MSC-Derived Exosomes in Wound Healing: Mechanisms, Clinical Translation, and the Future of Cell-Free Therapy
This article provides a comprehensive analysis of the role of mesenchymal stem cell (MSC)-derived exosomes in wound healing, tailored for researchers, scientists, and drug development professionals.
MSC-Derived Exosomes in Wound Healing: Mechanisms, Clinical Translation, and the Future of Cell-Free Therapy
Abstract
This article provides a comprehensive analysis of the role of mesenchymal stem cell (MSC)-derived exosomes in wound healing, tailored for researchers, scientists, and drug development professionals. It explores the foundational biology of exosomes and their mechanisms of action across the four stages of wound repair. The scope extends to methodological considerations for production and isolation, advanced application strategies using biomaterial scaffolds, and troubleshooting of key challenges such as heterogeneity and manufacturing. Finally, it offers a comparative validation of exosomes against conventional therapies and parent cells, synthesizing preclinical and clinical evidence to outline a clear pathway for clinical translation and regulatory approval of this promising cell-free therapeutic.
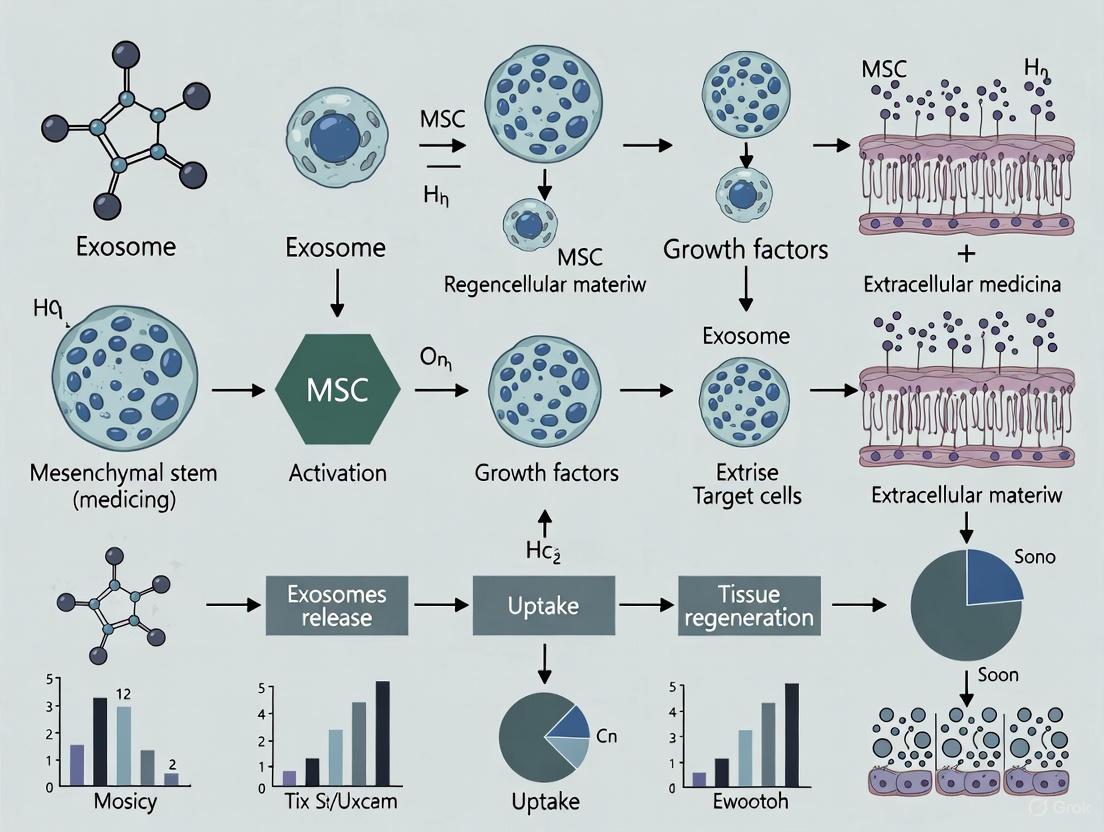
Unraveling the Biology: How MSC-Derived Exosomes Orchestrate Skin Regeneration
Biogenesis and Key Characteristics of MSC-Derived Exosomes
Mesenchymal stem cell (MSC)-derived exosomes have emerged as pivotal mediators of intercellular communication and promising cell-free therapeutic agents in regenerative medicine, particularly in the context of wound healing [1] [2]. These nanoscale extracellular vesicles transfer bioactive molecules—including proteins, lipids, and nucleic acids—from donor MSCs to recipient cells, thereby influencing various physiological and pathological processes [3] [4]. The therapeutic application of MSC-derived exosomes represents a paradigm shift from whole-cell therapies, offering enhanced stability, reduced immunogenicity, and lower risks of tumorigenicity [3] [1]. This technical guide comprehensively details the biogenesis, key characteristics, and functional mechanisms of MSC-derived exosomes, with specific emphasis on their role in promoting cutaneous wound repair through modulation of inflammation, angiogenesis, and extracellular matrix remodeling [1] [5].
Biogenesis of MSC-Derived Exosomes
The biogenesis of exosomes is a meticulously regulated, multi-step process that originates from the endosomal system [1] [6]. Understanding this biogenesis is fundamental to appreciating exosome function and harnessing their therapeutic potential.
Table 1: Key Stages in Exosome Biogenesis
| Stage | Cellular Process | Key Molecular Components |
|---|---|---|
| 1. Initiation | Invagination of the plasma membrane forms early sorting endosomes (ESEs) | Plasma membrane lipids and proteins |
| 2. MVB Formation | ESEs mature into late endosomes; inward budding creates intraluminal vesicles (ILVs) within multivesicular bodies (MVBs) | ESCRT complexes (ESCRT-0, -I, -II, -III) and associated proteins (Alix, TSG101) |
| 3. Fate Determination | MVBs are either trafficked to lysosomes for degradation or to the plasma membrane for exocytosis | Rab GTPases, SNARE proteins |
| 4. Secretion | MVBs fuse with the plasma membrane, releasing ILVs as exosomes into the extracellular space | SNARE complexes, cytoskeletal elements |
The biogenesis pathway comprises two primary mechanisms: the endosomal sorting complex required for transport (ESCRT)-dependent mechanism and ESCRT-independent mechanisms involving tetraspanins and lipids [6]. The ESCRT machinery, consisting of multiple protein complexes (ESCRT-0, -I, -II, -III), collaborates with accessory proteins to facilitate the inward budding of the endosomal membrane and vesicle scission [6]. Alternatively, ESCRT-independent biogenesis can occur through the organization of tetraspanin microdomains or the enzymatic conversion of sphingomyelin to ceramide, which promotes membrane invagination [6]. Following their formation, exosomes are released into the extracellular space upon fusion of MVBs with the plasma membrane, a process mediated by Rab GTPases and SNARE proteins [1] [6].
Diagram 1: Exosome Biogenesis Pathway
Key Characteristics and Molecular Composition
MSC-derived exosomes possess distinct physicochemical properties and carry a diverse molecular cargo that reflects their cellular origin and mediates their biological functions.
Physical and Structural Characteristics
MSC-derived exosomes are spherical, lipid bilayer-enclosed vesicles with diameters typically ranging from 30 to 150 nanometers [1] [6] [4]. Their size distinguishes them from other extracellular vesicles: microvesicles (50-1000 nm) and apoptotic bodies (800-5000 nm) [2] [6]. The lipid bilayer composition is rich in cholesterol, sphingomyelin, and ceramide, and contains lipid rafts that facilitate protein sorting and signaling [4]. This structure provides considerable stability and protects the internal cargo from degradation by extracellular RNases and other enzymes [1].
Molecular Cargo
The biological activity of MSC-derived exosomes is largely attributed to their diverse cargo, which includes proteins, nucleic acids, and lipids selectively packaged from the parent MSC.
Table 2: Characteristic Molecular Cargo of MSC-Derived Exosomes
| Cargo Type | Specific Components | Functional Roles |
|---|---|---|
| Surface Proteins | Tetraspanins (CD9, CD63, CD81), MHC class I, Integrins | Cell targeting, adhesion, immune recognition |
| Intracellular Proteins | ESCRT components (Alix, TSG101), Heat shock proteins (Hsp70, Hsp90), Rab GTPases | Vesicle biogenesis, protein folding, intracellular trafficking |
| Nucleic Acids | miRNAs (e.g., miR-21-5p, miR-26a-5p, miR-181c), mRNAs, lncRNAs, circRNAs | Post-transcriptional regulation, epigenetic reprogramming |
| Lipids | Cholesterol, sphingomyelin, ceramide, phosphatidylserine | Membrane structure, signal transduction |
The nucleic acid content, particularly microRNAs (miRNAs), represents a crucial functional component. miRNAs are short (∼22 nucleotides) non-coding RNAs that regulate gene expression at the post-transcriptional level by binding to target mRNAs [4]. MSC-derived exosomes have been shown to contain functionally significant miRNAs such as miR-26a-5p, which targets MAP2K4 in wound healing [7]; miR-181c, which attenuates burn-induced inflammation by downregulating TLR4 signaling [8]; and miR-21-5p, which promotes wound healing through the STAT3 pathway [9].
MSC-Derived Exosomes in Wound Healing: Mechanisms and Therapeutic Applications
The therapeutic potential of MSC-derived exosomes in wound healing stems from their ability to coordinately modulate multiple phases of the repair process, including inflammation, proliferation, and remodeling [1] [5].
Modulation of Inflammatory Responses
MSC-derived exosomes play a crucial role in tempering excessive inflammation, a common feature of chronic wounds. They promote the polarization of macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype [9], and directly modulate immune cell activity. For instance, exosomal miR-146a downregulates the NF-κB pathway, a key regulator of inflammatory responses [4]. Similarly, miR-181c in human umbilical cord MSC-derived exosomes has been shown to suppress the TLR4 signaling pathway, significantly reducing levels of pro-inflammatory cytokines TNF-α and IL-1β while increasing anti-inflammatory IL-10 in burn models [8].
Promotion of Angiogenesis
A critical aspect of wound healing is the re-establishment of vascular networks to supply oxygen and nutrients to the repairing tissue. MSC-derived exosomes robustly promote angiogenesis by transferring pro-angiogenic miRNAs to endothelial cells [1] [2]. For example, exosomes from antler MSCs containing miR-21-5p were found to stimulate the migration and tube formation of human umbilical vein endothelial cells (HUVECs) through the STAT3 signaling pathway [9]. These exosomal miRNAs enhance endothelial cell proliferation, migration, and the formation of new blood vessels, thereby improving perfusion in the wound bed.
Enhancement of Extracellular Matrix Remodeling
Proper synthesis, deposition, and organization of extracellular matrix (ECM) components are essential for effective wound healing with minimal scarring. MSC-derived exosomes modulate fibroblast behavior to optimize ECM remodeling [7] [9]. They promote fibroblast proliferation and migration while regulating collagen synthesis and maturation. Studies have demonstrated that exosomes from antler MSCs facilitate the conversion of collagen type III to collagen type I, resulting in restored epidermal thickness without aberrant hyperplasia and reduced scar formation [9]. Similarly, exosomes from miR-26a-5p-modified adipose MSCs upregulate collagen types I and III (Col1a1 and Col3a1) while downregulating inflammatory mediators [7].
Diagram 2: Exosome-Mediated Intercellular Communication in Wound Healing
Experimental Methodologies for MSC-Derived Exosome Research
Isolation and Purification Protocols
The isolation of high-purity exosomes is crucial for both research and therapeutic applications. Differential ultracentrifugation remains the most widely used method, involving sequential centrifugation steps to remove cells, debris, and larger vesicles, followed by high-speed ultracentrifugation (typically 100,000-120,000 × g) to pellet exosomes [9]. This method was successfully employed to isolate exosomes from antler MSCs, with the pellet resuspended in phosphate-buffered saline (PBS) for further analysis [9]. Alternative isolation techniques include size-exclusion chromatography, polymer-based precipitation, immunoaffinity capture using exosome-surface markers (e.g., CD63, CD81), and microfluidic technologies [2].
Characterization Techniques
Comprehensive characterization of isolated exosomes is essential to confirm their identity and quality. Standard characterization includes:
- Nanoparticle tracking analysis (NTA) to determine particle size distribution and concentration
- Transmission electron microscopy (TEM) for morphological assessment
- Western blot analysis for detection of exosomal markers (e.g., CD9, CD63, CD81, TSG101, Alix) and absence of negative markers (e.g., calnexin, GM130)
- Flow cytometry with bead-coupled antibodies for immunophenotyping [9]
Additionally, miRNA sequencing and proteomic analyses are employed to comprehensively profile exosomal cargo and identify potential functional components [7] [9].
Functional Validation Experiments
In vitro and in vivo models are utilized to validate the functional efficacy of MSC-derived exosomes in wound healing:
- Cellular assays: Proliferation (CCK-8 assay), migration (scratch assay), and tube formation assays using keratinocytes (HaCaT), fibroblasts, and endothelial cells (HUVECs) [9]
- Animal models: Full-thickness skin defect models in mice or rats to assess wound closure rates, histopathological analysis (H&E staining, Masson's trichrome for collagen), and immunohistochemistry for specific markers (e.g., CD31 for angiogenesis) [7] [9]
- Mechanistic studies: Gain- and loss-of-function experiments using miRNA mimics or inhibitors to establish causal relationships between specific exosomal components and observed functional effects [7] [8]
Table 3: Essential Research Reagents and Experimental Tools
| Reagent/Tool Category | Specific Examples | Research Application |
|---|---|---|
| Cell Culture Media | DMEM/F12 supplemented with exosome-depleted FBS | MSC expansion and exosome production without contaminating vesicles |
| Isolation Kits | Polymer-based precipitation kits, size-exclusion chromatography columns | Alternative exosome isolation methods beyond ultracentrifugation |
| Characterization Antibodies | Anti-CD9, CD63, CD81, TSG101, Alix | Western blot and flow cytometry validation of exosomal markers |
| Functional Assay Kits | CCK-8 proliferation assay, Transwell migration chambers, Matrigel tube formation assay | Assessment of exosome effects on cellular behaviors |
| Animal Models | Full-thickness excisional wound model in mice/rats | In vivo evaluation of exosome therapeutic efficacy |
| Analysis Reagents | H&E staining, Masson's trichrome, anti-CD31 antibodies | Histological assessment of wound healing and angiogenesis |
MSC-derived exosomes represent sophisticated natural nanoplatforms that coordinate multiple aspects of wound healing through their complex molecular cargo. Their biogenesis through the endosomal pathway results in stable vesicles capable of transferring functional proteins and regulatory RNAs to recipient cells. The documented roles of specific exosomal miRNAs, such as miR-26a-5p targeting MAP2K4, miR-181c suppressing TLR4 signaling, and miR-21-5p activating STAT3, provide mechanistic insights into how these vesicles modulate inflammation, promote angiogenesis, and enhance extracellular matrix remodeling. While challenges remain in standardization of isolation protocols and scalable production, the continued elucidation of MSC-derived exosome biogenesis and function solidifies their position as promising therapeutic agents in regenerative medicine and wound care. Future research directions include bioengineering approaches to enhance exosome targeting and payload capacity, ultimately improving their therapeutic efficacy for complex wound healing scenarios.
Exosomes, defined as nanoscale extracellular vesicles (EVs) with a diameter of 30-150 nm, are secreted by nearly all cell types and play a crucial role in intercellular communication [10]. These vesicles are formed via the endosomal pathway and carry a diverse cargo of proteins, lipids, nucleic acids (including DNA, mRNA, miRNA, and long non-coding RNA), and other bioactive molecules [11] [12] [13]. For researchers and drug development professionals, exosomes derived from mesenchymal stem cells (MSCs) represent a promising acellular therapeutic strategy that overcomes the limitations associated with whole-cell therapies, such as tumorigenic risk, immunogenicity, and ethical concerns [12] [14].
The therapeutic potential of MSC-derived exosomes is particularly relevant for wound healing, a complex process that, when impaired, results in chronic wounds or pathological scarring [14]. Chronic wounds—including diabetic foot ulcers, venous leg ulcers, and pressure ulcers—are characterized by a failure to proceed through an orderly and timely healing process, leading to prolonged inflammation, inability to re-epithelialize, and impaired angiogenesis [11] [14]. Current treatment options often fall short, necessitating innovative approaches that target the underlying pathophysiological mechanisms [11]. This whitepaper examines the role of exosomes within the precise sequence of wound healing phases, focusing on mechanistic insights and experimental methodologies relevant to therapeutic development.
The Four Phases of Wound Healing and Exosomal Mechanisms
The normal wound healing cascade comprises four precisely programmed and overlapping phases: hemostasis, inflammation, proliferation, and remodeling [14]. The following sections detail the cellular events of each phase and the specific contributions of MSC-derived exosomes, with summarized findings presented in Table 1.
Table 1: Key Effects of MSC-Derived Exosomes on the Four Phases of Wound Healing
| Healing Phase | Key Cellular Events | Exosomal Cargo & Mechanisms | Demonstrated Outcomes |
|---|---|---|---|
| Hemostasis | Platelet activation, fibrin clot formation | Delivery of pro-coagulant microRNAs; Surface tissue factor [14] [10] | Accelerated clot formation; Initial scaffold for cell migration |
| Inflammation | Neutrophil/monocyte recruitment; Macrophage differentiation (M1/M2) | lncRNAs (e.g., MEG3) regulating TGF-β; miRNAs inhibiting NF-κB; Promotion of M2 phenotype [12] [14] | Reduced pro-inflammatory cytokines (IL-1, TNF-α); Resolution of inflammation |
| Proliferation | Angiogenesis; Fibroblast proliferation; Re-epithelialization; ECM deposition | lncRNA KLF3-AS1 increasing VEGFA; miR-126-3p stimulating proliferation; Transfer of growth factors (VEGF, HGF) [11] [12] | Enhanced endothelial cell tube formation; Increased fibroblast migration/proliferation |
| Remodeling | ECM reorganization; Collagen cross-linking; Scar maturation | lncRNA-ASLNCS5088 suppressing miR-200c-3p; Regulation of MMPs/TIMPs; MEG3 reducing collagen [12] [14] | Balanced ECM deposition/degradation; Reduced fibrosis and pathological scarring |
Hemostasis Phase
The hemostasis phase begins immediately after injury and involves vasoconstriction, platelet activation, and fibrin clot formation to prevent further blood loss [14]. This phase establishes a provisional extracellular matrix (ECM) that serves as a scaffold for invading cells.
Exosomal Roles: Exosomes contribute to hemostasis by providing a pro-coagulant surface. Chargaff and West initially discovered that a "particulate fraction" of vesicles sedimented at high g-forces possessed high clotting potential [14]. MSC-derived exosomes can express surface tissue factor and phosphatidylserine, which promote thrombin generation and accelerate clot formation [10]. The clot also serves as a reservoir for exosomes, which are subsequently released to influence subsequent healing phases.
Inflammation Phase
The inflammation phase involves the recruitment of neutrophils and monocytes to the wound site, with subsequent differentiation of monocytes into macrophages [14]. A critical transition from a pro-inflammatory (M1) to an anti-inflammatory, pro-resolving (M2) macrophage phenotype is essential for normal healing [12] [14]. Chronic wounds are characterized by a failure to resolve this inflammatory phase.
Exosomal Roles: MSC-derived exosomes play a pivotal role in modulating the immune response. They can promote the polarization of macrophages toward the M2 phenotype, which reduces inflammation and supports tissue repair [12]. This occurs through exosomal transfer of long non-coding RNAs (lncRNAs) such as MEG3, which reduces fibrosis-related protein and collagen expression [12]. Additionally, exosomes can carry miRNAs that inhibit the NF-κB signaling pathway, a key driver of pro-inflammatory cytokine production [14]. By regulating the balance between M1 and M2 macrophages, exosomes help resolve inflammation and create a microenvironment conducive to proliferation.
Proliferation Phase
The proliferation phase is characterized by the formation of granulation tissue, which involves the in-growth of fibroblasts and blood vessels, as well as re-epithelialization [11] [14]. Key processes include angiogenesis, fibroblast proliferation, and ECM deposition.
Exosomal Roles in Angiogenesis: MSC-derived exosomes significantly promote the formation of new blood vessels—a process critical for delivering oxygen and nutrients to the healing tissue. They achieve this by transferring pro-angiogenic factors and genetic materials. For instance, exosomal lncRNA KLF3-AS1 from bone marrow MSCs (BMSCs) has been shown to increase the expression of VEGFA—a potent angiogenic factor—by sponging a regulatory miRNA [12]. Hypoxic preconditioning of parent MSCs further enhances the angiogenic capacity of their exosomes by upregulating cargo such as HIF-1α and VEGF [11] [14].
Exosomal Roles in Cell Proliferation and Migration: Exosomes directly stimulate the proliferation and migration of fibroblasts and keratinocytes, the key cellular players in tissue rebuilding. Engineered exosomes overexpressing specific miRNAs, such as miR-126-3p, have demonstrated enhanced stimulating effects on the proliferation of epidermal fibroblasts and vascular endothelial cells [11]. Exosomes also carry growth factors like VEGF and HGF, which activate recipient cells via paracrine signaling [12].
Remodeling Phase
The final remodeling phase can last for months to years and involves the reorganization and maturation of the ECM, with a shift from collagen type III to type I, and cross-linking of collagen fibers [14]. An imbalance in this phase can lead to either weak wounds or pathological scarring (hypertrophic scars and keloids).
Exosomal Roles: MSC-derived exosomes contribute to balanced ECM remodeling by regulating the activity of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs). They can mitigate excessive scarring; for example, exosomes from human BMSCs containing lncRNA MEG3 have been shown to prevent keloid formation by reducing collagen expression [12]. Conversely, in a TGF-β1-rich environment, exosomes from M2 macrophages containing lncRNA-ASLNCS5088 can promote fibroblast activation and ECM production, which is necessary for tissue repair but must be carefully controlled to prevent fibrosis [12]. This dual potential highlights the importance of precise exosomal engineering for therapeutic applications.
Experimental Protocols for Exosome Research
The isolation and characterization of exosomes are critical for research and therapeutic development. Below are detailed methodologies for key experimental procedures.
Isolation of Exosomes from Human Plasma via Ultracentrifugation
Ultracentrifugation remains a widely used benchmark method for exosome isolation [15] [13].
- Sample Collection: Collect whole blood (e.g., 9 mL) into citrate tubes via venipuncture.
- Plasma Separation: Centrifuge the sample at 1,500 × g for 20 minutes at 4°C to separate cells from plasma. Transfer the supernatant to a new tube.
- Cell-Free Plasma: Centrifuge the supernatant at 2,800 × g for 20 minutes at 4°C to remove all remaining cells. Transfer the resulting cell-free plasma (CFP) to ultracentrifugation tubes (1 mL per tube).
- Exosome Pellet: Centrifuge the CFP at 100,000 × g for 90 minutes at 4°C to pellet the exosomes. Carefully remove 900 µL of supernatant.
- Wash Step: Re-suspend the pellet in the remaining 100 µL. Add 900 µL of phosphate-buffered saline (PBS) to wash. Centrifuge again at 100,000 × g for 30 minutes at 4°C.
- Final Resuspension: Remove 900 µL of supernatant and re-suspend the final exosome pellet in the remaining 100 µL of PBS.
- Filtration (Optional): For particle measurement, a fraction (5-20 µL) of the suspension can be diluted in 40 mL of distilled water and filtered through a 450 nm filter to separate exosomes from larger particles [15].
Characterization via Nanoparticle Tracking Analysis (NTA)
Nanoparticle Tracking Analysis (NTA) is used to determine the size distribution and concentration of isolated exosomes [15] [13].
- Instrument Startup: Initialize the NTA instrument (e.g., ZetaView) and perform an automated startup procedure, including a cell quality check and auto-alignment.
- System Flushing: Flush the instrument's cell channel with 10 mL of distilled water using a syringe to ensure it is free of air bubbles and contaminants.
- Sample Injection: Inject the prepared exosome suspension into the channel.
- Parameter Adjustment: Adjust key software parameters:
- Sensitivity: Determine the optimal sensitivity level by generating a "Number of Particles vs. Sensitivity" curve. Select a sensitivity level just before the curve's maximum slope.
- Focus and Camera Shutter/Frame Rate: Manually adjust the focus for sharp particle images. Set the camera shutter to 100 and the frame rate to 30 frames per second as potential starting points [15].
- Measurement and Analysis: Initiate the measurement. The software will track the Brownian motion of particles, calculating their size and concentration based on the Stokes-Einstein equation. Results are displayed as a size distribution profile and concentration measurement.
Functional Analysis: In Vitro Tube Formation Assay
This assay evaluates the pro-angiogenic capacity of exosomes by measuring their ability to promote endothelial cell network formation.
- Matrigel Coating: Thaw Matrigel on ice and coat the wells of a pre-chilled 96-well plate (50-100 µL per well). Incubate the plate at 37°C for 30-60 minutes to allow polymerization.
- Cell Preparation: Harvest human umbilical vein endothelial cells (HUVECs) and re-suspend them in serum-free medium. Seed the cells onto the surface of the polymerized Matrigel at a density of 1-2 x 10^4 cells per well.
- Exosome Treatment: Immediately add the test sample (e.g., MSC-derived exosomes, hypoxic preconditioned exosomes, or PBS as a negative control) to the seeded cells.
- Incubation: Incubate the plate at 37°C with 5% CO2 for 4-18 hours.
- Imaging and Quantification: Capture images of the tubular networks using an inverted light microscope. Quantify the pro-angiogenic effect by measuring parameters such as the total tube length, number of branching points, and number of meshes per field of view using image analysis software.
Research Reagent Solutions Toolkit
Table 2: Essential Reagents and Tools for Exosome Research
| Reagent / Tool | Function / Application | Notes / Key Characteristics |
|---|---|---|
| Ultracentrifuge | Isolation of exosomes from biofluids/cell media via high g-forces [15] | Essential for classic ultracentrifugation protocol; requires significant bench time. |
| NTA Instrument (e.g., ZetaView) | Measures exosome size distribution and concentration [15] [13] | Provides real-time analysis ideal for particles in the 70-160 nm range. |
| Transmission Electron Microscope (TEM) | Visualizes exosome morphology and confirms cup-shaped structure [13] | Requires extensive sample preparation (fixation, negative staining). |
| CD63, CD9, CD81 Antibodies | Western Blot (WB) and Immunoaffinity Capture for exosome identification/isolation [10] [13] | Tetraspanins are common exosome surface markers for characterization. |
| TSG101 Antibody | Western Blot for identification of exosomal markers [13] | An endosomal-related protein commonly used to confirm exosomal identity. |
| Size-Exclusion Chromatography (SEC) Kit | Isolation of exosomes based on size [13] | Offers excellent purity and is scalable; an alternative to ultracentrifugation. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | In vitro model for angiogenesis (tube formation) assays [11] | Standard cell model for testing the pro-angiogenic capacity of exosomes. |
| Matrigel | Basement membrane matrix for tube formation assays [11] | Provides a substrate for endothelial cells to form tubular networks. |
| 6-Bromo-5-fluoroquinoxaline | 6-Bromo-5-fluoroquinoxaline | |
| Copper chlorophyllin B | Copper Chlorophyllin B Reagent|RUO | High-purity Copper Chlorophyllin B for research. Explore its applications in antiviral, antioxidant, and cancer research. For Research Use Only. Not for human use. |
Visualization of Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate key signaling pathways and experimental workflows discussed in this whitepaper. The color palette is restricted to the specified brand colors for visual consistency.
Exosomal Regulation of Macrophage Polarization
Pro-Angiogenic Signaling by Exosomal lncRNA KLF3-AS1
Experimental Workflow for Exosome Isolation & Characterization
Mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as pivotal mediators of tissue regeneration, primarily through their sophisticated molecular cargo delivery system. These nanoscale vesicles transport proteins, microRNAs (miRNAs), and lipids that collectively orchestrate the complex process of wound healing. The therapeutic efficacy of MSC-Exos in cutaneous wound repair stems from their ability to modulate inflammation, promote angiogenesis, stimulate cellular proliferation, and facilitate extracellular matrix (ECM) remodeling. This whitepaper provides a comprehensive analysis of the specific molecular constituents within MSC-Exos, their mechanistic roles in wound healing pathways, and the experimental methodologies essential for advancing this promising field toward clinical applications. Understanding these key molecular cargos is fundamental to harnessing the full regenerative potential of exosome-based therapies for acute and chronic wounds.
Exosomes are nanosized extracellular vesicles (30-150 nm in diameter) bounded by a lipid bilayer and formed via the endosomal pathway, specifically through the inward budding of multivesicular bodies (MVBs) that subsequently fuse with the plasma membrane for release [16]. As critical mediators of intercellular communication, MSC-Exos mirror the therapeutic potential of their parent cells while offering advantages such as lower immunogenicity, minimal tumorigenic risk, and enhanced stability [17]. Their cargo—comprising proteins, nucleic acids (including miRNAs and long non-coding RNAs), and lipids—is selectively packaged and transferred to recipient cells, thereby modulating key physiological processes in wound healing [18] [12].
The functional significance of these molecular cargos is particularly evident in chronic wound environments, where MSC-Exos have demonstrated capacity to rescue impaired healing processes. For diabetic wounds characterized by delayed closure and disrupted immune responses, MSC-Exos delivered via hydrogels can overcome the limitations of rapid diffusion and poor retention, enabling sustained therapeutic effects through their diverse biomolecular constituents [19]. The following sections provide a detailed examination of these cargo components, their quantitative profiles, functional mechanisms, and the experimental approaches used to characterize their roles in wound healing.
Comprehensive Analysis of Molecular Cargos
Protein Cargo: Composition and Functional Significance
Table 1: Key Protein Cargos in MSC-Derived Exosomes and Their Roles in Wound Healing
| Protein Category | Specific Examples | Functional Roles in Wound Healing | Mechanistic Insights |
|---|---|---|---|
| Tetraspanins | CD9, CD63, CD81 | Facilitate cellular uptake and target cell interaction [20] | Mediate exosome adhesion and fusion with recipient cell membranes; serve as canonical exosome markers |
| Endosomal Biogenesis Proteins | ALIX, TSG101 | Regulate exosome formation and cargo sorting [20] | Part of ESCRT-dependent and independent biogenesis pathways; ensure proper vesicle formation |
| Heat Shock Proteins | HSP70, HSP90 | Promote cell survival under stress conditions [20] | Enhance cellular stress resistance in the wound microenvironment; facilitate protein folding |
| Growth Factors & Cytokines | VEGF, FGF, TGF-β, IL-10 | Stimulate angiogenesis and modulate immune responses [18] | VEGF and FGF promote blood vessel formation; TGF-β and IL-10 suppress excessive inflammation |
| Anti-inflammatory Factors | IL-10, TGF-β | Control inflammatory phase resolution [18] | Shift macrophages from pro-inflammatory M1 to anti-inflammatory M2 phenotype; reduce pro-inflammatory cytokine production |
The protein cargo of MSC-Exos comprises both universal exosome markers and specialized functional proteins that directly contribute to wound repair. Tetraspanins (CD9, CD63, CD81) not only serve as identification markers but also facilitate membrane fusion and cellular uptake, ensuring efficient cargo delivery to target cells in the wound bed [20]. The growth factors and cytokines carried by MSC-Exos, particularly those derived from adipose tissue MSC-Exos (ADSC-Exos), play crucial roles in coordinating the healing process. Vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) directly stimulate angiogenesis, while transforming growth factor-β (TGF-β) and interleukin-10 (IL-10) modulate the immune response by suppressing excessive inflammation and promoting transition to the proliferative phase of healing [18].
The biogenesis proteins ALIX and TSG101, in addition to their role in exosome formation, may indirectly influence wound healing by ensuring the proper packaging of therapeutic cargo. Heat shock proteins (HSP70, HSP90) contribute to cellular protection in the often hostile wound microenvironment, particularly in chronic wounds characterized by elevated oxidative stress [20]. This diverse protein portfolio enables MSC-Exos to simultaneously address multiple pathological aspects of impaired wound healing.
miRNA Cargo: Regulatory Networks and Mechanisms
Table 2: Key miRNA Cargos in MSC-Derived Exosomes and Their Functions in Wound Healing
| miRNA | Target Genes/Pathways | Primary Functions in Wound Healing | Experimental Evidence |
|---|---|---|---|
| miR-26a-5p | MAP2K4 (MAPK signaling) [7] | Inhibits inflammation, enhances angiogenesis, promotes ECM synthesis [7] | Downregulates Il6, Il1β, Tnf-α; upregulates Col1a1, Cd31, Col3a1 in mouse models |
| miR-23a-3p | Angiogenesis pathways [21] | Promotes vascular development and tube formation | Targets >90 genes in circulatory system development; confirmed in HUVEC assays |
| miR-29b-3p | COL1A1, TGF-β pathway [21] | Anti-fibrotic; reduces excessive collagen deposition | Directly targets collagen isoforms; inhibits TGF-β signaling in cardiac fibroblasts |
| Let-7i | TGF-β pathway, fibrotic genes [21] | Anti-fibrotic; modulates ECM remodeling | Targets multiple collagen genes; reduces scar formation |
| miR-130a-3p | Angiogenesis pathways [21] | Stimulates blood vessel formation | Targets vascular development genes; promotes endothelial cell function |
| miR-144-3p | Angiogenesis pathways [21] | Promotes vascular development | Targets >90 genes in circulatory system development |
MicroRNAs represent one of the most biologically active components of MSC-Exos, functioning as master regulators of gene expression in recipient cells. Systems-level analyses have revealed that the top 23 miRNAs in MSC-Exos account for approximately 79.1% of the total miRNA content and collectively target 5,481 genes involved in critical wound healing processes [21]. These miRNA networks predominantly regulate pathways related to cardiovascular development, angiogenesis, inflammation control, and extracellular matrix organization.
A notable example is miR-26a-5p, identified as a hub miRNA in ADSC-derived exosomes, which accelerates wound healing by targeting MAP2K4, a key regulator of the MAPK signaling cascade [7]. This targeting results in downstream suppression of pro-inflammatory cytokines (IL-6, IL-1β, TNF-α) while simultaneously enhancing expression of collagen genes (Col1a1, Col3a1) and the endothelial marker CD31, thereby coordinating inflammation resolution with tissue regeneration [7].
The miR-29 family and Let-7 miRNAs exhibit potent anti-fibrotic activity by directly targeting multiple collagen isoforms and TGF-β signaling components, preventing excessive scar formation during the remodeling phase [21]. Additionally, angiogenic miRNAs like miR-23a-3p, miR-130a-3p, and miR-144-3p collectively target over 90 genes involved in vascular development, stimulating the robust angiogenesis necessary for nutrient delivery and waste removal in healing tissue [21].
Diagram 1: miRNA-Mediated Regulatory Networks in Wound Healing. This diagram illustrates how specific exosomal miRNAs target key genes and pathways to coordinate multiple aspects of wound repair.
Lipid Cargo: Structural and Functional Roles
While less extensively characterized than proteins and miRNAs, the lipid composition of MSC-Exos contributes significantly to their stability and function. The lipid bilayer not only provides structural integrity but also facilitates membrane fusion with target cells and participates in signal transduction. MSC-Exos contain a diverse lipid profile including cholesterol, sphingomyelin, phosphatidylserine, and ceramides that contribute to their biological activities [20].
