Overcoming the Vascularization Bottleneck: Advanced Strategies for Engineering Thick, Clinically Relevant Tissues
The inability to create functional, perfusable vascular networks remains a primary obstacle in tissue engineering, preventing the clinical translation of thick, metabolically active tissues and organs.
Overcoming the Vascularization Bottleneck: Advanced Strategies for Engineering Thick, Clinically Relevant Tissues
Abstract
The inability to create functional, perfusable vascular networks remains a primary obstacle in tissue engineering, preventing the clinical translation of thick, metabolically active tissues and organs. This article provides a comprehensive analysis for researchers and drug development professionals, covering the foundational biology of vascularization, cutting-edge engineering methodologies from 3D bioprinting to self-assembly, and critical troubleshooting of persistent bottlenecks like cell source limitations and immune integration. It further explores advanced validation techniques using in vitro microphysiological systems for disease modeling and drug screening. By synthesizing insights across these four core intents, this review aims to equip the field with an interdisciplinary roadmap to overcome diffusion limits and achieve the grand challenge of engineering scalable, vascularized human tissues.
The Biological Imperative: Why Vascularization is the Gatekeeper to Thick Tissue Engineering
Frequently Asked Questions (FAQs)
Q1: What is the 100-200 µm diffusion limit and why is it a critical bottleneck in tissue engineering? The 100-200 µm diffusion limit refers to the maximum distance oxygen and nutrients can effectively travel through biological materials to reach cells before being consumed. This creates a critical barrier because in tissue-engineered constructs thicker than this, cells located in the core region face oxygen deprivation and nutrient shortage, leading to hypoxia (oxygen levels <5%) and ultimately cell death via apoptosis or necrosis. This phenomenon severely restricts the size and clinical applicability of engineered tissues [1] [2] [3].
Q2: How does the initial inflammatory response after implantation further exacerbate hypoxia? Following implantation, the host's inflammatory response increases the local metabolic demand for oxygen, creating a paradoxical situation where oxygen demand rises precisely when its supply is most limited. Furthermore, before the implanted tissue achieves functional connection to the host's blood vessels (anastomosis), the tissue is depleted of oxygen, resulting in hypoxic (<5% dissolved oxygen) followed by anoxic (<0.5% dissolved oxygen) microenvironments in the scaffold's core [1].
Q3: What are the primary differences between hypoxia and hyperoxia, and why is the balance crucial? Hypoxia is a condition of insufficient oxygen supply, which forces cells to rely on inefficient anaerobic respiration, leading to acidification from lactic acid build-up and the initiation of apoptosis. Hyperoxia is an excess of oxygen, which can lead to overproduction of reactive oxygen species (ROS), causing significant oxidative damage to cells. A precise balance is crucial because both extremes are detrimental to cell survival, function, and integration of tissue constructs [2] [3].
Q4: Beyond oxygen, what other transport limitations exist in large tissue constructs? The diffusion challenge extends beyond oxygen. Cells in the core of large constructs also suffer from:
- Nutrient Deprivation: Essential nutrients like glucose are consumed by cells on the construct's periphery, failing to reach the center.
- Waste Accumulation: Metabolic waste products (e.g., lactic acid) build up in the core, leading to toxic microenvironments and low pH.
- Impaired Signaling: Diffusion limitations can disrupt vital paracrine signaling between cells, affecting tissue development and repair [2].
Q5: What key signaling pathway is activated by hypoxic conditions, and what is its dual role? The primary pathway activated by hypoxia is mediated by Hypoxia-Inducible Factors (HIFs). Under normal oxygen levels, HIF subunits are constantly degraded. In hypoxia, HIFs stabilize, move to the nucleus, and bind to Hypoxia Response Elements (HREs), activating genes involved in angiogenesis (like VEGF), cell survival, and metabolism. While this is a protective cellular response, its chronic activation in tissue constructs can indicate unresolved diffusion limitations and may promote unfavorable outcomes like inflammation [4] [3].
Diagram Title: HIF Signaling Pathway in Hypoxia
Troubleshooting Guides
Guide 1: Diagnosing and Mitigating Hypoxia in 3D Constructs
Problem: Cell death and necrotic core formation in thick (>200 µm) tissue constructs.
Symptoms:
- Significant increase in apoptotic markers (e.g., activated caspase-3) in the construct's core after 48-72 hours in culture [2].
- Low pH and buildup of lactic acid in the culture medium, indicating a shift to anaerobic metabolism [2].
- Upregulation of hypoxia markers (e.g., HIF-1α stabilization) and downstream genes like VEGF in the core region [3].
- Poor cell viability specifically in the central regions of the scaffold, while periphery cells remain healthy.
Solutions and Methodologies:
Table 1: Strategies to Overcome the Oxygen Diffusion Limit
| Strategy | Mechanism of Action | Key Experimental Protocols | Advantages | Limitations |
|---|---|---|---|---|
| Oxygen-Generating Biomaterials (OGBs) [1] | Solid peroxides (e.g., CaO₂, MgO₂) react with water to release oxygen over time. | 1. Incorporate CaO₂ particles (5-50 µm) into polymers like PLGA or PCL.2. Fabricate scaffolds via solvent casting/particulate leaching or electrospinning.3. Validate oxygen release using a dissolved oxygen meter over 10-14 days in PBS at 37°C.4. Assess cell viability under hypoxic conditions (1-5% O₂) vs. control scaffolds. | Provides sustained, localized oxygen supply for up to 10 days. Can be tailored for controlled release kinetics. | Risk of burst release and toxic ROS generation. pH shifts may occur. Release kinetics depend on scaffold porosity and hydration. |
| Perfluorocarbons (PFCs) [1] [3] | Chemically inert compounds with high oxygen solubility act as synthetic oxygen carriers. | 1. Emulsify PFCs or incorporate PFC-nanoparticles into hydrogels or scaffolds.2. Pre-saturate scaffolds with oxygen before cell seeding or during culture.3. Measure oxygen tension within the construct using microsensors or fluorescent probes. | High oxygen-dissolving capacity (e.g., 20x greater than water). Biocompatible and inert. Linear oxygen release relative to partial pressure. | May require pre-saturation. Can be expensive. Long-term biocompatibility of some formulations requires further study. |
| Prevascularization Strategies [4] [2] | Creating a primitive vascular network within the construct in vitro before implantation. | 1. Co-culture endothelial cells (ECs) with supportive cells (e.g., fibroblasts, MSCs) in a 3D scaffold (e.g., fibrin, collagen).2. Use patterned scaffolds or bioprinting to create channeled architectures.3. Supplement with pro-angiogenic factors (VEGF, bFGF) to promote vessel maturation.4. Apply shear stress in a bioreactor to enhance endothelial network formation. | Creates a native-like transport system. Promotes rapid anastomosis with host vasculature upon implantation. | Technically complex and time-consuming. Ensuring functionality and stability of the engineered network is challenging. |
| Bioreactor-Enhanced Culturing [2] | Uses convective flow to perfuse media through the construct, overcoming diffusion limits. | 1. Place the construct in a perfusion bioreactor system.2. Optimize flow rates to ensure sufficient nutrient delivery and waste removal without causing shear stress damage.3. Monitor metabolic parameters (glucose, lactate, O₂) in the inlet and outlet media in real-time. | Ensures uniform cell distribution and viability throughout large constructs. Mimics physiological shear forces. | Requires specialized, often costly equipment. Optimization of flow dynamics is necessary for each construct type. |
Diagram Title: Troubleshooting Workflow for Hypoxic Constructs
Guide 2: Designing Experiments to Quantify Diffusion and Cell Viability
Objective: Accurately measure oxygen gradients and their correlation with cell survival in a 3D scaffold.
Experimental Workflow:
Scaffold Fabrication & Instrumentation:
- Fabricate scaffolds with a known, reproducible geometry (e.g., 5mm diameter x 2mm thick discs).
- If possible, embed optical fluorescent oxygen sensors (e.g., based on ruthenium complexes) at different depths within the scaffold during fabrication [5].
Cell Seeding and Culture:
- Seed scaffolds at a clinically relevant cell density (e.g., 10-50 million cells/mL). Ensure uniform seeding using dynamic methods (e.g., orbital shaking or perfusion) [6].
- Culture under standard (normoxic) and controlled hypoxic (e.g., 1-2% O₂) conditions in an incubator to simulate pre-vascularization conditions.
Real-Time Oxygen Mapping:
- Use a fiber-optic oxygen microsensor to manually profile the oxygen tension from the surface to the core of the scaffold at predetermined time points (e.g., days 1, 3, 7) [5].
- Alternatively, use a fluorescence lifetime imaging microscope (FLIM) to read the embedded oxygen sensors non-invasively and create a 2D oxygen map.
Endpoint Viability and Hypoxia Analysis:
- Viability Staining: Perform a live/dead assay (e.g., Calcein-AM/Propidium Iodide) on cross-sectioned scaffold slices. Quantify the ratio of live to dead cells as a function of distance from the surface.
- Hypoxia Staining: Immunofluorescence staining for HIF-1α or use pimonidazole hydrochloride, a hypoxic marker that forms protein adducts in cells with oxygen tension <1.3%. Co-stain with DAPI for nuclei [5].
- Histological Analysis: Process scaffolds for histology (H&E staining) to identify pyknotic nuclei and necrotic regions.
Data Correlation:
- Correlate the measured oxygen gradients with the spatial distribution of cell death and hypoxia markers. This data can be used to validate mathematical models of oxygen diffusion and consumption in your specific scaffold [5].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating and Overcoming Diffusion Limits
| Item / Reagent | Function / Application | Key Considerations & Examples |
|---|---|---|
| Calcium Peroxide (CaO₂) | Oxygen-generating material. Releases O₂ upon hydrolysis. | Considerations: Purity affects O₂ release kinetics. Can increase pH and generate H₂O₂. Use in composite polymers (PLGA, PCL) to control release [1]. |
| Perfluorocarbons (PFCs) | Synthetic oxygen carriers with high O₂ solubility. | Examples: Perfluorodecalin, Perfluoro-15-crown-5-ether. Can be used as emulsions or encapsulated in nanoparticles for integration into hydrogels [1] [3]. |
| Pimonidazole HCl | A chemical probe that forms irreversible adducts in hypoxic cells (<1.3% O₂). | Application: Detected via specific antibodies; allows for immunohistochemical identification and quantification of hypoxic regions in fixed tissue constructs [5]. |
| Hydrogel ECM Models (e.g., MaxGel) | A model extracellular matrix hydrogel for studying diffusion. | Application: Used in Multiple Particle Tracking (MPT) analysis to study how nanoparticle shape and size affect diffusion through biological gels, informing drug delivery system design [7]. |
| Recombinant VEGF / bFGF | Pro-angiogenic growth factors. | Application: Added to culture media to induce and stabilize the formation of endothelial tubules in prevascularization strategies [4] [2]. |
| HIF-1α Antibody | For immunofluorescence detection of stabilized HIF-1α protein. | Application: A key marker for confirming cellular hypoxic response. Nuclear localization indicates pathway activation [3]. |
| Dissolved Oxygen Probe | For measuring oxygen concentration in solution or culture media. | Considerations: Essential for validating the oxygen release profile from OGBs or O₂-saturated PFCs in real-time [1]. |
| Matrigel | Basement membrane extract for tubule formation assays. | Application: Used in standard in vitro angiogenesis assays where endothelial cells form capillary-like tubule networks [4]. |
Diagnostic Techniques & Quantitative Biomarkers
How can I non-invasively monitor vascularization and predict implant failure in real-time?
Ultrasound-guided photoacoustic (US/PA) imaging is an emerging, non-invasive technology that allows for longitudinal monitoring of vascular changes around subcutaneous implants. It can detect signs of vascular compromise approximately 2–4 weeks before visible skin necrosis occurs [8].
The table below summarizes key quantitative biomarkers measurable with this technique.
Table 1: Key Biomarkers for Photoacoustic Imaging Monitoring
| Biomarker | Wavelength (nm) | Measured Parameter | Significance in Predicting Failure |
|---|---|---|---|
| PA Vasculature | 532 nm | Vascular density and structure | Most sensitive biomarker; reduction of up to 48% correlates strongly with skin health (R >0.85) [8] |
| Total Hemoglobin | 700-950 nm | Hemoglobin concentration | Indicates local blood volume and oxygen-carrying capacity [8] |
| Spatial Hemoglobin Maps | 700-950 nm | Local distribution of vasculature | Local reductions precede specific sites of skin breakdown (dehiscence) [8] |
Experimental Protocol: Longitudinal US/PA Imaging
- Animal Model: Subcutaneous implantation in SKH1-Elite hairless mice (or similar).
- Implant Types: 3D-printed porous poly-ɛ-caprolactone implants (e.g., unimodal cube, bimodal cube, unimodal dome) [8].
- Imaging Schedule: Perform US/PA imaging bi-weekly over a 12-week period [8].
- Data Correlation: Correlate PA biomarkers (vasculature at 532 nm, total hemoglobin) with a clinical skin health score (e.g., a modified National Pressure Injury Advisory Panel system) [8].
Figure 1: Experimental workflow for longitudinal photoacoustic monitoring of implant integration, showing key biomarkers and their prognostic outcomes.
Evidence-Based Graft Selection
What does the evidence say about vascularized vs. non-vascularized bone grafts for repairing non-union fractures?
In the context of scaphoid nonunion fractures, a meta-analysis of 62 studies demonstrates superior outcomes for vascularized bone grafts (VBGs) compared to non-vascularized bone grafts (NVBGs). VBGs directly address the core problem of poor blood supply, leading to faster and more reliable healing [9].
Table 2: Comparative Efficacy of Bone Graft Types for Scaphoid Nonunion
| Graft Type | Union Rate | Time to Healing | Key Functional Outcomes | Considerations & Drawbacks |
|---|---|---|---|---|
| Vascularized Bone Graft (VBG) | Significantly Higher | Shorter | Better grip strength and functional wrist scores (MMWS) [9] | Higher technical complexity, longer surgery, risk of donor-site morbidity [9] |
| Non-Vascularized Bone Graft (NVBG) | Lower | Longer | Improved but generally inferior to VBG outcomes [9] | Donor-site morbidity (5-10%), higher risk of graft failure in avascular environments [9] |
| Bone Biomaterial Graft | Promising, comparable to NVBG | Data Limited | Potential for good functional recovery [9] | Emerging technology; limited clinical data; requires more validation [9] |
Conclusion for Clinical Practice: VBGs are strongly indicated for complex cases with compromised blood supply (e.g., proximal pole fractures). NVBGs may suffice for simpler, well-vascularized non-unions. Bone biomaterials represent a promising less-invasive alternative but are not yet a gold standard [9].
Therapeutic Strategies & Molecular Pathways
What signaling pathways can be targeted to enhance osteogenesis and vascularization in smart implants?
"Smart" bone implants are engineered to actively promote healing by releasing bioactive ions or molecules that influence key cellular signaling pathways. These pathways regulate bone-forming cells (osteoblasts), blood vessel-forming cells (endothelial cells), and immune cells [10].
Table 3: Key Signaling Pathways and Smart Implant Strategies for Bone Repair
| Signaling Pathway | Implant Material / Strategy | Molecular/Cellular Mechanism | Outcome |
|---|---|---|---|
| BMP/Smad | Silica-coated GO/GelMA scaffold [10] | Adsorbs and releases endogenous BMPs; released Si⁺ ions upregulate BMP2 [10] | Enhanced osteogenic differentiation of BMSCs [10] |
| Wnt/β-catenin | Mg-1Ca/PCL scaffolds [10] | Release of Mg²⁺ ions activates the canonical Wnt pathway [10] | Promotes proliferation and osteogenesis of human BMSCs [10] |
| TGF-β | Nano-Mg(OH)₂ films on Ti [10] | Release of Mg²⁺ and creation of a weakly alkaline microenvironment [10] | Promotes osteogenesis in murine mesenchymal cells [10] |
| MAPK | Hydrogel delivery of Mg²⁺ and Zn²⁺ [10] | Synergistic release of ions upregulates the MAPK pathway [10] | Enhanced osteogenesis of human BMSCs [10] |
| Angiogenesis | Biomaterials incorporating VEGF [9] | Delivery of Vascular Endothelial Growth Factor (VEGF) [9] | Stimulates new blood vessel formation at the implant site [9] |
Figure 2: Signaling pathways activated by smart implant materials, leading to enhanced bone and blood vessel formation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for Vascularized Implant Research
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| 3D-Printed Porous Polymers | Fabrication of subcutaneous implants for studying tissue integration and vascularization. | Poly-ɛ-caprolactone (PCL) implants (unimodal/bimodal cubes, domes) [8]. |
| Bioactive Ions & Delivery Systems | To create "smart" implants that release osteogenic and angiogenic factors. | Mg²⁺, Zn²⁺, Si⁺ ions; delivery via hydrogels, nano-films, or composite scaffolds (e.g., Mg-1Ca/PCL) [10]. |
| Growth Factors | Directly stimulate bone and blood vessel growth. | Bone Morphogenetic Protein-2 (BMP-2) for osteogenesis; Vascular Endothelial Growth Factor (VEGF) for angiogenesis [9]. |
| Extracellular Matrix (ECM) Gels | Provide a 3D, biologically active scaffold for in vitro and in vivo cell growth and vessel formation. | Matrigel; brain-derived ECM for stroke models; bladder-derived ECM [11] [12]. |
| Mesenchymal Stromal Cells (MSCs) | Cell-based therapy to promote vascular regeneration via paracrine signaling. | Adipose-derived or bone marrow-derived MSCs; can be delivered peri-adventitially with a collagen scaffold [11]. |
Frequently Asked Questions (FAQs)
What are the primary bottlenecks in achieving vascular regeneration for clinical applications?
The major bottlenecks include:
- Elastin Regeneration: In conditions like aortic aneurysms, protecting existing elastin and stimulating new elastin production remains a significant challenge. Current research explores stabilizers like PGG (penta galloyl glucose) and cell-based therapies [11].
- Integration with Host Vasculature: Ensuring that pre-formed vascular networks in implants rapidly connect with the host's blood circulation upon implantation is critical for the survival of thick tissue constructs [12].
- Biomaterial Limitations: The foreign body response, suboptimal biocompatibility, and variable resorption rates of biomaterials can hinder vascular integration [9].
- Spatial Complexity: Recapitulating the organ-specific density and architecture of vasculature (e.g., over 2000 capillaries/mm³ in organs like the heart and liver) is technically demanding [12].
Beyond bone, what is the significance of a necrotic core in other tissues like tumors?
A necrotic core is not merely a passive zone of cell death. In tumors, it actively promotes metastasis. Research has shown that the necrotic microenvironment is rich in factors like angiopoietin-like 7 (A-7), which remodels the tumor surroundings, induces the formation of dilated, leaky blood vessels, and facilitates the escape of circulating tumor cells (CTCs) to other parts of the body [13]. Suppressing A-7 in models dramatically reduced necrosis, CTC count, and metastasis, highlighting it as a potential therapeutic target [13].
What advanced in vitro models are available to study vascularization before animal testing?
Several 3D models provide more physiologically relevant platforms:
- Organs-on-a-Chip (OOaC): Microfluidic devices that can mimic blood flow, shear stress, and oxygen gradients, allowing for the formation of perfusable vascular networks [12].
- 3D Bioprinting: Enables the precise deposition of cells (e.g., endothelial cells, pericytes) and biomaterials ("bioinks") to create complex, predefined vascular-like structures [12].
- Spheroids and Organoids: 3D cell cultures that can self-assemble and be coaxed to develop internal endothelial networks. These can also be integrated into larger bioreactors for perfusion [12].
FAQs: Core Concepts and Definitions
Q1: What is the fundamental difference between vasculogenesis and angiogenesis?
A1: Vasculogenesis is the de novo formation of a primitive vascular network from progenitor cells called angioblasts, which differentiate into endothelial cells [14] [15]. In contrast, angiogenesis is the growth of new capillaries from pre-existing blood vessels [14] [15]. In the embryo, both processes occur, while in adults, new vessel formation primarily happens through angiogenesis, except in certain pathological conditions where vasculogenesis can re-occur [15].
Q2: What are the key growth factors and their primary roles in these processes?
A2: The key growth factors are members of the Vascular Endothelial Growth Factor (VEGF) and Fibroblast Growth Factor (FGF) families [14] [15]. Their roles are outlined below:
- Table: Key Growth Factors in Vascular Development
| Growth Factor/Receptor | Primary Role | Key Evidence |
|---|---|---|
| VEGF-A | Crucial for vasculogenesis and the growth phase of angiogenesis; promotes endothelial cell proliferation, migration, and permeability [14]. | Heterozygous knockout mice die in utero with aberrant blood vessel formation [15]. |
| VEGF-R2 (flk-1/KDR) | Essential for the differentiation of angioblasts; a very early marker of endothelial commitment [14] [15]. | Knockout mice show early defects in angioblastic lineages and die by E8.5 [15]. |
| VEGF-R1 (flt-1) | Appears to play a role after VEGF-R2, involved in the correct assembly of endothelial cells into functional vessels [14] [15]. | Knockout mice produce angioblasts but fail to form proper vessels and die at E8.5 [15]. |
| FGF2 (bFGF) | Implicated in vasculogenesis and is a potent angiogenic factor [14] [15]. | Strictly required for the formation of vascular structures in quail blastodisc cultures [15]. |
| TGF-β, PDGF-BB, Angiopoietin-1 | Critical for the stabilization phase of angiogenesis; inhibit proliferation, recruit pericytes/SMCs, and promote vessel maturation [14] [15]. | Gene inactivation leads to lethality due to edemas and hemorrhages from defective vascular maturation [15]. |
Q3: What are the main in vitro models used to study vasculogenesis?
A3: The primary models are:
- Embryonic Stem (ES) Cell-Derived Embryoid Body (EB) Assay: When murine ES cells are cultured without leukemia inhibitory factor (LIF), they form three-dimensional embryoid bodies. Within these EBs, a primitive vascular plexus forms, recapitulating the differentiation of angioblasts, endothelial cell assembly, and vascular morphogenesis [15].
- Blastodisc Cultures: Adherent or suspension cultures of dissociated cells from quail blastodiscs can generate both hematopoietic and endothelial cells that aggregate into blood islands and vascular structures, dependent on FGF2 [15].
Troubleshooting Guides for Common Experimental Challenges
Q1: My endothelial cells in 3D culture are failing to form stable, mature vessels. The structures regress or undergo apoptosis. What could be wrong?
A1: Vessel regression often indicates a failure in the transition from the growth phase to the stabilization phase [15].
- Problem: Lack of vessel stabilization.
- Possible Causes and Solutions:
- Cause 1: Deficiency in stabilization factors. The culture environment may be rich in pro-growth factors like VEGF but lacking factors that promote maturation.
- Solution: Add critical stabilization factors to your medium, such as TGF-β, PDGF-BB (for pericyte recruitment), and Angiopoietin-1 [15].
- Cause 2: Incorrect timing of factor presentation. Presenting growth and stabilization factors simultaneously can be counterproductive.
- Solution: Develop a timed protocol. First, provide pro-angiogenic factors (VEGF, FGF) to promote sprouting. Then, switch to or add stabilization factors (TGF-β, PDGF-BB) to halt proliferation and promote mural cell coverage and basement membrane reconstruction [14] [15].
- Cause 3: Lack of proper co-culture. Vessels require pericytes or smooth muscle cells for stability.
- Solution: Establish a co-culture system with pericytes or smooth muscle cells to invest the endothelial tubes [14].
Q2: I am not observing any vascular sprouting (angiogenesis) in my assay. What are the potential issues?
A2: A lack of sprouting suggests a failure in the initial activation phase.
- Problem: Absence of angiogenic sprouting.
- Possible Causes and Solutions:
- Cause 1: Insufficient pro-angiogenic stimulus.
- Solution: Ensure your growth factors (e.g., VEGF-A or FGF2) are present at an effective concentration and are bioavailable [14] [15].
- Cause 2: Over-stabilized initial endothelium. The pre-existing vessel monolayer might be too quiescent.
- Solution: Use a pro-angiogenic matrix (like Matrigel or fibrin) that supports migration and invasion. You can also gently wound the monolayer to initiate the process [15].
- Cause 3: Inadequate matrix degradation. Sprouting requires local degradation of the extracellular matrix (ECM).
- Solution: Verify that the protease systems (e.g., matrix metalloproteinases) are active. The basal lamina of the "mother" vessel must be dissolved for migration to occur [14].
Q3: My 3D bioprinted cardiac construct lacks sufficient integration with the host vasculature after implantation. How can I improve this?
A3: This is a key challenge in tissue engineering of thick tissues [16].
- Problem: Poor host-graft vascular integration.
- Possible Causes and Solutions:
- Cause 1: The implanted construct lacks a pre-formed microvascular network. Relying solely on host vessel ingrowth is too slow for thick tissues.
- Solution: Pre-vascularize the construct by 3D bioprinting with bioinks containing endothelial cells (e.g., using a layer-by-layer grid method) to create an internal microvascular network. This network can then anastomose (connect) with the host's invading vessels, as demonstrated in recent studies [16].
- Cause 2: The bioink or construct environment is not conducive to vascular survival and remodeling.
- Solution: Optimize bioink composition to ensure long-term stability and functionality. It must support both cardiomyocyte and endothelial cell viability and allow for the release of angiogenic factors to attract host vessels [16].
Essential Research Reagent Solutions
The following table lists key reagents and their functions for setting up experiments in vascular development and engineering.
- Table: Essential Research Reagents for Vascular Engineering
| Reagent / Material | Function / Application |
|---|---|
| VEGF-A | The primary pro-angiogenic factor; induces endothelial cell proliferation, permeability, and migration. Essential for initiating vasculogenesis and angiogenesis [14] [15]. |
| FGF2 (bFGF) | A potent angiogenic factor; crucial for in vitro vasculogenesis models and endothelial cell proliferation [15]. |
| TGF-β & PDGF-BB | Vessel stabilization factors; TGF-β inhibits endothelial proliferation and PDGF-BB recruits pericytes/smooth muscle cells to stabilize nascent vessels [15]. |
| Embryonic Stem (ES) Cells | Used in the Embryoid Body (EB) assay to model embryonic vasculogenesis and study endothelial differentiation de novo [15]. |
| Specialized Bioinks | Hydrogels for 3D bioprinting that support the encapsulation and survival of endothelial and parenchymal cells (e.g., cardiomyocytes) and enable the fabrication of microvascular networks [16]. |
| Integrin αvβ3 Inhibitors | Used to study the role of adhesion molecules in tumor angiogenesis; however, its role is less crucial in developmental angiogenesis [15]. |
| VE-Cadherin Antibodies | For studying and blocking endothelial cell-cell adhesion, which is essential for vessel integrity and tube formation [15]. |
Key Experimental Protocols & Workflows
A. Protocol: Murine ES Cell Embryoid Body (EB) Assay for Vasculogenesis
This protocol allows for the in vitro study of the entire vasculogenesis process [15].
- Maintenance of Undifferentiated ES Cells: Culture mouse ES cells on a feeder layer or in gelatinized flasks with media supplemented with Leukemia Inhibitory Factor (LIF).
- EB Formation (Differentiation Initiation): Harvest ES cells and transfer them to non-adherent bacterial-grade Petri dishes. Culture in media without LIF. Cells will aggregate to form simple embryoid bodies.
- Maturation and Vasculogenesis: Continue culturing EBs for up to 10-15 days. During this period, they may develop into cystic EBs. Spontaneous differentiation will occur, leading to the formation of blood islands and vascular channels within the EB walls.
- Analysis: Fix EBs and analyze vascular structure formation via immunohistochemistry for endothelial markers (e.g., PECAM-1, VE-cadherin, Flk-1) [15].
B. Protocol: General Workflow for a Sprouting Angiogenesis Assay
This workflow outlines the steps for assessing pro- or anti-angiogenic compound effects.
- Endothelial Cell Plating: Plate human umbilical vein endothelial cells (HUVECs) or a similar cell type onto a layer of gelled extracellular matrix (e.g., Matrigel, Collagen) in a multi-well plate.
- Tube Formation (Initial Morphogenesis): Allow cells to form capillary-like tube networks over 4-18 hours.
- Compound Treatment: Add the test compound (angiogenic factor, inhibitor, etc.) to the medium.
- Incubation and Sprouting Assessment: Incubate for a further 6-48 hours. Quantify changes in the network by measuring parameters like total tube length, number of branch points, or number of sprouts using microscopy and image analysis software.
- Validation with Specific Assays: Follow up with targeted assays to understand the mechanism:
- Proliferation: Quantitate tritiated thymidine incorporation or perform cell counting [15].
- Migration: Use a Boyden chamber or a linear "wound healing" assay across a monolayer [15].
- Proteolysis: Test using zymographic assays for matrix metalloproteinases (MMPs) [15].
- Apoptosis: Measure by the TUNEL method or quantitation of caspases [15].
Signaling Pathways in Vascular Development
The following diagram summarizes the core signaling pathways involved in the sequential processes of vasculogenesis and angiogenesis, highlighting the key factors and their primary functions.
