Optimizing iPSC-Cardiomyocyte Differentiation: Protocols, Challenges, and Clinical Applications
This article provides a comprehensive analysis of current protocols for differentiating human induced pluripotent stem cells (iPSCs) into cardiomyocytes (iPSC-CMs).
Optimizing iPSC-Cardiomyocyte Differentiation: Protocols, Challenges, and Clinical Applications
Abstract
This article provides a comprehensive analysis of current protocols for differentiating human induced pluripotent stem cells (iPSCs) into cardiomyocytes (iPSC-CMs). It explores foundational biological principles, compares methodological approaches including 2D monolayer and 3D suspension systems, addresses critical troubleshooting and optimization strategies for improving yield and maturity, and examines validation techniques for functional assessment. Targeting researchers, scientists, and drug development professionals, the content synthesizes recent advances in protocol standardization, cost-reduction strategies, and clinical translation requirements, offering practical guidance for implementing robust cardiac differentiation workflows.
Understanding Cardiac Differentiation: From Developmental Biology to Protocol Design
The Wnt/β-catenin pathway, an evolutionarily conserved signaling cascade, serves as a fundamental regulatory mechanism governing cardiac specification and development. This pathway plays an indispensable role in the intricate process of differentiating induced pluripotent stem cells (iPSCs) into cardiomyocytes, a capability that has revolutionized cardiovascular research and drug development. The dynamic and temporally precise manipulation of Wnt/β-catenin signaling has become the cornerstone of modern protocols for generating human iPSC-derived cardiomyocytes (hiPSC-CMs), enabling researchers to create clinically relevant models for studying heart development, disease mechanisms, and potential regenerative therapies [1] [2]. This application note delineates the core signaling mechanisms and provides detailed methodologies for exploiting this pathway to enhance cardiac differentiation efficiency, reproducibility, and maturation, framed within the context of advancing iPSC-derived cardiomyocytes research.
Core Signaling Mechanism
The canonical Wnt/β-catenin pathway is a finely tuned signaling cascade that dictates cell fate through the regulation of β-catenin stability and nuclear translocation. In the absence of Wnt ligands, a cytoplasmic destruction complex—comprising Axin, Adenomatous Polyposis Coli (APC), Casein Kinase 1α (CK1α), and Glycogen Synthase Kinase 3β (GSK-3β)—orchestrates the phosphorylation of β-catenin, marking it for ubiquitination and proteasomal degradation. This process maintains low cytoplasmic β-catenin levels, preventing nuclear translocation and the activation of target genes.
Upon binding of Wnt ligands to their Frizzled (FZD) receptors and Low-Density Lipoprotein Receptor-Related Protein 5/6 (LRP5/6) co-receptors, the signal is transduced intracellularly via Dishevelled (DVL). This activation leads to the inhibition of the destruction complex, allowing β-catenin to accumulate in the cytoplasm and subsequently translocate to the nucleus. Within the nucleus, β-catenin partners with T-cell factor/lymphoid enhancer-binding factor (TCF/LEF) transcription factors to activate the expression of downstream target genes crucial for cell proliferation, differentiation, and survival [3] [4].
The following diagram illustrates the core components and state transitions of the Wnt/β-catenin signaling pathway:
Diagram 1: The core mechanism of the Wnt/β-catenin signaling pathway, showing both OFF and ON states.
In the context of cardiac development, Wnt/β-catenin signaling exhibits stage-specific effects. During early embryogenesis, it is required for the formation of mesodermal precursors. However, for these precursors to commit to a cardiac lineage, Wnt/β-catenin signaling must be repressed, allowing for the specification of cardiogenic mesoderm and the formation of the first and second heart fields. Subsequently, reactivation of the pathway promotes the expansion of multipotent Isl1+ cardiovascular progenitors and drives the proliferation of early ventricular myocytes in the compact myocardium [4]. Finally, for terminal differentiation to occur, Wnt/β-catenin signaling must again be downregulated. This precise temporal control is ingeniously replicated in vitro to direct iPSCs through the stages of cardiac specification.
Application in Cardiac Differentiation Protocols
The GiWi Protocol: A Standardized Approach
The most widely adopted method for differentiating iPSCs into cardiomyocytes is the GiWi protocol, which leverages sequential pharmacological manipulation of the Wnt/β-catenin pathway. This protocol involves an initial activation of Wnt signaling using a GSK-3β inhibitor (such as CHIR99021, termed "Gi") to specify mesodermal fate, followed by its inhibition (using compounds like IWP2 or IWR-1, termed "Wi") to promote cardiac mesoderm formation and cardiomyocyte differentiation [5] [2]. The robustness of this strategy stems from its recapitulation of the endogenous signaling dynamics observed during embryonic heart development.
The following diagram outlines the key stages and critical timing of this standard workflow:
Diagram 2: The core workflow of the GiWi cardiac differentiation protocol.
Advanced Protocol Optimization
Recent advancements have focused on improving the efficiency, purity, and scalability of the GiWi protocol. Key optimizations include:
- Metabolic Substrate Regulation: Emerging evidence indicates that the effect of Wnt/β-catenin signaling on downstream targets like Connexin 43 (Cx43) is modulated by the primary metabolic substrate. Cx43 downregulation occurs primarily in glucose-rich media, mimicking the metabolic state of heart failure, but not in lipid-rich media, which resembles healthy adult hearts [6]. This finding is critical for modeling disease-specific phenotypes.
- Progenitor Cell Reseeding: Detaching and reseeding cardiac progenitor cells (specifically EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitors) at a lower density during differentiation has been shown to improve cardiomyocyte purity by an absolute 10-20% without negatively impacting contractility, sarcomere structure, or the expression of junctional proteins like Cx43 [5].
- Suspension Culture System: Transitioning from traditional monolayer cultures to stirred suspension bioreactors ad-dresses issues of scalability and reproducibility. This system allows for better control of the microenvironment (pH, O₂, nutrients), yields high-purity cardiomyocytes (~94% TNNT2+), and results in cells that exhibit more mature functional properties and higher viability after cryopreservation (>90%) [2].
Key Research Reagent Solutions
The successful implementation of cardiac differentiation protocols relies on a suite of critical reagents. The table below details essential materials, their specific functions, and relevant application notes.
Table 1: Essential Research Reagents for Cardiac Differentiation via the Wnt/β-catenin Pathway
| Reagent Category | Example | Function in Protocol | Application Notes |
|---|---|---|---|
| Wnt Pathway Activator | CHIR99021 (GSK-3β inhibitor) | Activates β-catenin signaling to induce mesoderm specification from hiPSCs. | Concentration & duration are critical; typically 6-7 μM for 24-48 hours [5] [2]. |
| Wnt Pathway Inhibitor | IWP2/IWR-1 (Porcupine inhibitor) | Inhibits Wnt ligand secretion to suppress signaling, promoting cardiac progenitor formation. | Added 24-48 hours after CHIR99021 washout [2]. |
| Base Culture Medium | RPMI 1640 | Serves as the basal medium for the differentiation process. | Often supplemented with B-27 (with or without insulin) [1] [7]. |
| Pluripotency Maintenance Medium | Essential 8 (E8) / StemFit AK03 | Chemically defined media for the routine culture of hiPSCs prior to differentiation. | Quality of pre-culture medium impacts differentiation efficiency [7]. |
| Extracellular Matrix | Matrigel / iMatrix-511 / Laminin-521 | Coats culture surfaces to support hiPSC attachment, survival, and self-renewal. | Recombinant proteins like iMatrix-511 offer a more defined alternative to Matrigel [7]. |
| Cell Survival Supplement | Y-27632 (ROCK inhibitor) | Enhances single-cell survival after passaging or thawing by inhibiting apoptosis. | Typically used for 24 hours post-passage or post-thaw [1]. |
Quantitative Data and Protocol Outcomes
Robust differentiation protocols yield predictable and quantifiable outcomes. The following table summarizes key performance metrics from optimized studies, providing benchmarks for researchers.
Table 2: Quantitative Outcomes of Optimized Cardiac Differentiation Protocols
| Protocol Parameter | Monolayer Differentiation (Standard GiWi) | Optimized Suspension Bioreactor | Notes and Context |
|---|---|---|---|
| Cardiomyocyte Purity (% TNNT2+) | 70 - 90% (high variability) [5] | ~94% (high consistency) [2] | Purity can be increased by progenitor reseeding [5]. |
| Yield (Cells per mL of culture) | Lower, scales linearly with surface area [2] | ~1.2 million cells/mL [2] | Bioreactor systems offer superior scalability. |
| Onset of Beating | Differentiation Day 7-8 [2] | Differentiation Day 5 [2] | Earlier beating suggests potentially faster maturation. |
| Post-Cryopreservation Viability | Often lower; functional properties can be impacted [2] | >90% [2] | High viability is crucial for experimental planning and biobanking. |
| Primary Metabolic Substrate Effect | Wnt activation reduces Cx43 in glucose-rich media, but not lipid-rich media [6] | Data specifically comparing substrates in suspension is limited. | Critical for modeling arrhythmogenic disease states. |
| Inter-Batch Variability | Moderate to High [2] | Low [2] | Suspension systems in bioreactors enhance reproducibility. |
Detailed Experimental Protocol
Optimized Suspension Culture Cardiac Differentiation
This protocol is adapted from recent studies demonstrating high efficiency and reproducibility across multiple hiPSC lines [2].
Initial Preparation and hiPSC Quality Control:
- Starting Material: Use a quality-controlled master cell bank of hiPSCs. Confirm pluripotency marker expression (e.g., >70% SSEA4+ via FACS) and normal karyotype.
- Critical Step: The success of differentiation is highly dependent on the quality and maintenance of hiPSCs. Use low-passage cells and maintain them in a pluripotent state in defined media like E8 on recombinant vitronectin or Matrigel.
Differentiation in Stirred Suspension Bioreactor:
- Formation of Embryoid Bodies (EBs): Dissociate hiPSCs to single cells and seed them into a stirred bioreactor system (e.g., a 250 mL vessel) containing an appropriate volume of pre-warmed medium (e.g., E8 supplemented with 10 µM Y-27632). Set the stir speed to maintain a homogeneous suspension without subjecting the cells to excessive shear stress.
- Mesoderm Specification (Wnt Activation): After approximately 24 hours, monitor EB size. When the average EB diameter reaches 100 µm, add CHIR99021 to a final concentration of 7 µM. Continue stirring for 24 hours.
- Wnt Inhibition and Cardiac Specification: At the end of the 24-hour CHIR99021 incubation (Differentiation Day 1), perform a complete medium exchange to remove the compound. Allow the cells to incubate for 24 hours without Wnt modulators. On Differentiation Day 3, add the Wnt inhibitor IWR-1 to a final concentration of 5 µM for 48 hours.
- Cardiomyocyte Maturation: After 48 hours of IWR-1 treatment (Differentiation Day 5), perform another medium exchange to remove the inhibitor and transition to a maintenance medium, such as RPMI 1640 supplemented with B-27. Continue feeding the cells every 2-3 days. Spontaneous contractions are typically observed from day 5 onwards.
Harvesting and Cryopreservation:
- Cardiomyocytes can be harvested between days 12-15 for experimentation or cryopreserved. Use a gentle dissociation enzyme. For cryopreservation, use controlled-rate freezing and store in liquid nitrogen. Thaw cells rapidly and plate in the presence of a ROCK inhibitor to maximize viability and recovery.
Progenitor Reseeding to Enhance Purity
This supplementary technique can be integrated into standard monolayer or suspension protocols to significantly increase cardiomyocyte purity [5].
- Differentiate hiPSCs according to your standard GiWi protocol.
- On approximately day 5-7, identify and isolate the ISL1+/NKX2-5+ cardiac progenitor cell population.
- Gently detach the progenitor cells and reseed them at a lower density. A reseeding ratio of 1:2.5 to 1:5 (initial surface area to reseeded surface area) has been shown to be effective.
- Continue the differentiation protocol. This physical separation and reduction in density have been demonstrated to improve terminal CM purity by an absolute 10-20%.
The Wnt/β-catenin pathway is not merely a participant but a central conductor of cardiac specification, whose precise temporal manipulation enables the robust generation of hiPSC-derived cardiomyocytes. The standardized GiWi protocol, augmented by recent optimizations in metabolic control, progenitor cell handling, and suspension culture technology, provides researchers with a powerful and reproducible toolkit. These advances are pivotal for enhancing the translational value of hiPSC-CMs in disease modeling, drug screening, and the future development of regenerative therapies, pushing the boundaries of cardiovascular research.
The differentiation of induced pluripotent stem cells (iPSCs) into functional cardiomyocytes represents a cornerstone of modern cardiovascular research, disease modeling, and regenerative medicine. This process meticulously recapitulates key stages of embryonic heart development, transitioning through well-defined pluripotent, mesodermal, cardiac progenitor, and functionally mature states [8]. The ability to generate human iPSC-derived cardiomyocytes (iPSC-CMs) provides an unparalleled opportunity to replace lost cardiomyocytes via cellular therapy, in addition to their promise for drug discovery and disease modeling applications [5]. Since the earliest protocols were developed, significant advancements have been made in understanding the signaling pathways and culture conditions that guide this differentiation efficiently. However, challenges remain in achieving consistent high purity and full functional maturity, driving continued optimization of differentiation protocols [9] [5]. This application note provides a detailed roadmap of the developmental stages, supported by structured data, experimental protocols, and visual guides to empower researchers in this critical field.
The Roadmap of Cardiac Differentiation
The journey from a pluripotent stem cell to a contracting cardiomyocyte is driven by the sequential activation and inhibition of key signaling pathways, primarily the canonical Wnt/β-catenin pathway [8]. The process can be conceptually divided into two major transcriptional waves: an initial wave driven by factors like c-Myc and Klf4, followed by a second wave governed by Oct4, Sox2, and Klf4, which establishes stable pluripotency or commits cells to a new fate [10].
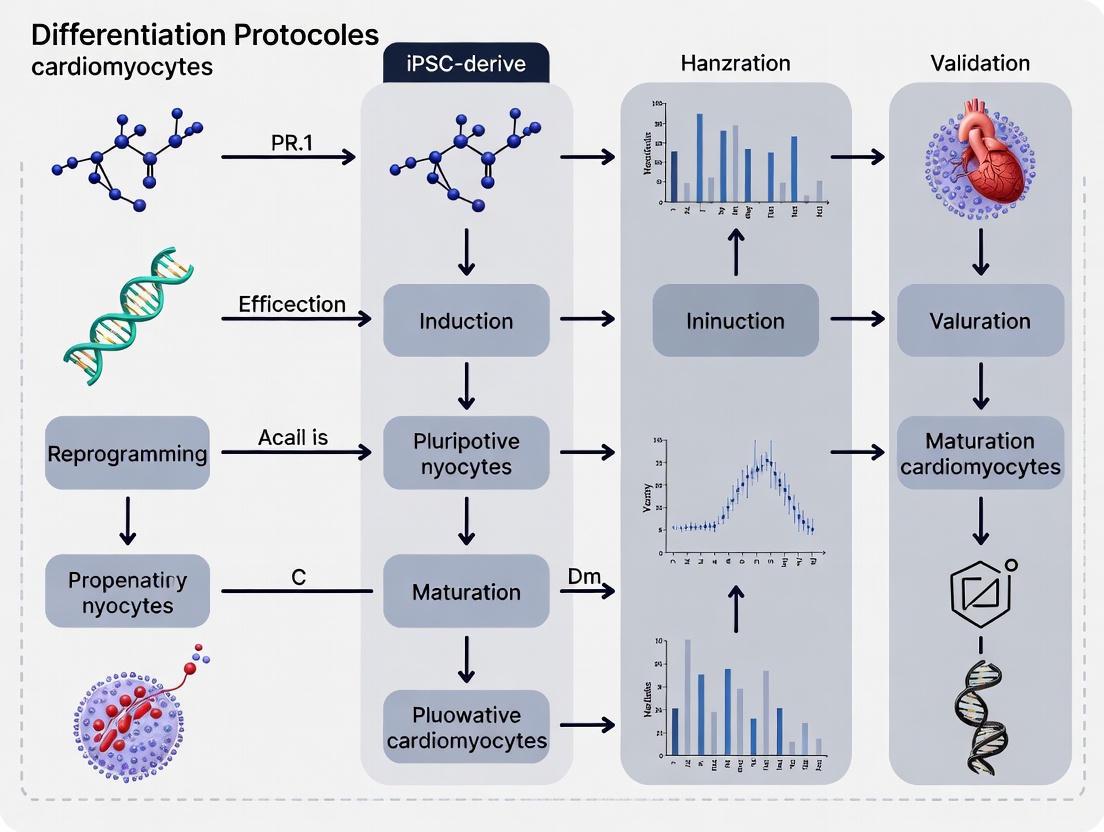
The diagram below illustrates the core signaling pathway and morphological stages involved in directing iPSCs towards a cardiac fate.
Figure 1: Core Signaling Pathway and Morphological Stages in Cardiac Differentiation. This workflow outlines the key developmental transitions and the central role of biphasic Wnt modulation in guiding iPSCs to functional cardiomyocytes.
Quantitative Data on Differentiation Markers and Efficiencies
Tracking the expression of stage-specific markers is crucial for monitoring differentiation progression and assessing protocol efficiency. The following tables summarize key quantitative data on marker expression and the impact of recent protocol optimizations.
Table 1: Expression of Key Markers During Cardiac Differentiation from iPSCs
| Developmental Stage | Key Markers | Expression Notes | Reference |
|---|---|---|---|
| Pluripotency | Oct4, Sox2, Nanog, c-Myc, Klf4, Lin28 | Significantly higher expression of Oct4 and c-Myc in iPSCs vs. bone-marrow MSCs. [11] | |
| Mesoderm | EOMES, MESP1, T (Brachyury) | Induced by Wnt activation (e.g., CHIR99021). Cryopreservation at this stage is possible. [5] | |
| Cardiac Progenitor | ISL1, NKX2-5, KDR, PDGFRα | ISL1+ progenitors are multipotent. Cryopreservation viable with high cell recovery. [5] [8] | |
| Early Cardiomyocyte | Cardiac Troponin T (cTnT), MYL2 (MLC2v), MYL7 (MLC2a) | Baseline purity can be highly variable (30-70% cTnT+). [5] | |
| Mature Cardiomyocyte | Atrial Natriuretic Peptide (ANP), Pro-B-type Natriuretic Peptide (proBNP), Connexin 43 (Cx43) | ANP and BNP indicate hormonal function. Junctional Cx43 is critical for electromechanical coupling. [7] [8] |
Table 2: Impact of Protocol Optimization on Differentiation Efficiency
| Optimization Strategy | Key Parameter Changed | Reported Outcome | Reference |
|---|---|---|---|
| Progenitor Reseeding | Detaching and reseeding ISL1+/NKX2-5+ CPCs at lower density (1:2.5 ratio) | ↑ CM purity by 10-20% (absolute) without negatively affecting CM number, contractility, or sarcomere structure. [5] | |
| Pre-culture Medium | Using a medium similar to E8 medium prior to differentiation induction | Achieved high cTnT positivity (up to 91%) and promoted cardiac tissue formation with high ANP expression. [7] | |
| Cryopreservation of Progenitors | Freezing EOMES+ mesoderm or ISL1+/NKX2-5+ CPCs for later differentiation | High cell recovery (70-90%) and retained differentiation capacity, enabling on-demand CM production. [5] |
Experimental Protocols
GiWi Protocol for Directed Cardiomyocyte Differentiation
This is a widely used, small molecule-based protocol that relies on biphasic modulation of the Wnt signaling pathway [5] [8].
Key Materials:
- Cell Line: Human iPSCs (e.g., WTC11 line).
- Basal Medium: RPMI 1640.
- Small Molecules: CHIR99021 (GSK3 inhibitor, Wnt activator), IWP2 (Wnt inhibitor).
- Supplements: B-27 Supplement (with and without insulin).
Detailed Procedure:
- Mesoderm Induction (Day 0): When iPSCs reach ~80-90% confluency, initiate differentiation by replacing the maintenance medium with RPMI 1640 + B-27 Supplement (minus insulin) supplemented with CHIR99021. The optimal concentration (typically 6-12 µM) must be determined for each cell line [5] [8].
- Wnt Inhibition (Day 3): After 72 hours, replace the medium with RPMI 1640 + B-27 Supplement (minus insulin) supplemented with IWP2 (e.g., 5 µM).
- Metabolic Selection (Day 5): On day 5, change the medium to RPMI 1640 + B-27 Supplement (with insulin). This medium supports the survival of cardiomyocytes over non-myocyte cells.
- Maintenance and Maturation (Day 7 onwards): Continue feeding the cells every 2-3 days with RPMI 1640 + B-27 Supplement (with insulin). Spontaneous contractions are typically observed between days 8 and 10.
Protocol Enhancement: Progenitor Reseeding
To improve cardiomyocyte purity and reduce batch-to-batch variability, integrate the following reseeding step into the GiWi protocol [5].
Key Materials:
- Enzymatic Dissociation Reagent: TrypLE Select Enzyme.
- ROCK Inhibitor: Y-27632.
- Coating Matrix: Defined matrices like fibronectin, vitronectin, or laminin-111.
Detailed Procedure:
- Progenitor Harvest (Day 5): On day 5 of the standard GiWi protocol, corresponding to the ISL1+/NKX2-5+ cardiac progenitor stage, wash the cells with D-PBS(-) and dissociate them using TrypLE Select Enzyme.
- Reseeding: Count the cells and reseed them at a lower density onto a fresh plate pre-coated with an appropriate ECM. A reseeding ratio of 1:2.5 (initial surface area to reseeded surface area) is optimal, significantly improving purity without reducing total cardiomyocyte yield [5].
- Recovery: Include Y-27632 (10 µM) in the medium for the first 24 hours post-reseeding to enhance cell survival.
- Continued Differentiation: After 24 hours, resume the standard differentiation protocol from the metabolic selection step.
The following diagram contrasts the standard protocol with the enhanced reseeding method.
Figure 2: Workflow Comparison: Standard vs. Enhanced Differentiation Protocol. The enhanced protocol incorporates a critical reseeding step at the cardiac progenitor stage to significantly increase the purity of the resulting cardiomyocyte population.
The Scientist's Toolkit: Essential Research Reagents
A successful differentiation experiment relies on a suite of high-quality, well-characterized reagents. The following table details essential materials and their functions.
Table 3: Key Research Reagent Solutions for iPSC-CM Differentiation
| Reagent Category | Specific Examples | Function in Protocol | Notes |
|---|---|---|---|
| Small Molecule Inducers | CHIR99021, CHIR 99021 | Glycogen synthase kinase-3 (GSK3) inhibitor. Activates Wnt signaling to induce mesoderm formation. [5] [8] | Concentration is cell line-specific and critical for efficiency. |
| Small Molecule Inhibitors | IWP2, IWP-2 | Porcupine inhibitor. Suppresses Wnt signaling to drive cardiac progenitor specification. [5] [8] | Used after mesoderm induction. |
| Cell Culture Media | StemFit AK03/AK03N, Essential 8 Medium, RPMI 1640 | Maintenance of pluripotency (StemFit, E8) and as a basal medium for differentiation (RPMI). [7] | Pre-culture medium composition can impact final differentiation efficiency. [7] |
| Supplements | B-27 Supplement (With/Without Insulin) | Provides hormones, growth factors, and antioxidants. The "minus insulin" formulation is used for metabolic selection of CMs. [5] [8] | Critical for cell survival and lineage selection. |
| Extracellular Matrices | iMatrix-511 (Laminin-511), Laminin-521, Fibronectin, Vitronectin | Coats culture surfaces to support iPSC attachment, survival, and organization. [5] [8] | Reseeding allows transition to defined matrices like fibronectin. [5] |
| Dissociation Reagents | TrypLE Select Enzyme | Enzymatically dissociates cell colonies into single cells for passaging or reseeding. | Gentler on cells than traditional trypsin. |
| Detection Antibodies | Anti-cardiac Troponin T (cTnT), Anti-ANP, Anti-NKX2-5, Anti-ISL1 | Immunocytochemistry or flow cytometry analysis to identify and quantify specific cell types and assess purity at different stages. [7] [5] | Essential for quality control and protocol validation. |
Within the broader scope of optimizing differentiation protocols for iPSC-derived cardiomyocytes research, the precise tracking of differentiation efficiency and lineage commitment is paramount. The successful generation of cardiomyocytes for disease modeling, drug development, and regenerative medicine relies on robust methods to monitor the stepwise progression from pluripotency through mesoderm and cardiac progenitor stages to functional cardiomyocytes. This application note details the key molecular markers and signaling pathways that serve as critical benchmarks for assessing the quality and trajectory of cardiac differentiation, providing researchers with a validated toolkit for protocol evaluation and optimization.
