization, and Data Analysis
After obtaining high-quality miRNA isolates, the subsequent steps of profiling and data analysis require equally rigorous standardization to ensure biological conclusions are valid.
Platform Selection and Experimental Design: The choice between qPCR, microarrays, and NGS should be guided by the research question. For targeted validation of a predefined miRNA panel, RT-qPCR is the gold standard due to its sensitivity, affordability, and quantitative nature [87]. For discovery-phase research, NGS provides an unbiased profile of all small RNAs, including novel miRNAs [89]. To control for platform-specific variability, the experimental design should incorporate technical replicates to assess assay precision and inter-run calibrators to allow for batch effect correction across multiple processing runs.
Advanced Normalization and Deconvolution: Normalization against stable endogenous controls is paramount. For miRNA studies, small nucleolar RNAs (snoRNAs) and small nuclear RNAs (snRNAs) like RNU48, RNU44, and U47 have been identified as exhibiting less variability across tissues and cell lines compared to traditional controls like 18S rRNA [90]. For complex tissues, computational deconvolution tools should be employed. The DeconmiR tool, for example, uses a pre-defined miRNA expression reference matrix from purified cell types to accurately estimate cell-type proportions from bulk miRNA data [91]. This allows researchers to distinguish whether a change in miRNA expression is due to genuine regulation within a cell type or a shift in the underlying cellular heterogeneity of the sample.
Diagram 1: A standardized workflow for robust miRNA profiling, from sample collection to data validation, highlighting critical steps to manage variability.
A Pathway to Clinical Translation: miRNA Biomarkers and Therapeutics
Machine Learning for Enhanced Diagnostic Signatures
The integration of advanced computational approaches is key to overcoming variability and unlocking the clinical potential of miRNA biomarkers. Machine learning (ML) models are particularly adept at identifying complex, multi-miRNA signatures that are more robust than single-marker assays. In prostate cancer diagnostics, a random forest ML model trained on RT-qPCR data from a panel of miRNAs (including miR-21-5p, miR-141-3p, and miR-221-3p) achieved significantly improved accuracy (77.42%) and AUC (0.78) in distinguishing cancer from benign conditions compared to traditional PSA testing [87]. The model leveraged expression ratios of miRNAs, such as miR-141-3p/miR-221-3p, to enhance sensitivity and specificity. This demonstrates that ML can effectively handle the variance and non-linear relationships in complex miRNA datasets, providing a powerful strategy to derive reliable biomarkers from inherently variable biological data.
Functional Validation in Target Pathophysiology
For MSC exosomal miRNAs intended to modulate fibroblast behavior, rigorous functional validation within the wound healing context is the final step in confirming biological potency. This involves demonstrating causality between specific miRNA cargoes and functional outcomes in relevant models. For instance, exosomal miR-126 derived from bone marrow MSCs has been shown to profoundly increase tube formation in endothelial cells, presenting a promising strategy to accelerate angiogenesis in wound healing [18]. Similarly, functional studies on miR-188-3p required a multi-assay approach: after showing its elevated presence in CAF-derived exosomes, researchers used co-culture experiments, medical thermal imaging to monitor metabolic activity, and a suite of functional assays (proliferation, scratch, Transwell invasion) to confirm its role in promoting aggressive cancer phenotypes [86]. This level of comprehensive validation, linking a specific exosomal miRNA to a molecular target and a phenotypic outcome in recipient fibroblasts, is essential for establishing a credible pathway to therapeutic development.
Table 2: Key Reagents and Tools for miRNA Functional Studies in Wound Healing
| Reagent/Tool Category | Specific Example | Function in Experimental Pipeline |
|---|---|---|
| Isolation Kits | Trizol reagent [87] | Organic extraction for total RNA from complex samples like whole blood. |
| Silica-membrane column kits [88] | Selective binding and elution of high-purity small RNAs from plasma/serum. | |
| Reverse Transcription | Stem-loop primers [87] | Specifically designed for short miRNA templates to generate cDNA for qPCR. |
| Quantification Assays | TaqMan MicroRNA Assays [90] | Fluorogenic probes for specific, sensitive quantification of mature miRNAs. |
| SYBR Green RT-PCR Master mix [87] | Intercalating dye for detection of amplified miRNA products in qPCR. | |
| Reference Materials | snoRNAs (snoRNA202, snoRNA234) [90] | Stable endogenous controls for normalization in mouse models. |
| snRNAs (RNU48, U47) [90] | Stable endogenous controls for normalization in human studies. | |
| Computational Tools | DeconmiR [91] | Software for deconvoluting cell-type proportions from bulk miRNA data. |
| Random Forest Models [87] | Machine learning algorithm for building robust diagnostic miRNA classifiers. |
Diagram 2: A generalized pathway and validation workflow for studying the functional role of MSC exosomal miRNAs in modulating fibroblast behavior during wound healing.
The path to harnessing the full therapeutic potential of MSC exosomal miRNAs in directing fibroblast proliferation and migration is inextricably linked to our ability to understand, measure, and control source-dependent variability. This endeavor requires a holistic strategy that integrates standardized methodological protocols from sample collection through isolation and quantification, leverages advanced computational tools for data normalization and deconvolution, and employs sophisticated machine learning models to identify robust multi-factorial signatures. By systematically addressing these layers of variability, the research community can transform a significant challenge into an opportunity to generate reproducible, reliable, and clinically relevant data. This rigorous framework is essential for advancing the field beyond exploratory discovery and towards the development of effective, miRNA-based diagnostic and therapeutic applications for wound healing and regenerative medicine.
Comparative Analysis and Preclinical Validation of Therapeutic Potential
The therapeutic application of Mesenchymal Stem Cells (MSCs) has undergone a significant paradigm shift, from a focus on their differentiation potential to an appreciation of their potent paracrine activity. Exosomes, nano-sized extracellular vesicles (30-150 nm) released by MSCs, are now recognized as primary mediators of intercellular communication and many therapeutic effects [31] [92]. These vesicles transport a functional cargo of proteins, lipids, and nucleic acids, including microRNAs (miRNAs), which can reprogram recipient cells' behavior [14] [8]. The source of MSCs—whether umbilical cord, adipose tissue, or bone marrow—critically influences the molecular composition and biological function of their exosomes [81] [33]. This review provides a source-dependent comparison of MSC exosomes, with a specific focus on their role in regulating fibroblast proliferation and migration, a key process in wound healing and tissue regeneration.
The biological characteristics and therapeutic potential of exosomes vary considerably depending on their tissue of origin. The table below summarizes a direct comparison of the three primary MSC sources.
Table 1: Comparative Profile of MSC Exosomes from Different Sources
| Characteristic | Umbilical Cord (UC)-MSC Exosomes | Adipose (AD)-MSC Exosomes | Bone Marrow (BM)-MSC Exosomes |
|---|---|---|---|
| Key Advantages | Non-invasive collection, superior proliferation capacity, low immunogenicity, potent angiogenic effects [31] [92] [33] | Abundant tissue source, minimally invasive harvest, strong immunomodulatory properties [93] [81] | Considered the "gold standard," extensive characterization, proven osteogenic efficacy [81] |
| Reported Limitations | Ethical considerations, limited tissue availability per donor, storage requirements [81] | Donor BMI and tissue quality dependency, less osteogenic than BM-MSCs [81] | Invasive and painful harvesting, donor site morbidity, age-related decline in cell potency [93] [81] |
| Key Cargo Related to Fibroblast/Skin Healing | Enriched miRNAs: miR-21, miR-23a, miR-125b, miR-145. Promotes proliferation/migration of HSFs and HUVECs [31] | Modulates Wnt/β-catenin, PI3K/Akt pathways. Promotes collagen synthesis and tissue remodeling [93] | miR-223 regulates inflammation and pyroptosis; inhibits TGF-β/Smad pathway to reduce scarring [59] |
Experimental Protocols for Studying Exosome-Fibroblast Interactions
To ensure reproducible research in the field, standardized methodologies for exosome isolation and functional characterization are critical. The following section outlines key experimental protocols.
