MSC-Derived Exosomes vs. Whole Cell Therapy: A Comparative Analysis of Functional Outcomes and Clinical Translation
This article provides a comprehensive analysis of the functional outcomes of mesenchymal stem cell (MSC)-derived exosomes compared to whole cell MSC therapy.
MSC-Derived Exosomes vs. Whole Cell Therapy: A Comparative Analysis of Functional Outcomes and Clinical Translation
Abstract
This article provides a comprehensive analysis of the functional outcomes of mesenchymal stem cell (MSC)-derived exosomes compared to whole cell MSC therapy. Aimed at researchers, scientists, and drug development professionals, it explores the foundational biology of both therapeutic agents, detailing the paracrine mechanisms of MSCs and the biogenesis, cargo, and cell-free nature of exosomes. The review covers methodological advances in production and isolation, alongside diverse preclinical and clinical applications in neurodegenerative, autoimmune, cardiovascular, and pulmonary diseases. It critically addresses key challenges in standardization, dosing, and manufacturing scalability. Finally, the article synthesizes evidence from clinical trials and advanced imaging studies to present a balanced comparison of safety, efficacy, and therapeutic potential, offering a roadmap for the future of regenerative medicine.
Unlocking the Biology: From MSC Paracrine Action to Exosome Biogenesis
For decades, the therapeutic mechanism of mesenchymal stem cells (MSCs) was attributed to their ability to engraft at injury sites and differentiate into functional tissue cells. However, a paradigm shift has occurred with the emergence of the paracrine hypothesis, which posits that MSCs exert their primary therapeutic effects through the secretion of bioactive molecules rather than through direct cellular replacement [1]. This cell-free mechanism is primarily mediated through extracellular vesicles (EVs), especially exosomes, which carry a complex cargo of proteins, lipids, and nucleic acids [2] [3]. This guide objectively compares the functional outcomes of MSC-derived exosomes versus whole cell therapy, providing researchers with experimental data and methodologies relevant to drug development.
The Scientific Foundation of the Paracrine Hypothesis
From Engraftment to Secretome: An Evolving Paradigm
The traditional view held that systemically administered MSCs would migrate to damaged tissues, engraft, and differentiate into specific cell types to repair defects. However, tracking studies revealed that most infused MSCs exhibit poor long-term engraftment and survival at injury sites, despite observed therapeutic benefits [3] [1]. This discrepancy led researchers to investigate alternative mechanisms, ultimately identifying the MSC secretome – the collection of factors these cells secrete – as the primary driver of their therapeutic effects [1].
The secretome includes both soluble factors (growth factors, cytokines, chemokines) and insoluble factors contained within extracellular vesicles [3]. These vesicles, particularly exosomes (30-150 nm in diameter), have emerged as crucial mediators of intercellular communication, transferring functional biomolecules to recipient cells [4]. MSC-derived exosomes (MSC-Exos) contain diverse cargo including cytokines, growth factors, signaling lipids, mRNAs, and regulatory miRNAs that can alter target cell metabolism and function [2]. This discovery has fundamentally reshaped our understanding of MSC therapeutics and opened new avenues for cell-free regenerative approaches.
Key Paracrine Mediators and Their Functions
Table 1: Key Bioactive Components of the MSC Paracrine Secretome
| Component Category | Key Examples | Primary Functions |
|---|---|---|
| Soluble Factors | VEGF, HGF, TGF-β, PGE2, IDO | Angiogenesis, antifibrotic effects, immunomodulation, tissue repair [1] |
| Extracellular Vesicles | Exosomes, Microvesicles | Intercellular communication, cargo delivery (proteins, RNAs, lipids) [4] [3] |
| Mitochondria | Whole mitochondria | Mitochondrial transfer to damaged cells, restoration of bioenergetics [1] |
MSCs engage with parenchymal cells and facilitate the restoration and rejuvenation of damaged tissues through direct cell-cell contact and the release of these signaling molecules [4]. Damage-associated molecular patterns (DAMPs) and alarmins generated by damaged cells trigger MSC activation, which in turn prevents apoptosis of unaffected parenchymal cells, promoting survival and multiplication [4]. The composition of the MSC secretome is not static but dynamically responsive to the local microenvironment, indicating that MSC exosome content can be altered when MSCs are cultured with tumor cells or in specific in vivo environments [2].
Comparative Analysis: MSC-Derived Exosomes vs. Whole Cell Therapeutics
Mechanism of Action Comparison
Table 2: Functional Comparison of MSC vs. MSC-Exos Therapies
| Parameter | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Primary Mechanism | Direct differentiation (limited) & paracrine signaling [1] | Pure paracrine effect via biomolecule transfer [2] [5] |
| Immunomodulation | Inhibits T-cell proliferation, promotes M2 macrophage polarization [1] | Suppresses B-cell maturation, inhibits DC maturation, modulates T-cells [4] |
| Tissue Repair | Secretes trophic factors (VEGF, bFGF, HGF) [1] | Transfers regenerative miRNAs and proteins [3] [6] |
| Mitochondrial Transfer | Direct donation via tunneling nanotubes [1] | Not demonstrated; primarily biomolecule transfer |
| Biodistribution | Often trapped in lung microvasculature; limited target tissue homing [5] | Superior tissue penetration; crosses biological barriers including blood-brain barrier [3] |
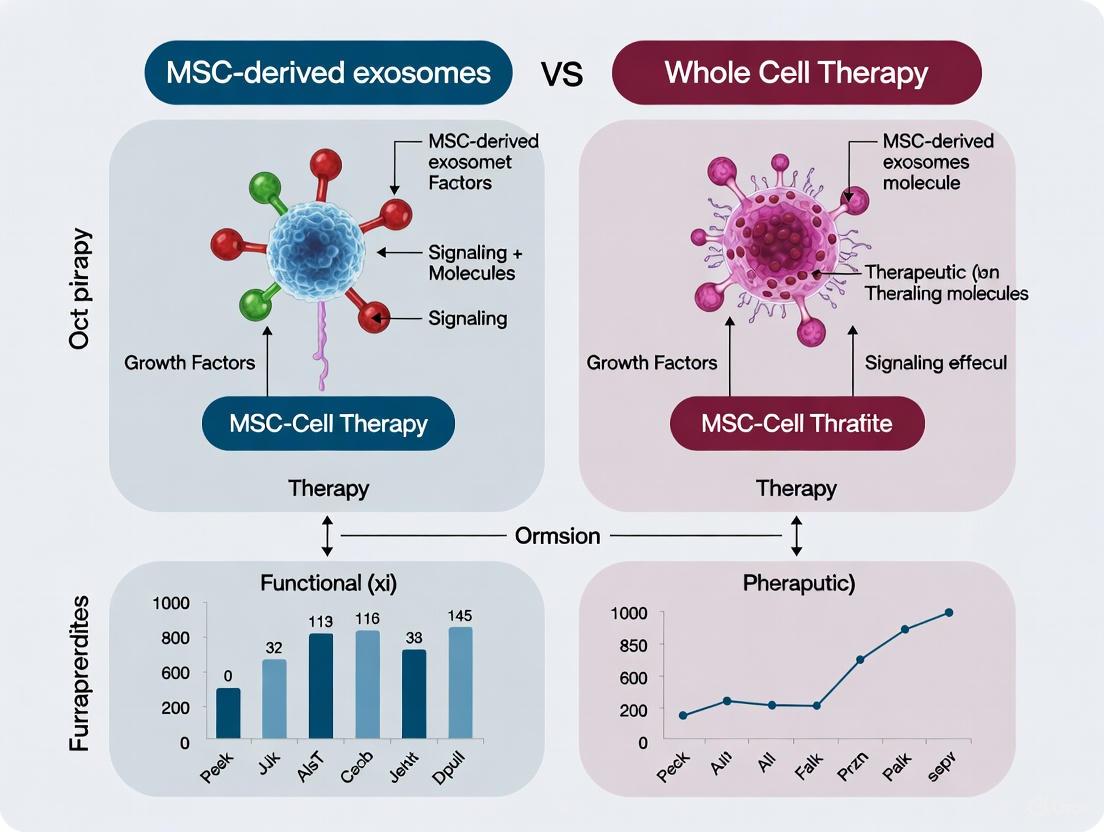
The following diagram illustrates the central hypothesis that MSCs primarily function through paracrine signaling, with exosomes as key mediators:
Therapeutic Efficacy and Clinical Translation
Table 3: Clinical Translation Status Comparison
| Aspect | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Clinical Trial Volume | ~1,742 registered trials worldwide [7] | 64 registered clinical trials [3] |
| Approved Products | 10 approved products (Alofisel, Prochymal, etc.) [7] | None yet fully approved |
| Standardization | Established but heterogeneous [5] | Limited standardization; methods evolving [3] |
| Administration Routes | Intravenous, local implantation [5] | IV, inhalation, local; more versatile [5] |
| Safety Profile | Infusion-related toxicities, pulmonary entrapment [5] | Higher safety profile; reduced adverse effects [3] |
The therapeutic efficacy of both approaches has been demonstrated across multiple disease models. MSC-derived exosomes have shown significant benefits in animal models of neurological disorders (epilepsy, Parkinson's disease, stroke), autoimmune diseases (multiple sclerosis, rheumatoid arthritis, type 1 diabetes), and conditions requiring tissue regeneration (cardiac, hepatic, and renal) [5]. Whole MSC therapies have demonstrated clinical efficacy in graft-versus-host disease (GVHD), Crohn's disease, and myocardial infarction [1] [7].
Experimental Evidence and Methodologies
Key Experimental Models Demonstrating Paracrine Effects
Transwell Coculture Systems
Protocol Overview: This methodology examines paracrine communication without direct cell-cell contact. MSCs are cultured in the upper chamber while target cells (e.g., myogenic cells, immune cells) are placed in the lower chamber, separated by a semi-permeable membrane [8].
Key Findings: In studies examining muscle regeneration, both iPSC-derived MSCs (iMSCs) and bone marrow-derived MSCs (BM-MSCs) promoted the proliferation and differentiation of human myogenic cells in this system [8]. The fusion index of human myogenic cells increased significantly when cocultured with MSCs, demonstrating enhanced maturation through paracrine factors alone.
Data Interpretation: This experimental setup provides direct evidence for the paracrine hypothesis by eliminating the possibility of direct differentiation or cell-cell contact. The results confirm that soluble factors and vesicles secreted by MSCs can independently mediate therapeutic effects.
Substrate Mechanical Properties Studies
Protocol Overview: MSCs are cultured on polyacrylamide hydrogels of varying stiffness (0.2 kPa vs. 100 kPa) to investigate how mechanical cues influence paracrine activity [9].
Key Findings: Conditioned medium from MSCs cultured on soft substrates (0.2 kPa) promoted MSC osteogenesis and adipogenesis, enhanced angiogenesis, and increased macrophage phagocytosis. In contrast, conditioned medium from stiff substrates (100 kPa) boosted MSC proliferation [9]. Proteomic analysis identified differential secretion of IL-6, OPG, TIMP-2, MCP-1, and sTNFR1 based on substrate stiffness.
Data Interpretation: These findings demonstrate that the MSC secretome is not static but dynamically responsive to physical microenvironmental cues. This has significant implications for manufacturing potent MSCs for specific clinical applications and designing biomaterials that optimize MSC activity after delivery.
The following diagram illustrates the experimental workflow for evaluating paracrine effects:
Immunomodulatory Mechanisms of MSC-Exosomes
MSC-derived exosomes exert comprehensive effects on both innate and adaptive immune systems. The following diagram details their key immunomodulatory pathways:
Specific immunomodulatory effects include:
- B-cell Regulation: MSC-exosomes are internalized by activated B cells, resulting in inhibition of B cell proliferation, differentiation, antibody production, and maturation of memory B cells [4]. They prompt B cells to downregulate the PI3K/Akt signaling pathway via miR-155-5p, inhibiting B cell proliferation and diminishing activation potential [4].
- Macrophage Polarization: MSC-exosomes guide macrophage polarization by converting pro-inflammatory M1 macrophages into anti-inflammatory M2 phenotypes through signaling molecules like interleukin-10 (IL-10) and transforming growth factor-beta (TGF-β) [1].
- T-cell Modulation: MSC-exosomes inhibit T-cell proliferation through the secretion of immunosuppressive agents such as prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), and programmed death-ligand 1 (PD-L1), thereby tempering overactive immune responses [1].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Key Research Reagents and Experimental Solutions
| Reagent/Solution | Function in Paracrine Research | Application Examples |
|---|---|---|
| Transwell Systems | Permeable supports for coculture without direct contact | Studying paracrine effects on target cells [8] |
| Polyacrylamide Hydrogels | Tunable stiffness substrates | Investigating mechanotransduction on secretome [9] |
| Ultracentrifugation | Gold standard for exosome isolation | MSC-Exos purification for functional studies [5] |
| Tangential Flow Filtration | Scalable EV purification | Clinical-grade exosome production [5] |
| CD73/CD90/CD105 Antibodies | MSC characterization markers | Confirming MSC phenotype per ISCT criteria [1] |
| Cytokine Array Kits | Multiplex secretome analysis | Identifying key paracrine factors [8] |
| Alizarin Red/Oil Red O | Differentiation capacity assessment | Verifying MSC multipotency [8] |
The selection of appropriate reagents and methodologies is critical for rigorous investigation of MSC paracrine activities. Researchers should implement quality control measures including:
- Characterization Standards: Follow MISEV2018 guidelines for extracellular vesicle characterization, including positive markers (CD63, CD81, CD9) and negative markers [5].
- Potency Assays: Establish disease-relevant functional assays rather than relying solely on particle count or protein content [5].
- GMP Compliance: Implement good manufacturing practice standards for clinical-grade production, including monitoring of cell culture environment, cultivation system, and culture medium [5].
The evidence supporting the paracrine hypothesis has transformed our approach to MSC therapeutics, shifting focus from cell replacement to biomolecule delivery. MSC-derived exosomes represent a promising cell-free therapeutic tool with significant advantages in safety, standardization, and manufacturing. However, whole cell therapies maintain unique capabilities such as mitochondrial transfer and dynamic response to local microenvironments.
Future research directions should address key challenges in MSC-exosome therapeutics, including standardization of production processes, enhancement of targeting capabilities for in vivo delivery, and generation of comprehensive long-term biodistribution data [3]. Interdisciplinary technologies such as 3D dynamic culture, genetic engineering, and intelligent slow-release systems are expected to facilitate the transition of MSC-exosomes from laboratory tools to clinically approved "programmable nanomedicines" [3].
For drug development professionals, the evolving landscape suggests a complementary rather than exclusive approach to whole cell versus exosome therapies. The choice between these modalities should be guided by specific clinical indications, mechanism of action requirements, and manufacturing considerations. As the field advances, the paracrine hypothesis continues to open new avenues for precision medicine in regenerative applications.
Exosomes, nanosized extracellular vesicles formed within multivesicular bodies (MVBs) and released via fusion with the plasma membrane, have emerged as pivotal mediators of intercellular communication. This review delineates the fundamental biological principles of exosomes, focusing on their complex biogenesis, diverse molecular cargo, and functional roles. Particular emphasis is placed on exosomes derived from mesenchymal stromal/stem cells (MSCs) and their emerging potential as cell-free therapeutic agents. Within the context of a broader thesis on functional outcomes, this article provides a direct comparison between MSC-derived exosomes and whole cell therapy, evaluating their respective mechanisms, therapeutic efficacy, and practical applications in regenerative medicine and immunomodulation. By synthesizing current scientific evidence, we aim to provide researchers and drug development professionals with a comprehensive framework for understanding exosomes as key MSC messengers and their translational potential.
Exosomes are small, membrane-bound extracellular vesicles with a diameter typically ranging from 30 to 150 nanometers, though some sources extend this range to 200 nm [10] [11]. First discovered in the 1980s during studies of reticulocyte maturation, exosomes were initially regarded as cellular waste disposal mechanisms [12] [13]. The term "exosome" was coined by Rose Johnstone in 1987, reflecting the process that seemed akin to reverse endocytosis, with internal vesicular contents released rather than external molecules internalized [13] [14]. However, over the past two decades, extensive research has revealed that exosomes play crucial roles in intercellular communication by transferring functional proteins, lipids, nucleic acids, and other bioactive molecules between cells [10] [15].
These vesicles are now recognized as key mediators in various physiological and pathological processes, including immune responses, tissue repair, central nervous system communication, and cancer progression [10]. The composition of exosomes reflects their cell of origin and their biological status, making them valuable as potential diagnostic biomarkers and therapeutic vehicles [15] [16]. Among different exosome sources, those derived from mesenchymal stromal/stem cells (MSCs) have garnered significant research interest due to their robust immunomodulatory and regenerative properties, positioning them as promising cell-free therapeutic alternatives to whole cell therapy [11] [2] [5].
Exosome Biogenesis: From Endocytosis to Secretion
Exosome biogenesis is a complex, multi-step process that occurs within the endosomal system, culminating in the release of intraluminal vesicles (ILVs) into the extracellular space as exosomes. This sophisticated cellular machinery involves several coordinated stages:
Endocytosis and Early Endosome Formation
The biogenesis pathway initiates with the inward budding of the plasma membrane, forming early endosomes that encapsulate extracellular components and membrane proteins [12] [10]. These early endosomes serve as the sorting stations for cargo destined for various intracellular destinations, including degradation, recycling, or secretion.
MVB Formation and ILV Generation
Early endosomes mature into late endosomes or multivesicular bodies (MVBs) through a process characterized by the inward budding of the endosomal membrane, generating numerous intraluminal vesicles (ILVs) within the lumen of the organelles [12] [13] [15]. These ILVs eventually become exosomes upon secretion. The formation of ILVs is mediated through several distinct but sometimes overlapping molecular mechanisms:
ESCRT-Dependent Pathway
The Endosomal Sorting Complex Required for Transport (ESCRT) machinery is a well-characterized pathway for ILV formation [12] [10] [16]. Comprising four complexes (ESCRT-0, -I, -II, -III) and associated proteins (particularly VPS4 ATPase), this system works sequentially to mediate membrane budding and scission. ESCRT-0, consisting of Hrs and STAM, recognizes and clusters ubiquitinated cargo proteins. ESCRT-I and -II are then recruited to drive membrane deformation, while ESCRT-III forms filaments that constrict the membrane neck before VPS4-mediated ATP hydrolysis enables membrane fission and ILV release [12] [16].
ESCRT-Independent Pathways
Several ESCRT-independent mechanisms also contribute to exosome biogenesis. The most studied involves neutral sphingomyelinase 2 (nSMase2), which catalyzes the conversion of sphingomyelin to ceramide [12]. Ceramide molecules possess cone-shaped structures that spontaneously induce membrane curvature, facilitating ILV formation. This pathway has been shown to mediate the sorting of specific cargoes, such as proteolipid protein in oligodendroglia cells and certain RNAs in cancer cells [12]. Other ESCRT-independent mechanisms involve tetraspanin proteins (CD63, CD9, CD81) and lipids like lysobisphosphatidic acid (LBPA), which can promote ILV formation through specific molecular interactions [12] [10].
MVB Fate and Exosome Release
Once formed, MVBs face one of two potential fates: degradation through fusion with lysosomes or autophagosomes, or secretion through fusion with the plasma membrane [12] [13]. The fate decision appears to depend on specific MVB subpopulations, with only certain MVBs destined for exosome release [13]. For instance, in B-lymphocytes, cholesterol-rich MVBs are more likely to fuse with the plasma membrane and release exosomes [13]. The transport of MVBs to the plasma membrane involves the cytoskeletal network and Rab GTPase proteins, while SNARE complexes facilitate the fusion process itself [10]. Upon fusion, ILVs are released into the extracellular space as exosomes, ready to participate in intercellular communication.
Table 1: Key Molecular Machinery in Exosome Biogenesis
| Biological Process | Key Molecular Components | Primary Function |
|---|---|---|
| Cargo Recognition | ESCRT-0 (Hrs, STAM), Ubiquitin | Identifies and clusters cargo proteins for sorting |
| Membrane Budding | ESCRT-I/-II, Ceramide, Tetraspanins | Mediates inward budding of endosomal membrane |
| Vesicle Scission | ESCRT-III, VPS4 ATPase | Executes membrane abscission to form ILVs |
| MBV Transport | Rab GTPases, Cytoskeletal Elements | Moves MVBs to plasma membrane |
| Membrane Fusion | SNARE Proteins, Annexins | Mediates fusion of MVBs with plasma membrane |
Figure 1: Exosome Biogenesis Pathways. This diagram illustrates the key steps in exosome formation, including both ESCRT-dependent and ESCRT-independent mechanisms, culminating in MVB fusion with the plasma membrane and exosome release.
Molecular Composition of Exosomes
Exosomes possess a sophisticated molecular architecture that reflects their biogenesis pathway and cellular origin. Their composition is not random; rather, it represents a selective enrichment of specific biomolecules that define exosome identity and function.
Protein Cargo
Exosomes carry a diverse array of proteins that can be broadly categorized into three groups:
Conserved Universal Proteins: These include proteins involved in exosome biogenesis such as ESCRT components (TSG101, Alix), tetraspanins (CD9, CD63, CD81), heat shock proteins (HSP70, HSP90), fusion proteins (Annexins, Rab GTPases), and cytoskeletal components [10] [15] [16]. These molecules are commonly used as exosome markers for identification and characterization.
Cell-Type-Specific Proteins: Exosomes carry proteins characteristic of their cell of origin. For instance, MSC-derived exosomes contain factors related to immunomodulation and tissue repair, while exosomes from antigen-presenting cells may carry MHC class I and II molecules [10] [11].
Context-Dependent Proteins: The protein profile of exosomes can change based on the physiological or pathological state of the parent cell. Cancer-derived exosomes, for example, often contain oncoproteins, growth factors, and matrix metalloproteinases that facilitate tumor progression [12] [16].
Nucleic Acid Cargo
Exosomes are rich in various nucleic acid species that can be transferred to recipient cells to alter gene expression and cellular function:
RNAs: Exosomes contain diverse RNA populations, including messenger RNAs (mRNAs), microRNAs (miRNAs), long non-coding RNAs (lncRNAs), transfer RNAs (tRNAs), ribosomal RNAs (rRNAs), and other non-coding RNAs [10] [15] [16]. miRNAs are among the most studied exosomal RNAs, with demonstrated roles in post-transcriptional regulation in recipient cells.
DNA Content: Exosomes can carry various forms of DNA, including single-stranded DNA, double-stranded DNA, mitochondrial DNA, and even genomic DNA fragments, particularly from cancer cells [15] [16]. This DNA content has implications for both disease diagnosis and progression.
Lipid Composition
The lipid bilayer of exosomes is enriched in specific lipid species that contribute to their structure and function:
Table 2: Major Lipid Components of Exosomes
| Lipid Category | Specific Molecules | Functional Significance |
|---|---|---|
| Structural Lipids | Cholesterol, Phosphatidylserine, Phosphatidylcholine | Membrane integrity, rigidity, and stability |
| Sphingolipids | Ceramide, Sphingomyelin | Membrane curvature, microdomain formation, signaling |
| Glycolipids | Gangliosides, Glycosphingolipids | Cell recognition, adhesion, and receptor function |
| Phospholipids | Lysobisphosphatidic acid (LBPA) | Endosomal membrane organization, Alix interaction |
This unique lipid composition not only provides structural stability but also facilitates exosome uptake by recipient cells and participates in cellular signaling pathways [10] [15].
MSC-Derived Exosomes as Therapeutic Agents
Mesenchymal stromal/stem cells (MSCs) have demonstrated significant potential in regenerative medicine and immunomodulation. However, growing evidence indicates that many of their therapeutic effects are mediated primarily through paracrine factors, with exosomes emerging as key mediators [11] [2] [14]. MSC-derived exosomes (MSC-Exos) retain the biological activity of their parent cells while offering several advantages as cell-free therapeutics.
Functional Mechanisms of MSC-Exos
MSC-Exos exert their therapeutic effects through multiple interconnected mechanisms:
Immunomodulation: MSC-Exos can modulate immune responses by transferring regulatory molecules to immune cells. They have been shown to promote anti-inflammatory M2 macrophage polarization, suppress T-cell proliferation, and increase regulatory T-cell populations through the transfer of miRNAs like miR-21, miR-146a, and miR-181, as well as immunomodulatory proteins [11] [17].
Tissue Regeneration: MSC-Exos enhance tissue repair by stimulating angiogenesis, cell proliferation, and differentiation while inhibiting apoptosis. For instance, in wound healing models, MSC-Exos accelerate re-epithelialization, collagen deposition, and neovascularization by activating Wnt/β-catenin and AKT signaling pathways [17].
Anti-fibrotic Effects: In models of organ fibrosis (liver, kidney, lung), MSC-Exos have demonstrated the ability to reduce fibrotic tissue formation by decreasing the activation of profibrotic pathways and reducing extracellular matrix deposition [11].
Neuroprotection: MSC-Exos support neuronal survival and regeneration in neurological disorders by transferring neuroprotective factors, promoting neurite outgrowth, and modulating inflammatory responses in the central nervous system [5].
Comparative Analysis: MSC-Exos vs. Whole Cell Therapy
The transition from MSC-based cell therapy to exosome-based cell-free therapy represents a paradigm shift in regenerative medicine. The table below provides a direct comparison of these two approaches:
Table 3: Functional Comparison: MSC-Derived Exosomes versus Whole Cell Therapy
| Parameter | MSC-Derived Exosomes | Whole MSC Therapy |
|---|---|---|
| Therapeutic Cargo | Proteins, lipids, nucleic acids (pre-packaged) | Live cells producing various factors |
| Immunogenicity | Low (reduced MHC expression) | Moderate to high (risk of immune recognition) |
| Tumor Risk | Minimal (non-replicative) | Potential concern with uncontrolled differentiation |
| Delivery Safety | Reduced risk of vascular occlusion (nanoscale) | Risk of pulmonary embolism (microscale cells) |
| Production & Storage | More stable, suitable for off-the-shelf use | Cryopreservation challenges, viability concerns |
| Dosing Precision | Quantifiable by particle count or protein content | Challenging (cell number ≠ functional potency) |
| Manufacturing | Scalable under GMP conditions | Complex expansion, higher contamination risk |
| Regulatory Pathway | Evolving as biological products/bioengineered drugs | Complex cellular therapy regulations |
| Targeting Potential | Modifiable surface for enhanced specificity | Limited homing efficiency, poor target retention |
| Mechanistic Clarity | Defined molecular cargoes | Multiple overlapping mechanisms |
Clinical Translation of MSC-Exos
The therapeutic potential of MSC-Exos is being actively explored in clinical settings. As of 2023, seven clinical studies have been published, and at least 14 clinical trials are registered, investigating MSC-Exos for conditions including acute respiratory distress syndrome (ARDS), kidney diseases, graft-versus-host disease (GvHD), osteoarthritis, stroke, Alzheimer's disease, and type 1 diabetes [5]. These studies utilize MSC-Exos from various sources, with adipose tissue being the most common (7 studies), followed by bone marrow (5 studies) and umbilical cord (4 studies) [5].
Dosing in these clinical studies varies considerably, with some calculating exosome amount by weight (micrograms), others by particle number, and some simply stating the number of MSCs used to generate the exosomes [5]. This highlights the need for standardization in exosome quantification and dosing protocols for clinical applications.
Experimental Methodologies in Exosome Research
Robust experimental protocols are essential for advancing exosome research and therapeutic applications. This section outlines key methodologies for exosome isolation, characterization, and functional analysis.
Exosome Isolation Techniques
Several methods are employed for exosome isolation, each with distinct advantages and limitations:
Ultracentrifugation-Based Methods
Differential Ultracentrifugation (DUC): This remains the gold standard and most widely used method (approximately 56% of studies) [14]. The protocol involves sequential centrifugation steps: (1) 300 × g for 10 min to remove cells; (2) 2,000 × g for 10 min to remove cell debris; (3) 10,000 × g for 30 min to remove larger vesicles and organelles; and (4) 100,000-120,000 × g for 70 min to pellet exosomes. The final pellet is resuspended in PBS or appropriate buffer [14]. While suitable for large volumes, DUC may co-isolate non-exosomal components like protein aggregates and lipoproteins.
Density Gradient Ultracentrifugation (DGUC): This method provides higher purity by separating vesicles based on buoyant density in iodixanol, CsCl, or sucrose gradients [14]. Exosomes typically band at densities of 1.13-1.19 g/ml in sucrose gradients. Though more time-consuming, DGUC effectively separates exosomes from soluble proteins and other contaminants.
Alternative Isolation Methods
Tangential Flow Filtration (TFF): This size-based filtration method uses hollow fiber membranes to concentrate and purify exosomes from large volume samples [5]. TFF offers advantages for scalable GMP-compliant production and has been used in some clinical trials [5].
Precipitation Methods: Commercial polymer-based kits precipitate exosomes by reducing their solubility. While user-friendly and rapid, these methods may co-precipitate non-vesicular contaminants.
Immunoaffinity Capture: Antibodies against exosome surface markers (CD9, CD63, CD81) enable highly specific isolation but may select subpopulations and are less suitable for large-scale preparation.
Exosome Characterization
Comprehensive exosome characterization should include multiple complementary approaches, following MISEV2018 guidelines [5]:
Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration based on Brownian motion.
Electron Microscopy: Visualizes exosome morphology, typically showing cup-shaped structures after chemical fixation and dehydration.
Western Blotting: Confirms presence of exosome markers (CD9, CD63, CD81, TSG101, Alix) and absence of negative markers (calnexin, GM130).
Flow Cytometry: Enumerates exosomes and detects surface markers using antibody-conjugated beads or high-sensitivity flow cytometers.
Functional Assays for MSC-Exos
To evaluate the therapeutic potential of MSC-Exos, researchers employ various functional assays:
In Vitro Uptake Studies: Fluorescent labeling (PKH67, DID) followed by confocal microscopy or flow cytometry to track exosome internalization by recipient cells.
Migration/Proliferation Assays: Scratch/wound healing assays, Transwell migration chambers, and MTT/XTT assays to assess effects on cell motility and growth.
Angiogenesis Assays: Tube formation assays using endothelial cells on Matrigel to evaluate pro-angiogenic properties.
Immunomodulation Assays: Mixed lymphocyte reactions, T-cell proliferation assays, and macrophage polarization studies to assess immune regulatory functions.
Animal Disease Models: In vivo administration in clinically relevant models (e.g., myocardial infarction, skin wounds, neurological disorders) to evaluate therapeutic efficacy.
