Optimizing MSC Exosome Therapy for Wound Healing: A Comprehensive Guide to Dosing and Administration Routes
This article provides a critical analysis of current strategies for dosing and administering mesenchymal stem cell-derived exosomes (MSC-Exos) in wound therapy.
Optimizing MSC Exosome Therapy for Wound Healing: A Comprehensive Guide to Dosing and Administration Routes
Abstract
This article provides a critical analysis of current strategies for dosing and administering mesenchymal stem cell-derived exosomes (MSC-Exos) in wound therapy. Tailored for researchers and drug development professionals, it synthesizes findings from recent clinical trials and preclinical studies to establish foundational principles of MSC-Exo biology and therapeutic mechanisms. The content explores methodological considerations for production and characterization, identifies key challenges in standardization and optimization, and offers comparative validation of different approaches. By integrating the latest evidence, this review aims to support the development of safe, effective, and standardized MSC-Exo therapies to advance regenerative medicine for wound healing.
The Science Behind MSC Exosomes: Mechanisms and Sources for Wound Repair
The therapeutic benefits of mesenchymal stem cells (MSCs) were initially attributed to their direct differentiation and replacement of damaged cells. However, emerging evidence demonstrates that these effects are primarily mediated through robust paracrine activity, with extracellular vesicles—particularly exosomes (Exos)—serving as crucial delivery vehicles for bioactive molecules [1] [2]. MSC-derived exosomes (MSC-Exos) are nanoscale (30-150 nm), lipid bilayer-enclosed vesicles that facilitate intercellular communication by transferring functional proteins, nucleic acids, and lipids to recipient cells [1] [3]. In the context of wound healing, MSC-Exos have demonstrated remarkable abilities to modulate immune responses, promote angiogenesis, stimulate cellular proliferation and migration, and regulate extracellular matrix (ECM) remodeling [1] [4]. Their composition reflects their parent cells, carrying specific therapeutic cargos that collectively address the multifaceted challenges of impaired wound healing, offering a promising cell-free therapeutic alternative with advantages including low immunogenicity, absence of tumorigenic risk, and enhanced stability [5] [2].
Key Therapeutic Cargos of MSC-Exos
The therapeutic efficacy of MSC-Exos is mediated by their diverse cargo, which includes proteins, miRNAs, lipids, and other nucleic acids. These components work in concert to regulate multiple signaling pathways in recipient cells within the wound microenvironment.
Table 1: Key Protein Cargos in MSC-Exos and Their Functions in Wound Healing
| Protein Cargo | Function in Wound Healing | Mechanism of Action |
|---|---|---|
| Cytokines (IL-10, TGF-β1) [4] | Immunomodulation | Polarization of macrophages toward anti-inflammatory M2 phenotype; reduction of pro-inflammatory cytokines |
| Growth Factors (VEGF, HGF) [4] | Angiogenesis | Stimulation of endothelial cell proliferation and migration; formation of new blood vessels |
| Heat Shock Proteins (HSP70, HSP90) [3] | Cytoprotection | Protection of cells against stress and apoptosis; promotion of cell survival |
| ECM Proteins [3] | Tissue Remodeling | Structural support for cell migration and tissue regeneration |
| Transcription Factors [3] | Epigenetic Regulation | Modulation of gene expression in recipient cells to promote repair processes |
Table 2: Key miRNA Cargos in MSC-Exos and Their Therapeutic Roles
| miRNA Cargo | Therapeutic Role | Target Pathways/Genes |
|---|---|---|
| miR-21 [6] | Anti-apoptosis, Neuroprotection | PTEN/PDCD4 signaling pathway |
| miR-133b [6] | Axon Regeneration, Neural Recovery | Not specified; promotes expression of neurofilament, GAP-43 |
| miR-200c-3p [4] | ECM Remodeling, Anti-fibrotic | Regulates glutaminase; targeted by lncRNA-ASLNCS5088 |
| Anti-ferroptotic miRNAs [3] | Antioxidant, Cell Protection | Regulation of GPX4, SLC7A11; inhibition of lipid peroxidation |
Beyond proteins and miRNAs, MSC-Exos contain long non-coding RNAs (lncRNAs) that play pivotal regulatory roles. For instance, the lncRNA KLF3-AS1 from bone marrow MSC-Exos promotes angiogenesis by increasing VEGFA expression [4], while lncRNA MEG3 helps prevent keloid formation by reducing fibrosis-related protein and collagen expression [4]. The lipid components of the exosomal membrane itself are functional, contributing to membrane stability, cellular uptake, and signaling processes such as the resolution of inflammation [3].
Experimental Protocols for MSC-Exos Research
Protocol 1: Production and Isolation of MSC-Exos Using an Upscaling Approach
Principle: Efficient production of high-quality MSC-Exos is a prerequisite for therapeutic and research applications. This protocol describes a 3D culture-based upscaling method, which significantly enhances exosome yield compared to conventional 2D cultures [7].
Materials:
- Source Cells: Canine Adipose-Derived MSCs (cAD-MSCs) or human MSCs from bone marrow, adipose tissue, or umbilical cord [2] [7]
- Exosome-Collecting Medium: In-house serum-free medium (e.g., VSCBIC-3) or commercial serum-free alternatives [7]
- Culture System: Microcarrier-based 3D bioreactor system or conventional 2D flasks for comparison
- Isolation Equipment: Tangential Flow Filtration (TFF) system with appropriate molecular weight cut-off filters [2] [7]
- Characterization Instruments: Nanoparticle Tracking Analysis (NTA) system, Transmission Electron Microscope (TEM), Western blot apparatus [2]
Procedure:
- Cell Culture and Expansion: Culture MSCs in growth medium (e.g., DMEM with 10% FBS) until ~80% confluence. Use early passages (P3-P5) to avoid senescence [2].
- Conditioning with Exosome-Collecting Medium: Replace growth medium with serum-free exosome-collecting medium (e.g., VSCBIC-3). Maintain cells for 48-72 hours.
- Conditioned Medium (CM) Harvesting: Collect the CM and centrifuge at 2,000 × g for 30 minutes to remove cells and debris. Follow with a 10,000 × g centrifugation for 45 minutes to eliminate larger vesicles and apoptotic bodies [2] [7].
- Exosome Concentration and Purification (TFF): Concentrate and purify the clarified CM using a TFF system. This method is scalable and maintains exosome integrity better than ultracentrifugation [2].
- Post-Isolation Processing: Concentrate the purified exosome suspension. Aliquot and store at -80°C. Avoid repeated freeze-thaw cycles.
Validation and Quality Control:
- Yield Quantification: Use NTA to determine particle concentration and size distribution (expected peak: 30-150 nm) [8] [2].
- Purity Assessment: Confirm the presence of exosomal markers (CD63, CD81, CD9, TSG101, Alix) and the absence of negative markers (e.g., calnexin) via Western blot [2].
- Morphology: Verify spherical, cup-shaped morphology using TEM [2].
Diagram 1: MSC-Exos isolation and characterization workflow.
Protocol 2: In Vitro Bioactivity Assessment for Wound Healing
Principle: This protocol assesses the functional effects of isolated MSC-Exos on key cellular processes in wound healing, including fibroblast migration and proliferation.
Materials:
- Test Cells: Primary dermal fibroblasts
- MSC-Exos Preparations: Isolated MSC-Exos and a negative control (e.g., PBS)
- Equipment: Cell culture incubator, microscope, materials for scratch assay (e.g., pipette tip), cell proliferation assay kit (e.g., resazurin-based) [7]
- Analysis Tools: RT-qPCR system, primers for wound healing-related genes (e.g., collagen types I and III, fibronectin, α-SMA) [7]
Procedure:
- Fibroblast Culture: Seed fibroblasts in appropriate growth medium in multi-well plates. Allow to adhere and reach ~90% confluence.
- Scratch Assay / Migration Test: Create a uniform scratch in the cell monolayer using a sterile pipette tip. Wash to remove dislodged cells.
- Exosome Treatment: Add MSC-Exos (e.g., 10-100 μg/mL based on protein content) to the treatment wells. Use serum-free medium with PBS as a negative control.
- Incubation and Monitoring: Incubate cells and capture images of the scratch at regular intervals (0, 12, 24 hours) under a microscope.
- Proliferation Assay: In a separate plate, seed fibroblasts at a lower density. Treat with MSC-Exos or control. After 24-72 hours, measure cell proliferation using a resazurin assay [7].
- Gene Expression Analysis: Post-treatment (e.g., 24 hours), lyse fibroblasts and extract RNA. Perform RT-qPCR to analyze the expression of genes related to wound healing [7].
Data Analysis:
- Migration: Calculate the percentage of wound closure at each time point compared to the initial scratch area.
- Proliferation: Compare fluorescence/absorbance values between treated and control groups.
- Gene Expression: Analyze fold-changes in gene expression using the 2^(-ΔΔCt) method.
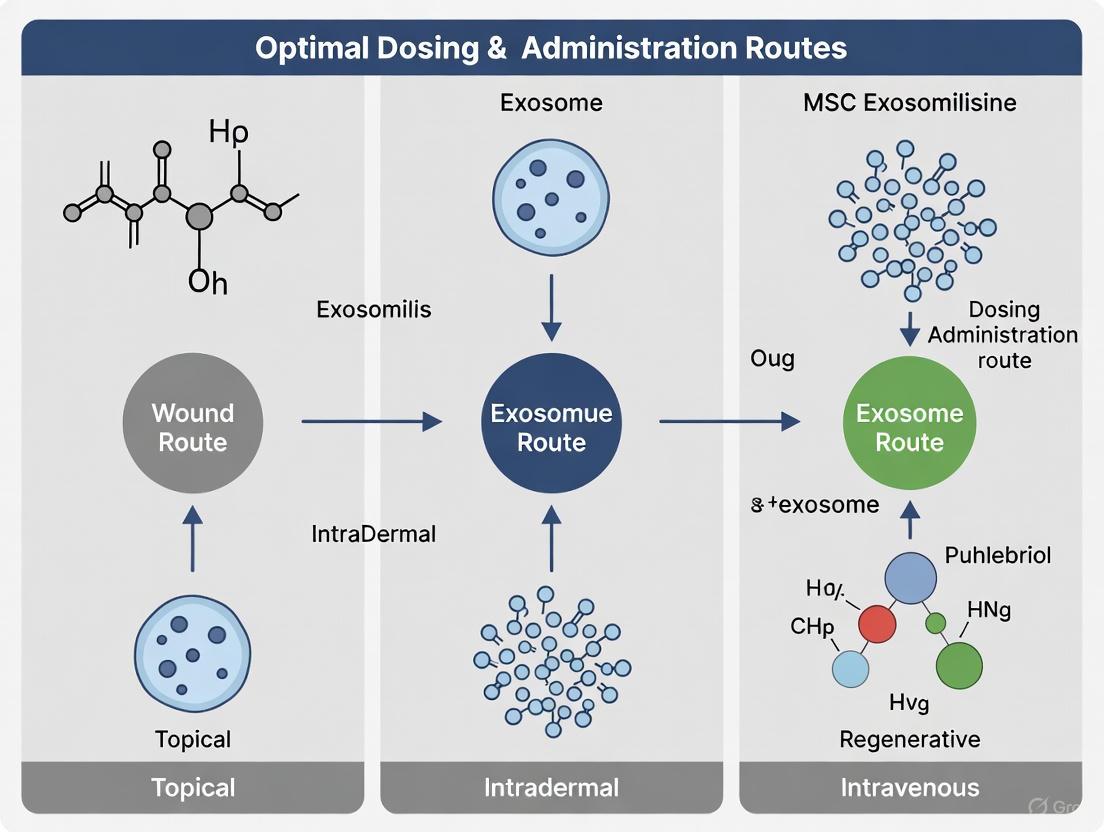
Dosing and Administration Considerations for Wound Therapy
Translating MSC-Exos bioactivity into clinical efficacy requires careful consideration of dosing and administration routes, which are critical elements of the user's thesis context.
Table 3: MSC-Exos Dosing in Preclinical and Clinical Studies
| Context | Reported Dose Range | Quantification Method | Administration Route |
|---|---|---|---|
| Preclinical (Rodent Models) [8] | 10 - 100 μg protein (approx. 2.0 x 10^10 - 2.0 x 10^11 particles) | Protein content (Bradford assay), Particle count (NTA) | Intravenous, Local injection |
| Clinical (Human Trials) [8] | Broad range: ~10^8 - 10^13 particles total dose | Particle count (NTA), Protein content, Cell-equivalent | Intravenous, Inhalation, Local/topical |
| Proposed "Working Range" (Human) [8] | 1 x 10^10 - 6 x 10^12 particles total dose | Particle count (NTA) | Route-dependent |
The administration route profoundly influences the required effective dose due to differences in bioavailability, distribution, and retention at the target site [8]. For cutaneous wound healing, local administration (e.g., topical application via hydrogels, direct injection) is often favored as it maximizes delivery to the wound site while minimizing systemic exposure and potential off-target effects [9] [2]. Evidence suggests that local application can achieve therapeutic effects at significantly lower doses compared to systemic routes like intravenous infusion [9]. The optimal dosing regimen (single vs. multiple doses) must be determined empirically for each specific wound type and exosome preparation.
Diagram 2: Key factors influencing MSC-Exos therapeutic efficacy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for MSC-Exos Wound Healing Studies
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Serum-Free Exosome Production Media | Provides nutrients for MSCs during exosome production without contaminating bovine exosomes. | Commercial serum-free media; In-house formulations (e.g., VSCBIC-3) [7]. |
| Tangential Flow Filtration (TFF) System | Scalable isolation and concentration of exosomes from large volumes of conditioned medium. | Preferable to ultracentrifugation for large-scale, GMP-compliant production [2] [7]. |
| Nanoparticle Tracking Analyzer (NTA) | Measures the size distribution and concentration of exosomes in a solution. | Essential for dose quantification and characterization (e.g., ZetaView, NanoSight) [8] [2]. |
| Exosomal Surface Marker Antibodies | Characterizing exosomes and confirming identity via specific surface proteins. | Antibodies against CD63, CD81, CD9, TSG101, Alix. Negative marker: Calnexin [6] [2]. |
| In Vitro Wound Healing Assay Kits | Functional validation of exosome bioactivity on target cells. | Scratch assay kits; Cell migration and proliferation assay kits (e.g., resazurin) [7]. |
| Biomaterial Scaffolds / Hydrogels | Serve as delivery vehicles for sustained release and localization of exosomes at the wound site. | Chitosan, collagen, hyaluronic acid-based hydrogels. Protect exosomes and enhance retention [5]. |
The field of regenerative medicine is undergoing a significant transformation, moving from whole cell-based therapies toward cell-free approaches utilizing exosomes and extracellular vesicles (EVs). Mesenchymal stem cell (MSC)-derived exosomes have emerged as promising therapeutic agents that retain many of the beneficial properties of their parent cells while exhibiting superior safety profiles. These nanoscale vesicles (30-150 nm) mediate intercellular communication by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating immune responses and promoting tissue repair [10] [11]. This application note details the comparative advantages of MSC-derived exosomes, with a specific focus on their low immunogenicity and tumorigenicity relative to cell-based therapies, providing essential guidance for researchers developing exosome-based wound therapeutics.
The therapeutic benefits of MSCs were originally attributed to their differentiation potential and engraftment capabilities. However, accumulating evidence indicates that most administered MSCs exhibit limited long-term survival in host tissues, suggesting their effects are predominantly mediated through paracrine signaling [12]. MSC-derived exosomes contain a complex cargo of growth factors, cytokines, and regulatory RNAs that can modulate inflammation, promote angiogenesis, and stimulate regeneration—key processes in wound healing—without the risks associated with whole-cell transplantation [13] [12]. This paradigm shift toward acellular therapies addresses critical safety concerns while maintaining therapeutic efficacy.
Comparative Safety Profiles: Exosomes Versus Cell-Based Therapies
Immunogenicity
A primary advantage of MSC-derived exosomes is their low immunogenicity, which enables allogeneic administration without provoking significant immune responses. Unlike whole MSCs, which express Major Histocompatibility Complex (MHC) molecules that can trigger immune recognition and rejection, exosomes have reduced immunostimulatory properties [14] [15]. This characteristic makes them suitable for off-the-shelf therapeutics that don't require patient matching.
- Immune Cell Modulation: MSC-derived exosomes modulate immune responses through multiple mechanisms, including promoting macrophage polarization toward anti-inflammatory M2 phenotypes, suppressing T-cell proliferation, and regulating dendritic cell maturation [10] [16]. These immunomodulatory effects are particularly beneficial in wound healing, where controlling excessive inflammation is crucial for optimal tissue repair.
- Composition Advantages: The lipid bilayer membrane of exosomes protects their cargo from degradation while minimizing immune activation. Their small size and lack of complete cellular machinery contribute to their stealth properties, allowing wider biodistribution and longer circulation times compared to cellular therapies [17] [11].
Tumorigenicity
The risk of tumor formation represents a significant concern with stem cell-based therapies, particularly those utilizing cells with high proliferative potential. MSC-derived exosomes address this concern through several inherent characteristics:
- Non-Replicative Nature: As acellular vesicles, exosomes cannot self-replicate or form teratomas, effectively eliminating the risk of uncontrolled growth associated with undifferentiated stem cells [14] [15]. This fundamental difference in biology provides a critical safety advantage for clinical applications.
- Regulatory Cargo: Exosomes derived from MSCs typically lack oncogenic factors and may even deliver tumor-suppressive molecules. Multiple studies have demonstrated that MSC-derived exosomes do not induce tumor formation in appropriate experimental models [11] [15]. However, researchers should note that exosome cargo can vary based on cell source and culture conditions, emphasizing the need for thorough characterization.
Table 1: Comparative Safety Profiles of MSC-Based Therapies
| Safety Parameter | Whole MSC Therapy | MSC-Derived Exosomes |
|---|---|---|
| Immunogenicity | Moderate to high; risk of immune rejection | Low; suitable for allogeneic use |
| Tumorigenic Potential | Low but documented risk of differentiation complications | Minimal; non-replicative vesicles |
| Infusion Toxicity | Risk of cell clumping and embolization | Reduced risk due to nanoscale size |
| Long-term Engraftment | Potential for unwanted differentiation | No engraftment risk |
| Storage Stability | Limited; requires cryopreservation | High stability; lyophilization possible |
Quantitative Assessment of Safety Parameters
Immunogenicity Metrics
Recent meta-analyses of preclinical studies provide compelling quantitative evidence supporting the low immunogenicity of MSC-derived exosomes. Systematic evaluation of multiple murine models reveals consistent patterns of immune tolerance:
- Cytokine Profile Modulation: Treatment with MSC-exosomes significantly reduces pro-inflammatory cytokines including TNF-α (SMD: -0.880; 95% CI: -1.623 to -0.136) and IL-17A (SMD: -2.390; 95% CI: -4.522 to -0.258) while elevating anti-inflammatory mediators such as IL-10 and TGF-β [14]. This immunomodulatory activity is particularly relevant for chronic wounds characterized by persistent inflammation.
- Dose-Response Relationship: Studies examining different administration routes have identified that nebulization therapy achieved therapeutic effects at approximately 10^8 particles, significantly lower than intravenous routes, demonstrating high bioavailability with minimal immune activation [9].
Tumorigenicity Assessment
Comprehensive analysis of tumor formation across animal studies and early-phase clinical trials confirms the favorable safety profile of MSC-derived exosomes:
- Zero Tumor Incidence: A review of 66 registered clinical trials involving MSC-EVs and Exos reported no cases of tumor formation directly attributable to exosome administration [9]. This finding is particularly significant given that many of these trials utilized allogeneic exosome sources without HLA matching.
- Long-term Safety: Follow-up studies in murine models extending to 6 months post-treatment have documented absent tumorigenicity even with repeated administrations of MSC-derived exosomes [14]. The non-replicative nature of exosomes provides a fundamental safety advantage over living cell therapies.
Table 2: Efficacy and Safety Outcomes of MSC-Exosomes in Preclinical Models
| Disease Model | Exosome Source | Dose Range | Immunogenicity Markers | Tumor Incidence |
|---|---|---|---|---|
| Psoriasis (IMQ-induced) | Human UCMSC | 1×10^8 particles | ↓ Epidermal thickness, ↓ TNF-α, ↓ IL-17A | 0/6 animals |
| Osteoarthritis | BMSC, ADSC, UCMSC | 50-1000 μg/mL | ↓ NF-κB, ↓ MAPK signaling | Not detected |
| Retinal Injury | BMSC | 50 μg/mL | ↓ Apoptotic cells, ↑ Cell viability | 0/5 donors |
| Myocardial Injury | iPSC | 10^10 particles | Improved function, ↓ Inflammation | Not reported |
Experimental Protocols for Safety Assessment
Protocol: Immunogenicity Assessment
Objective: To evaluate the immune response following administration of MSC-derived exosomes in a wound healing model.
Materials:
- MSC-derived exosomes (characterized per MISEV guidelines)
- Control articles (vehicle buffer, whole MSCs)
- Animal wound model (e.g., diabetic mouse excisional wound)
- Multiplex cytokine assay platform
- Flow cytometry equipment with immune cell markers
Procedure:
- Administration: Apply exosomes (10^8-10^10 particles/wound) topically to full-thickness wounds every 48 hours until closure.
- Sample Collection: At days 3, 7, and 14 post-wounding, collect:
- Wound tissue homogenates for cytokine analysis
- Peripheral blood for immune cell profiling
- Draining lymph nodes for lymphocyte activation assessment
- Cytokine Profiling: Quantify pro-inflammatory (TNF-α, IL-1β, IL-6, IL-17) and anti-inflammatory (IL-10, TGF-β) cytokines using multiplex immunoassay.
- Immune Cell Phenotyping: Analyze T-cell populations (CD4+, CD8+, Tregs), macrophage polarization (M1/M2 ratio), and dendritic cell activation markers by flow cytometry.
- Histological Assessment: Evaluate immune cell infiltration in wound sections using H&E staining and immunohistochemistry for CD45+ cells.
Acceptance Criteria: Exosome-treated groups should show significantly reduced pro-inflammatory cytokines and increased regulatory T-cell populations compared to MSC-treated groups while maintaining comparable wound closure rates.
Protocol: Tumorigenicity Assessment
Objective: To assess the potential for tumor formation following repeated administration of MSC-derived exosomes.
Materials:
- Test articles: MSC-derived exosomes from multiple donors
- Control articles: Vehicle buffer, pluripotent stem cell-derived exosomes
- Immunodeficient mouse model (e.g., NOD/SCID)
- In vivo imaging system (IVIS)
- Histopathology equipment
Procedure:
- Study Design: Randomize immunodeficient mice (n=10/group) to receive:
- Test article: MSC-derived exosomes (10^10 particles/dose)
- Negative control: Vehicle buffer
- Positive control: Pluripotent stem cell-derived exosomes
- Dosing Regimen: Administer test articles via subcutaneous injection adjacent to wound sites twice weekly for 8 weeks.
- In Vivo Monitoring:
- Weekly palpation for mass formation
- Biweekly IVIS imaging (if exosomes are labeled)
- Monthly body weight and clinical observations
- Terminal Assessment:
- Necropsy with gross examination of organs and injection sites
- Histopathological evaluation of all major organs and any suspicious masses
- Assessment of metastatic potential through lung and liver sections
- Cell Transformation Assay: Evaluate potential procarcinogenic effects using in vitro soft agar colony formation assays with recipient cells exposed to exosomes.
Acceptance Criteria: No gross or histological evidence of tumor formation at injection sites or distant organs in exosome-treated groups beyond background levels observed in negative controls.
Signaling Pathways in Exosome-Mediated Safety and Efficacy
The therapeutic effects and safety profile of MSC-derived exosomes are mediated through specific signaling pathways that modulate cellular responses without inducing excessive immune activation or proliferation.
Pathway Analysis:
- NF-κB and MAPK Suppression: MSC-derived exosomes significantly reduce phosphorylation of p65 (pp65) and MAPK pathway components (p38, JNK, ERK) compared to IL-1β-stimulated controls, attenuating inflammatory signaling without complete pathway inhibition [10]. This balanced modulation is critical for controlling excessive inflammation in chronic wounds while maintaining essential immune functions.
- Immunomodulatory Cargo: Exosomes from umbilical cord and bone marrow MSCs demonstrate superior efficacy in delivering anti-inflammatory miRNAs (e.g., miR-146a-5p, miR-150-5p) that target key pro-inflammatory mediators while avoiding complete immune suppression [10] [11]. This targeted approach reduces immunogenicity while preserving host defense mechanisms.
- Proliferation Regulation: Unlike whole MSCs that retain proliferative capacity, exosomes transfer regulatory RNAs that modulate cell cycle progression without driving uncontrolled division. Studies confirm that exosome-treated cells maintain normal contact inhibition and do not form colonies in soft agar assays [14] [15].