A fundamental roadblock in tissue engineering is the inability to rapidly form functional vascular networks within thick, engineered tissues (>1 cm³). Without these networks, cells in the core of the construct perish due to hypoxia and insufficient nutrient supply, as the diffusion limit of oxygen is only 100–200 μm [4] [17]. This diffusion limit leads to necrosis and ultimate implant failure [4]. Overcoming this requires a deep understanding of the key cellular players responsible for building stable, functional blood vessels: Endothelial Cells (ECs), which form the vessel lining, and Mural Cells (Pericytes and Vascular Smooth Muscle Cells (vSMCs)), which provide structural support and stability [18] [19]. This technical support center provides targeted guidance for researchers aiming to harness these interactions to overcome vascularization limitations.
Core Concepts: Cellular Functions and Signaling Pathways
What are the distinct roles of endothelial cells, pericytes, and vascular smooth muscle cells?
The stability and function of blood vessels rely on the coordinated interactions between endothelial and mural cells. The table below summarizes their distinct roles and characteristics.
Table 1: Key Characteristics of Vascular Cells.
| Cell Type | Location | Primary Functions | Key Identification Markers |
|---|---|---|---|
| Endothelial Cells (ECs) | Inner lining of all vessels (Tunica Intima) | Form a non-thrombogenic barrier; regulate vascular tone and permeability; initiate angiogenesis [6]. | VE-cadherin [19], CD31 [17] |
| Pericytes | Microvasculature (capillaries, post-capillary venules) embedded within the basement membrane [18] | Stabilize capillaries; regulate blood flow; induce blood-brain barrier properties [18] [19]. | PDGFR-β, NG2, CD13, α-SMA, Desmin [18] |
| Vascular Smooth Muscle Cells (vSMCs) | Larger vessels (arteries, veins) in the Tunica Media [18] | Provide structural strength and contractility; regulate vessel diameter and blood pressure [20] [6]. | α-SMA, SMMHC, SM22, Calponin, Desmin [21] |
How do these cells communicate to stabilize vessels?
Stable vascular maturation depends on precise bidirectional signaling between ECs and mural cells. The following diagram illustrates the key signaling pathways involved.
Diagram 1: Key EC-Pericyte Signaling Pathways for Vessel Stabilization.
The PDGF-BB/PDGFR-β axis is a primary recruitment signal where ECs secrete PDGF-BB, attracting PDGFR-β-positive pericytes [18] [19]. Subsequently, pericytes secrete Angiopoietin-1 (Ang-1), which binds to Tie2 receptors on ECs, promoting vessel quiescence and stability [18]. Additional factors like Endothelin-1 and PDGF-DD from ECs further support pericyte recruitment and proliferation [18]. Direct physical contact through adherens junctions (e.g., N-cadherin) and gap junctions (e.g., Connexin 43) is equally critical for communication and stabilization [18] [19]. A major function of this cross-talk is the coordinated production and maintenance of the vascular basement membrane, which is essential for preventing abnormal vessel expansion and elasticity [19].
The Scientist's Toolkit: Essential Research Reagents
Successful experimentation requires high-quality, well-characterized reagents. The following table lists essential tools for studying vascular cells.
Table 2: Essential Research Reagents for Vascular Cell Biology.
| Reagent / Material | Function / Application | Key Considerations & Examples |
|---|---|---|
| Hydrogels | Provide a 3D extracellular matrix (ECM)-mimetic environment for cell culture and vessel formation [18]. | Collagen-I: Natural, fibrous, tunable stiffness [18]. Matrigel: Basement membrane extract; contains laminin and collagen IV [18]. GelMA (Gelatin Methacryloyl): Tunable, photopolymerizable [22]. |
| Growth Factors & Cytokines | Direct cell differentiation, proliferation, migration, and network formation. | PDGF-BB: Critical for pericyte/vSMC recruitment and proliferation [18] [21]. VEGF: Key driver of endothelial cell angiogenesis [18] [4]. TGF-β: Involved in mural cell differentiation and stabilization [19]. |
| Cell Isolation Reagents | Enzymatic digestion of tissues to isolate primary cells. | Collagenase: Digests collagen in connective tissue. Elastase: Breaks down elastic fibers in vessels [20]. Trypsin/TrypLE: Used for passaging adherent cells [21] [20]. |
| Cell Culture Media | Supports the growth and maintenance of specific cell types. | SmBm BulletKit: Commercial medium optimized for smooth muscle cells [20]. Endothelial Cell Growth Medium: Typically supplemented with VEGF, FGF, and EGF. |
| Antibodies for Characterization | Identify and confirm cell identity via immunofluorescence, flow cytometry. | α-SMA (Alpha-Smooth Muscle Actin): Marks contractile mural cells [21] [17]. NG2 (CSPG4): A common pericyte marker [18]. HuCD31/CD31 (PECAM-1): Specific for endothelial cells [17]. |
Troubleshooting Guides & FAQs
Common Co-Culture Challenges
Q: In my 3D hydrogel co-culture, pericytes are not associating with the endothelial tubes. What could be wrong?
- A: This is typically a signaling or timing issue. Consider the following:
- Confirm Growth Factor Activity: Ensure your culture medium contains adequate PDGF-BB, the primary EC-derived chemoattractant for pericytes. Check the concentration and bioactivity of your stock [18].
- Optimize Seeding Timing: In some protocols, adding pericytes after ECs have begun to form tubules (e.g., 24-48 hours later) is more effective than co-seeding simultaneously, as it mimics the physiological sequence of events.
- Check Matrix Stiffness: The biomechanical properties of your hydrogel (e.g., Collagen-I, Fibrin) profoundly affect cell behavior. An inappropriate stiffness can inhibit both EC network formation and pericyte migration. Stiffness should mimic that of native soft tissues [18] [22].
Q: My engineered microvessels are unstable and regress after a few days in culture. How can I improve longevity?
- A: Vessel regression indicates a lack of maturation signals.
- Enhance Mural Cell Coverage: Ensure you have a sufficient ratio and viable population of pericytes or vSMCs. These cells provide essential survival signals like Angiopoietin-1 [18] [19].
- Promote Basement Membrane Formation: The cross-talk between ECs and pericytes is crucial for depositing a robust basement membrane (containing collagen IV, laminin). Allow sufficient culture time (7-14 days) for this matrix to assemble, as it is critical for mechanical stability [19].
- Introduce Physiological Cues: Use advanced platforms like microfluidic chips that provide interstitial flow, which has been shown to enhance vessel maturation and stability [18].
Cell Sourcing and Characterization Issues
Q: What are the best sources for obtaining pericytes and how can I confirm their identity?
- A: Pericytes can be sourced from multiple places, but they require validation with a panel of markers due to the lack of a single unique identifier.
- Primary Isolation: Can be isolated from microvessel-rich tissues like brain, retina, or adipose tissue [18]. This can yield tissue-specific pericytes but may involve complex isolation procedures.
- Stem Cell Differentiation: Human-induced pluripotent stem cells (iPSCs) can be differentiated into pericytes, offering a scalable and patient-specific source [18].
- Validation: Use a combination of positive and negative markers. Positive markers include PDGFR-β, NG2, and CD13. Assess the expression of cytoskeletal proteins like α-SMA and Desmin. Confirm the absence of endothelial (e.g., VE-cadherin) and fibroblast markers [18] [21].
Q: My isolated vascular smooth muscle cells (vSMCs) are not expressing contractile markers. What is happening?
- A: VSMCs can undergo phenotypic modulation from a contractile to a synthetic/proliferative state in culture.
- Culture Conditions: Standard culture conditions on plastic with high serum promote the synthetic phenotype. To induce the contractile phenotype, reduce serum concentration and use specialized media (e.g., SmBm) [20].
- Use of TGF-β1: Treating cells with recombinant TGF-β1 is a well-established method to upregulate the expression of contractile genes like α-SMA, calponin, and SM22 [20].
- Passage Number: The contractile phenotype is often lost at higher passages. Use low-passage cells for experiments requiring a contractile phenotype.
In Vivo Integration Challenges
Q: After implantation, my prevascularized construct fails to anastomose with the host circulation. What host factors should I consider?
- A: The host environment is critical for successful integration, and the choice of animal model can drastically alter outcomes.
- Animal Model Discrepancies: Studies show identical engineered tissues can have divergent vascularization and engraftment in athymic nude mice versus athymic rats. Mice may support better guided vascularization, while rats might support better survival of certain cell types like cardiomyocytes [17].
- Implantation Site: The anatomic location (e.g., subcutaneous space, intraperitoneal fat pad, epicardial surface of the heart) influences vascular ingrowth, inflammatory response, and the stability of the implanted construct [17].
- Host Inflammation: A strong inflammatory response can degrade the graft and disrupt patterned vessels. Strategies to modulate the host immune response may be necessary for successful anastomosis [17].
Detailed Experimental Protocol: Establishing a 3D EC-Pericyte Co-Culture in Collagen-I Hydrogel
This protocol is adapted from methods used to investigate EC-pericyte interactions and capillary network co-assembly [18].
Diagram 2: Workflow for 3D EC-Pericyte Co-Culture.
Materials
- High-concentration Rat Tail Collagen-I (e.g., ~8-10 mg/mL)
- Endothelial Cells (e.g., HUVECs, human retinal ECs)
- Pericytes (e.g., primary human brain or iPSC-derived)
- Cell culture medium (e.g., EGM-2 for ECs, pericyte growth medium, or a shared co-culture medium)
- Neutralization Solution (e.g., 0.1-1M NaOH, 10x PBS)
- Sterile tissue culture plates (e.g., 24-well plate)
Step-by-Step Procedure
- Prepare Collagen-I Working Solution: On ice, mix the high-concentration Collagen-I with neutralization solution and 10x PBS according to the manufacturer's instructions to achieve a final working concentration of 2.5 - 3.0 mg/mL at a physiological pH (pink color). Keep on ice to prevent premature polymerization [18].
- Seed Cells and Polymerize Hydrogel: Quickly mix the cell suspensions (e.g., a 3:1 or 5:1 ratio of ECs to Pericytes) with the neutralized collagen solution. Gently pipette the cell-collagen mixture into the wells of a culture plate. Incubate the plate at 37°C for 30-45 minutes to allow for complete gel polymerization.
- Add Culture Medium: After polymerization, carefully add pre-warmed culture medium on top of the hydrogel without disturbing it. The medium can be supplemented with pro-angiogenic factors like VEGF (50 ng/mL) and other relevant factors identified in studies, such as SCF, IL-3, and SDF-1α [18].
- Maintain and Monitor Culture: Change the culture medium every 48 hours. Observe the development of endothelial tubular networks and pericyte association daily using an inverted light microscope.
- Analyze Networks: After 7-14 days in culture, fix the constructs and perform immunostaining for markers like CD31 (ECs) and NG2 or α-SMA (Pericytes) to visualize network morphology and pericyte coverage. Quantify parameters such as branch length, junction numbers, and pericyte association index.
Expected Outcomes
Within 3-7 days, you should observe extensive EC tubular networks. Pericytes should migrate along and wrap around these tubes, leading to more mature and stable structures compared to EC-only cultures.
Advanced Models: From Microfluidics to Application
To truly overcome the limitation of vascularizing thick tissues, moving beyond simple hydrogels to more sophisticated models is essential.
- Microfluidic Vasculature-on-a-Chip: These platforms allow for the precise control of physiochemical cues, such as interstitial flow and shear stress, which are critical for guiding angiogenesis and enhancing barrier function [18]. They enable high-resolution, real-time imaging of the dynamic interactions between ECs and pericytes during vascular morphogenesis.
- Guided Vascularization In Vivo: For implantation, research shows that pre-patterning endothelial cells into specific geometries (e.g., parallel "cords") within engineered tissues can act as "railroad tracks," guiding the formation of chimeric host-graft vessels that efficiently anastomose with the host circulation [17]. This approach has been shown to improve the survival of embedded functional cells, such as hepatocytes and cardiomyocytes [17].
- Bioreactors for Maturation: The use of dynamic bioreactor systems that provide pulsatile flow and mechanical conditioning is a final, critical step for developing implantable large-scale blood vessels with sufficient mechanical strength to withstand physiological blood pressures [6].
Frequently Asked Questions (FAQs)
Q1: What is the primary cellular mechanism by which engineered vascular networks connect to the host circulation? Engineered vascular networks connect to the host vasculature through a previously unidentified process called "wrapping-and-tapping" anastomosis [23] [24]. This process does not rely on tip cell connections or vacuole fusion. Instead, at the host-implant interface, implanted endothelial cells (ECs) first wrap around nearby host vessels [23]. These wrapping ECs then express high levels of matrix metalloproteinase-14 (MMP-14) and matrix metalloproteinase-9 (MMP-9), which facilitate the reorganization of the host vessel's basement membrane and pericytes, and the localized displacement of the underlying host endothelium [23]. In this way, the implanted ECs effectively replace segments of the host vessel wall to directly tap into the host blood supply and divert flow into the implanted network [23] [24].
Q2: My implanted tissues vascularize poorly in my current animal model. Could the host species or anatomic location be the cause? Yes, the host model and anatomic implant location are critical factors that can lead to divergent outcomes, even when using identical engineered tissues [17]. For instance, guided vascular networks formed and anastomosed robustly in both the intraperitoneal space and on the heart of athymic nude mice [17]. However, the same tissues elicited substantive inflammatory changes when implanted onto the hearts of athymic rats, which disrupted vascular patterning and led to graft degradation [17]. This underscores that the host environment can override the intrinsic vascularization capacity of an engineered tissue.
Q3: Besides endothelial cells, what other cell types are crucial for building stable, implantable vascular networks? Creating stable, implantable vasculature requires a multi-lineage approach that recapitulates the structure of native blood vessels.
- Smooth Muscle Cells (SMCs) and Pericytes: These cells provide structural support and are effectors of vascular tone. They form the tunica media around larger vessels, while pericytes abut the endothelium in capillaries [25] [6]. The presence of α-smooth muscle actin (α-SMA)+ cells partially or fully encircling engineered endothelial lumens is a marker of mature, stabilized microvessels [17].
- Stromal Cells/Fibroblasts: These cells are a key component of the tunica adventitia, providing connective tissue and ECM to maintain the overall vessel structure [6]. The inclusion of mesenchymal precursor cells or fibroblasts with endothelial cells significantly enhances the formation of perfused, vascular networks in vivo [23] [25].
Q4: How quickly can I expect blood perfusion to be established in a prevascularized implant? In optimized models, anastomosis between host vessels and implanted EC networks can occur as early as two weeks after implantation [23]. The "wrapping-and-tapping" mechanism facilitates this rapid connection. Furthermore, studies have shown that by 7 days post-implantation, a high percentage of pre-patterned endothelial cords can become associated with lumens containing host red blood cells, indicating successful anastomosis and perfusion [17].
Q5: What are the major structural requirements for an engineered tissue to integrate successfully with the host vasculature? Successful integration depends on recapitulating key structural and biological features:
- Trilaminate Structure: Ideal engineered vessels mimic native anatomy with a tunica intima (endothelial cell layer for anti-thrombogenicity), a tunica media (smooth muscle cells for mechanical strength), and a tunica adventitia (fibroblasts in connective tissue for structural integrity) [25] [6].
- Mechanical Properties: The construct must have sufficient mechanical strength to withstand physiologic blood pressures (approximately 2000–3000 mmHg burst strength for arteries) and surgical handling, such as stitching during implantation [6].
- Non-thrombogenic Surface: The luminal surface must be lined with a confluent layer of endothelial cells to prevent clot formation and ensure patency [25] [6].
Troubleshooting Guide
Problem 1: Lack of Perfusion in Engineered Grafts
| Symptom | Possible Cause | Solution |
|---|---|---|
| No blood flow in implanted networks 2+ weeks post-implantation. | Insufficient or unstable anastomosis with host vasculature. | Co-implant stromal cells (e.g., 10T1/2, MSCs) with ECs at a ratio of 1:4 (stromal:EC) to enhance network stability and anastomosis [23]. |
| Graft necrosis or central cell death. | Delayed perfusion; diffusion limit of oxygen (100-200 μm) exceeded [17]. | Pre-form patterned endothelial networks (e.g., "cords") within the graft to act as "railroad tracks" for guided host-graft vessel formation and faster perfusion [17]. |
| Inflammatory degradation of the graft. | Host-dependent foreign body response or inflammation [17]. | Consider switching host animal models (e.g., from rat to mouse) or anatomic location based on pilot studies [17]. Use immunodeficient models to minimize rejection. |
Problem 2: Host-Dependent Variability in Vascularization & Engraftment
| Symptom | Possible Cause | Solution |
|---|---|---|
| Robust vascularization but sparse survival of co-implanted functional cells (e.g., cardiomyocytes). | Host factors that differentially support vascularization vs. parenchymal cell engraftment [17]. | Athymic mice supported robust guided vascularization but relatively sparse cardiac grafts, while athymic rats supported >3-fold larger cardiomyocyte grafts despite disrupted vessels [17]. Test multiple host models for your specific cell type. |
| Patterned vascular networks fail to form; severe inflammation at implant site. | Aggressive host inflammatory response degrading the graft or disrupting patterning [17]. | This was observed in athymic rats [17]. Pre-assess the host inflammatory response to your biomaterial in the target anatomic location before large-scale studies. |
Experimental Protocols
Protocol 1: Investigating Anastomosis via the Cranial Window Model
This protocol is adapted from methods used to discover the "wrapping-and-tapping" mechanism [23].
Cell Preparation:
- Culture Human Umbilical Vein Endothelial Cells (HUVECs) in endothelial growth medium.
- Culture mouse mesenchymal precursor cells (e.g., 10T1/2) in Dulbecco's Modified Eagle Medium (DMEM) with 10% FBS.
- Optionally, transduce HUVECs with a fluorescent protein (e.g., GFP) using retrovirus for in vivo tracking.
Construct Fabrication:
- Suspend 8x10⁵ HUVECs and 2x10⁵ 10T1/2 cells in 1 mL of ice-cold rat-tail type I collagen (1.5 mg/mL) solution mixed with human plasma fibronectin (90 μg/mL).
- Adjust pH to 7.6 using 1N NaOH.
- Pipette the cell suspension into a multi-well plate and incubate at 37°C for 30 minutes to allow collagen polymerization.
- Cover the solidified gel with culture medium and culture for 18-24 hours.
Implantation:
- Use a 4-mm biopsy punch to create disk-shaped gels for implantation.
- Implant the gel into a cranial window preparation in a severe combined immunodeficient (SCID) mouse [23].
Intravital Imaging & Analysis:
- Visualize host vasculature by intravenous injection of a fluorescently labeled mouse-specific CD31 antibody.
- Track blood flow by injecting mouse red blood cells labeled with lipophilic carbocyanine dyes (DiI or DiD).
- Use confocal laser-scanning microscopy for intravital imaging at various time points (e.g., from day 3 to 7 and beyond) to observe the wrapping and tapping process.
Protocol 2: Assessing Guided Vascularization with Endothelial Cords
This protocol details the creation of tissues with patterned endothelial cords for improved perfusion [17].
Cord Patterning:
- Suspend HUVECs and stromal cells in a collagen solution.
- Pipette the cell-collagen suspension into a polydimethylsiloxane (PDMS) mold containing an array of parallel microchannels.
- Allow the collagen to polymerize, forming solid "endothelial cords" within the channels.
Tissue Encapsulation:
- Carefully encapsulate the patterned cord structure within a fibrin hydrogel to create the final 3D engineered tissue.
Implantation and Analysis:
- Implant the engineered tissue into the desired animal model (e.g., sutured to the intraperitoneal gonadal fat pad or the epicardial surface of the heart in athymic nude mice).
- For analysis, perfuse the animal with a biotinylated lectin intravenously prior to harvest to label perfused vessels.
- Harvest tissues at set time points (e.g., 3 and 7 days).
- Fix, section, and perform immunohistochemistry for human CD31 (to identify graft-derived endothelium) and mouse-specific markers (e.g., TER-119 for red blood cells) to confirm perfusion and pattern retention.
Research Reagent Solutions
| Reagent / Material | Function / Explanation |
|---|---|
| HUVECs & Stromal Cells (10T1/2) | Foundation for self-assembling vascular networks; stromal cells enhance stability and anastomosis [23]. |
| Collagen-Fibronectin Matrix | A natural hydrogel that supports 3D cell organization, lumenogenesis, and matrix remodeling crucial for anastomosis [23]. |
| Patterned PDMS Molds | Used to create "endothelial cords," which guide the formation of structured, parallel vascular networks in vivo [17]. |
| Fluorescently Labeled Antibodies (e.g., α-mCD31) | Allows for clear visualization and distinction of the host vasculature during live imaging [23]. |
| Labeled Red Blood Cells (DiI/DiD) | Enable direct tracking and confirmation of blood flow and perfusion within the engineered networks [23]. |
| Matrix Metalloproteinase (MMP) Inhibitors | Tool to investigate the mechanistic role of MMP-14 and MMP-9 in the "wrapping-and-tapping" anastomosis process [23]. |
Process Diagrams
Building the Vascular Blueprint: From Prevascularization to 3D Bioprinting Strategies
A major obstacle in engineering thick, clinically relevant tissues is the diffusion limit of oxygen and nutrients, which is approximately 100–200 μm [4]. Without a functional vascular network, cells in the core of these constructs suffer from hypoxia and insufficient nutrient supply, leading to necrosis and ultimate graft failure [4]. Cell-based prevascularization is a promising strategy to overcome this limitation. This approach involves the co-culturing of endothelial cells (ECs) and supportive stromal cells within three-dimensional (3D) scaffolds before implantation, aiming to pre-form organized vascular networks that can rapidly anastomose with the host circulation upon grafting [4] [26] [25]. This technical support center provides targeted troubleshooting and foundational protocols to help researchers navigate the challenges of creating robust, pre-vascularized tissues.
Frequently Asked Questions (FAQs)
1. What is the primary goal of prevascularizing a tissue-engineered construct? The primary goal is to create an integrated, self-assembled network of vessel-like structures within the tissue construct in vitro that, after implantation, can quickly connect to the host's blood circulation. This anastomosis provides immediate perfusion, overcoming the diffusion limit and ensuring the survival and function of cells throughout a thick tissue graft [4] [17].
2. Why is it necessary to co-culture endothelial cells with support cells? Endothelial cells alone often form unstable and transient tubular structures. Co-culturing them with support cells—such as mesenchymal stem cells (MSCs), fibroblasts, or pericytes—is crucial because these cells provide vital paracrine signals and physical support that stabilize the newly formed vascular networks, promote lumen formation, and enhance maturation by recruiting perivascular cells [4] [25].
3. What are the critical host-related factors affecting implant success? The host animal model and anatomic implantation site critically influence vascularization and engraftment. Studies show significant differences in outcomes between immunodeficient athymic nude mice and rats. Mice may support better guided vascularization of human microvessels, while rats might support better cardiomyocyte survival but exhibit more disruptive inflammation or degraded vascular patterning depending on the implant site [17].
4. How can I assess the functionality of the pre-formed networks in vitro? While full functionality (blood perfusion) can only be confirmed in vivo, several in vitro assays can indicate potential functionality. These include immunostaining for endothelial markers (e.g., CD31) to visualize network morphology, and measuring the expression of key angiogenic growth factors like VEGF, bFGF, and angiopoietins [4].
Troubleshooting Guides
Common Experimental Issues and Solutions
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Poor Network Formation | Incorrect EC-to-support cell ratio; Suboptimal scaffold stiffness; Lack of pro-angiogenic factors. | Systemically test cell ratios (e.g., 1:1 to 1:5 ECs/Support); Tune scaffold mechanical properties to mimic native ECM; Incorporate angiogenic factors (VEGF, bFGF). |
| Networks Are Unstable/Regress | Lack of continuous biochemical cues; Insufficient ECM remodeling; Absence of mechanical stabilization. | Use a sustained-release hydrogel for growth factors; Incorporate enzymes for ECM degradation (e.g., MMP-sensitive peptides); Apply cyclic mechanical strain during culture. |
| Low Cell Viability in Construct Core | Scaffold thickness exceeds oxygen diffusion limit; High cell seeding density; Pre-formed networks are not perfusable. | Use a bioreactor for enhanced medium perfusion during culture; Pattern internal channels to mimic a rudimentary flow circuit; Optimize cell seeding density. |
| Lack of Host Anastomosis In Vivo | Host inflammatory response; Mismatch in vessel maturity; Surgical model or site is not optimal. | Use immunodeficient host models; Assess pericyte coverage (α-SMA) pre-implantation; Test different anatomic implant sites (e.g., intraperitoneal vs. epicardial). |
Quantitative Data for Experimental Planning
Table: Key Growth Factors in Prevascularization [4]
| Growth Factor | Primary Role in Angiogenesis |
|---|---|
| VEGF (Vascular Endothelial Growth Factor) | Promotes EC proliferation, migration, and survival; increases vascular permeability. |
| bFGF (Basic Fibroblast Growth Factor) | Stimulates proliferation of ECs and support cells; promotes ECM degradation. |
| PDGF (Platelet-Derived Growth Factor) | Recruits and stabilizes support cells (pericytes, SMCs) around nascent vessels. |
| TGF-β1 (Transforming Growth Factor Beta-1) | Modulates EC proliferation and stimulates ECM production by support cells. |
Table: Host Model Comparison for In Vivo Implantation [17]
| Host Model / Implant Site | Observed Vascular Outcomes | Cell Engraftment Survival |
|---|---|---|
| Athymic Nude Mouse (IP) | Robust, guided vascularization; patterned vessels anastomose with host. | Sparse cellular grafts. |
| Athymic Nude Mouse (Epicardial) | Robust, guided vascularization; patterned vessels anastomose with host. | Sparse cellular grafts. |
| Athymic Rat (Abdomen) | Substantial inflammation; graft degradation. | Not specified. |
| Athymic Rat (Epicardial) | Disrupted vascular patterning. | >3-fold larger cardiomyocyte grafts vs. mice. |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Prevascularization Experiments
| Reagent / Material | Function / Application | Example |
|---|---|---|
| Endothelial Cells (ECs) | Form the inner lining of the vascular tubes. | HUVECs, induced pluripotent stem cell-derived ECs. |
| Support / Stromal Cells | Stabilize EC networks and promote maturation. | Mesenchymal Stem Cells (MSCs), fibroblasts, pericytes. |
| 3D Scaffold / Hydrogel | Provides a 3D environment for cell growth and network formation. | Fibrin, collagen gels, synthetic PEG-based hydrogels. |
| Angiogenic Growth Factors | Stimulate EC sprouting, tube formation, and network stability. | VEGF, bFGF (FGF-2), PDGF-BB. |
| Temperature-Responsive Dishes | Enable harvest of intact, contiguous cell sheets for layering. | Poly(N-isopropylacrylamide) grafted dishes. |
Detailed Experimental Protocols
Methodology: This protocol uses temperature-responsive culture dishes to create and stack 2D co-culture sheets into a 3D tissue.
- Surface Preparation: Use temperature-responsive culture dishes (e.g., grafted with poly(N-isopropylacrylamide)).
- Cell Seeding and Co-culture: Seed and culture a mixture of endothelial cells (e.g., HUVECs) and the target parenchymal cell (e.g., cardiomyocytes, fibroblasts). Culture until a confluent, contiguous cell sheet is formed.
- Cell Sheet Harvest: Reduce the culture temperature (e.g., to below 32°C). The surface becomes hydrophilic, allowing the intact cell sheet to detach spontaneously without enzyme treatment. The sheet preserves its deposited extracellular matrix and cell-cell junctions.
- 3D Stratification: Using a manipulator, gently transfer the harvested cell sheet onto a previously deposited sheet. A plunger coated with a fibrin gel can be used to handle and stack the delicate sheets. Repeat this process to create multi-layered, 3D tissues.
- Maturation and Analysis: Culture the layered construct to allow for the self-organization and formation of endothelial network structures throughout the 3D tissue.
Methodology: This protocol pre-patterns endothelial cells into defined geometries to guide vascular network formation.
- Cord Fabrication: Suspend human umbilical vein endothelial cells (HUVECs) and stromal cells (e.g., MSCs) in a collagen solution.
- Molding: Pipette the cell-collagen suspension into a polydimethylsiloxane (PDMS) mold featuring an array of parallel micro-channels (e.g., 50-100 µm apart). Allow the collagen to gel, forming solid "endothelial cords" within the channels.
- Tissue Encapsulation: Carefully encapsulate the entire patterned cord structure within a fibrin-based hydrogel. This bulk hydrogel can also be seeded with other cell types, such as cardiomyocytes.
- In Vitro Culture: Maintain the construct in culture to allow for preliminary network maturation.
- Implantation and Analysis: Implant the engineered tissue in vivo (e.g., suture to the epicardial surface of the heart or intraperitoneal site). Upon explantation, the guided formation of patterned, chimeric host-graft vessels can be analyzed.
Signaling Pathways and Experimental Workflows
Frequently Asked Questions (FAQs)
Q1: Why is scaffold-based vascularization critical for engineering thick tissues? Without a built-in vascular network, thick tissue constructs (>1-2 mm) face central necrosis because oxygen and nutrients cannot diffuse more than 100–200 μm from the nearest blood vessel [27] [4]. Scaffolds provide the initial 3D template to guide the formation of this essential, life-sustaining vascular network, thereby overcoming this diffusion limit and ensuring cell viability throughout the construct post-implantation [4].
Q2: What are the primary scaffold properties that influence angiogenesis? The key properties can be categorized as follows:
- Architectural: High porosity and pore interconnectivity are vital for cell migration, tissue infiltration, and formation of interconnected vascular networks. Recommended pore sizes often range from 150 to 500 μm for optimal vascularization [28] [29].
