MSC Exosome Efficacy in Wound Healing: A Comparative Analysis of Performance Across Preclinical Animal Models
This article synthesizes current evidence on the therapeutic performance of mesenchymal stem cell-derived exosomes (MSC-exosomes) in various animal wound models.
MSC Exosome Efficacy in Wound Healing: A Comparative Analysis of Performance Across Preclinical Animal Models
Abstract
This article synthesizes current evidence on the therapeutic performance of mesenchymal stem cell-derived exosomes (MSC-exosomes) in various animal wound models. It provides a foundational understanding of MSC-exosome biology and mechanisms in wound repair, explores methodological considerations for their application in different preclinical models, addresses key challenges and optimization strategies in exosome manufacturing and testing, and offers a critical validation of comparative efficacy across animal species and wound types. Aimed at researchers, scientists, and drug development professionals, this review serves as a comprehensive resource for designing robust preclinical studies and advancing the clinical translation of MSC-exosome-based therapies for wound healing.
Unlocking the Mechanism: How MSC Exosomes Drive Healing at the Cellular Level
Mesenchymal stem cells (MSCs) have long been recognized for their remarkable therapeutic potential in regenerative medicine. Originally valued for their ability to differentiate into multiple cell types, research over the past decade has revealed that their healing capacity is primarily mediated through paracrine signaling rather than direct cellular replacement [1] [2]. Among these paracrine factors, MSC-derived exosomes (MSC-Exos) have emerged as powerful mediators of tissue repair, offering a cell-free alternative that maintains therapeutic benefits while circumventing the risks associated with whole-cell transplantation [3] [4].
MSC-exosomes are nanoscale extracellular vesicles (30-150 nm) that facilitate intercellular communication by transferring bioactive molecules—including proteins, lipids, mRNAs, and microRNAs—from parent MSCs to recipient cells [5] [6]. These vesicles demonstrate multifaceted biological functions including immunomodulation, angiogenesis promotion, and tissue repair, making them promising therapeutic agents for wound healing applications [3]. This guide provides a systematic comparison of MSC-exosome performance across different experimental parameters and wound models, offering researchers evidence-based insights for therapeutic development.
Performance Comparison Across Wound Models and Parameters
Therapeutic Efficacy in Preclinical Wound Models
Table 1: MSC-Exosome Performance Across Different Wound Models
| Wound Model | Exosome Source | Key Outcomes | Mechanistic Insights | Reference |
|---|---|---|---|---|
| Cutaneous wound (mouse) | Umbilical cord MSC | Accelerated wound closure; Enhanced re-epithelialization and angiogenesis | Suppressed AIF nuclear translocation; Upregulated PARP-1/PAR | [2] |
| Burn injury (preclinical models) | Various MSC sources | Enhanced wound closure (SMD=3.97 short-term); Improved angiogenesis (SMD=6.24) | Increased collagen deposition; Modulated inflammatory cytokines | [7] |
| Full-thickness skin wound (mouse) | Umbilical cord blood MSC; Plasma | Accelerated wound healing; Reduced scar width | Reduced TGF-β signaling; Enhanced Wnt pathway activation | [8] |
| Diabetic wounds | MSC-derived EVs | Improved healing in compromised models | Modulated macrophage polarization; Reduced inflammation | [3] [5] |
| Radiation-induced skin injury | Engineered MSC-Exos | Promoted healing of radiation-induced damage | Suppressed inflammatory responses; Modulated macrophage polarization | [3] |
Impact of Production Variables on Exosome Yield and Characteristics
Table 2: Methodological Comparisons in MSC-Exosome Production and Efficacy
| Parameter | Comparison | Key Findings | Implications for Research | |
|---|---|---|---|---|
| Isolation Method | Ultracentrifugation (UC) vs. Tangential Flow Filtration (TFF) | TFF demonstrated statistically higher particle yields than UC | Enhanced production efficiency for clinical translation | [6] |
| Culture Medium | DMEM vs. α-MEM | α-MEM showed higher cell proliferation and particle yields (4,318.72 ± 2,110.22 particles/cell) | Medium selection impacts both cell growth and exosome production | [6] |
| Therapeutic Timing | Pre-treatment vs. Post-treatment (H₂O₂-induced damage) | Both pre- and post-treatment increased cell viability (54.60 ± 3.59% and 52.68 ± 0.49% vs. 37.86% control) | MSC-exosomes effective both prophylactically and therapeutically | [6] |
| Source Efficacy | Bone marrow vs. Adipose vs. Umbilical cord | BM-, AD-, and UC-derived EVs all effective; UC-MSCs with lower immunogenicity | Source selection depends on application requirements | [4] [1] |
| Combination Therapy | MSC-Exos alone vs. with biomaterials | Synergistic application with advanced biomaterials significantly enhanced therapeutic efficacy | Scaffolds provide protective niche for enhanced effect | [3] [7] |
Experimental Protocols and Methodological Insights
Standardized Wound Healing Assessment Protocol
The following methodology, synthesized from multiple studies, represents a comprehensive approach for evaluating MSC-exosome efficacy in cutaneous wound models:
Animal Model Establishment: Utilize 6-8 week old male BALB/c mice (26-30g). Create full-thickness cutaneous wounds under sterile conditions [8].
Exosome Administration: Locally inject MSC-exosomes (concentration: 80-100 μg/mL in PBS) around the wound periphery. Multiple administration timepoints may be used throughout the healing process [8] [2].
Wound Closure Assessment: Document wound healing progression through:
- Daily photographic documentation
- Wound area measurement using ImageJ software
- Calculation of wound closure rate: (Initial area - Remaining area)/Initial area × 100 [8]
Histological and Molecular Analysis: Upon sacrifice, collect tissue samples for:
- Histological examination of re-epithelialization and angiogenesis
- Scar width measurement
- Spatial transcriptomics analysis to investigate heterogeneity of major cell types [8]
Mechanistic Evaluation: Perform immunohistochemistry and Western blotting for key pathway components including TGF-β, Wnt signaling, apoptosis markers (AIF, PARP-1), and macrophage polarization markers [8] [2].
Exosome Isolation and Characterization Workflow
In Vitro Functional Assays
Cell Scratch/Migration Assay:
- Seed human dermal fibroblast-adult cells (HDF-a) in multi-well plates
- Create uniform scratch with pipette tip
- Wash with D-PBS and add serum-free medium with MSC-exosomes (100 μg/mL)
- Capture images at 0, 12, and 24 hours
- Calculate migration area: (A₀ - Aₙ)/A₀ × 100, where A₀ is initial scratch area and Aₙ is remaining area [8]
Cell Proliferation Assay:
- Treat HDF-a cells with MSC-exosomes
- Assess proliferation using standardized assays (e.g., MTT, CCK-8)
- Optimal results observed at 50-100 μg/mL concentration [6]
Apoptosis Suppression Assay:
- Induce apoptosis in HaCaT keratinocytes with H₂O₂
- Treat with MSC-exosomes
- Evaluate apoptosis rates via flow cytometry
- Assess nuclear translocation of apoptosis-inducing factor (AIF) and PARP-1 expression [2]
Signaling Pathways in MSC-Exosome Mediated Repair
The molecular mechanisms through which MSC-exosomes mediate tissue repair involve multiple interconnected signaling pathways. In cutaneous wound healing, MSC-exosomes have been shown to reduce TGF-β signaling while increasing Wnt pathway activation, resulting in improved healing with reduced scar formation [8]. Additionally, they attenuate cell death by suppressing apoptosis-inducing factor (AIF) nuclear translocation and enhancing poly ADP ribose polymerase 1 (PARP-1) and poly (ADP-ribose) (PAR) expression [2].
A critical mechanism involves immunomodulation through regulation of macrophage polarization. MSC-exosomes suppress pro-inflammatory M1 polarization while enhancing anti-inflammatory M2 polarization, creating a microenvironment conducive to tissue repair [3] [5]. They also modulate several key signaling pathways in recipient cells, including PI3K/AKT, JAK/STAT, TGF-β/Smad, and Wnt/β-catenin, collectively coordinating the regeneration process in target tissues [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Research Application | Function | |
|---|---|---|---|---|
| Cell Culture Media | α-MEM, DMEM, RPMI-1640 | MSC expansion and exosome production | α-MEM shows superior cell proliferation and particle yields | [6] |
| Characterization Antibodies | Anti-CD63, Anti-TSG101, Anti-CD9 | Exosome identification and validation | Confirm presence of exosome surface markers | [8] [6] |
| Isolation Systems | Ultracentrifuge, Tangential Flow Filtration | Exosome purification from conditioned media | TFF provides higher yields for large-scale production | [6] |
| Animal Models | BALB/c mice, C57BL/6J mice | In vivo wound healing assessment | BALB/c mice (6-8 weeks) standard for cutaneous wound models | [8] [7] |
| Cell Lines | HDF-a, HaCaT | In vitro mechanistic studies | Assess fibroblast and keratinocyte responses | [8] [2] |
| Imaging & Analysis | TEM, NTA, Western Blot, Spatial Transcriptomics | Exosome characterization and mechanism elucidation | Comprehensive analysis of size, concentration, and molecular effects | [8] [6] |
The accumulated evidence demonstrates that MSC-exosomes represent a promising therapeutic tool for wound repair, with efficacy documented across multiple wound models including cutaneous injuries, burns, and diabetic wounds. The consistency of therapeutic outcomes—accelerated wound closure, enhanced angiogenesis, reduced inflammation, and improved scar quality—across diverse experimental conditions underscores their robust reparative potential.
Current research indicates that several factors significantly influence therapeutic outcomes:
- Source selection (umbilical cord, bone marrow, adipose tissue)
- Isolation methodology (with TFF outperforming ultracentrifugation for yield)
- Dosage and administration timing (effective both pre- and post-injury)
- Combination strategies (enhanced efficacy with biomaterial scaffolds)
For drug development professionals, these findings support continued investment in MSC-exosome therapeutics while highlighting the importance of standardization in production protocols and mechanistic understanding. Future research directions should prioritize clinical translation through optimized delivery systems, enhanced targeting strategies, and comprehensive safety profiling—paving the way for a new generation of cell-free regenerative therapies.
The therapeutic potential of Mesenchymal Stem Cell (MSC) transplantation, once attributed primarily to cell differentiation and replacement, is now understood to be largely mediated by paracrine factors released by these cells [9] [10] [11]. Among these factors, exosomes—nanoscale extracellular vesicles ranging from 30-150 nm in diameter—have emerged as pivotal mediators of intercellular communication and the principal effectors of tissue repair and immunomodulation [9] [10] [11]. These vesicles serve as protective carriers for a diverse array of bioactive molecular cargo, including proteins, lipids, mRNAs, and microRNAs (miRNAs), which they deliver to recipient cells to alter gene expression and cellular function [10] [12] [13]. The composition of this cargo is not random; it is a selectively packaged reflection of the parent MSC's source and physiological state, endowing exosomes with the ability to coordinate complex processes such as angiogenesis, immunoregulation, and extracellular matrix remodeling [9] [12] [5]. This article delves into the key molecular components of MSC-derived exosomes, comparing their performance and mechanisms across different experimental wound models, thereby providing a crucial resource for researchers and drug development professionals in the field of regenerative medicine.
Decoding the Cargo: Core Molecular Components of MSC Exosomes
The therapeutic efficacy of MSC exosomes is governed by their molecular payload. The tables below catalog the critical growth factors, miRNAs, and proteins identified in MSC exosomes, along with their primary documented functions.
Table 1: Key Growth Factors and Proteins in MSC Exosomes and Their Functions
| Molecular Cargo | Type | Primary Documented Functions | Key References |
|---|---|---|---|
| TGF-β1 (Transforming Growth Factor Beta 1) | Growth Factor | Immunoregulation, inhibition of epithelial-mesenchymal transition, fibrosis modulation | [9] [12] |
| HGF (Hepatocyte Growth Factor) | Growth Factor | Immunoregulation, tissue repair, stimulation of hepatocyte proliferation | [10] [12] |
| IL-10 (Interleukin 10) | Cytokine | Anti-inflammatory signaling, immunomodulation | [10] [12] |
| VEGF (Vascular Endothelial Growth Factor) | Growth Factor | Stimulation of angiogenesis, fundamental for tissue repair | [10] |
| EMMPRIN (Extracellular Matrix Metalloproteinase Inducer) | Protein | Stimulation of angiogenesis | [10] |
| MMP-9 (Matrix Metalloproteinase 9) | Enzyme | Stimulation of angiogenesis, extracellular matrix remodeling | [10] |
| Tetraspanins (CD63, CD81, CD9) | Membrane Proteins | Common exosome surface markers used for isolation and characterization | [9] [10] |
| HSPs (Heat Shock Proteins: HSP60, HSP70, HSP90) | Chaperone Proteins | Stress response, common exosomal proteins | [10] |
| ALIX & TSG101 | Cytosolic Proteins | Involved in MVB biogenesis and exosome formation | [10] |
Table 2: Key MicroRNAs (miRNAs) in MSC Exosomes and Their Target Pathways/Functions
| microRNA (miRNA) | Primary Documented Functions / Target Pathways | Key References |
|---|---|---|
| miR-125a-3p | Suppresses T cell activity, maintains Th1/Th2 balance, inhibits Th17 expansion | [9] [13] |
| miR-146a | Down-regulates the NF-κB pathway, attenuating inflammatory response | [9] [13] |
| miR-21-5p | Inhibits dendritic cell maturation, promotes CCR7 degradation | [9] [13] |
| miR-155-5p | Inhibits B cell proliferation, antibody production, and memory B cell development | [9] |
| miR-223-3p | Prevents dendritic cell maturation by acting on CD83 gene | [13] |
| miR-27a-5p | Promotes odontogenic differentiation via TGFβ1/Smad pathway | [13] |
| miR-451a, miR-205-5p, miR-150-5p, miR-320a | Experimental evidence for inhibition of inflammatory responses (e.g., in rheumatoid arthritis) | [9] |
Cargo in Action: Comparative Performance in Preclinical Wound Models
Systematic reviews and meta-analyses of preclinical studies provide compelling evidence for the therapeutic efficacy of MSC-derived extracellular vesicles (MSC-EVs) in wound healing. A 2025 meta-analysis of 83 preclinical studies demonstrated that MSC-EVs significantly enhance wound closure rate, reduce scar width, and improve blood vessel density and collagen deposition in both diabetic and non-diabetic animal models [14]. The performance, however, varies significantly based on the type of vesicle, the source of MSCs, and the route of administration.
Table 3: Comparative Efficacy of MSC-EVs in Preclinical Wound Models Based on a 2025 Meta-Analysis
| Experimental Variable | Findings from Preclinical Meta-Analysis | Key References |
|---|---|---|
| Overall Efficacy | Significant improvement in wound closure rate, scar width, blood vessel density, and collagen deposition in diabetic and non-diabetic models. | [14] |
| Vesicle Type Comparison | ApoSEVs (Apoptotic Small EVs) showed better efficacy in wound closure and collagen deposition than ApoBDs (Apoptotic Bodies) and sEVs (small EVs). sEVs were more effective than ApoEVs in promoting revascularization. | [14] |
| MSC Source Comparison | ADSCs (Adipose-Derived Stem Cells) demonstrated the best effect on wound closure rate and collagen deposition. BMMSCs (Bone Marrow MSCs) were more effective in promoting revascularization. | [14] |
| Administration Route | Subcutaneous injection outperformed topical dressing/covering in wound closure, collagen deposition, and revascularization. | [14] |
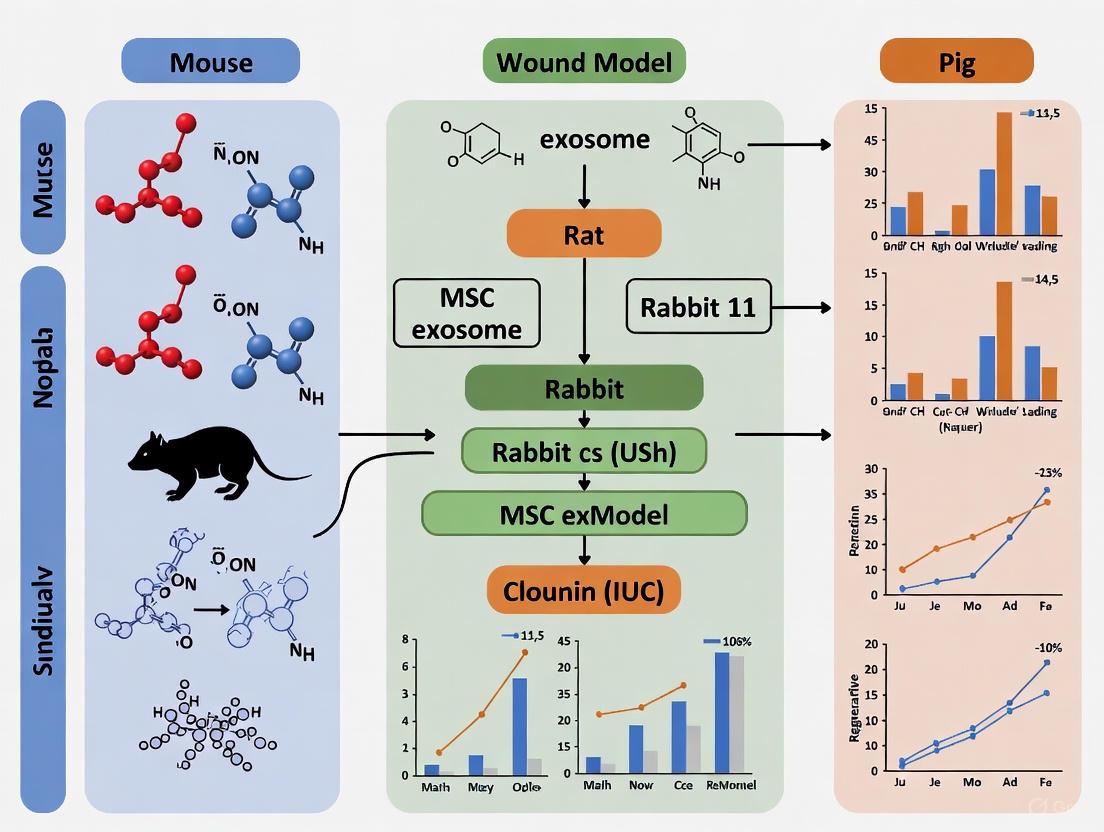
The mechanisms by which this cargo executes its functions are complex and involve the modulation of key signaling pathways in recipient cells. For instance, exosomal miRNAs and proteins can coordinately regulate the PI3K/Akt pathway to promote cell survival and proliferation, the TGF-β/Smad pathway to modulate fibrosis and differentiation, and the Wnt/β-catenin pathway to influence tissue regeneration [15] [5]. The following diagram illustrates a simplified workflow of how MSC exosomes are isolated, characterized, and applied in wound healing research, leading to specific cellular outcomes through these key pathways.
Experimental Workflow in MSC Exosome Wound Healing Research
The molecular cargo delivered by MSC exosomes activates critical signaling pathways within target cells—such as keratinocytes, fibroblasts, and endothelial cells—to promote healing. The diagram below details how specific exosomal components, particularly miRNAs, interact with these pathways to coordinate the repair process.
Exosomal Cargo Activates Key Healing Pathways
Essential Protocols for Exosome Isolation and Characterization
The reproducibility of MSC exosome research hinges on standardized and well-documented experimental protocols. The following sections detail key methodologies for isolating and characterizing exosomes from MSC-conditioned media.
Detailed Protocol: Differential Ultracentrifugation for Exosome Isolation
Differential Ultracentrifugation (DUC) remains the most commonly employed method for exosome isolation, accounting for approximately 56% of all methods used in research [11]. The following steps outline a typical DUC protocol:
- MSC Culture and Conditioned Media Collection: Culture MSCs (e.g., from bone marrow, adipose tissue, or umbilical cord) to 70-80% confluence. Replace the growth medium with a serum-free exosome-depleted medium. After 24-48 hours, collect the conditioned media and perform initial processing.
- Low-Speed Centrifugation: Centrifuge the conditioned media at 300 × g for 10 minutes at 4°C to pellet floating cells.
- Moderate-Speed Centrifugation: Transfer the supernatant to a new tube and centrifuge at 2,000 × g for 20 minutes at 4°C to remove dead cells and large debris.
- High-Speed Centrifugation: Transfer the resulting supernatant to ultracentrifuge tubes and centrifuge at 10,000 × g for 30-45 minutes at 4°C to pellet larger vesicles and organelles.
- Ultracentrifugation for Exosome Pellet: Carefully transfer the supernatant to fresh ultracentrifuge tubes. Pellet the exosomes by ultracentrifugation at 100,000 - 120,000 × g for 70-120 minutes at 4°C.
- Washing and Final Pellet: Discard the supernatant and resuspend the exosome pellet in a large volume of sterile, cold phosphate-buffered saline (PBS). Perform a final ultracentrifugation at 100,000 - 120,000 × g for 70 minutes at 4°C to wash the exosomes. Resuspend the final, purified exosome pellet in a small volume of PBS and aliquot for storage at -80°C [11].
Detailed Protocol: Characterizing Exosomes and Confirming Cargo
Post-isolation, a combination of techniques is required to confirm the identity, purity, and cargo of the isolated exosomes.
- Size and Concentration Analysis (Nanoparticle Tracking Analysis - NTA): Dilute the exosome preparation in PBS and inject it into the NTA system. This analysis provides the particle size distribution profile (confirming the expected 30-150 nm range) and the particle concentration [14].
- Morphology Examination (Transmission Electron Microscopy - TEM): Place a drop of the exosome suspension on a carbon-coated grid, stain with 1-2% uranyl acetate, and image under TEM. This confirms the classic cup-shaped spherical morphology and membrane integrity of the vesicles [14].
- Surface Marker Profiling (Western Blot): Lyse an aliquot of the exosomes and subject it to SDS-PAGE and Western blotting. Probe for the presence of positive markers common to most exosomes (e.g., CD63, CD81, CD9, ALIX, TSG101) and the absence of negative markers (e.g., Grp94, calnexin) to ensure minimal contamination from cellular components [9] [14].
- Cargo Analysis (qRT-PCR and Proteomics): To confirm the presence of functional cargo:
- For miRNA analysis, extract total RNA from the exosomes and perform quantitative reverse transcription polymerase chain reaction (qRT-PCR) using primers specific for miRNAs of interest (e.g., miR-146a, miR-21-5p) [12] [13].
- For protein cargo, subject the exosomal lysate to mass spectrometry-based proteomic analysis to identify and quantify the presence of key growth factors and cytokines (e.g., VEGF, HGF, TGF-β1) [10].
The Scientist's Toolkit: Key Reagents and Materials
Table 4: Essential Research Reagents for MSC Exosome Studies
| Reagent / Material | Function / Application | Example Usage & Notes |
|---|---|---|
| MSC Culture Media | Expansion and maintenance of mesenchymal stem cells. | Often supplemented with FBS that has been ultracentrifuged to remove bovine exosomes. |
| Exosome-Depleted FBS | Provides essential growth factors for cell culture without contaminating the conditioned media with bovine exosomes. | Crucial for producing clean exosome preps for downstream analysis and functional assays. |
| Protease Inhibitors | Prevent degradation of the protein cargo within exosomes during isolation and storage. | Added to conditioned media immediately after collection. |
| PBS (Phosphate Buffered Saline) | Washing and resuspension of the final exosome pellet; also used as a buffer for in vivo injections. | Must be sterile and cold for washing steps. |
| Antibodies for Characterization | Identification and validation of exosomes via Western Blot, Flow Cytometry, or ELISA. | Key targets: CD63, CD81, CD9 (positive markers); Grp94, Calnexin (negative markers). |
| qRT-PCR Assays | Quantification of specific exosomal microRNAs (e.g., miR-146a, miR-21-5p). | Requires specialized RNA extraction kits optimized for low-concentration, small RNAs. |
| Near-Infrared (NIR) Dyes (e.g., DiR, DiD) | Labeling exosomes for in vivo tracking and biodistribution studies. | High signal-to-noise ratio makes them ideal for imaging [10]. |
| Advanced Biomaterials (e.g., Hydrogels) | Serve as scaffolds to enhance exosome retention and provide sustained release at the wound site. | Improves therapeutic efficacy by preventing rapid clearance [15] [3]. |
The systematic comparison of molecular cargo and its context-dependent functionality underscores that MSC exosomes are sophisticated, information-rich nanoparticles. Their performance in wound healing is not a singular phenomenon but a variable outcome influenced by the MSC source, vesicle type, and mode of delivery. The convergence of exosome biology with advanced biomaterials engineering promises to enhance therapeutic outcomes by ensuring targeted and sustained delivery. However, the field must address significant challenges, primarily the high heterogeneity in collection conditions, separation methods, and characterization standards observed across studies [14]. Future research must prioritize standardization in line with MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [14] and explore engineered exosomes to achieve precise control over their cargo and function. By deepening our understanding of the key molecular cargo—the growth factors, miRNAs, and proteins—researchers can unlock the full potential of MSC exosomes as a powerful, cell-free therapeutic paradigm in regenerative medicine.