Key Molecular Markers of Cardiac Lineage Commitment
The differentiation of human induced pluripotent stem cells (hiPSCs) into cardiomyocytes recapitulates key stages of embryonic heart development, with each stage defined by a unique transcriptional and proteomic signature. Tracking these markers allows researchers to quantify differentiation efficiency and confirm the successful derivation of the target cell type.
Table 1: Key Molecular Markers for Tracking iPSC-to-Cardiomyocyte Differentiation
| Differentiation Stage | Key Markers | Function & Significance | Expression Dynamics |
|---|---|---|---|
| Pluripotency | OCT4 (POU5F1), NANOG, SOX2 | Core transcription factors maintaining self-renewal and pluripotency [12]. | High in undifferentiated iPSCs; rapidly downregulated upon differentiation initiation [12] [13]. |
| Early Mesoderm / Primitive Streak | T (Brachyury), MIXL1, EOMES | Mesoderm formation and specification; T is a classic marker for nascent mesoderm [12] [13]. | Peak expression around day 2 of differentiation [12]. |
| Cardiac Mesoderm & Progenitors | MESP1, ISL1, GATA4, NKX2-5, TBX5 | Critical transcription factors for cardiac lineage commitment. ISL1 marks cardiac precursors, while NKX2-5 and TBX5 are fundamental for heart field patterning and chamber formation [12] [14]. | Activated after mesoderm formation; highest in cardiac progenitor clusters [12] [14]. |
| Differentiated Cardiomyocytes | TNNT2 (cTnT), MYH6 (α-MHC), MYL7 (MLC2a), TTN | Sarcomeric structural proteins essential for cardiomyocyte contractility [12] [15]. | Significantly increased in mature cardiomyocyte clusters (e.g., from day 10 onward) [12]. |
| Cardiomyocyte Subtypes | MYL2 (MLC2v), TBX5 | MYL2: Marker for ventricular cardiomyocytes [14].TBX5: Lineage tracer for First Heart Field (FHF)-derived left ventricular cardiomyocytes [14]. | Used to confirm subtype specification; one study showed >90% of derived cardiomyocytes were TBX5-lineage positive, indicating a strong FHF/LV bias [14]. |
The transition through these stages can be visualized at single-cell resolution. Single-cell RNA sequencing (scRNA-seq) of differentiating iPSCs has successfully identified distinct cell clusters, including pluripotent stem cells, primitive streak mesoderm, cardiac progenitors, and definitive cardiomyocytes, based on the expression patterns of these markers [12]. Furthermore, proteomic analyses have confirmed that the differentiation process is mediated by extensive proteome reorganization, with proteins involved in DNA replication decreasing as proteins for muscle contraction and metabolism increase [13].
Experimental Protocols for Marker Analysis
Monolayer Cardiac Differentiation Protocol
This is a widely adopted, chemically defined protocol for directed cardiac differentiation.
Key Reagents:
Detailed Procedure:
- Culture hiPSCs: Maintain hiPSCs in a defined medium such as mTeSR Plus or E8 on a substrate like GelTrex until they reach 80-90% confluency [15].
- Initiate Differentiation (Day 0): Replace the medium with RPMI 1640 supplemented with B-27 without insulin. Add CHIR99021 at a final concentration of 6-12 µM for 24 hours to activate Wnt signaling and induce mesendoderm [15] [16].
- Recovery Phase (Day 2): After 24 hours of CHIR99021 treatment, replace the medium with fresh RPMI/B-27 without insulin. Do not add any small molecules. Allow the cells to recover for 48 hours [15].
- Cardiac Specification (Day 3): Add IWR-1 at a final concentration of 5 µM in RPMI/B-27 without insulin to inhibit Wnt signaling and promote cardiac mesoderm and progenitor formation. Incubate for 48 hours [15] [16].
- Maturation (Day 5 onwards): On day 5, replace the medium with RPMI/B-27 without insulin. Change the medium every 2-3 days. Spontaneously beating cells are typically observed between day 7 and day 10 [15] [16].
Flow Cytometry for Quantifying Differentiation Efficiency
Flow cytometry is a standard method for quantifying the percentage of cells expressing specific markers, such as cardiac troponin T (TNNT2), to assess differentiation efficiency and purity [15].
- Procedure:
- Cell Harvest: On the desired day of differentiation (e.g., day 12-15), dissociate the cells into a single-cell suspension using a gentle enzyme like Accutase [15].
- Fixation and Permeabilization: Fix the cells with 4% paraformaldehyde for 15 minutes at room temperature. Permeabilize the cells using ice-cold 90% acetone for 20 minutes on ice or with a commercial permeabilization buffer.
- Antibody Staining: Incubate the cells with a primary antibody against the target intracellular protein (e.g., anti-cardiac Troponin T). Use an isotype-matched antibody as a negative control. After washing, incubate with a fluorescently conjugated secondary antibody if required.
- Analysis: Analyze the stained cells using a flow cytometer. The percentage of TNNT2-positive cells is a direct measure of cardiomyocyte differentiation purity, with efficiencies often exceeding 85-90% using optimized protocols [15].
Single-Cell RNA Sequencing (scRNA-seq) for Lineage Trajectory Analysis
scRNA-seq provides an unbiased, high-resolution view of the heterogeneity within a differentiating cell population and allows for the reconstruction of differentiation trajectories [12].
- Workflow:
- Sample Collection: Collect cells at multiple time points during differentiation (e.g., day 0, 2, 4, 7, 10) [12].
- Single-Cell Isolation and Library Prep: Create a single-cell suspension and use a platform like the 10x Genomics Chromium to barcode and capture individual cell transcripts. Prepare sequencing libraries according to the manufacturer's protocol.
- Bioinformatic Analysis:
- Quality Control: Filter out low-quality cells, doublets, and cells with high mitochondrial gene content [12].
- Clustering and Visualization: Use tools like Seurat to perform log-normalization, dimensionality reduction (PCA, UMAP/t-SNE), and cluster cells based on transcriptional similarity [12].
- Marker Identification: Identify differentially expressed genes that define each cluster, allowing for the annotation of cell types (e.g., pluripotent, mesoderm, cardiomyocyte) [12].
- Pseudotime Analysis: Utilize algorithms like Monocle to order cells along a hypothetical differentiation timeline, revealing the continuous progression from one state to another and identifying branching points in the lineage commitment [12].
Signaling Pathways Governing Cardiac Commitment
Cardiac differentiation is orchestrated by the precise temporal regulation of key signaling pathways. Understanding this dynamics is crucial for optimizing protocols.
The diagram above illustrates the core biphasic Wnt/β-catenin signaling model, which is fundamental to most contemporary cardiac differentiation protocols [16] [1]. Initial activation of Wnt signaling using a GSK-3β inhibitor like CHIR99021 is essential for driving mesoderm formation. Subsequently, the precise inhibition of Wnt signaling at the cardiac mesoderm stage, using compounds like IWR-1, is critical for the specification of cardiac progenitors and their subsequent differentiation into beating cardiomyocytes [16] [1]. Recent research has identified Beclin1 (Becn1) as a key upstream regulator of this process. Becn1 deficiency was shown to enhance cardiomyocyte yield by eliciting a biphasic Wnt response (early activation followed by later suppression) and sustaining BMP pathway activation, thereby promoting cardiac lineage commitment [16].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Reagents for iPSC-Cardiomyocyte Differentiation Research
| Reagent Category | Specific Example | Function in Protocol |
|---|---|---|
| hiPSC Culture Media | mTeSR Plus, Essential 8 (E8) | Chemically defined, xeno-free media for the maintenance of hiPSCs in a pluripotent state [1]. |
| Basal Differentiation Media | RPMI 1640 | A standard basal medium used during the cardiac induction phase [15] [16]. |
| Differentiation Supplements | B-27 Supplement (Without Insulin) | Provides essential lipids, hormones, and vitamins to support cell survival and cardiac differentiation [15] [16]. |
| Wnt Pathway Modulators | CHIR99021 (Activator)IWR-1 (Inhibitor) | Small molecules used to precisely control the biphasic Wnt signaling pathway for directed differentiation [16]. |
| Extracellular Matrix | GelTrex, Matrigel | A basement membrane matrix used to coat culture vessels, providing a substrate for hiPSC attachment and growth [15] [1]. |
| Cell Dissociation Agents | Accutase, EDTA | Enzymatic (Accutase) or non-enzymatic (EDTA) reagents used for passaging hiPSCs or harvesting differentiated cells [15] [1]. |
| Lineage Tracing Tools | TBX5/MYL2 Reporter Lines | Genetically engineered hiPSC lines that allow for the identification and isolation of specific cardiomyocyte subtypes (e.g., FHF-derived left ventricular cells) [14]. |
The systematic application of molecular marker tracking, through both established protein-based techniques and cutting-edge transcriptomic and proteomic analyses, provides an indispensable framework for advancing iPSC-derived cardiomyocyte research. By integrating the analysis of stage-specific markers with a deep understanding of the underlying signaling dynamics, researchers can reliably assess differentiation efficiency, understand lineage commitment, and consistently generate high-quality cardiomyocytes for therapeutic and drug development applications. The tools and protocols outlined here serve as a foundation for ongoing efforts to enhance the maturity, purity, and functional fidelity of hiPSC-derived cardiomyocytes.
The successful differentiation of human induced pluripotent stem cells into cardiomyocytes (hiPSC-CMs) represents a landmark achievement in cardiovascular research, yet the functional immaturity of these cells remains a significant limitation for therapeutic applications and drug screening [17] [18]. A defining characteristic of this immaturity is their metabolic profile, which resembles fetal cardiomyocytes rather than adult cells [17] [19]. While adult cardiomyocytes primarily rely on oxidative phosphorylation fueled by fatty acid oxidation to meet their substantial energy demands, hiPSC-CMs depend predominantly on glycolytic metabolism,
similar to early developmental stages [17] [20]. This metabolic immaturity directly impacts contractile function, calcium handling, and electrophysiological properties, limiting the utility of hiPSC-CMs in modeling adult cardiac diseases and predicting drug responses [21] [18].
The metabolic transition from glycolysis to oxidative phosphorylation is not merely a consequence of maturation but may actually drive the maturation process itself [19]. During perinatal development, cardiomyocytes undergo a significant metabolic switch triggered by changes in oxygen tension, nutrient availability, and hormonal signaling [19]. Recapitulating this switch in vitro is therefore crucial for generating hiPSC-CMs with adult-like phenotypes. This Application Note outlines the fundamental principles of cardiac metabolic maturation and provides detailed protocols to enhance this process in hiPSC-CMs, with the goal of supporting more physiologically relevant research models in drug development and disease modeling.
Biological Fundamentals of the Cardiac Metabolic Switch
Metabolic Transitions During Cardiac Development
The developing heart exhibits remarkable metabolic plasticity, adapting to changing nutrient availability and energy demands throughout gestation and into postnatal life. Fetal cardiomyocytes primarily utilize glucose and lactate as energy sources through glycolysis, even in the presence of oxygen - a phenomenon similar to the Warburg effect observed in cancer cells [17]. This glycolytic dominance supports both ATP production and anabolic processes required for rapid cellular proliferation during development [19].
The postnatal period marks a critical window for metabolic maturation. As oxygen availability increases and nutritional sources shift, cardiomyocytes undergo a profound metabolic reprogramming characterized by:
- A shift from glycolysis to fatty acid oxidation as the primary ATP source [17]
- Mitochondrial biogenesis and structural maturation [20] [19]
- Enhanced oxidative capacity through increased cristae density and electron transport chain complexity [19] [22]
This transition is quantitatively summarized in Table 1, which compares the metabolic profiles of cardiomyocytes at different developmental stages.
Table 1: Metabolic Properties of Cardiomyocytes at Different Developmental Stages
| Metabolic Parameter | Fetal Cardiomyocytes | hiPSC-CMs (Immature) | Adult Cardiomyocytes |
|---|---|---|---|
| Primary ATP Source | Glycolysis (≈80%) [17] | Glycolysis/Lactate Oxidation [17] | Fatty Acid Oxidation (≈70%) [17] |
| Mitochondrial Morphology | Small, round, peripheral [19] | Small, fragmented, perinuclear [19] [22] | Large, elongated, intermyofibrillar [19] |
| Mitochondrial Dynamics | Fission-dominated [17] | Fission-dominated [20] | Fusion-dominated [17] [20] |
| Sarcomere Organization | Poorly organized [18] | Disorganized, random orientation [21] [18] | Highly organized, aligned [21] [18] |
| Oxidative Capacity | Low [19] | Intermediate [22] | High [19] [22] |
Molecular Regulation of Metabolic Maturation
The metabolic switch is orchestrated by sophisticated molecular sensing systems that detect changes in nutrient availability and energy status [19]. Key regulators include:
- PGC-1α: A master regulator of mitochondrial biogenesis that is upregulated after birth, driving the expression of nuclear and mitochondrial genes encoding oxidative phosphorylation components [20] [22].
- AMPK: Activated under low-energy conditions, AMPK promotes catabolic pathways and mitochondrial biogenesis while inhibiting anabolic processes [19].
- mTOR: Integrates signals from growth factors, nutrients, and energy status to coordinate cell growth with metabolic activity [19].
- HIF-1α: Stabilized under hypoxic conditions, HIF-1α promotes glycolytic metabolism and is downregulated after birth with increased oxygen availability [19].
These sensors converge on mitochondrial dynamics, regulating the balance between fission (mediated by Drp1) and fusion (mediated by Mfn1/2 and Opa1) [20]. The postnatal period is characterized by a shift toward mitochondrial fusion, forming the interconnected networks characteristic of adult cardiomyocytes [17] [20]. Additionally, mitophagy (selective mitochondrial autophagy) and mitochondrial biogenesis work in concert to ensure a healthy, functional mitochondrial population capable of meeting the high energy demands of the mature heart [17].
Figure 1: Molecular Regulation of Cardiomyocyte Metabolic Switch. The transition from fetal to adult metabolic phenotypes is triggered by postnatal environmental changes and mediated by key regulators including HIF-1α and PGC-1α.
Experimental Strategies for Enhancing Metabolic Maturation
Integrated Metabolic Maturation Protocol
Recent research demonstrates that a combinatorial approach integrating multiple maturation stimuli yields the most significant improvements in hiPSC-CM metabolic maturity [21]. The protocol outlined below systematically combines metabolic, structural, and electrophysiological conditioning to promote adult-like characteristics.
Protocol: Comprehensive Metabolic Maturation of hiPSC-CMs
Time Commitment: 4-6 weeks post-cardiac differentiation Key Materials:
- hiPSC-derived cardiomyocytes (≥90% purity)
- Metabolic Maturation Medium (see Table 2)
- Nanopatterned culture surfaces
- Electrostimulation system (e.g., C-Pace EP Culture Pacer)
Procedure:
Cardiomyocyte Differentiation and Plating
- Differentiate hiPSCs into cardiomyocytes using your preferred method (e.g., small molecule-directed differentiation)
- At day 15-20 post-differentiation, dissociate cardiomyocytes and plate at appropriate density (50,000-100,000 cells/cm²) onto nanopatterned surfaces
Metabolic Conditioning
- Replace standard maintenance medium with Metabolic Maturation Medium (detailed in Table 2)
- Supplement with 100-200 µM palmitate conjugated to BSA (1:5-1:7 molar ratio)
- Add 1-2 nM triiodothyronine (T3) and 10-20 nM dexamethasone
- Culture for 4-6 weeks with medium changes every 2-3 days
Structural Conditioning via Nanopatterning
- Use culture surfaces with parallel ridge-groove patterns (800-1200 nm width, 200-400 nm depth)
- Align cardiomyocytes according to manufacturer's instructions
- Maintain patterned culture throughout the maturation period
Electrophysiological Conditioning
- Beginning 3-5 days after metabolic medium initiation, apply electrical field stimulation
- Use rectangular pulses (2 ms duration, 5-7 V/cm amplitude)
- Gradually increase stimulation frequency from 0.5 Hz to 2 Hz over 7-10 days
- Maintain at 2 Hz for the remainder of the maturation period
Quality Control and Validation
- Assess metabolic maturation via oxygen consumption rate (Seahorse XF Analyzer)
- Evaluate structural maturation via immunostaining for sarcomeric proteins (α-actinin, cTnI)
- Confirm electrophysiological maturation via patch clamp analysis
Table 2: Metabolic Maturation Medium Composition
| Component | Concentration | Function | Rationale |
|---|---|---|---|
| Basal Medium | RPMI 1640 or DMEM without glucose | Base formulation | Eliminates reliance on glycolytic metabolism |
| Fatty Acids | 100-200 µM palmitate conjugated to BSA | Primary oxidative substrate | Promotes mitochondrial fatty acid oxidation capacity |
| L-Carnitine | 1-2 mM | Fatty acid transport | Facilitates fatty acid import into mitochondria |
| Triiodothyronine (T3) | 1-2 nM | Thyroid hormone | Enhances mitochondrial biogenesis and oxidative metabolism |
| Dexamethasone | 10-20 nM | Glucocorticoid | Promotes metabolic maturation and ion channel expression |
| Insulin | 10-20 µg/L | Growth factor | Regulates glucose and lipid metabolism |
| Albumin | 1-2 mg/mL | Fatty acid carrier | Facilitates lipid delivery and prevents detergent effects |
| Glucose | 1-2 mM | Minimal energy source | Prevents complete glucose deprivation while encouraging oxidative metabolism |
Essential Research Reagent Solutions
Table 3: Key Research Reagents for hiPSC-CM Metabolic Maturation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Metabolic Substrates | Palmitate, oleate, linoleate conjugated to BSA | Induce fatty acid oxidation | Use 100-200 µM in 1:5-7 fatty acid:BSA ratio; test different fatty acid profiles |
| Hormonal Supplements | Triiodothyronine (T3), dexamethasone, insulin | Activate nuclear receptors to drive metabolic maturation | T3 (1-2 nM), dexamethasone (10-20 nM), insulin (10-20 µg/L) |
| Metabolic Modulators | Etomoxir (optional), AMPK activators (AICAR) | Fine-tune metabolic pathways | Use etomoxir with caution (≤5 µM) to partially inhibit CPT1 without complete blockade |
| Structural Engineering | Nanopatterned surfaces (800-1200 nm grooves) | Promote sarcomere alignment and structural maturity | Commercial options available; optimal alignment with 800 nm patterns |
| Electrostimulation Systems | C-Pace EP Culture Pacer, custom setups | Mimic physiological electrical activity | 2 Hz frequency, 2 ms duration, 5-7 V/cm amplitude for 4+ weeks |
| Maturation Media | Commercial maturation media, custom formulations | Provide optimized substrate and hormone combinations | Consider glucose-free or low-glucose formulations with fatty acid supplementation |
Validation and Analytical Methods for Metabolic Maturation
Functional Metabolic Assessment
Comprehensive validation of hiPSC-CM metabolic maturation requires multiple complementary approaches:
Mitochondrial Function Analysis:
- Seahorse XF Cell Mito Stress Test: Measure basal respiration, ATP-linked respiration, proton leak, and maximal respiratory capacity [21] [22]
- Fatty Acid Oxidation Assays: Use ¹⁴C-labeled or ¹³C-labeled fatty acids to quantitatively assess oxidation rates [22]
- Glycolytic Rate Assay: Determine glycolytic versus oxidative ATP production rates [22]
Structural and Molecular Validation:
- Transmission Electron Microscopy: Evaluate mitochondrial ultrastructure, cristae density, and spatial organization [17] [19]
- Immunofluorescence Microscopy: Assess sarcomere organization (α-actinin), T-tubule formation (BIN1, caveolin-3), and mitochondrial networks (TOM20) [21] [18]
- Gene Expression Analysis: Quantify maturation markers (MYH7, TNNI3), metabolic enzymes (CPT1B, PDK4), and mitochondrial biogenesis regulators (PGC-1α, TFAM) [21]
Electrophysiological Assessment:
- Patch Clamp Electrophysiology: Measure action potential parameters, ion current densities, and the presence of mature characteristics like the "notch-and-dome" morphology [21]
- Calcium Transient Imaging: Assess calcium handling properties and sarcoplasmic reticulum function [18]
Expected Outcomes and Benchmarking
Successful metabolic maturation should yield hiPSC-CMs with:
- Increased oxygen consumption rates (2-3 fold increase in basal and maximal respiration) [21] [22]
- Shift in fuel dependence from glucose to fatty acids (50-70% of ATP from fatty acid oxidation) [17] [22]
- Enhanced mitochondrial content and cristae density [19]
- Improved structural organization with aligned sarcomeres and elongated cell morphology [21]
- Adult-like electrophysiological properties including more negative resting membrane potentials (-65 to -75 mV), faster upstroke velocities (>100 V/s), and presence of phase 1 repolarization notch [21]
Figure 2: Integrated Workflow for hiPSC-CM Metabolic Maturation. The combinatorial approach systematically applies metabolic, structural, and electrophysiological conditioning over 4-6 weeks to achieve comprehensive maturation.
Applications in Disease Modeling and Drug Development
Metabolically mature hiPSC-CMs enable more physiologically relevant modeling of cardiac diseases and improved drug screening applications. Metabolic maturation is particularly crucial for modeling conditions like diabetic cardiomyopathy, ischemia-reperfusion injury, and inherited metabolic disorders that directly affect cardiac energy metabolism [17] [18]. Additionally, mature hiPSC-CMs demonstrate adult-like pharmacological responses, reducing false positives and negatives in cardiotoxicity screening [21] [18].
The integration of metabolic maturation protocols into standard hiPSC-CM differentiation workflows represents a critical advancement toward more predictive in vitro models. These approaches will enhance the translational potential of hiPSC-CMs in regenerative medicine, disease modeling, and drug discovery applications, ultimately contributing to improved safety and efficacy in cardiovascular therapeutic development.
Protocol Implementation: 2D, 3D, and Scalable Differentiation Systems
The derivation of cardiomyocytes from human induced pluripotent stem cells (hiPSCs) represents a cornerstone of modern cardiovascular research, offering unprecedented opportunities for disease modeling, drug screening, and regenerative therapies. The efficacy of these applications is fundamentally governed by the choice of differentiation platform—primarily two-dimensional monolayer culture or three-dimensional suspension systems. Within the context of advancing differentiation protocols for iPSC-derived cardiomyocytes research, this application note provides a systematic comparison of these foundational technologies. We present quantitative data on their performance characteristics, detailed experimental methodologies for implementation, and a structured analysis of their respective advantages and limitations to guide protocol selection for specific research objectives.
Comparative Performance Analysis
The selection between monolayer and suspension culture systems necessitates a careful evaluation of performance metrics aligned with research goals. Table 1 summarizes key quantitative and qualitative parameters from recent studies to inform this decision-making process.