- Mechanical: Stiffness and elasticity must be appropriate for the target tissue, as these properties directly influence cell behavior, including endothelial cell sprouting and differentiation [27] [28].
- Biological: Biocompatibility ensures cell adhesion and survival without a severe immune response. Biodegradability at a rate matching new tissue formation is crucial to prevent the scaffold from obstructing growth [30] [28].
Q3: Which cell sources are most promising for building vascular networks within scaffolds? Common cell sources include:
- Mature Vascular Cells: Autologous Endothelial Cells (ECs) and Smooth Muscle Cells (SMCs), which are directly functional but have limited expansion capability [31] [32].
- Progenitor/Stem Cells: Endothelial Progenitor Cells (EPCs) and Mesenchymal Stem Cells (MSCs) offer greater proliferative potential and can differentiate into vascular lineages [32].
- Pluripotent Stem Cells (PSCs): Both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) provide an unlimited, self-renewing source for generating ECs and SMCs, though oncogenic risk must be managed [32].
Q4: What key biochemical signals should be incorporated into scaffolds to promote angiogenesis?
- Vascular Endothelial Growth Factor (VEGF) is a primary stimulator for EC migration and proliferation [32] [4].
- Basic Fibroblast Growth Factor (FGF-2) promotes vessel sprouting and mural cell recruitment [32].
- Platelet-Derived Growth Factor (PDGF) helps stabilize new vessels by recruiting supporting pericytes or smooth muscle cells [32] [4].
Troubleshooting Guides
Problem: Poor Cell Seeding and Inhomogeneous Distribution
| Potential Cause | Solution | Underlying Principle |
|---|---|---|
| Low Scaffold Porosity/Interconnectivity | Optimize fabrication parameters to increase pore size and interconnection. Use techniques like porogen leaching or 3D-bioprinting for precise control [28] [29]. | Enhances cell penetration and uniform distribution. Interconnected pores allow for nutrient/waste exchange in deep regions [30]. |
| Hydrophobic Scaffold Surface | Functionalize material with cell-adhesive peptides (e.g., RGD sequence) or natural polymers like collagen or fibronectin [31] [28]. | Increases initial cell attachment by mimicking the natural extracellular matrix (ECM), improving seeding efficiency [28]. |
| Static Seeding Methods | Utilize dynamic seeding in a bioreactor, where the cell suspension is perfused or agitated [31]. | Promotes higher and more uniform cell distribution by actively driving cells into the scaffold's pores [31]. |
Problem: Inadequate or Immature Vascular Network Formation
| Potential Cause | Solution | Underlying Principle |
|---|---|---|
| Lack of Pro-Angiogenic Signals | Incorporate sustained-release systems for growth factors (e.g., VEGF, FGF) within the scaffold material [32] [4]. | Provides a continuous, localized signal to guide and stimulate the multi-stage process of angiogenesis [32]. |
| Absence of Supporting Cells | Co-culture ECs with pericytes or MSCs within the scaffold [32] [33]. | Recapitulates the natural cellular environment; supporting cells stabilize nascent vessels and prevent regression [32]. |
| Suboptimal Scaffold Stiffness | Tune the mechanical properties of the scaffold to match the compliance of the native target tissue [27] [28]. | Cells sense and respond to substrate stiffness (mechanotransduction). An appropriate mechanical environment is crucial for proper EC and SMC function [28]. |
Problem: Scaffold Degradation Outpaces Tissue Formation
| Potential Cause | Solution | Underlying Principle |
|---|---|---|
| Overly Fast Degradation Rate | Select a biomaterial with a slower degradation profile or increase crosslinking density [30] [28]. | The scaffold must provide mechanical support long enough for the new tissue and vascular network to become self-supporting [30]. |
| High Inflammatory Response | Use more biocompatible or purer materials. Consider decellularized ECM scaffolds to minimize immune rejection [27] [30]. | A severe inflammatory response can accelerate scaffold degradation through the release of enzymes and reactive oxygen species [30]. |
Experimental Protocols
Protocol: Fabrication of a Porous Angiogenic Scaffold via Porogen Leaching
This is a widely used method to create scaffolds with high, interconnected porosity [28].
Workflow Diagram: Porogen Leaching Scaffold Fabrication
Materials:
- Biomaterial: e.g., PLGA, PCL, or Chitosan.
- Solvent: e.g., Chloroform (for synthetic polymers) or Aqueous Acetic Acid (for Chitosan).
- Porogen: Sodium Chloride (NaCl) or Sucrose crystals, sieved to a specific size range (e.g., 150-250 μm).
- Equipment: Glass vial, magnetic stirrer, Teflon mold, lyophilizer, UV lamp.
Step-by-Step Method:
- Prepare Polymer Solution: Dissolve your chosen polymer in a suitable solvent at a concentration of 5-10% w/v under constant stirring until a clear solution is obtained.
- Incorporate Porogen: Add the sieved porogen particles to the polymer solution at a high weight ratio (e.g., 70-90% porogen to polymer). Mix thoroughly to ensure a homogeneous suspension.
- Cast the Mixture: Pour the polymer-porogen mixture into a pre-defined mold (e.g., Teflon dish). Spread evenly.
- Evaporate Solvent: Place the mold in a fume hood for 24-48 hours to allow the solvent to evaporate completely, forming a solid composite.
- Leach Out Porogen: Immerse the solid composite in deionized water for 48 hours, changing the water every 6-8 hours to fully dissolve and leach out the porogen particles.
- Dry and Sterilize: Remove the now-porous scaffold from the water and freeze-dry it. Sterilize under UV light for 1 hour per side or using ethanol immersion before cell culture.
Protocol: Assessing Angiogenesis in a 3D Scaffold
Workflow Diagram: Angiogenesis Assessment Pipeline
Materials:
- Cells: Human Umbilical Vein Endothelial Cells (HUVECs), optionally with Mesenchymal Stem Cells (MSCs) or fibroblasts in co-culture.
- Scaffold: Your fabricated 3D scaffold.
- Culture Media: Endothelial Cell Growth Medium.
- Fixative: 4% Paraformaldehyde (PFA).
- Staining Antibodies: Primary antibody against CD31/PECAM-1 (endothelial cell marker) and a fluorescently-labelled secondary antibody.
- Equipment: Confocal microscope, cell culture incubator, qPCR machine.
Step-by-Step Method:
- Cell Seeding: Seed HUVECs (with or without supporting cells) onto the sterile scaffold using a high-density suspension. Allow 2-4 hours for cell attachment before adding culture media.
- Culture: Maintain the cell-scaffold constructs in culture for 7-14 days, changing the media every 2-3 days.
- Fixation: At the desired time point, carefully wash the constructs with PBS and fix with 4% PFA for 30-60 minutes.
- Immunostaining:
- Permeabilize and block the fixed constructs.
- Incubate with primary anti-CD31 antibody overnight at 4°C.
- Wash and incubate with a fluorescent secondary antibody.
- Counterstain nuclei with DAPI and the actin cytoskeleton with Phalloidin.
- Imaging and Analysis: Image the entire scaffold using a confocal microscope with Z-stacking capability. Use image analysis software (e.g., ImageJ with Angiogenesis Analyzer plugin) to quantify key parameters from the 3D reconstructions.
Key Quantitative Measures for Analysis:
- Total Tube Length: The combined length of all CD31-positive structures.
- Number of Branch Points: Points where three or more tubules intersect.
- Number of Meshes: Closed loops formed by the tubular network.
Research Reagent Solutions
A table of essential materials for scaffold-based angiogenesis studies.
| Category | Item / Reagent | Primary Function in Angiogenesis Research |
|---|---|---|
| Biomaterials (Natural) | Collagen [30] [29] | Highly biocompatible; mimics native ECM; promotes cell adhesion and tubulogenesis. |
| Chitosan [30] [29] | Biodegradable polysaccharide; can be modified to enhance bioactivity and control degradation. | |
| Fibrin [27] | Natural hydrogel derived from blood clot; inherently pro-angiogenic; used as a matrix for EC network formation. | |
| Biomaterials (Synthetic) | PLGA [27] [30] | Tunable degradation and mechanical properties; excellent for controlled release of growth factors. |
| PEG [27] [33] | "Blank slate" hydrogel; highly modifiable with bioactive peptides (e.g., RGD, VEGF-mimetic). | |
| Cells | HUVECs [32] [4] | Standard primary EC model; robustly forms tubular structures in 3D cultures. |
| Mesenchymal Stem Cells (MSCs) [32] | Pericyte-like function; stabilizes new vessels; secretes pro-angiogenic paracrine factors. | |
| Induced Pluripotent Stem Cells (iPSCs) [32] [33] | Source for generating autologous ECs and SMCs; unlimited expansion potential. | |
| Bioactive Factors | Vascular Endothelial Growth Factor (VEGF) [32] [4] | Key mitogen and chemoattractant for ECs; essential for initiation of angiogenesis. |
| Basic Fibroblast Growth Factor (FGF-2) [32] | Promotes EC proliferation and protease production; works synergistically with VEGF. | |
| RGD Peptide [28] | Cell-adhesive ligand; grafted onto materials to enhance integrin-mediated cell attachment. |
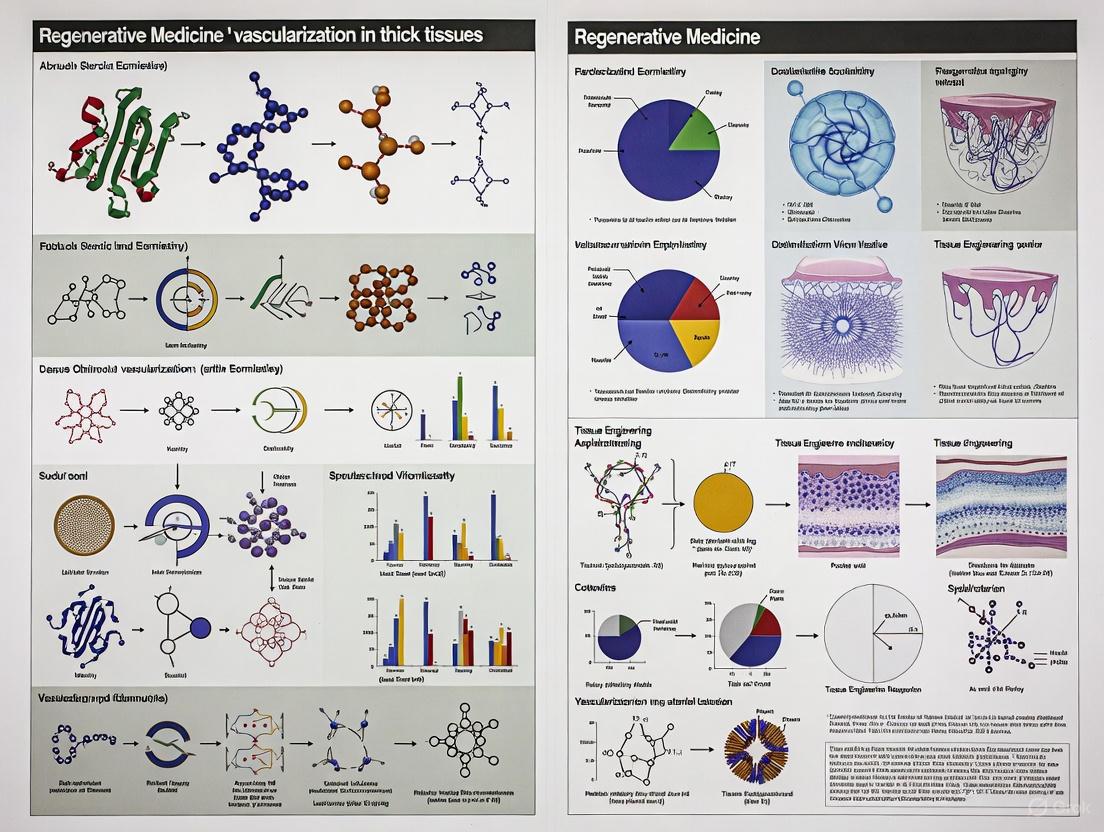
A critical obstacle in tissue engineering is the inability to develop large-scale, functional tissues that fully mimic native organs. A primary reason for this limitation is the lack of integrated, perfusable vascular networks, which are essential for delivering oxygen and nutrients to cells and removing waste products. The diffusion limit of oxygen and nutrients is approximately 100–200 µm from a blood vessel, meaning that cells located beyond this distance in a thick tissue construct will face hypoxia, nutrient deficiency, and eventual necrosis [4] [34]. Consequently, engineered tissues exceeding a few hundred micrometers in thickness require an internal vascular system to remain viable [35].
Advanced biofabrication, particularly 3D bioprinting, has emerged as a promising strategy to overcome this bottleneck. This technical support document provides a foundational guide and troubleshooting resource for researchers aiming to implement these sophisticated biofabrication strategies in their work on thick tissue constructs.
Core Bioprinting Strategies for Vascular Networks
Several 3D bioprinting strategies have been developed to create the hierarchical, branched structures characteristic of native vasculature. The table below summarizes the key approaches, their core principles, and associated technical considerations.
Table 1: Core 3D Bioprinting Strategies for Fabricating Vascular Networks
| Strategy | Fundamental Principle | Key Advantages | Inherent Challenges |
|---|---|---|---|
| Sacrificial Bioprinting | A fugitive bioink (e.g., Pluronic F-127, carbohydrate glass) is printed into a network, embedded in a cell-laden hydrogel, and then liquefied and removed to create hollow channels [35] [34]. | Creates complex, free-form channel geometries; allows for subsequent endothelialization. | Requires a multi-step process; removal of sacrificial material can be incomplete in large constructs. |
| Direct Coaxial Extrusion | Uses a concentric multilayered nozzle to directly deposit a hollow, tubular filament in a single step. An inner core solution (e.g., CaCl₂) can crosslink a shell bioink (e.g., alginate-GelMA blend) [36]. | One-step fabrication of perfusable tubes; enables continuous fabrication. | Limited to simpler, often straight or gently curving geometries; requires specialized nozzle systems. |
| Embedded Bioprinting (e.g., FRESH) | Bioinks are printed within a temporary support bath (e.g., a yield-stress gelatin slurry), which holds the soft ink in place until crosslinking is complete [34]. | Enables printing of complex, overhanging structures with high fidelity using low-viscosity bioinks. | Support bath removal required; potential for contamination; process can be slow. |
The following workflow diagram illustrates a generalized experimental process for creating vascularized tissues, integrating elements from sacrificial and direct bioprinting approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful bioprinting of vascular networks relies on a carefully selected suite of materials. The following table catalogs key reagents and their specific functions in the biofabrication process.
Table 2: Essential Research Reagents for Vascular Bioprinting
| Reagent/Material | Core Function | Application Notes |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | A photopolymerizable hydrogel providing natural cell-adhesive motifs (e.g., RGD sequences) to support cell spreading and proliferation [36] [35]. | Degree of functionalization and concentration tune mechanical properties. A common concentration is 8-10% (w/v) [35]. |
| Sodium Alginate | A natural polysaccharide used to provide immediate structural integrity via rapid ionic crosslinking with calcium ions (Ca²⁺) [36] [37]. | Blended with other hydrogels (e.g., GelMA) to improve bioink shear-thinning and shape fidelity during printing [36]. |
| 4-arm Poly(Ethylene Glycol)-Tetra-Acrylate (PEGTA) | A synthetic polymer used to enhance the mechanical strength and crosslinking density of bioinks due to its branched, tetravalent structure [36]. | Increases mechanical robustness without significantly compromising the porous structure needed for cell growth [36]. |
| Pluronic F-127 | A thermoreversible polymer widely used as a sacrificial bioink. It is solid at room temperature and liquefies when cooled, allowing for easy removal [35]. | A concentration of 40% (w/v) is often used to achieve a balance between printability and post-printing stability [35]. |
| Calcium Chloride (CaCl₂) | A crosslinking agent used to ionically crosslink alginate-containing bioinks, providing immediate stability after deposition [36]. | Often delivered coaxially during direct printing of hollow tubes or used as an immersion bath post-printing. |
| Irgacure 2959 | A photoinitiator used to catalyze the covalent crosslinking of methacrylated polymers (like GelMA) and PEGTA upon exposure to UV light [36] [35]. | Concentration is typically 0.25% (w/v); enables permanent stabilization of the printed construct [36]. |
Detailed Experimental Protocol: Direct 3D Bioprinting of Perfusable Constructs
This protocol is adapted from a cited study that describes a versatile strategy for depositing perfusable vascular structures in a single-step process using a multilayered coaxial extrusion system and a specially designed bioink [36].
Bioink Preparation
- Prepare Base Solution: Dissolve GelMA (5-7% w/v), sodium alginate (1-3% w/v), and 4-arm PEGTA (1-3% w/v) in de-ionized water supplemented with 10% (v/v) FBS and 25 mM HEPES buffer.
- Add Photoinitiator: Incorporate 0.25% (w/v) Irgacure 2959 into the solution. Sterilize the blend by passing it through a 0.22-µm filter and store at 37°C until use.
- Prepare Crosslinkers: Dissolve CaCl₂ in a 10% (v/v) FBS solution at a 0.3 M concentration for ionic crosslinking. Prepare a 20 mM EDTA solution in PBS as a calcium chelator for control purposes.
Bioprinting Process
- Setup: Employ a bioprinter equipped with a custom multilayered coaxial nozzle. Load the blend bioink into the outer cartridge and the CaCl₂ solution into the inner cartridge.
- Printing: Co-extrude the bioink and crosslinker simultaneously. The inner CaCl₂ stream instantly ionically crosslinks the alginate in the bioink shell, forming a stable hollow tube upon deposition.
- Photocrosslinking: After printing the desired structure, expose the entire construct to UV light (e.g., 365 nm wavelength) to covalently crosslink the GelMA and PEGTA components, permanently fixing the morphology and enhancing mechanical strength.
Post-Printing Culture & Maturation
- Transfer to Bioreactor: Carefully transfer the bioprinted construct to a perfusion bioreactor system.
- Perfusion Culture: Connect the inlet and outlet of the perfusable channels to the bioreactor's flow system. Initiate perfusion with culture medium at a low, physiologically relevant shear stress to promote endothelial cell maturation and alignment.
- Long-term Culture: Maintain the construct under dynamic perfusion for up to 14-21 days to allow for tissue remodeling and the formation of a biologically relevant vessel [35].
Troubleshooting Guide & FAQs
This section addresses common experimental challenges encountered during the 3D bioprinting of vascular networks.
Bioink Performance and Printability
Question: My bioink does not extrude smoothly, and the printed structure collapses or lacks resolution. What are the potential causes and solutions?
Table 3: Troubleshooting Bioink Printability and Structural Fidelity
| Observed Problem | Potential Root Cause | Recommended Solution |
|---|---|---|
| Poor extrusion/clogging | Bioink viscosity is too high. | Slightly increase printing temperature or dilute the bioink moderately while maintaining gelation capacity. |
| Filament spreading or collapse | Bioink viscosity is too low; crosslinking is too slow. | Increase bioink polymer concentration (e.g., GelMA/alginate); optimize CaCl₂ concentration and flow rate for faster ionic gelation [36]. |
| Lack of fusion between layers | Gelation is too rapid. | Slightly reduce the crosslinker concentration or flow rate to allow for better interlayer bonding. |
| Cell viability is low post-printing | Excessive shear stress during extrusion; cytotoxic crosslinking conditions. | Optimize printing pressure and nozzle diameter to reduce shear. For photocrosslinking, ensure UV intensity and exposure time are minimized while achieving sufficient crosslinking [37]. |
Question: Why is my sacrificial bioprinting process failing to create clean, continuous channels?
- Incomplete Removal of Sacrificial Ink: Ensure the sacrificial material (e.g., Pluronic F-127) is fully liquefied and evacuated. This can be achieved by flushing the channels with cold culture medium or a specific solvent. The viscosity and concentration of the sacrificial ink are critical; for instance, 40% Pluronic F-127 offers a good balance of printability and easy removal [35].
- Channel Collapse During Removal: The surrounding matrix hydrogel may lack sufficient mechanical strength to support the void space left after sacrificial ink removal. Consider increasing the concentration of the matrix hydrogel (e.g., 8% GelMA) or incorporating a secondary reinforcing polymer to improve its structural integrity [35].
Vascular Network Functionality
Question: After successful printing and endothelial seeding, my channels occlude with cells or fail to form a confluent, stable endothelium. How can this be addressed?
- Optimize Seeding Density: Ensure a sufficiently high density of endothelial cells (e.g., HUVECs) is introduced into the channel to promote rapid coverage and confluence.
- Apply Physiological Perfusion: Static culture is insufficient. Implement dynamic perfusion using a bioreactor. The application of physiological shear stress is crucial for guiding endothelial cell alignment, promoting the formation of strong cell-cell junctions, and maintaining a non-thrombotic, quiescent phenotype [34] [6]. Start with low flow rates and gradually increase to physiological levels.
- Use Support Cells: Co-culture endothelial cells with perivascular cells (e.g., mesenchymal stem cells or fibroblasts) either encapsulated in the surrounding matrix or introduced via perfusion. These cells provide vital paracrine signals that stabilize the nascent vasculature and prevent regression [36] [4].
Question: How can I quantitatively assess the quality and function of the bioprinted vascular networks?
- Immunofluorescence Staining: Confirm the presence and organization of endothelial markers like CD31/PECAM-1 (for cell-cell junctions) and VE-Cadherin. Assess vessel maturity by staining for α-Smooth Muscle Actin (α-SMA) in supporting cells [36] [38].
- Permeability Assays: Evaluate the barrier function of the endothelium by measuring the diffusion of fluorescently-labeled dextran molecules of varying sizes across the vessel wall into the surrounding matrix [38].
- Perfusion Validation: Demonstrate the perfusability of the network by flowing fluorescent beads or dye through the channels and visualizing their trajectory using confocal microscopy, confirming the absence of blockages and the interconnectivity of the network [35].
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Sacrificial Material Clearance Failures in Embedded Microchannels
Problem: Incomplete or failed clearance of sacrificial material from embedded 3D-printed microchannels, leading to blocked fluid pathways.
Solutions:
- Issue: Low Clearance Efficiency in Small Channels
- Explanation: Clearance performance drops significantly in channels with printed widths below ~200 µm due to increased flow resistance and material adhesion [39].
- Solution: Optimize channel design to maintain widths above 200 µm where possible. For critical smaller channels, implement extended flushing protocols with increased pressure.
Issue: Sacrificial Wax Remains After Standard Protocol
- Explanation: Standard thermal or chemical protocols alone are often insufficient for embedded channels with limited access ports [39].
- Solution: Implement a multi-step clearance procedure: (1) Mechanical removal of exterior wax; (2) 1-hour sonication in 10% NaOH; (3) Oriented baking at 80°C for ≥4 hours for gravitational drainage; (4) Flushing with 10% NaOH solution; (5) Final water and air flushing until effluent runs clear [39].
Issue: Optical Overexposure in SLA-Printed Channels
- Explanation: Square-profile optical beams are difficult to achieve, causing overexposure that compromises channel boundaries during printing [39].
- Solution: Consider printers using UV-cured sacrificial materials (e.g., composite wax) that avoid this issue, or adjust printer settings to minimize overexposure effects [39].
Table: Sacrificial Material Clearance Efficiency vs. Channel Width
| Printed Channel Width (µm) | Expected Clearance Efficiency | Recommended Action |
|---|---|---|
| < 200 | ~40% or lower | Redesign if possible; use enhanced protocols |
| 200-500 | ~40-75% | Standard clearance protocol |
| > 500 | >75% | Standard protocol typically sufficient |
Guide 2: Resolving Microfluidic Device Design and Fabrication Problems
Problem: Device failures stemming from design, fabrication, or material incompatibility issues.
Solutions:
- Issue: Recurring Blockages in Microchannels
- Explanation: Blockages often result from particle accumulation, bubble entrapment, or poor surface properties that disrupt flow [40].
- Solution: Implement design iterations with computational fluid dynamics (CFD) simulation. Incorporate bubble traps and filters. Optimize surface wettability for your specific fluids [40].
Issue: Structural Failure or Material Degradation
- Explanation: Material incompatibility with reagents or inadequate structural strength can cause fractures, deformations, or chemical degradation [40].
- Solution: Conduct thorough material compatibility testing. Select materials with sufficient strength for your operating pressures and chemical environment [40].
Issue: Overly Complex Designs That Are Difficult to Fabricate
Issue: Lack of Proper Simulation Leading to Unpredicted Fluid Behavior
Guide 3: Managing Host Integration Challenges for Implanted Vascularized Tissues
Problem: Engineered tissues with vascular networks fail to properly integrate with host circulation after implantation.
Solutions:
- Issue: Disrupted Vascular Patterning Post-Implantation
- Explanation: Host inflammatory responses can degrade grafts or disrupt predefined vascular architecture, varying significantly between model organisms [17].
- Solution: Pre-test engineered tissues in relevant animal models and implant locations. Consider using immunodeficient athymic nude mice, which showed robust guided vascularization with retained patterning in both abdominal and cardiac implant sites [17].
Issue: Limited Survival of Implanted Cells
- Explanation: Cells may suffer hypoxia before host-graft anastomosis is complete, especially in thicker tissues [17].
- Solution: Use endothelial cord patterning as "railroad tracks" to guide rapid host-graft vessel formation. Incorporate stromal cells to enhance vascular self-assembly and anastomosis [17].
Issue: Insufficient Mechanical Strength for Surgical Handling
- Explanation: Engineered vascular conduits may lack the burst strength to withstand physiological pressures or suturing during implantation [6].
- Solution: Utilize dynamic maturation in bioreactors to improve mechanical properties. Consider electrospun polycaprolactone (PCL) with macropores for suturable grafts that support angiogenesis [43].
Frequently Asked Questions (FAQs)
Q: What are the most critical factors for successfully clearing sacrificial material from 3D-printed microfluidic devices? A: Success depends on three key factors: (1) Channel design - maintain widths >200 µm for ~40-75% clearance efficiency; (2) Multi-step protocol - combine thermal, chemical, and mechanical methods; (3) Material selection - use dedicated sacrificial materials like SUP706B wax rather than uncured resin for embedded channels [39].
Q: Why do my engineered tissues with pre-formed vascular networks fail to connect to the host's circulation? A: This common failure can stem from several factors: (1) Host model differences - athymic mice support better guided vascularization than rats for some applications; (2) Inflammatory responses that degrade the graft; (3) Lack of proper anastomosis signals - include both endothelial and stromal cells to enhance connection to host circulation [17].
Q: What mechanical properties should I target for implantable vascular conduits? A: Aim for burst strengths of 2000-3000 mmHg to match human saphenous vein and internal mammary artery. Use natural ECM components like collagen and elastin in your biomaterial backbone, and condition constructs in bioreactors to achieve these mechanical properties [25] [6].
Q: How can I prevent blockages in complex microfluidic networks? A: Implement three key strategies: (1) Simplify designs to minimize unnecessary complexity; (2) Use CFD simulation to predict and optimize flow dynamics before fabrication; (3) Incorporate appropriate filters and bubble traps in your design; (4) Select materials with suitable surface properties to prevent adhesion [40] [41].
Q: What are the advantages of guided vascularization over random self-assembly for tissue engineering? A: Guided vascularization using patterned endothelial cords provides: (1) Controlled vessel architecture rather than irregular networks; (2) Reduced thrombosis susceptibility; (3) Faster perfusion onset preventing hypoxic cell death; (4) Better support for functional cells like cardiomyocytes or hepatocytes within engineered tissues [17].
Experimental Protocols
Protocol 1: Sacrificial Material Clearance from 3D-Printed Microfluidics
This protocol enables clearance of sacrificial wax from embedded microchannels with ~40-75% efficiency for channels ≥200 µm [39].
Materials:
- 3D-printed chips (VeroClear-RGD810 with SUP706B sacrificial material)
- NaOH solution (10% by mass in water)
- Sonicator bath
- Oven capable of maintaining 80°C
- 1 mL syringe with 23-gauge luer-stub adapter
- Mineral oil (for optical clarity)
Method:
- Mechanical Pre-clearing: Remove sacrificial material from the chip exterior by careful rubbing and scraping.
- Sonication: Submerge chip in 10% NaOH solution and sonicate for 1 hour.
- Rinse: Remove chip and rinse with water to eliminate NaOH from outer surfaces.
- Thermal Drainage: Orient chip to promote gravitational drainage and bake at 80°C for minimum 4 hours.
- Cooling: Allow chip to cool to room temperature.
- Chemical Flushing: Flush 10% NaOH solution through channels using static pressure applied via syringe.
- Rinse Flushing: Flush with water until exiting fluid appears clear (not milky).
- Air Drying: Flush air through channels to remove residual water.
- Optical Assessment: Add mineral oil to top surface to smooth roughness and image under microscope.
Protocol 2: Creating and Implanting Engineered Tissues with Patterned Vascular Networks
This method creates pre-vascularized tissues with guided architecture that can anastomose with host circulation [17].
Materials:
- HUVECs (Human Umbilical Vein Endothelial Cells)
- Stromal cells
- Collagen solution
- Fibrin hydrogel
- PDMS mold with parallel channels (50-100 µm spacing)
- Immunodeficient athymic nude mice
- Surgical instruments for implantation
Method:
- Cord Formation: Suspend HUVECs and stromal cells in collagen within PDMS mold with parallel channels to form "endothelial cords."
- Tissue Encapsulation: Encapsulate the cords within fibrin hydrogel to create engineered tissues.