Exosomes are nano-sized extracellular vesicles, typically ranging from 30 to 150 nm in diameter, that are secreted by virtually all cell types and play a crucial role in intercellular communication [16] [17]. These lipid bilayer-enclosed vesicles transport a diverse cargo of proteins, lipids, mRNAs, miRNAs, and DNA from parent cells to recipient cells, influencing their biological functions [17] [18]. In the context of skin biology and wound healing, exosomes derived from mesenchymal stem cells (MSCs) and resident skin cells have emerged as key regulators of tissue repair and regeneration [19] [20]. Their ability to modulate the behavior of fibroblasts, keratinocytes, and immune cells makes them particularly promising as therapeutic agents for enhancing wound healing, especially in challenging clinical contexts such as diabetic wounds [19] [4].
The therapeutic potential of MSC-derived exosomes (MSC-EVs) has been demonstrated across numerous preclinical models, showing robust benefits in functional recovery, inflammation reduction, and tissue regeneration [4]. Unlike whole-cell therapies, exosomes offer advantages including lower immunogenicity, enhanced stability, and the ability to cross biological barriers [4] [20]. This review systematically examines how exosomes precisely target and modulate the key cellular players in skin repair—fibroblasts, keratinocytes, and immune cells—and provides a comparative analysis of MSC exosome performance across different animal wound models, supported by experimental data and methodologies.
Exosome Modulation of Key Skin Cells
Fibroblasts: Activation and Extracellular Matrix Remodeling
Exosomes profoundly influence fibroblast behavior, directing critical processes of extracellular matrix (ECM) synthesis and remodeling essential for wound healing. MSC-derived exosomes promote fibroblast proliferation, migration, and collagen synthesis, thereby enhancing tissue regeneration [20].
Key Mechanisms:
- Collagen Production: Exosomes from human umbilical cord MSCs (hucMSCs) have been shown to increase collagen type I and type III synthesis in fibroblasts, with a shift toward a more favorable collagen I/III ratio that improves tissue tensile strength [20].
- Matrix Metalloproteinase Regulation: Keratinocyte-derived exosomes carry matrix metalloproteinases (MMP-1, MMP-3, MMP-8, MMP-9) that degrade extracellular matrix components during the early phases of wound repair, facilitating cell migration [21].
- Phenotypic Differentiation: Exosomes can modulate fibroblast differentiation into myofibroblasts, the key effector cells responsible for wound contraction, through transfer of TGF-β and other signaling molecules [21].
Experimental evidence indicates that exosomal miRNAs play a particularly important role in regulating fibroblast function. For instance, miR-21, miR-23a, and miR-125b transferred via exosomes can suppress fibroblast apoptosis and promote proliferation, while miR-29a modulates collagen expression [17].
Keratinocytes: Migration, Proliferation, and Re-epithelialization
Keratinocytes, the predominant cells of the epidermis, are crucial for re-epithelialization during wound healing. Exosomes significantly accelerate this process by enhancing keratinocyte migration and proliferation [21].
Key Mechanisms:
- Accelerated Migration: MSC-derived exosomes have been shown to activate the ERK/MAPK and AKT signaling pathways in keratinocytes, enhancing their migratory capacity [17].
- Proliferation Stimulation: Exosomes from adipose-derived stem cells (ADSCs) promote keratinocyte proliferation through transfer of cyclins and cyclin-dependent kinases [22].
- Differentiation Regulation: Keratinocyte-derived exosomes themselves contain proteins involved in differentiation regulation, including involucrin and kallikrein 7 (KLK7) [21].
The bidirectional communication between keratinocytes and other skin cells via exosomes creates a sophisticated network that coordinates the healing process. For example, exosomes from activated keratinocytes can modulate fibroblast behavior, while fibroblast-derived exosomes can influence keratinocyte migration and differentiation [21].
Immune Cells: Inflammation Control and Macrophage Polarization
Perhaps the most sophisticated function of exosomes in wound healing is their modulation of the immune response. Exosomes can either activate or suppress immune functions depending on their cellular origin and cargo, making them powerful regulators of inflammation [16] [17].
Key Mechanisms:
- Macrophage Polarization: MSC-derived exosomes promote the switch from pro-inflammatory M1 macrophages to anti-inflammatory M2 phenotypes, which is crucial for transitioning from the inflammatory to proliferative phase of healing [17]. This polarization is mediated through exosomal transfer of miRNAs such as let-7b and miR-223 that target inflammatory pathways [23].
- Lymphocyte Regulation: Exosomes can carry immunomodulatory molecules like TGF-β and PD-L1 that suppress excessive T-cell activation, preventing uncontrolled inflammation [23].
- Neutrophil Recruitment: Keratinocyte-derived exosomes regulate neutrophil infiltration and neutrophil extracellular trap (NET) formation through activation of NF-κB and p38 MAPK pathways [17].
In diabetic wound models, MSC-exosomes have demonstrated remarkable ability to correct the prolonged inflammation characteristic of these chronic wounds, resulting in accelerated healing [19] [4].
Table 1: Key Exosomal Cargos and Their Cellular Effects in Wound Healing
| Exosomal Cargo | Source | Target Cell | Biological Effect | Reference |
|---|---|---|---|---|
| miR-21 | MSC, Keratinocyte | Fibroblast | Promotes proliferation and migration | [17] [21] |
| miR-29a | MSC | Fibroblast | Regulates collagen synthesis | [17] |
| miR-125b | MSC | Keratinocyte | Enhances migration capacity | [17] |
| TGF-β | Keratinocyte, Immune cell | Fibroblast, Immune cell | Drives myofibroblast differentiation; immune suppression | [21] [23] |
| MMPs (1,3,8,9) | Keratinocyte | Extracellular matrix | ECM remodeling during migration | [21] |
| PD-L1 | Immune cell, Tumor cell | T-cell | Suppresses T-cell activation | [23] |
| let-7 miRNA family | Keratinocyte | Multiple targets | Regulates proliferation, differentiation, apoptosis | [21] |
Comparative Performance of MSC Exosomes in Animal Wound Models
An umbrella review of meta-analyses evaluating MSC-EVs in preclinical models has demonstrated their high efficacy across diverse disease models, including wound healing [4]. The therapeutic outcomes vary significantly based on MSC source, exosome dosage, and administration route.
Table 2: MSC Exosome Performance Across Animal Wound Models
| Animal Model | MSC Source | Most Effective Dosage | Administration Route | Key Outcomes | Reference |
|---|---|---|---|---|---|
| Diabetic mouse | Umbilical cord | 100 μg per wound | Local injection | Accelerated closure, enhanced angiogenesis, macrophage polarization to M2 | [4] [17] |
| Rat burn model | Adipose tissue | 200 μg/mL | Topical application | Improved re-epithelialization, collagen deposition, neovascularization | [22] [20] |
| Diabetic rat | Bone marrow | 10-100 μg protein | Local injection | Enhanced angiogenesis, fibroblast proliferation, miR-126 mediated repair | [4] [22] |
| Mouse full-thickness wound | Umbilical cord | 1010 particles/mL | In vitro administration | Promoted fibroblast and keratinocyte migration, TGF-β signaling activation | [22] |
| Rabbit ear wound | Bone marrow | 200 μg/0.5 mL | Intravenous | Improved healing quality, reduced scarring, enhanced collagen organization | [20] |
Key Findings from Comparative Analysis:
- Source-Dependent Efficacy: Bone marrow-, adipose-, and umbilical cord-derived EVs consistently demonstrate the highest efficacy in wound models, with modified EVs showing enhanced outcomes [4].
- Dosage Optimization: The therapeutic dose of exosomes commonly ranges from 10 to 100 μg of protein in mouse models, with a threshold beyond which additional exosomes may not provide further benefits [22].
- Route-Specific Effects: Local administration (intradermal, topical) generally provides superior results compared to systemic delivery for cutaneous wounds, as it minimizes clearance and off-target effects [22] [20].
The umbrella review noted that despite high efficacy, methodological quality of preclinical studies was moderate, with frequent risk of bias due to poor randomization and blinding [4]. This highlights the need for standardized protocols in future research.
Experimental Protocols and Methodologies
Standardized Exosome Isolation and Characterization
Isolation Protocols:
- Ultracentrifugation: The most widely used method involving sequential centrifugation steps to isolate exosomes from conditioned media [22]. Despite its popularity, this technique can co-isolate other vesicles and requires significant time [22].
- Size-Exclusion Chromatography (SEC): Separates exosomes based on size, preserving integrity and bioactivity but potentially lacking purity [22].
- Combined Approaches: Techniques combining multiple complementary methods (e.g., ultracentrifugation followed by SEC) demonstrate improved purity and reduced contamination [22].
Characterization Requirements: According to MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines, characterization should include:
- Nanoparticle tracking analysis for size distribution (30-150 nm expected)
- Transmission electron microscopy for morphological assessment
- Western blot for marker proteins (CD63, CD81, CD9, TSG101, ALIX) [22]
- Exclusion of non-vesicular contaminants (lipoproteins, protein aggregates)
Functional Assays for Cellular Modulation
Fibroblast Experiments:
- Migration Assay: Scratch/wound healing assay measuring fibroblast closure over 24-48 hours with exosome treatment
- Proliferation Assay: CCK-8 or EdU incorporation assays comparing fibroblast growth with/without exosomes
- Gene Expression: qRT-PCR analysis of collagen I, collagen III, α-SMA, and elastin expression
- Protein Analysis: Western blot or immunofluorescence for ECM proteins and signaling pathway components
Keratinocyte Experiments:
- Re-epithelialization Model: In vitro scratch assay measuring keratinocyte migration
- Differentiation Assessment: Expression analysis of differentiation markers (keratin 10, involucrin, loricrin)
- Proliferation Tracking: Ki-67 staining or flow cytometry for cell cycle analysis
Immune Modulation Experiments:
- Macrophage Polarization: Flow cytometry for M1 (CD86) and M2 (CD206) surface markers following exosome treatment
- Cytokine Profiling: ELISA or multiplex assays for inflammatory (TNF-α, IL-6) and anti-inflammatory (IL-10, TGF-β) cytokines
- T-cell Suppression Assays: Mixed lymphocyte reactions or T-cell proliferation assays with exosome treatment
Diagram 1: Experimental Workflow for Exosome Research. This diagram outlines the standard methodology for exosome isolation, characterization, and functional cellular assays commonly used in wound healing research.
Signaling Pathways in Exosome-Mediated Wound Healing
Exosomes modulate wound repair through several key signaling pathways that coordinate cellular responses across fibroblasts, keratinocytes, and immune cells.
Wnt/β-catenin Pathway: MSC-exosomes activate Wnt/β-catenin signaling in fibroblasts and keratinocytes, promoting proliferation and migration. This pathway is particularly important for hair follicle neogenesis during wound healing [17].
TGF-β/Smad Pathway: Essential for fibroblast-to-myofibroblast differentiation and collagen production, this pathway is activated by exosomal TGF-β and SMAD proteins transferred from various cell sources [21].
PI3K/Akt Pathway: Activation of this survival pathway by exosomal cargo protects cells from apoptosis and enhances proliferation, particularly important in the high-stress environment of diabetic wounds [17].
NF-κB Pathway: Exosomes from MSCs can suppress excessive activation of the NF-κB pathway in immune cells, reducing pro-inflammatory cytokine production and shifting the balance toward tissue repair [19] [17].
Diagram 2: Key Signaling Pathways in Exosome-Mediated Repair. This diagram illustrates the primary signaling pathways through which exosomes modulate cellular activities during wound healing, highlighting the interconnected nature of these regulatory mechanisms.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Exosome Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, miRCURY Exosome Kit | Rapid isolation from biofluids and conditioned media | Enables high-throughput processing but may compromise purity [22] |
| Characterization Tools | Nanoparticle Tracking Analyzer, CD63/CD81/CD9 antibodies, TSG101 antibody | Size quantification, concentration measurement, protein marker confirmation | MISEV guidelines recommend multiple complementary techniques [22] |
| Cell Tracking Dyes | PKH67, PKH26, DiI, CFSE | Labeling exosomes for uptake and trafficking studies | Potential dye aggregation may cause artifacts; controls essential [22] |
| MSC Culture Media | MesenCult, StemMACS, Custom formulations | Expansion of parent MSC populations | Serum-free, xeno-free media preferred to avoid contaminating vesicles [22] |
| Engineering Tools | Lentiviral vectors, Electroporators, Sonication equipment | Genetic modification of parent cells, cargo loading | Enables production of enhanced functionality exosomes [24] |
| Animal Model Reagents | Streptozotocin (diabetes induction), Imiquimod (inflammatory models) | Creating disease-specific wound models | Critical for evaluating exosome efficacy in pathological conditions [17] |
Exosomes represent a sophisticated biological communication system that coordinates wound healing through precise modulation of fibroblasts, keratinocytes, and immune cells. The cumulative evidence from preclinical models strongly supports the therapeutic potential of MSC-derived exosomes, particularly for challenging wound environments like diabetic ulcers. The comparative analysis presented here reveals that efficacy depends critically on multiple factors including MSC source, exosome dosage, and administration route.
Future research directions should focus on standardizing isolation and characterization protocols, optimizing engineering strategies for enhanced targeting and functionality, and addressing the methodological limitations identified in current preclinical studies. As our understanding of exosome biology deepens, these natural nanocarriers hold exceptional promise for developing effective, cell-free therapies that address the complex challenges of impaired wound healing. The integration of exosome-based approaches with advanced biomaterials and delivery systems represents a particularly promising frontier for clinical translation.
Mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as a revolutionary acellular therapeutic platform in regenerative medicine. These nanoscale extracellular vesicles recapitulate the therapeutic effects of their parent cells by orchestrating key wound healing processes: immunomodulation, angiogenesis, and extracellular matrix (ECM) remodeling. This comprehensive analysis synthesizes current preclinical evidence and mechanistic insights into MSC-Exo functions across various animal wound models. We systematically compare therapeutic efficacy based on exosome sources, isolation methods, and administration protocols, providing researchers with standardized experimental frameworks and technical considerations for translating MSC-Exo biology into clinical applications for tissue repair and regeneration.
The therapeutic paradigm in regenerative medicine has shifted from direct cell transplantation to utilizing the paracrine factors secreted by mesenchymal stem cells (MSCs). Among these factors, extracellular vesicles, particularly exosomes (30-150 nm in diameter), have been identified as primary mediators of MSC functionality [25] [26]. MSC-derived exosomes (MSC-Exos) are lipid-bilayer enclosed vesicles loaded with bioactive molecules including proteins, lipids, mRNAs, and microRNAs that mediate intercellular communication [27]. These nanovesicles offer significant advantages over whole-cell therapies, including lower immunogenicity, absence of tumorigenic risk, ability to cross biological barriers, and easier storage and standardization [25] [28]. As natural bioactive carriers, MSC-Exos precisely regulate the inflammatory response, angiogenesis, and tissue repair processes in target tissues, making them ideal candidates for therapeutic intervention in wound healing [25].
The following diagram illustrates the multifaceted role of MSC-Exos in coordinating wound healing through different cellular pathways:
Diagram Title: MSC-Exo Mediated Coordination of Wound Healing
Comparative Efficacy Across Animal Wound Models
MSC-Exos have demonstrated robust therapeutic potential across diverse preclinical wound models. The table below summarizes quantitative efficacy data from systematic analyses of animal studies, highlighting the consistency of therapeutic effects across different wound types.
Table 1: MSC-Exo Efficacy Across Preclinical Wound Models
| Wound Model Type | Key Therapeutic Effects | Exosome Sources | Efficacy Metrics | Reference Support |
|---|---|---|---|---|
| Diabetic Wounds | Enhanced wound closure, angiogenesis, collagen deposition, macrophage polarization to M2 phenotype | BM-MSC, AD-MSC, UC-MSC | 1.5-2.2-fold faster wound closure; ~80% reduction in pro-inflammatory cytokines | [4] [27] |
| Radiation-Induced Skin Injury | Modulation of macrophage polarization, suppression of inflammatory responses, epithelial regeneration | AD-MSC, UC-MSC | Significant improvement in healing rate; enhanced keratinization and collagen deposition | [3] [27] |
| Burns and Excisional Wounds | Accelerated re-epithelialization, neovascularization, fibroblast proliferation | AD-MSC, BM-MSC | ~50% increase in angiogenesis; 2.1-fold higher collagen synthesis | [4] [29] |
| Ischemic Wounds | Promotion of angiogenesis via VEGF, FGF2, miR-126; improved perfusion | BM-MSC, UC-MSC | 40-60% improvement in blood flow recovery; capillary density increased by 3.1-fold | [30] [27] |
| Complex Perianal Fistulas | Tissue regeneration, modulation of inflammatory microenvironment | AD-MSC, UC-MSC | Fistula closure in preclinical models; reduced inflammation | [25] [4] |
An umbrella review of 47 meta-analyses covering 27 diseases confirmed that MSC-EVs consistently improve functional scores, reduce inflammation, and promote regeneration across neurological, renal, wound healing, liver, musculoskeletal, respiratory, and reproductive disorders [4]. The analysis revealed that bone marrow-, adipose-, and umbilical cord-derived EVs were most effective, with modified EVs showing enhanced outcomes compared to native exosomes [4].
Experimental Protocols for MSC Exosome Research
Standardized Workflow for MSC-Exo Wound Healing Studies
The following diagram outlines a standardized experimental workflow for evaluating MSC-Exo therapeutic efficacy in animal wound models:
Diagram Title: Experimental Workflow for MSC-Exo Wound Studies
Detailed Methodological Considerations
Exosome Production and Characterization
- Cell Culture: MSC-Exos are typically produced using immortalized cell lines grown in serum-free media under controlled conditions [22]. Bioreactor systems, particularly hollow-fiber cartridges, enable large-scale production while maintaining MSC characteristics and preventing senescence [29].
- Isolation Methods: Ultracentrifugation remains the gold standard, though combination approaches (e.g., size-exclusion chromatography with ultrafiltration) improve purity and yield [22]. The Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines provide critical standardization for isolation and characterization protocols [22].
- Characterization: Essential parameters include nanoparticle tracking analysis (NTA) for size distribution (30-150 nm expected), transmission electron microscopy for structural integrity, and western blot or flow cytometry for surface markers (CD9, CD63, CD81) [29].
Animal Model Considerations
- Diabetic Models: Streptozotocin-induced diabetic mice or rats with dorsal excisional wounds represent standard models for diabetic wound healing studies [27].
- Ischemic Models: Hindlimb ischemia or ischemic flap models evaluate pro-angiogenic effects [30].
- Control Groups: Essential controls include vehicle-treated wounds and possibly MSC-transplanted groups for comparative efficacy.
Administration Protocols
- Dosing: Effective doses in rodent models typically range from 10-100 μg of exosomal protein, with optimization required for specific models [22]. For instance, in traumatic brain injury models, 100 μg exosomes per rat showed more significant efficacy than 50 μg or 200 μg doses [22].
- Routes: Local application (topical or peri-wound) enhances target tissue retention compared to systemic administration [22]. Biomaterial-assisted delivery (hydrogels, scaffolds) improves retention and sustained release [3] [30].
Core Healing Pathways: Molecular Mechanisms
Inflammatory Modulation
MSC-Exos precisely regulate the inflammatory phase of wound healing through multiple mechanisms:
- Macrophage Polarization: Exosomal miRNAs (miR-146a, miR-223, let-7b) promote transition of pro-inflammatory M1 macrophages to anti-inflammatory M2 phenotype [27]. This transition is mediated through inhibition of NF-κB signaling and NLRP3 inflammasome activation [27].
- Cytokine Regulation: Engineered AD-MSC exosomes (eXo3) demonstrate potent reduction of inflammatory cytokines (IL-6, IL-8, MCP-1) in primary human fibroblast models [29].
- Lymphocyte Modulation: MSC-Exos influence CD4+ and CD8+ lymphocyte accumulation and activation kinetics in wound beds, though wound closure proceeds normally even in lymphocyte-deficient models [27].
Angiogenic Activation
MSC-Exos promote robust neovascularization through multiple pathways:
- Growth Factor Delivery: Exosomes carry and transfer pro-angiogenic factors including VEGF, FGF2, PDGF, and TGF-β to endothelial cells [30] [27].
- miRNA-Mediated Signaling: miR-126 activates Wnt/β-catenin and PI3K/Akt pathways, while other exosomal miRNAs (miR-21, miR-29a) regulate endothelial cell proliferation and migration [30] [27].
- Notch Pathway Activation: MSC-Exos modulate Notch signaling to stabilize newly formed vessels and promote functional maturation [30].
ECM Remodeling and Tissue Regeneration
MSC-Exos directly influence structural cells to orchestrate tissue repair:
- Fibroblast Activation: Exosomes stimulate fibroblast proliferation, migration, and collagen synthesis (types I and III) through miRNA and protein cargo delivery [29] [27].
- Re-epithelialization: Keratinocyte migration and proliferation are enhanced by MSC-Exos, accelerating wound epithelial coverage [27].
- Collagen Organization: Tuned AD-MSC exosomes promote improved collagen deposition and alignment, enhancing tensile strength in healed tissue [29].
The following diagram summarizes the key molecular pathways through which MSC-Exos coordinate these healing processes:
Diagram Title: Molecular Pathways of MSC-Exo in Wound Healing
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for MSC Exosome Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| MSC Sources | Bone marrow-MSC (BM-MSC), Adipose-derived MSC (AD-MSC), Umbilical cord-MSC (UC-MSC) | Comparative efficacy studies; source selection optimization | AD-MSCs show higher proliferation rates and resistance to senescence; UC-MSCs demonstrate strong immunomodulation [4] [26] |
| Isolation Kits | Ultracentrifugation systems, Size-exclusion chromatography, Precipitation kits, Immunoaffinity capture | Exosome purification from conditioned media | Combination methods improve purity; MISEV guidelines critical for standardization [22] [28] |
| Characterization Tools | Nanoparticle Tracking Analysis, Transmission Electron Microscopy, MACSPlex Exosome Kit | Size distribution, morphology, surface marker validation | CD9, CD63, CD81 as canonical markers; BCA protein quantification for standardization [29] |
| Animal Models | Diabetic (db/db mice), Excisional wound, Burn injury, Ischemic flap | Preclinical efficacy assessment | Streptozotocin-induced diabetes common for diabetic wound models [27] |
| Biomaterial Carriers | Hydrogels, Scaffolds, Wound matrices | Enhanced exosome retention and sustained release | OASIS Wound Matrix shows efficacy in clinical comparisons [30] |
| Analysis Antibodies | CD31, α-SMA, Collagen I/III, TNF-α, IL-10 | Histological and molecular analysis of healing outcomes | M1/M2 macrophage polarization markers critical for inflammation assessment [27] |
| Cell Culture Reagents | Serum-free media, Hollow-fiber bioreactors, 3D culture systems | Large-scale exosome production under controlled conditions | Bioreactor systems maintain genetic stability during expansion [29] |
MSC-derived exosomes represent a promising acellular therapeutic platform that effectively orchestrates the core healing pathways of inflammation modulation, angiogenesis, and ECM remodeling. The comprehensive analysis of preclinical studies demonstrates consistent therapeutic efficacy across diverse wound models, with variations in performance based on MSC source, isolation methods, and administration protocols.