Figure 2: Experimental Workflow for Exosome Research. This diagram outlines the key steps in exosome isolation, characterization, and functional analysis, highlighting major methodological approaches at each stage.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful exosome research requires specialized reagents and materials for isolation, characterization, and functional analysis. The following table details essential tools for working with MSC-derived exosomes:
Table 4: Essential Research Reagents for Exosome Studies
| Category | Specific Reagents/Materials | Primary Application | Technical Notes |
|---|---|---|---|
| Isolation Materials | Polycarbonate ultracentrifuge bottles/tubes, 0.22μm filters, Sucrose/iodixanol gradients, Tangential Flow Filtration systems | Exosome purification | Choose appropriate tube materials compatible with high g-forces; pre-clear samples to reduce contaminants |
| Characterization Antibodies | Anti-CD63, Anti-CD9, Anti-CD81, Anti-TSG101, Anti-Alix, Negative markers (Calnexin, GM130) | Exosome identification and validation | Combine multiple positive markers for definitive identification; include negative controls |
| Visualization Reagents | PKH67/PKH26 lipophilic dyes, DID membrane labels, Colloidal gold (EM), Uranyl acetate (negative staining) | Exosome tracking and morphology | Optimize dye concentration to avoid aggregation artifacts; use appropriate fixation for EM |
| Functional Assay Kits | MTT/XTT cell proliferation kits, Transwell migration chambers, Matrigel for tube formation, ELISA cytokine panels | Assessment of exosome bioactivity | Include appropriate controls (e.g., donor cell-conditioned media, heat-inactivated exosomes) |
| Molecular Analysis Tools | RNA isolation kits (with small RNA protection), Protease inhibitors, BCA/ Bradford protein assays, RNA sequencing libraries | Cargo analysis | Implement rigorous quality control for RNA/protein extraction from limited exosome samples |
| Animal Study Materials | In vivo imaging systems, Fluorescent dyes (DIR/DID), IVIS imaging chambers, Tissue fixation/permeabilization buffers | In vivo tracking and efficacy | Consider route of administration (IV, local, inhalation) based on target tissue |
Exosomes represent sophisticated natural nanovehicles that play essential roles in intercellular communication, particularly as key messengers for MSC-mediated therapeutic effects. Their defined biogenesis pathways, selective cargo loading mechanisms, and ability to horizontally transfer bioactive molecules position them as crucial components of the MSC paracrine system. The comparative analysis presented in this review demonstrates that MSC-derived exosomes offer significant advantages over whole cell therapies, including reduced risks, improved safety profiles, and more precise therapeutic targeting.
As the field advances, standardizing isolation protocols, enhancing exosome engineering for specific targeting, and establishing regulatory frameworks will be critical for clinical translation. The ongoing clinical trials with MSC-derived exosomes highlight the growing interest in this cell-free therapeutic approach. For researchers and drug development professionals, understanding the fundamental biology of exosomes and their functional comparison with whole cell therapies provides a foundation for developing next-generation regenerative medicines that leverage the natural communicative properties of these remarkable extracellular vesicles.
The field of regenerative medicine is witnessing a paradigm shift from whole-cell therapies toward cell-free approaches utilizing extracellular vesicles (EVs). Mesenchymal stromal/stem cells (MSCs) have been central to this evolution, with their therapeutic effects increasingly attributed to paracrine signaling rather than direct cell replacement [18]. This guide provides a detailed comparison of the physical and functional properties of MSC-derived exosomes (MSC-Exos) versus whole MSC therapies, offering researchers a scientific framework for therapeutic development. MSC-Exos represent a distinct class of nanoscale biologics with unique biophysical characteristics that fundamentally differentiate them from cellular therapeutics [19] [18]. Understanding these differences is critical for selecting appropriate therapeutic platforms for specific applications in drug development.
Physical and Biological Properties Comparison
Table 1: Comparative physical and biological properties of MSC-derived exosomes versus whole MSCs
| Property | MSC-Derived Exosomes | Whole MSC Therapeutics |
|---|---|---|
| Size Range | 30-150 nm [18] [20] | 15-30 μm (cellular scale) [19] |
| Structure | Lipid bilayer vesicles, no organelles [20] | Complete cellular structure with organelles [19] |
| Biogenesis | Endosomal pathway via multivesicular bodies [18] [20] | Cell division and differentiation [19] |
| Cargo Content | Proteins, lipids, nucleic acids (miRNA, mRNA) [18] | Complete cellular machinery, organelles, genetic material [19] |
| Primary Mechanism | Paracrine signaling via biomolecule transfer [18] | Direct differentiation and paracrine signaling [19] |
| Blood-Brain Barrier Penetration | Demonstrated capability [21] [22] | Limited without disruption [18] |
| Storage Requirements | -80°C with stabilizers; avoid freeze-thaw cycles [23] | Cryopreservation with DMSO; requires viability testing [18] |
| Circulation Half-life | Approximately 10-30 minutes post-IV injection [21] | Short persistence; rapid clearance after administration [18] [24] |
| Immunogenicity | Low; lack MHC complexes [18] | Low but present; risk of immune rejection [18] |
| Tumorigenic Risk | Minimal; non-replicative [18] | Theoretical concerns despite low probability [18] |
| Scalable Production | Challenging; requires advanced bioreactor systems [18] | Established expansion protocols [18] |
Experimental Methodologies for Characterization
Isolation and Purification Protocols
MSC-Exos Isolation Techniques
- Ultracentrifugation: Considered the gold standard; involves sequential centrifugation steps to remove cells, debris, and larger vesicles, followed by high-speed centrifugation (100,000-120,000 × g) to pellet exosomes [23]. Limitations include time consumption, requirement for large sample volumes, and potential for protein co-precipitation [23].
- Size-Exclusion Chromatography: Separates vesicles based on hydrodynamic radius; preserves vesicle integrity and functionality while providing high purity by effectively removing contaminating proteins [23].
- Polymer-Based Precipitation: Utilizes hydrophilic polymers to decrease exosome solubility; enables rapid processing with good recovery but may yield lower purity with co-precipitation of contaminants [23].
- Tangential Flow Filtration: Suitable for large-scale production; uses membrane filters with specific molecular weight cutoffs to concentrate and purify exosomes from large volume samples [23].
MSC Culture and Expansion
- Source Materials: Isolate MSCs from bone marrow, adipose tissue, umbilical cord, or placental compartments [18] [25].
- Culture Conditions: Maintain in serum-free or xeno-free media with essential growth factors (FGF-2, PDGF) at 37°C with 5% CO₂ [18].
- Characterization: Verify MSC identity through flow cytometry for CD73, CD90, CD105 positivity and CD34, CD45 negativity; demonstrate trilineage differentiation potential (osteogenic, adipogenic, chondrogenic) [23].
Characterization Techniques
Physical Characterization
- Nanoparticle Tracking Analysis: Quantifies particle concentration and size distribution by tracking Brownian motion [23].
- Dynamic Light Scattering: Determines hydrodynamic diameter and size distribution [23].
- Transmission Electron Microscopy: Visualizes ultrastructure and morphology; confirms cup-shaped morphology characteristic of exosomes [23].
- Resistive Pulse Sensing: Measures particle size distribution and concentration based on electrical impedance [23].
Molecular Characterization
- Western Blot: Detects exosomal markers (CD9, CD63, CD81, TSG101, ALIX) and absence of negative markers (GM130, calnexin) [23].
- RNA Sequencing: Profiles miRNA, mRNA, and other RNA species in exosomal cargo [24].
- Proteomic Analysis: Identifies protein composition through mass spectrometry [18].
- Lipidomic Analysis: Characterizes lipid composition of exosomal membranes [18].
Therapeutic Mechanisms and Signaling Pathways
MSC-Exos Mechanisms of Action
Diagram 1: MSC-Exos therapeutic mechanisms via biomolecule transfer
MSC-Exos exert therapeutic effects through multiple interconnected mechanisms. They facilitate intercellular communication by transferring functional miRNAs, proteins, and lipids to recipient cells, modulating key biological processes including immunoregulation, tissue repair, and cellular metabolism [18] [24]. Specific miRNAs such as miR-146a, miR-21, and miR-181a play crucial roles in mediating these effects, particularly in modulating inflammatory responses and promoting tissue regeneration [24].
Whole MSC Therapeutic Mechanisms
Diagram 2: Whole MSC therapeutic mechanisms and limitations
Whole MSCs function through more complex mechanisms including direct differentiation into tissue-specific cells, extensive paracrine signaling, cell-cell contact mediated effects, and even mitochondrial transfer to damaged cells [19] [18]. However, these mechanisms are constrained by practical limitations including low engraftment rates, short in vivo lifespan, and potential safety concerns that have motivated the shift toward MSC-Exos [18] [24].
Research Reagent Solutions Toolkit
Table 2: Essential research reagents and materials for MSC and MSC-Exos research
| Category | Specific Reagents/Materials | Research Application | Technical Notes |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kits, ExoQuick-TC | MSC-Exos precipitation from conditioned media | Polymer-based; suitable for small volumes [23] |
| Chromatography | qEV Original Columns, SEPAX Nanobio Analyzer | Size-based MSC-Exos separation | Preserves vesicle integrity; ideal for functional studies [23] |
| Characterization | CD9/CD63/CD81 antibodies, TSG101, ALIX | MSC-Exos identification via Western blot | Confirm exosomal markers; check for contaminants [23] |
| Cell Culture | Serum-free MSC media, FGF-2, PDGF-AB | MSC expansion and conditioning | Maintain stemness; prevent differentiation [18] |
| Preconditioning | LPS, TNF-α, IL-1β, hypoxia chambers | Enhance therapeutic potential of MSC-Exos | Modifies miRNA content (e.g., increases miR-146a) [24] |
| Storage | Trehalose, BSA, DMSO, cryovials | Preservation of MSC-Exos and MSCs | Avoid freeze-thaw cycles; use stabilizers for MSC-Exos [23] |
| Imaging | NIR-II fluorescent probes, lipophilic dyes | In vivo tracking of MSC-Exos biodistribution | Real-time visualization of pharmacokinetics [23] |
| Engineering | CRISPR/Cas9 systems, transfection reagents | Genetic modification of MSCs for enhanced MSC-Exos production | Modify parent MSCs to alter MSC-Exos cargo [21] |
Discussion and Future Perspectives
The comparative analysis reveals distinct advantages and limitations for both therapeutic platforms. MSC-Exos offer significant safety benefits with lower immunogenicity and tumorigenic potential, coupled with enhanced biodistribution capabilities including blood-brain barrier penetration [21] [18]. However, challenges remain in scalable production, standardization, and rapid clearance post-administration [21] [18].
Whole MSCs provide the complete cellular machinery for complex tissue integration but face challenges with inconsistent engraftment, potential embolic risks, and storage complications [18]. Current research focuses on engineering approaches to enhance MSC-Exos targeting and therapeutic efficacy through surface modifications and cargo loading [21]. Genetic engineering of parent MSCs enables production of MSC-Exos with enhanced therapeutic cargo, while chemical modification and membrane fusion techniques allow for improved tissue-specific targeting [21]. These advancements position MSC-Exos as increasingly viable alternatives to whole-cell therapies across multiple therapeutic domains, particularly for neurological disorders, cardiovascular diseases, and immune modulation [21] [18] [22].
The field of regenerative medicine has been significantly shaped by the therapeutic potential of mesenchymal stem cells (MSCs), which have demonstrated robust capabilities in modulating immune responses and promoting tissue repair. However, the clinical application of whole MSC therapies faces significant challenges, including low cell survival rates after transplantation, potential immune rejection, and ethical concerns [26]. In recent years, a paradigm shift has occurred towards understanding that many of the therapeutic benefits of MSCs are mediated through their paracrine activity, particularly via the release of extracellular vesicles [5]. Among these vesicles, exosomes—nanosized extracellular vesicles (30-150 nm in diameter) released by MSCs—have emerged as a promising cell-free therapeutic alternative [26] [3].
MSC-derived exosomes (MSC-Exos) are lipid-bilayer enclosed vesicles that carry a diverse array of bioactive molecules, including proteins, lipids, and nucleic acids (such as mRNA and microRNA), which they transfer to recipient cells to affect cellular processes [26] [27]. These "tiny giants of regeneration" share many therapeutic benefits with their parent MSCs but offer significant advantages, including lower immunogenicity, enhanced biological barrier penetration, avoidance of infusion-related toxicities, and easier storage stability [3]. This review comprehensively compares the mechanisms of action of MSC-derived exosomes against whole cell therapy across three critical domains: immunomodulation, tissue repair, and cross-barrier delivery, providing researchers and drug development professionals with an evidence-based assessment of these complementary therapeutic approaches.
Comparative Mechanisms of Action
Immunomodulatory Mechanisms
Whole MSC Immunomodulation: Whole MSCs exert their immunomodulatory effects through direct cell-cell contact and secretion of soluble factors. They interact with parenchymal cells and facilitate restoration of damaged tissues through the release of signaling molecules [4]. When activated by damage-associated molecular patterns (DAMPs) and alarmins generated by damaged cells, MSCs inhibit apoptosis of unaffected parenchymal cells while suppressing inflammatory activity of monocytes, neutrophils, T lymphocytes, and natural killer (NK) cells [4]. Crucially, MSCs stimulate the production and development of immunosuppressive T regulatory cells (Tregs), resulting in the overall reduction of inflammation [4]. The immunomodulatory function of whole MSCs is dynamic and depends on the inflammatory microenvironment, requiring viable, functional cells that can respond to environmental cues.
MSC-Exos Immunomodulation: MSC-derived exosomes mediate immunomodulation through the transfer of bioactive molecules that regulate both innate and adaptive immune responses [4]. These nano-sized vesicles facilitate signal transmission via receptor-ligand interactions or endocytosis in recipient cells, delivering physiologically active chemicals, cytokines, chemokines, and immuno-regulatory factors to modulate cellular activity [4]. The mechanisms are more targeted and specific compared to whole MSCs:
B-Cell Regulation: MSC-Exos are internalized by activated CD19+/CD86+ B cells, resulting in the inhibition of B cell proliferation, differentiation, antibody production, and maturation of memory B cells [4]. They demonstrate dose-dependent anti-inflammatory effects by suppressing B cell maturation and promoting regulatory B cells (Bregs) in lymph nodes within disease models [4]. MSC-Exos prompt B cells to downregulate the PI3K/Akt signaling pathway via miR-155-5p, inhibiting B cell proliferation and diminishing the activation potential of B lymphocytes [4].
T-Cell Regulation: MSC-Exos carry anti-inflammatory molecules, including IL-10 and TGF-β, which help suppress excessive immune responses and modulate T-cell activity [27]. They inhibit T-cell proliferation and inflammatory responses through the transfer of specific miRNAs and proteins that alter signaling pathways in recipient immune cells [4].
Macrophage Polarization: MSC-Exos promote the transition of pro-inflammatory M1 macrophages to anti-inflammatory M2 phenotypes, supporting the resolution of inflammation and transition to tissue repair phases [28]. This polarization is crucial for orchestrating the transition from inflammatory to regenerative environments in damaged tissues.
Table 1: Comparative Analysis of Immunomodulatory Actions
| Immune Component | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| B-cells | Moderate suppression via direct contact and soluble factors | Strong suppression of proliferation, differentiation, and antibody production via miR-155-5p/PI3K/Akt pathway |
| T-cells | Direct interaction and stimulation of Treg production; context-dependent effects | Inhibition of proliferation via miRNA transfer; promotion of anti-inflammatory cytokine profiles |
| Macrophages | Paracrine signaling inducing M1 to M2 transition | Efficient macrophage polarization via exosomal cargo transfer |
| NK Cells | Suppression of inflammatory activity | Modulation of IFN-γ production and cytotoxic activity |
| Therapeutic Consistency | Variable based on cell viability and microenvironment | More consistent due to stable cargo composition |
| Onset of Action | Slower (requires cell engraftment and activation) | Faster (immediate delivery of bioactive molecules) |
Tissue Repair and Regenerative Mechanisms
Whole MSC Tissue Repair: Whole MSCs promote tissue repair through multiple parallel mechanisms. The primary approaches include direct differentiation into target cell types to replace damaged cells, secretion of growth factors and cytokines that promote endogenous repair processes, and extensive paracrine signaling that modulates the tissue microenvironment [29]. MSCs have the capability to differentiate into multiple cell types, including osteoblasts, chondrocytes, and adipocytes, making them ideal for repairing damaged tissues [29]. In the complex process of tissue repair, which involves hemostasis, inflammation, repair, and remodeling phases, MSCs participate by interacting with various immune cells to modulate the tissue microenvironment [28]. However, the effectiveness of whole MSCs depends on their successful migration to injury sites, adhesion, survival, retention, and functional integration into host tissues—factors that have proven challenging to control in clinical applications [3].
MSC-Exos Tissue Repair: MSC-derived exosomes promote tissue repair through the coordinated delivery of regenerative cargo to injured cells. As natural bioactive molecular carriers, MSC-Exos precisely regulate the inflammatory response, angiogenesis, and tissue repair processes in target tissues by delivering functional RNA, proteins, and other signaling elements [3]. The mechanisms include:
Anti-apoptotic Effects: MSC-Exos deliver miRNAs and proteins that inhibit programmed cell death in injured tissues, promoting cell survival and maintaining tissue architecture [27].
Angiogenic Induction: Through transfer of pro-angiogenic factors (such as miRNAs, proteins, and lipids), MSC-Exos stimulate the formation of new blood vessels, enhancing oxygen and nutrient supply to regenerating tissues [27] [3].
Stem Cell Recruitment and Activation: MSC-Exos promote the maintenance and recruitment of endogenous stem cells, amplifying the body's innate regenerative capacity without requiring exogenous cell engraftment [5].
Extracellular Matrix Remodeling: By delivering matrix metalloproteinases (MMPs) and their inhibitors, MSC-Exos facilitate the balanced remodeling of extracellular matrix components essential for functional tissue restoration [28].
Oxidative Stress Reduction: MSC-Exos contain and transfer antioxidant molecules that mitigate oxidative damage in inflamed or injured tissues, creating a more favorable microenvironment for regeneration [28].
Table 2: Tissue Repair Mechanisms Comparison
| Repair Mechanism | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Cell Replacement | Direct differentiation and integration | Indirect stimulation of endogenous stem cells |
| Paracrine Signaling | Broad secretion of soluble factors | Targeted delivery via vesicular cargo |
| Angiogenesis | Factor secretion and sometimes pericyte-like function | Efficient induction via miRNA/protein transfer |
| Anti-apoptotic Effect | Moderate through secreted factors | Potent via direct delivery of anti-apoptotic miRNAs |
| Extracellular Matrix Modulation | Cell-mediated and paracrine actions | Delivery of MMPs and TIMPs for balanced remodeling |
| Therapeutic Window | Limited by cell survival | Extended due to sustained bioactivity of cargo |
Cross-Barrier Delivery Capabilities
Whole MSC Barrier Penetration: Whole MSCs, with diameters typically ranging from 30-60 μm, face significant challenges in traversing biological barriers [5]. After systemic administration, MSCs often become physically trapped in the lung microvasculature, with only a small percentage reaching the intended target tissues [5]. This limited barrier penetration necessitates higher cell doses to achieve therapeutic effects, increasing the risk of infusion-related toxicities, including pulmonary embolism [5]. While some MSCs can migrate to sites of injury following inflammatory cues, their relatively large size fundamentally limits their ability to cross tight physiological barriers like the blood-brain barrier (BBB) or penetrate deep into avascular or densely structured tissues.
MSC-Exos Barrier Penetration: MSC-derived exosomes demonstrate superior capabilities in crossing biological barriers, primarily due to their nanoscale size (30-150 nm) and natural biocompatibility [3] [30]. Their small dimensions and biological properties allow them to traverse protective barriers, including the blood-brain barrier, without causing embolism or transmission of infections [3]. The blood-brain barrier, which restricts the development of drug delivery systems for the brain, hinders the potential applications of numerous pharmaceutical agents for treating central nervous system diseases [31]. MSC-Exos overcome this limitation through multiple mechanisms:
Transcellular Penetration: Their lipid bilayer membrane enables fusion with cellular membranes, facilitating direct delivery of contents into the cytoplasm of target cells [3].
BBB Transcytosis: MSC-Exos can utilize various transcytosis mechanisms, including receptor-mediated transcytosis, to cross the tightly joined endothelial cells of the BBB [31] [30].
Enhanced Tissue Distribution: The small size of exosomes allows for more homogeneous distribution within tissues and access to compartments inaccessible to whole cells [3].
Multiple Administration Routes: MSC-Exos can be administered via various routes, including intravenous infusion, inhalation, or local administration, with studies showing different accumulation patterns based on the delivery method [5].
Table 3: Cross-Barrier Delivery Capabilities
| Delivery Parameter | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Size Profile | 30-60 μm (cells) | 30-150 nm (vesicles) |
| BBB Penetration | Minimal to none | Efficient via transcytosis mechanisms |
| Lung Entrapment | Significant (~80% after IV administration) | Minimal due to nanoscale size |
| Tissue Distribution | Limited to perfused areas with appropriate cues | Wide distribution including avascular areas |
| Administration Routes | Primarily intravenous or local implantation | IV, inhalation, local, and even oral delivery possible |
| Targeting Efficiency | Limited homing relying on inflammatory signals | Enhancable via surface engineering |
Experimental Models and Methodologies
Standardized Isolation and Characterization Protocols
The isolation and characterization of MSC-derived exosomes require standardized methodologies to ensure reproducibility and reliability of experimental results. The most commonly used techniques include:
Isolation Methods:
- Ultracentrifugation: This remains the most frequently used method for isolating MSC-Exos in clinical trials. Suspension components are separated using centrifugation based on their sizes, shapes, densities, centrifugal vigor, and solvent stickiness. Significant centrifugal forces of up to 1,000,000×g are utilized in ultracentrifugation to separate MSC-Exos from various sample components [5].
- Tangential Flow Filtration (TFF): This method concentrates conditioned medium and purifies MSC-Exos based on vesicle sizes. A cell culture medium is filtered with a sterile hollow fiber polyether-sulfone membrane with a specific pore size (in µm) to remove cell debris and retain biomolecules. After washing with sterile phosphate-buffered saline (PBS), the MSC-Exos are concentrated and diafiltrated using a sucrose buffer [5].
- Size-Exclusion Chromatography: This technique separates vesicles based on size through a porous stationary phase, providing high purity exosome preparations suitable for therapeutic applications [30].
Characterization Protocols: MSC-Exos intended for research or clinical applications should meet the minimal characterization criteria for extracellular vesicles as stated in the MISEV2018 guidelines, which include both marker and physical characterizations [5]. Marker characterization should be evaluated by:
- Positive presence of transmembrane proteins (e.g., CD9, CD63, CD81)
- Presence of cytosolic proteins (e.g., TSG101, Alix)
- Negative markers (e.g., absence of endoplasmic reticulum proteins such as calnexin) Physical characterization includes:
- Nanoparticle tracking analysis (NTA) for size distribution and concentration
- Transmission electron microscopy (TEM) for morphological assessment
- Dynamic light scattering (DLS) for hydrodynamic diameter measurement [5]
In Vitro and In Vivo Experimental Models
Immunomodulation Assays:
- T-cell and B-cell Proliferation Assays: MSC-Exos are co-cultured with activated immune cells using mitogens like phytohemagglutinin (PHA) or anti-CD3/CD28 antibodies. Proliferation is measured via 3H-thymidine incorporation or CFSE dilution using flow cytometry [4].
- Macrophage Polarization Models: Human monocyte cell lines (THP-1) or primary monocytes are differentiated into macrophages and treated with MSC-Exos alongside polarizing cytokines (IFN-γ/LPS for M1; IL-4/IL-13 for M2). Polarization is assessed via surface marker expression (CD80/CD86 for M1; CD206/CD163 for M2) and cytokine secretion profiles [28] [4].
- Mixed Lymphocyte Reaction (MLR): This assay evaluates the effect of MSC-Exos on T-cell activation in response to allogeneic antigens, measuring the suppression of proliferation and inflammatory cytokine production [4].
Tissue Repair Models:
- Wound Healing Assays: In vitro scratch assays using fibroblast or epithelial cell lines evaluate the effect of MSC-Exos on cell migration and gap closure rates [3].
- Angiogenesis Assays: Tube formation assays using human umbilical vein endothelial cells (HUVECs) on Matrigel quantify the pro-angiogenic potential of MSC-Exos by measuring tube length, branching points, and network complexity [3].
- Organoid and 3D Culture Models: Complex 3D tissue models incorporating multiple cell types provide more physiologically relevant systems for evaluating the regenerative effects of MSC-Exos on tissue morphogenesis and function [3].
Blood-Brain Barrier Penetration Studies:
- In Vitro BBB Models: Transwell systems with brain microvascular endothelial cells cultured on porous membranes recreate the BBB. The permeability of fluorescently labeled MSC-Exos is measured and compared to whole MSCs [31] [30].
- In Vivo Tracking Studies: MSC-Exos are labeled with near-infrared dyes or radioactive tags and administered to animal models. Biodistribution is tracked using imaging systems (IVIS, PET) and ex vivo tissue analysis [30].
- Disease-Specific Animal Models: Neurological disorder models (stroke, Alzheimer's, Parkinson's) are used to evaluate the therapeutic efficacy of MSC-Exos compared to whole MSCs, assessing functional recovery, biomarker modulation, and target engagement [31] [30].
Signaling Pathways and Molecular Mechanisms
Key Signaling Pathways in Immunomodulation
The immunomodulatory effects of MSC-derived exosomes are mediated through several key signaling pathways that regulate immune cell function and inflammatory responses:
Diagram 1: Immunomodulatory Signaling Pathways Activated by MSC-Derived Exosomes
Tissue Repair and Regenerative Pathways
MSC-derived exosomes activate multiple interconnected signaling pathways that coordinate tissue repair processes:
Diagram 2: Tissue Repair Pathways Activated by MSC-Derived Exosomes
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for MSC-Exosome Studies
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, exoEasy Maxi Kit | Exosome purification from conditioned media | Rapid isolation with minimal equipment requirements |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, Alix, Calnexin | Western blot, flow cytometry, immuno-EM | Confirmation of exosomal identity and purity |
| Tracking Dyes | PKH67, PKH26, DiD, DiR, CFSE | In vitro and in vivo tracking | Visualization of exosome uptake and biodistribution |
| Cell Culture Media | Serum-free MSC media, exosome-depleted FBS | MSC expansion and exosome production | Ensuring consistent exosome yield without serum contaminants |
| Analysis Instruments | Nanoparticle Tracking Analyzer, DLS, TEM | Physical characterization | Size distribution and morphological assessment |
| ELISA/Kits | TNF-α, IL-10, TGF-β, IFN-γ ELISA kits | Immunomodulation assessment | Quantification of inflammatory mediators |
| Animal Models | CIA mice, EAE mice, stroke models | In vivo efficacy testing | Disease-specific therapeutic evaluation |
The comparative analysis of MSC-derived exosomes versus whole cell therapy reveals a complex landscape of complementary mechanisms with distinct advantages for each approach. Whole MSC therapies offer the potential for direct cellular integration and dynamic response to microenvironments but face significant challenges related to cell viability, consistency, and biological barrier penetration. In contrast, MSC-derived exosomes provide a cell-free alternative with enhanced targetability, superior safety profile, and remarkable stability, though they may lack the adaptive responsiveness of living cells.
From a functional outcomes perspective, MSC-exosomes demonstrate particular strength in applications requiring precise immunomodulation, efficient biological barrier crossing (especially CNS targets), and reduced risk of infusion-related adverse events. Whole MSC therapies may still hold advantages in scenarios requiring continuous, adaptive paracrine signaling or direct cellular integration, though the evidence for meaningful long-term engraftment remains limited.
For researchers and drug development professionals, the choice between these therapeutic modalities should be guided by specific disease pathophysiology, target tissue accessibility, and desired mechanism of action. Future research directions should focus on standardizing isolation protocols, engineering exosomes for enhanced targeting, and conducting direct comparative studies in disease-relevant models. As the field advances, MSC-derived exosomes represent a promising next-generation therapeutic tool that may overcome many of the limitations associated with whole cell therapies while harnessing the fundamental regenerative capabilities of mesenchymal stem cells.
From Bench to Bedside: Production, Isolation, and Therapeutic Applications
The field of regenerative medicine is undergoing a significant transformation, moving from whole cell-based therapies toward acellular strategies that offer enhanced safety and scalability. Within this context, Mesenchymal Stem Cell (MSC)-derived exosomes have emerged as a potent therapeutic alternative, mirroring the regenerative and immunomodulatory functions of their parent cells without the associated risks of immunogenicity, infusion toxicity, or tumorigenicity [32] [3]. The efficacy of these exosomes, however, is critically dependent on the methods used for their production and isolation. This guide provides a objective comparison of two core isolation techniques—ultracentrifugation (UC) and tangential flow filtration (TFF)—framed within the broader thesis that MSC-derived exosomes represent a superior functional outcome to whole cell therapy for research and clinical applications.
The Superiority of MSC-Derived Exosomes Over Whole Cell Therapy
The therapeutic application of MSCs, while promising, is fraught with challenges that hinder clinical translation. MSC-derived exosomes present a viable solution to these limitations, offering a more controlled and safer therapeutic profile.
Table 1: Functional Advantages of MSC-Derived Exosomes vs. Whole Cell Therapy
| Aspect | Whole MSC Therapy | MSC-Derived Exosome Therapy | Key Advantage of Exosomes |
|---|---|---|---|
| Immunogenicity | Higher risk of immune rejection [3] | Low immunogenicity; non-immunogenic [32] [3] | Reduced risk of adverse reactions |
| Tumorigenic Risk | Potential for ectopic tissue formation or uncontrolled differentiation [32] | No risk of tumorigenicity [32] [33] | Enhanced safety profile |
| Delivery & Engraftment | Poor engraftment; cells can lodge in lung microvasculature [33] | Can cross biological barriers; no risk of vascular occlusion [3] | Superior biodistribution and targeting |
| Storage & Stability | Requires cryopreservation; sensitive to freeze-thaw cycles [3] | Stable at -80°C for long periods; retains activity [3] | Simplified logistics and storage |
| Production Scalability | Difficult to scale; senesce during in vitro expansion [33] | Scalable production using bioreactors and advanced isolation [34] [3] | More feasible for industrial production |
| Therapeutic Mechanism | Complex, paracrine and cell-contact dependent [3] | Defined, primarily via delivery of cargo (proteins, RNA) [3] [33] | More predictable and reproducible effects |
The consensus from recent literature is that the therapeutic benefits of MSCs are largely mediated by their paracrine secretions, with exosomes being a key effector [3] [33]. These nanosized vesicles act as natural delivery systems, transferring functional proteins, lipids, and nucleic acids to recipient cells to promote processes like tissue regeneration, immunomodulation, and angiogenesis [32] [33]. This positions exosomes as the active pharmaceutical ingredient, making their high-quality, scalable isolation a paramount research and clinical objective.