Research Reagent Solutions for Exosome Studies
Table 3: Essential Research Reagents for MSC-Exosome Wound Therapy Studies
| Reagent Category | Specific Examples | Research Application | Safety Assessment Utility |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, miRCURY Exosome Kit | Rapid exosome purification | Standardized yield for dosing |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-CD9, Anti-Alix, Anti-Calnexin | Exosome identification and purity assessment | Confirmation of minimal cellular contaminants |
| Nanoparticle Tracking | ZetaView PMX 110, NanoSight NS300 | Size distribution and concentration analysis | Batch-to-batch consistency |
| Cytokine Arrays | Proteome Profiler Array, Luminex Assays | Inflammatory mediator profiling | Immunogenicity potential |
| Cell Fate Assays | Annexin V Apoptosis Kit, CellTiter-Glo Viability | Functional response assessment | Tumorigenicity screening |
MSC-derived exosomes represent a transformative approach in regenerative medicine, offering significant advantages in safety profiles and manufacturing control compared to traditional cell-based therapies. Their inherently low immunogenicity and tumorigenicity, combined with demonstrated efficacy in modulating key wound healing processes, position them as ideal candidates for next-generation wound therapeutics. The experimental frameworks and safety assessment protocols outlined in this document provide researchers with standardized methodologies for advancing exosome-based wound therapy development.
As the field progresses toward clinical translation, attention to standardized characterization, potency assays, and scalable manufacturing will be essential for realizing the full potential of these promising acellular therapeutics. Future research directions should focus on engineering approaches to enhance target specificity and therapeutic payload, further improving the already favorable benefit-risk profile of MSC-derived exosomes in wound healing applications.
Application Notes: Comparative Therapeutic Profiles
The therapeutic efficacy of mesenchymal stem cell-derived exosomes (MSC-Exos) in wound healing exhibits significant source-dependent variability, influencing their mechanistic actions and clinical applicability. The table below summarizes the comparative therapeutic profiles of exosomes derived from adipose tissue (ADSC-Exos), bone marrow (BMSC-Exos), and umbilical cord (UCMSC-Exos).
Table 1: Comparative Analysis of MSC-Exos from Different Sources
| Parameter | Adipose (ADSC-Exos) | Bone Marrow (BMSC-Exos) | Umbilical Cord (UCMSC-Exos) |
|---|---|---|---|
| Key Therapeutic Strengths | Potent immunomodulation; Enhanced angiogenesis; Superior collagen deposition [18] [19] [20]. | Effective neuroprotection; Cartilage/bone repair; Established research history [16]. | Superior proliferation & migration; High angiogenic capacity; Low immunogenicity [21] [14]. |
| Proposed Primary Mechanisms in Wound Healing | Deliver anti-inflammatory miRNAs (e.g., miR-126); Promote M2 macrophage polarization; Activate PI3K/Akt pathway [18] [19]. | Inhibit TGF-β/Smad pathway to reduce scarring; Modulate inflammatory response [21]. | Enrich specific miRNAs to inhibit TGF-β/Smad; Promote fibroblast functions & tube formation [21]. |
| Evidence Level (Wound Healing) | Extensive preclinical data; Prominent in meta-analyses [20]. | Strong preclinical evidence [20]. | Strong preclinical evidence; Promising clinical data [21]. |
| Considerations for Dosing & Administration | High yield facilitates frequent/repeated dosing [19]. | Well-established isolation protocols [16]. | High proliferative capacity ensures exosome supply; Often used allogeneically [21] [16]. |
Experimental Protocols
Protocol: Isolation and Characterization of MSC-Exos
This standard protocol for isolating exosomes from MSC culture supernatant via ultracentrifugation is adapted from multiple methodologies detailed in the search results [21] [14] [22].
Key Research Reagent Solutions:
- Mesenchymal Stem Cells: Source from adipose tissue, bone marrow, or umbilical cord, characterized per ISCT guidelines (plastic adherence, trilineage differentiation, surface marker expression) [16] [20].
- Culture Medium: Use MSC NutriStem XF Basal Medium supplemented with human platelet lysate or other serum-free, exosome-depleted media to avoid contaminating vesicles [21].
- Isolation Reagents: Phosphate-Buffered Saline (PBS), sterile and pre-cooled for dilution and resuspension steps.
- Characterization Reagents:
Procedure:
- Cell Culture and Supernatant Collection: Culture MSCs until 80% confluency. Replace with fresh culture medium. After 48-72 hours, collect the conditioned medium.
- Pre-Clearing Centrifugation:
- Centrifuge the medium at 2,000 × g for 30 minutes at 4°C to remove cells and large debris.
- Transfer the supernatant to a new tube and centrifuge at 10,000 × g for 45 minutes at 4°C to remove apoptotic bodies and larger vesicles.
- Carefully filter the supernatant through a 0.22 µm pore filter to sterilize and remove remaining particulates.
- Ultracentrifugation:
- Transfer the filtered supernatant to ultracentrifuge tubes. Balance tubes precisely.
- Perform ultracentrifugation at 110,000 × g to 120,000 × g for 70-90 minutes at 4°C.
- Discard the supernatant carefully. The exosome pellet may not always be visible.
- Resuspend the pellet in a large volume of PBS (e.g., 30-35 mL) and perform a second ultracentrifugation under the same conditions to wash the exosomes.
- Discard the supernatant and resuspend the final, purified exosome pellet in 100-500 µL of PBS.
- Characterization:
- Nanoparticle Tracking Analysis (NTA): Dilute the exosome suspension and inject it into the NTA system to determine particle size distribution (expected peak ~30-150 nm) and concentration [21] [14].
- Transmission Electron Microscopy (TEM): Fix a small volume of exosomes on a grid, negative stain with uranyl acetate, and image to confirm a cup-shaped spherical morphology with a size of approximately 30-150 nm [21] [14].
- Western Blotting: Lyse exosomes and analyze proteins for the presence of positive markers (e.g., CD9, CD63, TSG101, Alix) and the absence of the negative endoplasmic reticulum marker Calnexin [14].
Protocol: In Vivo Assessment of MSC-Exos in a Murine Wound Healing Model
This protocol outlines the methodology for evaluating the efficacy of MSC-Exos using a full-thickness excisional wound model in mice, as commonly employed in the cited studies [14] [20] [22].
Procedure:
- Animal Model Preparation:
- Use 6-8 week-old male BALB/c mice. Anesthetize the animals according to approved institutional protocols.
- Create one or more full-thickness excisional wounds on the dorsum using a sterile biopsy punch. The wound area should be recorded (e.g., by photography) immediately post-creation (Day 0).
- Treatment Administration:
- Randomly assign mice to experimental groups: Vehicle Control (e.g., PBS), and treatment groups (e.g., ADSC-Exos, UCMSC-Exos).
- The primary and most effective route for wound healing is local subcutaneous injection around the wound periphery [20].
- A common effective dose, based on particle count, is 1 × 10^8 particles in a volume of 25-50 µL PBS per wound, administered daily or every other day [14] [22]. Dosing frequency and total number of administrations should be optimized based on the study design.
- Efficacy Monitoring:
- Wound Closure Rate: Monitor and photograph wounds daily. Use image analysis software (e.g., ImageJ) to calculate the percentage reduction in wound area over time.
- Histological Analysis: After euthanasia at a predetermined endpoint (e.g., Day 7-14), harvest wound tissue.
- Fix samples in formalin, embed in paraffin, and section.
- Perform Hematoxylin and Eosin (H&E) staining to evaluate tissue architecture, epidermal thickness, and re-epithelialization.
- Perform Masson's Trichrome staining to assess collagen deposition, organization, and scar width.
- Immunohistochemistry/Immunofluorescence: Stain tissue sections with antibodies against specific markers to evaluate key processes.
- CD31: To quantify blood vessel density and angiogenesis.
- α-Smooth Muscle Actin (α-SMA): To identify myofibroblasts and assess scar formation.
Signaling Pathways in MSC-Exos Mediated Wound Healing
MSC-Exos from different sources promote wound healing through complex, interconnected signaling pathways, primarily driven by their cargo of miRNAs, proteins, and cytokines.
The Scientist's Toolkit: Essential Materials for MSC-Exos Wound Healing Research
Table 2: Key Research Reagents and Equipment
| Item | Function/Application | Examples/Notes |
|---|---|---|
| Ultracentrifuge | Isolation of exosomes from conditioned media or biofluids via high-speed centrifugation. | Beckman Coulter Optima series with fixed-angle rotors (e.g., Type 50.2 Ti) [14]. |
| Nanoparticle Tracking Analyzer (NTA) | Measures the size distribution and concentration of exosomes in suspension. | ZetaView PMX 110 system (Particle Metrix); Malvern Panalytical NanoSight [21] [14]. |
| Transmission Electron Microscope (TEM) | Visualizes the morphology and ultrastructure of isolated exosomes. | Hitachi HT-7700; samples are negative-stained with uranyl acetate [21] [14]. |
| Specific Antibodies | Characterizes exosomes and analyzes tissue response via Western Blot (WB) and Immunohistochemistry (IHC). | WB: Anti-CD9, CD63, TSG101, Alix, Calnexin (negative control) [14]. IHC/IF: Anti-CD31 (vessels), α-SMA (myofibroblasts) [22]. |
| PKH67 / PKH26 Fluorescent Dyes | Labels the lipid membrane of exosomes for in vitro and in vivo tracking and uptake studies. | Labeled exosomes can be visualized after co-culture with cells (e.g., fibroblasts) to confirm internalization [22]. |
| Animal Model | In vivo testing of exosome therapeutic efficacy. | BALB/c or C57BL/6 mice; full-thickness excisional wound model is standard [20] [22]. |
Application Notes: Core Biological Functions and Therapeutic Mechanisms
Mesenchymal stem cell-derived exosomes (MSC-Exos) are nanoscale extracellular vesicles (30-150 nm in diameter) that serve as primary mediators of the therapeutic effects of their parent cells [23]. They function as sophisticated natural delivery systems, transferring bioactive cargo—including proteins, lipids, mRNAs, and microRNAs (miRNAs)—to recipient cells, thereby orchestrating key processes in tissue repair [23] [24]. Their cell-free nature confers significant advantages, including lower immunogenicity, a high safety profile, and the ability to avoid entrapment in lung microvasculature, which poses a risk when administering whole cells [23] [25]. The following sections detail the mechanistic basis of their three core inherent biological functions.
Immunomodulation
MSC-Exos exert profound immunomodulatory effects by interacting with a wide array of immune cells, facilitating a shift from a pro-inflammatory to an anti-inflammatory and pro-healing state [24]. This immunomodulation is a cornerstone of their effectiveness in treating inflammatory conditions and creating a conducive environment for tissue regeneration.
Key Mechanisms:
- Macrophage Polarization: MSC-Exos promote the polarization of macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype [24]. This shift is mediated through the delivery of specific miRNAs (e.g., let-7b, miR-146a, miR-181c) and bioactive proteins like Prostaglandin E2 (PGE2) and TNF-stimulated gene 6 (TSG-6) [24]. M2 macrophages subsequently secrete immunosuppressive factors such as IL-10 while reducing levels of pro-inflammatory cytokines like TNF-α, IL-1β, IL-12, IL-6, and IFN-γ [24].
- Lymphocyte Regulation: MSC-Exos modulate adaptive immune responses by suppressing the proliferation and activation of pro-inflammatory T cells (e.g., Th1 and Th17) and promoting the expansion and function of regulatory T cells (Tregs) [24]. This regulation helps restore immune homeostasis and dampens excessive immune reactions that can impede healing [26].
- Anti-inflammatory Signaling: The cargo within MSC-Exos, including miR-21, miR-146a, and miR-182, can inhibit key pro-inflammatory signaling pathways, such as the Toll-like Receptor (TLR) and NF-κB pathways, further contributing to inflammation resolution [24].
Angiogenesis
The promotion of new blood vessel formation is critical for supplying oxygen and nutrients to regenerating tissue. MSC-Exos robustly stimulate angiogenesis through the delivery of pro-angiogenic factors and genetic materials [27] [26].
Key Mechanisms:
- Growth Factor and miRNA Delivery: MSC-Exos are enriched with pro-angiogenic factors such as Vascular Endothelial Growth Factor (VEGF), Hepatocyte Growth Factor (HGF), and Insulin-like Growth Factor-1 (IGF-1) [26]. They also carry specific miRNAs (e.g., miR-126, miR-130a, miR-132) that are known to enhance angiogenic signaling [26].
- Activation of Signaling Pathways: A principal mechanism involves the transfer of Wnt4 to endothelial cells, which stimulates the Wnt/β-catenin signaling pathway [26]. This, in turn, activates the AKT pathway, promoting endothelial cell proliferation, migration, and survival, and ultimately leading to the formation of new vascular structures [26].
- Direct Pro-angiogenic Effect: The exosomal cargo directly targets endothelial cells, encouraging tube formation and enhancing cell-to-cell communication, which is vital for establishing a functional vascular network in the wound bed [27].
Fibroblast Activation
Fibroblasts are the primary cells responsible for depositing the extracellular matrix (ECM) that forms the structural basis of new tissue. MSC-Exos directly activate fibroblasts, driving the proliferative phase of wound healing [26].
Key Mechanisms:
- Proliferation and Migration Stimulation: MSC-Exos enhance fibroblast proliferation and migration by upregulating the expression of genes and proteins critical for cell division and motility, including N-cadherin, cyclin-1, and Proliferating Cell Nuclear Antigen (PCNA) [26].
- Collagen Synthesis: Treatment with MSC-Exos leads to a significant increase in the production of Collagen I and Collagen III, the main structural components of the ECM, thereby improving the tensile strength of the healing wound [26].
- Pathway Activation: The therapeutic effects on fibroblasts are mediated through the activation of key signaling pathways, including ERK and AKT, which are stimulated by exosomal components [26].
Table 1: Summary of Key Molecular Mediators in MSC-Exos Functions
| Biological Function | Key Molecular Mediators | Primary Effects |
|---|---|---|
| Immunomodulation | let-7b, miR-146a, PGE2, TSG-6, IL-10 | Macrophage polarization to M2; Treg induction; Suppression of TNF-α & IL-1β [24] |
| Angiogenesis | Wnt4, miR-126, miR-130a, VEGF, HGF | Activation of Wnt/β-catenin & AKT pathways; Endothelial cell proliferation [27] [26] |
| Fibroblast Activation | PCNA, N-cadherin, Collagen I, Collagen III | Enhanced fibroblast proliferation, migration, and ECM synthesis [26] |
Experimental Protocols for Validating Biological Functions
To empirically validate the inherent functions of MSC-Exos, standardized in vitro and in vivo protocols are essential. The following sections provide detailed methodologies for assessing immunomodulation, angiogenesis, and fibroblast activation.
Protocol: In Vitro Assessment of Macrophage Polarization
This protocol evaluates the immunomodulatory capacity of MSC-Exos by measuring their ability to induce a shift from M1 to M2 macrophages [24].
Research Reagent Solutions:
- Primary Human Monocytes: Source cells for deriving macrophages.
- MSC-Exos Preparation: Isolated from human bone marrow or adipose tissue-derived MSCs (100 µg/mL stock concentration).
- LPS & IFN-γ: For M1 macrophage polarization (e.g., 100 ng/mL LPS + 20 ng/mL IFN-γ).
- IL-4 & IL-13: For classical M2 macrophage polarization (positive control).
- Flow Cytometry Antibodies: Anti-CD86 (M1 marker) and Anti-CD206 (M2 marker).
- ELISA Kits: For quantifying TNF-α (pro-inflammatory) and IL-10 (anti-inflammatory) cytokines.
Procedure:
- Macrophage Differentiation: Isolate peripheral blood mononuclear cells (PBMCs) from human blood. Differentiate monocytes into naïve macrophages (M0) by culturing in RPMI-1640 medium supplemented with 50 ng/mL Macrophage Colony-Stimulating Factor (M-CSF) for 6 days.
- M1 Polarization: Polarize the M0 macrophages towards an M1 phenotype by treating with 100 ng/mL LPS and 20 ng/mL IFN-γ for 48 hours.
- Exosome Treatment: Divide the M1-polarized macrophages into three groups:
- Test Group: Treat with MSC-Exos (50 µg/mL).
- Positive Control: Treat with 20 ng/mL IL-4 and IL-13.
- Negative Control: Treat with PBS. Incubate for 48 hours.
- Flow Cytometry Analysis: Harvest the macrophages. Stain cells with fluorescently labeled anti-CD86 and anti-CD206 antibodies. Analyze using flow cytometry to determine the percentage of CD86+ (M1) and CD206+ (M2) populations.
- Cytokine Secretion Profiling: Collect cell culture supernatants. Use ELISA kits to quantify the secretion levels of TNF-α and IL-10, following the manufacturer's instructions.
- Data Interpretation: Successful immunomodulation is indicated by a statistically significant decrease in CD86+ cells and TNF-α secretion, coupled with an increase in CD206+ cells and IL-10 secretion in the test group compared to the negative control.
Protocol: In Vitro Tubule Formation Assay (Angiogenesis)
This protocol assesses the pro-angiogenic potential of MSC-Exos by measuring their ability to stimulate human umbilical vein endothelial cells (HUVECs) to form capillary-like tubule structures in vitro [27].
Research Reagent Solutions:
- HUVECs: Primary human umbilical vein endothelial cells (passage 3-5).
- Growth Factor-Reduced Matrigel: Extracellular matrix substitute for tubule formation.
- MSC-Exos Preparation: As per Protocol 2.1.
- VEGF: Positive control (e.g., 50 ng/mL).
- Microscope with Image Analysis Software: For quantifying tubule formation.
Procedure:
- Matrigel Coating: Thaw Growth Factor-Reduced Matrigel on ice. Coat each well of a pre-chilled 96-well plate with 50 µL of Matrigel. Incubate the plate at 37°C for 30-60 minutes to allow polymerization.
- Cell Seeding and Treatment: Trypsinize and harvest HUVECs. Resuspend cells in serum-free medium and seed onto the polymerized Matrigel at a density of 1.5 x 10^4 cells per well.
Immediately add treatments to the wells:
- Test Group: Serum-free medium containing MSC-Exos (50 µg/mL).
- Positive Control: Serum-free medium containing 50 ng/mL VEGF.
- Negative Control: Serum-free medium only.
- Incubation: Incubate the plate at 37°C with 5% CO2 for 6-8 hours to allow tubule networks to form.
- Image Acquisition and Analysis: After incubation, capture images of the tubule networks using an inverted microscope (4x or 10x objective) in at least three random fields per well.
Use image analysis software (e.g., ImageJ with the Angiogenesis Analyzer plugin) to quantify the following parameters:
- Total Tubule Length: The combined length of all formed tubules.
- Number of Junctions: The number of branch points in the network.
- Number of Meshes: The number of enclosed areas within the network.
- Data Interpretation: A significant increase in total tubule length, number of junctions, and number of meshes in the MSC-Exos-treated group compared to the negative control indicates potent pro-angiogenic activity.
Protocol: In Vitro Fibroblast Proliferation and Migration (Scratch Assay)
This protocol evaluates the effect of MSC-Exos on the proliferative and migratory capacity of human dermal fibroblasts, which are critical for wound closure and ECM deposition [26].
Research Reagent Solutions:
- Human Dermal Fibroblasts (HDFs): Primary cells (passage 3-7).
- MSC-Exos Preparation: As per Protocol 2.1.
- Mitomycin C: (e.g., 10 µg/mL) to inhibit cell proliferation for migration-specific assays (optional).
- Cell Culture Inserts: For a standardized scratch (optional).
- Image Analysis Software.
Procedure:
- Cell Seeding: Seed HDFs in a 12-well plate at a high density (e.g., 2.5 x 10^5 cells/well) and culture until they form a 100% confluent monolayer.
- Creating a "Scratch": Use a sterile 200 µL pipette tip to create a straight, vertical scratch ("wound") through the cell monolayer. Gently wash the wells with PBS to remove detached cells. Alternatively, use a culture-insert to create a uniform gap.
- Exosome Treatment: Add serum-free medium containing MSC-Exos (50 µg/mL) to the test group. The control group receives serum-free medium only. To isolate the effect on migration from proliferation, pre-treat cells with 10 µg/mL Mitomycin C for 2 hours before creating the scratch.
- Image Acquisition: Immediately after creating the scratch (T=0h), capture images of the wound area using an inverted microscope (4x objective). Mark the plate to ensure imaging of the same locations at later time points.
- Incubation and Final Imaging: Incubate the plate for 24-48 hours. Capture images of the same locations at the end of the incubation period (T=24h or 48h).
- Wound Closure Analysis: Measure the width of the scratch at T=0h and T=24/48h using image analysis software. Calculate the percentage of wound closure using the formula:
% Wound Closure = [(Area T=0 - Area T=24) / Area T=0] x 100 - Data Interpretation: A significantly higher percentage of wound closure in the MSC-Exos-treated group compared to the control group indicates enhanced fibroblast migration and/or proliferation.
Table 2: Summary of Key Experimental Parameters for Functional Assays
| Assay | Cell Type | MSC-Exos Dose | Key Readouts | Critical Reagents |
|---|---|---|---|---|
| Macrophage Polarization | Human monocyte-derived macrophages | 50 µg/mL | CD86+/CD206+ ratio; TNF-α/IL-10 secretion [24] | M-CSF, LPS, IFN-γ, IL-4/IL-13 |
| Tubule Formation | HUVECs (Passage 3-5) | 50 µg/mL | Total tubule length; Number of junctions [27] | Growth Factor-Reduced Matrigel, VEGF |
| Scratch Assay | Human Dermal Fibroblasts | 50 µg/mL | Percentage of wound closure at 24h [26] | Mitomycin C (optional) |
Visualization of Signaling Pathways and Experimental Workflows
MSC Exosome Mediated Immunomodulation Pathway
MSC Exosome Mediated Angiogenesis Pathway
Experimental Workflow for Functional Validation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for MSC-Exos Functional Studies
| Reagent / Material | Function / Application | Example Usage in Protocols |
|---|---|---|
| Bone Marrow or Adipose-derived MSCs | Cellular source for exosome production and isolation [16] [20]. | Culture and expand MSCs to ~80% confluency for exosome collection. |
| Ultracentrifugation System | Gold-standard method for isolating and purifying exosomes from conditioned medium [23]. | Pellet exosomes at 100,000-120,000 x g for 70-120 minutes. |
| Nanoparticle Tracking Analysis (NTA) | Characterizes exosome size distribution and concentration [23] [24]. | Dilute exosome sample in PBS and analyze to confirm a size peak of 30-150 nm. |
| CD63, CD81, TSG101 Antibodies | Western Blot detection of positive exosomal protein markers for validation [25] [24]. | Confirm exosome identity post-isolation via immunoblotting. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | In vitro model for studying exosome-induced angiogenesis [27]. | Seed on Matrigel for tubule formation assay (Protocol 2.2). |
| Growth Factor-Reduced Matrigel | Synthetic basement membrane matrix for 3D tubule formation assays [27]. | Coat wells and allow to polymerize for HUVEC seeding. |
| Human Dermal Fibroblasts (HDFs) | In vitro model for studying exosome effects on proliferation, migration, and ECM production [26]. | Create a confluent monolayer for the scratch/wound healing assay. |
| Flow Cytometry Antibodies (CD86, CD206) | Quantification of macrophage surface markers to determine M1/M2 polarization status [24]. | Stain and analyze macrophages after exosome treatment (Protocol 2.1). |
| ELISA Kits (TNF-α, IL-10, etc.) | Quantification of secreted pro- and anti-inflammatory cytokines in cell culture supernatants [25] [24]. | Measure cytokine levels from macrophage culture media. |
From Production to Patient: MSC Exosome Isolation, Characterization, and Delivery Methods
Within advanced therapeutic medicinal products, mesenchymal stem cell (MSC)-derived exosomes represent a promising cell-free therapeutic paradigm, particularly for wound therapy. A pivotal challenge in translating this promise into clinical reality is the establishment of robust, reproducible, and scalable Good Manufacturing Practice (GMP)-grade production processes. The quality, safety, and efficacy of the final exosome product are profoundly influenced by the upstream isolation and downstream purification strategies employed. This application note details standardized protocols for three cornerstone technologies—Ultracentrifugation, Tangential Flow Filtration (TFF), and Chromatography—framed within the specific context of producing MSC exosomes for wound healing research and development. Adherence to these GMP-compliant methodologies ensures the consistent production of exosomes with defined characteristics, which is a critical prerequisite for meaningful investigation into optimal dosing and administration routes.
Ultracentrifugation for Exosome Isolation
Ultracentrifugation remains a widely used benchmark technique for the isolation of exosomes from conditioned cell culture media. Its principle relies on the sequential application of centrifugal forces to separate particles based on their size, density, and shape.
Application Notes and Protocol
Differential ultracentrifugation is the most common approach, though it requires specialized equipment and can subject exosomes to high shear forces [28]. The following protocol is adapted for GMP-compliant production of MSC exosomes.