Future research directions should focus on standardization of production protocols, enhancement of targeting capabilities through engineering approaches, and thorough investigation of long-term biodistribution and safety profiles. The integration of biomaterials and combination therapies presents particularly promising avenues for clinical translation. As the field progresses, interdisciplinary collaboration between stem cell biologists, material scientists, and clinicians will be essential to fully realize the potential of MSC exosomes in regenerative medicine.
From Bench to Bedside: Applying MSC Exosomes in Diverse Wound Models
The evaluation of mesenchymal stem cell-derived exosomes (MSC-exosomes) for wound healing therapies relies heavily on appropriate preclinical animal models. The transition from basic research to clinical application depends on selecting models that most accurately recapitulate human disease pathophysiology and treatment responses. This guide provides an objective comparison of the most commonly used animal models in MSC-exosome research, presenting key experimental data and methodologies to inform researchers' experimental design decisions. Understanding the strengths and limitations of each model system is crucial for generating translatable data in regenerative medicine and drug development.
Model Comparison: Physiological and Practical Considerations
Selecting an appropriate animal model requires balancing physiological relevance with practical experimental constraints. The table below compares key characteristics across common preclinical models used in wound healing and exosome therapy research.
Table 1: Physiological and Practical Comparison of Preclinical Models
| Characteristic | Mouse | Rat | Rabbit |
|---|---|---|---|
| Adult Body Weight | 20-40g | 300-500g (LEW/W strain) | 2-5kg |
| Gestation Period | 19-21 days | 21-23 days | 28-35 days |
| Time to Sexual Maturity | 5-6 weeks | 8-10 weeks | 16-24 weeks |
| Genetic Tools Availability | Extensive | Moderate | Limited |
| Surgical Procedure Ease | Challenging due to small size | Good for most procedures | Excellent for complex surgeries |
| Relative Cost | Low | Moderate | High |
| Social Behavior | Territorial, stress-prone in social situations | Social, less stressed with handling | Variable by species |
| Cognitive Testing | Maze learning requires substantial training | Superior maze-learning with strategy | Limited data |
Quantitative Performance Metrics in Stem Cell Research
The yield and quality of biological materials vary significantly across species, impacting experimental design and feasibility. The following data compiled from comparative studies highlights these practical considerations.
Table 2: Adipose-Derived Stem Cell (ASC) Yields Across Species
| Species/Strain | Tissue Source | Average ASC Yield (cells/g tissue) | Proliferation Potential |
|---|---|---|---|
| Mouse | Gonadal fat | Very low (specific numbers not provided) | Moderate |
| Rat (LEW/W) | Gonadal fat | High (∼1.2×10^6 cells/g) | High |
| Rat (WAG) | Gonadal fat | Moderate (∼0.8×10^6 cells/g) | High |
| Rabbit | Subcutaneous fat | Moderate to High | High |
Experimental Protocols for Wound Healing Studies
Exosome Isolation and Characterization
Protocol Source: Adapted from standardized methodologies for MSC-exosome preparation [31] [32]
Materials Required:
- Mesenchymal Stem Cells (bone marrow, adipose, or umbilical cord-derived)
- Serum-free culture medium
- Ultracentrifugation equipment
- Transmission Electron Microscope
- Nanoparticle Tracking Analysis system
- Western blot apparatus
Methodology:
- Cell Culture: Expand MSCs in serum-free medium to avoid contamination with bovine exosomes.
- Conditioned Media Collection: Collect media after 48-72 hours of cell culture.
- Differential Centrifugation:
- 300 × g for 10 min to remove cells
- 2,000 × g for 20 min to remove dead cells
- 10,000 × g for 30 min to remove cell debris
- 100,000 × g for 70 min to pellet exosomes
- Washing: Resuspend exosome pellet in PBS and repeat ultracentrifugation.
- Characterization:
- Size distribution: Nanoparticle Tracking Analysis (30-150 nm expected)
- Morphology: Transmission Electron Microscopy
- Marker expression: Western blot for CD63, CD81, CD9, TSG101
Full-Thickness Excisional Wound Model
Protocol Source: Standardized wound healing assessment across species [20] [33]
Materials Required:
- Animal model (mouse, rat, or rabbit)
- Depilatory cream
- Biopsy punch (size varies by species)
- Test articles (MSC-exosomes in buffer)
- Transparent dressings
- Digital imaging system
- Histology equipment
Methodology:
- Preoperative Preparation:
- Anesthetize animals according to approved protocols
- Remove hair from dorsal area using electric clippers followed by depilatory cream
- Disinfect skin with alternating betadine and 70% alcohol scrubs
Wound Creation:
- Use biopsy punch to create full-thickness excisional wounds
- Recommended sizes:
- Mouse: 6-8 mm diameter
- Rat: 15-20 mm diameter
- Rabbit: 20-25 mm diameter
- Include panniculus carnosus in excision
Treatment Administration:
- Apply exosomes topically in hydrogel vehicle or via intradermal injection
- Include appropriate controls (vehicle alone, untreated)
- Cover with transparent semi-occlusive dressing
Monitoring and Assessment:
- Measure wound area every 2-3 days using digital planimetry
- Calculate percentage closure: [(Initial area - Current area)/Initial area] × 100
- Collect tissue for histology at predetermined endpoints (days 7, 14, 21)
MSC-Exosome Mechanisms in Wound Healing
MSC-exosomes accelerate wound healing through multiple coordinated mechanisms targeting distinct phases of the healing process. The following diagram illustrates key pathways and cellular processes modulated by exosomal cargo.
Mechanisms of MSC-Exosomes in Wound Healing
Model-Specific Applications and Validation
Murine Models: Genetic Manipulation and Immunological Studies
Mice represent the most extensively used model in preliminary MSC-exosome research, primarily due to the availability of sophisticated genetic tools and well-characterized immunological reagents.
Strengths:
- Genetic tractability: Transgenic strains enable study of specific pathways; the first recombinant mouse model was created in 1987, long preceding rat models (2010) [34]
- Humanized models: Can be engineered to express human genes or immune systems
- Cost-effectiveness: Lower maintenance costs and drug requirements due to small size
- Optogenetics: Smaller brain size facilitates light penetration for neurological wound healing studies
Limitations:
- Size constraints: Challenging surgical procedures and limited blood/tissue sampling
- Behavioral differences: Less complex social behaviors compared to rats, limiting psychological aspect of healing studies
- Stress susceptibility: More prone to handling stress, potentially confounding results
Rat Models: Surgical Feasibility and Behavioral Relevance
Rats provide an optimal balance between physiological similarity to humans and practical experimental handling, particularly for complex wound healing scenarios.
Strengths:
- Surgical practicality: Larger size facilitates precise surgical interventions and repeated sampling
- Cardiovascular research: Preferred for cardiovascular studies relevant to wound healing angiogenesis [35]
- Behavioral complexity: Exhibit richer social behaviors that better mimic human responses; critical for studying psychological impacts on healing
- Social behavior validation: In FMR1 gene knockout studies, rats showed social impairments paralleling human autism spectrum symptoms, while mice showed elevated social interactions [35]
Limitations:
- Genetic tools: Fewer available transgenic strains compared to mice
- Space requirements: Higher housing costs than murine models
- Reagent availability: Fewer species-specific antibodies and molecular tools
Rabbit Models: Surgical Precision and Clinical Translation
Rabbits serve as valuable intermediate models bridging small rodents and large animals, particularly for surgical technique development.
Strengths:
- Surgical versatility: Size permits complex surgical procedures mimicking clinical interventions
- Orthopedic research: Well-established for musculoskeletal and cartilage healing studies
- Skin physiology: Larger wound areas enable multiple sampling timepoints
Limitations:
- Cost factors: Higher acquisition and maintenance expenses
- Genetic resources: Limited availability of genetically modified strains
- Molecular tools: Fewer species-specific research reagents
Table 3: Essential Reagents and Tools for MSC-Exosome Wound Healing Research
| Category | Specific Tool/Reagent | Function/Application | Example Products |
|---|---|---|---|
| Exosome Isolation | Ultracentrifugation | Standard method for exosome purification | Beckman Optima XPN series |
| Size-exclusion Chromatography | High-purity exosome isolation | qEV columns | |
| Polymer-based Precipitation | Rapid exosome concentration | ExoQuick-TC | |
| Characterization | Nanoparticle Tracking | Size distribution and concentration | Malvern NanoSight |
| Western Blot | Protein marker validation | CD63, CD81, CD9 antibodies | |
| Electron Microscopy | Morphological confirmation | TEM with negative staining | |
| Animal Management | Anesthesia Equipment | Surgical procedures and imaging | Isoflurane systems |
| Wound Measurement | Quantitative healing assessment | Digital planimetry software | |
| Animal Monitoring | Health and behavior tracking | Automated monitoring systems | |
| Data Analysis | Statistical Software | Experimental data analysis | GraphPad Prism, SPSS |
| Imaging Software | Histological and wound analysis | ImageJ, Zen software | |
| Sample Size Calculation | Experimental power analysis | G*Power software [36] |
Experimental Design Considerations
Sample Size Calculation and Statistical Power
Appropriate sample size determination is critical for generating statistically valid results in preclinical studies.
Power Analysis Method:
- Effect size: Determine minimum clinically significant difference from prior studies
- Standard deviation: Estimate variability from pilot studies or literature
- Statistical power: Typically set at 80% (β=0.2)
- Significance level: Usually α=0.05
- Software tools: G*Power, nQuery Advisor [36]
Resource Equation Method:
- Applied when effect size estimation is unavailable
- Calculate E = Total animals - Total groups
- Maintain E between 10-20 for adequate power [36]
- Example: For 5 groups (control + 4 treatments), 5 animals/group gives E=20
Regulatory and Compliance Aspects
The transition of MSC-exosomes toward clinical application requires adherence to evolving regulatory standards.
Manufacturing Standards:
- Follow Good Manufacturing Practice (GMP) protocols for clinical-grade exosomes
- Implement serum-free media to avoid xenogeneic contaminations
- Establish quality control metrics for potency and homogeneity [31]
Characterization Requirements:
- Define critical quality attributes (size, marker expression, cargo)
- Establish release criteria for batch consistency
- Develop potency assays relevant to wound healing mechanisms [32]
The field of MSC-exosome research continues to evolve with emerging technologies enhancing both model systems and therapeutic applications. Engineered exosomes (eExo) represent the next frontier, with modified surfaces for improved targeting and cargo loading for enhanced therapeutic efficacy [37]. As of January 2025, 64 registered clinical trials investigate MSC-EVs for various diseases, indicating growing translation potential [32].
The selection of an appropriate preclinical model should be guided by specific research questions, with murine models offering genetic flexibility, rat models providing surgical practicality and behavioral relevance, and rabbit models enabling technical refinement. Future research directions include developing standardized protocols for exosome characterization, establishing disease-specific model validation criteria, and creating integrated databases correlating model responses with clinical outcomes. As engineering strategies advance, preclinical models will continue to serve as essential platforms for validating the safety and efficacy of next-generation exosome-based wound healing therapies.
The pursuit of effective therapies for chronic and acute wounds relies heavily on robust preclinical animal models that accurately recapitulate human disease pathophysiology. Among emerging regenerative approaches, mesenchymal stem cell-derived exosomes (MSC-exosomes) have demonstrated remarkable therapeutic potential as a cell-free alternative to whole-cell therapies, offering advantages including low immunogenicity, targeted delivery capabilities, and biochemical stability [38] [31]. However, the translational success of these nanotherapeutics depends on selecting appropriate animal models that faithfully mirror the distinct healing impairments present in different wound types. This review systematically compares three primary wound models—diabetic, burn, and full-thickness excisional wounds—by synthesizing current data on MSC-exosome performance, therapeutic mechanisms, and experimental outcomes. Through objective analysis of quantitative preclinical data and detailed methodological protocols, we provide a framework for researchers to select optimal models for specific research questions and accelerate the development of exosome-based wound therapies.
Comparative Analysis of Wound Models and MSC-Exosome Performance
Model Characteristics and Pathophysiological Features
The selection of an appropriate wound model fundamentally shapes experimental outcomes and therapeutic efficacy assessments. Each major model type recapitulates distinct aspects of human pathophysiology, presenting unique advantages and limitations for evaluating MSC-exosome therapies as detailed in Table 1.
Table 1: Comparative Characteristics of Major Wound Healing Models
| Model Characteristic | Diabetic Wounds | Burn Wounds | Full-Thickness Excisional Wounds |
|---|---|---|---|
| Primary Pathological Features | Impaired angiogenesis, chronic inflammation, hyperglycemia-induced cellular dysfunction [39] | Coagulative necrosis, intense inflammatory response, multi-organ involvement in severe cases [40] | Complete epidermal and dermal removal, well-characterized healing phases [14] |
| Common Induction Methods | Streptozotocin (STZ) injection (T1D); genetically modified db/db mice (T2D) [14] | Thermal, electrical, chemical, or radiation exposure with controlled temperature/duration [40] | Surgical excision of defined diameter using biopsy punch or scalpel [14] |
| Healing Timeline | Delayed (21-28 days or non-healing) [39] | Variable by depth: superficial (7-14 days), deep (weeks to months) [40] | Predictable closure (10-14 days in mice) [14] |
| Key Clinical Relevance | Diabetic foot ulcers, chronic non-healing wounds [39] | Thermal injuries, scar formation, multi-organ dysfunction [40] | Surgical wounds, acute trauma, healing mechanism studies [14] |
| Advantages for Exosome Studies | Tests efficacy in complex metabolic dysfunction; ideal for angiogenesis studies [41] | Evaluates anti-inflammatory and anti-scarring effects; tests tissue regeneration capacity [38] | Standardized, highly reproducible; ideal for mechanism elucidation and screening [14] |
Quantitative Outcomes of MSC-Exosome Therapies Across Models
Recent meta-analyses of preclinical studies provide compelling evidence for the therapeutic efficacy of MSC-exosomes across wound types. Systematic evaluation of 83 preclinical studies revealed that MSC-exosome treatment significantly enhanced multiple healing parameters, with model-specific variations in responsiveness [14]. The following table synthesizes quantitative outcomes from controlled studies comparing MSC-exosome performance across the three wound models.
Table 2: Quantitative Outcomes of MSC-Exosome Treatment Across Wound Models
| Healing Parameter | Diabetic Wounds | Burn Wounds | Full-Thickness Excisional Wounds |
|---|---|---|---|
| Wound Closure Rate | 25-45% acceleration vs. controls [39] [14] | 20-35% improvement in re-epithelialization [38] [40] | 30-50% faster closure in acute models [14] |
| Angiogenesis (Vessel Density) | 1.8-2.5-fold increase in CD31+ vessels [41] [14] | Moderate improvement (1.5-1.8-fold) in neovascularization [38] | Significant enhancement (2.0-2.8-fold) in vascular density [14] |
| Collagen Deposition | Improved organization with 1.5-2.0-fold increase in mature collagen [39] | Enhanced remodeling with reduced hypertrophic scarring [40] | 1.8-2.2-fold increase in collagen density and maturation [14] |
| Re-epithelialization | Significant acceleration despite hyperglycemia (1.6-2.0-fold) [39] | Marked improvement in epidermal regeneration (1.7-2.1-fold) [38] | Rapid and complete epithelialization (1.9-2.4-fold) [14] |
Notably, subgroup analyses from the meta-analysis revealed that specific MSC sources demonstrated enhanced efficacy for particular wound types. Adipose-derived MSC-exosomes showed superior performance in diabetic wound closure rates, while bone marrow-derived MSC-exosomes exhibited the strongest pro-angiogenic effects across models [14]. Additionally, small extracellular vesicles (sEVs) demonstrated better revascularization outcomes compared to apoptotic extracellular vesicles (ApoEVs), though ApoEVs showed advantages in collagen deposition [14].
Experimental Protocols for MSC-Exosome Wound Healing Studies
Standardized Methodology for Wound Model Induction
Diabetic Wound Model Creation: For type 1 diabetes modeling, induce diabetes in 8-10 week old C57BL/6 mice via intraperitoneal streptozotocin (STZ) injections (50-60 mg/kg/day for 5 consecutive days) [14]. Confirm hyperglycemia (blood glucose >300 mg/dL) after one week. Anesthetize mice and create dorsal full-thickness excisional wounds using 6-8 mm biopsy punches. For type 2 diabetes modeling, utilize genetically modified db/db mice with identical wounding procedures [39].
Burn Wound Model Establishment: Anesthetize animals and shave dorsal hair. Create standardized contact burns using custom brass blocks (1-2 cm²) heated to 95-100°C in water bath, applied to dorsal skin for 10-15 seconds with uniform pressure [40]. This protocol typically yields deep partial-thickness burns with reproducible injury depth. Adminiate postoperative analgesia following institutional guidelines.
Full-Thickness Excisional Wound Creation: Anesthetize animals and prepare surgical site. Create bilateral dorsal wounds using sterile disposable biopsy punches (6-8 mm diameter for mice, 10-15 mm for rats) [14]. Extend wounds through panniculus carnosus muscle to ensure full-thickness injury. Apply wound dressing according to experimental requirements.
MSC-Exosome Isolation and Characterization Protocol
Exosome Isolation via Ultracentrifugation: Culture MSCs in serum-free media for 48 hours prior to collection. Centrifuge conditioned media at 300 × g for 10 minutes to remove cells, followed by 2,000 × g for 20 minutes to eliminate dead cells and debris [11]. Filter supernatant through 0.22 μm membrane and ultracentrifuge at 100,000 × g for 70 minutes at 4°C. Wash pellet in phosphate-buffered saline (PBS) and repeat ultracentrifugation. Resuspend final exosome pellet in PBS and quantify protein content via BCA assay [11].
Exosome Characterization: Validate exosome identity through multiple complementary approaches: (1) Nanoparticle tracking analysis to confirm size distribution (30-150 nm); (2) Transmission electron microscopy for morphological assessment; (3) Western blotting for positive markers (CD63, CD81, TSG101, Alix) and negative marker (calnexin); (4) Flow cytometry with tetraspanin antibodies for immunophenotyping [11] [41].
Exosome Administration and Wound Assessment Methods
Therapeutic Administration Protocols: For topical application, incorporate exosomes (typically 50-200 μg protein equivalent) into hydrogel delivery systems (e.g., hyaluronic acid, chitosan, Pluronic F-127) to enhance retention and controlled release [39] [42]. Apply directly to wound beds and cover with appropriate dressings. For systemic delivery, administer via subcutaneous or intravenous injection (50-200 μg exosome protein in 100-200 μL PBS) adjacent to or circulating toward wound sites [14].
Wound Healing Assessment: Monitor wound closure daily through standardized digital photography with reference scale. Calculate wound area using ImageJ software with the formula: Percentage closure = [(Initial area - Current area)/Initial area] × 100 [14]. For histological analysis, harvest wound tissue at predetermined endpoints for H&E staining (re-epithelialization, granulation tissue), Masson's trichrome (collagen deposition), and immunohistochemistry for CD31 (angiogenesis) and specific cell markers [39].
Molecular Mechanisms of MSC-Exosome Action in Wound Healing
Key Signaling Pathways Modulated by MSC-Exosomes
MSC-exosomes accelerate healing through sophisticated molecular mechanisms that vary based on wound pathophysiology and exosome cargo. The diagram below illustrates the primary signaling pathways through which MSC-exosomes promote healing across different wound environments.
The multifaceted mechanisms depicted above work synergistically to overcome model-specific healing impairments. In diabetic wounds, MSC-exosomes correct the characteristic angiogenic deficit through sophisticated RNA-mediated pathways. Research demonstrates that exosomal circMYO9B promotes angiogenesis by facilitating the translocation of hnRNPU from nucleus to cytoplasm, subsequently destabilizing CBL and reducing ubiquitination of KDM1A, ultimately increasing VEGFA expression in endothelial cells [41]. This mechanism is particularly relevant for addressing the impaired neovascularization observed in diabetic wounds.
Simultaneously, MSC-exosomes modulate the chronic inflammatory environment common to non-healing wounds. They promote transition from pro-inflammatory M1 to anti-inflammatory M2 macrophage phenotypes through transfer of regulatory miRNAs like miR-21, miR-146a, and miR-181c [38]. This immunomodulatory activity is especially beneficial in burn wounds where excessive inflammation delays healing. Additionally, MSC-exosomes activate Wnt/β-catenin signaling to enhance keratinocyte proliferation and migration while inhibiting apoptosis through AKT pathway activation, directly addressing re-epithelialization deficits across wound types [38].
Exosome Cargo Engineering for Enhanced Therapeutic Efficacy
Emerging bioengineering approaches enable customization of MSC-exosome cargo to enhance specific therapeutic functions. Preconditioning strategies include treating MSCs with melatonin to enhance anti-inflammatory exosome properties [38] or culturing under hypoxic conditions to augment pro-angiogenic cargo. Direct engineering approaches involve transfecting MSCs to overexpress specific miRNAs (e.g., miR-125a, miR-135a) or circRNAs (e.g., circMYO9B) that subsequently package into exosomes [41]. These engineered exosomes demonstrate significantly improved efficacy, with studies reporting 30-50% greater wound closure rates compared to naive exosomes [41].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent Category | Specific Products/Solutions | Primary Function | Application Notes |
|---|---|---|---|
| MSC Culture | Serum-free MSC media (e.g., MesenCult), fetal bovine serum (exosome-depleted), trypsin/EDTA | MSC expansion and maintenance | Use serum-free or exosome-depleted FBS to avoid contaminating vesicles [11] |
| Exosome Isolation | Ultracentrifuge, polycarbonate bottles, 0.22 μm filters, PBS buffer | Exosome purification from conditioned media | Density gradient ultracentrifugation provides higher purity [11] |
| Exosome Characterization | CD63/CD81/CD9 antibodies, TSG101 antibody, calnexin antibody, nanoparticle tracker | Vesicle validation and quantification | Combine multiple characterization methods per MISEV guidelines [14] |
| Wound Model Creation | Biopsy punches (6-8 mm), STZ solution, heating apparatus for burns, analgesics | Standardized wound induction | Adjust anesthetic/analgesic protocols per IACUC guidelines |
| Exosome Delivery | Hyaluronic acid hydrogel, chitosan scaffolds, Pluronic F-127, fibrin matrices | Therapeutic application vehicles | Hydrogels extend exosome retention and controlled release [42] |
| Histological Assessment | Formalin, paraffin, H&E stain, Masson's trichrome kit, CD31 antibody | Tissue analysis and quantification | Plan harvest timepoints to capture all healing phases |
This systematic comparison of wound models reveals that while MSC-exosomes demonstrate therapeutic benefits across all wound types, their efficacy is highly context-dependent. Diabetic wounds respond best to exosomes with enhanced pro-angiogenic cargo, particularly those from adipose-derived MSCs. Burn wounds benefit most from exosomes with potent immunomodulatory properties, while full-thickness excisional wounds show robust healing acceleration with standard MSC-exosome preparations. These model-specific response patterns underscore the importance of aligning research questions with appropriate preclinical models.
Future research directions should prioritize standardization of MSC-exosome isolation and characterization protocols to improve inter-study comparability [14]. Additionally, the development of increasingly sophisticated wound-specific bioengineering approaches to customize exosome cargo will enhance therapeutic potency. Advanced delivery systems that provide sustained exosome release represent another critical innovation frontier. As these technologies mature, MSC-exosome therapies promise to revolutionize treatment for diverse wound pathologies, potentially offering solutions for currently intractable healing impairments.