Table 1: Quantitative Comparison of Monolayer vs. Suspension Culture for hiPSC-CM Differentiation
| Performance Parameter | Monolayer Culture | Suspension Culture (Stirred Systems) | Citations |
|---|---|---|---|
| Scalability & Yield | Limited by surface area; linear scaling. | High; ~1.2 - 1.5 million cells/mL; scalable to liter volumes. | [2] [23] |
| Cardiomyocyte Purity | Variable; can be high but significant inter-batch variability. | High and consistent; ~94% - >98% TNNT2+ cells. | [2] [23] |
| Inter-Batch Variability | Higher due to local heterogeneity in cell seeding and environment. | Lower; improved reproducibility across lines and batches. | [2] |
| Cell Maturity Phenotype | Fetal-like; less mature functional properties. | Enhanced structural and functional maturity; earlier contraction onset (dd5). | [2] [24] |
| Ventricular Subtype Purity | Mixed cardiac subtypes. | Predominantly ventricular identity (~83% MLC2v+). | [2] |
| Post-Cryopreservation Viability | Reported negative impact on function (contraction, electrophysiology). | High viability (>90%) after cryo-recovery. | [2] |
| Process Control & Monitoring | Simple but static; suboptimal nutrient/pH distribution. | Controlled monitoring/adjustment of O₂, CO₂, pH, temperature. | [2] |
| Relative Cost & Accessibility | Low equipment cost; accessible to all labs. | Higher initial investment in bioreactor equipment. | [25] |
Detailed Experimental Protocols
Protocol A: Suspension Culture Differentiation in Stirred Systems
This protocol, adapted from recent high-efficiency studies, describes the differentiation of hiPSCs into cardiomyocytes in a stirred suspension bioreactor system [2] [23].
Key Reagent Solutions:
- Small Molecule Inhibitors: CHIR99021 (GSK-3 inhibitor, Wnt activator), IWR-1 (Wnt inhibitor).
- Basal Media: RPMI 1640.
- Supplements: B-27 Supplement (with and without insulin).
Step-by-Step Workflow:
- hiPSC Expansion & Quality Control: Expand hiPSCs in suspension as aggregates in an appropriate medium (e.g., TeSR-E8 3D). Use quality-controlled master cell banks and confirm pluripotency (e.g., >70% SSEA4+ by flow cytometry) prior to differentiation [2] [26].
- Aggregate Formation & Mesoderm Induction (Day 0):
- Form embryoid bodies (EBs) in a stirred bioreactor or spinner flask.
- Monitor EB diameter. Initiate differentiation by adding CHIR99021 (e.g., 7 µM) in RPMI/B-27 without insulin when the majority of EBs reach ~100 µm [2].
- Critical Timing: Adding CHIR to EBs that are too small (<100 µm) or too large (>300 µm) reduces differentiation efficiency.
- Wnt Inhibition & Cardiac Specification (Days 1-5):
- At 24 hours (Day 1), replace medium with fresh RPMI/B-27 without insulin.
- At 72 hours (Day 3), add the Wnt inhibitor IWR-1 (e.g., 5 µM) to the culture.
- On Day 5, perform a full medium change to RPMI/B-27 without insulin.
- Metabolic Selection & Maturation (Days 7-12+):
- On Day 7, switch to RPMI 1640 supplemented with B-27 with insulin (RPMI/B-27+).
- On Day 9, implement metabolic selection by replacing the medium with glucose-free RPMI 1640 supplemented with B-27 with insulin and 4 mM lactate for 48-72 hours. This selectively eliminates non-cardiomyocytes [23].
- Return to RPMI/B-27+ maintenance medium. Spontaneous contractions are typically observed from Day 5 onwards [2].
Protocol B: Monolayer Differentiation
This standard protocol is provided for comparative purposes and is typically performed in multi-well plates or culture flasks.
Key Reagent Solutions:
- Coating Matrix: Matrigel or Geltrex.
- Small Molecule Inhibitors: CHIR99021, IWR-1.
- Basal Media & Supplements: As in Protocol A.
Step-by-Step Workflow:
- hiPSC Culture & Seeding:
- Maintain hiPSCs on a matrix-coated surface in a pluripotency medium until high confluence.
- Critical Parameter: Achieving a uniform and optimal cell density at the start of differentiation is crucial and a major source of variability [2].
- Mesoderm Induction (Day 0): Add CHIR99021 (typically at a higher concentration or longer duration than in suspension, e.g., 6-12 µM for 24-48 hours) in RPMI/B-27 without insulin [2] [27].
- Wnt Inhibition & Cardiac Specification (Days 2-5):
- At 24-48 hours after CHIR addition, replace the medium with fresh RPMI/B-27 without insulin.
- At 72 hours (Day 3), add IWR-1 (e.g., 5 µM) in RPMI/B-27 without insulin.
- On Day 5, replace the medium with fresh RPMI/B-27 without insulin.
- Metabolic Selection & Maturation (Days 7-12+):
- On Day 7, switch to RPMI/B-27+ medium.
- Metabolic selection with lactate-containing media can be applied from approximately Day 10-14 to enrich for cardiomyocytes.
- Spontaneous contractions typically begin around Day 7-8 [2].
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Research Reagent Solutions for hiPSC-CM Differentiation
| Reagent/Material | Function in Protocol | Examples & Notes |
|---|---|---|
| CHIR99021 | GSK-3 inhibitor; activates Wnt signaling to initiate mesoderm formation. | Critical for both monolayer and suspension; concentration and timing vary between systems [2] [23]. |
| IWR-1 | Tankyrase inhibitor; suppresses Wnt signaling to promote cardiac specification. | Used after CHIR; part of the standard GiWi protocol [23]. |
| B-27 Supplement | Serum-free supplement providing hormones, lipids, and trace elements. | Essential for cardiomyocyte survival and maturation; "without insulin" is used during differentiation, "with insulin" for maintenance [23]. |
| RPMI 1640 Medium | Basal, defined medium for cardiac differentiation and maintenance. | Provides a consistent, undefined environment [23]. |
| Lactate | Metabolic selection agent. | Cardiomyocytes metabolize lactate, while undifferentiated cells rely on glycolysis and die in lactate-only media [23]. |
| Y-27632 (ROCKi) | ROCK inhibitor; enhances cell survival after passaging or thawing. | Often added during the first 24 hours after seeding cells for differentiation [28]. |
| Vertical-Wheel Bioreactor | Low-shear suspension culture vessel. | Enables high-fold expansion of hiPSCs prior to differentiation [26]. |
| Spinner Flasks / Bioreactors | Suspension culture vessels for scalable differentiation. | A more economical and scalable alternative to large bioreactors [2]. |
Signaling Pathways and Workflow
The following diagram illustrates the core Wnt signaling manipulation strategy (GiWi method) common to both monolayer and suspension protocols, highlighting key divergences in the process workflow.
The choice between monolayer and suspension culture systems is not a matter of superior versus inferior, but rather context-dependent suitability. Monolayer differentiation remains a robust, accessible, and powerful method for foundational research, high-content imaging, and experiments where lower cell numbers are sufficient. In contrast, suspension culture in stirred systems presents a compelling platform for applications demanding high scalability, superior reproducibility, and enhanced cardiomyocyte maturity, such as drug discovery, toxicology screening, and clinical translation. Researchers must weigh the quantitative advantages of suspension culture against the practical simplicity of monolayer systems, aligning their choice with the specific goals and constraints of their research program in iPSC-derived cardiomyocytes.
The directed differentiation of human induced pluripotent stem cells (hiPSCs) into cardiomyocytes represents a cornerstone of modern cardiovascular research, disease modeling, and drug development. Among the various strategies developed, temporal modulation of the Wnt/β-catenin signaling pathway using small molecules has emerged as a predominant method due to its high efficiency, reproducibility, and applicability across multiple cell lines [2] [29]. This approach, commonly known as the GiWi protocol, involves sequential application of a glycogen synthase kinase-3 (GSK3) inhibitor—typically CHIR99021 (CHIR)—followed by Wnt pathway inhibitors such as IWP2 or IWR-1 [30] [29]. The philosophical foundation of this strategy rests upon recapitulating developmental cardiac ontogeny, where Wnt signaling exhibits a biphasic role: early activation promotes mesoderm formation, while subsequent inhibition drives cardiac specification [31] [29]. This application note provides a comprehensive technical resource detailing protocol implementations, signaling mechanisms, and practical considerations for optimizing cardiomyocyte differentiation using CHIR99021 and Wnt inhibitors.
Scientific Foundation: Signaling Pathways and Molecular Mechanisms
The Biphasic Wnt Signaling Model in Cardiac Differentiation
The mechanistic basis of GiWi differentiation centers on precise temporal control of canonical Wnt signaling. During early differentiation, GSK3 inhibition by CHIR99021 leads to β-catenin stabilization and nuclear translocation, where it forms complexes with T-cell factor (TCF) transcription factors to activate mesodermal gene programs [31] [32]. The subsequent inhibition of Wnt secretion using small molecules like IWP2 prevents endogenous Wnt ligands from sustaining signaling, thereby allowing for cardiac specification from the newly formed mesoderm [30] [29]. Research demonstrates that this biphasic modulation not only directs lineage specification but also influences the maturation state of the resulting cardiomyocytes [33]. The timing of Wnt activation and inhibition critically affects the expression of genes important for structural, metabolic, and functional maturation, with specific protocols generating cardiomyocytes with more adult-like properties [33].
Key Signaling Modulators and Their Cellular Targets
Table 1: Core Small Molecules in GiWi Cardiac Differentiation
| Small Molecule | Primary Target | Functional Role | Typical Working Concentration |
|---|---|---|---|
| CHIR99021 | GSK3α/GSK3β | Activates Wnt/β-catenin signaling; induces mesendoderm | 2-12 µM [30] [31] [33] |
| IWP2 | Porcupine (PORCN) | Inhibits Wnt ligand secretion; promotes cardiac specification | 2-5 µM [30] [33] |
| IWR-1-endo | Tankyrase (TNKS) | Stabilizes AXIN; promotes β-catenin degradation | 5 µM [2] [33] |
| XAV939 | Tankyrase (TNKS) | Inhibits Wnt/β-catenin signaling via AXIN stabilization | 5 µM [33] |
The molecular interplay between GSK3 inhibition and downstream effectors extends beyond lineage specification to critically influence cell fate decisions between proliferation and maturation. Recent investigations reveal that CHIR99021-mediated Wnt activation, particularly when combined with insulin/PI3K-AKT signaling, promotes robust proliferation of immature hiPSC-cardiomyocytes by modulating TCF and FOXO transcription factors [32]. Conversely, withdrawal of these pathway activators rapidly induces cell-cycle exit and facilitates structural and metabolic maturation, characterized by increased organization of sarcomeres and mitochondria, and a shift toward adult myosin heavy chain isoform expression (MYH7) [32]. This molecular understanding enables researchers to strategically manipulate culture conditions to either expand cardiomyocyte populations or direct them toward more mature phenotypes suitable for specific applications.
Experimental Protocols and Workflows
Core Monolayer Differentiation Protocol
The following protocol, adapted from established methodologies [30] [29], provides a robust foundation for GiWi-based cardiac differentiation in monolayer cultures:
hPSC Culture and Quality Control: Maintain hPSCs in defined culture medium such as mTeSR1 or E8 on Matrigel-coated or Synthemax plates. Prior to differentiation, ensure cells exhibit uniform undifferentiated morphology and express pluripotency markers (OCT4 >95% by flow cytometry) [29]. Passage cells using enzyme-free methods (e.g., Versene) and seed onto matrix-coated plates at a density sufficient to achieve 80-90% confluency at the time of differentiation initiation [30] [29].
Differentiation Initiation (Day 0): Replace maintenance medium with cardio differentiation medium (e.g., RPMI 1640 supplemented with human recombinant albumin and L-ascorbic acid 2-phosphate). Add CHIR99021 at a concentration optimized for the specific cell line (commonly 4-8 µM) [30] [33]. Incubate for 24-48 hours to induce mesendoderm formation.
Wnt Pathway Inhibition (Day 2 or 3): Without medium change, add the Wnt inhibitor IWP2 (typically 2-5 µM) or IWR-1 (5 µM) directly to the culture. Alternatively, replace medium with fresh cardio differentiation medium containing the Wnt inhibitor. Incubate for 48 hours [30] [2].
Cardiac Specification and Maturation (Day 5 onward): Replace medium with cardio culture medium (e.g., RPMI 1640 supplemented with B27 supplement). Continue culture, changing medium every 2-3 days. Spontaneously contracting cells typically appear between days 8-12 [30] [29].
Cardiomyocyte Analysis and Maintenance: At day 15-20, cardiomyocytes can be dissociated using collagenase B and trypsin/EDTA for replating or analysis. For long-term culture and maturation, maintain cells in RPMI/B27 medium for up to 90 days [30].
Diagram 1: Core workflow for monolayer GiWi cardiac differentiation.
Advanced Suspension Culture Protocol
For large-scale production, recent advancements have adapted the GiWi principle to stirred suspension systems, offering improved scalability, reproducibility, and functional maturity [2]:
hPSC Expansion and EB Formation: Dissociate high-quality hPSCs (SSEA4+ >70%) to single cells and transfer to low-attachment plates or bioreactors in medium containing Rho-kinase inhibitor (Y-27632). Allow embryoid body (EB) formation for 24 hours with agitation [2].
Mesoderm Induction: When EB diameter reaches approximately 100 µm (typically at 24 hours), add CHIR99021 (7 µM) to the suspension culture. Incubate for 24 hours with continuous agitation [2].
Cardiac Specification: After a 24-hour gap without small molecules, add IWR-1 (5 µM) to the culture for 48 hours. Subsequently, transition to RPMI 1640 supplemented with B27 for cardiomyocyte maturation with continuous agitation [2].
Harvesting and Cryopreservation: Monitor EB contraction starting around differentiation day 5. At day 15-20, harvest bioreactor-derived cardiomyocytes (bCMs) using enzymatic digestion. Cryopreserve with controlled freeze/thaw protocols, achieving >90% viability post-recovery [2].
Critical Parameters for Protocol Optimization
Quantitative Comparison of GiWi Protocol Variations
Table 2: Key Variable Parameters and Their Impact on Differentiation Outcomes
| Parameter | Impact on Differentiation | Optimization Guidance | Reported Outcome Range |
|---|---|---|---|
| CHIR99021 Concentration | Lineage specificity; Cytotoxicity [31] | Cell line-specific titration (4-12 µM); Higher density cultures often require lower concentrations [31] | 2-12 µM [30] [31] [2] |
| Cell Seeding Density/Confluency | Differentiation efficiency; Cell death [31] | 80-90% confluency for monolayer; EB size of 100 µm for suspension [30] [2] | Monolayer: 80-90% [30]; Suspension: ~100 µm EB diameter [2] |
| CHIR Duration | Mesoderm patterning; Efficiency [33] | 24-48 hours; Longer durations may enhance efficiency but require timing adjustments [30] [2] [33] | 24 hours [2] to 48 hours [30] |
| Wnt Inhibitor Timing | Cardiac specification efficiency; Purity [33] | Start 24-48 hours after CHIR initiation; Critical window for mesoderm to cardiac progenitor transition [2] [33] | Day 1-3 [30] [2] [33] |
| Insulin Timing | Differentiation yield vs. proliferation [32] [29] | Exclude during first 5 days to enhance yield; Include for proliferation of immature CMs [32] [29] | B27 without insulin for first 5 days [29] |
Troubleshooting and Mitigation Strategies
Several critical factors necessitate optimization to achieve consistent, high-yield cardiac differentiation:
Cell Line Variability and Pluripotency Status: Differentiation efficiency strongly correlates with input hiPSC quality. Consistently use hiPSCs with >70% SSEA4 expression and normal karyotype. Establish master cell banks to ensure consistency [2]. Different hPSC lines show substantial variation in cell-cycle profiles, which significantly impacts their response to CHIR99021 and subsequent differentiation efficiency [31].
CHIR99021 Cytotoxicity and Cell Density: H PSCs with higher percentages of cells in the G1 phase of the cell cycle (often associated with high culture density) exhibit increased cell death upon CHIR99021 exposure and require lower doses for cardiac induction [31]. Monitor culture confluency closely before differentiation initiation.
Cell Death Management: Substantial cell loss during the initial stage of differentiation, primarily through ferroptosis, can limit efficiency. The addition of ferrostatin-1 (1 µM), a ferroptosis inhibitor, during the first 48 hours of differentiation increases robustness and cell yield [34].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for GiWi Cardiac Differentiation
| Reagent Category | Specific Products | Function in Protocol |
|---|---|---|
| GSK3 Inhibitors | CHIR99021 (Millipore, Axon Medchem) [30] | Activates Wnt/β-catenin signaling; induces mesendoderm commitment |
| Wnt Secretion Inhibitors | IWP2 (Millipore, Tocris) [30] | Inhibits Porcupine-mediated Wnt ligand secretion; promotes cardiac specification |
| Tankyrase Inhibitors | IWR-1-endo (Cayman), XAV939 (Cayman) [33] | Stabilizes AXIN protein; promotes β-catenin degradation; inhibits Wnt signaling |
| Basal Media | RPMI 1640 with GlutaMAX and HEPES (Thermo Fisher) [30] | Chemically defined base medium for differentiation |
| Supplements | B-27 Supplement minus insulin (Thermo Fisher) [29] | Defined supplement for cardiac differentiation; insulin-free version enhances yield |
| Extracellular Matrices | Matrigel (Corning), Synthemax (Corning), iMatrix-511 [33] [29] [35] | Defined substrates for hPSC attachment and monolayer differentiation |
| Pro-survival Reagents | Y-27632 (ROCK inhibitor), Thiazovivin [30] | Enhances cell survival after passaging and during dissociation |
| Ferroptosis Inhibitors | Ferrostatin-1 [34] | Reduces cell death during initial differentiation stage; increases yield |
Advanced Applications and Future Directions
Expansion of hiPSC-Derived Cardiomyocytes
Beyond directed differentiation, CHIR99021 plays a crucial role in expanding hiPSC-derived cardiomyocyte populations. Combined activation of Wnt/β-catenin via CHIR99021 (3 µM) and insulin/PI3K-AKT signaling promotes robust proliferation of immature cardiomyocytes, achieving proliferation rates of ~38% (Ki67+/cTnT+) compared to 1.5% in unstimulated controls [32]. This expansion capability addresses a critical scalability challenge in producing clinically relevant quantities of human cardiomyocytes. Importantly, recent evidence suggests that Wnt-driven proliferation transcends disease-specific molecular lesions, demonstrating preserved responsiveness in cardiomyocytes derived from patients with inherited cardiomyopathies including Pompe disease (GAA mutations), catecholaminergic polymorphic ventricular tachycardia (RYR2 mutations), and long QT syndrome (KCNQ1 mutations) [36]. This genetic agnosticism enables standardized manufacturing approaches across diverse patient populations.
Cardiac Organoid Generation in Suspension Culture
Minor modifications to the GiWi protocol enable generation of complex 3D cardiac organoids entirely in suspension culture [2]. These bioreactor-derived cardiac organoids (bCOs) primarily consist of cardiomyocytes and model aspects of ventricular wall and chamber formation, providing advanced platforms for studying embryonic heart development, congenital malformations, and injury responses [2]. The suspension culture approach facilitates scaling of organoid production compared to static methods limited to one organoid per well, thereby increasing throughput for screening applications.
Diagram 2: Multifaceted cellular responses to CHIR99021 determined by context.
Stirred Bioreactor Systems for Scalable, High-Yield CM Production
Human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) represent a transformative resource for cardiovascular disease modeling, drug discovery, and regenerative therapies [37]. The transition from laboratory research to industrial and clinical applications necessitates a paradigm shift from traditional 2D culture to scalable, reproducible, and cost-effective manufacturing systems [37] [38]. Stirred-tank bioreactors offer an advanced technological platform that enables three-dimensional (3D) aggregate culture with precise control over critical process parameters, including pH, dissolved oxygen (DO), and temperature [39]. This application note delineates optimized protocols and key engineering parameters for the implementation of stirred bioreactor systems to achieve robust, large-scale production of high-quality hiPSC-CMs.
Bioreactor Protocol for hiPSC Expansion and Cardiac Differentiation
The production of hiPSC-CMs in stirred bioreactors is a biphasic process, beginning with the expansion of high-quality hiPSCs as 3D aggregates, followed by directed cardiac differentiation [37] [39]. The workflow from cell thawing to functional characterization is illustrated below.
Detailed Experimental Methodology
hiPSC Expansion in Stirred Bioreactors
Initial Bioreactor Setup and Inoculation:
- Cell Lines: Utilize quality-controlled hiPSC master cell banks that have been karyotyped and tested for mycoplasma [2]. The pluripotency status should be confirmed (e.g., >70% SSEA4+ via FACS) prior to differentiation [2].
- Bioreactor Systems: The protocol can be implemented across scales using systems such as the DASbox Mini Bioreactor System (100-250 mL working volume) for process development and the BioFlo 320 (1.25-3.75 L working volume) for scaled-up manufacturing [39].
- Culture Medium: Use a defined, xeno-free medium such as Essential 8 (E8) [38]. To enhance aggregate stability and control size, consider media additives optimized via Design of Experiments (DoE), which may include Heparin Sodium Salt (HS), Polyethylene Glycol (PEG), and Poly (vinyl alcohol) (PVA) [38].
- Inoculation and Aggregation: Dissociate hiPSCs to single cells using TrypLE or Accutase and inoculate the bioreactor at a density of approximately 0.5 - 2.0 x 10^6 cells/mL in the presence of a ROCK inhibitor (e.g., 10 µM Y-27632) to enhance cell survival [38] [39].
Process Parameters for Expansion:
- Stirring Speed: Maintain at 40-60 RPM to ensure homogeneous mixing while minimizing shear stress on the aggregates [38]. This can be achieved with a vertical wheel bioreactor system.
- Physicochemical Conditions: Control temperature at 37°C, dissolved oxygen (DO) at 30-50%, and pH between 7.2 and 7.4 [39].
- Monitoring: Sample the culture daily to monitor cell count, viability, and aggregate size distribution. The target aggregate size for initiating differentiation is 100-200 µm in diameter [2] [39]. Aggregates smaller than 100 µm may disintegrate, while those larger than 300 µm exhibit reduced differentiation efficiency due to diffusion limitations [2].
- Endpoint: Expansion typically lasts 3-4 days, achieving a final cell density suitable for differentiation initiation. Over 90% of cells should express pluripotency markers (SOX-2, OCT-3/4, NANOG) at harvest [39].
Cardiac Differentiation Protocol
Directed Differentiation via Wnt Pathway Modulation: This protocol is based on the widely used GiWi method, which involves sequential activation and inhibition of the Wnt/β-catenin signaling pathway [2]. The schematic below details the molecular signaling and cell fate transitions during this process.
Protocol Steps:
- Day 0 (Mesoderm Induction): Add the GSK-3β inhibitor CHIR99021 to the culture medium at a concentration of 7 µM to activate Wnt signaling. The optimal treatment duration is 24 hours [2].
- Day 1-3 (Cardiac Specification): After a 24-hour gap following CHIR99021 removal, add the Wnt inhibitor IWP-1 or IWR-1 at 5 µM for 48 hours to direct cells toward the cardiac lineage [2].
- Day 5-15+ (Cardiac Maturation): Continue culture in a maintenance medium without differentiation factors. Spontaneous contractions are typically observed around day 5 [2]. The cells can be harvested as early as day 10 or maintained for up to 30+ days to promote further maturation, characterized by increased expression of ventricular markers like MYH7 and MLC2v [2].
Quantitative Performance Data
Key Outcomes from Optimized Bioreactor Differentiation
Stirred suspension bioreactor protocols demonstrate significant improvements in yield, purity, and functional maturity of hiPSC-CMs compared to traditional monolayer differentiation.