- Surgical Implantation: Sutured tissues onto either intraperitoneal gonadal fat pad or epicardial surface of heart in athymic nude mice.
- Maturation: Allow 7 days for host-graft anastomosis and vascular maturation.
- Analysis: Explant tissues and analyze via H&E staining, Sirius Red staining, and immunostaining for huCD31 and TER-119 to confirm perfused vessels.
Research Reagent Solutions
Table: Essential Materials for Sacrificial and Microfluidic Techniques
| Item | Function/Application | Specific Examples/Notes |
|---|---|---|
| SUP706B Sacrificial Material | Forms sacrificial elements in 3D-printed microfluidics | Proprietary composite wax for Stratasys printers; avoids optical overexposure issues [39] |
| VeroClear-RGD810 | Transparent structural material for 3D-printed devices | Provides optical clarity, chemical resistance, and rigidity [39] |
| NaOH Solution (10%) | Chemical clearing of sacrificial material | Dissolves residual wax after thermal treatment [39] |
| HUVECs | Forming engineered vascular networks | Human umbilical vein endothelial cells; create lumenized structures [17] |
| Fibrin Hydrogel | 3D matrix for cell encapsulation in engineered tissues | Supports vascular network formation and tissue integration [17] |
| Electrospun Polycaprolactone (PCL) | Macroporous scaffold for suturable vascular grafts | Supports angiogenesis; has mechanical properties comparable to native vessels [43] |
| Collagen & Elastin | Natural ECM components for vascular grafts | Provides characteristic mechanical properties of native arteries [25] |
In Vivo Prefabrication is an advanced strategy in regenerative medicine where the host's own body is used as a living bioreactor to cultivate vascularized tissue flaps. This approach leverages the body's innate regenerative capacity to create bioengineered tissues with pre-existing vascular networks, effectively overcoming the critical challenge of vascularization in thick tissue constructs [44]. The process involves implanting scaffolds, cells, and/or growth factors into a well-vascularized site within the body, allowing the host's circulatory system to infiltrate and nourish the developing tissue. After a maturation period, this newly formed, vascularized tissue can be harvested as a flap and transferred to reconstruct a defect at a distant site [44] [45]. This method bridges the gap between conventional reconstructive surgery and tissue engineering, providing a solution to the perfusion limitations that often plague large engineered tissues [44].
Troubleshooting Guide: Common Experimental Challenges
Table 1: Frequently encountered problems, their potential causes, and solutions in in vivo prefabrication models.
| Problem | Potential Causes | Recommended Solutions & Verification Methods |
|---|---|---|
| Flap Necrosis | - Vascular Compromise: Pedicle thrombosis, kinking, or mechanical compression [46].- Insufficient Pre-vascularization: Inadequate time for vascular ingrowth into the construct [44].- Poor Scaffold Design: Limited porosity or bio-incompatibility hindering diffusion and vascularization [47]. | - Verify Pedicle Patency: Use intra- and post-operative Doppler ultrasound to confirm blood flow [48].- Optimize Implantation Period: Extend the in vivo maturation period (typically 4-8 weeks) to allow for robust vascular network formation [44] [45].- Ensure Scaffold Quality: Use scaffolds with high porosity (>90%) and interconnectivity to facilitate rapid vascular invasion [47]. |
| Inadequate Tissue Formation | - Poor Cell Survival: Hypoxia and nutrient deficiency at the construct core [44].- Suboptimal Bioreactor Site: The chosen implantation site (e.g., subcutaneous, muscle, chamber) may not provide a sufficient regenerative niche [44].- Inappropriate Scaffold Degradation: Scaffold breaks down too quickly or too slowly for the intended tissue growth [25]. | - Apply the "Chamber" Technique: Use an isolated, protected space around a vascular pedicle to create a highly angiogenic microenvironment [45].- Utilize an Arteriovenous Loop (AVL): This model generates a large, highly vascularized, and isolated tissue platform ideal for engineering various tissues [45].- Match Scaffold Degradation Rate: Select biomaterials whose degradation kinetics align with the rate of new tissue formation (e.g., specific collagen cross-linking densities) [25]. |
| Unpredictable Flap Viability upon Transfer | - Unreliable Vascular Pedicle: The newly formed vasculature may not be robust enough to survive as an independent flap [44].- Poor Integration: Lack of functional anastomosis between the host's pedicle and the engineered tissue vasculature. | - Pre-transfer "Delay" Procedure: Ligate minor feeding vessels 1-2 weeks before flap harvest to condition the tissue to rely solely on the main vascular pedicle [44].- Confirm Vascular Integration: Use perfusion CT or micro-CT angiography post-maturation to visualize and quantify the 3D vascular network integrated with the pedicle before transfer [45]. |
| Post-operative Monitoring Difficulties | - Difficulty distinguishing arterial insufficiency from venous congestion, especially in buried flaps [49] [46].- Subjectivity of clinical signs like color, temperature, and capillary refill. | - Employ Infrared Thermal Imaging: Use a FLIR camera to detect temperature differences. A lower perforator temperature versus the flap's average indicates vascular compromise [49].- Use Combined Monitoring: Integrate clinical assessment with tools like implantable Doppler and near-infrared spectroscopy (NIRS) for continuous, objective data [46]. |
Troubleshooting Workflow
When facing experimental failure, follow this logical pathway to diagnose and address the issue.
Frequently Asked Questions (FAQs)
Q1: What are the primary advantages of using an in vivo bioreactor over an in vitro system for fabricating vascularized flaps?
The key advantage is the ability to recapitulate a complex, native regenerative microenvironment that is difficult to mimic in a lab. The in vivo bioreactor provides a constant stream of the host's own stem cells and native biochemical signals for tissue growth [44]. It ensures the simultaneous development of a functional, hierarchically branched neurovascular network within the engineered tissue, which is critical for survival upon transfer and long-term integration [44] [45]. Furthermore, it often bypasses the need for excessive ex vivo cell manipulation, preserving their functional properties and reducing regulatory hurdles [44].
Q2: How do I choose the most appropriate in vivo bioreactor model for my research (e.g., AV Loop vs. Chamber vs. simple implantation)?
The choice depends on the volume and type of tissue you aim to engineer.
- Simple Implantation: Suitable for thin scaffolds or cell-loaded matrices where rapid vascularization from the surrounding tissue is sufficient.
- Vascularized Chamber: Ideal for generating larger, isolated volumes of tissue. The chamber protects the construct and creates a controlled, highly angiogenic space around a vascular pedicle [45].
- Arteriovenous Loop (AVL): Best for engineering the largest volumes of tissue. The AVL creates a new microcirculation within a protected chamber, resulting in significant, axially vascularized tissue blocks that can exceed 1 cm³ [45].
Q3: What are the critical timeframes for in vivo maturation before flap transfer, and how can I determine if my construct is ready?
Maturation periods are species- and model-dependent but generally range from 4 to 8 weeks [44] [45]. readiness should not be determined by time alone. The construct is ready when it has a mature, perfusable vascular network integrated with the central pedicle. This can be verified through:
- Non-invasive imaging: Micro-CT angiography or perfusion MRI to visualize and quantify the 3D vascular network [45].
- Direct observation: The construct should have a robust, tissue-specific appearance and bleed from the periphery upon needle prick, indicating established perfusion.
Q4: My construct appears viable but is much smaller than expected. How can I enhance the volume of tissue generated?
To increase tissue volume, focus on enhancing the regenerative niche and providing robust mechanical and biological cues:
- Combine with Osteogenic Factors: For bone grafts, combine the AV loop with BMP-2 to significantly boost bone formation [44].
- Incorporate Pro-angiogenic Cells: Seeding scaffolds with human adipose-derived stem cells (ASCs) and VEGF-releasing microspheres has been shown to enhance vascularized flap volume [45].
- Optimize the Scaffold Microenvironment: Use a collagen-chitosan scaffold with a flow-through vascular pedicle to support larger tissue volumes [45].
The Scientist's Toolkit: Essential Research Reagents & Models
Table 2: Key materials, models, and their applications in vascularized flap prefabrication research.
| Category / Item | Function & Rationale | Example Application |
|---|---|---|
| Scaffold Materials | Provides a 3D structural template for cell attachment, proliferation, and tissue ingrowth. | |
| • Collagen-Chitosan Matrix | Biocompatible and biodegradable blend that supports cell infiltration and neovascularization. | Used in conjunction with a flow-through vascular pedicle and ASCs to engineer soft tissue flaps [45]. |
| • Porous β-Tricalcium Phosphate (β-TCP) | Osteoconductive ceramic that provides mechanical support and guides bone formation. | Implanted around an arteriovenous bundle in a muscular site to prefabricate vascularized bone grafts [44]. |
| Cell Sources | Provides living building blocks and secretes trophic factors to drive tissue formation and vascularization. | |
| • Adipose-Derived Stem Cells (ASCs) | Multipotent stromal cells that promote angiogenesis and modulate inflammation via paracrine signaling. | Seeded onto scaffolds with VEGF-releasing microspheres to enhance volume and vascularity of engineered flaps [45]. |
| • Induced Pluripotent Stem Cells (iPSCs) | Offer potential for generating patient-specific endothelial cells (ECs) and smooth muscle cells (SMCs). | Differentiated iPSC-SMCs delivered via collagen scaffold to an aneurysm site for vascular regeneration [11]. |
| Growth Factors & Delivery | Provides biochemical cues to direct cell differentiation, proliferation, and angiogenesis. | |
| • Bone Morphogenetic Protein-2 (BMP-2) | Potent osteoinductive signal that initiates and accelerates bone formation. | Combined with an AV loop model to generate significant volumes of vascularized bone tissue [44]. |
| • Vascular Endothelial Growth Factor (VEGF) | Key signaling protein that stimulates the growth of new blood vessels (angiogenesis). | Incorporated into PLGA/PEG microspheres for sustained, localized release within the scaffold [45]. |
| In Vivo Bioreactor Models | Surgical models that define the anatomical site and conditions for in vivo tissue cultivation. | |
| • Arteriovenous Loop (AVL) | Creates a de novo, isolated, and axially vascularized tissue platform in a protected chamber. | Used to generate large volumes of vascularized adipose, bone, and cardiac tissue for reconstruction [45]. |
| • Vascularized Chamber | A protected space created around a vascular pedicle to induce a highly angiogenic microenvironment. | Ideal for studying the dynamics of in vivo angiogenesis and supporting transplanted bioengineered constructs [45]. |
Detailed Experimental Protocols
Protocol 1: Establishing a Rodent Arteriovenous Loop (AVL) Model
This protocol is foundational for generating large, axially vascularized tissue constructs de novo [45].
- Anesthesia & Preparation: Anesthetize the rodent (e.g., rat) and shave the surgical site (typically the groin or back). Maintain sterile technique throughout.
- Vessel Dissection: Through a skin incision, carefully isolate the femoral artery and vein (or other suitable vessels) using microsurgical techniques under a microscope.
- AV Loop Creation: Transect the artery and vein. Anastomose the proximal end of the artery to the distal end of the vein, creating a closed-loop shunt. This is typically done with 10-0 or 11-0 nylon sutures.
- Chamber Implantation: Place the AV loop into a non-collapsible chamber (e.g., a Teflon or polycarbonate cylinder). The chamber serves to protect the loop and define the space for tissue growth.
- Scaffold Seeding: Implant the chosen scaffold (e.g., a fibrin gel, Matrigel, or a porous synthetic scaffold) into the chamber, ensuring it surrounds the AV loop.
- Closure & Recovery: Close the surgical site and provide appropriate post-operative analgesia and care. The typical maturation period is 4-8 weeks.
Protocol 2: Monitoring Flap Viability with Infrared Thermal Imaging
This non-invasive protocol aids in the early detection of vascular compromise [49].
- Standardize Environment: Perform imaging in a temperature-controlled room (e.g., 18–22°C) with stable humidity (50–55%). Allow the subject to acclimate for 10 minutes to reduce temperature bias.
- Image Acquisition: Use a calibrated thermal imaging camera (e.g., FLIR C5). Capture images from a consistent distance (e.g., 40 cm) from the flap at regular post-operative intervals (e.g., days 0, 1, 2, 3, and 7).
- Image Analysis: Use dedicated software (e.g., FLIR Thermal Studio) to analyze the images.
- Mark the total flap area and record the average temperature (ATF).
- Mark the perforator point (PF) and a point on normal skin 2 cm proximal to the flap (NS).
- Interpretation:
- Calculate the temperature difference between normal skin and the perforator (dT = NS - PF).
- A consistently higher dT in the necrosis group is a sign of compromise.
- A lower perforator temperature compared to the flap's average (PF - ATF) is a strong indicator of vascular compromise and potential flap failure [49].
Vascular Regeneration Signaling Pathway
The following diagram illustrates the key molecular and cellular interactions that are harnessed in vivo to drive vascularization.
A major hurdle in engineering thick, clinically relevant tissues is the inability to create functional, perfusable vascular networks. Without a robust blood supply, cells in the core of engineered constructs rapidly succumb to hypoxia and nutrient deficiency, leading to cell death and graft failure. While primary endothelial cells (ECs) are the natural building blocks for vasculature, their use is constrained by limited expansion potential, donor-site morbidity, and batch-to-batch variability. This technical support document explores three promising alternative cell sources—Induced Pluripotent Stem Cells (iPSCs), Endothelial Progenitor Cells (EPCs), and Mesenchymal Stem Cells (MSCs)—framed within the overarching goal of overcoming vascularization limitations. The following sections provide a comparative analysis, detailed protocols, and troubleshooting guides to support your research.
Cell Source Comparison and Selection Guide
Selecting the appropriate cell source is critical for experimental success. The table below summarizes the key characteristics, advantages, and challenges of iPSCs, EPCs, and MSCs to guide your decision-making.
Table 1: Comparison of Alternative Cell Sources for Vascularization Studies
| Cell Source | Key Characteristics & Markers | Differentiation Potential | Major Advantages | Primary Challenges & Risks |
|---|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Pluripotency Markers: OCT4, SOX2, NANOG [50]Derived EC Markers: VE-Cadherin, PECAM1 (CD31) [51] | Can differentiate into all adult cell types, including endothelial cells, neural cells, and vascular smooth muscle cells [52]. | • Unlimited expansion in vitro [52]• No ethical concerns (vs. ESCs) [52] [53]• Source for autologous therapy [50] | • Tumorigenicity risk from residual undifferentiated cells [52]• Genetic/epigenetic alterations from reprogramming [52]• Complex, multi-step differentiation protocols [51] |
| Endothelial Progenitor Cells (EPCs) | Common Markers: CD31, VE-Cadherin, VEGFR2, CD34 [54] | Primarily differentiate into mature endothelial cells; contribute to angiogenesis [52]. | • High angiogenic potential [52]• Can be isolated from adipose tissue (relatively accessible) [54]• Promote CNS remyelination via BDNF secretion [52] | • Low abundance in peripheral blood [54]• Difficult isolation and purification from some tissues [54]• Overlap in marker expression with hematopoietic cells [54] |
| Mesenchymal Stem Cells (MSCs) | Defining Markers: CD73, CD90, CD105 [55] [53]Lack: CD34, CD45 [51] | Multipotent: Can differentiate into osteocytes, adipocytes, chondrocytes, and, with specific cues, endothelial cells [53]. | • Strong immunomodulatory properties [52] [53]• Readily available from multiple tissues (bone marrow, adipose) [53]• Low immunogenicity, suitable for allogeneic use [53] | • Aging and senescence during in vitro expansion [51]• Donor-dependent variability in potency [52]• Relatively lower direct angiogenic potential compared to EPCs [52] |
Detailed Experimental Protocols
Protocol 1: Differentiation of iPSCs into Endothelial Cells via an MSC Intermediate
This two-step protocol leverages the expansion capacity of MSCs to generate functional endothelial cells.
Table 2: Key Reagents for iPSC to Endothelial Cell Differentiation
| Reagent | Function/Description | Example Catalog Number |
|---|---|---|
| SB431542 | TGF-β inhibitor; critical for initial differentiation of iPSCs into MSCs. | N/A |
| Collagen from Rat Tail | Substrate for coating cultureware to enhance cell adhesion. | Sigma C7661 [56] |
| Recombinant Human VEGF | Key growth factor for endothelial differentiation and survival. | N/A |
| Ascorbic Acid | Enhances endothelial differentiation and maturation. | N/A |
| CD31 MicroBeads | For magnetic-activated cell sorting (MACS) to purify CD31+ endothelial cells. | Miltenyi Biotec Human CD31 Kit [54] |
| Endothelial Cell Medium (e.g., M131) | Specialized medium formulated for endothelial cell growth. | Gibco M131 [54] |
Workflow Description: The process begins with human iPSCs cultured on a collagen-coated surface. The first step induces differentiation into iPSC-derived Mesenchymal Stem Cells (iMSCs) using SB431542. These iMSCs are then transduced with the transcription factor ER71 (ETV2) and simultaneously treated with a combination of a TGF-β inhibitor, VEGF, and ascorbic acid. This crucial second step drives the directed differentiation into functional endothelial cells. The final population can be purified using magnetic beads against the surface marker CD31 to yield a highly pure population of MSC-derived Induced Endothelial Cells (MiECs) [51].
Protocol 2: Isolation and Culture of Endothelial Progenitor Cells from Human Adipose Tissue
This protocol optimizes the yield of EPCs from a readily accessible tissue source.
Workflow Description: The process starts with a small (1-2g) sample of human omental or subcutaneous adipose tissue. The tissue is minced and digested with Type I Collagenase to break down the extracellular matrix. The resulting digest is filtered through a 250µm strainer. The filtered fraction (SVF-I) is often depleted of ECs/EPCs. The key cell population is retained on the 250µm strainer (SVF-II). This SVF-II fraction undergoes a second digestion with trypsin/EDTA to dissociate cell clusters, followed by filtration through a 70µm strainer. The cells from this filtrate are then subjected to magnetic-activated cell sorting (MACS) using anti-human CD31 microbeads. The positively selected CD31+ population is plated on attachment factor-coated dishes in a specialized microvascular endothelial growth medium (M131) supplemented with growth factors to selectively expand the Adipose Tissue-derived EPCs (AT-EPCs) [54].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Vascularization Research
| Reagent / Material | Primary Function | Application Notes |
|---|---|---|
| Silk Fibroin-coated PLLA Scaffolds | Provides a biocompatible, porous scaffold for 3D tissue culture and vascular graft engineering. | Enhances cell adhesion and proliferation of iMSCs compared to uncoated scaffolds [55]. |
| NG2 Antibody-Conjugated Magnetic Beads | Isolation of primary pericytes from various mouse tissues (e.g., brain, lung, bone). | Critical for studying pericyte-EC interactions in vascular stabilization; culture under physioxic O₂ tension (5%) is essential [56]. |
| ER71/ETV2, KLF2, TAL1 Transcription Factors | Master regulators for direct reprogramming of fibroblasts or MSCs into endothelial cells. | Forced expression drives endothelial fate; ER71 alone can be sufficient when combined with VEGF and TGF-β inhibition [51]. |
| Stem Cell-Derived Exosomes (e.g., from iPSCs) | Act as paracrine messengers, transferring bioactive molecules (RNA, proteins) to recipient cells. | Can mimic therapeutic effects of parent cells (e.g., pro-regenerative, anti-inflammatory); lower risk of immune rejection vs. whole cells [52] [50]. |
| SimVascular Open-Source Software | Algorithmic design of organ-scale, computationally-generated vascular trees for biomanufacturing. | Enables rapid (hours vs. months) design of complex, perfusable vascular networks that can be translated to 3D bioprinting instructions [57]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: My iPSC-derived endothelial cells show poor survival after seeding onto 3D scaffolds. What can I do? A1: This is a common challenge. Ensure your scaffolds are pre-treated with extracellular matrix proteins (e.g., Collagen I, Fibronectin) to enhance cell adhesion. Optimize the seeding protocol by using a low-viscosity cell suspension and allowing adequate time for attachment under static conditions before initiating perfusion. Supplementing the medium with a higher concentration of VEGF (e.g., 50-100 ng/mL) and using ROCK inhibitor (Y-27632) for the first 24-48 hours can significantly improve initial cell survival and recovery.
Q2: How can I confirm the functional potency of my isolated EPCs beyond surface marker expression? A2: Surface marker analysis (e.g., CD31, VE-Cadherin) must be complemented with functional assays. The gold standard is the in vitro Tube Formation Assay on Matrigel or other basement membrane extracts, where functional EPCs will self-organize into capillary-like networks within hours. Another key assay is Acetylated LDL Uptake, where EPCs actively ingest fluorescently-labeled acLDL, a characteristic function of endothelial lineage cells [54].
Q3: I'm concerned about tumorigenicity in my iPSC-EC products. What quality controls can I implement? A3: Tumorigenicity risk is a primary concern. Implement stringent quality control measures:
- Residual Pluripotent Cell Detection: Use highly sensitive flow cytometry or qPCR to check for the presence of pluripotency markers (OCT4, NANOG) in the final differentiated product.
- Karyotype Analysis: Perform regular karyotyping to ensure genetic stability after long-term culture.
- Functional Purity: Use magnetic (MACS) or fluorescence-activated cell sorting (FACS) to purify the target endothelial population (e.g., CD31+ cells) and remove undifferentiated progenitors [52].
Q4: What is the biggest advantage of using MSCs for vascularization studies compared to iPSCs? A4: The most significant advantage is their favorable safety profile and established clinical use. MSCs are not pluripotent and therefore do not carry the same tumorigenic risks as iPSCs. Their well-documented immunomodulatory properties and proven safety in numerous clinical trials make them a more straightforward choice for allogeneic, off-the-shelf therapies in the near term [53].
Troubleshooting Common Problems
Problem: Low Yield of EPCs from Adipose Tissue Digestion.
- Potential Cause: Inefficient enzymatic digestion or loss of cells during filtration.
- Solution: Optimize collagenase concentration and digestion time. Use a sequential filtration strategy (250µm followed by 70µm) as described in Protocol 2, and ensure the SVF-II fraction (retained on the 250µm filter) is processed, as it is enriched for EPCs [54].
Problem: Differentiated Endothelial Cells Exhibit an Unstable Phenotype and Lose Markers in Culture.
- Potential Cause: Lack of proper biomechanical and biochemical cues, or contamination with rapidly proliferating fibroblasts/MSCs.
- Solution: Culture cells under physiological shear stress using a bioreactor system. Use purified populations (CD31+ sorted) and maintain cells on endothelial-specific ECM coatings. The medium must be consistently supplemented with key growth factors like VEGF and FGF-2.
Problem: Engineered Vascular Networks Fail to Anastomose with Host Circulation Upon Implantation.
- Potential Cause: Poor bioactivity of the endothelial lumen or a lack of pro-angiogenic signals.
- Solution: Pre-implant "pre-conditioning" of the constructs with pro-angiogenic factors (SDF-1, VEGF). Consider co-seeding with supportive cells like pericytes [56] to enhance vessel maturity and stability, which improves the likelihood of successful anastomosis.
Navigating the Bottlenecks: Troubleshooting Scalability, Integration, and Function
Troubleshooting Guide: Cell Source Challenges
This guide addresses common obstacles in sourcing and expanding cells for vascularized tissue constructs, providing targeted solutions for researchers.
| Challenge | Root Cause | Recommended Solution | Key Considerations |
|---|---|---|---|
| Low Cell Expansion | Suboptimal seeding density; donor-specific intrinsic factors [58]. | Systematically test seeding densities (e.g., 0.5-2.5 x 10⁶ cells/cm²); perform donor pre-screening [58]. | An optimal density of 2.0 x 10⁶ cells/cm² was identified for NK cells; expansion rates can vary significantly between donors [58]. |
| High Donor-to-Donor Variability | Genetic polymorphisms (SNPs); age; health status; prior patient treatment [58] [59]. | Genotype donors for high-priority SNPs (e.g., in KLRK1, FCGR3A); use sequential processing to enrich target cells [58] [59]. | In CAR-T manufacturing, mononuclear cell product content and manufacturing success rates vary by clinical indication [59]. |
| Loss of Phenotypic Stability | Inadequate culture conditions; spontaneous differentiation during expansion [60]. | Optimize culture media with specific growth factors; use bioreactors for parameter control; employ genetic modification [60]. | |
| Inconsistent Seeding & Counting | Cell counting inaccuracies; heterogeneous cell preparations; inappropriate suspension medium [61]. | Use automated cell counters; standardize counting protocols; use culture medium over salt solutions to maintain cell concentration [61]. | The presence of DMSO or saline/PBS can reduce stained cell counts and viability, leading to inaccurate dosing [61]. |
Frequently Asked Questions (FAQs)
Q1: How does donor variability specifically impact the manufacturing of cell therapies?
Donor variability is a primary driver of inconsistency in cell therapy manufacturing. The apheresis product, the starting material for therapies like CAR-T cells, is a direct reflection of the donor's cell populations at the time of collection [59]. Factors such as the patient's clinical indication, prior treatments, and demographics can lead to significant differences in the yield, purity, and composition of the collected mononuclear cells [59]. For instance, patients with chronic lymphocytic leukemia (CLL) often present with lymphocytosis, while lymphoma patients may have lymphopenia, directly impacting the number of T cells available for manufacturing and the subsequent success of the expansion process [59].
Q2: What are the best practices for ensuring accurate cell counting and seeding?
Accurate cell counting is fundamental for reproducible seeding and reliable experimental outcomes. Key strategies include:
- Method Selection: Move beyond manual hemocytometers to automated systems (e.g., image-based or impedance counters) for improved speed, precision, and reduced operator-dependent variation [61].
- Medium Choice: Use culture medium instead of salt solutions like PBS or saline as the suspension vehicle, as the latter can reduce observed cell concentration by nearly 40% [61].
- Viability Assessment: Be aware that the presence of cryoprotectants like DMSO can interfere with fluorescent dye-based viability assays, potentially leading to an underestimation of cell count and viability [61]. Always use a viability dye to exclude dead cells during analysis for a more accurate picture [62].
Q3: Beyond genetic factors, what other mechanisms contribute to donor variability?
While genetic single-nucleotide polymorphisms (SNPs) can explain some donor differences—for instance, those affecting NK cell receptor expression and function [58]—other non-genetic mechanisms play a significant role. These include the epigenetic priming of cells and the presence of adaptive NK-cell differentiation [58]. This means that a donor's immunological history and environmental exposures can create functional variability that is not encoded in their DNA sequence.
Q4: What strategies can be used to mitigate the effects of donor variability in research?
- Donor Screening and Selection: When possible, pre-screen donors for known genetic variants (SNPs) that impact your cell system of interest [58].
- Blended Donor Pools: For allogeneic therapies, creating cell banks from pooled donors can help average out individual donor variations.
- Process Control: Implement robust and standardized manufacturing processes with strict control over culture conditions, including media, growth factors, and physical parameters, to minimize process-induced variability [60] [59].
Experimental Protocol: Optimizing NK Cell Expansion
The following detailed protocol, adapted from a recent study, outlines a method for investigating the impact of seeding density and donor variability on NK cell expansion and phenotype [58].
1. NK Cell Isolation:
- Source: Obtain buffy coats from healthy donors.
- Enrichment: Use a human NK Cell Enrichment Cocktail. Add the cocktail directly to the buffy coat, then isolate cells by density-gradient centrifugation using SepMate-50 tubes and Lymphoprep [58].
2. Seeding and Culture in G-Rex System:
- Seeding Densities: Seed NK cells in a G-Rex 24-well plate (growth surface: 2 cm²/well) at a range of densities (e.g., 0.5, 1.0, 2.0, and 2.5 × 10⁶ cells/cm²) [58].
- Culture Medium: Use NK MACS Basal Medium supplemented with NK MACS Supplement, 1% penicillin–streptomycin, 5% human AB serum, and 500 U/mL of IL-2 Premium Grade [58].
- Maintenance: Maintain cultures at 37°C and 5% CO₂ for up to 49 days. Change medium and IL-2 every 3-4 days.
3. Longitudinal Monitoring via Flow Cytometry:
- Sampling: On each measurement day, carefully remove 6 mL of supernatant, resuspend the remaining 2 mL, and collect a 200 µL sample for analysis [58].
- Staining Panel: Use an 8-color antibody panel to characterize key markers. A recommended panel includes [58]:
- CD45 (hematopoietic cells)
- CD3 (exclude T cells)
- CD56 (identify NK cells)
- CD16a (Fc receptor for ADCC)
- NKp46 (natural cytotoxicity receptor)
- NKG2D (stress-induced ligand receptor)
- ICAM-1 (adhesion and synapse formation)
- Acquisition: Perform data acquisition on a flow cytometer (e.g., Gallios Cell Analyzer) [58].
- Troubleshooting Flow Cytometry:
- High Background: Ensure adequate Fc receptor blocking, include a viability dye to exclude dead cells, and titrate all antibodies to optimal concentrations [62].
- Low Signal: Confirm the antibody is validated for the application, check that fluorophores are protected from light, and ensure proper fixation/permeabilization for intracellular targets [62].
- Unusual Scatter: Avoid harsh vortexing and ensure sample is not contaminated or full of debris [62].
4. Targeted Genetic Analysis:
- DNA Extraction: Extract DNA from cryopreserved donor cells.
- SNP Sequencing: Perform targeted SNP sequencing on genes encoding key receptors (e.g., IL2RA, IL2RB, FCGR3A, NCR1, KLRK1, ICAM-1) to correlate genetic variation with phenotypic outcomes [58].