The lipid composition enables MSC-Exos to withstand enzymatic degradation in the proteolytic wound environment, ensuring the protected delivery of their cargo to recipient cells. Specific lipid components also participate directly in signaling processes; for instance, phosphatidylserine externalization can mediate immunomodulatory effects, while ceramides play a role in organizing membrane microdomains that cluster specific proteins and facilitate their sorting into exosomes [20]. This lipid-mediated cargo sorting represents a crucial mechanism for ensuring the therapeutic composition of MSC-Exos.
Experimental Methodologies for Cargo Analysis
Exosome Isolation and Characterization Techniques
Table 3: Standard Methodologies for MSC-Exosome Isolation and Characterization
| Method Category | Specific Technique | Key Parameters | Advantages | Limitations |
|---|---|---|---|---|
| Isolation | Ultracentrifugation | Sequential spins: 300×g, 2000×g, 100,000×g [16] | Gold standard; no reagent requirement | Time-consuming; potential protein contamination |
| Isolation | Size Exclusion Chromatography (SEC) | Porous bead matrix [16] | Preserves exosome integrity; good purity | May not completely remove co-eluting proteins |
| Isolation | Immunoaffinity Capture | Antibodies against CD63, CD81, CD9 [16] | High specificity for exosome subpopulations | Lower yield; selective for surface markers |
| Characterization | Nanoparticle Tracking Analysis (NTA) | Hydrodynamic diameter measurement [21] | Size distribution and concentration | Size differences between hydrated vs. dry states |
| Characterization | Transmission Electron Microscopy (TEM) | Morphological visualization [21] | Direct imaging; size confirmation (~55.5±11.1 nm) | Sample dehydration may alter apparent size |
| Characterization | Western Blotting | Protein markers: CD63, CD81, CD9, TSG101 [20] | Confirms exosomal identity | Semi-quantitative; dependent on antibody quality |
Standardized isolation and characterization are prerequisites for reliable exosome research. Ultracentrifugation remains the most widely used isolation technique, employing sequential centrifugation steps to remove cells, debris, and larger vesicles before pelleting exosomes at high speeds (100,000×g or higher) [16]. Alternative methods include size exclusion chromatography (SEC), which separates vesicles based on size while preserving structural integrity, and immunoaffinity capture using antibodies against surface tetraspanins (CD63, CD81, CD9) for highly specific isolation of exosome subpopulations [16].
Comprehensive characterization requires multiple orthogonal techniques. Nanoparticle tracking analysis (NTA) measures the hydrodynamic diameter and concentration of exosomes in suspension (typically ~98 nm), while transmission electron microscopy (TEM) provides detailed morphological information and precise size measurements (approximately 55.5±11.1 nm) [21]. Western blotting confirms the presence of characteristic exosomal markers (tetraspanins, ALIX, TSG101) and absence of negative markers to ensure isolation purity [20].
Diagram 2: Experimental Workflow for MSC-Exosome Isolation and Characterization. This diagram outlines the standard methodologies for obtaining and validating exosomes prior to cargo analysis.
Cargo Profiling and Functional Validation
miRNA Profiling: High-throughput techniques such as NanoString nCounter analysis and RNA sequencing enable comprehensive miRNA profiling. The standard protocol involves RNA extraction from purified exosomes using TRIzol or commercial kits, followed by quality assessment and library preparation. Bioinformatics analysis then identifies highly abundant miRNAs and predicts their target genes and pathways using databases such as miRDIP and functional enrichment tools like PANTHER [21].
Protein Analysis: Western blotting confirms the presence of specific exosomal proteins using antibodies against tetraspanins (CD63, CD81, CD9) and biogenesis markers (ALIX, TSG101) [20]. For comprehensive profiling, mass spectrometry provides an unbiased analysis of the entire protein cargo, revealing both constitutive and cell source-specific proteins that contribute to wound healing functions.
Functional Assays: In vitro validation includes:
- Angiogenesis assays: Tube formation using HUVECs on Matrigel to assess pro-angiogenic effects [21]
- Fibroblast proliferation/migration: Scratch assays and cell counting kits to measure effects on dermal fibroblasts [22]
- Collagen production: ELISA or qRT-PCR to quantify collagen I and III expression in TGF-β-stimulated fibroblasts [21]
- Anti-inflammatory effects: Macrophage polarization assays measuring cytokine levels (IL-6, IL-1β, TNF-α) via ELISA [7]
In vivo validation typically employs rodent wound models (e.g., full-thickness excisional wounds, diabetic db/db mice) with measurements of wound closure rate, histopathological analysis of re-epithelialization, collagen maturity, and capillary density [19] [7].
Advanced Engineering and Delivery Strategies
Biomaterial-Assisted Delivery Systems
To overcome the challenges of rapid clearance and limited retention in dynamic wound environments, advanced delivery systems have been developed. Injectable hydrogels, particularly those based on hyaluronic acid (HA), have demonstrated excellent efficacy for sustained exosome delivery. These systems exhibit desirable cytocompatibility, biodegradability, and skin-like rheology while their porous structure enables in situ retention of exosomes, significantly enhancing therapeutic efficacy in chronic wound models [19].
The HA-based hydrogel system allows for in situ cross-linking, creating a scaffold that progressively releases functional exosomes while maintaining a moist wound environment conducive to healing. This approach addresses the critical limitation of direct exosome application, which often results in rapid diffusion away from the wound site before exerting their full therapeutic effects [19].
Engineered Exosomes for Enhanced Therapeutics
Genetic modification of parent MSCs represents a powerful strategy to enhance the therapeutic potential of their exosomes. Overexpression of specific miRNAs, such as miR-26a-5p in ADSCs, creates exosomes with enriched cargo that more potently modulates healing processes [7]. Preconditioning strategies, including hypoxic treatment and pharmacological priming, can further optimize exosome cargo composition by activating specific cellular pathways that enhance their regenerative properties [18].
These engineering approaches enable the production of "designer exosomes" with tailored cargo profiles optimized for specific aspects of wound repair, such as enhanced anti-inflammatory activity, superior angiogenic potential, or improved collagen remodeling capabilities.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for MSC-Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Primary Applications | Technical Considerations |
|---|---|---|---|
| Isolation Kits | Ultracentrifugation kits, SEC columns, Polymer-based precipitation kits | Exosome isolation from conditioned media | Selection depends on required purity, yield, and downstream applications |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, ALIX | Western blot, immunoaffinity capture, flow cytometry | Essential for confirming exosomal identity and purity |
| Cell Culture Media | MesenGro hMSC medium, DMEM with 10% FBS | MSC expansion and exosome production | Use exosome-depleted FBS for production phases |
| miRNA Analysis Tools | NanoString nCounter, miRNA sequencing kits, qRT-PCR assays | miRNA profiling and validation | NanoString provides digital counting without amplification bias |
| Functional Assay Kits | Tube formation assay (Matrigel), cell proliferation kits, ELISA collagen kits | In vitro validation of exosome effects | HUVEC tube formation assesses angiogenic potential |
| Animal Models | Diabetic db/db mice, full-thickness excisional wounds | In vivo therapeutic efficacy | Diabetic models critical for chronic wound healing studies |
| Hydrogel Systems | Hyaluronic acid-based injectable hydrogels | Delivery vehicle for sustained release | Provides scaffold structure and prolongs exosome retention |
| Donepezil Benzyl Chloride | Donepezil Benzyl Chloride, MF:C31H36ClNO3, MW:506.1 g/mol | Chemical Reagent | Bench Chemicals |
| Diisooctyl glutarate | Diisooctyl glutarate, CAS:28880-25-3, MF:C21H40O4, MW:356.5 g/mol | Chemical Reagent | Bench Chemicals |
This toolkit comprises essential reagents and models that form the foundation of rigorous MSC-Exos research in wound healing. Isolation methods must be selected based on specific research needs, with ultracentrifugation remaining the benchmark for many applications, while newer techniques like size exclusion chromatography offer advantages in preserving exosome integrity [16]. Characterization antibodies against tetraspanins (CD63, CD81, CD9) and biogenesis markers (TSG101, ALIX) are indispensable for confirming exosomal identity and ensuring preparation purity [20].
For functional analysis, HUVEC tube formation assays on Matrigel provide robust assessment of angiogenic potential, while fibroblast proliferation and collagen production assays evaluate effects on ECM synthesis [22] [21]. Animal models, particularly diabetic mouse models, are essential for validating therapeutic efficacy in physiologically relevant systems that mimic human chronic wounds [19] [7]. Finally, hydrogel delivery systems, especially hyaluronic acid-based formulations, have emerged as critical tools for enhancing exosome retention and sustained release in wound environments [19].
The molecular cargos of MSC-derived exosomes—proteins, miRNAs, and lipids—represent a sophisticated biological delivery system that coordinately regulates the complex process of wound healing. Through their diverse biomolecular constituents, MSC-Exos modulate inflammation, stimulate angiogenesis, promote cellular proliferation, and guide extracellular matrix remodeling, making them promising therapeutic agents for both acute and chronic wounds.
Future research directions should focus on standardizing isolation protocols to ensure reproducible cargo profiles, optimizing engineering strategies to enhance specific therapeutic functions, and addressing scalability challenges for clinical translation. As our understanding of these molecular cargos deepens, the potential for developing precision exosome-based therapies that target specific pathological aspects of non-healing wounds becomes increasingly feasible. The integration of biomaterial science with exosome biology, particularly through advanced delivery systems like injectable hydrogels, represents a promising avenue for maximizing the clinical impact of MSC-Exos in regenerative medicine.
The systematic characterization of MSC-Exos cargo composition and function, as outlined in this technical guide, provides a foundation for advancing these novel therapeutics from bench to bedside, potentially offering new solutions for the significant clinical challenge of impaired wound healing.
Exosome-Mediated Intercellular Communication with Fibroblasts, Keratinocytes, and Immune Cells
Exosomes, nano-sized extracellular vesicles secreted by nearly all cell types, have emerged as pivotal mediators of intercellular communication within the skin microenvironment. These vesicles facilitate the transfer of bioactive molecules—including proteins, lipids, and nucleic acids—between mesenchymal stem cells (MSCs), structural skin cells, and immune cells, thereby orchestrating complex processes essential for wound healing and tissue regeneration. This whitepaper delineates the specific mechanisms through which MSC-derived exosomes modulate the functions of fibroblasts, keratinocytes, and immune cells, highlighting the key signaling pathways involved. Furthermore, it provides a detailed compendium of experimental methodologies for investigating these interactions and discusses the translational potential of engineered exosomes as next-generation therapeutic agents in regenerative dermatology.
Exosomes are lipid bilayer vesicles, typically 30-150 nm in diameter, that originate from the endosomal system and are secreted by virtually all cell types into the extracellular environment [23] [14]. They are enriched in a conserved set of biomarker proteins, including tetraspanins (CD63, CD81, CD9), heat shock proteins (HSP70, HSP90), and biogenesis-related proteins (ALIX, TSG101) [23]. Their cargo, comprising proteins, lipids, mRNAs, microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), reflects their parental cell's physiological state and endows them with the capacity to regulate fundamental cellular processes in recipient cells [23].
The skin, being the body's largest organ, relies on intricate communication between its constituent cells—keratinocytes, fibroblasts, melanocytes, and resident immune cells—to maintain barrier function and execute coordinated wound healing responses [23]. Exosomes have been identified as crucial signaling intermediaries in this network. The dysregulation of exosome-mediated communication is implicated in the pathogenesis of various inflammatory and autoimmune skin diseases, while the therapeutic application of MSC-derived exosomes presents a promising cell-free strategy for promoting skin regeneration and resolving chronic wounds [23] [24].
This review is framed within the context of a broader thesis on the role of MSC-derived exosomes in wound healing research, focusing specifically on their multifaceted interactions with fibroblasts, keratinocytes, and immune cells.
Mechanisms of MSC-Exosome Communication with Skin Cells
Communication with Fibroblasts
Fibroblasts are the primary architects of the extracellular matrix (ECM), and their regulation is critical for effective wound healing and prevention of pathological scarring. MSC-derived exosomes (MSC-exos) modulate fibroblast behavior through the targeted delivery of molecular cargo, primarily miRNAs.
A pivotal study demonstrated that exosomes derived from miR-26a-5p-modified adipose-derived MSCs (AMSCs) significantly accelerated wound healing in a mouse skin defect model [7]. These engineered exosomes functioned by delivering miR-26a-5p to dermal fibroblasts, where it directly targeted and downregulated MAP2K4, a key upstream kinase in the MAPK signaling cascade. This downregulation led to a suppression of pro-inflammatory cytokines (Il6, Il1β, Tnf-α) and a concurrent upregulation of crucial ECM components, including Col1a1, Col3a1, and α-SMA, thereby enhancing collagen synthesis and tissue remodeling [7]. The table below summarizes the key quantitative findings from this study.
Table 1: Effect of miR-26a-5p-Overexpressing AMSC Exosomes on Wound Healing Markers in Vivo
| Parameter Measured | Effect vs. Control | Proposed Mechanism |
|---|---|---|
| Wound Closure Rate | Significantly increased | Enhanced proliferation and matrix synthesis |
| MAP2K4 Expression | Down-regulated | Direct targeting by miR-26a-5p |
| Inflammatory Markers (Il6, Il1β, Tnf-α) | Down-regulated | Inhibition of MAPK pathway |
| ECM Components (Col1a1, Col3a1, Col2a1) | Up-regulated | Enhanced fibroblast synthetic activity |
| Angiogenesis Marker (Cd31) | Up-regulated | Improved neovascularization |
Beyond modulating individual genes, MSC-exos possess broader anti-fibrotic properties. They have been shown to mitigate the progression of pathological scarring, such as keloids and hypertrophic scars, by counteracting the triggers of fibrosis: immune dysregulation, mechanical stress, and hypoxia [14]. They achieve this by regulating key pro-fibrotic pathways, including NF-κB and TGF-β1, and by modulating the activity of mechanosensors like YAP/TAZ [14].
Communication with Keratinocytes
Keratinocytes, the predominant cells of the epidermis, are responsible for re-epithelialization, a critical step in wound closure. MSC-exos directly promote the proliferation and migration of keratinocytes, facilitating the restoration of the epidermal barrier.
The cargo within MSC-exos is instrumental in this process. Specific miRNAs, such as miR-21-3p and miR-31-5p, have been identified as upregulated during wound healing and are associated with enhanced keratinocyte function [7]. Furthermore, exosomes from human umbilical cord MSCs (hUCMSCs) and epidermal stem cells (ESCs) have demonstrated efficacy in improving the skin environment and promoting epithelial regeneration [23] [25]. The ability of topically applied exosomes to localize within the stratum corneum of human skin underscores their potential for direct therapeutic application in cutaneous wounds [23].
Communication with Immune Cells
The immunomodulatory capacity of MSC-exos is a cornerstone of their therapeutic effect, primarily achieved through the regulation of macrophage polarization. In the wound microenvironment, a shift from a pro-inflammatory M1 phenotype to an anti-inflammatory, pro-healing M2 phenotype is essential for the resolution of inflammation and the transition to the proliferation phase.
MSC-exos are potent inducers of this M1-to-M2 transition. They carry specific miRNAs that modulate key signaling pathways in macrophages. For instance, miR-146a delivered by exosomes has been shown to reduce cartilage degradation in osteoarthritis by shifting synovial macrophages towards the M2 phenotype via the TLR4/TRAF6/NF-κB pathway [26]. Similarly, in the context of skin, this polarization leads to increased secretion of anti-inflammatory cytokines like IL-10 and IL-4, which collectively alleviate inflammation and promote a regenerative microenvironment [27]. This immunomodulatory effect not only accelerates healing but also reduces the risk of fibrosis and scarring.
Table 2: MSC-Exosome Cargo and Their Immunomodulatory Targets
| Exosomal Cargo | Source Cell | Target Immune Cell/Pathway | Biological Outcome | Reference Context |
|---|---|---|---|---|
| miR-146a | Fibroblast-like synoviocytes | Macrophage; TLR4/TRAF6/NF-κB pathway | M2 polarization; Reduced inflammation | [26] |
| miR-26a-5p | Engineered AMSCs | MAP2K4 pathway | Downregulation of Il6, Il1β, Tnf-α | [7] |
| TSG-6, PGE2, IDO | MSC Spheroids | T-cells; Macrophages | Suppression of immune cell proliferation; M2 polarization | [27] |
| let-7a miRNA | Hypoxic Tumor Cells | Macrophage Metabolism | Induction of OXPHOS, M2-like polarization | [28] |
The following diagram illustrates the central signaling pathways through which MSC-derived exosomes influence fibroblasts, keratinocytes, and macrophages to promote wound healing.
Experimental Protocols for Studying Exosome-Cell Interactions
To investigate the mechanisms outlined above, robust and standardized experimental protocols are essential. Below is a detailed methodology for a key experiment that validates the functional role of exosomal miRNA in modulating fibroblast behavior, based on the study by Frontiers in Bioengineering and Biotechnology [7].
Detailed Protocol: Validating Exosomal miRNA Function in Fibroblasts
Objective: To investigate the mechanism by which miR-26a-5p-enriched AMSC-exos promote wound healing by targeting MAP2K4 in fibroblasts.
Materials:
- Primary human dermal fibroblasts
- Adipose-derived MSCs (AMSCs)
- miR-26a-5p agomir (mimic) and antagomir (inhibitor)
- Transfection reagent (e.g., Lipofectamine)
- Exosome isolation kit (e.g., ultracentrifugation or commercial precipitation kit)
- Antibodies for characterization (CD63, CD81, TSG101)
- Dual-luciferase reporter assay system
Methodology:
Exosome Isolation and Engineering:
- Culture AMSCs and transfect them with miR-26a-5p agomir or a scrambled control using an appropriate transfection reagent.
- 48 hours post-transfection, collect the conditioned media.
- Isolate exosomes via sequential ultracentrifugation: centrifuge media at 300 × g for 10 min (remove cells), then 2,000 × g for 20 min (remove dead cells), followed by 10,000 × g for 30 min (remove cell debris). Finally, ultracentrifuge at 100,000 × g for 70 min to pellet exosomes.
- Wash the pellet in phosphate-buffered saline (PBS) and repeat the ultracentrifugation.
- Resuspend the final exosome pellet in PBS and store at -80°C.
Exosome Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the size distribution and concentration of isolated exosomes.
- Transmission Electron Microscopy (TEM): Visualize the morphology and confirm the cup-shaped structure of exosomes.
- Western Blotting: Confirm the presence of positive exosomal markers (CD63, CD81, TSG101) and the absence of a negative marker (e.g., Calnexin).
Functional In Vitro Assay:
- Treat primary human dermal fibroblasts with the following:
- Group 1: PBS (Control)
- Group 2: Exosomes from control AMSCs (Ctrl-Exos)
- Group 3: Exosomes from miR-26a-5p-overexpressing AMSCs (miR-26a-5p-Exos)
- Group 4: miR-26a-5p agomir directly
- Incubate for 24-48 hours.
- Treat primary human dermal fibroblasts with the following:
Downstream Analysis:
- Dual-Luciferase Reporter Assay: Clone the wild-type and mutant 3'UTR of the MAP2K4 gene into a luciferase reporter vector. Co-transfect these constructs with miR-26a-5p agomir or control into HEK293T cells. Measure luciferase activity after 48 hours to confirm direct binding.
- qRT-PCR: Isolve total RNA from treated fibroblasts. Quantify the mRNA expression levels of MAP2K4, inflammatory cytokines (Il6, Il1β, Tnf-α), and ECM genes (Col1a1, Col3a1).
- Western Blotting: Analyze protein expression levels of MAP2K4 and other relevant pathway components.
In Vivo Validation:
- Utilize a mouse skin defect model.
- Create full-thickness excisional wounds on the dorsum of mice.
- Topically apply the following to the wounds daily:
- Group A: PBS
- Group B: Ctrl-Exos
- Group C: miR-26a-5p-Exos
- Monitor and photograph wounds daily to calculate the wound closure rate.
- Harvest wound tissues on specific days post-injury for histological analysis (H&E staining, Masson's trichrome for collagen) and immunohistochemistry (for CD31, α-SMA, etc.).
The following diagram outlines the core workflow of this experimental protocol.
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing research in exosome-mediated communication requires a suite of reliable and well-characterized reagents. The table below details essential tools for isolating, characterizing, and functionally analyzing exosomes and their interactions with target cells.
Table 3: Key Research Reagent Solutions for Exosome Studies
| Reagent/Material | Primary Function | Specific Examples & Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source of therapeutic exosomes | Adipose-derived MSCs (AMSCs), human umbilical cord MSCs (hUCMSCs). hUCMSCs offer superior immunomodulatory properties and minimal donor variation [27]. |
| Transfection Reagents | Engineering exosome cargo | For modifying parent MSCs with miRNA agomirs/antagomirs or plasmid DNA (e.g., Lipofectamine, electroporation systems). |
| Ultracentrifuge | Gold-standard exosome isolation | Enriches exosomes from conditioned media via high-speed centrifugation [7]. |
| Commercial Kits | Alternative exosome isolation | Polymer-based precipitation kits (e.g., ExoQuick-TC). Useful for smaller sample sizes but may co-precipitate contaminants. |
| Nanoparticle Tracker | Physicochemical characterization | Instruments like Malvern Nanosight for determining exosome size distribution and concentration (NTA) [7]. |
| Antibodies for Markers | Confirm exosome identity | Anti-tetraspanins (CD63, CD81, CD9), anti-biogenesis markers (TSG101, ALIX). Negative control: Calnexin or GM130. |
| Dual-Luciferase Reporter Assay | Validate direct miRNA-mRNA binding | System to clone the 3'UTR of a putative target gene (e.g., MAP2K4) and confirm direct interaction with an exosomal miRNA [7]. |
| Animal Wound Models | In vivo functional validation | Mouse or rat models of full-thickness excisional wounds or diabetic ulcers to test the therapeutic efficacy of exosomes [7]. |
| Hydrogel Delivery Systems | Application in vivo | Pluronic F-127 or gelatin sponge/polydopamine scaffolds (GS-PDA) for sustained release and improved retention of exosomes at the wound site [7] [14]. |
| 3-Ethyl-4-methylhexane | 3-Ethyl-4-methylhexane, CAS:3074-77-9, MF:C9H20, MW:128.25 g/mol | Chemical Reagent |
| Psoralen-c 2 cep | Psoralen-c 2 cep | Psoralen-c 2 cep (CAS 126221-83-8) is a high-purity biochemical for research into nucleic acid interactions. This product is For Research Use Only and is not for human or veterinary use. |
The evidence is compelling that MSC-derived exosomes serve as master regulators of cutaneous wound healing by orchestrating the activities of fibroblasts, keratinocytes, and immune cells through sophisticated paracrine communication. By shuttling specific miRNAs and other bioactive molecules, they precisely modulate key signaling pathways such as MAPK and NF-κB, leading to reduced inflammation, enhanced ECM synthesis, accelerated re-epithelialization, and a pro-regenerative immune environment.
The future of this field lies in moving beyond natural exosomes toward precision engineering. Strategies such as loading exosomes with specific therapeutic miRNAs (e.g., miR-26a-5p) or modifying their surface to enhance tissue targeting are already under investigation [7] [14]. Furthermore, overcoming the challenge of effective delivery through the use of biomaterial-based scaffolds (e.g., hydrogels) that ensure controlled and sustained release at the wound site will be crucial for clinical translation [24]. As we deepen our understanding of exosome biology and refine engineering and delivery techniques, MSC-derived exosomes are poised to revolutionize regenerative medicine, offering a potent, cell-free, and scalable therapeutic paradigm for treating acute and chronic skin wounds.
Chronic wounds, including diabetic foot ulcers (DFUs), venous leg ulcers (VLUs), and pressure ulcers (PUs), represent a significant and growing global health challenge, affecting an estimated 2% of the world's population and approximately 6.5 million patients in the United States alone [29]. These wounds are characterized by a failure to progress through the normal stages of wound healing—hemostasis, inflammation, proliferation, and remodeling—often remaining in a state of persistent inflammation and impaired tissue repair [30] [31]. The economic burden is substantial, with annual treatment costs in the U.S. estimated at $20–25 billion [29].
Within the broader thesis on the role of mesenchymal stem cell (MSC)-derived exosomes in wound healing research, this review focuses on the core pathophysiological drivers of chronic wounds, specifically the mechanisms underlying persistent inflammation and impaired angiogenesis. Recent advances in "omics" technologies have deepened our understanding of chronic wound pathology at cellular and molecular levels, revealing specific dysregulations in keratinocytes, fibroblasts, immune cells, and endothelial cells [29]. Concurrently, MSC-derived exosomes have emerged as a promising cell-free therapeutic alternative, demonstrating the ability to modulate these pathological processes and promote healing [31] [1].
This technical guide provides an in-depth analysis of the molecular mechanisms perpetuating chronic wounds, with particular emphasis on how MSC-exosomes target these pathways. We summarize quantitative data in structured tables, detail experimental methodologies, visualize key signaling pathways, and catalog essential research reagents to support ongoing drug development and basic research efforts in this field.
Pathophysiological Hallmarks of Chronic Wounds
Persistent Inflammation and Immune Dysregulation
In normal wound healing, the inflammatory phase is transient, characterized by sequential recruitment of neutrophils and monocytes/macrophages that clear debris and pathogens before transitioning to a pro-reparative state [30] [31]. In chronic wounds, this process becomes dysregulated, leading to a state of persistent inflammation that prevents progression to proliferation and remodeling phases.
Cellular Dysregulation:
- Neutrophils: Show reduced infiltration and migration across endothelial cells but remain in the wound for extended periods, releasing proteases such as matrix metalloproteinases (MMPs) and reactive oxygen species (ROS) that damage newly formed tissue [30].
- Macrophages: Exhibit impaired transition from pro-inflammatory M1 to anti-inflammatory M2 phenotypes. The M1 macrophage profile persists, characterized by uncontrolled production of inflammatory mediators including TNF-α, IL-1β, and IL-6 [30] [31]. Reduced induction of the M2 macrophage profile limits the production of reparative factors such as IL-10, VEGF, PDGF, and FGFs [30].
- Lymphocytes: Abnormal T-cell function contributes to the dysregulated immune response, though the exact mechanisms in chronic wounds are still being elucidated [31].
Molecular Mediators: Chronic wounds exhibit dysregulated cytokine/growth factor levels with increased pro-inflammatory signaling. Key mediators include sustained elevated levels of TNF-α, IL-1β, and IL-6, which perpetuate the inflammatory state [31]. Protease activity is significantly increased, with MMP levels exceeding their tissue inhibitors (TIMPs), causing degradation of the extracellular matrix (ECM), growth factors, and receptors [29] [30].
Table 1: Comparative Analysis of Inflammatory Phase in Acute vs. Chronic Wounds
| Aspect | Acute Wounds | Chronic Wounds | Key References |
|---|---|---|---|
| Inflammation Duration | Transient (days) | Persistent (weeks to months) | [30] [31] |
| Neutrophil Activity | Timely infiltration and clearance | Prolonged persistence, impaired migration | [30] |
| Macrophage Polarization | Balanced M1 to M2 transition | Sustained M1 phenotype, impaired M2 transition | [30] [31] |
| Cytokine Profile | Coordinated pro- and anti-inflammatory signals | Dominance of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) | [31] |
| Protease Activity | Balanced MMP/TIMP ratio | Elevated MMPs, degraded growth factors & ECM | [29] [30] |
Impaired Angiogenesis
Angiogenesis, the formation of new blood vessels from existing vasculature, is crucial for delivering oxygen and nutrients to the healing wound. In chronic wounds, this process is severely compromised, contributing to tissue hypoxia and impaired repair.
Dysfunctional Endothelial Cells: Endothelial cells in chronic wounds exhibit reduced proliferative and migratory capacity, impairing new blood vessel formation [29]. The diabetic microenvironment, characterized by hyperglycemia, further damages endothelial cells through increased oxidative stress and the formation of advanced glycation end products (AGEs) [32].
Molecular Mechanisms of Impaired Angiogenesis:
- Growth Factor Dysregulation: Despite the pro-inflammatory environment, the bioavailability and activity of key angiogenic growth factors, particularly VEGF, are often reduced due to increased degradation and impaired signaling [29] [32].
- Oxidative Stress: Chronic hyperglycemia in diabetic wounds promotes excessive production of reactive oxygen species (ROS), causing mitochondrial dysfunction in endothelial cells and reducing their capacity to form vessels [32].
- Altered Nitric Oxide (NO) Bioavailability: Changes in amino acid metabolism, particularly arginine deficiency, compromise NO synthesis, a critical mediator of vasodilation and angiogenesis [32].
Table 2: Mechanisms of Impaired Angiogenesis in Chronic Wounds
| Mechanism | Pathophysiological Consequences | Impact on Healing | References |
|---|---|---|---|
| Endothelial Cell Dysfunction | Reduced proliferation and migration | Failed neovascularization, tissue hypoxia | [29] |
| VEGF Signaling Impairment | Decreased growth factor bioavailability | Insufficient angiogenic stimulus | [29] [32] |
| Oxidative Stress | Mitochondrial damage, cellular senescence | Compromised endothelial cell function | [32] |
| Reduced NO Bioavailability | Impaired vasodilation & endothelial signaling | Dysfunctional microcirculation | [32] |
MSC-Derived Exosomes as a Therapeutic Modality
Biogenesis and Composition of MSC-Exosomes
Exosomes are nano-sized extracellular vesicles (30-150 nm in diameter) of endocytic origin, secreted by virtually all cell types, including MSCs [30] [1]. Their biogenesis begins with the inward budding of the endosomal membrane, forming intraluminal vesicles within multivesicular bodies. These multivesicular bodies subsequently fuse with the plasma membrane, releasing the vesicles as exosomes into the extracellular space [1].
MSC-exosomes inherit specific biological components from their parent cells, including proteins, lipids, mRNA, and miRNA, which enable them to mediate intercellular communication [1]. They function as natural transporters of these bioactive molecules, which can be internalized by recipient cells through endocytosis, membrane fusion, or ligand-receptor interactions, thereby altering the recipient cell's phenotype and function [30] [1].
Mechanisms of Action in Targeting Chronic Wound Pathophysiology
Extensive research demonstrates that MSC-exosomes can mitigate the core pathophysiological features of chronic wounds through multiple mechanisms.
Modulation of Inflammation: MSC-exosomes facilitate the transition of macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype [31]. This immunomodulatory effect is partly mediated by exosomal miRNAs, such as miR-146a and miR-223, which inhibit key pro-inflammatory signaling pathways like NF-κB and suppress NLRP3 inflammasome activation [31]. Furthermore, exosomes from preconditioned MSCs can enhance anti-inflammatory polarization via let-7b signaling [31].
Promotion of Angiogenesis: MSC-exosomes are enriched with pro-angiogenic factors and miRNAs that stimulate new blood vessel formation. They promote the proliferation, migration, and tube formation of endothelial cells [31] [33]. Specific exosomal miRNAs, including miR-126-3p, directly target genes that inhibit angiogenesis, such as PIK3R2, thereby activating the PI3K/AKT signaling pathway, a key regulator of endothelial cell survival and vascular maturation [33].
Enhancement of Cell Proliferation and Migration: MSC-exosomes enhance the activity of keratinocytes and fibroblasts, which are critical for re-epithelialization and ECM reconstruction. They activate pathways such as AKT and ERK/MAPK in these cells, boosting their proliferative and migratory capacity [33]. This helps overcome the hyperproliferative but non-migratory phenotype of keratinocytes observed at the non-healing edge of chronic ulcers [29].
The following diagram illustrates the multifaceted therapeutic mechanisms of MSC-derived exosomes in the chronic wound microenvironment:
Therapeutic Mechanisms of MSC-Exosomes in Chronic Wounds.
Engineering and Delivery Strategies for Enhanced Efficacy
Natural exosomes face challenges such as rapid clearance and limited targeting. Bioengineering approaches are being developed to overcome these limitations and enhance therapeutic potential.
Content Engineering: Genetic modification of parent MSCs can enrich exosomes with specific therapeutic miRNAs or proteins. For instance, ADSC-exosomes overexpressing miR-21-5p have been shown to significantly promote diabetic wound healing through enhanced re-epithelialization, collagen remodeling, and angiogenesis [33]. Similarly, miR-146a-modified ADSC-exosomes promoted fibroblast proliferation and migration and stimulated neovascularization [33].
Delivery Systems: To address the rapid clearance of exosomes, hydrogel-based scaffolds and other biocompatible materials are being investigated for sustained release [34]. These systems prolong the presence of therapeutic exosomes at the wound site, maintaining optimal concentrations and improving functional outcomes.
Experimental Models and Methodologies
Standardized Experimental Workflow
A typical research workflow for evaluating the efficacy of MSC-exosomes in wound healing involves a sequence of critical steps, from exosome isolation to functional validation in vivo. The following diagram outlines this standardized protocol:
Workflow for MSC-Exosome Wound Healing Research.
Detailed Methodological Protocols
1. Isolation and Characterization of MSC-Exosomes:
- Cell Culture: Culture MSCs from selected sources (e.g., bone marrow, adipose tissue, umbilical cord) in serum-free media to avoid contamination with bovine exosomes. Expand cells to 70-80% confluence [1] [33].
- Exosome Isolation: Collect conditioned media and perform sequential centrifugation: 300 × g for 10 min to remove cells; 2,000 × g for 20 min to remove dead cells; 10,000 × g for 30 min to remove cell debris; and finally, ultracentrifugation at 100,000 × g for 70 min to pellet exosomes [1] [33].
- Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the size distribution and concentration of exosomes.
- Western Blotting: Confirm the presence of exosomal markers (CD63, CD81, TSG101) and absence of negative markers (e.g., GM130) [1] [33].
- Transmission Electron Microscopy (TEM): Visualize the morphology and ultrastructure of exosomes.
2. In Vitro Functional Assays:
- Cell Migration Assay (Scratch Assay): Culture fibroblasts or keratinocytes to confluence. Create a uniform scratch and treat with MSC-exosomes. Monitor and quantify cell migration into the scratch area over 24-48 hours [33].
- Tube Formation Assay:
- Materials: Matrigel matrix, endothelial cells (e.g., HUVECs), MSC-exosomes, tissue culture plates.
- Protocol: Coat plates with Matrigel and allow polymerization. Seed HUVECs on the Matrigel and treat with MSC-exosomes. After 4-18 hours, image the tubes and quantify parameters like total tube length, number of nodes, and branching points [33].
- Gene Expression Analysis: Isulate RNA from exosome-treated cells and perform qRT-PCR to analyze the expression of genes related to angiogenesis (VEGF, Ang-1), inflammation (IL-1β, IL-6, IL-10), and ECM remodeling (Collagen I, III, MMPs, TIMPs) [33].
3. In Vivo Efficacy Testing:
- Diabetic Wound Model:
- Animals: Use genetically diabetic mice (e.g., db/db mice) or induce diabetes in C57BL/6 mice with streptozotocin.
- Wound Creation: Anesthetize mice and create one or two full-thickness excisional wounds on the dorsum using a biopsy punch.
- Treatment: Randomize animals into groups. Apply MSC-exosomes (e.g., 100 µg in 50 µL PBS) topically to the wound bed every other day. Control groups receive vehicle alone.