Optimizing the Starting Material: Culture Media and Systems
The yield and potency of exosomes are profoundly influenced by the culture conditions of the parent MSCs.
- 3D Culture Systems: Transitioning from traditional 2D flasks to 3D cultures, such as microcarrier-based bioreactors, has been shown to dramatically increase exosome yield. One study demonstrated that 3D culture yielded 20-fold more exosomes than 2D culture when combined with differential ultracentrifugation. When further paired with TFF, the yield was 7-fold higher than the 3D-UC output [34].
- Media Composition and Stimulation: The biochemical environment, including oxygen tension and the presence of specific cytokines (e.g., IFN-γ, TNF-α), can influence the cargo and subsequent biological activity of the harvested exosomes [3]. For consistent results, the use of EV-depleted fetal bovine serum (FBS) in culture media is essential to avoid contamination with bovine vesicles [35].
Head-to-Head Comparison: Ultracentrifugation vs. Tangential Flow Filtration
The isolation method is a critical determinant of exosome yield, purity, and, most importantly, biological functionality. The following experimental data and workflows compare the two primary techniques.
Experimental Protocols for Direct Comparison
To ensure a fair comparison, studies have directly contrasted UC and TFF, often with a subsequent polishing step like Size Exclusion Chromatography (SEC) to enhance purity.
Protocol for Ultracentrifugation (UC-SEC):
- Clarification: Conditioned media is centrifuged at 500 × g for 10 minutes to remove detached cells [35].
- Filtration: The supernatant is filtered through a 0.22 µm filter to remove large debris and particles [35].
- Ultracentrifugation: The clarified media is centrifuged at high force (e.g., 100,000 × g) for 70-120 minutes at 4°C to pellet crude exosomes [36] [35].
- Washing (Optional): The pellet is resuspended in PBS and subjected to a second round of ultracentrifugation [35].
- Size Exclusion Chromatography (SEC): The final pellet is resuspended and loaded onto a SEC column (e.g., qEV columns) to separate exosomes from contaminating proteins [36].
Protocol for Tangential Flow Filtration (TFF-SEC):
- Clarification & Filtration: Identical to the UC protocol (steps 1-2) [35].
- Concentration & Diafiltration: The clarified media is processed through a TFF system. The flow is directed tangentially across a membrane (typically with a pore size of 100-500 kDa), concentrating the exosomes and simultaneously exchanging the buffer (e.g., from culture media to PBS) [36] [37].
- Size Exclusion Chromatography (SEC): The concentrated retentate is then purified using SEC to remove soluble protein contaminants, yielding a pure exosome preparation [36] [35].
Quantitative Performance Data
Direct comparisons in rigorous studies reveal clear performance differences between the two isolation methodologies.
Table 2: Experimental Outcome Comparison: UC-SEC vs. TFF-SEC
| Performance Metric | Ultracentrifugation-SEC (UC-SEC) | Tangential Flow Filtration-SEC (TFF-SEC) | Experimental Details |
|---|---|---|---|
| Particle Yield | Baseline (Reference) | Up to 23-fold higher than UC-SEC [36] | Tunable Resistive Pulse Sensing (qNano) analysis [36] |
| Process Time | > 4 hours [36] [37] | < 4 hours; >40% time saving [36] [37] | For processing large volume samples [36] |
| Cost & Scalability | Limited scale; high cost for large volumes [36] | Highly scalable; cost < one tenth of UC [36] | Suitable for industrial-scale production [36] [37] |
| Exosome Integrity | Risk of damage/aggregation from high g-forces [36] [35] | Gentle process; preserves integrity & function [36] [37] | TEM shows cup-shaped morphology for both [36] |
| Purity | Moderate; co-isolation of contaminants [35] [37] | Similar particle-to-protein ratio; high purity with SEC [36] | Nano-flow cytometry confirmed specific markers [36] |
| Functional Potency | N/A | 7x more potent in siRNA delivery to neurons [34] | Comparison of 3D-TFF-exosomes vs 2D-UC-exosomes [34] |
The data consistently demonstrates that TFF surpasses UC in critical areas for research and development: it provides a substantially higher yield of functional exosomes in a shorter time and at a lower cost, making it inherently more scalable [36] [34] [35].
The Scientist's Toolkit: Essential Reagents and Materials
Successful isolation of MSC-derived exosomes requires specific reagents and equipment to ensure quality and reproducibility.
Table 3: Key Research Reagent Solutions for Exosome Isolation
| Item | Function in Protocol | Example / Specification |
|---|---|---|
| EV-Depleted FBS | Provides growth nutrients for MSC culture without contaminating the sample with bovine vesicles [35]. | Ultracentrifuged or commercially available EV-depleted FBS. |
| TFF System & Membranes | Concentrates and purifies exosomes from large volumes of conditioned media via cross-flow filtration [37]. | Systems from Pall (Minimate), Spectrum Labs; 100-500 kDa MWCO membranes. |
| Size Exclusion Columns | Polishing step to remove contaminating proteins and other soluble factors from exosome preparations [36]. | qEV columns (Izon Science) or Sepharose-based CL-2B columns. |
| Ultracentrifuge & Rotors | High-speed centrifugation to pellet exosomes based on density and size (for UC protocol) [35]. | Beckman Coulter Optima XPN with Type 50.2 Ti fixed-angle rotor. |
| Characterization Reagents | Validate exosome identity, size, and concentration after isolation. | Antibodies for tetraspanins (CD63, CD81, CD9); NTA for size distribution. |
Within the evolving paradigm that prioritizes MSC-derived exosomes over whole cell therapy, the choice of isolation technique is a cornerstone of successful research and translation. The experimental data leads to a clear conclusion: Tangential Flow Filtration (TFF), coupled with a polishing step like SEC, presents a superior isolation strategy for most applications, particularly those requiring scalability, high yield, and preserved biological function.
While ultracentrifugation remains a widely used benchmark, its drawbacks in yield, scalability, and potential for vesicle damage are significant [36] [35]. TFF effectively addresses these limitations, enabling the robust production of functional exosomes necessary for both advanced in vitro studies and the growing pipeline of clinical trials [3] [33]. For researchers aiming to optimize the production of therapeutic MSC-derived exosomes, investing in TFF methodology is a rational and data-supported decision.
In the evolving landscape of regenerative medicine, mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as a promising cell-free therapeutic tool, offering significant advantages over whole MSC therapy. These nano-sized extracellular vesicles (30-150 nm in diameter) encapsulate the therapeutic paracrine potential of their parent cells—carrying proteins, lipids, mRNAs, and microRNAs—while mitigating risks associated with whole-cell transplantation, such as infusion-related toxicities, pulmonary embolism, and tumorigenicity [2] [3] [5]. The efficacy of these "tiny giants of regeneration," however, is profoundly influenced by the administration route, which determines their biodistribution, targeting efficiency, and therapeutic potency [38] [5]. This guide provides a detailed comparative analysis of the three primary administration routes—intravenous infusion, local injection, and nebulized inhalation—to inform preclinical and clinical protocol development.
Comparative Analysis of Administration Routes
Table 1: Direct Comparison of MSC-Derived Exosome Administration Routes
| Parameter | Intravenous Infusion | Local Injection | Nebulized Inhalation |
|---|---|---|---|
| Key Characteristics | Systemic delivery; broad distribution [5] | Direct targeting to a specific site [5] | Local delivery to the respiratory tract [39] |
| Primary Advantages | Suitable for systemic conditions (e.g., GvHD, systemic lupus) [5] | High local concentration; avoids first-pass metabolism [5] | Non-invasive; direct targeting to lungs; superior safety profile [38] [39] [40] |
| Key Limitations | Rapid clearance; potential accumulation in liver/spleen; lower disease-site bioavailability [5] | Invasive; not suitable for disseminated diseases [5] | Limited application to respiratory diseases [39] |
| Typical Doses in Clinical Trials | Varied units (μg, particle number); often higher doses required [38] [5] | Dependent on target tissue/organ [5] | ~10^8 particles (notably lower than IV doses for similar efficacy in lung diseases) [38] |
| Common Clinical Applications | GvHD, ARDS, stroke, type 1 diabetes [5] | Osteoarthritis, wound healing, Alzheimer's disease (intranasal) [5] | ARDS, COVID-19, lung fibrosis, bronchopulmonary dysplasia [38] [39] |
| Therapeutic Efficacy | Well-documented for immunomodulation [5] | High efficacy in localized tissue repair [3] [5] | High clinical efficacy rates in lung diseases; can achieve effects at lower doses than IV [38] [41] |
Detailed Experimental Protocols and Methodologies
The following section outlines standard experimental protocols for evaluating administration routes, reflecting current practices in clinical trials and preclinical studies.
Protocol for Intravenous Infusion of MSC-Exos
This protocol is commonly employed for systemic conditions like graft-versus-host disease (GvHD) and acute respiratory distress syndrome (ARDS) [5].
Exosome Production and Isolation:
- Cell Source: Human bone marrow, adipose tissue, or umbilical cord-derived MSCs are cultured under GMP-grade conditions [5] [42].
- Isolation Method: Ultracentrifugation is the most frequently used method. Conditioned medium is sequentially centrifuged at low speeds (e.g., 2,000 × g) to remove cells and debris, followed by high-speed ultracentrifugation (e.g., 100,000 × g) to pellet exosomes [5] [42]. Tangential Flow Filtration (TFF) is also used for its scalability [5].
- Characterization: Isolated exosomes must be characterized per MISEV2018 guidelines. This includes nanoparticle tracking analysis (NTA) for size and concentration, transmission electron microscopy (TEM) for morphology, and flow cytometry or Western blot for surface markers (e.g., CD9, CD63, CD81) [5] [42].
Formulation and Dosing:
Administration Technique:
- The exosome suspension is administered via slow bolus injection into the tail vein of mice or a peripheral vein in humans [5].
- Monitoring for potential adverse effects, such as cytokine release syndrome, is recommended.
Protocol for Nebulized Inhalation of MSC-Exos
This route is optimized for treating respiratory diseases, offering targeted delivery with potentially lower effective doses [38] [39].
Exosome Preparation for Aerosolization:
- Exosomes are isolated and characterized as described in the IV protocol.
- A critical quality control step is assessing exosome integrity and biological activity post-nebulization. Techniques like NTA and functional assays are used to confirm stability after passing through the nebulizer [39].
Nebulization and Delivery:
- The exosome suspension is loaded into a vibrating-mesh or jet nebulizer. These devices generate an aerosol with a particle size distribution (typically 1-5 μm) suitable for deep lung deposition [39].
- In rodent studies, animals are placed in a sealed inhalation chamber connected to the nebulizer. For clinical use, patients use a standard mouthpiece or mask.
Dosing Considerations:
- Clinical data suggest that nebulization therapy can achieve therapeutic effects at doses around 10^8 particles, which is significantly lower than the doses typically required for intravenous routes in treating lung diseases [38].
Mechanisms of Action and Therapeutic Signaling Pathways
The therapeutic effect of MSC-Exos is mediated by their cargo, which is transferred to recipient cells via three primary interaction types: A) complete fusion with the target cell membrane, B) internalization via endocytosis, and C) receptor-ligand binding to signal through surface receptors [3]. The administration route directly influences which pathways are activated by determining the primary target cells.
Diagram 1: Exosome Therapeutic Pathways by Administration Route. The route determines the primary target cells, which subsequently internalize exosomes and trigger distinct therapeutic outcomes through cargo transfer.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Exosome Administration Studies
| Item Name | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source for exosome production. Biological activity varies by tissue source [2] [42]. | Bone marrow, adipose tissue, or umbilical cord-derived MSCs. Source impacts exosome cargo and function [5] [42]. |
| Ultracentrifugation System | Gold-standard method for laboratory-scale exosome isolation from conditioned media [5] [42]. | Requires high-speed centrifuges capable of ≥100,000 × g. Can cause exosome aggregation [5] [42]. |
| Tangential Flow Filtration (TFF) | Scalable, GMP-compatible method for isolating and concentrating exosomes [5]. | Suitable for large-scale clinical production. Often used with hollow fiber polyethersulfone membranes [5]. |
| Nanoparticle Tracking Analyzer (NTA) | Characterizes exosome size distribution and concentration in solution [38] [5]. | Essential for quality control and dose standardization (e.g., particle number per dose) [38]. |
| Flow Cytometer | Detects and validates exosome surface markers for characterization [5] [42]. | Antibodies against tetraspanins (CD9, CD63, CD81) are commonly used for identification [5] [42]. |
| Vibrating-Mesh Nebulizer | Generates exosome-containing aerosol for inhalation studies without significant degradation [39]. | Preferable over jet nebulizers for better preservation of exosome integrity [39]. |
The choice of administration route for MSC-derived exosomes is a critical determinant of therapeutic success, dictated by the target pathology. Intravenous infusion remains indispensable for systemic immunomodulation, local injection excels in focused regenerative applications, and nebulized inhalation represents a paradigm of efficiency for respiratory diseases, achieving potent effects with remarkably lower doses. Future progress hinges on standardizing dose metrics (moving from μg to particle number), developing scalable GMP production, and engineering "smart" exosomes with enhanced tissue targeting [38] [3] [5]. As these cell-free therapies mature, rational route selection will be fundamental to harnessing their full potential in precision regenerative medicine.
The treatment of neurodegenerative diseases presents a formidable challenge, primarily due to the restrictive nature of the blood-brain barrier (BBB) and complex cell death mechanisms such as ferroptosis. Mesenchymal stem cell (MSC) transplantation has been extensively evaluated as a cellular therapy in clinical trials for neurological disorders, leveraging their immunomodulatory and regenerative properties [2]. However, a paradigm shift is occurring toward cell-free therapies, with MSC-derived exosomes (MSC-Exos) emerging as a promising alternative. These nanoscale extracellular vesicles (30-150 nm in diameter) retain the therapeutic potential of their parent cells while offering superior biocompatibility, reduced immunogenicity, and the ability to cross biological barriers [11] [5]. Particularly relevant for neurodegenerative diseases is their capacity to deliver bioactive cargo that can modulate ferroptosis—a regulated cell death pathway driven by iron-dependent lipid peroxidation that has been implicated in Alzheimer's disease, Parkinson's disease, and other neurological conditions [43] [44]. This review provides a comprehensive comparison between MSC-derived exosomes and whole cell therapies, focusing on their respective capabilities for ferroptosis modulation and BBB penetration, with implications for functional outcomes in neurodegenerative disease treatment.
Ferroptosis in Neurodegeneration: Mechanisms and Therapeutic Targets
Molecular Pathways of Ferroptosis
Ferroptosis is distinct from other forms of regulated cell death morphologically, biochemically, and genetically. The core molecular machinery involves three interconnected pathways: iron metabolism dysregulation, lipid peroxidation accumulation, and failure of antioxidant defense systems [44]. Intracellular iron homeostasis is maintained through precise regulation of iron uptake, storage, and efflux. Under pathological conditions, excess ferrous iron (Fe²⁺) catalyzes the Fenton reaction, generating hydroxyl radicals that initiate oxidative damage [44]. The antioxidant defense system, centered on glutathione peroxidase 4 (GPX4) and glutathione (GSH), becomes compromised in neurodegenerative states. System Xc⁻, a cystine/glutamate antiporter composed of SLC7A11 and SLC3A2 subunits, imports cystine for GSH synthesis. When this system is impaired, GSH depletion occurs, reducing GPX4 activity and allowing lethal lipid peroxides to accumulate [43] [44]. Additionally, enzymes such as acyl-CoA synthetase long-chain family member 4 (ACSL4) facilitate the esterification of polyunsaturated fatty acids into membrane phospholipids, rendering them more susceptible to peroxidation [44].
Experimental Models and Assessment Methodologies
Research into ferroptosis employs various experimental models and assessment techniques, as detailed in the table below.
Table 1: Experimental Models and Methods for Ferroptosis Research
| Model System | Key Readouts | Technical Approaches |
|---|---|---|
| In Vitro Cellular Models | Cell viability, Lipid ROS, GSH/GSSG ratio | CCK-8 assay, C11-BODIPY 581/591 staining, GSH assay kit [44] |
| Animal Models | Behavioral deficits, Histopathological changes, Biochemical alterations | Morris water maze, Immunohistochemistry, ELISA, Western blot [45] [44] |
| Molecular Analysis | Gene/protein expression of ferroptosis regulators | qRT-PCR, RNA sequencing, Western blotting [43] [44] |
Comparative Therapeutic Mechanisms: MSC-Exosomes versus Whole Cell Therapies
Biodistribution and Blood-Brain Barrier Penetration
The ability to reach pathological sites in the brain is a critical differentiator between MSC-Exosomes and whole cell therapies.
Table 2: BBB Penetration and Biodistribution Profiles
| Characteristic | MSC-Exosomes | Whole MSC Therapy |
|---|---|---|
| Size | 30-150 nm [5] [46] | 30-60 μm [5] |
| Primary Transport Mechanism | Transcytosis across endothelial cells [46] | Paracellular migration through impaired BBB, adhesion to endothelium [47] |
| Systemic Distribution | Wider biodistribution; can cross intact BBB [46] | Primarily trapped in lung microvasculature; limited brain engraftment [5] [11] |
| Therapeutic Implications | Can be administered prophylactically or in early disease | Largely restricted to acute phases with significant BBB disruption |
MSC-Exos achieve brain penetration primarily through transcytosis, with several hypothesized pathways: (1) binding to G protein-coupled receptors on the cell surface to induce signaling cascades; (2) internalization by adhesion and fusion with the cell membrane to release contents; (3) micropinocytosis via inverse membrane invagination; (4) receptor-mediated transcytosis through endocytosis and multivesicular body storage; or (5) lipid raft-mediated uptake influencing membrane fluidity [46]. Their nano-scale size enables them to cross the BBB without requiring its breakdown, facilitating targeted delivery to the brain parenchyma [44].
In contrast, intravenously administered whole MSCs (30-60 μm in diameter) face significant trafficking limitations. A substantial proportion become trapped in the lung microvasculature, reducing the number of cells reaching the brain [5] [11]. Those that do reach cerebral vasculature employ a leukocyte-like, multistep homing process: initial tethering and rolling along endothelial walls via selectins, activation by chemokines such as stromal cell-derived factor-1 (SDF-1), firm adhesion through integrin/VCAM-1 interactions, and final transmigration via secretion of matrix metalloproteinases (MMPs) to degrade the endothelial basement membrane [47]. This process predominantly occurs when the BBB is compromised, such as following acute injury or in advanced disease stages, limiting the therapeutic window for whole cell approaches.
Ferroptosis Modulation Capabilities
Both MSC-Exosomes and whole MSCs possess ferroptosis-modulating activity, though through distinct mechanisms and with different efficiency profiles.
Table 3: Comparative Ferroptosis Modulation Mechanisms
| Mechanism | MSC-Exosomes | Whole MSCs |
|---|---|---|
| Antioxidant Delivery | Direct transfer of GPX4, anti-ferroptotic miRNAs [43] [44] | Paracrine secretion of factors; requires cell viability and engraftment [11] |
| Iron Homeostasis | Delivery of iron-regulating miRNAs and proteins [43] | Secretion of iron-regulating factors (limited evidence) |
| Lipid Peroxidation Suppression | Specific miRNAs targeting ACSL4/LPCAT3 [44] | Broad anti-inflammatory effects potentially reducing oxidative stress |
| Therapeutic Specificity | Targeted via engineering; cargo reflects parent cell status [2] [43] | Influenced by local microenvironment; potential undesirable polarization |
MSC-Exos contain a sophisticated cargo of biomolecules that directly counter ferroptotic pathways. They are enriched with antioxidant enzymes, including GPX4, which directly reduces phospholipid hydroperoxides to nontoxic alcohols [44]. Additionally, they carry specific microRNAs (e.g., miR-27a-3p) that downregulate ferroptosis promoters such as ACSL4, thereby reducing membrane phospholipid susceptibility to peroxidation [43]. These vesicles also modulate iron homeostasis by transferring molecules that regulate ferritinophagy and iron storage, thus limiting the catalytic iron pool available for Fenton chemistry [44]. The exosomal cargo is not static but dynamically reflects the physiological state of the parent MSCs, potentially allowing for preconditioning strategies to enhance anti-ferroptotic activity [2].
Whole MSCs exert anti-ferroptotic effects primarily through paracrine signaling, releasing a cocktail of trophic factors, cytokines, and vesicles that collectively reduce oxidative stress and inflammation in the brain microenvironment [11]. While this approach can be beneficial, it is less specific than exosome-mediated targeting and depends heavily on MSC survival, engraftment, and correct phenotypic polarization in the host tissue—factors that are often suboptimal in the inflammatory milieu of neurodegenerative diseases. There is also evidence that MSCs can adopt a pro-tumorigenic phenotype in certain contexts, raising safety concerns for chronic administration [2] [11].
Experimental Models and Functional Outcomes
Quantitative Assessment of Therapeutic Efficacy
Preclinical studies across various neurological disease models provide compelling data on the comparative efficacy of both therapeutic approaches.
Table 4: Quantitative Efficacy Metrics in Preclinical Models
| Disease Model | MSC-Exosome Treatment Outcomes | Whole MSC Treatment Outcomes |
|---|---|---|
| Alzheimer's Disease | ~45% reduction in Aβ plaques in APP/PS1 mice; cognitive recovery to wild-type levels [45] | Moderate reduction in Aβ; variable cognitive improvement [47] |
| Stroke (Ischemic) | Significant reduction in infarct volume; improved functional recovery via GPX4–GSH axis [44] | Limited consistent efficacy; cell engraftment issues [11] |
| Parkinson's Disease | Protection of dopaminergic neurons; reduced lipid peroxides [44] | Moderate functional improvement; poor long-term cell survival |
| Cognitive Assessment | Performance indistinguishable from wild-type for 6 months post-treatment [45] | Transient improvement with potential decline |
In Alzheimer's disease models, MSC-Exos have demonstrated remarkable efficacy. One study utilizing LRP1-targeted polymersomes to enhance Aβ clearance observed approximately 45% reduction in brain Aβ levels within hours of treatment, with an 8-fold increase in plasma Aβ, indicating efficient clearance across the BBB [45]. Critically, treated AD mice exhibited cognitive performance indistinguishable from wild-type controls in spatial learning and memory tests, with benefits persisting for up to 6 months post-treatment [45]. This suggests that MSC-Exos not only clear pathological protein aggregates but also facilitate lasting functional recovery—a crucial outcome measure for neurodegenerative therapies.
The functional benefits of MSC-Exos in ferroptosis-driven pathology are particularly notable in stroke models. These nanovesicles restore redox balance by enhancing the GPX4-GSH axis, reducing infarct volume, and improving neurological function [44]. Their multi-targeted approach simultaneously addresses iron dysregulation, lipid peroxidation, and antioxidant depletion—key pillars of ferroptotic cell death. Whole MSCs have shown more variable outcomes in similar models, with functional improvements often not correlating with long-term cell engraftment, supporting the notion that their benefits are primarily paracrine rather than through structural integration [11].
Safety and Manufacturing Considerations
The translational potential of therapeutic platforms extends beyond efficacy to encompass safety profiles and manufacturing feasibility.
Table 5: Safety and Manufacturing Comparison
| Parameter | MSC-Exosomes | Whole MSC Therapy |
|---|---|---|
| Tumorigenic Risk | Minimal (non-replicative) [11] | Potential concern (particularly with immortalized lines) [2] |
| Immunogenicity | Low; avoids immune rejection [5] [11] | Moderate; requires matching or immunosuppression |
| Storage & Stability | Lyophilization possible; more stable [5] | Requires cryopreservation; viability concerns |
| Production Scalability | Potentially scalable with TFF systems [5] | Limited by cell expansion capacity and senescence [11] |
| Quality Control | Standardized characterization possible (MISEV guidelines) [5] | Variable potency with passages; senescence issues [11] |
MSC-Exos present significant safety advantages as acellular therapeutics. Their non-replicative nature essentially eliminates the risk of tumor formation associated with whole cell therapies [11]. Additionally, they exhibit low immunogenicity, minimizing concerns about immune rejection and enabling allogeneic applications without matching requirements [5]. From a manufacturing perspective, exosomes can be isolated using scalable methods such as tangential flow filtration (TFF) and characterized according to MISEV2018 guidelines, promoting batch-to-batch consistency [5]. They can also be lyophilized for enhanced stability, simplifying storage and distribution [5].
Whole MSCs face greater manufacturing and safety challenges. Their therapeutic potency can vary with donor age, tissue source, and passage number, with senescence occurring after limited population doublings [11]. Although immortalized MSC lines offer a potential solution, they raise additional safety concerns regarding tumorigenicity [2]. Clinical administration of whole cells carries risks of infusion-related toxicities, including pulmonary embolism from cells trapped in lung capillaries—a concern not applicable to nano-scale exosomes [5].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing research on MSC-exosomes and ferroptosis requires specialized reagents and methodologies.
Table 6: Essential Research Reagents and Tools
| Reagent/Tool | Function/Application | Experimental Context |
|---|---|---|
| PHK26/DiD Fluorescent Dyes | Labeling exosomes for tracking and uptake studies [46] | Visualizing exosome transport across BBB models |
| C11-BODIPY 581/591 | Sensitive detection of lipid peroxidation [44] | Measuring ferroptosis in cellular models |
| Ferrostatin-1 | Specific ferroptosis inhibitor (reference compound) [43] | Validating ferroptosis pathways; control experiments |
| GPX4 Antibody | Detection of GPX4 protein expression | Western blot, immunohistochemistry for ferroptosis assessment |
| CD63/CD81/CD9 Antibodies | Exosome characterization (tetraspanin markers) [11] | Flow cytometry, immunoblotting for vesicle validation |
| TSG101 & Alix Antibodies | Identification of exosome biogenesis markers [46] | Confirming exosome isolation by Western blot |
| LRP1-Targeting Ligands | Enhancing BBB penetration (e.g., angiopep-2) [45] | Engineering exosomes for improved brain delivery |
| Ultracentrifugation System | Gold-standard exosome isolation [5] | Purifying exosomes from conditioned media |
| Tangential Flow Filtration | Scalable exosome purification [5] | Large-scale production for therapeutic applications |
The accumulating evidence positions MSC-derived exosomes as a superior therapeutic platform for targeting ferroptosis in neurodegenerative diseases compared to whole cell therapies. Their innate ability to cross the intact blood-brain barrier via transcytosis mechanisms, combined with their multi-faceted anti-ferroptotic cargo and favorable safety profile, addresses critical limitations of whole cell approaches. The functional outcomes observed in preclinical models—including significant reduction in pathological protein aggregates, protection against ferroptotic cell death, and lasting cognitive recovery—underscore their potential as a transformative therapeutic paradigm.
Future research directions should focus on optimizing exosome engineering for enhanced brain targeting, standardizing production protocols for clinical-grade manufacturing, and validating specific anti-ferroptotic cargo responsible for therapeutic effects. As the field progresses toward clinical translation, MSC-exosomes represent a promising cell-free platform that effectively merges targeted delivery with disease-modifying potential for neurodegenerative conditions characterized by ferroptotic pathology.
The therapeutic landscape for autoimmune and inflammatory disorders is undergoing a significant transformation, shifting from conventional broad-spectrum immunosuppression toward precision medicine strategies that restore immune homeostasis. Among the most promising advancements are therapies based on mesenchymal stem cells (MSCs) and their derived exosomes. The table below provides a high-level comparison of these two interrelated therapeutic approaches.
Table 1: Core Comparison of MSC-Based Therapeutic Platforms
| Feature | MSC Whole Cell Therapy | MSC-Derived Exosomes (MSC-Exos) |
|---|---|---|
| Therapeutic Entity | Live, intact cells [2] | Cell-free, nanosized vesicles (30-150 nm) [24] [48] |
| Primary Mechanism | Direct differentiation; paracrine signaling (secretion of soluble factors and vesicles) [23] | Paracrine mediation; transfer of bioactive cargo (proteins, lipids, miRNAs) [2] [23] |
| Key Advantages | Multimodal action; homing to injury sites [49] | Lower immunogenicity; no risk of tumorigenesis or ectopic tissue formation; inherent targeting; superior stability [24] |
| Major Challenges | Low engraftment/short lifespan; immunogenic responses; risk of malignant transformation; pulmonary entrapment [24] [23] | Cargo variability; lack of standardized isolation/purification methods; scalable production [24] [48] |
| Clinical Safety Profile | Risks of immune rejection, transient fever, and administration-related effects [49] | Inherently safer profile; no risk of cell proliferation-related complications [24] |
| Manufacturing & Storage | Complex; requires stringent viability control; limited shelf-life [49] | More amenable to storage, sterilization, and off-the-shelf use [24] |
Mechanisms of Action: A Detailed Functional Comparison
Understanding the distinct mechanistic pathways through which MSC whole cell therapy and MSC-derived exosomes operate is crucial for selecting the appropriate therapeutic platform for specific autoimmune pathologies.
Immunomodulatory Pathways
Both MSCs and MSC-Exos are potent immunomodulators, but they achieve this through different cellular interactions and molecular deliveries.
MSC Whole Cell Mechanisms: MSCs are dynamic immune orchestrators. They modulate the local microenvironment by direct cell-to-cell contact and the secretion of soluble factors like prostaglandin E2 (PGE2) and indoleamine 2,3-dioxygenase (IDO) [49]. A key function is their ability to promote the expansion of regulatory T cells (Tregs), which are critical for maintaining immune tolerance, while simultaneously suppressing the activity of pro-inflammatory T-helper 1 (Th1) and Th17 cells [49]. Their homing capacity, mediated by the CXCR4/SDF-1 axis, allows them to migrate to sites of inflammation and exert these effects locally [49].
MSC-Exosome Mechanisms: MSC-Exos function as a refined, molecular-level communication system. Their immunomodulatory effects are largely mediated by their cargo, particularly microRNAs (miRNAs). Key miRNAs and their roles include:
- miR-21 & miR-146a: These are pivotal miRNAs in suppressing inflammatory responses. Preconditioning MSCs with inflammatory cytokines like TNF-α or IL-1β can enhance the loading of these miRNAs into exosomes, amplifying their anti-inflammatory effect upon delivery to recipient immune cells [24].