Visualizing the Challenge: Donor Variability in Cell Expansion
The following diagram illustrates the core concepts of donor variability and the strategies to manage it.
The Scientist's Toolkit: Key Reagents & Materials
The table below lists essential reagents and their functions for conducting the NK cell expansion experiment detailed above.
| Item | Function / Application in the Protocol |
|---|---|
| G-Rex Culture System | A gas-permeable culture vessel that enhances nutrient availability and gas exchange, supporting efficient and scalable cell expansion [58]. |
| RosetteSep Human NK Cell Enrichment Cocktail | Antibody cocktail for the negative selection and isolation of highly pure NK cells directly from buffy coats [58]. |
| NK MACS Medium with IL-2 | Specialized basal medium and supplement, used with recombinant IL-2, to provide optimal nutrients and signaling for NK cell proliferation and survival [58]. |
| Flow Cytometry Antibodies (CD45, CD3, CD56, CD16a, etc.) | Fluorophore-conjugated antibodies used in an 8-color panel to longitudinally monitor NK cell identity, purity, and receptor phenotype during expansion [58]. |
| Magnetic-Activated Cell Sorting (MACS) | Technology for isolating specific cell types from a heterogeneous population, crucial for ensuring a homogeneous starting population or depleting contaminants [60]. |
Troubleshooting Guides
Common Experimental Challenges and Solutions
Problem: Engineered vessels lack mechanical strength and rupture under perfusion.
- Potential Cause 1: The scaffold material is too soft or degrades too quickly.
- Solution: Optimize the cross-linking density of your hydrogel or use a composite bioink. Incorporate materials like methacrylated gelatin (GelMA) to allow for UV-crosslinking, which increases stiffness and stability [63].
- Potential Cause 2: Absence of a supportive tunica media layer.
Problem: Poor vascular network integration with host tissue after implantation.
- Potential Cause 1: The preformed vascular network lacks alignment and morphological matching with host vessels at the implantation site.
- Solution: Incorporate mechanical cues such as stiffness gradients or anisotropic structures into your scaffold. These cues guide endothelial cell alignment parallel to the gradient or grooves, promoting better integration [65].
- Potential Cause 2: Insufficient or delayed inosculation (connection) between the preformed and host vasculature.
Problem: Inconsistent and leaky endothelial barriers in microvessels.
- Potential Cause 1: Endothelial cells (ECs) are not forming stable, mature junctions.
- Potential Cause 2: Lack of pericyte coverage.
Problem: Limited capillary formation and perfusion in thick tissue constructs.
- Potential Cause: The construct relies solely on host vessel ingrowth, which is slow (~5 μm/h), leading to core necrosis.
- Solution: Implement a prevascularization strategy. Create a hierarchical network by integrating 3D-bioprinted larger, perfusable channels (using techniques like sacrificial writing) with self-assembled micro-capillaries. This provides an immediate perfusion pathway and supports the viability of the surrounding tissue [65] [64].
Frequently Asked Questions (FAQs)
Q1: What are the key mechanical properties I should match when engineering a blood vessel? The primary mechanical properties to consider are:
- Non-linearity: The vessel's stress-strain response should be J-shaped, compliant at low pressures and stiff at high pressures.
- Anisotropy: Properties differ along the circumferential and axial directions.
- Compliance: The ability to expand and contract with pulse pressure is critical to prevent compliance mismatch with native tissue [67].
- Strength: The vessel must withstand physiological burst pressures [67] [68].
Q2: How can I apply physiological mechanical stimuli to my vascular constructs in vitro? Two main methods are used:
- Perfusion Bioreactors: Apply controlled fluid flow to generate shear stress on the endothelium, crucial for barrier function and anti-inflammatory phenotypes [65] [66].
- Cyclic Stretch Bioreactors: Apply rhythmic stretching to mimic the circumferential strain from pulsatile blood pressure, which promotes alignment and maturation of SMCs [65] [68].
Q3: My scaffold supports good EC growth, but vessels regress. Why? Vessel regression often indicates a lack of maturation signals. Ensure your culture system includes:
- Mural Cells: Co-culture with pericytes or SMCs is vital for stability.
- Appropriate ECM: A basement membrane containing collagen IV and laminin provides essential biochemical cues.
- Sustained Mechanical Stimulation: Continuous perfusion and cyclic stretch are necessary to maintain a quiescent, stable phenotype [65] [63].
Q4: What is the most effective cell source for creating vascular networks? The choice depends on your application:
- HUVECs: are widely used for macrovessel models due to easy access and well-characterized behavior [65].
- Stem Cells: (iPSCs, MSCs) are advantageous for creating patient-specific models and have self-renewal capacity. iPSC-derived ECs are particularly promising for microvascular networks [69] [65].
- Co-cultures: Using ECs with supporting cells (fibroblasts, MSCs) is often essential to recapitulate the complex cellular crosstalk in native vasculature [4] [65].
Table 1: Target Ranges for Key Mechanical and Structural Properties in Engineered Vasculature
| Property | Native / Target Value | Engineering Consideration |
|---|---|---|
| Shear Stress (Laminar) | 10-70 dyn/cm² [66] | Aim for ~15-20 dyn/cm² in perfusion bioreactors to promote an anti-inflammatory endothelial phenotype [66]. |
| Burst Pressure | >1200 mmHg (native artery) [68] | A key metric for graft integrity; should match or exceed native vessel pressure [67]. |
| Scaffold Stiffness | Physiologically relevant range (e.g., matching tissue of interest) | Optimize substrate stiffness to promote EC tubulogenesis, but avoid excessively stiff materials that can disrupt cell-cell junctions [65]. |
| Vessel Diameter (Capillaries) | 5-10 μm [66] [68] | Use high-resolution bioprinting (e.g., laser-based, microfluidics) or self-assembly to achieve micro-scale diameters for nutrient exchange [66]. |
| Oxygen Diffusion Limit | ~100-200 μm [4] | Ensure the distance between any cell and a perfusable vessel is within this range to prevent hypoxia and necrosis [4]. |
| Host Vessel Ingrowth Rate | ~5 μm/h [65] | Prevascularization is necessary for large constructs, as relying on host ingrowth alone is too slow for clinical relevance [65]. |
Table 2: Key Growth Factors and Their Roles in Vascular Maturity
| Growth Factor | Primary Function in Vascularization | Common Experimental Use |
|---|---|---|
| VEGF (Vascular Endothelial Growth Factor) | Key regulator of endothelial proliferation, migration, and permeability; critical for initiating angiogenesis [4] [69]. | Used to initiate vessel sprouting; slow, sustained release is more effective than rapid bolus delivery [69]. |
| PDGF-BB (Platelet-Derived Growth Factor-BB) | Crucial for recruiting pericytes and smooth muscle cells to stabilize newly formed vessels [63]. | Co-delivery with VEGF enhances the formation of mature, stabilized vascular networks [63]. |
| bFGF (Basic Fibroblast Growth Factor) | Promotes proliferation of endothelial cells and smooth muscle cells; involved in angiogenesis and vessel maturation [4] [69]. | Often used in combination with VEGF to promote robust vascular growth and remodeling [69]. |
Experimental Protocols
Protocol 1: Coaxial Bioprinting of a Multilayer Blood Vessel
This protocol outlines the methodology for creating a biomimetic, dual-layer blood vessel using coaxial bioprinting, based on the co-SWIFT technique [64].
Materials:
- Bioinks:
- Shell Ink: A collagen-based bioink supplemented with Smooth Muscle Cells (SMCs).
- Core Ink: A sacrificial gelatin-based bioink.
- Equipment: Coaxial printhead bioprinter, temperature-controlled stage (~37°C), perfusion bioreactor.
- Matrix: A dense, living cellular matrix (e.g., cardiac organ building blocks - OBBs) or a porous collagen-based matrix (e.g., uPOROS).
Step-by-Step Method:
- Preparation: Load the shell and core inks into their respective reservoirs in the coaxial printhead. Maintain the matrix at 37°C.
- Printing: Program the printer to create the desired vascular architecture. Extrude the bioinks into the matrix. The core ink is fully surrounded by the cell-laden shell ink during deposition.
- Cross-linking: After printing, incubate the construct at 37°C. This simultaneously cross-links the collagen in the shell/matrix and liquefies the sacrificial gelatin core ink.
- Evacuation: Gently perfuse the vascular network with culture medium to evacuate the liquefied core ink, resulting in an open, perfusable lumen.
- Endothelialization: Perfuse the lumen with a suspension of Endothelial Cells (ECs). The ECs will adhere to the inner surface of the SMC-lined channel, forming a confluent endothelium.
- Maturation: Transfer the construct to a perfusion bioreactor and culture under physiological flow conditions for 5-7 days to promote tissue maturation and function.
Protocol 2: Prevascularizing a Dense Tissue Construct using Sacrificial Molding
This protocol describes a method to create a perfusable, branched vascular network within a thick tissue construct [64].
Materials:
- Sacrificial Material: Gelatin or carbohydrate glass.
- Encapsulating Matrix: A hydrogel such as fibrin or collagen, mixed with the primary parenchymal cells of interest (e.g., cardiomyocytes, hepatocytes).
- Equipment: Bioprinter or micromolding setup, 37°C incubator, perfusion system.
Step-by-Step Method:
- Fabricate Sacrificial Network: 3D print a network of the sacrificial material.
- Embed in Matrix: Encapsulate the printed network within the cell-laden hydrogel matrix. Cross-link the matrix.
- Sacrifice and Remove: Cool the construct to liquefy the sacrificial material (if using gelatin) or flush with aqueous solution to dissolve it. This leaves behind hollow, interconnected channels within the tissue.
- Endothelial Seeding: Perfuse the channels with a high-density suspension of ECs, allowing them to adhere and form a continuous endothelial lining.
- Perfusion Culture: Connect the construct to a perfusion bioreactor to provide nutrient flow and apply mechanical stimulation, promoting vessel maturity and tissue function.
Signaling Pathway Diagrams
Mechanical Cues in Vascular Maturation
Biochemical Signaling for Vessel Stability
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Engineering Mature Vasculature
| Item | Function & Rationale |
|---|---|
| GelMA (Methacrylated Gelatin) | A tunable hydrogel; UV cross-linking allows precise control over scaffold stiffness and degradation, supporting both cell viability and mechanical integrity [63]. |
| HUVECs (Human Umbilical Vein Endothelial Cells) | A standard model for macrovessel endothelium; readily available and well-characterized for studying barrier function and angiogenesis [65]. |
| Induced Pluripotent Stem Cells (iPSCs) | Provide a patient-specific cell source for deriving both ECs and supporting cells, crucial for personalized medicine and disease modeling [69] [65]. |
| Pericytes / Vascular Smooth Muscle Cells (SMCs) | Supporting cells that are co-cultured with ECs to enhance vessel stability, maturity, and barrier function via paracrine signaling and direct contact [65] [63]. |
| VEGF & PDGF-BB Growth Factors | Used in combination to first promote vessel formation (VEGF) and then recruit stabilizing cells (PDGF-BB), mimicking the natural sequence of vascular maturation [69] [63]. |
| Perfusion Bioreactor | A critical device for applying physiological shear stress to endothelial layers, promoting alignment, improving barrier function, and enhancing vessel maturity [65] [66]. |
FAQs: Core Concepts for Researchers
FAQ 1: What is the single most critical factor for achieving rapid anastomosis in pre-vascularized constructs? The most critical factor is the maturation degree of the engineered vessel networks before implantation. Constructs bearing mature, complex vessel networks, characterized by elongated and branched structures, a continuous basement membrane (e.g., Collagen IV), and close association with mural cells (e.g., α-SMA-positive cells), demonstrate significantly superior integration. Compared to immature constructs, mature networks can lead to an approximately eightfold increase in host vessel penetration and a sixfold increase in graft perfusion, while also preventing clot accumulation [70] [71].
FAQ 2: How does the choice of host animal model impact experimental outcomes? The host model is a critical variable. Identical engineered tissues can yield divergent results in different immunodeficient hosts. For example:
- Athymic Nude Mice: Support robust guided vascularization of human microvessels carrying host blood, making them suitable for studying vascular patterning and integration [17].
- Athymic Rats: May produce substantive inflammatory changes that degrade grafts or disrupt vascular patterning. However, they can support >3-fold larger human cardiomyocyte grafts compared to mice, indicating host-dependent factors for different cell types [17]. Researchers must select a host model that aligns with their primary endpoint—vascular architecture versus parenchymal cell survival.
FAQ 3: What are the key advantages of using patterned, perfusable microvessels over self-assembled networks? Pre-patterned microvessel (µV) grafts enable rapid and functional anastomosis. In infarcted rat hearts, these constructs demonstrated:
- A 6-fold greater vascular density than self-assembled controls.
- 2.5-fold higher vascular velocities and >20-fold higher volumetric perfusion rates at 5 days post-implantation.
- Enhanced survival and density of co-implanted cells, such as cardiomyocytes [72]. The pre-formed architecture provides a "railroad track" for host vessels to connect to, accelerating perfusion.
FAQ 4: Which cell sources show promise for clinical translation in vascularized constructs? While Human Umbilical Vein Endothelial Cells (HUVECs) are commonly used, human pluripotent stem cell-derived endothelial cells (hESC-ECs or iPSC-ECs) are emerging as a promising autologous source. These cells can be differentiated at high purity (>98% CD31+), exhibit robust angiogenic potential, and form functional, anastomosing networks in vitro and in vivo, overcoming the limitations of immunogenicity and poor survival associated with primary lines [72] [73].
Troubleshooting Guides
Problem 1: Poor Host Vessel Invasion and Graft Perfusion
| Potential Cause | Diagnostic Tests | Corrective Action |
|---|---|---|
| Immature engineered vasculature [70] | Immunostaining for maturity markers (VE-cadherin, α-SMA, Collagen IV) after in vitro culture. | Extend the in vitro pre-culture period (e.g., to 14 days) to allow for vessel maturation and basement membrane formation [70]. |
| Lack of architectural guidance [72] [17] | Confocal imaging of pre-implant construct architecture. | Implement patterning techniques (e.g., lithography, microfluidics) to create defined, perfusable channel networks that guide host vessel ingrowth [72]. |
| Thrombus formation [70] | Histological analysis (H&E) for clots; staining for coagulation factors (vWF, TF). | Ensure vessel maturity, as mature networks naturally suppress thrombus formation. Alternatively, incorporate anti-thrombotic agents (e.g., dipyridamole) into the scaffold [70] [74]. |
Problem 2: Graft Degradation or Disruption Post-Implantation
| Potential Cause | Diagnostic Tests | Corrective Action |
|---|---|---|
| Excessive host inflammatory response [17] | H&E staining for immune cell infiltration; Sirius Red for collagen deposition. | Consider switching host animal models (e.g., from rat to mouse for vascular patterning studies) or implant location. Utilize more robust, bioinert, or immune-modulating scaffold materials [17]. |
| Insufficient mechanical integrity [6] [74] | Burst strength and suture retention testing in vitro. | Use reinforced scaffolds (e.g., electrospun PCL/PDO with 3D-printed coils) or hydrogels with higher mechanical strength. Condition constructs in bioreactors that simulate physiological pressures [6] [74]. |
Table 1: Impact of Vessel Maturity on Anastomosis and Perfusion (14 days post-implantation) [70]
| In Vitro Maturation Time | Host Vessel Penetration (Middle Graft Region) | Graft Perfusion Level | Thrombus Formation | Key Molecular Markers |
|---|---|---|---|---|
| 1 Day (Immature) | Low (Baseline) | Low (Baseline) | Increased | Elevated vWF and TF |
| 14 Days (Mature) | ~8-fold increase | ~6-fold increase | Prevented | Continuous Collagen IV, high α-SMA association |
Table 2: Performance of Patterned Microvessel (µV) Grafts in Cardiac Repair [72]
| Parameter | Self-Assembled Constructs | Patterned, Perfusable µV Grafts | Improvement Factor |
|---|---|---|---|
| Vascular Density | Baseline | 6-fold greater | 6x |
| Vascular Velocity | Baseline | 2.5-fold higher | 2.5x |
| Volumetric Perfusion Rate | Baseline | >20-fold higher | >20x |
Detailed Experimental Protocols
Protocol 1: Generating Mature Pre-vascularized Constructs
This protocol is adapted from methods used to create constructs that showed enhanced anastomosis [70] [75].
Key Reagents & Materials:
- Cells: Human Umbilical Vein Endothelial Cells (HUVECs) and human dermal fibroblasts (HDFs) or similar stromal cells.
- Scaffold: ~800-µm-thick PLLA/PLGA scaffolds with 212-600 µm pore sizes, or fibrin/collagen-based hydrogels.
- Culture Media: Endothelial cell growth medium (e.g., EGM-2) supplemented with appropriate angiogenic factors (VEGF, FGF).
Workflow:
- Cell Seeding: Co-culture HUVECs (e.g., GFP-labeled) and fibroblasts on the 3D scaffold at a defined ratio (e.g., 1:1).
- In Vitro Maturation: Culture the constructs for a critical period of 14 days.
- Monitor regularly (e.g., every 3-4 days) for vessel network formation using confocal microscopy.
- Confirm maturity after 14 days via immunostaining for VE-cadherin (junctional integrity), α-SMA (mural cell association), and Collagen IV (basement membrane) [70].
- Pre-Implantation Validation: Ensure the construct has flourishing, branched vessel networks with a fourfold increase in junction points compared to day 1 [70].
Protocol 2: Assessing Anastomosis and Perfusion In Vivo
This protocol describes common methods for evaluating the success of host-graft integration [70] [72] [17].
Key Reagents & Materials:
- Immunodeficient host animal (e.g., Athymic Nude mouse or rat).
- Dorsal window chamber or surgical tools for graft implantation.
- Species-specific antibodies: e.g., Alexa-647-anti-CD31 for staining host mouse vasculature, and anti-human CD31 (huCD31) for graft vasculature.
- Intravenous tracers: Fluorescent lectin (e.g., Isolectin B4) or fluorescent beads to mark perfused vessels.
Workflow:
- Construct Implantation: Implant the mature, pre-vascularized construct into the chosen model (e.g., intraperitoneal fat pad, epicardial heart surface, or dorsal skinfold chamber).
- Host Vasculature Labeling: At designated timepoints (e.g., 7, 10, 14 days), intravenously inject host-specific endothelial markers (Alexa-647-anti-CD31) or perfusion tracers (fluorescent lectin) [70] [17].
- Tissue Harvest and Analysis:
- Histology: Harvest the graft and process for frozen or paraffin sections.
- Immunofluorescence: Co-stain for host and graft endothelium (huCD31/mCD31) and red blood cells (TER-119) to identify anastomosis sites and perfused vessels [17].
- Imaging: Use confocal microscopy or Optical Microangiography (OMAG) to quantify vascular density, perfusion rates, and the depth of host vessel penetration into different graft regions (outer, middle, center) [70] [72].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Engineering Vascularized Constructs
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| HUVECs [70] [75] | Primary endothelial cell source for forming vessel networks. | Readily available but has potential immunogenic issues in vivo; consider stem cell-derived ECs for translation [72]. |
| hPSC-derived ECs [72] | Autologous, patient-specific endothelial cell source with high angiogenic potential. | Requires robust differentiation protocol; purity (>98% CD31+) is critical for consistent results [72]. |
| PLLA/PLGA Scaffolds [70] | Biodegradable synthetic polymer scaffold providing 3D structure for cell growth. | Pore size (212-600 µm) and thickness (~800 µm) are crucial for nutrient diffusion and network infiltration [70]. |
| Fibrin/Collagen Hydrogels [72] [17] | Natural hydrogel matrices that support cell self-assembly and tubulogenesis. | Mechanical properties can be tuned; allows for embedding of both vascular and parenchymal cells [17]. |
| Anti-α-SMA Antibody [70] | Marker for smooth muscle cells and pericytes; indicates vessel maturity and stability. | Association of α-SMA+ cells with CD31+ vessels is a key metric for a mature, stable network [70]. |
| Anti-Collagen IV Antibody [70] | Marker for the vascular basement membrane; a hallmark of mature, stabilized vessels. | A continuous basement membrane around engineered vessels is a sign of advanced maturation [70]. |
Frequently Asked Questions & Troubleshooting Guides
This technical support center provides practical guidance for researchers tackling immunogenic challenges in vascular graft development. The FAQs and troubleshooting guides below are based on current literature and are framed within the broader context of overcoming vascularization limitations in thick tissue engineering.
FAQ: Common Immunogenic Challenges
What are the primary immune-related causes of tissue-engineered vascular graft (TEVG) failure?
The primary immune-related cause of TEVG failure is stenosis, or the pathological narrowing of the graft lumen. This is not typically a direct adaptive immune rejection (like T-cell-mediated rejection), but rather an exuberant innate immune response driven by host macrophages, Natural Killer (NK) cells, and platelets in response to the implanted scaffold [76]. This inflammatory process leads to excessive neotissue formation, which occludes the graft.
How does the choice of scaffold material influence the host immune response?
The scaffold material is a major determinant of the host immune response.
- Synthetic polymers (e.g., PGA/PLA) can trigger a foreign body response and chronic inflammation, leading to stenosis [76] [77].
- Decellularized animal tissues retain native extracellular matrix (ECM) but may carry xenogeneic antigens, risking immune recognition [78].
- Decellularized plant-based scaffolds (e.g., from parsley stems, apple, or spinach leaves) are composed primarily of cellulose. Cellulose is bio-inert in mammals and elicits only a mild, resolvable foreign body reaction, presenting a potentially low-immunogenic alternative [78].
What strategies can be used to create a non-thrombogenic graft surface?
A functional, confluent endothelial layer is the primary strategy for preventing thrombosis.
- Pre-seeding with Endothelial Cells: Seeding the graft lumen with autologous or stem cell-derived endothelial cells (e.g., hiPSC-ECs) before implantation creates a natural blood-contacting barrier [77].
- Shear Stress Conditioning: Conditioning the seeded graft in a perfusion bioreactor under physiological flow rates is crucial. This "trains" the endothelial cells, promoting a quiescent, anti-thrombotic phenotype characterized by increased expression of eNOS, TFPI, and tPA [77].
- Surface Modifications: Immobilizing anti-thrombogenic molecules like VEGF on synthetic polymer surfaces can enhance endothelial cell adhesion and migration [78].
Is it possible to modulate the host immune response after graft implantation?
Yes, post-implant immunomodulation is a viable strategy. Research in murine models has shown that systemic administration of:
- Anti-platelet therapy (e.g., Aspirin and Clopidogrel) significantly reduces stenosis [76].
- NK cell–neutralizing antibodies also improves graft patency, directly implicating these innate immune cells in the stenotic process [76].
Troubleshooting Guide: Common Experimental Problems
Problem: Significant stenosis observed in small-diameter TEVG implants in animal models.
| Possible Cause | Investigation Methods | Proposed Solutions |
|---|---|---|
| Overactive innate immune response [76] | Histology (H&E) for luminal diameter; IHC for macrophages (F4/80) & NK cells (NK1.1); qPCR for pro-inflammatory cytokines (TNF-α, CCL3) [76] | Pre-implant scaffold seeding; Systemic anti-platelet therapy; NK cell depletion [76] |
| Scaffold material triggering intense inflammation [78] [77] | Histology for general structure and cellular infiltration; IHC for immune cell markers | Switch to a low-immunogenicity material (e.g., decellularized plant cellulose); Use anti-inflammatory biomaterial coatings [78] |
| Lack of a confluent endothelial layer [78] [77] | IHC for endothelial markers (vWF); Scanning Electron Microscopy (SEM) | Improve endothelial cell seeding density & viability; Implement pre-implant shear stress conditioning in a bioreactor [77] |
| Compliance mismatch with native vessel [78] [79] | Burst pressure testing; Tensile testing | Redesign scaffold architecture/mechanics; Use composite materials to better match native vessel compliance [78] |
Problem: Poor endothelialization and thrombus formation on the graft lumen.
| Possible Cause | Investigation Methods | Proposed Solutions |
|---|---|---|
| Inadequate shear stress conditioning [77] | IHC for endothelial maturation markers (KLF2, eNOS); Thrombus assessment | Implement a graduated shear stress training regimen in a perfusion bioreactor (e.g., 15 dynes/cm² down to 5 dynes/cm²) [77] |
| Suboptimal scaffold surface for cell adhesion [78] [80] | SEM for cell morphology & attachment; Water contact angle measurement for wettability | Modify surface topography (e.g., via electrospun aligned fibers); Treat surface with ECM-derived peptides (e.g., RGD) to improve cell adhesion [80] |
| Static vs. dynamic cell culture [77] [66] | Compare endothelial coverage and thrombogenicity between static and flow-conditioned grafts | Always use perfusion bioreactors for maturation; They simulate physiological hemodynamics and enhance cell integration and function [78] [66] |
Problem: Inconsistent results between batches of decellularized scaffolds.
| Possible Cause | Investigation Methods | Proposed Solutions |
|---|---|---|
| Inefficient or variable decellularization [78] | DNA quantification; Histology (DAPI staining) for residual nuclear material | Standardize protocol (e.g., SDS concentration, duration, perfusion pressure); Validate with DNA removal and ECM preservation checks [78] |
| Loss of key ECM components and mechanical properties [78] | Mechanical testing (tensile strength, compliance); Biochemical assays for ECM components | Optimize decellularization agents (e.g., try Triton X-100 after SDS); Avoid harsh detergents that damage the ECM microstructure [78] |
| Source plant/animal tissue variability [78] | Document source species, age, and anatomical location | Establish strict quality control for source tissues; Use in-bred or genetically uniform source organisms where possible [78] |
Key Quantitative Data on Immune Cell Impact on TEVG Stenosis
The following table summarizes critical data from a foundational study investigating the role of specific immune cells in TEVG performance in a murine model [76].
Table: Impact of Immune Cell Depletion on TEVG Luminal Patency
| Mouse Model (C.B-17 Background) | Key Immune System Characteristics | Average Luminal Diameter (mm) at 10 Weeks | P-value vs. Wild-Type |
|---|---|---|---|
| Wild-Type (WT) | Fully functional immune system | 0.071 ± 0.035 | (Control) |
| SCID | Lacks T and B lymphocytes (No adaptive immunity) | 0.137 ± 0.032 | Not Significant |
| SCID/beige (bg) | Lacks T/B cells; also has NK cell and platelet dysfunction | 0.804 ± 0.039 | < 0.001 |
| WT + Anti-NK1.1 Antibody | NK cells neutralized by systemic treatment | 0.356 ± 0.151 | < 0.001 |
| WT + Aspirin/Plavix | Platelet function inhibited by systemic treatment | 0.452 ± 0.130 | < 0.001 |
Detailed Protocol: Perfusion Bioreactor Conditioning for Enhanced Endothelialization
This protocol is adapted from recent work on engineering endothelialized vascular conduits [77].
Objective: To mature and fortify a pre-seeded TEVG by exposing it to physiological shear stress, thereby promoting an anti-thrombotic endothelial phenotype.
Materials:
- Perfusion bioreactor system with pulsatile flow capability
- Sterile cell culture media
- TEVG construct seeded with endothelial cells (e.g., hiPSC-ECs or HUVECs)
- Luer-lock connectors or custom fittings compatible with the graft diameter
- 37°C, 5% CO2 incubator
Method:
- Seeding: Seed the luminal surface of your TEVG (e.g., a decellularized human umbilical artery or a polymeric scaffold) with endothelial cells at a high density. Culture under static conditions for 1-2 days to allow initial attachment.
- Assembly: Aseptically connect the seeded TEVG to the perfusion bioreactor system. Ensure all connections are secure to prevent leaks.
- Conditioning Protocol:
- Initiate flow with a low, non-detaching shear stress (e.g., 1-2 dynes/cm²) for the first 24 hours.
- Gradually ramp up the shear stress to an arterial level of 15 dynes/cm² over the next 48 hours.
- Maintain at 15 dynes/cm² for 24-48 hours to promote endothelial maturation and alignment.
- If the graft is destined for a venous environment, gradually ramp down the shear stress to a venous level of 5 dynes/cm² and maintain for another 24-48 hours [77].
- Monitoring: Monitor the system daily for flow rates, pressure, and any air bubbles. Collect effluent media for analysis (e.g., NO production, cell viability markers).
- Harvesting: After 5-7 days of total conditioning, the graft is ready for assessment (e.g., histology, IHC, mechanical testing) or implantation.