Detailed Experimental Protocol:
- Conditioned Media Harvesting: Collect conditioned media from serum-free cultures of MSCs (e.g., bone marrow, adipose, or umbilical cord-derived). Centrifuge at 300 × g for 10 minutes to remove live cells.
- Cellular Debris Removal: Transfer the supernatant to new tubes and centrifuge at 2,000 × g for 20 minutes to eliminate dead cells.
- Large Particle Clearance: Further clarify the supernatant by centrifugation at 10,000 × * g for 30 minutes to remove large vesicles and apoptotic bodies.
- Exosome Pelletion: Transfer the resulting supernatant to ultracentrifuge tubes. Pellet the exosomes via ultracentrifugation at ≥100,000 × g for 70 minutes at 4°C.
- Washing (Optional): Resuspend the pellet in a large volume of sterile, cold phosphate-buffered saline (PBS) and repeat the ultracentrifugation step (100,000 × g, 70 minutes) to enhance purity.
- Final Resuspension: Gently resuspend the final exosome pellet in a small volume of PBS or a formulation buffer suitable for wound therapy applications (e.g., containing cryoprotectants). Aliquot and store at –65°C to –85°C [29].
Table 1: Quantitative Parameters for Ultracentrifugation-Based Exosome Isolation
| Parameter | Typical Value/Description | GMP Consideration |
|---|---|---|
| Starting Material | Serum-free MSC conditioned media | Use of GMP-grade cell lines and media components is mandatory [29]. |
| G-Force for Exosome Pellet | ≥100,000 × g | Equipment must be validated and undergo regular calibration [30]. |
| Duration | 70-120 minutes | Process parameters must be fixed and documented in batch records. |
| Yield | Variable; highly dependent on MSC source and culture | In-process controls to monitor consistency between batches. |
| Purity | Moderate to high; potential for co-precipitation of proteins | Orthogonal characterization (e.g., NTA, CD63/81 detection) required for release [29]. |
GMP Data Integrity and Software
For AUC, which is used for the biophysical characterization of isolated exosomes, GMP compliance requires specialized software to address data integrity. Modern solutions like UltraScan GMP software provide automated workflows, role-based user management, electronic signatures, and comprehensive audit trails, which are essential for regulatory compliance and moving AUC towards full GMP validation [31] [32].
Tangential Flow Filtration for Scalable Purification
Tangential Flow Filtration (TFF) is a scalable and gentle separation technique ideal for processing large volumes of conditioned media. In TFF, the feed flow moves parallel to the filter membrane, continuously sweeping away retained particles and minimizing membrane fouling, making it suitable for concentrating and purifying exosomes.
Application Notes and Protocol
TFF is highly advantageous for GMP manufacturing as it can be integrated into a fully closed system, reducing contamination risk and facilitating scale-up for clinical trial material production [29]. Its market growth, with a projected CAGR of 12.13%-12.44%, underscores its adoption in bioprocessing [33] [34].
Detailed Experimental Protocol:
- System Setup and Equilibration: Assemble a single-use TFF system with a membrane pore size of 300-500 kDa or 0.1 µm. Flush and equilibrate the system with PBS or a suitable buffer.
- Clarified Media Processing: Pump the clarified conditioned media (pre-cleared by steps 1-3 in 1.1) through the TFF system. The exosomes are retained (retentate) while small molecules and contaminants pass through the membrane (permeate).
- Diafiltration: Continuously add diafiltration buffer (e.g., PBS) to the retentate at the same rate as the permeate flow. This step exchanges the solution and removes soluble impurities. Typically, 5-10 volume exchanges are performed.
- Concentration: Once diafiltration is complete, stop the buffer input and continue circulating the retentate until the desired exosome concentration is achieved.
- Product Recovery: Recirculate the retentate briefly in the reverse direction or use a flush to recover the concentrated exosome product from the system.
- Sterile Filtration: The final concentrate is passed through a 0.22 µm sterile filter into a sterile bag. The product is aliquoted and stored at –65°C to –85°C [29].
Table 2: Quantitative Parameters for TFF-Based Exosome Purification
| Parameter | Typical Value/Description | GMP Consideration |
|---|---|---|
| Membrane Material | Polyethersulfone (PES), Regenerated Cellulose | Use of GMP-grade, single-use membranes to prevent cross-contamination [33] [29]. |
| Pore Size / MWCO | 300-500 kDa or 0.1 µm | Membrane selection validation is critical for yield and purity. |
| Volume Reduction | 10- to 50-fold concentration | Process consistency must be demonstrated across batches. |
| Diafiltration Volumes | 5-10 volumes | Ensures effective removal of process-related impurities. |
| Scale | From 100 mL to >100 L | A closed-system design supports scalable, aseptic processing [29]. |
Chromatography for High-Purity Exosome Preparation
Chromatography offers high-resolution purification of exosomes based on intrinsic properties such as size, charge, or affinity, and is invaluable for obtaining a highly pure product for therapeutic use.
Application Notes and Protocol
Among various modes, Anion Exchange Chromatography (AEC) is particularly effective, exploiting the inherent negative surface charge of exosomes. This method can be combined with TFF or ultrafiltration to create a powerful two-dimensional purification strategy [28].
Detailed Experimental Protocol:
- Sample Preparation: The exosome sample, preferably pre-concentrated using TFF or ultrafiltration, is diluted with a binding buffer (e.g., 20-50 mM Tris-HCl, pH ~8.0) to ensure a low ionic strength.
- Column Equilibration: Equilibrate an AEC column (e.g., quaternary amine resin) with 5-10 column volumes (CV) of binding buffer.
- Sample Loading: Load the prepared exosome sample onto the column at a controlled flow rate. Exosomes bind to the positively charged resin.
- Washing: Wash the column with 5-10 CV of binding buffer to remove unbound or weakly bound contaminants.
- Elution: Elute the purified exosomes using a linear or step-wise gradient of elution buffer (binding buffer with increasing NaCl concentration, typically up to 1-2 M). Exosomes typically elute at specific salt concentrations.
- Fraction Collection & Buffer Exchange: Collect the eluate in fractions. Pool the fractions containing exosomes and perform a buffer exchange into a storage buffer like PBS using TFF or size-exclusion chromatography.
Table 3: Quantitative Parameters for AEC-Based Exosome Purification
| Parameter | Typical Value/Description | GMP Consideration |
|---|---|---|
| Chromatography Type | Anion Exchange (AEC) | Columns and resins must be GMP-grade. Lifecycle and cleaning validation are required [30]. |
| Binding Buffer | Low salt buffer (e.g., 20 mM Tris, pH 8.0) | All reagents require certificates of analysis (CoA) [29]. |
| Elution Method | Linear NaCl gradient (e.g., 0 to 2 M) | Method robustness and reproducibility must be established. |
| Yield | Can be lower than TFF but offers higher purity | Balance between yield and purity is a key process decision. |
| Purity | Very high, separation from protein aggregates | Excellent for removing co-isolated impurities from other methods. |
Integrated Workflow and Dosing Considerations for Wound Therapy
For clinical translation, these techniques are often combined into an integrated, closed-system workflow to maximize product yield, purity, and safety.
Workflow Diagram
This integrated process ensures a consistent and well-characterized exosome product, which is the foundation for reliable dosing studies.
Dosing and Administration in Wound Therapy
The production process directly influences the critical quality attributes (CQAs) of the exosome product, which in turn impacts therapeutic dosing. Research indicates that administration route is a key determinant of the effective dose. For instance, topical application for wound healing may require different dosing compared to intravenous routes. Clinical trials for MSC-EVs have shown that aerosolized inhalation can achieve therapeutic effects at doses around 10⁸ particles, which is significantly lower than doses required for intravenous infusion [9]. This highlights the importance of standardizing dose units (e.g., particle number, protein content) and developing potency assays linked to the wound healing mechanism (e.g., angiogenesis, fibroblast proliferation) [9] [29].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents essential for implementing the GMP-grade protocols described above.
Table 4: Essential Materials for GMP-Grade MSC Exosome Production
| Item | Function / Role | GMP-Grade Consideration |
|---|---|---|
| GMP-Grade MSC Cell Bank | Source and starting material for exosome production. | Well-defined, characterized, and tested for adventitious agents to ensure batch-to-b consistency [29]. |
| Chemically Defined, Serum-Free Media | Supports MSC expansion and vesiculation without introducing foreign contaminants. | Eliminates variability and safety risks associated with animal sera; requires CoA [29]. |
| Single-Use TFF Cassettes | For concentration and purification of exosomes from large volumes of media. | Prevents cross-contamination, reduces cleaning validation, and supports a closed system [33] [29]. |
| Chromatography Resins & Columns | High-resolution purification based on charge (AEC) or other properties. | Must be qualified for intended use. Documentation for traceability and leachables testing is critical [30]. |
| Reference Standards & Buffers | Used in system suitability testing, calibration, and as process buffers. | All reagents must have Certificates of Analysis (CoA) confirming identity, purity, and strength [29] [30]. |
| Nanoparticle Tracking Analysis (NTA) | Instrument for characterizing particle size and concentration. | Part of quality control for identity and quantity; requires regular calibration and method validation [9] [29]. |
| ELISA/Ligand Blinding Assays | Detection of specific surface markers (e.g., CD9, CD63, CD81). | Used as a purity and identity test; assays must be validated for accuracy, precision, and specificity [29]. |
For researchers and drug development professionals advancing mesenchymal stem cell exosome (MSC-exosome) wound therapies, standardized characterization is not merely a preliminary step but the fundamental basis for generating reproducible, reliable, and clinically translatable data. The inherent heterogeneity of extracellular vesicle (EV) preparations, including exosomes, presents a significant challenge in correlating therapeutic efficacy with specific biological entities [9] [28]. The Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines, established by the International Society for Extracellular Vesicles (ISEV), provide a critical framework to overcome this challenge by defining the minimal biochemical, biophysical, and functional criteria required to robustly claim the presence of EVs in isolates [35] [36]. Adherence to these guidelines is particularly crucial in the context of wound therapy research, where understanding the relationship between exosome characteristics, dosing parameters, and mechanisms of action—such as promoting angiogenesis, modulating inflammation, and enhancing fibroblast proliferation—is essential for developing effective treatments [37] [13].
This application note details practical protocols for characterizing MSC-exosomes according to MISEV principles, with a specific focus on nanoparticle tracking analysis (NTA) and surface marker characterization—two core techniques mandated for establishing vesicle identity, quantity, and purity. Furthermore, it contextualizes these characterization data within the broader scope of optimizing dosing and administration routes for cutaneous wound healing applications.
Core Principles of the MISEV Guidelines
The MISEV guidelines have evolved through several iterations (MISEV2014, MISEV2018, and the latest MISEV2023) to address the growing complexity and methodological diversity in EV research [36]. The fundamental principle underpinning these guidelines is the need for comprehensive reporting of experimental conditions, from sample collection and pre-processing through to separation, concentration, and characterization [36]. For MSC-exosomes intended for wound healing, this begins with detailed documentation of the parental cell source (e.g., bone marrow, adipose tissue, umbilical cord), culture conditions, and the methods used to harvest the cell culture medium [9] [16].
MISEV2023 recommends a multifaceted approach to characterization, requiring researchers to:
- Define the presence of EVs by quantifying transmembrane or GPI-anchored proteins (Category 1, e.g., tetraspanins CD63, CD81, CD9) and cytosolic proteins (Category 2, e.g., TSG101, flotillins) [35] [36].
- Assess sample purity by testing for common co-isolated contaminants (Category 3), such as apolipoproteins in blood-derived EVs or albumin from culture medium supplements [35].
- Report quantitative metrics using at least two different, complementary techniques, such as NTA for particle concentration and size, and a protein assay for total mass [8].
The MISEV guidelines emphasize that no single isolation method is perfect, and the choice of technique—whether differential ultracentrifugation, size-exclusion chromatography (SEC), or others—must be reported along with its specific performance metrics for the given sample type [28] [36]. This rigorous reporting, potentially facilitated by the EV-TRACK knowledgebase, ensures that experimental outcomes in wound healing models can be properly interpreted and reproduced across different laboratories [36].
Experimental Protocols for MISEV-Compliant Characterization
Nanoparticle Tracking Analysis (NTA) for Concentration and Size
Principle: NTA utilizes light scattering and Brownian motion to determine the hydrodynamic diameter and particle concentration of a vesicle preparation in liquid suspension [8]. This provides a critical quantitative parameter for dosing in therapeutic applications.
Sample Preparation:
- Isolate MSC-exosomes from conditioned culture medium using a standardized method (e.g., SEC or ultracentrifugation). The culture medium should be devoid of serum-derived EVs or supplemented with EV-depleted serum [28].
- Resuspend the final exosome pellet in a filtered (0.1 µm), particle-free phosphate-buffered saline (PBS).
- For wound healing studies, note that the biological source of MSCs (e.g., adipose tissue vs. bone marrow) can influence the resulting exosome size distribution [9].
Instrument Calibration and Measurement:
- Calibrate the NTA instrument (e.g., Malvern Nanosight NS300) using latex beads of a known size (e.g., 100 nm) according to the manufacturer's protocol.
- Dilute the exosome sample to achieve an optimal concentration of 20-100 particles per frame, ensuring accurate tracking while minimizing coincidence errors. The required dilution factor (often between 1:100 and 1:10,000) must be empirically determined and recorded.
- Perform five recordings of 60 seconds each per sample, ensuring the camera level and detection threshold are kept consistent across all samples within an experiment.
Data Analysis and Reporting (MISEV Compliance):
- Report the mode, mean, and D10/D90 diameters to describe the particle size distribution.
- Report the final particle concentration in particles per milliliter (particles/mL), applying the appropriate dilution factor.
- A representative screenshot of the particle movement video and the size distribution graph should be retained for publication.
- MISEV requires reporting the yield of particles (e.g., particles per cell, or per mL of culture medium) [8] [36].
Surface Marker Analysis by Liquid Chromatography Tandem Mass Spectrometry (LC-MS/MS)
Principle: While Western blotting is conventionally used, targeted LC-MS/MS offers a high-throughput, multiplexed, and quantitative approach to confirm the presence of EV-associated proteins and absence of contaminants, as recommended by MISEV to enhance rigor [35]. This is especially valuable for characterizing clinical-grade MSC-exosome batches for wound therapy.
Sample Preparation:
- Lyse a volume of MSC-exosome preparation containing 5-20 µg of total protein (quantified by a compatible assay like BCA).
- Reduce, alkylate, and digest the proteins into peptides using a protease (typically trypsin).
- Desalt the resulting peptides using C18 solid-phase extraction tips.
Targeted LC-MS/MS Analysis (Multiple Reaction Monitoring - MRM):
- Separate the peptides using reverse-phase liquid chromatography.
- On a triple quadrupole mass spectrometer, program MRM transitions to detect and quantify specific peptides representing:
- Category 1 (Transmembrane) Proteins: CD9, CD63, CD81.
- Category 2 (Cytosolic) Proteins: TSG101, Flotillin-1, Flotillin-2.
- Category 3 (Contaminants): Apolipoproteins (APOA1, APOB), Albumin (ALB).
- Use stable isotope-labeled (SIL) versions of the target peptides as internal standards for precise quantification [35].
Data Analysis and Reporting (MISEV Compliance):
- Quantify the abundance of each target protein in the sample.
- Calculate the ratio of EV-positive markers (e.g., CD81) to contaminant proteins (e.g., APOA1) to establish a purity index for the preparation.
- Report the presence of at least three EV-positive protein markers (preferably two transmembrane and one cytosolic) and the absence or low abundance of contaminants relevant to the sample source (e.g., culture medium supplements) [35] [36].
The workflow below illustrates the integrated process of sample preparation, characterization, and data analysis for MSC-exosomes, culminating in the critical link to functional wound healing studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and instruments required for the standardized characterization of MSC-exosomes for wound therapy research.
Table 1: Key Research Reagents and Solutions for MSC-Exosome Characterization
| Item | Function/Application | Specific Examples & Notes |
|---|---|---|
| Particle-Free PBS | Diluent and suspension buffer for exosomes prior to NTA. | Must be filtered through a 0.1 µm filter to eliminate background particulate interference. |
| Size Standard Beads | Calibration of NTA instrument for accurate size measurement. | 100 nm polystyrene latex beads; essential for protocol standardization. |
| Trypsin, Sequencing Grade | Proteolytic enzyme for digesting exosome proteins into peptides for LC-MS/MS. | High-purity grade ensures reproducible and efficient digestion. |
| Stable Isotope-Labeled (SIL) Peptides | Internal standards for absolute quantification of proteins in targeted LC-MS/MS. | Allows precise measurement of EV markers (e.g., CD9, CD81) and contaminants [35]. |
| C18 Desalting Tips | Desalting and cleaning of peptide mixtures prior to LC-MS/MS analysis. | Improves sample quality and instrument performance. |
| NTA Instrument | Measurement of particle size distribution and concentration. | Instruments such as the Malvern Panalytical Nanosight NS300. |
| Triple Quadrupole Mass Spectrometer | Targeted, quantitative analysis of specific protein markers via MRM. | Enables multiplexed, high-sensitivity quantification of the EV proteome [35]. |
Integrating Characterization Data with Dosing and Administration in Wound Healing
Robust characterization directly informs the optimization of dosing and administration routes for MSC-exosome therapies. Clinical data reveal that the effective dose is highly dependent on the administration route. For instance, aerosolized inhalation for respiratory diseases can achieve therapeutic effects at doses around 10^8 particles, which is significantly lower than the doses typically required for intravenous routes [9]. This underscores the existence of a narrow, route-dependent effective dose window.
For topical application to wounds, characterizing the particle number and protein content becomes paramount for establishing a dose-response relationship. A working range for total MSC-EV dose in humans has been proposed, spanning from ~1 × 10^10 particles (an absolute minimum based on rodent studies) to an upper limit of ~6 × 10^12 particles (based on endogenous EV levels in human blood) [8]. The table below summarizes how characterization parameters feed into dosing considerations for wound therapy.
Table 2: Linking Characterization Data to Dosing Parameters in Wound Therapy
| Characterization Parameter | Influence on Dosing Strategy | Considerations for Wound Therapy |
|---|---|---|
| Particle Concentration (NTA) | Enables dosing based on absolute particle number. | Facilitates precise and reproducible dosing in animal models and clinical trials (e.g., particles/cm² of wound area) [8]. |
| Protein Content (e.g., BCA Assay) | Allows alternative dosing based on total protein mass. | Common but can be confounded by co-isolated protein contaminants; must be interpreted alongside purity metrics [8]. |
| Size Distribution (NTA) | May influence tissue penetration and retention within the wound bed. | Smaller vesicles (30-150 nm) may diffuse more readily through the wound extracellular matrix [28]. |
| Purity Ratio (e.g., CD81/APOA1 from LC-MS/MS) | Ensures that the therapeutic effect is attributed to exosomes and not contaminants. | High-purity preparations reduce the risk of unintended side effects and improve batch-to-batch consistency [35] [13]. |
| Surface Marker Profile | Correlates specific molecular signatures with therapeutic potency. | Certain marker combinations may be linked to enhanced pro-angiogenic or anti-inflammatory activity, guiding potency assay development [37] [13]. |
Adherence to MISEV guidelines through standardized application of NTA and surface marker analysis is not an end in itself, but a prerequisite for generating meaningful data that can accelerate the clinical translation of MSC-exosome wound therapies. By providing a robust and reproducible framework for defining the identity, quantity, and purity of exosome preparations, researchers can confidently correlate these critical quality attributes (CQAs) with biological activity in wound healing models. This disciplined approach is the cornerstone for establishing reliable potency assays, optimizing dosing regimens based on particle number and route of administration, and ultimately developing effective, off-the-shelf regenerative therapies for patients suffering from chronic wounds [9] [13].
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a paradigm shift in regenerative medicine, particularly for challenging wound healing scenarios such as diabetic foot ulcers and other chronic wounds [38] [39]. While the therapeutic potential of these nanovesicles is well-established, the optimal delivery strategy remains a critical translational challenge. The selection between subcutaneous injection and topical dressing/covering transcends mere application methodology; it directly influences the bioavailability, biodistribution, and ultimate therapeutic efficacy of MSC-Exos at the wound site [20]. Route selection impacts key pharmacokinetic parameters, including retention time, penetration depth into wound tissue, and the ability to sustain a therapeutic microenvironment conducive to the complex processes of regeneration [40]. This document provides a structured comparison of these two primary administration routes, synthesizing current preclinical and clinical evidence to guide researchers in aligning delivery strategies with specific wound healing objectives and experimental models.
Quantitative Efficacy Comparison of Administration Routes
A comprehensive meta-analysis of preclinical studies provides direct comparative data on the efficacy of subcutaneous injection versus topical dressing/covering for MSC-EVs in wound healing. The table below summarizes the key outcome measures, demonstrating route-dependent therapeutic profiles [20].
Table 1: Efficacy Comparison of Subcutaneous Injection vs. Topical Dressing/Covering from Preclinical Meta-Analysis
| Administration Route | Wound Closure Rate | Revascularization (Blood Vessel Density) | Collagen Deposition | Key Advantages |
|---|---|---|---|---|
| Subcutaneous Injection | Superior Improvement | Greater Improvement | Greater Improvement | Enhanced deep tissue delivery; superior stromal remodeling. |
| Topical Dressing/Covering | Effective | Effective | Effective | Simpler application; less invasive; suitable for large surface areas. |
The underlying mechanism for the enhanced performance of subcutaneous injection appears to be its ability to deliver exosomes deeper into the wound bed, facilitating more robust interactions with dermal and stromal components critical for regeneration [20]. Topical application, while effective, may be more susceptible to clearance and may not achieve the same penetration depth, potentially limiting its access to key cellular targets in the deeper dermal layers.
Experimental Protocols for Route-Specific Administration
Protocol for Subcutaneous Injection
The subcutaneous route delivers exosomes directly into the tissue surrounding the wound, promoting diffusion throughout the wound bed from the inside out [20].
Materials:
- Purified MSC-Exos suspension in PBS
- Insulin syringe (e.g., 0.3-0.5 mL, 29-31 gauge)
- Animal restraint device (if applicable)
- Sterile swabs and disinfectant
Procedure:
- Exosome Preparation: Thaw the purified MSC-Exos suspension on ice and dilute to the desired working concentration in sterile, endotoxin-free PBS. Gently mix by pipetting; avoid vortexing to preserve vesicle integrity [39].
- Site Preparation: Identify multiple injection sites around the perimeter of the wound, approximately 3-5 mm from the wound edge. Cleanse the area with a disinfectant according to standard aseptic techniques.
- Administration: Using an insulin syringe, slowly administer a volume of 20-50 µL per injection site. The number of sites should be adjusted based on wound size to ensure even distribution (e.g., 4-8 sites for a standard murine dorsal wound) [20].
- Post-Procedure: Apply gentle pressure if needed. The treatment frequency can vary from a single injection to multiple injections spaced days apart, depending on the experimental design.
Protocol for Topical Application with Hydrogel
Topical application often utilizes a hydrogel vehicle to retain exosomes at the wound site, protect them from the environment, and provide a moist healing environment [40] [39].
Materials:
- Purified MSC-Exos
- Biocompatible hydrogel (e.g., Hyaluronic Acid-based, Carboxymethyl Cellulose (CMC) gel)
- Sterile PBS
- Wound dressing (e.g., Tegaderm, non-adhesive gauze)
Procedure:
- Exosome-Hydrogel Formulation: Mix the purified MSC-Exos pellet thoroughly with the hydrogel matrix. A typical ratio for a hyaluronic acid hydrogel is 100-500 µg of exosome protein per mL of hydrogel precursor solution [40]. Ensure homogenous distribution by gentle stirring.
- Wound Bed Preparation: Gently cleanse the wound with sterile saline to remove debris and exudate. Pat the surrounding skin dry.
- Application: Apply a uniform layer of the exosome-loaded hydrogel directly onto the entire wound surface, ensuring complete coverage and contact with the wound bed.
- Dressing: Cover the hydrogel with a sterile, non-adhesive wound dressing to secure the formulation in place and maintain a moist environment. The dressing should be changed, and the gel reapplied according to the treatment schedule (e.g., weekly in clinical settings) [39].
Dosing Considerations Across Administration Routes
Dosing is a critical parameter that is intrinsically linked to the administration route. The following table summarizes key dosing considerations and findings from the literature.
Table 2: Dosing Parameters for Subcutaneous and Topical Administration Routes
| Parameter | Subcutaneous Injection | Topical Dressing/Covering |
|---|---|---|
| Reported Effective Dose (Preclinical) | Varies by model; e.g., 100-200 µg exosome protein per wound in multiple injections [20] | Varies by model and vehicle; e.g., 100-500 µg exosome protein per mL hydrogel [40] |
| Clinical Dose Example | Not yet standardized in clinical trials for wounds | 1.4x1010 particles/mL gel applied weekly [39] |
| Dose Frequency (Clinical) | N/A | Weekly application for 4 weeks [39] |
| Critical Consideration | Dose must be divided across multiple injection sites for uniform effect. | The retention capacity of the hydrogel vehicle is a key determinant of efficacy. |
A critical insight from clinical studies of MSC-EVs in other indications is that the effective dose is highly route-dependent. For instance, nebulization for lung diseases achieved efficacy at doses significantly lower than those required for intravenous routes [9]. This underscores the necessity for route-specific dose-finding studies in wound healing.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials essential for conducting research on MSC exosome-based wound therapies.