- miR-125a & miR-181a: These miRNAs facilitate tissue repair and modulate inflammatory pathways, further contributing to the restoration of immune homeostasis [24].
By transferring this specific genetic material, MSC-Exos can reprogram the behavior of immune cells, such as macrophages, shifting them from a pro-inflammatory (M1) to an anti-inflammatory (M2) phenotype [50].
Tissue Repair and Regenerative Potential
Beyond immunomodulation, promoting the repair of tissue damaged by chronic inflammation is a critical therapeutic goal.
MSC Whole Cell Mechanisms: MSCs possess inherent regenerative potential due to their capacity to differentiate into multiple cell lineages, such as osteoblasts, chondrocytes, and adipocytes [23]. In theory, they can directly replace damaged cells. Furthermore, they secrete a wide array of growth factors that promote endogenous repair processes, including angiogenesis and progenitor cell proliferation [49].
MSC-Exosome Mechanisms: MSC-Exos promote tissue repair indirectly. They transport anabolic factors and regulatory RNAs that activate endogenous repair pathways in resident cells. For instance, in rheumatoid arthritis (RA), MSC-derived exosomes have been shown to carry factors that can facilitate joint repair and regeneration, reducing pain and inflammation [50]. In osteoarthritis (OA), exosomes from human MSCs carrying miR-92a-3p have been demonstrated to enhance chondrogenesis and suppress cartilage degradation by targeting WNT5A [48].
The diagram below illustrates the key mechanistic differences in how these two therapeutics target and resolve inflammation and tissue damage in an autoimmune context.
Comparative Therapeutic Efficacy: Analysis of Experimental and Clinical Data
The theoretical mechanisms are supported by a growing body of experimental and clinical data, which helps quantify the functional outcomes of each therapeutic approach.
Preclinical and Clinical Outcomes in Autoimmune Models
Data from animal models and human trials provide critical insights into the efficacy and durability of responses. The following table summarizes key findings across multiple autoimmune and inflammatory conditions.
Table 2: Comparative Therapeutic Efficacy Across Disease Models
| Disease Model | MSC Whole Cell Therapy Outcomes | MSC-Exosome Outcomes | Key Mechanisms & Notes |
|---|---|---|---|
| Systemic Lupus Erythematosus (SLE) | Clinical trials show immunomodulation and disease activity reduction [49]. | Not explicitly detailed in search results. | MSC therapy is a key focus in global clinical trials for SLE [49]. |
| Rheumatoid Arthritis (RA) | Reduction of inflammation and pain in clinical trials [50]. | Reduction of inflammation and pain; promotion of joint repair/regeneration [50]. | MSC-Exos transport anti-inflammatory substances and growth factors [50]. |
| Osteoarthritis (OA) | Not explicitly detailed in search results. | Promoted chondrocyte viability; suppressed cartilage degradation (e.g., via miR-92a-3p/WNT5A); reduced inflammation [48]. | MSC-Exo miRNA cargo (e.g., miR-361-5p) can inactivate NF-κB pathway [48]. |
| Multiple Sclerosis & Scleroderma | Hematopoietic stem cell (HSC) transplantation shows long-term remission potential [49]. | Not explicitly detailed in search results. | HSC therapy re-establishes immune tolerance [49]. |
| Crohn’s Disease (CD) | 85 global clinical trials focused on MSC therapy [49]. | Not explicitly detailed in search results. | CD is the most studied autoimmune disease for stem cell therapy [49]. |
Impact of Preconditioning on Exosome Efficacy
A significant advancement in the field is the use of preconditioning strategies to enhance the therapeutic potency of MSC-Exos. By exposing parent MSCs to specific stimuli, the miRNA content and functional properties of the secreted exosomes can be optimized [24].
Table 3: Preconditioning Strategies for Enhancing MSC-Exosome Efficacy
| Preconditioning Stimulus | Dosage Example | Resulting miRNA Cargo Changes | Documented Functional Outcome |
|---|---|---|---|
| Lipopolysaccharide (LPS) | 0.1 - 1.0 μg/mL [24] | Upregulation of miR-222-3p, miR-181a-5p, miR-150-5p [24] | Mitigation of inflammatory damage [24]. |
| TNF-α (Inflammatory Cytokine) | 10 - 20 ng/mL [24] | Significant increase in miR-146a; higher doses increase miR-34 [24] | Enhanced immunomodulatory effects; promotion of macrophage polarization [24]. |
| IL-1β (Inflammatory Cytokine) | Not specified [24] | Increased miR-146a in EVs [24] | Improved outcomes in sepsis models; macrophage polarization [24]. |
| Hypoxia | Not specified [24] | Altered miRNA expression profiles [24] | Optimization of therapeutic potential for tissue repair and immunomodulation [24]. |
Experimental Protocols: Key Methodologies for Research and Validation
For researchers aiming to replicate or build upon these findings, standardized protocols are essential. Below is a detailed methodology for a key experiment evaluating the immunomodulatory effects of preconditioned MSC-Exos.
Detailed Protocol: Evaluating Preconditioned MSC-Exos in Macrophage Polarization
Objective: To isolate and characterize exosomes from TNF-α-preconditioned MSCs and assess their ability to polarize macrophages from an M1 (pro-inflammatory) to an M2 (anti-inflammatory) phenotype.
Step 1: MSC Preconditioning and Exosome Isolation
- Cell Culture: Culture human umbilical cord MSCs (hucMSCs) in standard media.
- Preconditioning: Stimulate MSCs at ~80% confluency with 10-20 ng/mL of recombinant human TNF-α for 24-48 hours [24].
- Exosome Isolation: Collect conditioned media. Differential centrifugation is the gold-standard method:
- Centrifuge at 300 × g for 10 min to remove cells.
- Centrifuge supernatant at 2,000 × g for 20 min to remove dead cells.
- Centrifuge at 10,000 × g for 30 min to remove cell debris.
- Ultracentrifugate the final supernatant at 100,000 × g for 70 min to pellet exosomes [23].
- Characterization: Validate exosome identity using Nanoparticle Tracking Analysis (NTA) for size/concentration (30-150 nm) and Western Blotting for positive markers (CD63, CD81, TSG101) and a negative marker (calnexin) [23]. miRNA cargo can be profiled via RT-qPCR or next-generation sequencing for miR-146a and others [24].
Step 2: Macrophage Polarization Assay
- Macrophage Generation: Differentiate human monocytic THP-1 cells into M0 macrophages using PMA.
- M1 Polarization: Stimulate M0 macrophages with 100 ng/mL LPS and 20 ng/mL IFN-γ for 24 hours to establish an M1 phenotype.
- Exosome Treatment: Treat M1 macrophages with isolated MSC-Exos (e.g., 50 μg/mL) for 48 hours.
- Flow Cytometry Analysis: Analyze surface markers to confirm polarization shift. Key markers include:
- M1 Markers: CD80, CD86
- M2 Markers: CD206, CD209
- Cytokine Profiling: Use ELISA to measure cytokine levels in the supernatant. Expect a decrease in M1-associated cytokines (TNF-α, IL-6, IL-12) and an increase in M2-associated cytokines (IL-10, TGF-β).
The workflow for this experimental protocol is summarized in the following diagram.
The Scientist's Toolkit: Essential Research Reagent Solutions
To conduct the aforementioned research, specific high-quality reagents and tools are required. The following table catalogs essential solutions for working with MSC-derived exosomes.
Table 4: Key Research Reagent Solutions for MSC-Exosome Research
| Reagent / Solution | Function / Application | Specific Examples / Notes |
|---|---|---|
| MSC Culture Media | Expansion and maintenance of parent mesenchymal stem cells. | Commercially available, serum-free, xeno-free media optimized for MSC growth. |
| Preconditioning Agents | Priming MSCs to alter exosome cargo and enhance therapeutic potency. | Recombinant human cytokines (TNF-α, IL-1β); LPS; agents to induce hypoxia [24]. |
| Exosome Isolation Kits | Purification of exosomes from conditioned cell culture media. | Polymer-based precipitation kits offer scalability; affinity capture kits provide specificity (e.g., for CD63). Ultracentrifugation remains the gold standard [23]. |
| Exosome Characterization Tools | Validation of exosome identity, size, concentration, and cargo. | NTA: For size/distribution (e.g., ZetaView, NanoSight). WB Antibodies: Against tetraspanins (CD9, CD63, CD81) and markers (TSG101, ALIX). RT-qPCR Assays: For miRNA cargo quantification (e.g., miR-146a, miR-21) [23]. |
| Cell Lines for Functional Assays | In vitro validation of exosome immunomodulatory function. | Human monocytic cell line (THP-1) for macrophage polarization assays; primary immune cells (T-cells, B-cells). |
| Flow Cytometry Antibodies | Phenotyping immune cells and assessing polarization states. | Antibody panels for M1 (CD80, CD86) and M2 (CD206, CD209) macrophage markers; T-cell markers (CD4, CD25, FoxP3 for Tregs). |
The comparative analysis of MSC whole cell therapy and MSC-derived exosomes reveals a clear evolutionary path in regenerative immunology. While whole MSC therapy offers the potential for direct cellular interaction and multi-faceted repair, its clinical translation is hampered by significant safety and logistical challenges. In contrast, MSC-derived exosomes present a safer, more refined, and engineerable "cell-free" therapeutic platform. Their efficacy, particularly when enhanced through preconditioning strategies, positions them as a superior candidate for next-generation treatments aimed at restoring immune homeostasis in autoimmune and inflammatory disorders. Future success hinges on overcoming challenges related to production scalability, cargo standardization, and the development of robust engineering protocols for precision targeting.
Promising Results in Cardiovascular Repair, Lung Diseases, and Ocular Conditions
The field of regenerative medicine has been significantly shaped by research into mesenchymal stem cells (MSCs), which possess notable regenerative, reparative, and immunomodulatory capacities. However, the therapeutic application of whole MSCs faces challenges including suboptimal biocompatibility, potential for host immune rejection, risk of tumor formation, and difficulties with targeted delivery to specific tissues. In recent years, MSC-derived exosomes have emerged as a promising cell-free therapeutic alternative, demonstrating comparable or superior functional outcomes across multiple disease models while mitigating the risks associated with whole cell transplantation [2] [51] [52]. This guide objectively compares the therapeutic performance of MSC-derived exosomes against whole MSC therapy in cardiovascular, pulmonary, and ocular conditions, supported by experimental data and detailed methodologies.
Comparative Therapeutic Performance Data
The tables below summarize quantitative data from preclinical and clinical studies comparing the efficacy of MSC-derived exosomes and whole MSC therapy across three therapeutic areas.
Table 1: Comparative Outcomes in Cardiovascular Disease Models
| Disease Model | Therapeutic Agent | Key Outcomes | Proposed Mechanisms | Source/Study |
|---|---|---|---|---|
| Myocardial Ischemia/Reperfusion Injury | MSC-derived Exosomes | Restored impaired autophagic flux, reduced infarct size, improved cardiac function | Activation of AMPK/mTOR and Akt/mTOR signaling pathways; transfer of miRNAs (e.g., miR-455-3p, miR-125b-5p) [53]. | Liu et al. [53] |
| Drug-Induced Cardiotoxicity | MSC-derived Exosomes | Suppressed excessive autophagy, reduced apoptosis, preserved mitochondrial function | Modulation of autophagic flux via exosomal cargo (e.g., GDF-15, OPTN) [53]. | Xiong et al. [53] |
| Heart Failure | Whole MSC Therapy | Improved cardiac function, reduced scar tissue, paracrine signaling | Direct differentiation and paracrine factor secretion; limited by graft rejection and tumor formation risk [54] [51]. | Frontiers Review [54] |
Table 2: Comparative Outcomes in Lung Disease Models
| Disease Model | Therapeutic Agent | Key Outcomes | Proposed Mechanisms | Source/Study |
|---|---|---|---|---|
| Oleic Acid-Induced Acute Lung Injury (Rat) | BMSCs (Whole Cells) | Significant restoration of histopathological parameters (bleeding, leukocyte infiltration, edema, hyperplasia) | Downregulation of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) and apoptotic signals; upregulation of anti-inflammatory cytokines (IL-4, IL-10) [55]. | Önsöz et al. [55] |
| Oleic Acid-Induced Acute Lung Injury (Rat) | BMSC-derived Exosomes | Restored histopathological parameters, but with less efficacy than whole BMSCs | Carried regenerating agents (miRNA, siRNA, ceramide); downregulation of inflammatory cytokines [55]. | Önsöz et al. [55] |
| Chronic Lung Diseases (COPD, PF, ALI/ARDS) | Engineered MSC-Exosomes | Enhanced targeted drug delivery, increased potency, improved ability to cross physiological barriers | Engineered modifications for specific targeting and enhanced biological effects; acts as a cell-free therapeutic agent [56] [57]. | Hu et al. [56] |
Table 3: Comparative Outcomes in Ocular Disease Models
| Disease Model | Therapeutic Agent | Key Outcomes | Proposed Mechanisms | Source/Study |
|---|---|---|---|---|
| Various Anterior/Posterior Segment Diseases | MSC-derived Exosomes | Rapid penetration of ocular barriers, efficient delivery of therapeutic factors, neuroprotection, immunomodulation | Nano-size (30-150 nm) enables penetration of blood-retinal barrier; cargo (miRNAs) modulates immune response and promotes repair; lower risk of immune rejection and vitreous opacification [58] [52]. | Pharmaceutics Review [58] [52] |
| Chronic Ophthalmic Pathologies | Whole MSC Therapy | Regenerative and immunomodulatory effects; limited by suboptimal biocompatibility, penetration, and delivery risks | Direct cell action; limited by risks of allogeneic rejection, unwanted differentiation, and vessel occlusion upon intravenous injection [52]. | Pharmaceutics Review [52] |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for evaluating the cited data, this section outlines the key methodologies from the featured studies.
This protocol directly compares whole BMSCs and their derivative exosomes in the same disease model.
Step 1: Induction of Acute Lung Injury
- Animal Model: Adult male Wistar Albino rats (220-270 g).
- Injury Induction: Intravenous (i.v.) administration of oleic acid solution (60 mg/kg dissolved in ethanol and saline) via the tail vein.
- Control Group: Administered a vehicle control (alcohol and saline solution).
Step 2: Therapeutic Intervention
- Timing: Therapeutics administered 2 hours after oleic acid injection to avoid direct destruction by the fatty acid.
- Treatment Groups:
- BMSC Group: Received 1 x 10^6 rat BMSCs (in PBS) via tail vein injection.
- Exosome Group: Received an exosome fraction (isolated from 1 x 10^6 BMSCs using a commercial kit) in PBS via tail vein injection.
- Source of BMSCs: Isolated from rat femur and tibia bones, cultured in Alpha MEM medium with 10% FBS, and used at passage 3 (P3) or 4 (P4).
Step 3: Outcome Assessment
- Timing: Rats were sacrificed 24 hours post-treatment under deep anesthesia.
- Primary Analysis: Lung tissues were collected and stained with hematoxylin and eosin (H&E).
- Histopathological Evaluation: A blinded examination scored H&E-stained samples for parameters of bleeding, leukocyte infiltration, edema, and hyperplasia.
This methodology focuses on elucidating the mechanism of action for exosomes in cardiovascular repair.
Step 1: Exosome Isolation and Characterization
- Source: Exosomes are isolated from the culture medium of MSCs (source can vary: bone marrow, adipose tissue, umbilical cord).
- Isolation Method: Ultracentrifugation or commercial kits are standard. Isolated exosomes are characterized for size (30-150 nm) and surface markers (e.g., CD63, CD81, CD9) typically via dynamic light scattering (DLS) or nanoparticle tracking analysis (NTA) and flow cytometry.
- Cargo Analysis: The exosomal content (e.g., miRNAs like miR-455-3p, miR-125b-5p; proteins like GDF-15) is profiled using techniques like RNA sequencing and mass spectrometry.
Step 2: In Vitro/In Vivo Modeling of Cardiac Stress
- In Vitro Model: Cardiomyocytes are subjected to hypoxia/reoxygenation or specific drug treatments (e.g., doxorubicin) to simulate ischemia/reperfusion injury or cardiotoxicity.
- In Vivo Model: Animal models (e.g., mouse, rat) of myocardial infarction (via coronary artery ligation) or ischemia/reperfusion injury are used.
Step 3: Therapeutic Intervention and Mechanistic Evaluation
- Treatment: Models are treated with MSC-derived exosomes vs. controls (e.g., whole MSCs, vehicle).
- Functional Assays: Cardiac function is assessed via echocardiography (e.g., ejection fraction, fractional shortening).
- Molecular Analysis:
- Autophagy Flux Assessment: Western blotting for key autophagy markers LC3-II and p62/SQSTM1.
- Signaling Pathway Analysis: Western blotting or immunohistochemistry to analyze the activity of key pathways (e.g., AMPK/mTOR, Akt/mTOR) in heart tissue or cells.
- Gene Expression: qRT-PCR to measure the levels of specific miRNAs or mRNAs involved in autophagy and apoptosis.
Signaling Pathways and Mechanisms of Action
The therapeutic effects of MSC-derived exosomes are mediated through complex signaling pathways that modulate key cellular processes like autophagy. The diagram below illustrates how exosomes act as "autophagic rheostats" in the context of cardiovascular aging and repair.
Diagram: Exosome-Mediated Autophagy Regulation in Cardiac Repair. MSC-derived exosomes deliver cargo that modulates mTOR signaling pathways, restoring balanced autophagy to promote cardiomyocyte survival and function.
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents and materials essential for conducting research in the field of MSC-exosome biology and therapy.
Table 4: Essential Research Reagents for MSC-Exosome Studies
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source material for exosome production and whole-cell therapy comparisons. | Source (e.g., Bone Marrow, Adipose Tissue, Umbilical Cord) can influence exosome content and therapeutic effect [51] [57]. |
| Exosome-Depleted Fetal Bovine Serum (FBS) | Used in MSC culture media to prevent contamination of isolated exosomes with bovine vesicles. | Critical for obtaining pure, host-derived exosome preparations for downstream analysis and application [55]. |
| Exosome Isolation Kits | For purifying exosomes from cell culture supernatant or biological fluids. | Kits (e.g., based on precipitation) provide a standardized and accessible method, though ultracentrifugation remains a gold standard [55]. |
| Characterization Tools (NTA, Flow Cytometry) | To confirm exosome identity, size (30-150 nm), and concentration. | Nanoparticle Tracking Analysis (NTA) for size/distribution; flow cytometry for surface marker detection (CD63, CD81, CD9) [55] [52]. |
| Model Organisms | For in vivo testing of therapeutic efficacy (e.g., rat models for lung injury, mouse models for MI). | Choice of model must accurately reflect the human disease pathology being studied [53] [55]. |
| Pathway-Specific Antibodies | For mechanistic studies via Western Blot or IHC (e.g., anti-LC3, anti-p62, anti-phospho-AMPK/Akt/mTOR). | Essential for validating the modulation of specific signaling pathways like autophagy in response to exosome treatment [53]. |
Navigating Clinical Hurdles: Standardization, Dosing, and Safety
Mesenchymal stem cells (MSCs) and their derived exosomes have emerged as highly promising therapeutic agents in regenerative medicine, offering significant potential for treating a wide spectrum of diseases, from autoimmune and inflammatory disorders to neurodegenerative conditions and orthopedic injuries [59]. Their therapeutic value lies in their unique biological properties—multipotent differentiation capabilities, immunomodulatory functions, and potent paracrine activity [60]. However, as the field transitions from preclinical research to clinical applications, a critical challenge has emerged: a profound lack of harmonized protocols for the isolation and characterization of these complex biological entities. This standardization crisis threatens to undermine the reproducibility, reliability, and clinical translation of research findings, creating significant barriers to the development of consistent, effective therapies.
The therapeutic paradigm has shifted from viewing MSCs primarily as differentiation-capable units to recognizing their role as secretory powerhouses. Their beneficial effects are now largely attributed to their potent paracrine capacity, particularly through the secretion of extracellular vesicles, including exosomes [61]. These nano-sized vesicles (30-150 nm in diameter) effectively encapsulate the therapeutic properties of their parent MSCs, containing a diverse cargo of proteins, lipids, and nucleic acids that mediate intercellular communication [42]. As interest increasingly turns toward these cell-free therapeutic agents, the field faces a dual standardization challenge: establishing consistent protocols for both the parental MSCs and the exosomes they produce.
Comparative Analysis: MSC vs. MSC-Derived Exosome Therapeutics
Table 1: Fundamental Comparison of MSC Therapy vs. MSC-Derived Exosome Therapy
| Characteristic | MSC Whole-Cell Therapy | MSC-Derived Exosome Therapy |
|---|---|---|
| Physical Nature | Live, nucleated cells (10-100 μm) [19] | Extracellular vesicles (30-150 nm) [61] [42] |
| Therapeutic Mechanism | Direct differentiation; Cell-cell contact; Paracrine secretion [59] | Cargo transfer (proteins, lipids, nucleic acids); Paracrine signaling without cells [19] [33] |
| Key Advantages | Self-renewing; Multipronged mechanism of action [60] | Lower immunogenicity; Cannot form tumors; Cross biological barriers; Higher stability [61] [33] |
| Major Challenges | Heterogeneity; Senescence during expansion; Pulmonary entrapment; Risk of ectopic tissue formation [62] [33] | Cargo variability; Scalable production; Complex isolation and characterization [42] |
| Standardization Hurdles | Donor/source variability; Expansion conditions; Passage number; Characterization markers [62] [60] | Isolation method purity; Cargo profiling; Functional potency assays; Dosing metrics [42] |
The divergence in physical and biological properties between MSCs and their exosomes necessitates distinct regulatory and manufacturing frameworks. MSC therapies face challenges related to cellular heterogeneity, viability, and potential adverse effects post-transplantation. In contrast, exosome therapies, while circumventing cell-based risks, introduce complexities in vesicle isolation, cargo standardization, and the development of potency assays that reliably predict their therapeutic function [33] [42]. The resolution of the standardization crisis is therefore not a one-size-fits-all endeavor but requires tailored approaches for each therapeutic modality.
The MSC Isolation and Characterization Landscape
Source-Dependent Variability
MSCs can be isolated from a diverse range of tissues, including bone marrow (BM), adipose tissue (AT), umbilical cord (UC), and dental pulp, among others [59]. This source diversity is a significant contributor to the standardization crisis. While the International Society for Cellular Therapy (ISCT) has established minimal defining criteria—plastic adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-), and trilineage differentiation potential—the functional and compositional characteristics of MSCs are profoundly influenced by their tissue of origin [59] [60]. For instance, umbilical cord-derived MSCs (UC-MSCs) are known for their enhanced proliferation and lower immunogenicity, while bone marrow-derived MSCs (BM-MSCs) have been the most extensively studied and are recognized for their strong immunomodulatory effects [59].
Protocol Inconsistencies in Clinical Trials
An analysis of 47 clinical trials utilizing bone marrow-derived MSCs revealed a striking lack of consensus in isolation and expansion protocols, which directly impacts the critical quality attributes (CQAs) of the final cellular product [62].
Table 2: Variability in MSC Isolation and Expansion Protocols in Clinical Trials
| Process Step | Methodological Options in Use | Impact on Critical Quality Attributes (CQAs) |
|---|---|---|
| BM Sample Processing | • Ficoll density gradient (62%)• Whole BM cells (16%)• Percoll density gradient (9%) [62] | Initial Purity & Yield: Whole BM method yields greater CFU-F number vs. gradient methods affecting initial MSC population and contaminating cells. [62] |
| Isolation Technique | • Plastic adherence (vast majority)• Fluorescence-activated cell sorting (FACS)• Magnetic-activated cell sorting (MACS) [62] | Population Homogeneity: Plastic adherence yields heterogeneous mix; FACS/MACS offer higher purity but are less common due to cost, labor, and lack of a single specific marker. [62] [60] |
| Culture Flask Type | • Corning (27%)• Falcon (27%)• Nunc (23%)• Greiner (18%) [62] | Adhesion & Expansion Efficiency: Significant differences in acquired MSC numbers due to surface treatment variations. [62] |
| Cell Seeding Density | Wide variability reported across studies [62] | Growth Kinetics & Senescence: Inappropriate density affects adherence, contamination by other cells, and initial growth, potentially leading to premature senescence. [62] |
| Passage Number | Inconsistent use, often up to passage 5 [62] | Potency & Differentiation Potential: Therapeutic properties (e.g., cardioprotective effect) can be significantly reduced in higher passages (e.g., P5 vs. P3). [62] |
The choice of isolation method exemplifies the core of the standardization crisis. While the majority of trials use simple plastic adherence for its ease and cost-effectiveness, this results in a heterogeneous initial cell population containing not only MSCs but also hematopoietic cells, endothelial cells, and others [62]. Although fluorescence-activated cell sorting (FACS) and magnetic-activated cell sorting (MACS) can provide more purified populations, they are hampered by the lack of a single unique surface marker for MSCs, high cost, and technical demands, making them unsuitable for many clinical applications [60].
The Compounding Complexity of Exosome Isolation and Characterization
The standardization challenges are magnified for MSC-derived exosomes. These nanoparticles serve as sophisticated communication vehicles, carrying a functional cargo of proteins, miRNAs, and lipids from their parent cells. However, their small size and heterogeneous composition make consistent isolation and characterization particularly difficult.
Isolation Techniques and Purity Concerns
No single isolation method is perfect, and each technique co-isolates different non-exosome components, directly impacting the functional properties of the final product and the interpretation of experimental results [42].
Table 3: Common Exosome Isolation Techniques and Their Limitations
| Technique | Principle | Advantages | Disadvantages & Standardization Challenges |
|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation steps at high speeds (up to 100,000 g) to pellet exosomes based on density and size. [42] | Widely used; no requirement for specific labels; suitable for large volumes. | Can cause exosome aggregation and damage; co-precipitation of protein aggregates and other contaminants; yield and purity are highly protocol-dependent. [42] |
| Size-Exclusion Chromatography (SEC) | Separates exosomes from smaller soluble proteins and larger vesicles based on hydrodynamic volume as they pass through a porous stationary phase. [42] | Better preservation of exosome integrity and function; good separation from contaminants. | May not completely separate exosomes from co-eluting proteins and lipoproteins; sample dilution can occur. [42] |
| Immunoaffinity Capture | Uses antibodies against exosome surface markers (e.g., CD9, CD63, CD81) to selectively capture exosomes. [42] | High specificity and purity for subpopulations expressing the target antigen. | Lower yield; cost; captures only a specific subset of exosomes; highly dependent on antibody specificity and efficiency. [42] |
| Tangential Flow Filtration (TFF) | Uses a pump and filters to circulate the sample, retaining exosomes while allowing smaller molecules to pass through. | Scalable for industrial production; higher processing capacity. | Membrane fouling can occur; definition of "pure" exosome fractions remains debated. [42] |
The International Society for Extracellular Vesicles (ISEV) has recommended the generic term "extracellular vesicles (EVs)" to encompass the heterogeneity of vesicle populations, acknowledging that most common isolation methods yield a mixture of vesicle types [42]. This inherent complexity means that what many studies refer to as "exosomes" are often preparations enriched in small EVs, but not pure exosome populations. This lack of precise definition is a fundamental barrier to standardizing both research and therapeutic applications.
Characterization Hurdles and Functional Potency
Characterizing exosomes goes beyond mere physical identification; it requires a deep understanding of their molecular cargo and functional potency. The molecular composition of exosomes—including over 850 gene products and 150 microRNAs (miRNAs)—varies significantly depending on the source of the MSCs (e.g., BM, AT, UC) and external stimuli they encountered [33] [42]. For instance, miR-146a-5p was found to be uniquely upregulated in the cellular compartment of TNF-α-stimulated MSCs, while miR-150-5p was significantly downregulated, and these differences were reflected differently in the exosome compartment [19]. This dynamic nature of the exosome cargo makes it difficult to establish stable reference materials or universal quality control metrics.
Furthermore, the field lacks universally accepted and standardized assays to measure the functional potency of MSC-derived exosomes. While their therapeutic effects—such as immunomodulation, promotion of angiogenesis, and tissue repair—are well-documented in preclinical models, translating these into reliable in vitro potency assays for batch-to-batch quality control remains a significant hurdle [33].
Experimental Data: Highlighting Therapeutic Potential and Methodological Divergence
Functional Outcomes in Disease Models
Despite the standardization crisis, compelling experimental data demonstrates the therapeutic potential of both MSCs and their exosomes, underscoring why resolving these methodological issues is so critical.
Multiple Sclerosis (MS): In MS research, MSC-derived exosomes have shown promise in addressing two major treatment gaps: alleviating chronic innate inflammation and promoting remyelination. In vitro studies demonstrate that these exosomes can modulate activated microglia from an inflammatory (M1) to an anti-inflammatory (M2) phenotype. Rodent models of experimental autoimmune encephalomyelitis (EAE) have shown potent immunomodulation and remyelination following exosome administration, leading to improved functional outcomes [61]. This is significant because chronic microglial activation, sealed behind an intact blood-brain barrier, is difficult to target with conventional drugs or even whole MSCs, which may get trapped in the lungs [61].
Spinal Cord Injury (SCI): A recent clinical study on chronic SCI patients treated with either bone marrow or Wharton's jelly-derived MSCs reported significant improvements in quality of life (QoL), particularly in bowel and bladder function. The study used standardized questionnaires like the Neurogenic Bowel Dysfunction Score (NBDS) and Wexner Score, showing statistically significant improvements up to one year post-treatment [63]. This highlights that functional recovery, measured by patient-reported outcomes, can be a sensitive indicator of therapeutic efficacy, even for a condition often considered irreversible.
Immunomodulation: The immunomodulatory功能 of MSC exosomes is a key mechanism of action. They have been shown to suppress the proliferation of pro-inflammatory Th1 cells and promote the expansion of regulatory T cells (Tregs). In a contact hypersensitivity model, exosomes from UC-MSCs decreased Th1 cells and IFN-γ secretion while increasing Treg induction [33]. This fine-tuning of the immune response underscores their potential as treatments for autoimmune diseases.
Detailed Experimental Protocol: Isolating and Testing MSC Exosomes in an EAE Model
To illustrate the interconnectedness of methodology and outcome, the following workflow details a typical experiment demonstrating the therapeutic effect of MSC-derived exosomes in a murine EAE model, highlighting steps where protocol choices significantly impact results [61].
Critical Methodological Notes:
- MSC Pre-conditioning: Inflammatory priming (e.g., with IFN-γ) can enhance the immunomodulatory cargo of the resulting exosomes, potentially increasing their therapeutic efficacy [33].