Table 1: Performance Metrics of Bioreactor-Derived Cardiomyocytes (bCMs)
| Performance Metric | Monolayer Differentiation (mCMs) | Bioreactor Differentiation (bCMs) | Measurement Context |
|---|---|---|---|
| Average Yield | Lower than bCMs [2] | ~1.21 million cells/mL [2] | Across 25 differentiations of 14 hiPSC lines [2] |
| Cardiomyocyte Purity | ~90% (TNNT2+), higher inter-batch variability [2] | ~94% (TNNT2+) [2]; 87.4% ± 5.9% (cTNT+) [39] | Flow cytometry analysis [2] [39] |
| Ventricular Subtype | Information missing | 83.4% (MLC2v+) [2]; 84% ± 5.6% (cTNT+ MLC2v+) [39] | Flow cytometry and immunostaining [2] [39] |
| Cryopreservation Viability | Reported negative impact on function [2] | >90% viability post-thaw [2] | Post-cryorecovery assessment [2] |
| Onset of Contraction/Beating | Differentiation Day 7 [2] | Differentiation Day 5 [2]; Regular beat rate: 2.1 ± 0.14/s [39] | Microscopic observation and MEA analysis [2] [39] |
Critical Bioprocess Parameters and Their Optimization
Successful scale-up requires precise control and monitoring of engineering parameters. The following table summarizes key parameters and their optimized ranges for robust hiPSC-CM production.
Table 2: Critical Process Parameters for Scalable hiPSC-CM Production
| Process Parameter | Optimal Range / Type | Impact on Culture & Rationale |
|---|---|---|
| Aggregate Size at Diff. | 100 - 200 µm [2] | Critical for efficient differentiation. Smaller aggregates (<100µm) are unstable; larger ones (>300µm) have necrotic cores due to diffusion limits [2]. |
| Stirring Speed/Mixing | 40 - 60 RPM [38] | Ensures homogeneity and adequate mass transfer while minimizing shear-induced cell damage and aggregate disruption [38]. |
| Dissolved Oxygen (DO) | 30 - 50% [39] | Controlled via sparging or surface aeration. Oxygen transfer rate (OTR) must balance cellular oxygen uptake rate (OUR) to prevent hypoxia [40]. |
| pH | 7.2 - 7.4 [39] | Tight control is essential for maintaining optimal enzyme activity and cell metabolism throughout the process [39]. |
| Critical Quality Attributes | Pluripotency (>90% OCT4+ pre-diff) [39] | High-quality input cells are essential for successful and consistent cardiac differentiation outcomes [2]. |
| Process Optimization Method | Design of Experiments (DoE) [38] | Systematically evaluates multiple factor interactions (e.g., media additives) to optimize outcomes like growth, pluripotency, and aggregate stability [38]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of a stirred bioreactor process relies on a set of defined reagents, equipment, and methodological tools.
Table 3: Key Research Reagent Solutions for Bioreactor-based hiPSC-CM Production
| Category / Item | Function / Purpose | Example Specifications / Notes |
|---|---|---|
| hiPSC Culture Medium | Supports expansion and maintenance of pluripotency in 3D aggregates. | Defined, xeno-free media (e.g., Essential 8). DoE can be used to optimize additives like PEG for aggregate stability [38]. |
| Small Molecule Inducers | Directs cell fate through targeted signaling pathways. | CHIR99021 (GSK-3β inhibitor for Wnt activation); IWP-2/IWR-1 (Wnt inhibitors for cardiac specification) [2]. |
| Quality Control Antibodies | Characterizes cell populations at various stages via flow cytometry. | Pluripotency: Anti-OCT-3/4, SOX-2, NANOG. Cardiac: Anti-cTNT/TNNT2, MLC2v, α-actinin [39]. |
| Bioreactor Systems | Provides a controlled environment for scalable 3D cell culture. | DASbox (100-250 mL for process development); BioFlo 320 (1.25-3.75 L for production) [39]. |
| Functional Assay Platform | Assesses electrophysiological maturity and drug responses of hiPSC-CMs. | Multi-electrode array (MEA) systems (e.g., Maestro). Metrics: Beat rate, field potential duration (FPD), spike amplitude [39]. |
| Process Optimization Tool | Statistically guided screening of multiple process variables efficiently. | Design of Experiments (DoE) software (e.g., MODDE). Used to model and optimize media compositions and process parameters [38]. |
Stirred-tank bioreactor systems represent a robust and scalable platform for the mass production of functionally mature hiPSC-derived cardiomyocytes. By implementing the protocols and adhering to the critical process parameters outlined in this application note, researchers can achieve high-yield, reproducible differentiations with purities exceeding 90% TNNT2+ cells and yields of approximately 1.2 million cardiomyocytes per mL. The ability to control aggregate size, modulate signaling pathways with small molecules, and employ statistical tools for process optimization is paramount to success. This scalable bioprocess methodology paves the way for the widespread application of hiPSC-CMs in drug discovery, disease modeling, and the advancement of clinical regenerative therapies.
Cost-Effective, Protein-Free Formulations for Enhanced Accessibility
The use of human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) has become indispensable for cardiovascular disease modeling, drug discovery, and safety pharmacology. However, their widespread adoption, especially for clinical translation, has been hampered by the high cost and compositional complexity of traditional differentiation media. These protocols often rely on protein-rich supplements, such as B27 or recombinant human albumin, which introduce significant batch-to-batch variability, increase economic burden, and raise regulatory concerns for therapeutic applications [41] [42]. This application note details the development and implementation of novel, cost-effective, and entirely protein-free media formulations for the cardiac differentiation of hiPSCs. By eliminating xenogeneic components and complex supplements, these protocols enhance process robustness, reduce variability, and significantly improve scalability, thereby enriching the utility of hiPSC-CMs in both research and clinical realms [41] [43].
Research Reagent Solutions: Core Components for Protein-Free Differentiation
The successful implementation of protein-free cardiac differentiation protocols relies on a minimal set of key reagents designed to replace the functions of albumin and other proteins. The table below outlines these essential components and their functions.
Table 1: Essential Reagents for Protein-Free Cardiomyocyte Differentiation
| Reagent Category | Specific Example(s) | Function in the Protocol |
|---|---|---|
| Basal Medium | RPMI 1640 or DMEM/F12 [41] [42] | Serves as the foundation, providing essential salts, vitamins, and energy sources. |
| Antioxidant/Survival Factor | L-ascorbic acid 2-phosphate (AA-2P) [41] [42] | Enhances cell survival and promotes robust differentiation. |
| Shear-Protectant/Albumin Replacement | Pluronic F-68 or specific Polyvinyl Alcohol (PVA) [42] | Protects cells from shear stress in suspension culture, replacing the shear-protectant function of albumin. |
| Small Molecule Inducers | CHIR99021 (CHIR), IWR-1 [2] | Critically modulate Wnt signaling pathway; CHIR activates for mesoderm induction, IWR-1 inhibits for cardiac specification. |
| Xeno-Free Matrix | Recombinant human vitronectin [41] | Provides a defined, animal-free substrate for adherent culture of hPSCs prior to differentiation. |
Quantitative Comparison of Protocol Performance
The adoption of protein-free and minimal-component media formulations has demonstrated performance metrics that are competitive with, and in some cases superior to, traditional protein-based protocols. The following table summarizes key quantitative outcomes from recent studies.
Table 2: Performance Metrics of Cost-Effective Differentiation Protocols
| Protocol Description | Reported Cardiomyocyte Purity | Reported Yield | Scalability | Key Advantages |
|---|---|---|---|---|
| 2-Component Protocol (DMEM/F12 + AA-2P) [41] | >80% | Information Missing | Enhanced scalability in directed differentiations | Minimal components, protein-free, cost-effective, decreased variability. |
| Protein-Free Suspension Culture (RPMI + AA-2P + PF-68/PVA) [42] | 85% to 99% | >1.3 × 10^9 CMs per 2000 mL batch | Successfully scaled to 2000 mL stirred-tank bioreactor | Chemically defined, eliminates albumin, reduces cost, suitable for clinical translation. |
| Stirred Suspension Bioreactor (Small molecules) [2] | ~94% | ~1.21 million cells per mL | Scalable from mL to liter scales | High purity and viability post-cryopreservation, more mature functional properties. |
Experimental Workflow for Protein-Free Cardiac Differentiation
The following diagram illustrates the generalized workflow for the protein-free differentiation of hiPSCs into cardiomyocytes, integrating steps for both adherent and suspension culture formats.
Detailed Methodology: A Two-Component Protein-Free Protocol
This section provides a step-by-step guide for a minimal-component, protein-free differentiation protocol, adapted from established methods [41].
Basic Protocol 1: hPSC Culture in Preparation for Differentiation
Objective: To maintain hPSCs in a proliferative, undifferentiated state using a xeno-free substrate.
Materials:
- Recombinant human vitronectin (VTN-N)
- DMEM/F12 basal medium
- Essential 8 (E8) medium
- 1x phosphate-buffered saline (PBS), without Ca2+/Mg2+
- Y-27632 Rho kinase inhibitor
- Cell Dissociation Buffer (CDB) or similar enzyme-free solution
Procedure:
- Coating Culture Plates: Thaw an aliquot of recombinant human vitronectin overnight at 4°C. Dilute it in cold PBS to the manufacturer's recommended working concentration. Add sufficient volume to cover the culture surface (e.g., 2 mL/well for a 6-well plate). Incubate coated plates for at least 1 hour at room temperature.
- Seeding hPSCs: Prior to seeding, aspirate the vitronectin solution from the plate. Do not allow the coated surface to dry. Wash the plate once with DMEM/F12. Harvest hPSCs as small clumps or single cells using CDB. For single-cell passaging, resuspend the cell pellet in E8 medium supplemented with 10 µM Y-27632. Seed cells at an appropriate density (e.g., ~1.25 x 10^5 cells/cm²) onto the coated plates and place them in a 37°C, 5% CO2 incubator.
- Maintenance: Change the E8 medium daily. Cells should be passaged upon reaching 70-80% confluence, typically every 3-4 days, to prevent spontaneous differentiation and maintain optimal growth.
Basic Protocol 2: hPSC-CM Differentiation via Wnt Modulation
Objective: To efficiently differentiate hPSCs into cardiomyocytes using a two-component, protein-free medium.
Materials:
- DMEM/F12 basal medium
- L-ascorbic acid 2-phosphate (AA-2P)
- CHIR99021 (CHIR)
- IWR-1
Procedure:
- Preparation: Pre-make stock solutions of AA-2P (213 µg/mL in DMEM/F12), CHIR99021 (e.g., 7 µM in DMSO), and IWR-1 (e.g., 5 µM in DMSO). The protein-free differentiation medium is DMEM/F12 supplemented with 213 µg/mL AA-2P.
- Initiation of Differentiation (Day 0): When hPSC cultures reach >90% confluence, aspirate the E8 medium and wash once with DMEM/F12. Add the protein-free differentiation medium (DMEM/F12 + AA-2P) containing the GSK-3β inhibitor and Wnt activator, CHIR99021. The optimal concentration (e.g., 6-8 µM) should be determined for each cell line.
- Wnt Inhibition (Day 3): After 72 hours of CHIR99021 exposure, aspirate the medium. Wash the cells once with DMEM/F12 to remove residual CHIR. Add fresh protein-free differentiation medium (DMEM/F12 + AA-2P) containing the Wnt inhibitor IWR-1. The optimal concentration (e.g., 5 µM) should be determined for each cell line.
- Medium Refresh (Day 5): Aspirate the medium containing IWR-1 and replace it with fresh protein-free differentiation medium (DMEM/F12 + AA-2P) without any small molecules.
- Maturation (Day 7 Onwards): Continue to refresh the protein-free differentiation medium every 2-3 days. Spontaneously contracting cells are typically observed between days 8-10.
Basic Protocol 3: Characterization of hPSC-CMs by Immunofluorescence
Objective: To confirm the successful differentiation and sarcomeric organization of hPSC-CMs.
Materials:
- 4% paraformaldehyde (PFA) in PBS
- Permeabilization/Blocking buffer (e.g., 0.1% Triton X-100, 5% normal serum in PBS)
- Primary antibodies: Anti-cardiac Troponin T (cTnT), Anti-α-Actinin (sarcomeric)
- Secondary antibodies (species-specific, fluorophore-conjugated)
- DAPI (4',6-diamidino-2-phenylindole) for nuclear counterstaining
- Fluorescent mounting medium
Procedure:
- Fixation: Aspirate the culture medium from the differentiated cells and wash gently with PBS. Fix the cells by adding 4% PFA for 15 minutes at room temperature.
- Permeabilization and Blocking: Aspirate the PFA and wash the cells three times with PBS for 5 minutes each. Incubate the cells with permeabilization/blocking buffer for 60 minutes at room temperature to block non-specific antibody binding.
- Primary Antibody Incubation: Prepare the primary antibodies (e.g., anti-cTnT and anti-α-Actinin) in blocking buffer at the manufacturer's recommended dilution. Aspirate the blocking buffer and add the primary antibody solution. Incubate overnight at 4°C.
- Secondary Antibody Incubation: The next day, retrieve the plate and wash three times with PBS for 5 minutes each. Prepare the fluorophore-conjugated secondary antibodies in blocking buffer, protected from light. Add the secondary antibody solution and incubate for 1 hour at room temperature in the dark.
- Counterstaining and Mounting: Wash the cells three times with PBS in the dark. Add a DAPI solution for 5-10 minutes to stain nuclei. Perform a final wash with PBS. Add a drop of fluorescent mounting medium and carefully apply a coverslip.
- Imaging: Image the stained cells using a fluorescent or confocal microscope. Successful differentiation is indicated by a high percentage of cells positive for cTnT and α-actinin, with the latter showing organized cross-striations, characteristic of mature sarcomeres.
Key Signaling Pathways in Cardiac Differentiation
The core biochemical logic driving efficient cardiac differentiation from hPSCs centers on the temporal control of the Wnt/β-catenin signaling pathway, as illustrated below.
Within the broader scope of differentiation protocols for iPSC-derived cardiomyocytes (iPSC-CMs) research, a significant challenge is the batch-to-batch variability and inefficiency of direct differentiation processes. The cryopreservation of intermediate cardiac progenitor cells represents a pivotal strategy to overcome these hurdles, enabling the creation of ready-to-use, fated progenitor banks for on-demand cardiomyocyte production. This Application Note details a validated protocol for the cryopreservation of EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitor cells, demonstrating improved terminal cardiomyocyte purity and facilitating flexible experimental and therapeutic workflows [5]. By standardizing this process, researchers can enhance reproducibility, streamline resource allocation, and accelerate drug discovery and disease modeling applications.
Recent investigations have established that specific progenitor stages during iPSC-CM differentiation are not only amenable to cryopreservation but that their subsequent thawing and reseeding can significantly enhance the final output. The table below summarizes the core quantitative findings from these studies.
Table 1: Key Experimental Outcomes from Cardiac Progenitor Cryopreservation and Reseeding
| Experimental Parameter | Result / Outcome | Significance / Implication |
|---|---|---|
| Improvement in CM Purity | Increase of 10–20% (absolute) in cTnT+ cells post-reseeding [5]. | Dramatically increases the number of differentiations meeting high-purity thresholds (≥70% cTnT+) for downstream applications. |
| CM Number | Maintained relative to control when reseeded at a 1:2.5 ratio (by surface area) [5]. | Enhances purity without sacrificing final cardiomyocyte yield. |
| Progenitor Stage Cryopreservation | EOMES+ mesoderm and ISL1+/NKX2-5+ CPCs are cryopreservable with high recovery [5]. | Enables banking of large, quality-controlled batches of CM-fated progenitors. |
| Terminal CM Properties | No negative impact on contractility, sarcomere structure, multinucleation, or junctional Cx43 expression [5]. | Confirms that the process does not compromise critical cardiomyocyte functionality and structure. |
| Myosin Heavy Chain Expression | Shift toward a more mature phenotype (increase in MYH7 single-positive CMs) [5]. | Suggests that the protocol may encourage a more developmentally advanced cardiomyocyte population. |
| Matrix Flexibility | Reseeding enables transition to defined ECMs (fibronectin, vitronectin, laminin-111) [5]. | Provides protocol flexibility and allows investigation of developmentally relevant extracellular matrices. |
Detailed Experimental Protocols
Protocol 1: Reseeding of Cardiac Progenitors to Enhance CM Purity
This protocol is adapted from studies demonstrating that detaching and reseeding progenitors at a lower density increases the purity of subsequent cardiomyocyte differentiation [5].
Key Materials:
- Cell Lines: Human Pluripotent Stem Cells (e.g., WTC11)
- Differentiation Reagents: CHIR99021 (GSK-3β inhibitor), IWP2 (Wnt inhibitor)
- Dissociation Agent: Accutase or enzyme-free dissociation buffer
- Reseeding Matrix: Matrigel, or defined matrices like fibronectin, vitronectin, or laminin-111
- Basal Media: RPMI 1640
- Supplement: B-27 Supplement (with and without insulin)
Methodology:
- Initiate Differentiation: Differentiate hPSCs toward the mesodermal lineage using a standard GiWi protocol. Activate Wnt signaling with CHIR99021 to specify cardiac mesoderm.
- Identify Progenitor Windows: Target two specific stages for intervention:
- EOMES+ Mesoderm: Typically appears after initial Wnt activation.
- ISL1+/NKX2-5+ Cardiac Progenitors (CPCs): Typically present upon Wnt inhibition (around Day 5 of differentiation).
- Detach Progenitors: At the desired stage, gently dissociate the cells using Accutase or an enzyme-free alternative.
- Reseed at Optimized Density: Centrifuge the cell suspension, resuspend in fresh medium, and reseed the progenitors onto fresh matrix-coated plates. A 1:2.5 to 1:5 reseeding ratio (initial vs. final surface area) has been shown to be optimal [5].
- Continue Differentiation: After reseeding, continue the standard differentiation protocol to terminal cardiomyocytes.
- Assess Outcomes: At terminal differentiation (Day 12-16), analyze CM purity via flow cytometry for cTnT and assess functionality via contractility analysis (e.g., MUSCLEMOTION) and sarcomere structure (immunostaining for ACTN2) [5].
Figure 1: Workflow for progenitor reseeding and cryopreservation. Key intervention points at the EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitor cell (CPC) stages are shown.
Protocol 2: Cryopreservation of Cardiac Progenitor Cells
This protocol enables the long-term storage of cardiac progenitors, forming a master bank for on-demand CM production [5].
Key Materials:
- Cryoprotective Agent (CPA): Standard: 10% DMSO in culture-grade FBS or serum-free freezing medium. Advanced: DMSO-free CPA cocktails (e.g., trehalose, glycerol, isoleucine mixtures) [44].
- Controlled-Rate Freezer (optional but recommended)
- Cryogenic Vials
- Liquid Nitrogen Storage System
Methodology:
- Generate and Identify Progenitors: Differentiate hPSCs to the desired EOMES+ or ISL1+/NKX2-5+ progenitor stage as in Protocol 1.
- Dissociate and Harvest: Gently dissociate the progenitor cultures into a single-cell or small-clump suspension.
- Prepare Freezing Suspension:
- Centrifuge the cell suspension and aspirate the supernatant.
- Resuspend the cell pellet in cold CPA at a pre-optimized concentration (e.g., 1-5 x 10^6 cells/mL).
- For DMSO-free methods, use the optimized osmolyte cocktail [44].
- Aliquot and Freeze:
- Quickly aliquot the cell suspension into cryovials.
- Use a controlled-rate freezer, cooling at approximately -1°C/min to -5°C/min until reaching at least -80°C before transferring to liquid nitrogen [44].
- Alternatively, use an isopropanol freezing chamber at -80°C overnight.
- Thaw and Use:
- Rapidly thaw cryovials in a 37°C water bath.
- Transfer the cell suspension to a tube containing pre-warmed culture medium dropwise to dilute the CPA.
- Centrifuge to remove the CPA and resuspend in fresh differentiation medium.
- Proceed immediately to the reseeding step (Protocol 1, Step 4) to continue differentiation.
Signaling Pathways and Workflow Logic
The differentiation and cryopreservation process hinges on the precise temporal modulation of key developmental signaling pathways. The following diagram illustrates the core signaling logic that guides progenitor fate and the points of cryopreservation intervention.
Figure 2: Signaling pathway modulation for cardiac differentiation. The canonical Wnt pathway is sequentially activated and inhibited to drive cardiac lineage specification from hPSCs. Cryopreservation can be introduced at the mesoderm or cardiac progenitor stages.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these protocols relies on a set of key reagents and materials. The following table details essential components and their functions.
Table 2: Essential Research Reagents for Cardiac Progenitor Cryopreservation
| Reagent / Material | Function / Application | Protocol Context |
|---|---|---|
| CHIR99021 | Small molecule GSK-3β inhibitor; activates Wnt signaling to induce mesoderm formation [5] [2]. | Differentiation Initiation |
| IWP2 | Small molecule Wnt inhibitor; promotes cardiac mesoderm specification to cardiac progenitors [5]. | Differentiation Specification |
| Defined Extracellular Matrices (e.g., Fibronectin, Vitronectin) | Provides a defined, reproducible substrate for cell adhesion and reseeding, supporting progenitor survival and differentiation [5]. | Cell Reseeding |
| DMSO (Dimethyl Sulfoxide) | Standard cryoprotectant; permeates cells to prevent ice crystal formation during freezing [45] [44]. | Conventional Cryopreservation |
| DMSO-Free CPA Cocktails (e.g., Trehalose/Glycerol/Isoleucine) | Mixtures of natural osmolytes that protect cells during freezing without DMSO's potential toxicity, enabling post-thaw recoveries >90% [44]. | Advanced Cryopreservation |
| ROCK Inhibitor (Y-27632) | Enhances survival of dissociated and thawed cells by inhibiting apoptosis [44]. | Post-Thaw Recovery |
| Cardiac Troponin T (cTnT) Antibody | Key marker for identifying and quantifying terminally differentiated cardiomyocytes via flow cytometry or immunostaining [5] [2]. | Outcome Assessment |
Overcoming Variability: Strategies for Enhanced Reproducibility and Maturation
Within cardiomyocyte differentiation research, the therapeutic and experimental promise of induced pluripotent stem cell (iPSC)-derived cardiomyocytes (iCMs) is fundamentally contingent upon the quality of the starting cell population. Robust characterization of input iPSCs and the establishment of rigorously tested Master Cell Banks (MCBs) are critical prerequisites for ensuring reproducible differentiation, reliable experimental data, and successful clinical translation. Inconsistencies in the quality of the starting iPSCs can lead to significant batch-to-batch variability in differentiation efficiency, compromising disease modeling, drug screening, and the development of cell therapies for conditions like myocardial infarction [5] [46]. This application note details the essential quality control (QC) parameters and experimental protocols for characterizing input iPSCs and establishing clinical-grade MCBs, providing a foundational framework for research and development in the field of iPSC-derived cardiomyocytes.
Quality Control for Input iPSC Characterization
Before initiating differentiation protocols, input iPSCs must undergo comprehensive characterization to confirm their identity, purity, and functional potential. The following parameters form the cornerstone of a robust QC strategy.
Core Characterization Assays
The table below summarizes the essential quality control tests for input iPSCs.
Table 1: Essential Quality Control Assays for Input iPSCs
| QC Category | Specific Test | Method(s) | Acceptance Criteria |
|---|---|---|---|
| Pluripotency Assessment | Marker Expression | Immunofluorescence, Flow Cytometry | Positive for OCT4, SOX2, NANOG, SSEA-4, TRA-1-60, TRA-1-81 [47] [48] |
| Alkaline Phosphatase Activity | Enzymatic staining | Positive staining [48] [49] | |
| Differentiation Potential | Trilineage Differentiation (In Vitro) | Directed differentiation to ectoderm, mesoderm, endoderm; qPCR/IF for lineage markers | Expression of markers for all three germ layers (e.g., SOX1, BRA, AFP) [46] [49] |
| Teratoma Formation (In Vivo) | Injection into immunodeficient mice; histology of formed teratomas | Presence of tissues from all three embryonic germ layers [50] [49] | |
| Genetic Integrity | Karyotype Analysis | G-banding | Normal karyotype (46, XX or XY) without major chromosomal abnormalities [46] [48] |
| Genomic Stability | Copy Number Variation (CNV) analysis | No major aberrations detected [50] | |
| Identity and Purity | Short Tandem Repeat (STR) Profiling | PCR | Matches donor material, unique profile [48] [49] |
| Mycoplasma Testing | PCR or culture method | Absence of mycoplasma contamination [46] [48] | |
| Safety | Sterility Testing | Culture method | Sterile [48] |
| Adventitious Virus Testing | PCR, TEM, in vitro inoculation | Absence of detectable viruses [48] |
Detailed Protocol: Trilineage Differentiation and Analysis
This protocol assesses the functional pluripotency of iPSCs by directing their differentiation toward the three germ layers in vitro, followed by analysis via quantitative PCR (qPCR) [46].