Table 3: Essential Research Reagents and Materials for MSC-Exos Wound Therapy Research
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Hyaluronic Acid (HA) Hydrogel | Biocompatible scaffold for topical exosome delivery; provides sustained release and moist wound environment [40]. | Can be modified for in-situ cross-linking. Critical for topical application protocols. |
| Carboxymethyl Cellulose (CMC) Gel | A vehicle used as a placebo control or for exosome delivery in clinical trials [39]. | Serves as the "exosome vehicle" in controlled studies. |
| Anti-CD63, CD81, CD9 Antibodies | Characterization of exosomes via flow cytometry or Western blot; markers for exosome identification and purity assessment [39]. | Essential for validating MISEV guidelines-compliant characterization. |
| Collagenase Type I | Enzymatic digestion of tissues (e.g., Wharton's Jelly) for the initial isolation of MSCs [39]. | First step in generating the parent MSCs for exosome production. |
| Density Gradient Medium | Improved purification of EVs by separating them based on buoyant density, enhancing purity [41] [28]. | Iodixanol or sucrose gradients are used as an alternative to ultracentrifugation. |
| Nanoparticle Tracking Analysis (NTA) | Instrumental technique for determining the size distribution and concentration of exosome preparations [9]. | Key for dose standardization (e.g., particle number). |
| FACS Melody or Equivalent | Flow cytometer for the immunophenotyping of MSCs and analysis of exosome-coated beads [39]. | Used to confirm MSC surface markers (CD73, CD90, CD105) and exosome markers. |
Workflow and Decision Pathway
The following diagram illustrates the experimental workflow for a comparative study of administration routes, from exosome preparation to outcome analysis.
Diagram: Workflow for Comparing Exosome Delivery Routes.
The choice between subcutaneous injection and topical dressing is not merely procedural but strategic, dictated by the specific wound pathophysiology and therapeutic goals. Subcutaneous injection demonstrates superior efficacy in enhancing wound closure, revascularization, and collagen deposition, making it the preferred route for deep, complex wounds where stromal remodeling is a priority [20]. In contrast, topical application offers a minimally invasive, practical approach suitable for superficial wounds, large surface areas, and clinical settings favoring ease of use and patient compliance [39]. Future research must focus on standardizing dose metrics and developing smart delivery systems that can further enhance the precision and longevity of exosome action at the wound site.
The transition of Mesenchymal Stem Cell-derived extracellular vesicles (MSC-EVs) from research tools to clinical therapeutics hinges on the development of robust, standardized quantification methods. Dosing for MSC-EV therapies remains a significant challenge in the field, with clinical trials reporting large variations in characterization, dose units, and outcome measures [9]. The lack of harmonized reporting standards directly impacts the ability to compare results across studies and establish reliable dose-effect relationships, particularly in wound healing applications [9] [20]. Proper quantification is not merely a technical requirement but a fundamental prerequisite for determining therapeutic efficacy, understanding pharmacokinetics, and ensuring patient safety. Currently, three principal methodologies have emerged for quantifying MSC-EVs: particle number concentration, protein content analysis, and lipid-based measurements. Each approach offers distinct advantages and limitations, influencing their suitability for different research and clinical applications. This protocol provides a comprehensive overview of these quantification strategies, their technical implementation, and their relevance to wound therapy research, with the aim of supporting the development of optimal dosing parameters for MSC exosome-based wound treatments.
Quantification Methodologies: Principles and Protocols
Particle Number Concentration
Principles and Applications: Particle number concentration quantification provides a direct measurement of extracellular vesicle count, typically expressed as particles per milliliter (particles/mL). This method is particularly valuable for establishing dose-response relationships in therapeutic applications, as it enables precise dosing based on the actual number of vesicles administered [9]. Nanoparticle Tracking Analysis (NTA) represents the current gold standard technique, allowing for both particle enumeration and size distribution analysis in a single measurement [42] [43]. The importance of this approach is highlighted by clinical evidence demonstrating that dose-response relationships are administration route-dependent, with nebulization therapy achieving therapeutic effects at approximately 10^8 particles, significantly lower than doses required for intravenous administration [9].
Experimental Protocol: Nanoparticle Tracking Analysis (NTA)
- Instrument Calibration: Perform routine calibration using latex beads of known concentration (e.g., 100 nm) to verify instrument performance and detection sensitivity [43].
- Sample Preparation: Dilute EV samples in 0.22-µm filtered phosphate-buffered saline (PBS) to achieve optimal concentration for analysis (typically 1×10^7 to 1×10^9 particles/mL) [44]. Maintain consistent dilution factors across experimental batches.
- Measurement Parameters: Configure NTA settings with a 532 nm laser, camera level set to 15, and detection threshold of 5 [44]. Capture three to five videos of 30-60 seconds each per sample to ensure statistical reliability.
- Data Analysis: Calculate mean particle concentration and size distribution using dedicated NTA software. Report mode, mean, and median sizes alongside particle concentration to fully characterize the EV population [42] [44].
Technical Considerations: NTA measurements can be influenced by sample purity, as protein aggregates or liposomal contaminants may interfere with accurate particle counting [43]. Samples with significant contamination require additional purification steps, such as size exclusion chromatography, prior to analysis. Additionally, NTA has limited sensitivity for particles below 50 nm, potentially underrepresenting smaller EV subpopulations [43].
Protein Content Analysis
Principles and Applications: Protein-based quantification measures the total protein content associated with extracellular vesicles, typically expressed as micrograms per milliliter (µg/mL). This approach assumes a correlation between protein content and vesicle quantity, though this relationship can be influenced by co-isolated contaminants and variations in EV cargo [43]. The protein quantification method is widely used due to its accessibility, cost-effectiveness, and familiarity to most laboratories. In wound healing research, protein-based dosing has been employed successfully, with studies demonstrating efficacy at concentrations such as 50 µg/mL in promoting cell proliferation and reducing apoptosis [42].
Experimental Protocol: Bicinchoninic Acid (BCA) Assay
- Standard Curve Preparation: Prepare albumin standards in the range of 0-60 µg/mL using the same buffer as EV samples to ensure matrix matching [43].
- Sample Preparation: Lyse EV samples with RIPA buffer (1:1 ratio) for 30 minutes on ice to release protein content [44]. Alternatively, use SDS-based lysis buffers for complete protein solubilization.
- Assay Procedure: Mix samples with BCA working reagent (1:8 ratio) and incubate at 37°C for 30 minutes [43]. Measure absorbance at 562 nm using a plate reader.
- Calculation: Determine protein concentration from the standard curve and apply appropriate dilution factors. Report results as µg protein/mL with reference to the standard used.
Technical Considerations: A significant limitation of protein-based quantification is the potential interference from co-isolated non-vesicular proteins, which can substantially impact accuracy [43]. The ratio of particle number to protein content serves as an important purity indicator, with higher ratios suggesting purer EV preparations [43]. This method should therefore be complemented with other quantification approaches when determining therapeutic doses.
Lipid-Based Measurements
Principles and Applications: Lipid-based quantification focuses on measuring membrane lipid components of extracellular vesicles, providing an alternative to protein-centric approaches. This method is particularly valuable for applications where membrane integrity and lipid composition are critical therapeutic factors, such as in drug delivery systems for wound healing [44]. While less commonly used than particle or protein measurements, lipid-based quantification offers complementary information about EV quantity and quality, especially for engineered EV formulations where membrane properties may be modified for enhanced therapeutic delivery.
Experimental Protocol: Fluorescent Lipid Staining and Quantification
- Lipid Staining: Incorporate fluorescent lipid dyes (e.g., rhodamine-PE, NBD-PS) during EV formation or use membrane-permeable dyes such as PKH67 for labeling intact vesicles [45].
- Standard Curve Generation: Prepare lipid standards of known concentration in the same buffer as EV samples. Create a standard curve correlating fluorescence intensity with lipid content.
- Measurement: Read fluorescence intensity using appropriate excitation/emission wavelengths for the selected dye. For high-throughput applications, adapt the protocol to 96-well plate formats.
- Calculation: Interpolate sample lipid content from the standard curve, applying necessary dilution factors.
Technical Considerations: Lipid-based methods require careful optimization of dye concentration to avoid self-quenching or membrane disruption. The choice of reference standard should reflect the lipid composition of MSC-EVs, which may vary based on source and isolation methods. This approach is particularly useful for hybrid nanoparticle systems engineered from MSC-EVs and synthetic lipids [45].
Table 1: Comparative Analysis of MSC-EV Quantification Methods
| Method | Principle | Common Units | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Particle Number | Direct counting of individual vesicles | particles/mL | Direct measurement of vesicle count; Correlates with therapeutic dose [9] | Affected by protein aggregates [43]; Limited detection <50 nm [43] |
| Protein Content | Colorimetric detection of proteins | µg/mL | Accessible and cost-effective; Familiar methodology | Influenced by co-isolated contaminants [43]; Variable cargo affects correlation [43] |
| Lipid-Based | Fluorescent detection of membrane lipids | µg lipid/mL | Focuses on membrane components; Useful for engineered EVs [45] | Requires specific optimization; Less established standards |
Integrated Workflow for Dose Quantification
The following workflow diagram illustrates the integrated process for comprehensive MSC-EV quantification, incorporating all three methods to ensure accurate dosing for wound therapy applications:
Research Reagent Solutions
Table 2: Essential Reagents for MSC-EV Quantification
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Instrumentation | NanoSight NS300 (Malvern) [44], Zetasizer Nano (Malvern) [43] | Particle concentration and size distribution analysis |
| Protein Assays | Micro BCA Protein Assay Kit (Thermo Fisher) [44], Pierce BCA Protein Assay [43] | Colorimetric quantification of EV-associated proteins |
| Lipid Stains | Rhodamine-PE, NBD-PS [45], PKH67 | Fluorescent labeling of EV membrane lipids |
| Separation Media | Size Exclusion Chromatography columns | Sample purification before quantification |
| Standards | Latex beads (100 nm) [43], Albumin standards [43] | Instrument calibration and assay standardization |
Technical Considerations for Wound Therapy Research
Method Selection and Integration
For wound therapy research, quantification method selection should align with specific research objectives and clinical translation goals. Particle counting provides the most direct measurement for dose-response studies, particularly important given the identified route-dependent efficacy in clinical applications [9]. Protein quantification remains valuable for comparative studies when consistent isolation methods are maintained. Lipid-based approaches gain importance when developing engineered EV formulations for enhanced wound healing capabilities.
The integration of multiple quantification methods provides a comprehensive characterization profile essential for establishing reproducible dosing protocols. The particle-to-protein ratio serves as a critical quality metric, with higher ratios indicating purer EV preparations with less contaminating protein [43]. This integrated approach supports the development of standardized dosing frameworks necessary for advancing MSC-EV therapies toward clinical application for wound healing.
Standardization Challenges
Significant challenges remain in standardizing quantification methods across different laboratories and studies. The variability in MSC sources, culture conditions, and isolation methods directly impacts quantification results and therapeutic dosing [42] [46]. Furthermore, the lack of universally accepted reference materials hampers cross-study comparisons and meta-analyses [43]. Addressing these challenges requires implementation of standardized reporting metrics that include detailed methodology descriptions, purity assessments, and orthogonal quantification approaches.
For wound therapy applications specifically, researchers should carefully document the MSC tissue source, as different sources (adipose tissue, bone marrow, umbilical cord) demonstrate variable efficacy in wound closure and tissue regeneration [20]. This source-dependent variability extends to EV characteristics and must be considered when determining therapeutic doses for wound healing applications.
Accurate quantification of MSC-derived extracellular vesicles represents a fundamental requirement for advancing wound therapy research and clinical applications. The three primary methods—particle number concentration, protein content analysis, and lipid-based measurements—each contribute valuable information for dose determination when appropriately implemented and interpreted. An integrated approach combining multiple quantification methods provides the most comprehensive assessment of EV preparations, enabling the development of optimized dosing strategies tailored to specific wound types and administration routes. As the field progresses toward standardized protocols and harmonized reporting, robust quantification methodologies will play an increasingly critical role in establishing MSC-EV therapies as reliable and effective treatments for wound healing.
The establishment of a defined clinical dose range is a critical step in the translational pathway of Mesenchymal Stem Cell (MSC) exosome therapies. For wound healing applications, a working range of 10^10 to 10^12 particles represents a therapeutically relevant window identified from emerging clinical data and preclinical evidence. This range balances biological efficacy with safety, providing a foundational framework for protocol development and standardization in regenerative medicine [9] [47].
Exosomes, the nanoscale extracellular vesicles (30-150 nm in diameter) secreted by MSCs, mediate therapeutic effects through their cargo of proteins, miRNAs, lipids, and other bioactive molecules [28] [47]. Unlike whole-cell therapies, exosomes offer a cell-free approach with lower immunogenicity, no risk of tumorigenesis, and enhanced stability [28]. Their efficacy, however, is profoundly influenced by both the absolute dose administered and the route of delivery, necessitating precise dose-response characterization for successful clinical application [9].
Quantitative Analysis of Clinical Dosing Data
Recent analyses of registered clinical trials provide crucial insights into the relationship between administration route, dose, and therapeutic outcome. The data underscore that the effective dose is not absolute but is intimately tied to the delivery method.
Table 1: Clinical Dose-Effect Relationships for MSC-EVs/Exosomes by Administration Route
| Administration Route | Typical Effective Dose (Particles) | Key Clinical Context | Therapeutic Indications |
|---|---|---|---|
| Aerosolized Inhalation | ~10^8 particles | Significantly lower dose required for efficacy compared to IV; direct delivery to lungs. | Respiratory diseases (COVID-19, ARDS) [9] |
| Intravenous (IV) Infusion | >10^10 particles | Higher dose required; first-pass lung trapping influences systemic bioavailability. | Systemic & inflammatory conditions [9] [48] |
| Local Application (e.g., Wound Site) | 10^10 - 10^12 particles (proposed) | Direct targeting to lesion; minimizes systemic exposure; based on preclinical wound healing models. | Cutaneous wound repair, diabetic ulcers [47] [5] |
The data reveal that nebulization therapy for respiratory diseases can achieve therapeutic effects at doses around 10^8 particles, which is substantially lower than the doses required for intravenous routes [9]. This suggests a relatively narrow and route-dependent effective dose window. For localized wound therapy, the proposed working range of 10^10 to 10^12 particles is extrapolated from systemic efficacy data and positive preclinical outcomes, aiming to ensure sufficient bioactive molecules reach the target tissue [47] [5].
Experimental Protocols for Dose Verification
Protocol: Isolation and Characterization of MSC Exosomes
This protocol ensures the production of a consistent and well-characterized exosome preparation for dose-response studies [28] [49].
Cell Culture and Conditioning:
- Culture human MSCs (from bone marrow, adipose tissue, or umbilical cord) in serum-free media to avoid contaminating bovine exosomes.
- At 70-80% confluence, replace media with a conditioned media formulation optimized for exosome production.
- Collect conditioned media after 48 hours and centrifuge at 2,000 × g for 30 minutes to remove cells and debris.
Exosome Isolation via Ultracentrifugation:
- Transfer the supernatant to ultracentrifuge tubes.
- Perform ultracentrifugation at 100,000 × g for 70 minutes at 4°C.
- Discard the supernatant and resuspend the pellet in a large volume of phosphate-buffered saline (PBS).
- Perform a second ultracentrifugation at 100,000 × g for 70 minutes to wash the exosomes.
- Finally, resuspend the pure exosome pellet in a small volume of PBS (e.g., 100-200 µL) and aliquot.
Characterization and Dosage Calculation:
- Nanoparticle Tracking Analysis (NTA): Dilute an aliquot of exosomes in PBS and inject into the NTA system. This determines the particle size distribution and concentration (particles/mL), which is used for accurate dosing.
- Protein Marker Analysis: Confirm the presence of exosomal surface markers (CD63, CD9, CD81) and the absence of negative markers (e.g., GM130) using Western Blot or flow cytometry.
- Transmission Electron Microscopy (TEM): Visualize the morphology and integrity of the exosomes.
Protocol: In Vivo Dose-Response Study in a Diabetic Wound Model
This protocol outlines the steps to validate the efficacy of the 10^10 to 10^12 particle range in a preclinical wound healing model [47] [5].
Animal Model Preparation:
- Use a genetically diabetic (e.g., db/db) mouse model.
- Anesthetize mice and create two full-thickness excisional wounds (e.g., 6 mm diameter) on the dorsum.
Treatment Groups and Dosing:
- Randomize animals into the following groups (n ≥ 8 per group):
- Group 1: Vehicle control (PBS).
- Group 2: Low-dose exosomes (1 × 10^10 particles in 50 µL PBS).
- Group 3: Mid-dose exosomes (5 × 10^11 particles in 50 µL PBS).
- Group 4: High-dose exosomes (1 × 10^12 particles in 50 µL PBS).
- Administer treatments via topical application directly onto the wound bed and surrounding tissue immediately post-wounding and every 3 days until closure.
- Randomize animals into the following groups (n ≥ 8 per group):
Efficacy Endpoint Analysis:
- Wound Closure Measurement: Digitally photograph wounds daily and calculate wound area as a percentage of the original area.
- Histological Analysis: Upon sacrifice, collect wound tissue for H&E staining (for re-epithelialization), Masson's Trichrome (for collagen deposition), and immunohistochemistry for CD31 (to assess angiogenesis) and α-SMA (to mark myofibroblasts).
Signaling Pathways in Exosome-Mediated Wound Healing
MSC exosomes promote wound healing by modulating key signaling pathways in target cells, such as fibroblasts, keratinocytes, and endothelial cells. The therapeutic cargo (e.g., miRNAs, proteins) within exosomes orchestrates a coordinated repair process.
Diagram 1: Key signaling pathways activated by MSC exosomes in wound healing. Exosomes deliver miRNAs and proteins that modulate the TGF-β, Wnt/β-catenin, AMPK/mTOR, and PI3K/Akt pathways in target cells like fibroblasts and keratinocytes. This coordinated signaling leads to essential repair processes, including extracellular matrix (ECM) remodeling, cell proliferation, reduced apoptosis, and new blood vessel formation [47] [48].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for MSC Exosome Wound Therapy Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Serum-Free Media | Culture of MSCs for exosome production. | Prevents contamination with serum-derived vesicles; essential for GMP-grade production [49]. |
| Differential Ultracentrifuge | Gold-standard isolation of exosomes from conditioned media. | Enables high-purity preparation; requires specialized, expensive equipment [28]. |
| Nanoparticle Tracking Analyzer | Quantification of exosome particle size and concentration. | Critical for standardizing doses (particles/mL) rather than protein mass [9] [49]. |
| CD63/CD9/CD81 Antibodies | Characterization of exosomes via Western Blot or Flow Cytometry. | Confirms identity and purity of isolated vesicles against MISEV guidelines [49]. |
| Diabetic (db/db) Mice | Preclinical model of impaired wound healing. | Gold-standard model for testing efficacy of exosome therapies in a pathologically relevant system [47]. |
| Hydrogel-based Scaffolds | Biocompatible material for topical exosome delivery. | Enhives exosome retention at the wound site, providing sustained release and improving efficacy [5]. |
Establishing a working dose range of 10^10 to 10^12 particles for MSC exosome wound therapy provides a critical benchmark for researchers and drug development professionals. This range is supported by clinical trends and is contingent upon rigorous characterization and a localized administration route. Future work must focus on standardizing isolation protocols, developing potency assays linked to specific cargo, and conducting well-controlled clinical trials to refine this dosing window for specific wound etiologies. The integration of exosomes with advanced biomaterial delivery systems holds particular promise for enhancing localized delivery and therapeutic outcomes within this defined dose spectrum [5].
Overcoming Clinical Translation Hurdles: Standardization and Bioengineering Solutions
In the rapidly advancing field of mesenchymal stem cell (MSC)-derived exosome therapy for wound healing, batch-to-batch variability represents a critical challenge that can significantly impact therapeutic efficacy and reproducibility. This variability stems from multiple factors including the biological source of MSCs, culture expansion conditions, and cell passage number, ultimately affecting the molecular cargo and functional properties of secreted exosomes. For wound therapy research, where consistent dosing and reliable administration routes are paramount for clinical translation, understanding and controlling these sources of heterogeneity is essential. This Application Note provides a detailed analysis of variability factors and standardized protocols to enhance reproducibility in MSC exosome research for wound healing applications.
Origins and Impact of MSC Heterogeneity
Tissue Source Variability
MSCs can be isolated from various tissues, each imparting distinct functional characteristics to their derived exosomes:
- Bone Marrow MSCs (BM-MSCs): Most extensively studied source with strong immunomodulatory effects [16]
- Adipose-derived MSCs (AD-MSCs): Easier to harvest with comparable therapeutic properties to BM-MSCs [16]
- Umbilical Cord MSCs (UC-MSCs): Enhanced proliferation capacity and lower immunogenicity [16]
- Functional Differences: AD-MSCs demonstrate superior immunosuppressive abilities, while BM-MSCs significantly enhance tubulogenesis and endothelial migration in vitro [50]
Comparative studies have revealed that MSC-exosomes from different tissue sources exhibit variations in angiogenic capability, with adipose tissue-derived exosomes showing better angiogenic potential than those from bone marrow [2]. These source-specific properties directly influence wound healing outcomes through different mechanisms of action.
Donor-Associated Variability
Donor-specific factors introduce substantial heterogeneity in MSC populations and their derived exosomes:
- Age: MSCs from older donors may exhibit reduced proliferative capacity and differentiation potential [51]
- Sex: Hormonal differences can influence MSC phenotype and function [52] [51]
- Health Status: Underlying medical conditions affect MSC characteristics and therapeutic potential [51]
Principal variance component analysis has demonstrated that the interaction between disease status and sex can contribute up to 31.7% of variance in transcriptomic data [52], highlighting the significant impact of donor biology on MSC properties.
Passage-Induced Variability
Long-term culture expansion significantly impacts MSC characteristics and exosome functionality:
- Cellular Senescence: Extended expansion leads to senescence-related changes, reduced trilineage differentiation capacity, and diminished anti-inflammatory properties of derived extracellular vesicles [53]
- Therapeutic Window: iPSC-derived MSCs (iMSCs) maintain prolonged effects compared to traditional MSCs, providing a wider therapeutic window despite batch-to-batch variability [53]
- Passage Effects: MSC expansion to passage five results in noticeable cellular senescence and reduction of stem-like properties [53]
For iPSC-derived MSCs, batch-to-batch variability in differentiation potential and EV biological properties presents challenges for therapeutic reliability [53], necessitating careful passage monitoring and standardization.
Table 1: Impact of MSC Source on Functional Properties Relevant to Wound Healing
| Tissue Source | Proliferation Capacity | Immunomodulatory Strength | Angiogenic Potential | Key Advantages |
|---|---|---|---|---|
| Bone Marrow | Moderate | Strong | High [50] | Most extensively characterized |
| Adipose Tissue | High | Strong [50] | Moderate | High yield, easy isolation |
| Umbilical Cord | High [16] | Moderate | Variable | Low immunogenicity |
| Dental Pulp | Moderate | Variable | Variable | Neural crest origin |
Quantifying and Addressing Variability in Manufacturing
Culture Condition Standardization
Harmonization of culture procedures has been demonstrated to minimize, though not completely eliminate, inter-laboratory variability [50]. Decentralized multicentre manufacturing studies show that implementation of standardized workflows improves reproducibility of MSC characteristics across independent facilities [50]. Key factors requiring standardization include:
- Culture Media Composition: Use of xeno-free supplements enhances MSC anti-inflammatory properties through secretion of chondroprotective molecules and EV-encapsulated therapeutic miRNA [53]
- Serum Supplements: Common lots of fetal bovine serum or defined serum-free formulations reduce batch effects [50]
- Seeding Densities: Optimization critical for consistent expansion (e.g., 300 cells/cm² for AD-MSCs vs. 3,000 cells/cm² for BM-/UC-MSCs) [50]
- Harvesting Criteria: Standardized confluence parameters (e.g., 70-80%) for culture passages and exosome collection [50]
Inter-laboratory studies emphasize that detailed protocols, identical reagents from the same providers, and specialized personnel training are critical for obtaining reproducible results across independent laboratories [54].