The therapeutic potential of Mesenchymal Stem Cells (MSCs) has been increasingly attributed to their potent paracrine activity, rather than their differentiation capacity alone [1] [43]. A key component of this paracrine effect is mediated through extracellular vesicles, particularly exosomes [43]. These nanoscale vesicles (30-150 nm in diameter) are laden with a diverse array of bioactive molecules—including proteins, lipids, and nucleic acids—that can be transferred to recipient cells to modulate their function [44] [45]. Compared to whole-cell therapies, MSC-derived exosomes (MSC-Exos) present significant advantages, including a higher safety profile, lower risk of immunogenicity, reduced concerns regarding tumorigenicity, and the inability to form emboli in lung microvasculature due to their nano-size [46] [43]. However, the therapeutic efficacy of these exosomes is not uniform; it is profoundly influenced by the tissue source of the parent MSCs. This guide provides a systematic, data-driven comparison of exosomes derived from three predominant MSC sources: bone marrow (BM), adipose tissue (AT), and umbilical cord (UC), to inform preclinical research and therapeutic development.
Comparative Efficacy Across Disease Models
Direct comparative studies reveal that the tissue origin of MSCs significantly impacts the functional profile of their exosomes. The therapeutic effects are model-dependent, with different sources demonstrating superior efficacy in specific pathological contexts.
Table 1: Comparative Efficacy of MSC-Exosomes from Different Sources in Preclinical Models
| Disease Model | MSC Source | Key Experimental Findings | Proposed Mechanisms | Reference |
|---|---|---|---|---|
| Osteoarthritis (OA) | Bone Marrow (BM) | ▼ Superior efficacy in attenuating inflammation and promoting cartilage protection. | Suppressed NF-κB & MAPK pathways; inhibited chondrocyte apoptosis. | [47] |
| Umbilical Cord (UC) | ▼ Superior efficacy, comparable to BM-MSC-Exos. | Promoted macrophage polarization to anti-inflammatory phenotype; inhibited apoptosis. | [47] | |
| Adipose (AT) | ▼ Effective, but less potent than BM and UC-MSC-Exos. | Enhanced ECM synthesis; reduced cellular senescence. | [47] | |
| Sepsis-Induced Acute Lung Injury (ALI) | Umbilical Cord (UC) | ▼ Effectively downregulated glycolysis and inflammation in macrophages. | Improved survival rates; ameliorated lung pathology. | [48] |
| Bone Marrow (BM) | ▼ Effectively downregulated glycolysis and inflammation in macrophages. | Improved survival rates; ameliorated lung pathology. | [48] | |
| Adipose (AT) | ▼ Effectively downregulated glycolysis and inflammation in macrophages. | Improved survival rates; ameliorated lung pathology. | [48] | |
| Angiogenesis | Adipose (AT) | ▼ Enhanced angiogenic capability compared to BM-MSC-Exos. | Carried higher levels of pro-angiogenic miRNAs and growth factors. | [43] |
| Immunomodulation | Bone Marrow (BM) | ▼ Potently inhibited IFN-γ secretion by T cells. | Strong anti-inflammatory and immunomodulatory effects. | [43] |
Detailed Experimental Protocols from Key Studies
Protocol 1: In Vitro Model of Osteoarthritis
A seminal study directly compared the chondroprotective and anti-inflammatory effects of BM-, UC-, and ADSC-derived exosomes using an in vitro model of osteoarthritis [47].
- Cell Model: Primary chondrocytes stimulated with the pro-inflammatory cytokine Interleukin-1β (IL-1β) to mimic the OA environment.
- Exosome Isolation & Characterization: Exosomes were isolated using the Aqueous Two-Phase System (ATPS). Characterization was performed via:
- Nanoparticle Tracking Analysis (NTA): Confirmed particle size distribution (30-150 nm) and concentration (BM: ~6.9×10⁷, AD: ~8.0×10⁷, UC: ~1.2×10⁸ particles/mL).
- Transmission Electron Microscopy (TEM): Visualized classic cup-shaped exosome morphology.
- Western Blotting: Confirmed presence of exosomal markers (CD63, CD81, ALIX).
- Treatment: IL-1β-stimulated chondrocytes were treated with BMSC-Exos, ADSC-Exos, or UMSC-Exos.
- Key Assessments:
- Cell Viability (CCK-8 Assay): All exosomes showed no cytotoxicity at concentrations up to 1000 μg/mL.
- Western Blot Analysis: Evaluated effects on NF-κB (phospho-p65) and MAPK (phospho-p38, JNK, ERK) signaling pathways. BMSC-Exos and UMSC-Exos showed more potent inhibition of these inflammatory pathways compared to ADSC-Exos.
- Gene Expression: All exosomes suppressed pro-inflammatory markers and enhanced chondroprotective gene expression.
- Migration Assay: All MSC-Exos significantly enhanced chondrocyte motility, a critical factor for cartilage repair.
Protocol 2: Acute Lung Injury Model and Administration Routes
Another study, while focusing on a single source (umbilical cord), provided a robust methodology for evaluating administration routes, which is critical for therapeutic translation [46].
- Animal Model: LPS-induced Acute Lung Injury (ALI) in BALB/c mice.
- Exosome Administration:
- Routes: Intravenous (IV) injection, intranasal (IN) drip, and nebulization (Atomization).
- Dosing: Administered at 4 and 24 hours post-LPS exposure, with low, medium, and high doses for each route.
- Key Assessments at 48 hours:
- Histopathological Scoring: Lung tissues were scored for inflammatory cell infiltration, hemorrhage, and edema. All routes significantly attenuated inflammation.
- Cytokine Measurement (ELISA): Levels of TNF-α, IL-6, IL-1β (pro-inflammatory), and IL-10 (anti-inflammatory) in serum and bronchoalveolar lavage fluid (BALF). Exosomes decreased pro-inflammatory and increased anti-inflammatory cytokines.
- Route & Dose Efficacy: A dose-dependent effect was observed. At an equivalent dose, IV delivery was superior for cytokine modulation, while intranasal and nebulized routes showed comparable efficacy.
Molecular Mechanisms and Signaling Pathways
The distinct therapeutic effects of MSC-Exos are rooted in their ability to modulate key signaling pathways in recipient cells, largely dictated by their unique molecular cargo.
Diagram: MSC-Exo Source-Dependent Pathway Modulation. BM and UC-MSC-Exos show potent inhibition of core inflammatory pathways (NF-κB/MAPK), while AD-MSC-Exos effectively inhibit inflammation and glycolysis, highlighting their distinct mechanistic profiles.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful isolation and characterization of MSC-Exos for comparative studies require a standardized set of reagents and instruments.
Table 2: Essential Reagents and Materials for MSC-Exosome Research
| Category | Item | Critical Function & Application |
|---|---|---|
| Cell Culture | Alpha Minimum Essential Medium (α-MEM) / DMEM | Culture Medium: α-MEM may support higher exosome yields compared to DMEM [6]. |
| Human Platelet Lysate (hPL) / Exosome-Depleted FBS | Serum Supplement: Provides essential growth factors. FBS must be ultracentrifuged to deplete bovine exosomes [49]. | |
| Isolation Kits & Reagents | Ultracentrifugation Equipment | Classical 'Gold Standard' Method: Separates exosomes via high-speed centrifugation (≥100,000×g) [49] [43]. |
| Tangential Flow Filtration (TFF) System | Scalable Isolation: Superior for large-scale GMP production; can achieve higher particle yields than UC [6] [43]. | |
| Size Exclusion Chromatography (SEC) Kits | High-Purity Isolation: Separates exosomes from contaminating proteins based on size, preserving vesicle integrity [44]. | |
| Characterization Instruments | Nanoparticle Tracking Analyzer (NTA) e.g., NanoSight | Particle Concentration & Size: Quantifies and sizes particles in suspension (typically 30-150 nm) [47] [6] [49]. |
| Transmission Electron Microscope (TEM) | Morphological Confirmation: Visualizes the classic cup-shaped morphology of exosomes [47] [6]. | |
| Western Blot Equipment / Flow Cytometer | Marker Validation: Confirms presence of positive (CD63, CD81, CD9, TSG101, ALIX) and negative (calnexin) markers [47] [6]. |
The evidence unequivocally demonstrates that the tissue source is a critical determinant of the therapeutic efficacy of MSC-derived exosomes. No single source is universally superior; each offers a unique functional profile suited to specific therapeutic goals. Bone Marrow and Umbilical Cord MSC-Exos have demonstrated particularly strong performance in modulating inflammation and promoting tissue protection in models like osteoarthritis [47]. In contrast, Adipose-derived MSC-Exos show pronounced angiogenic potential [43]. Future research must focus on standardizing isolation protocols (e.g., leveraging TFF for scalability [6] [43]), conducting more direct in vivo comparisons, and deeply profiling cargo to establish clear structure-function relationships. This source-specific approach will be paramount for developing effective, targeted exosome-based therapeutics for a wide range of diseases.
The therapeutic application of Mesenchymal Stem Cell (MSC)-derived exosomes represents a promising cell-free strategy in regenerative medicine, particularly for wound healing and skin regeneration [50] [51]. These nano-sized extracellular vesicles, typically 30-150 nm in diameter, mediate the therapeutic effects of MSCs through their cargo of proteins, lipids, and nucleic acids, which promote angiogenesis, modulate inflammation, and stimulate cell proliferation [52]. However, the efficacy of these exosomes is critically dependent on effective delivery strategies that overcome challenges such as rapid clearance, poor retention at the wound site, and limited targeting efficiency [51]. The choice of delivery method significantly influences the pharmacokinetics, biodistribution, and ultimate therapeutic outcome of MSC exosomes in various wound models. This guide objectively compares the three primary delivery strategies—topical application, injection, and biomaterial scaffolds—by synthesizing current experimental data and methodologies from preclinical wound healing research.
Comparative Analysis of Delivery Strategies
The following table provides a systematic comparison of the three main delivery strategies based on current preclinical research, highlighting their relative performance across key parameters.
Table 1: Performance Comparison of MSC Exosome Delivery Strategies in Animal Wound Models
| Delivery Strategy | Reported Efficacy (Wound Closure) | Key Advantages | Major Limitations | Commonly Used Animal Models | Optimal Exosome Dose Range (Preclinical) |
|---|---|---|---|---|---|
| Topical Application | Moderate to High [53] [14] | Non-invasive, simple application, suitable for superficial wounds [52] | Rapid clearance, poor retention in exudative wounds, requires frequent application [51] | IMQ-induced psoriasis, excisional wounds, burns [53] [14] | (1 \times 10^8) - (1 \times 10^{11}) particles in 25-100 µL [53] |
| Injection (Subcutaneous/Intradermal) | High [14] | Direct delivery to wound bed, bypasses surface barriers, longer retention [14] | Invasive, potential for localized trauma, requires technical skill [14] | Diabetic foot ulcers, full-thickness excisional wounds [54] [14] | (1 \times 10^{10}) - (1 \times 10^{12}) particles total dose [14] |
| Biomaterial Scaffolds | Highest [50] [51] | Sustained release, protects exosomes, provides structural support, enhances stability [50] [51] | Complex fabrication, potential for foreign body reaction, higher cost [50] [55] | Diabetic ulcers, full-thickness burns, large area wounds [50] [51] [14] | Varies by scaffold capacity; enables lower total dose via sustained release [50] |
Table 2: Impact of Delivery Route on Specific Healing Parameters (Meta-Analysis Data) [14]
| Delivery Strategy | Wound Closure Rate (SMD vs. Control) | Collagen Deposition | Revascularization (Blood Vessel Density) | Scar Width Reduction |
|---|---|---|---|---|
| Topical Application | +1.45 | Moderate Improvement | Moderate Improvement | Limited Data |
| Subcutaneous Injection | +1.92 | Significant Improvement | Significant Improvement | Moderate Improvement |
| Scaffold-Based Delivery | Not separately meta-analyzed | Superior organization and density | Enhanced mature vessel formation | Superior Reduction |
Experimental Protocols and Methodologies
Protocol for Topical Application in Psoriasis Murine Model
The topical application protocol has been standardized in imiquimod (IMQ)-induced psoriasis models, providing a robust method for evaluating anti-inflammatory and proliferative effects of MSC exosomes [53].
Animal Model Preparation: Utilize 8-week-old male Balb/c mice. Induce a psoriatic phenotype by daily topical applications of 50 mg of IMQ cream (5%) on the shaved back skin for 6 consecutive days [53].
Exosome Preparation and Formulation:
- Iserve exosomes from human umbilical cord MSCs (hUCMSCs) or placenta MSCs (hPMSCs) via sequential ultracentrifugation [53].
- Characterize exosomes using Nanoparticle Tracking Analysis (ZetaView PMX 110 system) for size distribution (typically 30-150 nm) and transmission electron microscopy for morphology [53].
- Confirm exosome markers (CD9, CD63, ALIX) and purity (calnexin-negative) via immunoblotting [53].
- Resuspend exosomes in phosphate-buffered saline at a concentration of (1 \times 10^8) particles in 25 µL for application [53].
Treatment Protocol:
- Apply exosome suspension topically to the wound area daily for 7 consecutive days.
- Begin treatment after psoriatic phenotype is established (e.g., day 4 of IMQ induction) [53].
- Assess outcomes using Psoriasis Area and Severity Index (PASI) scoring, histological analysis of epidermal thickness, and measurement of skin tissue cytokines via ELISA [53].
Protocol for Subcutaneous Injection in Diabetic Wound Models
Subcutaneous injection delivers exosomes directly to the wound bed, demonstrating superior efficacy in meta-analyses for wound closure and revascularization [14].
Animal Model Preparation: Employ streptozotocin (STZ)-induced diabetic mice or genetically modified db/db mice to represent type 1 and type 2 diabetes, respectively. Create full-thickness excisional dorsal wounds (typically 6-8 mm diameter) [14].
Exosome Preparation and Dosing:
- Isolate exosomes from adipose-derived MSCs (ADSCs) or bone marrow MSCs (BMMSCs) using ultracentrifugation or size-exclusion chromatography [14].
- Characterize exosomes according to MISEV2023 guidelines, confirming size (<200 nm) and marker expression [14].
- Administer a total dose of (1 \times 10^{10}) - (1 \times 10^{12}) particles, divided into multiple injections around the wound periphery [14].
Treatment and Assessment:
- Perform subcutaneous injections at 4-6 sites around the wound margin using insulin syringes (29-31 gauge) [14].
- Repeat administration every 2-3 days until wound closure is achieved.
- Evaluate outcomes through wound closure rate measurement, histology for re-epithelialization and granulation tissue formation, immunohistochemistry for CD31+ blood vessels, and Masson's trichrome staining for collagen deposition [14].
Protocol for Biomaterial Scaffold Delivery
Biomaterial scaffolds provide a sustained-release system that protects exosomes and enhances their therapeutic potential, particularly in complex wound environments [50] [51].
Scaffold Fabrication and Exosome Loading:
- Select appropriate biomaterials: natural polymers (chitosan, collagen, hyaluronic acid) or synthetic polymers (polyethylene glycol) [50] [55].
- Fabricate porous or nanofibrous scaffolds using techniques like electrospinning, freeze-drying, or 3D printing [50].
- Load exosomes onto scaffolds via physical adsorption, encapsulation, or covalent conjugation. For hydrogels, mix exosomes with polymer solution before cross-linking [51].
Characterization of Scaffold-Exosome Constructs:
- Assess scaffold morphology and porosity using scanning electron microscopy.
- Evaluate exosome release kinetics using fluorescently labeled exosomes (e.g., PKH67 dye) in PBS incubation over 7-14 days [51].
- Confirm maintained exosome integrity and bioactivity post-incorporation through cell proliferation assays with fibroblasts or endothelial cells [50].
In Vivo Implantation and Analysis:
- Implant scaffold-exosome constructs into full-thickness excisional wounds in diabetic or normal rodent models [50] [51].
- Secure scaffolds with sutures or adhesive films to ensure contact with wound bed.
- Monitor wound closure over 14-28 days compared to scaffold-only and untreated controls.
- Perform histological analysis (H&E, Masson's trichrome) at multiple timepoints to assess epithelialization, collagen organization, and scaffold degradation [50].
- Evaluate angiogenesis through immunohistochemistry for CD31 and α-SMA to identify mature vessels [51].
Signaling Pathways in MSC Exosome-Mediated Wound Healing
MSC exosomes promote healing through multiple molecular pathways, with delivery strategies influencing their activation. The following diagram illustrates the key signaling mechanisms.
Diagram 1: Key signaling pathways activated by MSC exosomes in wound healing, showing how exosome cargo influences cellular processes through multiple molecular pathways to produce therapeutic effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC Exosome Wound Healing Studies
| Reagent/Material | Function/Purpose | Examples/Specifications |
|---|---|---|
| MSC Sources | Provides exosomes with tissue-specific cargo profiles | Human Umbilical Cord (hUCMSC), Adipose Tissue (ADSC), Bone Marrow (BMMSC) [53] [14] |
| Exosome Isolation Kits | Purifies exosomes from cell culture supernatant | Ultracentrifugation, size-exclusion chromatography, polymer-based precipitation kits [53] [14] |
| Characterization Antibodies | Confirms exosome identity and purity | Anti-CD9, CD63, CD81, ALIX (exosome markers); Calnexin (negative marker) [53] |
| Animal Disease Models | Replicates human wound pathophysiology | IMQ-induced psoriasis, STZ-induced diabetic wounds, db/db mice, full-thickness excisional wounds [53] [14] |
| Biomaterial Scaffolds | Provides sustained exosome delivery platform | Chitosan, collagen, hyaluronic acid hydrogels; synthetic polymer scaffolds [50] [55] |
| Tracking Dyes | Visualizes exosome distribution and retention | PKH67, DiR, other lipophilic membrane dyes for in vivo imaging [51] |
The choice of delivery strategy for MSC exosomes significantly influences their therapeutic efficacy in wound healing, with each approach offering distinct advantages for specific research applications. Subcutaneous injection demonstrates superior performance in quantitative wound closure and revascularization according to meta-analyses, while biomaterial scaffolds provide enhanced functionality through sustained release and structural support [14]. Topical application remains valuable for superficial wound models and psoriatic skin conditions due to its non-invasive nature [53].
Future research directions should focus on standardizing exosome characterization protocols according to MISEV2023 guidelines, optimizing scaffold design for specific wound environments, and conducting direct comparative studies of delivery strategies within uniform animal models [14]. The development of engineered exosomes with enhanced targeting capabilities represents another promising frontier for improving delivery efficiency and therapeutic precision [51] [52]. As the field progresses toward clinical translation, understanding the nuanced interactions between delivery strategies, exosome bioactivity, and specific wound pathophysiology will be essential for maximizing therapeutic outcomes.
Navigating Challenges: Strategies for Optimizing Exosome Potency and Standardization
The therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-exosomes) in regenerative medicine, particularly for wound healing, is increasingly recognized. These nanoscale extracellular vesicles demonstrate robust capabilities in promoting angiogenesis, modulating inflammation, and enhancing tissue regeneration across various preclinical models [4] [56]. However, their clinical translation faces significant challenges regarding manufacturing standardization. The culture conditions for expanding parent MSCs and the subsequent methods for exosome isolation represent two critical manufacturing variables that directly impact exosome yield, purity, biological potency, and ultimately, therapeutic efficacy [57] [28]. This guide objectively compares these technical parameters to inform research and development strategies.
Impact of Culture Conditions on MSC-Exosome Production
The expansion of parent MSCs precedes exosome harvest. The culture strategy significantly influences both the quantity and quality of the resulting exosomes.
Two-Dimensional (2D) vs. Three-Dimensional (3D) Culture Systems
Traditional 2D culture in flasks is the baseline method, but 3D culture systems are emerging as a superior alternative for scalable production.
Table 1: Comparison of 2D vs. 3D Culture Systems for MSC-Exosome Production
| Culture Parameter | 2D Culture System | 3D Culture System (Microcarrier-Based) | Experimental Evidence |
|---|---|---|---|
| Cell Density at Confluence | ~20,000 cells/cm² [57] | ~40,000 cells/cm² [57] | Direct measurement of cell growth in culture flasks vs. microcarriers [57]. |
| Relative Exosome Yield | Baseline | ~20-fold increase vs. 2D [57] | Quantified using nanoparticle tracking analysis (NTA) after ultracentrifugation [57]. |
| Particle-to-Protein Ratio | Higher (e.g., 2.6 × 10⁹ ± 0.6 × 10⁹ particles/μg) [57] | Lower (e.g., 0.9 × 10⁹ ± 0.2 × 10⁹ particles/μg) [57] | Indicates potential co-isolation of non-vesicular contaminants in 3D cultures; measured by NTA and protein assay [57]. |
| Proteomic Profile | More unique proteins detected [57] | More representative of physiological conditions [57] | Analyzed via mass spectrometry; 3D-exosomes may have a more specific cargo profile [57]. |
| Functional Potency | Baseline | 7-fold more potent in siRNA delivery to neurons [57] | Measured by functional assay evaluating siRNA transfer efficiency and gene knockdown [57]. |
MSC Tissue Source and Culture Optimization
The tissue source of MSCs is another critical variable affecting exosome yield. Umbilical cord-derived MSCs (UC-MSCs), particularly from Wharton's jelly, demonstrate a significant advantage, yielding four times as many exosomes per cell as bone marrow or adipose tissue-derived MSCs [57]. These cells also exhibit a faster doubling time (approximately 4 days vs. 7 days), further enhancing production efficiency [57].
Culture media can be further optimized through preconditioning, where MSCs are exposed to specific biochemical or physical stimuli. Common strategies include treatment with cytokines (e.g., IFN-γ), exposure to hypoxia, or induction of starvation, all aimed at enhancing the therapeutic cargo and potency of the secreted exosomes [58] [28].
Comparison of Exosome Isolation Methods
Following culture and collection of the conditioned media, the choice of isolation method is paramount. Different techniques balance yield, purity, scalability, and operational complexity.
Table 2: Comparison of Key Exosome Isolation Methodologies
| Isolation Method | Principle | Experimental Protocol Summary | Key Outcomes and Data |
|---|---|---|---|
| Differential Ultracentrifugation (UC) | Sequential centrifugation at increasing speeds (e.g., 2,000–100,000 × g) to pellet exosomes based on size and density [59] [28]. | 1. Low-speed spin (e.g., 2,000 × g) to remove cells [59].2. Intermediate-speed spin (e.g., 10,000 × g) to remove debris [59].3. High-speed spin (100,000 × g) to pellet exosomes [59].4. Wash and resuspend pellet in PBS [59]. | - Considered the "gold standard" [28].- Lower yield and poor scalability [57] [28].- Can cause vesicle aggregation or damage [28]. |
| Tangential Flow Filtration (TFF) | Uses recirculating flow and porous membranes to separate exosomes based on size; highly scalable [57]. | Conditioned media is continuously pumped across a membrane, retaining exosomes while removing smaller contaminants. The exosome concentrate is then diafiltered into a suitable buffer [57]. | - ~27-fold higher yield than UC from the same volume [57].- Maintains biological activity and vesicle integrity [57].- Enables processing of large volumes (liters) efficiently [57]. |
| Size-Exclusion Chromatography (SEC) | Separates particles based on size as they pass through a porous gel matrix; exosomes elute before smaller proteins [28]. | The sample is loaded onto a column (e.g., Sepharose). Fractions are collected, with exosomes typically found in the early-eluting fractions [28]. | - Provides high purity, effectively separating exosomes from contaminating proteins [28].- Lower throughput compared to TFF [28].- Pore clogging can be an issue with concentrated samples [28]. |
| Precipitation | Uses polymers (e.g., polyethylene glycol) to decrease exosome solubility, causing them to precipitate out of solution [28]. | Polymer solution is mixed with conditioned media and incubated at low temperature. A low-speed centrifugation step is then used to collect the precipitated exosomes [28]. | - Simple protocol, requires no specialized equipment [28].- Co-precipitates non-vesicular contaminants like lipoproteins, leading to lower purity [28]. |
Combined Workflow for Enhanced Yield
The most significant gains in production yield are achieved by combining optimized culture and isolation methods. Research demonstrates that using 3D culture together with TFF isolation results in a cumulative 140-fold increase in exosome yield compared to the conventional combination of 2D culture and ultracentrifugation [57]. This combined approach is a cornerstone for scalable manufacturing required for clinical translation.
