Predicting Patient Response to Therapy: A Comprehensive Guide to Outcome Prediction Models in Clinical Research
This article provides a comprehensive overview of outcome prediction modeling for therapeutic response, tailored for researchers and drug development professionals.
Predicting Patient Response to Therapy: A Comprehensive Guide to Outcome Prediction Models in Clinical Research
Abstract
This article provides a comprehensive overview of outcome prediction modeling for therapeutic response, tailored for researchers and drug development professionals. It explores the foundational principles of using clinical and genomic data to forecast treatment outcomes, details advanced methodological approaches including deep learning and ensemble models, and addresses critical challenges such as model instability and bias. Furthermore, it offers a comparative analysis of algorithm performance and validation strategies to ensure model reliability and clinical utility, synthesizing insights from the latest research to guide the development of robust, clinically applicable prediction tools.
Core Principles and Data Foundations for Therapy Response Prediction
In the evolving field of precision medicine, defining the prediction goal is a critical first step in developing models that can forecast patient response to therapy. This foundational process requires precise specification of three core components: the target population, the outcome measures, and the clinical setting. These elements collectively determine the model's validity, generalizability, and ultimate clinical utility [1] [2]. Research demonstrates that machine learning (ML) approaches now achieve an average accuracy of 0.76 and area under the curve (AUC) of 0.80 in predicting treatment response for emotional disorders, highlighting the significant potential of well-defined prediction models [3].
The careful definition of these components directly addresses a key challenge in medical ML research: the demonstration of generalizability and regulatory compliance required for clinical implementation [1]. This guide systematically compares how contemporary research protocols define these core elements across different therapeutic domains, providing a framework for researchers developing prediction models for therapeutic response.
Comparative Analysis of Prediction Goal Definitions Across Studies
Table 1: Comparison of Target Population Definitions in Therapeutic Prediction Research
| Study/Model | Medical Domain | Inclusion Criteria | Exclusion Criteria | Sample Size | Data Sources |
|---|---|---|---|---|---|
| AID-ME Model [2] | Major Depressive Disorder (MDD) | Adults (≥18) with moderate-severe MDD; acute depressive episode | Bipolar depression, MDE from medical conditions, mild depression | 9,042 participants | 22 clinical trials from NIMH, academic partners, pharmaceutical companies |
| EoBC Prediction Study [4] | Early-Onset Breast Cancer | Women ≥18 to <40 years with non-metastatic invasive breast cancer | Metastatic cancer, malignancy 5 years prior to diagnosis | 1,827 patients | Alberta Cancer Registry, hospitalization databases, vital statistics |
| Stress-Related Disorders Protocol [5] | Stress-Related Disorders (Adjustment Disorder, Exhaustion Disorder) | Primary diagnosis of AD or ED; participants in RCT | N/A (protocol paper) | 300 participants | Randomized controlled trial data |
| Emotional Disorders Meta-Analysis [3] | Emotional Disorders (Depression, Anxiety) | Patients with emotional disorders receiving evidence-based treatments | Studies without ML for treatment response prediction | 155 studies (meta-analysis) | PubMed, PsycINFO (2010-2025) |
Table 2: Outcome Measures and Clinical Settings in Prediction Research
| Study/Model | Primary Outcome | Outcome Measurement Tool | Outcome Timing | Clinical Setting | Intervention Types |
|---|---|---|---|---|---|
| AID-ME Model [2] | Remission | Standardized depression rating scales | 6-14 weeks | Clinical trials (primary/psychiatric care) | 10 pharmacological treatments (8 antidepressants, 2 combinations) |
| EoBC Prediction Study [4] | All-cause mortality | Survival status | 5 and 10 years | Hospital-based cancer care | Surgical interventions, chemotherapy, radiation, hormone therapy |
| Stress-Related Disorders Protocol [5] | Responder status | Perceived Stress Scale-10 (PSS-10) with Reliable Change Index | Post-treatment | Internet-delivered interventions | Internet-based CBT vs. active control |
| Emotional Disorders Meta-Analysis [3] | Treatment response (responder vs. non-responder) | Various standardized clinical scales | Variable across studies | Multiple clinical settings | Psychotherapies, pharmacotherapies, other evidence-based treatments |
Experimental Protocols for Predictive Model Development
Data Sourcing and Participant Selection
The AID-ME study exemplifies a rigorous approach to data sourcing, utilizing clinical trial data from multiple sources including the NIMH Data Archive, academic researchers, and pharmaceutical companies through the Clinical Study Data Request platform [2]. Their protocol implemented strict inclusion/exclusion criteria: studies were required to focus on acute major depressive episodes in adults, with trial lengths between 6-14 weeks to align with clinical guidelines for remission assessment. Participants receiving medication doses below the minimum effective levels defined by CANMAT guidelines were excluded, as were those remaining in studies for less than two weeks, ensuring adequate outcome assessment [2].
The early-onset breast cancer study demonstrates a comprehensive registry-based approach, linking data from the Alberta Cancer Registry with hospitalization records, ambulatory care data, and vital statistics [4]. This population-based method captures complete clinical trajectories, though it presents challenges in data harmonization across sources. The protocol emphasized transparent reporting following TRIPOD guidelines for multivariable prediction models [4].
Machine Learning Methodologies and Validation
Recent systematic reviews of ML applications in major depressive disorder identify Random Forest (RF) and Support Vector Machine (SVM) as the most frequently used methods [1]. Models integrating multiple categories of patient data (clinical, demographic, molecular biomarkers) consistently demonstrate higher predictive accuracy than single-category models [1].
The stress-related disorders protocol employs a comparative methodology, testing four classifiers: logistic regression with elastic net, random forest, support vector machine, and AdaBoost [5]. This approach includes hyperparameter tuning using 5-fold cross-validation with randomized search, with dataset splitting (70% training, 30% testing) to evaluate model performance using balanced accuracy, precision, recall, and AUC [5].
For the emotional disorders meta-analysis, moderator analyses revealed that studies using robust cross-validation procedures exhibited higher prediction accuracy, and those incorporating neuroimaging data achieved superior performance compared to models using only clinical and demographic data [3].
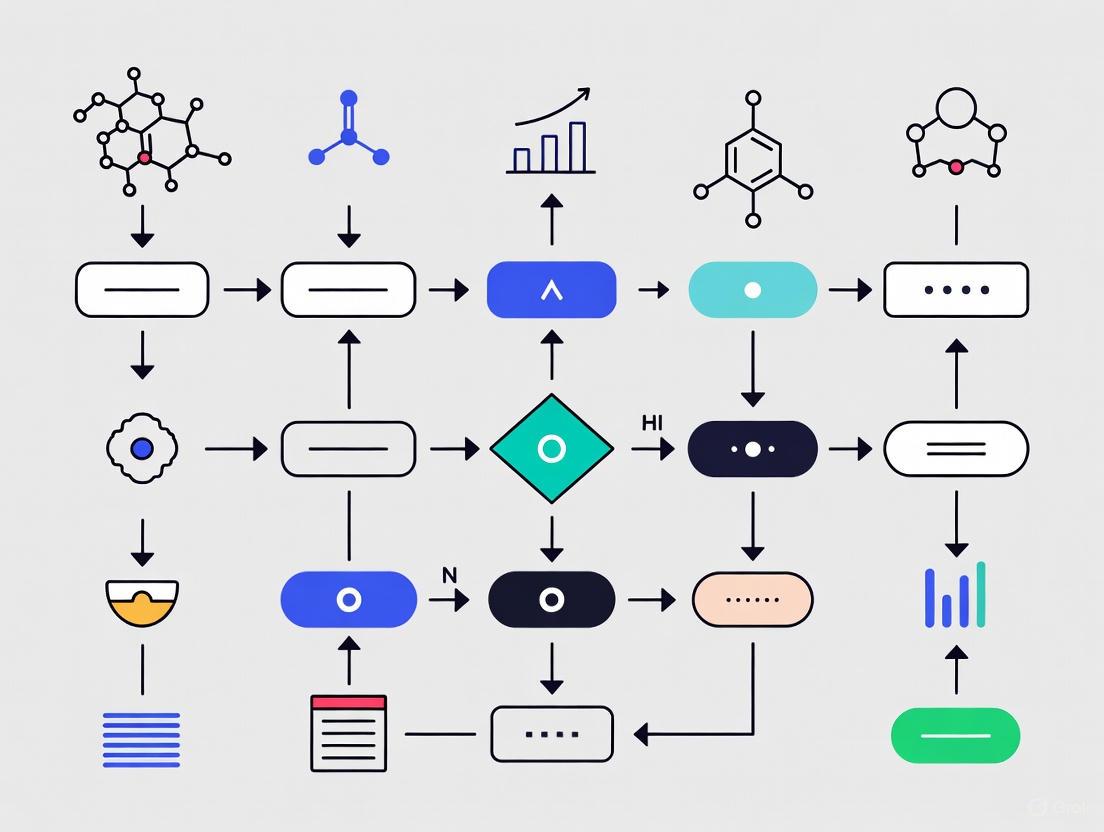
Diagram 1: Workflow for Defining Prediction Goals in Therapeutic Research
Performance Assessment and Validation Frameworks
The emotional disorders meta-analysis established comprehensive performance benchmarks, reporting mean sensitivity of 0.73 and specificity of 0.75 across 155 studies [3]. The stress-related disorders protocol proposes a balanced accuracy threshold of ≥67% as indicative of clinical utility [5].
Critical to performance assessment is the distinction between internal and external validation. The MDD systematic review found limited external validation of applied ML approaches, noting this as a significant barrier to clinical implementation [1]. Well-calibrated models are essential, as evidenced by the breast cancer study which evaluated both discrimination (AUC) and calibration, finding that PREDICT v2.1 overestimated 5-year mortality in high-risk groups despite good discrimination [4].
Research Reagent Solutions for Predictive Modeling
Table 3: Essential Research Materials and Computational Tools for Predictive Modeling
| Tool Category | Specific Examples | Function in Research | Implementation Considerations |
|---|---|---|---|
| Data Sources | Clinical trial data repositories (NIMH, CSDR), Cancer registries, Electronic Health Records | Provides structured, curated patient data with outcome measures | Data harmonization across sources; privacy-preserving access methods [2] [6] |
| Machine Learning Algorithms | Random Forest, Support Vector Machines, Deep Learning, LASSO Cox regression, Random Survival Forests | Pattern detection; handling complex nonlinear relationships in patient data | Algorithm selection based on data type and sample size; computational resources [1] [4] [3] |
| Validation Frameworks | k-fold cross-validation, bootstrapping, hold-out testing, time-dependent ROC analysis | Assess model performance and generalizability | Nested cross-validation preferred; external validation essential for clinical utility [4] [3] |
| Performance Metrics | AUC-ROC, Balanced Accuracy, Sensitivity, Specificity, Calibration plots (Emax, ICI) | Quantify predictive performance and clinical utility | Balance between discrimination and calibration; domain-specific thresholds [4] [3] [5] |
| Privacy/Compliance Tools | Tokenization, Clean Room technology, Expert Determination method, De-identification algorithms | Enable privacy-preserving analysis of sensitive health data | Compliance with GDPR, HIPAA; balance between data utility and privacy [6] |
Critical Considerations in Prediction Goal Definition
Methodological and Ethical Challenges
A significant finding across studies is that prediction models may yield "harmful self-fulfilling prophecies" when used for clinical decision-making [7]. These models can harm patient groups while maintaining good discrimination metrics post-deployment, creating an ethical challenge for implementation. This underscores the limitation of relying solely on discrimination metrics for model evaluation [7].
The systematic review of MDD prediction models identified ongoing challenges with regulatory compliance regarding social, ethical, and legal standards in the EU [1]. Key issues include algorithmic bias mitigation, model transparency, and adherence to Medical Device Regulation (MDR) and EU AI Act requirements [1] [6].
Domain-Specific Adaptations
The comparison reveals important domain-specific considerations in defining prediction goals. In oncology, prediction models must account for extended timeframes (5-10 year survival) and competing risks [4]. In mental health, standardized outcome measures with appropriate timing (6-14 weeks for depression remission) are critical, while also considering functional outcomes and quality of life measures [2] [5].
Diagram 2: Data Integration and Modeling Approaches in Therapeutic Prediction
Emerging Trends and Future Directions
Research indicates a shift toward multimodal data integration, combining clinical, demographic, molecular, and neuroimaging data to enhance predictive accuracy [1] [3]. There is also growing emphasis on privacy-preserving AI techniques that enable analysis without compromising patient confidentiality [6].
The field is moving beyond traditional clinical trial endpoints to incorporate real-world evidence and patient-reported outcomes, facilitated by technologies like wearable devices and digital biomarkers [8] [6]. This expansion of data sources enables more comprehensive prediction goals but introduces additional complexity in data standardization and harmonization.
Future research should focus on developing standardized frameworks for defining prediction goals across domains, addressing ethical implementation challenges, and demonstrating real-world clinical utility through impact studies rather than just performance metrics [1] [7].
In the pursuit of accurate outcome prediction modeling for patient response to therapy, researchers face a fundamental choice in data sourcing: highly controlled clinical trials or observational real-world data (RWD). This decision significantly influences the predictive models' development, validation, and ultimate clinical utility. Clinical trials, long considered the gold standard for establishing causal inference, generate data under standardized conditions that minimize variability and bias [9]. In contrast, real-world data, collected from routine clinical practice, offers insights into therapeutic performance across diverse patient populations and heterogeneous care settings, better reflecting clinical reality [10] [9].
The integration of both data types is increasingly crucial for comprehensive evidence generation throughout the medical product lifecycle. As regulatory agencies like the FDA recognize the value of RWD and its derived real-world evidence (RWE), understanding the complementary strengths and limitations of each source becomes essential for researchers, scientists, and drug development professionals aiming to build robust prediction models for therapeutic response [9].
Clinical Trial Data: The Controlled Environment
Clinical trials are prospective studies conducted according to strict protocols to evaluate the safety and efficacy of interventions under controlled conditions [11]. The data generated follows standardized collection procedures with prespecified endpoints and rigorous monitoring to ensure data integrity through principles like ALCOA (Attributable, Legible, Contemporaneous, Original, Accurate) [12].
Phase I trials focus primarily on safety and tolerability in small populations, often healthy volunteers, establishing preliminary pharmacokinetic and pharmacodynamic profiles [11]. Subsequent phases (II-IV) expand to larger patient populations to confirm efficacy and monitor adverse events. The controlled nature of these trials enables high internal validity through randomization, blinding, and protocol-specified comparator groups.
Real-World Data: The Clinical Practice Environment
Real-world data encompasses information collected from routine healthcare delivery outside the constraints of traditional clinical trials [10] [9]. According to regulatory definitions, RWD sources include electronic health records (EHRs), medical claims data, product and disease registries, patient-generated data from digital health technologies, and data from wearable devices [9].
Unlike clinical trial data, RWD is characterized by its heterogeneity in data collection methods, formats, and quality across different healthcare systems [13]. This diversity presents both opportunities and challenges for outcome prediction modeling, as it captures broader patient experiences but requires sophisticated methodologies to address inconsistencies and potential biases [10].
Comparative Analysis: Key Distinctions
Table 1: Fundamental Characteristics of Clinical Trial Data vs. Real-World Data
| Characteristic | Clinical Trial Data | Real-World Data |
|---|---|---|
| Data Collection Environment | Controlled, protocol-driven | Routine clinical practice |
| Patient Population | Strict inclusion/exclusion criteria; homogeneous | Broad, diverse; represents actual patients |
| Data Quality & Consistency | High consistency; standardized procedures | Variable quality; requires extensive curation |
| Sample Size | Limited by design and resources | Potentially very large |
| Follow-up Duration | Fixed by protocol | Potentially longitudinal over long term |
| Primary Strength | High internal validity; establishes efficacy | High external validity; establishes effectiveness |
| Primary Limitation | Limited generalizability; high cost | Potential biases; data heterogeneity |
Methodological Rigor and Data Integrity
Clinical trials employ systematic quality control measures throughout the data lifecycle. These include source data verification (SDV), rigorous training of all personnel, and independent monitoring committees (DMCs) that maintain confidentiality of interim results to prevent bias [12]. The implementation of risk-based monitoring approaches, as emphasized in ICH GCP E6(R2), further enhances data integrity while optimizing resource allocation [12].
Real-world data integrity faces different challenges, including variable documentation practices across healthcare settings and potential data missingness [13]. Ensuring RWD quality requires specialized methodologies such as validation studies to assess data accuracy, sophisticated statistical adjustments for confounding factors, and advanced data curation techniques to handle heterogeneous data structures [13] [10].
Applications in Outcome Prediction Modeling
Clinical Trial Data for Prediction Modeling
Clinical trials provide high-quality, structured data ideally suited for developing initial predictive models of treatment response. The detailed phenotyping of patients and standardized outcome assessments enable researchers to identify potential biomarkers and build multivariate prediction models with reduced noise.
The Nemati sepsis prediction model, developed using clinical trial data, demonstrates this application effectively. This early-warning system for sepsis development in ICU patients was built using carefully curated clinical trial data and subsequently validated in real-world settings, where it demonstrated improved patient outcomes [14].
Real-World Data for Prediction Modeling
RWD offers distinct advantages for model refinement and validation across broader populations. In oncology, for example, RWD from diverse sources enables researchers to develop more robust prediction models for rare cancer subtypes or special populations typically excluded from clinical trials [13] [15].
The FDA has acknowledged RWD's growing role in regulatory decision-making, including supporting hypotheses for clinical studies, constructing performance goals in Bayesian analyses, and generating evidence for marketing applications [9]. This regulatory recognition further validates RWD's utility in developing clinically relevant prediction models.
Experimental Protocols and Methodologies
Clinical Trial Data Collection Protocol
A standardized protocol for collecting clinical trial data for outcome prediction modeling includes these critical components:
- Protocol Development: Comprehensive study protocol specifying objectives, endpoints, sample size justification, randomization procedures, and statistical analysis plan [11].
- Site Selection and Training: Choosing qualified investigative sites with appropriate expertise and ensuring all personnel receive standardized training on the protocol and data collection procedures [12] [11].
- Data Collection Procedures: Implementing uniform data collection methods across all sites, including electronic data capture systems with built-in edit checks [12].
- Quality Control Measures: Establishing ongoing monitoring procedures, including source data verification, query resolution processes, and regular quality control audits [12].
- Endpoint Adjudication: Implementing blinded independent committee review for subjective endpoints to minimize assessment bias.
Table 2: Essential Research Reagents and Solutions for Clinical Data Research
| Research Tool | Function in Data Research |
|---|---|
| Electronic Data Capture (EDC) Systems | Standardized data collection across sites with audit trails |
| Clinical Trial Management Systems (CTMS) | Centralized management of trial operations and documentation |
| ALCOA+ Principles Framework | Ensures data integrity throughout collection process |
| Statistical Analysis Plans (SAP) | Pre-specified analytical approaches to minimize bias |
| Sample Size Calculation Tools | Determines adequate power for detecting predicted effects |
| Randomization Systems | Unbiased treatment allocation sequences |
Real-World Data Curation Protocol
Transforming raw real-world data into analyzable evidence requires a rigorous curation process:
- Data Source Evaluation: Assessing the suitability of RWD sources for the research question based on completeness, accuracy, and representativeness [9].
- Data Extraction and Harmonization: Extracting relevant variables from source systems and mapping to common data models to enable pooling and analysis [10].
