Paracrine Signaling: The Primary Mechanism Driving Adult Stem Cell Therapy
This article comprehensively reviews the paradigm shift in understanding adult stem cell therapy, where paracrine signaling is now recognized as a primary mechanism of action, surpassing the initial focus on...
Paracrine Signaling: The Primary Mechanism Driving Adult Stem Cell Therapy
Abstract
This article comprehensively reviews the paradigm shift in understanding adult stem cell therapy, where paracrine signaling is now recognized as a primary mechanism of action, surpassing the initial focus on direct differentiation. Tailored for researchers and drug development professionals, it explores the foundational biology of stem cell-secreted factors, methodologies for studying and harnessing these mechanisms, strategies to overcome therapeutic challenges, and the current clinical validation landscape. The synthesis of preclinical and clinical evidence underscores the potential of paracrine factor-based approaches, including cell-free therapies, to revolutionize regenerative medicine for conditions like heart failure, neurodegenerative disorders, and autoimmune diseases.
Deconstructing the Paracrine Secretome: Key Mediators and Mechanisms
The foundational paradigm of adult stem cell therapy has undergone a significant evolution over the past two decades. Initial research was predominantly anchored in the concept of direct differentiation, wherein transplanted stem cells were hypothesized to engraft and transdifferentiate into functional target cells, thereby directly regenerating damaged tissues. However, a confluence of animal studies and preliminary human trials has compellingly demonstrated that the functional benefits observed post-therapy are frequently disproportionate to the frequency of stem cell engraftment and direct differentiation. This discrepancy has catalyzed a paradigm shift towards the understanding that the secretion of bioactive molecules by stem cells—acting via paracrine mechanisms—plays a predominant role in mediating therapeutic effects. This whitepaper delineates the evidence driving this shift, details the core paracrine mechanisms involved, and outlines the advanced experimental and computational methodologies essential for profiling these complex signaling networks, thereby providing a strategic framework for researchers and drug development professionals in the field of regenerative medicine.
The initial premise of adult stem cell therapy was elegantly straightforward: the transplantation of stem cells would lead to their direct incorporation into damaged tissues, where they would differentiate into cardiomyocytes, vascular endothelial cells, or neurons to replace those that were lost or dysfunctional [1]. This direct differentiation hypothesis was supported by early, promising studies. For instance, research by Anversa's laboratory suggested that Lin− c-kit+ bone marrow-derived cells could regenerate a significant portion of infarcted mouse myocardium with newly formed cardiomyocytes [1]. Similarly, Tomita et al. showed that mesenchymal stem cells (MSCs) pretreated with 5-azacytidine could differentiate into cardiac-like muscle cells in cryoinjured rat hearts [1].
However, the reproducibility of these findings became a subject of intense scientific debate. Subsequent investigations frequently failed to detect substantial long-term engraftment or robust transdifferentiation of transplanted cells [1]. The central challenge to the direct differentiation model was the repeated observation that significant improvements in organ function—such as enhanced cardiac output after myocardial infarction—occurred despite a notably low number of newly generated, donor-derived functional cells [1]. This critical inconsistency necessitated a re-evaluation of the fundamental mechanisms of action.
The alternative hypothesis, which has now gained substantial traction, posits that the transplanted stem cells function as bioactive "factories," secreting a plethora of soluble factors that act locally on resident cells in a paracrine fashion. These factors are now understood to orchestrate therapeutic outcomes through cytoprotection, stimulation of neovascularization, modulation of the immune response, and activation of endogenous resident stem cells, rather than through large-scale direct replacement of lost tissue [1]. This whitepaper will explore the evidence for this paradigm shift and its implications for the future of regenerative medicine.
Establishing the Paracrine Hypothesis: Key Evidence
The transition from the direct differentiation model to the paracrine signaling paradigm is supported by multiple lines of rigorous experimental evidence.
Functional Benefits Without Significant Engraftment
A cornerstone of the paracrine argument is the dissociation between cell engraftment and functional recovery. In many animal models of disease, the administration of adult stem cells results in measurable functional improvement, even though the transplanted cells are only present transiently. This suggests that the cells initiate a reparative process during their short-term residence, rather than by becoming a permanent part of the organ architecture.
Efficacy of Conditioned Medium
Perhaps the most compelling evidence for the paracrine hypothesis comes from experiments utilizing conditioned medium (CM) collected from stem cell cultures. If the therapeutic effect were solely due to direct differentiation, then the cell-free CM should be ineffective. Contrarily, multiple studies have demonstrated that CM alone can recapitulate the benefits of whole-cell therapy.
- Cardioprotection: Culture medium conditioned by MSCs, particularly those overexpressing Akt-1 (Akt-MSCs), was shown to reduce apoptosis and necrosis in isolated rat cardiomyocytes subjected to low oxygen tension. This cytoprotective effect was also confirmed in vivo in a rat model of myocardial infarction [1].
- Neovascularization and Repair: Injection of CM from bone marrow mononuclear cells (BM-MNCs) into acutely infarcted hearts resulted in increased capillary density, decreased infarct size, and improved cardiac function compared to controls [1].
- Osteogenesis: Studies on dental-derived stem cells, such as SHEDs (stem cells from human exfoliated deciduous teeth), have indicated that they can mediate osteogenesis through paracrine mechanisms rather than solely through direct differentiation [2].
These findings collectively indicate that the soluble factors secreted by stem cells are both necessary and sufficient to elicit significant therapeutic effects.
Complex Paracrine Signaling in Pathophysiology
The importance of paracrine signaling is not limited to regenerative therapy but is also a critical mechanism in disease processes such as cancer metastasis. A stark example is the EGF/CSF-1 paracrine loop between mammary tumor cells and macrophages. Tumor cells secrete CSF-1, which activates macrophages and stimulates their secretion of EGF. The EGF, in turn, promotes the motility and invasiveness of the tumor cells [3]. This sophisticated cell-cell communication system highlights the potency of paracrine signaling and provides a rationale for targeting such pathways therapeutically. Computational modeling of this loop has shown it to be essential for the co-migration of these cell types, and blocking either the EGF or CSF-1 receptor drastically reduces cell invasion and intravasation [3].
Table 1: Key Experimental Evidence Supporting the Paracrine Hypothesis
| Experimental Approach | Key Finding | Implication |
|---|---|---|
| Cell Engraftment Tracking | Functional improvement occurs despite low long-term engraftment of transplanted cells [1]. | Therapeutic effects are not primarily due to direct tissue replacement by donor cells. |
| Conditioned Medium (CM) Studies | CM from MSCs and other stem cells reproduces therapeutic effects (e.g., cytoprotection, angiogenesis) in disease models [1] [2]. | Soluble factors secreted by cells are sufficient to mediate repair. |
| Genetic Manipulation | CM from Akt-overexpressing MSCs shows enhanced cytoprotective potency [1]. | The paracrine profile and efficacy of stem cells can be genetically modulated. |
| Receptor Blocking Studies | Blocking EGF or CSF-1 receptors disrupts tumor cell-macrophage co-migration and invasion [3]. | Validates specific ligand-receptor pairs as critical paracrine mediators and therapeutic targets. |
Core Mechanisms of Paracrine Action
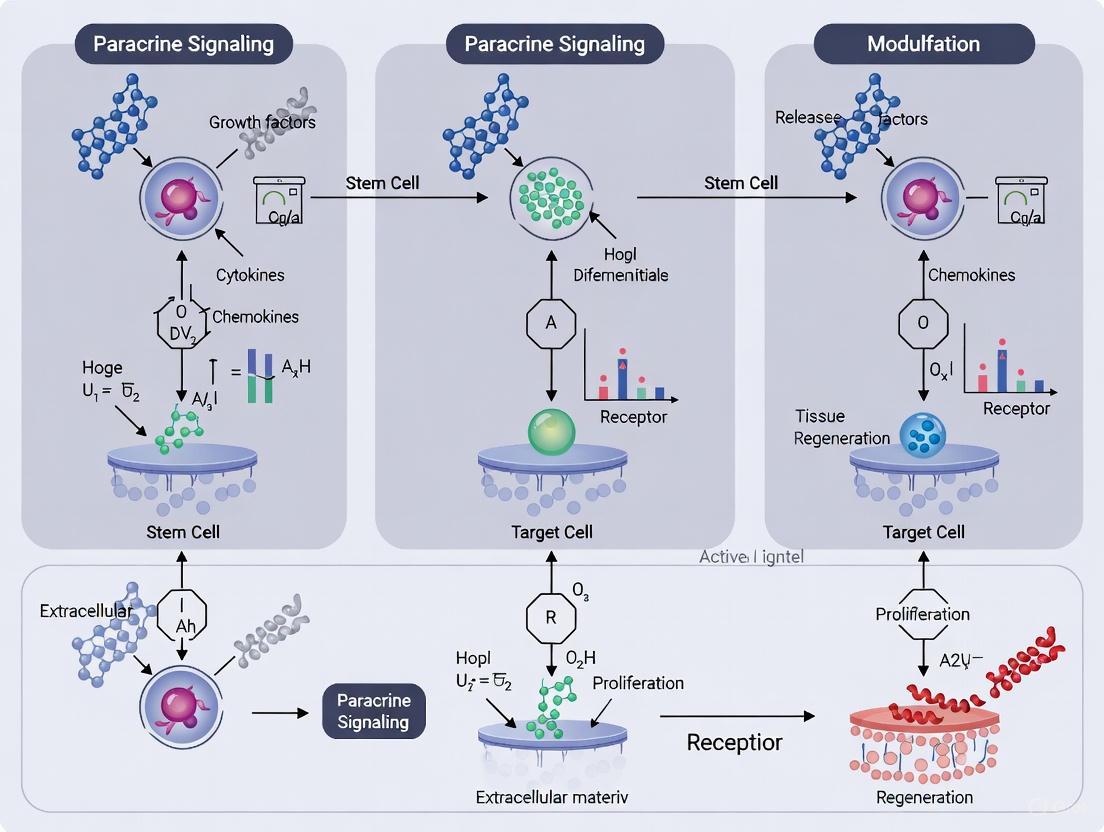
The paracrine factors released by adult stem cells orchestrate tissue repair through several coordinated mechanisms. The following diagram illustrates the key signaling pathways and their primary functions in cardiac repair, based on findings from adult stem cell therapy research.
The therapeutic impact of stem cell paracrine signaling is a summation of multiple distinct but interconnected biological processes.
Myocardial Protection (Cytoprotection)
An immediate effect of stem cell paracrine signaling in an ischemic environment is the protection of imperiled host cells from apoptosis and necrosis. Soluble factors such as Insulin-like Growth Factor-1 (IGF-1), Adrenomedullin (ADM), and Thymosin-β4 (TMSB4) have been identified as key mediators of this cytoprotection [1]. They act by activating pro-survival signaling cascades, such as the PI3K/Akt pathway, within endangered cardiomyocytes, thereby increasing their resistance to ischemic stress. This cytoprotective effect preserves viable tissue in the peri-infarct zone, which is critical for maintaining overall cardiac function and limiting adverse remodeling.
Stimulation of Neovascularization
A well-documented and reproducible effect of stem cell therapy is the enhancement of blood vessel formation in ischemic tissues, which restores oxygen and nutrient supply. This is largely driven by the secretion of potent angiogenic factors, including:
- Vascular Endothelial Growth Factor (VEGF)
- Basic Fibroblast Growth Factor (b-FGF or FGF2)
- Hepatocyte Growth Factor (HGF)
- Angiopoietin-1 (AGPT1) [1]
These factors promote the proliferation, migration, and tube formation of existing endothelial cells, leading to the formation of new capillaries (angiogenesis) and contributing to the stabilization of the newly formed vascular networks.
Activation of Endogenous Regeneration
Rather than solely acting as direct building blocks, transplanted stem cells can stimulate the body's own regenerative capacity. The release of factors like Stem Cell-Derived Factor-1 (SDF-1), Kit Ligand (Stem Cell Factor), HGF, and IGF-1 can activate resident tissue-specific stem and progenitor cells, such as resident cardiac stem cells (CSCs) [1]. This activation promotes the proliferation and differentiation of these endogenous pools, which then contribute to the regeneration of functional tissue in a more physiologically integrated manner.
Immunomodulation and Anti-Fibrotic Effects
The secretome of stem cells, particularly MSCs, has powerful effects on the immune system. Factors such as Transforming Growth Factor-β (TGF-β), prostaglandin E2 (PGE2), and interleukins can modulate the activity of T-cells, B-cells, and macrophages, polarizing them towards a more anti-inflammatory and pro-regenerative phenotype [2]. This suppression of detrimental inflammation creates a more favorable microenvironment for repair. Furthermore, by modulating the activity of fibroblasts and the deposition of extracellular matrix, paracrine signaling can also attenuate pathological fibrotic scarring, which impairs tissue compliance and function.
Table 2: Key Paracrine Factors and Their Functions in Tissue Repair
| Secreted Factor | Abbreviation | Primary Proposed Functions in Repair |
|---|---|---|
| Vascular Endothelial Growth Factor | VEGF | Angiogenesis, Cytoprotection, Cell proliferation & migration [1] |
| Insulin-like Growth Factor-1 | IGF-1 | Cytoprotection, Cell migration, Improved contractility [1] [4] |
| Hepatocyte Growth Factor | HGF | Cytoprotection, Angiogenesis, Cell migration [1] |
| Fibroblast Growth Factor-2 | FGF2 | Angiogenesis, Cell proliferation & migration [1] [4] |
| Stem Cell-Derived Factor-1 | SDF-1 | Progenitor cell homing [1] |
| Transforming Growth Factor-β | TGF-β | Immunomodulation, Vessel maturation, Cell proliferation [1] [5] [4] |
| Thymosin-β4 | TMSB4 | Cell migration, Cytoprotection [1] |
Advanced Methodologies for Profiling Paracrine Signaling
The investigation of paracrine mechanisms requires a sophisticated toolkit that moves beyond traditional cell culture and histology. The following workflow outlines a multi-faceted approach to experimentally validate paracrine effects, from in vitro conditioning to in vivo functional assessment.
Experimental Protocols for Paracrine Analysis
A. Generation of Conditioned Medium (CM)
Principle: To collect the soluble factors secreted by stem cells for use in downstream functional and analytical assays.
Detailed Protocol:
- Cell Culture: Culture the stem cells of interest (e.g., MSCs, DPSCs) to 70-80% confluence in standard growth medium.
- Wash: Thoroughly wash the cells with phosphate-buffered saline (PBS) to remove serum-derived proteins.
- Serum-Free Incubation: Incubate the cells with serum-free medium for 24-48 hours. To mimic the ischemic stress encountered after transplantation, hypoxia (e.g., 1% O₂) can be applied during this period, as it is known to increase the production of many therapeutic factors [1].
- Collection: Collect the medium and centrifuge (e.g., 2000 × g for 10 minutes) to remove any cellular debris.
- Concentration (Optional): Concentrate the CM using centrifugal filter units (e.g., 3-5 kDa molecular weight cutoff) to augment the concentration of secreted factors.
- Storage: Aliquot and store the CM at -80°C until use. A control medium (serum-free medium incubated without cells) must be prepared and processed identically.
B. In Vitro Functional Assays with CM
1. Cytoprotection Assay (e.g., Cardiomyocyte Apoptosis)
- Objective: To quantify the ability of CM to protect cells from induced apoptosis.
- Method:
- Isolate primary cardiomyocytes from neonatal rats or use a relevant cardiomyocyte cell line.
- Pre-treat cells with either CM or control medium for 1-2 hours.
- Expose the cells to a lethal insult, such as low oxygen tension (hypoxia) or hydrogen peroxide (H₂O₂) to simulate ischemia/reperfusion injury.
- After 12-24 hours, quantify apoptosis using TUNEL staining or by measuring the activity of executioner caspases (e.g., Caspase-3/7) with a luminescent assay [1].
2. Angiogenesis Assay (e.g., Endothelial Tube Formation)
- Objective: To assess the pro-angiogenic potential of CM.
- Method:
- Pre-chill µ-Slide Angiogenesis plates and pipette tips.
- Thaw Growth Factor Reduced Matrigel on ice and carefully pipette it into each well. Incubate the plate at 37°C for 30 minutes to allow polymerization.
- Seed Human Umbilical Vein Endothelial Cells (HUVECs) onto the surface of the Matrigel in either CM or control medium.
- Incubate for 4-16 hours and then image the formed capillary-like structures using a phase-contrast microscope.
- Quantify the total tube length, number of master junctions, and number of meshes per field using image analysis software (e.g., ImageJ with the Angiogenesis Analyzer plugin).
Computational Inference of Cell-Cell Communication
The advent of single-cell RNA-sequencing (scRNA-seq) has enabled the systematic inference of paracrine signaling networks within complex tissues. Tools like CellChat have been developed specifically for this purpose [6].
Principle: CellChat quantitatively infers intercellular communication probabilities by integrating scRNA-seq data with a manually curated database of ligand-receptor interactions (CellChatDB). This database includes heteromeric complexes and key co-factors, providing a more biologically accurate representation than simple ligand-receptor pairs [6].
Workflow:
- Input: A scRNA-seq dataset with cell group labels (either user-defined or identified computationally).
- Database Matching: CellChat overlays the gene expression data onto its knowledgebase of validated molecular interactions.
- Probability Calculation: The communication probability for each ligand-receptor pair between two cell groups is computed based on the average expression of the ligand in the "sender" population and the receptor (and its cofactors) in the "receiver" population, employing a mass action-based model.
- Statistical Validation: The significance of the inferred interactions is assessed by comparing them to a null distribution generated through random permutation of cell labels.
- Systems-Level Analysis: The resulting network is analyzed using methods from graph theory (e.g., centrality measures to identify key senders/receivers) and pattern recognition (to identify coordinated signaling modules) [6].
Application: This approach can delineate conserved and context-specific signaling pathways, predict key incoming/outgoing signals for specific cell types, and systematically compare communication networks across different biological conditions (e.g., healthy vs. diseased, pre- vs. post-treatment) [6].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Tools for Paracrine Signaling Research
| Reagent / Tool | Function / Application | Specific Examples / Notes |
|---|---|---|
| Serum-Free Media | Base for generating conditioned medium; eliminates confounding factors from serum. | DMEM, RPMI-1640. Must be optimized for cell type to maintain viability during conditioning. |
| Cytokine/Growth Factor Arrays | Multiplexed profiling of secreted proteins in conditioned medium. | Proteome Profiler Arrays; allow simultaneous detection of dozens of factors [1]. |
| ELISA Kits | Quantitative, specific measurement of individual secreted factors. | Commercial kits for VEGF, IGF-1, HGF, etc.; used for validating array results. |
| Extracellular Matrix (ECM) | Substrate for 3D functional assays like angiogenesis and cell migration. | Growth Factor Reduced Matrigel is standard for endothelial tube formation assays. |
| Primary Cells / Cell Lines | Targets for assessing CM bioactivity. | HUVECs (angiogenesis), primary cardiomyocytes (cytoprotection), fibroblast lines (fibrosis) [1] [5]. |
| scRNA-seq Platform | Generation of input data for computational inference of cell-cell communication. | 10x Genomics; required for tools like CellChat to map ligand-receptor expression to cell types [6]. |
| CellChat R Package | Computational inference and systems-level analysis of intercellular communication networks from scRNA-seq data. | Uses a curated database (CellChatDB) that includes heteromeric complexes [6]. |
| Neutralizing Antibodies / Small Molecule Inhibitors | Functional validation of specific ligand-receptor pairs. | e.g., anti-VEGF antibody, EGF/CSF-1 receptor inhibitors (e.g., Erlotinib, BLZ945) [3]. |
The paradigm shift from direct differentiation to paracrine signaling represents a fundamental maturation in our understanding of how adult stem cell therapies mediate their benefits. This refined model posits that stem cells are sophisticated signaling entities that orchestrate tissue repair by modulating the local microenvironment. This new understanding has profound implications for the future of regenerative medicine:
- Next-Generation Therapeutics: The focus is shifting from the cells themselves to their secreted products. This includes the development of "cell-free" therapies using engineered exosomes or purified combinations of key paracrine factors, which could offer improved safety, scalability, and storage profiles over live cell transplants.
- Potency Optimization: Strategies are being developed to enhance the therapeutic potency of stem cells through "priming" or genetic modification (e.g., Akt-overexpression) to boost the secretion of beneficial factors [1].
- Precision Targeting: As computational tools like CellChat [6] continue to map the complex signaling networks in health and disease, we can identify critical, context-specific nodal points for intervention. This will enable the development of highly targeted drugs, such as monoclonal antibodies or small molecules, to modulate these key paracrine pathways.
In conclusion, embracing the paracrine paradigm does not diminish the value of stem cell therapy but rather refines it. It provides a more robust and nuanced framework for explaining experimental observations and directs the field toward more controlled, predictable, and effective regenerative strategies. The future lies in harnessing and optimizing this sophisticated cellular communication system to develop a new generation of therapeutics for a wide range of degenerative diseases and injuries.
The therapeutic potential of adult stem cells, particularly Mesenchymal Stem Cells (MSCs), was initially attributed to their ability to differentiate and replace damaged cells. However, a paradigm shift has occurred in regenerative medicine, with growing evidence demonstrating that their benefits are predominantly mediated through paracrine signaling [7]. Rather than integrating into tissues, transplanted stem cells release a complex mixture of bioactive molecules that orchestrate repair processes. This mixture, collectively known as the secretome, has emerged as a critical mediator of tissue regeneration, immunomodulation, and cellular homeostasis [8] [7].
The secretome encompasses a diverse array of components, including soluble proteins, cytokines, growth factors, and Extracellular Vesicles (EVs) such as exosomes and microvesicles [7]. These elements act as a coordinated communication network, allowing stem cells to influence their local microenvironment. Upon release, these factors can modulate immune responses, enhance angiogenesis, protect surviving cells from apoptosis, and activate resident progenitor cells [1] [9]. This cell-free approach presents significant advantages over whole-cell therapies, including reduced risks of immune rejection, tumorigenicity, and simplified manufacturing and storage logistics [10] [7]. Cataloging these components and understanding their functions is essential for harnessing the full potential of secretome-based therapeutics in adult stem cell research and drug development.
Composition of the Stem Cell Secretome
The stem cell secretome is a highly complex biological entity. Its composition is dynamic and can be influenced by the source of the MSCs (e.g., bone marrow, umbilical cord, adipose tissue), the donor's health status, and the culture conditions used during production [11] [7]. The secretome can be broadly categorized into two functional delivery systems: soluble factors and encapsulated factors within extracellular vesicles.
Table 1: Major Soluble Factors in the MSC Secretome and Their Functions
| Factor Category | Key Examples | Primary Documented Functions | Therapeutic Context |
|---|---|---|---|
| Pro-angiogenic Factors | VEGF, HGF, IGF-1, FGF2 [1] [7] | Stimulate blood vessel formation, promote endothelial cell survival and migration. | Cardiac repair, wound healing, limb ischemia [1] |
| Immunomodulatory Factors | IL-10, TSG-6, PGE2, TGF-β [10] [7] | Suppress pro-inflammatory cytokine release, polarize macrophages to an M2 phenotype, inhibit T-cell proliferation. | Multiple sclerosis, Crohn's disease, GvHD, organ injury [11] [10] |
| Anti-apoptotic & Pro-survival Factors | IGF-1, HGF, bFGF, STC-1 [1] [7] | Activate pro-survival pathways (e.g., PI3K/Akt), reduce programmed cell death in stressed tissues. | Myocardial infarction, acute kidney injury, stroke [1] |
| Anti-fibrotic Factors | HGF, MMPs, decorin [11] [1] | Degrade excess extracellular matrix, inhibit TGF-β1 mediated pro-fibrotic signaling. | Liver fibrosis, pulmonary fibrosis, chronic kidney disease [11] |
Table 2: Key Components of Extracellular Vesicles (EVs) in the Secretome
| EV Component Type | Key Examples | Function & Mechanism | Experimental Evidence |
|---|---|---|---|
| Proteins | Tetraspanins (CD9, CD63, CD81), Annexins, Flotillins [12] | Define EV subtypes, facilitate membrane fusion and recipient cell uptake. | Single-particle imaging confirms distinct sEV subtypes based on tetraspanin composition [12] |
| Lipids | Cholesterol, Sphingomyelin, Phosphatidylserine [12] | Determine membrane fluidity/packing, influence stability and cellular uptake. | CD63+ sEVs exhibit greater membrane packing than CD81+ sEVs [12] |
| Nucleic Acids (RNAs) | mRNA, miRNA (e.g., miR-21, miR-146a), tRNA [7] | Modify gene expression in recipient cells; miR-21 modulates inflammatory pathways. | Engineered MSCs produce EVs with enriched miRNAs for targeted therapy [7] |
Extracellular Vesicles: Specialized Paracrine Carriers
Extracellular Vesicles (EVs), particularly small EVs (sEVs), are now recognized as primary effectors of the secretome's therapeutic function. These lipid-bilayer nanoparticles facilitate intercellular communication by transferring proteins, lipids, and nucleic acids to recipient cells [12] [7]. The internalization of sEVs by recipient cells is a regulated process. Recent research using single-particle tracking and super-resolution microscopy has shown that paracrine adhesion signaling facilitates sEV uptake. Binding of sEVs to the recipient cell plasma membrane triggers Ca2+ mobilization via Src family kinases and phospholipase Cγ, leading to the activation of calcineurin and dynamin, which promotes sEV internalization primarily via clathrin-independent endocytosis [12].
Methodologies for Secretome Analysis and Functional Characterization
Rigorous and standardized methodologies are required to isolate, characterize, and validate the secretome's composition and function. The following workflow outlines the key experimental stages, from cell culture to functional analysis.
Experimental Protocol: Secretome Collection and Analysis
1. Cell Culture and Pre-conditioning:
- Source and Culture: Isolate and culture MSCs from a chosen source (e.g., human gingiva, bone marrow, umbilical cord). Use defined, xeno-free culture medium to avoid contamination with animal serum-derived factors [10]. Cells are typically cultured to 70-80% confluence.
- Pre-conditioning: To enhance the therapeutic potency of the secretome, MSCs can be subjected to pre-conditioning stimuli. Common methods include exposure to hypoxic conditions (e.g., 1-3% O2) or priming with inflammatory cytokines (e.g., IFN-γ, TNF-α) [1] [8]. This mimics the inflammatory or ischemic microenvironment of damaged tissue and can significantly alter the secretome's composition, enriching it with beneficial factors [9].
2. Secretome Collection:
- Once MSCs reach the desired confluence, wash the cells thoroughly with phosphate-buffered saline (PBS) to remove residual serum.
- Incubate the cells with a serum-free basal medium for 24-48 hours.
- Collect the Conditioned Medium (CM), which contains the soluble secretome and EVs released by the cells [10].
3. Fractionation and Isolation:
- Concentration: The CM is concentrated using ultrafiltration devices (e.g., centrifugal filters with a 3-5 kDa molecular weight cut-off) [10].
- EV Isolation: Several techniques can be employed to isolate EVs from the soluble fraction:
- Ultracentrifugation: The gold standard, involving sequential centrifugation steps at high speeds (e.g., 100,000× g) to pellet EVs [12].
- Size-Exclusion Chromatography (SEC): Uses columns with porous beads to separate EVs from soluble proteins based on size. This method, using tools like qEVoriginal columns, is effective for obtaining high-purity EV preparations [10].
- Tangential Flow Filtration (TFF): A scalable method suitable for industrial-grade biomanufacturing of EVs for clinical applications [7].
4. Characterization and Analysis:
- Nanoparticle Tracking Analysis (NTA): Determines the particle size distribution and concentration of EVs in suspension [10].
- Transmission Electron Microscopy (TEM): Provides visual confirmation of EV morphology and size via negative staining [10] [12].