- Outcome Measures:
- Wound Closure: Digitally photograph wounds daily and calculate wound area as a percentage of original size.
- Histology: Harvest wound tissue at specified endpoints for H&E staining (re-epithelialization, granulation tissue), Masson's Trichrome (collagen deposition), and immunohistochemistry (CD31 for angiogenesis, F4/80 for macrophages) [33] [34].
Research Reagent Solutions
Table 3: Essential Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Research Function | Key References |
|---|---|---|---|
| MSC Sources | Bone Marrow-MSCs (BM-MSCs), Adipose-Derived Stem Cells (ADSCs), Human Umbilical Cord-MSCs (hUC-MSCs) | Provide biologically relevant exosomes for therapeutic testing; different sources may have varying potency. | [31] [33] |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-TSG101, Anti-Calnexin (negative control) | Confirm exosome identity and purity via Western Blot or flow cytometry. | [1] [33] |
| Cell Lines for In Vitro Assays | Human Umbilical Vein Endothelial Cells (HUVECs), Human Dermal Fibroblasts (HDFs), HaCaT Keratinocytes | Model the responses of key skin cell types (angiogenesis, ECM production, re-epithelialization). | [31] [33] |
| In Vivo Model Systems | db/db Mice, Streptozotocin-induced Diabetic Mice | Provide a pathophysiologically relevant model of impaired healing for testing therapeutic efficacy. | [33] [34] |
| Hydrogel Delivery Systems | Hyaluronic acid-based hydrogels, Chitosan scaffolds, Collagen matrices | Provide sustained release of exosomes at the wound site, enhancing retention and therapeutic effect. | [34] |
The pathophysiology of chronic wounds, dominated by persistent inflammation and failed angiogenesis, presents a complex therapeutic challenge. MSC-derived exosomes represent a promising cell-free therapeutic strategy that directly targets these core pathological mechanisms. Through their diverse cargo, they can reprogram the hostile wound microenvironment, shifting it from a state of chronic inflammation to one conducive to active repair, while simultaneously stimulating robust new blood vessel formation.
Future research should focus on standardizing isolation protocols, optimizing bioengineering strategies for enhanced targeting and potency, and conducting rigorous, large-animal preclinical studies to facilitate clinical translation. As a key component of the broader thesis on MSC-exosomes, the evidence presented in this review solidifies their position as a next-generation therapeutic modality with the potential to fundamentally change the management of chronic wounds.
From Lab to Bedside: Production, Isolation, and Advanced Delivery Systems for Exosome Therapies
Mesenchymal stem cells (MSCs) are nonhematopoietic, multipotent stem cells characterized by their capacity for self-renewal, multilineage differentiation, and immunomodulatory functions [35]. First identified in bone marrow, MSCs can now be isolated from numerous tissues, with bone marrow (BM), adipose tissue (AT), and umbilical cord (UC) being among the most clinically relevant sources [36]. The therapeutic potential of MSCs has been widely explored for conditions ranging from autoimmune and inflammatory disorders to orthopedic injuries and wound healing [35].
According to the International Society for Cellular Therapy (ISCT), defining criteria for MSCs include: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105 ≥95%) and lack of expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) ability to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [35] [36]. While MSCs from different sources generally meet these criteria, they exhibit significant functional heterogeneity.
Critically, the therapeutic mechanism of MSCs has undergone a paradigm shift. Initially valued for their differentiation potential, research now indicates their benefits are primarily mediated through paracrine signaling—the release of bioactive molecules such as growth factors, cytokines, and extracellular vesicles (EVs), particularly exosomes [24] [35] [37]. This review provides a comparative analysis of BM-, AT-, and UC-derived MSCs, framing the discussion within the advancing context of MSC-derived exosomes as key agents in wound healing and regenerative medicine.
Isolation Success, Proliferation, and Senescence
A critical factor in selecting an MSC source is its ease of isolation and expansion potential for therapeutic applications.
- Table 1: Comparative Growth and Expansion Potential of MSCs
Parameter Bone Marrow (BM)-MSCs Adipose Tissue (AT)-MSCs Umbilical Cord (UC)-MSCs Isolation Success Rate 100% [38] 100% [38] ~63% [38] Colony Frequency (CFU-F) 16.5 ± 4.4 [39] 6.4 ± 1.6 [39] 23.7 ± 5.8 [39] Proliferation Capacity Lowest; shortest culture period [39] [38] Intermediate; lower than UCB [39] Highest; longest culture period, highest expansion [39] [38] Population Doubling Time Longer [39] Intermediate [39] Shortest [39] Senescence Markers (p53, p21, p16) Higher expression [39] Higher expression [39] Significantly lower expression [39]
Experimental Protocol for Assessing Proliferation and Senescence:
- Population Doubling (PD) and PDT: Cells are cultured until growth cessation. PD is measured for each passage, and Population Doubling Time (PDT) is calculated to quantify proliferation speed [39].
- Colony-Forming Unit Fibroblast (CFU-F) Assay: A low density of MSCs is plated and cultured for 10-14 days. Colonies are then fixed, stained (e.g., with crystal violet), and counted to assess clonogenicity [39].
- Senescence-Associated β-Galactosidase (SA-β-Gal) Staining: Cells are fixed and incubated with a staining solution containing X-gal at pH 6.0. Senescent cells display blue pigmentation, and the percentage of positive cells is quantified [39].
- Western Blotting for Senescence Proteins: Cell lysates are prepared from MSCs at different passages. Proteins are separated by gel electrophoresis, transferred to a membrane, and probed with antibodies against p53, p21, and p16 to compare expression levels [39].
Immunophenotype and Multi-Lineage Differentiation
Despite their functional differences, MSCs from BM, AT, and UC share a core immunophenotype defined by the ISCT. They are consistently positive for CD29, CD44, CD73, CD90, CD105, and HLA-ABC, and negative for hematopoietic markers CD14, CD34, CD45, and HLA-DR [39] [36]. However, transcriptomic analyses reveal subtle differences in markers like CD106 (detected in AT-MSCs) and CD200 (detected specifically in UC-MSCs) [40].
All three sources demonstrate in vitro tri-lineage differentiation potential, a defining hallmark of MSCs [39] [41].
- Osteogenesis: Induced by culture in media containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate. Differentiation is confirmed by Alkaline Phosphatase (ALP) staining and mineral deposition detection by Alizarin Red S staining [39].
- Chondrogenesis: Induced in pellet or micromass culture using TGF-β superfamily members (e.g., TGF-β3) and ascorbate-2-phosphate. Proteoglycan synthesis is visualized by Safranin O staining [39].
- Adipogenesis: Induced with media containing dexamethasone, isobutylmethylxanthine (IBMX), indomethacin, and insulin. Lipid droplet accumulation is confirmed by Oil Red O staining [39]. Notably, one study found UC-MSCs lacked adipogenic capacity, highlighting potential source-specific variations [38].
Immunomodulatory and Paracrine Capacity
The therapeutic effects of MSCs are largely attributed to their immunomodulatory properties and secretome.
- Anti-inflammatory Effects: In a co-culture model with LPS-activated rat alveolar macrophages, UC-MSCs demonstrated superior anti-inflammatory activity, significantly reducing secretion of IL-1α, IL-6, and IL-8. This effect was partially mediated by the secretion of Angiopoietin-1 (Ang-1) [39].
- T-cell Proliferation Inhibition: In comparative studies, BM-MSCs most potently inhibited allogeneic T-cell proliferation, potentially linked to their higher secretion of immunosuppressive cytokines like IL-10 and TGFB1 [41].
- Gene Expression Profiles: BM-MSCs and AT-MSCs share similar gene expression profiles for both stemness-related genes (e.g., OCT4, NANOG) and lineage-related genes. The expression of genes like DLX5 appears associated with osteogenic potential [41].
The Exosome Frontier in Wound Healing
Exosomes as Primary Mediators of MSC Efficacy
MSC-derived exosomes are nanoscale extracellular vesicles (30-150 nm) that facilitate intercellular communication by transferring bioactive cargo—including proteins, lipids, mRNAs, and microRNAs (miRNAs)—to recipient cells [24] [37]. They are increasingly recognized as the principal effectors of MSC therapy, offering a cell-free alternative that circumvents risks associated with whole-cell transplantation, such as immune rejection and tumorigenicity [24] [37].
For wound healing, exosomes provide superior benefits in storage, safety, and tissue penetration compared to their parent MSCs [24]. Their therapeutic potential is particularly relevant for chronic wounds, which are characterized by a failure to progress through the normal stages of healing.
Mechanisms of Exosome Action in Cutaneous Repair
MSC-derived exosomes promote healing by influencing all phases of wound repair. The following diagram illustrates the key pathways and cellular processes involved in this complex mechanism.
Diagram Title: Exosomal miRNA Mechanism in Wound Healing
The molecular mechanisms by which exosomes exert their effects are becoming increasingly clear. For instance, exosomes derived from adipose mesenchymal stem cells (AMSCs) and loaded with miR-26a-5p have been shown to accelerate wound healing by targeting MAP2K4, a key regulator of the MAPK signaling cascade [7]. This targeting leads to:
- Inhibition of inflammation: Downregulation of pro-inflammatory cytokines IL-6, IL-1β, and TNF-α [7].
- Enhanced angiogenesis: Upregulation of CD31, a marker for endothelial cells and blood vessel formation [7].
- Improved ECM synthesis and remodeling: Increased expression of Collagen Type I (Col1a1), Collagen Type III (Col3a1), and α-Smooth Muscle Actin (α-Sma) [7].
Experimental Workflow for Exosome Research
The investigation of exosome functions follows a structured experimental pipeline, from isolation to functional validation in vivo.
Diagram Title: Workflow for Investigating MSC-Exosome Function
Detailed Experimental Protocol for Exosome Studies:
- MSC Culture and Modification: MSCs (e.g., AMSCs) are cultured in standard media. For mechanistic studies, cells are genetically modified (e.g., via lentiviral transduction) to overexpress a specific miRNA like miR-26a-5p [7].
- Exosome Isolation: Exosomes are harvested from the cell culture supernatant. Common methods include differential ultracentrifugation (sequential spins up to 100,000-120,000 x g) or using commercial polymer-based precipitation kits [7].
- Exosome Characterization:
- Nanoparticle Tracking Analysis (NTA): Determines the size distribution and concentration of isolated particles.
- Transmission Electron Microscopy (TEM): Visualizes the typical cup-shaped morphology of exosomes.
- Western Blotting: Confirms the presence of exosome marker proteins (CD63, CD81, TSG101) and the absence of negative markers (e.g., Calnexin) [7].
- In Vivo Functional Assay: A wound healing model, such as a mouse full-thickness skin defect, is established. Exosomes are administered topically, often with a carrier (e.g., Pluronic F-127 hydrogel) to enhance retention and bioavailability [7] [24].
- Tissue Analysis: Wound tissue is collected for:
- Quantitative PCR (qPCR): Measures gene expression levels of targets (e.g., MAP2K4, cytokines, ECM components).
- Enzyme-Linked Immunosorbent Assay (ELISA): Quantifies protein levels of inflammatory cytokines.
- Histological Staining (e.g., H&E, Masson's Trichrome): Assesses tissue morphology and collagen deposition [7].
The Scientist's Toolkit: Key Reagents and Materials
- Table 2: Essential Research Reagents for MSC and Exosome Studies
Reagent / Material Function / Application Examples / Details Culture Media In vitro expansion and maintenance of MSCs. Dulbecco's Modified Eagle Medium (DMEM), α-MEM, often supplemented with Fetal Bovine Serum (FBS) [36]. Induction Media Directing MSC differentiation into specific lineages. Contain specific inducters: Dexamethasone, IBMX, Insulin (Adipogenesis); TGF-β3, Ascorbate (Chondrogenesis); Dexamethasone, Ascorbate-2-phosphate, β-Glycerophosphate (Osteogenesis) [39] [41]. Isolation Kits Purifying exosomes from cell culture supernatant. Ultracentrifugation protocols; commercial kits like Total Exosome Isolation Kit [7]. Characterization Tools Validating exosome size, morphology, and markers. Nanoparticle Tracking Analyzer (size/concentration); Transmission Electron Microscope (morphology); antibodies for CD63, CD81, TSG101 (Western Blot) [7]. Delivery Scaffolds Enhancing exosome delivery and retention in vivo. Hydrogels (e.g., Pluronic F-127), Gelatin sponge/polydopamine (GS-PDA) scaffolds for controlled release [7] [24]. Animal Models In vivo functional testing of MSCs/exosomes. Mouse skin defect model for wound healing studies [7].
The choice of MSC source—Bone Marrow, Adipose Tissue, or Umbilical Cord—is not trivial, as each presents a unique balance of advantages and limitations. BM-MSCs are the gold standard with robust immunomodulation, AT-MSCs offer accessibility and high yield, and UC-MSCs provide superior proliferative capacity and primitive characteristics. The emerging paradigm, however, strongly points toward the secretome, and specifically MSC-derived exosomes, as the future of regenerative therapy.
For wound healing, exosomes represent a powerful, cell-free tool that can be engineered ("primed") for enhanced efficacy, such as by loading specific miRNAs like miR-26a-5p [7]. Future research must focus on standardizing isolation protocols, optimizing delivery systems for controlled release at the wound site, and conducting rigorous long-term safety studies [24] [37]. As these challenges are addressed, MSC-derived exosomes hold immense potential to revolutionize the treatment of chronic wounds and solidify the role of MSCs as indispensable bioreactors for next-generation therapeutics.
The field of regenerative medicine has increasingly recognized mesenchymal stem cell-derived exosomes (MSC-exosomes) as pivotal therapeutic agents for wound healing and tissue regeneration. These nanoscale extracellular vesicles (EVs), typically ranging from 30-150 nm in diameter, mediate the paracrine effects of their parent cells by transferring functional proteins, lipids, and nucleic acids to recipient cells [42] [43]. The efficacy of MSC-exosomes in modulating inflammation, promoting angiogenesis, and accelerating tissue repair has been demonstrated across multiple disease models, including diabetic ulcers, myocardial infarction, and neurological disorders [44] [6]. However, the translational potential of these vesicles is critically dependent on the isolation techniques employed, which directly influence exosome yield, purity, biological activity, and ultimately, therapeutic outcomes. Current challenges in the field stem from the lack of standardized isolation protocols, particularly when working with complex biological fluids where exosomes exist at low densities alongside contaminating proteins and lipoproteins [45] [46].
The selection of an appropriate isolation strategy represents a fundamental consideration in experimental design and therapeutic development. Techniques must be chosen based on the specific requirements of downstream applications, whether for diagnostic biomarker discovery, mechanistic studies, or therapeutic production. This technical guide provides a comprehensive comparison of three primary isolation methodologies—ultracentrifugation, precipitation, and chromatography—evaluating their respective advantages, limitations, and optimal applications within the context of MSC-derived exosome research for wound healing applications.
Core Isolation Techniques: Principles and Methodologies
Ultracentrifugation
Ultracentrifugation remains the most widely used and historically established method for exosome isolation, leveraging high gravitational forces to separate vesicles based on their size, density, and shape. The standard protocol involves sequential centrifugation steps to eliminate cells, debris, and larger vesicles, followed by high-speed ultracentrifugation (typically 100,000-120,000 × g) to pellet exosomes [47] [48]. When isolating exosomes from blood plasma for wound healing studies, researchers have found that conventional UC (e.g., 1-2 hours at 110,000 × g) often results in significant albumin contamination despite the majority of isolated particles falling within the expected size range for exosomes (30-150 nm) [47]. Modifications to protocol parameters, including longer centrifugation times, shorter sedimentation distances, or elevated temperatures (37°C), can increase exosomal yield but often fail to adequately address the purity issue [47].
The technical limitations of ultracentrifugation become particularly evident when processing MSC-conditioned media for therapeutic applications. The method's reliance on differential pelleting can lead to vesicle aggregation and damage, potentially compromising the biological activity of therapeutic exosomes [43]. Furthermore, the requirement for specialized equipment, lengthy processing times, and technical expertise presents challenges for standardization and scaling in therapeutic production. Despite these limitations, ultracentrifugation continues to serve as a reference method against which newer techniques are evaluated, particularly in research settings where purity requirements may be balanced against the need for comprehensive vesicle recovery.
Precipitation
Precipitation techniques employ hydrophilic polymers, typically polyethylene glycol (PEG), to alter the solubility of exosomes in solution, effectively forcing them out of suspension. Commercial kits based on this principle offer a user-friendly alternative to ultracentrifugation, requiring only standard laboratory centrifuges and minimal processing time [45] [48]. The standard protocol involves mixing the biological sample (e.g., MSC-conditioned media, plasma, or pericardial fluid) with a precipitation reagent at a predetermined ratio, followed by an incubation period (typically 1-12 hours at 4°C) and subsequent low-speed centrifugation (10,000 × g) to pellet the exosomes [45] [46].
Studies evaluating precipitation methods for isolating exosomes from biological fluids have consistently demonstrated high vesicle yields, making this approach particularly valuable when working with low-input samples. However, this advantage comes with a significant trade-off in purity. When used alone, precipitation methods co-precipitate non-vesicular contaminants, including proteins, lipoproteins, and nucleic acid complexes [45] [48]. This contamination profile presents particular challenges for proteomic analyses and functional studies, where the presence of non-exosomal biomolecules can confound results and interpretation. Additionally, the residual polymer in exosome preparations may inhibit downstream applications or influence biological activity in functional assays, a critical consideration for therapeutic development.
Chromatography
Size exclusion chromatography (SEC) separates exosomes from contaminating proteins based on hydrodynamic volume, with larger exosomes eluting earlier than smaller soluble proteins. This technique utilizes porous polymer beads that allow small molecules to enter pores while excluding larger vesicles, which consequently pass through the column more rapidly [47] [49]. The chromatographic process can be performed using various column matrices, with Sepharose CL-4B, Sephacryl S-400, and Sepharose 2B being among the most commonly employed [47]. Commercial systems such as qEV columns (Izon Science) have standardized this approach for exosome isolation.
Research comparing SEC with other isolation methods has demonstrated its superior performance in generating high-purity exosome preparations with minimal protein contamination. A comparative study of blood plasma isolation techniques found that SEC enabled the isolation of exosomes without significant albumin contamination, addressing a key limitation of ultracentrifugation approaches [47]. The gentle nature of size-based separation better preserves vesicle integrity and functionality, making it particularly suitable for downstream functional assays and therapeutic applications. The primary limitation of SEC lies in its relatively low capacity and potential for sample dilution, often necessitating a subsequent concentration step [45] [46]. Additionally, the initial investment in columns and equipment may present a barrier for some laboratories, though commercial options have increased accessibility.
Table 1: Comparative Analysis of Exosome Isolation Techniques
| Parameter | Ultracentrifugation | Precipitation | Size Exclusion Chromatography |
|---|---|---|---|
| Principle | Differential sedimentation based on size, density, and shape | Solubility reduction via volume-excluding polymers | Hydrodynamic volume separation through porous matrix |
| Typical Yield | Moderate | High | Low to moderate |
| Purity | Low to moderate (albumin contamination common) | Low (co-precipitation of contaminants) | High (minimal protein contamination) |
| Processing Time | 4-6 hours (ultracentrifugation steps) | 1-12 hours incubation + 1 hour centrifugation | 15-30 minutes (after column preparation) |
| Equipment Needs | Ultracentrifuge, fixed-angle/ swinging-bucket rotors | Standard laboratory centrifuge | Chromatography columns, fraction collector (optional) |
| Sample Volume | Medium to large (up to 30 mL per tube) | Small to large (flexible scaling) | Small (typically 500 µL per column) |
| Downstream Applications | Proteomics, functional studies (with contamination considerations) | RNA analysis, biomarker discovery | Functional studies, therapeutic development, proteomics |
| Cost Considerations | High equipment investment, low per-run cost | Low equipment investment, high per-run cost (kits) | Medium equipment investment, medium per-run cost |
| Key Advantages | No chemical additives; high sample capacity; established reference method | Simple protocol; high recovery; minimal equipment needs | High purity; maintained vesicle integrity; gentle processing |
| Key Limitations | Vesicle damage/aggregation; protein contamination; long processing time | Polymer contamination; co-precipitation of non-vesicular material; requires cleanup | Sample dilution; limited capacity; potential for vesicle retention |
| Benzo[c]picene | Benzo[c]picene|CAS 217-37-8|C26H16 | Bench Chemicals | |
| 2-Chloro-6-nitronaphthalene | 2-Chloro-6-nitronaphthalene, CAS:56961-37-6, MF:C10H6ClNO2, MW:207.61 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Technical Considerations
Integrated Approaches: Combination Methods
Recognizing the complementary strengths and limitations of individual isolation methods, researchers have developed integrated protocols that sequentially apply multiple techniques to achieve superior results. The most promising of these combination approaches involves precipitation followed by size exclusion chromatography (Precipitation+SEC) [45] [46]. This hybrid methodology leverages the high recovery of precipitation with the superior purity of SEC, effectively addressing the key limitations of each method when used independently.
In a comprehensive study comparing isolation protocols for exosome-like EVs from pericardial fluid, researchers demonstrated that precipitation alone resulted in high yields but low-purity exosomes, while SEC alone produced pure EVs but at low concentrations. Strikingly, the combination of precipitation followed by SEC yielded high-purity exosomes at substantially higher concentrations than SEC alone [46]. The sequential protocol involves first concentrating exosomes from the biological fluid using a precipitation reagent, resuspending the pellet, and then applying this concentrated sample to an SEC column for purification [45]. This approach effectively removes both the polymer from the precipitation reagent and soluble protein contaminants, resulting in a preparation suitable for even the most demanding downstream applications, including therapeutic development.
The Precipitation+SEC workflow is particularly valuable for processing biofluids with low exosome densities, such as wound drainage fluids, where maximizing recovery while maintaining purity is essential for meaningful analysis. This method also shows promise for standardizing isolation from MSC-conditioned media across different laboratory settings, as it reduces the technical variability associated with ultracentrifugation while avoiding the contamination issues of standalone precipitation.
Method Selection for Specific Research Applications
The optimal isolation strategy varies significantly depending on the specific requirements of the downstream application and the nature of the starting material. For discovery-phase proteomic analyses, where comprehensive vesicle coverage must be balanced with protein contamination concerns, SEC or combination methods generally provide the most reliable results [47] [49]. When evaluating RNA cargo or conducting biomarker discovery studies from limited clinical samples, precipitation methods may be preferred due to their high recovery rates, though follow-up validation with cleaner isolation methods is often necessary [48].
For functional studies in wound healing research, particularly those investigating the therapeutic effects of MSC-exosomes in in vitro or in vivo models, vesicle integrity and biological activity become paramount considerations. In these contexts, SEC or combination methods that minimize vesicle damage and avoid introducing inhibitory contaminants (such as polymer from precipitation reagents) are generally preferred [45] [43]. When developing exosomes as therapeutic agents, regulatory considerations further influence method selection, with scalability, reproducibility, and avoidance of exogenous chemicals being key determinants in process development.
Table 2: Technical Protocols for Exosome Isolation Techniques
| Isolation Method | Detailed Protocol Steps | Critical Parameters | Expected Outcomes |
|---|---|---|---|
| Ultracentrifugation | 1. Pre-clear sample: 2,000 × g, 30 min, 4°C2. Remove debris: 16,000 × g, 30 min, 4°C3. Ultracentrifugation: 110,000 × g, 2-4 h, 4°C4. Wash pellet: Resuspend in PBS, repeat UC5. Resuspend final pellet in appropriate buffer | Rotor type (fixed-angle vs swinging-bucket); sedimentation distance; acceleration/deceleration settings; resuspension technique | Yield: ~30-50% of total exosomesPurity: Significant albumin contamination commonSize range: 30-200 nm with some aggregates |
| Precipitation | 1. Pre-clear sample: 2,000 × g, 30 min, 4°C2. Mix sample with precipitation reagent (typically 1:1-1:2 ratio)3. Incubate: 4°C, 1 h to overnight4. Low-speed centrifugation: 10,000 × g, 1 h, 4°C5. Resuspend pellet in desired buffer | Sample-to-reagent ratio; incubation time and temperature; resuspension volume | Yield: ~60-80% of total exosomesPurity: Low, co-precipitation of non-vesicular materialSize range: 30-150 nm, may include protein aggregates |
| Size Exclusion Chromatography | 1. Pre-clear sample: 2,000 × g, 30 min, 4°C2. Equilibrate column with PBS or similar buffer3. Apply sample to column (typically 500 µL)4. Elute with PBS, collect sequential fractions5. Identify exosome-rich fractions (typically 7-10 for qEV columns)6. Concentrate if needed (ultrafiltration) | Column matrix selection; fraction volume; flow rate; buffer composition | Yield: ~20-40% of total exosomesPurity: High, minimal soluble protein contaminationSize range: 30-150 nm, minimal aggregation |
| Precipitation + SEC | 1. Isolate exosomes by precipitation as above2. Resuspend pellet in 500 µL PBS3. Apply to SEC column4. Elute and collect exosome-rich fractions5. Concentrate if needed | Volume adjustment between steps; complete resuspension of precipitation pellet | Yield: ~50-70% of total exosomesPurity: High, effectively removes polymer and contaminantsSize range: 30-150 nm, maintained vesicle integrity |
Research Reagent Solutions for Exosome Isolation
Table 3: Essential Research Reagents and Materials for Exosome Isolation
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Ultracentrifugation Rotors | Differential sedimentation of exosomes | Fixed-angle (e.g., Type 70 Ti) for high capacity; swinging-bucket (e.g., SW 55 Ti) for better resolution |
| Precipitation Reagents | Volume-excluding polymers for exosome precipitation | Total Exosome Isolation Reagent (Thermo Fisher); PEG-based solutions; Commercial kits |
| SEC Columns | Size-based separation of exosomes from contaminants | qEV columns (Izon Science); Sepharose CL-4B; Sephacryl S-400; Sepharose 2B |
| Ultrafiltration Devices | Concentration of dilute exosome preparations | Amicon Ultra centrifugal filters (Merck Millipore); 100 kDa molecular weight cut-off |
| Density Gradient Media | Enhanced purity through density separation | Sucrose cushions (30% sucrose/Tris/D2O); Iodixanol gradients |
| Characterization Instruments | Validation of exosome identity, size, and concentration | Nanoparticle tracking analysis (NTA); Dynamic light scattering (DLS); Transmission electron microscopy (TEM) |
| Immunoaffinity Beads | Antibody-based capture for specific exosome subpopulations | CD9, CD63, or CD81-conjugated magnetic beads; Cell-specific marker beads |
| Protease Inhibitors | Preservation of protein cargo during processing | Complete Mini EDTA-free tablets (Roche); PMSF; Aprotinin, Leupeptin cocktails |
Experimental Workflow Visualization
Diagram 1: Experimental workflow for exosome isolation and application.
The isolation and purification of MSC-derived exosomes represents a critical foundational step in wound healing research and therapeutic development. As this technical guide has detailed, each major isolation method—ultracentrifugation, precipitation, and size exclusion chromatography—offers distinct advantages and limitations that must be carefully considered within the context of specific research objectives and downstream applications. The emerging trend toward combination methods, particularly precipitation followed by SEC, demonstrates the field's progression toward protocols that balance the competing demands of yield, purity, and preservation of biological function.
For researchers investigating the role of MSC-exosomes in wound healing, method selection should be guided by the specific requirements of their experimental paradigm. Discovery-phase studies may prioritize comprehensive vesicle recovery, while mechanistic investigations and therapeutic development necessitate high-purity preparations with preserved biological activity. As the field advances, standardization of isolation protocols across laboratories will be essential for comparing results and accelerating clinical translation. The techniques detailed in this guide provide a foundation for these efforts, enabling researchers to isolate exosomes with the quality and consistency required to fully exploit their regenerative potential in wound healing applications.
Engineering and Modification of Exosomes for Enhanced Targeting and Potency
The therapeutic application of Mesenchymal Stem Cell-derived exosomes (MSC-exos) represents a paradigm shift in regenerative medicine, particularly in the challenging domain of wound healing. These naturally occurring nanovesicles (30-200 nm in diameter) have emerged as crucial mediators of the paracrine effects of their parent cells, transferring complex biological cargo—including proteins, lipids, and nucleic acids—to recipient cells [50] [33]. Within the context of wound healing, MSC-exos demonstrate remarkable capabilities to regulate inflammation, promote angiogenesis, enhance cellular proliferation and migration, and orchestrate extracellular matrix remodeling [50]. However, the native therapeutic potential of exosomes is often constrained by limited targeting specificity, rapid clearance, and variable cargo loading. This technical guide comprehensively addresses these challenges through advanced engineering strategies, focusing specifically on enhancing the targeting and potency of MSC-exos for wound healing applications, thereby providing researchers and drug development professionals with methodologies to transform these natural vesicles into precision therapeutic tools.
Core Principles of Exosome Biology and Function
Biogenesis and Natural Composition
Exosomes originate from the endosomal system, forming through the inward budding of the limiting membrane of multivesicular bodies (MVBs). These intraluminal vesicles are subsequently released into the extracellular space upon fusion of MVBs with the plasma membrane [51]. This biogenesis pathway imparts a consistent structural identity: a lipid bilayer membrane decorated with proteins and a hydrophilic core containing diverse biomolecules.
The molecular architecture of exosomes is characterized by several key components:
- Tetraspanins: Proteins such as CD9, CD63, and CD81 are enriched in exosomal membranes and serve as canonical markers for identification [52].
- Endosomal Sorting Complexes Required for Transport (ESCRT): This machinery, comprising ESCRT-0, -I, -II, -III complexes and associated proteins like ALIX and TSG101, plays a critical role in cargo sorting and vesicle formation [51].
- Lipid Composition: Exosomes are rich in cholesterol, sphingomyelin, and ceramide, which contribute to membrane rigidity and stability [51].
- Nucleic Acids: Exosomes carry various RNA species, including messenger RNA (mRNA), microRNA (miRNA), and long non-coding RNA (lncRNA), which can modulate gene expression in recipient cells [50] [33].
Table 1: Major Functional Cargos in MSC-Derived Exosomes for Wound Healing
| Cargo Type | Key Examples | Primary Functions in Wound Healing | Target Genes/Pathways |
|---|---|---|---|
| miRNAs | let-7b, miR-125a, miR-21-5p, miR-29a, miR-126-3p, miR-181c | Inflammation regulation, angiogenesis promotion, fibroblast proliferation, collagen remodeling | TLR4/NF-κB, PTEN, TGF-β/Smad, PI3K/Akt [50] [33] |
| Proteins | VEGF, TGF-β1, IL-10, HGF | Angiogenesis, immunomodulation, cell proliferation | Receptor-mediated signaling [33] |
| Lipids | Cholesterol, sphingomyelin, phosphatidylserine | Membrane stability, signal transduction | Cellular receptors [51] |
Native MSC-Exo Functions in Wound Healing Phases
The therapeutic efficacy of native MSC-exos in wound healing unfolds across the distinct but overlapping phases of repair:
Inflammation Regulation: MSC-exos modulate the immune response by promoting the polarization of macrophages toward the anti-inflammatory M2 phenotype. For instance, exosomal let-7b from human umbilical cord MSCs alleviates wound inflammation in rats by targeting the TLR4/NF-κB and STAT3/Akt signaling pathways [50]. Similarly, miR-181c downregulates the TLR4/NF-κB/P65 pathway, reducing pro-inflammatory cytokines like TNF-α and IL-1β while increasing anti-inflammatory IL-10 [50].
Angiogenesis Promotion: MSC-exos enhance the formation of new blood vessels, a critical process for delivering oxygen and nutrients to healing tissues. Adipose-derived MSC-exos containing miR-125a inhibit the angiogenic inhibitor DLL4, thereby promoting endothelial cell angiogenesis [50]. MiR-126 from bone marrow MSC-exos activates the PI3K/Akt pathway, enhancing capillary formation at wound sites [50].
Cellular Proliferation and Migration: MSC-exos directly enhance the activity of key skin cells. MiR-135a from amnion MSC-exos promotes fibroblast proliferation and migration by targeting LATS2 [50]. MiR-21 in adipose-derived MSC-exos upregulates PI3K/AKT/MMP-9 signaling, enhancing the migration and proliferation of keratinocytes (HaCaT cells) [50] [33].
Extracellular Matrix Remodeling: MSC-exos influence collagen deposition and tissue architecture to reduce scarring. MiR-29a from adipose-derived MSC-exos targets the TGF-β2/Smad3 pathway, reducing the expression of α-SMA, Col-I, and Col-III, which are associated with scar formation [50]. MiR-192-5p similarly inhibits the IL-17RA/Smad pathway, yielding comparable anti-fibrotic effects [50].
Engineering Strategies for Enhanced Targeting Precision
Understanding Native Biodistribution and Tropism
A critical foundation for engineering targeted exosomes is understanding their natural in vivo behavior. After systemic administration, exosomes typically show rapid clearance from the blood circulation (half-life of only a few minutes) and predominantly accumulate in the liver, spleen, and lungs [53] [54]. This biodistribution profile is influenced by several intrinsic factors:
- Cellular Origin: Exosomes inherit specific tropisms from their parent cells. For example, neural stem cell-derived exosomes show preferential brain targeting compared to MSC-derived exosomes, while tumor-derived exosomes may exhibit homing to their parental tumor tissue [53].
- Membrane Composition: The protein, lipid, and glycan makeup of the exosomal membrane significantly influences cellular interactions and targeting specificity [53].
Table 2: Factors Determining Native Biodistribution of Exosomes
| Factor | Impact on Biodistribution | Experimental Evidence |
|---|---|---|
| Cellular Origin | Determines baseline organotropism; exosomes tend to target tissues similar to their parent cells. | Neural stem cell exosomes show better brain targeting than MSC exosomes [53]. |
| Membrane Proteins | Surface ligands dictate interactions with recipient cells; tetraspanins and integrins are key players. | Tumor-derived exosome integrins direct organ-specific metastasis [53]. |
| Pathophysiological State | Disease conditions can alter exosome homing, often enhancing delivery to inflamed or damaged tissues. | Inflammatory environments increase exosome recruitment to wounded areas [50]. |
| Administration Route | Significantly affects distribution patterns and therapeutic efficacy. | In silicosis models, respiratory delivery was effective while intravenous was not [54]. |
Surface Modification Techniques for Active Targeting
To overcome the limitations of native biodistribution, researchers have developed sophisticated surface engineering strategies to direct exosomes to specific tissues and cell types relevant to wound healing.
Genetic Engineering of Parent Cells
This approach involves genetically modifying exosome-producing MSCs to express targeting ligands fused with exosomal surface proteins:
- Methodology: The most common strategy involves engineering MSCs to express fusion proteins where a targeting moiety (e.g., peptide, antibody fragment) is linked to an exosome-enriched transmembrane protein, such as Lamp2b, CD63, or PDGFR [55] [56]. The transfected cells subsequently produce exosomes displaying the targeting ligand on their surface.
- Application Example: For targeting skin cells in wound healing, researchers have expressed peptides with affinity for epidermal growth factor receptor (EGFR) or integrins abundant on keratinocytes and fibroblasts. The general workflow involves:
- Cloning the gene encoding the fusion protein (e.g., Lamp2b-RGD peptide) into an appropriate expression vector.