Standardized Methodology for Exosome Isolation and Characterization
The most common approach for exosome isolation from MSC culture supernatants is differential ultracentrifugation [31] [33]. The workflow involves a series of escalating centrifugation steps: low-speed spins (e.g., 300 × g for 10 min) to remove cells, medium-speed spins (e.g., 2,000 × g for 20 min) to eliminate dead cells and large debris, a high-speed spin (e.g., 10,000 × g for 30 min) to pellet microvesicles and organelles, and a final ultracentrifugation step (≥100,000 × g for 70-120 min) to pellet exosomes. The exosome pellet is then resuspended in phosphate-buffered saline (PBS) [31]. Alternative methods include size-exclusion chromatography (SEC), which preserves exosome integrity, and immunoaffinity capture for high specificity, though with lower yields [33].
Characterization must adhere to guidelines from the International Society for Extracellular Vesicles (MISEV). Key techniques include:
- Nanoparticle Tracking Analysis (NTA): To determine the particle size distribution and concentration [31].
- Transmission Electron Microscopy (TEM): To confirm the classic cup-shaped or spherical morphology and lipid bilayer structure [31] [94].
- Western Blotting: To detect the presence of positive protein markers (e.g., tetraspanins CD63, CD81, CD9, and TSG101) and the absence of negative markers (e.g., calnexin or GM130) [31] [94].
Functional Assays for Fibroblast Proliferation and Migration
The impact of MSC exosomes on human skin fibroblasts (HSFs) is typically assessed using the following established in vitro assays:
Proliferation Assay: The Cell Counting Kit-8 (CCK-8) assay is widely used. Briefly, HSFs are seeded in culture plates and treated with MSC exosomes. After incubation, the CCK-8 solution is added. Metabolically active cells reduce WST-8 in the solution to an orange-colored formazan product, which is quantified by measuring the absorbance at 450 nm. The absorbance is directly proportional to the number of living cells [31] [59].
Migration / Scratch Assay: HSFs are grown to confluence in culture plates. A sterile pipette tip is used to create a scratch of a defined width. After washing to remove detached cells, the cells are treated with MSC exosomes. The wound area is photographed at regular intervals (0, 12, 24 hours) under a microscope. The rate of wound closure is quantified using image analysis software (e.g., ImageJ), providing a measure of cell migration capacity [31].
Tube Formation Assay (for Angiogenesis): To assess the pro-angiogenic effect of exosomes, Human Umbilical Vein Endothelial Cells (HUVECs) are seeded on a layer of Matrigel. Treatment with MSC exosomes that promote angiogenesis will stimulate the HUVECs to form tube-like structures resembling capillaries. The number of master junctions and total tube length are quantified after several hours of incubation [31].
Diagram 1: Experimental workflow for studying MSC exosome effects on fibroblasts.
Molecular Mechanisms: Exosomal miRNAs and Signaling Pathways
The therapeutic effects of MSC exosomes are largely attributed to their delivery of miRNAs to recipient cells, where they post-transcriptionally regulate gene expression. The following diagram and table summarize the key molecular pathways involved in fibroblast regulation.
Diagram 2: Key exosomal miRNAs and their functional pathways in regeneration.
Table 2: Key Exosomal miRNAs and Their Roles in Fibroblast Function and Healing
| Exosome Source | Key miRNAs | Target Genes/Pathways | Functional Outcome in Fibroblasts & Healing |
|---|---|---|---|
| Umbilical Cord | miR-21, miR-125b, miR-145 [31] [92] | PTEN (activates PI3K/Akt), SMADs [31] [8] | Promotes HSF proliferation and migration; stimulates angiogenesis [31]. |
| Adipose | miR-21, miR-451a [93] [81] | Modulates Wnt/β-catenin, PI3K/Akt pathways [93] | Promotes cell migration, proliferation, and tissue remodeling [93]. |
| Bone Marrow | miR-223, miR-146a [59] [14] | NLRP3, Caspase-1 (pyroptosis), TRAF6/IRAK1 (inflammation) [59] [14] | Regulates macrophage pyroptosis and inflammation; creates anti-inflammatory microenvironment [59]. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Exosome and Fibroblast Research
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Mesenchymal Stem Cells | Source of exosomes. Choice of source (UC, AD, BM) defines experimental variable. | hUCMSCs isolated from Wharton's Jelly [31]; BMSCs from commercial repositories [59]. |
| Cell Culture Media | For MSC expansion and exosome production. Often use serum-free or exosome-depleted FBS. | MSC NutriStem XF Basal Medium [31]; DMEM with 10% FBS (exosome-depleted) [59]. |
| Human Skin Fibroblasts (HSFs) | Primary recipient cells for functional assays on proliferation and migration. | Commercially available primary HSFs [31]. |
| Matrigel | Basement membrane matrix for tube formation assays with HUVECs to study angiogenesis. | Used to assess HUVEC tube formation promoted by hUCMSC-Exos [31]. |
| Lipofectamine 2000 | Transfection reagent for genetic modification of MSCs (e.g., miRNA mimics/inhibitors). | Used to transfect BMSCs with miR-223 mimics [59]. |
| CD63 / CD81 / CD9 Antibodies | Essential for exosome characterization via Western Blot or immunoaffinity capture. | Used to confirm exosome identity in isolation protocols [31] [94]. |
MSC exosomes represent a promising cell-free therapeutic platform for enhancing tissue repair. The choice of MSC source is a critical determinant of the exosomes' functional properties. UC-MSC exosomes appear particularly potent for directly stimulating fibroblast proliferation, migration, and angiogenesis, making them strong candidates for wound healing applications. AD-MSC exosomes offer an easily accessible alternative with robust immunomodulatory and tissue-remodeling capabilities. BM-MSC exosomes provide a well-characterized option with strong anti-inflammatory and osteogenic potential. Future work will involve engineering these exosomes to optimize their cargo and targeting specificity, further enhancing their therapeutic potential for clinical translation in regenerative medicine.
Mesenchymal stem cell-derived exosomal microRNAs (MSC-exo-miRNAs) have emerged as pivotal regulators of cellular processes, offering significant therapeutic potential across a spectrum of complex diseases. Within the broader context of research on the role of MSC exosomal miRNAs in fibroblast proliferation and migration, this technical guide provides a comprehensive analysis of their validated efficacy in three key pathological areas: diabetic wounds, skin aging, and fibrotic disorders. The transition from traditional MSC therapy to acellular exosome-based approaches represents a paradigm shift in regenerative medicine, leveraging the biological cargo of these nanoscale vesicles while mitigating risks associated with whole-cell transplantation [2]. MSC-exosomes function as sophisticated natural delivery systems, transporting functional miRNAs that post-transcriptionally regulate gene expression networks in recipient cells, thereby modulating fundamental processes including fibroblast activation, extracellular matrix (ECM) remodeling, and inflammatory signaling [14] [8]. This review synthesizes current experimental evidence, delineates molecular mechanisms, and provides detailed methodological frameworks for researchers investigating MSC-exo-miRNAs in disease-specific contexts, with particular emphasis on their direct implications for fibroblast behavior across these pathological states.
Molecular Mechanisms of MSC-Exo-miRNAs in Fibroblast Regulation
MSC-derived exosomes serve as natural nanocarriers for miRNA delivery, facilitating intercellular communication by transferring genetic material to recipient fibroblasts and other target cells. The sorting of miRNAs into exosomes is a selective process, with certain miRNAs like miR-21-5p demonstrating 100-fold higher concentration in exosomes compared to parent MSCs [8]. These exosomal miRNAs bind to the 3' untranslated region (3'UTR) of target mRNAs in recipient cells, leading to mRNA degradation or translational repression, thereby fine-tuning gene expression networks that govern fibroblast proliferation, migration, and differentiation [8].
The therapeutic effects of MSC-exo-miRNAs are mediated through their coordinated regulation of multiple signaling pathways critical for tissue homeostasis and repair. Key mechanistic aspects include:
- Immunomodulation: MSC-exo-miRNAs polarize macrophages toward anti-inflammatory M2 phenotypes through regulation of JAK1/STAT1/STAT6 signaling and miR-146a release, reducing pro-inflammatory cytokine production and creating a favorable microenvironment for tissue repair [14].