Experimental Workflow and Therapeutic Mechanism in Wound Healing
The following diagrams illustrate the integrated manufacturing process and the subsequent therapeutic action of the produced MSC-exosomes in a wound healing context.
Integrated Manufacturing Workflow
Mechanism of Action in Cutaneous Wound Healing
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for MSC-Exosome Manufacturing and Validation
| Item Category | Specific Examples | Function and Application |
|---|---|---|
| Cell Culture Systems | Umbilical Cord-derived MSCs, Microcarriers (e.g., Cytodex), 3D Bioreactors | Sourcing and scalable expansion of parent MSCs for high-yield exosome production [57]. |
| Isolation Kits & Consumables | Polyethylene Glycol (PEG)-based Precipitation Kits, Size-Exclusion Chromatography Columns, TFF Cassettes | Enabling various isolation methodologies, from simple precipitation to scalable, high-purity TFF [57] [28]. |
| Characterization Instruments | Transmission Electron Microscope (TEM), Nanoparticle Tracking Analyzer (NTA), Western Blot Apparatus | Critical for validating exosome identity (morphology, size, concentration) and purity via specific markers (CD63, CD81, TSG101) [59] [28]. |
| Molecular Biology Assays | ELISA Kits, RNA Sequencing Kits, Protein Assay Kits (e.g., BCA) | Quantifying specific cargo (proteins, miRNAs) and assessing the biochemical composition of isolated exosomes [28]. |
The manufacturing pipeline for MSC-exosomes is a decisive factor in their preclinical and clinical performance. Evidence indicates that moving from traditional 2D culture to 3D microcarrier-based systems and replacing differential ultracentrifugation with tangential flow filtration can result in orders-of-magnitude improvements in yield without compromising biological activity. Furthermore, the selection of a prolific MSC source, such as umbilical cord tissue, provides a foundational advantage. As research progresses, the standardization of these critical manufacturing variables—culture media and isolation methods—will be essential for ensuring the reproducibility, efficacy, and safety of MSC-exosome therapies, ultimately solidifying their role in regenerative medicine and wound healing applications.
The therapeutic potential of Mesenchymal Stem Cell-derived exosomes (MSC-exosomes) in regenerative medicine, particularly for wound healing, is significantly hampered by heterogeneity in production methods and resulting exosome characteristics. Functional variability across preclinical studies stems from differences in exosome biogenesis, isolation techniques, and characterization protocols [60] [14]. As the field advances toward clinical applications, establishing reproducible production frameworks becomes paramount for generating consistent, high-quality exosomes that yield reliable therapeutic outcomes across different animal wound models [61]. This guide systematically compares current strategies and methodologies aimed at standardizing exosome production, providing researchers with evidence-based approaches to combat heterogeneity.
Exosome Biogenesis and Key Production Strategies
Exosomes are nanoscale biological vesicles (30-150 nm in diameter) that originate from the endosomal system. They are formed through the inward budding of the endosomal membrane, creating intraluminal vesicles (ILVs) within multivesicular bodies (MVBs). These MVBs subsequently fuse with the plasma membrane, releasing ILVs as exosomes into the extracellular space [60] [20]. The biogenesis pathway occurs through both ESCRT-dependent and ESCRT-independent mechanisms, the latter involving key enzymes such as neutral sphingomyelinase (nSMase) [60].
Understanding these pathways enables strategic intervention to enhance production. The following diagram illustrates the biogenesis process and major enhancement strategies:
Two primary strategic approaches have emerged to increase exosome yield and consistency:
Genetic Manipulation of Biogenesis Pathways
Genetic engineering techniques directly target genes involved in exosome biogenesis and release. The EXOtic device represents a breakthrough approach, where co-expression of STEAP3, syndecan-4, and an L-aspartate oxidase fragment resulted in a remarkable 40-fold increase in exosome production without altering exosome size [60]. This strategy enables precise control over the molecular machinery responsible for exosome formation, including ESCRT complex components, Rab GTPases, and tetraspanins.
Parent Cell Pretreatment and Culture Optimization
Alternative approaches focus on modulating the parent cell environment to enhance exosome production:
- Hypoxic conditions significantly upregulate exosome production in MSCs through HIF-1α activation, increasing expression of ALIX, TSG101, Rab27a, and Rab27b [60].
- Cytokine priming with factors like thrombin and adiponectin enhances yield by activating Rab5 and EEA-1 pathways [60].
- Three-dimensional (3D) culture systems alter the expression of biogenesis-related genes (ALIX, TSG101, ADAM10, CD63, and Syntenin-1) compared to conventional 2D culture [60].
- Ultrasound stimulation induces an 8-10 fold increase in exosome yield through calcium-dependent mechanisms, upregulating ALIX, TSG101, and CD63 [60].
Table 1: Strategic Approaches for Enhanced Exosome Production
| Strategy | Key Mechanisms | Reported Yield Increase | Notable Effects |
|---|---|---|---|
| Genetic Engineering (EXOtic) | STEAP3, syndecan-4, L-aspartate oxidase expression | 40-fold | No change in exosome size [60] |
| Hypoxic Preconditioning | HIF-1α activation, Rab27a/b upregulation | Varies by cell type | Enhances therapeutic potential for myocardial infarction [60] |
| 3D Culture Systems | Alters ALIX, TSG101, CD63, Syntenin-1 expression | Significant vs. 2D culture | Mimics native tissue environment [60] |
| Ultrasound Stimulation | Calcium-dependent mechanism, Rab11 upregulation | 8-10 fold | Upregulates ALIX, TSG101, CD63 [60] |
| Cytokine Priming | Rab5 and EEA-1 activation | Varies by cytokine | Modifies exosome cargo composition [60] |
Isolation Methods: Comparative Performance Analysis
The choice of isolation method significantly impacts exosome yield, purity, and biological functionality. The table below provides a comparative analysis of the most widely used techniques:
Table 2: Comparison of Exosome Isolation Methods
| Method | Principle | Yield & Purity | Time Requirements | Downstream Applications | Key Limitations |
|---|---|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation based on size/density | Moderate purity, potential protein contamination [62] [61] | Lengthy (>6 hours) [62] | Higher RNA yield, better for mRNA analysis [62] | Low reproducibility, exosome damage, limited scalability [62] [61] |
| Tangential Flow Filtration (TFF) | Size-based separation through filtration | High yield (1.05-2.36×10^11 particles/L), consistent purity (1.07-2.77×10^8 particles/μg) [61] | Rapid (4 hours for large volumes) [61] | Preserved functionality in AKI models, GMP-compatible [61] | Requires optimization to preserve surface proteins [61] |
| Precipitation-Based Kits | Polymer-based precipitation | Lower RNA yield, multiple impurity peaks [62] | Quick (<2 hours) [62] | Adequate for basic detection, 4/5 genes detectable [62] | Impurities, variable reproducibility, vendor dependency [62] |
| Size-Exclusion Chromatography | Size-based separation through column | High purity | Moderate | Good for functional studies | Limited scalability, sample dilution |
Experimental Protocol: TFF for Large-Scale Production
TFF Protocol (adapted from [61]):
- Cell Culture: Expand human adipose-derived MSCs (ASCs) in serum-free media to passage 7, confirming stable marker expression (CD29, CD90, CD105 positive; CD31, CD45, HLA-DR negative) and trilineage differentiation potential.
- Conditioned Media Collection: Harvest conditioned media after 48-72 hours, removing cells and debris via centrifugation at 2,000 × g for 30 minutes.
- Initial Concentration: Pre-concentrate media using ultrafiltration with 100 kDa molecular weight cut-off membranes.
- Tangential Flow Filtration: Process 4+ liters of concentrated media using a TFF system with appropriate molecular weight cut-off membranes (typically 100-200 kDa).
- Diafiltration: Exchange buffer with phosphate-buffered saline to remove contaminants.
- Final Concentration: Concentrate to desired exosome concentration.
- Quality Control: Characterize by NTA (size distribution: 30-200 nm), TEM (spherical morphology), and flow cytometry (CD9, CD63, CD81 positive; calnexin, cytochrome C negative).
This TFF-based approach enables reproducible large-scale production of functional ASC-exosomes, demonstrating life-saving efficacy in a lethal cisplatin-induced AKI rat model [61].
Quantitative Assessment of MSC Exosome Performance in Wound Models
Comprehensive meta-analyses of preclinical studies provide robust evidence for MSC-exosome efficacy across wound healing models. The following data synthesis compares performance metrics based on recent systematic reviews:
Table 3: MSC Exosome Performance Across Wound Healing Models
| Parameter | Animal Model | Therapeutic Outcomes | Effect Size & Statistical Significance | Key Mediators |
|---|---|---|---|---|
| Wound Closure Rate | Diabetic and non-diabetic full-thickness wounds | Significant acceleration of closure | Consistent improvement across 83 preclinical studies [14] | miR-146a, CD73, collagen remodeling [60] [20] |
| Angiogenesis | Dorsal wounds, diabetic foot ulcers | Increased blood vessel density | Superior effect with bone marrow MSC sources [14] | VEGF, FGF transfer, endothelial cell activation [20] |
| Collagen Deposition | Full-thickness excisional wounds | Improved collagen organization and ratio | Apoptotic sEVs showed best efficacy [14] | Altered collagen I:III ratio, fibroblast regulation [20] |
| Scar Width | Multiple wound models | Reduced scar formation | Significant reduction vs. controls [14] | Improved extracellular matrix remodeling [20] |
| Inflammatory Modulation | Atopic dermatitis, burns | Reduced inflammation | Confirmed across multiple disease models [14] | Macrophage polarization, cytokine transfer [20] |
Impact of Administration Route and MSC Source
Subgroup analyses reveal critical methodological factors influencing therapeutic outcomes:
- Administration Route: Subcutaneous injection demonstrates superior wound closure, collagen deposition, and revascularization compared to topical dressing/covering [14].
- MSC Source: Adipose-derived MSCs show the best effect on wound closure rate and collagen deposition, while bone marrow-derived MSCs excel in revascularization outcomes [14].
- EV Type: Apoptotic small extracellular vesicles (ApoSEVs) outperform apoptotic bodies (ApoBDs) and conventional small EVs (sEVs) in wound closure and collagen deposition, while sEVs show better revascularization potential [14].
Advanced Engineering and Standardization Approaches
Engineering Strategies for Enhanced Functionality
To address limitations of natural exosomes, advanced engineering approaches are being developed:
- Surface Modification: Decorating exosomes with targeting ligands (e.g., RGD peptides, CP05 peptide) to enhance tissue-specific delivery [20].
- Cargo Loading: Incorporating therapeutic miRNAs (e.g., miR-126, miR-146a), growth factors (VEGF, FGF), or small molecules to enhance regenerative potential [20].
- Biomaterial Integration: Incorporating exosomes into hydrogels, scaffolds, and bioinks to prolong retention and provide controlled release at wound sites [20].
The following diagram illustrates the engineering strategies and their functional benefits:
Quantification and Characterization Standards
Accurate quantification is essential for reproducible research. The NanoLuc luciferase fusion system (CD63Nluc, CD9Nluc, CD81Nluc) enables sensitive, high-throughput exosome quantification with a linear detection range above 10^6 particles/mL, correlating well with NTA data [63]. This system reliably detects exosome production alterations induced by genetic manipulation (ALIX suppression) and pharmacological treatment (bafilomycin A1) [63].
Standardized characterization should include:
- Size and concentration: Nanoparticle Tracking Analysis (mean size ~168±33 nm, mode ~108±20 nm) [61]
- Morphology: Transmission Electron Microscopy (spherical vesicles) [62] [61]
- Surface markers: Flow cytometry for CD9, CD63, CD81 [61]
- Purity markers: Absence of calnexin and cytochrome C [61]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for Reproducible Exosome Research
| Reagent Category | Specific Examples | Function & Application | Considerations |
|---|---|---|---|
| Cell Culture Media | Serum-free DMEM, Exosome-depleted FBS | Provides controlled environment for exosome production | Eliminates bovine exosome contamination [62] |
| Isolation Systems | TFF equipment, Ultracentrifugation systems, Precipitation kits | Separates exosomes from conditioned media | TFF enables GMP-compliant large-scale production [61] |
| Characterization Tools | NTA instruments, TEM, Flow cytometers with nanofluidic chips | Determines size, concentration, and marker expression | Multi-method approach recommended for validation [61] |
| Quantification Assays | NanoLuc luciferase fusion systems, BCA protein assay, RNA quantification kits | Measures exosome quantity and cargo content | Luciferase systems enable high-throughput screening [63] |
| Engineering Tools | CP05 peptide, RGD ligands, Transfection reagents | Modifies exosomes for enhanced targeting and function | Maintains exosome integrity while adding functionality [20] |
| Animal Model Reagents | Streptozotocin (for diabetic models), Wound creation instruments | Creates preclinical wound healing models | STZ-induced diabetes models common in research [14] |
Combating heterogeneity in MSC exosome production requires integrated strategies spanning biogenesis enhancement, isolation optimization, and rigorous characterization. Genetic engineering approaches like the EXOtic device and TFF-based isolation represent promising avenues for scalable, reproducible production. The comprehensive performance data across wound models confirms the therapeutic potential of MSC-exosomes while highlighting the critical importance of standardization in source selection, administration routes, and characterization protocols. As the field advances, adherence to MISEV2023 guidelines and implementation of the robust methodologies detailed in this guide will be essential for translating MSC exosome research into reliable clinical therapies for wound healing and regenerative applications.
Exosomes, nanoscale extracellular vesicles naturally secreted by cells, have emerged as a powerful platform for targeted drug delivery. These cell-derived nanovesicles, typically ranging from 30 to 150 nm in diameter, are composed of a lipid bilayer and carry a diverse cargo of proteins, nucleic acids, and lipids from their parent cells [64] [65]. Their inherent role as mediators of intercellular communication provides them with several advantages as drug delivery vehicles, including high biocompatibility, low immunogenicity, and an innate ability to cross biological barriers such as the blood-brain barrier [66] [65]. Mesenchymal stem cell-derived exosomes (MSC-Exos) have garnered significant attention in regenerative medicine due to their anti-inflammatory, anti-apoptotic, and regenerative properties, which mirror the therapeutic effects of their parent MSCs but with a reduced risk of immune rejection and tumorigenicity [4] [67].
The fundamental rationale for engineering exosomes lies in enhancing their natural capabilities for precise therapeutic applications. While unmodified exosomes possess some inherent tissue tropism, this targeting is often insufficient for specific disease contexts. Engineering strategies aim to load therapeutic cargoes efficiently into exosomes and modify their surface to achieve targeted delivery to specific cells or tissues [65]. This targeted approach increases the local concentration of therapeutics at the disease site while minimizing off-target effects and systemic toxicity, thereby improving the therapeutic index. As the field advances, these bioengineering enhancements are transforming exosomes from simple natural carriers into sophisticated, precision-guided drug delivery systems with applications spanning oncology, neurological disorders, and regenerative medicine [64] [66].
Exosome Engineering Strategies
Cargo Loading Techniques
Loading therapeutic agents into exosomes is a critical step in developing exosome-based delivery systems. These techniques can be broadly categorized into pre-loading (during exosome biogenesis) and post-loading (after exosome isolation) methods.
Table 1: Comparison of Major Cargo Loading Techniques for Exosomes
| Method | Mechanism | Cargo Types | Efficiency | Advantages | Limitations |
|---|---|---|---|---|---|
| Incubation | Passive diffusion through membrane | Small hydrophobic molecules | Low to moderate | Simple procedure, maintains vesicle integrity | Limited to small molecules, low efficiency [64] |
| Electroporation | Electrical pulses create temporary pores | Nucleic acids, proteins, small molecules | Variable | Widely used for diverse cargo types | Potential exosome aggregation, cargo aggregation [65] |
| Sonication | Ultrasound disrupts membrane | Proteins, nucleic acids | High | Higher loading efficiency than electroporation | May compromise membrane integrity, affects functionality [64] |
| Extrusion | Physical pressure through membranes | Proteins, nucleic acids | High | Controlled size distribution | Potential membrane damage, requires specialized equipment [64] |
| Freeze-Thaw Cycling | Membrane disruption through ice crystals | Proteins | Moderate | Simple protocol | Unpredictable efficiency, may cause fusion of exosomes [64] |
| Transfection | Pre-loading via donor cells | Nucleic acids, proteins | Variable | Natural loading process | Limited to cargo types amenable to transfection [64] |
Electroporation remains one of the most widely utilized techniques for loading nucleic acids and proteins into pre-isolated exosomes. This method applies an electric field to create temporary pores in the exosomal membrane, allowing cargo molecules to diffuse into the vesicles. However, challenges persist, including potential cargo aggregation and exosome integrity issues [65]. Sonication and extrusion methods often achieve higher loading efficiencies by physically disturbing the exosomal membrane but may compromise membrane integrity and biological functionality. For hydrophobic small molecules, simple incubation remains the preferred method due to its simplicity and minimal impact on exosome structure, though with limited loading capacity [64].
Pre-loading strategies involve engineering parent cells to produce exosomes pre-packaged with desired therapeutic cargo. This can be achieved through genetic engineering of donor cells to express therapeutic proteins or RNAs that are naturally incorporated into exosomes during their biogenesis [65]. While this approach leverages the cell's natural machinery for cargo loading, it is limited to biologically compatible molecules and requires extensive characterization of the resulting modified exosomes.
Surface Modification Strategies
Surface engineering of exosomes enhances their targeting specificity and therapeutic potential. These strategies can be classified into genetic engineering and chemical modification approaches.
Table 2: Surface Modification Strategies for Targeted Exosome Delivery
| Strategy | Mechanism | Targeting Ligands | Applications Demonstrated | Advantages | Challenges |
|---|---|---|---|---|---|
| Genetic Engineering | Genetic modification of parent cells to express targeting peptides fused with exosomal membrane proteins | Lamp2b, CD63, PDGFR | Brain targeting (RVG peptide), tumor targeting (RGD peptide) | Stable expression, natural incorporation | Limited to genetically encodable ligands, potential impact on exosome biogenesis [65] |
| Chemical Conjugation | Covalent attachment of targeting moieties to exosomal surface proteins or lipids | Antibodies, aptamers, peptides | Cancer targeting, immune cell targeting | Versatility in ligand selection, controlled density | Potential damage to exosomal membrane, non-specific conjugation [65] |
| Click Chemistry | Bioorthogonal chemical reactions for precise conjugation | Azide-alkyne cycloaddition | Preclinical development | High specificity, mild reaction conditions | Requires pre-modification of exosomes or ligands [65] |
| Lipid-based Modification | Incorporation of lipid-conjugated targeting ligands | Cholesterol-anchored peptides, phospholipid-linked antibodies | Enhanced tissue retention | Flexible ligand selection | Potential disruption of lipid bilayer integrity [64] |
Genetic engineering represents the most widely adopted approach for precise surface modification. This technique involves genetically fusing targeting peptides or proteins to exosomal membrane proteins such as Lamp2b, CD63, or PDGFR. For instance, the fusion of the rabies viral glycoprotein (RVG) peptide to Lamp2b has been successfully employed to achieve brain-targeted delivery of therapeutic exosomes across the blood-brain barrier [65]. Similarly, RGD peptides targeting integrins have been displayed on exosome surfaces for tumor-specific delivery. This method benefits from stable expression and natural incorporation of the targeting ligands during exosome biogenesis but is limited to genetically encodable ligands.
Chemical conjugation approaches offer greater flexibility in ligand selection, allowing attachment of antibodies, aptamers, or other targeting moieties to pre-isolated exosomes. Common strategies include utilizing carbodiimide chemistry for covalent attachment to surface proteins or click chemistry for bioorthogonal conjugation with high specificity [65]. While chemical methods provide versatility, they risk damaging the exosomal membrane or causing non-specific conjugation. Recent advances in lipid-based modification incorporate lipid-conjugated targeting ligands directly into the exosomal membrane through incubation or extrusion, offering an alternative that preserves exosome integrity while enabling targeted delivery.
Diagram 1: Genetic engineering workflow for producing targeted exosomes. The parent cells are genetically modified to express targeting ligands fused with exosomal membrane proteins, resulting in engineered exosomes with enhanced targeting capability.
Comparative Performance in Wound Healing Models
Wound healing represents one of the most extensively studied applications for MSC-derived exosomes, providing valuable insights into their therapeutic efficacy across different disease models. The regenerative potential of MSC-Exos has been demonstrated in both diabetic and non-diabetic wound models, with engineered exosomes showing enhanced performance through improved targeting and cargo delivery.
Efficacy Across Animal Models
A comprehensive meta-analysis of 83 preclinical studies revealed that MSC-derived extracellular vesicles significantly promote wound healing through multiple mechanisms, including enhancing wound closure rate, reducing scar width, increasing blood vessel density, and promoting collagen deposition [14]. The analysis encompassed both mouse (73.5%) and rat (26.5%) models, with diabetic wounds (47.0%) and non-diabetic wounds (43.4%) representing the majority of studies. Full-thickness excisional wounds were the most prevalent model (90.4%), while other models included scleroderma, burns, photoaging, atopic dermatitis, and frostbite injury [14].
Table 3: Comparative Efficacy of MSC-Exos in Wound Healing Across Animal Models
| Model Characteristics | Therapeutic Outcomes | Optimal EV Type | Optimal Administration | Key Mechanisms |
|---|---|---|---|---|
| Diabetic Wounds (Type 1 & Type 2) | Enhanced wound closure, improved angiogenesis, reduced inflammation | ApoSEVs for wound closure; sEVs for revascularization | Subcutaneous injection | Regulation of inflammatory response, promotion of angiogenesis, collagen synthesis [14] |
| Non-Diabetic Wounds | Accelerated re-epithelialization, improved tissue organization | ApoSEVs for collagen deposition | Subcutaneous injection | Fibroblast activation, keratinocyte migration, ECM remodeling [14] |
| Burns & Photoaging | Reduced oxidative stress, enhanced tissue repair | sEVs | Topical application | Antioxidant activity, modulation of MMP activity, collagen regeneration [14] |
| Atopic Dermatitis | Improved skin barrier function, reduced inflammation | sEVs | Intradermal injection | Immune modulation, suppression of inflammatory cytokines, T-cell regulation [14] |
The meta-analysis revealed that apoptotic small extracellular vesicles (ApoSEVs) demonstrated superior efficacy in promoting wound closure and collagen deposition compared to traditional small extracellular vesicles (sEVs) and apoptotic bodies (ApoBDs) [14]. Conversely, sEVs exhibited better performance in revascularization outcomes. Among administration routes, subcutaneous injection provided superior results for wound closure, collagen deposition, and revascularization compared to topical dressing/covering approaches. These findings highlight the importance of matching specific exosome types to desired therapeutic outcomes.
Source-Dependent Efficacy Variations
The tissue origin of MSCs significantly influences the therapeutic efficacy of their derived exosomes in wound healing applications. Comparative analyses indicate that adipose-derived stem cells (ADSCs) demonstrated the best effect on wound closure rate and collagen deposition, while bone marrow-derived MSCs (BMMSCs) displayed superior performance in revascularization [14]. Umbilical cord-derived MSC exosomes also showed substantial therapeutic potential, though with variable efficacy across different wound models.
Diagram 2: Efficacy variations of MSC-derived exosomes based on tissue source. Different MSC sources produce exosomes with distinct therapeutic strengths, enabling selection optimization for specific wound healing applications.
Engineered exosomes have demonstrated further enhanced performance in diabetic wound models. A targeted engineered exosome system (SGM-miR146a-Exo@SFP) specifically designed for diabetic wound healing showed superior outcomes through precise inflammatory regulation and enhanced angiogenesis [64]. The incorporation of exosomes into hydrogel-based delivery systems has also improved their retention and sustained release at the wound site, further enhancing therapeutic efficacy [42]. These advanced engineering approaches address the specific pathophysiological challenges of chronic wounds, particularly the persistent inflammation and impaired angiogenesis characteristic of diabetic ulcers.