- Transducing MSCs using viral vectors (e.g., lentivirus) or transfecting with non-viral methods.
- Selecting stable clones using antibiotics (e.g., puromycin).
- Iserving exosomes from the conditioned medium of these engineered cells via ultracentrifugation or tangential flow filtration.
- Validating surface modification through Western blot, flow cytometry, or immunogold electron microscopy [55] [56].
Direct Chemical Modification
Post-isolation chemical modification allows for direct conjugation of targeting ligands to exosome surfaces:
- Click Chemistry: This bioorthogonal approach utilizes highly specific and efficient reactions, such as the copper-catalyzed azide-alkyne cycloaddition (CuAAC). In this method, exosomal surface proteins are first functionalized with azide groups using chemical crosslinkers, followed by conjugation with alkyne-bearing targeting ligands (e.g., peptides, antibodies) [51] [55].
- Protocol Overview:
- Isolate and purify MSC-exos via ultracentrifugation (100,000× g for 70 minutes).
- Incubate exosomes with NHS-ester azide crosslinkers in PBS (pH 7.4) for 30-60 minutes at room temperature.
- Remove excess crosslinker using size exclusion chromatography or dialysis.
- React azide-labeled exosomes with alkyne-functionalized targeting ligands in the presence of a copper catalyst.
- Purify the conjugated exosomes via density gradient centrifugation [51].
- Considerations: While highly efficient, this method requires careful optimization to prevent exosome aggregation and maintain membrane integrity.
The following diagram illustrates the decision-making pathway for selecting appropriate targeting strategies based on research objectives and experimental constraints:
Engineering Strategies for Enhanced Therapeutic Potency
Cargo Loading Methodologies
Precise loading of therapeutic agents into MSC-exos is crucial for enhancing their potency in wound healing applications. Loading strategies can be broadly classified into passive and active methods, each with distinct advantages and limitations.
Passive Loading Techniques
Passive methods rely on physical principles to incorporate therapeutic cargo into exosomes:
- Simple Incubation: This straightforward approach involves co-incubating purified exosomes with therapeutic molecules, allowing diffusion across the membrane or integration into the lipid bilayer. Hydrophobic compounds (e.g., curcumin) typically show higher loading efficiency due to favorable partitioning into the membrane [56].
- Protocol Details:
- Isolate MSC-exos via ultracentrifugation.
- Resuspend exosome pellet in PBS containing the therapeutic agent (e.g., miRNA, small molecule drug).
- Incubate the mixture at room temperature for 5-30 minutes, or at 37°C for more complex cargos.
- Remove unincorporated cargo through repeated ultracentrifugation or size exclusion chromatography [56].
- Electroporation: This technique uses electrical pulses to create transient pores in the exosomal membrane, facilitating the entry of larger or charged molecules like siRNA and miRNAs.
- Mix exosomes with cargo in an electroporation buffer with low ionic strength.
- Apply electrical pulses at optimized voltage and capacitance (typically 100-500 V, 100-400 μF).
- Allow exosomes to recover on ice for 30-60 minutes to reseal membranes [51].
- Sonication: Ultrasound waves temporarily disrupt the exosomal membrane, enabling cargo loading.
- Mix exosomes with therapeutic cargo in a small volume.
- Subject the mixture to sonication using a probe sonicator at low amplitude (20-30% of maximum) for short durations (e.g., 30 seconds on, 30 seconds off for 3-6 cycles).
- Allow exosomes to recover at 37°C for 1 hour [51].
Active Loading Techniques
Active methods involve engineering the parent MSCs to package specific therapeutic molecules during exosome biogenesis:
- Genetic Modification for RNA Cargo: This approach entails transfecting MSCs with plasmids encoding precursor miRNAs or shRNAs, leading to the production of exosomes enriched with the desired RNA species.
- Design and clone miRNA sequence or shRNA expression cassette into an appropriate vector.
- Transduce MSCs using lentiviral or adenoviral vectors for stable expression.
- Select transduced cells using antibiotics and expand in culture.
- Harvest conditioned medium and isolate exosomes, which will be naturally enriched with the therapeutic RNA [50] [33].
- Optogenetic Control: Advanced systems enable precise spatiotemporal control over cargo loading. For instance, the CRY2/CIB1 system from Arabidopsis thaliana can be engineered such that cargo proteins fused to CRY2 are loaded into exosomes expressing CIB1 upon exposure to blue light [51].
Table 3: Cargo Loading Techniques for MSC-Derived Exosomes
| Method | Mechanism | Optimal Cargo Type | Loading Efficiency | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Simple Incubation | Diffusion along concentration gradient | Small hydrophobic molecules | Low to moderate | Simple, preserves exosome integrity | Low efficiency for hydrophilic/large molecules |
| Electroporation | Electrical field-induced membrane pores | Nucleic acids (siRNA, miRNA) | Moderate | Applicable to charged molecules | Potential exosome aggregation/damage |
| Sonication | Ultrasound-mediated membrane disruption | Proteins, small molecules | Moderate to high | Higher efficiency than incubation | Potential membrane damage, protein denaturation |
| Parent Cell Engineering | Endogenous sorting during biogenesis | Nucleic acids, proteins | High (biological) | Natural loading, sustainable production | Requires genetic modification of cells |
Preconditioning for Enhanced Bioactivity
Beyond direct engineering, the therapeutic potency of MSC-exos can be significantly enhanced through preconditioning of parent MSCs prior to exosome isolation:
- Hypoxic Preconditioning: Culturing MSCs under low oxygen tension (1-5% O₂) mimics the natural niche of stem cells and enhances the angiogenic potential of their exosomes. For example, hypoxia-preconditioned dental pulp stem cells secrete exosomes enriched with miR-210-3p, which induces M2 macrophage polarization by targeting NF-κB1 [50].
- Cytokine Priming: Incubating MSCs with specific inflammatory cytokines (e.g., IL-1β, TNF-α, IFN-γ) can enhance the immunomodulatory properties of their exosomes. MSCs pretreated with IL-1β produce exosomes with elevated miR-21, which induces M2 macrophage polarization by targeting programmed cell death factor 4 (PDCD4) [50].
- Pharmacological Preconditioning: Treatment with specific chemical agents can enhance exosome production and bioactivity. Deferoxamine-preconditioned bone marrow MSCs release exosomes with increased levels of miRNA-126, which promotes angiogenesis via the PTEN/PI3K/Akt pathway [50].
The following workflow outlines the integrated process of engineering and validating potent exosomes for wound healing applications, from parent cell manipulation to functional assessment:
Experimental Protocols for Key Validation Assays
Biodistribution and Pharmacokinetics Tracking
Accurate assessment of engineered exosome biodistribution is essential for validating targeting efficacy:
Isotopic Labeling with Zirconium-89 (â¸â¹Zr):
- Chelator Conjugation: Incubate purified engineered exosomes with the bifunctional chelator desferrioxamine (DFO) for 1 hour at room temperature using a mild crosslinking chemistry.
- Radiolabeling: Purify DFO-conjugated exosomes via size exclusion chromatography, then incubate with â¸â¹Zr (oxalate form) in HEPES buffer (pH 7.0-7.5) for 1 hour at 37°C.
- Purification: Remove unincorporated â¸â¹Zr using a PD-10 desalting column.
- Imaging: Administer â¸â¹Zr-labeled exosomes to wound-bearing animal models intravenously or locally. Acquire PET/CT images at multiple time points (e.g., 1, 4, 24, 48 hours post-injection) to quantify accumulation in wounds versus off-target organs [54].
Near-Infrared Fluorescent Labeling:
- Membrane Staining: Incubate engineered exosomes with lipophilic dyes (e.g., DiR, DiD) at 1-5 μM concentration for 20 minutes at 37°C.
- Purification: Remove unincorporated dye via ultracentrifugation (100,000× g for 70 minutes) or size exclusion chromatography.
- In Vivo Imaging: Administer labeled exosomes to animals and image at various time points using an IVIS imaging system. Quantify fluorescence intensity in regions of interest corresponding to wound sites and major organs [53].
Functional Validation in Wound Healing Models
Comprehensive assessment of engineered exosome efficacy requires rigorous in vitro and in vivo testing:
In Vitro Functional Assays:
- Cell Proliferation (CCK-8 Assay):
- Seed human dermal fibroblasts (HDFs) or human umbilical vein endothelial cells (HUVECs) in 96-well plates (3,000-5,000 cells/well).
- Treat with engineered MSC-exos (10-50 μg/mL) or controls.
- After 24-72 hours, add 10 μL CCK-8 solution to each well and incubate for 2-4 hours.
- Measure absorbance at 450 nm using a microplate reader [57].
- Cell Migration (Scratch Wound Assay):
- Seed HDFs or keratinocytes (HaCaTs) in 12-well plates to form confluent monolayers.
- Create a uniform scratch using a 200 μL pipette tip.
- Wash with PBS to remove detached cells and add serum-free medium containing engineered MSC-exos (10-50 μg/mL).
- Image the scratch at 0, 12, 24, and 48 hours using an inverted microscope.
- Quantify migration by measuring the percentage of wound closure using ImageJ software [57].
- Tube Formation Assay (Angiogenesis):
- Thaw Matrigel on ice and coat 96-well plates (50 μL/well), then polymerize at 37°C for 30 minutes.
- Seed HUVECs (1.5×10ⴠcells/well) in medium containing engineered MSC-exos (20-50 μg/mL).
- After 4-8 hours incubation, image tube networks using an inverted microscope.
- Quantify total tube length, number of branches, and number of complete loops using angiogenesis analysis software [50].
- Cell Proliferation (CCK-8 Assay):
In Vivo Wound Healing Models:
- Diabetic Wound Model:
- Induce diabetes in mice (e.g., C57BL/6) using streptozotocin injections (50 mg/kg for 5 consecutive days).
- After confirming hyperglycemia (>300 mg/dL), create full-thickness excisional wounds on the dorsal skin using a 6-8 mm biopsy punch.
- Apply engineered MSC-exos (100-200 μg in 50-100 μL PBS) topically to the wound bed or administer intravenously via tail vein every 2-3 days.
- Monitor wound closure daily by photographing wounds with a reference scale and planimetrically analyzing wound area using ImageJ software.
- Harvest wound tissues at various time points for histological analysis (H&E staining for re-epithelialization, Masson's trichrome for collagen deposition, CD31 immunohistochemistry for angiogenesis) [50] [33].
- Diabetic Wound Model:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Exosome Engineering and Validation
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, ExoQuick-TC, qEV size exclusion columns | Rapid exosome purification from cell culture media | Balance between yield, purity, and preservation of biological activity; critical for therapeutic applications [54] |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-CD9, Anti-TSG101, Anti-Calnexin | Confirm exosome identity and purity via Western blot, flow cytometry | Use combinations of positive and negative markers; calnexin should be absent in pure exosome preparations [52] |
| Labeling Dyes | DiI, DiD, DiR, PKH67, CFSE | Membrane labeling for uptake and tracking studies | Optimize concentration to avoid dye toxicity; include proper controls for dye transfer [53] |
| Engineering Tools | Lentiviral vectors, CRISPR/Cas9 systems, Click chemistry kits | Genetic modification of parent cells and direct exosome engineering | Ensure viral vectors are properly pseudotyped for MSC transduction; optimize MOI to maintain cell viability [51] [55] |
| Analysis Instruments | Nanoparticle Tracking Analyzer, DynaPro Nanostar, Transmission Electron Microscope | Size distribution, concentration, and morphological analysis | Use multiple complementary techniques for comprehensive characterization [54] [52] |
| Einecs 227-618-5 | Einecs 227-618-5, CAS:5908-95-2, MF:C24H29NO6, MW:427.5 g/mol | Chemical Reagent | Bench Chemicals |
| Caffeine, 8-(decylthio)- | Caffeine, 8-(decylthio)-, CAS:25837-26-7, MF:C18H30N4O2S, MW:366.5 g/mol | Chemical Reagent | Bench Chemicals |
The engineering of MSC-derived exosomes for enhanced targeting and potency represents a frontier in therapeutic development for wound healing and regenerative medicine. By leveraging sophisticated genetic, chemical, and biophysical approaches, researchers can now design exosomes with precision targeting capabilities and optimized therapeutic cargo, transforming these natural nanovesicles into powerful, cell-free therapeutics. As the field advances, key challenges remain in scaling production while maintaining quality, establishing standardized characterization protocols, and navigating regulatory pathways. Nevertheless, the continued refinement of engineering methodologies promises to unlock the full clinical potential of MSC-exos, offering new hope for patients with challenging wounds and establishing a platform technology with applications across the spectrum of regenerative medicine.
Mesenchymal stem cell-derived exosomes (MSC-Exo) have emerged as a potent cell-free therapeutic tool in regenerative medicine, particularly for wound healing. These nano-sized extracellular vesicles (30-150 nm in diameter) carry a diverse array of bioactive molecules—including proteins, lipids, mRNAs, and microRNAs—that mediate intercellular communication and modulate various biological processes critical to tissue repair [58] [59]. In the context of wound healing, MSC-Exo have been demonstrated to reduce inflammation, promote proliferation of endothelial cells and fibroblasts, inhibit apoptosis, enhance angiogenesis, and improve collagen deposition [58]. However, the clinical translation of exosome therapies faces significant challenges related to delivery efficiency. Direct application of free exosomes to wound sites often results in rapid diffusion and clearance, leading to poor retention at the target site and limited therapeutic efficacy [19].
To overcome these limitations, advanced delivery platforms have been developed to protect exosomes from degradation, provide controlled release kinetics, and maintain localized therapeutic concentrations at the wound site. Among these platforms, hydrogels, 3D-scaffolds, and injectable formulations have shown remarkable promise. These biomaterial-based systems can mimic the native extracellular matrix (ECM), provide structural support, and be engineered with specific physical and biological properties to enhance the regenerative potential of exosomes [60] [61]. This technical guide explores the fundamental principles, fabrication methodologies, and experimental evidence supporting these advanced delivery platforms, with a specific focus on their application in MSC-derived exosome delivery for wound healing research.
Hydrogel-Based Exosome Delivery Systems
Properties and Advantages of Hydrogels
Hydrogels are three-dimensional, hydrophilic polymer networks that exhibit high water content and biocompatibility, making them ideal scaffolds for tissue engineering and drug delivery applications. Their structural similarity to the native extracellular matrix (ECM) enables them to support cellular infiltration and tissue integration [61]. For exosome delivery, hydrogels offer distinct advantages: their porous structure allows for the encapsulation and retention of exosomes, their tunable physical properties enable controlled release kinetics, and their degradability can be matched to the rate of tissue regeneration [19] [60].
The table below summarizes key natural and synthetic polymers used in hydrogel fabrication for exosome delivery, along with their distinctive properties and applications in wound healing.
Table 1: Hydrogel Polymers for Exosome Delivery in Wound Healing
| Polymer Type | Specific Polymer | Key Properties | Wound Healing Applications | References |
|---|---|---|---|---|
| Natural Polymers | Hyaluronic Acid (HA) | Excellent biocompatibility, skin-like rheology, degradable by hyaluronidase | Injectable hydrogels for chronic wounds, promotes re-epithelialization | [19] |
| Chitosan & Derivatives (e.g., Q-CMC) | Inherent antibacterial properties, hemostatic, biocompatible | Antibacterial wound dressings for infected burns and scalds | [62] | |
| Alginate | Injectable, forms gentle gels with divalent cations, biocompatible | Microsphere encapsulation for sustained exosome release | [62] | |
| Gelatin/GelMA | Contains cell-adhesive motifs (e.g., RGD), photocrosslinkable | Bioink for 3D-printed scaffolds, promotes cell attachment | [63] | |
| Decellularized ECM (dECM) | Tissue-specific biochemical cues, highly biomimetic | 3D-printed bilayer scaffolds for osteochondral defects | [63] | |
| Synthetic Polymers | Poly(ethylene glycol) (PEG) | Highly tunable mechanical properties, chemically crosslinkable | Controlled release systems, triblock copolymers for small EVs | [61] |
Integration Strategies and Release Mechanisms
The method of integrating exosomes into hydrogels significantly impacts their stability, bioactivity, and release profile. Key integration strategies include:
- Physical Encapsulation: Simple mixing of exosomes with the hydrogel precursor solution before cross-linking. This method is straightforward but may lead to initial burst release if the hydrogel mesh size is too large [61].
- Covalent Conjugation: Exosomes can be surface-modified with functional groups (e.g., NHS esters, click chemistry handles) for covalent bonding to the hydrogel network. This strategy offers stronger retention but requires careful chemical modification to preserve exosome bioactivity [60].
- Affinity-Based Binding: Utilizing specific molecular interactions (e.g., streptavidin-biotin, heparin-sulfate proteoglycan interactions) to tether exosomes within the hydrogel. This allows for a more controlled release in response to cellular demand [64].
- Microsphere-Mediated Delivery: A advanced strategy involving the pre-encapsulation of exosomes within protective microspheres, which are then embedded within the bulk hydrogel. This double-encapsulation approach provides a secondary barrier, significantly prolonging release and protecting exosomes from harsh microenvironments, as demonstrated in an infected scald wound model using exosome-loaded calcium alginate microspheres (exo-CAMs) in a chitosan-alginate hydrogel [62].
The release of exosomes from hydrogels is governed by a combination of diffusion, hydrogel swelling, and polymer degradation. The degradation rate of natural polymers can be tuned via cross-linking density to achieve sustained release over days to weeks, which is crucial for the prolonged healing process of chronic wounds [60].
3D-Printed and Injectable Scaffolds for Complex Tissue Regeneration
3D-Printed Scaffolds with Spatial Specificity
For the regeneration of complex or multi-tissue defects, 3D printing (additive manufacturing) enables the fabrication of scaffolds with precise spatial architecture and heterogeneous composition. A seminal example is the development of a biomimetic double-layer scaffold for osteochondral (cartilage and bone) repair [63]. This scaffold was fabricated using a 3D bioprinting strategy that incorporated tissue-specific decellularized ECM (dECM)—cartilage dECM (DCM) for the chondrogenic layer and bone dECM (DBM) for the osteogenic layer—along with MSC-derived exosomes.
The workflow and regenerative effects of this sophisticated platform are illustrated in the following diagram:
This platform demonstrated the ability to promote rat bone marrow MSC attachment, spread, migration, proliferation, and lineage-specific differentiation in vitro. Furthermore, in a rat model, it accelerated the simultaneous regeneration of both cartilage and subchondral bone tissues, showcasing the power of combining spatial design with sustained biological cues [63].
Injectable Formulations for Minimally Invasive Delivery
Injectable hydrogels offer a clinically attractive delivery method for exosomes, as they can conform to irregular wound bed geometries and be administered in a minimally invasive manner. These formulations are designed to be liquid or low-viscosity solutions at room temperature but undergo rapid gelation in situ upon exposure to physiological conditions (temperature, pH, or ionic strength) [60].
A representative example is an injectable hyaluronic acid (HA)-based hydrogel for treating diabetic chronic wounds. This system exhibited excellent cytocompatibility, biodegradability, and skin-like rheology. The porous structure of the hydrogel allowed for in situ retention of MSC-derived exosomes, enabling a sustained therapeutic effect. In vivo studies confirmed the hydrogel's ability to accelerate wound closure, enhance angiogenesis, and promote re-epithelialization [19]. The therapeutic efficacy of exosome-laden injectable hydrogels in wound healing stems from their multi-faceted action, as visualized below:
Experimental Protocols and Analytical Methods
Protocol: Fabrication of an Exosome-Laden Injectable Hydrogel
The following protocol outlines the key steps for creating a hyaluronic acid-based injectable hydrogel loaded with MSC-derived exosomes, based on methodologies described in the literature [19].
Synthesis of Hydrogel Components:
- Modify hyaluronic acid (HA) to introduce functional groups for cross-linking (e.g., methacrylate groups for photopolymerization or aldehyde and hydrazide groups for Schiff base formation).
- Characterize the degree of substitution using proton nuclear magnetic resonance (¹H NMR).
Isolation and Characterization of MSC-Derived Exosomes:
- Culture MSCs from a chosen source (e.g., human umbilical cord, adipose tissue) in exosome-depleted media.
- Collect conditioned media and isolate exosomes via differential ultracentrifugation or size-exclusion chromatography.
- Characterize exosomes by:
- Dynamic Light Scattering (DLS): Determine particle size distribution.
- Flow Cytometry: Confirm presence of exosomal surface markers (CD63, CD81).
- Transmission Electron Microscopy (TEM): Visualize morphology.
- BCA Assay: Quantify total protein concentration.
Hydrogel Formation and Exosome Encapsulation:
- Resuspend the exosome pellet in the hydrogel precursor solution (e.g., modified HA solution) at the desired concentration.
- Mix thoroughly but gently to avoid damaging the exosomes.
- Add the cross-linker (e.g., FeCl₃ for ionic crosslinking) or initiate cross-linking (e.g., UV light for methacrylated polymers) to form the hydrogel.
In Vitro Release Kinetics Study:
- Incubate the exosome-laden hydrogel in phosphate-buffered saline (PBS) at 37°C under gentle agitation.
- Collect release medium at predetermined time points and replace with fresh PBS.
- Quantify the amount of exosomes released using a BCA protein assay or nanoparticle tracking analysis (NTA).
- Plot the cumulative release percentage over time to characterize the release profile.
Protocol: Evaluation of Wound Healing EfficacyIn Vivo
This protocol describes a standard rat model for evaluating the therapeutic effect of an exosome-hydrogel formulation on full-thickness skin wounds [65] [62].
Animal Model Establishment:
- Use adult male Wistar rats (e.g., 200-250 g).
- Anesthetize the animals and create a circular full-thickness skin defect (e.g., 15 mm diameter) on the dorsum.
- Apply a silicone ring splint around the wound and suture it in place to prevent wound contraction.
Experimental Groups and Treatment:
- Randomly divide rats into at least three groups:
- Group 1 (Treatment): Application of the exosome-laden hydrogel.
- Group 2 (Hydrogel Control): Application of the blank hydrogel (without exosomes).
- Group 3 (Vehicle Control): Injection of PBS or no treatment.
- Apply treatments topically or via subcutaneous injection around the wound bed.
- Randomly divide rats into at least three groups:
Monitoring and Analysis:
- Wound Closure Measurement: Photograph the wounds daily. Use image analysis software to calculate the wound area and determine the percentage of wound closure over time.
- Histological Analysis: On day 14 post-surgery, euthanize the animals and harvest the wound tissue.
- Fix tissues in formalin, embed in paraffin, and section.
- Perform staining:
- Hematoxylin and Eosin (H&E): Assess general tissue morphology and re-epithelialization.
- Masson's Trichrome: Evaluate collagen deposition and organization.
- Immunohistochemical Staining: Use antibodies against CD31 or CD34 to quantify neovascularization (angiogenesis).
The efficacy of integrated exosome delivery systems is demonstrated by quantitative data from preclinical studies. The table below consolidates key performance metrics from recent research.
Table 2: Quantitative Efficacy of Exosome-Laden Delivery Platforms in Preclinical Models
| Delivery Platform | Exosome Source | Disease Model | Key Quantitative Outcomes | References |
|---|---|---|---|---|
| HA-based Injectable Hydrogel | MSC | Diabetic Chronic Wound | Accelerated wound closure; Enhanced angiogenesis; Promoted re-epithelialization. | [19] |
| 3D-Printed dECM/GelMA Bilayer Scaffold | Human Adipose MSC | Rat Osteochondral Defect | Promoted BMSC migration & proliferation; Efficiently regenerated both cartilage and subchondral bone. | [63] |
| Exosome Microsphere/AgNP Hydrogel (HS-QAF-AgNPs) | Human Umbilical Cord MSC | Rat Scald Wound Model | Antibacterial effect; Promoted cell migration & proliferation; Stimulated angiogenesis; Accelerated wound closure. | [62] |
| Local Exosome Injection | Human Blood Serum | Rat Full-Thickness Wound | Accelerated wound closure; Improved collagen synthesis; Enhanced vessel formation & angiogenesis. | [65] |
The Scientist's Toolkit: Key Research Reagents and Materials
Successful implementation of research on exosome-integrated delivery platforms requires a suite of specialized reagents and materials.
Table 3: Essential Research Reagents for Exosome-Hydrogel Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Exosome Isolation Kits | Isolate exosomes from cell culture media or biological fluids. | Total Exosome Isolation kit (from serum); Size-exclusion chromatography columns; Polyethylene glycol (PEG)-based precipitation kits. |
| Characterization Antibodies | Confirm exosome identity via surface marker detection. | Anti-CD63, Anti-CD81 (for flow cytometry). |
| Hydrogel Polymers | Form the scaffold or matrix for exosome encapsulation and delivery. | Hyaluronic Acid (HA); Methacrylated Gelatin (GelMA); Chitosan (e.g., Q-CMC); Alginate; Decellularized ECM (dECM). |
| Crosslinking Agents | Initiate and sustain hydrogel formation. | FeCl₃ (ionic crosslinker); UV Light (for photopolymerization of GelMA); Genipin (for natural polymers). |
| Cell Assay Kits | Evaluate biological activity of exosomes and biocompatibility of constructs. | MTT assay (cytotoxicity); Scratch assay (cell migration); BCA assay (protein quantification). |
| Animal Model Supplies | Conduct in vivo wound healing studies. | Wistar rats; Ketamine/Xylazine (anesthesia); Silicone splints. |
| Propynyloxy | Propynyloxy, CAS:61244-93-7, MF:C3H2O, MW:54.05 g/mol | Chemical Reagent |
| 1,2,7-Trichloronaphthalene | 1,2,7-Trichloronaphthalene|RUO | 1,2,7-Trichloronaphthalene is a key synthetic intermediate for bioactive compounds and material science research. For Research Use Only. Not for human use. |
The integration of MSC-derived exosomes into advanced delivery platforms like hydrogels, 3D-scaffolds, and injectable formulations represents a paradigm shift in regenerative medicine, moving away from cell-based therapies toward more controllable and scalable cell-free approaches. These systems successfully address the critical challenges of poor retention and rapid clearance of freely delivered exosomes, thereby enhancing their therapeutic potential for complex wound healing applications.
Future developments in this field will likely focus on several key areas:
- Standardization and Scalability: Developing standardized, GMP-compliant protocols for exosome production and hydrogel fabrication is crucial for clinical translation [66].
- Smart Responsive Systems: Engineering "smart" hydrogels that respond to specific wound microenvironment cues (e.g., pH, enzyme activity, reactive oxygen species) to release exosomes on demand [61].
- Combinatorial Strategies: Combining exosomes with other therapeutic agents, such as antimicrobial nanoparticles (e.g., AgNPs) or growth factors, to create multifunctional dressings for infected or complex chronic wounds [62].
- Enhanced Characterization: Advancing analytical techniques to better monitor exosome retention, release, and functional status within the delivery matrix over time.
By leveraging the unique properties of biomaterials and the multifaceted regenerative signals of MSC-derived exosomes, researchers are paving the way for a new generation of highly effective therapies for wound healing and tissue regeneration.
The development of mesenchymal stem cell-derived exosomes (MSC-Exos) as therapeutics for wound healing represents a paradigm shift in regenerative medicine. Unlike traditional cell-based therapies, exosomes offer a cell-free approach with lower immunogenicity and enhanced safety profiles [33] [44]. However, their inherent complexity and heterogeneity present significant challenges for standardization and quality control. The current regulatory landscape reflects these challenges, with the U.S. Food and Drug Administration (FDA) emphasizing that exosome products used to treat diseases are regulated as drugs and biological products and must comply with premarket review and approval requirements [67].
Establishing robust potency assays and release criteria is particularly critical for MSC-Exos intended for wound healing applications. These exosomes facilitate cutaneous wound repair through multiple mechanisms, including promoting collagen synthesis, angiogenesis, re-epithelialization, and immunomodulation [68] [33] [69]. A comprehensive quality control framework must therefore capture this functional complexity while ensuring product consistency, safety, and efficacy.
Analytical Methods for Exosome Characterization
Critical Quality Attributes (CQAs) Assessment
A multi-parametric approach is essential for comprehensive exosome characterization. The following table summarizes key CQAs and their corresponding analytical methods:
Table 1: Critical Quality Attributes and Analytical Methods for MSC-Derived Exosomes
| Quality Attribute | Analytical Method | Target Specifications | Technical Considerations |
|---|---|---|---|
| Particle Concentration & Size Distribution | Nanoparticle Tracking Analysis (NTA) | 30-150 nm diameter [33] [44] | Method variability requires standardization [70] |
| Surface Marker Profile | Flow Cytometry | CD9, CD63, CD81 positive [69]; CD14, CD34, CD45, HLA-DR negative [44] | Use of calibrated fluorescent beads and validated antibodies |
| Morphology | Transmission Electron Microscopy (TEM) | Spherical, bilayer morphology | Artifacts possible from sample preparation |
| Total Protein Content | Bicinchoninic Acid (BCA) Assay | Particles/μg protein ratio [70] | Must combine with particle count for purity assessment |
| Purity Assessment | Multiple assays | High particle-to-protein ratio | Combination of NTA and protein quantification |
| Imaging | TEM | Cup-shaped morphology, bilayer structure | Qualitative assessment only |
Technical Considerations for CQA Implementation
The measurement of particle size and concentration demonstrates significant method-dependent variability, highlighting the need for standardized approaches and appropriate reference materials [70]. Surface marker analysis should employ calibrated instrumentation and validated antibody reagents to ensure reproducibility across manufacturing batches. Importantly, no single analytical method sufficiently characterizes exosomes; orthogonal approaches are necessary to build a complete quality profile.
Development of Potency Assays for Wound Healing Applications
Mechanism-Based Potency Assessment
Potency assays must reflect the multifaceted role of MSC-Exos in wound healing. The following mechanisms should be quantitatively measured:
3.1.1 Pro-Angiogenic Activity
- Tube Formation Assay: Quantify the ability of exosomes to promote capillary network formation by human umbilical vein endothelial cells (HUVECs) [68] [69]. Key metrics include total tube length, number of branches, and number of junctions.
- Experimental Protocol: Seed HUVECs on Matrigel matrix in 24-well plates. Treat with standardized exosome concentrations (e.g., 50-100 μg/mL). After 4-18 hours, capture images and analyze using automated image analysis software. Include VEGF as a positive control.
3.1.2 Fibroblast Proliferation and Migration
- Scratch Assay: Measure fibroblast migration into a created "wound" area [68] [69].
- Experimental Protocol: Create a confluent monolayer of human dermal fibroblasts. Scratch with a sterile pipette tip and treat with exosomes. Monitor closure through time-lapse microscopy. Calculate migration rate as percentage closure over time.
- Proliferation Assays: Utilize cell counting kits (e.g., CCK-8) to quantify dose-dependent fibroblast proliferation [68].
3.1.3 Extracellular Matrix Modulation
- Collagen Synthesis Measurement: Employ ELISA to quantify Type I and III collagen secretion by fibroblasts [68] [69]. Assess both protein secretion and mRNA expression via qRT-PCR.
- Scar Formation Markers: Evaluate the ratio of collagen I/III and TGF-β3/TGF-β1, as higher ratios correlate with reduced scar formation [33].
3.1.4 Anti-inflammatory Effects
- Macrophage Polarization Assay: Measure the ability of exosomes to shift macrophages from pro-inflammatory (M1) to anti-inflammatory (M2) phenotypes using flow cytometry for surface markers and cytokine profiling [71].
Quantitative Potency Metrics
Table 2: Potency Assays for Wound Healing Applications
| Biological Function | Assay Format | Key Metrics | Acceptance Criteria |
|---|---|---|---|
| Angiogenesis | Tube formation using HUVECs | Total tube length, branch points, junctions | Minimum 1.5-fold increase vs. control |
| Fibroblast Migration | Scratch assay | Percentage closure at 24h | Minimum 40% increase in migration rate |
| Fibroblast Proliferation | Cell counting/CCK-8 | Cell number after 48-72h | Dose-dependent response, EC50 calculation |
| Collagen Production | ELISA/qRT-PCR | Type I/III collagen secretion, mRNA expression | Significant increase vs. untreated control |
| Anti-inflammatory | Macrophage polarization | M2/M1 marker ratio, anti-inflammatory cytokines | Significant shift toward M2 phenotype |
| Anti-fibrotic | TGF-β signaling | TGF-β3/TGF-β1 ratio, MMP3/TIMP1 ratio | Increased ratio indicating reduced scarring |
Release Criteria and Specifications
Quality Control Release Tests
Establishing well-defined release specifications ensures consistent product quality across manufacturing batches:
Table 3: Proposed Release Criteria for MSC-Derived Exosomes
| Test Category | Test Method | Proposed Release Criteria | Rationale |
|---|---|---|---|
| Identity | Flow cytometry | Positive for CD9, CD63, CD81 (>70% of particles) | Confirms exosomal nature [69] |
| Identity | Flow cytometry | Negative for CD34, CD45 (<5% of particles) | Confirms absence of cellular contaminants [44] |
| Purity | NTA + BCA assay | Particle-to-protein ratio >2×10^9 particles/μg | Indicates minimal protein contamination [70] |
| Potency | Tube formation | ≥50% increase in tube length vs. control | Ensures pro-angiogenic activity [68] |
| Potency | Scratch assay | ≥40% improvement in migration vs. control | Ensures cell migration activity [68] |
| Safety | Endotoxin | <0.5 EU/mL | Meets pharmacopeial requirements |
| Safety | Sterility | No microbial growth in 14 days | Meets pharmacopeial requirements |
| Dosage | Particle count | Within 80-120% of target concentration | Ensures accurate dosing |
Batch-to-Batch Consistency Assessment
To demonstrate manufacturing consistency, compare critical parameters between consecutive batches using predefined acceptance criteria. Biochemical, biophysical, and functional assays should demonstrate high comparability (typically ≥70% similarity) between freshly prepared and previously manufactured batches [70].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Exosome Quality Control
| Reagent/Cell Line | Specific Example | Application in QC | Critical Function |
|---|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary HUVECs, passage 3-6 | Angiogenesis potency (tube formation) | Measure exosome pro-angiogenic capacity [68] [69] |
| Human Dermal Fibroblasts | Primary fibroblasts or cell lines (e.g., Hs27) | Migration (scratch assay) and proliferation assays | Assess fibroblast stimulation potential [68] |
| Macrophage Cell Line | THP-1 (with PMA differentiation) | Anti-inflammatory potency | Evaluate immunomodulatory capacity via polarization [71] |
| Characterization Antibodies | Anti-CD9, CD63, CD81, CD34, CD45 | Identity confirmation by flow cytometry | Verify exosome identity and purity [44] [69] |
| Extracellular Matrix | Matrigel or collagen-based matrices | Tube formation assay | Provide substrate for endothelial network formation [68] |
| Cell Viability/Proliferation Kits | CCK-8, MTT, WST assays | Proliferation potency | Quantify metabolic activity of stimulated cells [68] |
| Methyl glycyl-L-serinate | Methyl glycyl-L-serinate, CAS:66328-96-9, MF:C6H12N2O4, MW:176.17 g/mol | Chemical Reagent | Bench Chemicals |
| 3-Sulfanyl-D-isovaline | 3-Sulfanyl-D-isovaline, CAS:98119-54-1, MF:C5H11NO2S, MW:149.21 g/mol | Chemical Reagent | Bench Chemicals |
Regulatory Considerations and Standardization Challenges
Current Regulatory Framework
The global regulatory framework for exosomes is evolving, with approaches generally focusing on either elucidating constituent components within exosomes or examining their physiological effects [70]. In the United States, the FDA has clearly stated that no exosome products are currently approved, and clinics offering unapproved exosome products are "flouting federal statutes and FDA regulations" [67].