- Isolation Method Choice: Using ultracentrifugation vs. SEC will result in preparations of different purity. SEC often preserves exosome functionality better but may still include some co-eluting contaminants [42].
- Characterization Imperative: Without rigorous characterization using Nanoparticle Tracking Analysis (NTA) for size/concentration and Western Blot for specific markers (e.g., CD63, CD81), the material being injected cannot be accurately defined, complicating the interpretation of results and their replication.
- Dosing and Route: The optimal dose of exosomes (typically in the microgram range for mice) and the best administration route (intravenous vs. intranasal vs. local) are not standardized and can dramatically influence outcomes [61].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagent Solutions for MSC and Exosome Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| GMP-Grade Culture Media & Supplements | Expansion of MSCs for clinical-oriented research. | Moving away from Fetal Bovine Serum (FBS) to defined xeno-free media (e.g., with human platelet lysate) reduces immunogenicity and aligns with regulatory standards. [60] |
| CD Markers for Flow Cytometry | Characterization of MSC surface phenotype (ISCT criteria). | Essential panel: CD73, CD90, CD105 (positive); CD34, CD45, CD14, HLA-DR (negative). Critical for confirming identity and purity. [59] [60] |
| Collagenase / Enzymatic Mix | Isolation of MSCs from tissues (e.g., adipose tissue, umbilical cord). | Enzyme type, concentration, and digestion time must be optimized for each tissue source to maximize yield and viability. [60] |
| Isolation Kits & Columns | For purifying exosomes from conditioned media. | Includes kits for ultracentrifugation, SEC columns, or immunoaffinity pull-down. Choice dictates the purity-function relationship of the isolated vesicles. [42] |
| Characterization Antibodies | Identifying exosomes and specific cargo via Western Blot, ELISA. | Targets: Tetraspanins (CD9, CD63, CD81), ESCRT-related proteins (ALIX, TSG101). Cargo-specific antibodies (e.g., for miR-146a) for functional analysis. [19] [64] |
| Nanoparticle Tracking Analyzer | Physically characterizing isolated exosomes. | Provides size distribution and concentration measurements, a crucial step for quality control and dose standardization. [42] |
The "Standardization Crisis" is not an insurmountable obstacle but a call to action for the scientific community. Addressing it requires a multi-faceted approach: First, the widespread adoption of minimal experimental requirements for describing MSC sources and exosome isolation/characterization methods in publications. Second, a concerted effort to develop and validate scalable, reproducible isolation techniques like Tangential Flow Filtration combined with Size-Exclusion Chromatography (TFF-SEC) for exosomes [42]. Third, the establishment of robust, disease-relevant functional potency assays that can bridge the gap between in vitro characterization and in vivo efficacy.
The functional promise of MSC-derived exosomes as cell-free therapeutic agents capable of modulating immune responses, promoting remyelination, and enhancing quality of life in preclinical models is too great to be lost to irreproducibility [61] [33] [63]. By confronting the standardization crisis head-on through collaborative science, the field can unlock the full potential of these powerful biological nanoparticles and translate their promise into consistent and effective therapies for patients.
In regenerative medicine, Mesenchymal Stem/Stromal Cell (MSC) therapies have demonstrated significant potential for treating diverse conditions through immunomodulation and tissue repair capabilities. However, critical translational challenges including phenotypic instability, risks of immunological rejection, limited in vivo persistence, and potential tumorigenic concerns have hampered their clinical application [23]. These limitations have catalyzed a strategic pivot toward cell-free therapeutic approaches, particularly MSC-derived exosomes (MSC-Exos), which retain therapeutic benefits while circumventing cellular risks [24]. MSC-Exos are nanoscale vesicles (30-150 nm) that facilitate intercellular communication by transferring proteins, lipids, and nucleic acids, especially microRNAs (miRNAs), to recipient cells [65] [23]. This evolution from cellular to acellular therapies necessitates a fundamental re-evaluation of how we define, measure, and optimize biological activity and therapeutic potency.
The complex dose-effect relationship for MSC-Exos is intrinsically linked to administration routes and requires sophisticated potency assays that diverge significantly from those used for whole-cell therapies. Unlike living cells, exosomes function as biological couriers that transfer regenerative instructions without cellular transplantation [66]. Their mechanism of action depends heavily on delivery route, which determines biodistribution, cargo delivery efficiency, and ultimate therapeutic efficacy. This review systematically compares the functional outcomes of MSC-derived exosomes versus whole cell therapies, focusing on route-dependent efficacy and the evolving landscape of potency assays required to ensure product quality, manufacturing consistency, and predictable clinical outcomes.
Quantitative Comparison: MSC-Derived Exosomes vs. Whole Cell Therapies
Table 1: Comprehensive comparison of key characteristics between MSC-derived exosomes and whole cell therapies
| Characteristic | MSC-Derived Exosomes | Whole MSC Therapy |
|---|---|---|
| Physical Nature | Cell-free, nanoscale vesicles (30-150 nm) [24] | Live, nucleated cells (15-30 μm) |
| Therapeutic Cargo | Proteins, lipids, miRNAs, mRNAs [23] | Whole cell with secretory capacity and differentiation potential |
| Mechanism of Action | Paracrine signaling, cargo transfer, receptor mediation [23] | Direct differentiation, paracrine signaling, cell-cell contact |
| Immunogenicity | Lower risk (no cellular membranes, reduced MHC) [24] [23] | Moderate risk (despite low immunogenicity, rejection possible) |
| Tumorigenic Risk | Minimal (cannot replicate or form tumors) [24] [23] | Theoretical concern (proliferative and differentative capacity) |
| Biodistribution | Route-dependent, enhanced tissue penetration [23] | Often trapped in lung microvasculature, limited engraftment |
| Storage & Stability | -80°C for months; sensitive to freeze-thaw cycles [66] | Requires liquid nitrogen; complex thawing protocols [66] |
| Production Scalability | Technically challenging; requires standardization [65] | Established expansion protocols; donor-dependent variability |
| Dosing Metrics | Particle count (×10^9), protein mass (μg), RNA content [66] | Cell number, viability, passage number |
| Regulatory Pathway | Evolving framework for biologics [66] | More established but still complex cellular therapy pathway |
| Potency Assay Focus | Cargo composition, bioactivity, surface markers [24] | Viability, differentiation potential, secretory function |
Table 2: Route-dependent efficacy and dosing considerations for MSC-derived exosomes
| Administration Route | Advantages | Limitations | Optimal Dosing Range | Key Efficacy Evidence |
|---|---|---|---|---|
| Intravenous (IV) | Systemic distribution, access to multiple tissues [23] | Rapid clearance, potential sequestration by MPS | 100-200 billion particles/session [66] | Improved ejection fraction in cardiac studies [66] |
| Local/Topical | High local concentration, minimized systemic exposure | Limited to accessible tissues, potential leakage | Varies by tissue target | Enhanced tendon healing, dermatologic improvements [66] |
| Intranasal | Blood-brain barrier bypass, direct CNS delivery [65] | Limited dosing volume, mucosal clearance | Preclinical optimization ongoing | Neuroprotective effects in stroke models [66] |
| Intra-articular | Joint-specific delivery, prolonged retention | Technical expertise required, inflammatory potential | Orthopedic pilots showing functional improvement [66] | Faster tendon healing and pain reduction [66] |
Experimental Approaches for Evaluating Dose-Effect Relationships
Potency Assay Methodologies for MSC-Exosomes
The complex nature of MSC-Exos demands a multi-parametric approach to potency assessment that captures their biological activity and therapeutic potential. Unlike conventional biologics with single-mechanism actions, exosomes function through multiple parallel pathways, necessitating a potency assay matrix that collectively reflects their mechanism of action [67].
Cargo-Based Potency Assessment
- miRNA Profiling: Comprehensive miRNA sequencing identifies key therapeutic miRNAs (e.g., miR-21, miR-146, miR-125a) that can be quantified through RT-qPCR. Preconditioning strategies significantly alter miRNA profiles; for instance, LPS stimulation (0.1-1 μg/mL) upregulates miR-222-3p, miR-181a-5p, and miR-150-5p in a dose-dependent manner [24]. TNF-α preconditioning (10-20 ng/mL) increases miR-146a and miR-34 content, enhancing immunomodulatory potential [24].
- Protein Cargo Analysis: Western blotting for conserved exosome markers (CD9, CD63, CD81, ALIX, TSG101) confirms vesicle identity, while specific protein arrays quantify therapeutic proteins. The protein-to-particle ratio serves as a critical quality metric [23].
Functional Potency Bioassays
- Immunomodulation Assays: Co-culture systems with peripheral blood mononuclear cells (PBMCs) or macrophages measure cytokine secretion patterns (IL-10, TNF-α) following MSC-Exo treatment. These assays typically run for 24-72 hours and require standardized responder cell sources [24].
- Tissue Repair Models: In vitro scratch/wound healing assays using endothelial or epithelial cells quantify migration and proliferation rates following exosome treatment. Tube formation assays on Matrigel assess angiogenic potential [65].
Physical Characterization Methods
- Nanoparticle Tracking Analysis (NTA): Quantifies particle concentration and size distribution in phosphate-buffered saline, typically yielding 30-150 nm vesicles with minimal protein contaminants [66].
- Transmission Electron Microscopy (TEM): Visualizes ultrastructural morphology and membrane integrity using negative staining protocols [23].
Route-Dependent Efficacy Assessment Protocols
Evaluating how administration routes affect MSC-Exo efficacy requires sophisticated experimental designs that track biodistribution, retention, and ultimate biological effects.
Biodistribution and Pharmacokinetic Studies
- Fluorescent Labeling: DIR, DiD, or PKH dyes label exosome membranes for in vivo tracking. Newer NIR-II probes enable real-time in vivo tracking with enhanced resolution [23]. Animals are injected via different routes (IV, local, intranasal) and imaged at scheduled timepoints.
- Quantitative PCR for Human-specific miRNAs: Human MSC-Exos administered to animal models can be quantified in tissues using species-specific miRNA assays (e.g., hsa-miR-21-5p) to determine route-dependent biodistribution patterns.
Functional Outcome Measures
- Route-Controlled Experiments: Comparative studies administer identical exosome doses (e.g., 200 billion particles) via different routes to disease models, assessing functional outcomes through:
- Neurological: Modified Neurological Severity Score (mNSS) for stroke models, Morris water maze for cognitive function
- Cardiac: Echocardiography for ejection fraction and fractional shortening
- Orthopedic: Gait analysis, weight-bearing tests, histological scoring of tissue repair
Dose-Response Relationship Mapping
- Multi-Arm Studies: Establishing dose-effect curves requires multiple dose levels (e.g., 50, 100, 200 billion particles) administered via standardized routes with appropriate vehicle controls.
- Temporal Response Monitoring: Functional outcomes are measured at multiple timepoints (e.g., 7, 14, 28 days) to determine duration of effects and potential need for repeated dosing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagent solutions for MSC-exosome potency and efficacy studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, ExoQuick-TC, miRCURY Exosome Kit | Rapid exosome precipitation from cell conditioned media | Varying purity yields; may co-precipitate contaminants [23] |
| Characterization Instruments | NanoSight NTA, ZetaView, qNano | Particle concentration and size distribution | NTA provides concentration vs. DLS provides size [23] |
| Preconditioning Reagents | LPS (0.1-1 μg/mL), TNF-α (10-20 ng/mL), IFN-γ | Enhancing therapeutic miRNA content | Dose-dependent effects on cargo composition [24] |
| Tracking Dyes | PKH67, DIR, DiD, NIR-II probes | In vivo biodistribution studies | NIR-II offers superior depth penetration [23] |
| miRNA Analysis | miRCURY LNA miRNA PCR panels, TaqMan Advanced miRNA assays | Cargo potency assessment | Identifies key therapeutic miRNAs (e.g., miR-21, miR-146a) [24] |
| Cell-Based Assay Systems | PathHunter β-arrestin recruitment, HUVEC tube formation | Functional potency measurement | Reporter gene systems offer high throughput [68] |
| Reference Standards | MISEV2023-compliant controls, engineered reference materials | Assay standardization and reproducibility | Critical for inter-study comparisons [23] |
Mechanistic Insights: Signaling Pathways Underlying Route-Dependent Effects
The therapeutic efficacy of MSC-Exos is mediated through complex signaling pathways that are influenced by administration route and ultimately determine functional outcomes. Understanding these mechanisms is essential for rational therapy design.
Route-Dependent Signaling Activation
- Intravenous Administration: Systemically delivered exosomes interact with endothelial cells and immune cells, particularly through TGF-β-mediated immunomodulation and NF-κB pathway regulation. Their intrinsic hepatic tropism facilitates interaction with hepatocytes, but significant lung sequestration occurs [23].
- Local Administration: Direct tissue application enables high local concentration and sustained interaction with parenchymal cells, activating tissue-specific repair pathways including Wnt/β-catenin for regeneration and localized VEGF signaling for angiogenesis without systemic exposure [66].
- Intranasal Delivery: This route facilitates direct cerebrospinal fluid entry, enabling activation of neuroprotective pathways including BDNF signaling and modulation of neuronal excitability, particularly valuable for neurological applications [65].
Dose-Dependent Pathway Activation The intensity and duration of signaling pathway activation follows dose-dependent patterns that vary by administration route. Lower doses may achieve therapeutic effects locally but fail systemically, while excessively high doses via intravenous administration may activate unintended inflammatory pathways.
The transition from MSC-based cell therapy to MSC-derived exosome products represents a paradigm shift in regenerative medicine, demanding equally evolved approaches to potency assessment and dose optimization. The dose-effect relationship for MSC-Exos is fundamentally route-dependent, requiring careful consideration of administration method in both experimental design and clinical protocol development. Current evidence suggests that local administration typically requires lower absolute doses but achieves higher local concentrations, while systemic delivery necessitates higher doses to overcome distributional losses and achieve therapeutic effects at target sites.
The development of robust, clinically relevant potency assays remains the critical bottleneck in advancing MSC-Exos from investigational agents to approved therapeutics. Unlike traditional biologics with single mechanism of action, exosomes require a potency matrix approach that captures their multifaceted biological activities. The field is rapidly moving beyond simple physical characterization toward functional bioassays that reflect therapeutic mechanisms, with particular emphasis on miRNA profiling and immunomodulatory potential assessment. As regulatory frameworks evolve toward requiring comprehensive potency assessment [67], standardization of preconditioning strategies, isolation methods, and analytical techniques will be essential for establishing dose-effect relationships that are reproducible across laboratories and manufacturing facilities.
Future directions include developing route-specific potency assays that better predict in vivo performance, establishing international reference standards for cross-study comparisons, and implementing advanced engineering approaches to enhance target tissue delivery efficiency. By systematically addressing the interplay between administration route, dosage, and potency measurement, the field can accelerate the clinical translation of MSC-derived exosomes as truly targeted, potent, and predictable therapeutic agents.
In regenerative medicine, the therapeutic paradigm is shifting from whole Mesenchymal Stem Cell (MSC) transplantation toward cell-free approaches utilizing MSC-derived exosomes. These nano-sized extracellular vesicles (30-150 nm) mediate the paracrine effects of their parent cells, carrying bioactive cargoes like proteins, lipids, and nucleic acids to recipient cells [24]. However, this promising therapeutic platform faces a significant challenge: inherent variability in exosome function and composition based on donor characteristics and cellular source. This variability impacts therapeutic consistency, reproducibility, and clinical predictability, making its understanding essential for researchers and drug development professionals [69]. Unlike whole cell therapies, which carry risks of immunogenic responses, malignant transformation, and ectopic tissue formation, exosomes offer a safer profile as acellular entities that mitigate these risks while maintaining therapeutic efficacy [24]. This guide objectively compares the functional outcomes of MSC-derived exosomes versus whole cell therapies, focusing specifically on how donor and source variability influences exosome characteristics, and provides standardized experimental frameworks for quantifying this impact.
Donor and Source Variables Influencing Exosome Characteristics
Multiple factors related to the donor and cellular source significantly influence the molecular cargo, and consequently, the functional properties of exosomes. The following table summarizes the key variables and their documented impacts.
Table 1: Impact of Donor and Source Variables on Exosome Characteristics
| Variable Category | Specific Factor | Impact on Exosome Characteristics | Functional Consequence |
|---|---|---|---|
| Donor Physiology | Age | Exosomes from older donors show reduced anti-inflammatory and regenerative capabilities [69]. | Diminished osteogenic and lipogenic differentiation capacity compared to exosomes from younger donors [69]. |
| Donor Physiology | Health Status/Pathology | Cells from diseased individuals produce exosomes with altered molecular profiles [69]. | Exosomes from hypertrophic cardiomyopathy donors carried RNA profiles that dysregulated angiogenesis in endothelial cells [70]. |
| Cell Source | Tissue Origin (Anatomic Site) | Adipose-derived MSC exosomes from different anatomical locations contained different abundances of miRNAs [69]. | Variations in therapeutic efficacy for specific applications, such as wound healing or immunomodulation [71]. |
| Cell Source | Donor Site & Collection Method | Abdominal adipose tissue obtained by surgical excision versus lipoaspiration yielded exosomes with distinct characteristics [69]. | Altered functional performance in tissue regeneration models, though specific outcomes are source-dependent. |
| Cell Culture & Processing | Preconditioning (e.g., Hypoxia, Cytokines) | Preconditioning with hypoxia or inflammatory cytokines (TNF-α, IL-1β) alters miRNA profiles (e.g., increases miR-146a) [24]. | Enhanced pro-angiogenic potential and amplified immunomodulatory effects, such as promoting macrophage polarization [24]. |
Comparative Functional Outcomes: MSC-Exosomes vs. Whole Cell Therapies
When framed within the broader thesis of functional outcomes, MSC-derived exosomes demonstrate several advantages over whole cell therapies, while also presenting unique challenges related to variability.
Mechanisms of Action and Therapeutic Efficacy
The primary mechanism of action for whole MSC therapies was initially attributed to their differentiation and engraftment potential. However, evidence now indicates that their therapeutic benefits are largely mediated through paracrine signaling, a function that exosomes effectively replicate [2] [24]. In direct comparative preclinical studies, exosome-based interventions often achieve functional outcomes comparable to their cellular counterparts. For instance, in fat grafting models, graft retention rates were similar between EV-enriched and MSC-treated groups, with exosomes additionally resulting in reduced inflammation, earlier revascularization, and improved graft integrity [71]. A key functional advantage of exosomes is their ability to navigate biological barriers that whole cells cannot. Their nanoscale size and innate biocompatibility allow them to cross the blood-brain barrier, making them promising vehicles for treating central nervous system disorders [30].
Safety and Manufacturing Considerations
From a safety perspective, exosomes offer a superior profile. As acellular entities, they eliminate risks associated with whole-cell therapies, including immune rejection, malignant transformation, and pulmonary embolism [24]. They are also incapable of forming ectopic tissues, enhancing their clinical safety [24]. Regarding manufacturing, exosomes provide a distinct "off-the-shelf" advantage. They are more amenable to long-term storage and distribution than live cells, which require complex cryopreservation and viability protocols [71]. However, a significant challenge for exosome therapeutics is batch-to-batch consistency. The composition of exosomes is dynamic and highly sensitive to donor cell conditions, posing a greater hurdle for standardization compared to whole cells [69] [24].
Experimental Data: Quantifying Donor-Dependent Functional Variation
Key Study: Donor-Specific Variation in hiPSC Cardiomyocyte Exosomes
A comparative study exemplifies the direct impact of donor pathology on exosome function. Researchers generated human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) from six donors: three with left ventricular hypertrophy (LVH) and three with normal left ventricular mass (LVM) [70].
Experimental Protocol:
- Cell Culture & Exosome Production: hiPSC-CMs were cultured from donor cells. Exosomes were isolated from the cell culture medium via ultracentrifugation.
- Exosome Isolation & Characterization: The isolated exosomes were characterized using nanoparticle tracking analysis (NTA) for concentration and size distribution, and scanning electron microscopy (SEM) for morphology, as detailed in [72].
- RNA Sequencing: Intracellular and exosomal RNA from both LVH and LVM groups was subjected to sequence analysis.
- Functional Assay: hiPSC-derived endothelial cells (hiPSC-ECs) were treated with exosomes from the two donor groups. Functional endpoints included:
- Tube Formation Assay: To assess angiogenic capability.
- Migration Assay: To measure cell movement.
- Proliferation Assay: To quantify cell growth [70].
Results and Data Summary:
Table 2: Functional Outcomes of Endothelial Cells Treated with Donor-Derived Exosomes
| Treatment Group | Proliferation | Tube Formation | Migration | Exosomal RNA Profile |
|---|---|---|---|---|
| Exosomes from LVH Donors | Significantly Increased | Decreased | Decreased | Distinct expression patterns vs. normal LVM group [70]. |
| Exosomes from Normal LVM Donors | Baseline | Robust Angiogenesis | Robust Migration | Served as the baseline control profile [70]. |
The study concluded that exosomes from LVH-affected donors induced angiogenic dysregulation in recipient endothelial cells, despite promoting proliferation. This demonstrates that donor-specific disease phenotypes are captured and functionally transmitted by their exosomes [70].
Conceptual Workflow for Assessing Donor Variability
The following diagram illustrates the logical sequence and key decision points in a robust experimental workflow designed to assess donor-dependent impacts on exosome function.
The Scientist's Toolkit: Essential Reagents and Methods
To systematically address donor and source variability, researchers require a standardized toolkit for exosome isolation, characterization, and functional analysis.
Table 3: Essential Research Reagent Solutions for Exosome Variability Studies
| Item/Category | Specific Examples | Function in Experimental Protocol |
|---|---|---|
| Isolation Kits | Polymer-based precipitation kits (e.g., ExoQuick) | Rapid isolation of exosomes from biofluids or cell culture medium; useful for screening but may co-precipitate contaminants [69]. |
| Chromatography Media | Size-exclusion chromatography (SEC) columns (e.g., qEV columns) | High-purity isolation of exosomes based on size, preserving vesicle integrity and biological activity [69]. |
| Characterization Instruments | Nanoparticle Tracking Analyzer (e.g., ZetaView) | Measures exosome concentration and size distribution in a liquid suspension based on Brownian motion [72]. |
| Antibody Panels | Anti-CD63, CD81, CD9; Anti-Annexin A1 (microvesicle marker) | Confirm exosome identity (tetraspanins) and purity by distinguishing from other extracellular vesicles via immunoblot or flow cytometry [73]. |
| Cell Culture Supplements | Inflammatory cytokines (TNF-α, IL-1β), LPS, Hypoxia Mimetics | Preconditioning agents to modulate donor cell state and study its effect on subsequent exosome cargo and function [24]. |
| Functional Assay Kits | Tube Formation Assay, Migration Assay (e.g., Transwell), Proliferation Assay (e.g., CCK-8) | Quantify the functional impact of donor-derived exosomes on recipient cell behaviors like angiogenesis, migration, and growth [70]. |
The transition from MSC-based cell therapy to a cell-free exosome paradigm represents a significant advancement in regenerative medicine. However, the consistency and functional predictability of exosome therapeutics are profoundly influenced by donor physiology and cellular source. A donor's age, health status, and the anatomic origin of MSCs directly affect exosomal cargo, leading to measurable differences in functional outcomes such as angiogenic potential, immunomodulation, and tissue regeneration. To ensure the future clinical success and regulatory approval of exosome-based products, the field must adopt standardized, rigorous experimental protocols that systematically account for this variability. By identifying and controlling for these critical sources of heterogeneity, researchers can enhance batch-to-batch consistency, unlock the full potential of exosomes as targeted therapeutic agents, and fulfill their promise as the next frontier in regenerative medicine.
The field of regenerative medicine has witnessed a significant evolution, transitioning from whole-cell therapies toward advanced cell-free platforms. Mesenchymal stem cell (MSC) transplantation has undergone extensive evaluation in numerous clinical trials for diverse conditions, but concerns regarding tumorigenicity, immunogenicity, and cell senescence present substantial translational challenges [2] [11]. Concurrently, compelling evidence has revealed that the therapeutic benefits of MSCs are primarily mediated through their paracrine activity rather than direct cellular engraftment and differentiation [11]. This understanding has catalyzed the emergence of MSC-derived exosomes (MSC-Exos) as a promising cell-free therapeutic modality that retains the biological function of parent cells while potentially mitigating risks associated with whole-cell administration [2] [11] [5]. This review provides a comprehensive comparison between these therapeutic approaches, focusing on their safety profiles, functional outcomes, and translational potential within regenerative medicine.
Risk Comparison: MSC-Based versus Exosome-Based Therapies
Tumorigenicity and Senescence Concerns with Whole-Cell Therapies
Whole-cell MSC therapies carry inherent biological risks that must be carefully evaluated. While MSCs are generally considered to have low tumorigenic potential, the risk is not negligible, particularly with certain culture conditions or delivery methods [11]. The proliferation capacity of MSCs gradually weakens with increasing passages during in vitro culture, accompanied by differentiation potential loss and cellular aging, which directly impacts their therapeutic efficacy [11]. Furthermore, the self-renewal ability of MSCs in vivo cannot be fully controlled, creating concerns about potential unintended consequences [11]. A critical consideration is that MSCs have been found to potentially promote the growth of various cancer types [11], raising important safety considerations for their clinical application.
Despite these concerns, recent rigorous preclinical studies have demonstrated promising safety profiles for well-characterized MSC populations. A 2024 GLP-compliant study investigating allogeneic human umbilical cord MSCs (hUC-MSCs) found that single or multiple administrations up to 40 million cells per kilogram of body weight showed no adverse effects in terms of clinical symptoms, hematology parameters, or histology in healthy BALB/c mice [74]. Importantly, in a 26-week tumorigenicity assessment conducted in immunocompromised B-NDG mice, no signs of tumor formation were observed [74], providing robust evidence for the safety of these specific cell preparations when administered under controlled conditions.
Immunogenicity Profiles
Conventional cell therapies face significant immunogenicity challenges despite MSCs being historically characterized as "immunoprivileged." After systemic administration, host immune responses can recognize and clear transplanted cells, significantly limiting their engraftment and persistence [11]. Studies indicate that only a small number of administered MSCs reach target tissues due to the host's scavenging capacity, with many cells becoming trapped in lung microvasculature [11] [5]. This not only reduces therapeutic efficacy but may also initiate inflammatory responses.
In contrast, MSC-derived exosomes exhibit significantly lower immunogenicity compared to their cellular counterparts [11] [3]. As nanoscale vesicles, they largely avoid immune recognition and clearance, allowing for repeated administration without sensitization. Their biocompatible nature enables them to cross biological barriers like the blood-brain barrier without provoking significant immune reactions [11] [3]. This fundamental difference in immunogenic potential represents a key advantage for exosome-based therapeutics, particularly for conditions requiring repeated dosing or treatment of immunologically sensitive tissues.
Table 1: Comprehensive Risk Profile Comparison Between MSC and MSC-Exo Therapies
| Risk Parameter | Whole-Cell MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Tumorigenic Potential | Low but not negligible; dependent on source and culture conditions [11] | No replication capacity; significantly lower tumorigenic risk [11] [23] |
| Immunogenicity | Subject to host immune clearance; may trigger inflammatory responses [11] | Low immunogenicity; avoids immune recognition [11] [3] |
| Senescence Issues | Reduced potency with passages in vitro; aging affects functionality [11] | Not subject to senescence; consistent quality across batches [3] |
| Distribution & Engraftment | Limited target site delivery; pulmonary entrapment common [11] [5] | Superior tissue penetration; crosses biological barriers [11] [3] |
| Storage & Stability | Requires cryopreservation; sensitive to freeze-thaw cycles [11] | Stable at -80°C for extended periods; maintains bioactivity [3] |
| Oncogenic Modulation | May promote growth of certain cancers [11] | Lower risk profile; no evidence of supporting cancer growth [23] |
Functional Outcome Comparisons in Therapeutic Applications
Immunomodulatory Capacity
Both MSC and MSC-Exo therapies demonstrate significant immunomodulatory potential, though through distinct mechanisms of action. Whole-cell MSCs exert their effects through direct cell-cell contact and secretion of soluble factors, with their immunomodulatory function being highly regulated by the inflammatory environment [11]. When stimulated by inflammatory factors, MSCs produce numerous immunomodulatory factors, chemokines, and growth factors that regulate the tissue immune microenvironment [11]. Preclinical studies have confirmed that hUC-MSCs can reduce pro-inflammatory cytokines (IL-6 and TNF-α) in a dose-dependent manner [74], demonstrating their potent anti-inflammatory capabilities.
MSC-derived exosomes recapitulate many of these immunomodulatory functions while offering unique advantages. They contain cytokines, growth factors, signaling lipids, mRNAs, and regulatory miRNAs that collectively contribute to their therapeutic effects [2]. These vesicles facilitate intercellular communication by delivering their cargo to recipient cells, thereby altering cell or tissue metabolism at both short and long distances in the body [2]. The exosome content can be altered when MSCs are cultured under specific conditions, potentially allowing for production of vesicles tailored for particular therapeutic applications [2].
Regenerative Potential and Mechanisms
The regenerative capabilities of both therapeutic approaches have been extensively documented across various disease models. Whole-cell MSCs possess multidirectional differentiation potential, able to become osteoblasts, chondrocytes, or adipocytes in vitro [11]. This differentiation capacity has been leveraged for numerous regenerative applications, including treatment of osteoarthritis, pulmonary fibrosis, spinal cord injury, myocardial damage, and dental pulp regeneration [11].
MSC-derived exosomes promote regeneration through alternative mechanisms, primarily through modulation of endogenous repair pathways. They have demonstrated therapeutic potential in immune regulation and regeneration [11], with applications investigated in bone and joint regeneration, nerve function reconstruction, myocardial repair, and skin wound healing [3]. Their efficacy stems from the delivery of functional RNA, proteins, and other signaling elements that precisely regulate inflammatory response, angiogenesis, and tissue repair processes in target tissues [3].