- Quality Assessment and Validation: Implementing quality checks for data plausibility, completeness, and consistency across sources [13].
- Bias Assessment and Mitigation: Identifying potential selection, measurement, and confounding biases, then applying appropriate statistical adjustments [13].
- Privacy Protection: Implementing data anonymization or de-identification techniques while preserving data utility for analysis [13].
Figure 1: RWD Curation to Evidence Pipeline
Integrated Approaches and Future Directions
Hybrid Designs: Leveraging Both Worlds
Innovative trial designs that integrate clinical trial and RWD methodologies are emerging as powerful approaches for therapeutic response prediction. These include:
- Pragmatic Clinical Trials: Maintain randomization while implementing more inclusive eligibility criteria and flexible interventions to better reflect real-world practice [16].
- External Control Arms: Use carefully curated RWD to create historical controls when randomization to standard-of-care is impractical or unethical [9].
- Registry-Based Randomized Trials: Embed randomization within clinical registries to combine trial rigor with efficient long-term follow-up through RWD [9].
Artificial Intelligence and Advanced Analytics
AI and machine learning techniques are increasingly bridging the gap between clinical trial and real-world data by:
- Enhancing RWD Quality: Using natural language processing to extract structured information from unstructured clinical notes [13].
- Identifying Digital Phenotypes: Discovering novel patient subgroups and their differential treatment responses using unsupervised learning on multimodal RWD [15].
- Improving Generalizability: Testing prediction models developed in clinical trials against RWD to assess real-world performance and identify potential drift [14].
Figure 2: Data Integration for Prediction Modeling
The critical role of data sourcing in outcome prediction modeling for therapeutic response necessitates a purpose-driven approach rather than a universal preference for either clinical trials or real-world data. Clinical trial data provides the methodological foundation for establishing causal relationships and initial predictive signatures under controlled conditions. Meanwhile, real-world data offers the contextual validation needed to ensure these models perform effectively across diverse clinical settings and patient populations.
For researchers and drug development professionals, the most robust approach involves strategic integration of both data types throughout the therapeutic development lifecycle. This includes using clinical trial data for initial model development, followed by validation and refinement using carefully curated real-world data. As regulatory frameworks continue to evolve, with agencies like the FDA providing clearer pathways for RWD/RWE incorporation, this integrated approach will become increasingly essential for developing prediction models that are both scientifically valid and clinically actionable [9].
The future of outcome prediction modeling lies not in choosing between these data sources, but in developing sophisticated methodologies that leverage their complementary strengths while acknowledging and mitigating their respective limitations. This balanced approach will ultimately accelerate the development of more personalized and effective therapeutic interventions.
Predicting a patient's response to therapy remains a central challenge in modern precision medicine. While traditional models have relied on clinical variables alone, a growing consensus indicates that a holistic approach, integrating molecular-level omics data with clinical and demographic information, is needed to unveil the mechanisms underlying disease etiology and improve prognostic accuracy [17] [18]. This integrated approach leverages the fact that biological information flows through multiple regulatory layers—from genetic predisposition (genomics) to gene expression (transcriptomics), protein expression (proteomics), and metabolic function (metabolomics). Each layer provides a unique and complementary perspective on the patient's health status and disease pathophysiology [19] [20]. The integration of these diverse data types creates a more comprehensive model of the individual, which can lead to refined prognostic assessment, better patient stratification, and more informed treatment selection [17] [18]. This guide provides an objective comparison of the data types, computational methods, and their performance in therapy response prediction.
Data Landscape: Variables and Their Predictive Value
The predictive models discussed in this guide are built upon three primary categories of data, each contributing unique information.
Clinical and Demographic Variables
Clinical and demographic information often serves as the foundational layer for prognostic models. These variables typically include:
- Patient Phenotype: Age, sex, and body mass index.
- Disease Characteristics: Tumor stage, grade, and histology in oncology; symptom severity and functioning in mental health care.
- Treatment History: Prior therapies and treatment sequences. Clinical variables alone have demonstrated varying prognostic power across cancer types, with concordance indices (C-index) ranging from 0.572 to 0.819 in a pan-cancer analysis [18].
Omics Data Types and Repositories
Omics data provides a deep molecular characterization of the patient's disease state. Key data types and their sources include:
Table 1: Multi-Omics Data Types and Repositories
| Omics Data Type | Biological Information | Key Repositories |
|---|---|---|
| Genomics | DNA sequence and variation (germline and somatic) | TCGA, ICGC, CCLE [19] |
| Transcriptomics | RNA expression levels (coding and non-coding) | TCGA, TARGET, METABRIC [19] |
| Proteomics | Protein abundance and post-translational modifications | CPTAC [19] |
| Metabolomics | Small-molecule metabolite concentrations | Metabolomics workbench, OmicsDI [19] |
| Epigenomics | DNA methylation and chromatin modifications | TCGA [19] |
Among these, mRNA and miRNA expression profiles frequently demonstrate the strongest prognostic performance, followed by DNA methylation. Germline susceptibility variants (polygenic risk scores) consistently show lower prognostic power across cancer types [18].
Integrated Data Workflow
The process of integrating these disparate data types requires a structured framework to ensure interoperability and reproducibility. The following diagram illustrates a generalized workflow for multi-modal data integration.
Performance Comparison: Integrated Models vs. Single Data Type Models
Numerous studies have benchmarked the performance of integrative models against those using single data types. The following table summarizes key findings from comparative analyses.
Table 2: Performance Comparison of Integrative vs. Non-Integrative Models
| Study / Context | Integration Method | Comparison Baseline | Performance Metric | Result |
|---|---|---|---|---|
| Pan-Cancer Analysis [18] | Multi-omic kernel machine | Clinical variables alone | Concordance Index (C-index) | Integration improved prognosis over clinical-only in 50% of cancers (e.g., C-index for clinical: 0.572-0.819 vs. mRNA: 0.555-0.847) |
| Supervised Classification Benchmark [17] | DIABLO, SIDA, PIMKL, netDx, Stacking, Block Forest | Random Forest on single or concatenated data | Classification Accuracy | Integrative approaches performed better or equally well than non-integrative counterparts |
| Mental Health Care Prediction [21] | LASSO regression on routine care data | - | Area Under Curve (AUC) | AUC ranged from 0.77 to 0.80 in internal and external validation across 3 sites |
| Emotional Disorders Meta-Analysis [3] | Various Machine Learning models | - | Average Accuracy / AUC | ML models showed mean accuracy of 0.76 and mean AUC of 0.80 for predicting therapy response |
| Radiotherapy Response Prediction [22] | Multi-scale Dilated Ensemble Network (MDEN) | RNN, LSTM, 1D-CNN | Prediction Accuracy | Proposed MDEN framework outperformed individual deep learning models |
A critical finding from these comparisons is that the integration of multi-omics data with clinical variables can lead to substantially improved prognostic performance over the use of clinical variables alone in half of the cancer types examined [18]. Furthermore, integrative supervised methods consistently perform better or at least equally well as their non-integrative counterparts [17].
Experimental Protocols for Data Integration
To ensure reproducibility, this section outlines detailed methodologies for key integration experiments cited in this guide.
Protocol 1: Kernel Machine Learning for Pan-Cancer Prognosis
This protocol is derived from a study that integrated clinical and multi-omics data for prognostic assessment across 14 cancer types [18].
1. Data Acquisition and Preprocessing:
- Data Source: Download multi-omics data (somatic mutations, copy number, DNA methylation, mRNA/miRNA expression, RPPA) and clinical data from TCGA portal.
- Quality Control: Remove features with excessive missing values. Impute remaining missing values using appropriate methods (e.g., k-nearest neighbors).
- Data Normalization: Normalize each omics dataset to make features comparable (e.g., convert read counts to counts per million for RNA-Seq, use beta values for methylation).
2. Similarity Matrix Construction:
- For each omics data type and each patient pair, compute a linear kernel (similarity score).
- For a given omics profile
X(withpbiomarkers), the similarity between patientsiandjis calculated asK(i,j) = Σ (x_ik * x_jk) / pfork=1 to p. - This results in an
N x Nomic similarity matrix for each data type, whereNis the sample size.
3. Model Training and Validation:
- Outcome: Overall survival (time-to-event data).
- Integration: Use a kernel-based Cox proportional hazards model. The hazard for a patient is modeled based on the similarity of their omics profiles to all other patients.
- Clinical Variable Adjustment: Include clinical variables (e.g., age, sex, stage) as traditional covariates in the model.
- Validation: Perform cross-validation (e.g., 5-fold) and evaluate prognostic performance using the concordance index (C-index).
Protocol 2: Supervised Integrative Analysis with DIABLO
This protocol details the use of DIABLO (Data Integration Analysis for Biomarker discovery using Latent cOmponents) for classification problems, as featured in a benchmark study [17].
1. Experimental Setup:
- Input Data: Collect multiple matched omics datasets (
X1, X2, ..., Xm) from the sameNsamples and a categorical outcome vectorY(e.g., treatment responder vs. non-responder). - Design Matrix: Define a
m x mdesign matrix specifying whether omics views are connected (usually 1 for connected, 0 for not).
2. Model Training:
- Objective: DIABLO seeks
Hlinear combinations (components) of variables per view that are highly correlated across connected views and discriminatory for the outcome. - Optimization: It solves a sparse generalized canonical correlation analysis (sGCCA) problem for each component
h:maximize { Σ a_{ij} cov(X_i w_i^{(h)}, X_j w_j^{(h)}) }subject to penalties onw_i^{(h)}for variable selection. - Parameter Tuning: Use cross-validation to determine the number of components and the number of variables to select per view and per component to minimize prediction error.
3. Prediction and Evaluation:
- Classification: Project new samples into the latent space and classify them based on a weighted majority vote across views.
- Evaluation Metrics: Calculate classification accuracy, sensitivity, specificity, and area under the ROC curve (AUC) on a held-out test set.
Protocol 3: Cross-Site Validation in Mental Health Care
This protocol is based on a multisite study predicting undesired treatment outcomes in mental health care using routine outcome monitoring (ROM) data [21].
1. Data Standardization:
- Predictors: Extract a common set of variables from routine care data across all sites, including demographics (age, sex), diagnosis, baseline symptom severity (OQ-45.2 score), and early treatment response patterns.
- Outcome Definition: Define the undesired outcome (e.g., non-improvement) as improving less than a medium effect size on the Symptom Distress subscale between start and end of treatment.
2. Model Development:
- Algorithm: Apply Least Absolute Shrinkage and Selection Operator (LASSO) regression for model fitting and variable selection.
- Internal Validation: For each site, perform internal validation using cross-validation (e.g., 10-fold) within the site's own data.
3. External Validation:
- Process: Train a model on the complete dataset from one site (Site A) and then evaluate its performance on the untouched datasets from the other sites (Site B and C).
- Performance Reporting: Report the performance metrics (AUC, accuracy) for both internal and external validations to assess model robustness and generalizability.
Methodological Landscape: Choosing an Integration Strategy
The choice of integration methodology is critical and depends on the biological question, data structure, and desired outcome. The approaches can be broadly categorized as shown below.
Successfully implementing a multi-omics integration project requires a suite of computational tools, data resources, and analytical packages.
Table 3: Essential Research Reagent Solutions for Multi-Omics Integration
| Tool / Resource | Type | Primary Function | Key Features / Applications |
|---|---|---|---|
| TCGA / ICGC Portals [19] | Data Repository | Provides comprehensive, curated multi-omics and clinical data for various cancers. | Foundational data source for training and validating predictive models in oncology. |
| mixOmics (DIABLO) [17] | R Package | Performs supervised integrative analysis for classification and biomarker selection. | Uses sparse generalized CCA to identify correlated components across omics views that discriminate sample groups. |
| xMWAS [20] | R-based Tool | Performs association analysis and creates integrative networks across multiple omics datasets. | Uses PLS-based correlation to identify relationships between features from different omics types and visualizes them as networks. |
| WGCNA [20] | R Package | Identifies clusters (modules) of highly correlated genes/features from omics data. | Used to find co-expression networks; modules can be linked to clinical traits or used for integration with other omics. |
| LORIS & CBRAIN [23] | Data Management & HPC Platform | Manages, processes, and analyzes multi-modal data (imaging, omics, clinical) within a unified framework. | Automates workflows, ensures provenance tracking, and facilitates reproducible analysis across HPC environments. |
| SuperLearner / Stacking [17] | R Package | Implements ensemble learning (late integration) by combining predictions from multiple base learners. | Flexible framework for integrating predictions from omics-specific models into a final, robust prediction. |
| netDx [17] | R Package | Builds patient similarity networks using different omics data types for classification. | Uses prior biological knowledge (e.g., pathways) to define features and integrates them via patient similarity networks. |
Ethical Considerations and Bias Assessment in Model Foundations
The integration of advanced AI and foundational models into patient response to therapy research represents a paradigm shift in predictive healthcare. These large-scale artificial intelligence systems, trained on extensive multimodal and multi-center datasets, demonstrate remarkable versatility in predicting disease progression, treatment efficacy, and adverse events [24]. However, their clinical integration presents complex ethical challenges that extend far beyond technical performance metrics, particularly concerning patient data privacy, algorithmic bias, and model transparency [24]. The stakes are exceptionally high in medical applications, where model failures can directly impact patient outcomes and perpetuate healthcare disparities.
Current research reveals significant gaps in existing predictive frameworks. A recent systematic review of predictive models for metastatic prostate cancer found that most identified models require additional evaluation and validation in properly designed studies before implementation in clinical practice, with only one study among 15 having a low risk of bias and low concern regarding applicability [25]. This underscores the urgent need for rigorous ethical frameworks and bias assessment methodologies in medical AI systems. As foundational models become more prevalent in healthcare, establishing comprehensive guidelines for their ethical development and deployment is paramount to ensuring they enhance clinical decision-making without compromising ethical integrity or patient safety [24].
Comparative Analysis of Model Performance in Therapeutic Prediction
Quantitative Performance Metrics
The evaluation of predictive models for therapeutic response requires a multi-dimensional assessment approach. The table below summarizes key performance indicators across different model architectures as reported in recent literature:
Table 1: Performance comparison of AI models in medical prediction tasks
| Model Architecture | Clinical Application | Key Performance Metrics | Reported Performance | Limitations |
|---|---|---|---|---|
| Multi-scale Dilated Ensemble Network (MDEN) [22] | Patient response prediction during radiotherapy | Accuracy, Error Rate | 0.79-2.98% improvement over RNN, LSTM, 1DCNN | Requires extensive computational resources |
| Traditional Prognostic Models [25] | Metastatic prostate cancer treatment response | Risk of Bias, Applicability | Only 1 of 15 studies had low risk of bias | High risk of bias in many studies |
| Convolutional Neural Networks (CNN) [22] | Forecasting patient response to chemotherapy | Predictive Capacity | Widely used but limited by data scarcity | Requires large annotated datasets |
| Extreme Gradient Boosting (XGBoost) [22] | Radiation-induced fibrosis prediction | Model Generalizability | Effective for learning complex relationships | Demands exceptionally large data volumes |
| Neural Network Ensemble [22] | Radiation-induced lung damage prediction | ROC curves, Bootstrap Validation | Superior to Random Forests and Logistic Regression | Limited multi-institutional validation |
Bias Assessment Across Model Types
The evaluation of bias in predictive healthcare models requires careful consideration of multiple dimensions. The following table synthesizes bias assessment findings from recent research:
Table 2: Bias assessment in therapeutic prediction models
| Bias Category | Impact on Model Performance | Assessment Methodology | Mitigation Strategies |
|---|---|---|---|
| Data Collection Bias [24] | Perpetuates healthcare disparities across demographic groups | Historical data disparity analysis | Systematic bias detection and mitigation strategies |
| Annotation Bias [22] | Limits predictive accuracy and generalizability | Inter-annotator disagreement measurement | Multi-center, diverse annotator pools |
| Representation Bias [24] | Compromises diagnostic accuracy for underrepresented populations | Demographic parity metrics | Federated learning across diverse populations |
| Measurement Bias [25] | Impacts clinical applicability and real-world performance | PROBAST criteria for risk of bias | Robust validation in clinical settings |
| Algorithmic Bias [24] | Leads to discriminatory outcomes in treatment recommendations | Fairness-aware training procedures | Bias auditing and regulatory compliance strategies |
Experimental Protocols for Ethical Model Assessment
Comprehensive Bias Detection Framework
The systematic assessment of bias in foundational models for therapeutic prediction requires rigorous experimental protocols. A robust methodology should incorporate multiple complementary approaches:
Data Provenance and Characterization: The initial phase involves comprehensive audit trails for training data sources, with detailed documentation of demographic distributions, clinical settings, and data collection methodologies. This includes analyzing patient intrinsic factors such as lifestyle, sex, age, and genetics that significantly influence therapeutic outcomes [22]. Studies must explicitly report inclusion and exclusion criteria, with particular attention to underrepresented populations in medical datasets.
Multi-dimensional Bias Metrics: Implementation of quantitative bias metrics should span group fairness, individual fairness, and counterfactual fairness measures. Techniques include disparate impact analysis across racial, ethnic, gender, and socioeconomic groups, with statistical tests for significant performance variations across patient subgroups [24]. For metastatic prostate cancer models, this involves assessing whether prediction accuracy remains consistent across different disease stages, treatment histories, and comorbidity profiles [25].
Cross-institutional Validation: Given the sensitivity of medical models to data heterogeneity, rigorous external validation is essential. This involves testing model performance across multiple healthcare facilities with varying imaging devices, treatment protocols, and patient populations [24]. The PROBAST tool provides a structured approach for assessing risk of bias and applicability concerns in predictive model studies [25].
Performance Benchmarking Methodology
Standardized evaluation protocols are critical for meaningful comparison across therapeutic prediction models:
Stratified Performance Assessment: Models should be evaluated using stratified k-fold cross-validation with stratification across key demographic and clinical variables. This ensures representative sampling of patient subgroups and reliable performance estimation [22]. For radiotherapy response prediction, this includes stratification by cancer stage, treatment regimen, and prior therapy exposure.
Composite Metric Reporting: Beyond traditional accuracy metrics, comprehensive evaluation should include clinical utility measures such as calibration metrics, decision curve analysis, and clinical impact plots [25]. These assess how model predictions influence therapeutic decision-making and patient outcomes, providing a more complete picture of real-world applicability.
Robustness Testing: Models must undergo rigorous robustness evaluation against distribution shifts, adversarial examples, and data quality variations [24]. This is particularly crucial in medical contexts where model failures can have severe consequences. Techniques include stress testing with corrupted inputs, evaluating performance degradation with missing data, and assessing resilience to domain shifts between institutions.