Comprehensive MSC Characterization
International Society for Cellular Therapy (ISCT) criteria provide minimal standards for MSC characterization, though studies indicate only 18% of MSC studies explicitly refer to all criteria [51]. Comprehensive characterization should include:
- Surface Marker Expression: ≥95% expression of CD105, CD73, CD90; ≤2% expression of hematopoietic markers (CD45, CD34, CD14/CD11b, CD79a/CD19, HLA-DR) [16]
- Trilineage Differentiation: Osteogenic, adipogenic, and chondrogenic potential assessment across passages [53]
- Functional Potency Assays: Immunomodulatory and angiogenic potential specific to wound healing applications [50]
- Senescence Monitoring: β-galactosidase staining at critical passages (e.g., P2, P5, P10 for MSCs; P8, P12, P16 for iMSCs) [53]
Single-cell RNA sequencing has identified several MSC subpopulations with different functional characteristics, suggesting that heterogeneity exists even in clonal populations [51].
Figure 1: Sources and Impacts of MSC Variability on Exosome Therapeutics. Multiple factors contribute to exosome heterogeneity, creating challenges in therapeutic development that require comprehensive standardization strategies.
Experimental Protocols for Variability Assessment
Protocol: Assessment of Passage-Induced Senescence
Objective: Evaluate replicative senescence in MSCs across passages to establish critical quality attributes for exosome production.
Materials:
- Senescence β-Galactosidase Staining Kit (Cell Signaling Technology)
- MSC cultures at early (P2-P3), middle (P5-P6), and late (P10+) passages
- Phase contrast microscope with imaging capability
Procedure:
- Culture MSCs in harmonized culture conditions (MEM-α media with consistent FBS lot)
- Seed MSCs at optimized densities (300 cells/cm² for AD-MSCs; 3,000 cells/cm² for BM-/UC-MSCs)
- At target passages (P2, P5, P10 for MSCs; P8, P12, P16 for iMSCs), wash cells with PBS
- Fix cells with 1X Fixative Solution for 10-15 minutes at room temperature
- Wash cells twice with PBS
- Incubate with β-Galactosidase Staining Solution overnight at 37°C without CO₂
- Examine for development of blue color under phase contrast microscope
- Quantify percentage of senescent cells using ImageJ software across multiple fields
Interpretation: Establish passage limits where senescence exceeds 15-20% for consistent exosome production [53].
Protocol: Trilineage Differentiation Potential
Objective: Assess multilineage differentiation capacity as quality control for MSC functionality.
Materials:
- Adipogenic Differentiation Medium (PromoCell, C-28016)
- Osteogenic Differentiation Medium (PromoCell, C-28013)
- Chondrogenic differentiation supplements (TGF-β3, dexamethasone, ascorbate)
- Oil Red O, Alizarin Red S, and Alcian Blue staining solutions
Procedure: Adipogenic Differentiation:
- Seed MSCs at 5,700 cells/cm² in 24-well plates
- Culture in adipogenic differentiation medium for 21 days with medium changes every 3 days
- Fix with 3.7% PFA for 15 minutes and stain with Oil Red O for 10 minutes
- Quantify lipid droplet formation
Osteogenic Differentiation:
- Seed MSCs at 1.5×10⁴ cells/cm² in 24-well plates
- Culture in osteogenic medium (DMEM-HG with dexamethasone, β-glycerophosphate, ascorbic acid) for 21 days
- Fix with 3.7% PFA and stain with 2% Alizarin Red S solution
- Quantify calcium deposition
Chondrogenic Differentiation:
- Pellet 2.5×10⁵ MSCs in conical tubes
- Culture in chondrogenic medium with TGF-β3 for 21 days
- Process pellets for histology and stain with Alcian Blue for proteoglycan detection
Interpretation: Compare differentiation potential across passages and donors to establish acceptance criteria for MSC batches destined for exosome production [53] [50].
Table 2: Impact of Passage Number on MSC Properties and Exosome Functionality
| Passage Range | Senescence Markers | Differentiation Potential | Exosome Function | Recommended Use |
|---|---|---|---|---|
| P2-P4 (Early) | Low SA-β-Gal activity | High trilineage capacity | Maximum therapeutic effect | Primary exosome production |
| P5-P7 (Middle) | Moderate increase | Beginning decline | Reduced anti-inflammatory effects [53] | Limited production batches |
| P8+ (Late) | High SA-β-Gal activity | Significant reduction | Diminished wound healing potential | Research use only |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Standardized MSC Exosome Research
| Reagent/Category | Specific Product Examples | Function & Importance | Variability Considerations |
|---|---|---|---|
| Basal Media | MEM-α GlutaMAX [50] | Consistent nutrient base for MSC expansion | Lot-to-lot testing required for reproducibility |
| Xeno-Free Supplement | Purstem XFS [53] | Defined, animal-free supplement for clinical translation | Enhances anti-inflammatory properties of MSC-EVs |
| Serum Alternatives | Human platelet lysate, defined formulations | Reduce batch variability vs. FBS | Requires extensive qualification for exosome production |
| Dissociation Reagents | TrypLE Select [50] | Gentle, standardized cell passaging | Consistent activity reduces selection pressure |
| Cryopreservation Medium | FBS + 10% DMSO [50] | Maintain MSC viability and functionality post-thaw | Standardized cooling protocols critical |
| Exosome Isolation Kits | Ultracentrifugation protocols, TFF systems [2] | Reproducible particle recovery | Method significantly impacts exosome yield and purity |
Dosing and Administration Considerations for Wound Therapy
The variability in MSC exosome products directly impacts dosing strategies and administration route selection for wound healing applications:
- Dose Optimization: Nebulization therapy achieves therapeutic effects at approximately 10⁸ particles, significantly lower than intravenous routes [9]
- Route Selection: Local administration (e.g., topical for wounds) enables targeted delivery with potentially lower doses than systemic administration [2]
- Dosage Units: Standardization needed as studies report dosage by weight (μg), particle number, or parent cell equivalents [9] [2]
- Potency Assessment: Development of wound healing-specific potency assays (e.g., fibroblast migration, angiogenesis promotion) to correlate with clinical outcomes
Clinical evidence suggests a relatively narrow and route-dependent effective dose window for MSC-EV therapies [9], emphasizing the need for precise exosome characterization and dosing standardization.
Figure 2: Standardized Manufacturing Workflow for MSC Exosomes. The process highlights critical points where variability must be controlled through standardized protocols and quality attributes to ensure consistent therapeutic exosome products.
Addressing batch variability in MSC-derived exosomes requires a systematic, multi-factorial approach spanning from donor selection through final product characterization. For wound therapy applications, where dosing precision and administration route optimization are critical, implementation of standardized protocols for MSC culture, passage monitoring, and exosome isolation is fundamental. By adopting the harmonized procedures and quality control measures outlined in this Application Note, researchers can significantly enhance the reproducibility and therapeutic reliability of MSC exosome products, accelerating their clinical translation for wound healing applications. Future directions should focus on developing wound-specific potency assays, establishing clear critical quality attributes, and creating reference standards for cross-study comparisons.
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a paradigm shift in regenerative medicine, offering a cell-free alternative for treating chronic wounds. These nanovesicles, typically 30–150 nm in diameter, exert their effects through the transfer of bioactive cargo—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating inflammation, promoting angiogenesis, and stimulating tissue regeneration [2] [55]. However, a critical determinant of their therapeutic success lies in the strategic selection of administration routes, which directly governs their biodistribution, retention at the target site, and ultimate efficacy [56]. This Application Note provides a structured framework for researchers to optimize the delivery of MSC exosomes in wound healing applications, focusing on the interplay between administration pathways, biodistribution patterns, and functional outcomes.
Quantitative Analysis of Administration Routes
The route of administration is a primary driver of the pharmacokinetic profile of MSC-Exos. Different routes lead to significant variations in the required dose, local bioavailability, and systemic distribution, which must be considered during therapeutic design [9] [56].
Table 1: Comparative Analysis of MSC-Exos Administration Routes in Preclinical and Clinical Studies
| Administration Route | Typical Dose Range | Key Advantages | Key Limitations | Primary Evidence Source |
|---|---|---|---|---|
| Local/Topical(e.g., hydrogel, direct application) | Varies by wound size and carrier system [57] | • High local bioavailability• Minimal systemic exposure• Favorable wound microenvironment integration [57] | • Limited to accessible wounds• Potential need for specialized delivery systems (e.g., hydrogels) [57] | Preclinical wound models [57] |
| Intravenous (IV)(Systemic) | ~10⁸ particles and above [9] | • Broad systemic distribution• Suitable for multiple/comorbid conditions [2] | • Significant first-pass clearance by liver and spleen• Lower accumulation in target tissue• Higher dose required [58] [56] | Clinical trials for various diseases [9] [2] |
| Intratracheal (i.t.) / Inhalation | ~10⁸ particles [9] | • High retention in pulmonary tissue• Effective at lower doses compared to IV [9] [56] | • Primarily for respiratory indications• Requires specialized delivery devices | Clinical trials for lung diseases [9] |
The data underscores a fundamental principle: local administration routes enable a favorable biodistribution profile for wound healing. For instance, in a direct comparison of administration routes for an anti-inflammatory nanoparticle (P12), intratracheal instillation was superior to intravenous and intraperitoneal routes in reducing lung inflammation, achieved with a lower drug concentration. This enhanced efficacy was directly correlated with greater nanoparticle accumulation in the lungs and specific targeting of lung macrophages [56]. While this study focused on pulmonary delivery, the principle translates to wound care, where local application maximizes exosome availability at the injury site.
Table 2: Dose-Effect Relationship by Administration Route (Clinical Trial Data)
| Route | Disease Area | Reported Effective Dose | Therapeutic Outcome | Source / Clinical Trial Context |
|---|---|---|---|---|
| Inhalation | Respiratory Diseases | ~10⁸ particles | Achieved therapeutic effects at significantly lower doses than intravenous routes. [9] | Analysis of global MSC-EV clinical trials [9] |
| Intravenous | Various Systemic Diseases | >10⁸ particles | Requires higher doses to achieve therapeutic effect, likely due to sequestration in reticuloendothelial organs. [9] [58] | Analysis of global MSC-EV clinical trials [9] |
Experimental Protocols
Protocol: Evaluating Biodistribution and Wound Retention of Labeled MSC-Exos
Objective: To quantitatively assess the biodistribution and retention kinetics of MSC-Exos at a wound site following different administration routes in an animal model.
Materials:
- MSC-Exos: Isolated from human bone marrow-derived MSCs.
- Dye: Lipophilic fluorescent dye (e.g., DiR or DiD).
- Animal Model: e.g., Diabetic (db/db) mouse with a dorsal excisional wound.
- Imaging System: In vivo imaging system (IVIS) or similar.
- Tissue Processing: reagents for homogenization.
Method:
- Exosome Labeling and Characterization:
- Incubate purified MSC-Exos with a lipophilic fluorescent dye (e.g., 5 µM DiD) for 30 minutes at 37°C.
- Remove unincorporated dye using size-exclusion chromatography (e.g., PBS-equilibrated PD-10 columns) [55].
- Validate labeling efficiency and exosome integrity via Nanoparticle Tracking Analysis (NTA) and transmission electron microscopy (TEM).
In Vivo Administration and Imaging:
- Randomize wound-bearing animals into two groups (n=5-8/group):
- Group 1 (Local): Administer a fixed dose (e.g., 100 µg in 50 µL PBS) of DiD-labeled MSC-Exos topically to the wound bed via a pipette.
- Group 2 (Intravenous): Administer the same dose via tail vein injection.
- Acquire in vivo fluorescence images at predetermined time points (e.g., 1, 4, 12, 24, 48 hours) post-administration using standardized imaging parameters.
- Quantify the fluorescence signal intensity (radiance) specifically within the wound area and major organs (liver, spleen, lungs) using region-of-interest (ROI) analysis.
- Randomize wound-bearing animals into two groups (n=5-8/group):
Ex Vivo Validation:
- At the endpoint (e.g., 48 hours), euthanize the animals and harvest the wound tissue, liver, spleen, kidneys, and lungs.
- Image all excised organs ex vivo to confirm the in vivo biodistribution pattern.
- Homogenize tissues and quantify the exosome-derived fluorescence or use qPCR for a human-specific RNA marker to obtain absolute quantitative data.
Protocol: Functional Efficacy Testing in a Chronic Wound Model
Objective: To correlate the biodistribution data from Protocol 3.1 with functional healing outcomes.
Materials:
- MSC-Exos: Unlabeled, biologically active.
- Delivery Vehicle: e.g., Chitosan hydrogel [57].
- Animal Model: e.g., Diabetic (db/db) mouse with a dorsal excisional wound.
- Assessment Tools: Digital photography, planimetry software, histology reagents.
Method:
- Study Design:
- Randomize animals into three groups (n=8/group):
- Group 1: Local application of MSC-Exos loaded in hydrogel.
- Group 2: Intravenous injection of MSC-Exos in PBS.
- Group 3: Control (hydrogel only or PBS injection).
- Randomize animals into three groups (n=8/group):
Treatment and Monitoring:
- Administer exosomes every 3-4 days.
- Monitor wounds every other day via digital photography.
- Calculate wound closure percentage using planimetry software:
% Closure = [(Initial Area - Current Area) / Initial Area] * 100.
Endpoint Analysis:
- Harvest wound tissue at day 7 (proliferation phase) and day 14 (remodeling).
- Process for histology (H&E staining) to assess re-epithelialization and granulation tissue thickness.
- Perform immunohistochemistry for CD31 to quantify angiogenesis (vessel density) and for specific macrophages markers (e.g., CD86 for M1, CD206 for M2) to evaluate immunomodulation [57] [55].
Signaling Pathways in Exosome-Mediated Wound Healing
The therapeutic effects of MSC-Exos in wounds are mediated through the modulation of key signaling pathways in recipient cells, a process influenced by their successful delivery and uptake.
The diagram above illustrates the core mechanistic pathways activated upon successful intracellular delivery of MSC-Exos cargo. Key processes include:
- Immunomodulation: MSC-Exos promote a shift in macrophage phenotype from the pro-inflammatory M1 state to the anti-inflammatory, pro-repair M2 state. This is associated with a decrease in cytokines like TNF-α and an increase in IL-10, resolving chronic inflammation [57].
- Angiogenesis: Cargo such as vascular endothelial growth factor (VEGF) and regulatory miRNAs activate endothelial cells, stimulating the formation of new blood vessels crucial for supplying oxygen and nutrients to the healing tissue [57] [59].
- Cell Proliferation and Remodeling: Exosomes stimulate the proliferation and migration of fibroblasts and keratinocytes, enhancing extracellular matrix (ECM) deposition and promoting re-epithelialization to close the wound [59] [55].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for MSC-Exos Wound Therapy Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Bone Marrow-MSCs | A standard source for MSC-Exos isolation. | Well-characterized, robust immunomodulatory potential [2]. |
| Adipose Tissue-MSCs | A highly accessible source for MSC-Exos. | Yields exosomes with potent angiogenic capability [59] [2]. |
| Ultracentrifugation | The most common method for isolating MSC-Exos. | Considered the "gold standard"; requires significant technical expertise and equipment [2]. |
| Tangential Flow Filtration (TFF) | A scalable method for isolating and concentrating MSC-Exos. | More suitable for potential larger-scale production than ultracentrifugation [2]. |
| Nanoparticle Tracking Analysis (NTA) | Characterizes exosome particle size and concentration. | Essential for pre-dosing quantification and quality control [9] [2]. |
| Chitosan Hydrogel | A biocompatible delivery vehicle for local/topical application. | Provides sustained release of exosomes, protecting them from the harsh wound environment [57]. |
| Lipophilic Tracers (DiD, DiR) | Fluorescent labels for in vivo and in vitro tracking of exosomes. | Critical for biodistribution and cellular uptake studies [55] [56]. |
The route of administration is a critical variable that directly dictates the biodistribution, target site retention, and therapeutic efficacy of MSC exosomes in wound healing. Empirical evidence strongly supports the use of local delivery strategies to maximize bioavailability at the wound site and minimize non-specific systemic distribution. The protocols and frameworks outlined herein provide a foundation for rational design and optimization of exosome-based therapeutics, enabling researchers to make informed decisions that bridge the gap between preclinical promise and clinical reality. Future efforts must focus on standardizing dosing metrics and developing advanced delivery systems that further enhance wound retention and functional integration.
Mesenchymal stem cell (MSC) derived exosomes and extracellular vesicles (EVs) represent a paradigm shift in regenerative medicine, offering a cell-free therapeutic approach for wound healing. These nanoscale vesicles (30-150 nm) function as natural bioactive cargo carriers, delivering proteins, lipids, and nucleic acids that modulate inflammation, angiogenesis, and tissue repair processes [60] [38]. Compared to whole-cell therapies, MSC-exosomes exhibit lower immunogenicity, enhanced biological barrier penetration, superior stability, and no risk of tumorigenicity or thrombosis, positioning them as next-generation therapeutics for chronic wounds [41] [61] [62].
The therapeutic efficacy of native MSC-exosomes, however, is constrained by limitations in targeting specificity, cargo payload, and production consistency. Bioengineering strategies, particularly CRISPR-based gene editing and advanced biomimetic delivery systems, present innovative solutions to overcome these challenges, transforming native exosomes into precision nanotherapeutics [60] [63]. This document outlines specific application notes and protocols for implementing these bioengineering strategies within the critical context of optimizing dosing and administration routes for MSC-exosome wound therapy.
CRISPR/Cas9 Engineering of Parent MSCs
The CRISPR/Cas9 system enables precise genetic modification of parent MSCs to enhance the therapeutic cargo and functionality of their secreted exosomes. These modifications directly influence the potency of the final exosome product, which is a critical factor in determining optimal therapeutic dosing [60].
Protocol: Knock-in of Pro-Regenerative Factors
Aim: To stably integrate genes encoding therapeutic factors into specific genomic loci of parent MSCs, resulting in exosomes enriched with enhanced regenerative capacity.
Materials:
- Human MSCs: Umbilical cord (UC-MSCs) or adipose-derived (AD-MSCs) are preferred [20].
- CRISPR Plasmids: pX330-U6-Chimeric_BB-CBh-hSpCas9 (Addgene #42230) or equivalent.
- Donor Template: ssODN or pAAV vector containing IL-10 ORF or miR-146a precursor sequence flanked by ~800bp homology arms.
- Transfection Reagent: Lipofectamine CRISPRMAX Cas9 Transfection Reagent.
- Antibiotics: Puromycin dihydrochloride for selection.
- Validation Primers: For genomic DNA PCR and quantitative RT-PCR.
Procedure:
- Design gRNAs: Select gRNAs targeting the AAVS1 safe harbor locus (chr19:55,113,082-55,113,103, GRCh38/hg38) using the CRISPRscan algorithm.
- Prepare Donor Template: Clone the IL-10 gene (NCBI Gene ID: 3586) or miR-146a precursor (MI0000477) into the pAAV-MCS vector under control of the EF1α promoter.
- Transfect MSCs: Plate 2×10^5 MSCs per well in a 6-well plate. At 80% confluency, co-transfect with 1 µg of Cas9/gRNA plasmid and 1 µg of donor template using Lipofectamine CRISPRMAX.
- Select and Expand: At 48 hours post-transfection, apply 1 µg/mL puromycin selection for 72 hours. Culture surviving cells for 2 weeks to form colonies.
- Screen Clones: Pick individual colonies and expand. Validate integration via genomic PCR and Sanger sequencing. Confirm enhanced expression via ELISA (for IL-10) or qPCR (for miR-146a).
- Characterize Engineered Exosomes (eMSC-Exos): Iserve exosomes from validated clones and confirm cargo enrichment via Western blot (IL-10) or NanoString miRNA analysis (miR-146a) [60].
Application Note: Cargo Modulation and Dosing Implications
CRISPR-mediated enrichment of anti-inflammatory miR-146a or IL-10 in exosomes enhances their potency, potentially allowing for lower therapeutic doses to achieve the desired effect [60]. For instance, exosomes overexpressing miR-146a more effectively suppress NF-κB signaling in macrophages, resolving the chronic inflammation characteristic of diabetic wounds [60] [38]. Dosing studies must be re-evaluated for these engineered products, as their enhanced specific activity alters the dose-response relationship compared to native exosomes.
Biomimetic Delivery Systems for MSC Exosomes
Effective delivery is crucial for maximizing the therapeutic potential of exosomes at the wound site. The administration route directly determines bioavailability, biodistribution, and the required therapeutic dose [64] [20].
Protocol: Fabrication of Exosome-Loaded Hydrogel Scaffolds
Aim: To develop a chitosan-based hydrogel scaffold for the sustained release of MSC-exosomes at the wound site, improving local retention and prolonging therapeutic action.
Materials:
- Chitosan: Medium molecular weight, deacetylation degree ≥75% (Sigma-Aldrich 448877).
- Cross-linker: Glycerophosphate disodium salt hydrate (GP).
- MSC-Exosomes: Isolated via ultracentrifugation or tangential flow filtration, characterized per MISEV2023 guidelines [41] [61].
- Dialysis Membranes: MWCO 12-14 kDa.
- Rheometer: For characterizing gelation temperature and modulus.
Procedure:
- Prepare Chitosan Solution: Dissolve chitosan powder at 2% (w/v) in 0.1M acetic acid under constant stirring overnight. Adjust pH to 6.2 with 5M NaOH.
- Prepare GP Solution: Dissolve GP in DI water at 50% (w/v).
- Formulate Hydrogel: Cool the chitosan solution to 4°C. Slowly add GP solution dropwise to a final concentration of 8% (w/v) under vigorous stirring.
- Incorporate Exosomes: Mix the purified MSC-exosome pellet (dose range: 10^9 - 10^11 particles/mL final gel concentration) gently with the chitosan-GP solution on ice.
- Induce Gelation: Incubate the mixture at 37°C for 30 minutes to form a stable hydrogel.
- Characterize Release Profile: Place 1 mL of exosome-loaded hydrogel in 10 mL PBS at 37°C. Collect release medium at predetermined intervals (1, 3, 6, 12, 24, 48, 72h) and quantify exosome release via NTA or BCA protein assay [65].
Application Note: Administration Route and Dose Optimization
Biomimetic scaffolds localize exosomes to the wound bed, creating a sustained-release depot that minimizes systemic clearance. This localized delivery strategy can significantly enhance efficacy compared to topical application or injection alone, potentially reducing the frequency of administration and the total cumulative dose required for healing [65] [20]. Preclinical meta-analyses indicate that subcutaneous injection of MSC-exosomes improves wound closure and collagen deposition more effectively than simple topical application, highlighting the critical role of delivery method in dosing strategy [20].
Quantitative Dosing and Administration Data
The optimal dose of MSC-exosomes is highly dependent on the administration route, which influences bioavailability and biodistribution. The following tables synthesize current evidence from clinical and pre-clinical studies to guide dosing strategies.
Table 1: MSC-Exosome Dosing by Administration Route in Clinical Trials
| Administration Route | Therapeutic Dose Range (Particles) | Indication Examples | Dosing Frequency | Key Findings |
|---|---|---|---|---|
| Aerosolized Inhalation [64] | ~10^8 | Respiratory Distress, ARDS | Single dose to daily for 5 days | Achieves therapeutic effects at significantly lower doses than intravenous routes. |
| Intravenous Injection [64] | 10^10 - 10^13 | COVID-19, Ischemic Stroke | Single or multiple doses | Requires higher doses due to sequestration in liver, spleen, and lungs. |
| Localized/Wound Coverage [20] | 10^10 - 10^11 (in pre-clinical models) | Diabetic Foot Ulcers, Burn Wounds | Every 2-3 days | Sustained-release scaffolds (e.g., hydrogels) enhance retention and permit lower effective dosing. |
| Subcutaneous Injection [20] | 10^10 - 10^11 (in pre-clinical models) | Full-thickness skin wounds | Single or multiple injections | Meta-analysis shows superior wound closure and collagen deposition vs. topical dressing. |
Table 2: Research Reagent Solutions for MSC-Exosome Workflows
| Reagent / Material | Supplier Examples | Function / Application | Key Considerations |
|---|---|---|---|
| Lipofectamine CRISPRMAX | Thermo Fisher Scientific | Transfection of MSCs with CRISPR/Cas9 constructs for genetic engineering. | Optimized for stem cells; crucial for achieving high editing efficiency with low toxicity. |
| pX330 Cas9 Vector | Addgene | Core plasmid for expressing S. pyogenes Cas9 and a single-guide RNA. | Standardized backbone; enables rapid gRNA cloning and robust editing. |
| Chitosan (Medium MW) | Sigma-Aldrich | Natural polymer for forming thermosensitive hydrogel scaffolds. | Biocompatible, biodegradable, and forms a gel at body temperature for exosome delivery. |
| Differential Ultracentrifuge | Beckman Coulter | Isolation and purification of exosomes from MSC-conditioned media. | Considered the "gold standard" method, though can cause EV damage [41]. |
| Size Exclusion Chromatography (SEC) Columns | IZON Science (qEV columns) | Isolation of high-purity exosomes with minimal damage. | Yields higher purity exosomes than ultracentrifugation alone; better preserves integrity [41]. |
| Nanoparticle Tracking Analyzer (NTA) | Malvern Panalytical | Quantification of exosome particle size and concentration. | Essential for standardizing dose calculations in particles/mL prior to in vivo studies. |
Integrated Workflow and Signaling Pathways
The development of engineered MSC-exosome therapies involves a multi-stage bioengineering pipeline, from parent cell modification to final delivery. The therapeutic effect is mediated through key signaling pathways modulated by the exosomal cargo.