Key Validation Check:
- Perform IHC on conditioned grafts versus static controls. A successfully conditioned graft will show robust expression of Kruppel-like factor 2 (KLF2), eNOS, and TFPI, indicating a functional, thromboresistant endothelium [77].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents for Investigating Immune Response to Vascular Grafts
| Item | Function / Application | Example Use Case |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) [78] | Ionic detergent for decellularization; lyses cells and solubilizes nuclear and cytoplasmic components. | Effective removal of cellular material from plant or animal tissues to create a low-immunogenicity scaffold. |
| Anti-NK1.1 Antibody [76] | For in vivo neutralization/depletion of Natural Killer (NK) cells in murine models. | Investigating the specific role of NK cells in TEVG stenosis; testing NK depletion as a therapeutic strategy. |
| Anti-platelet Drugs (Aspirin/Clopidogrel) [76] | Systemic administration to inhibit platelet activation and aggregation. | Mitigating stenosis in TEVG implants by targeting the platelet component of the innate immune response. |
| Decellularized Plant Scaffolds [78] | Low-immunogenic, cellulose-based scaffold from sources like parsley, apple, or spinach. | Providing a biocompatible, cost-effective, and ethically uncontroversial alternative to synthetic or animal-derived grafts. |
| hiPSC-derived Endothelial Cells (hiPSC-ECs) [77] | Patient-specific cell source for creating a confluent, autologous endothelial layer on the graft lumen. | Generating a non-thrombogenic blood-contacting surface, crucial for small-diameter graft patency. |
| Perfusion Bioreactor [78] [77] [66] | Applies physiological pulsatile flow and shear stress to grafts during in vitro maturation. | "Training" endothelial cells to adopt a quiescent, anti-thrombotic phenotype before implantation. |
Visualizing Concepts and Workflows
Diagram 1: Key Innate Immune Drivers of Graft Stenosis
This diagram illustrates the cellular mechanism by which the innate immune system drives stenosis in Tissue-Engineered Vascular Grafts (TEVGs), as revealed in murine models [76].
Diagram 2: Strategies to Overcome Immunogenic Hurdles
This workflow chart outlines the main immunogenic challenges in vascular graft engineering and the corresponding strategies to overcome them, based on current research [78] [76] [77].
FAQs: Vascularization in Thick Tissues
FAQ 1: What is the primary mass transfer limitation in engineering thick tissues? The primary limitation is oxygen diffusion. Within the body, most cells are located within 100–200 µm of a capillary to ensure sufficient oxygen and nutrient supply. In vitro, diffusion constraints make constructing tissues beyond a few hundred microns in thickness impractical, leading to core necrosis in larger constructs [81].
FAQ 2: What are the prevailing strategic categories for vascularizing tissues? Current approaches fall into six major categories [81]:
- Scaffold Functionalization: Modifying scaffolds with angiogenic factors or designing them with enhanced porosity/channels.
- Cell-Based Techniques: Using co-cultures of endothelial cells to form pre-vascular networks.
- Bioreactor Designs: Using perfusion or rotating systems to improve nutrient transport during in vitro growth.
- MEMS-Related Approaches: Employing microelectromechanical systems (MEMS) and microfluidics to create vascular networks.
- Modular Assembly: Combining smaller, pre-vascularized tissue units (e.g., endothelial cell-coated hydrogels) into larger structures.
- In Vivo Systems: Leveraging the body's natural angiogenic potential via techniques like arteriovenous (AV) loops.
FAQ 3: Which key growth factors are used to promote vascularization, and what are their challenges? Commonly used growth factors and their functions are summarized in the table below [81].
Table 1: Key Pro-Angiogenic Growth Factors and Their Application
| Growth/Signaling Factor | Primary Function | Critical Issues in Application |
|---|---|---|
| Vascular Endothelial Growth Factor (VEGF) | Key initiator of endothelial capillary formation [81]. | Short half-life; rapid degradation; excessive amounts can cause vascular leakage [81]. |
| Basic Fibroblast Growth Factor (bFGF) | Induces proliferation of endothelial cells; initiator of capillary formation [81]. | Rapid diffusion requires controlled release; acts as a mitogen for many cell types [81]. |
| Platelet-Derived Growth Factor (PDGF) | Recruits smooth muscle cells to endothelial linings; promotes vessel maturation [81]. | High levels can destabilize vessels; linked to several diseases [81]. |
| Angiopoietin-1 | Promotes endothelial cell migration and stabilization of new capillaries [81]. | Overexpression can induce endothelial hyperplasia [81]. |
FAQ 4: How can large-scale tissue analysis overcome the limitations of current spatial transcriptomics platforms? Conventional platforms like Visium are limited by small capture areas (e.g., 6.5 mm × 6.5 mm). The iSCALE method addresses this by using a machine learning framework that leverages histology images from large-sized tissues ("mother image") and integrates information from multiple, smaller ST captures ("daughter captures"). This allows for the prediction of gene expression and annotation of cellular-level tissue architecture across entire large tissue sections, enabling the study of clinically relevant tissue sizes [82].
Troubleshooting Guides
Problem 1: Low Cell Viability in the Core of a Tissue Construct
- Potential Cause: Inadequate oxygen and nutrient diffusion due to the absence of a perfusable vascular network, leading to diffusion-limited mass transfer [81].
- Solutions:
- Incorporate Pro-Angiogenic Factors: Functionalize your scaffold with controlled-release systems for growth factors like VEGF or bFGF to encourage inward capillary growth [81].
- Pre-vascularize In Vitro: Seed endothelial cells in co-culture with your primary cell type to form capillary-like networks within the construct before implantation [81].
- Use Channeled Scaffolds: Design and fabricate scaffolds with built-in micro-channel networks that can be perfused, mimicking blood vessels [81].
- Apply Bioreactors: Culture constructs in perfusion bioreactors to enhance convective transport of oxygen and nutrients throughout the scaffold during maturation [81].
Problem 2: Failure of Engineered Vasculature to Anastomose with Host Blood Vessels
- Potential Cause: The pre-formed vascular networks within the implant may not be properly aligned, mature, or of a suitable size to connect with the host's circulatory system upon implantation [81].
- Solutions:
- Ensure Vessel Maturity: Co-deliver factors like PDGF that support the recruitment of perivascular cells (e.g., smooth muscle cells) to stabilize the newly formed endothelial tubes [81].
- Optimize Surgical Placement: Implant the tissue construct in close proximity to a robust host blood supply to facilitate rapid integration.
- Consider Modular Assembly: Utilize approaches that build tissues from small, pre-vascularized modules, which have shown a high capacity for anastomosis due to their dense vascular networks [81].
Problem 3: Inaccurate Spatial Profiling of Large Tissue Sections
- Potential Cause: Conventional spatial transcriptomics platforms have limited capture areas, making it impossible to profile an entire large biopsy or organ in a single capture [82].
- Solutions:
- Adopt an Advanced Computational Workflow: Implement the iSCALE framework. This involves taking multiple ST captures ("daughter captures") from the large tissue and using a semi-automatic algorithm to align them onto a whole-slide H&E image ("mother image"). A neural network then learns the relationship between histology and gene expression to predict spatial gene expression across the entire large section [82].
- Manual Stitching (Limited Utility): As a less sophisticated alternative, the 'visiumStitched' method attempts to extend the profiling window by manually aligning a few Visium captures, though this requires manual effort and only supports low-resolution analysis of directly measured regions [82].
Table 2: Quantitative Comparison of Vascularization Strategies
| Vascularization Strategy | Key Quantitative Metrics | Typical Experimental Outcomes |
|---|---|---|
| Scaffold Functionalization | Growth factor release kinetics (e.g., burst release vs. sustained over weeks); vessel density (vessels/mm²) [81]. | Increased capillary density in implant region; improved cell survival at construct core. |
| Cell-Based Techniques | Endothelial cell seeding density; capillary length per unit volume (mm/mm³); anastomosis rate with host vessels [81]. | Formation of interconnected, lumen-containing structures in vitro; functional connection to host circulation in vivo within days. |
| Bioreactor Designs | Perfusion flow rate (mL/min); shear stress (dyn/cm²); oxygen partial pressure (pO₂) measured within the construct [81]. | Enhanced uniformity of cell distribution; significantly higher cell viability and tissue maturation compared to static culture. |
| MEMS / Microfabrication | Channel diameter (µm); network geometry and branching angles; flow resistance [81]. | Recapitulation of capillary-scale networks; precise control over fluid flow paths. |
| iSCALE Prediction Accuracy | Pearson correlation coefficient (vs. ground truth); Root Mean Squared Error (RMSE) for top highly variable genes [82]. | High correlation (>0.45 for 50% of genes at 32µm resolution); accurate identification of fine-grained tissue structures like tertiary lymphoid structures [82]. |
Experimental Protocols
Protocol 1: Scaffold Functionalization with Dual Growth Factor Delivery This protocol outlines a method for incorporating two growth factors with different release kinetics to promote both rapid and sustained vascularization [81].
- Prepare Microspheres: Encapsulate PDGF into PLGA microspheres using a double-emulsion solvent evaporation technique to achieve slow, sustained release.
- Fabricate Composite Scaffold: Mix the PDGF-loaded microspheres with PLGA polymer particles and VEGF. Process this mixture to form a solid scaffold, resulting in VEGF being predominantly on the surface for rapid release.
- Implant and Evaluate: Implant the functionalized scaffold into the target site in an animal model.
- Analysis: Harvest the implant at various time points (e.g., 1, 2, 4 weeks). Quantify vascular ingrowth via histology (vessel counting on CD31-stained sections) and measure oxygen tension within the construct using oxygen-sensitive probes or dyes [81].
Protocol 2: iSCALE Workflow for Large Tissue Spatial Transcriptomics This protocol describes the steps to predict gene expression across large-sized tissues using the iSCALE framework [82].
- Tissue Preparation and Imaging: Obtain a large-sized tissue section and generate a high-resolution whole-slide H&E image (the "mother image").
- Generate Daughter Captures: From the same tissue block, prepare multiple adjacent sections that fit standard ST platform capture areas (e.g., Visium). Profile these "daughter captures" to obtain ground truth gene expression data.
- Spatial Alignment: Perform spatial clustering on the daughter ST data. Use this information in a semi-automatic algorithm to align each daughter capture onto the mother image accurately.
- Model Training and Prediction: Integrate the gene expression and spatial information from all aligned daughter captures. Extract global and local histological features from the mother image. Train a feedforward neural network to learn the relationship between image features and gene expression. Use the trained model to predict gene expression for every 8µm x 8µm superpixel across the entire mother image.
- Downstream Analysis: Leverage the predictions to automatically annotate cell types and identify enriched tissue regions, such as tertiary lymphoid structures, across the large tissue section [82].
Signaling Pathways & Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Vascularization and Large Tissue Analysis
| Research Reagent / Material | Function / Application |
|---|---|
| VEGF (Vascular Endothelial Growth Factor) | A critical cytokine for initiating the formation of new endothelial capillaries [81]. |
| PDGF (Platelet-Derived Growth Factor) | A key factor for recruiting smooth muscle cells to nascent vessels, promoting vessel maturation and stability [81]. |
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable polymer used to fabricate scaffolds and as a material for controlled-release microspheres of growth factors [81]. |
| Collagen & Alginate | Natural biopolymer hydrogels used as scaffolds; they are well-characterized and can be loaded or functionalized with growth factors [81]. |
| iSCALE Software Framework | A machine learning tool designed to predict super-resolution gene expression across large-sized tissues from H&E images and multiple ST captures [82]. |
| 10x Xenium / Visium HD | Commercial spatial transcriptomics platforms providing subcellular to cellular resolution data, useful as ground truth for benchmarking new methods [82]. |
| Oxygen-Sensitive Dyes/Probes | Tools for the quantitative measurement of oxygen concentration within 3D tissue constructs to validate models of oxygen diffusion [81]. |
Frequently Asked Questions (FAQs)
Q1: What are the core properties that an ideal biomaterial scaffold must possess? An ideal biomaterial scaffold must balance four key properties: excellent biocompatibility (ability to interact with host tissue without adverse effects), appropriate biodegradation rate (matching the rate of new tissue formation), sufficient mechanical strength (to withstand in vivo loads and maintain structural integrity), and bioactivity (to support cellular functions and vascularization) [83] [84].
Q2: Why is the degradation rate of a biomaterial critical, and how can I accurately measure it? The degradation rate is critical because it must synchronize with the rate of new tissue formation. If the material degrades too quickly, it loses mechanical support prematurely; if it degrades too slowly, it can impede tissue growth and lead to complications like fibrosis [85] [86]. Accurate measurement requires a multi-method approach, as summarized in Table 2.
Q3: How can I achieve sufficient mechanical strength in a scaffold without compromising its biodegradability and porosity? This is a central challenge in biomaterial design. Strategies include:
- Using Composite Materials: Combining a durable, slow-degrading polymer (e.g., PEK, PCL) with a bioactive, faster-degrading component (e.g., βTCP ceramic, gelatin hydrogel) [86] [87].
- Advanced Architectural Design: Employing triply periodic minimal surfaces (TPMS) like gyroid structures in 3D-printed scaffolds, which offer an excellent strength-to-weight ratio and enhance tissue integration [86].
- Post-Processing: Techniques like thermal annealing can toughen 3D-printed polymers to improve their mechanical performance [86].
Q4: What are the primary challenges in vascularizing thick tissue-engineered constructs? The primary challenges include:
- Recreating Hierarchical Networks: It is difficult to mimic the body's native network of arteries, veins, and capillaries, which have different diameters and cellular compositions [66].
- Providing Mechanical Cues: Vascular cells require appropriate mechanical stimuli (e.g., shear stress, cyclic stretch) to form stable, functional vessels, which is hard to replicate in static culture [66].
- Ensuring Perfusion: Engineered vessels must quickly anastomose (connect) with the host's circulatory system upon implantation to deliver nutrients and oxygen, preventing core cell death in thick tissues [83] [66].
Troubleshooting Guides
Problem 1: Rapid, Uncontrolled Biomaterial Degradation
| Symptom | Possible Cause | Solution |
|---|---|---|
| Loss of mechanical integrity before new tissue can bear load. | Material is too hydrophilic or has highly hydrolysable chemical bonds (e.g., ester groups). | Increase crosslinking density or switch to a polymer with a more stable backbone (e.g., blend PCL with PLA) [85]. |
| Premature scaffold collapse and inflammatory response. | Enzymatic activity in the implantation site is higher than anticipated. | Incorporate enzyme inhibitors into the scaffold or use a material less susceptible to enzymatic cleavage [83]. |
| Mistaking material dissolution for degradation. | Highly soluble polymer fractions are leaching out. | Use a combination of characterization techniques (see Table 2) to confirm chemical degradation, not just weight loss [85]. |
Experimental Protocol: Comprehensive Degradation Assessment
- Pre-degradation Characterization: Record initial mass, dimensions, and mechanical properties (e.g., compressive modulus). Analyze chemical structure via FTIR [85].
- Immersion: Immerse samples in degradation medium (e.g., PBS at pH 7.4, simulated body fluid, or specific enzymatic solutions) at 37°C. Use a sufficient volume-to-surface area ratio as per ASTM guidelines [85].
- Monitoring: At predetermined time points:
- Gravimetric Analysis: Remove samples, dry to constant weight, and calculate mass loss.
- pH Monitoring: Record changes in the degradation medium's pH.
- Mechanical Testing: Measure the compressive/tensile strength of samples.
- Morphological Examination: Use SEM to visualize surface erosion and pore structure changes.
- Chemical Analysis: Use GPC to track changes in molecular weight and HPLC/MS to identify degradation by-products [85].
Problem 2: Mechanical Failure or Stress Shielding
| Symptom | Possible Cause | Solution |
|---|---|---|
| Scaffold fractures under load. | Inherent mechanical properties of the material are insufficient for the application. | Select a higher-strength polymer (e.g., PEK for bone) or create a composite with bioceramics (e.g., HA, βTCP) [88] [86]. |
| Scaffold deforms or collapses over time (creep). | Material lacks long-term mechanical durability. | Utilize thermally toughened polymers (e.g., annealed PEK) and design architectures that distribute stress evenly [86]. |
| Lack of bone ingrowth or resorption around the implant. | Stress shielding: Scaffold is too stiff (e.g., like metal plates), shielding the surrounding tissue from mechanical stimuli. | Use a material with an elastic modulus matching the target tissue (e.g., PEK ~ bone) and design porous structures to lower overall stiffness [86]. |
Problem 3: Poor Vascularization in Thick Scaffolds
| Symptom | Possible Cause | Solution |
|---|---|---|
| Necrotic core in the scaffold post-implantation. | Lack of internal vascular network to transport nutrients and oxygen. | Pre-vascularization: Create microchannels within the scaffold using 3D printing or incorporate pro-angiogenic factors like VEGF [83] [66]. |
| Slow or insufficient integration with host blood vessels. | Scaffold lacks the necessary biochemical cues to attract endothelial cells. | Biofunctionalization: Coat the scaffold with peptides (e.g., RGD) to enhance cell adhesion or load it with extracellular vesicles from endothelial cells [83] [87]. |
| Engineered vessels are unstable and regress. | Missing perivascular support cells (e.g., VSMCs, pericytes). | Co-culture Systems: Seed scaffolds with both Vascular Endothelial Cells (VECs) and Vascular Smooth Muscle Cells (VSMCs)/pericytes to mimic native vessel structure [66]. |
Experimental Protocol: Fabricating a Pre-vascularized Scaffold via Co-culture
- Scaffold Preparation: Fabricate a porous, biodegradable scaffold (e.g., from collagen-chitosan composite) using 3D bioprinting to create a predefined channel network.
- Surface Functionalization: Treat the scaffold surface with RGD peptide solution to enhance cell adhesion [83].
- Cell Seeding:
- Day 1: Seed Human Umbilical Vein Endothelial Cells (HUVECs) into the microchannels under low perfusion flow to promote lining.
- Day 3: Seed Human Vascular Smooth Muscle Cells (HVSMCs) suspended in a fibrin gel around the endothelialized channels to provide support.
- Dynamic Culture: Transfer the construct to a bioreactor and subject it to cyclic radial stretching and pulsatile flow to mature the vessels and enhance their stability [66].
Data Presentation
Table 1: Mechanical and Degradation Properties of Common Biomaterial Classes
| Material Class | Example Materials | Tensile Strength (MPa) | Compressive Modulus (MPa) | Degradation Time | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Natural Polymers | Collagen, Chitosan, Silk Fibroin | 0.5 - 5 | 0.02 - 5 | Weeks - Months | Innate bioactivity, excellent biocompatibility [84] | Poor mechanical strength, rapid degradation [84] |
| Synthetic Polymers | PCL, PLA, PLGA | 20 - 50 | 0.1 - 2 | Months - Years | Tunable mechanics & degradation [88] | Hydrophobic, lacks bioactivity, acidic degradation products [88] |
| Bioceramics | Hydroxyapatite (HA), β-TCP | 40 - 100 (Compressive) | 500 - 1000 | Non-resorbable to >6 months | Osteoconductive, high compressive strength [87] | Brittle, low tensile strength [88] |
| High-Performance Polymers | PEEK, PEK | 90 - 100 | 3,000 - 4,000 | Non-resorbable | Excellent mechanical strength, radiolucency [86] | Bioinert, requires surface modification for integration [86] |
Table 2: Techniques for Assessing Biomaterial Degradation
| Assessment Type | Technique | Measured Parameter | Key Insight |
|---|---|---|---|
| Physical | Gravimetric Analysis | Mass Loss | Simple but can mistake solubility for degradation [85] |
| Scanning Electron Microscopy (SEM) | Surface Morphology & Erosion | Visualizes pitting, cracking, and pore structure changes [85] | |
| Mechanical | Compression/Tensile Testing | Young's Modulus, Ultimate Strength | Directly links degradation to functional performance loss [85] |
| Chemical | Gel Permeation Chromatography (GPC) | Molecular Weight Change | Confirms chain scission and polymer breakdown [85] |
| Fourier-Transform Infrared (FTIR) Spectroscopy | Chemical Bond Breakage | Identifies specific functional groups being hydrolyzed [85] | |
| High-Performance Liquid Chromatography (HPLC) / Mass Spectrometry (MS) | Degradation By-Product Identification | Crucial for evaluating by-product toxicity [85] |
Signaling Pathways and Workflows
Diagram: Scaffold Design and Optimization Workflow
Diagram: Key Signaling Pathways in Vascularization
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Biomaterial Research | Key Consideration |
|---|---|---|
| RGD Peptide | A short peptide sequence that promotes cell adhesion by binding to integrin receptors on cell surfaces. Used to biofunctionalize otherwise inert scaffolds [83]. | Density of peptide presentation is critical for effective cell signaling. |
| Gelatin Methacryloyl (GelMA) | A photopolymerizable hydrogel derived from gelatin. Serves as an excellent biodegradable carrier for cells (e.g., stem cells) and bioactive factors within a scaffold [86]. | Degree of methacrylation controls mechanical stiffness and degradation rate. |
| β-Tricalcium Phosphate (βTCP) | A bioactive and biodegradable ceramic. Acts as an osteoconductive filler and a reservoir for calcium ions, promoting bone formation in composite scaffolds [86] [87]. | Degradation rate and porosity can be tuned during synthesis. |
| Vascular Endothelial Growth Factor (VEGF) | A key signaling protein that stimulates angiogenesis (formation of new blood vessels). Incorporated into scaffolds to promote vascularization [66] [87]. | Requires controlled release kinetics; a sudden burst can be ineffective or harmful. |
| Polyetherketone (PEK) | A high-performance polymer with bone-like modulus and radiolucency. Used for load-bearing, non-resorbable scaffold frames that avoid stress-shielding [86]. | Requires surface modification (e.g., plasma treatment) to enhance biointegration. |
Bench to Bedside: Validating Function and Applying Vascularized Tissues in Research & Medicine
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary advantages of using vascularized MPS over traditional 2D models for drug screening? Vascularized MPS offer organ-level functionality and a more physiologically relevant environment for drug testing. Key advantages include:
- Enhanced Physiological Relevance: They replicate the blood-organ barrier, which is essential for mimicking organ-level drug delivery pharmacokinetics and studying immune cell interactions or tumor cell transmigration [89].
- Superior Nutrient/Waste Exchange: The integrated vasculature supports the survival and function of thicker, more complex 3D micro-tissues by ensuring efficient delivery of oxygen/nutrients and removal of waste, overcoming the ~200 µm diffusion limit that restricts traditional 3D cultures [4] [90] [91].
- Multi-Organ Interaction: They enable the creation of linked systems (e.g., intestine-liver-heart-lung) to study adsorption, distribution, metabolism, and excretion (ADME) of drugs, providing a more comprehensive evaluation of drug efficacy and toxicity [92] [93].
FAQ 2: My endothelial networks are unstable and regress quickly. What common factors should I investigate? The instability of vascular networks is often due to insufficient maturation and support. Focus on:
- Supportive Co-cultures: Incorporate pericytes, vascular smooth muscle cells, or mesenchymal stem cells (MSCs). These cells provide structural support and secrete stabilizing factors like Angiopoietin-1 (ANG-1) and Platelet-Derived Growth Factor (PDGF-BB), which enhance vessel maturity and longevity [90].
- Biomaterial Matrix: Ensure your hydrogel (e.g., fibrin or collagen) supports cell migration and network formation. The extracellular matrix provides essential guidance cues for endothelial and mural cells [4] [90].
- Soluble Factors: Use a defined cocktail of growth factors. VEGF is critical for initiating angiogenesis, but prolonged exposure to high concentrations can lead to immature, leaky vessels. Combining VEGF with other factors like FGF and PDGF promotes stabilization [90].
FAQ 3: How can I confirm that my in vitro vascular network has successfully connected to and is perfused by the host system after implantation? Successful anastomosis and perfusion can be confirmed through several methods:
- Histological Analysis: After explantation, stain tissue sections for host-specific red blood cell markers (e.g., TER-119 in mice) and human-specific endothelial markers (e.g., huCD31). The presence of host blood cells within graft-derived endothelial lumens is a direct indicator of functional connection [17].
- Intravital Imaging: Prior to harvest, intravenously inject a fluorescent lectin or dextran. The presence of the tracer within the vascular networks of the implanted construct under confocal microscopy demonstrates perfusion [17].
- Microscopic Observation: Direct observation of blood pooling in patterned endothelial cord structures within the explanted graft can serve as an initial morphological indicator of successful anastomosis [17].
Troubleshooting Guides
Table 1: Troubleshooting Vascular Network Formation
| Problem | Potential Cause | Solution | Reference |
|---|---|---|---|
| Poor or No Network Formation | Inadequate cell-to-cell interaction or signaling. | Co-culture endothelial cells with supporting stromal cells (e.g., fibroblasts, MSCs) in a 3D hydrogel like fibrin or collagen to promote spontaneous vasculogenesis. | [90] [91] |
| Suboptimal biochemical cues. | Supplement culture medium with a defined angiogenic growth factor cocktail (e.g., VEGF, FGF) to stimulate endothelial migration and tube formation. | [90] | |
| Uncontrolled, Disorganized Sprouting | Over-exposure to high concentrations of a single pro-angiogenic factor (e.g., VEGF). | Utilize sequential growth factor delivery; initiate sprouting with VEGF, then promote maturation and stability with PDGF-BB and ANG-1. | [90] |
| Vessel Regression and Instability | Lack of perivascular support. | Introduce pericytes or MSCs to the co-culture system. These cells are recruited by PDGF-BB and produce ECM and stabilizing factors. | [90] |
| Insufficient Perfusion in Patterned Channels | Lack of connectivity between patterned macrovessels and microvasculature. | Combine top-down patterning of "endothelial cords" with bottom-up vasculogenesis in the surrounding hydrogel bulk to create a hierarchical, perfusable network. | [17] [43] |
Table 2: Troubleshooting Multi-Organ MPS Integration and Function
| Problem | Potential Cause | Solution | Reference |
|---|---|---|---|
| Rapid Cell Death in Core of Tissue Construct | Construct thickness exceeds oxygen diffusion limit (~200 µm). | Incorporate a perfusable vascular network prior to implantation to ensure nutrient delivery to all cells. | [4] [90] [91] |
| Inconsistent Drug Response Between Chips | Variable "blood" flow distribution between organ compartments. | Design a vascular network with microchannel dimensions that accurately mimic in vivo blood flow distribution to ensure reproducible organ perfusion. | [94] |
| Unexpected High Drug Toxicity | Lack of functional excretion system to clear drugs and metabolites. | Integrate a dialysis membrane and a unidirectional flow chamber to simulate renal excretion, allowing dynamic control of drug and metabolite concentrations. | [94] |
| Failure of Host-Graft Anastomosis | Host inflammatory response degrading the graft. | Select an appropriate immunodeficient host model (e.g., athymic nude mice vs. rats), as the host biological response critically impacts vascularization and engraftment success. | [17] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Vascularized MPS
| Item | Function in Experiment | Example Application |
|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | Form the inner lining of the engineered vasculature (tunica intima). | Used in co-culture systems to create capillary-like networks within fibrin or collagen gels [90] [89]. |
| Mesenchymal Stem Cells (MSCs) | Act as perivascular support cells; secrete pro-angiogenic and stabilizing factors (VEGF, ANG-1). | Co-cultured with HUVECs to enhance the density, maturity, and stability of the formed vascular networks in vitro and in vivo [90]. |
| Fibrin Hydrogel | Serves as a biologically active 3D scaffold that supports cell invasion and capillary morphogenesis. | A common matrix for embedding endothelial and stromal cells to allow de novo formation of vascular networks through vasculogenesis [17] [90]. |
| Vascular Endothelial Growth Factor (VEGF) | Key signaling protein that stimulates endothelial cell migration, proliferation, and new blood vessel formation. | Added to culture medium to initiate angiogenesis; often used in combination with other factors for stable vessel formation [4] [90]. |
| Angiopoietin-1 (ANG-1) | Promotes vessel maturation and stability by mediating interactions between endothelial cells and surrounding support cells. | Used after initial VEGF-driven sprouting to stabilize newly formed vascular networks and prevent regression [90]. |
| Poly(dimethylsiloxane) (PDMS) | An elastomeric polymer used to fabricate microfluidic chips due to its gas permeability and optical clarity. | The base material for many organ-on-a-chip devices; its lipophilic nature can cause absorption of small molecule drugs, which may require mitigation strategies [93]. |
Experimental Protocols & Workflows
Protocol 1: Guided Vascularization via Endothelial Cord Patterning
This methodology creates pre-patterned vascular channels within engineered tissues to guide the formation of organized, perfusable networks upon implantation [17].
Detailed Methodology:
- Fabrication of PDMS Mold: Create a mold with parallel microchannels (e.g., 50-200 µm wide) using standard soft lithography techniques.
- Formation of Endothelial Cords: Suspend human endothelial cells (e.g., HUVECs) and stromal cells (e.g., fibroblasts) in a collagen solution. Pipette the cell-collagen mixture into the PDMS mold channels and incubate (37°C, 5% CO2) to allow gelation, forming solid "endothelial cords."
- Tissue Construct Encapsulation: Carefully extract the endothelial cords from the mold and encapsulate them within a larger fibrin-based hydrogel that may also contain parenchymal cells (e.g., cardiomyocytes, hepatocytes).
- Implantation and Analysis: Implant the composite engineered tissue into an immunodeficient host (e.g., mouse abdomen or epicardium). After 7-14 days, explant and analyze via:
- Immunofluorescence: Stain for human CD31 (huCD31) and host red blood cells (e.g., TER-119) to confirm the formation of chimeric, perfused vessels.
- Confocal Microscopy: Image cleared whole tissues to verify the retention of the patterned 3D vascular geometry.
The workflow for creating and validating these pre-vascularized tissues is as follows:
Protocol 2: Establishing an 18-Organ MPS with Physiological Support Systems
This protocol outlines the setup of a complex, multi-organ MPS featuring a biomimetic vascular network and an excretion system for long-term drug studies [94].
Detailed Methodology:
- Chip Fabrication and Assembly: Construct the MPS by laminating laser-ablated poly(methyl methacrylate) (PMMA) layers: an "organ" layer with 20 compartments, an "artery" layer, and a "vein" layer. Use porous membranes and hydrophobic PTFE layers to separate compartments and prevent leakage.