Visualization of Ethical Assessment Workflows
Comprehensive Bias Assessment Framework
Model Performance and Ethics Evaluation Workflow
Patient Response Prediction Pipeline
Essential Research Reagent Solutions
Table 3: Key research reagents and computational tools for ethical model development
| Research Reagent/Tool | Primary Function | Application in Therapeutic Prediction |
|---|---|---|
| PROBAST Tool [25] | Risk of bias assessment | Systematic evaluation of prediction model study quality |
| REE-COA Algorithm [22] | Feature selection and optimization | Enhances prediction performance by optimizing feature weights |
| Multi-scale Dilated Ensemble Network [22] | Patient response prediction | Integrates LSTM, RNN, and 1DCNN for improved accuracy |
| Federated Learning Framework [24] | Privacy-preserving model training | Enables multi-institutional collaboration without data sharing |
| Homomorphic Encryption [24] | Data privacy protection | Secures patient confidentiality during model training |
| Explainable AI Modules [24] | Model interpretability | Provides insights into model decisions for clinical trust |
| Bias Detection Toolkit [24] | Algorithmic fairness assessment | Identifies discriminatory patterns across patient demographics |
| CHARMS Checklist [25] | Data extraction standardization | Ensures consistent methodology in systematic reviews |
Discussion and Future Directions
The integration of comprehensive ethical frameworks into foundational models for therapeutic prediction represents both a moral imperative and a technical challenge. Current evidence suggests that without systematic bias assessment and mitigation strategies, AI models risk perpetuating and amplifying existing healthcare disparities [24]. The recent finding that only one of 15 predictive models for metastatic prostate cancer had a low risk of bias underscores the pervasive nature of this problem [25]. Furthermore, the heterogeneous nature of medical imaging data, with variations across imaging devices and institutional protocols, creates substantial challenges for developing unified models that can process and interpret diverse inputs effectively [24].
Future research must prioritize the development of standardized evaluation frameworks that simultaneously assess predictive performance and ethical implications. This includes advancing privacy-preserving technologies such as federated learning and homomorphic encryption to enable collaborative model development without compromising patient confidentiality [24]. Additionally, the implementation of explainable AI mechanisms is crucial for fostering clinician trust and facilitating regulatory compliance. As foundational models continue to evolve in medical imaging, maintaining alignment with core ethical principles while harnessing their transformative potential will require ongoing collaboration between AI researchers, clinical specialists, ethicists, and patients [24]. The establishment of clear guidelines for development and deployment, coupled with robust validation protocols, will be essential for realizing the promise of AI in personalized therapy while preserving the fundamental principles of medical ethics and patient-centered care.
Advanced Algorithms and Implementation in Clinical Workflows
The accurate prediction of patient response to therapy is a cornerstone of modern precision medicine, enabling more effective treatment personalization and resource allocation. The selection of an appropriate modeling approach is a critical step that researchers and drug development professionals must undertake, balancing model complexity, interpretability, and predictive performance. The modeling landscape spans traditional regression techniques, various machine learning algorithms, and advanced deep learning architectures, each with distinct strengths, limitations, and optimal application domains.
This guide provides an objective comparison of these approaches within the specific context of outcome prediction modeling for patient response to therapy research. We synthesize performance metrics across multiple therapeutic domains and present detailed experimental methodologies to inform model selection decisions. The comparative analysis focuses on practical implementation considerations, data requirements, and validation frameworks relevant to researchers working across the drug development pipeline—from early discovery to clinical application.
Comparative Performance of Modeling Approaches
Quantitative Performance Metrics Across Domains
Extensive research has evaluated the performance of different modeling approaches across various therapeutic domains. The table below synthesizes key performance indicators from multiple studies to enable direct comparison.
Table 1: Performance comparison of modeling approaches for therapeutic outcome prediction
| Modeling Approach | Application Domain | Accuracy (%) | AUC | Sensitivity | Specificity | Key Advantages | Citation |
|---|---|---|---|---|---|---|---|
| Cox Regression | SARS-CoV-2 mortality | 83.8 | 0.869 | - | - | Interpretable, established statistical properties | [26] |
| Artificial Neural Network (ANN) | SARS-CoV-2 mortality | 90.0 | 0.926 | - | - | Handles complex nonlinear relationships | [26] |
| Machine Learning (Multiple Algorithms) | Emotional disorders treatment response | 76.0 | 0.80 | 0.73 | 0.75 | Good balance of performance and interpretability | [3] [27] |
| Deep Learning (Sequential Models) | Heart failure preventable utilization | - | 0.727-0.778 | - | - | Superior for temporal pattern recognition | [28] |
| Logistic Regression | Heart failure preventable utilization | - | 0.681 | - | - | Computational efficiency, interpretability | [28] |
| Neural Networks (TensorFlow, nnet, monmlp) | Depression treatment remission | - | 0.64-0.65 | - | - | Moderate accuracy for psychological outcomes | [29] |
| Generalized Linear Regression | Depression treatment remission | - | 0.63 | - | - | Similar performance to complex models for this application | [29] |
| Multi-scale Dilated Ensemble Network | Radiotherapy patient response | - | - | - | - | Error minimization through ensemble approach | [22] |
Performance Analysis and Interpretation
The comparative data reveals several important patterns. First, deep learning approaches generally achieve superior performance for complex prediction tasks with large datasets and nonlinear relationships. The significant advantage of ANN over Cox regression for SARS-CoV-2 mortality prediction (90.0% vs. 83.8% accuracy, p=0.0136) demonstrates this capacity in clinical outcome prediction [26]. Similarly, for heart failure outcomes, deep learning models achieved precision rates of 43% at the 1% threshold for preventable hospitalizations compared to 30% for enhanced logistic regression [28].
However, this performance advantage is not universal. For depression treatment outcomes, neural networks provided only marginal improvement over generalized linear regression (AUC 0.64-0.65 vs. 0.63) [29], suggesting that simpler approaches may be adequate for certain psychological outcome predictions. The machine learning approaches for emotional disorders treatment response prediction show consistently good performance (76% accuracy, 0.80 AUC) [3] [27], positioning them as a balanced option between traditional regression and deep learning.
Experimental Protocols and Methodologies
Model Development Workflows
The predictive performance of different modeling approaches is heavily influenced by methodological choices during development. The following diagram illustrates a generalized experimental workflow for developing and comparing predictive models of treatment response.
Diagram 1: Model development workflow for 76px
Detailed Methodological Protocols
Traditional Regression Approaches
Cox regression and logistic regression models typically follow a structured development process. In the SARS-CoV-2 mortality prediction study, researchers used a parsimonious model-building approach with clinically relevant demographic, comorbidity, and symptomatology features [26]. The protocol included:
- Feature Selection: Predictors were chosen based on previously published literature and included age, sex, comorbidities, symptoms, and days of symptoms prior to admission.
- Data Splitting: The dataset was randomly split into training (80%) and test (20%) sets.
- Model Building: All predictors were initially included irrespective of univariable significance, with subsequent backward elimination of non-significant predictors.
- Validation: k-fold cross-validation was used on the training set with model selection based on the lowest Akaike information criterion (AIC) score and highest concordance index (c-index).
- Performance Assessment: Models were evaluated using accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and calibration metrics (Brier score) [26].
Deep Learning Approaches
Deep learning implementations require more specialized preprocessing and training protocols. In the SARS-CoV-2 study comparing ANN to Cox regression, the methodology included:
- Data Preprocessing: Feature-wise normalization was implemented, with each feature centered around zero by subtracting the mean and dividing by its standard deviation [26].
- Architecture Optimization: Hyperparameters (number and size of layers, batch size, dropout, regularization) were adjusted using k-fold cross-validation on the training set.
- Implementation: The TensorFlow machine learning library was used to construct the ANN [26].
- Validation Framework: The dataset was randomly split into training (80%) and test (20%) sets, with performance metrics calculated similarly to the Cox model for direct comparison.
For more complex deep learning applications such as predicting preventable utilization in heart failure patients, sequential models (LSTM, CNN with attention mechanisms) utilized temporal patient-level vectors containing 36 consecutive monthly vectors summing medical codes for each month [28]. This approach captured dynamic changes in patient status over time, which traditional models typically cannot leverage effectively.
Machine Learning Protocols for Emotional Disorders
The meta-analysis of machine learning for emotional disorder treatment response prediction revealed important methodological considerations [3] [27]:
- Data Requirements: Studies using more robust cross-validation procedures exhibited higher prediction accuracy.
- Predictor Selection: Neuroimaging data as predictors were associated with higher accuracy compared to clinical and demographic data alone.
- Outcome Balancing: Studies with larger responder rates and those that did not correct for imbalances in outcome rates were associated with higher prediction accuracy, though this may reflect methodological artifacts rather than true performance advantages.
Technical Implementation and Architecture
Deep Learning Architectures for Therapeutic Response Prediction
Advanced deep learning approaches employ sophisticated architectures tailored to specific data structures and prediction tasks. The following diagram illustrates architectural components of deep learning models used in therapeutic response prediction.
Diagram 2: Deep learning model architectures for 76px
Implementation Considerations
Data Requirements and Feature Engineering
The performance of different modeling approaches is heavily dependent on data quality and feature engineering:
- Traditional Models: Work effectively with structured clinical data (demographics, comorbidities, lab values) and require careful handling of confounding variables. Feature selection is often knowledge-driven based on clinical expertise [26] [28].
- Machine Learning: Can incorporate both knowledge-driven features and data-driven representations. Random forest models have demonstrated effectiveness with molecular fingerprints for drug response prediction [30].
- Deep Learning: Most effective with large sample sizes and can utilize raw data representations with minimal preprocessing. Sequential deep learning models excel with temporal data representations [28]. For drug permeation prediction, ANN models have shown RMSE values of 14.0, outperforming some traditional approaches [31].
Computational Requirements
Computational demands vary significantly across approaches:
- Traditional Regression: Can be implemented on standard computing resources with statistical software packages.
- Machine Learning: Requires moderate computational resources, with tree-based methods (random forests, gradient boosting) being more computationally intensive than linear models.
- Deep Learning: Often requires specialized hardware (GPUs) for efficient training, particularly for complex architectures like LSTM networks and ensemble approaches [22]. Training deep learning models for pharmaceutical applications has been successfully implemented using Tesla K20c GPU accelerators [32].
Research Reagent Solutions and Essential Materials
Successful implementation of predictive models requires appropriate computational tools and data resources. The table below details key solutions used across the cited studies.
Table 2: Essential research reagents and computational tools for predictive modeling
| Tool/Resource | Type | Primary Function | Example Applications | Citation |
|---|---|---|---|---|
| TensorFlow | Deep Learning Library | Neural network development and training | ANN for SARS-CoV-2 mortality prediction | [26] |
| Scikit-learn | Machine Learning Library | Traditional ML algorithms implementation | Drug permeation prediction | [31] |
| Python | Programming Language | Data preprocessing, model development, analysis | Heart failure utilization prediction | [28] |
| RDKit | Cheminformatics Library | Molecular fingerprint calculation | Drug discovery and ADME/Tox prediction | [32] |
| Electronic Health Records | Data Source | Clinical features and outcome labels | SARS-CoV-2 mortality, heart failure outcomes | [26] [28] |
| Patient-Derived Cell Cultures | Experimental System | Functional drug response profiling | Drug response prediction in precision oncology | [30] |
| FCFP6 Fingerprints | Molecular Descriptors | Compound structure representation | Drug discovery datasets, ADME/Tox properties | [32] |
The selection of modeling approaches for predicting patient response to therapy requires careful consideration of multiple factors, including dataset characteristics, performance requirements, and interpretability needs.
Based on the comparative evidence:
- Traditional regression models remain valuable for smaller datasets, when model interpretability is paramount, or when established clinical relationships exist. They provide a strong baseline against which to compare more complex approaches.
- Machine learning algorithms offer a balanced approach for medium-complexity problems, providing improved performance over traditional models while maintaining some interpretability. They are particularly effective when combining clinical and molecular data.
- Deep learning architectures deliver superior performance for complex problems with large datasets, particularly when dealing with temporal patterns, image data, or highly nonlinear relationships. However, they require substantial data and computational resources, and model interpretability remains challenging.
The optimal approach varies by application domain, with deep learning showing particular promise for mortality prediction and healthcare utilization forecasting, while traditional methods remain competitive for certain psychological treatment outcomes. Researchers should implement rigorous validation frameworks, including appropriate data partitioning and performance metrics relevant to the specific clinical context, when comparing modeling approaches for therapeutic response prediction.
Leveraging Ensemble and Multi-Scale Network Architectures for Enhanced Accuracy
In the pursuit of precision medicine, accurately predicting a patient's response to therapy is paramount for optimizing treatment outcomes and minimizing adverse effects. Traditional single-model approaches in machine learning often fall short in capturing the complex, multi-factorial nature of disease progression and therapeutic efficacy. Ensemble and multi-scale network architectures have emerged as powerful computational frameworks that address these limitations by integrating diverse data perspectives and model outputs. This guide provides a comparative analysis of these advanced architectures, detailing their methodologies, performance, and practical implementation for researchers and drug development professionals focused on outcome prediction modeling.
Comparative Performance Analysis of Ensemble and Multi-Scale Architectures
The table below summarizes the performance of various ensemble and multi-scale architectures as reported in recent scientific studies, providing a clear comparison of their capabilities in different therapeutic prediction contexts.
Table 1: Performance Comparison of Ensemble and Multi-Scale Architectures in Therapeutic Response Prediction
| Architecture Name | Application Context | Key Components | Reported Performance | Reference |
|---|---|---|---|---|
| Uncertainty-Driven Multi-Scale Ensemble | Pulmonary Pathology & Parkinson's Diagnosis | Bayesian Deep Learning, Multi-scale architectures, Two-level decision tree | Accuracy: 98.19% (pathology), 95.31% (Parkinson's) | [33] |
| Multi-scale Dilated Ensemble Network (MDEN) | Patient Response to Radiotherapy/Chemotherapy | LSTM, RNN, 1D-CNN, REE-COA optimization | Superior accuracy vs. RNN, LSTM, 1D-CNN | [22] |
| Multi-Model CNN Ensemble | COVID-19 Detection from Chest X-rays | Ensemble of VGGNet, GoogleNet, DenseNet, NASNet | Accuracy: 88.98% (3-class), 98.58% (binary) | [34] |
| Multi-Modal CNN for DDI (MCNN-DDI) | Drug-Drug Interaction Event Prediction | 1D CNN sub-models for drug features (target, enzyme, pathway, substructure) | Accuracy: 90.00%, AUPR: 94.78% | [35] |
| Multi-Scale Deep Learning Ensemble | Endometriotic Lesion Segmentation in Ultrasound | U-Net variants trained on multiple image resolutions | Dice Coefficient: 82% | [36] |
| Patient Knowledge Graph Framework (PKGNN) | Mortality & Hospital Readmission Prediction | GCN, Clinical BERT, BioBERT, BlueBERT on EHR data | Outperformed state-of-the-art baselines | [37] |
Detailed Experimental Protocols and Methodologies
Uncertainty-Driven Ensembles for Medical Image Classification
This approach employs a Bayesian Deep Learning framework to quantify uncertainty in classification decisions, using this metric to weight the contributions of different models within an ensemble.
- Architecture: The system integrates multiple deep learning architectures processing image data at various scales. The Bayesian nature of each classifier provides a principled measure of predictive uncertainty [33].
- Training: Individual networks are trained on medical image data (e.g., chest X-rays for pneumonia, neuroimages for Parkinson's). A two-level decision tree strategy is used for multi-class problems, such as dividing a 3-class classification (control vs. bacterial pneumonia vs. viral pneumonia) into two binary classifications [33].
- Inference & Fusion: During prediction, the uncertainty estimate of each classifier's decision is calculated. The final ensemble output is a weighted combination of all members' predictions, where the contribution of each model is inversely proportional to its uncertainty [33].
Multi-scale Dilated Ensemble Network for Radiotherapy Response
This framework predicts the likelihood of patients experiencing adverse long-term effects from radiotherapy and chemotherapy.
- Feature Selection: The Repeated Exploration and Exploitation-based Coati Optimization Algorithm (REE-COA) is employed to select the most predictive features from the collected patient data. This optimization aims to increase the correlation coefficient and minimize variance within the same classes [22].
- Ensemble Prediction: The selected weighted features are fed into the Multi-scale Dilated Ensemble Network (MDEN). This network integrates Long-Short Term Memory (LSTM), Recurrent Neural Network (RNN), and One-dimensional Convolutional Neural Networks (1D-CNN) to capture temporal and feature-level patterns [22].
- Output: The final prediction scores from LSTM, RNN, and 1D-CNN are averaged to produce a robust prediction of patient response, minimizing error rates and enhancing accuracy [22].
Multi-Modal CNN for Drug-Drug Interaction Prediction
The MCNN-DDI model predicts multiple types of interactions between drug pairs by integrating different data modalities.
- Input Representation: Four key drug features are used: chemical structure (SMILES), target proteins, involved enzymes, and biological pathways. Similarity matrices (e.g., Jaccard similarity) are computed for each feature type to represent drug pairs [35].
- Model Structure: Four separate 1D CNN sub-models are constructed, each dedicated to processing one type of similarity matrix. Each sub-model typically consists of an input layer with 5 kernels of filter size 1, followed by three dense layers with 1024, 512, and 256 neurons respectively [35].
- Fusion and Output: The representations learned by the four sub-models are concatenated. This fused representation is then used for the final prediction over 65 different DDI-associated events via an output layer of 65 neurons [35].
Conceptual Framework and Signaling Pathways
The following diagram illustrates the core logical workflow of an uncertainty-driven ensemble system, a representative architecture in this field.
Uncertainty-Driven Ensemble Workflow
The diagram below outlines the multi-modal data integration process for predicting complex biological outcomes like Drug-Drug Interactions.
Multi-Modal Data Integration for DDI Prediction
For researchers aiming to implement ensemble and multi-scale networks for therapeutic outcome prediction, the following computational tools and data resources are essential.
Table 2: Key Research Reagent Solutions for Ensemble Model Development
| Resource Name | Type | Primary Function | Relevance to Ensemble Models |
|---|---|---|---|
| Pre-trained CNN Models (VGGNet, GoogleNet, DenseNet, ResNet50, NASNet) | Software Model | Feature extraction and base classifier | Building blocks for creating robust model ensembles [34] [38] |
| BioBERT / Clinical BERT | NLP Model | Processing clinical text from EHRs and medical notes | Extracting semantic representations from unstructured data for patient graphs [37] |
| DrugBank / ChEMBL / BindingDB | Chemical & Bioactivity Database | Source of drug features (target, pathway, enzyme, structure) | Constructing multi-modal input features for DDI and drug response prediction [39] [35] |
| Graph Convolutional Network (GCN) | Software Library | Learning from graph-structured data (e.g., patient knowledge graphs) | Modeling complex relationships between patients, diagnoses, and treatments [37] |
| MIMIC-IV Dataset | Clinical Dataset | Large-scale EHR data from ICU patients | Benchmarking mortality and readmission prediction models [37] |
Feature Selection and Optimization Strategies for High-Dimensional Data
In the field of patient response to therapy research, high-dimensional data has become increasingly prevalent, particularly with the rise of genomic data, medical imaging, and electronic health records (EHRs). These datasets often contain thousands to tens of thousands of features, while sample sizes remain relatively small, creating significant analytical challenges. High-dimensional data typically exhibits characteristics such as high dimensionality, significant redundancy, and considerable noise, which traditional computational intelligence methods struggle to process effectively [40]. Feature selection (FS) has thus emerged as a critical step in predictive model development, aiming to identify the most relevant and useful features from original data to enhance model performance, reduce overfitting risk, and improve computational efficiency [40] [41].
The importance of feature selection in therapy response prediction extends beyond mere model improvement. In clinical and pharmaceutical research, identifying the most biologically significant features can provide valuable insights into disease mechanisms and treatment efficacy. For instance, in genomic studies, feature selection helps pinpoint genetic markers directly associated with treatment response, enabling more personalized therapeutic approaches [42]. Furthermore, by reducing dataset dimensionality, feature selection facilitates model interpretability—a crucial factor in clinical decision-making where understanding why a model makes certain predictions is as important as the predictions themselves [43].