- Western Blot: Confirms the presence of classic EV marker proteins (e.g., CD9, CD63, CD81, TSG101) and the absence of negative markers (e.g., calnexin) [10] [12].
- Proteomic and Transcriptomic Analysis: Liquid chromatography-mass spectrometry (LC-MS/MS) and next-generation RNA sequencing (RNA-Seq) are used to comprehensively profile the protein, miRNA, and mRNA content of the secretome and its subsets [10] [7].
5. Functional Validation (In Vitro and In Vivo):
- In Vitro Assays:
- Immunomodulation: Co-culture secretome-treated macrophages with inflammatory stimuli (e.g., LPS) and measure cytokine secretion (e.g., TNF-α, IL-10) via ELISA. Assess macrophage polarization flow cytometry [10].
- Myogenic/Cardiac Repair: Treat relevant progenitor cells (e.g., skeletal muscle progenitors, cardiomyocytes) with the secretome and quantify the expression of myogenic transcription factors (e.g., MyoD, Myogenin) via qPCR or immunofluorescence [10] [1].
- In Vivo Models:
- Administer the secretome/EVs into animal models of disease (e.g., rat tongue defect model for muscle regeneration [10], rodent myocardial infarction model for cardiac repair [1], or mouse models of BPD/NEC for neonatal disorders [7]).
- Evaluate outcomes through histological analysis, functional measurements (e.g., echocardiography), and assessment of scar size, inflammation, and angiogenesis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Secretome Research
| Reagent / Tool | Specific Example | Function in Secretome Research |
|---|---|---|
| Xeno-Free Cell Culture Medium | STEMCELL Technologies' StemiMacs MSC XF Medium | Provides a defined, animal-serum-free environment for MSC expansion to prevent contaminating bovine EVs in the secretome [10]. |
| Size-Exclusion Chromatography Columns | IZON Science's qEVoriginal columns (35 nm) | Isolates high-purity small Extracellular Vesicles (sEVs) from soluble proteins and other contaminants in conditioned medium [10]. |
| Ultrafiltration Devices | Amicon Ultra Centrifugal Filters (e.g., 10 kDa MWCO) | Concentrates the dilute conditioned medium collected from MSC cultures prior to further fractionation or analysis [10]. |
| Nanoparticle Tracking Analyzer | Malvern Panalytical's NanoSight NS300 | Characterizes the concentration and size distribution of EV preparations [10]. |
| Membrane Packing/Defect Probe | ApoC-TAMRA (Apolipoprotein C-I derived peptide) | Quantifies the membrane packing density and fluidity of different sEV subtypes, a key physical property [12]. |
| Tetraspanin Reporter Cell Lines | MSCs stably expressing CD63-mGFP and CD9-Halo7-TMR | Enables single-particle imaging and tracking of distinct sEV subpopulations released by donor cells [12]. |
Signaling Pathways Activated by the Secretome
The therapeutic effects of the secretome are mediated through the activation of multiple, interconnected signaling pathways in recipient cells. The following diagram summarizes the key signaling cascades triggered by secretome components leading to core therapeutic outcomes.
The activation of these pathways is initiated when ligands within the secretome, such as IGF-1, VEGF, and HGF, bind to their respective receptors on recipient cells. For instance, IGF-1 binding to the IGF-1 receptor triggers the PI3K/Akt pathway, a critical pro-survival signal that inhibits apoptosis in cardiomyocytes and neurons after injury [1]. Similarly, FGF2 activates the ERK1/2 pathway, promoting cell proliferation and tissue repair [1]. Furthermore, modulation of the Wnt/β-catenin and Notch signaling pathways by secretome components can influence the fate of resident stem cells, promoting endogenous regeneration [10]. A key anti-inflammatory mechanism involves the suppression of the NF-κB pathway by factors like TSG-6 and IL-10, leading to reduced production of pro-inflammatory cytokines such as TNF-α [7]. The transfer of regulatory miRNAs via EVs can also post-transcriptionally repress genes involved in cell death and inflammation, providing another layer of control [7].
The systematic cataloging of the stem cell secretome—encompassing its diverse cytokines, growth factors, and extracellular vesicles—has fundamentally advanced our understanding of paracrine mechanisms in adult stem cell therapy. Moving beyond the initial cell-replacement paradigm, the field now recognizes the secretome as a powerful, cell-free therapeutic agent capable of modulating inflammation, protecting at-risk tissue, and activating endogenous repair programs. The continued refinement of isolation protocols, analytical techniques, and functional assays, as outlined in this guide, is crucial for standardizing secretome-based products. As research progresses, the strategic engineering of MSCs to produce enriched or targeted secretomes holds the promise of a new class of highly effective, off-the-shelf regenerative medicines for a wide spectrum of diseases.
The therapeutic potential of adult stem cells, particularly Mesenchymal Stem/Stromal Cells (MSCs), extends far beyond their capacity for direct differentiation and tissue repopulation. A paradigm shift has occurred in the field, with research increasingly demonstrating that the primary mechanism through which MSCs exert their beneficial effects is paracrine signaling—the secretion of bioactive molecules that modulate the host environment [13]. These secreted factors, collectively known as the secretome, facilitate tissue repair and regeneration by orchestrating three core protective mechanisms: cytoprotection (enhancing cell survival), angiogenesis (promoting new blood vessel formation), and immunomodulation (regulating immune responses) [14] [15]. This in-depth technical guide synthesizes current research to elucidate these mechanisms, providing researchers and drug development professionals with a detailed framework of the molecular pathways, experimental methodologies, and reagent tools driving innovation in stem cell-based therapeutics.
The MSC secretome is a composite of soluble proteins (growth factors, cytokines, chemokines) and extracellular vesicles (EVs) such as exosomes and microvesicles, which carry proteins, lipids, and genetic material [14]. Its composition is not static; it varies significantly based on the tissue source of the MSCs (e.g., bone marrow, adipose tissue, umbilical cord) and is dynamically shaped by the local microenvironment [14] [16]. Preconditioning or "priming" of MSCs—through hypoxia, inflammatory cytokine exposure, or pharmacological agents—further alters the secretome's profile, enabling its optimization for specific clinical applications [14] [15] [17]. This cell-free, paracrine-based approach offers considerable advantages, including a reduced risk of immune rejection, elimination of concerns related to cell engraftment and persistence, and simpler regulatory and manufacturing pathways [14].
Molecular Mechanisms of Paracrine-Mediated Protection
Cytoprotection: Enhancing Cellular Survival and Homeostasis
Cytoprotection refers to the mechanisms that enhance the survival and function of endogenous cells in damaged or stressed tissues. The MSC secretome mitigates apoptosis and maintains cellular homeostasis through several coordinated strategies.
Anti-apoptotic Signaling: Secreted factors directly inhibit programmed cell death pathways. Molecules like VEGF, HGF, and IGF-1 activate intracellular pro-survival pathways such as PI3K/Akt in target cells, leading to the inactivation of pro-apoptotic proteins like Bad and caspase-9 [14] [13]. The transfer of specific microRNAs (e.g., miR-21) via EVs can also downregulate key apoptotic genes in recipient cells [14].
Oxidative Stress Reduction: MSCs secrete antioxidants and enzymes that scavenge reactive oxygen species (ROS), thereby reducing oxidative damage. For instance, extracellular vesicles carry superoxide dismutase and glutathione peroxidase, which directly neutralize free radicals [13]. Furthermore, the secretome can upregulate endogenous antioxidant defense systems in host cells.
Metabolic Support: In ischemic or nutrient-deprived environments, MSCs provide metabolic support by secreting metabolites, lipids, and enzymes that help sustain the energy production of stressed cells, preventing bioenergetic failure [13].
The following diagram illustrates the key cytoprotective pathways activated by the MSC secretome.
Angiogenesis: Orchestrating Vasculogenesis and Vascular Remodeling
Adequate blood supply is fundamental to tissue repair. The MSC secretome potently induces angiogenesis through a complex interplay of growth factors, cytokines, and EVs. Bone marrow-derived MSC (BM-MSC) and adipose tissue-derived MSC (AT-MSC) secretomes are particularly rich in pro-angiogenic factors [14].
Growth Factor-Driven Angiogenesis: Key secreted growth factors include Vascular Endothelial Growth Factor (VEGF), Basic Fibroblast Growth Factor (bFGF), Platelet-Derived Growth Factor (PDGF), and Transforming Growth Factor-β (TGF-β) [14]. These ligands bind to their respective receptors on endothelial cells (e.g., VEGFR, FGFR), activating the ERK/Akt signaling pathway and promoting endothelial cell proliferation, migration, and tube formation [14].
Extracellular Vesicle-Mediated Angiogenesis: EVs are now recognized as primary mediators. They are taken up by endothelial cells, transferring an active cargo that includes pro-angiogenic proteins (e.g., VEGF, FGF) and regulatory RNAs [14]. For example, EVs from hypoxia-preconditioned BM-MSCs are enriched with miR-125a, which suppresses the anti-angiogenic factor DLL4, thereby enhancing vessel sprouting [14]. Similarly, miR-30b promotes tube formation by targeting PDGFA [14].
Proteomic and Functional Heterogeneity: The angiogenic potential of the secretome is source-dependent. A comparative proteomic analysis revealed that AT-MSC-derived EVs contain higher levels of VEGF, von Willebrand factor (vWF), and TGF-β1, correlating with greater tubulogenic efficiency in vitro compared to BM-MSC EVs [14]. Furthermore, stimulation of MSCs with PDGF enhances EV release and upregulates angiogenic cargo such as c-kit and stem cell factor (SCF) [14].
Table 1: Key Pro-Angiogenic Factors in the MSC Secretome
| Molecule | Type | Primary Function in Angiogenesis | Key Signaling Pathway |
|---|---|---|---|
| VEGF | Growth Factor | Endothelial cell proliferation, migration, and permeability | VEGFR2 / PI3K-Akt |
| bFGF (FGF-2) | Growth Factor | Endothelial cell proliferation & tube formation | FGFR / ERK |
| Angiopoietin-1 | Growth Factor | Vessel maturation and stabilization | Tie2 / PI3K-Akt |
| PDGF | Growth Factor | Pericyte recruitment & vessel stabilization | PDGFR / ERK |
| IL-8 | Chemokine | Endothelial cell chemotaxis | CXCR1/2 |
| miR-125a | microRNA (in EVs) | Suppresses anti-angiogenic DLL4 | Notch Pathway |
| EMMPRIN | Protein (in EVs) | Induces matrix metalloproteinases (MMPs) | ERK/Akt |
Immunomodulation: Balancing the Immune Response
MSCs are potent regulators of the immune system, modulating both innate and adaptive immunity to resolve inflammation and create a pro-regenerative environment. This occurs via direct cell-cell contact and, more significantly, through paracrine signaling [13] [15].
Soluble Factor-Mediated Suppression: MSCs secrete a plethora of immunoregulatory molecules in response to inflammatory cues. Key among these are Prostaglandin E2 (PGE2), Indoleamine 2,3-dioxygenase (IDO), TGF-β, HGF, and IL-10 [13] [15]. These factors collectively suppress the proliferation and effector functions of pro-inflammatory T cells (Th1, Th17) and natural killer (NK) cells, while promoting the expansion and activity of regulatory T cells (Tregs) [13].
Extracellular Vesicle-Driven Modulation: MSC-derived EVs carry immunomodulatory cargo that mirrors their parental cells. They can induce a shift in macrophages from a pro-inflammatory M1 phenotype to an anti-inflammatory, pro-healing M2 phenotype [14] [13]. This is partly mediated by the transfer of CD73 to recipient immune cells, which catalyzes the production of anti-inflammatory adenosine from extracellular ATP [15]. EVs also modulate dendritic cell maturation and B cell antibody production [15].
Dynamic and Context-Dependent Action: The immunomodulatory function of MSCs is not universally suppressive but is highly adaptable to the host's inflammatory state. In a low-inflammatory context, MSCs may have a neutral or mildly stimulatory effect. However, in a high-inflammatory milieu (e.g., high levels of IFN-γ and TNF-α), they become powerfully immunosuppressive, a phenomenon known as "licensing" [15]. This dynamic regulation makes them attractive for treating autoimmune diseases and mitigating graft-versus-host disease (GVHD) [13].
The diagram below summarizes the complex immunomodulatory network orchestrated by the MSC secretome.
Experimental Protocols for Investigating Paracrine Mechanisms
Isolation and Characterization of the MSC Secretome
Objective: To collect, concentrate, and characterize the protein and extracellular vesicle components of the MSC-conditioned medium (CM).
Detailed Methodology:
MSC Culture and Conditioning:
- Culture MSCs from a chosen source (e.g., bone marrow, adipose tissue) in standard media until 70-80% confluent.
- Wash cells thoroughly with PBS to remove serum contaminants.
- Incubate with a serum-free, defined basal medium (e.g., DMEM/F-12) for 24-48 hours. Preconditioning with hypoxia (1-3% O₂) or inflammatory cytokines (e.g., 10-50 ng/mL IFN-γ or TNF-α) can be applied during this period to modulate secretome composition [14] [15].
- Collect the conditioned medium (CM).
Processing of Conditioned Medium:
- Centrifuge CM at 2,000 × g for 20 minutes to remove dead cells and debris.
- Concentrate the supernatant using ultrafiltration centrifugal devices (e.g., 3 kDa molecular weight cut-off) or tangential flow filtration.
- For EV isolation, subject the concentrated CM to differential ultracentrifugation:
- Centrifuge at 10,000 × g for 30 minutes to remove apoptotic bodies and large vesicles.
- Centrifuge the resulting supernatant at 100,000 × g for 70-120 minutes to pellet EVs.
- Resuspend the EV pellet (containing exosomes and microvesicles) in PBS or a suitable buffer [14]. Alternative purification methods include size-exclusion chromatography or density gradient ultracentrifugation.
Secretome Characterization:
- Protein Quantification: Use colorimetric assays like BCA or Bradford to determine total protein concentration.
- EV Characterization: Perform Nanoparticle Tracking Analysis (NTA) to determine particle size and concentration. Confirm the presence of EV markers (e.g., CD63, CD81, TSG101) and the absence of negative markers (e.g., Calnexin) via western blot, in accordance with MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [14].
- Proteomic Analysis: Utilize liquid chromatography with tandem mass spectrometry (LC-MS/MS) to identify and quantify the protein components of the secretome and EV cargo [14].
In Vitro Functional Assays for Core Protective Mechanisms
Objective: To quantitatively evaluate the cytoprotective, angiogenic, and immunomodulatory potential of the isolated secretome/EVs.
Detailed Methodology:
Table 2: Key In Vitro Functional Assays for Paracrine Activity
| Mechanism | Assay | Protocol Outline | Key Readouts |
|---|---|---|---|
| Cytoprotection | Hydrogen Peroxide (H₂O₂) Challenge | 1. Seed target cells (e.g., cardiomyocytes, neurons) in a plate.2. Pre-treat with MSC secretome/EVs for 4-24h.3. Induce oxidative stress with H₂O₂ (e.g., 100-500 µM) for several hours.4. Assess cell viability. | - Cell Viability: MTT, MTS, or Calcein-AM assay.- Apoptosis: Caspase-3/7 activity assay or Annexin V/PI staining by flow cytometry. |
| Angiogenesis | Tube Formation Assay | 1. Coat a plate with a basement membrane matrix (e.g., Matrigel or Geltrex).2. Seed human umbilical vein endothelial cells (HUVECs) or human microvascular endothelial cells (HMEC-1) on the matrix.3. Treat with MSC secretome/EVs.4. Incubate for 4-16 hours and image. | - Total Tube Length: Quantified using image analysis software (e.g., ImageJ Angiogenesis Analyzer).- Number of Nodes & Junctions. |
| Immunomodulation | T Cell Proliferation Assay | 1. Isolate peripheral blood mononuclear cells (PBMCs) from human blood.2. Label T cells with a cell division tracker (e.g., CFSE).3. Activate T cells with anti-CD3/CD28 beads or mitogens (e.g., PHA).4. Coculture with MSC secretome/EVs or MSCs in a transwell system for 3-5 days.5. Analyze by flow cytometry. | - % of Divided T Cells: CFSE dilution.- Cytokine Profiling: ELISA for IFN-γ, TNF-α, IL-10 in supernatant. |
The following diagram maps the workflow for a comprehensive in vitro and in vivo validation of paracrine functions.
Advanced Spatial Analysis of the Stem Cell Niche
Objective: To identify and characterize in vivo stem cell niches and their paracrine signaling activities using spatially resolved omics technologies.
Detailed Methodology:
Advanced computational tools like NicheCompass are designed to model cellular communication and identify functional niches from spatial omics data [18]. The protocol involves:
Data Acquisition and Preprocessing: Generate high-resolution spatial transcriptomic or multi-omic data (e.g., using 10x Visium, MERFISH, or seqFISH). Construct a spatial neighborhood graph where nodes represent cells/spots and edges represent spatial proximity [18].
Model Application and Niche Identification: Input the data into NicheCompass, which uses a graph neural network to learn cell embeddings that encode signaling events based on prior knowledge (e.g., ligand-receptor pairs) and de novo spatial gene programs. Cluster these embeddings to identify spatially contiguous cell communities (niches) with coordinated functions [18].
Quantitative Niche Characterization: Characterize the identified niches by analyzing the activity of specific signaling pathways (e.g., Fgf17, Calca, Cthrc1) that define their identity and functional state. This allows for the quantitative dissection of how stem cells and their neighbors communicate via paracrine signals within the tissue architecture [18].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying MSC Paracrine Mechanisms
| Reagent / Tool | Category | Specific Example(s) | Research Application |
|---|---|---|---|
| Fura-2 AM | Calcium Indicator | Invitrogen Fura-2 AM [19] | Multicellular Ca²⁺ imaging to study intercellular communication, such as gap-junctional vs. paracrine wave propagation. |
| Carbenoxolone (CBX) | Gap Junction Blocker | Sigma-Aldrich C4790 [19] | Pharmacologically disrupts direct cell-cell communication via connexin channels, allowing isolation of paracrine effects. |
| Apyrase | ATP-hydrolyzing Enzyme | Sigma-Aldrich A6237 [19] | Degrades extracellular ATP, a key purinergic signaling molecule, to investigate ATP-mediated paracrine pathways. |
| Matrigel / Geltrex | Basement Membrane Matrix | Corning Matrigel [14] | Provides a physiological substrate for in vitro endothelial tube formation assays to assess angiogenic potential. |
| CD63 / CD81 / TSG101 Antibodies | EV Markers | Abcam, System Biosciences [14] | Western blot validation of extracellular vesicle isolates to confirm successful purification and characterization. |
| Recombinant Cytokines (IFN-γ, TNF-α) | Preconditioning Agents | PeproTech [15] | "Prime" or "license" MSCs to enhance the immunomodulatory potency of their secretome prior to collection. |
| Cell Tracker Dyes (CFSE, PKH67) | Cell Labeling | Thermo Fisher Scientific [15] | Track cell proliferation (CFSE) or the uptake and trafficking of secreted EVs (PKH67) in co-culture systems. |
| NicheCompass | Computational Tool | Python Package [18] | Identify and quantitatively characterize stem cell niches and their paracrine signaling from spatial omics data. |
The profound therapeutic impact of adult stem cells is largely mediated by their paracrine activity, which coordinately regulates cytoprotection, angiogenesis, and immunomodulation. The move towards using the defined secretome and its components, particularly extracellular vesicles, represents a pivotal shift from cell-based to cell-free therapeutics, mitigating key clinical risks while retaining efficacy. As the field progresses, the challenge lies in standardizing the production and characterization of these complex biological products, understanding their context-dependent actions, and translating robust preclinical findings into effective clinical therapies. By leveraging the advanced experimental and computational tools detailed in this guide, researchers are poised to unlock the full potential of paracrine signaling, heralding a new era of precision regenerative medicine.
The therapeutic application of adult stem cells has undergone a significant paradigm shift, moving from a focus on direct cell differentiation and replacement toward understanding their potent secretome-mediated effects. Paracrine signaling—the process by which cells release biologically active factors that influence neighboring and distant cells—is now recognized as a primary mechanism through which transplanted stem cells exert their reparative and regenerative effects [20]. These secreted factors create a dynamic tissue microenvironment that coordinately regulates processes including cell survival, angiogenesis, immunomodulation, and endogenous regeneration in a temporal and spatial manner [20]. This in-depth technical guide examines the unique paracrine fingerprints of three clinically significant adult stem cell types: Mesenchymal Stem Cells (MSCs), Cardiac Stem Cells (CSCs), and Endothelial Progenitor Cells (EPCs), providing researchers with a comparative analysis of their secretory profiles, signaling pathways, and methodological considerations for experimental investigation.
Molecular Composition of Stem Cell Secretomes
Defining the Paracrine Fingerprint
The "paracrine fingerprint" of a stem cell type encompasses the complete repertoire of molecules it secretes, including growth factors, cytokines, chemokines, and extracellular vesicles (EVs) containing proteins, lipids, and nucleic acids. These fingerprints are highly cell-type-specific and are influenced by both the tissue of origin and the surrounding microenvironmental conditions [20] [13] [21]. The therapeutic potential of these secretomes is largely mediated through their modulation of key biological processes in recipient tissues.
Comparative Secretome Profiles
Table 1: Key Paracrine Factors Secreted by Different Stem Cell Types and Their Primary Functions
| Stem Cell Type | Key Secreted Factors | Primary Biological Functions |
|---|---|---|
| MSCs | VEGF, HGF, FGF, IGF-1, Sfrp2, HASF, PGE2, IL-6, IDO, TGF-β [20] [13] | Cytoprotection, immunomodulation, angiogenesis, anti-fibrosis, stimulation of endogenous stem cells [20] [13] [22] |
| CSCs | Not fully characterized in search results; likely cardiac-specific regenerative factors [23] | Cardiomyocyte proliferation, protection, and survival; cardiac repair [23] [24] |
| EPCs | Angiogenic cytokines; pro-inflammatory factors (MCP-1); tissue factor (under LPS stimulation) [20] [25] | Neovascularization, vascular repair, endothelial regeneration [20] [25] |
Table 2: Extracellular Vesicle Characteristics and Cargo
| Stem Cell Type | EV Cargo Components | Documented Effects |
|---|---|---|
| MSCs | miRNAs, growth factors, cytokines [22] | Anti-apoptotic, anti-inflammatory, angiogenic; improved cardiac function in MI models [22] |
| EPCs | Pro-angiogenic miRNAs and proteins [25] | Enhanced endothelial cell migration and tubule formation [25] |
| CSCs | Information limited in search results | Information limited in search results |
Mesenchymal Stem Cells (MSCs): Versatile Paracrine Communicators
Secretome Profile and Mechanisms of Action
MSCs release a diverse array of bioactive molecules that mediate their extensive therapeutic effects. Key identified factors include secreted frizzled related protein 2 (Sfrp2) and hypoxic induced Akt regulated stem cell factor (HASF), both of which demonstrate significant cytoprotective effects by inhibiting caspase activity and preventing apoptosis in cardiomyocytes [20]. The immunomodulatory strength of MSCs is mediated through factors like prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), and transforming growth factor-beta (TGF-β), which collectively inhibit T-cell proliferation, prevent dendritic cell maturation, and modulate macrophage polarization toward a regenerative M2 phenotype [20] [13].
Regulatory Signaling Pathways
The paracrine activity of MSCs is finely regulated by several intrinsic signaling pathways. The Akt signaling pathway is particularly crucial, as its activation significantly enhances the cytoprotective capabilities of MSC-conditioned media [20]. Additionally, the Wnt/β-catenin pathway interacts with MSC-derived Sfrp2 to modulate apoptotic signaling in target cells [20]. Research indicates that transcriptional regulators including Twist1/2, OCT4, and SOX2 play important roles in maintaining MSC stemness and secretory capacity, with their expression influencing the therapeutic potential of MSCs during ex vivo expansion [26].
Figure 1: Key regulatory pathways and mechanisms governing the paracrine functions of MSCs. Transcription factors Twist and OCT4 enhance secretome production. The Akt pathway, activated by hypoxic conditions, upregulates key factors Sfrp2 and HASF which inhibit apoptosis via Wnt inhibition and PKCε activation, respectively. The resulting secretome drives core therapeutic effects.
Endothelial Progenitor Cells (EPCs): Vascular Regeneration Specialists
Defining EPC Populations
EPCs are bone marrow-derived cells that circulate in the bloodstream and contribute to adult vasculogenesis and endothelial repair [25]. There is ongoing debate regarding their precise definition, but researchers commonly identify EPCs by their surface marker expression, particularly CD34+CD133+KDR+ triple-positive cells [25]. These cells exhibit high clonogenic potential, which serves as a predictor of their angiogenic capability [25]. Subpopulations with lineage-negative markers (e.g., CD14−/CD45−) have also been identified and may possess enhanced angiogenic capacity [25].
Paracrine Mechanisms in Vascular Repair
While EPCs can directly incorporate into nascent vessels, their paracrine activity significantly contributes to vascular regeneration. EPCs secrete a cocktail of pro-angiogenic cytokines that promote the migration, proliferation, and tubulogenesis of mature endothelial cells [25]. Interestingly, in contrast to MSCs, EPCs can secrete pro-inflammatory cytokines like MCP-1 and, under specific conditions such as lipopolysaccharide (LPS) stimulation, the procoagulant protein tissue factor [20]. This highlights the context-dependent nature of EPC paracrine activity and underscores the importance of understanding their functional state before therapeutic application.
Cardiac Stem Cells (CSCs): Cardiac-Specific Regenerative Signaling
Paracrine Role in Heart Repair
CSCs reside within the heart and possess the ability to differentiate into major cardiac lineages, including cardiomyocytes, endothelial cells, and smooth muscle cells [23] [24]. While the specific factors comprising the CSC secretome are not fully detailed in the provided search results, their therapeutic benefits in advanced heart failure are increasingly attributed to paracrine mechanisms [23]. Clinical trials using cardiosphere-derived cells (CDCs), a CSC-containing population, have demonstrated safety and signals of efficacy, with recent attention shifting toward their paracrine signaling effects [23].
Mechanisms of Cardiac Repair
The CSC paracrine factors are believed to promote cardiomyocyte proliferation and survival, stimulate angiogenesis, and activate endogenous repair mechanisms [23] [24]. These combined actions can potentially reduce infarct size, improve ventricular remodeling, and enhance cardiac function after injury. The direct comparison of CSC secretomes with those of MSCs and EPCs remains an important area of ongoing research, as understanding these differences is crucial for selecting the optimal cell type for specific cardiac pathologies.
Experimental Approaches for Paracrine Analysis
Standardized Methodologies for Secretome Characterization
Table 3: Essential Reagents and Methodologies for Paracrine Factor Analysis
| Research Tool | Specific Application | Technical Purpose |
|---|---|---|
| Conditioned Media Collection | Culture in serum-free/XF media for 24-48h; concentration via ultrafiltration [20] [21] | Source of soluble paracrine factors for functional assays |
| High-Throughput ELISA/Multiplex Assays | Quantification of VEGF, HGF, IGF-1, FGF, cytokines (PGE2, IL-6) [20] [21] | Comprehensive protein-level secretome profiling |
| EV Isolation (Ultracentrifugation/SEC) | Separation of sEVs (50-150 nm) from conditioned media [22] | Isolation of vesicular fraction of secretome |
| Nanoparticle Tracking Analysis | Characterization of EV size distribution and concentration (e.g., ZetaView, NanoSight) [21] | Quantitative and qualitative EV analysis |
| miRNA qRT-PCR Arrays | Profiling of EV-embedded miRNAs (e.g., miR-21, miR-146a) [21] [22] | Functional RNA cargo characterization |
| Flow Cytometry | Immunophenotyping of surface markers (CD73, CD90, CD105 for MSCs; CD34, CD133, KDR for EPCs) [25] [13] [21] | Cell population identification and purity assessment |
Functional Assays for Paracrine Activity Validation
- In Vitro Cytoprotection Assay: Subject cardiomyocytes or other target cells to hypoxia/reoxygenation injury. Treat with conditioned media (CM) from stem cells. Quantify apoptosis rates using TUNEL staining or caspase-3/7 activity assays [20].