Table 2: Experimentally Demonstrated Efficacy Across Disease Models
| Disease Model | MSC Therapy Outcomes | MSC-Exo Therapy Outcomes |
|---|---|---|
| Acute Lung Injury | Not specifically quantified in results | Significant attenuation of pulmonary inflammation; reduced pro-inflammatory cytokines (TNF-α, IL-6, IL-1β); increased IL-10 [75] |
| Graft-versus-Host Disease | Beneficial with multiple infusions (8 infusions of 2×10⁶ cells/kg) [74] | Investigated in clinical trials; emerging as promising approach [5] |
| GLOBAL ANTI-INFLAMMATORY EFFECT | Reduces pro-inflammatory cytokines (IL-6, TNF-α) in dose-dependent manner [74] | Decreases TNF-α, IL-6, IL-1β while increasing anti-inflammatory IL-10 [75] |
| Stroke | High doses explored (up to 1.2×10⁹ cells/subject) [74] | Effective in animal models; clinical trials ongoing [5] |
| GENERAL SAFETY PROFILE | No adverse effects at 40×10⁶ cells/kg in mice; no tumor formation in 26-week study [74] | No microvascular occlusion risk; lower immunogenicity [5] [75] |
Experimental Data and Methodological Considerations
Dosing and Administration Optimization
The route of administration and dosing parameters significantly influence therapeutic outcomes for both modalities. For whole-cell therapies, studies have explored various dosing regimens, with evidence supporting multiple administrations at short intervals to maximize reparative and immunomodulatory effects [74]. In GvHD patients, protocol of 8 infusions of 2×10⁶ cells/kg MSCs each within a 4-week period demonstrated benefits [74], while studies in stroke have explored doses up to 1.2×10⁹ cells per subject (approximately 17×10⁶ cells/kg) [74].
For exosome therapies, systematic comparisons of administration routes have identified important efficacy differences. In LPS-induced acute lung injury models, intravenous delivery of exosomes (5×10⁸ particles) demonstrated superior therapeutic efficacy compared to intranasal and nebulized routes [75]. Dose-dependent effects have been consistently observed, with higher doses generally producing enhanced responses across administration routes [75]. However, the optimal dosing paradigm appears to be route-dependent, as some studies have shown that the highest therapeutic efficacy was not necessarily achieved with the highest dose [5], emphasizing the need for careful optimization.
Experimental Workflows and Characterization Standards
Rigorous characterization and standardized production methods are essential for both therapeutic approaches. For whole-cell therapies, the International Society for Cellular Therapy (ISCT) has established minimum criteria for identifying human MSCs, including plastic adherence, specific surface marker expression (CD105+, CD73+, CD90+, with ≤2% expression of hematopoietic markers CD45, CD34, CD14 or CD11b, CD79a or CD19, and HLA-DR), and tri-lineage differentiation potential [11].
For exosome therapies, the International Society for Extracellular Vesicles (ISEV) has established guidelines (MISEV2023) that define standard characterization criteria [23]. These include comprehensive assessment of physical properties, biochemical composition, and functional properties. Standardized isolation methods are critical, with ultracentrifugation remaining the most commonly used technique [3] [5], though tangential flow filtration systems are gaining prominence for clinical applications [5].
Diagram: Comparative profiles of MSC and exosome therapeutics, highlighting key challenges and advantages for each platform.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing both whole-cell and exosome therapies requires specialized reagents and methodologies to ensure product quality, safety, and efficacy. The following toolkit outlines critical components for research and development in this field:
Table 3: Essential Research Reagents and Methodologies for MSC and Exosome Research
| Tool Category | Specific Reagents/Methods | Research Application | Therapeutic Relevance |
|---|---|---|---|
| Cell Characterization | Flow cytometry antibodies (CD105, CD73, CD90, hematopoietic markers) [11] | MSC phenotype verification | Quality control for cellular products |
| Differentiation Assays | Osteogenic, chondrogenic, adipogenic induction media [11] | Tri-lineage differentiation potential assessment | Functional potency evaluation |
| Exosome Isolation | Ultracentrifugation, Tangential Flow Filtration, Size-exclusion chromatography [23] [5] | Vesicle purification from conditioned media | GMP-compatible production methods |
| Vesicle Characterization | Nanoparticle tracking analysis, Transmission electron microscopy, Western blot (CD63, CD81, CD9, TSG101) [23] | Physical and biochemical vesicle properties | Product identity and batch consistency |
| Functional Assays | Lymphocyte proliferation assays, Cytokine quantification (ELISA), Animal disease models [74] [75] | Immunomodulatory and regenerative capacity assessment | Preclinical efficacy demonstration |
| Storage Solutions | Trehalose, Albumin stabilizers, Cryopreservation media [23] | Preserving vesicle integrity and functionality | Maintaining product stability and potency |
The comprehensive comparison between whole-cell MSC therapies and MSC-derived exosomes reveals a complementary rather than competitive relationship in the regenerative medicine landscape. Whole-cell therapies offer the advantage of sustained paracrine signaling and direct cellular interactions, with established protocols and growing safety data supporting their use in controlled settings [74]. Conversely, MSC-derived exosomes provide a cell-free alternative with lower risks of tumorigenicity and immunogenicity, superior tissue penetration, and more flexible administration routes [11] [3] [5].
The choice between these therapeutic platforms should be guided by specific clinical indications, risk-benefit considerations, and practical manufacturing constraints. Whole-cell approaches may be preferable for conditions requiring sustained secretory activity and structural support, while exosome-based strategies offer advantages for targeting immunologically sensitive tissues or crossing biological barriers. As the field advances, the development of standardized production protocols, rigorous characterization standards, and comprehensive safety assessment will be crucial for both modalities [23] [5]. Ultimately, the evolution of both whole-cell and cell-free therapeutic approaches will expand the arsenal of regenerative medicine, enabling more precise and effective treatments for a wide range of debilitating conditions.
The field of regenerative medicine is undergoing a significant paradigm shift from whole-cell therapies toward cell-free approaches, with mesenchymal stem cell-derived exosomes (MSC-Exos) emerging as a promising therapeutic alternative. Exosomes are nanoscale extracellular vesicles (30-150 nm in diameter) secreted by cells that facilitate intercellular communication by transferring proteins, lipids, and nucleic acids to recipient cells [76] [3]. Compared to whole MSC therapies, which face challenges including poor engraftment, infusional toxicity, and potential tumorigenicity, MSC-Exos offer a potentially superior safety profile while retaining therapeutic benefits [23] [33] [5]. This review systematically evaluates the safety profile of MSC-derived exosomes, focusing on their low immunogenicity and manageable toxicity, through a comprehensive analysis of current experimental data and clinical evidence.
Comparative Safety Profiles: MSC-Exos versus Whole Cell Therapies
The therapeutic advantages of MSC-Exos over their cellular counterparts are particularly evident in their improved safety characteristics, as summarized in Table 1.
Table 1: Comparative Safety Profiles: MSC vs. MSC-Derived Exosomes
| Safety Parameter | MSC Therapy | MSC-Exos Therapy | Experimental Evidence |
|---|---|---|---|
| Immunogenicity | Low but present; risks of allogeneic rejection | Very low; no MHC-II, low immunogenicity confirmed in models [77] [3] | No significant changes in immunoglobulins or lymphocytes in mice [77] |
| Infusion Toxicity | Risk of pulmonary embolism due to cell size and aggregation [33] [5] | No embolization; nanoscale size prevents capillary blockage [3] [5] | Preclinical models show no lung entrapment [5] |
| Tumorigenic Risk | Theoretical risk of uncontrolled differentiation or division [77] [23] | No replication capacity; significantly mitigated risk [3] [33] | No tumor formation in safety studies [77] |
| In Vivo Persistence | Variable engraftment and survival | Controlled, finite lifespan; no long-term persistence concerns [3] | Short circulation half-life without accumulation [78] |
| Storage & Handling | Requires cryopreservation; sensitive to freeze-thaw | Stable at -80°C for extended periods; retains bioactivity [3] [78] | Maintained size and concentration over 30 days at -20°C [78] |
Mechanisms Underlying Low Immunogenicity
The low immunogenicity of MSC-Exos stems from their inherent biological properties. Unlike whole cells, exosomes lack the complete major histocompatibility complex (MHC) machinery necessary to provoke robust immune responses [33]. Experimental data demonstrates that MSC-Exos do not stimulate significant immune activation even at high concentrations.
A dedicated immunological safety study in mice evaluated the effects of high-dose intravenous administration of human umbilical cord MSC-derived exosomes (hucMSC-exosomes). When mice received tail vein injections of 6 × 10^10 particles, researchers observed no significant changes in blood composition, immunoglobulin levels (IgA, IgM, IgG), key cytokines (IFN-γ, IL-10), or lymphocyte subpopulations (CD4+, CD8+ T cells, CD19+ B cells) throughout the 14-day observation period. Critically, immune organs including the thymus, spleen, and bone marrow showed no pathological alterations, confirming the low immunogenic potential of these vesicles [77].
The following diagram illustrates the key experimental workflow and findings from this immunological safety assessment:
Experimental Evidence: Assessing Exosome Toxicity Profiles
In Vivo Toxicology Studies
Rigorous preclinical safety assessments have provided substantial evidence supporting the favorable toxicity profile of MSC-Exos. In an acute toxicity study conducted in accordance with ISO 10993-11 guidelines, rats received tail vein injections of exosomes derived from canine adipose-derived MSCs (cAD-MSCs). The study reported no adverse effects on clinical parameters, organ health, or body weight, supporting the physiological safety of exosomes even at high concentrations [78].
The biodistribution and clearance pathways of exosomes contribute significantly to their safety profile. Their nanoscale dimensions (typically 30-150 nm) prevent vascular occlusion and enable efficient clearance through physiological mechanisms, unlike larger MSC cells which can become trapped in lung microvasculature and cause embolization [3] [5]. This fundamental difference in physical properties underlies the reduced infusion-related toxicity observed with exosome therapies.
Analytical Characterization for Safety Assurance
Comprehensive characterization of MSC-Exos is essential for ensuring batch-to-batch consistency and safety. Standardized assessments include:
- Physical Characterization: Size distribution analysis via Nanoparticle Tracking Analysis (NTA) typically shows a peak size of 80-150 nm [77] [78], with morphological confirmation using Transmission Electron Microscopy (TEM) revealing the classic cup-shaped structure [78].
- Molecular Marker Profiling: Western blot analysis confirms the presence of tetraspanins (CD9, CD63, CD81) and absence of negative markers (e.g., Calnexin) [77].
- Stability Testing: Studies demonstrate that MSC-Exos maintain structural integrity and bioactivity when stored at -80°C, with minimal degradation over time [78].
Table 2: Standardized Exosome Characterization Parameters
| Characterization Method | Parameters Assessed | Expected Results | Safety Significance |
|---|---|---|---|
| Nanoparticle Tracking Analysis (NTA) | Size distribution, concentration | 30-150 nm, high particle count [78] | Ensures proper size to prevent embolization |
| Transmission Electron Microscopy (TEM) | Morphology, structural integrity | Cup-shaped vesicles, intact membranes [78] | Confirms structural normality |
| Western Blot | Surface and intravesicular markers | CD9/CD63/CD81 positive, Calnexin negative [77] | Verifies exosome identity and purity |
| Zeta Potential Analysis | Surface charge, colloidal stability | Negative surface charge (-15 to -25 mV) [78] | Indicates suspension stability |
| Flow Cytometry | Surface marker quantification | CD9 positive populations [78] | Additional marker confirmation |
Clinical Translation: From Bench to Bedside
Current Clinical Trial Landscape
The promising preclinical safety data has facilitated the transition of MSC-Exos into clinical testing. As of January 2025, 64 registered clinical trials are evaluating MSC-derived extracellular vesicles for various conditions, including severe COVID-19, ischemic stroke, and complex wound healing [3]. Completed studies have begun to generate initial human safety data.
In published clinical studies utilizing MSC-Exos for conditions such as graft-versus-host disease (GvHD) and dry eye associated with chronic GvHD, no severe adverse events related to exosome administration have been reported [33] [5]. The routes of administration in these trials have included intravenous infusion, inhalation, and local application, with all methods demonstrating acceptable tolerability profiles.
Manufacturing and Standardization Considerations
The production methodology for therapeutic exosomes significantly influences their safety characteristics. Current approaches include:
- Ultracentrifugation: The most commonly used method in clinical trials, employing high centrifugal forces (up to 1,000,000×g) to isolate exosomes [5].
- Tangential Flow Filtration (TFF): A scalable alternative that separates vesicles based on size using polyethersulfone membranes, offering advantages for manufacturing consistency [5].
- Three-Dimensional (3D) Culture Systems: Emerging bioreactor technologies that enhance exosome yield and functionality while maintaining safety profiles [78].
The following diagram outlines the key steps in exosome biogenesis, isolation, and quality control:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Exosome Safety Evaluation
| Reagent/Equipment | Specific Example | Research Application | Safety Assessment Role |
|---|---|---|---|
| Flow Cytometry Antibodies | Anti-CD4, CD8, CD19 [77] | Immune cell profiling | Quantifies effects on lymphocyte populations |
| ELISA Kits | IgA, IgM, IgG, IFN-γ, IL-10 assays [77] | Cytokine and immunoglobulin measurement | Detects immune activation or suppression |
| Cell Culture Media | DMEM-10FBS, serum-free media [78] | MSC expansion and exosome production | Ensures consistent exosome production |
| Characterization Instruments | NTA (Malvern), TEM (Hitachi) [77] [78] | Physical characterization | Verifies exosome identity and purity |
| Animal Models | C57BL/6 mice, Sprague-Dawley rats [77] [78] | In vivo safety assessment | Evaluates systemic toxicity and immunogenicity |
The comprehensive safety profile of MSC-derived exosomes, characterized by their low immunogenicity and manageable toxicity, positions them as promising candidates for the next generation of cell-free therapeutics. Extensive preclinical evidence demonstrates their favorable safety characteristics compared to whole cell therapies, particularly regarding reduced infusion-related risks, minimal immunogenic responses, and absence of tumorigenic potential. Ongoing clinical trials continue to validate these findings in human patients, supporting the potential for broader clinical application. However, standardization of production methods, establishment of potency metrics, and long-term biodistribution studies remain important challenges to address as the field advances toward regulated therapeutic applications.
Evidence and Decision-Making: Clinical Trials and Direct Comparisons
The therapeutic landscape for regenerative medicine is undergoing a significant transformation from whole-cell therapies toward cell-free approaches utilizing mesenchymal stem cell-derived exosomes (MSC-Exos). As of January 2025, 64 registered clinical trials worldwide are evaluating MSC-Exos for conditions ranging from neurodegenerative diseases to orthopedic disorders, respiratory conditions, and autoimmune diseases. This comprehensive analysis reviews the global clinical trial landscape for MSC-Exos, examining their therapeutic mechanisms, production methodologies, and functional outcomes compared to conventional MSC therapies. The data reveal a paradigm shift toward cell-free regenerative strategies that maintain therapeutic efficacy while addressing critical safety concerns associated with whole-cell transplantation, positioning MSC-Exos as next-generation biotherapeutics with applications across multiple medical specialties.
Mesenchymal stem cells (MSCs) have long been regarded as promising therapeutic agents in regenerative medicine due to their multipotent differentiation capacity, immunomodulatory properties, and trophic factor secretion [23] [79]. However, translational challenges including phenotypic instability, risks of immunological rejection, limited in vivo persistence, pulmonary microvascular entrapment, and potential tumorigenic concerns have constrained their clinical application [23] [3]. Emerging evidence indicates that the therapeutic benefits of MSCs are primarily mediated through paracrine signaling mechanisms rather than direct cellular engraftment and differentiation [3] [5].
Exosomes, nanoscale extracellular vesicles (30-150 nm) secreted by most cell types, serve as crucial mediators of intercellular communication by transporting bioactive molecules including proteins, lipids, mRNA, and microRNA [23] [42]. MSC-derived exosomes (MSC-Exos) recapitulate many therapeutic effects of their parent cells while offering significant advantages as cell-free therapeutic entities [80] [5]. These advantages include lower immunogenicity, minimal risk of tumor formation, absence of microvascular entrapment, intrinsic tissue tropism, and enhanced biological barrier penetration [23] [3].
Table 1: Comparative Analysis: MSC-Exos vs. Whole Cell MSC Therapy
| Characteristic | MSC-Exos | Whole Cell MSC Therapy |
|---|---|---|
| Size | 30-150 nm | 30-60 μm |
| Immunogenicity | Low (no MHC molecules) | Low but present (reduced MHC expression) |
| Tumorigenic Risk | Minimal (non-replicative) | Present (especially with poor differentiation control) |
| Administration Risks | No microvascular entrapment | Pulmonary embolism risk |
| Storage Stability | Stable at -80°C for extended periods | Limited, requires careful cryopreservation |
| Production Scalability | Challenging but feasible with advanced systems | Limited by cell expansion capacity |
| Therapeutic Mechanism | Cargo delivery, receptor signaling | Differentiation, paracrine signaling, cell-cell contact |
| Regulatory Status | 64 registered clinical trials | >2,300 registered clinical trials |
| FDA Approval Status | Generally recognized as safe for many applications | Limited FDA-approved applications |
Global Clinical Trial Landscape for MSC-Exos
Current Registration Statistics and Distribution
The clinical investigation of MSC-Exos has expanded significantly in recent years. As of January 2025, there are 64 registered clinical trials evaluating MSC-derived extracellular vesicles for various medical conditions, according to ClinicalTrials.gov records [3]. This represents a substantial increase from the 21 registered clinical studies documented in a 2023 systematic review [5], reflecting accelerating research interest and investment in exosome-based therapeutics.
The geographic distribution of these trials shows concentrated research activities in Asia, North America, and Europe, with emerging contributions from Middle Eastern countries. The trial distribution across medical specialties demonstrates the versatile therapeutic potential of MSC-Exos, with notable concentrations in orthopedics, neurology, pulmonology, and immunology [3] [5].
MSC-Exos used in clinical trials originate from various tissue sources, each with potential implications for therapeutic efficacy and manufacturing consistency.
Table 2: MSC Sources in Clinical Trials and Their Applications
| Tissue Source | Prevalence in Clinical Trials | Notable Therapeutic Applications | Reported Advantages |
|---|---|---|---|
| Adipose Tissue | Most frequent (7 studies) | Orthopedic conditions, wound healing | Abundant source, angiogenic potential |
| Bone Marrow | Intermediate (5 studies) | GvHD, neurological disorders | Immunomodulatory potency |
| Umbilical Cord | Emerging (4 studies) | ARDS, stroke, Alzheimer's disease | Proliferative capacity, neonatal properties |
| Other Sources | Limited (dental pulp, placenta) | Exploratory applications | Tissue-specific potentials |
Adipose tissue has emerged as the predominant source in clinical studies, followed by bone marrow and umbilical cord-derived MSCs [5]. Comparative preclinical studies suggest that MSC-Exos from different sources exhibit variations in cargo composition and functional efficacy. For instance, adipose tissue-derived exosomes demonstrate enhanced angiogenic capability, while bone marrow-derived exosomes show superior immunomodulatory effects through inhibition of IFN-γ secretion by T cells [5].
Administration Routes and Dosing Strategies
Clinical trials have employed various administration routes for MSC-Exos, reflecting disease-specific therapeutic requirements and biodistribution considerations:
- Intravenous (IV) infusion: The most common systemic delivery approach, used in 6 registered studies [5]
- Inhalation/Nebulization: Employed for respiratory conditions including ARDS and COVID-19 [75] [5]
- Local administration: Direct application to affected tissues (5 studies), including intra-articular injection for osteoarthritis and topical application for wound healing [5]
Dosing strategies vary considerably across trials, with exosomes quantified by particle number (ranging from 10⁸ to 10¹¹ particles), protein weight (micrograms), or the cell equivalent from which exosomes were derived [75] [5]. This heterogeneity in dosage reporting presents challenges for cross-trial comparisons and underscores the need for standardized quantification protocols.
Methodological Framework: Production and Characterization of Clinical-Grade MSC-Exos
Isolation and Purification Techniques
The transition from laboratory-scale exosome isolation to clinically applicable production requires rigorous standardization and quality control. Current clinical trials primarily utilize two isolation methodologies:
- Ultracentrifugation: remains the most widely used technique (employed in all except two published clinical trials), involving sequential centrifugation steps up to 1,000,000×g to separate exosomes based on size and density [5]
- Tangential Flow Filtration (TFF): an emerging scalable alternative that utilizes size-based filtration through hollow fiber membranes, employed by Cho et al. and Kwon et al. in clinical studies for its superior preservation of exosome integrity and scalability [5]
Additional techniques including size exclusion chromatography, precipitation methods, and immunoaffinity capture are utilized in research settings but show limited application in current clinical trials due to scalability or purity concerns [23] [42].
Characterization and Quality Control Standards
Clinical-grade MSC-Exos must adhere to the Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines established by the International Society for Extracellular Vesicles [23] [5]. Characterization encompasses:
- Physical properties: Size distribution and concentration analyzed via Nanoparticle Tracking Analysis (NTA) or Tunable Resistive Pulse Sensing (TRPS)
- Morphological assessment: Transmission Electron Microscopy (TEM) confirming classic cup-shaped morphology
- Biomarker profiling: Surface markers (CD63, CD9, CD81) and MSC-specific markers (CD73, CD90, CD105) via western blot or flow cytometry
- Cargo analysis: RNA and protein content profiling through next-generation sequencing and mass spectrometry [23] [5] [81]
Diagram Title: Clinical-Grade MSC-Exosome Production Workflow
Storage and Stability Protocols
Maintaining exosome integrity during storage is critical for therapeutic consistency. Clinical protocols typically recommend:
- Short-term storage: 4°C for ≤24-48 hours
- Long-term preservation: -80°C with minimized freeze-thaw cycles
- Stabilization solutions: Addition of trehalose or BSA to plain PBS to prevent exosome loss through surface adhesion [23]
Functional Outcome Comparison: MSC-Exos vs. Whole Cell Therapy
Safety Profiles and Adverse Event Reduction
MSC-Exos demonstrate substantially improved safety profiles compared to whole cell therapies:
- Elimination of infusion-related toxicities: Nanoscale size (30-150 nm) prevents pulmonary microvascular entrapment that occurs with MSC administration (cells measuring 30-60 μm) [23] [5]
- Reduced immunogenic potential: Absence of cellular machinery and minimal MHC expression minimizes immune rejection risks [80] [3]
- Elimination of tumorigenic concerns: Non-replicative nature prevents unintended proliferation and differentiation [23] [81]
- Avoidance of thrombotic complications: Lower tissue factor expression compared to parent cells reduces coagulation risks [81]
Clinical reports consistently note excellent tolerability of MSC-Exos with minimal adverse events, even at high doses, addressing a critical limitation of cellular therapies [3] [5].
Therapeutic Efficacy Across Disease Models
Respiratory Diseases
In a murine model of LPS-induced acute lung injury (ALI), MSC-Exos administration significantly attenuated pulmonary inflammation, reducing pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) while increasing anti-inflammatory IL-10 [75]. Intravenous delivery demonstrated superior efficacy compared to intranasal and nebulized routes at equivalent doses (5×10⁸ particles), highlighting the importance of administration route optimization [75].
Neurological Disorders
MSC-Exos show exceptional promise in neurological applications due to their ability to cross the blood-brain barrier, a significant advantage over cellular therapies [79] [81]. Mechanisms include:
- Neurovascular regeneration: Promotion of angiogenesis through VEGF signaling and angiopoietin/Tie2 system activation [79]
- Neuroinflammation modulation: Suppression of microglial activation and pro-inflammatory cytokine secretion [81]
- Neurogenesis enhancement: Facilitation of endogenous neural stem cell proliferation and differentiation [79]
Orthopedic and Joint Disorders
Clinical trials for osteoarthritis demonstrate that MSC-Exos effectively mitigate cartilage degradation, reduce pain, and improve joint function through immunomodulation and trophic factor delivery, with effects persisting for months post-treatment [5].
Mechanisms of Action: Comparative Molecular Pathways
MSC-Exos exert therapeutic effects through distinct yet overlapping mechanisms compared to whole cell therapies:
Diagram Title: Comparative Therapeutic Mechanisms of MSC-Exos vs. Whole Cell MSCs
The hierarchical translation of therapeutic effects occurs through tissue-specific responses and cell-specific molecular signaling pathways, with MSC-Exos demonstrating more targeted activity compared to the broader mechanisms of whole cell therapies [80].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Tools for MSC-Exos Investigation
| Reagent/Technology | Primary Function | Application Examples | Considerations |
|---|---|---|---|
| CD63/CD81/CD9 Antibodies | Exosome detection and quantification | Immunoaffinity capture, flow cytometry, western blot | Specificity for exosome subpopulations |
| NTA Instrumentation | Size distribution and concentration analysis | Quality control, dosing standardization | Instrument-dependent variability |
| Ultracentrifugation Systems | Exosome isolation from conditioned media | Research-scale production | Potential for vesicle damage, low throughput |
| Tangential Flow Filtration | Scalable exosome purification | Clinical-grade manufacturing | Preserves vesicle integrity, suitable for scale-up |
| RNA Isolation Kits (EV-specific) | Cargo analysis from exosome samples | miRNA profiling, biomarker discovery | Optimization needed for small RNA yields |
| MSC Culture Media (Xeno-free) | GMP-compliant cell expansion | Clinical trial material preparation | Impacts exosome yield and cargo composition |
| Cryopreservation Solutions | Long-term exosome storage | Biobanking, product stability studies | Trehalose preferred for membrane protection |
| Liquid Chromatography-Mass Spectrometry | Proteomic and lipidomic profiling | Cargo characterization, potency assays | Identifies therapeutic cargo molecules |
Challenges and Future Directions in MSC-Exos Clinical Translation
Standardization and Manufacturing Scalability
The clinical translation of MSC-Exos faces several significant challenges:
- Heterogeneity management: Donor-specific variations, culture conditions, and isolation methods contribute to product variability [23] [3]
- Potency assay development: Lack of standardized correlation between physical characteristics and biological activity [5]
- Manufacturing scalability: Transition from laboratory techniques to industrially relevant production volumes while maintaining consistency [42] [3]
Emerging solutions include 3D dynamic culture systems, genetic engineering of parent cells, immobilized cell culture technologies, and improved downstream processing methodologies [3].
Targeted Delivery and Engineering Strategies
Future research directions focus on enhancing MSC-Exos therapeutic precision through:
- Surface modification: Incorporation of targeting ligands (peptides, antibodies) for tissue-specific delivery [23] [3]
- Cargo loading: Development of efficient methods for therapeutic molecule encapsulation (drugs, nucleic acids, proteins) [23] [5]
- Hybrid systems: Integration with biomaterials and controlled-release platforms for sustained local delivery [3]
These engineering approaches aim to transform MSC-Exos from naturally occurring vesicles to programmable nanomedicines with enhanced therapeutic efficacy [3].
The global landscape of registered clinical trials for MSC-derived exosomes demonstrates a rapid expansion of this innovative therapeutic platform across diverse medical specialties. MSC-Exos represent a paradigm shift from cellular to cell-free therapies, addressing critical limitations of whole cell approaches while maintaining therapeutic efficacy through sophisticated intercellular communication mechanisms. As research advances, standardization of manufacturing protocols, development of potency assays, and implementation of engineering strategies for enhanced targeting will be crucial for realizing the full clinical potential of MSC-Exos. The ongoing transition from injectable regenerative factors to programmable nanomedicines positions MSC-Exos as transformative agents in the evolving landscape of regenerative medicine, offering new solutions for precision therapy across a spectrum of debilitating conditions.
Ischemic stroke remains a leading cause of death and long-term disability worldwide, creating an urgent need for novel therapeutic strategies that extend beyond the narrow time window of conventional thrombolytic therapies [82]. In recent years, stem cell-based interventions have emerged as promising approaches for promoting repair and recovery in the subacute and chronic phases of ischemic stroke [83]. Among these, therapies utilizing mesenchymal stem cells (MSCs) and their derived exosomes have demonstrated particular potential for improving functional outcomes through multiple mechanisms including neurogenesis, angiogenesis, and immunomodulation [79] [82]. This review systematically compares the functional outcomes associated with MSC-based whole cell therapy versus cell-free exosome approaches, leveraging insights from advanced MRI techniques and standardized clinical endpoints to objectively evaluate their therapeutic profiles within the context of ischemic stroke recovery.
Therapeutic Mechanisms of Action
MSC Whole Cell Therapy Mechanisms
Mesenchymal stem cells are multipotent adult stem cells isolated from various tissues including bone marrow, adipose tissue, and umbilical cord blood [79] [83]. According to International Society for Cellular Therapy criteria, MSCs are defined by their plastic-adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD45-, CD34-, CD14- or CD11b-, CD79α- or CD19-), and ability to differentiate into osteoblasts, adipocytes, and chondrocytes in vitro [79]. When transplanted into ischemic brain tissue, MSCs promote functional recovery through multiple distinct mechanisms [79] [83]:
- Paracrine Signaling: MSCs secrete various trophic factors including vascular endothelial growth factor (VEGF), brain-derived neurotrophic factor (BDNF), fibroblast growth factor-2 (FGF-2), and insulin-like growth factor-1 (IGF-1) that promote endogenous repair processes [79] [83].
- Angiogenesis Promotion: Experimental studies demonstrate that MSC transplantation significantly increases VEGF expression and promotes vascular remodeling, enhancing cerebral blood flow and nutrient delivery to ischemic regions [79].
- Immunomodulation: MSCs create a localized anti-inflammatory state by secreting IL-10, IL-6, and nitric oxide, while also inhibiting T-cell proliferation, natural killer cells, and dendritic cells [83].
- Neurogenesis Enhancement: MSCs promote the generation of new functional neurons from endogenous neural stem cells (NSCs) and neural progenitor cells (NPCs), primarily in the subventricular zone and hippocampal subgranular zone [79].
MSC-Derived Exosome Mechanisms
Exosomes are nanosized extracellular vesicles (30-150 nm in diameter) secreted by most cell types, including MSCs [82]. These specialized vesicles contain proteins, lipids, miRNAs, mRNAs, and other bioactive factors that facilitate intercellular communication [79] [82]. MSC-derived exosomes exert therapeutic effects through several key mechanisms:
- Cross-BBB Capability: Their small size and lipid bilayer membrane allow exosomes to cross the blood-brain barrier efficiently, facilitating targeted delivery of therapeutic cargo to the ischemic brain [82] [84].
- Cargo-Mediated Regulation: Exosomes transfer miRNAs, proteins, and other bioactive molecules to recipient cells, modulating gene expression and cellular functions. This includes promoting neuronal survival, reducing inflammation and apoptosis, and enhancing angiogenesis [82].
- White Matter Remodeling: Studies using diffusion tensor imaging (DTI) have demonstrated that MSC-exosomes significantly increase fractional anisotropy values, fiber length, and fiber number ratios, indicating enhanced white matter integrity and remodeling after stroke [84].
- Multiphase Action: Exosomes secreted under different stress conditions exhibit distinct characteristics and functions, making them potential dynamic biomarkers and therapeutic agents for different stages of stroke progression [79].