Taxonomy of Feature Selection Methodologies
Filter Methods
Filter methods represent the most straightforward approach to feature selection, ranking features based on statistical measures without incorporating any learning algorithm. These methods evaluate features solely on their intrinsic characteristics and their relationship to the target variable. Common statistical measures used in filter methods include Pearson correlation coefficient, chi-squared test, information gain, and Fisher score [44] [45]. The recently proposed weighted Fisher score (WFISH) method enhances traditional Fisher scoring by assigning weights based on gene expression differences between classes, prioritizing informative features while reducing the impact of less useful ones [42].
Filter methods offer several advantages, including computational efficiency, scalability to very high-dimensional datasets, and independence from specific learning algorithms [46]. However, their primary limitation lies in the inability to capture feature dependencies and interactions with learning algorithms, potentially leading to suboptimal model performance [46]. They also tend to select large numbers of features, which may include redundant variables [44].
Wrapper Methods
Wrapper methods employ a specific learning algorithm to evaluate feature subsets, using the model's performance as the objective function for subset selection. This approach typically yields feature subsets that perform well with the chosen classifier. Common wrapper techniques include sequential feature selection, genetic algorithms (GA), and other metaheuristic algorithms such as Particle Swarm Optimization (PSO) and Differential Evolution (DE) [47] [45].
While wrapper methods generally achieve higher accuracy in feature selection and better capture feature interactions compared to filter methods, they come with significant computational demands, particularly for high-dimensional datasets [47]. They are also more prone to overfitting, especially with limited samples, and the selected feature subsets may not generalize well to other classifiers [45]. Recent innovations in wrapper methods include the development of enhanced algorithms such as the Q-learning enhanced differential evolution (QDEHHO), which dynamically balances exploration and exploitation during the search process [47].
Embedded Methods
Embedded methods integrate the feature selection process directly into model training, combining advantages of both filter and wrapper approaches. These methods perform feature selection as part of the model construction process, often through regularization techniques that penalize model complexity. Examples include LASSO regression, which uses L1 regularization to drive less important feature coefficients to zero, and tree-based methods like Random Forests that provide inherent feature importance measures [44] [45].
Embedded methods strike a balance between computational efficiency and selection performance, automatically selecting features while optimizing the model [46]. However, they are model-specific, meaning the feature selection is tied to a particular algorithm and may not transfer well to other modeling approaches [47]. Additionally, they may struggle with high-dimensional datasets containing substantial noise [47].
Hybrid Methods
Hybrid methods attempt to leverage the strengths of multiple approaches, typically combining the computational efficiency of filter methods with the performance accuracy of wrapper methods. These approaches often begin with a filter method to reduce the feature space, then apply a wrapper method to the pre-selected subset [46]. The recently developed FeatureCuts algorithm exemplifies this approach by first ranking features using a filter method (ANOVA F-value), then applying an adaptive filtering method to find the optimal cutoff point before final selection with PSO [46].
While hybrid methods can achieve superior performance with reduced computation time, they face challenges in determining the optimal transition point between methods [46]. The effectiveness of these methods depends heavily on properly balancing the components and avoiding the pitfalls of either approach when combined.
Table 1: Comparison of Feature Selection Methodologies
| Method Type | Key Characteristics | Advantages | Disadvantages | Representative Algorithms |
|---|---|---|---|---|
| Filter Methods | Uses statistical measures independent of learning algorithm | Fast computation; Scalable; Model-agnostic | Ignores feature interactions; May select redundant features | WFISH [42], Pearson Correlation [47], Fisher Score [47] |
| Wrapper Methods | Evaluates subsets using specific learning algorithm | High accuracy; Captures feature interactions | Computationally expensive; Risk of overfitting | QDEHHO [47], TMGWO [41], BBPSO [41] |
| Embedded Methods | Integrates selection with model training | Balanced performance; Model-specific optimization | Algorithm-dependent; Limited generalizability | LASSO [44], Random Forest [44], SCAD [44] |
| Hybrid Methods | Combines multiple approaches | Superior performance; Reduced computation | Complex implementation; Parameter tuning challenges | FeatureCuts [46], Fisher+PSO [45] |
Comparative Performance Analysis of Feature Selection Algorithms
Experimental Framework and Evaluation Metrics
To objectively compare feature selection strategies, we established a standardized evaluation framework using multiple benchmark datasets relevant to therapy response prediction. The experimental design incorporated three well-known medical datasets: the Wisconsin Breast Cancer Diagnostic dataset, the Sonar dataset, and the Differentiated Thyroid Cancer recurrence dataset [41]. These datasets represent diverse medical scenarios with varying dimensionalities and sample sizes, providing a comprehensive testbed for algorithm performance.
Performance evaluation employed multiple metrics to assess different aspects of feature selection effectiveness. Classification accuracy measured the predictive performance of models built on selected features, while precision and recall provided additional insights into model behavior [41]. The feature selection score (FS-score) was used in some studies as a composite metric balancing both model performance and feature reduction percentage, calculated as the weighted harmonic mean of these two factors [46]. Computational efficiency was assessed through training time and resource requirements, particularly important for high-dimensional biomedical data [46].
Performance Comparison Across Methodologies
Recent comparative studies have yielded insightful results regarding the performance of various feature selection approaches. Hybrid methods have demonstrated particularly strong performance, with the FeatureCuts algorithm achieving approximately 15 percentage points more feature reduction with up to 99.6% less computation time while maintaining model performance compared to state-of-the-art methods [46]. When integrated with wrapper methods like PSO, FeatureCuts enabled 25 percentage points more feature reduction with 66% less computation time compared to PSO alone [46].
Among wrapper methods, the Two-phase Mutation Grey Wolf Optimization (TMGWO) hybrid approach achieved superior results, outperforming other experimental methods in both feature selection and classification accuracy [41]. Similarly, the weighted Fisher score (WFISH) method demonstrated consistently lower classification errors compared to existing techniques when applied to gene expression data with random forest and kNN classifiers [42].
Table 2: Performance Comparison of Feature Selection Algorithms on Medical Datasets
| Algorithm | Type | Average Accuracy | Feature Reduction | Computational Efficiency | Best Use Cases |
|---|---|---|---|---|---|
| TMGWO | Wrapper | 98.85% [41] | High | Moderate | High-dimensional classification with balanced data |
| WFISH | Filter | Lower classification errors vs benchmarks [42] | Moderate | High | Gene expression data with RF/kNN classifiers |
| FeatureCuts | Hybrid | Maintains model performance [46] | 15-25% higher reduction [46] | 66-99.6% faster [46] | Large-scale enterprise datasets |
| QDEHHO | Wrapper | High accuracy [47] | High | Low | Complex medical data with nonlinear relationships |
| LASSO | Embedded | Varies by dataset [44] | High | High | Linear models with implicit feature selection |
| Random Forest | Embedded | High with important features [44] | Moderate | Moderate | Nonlinear data with interaction effects |
Domain-Specific Performance in Therapy Response Prediction
In the specific context of outcome prediction modeling for patient response to therapy, feature selection performance varies based on data characteristics and clinical objectives. For genomic data with extremely high dimensionality (where features far exceed samples), filter methods like WFISH and SIS (Sure Independence Screening) have shown particular utility [42] [44]. The WFISH approach specifically leverages differential gene expression between patient response categories to assign feature weights, enhancing identification of biologically significant genes [42].
For integrated multi-omics data combining genomic, transcriptomic, and clinical features, hybrid methods typically deliver the most robust performance. These complex datasets benefit from the initial feature reduction of filter methods followed by the refined selection of wrapper methods. The QDEHHO algorithm, which combines differential evolution with Q-learning and Harris Hawks Optimization, has demonstrated effectiveness in handling such complex biomedical data by dynamically adapting its search strategy [47].
Advanced Optimization Strategies for High-Dimensional Data
Metaheuristic Optimization Approaches
Metaheuristic algorithms have gained significant traction for feature selection in high-dimensional spaces due to their powerful global search capabilities. These nature-inspired algorithms include Particle Swarm Optimization (PSO), Differential Evolution (DE), Grey Wolf Optimization (GWO), and Harris Hawks Optimization (HHO) [47]. Recent advances have focused on enhancing these algorithms to address limitations such as premature convergence and parameter sensitivity.
The QDEHHO algorithm represents a sophisticated example of this trend, where DE serves as the backbone search framework, Q-learning adaptively selects mutation strategies and parameter combinations, and HHO provides directional masks to guide the crossover process [47]. This design enables dynamic balancing between exploration (global search) and exploitation (local refinement), achieving robust search in early phases and precise refinement in later phases [47]. Similarly, the TMGWO approach incorporates a two-phase mutation strategy that enhances the balance between exploration and exploitation [41].
Adaptive and Automated Feature Selection
A significant challenge in feature selection, particularly for hybrid methods, is determining the optimal cutoff point for initial feature filtering. Current approaches may use fixed cutoffs (e.g., top 5% of features), mean filter scores, or test arbitrary feature numbers [46]. The FeatureCuts algorithm addresses this challenge by reformulating cutoff selection as an optimization problem, using a Bayesian Optimization and Golden Section Search framework to adaptively select the optimal cutoff with minimal overhead [46].
This automated approach is particularly valuable in therapy response prediction research, where researchers may lack the expertise or computational resources for extensive parameter tuning. By systematically evaluating the trade-off between feature reduction and model performance, FeatureCuts achieves approximately 99.6% reduction in computation time while maintaining competitive performance compared to traditional methods [46].
Experimental Protocols and Research Workflows
Standardized Experimental Protocol for Feature Selection
Implementing a robust experimental protocol is essential for reliable feature selection in therapy response prediction. Based on methodologies from recent studies, we propose the following standardized workflow:
Data Preprocessing: Handle missing values through appropriate imputation methods. Normalize or standardize features to ensure comparability, especially for regularized models [48].
Initial Feature Ranking: Apply filter methods (e.g., ANOVA F-value, Fisher score) to rank features according to their statistical relationship with the therapy response variable [46].
Feature Subset Selection: Implement appropriate selection strategy based on methodology:
- For filter methods: Select top-k features based on established cutoff points or optimization algorithms like FeatureCuts [46]
- For wrapper methods: Apply metaheuristic algorithms to search for optimal feature subsets [47]
- For embedded methods: Train models with built-in feature selection capabilities [44]
- For hybrid methods: Combine filter and wrapper approaches, using the filter to reduce search space for the wrapper method [46]
Model Training and Validation: Train predictive models using the selected features and evaluate performance through cross-validation or hold-out validation sets [41]. Employ multiple metrics including accuracy, precision, recall, and clinical relevance.
Biological Validation: Where possible, validate selected features against known biological mechanisms or through experimental follow-up [42].
Feature Selection Workflow for Therapy Response Prediction: This diagram illustrates the standardized experimental protocol for implementing feature selection in patient response to therapy research.
Validation Strategies for Therapy Response Prediction
Robust validation is particularly crucial in medical applications where model decisions may impact patient care. Recommended validation strategies include:
Nested Cross-Validation: Implement inner loops for feature selection and parameter tuning with outer loops for performance estimation to prevent optimistic bias [41].
Multi-Cohort Validation: Validate selected features and models across independent patient cohorts when available to assess generalizability [42].
Clinical Relevance Assessment: Evaluate whether selected features align with known biological mechanisms or clinically actionable biomarkers [43].
Stability Analysis: Assess the consistency of selected features across different data resamples or algorithmic runs [47].
Implementing effective feature selection strategies requires both computational tools and domain knowledge. The following table outlines key resources for researchers developing therapy response prediction models.
Table 3: Research Reagent Solutions for Feature Selection Experiments
| Resource Category | Specific Tools/Resources | Function/Purpose | Application Context |
|---|---|---|---|
| Computational Frameworks | Scikit-learn, WEKA, R Caret | Implementation of feature selection algorithms | General-purpose machine learning and feature selection |
| Specialized FS Algorithms | TMGWO, WFISH, FeatureCuts, QDEHHO | Advanced feature selection for high-dimensional data | Specific high-dimensional scenarios (genomics, medical imaging) |
| Biomedical Data Repositories | TCGA, GEO, UK Biobank | Source of high-dimensional biomedical data | Access to real-world datasets for method development and validation |
| Performance Metrics | FS-score, Accuracy, Precision, Recall | Objective evaluation of selection effectiveness | Comparative algorithm assessment |
| Visualization Tools | Graphviz, Matplotlib, Seaborn | Diagramming workflows and result presentation | Experimental protocol documentation and result communication |
| Validation Frameworks | Nested Cross-Validation, Bootstrapping | Robust performance estimation | Preventing overoptimistic performance estimates |
Feature selection remains an indispensable component in developing robust therapy response prediction models from high-dimensional biomedical data. Our comprehensive comparison reveals that while each methodology offers distinct advantages, hybrid approaches generally provide the most favorable balance of performance and efficiency for medical applications. Methods like FeatureCuts and QDEHHO demonstrate how combining multiple strategies can overcome limitations of individual approaches.
The evolving landscape of feature selection is increasingly shaped by emerging artificial intelligence paradigms. The integration of reinforcement learning with traditional optimization algorithms, as seen in QDEHHO, represents a promising direction for adaptive feature selection [47]. Similarly, the need for explainable AI in clinical settings has stimulated research into interpretable feature selection methods that provide both predictive accuracy and biological insight [43].
As high-dimensional data continues to grow in volume and complexity within healthcare, feature selection methodologies will play an increasingly critical role in translating these data into clinically actionable knowledge. Future research should focus on developing more adaptive, automated, and interpretable feature selection strategies specifically tailored to the unique challenges of therapy response prediction.
Integrating Predictions into Clinical Decision Support Systems (CDSS)
Clinical Decision Support Systems are undergoing a fundamental transformation, shifting from static, rule-based reference tools to dynamic, predictive partners in clinical care. This evolution is largely driven by advances in artificial intelligence and machine learning that enable these systems to forecast patient-specific outcomes and therapy responses with increasing accuracy. By 2025, the CDSS market reflects this shift, with an expected value surpassing $2.2 billion and projected growth to $8.22 billion by 2034, demonstrating significant investment in these advanced capabilities [49] [50].
The integration of predictive models represents a crucial advancement in healthcare technology, moving clinical decision-making from a reactive to a proactive paradigm. Modern CDSS can now analyze complex patient data patterns to predict complications, treatment responses, and disease trajectories before they become clinically apparent. This capability is particularly valuable in therapeutic areas like oncology, where predicting individual patient responses to targeted therapies can significantly influence treatment selection and monitoring strategies [51]. For researchers and drug development professionals, understanding these integrated systems is essential for designing more targeted therapies and companion diagnostic tools that align with evolving clinical decision architectures.
Comparative Analysis of Predictive Modeling Approaches in CDSS
Performance Comparison of Machine Learning Algorithms
Different predictive modeling approaches offer distinct advantages for integration into clinical decision support systems. The table below summarizes experimental performance data from recent implementations across healthcare domains:
Table 1: Performance comparison of predictive modeling approaches in CDSS
| Model Type | Clinical Application | Dataset Size | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Random Forest | Predicting complications from Bevacizumab therapy in solid tumors | 395 patient records | Accuracy: 70.63%, Sensitivity: 66.67%, Specificity: 73.85%, AUC-ROC: 0.75 | [51] |
| Multi-scale Dilated Ensemble Network (MDEN) | Predicting patient response to radiotherapy | Not specified | Superior accuracy compared to RNN, LSTM, and 1DCNN by 0.79-2.98% | [22] |
| Logistic Regression-based Risk Score | Stratifying risk for targeted therapy complications | 395 patient records | AUC-ROC: 0.720 | [51] |
| AI-CDSS for Sepsis Detection | Early hospital sepsis prediction | Not specified | Prediction up to 12 hours before clinical signs, reduced mortality | [52] |
Methodological Protocols for Predictive Model Development
Machine Learning Protocol for Oncology CDSS
A 2025 prospective observational study detailed a comprehensive protocol for developing a CDSS predicting complications from Bevacizumab in solid tumors [51]:
Patient Selection and Data Collection: The study consecutively included 395 records from patients treated with Bevacizumab or its biosimilars for solid malignant tumors. Data extraction occurred from medical records and hospital electronic databases with a minimum follow-up period of 6 months.
Variable Selection: Researchers collected pretherapeutic variables including demographic data, medical history, tumor characteristics, and laboratory findings. Specific predictors identified as significant included age ≥65, anemia, elevated urea, leukocytosis, tumor differentiation, and stage.
Model Training and Validation: Multiple machine learning models (logistic regression, Random Forest, XGBoost) were trained using both 70/30 and 80/20 data splits. The models were compared using accuracy, AUC-ROC, sensitivity, specificity, F1-scores, and error rate.
Implementation: The best-performing model (Random Forest with 80/20 split) was translated into an interactive HTML form for clinical use, providing individual risk levels and stratifying patients into low-, intermediate-, or high-risk categories.
Deep Learning Framework for Radiotherapy Response Prediction
A separate 2025 study implemented a sophisticated deep learning approach for predicting patient response to radiotherapy [22]:
Architecture Design: The Multi-scale Dilated Ensemble Network (MDEN) integrated Long-Short Term Memory (LSTM), Recurrent Neural Network (RNN), and One-dimensional Convolutional Neural Networks (1DCNN) architectures, with final prediction scores averaged across models.
Feature Optimization: The Repeated Exploration and Exploitation-based Coati Optimization Algorithm (REE-COA) selected optimal features by increasing correlation coefficients and minimizing variance within the same classes.
Performance Validation: The model was evaluated against individual component algorithms (RNN, LSTM, 1DCNN) and demonstrated superior performance in minimizing error rates while enhancing prediction accuracy.
Visualizing Predictive Model Integration in CDSS
Workflow for Predictive Model Integration
The following diagram illustrates the end-to-end workflow for integrating predictive models into clinical decision support systems:
Predictive Model Integration Workflow in CDSS: This diagram illustrates the comprehensive process from data acquisition to clinical application, highlighting the key stages of integrating predictive analytics into clinical decision support systems.
Ensemble Architecture for Predictive Modeling
The following visualization depicts the ensemble deep learning architecture used in advanced prediction systems:
Ensemble Deep Learning Architecture for Response Prediction: This visualization shows the multi-scale dilated ensemble network (MDEN) framework that combines predictions from LSTM, RNN, and 1D-CNN models through an averaging layer to generate final patient response predictions.
Research Reagent Solutions for Predictive CDSS Development
The development and implementation of predictive clinical decision support systems require specific technical components and methodological approaches. The table below details essential research reagents and their functions in creating these advanced systems:
Table 2: Essential research reagents and computational tools for predictive CDSS development
| Research Reagent/Tool | Function in Predictive CDSS Development | Application Example |
|---|---|---|
| Machine Learning Algorithms (RF, XGBoost) | Statistical pattern recognition for risk prediction | Predicting complications from targeted therapies [51] |
| Deep Learning Architectures (LSTM, RNN, 1D-CNN) | Complex temporal and sequential data analysis | Radiotherapy response prediction through ensemble modeling [22] |
| Feature Selection Algorithms (REE-COA) | Optimization of predictive features while reducing dimensionality | Weight optimization for improved prediction accuracy [22] |
| DICOMWeb-Compatible Image Archives | Standardized medical imaging data storage and retrieval | Orthanc, DCM4CHEE for medical imaging integration [53] |
| OpenID Connect Authentication | Secure, standards-based access to clinical data APIs | AWS HealthImaging integration with OHIF Viewer [54] |
| Interactive HTML Forms | Clinical translation of predictive models into usable tools | Risk stratification interface for oncology applications [51] |
Implementation Challenges and Adoption Considerations
Technical and Workflow Barriers
Despite their potential, integrated predictive CDSS face significant implementation challenges that researchers and developers must address:
Algorithmic Bias and Generalizability: Predictive models may demonstrate unequal performance across patient populations. A 2019 study found that healthcare prediction algorithms trained primarily on data from white patients systematically underestimated the care needs of black patients [52]. Similar disparities have been observed for gender minorities and patients with rare diseases.