Current Good Manufacturing Practices (cGMP) provide the foundation for quality systems, emphasizing rigorous process controls, validation protocols, and comprehensive documentation [70]. However, specific regulatory guidelines tailored to exosome-based therapeutics are still under development, creating challenges for sponsors seeking marketing authorization.
Key Standardization Challenges
6.2.1 Manufacturing Consistency Exosome secretion is sensitive to culture conditions, including cell passage number, culture method, and medium composition. Even minor variations can significantly alter exosome characteristics, creating substantial batch-to-batch variability [70]. Development of standardized culture conditions and process controls is essential to mitigate this challenge.
6.2.2 Analytical Method Standardization Different methods for particle characterization (e.g., NTA, TRPS, resistive pulse sensing) can yield significantly varying results for the same sample [70]. This highlights the urgent need for standardized methodologies and international reference materials to enable cross-laboratory comparisons and data harmonization.
6.2.3 Stability and Storage Liquid-based exosomes are highly susceptible to degradation and alteration within hours after production [70]. Cryopreservation and lyophilization technologies offer potential solutions, but further investigation is required to confirm that post-preservation exosomes maintain equivalence to their original state.
The development of robust potency assays and release criteria for MSC-derived exosomes represents a critical milestone in advancing these promising therapeutics toward clinical application for wound healing. A comprehensive quality control framework must encompass identity, purity, safety, and potency attributes, with particular emphasis on mechanism-based functional assays that reflect the multifaceted role of exosomes in promoting wound repair.
While significant challenges remain in standardization and regulatory alignment, the establishment of scientifically rigorous and clinically relevant quality standards will accelerate the legitimate development of exosome-based wound healing therapies. Continued collaboration between researchers, manufacturers, and regulatory agencies is essential to build consensus on testing methodologies, acceptance criteria, and manufacturing standards that will ultimately ensure the consistent quality, safety, and efficacy of MSC-derived exosome products.
Navigating the Hurdles: Overcoming Heterogeneity, Scalability, and Regulatory Challenges
Addressing Exosome Heterogeneity and Cargo Variability
Exosomes derived from mesenchymal stem cells (MSCs) represent a promising cell-free therapeutic paradigm for wound healing, leveraging their innate abilities to modulate immune responses, promote angiogenesis, and facilitate tissue regeneration. However, their inherent heterogeneity and cargo variability present significant challenges for clinical translation, impacting therapeutic consistency, reproducibility, and predictability. This technical guide delves into the molecular and cellular origins of exosome heterogeneity, systematically outlines robust methodologies for its characterization and quantification, and proposes a standardized framework to mitigate its effects. Within the context of wound healing research, we synthesize current data on MSC-exosome variability and provide detailed experimental protocols to equip researchers with the tools necessary for advancing reproducible and efficacious exosome-based therapies.
Exosomes are nanoscale extracellular vesicles (30-150 nm in diameter) of endocytic origin, secreted by virtually all cell types and present in all biological fluids [72]. They are formed through the inward budding of the endosomal membrane, creating intraluminal vesicles within multivesicular bodies, which are subsequently released into the extracellular space upon fusion of these bodies with the plasma membrane [73]. Exosome heterogeneity refers to the substantial variations in exosome size, surface molecular composition, and biomolecular cargo observed between exosomes derived from different cellular sources, different subpopulations of the same cell type, and even within a single cell's secretory output [74] [73]. This heterogeneity is not merely random noise; it is a biologically consequential feature influenced by the physiological state, pathological conditions, and microenvironment of the parent cell [75].
In the specific context of MSC-derived exosomes for wound healing, this variability manifests in several critical ways. The proteomic, lipidomic, and nucleic acid content of MSC-exosomes can shift dramatically based on the MSC tissue source (e.g., bone marrow vs. umbilical cord), passage number, culture conditions, and exposure to inflammatory cytokines or hypoxia [74] [72]. For instance, exosomes derived from human induced pluripotent stem cell-derived MSCs (hiPSC-MSCs) have been shown to be enriched with pro-angiogenic and pro-migratory factors that facilitate cutaneous wound healing [22]. Conversely, understanding and controlling this heterogeneity is paramount for developing exosome-based therapeutics with reliable dose-response relationships and predictable clinical outcomes for chronic wounds.
The variability observed in exosome populations stems from a complex interplay of intrinsic and extrinsic factors.
- Cellular Origin and State: The molecular signature of an exosome is a reflection of its parent cell. MSCs from different tissues (e.g., bone marrow, adipose tissue, umbilical cord) produce exosomes with distinct cargo profiles and functional properties [74] [72]. Furthermore, the cell's metabolic state, cell cycle stage, and exposure to stress (e.g., oxidative stress, hypoxia) directly influence exosome biogenesis and cargo sorting [73].
- Biogenesis Pathways: Exosomes can be generated via both ESCRT (Endosomal Sorting Complexes Required for Transport)-dependent and ESCRT-independent pathways (e.g., involving tetraspanins or ceramide) [73]. The choice of biogenesis pathway can determine which cargo is selectively enriched into the nascent vesicles, leading to populations of exosomes with different functional potentials from the same cell [73].
- Post-Secretion Modifications: Once released, exosomes can undergo surface modifications, aggregate with other vesicles, or have their cargo degraded over time, adding another layer of heterogeneity. Storage conditions, such as repeated freeze-thaw cycles, can exacerbate this variability [17].
Implications for Wound Healing Research and Therapy
For researchers focusing on MSC-exosomes in wound healing, heterogeneity poses several direct challenges:
- Therapeutic Reproducibility: Variations in anti-inflammatory or pro-angiogenic cargo (e.g., miRNAs like miR-21-5p or proteins like TSG101) between exosome batches can lead to inconsistent results in promoting re-epithelialization, angiogenesis, and collagen synthesis in diabetic or chronic wound models [19] [22] [57].
- Dosing and Potency Assessment: The functional unit of an exosome therapeutic is not merely its particle number or protein quantity, but its bioactive cargo. Heterogeneity complicates the establishment of a standardized potency assay, as the critical therapeutic molecules may vary [76] [77].
- Mechanistic Studies: Inconsistent exosome preparations can obscure structure-activity relationships, making it difficult to pinpoint which specific exosome components are responsible for observed therapeutic effects in wound healing [74] [73].
Table 1: Key Sources and Functional Impacts of MSC-Exosome Heterogeneity in Wound Healing
| Source of Heterogeneity | Impact on Exosome Characteristics | Potential Consequence in Wound Healing |
|---|---|---|
| MSC Tissue Source (e.g., Umbilical Cord vs. Bone Marrow) | Varying levels of immunomodulatory miRNAs (e.g., let-7b-5p) and pro-angiogenic factors [74] [57] | Differences in the rate of inflammation reduction and new blood vessel formation |
| Cell Culture Conditions (e.g., Hypoxia, 3D vs. 2D) | Altered cargo loading; upregulation of specific growth factors and miRNAs [74] | Enhanced or diminished promotion of fibroblast migration and collagen production |
| Biogenesis Pathway (ESCRT-dependent vs. independent) | Selective enrichment of different protein and RNA cargoes [73] | Changes in the ability to modulate specific signaling pathways (e.g., Wnt/β-catenin) in target cells [57] |
| Isolation Method (e.g., Ultracentrifugation vs. Precipitation) | Co-isolation of non-exosomal contaminants; variable yield and purity [76] [72] | Introduction of confounding variables; inaccurate attribution of therapeutic effects |
Quantitative Assessment of Variability
A critical step in managing heterogeneity is its rigorous quantification. A landmark study by Tiruvayipati et al. (2020) systematically evaluated the qualitative (presence/absence) and quantitative (abundance) variability of proteins in exosome-enriched extracellular vesicles (EE-EVs) from lung adenocarcinoma cell lines, providing a robust framework applicable to MSC-exosomes [76] [77].
Experimental Design for Variability Assessment
The researchers designed a replicate strategy to disentangle technical noise from biological variation.
- Biological Replicates (BRs): Defined as exosomes isolated from different passages of the same cell line, informing on the reproducibility of the biological phenomenon [77].
- Technical Replicates (TRs): Defined as multiple aliquots from the same exosome isolation lysate, assessing the reproducibility of the analytical assay (LC/MS/MS) [77].
Table 2: Summary of Quantitative Variability in Exosomal Protein Cargo [77]
| Cell Line | Qualitative Variability (Protein Presence/Absence) | Quantitative Variability (Protein Abundance) |
|---|---|---|
| H1993 | Higher among Biological Replicates (BRs) vs. Technical Replicates (TRs) | Low variability across both TRs and BRs |
| A549 | Higher among Biological Replicates (BRs) vs. Technical Replicates (TRs) | Low variability across both TRs and BRs |
| H1975 | Higher among Biological Replicates (BRs) vs. Technical Replicates (TRs) | Significant quantitative variability observed |
Key Finding: The study concluded that variability was largely qualitative (which proteins are detected) and was more pronounced among biological replicates than technical replicates. This underscores that the biological state of the cell is a major driver of heterogeneity. However, for the most abundant proteins, quantitative variability was generally low, except in specific cases like the H1975 cell line [77]. This replicate strategy successfully identified 90% of the most abundant proteins, validating its utility for core exosome analysis.
Detailed Protocol: Assessing Protein Cargo Variability
This protocol is adapted from Tiruvayipati et al. for application with MSC-exosomes [77].
Objective: To determine the qualitative and quantitative variability in the protein cargo of MSC-derived exosomes.
Materials:
- Human MSCs (e.g., from bone marrow or umbilical cord)
- Standard cell culture media and reagents
- Ultracentrifugation equipment (or alternative isolation kit)
- RIPA Lysis Buffer with protease/phosphatase inhibitors
- BCA Protein Assay Kit
- Liquid Chromatography-Tandem Mass Spectrometry (LC/MS/MS) access
Methodology:
- Cell Culture and Exosome Isolation:
- Culture MSCs to 85-95% confluency in multiple T175 flasks.
- Replace medium with exosome-depleted serum medium.
- After 48 hours, collect conditioned medium.
- Isolate exosomes using a standardized method (e.g., sequential ultracentrifugation: 300 × g for 10 min, 2,000 × g for 10 min, 10,000 × g for 30 min, and 100,000 × g for 70 min) [57] [72].
- Repeat the entire process across three different cell passages to generate three biological replicates (BR1, BR2, BR3).
Sample Preparation for Proteomics:
- Lysate each exosome pellet (BR1, BR2, BR3) in RIPA buffer.
- Determine protein concentration using the BCA assay.
- For each biological replicate lysate, divide into three equal aliquots. These are your technical replicates (TR1, TR2, TR3 for each BR).
- Process all nine samples (3 BRs × 3 TRs) for LC/MS/MS analysis using standardized protein digestion protocols.
Data Analysis:
- Use customized bioinformatics and biostatistical workflows to analyze LC/MS/MS data.
- Qualitative Analysis: Compare the lists of identified proteins across all replicates. Calculate the percentage overlap.
- Quantitative Analysis: Compare the normalized abundance (e.g., label-free quantitation intensity) of the identified proteins across replicates. Calculate coefficients of variation (CV) for proteins within TRs and between BRs.
Interpretation: This design allows researchers to distinguish variability introduced by the measurement technique (low variability among TRs) from true biological variation (potentially higher variability among BRs). A successful, consistent preparation will show high quantitative correlation among TRs and a core set of consistently identified proteins across BRs.
Strategies to Mitigate Heterogeneity
A multi-pronged approach is required to standardize exosome populations for therapeutic applications.
Standardization of Production and Isolation
- Cell Source and Culture Standardization: Utilize well-characterized MSC banks at low passage numbers. Control critical culture parameters such as oxygen tension, serum batches (preferably exosome-depleted), and confluence at the time of harvest [72].
- Refined Isolation Techniques: While differential ultracentrifugation (DUC) is common, it co-isolates contaminants. Density gradient ultracentrifugation (DGUC) or size-exclusion chromatography (SEC) can yield purer exosome preparations [72] [17]. The choice of method should be validated and consistently applied.
Cargo Engineering and Loading
To overcome the limitations of natural heterogeneity, engineering approaches can create exosomes with defined and potent cargo.
- Parent Cell Engineering: Genetically modify MSCs to overexpress specific therapeutic miRNAs (e.g., miR-21-5p for activating Wnt/β-catenin pathway in hair follicle regeneration [57]) or proteins, ensuring their enrichment in secreted exosomes.
- Direct Cargo Loading: Post-isolation, therapeutic molecules can be loaded into exosomes using techniques such as electroporation, sonication, or saponin-mediated permeabilization [74]. This allows for precise dosing, transforming exosomes into targeted drug delivery vehicles.
The following diagram illustrates a standardized workflow that integrates production, isolation, and engineering strategies to minimize heterogeneity and create more consistent exosome therapeutics for wound healing.
Diagram: A standardized workflow for producing consistent MSC-exosome therapeutics, incorporating quality control and engineering strategies to address heterogeneity.
The Scientist's Toolkit: Key Reagents and Materials
The following table catalogues essential reagents and materials critical for research into exosome heterogeneity and its application in wound healing.
Table 3: Research Reagent Solutions for Exosome Studies
| Reagent/Material | Function/Application | Example from Search Context & Notes |
|---|---|---|
| Exosome-Depleted FBS | Cell culture supplement that minimizes contamination of the conditioned medium with bovine exosomes. | Used during the conditioning phase prior to exosome harvest [77] [57]. Critical for obtaining pure MSC-exosome preps. |
| Ultracentrifugation Equipment | Gold-standard method for isolating exosomes from large volumes of conditioned media via high-speed centrifugation. | Used in multiple studies for exosome purification [22] [57] [72]. Requires optimization to avoid co-pelleting contaminants. |
| CD63, CD81, CD9 Antibodies | Tetraspanin markers used to confirm the identity of isolated exosomes via Western Blot or flow cytometry. | Listed as characteristic exosome surface proteins [76] [73]. Essential for quality control. |
| ALIX / TSG101 Antibodies | Proteins associated with the ESCRT pathway and exosome biogenesis; used as additional positive markers for exosomes. | Commonly detected in exosome preparations to verify endosomal origin [73] [72]. |
| LC/MS/MS System | High-throughput platform for identifying and quantifying proteins in exosome cargo (proteomic analysis). | Key technology used to assess protein cargo variability in replicates [76] [77]. |
| Nanoparticle Tracking Analysis (NTA) | Instrumentation (e.g., ZetaView, NanoSight) to determine exosome particle size distribution and concentration. | Recommended for characterizing exosome size and concentration according to MISEV guidelines [17]. |
| Transmission Electron Microscopy (TEM) | Imaging technique used to visualize the morphology and ultrastructure of isolated exosomes. | Used to confirm the cup-shaped morphology and size of exosomes [57] [17]. |
| RIPA Lysis Buffer | A buffer used to lyse exosomes and extract total protein for downstream analysis like Western Blot or BCA assay. | Used for lysing exosome pellets prior to protein quantification and analysis [77] [57]. |
| miRNA Inhibitors/Mimics | Synthetic oligonucleotides used to manipulate miRNA levels in parent MSCs to study functional cargo. | Useful for validating the role of specific miRNAs (e.g., miR-21-5p, let-7b-5p) in exosome function [57]. |
Exosome heterogeneity is not an insurmountable barrier but a fundamental property that must be systematically understood and controlled. For the field of MSC-exosome therapy in wound healing to mature, researchers must adopt rigorous, quantitative frameworks for assessing variability, standardize production and isolation pipelines, and leverage bioengineering to create defined therapeutic products. By implementing the detailed experimental protocols and strategic guidelines outlined in this document, the scientific community can enhance the reproducibility, efficacy, and safety of exosome-based therapies, ultimately accelerating their translation from the bench to the bedside for treating debilitating chronic wounds.
The field of regenerative medicine is increasingly focusing on mesenchymal stem cell-derived exosomes (MSC-exosomes) as a promising cell-free therapeutic strategy for challenging wound healing scenarios. Chronic wounds, characterized by prolonged inflammation and inability to re-epithelialize, represent a significant clinical burden where conventional treatments often fall short [14]. MSC-exosomes have demonstrated remarkable capacities to modulate immune responses, promote angiogenesis, support cell proliferation, and facilitate extracellular matrix remodeling—addressing multiple pathological aspects of non-healing wounds simultaneously [19] [24] [33].
Despite their considerable therapeutic potential, the clinical translation of MSC-exosomes faces a critical bottleneck: the development of robust, scalable, and compliant Good Manufacturing Practice (GMP) production processes [78]. Unlike small molecule pharmaceuticals, exosomes are complex biological nanoparticles requiring sophisticated manufacturing approaches that preserve their structural integrity and biological functionality while ensuring batch-to-batch consistency [79]. This technical guide examines current strategies and methodologies for scaling up GMP manufacturing of MSC-derived exosomes, with particular emphasis on their application in wound healing research and therapy development.
Upstream Process Development: From Static Culture to Scalable Bioreactors
Cell Line Selection and Culture Optimization
The foundation of any successful exosome production process begins with carefully selected and characterized mesenchymal stem cell lines. Common sources include bone marrow-derived MSCs (BM-MSCs), adipose-derived stem cells (ADSCs), and human umbilical cord MSCs (hUCMSCs), each offering distinct advantages in terms of expansion potential and secretory profile [78] [33]. For GMP compliance, comprehensive cell banking and rigorous characterization are essential, including verification of standard MSC surface markers (CD73, CD90, CD105 ≥95%; CD34, CD45, HLA-DR ≤2%) and differentiation potential [57].
Culture medium optimization represents a critical parameter for maximizing both cell growth and exosome yield. Recent advances have shifted toward chemically defined, xeno-free media formulations to eliminate animal-derived components and enhance product consistency [79]. For instance, human platelet lysate has emerged as an effective supplement for MSC expansion, though exosome production phases may utilize specialized, protein-free formulations to facilitate downstream purification [78].
Scalable Expansion Systems
Transitioning from laboratory-scale flask cultures to industrial-grade bioreactor systems is essential for achieving clinically relevant exosome quantities. The table below compares various cultivation systems used in GMP-compliant exosome production:
Table 1: Comparison of Upstream Cultivation Systems for MSC-Exosome Production
| System Type | Scale Capacity | Key Advantages | Reported Exosome Yield | Reference |
|---|---|---|---|---|
| T-Flasks (Static) | < 1L | Simple operation, low capital investment | Baseline | [78] |
| Cell Factory Stacks | 1-10L | Increased surface area, closed system | 2-3x over flasks | [78] |
| iCELLis Fixed-Bed Bioreactor | Up to 500L | High volumetric productivity, scalability | High (process-specific) | [79] |
| Hollow Fiber Bioreactor | 10-100L | High cell density, continuous harvesting | 10-20x over flasks | [78] |
Fixed-bed bioreactors like the iCELLis system have demonstrated particular promise for scalable adherent cell culture, with documented success in processes capable of scaling up to 500L production volumes [79]. These systems maintain cells in a three-dimensional environment that better mimics physiological conditions while providing enhanced surface area for cell attachment and growth. Process parameter optimization—including seeding density, nutrient feeding strategies, and harvest timing—enables maximization of both cell biomass and exosome secretion rates.
Downstream Processing: Purification and Formulation Strategies
Primary Recovery and Clarification
The initial downstream processing steps focus on separating exosomes from cells and cellular debris in the conditioned media. A typical protocol begins with low-speed centrifugation (300-2,000 × g) to remove intact cells, followed by higher-speed centrifugation (10,000-30,000 × g) to eliminate apoptotic bodies and large vesicles [78] [57]. Subsequent microfiltration through 0.22 µm filters effectively removes remaining particulates while allowing exosomes to pass through into the filtrate [79].
Concentration and Purification
Tangential Flow Filtration has emerged as the industry standard for concentrating exosomes from large volumes of clarified conditioned media while maintaining their structural integrity. This method utilizes membranes with specific molecular weight cut-offs (typically 100-500 kDa) to retain exosomes while removing soluble proteins and small molecules [78] [79]. Following concentration, chromatographic purification strategies—particularly size exclusion chromatography—enable separation of exosomes from co-purifying proteins and nucleic acids based on hydrodynamic volume differences [79].
Ultracentrifugation, while historically the most common laboratory-scale purification method, presents significant limitations for large-scale GMP implementation due to limited scalability, potential for vesicle damage, and prolonged processing times. However, it may still be incorporated as a final polishing step in some processes [78]. The table below summarizes key purification methodologies and their performance characteristics:
Table 2: Downstream Purification Technologies for MSC-Derived Exosomes
| Method | Principle | Recovery Efficiency | Scalability | GMP Suitability |
|---|---|---|---|---|
| Ultracentrifugation | Density-based separation | Moderate (60-80%) | Limited | Moderate (with optimization) |
| Tangential Flow Filtration | Size-based separation | High (70-90%) | Excellent | Excellent |
| Size Exclusion Chromatography | Hydrodynamic volume separation | High (60-85%) | Good | Excellent |
| Precipitation | Solubility shift | Variable (40-95%) | Good | Moderate (additive removal concern) |
Formulation and Final Fill
The final processing steps involve diafiltration into an appropriate formulation buffer that ensures exosome stability during storage. Common formulation components include cryoprotectants (e.g., trehalose, sucrose) and buffers that maintain physiological pH and osmolarity [79]. A terminal 0.2 µm filtration step ensures sterility before aseptic filling into final containers, typically conducted under Grade A conditions to maintain product safety [78].
Analytical Characterization and Quality Control
Robust analytical characterization is fundamental to GMP manufacturing, providing critical quality attributes for identity, potency, purity, and safety. The following diagram illustrates a comprehensive quality control workflow for GMP-produced exosomes:
Diagram 1: Quality Control Workflow for GMP Exosomes
The analytical methods employed must comply with GMP principles of validation, accuracy, and precision. Nanoparticle Tracking Analysis provides quantitative data on particle size distribution and concentration, while transmission electron microscopy confirms characteristic exosome morphology [78] [57]. Identity testing includes detection of tetraspanin markers (CD9, CD63, CD81) via Western blot or flow cytometry, complemented by assessment of MSC-specific markers and absence of contaminants from parental cells [78] [79].
Safety testing encompasses standard sterility assays, mycoplasma testing, and endotoxin measurement to ensure the final product meets regulatory requirements for parenteral administration. Additionally, potency assays—particularly relevant for wound healing applications—may include in vitro assessments of angiogenesis (e.g., endothelial tube formation), fibroblast migration, or anti-inflammatory activity to demonstrate biological functionality [19] [33].
Process Integration and Technology Transfer
Successful technology transfer from development to GMP manufacturing requires careful planning and documentation. A typical integrated process follows this workflow:
Diagram 2: Integrated GMP Manufacturing Workflow
Strategic partnerships between academic institutions, technology providers, and contract development and manufacturing organizations have proven highly effective in accelerating process development and GMP implementation [80]. These collaborations leverage complementary expertise in stem cell biology, bioprocess engineering, and regulatory compliance to establish robust manufacturing platforms. For instance, the partnership between Waisman Biomanufacturing and RoosterBio exemplifies this integrated approach, combining optimized MSC bioprocess products with established GMP manufacturing capabilities to provide end-to-end solutions for exosome therapeutic development [80].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for MSC-Exosome Production and Characterization
| Reagent/Material | Function | Application Example | Reference |
|---|---|---|---|
| TrypLE Select Enzyme | Cell dissociation | Gentle detachment of adherent MSCs | [57] |
| Chemically Defined Media | Cell nutrition | Xeno-free expansion and production | [79] |
| Human Platelet Lysate | Media supplement | Serum alternative for MSC culture | [78] |
| Ultrafiltration Membranes | Concentration | Tangential flow filtration systems | [79] |
| Size Exclusion Columns | Purification | Chromatographic separation of exosomes | [78] |
| Antibody Panels | Characterization | Flow cytometry (CD9, CD63, CD81) | [57] |
The successful scale-up of GMP manufacturing processes for MSC-derived exosomes represents a critical enabler for translating promising preclinical results in wound healing into clinically viable therapeutics. Through implementation of scalable bioreactor platforms, robust purification methodologies, and comprehensive quality control systems, researchers and manufacturers can overcome the historical challenges associated with exosome production. As these technologies continue to evolve, they will undoubtedly accelerate the development of innovative exosome-based treatments for chronic wounds and other applications in regenerative medicine, ultimately fulfilling the potential of these remarkable biological nanoparticles as next-generation therapeutics.
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a promising cell-free paradigm for advancing wound healing treatments. These nanoscale extracellular vesicles facilitate tissue repair through their cargo of proteins, mRNAs, and miRNAs, which modulate inflammation, promote angiogenesis, and stimulate cellular proliferation [81] [71]. However, the translational potential of MSC-Exos is constrained by significant pharmacokinetic challenges: rapid systemic clearance, limited retention at the target site, and undefined dosing parameters [82] [83]. Achieving therapeutic efficacy requires sophisticated strategies to overcome these biological barriers, ensuring that sufficient exosome concentrations are maintained within the wound microenvironment for clinically relevant durations. This review examines current advancements in optimizing the biodistribution, dosing, and wound site retention of MSC-Exos, providing a technical framework for researchers and drug development professionals working in wound healing applications.
Biodistribution and Clearance Dynamics
The biodistribution profile of MSC-Exos is critically influenced by the route of administration, which directly dictates their absorption, distribution, metabolism, and elimination (ADME) characteristics [82]. Following intravenous administration, MSC-Exos typically exhibit rapid clearance from circulation, often within hours, primarily through uptake by mononuclear phagocytic system cells in the liver and spleen [82]. This rapid elimination necessitates consideration of prolonged dosing regimens involving multiple administrations to maintain therapeutic levels.
Route-Specific Distribution Patterns: Preclinical studies most commonly utilize intravenous injection, direct site-specific injection, or subcutaneous administration [82]. Local injection around wound sites offers the advantage of direct delivery, potentially enhancing local concentration and reducing systemic exposure. However, even with local administration, exosomes may undergo rapid diffusion away from the wound site or be cleared from the tissue, limiting their therapeutic window [83]. A recent innovation to address this challenge involves the use of hyaluronic acid-based injectable hydrogel systems that create a reservoir for sustained local release, significantly improving retention at the wound site [19].
Dosing Strategies and Quantification Methods
Establishing standardized dosing protocols for MSC-Exos remains challenging due to variability in quantification methods and reporting units across studies. Doses have been reported using multiple metrics: particle number, protein content, or the equivalent cell number used for production [82].
Current Dosing Range in Clinical Applications
Table 1: MSC-Exo Dosing in Clinical Trials and Preclinical Studies
| Indication | Administration Route | Doses per Regimen | Dose Interval | Dose (Particle Number) | Dose (Protein Content) |
|---|---|---|---|---|---|
| Alzheimer's Disease [82] | Nasal Drip | 24 | Twice weekly | 1-4 × 10^9 | 5-20 µg |
| ARDS [82] | Intravenous | 1 | N/A | 8 × 10^11 | N/A |
| ARDS [82] | Inhalation | 7 | Daily | 0.2-1.6 × 10^9 | N/A |
| cGVHD [82] | Eye Drop | 56 | 4x daily over 14 days | 2 × 10^10 | 10 µg |
| Chronic Kidney Disease [82] | Intravenous | 2 | Weekly | 1.3 × 10^13 | 6.6 mg |
| General Safety [82] | Inhalation | 1 | N/A | 0.2-1.6 × 10^9 | N/A |
| Preclinical Rodent Studies [82] | Various | Varies | Varies | ~1.4 × 10^10 (average) | 70 µg (average) |
Unit Conversion and Working Range
Consensus is emerging around a "working range" for human MSC-Exo dosing. Based on analysis of preclinical and clinical data, a reasonable total dose ranges from 1 × 10^10 to 6 × 10^12 particles [82]. This range is derived from several key considerations. Preclinical rodent studies typically use approximately 1.4 × 10^10 particles per dose, establishing a likely minimum for human applications. The upper limit is informed by the estimated 6 × 10^12 endogenous vesicles naturally present in human circulation, providing a physiological reference point [82].
Conversion between quantification methods remains challenging but essential for cross-study comparisons. A commonly used approximation suggests that 1 µg of exosome protein equates to approximately 2 × 10^9 particles [82]. However, this ratio can vary based on exosome isolation methods and cellular source, highlighting the need for comprehensive characterization according to MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [82].
Advanced Formulation Strategies for Enhanced Retention
Hydrogel-Based Delivery Systems
A promising approach to improve wound site retention involves incorporating MSC-Exos into biomaterial scaffolds. Recent research has demonstrated that hyaluronic acid-based injectable hydrogels can effectively encapsulate exosomes and create a sustained-release system at the wound site [19]. These hydrogel systems exhibit excellent cytocompatibility, biodegradability, and skin-like rheology properties, making them ideal for wound healing applications [19]. The porous structure of the hydrogel allows for in situ retention of exosomes while permitting controlled release and interaction with surrounding tissues.
Table 2: Research Reagent Solutions for Exosome Delivery Systems
| Reagent/Material | Function | Application Example |
|---|---|---|
| Hyaluronic Acid (HA) | Base polymer for injectable hydrogel formation | Creates biodegradable scaffold with skin-like rheology [19] |
| MSC-Derived Exosomes | Active therapeutic cargo | Promotes angiogenesis, collagen synthesis, and immunomodulation [71] |
| Conditioned Medium | Source of MSC-Exos | Collected from MSC cultures after 48-72 hours [22] |
| Differential Centrifugation | Exosome isolation method | Sequential centrifugation at 300 × g, 2000 × g, then 100,000 × g [22] |
| Nanoparticle Tracking Analysis (NTA) | Particle quantification | Measures exosome concentration and size distribution [82] |
| Bradford Assay | Protein quantification | Alternative method for estimating exosome dose [82] |
In vivo studies confirm that MSC-Exo-loaded hydrogels significantly accelerate wound closure, enhance angiogenesis, and promote re-epithelialization compared to free exosomes [19]. The hydrogel system maintains exosomes within the wound bed, facilitating sustained paracrine signaling that modulates the inflammatory response and supports tissue regeneration throughout the healing process.
Bioengineering Strategies for Improved Targeting
Beyond simple encapsulation, advanced bioengineering approaches are being developed to enhance the targeting capabilities of MSC-Exos. These include genetic engineering of parent MSCs to express specific surface ligands, direct modification of exosome membranes, and creation of hybrid exosomes combining MSC-Exos with synthetic materials [83]. These strategies aim to improve the binding affinity of exosomes for specific cell types in the wound environment, such as endothelial cells, fibroblasts, or immune cells, thereby increasing their local retention and cellular uptake efficiency.
Experimental Protocols for Pharmacokinetic Assessment
Protocol: Evaluating Wound Retention Using Hydrogel Delivery
Objective: Assess the retention and therapeutic efficacy of MSC-Exos delivered via hyaluronic acid hydrogel in a diabetic wound model.
Materials:
- MSC-Exos isolated from human iPSC-MSCs (characterized by NTA and western blot)
- Hyaluronic acid hydrogel solution (sterile, injectable)
- Diabetic rodent wound model
- Imaging system for tracking labeled exosomes
Methodology:
- Exosome Isolation and Labeling: Isolate MSC-Exos from conditioned medium using differential centrifugation [22]. Label with near-infrared fluorescent dye for tracking.
- Hydrogel Preparation: Mix MSC-Exos (≥1 × 10^10 particles) with HA hydrogel precursor under sterile conditions.
- Wound Application: After creating full-thickness excisional wounds, inject the MSC-Exo-hydrogel composite subcutaneously around the wound margins [19].
- Retention Assessment: Use fluorescence imaging at 0, 6, 12, 24, 48, and 72 hours post-application to quantify signal intensity remaining at the wound site.
- Efficacy Endpoints: Measure wound closure rate daily, assess histology for re-epithelialization and angiogenesis at day 7 and 14, and analyze collagen deposition using Masson's trichrome staining [19] [22].
Protocol: Dose-Response Relationship Establishment
Objective: Determine the optimal MSC-Exo dose for maximal wound healing response.
Materials:
- MSC-Exos quantified by both NTA and protein assay
- Animal wound model (n=6-8 per group)
- Materials for molecular analysis (qPCR, ELISA)
Methodology:
- Dose Preparation: Prepare MSC-Exo suspensions at four concentrations: 1 × 10^9, 5 × 10^9, 1 × 10^10, and 5 × 10^10 particles in saline.
- Administration: Administer exosomes via local perimeter injection immediately after wound creation and every 48 hours thereafter.
- Assessment: Monitor wound closure kinetics daily. At day 10, harvest tissue for analysis of angiogenesis (CD31 immunohistochemistry), collagen maturity (picrosirius red), and cytokine expression (qPCR for VEGF, TGF-β, IL-10) [71] [22].
- Statistical Analysis: Use non-linear regression to model the dose-response relationship and identify the EC50 for each parameter.
Visualization of Key Concepts
Diagram 1: Pharmacokinetic Optimization Workflow for MSC-Exo Wound Therapy. This flowchart outlines the critical stages in developing effective MSC-Exo-based wound treatments, highlighting key decision points and their impact on therapeutic outcomes.
Diagram 2: Molecular Mechanisms of MSC-Exos in Wound Healing. This diagram illustrates the key signaling pathways through which MSC-Exos exert their therapeutic effects following successful delivery and retention at the wound site.
Optimizing the pharmacokinetic profile of MSC-derived exosomes is paramount for realizing their full therapeutic potential in wound healing applications. The integration of advanced delivery systems, particularly hydrogels that provide sustained local release, represents a significant advancement in overcoming the limitation of rapid clearance. Simultaneously, standardized dosing protocols and comprehensive characterization are essential for translating preclinical findings into clinically viable treatments. Future research directions should focus on developing more sophisticated engineering approaches to enhance target specificity, establishing clinically relevant pharmacokinetic-pharmacodynamic models, and validating these optimization strategies in large animal models and human trials. As these advancements mature, MSC-Exo-based therapies are poised to become a transformative modality in the management of complex wounds.
The transition of mesenchymal stem cell-derived exosomes (MSC-Exos) from laboratory research to clinical applications in wound healing necessitates rigorous safety evaluation. As cell-free therapeutics, MSC-Exos present distinct safety considerations compared to their parent cells. This whitepaper provides a comprehensive technical framework for assessing the immunogenicity, tumorigenicity, and long-term toxicity profiles of MSC-Exos within the context of wound healing research. We synthesize current methodologies, experimental protocols, and safety data, highlighting the inherent advantages of these nanovesicles while addressing persistent challenges. By establishing standardized assessment paradigms, this guide aims to support researchers and drug development professionals in advancing safe, effective MSC-Exo-based therapies for cutaneous wound repair.
The therapeutic application of mesenchymal stem cell-derived exosomes represents a paradigm shift in regenerative medicine, particularly for complex wound healing. As the field moves toward clinical translation, comprehensive safety profiling becomes paramount for regulatory approval and clinical adoption [81]. MSC-Exos offer distinct safety advantages over whole-cell therapies, including reduced immunogenicity, absent tumorigenic risk from replication, and eliminated risk of pulmonary embolism associated with cell administration [42]. However, their nanoscale properties, complex cargo, and potential for bioengineering modifications necessitate specialized safety assessment frameworks.