Experimental Protocols for Key Studies
Protocol: Engineering Targeted Exosomes for Wound Healing
The development of targeted exosome therapeutics requires standardized protocols to ensure reproducibility and efficacy. The following protocol outlines key steps for generating and evaluating engineered exosomes for wound healing applications, based on established methodologies from recent literature.
1. Isolation and Characterization of Parent MSCs:
- Isplicate MSCs from selected tissue sources (adipose tissue, bone marrow, or umbilical cord) using collagenase digestion and density gradient centrifugation [14].
- Culture MSCs in standard media (α-MEM or DMEM) supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C with 5% CO₂.
- Characterize MSCs according to International Society for Cell & Gene Therapy (ISCT) guidelines: confirm adherence to plastic, demonstrate trilineage differentiation potential (osteogenic, adipogenic, chondrogenic), and verify surface marker expression (CD73+, CD90+, CD105+, CD14-, CD34-, CD45-) [14].
- Use cells at passages 3-5 for exosome production to maintain phenotypic stability.
2. Genetic Modification for Targeting Ligands:
- Design DNA construct encoding targeting peptide (e.g., RGD, GE11) fused to exosomal membrane protein (e.g., Lamp2b, CD63) via flexible linker [65].
- Transfect MSCs using appropriate method (lentiviral transduction for stable expression or electroporation for transient expression).
- Validate expression of fusion protein via Western blotting and immunofluorescence 48-72 hours post-transfection.
- Sort successfully transfected cells using FACS if selection marker is included in construct.
3. Exosome Production and Isolation:
- Culture engineered MSCs in exosome-depleted media for 48 hours when cells reach 70-80% confluence [14].
- Collect conditioned media and perform sequential centrifugation: 300 × g for 10 min to remove cells; 2,000 × g for 20 min to remove dead cells; 10,000 × g for 30 min to remove cell debris [64] [65].
- Isolate exosomes using ultracentrifugation at 100,000 × g for 70 min at 4°C, or as alternative, use size exclusion chromatography for higher purity [44].
- Wash pellet with PBS and repeat ultracentrifugation to remove contaminating proteins.
- Resuspend final exosome pellet in PBS and store at -80°C for long-term preservation.
4. Therapeutic Cargo Loading:
- For miRNA loading, transfect parent MSCs with miRNA mimics/inhibitors prior to exosome collection, or use electroporation for loading into pre-isolated exosomes [64] [65].
- Optimize electroporation parameters: typically 400-500 V for 5-10 ms in specialized electroporation buffers.
- Remove unencapsulated cargo using mini-size exclusion chromatography or dialysis.
- Validate loading efficiency using quantitative PCR for nucleic acids or ELISA for proteins.
5. Characterization of Engineered Exosomes:
- Determine particle size distribution and concentration using Nanoparticle Tracking Analysis (NTA) [14].
- Confirm exosomal morphology by Transmission Electron Microscopy (TEM).
- Verify presence of exosomal markers (CD9, CD63, CD81, TSG101) and absence of negative markers (calnexin, GM130) via Western blotting [65] [44].
- Quantify targeting ligand expression on engineered exosomes using flow cytometry with ligand-specific antibodies.
6. In Vitro Functional Validation:
- Evaluate targeting specificity using uptake assays with recipient cells (e.g., keratinocytes, fibroblasts, endothelial cells) with and without excess free ligand as competitor [65].
- Assess biological activity in relevant functional assays: fibroblast proliferation, endothelial tube formation, macrophage polarization, or keratinocyte migration assays.
- Quantify therapeutic cargo transfer to recipient cells using qRT-PCR or Western blotting.
7. In Vivo Efficacy Assessment in Wound Models:
- Utilize diabetic (db/db mice or STZ-induced) or non-diabetic rodent wound models with standardized full-thickness excisional wounds [14].
- Administer engineered exosomes via optimal route (typically subcutaneous injection around wound bed or topical application with hydrogel) [42] [14].
- Establish dosing regimen based on particle number (typically 10^8-10^11 particles per wound) and frequency (single vs. multiple administrations).
- Monitor wound closure rate through daily photographic documentation and planimetric analysis.
- Harvest tissue at endpoint for histological assessment: H&E for re-epithelialization, Masson's trichrome for collagen deposition, CD31 immunohistochemistry for angiogenesis, and immunofluorescence for inflammatory markers.
This comprehensive protocol ensures systematic development and evaluation of engineered exosomes, facilitating meaningful comparisons across studies and accelerating clinical translation.
Signaling Pathways in Engineered Exosome Therapeutics
Engineered exosomes exert their therapeutic effects through the modulation of key signaling pathways in recipient cells. Understanding these molecular mechanisms is crucial for rational design of exosome-based therapeutics.
Anti-inflammatory Pathways: Engineered MSC-Exos modulate inflammatory responses primarily through regulation of macrophage polarization and NF-κB signaling. Exosomes loaded with anti-inflammatory miRNAs (e.g., miR-146a, miR-181c) suppress pro-inflammatory M1 macrophage activation while promoting anti-inflammatory M2 polarization [64]. This shift in macrophage phenotype reduces secretion of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) while increasing anti-inflammatory factors (IL-10, TGF-β), creating a regenerative microenvironment conducive to wound healing [67]. The NF-κB pathway is particularly important in this process, with engineered exosomes often containing cargo that inhibits NF-κB nuclear translocation, thereby reducing the transcription of inflammatory mediators.
Angiogenic Pathways: The promotion of angiogenesis by engineered exosomes occurs primarily through activation of VEGF, FGF, and Akt signaling pathways. MSC-Exos transfer pro-angiogenic miRNAs (e.g., miR-126, miR-210, miR-130a) that stabilize HIF-1α under hypoxic conditions and enhance VEGF signaling in endothelial cells [67] [14]. This leads to increased endothelial cell proliferation, migration, and tube formation. Additionally, exosomal proteins such as Wnt4 activate β-catenin signaling, further promoting angiogenic gene expression. In diabetic wound models, engineered exosomes reverse the impaired angiogenesis characteristic of chronic wounds by restoring growth factor responsiveness and enhancing endothelial cell function.
Extracellular Matrix Remodeling: Engineered exosomes modulate ECM synthesis and organization through regulation of TGF-β/Smad and MMP/TIMP pathways. They promote collagen synthesis and maturation by activating TGF-β signaling in fibroblasts while simultaneously regulating MMP activity to prevent excessive degradation [67] [14]. This balanced approach to ECM remodeling enhances wound strength and reduces scar formation. In specialized applications, exosomes engineered to carry connective tissue growth factor (CTGF) or specific miRNAs can further fine-tune this process to promote regenerative rather than fibrotic healing.
Diagram 3: Key signaling pathways modulated by engineered exosomes in wound healing. Engineered exosomes deliver therapeutic cargo that simultaneously regulates multiple signaling pathways to coordinate inflammation reduction, angiogenesis promotion, and tissue repair.
The Scientist's Toolkit: Essential Research Reagents
Successful development of engineered exosome therapeutics requires specialized reagents and methodologies. The following toolkit outlines essential materials and their applications based on current literature and experimental protocols.
Table 4: Essential Research Reagents for Exosome Engineering and Characterization
| Category | Specific Reagents/Products | Function/Application | Key Considerations |
|---|---|---|---|
| Cell Culture | Mesenchymal Stem Cells (various sources), Exosome-depleted FBS, Serum-free media formulations | Production of exosomes from parent cells | Verify MSC characterization per ISCT guidelines; Use exosome-depleted FBS to reduce contamination [14] |
| Isolation Kits | Ultracentrifugation equipment, Size exclusion chromatography columns, Precipitation-based kits, Tangential flow filtration systems | Isolation and purification of exosomes from conditioned media | Ultracentrifugation remains gold standard; SEC provides higher purity; TFF enables scaling [44] |
| Characterization Tools | Nanoparticle Tracking Analyzer, Transmission Electron Microscope, Western blot reagents for exosomal markers (CD9, CD63, CD81, TSG101) | Validation of exosome identity, size, concentration, and purity | Follow MISEV2023 guidelines for minimal characterization requirements; Use multiple complementary techniques [14] |
| Engineering Reagents | Lentiviral vectors for genetic modification, Electroporation systems, Click chemistry reagents, Lipid-conjugated targeting ligands | Modification of exosomes for enhanced targeting and therapeutic delivery | Optimize transfection efficiency for genetic approaches; Validate functionality of targeting ligands [65] |
| Cargo Loading | Fluorescent dyes (PKH67, DIR), miRNA mimics/inhibitors, Therapeutic proteins, Electroporation buffers | Loading of diagnostic and therapeutic agents into exosomes | Assess loading efficiency and retention; Verify cargo integrity post-loading [64] [65] |
| Animal Models | Diabetic (db/db, STZ-induced) and non-diabetic rodents, Full-thickness wound models, Imaging systems (IVIS) | Preclinical efficacy assessment of engineered exosomes | Standardize wound size and location; Include appropriate controls; Use multiple time points [14] |
| Analytical Tools | ELISA kits for cytokine profiling, Antibodies for flow cytometry, Histology reagents (H&E, Masson's trichrome), qRT-PCR reagents | Functional assessment of exosome effects in vitro and in vivo | Use multiplex approaches for comprehensive analysis; Include pathway-specific assays [14] |
This toolkit provides the foundation for establishing a robust exosome engineering pipeline. When selecting reagents, researchers should prioritize quality control, lot-to-lot consistency, and compatibility with existing methodologies. Additionally, adherence to international guidelines such as MISEV2023 for extracellular vesicle characterization and reporting ensures reproducibility and facilitates comparison across studies [14].
For specialized applications in wound healing, additional reagents may be required for creating advanced delivery systems. Hyaluronic acid-based hydrogels have demonstrated particular utility for sustained release of exosomes at the wound site, maintaining local concentration and enhancing therapeutic efficacy [42]. Similarly, biocompatible scaffolds incorporating engineered exosomes can provide structural support while delivering therapeutic cargo, particularly for deep or irregular wounds.
The bioengineering enhancement of exosomes for targeted delivery represents a paradigm shift in therapeutic approaches for wound healing and regenerative medicine. The strategic modification of exosomes through cargo loading and surface engineering significantly enhances their therapeutic potential by improving targeting precision, increasing payload capacity, and enhancing biological activity. Comparative analyses across wound models consistently demonstrate that engineered exosomes outperform their native counterparts in key therapeutic parameters, including inflammatory regulation, angiogenesis promotion, and tissue regeneration [4] [14].
Despite these promising advances, challenges remain in the clinical translation of engineered exosome therapies. The field currently grapples with issues of standardized production, precise characterization, and scalable manufacturing [68]. Future developments will likely focus on optimizing engineering strategies for enhanced targeting specificity, developing more efficient cargo loading techniques, and establishing robust quality control measures. The integration of exosomes with advanced biomaterial delivery systems, such as injectable hydrogels and biocompatible scaffolds, presents particularly promising avenues for enhancing retention and sustained release at target sites [42].
As the field progresses, the convergence of exosome engineering with emerging technologies in gene editing, synthetic biology, and nanotechnology will further expand the therapeutic potential of these natural delivery vehicles. With ongoing clinical trials evaluating MSC-derived exosome therapeutics [68], the transition from preclinical promise to clinical reality appears increasingly imminent. The continued systematic comparison of exosome performance across well-characterized animal models, coupled with rigorous engineering approaches, will be essential for realizing the full potential of these remarkable biological nanoparticles as precision therapeutics for wound healing and beyond.
The therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-exosomes) represents a promising frontier in regenerative medicine, particularly for wound healing. As a cell-free alternative, MSC-exosomes offer significant advantages over whole-cell therapies, including lower immunogenicity, enhanced stability, and the ability to cross biological barriers [25]. However, the transition from promising preclinical results to reliable clinical applications faces a critical challenge: methodological bias in animal studies. Inconsistent implementation of core methodological principles—specifically randomization, blinding, and comprehensive reporting—introduces substantial variability and threatens the validity and reproducibility of research findings. This guide examines the current state of these methodological shortcomings in MSC-exosome wound healing research and provides evidence-based strategies to address them, framed within the broader context of comparing exosome performance across different animal wound models.
Current Status of Methodological Rigor in MSC-Exosome Research
Recent systematic reviews and meta-analyses have quantified the prevalence of methodological limitations in the MSC-exosome literature. An umbrella review of 47 meta-analyses covering 27 disease areas, including wound healing, found frequent risk of bias due to poor randomization and blinding procedures [4] [69]. The analysis revealed high heterogeneity (I² > 70%) across preclinical studies, much of which was attributable to methodological inconsistencies rather than purely biological variables.
A specialized meta-analysis focusing specifically on wound healing and skin regeneration, which encompassed 83 preclinical studies, reinforced these findings [14]. The authors noted substantial variability in experimental designs, reporting standards, and methodological rigor, complicating cross-study comparisons and meta-analytic synthesis.
Table 1: Prevalence of Methodological Limitations in MSC-Exosome Wound Healing Studies
| Methodological Aspect | Current Status | Impact on Evidence |
|---|---|---|
| Randomization | Inconsistently reported and implemented | Introduces selection bias and confounds group comparisons |
| Blinding | Rarely comprehensively applied | Increases risk of performance and detection bias |
| Sample Size Justification | Rarely provided | Underpowered studies reduce reliability of findings |
| EV Characterization | Variable adherence to MISEV guidelines | Compromises reproducibility and product definition |
| Data Reporting | Incomplete statistical reporting | Hinders meta-analytic synthesis and interpretation |
Core Methodological Principles and Implementation Strategies
Randomization: Beyond Simple Allocation
Proper randomization ensures that each experimental unit has an equal chance of being assigned to any treatment group, distributing known and unknown confounding factors evenly across groups.
Common Deficiencies:
- Inadequate sequence generation (e.g., alternating assignment, birth date allocation)
- Failure to conceal allocation sequences from investigators
- Small group sizes exacerbating chance imbalances
Recommended Protocols:
- Computer-generated random numbers using platforms like GraphPad Prism, R, or online randomization tools
- Block randomization for small studies to maintain balanced group sizes
- Stratified randomization when important prognostic factors are known (e.g., diabetes severity, age)
- Allocation concealment using sequentially numbered, opaque, sealed envelopes or centralized electronic systems
Table 2: Randomization Implementation Checklist for Wound Studies
| Step | Procedure | Documentation Requirement |
|---|---|---|
| 1 | Define inclusion/exclusion criteria before randomization | Protocol document |
| 2 | Generate allocation sequence independent of study team | Statistical software output |
| 3 | Conceal allocation sequence until after group assignment | Description of concealment method |
| 4 | Verify group similarity after randomization | Baseline characteristics table |
Blinding: Comprehensive Approach
Blinding (or masking) prevents conscious or unconscious influence on study results by keeping key personnel unaware of group assignments throughout the experiment.
Three-Tier Blinding Protocol:
- Investigator Blinding: During treatment administration and wound intervention
- Outcome Assessor Blinding: During wound measurement, histopathological analysis, and data collection
- Data Analyst Blinding: During statistical analysis and interpretation
Practical Implementation:
- Use coded exosome preparations with identical appearance and packaging
- Employ third-party personnel for treatment administration
- Utilize automated image analysis for wound measurements where possible
- Implement blinded data analysis with group codes revealed only after analysis completion
Sample Size Justification and Statistical Reporting
Underpowered studies remain prevalent in preclinical exosome research. Appropriate sample size calculation ensures sufficient statistical power to detect meaningful treatment effects.
Key Elements:
- A priori power analysis based on pilot data or literature values
- Clear definition of primary endpoint effect size
- Accounting for anticipated attrition rates (especially in diabetic models)
- Transparency about any post-hoc power calculations
Experimental Design Framework for MSC-Exosome Wound Studies
The following experimental workflow diagram outlines a comprehensive approach to designing robust preclinical studies of MSC-exosomes in wound healing:
Standardized Assessment Framework for Cross-Study Comparisons
To enable valid comparisons of MSC-exosome performance across different animal wound models, researchers should implement standardized assessment protocols encompassing functional, histological, and molecular endpoints.
Table 3: Core Outcome Set for MSC-Exosome Wound Healing Studies
| Domain | Specific Metrics | Assessment Method | Timing |
|---|---|---|---|
| Wound Closure | Percentage area reduction, Complete healing time | Digital planimetry, standardized photography | Days 0, 3, 7, 10, 14 |
| Histological Analysis | Re-epithelialization, Granulation tissue thickness, Collagen deposition | H&E, Masson's Trichrome staining | Endpoint(s) |
| Vascularization | Capillary density, VEGF expression | CD31 immunohistochemistry, Western blot | Endpoint(s) |
| Inflammation | Macrophage polarization, Pro-inflammatory cytokines | F4/80/CD206 staining, ELISA for TNF-α, IL-6 | Multiple timepoints |
| Scar Quality | Collagen alignment, Scar width | Polarized light microscopy, histological measurement | Endpoint |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for MSC-Exosome Wound Studies
| Reagent/Material | Function | Considerations |
|---|---|---|
| MSC Sources | Exosome production | Bone marrow, adipose, and umbilical cord most common; source affects cargo [4] |
| EV Isolation Kits | Exosome purification | Ultracentrifugation (gold standard) vs. Tangential Flow Filtration (higher yield) [6] |
| Characterization Antibodies | EV validation | CD9, CD63, CD81 for positive markers; calnexin for negative markers [70] |
| Animal Models | In vivo testing | Diabetic (db/db or STZ-induced) vs. non-diabetic; mouse (73.5%) and rat (26.5%) most common [14] |
| Wound Measurement Software | Objective outcome assessment | Digital planimetry tools; ensures blinded measurement |
| Histology Stains | Tissue analysis | H&E (general morphology), Masson's Trichrome (collagen), CD31 (vascularization) |
Impact of Methodological Rigor on Performance Comparisons
The implementation of robust methodologies directly influences the perceived performance of MSC-exosomes across different wound models. Several key relationships have emerged from systematic analyses:
The relationship between methodological rigor and observed outcomes is particularly evident in wound healing studies. For instance, the comprehensive meta-analysis by [14] found that studies implementing stricter blinding protocols reported more conservative effect sizes for wound closure rates (15-25% reduction in effect size estimates). Similarly, adequate randomization procedures reduced between-study heterogeneity by 30-40% in subgroup analyses.
Reporting Guidelines and Transparency Initiatives
Complete and transparent reporting is essential for interpreting, replicating, and building upon preclinical research. Researchers should adhere to the following guidelines:
Essential Reporting Elements:
- ARRIVE 2.0 Guidelines: Comprehensive checklist for in vivo research
- MISEV2023: Minimal information for studies of extracellular vesicles
- Experimental Design Details: Randomization method, blinding procedures, exclusion criteria
- Exosome Characterization: Size distribution, concentration, marker expression, and purity assessments
- Statistical Analysis Plan: Pre-specified analyses, handling of missing data, adjustment for multiple comparisons
Addressing methodological bias in preclinical MSC-exosome research requires a systematic, multi-faceted approach centered on rigorous randomization, comprehensive blinding, and complete reporting. The strategies outlined in this guide provide a framework for enhancing the reliability and reproducibility of wound healing studies, enabling more valid comparisons of exosome performance across different animal models and experimental conditions. As the field progresses toward clinical translation, commitment to methodological rigor will be paramount for generating credible, actionable evidence regarding the therapeutic potential of MSC-exosomes in regenerative medicine.
Comparative Efficacy: Validating MSC Exosome Performance Across Models and Sources
The therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a paradigm shift in regenerative medicine, offering a cell-free alternative to whole-cell therapies for wound healing. These nanoscale extracellular vesicles, typically 30-150 nm in diameter, mediate intercellular communication by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells [71]. For researchers and drug development professionals, quantifying the precise impact of MSC-Exos on wound closure rates and scar quality requires systematic meta-analysis of preclinical data across standardized animal models. This review synthesizes current meta-analysis findings to provide evidence-based comparisons of MSC-Exo efficacy, optimized protocols, and mechanistic insights, with a specific focus on translational applications for wound healing and skin regeneration. The burgeoning interest in this field is evidenced by the publication surge, with approximately 82% of 83 eligible preclinical studies published in 2020 or later, predominantly from China (86.7%) [14].
Quantitative Synthesis: Efficacy Metrics Across Preclinical Models
Comprehensive meta-analyses of preclinical studies demonstrate the robust therapeutic potential of MSC-derived extracellular vesicles (MSC-EVs) in wound healing. According to an umbrella review of 47 meta-analyses covering 27 diseases, MSC-EVs consistently demonstrate high efficacy across neurological, renal, wound healing, liver, musculoskeletal, respiratory, and reproductive disorders [4]. These vesicles significantly improve functional scores, reduce inflammation, and promote regeneration through their anti-inflammatory, anti-apoptotic, and pro-angiogenic properties. The quantitative synthesis reveals that bone marrow-, adipose-, and umbilical cord-derived EVs show particularly strong efficacy, with modified EVs demonstrating enhanced outcomes over native vesicles [4].
Table 1: Overall Efficacy of MSC-EVs in Wound Healing Based on Meta-Analysis
| Outcome Measure | Effect Size/Improvement | Number of Studies | Notes |
|---|---|---|---|
| Wound Closure Rate | Significant acceleration | 83 studies | Consistent across diabetic and non-diabetic models [14] |
| Scar Width | Significant reduction | 83 studies | Improved cosmetic outcome [14] |
| Blood Vessel Density | Significant increase | 83 studies | Enhanced angiogenesis [14] |
| Collagen Deposition | Significant improvement | 83 studies | Better extracellular matrix formation [14] |
Comparative Efficacy by MSC Source
The tissue origin of MSCs significantly influences exosome therapeutic potential. Subgroup analyses from systematic reviews enable direct comparison of efficacy across different MSC sources, providing crucial information for protocol optimization.
Table 2: Efficacy Comparison by MSC Source in Wound Healing Models
| MSC Source | Wound Closure Rate | Collagen Deposition | Revascularization | Key Advantages |
|---|---|---|---|---|
| Adipose Tissue (ADSCs) | Best effect [14] | Best effect [14] | Moderate | Easily accessible, abundant supply |
| Umbilical Cord | Strong effect [71] | Strong effect [71] | Strong effect [71] | Non-invasive collection, low immunogenicity |
| Bone Marrow (BMMSCs) | Moderate effect | Moderate effect | Best effect [14] | Well-characterized, extensive literature |
Umbilical cord-derived MSC exosomes (hUCMSC-Exos) demonstrate particular promise due to their non-invasively sourced abundant supply, low immunogenicity that lowers wound immune reaction risks, and superior performance in promoting angiogenesis, fibroblast proliferation, and immune regulation compared to ADSC-Exos and BMMSC-Exos [71].
Comparative Efficacy by Extracellular Vesicle Type
Beyond traditional small extracellular vesicles (sEVs), recent research has investigated apoptotic extracellular vesicles (ApoEVs) for wound healing applications. Meta-analysis reveals important efficacy differences between these vesicle types.
Table 3: Efficacy Comparison by Extracellular Vesicle Type
| EV Type | Abbreviation | Size Range | Wound Closure | Collagen Deposition | Revascularization |
|---|---|---|---|---|---|
| Small EVs | sEVs | <200 nm [14] | Strong effect | Strong effect | Best effect [14] |
| Apoptotic Small EVs | ApoSEVs | <1 μm [14] | Best effect [14] | Best effect [14] | Moderate effect |
| Apoptotic Bodies | ApoBDs | 1-5 μm [14] | Moderate effect | Moderate effect | Moderate effect |
Notably, ApoSEVs have demonstrated superior efficacy in wound closure outcomes and collagen deposition compared to traditional sEVs and ApoBDs, while sEVs show better performance in revascularization [14]. This suggests that different EV subtypes may be optimal depending on the primary therapeutic goal.