- Tube Formation Assay: Plate endothelial cells (e.g., HUVECs) on Matrigel and treat with stem cell CM or EVs. Measure tubule length, number of nodes, and closed structures after 4-18 hours to assess angiogenic potential [25].
- Immune Cell Modulation Assay: Co-culture stem cell CM with activated T-cells (e.g., using anti-CD3/CD28 antibodies). Measure T-cell proliferation via CFSE dilution or 3H-thymidine incorporation to quantify immunomodulatory capacity [20] [13].
- In Vivo Efficacy Testing: Utilize rodent myocardial infarction models (e.g., permanent LAD ligation). Administer stem cell CM, EVs, or cells via intramyocardial or intravenous injection. Assess functional outcomes by echocardiography (ejection fraction, fractional shortening) and histological analysis (infarct size, capillary density) [20] [22].
Figure 2: Comprehensive experimental workflow for the isolation, characterization, and functional validation of stem cell paracrine factors. The process begins with conditioned media collection, followed by parallel analysis of soluble proteins and extracellular vesicles, culminating in functional assays that inform an integrated paracrine fingerprint.
Technical Considerations and Challenges
Critical Variables Affecting Secretome Composition
The paracrine fingerprint of any stem cell population is not static but is significantly influenced by multiple technical and biological variables that researchers must carefully control and document:
- Culture Conditions: The choice of expansion media (e.g., FBS, human platelet lysate, or serum/xeno-free formulations) creates divergent secretome signatures, with demonstrated functional consequences on immune cells and chondrocytes [21].
- Oxygen Tension: Physiological hypoxia (e.g., 1-5% O2) often enhances the secretion of cytoprotective factors like HASF and influences the expression of transcriptional regulators such as OCT4 [20] [26].
- Passage Number and Donor Variability: Increasing passage number leads to replicative senescence and reduced secretory function, while donor-specific characteristics introduce inherent variability in secretome potency [26].
- Cell Source and Purity: The tissue origin of MSCs (e.g., bone marrow, adipose, umbilical cord) affects their secretory profile, and the definition and purification of EPC subpopulations (e.g., early vs. late EPCs) remain challenging [26] [25] [13].
Translation to Clinical Applications
The progression of stem cell paracrine biology toward clinical therapy requires addressing several key challenges. Standardization of manufacturing protocols according to Good Manufacturing Practice (GMP) guidelines is essential for consistent secretome production [21] [27]. Additionally, developing robust potency assays that reliably predict the therapeutic efficacy of a given secretome remains a significant hurdle in the field [27]. Finally, the shift toward using the acellular secretome or isolated EVs as biologicals—which offers advantages in safety, storage, and dosing—requires the development of appropriate regulatory frameworks [22] [27].
The distinct paracrine fingerprints of MSCs, EPCs, and CSCs represent a sophisticated biological communication system that can be harnessed for therapeutic purposes. MSCs demonstrate remarkable versatility through their immunomodulatory and cytoprotective secretome, EPCs specialize in orchestrating vascular repair, and CSCs likely secrete factors tailored to the cardiac regenerative niche. For researchers advancing this field, meticulous attention to cell source, culture conditions, and characterization methodologies is paramount. Future directions will focus on engineering these native secretomes for enhanced potency and specificity, potentially through genetic modification or preconditioning strategies, and standardizing EV-based products as next-generation acellular therapeutics for regenerative medicine.
From Bench to Bedside: Methodologies and Therapeutic Applications
The therapeutic potential of adult stem cells, particularly mesenchymal stromal cells (MSCs), is now largely attributed to their paracrine activity rather than direct differentiation and engraftment. These cells release a complex mixture of bioactive molecules, collectively known as the secretome, which includes proteins, growth factors, cytokines, chemokines, and extracellular vesicles (EVs) containing proteins, RNA, and lipids [28] [13] [29]. This secretome mediates intercellular communication, modulating immune responses, promoting tissue repair, and enhancing angiogenesis [30] [13]. Consequently, precise characterization of the secretome is fundamental to understanding the mechanisms of action in stem cell therapies. This technical guide details the core analytical techniques—proteomics and RNA sequencing—used to profile the secretome, providing a framework for researchers and drug development professionals to decipher this critical cellular "sign language" [31].
Core Analytical Techniques for Secretome Profiling
Proteomic Analysis of the Secretome
Proteomic technologies enable the comprehensive identification and quantification of proteins within a secretome. The typical workflow involves separating complex protein mixtures followed by mass spectrometry (MS) analysis.
Methodology and Workflow:
- Sample Preparation: Secretomes are collected from serum-free cell culture conditioned media to avoid contamination from serum proteins, particularly those from fetal bovine serum (FBS) [29]. Proteins are then concentrated and digested into peptides.
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): This is the cornerstone of modern secretome proteomics. As utilized in key studies, high-resolution two-dimensional LC-MS/MS allows for the separation of thousands of peptides and their subsequent identification by mass analysis [32].
- Data Analysis: Computational pipelines are used to match acquired mass spectra to protein sequence databases, enabling identification and label-free or label-based quantification. This reveals proteins that are differentially secreted under various conditions (e.g., resting vs. inflamed) [32] [31].
Key Applications:
- Defining Phenotypic Signatures: Proteomics can distinguish between different MSC activation states. For instance, resting MSC secretomes are rich in extracellular matrix (ECM) and pro-regenerative proteins, whereas secretomes from MSCs licensed with IFN-γ and TNF-α are enriched for immunomodulatory and chemotactic factors like IDO [32].
- Comparing Cellular Sources: Proteomic profiling reveals that secretome composition varies significantly with the MSC source. Induced pluripotent stem cell-derived MSCs (iMSCs) and umbilical cord-derived MSCs (UC-MSCs) show signatures related to proliferative potential, while adult tissue-derived MSCs (from bone marrow or adipose tissue) express higher levels of fibrotic and ECM-related proteins [32].
RNA Sequencing of Extracellular Vesicles
While the cellular secretome includes soluble factors, a significant portion of its regulatory capacity is housed within extracellular vesicles (EVs), such as exosomes and microvesicles. These vesicles carry nucleic acids, including RNA, which can be delivered to recipient cells to alter their function.
Methodology and Workflow:
- EV Isolation: EVs are purified from conditioned media using techniques like ultracentrifugation, density gradient separation, or size-exclusion chromatography [28].
- RNA Extraction and Library Preparation: RNA is isolated from the EV pellet. For single-cell RNA sequencing (scRNA-Seq), systems like the 10x Genomics Chromium Controller or Parse Biosciences' Evercode kit are used to barcode RNA from thousands of individual cells or vesicles, preserving the resolution of cellular heterogeneity [33].
- Sequencing and Bioinformatic Analysis: Next-generation sequencing is performed, followed by alignment and quantification of transcripts. This can identify the repertoire of mRNAs, microRNAs (miRNAs), and other non-coding RNAs contained within EVs [28] [33].
Key Applications:
- Mechanistic Insight: Sequencing of EV-derived RNA can reveal how MSCs influence recipient cells. For example, MSC-EVs contain miRNAs and mRNAs that regulate processes such as angiogenesis, immune modulation, and oxidative stress response in injured tissues [28].
- Functional Phenotyping: Technologies like the Bruker IsoSpark system integrate secretome analysis with single-cell resolution, allowing researchers to link the secretion of specific cytokines (a functional output) to individual cells within a heterogeneous population [33] [34].
Table 1: Comparison of Core Secretome Profiling Techniques
| Feature | Proteomics (LC-MS/MS) | RNA Sequencing (of EVs) |
|---|---|---|
| Primary Focus | Identifies and quantifies proteins, cytokines, and growth factors. | Identifies and quantifies RNA species (mRNA, miRNA, etc.). |
| Key Technology | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS). | Next-Generation Sequencing (NGS), e.g., 10x Genomics, Parse Biosciences. |
| Sample Type | Cell-conditioned media (serum-free). | Isolated Extracellular Vesicles (EVs). |
| Reveals | Direct effector molecules and post-translational modifications. | Regulatory codes and potential for altering recipient cell gene expression. |
| Information Gained | Functional protein composition and signaling pathways (e.g., VEGF, IL-6). | Cargo that can modulate protein synthesis in target cells. |
Integrated Experimental Workflows
Modern secretome analysis often integrates multiple omics technologies to build a comprehensive picture of paracrine signaling. The following diagram illustrates a generalized workflow for a multi-omics secretome study.
Diagram Title: Integrated Multi-Omics Secretome Analysis Workflow
Critical Research Reagents and Solutions
The following table details key reagents and tools essential for conducting secretome profiling experiments, as derived from the cited methodologies.
Table 2: Research Reagent Solutions for Secretome Profiling
| Item | Function / Application | Examples / Specifications |
|---|---|---|
| MSC Culture Media | Expansion and maintenance of mesenchymal stromal cells. | DMEM/RPMI-1640, supplemented with MSC-qualified FBS [32] [30]. For secretome collection, serum-free media is critical [29]. |
| Inflammatory Cytokines | For licensing MSCs to an immunomodulatory (MSC2) phenotype. | Recombinant human IFN-γ and TNF-α (e.g., 15 ng/mL each for 48h) [32]. |
| Proteomic Kits | Sample preparation for LC-MS/MS. | Trypsin/Lys-C for protein digestion, TMT/Isobaric tags for multiplexed quantification. |
| EV Isolation Kits | Purification of extracellular vesicles from conditioned media. | Ultracentrifugation protocols; commercial kits based on precipitation or size-exclusion [28]. |
| Single-Cell Barcoding | Partitioning cells/vesicles for RNA-Seq. | 10x Genomics Chromium (GemCode tech); Parse Biosciences Evercode (split-pool combinatorial barcoding) [33]. |
| Cytokine Panels | Multiplexed protein detection at single-cell resolution. | Bruker IsoCode Chips (32-plex panels for Human/Mouse Adaptive/Innate immunity) [34]. |
Signaling Pathways and Experimental Findings
Secretome profiling has been instrumental in mapping the molecular pathways activated by paracrine signaling. A prime example is the inflammatory licensing of MSCs, a key process that enhances their immunomodulatory function.
Diagram Title: MSC Inflammatory Licensing and Secretome Shift
This pathway, validated by proteomic studies [32], shows how environmental cues reshape the MSC secretome. The licensed MSC2 phenotype is defined by a marked upregulation of IDO secretion and surface HLA expression, alongside a broader shift toward an anti-inflammatory and pro-regenerative protein profile [32]. This demonstrates how secretome analysis directly illuminates the mechanisms behind observed therapeutic effects, such as the suppression of T-cell proliferation and polarization of macrophages toward an M2 reparative state [30] [13].
The synergistic application of proteomics and RNA sequencing provides an unparalleled, multi-dimensional view of the stem cell secretome. These techniques move beyond cataloging secreted factors to revealing the dynamic and regulated nature of paracrine communication. As standardization in secretome production and analysis improves [29], these profiling technologies will be crucial for qualifying potency, ensuring batch-to-batch consistency, and rationally designing the next generation of cell-free regenerative therapeutics. For drug development professionals, mastering these analytical techniques is no longer optional but essential for leveraging the full potential of paracrine signaling in adult stem cell research.
The paradigm of adult stem cell therapy has undergone a significant shift over the past decade. Initially, the therapeutic potential of stem cells was attributed primarily to their ability to engraft and differentiate into tissue-specific cells to replace damaged areas [20]. However, substantial evidence now supports that stem cells exert their reparative and regenerative effects largely through the release of biologically active molecules that act in a paracrine fashion on resident cells [20]. This paracrine hypothesis posits that transplanted stem cells create a tissue microenvironment where secreted factors influence cell survival, inflammation, angiogenesis, repair, and regeneration in a temporal and spatial manner [20]. The validation of this mechanism relies on robust functional assays that can demonstrate these effects both in controlled laboratory settings (in vitro) and in living organisms (in vivo).
The development of the paracrine hypothesis emerged from observations that functional improvement occurred despite poor cellular survivability and minimal engraftment of transplanted cells [20] [1]. Critical evidence came from studies showing that administration of conditioned medium (CM) from cultured stem cells could recapitulate the therapeutic benefits of the cells themselves [20] [1]. This discovery redirected research focus toward identifying the specific factors responsible for these effects and developing assays to quantify their biological activities. This guide provides a comprehensive technical framework for validating these paracrine effects through established functional assays.
Key Paracrine Mechanisms and Their Assay Targets
Stem cell paracrine signaling mediates therapeutic effects through multiple interconnected mechanisms. The table below summarizes the primary mechanisms, their functional outcomes, and key factors involved, providing critical targets for assay development.
Table 1: Key Paracrine Mechanisms and Assay Targets
| Mechanism | Functional Outcome | Key Soluble Factors | Affected Cell Types |
|---|---|---|---|
| Survival/Cytoprotection | Reduced apoptosis and necrosis in injured tissue [20] [1] | Sfrp2, HASF, VEGF, HGF, IGF-1, Akt1 [20] [1] | Cardiomyocytes, Neurons |
| Immunomodulation/Inflammation | Damped inflammatory response; macrophage polarization [20] | PGE2, IL-6, TGF-β, IL-1ra, TSG-6 [20] | T-cells, B-cells, Macrophages, Dendritic cells |
| Neovascularization | Increased capillary density; improved blood flow [1] | VEGF, FGF2, HGF, Angiopoietin-1 [20] [1] | Endothelial cells, Pericytes |
| Tissue Regeneration | Activation and differentiation of resident stem cells [1] | IGFBP5, CTGF, SDF-1 [1] [35] | Resident tissue-specific stem and progenitor cells |
These mechanisms are not isolated; paracrine factors are often pleiotropic, acting on multiple cell types and processes simultaneously [20]. Furthermore, the composition of the secretome can be dynamically influenced by the local microenvironment, such as hypoxia, which can upregulate the production of beneficial factors [20] [36]. The following sections detail the assays used to quantify these functional outcomes.
In Vitro Validation Assays
In vitro assays provide a controlled system for deconstructing complex paracrine interactions and establishing direct causal relationships between secreted factors and cellular responses.
Conditioned Medium (CM) Preparation
The foundation of in vitro paracrine studies is the production of high-quality conditioned medium.
Detailed Protocol: CM from Mesenchymal Stem Cells (MSCs)
- Cell Culture: Expand human Adipose-derived MSCs (Ad-MSCs) in standard culture medium (e.g., DMEM with 10% FBS) until 70-80% confluency [36].
- Serum Deprivation: Wash the cell monolayer twice with 1X Phosphate-Buffered Saline (PBS) to remove residual serum. Incubate the cells in a serum-free medium (e.g., OPTIMEM) under defined conditions (e.g., normoxia or hypoxia at 2% O2) for 24 hours [36].
- Collection and Clarification: Collect the medium and centrifuge at 1200 × g for 10 minutes to remove cellular debris [36].
- Concentration and Standardization: Adjust the protein concentration of the clarified supernatant (e.g., to 100-200 µg/mL) using serum-free medium. Sterilize by filtration through a 0.22 µm filter and store at -20°C until use [36].
Functional Cellular Assays
Survival/Cytoprotection Assay
This assay tests the ability of CM to protect cells from injury-induced death.
Protocol:
- Induce Injury: Subject recipient cells (e.g., cardiomyocytes or photoreceptors) to a lethal insult, such as oxygen-glucose deprivation, hydrogen peroxide, or exposure to cytotoxic drugs [20] [35].
- Apply CM: Treat the injured cells with the test CM, control medium (unconditioned), or purified candidate factors.
- Quantify Viability:
- Apoptosis Assay: Measure caspase-3/7 activity using luminescent or fluorescent substrates [20].
- Necrosis Assay: Use membrane integrity dyes like propidium iodide.
- Metabolic Activity: Employ MTT or WST-1 assays as a proxy for cell health.
Table 2: Key Outcomes from Cytoprotection Assays
| CM Source | Injury Model | Target Cell | Key Identified Factor(s) | Effect on Viability |
|---|---|---|---|---|
| Akt1-overexpressing MSCs [20] | Hypoxia/Reoxygenation | Rat cardiomyocytes | Sfrp2, HASF [20] | Significant reduction in caspase-3 activity and apoptosis [20] |
| Retinal Mueller Glial Cells [35] | Serum starvation | Primary photoreceptors | IGFBP5, CTGF [35] | Significant increase in photoreceptor survival [35] |
| Bone Marrow Mononuclear Cells [20] | Ischemia | Cardiomyocytes | VEGF, PDGF, IGF-1 [20] | Inhibition of apoptosis; preserved contractility [20] |
Migration and Wound Healing Assay
This assesses the chemoattractant or pro-migratory capacity of paracrine factors, crucial for recruitment of progenitor cells and vascular healing.
Protocol (Wound Healing/Scratch Assay):
- Create a "Wound": Culture recipient cells (e.g., endothelial cells or myoblasts) to full confluency in a multi-well plate. Create a scratch in the monolayer using a sterile pipette tip.
- Apply CM: Wash away dislodged cells and add test CM or controls.
- Image and Quantify: Capture images of the scratch at 0, 12, 24, and 48 hours. Use image analysis software (e.g., Fiji/ImageJ) to measure the change in wound area over time, calculating the rate of migration [37].
Non-Contact Co-Culture System
This system models paracrine interactions between two distinct cell types without direct physical contact.
Protocol (for Neural Crest Cell - Myoblast signaling) [37]:
- Cell Preparation: Culture signal-sending cells (e.g., Neural Crest Cells, NCCs) and signal-receiving cells (e.g., C2C12 myoblasts) separately.
- Co-Culture Setup: Seed the signal-receiving cells in the bottom of a multi-well plate. Place a cell culture insert with a porous membrane (permeable to proteins but not cells) into the well. Seed the signal-sending cells onto this insert.
- Phenotypic Analysis: After an appropriate incubation period (e.g., 24-72 hours), fix and immunostain the signal-receiving cells in the bottom well for morphological changes. For example, stain for F-actin with phalloidin to visualize increased filopodia and lamellipodia formation, a hallmark of noncanonical Wnt activation [37].
- Molecular Analysis: Recover the signal-receiving cells for downstream analysis, such as Western blotting to detect phosphorylation of key signaling proteins.
In Vivo Validation Assays
In vivo models are essential for confirming that paracrine effects observed in vitro translate to functional tissue repair in a complex physiological environment.
Small Animal Disease Models
Protocol: Myocardial Infarction Model in Rodents [20]
- Induce Injury: Anesthetize the animal and surgically occlude a coronary artery to induce a controlled myocardial infarction.
- Administer Treatment: Immediately following injury, inject the test article directly into the ischemic border zone or systemically. Test articles can include:
- Cells: e.g., 1-2 million MSCs in saline.
- Conditioned Medium: e.g., 50-100 µL of concentrated CM.
- Purified Protein: e.g., a single dose of HASF protein [20].
- Functional Endpoint Analysis:
- Histology: After a set period (e.g., 4 weeks), harvest hearts. Analyze sections for infarct size (Masson's Trichrome stain), apoptosis (TUNEL assay), and capillary density (CD31+ immunostaining) [20].
- Functional Imaging: Use echocardiography to measure functional parameters like Left Ventricular Ejection Fraction (LVEF) and Left Ventricular End-Systolic Volume (LVESV) at baseline and endpoint to quantify improvement.
Protocol: Bone Defect Model in Rabbits [36]
- Create Defect: Surgically create a critical-sized (e.g., 10 mm diameter) bicortical defect in the rabbit mandible.
- Apply Treatment: Implant a scaffold (e.g., Human Blood Plasma Hydrogel, HBPH) containing the test article into the defect. Test articles include:
- Ad-MSCs: e.g., 60,000 cells in HBPH.
- CM: e.g., HBPH mixed with CM.
- Control: Empty scaffold or scaffold with non-conditioned medium.
- Outcome Assessment:
- Radiographic/Micro-CT: Periodically image the defect to quantify new bone mineral density and volume.
- Histomorphometry: Upon termination, perform undecalcified histology (e.g., Van Gieson stain) to measure the percentage of new bone formation within the defect [36].
Table 3: In Vivo Outcomes of Paracrine-Based Therapies
| Disease Model | Treatment | Key Results | Implied Mechanism |
|---|---|---|---|
| Myocardial Infarction (Rat) [20] | CM from Akt-MSCs | Reduced infarct size; improved LV function; fewer TUNEL+ cells [20] | Cytoprotection; Anti-apoptosis |
| Bone Defect (Rabbit) [36] | Ad-MSC-CM in HBPH | Induced bone regeneration in mandibular defect, comparable to cell transplant [36] | Activation of endogenous regeneration |
| Myocardial Infarction (Porcine) [20] | CM from MSCs | Reduced infarct size; preserved cardiac function [20] | Cytoprotection |
Analytical Techniques for Factor Identification
Identifying the specific bioactive molecules within CM is a critical step in understanding and optimizing paracrine therapy.
Protein Identification Workflow
A multi-step functional proteomics approach is required to isolate and identify low-abundance cytokines.
Protocol: Integrated Workflow for Candidate Identification [35]
- Functional Screening: Use a high-content survival assay (e.g., primary photoreceptor survival) to confirm bioactivity of the starting CM [35].
- Fractionation: Subject the active CM to sequential fractionation:
- Size-Based: Use size-exclusion chromatography (e.g., SEC-HPLC).
- Charge-Based: Follow with ion-exchange chromatography.
- Hydrophobicity-Based: Finally, use reverse-phase liquid chromatography (RPLC) [35].
- Activity Tracking: After each fractionation step, test all fractions for biological activity using the functional assay from step 1. This ensures only fractions retaining the desired activity are advanced.
- Mass Spectrometry: Analyze the final active fraction using techniques like Q-TOF MS/MS or MALDI MS/MS to identify the proteins present [35].
- Validation: Clone and express candidate genes (e.g., in HEK293 cells) and test the conditioned medium from these cells in the original functional assay to confirm bioactivity [35].
Quantification of Signaling Pathways
Once candidate pathways are identified, their activation in recipient cells can be quantified.
Techniques:
- Phospho-Specific ELISA Kits: These kits allow quantitative measurement of the phosphorylation status of key signaling proteins (e.g., Akt, CREB, STAT3, ERK), providing a direct readout of pathway activation. They are highly sensitive, quantitative, and suitable for high-throughput screening [38].
- Multiplex Immunoassays (e.g., ProcartaPlex): These bead-based assays enable the simultaneous quantification of multiple phosphorylated and total proteins from a single small-volume sample, providing a broader view of signaling network activation [38].
- Western Blotting: A standard method for semi-quantitatively detecting specific proteins and their post-translational modifications, useful for validation and visual confirmation [38].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Paracrine Studies
| Reagent / Kit | Primary Function | Application Context | Key Features |
|---|---|---|---|
| Conditioned Medium [20] [36] | Source of paracrine factors | In vitro and in vivo functional assays; factor identification | Can be hypoxic-preconditioned; concentrated; standardized by protein content |
| Phospho-Specific ELISA Kits [38] | Quantify pathway activation | Analysis of recipient cell signaling (Akt, STAT, CREB pathways) | High sensitivity and specificity; quantitative; pre-coated plates |
| ProcartaPlex Multiplex Assays [38] | Simultaneously quantify multiple analytes | Measuring panels of cytokines/growth factors in CM; phospho/total protein | High-throughput; minimal sample volume; up to 80-plex |
| Human Angiogenesis Antibody Array [36] | Semi-quantitative protein profiling | Screening CM for the presence of dozens of angiogenic factors | Membrane-based array; good for initial secretome characterization |
| Cell Culture Inserts [37] | Enable non-contact co-culture | Modeling paracrine signaling between two distinct cell types | Porous membrane (0.4-8 µm); prevents cell mixing |
| Human Blood Plasma Hydrogels (HBPH) [36] | Biocompatible delivery scaffold | In vivo delivery of cells or CM in bone defect models | Biodegradable; histocompatible; allows cell visualization |
The shift from a differentiation-based to a paracrine-centric understanding of stem cell therapy has necessitated the development of sophisticated functional assays. The integrated use of in vitro systems—like conditioned medium experiments and non-contact co-cultures—with robust in vivo disease models provides a powerful framework for validating paracrine effects. The ongoing challenge lies in fully deconvoluting the complex mixture of factors secreted by stem cells and understanding their temporal and spatial interactions. The protocols and tools outlined in this guide provide a foundation for researchers to rigorously test the paracrine hypothesis, with the ultimate goal of developing more effective and safe cell-free therapeutic interventions for regenerative medicine.
Conditioned Medium and Cell-Free Therapies as Novel Biologics
The field of regenerative medicine is undergoing a fundamental transformation, moving away from the traditional concept of stem cell differentiation and engraftment toward a new paradigm centered on paracrine signaling as the primary therapeutic mechanism. Mesenchymal stem cells (MSCs), particularly those derived from adipose tissue (ADSCs), have demonstrated remarkable therapeutic potential in treating diverse conditions from diabetic wounds to myocardial infarction. However, a growing body of evidence suggests that the transplanted cells themselves do not significantly engraft or differentiate in target tissues but rather exert their beneficial effects through secreted bioactive factors [1] [20] [13]. This understanding has catalyzed the development of cell-free therapies utilizing conditioned medium (CM) – the liquid medium enriched with a stem cell's secretome – which contains a complex cocktail of growth factors, cytokines, and extracellular vesicles that coordinate tissue repair [39] [16].
This shift addresses significant challenges associated with cell-based therapies, including low engraftment efficiency, potential immunogenicity, and the harsh pathological microenvironment of chronic disease states that limits transplanted cell survival [39] [20]. Conditioned medium therapies effectively bypass these limitations while harnessing the full repertoire of therapeutic molecules produced by stem cells, offering a promising new class of biologics with enhanced safety profiles and manufacturing advantages.
The Scientific Foundation: Paracrine Mechanisms of Action
Historical Development of the Paracrine Hypothesis
The paracrine hypothesis emerged from observations in both cardiac and wound healing research where significant functional improvements occurred despite minimal long-term engraftment of administered stem cells. Initial studies proposed that bone marrow-derived cells could transdifferentiate into cardiomyocytes; however, subsequent research could not reproduce these findings, revealing instead that the functional benefits were mediated by soluble factors released by the cells [20]. Seminal experiments demonstrated that administering conditioned medium from cultured MSCs could recapitulate the therapeutic benefits of the cells themselves, providing direct evidence for the paracrine hypothesis [1] [20].
Key Paracrine Mechanisms in Tissue Repair
Stem cell-derived paracrine factors facilitate tissue repair through several coordinated mechanisms:
- Cytoprotection: Paracrine factors activate pro-survival pathways in endangered native cells, reducing apoptosis and necrosis. Key molecules include secreted frizzled related protein 2 (Sfrp2), which inhibits caspase-3 activity, and hypoxic induced Akt regulated stem cell factor (HASF), which prevents mitochondrial pore opening [20].
- Immunomodulation: MSCs release factors that dampen deleterious inflammatory responses by inhibiting T-cell proliferation, preventing dendritic cell maturation, and switching macrophages from a pro-inflammatory M1 to a reparative M2 phenotype [20] [13]. This includes downregulation of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 [39] [20].
- Angiogenesis: Conditioned medium is enriched with pro-angiogenic factors including vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and hepatocyte growth factor (HGF) that stimulate new blood vessel formation, crucial for oxygenating and nourishing damaged tissues [39] [1].
- Activation of Endogenous Stem Cells: Paracrine signals can mobilize and activate resident tissue-specific stem cells, enhancing the body's innate regenerative capacity [1].