- Microtissue Loading: Place freshly harvested rat microtissues (representing 18 organs) into their respective compartments in the "organ" layer. Use a customized culture medium to maintain viability.
- Initiation of "Blood" Circulation: Connect the chip to a peristaltic pump. Circulate culture medium ("blood") from a reservoir to the "lung" compartment for oxygenation, then through the "left heart," "aorta," and the vascular network to perfuse all organ compartments. "Venous blood" returns to the reservoir via the "vein" layer.
- Integration of Excretion System: Activate the micro-stirrer in the "kidney-1" compartment. The stirrer enhances mass transfer of small molecule wastes and drugs from the "artery" through a dialysis membrane into the kidney compartment, from where they are removed by a unidirectional flow.
- Drug Testing and Pharmacokinetic (PK) Analysis: Introduce the drug candidate into the circulation system. Collect effluent from the excretion system and samples from specific organ compartments at timed intervals. Analyze drug and metabolite concentrations to establish PK profiles and assess organ-specific toxicity.
The structure and fluid path of this complex system are illustrated below:
Key Signaling Pathways in Vascularization
Successful in vitro vascularization requires recapitulating the key signaling events that govern blood vessel formation in vivo. The diagram below summarizes the core pathway and critical interactions:
Technical Troubleshooting Guides
Troubleshooting Engineered Vasculature for Disease Modeling
| Problem Phenomena | Potential Root Cause | Diagnostic Steps | Solution & Prevention |
|---|---|---|---|
| Poor cell viability/engraftment in aneurysm models [11] | Lack of proper ECM cues; Inadequate cell localization; Host inflammatory response. | Check cell viability pre-implantation; Analyze scaffold for cell adhesion motifs; Monitor inflammatory markers post-implantation. | Use bioengineered scaffolds (e.g., collagen) to promote localization and survival [11]; Implement peri-adventitial delivery for better engraftment [11]. |
| Insufficient mechanical strength in engineered vessels [31] | Suboptimal ECM production (lack of elastin/collagen); Inadequate dynamic conditioning. | Perform tensile strength testing; Conduct histological staining for elastin/collagen. | Use dynamic bioreactors for mechanical maturation; Apply pulsatile flow to condition vessels and improve ECM production [31]. |
| Failure to recapitulate three-layer vessel structure [31] | Static cell seeding methods; Incorrect cell distribution; Lack of appropriate biomolecular cues. | Perform cross-sectional histology; Immunostain for EC (CD31), SMC (α-SMA), and FB markers. | Employ advanced biofabrication (e.g., 3D bioprinting) for precise cell placement; Use biomaterials with adhesion peptides (e.g., RGD) [31]. |
| Low contrast in histological images [95] | Improper fixation/ decalcification; Incorrect staining protocols; Suboptimal sample preparation. | Review pre-analytical protocols; Use control samples. | Optimize fixation and decalcification times; Use specialized films for sectioning hard samples; Validate with standardized staining protocols [95]. |
| High thrombogenicity in engineered vessel lumen [31] | Absence or incomplete endothelial cell layer; Non-hemocompatible biomaterial surface. | Assess EC coverage (CD31 staining); Perform platelet adhesion tests. | Ensure confluent EC layer on lumen; Use specially designed biomaterials that promote anti-thrombogenic surface [31]. |
Troubleshooting Specific Disease Models
| Disease Context | Common Challenge | Recommended Solution |
|---|---|---|
| Abdominal Aortic Aneurysm (AAA) | Inability to initiate elastin regeneration; Uncontrolled inflammation [11]. | Utilize PGG-loaded nanoparticles to stabilize existing elastin against MMP degradation [11]. |
| Ischemic Stroke | Difficulty localizing therapeutics to brain lesion; Inefficient blood-brain barrier (BBB) repair [11]. | Employ biomimetic (e.g., RBC membrane) or magnetic nanovesicles for targeted delivery to ischemic site [11]. |
| Peripheral Artery Disease (PAD) | Limited durability of regenerative interventions; Diffuse infrainguinal disease [96]. | For preclinical models, consider surgical bypass with saphenous vein conduit in settings where endovascular durability is limited [96]. |
Frequently Asked Questions (FAQs)
Q1: What is the minimum sample size I should use for my in vivo animal model to ensure statistically meaningful results? While the ideal sample size depends on the model and variability, a common mistake is using only one sample per group [97]. For animal models with greater inherent variability, such as mice, a minimum of five to ten samples per group is recommended. For more controlled systems like cell lines, a minimum of three samples is a starting point. Always perform a power analysis specific to your assay [97].
Q2: My engineered vascular constructs lack mechanical strength. How can I improve this before implantation? The use of dynamic bioreactor systems for maturation is crucial. These systems subject the constructs to physiological-like conditions, including pulsatile flow and pressure, which stimulates cells to produce and organize a more robust extracellular matrix, thereby enhancing mechanical properties such as burst pressure [31].
Q3: How can I better assess cell viability and distribution within my opaque 3D-bioprinted vascular scaffold? Standard microscopy faces challenges with opaque scaffolds. Techniques like confocal microscopy allow you to capture images at different depths within the construct to assess 3D cell viability and distribution [95]. Additionally, flow cytometry can be used to dissociate cells from the scaffold and perform multiparametric analysis of cell viability, proliferation, and immunophenotype [95].
Q4: What are the key considerations when selecting a cell source for engineering a trilayered blood vessel? The key is to recapitulate the three primary cell types: Endothelial Cells (ECs) for the intima, Smooth Muscle Cells (SMCs) for the media, and Fibroblasts (FBs) for the adventitia [31]. Sources can include primary cells or stem cell-derived progenitors (e.g., iPSC-derived SMCs). The choice involves balancing authenticity, scalability, and clinical translatability [11] [31].
Q5: In my stroke model, therapeutics do not efficiently reach the ischemic lesion. What advanced delivery strategies can I use? Traditional systemic delivery is often inefficient. Emerging strategies include using extracellular nanovesicles derived from mesenchymal stem cells with magnetic properties for targeted delivery, or biomimetic nanovesicles composed of red blood cell membranes, which have shown promise in improving localization to the ischemic brain and promoting repair [11].
Experimental Protocols & Workflows
Detailed Protocol: Assessing Engineered Vasculature In Vivo
This protocol outlines the key steps for implanting and analyzing engineered vascular constructs in a pre-clinical model, such as a murine AAA model [11].
1. Pre-Implantation Construct Maturation:
- Culture the engineered vessel in a bioreactor under dynamic conditions (pulsatile flow, ~2,000-3,000 mmHg) for a minimum of 2-4 weeks to enhance ECM deposition and mechanical strength [31].
- Perform quality control checks: Assess cell viability via live/dead staining and confirm trilayered structure via histology (H&E, Masson's Trichrome) on a representative sample [95].
2. Surgical Implantation (e.g., Peri-adventitial Delivery for AAA):
- Anesthetize and prepare the animal following approved IACUC protocols.
- For peri-adventitial delivery, perform a laparotomy to access the abdominal aorta.
- Wrap the engineered vascular construct or cell-laden scaffold around the exposed aorta.
- Secure the construct in place with bioabsorbable sutures or adhesive.
- Close the surgical site in layers [11].
3. Post-Op Monitoring & Analysis:
- Monitor animals for signs of distress, inflammation, or graft failure.
- At the experimental endpoint, harvest the tissue.
- Perfusion-fix the vascular system (e.g., with 4% PFA) at physiological pressure for optimal histology.
- Process the explanted construct and host tissue for analysis [95].
Core Analysis Workflow
The following diagram illustrates the primary workflow for analyzing an explanted engineered vascular construct, integrating multiple methods to form a comprehensive assessment.
Research Reagent Solutions
The table below catalogues essential materials and reagents for engineering and analyzing vascular tissues, as featured in the cited research.
| Reagent / Material | Function & Application in Vascular Engineering |
|---|---|
| PGG (Penta Galloyl Glucose) Nanoparticles [11] | Elastin stabilization; used in AAA models to inhibit protease-mediated degradation and halt aneurysm progression. |
| Biomimetic Nanovesicles (RBC/Platelet membrane) [11] | Targeted drug/therapeutic delivery; particularly for crossing the BBB in stroke models and promoting angiogenesis. |
| Adipose-derived Mesenchymal Stromal Cells (ASCs) [11] [95] | Cell source for regeneration; can differentiate towards vascular lineages and secrete paracrine factors to modulate inflammation and promote repair. |
| Urinary Bladder/Brain-derived ECM [11] | Bioactive scaffold material; supports endogenous cell infiltration and reduces lesion volume in stroke and brain injury models. |
| RGD-peptide modified Biomaterials [31] | Enhances cell adhesion; critical for improving endothelial and smooth muscle cell attachment and survival within engineered scaffolds. |
| Safranin-O / Fast Green Stain [95] | Histological assessment; used to quantify proteoglycan content in neotissue, a key component of a healthy ECM. |
| Dynamic Bioreactor Systems [31] | In vitro maturation; provides pulsatile flow and mechanical conditioning to enhance the mechanical strength and biological function of engineered vessels. |
Signaling Pathways in Vascular Pathologies and Regeneration
The diagram below summarizes key signaling interactions involved in vascular diseases like AAA and the regenerative approaches targeting them.
A fundamental hurdle in engineering thick, complex tissues is the lack of integrated vascular networks. Cells located more than 200 micrometers from a nutrient source cannot survive, leading to central necrosis in un-vascularized constructs [91]. Prevascularization—the incorporation of functional vascular networks within a tissue construct in vitro before implantation—has emerged as a vital strategy to overcome this limitation. Prevascularized constructs demonstrate enhanced anastomosis with host vasculature post-implantation, improving cell survival, graft integration, and functional outcomes [91] [98]. This technical support center provides a comparative analysis of prevailing prevascularization techniques, detailed protocols, and troubleshooting guides to aid researchers in selecting and optimizing strategies for their specific applications.
Technique Comparison: Advantages, Disadvantages, and Clinical Readiness
The table below summarizes the core prevascularization techniques, their key features, and their current stage of development.
Table 1: Comparative Analysis of Prevascularization Techniques
| Technique | Key Principle | Advantages | Disadvantages/Challenges | Representative Clinical Readiness |
|---|---|---|---|---|
| 3D Bioprinting | Precision deposition of cells and biomaterials to create vascular channels [99]. | High spatial control; ability to create complex, anatomically accurate architectures [99]. | Shear stress can reduce cell viability; resolution limits for capillaries [99]. | Preclinical research for vascularized bone and liver [99] [100]. |
| Microfluidics | Fabrication of micron-scale channels within biomaterials to guide vascular formation [91]. | Can create perfusable networks with near-physiological flow dynamics. | Limited thickness of constructs; complexity in scaling up. | Primarily used for advanced in vitro modeling [91]. |
| Cell Sheet Engineering | Stacking of thin, confluent cell layers containing endothelial and other cells [91]. | Preserves native extracellular matrix and cell-cell junctions. | Manual process; limited scalability for large organs. | Clinical use in avascular tissues like cornea and skin [91]. |
| Sacrificial Molding | 3D printing of a temporary template (e.g., sugar, gelatin) which is later removed to leave hollow channels [100] [91]. | Can generate complex, free-form vascular networks. | Difficulty in completely removing material; potential cytotoxicity. | Preclinical development for various tissues, including liver [100]. |
| In Vivo Prevascularization | Implanting a construct into a highly vascularized site in the body (e.g., AV loop) to allow host vessel ingrowth [98]. | Generates a mature, functional vascular network from the host. | Requires two separate surgeries; not a purely in vitro strategy. | Established preclinical models; used in complex graft fabrication [98]. |
Deeper Dive into 3D Bioprinting Modalities
Within 3D bioprinting, several technologies offer distinct trade-offs between resolution, speed, and biocompatibility, making them suitable for different aspects of vascularization.
Table 2: Comparison of 3D Bioprinting Technologies for Vascularization
| Technology | Characteristics | Advantages | Disadvantages | Best Use in Vascularization |
|---|---|---|---|---|
| Inkjet Bioprinting | Droplet-based, non-contact printing [99]. | Fast, low-cost, high cell viability (>85%) [99]. | Limited to low-viscosity bioinks; risk of nozzle clogging [99]. | Precise patterning of endothelial cells or growth factors [99]. |
| Extrusion Bioprinting | Continuous filament extrusion via pneumatic or piston force [99]. | Versatile; prints high-viscosity bioinks and high cell loads; can create large constructs [99]. | Lower resolution; shear stress can reduce viability (40-90%) [99]. | Fabricating bulk scaffold structure with integrated macroscale channels [99]. |
| Laser-Assisted Bioprinting | Nozzle-free; uses laser pulses to eject droplets [99]. | Highest resolution; very high cell viability (>95%); handles high-viscosity inks [99]. | Expensive; slow throughput; complex setup [99]. | High-precision placement of single cells or micro-vascular patterns [99]. |
Experimental Protocols for Key Techniques
Protocol: Co-culture Prevascularization in a 3D Construct
This protocol describes creating a self-assembled microvascular network within a hydrogel by co-culturing endothelial and support cells [98].
- Cell Preparation: Expand human umbilical vein endothelial cells (HUVECs) and mesenchymal stem cells (MSCs) or 10T1/2 cells in standard culture conditions.
- Hydrogel Preparation: Prepare a collagen/fibronectin hydrogel solution on ice.
- Cell Encapsulation: Trypsinize, count, and resuspend HUVECs and MSCs at a desired ratio (e.g., 4:1) in the hydrogel solution at a final concentration of 5-10 million cells/mL.
- Gelation: Pipette the cell-laden hydrogel into the desired culture vessel (e.g., multi-well plate) and incubate at 37°C for 30-45 minutes to induce polymerization.
- Culture and Maintenance: After gelation, carefully overlay with endothelial cell growth medium. Change the medium every 2-3 days.
- Network Monitoring: Monitor the formation of capillary-like structures over 7-14 days using phase-contrast microscopy or fluorescent labeling.
Protocol: Sacrificial Molding for Perfusable Channel Networks
This protocol outlines the creation of a perfusable vascular network using a sacrificial material [100].
- Template Design and Printing: Design a branched 3D network. 3D print the network using a sacrificial material like carbohydrate glass or gelatin.
- Embedding in Hydrogel: Place the sacrificial template in a mold and encapsulate it within a cell-laden hydrogel (e.g., fibrin, collagen, or PEG-GelMA [100]).
- Cross-linking: Allow the surrounding hydrogel to cross-link completely.
- Sacrificial Removal:
- For Gelatin: Cool the entire construct to 4°C to liquefy the gelatin, then gently flush it out using a syringe and cold culture medium.
- For Carbohydrate Glass: Dissolve the template by perfusing the construct with aqueous solution or culture medium.
- Endothelial Seeding: Introduce a suspension of endothelial cells (e.g., HUVECs) into the resulting hollow channels and allow them to adhere under static conditions or low flow for 4-6 hours.
- Perfusion Culture: Connect the construct to a perfusion bioreactor system. Initiate a low flow rate to condition the endothelium, gradually increasing it to physiological levels over several days.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Prevascularization Experiments
| Reagent / Material | Function / Application | Example |
|---|---|---|
| Endothelial Cells | Form the lumen and lining of blood vessels. | HUVECs, Endothelial Colony Forming Cells (ECFCs), induced pluripotent stem cell-derived ECs [98]. |
| Support Cells | Stabilize vascular structures and promote maturation. | Mesenchymal Stem Cells (MSCs), Pericytes, 10T1/2 cells [98]. |
| Pro-Angiogenic Growth Factors | Stimulate endothelial cell proliferation and tubule formation. | Vascular Endothelial Growth Factor (VEGF), basic Fibroblast Growth Factor (FGF-2) [99] [98]. |
| Hydrogels | Mimic the extracellular matrix; provide a 3D environment for cell growth and network formation. | Collagen Type I, Fibrin, Gelatin Methacryloyl (GelMA), Poly(ethylene glycol) (PEG)-based hydrogels [100] [98]. |
| Sacrificial Materials | Used to create temporary, patterned structures that are later removed to form hollow channels. | Gelatin, Carbohydrate glass, Pluronic F127 [100]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q: My co-culture vascular networks are unstable and regress after a week. What could be the cause?
- A: Network instability is often due to a lack of mechanical stability in the hydrogel or the absence of necessary maturation cues. Ensure your hydrogel is sufficiently cross-linked. Incorporating support cells like MSCs or pericytes is crucial, as they secrete factors that stabilize new vessels. Adding a defined mixture of angiogenic factors (e.g., VEGF and FGF-2) can also promote persistence.
Q: When using sacrificial molding, my channels collapse after the template is removed. How can I prevent this?
- A: Channel collapse indicates that the surrounding matrix lacks the mechanical strength to withstand the removal process and subsequent perfusion. Increase the polymer or cross-linker concentration of your hydrogel. Alternatively, use a composite or double-network hydrogel designed for higher stiffness and toughness.
Q: What is the difference between "prevascularization" and "vascularization"?
- A: Prevascularization specifically refers to the process of creating a vascular network in vitro within a tissue construct before it is implanted. Vascularization is a broader term that can refer to this, or to the process of host blood vessels growing into an implant after it is placed in vivo (a process which can be slow and inefficient for large grafts) [91].
Q: My bioprinted endothelial cells have low viability. What are the main culprits?
- A: Low viability in bioprinting is frequently caused by shear stress during the extrusion process [99]. Optimize your printing parameters: use a larger nozzle diameter, reduce the printing pressure, and use a bioink with lower viscosity if possible. For laser-assisted bioprinting, viability is typically higher, but the trade-off is cost and speed [99].
Decision Matrix: Choosing a Prevascularization Strategy
This diagram illustrates the logical workflow for selecting the most appropriate prevascularization technique based on key research requirements.
FAQs on Quantifying Tissue Perfusion and Vascularization
Q1: What non-invasive techniques can I use to assess perfusion and endothelial function in my engineered tissue constructs?
You can adapt several clinical non-invasive techniques to assess vascular function in 3D tissues. Flow-Mediated Dilation (FMD) is a key method that uses high-resolution ultrasound to measure the brachial artery's diameter change in response to increased shear stress and reactive hyperemia, providing a readout of endothelium-dependent vasodilation [101] [102]. Additionally, Pulse Wave Velocity (PWV), specifically carotid-femoral PWV (cfPWV), is a gold-standard technique for assessing arterial stiffness, an important marker of vascular health [102]. The Table 1 below summarizes the primary non-invasive methods.
Table 1: Non-Invasive Methods for Assessing Vascular Function
| Method | Primary Metric | What It Assesses | Key Advantages |
|---|---|---|---|
| Flow-Mediated Dilation (FMD) | Percentage change in arterial diameter [102] | Endothelium-dependent vasodilation (largely NO-mediated) [101] | Non-invasive, widely used, strong prognostic value [101] [102] |
| Pulse Wave Velocity (PWV) | Speed of the pulse wave between two arterial sites (e.g., carotid-femoral) [102] | Arterial stiffness [102] | Gold-standard, simple to perform, high reproducibility [102] |
| Reactive Hyperemia Index (RHI) | Post-occlusion increase in peripheral blood flow [102] | Microvascular endothelial function [102] | Assesses microvascular bed, automated analysis [102] |
Q2: My lab specializes in ex vivo tissue analysis. What are the best practices for measuring vascular function in isolated vessels?
For ex vivo assessment, pressure myography and wire myography are the two principal techniques. The consensus in the field is that pressure myography more closely mimics physiological conditions because the vessel is cannulated and pressurized, as it is in vivo [103]. This setup allows for the study of critical physiological phenomena like the myogenic response (pressure-induced constriction) and flow-mediated dilation by controlling intraluminal flow and shear stress [103]. Wire myography, where a vessel ring is mounted on two wires to measure tension, is a powerful alternative, especially when vessel length is limited. It allows for high-throughput pharmacological testing of vasoactive compounds on segments from the same artery [103]. Key differences are summarized in Table 2 below.
Table 2: Comparison of Ex Vivo Vascular Function Assessment Techniques
| Characteristic | Pressure Myography | Wire Myography |
|---|---|---|
| Physiological Relevance | High (mimics in vivo pressure and flow) [103] | Moderate (vessel is stretched, not pressurized) [103] |
| Key Measurable Responses | Myogenic tone, flow-mediated dilation, pharmacological responses [103] | Pharmacologically-induced contraction and relaxation [103] |
| Best For | Studying resistance arteries, myogenic response, and shear stress [103] | Pharmacological studies, comparing vessel segments, when vessel length is short [103] |
| Limitations | Requires more specialized equipment and skill [103] | Cannot directly study myogenic response or flow; may activate different endothelial pathways [103] |
Q3: What are the critical signaling pathways and biomarkers I should monitor to assess endothelial cell barrier function?
Endothelial barrier function is compromised in many pathologies, and its assessment is crucial. Key biomarkers of endothelial damage and activation include endocan (associated with glycocalyx disruption), von Willebrand factor (vWF) (a pro-coagulant mediator), and circulating adhesion molecules like ICAM [101]. The integrity of the barrier is regulated by signaling pathways centered on Nitric Oxide (NO) bioavailability. Reduced NO, often due to oxidative stress, leads to endothelial dysfunction, a pro-inflammatory, and pro-coagulant state [101]. The following diagram illustrates the core signaling and key biomarkers involved in endothelial barrier function.
Figure 1: Signaling and Biomarkers in Endothelial Barrier Function.
Q4: Which metabolic pathways and functional readouts are most indicative of mature tissue function, particularly in engineered myocardium?
A switch from glycolytic to oxidative metabolism is a hallmark of mature tissue function, especially in energy-demanding tissues like the myocardium. Key pathways to assess include AMPK/Sirt1 signaling, which is linked to the NAD+/NADH ratio and senses cellular energy status, and PGC-1α/PPAR activity, which is a master regulator of mitochondrial biogenesis and oxidative metabolism [104]. A functional engineered myocardium should demonstrate key adult features, including extensive mitochondrial biogenesis, efficient calcium handling for proper electrophysiology, and strong contractile kinetics and dynamics [104]. The metabolic maturation is critically regulated by oxygenation and involves a shift in specific signaling pathways, as shown below.
Figure 2: Key Pathways in Myocardial Metabolic Maturation.
Research Reagent Solutions
Table 3: Essential Reagents for Vascular and Metabolic Function Assessment
| Reagent / Material | Function in Assessment |
|---|---|
| Iohexol | A non-radioactive exogenous filtration marker used to measure glomerular filtration rate (GFR) via plasma clearance protocols, crucial for assessing kidney perfusion and filtration [105]. |
| Acetylcholine (ACh) | Used in ex vivo myography and invasive clinical studies to assess endothelium-dependent vasodilation. Its action is primarily mediated by the release of nitric oxide from endothelial cells [101] [103]. |
| Sodium Nitroprusside | A direct nitric oxide donor used to assess endothelium-independent vasodilation. This control confirms that the vascular smooth muscle is capable of relaxing, isolating the role of the endothelium [101] [103]. |
| Dextran | Used in pressure myography to increase the viscosity of the perfusate, allowing for the manipulation of shear stress on the endothelial layer without changing the intraluminal flow rate, to study flow-mediated dilation [103]. |
| Phenylephrine | A synthetic vasoconstrictor commonly used in wire myography to pre-constrict isolated vessel rings before testing the vasodilatory capacity of various compounds [103]. |
A paramount obstacle in engineering thick, functional tissues is the establishment of a robust and functional vascular network. Without adequate blood supply, cells within large constructs (>1 cm³) suffer from insufficient oxygen, nutrients, and waste removal, leading to core necrosis and ultimate implant failure [31] [106]. This technical support document details current strategies and troubleshooting guides, framed within a thesis on overcoming vascularization limitations, to aid researchers in developing viable regenerative therapies for bone, cardiac, and soft tissue repair.
Bone Tissue Repair
Experimental Protocols for Enhanced Bone Regeneration
Protocol: Implementing a Resistance Rehabilitation Model in Segmental Bone Defects This protocol is based on a study demonstrating that controlled mechanical loading significantly improves bone healing in a rodent model [107].
- 1. Animal Model and Surgery:
- Create a 2 mm segmental bone defect in the femur of a Sprague Dawley rat.
- Stabilize the defect using a custom fixation plate, ideally instrumented with a wireless strain sensor to monitor local strain environments.
- 2. Postoperative Recovery:
- Allow all animals to recover under sedentary conditions for 1 week.
- 3. Rehabilitation Groups:
- Sedentary Control Group: Animals remain in standard cages without scheduled exercise.
- No-Resistance Rehabilitation Group: Animals have access to a free-running wheel.
- Resistance Rehabilitation Group: Animals have access to a running wheel with a programmable brake that applies resistance, increasing the mechanical load.
- 4. Monitoring and Analysis:
- Longitudinal Analysis: Monitor bone formation weekly via radiographs.
- Endpoint Analysis (e.g., 8 weeks):
- Micro-CT: Quantify bone volume (BV) and tissue mineral density (TMD) within the defect region.
- Mechanical Testing: Perform torsion testing to failure on explanted femurs to determine failure torque and torsional stiffness.
- Histology: Process and stain sections with Hematoxylin & Eosin (H&E) and Safranin O/Fast Green to evaluate tissue morphology and the presence of cartilage, indicative of endochondral ossification.
Protocol: Utilizing 3D-Printed Scaffolds with Cranial-Specific Stem Cells for Craniofacial Reconstruction This protocol uses a biofabrication approach to create cell-laden bone grafts [108].
- 1. Cell Source and Differentiation:
- Generate induced pluripotent stem cells (iPSCs).
- Differentiate iPSCs into cranial-specific mesenchymal stem cells (MSCs) or iPSC-derived notochordal cells using established developmental cues.
- 2. Bioink Preparation:
- Suspend the cranial-specific stem cells in a sterile, biocompatible bioink. The bioink must be printable and support cell viability and differentiation. (Example biomaterials: hyaluronic acid-based hydrogels, collagen, or other GMP-compliant hydrogels).
- Add the osteogenic protein BMP6 to the bioink-cell mixture to enhance bone formation.
- 3. 3D Bioprinting:
- Use a bioprinter to fabricate a scaffold in the shape and dimensions of the cranial bone injury.
- 4. Implantation:
- Implant the 3D-bioprinted construct into the cranial defect.
- 5. Assessment:
- Monitor healing over time using medical imaging (e.g., micro-CT).
- Upon explanation, assess osseointegration and new bone formation via histology and mechanical testing.
Troubleshooting Guide for Bone Repair
FAQ 1: Our tissue-engineered bone constructs fail to integrate and show central necrosis after implantation. What is the primary issue? This is a classic symptom of insufficient vascularization. The core of the construct is not receiving adequate oxygen or nutrients. To address this:
- Strategy 1: Incorporate Pro-Angiogenic Factors. Seed scaffolds with mesenchymal stem cells (MSCs), which secrete pro-angiogenic factors [109] [110]. Alternatively, load the scaffold with sustained-release systems containing VEGF or BMPs.
- Strategy 2: Design Pre-vascularized Constructs. Use 3D bioprinting to create channels within the scaffold and seed them with endothelial cells (ECs) to create a rudimentary network that can anastomose with the host vasculature [31].
- Strategy 3: Utilize Photosynthetic Biomaterials. As demonstrated in soft tissue repair, oxygen-generating scaffolds can locally ameliorate hypoxia, supporting cell survival until host vasculature invades [111].
FAQ 2: Our rehabilitation model does not yield consistent improvements in bone healing. What parameters should we optimize? The key is the local strain environment within the regenerative niche, not just the external activity.
- Solution: Implement implantable strain sensors to directly measure the local mechanical environment in real-time [107]. Couple this data with subject-specific finite element models to calculate tissue-level strains.
- Optimization: Adjust rehabilitation intensity (e.g., resistance level) based on sensor data to ensure the strain magnitude is within a range known to promote endochondral ossification (often associated with higher strains) rather than fibrous tissue formation (associated with lower strains) [107].
Cardiac Tissue Repair
Experimental Protocols for Myocardial Repair
Protocol: Employing Stem Cell-Derived Extracellular Vesicles (Stem-EVs) for Cardiac Repair Given the challenges of cell-based therapies, including arrythmias and poor cell retention, Stem-EVs represent a promising cell-free alternative [112].
- 1. EV-Producing Cell Culture:
- Expand human Mesenchymal Stem Cells (MSCs) or other relevant stem cells under GMP-compliant conditions.
- 2. Extracellular Vesicle Isolation:
- Collect conditioned media from the cell cultures.
- Isolate small EVs (sEVs, 50-150 nm) via sequential ultracentrifugation, density gradient centrifugation, or size-exclusion chromatography. Adhere to MISEV2023 guidelines for characterization [112].
- 3. EV Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine particle size and concentration.
- Transmission Electron Microscopy (TEM): Confirm vesicle morphology.
- Western Blot: Analyze markers associated with exosomes (e.g., CD63, CD81, TSG101) and absence of negative markers (e.g., calnexin).
- 4. In Vivo Administration:
- In an animal model of acute myocardial infarction (MI), administer Stem-EVs via intramyocardial or intravenous injection immediately post-MI.
- 5. Outcome Assessment:
- Functional: Measure left ventricular ejection fraction (LVEF) and end-systolic volume by echocardiography.
- Histological: Quantify infarct size, apoptosis (TUNEL assay), capillary density (CD31 staining), and inflammation.
Protocol: In Vivo Reprogramming of Cardiac Fibroblasts to Cardiomyocytes This protocol aims to directly convert scar-forming fibroblasts into contractile cardiomyocytes within the injured heart [112] [110].