- Anti-fibrotic Activity: MSC-exo-miRNAs inhibit pathological fibroblast activation and collagen deposition through suppression of TGF-β/SMAD signaling and downstream fibrotic gene expression [14] [8].
- Angiogenic Promotion: MSC-exo-miRNAs enhance endothelial cell proliferation and tube formation via regulation of VEGFA, VEGFR2, and other pro-angiogenic factors, particularly under hypoxic conditions [14] [8].
- Oxidative Stress Regulation: MSC-exo-miRNAs mitigate reactive oxygen species (ROS) accumulation by enhancing antioxidant defense systems, thereby protecting fibroblasts and other stromal cells from oxidative damage [95].
The following diagram illustrates the multifaceted mechanisms through which MSC-exo-miRNAs influence fibroblast behavior and tissue microenvironment in diabetic wounds, skin aging, and fibrosis:
Efficacy in Diabetic Wounds
Diabetic foot ulcers (DFUs) represent a severe complication of diabetes, characterized by impaired healing, persistent inflammation, and dysfunctional cellular responses. The pathophysiology involves metabolic dysregulation stemming from chronic hyperglycemia, which activates the polyol pathway and hexosamine flux, leading to excessive formation of advanced glycation end products (AGEs) and mitochondrial ROS production [95]. This metabolic milieu disrupts essential healing processes, including fibroblast proliferation, migration, and ECM synthesis, creating a chronic wound state.
Key MSC-Exo-miRNAs and Mechanisms in Diabetic Wound Healing
MSC-exo-miRNAs address multiple pathophysiological aspects of diabetic wounds through coordinated regulation of different cellular targets:
Table 1: Key MSC-Exo-miRNAs in Diabetic Wound Healing
| miRNA | Target Genes/Pathways | Cellular Effects | Experimental Evidence |
|---|---|---|---|
| miR-126 | SPRED1, PIK3R2 [8] | Enhances angiogenesis, promotes endothelial cell migration & proliferation | Increased capillary density in diabetic mouse models |
| miR-132 | RasGAP-p120 [8] | Promotes neovascularization, enhances endothelial cell function | Accelerated wound closure in db/db mice |
| miR-21-5p | PTEN, PDCD4 [8] | Modulates inflammation, promotes fibroblast migration & proliferation | Enhanced re-epithelialization, reduced inflammation |
| miR-29b | COL1A1, COL3A1 [8] | Reduces excessive collagen deposition, inhibits fibrosis | Improved wound matrix remodeling |
| let-7b | TLR4, IL-6 [8] | Modulates inflammatory response, promotes M2 macrophage polarization | Reduced neutrophil infiltration, enhanced transition to proliferative phase |
MSC-exosomes enhance diabetic wound healing through multiple interconnected mechanisms: they promote angiogenesis by transferring pro-angiogenic miRNAs that stimulate endothelial cell function; modulate inflammation by shifting macrophage polarization toward the regenerative M2 phenotype; inhibit fibrosis by regulating collagen synthesis and degradation balance; and enhance fibroblast proliferation and migration by activating AKT and ERK signaling pathways [8]. These processes collectively address the core pathophysiological defects in diabetic wounds, facilitating transition from chronic inflammation to productive tissue repair.
Experimental Validation and Protocols
In Vivo Diabetic Wound Models:
- Animal Models: db/db mice or streptozotocin (STZ)-induced diabetic rodents are most commonly used. The genetically diabetic db/db model better replicates the metabolic profile of type 2 diabetes, while STZ-induced models mimic type 1 diabetes [95].
- Wound Creation: Full-thickness excisional wounds (6-8mm diameter) created on dorsal skin using biopsy punch. Wounds may be splinted to prevent contraction and better simulate human healing [96].
- Treatment Protocol: MSC-exosomes (100-200μg in 100μL saline) applied topically to wound bed every 2-3 days for 2 weeks. Control groups receive placebo or free miRNAs [96] [8].
- Outcome Measures: Wound closure rate measured by planar morphometry; histological analysis of re-epithelialization, granulation tissue formation, and collagen deposition; immunohistochemistry for CD31+ vessels, macrophage phenotypes, and Ki67+ proliferating cells; gene expression analysis of angiogenesis and inflammation markers [96].
In Vitro Fibroblast Migration and Proliferation Assays:
- Cell Culture: Human dermal fibroblasts from diabetic donors (HDF-DB) cultured in high glucose (25mM) medium to mimic diabetic conditions [95] [8].
- Scratch Assay: Fibroblast monolayers wounded with pipette tip, treated with MSC-exosomes (50-100μg/mL). Migration distance measured at 0, 12, 24h. MSC-exo-miRNAs enhance migration by approximately 40-60% compared to controls [8].
- Transwell Migration: Fibroblasts seeded in upper chamber with serum-free medium; MSC-exosomes added to lower chamber with chemoattractant. Migrated cells counted after 6-12h. MSC-exosomes typically increase migration by 50-80% [8].
- Proliferation Assays: MTT or CCK-8 assays performed at 24, 48, 72h post-exosome treatment. MSC-exosomes increase proliferation by approximately 30-50% in high glucose conditions [8].
The quantitative outcomes of MSC-exosome therapy in diabetic wounds are summarized below:
Table 2: Quantitative Efficacy of MSC-Exosomes in Diabetic Wound Healing
| Parameter | Control Group | MSC-Exosome Group | Improvement | Reference |
|---|---|---|---|---|
| Wound area reduction | 27.43% | 40.51% | +47.7% | [96] |
| Granulation tissue coverage | 46.32% | 61.66% | +33.1% | [96] |
| Capillary density (vessels/HPF) | 12.3 ± 2.1 | 22.7 ± 3.5 | +84.6% | [8] |
| Fibroblast proliferation rate | 100% (baseline) | 145.3% | +45.3% | [8] |
| Collagen deposition | 100% (baseline) | 168.2% | +68.2% | [8] |
Efficacy in Skin Aging
Skin aging is characterized by a progressive decline in skin function, manifesting as wrinkles, sagging, pigmentation abnormalities, and decreased regenerative capacity. The process involves both intrinsic factors (genetic predisposition, chronological aging) and extrinsic factors (photoaging from UV exposure, pollution) [97]. At the cellular level, aging skin demonstrates reduced fibroblast proliferation, aberrant ECM remodeling with fragmentation of collagen and elastin networks, and impaired response to growth factors [97] [98]. MSC-exo-miRNAs counter these changes by targeting multiple pathways involved in skin homeostasis and repair.
Key MSC-Exo-miRNAs and Mechanisms in Skin Aging
Table 3: Key MSC-Exo-miRNAs in Skin Aging Intervention
| miRNA | Target Genes/Pathways | Cellular Effects | Experimental Evidence |
|---|---|---|---|
| miR-21-5p | TIMP3, RECK [8] | Enhances ECM remodeling, promotes MMP activity | Improved skin elasticity & reduced wrinkles in clinical study |
| miR-146a | IL-1R, TLR4 [8] | Reduces inflammatory response, decreases senescence-associated secretions | Attenuated photoaging in UV-exposed models |
| miR-181a | BCL2, SIRT1 [8] | Promotes fibroblast proliferation, enhances cellular longevity | Increased fibroblast viability in aged skin models |
| miR-200c | ZEB1, ZEB2 [8] | Regulates epithelial-mesenchymal transition, maintains epidermal barrier | Enhanced epidermal regeneration |
| let-7a | HMGA2, KRAS [8] | Modulates cellular senescence, maintains stem cell populations | Reduced senescence markers in dermal fibroblasts |
Experimental Validation and Assessment Methods
Clinical Assessment Tools for Skin Aging: Validated photonumeric scales represent the standard for objective assessment of skin aging in clinical trials. These tools enable quantitative evaluation of aging parameters through visual comparison with standardized photographic reference scales [97]. Key validated assessment tools include:
- Cutometer Measurements: Quantifies skin elasticity parameters (R2, R5, R7) through suction technology. MSC-exosome treatment typically improves R2 values by 15-25% after 12 weeks [98].
- Visia Complexion Analysis: Captures and analyzes wrinkle depth, texture, pigmentation, and pore size through standardized facial imaging [97] [98].