Materials:
- StemMACS Trilineage Differentiation Kit (Miltenyi Biotec): Provides optimized media and supplements for directed differentiation.
- iPSCs cultured in feeder-free conditions (e.g., on iMatrix-511).
- Fixation Solution: 4% Paraformaldehyde (PFA) in PBS.
- qPCR Reagents: iTaq Universal SYBR Green Supermix (Bio-Rad), primers for germ layer markers.
Procedure:
- Cell Preparation: Harvest and count iPSCs. Seed the cells onto a suitable extracellular matrix (e.g., iMatrix-511) at a density optimized for differentiation (e.g., 1-2 x 10^4 cells/cm²).
- Directed Differentiation: Follow the manufacturer's instructions for the Trilineage Differentiation Kit. Typically, this involves:
- Ectoderm Induction: Culture cells in ectoderm induction medium for 7 days.
- Mesoderm Induction: Culture cells in mesoderm induction medium for 7 days.
- Endoderm Induction: Culture cells in endoderm induction medium for 7 days.
- RNA Extraction: On day 7, lyse cells from each differentiation lineage and extract total RNA using a commercial kit (e.g., RNeasy Mini Kit, Qiagen).
- cDNA Synthesis: Reverse-transcribe 1 µg of total RNA into cDNA using a cDNA synthesis kit (e.g., iScript cDNA Synthesis Kit, Bio-Rad).
- Quantitative PCR (qPCR):
- Prepare qPCR reactions using SYBR Green Supermix and primers specific for germ layer markers.
- Germ Layer Markers:
- Ectoderm: SOX1, PAX6
- Mesoderm: BRA (Brachyury), TBX6
- Endoderm: SOX17, AFP
- Include a housekeeping gene (e.g., GAPDH) for normalization.
- Run the qPCR program: initial denaturation at 95°C for 3 min; 40 cycles of 95°C for 10 sec and 60°C for 30 sec.
- Data Analysis: Calculate the relative gene expression using the 2^(-ΔΔCt) method. Differentiated cultures should show significant upregulation of germ layer-specific markers compared to undifferentiated iPSCs.
Establishment and Qualification of Master Cell Banks
A Master Cell Bank (MCB) is a collection of cryopreserved cells of uniform composition derived from a single source, intended for use in production. Its establishment under GMP-compliant conditions is critical for clinical applications [51] [52].
MCB Release Criteria
MCBs require an expanded battery of tests to ensure safety, identity, and suitability for manufacturing. The following table outlines typical release criteria.
Table 2: Master Cell Bank (MCB) Release Criteria
| Test Category | Test Item | Method | Release Criteria |
|---|---|---|---|
| Safety | Sterility | Culture Method | No microbial growth [48] |
| Mycoplasma | PCR/Culture Method | Absence of mycoplasma [46] [48] | |
| Adventitious Viruses | In vitro & in vivo assays, TEM | Absence of detectable viruses [48] | |
| Identity | Cell Morphology | Microscopic observation | Characteristic iPSC morphology [48] |
| STR Analysis | PCR | Matches donor and seed stock [48] | |
| Genetic Integrity | Karyotype | G-banding (≥20 metaphases) | Normal female/male karyotype [48] |
| Potency/Purity | Pluripotency Markers | Flow Cytometry | High expression (e.g., >80% positive for SOX2, NANOG, etc.) [48] |
| Viability | Trypan Blue/AOPI Staining | >80% post-thaw viability [48] |
Workflow for MCB Generation
The process of generating a GMP-compliant MCB is a multi-step procedure that integrates rigorous quality control at every stage. The workflow below visualizes this process from donor selection to the qualified MCB.
Diagram 1: MCB Generation and Qualification Workflow
Application in Cardiomyocyte Differentiation
The quality of the input iPSC MCB has a direct and measurable impact on the efficiency and reliability of cardiomyocyte differentiation protocols.
Protocol for Enhanced iCM Purity via Progenitor Reseeding
Recent research demonstrates that protocol adaptations, such as reseeding cardiac progenitors, can significantly improve the purity of the resulting cardiomyocyte populations. The following protocol, adapted from a 2025 study, can increase cardiomyocyte purity by an absolute 10-20% [5].
Materials:
- Cardiac Differentiation Kit: e.g., StemMACS CardioDiff Kit XF (Miltenyi Biotec).
- Extracellular Matrix: iMatrix-511 (Takara) or defined alternatives (Fibronectin, Vitronectin, Laminin-111).
- Cell Dissociation Reagent: Accutase or TrypLE Select.
- Small Molecule Inhibitors: CHIR99021 (GSK-3 inhibitor), IWP2 (Wnt inhibitor).
Procedure:
- Initiate Differentiation: Differentiate iPSCs into cardiomyocytes using a standard small molecule-based protocol (e.g., GiWi protocol) [5].
- Generate Cardiac Progenitors:
- Activate Wnt signaling with CHIR99021 to specify mesoderm.
- Inhibit Wnt signaling with IWP2 to promote cardiac mesoderm and progenitor formation.
- Detach and Reseed Progenitors:
- On day 5 of differentiation, dissociate the cells containing EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitors (CPCs) using a gentle enzyme.
- Reseed the dissociated progenitors at a lower density. A 1:2.5 or 1:5 ratio (initial surface area to reseeded surface area) has been shown to be optimal [5].
- This reseeding step allows for a change to a defined extracellular matrix.
- Continue Differentiation: Continue the differentiation protocol in cardiomyocyte maintenance media until day 10-17.
- Assess Purity: Analyze the resulting cells on day 16-18 via flow cytometry for cardiac Troponin T (cTnT) to confirm increased purity.
Signaling in Cardiac Differentiation
The canonical Wnt signaling pathway is central to the directed differentiation of iPSCs into cardiomyocytes. The following diagram illustrates the key stages of the process and the critical signaling events.
Diagram 2: Signaling Pathway in iPSC-CM Differentiation
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these protocols relies on high-quality, well-characterized reagents. The table below lists key solutions used in the featured experiments and the broader field.
Table 3: Research Reagent Solutions for iPSC Characterization and Cardiomyocyte Differentiation
| Reagent Category | Example Product | Function / Explanation |
|---|---|---|
| Reprogramming System | CytoTune-iPSC Sendai Reprogramming Kit [46] | Non-integrating viral vector for safe generation of iPSCs from somatic cells. |
| Reprogramming System | mRNA-LNP Reprogramming Cocktail [48] | Non-integrating, non-viral method for footprint-free iPSC generation. |
| iPSC Culture Medium | StemFit AK03 / AK03N (Ajinomoto) [7] | Xeno-free, chemically defined medium for the stable maintenance of iPSCs. |
| iPSC Culture Medium | TeSR / mTeSR Plus (STEMCELL Technologies) [47] | Widely used, serum-free medium for feeder-free culture of iPSCs. |
| Cardiac Differentiation Kit | StemMACS CardioDiff Kit XF (Miltenyi Biotec) [46] | Xeno-free kit providing optimized media for directed cardiac differentiation. |
| Extracellular Matrix | iMatrix-511 (Laminin-511 E8 fragment) [46] [7] | Recombinant laminin fragment that supports robust feeder-free iPSC adhesion and growth. |
| Small Molecule Inhibitor | CHIR 99021 [5] [7] | GSK-3 inhibitor that activates Wnt signaling to drive mesoderm formation. |
| Small Molecule Inhibitor | IWP2 [5] | Porcupine inhibitor that blocks Wnt secretion, crucial for cardiac progenitor specification. |
| Cell Dissociation Reagent | TrypLE Select [7] | Animal-origin-free recombinant enzyme for gentle passaging and dissociation of cells. |
| Cryopreservation Medium | CryoStor CS10 [47] | GMP-manufactured, serum-free cryopreservation medium optimized for cell recovery. |
Optimizing Cell Seeding Density and Embryoid Body Size Parameters
The following table consolidates key quantitative parameters for embryoid body (EB) formation from recent studies, highlighting the direct relationship between initial cell number, resulting EB size, and its impact on differentiation efficiency.
Table 1: Experimentally Determined Parameters for EB Formation and Differentiation Outcomes
| Initial Seeding Number (cells/EB) | Resulting EB Diameter (μm) | Differentiation Target | Differentiation Outcome / Key Finding | Citation |
|---|---|---|---|---|
| 200 - 1,000 cells per microwell | 157.2 ± 29.4 to 381.3 ± 115.7 | Neural / General | EB size can be precisely controlled by input cell number and microwell size. | [53] |
| 400 cells per microwell | 157.2 ± 29.4 (Homogeneous) | Neural Stem Cells (NSCs) | Enabled rapid NSC differentiation within 4 days. | [53] |
| ~100 μm diameter target | ~100 μm | Cardiomyocytes | EBs <100 μm fell apart; optimal for initiating cardiac differentiation. | [2] |
| >300 μm diameter | >300 μm | Cardiomyocytes | EBs >300 μm differentiated less efficiently due to diffusion limits. | [2] |
| 250 cells per well (aggregation) | 235.7 ± 42.23 | Retinal Organoids | Highly homogeneous EBs in shape and size. | [54] |
| Clumps (non-forced aggregation) | 237.5 ± 52.36 | Retinal Organoids | Heterogeneous EBs in shape and size. | [54] |
| 9,000 cells per aggregate | Not Specified | Neural Embryoid Bodies (NEBs) | Standard seeding density for NEB formation in ultra-low attachment plates. | [55] |
Detailed Experimental Protocols
Protocol 1: Forming Homogeneous EBs Using Microwell Arrays
This protocol utilizes the EZSPHERE system to generate uniform EBs for highly reproducible differentiation [53].
Key Reagents and Materials:
- Cell Line: Human iPSCs or ESCs.
- Microwell Vessel: EZSPHERE dish (e.g., #900 type: 500 μm diameter, 100 μm depth microwells).
- Basal Medium: Chemically defined medium, such as mTeSR1.
- Dissociation Reagent: Enzyme-free dissociation buffer or Accutase.
- ROCK Inhibitor: Y-27632.
Step-by-Step Methodology:
- Pre-culture and Dissociation: Maintain hiPSCs in a pluripotent state using standard 2D culture. Dissociate the cells into a single-cell suspension using an appropriate dissociation reagent.
- Cell Seeding Calculation and Preparation: Calculate the total number of cells required based on the desired EB size. The literature shows a correlation between input cell number and EB diameter [53]. For example, seeding 400 cells per microwell resulted in EBs of 157.2 ± 29.4 μm in diameter. Resuspend the cell pellet in culture medium supplemented with 10 μM ROCK inhibitor to enhance cell survival after dissociation.
- Microwell Seeding: Seed the cell suspension into the EZSPHERE dish. The design of the microwells will cause the cells to spontaneously drop into individual microwells.
- EB Formation: Within 3-4 hours of seeding, the cells will aggregate at the bottom of each microwell to form a single, homogeneous EB per well.
- EB Culture and Analysis: Culture the EBs in the microwells for the desired duration. The uniformity of the population can be confirmed by measuring EB diameters using image analysis software (e.g., ImageJ), which should show a tight Gaussian distribution [53].
- Downstream Differentiation: Proceed with lineage-specific differentiation protocols directly in the microwell system or transfer the uniform EBs to suspension culture for further development.
Protocol 2: Optimized Cardiac Differentiation in Stirred Suspension Bioreactors
This protocol outlines the critical EB size control steps for efficient and reproducible generation of iPSC-derived cardiomyocytes (hiPSC-CMs) in a controlled bioreactor environment [2].
Key Reagents and Materials:
- Cell Line: High-quality human iPSCs (SSEA4+ >70%).
- Bioreactor: Stirred suspension bioreactor or economical spinner flask.
- Small Molecule Inducers: CHIR99021 (GSK3-β inhibitor, Wnt activator), IWP2 or IWR-1 (Wnt inhibitor).
- Cardiac Differentiation Medium: RPMI 1640 medium supplemented with B-27 supplement (without insulin).
Step-by-Step Methodology:
- Quality Control of Input Cells: Ensure the pluripotency of the starting hiPSC population, as a high SSEA4 positivity (>70%) is correlated with successful cardiac differentiation [2].
- Inoculation and EB Formation: Seed a single-cell suspension of hiPSCs into the stirred bioreactor system. The agitation promotes the formation of EBs of relatively uniform size.
- EB Size Monitoring and Critical Threshold: Monitor the size of the EBs closely. The optimal window for initiating cardiac differentiation is when the EB diameter reaches approximately 100 μm. EBs smaller than this threshold are prone to disintegration upon subsequent chemical induction, while EBs larger than 300 μm differentiate less efficiently, likely due to impaired diffusion of signaling molecules and nutrients within the core [2].
- Mesoderm Induction: Once the target EB size is achieved, initiate differentiation by adding the Wnt pathway activator CHIR99021 (e.g., 7 μM) to the medium. In this optimized protocol, the CHIR99021 induction period is 24 hours.
- Cardiac Mesoderm Specification: After a 24-hour gap following CHIR99021 removal, add the Wnt inhibitor IWR-1 (e.g., 5 μM) or IWP2 to the culture for 48 hours to direct the cells toward a cardiac lineage.
- CM Maturation: Following the differentiation phase, maintain the EBs in culture for several weeks, feeding with appropriate medium to support cardiomyocyte maturation. Contractions are typically observed around differentiation day 5 [2].
Signaling Pathway and Experimental Workflow
The diagram below illustrates the logical workflow and key signaling decisions for optimizing EB formation and subsequent cardiac differentiation, integrating critical size checkpoints.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and their functions for successful EB formation and differentiation.
Table 2: Key Reagents for EB Formation and Cardiac Differentiation
| Reagent / Tool | Function / Role in Protocol | Example Usage Context | |
|---|---|---|---|
| ROCK Inhibitor (Y-27632) | Enhances survival of single cells after dissociation by inhibiting apoptosis. | Added to medium after passaging hiPSCs or during initial EB aggregation. | [54] [56] [2] |
| CHIR99021 | Glycogen synthase kinase-3β (GSK-3β) inhibitor; activates Wnt signaling to specify mesoderm lineage. | Used at the start of differentiation (Day 0) for a defined period (e.g., 24-48 hours). | [5] [2] [44] |
| IWP2 / IWR-1 | Small molecule inhibitors of Wnt production and signaling; promotes cardiac mesoderm specification. | Added after CHIR99021 priming (e.g., Day 2-4) to inhibit Wnt pathway. | [2] [44] |
| Microwell Arrays (e.g., EZSPHERE) | Provides a microfabricated physical scaffold to form thousands of uniformly sized EBs simultaneously. | Used for high-throughput, homogeneous EB formation by seeding single-cell suspensions. | [53] [57] |
| Stirred Bioreactors/Spinner Flasks | Provides controlled agitation and monitoring (O₂, pH, temperature) for scalable EB culture and differentiation. | Enables large-scale production of hiPSC-CMs from EBs with improved reproducibility. | [2] |
| Extracellular Matrices (e.g., Laminin-511, Vitronectin) | Defined substrates for the maintenance of pluripotent stem cells prior to EB formation. | Used to coat tissue culture surfaces for 2D expansion of hiPSCs. | [56] [2] |
Within the broader thesis of optimizing differentiation protocols for induced pluripotent stem cell (iPSC)-derived cardiomyocyte (CM) research, achieving high-purity CM populations is a critical determinant of success for disease modeling, drug screening, and cell therapy applications [5]. Current directed differentiation strategies often result in variable and unsatisfactory CM purity, plagued by batch-to-batch and line-to-line variability [5]. This application note details a robust protocol adaptation—progenitor reseeding—that consistently improves cardiomyocyte purity by 10–20% (absolute) across multiple cell lines. This method enhances the efficiency of differentiation protocols without requiring terminal purification steps, thereby increasing the yield of functional CMs for downstream applications [5].
Reseeding Cardiac Progenitors Significantly Enhances CM Purity
Reseeding involves detaching and replating cardiac progenitor cells at a lower density at a specific time during differentiation. Systematic investigation of different reseeding ratios reveals a clear optimal range for maximizing CM purity while maintaining cell yield.
Table 1: Impact of Reseeding Ratio on CM Purity and Yield
| Reseeding Ratio (Initial:Reseeded Surface Area) | Absolute Change in cTnT+ Purity | Impact on CM Number Relative to Control | Cell Confluency on Day 16 |
|---|---|---|---|
| 1:1 | Significant increase | Significant decrease | 100% |
| 1:2.5 | ~12% increase | Unchanged | 100% |
| 1:5 | ~15% increase | Significant decrease | 100% |
| 1:10 | Significant decrease | Significant decrease | ~60% |
Data adapted from [5]. The 1:2.5 ratio provides the optimal balance, significantly improving purity without reducing the final cardiomyocyte count.
Cryopreservation of Progenitors for On-Demand CM Production
A significant advantage of this reseeding strategy is the compatibility of specific cardiac progenitors with cryopreservation. This facilitates the creation of master cell banks for on-demand CM production, enhancing experimental flexibility and reproducibility.
Table 2: Cryopreservation Potential of Cardiac Progenitors
| Progenitor Stage | Recovery Post-Cryopreservation | Ability to Differentiate into CMs | CM Purity After Reseeding Cryopreserved Cells |
|---|---|---|---|
| EOMES+ Mesoderm Progenitors | High (70–90%) | Retained | Improved compared to non-cryopreserved controls |
| ISL1+/NKX2-5+ Cardiac Progenitors | High (70–90%) | Retained | Improved compared to non-cryopreserved controls |
Data synthesized from [5]. This allows for the creation of large, quality-controlled batches of CM-fated progenitors, enabling more predictable and efficient differentiation workflows.
Experimental Protocol: Progenitor Reseeding for Enhanced CM Purity
This protocol is designed as an adaptation to existing GiWi (CHIR99021 and IWP2)-based hPSC-CM differentiation protocols [5].
Materials and Reagents
- Cell Lines: Human Pluripotent Stem Cells (hPSCs), e.g., WTC11 [5].
- Culture Vessels: Matrigel-coated plates or flasks.
- Extracellular Matrices: Matrigel, iMatrix-511, or defined alternatives (Fibronectin, Vitronectin, Laminin-111) [5].
- Key Reagents:
- CHIR99021: A GSK-3 inhibitor used for Wnt activation to induce mesoderm.
- IWP2/IWR-1: Wnt inhibitors used to direct cardiac mesoderm specification.
- RPMI 1640 Medium: Basal medium for differentiation.
- B-27 Supplement (With and Without Insulin): Used in differentiation and maintenance media.
- Accutase: Enzyme for cell detachment.
- Y-27632 (ROCK inhibitor): Improves cell survival after dissociation.
Step-by-Step Procedure
- Initiate Differentiation: Begin your standard GiWi protocol. Differentiate hPSCs towards the cardiac lineage using CHIR99021 to activate Wnt signaling, followed by a Wnt inhibitor like IWP2 after a defined gap [5].
- Monitor Progenitor Stage: On differentiation day 5, identify the target population of ISL1+/NKX2-5+ cardiac progenitors (CPCs). The optimal reseeding window is between the EOMES+ mesoderm and ISL1+/NKX2-5+ CPC stages [5].
- Detach Progenitors:
- Aspirate the differentiation medium.
- Wash the cells gently with DPBS.
- Add Accutase to dissociate the cells into a single-cell suspension. Incubate at 37°C until cells detach.
- Neutralize the Accutase with an appropriate volume of complete medium.
- Collect the cell suspension and centrifuge.
- Resuspend the cell pellet in fresh cardiomyocyte maintenance medium (e.g., RPMI/B-27 with insulin) supplemented with 10 µM Y-27632.
- Reseed Progenitors:
- Plate the dissociated progenitor cells onto fresh Matrigel-coated plates at the optimal ratio of 1:2.5 (initial differentiation surface area to reseeded surface area). For example, if differentiating in one well of a 6-well plate (~10 cm²), reseed the progenitors onto 2.5 wells of a 6-well plate.
- Ensure even distribution of cells.
- Continue Differentiation:
- Twenty-four hours after reseeding, replace the medium with fresh cardiomyocyte maintenance medium without Y-27632.
- Continue the culture, refreshing the medium every 2-3 days.
- Spontaneously beating cardiomyocytes are typically observed within days after reseeding.
- (Optional) Cryopreservation of Progenitors: After step 3, instead of reseeding immediately, the progenitor cell pellet can be resuspended in a suitable cryopreservation medium. Freeze the vials using a controlled-rate freezer. Upon thawing, resume the protocol from step 4.
Diagram 1: Experimental workflow for progenitor reseeding and cryopreservation. The process integrates into standard GiWi differentiation, with a key decision point at the progenitor stage for immediate reseeding or banking.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Progenitor Reseeding and Cardiac Differentiation
| Reagent / Tool | Function in Protocol | Example Product / Note |
|---|---|---|
| CHIR99021 | GSK-3 inhibitor; activates Wnt signaling to induce mesoderm. | Critical for initial differentiation phase. |
| IWP2 / IWR-1 | Wnt inhibitor; promotes cardiac mesoderm specification from nascent mesoderm. | Used after CHIR99021 pulse. |
| Accutase | Enzyme for gentle, effective dissociation of progenitor cells into single cells for reseeding. | Preferable to trypsin for better cell viability. |
| Y-27632 | ROCK inhibitor; significantly improves survival of dissociated and cryopreserved progenitor cells. | Add to medium during reseeding and after thawing. |
| B-27 Supplement | Serum-free supplement used in basal medium to support cardiomyocyte survival and maturation. | Use "with insulin" for maintenance, "without insulin" for specific differentiation stages. |
| Extracellular Matrices | Provides a defined substrate for cell adhesion and growth. Enables protocol transition to xeno-free conditions. | Matrigel, iMatrix-511, or defined proteins (Fibronectin, Vitronectin). |
| Flow Cytometry Antibodies | Quantification of CM purity (e.g., cTnT) and progenitor stage identification (e.g., ISL1, NKX2-5). | Anti-cTnT, Anti-ISL1, Anti-NKX2-5. |
Discussion and Concluding Remarks
The progenitor reseeding strategy addresses a central challenge in iPSC-CM research: the variability and insufficient purity of cardiomyocyte differentiations. By simply detaching and reselecting ISL1+/NKX2-5+ cardiac progenitors at a lower, optimized density, researchers can reliably achieve a significant boost in CM purity. This method is effective across multiple cell lines and is compatible with cryopreservation, enabling the creation of progenitor biobanks for on-demand production of high-quality CMs [5]. This protocol enhancement, framed within the ongoing optimization of iPSC differentiation systems, provides a simple yet powerful tool to advance the reproducibility and scalability of iPSC-CMs for basic research, drug development, and future clinical applications.
Within the context of developing robust differentiation protocols for human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs), the control of oxygen tension is a critical, yet often underreported, parameter. Achieving a mature, adult-like cardiomyocyte phenotype in vitro requires careful mimicry of the physiological environment, which includes replicating the dynamic oxygen conditions present during embryonic heart development. In vivo, cardiomyocytes develop in a relatively hypoxic environment, and the transition to higher oxygen levels at birth triggers key maturational events [58]. This application note provides a detailed overview of oxygen handling practices, summarizes key quantitative data, and offers standardized protocols to enhance the maturity and reproducibility of hiPSC-CMs for research and drug development applications.