Workflow Integration and Alert Fatigue: CDSS adoption by nurses and physicians is significantly influenced by workflow alignment. A 2025 qualitative study identified 26 distinct factors affecting nurse adoption, with alert fatigue, poor design, and limited digital proficiency as key barriers. Value tensions emerge between standardization and professional autonomy, and between enhanced decision support and increased administrative burden [55].
System Integration Complexities: Variations in healthcare data standards and legacy EHR systems create significant integration challenges. The FITT (Fit Between Individuals, Tasks, and Technology) framework emphasizes that successful implementation depends on alignment between user characteristics, task demands, technology features, and organizational context [55].
Ethical Framework and Validation Requirements
The integration of predictive models into clinical decision support necessitates robust ethical and validation frameworks:
Transparency and Explainability: Research indicates that physician trust in AI tools increases when results align with randomized controlled trial outcomes, highlighting the importance of model explainability [51]. Regulatory frameworks increasingly require transparency in algorithmic decision-making.
Continuous Validation and Calibration: Predictive models require ongoing validation using separate datasets not used during training. Appropriate metrics must be applied to assess sensitivity, specificity, precision, and other accuracy indicators throughout the model lifecycle [52].
Patient Involvement in Development: Public and Patient Involvement (PPI) in predictive model development helps identify which health risks merit prediction tools and ensures models align with patient realities. Patients can provide valuable feedback on outcome measures and whether model outputs resonate with lived experiences [52].
Future Directions in Predictive CDSS Integration
The integration of predictive analytics into clinical decision support continues to evolve with several emerging trends:
Generative AI and Conversational Interfaces: Dynamic AI combinations, particularly conversational AI and generative AI, are being integrated to provide clinicians with more natural access to relevant information and administrative support [56].
Real-time Data Integration for Critical Conditions: Emerging opportunities exist for CDSS that incorporate real-time data streams for critical conditions, enabling more dynamic and responsive prediction systems [56].
Expansion to Home-based Care Settings: Point-of-care CDSS for home-based treatment represents a growing application area, extending predictive capabilities beyond traditional clinical environments [56].
Multimodal Data Fusion: Advanced CDSS increasingly incorporate diverse data types including genomic insights, patient-reported outcomes, and social determinants of health to create more comprehensive prediction models [49].
For researchers and drug development professionals, these advancements highlight the growing importance of developing therapies with companion predictive tools that can integrate seamlessly into evolving CDSS architectures, ultimately supporting more personalized and effective patient care.
Addressing Instability, Data Challenges, and Model Degradation
Mitigating Model Instability and the 'Multiverse of Madness' in Small Datasets
In the field of patient response to therapy research, clinical prediction models are developed to inform individual diagnosis, prognosis, and treatment selection. However, a critical challenge often overlooked is the "multiverse of madness" in model development – the concept that for any prediction model developed from a sample dataset, there exists a multiverse of other potential models that could have been developed from different samples of the same size from the same overarching population [57]. This multiverse represents the epistemic uncertainty in model development, where the same modeling process applied to different samples yields varying models with different predictions for the same individual [57].
The instability arising from this multiverse is particularly pronounced when working with small datasets, a common constraint in therapy response research due to the challenges in recruiting participants for clinical trials [57] [58]. When sample sizes are limited, individual predictions can vary dramatically across the multiverse of possible models, potentially leading to different clinical decisions for the same patient [57]. This article examines the nature of this instability, compares methodological approaches for addressing it, and provides evidence-based strategies for mitigating its effects in patient response prediction research.
Understanding the 'Multiverse of Madness' in Clinical Prediction
Conceptual Framework and Terminology
The "multiverse of madness" metaphor describes the phenomenon where numerous equally plausible models can emerge from the same underlying population depending on the specific sample used for development [57]. This occurs because of the inherent variability across random samples of the same size taken from a particular population [57]. The concept is strongly related to epistemic uncertainty (reducible uncertainty), which refers to uncertainty in predictions arising from the model production itself, as opposed to aleatoric uncertainty (irreducible uncertainty) that refers to residual uncertainty that cannot be explained by the model [57].
In practical terms, this means that a prediction model created using regression or machine learning methods is dependent on the sample and size of data used to develop it. If a different sample of the same size were used from the same overarching population, the developed model could be very different – in terms of included predictors, predictor effects, regression equations, or tuning parameters – even when applying identical model development methods [57].
Impact on Patient Response Prediction Research
In therapy response prediction, instability matters because model predictions guide individual counseling, resource prioritization, and clinical decision making [57]. For example, a model might be used to classify patients as likely responders or non-responders to specific therapies like cognitive behavioral therapy, potentially influencing treatment pathways [59] [60] [61].
Consider a scenario where a model suggests a patient's probability of responding to therapy is above a clinical decision threshold (e.g., 60%), but alternative models from the multiverse suggest probabilities below this threshold. This creates a "multiverse of madness" for clinicians who must determine which prediction to trust when making treatment decisions [57]. The problem is particularly acute in mental health research, where sample sizes are often limited and multiple outcome measures may be considered [60].
Methodological Approaches for Examining Instability
Bootstrapping and Instability Analysis
Bootstrapping provides a practical method for examining the multiverse of models and quantifying instability at the individual prediction level [57]. The process involves:
- Taking B bootstrap samples (e.g., 500) from the original dataset, each of the same size as the original development data
- Developing a prediction model in each bootstrap sample using exactly the same development process
- Generating predictions for each individual from each of the B models
- Quantifying the variability (instability) in predictions at the individual level [57]
The results can be presented using a prediction instability plot – a scatter of the B predicted values for each individual against their predicted value from the original developed model, with uncertainty intervals (e.g., 95% using the 2.5th and 97.5th percentiles) [57]. The mean absolute prediction error (MAPE) can be calculated for each individual, representing the mean of the absolute difference between the bootstrap model predictions and the original model prediction [57].
Figure 1: Workflow for Bootstrap Instability Analysis
Applied Example in Mental Health Research
A recent study on predicting depression treatment response exemplifies how instability can be examined in therapy response research [60]. The researchers used elastic net models to predict response to internet-delivered cognitive behavioral therapy (iCBT) based on 85 baseline features in 776 patients. They developed models on a training set (N=543) and validated performance in a hold-out sample (N=233) [60].
While the study did not explicitly report instability metrics, its approach of evaluating multiple outcome measures (16 individual symptoms, 4 latent factors, and total scores) highlights the potential for variability in predictions depending on how outcomes are defined [60]. The results showed substantial variability in model performance across different symptoms (R²: 2.1%-44%), suggesting that the predictability of treatment response may vary considerably depending on which aspect of depression is being predicted [60].
Comparative Analysis of Modeling Approaches
Statistical Logistic Regression vs. Machine Learning
The choice between statistical logistic regression and machine learning approaches involves important trade-offs concerning model instability, particularly in small datasets:
Table 1: Comparison of Modeling Approaches in Small Datasets
| Aspect | Statistical Logistic Regression | Supervised Machine Learning |
|---|---|---|
| Learning process | Theory-driven; relies on expert knowledge for model specification | Data-driven; automatically learns relationships from data [58] [62] |
| Assumptions | High (linearity, independence) | Low; handles complex, nonlinear relationships [58] [62] |
| Sample size requirement | Lower; more efficient with limited data [58] [62] | Higher; data-hungry, requires more events per predictor [58] [62] |
| Interpretability | High; white-box nature, coefficients directly interpretable [58] [62] | Low; black-box nature, requires post hoc explanation methods [58] [62] |
| Performance in small samples | More stable due to fewer parameters and stronger assumptions [58] | Prone to overfitting and instability without sufficient data [58] |
| Handling of complex relationships | Limited unless manually specified | Automated handling of interactions and nonlinearities [58] [62] |
The fundamental difference between these approaches lies in their learning philosophy. Statistical logistic regression operates under conventional statistical assumptions, employs fixed hyperparameters without data-driven optimization, and uses prespecified candidate predictors based on clinical or theoretical justification [58] [62]. In contrast, machine learning-based logistic regression involves hyperparameter tuning through cross-validation, may select predictors algorithmically, and shifts focus decisively toward predictive performance [58] [62].
Performance Metrics Across Modeling Paradigms
Recent meta-analyses provide insights into the performance of different modeling approaches in mental health applications:
Table 2: Performance Comparison in Mental Health Treatment Response Prediction
| Model Type | Average Accuracy | Average AUC | Key Moderating Factors |
|---|---|---|---|
| Machine Learning (across emotional disorders) | 0.76 [3] [61] | 0.80 [3] | Robust cross-validation, neuroimaging predictors [3] |
| Elastic Net (depression symptoms) | Variable (R²: 2.1%-44%) [60] | Not reported | Outcome measure selection, baseline symptom severity [60] |
| Traditional Logistic Regression | Context-dependent [58] | No consistent advantage over ML [58] | Sample size, data quality, linearity of relationships [58] |
A large meta-analysis of machine learning for predicting treatment response in emotional disorders found an overall mean prediction accuracy of 76% and AUC of 0.80 across 155 studies [3]. However, this analysis also identified important moderators: studies using more robust cross-validation procedures exhibited higher prediction accuracy, and those using neuroimaging data as predictors achieved higher accuracy compared to those using only clinical and demographic data [3].
Experimental Evidence: Sample Size Effects on Instability
Case Study: Myocardial Infarction Mortality Prediction
A compelling demonstration of sample size effects on instability comes from a study using the GUSTO-I dataset with 40,830 participants, of which 2,851 (7%) died by 30 days [57]. Researchers developed a logistic regression model with lasso penalty considering eight predictors [57].
When using the full dataset (approximately 356 events per predictor parameter), bootstrap analysis revealed low variability in individual predictions with an average MAPE across individuals of 0.0028 and largest MAPE of 0.027 [57]. However, when using a random subsample of 500 participants with only 35 deaths (about 4 events per predictor parameter), the same analysis revealed huge variability in individual predictions [57]. An individual with an estimated 30-day mortality risk of 0.2 from the original model had a wide range of alternative predictions from about 0 to 0.8 across the multiverse, with an average MAPE of 0.023 and largest MAPE of 0.14 [57].
This case illustrates how apparently good discrimination performance (c-statistic of 0.82 in the small sample) can mask substantial instability in individual predictions when sample sizes are inadequate [57].
Sample Size Recommendations for Stability
Adherence to minimum sample size recommendations is one way to mitigate instability concerns [57] [58]. A 2023 systematic review reported that 73% of binary clinical prediction models using statistical logistic regression had sample sizes below the recommended minimum threshold [58]. Machine learning algorithms are generally more data-hungry than logistic regression to achieve stable performance – for example, random forest may require more than 20 times the number of events per candidate predictor compared to statistical logistic regression [58].
Figure 2: Sample Size Impact on Prediction Stability
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing robust modeling practices requires specific methodological tools and approaches. The following table details key "research reagent solutions" for addressing instability in therapy response prediction research:
Table 3: Essential Methodological Tools for Mitigating Instability
| Research Reagent | Function | Application Context |
|---|---|---|
| Bootstrap Resampling | Examines the multiverse of models by creating multiple samples with replacement [57] | Quantifying prediction instability for any modeling approach |
| Cross-Validation Procedures | Provides robust performance estimation and hyperparameter tuning [3] [58] | Preventing overfitting, especially in machine learning applications |
| Elastic Net Regression | Balances variable selection and regularization through L1 and L2 penalties [60] | When dealing with correlated predictors and limited sample sizes |
| Instability Plots | Visualizes variability in individual predictions across bootstrap models [57] | Communicating uncertainty in predictions to stakeholders |
| SHAP (Shapley Additive Explanations) | Provides post hoc interpretability for complex machine learning models [58] [62] | Explaining black-box model predictions to clinical audiences |
| TRIPOD+AI Statement | Reporting guidelines for prediction model studies [63] | Ensuring transparent and complete reporting of modeling procedures |
Integrated Strategies for Mitigating Instability
Data Quality Over Model Complexity
Rather than focusing solely on algorithmic sophistication, researchers should prioritize data quality as a primary strategy for reducing instability [58] [62]. The "no free lunch" theorem suggests there is no universal best modeling approach, and performance depends heavily on dataset characteristics and data quality [58] [62]. Efforts to improve data completeness, accuracy, and relevance are more likely to enhance reliability and real-world utility than pursuing model complexity alone [58].
Multimodal Data Integration
Studies incorporating neuroimaging data have demonstrated higher prediction accuracy for treatment response [3] [61]. Integrating multiple data types (e.g., clinical, neuroimaging, cognitive, genetic) may enhance stability by providing complementary information about underlying mechanisms [3]. However, such approaches require careful handling of missing data and appropriate sample sizes to avoid exacerbating instability issues.
Outcome Definition Considerations
Research on depression treatment response suggests that predictability varies substantially across different symptoms and outcome definitions [60]. Rather than relying solely on aggregate scores, researchers should consider modeling individual symptoms or latent factors, which may show different patterns of predictability and stability [60]. This approach aligns with moves toward more personalized and precise psychiatry.
Transparency and Reporting Standards
Enhancing transparency in modeling procedures is crucial for addressing instability concerns [58]. This includes clear documentation of data preprocessing steps, sample size justifications, modeling decisions, hyperparameter tuning strategies, feature selection techniques, and model evaluation methods [58] [62]. Adherence to reporting guidelines such as TRIPOD+AI helps ensure that instability and other limitations are appropriately communicated [63].
Model instability arising from the "multiverse of madness" presents a significant challenge in therapy response prediction research, particularly when working with small datasets. Through comparative analysis of methodological approaches and experimental evidence, we have identified that instability is fundamentally driven by inadequate sample sizes relative to model complexity, rather than by specific algorithmic choices.
The most effective strategies for mitigating instability include prioritizing data quality over model complexity, ensuring adequate sample sizes through collaborative data sharing, employing bootstrap methods to quantify and communicate instability, and maintaining methodological transparency throughout the modeling process. By addressing these challenges directly, researchers can develop more stable and reliable prediction models that ultimately enhance personalized treatment approaches in mental health care.
Handling Missing Data, Sparse Outcomes, and Irregular Time Series
In patient response to therapy research, the quality and structure of data directly influence the reliability of outcome prediction models. Real-world clinical data, derived from sources such as electronic health records (EHRs) and clinical trials, is often characterized by three pervasive challenges: missing data, sparse outcomes, and irregular time series. Missing data is present in almost every clinical study and, if handled improperly, can compromise analyses and bias results, threatening the scientific integrity of conclusions [64] [65]. Sparse outcomes, where positive clinical events of interest are rare, can lead to models that are not suitable for predicting these events [66]. Furthermore, clinical time series are often irregularly sampled, with uneven intervals between observations due to varying patient visit schedules and clinical priorities, which complicates the application of traditional time-series models [67] [68]. This guide objectively compares the performance of contemporary statistical and advanced machine learning methods designed to overcome these challenges, providing researchers with evidence-based protocols to enhance their predictive modeling efforts.
Comparative Analysis of Methods for Handling Missing Data
Understanding Missing Data Mechanisms
The choice of an appropriate method for handling missing data first requires an understanding of the underlying missingness mechanism [69]. The three primary classifications are:
- Missing Completely at Random (MCAR): The probability of data being missing is unrelated to any observed or unobserved variables. A complete case analysis can be valid in this scenario.
- Missing at Random (MAR): The probability of missingness may depend on observed data but not on unobserved data. Multiple imputation methods are typically valid under MAR.
- Missing Not at Random (MNAR): The probability of missingness depends on the unobserved data itself. This is the most complex scenario and requires specialized methods like pattern mixture models [64] [65].
Performance Comparison of Missing Data Imputation Methods
A 2024 systematic review and a 2025 simulation study provide robust evidence for comparing the performance of various imputation methods under different conditions [64] [69]. The following table synthesizes key findings on their performance relative to data characteristics.
Table 1: Comparison of Missing Data Handling Methods
| Method Category | Specific Method | Optimal Missing Mechanism | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Single Imputation | Last Observation Carried Forward (LOCF) | Limited utility | Simple, straightforward | Well-documented to bias treatment effect estimates [64] |
| Model-Based (No Imputation) | Mixed Model for Repeated Measures (MMRM) | MAR | Utilizes all available data without imputation; High power, low bias [64] | Model assumptions must be met |
| Multiple Imputation | Multiple Imputation by Chained Equations (MICE) | MAR | Leads to valid estimates including uncertainty; Good performance [64] [70] | Implementation complexity |
| Control-Based Pattern Mixture Models (PPMs) | Jump-to-Reference (J2R), Copy Reference (CR) | MNAR | Superior under MNAR; Provides conservative estimates [64] | Less powerful than MMRM/MICE under MAR |
| Machine Learning | Random Forest (RF) for Imputation | MAR | Can model complex, non-linear relationships [66] | Risk of overfitting; requires careful tuning |
The systematic review by et al. (2024) emphasizes that Multiple Imputation (MI) is generally advantageous over single imputation methods like LOCF because it accounts for the uncertainty of the imputed values, leading to more unbiased estimates [69] [70]. Furthermore, research funded by the Patient-Centered Outcomes Research Institute (PCORI) confirmed that MI outperformed complete-case analysis and single imputation methods in most longitudinal study scenarios, with performance further improved by including auxiliary variables related to the missingness mechanism [70].
For the specific context of Missing Not at Random (MNAR) data, such as when patients in a clinical trial drop out due to side effects or lack of efficacy, control-based Pattern Mixture Models (PMMs) like Jump-to-Reference (J2R) are recommended. A 2025 simulation study on Patient-Reported Outcomes (PROs) found that PPM methods were superior to others under MNAR mechanisms, as they provide a more conservative and often clinically plausible estimate of the treatment effect [64].
Experimental Protocol for Comparing Imputation Methods
To validate the performance of different imputation methods in a specific dataset, researchers can adopt a simulation-based evaluation protocol as used in state-of-the-art studies [64] [70]:
- Start with a Complete Dataset: Identify a real, complete dataset (e.g., from a clinical trial) to serve as a gold standard.
- Induce Missingness: Artificially generate missing values in this complete dataset under various controlled conditions, including:
- Different mechanisms (MCAR, MAR, MNAR).
- Different missing rates (e.g., 10%, 30%, 50%).
- Different patterns (monotonic vs. non-monotonic).
- Apply Imputation Methods: Apply the candidate methods (e.g., MMRM, MICE, PPMs) to the datasets with induced missingness.
- Evaluate Performance: Compare the results from each method against the "true" results from the original complete dataset. Key metrics include:
- Bias: The deviation of the estimated treatment effect from the true value.
- Statistical Power: The ability to detect a true effect.
- Coverage Probability: The proportion of times the confidence interval contains the true value.