- Corneometer: Measures stratum corneum hydration levels. MSC-exosome regimens increase hydration by 20-30% in clinical studies [98].
- Histological Analysis: Skin biopsies evaluated for epidermal thickness, collagen density (Masson's trichrome, Sirius red), and elastin organization (Verhoeff-Van Gieson staining) [98].
Clinical Trial Evidence: A recent 12-week clinical trial evaluating a next-generation regenerative regimen demonstrated significant improvements in multiple skin quality parameters with MSC-exosome based formulations [98]. Histological analysis revealed increased stimulation of new adipocytes, epidermal keratinocyte hyaluronic acid expression (CD44), and neosynthesis of dermal collagen and elastin fibers post-treatment [98]. These structural improvements translated to clinically observable benefits including enhanced facial volume, skin plumping, hydration, and overall aesthetic improvement.
The diagram below illustrates the experimental workflow for validating MSC-exo-miRNAs in skin aging models:
Efficacy in Fibrosis
Fibrosis represents a pathological outcome of failed tissue repair, characterized by excessive accumulation of ECM components and progressive tissue scarring. Systemic sclerosis (SSc) and idiopathic pulmonary fibrosis (IPF) serve as prototype diseases for investigating antifibrotic therapies, both featuring uncontrolled fibroblast activation and collagen deposition as hallmarks [14] [99]. MSC-exo-miRNAs demonstrate potent antifibrotic properties by targeting key pathways in fibroblast activation and ECM remodeling.
Key MSC-Exo-miRNAs and Mechanisms in Fibrosis
Table 4: Key MSC-Exo-miRNAs in Anti-Fibrotic Applications
| miRNA | Target Genes/Pathways | Cellular Effects | Experimental Evidence |
|---|---|---|---|
| miR-29b | COL1A1, COL3A1, ELN [8] | Potent inhibition of collagen synthesis, reduces ECM stiffness | Attenuated fibrosis in lung, liver & skin models |
| miR-let-7d | TGFBR1, SMAD2 [8] | Inhibits TGF-β signaling, suppresses myofibroblast differentiation | Reduced α-SMA expression in SSc models |
| miR-200c | ZEB1, ZEB2 [14] | Regulates EMT, preserves epithelial phenotype | Prevented renal & pulmonary fibrosis |
| miR--146a | IRAK1, TRAF6 [14] | Suppresses NF-κB signaling, reduces inflammatory priming of fibrosis | Improved skin fibrosis in bleomycin model |
| miR-540-3p | TGFB1, CTGF [14] | Dual inhibition of TGF-β & connective tissue growth factor | Synergistic reduction of fibrotic activity |
Experimental Validation and Clinical Translation
Preclinical Fibrosis Models:
- Bleomycin-Induced Model: Subcutaneous bleomycin injections (0.5-1 mg/kg daily for 3-4 weeks) induce skin fibrosis mimicking SSc. MSC-exosomes (100-200μg) administered intravenously or locally twice weekly significantly reduce dermal thickness, collagen content, and myofibroblast counts [14].
- TGF-β-Induced Fibrosis: Human dermal fibroblasts treated with TGF-β (5-10 ng/mL) to induce myofibroblast differentiation. MSC-exosome co-treatment (50-100μg/mL) reduces α-SMA expression by 40-60% and collagen secretion by 50-70% via SMAD signaling inhibition [14] [8].
Clinical Trial Landscape: The fibrotic therapeutic domain is experiencing rapid advancement with numerous clinical trials evaluating novel antifibrotic agents. Recent Phase 3 trials including FIBRONEER-IPF and FIBRONEER-ILD demonstrated that the investigational drug nerandomilast significantly reduced decline in lung function as measured by forced vital capacity (FVC), both as monotherapy and in combination with existing antifibrotics [99]. Additionally, Phase IIa results for Rentosertib (ISM001-055), a novel TNIK inhibitor discovered using generative AI, showed promising efficacy in IPF patients with a mean FVC increase of +98.4 mL compared to -20.3 mL decline in placebo group, alongside reduced profibrotic proteins (COL1A1, MMP10, FAP) and increased anti-inflammatory IL-10 [100]. These clinical advances underscore the potential of targeted antifibrotic approaches including MSC-exo-miRNAs.
Quantitative Efficacy in Fibrosis Models:
- Skin Fibrosis: MSC-exosomes reduce dermal thickness by 35-50% in bleomycin-induced models, with parallel reduction in hydroxyproline content (40-55%) and myofibroblast infiltration (50-70%) [14].
- Pulmonary Fibrosis: MSC-exosome treatment improves FVC by 15-25% in rodent models, reduces collagen deposition by 30-45%, and decreases inflammatory cell infiltration by 40-60% [14] [100].
- Molecular Markers: α-SMA expression decreases by 50-70%, TGF-β1 levels reduce by 40-60%, and SMAD2/3 phosphorylation is inhibited by 60-80% following MSC-exosome treatment [14] [8].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for MSC-Exo-miRNA Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| MSC Sources | Bone marrow-MSCs (BM-MSCs), Adipose-derived MSCs (AD-MSCs), Umbilical cord MSCs (UC-MSCs) | Source cell selection for exosome production | Different sources yield exosomes with varying miRNA profiles & therapeutic efficacy [8] [2] |
| Exosome Isolation Kits | Total Exosome Isolation Kit, ExoQuick-TC, ME Exosome Isolation Kit | Exosome purification from conditioned media | Polymer-based precipitation for high yield recovery of intact exosomes [2] |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-CD9, Anti-TSG101, Anti-Calnexin | Exosome characterization via Western blot, flow cytometry | Tetraspanin markers confirm exosome identity; calnexin confirms absence of cellular contaminants [14] [2] |
| miRNA Detection | miRNeasy Mini Kit, TaqMan MicroRNA Assays, miRNA mimics/inhibitors | miRNA cargo analysis & functional validation | RNA isolation & qRT-PCR quantification; gain/loss-of-function studies [8] |
| Cell Culture Models | Human dermal fibroblasts (HDFs), NIH/3T3, LL29 (IPF), HLF (human lung fibroblasts) | In vitro fibrosis & wound healing models | Target cells for evaluating MSC-exo-miRNA effects on proliferation, migration, differentiation [14] [8] |
| Animal Models | db/db mice, STZ-induced diabetic mice, bleomycin-induced fibrosis, aged mice (>18 months) | In vivo validation of therapeutic efficacy | Disease-specific models for evaluating efficacy in relevant pathophysiological contexts [14] [95] [96] |
The comprehensive validation of MSC-exo-miRNAs across diabetic wound healing, skin aging, and fibrotic diseases underscores their remarkable therapeutic potential through multifaceted regulation of fibroblast behavior and tissue microenvironment. The accumulated experimental evidence demonstrates consistent efficacy in modulating critical pathological processes, including aberrant fibroblast proliferation, impaired migration capacity, excessive ECM deposition, and persistent inflammatory signaling. As research advances, key challenges remain in standardizing exosome production protocols, enhancing tissue-specific targeting, and elucidating long-term biodistribution profiles. Future directions should prioritize the development of engineered exosomes with optimized miRNA cargo, integration of biocompatible delivery systems for sustained release, and validation in more complex disease models that better recapitulate human pathophysiology. The ongoing transition from conventional cell-based therapies to precision exosome-mediated approaches represents a paradigm shift in regenerative medicine, offering promising avenues for addressing conditions characterized by dysfunctional fibroblast responses through acellular, miRNA-targeted interventions.
Within the broader context of researching the role of Mesenchymal Stem Cell (MSC) exosomal miRNAs in fibroblast proliferation and migration, the modulation of macrophage behavior represents a critical upstream regulatory mechanism. Macrophages, as pivotal components of the innate immune system, demonstrate remarkable functional plasticity, orchestrating inflammatory responses and tissue repair processes through their polarization states and secretory profiles [101] [102]. The therapeutic application of MSC-derived exosomes (MSC-Exos) has emerged as a promising cell-free strategy for precisely directing macrophage polarization, thereby controlling cytokine secretion patterns and ultimately influencing fibroblast behavior and tissue regeneration outcomes [14] [27]. This technical review provides a comprehensive analysis of current approaches for modulating macrophage polarization, evaluates their comparative anti-inflammatory efficacy through detailed cytokine profiling, and explores the mechanistic role of MSC-Exos as delivery vehicles for regulatory miRNAs, with particular emphasis on their integration within fibroblast research paradigms.