Current Landscape and Quantitative Data
A scoping review of the literature from the past 15 years reveals that oxygen handling practices during hiPSC-CM differentiation are highly variable and frequently underreported [58]. Among the research articles analyzed, only 34% explicitly reported the oxygen conditions used during hPSC culture, and a mere 16% reported the conditions during cardiomyocyte differentiation [58]. This lack of reporting hinders protocol standardization and reproducibility. The identified approaches can be categorized into six main methods, summarized in Table 1.
Table 1: Categorization of Oxygen Handling Practices in hiPSC-CM Differentiation
| Category | Description | Reported Prevalence |
|---|---|---|
| 1 | Differentiation entirely under atmospheric oxygen (~20% O₂) | Among studies that do report conditions, a convergence towards common protocols is seen [58]. |
| 2 | Differentiation entirely under physiological hypoxia (~1-5% O₂) | |
| 3 | Hypoxia-to-normoxia switch post-differentiation | |
| 4 | Normoxia-to-hypoxia switch during differentiation | |
| 5 | Hypoxia during early differentiation, normoxia later | |
| 6 | Use of triple-gas incubators (O₂, CO₂, N₂) for precise control |
The physiological rationale for controlling oxygen tension is strong. Human pluripotent stem cells in their native niche reside in a low-oxygen environment, which helps maintain genomic stability and reduce oxygen-induced damage [58]. During early embryonic development, cells rely predominantly on glycolysis. As differentiation progresses towards a cardiac fate, a metabolic shift occurs towards oxidative phosphorylation, a process driven by mitochondrial expansion and changes in oxygen availability [58]. Therefore, recapitulating these metabolic cues in vitro is essential for guiding cells towards a more mature phenotype.
Experimental Protocols for Oxygen Handling
Protocol 1: Hypoxic Conditioning in Monolayer Culture
This protocol is designed for differentiating hiPSC-CMs in standard 2D culture formats under controlled, low-oxygen conditions.
Key Materials:
- Quality-controlled hiPSC line (Pluripotency marker SSEA4 >70% by FACS is recommended for high differentiation efficiency) [2].
- Triple-gas incubator (capable of precise control of O₂, CO₂, and N₂).
- Chemically defined cardiac differentiation media.
- Oxygen sensor or analyzer for incubator calibration.
Methodology:
- hiPSC Maintenance (Hypoxia): Maintain undifferentiated hiPSCs in a humidified incubator at 5% O₂, 5% CO₂, and 37°C. Culture cells on recombinant vitronectin or laminin in chemically defined media. Perform daily media changes.
- Cardiac Differentiation: Initiate differentiation using a standard Wnt modulation protocol (e.g., with CHIR99021 and IWR-1) [2].
- For the first 4-6 days of differentiation, maintain cultures at 5% O₂.
- On differentiation day ~7, switch the cultures to a normoxic environment (20% O₂) for the remaining maturation period (up to 30-90 days). This switch aims to mimic the postnatal increase in oxygen tension, promoting metabolic maturation.
- Monitoring: Monitor the onset of spontaneous contraction. In optimized suspension protocols, contraction can be observed as early as day 5 [2]. Confirm cardiomyocyte identity and purity via flow cytometry for cardiac troponin T (TNNT2; expected >90%) [2] and functional analysis.
Protocol 2: Oxygen Control in Stirred Suspension Bioreactors
This protocol leverages suspension culture to improve scalability and reproducibility, integrating oxygen control throughout the process [2].
Key Materials:
- Stirred-tank bioreactor system (e.g., DASbox Mini Bioreactor System) or economical spinner flasks.
- Integrated dissolved oxygen (DO) probe.
- Gas mixing system (O₂, CO₂, N₂).
- hiPSCs qualified for suspension culture.
Methodology:
- Inoculation and EB Formation: Dissociate hiPSCs to single cells and seed into the bioreactor. Allow embryoid bodies (EBs) to form under continuous agitation.
- Oxygen Setpoint Control:
- Set the dissolved oxygen (DO) setpoint to ~20-40% air saturation (equivalent to ~4-8% O₂) throughout the entire differentiation process. The bioreactor's gas mixing system will automatically maintain this level by sparging with N₂ or air.
- Continuously monitor the pH and adjust CO₂ sparging to maintain a pH of ~7.2-7.4.
- Differentiation: Initiate differentiation with CHIR99021 when the average EB diameter reaches ~100 µm (typically at 24 hours post-inoculation). This ensures optimal molecule diffusion [2]. Follow with IWR-1 treatment according to established timelines.
- Harvesting and Analysis: On day 15, harvest the hiPSC-CMs (bioreactor-derived CMs, or bCMs). Expected yield is ~1.2 million cells per mL with >90% TNNT2+ purity [2]. bCMs typically show a predominantly ventricular identity and higher functional maturity compared to monolayer-derived CMs [2].
Signaling Pathways and Workflow Diagrams
The following diagrams illustrate the key signaling pathways influenced by oxygen and the integrated experimental workflows.
Oxygen Signaling in Cardiac Maturation
Experimental Workflows for Oxygen Control
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Oxygen-Controlled hiPSC-CM Differentiation
| Item | Function/Description | Example/Note |
|---|---|---|
| Triple-Gas Incubator | Precisely controls O₂, CO₂, and N₂ levels to maintain hypoxic or normoxic conditions. | Essential for Protocol 1. Requires regular calibration of the oxygen sensor. |
| Stirred-Tank Bioreactor | Provides scalable suspension culture with integrated monitoring and control of dissolved oxygen (DO), pH, and temperature. | Systems like DASbox or simpler spinner flasks can be used [2]. Core for Protocol 2. |
| Small Molecule Inducers | Chemically defined molecules for directed cardiac differentiation via Wnt pathway modulation. | CHIR99021 (Wnt activator) and IWR-1 (Wnt inhibitor) [2]. More cost-effective and consistent than growth factors. |
| Dissolved Oxygen Probe | Measures the actual concentration of oxygen dissolved in the culture medium in real-time. | Critical for bioreactor systems to maintain a set DO percentage. |
| Synthetic Polymer Nanofibers | Scaffolds that mimic the cardiac extracellular matrix, promoting cell alignment and mature morphology. | Poly(ε-caprolactone) (PCL) and Polyurethane (PU) nanofibrous mats can support 3D culture models [59]. |
| Antibodies for Characterization | Validate cardiomyocyte identity, purity, and maturity via flow cytometry or immunocytochemistry. | Anti-cardiac Troponin T (TNNT2) for purity, Anti-MYL2 (MLC2v) for ventricular identity, Anti-ACTN2 for sarcomeric organization [2]. |
The transition to xenogeneic-free culture systems is a critical step in advancing human induced pluripotent stem cell-derived cardiomyocyte (hiPSC-CM) research from preclinical discovery to clinical application. The use of animal-derived components, such as fetal bovine serum (FBS), poses significant risks including immune reactions, batch-to-batch variability, and potential pathogen transmission [60] [61]. For hiPSC-CMs destined for therapeutic use in drug development or regenerative medicine, establishing robust, chemically-defined, and Good Manufacturing Practice (GMP)-compliant differentiation protocols ensures product safety, quality, and reproducibility [62]. This application note details standardized methodologies and key considerations for implementing xenogeneic-free systems within the context of hiPSC-cardiomyocyte differentiation protocols.
Key Reagent Solutions for Xenogeneic-Free Cardiomyocyte Production
The foundation of a successful xenogeneic-free protocol lies in the identification and qualification of GMP-compliant reagents that support both pluripotent stem cell maintenance and efficient cardiac differentiation. The table below summarizes essential reagent solutions and their functions.
Table 1: Key Research Reagent Solutions for Xenogeneic-Free hiPSC-CM Differentiation
| Reagent Category | Specific Examples | Function & Rationale |
|---|---|---|
| Basal Media | DMEM/F12, Knockout DMEM [1] [62] | Chemically-defined base media that supports hiPSC expansion and differentiation. |
| Xenogeneic-Free Supplements | Human Platelet Lysate (hPL) [63] [60] [61], Pooled Human Serum (HS) [60] | Replaces FBS to provide essential growth factors and adhesion proteins, reducing immunogenicity risks. |
| Cell Dissociation Agents | Animal-free trypsin substitutes [61], TrypLE [60], EDTA [1] | Enzymatic or non-enzymatic solutions for cell passaging that avoid animal-derived trypsin. |
| Extracellular Matrices | Recombinant Vitronectin Peptides (e.g., Synthemax II-SC) [1], Laminin-521 [1] | Defined, human-derived or synthetic substrates that replace Matrigel for cell attachment and growth. |
| Small Molecule Inducers | CHIR99021 (CHIR), IWR-1 [2] | Critically used in Wnt pathway modulation for highly efficient cardiac differentiation; preferred over growth factors for cost and lot consistency [2]. |
Quantitative Comparison of Culture Systems
Transitioning from research-grade to GMP-compliant systems requires careful evaluation of performance metrics. The following table summarizes quantitative data from studies comparing traditional and xenogeneic-free systems for culturing mesenchymal stromal cells and hiPSC-derived cardiomyocytes.
Table 2: Performance Metrics of Xenogeneic-Free vs. Traditional Culture Systems
| Cell Type / System | Expansion/Fold Increase | Purity / Characterization | Key Findings |
|---|---|---|---|
| MSC(WJ) in STR with hPL [63] | 30.1 ± 0.740-fold cell expansion in 7 days; (1.26 ± 0.186) x 10⁴ EVs/cell/day [63] | High EV purity: (5.53 ± 1.55) x 10⁹ particles/µg; Mean EV diameter: 115 ± 4.88 nm [63] | Successfully produced clinically relevant numbers of extracellular vesicles under xenogeneic-free conditions. |
| Fetal Pancreatic MSCs with Human Serum [60] | Higher proliferative effect compared to FBS [60] | Senescence occurred earlier in FBS-supplemented cultures [60] | Human serum is an effective, clinically superior alternative to FBS for MSC expansion. |
| hiPSC-CMs in Stirred Suspension [2] | ~1.21 million cells/mL; ~2.4 hiPSC-CMs/input hiPSC [2] | ~94% TNNT2+ purity; Earlier contraction (dd5) and higher expression of ventricular markers [2] | Suspension bioreactor system enabled scalable production of functionally mature CMs with low batch variability. |
Protocol: Xenogeneic-Free hiPSC Culture and Cardiomyocyte Differentiation
This section provides a detailed, step-by-step protocol for the xenogeneic-free culture of hiPSCs and their differentiation into cardiomyocytes using a scalable stirred suspension system, adapted from current methodologies [2].
Xenogeneive-Free Culture of hiPSCs
- Cell Thawing and Seeding: Thaw hiPSCs from a qualified, GMP-compliant master cell bank. Pre-coat culture vessels with a defined substrate such as recombinant vitronectin (e.g., Synthemax II-SC) or diluted laminin-521 [1].
- Maintenance Medium: Use a fully defined, xenogeneic-free medium such as Essential 8 or a commercial equivalent. These media are typically serum-free and albumin-free, containing only recombinant proteins and small molecules [1].
- Passaging: Upon reaching ~85% confluency, passage cells using a non-enzymatic method such as 0.5 mM EDTA in DPBS⁻/⁻ or an animal-free recombinant trypsin substitute [1] [61]. After dissociation, add a Rho kinase inhibitor (e.g., 10 µM Y27632 or 2 µM thiazovivin) to the medium for the first 24 hours post-passaging to enhance cell survival [1].
- Quality Control: Regularly monitor pluripotency marker expression (e.g., SSEA4 via FACS). Successful cardiac differentiation efficiencies of >90% are strongly correlated with high SSEA4 expression (>70%) in the starting hiPSC population [2].
Stirred Suspension Cardiac Differentiation
The following workflow outlines the key stages for differentiating hiPSCs into cardiomyocytes in a stirred-tank bioreactor, a system that offers superior control and scalability compared to traditional monolayer cultures [2].
Diagram 1: Suspension Differentiation Workflow
- Embryoid Body (EB) Formation: Seed high-quality hiPSCs into a stirred-tank bioreactor. The system should continuously monitor and adjust temperature, O₂, CO₂, and pH. Allow cells to spontaneously aggregate into EBs [2].
- Mesoderm Induction: Initiate differentiation by adding the Wnt pathway activator CHIR99021. The optimal timing for addition is when the average EB diameter reaches ~100 µm; EBs smaller than 100 µm may disintegrate, while larger EBs show reduced differentiation efficiency due to diffusion limits [2]. A concentration of 7 µM CHIR99021 is typically effective.
- Specification: After a 24-hour incubation with CHIR, replace the medium to remove the compound and continue culture for a 24-hour gap without any differentiation factors [2].
- Cardiac Specification: Add the Wnt inhibitor IWR-1 at a concentration of 5 µM and incubate for 48 hours to promote cardiac lineage specification [2].
- Maturation and Harvest: Continue culture for up to 15 days, with medium changes as needed. Spontaneous contractions are typically observed by differentiation day 5. Cells can be harvested as a bulk population of cardiomyocytes (bCMs) or used to form cardiac organoids directly in suspension [2].
Signaling Pathways in Cardiac Differentiation
The canonical Wnt signaling pathway is the primary regulator of efficient cardiac differentiation. The following diagram illustrates the temporal control of this pathway used in the aforementioned protocol.
Diagram 2: Wnt Pathway in Cardiac Differentiation
- Wnt Activation Phase: Addition of CHIR99021 activates β-catenin signaling, driving hiPSCs toward a primitive streak and mesodermal fate [2].
- Basal Signaling Phase: The withdrawal of CHIR allows endogenous signaling dynamics to proceed, enabling the transition to cardiac mesoderm.
- Wnt Inhibition Phase: Addition of IWR-1, which stabilizes Axin and promotes β-catenin degradation, robustly specifies cardiac lineage and initiates cardiomyocyte differentiation [2].
The adoption of xenogeneic-free, GMP-compliant systems is no longer a future aspiration but a present necessity for the clinical translation of hiPSC-cardiomyocyte research. By integrating defined reagents like human platelet lysate, recombinant matrices, and small molecule inducers into robust and scalable platforms such as stirred-tank bioreactors, researchers can achieve high-yield production of functionally mature cardiomyocytes. These standardized protocols ensure the safety, reproducibility, and quality required for advanced drug development and regenerative medicine applications.
Functional Characterization and Protocol Performance Assessment
The generation of cardiomyocytes from human induced pluripotent stem cells (iPSC-CMs) represents a transformative advancement for cardiovascular research, offering unprecedented opportunities for disease modeling, drug screening, and regenerative therapies [64]. However, the translational potential of iPSC-CMs is significantly hampered by protocol variability and inconsistent functional outcomes across different cell lines [2] [58]. This variability underscores the critical need for systematic, morpho-functional comparisons of differentiation methodologies to establish robust and reproducible approaches.
The fundamental challenge lies in the limited comparative data on how different differentiation protocols perform across multiple iPSC lines, particularly from both healthy donors and patients with inherited cardiac conditions [64]. While numerous cardiac differentiation protocols have been developed, most employ temporal modulation of the Wnt/β-catenin pathway as their core mechanistic principle [2]. Understanding how protocol variations impact the structural, molecular, and functional properties of resulting cardiomyocytes is essential for advancing both basic research and clinical applications.
This application note provides a comprehensive morpho-functional analysis of differentiation protocol efficiency across multiple iPSC lines, with specific focus on two established monolayer-based serum-free protocols that utilize distinct small molecules for Wnt pathway inhibition. Within the broader context of iPSC-CM research standardization, we present quantitative data, detailed methodologies, and analytical frameworks to guide protocol selection and optimization.
Comparative Performance Analysis of Differentiation Protocols
Protocol Architectures and Experimental Design
We evaluated two monolayer-based serum-free differentiation protocols that employ a sequential two-step procedure for cardiac specification. Both protocols initiate with mesoderm induction through activation of the Wnt/β-catenin pathway using the GSK3 inhibitor CHIR99021 [64] [65]. The protocols diverge in the second step, where cardiac fate specification is achieved through inhibition of the canonical Wnt pathway using different small molecules:
- Protocol A: Utilizes IWP-2 as the Wnt inhibitor [64]
- Protocol B: Employs Wnt-C59 as the Wnt inhibitor [64]
The experimental design incorporated one iPSC clone from four individuals (two controls and two Brugada syndrome patients carrying SCN5A mutations), with each line differentiated in four to six replicates per protocol [64]. This approach enabled assessment of both protocol efficiency and line-to-line variability.
Quantitative Comparison of Differentiation Outcomes
Table 1: Morpho-Functional Characteristics of iPSC-CMs Generated with Protocol A vs. Protocol B
| Parameter | Protocol A (IWP-2) | Protocol B (Wnt-C59) |
|---|---|---|
| Differentiation Efficiency (% cACT+ cells) | 90.2 ± 4.1% [64] | 95.9 ± 4.1% [64] |
| Contracting Area | 11 ± 1% [64] | 33 ± 5.6% [64] |
| Success Rate (replicates producing contracting CMs) | 7/18 replicates [64] | 15/18 replicates [64] |
| Growth Morphology | Patches of monolayer & 3D cell clumps [64] | Primarily flat monolayer [64] |
| Cell Survival After Dissociation | >50% with smooth membrane [64] | >50% with smooth membrane [64] |
| Accessibility for Patch-Clamp | Lower (avg. 6.7 recordings/line) [64] | Higher (avg. 10.7 recordings/line) [64] |
| Gene Expression Similarity to Ventricular Tissue | Lower similarity [64] | Higher similarity [64] |
Table 2: Action Potential Properties of iPSC-CMs
| Action Potential Parameter | Protocol A (BrS Patient 2) | Protocol B (BrS Patient 1) | Protocol B (BrS Patient 2) |
|---|---|---|---|
| APD50 (ms) | 422.08 [64] | 351.51 ± 24.84 [64] | 273.7 ± 40.83 [64] |
| APD90 (ms) | 501.8 [64] | 509.95 ± 27.91 [64] | 422.3 ± 10.9 [64] |
| APA (mV) | 114.5 [64] | 90.8 ± 5.1 [64] | 86.7 ± 17.3 [64] |
| RMP (mV) | -59.3 [64] | -59.6 ± 3.1 [64] | -58.3 ± 5.4 [64] |
| Beats Per Minute | 8 [64] | 17 ± 1.12 [64] | 27 ± 3 [64] |
Analysis of cardiac-specific gene expression revealed significant differences between protocols. Protocol B generated cells with expression patterns more closely resembling human left ventricular tissue, showing significantly higher relative expression of key cardiac markers including MYH6, MYH7, and RYR2 [64]. Both protocols produced cells expressing cardiac proteins (cACT, cTNNI, and Nkx2.5), but Protocol B yielded better organized sarcomeric structures with cTNNI displaying clear cytoskeletal patterning rather than predominantly peri-nuclear localization [64].
Experimental Methodologies
iPSC Culture and Quality Control
High-quality input iPSCs are critical for successful and consistent cardiac differentiation [2]. The following methodology ensures optimal starting material:
- Culture Conditions: Maintain iPSCs in Essential 8 medium on Geltrex-coated plates with daily medium changes [66]. For suspension culture, use recombinant protein-based substrates rather than animal-derived feeders to enhance reproducibility [58].
- Quality Assessment: Prior to differentiation, validate pluripotency marker expression (SSEA4 >70% via FACS) and ensure appropriate colony morphology (bright small round cells forming compact colonies with defined edges) [64] [2].
- Karyotyping and Mycoplasma Testing: Perform routine karyotyping and mycoplasma testing to ensure genetic integrity and absence of contamination [2].
- Oxygen Conditions: Explicitly control and report oxygen conditions during iPSC culture, as this parameter significantly impacts genomic stability and differentiation efficiency but is frequently underreported [58].
Cardiac Differentiation Protocols
Base Differentiation Media Formulation:
- Cardiac Differentiation Medium (C-diff): RPMI 1640 with Glutamax and HEPES, supplemented with 0.2 mg/ml ascorbic acid 2-phosphate and 0.5 mg/ml human recombinant albumin [66].
- Maintenance Medium: RPMI 1640 with 2% B27 supplement [66].
Protocol A (IWP-2-based) Procedure:
- Day 0: Replace maintenance medium with C-diff supplemented with 4 µM CHIR99021 [66].
- Day 2: Exchange medium to C-diff containing 5 µM IWP-2 [66].
- Day 4: Change to base C-diff medium without small molecules.
- Day 6: Refresh with C-diff medium.
- Day 8+: Maintain cells in RPMI 1640 with 2% B27 supplement, changing medium every 2-3 days [66].
Protocol B (Wnt-C59-based) Procedure:
- Day 0: Initiate differentiation with C-diff containing CHIR99021 (concentration optimized per cell line).
- Day 2: Replace medium with C-diff containing Wnt-C59.
- Day 4: Transition to basal C-diff medium.
- Day 6: Refresh with C-diff medium.
- Day 8+: Culture in RPMI 1640 with 2% B27 supplement with regular medium changes [64].
First contractions typically appear between days 8-10 post-differentiation initiation [66].
Functional Characterization Methods
Electrophysiological Analysis:
- Patch-Clamp Recording: Perform action potential recordings on dissociated single cells or monolayers. For single-cell recordings, dissociate cells using collagenase B and trypsin/EDTA, then plate on appropriate substrates [64] [66].
- Parameters Measured: Action potential duration at 50% and 90% repolarization (APD50, APD90), action potential amplitude (APA), resting membrane potential (RMP), and beating rate (BPM) [64].
Calcium Transient Imaging:
- Use optical dyes (e.g., Cal-520, Fluo-4) to record calcium transients [64].
- Analyze calcium transient duration (CTD), time of rise and decay, and synchronization with contractile activity [64].
Contractility Assessment:
- Employ video-based motion analysis systems (e.g., Maia software) to quantify beating parameters [66].
- Extract features including displacement, relaxation-rise time, beating duration, contraction time, relaxation time, and maximum contraction/relaxation velocities [66].
Molecular Characterization
Immunocytochemistry:
- Fix cells and stain for cardiac markers including cardiac troponin T (cTnT), cardiac α-actinin (cACT), cardiac troponin I (cTNNI), and Nkx2.5 [64].
- Visualize sarcomeric organization and quantify differentiation efficiency based on percentage of positive cells.
Gene Expression Analysis:
- Extract RNA and perform qPCR for key cardiac structural and ion channel genes [64].
- Assess expression of GJA1, KCNJ2, MYH6, MYH7, RYR2, TNNI3, and other markers relative to human ventricular tissue [64].
Signaling Pathways and Experimental Workflow
Wnt Signaling Pathway in Cardiac Differentiation
Experimental Workflow for Protocol Comparison
Research Reagent Solutions
Table 3: Essential Research Reagents for iPSC-CM Differentiation and Characterization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Wnt Pathway Activators | CHIR99021 [64] [66] | GSK3 inhibitor; activates Wnt/β-catenin signaling | Critical for mesoderm induction; concentration requires optimization per cell line |
| Wnt Pathway Inhibitors | IWP-2 [64], Wnt-C59 [64] | Inhibits Wnt secretion and signaling | Drives cardiac specification; different inhibitors impact maturity and functionality |
| Basal Media | RPMI 1640 [66], DMEM [66] | Foundation for differentiation media | Chemically defined formulations enhance reproducibility |
| Media Supplements | B27 supplement [66], Ascorbic acid [66] | Supports cell survival and differentiation | Serum-free supplements reduce batch-to-batch variability |
| Extracellular Matrices | Geltrex [66], Fibronectin [67], Matrigel [67] | Provides structural support and signaling cues | Composite matrices (e.g., fibronectin-Matrigel) enhance maturation |
| Characterization Antibodies | Anti-cTnT [64] [2], Anti-cACT [64], Anti-Nkx2.5 [64] | Identifies cardiac-specific proteins | Essential for quantifying differentiation efficiency |
| Functional Assay Reagents | Calcium-sensitive dyes [64], Electrophysiology solutions [64] | Enables functional characterization | Critical for assessing electrophysiological maturity |
The comprehensive morpho-functional analysis presented herein demonstrates that both Protocol A (IWP-2-based) and Protocol B (Wnt-C59-based) can successfully generate functional cardiomyocytes from iPSCs, but with significant differences in efficiency, maturity, and experimental utility across multiple cell lines.