- 1. Vector Design:
- Create a lentiviral or adeno-associated viral (AAV) vector expressing cardiac reprogramming factors. The classic combination is GMT (GATA4, Mef2C, Tbx5) or GHMT (GATA4, Hand2, Mef2C, Tbx5).
- 2. Viral Production and Purification:
- Produce high-titer, clinical-grade viral vectors.
- 3. In Vivo Delivery:
- In a murine MI model, directly inject the viral vector into the border zone of the infarct.
- 4. Efficiency and Safety Analysis:
- Lineage Tracing: Use cardiac fibroblast-specific reporters (e.g., Tcf21-MerCreMer) to confirm the origin of newly formed induced cardiomyocytes (iCMs).
- Functional Assessment: Use electrophysiology to assess the electrical integration of iCMs and monitor for arrythmias.
- Histology: Stain for cardiomyocyte markers (e.g., cTnT, α-actinin) and scar tissue (Masson's Trichrome).
Troubleshooting Guide for Cardiac Repair
FAQ 1: Transplanted cardiomyocytes show poor long-term survival and integration, often causing arrythmias. What are the alternatives? Cell-based therapies face significant hurdles. Consider these alternatives:
- Alternative 1: Use Stem Cell-Derived Extracellular Vesicles (Stem-EVs). Stem-EVs carry cardioprotective cargo (miRNAs, proteins) that reduce apoptosis, inflammation, and fibrosis, while promoting angiogenesis, without the risks of tumorigenicity or arrythmias [112].
- Alternative 2: Optimize In Vivo Reprogramming. While efficiency is currently low, focus on improving viral tropism for cardiac fibroblasts and using cell-specific promoters to enhance the safety and efficacy of direct reprogramming [112] [110].
- Alternative 3: Engineer "Safer" Cell Products. Use purified iPSC-derived cardiomyocyte progenitors or pacemaker cells instead of fully differentiated cells to potentially reduce arrythmogenic risk.
FAQ 2: How can we enhance the therapeutic potency and targeting of Stem-EVs? Native EVs can have limited specificity. Engineering can overcome this.
- Solution 1: Surface Modification. Engineer parental cells to express targeting ligands (e.g., cardiac homing peptides) on the EV surface to improve their retention in the heart [112].
- Solution 2: Cargo Loading. Actively load EVs with specific therapeutic miRNAs or siRNAs (e.g., targeting pro-fibrotic or cell-cycle arrest pathways) to enhance their regenerative capacity [112].
- Solution 3: Biomaterial-Assisted Delivery. Incorporate EVs into a hydrogel that allows for sustained, localized release at the site of myocardial injury.
Soft Tissue & Vascular Repair
Experimental Protocols for Dermal and Vascular Regeneration
Protocol: Applying a Photosynthetic Scaffold for Dermal Regeneration This innovative approach addresses the critical challenge of hypoxia in wound healing [111].
- 1. Scaffold Fabrication:
- Use a clinically approved dermal regeneration template (e.g., Integra) as the base scaffold.
- Seed the scaffold with photosynthetic Chlamydomonas reinhardtii microalgae, suspended in a fibrin sealant (e.g., Evicel).
- Culture the construct under constant illumination for 4 days to allow algal growth.
- Perform rigorous microbiology tests to ensure sterility.
- 2. Surgical Implantation (First Surgery):
- Debride the wound (e.g., full-thickness skin defect) to create a clean, vascularized wound bed.
- Sutured the photosynthetic scaffold onto the wound.
- Cover the area with an FDA-approved illumination device that emits blue light to stimulate photosynthesis for a prescribed period (e.g., 7 days).
- 3. Secondary Grafting (Second Surgery):
- After a period of dermal regeneration (e.g., 21 days), implant a split-thickness autograft on top of the newly formed, vascularized bed.
- 4. Postoperative Care and Assessment:
- Monitor for wound closure, infection, and contracture.
- Assess long-term outcomes through clinical appearance, functionality, and patient-reported quality of life.
Protocol: 3D Bioprinting of a Tissue-Engineered Vascular Graft (TEVG) This protocol outlines the creation of a biomimetic, multi-layered blood vessel [31] [106].
- 1. Cell Sourcing:
- Differentiate iPSCs into endothelial cells (ECs) for the tunica intima and smooth muscle cells (SMCs) for the tunica media. Alternatively, use primary cells if available.
- 2. Bioink Formulation:
- Formulate two separate bioinks:
- Bioink 1 (Intima): A soft hydrogel (e.g., gelatin methacryloyl) containing ECs.
- Bioink 2 (Media): A tougher, more elastic hydrogel (e.g., fibrin-based hydrogel with SMCs).
- Formulate two separate bioinks:
- 3. 3D Bioprinting Process:
- Use a coaxial bioprinting system to print a tubular structure.
- The core nozzle deposits Bioink 1 (ECs) to form the inner lining.
- The outer nozzle simultaneously deposits Bioink 2 (SMCs) to form the medial layer.
- 4. Dynamic Maturation in a Bioreactor:
- Transfer the printed TEVG to a pulsatile flow bioreactor.
- Condition the TEVG with cyclical radial distension and gradual increases in flow rate and pressure to mimic physiological conditions and improve mechanical strength and ECM organization.
- 5. Implantation and Analysis:
- Implant the TEVG as an interpositional graft in an animal model (e.g., rodent or porcine).
- Monitor patency over time using ultrasound.
- Upon explanation, assess tissue structure, ECM composition, and immune response.
Troubleshooting Guide for Soft Tissue & Vascular Repair
FAQ 1: Our tissue-engineered skin and vascular grafts fail due to hypoxia before host integration. How can we improve oxygen delivery? Traditional scaffolds rely on diffusion, which is insufficient.
- Solution: Implement Oxygen-Generating Systems. The use of photosynthetic scaffolds, as detailed in the protocol above, provides a continuous, local source of oxygen directly at the wound site, independent of host blood supply [111]. This has been shown to support cell survival and enhance graft take in large full-thickness defects.
FAQ 2: Our tissue-engineered blood vessels have low patency rates, often failing due to thrombosis or mechanical failure. This is a common challenge in Vascular Tissue Engineering (VTE). The graft must be non-thrombogenic and possess native-like mechanical properties.
- Strategy 1: Ensure a Confluent Endothelium. A intact and functional endothelial layer (tunica intima) is critical for preventing thrombosis. Ensure high EC viability and confluence during fabrication and maturation [31].
- Strategy 2: Recapitulate the Three-Layer Structure. Native vessels have three distinct layers (intima, media, adventitia). Use co-axial 3D bioprinting or other advanced fabrication techniques to mimic this structure, which is essential for mechanical strength and vasoactivity [31].
- Strategy 3: Implement Dynamic Mechanical Conditioning. Mature the TEVG in a pulsatile flow bioreactor that mimics blood pressure and flow. This conditioning promotes SMC alignment, ECM deposition, and strengthens the graft, preventing mechanical failure upon implantation [31] [106].
The Scientist's Toolkit: Key Reagents & Materials
The following table catalogues essential materials used in the featured regenerative medicine approaches.
Table 1: Research Reagent Solutions for Regenerative Medicine
| Item | Function / Rationale | Example Application / Note |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source for cell therapy & paracrine signaling; can differentiate into osteoblasts, chondrocytes; secretes pro-angiogenic factors. | Bone regeneration [109]; Cardiac repair (via paracrine effects) [110]. |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific cell source; can be differentiated into any cell type (e.g., cardiomyocytes, cranial MSCs, endothelial cells). | Personalized bone [108] and cardiac [112] tissue engineering. |
| Photosynthetic Microalgae (C. reinhardtii) | Provides localized, continuous oxygen production via photosynthesis to mitigate hypoxia in avascular wounds. | Dermal regeneration scaffolds [111]. |
| Bone Morphogenetic Protein (BMP6) | Potent osteoinductive growth factor; stimulates osteoblast differentiation and bone formation. | Enhancing osteogenesis in 3D-printed cranial constructs [108]. |
| Extracellular Vesicles (sEVs/exosomes) | Cell-free therapeutic; mediates intercellular communication by transferring bioactive cargo (miRNA, proteins); non-immunogenic. | Cardioprotection and repair post-MI [112]. |
| Fibrin Sealant | Natural hydrogel scaffold; excellent biocompatibility and cell adhesion properties; used as a bioink component or cell carrier. | Embedding microalgae in scaffolds [111]; Component of vascular bioinks [31]. |
| 3D Bioprinter & Bioinks | Enables fabrication of complex, patient-specific 3D structures with spatially controlled cell placement. | Creating vascular grafts [31] and cranial bone scaffolds [108]. |
| Pulsatile Flow Bioreactor | Provides dynamic mechanical conditioning (pressure, flow) to mature tissue constructs and improve ECM organization and strength. | Essential for maturation of TEVGs [31]. |
Visualizing Key Concepts and Workflows
Signaling Pathways in Injury Detection and Stem Cell Recruitment
The initial response to tissue injury is coordinated by Damage-Associated Molecular Patterns (DAMPs), which activate a signaling cascade leading to stem cell recruitment [113].
Workflow for Engineering a Vascularized Tissue Construct
This diagram outlines a generalized, integrated workflow for creating an implantable, pre-vascularized tissue construct, combining elements from bone, cardiac, and vascular protocols.
Technical Support Center: Troubleshooting Vascularization in Engineered Tissues
This technical support center addresses common experimental challenges in vascularized tissue engineering, providing targeted solutions for researchers developing implantable tissues. The guidance is framed within the broader thesis of overcoming perfusion limitations in thick tissue constructs.
Frequently Asked Questions & Troubleshooting Guides
FAQ 1: Our engineered tissues develop a necrotic core shortly after implantation. How can we improve oxygen and nutrient diffusion?
- Problem: Central necrosis in thick tissue constructs (>100-200 µm) due to oxygen diffusion limits.
- Solution: Implement a pre-vascularization strategy to create an internal capillary network before implantation.
- Protocol: Guided Vascularization via Endothelial Patterning
- Prepare "Endothelial Cords": Suspend human umbilical vein endothelial cells (HUVECs) and supporting stromal cells (e.g., human fibroblasts) at a 4:1 ratio in neutralized Type I collagen solution (2-3 mg/mL).
- Pattern Cords: Pipette the cell-collagen suspension into a polydimethylsiloxane (PDMS) mold containing parallel microchannels (100-200 µm diameter). Incubate for 30 minutes at 37°C to allow gelation.
- Encapsulate Cords: Gently extrude the polymerized collagen cords and encapsulate them within a fibrin hydrogel (10-20 mg/mL) containing your primary tissue-specific cells (e.g., cardiomyocytes, hepatocytes).
- Implant and Analyze: Suturing the construct to the target organ. Upon explanation, anastomosis to host circulation can be confirmed via immunostaining for human CD31 (huCD31) and host species-specific red blood cell markers (e.g., Ter-119 for mouse). Perfusion can be assessed by intravenous injection of fluorescent lectin prior to harvest [17].
FAQ 2: Our tissue-engineered vascular grafts (TEVGs) are prone to thrombosis. How can we enhance their thromboresistance?
- Problem: Early thrombosis occludes the lumen of implanted vascular grafts.
- Solution: Recreate a functional, confluent endothelial layer on the luminal surface to provide a natural anti-thrombotic barrier.
- Protocol: Seeding a Non-Thrombogenic Intima
- Luminal Coating: For acellular scaffolds or TEVGs, coat the lumen with proteins that enhance endothelial cell adhesion, such as fibronectin or collagen. For synthetic polymers, consider covalent binding of Arg-Gly-Asp (RGD) peptides.
- Dynamic Seeding: Introduce a high-density suspension of endothelial cells (ECs) into the graft lumen. Use a bioreactor system to rotate the graft, ensuring all surfaces are exposed to the cells for 1-2 hours.
- Maturation under Flow: Transfer the seeded graft to a flow bioreactor. Condition the construct with gradually increasing physiological shear stress for 7-14 days to promote endothelial maturation, monolayer formation, and production of anti-thrombotic factors [31] [114].
FAQ 3: The implanted vascular networks fail to connect with the host's circulatory system. What factors promote stable anastomosis?
- Problem: Pre-formed graft vasculature fails to anastomose with host blood vessels, leading to avascular implants.
- Solution: Optimize the host environment and graft design to promote integration.
- Troubleshooting Checklist:
- Confirm Host Model Suitability: Recognize that the host animal model significantly impacts engraftment. Athymic nude mice may support better guided vascularization, while athymic rats might support superior parenchymal cell (e.g., cardiomyocyte) survival [17].
- Incorporate Pro-Angiogenic Signals: Load your scaffold with sustained-release vehicles (e.g., nanoparticles, microspheres) containing vascular endothelial growth factor (VEGF) and other angiogenic factors (e.g., FGF, PDGF) to actively recruit host vasculature [115] [4].
- Ensure Scaffold Porosity: Verify your scaffold has interconnected pores greater than 100 µm to facilitate host cell and vessel invasion [115].
FAQ 4: How can we create a patient-specific, autologous vascular graft without complex manufacturing?
- Problem: Limited availability of autologous vessels and high complexity of in vitro TEVG manufacturing.
- Solution: Utilize in-body tissue architecture (iBTA) to harness the body's innate regenerative capacity.
- Protocol: In Vivo Generation of "Biotube" Grafts
- Implant Mold: Subcutaneously implant a specially designed, sterile, cylindrical mold (e.g., the BTM1 device made of stainless steel and plastic) in a patient.
- Harvest Autologous Tissue: After 1-3 months, a connective tissue capsule (the "Biotube") forms around the mold. Surgically remove the mold and the encapsulated Biotube.
- Implant: The acellular Biotube, composed of the patient's own collagen and fibroblasts, can be used as a vascular graft. Upon implantation, it remodels and endothelializes, forming a three-layered vascular structure [116].
Key Signaling Pathways in Vascularization and Bone Regeneration
Understanding the molecular cues is critical for directing successful vascularization. The diagram below illustrates key pathways, particularly in the context of vascularized bone regeneration.
Quantitative Data for Pre-Clinical and Clinical Endpoints
Defining success requires measurable endpoints. The table below summarizes key quantitative metrics from recent research.
Table 1: Key Quantitative Metrics for Vascularized Tissue Implants
| Parameter | Target Value / Observation | Significance / Clinical Correlation | Source |
|---|---|---|---|
| Oxygen Diffusion Limit | 100-200 µm | Defines maximum tissue thickness without vasculature; core necrosis occurs beyond this. | [117] [4] |
| Capillary Distance in Vivo | 60-300 µm | Physiological target for capillary network density in implanted tissues. | [117] |
| In Vivo Anastomosis Time | ~7 days | Time for pre-formed human endothelial cords to form perfused vessels with host blood in mouse models. | [17] |
| Biotube Graft Patency (First-in-Human) | 3 years (case report) | Demonstrated long-term patency of an iBTA-generated vascular graft in a dialysis shunt. | [116] |
| Mechanical Strength (Target) | Withstand 2,000–3,000 mmHg pressure | Target burst pressure for engineered vessels to resist physiological blood pressure. | [31] |
| Host-Dependent Cell Survival | >3-fold increase in cardiomyocyte graft size in rats vs. mice | Highlights host model as a critical variable for defining engraftment success. | [17] |
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Vascularization Experiments
| Item | Function / Application | Example & Notes |
|---|---|---|
| HUVECs | Forming the endothelial lining of vessels; primary cell source for in vitro vascular networks. | Human Umbilical Vein Endothelial Cells; widely used model. iPSC-ECs for patient-specific applications. |
| Supportive Stromal Cells | Enhance vascular stability, maturation, and prevent regression. | Human fibroblasts or mesenchymal stem cells (MSCs). Typically used in a 1:4 ratio with ECs. |
| Fibrin Hydrogel | A natural, cell-friendly hydrogel for 3D encapsulation of cells and patterned vascular structures. | Excellent biocompatibility and enables cell-driven remodeling. Common working concentration: 10-20 mg/mL. |
| Type I Collagen Hydrogel | Used for creating initial pre-patterned "endothelial cords" and as a major ECM component. | Provides structural integrity and bioadhesive signals. Neutralized before use. |
| VEGF & BMP-2 | Key cytokines to induce angiogenesis (VEGF) and couple it with osteogenesis (BMP-2) in bone models. | Often loaded into scaffolds via microparticles for sustained release. |
| PDMS Molds | For micro-patterning cells and hydrogels into specific geometries, such as parallel channels. | Enables creation of guided vascular networks instead of random self-assembly. |
| Flow Bioreactor | Provides physiological mechanical conditioning (shear stress) for maturing TEVGs in vitro. | Crucial for developing a confluent, functional, and anti-thrombogenic endothelial monolayer. |
| iBTA Mold (e.g., BTM1) | A medical device mold for the in vivo creation of completely autologous tissue grafts (Biotubes). | Enables scaffold-free, patient-specific graft generation without complex manufacturing [116]. |
Conclusion
Overcoming vascularization limitations requires a synergistic, interdisciplinary approach that integrates foundational biology with cutting-edge engineering. The convergence of advanced biofabrication like 4D bioprinting, the strategic use of iPSC-derived cells, and the development of smart, instructive biomaterials represents the most promising path forward. Future research must prioritize the creation of fully integrated, hierarchically branched vascular trees that can rapidly anastomose with host circulation, a feat that will unlock the fabrication of complex, metabolically demanding organs. The validation of these technologies through physiologically relevant in vitro microsystems will not only accelerate regenerative medicine but also revolutionize disease modeling and drug development. By systematically addressing the bottlenecks outlined across biological, methodological, and translational domains, the field is poised to finally breach the vascularization barrier and realize the full clinical potential of tissue engineering.
References
- 1. Insight on Oxygen-Supplying Biomaterials Used to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10295847/]
- 2. Oxygen and nutrient delivery in tissue engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC6852121/]
- 3. Controlled oxygen delivery to power tissue regeneration [https://www.nature.com/articles/s41467-024-48719-x]
- 4. Vascularization strategies in tissue engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8419139/]
- 5. Analytic Models of Oxygen and Nutrient Diffusion, Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5029285/]
- 6. Vascular Tissue Engineering: Challenges and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.721843/full]
- 7. Shaping nanoparticle diffusion through biological barriers ... [https://www.sciencedirect.com/science/article/pii/S2666934X21000246]
- 8. Ultrasound-Guided Photoacoustic Monitoring of Vascular ... [https://www.sciencedirect.com/science/article/pii/S0301562925003114]
- 9. A systematic review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12269465/]
- 10. Advancement in smart bone implants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146007/]
- 11. Overcoming big bottlenecks in vascular regeneration [https://www.nature.com/articles/s42003-024-06567-x]
- 12. In Vitro Strategies to Vascularize 3D Physiologically Relevant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8498873/]
- 13. Dead to me? Insights into a tumor's necrotic core [https://www.fredhutch.org/en/news/center-news/2023/02/new-research-insights-into-cancer-tumor-necrotic-core-.html]
- 14. Vasculogenesis and Angiogenesis: Molecular and Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548208/]
- 15. In Vitro Models of Vasculogenesis and Angiogenesis [https://www.nature.com/articles/3780252]
- 16. Medina et al., titled “3D bioprinting of ... [https://www.facebook.com/cellink3d/posts/creating-cardiac-tissue-of-clinically-relevant-size-has-been-a-longstanding-chal/1375579857905266/]
- 17. Engineered tissue vascularization and engraftment ... [https://www.nature.com/articles/s41598-022-23895-2]
- 18. THE ROLE OF MURAL CELLS IN VASCULAR BIOLOGY ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9989888/]
- 19. Interactions between mural cells and endothelial ... - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5278630/]
- 20. Vascular Smooth Muscle Cell Isolation and Culture from ... [https://en.bio-protocol.org/en/bpdetail?id=2045&type=0]
- 21. Isolation and Cultivation of Vascular Smooth Muscle Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10614493/]
- 22. A strategy to engineer vascularized tissue constructs by ... [https://www.sciencedirect.com/science/article/pii/S1742706121007443]
- 23. Engineered blood vessel networks connect to host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3208287/]
- 24. Engineered blood vessel networks connect to host ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/21835951/]
- 25. Vascular tissue engineering: progress, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5849079/]
- 26. Pre-vascularization of in vitro three-dimensional tissues ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961210001377]
- 27. Cell-Seeded Biomaterial Scaffolds: The Urgent Need for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8927652/]
- 28. Scaffolding in tissue engineering: general approaches and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2587658/]
- 29. Development of Scaffolds from Bio-Based Natural ... [https://www.mdpi.com/2310-2861/9/2/100]
- 30. The biomaterialist's task: scaffold biomaterials and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4295700/]
- 31. Vascular Tissue Engineering: Challenges and Requirements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8522984/]
- 32. Vascular tissue engineering: biodegradable scaffold platforms ... [https://stemcellres.biomedcentral.com/articles/10.1186/scrt156]
- 33. Scaffold-based developmental tissue engineering strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8050778/]
- 34. Three-Dimensional Printing and Bioprinting Strategies for ... [https://www.mdpi.com/2073-4360/17/17/2337]
- 35. 3D bioprinting for the production of a perfusable ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1484738/full]
- 36. Direct 3D bioprinting of perfusable vascular constructs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5300870/]
- 37. Advanced Strategies for 3D Bioprinting of Tissue and Organ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8708555/]
- 38. Bioprinting in Vascularization Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6305822/]
- 39. A Solution to the Clearance Problem of Sacrificial Material ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9865861/]
- 40. Typical Failure Modes In Microfluidics [https://www.alineinc.com/typical-failure-modes-in-microfluidics/]
- 41. Eden Materials - 3 common mistakes in microfluidics design [https://www.linkedin.com/posts/edenmaterials-fluidevice_3-common-mistakes-in-microfluidics-design-activity-7372260412211511296-aBEF]
- 42. Microfluidics System Development: Challenges and ... [https://mantadesign.com/microfluidics-system-development/]
- 43. Hierarchically vascularized and suturable tissue constructs ... [https://www.sciencedirect.com/science/article/pii/S1742706124005798]
- 44. Bone Graft Prefabrication Following the In Vivo Bioreactor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5078640/]
- 45. Review The Vascularised Chamber as an In Vivo Bioreactor [https://www.sciencedirect.com/science/article/abs/pii/S0167779918301446]
- 46. Ischaemic & Congested Flap: Diagnosis, Management & ... [https://www.theplasticsfella.com/ischaemic-and-congested-flap/]
- 47. In Vitro and In Vivo Bioreactor Strategies for Bone Defect ... [https://biomedres.us/fulltexts/BJSTR.MS.ID.004082.php]
- 48. Strategies for Avoiding Complications with Vascularized Bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2884885/]
- 49. An Experimental and Clinical Study of Flap Monitoring with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11273470/]
- 50. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 51. Directed differentiation of human mesenchymal stromal ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225005253]
- 52. Induced pluripotent stem cells in the treatment of ischemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371394/]
- 53. MSCs vs. iPSCs: Potential in therapeutic applications [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1005926/full]
- 54. Isolation of endothelial progenitor cells from human ... [https://www.nature.com/articles/s41366-025-01884-5]
- 55. Blood vessels bioengineered from induced pluripotent ... [https://pubmed.ncbi.nlm.nih.gov/40771988/]
- 56. Isolation and Culture of Primary Pericytes from Mouse - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021682/]
- 57. Science:开发出设计和三维打印复杂血管树的新工具 [https://news.bioon.com/article/b5ef884083dd.html]
- 58. Donor Variability and Seeding Density Shape NK-Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384078/]
- 59. Addressing Variability in Donor Tissues and Cells - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK544028/]
- 60. Challenges to Cell Expansion for Allogenic Cell Therapies [https://www.biopharminternational.com/view/challenges-to-cell-expansion-for-allogenic-cell-therapies]
- 61. Challenges of Cell Counting in Cell Therapy Products - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11520012/]
- 62. Flow Cytometry Troubleshooting Guide [https://fluorofinder.com/flow-cytometry-troubleshooting/]
- 63. Bioprinting Vascularized Constructs for Clinical Relevance [https://www.mdpi.com/2310-2861/11/8/636]
- 64. 3D-printed blood vessels bring artificial organs closer to reality [https://wyss.harvard.edu/news/3d-printed-blood-vessels-bring-artificial-organs-closer-to-reality/]
- 65. Mechanical strategies to promote vascularization for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11441985/]
- 66. Engineering in vitro vascular microsystems [https://www.nature.com/articles/s41378-025-00956-w]
- 67. The mechanical characterization of blood vessels and their ... [https://www.sciencedirect.com/science/article/pii/S2590006421000144]
- 68. Bioprinting for vascular and vascularized tissue biofabrication [https://www.sciencedirect.com/science/article/abs/pii/S1742706117300351]
- 69. 3D Bioprinting for Vascularization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215405/]
- 70. Mature vessel networks in engineered tissue promote graft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6386696/]
- 71. Mature vessel networks in engineered tissue promote graft-host ... [https://www.omicsdi.org/dataset/biostudies-literature/S-EPMC6386696]
- 72. Patterned human microvascular grafts enable rapid ... [https://www.nature.com/articles/s41467-019-08388-7]
- 73. Current Strategies for Engineered Vascular Grafts and ... [https://www.mdpi.com/2073-4360/15/9/2015]
- 74. Rapid remodeling observed at mid-term in-vivo study of a ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-022-00313-9]
- 75. Pre-vascularized dermis model for fast and functional ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961218307956]
- 76. The innate immune system contributes to tissue- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4447224/]
- 77. Engineering the Future of Stem Cells in Vascular ... [https://link.springer.com/article/10.1007/s12015-025-10968-8]
- 78. Engineering vascular grafts from decellularized plants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344396/]
- 79. Can the GORE-TEX ® Vascular Grafts be resterilized? [https://www.goremedical.com/ap/products/vgbifur---faq/faq]
- 80. Development of Electrospinning Setup for Vascular Tissue- ... [https://pubmed.ncbi.nlm.nih.gov/39825992/]
- 81. Vascularization Strategies for Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2817665/]
- 82. Scaling up spatial transcriptomics for large-sized tissues [https://www.nature.com/articles/s41592-025-02770-8]
- 83. Frontiers | Biomaterials in tissue repair and regeneration: key insights from extracellular matrix biology [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 84. Frontiers | Recent advances in bionic scaffolds for cartilage tissue engineering [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1625550/full]
- 85. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 86. Mechanobiologically-optimized non-resorbable artificial ... [https://www.nature.com/articles/s41467-025-64466-z]
- 87. Frontiers | Editorial: Biomaterials and biological regulation for bone tissue remodeling and regeneration [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1582215/full]
- 88. Material synthesis and design optimization of biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954756/]
- 89. Vascularized microfluidic organ-chips for drug screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6082713/]
- 90. State-of-the-Art Strategies for the Vascularization of Three- ... [https://www.vsijournal.org/journal/view.html?doi=10.5758/vsi.2019.35.2.77]
- 91. In vitro pre-vascularization strategies for tissue engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7575626/]
- 92. Dynamic microphysiological system chip platform for high- ... [https://www.sciencedirect.com/science/article/pii/S2452199X24001853]
- 93. Microphysiological Systems (“Organs‐on‐Chips”) for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5504483/]
- 94. An eighteen-organ microphysiological system coupling a ... [https://www.nature.com/articles/s41378-025-00933-3]
- 95. Modern experimental methods for assessing the effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318997/]
- 96. Society for Vascular Surgery practice guidelines for atherosclerotic... [https://pubmed.ncbi.nlm.nih.gov/25638515/]
- 97. Top Mistakes in Experimental Design for Biologists [https://bigomics.ch/blog/common-mistakes-biologists-make-when-designing-experiments-and-analyzing-data/]
- 98. A short discourse on vascular tissue engineering [https://www.nature.com/articles/s41536-017-0011-6]
- 99. Preclinical Evaluation and Advancements in Vascularized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292946/]
- 100. 3D bioprinted thick hepatic constructs with vascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049840/]
- 101. Methods to evaluate vascular function: a crucial approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9120812/]
- 102. Noninvasive Assessment of Vascular Function [https://www.sciencedirect.com/science/article/pii/S2772374724003636]
- 103. Guidelines for the measurement of vascular function and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321813/]
- 104. Harnessing conserved signaling and metabolic pathways ... [https://www.nature.com/articles/s41536-022-00246-3]
- 105. A Comprehensive Framework for Kidney Function Assessment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446987/]
- 106. Mitigating challenges and expanding the future of vascular ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.1079421/full]
- 107. Early resistance rehabilitation improves functional ... [https://www.nature.com/articles/s41536-024-00377-9]
- 108. Mining Cell Therapy to Repair Injured Bones and Tendons [https://www.cedars-sinai.org/newsroom/mining-cell-therapy-to-repair-injured-bones-and-tendons/]
- 109. Bone regeneration: stem cell therapies and clinical studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4373328/]
- 110. Therapeutic approaches for cardiac regeneration and repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC6241533/]
- 111. Case report: Long-term follow-up of a large full-thickness ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1004155/full]
- 112. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 113. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 114. Ink-structing the future of vascular tissue engineering [https://link.springer.com/article/10.1007/s42242-024-00270-w]
- 115. Recent advancement in vascularized tissue-engineered bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679779/]
- 116. Safety and efficacy of an iBTA-induced autologous Biotube ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0335900]
- 117. 3D Bioprinting of Vascularized Tissues for in vitro and in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.664188/full]