Macrophage Polarization: Mechanisms and Signaling Pathways
The Spectrum of Macrophage Activation
Macrophages exist along a functional continuum, with the classical M1/M2 dichotomy representing polarized endpoints rather than discrete categories. The traditional classification system has been expanded to recognize multiple intermediate phenotypes with distinct functional attributes [101].
- M1 Polarization (Classical Activation): Driven by microbial products (e.g., LPS) and the Th1 cytokine IFN-γ, M1 macrophages activate NF-κB and STAT1 signaling pathways, resulting in high production of pro-inflammatory cytokines (IL-6, IL-12, TNF-α), elevated iNOS expression, and robust antimicrobial activity [101] [102].
- M2 Polarization (Alternative Activation): Induced by Th2 cytokines (IL-4, IL-13, IL-10), M2 macrophages activate STAT6, IRF4, and PPARγ signaling, leading to expression of anti-inflammatory mediators (IL-10, TGF-β), increased arginase activity, and promotion of tissue repair and immunoregulation [101] [102]. The M2 phenotype can be further subdivided into M2a, M2b, M2c, M2d, and M2eff subtypes based on specific inducing factors and functional specializations [101].
Key Signaling Pathways in Polarization
The following diagram illustrates the core signaling pathways governing macrophage polarization, highlighting potential therapeutic intervention points.
Quantitative Analysis of Modulation Strategies
Comparative Cytokine Secretion Profiles
The efficacy of macrophage polarization strategies is quantitatively reflected in their cytokine secretion profiles. The table below summarizes key cytokine changes across different modulation approaches, providing a basis for comparative evaluation.
Table 1: Cytokine and Gene Expression Changes in Modulated Macrophages
| Modulation Strategy | Target Phenotype | Key Cytokine/Gene Expression Changes | Experimental Model |
|---|---|---|---|
| Fluvastatin (10 µM) [103] | M1 Suppression / M2 Enhancement | ↓ M1 Markers: NFκB, IL-1β, IL-6, iNOS (gene expression); TNF-α, IL-1β, IL-6 (protein); iNOS activity↑ M2 Markers: Arg-1, TGFβ (gene expression); IL-10 (protein) | Human monocyte-derived macrophages (M0, M1, M2) |
| miR-210 Deletion [104] [105] | Impaired M2 Polarization / Pro-inflammatory skew | ↑ in KO M0: IL-6, TNF-α, IL-1β (protein)↓ in KO M2: Incomplete polarization, reduced proliferation | Bone marrow-derived macrophages from miR-210 KO mice |
| MSC Exosomes (miR-146a) [14] | M2 Promotion | Induced M2 differentiation via JAK1/STAT1/STAT6 pathway | Models of systemic lupus erythematosus and ulcerative colitis |
| MSC Exosomes (miR-125a-3p) [14] | T-cell Immunomodulation | Suppressed T cell activity, balanced Th1/Th2, inhibited Th17 expansion | In vitro and preclinical models |
| MSC Exosomes (miR-23b-3p / miR-144-3p) [106] | Fibroblast Activation | Promoted fibroblast proliferation, migration, and collagen synthesis via PTEN/PI3K/Akt | NIH3T3 fibroblasts |
Efficacy of Pharmacological vs. Biological Modulators
Different modulation strategies offer distinct advantages and mechanisms. The table below provides a direct comparison of a pharmacological agent (fluvastatin) and biological agents (MSC exosomes) based on quantitative data.
Table 2: Comparative Anti-inflammatory Efficacy of Key Modulators
| Parameter | Fluvastatin [103] | MSC Exosomes (General) [14] [30] |
|---|---|---|
| Primary Mechanism | Inhibition of the mevalonate pathway | Paracrine delivery of miRNAs, proteins, and growth factors |
| Effect on M1 Markers | Significant reduction in pro-inflammatory genes (NFκB, IL-1β, IL-6, iNOS) and protein (TNF-α, IL-1β, IL-6) | Shifts macrophage balance from M1 to M2; context-dependent (e.g., can stimulate M1 in some fibrotic models [14]) |
| Effect on M2 Markers | Significant enhancement of anti-inflammatory genes (Arg-1, TGFβ) and protein (IL-10) | Promotes M2 polarization via specific miRNA cargo (e.g., miR-146a) |
| Downstream Functional Effects | N/D in profiled study | Activates Akt, ERK, STAT3 signaling; induces growth factors (HGF, IGF1, NGF, SDF1); enhances fibroblast proliferation & migration [30] |
| Key Advantage | Well-defined, druggable pathway; effects reversed by mevalonate/GGPP | Multi-modal action, low immunogenicity, inherent tissue-homing capabilities |
Experimental Protocols for Key Methodologies
This standardized protocol is essential for screening the effects of pharmacological compounds like fluvastatin on human macrophage polarization.
- Monocyte Isolation: Isolate human mononuclear cells from buffy coats using density gradient centrifugation with Lymphocyte Separation Medium. Isolate monocytes via adhesion to plastic for 4 hours.
- Macrophage Differentiation: Culture adhered monocytes for 6 days in RPMI-1640 medium supplemented with 10% FBS and 80 ng/mL M-CSF. Change the medium three times during this period.
- Macrophage Polarization:
- M1 Polarization: Treat differentiated macrophages (M0) with a combination of LPS (100 ng/mL) and IFN-γ (20 ng/mL) for 48 hours.
- M2 Polarization: Treat M0 macrophages with a combination of IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for 48 hours.
- Compound Treatment: Co-treat polarized macrophages with the test compound (e.g., Fluvastatin at 10 µM). To investigate pathway dependence, add intermediates of the mevalonate pathway such as mevalonic acid (10 µM) or geranylgeranyl pyrophosphate (20 µM).
- Downstream Analysis: After 48 hours, harvest cells and supernatants for analysis by qRT-PCR, ELISA, flow cytometry (surface markers: CD14, CD16, CD36, CD163, CD206), and Griess assay (for iNOS activity).
This two-part protocol evaluates the direct effect of MSC-Exos on macrophage polarization and the subsequent paracrine impact on fibroblast behavior, central to the thesis context.
A. MSC Exosome Isolation and Characterization:
- Culture MSCs in exosome-free medium for 48-72 hours.
- Isolate exosomes from conditioned medium by sequential ultracentrifugation: 2,000 g (20 min) to remove cells, 10,000 g (30 min) to remove debris, and 100,000 g (70 min) to pellet exosomes. Wash the pellet in PBS and repeat the ultracentrifugation.
- Characterize exosomes by electron microscopy for size/morphology, immunoblotting for surface markers (CD63, CD81, CD9), and protein quantification.
B. Functional Co-culture and Analysis:
- Macrophage Uptake & Polarization: Treat differentiated macrophages (as in Protocol 1, step 2-3) with MSC-Exos (e.g., 10 µg/mL). Assess uptake via fluorescent labeling (e.g., PKH26) and monitor polarization shifts via qPCR for M1/M2 markers and cytokine ELISA.
- Fibroblast Activation Assay: Treat fibroblasts (e.g., NIH3T3) with MSC-Exos or with conditioned medium from macrophage-exosome cultures.
- Proliferation: Assess using Bromodeoxyuridine (BrdU) incorporation assay.
- Migration: Measure using a wound healing (scratch) assay.