Experimental Workflow Diagram
Diagram Title: MSC-Exosome Bioengineering Pipeline
Key Signaling Pathways in Exosome-Mediated Repair
Diagram Title: Key Signaling Pathways in Wound Repair
Concluding Remarks
The integration of CRISPR editing and biomimetic delivery systems marks a significant advancement in MSC-exosome therapy for wound healing. Engineering exosomes to carry enhanced levels of specific therapeutic cargo, such as anti-inflammatory miRNAs and growth factors, increases their intrinsic potency. Concurrently, sophisticated delivery systems like hydrogels improve localization and retention at the wound site, thereby enhancing bioavailability.
These bioengineering strategies are intrinsically linked to the optimization of dosing and administration. Enhanced potency and improved delivery can lower the total therapeutic dose required and extend the duration of action, directly addressing the challenges of rapid clearance and variable biodistribution. Future research must focus on standardized characterization of engineered exosome products, rigorous dose-escalation studies for each administration route, and the development of potency assays that correlate specific cargo profiles with in vivo efficacy. This integrated approach will accelerate the clinical translation of engineered MSC-exosomes from a promising therapeutic concept to a robust, off-the-shelf regenerative medicine product.
The transition of mesenchymal stem cell (MSC) exosome therapies from laboratory research to industrial-scale production represents a critical juncture in regenerative medicine. While exosomes offer significant advantages over whole-cell therapies, including reduced risks of immunogenicity and tumorigenesis, their clinical translation is hampered by substantial manufacturing challenges [66] [60]. The inherent variability of primary MSCs, low yield of exosomes using conventional methods, and lack of standardized protocols create significant bottlenecks in producing consistent, clinically viable exosome products [67] [68]. For wound therapy applications specifically, where dosing parameters and administration routes are being actively refined, the ability to produce standardized exosome preparations at scale becomes paramount for both clinical validation and eventual therapeutic use [9] [60]. This application note examines these scalability challenges and presents emerging solutions for industrial-scale production of MSC exosomes, with particular emphasis on implications for dosing optimization in wound healing applications.
Key Production Challenges and Yield Limitations
Critical Scalability Barriers
The path to industrial-scale exosome production faces multiple interconnected challenges that impact both the quantity and quality of the final therapeutic product:
Donor Variability and Finite Expansion Capacity: Primary MSCs derived from bone marrow, adipose tissue, or umbilical cord tissue exhibit significant donor-to-donor variability and limited expansion capacity in vitro, leading to batch-to-batch inconsistencies that complicate standardized therapeutic development [68] [66]. This variability directly impacts exosome characteristics and potency, creating significant challenges for dose optimization studies.
Low Yield with Conventional Methods: Traditional two-dimensional (2D) culture systems produce insufficient exosome yields for large-scale clinical applications. Estimates indicate that one patient treatment requires approximately 100 μg/kg of exosomes per administration, creating substantial production demands for clinical trials and broader therapeutic use [67].
Process Standardization Gaps: The absence of standardized Good Manufacturing Practice (GMP)-grade protocols for exosome isolation, purification, and characterization contributes to product heterogeneity. Current isolation techniques, including ultracentrifugation, precipitation, and ultrafiltration, produce variable yields and purity levels, with ultracentrifugation yielding only approximately 5-25% recovery of exosomes [69] [66].
Storage and Stability Concerns: Exosome integrity and functionality can be compromised during storage, particularly at temperatures of 4°C and -20°C, with degradation of key marker proteins like CD63 and HSP70 observed after 10 days at 4°C [66]. These stability issues present significant hurdles for product shelf-life and distribution.
Quantitative Production Challenges
Table 1: Key Production Challenges in MSC Exosome Manufacturing
| Challenge Category | Specific Issue | Impact on Scalability |
|---|---|---|
| Cell Source Limitations | Donor variability in primary MSCs [68] | Batch-to-batch inconsistency in exosome potency and composition |
| Finite expansion capacity of primary MSCs [66] | Limited scale-up potential for large-volume production | |
| Process Limitations | Low yield of conventional 2D culture systems [67] | Insufficient production for clinical dosing requirements |
| Ultracentrifugation recovery rates of ~5-25% [69] | Significant product loss during processing | |
| Characterization Gaps | Lack of standardized potency assays [9] | Difficulty correlating production metrics with therapeutic efficacy |
| Heterogeneity in dose units across studies [9] | Challenges in dose optimization and cross-study comparisons | |
| Storage & Stability | Degradation at -20°C and 4°C [66] | Limited shelf-life and distribution challenges |
Emerging Solutions for Scalable Production
Advanced Bioreactor Systems
Bioreactor technology represents a fundamental advancement in exosome production scalability, enabling higher-density cell cultures with improved process control:
Fixed-Bed Bioreactor Systems: These systems provide uniform nutrient perfusion and minimal shear stress, supporting GMP-compatible production. Recent implementations have demonstrated capacity for continuous expansion of induced MSCs (iMSCs) with yields of approximately 1.2 × 10¹³ EV particles per day, representing orders of magnitude improvement over conventional flask-based culture [68].
Suspension Bioreactor Cultures: Utilizing microcarriers for adherent cell growth, suspension systems enable large-volume production with the potential for automation integration. One scalable biomanufacturing strategy reported expansion of iMSCs for up to 20 days in 3D culture, yielding >5 × 10⁸ cells per production batch [68].
Process Monitoring and Control: Advanced bioreactor systems incorporate real-time monitoring of critical process parameters (pH, dissolved oxygen, metabolite levels) to maintain optimal production conditions and enhance batch consistency [68].
To overcome the limitations of primary MSCs, researchers are developing more consistent and scalable cell sources:
Induced MSC (iMSC) Platforms: Derived from extended pluripotent stem cells (EPSCs) or induced pluripotent stem cells (iPSCs), iMSCs offer unlimited expansion capacity, reduced batch-to-batch variability, and opportunities for genetic engineering to enhance therapeutic potential [68]. These cells maintain phenotypic stability through multiple passages while producing exosomes with characteristics comparable to primary MSC-derived exosomes.
Genetically Engineered MSC Lines: Synthetic biology approaches, such as the exosome-to-cell (EXOtic) device, can enhance exosome production by manipulating biogenesis pathways. One study demonstrated that co-expression of STEAP3, syndecan-4, and an L-aspartate oxidase fragment resulted in a 40-fold increase in exosome production without altering exosome size characteristics [67].
Yield Optimization Strategies
Table 2: Strategies for Enhancing MSC Exosome Yield
| Strategy Type | Specific Approach | Reported Yield Improvement |
|---|---|---|
| Genetic Engineering | EXOtic device (STEAP3, syndecan-4, L-aspartate oxidase) [67] | 40-fold increase in production |
| 3D Culture Systems | Bioreactor-based expansion [68] | >5 × 10⁸ cells/batch; ~1.2 × 10¹³ particles/day |
| Preconditioning Strategies | Hypoxic conditions (1% O₂) [70] | Enhanced production and therapeutic potential |
| Inflammatory cytokine priming (TNF-α, IL-1β) [70] | Altered miRNA profiles and increased potency | |
| Process Optimization | Tangential flow filtration [69] | Improved recovery rates and processing volumes |
| Serum-free, chemically defined media [66] | Reduced contamination and improved consistency |
Experimental Protocols for Scalable Production
Bioreactor-Based Production Workflow
Objective: Establish a scalable, GMP-compliant process for industrial-scale production of MSC exosomes.
Materials:
- Induced MSCs (iMSCs) derived from EPSCs/iPSCs
- Fixed-bed or suspension bioreactor system
- Serum-free, chemically defined culture media
- Tangential Flow Filtration (TFF) system
- Nanoparticle Tracking Analysis (NTA) system
- CD63, CD81, TSG101 antibodies for characterization
Methodology:
- Cell Expansion Phase:
- Inoculate bioreactor with iMSCs at density of 1-2 × 10⁵ cells/mL
- Maintain culture parameters: pH 7.2-7.4, dissolved oxygen 30-50%, temperature 37°C
- Implement continuous perfusion feeding strategy with metabolite monitoring
- Culture for 10-20 days, monitoring cell density and viability
Harvesting and Clarification:
- Collect conditioned media continuously or at batch endpoint
- Remove cells and debris through sequential filtration (0.45μm → 0.22μm)
- Concentrate clarified media 10-20× using tangential flow filtration
Exosome Isolation and Purification:
- Isolate exosomes using size-exclusion chromatography or density gradient centrifugation
- Concentrate purified exosomes using centrifugal devices (100kDa MWCO)
- Perform buffer exchange into formulation buffer (e.g., PBS with trehalose)
Quality Control and Characterization:
- Quantify particle concentration and size distribution via NTA (expect 70-150nm)
- Confirm exosome markers (CD63, CD81, TSG101) via western blot or flow cytometry
- Assess purity (protein/particle ratio) and sterility
- Evaluate functionality through in vitro potency assays
Preconditioning Protocol for Enhanced Potency
Objective: Enhance therapeutic potency of MSC exosomes through cytokine preconditioning for improved wound healing efficacy.
Materials:
- Primary MSCs or iMSCs at 70-80% confluence
- Serum-free basal media
- Recombinant human TNF-α and IL-1β
- miRNA extraction and analysis kits
- Western blot equipment for protein characterization
Methodology:
- Preconditioning Stimulation:
- Prepare preconditioning media: serum-free basal media supplemented with:
- TNF-α: 10-20 ng/mL
- IL-1β: 10 ng/mL
- Remove standard culture media from MSC cultures
- Add preconditioning media and incubate for 24-48 hours at 37°C, 5% CO₂
- Include control cells with standard media only
- Prepare preconditioning media: serum-free basal media supplemented with:
Exosome Collection and Analysis:
- Collect conditioned media after preconditioning period
- Isolate exosomes using standardized protocol (e.g., ultracentrifugation)
- Characterize miRNA cargo changes via qPCR or RNA sequencing
- Focus on key wound-healing miRNAs: miR-146a, miR-21, miR-126, miR-181a
- Confirm protein marker expression (CD63, CD81, Alix)
Potency Validation:
- Evaluate enhanced immunomodulatory potential via macrophage polarization assays
- Assess pro-angiogenic effects using endothelial tube formation assays
- Test improved wound closure in in vitro scratch assays
Implications for Dosing and Administration in Wound Therapy
The scalability of exosome production directly influences dosing strategies and administration route optimization in wound healing applications. Current clinical evidence suggests that administration route significantly impacts dose requirements, with aerosolized inhalation achieving therapeutic effects at approximately 10⁸ particles, substantially lower than intravenous routes [9]. As production methods improve and enable more consistent exosome characterization, precise dose-response relationships can be established, potentially reducing the long-term cost of clinical trials and avoiding ineffective dosing regimens [9].
For wound healing specifically, the ability to produce exosomes at scale enables exploration of optimal administration methods. Research indicates that subcutaneous injection demonstrates superior wound closure outcomes compared to topical application, with enhanced collagen deposition and revascularization [20]. Furthermore, comparative studies of exosomes from different MSC sources reveal that adipose-derived stem cells (ADSCs) show the best effect on wound closure rate, while bone marrow MSCs demonstrate superior revascularization potential [20]. These findings highlight how scalable production platforms enable systematic optimization of both the production source and administration approach for specific therapeutic outcomes.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Scalable MSC Exosome Production
| Reagent Category | Specific Product/Technology | Function & Application |
|---|---|---|
| Cell Culture Systems | Serum-free, xeno-free media [66] | Eliminates exogenous vesicle contamination and improves consistency |
| Fixed-bed and suspension bioreactors [68] | Enables high-density cell culture for increased exosome yield | |
| Microcarriers for 3D culture [68] | Supports scalable expansion of adherent MSCs | |
| Isolation & Purification | Tangential Flow Filtration (TFF) [69] | Scalable concentration and buffer exchange for large volumes |
| Size Exclusion Chromatography (SEC) [69] | High-purity exosome separation based on hydrodynamic radius | |
| Density gradient centrifugation [69] | Separation based on buoyant density for high-purity isolates | |
| Characterization Tools | Nanoparticle Tracking Analysis (NTA) [69] | Quantifies particle concentration and size distribution |
| Western blot markers (CD63, CD81, TSG101) [69] | Confirms exosome identity and purity | |
| miRNA sequencing and qPCR [70] | Analyzes therapeutic cargo and batch consistency | |
| Storage & Formulation | Cryoprotectants (trehalose) [66] | Maintains exosome integrity during freeze-thaw cycles |
| PBS-based formulation buffers [66] | Provides stable storage medium for final product |
The transition from laboratory-scale to industrial-scale production of MSC exosomes represents a critical pathway for realizing the full therapeutic potential of these nanovesicles in wound healing and other regenerative applications. While significant challenges remain in standardization, yield optimization, and characterization, emerging technologies in bioreactor design, alternative cell sources, and engineered production systems offer promising solutions. The continued development of scalable, GMP-compliant production platforms will be essential for establishing robust dosing guidelines and administration protocols that maximize therapeutic efficacy while ensuring manufacturing feasibility and economic viability. As these production methodologies mature, they will fundamentally enable the clinical translation of MSC exosome therapies from experimental approaches to mainstream regenerative treatments.
Evidence-Based Practice: Analyzing Preclinical and Clinical Trial Outcomes
Diabetic foot ulcers (DFUs) represent a severe and pervasive complication of diabetes mellitus, with a lifetime incidence affecting up to a quarter of this patient population [71]. These chronic wounds are characterized by a persistent, hyper-inflammatory environment that prevents progression to regenerative wound closure, often leading to frequent hospitalizations, diminished quality of life, and high risk of lower-extremity amputation [71] [72]. The complex pathophysiology of diabetic wounds involves multiple factors, including decreases in growth factor production, impaired angiogenesis, macrophage dysfunction, and reduced keratinocyte and fibroblast migration and proliferation [72]. Critically, the wound healing process in diabetic models remains stalled in the inflammatory phase, preventing transition to the regenerative phase essential for tissue repair [72].
Mesenchymal stem cell-derived extracellular vesicles (MSC-EVs), particularly exosomes, have emerged as promising cell-free therapeutic agents due to their immunomodulatory and regenerative properties [9] [73]. These nano-sized membrane-bound structures carry bioactive molecules such as microRNAs, proteins, and lipids that mediate intercellular communication and recapitulate many therapeutic effects of their parent cells [73]. Unlike whole-cell therapies, MSC-EVs offer advantages including lower immunogenicity, enhanced stability, ability to cross biological barriers, and no risk of tumorigenesis or thrombosis [9] [73]. Current research focuses on optimizing dosing and administration routes to maximize their therapeutic potential for wound healing applications across different disease models.
This meta-analysis examines the comparative efficacy of MSC-EV therapies in diabetic versus non-diabetic wound models, with particular emphasis on dose-response relationships and administration pathways. Understanding these parameters is crucial for developing standardized protocols that can enhance clinical translation and therapeutic outcomes.
Comprehensive Meta-Analysis of Preclinical Data
Therapeutic Efficacy Across Wound Models
Table 1: Comparative Efficacy of Advanced Therapies in Diabetic Wound Models
| Intervention | Healing Rate vs. Control | Healing Time Reduction vs. Control | Amputation Rate Reduction vs. Control | SUCRA Ranking |
|---|---|---|---|---|
| Stem Cells (SC) | OR = 5.71 [74] | Not specified | OR = 0.12 [74] | 89.7% [74] |
| Amniotic Membrane Therapy (AMT) | OR = 5.11 [74] | -26.91 days [74] | Not specified | 89.2% [74] |
| Platelet-Rich Plasma (PRP) | RR = 1.42 [74] | -21.65 days [74] | OR = 0.35 (HBOT) [74] | 73.2% (amputation) [74] |
| Negative Pressure Wound Therapy (NPWT) | Risk Ratio = 1.46 [71] | -16.79 days [74] | Risk Ratio = 0.69 [71] | Not specified |
| Low-Level Laser Therapy (LLLT) | Not specified | Not specified | Not specified | 93.9% (PAR) [74] |
| Extracorporeal Shockwave Therapy (ESWT) | Not specified | Not specified | Not specified | 84.0% (PAR) [74] |
Recent network meta-analyses evaluating 12 interventions for diabetic foot ulcers revealed that stem cell therapy and amniotic membrane therapy demonstrated superior efficacy in improving wound healing rates compared to other advanced therapies [74]. The surface under the cumulative ranking curve (SUCRA) values indicated SC (89.7%) and AMT (89.2%) as highest-ranking interventions, while conventional standard of care (SOC) ranked lowest (10.4%) [74]. These findings highlight the significant potential of biologically active therapies, particularly those with immunomodulatory properties, for managing complex diabetic wounds.
MSC-based therapies demonstrate robust therapeutic potential across diverse preclinical models, supported by evidence from numerous meta-analyses covering neurological, renal, wound healing, liver, musculoskeletal, respiratory, and reproductive disorders [73]. These therapies significantly improve functional scores, reduce inflammation, and promote regeneration through multiple mechanisms, including anti-inflammatory, anti-apoptotic, and pro-angiogenic actions [73]. The therapeutic effects are largely mediated through paracrine signaling via extracellular vesicles rather than direct cell differentiation and engraftment [16].
Dose-Response Relationships and Administration Routes
Table 2: MSC-EV Dosing Strategies by Administration Route
| Administration Route | Effective Dose Range | Therapeutic Indications | Source Efficacy | Dosing Frequency |
|---|---|---|---|---|
| Aerosolized Inhalation | ~10^8 particles [9] | Respiratory diseases, COVID-19 [9] | BM-, AD-, UC-MSCs [9] | Single to multiple doses |
| Intravenous Infusion | Higher than inhalation [9] | Systemic, neurological disorders [73] | BM-, AD-, UC-MSCs [73] | Single to multiple doses |
| Topical Application | Variable, depending on formulation [73] | Diabetic wounds, skin injuries [73] | UC-, AD-MSCs [73] | Weekly or bi-weekly |
| Local Injection | 10^6-10^9 particles [73] | Joint disorders, localized injuries [73] | BM-, AD-MSCs [73] | Single to multiple doses |
Comprehensive analysis of global clinical trials registered between 2014 and 2024 revealed that administration route significantly influences effective dosing of MSC-EVs [9]. Notably, nebulization therapy achieved therapeutic effects at doses around 10^8 particles, significantly lower than those required for intravenous routes, suggesting a relatively narrow and route-dependent effective dose window [9]. This has important implications for preclinical study design and clinical translation, emphasizing the need for route-specific dose optimization.
The tissue source of MSCs significantly influences the biological functions and characteristics of derived EVs, affecting their size, composition, and therapeutic efficacy [9]. Bone marrow-, adipose-, and umbilical cord-derived EVs have demonstrated particularly high efficacy, with modified EVs showing enhanced outcomes across various disease models [73]. This variability necessitates careful consideration of EV source when designing preclinical studies and interpreting results across different wound models.
Experimental Protocols and Methodologies
Preclinical Wound Model Establishment
Diabetic Mouse Model Protocol:
- Utilize male B6.Cg-m+/+Leprdb/J mice (db/db) aged 8-12 weeks from Jackson Laboratories (Strain Code 000697) [72].
- House mice individually on a 12-hour light-dark cycle at 20-24°C with 30-70% humidity with ad libitum access to food and water [72].
- Acclimate for approximately one week prior to study initiation.
- Randomize into treatment groups based on blood glucose values prior to surgical wounding [72].
- Create two full-thickness 6 mm wounds through the panniculus over the shoulders using a punch biopsy tool [72].
- Apply silicone splints secured with non-absorbable suture and surgical glue to prevent skin contracture [72].
- Replace splint sutures as needed, taking care not to disrupt wound healing.
- Administer non-steroidal anti-inflammatory drugs once daily for 3 days post-wounding.
Aged Non-Diabetic Mouse Model Protocol:
- Utilize male and female C57BL/6J mice at 77 weeks of age from Jackson Laboratories [72].
- House and acclimate as described for diabetic models.
- Randomize into treatment groups prior to surgical wounding using same wound creation protocol [72].
- Note: Aged non-diabetic mice demonstrate similar natural wound healing deficiencies as young diabetic mice, providing a comparable model for chronic wound healing studies [72].
MSC-EV Isolation and Characterization Protocol
EV Isolation Methodology:
- Culture MSCs from selected sources (bone marrow, adipose tissue, or umbilical cord) under standardized conditions [9] [16].
- Isolate extracellular vesicles from conditioned media using differential centrifugation or ultracentrifugation techniques [9].
- Characterize EVs using nanoparticle tracking analysis (NTA) for size and concentration determination [9].
- Confirm surface markers using flow cytometry [9].
- Verify EV morphology using electron microscopy [9].
Quality Control Parameters:
- Confirm diameter range of 30-150 nm for exosomes [9].
- Verify expression of characteristic surface markers (CD73, CD90, CD105) while lacking hematopoietic markers (CD34, CD45, CD14, CD19, HLA-DR) per International Society for Cellular Therapy guidelines [16].
- Ensure absence of cellular debris through appropriate purification steps.
- Quantify using standardized particle counting methods.
Dosing and Administration Protocols
Nebulization Administration:
- Utilize dose range of approximately 10^8 particles for respiratory applications [9].
- Suspend EVs in appropriate isotonic solution compatible with nebulization equipment.
- Administer using standardized nebulization protocols with particle size optimization.
- Monitor deposition and distribution using appropriate tracking methods.
Topical Wound Application:
- Incorporate EVs into appropriate delivery vehicles (hydrogels, methylcellulose wafers, or specialized dressings) [72].
- For plasmid-based therapies, prepare methylcellulose wafers by mixing plasmid DNA in 1% methylcellulose and spotting in 50 μL droplets [72].
- Air dry wafers for maximum 5 hours prior to application [72].
- Apply directly to wound bed, ensuring complete contact with wound surface.
- Re-dose as needed based on treatment protocol, typically weekly [72].
Intravenous Administration:
- Utilize higher dose ranges compared to inhalation routes [9].
- Suspend in sterile, pyrogen-free saline solution.
- Administer via tail vein injection in rodent models.
- Monitor systemic distribution and potential immune responses.
Assessment and Evaluation Methods
Wound Measurement Protocol:
- Capture standardized digital images of wounds at regular intervals (daily or every other day).
- Use calibrated reference scales in all images.
- Measure wound areas using image analysis software (ImageJ or equivalent).
- Calculate wound closure percentage: [(Initial area - Current area)/Initial area] × 100.
- Document complete closure time (number of days until full re-epithelialization).
Histological Analysis:
- Collect wound tissue samples at predetermined endpoints.
- Process for hematoxylin and eosin staining for general morphology.
- Perform Masson's trichrome staining for collagen deposition assessment.
- Conduct immunohistochemistry for specific markers (CD31 for angiogenesis, CD68 for macrophages, α-SMA for myofibroblasts).
- Score histological parameters using standardized semi-quantitative methods.
Molecular Analysis:
- Extract RNA and protein from wound tissue at various healing stages.
- Analyze gene expression of inflammatory markers (IL-1β, TNF-α, IL-6), growth factors (VEGF, FGF, TGF-β), and matrix components (collagen I, III) using qRT-PCR.
- Measure protein levels via ELISA or Western blotting.
- Evaluate macrophage polarization using specific markers (iNOS for M1, Arg-1 for M2).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for MSC Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Research Function | Considerations |
|---|---|---|---|
| MSC Sources | Bone Marrow (BM-MSCs), Adipose (AD-MSCs), Umbilical Cord (UC-MSCs) [16] | Therapeutic agent origin; Different efficacy profiles [73] | BM-MSCs: High differentiation; AD-MSCs: Easier harvest; UC-MSCs: Lower immunogenicity [16] |
| EV Isolation Kits | Ultracentrifugation systems, Precipitation kits, Size-exclusion chromatography | MSC-EV purification from conditioned media [9] | Method affects yield, purity, and functionality; Standardization needed [9] |
| Characterization Tools | Nanoparticle Tracking Analysis (NTA), Flow Cytometry, Electron Microscopy [9] | EV quantification, size distribution, morphology, and marker confirmation [9] | Essential for quality control and reproducibility |
| Animal Models | db/db mice (diabetic), Aged C57BL/6J (non-diabetic) [72] | Preclinical efficacy testing in pathologically relevant systems | Diabetic and aged models show similar healing impairment [72] |
| Wound Measurement Tools | Digital calipers, DSLR cameras with scale, ImageJ software | Standardized wound area quantification and healing rate calculation | Critical for objective endpoint assessment |
| Molecular Biology Assays | qRT-PCR, ELISA, Western Blot, Immunohistochemistry | Mechanism analysis: angiogenesis, inflammation, matrix remodeling | Multiplex approaches recommended for comprehensive profiling |
| Delivery Matrices | Methylcellulose wafers, Hydrogels, Collagen scaffolds [72] | EV stabilization and controlled release at wound site | Affects bioavailability and retention |
Discussion and Clinical Translation Challenges
The meta-analysis of preclinical data reveals several critical considerations for optimizing MSC exosome therapy in wound healing applications. First, significant differences in therapeutic efficacy emerge between diabetic and non-diabetic wound models, necessitating model-specific dosing strategies. Second, the administration route profoundly influences effective dosing, with topical and inhalation routes requiring significantly different quantities than systemic administration [9]. Third, the source of MSCs considerably impacts EV characteristics and functionality, with bone marrow-, adipose-, and umbilical cord-derived EVs showing distinct efficacy profiles across different wound models [73] [16].