This protocol allows for a direct, quantitative comparison of how each method performs under specific challenging conditions relevant to the research at hand.
Figure 1: Experimental protocol for comparing missing data imputation methods, based on simulation studies [64] [70].
Addressing Sparsity in Outcomes and Features
The Challenge of Data Sparsity
In clinical prediction models, sparsity manifests in two primary forms: sparse outcomes (e.g., a rare disease or a low-incidence adverse event) and sparse features (where most values in a clinical variable are zero or missing) [66]. Sparse outcomes create imbalanced datasets where machine learning models may become biased toward the majority class, failing to learn the patterns of the rare event. Sparse features, common in EHRs due to the large number of potential laboratory tests, medications, and diagnoses, increase computational memory and can reduce a model's generalization ability [66].
Technical Solutions for Sparsity and Imbalance
A 2023 study proposed a systematic machine learning approach to tackle missing, imbalanced, and sparse features simultaneously in emergency medicine data [66]. The workflow included:
- Random Forest (RF) for Missing Values: The study used a Random Forest model to perform single imputation for both continuous and discrete variables, reporting a median R² of 0.623 for continuous variables.
- K-means for Imbalanced Data: To address class imbalance in outcomes, the researchers used k-means clustering. This technique helps in identifying and potentially resampling the data to create a more balanced distribution for model training.
- Principal Component Analysis (PCA) for Sparse Features: PCA was employed to reduce the dimensionality of the feature space, thereby mitigating the challenges posed by sparse features and improving model generalization.
The case study results demonstrated that a logistic regression model built on data processed with this approach achieved a recall of 0.746 and an F1-score of 0.73, significantly outperforming a model built on the raw, unprocessed data [66].
Modeling Irregular Clinical Time Series
The Nature of Irregular Time Series in Healthcare
Clinical time series are inherently irregular. The intervals between patient measurements are not fixed but depend on clinical need, patient condition, and hospital schedules [67] [68]. This irregularity is not merely noise; it often contains valuable information. For instance, shorter intervals between tests may indicate a more critical or unstable patient state, while longer intervals may suggest stability [67]. This informatively sampled data poses a significant challenge for classical time-series models that assume regular, equally spaced observations.
Advanced Architectures for Irregular Time Series
Recent advancements have introduced sophisticated models designed specifically to capture the continuous dynamics of irregularly sampled data. Key architectures include:
- TrajGPT: This model employs a Selective Recurrent Attention (SRA) mechanism with a data-dependent decay, allowing it to adaptively filter out irrelevant past information based on the current context. By being interpreted as discretized ordinary differential equations (ODEs), TrajGPT can effectively capture underlying continuous dynamics, enabling interpolation and extrapolation of health trajectories from partially-observed data [71].
- Multi-Level Transfer Learning (MLTL): This framework categorizes time series based on patient conditions (e.g., stable vs. unstable) and performs predictions tailored to these categories. It uses a pre-training task to capture correlations among clinical indicators, thereby enhancing the information density of sparse series. Empirical results showed that even with 80% of indicator values missing, MLTL achieved a significant 9.4% reduction in mean absolute error (MAE) compared to mainstream methods [67].
- Digital Twin—Generative Pretrained Transformer (DT-GPT): This approach fine-tunes a large language model (LLM) on EHR data to forecast clinical trajectories. A key advantage is its ability to handle raw EHR data "without requiring data imputation or normalization," thus directly addressing challenges of missingness and noise. Benchmarking on ICU and cancer datasets showed that DT-GPT outperformed state-of-the-art models like Temporal Fusion Transformers and LSTMs, reducing the scaled MAE by 1.3% to 3.4% [72].
Table 2: Performance of Advanced Time-Series Models on Benchmark Datasets
| Model | Core Innovation | Dataset | Key Performance Metric | Result vs. Baseline |
|---|---|---|---|---|
| TrajGPT [71] | Selective Recurrent Attention (SRA) & ODEs | Healthcare EHRs | Forecasting & Classification | Excels in trajectory forecasting and phenotype classification in zero-shot settings. |
| MLTL [67] | Condition-based categorization & transfer learning | Clinical benchmark datasets | Mean Absolute Error (MAE) | 9.4% reduction in MAE even with 80% data missing. |
| DT-GPT [72] | Fine-tuned LLM for clinical data | NSCLC (Cancer) | Scaled MAE | 0.55 vs 0.57 for LightGBM (3.4% improvement). |
| DT-GPT [72] | Fine-tuned LLM for clinical data | ICU (MIMIC-IV) | Scaled MAE | 0.59 vs 0.60 for LightGBM (1.3% improvement). |
| DT-GPT [72] | Fine-tuned LLM for clinical data | Alzheimer's Disease | Scaled MAE | 0.47 vs 0.48 for TFT (1.8% improvement). |
The following diagram illustrates the core architecture of TrajGPT, which enables it to effectively handle irregular time series.
Figure 2: TrajGPT architecture for irregular time-series representation learning [71].
This section details essential computational and methodological "reagents" required to implement the solutions discussed in this guide.
Table 3: Research Reagent Solutions for Advanced Outcome Prediction
| Tool/Resource Name | Type | Primary Function | Relevance to Challenge |
|---|---|---|---|
| SimTimeVar / SimulateCER [70] | R Software Package | Simulates longitudinal studies with time-varying covariates and missing data. | Enables method validation by creating realistic test datasets with known properties. |
| Multiple Imputation by Chained Equations (MICE) | Statistical Algorithm | Creates multiple plausible imputations for missing data. | Handles MAR data, accounting for imputation uncertainty. |
| Control-Based Pattern Mixture Models (PMMs) | Statistical Framework | Provides conservative estimates for missing data under MNAR. | Sensitivity analysis for scenarios where missingness is related to the outcome. |
| Random Forest Imputation [66] | Machine Learning Algorithm | Single imputation using non-linear relationships in the data. | Addresses missingness in complex datasets with non-linear patterns. |
| Principal Component Analysis (PCA) [66] | Dimensionality Reduction Technique | Reduces feature space by creating composite components. | Mitigates issues caused by sparse features, improving model generalization. |
| TrajGPT [71] | Pre-trained Transformer Model | Learns representations from irregular time series for forecasting and classification. | Directly models irregularly sampled clinical data without the need for resampling. |
| DT-GPT [72] | Fine-tuned Large Language Model | Forecasts multivariable clinical trajectories from EHR data. | Handles raw, messy clinical data with missingness and noise for end-to-end prediction. |
The evolution of methods for handling imperfect clinical data has progressed from traditional statistical imputations to sophisticated machine learning and generative AI models. Evidence consistently shows that Multiple Imputation techniques are generally superior to single imputation for MAR data, while Pattern Mixture Models are essential for sensitivity analyses under MNAR assumptions [64] [69] [65]. For the challenges of sparse outcomes and irregular time series, systematic preprocessing (using methods like RF and PCA) and advanced architectures (like TrajGPT and DT-GPT) demonstrate significant performance improvements by directly embracing the complex, informatively sampled nature of clinical data [66] [67] [72].
A promising future direction lies in the application of large language models (LLMs), such as DT-GPT, which show a remarkable ability to work with heterogeneous EHR data without extensive preprocessing and to perform zero-shot forecasting [72]. As these models continue to mature, they offer a path toward more robust, generalizable, and actionable digital twins and predictive models in patient response to therapy research, ultimately enhancing clinical decision-making and drug development.
Monitoring and Correcting for Model Shift and Performance Decay Over Time
Artificial intelligence (AI) is increasingly integrated into modern healthcare, offering powerful support for clinical decision-making, from disease diagnosis and patient monitoring to treatment outcome prediction [73]. However, in real-world settings, AI systems frequently experience performance degradation over time due to factors such as shifting data distributions, changes in patient characteristics, evolving clinical protocols, and variations in data quality [73]. This phenomenon, known as model drift, compromises model reliability and poses significant safety concerns, increasing the likelihood of inaccurate predictions or adverse patient outcomes [73].
Ensuring the long-term safety and reliability of machine learning (ML) models requires more than pre-deployment evaluation; it demands robust, continuous post-deployment monitoring and correction strategies [73]. This comparison guide provides researchers, scientists, and drug development professionals with a comprehensive framework for detecting, analyzing, and correcting performance decay in predictive models for patient response to therapy, enabling the development of AI systems that maintain accuracy and relevance in dynamic clinical environments.
Understanding Performance Degradation: Causes and Evidence
Defining Data and Model Drift
Performance degradation in AI, or model drift, occurs when models exhibit reduced effectiveness in real-world applications compared to their performance during initial training or testing [73]. The underlying assumption in classic ML theory that training and test data are drawn from the same underlying distribution rarely holds in clinical practice [73]. Two primary types of variation lead to model degradation:
- Cross-environment variation: An AI model trained in one environment encounters significantly different data distributions when applied to new environments. Demographic differences, variations in medical practices, device settings, or disease prevalence across geographic regions can trigger this spatial variation [73].
- Within-environment variation: Also known as temporal variation, this "AI aging" phenomenon occurs when a model deployed in a fixed environment experiences performance decline over time due to gradual shifts in the underlying data distribution [73].
Documented Cases of Performance Decay in Clinical Models
Substantial empirical evidence demonstrates the pervasive nature of model degradation in healthcare applications:
- Cardiac Surgery Risk Prediction: A study investigating performance drift in machine learning models for cardiac surgery risk prediction using a large UK dataset from 2012–2019 found strong evidence of performance degradation over time, attributed to changes in data distributions and variable importance [73].
- In-Hospital Mortality Prediction: An empirical evaluation of the long-term performance degradation of ML models predicting in-hospital mortality at emergency admission analyzed 1.83 million patient discharge records. The study tracked degradation across key metrics—including Area Under the Receiver Operator Characteristic Curve (AUC), accuracy, precision, and recall—finding that while ML models can remain effective for over a year post-training, gradual performance decline necessitates strategic retraining [73].
- Acute Kidney Injury (AKI) Prediction: Research on models predicting AKI over nine years demonstrated that while discriminatory performance may remain stable, calibration drift can significantly undermine clinical utility [73]. Similar findings were reported for models predicting 30-day hospital mortality, where multiple regression and machine learning models exhibited calibration drift [73].
- Large Language Models (LLMs) in Medicine: Even advanced AI models are not immune to degradation. When GPT-4's performance was reassessed on the American College of Radiology in-training examination several months after initial testing, it chose a different answer 25.5% of the time, indicating substantial temporal variability [73]. A broader evaluation highlighted how GPT-4 and GPT-3.5 exhibit performance drift across various tasks, including following user instructions [73].
Detection Methods: Comparing Approaches for Identifying Model Drift
Effective monitoring requires robust detection methods for both data and model performance changes. The table below compares key techniques for detecting degradation in clinical prediction models.
Table 1: Comparison of Detection Methods for Model Performance Degradation
| Method Category | Specific Techniques | Key Strengths | Key Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Data Distribution Monitoring | Population stability index (PSI), Kullback-Leibler (KL) divergence, Kolmogorov-Smirnov test, Maximum Mean Discrepancy (MMD) | Early warning of input data shifts before performance degradation manifests; applicable to all feature types | Does not directly measure performance impact; may flag clinically irrelevant changes | Baseline monitoring for all deployed models; preprocessing data quality checks |
| Performance Monitoring | AUC-ROC tracking, precision/recall drift, calibration curve analysis, Brier score decomposition | Directly measures impact on prediction quality; clinically interpretable metrics | Requires ongoing ground truth labels, which may be delayed in healthcare settings | Models with reliable outcome data collection; quarterly performance reviews |
| Model-Based Detection | Feature importance shift analysis, residual pattern monitoring, uncertainty quantification | Identifies specific mechanisms of failure; explains which relationships have changed | Computationally intensive; requires access to model internals | High-stakes applications requiring explainability; diagnostic models |
| LLM-Specific Monitoring | Output consistency scoring, embedding drift detection, prompt adherence tracking | Specialized for generative AI systems; captures semantic and behavioral shifts | Emerging methodology with limited standardization | Clinical documentation assistants; patient communication tools |
Statistical Protocols for Drift Detection
Implementing effective detection requires standardized statistical protocols. The following methodology provides a framework for monitoring clinical prediction models:
Experimental Protocol: Quarterly Model Performance Assessment
- Data Collection: Extract recent inference data from the past quarter (minimum n=200 cases for adequate power) along with corresponding ground truth outcomes [73].
- Baseline Comparison: Calculate key performance metrics (AUC, accuracy, precision, recall, calibration) on the recent data and compare against original validation performance [73].
- Statistical Testing: Apply appropriate statistical tests based on data characteristics:
- For AUC comparison: Use DeLong's test for ROC curves
- For calibration assessment: Use Hosmer-Lemeshow goodness-of-fit test
- For distribution shifts: Use population stability index (PSI) with threshold of >0.1 indicating mild drift, >0.25 indicating significant drift [73]
- Clinical Significance Evaluation: Determine if observed performance changes exceed predetermined clinical thresholds (e.g., >5% decrease in sensitivity for critical conditions).
- Reporting: Document findings in model cards with specific recommendations for intervention if degradation is detected.
This systematic approach enables researchers to distinguish random variation from meaningful degradation and initiate appropriate correction protocols.
Correction Strategies: Comparing Approaches for Model Recovery
When performance degradation is detected, various correction strategies can restore model effectiveness. The table below compares the primary approaches for clinical prediction models.
Table 2: Comparison of Correction Strategies for Degraded Clinical Models
| Strategy | Technical Approach | Data Requirements | Implementation Complexity | Typical Effectiveness |
|---|---|---|---|---|
| Full Retraining | Complete model rebuild with recent data | Substantial new labeled data (1000+ samples) | High (requires MLOps pipeline) | High (resets model to current environment) |
| Fine-Tuning/Transfer Learning | Update parameters of existing model with new data | Moderate new labeled data (100-500 samples) | Medium (requires careful tuning) | Medium-High (preserves some original learning) |
| Ensemble Methods | Combine predictions from original and newly trained models | Moderate new labeled data (200-800 samples) | Medium (managing multiple models) | High (robust to various drift types) |
| Threshold Adjustment | Modify classification thresholds to restore calibration | Minimal new data (50-100 samples) | Low (simple implementation) | Low-Medium (addresses calibration only) |
| Test-Time Adaptation | Adjust model during inference without retraining | Unlabeled data during deployment | Medium-High (emerging technique) | Variable (depends on method and data) |
Protocol for Strategic Model Correction
Selecting the appropriate correction strategy requires systematic evaluation of the degradation characteristics:
Experimental Protocol: Model Correction Selection Framework
Root Cause Analysis:
- Determine if degradation stems from data quality issues, data distribution shifts, or concept drift
- Analyze feature importance changes to identify specific shifted relationships
- Assess whether degradation affects discrimination, calibration, or both [73]
Data Resource Assessment:
- Inventory available recent labeled data
- Evaluate data quality and representativeness
- Determine labeling timeline and costs for additional data collection
Intervention Selection:
- For calibration drift only: Implement threshold adjustment or Platt scaling
- For moderate distribution shifts with limited data: Apply fine-tuning with regularization
- For major concept drift or substantial data: Initiate full retraining pipeline
- For critical applications requiring stability: Deploy ensemble approach
Validation Protocol:
- Hold out temporal validation set from most recent period
- Assess performance on both recent data and original validation set
- Conduct fairness analysis across patient subgroups
- Implement ongoing monitoring with tighter control limits post-correction
This structured approach ensures appropriate matching of correction strategies to specific degradation scenarios while maximizing resource efficiency.
Visualization Frameworks for Monitoring and Correction Workflows
Comprehensive Model Health Monitoring System
The following diagram illustrates an integrated framework for detecting and addressing model performance degradation in clinical settings:
Model Health Monitoring Framework
Correction Strategy Decision Pathway
The following workflow provides a detailed decision pathway for selecting the appropriate correction strategy based on degradation characteristics and available resources:
Correction Strategy Decision Pathway
Maintaining clinical AI models requires specialized tools and methodologies. The table below details key research reagent solutions for implementing effective monitoring and correction protocols.
Table 3: Essential Research Reagent Solutions for Model Maintenance
| Tool Category | Specific Solutions | Primary Function | Implementation Considerations |
|---|---|---|---|
| Drift Detection Libraries | Amazon SageMaker Model Monitor, Evidently AI, Alibi Detect, NannyML | Automated statistical testing for data and model drift | Compatibility with existing MLOps stack; regulatory compliance for healthcare data |
| Performance Monitoring Platforms | Weights & Biases, MLflow, Neptune AI, TensorBoard | Tracking experiment metrics and model performance over time | Integration with clinical data warehouses; HIPAA compliance requirements |
| Data Validation Frameworks | Great Expectations, TensorFlow Data Validation, Deequ | Automated data quality assessment and anomaly detection | Handling of PHI; validation against clinical data standards |
| Model Interpretability Tools | SHAP, LIME, Captum, InterpretML | Explaining model predictions and identifying feature contribution changes | Clinical relevance of explanations; usability for healthcare professionals |
| Continuous Retraining Infrastructure | Kubeflow Pipelines, Apache Airflow, Azure Machine Learning pipelines | Orchestrating end-to-end retraining workflows | Governance and validation requirements for clinical models; version control |
Model shift and performance decay present significant challenges for outcome prediction modeling in patient response to therapy research. The comparison frameworks presented in this guide demonstrate that effective maintenance requires continuous performance monitoring, early degradation detection, and appropriate correction strategies tailored to the specific type and severity of drift encountered. By implementing systematic detection protocols and strategic correction workflows, researchers and drug development professionals can create AI systems that not only demonstrate initial efficacy but maintain their performance and safety throughout their operational lifespan in dynamic clinical environments. As AI becomes increasingly embedded in therapeutic development and clinical decision-making, robust approaches to monitoring and maintenance will become essential components of the research infrastructure, ensuring that predictive models remain accurate, reliable, and clinically valuable over time.
Optimizing Computational Efficiency and Scalability for Large-Scale Data
In the field of outcome prediction modeling for patient response to therapy, researchers face an unprecedented computational challenge. The convergence of multi-omics data, high-throughput drug screening, and complex mechanistic models has created a data deluge that traditional computational approaches cannot efficiently process. For drug development professionals seeking to build accurate predictive models, the scalability and efficiency of computational infrastructures have become as crucial as the biological insights themselves. The paradigm is shifting from simply collecting massive datasets to implementing sophisticated computational frameworks that can extract meaningful patterns within feasible timeframes and resource constraints.
The critical importance of this optimization is underscored by the emergence of precision oncology approaches that leverage patient-derived cell cultures and complex machine learning models to predict individual drug responses. These methodologies require processing highly dimensional data from diverse sources, including genomic profiles, drug sensitivity screens, and clinical outcomes [30]. Similarly, in colorectal liver metastasis research, the integration of deep learning models for prognosis prediction and drug response modeling demands substantial computational resources to analyze multi-omics datasets and identify potential therapeutic candidates [74]. This article provides a comprehensive comparison of computational frameworks and optimization methodologies that enable researchers to overcome these scalability challenges in therapeutic response prediction.
Comparative Analysis of Large-Scale Optimization Algorithms
Interior-Point Methods vs. Newton-Type Algorithms
For researchers handling large-scale nonlinear optimization problems in therapeutic modeling, selecting the appropriate algorithm significantly impacts both computational efficiency and result accuracy. A recent head-to-head evaluation provides insightful performance data comparing the Improved Inexact-Newton–Smart (INS) algorithm against a primal-dual interior-point framework for large-scale nonlinear optimization [75].