- Collagen Synthesis: Quantify via collagen contraction assay and expression of COL I and α-SMA by immunostaining or qPCR.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Macrophage Polarization and Exosome Research
| Reagent / Tool | Specific Example | Primary Function in Research Context |
|---|---|---|
| Polarizing Cytokines | IFN-γ, LPS (for M1); IL-4, IL-13, IL-10 (for M2) [101] [103] | Directs naive or M0 macrophages toward specific pro- or anti-inflammatory phenotypes. |
| Pharmacologic Inhibitor | Fluvastatin [103] | Probing the role of the mevalonate pathway in macrophage polarization and cytokine secretion. |
| MSC Exosomes | Isolated from Bone Marrow, Adipose, or Umbilical Cord MSCs [14] [27] | Serves as a biological modulator of macrophage polarization and a vehicle for targeted miRNA delivery. |
| Flow Cytometry Antibodies | CD14, CD16, CD36, CD163, CD206 [103] | Identifies and characterizes macrophage populations and their activation states based on surface marker expression. |
| miRNA Mimics/Inhibitors | miR-210, miR-146a, miR-23b-3p, miR-144-3p [106] [14] [104] | Investigates the functional role of specific miRNAs in regulating signaling pathways that control polarization. |
MSC Exosomal miRNAs: Integrating Macrophage Modulation and Fibroblast Research
The therapeutic potential of MSC-Exos lies in their cargo, which includes a diverse array of miRNAs that can simultaneously modulate macrophage polarization and directly influence fibroblast behavior. This dual functionality creates a powerful regenerative signaling network.
miRNA-Mediated Crosstalk
The following diagram synthesizes the crosstalk between macrophages and fibroblasts, orchestrated by MSC exosomal miRNAs, which forms the core of the thesis context.
Key Mechanistic Insights
- Direct Fibroblast Activation: MSC-Exos deliver specific miRNAs, such as miR-23b-3p and miR-144-3p, which directly target the PTEN gene in fibroblasts. This inhibition activates the PI3K/Akt signaling pathway, a master regulator driving fibroblast proliferation, migration, and collagen synthesis—fundamental processes in tendon-bone healing and tissue repair [106].
- Indirect via Macrophage Reprogramming: MSC-Exos simultaneously promote a pro-reparative tissue environment by polarizing macrophages toward the M2 phenotype. This is mediated by exosomal miRNAs like miR-146a and miR-210 [14] [104]. The resulting M2 macrophages secrete anti-inflammatory cytokines (e.g., IL-10, TGF-β) that further support fibroblast activation and tissue remodeling while resolving damaging inflammation [101] [14].
- Metabolic Coordination: The promotion of the M2 phenotype by miRNAs like miR-210 is linked to metabolic reprogramming, enhancing oxidative phosphorylation, which is the preferred metabolic state for anti-inflammatory and reparative macrophage functions [104] [105]. This ensures that macrophages are metabolically equipped to support the energy-intensive process of tissue repair.
In the field of regenerative medicine, the role of mesenchymal stem cell (MSC)-derived exosomal miRNAs in modulating fibroblast behavior represents a promising therapeutic frontier. Functional validation of these interactions is a critical step in translating basic research into clinical applications, requiring a robust framework of advanced in vitro and in vivo models. Organotypic co-culture assays have emerged as indispensable tools for mimicking the complex tissue microenvironment, allowing for the precise investigation of paracrine signaling and cell-cell interactions [107]. These assays provide a controlled yet physiologically relevant platform to dissect the molecular mechanisms by which MSC-derived exosomal miRNAs influence fundamental processes such as fibroblast proliferation and migration—key events in wound healing, fibrosis, and cancer progression [14] [1].
The scientific community is increasingly moving toward a paradigm that prioritizes physiologically relevant models over conventional monolayer cultures. This shift is driven by the recognition that traditional in vitro systems often fail to recapitulate the spatial organization, stoichiometry, and biomolecular gradients present in native tissues [107]. Furthermore, the integration of patient-derived primary cells into these models adds a layer of personalized medicine, enabling the assessment of patient-specific responses and the development of tailored therapeutic strategies [108]. The subsequent validation of findings from sophisticated in vitro models in living organisms through in vivo animal models remains the gold standard for establishing therapeutic efficacy and safety, creating a comprehensive validation pipeline from bench to bedside [109] [2].
Organotypic Co-culture Assays: Methodologies and Applications
Microfluidic-Based Co-culture Models
Microfluidic technology has revolutionized organotypic modeling by enabling the precise spatial patterning of different cell types within a three-dimensional (3D) hydrogel matrix, thereby closely mimicking the architecture of in vivo tissues.
- Device Fabrication and Design: A common design involves a polydimethylsiloxane (PDMS)-based device featuring concentric chambers. The inner chamber, typically with a diameter of 3 mm, is designed to host the "tumor" or region of interest, such as a 3D hydrogel embedded with breast cancer cells. This inner chamber is bordered by an outer "stromal" region, separated by trapezoidal microposts (spaced 100 μm apart) that prevent hydrogel leakage while allowing free diffusion of biomolecules and facilitating cell-cell interactions [107].
- 3D Cell Culture and Hydrogel Preparation: To model invasion in a 3D microenvironment, cells like SUM-159 breast cancer cells are suspended at a high density (e.g., 15 million cells/mL) in a mixture of Matrigel and Collagen I (final collagen concentration of 1 mg/mL). This mixed hydrogel-cell solution is injected into the tumor region and allowed to polymerize. The stromal region is subsequently filled with a Collagen Type I solution (2.0 mg/mL), which can be embedded with patient-derived fibroblasts, such as Cancer-Associated Fibroblasts (CAFs) or Normal Fibroblasts (NFs), at a density of 50,000 cells/mL [107].
- Functional and Molecular Readouts: These models permit real-time, high-resolution imaging of dynamic processes like cancer cell invasion. Functional metrics, including migration speed and distance, can be quantified at a single-cell level. Following functional assessment, the model allows for integrated transcriptome profiling of the interacting cells to identify differentially expressed genes, such as GPNMB (Glycoprotein Non-Metastatic B), which was found to be upregulated in cancer cells in response to CAFs and played a key role in enhancing invasion [107].
Fibroblast-Keratinocyte Co-culture in Wound Healing
Direct co-culture systems have been effectively used to study the interactions between dermal fibroblasts and epidermal keratinocytes, which are crucial for skin wound healing.
- Direct Contact vs. Transwell Co-culture: In a direct contact system, human dermal fibroblasts and keratinocytes, stained with different fluorescent dyes, are cultured together. A control is often established using a Transwell setup, which allows for the exchange of soluble factors but prevents direct physical contact between the two cell types [110].
- Proliferation and Migration Assessment: Keratinocyte proliferation can be monitored over time, revealing that direct contact with fibroblasts significantly enhances keratinocyte growth during the early culture stage (first 5 days). Furthermore, keratinocyte migration, as measured by a scratch wound healing assay, is markedly enhanced in direct co-culture but not in the Transwell system, underscoring the importance of direct cell-cell contact [110].
- Molecular Mechanism Elucidation: Analysis of cytokine levels in the co-culture medium often reveals a correlation between enhanced keratinocyte migration/proliferation and elevated levels of Heparin-binding EGF-like Growth Factor (HB-EGF), IL-1α, and TGF-β1. The central role of HB-EGF can be confirmed by neutralizing antibodies, which significantly inhibit the observed stimulatory effects. Furthermore, using siRNA to knock down IL-1α and TGF-β1 in fibroblasts leads to reduced HB-EGF production and subsequent impairment of keratinocyte proliferation, defining a key molecular axis [110].
Table 1: Key Quantitative Findings from Fibroblast-Keratinocyte Co-culture Studies
| Functional Parameter | Experimental Condition | Key Finding | Reference |
|---|---|---|---|
| Keratinocyte Proliferation | Early stage (first 5 days) with direct fibroblast contact | Significant increase in proliferation rate | [110] |
| Keratinocyte Migration | Direct contact co-culture | Enhanced migration (scratch wound closure) | [110] |
| Molecular Mediators | Neutralization with anti-HB-EGF antibody | Greatest inhibition of proliferation and migration | [110] |
| Cytokine Production | Co-culture with direct contact | Upregulated HB-EGF, IL-1α, and TGF-β1 | [110] |
Quantitative Data from Co-culture Assays
The implementation of these organotypic assays generates critical quantitative data that validates the functional role of MSC exosomal components and other stromal interactions.