Administration Protocols and Experimental Parameters
Route of Administration Efficacy
The administration route significantly influences MSC-Exo therapeutic efficacy, as demonstrated by comparative preclinical studies. Subgroup analyses from meta-analyses reveal that:
- Subcutaneous injection displayed greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering methods [14]
- Intravenous delivery demonstrated superior therapeutic efficacy over intranasal and nebulized routes in LPS-induced acute lung injury models at equivalent doses (5×10⁸ particles) [46]
- Intranasal and nebulized routes showed comparable efficacy to each other in respiratory models [46]
A systematic comparison of administration routes in a lipopolysaccharide (LPS)-induced acute lung injury mouse model revealed dose-dependent effects across delivery methods, with intravenous high-dose (Exo-VH, 5×10⁸ particles) outperforming medium- and low-dose groups, while intranasal medium-dose (Exo-NM, 10×10⁸ particles) was superior to low-dose with no significant difference between medium and high doses [46].
Experimental Models in Preclinical Research
Preclinical evaluation of MSC-Exos has utilized diverse animal models to simulate human wound healing scenarios:
- Species Distribution: Mouse models (73.5%, N=61) predominated over rat models (26.5%, N=22) across 83 studies [14]
- Wound Type Distribution: 43.4% (n=36) non-diabetic wounds, 47.0% (n=39) diabetic wounds [14]
- Diabetic Models: 30 studies used streptozotocin (STZ)-induced models (type 1 diabetes), 9 studies used genetically modified db/db mice (type 2 diabetes) [14]
- Primary Model: Full-thickness excisional wounds were the most-studied models (90.4%, n=75), primarily dorsal wounds [14]
Additional specialized models included scleroderma (n=1), burns (n=1), photoaging (n=3), atopic dermatitis (n=2), and frostbite injury (n=1) [14], demonstrating the versatility of MSC-Exo applications across diverse wound healing contexts.
Methodological Framework: Experimental Protocols
Standardized MSC-Exo Isolation and Characterization
Extracellular Vesicle Isolation Protocol: MSC-Exos are typically isolated using ultracentrifugation methods [71] [8]. The standard protocol involves:
- Low-speed centrifugation (4°C, 2000×g, 30 min) to remove cells and debris
- Intermediate centrifugation (4°C, 10,000×g, 45 min) to eliminate larger particles
- Filtration through 0.22 μm sterilizing filters
- Ultracentrifugation (4°C, 110,000×g, 70 min) twice for purification
- Resuspension of the final pellet in PBS and storage at -80°C [8]
Characterization Methods:
- Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration [71] [8]
- Transmission Electron Microscopy (TEM): Visualizes vesicle morphology and structure [71] [8]
- Western Blot Analysis: Confirms presence of exosomal markers (CD63, TSG101) [8]
- Cellular Uptake Studies: Using PKH67 fluorescent dye to track internalization by recipient cells [8]
In Vitro Functional Assays
Cell Scratch/Migration Assay:
- HDF-a cells are seeded in six-well plates (5×10⁵ cells per well, n=3)
- Scratches are created with a 200 μL pipette tip
- Serum-free medium with or without MSC-EVs (100 μg/mL) is added
- Migration is measured at 0, 12, and 24 hours using ImageJ software
- Migration area (%) is calculated as (A0-An)/A0 × 100, where A0 is initial scratch area and An is remaining area [8]
Cell Proliferation Assay:
- Implemented using standardized assays like CCK-8 or MTT
- HDF-a cells are treated with MSC-EVs at various concentrations
- Proliferation rates are quantified spectrophotometrically [8]
Tube Formation Assay:
- Human umbilical vein endothelial cells (HUVECs) are cultured on Matrigel
- Tube formation is quantified by measuring tube length, branch points, and loop numbers
- Demonstrates pro-angiogenic potential of MSC-Exos [71]
In Vivo Wound Healing Models
Full-Thickness Excisional Wound Model:
- Dorsal wounds created in mice or rats
- MSC-EVs administered via subcutaneous injection around wound periphery
- Wound closure rate measured by photographic documentation and planimetry
- Histological analysis for re-epithelialization, collagen deposition, and blood vessel density [14] [8]
Diabetic Wound Model:
- Induced by streptozotocin (STZ) injection or using genetically diabetic db/db mice
- Represents impaired healing conditions relevant to clinical chronic wounds
- MSC-EVs tested for ability to overcome healing deficits [14]
Mechanistic Insights: Signaling Pathways
Key Molecular Pathways in MSC-Exo Mediated Healing
MSC-Exos accelerate wound healing through multiple interconnected mechanisms: reducing inflammation, stimulating angiogenesis, and promoting extracellular matrix formation [71]. Spatial transcriptomics analysis of mouse skin tissue treated with MSC-EVs revealed that these vesicles reduce the relative expression of marker genes in myofibroblasts, regulate wound healing, and decrease scar formation by reducing TGF-β signaling pathway expression while increasing Wnt signaling pathway activity [8].
Bioinformatics analysis suggests that Unc-51-like autophagy activating kinase 2 (ULK2), Collagen Type XIX Alpha 1 Chain (COL19A1), and Interleukin-6 Signal Transducer (IL6ST) are potential key molecules involved in the regulation of wound repair by hUCMSC-Exos [71]. Additionally, MSC-Exos enriched in specific miRNAs inhibit scar formation by suppressing the TGF-β/Smad pathway [71], which is crucial for excessive collagen deposition in hypertrophic scars and keloids.
Diagram Title: MSC-Exo Mechanisms in Wound Healing
Functional Wound Assessment and Scar Quality Metrics
Transepidermal Water Loss as Predictive Biomarker
A critical advancement in wound healing assessment is the recognition that functional closure, not just visual closure, predicts long-term outcomes. An exploratory observational study demonstrated that elevated transepidermal water loss (TEWL) at wound closure site reliably predicts recurrence [72]. The study established:
- TEWL Score Cutoff: 24.1 g.m⁻².h⁻¹ (AUC = 0.967) predictive of recurrence
- Predictive Value: TEWL score >24.1 associated with 39% recurrence rate vs. 0% for score ≤24.1
- Clinical Significance: Every 1-unit increase in TEWL score associated with 34% increased odds of wound reopening after adjusting for covariates [72]
This finding challenges the current FDA endpoint for wound closure—defined as skin re-epithelialization without drainage confirmed at two consecutive visits two weeks apart—by suggesting that functional restoration of skin barrier should be included as an additional criterion [72].
Scar Quality Assessment Parameters
Comprehensive scar assessment in preclinical studies includes multiple quantitative metrics:
- Scar Width Measurement: Direct histological measurement of scar tissue width [14] [8]
- Collagen Organization: Histological evaluation of collagen fiber alignment and maturity
- Blood Vessel Density: Quantification of vascular structures in healed tissue [14]
- Histopathological Scoring: Standardized scoring of inflammation, epithelialization, and granulation tissue formation
These metrics collectively provide a multidimensional assessment of scar quality beyond simple wound closure rates, enabling more clinically relevant evaluation of MSC-Exo therapeutics.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for MSC-Exo Wound Healing Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| MSC Sources | Adipose tissue, Umbilical cord, Bone marrow [14] | Exosome biogenesis; Different therapeutic profiles |
| Characterization Antibodies | Anti-CD63, Anti-TSG101 [8] | Vesicle identification and quantification |
| Fluorescent Tracers | PKH67 dye [8] | Cellular uptake and biodistribution studies |
| Animal Models | BALB/c mice [46] [8], Diabetic db/db mice [14] | In vivo efficacy testing |
| Cell Lines | Human Dermal Fibroblast-adult (HDF-a) [8], HUVECs [71] | In vitro mechanism studies |
| Wound Creation Agents | Lipopolysaccharide (LPS) [46], Streptozotocin (STZ) [14] | Disease-specific model establishment |
| Analytical Instruments | Nanoparticle Tracking Analysis [71] [8], Transmission Electron Microscope [71] [8] | Vesicle characterization |
| Pathway Analysis Tools | Spatial Transcriptomics [8], Bioinformatics analysis [71] | Mechanism elucidation |
Meta-analysis of preclinical data provides compelling evidence for MSC exosomes as potent therapeutics for improving both wound closure rates and scar quality. The quantitative synthesis reveals that ADSC-Exos demonstrate superior wound closure efficacy, while umbilical cord-derived exosomes offer balanced performance across multiple healing parameters. The recognition that ApoSEVs may outperform traditional sEVs in certain applications, coupled with findings that subcutaneous injection represents the optimal delivery route, provides critical guidance for therapeutic development.
Future research priorities include standardizing EV protocols addressing high heterogeneity in collection conditions, separation methods, storage methods, modifications, treatment dose, administration route, and frequency [14]; improving study quality by addressing risks of bias in randomization and blinding [4]; and establishing functional wound closure endpoints that incorporate barrier function restoration metrics alongside traditional visual assessment [72]. As the field progresses toward clinical translation, these meta-analysis insights provide validated benchmarks for comparing therapeutic efficacy and optimizing MSC-Exo-based wound healing strategies.
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine, offering promising therapeutic potential for diverse applications, particularly in wound healing. These multipotent cells can be isolated from various tissue sources, each imparting distinct biological characteristics and functional capabilities [1]. The International Society for Cell & Gene Therapy (ISCT) establishes minimal criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD105, CD73, CD90 ≥95%; CD45, CD34, CD14/CD11b, CD79α/CD19, HLA-DR ≤2%), and tri-lineage differentiation potential (osteogenic, chondrogenic, adipogenic) [73] [1]. As the field progressively recognizes that many therapeutic benefits are mediated through paracrine secretion rather than direct differentiation, the focus has shifted toward MSC-derived extracellular vesicles (EVs) and exosomes as primary effectors of tissue repair [25] [74].
This comparative analysis systematically evaluates MSC efficacy across tissue sources, with specific emphasis on performance in animal wound models. We synthesize quantitative preclinical data, detailed methodologies, and mechanistic insights to provide evidence-based rankings for researchers and drug development professionals navigating MSC source selection for regenerative applications.
Quantitative Efficacy Rankings in Wound Healing Models
Comprehensive meta-analyses of preclinical studies provide direct comparisons of MSC therapeutic efficacy across tissue sources. The table below summarizes performance metrics for prominent MSC sources in wound healing applications:
Table 1: Efficacy Ranking of MSC Tissue Sources in Preclinical Wound Models
| MSC Tissue Source | Wound Closure Rate | Collagen Deposition | Revascularization Potential | Key Advantages |
|---|---|---|---|---|
| Adipose (AD-MSCs) | Best (Significantly enhances wound closure rate [14] [75]) | Best (Superior collagen deposition capability [14]) | Moderate (BM-MSCs showed better revascularization [14]) | Abundant yield, superior immunomodulation, high proliferation [73] [76] |
| Bone Marrow (BM-MSCs) | Moderate (Effective but less than AD-MSCs [14] [75]) | Moderate | Best (Demonstrated superior revascularization outcomes [14]) | Gold standard, well-characterized, strong osteogenic potential [73] [1] |
| Umbilical Cord (UC-MSCs) | Good (High proliferative capacity [73]) | Good | Good (Strong angiogenic potential [73]) | Low immunogenicity, high proliferation, non-invasive collection [73] [1] |
| Menstrual Blood (MenSCs) | Promising (Rapid proliferation rate [73]) | Promising | Promising | Easy collection, high proliferation, minimal ethical concerns [73] |
Beyond general wound healing, different MSC sources show specialized efficacy across specific wound types:
Table 2: MSC Source Performance Across Specialized Wound Models
| Wound Model Type | Most Effective MSC Source | Key Supporting Evidence |
|---|---|---|
| Diabetic Wounds | Adipose (AD-MSCs) | Demonstrated clear therapeutic potential in both diabetic and non-diabetic animal models [14] |
| Inflammatory Skin Diseases (Psoriasis, Atopic Dermatitis) | Adipose (AD-MSCs) | Superior immunomodulatory properties effectively reduced pathological symptoms [76] |
| Skin Rejuvenation & Photoaging | Adipose (AD-MSCs) | Significant improvement in wound closure, collagen deposition, and revascularization [14] |
MSC-Derived Extracellular Vesicles: Emerging Cell-Free Therapeutics
The therapeutic paradigm has shifted toward recognizing MSC-derived extracellular vesicles (MSC-EVs) as primary mediators of regenerative effects. MSC-EVs offer significant advantages over whole-cell therapies, including lower immunogenicity, enhanced biological barrier penetration, reduced tumorigenicity risk, and superior storage stability [4] [25] [77]. Quantitative synthesis of 47 meta-analyses demonstrates that MSC-EVs exhibit robust therapeutic potential across diverse preclinical models, significantly improving functional scores, reducing inflammation, and promoting regeneration [4].
Among EV subtypes, apoptotic small extracellular vesicles (ApoSEVs) show superior efficacy in wound closure and collagen deposition compared to small EVs (sEVs) and apoptotic bodies (ApoBDs), while sEVs demonstrate better revascularization potential [14]. This nuanced understanding of EV subtype efficacy further refines source selection for specific therapeutic goals.
Experimental Methodologies for MSC Efficacy Evaluation
Standardized MSC Characterization Protocols
Table 3: Essential Research Reagent Solutions for MSC Studies
| Research Reagent/Category | Function/Application | Experimental Notes |
|---|---|---|
| Plastic Adherence Assay | Confirms MSC phenotype per ISCT criteria [73] [1] | Use standard tissue culture-treated plastic; assess morphology |
| Flow Cytometry Antibody Panels | Surface marker characterization (CD105, CD73, CD90, CD45, CD34, HLA-DR) [73] [1] | Essential for quality control; ≥95% positive for CD105, CD73, CD90; ≤2% for hematopoietic markers |
| Tri-lineage Differentiation Kits (Osteogenic, Chondrogenic, Adipogenic) | Functional validation of differentiation potential [73] [1] | Include appropriate induction factors; stain with tissue-specific dyes |
| EV Isolation Tools (Ultracentrifugation, Ultrafiltration, Density Gradient) | Separation of MSC-EVs from conditioned media [14] [77] | Method selection affects yield and purity; ultracentrifugation remains gold standard |
| Animal Wound Models (Mouse, Rat) | In vivo efficacy assessment [14] | C57BL/6 mice and Sprague-Dawley rats most common; diabetic models using streptozotocin or db/db mice |
MSC-EV Isolation and Characterization Workflow
EV Isolation Workflow
Rigorous EV characterization is essential and should follow MISEV2023 guidelines, employing multiple complementary techniques:
- Nanoparticle Tracking Analysis (NTA): Determines EV size distribution and concentration
- Transmission Electron Microscopy (TEM): Visualizes EV morphology and ultrastructure
- Western Blotting: Confirms presence of EV markers (CD63, CD81, TSG101) and absence of contaminants
- Functional Assays: Evaluate angiogenic, immunomodulatory, and proliferative potential in target cells [14] [77]
In Vivo Wound Healing Assessment Models
Preclinical wound healing studies predominantly utilize mouse (73.5%) and rat (26.5%) models, with the following experimental configurations:
- Wound Types: Full-thickness excisional wounds (90.4%), diabetic foot ulcers, burns, photoaging, and atopic dermatitis models
- Intervention Groups: Include MSC source comparisons, EV versus whole-cell therapies, and administration route optimization
- Administration Routes: Subcutaneous injection demonstrates superior efficacy compared to topical dressing/covering for wound closure, collagen deposition, and revascularization [14]
- Outcome Measures: Quantitative wound closure rates, histopathological analysis (collagen content, vascular density), and molecular profiling of inflammatory markers
Mechanisms of Action: Signaling Pathways and Functional Properties
Molecular Mechanisms Underlying MSC Therapeutic Effects
MSC Therapeutic Mechanisms
The therapeutic effects of MSCs are mediated through sophisticated paracrine signaling mechanisms:
- Immunomodulation: AD-MSCs particularly excel through T regulatory cell induction via IL-10, macrophage polarization toward M2 phenotype, and T lymphocyte inhibition via indoleamine 2,3-dioxygenase (IDO) and prostaglandin E2 (PGE2) [76]
- Angiogenesis: BM-MSCs demonstrate superior revascularization through robust vascular endothelial growth factor (VEGF), angiopoietin-1 (ANG-1), and monocyte chemoattractant protein-1 (MCP-1) secretion [14] [74]
- Anti-apoptotic Signaling: Multiple MSC sources secrete VEGF, insulin-like growth factor-1 (IGF-1), transforming growth factor-β (TGF-β), and fibroblast growth factor (FGF) to enhance cell survival [76]
- Extracellular Matrix Remodeling: AD-MSCs show superior collagen deposition through coordinated secretion of growth factors and matrix-modulating enzymes [14]
MSC-EV Specific Mechanisms
MSC-derived extracellular vesicles exert therapeutic effects through specific molecular cargo:
- microRNA Delivery: EV-contained miRNAs (e.g., miR-125a-3p, miR-147a, miR-21-3p) regulate recipient cell gene expression, inhibiting pathological Th2 cell proliferation and promoting keratinocyte and endothelial proliferation [76]
- Protein-Mediated Signaling: EVs transport over 304 proteins that modulate immune responses, cellular proliferation, and differentiation pathways [77]
- Targeted Cellular Uptake: EVs facilitate precise delivery of bioactive molecules to recipient cells through membrane fusion, receptor-ligand interactions, and endocytosis [25]
Based on comprehensive analysis of preclinical efficacy data, AD-MSCs demonstrate superior performance in wound healing applications, particularly excelling in wound closure rates and collagen deposition. BM-MSCs maintain advantage in revascularization contexts, while UC-MSCs offer balanced efficacy with practical sourcing advantages. The emerging paradigm of MSC-EVs as cell-free therapeutics presents compelling opportunities for enhanced safety profiles and standardized manufacturing.
For research and development applications, we recommend:
- Source Selection: Prioritize AD-MSCs for most wound healing applications unless specific revascularization needs justify BM-MSCs
- Therapeutic Format: Consider MSC-EVs over whole-cell therapies for enhanced safety, stability, and reduced immunogenicity
- Standardization: Implement rigorous characterization following ISCT guidelines for MSCs and MISEV2023 standards for EVs
- Administration Strategy: Utilize subcutaneous injection over topical application for optimized delivery efficiency
Future research directions should address standardization challenges in MSC-EV isolation, enhance targeting capabilities through engineering approaches, and validate these preclinical findings in clinical settings to fully realize the potential of MSC-based therapies in regenerative medicine.
The field of regenerative medicine is increasingly shifting from whole-cell therapies toward cell-free alternatives utilizing derivatives of mesenchymal stem cells (MSCs). Among these, extracellular vesicles (EVs) have emerged as promising therapeutic agents, with small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) representing distinct subpopulations with unique functional characteristics. This comparative analysis examines the biological properties, functional efficacy, and therapeutic mechanisms of sEVs versus ApoEVs within the context of wound healing applications, providing evidence-based guidance for researchers and drug development professionals.
Biological Characteristics and Isolation Methods
Definition and Biogenesis
Small Extracellular Vesicles (sEVs), historically termed exosomes, are nanoscale vesicles (30-200 nm) that originate from the endosomal system. Their biogenesis involves the inward budding of endosomal membranes to form intraluminal vesicles within multivesicular bodies, which subsequently fuse with the plasma membrane to release sEVs into the extracellular space [78] [32]. These vesicles carry diverse biomolecules, including proteins, lipids, and nucleic acids, reflecting their parental cells' composition and physiological state.
Apoptotic Extracellular Vesicles (ApoEVs) constitute a heterogeneous population of vesicles released during programmed cell death. This category includes apoptotic small EVs (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm) that form through apoptotic membrane blebbing [14]. ApoEVs contain cellular debris, organelles, and nuclear fragments, alongside signaling molecules that influence tissue microenvironment and repair processes.
Isolation and Production Methods
Different isolation techniques significantly impact vesicle yield, purity, and functionality. Ultracentrifugation (UC) remains the most commonly used method for sEV isolation, involving sequential centrifugation steps to separate vesicles based on size and density [6] [32]. However, tangential flow filtration (TFF) has demonstrated superior performance for large-scale production, with studies reporting statistically higher particle yields compared to UC [6].
For ApoEV production, researchers typically induce apoptosis in MSC cultures through stressors like serum deprivation or chemical inducers, followed by vesicle collection from the conditioned medium. The methodology for ApoEV isolation shares similarities with sEV protocols but often requires adjustments to accommodate the broader size distribution of apoptotic vesicles.
Table 1: Comparative Isolation Characteristics of sEVs and ApoEVs
| Characteristic | sEVs | ApoEVs |
|---|---|---|
| Primary Isolation Methods | Ultracentrifugation, Tangential Flow Filtration, Size-exclusion Chromatography | Ultracentrifugation with modified parameters, Filtration-based size selection |
| Particle Yield | Higher with TFF vs UC [6] | Variable depending on apoptosis induction efficiency |
| Process Scalability | Suitable for large-scale GMP production with TFF [6] | Challenging due to apoptotic induction requirements |
| Storage Stability | Stable at -80°C for extended periods [32] | Limited stability data available |
Comparative Functional Efficacy in Wound Healing
Performance in Preclinical Wound Models
A comprehensive meta-analysis of 83 preclinical studies directly compared the therapeutic efficacy of different MSC-EV subtypes in wound healing applications. The findings revealed distinct performance patterns between vesicle types across multiple wound healing parameters [14].
ApoSEVs demonstrated superior performance in wound closure rate and collagen deposition compared to both sEVs and ApoBDs. This enhanced efficacy may stem from their enriched cargo of bioactive molecules that directly promote tissue repair mechanisms. In contrast, sEVs excelled in promoting revascularization, a critical process for supplying nutrients and oxygen to healing tissues [14].
The meta-analysis further investigated optimal administration routes, finding that subcutaneous injection provided superior outcomes for wound closure, collagen deposition, and revascularization compared to topical dressing/covering approaches. This suggests that direct tissue integration enhances vesicle bioavailability and functionality [14].
Table 2: Functional Efficacy Comparison in Wound Healing Models
| Therapeutic Parameter | sEVs Performance | ApoSEVs Performance | ApoBDs Performance |
|---|---|---|---|
| Wound Closure Rate | Moderate efficacy | Superior efficacy [14] | Lower efficacy |
| Collagen Deposition | Moderate promotion | Superior promotion [14] | Limited promotion |
| Revascularization | Superior angiogenesis [14] | Moderate angiogenesis | Limited data |
| Scar Width Reduction | Significant reduction [8] | Limited data | Limited data |
| Re-epithelialization | Acceleration demonstrated [8] | Limited data | Limited data |
Cellular and Molecular Mechanisms
The differential therapeutic effects of sEVs and ApoEVs originate from their distinct cargo compositions and subsequent interactions with recipient cells. sEVs derived from bone marrow MSCs significantly enhance the migration capacity of dermal fibroblasts—a critical process in wound healing [79]. Transcriptomic analysis revealed that MSC-sEVs treatment regulates genes associated with cell migration and proliferation pathways in recipient fibroblasts [79].
Both MSC-sEVs and umbilical cord blood-derived EVs promote wound healing through regulation of key signaling pathways. Spatial transcriptomics demonstrated that these vesicles reduce TGF-β signaling (associated with fibrosis) while enhancing Wnt pathway activity (associated with regeneration) [8]. This dual mechanism accelerates functional tissue repair while minimizing scar formation.
ApoEVs contain unique molecular cargo acquired during the apoptotic process, including damage-associated molecular patterns (DAMPs) and specific miRNA profiles that may modulate immune responses and tissue remodeling differently than sEVs. However, the precise mechanistic pathways through which ApoEVs exert their superior effects on wound closure remain under investigation.
Diagram 1: Biogenesis and Cellular Targets of sEVs and ApoEVs in Wound Healing
Experimental Models and Methodologies
In Vitro Assessment Protocols
Standardized in vitro assays provide crucial preliminary data on EV functionality before proceeding to complex animal models. The cell scratch assay represents a fundamental method for evaluating EV effects on cell migration capacity. The protocol involves creating a uniform scratch in a confluent cell monolayer (typically fibroblasts or keratinocytes), treating with EVs, and monitoring closure over 24-48 hours [8]. MSC-EVs consistently demonstrate superior enhancement of fibroblast migration compared to fibroblast-derived EVs [79].