Current challenges in clinical translation include lack of standardized protocols for EV isolation and purification, significant heterogeneity in dosing units and outcome measures across studies, and insufficient understanding of optimal dosing frequencies and treatment durations [9]. Additionally, the field faces methodological limitations in preclinical studies, including poor randomization and blinding procedures, which contribute to high heterogeneity and potential bias in meta-analyses [73]. Future research directions should focus on developing standardized dosing frameworks, establishing potency assays, harmonizing clinical protocols, and exploring combination therapies that might synergize with MSC-EV treatment.
The promising therapeutic efficacy of MSC-EVs across diverse preclinical models, particularly their demonstrated ability to accelerate wound healing in both diabetic and aged non-diabetic models [72], supports their continued development as a versatile regenerative therapy. However, successful clinical translation will require addressing current methodological challenges and establishing robust, standardized protocols that ensure consistent product quality and therapeutic outcomes.
Extracellular vesicles (EVs) are lipid bilayer-enclosed particles secreted by cells that play a crucial role in intercellular communication by transferring proteins, lipids, and nucleic acids [75]. Within regenerative medicine, mesenchymal stem cell-derived EVs (MSC-EVs) have emerged as promising cell-free therapeutic agents, particularly for wound healing and skin regeneration [76] [23]. MSC-EVs can be broadly categorized into two main types based on their biogenesis and cellular origin: small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs). sEVs (typically <200 nm in diameter) are primarily derived from the endosomal system of viable cells, whereas ApoEVs are produced during programmed cell death and encompass a broader size range, including apoptotic small EVs (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm) [76] [77] [78]. Understanding the comparative efficacy of these EV subpopulations is essential for optimizing therapeutic strategies in wound management.
Biological Characteristics and Mechanisms of Action
Biogenesis and Cargo Composition
The biogenesis pathways of sEVs and ApoEVs fundamentally differ, resulting in distinct cargo compositions and functional properties. sEVs are generated through the inward budding of endosomal membranes, forming intraluminal vesicles within multivesicular bodies (MVBs) that subsequently fuse with the plasma membrane for release [75]. This process involves the endosomal sorting complex required for transport (ESCRT) machinery and is characterized by specific markers such as tetraspanins (CD9, CD63, CD81), ALIX, and TSG101 [77] [75]. In contrast, ApoEVs are produced during apoptosis through caspase-mediated cell disassembly, which includes membrane blebbing and formation of apoptopodia [77] [78]. The molecular driver of ApoEV formation is ROCK1 activation following cleavage by caspase-3 [77]. ApoEVs typically display phosphatidylserine on their surfaces as a key "eat-me" signal and can contain diverse cargo, including intact organelles, nuclear fragments, and cytoplasmic components [77] [78].
Signaling Pathways and Functional Mechanisms
Both sEVs and ApoEVs facilitate tissue repair through complex signaling mechanisms, though their specific pathways and functional emphases differ. sEVs primarily promote angiogenesis, modulate inflammation, and stimulate collagen synthesis through the transfer of growth factors, miRNAs, and cytokines [76] [23]. ApoEVs exert their effects through efferocytosis (the phagocytosis of apoptotic material) by immune cells, particularly macrophages, leading to potent immunomodulation and activation of regenerative programs [79] [78]. Recent evidence indicates that ApoEVs from MSCs can inhibit the TGF-β/SMAD2/3 pathway, reducing fibrosis and inflammation in chronic disease models [79]. The diagram below illustrates the key signaling pathways through which sEVs and ApoEVs mediate their therapeutic effects in wound healing.
Comparative Efficacy Analysis
Quantitative Efficacy Metrics in Wound Healing
Recent meta-analyses of preclinical studies provide direct comparative data on the efficacy of different MSC-EV subtypes across key wound healing parameters. The table below summarizes the therapeutic outcomes of sEVs, ApoSEVs, and ApoBDs in animal models of wound healing, based on a comprehensive analysis of 83 studies [76].
Table 1: Comparative Efficacy of MSC-EV Subtypes in Wound Healing Parameters
| EV Subtype | Wound Closure Rate | Scar Width Reduction | Blood Vessel Density | Collagen Deposition |
|---|---|---|---|---|
| sEVs (<200 nm) | Moderate efficacy | Moderate efficacy | Superior efficacy | Moderate efficacy |
| ApoSEVs (<1 μm) | Superior efficacy | Not fully characterized | High efficacy | Superior efficacy |
| ApoBDs (1-5 μm) | Lower efficacy | Not fully characterized | Moderate efficacy | Lower efficacy |
Impact of MSC Source and Administration Route
The therapeutic efficacy of MSC-EVs is significantly influenced by both the tissue source of parent MSCs and the method of administration. A comparative analysis reveals that adipose-derived stem cells (ADSCs) demonstrate the best effect on wound closure rate and collagen deposition, while bone marrow MSCs (BMMSCs) show superior performance in revascularization [76]. Regarding administration routes, subcutaneous injection consistently demonstrates better outcomes for wound closure, collagen deposition, and revascularization compared to topical dressing/covering approaches [76]. The diagram below illustrates the workflow for a comparative study evaluating these critical variables in EV efficacy.
Dosing and Administration Protocols
EV Quantification and Dosing Standards
Establishing standardized dosing protocols remains a significant challenge in EV therapy due to heterogeneity in quantification methods across studies. The table below summarizes the current dosing approaches and ranges used in preclinical and clinical studies, highlighting the need for harmonization in the field [8].
Table 2: MSC-EV Dosing Strategies and Quantification Methods
| Quantification Method | Typical Dose Range (Preclinical) | Typical Dose Range (Clinical) | Advantages | Limitations |
|---|---|---|---|---|
| Particle Concentration (NTA) | 10⁹ - 10¹¹ particles/dose | 10¹⁰ - 10¹² particles/dose | Direct EV counting | Does not reflect bioactive content |
| Protein Content (Bradford/BCA) | 10-250 μg/dose | 100 μg/kg - 6.6 mg total | Standardized protein quantitation | Contamination by non-EV proteins |
| Cell Equivalents | EV yield from 10⁶ - 10⁸ cells | EV yield from 10⁷ - 10⁹ cells | Production scalability | Indirect measurement, high variability |
Based on analysis of preclinical and clinical data, a working range for effective MSC-EV dose in humans falls between 1 × 10¹⁰ and 6 × 10¹² total particles per dose regimen, though optimal dosing is highly dependent on specific administration route and disease indication [8].
Comparative Administration Strategies
The route of administration significantly influences the distribution and therapeutic efficacy of MSC-EVs. For wound healing applications, subcutaneous injection around the wound periphery has demonstrated superior outcomes compared to topical application for both sEVs and ApoEVs [76]. Intravenous administration results in rapid systemic distribution but may lead to significant accumulation in hepatic and splenic tissues, reducing targeted delivery to wound sites [23] [8]. Recent advances include engineered scaffolds and hydrogels that improve EV retention at wound sites for sustained release, potentially enhancing the efficacy of both sEV and ApoEV therapies [80].
Experimental Protocols
Protocol 1: Isolation and Characterization of MSC-sEVs and ApoEVs
Principle: sEVs are isolated from conditioned medium of viable MSCs, while ApoEVs are obtained from MSCs undergoing apoptosis induced by chemical inducers.
Materials:
- MSC culture medium (LG-DMEM with 10% EV-depleted FBS)
- Ultracentrifugation equipment
- Staurosporine (0.5 μM working concentration)
- PKH26 dye for labeling
- Antibodies for characterization (CD63, CD81, Annexin V, caspase-3)
Procedure:
- MSC Culture: Culture MSCs from selected sources (adipose, bone marrow, umbilical cord) to 80% confluence [79].
- sEV Production: Collect conditioned medium after 48 hours of culture with viable MSCs. Centrifuge at 300 × g for 10 min, then 2000 × g for 20 min to remove cells and debris [76] [79].
- ApoEV Induction: Treat MSCs with 0.5 μM staurosporine for 4-6 hours to induce apoptosis. Confirm apoptosis by flow cytometry using Annexin V/PI staining [79].
- EV Isolation: Ultracentrifuge both conditioned media at 100,000 × g for 70 min at 4°C. Resuspend pellets in PBS and filter through 0.22-μm membranes [79].
- Characterization:
Protocol 2: In Vitro Efficacy Assessment for Wound Healing Applications
Principle: Evaluate the functional effects of sEVs and ApoEVs on key cellular processes involved in wound healing.
Materials:
- HuH7 cell line (oxidative stress model)
- THP-1 cell line (macrophage polarization)
- Primary human T-cells (immunomodulation)
- MitoSOX Red (mitochondrial ROS)
- Seahorse XF Analyzer (mitochondrial function)
- CFSE dye (T-cell proliferation)
Procedure:
- Immunomodulation Assay:
- Isolate human PBMCs and label with CFSE
- Treat with sEVs or ApoEVs (10⁹ particles/mL) for 72 hours
- Assess T-cell proliferation by flow cytometry
- Measure T-regulatory cell differentiation (CD4+CD25+FoxP3+) [79]
Macrophage Polarization Assay:
- Differentiate THP-1 monocytes into M0 macrophages with PMA
- Treat with sEVs or ApoEVs for 48 hours
- Analyze M1 (CD80+ iNOS+) and M2 (CD206+ Arg1+) markers by flow cytometry
- Measure cytokine secretion (IL-10, TGF-β for M2; TNF-α, IL-6 for M1) [79]
Oxidative Stress Protection:
- Treat HuH7 cells with H₂O₂ to induce oxidative stress
- Co-treat with sEVs or ApoEVs (10⁹ particles/mL) for 24 hours
- Measure mitochondrial ROS using MitoSOX Red
- Assess mitochondrial respiration using Seahorse XF Analyzer [79]
Protocol 3: In Vivo Evaluation in Diabetic Wound Model
Principle: Assess comparative efficacy of sEVs and ApoEVs in a physiologically relevant wound healing model.
Materials:
- db/db mice (type 2 diabetes model) or STZ-induced diabetic mice
- Wound creation apparatus (4-6 mm biopsy punch)
- EV formulations for administration
- Histology reagents (H&E, Masson's trichrome)
Procedure:
- Wound Creation: Anesthetize mice and create full-thickness excisional wounds on dorsal skin [76].
- Treatment Groups:
- Group 1: sEVs (10¹⁰ particles in 50 μL PBS, subcutaneous)
- Group 2: ApoSEVs (10¹⁰ particles in 50 μL PBS, subcutaneous)
- Group 3: ApoBDs (10¹⁰ particles in 50 μL PBS, subcutaneous)
- Group 4: Vehicle control (PBS only)
- Administration: Administer treatments every 3 days until wound closure [76].
- Outcome Measures:
- Daily wound closure measurement (planimetry)
- Histological analysis at day 10 (H&E for re-epithelialization, Masson's trichrome for collagen)
- Immunofluorescence for CD31 (vascular density) and α-SMA (myofibroblasts)
- RNA analysis of fibrotic (TGF-β, collagen I/III) and inflammatory (TNF-α, IL-10) markers [76] [79]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC-EV Research
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| MSC Source Reagents | Bone marrow aspirate, Adipose tissue, Wharton's Jelly | MSC isolation and expansion | Provide tissue-specific MSC populations for comparative studies |
| EV Induction Agents | Staurosporine (0.5 μM), Other caspase activators | ApoEV production | Induce controlled apoptosis for ApoEV generation |
| EV Isolation Kits | Ultracentrifugation reagents, Size-exclusion columns, Polymer-based precipitation | EV purification from conditioned media | Iserate EV subpopulations with minimal contamination |
| Characterization Antibodies | CD63, CD81, CD9, ALIX, TSG101, Annexin V, phosphatidylserine | EV characterization and quantification | Confirm EV identity and subcellular origin |
| Functional Assay Kits | MitoSOX Red, CFSE proliferation kit, Seahorse XF assay kits | In vitro efficacy assessment | Evaluate mitochondrial function, immunomodulation, and cellular responses |
| Animal Models | db/db mice, STZ-induced diabetic mice, Full-thickness wound models | In vivo efficacy studies | Provide physiologically relevant wound healing environments |
The comparative analysis of sEVs and ApoEVs reveals a complementary therapeutic profile, with each EV subtype exhibiting distinct advantages for specific wound healing parameters. sEVs demonstrate superior efficacy in promoting revascularization, while ApoSEVs show enhanced performance in wound closure rates and collagen deposition. The emerging evidence that apoptosis induction can serve as a priming strategy to enhance the immunomodulatory and regenerative potential of MSC-EVs represents a significant advancement in the field [79]. Future research directions should focus on standardizing isolation protocols, engineering EVs for enhanced targeting, and conducting direct comparative studies in clinically relevant models. The optimal translation of MSC-EV therapies will likely involve strategic selection of EV subtype, MSC source, and administration route based on specific wound healing deficiencies present in different patient populations.
The transition of mesenchymal stem cell-derived exosomes (MSC-Exos) from preclinical promise to clinical application hinges on a rigorous understanding of their safety profile, tolerability, and dose-response relationships. As a cell-free therapeutic strategy, MSC-Exos offer significant advantages over whole cell therapies, including lower immunogenicity, reduced risk of infusion-related toxicities, and the absence of tumorigenic potential [81] [2]. Current clinical evaluation is focused on establishing standardized frameworks for dosing and administration that can reliably translate therapeutic efficacy from animal models to human patients. This application note synthesizes the latest clinical trial data and experimental protocols to provide evidence-based guidance for researchers and drug development professionals working in the field of regenerative medicine, with particular emphasis on wound therapy applications.
Current Clinical Trial Landscape and Safety Profile
Safety and Tolerability of MSC-Exos
The favorable safety profile of MSC-Exos constitutes one of their most significant therapeutic advantages. Clinical studies consistently report that MSC-Exos exhibit low immunogenicity and do not elicit significant adverse immune reactions upon administration [81] [2]. Their nanoscale size (30-150 nm) prevents aggregation in pulmonary microvasculature, effectively avoiding the risk of pulmonary embolism that can occasionally occur with whole MSC infusions [2]. Furthermore, unlike viable cells, exosomes lack the capacity for replication, thereby eliminating tumorigenicity concerns associated with some stem cell therapies [62] [81].
Table 1: Completed Clinical Trials Demonstrating MSC-Exos Safety and Efficacy
| Condition | Exosome Source | Administration Route | Dose | Safety Outcomes | Efficacy Findings |
|---|---|---|---|---|---|
| GvHD [81] | MSC (unspecified) | Not specified | Not specified | Significant symptom improvement | Reduced steroid dosage |
| Cochlear Implant Inflammation [81] | Umbilical Cord MSC | Inner ear | Not specified | Safe and well tolerated | Improved speech perception |
| COVID-19 [9] | Various MSC sources | Aerosolized inhalation | ~10⁸ particles | Safe and well tolerated | Therapeutic effects observed |
Clinical Administration Routes and Tolerability
The route of administration significantly influences both the safety profile and therapeutic efficacy of MSC-Exos. Intravenous infusion and aerosolized inhalation have emerged as the predominant methods in clinical trials, particularly for systemic and respiratory conditions, respectively [9] [2]. Local administration routes—including topical application for dermatological conditions, intra-articular injection for osteoarthritis, and inner ear application for auditory disorders—have demonstrated excellent tolerability with minimal localized reactions [81] [14]. The choice of administration pathway must align with both the target tissue and the specific biophysical properties of the exosome preparation.
Dose-Response Relationships in Clinical Applications
Analysis of Effective Dosing Ranges
Dose-response relationships for MSC-Exos exhibit significant route-dependent variation, necessitating careful consideration of administration method when determining therapeutic dosing. Analysis of global clinical trials registered between 2014 and 2024 reveals that nebulization therapy achieves therapeutic effects at doses approximately as low as 10⁸ particles, substantially lower than those required for intravenous routes [9]. This suggests a relatively narrow and route-dependent effective dose window that must be carefully optimized for each clinical indication.
Table 2: Dose-Response Relationships by Administration Route
| Administration Route | Typical Effective Dose Range | Key Clinical Applications | Dose-Response Considerations |
|---|---|---|---|
| Aerosolized Inhalation [9] | ~10⁸ particles | Respiratory diseases (COVID-19, ARDS) | Lower dose requirement due to direct target tissue delivery |
| Intravenous Infusion [9] [2] | Higher than inhalation (precise range not specified) | Systemic applications, GvHD | Higher doses needed due to distribution throughout circulation |
| Topical Application [14] | 10⁸ particles in 25 µL PBS | Dermatological conditions, wound healing | Direct application enables localized effect with moderate dosing |
Dosing Standardization Challenges
A critical challenge in establishing definitive dose-response relationships is the lack of harmonized reporting standards across clinical trials [9]. Significant variations exist in how MSC-Exos doses are quantified, with different studies using weight (μg), particle number, or parent cell equivalents [2]. This methodological heterogeneity complicates cross-trial comparisons and underscores the urgent need for standardized dosing frameworks and potency assays to advance the clinical translation of MSC-Exos therapies [9].
Experimental Protocols for Dose-Response Studies
Murine Model for Psoriasis Dose-Response Investigation
Protocol Objective: To evaluate the therapeutic efficacy and optimal dosing of human placenta MSC (hPMSC) and human umbilical cord MSC (hUCMSC) exosomes in an imiquimod (IMQ)-induced psoriasis murine model [14].
Materials and Reagents:
- Exosomes isolated from hPMSCs or hUCMSCs
- 8-week-old male Balb/c mice
- IMQ cream (5% Aldara cream)
- Phosphate-buffered saline (PBS)
- Zoletil/Rompun anesthetic mixture
Methodology:
- Psoriasis Induction: Apply 50 mg IMQ cream topically to shaved skin daily for 6 consecutive days
- Exosome Treatment: Dissolve exosomes in PBS and apply topically daily for 7 days
- Dosage: Administer 1×10⁸ particles in 25 µL PBS for both hUCMSC and hPMSC exosomes
- Clinical Assessment: Evaluate PASI scores (erythema, scaling, skin thickening) on scale of 0-4
- Histological Analysis: Measure epidermal thickness after tissue fixation and staining
- Cytokine Measurement: Quantify skin tissue cytokines using ELISA
Key Findings: Both hPMSC and hUCMSC exosomes significantly reduced epidermal thickness and clinical severity scores compared to controls, with no significant difference observed between the two exosome sources [14].
MSC-Exos Isolation and Characterization Protocol
Protocol Objective: To isolate, purify, and characterize MSC-Exos for clinical trial applications under GMP-grade conditions [2] [14].
Materials and Reagents:
- MSC culture medium (serum-free, xeno-free)
- Ultracentrifugation equipment (Beckman Coulter Optima L-90K)
- Tangential Flow Filtration system (hollow fiber polyethersulfone membrane)
- PBS sucrose buffer
- Nanoparticle Tracking Analysis system (ZetaView PMX 110)
- Transmission Electron Microscopy equipment
- Antibodies for CD9, CD63, CD81, ALIX, Calnexin
Isolation Methods:
- Ultracentrifugation Protocol [2] [14]:
- Harvest conditioned medium from MSC cultures
- Sequential centrifugation: 300×g (10 min), 2,000×g (10 min), 10,000×g (30 min)
- Ultracentrifugation: 100,000×g for 90 minutes at 4°C
- Resuspend pellet in PBS and repeat ultracentrifugation
- Final resuspension in PBS or sucrose buffer storage solution
- Tangential Flow Filtration Alternative [2]:
- Filter culture medium through sterile hollow fiber membrane
- Wash with sterile PBS multiple times
- Concentrate and diafiltrate using sucrose buffer
- Final purification step
Characterization Requirements (per MISEV2018/2023 guidelines):
- Physical Characterization: NTA for size distribution (30-150 nm) and concentration; TEM for morphological analysis
- Marker Characterization: Western blot for positive markers (CD9, CD63, CD81, ALIX) and negative marker (Calnexin) to assess purity
- Bioactivity Assessment: Functional assays relevant to intended therapeutic application
Signaling Pathways and Therapeutic Mechanisms
MSC-Exos exert their therapeutic effects through the transfer of bioactive molecules that modulate key signaling pathways involved in inflammation, fibrosis, and tissue repair. Two particularly relevant pathways for wound healing applications are:
Diagram 1: MSC-Exos Modulation of TGF-β Signaling in Fibrosis. MSC-Exos deliver miRNAs and PTEN that suppress TGF-β pathway activation, subsequently reducing Smad2/3-dependent signaling, myofibroblast differentiation, and excessive ECM deposition that characterizes fibrotic conditions [48].
Diagram 2: MSC-Exos Regulation of Wnt/β-catenin Pathway. MSC-Exos downregulate β-catenin gene expression while enhancing Wnt5a/BMP2-driven signaling, which collectively inhibits Wnt/β-catenin dependent collagen deposition and epithelial-mesenchymal transition in fibrotic tissues [48].
Research Reagent Solutions for MSC-Exos Studies
Table 3: Essential Research Reagents for MSC-Exos Investigation
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| MSC Sources [16] [2] | Bone Marrow, Adipose Tissue, Umbilical Cord | Therapeutic exosome production | Umbilical cord sources show enhanced proliferation; adipose tissue is commonly used in clinical studies |
| Isolation Methods [2] | Ultracentrifugation, Tangential Flow Filtration | Exosome separation and purification | Ultracentrifugation remains most common; TFF offers scalability advantages |
| Characterization Tools [2] [14] | NTA, TEM, Western Blot | Physical and biomarker characterization | Essential for verifying exosome identity, size, and purity per MISEV guidelines |
| Surface Markers [2] [82] | CD9, CD63, CD81, ALIX | Positive exosome identification | Confirm vesicular identity; absence of calnexin indicates purity |
| Animal Models [14] | IMQ-induced psoriasis, Bleomycin-induced PF | Preclinical efficacy testing | Enable dose-response evaluation in pathologically relevant contexts |
The establishment of robust safety profiles, tolerability data, and dose-response relationships is paramount for the clinical advancement of MSC-exosome therapies. Current evidence indicates that MSC-Exos present a favorable safety profile with low immunogenicity and minimal infusion-related toxicities. The demonstrated route-dependent efficacy, particularly the enhanced efficiency of aerosolized inhalation, provides critical insights for therapeutic optimization. Future research priorities include the development of standardized dosing metrics, potency assays, and GMP-compliant manufacturing protocols to facilitate consistent clinical outcomes. The ongoing integration of bioengineering approaches with traditional MSC-Exos applications holds significant promise for enhancing targeting specificity and therapeutic efficacy in wound healing and other regenerative applications.
Mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as promising cell-free therapeutic agents in regenerative medicine, particularly for wound healing. These nanoscale vesicles (30-150 nm in diameter) transfer bioactive cargoes—including proteins, lipids, and nucleic acids—to recipient cells, modulating inflammation, promoting angiogenesis, and facilitating tissue repair [19] [2]. The therapeutic profile of MSC-Exos varies significantly depending on their tissue of origin, with adipose-derived (ADSC) and bone marrow-derived (BM-MSC) exosomes representing the most extensively studied types [2]. Understanding their source-specific performance is crucial for developing optimized, effective wound therapies. This application note details the comparative mechanisms, efficacy, and protocols for using ADSC-Exos and BM-MSC-Exos in wound healing research, providing a framework for their rational selection and application.
Comparative Analysis: ADSC-Exos vs. BM-MSC-Exos
The therapeutic efficacy of exosomes in wound healing is profoundly influenced by the biological characteristics of their parent cells. The table below summarizes the key comparative aspects of ADSC-Exos and BM-MSC-Exos.