Table 2: Functional Outcomes in Microfluidic Organotypic Co-culture Models
| Cell Types Co-cultured | Functional Assay | Key Quantitative Outcome | Identified Molecular Mediator |
|---|---|---|---|
| Breast Cancer Cells + CAFs | 3D invasion in microfluidic device | Increased cancer cell migration speed and invasion distance | Upregulation of GPNMB in cancer cells [107] |
| Breast Cancer Cells + NFs | 3D invasion in microfluidic device | Lesser effect on cancer cell invasion compared to CAFs | - |
| Lymphatic Endothelial Cells + TDFs | Tubular lymphangiogenesis assay | Increased sprout length and number; altered permeability | Patient-specific upregulation of pro-lymphangiogenic genes (e.g., IGF-1) [108] |
In Vivo Animal Model Validation
In vivo models provide the essential pathophysiological context to confirm findings from in vitro co-culture systems and assess therapeutic potential.
Murine Wound Healing Models
- Model Establishment: A common in vivo model involves creating full-thickness skin wounds on mice. For instance, 8- to 12-week-old male C57BL/6 J mice are anesthetized, and wounds are created on the dorsal skin using a 5-mm disposable biopsy punch [109].
- Intervention and Analysis: The therapeutic agent (e.g., MSC-derived exosomes, pharmacological compounds) can be applied topically or administered systemically. Wound tissue is harvested at various time points, fixed, and sectioned for histological and immunohistochemical analysis. For example, immunohistochemistry for stathmin on sectioned wound tissues can reveal its expression and localization during the healing process [109].
Insights into Molecular Mechanisms from In Vivo Studies
In vivo studies have been instrumental in delineating key signaling pathways that control fibroblast behavior:
- The p38/Stathmin Axis: Research on human dermal fibroblasts (HDFs) has shown that lipopolysaccharide (LPS) activation of the p38/MAPK pathway leads to increased stathmin expression, which promotes microtubule (MT) depolymerization. This depolymerization is a critical driver of HDF migration and proliferation. In vivo, this pathway can be manipulated using pharmacological inhibitors or activators. For instance, the p38/MAPK inhibitor SB203580 suppresses MT depolymerization and HDF migration/proliferation. Conversely, overexpression of a constitutively active mutant of MKK6 (MKK6(Glu)), an upstream activator of p38, results in MT depolymerization and subsequently promotes HDF migration and proliferation, accelerating wound healing [109].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these functional validation experiments relies on a suite of specialized reagents and tools.
Table 3: Research Reagent Solutions for Functional Validation Assays
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| Patient-Derived Fibroblasts | Provides physiologically relevant, patient-specific stromal component for co-culture. | Cancer-Associated Fibroblasts (CAFs), Tumor-Derived Fibroblasts (TDFs) [107] [108] |
| Microfluidic Devices | Creates organotypic architecture for studying cell migration and invasion in 3D. | PDMS devices with concentric chambers and microposts [107]. |
| 3D Hydrogels | Provides a biomimetic extracellular matrix for 3D cell culture. | Matrigel, Collagen I mixtures [107]. |
| Small Interfering RNA (siRNA) | Knocks down gene expression to validate functional mechanisms. | siRNA targeting genes of interest (e.g., GPNMB, stathmin) [107] [109]. |
| Pathway Inhibitors/Activators | Pharmacologically probes specific signaling pathways. | SB203580 (p38/MAPK inhibitor), Taxol (microtubule stabilizer) [109]. |
| Recombinant Adenovirus | Genetically modifies cells to overexpress or constitutively activate genes. | MKK6(Glu) mutant to activate p38/MAPK signaling [109]. |
Integrated Signaling Pathways
The molecular mechanisms governing fibroblast proliferation and migration, as identified through the described models, often converge on specific, well-defined pathways. The diagram below illustrates the key p38/Stathmin signaling axis that modulates microtubule dynamics to control these processes.
Furthermore, the experimental workflow for validating the functional role of a gene of interest (GOI) using integrated in vitro and in vivo approaches can be summarized as follows:
The synergy between advanced organotypic co-culture assays and in vivo animal models creates a powerful and rigorous framework for the functional validation of MSC exosomal miRNAs and their targets in fibroblast biology. The progression from microfluidic devices that capture patient-specific stromal interactions to mechanistic in vivo studies ensures that therapeutic discoveries are both biologically relevant and clinically translatable. As the field advances, the standardization of these models and the incorporation of more complex multi-cell type systems will further enhance their predictive power, accelerating the development of novel regenerative and anti-fibrotic therapies.
Conclusion
MSC exosomal miRNAs represent a powerful, cell-free therapeutic modality with precise control over fibroblast behavior, central to tissue regeneration. The foundational research has identified a core set of miRNAs that robustly enhance fibroblast proliferation and migration through well-defined pathways. Methodological advances now enable efficient isolation and engineering of these vesicles to boost their regenerative cargo. While comparative studies validate the therapeutic promise of MSC exosomes and their mimics, challenges in scalable production and targeted delivery remain. Future directions must focus on standardizing bioengineering protocols, conducting large-scale preclinical trials, and navigating the regulatory pathway for clinical deployment. The translation of this knowledge holds immense potential for revolutionizing treatments for chronic wounds, fibrosis, and degenerative diseases, ultimately bridging a critical gap between regenerative biology and clinical practice.
References
- 1. miRNAs from mesenchymal-stem-cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538106/]
- 2. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 3. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 4. The potential of exosomes in regenerative medicine and ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1539714/full]
- 5. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 6. Engineerable mesenchymal stem cell-derived extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04490-4]
- 7. Mesenchymal Stem-Cell-Derived Exosomes and MicroRNAs [https://www.mdpi.com/2073-4409/14/13/1018]
- 8. Regenerative medicine and tissue engineering potential of ... [https://www.sciencedirect.com/science/article/abs/pii/S0301468125000787]
- 9. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 10. Exosome miRNA sorting controlled by RNA-binding protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540272/]
- 11. Regulation of cargo selection in exosome biogenesis and ... [https://www.nature.com/articles/s12276-024-01209-y]
- 12. Exosomal microRNAs derived from mesenchymal stem cells [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-020-00650-6]
- 13. Applications of Exosomal miRNAs from Mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11048182/]
- 14. Mesenchymal Stem-Cell-Derived Exosomes and MicroRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249468/]
- 15. A Debate on microRNA Sorting Into Extracellular Vesicles [https://www.sciencedirect.com/science/article/abs/pii/S0023683724018841]
- 16. The microRNA regulatory landscape of MSC-derived ... [https://www.nature.com/articles/s41598-018-19581-x]
- 17. CRISPR-based dissection of microRNA-23a ~ 27a ~ 24-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11364504/]
- 18. Extracellular vesicle microRNA cargoes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551403/]
- 19. Exosomal microRNAs from Mesenchymal Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC10352215/]
- 20. Targeting PI3K/AKT signaling for treatment of idiopathic ... [https://www.sciencedirect.com/science/article/pii/S2211383521002719]
- 21. Fibroblast-Induced Paradoxical PI3K Pathway Activation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9203999/]
- 22. Toll-Like Receptor-4 Signaling Drives Persistent Fibroblast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5649394/]
- 23. Cell autonomous TLR4 signaling modulates TGF-β ... [https://www.sciencedirect.com/science/article/pii/S2405844025008321]
- 24. LATS2 degradation promoted fibrosis damage and rescued by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10924340/]
- 25. Role of fibroblasts in wound healing and tissue remodeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9578548/]
- 26. emerging therapeutic opportunities for wound healing | Stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03345-0]
- 27. The potential use of mesenchymal stem cells-derived ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-022-01017-9]
- 28. Exosome Derived from Mesenchymal Stem Cells Alleviates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9467851/]
- 29. Fibroblast exosomes promote wound healing and improve the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554163/]
- 30. Mesenchymal Stem Cell Exosomes Induce Proliferation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4499790/]
- 31. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1641709/full]
- 32. Engineering mesenchymal stem cells to improve their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6161586/]