Table 1: Performance Comparison of Optimization Algorithms on Synthetic Benchmarks
| Performance Metric | Primal-Dual Interior-Point Method | Improved INS Algorithm | Performance Gap |
|---|---|---|---|
| Iteration Count | Approximately one-third fewer iterations | Higher iteration count | Interior-point method requires 33% fewer iterations |
| Computation Time | Approximately half the computation time | Nearly double the computation time | Interior-point method 50% faster |
| Solution Accuracy | Marginally higher accuracy | Slightly lower accuracy | Interior-point method more precise |
| Convergence Reliability | Stable performance across parameter changes | Sensitive to step length and regularization | Interior-point method more robust |
| Stopping Conditions | Met all primary stopping conditions | Succeeded in fewer cases under default settings | Interior-point method more reliable |
The interior-point method demonstrated superior performance across all key metrics, converging with roughly one-third fewer iterations and about one-half the computation time relative to the INS algorithm while attaining marginally higher accuracy [75]. This performance advantage stems from the interior-point method's transformation of constrained problems into a sequence of barrier subproblems that remain within the feasible region, enabling robust convergence for large-scale, structured models [75].
The INS algorithm, while generally less efficient, showed notable responsiveness to parameter tuning. With moderate regularization and step-length control, its iteration count and runtime decreased substantially, though not sufficiently to close the performance gap with the interior-point approach [75]. This suggests that INS may serve as a configurable alternative when specific problem structures favor its adaptive regularization capabilities, particularly for specialized optimization landscapes encountered in certain therapeutic response modeling scenarios.
Algorithmic Selection Guidelines for Therapeutic Research
The choice between these algorithmic approaches depends heavily on the specific requirements of the therapeutic modeling task:
- For high-dimensional omics data integration, where stability across diverse data types is crucial, interior-point methods provide more reliable convergence.
- For rapid screening applications where approximate solutions may suffice and problem structure is well-defined, tuned INS implementations may offer acceptable performance with potentially faster initial convergence.
- For resource-constrained environments, the stability of interior-point methods reduces the need for extensive computational parameter tuning, ultimately saving researcher time and computational resources.
Drug development professionals should note that interior-point methods have demonstrated particular strength in applications requiring high numerical precision, such as parameter estimation in pharmacokinetic-pharmacodynamic (PKPD) models and optimization of complex neural network architectures for drug response prediction [76] [77].
Scalable Infrastructure for Data-Intensive Therapeutic Research
Computational Demands of Modern Therapeutic Research
The exponential growth in biological data generation has created unprecedented computational requirements for therapeutic research. By 2030, global capital expenditures on data center infrastructure (excluding IT hardware) are expected to exceed $1.7 trillion, largely driven by AI applications in fields including drug discovery and precision medicine [78]. The United States alone will need to more than triple its annual power capacity over the next five years—from 25 gigawatts (GW) of demand in 2024 to more than 80 GW in 2030 to support computational needs for these data-intensive applications [78].
For research institutions and pharmaceutical companies, this escalating demand necessitates a fundamental rethinking of computational infrastructure strategies. Data center campuses are expanding from providing tens of megawatts of power to hundreds, with some even approaching gigawatt scale to support the hybrid facilities that host a mix of AI training, inferencing, and cloud workloads essential for modern therapeutic response prediction research [78].
Efficiency Optimization in Research Computing
The drive toward computational efficiency has become both an economic and practical necessity for research organizations. Modern data centers are now targeting power utilization efficiency (PUE) as low as 1.1, compared with current industry averages of 1.5 to 1.7, representing a substantial improvement in energy efficiency for computational research [78]. These efficiency gains directly impact the feasibility of large-scale therapeutic modeling efforts, particularly for resource-intensive tasks like:
- Cross-validation of predictive models across multiple patient cohorts
- Integration of diverse data modalities including genomic, transcriptomic, and proteomic data
- Simulation of drug response dynamics using complex mechanistic models
- Training of deep learning architectures on multi-omics datasets for response prediction
Adopting innovative design approaches could potentially reduce data center construction timelines by 10-20% and generate savings of 10-20% per facility, thereby increasing the accessibility of high-performance computing resources for therapeutic research organizations [78].
Specialized Computational Methods for Drug Response Prediction
Deep Learning Architectures for Response Prediction
The application of deep learning methods for drug response prediction (DRP) in cancer represents a particularly computationally intensive domain within therapeutic research. These models typically follow the formulation r = f(d, c), where f is an analytical model designed to predict the response r of cancer c to treatment by drug d, implemented through complex neural network architectures trained via backpropagation [77]. The computational burden scales significantly with model complexity, data dimensionality, and the number of compounds screened.
The field has witnessed substantial growth in deep learning-based DRP models, with at least 61 peer-reviewed publications now exploring diverse neural network architectures, feature representations, and learning schemes [77]. These approaches generally involve three computationally intensive components: (1) data preparation involving complex feature representation of drugs and cancers, (2) model development requiring specialized neural network architectures, and (3) performance analysis necessitating robust evaluation schemes [77].
Table 2: Computational Requirements for Deep Learning in Drug Response Prediction
| Model Component | Computational Demand | Key Considerations | Scalability Challenges |
|---|---|---|---|
| Data Preparation | High memory requirements for omics data | Dimensionality reduction techniques essential | Memory scaling with patient cohorts >10,000 |
| Model Training | GPU-intensive training cycles | Architecture selection impacts training time | Training time increases non-linearly with data size |
| Hyperparameter Optimization | Computationally expensive search process | Trade-off between exploration and resources | Combinatorial explosion with model complexity |
| Validation & Testing | Significant inference computation | Cross-validation strategies multiply resource needs | Model evaluation across multiple cell lines/datasets |
Transformational Machine Learning for Precision Oncology
A promising approach for scalable therapeutic response prediction is transformational machine learning (TML), which leverages historical screening data as descriptors to predict drug responses in new patient-derived cell lines [30]. This methodology uses a subset of a drug library as a probing panel, with machine learning models learning relationships between drug responses in historical samples and those in new samples. The trained model then predicts drug responses across the entire library for new cell lines, significantly reducing the experimental burden while maintaining predictive accuracy [30].
In validation studies, this approach has demonstrated excellent performance, with high correlations between predicted and actual drug activities (Rpearman = 0.873 for all drugs, 0.791 for selective drugs) and strong accuracy in identifying top-performing compounds (6.6 out of top 10 predictions correctly identified for all drugs) [30]. The computational efficiency of this method enables researchers to prioritize experimental validation on the most promising candidates, dramatically accelerating the drug discovery process.
Diagram 1: Computational workflow for drug response prediction modeling, illustrating the three major phases of data preparation, model development, and performance analysis that require optimization for large-scale therapeutic research [77].
Distributed Computing Frameworks for Large-Scale Therapeutic Modeling
Multi-Agent Reinforcement Learning for Scalable Decision-Making
As therapeutic models increase in complexity, distributed computing approaches have emerged as essential tools for scalable decision-making. Multi-agent reinforcement learning (MARL) provides a promising framework for distributed AI that decomposes complex tasks across collaborative nodes, enabling the scaling of AI models while maintaining performance [79]. This approach is particularly valuable for modeling complex biological systems where multiple components interact simultaneously, such as tumor microenvironment dynamics or multi-target therapeutic interventions.
The primary challenge in large-scale AI systems lies in achieving scalable decision-making that maintains sufficient performance as model complexity increases. Previous distributed AI technologies suffered from compromised real-world applicability due to massive requirements for communication and sampled data [79]. Recent advances in model-based decentralized policy optimization frameworks have demonstrated superior scalability in systems with hundreds of agents, achieving accurate estimations of global information through local observation and agent-level topological decoupling of global dynamics [79].
Data-Driven Optimization Paradigms
The integration of prediction with decision-making represents another frontier in computational optimization for therapeutic research. Data-driven optimization approaches have revolutionized traditional methods by creating a continuum from predictive modeling to decision implementation [80]. Three key methodologies have emerged as particularly relevant for therapeutic applications:
- Sequential optimization: Traditional approach separating prediction and optimization steps
- End-to-end learning: Integrated models that directly map input data to optimal decisions
- Direct learning: Approaches that bypass explicit prediction to directly learn decision policies
Breakthroughs in implicit differentiation techniques, surrogate loss functions, and perturbation methods have provided methodological guidance for achieving data-driven decision-making through prediction, enabling more efficient optimization of therapeutic intervention strategies [80].
Experimental Protocols and Research Reagent Solutions
Key Experimental Protocols in Computational Therapeutic Research
To ensure reproducibility and facilitate adoption of optimized computational methods, researchers should follow standardized experimental protocols:
Protocol for Benchmarking Optimization Algorithms:
- Problem Formulation: Define large-scale nonlinear optimization problem with specific constraints relevant to therapeutic modeling [75]
- Algorithm Configuration: Implement both interior-point and INS algorithms with appropriate parameter settings [75]
- Performance Metrics: Measure iteration count, computation time, solution accuracy, and convergence reliability [75]
- Sensitivity Analysis: Evaluate algorithm performance across different problem scales and conditioning levels [75]
- Validation: Verify results against known benchmarks and implement stopping conditions based on duality gap metrics [75]
Protocol for Drug Response Prediction Model Development:
- Data Preparation: Process multi-omics data from sources such as CCLE, GDSC, or TCGA, including normalization and batch effect correction [77] [74]
- Feature Representation: Implement appropriate representations for drugs (molecular fingerprints, descriptors) and cancers (genomic features, expression profiles) [77]
- Model Architecture Selection: Choose appropriate neural network architectures based on data characteristics and prediction tasks [77]
- Training & Validation: Implement cross-validation strategies and performance evaluation using metrics such as ROC curves and precision-recall analysis [30] [74]
- Experimental Validation: Conduct in vitro and in vivo assays to confirm computational predictions, such as Transwell assays or mouse models for candidate therapeutics [74]
Essential Research Reagent Solutions
Table 3: Key Computational Research Reagents for Therapeutic Response Modeling
| Resource Category | Specific Tools & Databases | Primary Function | Application in Therapeutic Research |
|---|---|---|---|
| Drug Sensitivity Databases | GDSC, CTRP, PRISM, CCLE [74] | Provide drug response data (e.g., IC50 values) across cancer cell lines | Training and validation of drug response prediction models |
| Genomic Data Repositories | TCGA, GEO, NCI GDC [74] | Host multi-omics data from patient samples and cell lines | Feature generation for predictive modeling |
| Deep Learning Frameworks | TensorFlow/Keras, PyTorch [77] | Enable implementation of complex neural network architectures | Building and training drug response prediction models |
| Optimization Libraries | Specialized implementations of interior-point and Newton-type algorithms [75] | Solve large-scale nonlinear optimization problems | Parameter estimation and model fitting in therapeutic applications |
| High-Performance Computing Infrastructure | Scalable data centers with advanced cooling technologies [78] | Provide computational resources for data-intensive tasks | Running large-scale simulations and complex model trainings |
Diagram 2: Distributed multi-agent learning architecture for scalable therapeutic modeling, demonstrating how complex computational tasks can be decomposed across collaborative nodes to improve efficiency and scalability [79].
The efficient optimization of computational resources has become an indispensable component of modern therapeutic response prediction research. As the field continues to grapple with increasingly complex and large-scale datasets, the strategic implementation of optimized algorithms, scalable infrastructure, and distributed computing frameworks will determine the pace of advancement in personalized medicine. The comparative analysis presented here provides researchers and drug development professionals with evidence-based guidance for selecting computational approaches that maximize efficiency while maintaining scientific rigor.
The integration of interior-point optimization methods, deep learning architectures specifically designed for drug response prediction, and scalable multi-agent reinforcement learning frameworks creates a powerful toolkit for addressing the most computationally challenging problems in therapeutic research. By adopting these optimized computational strategies and leveraging the experimental protocols and research reagents outlined in this review, researchers can significantly accelerate the development of predictive models for patient response to therapy, ultimately advancing the frontier of precision medicine and improving patient outcomes through more targeted and effective therapeutic interventions.
Benchmarking Performance and Ensuring Clinical Readiness
In outcome prediction modeling for patient response to therapy, validation is the process of assessing whether a model's predictions are accurate and reliable enough to support clinical decisions [81]. For researchers and drug development professionals, understanding the distinctions between internal, external, and temporal validation is fundamental to developing robust, clinically applicable models. Each framework serves a distinct purpose in the model lifecycle, from initial development to real-world implementation, and addresses different threats to a model's validity [82].
Validation ensures that a predictive tool does not merely capture patterns in the specific dataset used for its creation but can generate trustworthy predictions for new patients. This is particularly critical in therapeutic research, where models may influence treatment selection, patient stratification, or clinical trial design. The choice of validation strategy directly impacts the evidence base for a model's readiness for deployment in specific clinical contexts [83].
Comparative Analysis of Validation Frameworks
The table below provides a structured comparison of the three core validation frameworks, highlighting their distinct objectives, methodologies, and interpretations.
| Feature | Internal Validation | External Validation | Temporal Validation |
|---|---|---|---|
| Core Question | Is the model reproducible and not overfit to its development data? [81] | Does the model generalize to a different population or setting? [81] [82] | Does the model remain accurate over time at the original location? [82] |
| Core Methodology | Bootstrapping, Cross-validation [84] [81] [82] | Validation on data from a different location or center [85] [82] | Validation on data from the same location but a later time period [82] |
| Key Performance Aspects | Optimism-corrected discrimination and calibration [81] | Transportability of discrimination and calibration [85] [81] | Model stability; detection of performance decay due to "temporal drift" [82] |
| Interpretation of Results | Estimates performance in the underlying development population. A necessary first step [84]. | Assesses performance heterogeneity across locations. Not a single "yes/no" event [85] [86]. | Evidence for model's operational durability in a changing clinical environment [82]. |
| Primary Stakeholders | Model developers [82] | Clinical end-users at new sites; manufacturers; governing bodies [82] | Clinicians and hospital administrators at the implementing institution [82] |
| Role in Model Pipeline | Essential for any model development to quantify overfitting [84]. | Assesses transportability before broader implementation [81] [83]. | Required for ongoing monitoring and deciding when to update or retire a model [82]. |
Key Quantitative Metrics for Model Evaluation
Regardless of the validation framework, model performance is assessed using quantitative metrics that evaluate different aspects of predictive accuracy. The following table summarizes the key metrics used across therapeutic prediction research.
| Metric Category | Specific Metric | What It Measures | Interpretation in a Therapeutic Context |
|---|---|---|---|
| Discrimination | C-statistic (AUC) [81] | The model's ability to distinguish between patients with and without the outcome (e.g., responders vs. non-responders). | A value of 0.5 is no better than chance; 0.7-0.8 is considered acceptable; >0.8 is strong [85]. |
| Calibration | Calibration-in-the-large [81] | The agreement between the average predicted risk and the average observed outcome incidence. | A value >0 suggests the model overestimates risk on average; <0 suggests underestimation [85]. |
| Calibration | Calibration Slope [85] | The agreement across the range of predicted risks. | A slope of 1 is ideal; <1 suggests predictions are too extreme; >1 suggests predictions are not extreme enough [85]. |
| Clinical Usefulness | Net Benefit [81] | The clinical value of the model's predictions, weighing true positives against false positives, based on decision consequences. | Used to compare the model against "treat all" or "treat none" strategies across different probability thresholds [81]. |
Experimental Protocols for Validation
A robust validation strategy involves specific, well-established methodological protocols. The workflows below detail the standard procedures for implementing the core validation frameworks.
Internal Validation Protocol
Workflow Title: Internal Validation via Bootstrapping
The bootstrap procedure, the preferred method for internal validation, involves the following steps [84] [81]:
- Resampling: Draw a large number (e.g., 500-2000) of bootstrap samples from the original development dataset. Each sample is the same size as the original dataset, created by sampling patients with replacement.
- Model Development and Testing: For each bootstrap sample, develop a new model following the exact same steps (including any variable selection) as the original model. Then, test this model on the original dataset.
- Optimism Calculation: Calculate the optimism for each bootstrap sample as the performance on the bootstrap sample (apparent performance) minus the performance on the original dataset (test performance).
- Performance Adjustment: Average the optimism estimates from all iterations. Subtract this average optimism from the apparent performance of the original model to obtain an optimism-corrected performance estimate.
This protocol provides a reliable estimate of how the model is expected to perform in new samples from the same underlying population, correcting for the overoptimism that arises from model overfitting [84].
External & Temporal Validation Protocol
Workflow Title: External and Temporal Validation Workflow
The protocol for external and temporal validation focuses on testing the model on entirely new data [85] [82]:
- Validation Data Acquisition: Obtain a dataset that is external to the model's development data. For geographical validation, this data must come from a different hospital, region, or country. For temporal validation, the data should come from the same institution(s) but from a later, subsequent time period.
- Model Application: Apply the original, untrained model (with its pre-specified coefficients or parameters) to the new validation dataset to generate predictions.
- Performance Evaluation: Calculate performance metrics for discrimination (e.g., C-statistic) and calibration (e.g., calibration-in-the-large, calibration slope) on the validation dataset. For clinical usefulness, the Net Benefit should be calculated [81].
- Assessment of Heterogeneity/Stability: The core of the analysis involves comparing performance between the development and validation settings, or across multiple validation cohorts. Significant degradation in calibration indicates the model may not be directly transportable and requires updating [85]. For temporal validation, a "waterfall" design can be used, repeatedly testing the model on progressively newer data to monitor performance decay [82].
The Scientist's Toolkit: Essential Reagents for Validation
Successful execution of validation studies requires both methodological rigor and appropriate tools. The table below lists key conceptual and practical "reagents" essential for researchers in this field.
| Tool Category | Specific Tool/Technique | Primary Function |
|---|---|---|
| Statistical Software | R, Python | Provides the computational environment for implementing bootstrapping, cross-validation, and performance metric calculation [84] [81]. |
| Resampling Methods | Bootstrapping, Cross-Validation | The core engine for internal validation, used to estimate and correct for model optimism [84] [82]. |
| Performance Metrics | C-statistic, Calibration Plot, Net Benefit | Standardized measures to quantify a model's discrimination, calibration, and clinical value [81]. |
| Validation Framework | Internal-External Cross-Validation | A hybrid design used in multi-center studies where models are developed on all but one center and validated on the left-out center, iteratively [84] [82]. |
| Model Updating Methods | Recalibration, Model Revision | Techniques to adjust a model that fails in external validation, ranging from updating the intercept (recalibration) to re-estimating predictor effects (revision) [81]. |
| Reporting Guideline | TRIPOD/TRIPOD-AI | A checklist to ensure transparent and complete reporting of prediction model studies, including validation [84] [82]. |
Internal, external, and temporal validation are complementary frameworks that together build the evidence base for a prediction model's utility in patient response to therapy research. Internal validation is a non-negotiable first step that guards against overfitting. External validation investigates a model's transportability across geography and clinical domains, while temporal validation is crucial for ensuring a model's longevity and relevance in the face of evolving clinical practice.
A critical insight for researchers is that a model is never "fully validated" [85]. Instead, the goal is "targeted validation"—accumulating evidence of adequate performance for a specific intended use in a specific population and setting [83]. A principled, multi-faceted validation strategy is therefore indispensable for transforming a statistical model into a reliable tool that can genuinely support therapeutic decision-making.