Table 1: Source-Specific Characteristics of ADSC-Exos and BM-MSC-Exos
| Characteristic | Adipose-Derived (ADSC-Exos) | Bone Marrow-Derived (BM-MSC-Exos) |
|---|---|---|
| Source Tissue & Availability | Abundant, easily accessible via liposuction; high cell yield [19] [18] | Limited, invasive harvest; lower cell yield [12] |
| Key Strengths in Wound Healing | Superior angiogenic capacity; potent promotion of re-epithelialization and collagen organization [83] [2] | Robust immunomodulatory effects; strong anti-inflammatory capacity [2] |
| Typical Cargo Profile | Rich in pro-angiogenic factors (e.g., miR-205, miR-126) and anti-fibrotic miRNAs [18] | Enriched with immunomodulatory miRNAs (e.g., targeting IFN-γ pathways) [2] |
| Reported Optimal Dose (Wound Healing) | 200 µg/mL (identified in pre-clinical rat model) [83] | Specific optimal dose for wound healing less defined; pre-clinical studies often use 10–100 µg range [2] |
Optimal Dosing and Administration for Wound Healing
Determining an effective dose is critical for clinical translation. Evidence suggests a relatively narrow and route-dependent effective dose window for MSC-EVs [9] [64].
Establishing an Effective Dose
A seminal pre-clinical study systematically investigated the dose-response relationship for ADSC-Exos in wound healing. Using a rat model of dorsal circular defects, researchers found that 200 µg/mL of ADSC-Exos was the adequate and effective dose for maximizing re-epithelialization and angiogenesis. While higher doses (400 µg/mL) showed similar efficacy in some parameters, the 200 µg/mL dose was sufficient to promote well-organized collagen fibers, which is critical for scar regulation [83].
For BM-MSC-Exos, a specific optimal dose for wound healing is less clearly defined. Preclinical studies in various disease models often use a broad range of 10–100 µg of exosomes [2]. This highlights a significant gap in the literature and an area requiring further investigation for BM-MSC-Exos specifically in a wound healing context.
Administration Routes and Strategies
The route of administration directly influences the pharmacokinetics—absorption, distribution, metabolism, and elimination—of exosomes and thus the required therapeutic dose [8]. For cutaneous wound healing, local administration is the most direct and common strategy.
- Local Injection/Infiltration: Directly injecting exosomes into the wound periphery or bed ensures high local concentration. The optimal dose of 200 µg/mL for ADSC-Exos was established using this method [83].
- Biomaterial-Assisted Delivery: Incorporating exosomes into hydrogels, scaffolds, or advanced wound dressings can protect them from rapid clearance and provide sustained release, thereby prolonging their therapeutic activity at the wound site [19].
- Comparative Route Efficacy: Studies across diseases indicate that nebulization therapy for lung diseases can achieve effects with doses around 10^8 particles, significantly lower than intravenous routes, underscoring the principle that local delivery often requires a lower dose than systemic administration [9] [64].
Experimental Protocols for Wound Healing Research
Protocol: Isolating and Characterizing MSC-Exosomes
This protocol outlines the standard methodology for producing MSC-Exos under research-grade conditions.
Workflow: Exosome Isolation & Characterization
Materials:
- Mesenchymal Stem Cells: Human ADSCs or BM-MSCs (commercially available from ATCC or Lonza).
- Cell Culture Medium: Use exosome-depleted FBS to avoid contaminating bovine vesicles.
- Ultracentrifuge and Rotors (e.g., Type 70 Ti fixed-angle rotor, Beckman Coulter).
- Tangential Flow Filtration (TFF) System (e.g., from Repligen) for scalable concentration.
- Nanoparticle Tracking Analysis (NTA) Instrument (e.g., Malvern Panalytical NanoSight) to determine particle size and concentration.
- Transmission Electron Microscope (TEM) for morphological analysis.
- Antibodies: Anti-CD63, anti-CD81, anti-CD9, anti-TSG101, and negative marker Calnexin [2] [19].
Step-by-Step Procedure:
- Cell Culture and Conditioning: Expand ADSCs or BM-MSCs to 70-80% confluence. Replace standard medium with exosome-depleted medium. Culture for 24-48 hours, then collect the conditioned medium [2].
- Pre-Clearing: Centrifuge the conditioned medium at 2,000 × g for 30 minutes to remove cells and debris. Follow with filtration through a 0.22 µm filter [2].
- Concentration (Optional but Recommended): Concentrate the pre-cleared medium using a TFF system with a 100-500 kDa cutoff membrane. This step reduces processing volumes for ultracentrifugation [2].
- Exosome Isolation: Ultracentrifuge the concentrated medium at 100,000 × g for 70-120 minutes at 4°C. Carefully discard the supernatant and resuspend the exosome pellet in sterile phosphate-buffered saline (PBS) [2].
- Characterization:
- Physical Characterization: Use NTA to determine the particle size distribution and concentration. Use TEM to visualize the morphology and confirm the classic cup-shaped structure [2] [8].
- Molecular Characterization: Confirm the presence of exosomal markers (CD63, CD81, CD9, TSG101) and the absence of negative markers (e.g., Calnexin) via western blot or flow cytometry [2].
Protocol: Evaluating Efficacy in a Rodent Wound Healing Model
This protocol describes an in vivo experiment to assess the functional impact of different exosome sources and doses on wound closure.
Workflow: In Vivo Wound Healing Assay
Materials:
- Animals: Sprague-Dawley rats (e.g., 45 rats, 7-9 per group for statistical power) [83].
- Test Articles: Saline control, ADSC-Exos (e.g., 10 µg/mL, 100 µg/mL, 200 µg/mL), BM-MSC-Exos (e.g., 10 µg/mL, 100 µg/mL) in PBS.
- Anesthesia System (e.g., Isoflurane vaporizer).
- Wound Creation Tools: Biopsy punch (e.g., 6-8 mm diameter).
- Digital Camera and Planimetry Software (e.g., ImageJ) for wound area measurement.
- Histology Reagents: Formalin, paraffin, Hematoxylin and Eosin (H&E), Masson's Trichrome stain.
- Primary Antibodies for Immunohistochemistry: Anti-CD31 (angiogenesis marker), anti-α-SMA (myofibroblasts).
Step-by-Step Procedure:
- Wound Creation: Anesthetize rats and create full-thickness dorsal circular skin defects using a sterile biopsy punch [83].
- Randomization and Dosing: Randomly assign animals to different treatment groups. Administer treatments via local subcutaneous injection around the wound periphery on day 0. A typical dose volume is 100-200 µL per wound [83].
- Wound Closure Monitoring: Photograph wounds daily. Calculate wound area as a percentage of the original size using planimetry software to generate closure curves.
- Tissue Harvest and Analysis: Euthanize animals on day 14 (or other endpoints) and harvest wound tissue for analysis [83].
- Histopathology: Process tissue for H&E staining to assess epithelial tongue length and general morphology. Use Masson's Trichrome to evaluate collagen deposition and organization.
- Immunohistochemistry: Stain sections with anti-CD31 to quantify capillary density (angiogenesis) and anti-α-SMA to identify myofibroblasts.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for MSC-Exosome Wound Healing Research
| Item/Category | Function/Description | Example Suppliers |
|---|---|---|
| Human ADSCs & BM-MSCs | Parent cells for exosome production; ensure source-specific comparisons. | Lonza, ATCC, PromoCell |
| Exosome-Depleted FBS | Critical for cell culture to prevent contamination of research exosomes with bovine vesicles. | Thermo Fisher Scientific, System Biosciences |
| Ultracentrifuge | Gold-standard equipment for exosome isolation via high-speed centrifugation. | Beckman Coulter, Thermo Fisher Scientific |
| Nanoparticle Tracker | Characterizes exosome preparation by determining particle size and concentration (NTA). | Malvern Panalytical |
| Tetraspanin Antibodies | Validate exosome identity via detection of surface markers (CD63, CD81, CD9). | Abcam, System Biosciences, Thermo Fisher Scientific |
| Animal Wound Model | In vivo system for evaluating the therapeutic efficacy of exosomes. | Charles River, Jackson Laboratory |
Correlating Administration Route with Therapeutic Efficacy and Healing Speed
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a promising cell-free strategy in regenerative medicine. These nanovesicles, typically 30-150 nm in diameter, mediate intercellular communication by transferring proteins, mRNAs, and microRNAs to recipient cells, thereby exerting immunomodulatory, anti-inflammatory, and regenerative effects [47] [84]. Compared to whole-cell therapies, MSC-Exos offer significant advantages including lower immunogenicity, greater stability, absence of tumorigenicity risk, and no risk of microvascular occlusion [85] [9].
The route of administration critically influences the therapeutic efficacy and healing speed of MSC-Exos by affecting their biodistribution, bioavailability, and engagement with target tissues. Different administration methods result in varying pharmacokinetic profiles and tissue accumulation patterns, ultimately impacting treatment outcomes. This review synthesizes current evidence on how administration routes correlate with therapeutic efficacy, providing structured experimental protocols and analytical frameworks for researchers optimizing MSC-Exos therapies in wound healing and regenerative applications.
Quantitative Analysis of Administration Route Efficacy
Comparative Efficacy Across Administration Routes
Table 1: Comparative Efficacy of MSC-Exo Administration Routes in Preclinical Models
| Administration Route | Therapeutic Efficacy Findings | Optimal Dose Range | Model System | Key Outcome Measures |
|---|---|---|---|---|
| Intravenous (IV) | Superior lung injury score reduction and cytokine modulation compared to other routes at equivalent dose [85] | 5×10⁸ particles (high dose) | LPS-induced acute lung injury in mice | Histopathological scoring, pro-inflammatory cytokine levels (TNF-α, IL-6, IL-1β), anti-inflammatory IL-10 |
| Intranasal (IN) | Comparable efficacy to nebulization; superior to low-dose IV [85] | 10×10⁸ particles (medium dose) | LPS-induced acute lung injury in mice | BALF cytokine levels, inflammatory cell infiltration, alveolar hemorrhage reduction |
| Nebulization (Aerosol) | Achieved therapeutic effects at significantly lower doses than intravenous route [9] | ~10⁸ particles | Clinical trials for respiratory diseases | Pulmonary function tests, inflammation markers, radiographic improvement |
| Intramuscular | Significantly greater pain reduction when matched to patient preference [86] | 75 mg diclofenac (model drug) | Human acute low back pain trial | Numeric Pain Score (NPS) reduction, patient satisfaction |
| Oral | Effective but less than preference-matched administration [86] | 100 mg diclofenac (model drug) | Human acute low back pain trial | Numeric Pain Score (NPS) reduction, minimal clinically important difference |
Dose-Response Relationships by Administration Route
Table 2: Dose-Dependent Effects of MSC-Exos by Administration Route
| Administration Route | Dose Level | Efficacy Assessment | Statistical Significance |
|---|---|---|---|
| Intravenous | Low (1×10⁸ particles) | Moderate inflammation reduction | P<0.05 vs. model control |
| Medium (2×10⁸ particles) | Significant inflammation reduction | P<0.05 vs. low dose | |
| High (5×10⁸ particles) | Superior therapeutic efficacy | P<0.05 vs. medium dose | |
| Intranasal | Low (5×10⁸ particles) | Moderate efficacy | P<0.05 vs. model control |
| Medium (10×10⁸ particles) | Superior to low dose | P<0.05 vs. low dose | |
| High (15×10⁸ particles) | No significant improvement over medium | P>0.05 vs. medium dose | |
| Nebulization | Low (5×10⁸ particles) | Minimal therapeutic effect | P>0.05 vs. model control |
| Medium (10×10⁸ particles) | Significant improvement over low dose | P<0.05 vs. low dose | |
| High (15×10⁸ particles) | Enhanced efficacy over medium and low | P<0.05 vs. medium and low |
Experimental Protocols for Administration Route Evaluation
Protocol for Comparative Efficacy Assessment in Acute Lung Injury Model
Objective: To evaluate and compare the therapeutic efficacy of MSC-Exos administered via intravenous, intranasal, and nebulization routes in a lipopolysaccharide (LPS)-induced acute lung injury model [85].
Materials:
- Animals: Female BALB/c mice (6-8 weeks old, 19-21 g)
- LPS (Sigma-Aldrich, catalog no. L2630; strain 0111:B4)
- hUCMSC-Exos (Shandong Umbilical Cord Blood Stem Cell Bank)
- Anesthetic: pentobarbital sodium (40 mg/kg)
- ELISA kits for TNF-α, IL-6, IL-1β, and IL-10
Methods:
ALI Model Establishment:
- Anesthetize mice via intraperitoneal injection of pentobarbital sodium (40 mg/kg)
- Administer single intratracheal dose of 50 μl sterile saline containing 100 μg LPS
- Recover mice in 100% oxygen chamber
Experimental Group Allocation:
- Randomize mice into control, LPS model, and experimental groups (n=8) using randomization table
- Categorize experimental groups into nine subgroups (n=8 per subgroup) for different administration routes and doses
MSC-Exos Administration:
- Administer hUCMSC-Exos at 4 and 24 h post-LPS exposure via:
- Intravenous: Tail vein injection at low (1×10⁸), medium (2×10⁸), or high (5×10⁸) doses
- Intranasal: Nasal drip at low (5×10⁸), medium (10×10⁸), or high (15×10⁸) doses
- Nebulization: Atomization at low (5×10⁸), medium (10×10⁸), or high (15×10⁸) doses
- Administer hUCMSC-Exos at 4 and 24 h post-LPS exposure via:
Tissue Collection and Analysis:
- At 48 h post-treatment, euthanize mice and collect lung tissues
- Fix left lung tissues in 4% paraformaldehyde, paraffin-embed, and section into 4 μm-thick slices
- Perform H&E staining following standard histological techniques
- Assess histopathological damage using lung injury scoring system
- Collect bronchoalveolar lavage fluid (BALF) and serum for ELISA analysis
Data Analysis:
- Evaluate inflammatory cell infiltration, alveolar edema, hemorrhage, interstitial thickening
- Quantify pro-inflammatory (TNF-α, IL-6, IL-1β) and anti-inflammatory (IL-10) cytokine levels
- Perform statistical analysis with P<0.05 considered significant
Protocol for Administration Route Preference Assessment
Objective: To determine whether matching actual treatment with patient administration-route-preference improves therapeutic outcomes [86].
Materials:
- Patients: Adults with acute low back pain (aLBP)
- Analgesics: Diclofenac (Abitren Teva 75 mg/3 ml for IM; Betaren100 SR for PO)
- Assessment tool: Numeric Pain Score (NPS) scale (0-10)
Methods:
Patient Enrollment:
- Enroll literate adults (18-80 years) presenting with acute low back pain
- Exclude patients with radicular pain, known sensitivity to diclofenac, or "red flags" suggesting severe pathology
Preference Assessment:
- Ask patients to report their administration route preference (oral vs. intramuscular)
- Record initial numeric pain score (NPS)
Treatment Allocation:
- Regardless of patient preference, administer either PO or IM diclofenac according to treating physician's preference
- Utilize appropriate doses: 75 mg IM or 100 mg PO diclofenac
Outcome Measurement:
- Collect NPS (0-10) every 10 min during first hour post-administration
- Group patients as "matched" (received preferred route) or "non-matched" (received non-preferred route)
Statistical Analysis:
- Compare pain reduction between matched and non-matched groups
- Use parametric tests (chi-square, independent-sample t-test) and non-parametric alternatives as appropriate
- Consider P<0.05 statistically significant
Signaling Pathways and Molecular Mechanisms
Diagram 1: Molecular Mechanisms of MSC-Exo Therapeutic Action. This diagram illustrates key signaling pathways through which MSC-Exos exert their therapeutic effects across different administration routes, including inflammatory pathway modulation, immune cell regulation, and tissue repair mechanisms.
Experimental Workflow for Route Optimization
Diagram 2: Experimental Workflow for Administration Route Optimization. This workflow outlines the key steps in evaluating and comparing different MSC-Exo administration routes, from model establishment through data analysis and optimal route determination.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for MSC-Exo Administration Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Lipopolysaccharide (LPS) | Induction of acute lung injury model for efficacy testing | Sigma-Aldrich, catalog no. L2630; strain 0111:B4 [85] |
| Human Umbilical Cord Blood MSC-Exos | Therapeutic agent for experimental studies | Shandong Umbilical Cord Blood Stem Cell Bank; 30-150 nm particles [85] |
| ELISA Kits | Quantification of inflammatory cytokines in serum and BALF | TNF-α, IL-6, IL-1β, IL-10 specific kits [85] |
| Pentobarbital Sodium | Anesthesia for animal procedures prior to LPS administration | 40 mg/kg intraperitoneal injection [85] |
| Diclofenac | Model drug for administration route preference studies | Abitren Teva 75 mg/3 ml (IM); Betaren100 SR (PO) [86] |
| Paraformaldehyde | Tissue fixation for histopathological analysis | 4% solution for lung tissue preservation [85] |
| H&E Staining Reagents | Histological assessment of tissue architecture and inflammation | Hematoxylin and eosin following standard protocols [85] |
The administration route significantly influences the therapeutic efficacy and healing speed of MSC-Exos, with each method offering distinct advantages depending on the target pathology. Intravenous delivery demonstrates superior efficacy for systemic conditions and acute lung injury at optimal doses of 5×10⁸ particles, while nebulization achieves therapeutic effects at lower doses for respiratory conditions. Intranasal administration provides comparable efficacy to nebulization with practical advantages for certain applications. Beyond pharmacological considerations, patient administration route preference emerges as a significant factor influencing therapeutic outcomes, highlighting the importance of personalized approaches in MSC-Exo therapy optimization. These findings provide a framework for researchers to systematically evaluate administration routes for specific therapeutic applications of MSC-Exos in regenerative medicine.
Conclusion
The successful clinical translation of MSC exosome therapy for wound healing hinges on resolving critical challenges in standardization, dosing, and administration. Current evidence strongly supports the therapeutic potential of MSC-Exos, with route-dependent efficacy and source-specific performance characteristics. Intravenous and subcutaneous administration show distinct advantages for systemic and localized delivery, respectively, while adipose-derived MSC-Exos demonstrate particular promise for wound closure. Future research must prioritize establishing harmonized protocols for production, quantification, and characterization. Collaborative efforts integrating bioengineering, regulatory science, and clinical medicine are essential to develop off-the-shelf, engineered MSC-Exo therapies that fulfill their potential as transformative treatments for complex wounds.
References
- 1. Mesenchymal stem cell-derived exosomes: A novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 2. Mesenchymal stromal/stem cell (MSC)-derived exosomes in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03287-7]
- 3. Mesenchymal stem cell-derived exosomes as a potential ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04511-2]
- 4. Therapeutic potential of exosomal lncRNAs derived from ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04200-0]
- 5. Mesenchymal stem cell-derived exosomes: emerging ... [https://www.sciencedirect.com/science/article/pii/S2773041725000253]
- 6. Therapeutic potential of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11486650/]
- 7. Potential upscaling protocol establishment and wound ... [https://www.nature.com/articles/s41598-025-93219-7]
- 8. Establishing a Working Range for Effective MSC-EV Dose [https://www.roosterbio.com/blog/establishing-a-working-range-for-effective-msc-ev-dose/]
- 9. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 10. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 11. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 12. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 13. Optimizing mesenchymal stem cell extracellular vesicles ... [https://www.sciencedirect.com/science/article/pii/S2352320424001081]
- 14. A Murine Study and Meta-Analysis of Experimental Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467663/]
- 15. Mesenchymal Stem Cells vs Exosomes: A Comparison ... [https://celltexbank.com/mscs-vs-exosomes/]
- 16. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 17. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 18. Adipose-derived stem cell exosomes: multifaceted therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527763/]
- 19. Adipose-derived stem cell exosomes - Biomarker Research [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00801-2]
- 20. Mesenchymal stem cells-derived small extracellular vesicles ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 21. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620388/]
- 22. MSC-EVs and UCB-EVs promote skin wound healing and ... [https://www.nature.com/articles/s41598-025-87592-6]
- 23. Mesenchymal stromal/stem cell (MSC)-derived exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079493/]
- 24. Molecular and therapeutic effects of mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305160/]
- 25. Mesenchymal stem cells-derived extracellular vesicles for ... [https://www.nature.com/articles/s41598-024-54992-z]
- 26. Mesenchymal Stem Cells, Exosomes and Cutaneous ... [https://www.heraldopenaccess.us/openaccess/mesenchymal-stem-cells-exosomes-and-cutaneous-wound-healing]
- 27. Immunomodulatory and Regenerative Functions of MSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383523/]
- 28. Mesenchymal stem cell-derived extracellular vesicles [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1626996/full]
- 29. GMP‐Compliant Process for the Manufacturing of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365392/]
- 30. Meeting Industry Standards Good Chromatography Practices [https://gmpinsiders.com/good-chromatography-practices/]
- 31. Moving analytical ultracentrifugation software to a good ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7347214/]
- 32. UltraScan GMP Software for Biopharma to unlock ... [https://www.aucsolutions.com/gmp.php]
- 33. Tangential Flow Filtration Market Size, Growth Drivers 2025 [https://www.mordorintelligence.com/industry-reports/tangential-flow-filtration-market]
- 34. Tangential Flow Filtration Market Grows at 12.44% CAGR ... [https://www.towardshealthcare.com/insights/tangential-flow-filtration-market-sizing]
- 35. Addressing MISEV guidance using targeted LC‐MS/MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC11080780/]
- 36. Minimal Information for Studies of Extracellular Vesicles ... [https://www.mdpi.com/1999-4923/16/11/1394]
- 37. Mesenchymal stem cell-derived exosomes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8362559/]
- 38. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 39. The transforming role of wharton's jelly mesenchymal stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04690-y]
- 40. MSC-derived exosomes injectable hyaluronic acid ... [https://www.sciencedirect.com/science/article/pii/S0168365925006066]
- 41. Mesenchymal stem cell-derived extracellular vesicles [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399395/]
- 42. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 43. Limitations and challenges in the characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011935/]
- 44. Extracellular vesicles isolated from adipose tissue-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04435-x]
- 45. Hybrid lipid nanoparticles derived from human mesenchymal ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01405g]
- 46. Updated protocols for cell lysate, secretome, and exosome ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000568]
- 47. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 48. Engineerable mesenchymal stem cell-derived extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04490-4]
- 49. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]
- 50. Harmonised culture procedures minimise but do not eliminate ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03352-1]
- 51. The issue of heterogeneity of MSC-based advanced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1400347/full]
- 52. Reproducibility of PD patient-specific midbrain organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494858/]
- 53. Batch variability and anti-inflammatory effects of iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999995/]
- 54. Inter-laboratory variability of A549 epithelial cells grown ... [https://www.sciencedirect.com/science/article/pii/S088723332100103X]
- 55. Insights into optimizing exosome therapies for acute skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11283324/]
- 56. Administration route governs the therapeutic efficacy ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-021-00803-w]
- 57. Biological Nanoparticles for Enhancing Chronic Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564170/]
- 58. Pharmacokinetic characteristics of mesenchymal stem cells ... [https://www.nature.com/articles/s41392-024-01936-8]
- 59. Emerging Therapies in Chronic Wound Healing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619873/]
- 60. Optimizing mesenchymal stem cell extracellular vesicles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11228664/]
- 61. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 62. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 63. Advancements in engineered exosomes for wound repair [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1301362/full]
- 64. Trends in mesenchymal stem cell-derived extracellular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 65. Biomimetic scaffolds loaded with mesenchymal stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04012-8]
- 66. Applications, challenges and prospects of mesenchymal ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02596-z]
- 67. Current Strategies for Promoting the Large-scale Production of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10514529/]
- 68. A scalable platform for EPSC-Induced MSC extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04507-y]
- 69. The Opportunities and Challenges of Mesenchymal Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11640604/]
- 70. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 71. Efficacy and Safety of Negative Pressure Wound Therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619585/]
- 72. HOXA3 accelerates wound healing in diabetic and aged ... [https://www.nature.com/articles/s41598-023-36933-4]
- 73. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 74. Comparison of the efficacy of 12 interventions in ... [https://peerj.com/articles/19809/]
- 75. Extracellular vesicles as tools and targets in therapy for ... [https://www.nature.com/articles/s41392-024-01735-1]
- 76. Mesenchymal stem cells-derived small extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934660/]
- 77. Extracellular vesicles arising from apoptosis: forms, functions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10952477/]
- 78. Advances in biological functions and applications of apoptotic ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01251-9]
- 79. Uncovering the bequeathing potential of apoptotic ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04370-x]
- 80. Exploring Regulatory Frameworks for Exosome Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371722/]
- 81. Quality and Safety Considerations for Therapeutic Products ... [https://link.springer.com/article/10.1007/s11095-024-03757-4]
- 82. Mesenchymal Stem Cell-Derived Exosomes: Emerging as ... [https://www.mdpi.com/2218-273X/14/11/1353]
- 83. The Optimal Effective Dose of Adipose-Derived Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/39023411/]
- 84. Mesenchymal stem cell-derived exosomes: Toward cell-free therapeutic strategies in regenerative medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477653/]
- 85. Frontiers | Comparison of efficacy of exosomes derived from human umbilical cord blood mesenchymal stem cells in treating mouse acute lung injury via different routes [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1560915/full]
- 86. Matching actual treatment with patient administration-route ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-020-01594-w]