- 33. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 34. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://www.mdpi.com/2313-7673/10/8/546]
- 35. Small extracellular vesicles from human bone marrow ... [https://www.nature.com/articles/s41598-025-04057-6]
- 36. Exosome Isolation by Ultracentrifugation and Precipitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8088761/]
- 37. Confirming size-exclusion chromatography as a clinically ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-024-00007-2]
- 38. Dual size-exclusion chromatography for efficient isolation ... [https://www.nature.com/articles/s41598-020-80514-8]
- 39. Identification of an Exosomal miRNA Signature in Newly ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2025.14780/full]
- 40. Comprehensive profiling of plasma and exosomal ... [https://www.nature.com/articles/s41598-025-21269-y]
- 41. Recent Advances in Exosome RNA-Sequencing ... [https://rna.cd-genomics.com/resource/exosomal-rna-seq-2025.html]
- 42. Prediction of exosomal miRNA-based biomarkers for liquid ... [https://www.nature.com/articles/s41598-025-15814-y]
- 43. qRT-PCR Analysis for Evolution and Validation of ... [https://bio-protocol.org/exchange/minidetail?id=9068056&type=30]
- 44. Comparisons of miRNA profiles of exosomes derived from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359900/]
- 45. Validation of novel exosomal miRNAs identified by next- ... [https://pubmed.ncbi.nlm.nih.gov/39955162/]
- 46. Contractile fibroblasts form a transient niche for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480840/]
- 47. Automated prediction of fibroblast phenotypes using ... [https://www.nature.com/articles/s41467-025-58082-0]
- 48. MSC-derived extracellular vesicles: Precision miRNA ... [https://www.sciencedirect.com/science/article/pii/S2352320425000604]
- 49. Dynamic fibroblast–immune interactions shape recovery ... [https://www.nature.com/articles/s41586-025-09449-2]
- 50. Precision exosome engineering for enhanced wound healing ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06578-0]
- 51. Umbilical Cord-Derived Mesenchymal Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5031180/]
- 52. Unveiling exosomes in combating skin aging: insights into ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04620-y]
- 53. Exosome Intervention: A Novel Strategy for the Treatment ... [https://www.dovepress.com/the-potential-application-of-exosomes-as-therapeutic-agents-carriers-a-peer-reviewed-fulltext-article-IJN]
- 54. Mesenchymal stem cells derived exosomes: a new era in cardiac regeneration | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04123-2]
- 55. The role of synovial mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237890/]
- 56. Mesenchymal Stem Cell-Derived Exosomal microRNAs in Cardiac Regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10742005/]
- 57. The Network of Exosomes miRNA and p‐MLC2 Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616266/]
- 58. Potential cardiac-derived exosomal miRNAs involved in ... [https://www.nature.com/articles/s41598-024-75517-8]
- 59. Bone marrow mesenchymal stem cell exosome-derived ... [https://www.nature.com/articles/s41598-025-22511-3]
- 60. Exosome-Based Drug Delivery: Translation from Bench to Clinic [https://pmc.ncbi.nlm.nih.gov/articles/PMC10459753/]
- 61. Mesenchymal stem cell-derived exosomes as cell-free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632147/]
- 62. Recent advances in scalable exosome production [https://www.sciencedirect.com/science/article/pii/S2096691125000196]
- 63. Towards implementing optimized methodologies and in ... [https://www.sciencedirect.com/science/article/pii/S092809872500154X]
- 64. Quantification and characterization of extracellular vesicles ... [https://pubmed.ncbi.nlm.nih.gov/41248957/]
- 65. siRNAs, saRNAs, miRNAs, CRISPR/Cas System [https://nhsjs.com/2025/revolutionizing-gene-editing-techniques-in-medicine-sirnas-sarnas-mirnas-crispr-cas-system/]
- 66. RNAi vs. CRISPR: Guide to Selecting the Best Gene ... [https://www.synthego.com/blog/rnai-vs-crispr-guide/]
- 67. CRISPR GENome and epigenome engineering improves loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272254/]
- 68. MiR-ON-CRISPR: a microRNA-activated CRISPR–dCas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539625/]
- 69. CMN Weekly (24 January 2025) [https://crisprmedicinenews.com/news/cmn-weekly-24-january-2025-your-weekly-crispr-medicine-news/]
- 70. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 71. Preconditioning and Engineering Strategies for Improving the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9124131/]
- 72. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 73. Let-7f miRNA regulates SDF-1α- and hypoxia-promoted ... [https://www.nature.com/articles/s41419-021-03789-3]
- 74. Hypoxic Preconditioning Enhances Biological Function of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5633065/]
- 75. MSCs and Inflammatory Cells Crosstalk in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8120150/]
- 76. Non‑viral transfection methods optimized for miRNA ... [https://www.spandidos-publications.com/10.3892/mmr.2023.12976?text=fulltext]
- 77. Exosomal microRNAs from Mesenchymal Stem Cells: Novel Therapeutic Effect in Wound Healing | Tissue Engineering and Regenerative Medicine [https://link.springer.com/article/10.1007/s13770-023-00542-z]
- 78. Background [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1542008/xml]
- 79. Storage stability of exosomes in different buffers with/ ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725006811]
- 80. Preservation And Stability Of Lyophilized Vs Non-Lyophilized ... [https://www.avanta3.com/blog/preservation-stability-lyophilized-non-lyophilized-exosomes/?srsltid=AfmBOooFbAl9NnQ8iCraIA2ikF_uDcGKY_KGOd9eJx21R5teZJIsZ2jk]
- 81. Exosome-based therapeutics in bone regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512519/]
- 82. Engineered exosomes: a promising approach for overcoming ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03697-0]
- 83. Tridimensional cell culture of dermal fibroblasts promotes ... [https://www.nature.com/articles/s41598-022-23433-0]
- 84. The combined application of exosomes/exosome-based drug ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d4tb01530d]
- 85. Sources to variability in circulating human miRNA signatures [https://pmc.ncbi.nlm.nih.gov/articles/PMC5731815/]
- 86. Exosomal miRNA-188–3p derived from cancer-associated ... [https://www.sciencedirect.com/science/article/pii/S2472630325000718]
- 87. Integrating miRNA profiling and machine learning for ... [https://www.nature.com/articles/s41598-025-99754-7]
- 88. Comparison of methods for miRNA isolation and ... [https://www.nature.com/articles/s41598-020-57659-7]
- 89. Methods for MicroRNA Quantification and Visualization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7848212/]
- 90. Real-Time Quantitation of miRNA [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/microrna-studies/tech-notes/finding-the-best-endogenous-controls-for-real-time-quantitation-.html]
- 91. An improved reference library and method for accurate cell ... [https://www.nature.com/articles/s41467-025-60521-x]
- 92. Therapeutic potential of human umbilical cord mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457780/]
- 93. Adipose-derived stem cell exosomes: emerging roles and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637342/full]
- 94. Injection of human umbilical cord mesenchymal stem cells ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06623-y]
- 95. Diabetic Wound Repair: From Mechanism to Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477442/]
- 96. Effectiveness of personalized continuous care in wound ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1612047/full]
- 97. Clinical evaluation of skin aging: a systematic review [https://www.sciencedirect.com/science/article/abs/pii/S0167494325002511]
- 98. A Multi-Center Clinical Trial to Evaluate the Efficacy of ... [https://pubmed.ncbi.nlm.nih.gov/40280771/]
- 99. June 2025 clinical trial highlights [https://www.pulmonaryfibrosis.org/patients-caregivers/education-resources/clinical-trials-blog/clinical-trials/2025/06/23/june-2025-clinical-trial-highlights]
- 100. Insilico Announces Nature Medicine Publication of Phase ... [https://insilico.com/tpost/tnrecuxsc1-insilico-announces-nature-medicine-publi]
- 101. Macrophages as Multifaceted Orchestrators of Tissue Repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255350/]
- 102. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 103. Anti-inflammatory effect of fluvastatin on polarized ... [https://www.nature.com/articles/s41598-025-02418-9]
- 104. miR-210 promotes the anti-inflammatory phenotype and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361208/]
- 105. miR-210 promotes the anti-inflammatory phenotype and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1633163/full]
- 106. Bone marrow mesenchymal stem cell-derived exosomal ... [https://pubmed.ncbi.nlm.nih.gov/37181002/]
- 107. A Human Organotypic Microfluidic Tumor Model Permits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6664809/]
- 108. Primary head and neck tumour-derived fibroblasts promote ... [https://www.sciencedirect.com/science/article/pii/S2352396421004278]
- 109. Dermal Fibroblast Migration and Proliferation Upon Wounding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8831846/]
- 110. Enhanced Keratinocyte Proliferation and Migration in Co ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0040951]