Table 1: Key Paracrine Factors and Their Biological Functions
| Factor Category | Representative Molecules | Primary Documented Functions |
|---|---|---|
| Growth Factors | VEGF, bFGF, HGF, IGF-1, EGF | Angiogenesis, cell proliferation, migration, and survival [39] [1] [20] |
| Immunomodulatory Factors | PGE2, IL-1ra, TGF-β, IDO | Inhibition of T-cell proliferation, suppression of pro-inflammatory cytokine release, B-cell regulation [20] [13] |
| Anti-apoptotic Factors | Sfrp2, HASF, TIMPs | Inhibition of caspase activity, stabilization of mitochondrial membranes [20] |
| Extracellular Matrix Modulators | MMP-1, MMP-2, MMP-9, TIMP-1, TIMP-2 | Tissue remodeling, loosening matrix to facilitate cell migration and tubule formation [1] |
Experimental Evidence and Therapeutic Efficacy
Case Study: Diabetic Wound Healing
A compelling example of conditioned medium therapy comes from a 2025 study investigating ADSC-conditioned medium (ACM) for treating type 2 diabetic (T2D) wounds [39]. The research demonstrated that ACM significantly accelerated wound closure in a T2D rat model through dual mechanisms: stimulating vascularization and modulating the inflammatory microenvironment.
Experimental Protocol:
- ACM Preparation: ADSCs were cultured from rat adipose tissue and incubated in serum-free medium for 48 hours. The conditioned medium was collected, concentrated using a 3-kDa tangential flow filtration capsule, and quantified via BCA assay [39].
- In Vivo Model: A T2D rat model was established using a high-fat diet combined with streptozotocin (STZ) injections. Full-thickness skin defects were created and treated with daily intradermal injections of 100 µL ACM around the wound edges for 7 days [39].
- Analysis: Wound closure rate was measured, and tissue samples were analyzed by histopathology, q-PCR for inflammatory mediators, and transcriptome sequencing [39].
Key Findings:
- ACM significantly enhanced proliferation and angiogenesis of human umbilical vein endothelial cells (HUVECs) in vitro.
- ACM treatment in vivo accelerated wound closure and suppressed pro-inflammatory mediators (TNF-α, IL-1β, IL-6, COX-2, IL-12, IFN-γ).
- Transcriptome analysis revealed that ACM mediated its effects primarily by downregulating TNF and chemokine signaling pathways [39].
Table 2: Quantitative Therapeutic Effects of ACM on Diabetic Wounds [39]
| Parameter | Effect of ACM Treatment | Significance |
|---|---|---|
| Wound Closure Rate | Significantly Accelerated | p < 0.05 vs. control |
| HUVEC Proliferation | Enhanced | p < 0.05 vs. control |
| Angiogenic Markers | Upregulated EGF, bFGF, VEGF, KDR | p < 0.05 vs. control |
| Pro-inflammatory Cytokines | Suppressed TNF-α, IL-1β, IL-6, COX-2, IL-12, IFN-γ | p < 0.05 vs. control |
Functional Evidence Across Tissue Systems
The therapeutic potential of conditioned medium extends beyond wound healing. In cardiovascular disease, conditioned medium from Akt-modified MSCs reduced infarct size and improved cardiac function after myocardial infarction, with protective effects mediated through paracrine factors like Sfrp2 and HASF [20]. Furthermore, a 2025 study demonstrated that even AD-MSCs from type 2 diabetic donors retain robust biological activity, with their conditioned medium exhibiting enhanced pro-angiogenic potential compared to medium from healthy donor cells, supporting the feasibility of autologous therapies for diabetic patients [40].
Technical and Methodological Framework
Standardized Production of Conditioned Medium
The production of therapeutically active conditioned medium requires careful attention to cell source, culture conditions, and processing methods. The following workflow outlines a standardized protocol for generating ADSC-conditioned medium based on current research [39]:
Essential Research Reagents and Tools
Table 3: Essential Research Reagent Solutions for Conditioned Medium Studies
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Cell Isolation | Type I Collagenase, α-MEM medium, Fetal Bovine Serum (FBS) | Tissue digestion and primary cell culture establishment [39] |
| Cell Culture | Serum-free media, Human Platelet Lysate (hPL) | Production of conditioned medium without serum interference [39] [40] |
| Concentration | Tangential Flow Filtration (TFF) capsules, 3-kDa MWCO membranes | Concentrate conditioned medium while retaining bioactive factors [39] |
| Quality Assessment | BCA Assay Kit, ELISA Kits | Quantify total protein and specific factor concentration [39] |
| In Vitro Bioassays | CCK-8 Assay Kit, Matrigel, HUVECs | Assess cell viability, proliferation, and angiogenic potential [39] |
| Molecular Analysis | q-PCR reagents, Transcriptome Sequencing | Evaluate gene expression changes and pathway analysis [39] |
Critical Signaling Pathways
The therapeutic effects of conditioned medium are mediated through modulation of key signaling pathways. Research has identified several crucial pathways that are consistently regulated by MSC-derived secretomes:
Conditioned medium and cell-free therapies represent a novel class of biologics that effectively harness the paracrine potential of stem cells while overcoming the limitations of cell-based approaches. The scientific evidence demonstrates that these therapies target multiple pathological processes simultaneously – reducing inflammation, promoting angiogenesis, protecting vulnerable cells, and activating endogenous repair mechanisms.
Future development in this field will require standardization of production protocols, comprehensive characterization of secretome components, and rigorous clinical validation. As research progresses, conditioned medium therapies hold exceptional promise for treating a wide spectrum of diseases, from chronic wounds and cardiovascular conditions to autoimmune and degenerative disorders, potentially transforming the landscape of regenerative medicine.
The field of regenerative medicine has undergone a fundamental shift with the emergence of the paracrine hypothesis as a central mechanism for stem cell therapeutic efficacy. Initially, the regenerative potential of stem cells was attributed primarily to their ability to engraft and differentiate into target cell types [20]. However, both preclinical and clinical studies have consistently demonstrated that administered stem cells suffer from poor survivability and low engraftment rates, yet still produce significant functional benefits [20] [1]. This paradox led to the recognition that transplanted cells exert their therapeutic effects largely through the release of biologically active molecules that act on resident cells in a paracrine fashion [1] [41].
This paradigm shift has profound implications for clinical translation across medical specialties. The therapeutic effects are now understood to be mediated through a complex secretome comprising growth factors, cytokines, chemokines, and extracellular vesicles that influence cell survival, inflammation, angiogenesis, and endogenous repair processes in a temporal and spatial manner [20] [42]. This in-depth technical guide examines the clinical translation of adult stem cell therapies, with a specific focus on paracrine mechanisms, across three major therapeutic areas: cardiovascular, neurological, and orthopedic diseases.
Cardiovascular Diseases
Paracrine Mechanisms in Cardiac Repair
In cardiovascular medicine, the paracrine activities of stem cells mediate cardiac repair through multiple interconnected mechanisms. These include cytoprotection, neovascularization, immunomodulation, and stimulation of endogenous regeneration [1]. The seminal discovery that conditioned medium from mesenchymal stem cells (MSCs) could recapitulate the therapeutic benefits of the cells themselves provided compelling evidence for the paracrine hypothesis [20]. When administered to injured myocardium, stem cells secrete a diverse array of factors that create a regenerative microenvironment.
Table 1: Key Paracrine Factors in Cardiovascular Repair and Their Functions
| Paracrine Factor | Abbreviation | Primary Functions in Cardiac Repair |
|---|---|---|
| Vascular Endothelial Growth Factor | VEGF | Angiogenesis, cytoprotection, cell proliferation & migration [1] |
| Hepatocyte Growth Factor | HGF | Cytoprotection, angiogenesis, cell migration [20] [1] |
| Insulin-like Growth Factor-1 | IGF-1 | Cytoprotection, cell migration, contractility improvement [20] [1] |
| Fibroblast Growth Factor-2 | FGF2 | Cell proliferation & migration [1] |
| Secreted Frizzled Related Protein 2 | Sfrp2 | Cardiomyocyte protection via Wnt inhibition [20] |
| Hypoxic Induced Akt Regulated Stem Cell Factor | HASF | Mitochondrial protection, anti-apoptotic [20] |
Clinical Translation and Cardiovascular Applications
Cardiovascular diseases, particularly myocardial infarction (MI) and heart failure, represent a major focus for stem cell-based therapies. Bone marrow-derived mesenchymal stem cells (BM-MSCs) have been the most extensively studied, with over 100 active clinical trials in the United States alone [20]. The therapeutic potential of various stem cell types for cardiovascular applications is summarized below.
Table 2: Stem Cell Types in Cardiovascular Clinical Translation
| Cell Type | Tissue Source | Mechanism of Action | Clinical Trial Status |
|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone Marrow, Adipose Tissue, Umbilical Cord | Paracrine factor secretion (VEGF, HGF, IGF-1); Immunomodulation [20] [43] [24] | >100 active trials in US; Phase I/II for MI & HF [20] |
| Cardiac Stem Cells (CSCs) | Heart Tissue | Differentiation into cardiomyocytes & vascular cells; Paracrine signaling [1] [24] | Early clinical trials; Preclinical validation [1] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed Somatic Cells | Differentiation into cardiac cell types; Paracrine factors [24] | Preclinical stage; Safety concerns being addressed [24] |
| Bone Marrow Mononuclear Cells | Bone Marrow | Multiple mechanisms including paracrine signaling [1] | Multiple clinical trials completed [1] |
Experimental Protocols for Cardiovascular Applications
Standardized Protocol for MSC Preparation for Myocardial Infarction:
- Cell Isolation: Isplicate MSCs from bone marrow aspirate using density gradient centrifugation [43].
- Cell Expansion: Culture in DMEM/F12 medium supplemented with 10% FBS and 1% penicillin/streptomycin at 37°C with 5% CO₂ [43].
- Characterization: Verify MSC phenotype through flow cytometry for CD73, CD90, CD105 (≥95% positive) and CD34, CD45, HLA-DR (≤2% positive) [13].
- Pre-conditioning: Enhance paracrine activity through hypoxic preconditioning (1-2% O₂ for 24-48 hours) or cytokine priming (IFN-γ and TNF-α) [43].
- Quality Control: Assess viability (>90%), sterility, and endotoxin levels before administration [43] [13].
- Administration: Deliver cells via intramyocardial injection during cardiac surgery or intracoronary infusion via catheter-based systems [20] [24].
Paracrine Factor Analysis:
- Collect conditioned medium from cultured MSCs after 48 hours of serum-free culture [20] [1].
- Concentrate using centrifugal filters (3-10 kDa cutoff).
- Analyze paracrine factor profile using ELISA arrays for VEGF, HGF, IGF-1, FGF2, and Sfrp2 [20] [1].
- Validate functional activity through cardiomyocyte protection assays under hypoxic conditions [20].
Diagram 1: Paracrine signaling pathways in cardiovascular repair
Neurological Disorders
Paracrine Mechanisms in Neural Repair
The application of stem cell therapies for neurological disorders leverages multiple paracrine mechanisms to address complex neural damage. The central nervous system's limited regenerative capacity makes it particularly suitable for paracrine-based approaches that modulate the neural microenvironment [44]. Stem cells secrete a diverse array of factors that promote neuroprotection, immunomodulation, and endogenous repair.
Key paracrine mechanisms in neurological applications include:
- Neuroprotection: Secretion of brain-derived neurotrophic factor (BDNF), glial cell-derived neurotrophic factor (GDNF), and nerve growth factor (NGF) that enhance neuronal survival and synaptic connectivity [44].
- Immunomodulation: Regulation of microglial activation and polarization toward anti-inflammatory phenotypes, reducing neuroinflammation through IL-10, TGF-β, and TSG-6 [44].
- Angiogenesis: Promotion of vascular remodeling through VEGF and FGF2, restoring blood-brain barrier integrity and improving perfusion [44].
- Endogenous Stem Cell Activation: Stimulation of resident neural stem cells through cytokine networks that promote neurogenesis and gliogenesis [44].
Clinical Translation and Neurological Applications
Neurological disorders including Parkinson's disease (PD), Alzheimer's disease (AD), amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS), stroke, and spinal cord injury (SCI) represent major targets for stem cell therapies [44]. The translation of paracrine-based mechanisms to clinical applications has shown particular promise for these conditions.
Table 3: Stem Cell Applications in Neurological Disorders
| Neurological Condition | Cell Types Used | Primary Paracrine Mechanisms | Clinical Trial Phase |
|---|---|---|---|
| Parkinson's Disease | MSCs, NSCs, iPSC-derived dopaminergic neurons | Neurotrophic factor release (GDNF, BDNF); Immunomodulation [44] | Phase I/II trials [44] |
| Alzheimer's Disease | MSCs, NSCs | Anti-inflammatory cytokines; Amyloid-beta clearance facilitation [44] | Early phase trials [44] |
| Multiple Sclerosis | MSCs, Hematopoietic stem cells | T-cell modulation; Microglia polarization; Remyelination promotion [44] | Phase II/III trials [44] |
| Stroke | MSCs, NSCs | Neuroprotection; Angiogenesis; Anti-inflammation; Endogenous repair activation [44] | Phase I/II trials [44] |
| Spinal Cord Injury | MSCs, NSCs, Olfactory ensheathing cells | Neurotrophic support; Glial scar modulation; Axonal regeneration [44] | Phase I/II trials [44] |
Experimental Protocols for Neurological Applications
Standardized Protocol for MSC Intrathecal Administration for Neurological Disorders:
- Cell Source Selection: Utilize UC-MSCs for enhanced proliferation or BM-MSCs for established safety profile [44] [13].
- Manufacturing: Expand cells under GMP conditions using defined, xeno-free media [44].
- Potency Assays: Quantify secretion of BDNF, GDNF, VEGF, and PGE2 as critical quality attributes [44].
- Dose Preparation: Formulate at 1-2×10⁶ cells/kg in lactated Ringer's solution with 1% human serum albumin [44].
- Administration: Deliver via intrathecal injection using standard lumbar puncture technique [44].
- Monitoring: Assess neurological function using disorder-specific scales (UPDRS for PD, EDSS for MS, NIHSS for stroke) [44].
Extracellular Vesicle Isolation and Characterization:
- Collect conditioned medium from stem cells cultured in exosome-depleted FBS for 48 hours [42].
- Isolate vesicles using sequential ultracentrifugation (300g × 10 min, 2,000g × 20 min, 10,000g × 30 min, 100,000g × 70 min) [42].
- Characterize using nanoparticle tracking analysis (size distribution), Western blot (CD63, CD81, CD9), and TEM [42].
- Evaluate functional activity in vitro using neurite outgrowth assays with PC12 cells or primary neurons [42].
Orthopedic Diseases
Paracrine Mechanisms in Musculoskeletal Repair
In orthopedic applications, stem cell paracrine signaling plays a crucial role in modulating the bone and joint microenvironment to promote regeneration. The therapeutic effects are particularly mediated through immunomodulation and regulation of macrophage polarization [45] [46]. MSCs secrete factors that shift the balance from pro-inflammatory M1 macrophages to anti-inflammatory M2 phenotypes, creating a pro-regenerative environment [45].
The critical paracrine mechanisms in orthopedic repair include:
- Macrophage Polarization: Secretion of IL-10, TGF-β, and PGE2 that promote M2 macrophage differentiation, reducing inflammation and supporting tissue repair [45] [46].
- Osteogenic Differentiation: Release of BMP-2, BMP-6, and TGF-β that stimulate osteoblast differentiation and bone formation [45] [46].
- Chondroprotection: Production of TIMP-1, TIMP-2, and other factors that inhibit cartilage-degrading enzymes and promote cartilage matrix synthesis [46].
- Angiogenesis: Secretion of VEGF and PDGF that promote vascular invasion in bone repair [45] [46].
Clinical Translation and Orthopedic Applications
Orthopedic diseases including osteoarthritis (OA), bone fractures, cartilage degeneration, and orthopedic tumors represent promising targets for stem cell therapies [46]. The localized nature of many orthopedic conditions facilitates targeted delivery of stem cells and enhances the local concentration of paracrine factors.
Table 4: Stem Cell Applications in Orthopedic Diseases
| Orthopedic Condition | Cell Types Used | Primary Paracrine Mechanisms | Clinical Trial Status |
|---|---|---|---|
| Osteoarthritis | MSCs (BM, Adipose, Synovial) | Anti-inflammatory cytokines (IL-10, TGF-β); Cartilage protection; Immunomodulation [46] | Phase II/III trials; Clinical practice in some regions [46] |
| Bone Fractures/Non-union | MSCs (BM, Adipose), iPSCs | BMP secretion; Angiogenic factors; Macrophage polarization to M2 [45] [46] | Phase I/II trials [46] |
| Cartilage Defects | MSCs, Chondrocytes | ECM synthesis stimulation; Anti-catabolic factors; Immunomodulation [46] | Phase I/II trials [46] |
| Osteomyelitis/Bone Infection | MSCs with antimicrobial hydrogels | Macrophage reprogramming; Anti-inflammatory factors; Angiogenesis [45] | Preclinical and early clinical trials [45] |
Experimental Protocols for Orthopedic Applications
Standardized Protocol for Osteoarthritis Treatment:
- Cell Harvesting: Isolate MSCs from bone marrow aspirate (iliac crest) or adipose tissue (liposuction) [46].
- Processing: Use minimal manipulation or brief expansion (1-2 passages) to maintain stemness [46].
- Characterization: Confirm multipotency through osteogenic and chondrogenic differentiation assays [46] [13].
- Formulation: Prepare suspension at 10-50×10⁶ cells in physiological saline [46].
- Delivery: Administer via intra-articular injection using anatomical landmarks with ultrasound guidance [46].
- Rehabilitation: Implement controlled weight-bearing and physical therapy to enhance cell integration [46].
Macrophage Polarization Assay:
- Isplicate peripheral blood mononuclear cells (PBMCs) from healthy donors using Ficoll gradient [45].
- Differentiate monocytes to macrophages with M-CSF (50 ng/mL) for 6 days [45].
- Treat with MSC-conditioned medium (50% v/v) in the presence of IFN-γ (20 ng/mL) and LPS (100 ng/mL) to polarize toward M1 phenotype [45].
- Assess polarization via flow cytometry for M1 markers (CD80, CD86) and M2 markers (CD206, CD163) [45].
- Measure cytokine secretion using multiplex ELISA for TNF-α, IL-1β, IL-6 (M1) and IL-10, TGF-β (M2) [45].
Diagram 2: Paracrine-mediated macrophage polarization in orthopedic repair
The Scientist's Toolkit: Essential Research Reagents
Table 5: Essential Research Reagents for Studying Paracrine Mechanisms
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Surface Markers | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [13] | MSC characterization & quality control | Identity verification; Purity assessment [13] |
| Cytokine Priming Agents | IFN-γ, TNF-α, LPS [43] | Enhancement of immunomodulatory potency | MSC pre-conditioning; Secretome enrichment [43] |
| Growth Factors & Cytokines | VEGF, HGF, FGF2, BDNF, GDNF, BMP-2, IL-10, TGF-β [20] [1] | Functional assays; Mechanism studies | Angiogenesis; Neuroprotection; Osteogenesis [20] [44] [1] |
| Extracellular Vesicle Isolation Kits | Ultracentrifugation reagents; Size-exclusion chromatography; Polymer-based precipitation kits [42] | Paracrine factor concentration & analysis | Exosome isolation; miRNA/protein cargo analysis [42] |
| Macrophage Polarization Markers | CD80, CD86 (M1); CD206, CD163 (M2) [45] | Immunomodulation assessment | Flow cytometry; Mechanism validation [45] |
| Hypoxia Chamber/System | Hypoxic chambers (1-5% O₂); Chemical hypoxia mimetics [43] | Pre-conditioning to enhance paracrine effects | MSC secretome enhancement; Therapeutic potency improvement [43] |
The clinical translation of stem cell therapies across cardiovascular, neurological, and orthopedic diseases increasingly relies on harnessing paracrine mechanisms rather than cell replacement alone. The recognition that transplanted stem cells function primarily as "factories" of therapeutic factors represents a paradigm shift in regenerative medicine [20] [1] [41]. This understanding has led to innovative approaches including cell pre-conditioning, engineered hydrogels for sustained factor release, and development of cell-free therapies using extracellular vesicles [45] [42].
Future directions will focus on optimizing the therapeutic secretome through precise control of cell manufacturing, developing standardized potency assays based on paracrine factor profiles, and creating synergistic combinations of stem cells with biomaterials that enhance and sustain paracrine signaling [45] [43] [13]. As the field advances, the strategic manipulation of paracrine mechanisms will undoubtedly play an increasingly central role in realizing the full clinical potential of stem cell therapies across diverse disease domains.
Navigating Challenges and Enhancing Therapeutic Efficacy
The therapeutic potential of Mesenchymal Stem Cells (MSCs) in regenerative medicine is significantly shaped by their paracrine activity—the secretion of bioactive molecules that modulate immune responses, promote tissue repair, and activate endogenous regenerative pathways [47] [48] [13]. However, the efficacy of these paracrine-mediated therapies is not uniform, largely due to the profound heterogeneity of MSCs themselves. This heterogeneity arises from three primary sources: intrinsic biological differences between donors (donor variation), the anatomical and physiological context from which the cells are isolated (source), and the laboratory methods used to grow and prepare them (culture conditions) [48]. This variability compromises the potency, consistency, and clinical reproducibility of MSC-based treatments, presenting a major barrier to their widespread clinical translation [47] [48]. This guide details the mechanisms of this heterogeneity and provides standardized experimental frameworks to control for these variables, ensuring that research into the paracrine functions of MSCs is robust, reproducible, and predictive of clinical outcomes.
Quantifying the Dimensions of MSC Heterogeneity
The impact of donor, source, and culture conditions on MSC characteristics can be quantified through specific, measurable parameters. The following tables summarize key variables and their effects on MSC phenotype and function, which directly influence the composition and potency of the paracrine secretome.
Table 1: Impact of Donor and Tissue Source on MSC Properties
| Heterogeneity Factor | Specific Variables | Observed Impact on MSC Characteristics | Implications for Paracrine Signaling |
|---|---|---|---|
| Donor Variation | Age [48] [13] | MSCs from older donors may exhibit reduced proliferative capacity and differentiation potential [48] [13]. | Altered secretome profile, potentially diminishing pro-regenerative and immunomodulatory output. |
| Health Status [47] | Underlying diseases (e.g., diabetes, autoimmune conditions) can affect MSC functionality [47]. | Compromised therapeutic response and inconsistent paracrine effects in clinical applications. | |
| Genetic Background [48] | Natural genetic polymorphism influences cell surface marker expression and growth kinetics [48]. | Donor-specific secretome "fingerprints" leading to variable experimental and clinical outcomes. | |
| Tissue Source | Bone Marrow (BM) [13] | Considered the "gold standard"; strong osteogenic potential and well-characterized [13]. | A well-studied secretome, but cell harvest is invasive and yield decreases with donor age. |
| Adipose Tissue (AD) [13] | Easier to harvest in high yields; comparable immunomodulatory properties to BM-MSCs [13]. | A promising source for paracrine therapy, with a potent anti-inflammatory secretome. | |
| Umbilical Cord (UC) [13] | Enhanced proliferation capacity, lower immunogenicity, and younger cell population [13]. | A highly consistent and potent secretome, advantageous for allogeneic, off-the-shelf therapies. |
Table 2: Impact of Culture Conditions on MSC Properties
| Process Variable | Specific Parameters | Observed Impact on MSC Characteristics | Implications for Paracrine Signaling |
|---|---|---|---|
| Cell Culture & Expansion | Seeding Density [48] | High density can lead to contact inhibition and spontaneous differentiation; low density may promote rapid proliferation but alter phenotype. | Density can influence the metabolic state of cells, thereby changing the profile of secreted factors and vesicles. |
| Oxygen Tension [17] | Physiological (hypoxic) conditions (1-5% O₂) can enhance MSC proliferation, survival, and secretion of pro-angiogenic factors [17]. | Hypoxic preconditioning is a key strategy to boost the pro-regenerative potency of the MSC secretome. | |
| Culture Media Formulation | Use of fetal bovine serum (FBS) vs. xeno-free alternatives introduces batch-to-batch variability and immunogenic risks [48]. | Serum content directly introduces exogenous variables that can drastically alter the observed paracrine effects. | |
| Preservation & Administration | Cryopreservation Method | Freeze-thaw cycles can reduce cell viability and alter surface marker expression and homing ability. | Damaged cells may release inflammatory factors upon administration, counteracting the therapeutic secretome. |
| Route of Administration [48] | Intravenous, local injection, or intranasal delivery affect engraftment efficiency and distribution of cells and their secreted factors. | Determines the bioavailability of the paracrine signals at the target tissue site. |
Methodologies to Mitigate Heterogeneity and Standardize MSC Populations
To ensure that research on MSC paracrine signaling is reproducible, specific experimental strategies must be employed to control for the variables outlined above.
Strategic Cell Sourcing and Donor Screening
- Establish Rigorous Donor Criteria: For research, define and adhere to strict donor eligibility criteria based on age, sex, and health status. Maintain detailed records for all donor material to enable retrospective analysis of these variables on experimental outcomes [48] [13].
- Select Optimal Tissue Sources: Choose the MSC source based on the research question. UC-MSCs are often preferred for their consistency and proliferative capacity. When using BM-MSCs or AD-MSCs, pool cells from multiple donors (e.g., 3-5) to create a standardized research cell bank that averages out donor-specific effects [13].
Standardization of Culture and Expansion Protocols
- Adopt Defined, Xeno-Free Media: Transition from FBS to defined, serum-free or xeno-free media formulations. This eliminates a major source of batch-to-batch variability and enhances the translational relevance of the findings by reducing immunogenic risks [48].
- Control Passage Number and Seeding Density: Standardize the specific passage numbers (e.g., P3-P5) used for experiments, as prolonged culture leads to cellular senescence and alters secretome composition. Consistently use the same seeding density (e.g., cells/cm²) to ensure uniform growth conditions across experiments [48].
- Implement Preconditioning Strategies: Prime MSCs prior to application to enhance their paracrine activity. Common preconditioning protocols include:
- Hypoxic Preconditioning: Culture MSCs at 1-5% O₂ for 24-48 hours before harvesting conditioned medium or cells for therapy. This mimics the physiological niche and upregulates secretion of pro-survival and angiogenic factors like VEGF and HGF [17].
- Cytokine Priming: Incubate MSCs with inflammatory cytokines such as IFN-γ or TNF-α. This "licenses" the MSCs, boosting their immunomodulatory potency by enhancing the expression of key mediators like IDO and PGE2 [13] [17].
Analytical and Potency Assays
Moving beyond basic characterization, these functional assays are critical for linking MSC status to paracrine output.
- Secretome Analysis: Collect Conditioned Medium (CM) from standardized MSC cultures. Analyze the CM using proteomic arrays or mass spectrometry to quantify the levels of key paracrine factors (e.g., VEGF, IL-10, TGF-β, IDO). This provides a direct readout of the functional secretome [48] [13].
- Functional Potency Assays: Instead of relying solely on cell surface markers, implement bioassays that measure the intended biological function.
Diagram 1: A strategic workflow for addressing MSC heterogeneity, linking control strategies to functional quality control.
Experimental Protocol: Evaluating the Impact of Culture Conditions on Paracrine-Mediated Angiogenesis
This detailed protocol provides a methodology to systematically investigate how a specific variable—oxygen tension—affects the angiogenic capacity of the MSC secretome.
Objective: To compare the pro-angiogenic paracrine potential of MSCs expanded under standard (20%) versus physiological hypoxic (2%) O₂ tension.
Materials:
- Cell Line: Human Bone Marrow-MSCs (hBM-MSCs), passage 3-5, from a standardized bank.