Protocol B consistently outperformed Protocol A in several key metrics: higher success rate in generating contracting cardiomyocytes (15/18 vs. 7/18 replicates), larger contracting areas (33% vs. 11%), superior cell morphology for electrophysiological studies, and gene expression profiles more closely resembling human ventricular tissue [64]. These advantages make Protocol B particularly suitable for applications requiring high-quality, functionally mature cardiomyocytes, such as disease modeling and drug screening.
However, both protocols produced cells with immature characteristics compared to adult cardiomyocytes, including significantly lower expression of key ion channel genes (KCND3, KCNQ1) and structural genes (RYR2, TNNI3, TNNT2) relative to human left ventricular tissue [64]. This immaturity limitation underscores the need for further protocol refinement and maturation strategies.
Recent advances in suspension culture differentiation represent a promising direction for addressing scalability and reproducibility challenges [2]. Bioreactor-based approaches can yield approximately 1.2 million cardiomyocytes per milliliter with >90% purity and improved functional properties compared to monolayer-differentiated cells [2]. Additionally, the development of non-invasive maturity assessment methods using video-based motion analysis and machine learning algorithms offers new opportunities for quality control without compromising cell integrity [66].
Within the broader thesis context of optimizing iPSC-CM differentiation protocols, this analysis highlights the critical importance of systematic protocol comparison across multiple cell lines. The substantial variability observed between protocols and across different iPSC lines emphasizes that no single protocol is universally optimal. Researchers should select differentiation strategies based on their specific application requirements, considering the trade-offs between efficiency, maturity, scalability, and experimental accessibility.
Future work should focus on integrating the most effective elements of both protocols, optimizing timing and dosing of small molecules, incorporating advanced maturation strategies, and developing standardized quality assessment metrics. Such efforts will advance the field toward more reproducible, clinically relevant iPSC-CM models that faithfully recapitulate human cardiac physiology and pathology.
Within the broader scope of differentiation protocols for iPSC-derived cardiomyocytes (iPSC-CM) research, the functional validation of the resulting cells through electrophysiological profiling is a critical final step. The characterization of action potentials (AP) and calcium (Ca²⁺) transients provides the definitive evidence of successful differentiation and maturation, confirming that the cells recapitulate the fundamental electrophysiology of adult human cardiomyocytes [18]. These parameters are not only essential for basic research but are also crucial in drug discovery and safety pharmacology, as they can reveal pro-arrhythmic liabilities and other cardiotoxic effects of new compounds [68]. This application note details standardized protocols for the simultaneous optical recording of AP and Ca²⁺ transients, a powerful technique that correlates membrane electrical activity with the key event—calcium-induced calcium release—that initiates contraction [69] [70].
Materials and Methods
Cardiomyocyte Differentiation from iPSCs
Multiple robust differentiation protocols exist for generating iPSC-CMs. The core principle underlying many modern protocols is the temporal modulation of the Wnt/β-catenin signaling pathway [2] [68].
Protocol 1: Monolayer-based Differentiation (StemMACS CardioDiff Kit XF) [46] [68] This xeno-free, GMP-compatible protocol is suitable for clinical applications. iPSCs are seeded on iMatrix-511-coated plates. Differentiation is initiated by sequential media changes: 24 hours in Mesoderm Induction Media (MIM), 24 hours in Cardiomyocyte Maintenance Media (CMM), and 24 hours in Cardiac Induction Media (CIM). Cells are then maintained in CMM until day 10 or 17. Spontaneous contractions typically appear between days 6 and 10.
Protocol 2: Stirred Suspension Bioreactor Differentiation [2] This method offers superior scalability and batch-to-batch consistency. iPSCs are aggregated to form embryoid bodies (EBs) in a controlled bioreactor. When EBs reach an optimal diameter of ~100 µm, cardiac differentiation is induced by adding 7 µM CHIR99021 (a Wnt activator) for 24 hours. After a 24-hour gap, Wnt signaling is inhibited with 5 µM IWR-1 for 48 hours. This protocol yields approximately 1.2 million cells per mL with >90% purity (TNNT2+ cells) and is noted for its functional maturity and reduced inter-batch variability.
Protocol 3: Minimal Component, Protein-Free Differentiation [41] This cost-effective protocol uses only DMEM/F12 basal medium and L-ascorbic acid 2-phosphate (AA2P), alongside Wnt modulation. It eliminates expensive growth factors and xenobiotic components, reducing variability and enhancing scalability for basic research applications.
Simultaneous Optical Recording of AP and Ca²⁺ Transients
The following protocol, adapted from current methodologies, details the procedure for dual optical recording from single iPSC-CMs [69] [70].
Principle: This method utilizes two fluorescent indicators with distinct excitation/emission spectra to simultaneously record membrane potential and intracellular Ca²⁺ dynamics in a single cell.
Equipment and Reagents:
- Inverted epifluorescence microscope (e.g., Nikon Eclipse Ti-E) with a temperature-controlled stage incubator (e.g., Tokai Hit)
- High-speed camera (e.g., Hamamatsu ORCA-Flash4.0 or ImagEM X2 EMCCD)
- Multi-wavelength LED illumination system (e.g., X-Cite Turbo)
- Image splitting optics (e.g., W-VIEW GEMINI) to separate emission wavelengths
- 35 mm glass-bottom dishes
- Membrane potential dye: FluoVolt (Thermo Fisher Scientific)
- Ca²⁺ indicator: Calbryte 590 AM (AAT Bioquest) or Cal-520 AM (AAT Bioquest)
- Gey’s Balanced Salt Solution (GBSS) or custom Imaging Medium
- Pacing system (e.g., Myo-Pacer EP for field stimulation at 1-2 Hz)
Experimental Workflow:
Detailed Procedure:
- Cell Preparation: Seed purified and matured (≥day 60) iPSC-CMs onto fibronectin-coated 35 mm glass-bottom dishes at a density suitable for single-cell analysis [70]. Allow cells to adhere and recover for 48 hours before imaging.
- Dye Loading: On the day of recording, prepare the dye-loading solution in GBSS or Imaging Medium. The solution should contain 0.1% (v/v) FluoVolt and 10 µM Calbryte 590 AM (from a stock solution in DMSO with 0.02% Pluronic F-127). Replace the culture medium with the dye-loading solution and incubate for 40 minutes at 37°C protected from light [69].
- Wash and Recovery: After incubation, carefully replace the dye solution with pre-warmed GBSS or fresh Imaging Medium to remove excess dye. Allow the cells to recover for at least 20 minutes before imaging to ensure de-esterification of the AM esters and stabilization of the fluorescent signals.
- Microscope Setup and Imaging: Mount the dish on the stage-top incubator maintained at 37°C with 5% CO₂ supply. Configure the illumination system for simultaneous excitation: use a 475 nm LED (5% intensity) for FluoVolt and a 575 nm LED (25-100% intensity) for Calbryte 590. Use a dual-band filter set (e.g., FITC/TxRed) and image splitting optics equipped with 536/40 nm and 631/36 nm emission filters to direct the separate fluorescence signals to different regions of the camera [69]. Record videos at a high frame rate (≥100 fps) for 1 minute, both under spontaneous beating and during 1 Hz field stimulation.
- Drug Intervention (Optional): To assess drug effects, add compounds directly to the dish after an initial baseline recording. Use a gradual increase in concentration and record for 1 minute after each addition once the effect stabilizes [69].
Data Analysis
Fluorescence traces are analyzed for key parameters using custom automated software (e.g., in MATLAB or Python) [71] [70].
- Action Potential Analysis: Measure Action Potential Duration at 50% and 90% repolarization (APD50, APD90), amplitude, and resting membrane potential (if calibrated).
- Calcium Transient Analysis: Measure Calcium Transient Amplitude (ΔF/F0), Time to Peak (TTP), and Time to 50%//80% Decay (RT50/RT80).
Expected Results and Data Interpretation
Upon successful differentiation and maturation, iPSC-CMs exhibit characteristic AP and Ca²⁺ transient waveforms. The morphology of these signals evolves with the maturity of the cells.
Table 1: Typical Electrophysiological Parameters of maturing iPSC-CMs under 1 Hz Pacing [70]
| Parameter | Day 60 | Day 75 | Day 90 | Adult Human CMs |
|---|---|---|---|---|
| APD50 (ms) | ~300 | ~400 | ~500 | ~200-300 |
| APD90 (ms) | ~400 | ~500 | ~600 | ~300-400 |
| CaT Amplitude (ΔF/F0) | ~2.0 | ~2.2 | ~3.0 | ~4.0-6.0 |
| CaT Time to Peak (ms) | ~150 | ~120 | ~100 | ~50-100 |
| CaT RT50 (ms) | ~500 | ~400 | ~300 | ~200-300 |
| Presence of T-tubules | Rare | Rare | Emerging | Abundant [18] |
Table 2: Effects of Selected Drugs on iPSC-CM Electrophysiology [69] [68]
| Drug | Target / Class | Effect on APD | Effect on Ca²⁺ Transient |
|---|---|---|---|
| E4031 | hERG (IKr) Blocker | Profound prolongation | Can induce arrhythmic events |
| Nifedipine | L-type Ca²⁺ Channel Blocker | Shortening | Reduced amplitude |
| Flecainide | Na⁺ Channel Blocker | Can prolong APD | Can suppress abnormalities in CPVT models [69] |
| Moxifloxacin | IKr Blocker (mild) | Mild to moderate prolongation | Minimal direct effect |
| KN-93 | CaMKII Inhibitor | No significant change | Highly effective at reducing Ca²⁺ transient abnormalities [69] |
The relationship between AP and Ca²⁺ handling is fundamental. Maturation leads to a positive correlation between AP duration (APD) and Ca²⁺ transient duration, as longer APs allow for a greater Ca²⁺ influx through L-type channels, sustaining the transient [70]. This interplay is a key marker of mature Excitation-Contraction Coupling (ECC).
The Scientist's Toolkit
Table 3: Essential Reagents and Tools for Electrophysiological Profiling
| Item | Function / Description | Example |
|---|---|---|
| Membrane Potential Dyes | Fluorescent reporters that partition into the membrane and change fluorescence in response to changes in membrane potential. | FluoVolt [69], BeRST-1 [71] |
| Ca²⁺ Indicators | Fluorescent dyes that chelate Ca²⁺, resulting in a measurable increase in fluorescence intensity. | Calbryte 590 AM [69], Cal-520 AM [72], Rhod-2, GCaMP6f (genetically encoded) [71] |
| Wnt Pathway Modulators | Small molecules used in differentiation protocols to direct cardiac fate via temporal Wnt/β-catenin signaling control. | CHIR99021 (Activator) [2] [68], IWR-1 or Wnt-C59 (Inhibitor) [2] [68] |
| Metabolic Purification Agents | Compounds used to selectively eliminate non-cardiomyocytes, as CMs can utilize lactate as an energy source while undifferentiated cells cannot. | DL-Lactic Acid / Lactate [68] [72] |
| Automated Analysis Software | Custom or open-source code for high-throughput, user-independent quantification of AP and CaT parameters from fluorescence videos. | Custom MATLAB scripts [71] |
The detailed characterization of action potentials and calcium transients is a non-negotiable standard in the functional validation of iPSC-derived cardiomyocytes. The protocols outlined herein, from scalable differentiation to simultaneous optical recording and automated analysis, provide a robust framework for researchers. This framework is essential for accurate disease modeling, reliable cardiotoxicity screening, and the advancement of personalized medicine in cardiovascular research. As differentiation protocols continue to improve the maturity of iPSC-CMs, the fidelity of this electrophysiological profiling will only increase, solidifying its role as a cornerstone of iPSC-CM research.
Multi-Electrode Array (MEA) for Drug Response and Proarrhythmia Risk Assessment
The Comprehensive in Vitro Proarrhythmia Assay (CiPA) initiative has catalyzed the adoption of human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) as a physiologically relevant model for preclinical cardiotoxicity screening [73] [68]. Multi-Electrode Array (MEA) technology has emerged as a critical functional assay within this paradigm, enabling non-invasive, long-term recording of extracellular field potentials (EFPs) from spontaneously beating or electrically paced hiPSC-CM monolayers [73] [74]. This Application Note provides detailed protocols and analytical frameworks for implementing MEA-based proarrhythmia risk assessment, contextualized within evolving hiPSC differentiation methodologies that enhance the physiological relevance of these in vitro systems.
Key Principles of MEA Analysis in Cardiac Safety Pharmacology
MEA systems utilize microelectrodes embedded in culture surfaces to detect fluctuations in extracellular field potentials generated by cardiomyocyte networks [74] [75]. The cardiac field potential waveform closely correlates with the intracellular action potential, with key parameters providing functional insights into ion channel activity and repolarization reserve [75]. Field Potential Duration (FPD) serves as a surrogate for cardiac action potential duration and QT interval on the surface electrocardiogram, while FPD corrected (FPDc) for beating rate enables detection of drug-induced repolarization abnormalities [68] [76]. Spike amplitude reflects the integrity of sodium channel-mediated depolarization, and beat rate variability can indicate perturbations in pacemaker activity or conduction abnormalities [77].
The integration of hiPSC-CMs with MEA technology addresses critical limitations of conventional preclinical models, including species-specific differences in ion channel expression and the artificial nature of heterologously expressed single ion channel assays [68] [78]. Furthermore, patient-specific hiPSC-CMs enable the modeling of genetic predispositions to arrhythmias, facilitating personalized drug safety assessment [68] [79].
Experimental Workflow for MEA-Based Proarrhythmia Assessment
The following diagram illustrates the complete experimental workflow for MEA-based proarrhythmia assessment, from cardiomyocyte differentiation through data analysis:
hiPSC Culture and Cardiac Differentiation
Robust cardiac differentiation begins with quality-controlled hiPSCs. Multiple protocols exist, with contemporary methods favoring small molecule-directed differentiation via Wnt pathway modulation over spontaneous embryoid body formation [1] [2].
Monolayer Differentiation Protocol [68]:
- Culture Expansion: Maintain hiPSCs in defined media such as Essential-8 or B8 on growth factor-reduced Matrigel (1:800 dilution) with rigid 3-4 day passage schedules using EDTA dissociation [1].
- Differentiation Initiation (Day 0): At ~90% confluency, add 8 µM CHIR99021 (a GSK-3β inhibitor and Wnt activator) in cardiomyocyte differentiation medium (RPMI1640 with human albumin and L-ascorbic acid-2-phosphate) [68].
- Wnt Inhibition (Day 2): Replace medium with CDM containing 2 µM Wnt-C59 (a Wnt inhibitor) for 48 hours [68].
- Metabolic Selection (Day 7-10): Following spontaneous contraction onset, replace medium with glucose-free RPMI1640 containing 4 mM L-lactic acid for 4 days to enrich cardiomyocytes [68].
- Maturation (Day 10-30): Culture purified hiPSC-CMs in Advanced MEM medium supplemented with 100 ng/mL 3,3',5-triiodo-L-thyronine (T3) and 1 µM dexamethasone, changing medium every two days [68].
Suspension Bioreactor Differentiation [2]: For improved scalability and reproducibility, implement stirred suspension systems:
- Embryoid Body Formation: Aggregate hiPSCs in bioreactor systems with continuous monitoring of temperature, O₂, CO₂, and pH.
- Optimized Differentiation Timing: Add 7 µM CHIR99021 when embryoid bodies reach 100 µm diameter (typically 24 hours), followed by 5 µM IWR-1 (Wnt inhibitor) after 24-hour gap for 48 hours.
- Yield and Purity: This protocol generates ~1.21 million cells/mL with >90% TNNT2+ cardiomyocytes and predominantly ventricular identity [2].
hiPSC-CM Plating on MEA Plates
Proper cell plating ensures formation of a syncytium over electrodes for high-quality signal acquisition [73]:
- MEA Plate Coating: Apply 8 µL of 0.1 mg/mL Matrigel in DMEM/F12 directly covering electrode arrays. Incubate ≥1 hour at 37°C with 5% CO₂ while maintaining humidity with sterile water in plate edges [73].
- Cell Dissociation and Counting: At day 20-30 post-differentiation, dissociate hiPSC-CMs using TrypLE or 10X trypsin without phenol red. Count viable cells using trypan blue exclusion and hemocytometer [73] [68].
- Cell Plating: Plate approximately 4,000 cells/well in 48-well MEA plates in 8 µL droplets of plating media (RPMI1640 with 20% KnockOut Serum Replacement) directly onto coated electrodes [73].
- Culture Maintenance: After 2 hours attachment, carefully add 150 µL/well plating media. Replace with maintenance media (RPMI1640 with B27 + insulin) after 24 hours, changing media every 3 days until recording [73].
MEA Recording and Drug Application
Baseline Recording [73]:
- System Setup: Turn on MEA system (e.g., Maestro Pro, Axion Biosystems) at least 20 minutes before recording. Set environmental controls to 37°C and 5% CO₂.
- Signal Acquisition: Place MEA plate on recording area and allow signal offset. Record baseline spontaneous activity for 5 minutes using cardiac-specific EFP detection parameters.
- Electrical Pacing: Apply electrical pacing at 1 Hz, 1 ms duration, and 20 µA current density. Record paced activity for 5 minutes.
- Drug Preparation: Prepare serial dilutions in maintenance media pre-warmed to 37°C. Include vehicle control (e.g., DMSO at equivalent concentration).
- Drug Application: Add drug solutions according to predefined plate maps with 6 replicates per condition.
- Post-Compound Recording: Record electrically paced (1 Hz) activity for 20 minutes following drug addition to assess acute electrophysiological effects.
Quantitative Analysis of Drug Effects
MEA systems extract multiple parameters from cardiac field potentials for comprehensive proarrhythmia risk assessment. The following table summarizes key quantitative parameters and their physiological significance:
Table 1: Key Parameters for MEA-Based Proarrhythmia Risk Assessment
| Parameter | Description | Physiological Significance | Example Drug Effects |
|---|---|---|---|
| Field Potential Duration (FPD) | Time from depolarization spike to T-wave peak | Surrogate for action potential duration; prolonged FPD indicates repolarization impairment | E4031 (hERG blocker) concentration-dependently prolongs FPD [68] |
| Corrected FPD (FPDc) | FPD normalized for beating rate (e.g., using Fridericia's correction) | Detects repolarization abnormalities independent of rate changes | High/intermediate TdP risk drugs prolong FPDc; low/no risk drugs decrease FPDc [76] |
| Spike Amplitude | Magnitude of initial depolarization deflection | Reflects sodium channel function and cellular coupling | Flecainide (Na+ channel blocker) reduces spike amplitude [68] |
| Beat Rate | Frequency of spontaneous contractions | Indicates pacemaker activity and automaticity | Nifedipine (Ca2+ channel blocker) decreases beat rate [68] |
| Arrhythmic Events | Incidence of irregular beating patterns | Direct indicator of proarrhythmic potential | Quinidine induces early afterdepolarizations and irregular rhythms [68] |
Application of this analytical framework to various drug classes reveals distinct electrophysiological profiles, as demonstrated in the following table compiling experimental findings:
Table 2: Experimental Data on Drug Effects in hiPSC-CMs Using MEA Analysis
| Drug | Mechanism | TdP Risk Category | FPDc Response | Arrhythmic Events | Cell Line Sensitivity |
|---|---|---|---|---|---|
| E4031 | hERG blocker | High | Concentration-dependent prolongation | Induces EADs and irregular rhythms | Increased sensitivity in LQTS-derived lines [68] |
| Quinidine | Multi-channel blocker | Intermediate | Prolongation at therapeutic concentrations | Triggers irregular rhythms and EADs | Variable response across healthy lines [68] |
| Moxifloxacin | IKr blocker | Intermediate | Mild prolongation | Rare arrhythmic events | Consistent response across lines [68] |
| Flecainide | Na+ channel blocker | Low | Minimal effect or shortening | May induce conduction slowing | - |
| Nifedipine | L-type Ca2+ blocker | Low | Shortening | No proarrhythmic events | - |
| Ranolazine | Late Na+ current inhibitor | Low | Shortening | Suppresses arrhythmias | - |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of MEA-based cardiotoxicity assessment requires specific reagents and equipment. The following table details essential research solutions:
Table 3: Essential Research Reagent Solutions for MEA-Based Cardiotoxicity Assessment
| Item | Function | Example Specifications | Protocol Notes |
|---|---|---|---|
| hiPSC Culture Media | Maintain pluripotency and support expansion | Essential-8, B8, or StemMACS iPS-Brew XF | Use commercial or published formulations; monitor pluripotency markers (>70% SSEA4+) [1] [68] |
| Differentiation Inducers | Direct cardiac lineage specification | CHIR99021 (7-8 µM) for Wnt activation | Timing critical; initiate when EBs reach 100 µm diameter in suspension [68] [2] |
| Differentiation Inhibitors | Enhance cardiac purity and maturation | Wnt-C59 (2 µM) or IWR-1 (5 µM) for Wnt inhibition | Apply after 24-48 hour CHIR incubation [68] [2] |
| Extracellular Matrix | Support cell attachment and syncytium formation | Growth factor-reduced Matrigel (0.1 mg/mL) | Dilute in DMEM/F12; 1:800 dilution sufficient for hiPSC culture [73] [1] |
| Cell Dissociation Reagents | Generate single-cell suspensions for plating | TrypLE or trypsin without phenol red with EDTA | Use enzymatic dissociation post-differentiation for MEA plating [73] [68] |
| MEA Plates | Detect extracellular field potentials | 48-well plates with 16 electrodes/well | Electrodes optimized for detection and pacing; 200 µm spacing [73] |
| Cardiomyocyte Maintenance Media | Support long-term functional maturation | RPMI1640 with B27 + insulin supplement | Change every 3 days; final change 24h before recording [73] |
Advanced Analytical Approaches
Dual-Cardiotoxicity Evaluation
Beyond traditional FPD analysis, integrated assessment of electrophysiological and contractile parameters provides complementary cardiotoxicity insights [76]. This approach reveals that low/no TdP risk drugs more significantly reduce contractility than high/intermediate risk compounds, suggesting distinct mechanisms of cardiotoxicity that may be missed by focusing exclusively on proarrhythmic potential [76].
Spatiotemporal Analysis
Advanced signal processing platforms like PhysioMEA enable two-dimensional analysis of electrophysiological biomarker distributions across electrode arrays [77]. This reveals spatial heterogeneities in R- to S-peak amplitude (39.04% coefficient of variation) and maximal slope (46.95% coefficient of variation) that are not detectable in conventional one-dimensional analysis [77].
Disease-Specific Models
Incorporating patient-specific hiPSC-CMs enhances the predictive validity of MEA-based risk assessment. LQTS-derived cardiomyocytes show increased sensitivity to hERG blockers like E4031, demonstrating how genetic background modulates drug response [68] [79]. The following diagram illustrates the integration of disease-specific models in the proarrhythmia risk assessment workflow:
MEA-based proarrhythmia risk assessment represents a significant advancement in preclinical cardiotoxicity screening, combining the physiological relevance of hiPSC-CMs with the throughput required for drug development. The protocols detailed in this Application Note provide a framework for robust implementation of this technology, while emerging approaches—including dual-cardiotoxicity evaluation, spatiotemporal analysis, and patient-specific models—promise to further enhance its predictive validity. As differentiation protocols continue to evolve toward more mature cardiomyocyte phenotypes [2] [79], MEA technology will play an increasingly central role in ensuring cardiac safety while reducing reliance on animal testing.