This technical review examines the tripartite safety evaluation of MSC-Exos, with specific focus on implications for wound healing applications. We integrate current evidence, standardized experimental protocols, and emerging safety considerations to provide a structured approach for researchers developing MSC-Exo-based wound therapies.
Immunogenicity Profile of MSC-Derived Exosomes
Innate Immunogenicity Advantages
MSC-Exos exhibit inherently low immunogenicity, a characteristic inherited from their parent cells. Mesenchymal stem cells demonstrate low immunogenic potential due to reduced MHC-I expression and absence of MHC-II antigens under normal conditions [84]. This profile is largely retained by their secreted exosomes, making them promising cell-free therapeutics with minimal risk of immune rejection [85].
The nanoparticle characteristics of exosomes further contribute to their favorable immune profile. Their small size (30-150 nm) and endogenous lipid bilayer minimize recognition by pattern recognition receptors, reducing innate immune activation [42]. Additionally, MSC-Exos lack nuclei and cannot replicate, eliminating risks associated with cellular division and differentiation [71].
Immunomodulatory Mechanisms in Wound Healing
In the wound microenvironment, MSC-Exos demonstrate active immunomodulation rather than mere immune evasion. They participate in balancing inflammatory responses, which is crucial for transitioning chronic wounds from the inflammatory to proliferative phase [86]. The mechanisms include:
- Macrophage polarization: MSC-Exos promote the shift from pro-inflammatory M1 to anti-inflammatory M2 phenotypes, reducing excessive inflammation while promoting tissue repair [85].
- T-cell regulation: They inhibit pro-inflammatory T-helper 1 and 17 cell differentiation while promoting regulatory T-cell expansion [85].
- B-cell suppression: MSC-Exos impede B-cell proliferation, differentiation, and antibody production through transfer of TGF-β, PEG2, and IL1RA [85].
Table 1: Quantitative Effects of MSC-Exos on Immune Cell Populations in Preclinical Studies
| Immune Cell Type | Observed Effect | Magnitude of Effect | Experimental Model |
|---|---|---|---|
| B-cells | Inhibition of proliferation | 29.4% to 14% [85] | In vitro co-culture |
| B-cells | Inhibition of differentiation | 59.3% to 45.7% [85] | In vitro co-culture |
| Macrophages | Polarization to M2 phenotype | Significant increase [85] | Mouse inflammation models |
| T-cells | Suppression of activation | Dose-dependent inhibition [85] | Lymphocyte proliferation assays |
Experimental Assessment Protocols
In Vitro Immunogenicity Testing
Protocol: Immune Cell Activation Assay
- Isolate peripheral blood mononuclear cells (PBMCs) from human donors
- Co-culture PBMCs with MSC-Exos at varying concentrations (e.g., 10-100 μg/mL)
- Measure T-cell activation markers (CD69, CD25) via flow cytometry at 24, 48, and 72 hours
- Quantify cytokine secretion (IFN-γ, TNF-α, IL-2, IL-10) using ELISA or multiplex assays
- Compare responses to positive controls (e.g., phytohemagglutinin) and negative controls (media alone)
Protocol: Mixed Lymphocyte Reaction (MLR)
- Isolate PBMCs from two or more unrelated donors
- Label cells from one donor with CFSE dye
- Co-culture with irradiated stimulator cells from other donors ± MSC-Exos
- Analyze T-cell proliferation via CFSE dilution by flow cytometry after 5-7 days
- Include controls for allogeneic response and baseline proliferation
In Vivo Immunogenicity Assessment
Protocol: Repeat Administration Model
- Administer MSC-Exos via wound-relevant routes (topical, intradermal, subcutaneous)
- Utilize immunocompetent animal models (e.g., C57BL/6 mice)
- Implement biweekly administrations for 4-8 weeks
- Monitor for local and systemic immune responses
- Assess antibody production against exosomal proteins
- Evaluate histopathological changes at administration sites
Figure 1: Immunogenicity Assessment Workflow for MSC-Derived Exosomes
Tumorigenicity Assessment
Theoretical Safety Advantages
MSC-Exos demonstrate significantly reduced tumorigenic risk compared to whole cell therapies because they cannot replicate [42]. This fundamental difference eliminates concerns regarding uncontrolled cellular proliferation and teratoma formation associated with certain stem cell populations. The absence of nuclear material in properly isolated exosomes further minimizes theoretical risks of tumor initiation through genetic transfer [10].
However, nuanced considerations remain regarding their biodistribution patterns and potential to influence pre-existing malignant microenvironments. Studies note that exosome content can be altered when MSCs are cultured with tumor cells or in tumor microenvironments [81]. This highlights the importance of careful production controls and thorough tumorigenicity screening.
Experimental Assessment Frameworks
In Vitro Transformation Assays
Protocol: Cell Transformation Analysis
- Utilize immortalized but non-tumorigenic cell lines (e.g., NIH/3T3, HEK293)
- Treat with MSC-Exos at concentrations exceeding therapeutic levels (e.g., 100-500 μg/mL)
- Monitor for acquisition of transformation characteristics:
- Anchorage-independent growth in soft agar
- Loss of contact inhibition
- Morphological changes
- Increased proliferation rates
- Maintain cultures for 4-8 weeks with regular exosome supplementation
- Include positive controls (known oncogenes) and negative controls (vehicle alone)
Protocol: Gene Expression Profiling
- Extract RNA from exosome-treated cells
- Perform RNA sequencing or targeted PCR arrays for oncogenes/tumor suppressors
- Focus on pathways commonly dysregulated in cancer:
- p53 signaling
- Ras-MAPK pathway
- Myc network
- Cell cycle regulators
- Compare expression profiles to untreated controls
In Vivo Tumorigenicity Models
Protocol: Long-Term Tumor Formation Assay
- Utilize immunodeficient models (e.g., NOD/SCID mice) for sensitive detection
- Administer high doses of MSC-Exos via relevant routes (e.g., topical, systemic)
- Include positive control group (tumorigenic cells)
- Monitor for 6-12 months for:
- Local tumor formation at administration sites
- Distant tumor development
- Weight loss and other morbidity signs
- Conduct complete necropsy with histopathological analysis of major organs
Protocol: Tumor Promotion Study
- Employ models with pre-neoplastic lesions or genetically predisposed backgrounds
- Assess whether MSC-Exos accelerate tumor development or progression
- Evaluate effects on established tumors in oncological models
- Measure tumor incidence, latency, volume, and metastasis
Table 2: Tumorigenicity Assessment Parameters for MSC-Derived Exosomes
| Assessment Tier | Key Parameters | Acceptance Criteria | Recommended Duration |
|---|---|---|---|
| In Vitro | Anchorage-independent growth | No colony formation in soft agar | 4-8 weeks |
| Oncogene expression | No significant upregulation of major oncogenes | 48-72 hours | |
| Genomic stability | No chromosomal abnormalities | Multiple passages | |
| In Vivo | Local tumor formation | No nodules or masses at administration sites | 6-12 months |
| Distant tumor development | No evidence of systemic neoplasia | 6-12 months | |
| Tumor promotion | No acceleration of pre-neoplastic progression | Model-dependent |
Long-Term Toxicity Evaluation
Biodistribution and Accumulation Profiles
Understanding the long-term fate of administered MSC-Exos is crucial for comprehensive toxicity assessment. Current evidence suggests exosomes exhibit inherent hepatic tropism following systemic administration, with secondary distribution to spleen and kidneys [17]. Their nanoscale size enables biological barrier penetration, including the blood-brain barrier, raising important considerations for off-target effects [42].
For wound healing applications, local administration minimizes systemic exposure but necessitates evaluation of local retention and clearance kinetics. Studies incorporating NIR-II probes enable real-time in vivo tracking, providing critical pharmacokinetic data [17].
Comprehensive Toxicity Assessment Protocol
Protocol: Repeated Dose Toxicity Study
- Utilize two animal species (typically rodent and non-rodent)
- Administer MSC-Exos at three dose levels (low, anticipated therapeutic, high)
- Include recovery groups to assess reversibility of findings
- Duration: 14-28 days for short-term, up to 6 months for chronic toxicity
Assessment Endpoints:
- Clinical observations: Daily monitoring for signs of toxicity
- Body weight and food consumption: Weekly measurements
- Clinical pathology:
- Hematology (complete blood count, differential)
- Clinical chemistry (liver enzymes, renal parameters, electrolytes)
- Urinalysis
- Histopathology: Comprehensive tissue collection from all major organs
- Organ weights: Brain, liver, kidneys, spleen, heart
Specific Considerations for Wound Healing Applications
Local Toxicity Assessment:
- Evaluate effects on normal wound healing processes
- Assess potential for excessive fibrosis or scarring
- Monitor for aberrant angiogenesis
- Document effects on re-epithelialization
Off-Target Effects:
- Evaluate systemic exposure following topical administration
- Assess potential for immune system modulation beyond wound site
- Monitor for endocrine disruption
- Document neurological effects if systemic exposure occurs
Figure 2: Quality Control Cascade for MSC-Exosome Safety Profiling
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MSC-Exosome Safety Evaluation
| Reagent Category | Specific Examples | Research Application | Safety Relevance |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kits, Polymer-based precipitation reagents | Rapid exosome purification from conditioned media | Impacts purity, removes contaminating proteins |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, Calnexin | Confirm exosomal identity via western blot, flow cytometry | Verifies proper vesicle isolation, absence of cellular contaminants |
| Nanoparticle Tracking | NanoSight NS300, ZetaView systems | Size distribution and concentration analysis | Ensures proper vesicle size, detects aggregates |
| Endotoxin Detection | Limulus Amebocyte Lysate (LAL) assays | Quantify endotoxin contamination | Prevents pyrogenic responses in vivo |
| Viability Assays | MTT, Alamar Blue, ATP-based assays | Assess effects on cell viability | screens for acute cytotoxicity |
| Genomic Stability Assays | Comet assays, γH2AX staining, Karyotyping | Detect DNA damage and chromosomal abnormalities | Evaluates genotoxic potential |
| Cytokine Arrays | Multiplex cytokine/chemokine panels | Comprehensive immune profiling | Assesses immunomodulatory potency and potential for cytokine storms |
The comprehensive safety evaluation of MSC-derived exosomes for wound healing applications requires a multifaceted approach addressing immunogenicity, tumorigenicity, and long-term toxicity. Current evidence indicates a favorable safety profile for MSC-Exos, characterized by low immunogenicity, absent tumorigenic potential, and manageable toxicity risks. However, standardized assessment protocols and rigorous quality control throughout production remain essential as the field advances toward clinical translation.
Future directions should focus on establishing consensus guidelines for safety testing, developing improved tracking methodologies for long-term fate studies, and creating standardized panels for immunogenicity assessment. By addressing these challenges, researchers can fully leverage the therapeutic potential of MSC-Exos while ensuring the highest safety standards for patients suffering from complex wounds.
Regulatory Pathways and the Path to Clinical Approval for Exosome-Based Biologics
The transition of mesenchymal stem cell-derived exosomes (MSC-Exos) from promising wound healing agents to clinically approved biologics represents a critical challenge in regenerative medicine. This whitepaper provides a comprehensive analysis of the current global regulatory frameworks, manufacturing requirements, and preclinical development strategies essential for navigating clinical approval pathways. With no exosome products currently approved by the U.S. Food and Drug Administration and evolving international standards, developers must address unique challenges in characterization, quality control, and demonstration of efficacy. By integrating technical requirements with the specific context of wound healing applications, this guide serves as an essential resource for researchers and drug development professionals advancing exosome-based therapies toward clinical translation.
Exosome-based biologics represent a paradigm shift in therapeutic development, particularly for complex wound healing applications where MSC-Exos demonstrate significant promise in promoting angiogenesis, collagen synthesis, and immunomodulation [24] [71]. The global regulatory environment for these innovative products remains complex and fragmented, with no universally adopted technical guidelines specifically for exosome therapeutics [70] [87]. Regulatory agencies generally classify exosome products as biological medicinal products, subjecting them to premarket review and approval requirements similar to other biologics [70] [88]. This classification necessitates rigorous characterization, quality control, and demonstration of safety and efficacy through well-designed clinical trials.
The absence of specific regulatory guidelines for exosome products has created significant challenges for developers. In the United States, the FDA has issued public safety notifications clarifying that exosomes used to treat diseases in humans are regulated as drugs and biological products and must comply with premarket review and approval requirements [70] [89]. Similar approaches are emerging in Europe, Japan, and other regions, where exosomes are typically evaluated within existing frameworks for advanced therapy medicinal products or biologics [88]. The regulatory review of exosomes primarily follows two strategic approaches: one focused on elucidating constituent components within exosomes, and the other examining their physiological effects and mechanisms of action [70].
Global Regulatory Frameworks: A Comparative Analysis
Regional Regulatory Approaches
The regulatory landscape for exosome-based biologics varies significantly across major jurisdictions, reflecting different historical precedents, risk classifications, and technical requirements. Understanding these regional differences is essential for global development strategies and regulatory planning.
Table 1: Comparative Analysis of Regional Regulatory Frameworks for Exosome-Based Biologics
| Region/ Agency | Regulatory Classification | Key Emphasis Areas | Current Status | Notable Considerations |
|---|---|---|---|---|
| U.S. (FDA) | Biological medicinal products [70] | Molecular composition, structure, pharmacokinetics, therapeutic efficacy [70] | No approved exosome products; multiple clinical trials underway [89] | Requires premarket review and approval; has issued consumer safety notices about unapproved products [89] |
| Europe (EMEA) | Advanced therapy medicinal products (ATMPs) risk-based framework [88] | Quality management systems, robust validation protocols [70] | Evolving framework with emphasis on risk-based classification [88] | PIC/S GMP guidelines provide detailed requirements for organizational structures and training [70] |
| Japan (PMDA) | Biological products [88] | Manufacturing consistency, quality control | Actively developing regulatory approaches [88] | Alignment with international standards while addressing local requirements |
| South Korea (MFDS) | Innovative biologics [88] | Nonclinical evaluation, manufacturing controls | Growing clinical trial activity [90] | Emphasis on technological innovation with regulatory oversight |
Current Clinical Trial Landscape
The clinical development of exosome-based therapies is expanding rapidly, with over 301 clinical trials registered globally [89]. The temporal and spatial distribution of these trials generally mirrors publication trends, with significant concentrations in the United States, China, and European countries [90]. This growth reflects increasing interest in exosome therapeutics despite the regulatory challenges.
Multiple companies have advanced into clinical development phases, with several achieving important regulatory milestones. Aegle Therapeutics received FDA clearance for its Investigational New Drug (IND) application to initiate clinical trials for burn treatment using extracellular vesicles isolated from bone marrow-derived MSCs [89]. Similarly, Brexogen gained FDA approval to initiate a Phase 1 clinical trial of 'BRE-AD01,' an exosome-based therapy for atopic dermatitis, marking the first exosome trial for this indication and the first U.S. trial by a Korean company [89]. Other notable companies advancing in clinical development include Direct Biologics, Rion, and Kimera Labs, with active Phase I/II clinical trials for conditions ranging from diabetic foot ulcers to respiratory failure from COVID-19 [88].
Manufacturing and Quality Control Requirements
Current Good Manufacturing Practice (cGMP) Considerations
The manufacturing of exosome-based biologics requires adherence to cGMP standards, though specific regulatory guidance for exosomes remains under development [70] [87]. The inherent complexity and heterogeneity of exosomes present unique challenges for manufacturing standardization and quality control. Differences in GMP-based quality systems adopted by various countries have led to regulatory disparities, with the Pharmaceutical Inspection Convention and Current Good Manufacturing Practices (PIC/S GMP) providing more detailed requirements for organizational structures, responsibilities, and training programs compared to the focus on final product quality control in cGMP [70].
Manufacturing processes must address several critical factors that impact product quality and consistency:
- Source Material Considerations: The tissue source of parent MSCs (adipose, bone marrow, umbilical cord) significantly influences exosome efficacy and characteristics [70] [87].
- Culture Conditions: Variations in cell passage number, culture method, culture medium composition, and supplements can result in different exosome products even when originating from the same parent cell type [70].
- Production Scale Challenges: Large-scale GMP-grade manufacturing is extremely complex, with minor changes during cultivation potentially altering biological characteristics [70].
Analytical Characterization and Quality Control
Robust analytical characterization is essential for demonstrating product consistency, potency, and safety. The table below outlines key quality control parameters and methods for exosome-based biologics.
Table 2: Essential Quality Control Parameters for Exosome-Based Biologics
| Quality Attribute | Standard Analytical Methods | Key Challenges | Emerging Approaches |
|---|---|---|---|
| Identity/ Composition | Western blot (CD63, CD81, TSG101, Alix) [88] [87] | Heterogeneity of exosome populations | Single-vesicle analysis, multi-parameter characterization |
| Purity/ Impurities | Protein content (BCA), residual host cell DNA | Distinguishing exosomes from similar-sized particles | Orthogonal method combination |
| Quantity | Nanoparticle tracking analysis, tunable resistive pulse sensing | Method-dependent variability in particle concentration | Standardized reference materials |
| Potency | Cell-based assays, in vivo models [87] | Defining mechanism of action and relevant biomarkers | Pathway-specific reporter systems |
| Stability | Size distribution, particle concentration, functionality assessment after storage | Preservation of structural integrity and biological activity | Lyophilization, cryopreservation optimization |
The measurement of critical quality attributes presents significant methodological challenges. For instance, different analytical methods can yield significantly varying results for particle size and concentration measurements, highlighting the need for standardized approaches and orthogonal method combinations [70]. Similarly, demonstrating batch-to-batch consistency requires assessment against previously manufactured products using biochemical, biophysical, and functional assays [70].
Preclinical Development Considerations for Wound Healing Applications
Mechanism of Action Studies for Wound Healing
For MSC-Exos targeting wound healing applications, elucidating the mechanism of action is particularly critical for regulatory approval. MSC-Exos facilitate cutaneous wound healing through multiple coordinated processes including promoting collagen synthesis, angiogenesis, and immunomodulation [71] [22]. The diagram below illustrates the key signaling pathways through which MSC-Exos promote wound healing.
MSC-Exos demonstrate efficacy in diabetic foot ulcer models through multiple mechanisms, including immunomodulation, antioxidant effects, angiogenesis promotion, endothelial cell migration and proliferation, and collagen remodeling [71]. The therapeutic effects are mediated primarily through the transfer of bioactive molecules contained within exosomes, including proteins, mRNAs, microRNAs, and other non-coding RNAs [24] [87].
Essential Research Reagents and Experimental Systems
The development of exosome-based wound healing therapies requires specialized research reagents and experimental systems to evaluate efficacy, mechanism of action, and safety.
Table 3: Essential Research Reagent Solutions for Exosome Wound Healing Research
| Reagent/System Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Exosome Isolation Kits | Commercial purification kits, PEG-based precipitation | Isolation of exosomes from conditioned media | Rapid, standardized exosome isolation with minimal equipment requirements |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, Alix, Calnexin | Exosome characterization via Western blot, flow cytometry | Confirmation of exosome identity and assessment of specific markers |
| Cell Culture Models | Human dermal fibroblasts (HDFs), human umbilical vein endothelial cells (HUVECs) | In vitro assessment of exosome effects | Evaluation of proliferation, migration, collagen secretion, and tube formation |
| Animal Wound Models | Rat diabetic wound healing models, mouse excision models | In vivo efficacy assessment | Measurement of wound closure rates, re-epithelialization, collagen maturity, angiogenesis |
| Analytical Instruments | Nanoparticle tracking analyzer, electron microscope, flow cytometer | Physical characterization | Determination of particle size, concentration, and morphology |
Experimental Workflow for Wound Healing Applications
A comprehensive preclinical development program for MSC-Exos in wound healing should include in vitro and in vivo assessments aligned with the proposed mechanism of action. The following diagram illustrates a robust experimental workflow for evaluating the therapeutic potential of MSC-Exos in wound healing.
Detailed experimental protocols should include standardized methods for exosome isolation and characterization, such as sequential centrifugation approaches (300 × g for 10 minutes followed by 2000 × g for 10 minutes) to remove cells and debris [22]. Functional assays should evaluate dose-dependent effects on fibroblast proliferation, migration, collagen secretion, and endothelial tube formation, as these parameters directly correlate with wound healing efficacy [22]. Animal studies should employ appropriate wound models with detailed assessment of re-epithelialization, scar formation, collagen maturity, and angiogenesis through both histological and immunofluorescence methods [71] [22].
Clinical Development and Regulatory Strategy
Navigating the Approval Pathway
The path to clinical approval for exosome-based biologics requires careful planning and engagement with regulatory agencies throughout the development process. The following diagram outlines the key stages in the clinical development and regulatory approval pathway for exosome-based biologics.
Successful navigation of the regulatory pathway requires early and ongoing communication with regulatory agencies. Pre-IND meetings provide valuable opportunities to obtain feedback on manufacturing strategies, preclinical study designs, and proposed clinical trials [70] [87]. As development progresses, end-of-phase 2 and pre-BLA meetings help ensure alignment on Phase 3 trial designs and the completeness of marketing application packages.
Clinical Trial Design Considerations for Wound Healing
Designing clinical trials for exosome-based wound healing products requires careful consideration of several unique factors:
- Patient Population Selection: For diabetic foot ulcer trials, appropriate patient stratification based on ulcer characteristics (size, duration, vascular status) and standardization of conventional care are essential [71].
- Endpoint Selection: Regulatory-acceptable endpoints may include complete wound closure, time to closure, or percentage area reduction, with appropriate follow-up periods to assess durability of effect [71].
- Delivery Optimization: Preclinical and early clinical studies should establish optimal delivery methods (topical, localized injection), dosing frequency, and treatment duration [24].
- Safety Monitoring: Comprehensive safety evaluation should include assessment of systemic exposure, immunogenicity, and potential off-target effects, particularly for allogeneic exosome products [87].
The path to clinical approval for exosome-based biologics requires a strategic approach that addresses both technical and regulatory challenges. Key considerations for successful development include:
- Early Regulatory Engagement: Proactive communication with regulatory agencies through pre-IND and other milestone meetings is essential for aligning on development strategies and requirements.
- Robust Manufacturing and Characterization: Implementing well-controlled manufacturing processes and comprehensive analytical characterization from early development stages facilitates smoother regulatory review.
- Mechanism-Based Efficacy Demonstration: For wound healing applications, establishing clear relationships between exosome characteristics, mechanism of action, and therapeutic effects strengthens regulatory submissions.
- Global Development Strategy: Considering regional regulatory differences during development planning enables more efficient global registration and market access.
As the field continues to evolve, ongoing collaboration between industry, regulators, and academic researchers will be essential for developing appropriate standards and guidance specific to exosome-based biologics. With careful attention to regulatory requirements and strategic development planning, MSC-derived exosomes hold significant promise for advancing wound healing treatments and addressing unmet medical needs in this challenging clinical area.
Evidence and Efficacy: Preclinical Models, Clinical Trials, and Comparative Advantage Analysis
The therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-Exos) has emerged as a promising cell-free strategy for enhancing wound healing, particularly in complex and impaired wound environments. As natural nanoscale vesicles (30-150 nm) carrying bioactive cargo including proteins, lipids, and nucleic acids, MSC-Exos mediate intercellular communication and mirror many therapeutic effects of their parent cells [91]. Within the context of a broader thesis on the role of MSC-derived exosomes in wound healing research, this review provides a comprehensive technical assessment of their preclinical efficacy across three clinically challenging wound models: diabetic, burn, and infectious wounds. The compelling advantages of MSC-Exos over whole-cell therapies—including lower immunogenicity, reduced risk of tumorigenicity, superior biodistribution, and easier storage—position them as innovative biologics for regenerative medicine [92] [91] [1]. This whitepaper synthesizes current preclinical data, delineates underlying molecular mechanisms, and standardizes experimental methodologies to guide researchers and drug development professionals in advancing this promising therapeutic approach from bench to bedside.
Mechanisms of Action of MSC-Exos in Wound Healing
MSC-Exos accelerate wound repair through coordinated modulation of multiple pathological processes and cellular functions. Their efficacy stems from the delivery of a complex cargo of growth factors, cytokines, and genetic material to recipient cells in the wound microenvironment [91].
Immunomodulation and Inflammation Control: MSC-Exos polarize macrophages toward the anti-inflammatory M2 phenotype and suppress pro-inflammatory M1 macrophages by transferring regulatory miRNAs such as miR-21, miR-146a, and miR-181c. This shift resolves chronic inflammation, a key barrier to healing in diabetic and other chronic wounds [91] [93]. In infectious wound models, MSC-Exos have been shown to inhibit the NLRP3 inflammasome, suppressing Caspase-1-mediated pyroptosis and the subsequent release of IL-1β and IL-18 [94].
Angiogenesis Promotion: MSC-Exos are rich in pro-angiogenic factors (e.g., VEGF, FGF-2, HGF) and miRNAs (e.g., miR-125a, miR-126-3p) that activate signaling pathways such as AKT/HIF-1α and Wnt/β-catenin in endothelial cells. This stimulates proliferation, migration, and new blood vessel formation, critically addressing ischemia in diabetic wounds [33] [71].
Cell Proliferation and Migration: Exosomes derived from various MSC sources (e.g., adipose tissue, bone marrow, umbilical cord) significantly enhance the proliferation and migration of keratinocytes and fibroblasts, crucial for re-epithelialization and wound closure. This is mediated through the activation of ERK/MAPK, AKT, and Wnt/β-catenin signaling pathways [33] [91].
Extracellular Matrix (ECM) Remodeling: MSC-Exos regulate collagen synthesis and degradation by modulating fibroblast activity and the expression of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs). This promotes balanced ECM deposition and prevents excessive scar formation [33] [9] [93].
Table 1: Key Molecular Cargos in MSC-Exos and Their Functions in Wound Healing
| Molecular Cargo | Function in Wound Healing | Target/Pathway |
|---|---|---|
| miR-21-5p | Promotes angiogenesis, fibroblast migration, and re-epithelialization | STAT3, PTEN, PI3K/AKT [33] [9] |
| miR-126-3p | Enhances angiogenesis | Inhibits PIK3R2 [33] |
| miR-125a | Promotes endothelial cell function and angiogenesis | Inhibits PTEN [33] |
| miR-146a | Modulates inflammation | Targets inflammatory genes [91] |
| TSG-6 | Anti-inflammatory protein, inhibits pyroptosis | NLRP3/Caspase-1/GSDMD axis [94] |
| VEGF, FGF-2, HGF | Stimulate angiogenesis and cell proliferation | Endothelial cell receptors [91] |
Preclinical Efficacy in Specific Wound Models
Diabetic Wound Models
Diabetic foot ulcers (DFUs) are characterized by impaired healing due to persistent inflammation, vascular insufficiency, and cellular dysfunction. MSC-Exos have demonstrated significant efficacy in preclinical models of diabetic wounds [95] [71].
In a full-thickness skin defect model in diabetic rats, adipose-derived MSC exosomes (ADSC-Exos) enhanced the wound healing rate, promoted collagen deposition, and stimulated angiogenesis. The mechanism was linked to the exosomal transfer of miR-126-3p, which inhibits PIK3R2 and activates the PI3K/AKT signaling pathway [33]. Another study reported that ADSC-Exos ameliorate high-glucose-induced oxidative stress in human umbilical vein endothelial cells (HUVECs) and in diabetic mice by upregulating the SIRT3/SOD2 pathway, thereby reducing reactive oxygen species (ROS) production and improving mitochondrial function [33].
Furthermore, MSC-Exos pretreated with melatonin showed enhanced anti-inflammatory capacity, significantly suppressing pro-inflammatory cytokines (IL-1β, TNF-α) and promoting the anti-inflammatory cytokine IL-10 in diabetic rat wounds [91].
Table 2: Efficacy of MSC-Exos in Diabetic Wound Models
| Exosome Source | Animal Model | Key Outcomes | Proposed Mechanism |
|---|---|---|---|
| ADSC (overexpressing miR-21-5p) | Diabetic mice | Improved re-epithelialization, collagen remodeling, angiogenesis, and vascular maturation [33] | Activation of AKT/HIF-1α pathway |
| ADSC | Diabetic mice | Reduced ROS, improved mitochondrial function, promoted angiogenesis [33] | Modulation of SIRT3/SOD2 pathway |
| UC-MSC (Melatonin-pretreated) | Diabetic rats | Suppressed IL-1β and TNF-α, promoted IL-10, accelerated wound closure [91] | Enhanced anti-inflammatory cargo |
| BMSC | Diabetic rat | Promoted proliferation and migration of fibroblasts and keratinocytes [91] | Delivery of growth factors (FGF-2, VEGF, HGF) |
Burn Wound Models
Burn injuries disrupt skin's structural integrity and trigger a intense inflammatory response. MSC-Exos have proven effective in promoting healing across all phases of burn wound repair [93].
Studies have shown that MSC-Exos modulate the immune response by regulating macrophage polarization towards the M2 phenotype and inhibiting pro-inflammatory T helper cells, thereby accelerating the inflammatory phase [93]. During the proliferation phase, exosomes facilitate angiogenesis and wound contraction by delivering miRNAs to endothelial cells and regulating fibroblast and keratinocyte activity [93].
In rodent models, the systemic injection of stem cells not only accelerated burn wound healing but also effectively dampened inflammation and facilitated skin function recovery through the action of secreted cytokines, creating a conducive microenvironment for repair [93]. Bone marrow-derived MSC exosomes (BMSC-Exos) and adipose-derived MSC exosomes (ADSC-Exos) are the most frequently utilized sources in burn wound research [93].
Infectious Wound Models
Infectious wounds are characterized by bacterial presence and a heightened inflammatory state that prevents progression to healing. MSC-Exos exhibit potent anti-inflammatory properties that can mitigate this damage [94].
A compelling study modeling inflammatory bowel disease (a model of intense mucosal inflammation and barrier dysfunction) found that BMSC-derived exosomes enriched with the protein TSG-6 significantly alleviated intestinal inflammation and pyroptosis. These exosomes reduced NLRP3 inflammasome activation, suppressed Caspase-1-mediated Gasdermin D (GSDMD) cleavage, and decreased pro-inflammatory cytokine release (IL-1β, IL-18). Knockdown of TSG-6 in the exosomes abolished these protective effects, confirming its critical role [94]. This mechanism of inhibiting the NLRP3/Caspase-1/GSDMD pyroptosis axis is highly relevant for managing excessive inflammation in infectious skin wounds.
Furthermore, MSC-Exos can restore barrier integrity by upregulating tight junction proteins (e.g., ZO-1, occludin) and reducing epithelial permeability, which is crucial for containing infection and promoting healing [94].
Detailed Experimental Protocols
To ensure reproducibility and standardization in preclinical research, below are detailed methodologies for key experiments validating MSC-Exos efficacy.
Protocol for Establishing a Diabetic Mouse Wound Model
- Animal: Use 8-12 week old C57BL/6J mice.
- Induction of Diabetes: Administer streptozotocin (STZ) via intraperitoneal injection at 50 mg/kg daily for 5 consecutive days. Mice with stable blood glucose levels >16.7 mmol/L for over 2 weeks are selected for experiments [33].
- Wound Creation: Anesthetize the mice and shave the dorsal hair. Create one or two full-thickness excisional skin wounds (diameter 6-8 mm) on the dorsum using a sterile biopsy punch [33] [9].
- Exosome Administration: Dilute MSC-Exos in sterile PBS. Apply exosomes (e.g., 100 μg in 100 μL PBS) topially to the wound bed every other day. The control group receives an equal volume of PBS.
- Assessment: Monitor wound closure daily by photographing wounds and calculating the remaining wound area as a percentage of the original area. Harvest wound tissues at different time points for histological analysis (H&E staining for re-epithelialization, Masson's trichrome for collagen deposition) and immunohistochemical staining (e.g., CD31 for angiogenesis) [9].
Protocol for Isolating and Characterizing MSC-Exos
- Cell Culture: Culture MSCs (from bone marrow, adipose, or umbilical cord) in standard media supplemented with 10% FBS. For the final 24-48 hours before collection, replace the medium with serum-free medium or medium containing exosome-depleted FBS to avoid bovine exosome contamination [94] [9].
- Exosome Isolation (Differential Ultracentrifugation):
- Collect conditioned medium and centrifuge at 300 × g for 10 min to remove dead cells.
- Centrifuge supernatant at 2,000 × g for 30 min to remove cell debris.
- Centrifuge supernatant at 10,000 × g for 30 min to eliminate large vesicles.
- Filter the supernatant through a 0.22 μm filter.
- Ultracentrifuge the filtrate at 120,000 × g for 70-120 min at 4°C.
- Wash the pellet in PBS and repeat ultracentrifugation.
- Resuspend the final exosome pellet in sterile PBS [9] [91].
- Exosome Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the particle size distribution and concentration.
- Transmission Electron Microscopy (TEM): Visualize the typical cup-shaped morphology of exosomes.
- Western Blot: Confirm the presence of exosomal markers (CD9, CD63, CD81, TSG101) and the absence of negative markers (e.g., Calnexin) [91].
Protocol for In Vitro Wound Healing Assays
- Cell Proliferation Assay (CCK-8):
- Seed fibroblasts (e.g., NIH/3T3) or keratinocytes (e.g., HaCaT) in a 96-well plate.
- Treat cells with MSC-Exos (e.g., 50 μg/mL) or PBS control.
- At the desired time points, add CCK-8 reagent to each well and incubate for 1-4 hours.
- Measure the absorbance at 450 nm to determine cell viability/proliferation [9].
- Cell Migration Assay (Scratch Assay):
- Seed cells in a 12-well plate to form a confluent monolayer.
- Create a scratch in the monolayer using a sterile 200 μL pipette tip.
- Wash away detached cells and add fresh medium containing MSC-Exos or control.
- Photograph the scratch at 0, 12, and 24 hours. Quantify the migration distance or the percentage of wound closure [9].
- Tube Formation Assay (Angiogenesis Assay):
- Thaw Matrigel on ice and coat a 96-well plate.
- Seed HUVECs pretreated with MSC-Exos or control onto the Matrigel.
- Incubate for 4-8 hours and photograph the formed tubular structures.
- Quantify parameters like total tube length, number of nodes, and junctions [33].
Visualization of Key Signaling Pathways
The following diagrams illustrate the primary molecular mechanisms through which MSC-Exos promote wound healing.
Anti-inflammatory and Anti-pyroptosis Pathway
Figure 1: TSG-6 in MSC-Exos inhibits pyroptosis and inflammation.
Pro-angiogenic Signaling Pathway
Figure 2: MSC-Exos activate pro-angiogenic PI3K/AKT/HIF-1α signaling.