- Equipment: Hypoxic incubator (2% O₂, 5% CO₂, 37°C), normoxic incubator (20% O₂, 5% CO₂, 37°C), Class II biological safety cabinet, centrifuge.
- Reagents: Defined, serum-free MSC expansion medium, PBS, trypsin/EDTA, Growth Factor Reduced (GFR) Matrigel.
- Assay Cells: Human Umbilical Vein Endothelial Cells (HUVECs).
Procedure:
- Cell Culture and Preconditioning:
- Thaw and expand hBM-MSCs in serum-free medium under standard conditions (20% O₂) until 70-80% confluency.
- Split cells into two identical groups.
- Experimental Group: Culture in a hypoxic incubator at 2% O₂ for 48 hours.
- Control Group: Continue culture in a normoxic incubator at 20% O₂ for 48 hours.
- Conditioned Medium (CM) Collection:
- After 48 hours, wash both groups of MSCs with PBS and add fresh serum-free medium.
- Incubate for a further 24 hours under their respective oxygen conditions (2% or 20% O₂).
- Collect the culture supernatant from both groups. This is the Conditioned Medium (CM).
- Centrifuge the CM at 2,000 × g for 10 minutes to remove cell debris. Aliquot and store at -80°C.
- Tube Formation Assay:
- Thaw GFR Matrigel on ice overnight at 4°C. Coat a 96-well plate with 50 µL of Matrigel per well and polymerize at 37°C for 30 minutes.
- Trypsinize and harvest HUVECs. Resuspend 1.0 × 10⁴ HUVECs in 100 µL of either:
- Hypoxic MSC-CM
- Normoxic MSC-CM
- Fresh serum-free medium (negative control)
- Seed the HUVEC suspension onto the polymerized Matrigel.
- Incubate the plate at 37°C, 5% CO₂ for 4-8 hours.
- Image Acquisition and Quantification:
- Using an inverted microscope, capture images (10x objective) of three random fields per well at 6 hours.
- Analyze images with angiogenesis analysis software (e.g., ImageJ with Angiogenesis Analyzer plugin).
- Quantitative Measures: Total tube length per field, number of master junctions, number of meshes.
Expected Outcome: HUVECs treated with CM from hypoxic MSCs are expected to form a more extensive and interconnected tubular network, demonstrating enhanced paracrine-mediated angiogenic capacity compared to the normoxic control.
Diagram 2: Experimental workflow for evaluating the effect of oxygen preconditioning on MSC paracrine function.
The Scientist's Toolkit: Key Reagents for Heterogeneity Research
Table 3: Essential Research Reagents for Standardizing MSC Studies
| Reagent / Material | Specific Function | Role in Addressing Heterogeneity |
|---|---|---|
| Defined, Xeno-Free MSC Medium | Provides a consistent, serum-free nutrient base for cell growth, eliminating undefined serum components [48]. | Critical for standardizing the basal culture environment, removing FBS as a major source of technical variability and immunogenic risk. |
| Recombinant Human IFN-γ | A pro-inflammatory cytokine used to "license" or prime MSCs prior to experimentation or therapy [13] [17]. | Enhances and standardizes the immunomodulatory potency of MSCs by upregulating IDO and other key mediators, making responses more predictable. |
| Hypoxic Chamber / Incubator | Enables precise control of oxygen tension (typically 1-5% O₂) for cell culture [17]. | Allows for physiological preconditioning of MSCs, boosting the pro-regenerative quality of the secretome and improving in vivo survival. |
| Growth Factor Reduced Matrigel | A basement membrane extract that provides a substrate for endothelial cell tube formation [13]. | Essential for a standardized, quantitative in vitro bioassay to measure the angiogenic potency of the MSC secretome (via CM). |
| Antibody Panels for Flow Cytometry | Antibodies against CD73, CD90, CD105 (positive) and CD34, CD45, HLA-DR (negative) for MSC immunophenotyping [13]. | Verifies MSC identity and purity according to ISCT criteria, ensuring a baseline level of population homogeneity before experiments. |
| Proteomic Array Kits | Kits (e.g., from RayBiotech, R&D Systems) for multiplexed analysis of hundreds of secreted proteins in conditioned medium. | Provides a high-content, quantitative profile of the MSC secretome, directly linking cell state to functional paracrine output. |
The path to successful clinical translation of MSC therapies, particularly those reliant on paracrine mechanisms, depends on a rigorous and systematic approach to managing cellular heterogeneity. By acknowledging and actively controlling for the variables of donor, source, and culture conditions—through strategic sourcing, standardized protocols, functional preconditioning, and robust potency assays—researchers can transform MSCs from a variable biological material into a more consistent and predictable therapeutic agent. This disciplined framework is essential for unlocking the full potential of MSC-based paracrine therapies in regenerative medicine.
The therapeutic efficacy of adult stem cell therapies is largely mediated by paracrine signaling, a mechanism wherein transplanted cells secrete bioactive factors that orchestrate tissue repair, angiogenesis, and immune modulation. To overcome the limited secretory capacity of native stem cells in hostile diseased microenvironments, researchers have developed potent enhancement strategies. This whitepaper provides an in-depth technical analysis of two leading approaches: genetic modification to overexpress key paracrine factors and hypoxic preconditioning to physiologically augment the stem cell secretome. Within the context of cardiovascular and renal regenerative medicine, we summarize quantitative data on efficacy, detail standardized experimental protocols, visualize critical signaling pathways, and catalog essential research reagents. The evidence demonstrates that these strategies significantly enhance the paracrine activity of mesenchymal stem cells (MSCs), adipose-derived stem cells (ASCs), and other therapeutic cell types, leading to improved survival, neovascularization, and functional recovery in preclinical disease models.
Initially, the therapeutic potential of stem cell therapy was attributed to the direct differentiation and engraftment of transplanted cells to replace damaged tissues. However, a growing body of evidence now establishes that the primary mechanism is paracrine signaling [1]. In this paradigm, stem cells function as bioactive factories, secreting a multitude of cytokines, chemokines, and growth factors that act on neighboring cells in a paracrine fashion to elicit therapeutic effects [49] [1].
The recognized paracrine actions include:
- Cytoprotection: Enhancing survival of endangered host cells [1].
- Neovascularization: Stimulating the formation of new blood vessels [1] [50].
- Immunomodulation: Reducing detrimental inflammation [51].
- Activation of Endogenous Stem Cells: Promoting the body's own repair mechanisms [1].
- Attenuation of Pathological Remodeling: Limiting tissue scarring and dysfunction [1].
The composition and potency of this secretome are not fixed. The diseased microenvironment, often characterized by inflammation, fibrosis, and hypoxia, can impair the native secretory functions of therapeutic cells [51]. This pressing clinical challenge has driven the development of enhancement strategies designed to pre-emptively "arm" stem cells, boosting their paracrine output to ensure robust therapeutic efficacy post-transplantation.
Genetic Modification to Enhance Paracrine Signaling
Genetic modification involves the stable or transient introduction of genes encoding specific paracrine factors or upstream regulatory molecules into stem cells. This approach allows for a targeted amplification of desired signaling pathways.
Key Molecular Targets and Experimental Evidence
The selection of genetic targets is based on their central role in regulating survival, angiogenesis, and inflammation.
Table 1: Key Genetic Modification Targets for Enhancing Paracrine Signaling
| Target Gene | Class/Family | Primary Paracrine Effects | Validated Cell Types | Key Experimental Outcomes |
|---|---|---|---|---|
| Akt-1 (PKB) | Serine/Threonine Kinase | Cytoprotection, Angiogenesis [1] | MSCs [1] | Reduced apoptosis in cardiomyocytes; Enhanced cardiac function in infarcted hearts [1]. |
| VEGF-A | Growth Factor | Angiogenesis, Cell Survival [50] | MSCs, ASCs [50] | Increased capillary density; Improved cardiac function post-MI [50]. |
| HGF | Growth Factor | Cytoprotection, Angiogenesis, Cell Migration [1] [50] | MSCs [50] | Enhanced angiogenic potential; Tissue repair. |
| SDF-1 | Chemokine | Progenitor Cell Homing [50] | MSCs [50] | Improved stem cell recruitment and cardiac function. |
| ANG (Angiogenin) | Ribonuclease | Angiogenesis, Cell Proliferation [50] | ASCs [50] | Critical for in vivo angiogenic response; knockdown reduces vessel formation. |
| FGF2 (b-FGF) | Growth Factor | Cell Proliferation & Migration [1] | MSCs [1] | Promotes angiogenesis and tissue repair. |
Detailed Experimental Protocol: Genetic Modification of MSCs with Akt-1
This protocol outlines the steps to create MSCs that overexpress the Akt-1 gene, a potent enhancer of cytoprotective and angiogenic paracrine signals [1].
1. Cell Culture and Expansion:
- Cell Source: Human bone marrow-derived MSCs or adipose-derived ASCs.
- Culture Conditions: Maintain cells in Advanced MEM supplemented with 5-10% fetal calf serum (FCS) or platelet lysate, and 1% antibiotic-antimycotic solution at 37°C in a humidified atmosphere of 5% CO₂ [50] [51].
- Passaging: Harvest cells at 80-90% confluency using TrypLE Express and expand for 3-5 passages [51].
2. Viral Vector Preparation:
- Vector Choice: Utilize a lentiviral or retroviral vector system for stable gene expression.
- Vector Construction: Clone the human Akt-1 cDNA (or the constitutively active myristoylated form) into the vector under the control of a strong promoter (e.g., CMV or EF1α). Include a selectable marker (e.g., puromycin resistance or GFP).
3. Cell Transduction:
- Seed MSCs at a density of 5x10³ cells/cm².
- At 50-70% confluency, incubate cells with the viral supernatant containing polybrene (4-8 µg/mL) to enhance transduction efficiency.
- After 24 hours, replace the viral supernatant with fresh complete culture medium.
4. Selection and Expansion:
- 48-72 hours post-transduction, begin antibiotic selection (e.g., 1-2 µg/mL puromycin) for 5-7 days to eliminate non-transduced cells.
- Expand the polyclonal population of Akt-MSCs for subsequent experiments.
5. In Vitro Validation:
- Gene Expression: Confirm Akt-1 overexpression using qPCR.
- Protein Expression: Verify protein levels via Western blot.
- Secretome Analysis: Collect conditioned medium (CM) and quantify the enhanced secretion of paracrine factors (e.g., VEGF, HGF, IGF-1) using ELISA kits specific for each factor [1].
- Functional Assay: Validate the enhanced cytoprotective effect of Akt-MSC-CM on stressed cardiomyocytes in vitro using an apoptosis assay (e.g., TUNEL staining) [1].
Signaling Pathway Diagram: Akt-1 Mediated Paracrine Enhancement
Diagram Title: Genetic Akt-1 Modification Enhances Paracrine Signaling
Hypoxic Preconditioning to Enhance Paracrine Signaling
Hypoxic preconditioning (HPC) is a non-genetic, physiological strategy that involves exposing stem cells to brief, sublethal periods of low oxygen tension before transplantation. This process mimics a natural adaptive response, priming the cells to thrive in the harsh ischemic target tissue and robustly enhancing their paracrine profile [50] [51] [52].
Quantitative Evidence of HPC Efficacy
HPC has been demonstrated to consistently upregulate a spectrum of pro-angiogenic and pro-survival genes and proteins across multiple stem cell types.
Table 2: Quantitative Effects of Hypoxic Preconditioning on Stem Cell Paracrine Profile
| Cell Type | HPC Regimen | Key Upregulated Factors (Measured Change) | Downstream In Vivo Effect |
|---|---|---|---|
| Human ASCs [50] | <0.1% O₂, 24 hours | VEGF-A mRNA & Protein: Significantly increased [50]Angiogenin (ANG) mRNA & Protein: Significantly increased [50] | Increased angiogenesis in murine subcutaneous sponge model (% vascular volume: 6.0% vs 4.1% in normoxic control) [50]. |
| Human MSCs (from Healthy Donors) [51] | 1% O₂, 24 hours | EGF Release: Increased [51]SA-β-gal Activity (Senescence): Tended to decrease [51] | Improved proliferative capacity; Modest reduction in cellular senescence [51]. |
| Human MSCs (from HKD Patients) [51] | 1% O₂, 24 hours | HGF Release: Decreased [51]Senescence Gene Expression: A few genes upregulated [51] | Milder functional response compared to healthy MSCs. |
| MSCs (Various Preclinical Studies) [52] | 0.5-2% O₂, 12-72 hours | HIF-1α, Bcl-2, Bcl-xL, Angiopoietin-1: Increased [52] | Improved cell survival post-transplantation; Enhanced functional recovery in MI and kidney disease models [51] [52]. |
Detailed Experimental Protocol: Hypoxic Preconditioning of ASCs
This protocol is adapted from studies demonstrating enhanced angiogenic paracrine activity in human adipose-derived stem cells (ASCs) [50].
1. Cell Culture and Preparation:
- Isolate ASCs from human subcutaneous adipose tissue via collagenase digestion and centrifugation [51].
- Culture and expand ASCs in complete DMEM (low glucose) with 10% FCS and antibiotics. Use cells between passages 3-6.
- Seed ASCs at a density of 5x10³ cells/cm² and culture until they reach 80% confluency.
2. Hypoxic Conditioning:
- Pre-conditioning: Replace the growth medium with serum-free DMEM.
- Hypoxic Exposure: Place the culture flasks/plates into a dedicated hypoxic chamber (e.g., GENbox Jar) or a tri-gas incubator.
- Critical Parameters:
3. Collection of Conditioned Medium (CM):
- After the HPC period, collect the supernatant (now hypoxic ASC-conditioned medium, ASCCM).
- Centrifuge the CM at 875g for 10 minutes to remove cell debris.
- Filter the supernatant through a 0.2-µm filter.
- Concentration (Optional): For in vivo applications, concentrate the CM (e.g., 50x) using centrifugal filter columns with a 3-kDa molecular weight cutoff [50].
- Aliquot and store the CM at -80°C for subsequent functional assays.
4. Post-HPC Cell Harvest:
- For cells intended for transplantation, harvest using TrypLE Express after the HPC period and resuspend in an appropriate injection buffer.
- For RNA/Protein analysis, lyse cells directly to examine transcriptional changes (e.g., VEGF-A, ANG, GLUT-1) via qRT-PCR or protein via Western blot/ELISA.
5. Functional Validation:
- In Vitro Angiogenesis Assay: Test the HPC-CM on human umbilical vein endothelial cells (HUVECs) in a tube formation assay on Matrigel.
- In Vivo Angiogenesis Assay: Impregnate polyvinyl alcohol sponges with concentrated HPC-CM or normoxic-CM and implant subcutaneously in mice. After 2 weeks, harvest sponges and perform morphometric analysis of CD31-stained sections to quantify vascular volume [50].
- Antibody Neutralization: To confirm the specific contribution of factors like VEGF-A or ANG, pre-incubate the HPC-CM with neutralizing antibodies before the in vivo sponge assay [50].
Signaling Pathway Diagram: Hypoxic Preconditioning Mechanism
Diagram Title: Hypoxic Preconditioning Activates HIF-1α Pathway
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the described strategies requires a suite of validated reagents and tools.
Table 3: Research Reagent Solutions for Paracrine Enhancement Studies
| Reagent / Tool Category | Specific Examples | Function / Application |
|---|---|---|
| Cell Culture & Characterization | DMEM-low glucose, Advanced MEM, Fetal Calf Serum, Platelet Lysate, TrypLE Express [50] [51] | Culture and expansion of MSCs/ASCs. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD45, CD34, CD14) [51] | Immunophenotypic characterization of MSCs per ISCT guidelines. | |
| Genetic Modification | Lentiviral/Retroviral Vectors | Delivery and stable integration of target genes (Akt-1, VEGF, etc.). |
| Puromycin, G418 (Geneticin) | Selection of successfully transduced cells. | |
| Hypoxic Preconditioning | Tri-Gas Incubator, GENbox Jars [50] | Precise control and maintenance of hypoxic environments (<0.1% - 5% O₂). |
| Secretome Analysis | ELISA Kits (VEGF-A, HGF, ANG, IGF-1, EGF) [1] [50] [51] | Quantification of specific paracrine factors in conditioned media. |
| Amicon Ultra-15 Centrifugal Filters (3-kDa cutoff) [50] | Concentration of conditioned media for in vivo studies or proteomics. | |
| Functional Assays | HUVECs & Matrigel | In vitro tube formation assay to assess angiogenic potential of CM. |
| Neutralizing Antibodies (anti-VEGF-A, anti-ANG) [50] | To confirm the specific role of a paracrine factor in functional assays. | |
| In Vivo Validation | Polyvinyl Alcohol Sponges [50] | Subcutaneous implantation in mice to quantify in vivo angiogenesis. |
| Anti-CD31 Antibody [50] | Immunohistochemical staining to identify and quantify blood vessels. |
Genetic modification and hypoxic preconditioning are two powerful and complementary strategies for enhancing the paracrine potency of therapeutic stem cells. Genetic engineering offers precise, potent, and sustained overexpression of specific factors, while HPC provides a safer, more physiological boost to a broad spectrum of native paracrine signals. The choice between them depends on the specific clinical application, regulatory considerations, and the desired profile of the secretome. As the field advances, combination strategies and the application of these enhanced cells in clinical trials for conditions like ischemic heart disease and hypertensive kidney disease will be critical in realizing the full potential of paracrine-based regenerative medicine.
The therapeutic paradigm for adult stem cells, particularly mesenchymal stem cells (MSCs), has fundamentally shifted from a focus on cellular differentiation and replacement to an understanding that their primary mechanism of action occurs through paracrine signaling [20]. These cells function as bioreactors, secreting a complex cocktail of bioactive molecules—including growth factors, cytokines, chemokines, and extracellular vesicles—that modulate the host immune response, promote cytoprotection, enhance angiogenesis, and stimulate endogenous repair mechanisms [20] [13]. Consequently, the efficacy of any stem cell therapy is critically dependent on delivering a sufficient number of viable cells to the appropriate anatomical niche where they can exert these paracrine effects.
The dual challenges of targeted homing—the process by which cells navigate to injury sites—and route selection are thus central to clinical success. The route of administration directly influences the initial engraftment, distribution, and subsequent secretory profile of the cells, while the homing efficiency determines the fraction of delivered cells that ultimately participates in creating a reparative tissue microenvironment [20]. This guide provides a technical overview of current administration strategies, the molecular machinery governing homing, and the experimental frameworks used to optimize these parameters for research and clinical application.
Routes of Administration: A Technical Comparison
Selecting an administration route requires balancing invasiveness, targeting precision, cell viability, and clinical practicality. Each method presents a unique set of advantages and limitations for establishing a therapeutically productive paracrine niche.
Table 1: Comparison of Stem Cell Administration Routes
| Route | Technical Procedure | Therapeutic Rationale | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Intravenous (IV) | Infusion into peripheral vein | Systemic distribution via circulation; leverages innate homing signals [20] | Minimally invasive; allows broad systemic access for immunomodulation | High pulmonary first-pass effect; poor trafficking to solid tissues; potential emboli [13] |
| Local/Intra-Tissue | Direct injection into target tissue (e.g., myocardium, muscle, joint) | Focal delivery maximizes local paracrine concentration [20] | High local cell density; bypasses vascular barriers | Invasive; potential for injection-related tissue damage; limited diffusion from site |
| Intra-Arterial | Injection into artery supplying target organ | Direct regional delivery; reduces pulmonary sequestration | Improved organ-specific targeting vs. IV | Technically complex; risk of arterial embolism or vasospasm |
| Intrathecal | Injection into cerebrospinal fluid | Bypasses blood-brain/blood-nerve barriers | Direct access to central nervous system | Specialized procedure requiring significant clinical expertise |
The choice of route profoundly impacts the paracrine footprint. Local injection establishes a high-concentration gradient of secreted factors in a defined area, ideal for localized injuries. In contrast, systemic IV delivery is better suited for modulating widespread inflammatory or autoimmune conditions, though the low fraction of cells reaching the target site remains a significant constraint [20] [13].
The Molecular Machinery of Targeted Homing
The homing of systemically delivered MSCs to sites of injury is an active, multi-step process orchestrated by a cascade of molecular interactions, analogous to leukocyte trafficking. This process is critical for ensuring that cells dispatched into the circulation can extravasate and infiltrate the intended tissue to establish a functional paracrine unit.
The Homing Cascade: A Multi-Step Process
The journey from the vasculature to the injured tissue involves a coordinated sequence of events: initial tethering and rolling, activation, firm adhesion, and finally, transendothelial migration. The diagram below illustrates this complex molecular cascade and the key signaling pathways that regulate it internally.
Key Receptors, Ligands, and Signaling Pathways
The homing cascade is mediated by specific ligand-receptor interactions and intracellular signaling events. The SDF-1/CXCR4 axis is one of the most well-characterized pathways, where stromal-derived factor-1 (SDF-1) released from ischemic tissues binds to the CXCR4 receptor on MSCs, triggering intracellular signaling that leads to actin polymerization and directional migration [20]. Furthermore, key adhesion molecules like Vascular Cell Adhesion Molecule-1 (VCAM-1) on activated endothelium interact with Very Late Antigen-4 (VLA-4) on MSCs to mediate firm adhesion, a critical step for halting rolling cells on the vascular wall.
The internal signaling that governs MSC migration, proliferation, and secretion is complex, involving a network of tightly regulated pathways. These pathways integrate external homing signals into appropriate cellular responses, ultimately determining the success of the therapeutic intervention.
Table 2: Key Molecular Pairs in Stem Cell Homing
| Receptor on Stem Cell | Ligand in Tissue | Primary Function in Homing |
|---|---|---|
| CXCR4 | SDF-1 (CXCL12) | Chemoattraction; activation of integrins [20] |
| VLA-4 (α4β1 Integrin) | VCAM-1 | Mediates firm adhesion to activated endothelium |
| LFA-1 (αLβ2 Integrin) | ICAM-1 | Supports firm adhesion and transmigration |
| P-selectin Glycoprotein Ligand-1 (PSGL-1) | P-selectin, E-selectin | Mediates initial tethering and rolling |
| c-Met | HGF (Hepatocyte Growth Factor) | Chemoattraction and activation of motile machinery |
Experimental Protocols for Evaluating Homing and Paracrine Effects
Rigorous in vitro and in vivo models are essential for quantifying homing efficiency and optimizing delivery strategies. The following protocols represent standard methodologies in the field.
Protocol 1: Transwell Migration Assay (In Vitro)
Objective: To quantitatively measure the chemotactic response of MSCs toward a gradient of homing factors released from injured tissue.
Materials:
- Transwell plate: 24-well plate with cell culture inserts (polycarbonate membrane, 5-8 μm pore size).
- Chemoattractant: Conditioned media from target cell lines (e.g., hypoxic cardiomyocytes) or recombinant human SDF-1α.
- Serum-free basal medium: (e.g., DMEM).
- Cell staining solution: 4% paraformaldehyde (PFA), 0.1% Crystal Violet (in methanol).
- Imaging and quantification system: Microscope, camera, and image analysis software (e.g., ImageJ).
Methodology:
- Preparation: Place 500-600 μL of chemoattractant (test) or serum-free medium (negative control) into the lower chamber of the Transwell plate.
- Cell Seeding: Trypsinize, wash, and resuspend MSCs in serum-free medium. Seed 50,000-100,000 cells into the upper chamber of the Transwell insert.
- Incubation: Incubate the plate for 6-24 hours at 37°C in 5% CO₂ to allow for cell migration.
- Fixation and Staining: Carefully remove the non-migrated cells from the upper side of the membrane with a cotton swab. Fix the migrated cells on the lower side with 4% PFA for 10 minutes, then stain with 0.1% Crystal Violet for 15 minutes.
- Quantification: Wash the membrane, acquire images of multiple random fields under a microscope, and count the number of migrated cells. Express data as the fold-increase in migration compared to the negative control.
Protocol 2:In VivoCell Trafficking Using Bioluminescence Imaging (BLI)
Objective: To non-invasively monitor the real-time distribution, homing, and persistence of systemically administered MSCs in a living animal.
Materials:
- Luciferase-expressing MSCs: Stable cell line transduced with a firefly luciferase (Fluc) reporter gene.
- D-luciferin substrate: Potassium salt, dissolved in PBS (15 mg/mL).
- Animal model: Immunocompromised mice (e.g., NOD-scid) with a relevant injury model (e.g., myocardial infarction, stroke).
- Imaging system: In vivo bioluminescence imaging system (IVIS Spectrum or equivalent).
- Anesthesia system: Isoflurane vaporizer.
Methodology:
- Cell Preparation: Harvest and resuspend 1-2 x 10^6 luciferase-expressing MSCs in sterile PBS for injection.
- Administration: Inject cells into the animal via the chosen route (e.g., IV via tail vein).
- Image Acquisition: At predetermined time points (e.g., 4, 24, 48, 72 hours, 1 week post-injection), inject the animal intraperitoneally with D-luciferin (150 mg/kg). After 10 minutes (to allow for systemic distribution), anesthetize the animal and place it in the imaging chamber.
- Data Acquisition: Acquire images with a set exposure time (1-60 seconds). The resulting photon flux is displayed as a pseudocolor overlay on a grayscale photograph of the animal.
- Quantification: Use the imaging software to define regions of interest (ROIs) over the target organ and control areas. Quantify the signal as total flux (photons/second). Plot the kinetics of the homing signal to assess recruitment and retention.
The overall workflow for developing and testing an optimized delivery strategy, from pre-conditioning cells to final in vivo validation, can be summarized as follows:
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Homing and Delivery Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Recombinant Human SDF-1α | Establishes a chemotactic gradient in in vitro migration assays. | Positive control in Transwell migration experiments [20]. |
| AMD3100 (Plerixafor) | Small-molecule CXCR4 antagonist; inhibits SDF-1/CXCR4 axis. | Validating the specificity of SDF-1-mediated homing in vitro and in vivo. |
| Functional Blocking Antibodies | Antibodies against adhesion molecules (e.g., anti-VCAM-1, anti-VLA-4). | Mechanistic studies to block specific steps of the homing cascade. |
| Lentiviral Vectors | For stable genetic modification of MSCs (e.g., Luciferase, GFP). | Generating reporter cell lines for in vivo tracking and ex vivo detection [13]. |
| Matrigel Invasion Assay | Basement membrane matrix to model transendothelial migration. | Assessing the invasive capacity of MSCs through a simulated extracellular matrix. |
| Flow Cytometry Antibodies | Antibodies for surface markers (CD73, CD90, CD105, CXCR4, CD34). | Characterizing MSC phenotype and quantifying homing receptor expression pre-/post-transplantation [13] [53]. |
| High-Content Screening (HCS) Platforms | Automated microscopy and image analysis for phenotypic profiling. | Systematic evaluation of drug combinations or genetic modifications on MSC migration and secretome [54]. |
The optimization of delivery routes and the enhancement of targeted homing are not merely logistical concerns but are fundamental to unlocking the full paracrine potential of adult stem cell therapies. The future of the field lies in moving beyond naive cell administration toward engineered delivery strategies. This includes the pharmacological pre-conditioning of cells to boost homing receptor expression [55], the use of biomaterial scaffolds to localize cells and their secretory output, and the application of Quantitative and Systems Pharmacology (QSP) approaches to build predictive models that integrate cell pharmacokinetics with the dynamics of paracrine factor release [56]. By systematically addressing these delivery challenges, researchers can significantly improve the consistency and efficacy of stem cell-based treatments, ensuring that the reparative signals reach their intended targets.