Human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) represent a transformative platform for cardiovascular disease modeling, drug discovery, and regenerative medicine. However, their utility remains constrained by a persistent fetal-like phenotype that fails to fully recapitulate adult ventricular cardiomyocyte biology. This application note establishes a standardized framework for benchmarking hiP-CM maturity against native human ventricular tissue, providing researchers with quantitative metrics and validated protocols to enhance physiological relevance and experimental reproducibility.
Quantitative Benchmarking of iPSC-CMs Against Native Ventricular Tissue
Comprehensive maturity assessment requires multimodal evaluation across structural, functional, and molecular domains. The following tables provide definitive benchmarking parameters for comparing hiPSC-CMs to adult human ventricular myocardium.
Table 1: Structural and Metabolic Benchmarking Parameters
| Parameter | iPSC-CMs (Typical Range) | Adult Ventricular Cardiomyocytes | Citation |
|---|---|---|---|
| Cell Morphology | Rounded; 3,000-6,000 µm³ volume | Rod-shaped; ~40,000 µm³ volume | [18] |
| Sarcomere Organization | Disorganized, random orientation | Aligned, developed myofibrils | [80] [18] |
| Sarcomere Length | 1.7-2.0 µm | 2.0-2.2 µm | [80] [18] |
| T-Tubules | Largely absent | Highly developed network | [80] [18] |
| Mitochondrial Content | Low volume, perinuclear | ~30% of cell volume, interfibrillar | [80] |
| Primary Metabolism | Glycolysis | Fatty acid oxidation (>70%) | [80] [18] |
Table 2: Functional Benchmarking Parameters
| Parameter | iPSC-CMs (Typical Range) | Adult Ventricular Cardiomyocytes | Citation |
|---|---|---|---|
| Resting Membrane Potential | -44 to -65 mV | ~ -90 mV | [80] [21] |
| Action Potential Amplitude | <100 mV | 100-110 mV | [80] |
| Upstroke Velocity (Vmax) | 4-11 V/s | 250-300 V/s | [80] [21] |
| Conduction Velocity | 12-28 cm/s | 30-100 cm/s | [80] [21] |
| Contractile Stress | Variable, often lower | 25-60 mN/mm² | [80] |
| Excitation-Contraction Coupling | Delayed (poor RyR/LTCC coupling) | Rapid, coordinated (CICR) | [18] |
Experimental Protocols for Maturation and Assessment
Combined Maturation Protocol for Enhanced Ventricular Phenotype
A synergistic approach combining metabolic induction, structural alignment, and electrophysiological conditioning drives comprehensive maturation [21].
Workflow Overview:
Step-by-Step Methodology:
Cell Culture and Differentiation:
- Differentiate iPSCs to ventricular-like CMs using established small molecule protocols (e.g., Wnt activation/inhibition) [2].
- On differentiation day 15, harvest and plate cells for maturation experiments.
Metabolic Maturation (MM):
- Culture Medium: Replace standard B27 medium with lipid-enriched maturation medium [21] [66].
- Key Components: DMEM base supplemented with 0.5% AlbuMax I (lipid-rich BSA), 1.6 mM L-carnitine, 5 mM creatine, 2 mM taurine, 0.8 mM lactate, and insulin [66].
- Calcium Boost: Increase extracellular calcium concentration to promote electrophysiological maturation [21].
- Duration: Maintain culture for 21-28 days with medium changes every 48 hours.
Structural Maturation via Nanopatterning (NP):
- Substrate Preparation: Culture cells on nanopatterned surfaces with 2 μm line width to induce anisotropic sarcomere alignment [21].
- ECM Coating: Use defined substrates such as laminin-521 or synthetic vitronectin peptides instead of Matrigel for reproducibility [81].
- Outcome: Achieves organized myofibrils, elongated nuclei, and improved connexin 43 membrane localization.
Electrophysiological Maturation via Stimulation (ES):
- Apparatus: Use a carbon electrode system for field stimulation.
- Parameters: Apply 2 Hz rectangular pulses (2 ms duration, 5 V/cm) for 21-28 days [21].
- Outcome: Drives mitochondrial development, enhances calcium handling, and promotes adult-like action potential morphology.
Non-Invasive Maturity Assessment via Motion Analysis
A label-free method enables longitudinal tracking of maturation progress without compromising cellular integrity [66].
Workflow Overview:
Step-by-Step Methodology:
Video Acquisition:
- Culture iPSC-CMs in standard 2D format on Geltrex-coated plates.
- Record 30-second videos of spontaneous contraction using phase-contrast microscopy at 30-60 fps.
- Maintain consistent environmental control (37°C, 5% CO₂) during recording.
Motion Analysis:
- Process videos using specialized motion analysis software (e.g., Maia).
- Extract 10 key beating parameters: displacement, contraction time, relaxation time, beating duration, maximum contraction/relaxation velocities, and rise time.
Machine Learning Classification:
- Train a Support Vector Machine (SVM) classifier with labeled datasets (immature day 21 vs. mature day 42 CMs).
- Optimize hyperparameters via 5-fold cross-validation.
- Apply SHAP analysis to identify the most discriminative features: displacement, relaxation-rise time, and beating duration.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for iPSC-CM Maturation and Benchmarking
| Reagent Category | Specific Product/Component | Function | Citation |
|---|---|---|---|
| Culture Medium | Lipid-enriched Maturation Medium (MM) | Promotes metabolic shift to fatty acid oxidation | [21] [66] |
| Small Molecules | CHIR99021 (Wnt activator), IWP-2 (Wnt inhibitor) | Directs cardiac differentiation and patterning | [2] |
| Defined Substrates | Laminin-521, Synthemax II-SC | Xeno-free surface coating for reproducible differentiation | [1] [81] |
| Patterned Surfaces | Nanofabricated grooves (2 μm width) | Induces structural alignment and sarcomere organization | [21] |
| Electrostimulation | C-Pace EM Culture Pacer | Delivers controlled electrical conditioning | [21] |
| Analysis Software | Maia Motion Analysis | Quantifies contractile dynamics for maturity assessment | [66] |
Within the field of cardiovascular research and therapy, the differentiation of induced pluripotent stem cells into cardiomyocytes (iPSC-CMs) represents a cornerstone technology. However, the translational potential of these cells is critically dependent on the robustness of their manufacturing process. Batch-to-batch variability in iPSC-CM differentiations remains a significant challenge, leading to inconsistent experimental results, unreliable drug screening outcomes, and barriers to clinical application [5] [2]. This application note establishes a comprehensive framework of quantitative metrics and standardized protocols to rigorously assess and enhance the robustness of cardiac differentiation protocols, enabling researchers to achieve reproducible, high-quality iPSC-CM populations suitable for both basic research and therapeutic development.
Critical Quality Metrics for Assessing Batch Consistency
A multi-faceted approach is essential for comprehensive quality assessment. The following table summarizes the key quantitative metrics that should be tracked across multiple batches to evaluate differentiation robustness.
Table 1: Essential Metrics for Assessing iPSC-CM Differentiation Robustness
| Metric Category | Specific Parameter | Target Benchmark | Measurement Technique |
|---|---|---|---|
| Purity & Efficiency | Cardiomyocyte Purity (cTnT+/TNNT2+) | >90% [2] [82]; >70% (QC minimum) [39] | Flow Cytometry |
| Cardiogenic Mesoderm Induction (KDR+/PDGFR-α+) | ~95% [83] | Flow Cytometry | |
| Yield (Cells per mL or per input iPSC) | ~1.2 million/mL [2]; ~2.5 hiPSC-CMs/input iPSC [82] | Cell Counting | |
| Functional Maturity | Contractility (Beat Rate) | Regular and reproducible signals [39] | MUSCLEMOTION [5], MEA |
| Field Potential Duration (FPD on MEA) | 350-560 ms [84] [39] | Multi-Electrode Array (MEA) | |
| Metabolic Phenotype (Oxidative Capacity) | Shift from glycolysis to OXPHOS [22] | Seahorse XF Analyzer | |
| Structural & Molecular | Sarcomere Structure | Organized cTNT and alpha-actinin [39] | Immunofluorescence |
| Myosin Heavy Chain Isoform (MYH7/MYH6) | Increase in MYH7+ cells [5] | RT-qPCR, Flow Cytometry | |
| Mitochondrial Maturation | Increased cristae density, ATP production [22] | High-Content Imaging, PCR |
Detailed Experimental Protocols for Consistency Assessment
Protocol 1: Flow Cytometric Analysis of Differentiation Efficiency and Purity
This protocol outlines the steps for quantifying the emergence of progenitor populations and the final purity of iPSC-CMs, which are critical for tracking batch consistency [5] [83] [39].
Key Reagents:
- Dissociation Reagent: Accutase or TrypLE Select Enzyme [85] [46].
- Staining Buffer: PBS with 0.1% BSA and 0.5% Saponin for permeabilization [46].
- Primary Antibodies: Anti-cardiac Troponin T (cTnT/TNNT2) for CMs; Anti-KDR and Anti-PDGFR-α for cardiogenic mesoderm [83] [39].
- Fixation Solution: 4% methanol-free paraformaldehyde [85] [46].
Procedure:
- Cell Harvesting: At the desired timepoint (e.g., day 3-4 for progenitors, day 10-16 for CMs), dissociate 2D cultures or 3D aggregates into a single-cell suspension using the appropriate enzyme [83] [46].
- Fixation and Permeabilization: Resuspend the cell pellet in 4% PFA and incubate for 20 minutes at room temperature. Wash cells, then permeabilize with 0.5% Saponin in staining buffer for 20 minutes at 4°C [46].
- Antibody Staining: Incubate cells with primary antibodies diluted in staining buffer for 30 minutes at 4°C. After washing, incubate with appropriate fluorescently-labeled secondary antibodies if needed [46].
- Data Acquisition and Analysis: Acquire data using a flow cytometer (e.g., LSR Fortessa). Analyze using software such as FlowJo. Gate single cells using FSC-A/SSC-A and FSC-A/FSC-H, then determine the percentage of positive cells for the markers of interest compared to an unstained or isotype control [5] [46].
Protocol 2: Functional Characterization using Multi-Electrode Array (MEA)
Functional consistency is a key indicator of robust differentiation. This protocol details the use of MEA to assess the electrophysiological properties of iPSC-CM monolayers [84] [39].
Key Reagents and Equipment:
Procedure:
- Plate Preparation and Maturation: Thaw and plate cryopreserved iPSC-CMs or seed freshly dissociated cells onto MEA plates coated with an appropriate extracellular matrix (e.g., fibronectin). Culture the cells for 7-14 days to form a confluent, synchronously beating monolayer, with medium changes every 48-72 hours [84] [39].
- Baseline Recording: Place the MEA plate in the pre-warmed recording station. Record baseline field potentials for at least 2 minutes in a controlled environment (37°C, 5% CO₂). Ensure the system detects stable and regular beats.
- Data Analysis: The software will automatically calculate key parameters:
- Beat Rate: Beats per minute (BPM).
- Field Potential Duration (FPD): The time from the initial spike (depolarization) to the end of the repolarization wave, analogous to the QT interval in an ECG. Expected baseline is 350-560 ms [84] [39].
- Spike Amplitude: The magnitude of the initial depolarization signal.
- Pharmacological Challenge (Optional): To further validate functional maturity, perfuse the cells with known compounds like E-4031 to induce FPD prolongation and Early Afterdepolarizations (EADs), or isoproterenol to induce FPD shortening [84].
Protocol 3: Process Optimization using Statistical Design of Experiments (DoE)
For processes involving multiple interacting variables, a systematic DoE approach is superior to one-factor-at-a-time optimization for achieving robustness [83].
- Application Example: Optimizing the initial stage of cardiogenic mesoderm induction.
- Procedure:
- Factor Selection: Identify critical factors to test (e.g., concentrations of Activin A, BMP4, and CHIR99021) [83].
- Experimental Design: Create a design matrix (e.g., full factorial design) that defines the specific combinations of factor levels to be tested in a structured manner.
- Execution and Analysis: Run differentiations according to the design matrix. For each condition, measure the response variable (e.g., %KDR+/PDGFR-α+ cells via flow cytometry).
- Model Building and Prediction: Use statistical software to build a model that relates the factor levels to the outcome. This model can then predict the optimal factor concentrations (e.g., Activin A and CHIR99021) to achieve the target outcome (e.g., ~95% progenitor induction) with minimal variability [83].
Visualizing Workflows and Signaling Pathways
Quality Control and Batch Assessment Workflow
The following diagram illustrates the integrated workflow for producing and rigorously quality-checking iPSC-CM batches.
Core Cardiac Differentiation Signaling Pathway
The canonical Wnt modulation pathway is the foundation of most robust differentiation protocols. The following diagram outlines the key stages and molecular cues.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful and reproducible differentiation relies on a suite of well-defined reagents and tools.
Table 2: Key Research Reagent Solutions for Robust iPSC-CM Differentiation
| Reagent/Solution | Function | Example & Notes |
|---|---|---|
| Small Molecule Agonists/Antagonists | Direct cell fate via key signaling pathways. | CHIR99021 (GSK3i): Wnt activator for mesoderm induction [5] [2]. IWP2/IWR-1: Wnt inhibitors for cardiac specification [2] [82]. |
| Defined Culture Media | Provide a consistent, xeno-free environment for differentiation and maintenance. | RPMI/B27 (-Insulin): Base for many protocols [83]. Specialized Maintenance Media: Support long-term culture and maturation [85] [39]. |
| Extracellular Matrices (ECM) | Provide structural and biochemical support for cell attachment and growth. | Vitronectin (VTN-N), Laminin-111, Fibronectin: Defined matrices that support pluripotency and differentiation [5] [83] [46]. |
| Characterization Antibodies | Critical for quantifying differentiation efficiency and purity via flow cytometry and IF. | Anti-cTnT/TNNT2: Pan-cardiomyocyte marker. Anti-KDR & Anti-PDGFR-α: Markers for cardiogenic mesoderm [83]. Anti-MLC2v: Ventricular subtype marker [39]. |
| Cell Dissociation Enzymes | Generate single-cell suspensions for seeding, passaging, and analysis. | Accutase, TrypLE Select: Gentle, enzyme-based solutions for dissociating sensitive iPSCs and iPSC-CMs [85] [46]. |
Conclusion
The field of iPSC-cardiomyocyte differentiation has evolved toward more robust, scalable, and clinically applicable protocols. Key advancements include the standardization of Wnt pathway modulation, development of suspension bioreactor systems, implementation of cost-effective protein-free media, and improved purification strategies. Future directions must focus on enhancing cardiomyocyte maturity to better recapitulate adult phenotypes, establishing universal benchmarking standards, and addressing manufacturing challenges for clinical-scale production. As protocols become more reproducible and efficient, iPSC-CMs will play an increasingly vital role in disease modeling, drug discovery, and regenerative medicine, ultimately enabling personalized cardiac therapies and more accurate safety pharmacology assessments.
References
- 1. A review of protocols for human iPSC culture, cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405110/]
- 2. Efficient and reproducible generation of human iPSC ... [https://www.nature.com/articles/s41467-024-50224-0]
- 3. The WNT/β-catenin pathway regulates expression of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8874274/]
- 4. Wnt/β-Catenin Signaling during Cardiac Development and ... [https://www.mdpi.com/2308-3425/1/1/98]
- 5. Enhancing human pluripotent stem cell differentiation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124670/]
- 6. Wnt/β-catenin signaling regulates cardiac Cx43 in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519157/]
- 7. Effect of iPS cell culture medium on the differentiation ... [https://www.nature.com/articles/s41598-025-13259-x]
- 8. Reconstructing the heart using iPSCs: Engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8378256/]
- 9. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 10. A Molecular Roadmap of Reprogramming Somatic Cells ... [https://www.sciencedirect.com/science/article/pii/S0092867412014249]
- 11. Comparison of Differentiation of Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5396057/]
- 12. Single-cell RNA sequencing reveals key regulators and ... [https://www.nature.com/articles/s41598-024-79488-8]
- 13. Dynamic proteome profiling of differentiating human ... [https://www.nature.com/articles/s41598-025-24649-6]
- 14. Combined lineage and scRNA-seq reveals unexpected first... tracing [https://elifesciences.org/articles/80075]
- 15. Comparative analysis of the cardiomyocyte differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9950567/]
- 16. Beclin1 deficiency unlocks cardiac lineage commitment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613599/]
- 17. Metabolic Maturation in hiPSC-Derived Cardiomyocytes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389403/]
- 18. Human induced pluripotent stem cell-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1687840/full]
- 19. Mitochondria and metabolic transitions in cardiomyocytes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02252-6]
- 20. Energy Metabolism on Mitochondrial Maturation and Its Effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294643/]
- 21. Comprehensive promotion of iPSC-CM maturation by ... [https://www.nature.com/articles/s41467-025-58044-6]
- 22. Enhancing Mitochondrial Maturation in iPSC- ... [https://www.mdpi.com/2673-6411/5/3/23]
- 23. Bioreactor Suspension Culture: Differentiation and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.674260/full]
- 24. Metabolic Culture Medium Enhances Maturation of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346743/]
- 25. Scaling iPSC production in different 3D platforms ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X25000452]
- 26. Suspension culture improves iPSC expansion and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03382-9]
- 27. Human Pluripotent Stem Cells: Prospects and Challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4644514/]
- 28. Protocol for differentiating cardiomyocytes and generating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11835656/]
- 29. Directed cardiomyocyte differentiation from human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3612968/]
- 30. Directed Differentiation of iPSCs Into Cardiomyocytes [https://bio-protocol.org/exchange/minidetail?id=7360036&type=30]
- 31. Unraveling the Inconsistencies of Cardiac Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5989659/]
- 32. Glycogen synthase kinase-3 inhibition and insulin enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11784517/]
- 33. Temporal Control of the WNT Signaling Pathway During ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.714008/full]
- 34. Improving cardiac differentiation of human pluripotent stem ... [https://www.sciencedirect.com/science/article/pii/S2352320424000191]
- 35. Effect of iPS cell culture medium on the differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319073/]
- 36. Wnt pathway activation unlocks disease-neutral ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004975]
- 37. Considerations in designing systems for large scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055057/]
- 38. Addressing bioreactor hiPSC aggregate stability, maintenance ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03802-4]
- 39. Controlled, large-scale manufacturing of hiPSC-derived ... [https://www.axionbiosystems.com/resources/application-note/controlled-large-scale-manufacturing-hipsc-derived-cardiomyocytes]
- 40. Engineering Parameters in Bioreactor's Design: A Critical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755438/]
- 41. Minimal Component, Protein‐Free, and Cost‐effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11834755/]
- 42. Protein-free media for cardiac differentiation of hPSCs in 2000 ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03826-w]
- 43. Minimal Component, Protein-Free, and Cost-effective Human ... [https://pubmed.ncbi.nlm.nih.gov/39932462/]
- 44. DMSO-free cryopreservation of hiPSC-derived cardiomyocytes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04384-5]
- 45. Cryopreservation of Human Pluripotent Stem Cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5328614/]
- 46. Generation and purification of iPSC-derived cardiomyocytes ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04319-0]
- 47. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 48. - uBriGene iPSC Banks [https://www.ubrigene.com/ipsc-products/ipsc-banks/]
- 49. Human iPSC : barriers and opportunities | Journal of... banking [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-019-0578-x]
- 50. Stem iPSC Expansion, Cell and Characterization Banking [https://www.reprocell.com/research-stem-cell-services/ipsc-expansion-characterization-and-banking]
- 51. Bridging the Gap: Streamlining iPSC -Derived Cell Line Development... [https://www.cellistic.com/insights/bridging-the-gap-streamlining-ipsc-derived-cell-line-development-from-donor-cells-to-mcb]
- 52. and Regulatory Requirements for the Manufacture of Quality ... Master [https://pubmed.ncbi.nlm.nih.gov/39821060/]
- 53. Microfabric Vessels for Embryoid Body Formation and ... [https://www.nature.com/articles/srep31063]
- 54. The Analysis of Embryoid Body Formation and Its Role in ... [https://www.mdpi.com/1422-0067/25/3/1444]
- 55. Impact of photobiomodulation on neural embryoid body ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04088-2]
- 56. Size- and time-dependent growth properties of human ... [https://www.sciencedirect.com/science/article/abs/pii/S1389172317301597]
- 57. A microwell array system for stem cell culture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2253687/]
- 58. Oxygen Handling Practices for in Vitro Human Pluripotent ... [https://link.springer.com/article/10.1007/s12015-025-11004-5]
- 59. Hypoxia and re-oxygenation effects on human cardiomyocytes ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-024-00432-5]
- 60. Xeno-free protocol for GMP-compliant manufacturing of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9210668/]
- 61. Isolation and Culture of Human Adipose-Derived Stem Cells With an... [https://www.jove.com/t/65104/isolation-culture-human-adipose-derived-stem-cells-with-an-innovative]
- 62. GMP-compatible and xeno-free cultivation of mesenchymal ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-1119-3]
- 63. Continuous collection of human mesenchymal-stromal-cell-derived... [https://pubmed.ncbi.nlm.nih.gov/40275409/]
- 64. Morpho-functional comparison of differentiation protocols ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8890088/]
- 65. Cardiomyocyte Differentiation Service from iPSC [https://www.creative-bioarray.com/services/cardiomyocyte-differentiation.htm]
- 66. Non-invasive maturity assessment of iPSC-CMs based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409467/]
- 67. Cardiac regeneration revisited: Enhanced cardiomyocyte ... [https://pubmed.ncbi.nlm.nih.gov/41106300/]
- 68. Human induced pluripotent stem cell-cardiomyocytes for ... [https://www.kjpp.net/journal/view.html?doi=10.4196/kjpp.24.413]
- 69. Simultaneous optical recording of action potentials and ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1579815/full]
- 70. Optical Investigation of Action Potential and Calcium ... [https://www.mdpi.com/1422-0067/20/15/3799]
- 71. Robust, Automated Analysis of Electrophysiology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9527045/]
- 72. Differentiation, Maintenance, and Contraction Profiling of ... [https://bio-protocol.org/en/bpdetail?id=5222&type=0]
- 73. High-Throughput Analysis of Drug Safety Responses in Induced Pluripotent Stem Cell-Derived Cardiomyocytes Using Multielectrode Array - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12036537/]
- 74. Multielectrode Array (MEA) Assay for Profiling Electrophysiological Drug Effects in Human Stem Cell-Derived Cardiomyocytes - PubMed [https://pubmed.ncbi.nlm.nih.gov/27145112/]
- 75. hiPSCs Derived Cardiac Cells for Drug and Toxicity Screening and Disease Modeling: What Micro- Electrode-Array Analyses Can Tell Us - PubMed [https://pubmed.ncbi.nlm.nih.gov/31661896/]
- 76. Dual-cardiotoxicity evaluation of torsadogenic risk drugs ... [https://pubmed.ncbi.nlm.nih.gov/41043280/]
- 77. PhysioMEA: Signal processing platform for rate and rhythm ... [https://www.sciencedirect.com/science/article/pii/S0022282825002111]
- 78. Compound Testing of Human-Induced Pluripotent Stem ... [https://pubmed.ncbi.nlm.nih.gov/40307643/]
- 79. Arrhythmogenic Risk in iPSC-Derived Cardiomyocytes [https://www.mdpi.com/1648-9144/61/11/2056]
- 80. Induced pluripotent stem cell-derived cardiomyocyte in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376733/]
- 81. Differentiating Human Pluripotent Stem Cells to ... [https://www.mdpi.com/2306-5354/9/12/720]
- 82. Efficient and reproducible generation of human iPSC- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10925150/]
- 83. Engineering a controlled cardiac multilineage co ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04408-0]
- 84. Comprehensive suite of assays for assessment ... [https://www.sciencedirect.com/science/article/pii/S1056871925002928]
- 85. Integral approach to organelle profiling in human iPSC ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1644119/full]