Experimental Workflow for Preclinical Validation
Figure 3: Preclinical validation workflow for MSC-Exos.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for MSC-Exos Wound Healing Research
| Reagent/Material | Function/Application | Example/Note |
|---|---|---|
| MSC Culture Media | Expansion and maintenance of mesenchymal stem cells. | MEM-α or DMEM/F12, supplemented with 10% Exosome-Depleted FBS [94] [9]. |
| Exosome-Depleted FBS | Provides essential growth factors without contaminating bovine exosomes during exosome production. | Commercially available; prepared by ultracentrifugation of standard FBS [9]. |
| Differential Ultracentrifugation System | Gold-standard method for isolating exosomes from conditioned cell media. | Requires high-speed ultracentrifuge with fixed-angle and swinging-bucket rotors [91]. |
| Antibodies for Characterization | Identification and validation of exosomes via Western Blot, Flow Cytometry, or Immunofluorescence. | Anti-CD9, CD63, CD81 (positive markers); Anti-Calnexin (negative marker) [91]. |
| Streptozotocin (STZ) | Induces type 1 diabetes in rodent models for creating diabetic wound studies. | Administered via intraperitoneal injection; requires careful handling [33]. |
| Histological Stains | Evaluation of wound tissue architecture, collagen deposition, and re-epithelialization. | Hematoxylin and Eosin (H&E), Masson's Trichrome Stain [9]. |
| Antibodies for IHC/IF | Assessment of angiogenesis and cell proliferation in wound tissues. | Anti-CD31 (for endothelial cells), Anti-Ki67 (for proliferating cells) [9]. |
| Cell Lines for In Vitro Assays | Functional validation of exosome effects on key wound healing processes. | Human Umbilical Vein Endothelial Cells (HUVECs), HaCaT keratinocytes, NIH/3T3 fibroblasts [33] [9]. |
Preclinical data robustly validates the efficacy of MSC-derived exosomes as a versatile and potent therapeutic for enhancing healing in diabetic, burn, and infectious wound models. Their multifaceted mechanism of action, targeting inflammation, angiogenesis, proliferation, and remodeling, aligns perfectly with the complex pathophysiology of these challenging wounds.
Future work must focus on overcoming the hurdles of clinical translation. This includes standardizing isolation protocols to ensure batch-to-batch consistency, developing scalable production under Good Manufacturing Practice (GMP) conditions, and optimizing delivery systems—such as incorporation into hydrogel scaffolds for sustained release [95] [96] [91]. Furthermore, bioengineering approaches to create exosomes enriched with specific therapeutic miRNAs or proteins hold immense promise for enhancing their potency and homogeneity [96] [33] [91]. As research progresses, the successful translation of MSC-Exos from preclinical models to clinical applications will hinge on collaborative efforts between cell biologists, material scientists, and clinical researchers to realize the full potential of this cell-free therapy in regenerative medicine.
The field of regenerative medicine has increasingly recognized the therapeutic potential of mesenchymal stem cells (MSCs) for wound healing and tissue repair. Traditionally, the healing capabilities of MSCs were attributed to their ability to engraft at injury sites and differentiate into tissue-specific cells. However, emerging evidence indicates that the benefits are mediated primarily through paracrine signaling rather than direct cell replacement [72]. This revelation has catalyzed a paradigm shift toward cell-free therapeutic approaches, with MSC-derived exosomes (MSC-EXOs) emerging as a promising alternative.
Exosomes are nanoscale extracellular vesicles (30-150 nm in diameter) that function as crucial intermediaries in intercellular communication [85]. They are formed within multivesicular bodies (MVBs) inside cells and are released upon fusion of MVBs with the plasma membrane. These vesicles carry a functional cargo of proteins, lipids, mRNAs, and microRNAs from their parental cells, which they transfer to recipient cells to alter cellular functions [81] [4]. Within the context of wound healing research, MSC-EXOs represent a transformative approach that potentially retains the therapeutic benefits of MSCs while overcoming critical limitations associated with whole-cell therapies, particularly concerning immunogenicity and tumorigenic risk.
Comparative Advantages: MSC-Exosomes vs. Parental MSCs
Fundamental Biological Differences
The table below summarizes the core biological distinctions between MSC-derived exosomes and their parental MSCs.
Table 1: Fundamental Biological Comparison between MSCs and MSC-Derived Exosomes
| Characteristic | Parental MSCs | MSC-Derived Exosomes |
|---|---|---|
| Nature | Live, nucleated cells | Acellular, lipid-bilayer nanovesicles |
| Size | 15-30 μm (cell diameter) | 30-150 nm in diameter [85] [72] |
| Key Mechanism | Direct differentiation & paracrine signaling | Paracrine information transfer via bioactive cargo |
| Primary Cargo | Cellular organelles and nucleus | Proteins, lipids, mRNA, miRNA [4] |
| Replication Capacity | Yes | No |
Quantitative and Qualitative Assessment of Key Therapeutic Advantages
The translational appeal of MSC-EXOs is rooted in several practical advantages that address the significant challenges of cell-based therapies. The following table provides a comparative analysis of these critical parameters.
Table 2: Comparative Therapeutic Advantages of MSC-Exosomes over Parental MSCs
| Parameter | Parental MSCs | MSC-Derived Exosomes | Key Supporting Evidence |
|---|---|---|---|
| Immunogenicity | Low but present; risk of rejection upon repeated administration [1] | Very low; lack immunogenic MHC class II and co-stimulatory molecules [1] [85] | Safer for allogeneic and repeated use [1] |
| Tumorigenic Risk | Theoretical risk due to proliferative capacity and potential malignant transformation [17] [1] | Negligible; non-replicative and unable to form tumors [17] [1] | Cell-free nature eliminates risk of uncontrolled growth |
| Stability & Storage | Require cryopreservation; sensitive to freeze-thaw cycles; limited shelf-life [1] | High stability; can be stored at -80°C for long periods with minimal loss of function [1] [85] | More practical for clinical logistics and off-the-shelf availability |
| Biodistribution & Targeting | Prone to pulmonary entrapment; limited migration to target sites [17] [1] | Enhanced tissue penetration; can cross biological barriers (e.g., blood-brain barrier); intrinsic hepatic tropism [17] [1] | Higher efficacy in reaching diseased or injured tissues |
| Production Standardization | High variability due to donor differences, passage number, and culture conditions [17] | More reproducible production potential; cargo can be standardized and engineered [17] | Better batch-to-batch consistency for clinical manufacturing |
| Administration Safety | Risk of microvasculature occlusion (e.g., pulmonary embolism) [17] | Reduced safety risks; nanometer size prevents vessel blockage [17] | Favorable safety profile for intravenous delivery |
Deep Dive into Mechanisms: Lower Immunogenicity and Tumorigenic Risk
Mechanisms Underlying Low Immunogenicity
The low immunogenicity of MSC-EXOs is not merely a passive characteristic but an active biological property. The following diagram illustrates the key mechanisms through which MSC-EXOs avoid immune activation.
The immunomodulatory properties of MSC-EXOs extend beyond passive avoidance to active regulation. While parental MSCs naturally possess low immunogenicity due to reduced MHC-I and absent MHC-II expression [97], MSC-EXOs lack these complexes entirely, eliminating the risk of alloreactive T-cell activation [1]. Furthermore, they do not express co-stimulatory molecules (CD40, CD80, CD86), which are critical for initiating a robust adaptive immune response [4].
Beyond these passive attributes, MSC-EXOs actively modulate the immune landscape through their cargo. They carry immunosuppressive miRNAs—such as miR-21-5p, miR-146a, and miR-125a-3p—which can suppress T-cell proliferation, promote regulatory T-cell (Treg) survival, and inhibit dendritic cell maturation [4] [85]. This dual passive and active mechanism makes MSC-EXOs particularly advantageous for allogeneic applications and repeated dosing in chronic wound healing, where sustained treatment is often necessary.
Mechanisms Underlying Low Tumorigenic Risk
The theoretical tumorigenic risk of parental MSCs stems from their capacity for extended proliferation and the potential for malignant transformation after long-term culture or in the inflammatory wound microenvironment [1]. MSC-EXOs fundamentally circumvent this risk through their non-living, non-replicative nature.
It is crucial to note, however, that the bioactive cargo of MSC-EXOs can influence tumor growth in a context-dependent manner. Some studies suggest that MSC-EXOs in the tumor microenvironment might be co-opted to promote cancer progression [81]. This highlights the importance of careful characterization and quality control of exosome preparations, especially when derived from MSCs exposed to tumorigenic environments. For wound healing applications in non-cancerous contexts, the intrinsic non-replicative nature of MSC-EXOs provides a significant safety advantage.
Experimental Protocols for Validation
Assessing Immunogenicity: In Vitro and In Vivo Approaches
To empirically validate the low immunogenicity of MSC-EXOs, researchers employ a combination of immune cell activation assays.
A. Mixed Lymphocyte Reaction (MLR) Assay
- Purpose: To evaluate the potential of MSC-EXOs to stimulate T-cell proliferation in an allogeneic setting.
- Procedure:
- Isolate peripheral blood mononuclear cells (PBMCs) from multiple healthy donors.
- Label responder PBMCs with a cell proliferation dye (e.g., CFSE).
- Co-culture CFSE-labeled responder PBMCs with irradiated stimulator PBMCs from an allogeneic donor.
- Add varying concentrations of MSC-EXOs or parental MSCs to the co-culture.
- After 5-7 days, analyze T-cell proliferation by flow cytometry via CFSE dilution.
- Expected Outcome: MSC-EXO treated cultures will show significantly reduced T-cell proliferation compared to positive controls, and performance comparable to or better than parental MSCs [1].
B. Dendritic Cell (DC) Maturation Assay
- Purpose: To determine the effect of MSC-EXOs on the maturation and antigen-presenting function of DCs.
- Procedure:
- Generate immature DCs from human monocyte-derived CD14+ cells using GM-CSF and IL-4.
- Treat DCs with a maturation stimulus (e.g., LPS) in the presence or absence of MSC-EXOs.
- After 48 hours, analyze surface expression of maturation markers (CD83, CD86, HLA-DR) by flow cytometry.
- Measure secretion of pro-inflammatory cytokines (IL-12, TNF-α) in the supernatant by ELISA.
- Expected Outcome: MSC-EXO treatment will lead to downregulation of maturation markers and reduced secretion of pro-inflammatory cytokines, indicating suppressed DC maturation [4].
Assessing Tumorigenic Risk: Key Experimental Models
Evaluating the tumorigenic potential is a critical step in the preclinical safety profile of MSC-EXOs.
A. Soft Agar Colony Formation Assay
- Purpose: To assess the capacity of MSC-EXOs to induce anchorage-independent growth—a hallmark of cellular transformation.
- Procedure:
- Prepare a base layer of agar in cell culture medium in a multi-well plate.
- Mix target cells (e.g., a primary fibroblast line) with MSC-EXOs or parental MSCs in a top layer of soft agar.
- Culture for 2-4 weeks, replenishing media with fresh exosomes/MSCs periodically.
- Stain colonies with crystal violet and count.
- Expected Outcome: Cultures treated with MSC-EXOs should not form significant colonies, indicating no induction of transformation, unlike positive controls (e.g., oncogene-transformed cells).
B. In Vivo Tumor Formation Assay
- Purpose: The gold-standard test for evaluating tumorigenic potential in a living organism.
- Procedure:
- Utilize immunodeficient mice (e.g., NOD/SCID).
- Divide mice into three experimental groups:
- Group 1: Subcutaneous injection of parental MSCs.
- Group 2: Subcutaneous injection of MSC-EXOs (repeated doses).
- Group 3: Positive control (e.g., HeLa cells).
- Monitor injection sites for tumor formation over 2-4 months via palpation and caliper measurements.
- Perform histological analysis of the injection site and major organs at endpoint.
- Expected Outcome: The MSC-EXO group will show no evidence of tumor formation, confirming their non-tumorigenic nature [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for MSC-Exosome Isolation, Characterization, and Functional Assays
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| Exosome-Depleted FBS | Cell culture supplement for MSC expansion to prevent contamination with bovine exosomes during vesicle production. | Ultracentrifuged FBS (100,000-120,000 g for 18 hours) or commercially available exosome-depleted FBS is essential [98]. |
| Isolation Kits | Concentration and purification of exosomes from conditioned cell culture media. | Polymer-based precipitation kits (e.g., Total Exosome Isolation reagent) offer a user-friendly alternative to ultracentrifugation [72]. |
| Antibodies for Characterization | Identification of exosomal markers via Western blot, flow cytometry, or immuno-EM. | Anti-tetraspanins (CD63, CD81, CD9), Anti-TSG101, Anti-Alix, and Anti-HSP70/HSP90 are canonical markers [99] [72]. |
| Nanoparticle Tracking Analyzer | Quantification of exosome particle size and concentration in suspension. | Instruments like Malvern Nanosight provide critical data on exosome preparation quality (size distribution ~30-150 nm) [99]. |
| Cell Proliferation Dye | Tracking and quantification of immune cell proliferation in immunogenicity assays. | CFSE (Carboxyfluorescein succinimidyl ester) or similar dyes (e.g., CellTrace Violet) are used in Mixed Lymphocyte Reaction assays [1]. |
| ELISA Kits | Quantification of specific cytokines, growth factors, or exosomal cargo components. | Used to measure cytokine profiles (e.g., IL-10, TGF-β, TNF-α) in immunomodulation assays [4]. |
| miRNA Inhibitors/Mimics | Functional studies to investigate the role of specific exosomal miRNAs in wound healing pathways. | Tools for gain/loss-of-function experiments to validate miRNA-mediated mechanisms (e.g., miR-21-5p, miR-146a) [4]. |
The transition from parental MSCs to MSC-derived exosomes represents a significant evolution in regenerative medicine, particularly for complex processes like wound healing. The body of evidence convincingly demonstrates that MSC-EXOs possess a superior safety profile characterized by significantly lower immunogenicity and negligible tumorigenic risk compared to their cellular counterparts. These inherent advantages, coupled with their enhanced stability, targeted delivery potential, and ability to be engineered for precision therapy, firmly establish MSC-EXOs as a promising cell-free therapeutic tool.
For researchers and drug development professionals, this paradigm necessitates a refined focus on overcoming the remaining challenges of standardized production, scalable isolation, and comprehensive cargo profiling. As the field advances, the strategic application of MSC-EXOs is poised to unlock new, safer, and more effective therapeutic avenues for wound healing and beyond, marking a new chapter in translational regenerative medicine.
The therapeutic landscape for wound healing is undergoing a significant transformation, moving from conventional biologics and mechanical interventions to advanced acellular nanotherapeutics. Mesenchymal stem cell-derived exosomes (MSC-exos) are emerging as a superior cell-free therapeutic paradigm, addressing critical limitations of growth factors, skin grafts, and negative-pressure wound therapy (NPWT). This whitepaper provides a comparative analysis based on current scientific literature, detailing the mechanisms, efficacy, and practical applications of these technologies. It is structured to equip researchers and drug development professionals with actionable data and methodologies to advance the clinical translation of exosome-based wound healing solutions.
The challenge of chronic wounds, which affect millions globally and impose substantial economic burdens, has driven innovation in wound care beyond conventional therapies [34]. Mesenchymal stem cells (MSCs) have long been recognized for their regenerative potential, capable of self-renewal, immunomodulation, and multi-lineage differentiation. However, significant challenges related to their clinical use—including unpredictable growth, limited vascular transport efficiency, stringent storage requirements, and tumorigenicity concerns—have spurred the search for effective cell-free alternatives [24] [37].
The therapeutic effects of MSCs are now known to be mediated largely through paracrine signaling, primarily via their secretome, which includes extracellular vesicles and soluble factors, especially exosomes [24] [100]. Exosomes are nano-sized (30–150 nm) extracellular vesicles with a lipid bilayer, secreted by nearly all cell types. They act as intercellular communication vehicles by transferring bioactive cargo—such as proteins, lipids, and nucleic acids (including miRNAs and mRNAs)—between cells to influence recipient cells' physiological and pathological processes [10] [37]. Compared to whole-cell MSC therapy, exosomes offer superior benefits in storage, safety, biocompatibility, reduced immunogenicity, and enhanced tissue penetration capabilities, making them ideal acellular therapeutic agents [24] [34] [10]. This whitepaper situates MSC-exos within this evolving paradigm, analyzing their potential to overcome the limitations of established conventional therapies.
Analysis of Conventional Wound Healing Therapies
Growth Factors
- Mechanism of Action: Growth factors are signaling proteins that bind to specific cell surface receptors, activating intracellular pathways that regulate key wound healing processes, including cell proliferation, migration, and angiogenesis.
- Limitations and Challenges: Their clinical application is constrained by several factors. The harsh wound microenvironment (e.g., presence of proteases) can lead to rapid degradation of growth factors, significantly reducing their bioavailability and therapeutic half-life [34]. Furthermore, the delivery of a single growth factor often fails to recapitulate the complex, multi-factorial nature of the healing process, leading to suboptimal outcomes. The emergence of drug resistance and high production costs also limit their widespread use [7].
Skin Grafts
- Mechanism of Action: Skin grafts involve the transplantation of autologous or allogeneic skin to provide immediate wound coverage and facilitate re-epithelialization.
- Limitations and Challenges: A major challenge is suboptimal graft take, often due to factors like hematoma formation, infection, and poor vascularization at the graft bed. The integration of the graft with the native tissue is a critical and fragile process. Immune rejection is a significant risk for allogeneic grafts, and the procedure also creates a secondary donor site wound, adding to patient morbidity [101].
Negative-Pressure Wound Therapy (NPWT)
- Mechanism of Action: NPWT applies controlled sub-atmospheric pressure to a sealed wound environment through a specialized dressing. This promotes healing by removing excess exudate, reducing tissue edema, stimulating granulation tissue formation, and approximating wound edges.
- Limitations and Challenges: NPWT is a macroscopic management system that does not directly address the underlying cellular and molecular deficiencies in chronic wounds. Its efficacy can be limited in wounds with persistent biofilm infections [34]. A meta-analysis of randomized controlled trials highlighted that the effectiveness of NPWT for securing skin grafts is dependent on the specific negative pressure setting, with 80 mmHg showing improved graft take, while 125 mmHg did not, indicating a need for parameter optimization [101].
The Emergence of MSC-Derived Exosomes as a Novel Therapeutic
Mechanistic Basis for Exosome Efficacy
MSC-derived exosomes orchestrate wound healing by influencing all phases of the process. Their cargo, particularly microRNAs (miRNAs), regulates gene expression in recipient cells, driving therapeutic outcomes.
- Inflammation Phase: Exosomes modulate the immune response. For instance, exosomes from miR-26a-5p-modified adipose-derived MSCs downregulate pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, IFN-γ), accelerating the transition from the inflammatory to the proliferative phase [7].
- Proliferation Phase: They promote angiogenesis and cell proliferation. The same miR-26a-5p-enriched exosomes upregulate CD31 (a marker for endothelial cells) and enhance the synthesis of extracellular matrix (ECM) components like Collagen I, II, and III (Col1a1, Col2a1, Col3a1) and α-smooth muscle actin (α-Sma) [7].
- Remodeling Phase: Exosomes facilitate ECM reorganization by altering the ratio of matrix metalloproteinases (MMPs) to their tissue inhibitors (TIMPs), leading to improved collagen organization and tensile strength of the healed tissue [100].
The following diagram illustrates the multi-targeted mechanism by which MSC-exos, specifically those carrying miR-26a-5p, promote wound healing.
Quantitative Comparative Analysis of Therapeutic Modalities
The table below synthesizes quantitative data and key characteristics from the literature to provide a direct comparison between MSC-derived exosomes and conventional therapies.
Table 1: Comparative Analysis of MSC-Derived Exosomes and Conventional Wound Healing Therapies
| Therapeutic Modality | Key Efficacy Findings (from search results) | Primary Limitations | Key Advantages |
|---|---|---|---|
| MSC-Derived Exosomes | - Odds ratio for wound closure: 1.82 at 7 days; 2.29 at 14 days [100].- miR-26a-5p exosomes significantly enhance wound closure, downregulate IL-1β, IL-6, TNF-α, IFN-γ, and upregulate Col1a1, Cd31, Col3a1, α-Sma in vivo [7]. | - Rapid clearance from the body [34].- Requires optimized delivery systems for sustained release [24].- Standardization of isolation and characterization [100]. | - Multi-targeted action on inflammation, angiogenesis, ECM synthesis [7] [100].- Low immunogenicity [34] [10].- Native tissue penetration and biocompatibility [24].- Can be engineered and combined with biomaterials [24] [10]. |
| Growth Factors | - Not quantitatively detailed in results, but widely used. | - Susceptible to degradation in wound environment [34].- High cost, single-target action, potential drug resistance [7]. | - Direct activation of specific cellular pathways. |
| Skin Grafts | - NPWT (80mmHg) improves graft take vs. non-NPWT [101]. | - Risk of poor graft take, immune rejection, donor site morbidity [101]. | - Provides immediate wound coverage. |
| NPWT | - NPWT improves graft take percentage vs. non-NPWT (RR of re-operation) [101].- 80 mmHg pressure effective; 125 mmHg not [101]. | - Macroscopic management; doesn't address molecular pathology [34].- Limited efficacy against biofilms [34].- Parameter optimization is critical [101]. | - Effective exudate management and mechanical stimulation. |
Experimental Protocols for Evaluating Exosome Therapeutics
Protocol: In Vivo Evaluation of Exosome Efficacy in a Murine Model
This protocol is adapted from studies that successfully demonstrated the acceleration of wound healing using MSC-exos [7] [100].
Animal Model Establishment:
- Use 6-8 week-old male Sprague-Dawley or C57BL/6 mice.
- Anesthetize the animals and create full-thickness excisional dorsal wounds (e.g., 10 mm in diameter).
- Utilize an excisional splinting model to prevent wound contraction, mimicking human healing by re-epithelialization.
Experimental Groups:
- Group 1 (Control): Topical application of saline or buffer.
- Group 2 (Conventional Therapy): e.g., Povidone-Iodine (PI) hydrogel [102].
- Group 3 (Exosome Treatment): Topical application of MSC-exos (e.g., 0.2 mL of a standardized concentration) thrice over three weeks.
- Group 4 (Engineered Exosome): Topical application of exosomes from genetically modified MSCs (e.g., miR-26a-5p-overexpressing AMSCs) [7].
Treatment and Monitoring:
- Apply treatments directly to the wound bed according to the schedule.
- Perform weekly planimetric analysis by capturing wound images and calculating wound area using software (e.g., "Woundaries" or ImageJ) to track closure rates [103].
Endpoint Analysis (at 3 weeks post-operation):
- Histopathological Analysis: Harvest wound tissue, section, and stain with Hematoxylin and Eosin (H&E) for general morphology and Masson's Trichrome for collagen deposition assessment [102].
- Immunohistochemistry (IHC): Stain for specific markers like CD68 to quantify macrophage infiltration [102] or CD31 for angiogenesis [7].
- Molecular Analysis:
Protocol: Isolation and Characterization of MSC-Exos
Standardized isolation and characterization are critical for reproducibility and clinical translation [100].
- Cell Culture: Expand MSCs from a chosen source (e.g., adipose tissue, bone marrow) in culture flasks under standard conditions.
- Exosome Isolation:
- Ultracentrifugation (Gold Standard): Collect cell culture supernatant free of cells and debris. Centrifuge at progressively higher speeds (e.g., 2,000 × g for 30 min, 10,000 × g for 45 min), followed by ultracentrifugation at 100,000 × g for 70-120 min to pellet exosomes [100].
- Alternative Methods: Commercial exosome isolation kits or tangential flow filtration can also be used [100].
- Exosome Characterization:
- Nanoparticle Tracking Analysis (NTA): To determine the size distribution and concentration of the isolated particles (should be ~30-150 nm) [100].
- Transmission Electron Microscopy (TEM): To visualize the classic cup-shaped morphology and bilayer membrane structure of exosomes [100].
- Western Blot Analysis: To confirm the presence of exosomal marker proteins (e.g., CD63, CD9, CD81, TSG101) and the absence of negative markers (e.g., Grp94 from the endoplasmic reticulum) [100].
The following workflow diagram summarizes the key steps from exosome isolation to in vivo functional validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research into exosome-based wound healing requires a suite of specialized reagents and materials. The following table details key solutions for critical experimental steps.
Table 2: Essential Research Reagent Solutions for Exosome Wound Healing Studies
| Reagent/Material | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source of therapeutic exosomes. | Adipose-derived MSCs (AMSCs) are commonly used due to ease of isolation and strong paracrine potential [7]. Bone marrow and umbilical cord MSCs are also frequent sources [100]. |
| Exosome Isolation Kits | Simplified and standardized isolation of exosomes from cell culture media. | Commercial kits (e.g., from ThermoFisher, System Biosciences) offer an alternative to ultracentrifugation, though the latter remains the most reported method [100]. |
| Characterization Antibodies | Confirmation of exosome identity via Western Blot or Flow Cytometry. | Antibodies against tetraspanins: CD63, CD9, CD81; and the endosomal marker TSG101. Negative control: Grp94 [100]. |
| Hydrogel/Scaffold Biomaterials | Delivery vehicle for sustained release of exosomes at the wound site. | Chitosan hydrogel has demonstrated excellent biocompatibility and wound healing capabilities [102]. Pluronic F-127 and Gelatin sponge/Polydopamine (GS-PDA) scaffolds have been used to load and control the release of AMSC-exos [7] [10]. |
| qPCR Assays | Quantification of gene expression changes in wound tissue. | Assays for inflammatory cytokines (IL-1β, IL-6, TNF-α), ECM components (Col1a1, Col3a1), angiogenic markers (CD31), and target genes like MAP2K4 [102] [7]. |
| In Vivo Animal Model | Pre-clinical testing of therapeutic efficacy. | Murine (Rat/Mouse) full-thickness excisional wound model with splinting is critical to mimic human healing via re-epithelialization rather than contraction [102] [7] [100]. |
The comparative analysis presented in this whitepaper substantiates the position that MSC-derived exosomes represent a transformative therapeutic modality in wound healing. Their multi-targeted mechanistic approach, which concurrently regulates inflammation, promotes angiogenesis, and orchestrates ECM remodeling, addresses the core pathophysiological deficiencies in chronic wounds more comprehensively than single-target conventional therapies.
The future of this field lies in engineering and optimization. Key research frontiers include:
- Engineering Exosomes: Genetic modification of parent MSCs to produce exosomes enriched with specific therapeutic miRNAs (e.g., miR-26a-5p) or proteins to enhance their regenerative potency [7] [10].
- Advanced Delivery Systems: The development of sophisticated biomaterial scaffolds (e.g., chitosan hydrogels) for the controlled, localized, and sustained release of exosomes is paramount to overcoming the challenge of rapid clearance and maintaining therapeutic concentrations at the wound site [24] [34] [102].
- Standardization and Scalability: For successful clinical translation, the field must establish robust, scalable, and reproducible protocols for the isolation, characterization, and storage of MSC-exos, moving beyond the current reliance on ultracentrifugation [100] [10].
In conclusion, while growth factors, skin grafts, and NPWT remain valuable tools in the wound care arsenal, MSC-derived exosomes offer a paradigm shift towards a more integrated, biological, and efficacious treatment strategy. For researchers and drug development professionals, focusing on the bioengineering of exosomes and their delivery systems presents the most promising path to revolutionizing the standard of care for complex wound management.
Current Landscape of Clinical Trials and Emerging Commercial Products
The field of mesenchymal stem cell-derived exosomes (MSC-Exos) is transitioning from preclinical validation to clinical application, representing a paradigm shift in regenerative medicine for wound healing. This whitepaper details the current clinical trial landscape and emerging commercial products leveraging MSC-Exos for wound healing, particularly for complex conditions like diabetic foot ulcers (DFUs). The analysis reveals a rapidly maturing sector with multiple therapies in Phase II and III trials, advancing technologies for exosome engineering and delivery, and a robust pipeline of commercial products poised to address significant unmet medical needs in chronic wound management. Despite considerable progress, challenges in standardization, scalable manufacturing, and regulatory pathways remain active areas of development within the industry.
Mesenchymal stem cell-derived exosomes are nano-sized extracellular vesicles (typically 30-150 nm in diameter) that mediate intercellular communication by transferring functional molecular cargo—including proteins, lipids, mRNAs, and microRNAs—from parent MSCs to recipient cells [33] [44]. In the context of wound healing, MSC-Exos have demonstrated multifunctional capabilities including immunomodulation, angiogenesis promotion, collagen remodeling, and re-epithelialization [71] [30]. Compared to cell-based therapies, MSC-Exos offer significant advantages including lower immunogenicity, reduced risk of tumorigenicity, enhanced stability, and the ability to bypass the challenges associated with cell survival and engraftment [81] [44]. These properties position MSC-Exos as promising "cell-free" therapeutic agents for addressing the complex pathophysiology of chronic wounds.
Biological Mechanisms of Action in Wound Healing
MSC-Exos accelerate wound healing through coordinated modulation of multiple biological pathways and cellular processes across all phases of wound repair.
Key Signaling Pathways Modulated by MSC-Exos
Table 1: Key Signaling Pathways in MSC-Exo Mediated Wound Healing
| Pathway | Biological Effect | Molecular Mechanism |
|---|---|---|
| PI3K/AKT Pathway | Promotes fibroblast and keratinocyte proliferation and migration; reduces oxidative stress | Upregulates p-AKT/AKT levels; activates HIF-1α; modulates SIRT3/SOD2 under high glucose conditions [33] |
| TGF-β/Smad Pathway | Regulates extracellular matrix remodeling; modulates fibroblast activation | Increases TGF-β3/TGF-β1 ratio; affects collagen I/III deposition; prevents fibroblast differentiation to myofibroblasts [33] [71] |
| ERK/MAPK Pathway | Enhances cell mobility and activity; reduces scar formation | Increases cyclin-1 and PCNA expression; modulates MMP3/TIMP1 ratio [33] |
| NF-κB Pathway | Suppresses chronic inflammation; promotes M2 macrophage polarization | Reduces pro-inflammatory cytokines (TNF-α, IL-6, IL-1β); increases anti-inflammatory IL-10 [71] [104] |
| Wnt/β-Catenin Pathway | Accelerates re-epithelialization | Upregulates CK19 and PCNA markers; inhibits apoptosis under stress conditions [91] |
Cellular Targets and Functional Outcomes
MSC-Exos exert their therapeutic effects through precise modulation of key cell types involved in wound healing:
Fibroblasts: MSC-Exos enhance fibroblast proliferation and migration while regulating collagen synthesis and organization to promote functional tissue repair with reduced scarring [33]. ADSC-derived exosomes increase N-cadherin, cyclin-1, PCNA, and collagen I/III expression in recipient fibroblasts, particularly during early healing phases [33].
Keratinocytes: Exosomes from various MSC sources, particularly umbilical cord-derived MSCs, significantly promote keratinocyte migration and proliferation to accelerate re-epithelialization [104] [91]. This process is enhanced through activation of AKT/HIF-1α and ERK/MAPK signaling pathways [33].
Endothelial Cells: MSC-Exos promote angiogenesis by stimulating endothelial cell proliferation, migration, and tube formation [71]. This pro-angiogenic effect is mediated through transfer of specific miRNAs (miR-125a, miR-126-3p) and growth factors (VEGF, HGF) that activate key signaling pathways in endothelial cells [33] [91].
Immune Cells: MSC-Exos modulate the wound immune microenvironment by promoting the transition from pro-inflammatory M1 to anti-inflammatory M2 macrophages, suppressing T-cell proliferation, and enhancing regulatory T-cell differentiation through mechanisms involving IDO and Foxp3 upregulation [104] [91].
Figure 1: MSC-Exo Mechanisms in Wound Healing - This diagram illustrates the cellular targets, activated signaling pathways, and functional outcomes of MSC-derived exosomes in wound healing.
Current Clinical Trial Landscape
The clinical trial landscape for MSC-derived exosomes in wound healing applications is rapidly expanding, with several advanced trials demonstrating promising results.
Recent Clinical Trial Findings
A landmark 2025 randomized controlled clinical trial investigated Wharton's Jelly MSC-derived exosomes for diabetic foot ulcer healing in 110 patients with persistent DFUs [104]. Participants were divided into three groups: one receiving weekly topical application of WJ-MSC exosomes plus standard of care (SOC), a control group receiving SOC alone, and a placebo group receiving SOC plus carboxymethyl cellulose (the exosome vehicle) [104]. The findings demonstrated compelling evidence for exosome efficacy:
- Significantly Enhanced Complete Healing: The exosome-treated group showed a substantially higher percentage of patients achieving complete recovery compared to control groups [104].
- Accelerated Healing Timeline: The mean time to full recovery was 6 weeks (range: 4-8 weeks) in the exosome-treated group compared to 20 weeks (range: 12-28 weeks) in controls, representing approximately a 70% reduction in healing time [104].
- Excellent Safety Profile: The study reported no significant adverse events related to the exosome treatment, supporting the favorable safety profile of MSC-Exo therapies [104].
Table 2: Select Clinical Trials of MSC-Exo Therapies for Wound Healing
| Therapy/Source | Trial Phase | Patient Population | Key Findings | References |
|---|---|---|---|---|
| Wharton's Jelly MSC-Exos | Randomized Controlled Trial (n=110) | Diabetic Foot Ulcers | 62% fully recovered; mean recovery time 6 weeks vs 20 weeks in controls [104] | |
| ADSC-Exos | Preclinical/Phase I | Diabetic Wounds | Promoted collagen I/III formation, enhanced epithelialization, improved angiogenesis [33] | |
| hUC-MSC Exosomes | Preclinical/Phase I | Chronic Wounds | Enriched in miR-21, miR-23a, miR-125b, miR-145; reduced scar formation [104] | |
| BM-MSC Exosomes | Preclinical | Cutaneous Wounds | Superior effect on dermal fibroblast proliferation and migration [91] |
Source-Dependent Efficacy Profiles
Recent comparative studies have revealed that exosomes from different MSC sources exhibit distinct efficacy profiles and growth factor contents that may inform their clinical application:
- Bone Marrow MSC-Exos: Demonstrate particularly strong effects on dermal fibroblast proliferation and migration, making them potentially optimal for targeting dermal regeneration [91].
- Umbilical Cord MSC-Exos: Contain unique factors including TGF-β and show superior effects on keratinocyte migration and proliferation, suggesting enhanced epithelialization potential [104] [91].
- Adipose-Derived MSC-Exos: Rich in pro-angiogenic factors and demonstrate significant wound closure rates in diabetic models through enhanced vascularization [33].
These source-dependent variations highlight the potential for tailoring exosome therapies to specific wound types and healing phases.
Emerging Commercial Products and Pipeline
The commercial landscape for exosome-based wound therapies features several advanced candidates progressing through clinical development stages.
Table 3: Emerging Commercial MSC-Exo Products in Development
| Product/Company | Therapeutic Platform | Development Stage | Key Indications | Differentiating Features |
|---|---|---|---|---|
| ExoFlo (Direct Biologics) | BM-MSC derived extracellular vesicles | Phase III (EXTINGUISH ARDS); Phase I for UC & Crohn's [105] [106] | ARDS, Ulcerative Colitis, Crohn's | Rich in growth factors and extracellular vesicles; multiple administration routes [105] |
| AGLE-102 (Aegle Therapeutics) | MSC-derived exosomes with COL7 protein and mRNA | Phase I/II trial open for enrollment [105] [106] | Recessive Dystrophic Epidermolysis Bullosa (RDEB) | Delivers type VII collagen components; non-immunogenic; promotes functional regeneration [105] |
| CAP-1002 (Capricor Therapeutics) | Cardiosphere-derived cells producing exosomes | Phase III (HOPE-3 trial) fully enrolled [105] [106] | Duchenne Muscular Dystrophy (DMD) | Regulates immune activity and promotes cellular regeneration; successful pre-BLA meeting with FDA [105] |
| BRE-AD01 (Brexogen) | Stimulated stem cell-derived exosomes ('BxC') | Phase I clinical trial approved by FDA [105] | Atopic Dermatitis | Multiple mechanisms: suppresses type 2 immunity, modulates IL-31R, enhances skin barrier; superior preclinical efficacy vs. standard treatments [105] |
| ILB-202 (ILIAS Biologics) | Exosomes carrying super-repressor IκB (srIκB) | Phase I completed (Final Clinical Study Report) [105] [106] | Acute and Chronic Inflammatory Diseases | Directly targets core inflammatory signals in cytosol; minimizes off-target effects [105] |
Market Outlook and Commercialization Trends
The exosome therapies market is poised for substantial growth, with the 7MM (United States, EU4, United Kingdom, and Japan) expected to grow at a considerable CAGR through 2034 [106]. Key market dynamics include:
- Expanding Product Pipeline: There are currently more than 100 exosome therapies in various development phases (Phase III to Discovery), with approximately 15+ active human trials [106].