The therapeutic potential of adult stem cells, particularly mesenchymal stem cells (MSCs), in regenerative medicine is substantially constrained by a critical biological bottleneck: the poor survival and engraftment of transplanted cells. Studies indicate that up to 90% of transplanted stem cells undergo apoptosis within the initial days post-transplantation, primarily due to a hostile microenvironment characterized by ischemia, inflammation, and oxidative stress [57] [58]. This massive cell attrition compromises therapeutic efficacy, reproducibility, and stability—factors essential for any clinical intervention [57]. The paradigm of stem cell action has progressively shifted from a model of direct differentiation and tissue replacement to the understanding that a significant portion of their benefit is mediated through paracrine mechanisms [20] [1]. The efficacy of these paracrine signals—the secretion of growth factors, cytokines, and extracellular vesicles that modulate local cellular environments, promote tissue repair, and exert immunomodulatory effects—is intrinsically dependent on the presence and longevity of the viable donor cells [13] [9]. Therefore, overcoming the challenges of low engraftment and transient survival is not merely a technical obstacle but a fundamental prerequisite for harnessing the full paracrine potential of adult stem cell therapy. This whitepaper provides an in-depth technical analysis of the causes underlying poor cell engraftment and systematically details the latest advanced strategies being developed to enhance stem cell survival and functional integration within target tissues.
The Hostile Post-Transplantation Microenvironment: A Multi-Faceted Challenge
Upon transplantation, stem cells encounter a harsh environment that drastically differs from optimized in vitro culture conditions. This microenvironment inflicts irreversible cellular damage through several interconnected pathways, leading to the massive observed cell loss.
Metabolic and Ischemic Stress
Transplanted cells face an immediate metabolic crisis due to the absence of an established vascular network at the graft site. This results in severe hypoxia, nutrient deprivation (e.g., glucose, fatty acids, amino acids), and the accumulation of cytotoxic waste products [57] [58]. The oxygen tension in ischemic tissues, such as the heart after arterial occlusion, can plummet to near-anoxic conditions (0.2% pO₂) within minutes, inevitably causing cellular necrosis [57].
Oxidative Stress
The abrupt transition from in vitro culture to the pathological in vivo site generates excessive reactive oxygen species (ROS) that overwhelm the cells' intrinsic antioxidant defenses. This oxidative stress induces damage to lipids, proteins, and DNA, triggering apoptotic pathways [57].
Inflammatory and Immune Responses
The transplantation procedure and the underlying tissue injury create a pro-inflammatory milieu. While MSCs possess inherent immunomodulatory properties, the initial inflammatory onslaught can be detrimental to their survival before their paracrine signaling can adequately modulate the local immune response [20] [58].
The Complex Homing Process
For systemically administered cells to reach the parenchyma of the target tissue, they must successfully complete a multi-step homing process analogous to that of leukocytes. This process involves rolling, activation, adhesion, crawling, and transendothelial migration [58]. Each step presents a potential barrier, and the efficiency of this journey is often very low, with many cells trapped in non-target organs like the lungs [58].
The table below quantifies the key stressors in the post-transplantation microenvironment and their direct impacts on stem cell viability.
Table 1: Stressors in the Post-Transplantation Microenvironment and Their Impact on Cell Viability
| Stress Factor | Manifestation in Microenvironment | Direct Consequence on Stem Cells |
|---|---|---|
| Metabolic/Ischemic Stress | Severe hypoxia (0.2-0.9% pO₂), nutrient deprivation, waste accumulation [57] | Necrosis; energy crisis; disruption of ionic homeostasis [57] [58] |
| Oxidative Stress | Excessive reactive oxygen species (ROS) from ischemia-reperfusion and inflammation [57] | Oxidative damage to cellular macromolecules; apoptosis [57] |
| Inflammatory Response | Presence of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6, MCP-1) [20] | Activation of pro-death signaling pathways; exacerbation of oxidative stress [20] [57] |
| Inefficient Homing | Lack of adhesion molecule engagement; chemokine gradient insufficiency [58] | Failure to extravasate and reach target parenchyma; clearance in non-target organs [58] |
The following diagram illustrates the sequential journey of transplanted stem cells and the numerous hostile factors they encounter, which collectively lead to massive cell death and poor engraftment.
Strategic Approaches to Enhance Stem Cell Survival
To combat the high mortality rate, researchers have developed sophisticated strategies focused on preconditioning cells to withstand the harsh in vivo environment and providing direct physiological support.
Metabolic Preconditioning and "Stem Cell Domestication"
This strategy involves pre-adapting stem cells to adverse conditions in vitro to enhance their resilience upon transplantation.
- Hypoxic Preconditioning: Culturing MSCs at low oxygen tension (1-5% O₂) for 24-48 hours before transplantation activates hypoxia-inducible factor (HIF-1α), which upregulates pro-survival genes (e.g., VEGF, GLUT-1) and antioxidant enzymes (e.g., SOD2) [57]. This induces a metabolic reprogramming from oxidative phosphorylation to glycolysis, reducing oxygen consumption and enhancing resistance to ischemia. For example, MSCs preconditioned at 1% O₂ showed twice the survival rate under serum-deprived conditions compared to normoxic controls [57].
- Serum Deprivation/Starvation Mimicking: Transient serum deprivation induces protective autophagy, facilitating the removal of damaged proteins and organelles while upregulating protective heat shock proteins (e.g., HSP70) to reduce stress-induced injury [57].
Direct Oxygen and Metabolic Supplementation
Providing critical metabolic substrates directly to the transplantation site can bridge the gap until neovascularization occurs.
- Oxygen-Generating Biomaterials: Incorporating solid peroxides like calcium peroxide (CaO₂) or hydrogen peroxide (H₂O₂) into hydrogels allows for sustained oxygen release. PEGDA/CaO₂ microspheres can elevate dissolved oxygen for 16-20 hours, preserving MSC viability under oxygen-glucose deprivation [57].
- Perfluorocarbons (PFCs): These compounds have an oxygen solubility 15-20 times greater than water. When incorporated into hydrogels or scaffolds, they act as efficient oxygen reservoirs. PFC-laden scaffolds have been shown to increase bone formation by 2.5-fold in defect models [57].
- Exogenous Metabolic Substrates: Delivering key metabolites can support the tricarboxylic acid (TCA) cycle and oxidative phosphorylation, mitigating the energy crisis faced by the cells [57].
Genetic Modification to Enhance Paracrine Secretion and Resilience
Genetically engineering stem cells to overexpress specific genes can permanently enhance their cytoprotective and paracrine functions.
- Akt1 Overexpression: MSCs modified to overexpress the pro-survival gene Akt1 show greatly enhanced cytoprotective capabilities. The conditioned medium from these cells is sufficient to reduce infarct size and restore cardiac function in MI models, highlighting the potentiation of their paracrine profile [20] [1]. This modification leads to the identification and upregulation of novel paracrine factors like Sfrp2 and HASF [20].
- Enhancement of Antioxidant Defenses: Genetic modifications aimed at boosting the expression of antioxidant enzymes (e.g., superoxide dismutase, catalase) can better equip MSCs to manage the oxidative stress encountered post-transplantation [57].
Table 2: Experimental Protocols for Enhancing Stem Cell Survival
| Strategy | Detailed Experimental Protocol | Key Outcome & Mechanistic Insight |
|---|---|---|
| Hypoxic Preconditioning | Culture MSCs in a modular incubator chamber flushed with a gas mixture maintaining 1% O₂, 5% CO₂, and balance N₂ for 48 hours prior to transplantation [57]. | 2-fold increase in survival under serum deprivation. Mechanism: HIF-1α activation induces metabolic shift to glycolysis and upregulates pro-survival/antioxidant genes [57]. |
| Genetic Modification (Akt1) | Transduce MSCs with a lentiviral vector carrying the human Akt1 gene. Use conditioned media from these Akt-MSCs for in vitro cytoprotection assays or transplant cells directly in vivo [20] [1]. | Significant reduction in infarct size and restoration of cardiac function in MI models. Mechanism: Potentiated paracrine secretion of cytoprotective factors (Sfrp2, HASF) that inhibit caspase-3 and mitochondrial pore opening [20]. |
| Oxygen-Generating Hydrogels | Synthesize PEGDA hydrogels containing CaO₂ microparticles (e.g., 5-10 mg/mL). Encapsulate MSCs within the hydrogel matrix and transplant the construct in vivo [57]. | Prolonged cell viability (>14 days) under hypoxic culture. Mechanism: Sustained oxygen release from CaO₂ + H₂O -> Ca(OH)₂ + ½ O₂ counteracts local hypoxia [57]. |
Engineering Improved Engraftment and Homing
Enhancing the delivery and targeted integration of stem cells is equally critical as improving their survival. This involves material science and bioengineering approaches to create supportive matrices and modulate cell-surface interactions.
Matrix-Assisted Cell Transplantation (MACT)
MACT uses engineered biomaterials to create a protective, provisional microenvironment for the transplanted cells.
- Hyaluronic Acid (HyA)-Based Hydrogels: A tunable HyA hydrogel system can be engineered to independently control mechanical properties, cell-adhesion peptide density (e.g., RGD sequences), and degradation kinetics. Crucially, conjugating heparin within the hydrogel allows for the sequestration and sustained release of both exogenously added and endogenously produced growth factors (e.g., TGFβ1), significantly improving donor cell survival and participation in neovascularization in vivo [59].
- Mechanical and Biochemical Tuning: The modulus of the hydrogel can be matched to the target tissue to minimize mechanical mismatch, while the inclusion of adhesion peptides facilitates integrin-mediated signaling for cell survival and organization [59].
Enhancement of Homing Capability
Improving the homing efficiency of systemically delivered cells ensures a greater number reach the target tissue.
- Priming with Homing Factors: Pretreating MSCs with cytokines like SDF-1 can upregulate the expression of corresponding receptors (e.g., CXCR4), enhancing their chemotactic response to gradients established in injured tissues [58].
- Surface Engineering: Modifying the MSC surface to express homing ligands can improve their interaction with the vascular endothelium. For instance, engineering MSCs to express P-selectin glycoprotein ligand-1 (PSGL-1) and Sialyl-Lewis has been shown to increase rolling interactions and improve homing efficacy in models of multiple sclerosis [58]. The CD29/VCAM-1 interaction is also critical for MSC rolling on liver sinusoidal endothelial cells [58].
The following diagram synthesizes the multi-pronged strategic approach to overcoming the challenges of stem cell therapy, linking specific interventions to their biological mechanisms and desired outcomes.
The Scientist's Toolkit: Key Reagents and Materials
The experimental strategies discussed rely on a suite of specialized reagents and materials. The following table details essential components for implementing these advanced protocols.
Table 3: Research Reagent Solutions for Stem Cell Engraftment Studies
| Reagent/Material | Function/Application | Specific Example & Technical Note |
|---|---|---|
| Calcium Peroxide (CaO₂) | Solid peroxide for sustained oxygen generation within biomaterial scaffolds. Reacts with water to release oxygen [57]. | Example: Incorporated into PEGDA hydrogels at 5-10 mg/mL. Note: Release kinetics are dependent on local fluid volume and access; requires fine-tuning for specific applications [57]. |
| Thiolated Heparin (Heparin-SH) | Functionalized heparin for covalent incorporation into hydrogels. Enables sequestration and stabilized presentation of growth factors [59]. | Example: Conjugated into HyA hydrogels via Michael-type addition. Note: Crucial for coordinating the presentation of TGFβ1 and other heparin-binding factors to support CPC trophic functions [59]. |
| Acrylated Hyaluronic Acid (AcHyA) | A key building block for creating tunable, cell-compatible hydrogels for MACT. Provides a biocompatible and biodegradable backbone [59]. | Example: Functionalized with ~28% acrylation for crosslinking. Note: Allows independent control over mechanical properties and biofunctionalization when combined with crosslinkers and adhesion peptides [59]. |
| RGD-Adhesion Peptide | Synthetic peptide (e.g., CGGNGEPRGDTYRAY) grafted onto biomaterials to promote integrin-mediated cell adhesion and survival [59]. | Example: Reacted with AcHyA to create AcHyA-RGD derivative. Note: Density of RGD presentation can be independently varied to optimize cell-matrix interactions [59]. |
| Hypoxia-Inducible Factor (HIF-1α) Agonists | Small molecules (e.g., CoCl₂, DMOG) used to chemically mimic hypoxic preconditioning and stabilize HIF-1α. | Note: Provides a more scalable and controllable alternative to physical hypoxia chambers for pre-conditioning large cell batches. |
| Lentiviral Vectors (Akt1) | Delivery system for the stable genetic modification of stem cells to overexpress pro-survival genes like Akt1 [20] [1]. | Note: Potentiates the cytoprotective and reparative paracrine secretome of MSCs, a key mechanism for their therapeutic effect [20]. |
The challenge of low engraftment and transient survival represents a formidable yet surmountable barrier in adult stem cell therapy. The research community is moving beyond simple cell injection towards a new paradigm of "cell engineering"—where stem cells are actively preconditioned, genetically enhanced, or physically protected to withstand the transition from culture to patient. The interplay between developing cytoprotective strategies and refining delivery matrices is key. As these approaches mature and converge, the goal of achieving durable engraftment will transition from a major hurdle to a standard practice, thereby unlocking the full therapeutic potential of stem cell-derived paracrine signaling for treating a wide array of degenerative diseases and injuries.
Clinical Evidence and Comparative Analysis of Therapeutic Platforms
Systematic Review of Clinical Trial Outcomes in Advanced Heart Failure
Advanced heart failure (HF) remains a leading cause of global morbidity and mortality despite significant therapeutic innovations. This systematic review synthesizes recent clinical trial outcomes across pharmacological, device-based, and emerging regenerative therapies for advanced HF, with particular emphasis on the role of paracrine signaling mechanisms in adult stem cell therapies. We analyzed pivotal trials published within the last five years, focusing on interventions with practice-changing potential. Quantitative data on primary endpoints, mortality, hospitalization rates, and functional outcomes were extracted and tabulated. Furthermore, we delineate experimental methodologies and molecular mechanisms through which paracrine factors mediate cardiac repair, including cytoprotection, immunomodulation, angiogenesis, and endogenous regeneration. This review provides researchers and drug development professionals with a comprehensive evidence synthesis and mechanistic framework to guide future therapeutic development in advanced HF management.
Heart failure represents a complex clinical syndrome with escalating prevalence worldwide, characterized by high mortality, frequent hospitalizations, and substantially impaired quality of life. The therapeutic landscape has evolved substantially beyond the foundational four pillars of HF with reduced ejection fraction (HFrEF) therapy—beta-blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, and sodium-glucose cotransporter 2 (SGLT2) inhibitors [60] [61]. Recent years have witnessed the emergence of novel pharmacological agents, device strategies, and innovative biologic approaches targeting more advanced disease stages.
The contemporaneous understanding of myocardial repair mechanisms has expanded to include the pivotal role of paracrine signaling in regenerative therapy. Rather than directly replacing damaged cardiomyocytes through differentiation, accumulating evidence indicates that administered adult stem cells exert their therapeutic benefits predominantly through the secretion of bioactive molecules that modulate the local tissue microenvironment [20] [13]. This paracrine hypothesis posits that stem cells release growth factors, cytokines, and extracellular vesicles that influence resident cells through multiple mechanisms: promoting cardiomyocyte survival, attenuating maladaptive inflammation, stimulating angiogenesis, and potentially activating endogenous cardiac progenitor cells [20].
This systematic review aims to critically evaluate recent clinical trial outcomes in advanced HF through the conceptual lens of paracrine mechanisms. By integrating quantitative clinical outcomes with elucidated molecular pathways, we seek to provide a comprehensive resource that bridges translational gaps between observed clinical efficacy and underlying biological mechanisms in advanced HF therapeutics.
Recent Clinical Trial Outcomes in Advanced HF
Pharmacological Innovations
Table 1: Recent Pharmacological Clinical Trials in Advanced Heart Failure
| Trial/Agent | Patient Population | Primary Endpoint | Key Outcomes | Safety Profile |
|---|---|---|---|---|
| DIGIT-HF (Digitoxin) [61] | Symptomatic HFrEF on background therapy (n=1,212) | Composite: all-cause mortality or WHF hospitalization | Significant risk reduction (ARR 4.6%, NNT=22) | Well-tolerated in studied population |
| VICTORIA (Vericiguat) [61] | HFrEF with recent WHF (n>5,000) | Composite: CV death or HF hospitalization | Significant reduction, especially with moderate NT-proBNP elevation | Hypotension concerns manageable |
| VICTOR (Vericiguat) [61] | Stable ambulatory HFrEF with elevated NPs, no recent decompensation (n>6,000) | Composite: CV death or HF hospitalization | Non-significant reduction for primary endpoint; reduced CV and all-cause mortality | Similar to VICTORIA |
| STRONG-HF [61] | AHF with planned discharge (n=1,078) | All-cause death or HF readmission at 180 days | Absolute risk reduction 8.4% with rapid GDMT optimization | Tolerable with careful titration |
| Pooled Vericiguat [61] | HFrEF across spectrum (n>11,000) | Composite: HF hospitalization and CV death | Consistent risk reduction across clinical severity spectrum | Acceptable safety profile |
Recent pharmacological trials have focused on optimizing guideline-directed medical therapy (GDMT) in high-risk populations and introducing novel mechanistic approaches. The soluble guanylate cyclase (sGC) stimulator vericiguat has demonstrated particular promise in patients with recent worsening heart failure (WHF). Pooled analysis from VICTORIA and VICTOR trials encompassing over 11,000 patients with HFrEF demonstrated consistent reductions in the composite endpoint of heart failure hospitalization and cardiovascular death across a broad spectrum of clinical severity [61]. Vericiguat enhances cyclic guanosine monophosphate (cGMP) production, a crucial second messenger in the nitric oxide (NO) signaling pathway that promotes vasodilation and inhibits cardiac remodeling [60].
The DIGIT-HF trial reintroduced cardiac glycosides into contemporary HF management, demonstrating that digitoxin significantly reduced the composite endpoint of all-cause mortality or WHF hospitalization among symptomatic HFrEF patients receiving comprehensive background therapy, with an absolute risk reduction of 4.6% and number needed to treat of 22 [61].
The STRONG-HF trial paradigm challenged conventional approaches by demonstrating that rapid up-titration of GDMT before hospital discharge, coupled with close follow-up, significantly reduced 180-day all-cause mortality and HF readmission compared to usual care (absolute risk reduction 8.4%) [61]. This approach potentially mitigates neurohormonal activation that occurs during decompensation, highlighting the importance of timing in therapeutic optimization.
Device and Management Strategies
Table 2: Recent Non-Pharmacological Clinical Trials in Advanced Heart Failure
| Trial/Strategy | Patient Population | Intervention | Key Outcomes | Clinical Implications |
|---|---|---|---|---|
| ARRHYTHMIA MANAGEMENT [62] | Persistent AF with LVSD (n=119) | Catheter ablation | 60.5% met AIC criteria with LVEF recovery; AF burden <3.8% predicted AIC | Identified atrial septal fibrosis as predictor of AIC |
| HYPOTENSION PROFILING [62] | HFrEF (n=79) | ABPM vs. office BP | 46% had daytime SBP <90mmHg on ABPM vs. 3.8% office reading | Office BP underestimates hypotension prevalence |
| FLUID RESTRICTION (FRESH-UP) [61] | Chronic HF (n=192) | Liberal vs. restricted fluid intake | No QoL difference; reduced thirst distress with liberal intake | Liberal fluid intake potentially acceptable |
Recent trials have refined device-based and management approaches to advanced HF. In arrhythmia management, a post-hoc analysis of the DECAAF II trial demonstrated that among patients with persistent atrial fibrillation (AF) and left ventricular systolic dysfunction (LVSD) undergoing ablation, 60.5% fulfilled criteria for arrhythmia-induced cardiomyopathy (AIC), defined by left ventricular ejection fraction (LVEF) recovery to ≥50% with ≥10% absolute improvement [62]. Notably, patients with AIC showed significantly less atrial septal fibrosis (12.2% vs. 20.7%, p<0.001) on late gadolinium enhancement cardiac magnetic resonance imaging, while global left atrial fibrosis burden was not predictive [62].
The management of comorbidities has also evolved. The FRESH-UP trial challenged conventional fluid restriction in chronic HF patients, demonstrating that liberal fluid intake did not negatively impact quality of life while significantly reducing thirst distress compared to fluid restriction (up to 1500 mL daily) [61].
Profiling of hypotension in HFrEF revealed significant limitations in conventional office blood pressure measurements. While office systolic BP <90 mmHg was observed in only 3.8% of well-treated HFrEF patients, nearly half experienced postprandial hypotension and 46% had daytime episodes of systolic BP <90 mmHg on ambulatory BP monitoring [62]. This discrepancy underscores the need for more comprehensive hypotension assessment when titrating GDMT.
Phenotype-Specific Outcomes and Risk Stratification
Recent evidence emphasizes phenotype-specific therapeutic responses in advanced HF. A large individual patient data meta-analysis pooling 28,406 participants from eight randomized trials revealed a non-linear, phenotype-specific relationship between blood pressure and outcomes [62]. In HFrEF, low systolic BP (<120 mmHg) was consistently associated with increased risk of cardiovascular death and HF hospitalization (HR 1.71, 95% CI 1.60-1.82, p<0.001), whereas higher systolic BP (>140 mmHg) was not linked to worse outcomes. Conversely, in HF with mildly reduced or preserved ejection fraction (HFmrEF/HFpEF), both low and high systolic BP were associated with adverse outcomes, producing a U-shaped risk curve [62].
Emerging biomarkers continue to refine risk stratification. A systematic review and meta-analysis evaluating clonal hematopoiesis of indeterminate potential (CHIP) - acquired mutations in hematopoietic stem cells - demonstrated that carriers had significantly greater risk of new-onset HF compared to non-CHIP groups (HR 1.23, 95% CI 1.12-1.35, p<0.0001) [62]. Furthermore, among patients with preexisting HF, CHIP was associated with a significantly higher risk of the composite outcome of all-cause mortality and HF hospitalization (HR 1.84, 95% CI 1.25-2.70, p=0.002) [62]. Gene-specific CHIP subtypes revealed differential risks, with ASXL1, TET2, and JAK2 mutations associated with significantly increased HF risk, while DNMT3A demonstrated a non-significant effect [62].
Paracrine Mechanisms in Stem Cell Therapy: Molecular Insights
The Paracrine Hypothesis and Secretome Composition
The paradigm of stem cell-mediated cardiac repair has substantially evolved from initial concepts of direct differentiation toward the contemporary understanding of paracrine mechanisms. The paracrine hypothesis proposes that administered adult stem cells, particularly mesenchymal stem cells (MSCs), exert their therapeutic effects primarily through the secretion of bioactive molecules rather than direct engraftment and differentiation [20]. This conceptual shift emerged from observations that administered stem cells exhibited poor long-term survivability post-transplantation, yet still mediated significant functional improvements [20].
The stem cell secretome comprises a diverse array of biologically active factors including growth factors, cytokines, chemokines, and extracellular vesicles (EVs) containing proteins, lipids, and nucleic acids. Key identified paracrine factors include:
- Vascular endothelial growth factor (VEGF): Promotes angiogenesis and endothelial cell survival
- Basic fibroblast growth factor (bFGF): Stimulates fibroblast proliferation and tissue repair
- Hepatocyte growth factor (HGF): Exhibits mitogenic, morphogenic, and anti-apoptotic activities
- Insulin-like growth factor 1 (IGF-1): Mediates cellular growth, survival, and metabolism
- Secreted frizzled related protein 2 (Sfrp2): Attenuates Wnt/β-catenin signaling and exerts anti-apoptotic effects
- Hypoxia-induced Akt-regulated stem cell factor (HASF): Promotes cardiomyocyte survival through protein kinase C epsilon (PKCε) activation [20]
The composition and potency of the secretome can be modulated by preconditioning strategies, including hypoxia, pharmacological priming, and three-dimensional culture conditions, which enhance the production of therapeutic factors [13] [17].
Diagram 1: Paracrine Signaling Pathways in Stem Cell Therapy for Heart Failure. This diagram illustrates the sequential process from stem cell activation through paracrine factor secretion to mechanistic targets and ultimately clinical improvements in heart failure.
Molecular Mechanisms of Action
Paracrine factors mediate cardiac repair through multiple interconnected mechanisms that collectively attenuate adverse remodeling and promote tissue preservation:
Cytoprotection: Stem cell-derived factors directly enhance cardiomyocyte survival under ischemic and inflammatory stress. HASF protects cardiomyocytes from apoptosis by inhibiting mitochondrial pore opening and caspase activation through a PKCε-dependent mechanism [20]. Sfrp2 binds directly to Wnt3a, attenuating Wnt/β-catenin signaling and subsequent caspase activation in hypoxic cardiomyocytes [20]. Administration of conditioned media from Akt-overexpressing MSCs significantly reduced infarct size and improved cardiac function in rodent myocardial infarction models, validating the cytoprotective potential of the stem cell secretome [20].
Immunomodulation: MSCs profoundly influence the cardiac immune microenvironment through direct cell contact and paracrine factor release. They inhibit T-cell proliferation and cytotoxicity, prevent dendritic cell maturation, and modulate macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes [20] [13]. Key immunomodulatory molecules include transforming growth factor-β (TGF-β), hepatocyte growth factor (HGF), prostaglandin E2 (PGE2), interleukin-1 receptor antagonist (IL-1RA), and indoleamine 2,3-dioxygenase (IDO) [20] [13]. This immunomodulation attenuates maladaptive inflammation, reduces extracellular matrix degradation, and promotes tissue repair.
Angiogenesis: Paracrine factors stimulate neovascularization in ischemic myocardium through direct mitogenic effects on endothelial cells and mobilization of progenitor cells. VEGF and FGF promote endothelial cell proliferation, migration, and tube formation, while also enhancing endothelial nitric oxide synthase (eNOS) activity [20]. This angiogenic response improves perfusion of hibernating myocardium, reduces ischemic burden, and supports cardiomyocyte survival.
Endogenous Repair Activation: Emerging evidence suggests that stem cell-derived factors may activate resident cardiac progenitor cells and stimulate cell cycle re-entry in mature cardiomyocytes [20]. While the magnitude of this effect remains controversial, it represents a potential mechanism for genuine myocardial regeneration rather than solely damage mitigation.
Experimental Protocols and Methodologies
Stem Cell Isolation and Characterization
Mesenchymal Stem Cell Isolation from Bone Marrow:
- Sample Collection: Obtain bone marrow aspirate (typically 20-60 mL) from iliac crest under local anesthesia with informed consent.
- Density Gradient Centrifugation: Dilute marrow 1:1 with phosphate-buffered saline (PBS), layer over Ficoll-Paque PLUS (density 1.077 g/mL), centrifuge at 400 × g for 30 minutes at room temperature.
- Mononuclear Cell Collection: Carefully interface layer containing mononuclear cells, wash twice with PBS containing 2% fetal bovine serum (FBS).
- Plastic Adherence Selection: Resuspend cells in complete culture medium (α-MEM supplemented with 10% FBS, 1% penicillin/streptomycin, 2 mM L-glutamine), plate at density of 5 × 10^4 cells/cm².
- Culture Expansion: Incubate at 37°C with 5% CO₂, change medium after 48 hours then every 3-4 days, passage at 80-90% confluence using 0.25% trypsin-EDTA.
- Phenotypic Characterization: Passage 3-5 cells analyze by flow cytometry for CD73, CD90, CD105 (≥95% positive) and CD34, CD45, CD11b, CD19, HLA-DR (≤2% positive) per International Society for Cellular Therapy guidelines [13].
- Differentiation Capacity Verification: Induce adipogenic, osteogenic, and chondrogenic differentiation in specific induction media for 21 days, with appropriate staining (Oil Red O, Alizarin Red, Alcian Blue, respectively) to confirm multipotency [13].
Conditioned Media Preparation:
- Culture MSCs to 80% confluence in complete growth medium.
- Wash twice with PBS to remove serum components.
- Incubate with serum-free basal medium for 24-48 hours.