Table 1: Comparative Therapeutic Mechanisms of MSC Whole Cell vs. Exosome Therapies
| Mechanistic Aspect | MSC Whole Cell Therapy | MSC-Derived Exosomes |
|---|---|---|
| Primary Mode of Action | Direct paracrine signaling + potential cell replacement | Cargo-mediated intercellular communication |
| BBB Penetration | Limited without invasion | Excellent due to nanoscale size |
| Angiogenic Capacity | VEGF, Ang1/Tie2 upregulation; promotes vascular remodeling [79] | Pro-angiogenic miRNA transfer; enhances microvascular density [82] |
| Neurogenic Potential | Promotes NSC proliferation, migration, differentiation [79] | Stimulates neurogenesis via miRNA and growth factor delivery [84] |
| Immunomodulation | Direct suppression of T-cells, NK cells; induces M2 macrophages [83] | Reduces IL-1β; modulates inflammatory responses [84] |
| White Matter Repair | Indirect through trophic support | Direct enhancement of white matter integrity and remodeling [84] |
Figure 1: Comparative Mechanisms and Outcomes of MSC and Exosome Therapies in Ischemic Stroke
Assessment Methodologies for Functional Outcomes
Advanced MRI Techniques
Advanced neuroimaging techniques provide crucial biomarkers for predicting recovery and assessing therapeutic efficacy in ischemic stroke clinical trials [85].
- Diffusion-Weighted Imaging (DWI): Detects ischemic changes within minutes of onset by measuring water proton movement restrictions in ischemic tissue. DWI lesion volume serves as an early indicator of infarct size and strongly predicts functional outcome [85] [86].
- Diffusion Tensor Imaging (DTI): Visualizes white matter pathways and assesses damage to specific tracts, particularly the corticospinal tract. Fractional anisotropy values correlate with motor function recovery and can predict long-term outcome [85]. DTI parameters also relate to language performance when assessing damage to language pathways like the arcuate fasciculus [85].
- Perfusion-Weighted Imaging (PWI): Measures capillary perfusion and identifies the "ischemic penumbra" - potentially salvageable tissue at risk of infarction. The diffusion-perfusion mismatch helps identify patients who may benefit from extended therapeutic windows [86].
- Lesion Location Analysis: Advanced mapping techniques relate infarct location to specific neurological deficits, providing more accurate prognosis than lesion volume alone [85].
Clinical Endpoint Measures
Standardized clinical scales provide critical functional outcome measures in stroke trials:
- National Institutes of Health Stroke Scale (NIHSS): Quantifies neurologic deficit severity in acute stroke. Baseline NIHSS strongly predicts 3-month outcome [87] [85].
- Modified Rankin Scale (mRS): Assesses global functional independence and disability. Scores range from 0 (no symptoms) to 6 (death), with mRS ≤2 typically indicating functional independence [87] [88].
- Barthel Index (BI): Measures performance in activities of daily living including dressing, mobility, and bathing [87] [85].
- Fugl-Meyer Assessment (FMA): Specifically evaluates sensorimotor function in post-stroke patients [88].
Table 2: Advanced MRI Biomarkers for Predicting Functional Outcomes in Ischemic Stroke
| Imaging Modality | Key Parameters | Predictive Value for Functional Outcomes | Therapeutic Application |
|---|---|---|---|
| DWI | Lesion volume, ADC values | Predicts 3-month BI outcome; larger volumes correlate with poorer prognosis [85] | Early infarct delineation; treatment response assessment |
| DTI | Fractional anisotropy, tract integrity | Corticospinal tract damage predicts motor recovery; superior to lesion volume alone [85] | White matter integrity evaluation; MSC-exosome therapy monitoring [84] |
| PWI | CBF, CBV, MTT | Diffusion-perfusion mismatch identifies ischemic penumbra; predicts thrombolysis benefit [86] | Patient selection for extended window therapies |
| MRA/CTA | Vessel occlusion, collateral flow | Large vessel occlusion predicts 6-month mortality; collateral grade predicts good outcome [85] | Treatment planning and prognosis stratification |
Comparative Efficacy Analysis
Preclinical Evidence
Preclinical studies in rodent models of ischemic stroke provide compelling evidence for both MSC and exosome therapies:
- MSC Whole Cell Therapy: Multiple studies in immune-competent ischemic stroke rodent models demonstrate that MSC transplantation reduces infarct size, lessens motor deficits, improves spatial learning, and promotes functional recovery as measured by modified neurological severity scores (mNSS) [83]. MSC administration enhances angiogenesis and neurogenesis while reducing inflammation and apoptosis [79] [83].
- MSC-Derived Exosomes: In vivo tracking studies using near-infrared fluorescence imaging demonstrate that intravenously administered exosomes efficiently migrate to ischemic brain regions, peak at day 3 post-stroke, and localize within neurons [84]. DTI imaging reveals significant improvement in white matter integrity parameters, including increased fractional anisotropy values, fiber length, and fiber number ratios in exosome-treated animals [84]. Angiogenesis and neurogenesis are significantly improved, accompanied by reduced IL-1β expression [84].
Clinical Trial Data
Recent meta-analyses of randomized controlled trials provide insights into the clinical efficacy of stem cell therapies for ischemic stroke:
- Functional Outcomes: A 2020 systematic review including 9 RCTs and 7 non-randomized studies found stem cell-based therapies associated with better outcomes measured by NIHSS (MD -1.63, 95% CI -2.73 to -0.53) and Barthel Index (MD 14.68, 95% CI 1.12 to 28.24) in RCTs [87]. A 2025 meta-analysis of 18 RCTs with 1,026 patients confirmed these findings, showing SCT significantly improved mRS scores (MD -0.56, 95% CI -0.76 to -0.35) and Barthel Index scores (MD 12.00, 95% CI 4.00 to 20.00) [88].
- Timing Considerations: The therapeutic window for cell-based interventions appears broader than for thrombolytics. MSC transplantation in the subacute phase (several hours to days) abrogates early secondary cell death responses, while chronic phase treatment (days to weeks) triggers brain remodeling via angiogenesis, vasculogenesis, neurogenesis, and synaptogenesis [83].
Table 3: Clinical Efficacy Outcomes from Meta-Analyses of Stem Cell Therapies for Ischemic Stroke
| Outcome Measure | Number of Studies | Patient Population | Effect Size [MD (95% CI)] | Heterogeneity (I²) |
|---|---|---|---|---|
| NIHSS Improvement | 9 RCTs [87] | 740 participants | -1.63 (-2.73 to -0.53) | 60% |
| Barthel Index | 9 RCTs [87] | 740 participants | 14.68 (1.12 to 28.24) | 68% |
| mRS Improvement | 18 RCTs [88] | 1,026 patients | -0.56 (-0.76 to -0.35) | 30% |
| Fugl-Meyer Assessment | 18 RCTs [88] | 1,026 patients | 18.16 (6.58 to 29.75) | Not reported |
Figure 2: Multimodal Assessment Framework for Evaluating Stroke Recovery Interventions
Experimental Protocols and Research Tools
Standardized Experimental Models
- Animal Stroke Models: The middle cerebral artery occlusion (MCAO) model is widely used for ischemic stroke research [79]. Photothrombotic models offer advantages of simple procedures and low mortality rates [84].
- Cell Tracking Methodologies: Near-infrared fluorescence imaging using DiR-labeled exosomes enables in vivo tracking of biodistribution and migration patterns [84]. Magnetic resonance imaging provides longitudinal assessment of structural and functional recovery [84].
- Functional Assessment Timeline: Behavioral tests (grid walking, mNSS) are typically performed at baseline and periodically during follow-up periods, which often extend to 14 days in rodents and 3-6 months in clinical trials [87] [84].
Research Reagent Solutions
Table 4: Essential Research Tools for Investigating MSC and Exosome Therapies in Stroke
| Research Tool | Specific Application | Function and Utility |
|---|---|---|
| MSC Characterization | Cell surface marker analysis | Verification of CD73+, CD90+, CD105+, CD45- phenotype [79] |
| Exosome Isolation | Ultracentrifugation | Purification of exosomes from MSC-conditioned media [84] |
| Exosome Characterization | TEM, NTA, Western blot | Validation of exosome size (30-150 nm) and markers (CD9, CD63, Alix) [82] [84] |
| In Vivo Tracking | DiR fluorescent labeling | Near-infrared fluorescence imaging of exosome migration and distribution [84] |
| Angiogenesis Assessment | VEGF, Ang1/Tie2 measurement | Evaluation of pro-angiogenic signaling pathways [79] |
| White Matter Integrity | DTI with fractional anisotropy | Quantification of white matter remodeling and repair [85] [84] |
Clinical Translation Challenges
MSC Whole Cell Therapy Limitations
Despite promising results, MSC whole cell therapy faces several translational challenges:
- Delivery Complications: Intravascular administration carries embolism risks, while direct intracranial injection poses additional risks to already compromised brain tissue [83].
- Tumorigenic Potential: Although rare, the potential for uncontrolled proliferation remains a concern [82].
- Standardization Issues: Lack of well-defined release criteria for donor cells, varying timing, cell doses, and delivery routes complicate clinical translation [83].
- Immunogenic Response: While MSCs have low immunogenicity, immune responses against allogeneic stem cells remain possible [82].
Exosome Therapy Advantages and Challenges
MSC-derived exosomes present a promising cell-free alternative with distinct advantages:
- Reduced Risks: Exosomes eliminate risks associated with whole cell transplantation, including tumor formation and embolism [82] [2].
- Enhanced BBB Penetration: Their small size facilitates efficient crossing of the blood-brain barrier [82].
- Stability and Storage: Exosomes offer better storage stability compared to live cells [82].
- Standardization Hurdles: Clinical translation faces challenges in standardizing exosome isolation, optimal dosing, delivery methods, and long-term safety evaluation [79] [82].
- Manufacturing Scalability: Large-scale production of clinical-grade exosomes remains technologically challenging [82].
The comparative analysis of functional outcomes in ischemic stroke reveals distinct yet complementary profiles for MSC whole cell therapy and MSC-derived exosomes. While whole cell therapies offer the potential for multifactorial repair through direct paracrine signaling and possible cell replacement, exosome therapies provide a refined, cell-free approach with enhanced safety and targeted delivery capabilities. Advanced MRI techniques, particularly DTI for white matter integrity assessment and perfusion-diffusion mapping for penumbra identification, provide critical biomarkers for evaluating therapeutic efficacy beyond standard clinical scales. Future research directions should focus on optimizing delivery protocols, standardizing manufacturing processes, and identifying patient subgroups most likely to benefit from each approach. The integration of advanced imaging biomarkers with sensitive clinical outcome measures will be essential for advancing these promising therapies through the clinical translation pipeline and ultimately improving functional recovery for ischemic stroke patients.
The field of regenerative medicine is undergoing a fundamental transformation, moving away from whole-cell therapies toward cell-free approaches utilizing mesenchymal stem cell-derived exosomes (MSC-Exos). This paradigm shift is driven by growing recognition that many therapeutic benefits originally attributed to mesenchymal stem cells (MSCs) are actually mediated through their paracrine secretions rather than direct cell replacement [2] [11]. MSC-derived exosomes, nanoscale extracellular vesicles (30-150 nm in diameter), have emerged as principal effectors of MSC function, capable of recapitulating therapeutic benefits while overcoming significant limitations associated with whole-cell therapies [89] [11]. This comparative analysis objectively examines the efficacy, safety, and logistical profiles of MSC-derived exosomes versus whole MSC therapies, providing researchers and drug development professionals with evidence-based insights for therapeutic development.
The transition to exosome-based therapeutics represents more than a simple technical advancement—it constitutes a fundamental rethinking of MSC therapeutic activity. Seminal studies revealed that both implanted and intravenously administered MSCs yielded similar functional recovery despite minimal in vivo persistence or differentiation, pointing to secreted factors as the primary mechanism of action [89]. Subsequent research identified that the active fraction of the MSC secretome exceeded 1,000 kDa, leading to the characterization of extracellular vesicles as the key therapeutic components [89]. This review systematically compares these two therapeutic modalities across multiple domains critical to research and clinical translation.
Mechanisms of Action: Comparative Therapeutic Pathways
Whole MSC Therapeutic Mechanisms
Whole MSC therapies operate through two primary mechanistic pathways: direct cell engagement and paracrine signaling. The direct mechanisms include cellular differentiation into target tissues, cell-to-cell contact-dependent signaling, and physical integration into damaged tissues. However, growing evidence suggests that these direct mechanisms contribute minimally to functional recovery, with studies showing minimal long-term engraftment of administered MSCs in target tissues [90] [91]. Instead, the paracrine activity of MSCs—secretion of soluble factors, cytokines, and extracellular vesicles—appears to dominate their therapeutic effects [90] [11]. MSCs respond to local inflammatory environments by releasing immunomodulatory factors that alter tissue metabolism and promote regeneration through trophic effects on resident cells [11].
The immunomodulatory properties of MSCs deserve particular emphasis, as they represent one of their most therapeutically valuable features. When stimulated by inflammatory factors, MSCs produce numerous immunomodulatory factors, chemokines, and growth factors that regulate the tissue immune microenvironment [11]. This capability enables MSCs to modulate both innate and adaptive immune responses, making them promising candidates for treating autoimmune conditions, graft-versus-host disease, and other inflammation-driven pathologies [33].
MSC-Exos Therapeutic Mechanisms
MSC-derived exosomes function as sophisticated intercellular communicators that transfer bioactive cargo—including proteins, lipids, mRNAs, and regulatory miRNAs—to recipient cells [2] [5]. These nanosized vesicles (40-160 nm) mediate their effects through three principal mechanisms: membrane receptor binding, direct fusion with target cells, and endocytosis followed by cargo delivery [23]. Their therapeutic activities can be categorized into four unified mechanistic pillars across pathologies: (1) maintaining immunological-stromal homeostasis, (2) reprogramming metabolic circuitry, (3) determining cell fate, and (4) intercepting oncogenic signaling [23].
Exosomes execute these functions through their diverse molecular cargo. More than 304 proteins and 150 microRNAs have been identified in MSC-Exos, along with other bioactive molecules [5]. These components work in concert to mediate therapeutic effects including inhibition of apoptosis, immunomodulation, stimulation of angiogenesis, and recruitment of endogenous stem cells [5]. Notably, exosomes serve as natural delivery vehicles that protect their cargo from degradation and facilitate efficient cellular uptake [5].
Comparative mechanisms of MSC versus MSC-exosome therapies. Whole MSCs operate through direct cellular processes, while exosomes function via molecular cargo delivery and horizontal communication.
Efficacy Comparison: Therapeutic Outcomes Across Disease Models
Regenerative Capacity
Both MSC and MSC-Exos therapies demonstrate significant regenerative potential across diverse tissue types, though through different mechanistic emphasis. Whole MSC therapies have shown promise in cardiac regeneration following myocardial infarction, contributing to reduced scar mass, decreased infarct wall thickness, and improved cardiac function [90]. Similarly, in neurological applications, MSC transplantation has demonstrated therapeutic effects in sensory neuropathy models, reversing behavioral signs and reducing sciatic nerve ultrastructural alterations [91].
MSC-Exos recapitulate many of these regenerative benefits while exhibiting enhanced tissue targeting capabilities. In hepatic disease models, MSC-Exos demonstrate intrinsic hepatic tropism following systemic administration, enabling targeted cellular communication that promotes repair [23]. Their nanoscale size facilitates improved biodistribution and penetration into damaged tissues. In neurological disorders, MSC-Exos have shown efficacy in animal models of epilepsy, Parkinson's disease, and stroke, with the advantage of crossing the blood-brain barrier—a significant limitation for whole-cell therapies [5] [11].
Immunomodulatory Performance
The immunomodulatory capabilities of both therapeutic modalities represent one of their most valuable attributes, though with notable differences in mechanism and consistency. Whole MSCs dynamically respond to inflammatory environments by secreting factors that regulate immune cell activity, including T-cells, B-cells, natural killer cells, and macrophages [11] [33]. This dynamic responsiveness can be both an advantage and a limitation, as it introduces variability based on the host environment.
MSC-Exos provide more predictable immunomodulation through their defined cargo composition. They contain specific immunoregulatory molecules that suppress pro-inflammatory responses and promote regulatory immune phenotypes [33]. For instance, MSC-Exos have been shown to suppress IFN-γ secretion by T cells, inhibit Th1 cell proliferation, promote M2 macrophage polarization, and facilitate Treg induction [5] [33]. This consistent, defined immunomodulatory profile offers advantages for standardized therapeutic development.
Table 1: Comparative Efficacy in Preclinical Models
| Disease Category | MSC Therapeutic Effects | MSC-Exos Therapeutic Effects | Key Comparative Findings |
|---|---|---|---|
| Cardiac Injury | Reduced scar mass, improved cardiac function [90] | Enhanced angiogenesis, reduced apoptosis [90] | Comparable functional improvement; Exosomes avoid microvascular occlusion |
| Neurological Disorders | Migration to injury sites, neurotrophic support [91] | Blood-brain barrier penetration, anti-inflammatory effects [5] | Exosomes show superior distribution in CNS territories |
| Autoimmune Diseases | Dynamic immune modulation, tissue protection [33] | Consistent anti-inflammatory cargo delivery [33] | Exosomes provide more predictable response; Less host-dependent variation |
| Liver Diseases | Engraftment limitations, paracrine effects [23] | Intrinsic hepatic tropism, multi-mechanistic repair [23] | Exosomes demonstrate superior targeting and defined mechanisms |
| Renal Injury | Limited cell retention, paracrine-mediated repair [2] | Tubular cell proliferation, apoptosis inhibition [2] | Similar efficacy; Exosomes eliminate risks of aberrant differentiation |
Safety Profiles: Risk Assessment and Management
Whole MSC Safety Concerns
Whole MSC therapies present several significant safety considerations that have emerged through preclinical and clinical investigation. The most substantial risks include:
Tumorigenic Potential: As living, proliferative cells, MSCs carry a theoretical risk of malignant transformation or uncontrolled proliferation [11] [23]. While primary MSCs are generally considered to have low tumorigenic potential, the risk increases with extensive in vitro expansion and cellular senescence.
Vascular Occlusion: Following intravenous administration, MSCs (typically 30-60 μm in diameter) frequently become trapped in pulmonary microvasculature, potentially causing pulmonary embolism and associated complications [5] [11]. This physical lodging not only presents safety concerns but also significantly reduces the number of cells reaching target tissues.
Immunogenic Responses: Despite their immunomodulatory properties, allogeneic MSCs can still elicit host immune responses, potentially leading to rejection or reduced therapeutic efficacy upon repeated administration [33]. The immunogenicity of MSCs may increase with in vitro manipulation and culture duration.
Ectopic Tissue Formation: The differentiation capacity of MSCs, while therapeutically beneficial in some contexts, raises concerns about unintended differentiation into inappropriate tissues or contributions to pathological calcification [89].
MSC-Exos Safety Advantages
MSC-derived exosomes offer a markedly improved safety profile attributable to their acellular nature and nanoscale dimensions:
Eliminated Tumorigenic Risk: As non-living, non-replicative entities, MSC-Exos are incapable of uncontrolled proliferation or malignant transformation, addressing one of the most significant theoretical risks of cell-based therapies [89] [11].
Avoidance of Vascular Occlusion: With diameters of 30-150 nm, MSC-Exos readily traverse capillary networks without causing mechanical obstruction, significantly reducing the risk of pulmonary embolism or other vascular complications [5] [89].
Reduced Immunogenicity: MSC-Exos demonstrate lower immunogenic potential compared to their parent cells, minimizing risks of immune rejection and enabling repeat administration without sensitization [11] [33].
No Ectopic Tissue Formation: Lacking differentiation capacity, MSC-Exos cannot form inappropriate tissues, eliminating concerns about aberrant differentiation while still promoting regenerative processes through trophic effects [89].
Table 2: Comprehensive Safety Comparison
| Safety Parameter | Whole MSC Therapy | MSC-Exos Therapy | Clinical Implications |
|---|---|---|---|
| Tumorigenic Potential | Theoretical risk, especially with extensive culture [11] | No risk (non-replicative) [89] | Exosomes suitable for prolonged and immunocompromised use |
| Vascular Occlusion | Significant risk (30-60 μm cells) [5] | Minimal risk (30-150 nm vesicles) [5] | Exosomes enable safe systemic administration |
| Immunogenic Response | Low but present, increases with manipulation [33] | Very low immunogenicity [11] | Exosomes allow repeat dosing and allogeneic applications |
| Ectopic Differentiation | Possible risk [89] | No risk (no differentiation capacity) [89] | Exosomes eliminate differentiation concerns |
| Consistency Between Batches | High variability due to biological nature [33] | More consistent, but isolation methods vary [5] | Exosomes offer more predictable manufacturing |
| Storage and Stability | Requires cryopreservation, sensitive to freeze-thaw [11] | Lyophilization possible, superior stability [89] | Exosomes simplify logistics and extend shelf-life |
Production and Logistics: Practical Implementation Considerations
Manufacturing and Scalability
The manufacturing processes for whole MSCs and MSC-Exos differ significantly in complexity, scalability, and quality control requirements:
Whole MSC Manufacturing requires maintaining viable, proliferative cells throughout expansion and formulation. This process involves complex quality control to ensure phenotypic stability, differentiation potential, and absence of senescence [11]. MSC cultures face challenges with donor-dependent variation and phenotypic changes during extended passaging, creating batch-to-batch variability that complicates standardized therapeutic development [33]. Scaling MSC production necessitates substantial infrastructure for cell culture facilities, rigorous sterility testing, and comprehensive characterization of cellular properties.
MSC-Exos Manufacturing focuses on vesicle production, isolation, and purification. The most common isolation methods include:
- Ultracentrifugation: The historical gold standard, though limited by time consumption and batch variability [5] [23]
- Tangential Flow Filtration (TFF): Increasingly adopted for improved scalability and reproducibility [5]
- Chromatography: Effective for removing contaminants while preserving vesicle integrity [23]
- Polymer-based Precipitation: Enables scalable concentration but may compromise purity [23]
Exosome manufacturing benefits from the ability to use immortalized MSC lines as consistent production sources, overcoming donor variability concerns that plague whole-cell therapies [89]. Additionally, MSC-Exos can be produced under defined conditions that enhance consistency and enable more straightforward characterization of critical quality attributes (CQAs) [89].
Storage, Stability, and Distribution
Logistical considerations dramatically favor MSC-Exos over whole cell therapies:
Whole MSCs require cryopreservation at extremely low temperatures (-150°C to -196°C) and maintained throughout the distribution chain [11]. These cells are sensitive to freeze-thaw cycles, which can significantly impact viability and function. The requirement for continuous cold chain maintenance complicates distribution, increases costs, and limits accessibility in resource-constrained settings.
MSC-Exos demonstrate superior stability profiles, maintaining structural integrity and function after lyophilization (freeze-drying) and storage at refrigerated or ambient temperatures [89]. This dramatically reduces reliance on complex cold chain logistics, enabling broader geographic distribution, extended shelf lives, and point-of-care administration convenience. The stability of exosomes also supports the development of "off-the-shelf" formulations that can be readily deployed when needed.
Comparative production workflows for MSC versus MSC-exosome therapies, highlighting the simplified logistics and storage advantages of exosome-based approaches.
Clinical Translation: Current Status and Applications
Clinical Trial Landscape
The clinical development of both therapeutic modalities reflects their respective maturation levels and translational challenges:
Whole MSC Therapies have been investigated in numerous clinical trials across diverse conditions including graft-versus-host disease, osteoarthritis, spinal cord injury, myocardial damage, and COVID-19-associated acute respiratory distress syndrome [11] [33]. The FDA has approved nearly 60 clinical trials focused on MSC applications, establishing a substantial clinical evidence base [11]. However, clinical outcomes have shown variability, with some studies demonstrating promising results while others report limited efficacy or increased disease severity in certain contexts [33].
MSC-Exos Therapies represent a more recent therapeutic approach, with a rapidly expanding clinical trial portfolio. As of 2022, seven published clinical studies and 14 ongoing clinical trials were evaluating MSC-Exos for conditions including ARDS, kidney diseases, graft-versus-host disease, osteoarthritis, stroke, Alzheimer's disease, and type 1 diabetes [5]. The most common MSC sources in clinical trials are adipose tissue (7 studies), followed by bone marrow (5 studies) and umbilical cord (4 studies) [5]. These trials employ various administration routes including intravenous infusion, inhalation, and local administration, with doses calculated by weight (μg), particle number, or parent cell equivalents [5].
Regulatory Considerations
The regulatory pathways for these two therapeutic categories differ significantly:
Whole MSC Therapies are typically regulated as cellular products, requiring comprehensive characterization of viability, identity, potency, and safety. Regulatory challenges include addressing donor-to-donor variability, phenotypic stability during expansion, and comprehensive tumorigenicity assessments [11] [33]. The living nature of these products necessitates rigorous monitoring for potential adverse events including ectopic tissue formation, unintended differentiation, and immunogenic responses.
MSC-Exos Therapies are generally classified as biological products or non-living biological entities, which simplifies certain regulatory aspects while introducing others. Key regulatory considerations include establishing standardized characterization methods (following MISEV2018/2023 guidelines), defining critical quality attributes (CQAs), ensuring batch-to-batch consistency, and validating isolation methods [5] [23]. The non-replicative nature of exosomes eliminates concerns about uncontrolled proliferation but requires thorough characterization of cargo composition and biological activity.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Tools for MSC and MSC-Exos Investigation
| Reagent/Method | Primary Function | Application Notes |
|---|---|---|
| Flow Cytometry Panels | MSC surface marker characterization (CD73, CD90, CD105) [90] | Essential for validating MSC identity per ISCT criteria; Critical for quality control |
| Ultracentrifugation | Exosome isolation from conditioned media [5] | Historical gold standard; Consider combining with TFF for improved yield and purity |
| Tangential Flow Filtration (TFF) | Scalable exosome purification [5] | Increasingly adopted for clinical-grade production; Better scalability than ultracentrifugation |
| Nanoparticle Tracking Analysis | Exosome size and concentration quantification [23] | Vital for characterizing physical properties; Often combined with electron microscopy |
| miRNA Sequencing | Cargo profiling of MSC-Exos [24] | Critical for understanding mechanisms; Preconditioning strategies alter miRNA profiles |
| Preconditioning Reagents | Enhance therapeutic potential of MSC-Exos [24] | LPS, TNF-α, IL-1β, hypoxia mimicry; Modifies miRNA content and biological activity |
| Animal Disease Models | Efficacy assessment in relevant pathologies | Cardiac, neurological, autoimmune models; Essential for comparative efficacy studies |
The comparative analysis of MSC-derived exosomes versus whole MSC therapies reveals a compelling value proposition for exosome-based approaches across multiple domains. MSC-Exos demonstrate comparable therapeutic efficacy to their cellular counterparts in diverse disease models while offering superior safety profiles characterized by eliminated tumorigenic risk, reduced immunogenicity, and avoidance of vascular occlusion. From a practical perspective, MSC-Exos provide significant logistical advantages through enhanced stability, simplified storage requirements, and reduced dependence on cold chain infrastructure.
However, whole MSC therapies retain relevance in specific applications where direct cell-to-cell contact, temporary environmental modification, or cellular integration may provide therapeutic benefits not fully replicable by vesicles alone. The dynamic responsiveness of living MSCs to local environmental cues represents an advantage in certain complex pathological contexts.
For researchers and drug development professionals, the choice between these modalities should be guided by specific therapeutic objectives, target pathology, manufacturing capabilities, and regulatory considerations. MSC-Exos represent a promising cell-free alternative that addresses many limitations of cell-based therapies, particularly for conditions requiring precise molecular intervention, repeat administration, or systemic delivery. As manufacturing technologies advance and our understanding of exosome biology deepens, MSC-Exos are positioned to become increasingly prominent in the therapeutic landscape, potentially revolutionizing regenerative medicine through their unique combination of efficacy, safety, and practical advantages.
Future development should focus on standardizing isolation protocols, engineering exosomes for enhanced targeting and cargo delivery, and establishing robust potency assays that correlate with clinical outcomes. These advancements will accelerate the translation of MSC-Exos from promising experimental tools to mainstream therapeutic applications.
The field of regenerative medicine is undergoing a significant transformation, moving from whole-cell therapies toward advanced acellular approaches. Within this context, Mesenchymal Stem Cell (MSC)-derived exosomes have emerged as a promising alternative to whole cell therapies, offering a potentially superior safety profile with reduced risks of immune rejection, tumorigenicity, and ectopic tissue formation [2] [24]. These natural nanovesicles, typically measuring 30-150 nm in diameter, mediate intercellular communication by transferring proteins, lipids, and nucleic acids between cells [92] [76]. The integration of exosomes with gene editing technologies and bioengineering strategies represents a frontier in therapeutic development, creating synergistic platforms that enhance precision, efficacy, and applicability across diverse medical conditions. This comparison guide objectively analyzes the functional outcomes of engineered exosome therapies against conventional whole-cell approaches, providing researchers and drug development professionals with critical experimental data and methodological frameworks for advancing this promising field.
Exosomes as Natural Therapeutics: Composition and Biogenesis
Exosomes are extracellular vesicles generated through the endosomal pathway, specifically formed as intraluminal vesicles within multivesicular bodies (MVBs) that subsequently fuse with the plasma membrane for release [93] [94]. Their composition reflects their cellular origin, containing diverse biomolecules encapsulated within a phospholipid bilayer membrane.
- Key Components: Exosomes carry proteins (tetraspanins CD9, CD63, CD81, heat shock proteins, ESCRT components ALIX and TSG101), nucleic acids (miRNAs, mRNAs, circRNAs), lipids (cholesterol, sphingomyelin, phosphatidylserine), and metabolites [93] [76].
- Biogenesis Machinery: The Endosomal Sorting Complex Required for Transport (ESCRT) and associated proteins (ALIX, TSG101) play crucial roles in exosome formation and cargo sorting, with ESCRT-independent pathways involving tetraspanins and lipids like ceramide also contributing significantly [94].
The following diagram illustrates the biogenesis pathway and key engineering strategies for creating therapeutic exosomes.
Comparative Analysis: MSC-Derived Exosomes vs. Whole Cell Therapy
The transition from whole cell therapies to acellular exosome-based approaches presents distinct advantages and limitations. The table below provides a systematic comparison of key parameters relevant to research and therapeutic development.