- Strategic Collaborations: Partnerships between academic institutions and pharmaceutical companies are accelerating development, exemplified by collaborations between ExoXpert and Neucore Bio, and INOVIQ and Promega [106].
- Manufacturing Scale-Up: Companies like NurExone Biologic are securing master cell banks to ensure stable, scalable exosome production for clinical needs and eventual patient treatment [106].
- Intellectual Property Expansion: Continued patent issuance for novel exosome compositions, such as Aruna Bio's recent US Patent for neural exosomes, provides market protection and competitive advantages [106].
Experimental Protocols and Methodologies
Standardized protocols for exosome isolation, characterization, and functional testing are critical for research reproducibility and therapeutic development.
Standardized Isolation and Characterization Workflow
Figure 2: MSC-Exo Isolation & Characterization Workflow - This diagram outlines the standardized protocol for isolating and characterizing MSC-derived exosomes for research and therapeutic applications.
Detailed Methodological Protocols
MSC Culture and Exosome Production
- Cell Source Establishment: Isolate MSCs from Wharton's Jelly, adipose tissue, or bone marrow using collagenase (1 mg/ml type I) and hyaluronidase (0.7 mg/ml) digestion at 37°C for 1 hour, followed by centrifugation at 340×g [104]. Culture cells in DMEM/F12 supplemented with 15% FBS at 37°C with 5% CO₂, replacing media every 3-4 days [104].
- Exosome Production: At 70-80% confluence, culture MSC cells in serum-free media for 48 hours to collect conditioned media while preventing FBS-derived exosome contamination [104].
Exosome Isolation and Purification
- Differential Centrifugation: Subject conditioned media to sequential centrifugation: 10 minutes at 13,000×g to remove cells and debris, followed by 10 minutes at 45,000×g to eliminate larger vesicles [104].
- Ultracentrifugation: Pellet exosomes by ultracentrifugation at 110,000×g for 5 hours using a Beckman Coulter ultracentrifuge [104]. Resuspend the final pellet in PBS for therapeutic use or further analysis.
- Quality Control: Repeat isolation and characterization processes three times to confirm reproducibility and consistency [104].
Comprehensive Exosome Characterization
- Nanoparticle Tracking Analysis: Confirm exosome size distribution (30-150 nm) and concentration using nanoparticle tracking analysis [44] [104].
- Transmission Electron Microscopy: Assess exosome morphology and ultrastructure using TEM imaging [104].
- Surface Marker Validation: Confirm exosome identity using flow cytometry against tetraspanin markers CD9, CD63, CD81, and heat shock protein HSP70 [104] [91].
- Western Blot Analysis: Verify presence of exosomal protein markers (TSG101, Alix) and absence of negative markers (calnexin) [91].
Functional Assessment in Wound Healing Models
In Vitro Functional Assays
- Cell Proliferation and Migration: Assess exosome effects on dermal fibroblast and keratinocyte proliferation using MTT assays, and migration using scratch/wound healing assays [91]. Dose-dependent effects should be evaluated with exosome concentrations typically ranging from 10-100 μg/mL.
- Angiogenesis Assays: Test pro-angiogenic potential using human umbilical vein endothelial cell tube formation assays on Matrigel [33] [71].
- Gene Expression Analysis: Evaluate regulation of wound healing-related genes (collagen I/III, TGF-β, VEGF, α-SMA) using qRT-PCR and Western blotting [33].
In Vivo Efficacy Testing
- Diabetic Wound Models: Utilize streptozotocin-induced diabetic rodents with full-thickness excisional wounds [33] [104].
- Treatment Administration: Apply exosomes topically (incorporated in hydrogels) or via local injection. Recent clinical protocols used weekly topical applications for 4 weeks [104].
- Outcome Measures: Monitor wound closure rates weekly, with histological assessment of re-epithelialization, collagen deposition, capillary density, and immune cell infiltration at endpoint [33] [104].
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for MSC-Exo Wound Healing Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| MSC Sources | Bone Marrow MSCs, Adipose-derived MSCs, Umbilical Cord MSCs, Wharton's Jelly MSCs | Source selection for exosome production | Source impacts exosome cargo and functional properties; UC-MSCs show strong epithelialization effects [104] [91] |
| Isolation Kits | Differential Ultracentrifugation, Size-Exclusion Chromatography, Polymer-Based Precipitation | Exosome isolation and purification | Ultracentrifugation remains gold standard; kit-based methods offer faster processing but potential impurity co-isolation [91] |
| Characterization Antibodies | Anti-CD9, Anti-CD63, Anti-CD81, Anti-TSG101, Anti-Alix | Exosome identification and quantification | Tetraspanin markers essential for validation; flow cytometry with CD63 beads enables sensitive detection [104] |
| Delivery Systems | Chitosan/Silk Hydrogel, Pluronic F-127 Hydrogel, Carboxymethyl Cellulose Gel | Therapeutic exosome formulation | Hydrogels extend retention and provide sustained release; clinical trials used CMC-based vehicles [104] [91] |
| Cell Culture Assays | Scratch/Migration Assays, MTT/Proliferation Assays, Tube Formation Assays | In vitro functionality assessment | Dose-dependent responses typically observed between 10-100 μg/mL exosome protein concentration [91] |
| Animal Models | STZ-Induced Diabetic Mice, Full-Thickness Excisional Wounds | In vivo efficacy evaluation | Diabetic models essential for chronic wound healing assessment; multiple administration routes possible [33] [104] |
The clinical trial and commercial landscape for MSC-derived exosomes in wound healing has progressed substantially, with robust preclinical evidence supporting multiple mechanisms of action and several products advancing through clinical development. The recent positive results from randomized controlled trials demonstrate the significant potential of MSC-Exos to address the substantial unmet needs in chronic wound treatment, particularly for diabetic foot ulcers. As the field advances, key focus areas include standardization of isolation and characterization protocols, optimization of delivery systems for enhanced retention and bioavailability, and resolution of scalability challenges for commercial production. The continuing translation of MSC-derived exosome research into clinically available therapies holds exceptional promise for revolutionizing regenerative approaches to wound management.
The pursuit of optimal wound healing represents a significant challenge in regenerative medicine, focusing on the critical processes of angiogenesis, scar reduction, and re-epithelialization. Current therapeutic strategies increasingly recognize the limitations of conventional treatments in achieving functional and aesthetic tissue restoration. Within this context, mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as a promising cell-free therapeutic alternative, leveraging the innate paracrine signaling capabilities of their parent cells while overcoming challenges related to safety, storage, and standardized administration [24] [107]. These nano-sized extracellular vesicles facilitate intercellular communication by transferring bioactive cargo—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating multiple phases of the wound healing cascade [107]. This systematic review synthesizes current evidence on therapeutic outcomes in wound management, with a specific focus on the role of MSC-exosomes in coordinating angiogenesis, scar reduction, and re-epithelialization through multifaceted molecular mechanisms.
Therapeutic Outcomes in Wound Healing: A Quantitative Synthesis
Re-epithelialization
Re-epithelialization, the process of epidermal regeneration across the wound bed, is crucial for restoring barrier function. A 2025 meta-analysis of randomized controlled trials demonstrated that autologous skin cell suspensions significantly accelerate this process compared to standard treatments, reducing the mean time to re-epithelialization by -1.71 days (95% CI: -2.73 to -0.70; p=0.001) [108]. However, this acceleration did not translate to significant improvements in complete healing rates by the 4th week (RR=0.98, 95% CI: 0.94-1.02, p=0.24), suggesting that while initiation is faster, final barrier restoration follows a similar timeline to conventional care [108].
Table 1: Quantitative Outcomes for Re-epithelialization Therapies
| Therapeutic Intervention | Outcome Measure | Effect Size/Results | Statistical Significance | Source |
|---|---|---|---|---|
| Autologous Skin Cell Suspension | Time to Re-epithelialization | MD: -1.71 days | p=0.001 | [108] |
| Autologous Skin Cell Suspension | Complete Healing by Week 4 | RR: 0.98 | p=0.24 | [108] |
| Retinoid-based Therapies | Re-epithelialization Rate | Accelerated | Preclinical evidence | [109] |
| MSC-derived Exosomes | Re-epithelialization Quality | Improved tissue architecture | Multiple animal studies | [107] |
Angiogenesis
Therapeutic angiogenesis focuses on re-establishing microvascular networks to support healing tissues. Small extracellular vesicle (sEV) interventions consistently promote angiogenesis in both diabetic and non-diabetic animal models, regardless of the cell source or production protocol [107]. Specific mechanisms include the transfer of pro-angiogenic miRNAs, such as miR-26a-5p, which downregulates MAP2K4 and enhances expression of vascular markers including CD31 [7]. Retinoids further contribute to angiogenesis by stimulating endothelial cell activity and supporting the maturation of newly formed vessels [109].
Table 2: Quantitative Outcomes for Angiogenesis Therapies
| Therapeutic Intervention | Key Angiogenic Markers | Effect on Markers | Model System | Source |
|---|---|---|---|---|
| AMSC-exosomes (miR-26a-5p) | CD31, VEGF Pathways | Upregulated | Mouse skin defect model | [7] |
| AMSC-exosomes (miR-26a-5p) | MAP2K4, Inflammatory Cytokines | Downregulated | Mouse skin defect model | [7] |
| sEV Interventions | Multiple Angiogenic Factors | Promoted angiogenesis | Diabetic and non-diabetic animal models | [107] |
| Retinoids | Endothelial Cell Function | Stimulated | In vitro and animal models | [109] |
Scar Reduction
Scar management represents a complex therapeutic challenge, with current approaches ranging from mechanical modulation to biologically-based strategies. Silicone-based products remain foundational, maintaining hydration and occlusion to improve scar pliability [110]. Laser therapies, including fractional CO2 and picosecond systems, achieve efficacy rates up to 90% for atrophic acne scars through controlled thermal injury that stimulates collagen remodeling [111]. MSC-derived exosomes contribute to improved scar quality by modulating collagen deposition and enhancing extracellular matrix organization, though a 2025 meta-analysis found no significant differences in Patient and Observer Scar Assessment Scale (POSAS) or Vancouver Scar Scale scores compared to standard treatments [108] [110].
Table 3: Scar Reduction Efficacy Across Interventions
| Therapeutic Intervention | Primary Mechanism | Reported Efficacy | Evidence Level | Source |
|---|---|---|---|---|
| Autologous Skin Cell Suspension | Cellular Regeneration | No significant improvement in POSAS/VSS | Meta-analysis of RCTs | [108] |
| Fractional Laser (CO2/Er:YAG) | Collagen Remodeling | Up to 90% improvement | Clinical studies | [111] |
| Picosecond Laser | LIOB-induced Neocollagenesis | 32-45% scar volume reduction | Clinical studies | [111] |
| MSC-derived Exosomes | ECM Modulation | Improved collagen architecture | Preclinical studies | [24] [107] |
| Fractional RF Microneedling | Thermal Denaturation + HSP70/MMP-3 Upregulation | Significant texture improvement | Clinical trials | [111] |
Molecular Mechanisms of MSC-Exosomes in Wound Healing
Signaling Pathways in Angiogenesis and Scar Reduction
MSC-exosomes exert their therapeutic effects through sophisticated molecular signaling networks that coordinate multiple aspects of wound healing. The following diagram illustrates key pathways through which MSC-exosomes, particularly those enriched with miR-26a-5p, modulate angiogenesis and inhibit fibrosis:
Diagram 1: MSC-Exosome Mediated Regulation of Wound Healing. MSC-derived exosomes deliver miR-26a-5p which targets MAP2K4, suppressing the TGF-β/Smad pathway and reducing collagen overproduction while promoting angiogenesis [7].
The molecular cargo of MSC-exosomes directly influences critical wound healing pathways. As shown in Diagram 1, exosomal miR-26a-5p targets MAP2K4, an upstream regulator of the MAPK cascade, resulting in downstream suppression of pro-fibrotic TGF-β1/Smad signaling [7]. This inhibition attenuates myofibroblast differentiation and reduces excessive collagen deposition (COL1A1, COL3A1), thereby mitigating scar formation. Concurrently, miR-26a-5p enhances angiogenesis through upregulation of CD31 and other vascular markers while suppressing pro-inflammatory cytokines (IL-6, IL-1β, TNF-α) that impede healing [7].
Retinoid Signaling in Scarless Regeneration
Retinoids offer a complementary approach to scar management through well-defined nuclear signaling pathways:
Diagram 2: Retinoid Signaling in Wound Repair. Retinoids activate RAR/RXR heterodimers to regulate gene expression, suppressing TGF-β1/Smad signaling and myofibroblast differentiation while promoting ECM remodeling, angiogenesis, and appendage regeneration [109].
Retinoid signaling operates through nuclear receptor activation, as depicted in Diagram 2. All-trans retinoic acid (atRA) binds to retinoic acid receptors (RARs) that form heterodimers with retinoid X receptors (RXRs). These complexes then recognize retinoic acid response elements (RAREs) in promoter regions of target genes [109]. This signaling suppresses TGF-β1-driven myofibroblast differentiation and collagen overproduction while simultaneously promoting angiogenesis and potentially enabling hair follicle neogenesis—a hallmark of truly regenerative healing [109].
Experimental Protocols for Key Methodologies
MSC-Exosome Isolation and Modification
Protocol 1: Isolation and Characterization of MSC-derived Exosomes
- Source Cell Culture: Culture human umbilical cord mesenchymal stem cells (hUCMSCs) in serum-free media optimized for MSC expansion. Validate MSC identity through flow cytometry for CD73, CD90, CD105 positivity and CD34, CD45 negativity [27].
- sEV Isolation: Collect conditioned media after 48-72 hours. Perform sequential centrifugation: 300 × g for 10 min (remove cells), 2,000 × g for 20 min (remove debris), 10,000 × g for 30 min (remove apoptotic bodies), followed by ultracentrifugation at 100,000 × g for 70 min to pellet sEVs [107].
- sEV Characterization: Resuspend pellets in PBS and characterize using:
- Nanoparticle Tracking Analysis: Determine particle size distribution and concentration (30-200 nm expected) [107].
- Transmission Electron Microscopy: Confirm cup-shaped morphology.
- Western Blotting: Verify positive markers (CD63, CD81, TSG101) and negative markers (calnexin) [107].
- Protein Quantification: Use BCA assay to standardize therapeutic doses.
Protocol 2: Genetic Modification of MSC-Exosomes
- Preconditioning: Incubate MSCs with inflammatory cytokines (IFN-γ, TNF-α) to enhance immunomodulatory cargo through "licensing" [27].
- miRNA Overexpression: Transduce MSCs with lentiviral vectors encoding miR-26a-5p. Select stable populations with puromycin [7].
- Functional Validation: Isify exosomes and validate miR-26a-5p enrichment using qRT-PCR. Confirm target engagement through luciferase reporter assay with MAP2K4 3'UTR [7].
In Vivo Wound Healing Assessment
Protocol 3: Animal Model of Cutaneous Wound Healing
- Animal Selection: Utilize C57BL/6 mice (8-10 weeks, male). For diabetic models, induce diabetes with streptozotocin (50 mg/kg for 5 days) and confirm hyperglycemia (>300 mg/dL) [7].
- Wound Creation: Anesthetize mice and create full-thickness excisional wounds (6-8 mm diameter) on dorsal skin. Use sterile punch biopsy tool [7].
- Treatment Administration: Randomize animals to experimental groups:
- Outcome Measures:
- Wound Closure: Document with digital photography daily. Calculate wound area reduction using ImageJ software.
- Histological Analysis: Harvest tissue at days 7, 14, and 28 post-wounding. Process for H&E staining (re-epithelialization), Masson's trichrome (collagen content), and immunohistochemistry (CD31 for angiogenesis, α-SMA for myofibroblasts) [7].
- Molecular Analysis: Isify RNA from wound tissue for qRT-PCR analysis of MAP2K4, IL-6, IL-1β, TNF-α, Col1a1, Col3a1, and α-SMA [7].
- Scar Assessment: Evaluate scar tissue using Manchester Scar Scale or digital viscoelasticity meters at day 28 [110].
Research Reagent Solutions for Wound Healing Studies
Table 4: Essential Research Reagents for Wound Healing Investigation
| Reagent/Category | Specific Examples | Research Function | Key Applications | Source |
|---|---|---|---|---|
| Stem Cell Sources | hUCMSCs, ADMSCs, BMMSCs | Paracrine signaling, immunomodulation | Exosome production, cellular therapy | [27] |
| sEV Isolation Kits | Ultracentrifugation systems, Size-exclusion chromatography | sEV purification and concentration | Therapeutic sEV preparation | [107] |
| Characterization Antibodies | CD63, CD81, TSG101, CD9 | sEV marker identification | sEV characterization and validation | [107] |
| Angiogenesis Assays | Matrigel tube formation, CD31 immunohistochemistry | In vitro and in vivo vessel formation | Angiogenic capacity assessment | [112] [113] |
| Scar Assessment Tools | Vancouver Scar Scale, POSAS | Quantitative scar evaluation | Clinical and research outcome measures | [110] |
| Cytokine/Chemokine Arrays | IL-6, IL-1β, TNF-α, TGF-β1 ELISA | Inflammatory mediator quantification | Monitoring immune responses | [7] |
| Gene Expression Analysis | qRT-PCR primers (MAP2K4, collagen types) | Molecular pathway analysis | Mechanism of action studies | [7] |
| Biomaterial Scaffolds | Hydrogels, Gelatin sponge/polydopamine | sEV delivery and retention | Controlled release systems | [24] |
This systematic review demonstrates that MSC-derived exosomes represent a promising therapeutic modality for coordinating the complex processes of angiogenesis, scar reduction, and re-epithelialization in wound healing. The quantitative synthesis of current evidence reveals that while certain interventions like autologous skin cell suspensions significantly accelerate re-epithelialization, and laser therapies substantially improve scar appearance, MSC-exosomes offer a unique advantage through their ability to simultaneously modulate multiple healing phases. Their molecular cargo, particularly when engineered with specific miRNAs like miR-26a-5p, can target key signaling pathways such as MAP2K4 and TGF-β/Smad to suppress fibrosis while promoting angiogenesis and regeneration. Future research directions should focus on optimizing exosome engineering, delivery systems, and dosage regimens to enhance therapeutic efficacy and facilitate clinical translation for improved wound management outcomes.
Conclusion
MSC-derived exosomes represent a paradigm shift in regenerative medicine, offering a powerful, cell-free therapeutic strategy for wound healing. They coordinate the complex process of skin repair through multifaceted mechanisms, including immunomodulation, angiogenesis promotion, and extracellular matrix remodeling. Their advantages over whole-cell therapies—such as superior safety profile, stability, and scalability—position them as a leading candidate for next-generation treatments. Future efforts must focus on standardizing manufacturing protocols, elucidating precise structure-function relationships of exosomal cargo, and conducting robust, controlled clinical trials. The successful translation of exosome-based therapies will require a collaborative framework involving basic scientists, clinical researchers, bioengineers, and regulators to fully realize their potential in transforming the standard of care for acute and chronic wounds.
References
- 1. - Mesenchymal : A novel and potential... stem cell derived exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 2. - MSC : roles and potential for tissue rep derived extracellular vesicles [https://www.dovepress.com/msc-derived-extracellular-vesicles-roles-and-molecular-mechanisms-for--peer-reviewed-fulltext-article-IJN]
- 3. Mesenchymal stem cell- derived : A paradigm shift in clinical... exosomes [https://pubmed.ncbi.nlm.nih.gov/40414452/]
- 4. Exosomal microRNAs derived from mesenchymal stem cells... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-020-00650-6]
- 5. Mesenchymal stem cell-derived exosomes: An emerging therapeutic strategy for normal and chronic wound healing - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8362559/]
- 6. Bioengineered MSC-derived exosomes in skin wound repair and regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009159/]
- 7. Frontiers | Exosomes from miR-26a-5p-modified adipose... derived [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1662095/full]
- 8. Exosome Derived From Human Umbilical Cord Mesenchymal Stem Cell Mediates MiR-181c Attenuating Burn-induced Excessive Inflammation - PubMed [https://pubmed.ncbi.nlm.nih.gov/27428420/]
- 9. from antler Exosomes promotes... derived mesenchymal stem cells [https://www.dovepress.com/exosomes-derived-from-antler-mesenchymal-stem-cells-promote-wound-heal-peer-reviewed-fulltext-article-IJN]
- 10. and Their Bioengineering Strategies in the Cutaneous... Exosomes [https://www.ijbs.com/v19p1430.htm]
- 11. Microenvironmental cue-regulated exosomes as therapeutic strategies... [https://www.nature.com/articles/s41427-022-00419-y?error=cookies_not_supported&code=e211ed4f-4d92-488d-8819-7546a41d805a]
- 12. Therapeutic potential of exosomal lncRNAs derived from stem cells in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11816792/]
- 13. Analysis: Cutting-Edge Research... - Creative Proteomics Exosome [https://www.creative-proteomics.com/resource/exosome-analysis-technology-proteomic-profiling.htm]
- 14. Precision exosome engineering for enhanced wound and... healing [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06578-0]
- 15. An Innovative Method for Exosome Quantification and Size... [https://www.jove.com/t/50974/an-innovative-method-for-exosome-quantification-and-size-measurement]
- 16. Stem cell derived exosome trilogy: an epic comparison of human MSCs, ESCs and iPSCs | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 17. Mesenchymal stem cell-derived exosomes as cell-free therapeutics: mechanistic insights and engineering strategies for liver disease treatment | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04747-y]
- 18. Adipose-derived stem cell exosomes: mechanisms and therapeutic potentials in wound healing | Biomarker Research | Full Text [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00801-2]
- 19. - MSC injectable hyaluronic acid hydrogel for... derived exosomes [https://pubmed.ncbi.nlm.nih.gov/40581219/]
- 20. Lipid, Protein, and MicroRNA Composition Within Mesenchymal Stem Cell-Derived Exosomes - PubMed [https://pubmed.ncbi.nlm.nih.gov/29782191/]
- 21. The microRNA regulatory landscape of MSC-derived exosomes: a systems view | Scientific Reports [https://www.nature.com/articles/s41598-018-19581-x]
- 22. released from human induced pluripotent stem... Exosomes [https://link.springer.com/article/10.1186/s12967-015-0417-0]
- 23. : The emerging mechanisms and potential clinical... Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929203/]
- 24. -derived Stem in cell : exosomes insights... wound healing mechanistic [https://pubmed.ncbi.nlm.nih.gov/41017563/]
- 25. longlifenutri.com/blogs/news/therapeutic-potential-of- exosomes -in... [https://www.longlifenutri.com/blogs/news/therapeutic-potential-of-exosomes-in-wound-healing-advanced-regenerative-care]
- 26. Editorial: Exosome-mediated intercellular communications: immune stimulation and suppression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700974/]
- 27. The Promising Role of Human Umbilical Cord Mesenchymal ... Stem [https://www.jwmr.org/journal/view.php?doi=10.22467/jwmr.2025.03258]
- 28. Decoding the Tumor Microenvironment: Exosome-Mediated Macrophage Polarization and Therapeutic Frontiers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223767/]
- 29. Molecular Pathophysiology of Chronic : Current State and... Wounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC10024648/]
- 30. Mesenchymal stem cell-derived exosomes: An emerging therapeutic strategy for normal and chronic wound healing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8362559/]
- 31. Therapeutic Potential of Stem Cell-Derived Exosomes in Skin Wound Healing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 32. Mechanisms and therapeutic opportunities in metabolic aberrations of... [https://www.nature.com/articles/s41419-025-07583-3?error=cookies_not_supported&code=12e33f3b-985c-49cd-851c-22170df04a91]
- 33. Stem cell-derived exosomes: emerging therapeutic opportunities for wound healing | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03345-0]
- 34. Nanomanaging Chronic Wounds with Targeted Exosome Therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945274/]
- 35. Mesenchymal stem cells in treating human diseases: molecular mechanisms and clinical studies | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02313-9]
- 36. Human mesenchymal stem cells - current trends and future prospective - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4413017/]
- 37. Therapeutic potential and mechanisms of mesenchymal ... stem [https://link.springer.com/article/10.1186/s12951-023-01778-6]
- 38. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue - PubMed [https://pubmed.ncbi.nlm.nih.gov/16410387/]
- 39. Analysis of Human Comparative from... Mesenchymal Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3794764/]
- 40. Transcriptomic Heterogeneity of Human Mesenchymal Stem Cells Derived from Bone Marrow, Dental Pulp, Adipose Tissue, and Umbilical Cord - PubMed [https://pubmed.ncbi.nlm.nih.gov/37384924/]
- 41. Comparison of molecular profiles of human mesenchymal stem cells derived from bone marrow, umbilical cord blood, placenta and adipose tissue - PubMed [https://pubmed.ncbi.nlm.nih.gov/26719857/]
- 42. Frontiers | The tiny giants of regeneration: MSC-derived extracellular vesicles as next-generation therapeutics [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 43. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? | Cell Death & Disease [https://www.nature.com/articles/s41419-022-05034-x]
- 44. The application of mesenchymal stromal cells (MSCs) and their derivative exosome in skin wound healing: a comprehensive review | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02697-9]
- 45. Combination of precipitation and size exclusion chromatography as... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10161387/]
- 46. Combination of precipitation and size exclusion chromatography as... [https://www.ntno.org/v07p0345.htm]
- 47. of Isolation from Blood Plasma: Qualitative and... Exosomes [https://pubmed.ncbi.nlm.nih.gov/26690353/]
- 48. Evaluation of immune and chemical precipitation ... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0242732]
- 49. Novel Methods for Exosome Isolation Based on Precipitation and... [https://link.springer.com/chapter/10.1007/978-3-031-89270-7_5]
- 50. Exosomal microRNAs from Mesenchymal Stem Cells: Novel... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10352215/]
- 51. Engineering Exosomes for Therapeutic Applications: Decoding Biogenesis, Content Modification, and Cargo Loading Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11268655/]
- 52. Integrative Modeling and Visualization of Exosomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9139774/]
- 53. Biodistribution of Exosomes and Engineering Strategies for Targeted ... [https://link.springer.com/article/10.1007/s13770-021-00361-0]
- 54. Frontiers | Mesenchymal stem cell- derived subpopulations... exosome [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1550447/full]
- 55. : advanced nanocarriers for Engineered therapy... exosomes targeted [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00334-1]
- 56. Engineering exosomes as refined biological nanoplatforms for drug delivery | Acta Pharmacologica Sinica [https://www.nature.com/articles/aps201712]
- 57. Human umbilical cord mesenchymal stem cell- derived ... exosomes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04538-5]
- 58. Exosomes derived from mesenchymal stem cells: A promising cell-free therapeutic tool for cutaneous wound healing - PubMed [https://pubmed.ncbi.nlm.nih.gov/36681232/]
- 59. - MSC in tissue regeneration | Frontiers derived ... exosomes Research [https://www.frontiersin.org/research-topics/30764/msc-derived-exosomes-in-tissue-regeneration/magazine]
- 60. Exosome-Laden Hydrogels: A Novel Cell-free Strategy for In-situ Bone Tissue Regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9011111/]
- 61. Hydrogels for Exosome Delivery in Biomedical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9223116/]
- 62. Frontiers | Exosome microsphere/nano silver loaded injectable ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1550276/full]
- 63. Printing of Microenvironmentâ€Specific Bioinspired and... 3 D [https://pmc.ncbi.nlm.nih.gov/articles/PMC10502685/]
- 64. Exosome-Integrated Hydrogels for Bone Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675329/]
- 65. Enhancing the wound process through local healing of... injection [https://pmc.ncbi.nlm.nih.gov/articles/PMC11237357/]
- 66. in skin care: Promise and challenges revealed in new study Exosomes [https://www.cosmeticsdesign.com/Article/2025/01/22/exosomes-in-skin-care-promise-and-challenges-revealed-in-new-study/]
- 67. Public Safety Notification on Exosome Products | FDA [https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/public-safety-notification-exosome-products]
- 68. from human induced pluripotent stem... Exosomes released [https://pubmed.ncbi.nlm.nih.gov/25638205/]
- 69. from human induced pluripotent stem... Exosomes released [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-015-0417-0]
- 70. Regulation of exosomes as biologic medicines: Regulatory challenges faced in exosome development and manufacturing processes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11307316/]
- 71. Mesenchymal Stem Cell- derived Hold Promise in the... Exosomes [https://www.dovepress.com/mesenchymal-stem-cell-derived-exosomes-hold-promise-in-the-treatment-o-peer-reviewed-fulltext-article-IJN]
- 72. Mesenchymal stem cell derived- exosomes : a modern approach in... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02622-3]
- 73. Regulation of cargo selection in exosome biogenesis and its biomedical applications in cancer | Experimental & Molecular Medicine [https://www.nature.com/articles/s12276-024-01209-y]
- 74. The Opportunities and Challenges of Mesenchymal Stem Cells-Derived... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11640604/]
- 75. The role of exosome heterogeneity in epithelial ovarian cancer - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2667394022000144]
- 76. Variability in protein cargo detection in technical and biological replicates of exosome-enriched extracellular vesicles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7051218/]
- 77. in protein Variability detection in technical and... | PLOS One cargo [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228871]
- 78. Exosomes in clinical trial and their production in compliance with good manufacturing practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7137364/]
- 79. Development of a Scalable GMP Manufacturing Process for Therapeutic Exosomes - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1465324925002579]
- 80. Waisman Biomanufacturing & RoosterBio Announce Collaboration for GMP Manufacturing of Cell & Exosome Therapies - RoosterBio [https://www.roosterbio.com/press_release/waisman-biomanufacturing-roosterbio-announce-collaboration-for-gmp-manufacturing-of-cell-exosome-therapies/]
- 81. Concise Review: MSC - Derived for Cell-Free Therapy Exosomes [https://pubmed.ncbi.nlm.nih.gov/28294454/]
- 82. Establishing a Working Range for Effective MSC -EV Dose - RoosterBio [https://www.roosterbio.com/blog/establishing-a-working-range-for-effective-msc-ev-dose/]
- 83. Frontiers | Bioengineered MSC - derived in skin exosomes ... wound [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1029671/full]
- 84. Advances in mesenchymal stem cell and exosome-based therapies for aging and age-related diseases | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 85. Frontiers | Mesenchymal - stem as a plausible... cell derived exosomes [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1563427/full]
- 86. Synergistic effects of mesenchymal stem cells and their secretomes with scaffolds in burn wound healing: a systematic review and meta-analysis of preclinical studies | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06712-y]
- 87. Extracellular vesicle-based drug overview: research landscape, quality control and nonclinical evaluation strategies | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02312-w]
- 88. Exploring Regulatory Frameworks for Exosome Therapy: Insights and Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371722/]
- 89. Exosomes: Company Spotlights from "A" to "Z" [https://bioinformant.com/exosomes/]
- 90. Past, present, and future of exosomes research in cancer: A bibliometric and visualization analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988232/]
- 91. Therapeutic potential of mesenchymal stem cell-derived exosomes for regenerative medicine applications | Clinical and Experimental Medicine [https://link.springer.com/article/10.1007/s10238-023-01282-z]
- 92. Frontiers | Mesenchymal stromal/ stem - cell as... derived exosomes [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1549096/full]
- 93. and Exosomes Therapy Advancements Accelerated and... Stem Cell [https://www.longdom.org/open-access/exosomes-and-stem-cell-therapy-advancements-accelerated-and-improved-burn-wound-healing-108240.html]
- 94. Frontiers | Bone marrow mesenchymal stem cell-derived exosomes alleviate DSS-induced inflammatory bowel disease in mice through inhibiting intestinal epithelial cell pyroptosis via delivery of TSG-6 [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1601591/full]
- 95. Advances in the Role of Stem - Cell in Derived ... Exosomes Diabetic [https://pubmed.ncbi.nlm.nih.gov/40821749/]
- 96. [Research advances on improving the therapeutic efficacy of...] [https://pubmed.ncbi.nlm.nih.gov/37805701/]
- 97. iPSC-Derived MSCs Are a Distinct Entity of MSCs with Higher Therapeutic Potential than Their Donor-Matched Parental MSCs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9821152/]
- 98. Mesenchymal stem cells-derived exosomes ameliorate blue light stimulation in retinal pigment epithelium cells and retinal laser injury by VEGF-dependent mechanism - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902357/]
- 99. Frontiers | Therapeutic application of mesenchymal -derived... stem cell [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1428793/full]
- 100. Role of Exosomes in Dermal Wound Healing: A Systematic Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9400548/]
- 101. - Negative in pressure : A systematic... wound therapy skin grafts [https://pubmed.ncbi.nlm.nih.gov/33814213/]
- 102. Comparative Analysis of Antibacterial and Wound Healing Activities of Chitosan and Povidone-Iodine-Based Hydrogels - PubMed [https://pubmed.ncbi.nlm.nih.gov/38198629/]
- 103. A toolkit for the quantitative evaluation of chronic wounds evolution for early detection of non-healing wounds - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0965206X21000279]
- 104. The transforming role of wharton’s jelly mesenchymal stem... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04690-y]
- 105. 5 Exosome Therapies in the Clinical Pipeline [https://www.delveinsight.com/blog/5-promising-exosome-based-therapies]
- 106. Exosome Therapies Market Poised for Explosive Growth During the Study Period (2025-2034) | DelveInsight [https://www.prnewswire.com/news-releases/exosome-therapies-market-poised-for-explosive-growth-during-the-study-period-20252034--delveinsight-302348895.html]
- 107. Efficacy and safety of small extracellular vesicle interventions in wound... [https://www.thno.org/v12p6455.htm]
- 108. Effect of Autologous Skin Cell Suspensions Versus Standard... [https://pubmed.ncbi.nlm.nih.gov/40142341/]
- 109. Frontiers | Retinoids in scarless skin regeneration: from molecular... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1683851/full]
- 110. A Comparative Analysis of the Advances in Scar Reduction: Techniques, Technologies, and Efficacy in Plastic Surgery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11392586/]
- 111. Frontiers | Advances in the treatment of acne scars [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1643035/full]
- 112. A novel quantitative assay based on visualized... angiogenesis [https://link.springer.com/article/10.1007/s10456-024-09967-z]
- 113. sciencedirect.com/topics/medicine-and-dentistry/ angiogenesis [https://www.sciencedirect.com/topics/medicine-and-dentistry/angiogenesis]