- Collect conditioned medium, centrifuge at 2000 × g for 10 minutes to remove cellular debris.
- Concentrate using 3-kDa cutoff centrifugal filters (20-50× concentration).
- Store at -80°C for subsequent experiments [20].
In Vitro and In Vivo Assessment of Paracrine Effects
In Vitro Cardiomyocyte Protection Assay:
- Cardiomyocyte Culture: Isolate neonatal rat ventricular cardiomyocytes or use H9c2 cardiomyoblast cell line.
- Hypoxia/Reoxygenation Injury: Place cells in anaerobic chamber (1% O₂, 5% CO₂, 94% N₂) with glucose-free medium for 6-12 hours, followed by reoxygenation with normal medium for 12-24 hours.
- Treatment Groups: (1) Control medium, (2) MSC-conditioned medium, (3) Concentrated conditioned medium with/without specific factor neutralization antibodies.
- Viability Assessment: Measure by MTT assay or Calcein-AM staining.
- Apoptosis Quantification: TUNEL staining, caspase-3/7 activity assay, Annexin V/propidium iodide flow cytometry.
- Mechanistic Studies: Western blotting for Akt, ERK, STAT3, and Bcl-2 family proteins; mitochondrial membrane potential with JC-1 dye [20].
In Vivo Myocardial Infarction Model:
- Surgical Procedure: Anesthetize rodent (mouse/rat), intubate, maintain on ventilator.
- Left Anterior Descending Coronary Artery Ligation: Perform left thoracotomy, identify LAD, ligate with 7-0 prolene suture.
- Treatment Administration: Direct intramyocardial injection of MSCs (1-5 × 10^5 cells) or concentrated conditioned medium (50-100 µL) at multiple peri-infarct sites immediately post-ligation.
- Functional Assessment: Serial echocardiography at 1, 2, and 4 weeks post-infarction to measure LVEF, LV dimensions, wall motion.
- Histological Analysis: Harvest hearts at study endpoint, section, stain with Masson's trichrome for fibrosis assessment, immunohistochemistry for capillary density (CD31+), macrophage polarization (CD68+/CD206+), and cardiomyocyte apoptosis (TUNEL/α-actinin double staining) [20].
Diagram 2: Experimental Workflow for Paracrine Mechanism Studies. This diagram outlines the comprehensive experimental pipeline from stem cell preparation through in vitro validation to in vivo assessment and final analysis in paracrine mechanism research.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Studying Paracrine Mechanisms in Stem Cell Therapy
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Stem Cell Markers | CD73, CD90, CD105 antibodies | MSC characterization by flow cytometry | Identification and purification of MSCs per ISCT criteria [13] |
| Negative Markers | CD34, CD45, HLA-DR antibodies | Purity assessment and hematopoietic exclusion | Confirmation of mesenchymal lineage [13] |
| Differentiation Kits | Adipogenic, osteogenic, chondrogenic induction media | Multipotency verification | Demonstration of trilineage differentiation capacity [13] |
| Cytokine Arrays | Proteome profiler arrays, Luminex kits | Secretome characterization | Comprehensive analysis of paracrine factor secretion [20] |
| Extracellular Vesicle Isolation | Ultracentrifugation, size exclusion chromatography, polymer-based precipitation | EV isolation and characterization | Isolation of vesicular fraction of secretome [13] |
| Cell Tracking Agents | CM-Dil, GFP-lentivirus, BrdU | Cell fate tracking post-transplantation | Monitoring of cell retention, distribution, and viability [20] |
| Apoptosis Assays | TUNEL kit, Annexin V/PI, caspase-3/7 activity assays | Cardiomyocyte protection assessment | Quantification of anti-apoptotic effects [20] |
| Angiogenesis Assays | Matrigel tube formation, chick chorioallantoic membrane assay | Neovascularization assessment | Evaluation of pro-angiogenic paracrine effects [20] |
| Signal Transduction Inhibitors | Wnt, TGF-β, NF-κB pathway inhibitors | Mechanistic studies | Dissection of specific signaling pathways [17] |
Integration of Clinical Outcomes and Paracrine Mechanisms
The convergence of clinical trial data and mechanistic studies provides compelling evidence that paracrine signaling represents a fundamental biological process underlying the therapeutic effects of diverse HF interventions. Pharmacological agents like vericiguat directly modulate signaling pathways (NO-sGC-cGMP axis) that intersect with paracrine mechanisms, enhancing cardiomyocyte function and vascular homeostasis [60]. Similarly, the benefits of SGLT2 inhibitors may partially derive from pleiotropic effects that mimic or enhance endogenous protective signaling [60].
In stem cell-based approaches, the recognition of paracrine mechanisms has shifted therapeutic strategies from differentiation-focused paradigms to secretion-enhanced approaches. Engineering MSCs to overexpress Akt enhances their paracrine potency and cytoprotective efficacy [20]. Similarly, preconditioning with hypoxia or pro-inflammatory cytokines augments the immunomodulatory capacity of MSCs, potentially enhancing their therapeutic effectiveness in the inflammatory milieu of failing myocardium [13] [17].
The molecular pathways activated by paracrine factors—including PI3K/Akt, JAK/STAT, Wnt/β-catenin, and NF-κB signaling—represent promising targets for pharmacological modulation. Small molecule approaches targeting these pathways may potentially recapitulate beneficial aspects of the stem cell secretome without the complexities of cell-based therapy [17]. Furthermore, combination strategies employing both pharmacological agents and stem cell therapy may produce synergistic effects through complementary mechanisms.
This systematic review demonstrates substantial progress in advanced HF therapeutics, with recent clinical trials yielding important new options for this high-risk population. Simultaneously, elucidation of paracrine mechanisms has provided a conceptual framework unifying diverse therapeutic approaches through their effects on fundamental biological processes promoting myocardial repair.
Future directions should include optimized cell engineering strategies to enhance paracrine potency, development of biomaterial-based delivery systems for sustained release of paracrine factors, and identification of patient subpopulations most likely to respond to specific therapeutic approaches. The integration of targeted pharmacological modulation with enhanced paracrine therapy represents a promising frontier for advancing HF treatment beyond current limitations.
As the field progresses, standardized methodologies for secretome characterization, potency assays, and mechanism-of-action studies will be essential for translating promising preclinical findings into clinical applications. By leveraging insights from both clinical trials and mechanistic studies, the next generation of HF therapies can more effectively target the fundamental pathological processes driving disease progression, ultimately improving outcomes for patients with advanced heart failure.
The field of regenerative medicine has been revolutionized by advanced understanding of adult stem cell therapeutics, with mesenchymal stromal/stem cells (MSCs), bone marrow stromal cells (BMSCs, often abbreviated as BMCs in clinical contexts), and cancer stem cells (CSCs) representing distinct cellular entities with critical roles in tissue repair and disease pathogenesis. Within this landscape, paracrine signaling has emerged as a fundamental mechanism whereby these cells exert their biological effects through secretion of soluble factors rather than direct cellular differentiation [1] [13]. This whitepaper provides a comprehensive technical analysis of the safety and efficacy profiles of these cell types, with particular emphasis on their paracrine-mediated activities, which include immunomodulation, trophic support, and pathological processes. Understanding these mechanisms is essential for researchers and drug development professionals aiming to develop targeted therapeutic strategies for a range of conditions from inflammatory diseases to cancer.
Defining the Cellular Entities
Mesenchymal Stromal/Stem Cells (MSCs)
MSCs are non-hematopoietic, multipotent stem cells initially identified in bone marrow but since isolated from various tissues including adipose tissue, umbilical cord, and placental tissue [13]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105 ≥95%) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) capacity for in vitro differentiation into osteogenic, chondrogenic, and adipogenic lineages [13]. Their therapeutic potential is largely mediated through paracrine secretion of bioactive molecules including growth factors, cytokines, and extracellular vesicles [13].
Bone Marrow Stromal Cells (BMCs)
BMCs (frequently used interchangeably with BMSCs - bone marrow stromal cells) represent the original MSC population first isolated from bone marrow aspirates [63] [13]. While the terms MSC and BMC are often used interchangeably in literature, BMCs specifically refer to the stromal cell fraction derived from bone marrow, whereas MSCs can be sourced from multiple tissues. BMCs function as trophoblast cells that facilitate the differentiation of hematopoietic stem cells into granulocytes, macrophages, and megakaryocytes through secretion of growth factors including colony stimulating factor 1 (CSF-1), granulocyte-macrophage (GM)-CSF, granulocyte (G)-CSF, interleukin (IL)-6, c-kit ligand, and IL-3 [13].
Cancer Stem Cells (CSCs)
CSCs constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [64]. First identified in acute myeloid leukemia (AML) in 1997, CSCs are characterized by self-renewal capacity, enhanced survival mechanisms, and resistance to conventional therapies [64] [65]. They exhibit dynamic interactions with their microenvironment, facilitating metabolic symbiosis and further promoting CSC survival and drug resistance [64]. Unlike MSCs and BMCs, CSCs represent a pathological entity that contributes to disease persistence and recurrence.
Table 1: Defining Characteristics of Stem Cell Types
| Characteristic | MSCs | BMCs | CSCs |
|---|---|---|---|
| Origin | Multiple tissues (BM, adipose, UC, placenta) | Specifically bone marrow | Tumor cell subpopulation |
| Key Markers | CD73, CD90, CD105 | CD73, CD90, CD105 | CD44, CD133, ALDH activity |
| Primary Functions | Immunomodulation, tissue repair | Hematopoietic support, tissue repair | Tumor initiation, metastasis, recurrence |
| Therapeutic Role | Regenerative medicine, immunomodulation | Regenerative medicine, hematopoietic support | Therapeutic target |
| Paracrine Signaling | Extensive soluble factor secretion | Growth factor secretion | Tumor microenvironment modulation |
Paracrine Mechanisms and Molecular Signaling
Paracrine Actions of MSCs and BMCs
The paracrine hypothesis represents a paradigm shift in understanding MSC and BMC therapeutic mechanisms, suggesting that functional benefits observed after stem-cell transfer are related to secretion of soluble factors that act in a paracrine fashion to protect tissues, attenuate pathological remodeling, induce neovascularization, and promote regeneration [1]. These paracrine factors may influence adjacent cells through several established mechanisms:
Myocardial protection: MSCs release cytoprotective molecules that increase cardiomyocyte survival. Conditioned medium from hypoxic MSCs reduces apoptosis and necrosis of isolated rat cardiomyocytes exposed to low oxygen tension [1].
Neovascularization: MSC secretion of vascular endothelial growth factor (VEGF), basic fibroblast growth factor (b-FGF), hepatocyte growth factor (HGF), and insulin growth factor I (IGF-I) significantly increases in injured hearts treated with MSCs, promoting angiogenesis [1].
Immunomodulation: MSCs interact with various immune cells (T cells, B cells, dendritic cells, macrophages) modulating immune responses through both direct cell-cell interactions and release of immunoregulatory molecules [13].
The secretome of MSCs includes a broad variety of cytokines, chemokines, and growth factors that may potentially be involved in tissue repair, with hypoxic stress increasing the production of several of these factors [1]. Importantly, the composition of this secretome varies depending on the MSC source. For example, comparative studies between endometrial regenerative cells (ERC) and BMSCs show that IL-8 and ICAM-1 levels are greater in ERC supernatants, while HGF, VEGF, IL-6, CXCL12, TGFB1 and TGFB2 are greater in BMSC supernatants [66].
CSC Signaling Pathways and Microenvironment Interactions
CSCs utilize multiple signaling pathways to maintain their stem-like properties and resistance mechanisms. Key regulatory pathways include WNT/β-Catenin, hedgehog, Notch, NF-κB, JAK/STAT, TGF-β, PI3K/AKT, and PPAR pathway, along with extensive crosstalk between these pathways [65]. CSCs constantly interact with their surrounding environment, including supportive tissue, immune cells, and extracellular matrix components, increasing complexity and further affecting how a tumor grows and responds to treatment [64].
CSCs exhibit metabolic plasticity that allows them to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling survival under diverse environmental conditions [64]. Furthermore, their ability to create many kinds of cells within a single tumor leads to intratumoral heterogeneity, making cancer challenging to treat because different cell groups may not respond similarly to therapy [64].
Figure 1: CSC Signaling Pathways and Functional Outcomes. CSCs utilize multiple interconnected signaling pathways to maintain their stem-like properties, influenced by environmental factors and leading to therapeutic resistance and disease progression.
Safety and Efficacy Profiles
Clinical Safety and Efficacy of MSCs and BMCs
MSC therapies have been employed in more than 800 registered clinical studies across the globe with over 55,000 publications readily available [67]. Meta-analyses of clinical trials with first-generation MSC products have demonstrated safety, though clinical efficacy and understanding of underlying mechanisms of action still need improvement [67].
Safety Profile: MSC infusion procedures have exhibited an excellent safety profile, with over 10,000 patients treated in a controlled clinical setting [63]. A recent meta-analysis of stem cell-based therapies for acute respiratory distress syndrome (ARDS) found no significant differences in adverse events or serious adverse events between the stem cell-based therapy group and the control group [68].
Efficacy Outcomes:
- ARDS Treatment: Stem cell-based therapy significantly reduced all-cause mortality within one month (RR = 0.74, 95% CI = 0.63-0.87, p = 0.0003) and was well tolerated in ARDS patients [68]. High dose MSCs (over 1 × 10^6 cells/kg or 7 × 10^7 cells per infusion) were associated with reduction of all-cause mortality in ARDS (RR = 0.70, 95% CI = 0.55-0.89) [68].
- Graft-versus-Host Disease: A phase I study of iPSC-derived MSCs (CYP-001) in steroid-resistant acute GvHD demonstrated safety and tolerability with no serious adverse events assessed as related to CYP-001 [69]. Overall response, complete response and overall survival rates by day 100 were 86.7%, 53.3%, and 86.7%, respectively [69].
The efficacy of MSCs is influenced by multiple factors including donor characteristics, tissue source, isolation methods, culture conditions, and delivery methods [67]. Additionally, the therapeutic application can utilize either autologous or allogeneic MSCs, with the decision representing a fundamental clinical choice [63].
Table 2: Clinical Safety and Efficacy Evidence for MSCs/BMCs
| Condition | Study Design | Safety Outcomes | Efficacy Outcomes |
|---|---|---|---|
| ARDS | Meta-analysis of 31 studies (1,773 patients) [68] | No significant differences in AE (RR=1.08, 95% CI=0.97-1.21) or SAE (RR=0.94, 95% CI=0.80-1.11) | Significant reduction in all-cause mortality within one month (RR=0.74, 95% CI=0.63-0.87, p=0.0003) |
| Steroid-resistant aGvHD | Phase I, open-label trial of iPSC-derived MSCs (CYP-001) [69] | No related serious adverse events; well tolerated | Day 100: OR=86.7%, CR=53.3%, OS=86.7% |
| Multiple Sclerosis | Phase I (4 patients) with ERC [66] | Safe for allogeneic use; no teratoma risk | Prevented disease progression |
| Critical Limb Ischemia | Preclinical models with ERC [66] | Favorable safety profile | Stimulation of angiogenesis |
Therapeutic Challenges Posed by CSCs
CSCs contribute significantly to treatment failure through multiple resistance mechanisms:
Therapy resistance: CSCs possess several mechanisms to resist treatments, including strong DNA repair systems, drug efflux capabilities, and dormancy to protect them from therapies targeting rapidly dividing cells [64].
Tumor recurrence: Due to their ability to survive conventional cancer treatments and remain in resistant or dormant states, CSCs frequently cause cancer recurrence. Even if most of a tumor is destroyed, remaining CSCs can restart tumor growth, often in a more aggressive form [64].
Metabolic adaptability: Recent advances reveal that metabolic plasticity allows CSCs to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources, enabling survival under diverse environmental conditions [64].
The clinical challenge is compounded by the lack of universal CSC markers. Although surface proteins such as CD44 and CD133 have been widely used to isolate CSC populations, these markers are not exclusive to CSCs and are often expressed in normal stem cells or non-tumorigenic cancer cells [64]. Furthermore, their expression varies across tumor types, reflecting the influence of tissue origin and microenvironmental context on CSC phenotypes [64].
Experimental Models and Methodologies
Key Experimental Protocols for Evaluating Paracrine Effects
Mixed Leukocyte Reaction (MLR) Inhibition Assay: This protocol evaluates the immunomodulatory properties of MSCs/BMCs by measuring their ability to suppress immune cell proliferation [66].
Protocol Steps:
- Isolate peripheral blood mononuclear cells (PBMCs) from donors via Ficoll separation
- Plate PBMCs in 96-well plates at 1×10^5 responders per well
- Co-culture responders with 2500 cGy irradiated stimulator PBMCs at 1×10^5 cells/well
- Add test MSCs/BMCs at varying concentrations (e.g., 10^4 and 10^5 cells/well)
- Incubate plates for 6 days in humidified 5% CO2 at 37°C
- Add 0.5 μCi of 3H-thymidine to each well for 4 hours before harvest
- Measure lymphocyte proliferation using liquid scintillation counting
- Calculate suppression percentage compared with proliferative response without MSCs/BMCs
Conditioned Medium (CM) Preparation for Paracrine Studies: This methodology isolates the soluble fraction of MSC secretion to evaluate paracrine effects without cellular presence [1].
Protocol Steps:
- Culture MSCs to 70-80% confluence in standard complete medium
- Replace with serum-free medium for 24-48 hours
- Collect supernatant and centrifuge at 2000 × g for 10 minutes to remove cellular debris
- Concentrate using centrifugal filter devices (e.g., 3-kDa cutoff)
- Sterilize using 0.22-μm filters
- Store at -80°C until use
- Apply to target cells (e.g., cardiomyocytes under hypoxia) to evaluate cytoprotective effects
Figure 2: Experimental Workflow for Stem Cell Characterization. Comprehensive evaluation of stem cell properties involves sequential processes from isolation through in vitro and in vivo functional assays.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Cell Isolation | Ficoll separation media, collagenase enzymes, magnetic bead-based kits (e.g., CD34+ isolation) | Isolation of specific cell populations from complex tissues |
| Culture Media | Alpha MEM, DMEM/F12, MSC-qualified FBS, gentamicin | Optimized expansion while maintaining stem cell properties |
| Characterization Antibodies | Anti-CD73, CD90, CD105, CD34, CD45, CD14, CD19, HLA-DR | Phenotypic verification per ISCT criteria |
| Differentiation Kits | Osteogenic: dexamethasone, β-glycerophosphate, ascorbate; Adipogenic: IBMX, indomethacin, insulin | Multilineage differentiation potential assessment |
| Cytokine Arrays | Proteome Profiler Array, SearchLight Protein Array | Comprehensive secretome analysis |
| Animal Models | SCID mice, NOD/SCID models, disease-specific models (ARDS, MI, GvHD) | In vivo safety and efficacy evaluation |
Emerging Trends and Future Perspectives
Advanced Therapeutic Development
The field is moving toward next-generation MSC therapies with efforts underway to improve product design and delivery, safety and potency assessment, and understanding of exact mechanisms of action [67]. Key advancements include:
iPSC-derived MSCs: Induced pluripotent stem cell-derived MSCs potentially overcome challenges with scalability and interdonor variability observed in conventional manufacturing approaches [69].
Extracellular Vesicles (EVs): MSC-derived EVs and secretomes demonstrate preliminary efficacy in treatment of conditions like ARDS (RR = 0.63, 95% CI = 0.46-0.86, p = 0.003) [68], offering a cell-free therapeutic alternative.
Manufacturing Optimization: Adjustments in manufacturing include cell expansion conditions, culture media composition, and cell priming to enhance therapeutic potential [67].
CSC-Targeted Therapeutic Strategies
Emerging strategies to overcome CSC-mediated therapy resistance include:
Dual metabolic inhibition: Targeting multiple energy pathways simultaneously to overcome CSC metabolic plasticity [64].
Synthetic biology-based interventions: Engineered approaches to specifically target CSC vulnerabilities [64].
Immune-based approaches: CAR-T cells targeting CSC markers such as epithelial cell adhesion molecule (EpCAM) have demonstrated effectiveness in eliminating CSCs in preclinical models [64].
The safety and efficacy profiles of MSCs, BMCs, and CSCs reflect their distinct biological roles and mechanisms of action. MSCs and BMCs demonstrate favorable safety profiles and promising efficacy in regenerative and immunomodulatory applications, largely mediated through paracrine signaling mechanisms. In contrast, CSCs represent therapeutic targets due to their role in tumor recurrence and treatment resistance. Future progress will depend on continued elucidation of paracrine mechanisms, optimization of manufacturing processes, and development of targeted approaches that address the unique challenges posed by each cell type. Researchers and drug development professionals should consider these distinct profiles when designing therapeutic strategies for various disease contexts.
The therapeutic application of adult stem cells (ASCs) has long been predicated on two principal mechanisms of action: direct differentiation, wherein stem cells replace damaged tissue by becoming functional target cells, and paracrine signaling, a bystander effect where stem cells secrete bioactive factors that orchestrate repair. Initial therapeutic hypotheses emphasized direct differentiation and cell replacement as the primary pathway for functional recovery. However, a substantial body of recent evidence has prompted a paradigm shift, revealing that the secretion of soluble factors—the paracrine effect—may be the predominant mechanism underlying the observed benefits of ASC therapy. This review provides a comparative assessment of these two mechanisms within the context of adult stem cell therapy research, synthesizing current understanding of their relative contributions, benefits, and translational implications for researchers and drug development professionals.
The foundational premise of regenerative medicine is the restoration of lost or damaged tissue. In the context of adult stem cell therapy, particularly for conditions like acute myocardial infarction, this was initially conceptualized as the direct engraftment and differentiation of transplanted cells into cardiomyocytes and vascular cells [1]. Early animal studies supported this, suggesting that bone marrow-derived cells could transdifferentiate into cardiac lineages and significantly regenerate infarcted myocardium [1].
However, the scientific consensus has been fundamentally challenged and refined over the past decade. A growing body of evidence indicates that the frequency of permanent stem cell engraftment and direct transdifferentiation is often too low to account for the significant functional improvements observed in preclinical and clinical studies [1] [48]. This discrepancy led to the advancement of an alternative hypothesis: the transplanted stem cells act as medicinal biofactories, releasing a portfolio of soluble factors that, acting in a paracrine fashion, are the primary mediators of cardiac repair and regeneration [1]. This paracrine hypothesis has since been validated in numerous other therapeutic contexts, including neurological disorders, musculoskeletal repair, and urological conditions [48] [70]. The field now recognizes paracrine signaling not merely as a secondary effect, but as a central mechanism orchestrating a multifaceted therapeutic response.
Comparative Mechanism Analysis: Direct Differentiation vs. Paracrine Signaling
Core Principles and Therapeutic Objectives
Direct Differentiation: This mechanism is defined by the capacity of an undifferentiated or partially committed stem cell to undergo a process of specialization into a mature, functional cell type of a specific tissue, such as a cardiomyocyte, neuron, or chondrocyte [48]. The primary therapeutic objective is structural replacement—literally rebuilding lost tissue by supplying new, functional cells that integrate into the host architecture [1] [71].
Paracrine Signaling: This mechanism involves the secretion of a broad spectrum of bioactive molecules from the stem cells into the surrounding microenvironment. These factors then exert effects on neighboring host cells. The therapeutic objective is not direct replacement, but rather biological modulation, whereby the secretome influences key repair processes such as cell survival, blood vessel formation, and modulation of the immune response [1] [48] [70].
Key Signaling Pathways and Molecular Mediators
The therapeutic effects of paracrine signaling are mediated by a complex cocktail of factors. The table below summarizes the key classes of molecules and their primary proposed functions in tissue repair.
Table 1: Key Paracrine Factors Secreted by Adult Stem Cells and Their Proposed Functions
| Secreted Factor | Abbreviation | Primary Proposed Functions in Repair |
|---|---|---|
| Vascular Endothelial Growth Factor | VEGF | Angiogenesis, cytoprotection, cell proliferation & migration [1] |
| Hepatocyte Growth Factor | HGF | Cytoprotection, angiogenesis, cell migration [1] |
| Insulin-like Growth Factor-1 | IGF-1 | Cytoprotection, cell migration, improved contractility [1] |
| Fibroblast Growth Factor-2 | FGF-2 | Cell proliferation & migration, angiogenesis [1] |
| Brain-Derived Neurotrophic Factor | BDNF | Neuronal survival & repair (e.g., in ED models) [70] |
| Transforming Growth Factor-β | TGF-β | Vessel maturation, immunomodulation, cell proliferation [1] [17] |
| Monocyte Chemoattractant Protein-1 | MCP-1 | Immune cell recruitment & modulation [1] |
| Extracellular Vesicles / Exosomes | EVs | Intercellular communication, transfer of miRNAs, proteins, and lipids [72] [73] |
These factors activate crucial signaling pathways in recipient cells. The following diagram illustrates the core signaling logic by which transplanted stem cells, via their secretome, influence key repair processes in the host tissue.
In contrast, direct differentiation relies on the stem cell's intrinsic developmental programming, often involving pathways like Wnt, Notch, BMP, and Hedgehog, to guide its transformation into a specific terminal cell type [17]. The therapeutic outcome is contingent upon this successful differentiation and subsequent functional integration.
Quantitative Benefit Analysis: A Structured Comparison
The relative advantages and challenges of direct differentiation versus paracrine signaling can be quantitatively and qualitatively assessed across several critical parameters for therapeutic development.
Table 2: Comparative Analysis of Direct Differentiation vs. Paracrine Signaling
| Parameter | Direct Differentiation | Paracrine Signaling |
|---|---|---|
| Primary Therapeutic Goal | Structural tissue replacement [1] [48] | Functional modulation & endogenous repair [1] [48] |
| Therapeutic Onset | Slow (Days to weeks, requires integration) | Rapid (Hours to days) [1] |
| Engraftment Requirement | High, stable, and long-term | Low to moderate; effects can be transient [48] |
| Key Evidence | Historical histology (e.g., putative new cardiomyocytes); now debated [1] [48] | Conditioned medium experiments reproduce benefits; factor profiling [1] |
| Major Risk/Challenge | Potential for aberrant differentiation; arrhythmogenesis (cardiac) | Limited by cell survival in hostile microenvironment [48] |
| Tumorigenic Potential | Theoretical risk of teratoma (if pluripotent) or mis-differentiation | Lower, but potential if pro-angiogenic/growth signals are dysregulated [74] |
| Therapeutic Breadth | Narrow, tissue-specific | Broad, applicable across multiple disease etiologies [48] [70] |
| Dosing Strategy | Complex (depends on engraftment efficiency) | Potentially simpler; can be augmented via preconditioning [48] |
Experimental Protocols for Mechanistic Validation
Protocol 1: Validating Paracrine Effects via Conditioned Medium Experiments
Objective: To isolate and confirm the therapeutic effects of stem cell-secreted factors, independent of the cells themselves.
Methodology:
- Cell Culture & Conditioning: Culture therapeutic stem cells (e.g., Mesenchymal Stem Cells, MSCs) to 70-80% confluence. Replace growth medium with a defined, serum-free basal medium. Condition for 24-48 hours under normoxic or disease-relevant (e.g., hypoxic, inflammatory cytokine-primed) conditions [1] [48].
- Collection & Concentration: Collect the medium, now termed "Conditioned Medium" (CM). Centrifuge to remove cellular debris. The CM can be used directly or concentrated using centrifugal filters (e.g., 3kDa cutoff) to enrich for secreted factors [1].
- Therapeutic Testing:
- In Vitro: Apply the CM to target cells (e.g., cardiomyocytes, neurons) under stress (e.g., hypoxia, toxin-induced apoptosis). Assess for cytoprotection (reduced apoptosis via TUNEL/Caspase assays), proliferation (BrdU/Ki67), or migration (scratch assay) [1].