Table 1: Functional Comparison of MSC-Derived Exosomes vs. Whole Cell Therapies
| Parameter | MSC-Derived Exosomes | Whole MSC Therapy |
|---|---|---|
| Therapeutic Cargo | Proteins, lipids, miRNAs, mRNAs, non-coding RNAs [2] [76] | Whole cells with secretory capability and differentiation potential |
| Immunogenicity | Low risk, immunologically privileged [24] [95] | Moderate to high risk of immune rejection [24] |
| Tumorigenic Risk | Minimal, no risk of ectopic tissue formation [24] | Present due to proliferative capacity and differentiation potential [24] |
| Delivery Efficiency | Superior tissue penetration (30-150 nm size) [92] | Limited by cell size and engraftment efficiency [24] |
| Storage & Stability | Long-term storage without loss of viability [96] | Complex cryopreservation requirements [96] |
| Manufacturing Scalability | Challenging but improving with advanced chromatography [94] | Complex, expensive expansion processes [96] |
| Regulatory Pathway | Evolving as biological product/devices [97] [95] | Complex cellular therapy regulations |
| Dosing Precision | Controllable, quantifiable vesicle dosing [96] | Variable, dependent on cell viability and function |
Synergistic Integration with Gene Editing Technologies
Exosome-Mediated CRISPR/Cas9 Delivery
The combination of exosomes with gene editing technologies represents a particularly promising synergy, addressing critical delivery challenges associated with CRISPR/Cas9 systems. Research by McAndrews et al. demonstrated that exosomes can be engineered to deliver CRISPR/Cas9 machinery targeting oncogenic mutations, such as KrasG12D in pancreatic cancer [98].
- Delivery Advantage: Exosomes circumvent limitations of viral vectors (immunogenicity, insertional mutagenesis) and synthetic nanoparticles (toxicity, accelerated clearance) [98].
- Experimental Workflow: The study utilized HEK293T cell-derived exosomes loaded with CRISPR/Cas9 plasmid DNA targeting KrasG12D using the commercial transfection reagent Exo-Fect [98].
- Functional Outcomes: This approach achieved significant suppression of KrasG12D expression, inhibited cancer cell proliferation, and suppressed tumor growth in syngeneic subcutaneous and orthotopic pancreatic cancer models [98].
The experimental workflow below details the methodology for implementing exosome-mediated gene editing.
Experimental Outcomes and Validation Data
The quantitative outcomes from exosome-mediated gene editing experiments provide compelling evidence for this synergistic approach. The table below summarizes key experimental findings from the pancreatic cancer gene editing study.
Table 2: Experimental Outcomes of Exosome-Mediated KrasG12D Targeting [98]
| Experimental Parameter | Methodology | Result |
|---|---|---|
| Exosome Characterization | Nanoparticle tracking analysis, Western blot (CD81, Alix) | Size range 30-150 nm, positive for exosomal markers |
| Plasmid Loading Efficiency | qPCR for GFP copy number, DNase protection assay | Successful encapsulation with nuclease resistance |
| Gene Editing Efficiency | T7/surveyor mismatch detection assay | Successful Cas9-mediated cleavage and gene editing |
| KrasG12D Suppression | Quantitative PCR (qPCR) | Significant mRNA suppression, particularly with sgRNA2 |
| Functional Impact In Vitro | Cell proliferation assays | Inhibited cancer cell proliferation |
| Functional Impact In Vivo | Syngeneic subcutaneous and orthotopic models | Suppressed tumor growth |
Bioengineering Strategies for Enhanced Therapeutic Potential
Preconditioning for Cargo Enhancement
Preconditioning of parent MSCs represents a powerful bioengineering approach to modulate exosome cargo and enhance therapeutic efficacy. Various stimuli can significantly alter the miRNA profile of resulting exosomes, tailoring them for specific applications.
- Hypoxia: Enhances pro-angiogenic factors including miR-126 [96] [24].
- Inflammatory Cytokines (TNF-α, IL-1β): Upregulates immunomodulatory miRNAs (miR-146a, miR-181a) [24].
- Lipopolysaccharide (LPS): At varying concentrations (0.1-1 μg/mL) induces dose-dependent miRNA profiles (miR-222-3p, miR-181a-5p, miR-150-5p) that mitigate inflammatory damage [24].
Engineered Exosomes and Advanced Loading Techniques
Beyond preconditioning, direct engineering of exosomes enables precise control over their targeting capabilities and cargo composition.
- Surface Modification: Incorporation of targeting ligands (peptides, antibodies, DARPins) enhances tissue-specific delivery [94] [76].
- Cargo Loading: Multiple strategies exist for loading therapeutic molecules, including:
- Hybrid and Artificial Exosomes: Fusion of natural exosomes with synthetic liposomes creates hybrid systems combining natural functionality with engineering control [94].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research at the intersection of exosome biology, gene editing, and bioengineering requires specific reagents and methodologies. The following table details essential components for developing engineered exosome therapeutics.
Table 3: Essential Research Reagents and Materials for Exosome Engineering
| Category | Specific Examples | Research Application |
|---|---|---|
| Isolation Tools | Ultracentrifugation, Size-exclusion chromatography, Immunoaffinity capture (CD63/CD81 antibodies), Cation/anion exchange chromatography [93] [94] | High-purity exosome isolation with maintained bioactivity |
| Characterization Reagents | Antibodies against CD9, CD63, CD81, ALIX, TSG101, HSP70; Calnexin/β-actin for purity assessment [93] [76] | Vesicle identification, quantification, and purity validation |
| Loading/Engineering Materials | Exo-Fect, Electroporation systems, Optogenetic modules (CRY2/CIB1), Liposome preparations [98] [94] | Therapeutic cargo encapsulation and surface functionalization |
| Gene Editing Components | CRISPR/Cas9 plasmids (LentiCRISPR V2, PX458), sgRNAs, RNP complexes, Reporter constructs (GFP) [98] | Genetic modification of parent cells or direct therapeutic payload |
| Preconditioning Agents | LPS, TNF-α, IL-1β, IFN-γ, Hypoxia chambers, Chemical stimuli [24] | Enhancement of native therapeutic potential through cargo modulation |
| Analytical Assays | Nanoparticle tracking analysis, Western blot, qPCR, T7/surveyor assay, miRNA sequencing, Functional proliferation assays [98] [93] | Comprehensive validation of engineering success and efficacy |
Clinical Translation and Safety Profiles
The clinical translation of exosome-based therapies is advancing, with growing evidence supporting their safety and potential efficacy. A large-scale retrospective analysis of 608 patients treated with amniotic-derived exosomes reported no serious adverse events, with a 95% confidence interval for serious adverse event rate of 0%-0.63% [95]. Common transient side effects included tiredness (10%) and general joint pain (10%), with satisfactory symptom relief reported by 85% of patients [95].
Compared to whole cell therapies, exosomes present a favorable safety profile with minimal risks of immunogenic responses, malignant transformation, or transmission of infectious pathogens [24]. Their acellular nature circumvents many ethical and regulatory hurdles associated with stem cell therapies, potentially accelerating clinical implementation [95].
The integration of exosome biology with gene editing and bioengineering represents a paradigm shift in therapeutic development, offering unprecedented opportunities for precision medicine. MSC-derived exosomes demonstrate significant advantages over whole cell therapies in terms of safety, manufacturability, and engineering flexibility. The synergistic potential of these technologies is particularly evident in applications requiring targeted delivery, such as oncology and regenerative medicine.
Future research directions should focus on standardizing isolation protocols, enhancing scalable manufacturing processes, developing more precise targeting systems, and establishing comprehensive regulatory frameworks. As the field continues to mature, engineered exosome platforms are poised to become powerful tools in the therapeutic arsenal, potentially surpassing the capabilities of both conventional biologics and whole cell therapies for a wide range of applications.
Analyzing the Risk-Benefit Profile for Specific Disease Indications
The therapeutic application of mesenchymal stem cells (MSCs) has represented a cornerstone of regenerative medicine for decades, offering promise for conditions ranging from autoimmune diseases to tissue injury. However, a paradigm shift is underway as research increasingly demonstrates that many therapeutic benefits originate not from the cells themselves but through their paracrine activity [99] [14]. This recognition has catalyzed the emergence of MSC-derived exosomes (MSC-Exos) as a novel cell-free therapeutic platform. Exosomes are nanosized extracellular vesicles (30-150 nm) that mediate intercellular communication by transferring functional proteins, lipids, and nucleic acids from parent MSCs to recipient cells [23] [33]. This article provides a comprehensive risk-benefit analysis of MSC-derived exosomes versus whole cell therapy across specific disease indications, framing this comparison within the broader context of functional outcomes in regenerative medicine.
Table 1: Fundamental Characteristics of MSC Therapy vs. MSC-Derived Exosomes
| Parameter | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Nature | Living, replicating cells | Non-living, non-replicating nanovesicles |
| Primary Mechanism | Direct differentiation & paracrine signaling | Paracrine signaling & biomolecule transfer |
| Therapeutic Cargo | Secreted factors, vesicles, differentiation potential | Pre-packaged proteins, miRNAs, mRNAs, lipids |
| Typical Size | 15-30 μm (cellular) | 30-150 nm (vesicular) |
| Immunogenicity | Low but present; risk of rejection | Very low; no MHC expression |
| Tumorigenic Risk | Theoretical concern with uncontrolled differentiation | Minimal to none |
| Administration Safety | Risk of microvascular occlusion | No occlusion risk due to nano-size |
Comparative Mechanistic Profiles and Therapeutic Actions
Mechanisms of Action: Cellular Differentiation vs. Precision Signaling
The therapeutic mechanisms of whole MSCs and their derived exosomes diverge significantly. MSCs exhibit a dual mechanism: direct differentiation into target tissue lineages and paracrine signaling through secreted factors and vesicles [100]. In contrast, MSC-Exos function exclusively through sophisticated paracrine signaling, transferring bioactive cargo to recipient cells to reprogram their function [23] [17]. These vesicles naturally encapsulate a diverse cargo including tetraspanins (CD9, CD63, CD81), heat shock proteins, and nucleic acids that mediate their effects [23].
The diagram below illustrates the four-pillar mechanistic framework through which MSC-derived exosomes exert their therapeutic effects across liver pathologies, representing a model applicable to multiple disease contexts:
Disease-Specific Risk-Benefit Profiles
The risk-benefit calculus for MSC versus MSC-Exo therapies varies significantly across disease contexts, with each approach demonstrating distinct advantages in specific indications.
Table 2: Disease-Specific Risk-Benefit Analysis of MSC vs. MSC-Exo Therapies
| Disease Area | Whole MSC Therapy Benefits | MSC-Exo Therapy Benefits | Key Risks & Limitations |
|---|---|---|---|
| Immune Disorders (GvHD, Diabetes T1) | Potent immunomodulation via direct cell contact [33] | Specific miRNA transfer (e.g., miR-146a) suppresses Th1 cells; induces Tregs [33] | MSC: Infusional toxicity, pulmonary entrapment [33] [17] |
| Liver Diseases | Direct hepatic differentiation potential [23] | Intrinsic hepatic tropism; intercepts oncogenic signaling [23] | MSC: Limited engraftment, oncogenic concerns [23] |
| Wound Healing & Cutaneous Repair | Direct cell participation in early wound bed [99] | Accelerates re-epithelialization via Wnt/β-catenin; modulates inflammation [17] | MSC: Heterogeneous delivery outcomes [99] |
| Bone/Cartilage Repair | Direct differentiation into osteoblasts/chondrocytes [17] | Stimulates endogenous osteogenesis; enhances matrix synthesis [17] | MSC: Ectopic tissue formation risk [17] |
| Neurological Conditions | Structural integration potential in some models | Crosses BBB; transfers neuroprotective miRNAs [14] | MSC: Limited migration to CNS; poor survival |
Experimental Models and Functional Outcome Assessment
Methodological Approaches for Comparative Studies
Robust experimental protocols are essential for directly comparing the efficacy and safety profiles of MSC versus MSC-Exo therapies. The workflow below outlines a standardized approach for such comparative studies:
Quantitative Functional Outcomes in Preclinical Models
Preclinical investigations have yielded substantial quantitative data demonstrating the therapeutic potential of both approaches across disease models, with MSC-Exos frequently matching or exceeding the functional outcomes achieved with whole cell therapy while demonstrating superior safety profiles.
Table 3: Comparative Functional Outcomes in Preclinical Studies
| Disease Model | MSC Therapy Outcomes | MSC-Exo Therapy Outcomes | Reference |
|---|---|---|---|
| Diabetic Wound Healing | Accelerated wound closure; reduced inflammation | Enhanced re-epithelialization; increased collagen deposition; superior angiogenesis via miR-125a | [17] |
| Myocardial Injury | Improved ejection fraction; reduced scar size | Comparable functional improvement; targeted miRNA delivery | [33] [19] |
| Graft-versus-Host Disease | 50-60% response rates in steroid-refractory patients | Increased Treg induction; suppressed Th1 proliferation via CD39/adenosine pathway | [33] |
| Liver Fibrosis | Reduced collagen deposition; functional improvement | Attenuated inflammation; decreased fibrotic markers; metabolic reprogramming | [23] |
| Osteoarthritis | Cartilage protection; pain reduction | Enhanced chondrocyte proliferation; increased matrix synthesis; anti-inflammatory effects | [17] |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing research in this field requires specific reagents and methodologies tailored to the unique challenges of working with both cellular and vesicular therapeutics.
Table 4: Essential Research Toolkit for MSC and MSC-Exo Studies
| Reagent/Methodology | Function & Application | Technical Considerations |
|---|---|---|
| Ultracentrifugation | Gold standard exosome isolation via high-speed centrifugation [23] [14] | Time-consuming; potential for vesicle damage; requires optimization |
| Nanoparticle Tracking Analysis (NTA) | Quantifies exosome size distribution and concentration [23] | Essential for characterization; requires specialized equipment |
| Tetraspanin Antibodies (CD9, CD63, CD81) | Exosome identification and characterization via Western blot/flow cytometry [23] [42] | Critical for quality control; confirms exosomal identity |
| Transwell Migration Assays | Evaluates MSC migratory capacity toward injury signals [33] | Models homing potential; key for efficacy assessment |
| miRNA Sequencing & PCR | Cargo analysis and functional mechanism elucidation [23] [33] | Identifies active components; reveals mechanistic pathways |
| 3D Biomaterial Scaffolds | Enables sustained localized delivery for both MSCs and exosomes [17] | Enhances retention and therapeutic efficacy in tissue engineering |
Clinical Translation Landscape and Regulatory Considerations
Clinical Trial Progress and Regulatory Status
The translation of these therapeutic approaches from bench to bedside has progressed at different rates. Whole MSC therapy has advanced significantly, with over 1,000 registered clinical trials worldwide and several approved products internationally [101] [100]. These include Alofisel (darvadstrocel) for Crohn's perianal fistulas and Remestemcel-L for pediatric graft-versus-host disease [100]. In contrast, MSC-derived exosome therapies remain predominantly in earlier stages of clinical investigation, with approximately 16 registered clinical trials underway as of 2021 [33]. These pioneering trials focus on indications including dry eye in chronic GVHD, type 1 diabetes, periodontitis, and multiple organ dysfunction syndrome [33].
The regulatory pathway for MSC-Exos presents distinct challenges compared to whole cell therapies. While MSC products are typically regulated as biological drugs or advanced therapy medicinal products (ATMPs), the classification of exosomes remains less standardized [23] [100]. The field is addressing challenges including heterogeneity in isolation methods, cargo standardization, scalable production, and potency assay development [23] [42]. Resolving these issues is crucial for progressing MSC-Exo therapies through the clinical development pipeline.
The risk-benefit analysis of MSC-derived exosomes versus whole cell therapy reveals a complex landscape where the optimal therapeutic approach is highly indication-dependent. Whole MSC therapy maintains advantages in contexts where direct cellular differentiation and structural integration are required for functional recovery. In contrast, MSC-derived exosomes offer a compelling alternative with superior safety profiles, enhanced targeting capabilities, and reduced complexity for applications where paracrine signaling mediates the primary therapeutic effects.
Future research directions should focus on optimizing exosome engineering strategies to enhance target specificity and therapeutic potency [23]. Additionally, standardized protocols for large-scale production and comprehensive characterization are essential for clinical translation [42] [14]. As the field progresses, the complementary application of both therapeutic modalities may offer the most promising approach, leveraging the unique advantages of each to address the complex challenges of regenerative medicine. The ongoing evolution from cell-based to cell-free therapeutics represents not a replacement of one modality by another, but rather a maturation of the regenerative medicine arsenal, enabling more precise matching of therapeutic approaches to specific disease indications and patient needs.
Conclusion
The comparison between MSC-derived exosomes and whole cell therapy reveals a paradigm shift toward cell-free regenerative strategies. Exosomes offer a compelling profile, harnessing the core therapeutic mechanisms of MSCs—such as immunomodulation and tissue repair—while mitigating critical risks associated with whole cells, including tumorigenicity, immunogenicity, and pulmonary embolism. Their stability, ability to cross biological barriers, and suitability as drug delivery vehicles provide distinct advantages. However, the clinical translation of exosome therapies is currently hampered by a lack of standardized manufacturing protocols, undefined dosing metrics, and incomplete understanding of their in vivo trafficking. Future progress hinges on collaborative efforts to establish robust potency assays, scalable GMP-compliant production, and well-designed clinical trials that leverage advanced monitoring techniques. Ultimately, both modalities will likely find their niche, with the choice depending on the specific pathophysiology of the target disease, paving the way for a new era of precise and effective regenerative medicine.
References
- 1. Frontiers | From bench to bedside: translating mesenchymal stem cell... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1639439/full]
- 2. Concise Review: MSC - Derived for Exosomes -Free Cell Therapy [https://pubmed.ncbi.nlm.nih.gov/28294454/]
- 3. Frontiers | The tiny giants of regeneration: MSC-derived extracellular vesicles as next-generation therapeutics [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 4. Frontiers | Mesenchymal stem cell-derived exosomes as a plausible immunomodulatory therapeutic tool for inflammatory diseases [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1563427/full]
- 5. Mesenchymal stromal/stem cell (MSC)-derived exosomes in clinical trials | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03287-7]
- 6. Advances in mesenchymal stem cell and exosome-based therapies for aging and age-related diseases - PubMed [https://pubmed.ncbi.nlm.nih.gov/40713733/]
- 7. MSC-Derived Therapeutics and Exosomes as Rising Stars in Advanced Therapeutics | BioInformant [https://bioinformant.com/msc-therapeutics-and-msc-derived-exosomes/]
- 8. Mesenchymal stem cells derived from human induced pluripotent stem... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02594-1]
- 9. Substrate mechanical properties bias MSC paracrine activity and... [https://pubmed.ncbi.nlm.nih.gov/37422008/]
- 10. The exosome journey: from biogenesis to uptake and intracellular... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-021-00730-1]
- 11. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? | Cell Death & Disease [https://www.nature.com/articles/s41419-022-05034-x]
- 12. : machinery, regulation, and therapeutic... Exosome biogenesis [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01671-0]
- 13. Current knowledge on exosome and release - PMC biogenesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC5756260/]
- 14. Mesenchymal stem cell derived-exosomes: a modern approach in translational medicine | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02622-3]
- 15. Regulation of cargo selection in exosome biogenesis and its... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11059157/]
- 16. Regulation of cargo selection in exosome and its... biogenesis [https://www.nature.com/articles/s12276-024-01209-y?error=cookies_not_supported&code=99ef3af4-cece-4256-b86f-878de064bccb]
- 17. Therapeutic potential of mesenchymal stem cell-derived exosomes for regenerative medicine applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10907468/]
- 18. Mesenchymal stem cell-derived exosomes: A paradigm shift in clinical therapeutics - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0014482725002125]
- 19. Stem Exosomes : Differences & Utility ( vs ) Cells 2025 [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 20. Extracellular vesicles : a rising star for therapeutics and drug delivery [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-023-01973-5]
- 21. Targeted delivery of extracellular vesicles: the mechanisms, techniques and therapeutic applications | Molecular Biomedicine [https://link.springer.com/article/10.1186/s43556-024-00230-x]
- 22. Frontiers | Extracellular vesicles as vital players in drug delivery: a focus on clinical disease treatment [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1600227/full]
- 23. Mesenchymal stem cell -derived exosomes as cell -free therapeutics... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04747-y]
- 24. Frontiers | Optimizing therapeutic : preconditioning... outcomes [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 25. potential of extracellular Therapeutic for treating human... vesicles [https://www.oaepublish.com/articles/evcna.2025.07]
- 26. "Mesenchymal stem cell- derived ( exosomes - MSC ) in..." exosomes [https://pubmed.ncbi.nlm.nih.gov/40499318/]
- 27. The Functions and Application of MSCs- Derived Exosomes [https://www.linkedin.com/pulse/functions-application-mscs-derived-exosomes-jack-huang-md-phd-e0t0e]
- 28. for Immunomodulation and Regeneration - PMC Tissue Repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC10219918/]
- 29. Advanced Tissue Techniques Repair [https://www.numberanalytics.com/blog/advanced-tissue-repair-techniques]
- 30. Engineering Exosomes for CNS Disorders: Advances, Challenges, and Therapeutic Potential - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989722/]
- 31. Frontiers | Strategies for delivering drugs across the blood-brain barrier for the treatment of neurodegenerative diseases [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 32. Clinical applications of stem cell-derived exosomes | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-023-01704-0]
- 33. Therapeutic Features and Updated Clinical Trials of Mesenchymal Stem Cell (MSC)-Derived Exosomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7916919/]
- 34. Produced from 3D Cultures of Exosomes by MSCs ... Tangential Flow [https://pubmed.ncbi.nlm.nih.gov/30341012/]
- 35. analysis of Comparative and... tangential flow filtration [https://pmc.ncbi.nlm.nih.gov/articles/PMC9486818/]
- 36. Pairing Tangential and Size Exclusion... Flow Filtration [https://www.izon.com/news/pairing-tangential-flow-filtration-and-size-exclusion-chromatography]
- 37. : A Guide to EVs Research Exosome Isolation [https://www.rocker.com.tw/en/application/exosome-isolation/]
- 38. Frontiers | Trends in mesenchymal stem cell- derived extracellular... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 39. Therapeutic Potential of Mesenchymal Stem Cells and Their Products... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7915745/]
- 40. Frontiers | Efficacy and safety of nebulized vs.... inhalation [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1654973/full]
- 41. [Clinical efficacy and safety of intravenous colistin sulfate...] [https://pubmed.ncbi.nlm.nih.gov/41146504/]
- 42. Stem cell derived exosome trilogy: an epic comparison of human... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 43. Mesenchymal stem cell- derived as a potential therapeutic... exosomes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04511-2]
- 44. Frontiers | Exosome -based modulation of ferroptosis in neurological... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1677808/full]
- 45. Rapid amyloid-β clearance and cognitive recovery through multivalent... [https://www.nature.com/articles/s41392-025-02426-1?error=cookies_not_supported&code=e283f8a0-36f7-4b83-b945-41400dec70ae]
- 46. Insights into Exosome Transport through the Blood–Brain Barrier and the Potential Therapeutical Applications in Brain Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10144189/]
- 47. Mesenchymal Stem Cells Cross the Blood Brain Barrier (BBB) [https://www.dvcstem.com/post/msc-bbb]
- 48. International Journal of Molecular Medicine [https://www.spandidos-publications.com/10.3892/ijmm.2025.5484]
- 49. Frontiers | Global clinical trials on stem cell for autoimmune... therapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 50. Review of mesenchymal stem cell-derived exosomes and their potential therapeutic roles in treating rheumatoid arthritis - PubMed [https://pubmed.ncbi.nlm.nih.gov/39948229/]
- 51. Mesenchymal stem cells derived exosomes: a new era in cardiac regeneration | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04123-2]
- 52. Mesenchymal Stem Cell-Derived Exosomes in Ophthalmology: A Comprehensive Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10142951/]
- 53. MSC-Derived Exosomes in Preserving Autophagy through Key Signaling Pathways: A Preventive Strategy against Cardiovascular Aging | Cell Biochemistry and Biophysics [https://link.springer.com/article/10.1007/s12013-025-01913-0]
- 54. Frontiers | Current state of heart failure treatment: are mesenchymal... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1518036/full]
- 55. of bone marrow stem Comparison and cells - cell ... derived exosomes [https://www.hippokratia.gr/comparison-of-bone-marrow-stem-cells-and-cell-derived-exosomes-on-oleic-acidinduced-lung-injury-in-rats/]
- 56. Advancements in engineered mesenchymal stem cell exosomes for chronic lung disease treatment - PubMed [https://pubmed.ncbi.nlm.nih.gov/38071321/]
- 57. Mesenchymal stem cell-derived exosomes in various respiratory diseases | JIR [https://www.dovepress.com/mesenchymal-stem-extracellular-vesicles-in-various-respiratory-disease-peer-reviewed-fulltext-article-JIR]
- 58. Mesenchymal Stem Cell - Derived in Ophthalmology... Exosomes [https://pubmed.ncbi.nlm.nih.gov/37111652/]
- 59. Mesenchymal stem cells in treating human diseases: molecular mechanisms and clinical studies | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02313-9]
- 60. Mesenchymal Stem Cell and Its Clinical... | IntechOpen Therapy [https://www.intechopen.com/online-first/1228919]
- 61. The Therapeutic Potential of Exosomes from Mesenchymal Stem... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11477223/]
- 62. Mesenchymal Stem Cells for Regenerative Therapy : Optimization of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3912818/]
- 63. Functional improvements correlate with enhanced quality of life following mesenchymal stromal cell therapy in chronic spinal cord injury | Scientific Reports [https://www.nature.com/articles/s41598-025-23142-4]
- 64. New therapeutic approaches of mesenchymal stem cells-derived... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-021-00736-4]
- 65. Exosomes: from basic research to clinical diagnostic and therapeutic applications in cancer | Cellular Oncology [https://link.springer.com/article/10.1007/s13402-024-00990-2]
- 66. Exosome IV Therapy 2025: Safety, Cost, Benefits - HealthE1 Mobile Medical [https://healthe1medical.com/exosome-iv-therapy-2025/]
- 67. Analysis of the measurements used as potency tests for the 31 US FDA-approved cell therapy products | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06253-4]
- 68. Accelerating Biologic and Biosimilar Drug Development: Ready-to-Use... [https://www.bioprocessintl.com/assays/accelerating-biologic-and-biosimilar-drug-development-ready-to-use-cell-based-assays-for-potency-and-lot-release-testing]
- 69. Exosome Source Matters: A Comprehensive Review from the Perspective of Diverse Cellular Origins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858990/]
- 70. -specific phenotypic variation in hiPSC cardiomyocyte-derived... Donor [https://pubmed.ncbi.nlm.nih.gov/33416449/]
- 71. Evolving Role of Exosomes in Plastic and Reconstructive Surgery and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11326466/]
- 72. An Innovative Method for Exosome Quantification and Size Measurement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354536/]
- 73. Reassessment of Exosome Composition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6664447/]
- 74. Preclinical assessments of safety and tumorigenicity of very high doses of allogeneic human umbilical cord mesenchymal stem cells | In Vitro Cellular & Developmental Biology - Animal [https://link.springer.com/article/10.1007/s11626-024-00852-z]
- 75. Frontiers | Comparison of efficacy of exosomes from human... derived [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1560915/full]
- 76. : a review of biologic function, diagnostic and targeted... Exosomes [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-01055-0]
- 77. Immunological Safety Evaluation of Exosomes Derived From Human Umbilical Cord Mesenchymal Stem Cells in Mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049250/]
- 78. Scalable production of anti-inflammatory exosomes from three-dimensional cultures of canine adipose-derived mesenchymal stem cells: production, stability, bioactivity, and safety assessment | BMC Veterinary Research | Full Text [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-025-04517-1]
- 79. Frontiers | Mesenchymal and stem in ischemic brain... cells exosomes [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1639756/full]
- 80. Clinical applications of stem -derived cell exosomes [https://pubmed.ncbi.nlm.nih.gov/38212307/]
- 81. Mesenchymal stem cell exosome therapy: current research status in the treatment of neurodegenerative diseases and the possibility of reversing normal brain aging | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04160-5]
- 82. Mesenchymal stem cell‐ derived : Shaping the next era of... exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10811806/]
- 83. Mesenchymal stem cell-based therapy for ischemic stroke [https://cnjournal.biomedcentral.com/articles/10.1186/s41016-016-0053-4]
- 84. In vivo Monitoring and Assessment of Exogenous Mesenchymal Stem Cell-Derived Exosomes in Mice with Ischemic Stroke by Molecular Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7680167/]
- 85. Imaging for Prediction of Functional Outcome and Assessment of Recovery in Ischemic Stroke - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3981064/]
- 86. Magnetic Resonance Imaging in Acute Ischemic Stroke - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9399663/]
- 87. Stem cell-based therapies for ischemic stroke: a systematic review and meta-analysis of clinical trials | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01762-z]
- 88. Safety and Efficacy of Stem Cell Therapy in Ischemic Stroke: A Comprehensive Systematic Review and Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943215/]
- 89. Rethinking miRNAs in MSC -sEV therapeutics: implications for... [https://www.oaepublish.com/articles/evcna.2025.55]
- 90. Stem Cell-Based Therapy and Cell-Free Therapy as an Alternative Approach for Cardiac Regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10635745/]
- 91. Cell-free therapy: a neuroregenerative approach to sensory neuropathy? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6524517/]
- 92. and Their Exosomes Strategies in the Cutaneous... Bioengineering [https://www.ijbs.com/v19p1430.htm]
- 93. Exosome Processing and Characterization Approaches for Research and Technology Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9130923/]
- 94. Engineering Exosomes for Therapeutic Applications: Decoding Biogenesis, Content Modification, and Cargo Loading Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11268655/]
- 95. Amniotic- Derived in Clinical Practice: Safety and... Exosomes [https://www.fortunejournals.com/articles/amnioticderived-exosomes-in-clinical-practice-safety-and-outcomes-in-608-patients.html]
- 96. Frontiers | Exosomes : the future of acellular nanotherapeutics in... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1607605/full]
- 97. Clinical Applications of Exosomes: A Critical Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11277529/]
- 98. Exosome-mediated delivery of CRISPR/Cas9 for targeting of oncogenic KrasG12D in pancreatic cancer | Life Science Alliance [https://www.life-science-alliance.org/content/4/9/e202000875]
- 99. Mesenchymal stromal cells - exosomes : a promising cell -free... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6933895/]
- 100. Mesenchymal stromal cell therapy: Progress to date and future outlook - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1525001625000930]
- 101. A Brief Overview of Global Trends in MSC-Based Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8958818/]