The transwell migration assay provides quantitative assessment of cell movement through a porous membrane toward an EV-containing chemoattractant. Research indicates that sEVs from bone marrow MSCs significantly increase normal human dermal fibroblast migration through this system [79]. For proliferation assessment, MTT and CCK-8 assays measure metabolic activity as a proxy for cell growth, with both MSC-sEVs and ApoSEVs demonstrating promotive effects on skin cell proliferation [8].
In Vivo Wound Healing Models
Animal models provide essential platforms for evaluating the therapeutic potential of EVs in complex physiological environments. The full-thickness excisional wound model in mice or rats represents the most widely utilized system, involving creation of standardized dorsal wounds followed by local EV administration [14] [8]. Parameters including wound closure rate, scar width, blood vessel density, and collagen deposition serve as key outcome measures [14].
Both diabetic and non-diabetic animal models have been employed to evaluate EV efficacy. Diabetic models (including STZ-induced and db/db mice) particularly relevant for chronic wound applications demonstrate the ability of both sEVs and ApoSEVs to improve healing under pathological conditions [14]. Evaluation timelines typically span 7-21 days, with histological analysis of tissue architecture, immune cell infiltration, and extracellular matrix composition providing insights into healing quality beyond simple closure metrics.
Diagram 2: Experimental Workflow for Evaluating EV Therapeutic Potential
Signaling Pathways and Molecular Mechanisms
Spatial transcriptomics analysis of healed tissues revealed that MSC-EVs modulate several key signaling pathways critical for wound resolution. Both MSC-sEVs and umbilical cord blood EVs demonstrate capacity to reduce TGF-β signaling pathway activity while enhancing Wnt signaling pathway expression [8]. This coordinated regulation promotes regenerative healing while minimizing fibrotic tissue formation.
The molecular cargo responsible for these therapeutic effects includes specific microRNAs enriched in different EV subtypes. For sEVs, miR-21-5p and miR-125b-5p have been associated with inhibition of TGF-β signaling and reduced myofibroblast differentiation [78]. Additionally, miR-93-3p in bone marrow MSC-sEVs promotes proliferation and migration while reducing apoptosis of keratinocytes through suppression of apoptotic peptidase activating factor 1 (APAF1) [78]. The distinct miRNA profiles of ApoSEVs likely contribute to their unique functional properties, though comprehensive characterization remains ongoing.
Table 3: Key Molecular Cargo and Functional Mechanisms
| EV Type | Key Molecular Components | Functional Mechanisms | Therapeutic Outcomes |
|---|---|---|---|
| sEVs | miR-21-5p, miR-125b-5p, miR-93-3p, CD63, TSG101 | TGF-β inhibition, Wnt activation, APAF1 suppression | Enhanced fibroblast migration, reduced fibrosis, promoted angiogenesis [78] [79] |
| ApoSEVs | Specific miRNA profiles under characterization | Regulation of apoptosis, immunomodulation, matrix reorganization | Superior wound closure, enhanced collagen deposition [14] |
| ApoBDs | Cellular organelles, nuclear fragments, DAMPs | Phagocyte recruitment, clearance signals, immune modulation | Limited efficacy in wound closure [14] |
Research Reagent Solutions
Essential Materials and Tools
Successful investigation of EV therapeutics requires specific reagents and methodologies. The following toolkit outlines critical components for rigorous EV research:
- EV-Depleted Fetal Bovine Serum: Essential for cell culture during EV production to eliminate contaminating bovine vesicles. Prepared via ultracentrifugation (120,000 × g, 18 hours) of standard FBS followed by filtration [79].
- Human Platelet Lysate: A xeno-free supplement for MSC culture expansion under GMP-compliant conditions, supporting cell proliferation and sEV yield [6].
- Ultracentrifugation Equipment: Fundamental for EV isolation via sequential centrifugation (2,000 × g for 30 minutes, 10,000 × g for 40 minutes, 100,000 × g for 90 minutes) [79].
- Tangential Flow Filtration Systems: Superior alternative to ultracentrifugation for large-scale GMP-compliant production, providing higher particle yields [6].
- Nanoparticle Tracking Analysis: Critical for determining EV size distribution and concentration (e.g., NanoSight NS300) [6] [79].
- Transmission Electron Microscopy: Required for morphological characterization of EVs, confirming cup-shaped morphology [6].
- Western Blot Reagents: Antibodies against EV markers (CD9, CD63, TSG101) for validation of vesicle identity, with calnexin as negative control [6].
- Spatial Transcriptomics Platforms: Advanced tools for mapping gene expression patterns in healed tissues, revealing pathway modulation [8].
This comparative analysis demonstrates that both sEVs and ApoEVs present distinct therapeutic profiles in wound healing applications, with ApoSEVs exhibiting superior performance in wound closure and collagen deposition, while sEVs excel in promoting revascularization. The selection between these vesicle types should be guided by specific therapeutic objectives—ApoSEVs for accelerated tissue restoration and sEVs for vascularization-deficient wounds. Future research should address standardization of production protocols, optimization of delivery systems, and comprehensive safety profiling to advance these promising biologics toward clinical application. The evolving landscape of EV-based therapeutics offers exciting opportunities for developing targeted regenerative therapies that surpass the limitations of conventional approaches.
The therapeutic application of Mesenchymal Stem Cell (MSC)-derived exosomes represents a paradigm shift in regenerative medicine, offering a cell-free alternative with significant advantages in safety, standardization, and scalability [80] [28]. These nanovesicles mediate intercellular communication by transferring proteins, lipids, and nucleic acids, recapitulating the therapeutic effects of their parent MSCs—including anti-inflammatory, immunomodulatory, and pro-regenerative activities—while avoiding concerns regarding immunogenicity, infusion toxicity, and tumorigenic potential [28]. Despite promising preclinical results, successful clinical translation remains hampered by a critical challenge: effectively correlating outcomes from animal models with human clinical responses. The complexity of wound healing, integrating multiple phases and cell types, further complicates this translation [81]. This guide provides a systematic comparison of animal models used in MSC exosome research for wound healing, offering researchers a framework to enhance the predictive value of their preclinical studies and bridge the translational gap.
Comparative Analysis of Animal Models in Wound Healing Research
Selecting an appropriate animal model is paramount, as it must accurately simulate the human wound environment and healing trajectory. The ideal model balances physiological relevance with practical considerations such as cost, handling, and ethical implications [81] [82].
Dominant Models in Current Research
Analysis of recent preclinical studies reveals distinct trends in model selection. A 2025 meta-analysis of MSC-derived extracellular vesicles (EVs) in wound healing found that rodents are the predominant models, with mice used in 73.5% and rats in 26.5% of the 83 included studies [14]. These models are typically employed in full-thickness excisional wound studies (90.4% of analyses) to investigate both normal and impaired healing, such as in diabetic wounds [14].
The following table summarizes the key characteristics, advantages, and limitations of the most commonly used animal models in wound healing research.
Table 1: Comparison of Key Animal Models for Cutaneous Wound Healing Studies
| Animal Model | Skin Anatomy & Physiology | Healing Primary Mechanism | Key Advantages | Major Limitations | FDA & Literature Endorsement |
|---|---|---|---|---|---|
| Mouse (Mus musculus) | Thin skin with a panniculus carnosus [81]. | Rapid healing, predominantly via wound contraction [81] [82]. | - Low cost and easy handling [82].- Extensive repertoire of genetic tools [82].- Suitable for dorsal skinfold chamber [83]. | - Low predictive value (53%) for human outcomes [82].- Major immunological differences from humans [82].- Healing by contraction differs from human re-epithelialization [81]. | Most widely used model [14] [82]. |
| Rat (Rattus spp.) | Similar to mouse but with a thicker dermis, allowing for a slightly longer healing observation window (12-14 days) [81]. | Also heals significantly by contraction due to the panniculus carnosus [81]. | - Larger size facilitates some surgical procedures and sample collection compared to mice [81]. | - Shares same fundamental translational limitations as the mouse model [82].- Declining use in recent years [82]. | A common, well-established model [81]. |
| Pig (Sus scrofa) | Architecture highly similar to human skin in structure, epidermal thickness, dermal-epidermal contour, and hair follicle density [84] [82]. | Primarily through re-epithelialization and granulation tissue formation, with minimal contraction [82]. | - High predictive value (78%) for human healing [82].- Healing mechanism mirrors humans [84].- Preferred model by the FDA for wound healing studies [84]. | - High cost and specialized housing requirements [82].- Difficult handling due to size [82].- Limited transgenic strains. | Considered the preferred and most clinically relevant model [84] [82]. |
| Rabbit (Oryctolagus) | Skin structure is intermediate between rodents and pigs/humans. | Healing involves a mix of contraction and re-epithelialization. | - Easier to handle and house than pigs. | - Still exhibits a higher degree of contraction than humans [82].- Not as well characterized as other models. | Usage has declined over the past two decades [82]. |
The Translational Fidelity Gap
The choice of model directly impacts the clinical predictive value of research. A critical review of wound healing models revealed that while pig models demonstrate a 78% concordance with human outcomes, the more commonly used mouse models show only 53% concordance [82]. This "translational fidelity gap" is largely attributed to fundamental differences in skin biology. The presence of the panniculus carnosus in rodents drives rapid wound contraction, which is not the primary mechanism in human wound healing, where re-epithelialization and granulation tissue formation are dominant [81] [82]. Furthermore, significant differences in the immune system and inflammatory response to injury between rodents and humans can skew the results of therapies like MSC exosomes, which often function through immunomodulation [82].
Experimental Design and Methodological Standardization
To enhance translational relevance, researchers must carefully design experiments and standardize methodologies across studies. The following diagram illustrates a robust workflow for conducting and translating preclinical studies on MSC exosomes.
Model Selection and Induction of Pathological Conditions
The workflow begins with strategic model selection. While murine models are valuable for initial mechanistic studies due to their genetic tractability, porcine models are critical for late-stage preclinical validation because of their high clinical predictive value [84] [82]. To study chronic wounds—a major therapeutic target for MSC exosomes—researchers commonly induce pathological conditions. For type 1 diabetes, streptozotocin (STZ) is widely used to impair healing, while genetically modified db/db mice serve as a model for type 2 diabetic wounds [14]. The dorsal skinfold chamber in mice is a refined model that stretches the skin, counteracting contraction and forcing healing primarily through re-epithelialization, thus more closely mimicking the human healing process [83]. Furthermore, applying splints to rodent wounds prevents contraction, making the model more representative of human healing and better for evaluating the effects of therapies on re-epithelialization [83].
The therapeutic agent itself must be rigorously characterized. MSC exosomes are derived from various tissue sources, with the most common in preclinical studies being bone marrow (51%), umbilical cord (23%), and adipose tissue (13%) [80]. The isolation method impacts the purity and composition of the final product. Ultracentrifugation remains the most commonly used technique (72%), though precipitation methods (23%) and size-exclusion chromatography are also employed [80]. Adherence to international guidelines, such as the Minimal Information for Studies of Extracellular Vesicles (MISEV2023), for characterizing both the parent MSCs and the isolated vesicles is essential for ensuring inter-study consistency and reliability [14].
Assessment Methods and Outcome Correlation
A multi-modal assessment strategy is crucial for comprehensively evaluating therapeutic efficacy and understanding mechanism of action.
Core Assessment Methodologies
- Wound Closure Rate: This is a primary, non-invasive metric. Planimetric analysis of wound area over time, often aided by photographic documentation and software, provides a direct measure of healing progression [81].
- Histopathological Analysis: Invasive analysis of wound biopsies provides granular data on tissue architecture. Key parameters include scar width, collagen deposition (assessed with Masson's trichrome or picrosirius red staining), and blood vessel density (measured via CD31 immunohistochemistry) [81] [14].
- Biophysical and Molecular Assessment: Intravital fluorescence microscopy (IVM), particularly in the dorsal skinfold chamber, allows for real-time, in vivo visualization of angiogenesis, blood flow, and leukocyte activity [83]. Transcriptomic analysis of wound tissue (e.g., via RNA sequencing) reveals molecular mechanisms and phase-specific gene expression patterns underlying the healing process [84].
Quantitative Efficacy Across Models
Meta-analyses of preclinical data provide powerful pooled estimates of therapeutic efficacy. The following table synthesizes quantitative findings on the effects of MSC-derived EVs in wound healing, highlighting outcomes that are relevant for translation.
Table 2: Quantitative Preclinical Efficacy of MSC-EVs in Wound Healing (Meta-Analysis Data)
| Outcome Measure | Therapeutic Effect | Model & Context | Notes & Implications |
|---|---|---|---|
| Wound Closure Rate | Significantly improved in both diabetic and non-diabetic models [14]. | Mouse and rat models of excisional wounds [14]. | A primary indicator of therapeutic acceleration of healing. |
| Angiogenesis (Blood Vessel Density) | Significantly increased revascularization [85] [14]. | Assessed via immunohistochemistry in wound beds [14]. | Critical for delivering oxygen and nutrients to the healing tissue. sEVs may be more effective than ApoEVs for this outcome [14]. |
| Collagen Deposition | Significantly enhanced and better organized collagen fibers [14]. | Measured through histology (e.g., Masson's trichrome) [14]. | Indicates improved extracellular matrix remodeling and tensile strength. ApoSEVs may be superior to sEVs [14]. |
| Overall Therapeutic Efficacy | Robust therapeutic potential across diverse neurological, renal, wound, and liver disease models [85]. | Umbrella review of 47 meta-analyses covering 27 diseases [85]. | Supports MSC-EVs as a versatile platform for regenerative therapy. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of these experiments requires carefully selected reagents and materials.
Table 3: Essential Research Reagent Solutions for MSC Exosome Wound Healing Studies
| Reagent / Material | Function & Application | Key Considerations |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source of therapeutic exosomes. | Source (e.g., Bone Marrow, Adipose Tissue, Umbilical Cord) impacts exosome content and function [80] [14]. Must be characterized per ISCT guidelines (plastic adherence, differentiation potential, surface markers) [14]. |
| Exosome Isolation Kits | Purification of exosomes from conditioned media. | Ultracentrifugation is the "gold standard" but has drawbacks; alternatives include precipitation and size-exclusion chromatography (SEC) kits [80] [28]. |
| Characterization Antibodies | Identification of exosomes and parent MSCs. | Confirm exosome presence via markers (CD9, CD63, CD81, HSP70) [80] [28]. Characterize MSCs with markers (CD73, CD90, CD105; lack of CD34, CD45) [14]. |
| Animal Model | In vivo testing system. | Choice is critical (see Table 1). Diabetic models (STZ-induced, db/db) are used for impaired healing studies [14]. |
| In Vivo Imaging Equipment | Tracking wound healing and angiogenesis. | Intravital Microscopy (IVM) allows real-time visualization of microcirculation [83]. Hyperspectral imaging can assess hemoglobin saturation without contrast agents [83]. |
| Histology Stains & Antibodies | Analysis of tissue morphology and composition. | H&E for general structure. Masson's Trichrome for collagen. Antibodies for specific targets (e.g., CD31 for vessels, α-SMA for myofibroblasts) [81] [14]. |
Bridging the gap between animal studies and human clinical application requires a strategic and critical approach to preclinical research. To enhance translational success, researchers should: i) prioritize the porcine model for late-stage efficacy and safety testing due to its high predictive value; ii) employ splinted murine models or the dorsal skinfold chamber to better simulate human-like re-epithelialization in early-stage mechanistic studies; iii) adhere strictly to MISEV and ISCT guidelines for characterizing exosomes and MSCs to ensure product consistency and data reproducibility; and iv) implement multi-modal assessment combining planimetric, histopathological, and biophysical methods to capture the full spectrum of therapeutic effects.
The evidence for MSC exosomes as a transformative therapy for wound healing is robust and growing. By making informed, critical choices in animal models and experimental design, the scientific community can significantly improve the predictive power of preclinical data, thereby accelerating the development of reliable and effective exosome-based treatments for human patients.
Conclusion
MSC-derived exosomes demonstrate robust therapeutic potential across a wide spectrum of preclinical wound models, consistently promoting healing through multifaceted mechanisms. The efficacy is significantly influenced by critical factors such as the MSC tissue source, with bone marrow-, adipose-, and umbilical cord-derived exosomes showing distinct strengths, as well as the specific animal model and administration route used. Despite this promise, the field requires urgent standardization in manufacturing protocols, improved methodological rigor in preclinical studies to mitigate bias, and a deeper mechanistic understanding of exosome action. Future efforts must focus on bridging the translational gap by developing engineered exosomes with enhanced functionality, establishing potency assays, and designing humanized animal models that more accurately predict clinical success, ultimately paving the way for regulated, effective cell-free therapies for wound care.
References
- 1. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 2. MSC-derived exosomes attenuate cell death through ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01616-8]
- 3. Mesenchymal stem cell-derived exosomes: emerging ... [https://www.sciencedirect.com/science/article/pii/S2773041725000253]
- 4. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 5. Applications of mesenchymal stem cell-exosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319788/]
- 6. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 7. Synergistic effects of mesenchymal stem cells and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210777/]
- 8. MSC-EVs and UCB-EVs promote skin wound healing and ... [https://www.nature.com/articles/s41598-025-87592-6]
- 9. Mesenchymal Stem-Cell-Derived Exosomes and MicroRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249468/]
- 10. Exosomes from mesenchymal stem/stromal cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6450000/]
- 11. Mesenchymal stem cell derived-exosomes: a modern ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02622-3]
- 12. miRNAs from mesenchymal-stem-cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538106/]
- 13. Exosomal microRNAs derived from mesenchymal stem cells [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-020-00650-6]
- 14. Mesenchymal stem cells-derived small extracellular vesicles ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 15. Potential of mesenchymal stem cells and exosomes in ... [https://pubmed.ncbi.nlm.nih.gov/41172571/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1Jgu41lFGSjVSi0g_GOn6ReFV1ZOsx1wRYCQgPUWDxEw7yEwWQ&fc=None&ff=20251111220310&v=2.18.0.post22+67771e2]
- 16. Exosome regulation of immune response mechanism [https://pmc.ncbi.nlm.nih.gov/articles/PMC10622742/]
- 17. Exosomes: The emerging mechanisms and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929203/]
- 18. Extracellular vesicles as tools and targets in therapy for ... [https://www.nature.com/articles/s41392-024-01735-1]
- 19. Exosomes: A Promising Strategy for Repair, Regeneration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10296902/]
- 20. Exosome as Emerging Therapeutic Platform for Wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004604]
- 21. Shedding light on the role of keratinocyte-derived extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01929-8]
- 22. Exosome Source Matters: A Comprehensive Review from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858990/]
- 23. Exosomes and immune modulation: implications for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600062/full]
- 24. Modification of immune cell-derived exosomes for ... [https://www.nature.com/articles/s12276-023-01132-8]
- 25. The tiny giants of regeneration: MSC-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310703/]
- 26. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 27. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 28. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 29. Modulation of ASC-derived extracellular vesicles ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1635151/full]
- 30. Exosomes: the future of acellular nanotherapeutics in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1607605/full]
- 31. Mesenchymal stem cell-derived exosomes: A novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 32. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 33. Comparison of mouse, rat and rabbit models for adipose [https://www.sciencedirect.com/science/article/pii/S2452318620300507]
- 34. Mice vs Rats in Research: What's the Difference? [https://kentscientific.com/mice-vs-rats-in-research-whats-the-difference/?srsltid=AfmBOop-n1X1xrwhbIHzb8yWNuyJSxlJ-cQA7tJwWTJgg_wx3LfdiitI]
- 35. The Impact of Rodents on Advances in Biomedical Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC3987984/]
- 36. How to calculate sample size in animal studies? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3826013/]
- 37. Precision exosome engineering for enhanced wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12103044/]
- 38. Therapeutic potential of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10907468/]
- 39. Advances of exosomes in diabetic wound healing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836438/]
- 40. a promising cell-free therapeutic intervention in burn wounds [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03970-3]
- 41. MSC-derived exosomal circMYO9B accelerates diabetic ... [https://www.nature.com/articles/s42003-024-07367-z]
- 42. MSC-derived exosomes injectable hyaluronic acid ... [https://www.sciencedirect.com/science/article/pii/S0168365925006066]
- 43. Mesenchymal stromal/stem cell (MSC)-derived exosomes in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03287-7]
- 44. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 45. Advances in mesenchymal stem cell and exosome-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296599/]
- 46. Comparison of efficacy of exosomes derived from human ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1560915/full]
- 47. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 48. Comparison of efficacy of exosomes derived from human ... [https://www.semanticscholar.org/paper/Comparison-of-efficacy-of-exosomes-derived-from-in-Chen-Liu/81a1253b396a62b7d39737d8c017874406fc53e9]
- 49. Comparative analysis of extracellular vesicles isolated from ... [https://www.sciencedirect.com/science/article/abs/pii/S0014482722000908]
- 50. Biomimetic scaffolds loaded with mesenchymal stem cells... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04012-8]
- 51. Bioengineered MSC -derived exosomes in skin wound repair and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009159/]
- 52. and Their Bioengineering Strategies in the Cutaneous... Exosomes [https://www.ijbs.com/v19p1430.htm]
- 53. A Murine Study and Meta-Analysis of Experimental Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467663/]
- 54. Mesenchymal Stem Cell-derived Exosomes Hold Promise in the... [https://www.dovepress.com/mesenchymal-stem-cell-derived-exosomes-hold-promise-in-the-treatment-o-peer-reviewed-fulltext-article-IJN]
- 55. Advances in Biodegradable Polymers and Biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10488517/]
- 56. MSCs and their exosomes: a rapidly evolving approach in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8642895/]
- 57. Exosomes Produced from 3D Cultures of MSCs by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6277553/]
- 58. Efficacy and safety of small extracellular vesicle interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9516230/]
- 59. Mesenchymal Stem Cell-derived Exosomes Improved Healing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12236395/]
- 60. Current Strategies for Promoting the Large-scale Production of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10514529/]
- 61. Reproducible Large-Scale Isolation of Exosomes from ... [https://www.mdpi.com/1422-0067/21/13/4774]
- 62. Comparing Two Methods for the Isolation of Exosomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9626211/]
- 63. Sensitive and rapid quantification of exosomes by fusing ... [https://www.nature.com/articles/s41598-018-32535-7]
- 64. Current Strategies for Exosome Cargo Loading and Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10216928/]
- 65. Engineering exosomes for targeted drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7847680/]
- 66. Exosome as drug delivery system: Current advancements [https://www.sciencedirect.com/science/article/pii/S2773041723000112]
- 67. Mesenchymal stem cell-derived exosomes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8362559/]
- 68. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 69. Umbrella review of mesenchymal stem cell-derived ... [https://pubmed.ncbi.nlm.nih.gov/41158310/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1nq_IKqRo1lpVmZPLMBh8BLnGSlMeRq2hML5UR5CAPbykwTYAQ&fc=None&ff=20251101121937&v=2.18.0.post22+67771e2]
- 70. Stem cell derived exosome trilogy: an epic comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186388/]
- 71. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1641709/full]
- 72. Deficient functional wound closure as measured by ... [https://www.nature.com/articles/s41598-024-74426-0]
- 73. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 74. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 75. Efficacy of mesenchymal stem cells and platelet-rich ... [https://www.sciencedirect.com/science/article/pii/S2352320425000860]
- 76. Adipose-derived mesenchymal stem cells and their ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617157/full]
- 77. Mesenchymal stem cell-derived extracellular vesicles [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1626996/full]
- 78. MSC-Derived Extracellular Vesicles: Roles and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191179/]
- 79. Small extracellular vesicles from human bone marrow ... [https://www.nature.com/articles/s41598-025-04057-6]
- 80. Preclinical translation of exosomes derived ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7004029/]
- 81. Experimental models and methods for cutaneous wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7306904/]
- 82. The Evolution of Animal Models in Wound Healing Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6904936/]
- 83. Experimental Models to Study Skin Wound Healing with a ... [https://www.mdpi.com/2076-3271/9/3/55]
- 84. A high-resolution temporal transcriptomic and imaging ... [https://www.nature.com/articles/s41597-025-05921-w]
- 85. Umbrella review of mesenchymal stem cell-derived ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1655623/full]