- In Vivo: Administer the CM (e.g., via intramyocardial injection in myocardial infarction models, intrathecal injection for neurological models) in place of live cells. Compare functional outcomes (e.g., ejection fraction, nerve conduction velocity) and histological endpoints (e.g., infarct size, capillary density, neuronal survival) against controls receiving non-conditioned medium [1].
Protocol 2: Fate Mapping for Direct Differentiation
Objective: To definitively trace the fate of transplanted stem cells and quantify their direct differentiation into target tissue cells.
Methodology:
- Cell Labeling: Label donor stem cells with a durable, heritable marker. The gold standard is genetic fate mapping using Cre-lox technology in transgenic animals. For human cells, lentiviral transduction with a constitutive promoter driving a fluorescent protein (e.g., GFP, tdTomato) or a human-specific nuclear antigen (e.g., HUNu) is common [48].
- Transplantation & Maturation: Transplant the labeled cells into the injured host tissue (e.g., murine infarcted heart, rat injured spinal cord). Allow a sufficient period for potential engraftment and differentiation (weeks to months).
- Histological Analysis & Lineage Tracing: Harvest the tissue and perform immunohistochemistry/immunofluorescence. Co-localization of the donor cell marker (GFP) with specific, mature lineage markers (e.g., cTnT for cardiomyocytes, MAP2 for neurons, CD31 for endothelial cells) is required to claim differentiation.
- Critical Controls: Include controls for:
- Cell Fusion: Use methodologies to detect polyploidy or the presence of both donor and host genomes.
- Antibody Specificity: Ensure no false-positive signal from non-specific antibody binding.
- Engraftment Quantification: Report the total number of engrafted donor cells and the percentage that have co-localized with lineage markers. Modern lineage tracing studies often show this percentage is very low [48].
The experimental workflow for definitively distinguishing between these two mechanisms in a preclinical study integrates both approaches, as illustrated below.
The Scientist's Toolkit: Essential Research Reagents
Research into stem cell mechanisms requires a specific set of reagents and tools to dissect these complex biological processes.
Table 3: Key Research Reagent Solutions for Mechanistic Studies
| Research Reagent / Tool | Primary Function in Analysis | Specific Examples |
|---|---|---|
| Conditioned Medium (CM) | Serves as a cell-free therapeutic to isolate paracrine effects; used in both in vitro and in vivo functional assays [1]. | CM from hypoxic MSCs, CM from cytokine-primed MSCs. |
| Genetic Fate Mapping Systems | Provides definitive, heritable labeling of donor cells for in vivo tracking of engraftment, survival, and differentiation; gold standard for lineage tracing [48]. | Cre-lox models (e.g., Rosa26-lox-STOP-lox-tdTomato), Lentiviral GFP/TdTomato. |
| Cytokine & Growth Factor Arrays | Profiling the composition of the stem cell secretome; identifies key paracrine mediators present in CM [1]. | Proteome Profiler Arrays (e.g., Human XL Cytokine Array), ELISAs for VEGF, HGF, IGF-1. |
| Pathway-Specific Agonists/Antagonists | Pharmacological modulation of specific signaling pathways to validate their functional role in the observed therapeutic effect [17]. | SB431542 (TGF-β inhibitor), IWP-2 (Wnt inhibitor), recombinant growth factors (e.g., rhVEGF). |
| Small Interfering RNA (siRNA) / shRNA | Gene knockdown in stem cells to selectively deplete specific paracrine factors, establishing a causal link between factor secretion and function. | siRNA targeting VEGF in MSCs, shRNA against BDNF. |
| Extracellular Vesicle Isolation Kits | Isolation of exosomes and other EVs from CM to determine their specific contribution to the total paracrine effect. | Ultracentrifugation protocols, commercial kits (e.g., ExoQuick, Total Exosome Isolation kit). |
| In Vivo Disease Models | Preclinical testing platform to evaluate the therapeutic efficacy and mechanism of action of stem cells or their derivatives. | Rodent models of myocardial infarction, spinal cord injury, erectile dysfunction, stroke [1] [70]. |
The comparative assessment firmly establishes that while the concept of direct differentiation remains theoretically powerful for long-term structural repair, the paracrine signaling mechanism offers a more versatile, rapid, and broadly applicable therapeutic profile that underpins many of the functional benefits observed in adult stem cell therapies. The paradigm has shifted from "cell replacement" to "cell-as-a-drug" or "cell-as-a-biologic facilitator."
This refined understanding directly informs future therapeutic strategies. Research is now focused on enhancing the paracrine effect through the preconditioning of stem cells (e.g., with hypoxia or cytokines) [48], genetic modification to overexpress beneficial factors (e.g., Akt-overexpressing MSCs) [1], and the move towards cell-free therapies utilizing purified exosomes or manufactured secretome formulations [72] [48]. These approaches aim to capitalize on the benefits of paracrine signaling—such as a superior safety profile and logistical simplicity—while overcoming challenges related to cell survival and manufacturing. For researchers and drug developers, the future lies in strategically manipulating the stem cell secretome to create optimized, reproducible, and effective regenerative medicines for a wide spectrum of diseases.
Regenerative medicine is undergoing a significant transformation, moving from whole-cell therapies toward refined cell-free derivative products. This evolution is particularly evident in the context of paracrine signaling, which has emerged as a fundamental mechanism explaining the therapeutic effects of adult stem cell therapy. Initially, the regenerative potential of stem cells was attributed primarily to their ability to differentiate into target cell types, such as cardiomyocytes following myocardial infarction [1]. However, a growing body of evidence now suggests that transplanted stem cells function predominantly as biochemical factories, secreting a complex cocktail of bioactive molecules that orchestrate repair processes through paracrine mechanisms [1] [75]. These secreted factors include cytokines, growth factors, and extracellular vesicles (EVs) like exosomes, which collectively mediate cytoprotection, neovascularization, immunomodulation, and endogenous regeneration [1].
This whitepaper provides an in-depth technical analysis comparing traditional cell-based therapies with emerging cell-free therapeutic products, with a specific focus on the implications of paracrine signaling mechanisms for research and drug development. We examine the underlying biology, manufacturing considerations, therapeutic applications, and future directions for both therapeutic modalities, providing researchers and drug development professionals with a comprehensive framework for strategic decision-making in this rapidly evolving field.
The Central Role of Paracrine Signaling in Stem Cell Therapeutics
Historical Context and Mechanistic Insights
The paradigm shift from differentiation-based to paracrine-mediated mechanisms began when researchers observed that the functional benefits of stem cell transplantation often exceeded what could be explained by the relatively low rates of cell engraftment and direct differentiation [1] [41]. Seminal studies demonstrated that conditioned medium (CM) from mesenchymal stem cells (MSCs) could recapitulate many therapeutic effects of the cells themselves, including reduced infarct size, improved cardiac function, and enhanced capillary density in infarcted hearts [1]. This provided compelling evidence that secreted factors, rather than the cells themselves, were primarily responsible for the observed therapeutic outcomes.
Paracrine factors exert their effects through multiple interconnected mechanisms. The table below summarizes the key functional categories of paracrine signaling and their physiological effects.
Table 1: Key Paracrine Signaling Mechanisms and Their Therapeutic Effects
| Signaling Mechanism | Key Mediators | Primary Physiological Effects | Therapeutic Applications |
|---|---|---|---|
| Cytoprotection | IGF-1, HGF, ADM, TMSB4 [1] | Reduces apoptosis and necrosis in ischemic cardiomyocytes [1] | Myocardial infarction, ischemic injury |
| Neovascularization | VEGF, FGF2, HGF, ANG [1] | Stimulates angiogenesis and arteriogenesis | Ischemic diseases, wound healing |
| Immunomodulation | TGF-β, PGE2, IL-6 [75] | Modulates T-cell and macrophage function | Autoimmune diseases, graft-versus-host disease |
| Activation of Endogenous Stem Cells | SDF-1, KITLG [1] | Recruits and activates resident stem cells | Tissue regeneration, organ repair |
| Extracellular Matrix Remodeling | MMPs, TIMPs, CTGF [1] | Regulates fibrosis and tissue architecture | Fibrotic diseases, myocardial remodeling |
The following diagram illustrates the complex paracrine signaling network through which transplanted stem cells, particularly MSCs, orchestrate tissue repair. This network forms the biological basis for both cell-based and cell-free therapeutic approaches.
Experimental Evidence Supporting Paracrine Mechanisms
Critical proof-of-concept studies have demonstrated that administration of conditioned medium from various stem cell types can produce therapeutic benefits comparable to cell transplantation. In one foundational experiment, conditioned medium from Akt-modified MSCs (Akt-MSCs) significantly reduced apoptosis in isolated cardiomyocytes exposed to low oxygen tension in vitro [1]. Subsequent in vivo studies confirmed that injection of this conditioned medium into infarcted hearts reduced apoptosis, promoted angiogenesis, and improved cardiac function without significant cell engraftment [1]. Similar findings have been reported with conditioned medium from bone marrow mononuclear cells (BM-MNCs), which increased capillary density and decreased infarct size when injected into acutely infarcted hearts [1].
The potency of paracrine signaling is further enhanced under hypoxic conditions. Studies have shown that hypoxic preconditioning of MSCs significantly increases the production and secretion of key trophic factors such as VEGF, FGF2, HGF, and IGF-1, resulting in a more potent secretome with enhanced therapeutic capacity [1]. This phenomenon has important implications for both cell-based and cell-free therapeutic manufacturing, suggesting that environmental conditioning can be leveraged to enhance product efficacy.
Cell-Based Therapies: Current Status and Technical Hurdles
Cell-based therapies involve the administration of living cells as therapeutic agents. Multiple cell types have been investigated for regenerative applications, each with distinct advantages and limitations.
Table 2: Comparison of Primary Cell Types for Cell-Based Therapies
| Cell Type | Key Markers | Differentiation Potential | Therapeutic Advantages | Technical Challenges |
|---|---|---|---|---|
| Bone Marrow MSCs (BM-MSCs) | CD73, CD90, CD105, CD44 [75] | Osteogenic, chondrogenic, adipogenic [75] | Immunomodulatory, well-characterized [75] | Invasive extraction, low yield [75] |
| Adipose-Derived MSCs (AdMSCs) | CD13, CD29, CD44, CD73, CD90 [75] | Osteogenic, chondrogenic, adipogenic [75] | Abundant tissue source, high yield [75] | Variable quality based on donor [75] |
| Cardiac Stem Cells (CSCs) | c-kit, Sca-1 [1] | Cardiomyocytes, endothelial cells, smooth muscle cells [1] | Tissue-specific differentiation, autologous [1] | Limited quantity, difficult isolation [1] |
| Induced Pluripotent Stem Cells (iPSCs) | Oct4, Nanog, Sox2 [76] | Virtually all cell types [76] | Patient-specific, unlimited expansion [76] | Tumorigenicity risk, complex differentiation [76] |
Manufacturing and Regulatory Challenges
The translation of cell-based therapies from research to clinical application faces significant technical hurdles. Manufacturing living cellular products requires maintaining strict aseptic processing conditions throughout expansion, manipulation, and formulation. The viability and potency of the final product must be rigorously controlled, necessitating robust analytical methods and release criteria [77]. Cryopreservation and cold chain logistics present additional complexities, as cell viability is sensitive to freezing and thawing parameters as well as transportation conditions [77].
From a regulatory perspective, cell-based products are subject to stringent requirements due to concerns about tumorigenicity, immunogenicity, and the potential for uncontrolled differentiation [77]. Allogeneic approaches, while offering off-the-shelf availability, face additional challenges related to host immune rejection, often requiring concomitant immunosuppression [77]. These complex manufacturing and regulatory hurdles have contributed to the high costs associated with cell-based therapies, limiting their widespread accessibility and commercial viability [78].
Cell-Free Derivative Products: Emerging Opportunities
The Secretome and Extracellular Vesicles
Cell-free derivative products primarily consist of the secretome - the complete set of molecules secreted by cells - with particular emphasis on extracellular vesicles (EVs) such as exosomes. The MSC-derived secretome contains a diverse array of bioactive components, including growth factors, cytokines, chemokines, lipids, and regulatory RNAs, which collectively facilitate cardiac repair through mechanisms comparable to MSCs but without the associated risks of cell therapy [75].
Exosomes, typically 30-150 nm in diameter, are membrane-bound vesicles that carry proteins, lipids, and nucleic acids (including mRNA, miRNA, and other non-coding RNAs) from donor to recipient cells [76] [75]. They serve as protected delivery vehicles for bioactive molecules, facilitating intercellular communication and mediating many of the paracrine effects previously attributed to the parent cells. The table below compares key characteristics of cell-based and cell-free therapeutic approaches.
Table 3: Technical Comparison of Cell-Based vs. Cell-Free Therapeutic Approaches
| Parameter | Cell-Based Therapy | Cell-Free Derivatives |
|---|---|---|
| Mode of Action | Direct differentiation & paracrine signaling [1] | Primarily paracrine signaling [75] |
| Manufacturing Complexity | High (viability, sterility, characterization) [77] | Moderate (purification, characterization) |
| Storage & Stability | Cryopreservation, limited shelf life [77] | Potentially lyophilized, longer shelf life [75] |
| Dosing Strategy | Complex (cell number, viability) [77] | Standardized (protein/vesicle concentration) |
| Tumorigenic Risk | Present (especially with pluripotent cells) [76] | Negligible [75] |
| Immunogenicity | Variable (allogeneic vs. autologous) [77] | Low (especially with EV products) [75] |
| Scalability | Challenging (bioreactor expansion) [78] | More straightforward (conditioned media production) |
| Regulatory Pathway | Complex (advanced therapy medicinal product) [77] | Evolving (potentially as biological products) |
Manufacturing Considerations for Cell-Free Products
The production of cell-free derivatives begins with the generation of conditioned medium from appropriate cell sources under controlled culture conditions. Subsequent purification steps typically involve differential centrifugation, ultrafiltration, chromatography, or precipitation methods to concentrate the bioactive components, particularly EVs [75]. Compared to cell-based products, cell-free derivatives offer advantages in storage stability and distribution, as they may potentially be lyophilized and reconstituted, eliminating the need for complex cold chain logistics [75].
Quality control for cell-free products focuses on characterizing the molecular composition (proteomic, lipidomic, and transcriptomic profiles), quantifying specific therapeutic factors, and establishing potency through in vitro bioassays [75]. The defined nature of these products facilitates batch-to-batch consistency and more straightforward potency standardization compared to living cell products.
Experimental Approaches and Methodologies
Standardized Protocol for Paracrine Factor Analysis
To investigate the paracrine-mediated effects of stem cells and their derivatives, researchers can employ the following standardized protocol for collecting and analyzing the secretome:
1. Cell Culture and Conditioning:
- Culture MSCs (from bone marrow, adipose tissue, or other sources) to 80% confluence in standard culture flasks.
- Replace growth medium with serum-free basal medium to eliminate interference from serum-derived factors.
- Subject cells to normoxic (21% O₂) or hypoxic (1-3% O₂) conditions for 24-72 hours to condition the medium.
- Collect conditioned medium and centrifuge at 2,000 × g for 10 minutes to remove cell debris.
2. Secretome Concentration and Fractionation:
- Concentrate conditioned medium using 3-10 kDa molecular weight cut-off ultrafiltration devices.
- For extracellular vesicle isolation, subject the concentrated conditioned medium to differential ultracentrifugation: 10,000 × g for 30 minutes (to remove apoptotic bodies) followed by 100,000 × g for 70 minutes to pellet exosomes.
- Resuspend the exosome pellet in phosphate-buffered saline or appropriate buffer for downstream applications.
3. Functional Characterization:
- Protein Quantification: Determine total protein concentration using BCA or Bradford assay.
- Vesicle Characterization: Analyze exosome size distribution and concentration using nanoparticle tracking analysis (NTA).
- Molecular Profiling: Characterize protein content by Western blotting for exosomal markers (CD9, CD63, CD81) or multiplex immunoassays for specific growth factors and cytokines.
- Functional Assays: Evaluate biological activity using in vitro angiogenesis assays (tube formation), cytoprotection assays (hypoxia/reoxygenation models), or immunomodulation assays (T-cell suppression).
The Scientist's Toolkit: Essential Research Reagents
The table below outlines key reagents and methodologies essential for research in cell-based and cell-free therapeutics.
Table 4: Essential Research Reagents and Platforms for Paracrine Mechanism Studies
| Research Tool Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Cell Isolation & Culture | Collagenase digestion kits, defined culture media, hypoxia chambers [75] | Isolation and expansion of MSCs from tissues, conditioning of cells | Maintain differentiation potential, avoid senescence [75] |
| Extracellular Vesicle Isolation | Differential centrifugation kits, size-exclusion chromatography, polymer-based precipitation [75] | Isolation of exosomes and other EVs from conditioned medium | Minimize co-isolation of proteins, maintain vesicle integrity |
| Molecular Characterization | Multiplex immunoassays, Western blot reagents, RNA extraction kits (for EV RNA) [75] | Proteomic and transcriptomic analysis of secretome | Sufficient sensitivity for low-abundance factors |
| Functional Assays | Tube formation assays (Matrigel), T-cell proliferation kits, apoptosis detection reagents [1] [75] | Assessment of angiogenesis, immunomodulation, cytoprotection | Include appropriate controls (non-conditioned medium) |
| In Vivo Models | Myocardial infarction (ligation/reperfusion), hindlimb ischemia, skin wound models [1] | Evaluation of therapeutic efficacy in disease contexts | Consider route of administration (intravenous, local) |
Future Perspectives and Research Directions
Engineering Strategies for Enhanced Therapeutics
The future landscape of both cell-based and cell-free therapies will be shaped by advanced engineering approaches aimed at enhancing product efficacy and specificity. For cell-based therapies, genetic engineering techniques such as CRISPR-Cas9 and synthetic biology circuits are being employed to create "smart" cells that can sense disease environments and respond with precisely controlled therapeutic outputs [77]. Similarly, parent cells can be genetically modified to enhance the potency of their secretome before collection of conditioned medium for cell-free products [1].
Biomaterial-assisted delivery represents another promising strategy for both therapeutic modalities. Cells or cell-free derivatives can be encapsulated in biomaterial matrices that provide protective microenvironments and control the spatiotemporal release of therapeutic factors [77]. For cell-free approaches specifically, engineering extracellular vesicles to display specific targeting ligands or carry customized therapeutic cargo (such as specific miRNAs or proteins) will enable more precise targeting and enhanced therapeutic efficacy [75].
The following diagram illustrates a potential integrated manufacturing workflow for both cell-based and cell-free therapeutic products, highlighting shared and divergent processes in their production pipelines.
Clinical Translation and Commercial Considerations
The translation of both cell-based and cell-free therapies faces significant funding challenges, with venture capital for cell and gene therapies dropping from $8.2 billion in 2021 to $1.4 billion in 2024 [78]. This funding environment has increased pressure on developers to demonstrate clear clinical impact and commercial viability. Cell-free derivatives may face lower regulatory hurdles and manufacturing costs, potentially accelerating their path to clinical application and commercial success [75].
Future clinical applications will likely see both therapeutic modalities occupying complementary niches rather than competing directly. Cell-based therapies may be preferred for situations requiring sustained, long-term secretion of therapeutic factors or structural integration, while cell-free approaches may be optimal for acute interventions, repeat dosing regimens, and conditions where safety concerns preclude cell transplantation [75]. The continued elucidation of paracrine mechanisms will be essential for rationally designing both cell-based and cell-free products with enhanced therapeutic profiles.
The evolving landscape of regenerative medicine is increasingly embracing both cell-based therapies and cell-free derivative products as complementary therapeutic modalities. The recognition that paracrine signaling mediates many of the therapeutic benefits of stem cells has fundamentally reshaped this field, providing a mechanistic foundation for cell-free approaches based on the stem cell secretome and extracellular vesicles. While cell-based therapies continue to offer unique capabilities for structural integration and sustained factor delivery, cell-free derivatives present distinct advantages in terms of safety profile, manufacturing scalability, and regulatory pathway.
For researchers and drug development professionals, strategic decisions regarding therapeutic modality selection should be guided by the specific clinical indication, mechanistic requirements, and practical constraints of each application. The continued advancement of both approaches will depend on deepening our understanding of paracrine mechanisms, refining manufacturing processes, and developing robust characterization methods. As both fields evolve, they hold tremendous promise for addressing currently intractable diseases through uniquely powerful modes of action rooted in the fundamental biology of cellular communication and repair.
Conclusion
The evidence firmly establishes paracrine signaling as a central mechanism by which adult stem cells mediate tissue repair and functional recovery. This paradigm shift, supported by a growing body of preclinical and clinical data, redirects therapeutic strategy from cell replacement to the targeted delivery of bioactive secretomes. Future directions must focus on standardizing characterization of paracrine factors, developing potent enhancement strategies like genetic modification and preconditioning, and advancing cell-free therapies such as exosomes for improved safety and scalability. For researchers and drug developers, the challenge and opportunity lie in systematically harnessing this complex signaling network to create a new generation of precise, effective, and off-the-shelf regenerative biologics.
References
- 1. Paracrine mechanisms in adult stem cell signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2667788/]
- 2. Comparative analysis of dental-derived stem cells and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1717849/full]
- 3. 3-D individual cell based computational modeling of tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5013833/]
- 4. Paracrine Signalling - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/paracrine-signalling]
- 5. Paracrine effect of fibroblasts on the proliferation and ... [https://www.sciencedirect.com/science/article/abs/pii/S030090842500269X]
- 6. Inference and analysis of cell-cell communication using ... [https://www.nature.com/articles/s41467-021-21246-9]
- 7. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 8. Mesenchymal stem cell secretome for regenerative medicine [https://www.sciencedirect.com/science/article/pii/S2090123224001814]
- 9. Adult Stem Cell Paracrine Mechanisms : Signaling and Therapy [https://drstemcellsthailand.com/stem-cell-paracrine/]
- 10. Secretome enriched with small extracellular vesicles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150548/]
- 11. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 12. Uptake of small extracellular vesicles by recipient cells is ... [https://www.nature.com/articles/s41467-025-57617-9]
- 13. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 14. Paracrine Mechanisms of Mesenchymal Stromal Cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7085399/]
- 15. Mesenchymal Stem/Stromal Cells and Their Paracrine Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875256/]
- 16. Effects of microenvironment and biological behavior on the ... [https://www.sciencedirect.com/science/article/pii/S235230422300140X]
- 17. Pharmacological modulation of stem cells signaling ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 18. Quantitative characterization of cell niches in spatially ... [https://www.nature.com/articles/s41588-025-02120-6]
- 19. Gap Junctional Versus Paracrine Signaling in the Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637001/]
- 20. Emerging Concepts in Paracrine Mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4874329/]
- 21. Cell culture expansion media choice affects secretory ... [https://www.sciencedirect.com/science/article/pii/S235232042500015X]
- 22. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 23. A comprehensive review of clinical trials and Progress in ... [https://pubmed.ncbi.nlm.nih.gov/41079454/]
- 24. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 25. Unlocking the potential of endothelial progenitor cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497398/]
- 26. Understanding the molecular basis of mesenchymal stem ... [https://www.nature.com/articles/s41419-025-08094-x]
- 27. Advancing regenerative therapies with umbilical cord ... [https://pubmed.ncbi.nlm.nih.gov/41036706/]
- 28. Exploring the therapeutic potential of MSC-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398063/]
- 29. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 30. Mesenchymal stromal cells modulate neutrophil phenotype ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04684-w]
- 31. Secretome Analysis: Reading Cellular Sign Language to ... [https://www.sciencedirect.com/science/article/pii/S1535947623002037]
- 32. Proteomic profiling of iPSC and tissue-derived MSC ... [https://www.nature.com/articles/s41536-024-00382-y]
- 33. Single-cell genomics and proteomics analysis | Yale Research [https://research.yale.edu/cores/single-cell-genomics-and-proteomics-analysis]
- 34. Single-Cell Secretome [https://brukercellularanalysis.com/products/chips/single-cell-secretome/]
- 35. Identification of Paracrine Neuroprotective Candidate ... [https://www.sciencedirect.com/science/article/pii/S1535947620313360]
- 36. Paracrine Effect of Mesenchymal Stem Cells Derived from ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0107001]
- 37. Modeling Paracrine Noncanonical Wnt Signaling In Vitro [https://pmc.ncbi.nlm.nih.gov/articles/PMC9253518/]
- 38. Cell Signaling ELISA Kits and Multiplex Immunoassays [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/immunoassay-research-areas/cell-signaling-elisa-kits-immunoassays.html]
- 39. Mesenchymal stem cell-conditioned medium accelerates ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1659444/full]
- 40. Comparison of biological properties of human adipose tissue ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02943-x]
- 41. Paracrine mechanisms in adult stem cell signaling and therapy [https://pubmed.ncbi.nlm.nih.gov/19028920/]
- 42. Paracrine Signalling - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/paracrine-signalling]
- 43. Translational potential of mesenchymal stem cells in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03885-z]
- 44. Stem cell therapies for neurological disorders - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11270957/]
- 45. From macrophage polarization to clinical translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504304/]
- 46. Advances in cell therapy for orthopedic diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567640/full]
- 47. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 48. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 49. Current status and new horizons in stem cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406451/]
- 50. Hypoxic Conditioning Enhances the Angiogenic Paracrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3653395/]
- 51. The impact of hypoxia preconditioning on mesenchymal stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03778-1]
- 52. A nonpharmacological approach in COVID-19 prevention [https://www.sciencedirect.com/science/article/pii/S1201971220324942]
- 53. Mesenchymal Stem Cell Therapy and Its Clinical ... [https://www.intechopen.com/online-first/1228919]
- 54. Quantitative phenotypic and pathway profiling guides ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2014.00118/full]
- 55. Pharmacological modulation of stem cells signaling pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210473/]
- 56. Applying quantitative and systems pharmacology to drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11483046/]
- 57. Modulation of Stem Cell Survival and Engraftment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439257/]
- 58. Enhancing mesenchymal stem cell survival and homing ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03476-4]
- 59. Enhanced Survival and Engraftment of Transplanted Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4457539/]
- 60. Advances in HFrEF Pharmacological Therapy 2025 [https://www.cfrjournal.com/articles/pharmacological-therapy-hfref-2025-navigating-new-advances-and-old-unmet-needs-eternal?language_content_entity=en]
- 61. Update on clinical heart failure trials [https://link.springer.com/article/10.1007/s00392-025-02784-4]
- 62. What's new in heart failure? September 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502451/]
- 63. Mesenchymal stem cell perspective: cell biology to clinical ... [https://www.nature.com/articles/s41536-019-0083-6]
- 64. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 65. Cancer stem cells: advances in knowledge and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224386/]
- 66. Comparison of endometrial regenerative cells and bone ... [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-10-207]
- 67. Editorial: Safety, Efficacy and Mechanisms of Action ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7040069/]
- 68. Efficacy and safety of mesenchymal stem/stromal cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481956/]
- 69. Production, safety and efficacy of iPSC-derived ... [https://www.nature.com/articles/s41591-020-1050-x]
- 70. Advances in stem cell therapy for erectile dysfunction [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1519095/full]
- 71. A Comprehensive Review of Adult Stem Cell Research ... [https://www.openaccessjournals.com/articles/a-comprehensive-review-of-adult-stem-cell-research-advances-16812.html]
- 72. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 73. Top Stem Cell Applications in 2026 [https://bioinformant.com/stem-cell-applications/]
- 74. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 75. Stem Cell-Based Therapy and Cell-Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10635745/]
- 76. - Cell and Selected Based - Cell for Myocardial... Free Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC9499607/]
- 77. Engineering the next generation of cell-based therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9149674/]
- 78. Budget blues: where are cell and gene therapies heading? [https://www.labiotech.eu/trends-news/european-cell-gene-therapy-summit-2025-funding-challenges/]