In the field of patient response to therapy research, the successful implementation of clinical prediction models hinges on the rigorous evaluation of three cornerstone performance metrics: discrimination, calibration, and clinical utility. These metrics are indispensable for researchers and drug development professionals to validate the reliability, accuracy, and practical impact of prognostic tools before they can be translated into clinical practice or used to stratify patients in clinical trials.
The table below summarizes the core definitions and common measures for each of these key metrics.
| Metric | Definition | Common Measures & Assessments |
|---|---|---|
| Discrimination | The model's ability to distinguish between patients who do and do not experience the outcome of interest (e.g., response vs. non-response to a therapy) [87]. | Area Under the Receiver Operating Characteristic Curve (AUROC) [87] [1]. Values range from 0.5 (no discrimination) to 1.0 (perfect discrimination). |
| Calibration | The agreement between the predicted probabilities of an outcome generated by the model and the actual observed outcomes in the population [87]. | Calibration-in-the-large (assesses overall over- or under-prediction), Calibration plots [87]. Poor calibration requires recalibration for the target population [87]. |
| Clinical Utility | The degree to which a prediction model improves decision-making and leads to better patient outcomes and more efficient resource allocation in a real-world clinical setting [87]. | Decision Curve Analysis (DCA) [87]. Quantifies the net benefit of using the model across different threshold probabilities for clinical intervention. |
Comparative Performance in Practice: A Validation Case Study
A 2025 external validation study of two models predicting cisplatin-associated acute kidney injury (C-AKI) provides a concrete example of how these metrics are applied and compared [87]. This study evaluated models by Motwani et al. and Gupta et al. in a Japanese cohort, offering a template for model comparison.
Experimental Protocol & Performance Data
- Objective: To evaluate and compare the external validity of the Motwani and Gupta C-AKI prediction models in a population different from their original development cohorts [87].
- Cohort: A retrospective cohort of 1,684 patients treated with cisplatin at a single Japanese university hospital [87].
- Outcome Definitions:
- Methodology: The performance of each model was assessed for discrimination (AUROC), calibration, and clinical utility (Decision Curve Analysis). Logistic recalibration was also performed to adapt the models to the local population [87].
The quantitative results from this validation study are summarized in the table below.
| Model / Metric | Discrimination for C-AKI (AUROC) | Discrimination for Severe C-AKI (AUROC) | Calibration (Pre-Recalibration) | Net Benefit (from DCA) |
|---|---|---|---|---|
| Motwani et al. | 0.613 [87] | 0.594 [87] | Poor [87] | Lower than Gupta model for severe C-AKI [87] |
| Gupta et al. | 0.616 [87] | 0.674 [87] | Poor [87] | Highest clinical utility for severe C-AKI [87] |
| Recalibrated Models | - | - | Improved [87] | Greater net benefit [87] |
Key Findings and Implications
The case study demonstrates that while the models showed similar discriminatory ability for general C-AKI, the Gupta model was significantly superior for predicting severe C-AKI, a clinically more critical outcome [87]. Furthermore, the poor initial calibration of both models underscores that high discrimination does not guarantee accurate probability estimates, and recalibration is an essential step before clinical implementation in a new population [87]. Finally, DCA confirmed that the Gupta model provided the greatest net benefit for predicting severe C-AKI, highlighting its superior clinical utility for this specific purpose [87].
Model Evaluation Workflow
Successfully navigating the evaluation of prediction models requires a suite of methodological tools and resources. The following toolkit outlines key solutions for conducting robust validation studies.
Research Toolkit Components
Research Reagent Solutions for Performance Evaluation
| Tool / Resource | Function in Evaluation |
|---|---|
| R or Python (scikit-learn) | Statistical computing environments used to calculate AUROC, create calibration plots, and perform statistical tests for comparing models [87]. |
| Decision Curve Analysis (DCA) | A specific methodological tool to quantify the clinical utility of a model by integrating the relative harms of false positives and false negatives, providing an estimate of net benefit [87]. |
| TRIPOD+AI Guidelines | A reporting framework that ensures transparent and complete reporting of clinical prediction models, which is essential for critical appraisal and replication [88]. |
| Algorithmic Fairness Metrics | A set of quantitative tools (e.g., equalized odds, predictive parity) used to evaluate potential performance disparities across different demographic groups (e.g., sex, race/ethnicity) to ensure equitable application [89]. |
The pathway to trustworthy and effective patient response prediction models in therapy research is paved with the rigorous assessment of discrimination, calibration, and clinical utility. As demonstrated, these metrics provide complementary insights: a model with excellent discrimination can still be clinically useless if poorly calibrated, and a well-calibrated model must demonstrate superior net benefit over simple alternative strategies to warrant adoption. For researchers and drug developers, a comprehensive evaluation strategy that includes external validation, recalibration for new populations, and a critical analysis of fairness is not just a best practice—it is a fundamental requirement for building models that can genuinely advance personalized medicine and therapeutic outcomes.
Comparative Analysis of Machine Learning and Deep Learning Algorithms
In the evolving field of therapeutic outcome prediction, selecting the appropriate algorithmic approach is a critical determinant of research success. Machine Learning (ML) and Deep Learning (DL), while both branches of artificial intelligence, offer distinct capabilities and limitations for modeling patient responses to therapy [90]. The choice between these paradigms impacts not only predictive accuracy but also practical considerations around data requirements, computational resources, and interpretability—factors of paramount importance in clinical research and drug development [91].
This comparative analysis examines ML and DL algorithms specifically within the context of patient response prediction, synthesizing evidence from recent healthcare applications to guide researchers in selecting optimal methodologies for their specific therapeutic contexts.
Fundamental Conceptual Differences
ML and DL differ fundamentally in their learning approaches and architectural complexity. ML algorithms typically require researchers to predefine and engineer relevant features from input data, whereas DL algorithms automatically learn hierarchical feature representations directly from raw data through multiple neural network layers [91].
Machine Learning Approach
Machine learning employs simpler, more interpretable algorithms to identify patterns in data. These include linear models, decision trees, random forests, and support vector machines (SVMs) [90]. In healthcare applications, ML models effectively analyze structured clinical data, demographic information, and pre-selected biomarkers to predict treatment outcomes [92]. Their relative architectural simplicity enables faster training times and lower computational requirements, making them accessible with standard computing infrastructure [90].
Deep Learning Approach
Deep learning utilizes artificial neural networks with multiple hidden layers that mimic human brain functions to analyze data with high dimensionality [90]. Architectures such as Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs), Long Short-Term Memory (LSTM) networks, and Transformers excel at processing complex, unstructured data types including medical images, clinical free-text notes, and physiological signals [93] [94]. This capability makes DL particularly suited for applications requiring automatic feature extraction from raw, high-dimensional inputs [90].
Comparative Performance in Healthcare Applications
Predictive Performance in Mental Health Treatment Response
Substantial evidence demonstrates the application of both ML and DL in predicting patient responses to therapies, particularly in mental health disorders. A systematic review and meta-analysis of ML applications for predicting treatment response in emotional disorders (including depression and anxiety) revealed an average prediction accuracy of 0.76, with an area under the curve (AUC) average of 0.80 across 155 studies [3]. These models utilized various data types, with studies incorporating neuroimaging predictors demonstrating higher accuracy compared to those using only clinical and demographic data [3].
In direct comparative studies, conventional ML algorithms have demonstrated competitive performance against more complex DL models for specific data types. A systematic review on machine learning approaches for predicting therapeutic outcomes in Major Depressive Disorder (MDD) identified Random Forest (RF) and Support Vector Machine (SVM) as the most frequently used ML methods [95]. Models integrating multiple categories of patient data demonstrated higher predictive accuracy than single-category models [95].
Table 1: Comparative Performance of ML and DL in Treatment Response Prediction
| Study Focus | Best Performing Algorithms | Performance Metrics | Data Characteristics |
|---|---|---|---|
| Emotional Disorders Treatment Response [3] | Multiple ML Models | Mean accuracy: 0.76, Mean AUC: 0.80 | Clinical, demographic, and neuroimaging data from 155 studies |
| Mental Illness Prediction from Clinical Notes [94] | CB-MH (Custom DL) vs. SVM (ML) | DL F1: 0.62, ML F1: Not specified | 150,085 clinical notes; free-text descriptions |
| Alzheimer's Disease Prediction [96] | Logistic Regression (ML) with mRMR feature selection | Accuracy: 99.08% | Longitudinal dataset of 150 people |
| Cerebral Aneurysm Treatment Outcome [96] | Extreme Gradient Boosting (XGBoost) | AUC ROC: 0.72 ± 0.03 | Dataset of 344 patients' preoperative characteristics |
For mental illness prediction from free-text clinical notes, a comprehensive comparison of seven DL and two conventional ML models demonstrated that a custom DL architecture (CB-MH) incorporating multi-head attention achieved the best F1 score (0.62), while another attention model performed best for F2 (0.71) [94]. This study utilized 150,085 psychiatry clinical notes spanning 10 years, providing robust evidence for DL's capabilities with unstructured textual data [94].
Performance in Time-Series and High-Stationarity Data
Beyond healthcare-specific applications, comparative analyses in other domains provide insights relevant to therapeutic monitoring and longitudinal outcome tracking. Research on high-stationarity data (characterized by consistent statistical properties over time) has demonstrated that ML algorithms can outperform DL models for certain prediction tasks [97].
A vehicle flow prediction study found that the XGBoost algorithm (ML) outperformed RNN-LSTM (DL) and other competitors, particularly in terms of MAE and MSE metrics [97]. This highlights how shallower algorithms can sometimes achieve better adaptation to specific time-series patterns compared to deeper models that may develop smoother, less accurate predictions [97].
Table 2: Algorithm Performance Across Data Types and Domains
| Data Type | Best Performing Algorithm | Key Findings | Domain |
|---|---|---|---|
| Highly Stationary Time-Series [97] | XGBoost (ML) | Outperformed RNN-LSTM in prediction accuracy | Vehicle flow prediction |
| Financial Time-Series [98] | LSTM (DL) | R-squared: 0.993 with 60-day window | Market price forecasting |
| Medical Imaging [96] | Ensemble Deep Learning | Over 90% accuracy in gastric cancer detection | Medical diagnostics |
| Physiological Signals [96] | Custom Deep Learning | Mean absolute error of 2 breaths/min at 7s window | Respiratory rate estimation |
Conversely, in financial market prediction—a domain with complex temporal dependencies—LSTM networks have demonstrated superiority over both Support Vector Regression (SVR) and basic RNNs, achieving an R-squared value of 0.993 when using a 60-day window with technical indicators [98]. This suggests DL's advantage in capturing complex temporal patterns in noisy, non-stationary environments.
Methodological Considerations for Therapeutic Outcome Prediction
Data Requirements and Feature Engineering
The fundamental differences in data requirements between ML and DL significantly impact their applicability in therapeutic research settings. ML algorithms generally achieve optimal performance with smaller, structured datasets and benefit substantially from domain knowledge-driven feature selection [90] [92]. For instance, in predicting antidepressant treatment response, ML models effectively incorporate clinically relevant features such as demographic characteristics, symptom severity scores, genetic markers, and neuroimaging data [95].
In contrast, DL models require large volumes of data (often thousands to millions of examples) to effectively train their numerous parameters and avoid overfitting [90]. However, they automatically learn relevant features from raw data, reducing the need for manual feature engineering [91]. This capability makes DL particularly valuable for analyzing complex biomedical data types such as medical images [93], raw text from clinical notes [94], and physiological signals [96].
Interpretability and Explainability
Interpretability remains a crucial consideration in healthcare applications, where understanding model decisions is often as important as prediction accuracy itself. ML models generally offer superior interpretability; their decision-making processes can typically be traced and understood by humans [90]. For example, linear models provide clear coefficient estimates, while decision trees offer transparent branching logic—features essential for clinical adoption and regulatory approval [92].
DL models, particularly those with deep and complex architectures, often function as "black boxes" with limited interpretability [90]. The intricate web of nonlinear transformations in deep neural networks makes pinpointing the exact reasons for specific decisions challenging [90]. This opacity poses significant challenges in healthcare contexts where regulatory compliance and ethical considerations require clear justification of algorithmic decisions [92]. Nevertheless, emerging explainable AI techniques such as Integrated Gradients are being applied to illuminate DL model decisions in mental health prediction [94].
Computational Resource Requirements
Computational demands represent another critical differentiator between ML and DL approaches. ML can typically run on lower-end hardware, making it more accessible and cost-effective for research settings with limited infrastructure [90]. Most ML tasks can be performed on standard CPUs without specialized processing units [90].
DL training necessitates advanced hardware—primarily GPUs or TPUs—to manage the significant computational demands of training expansive neural networks [90] [91]. The intensive computational requirements stem from the need to perform numerous matrix multiplications quickly, which GPUs and TPUs are specially designed to handle [90]. This hardware dependency increases both the financial cost and technical complexity of DL implementation [91].
Table 3: Resource Requirements and Methodological Considerations
| Parameter | Machine Learning | Deep Learning |
|---|---|---|
| Data Requirements | Effective with smaller datasets (thousands of data points) [90] | Requires large datasets (thousands to millions of examples) [90] |
| Feature Engineering | Manual feature engineering required [91] | Automatic feature extraction from raw data [91] |
| Hardware Dependencies | Can run on standard CPUs [90] | Requires GPUs/TPUs for efficient training [90] [91] |
| Training Time | Shorter (seconds to hours) [90] | Longer (hours to weeks) [90] |
| Interpretability | Generally more interpretable [90] | Often acts as "black box" [90] |
| Implementation Cost | More economical [90] | More expensive due to hardware and data needs [90] |
Experimental Protocols for Algorithm Comparison
Mental Health Prediction from Clinical Text Protocol
A rigorous comparison methodology for mental illness prediction from free-text clinical notes exemplifies robust experimental design in healthcare ML/DL research [94]:
Dataset: 150,085 de-identified clinical notes from psychiatry outpatient visits over 10 years, with ICD-9 diagnosis codes grouped into 8 categories including Unipolar Depression (51%), Anxiety Disorders (23%), and Substance Use Disorders (19%) [94].
Data Splitting: Patient-level split with 65% training, 15% validation, and 20% testing sets, ensuring all records from a single patient resided in only one split [94].
Compared Models:
- Conventional ML: SVM, Logistic Regression
- DL Models: LSTM, BiLSTM, CNN, CNN-BiLSTM, BERT, attention-enhanced variants
- Custom DL: CB-MH (Convolution BiLSTM with Multi-Headed attention)
Evaluation Metrics: F1 and F2 scores, with detailed error analysis using Integrated Gradients interpretability method [94].
This protocol highlights the importance of appropriate data splitting (patient-level rather than note-level), comprehensive model comparison, and thorough error analysis in therapeutic prediction research.
Treatment Response Prediction for Emotional Disorders Protocol
A systematic review and meta-analysis established methodological standards for evaluating prediction models in emotional disorders [3]:
Literature Search: Comprehensive search across PubMed and PsycINFO (2010-2025) following PRISMA guidelines, identifying 155 studies meeting inclusion criteria [3].
Data Extraction: Standardized extraction of sample size, treatment type, predictor modalities, ML methods, and prediction accuracy metrics [3].
Quality Assessment: Evaluation of cross-validation robustness, with moderator analyses indicating that studies using more robust cross-validation procedures exhibited higher prediction accuracy [3].
Performance Synthesis: Meta-analytic techniques to synthesize findings and identify moderators of prediction accuracy, including the impact of neuroimaging predictors versus clinical and demographic data alone [3].
Research Workflow and Algorithm Selection Framework
The following diagram illustrates a systematic workflow for selecting and evaluating ML versus DL approaches in therapeutic outcome prediction research:
Table 4: Essential Research Resources for ML/DL in Therapeutic Prediction
| Resource Category | Specific Tools & Techniques | Application in Therapeutic Prediction |
|---|---|---|
| ML Algorithms | Random Forest, SVM, XGBoost, Logistic Regression [95] | Structured data analysis, clinical-demographic prediction [3] [95] |
| DL Architectures | CNN, RNN, LSTM, BERT, Transformer [94] | Medical imaging, clinical text, time-series data [93] [94] |
| Interpretability Methods | Integrated Gradients, SHAP, Attention Weights [94] | Model decision explanation, biomarker identification [94] |
| Validation Frameworks | Time-series cross-validation, Patient-level splitting [94] | Robust performance estimation, prevention of data leakage [94] |
| Data Modalities | Clinical records, Neuroimaging, Genetic markers, Clinical text [3] [95] | Multimodal predictor integration for enhanced accuracy [3] [95] |
| Computational Infrastructure | CPU clusters, GPU accelerators (for DL) [90] [91] | Model training and experimentation [90] |
The comparative analysis of machine learning and deep learning algorithms for therapeutic outcome prediction reveals a context-dependent landscape without universal superiority of either approach. ML algorithms, particularly Random Forest, SVM, and XGBoost, demonstrate strong performance with structured clinical data, offering advantages in interpretability, computational efficiency, and implementation with smaller sample sizes [95]. These characteristics make ML particularly suitable for research settings with limited data availability or where model interpretability is prioritized for clinical translation.
Conversely, DL architectures excel with complex, high-dimensional data types including medical images, clinical free-text, and physiological signals [93] [96] [94]. Their capacity for automatic feature extraction reduces manual engineering efforts and can uncover subtle patterns inaccessible to conventional methods [91]. However, these advantages come with substantial computational requirements and increased model opacity that may challenge regulatory approval and clinical adoption [90] [92].
The emerging paradigm for optimal therapeutic outcome prediction increasingly leverages hybrid approaches that combine the strengths of both methodologies [91]. Such integrated frameworks may employ DL for initial feature extraction from raw data streams, with ML models providing interpretable predictions for clinical decision support. Future advances will likely focus on enhancing DL interpretability, developing efficient learning techniques for data-limited scenarios, and establishing robust validation frameworks that ensure reliable performance across diverse patient populations—critical steps toward translating algorithmic predictions into improved therapeutic outcomes.
Assessing Real-World Impact and Generalizability Across Populations
For researchers in precision psychiatry and drug development, a central challenge is that machine learning models demonstrating excellent performance in controlled research cohorts often fail when applied to the diverse populations and settings encountered in real-world clinical practice [99]. This limitation directly impacts the development of robust outcome prediction models for patient response to therapy. Concerns about generalizability arise partly from sampling effects and data disparities between research cohorts and real-world populations [99]. Traditionally, randomized controlled trials (RCTs) have been the gold standard for clinical evidence generation, yet they typically involve highly selective patient populations that don't fully represent real-world diversity [100] [101]. The integration of real-world data (RWD) and advanced analytical approaches like causal machine learning (CML) is creating new paradigms for developing more generalizable predictive models that maintain performance across diverse populations and healthcare settings [102] [103].
Performance Comparison of Prediction Modeling Approaches
Different methodological approaches to outcome prediction modeling demonstrate varying strengths and limitations regarding real-world impact and generalizability. The table below summarizes the comparative performance of traditional RCT-based models, RWD-enabled models, and emerging CML approaches.
Table 1: Performance comparison of prediction modeling approaches for patient response to therapy
| Modeling Approach | Generalizability Strength | Data Sources | Key Limitations | Representative Performance Metrics |
|---|---|---|---|---|
| Traditional RCT-Based Models | Low (Highly selective populations) [101] | Controlled clinical trial data [100] | Limited diversity, artificial settings [100] [101] | Internal validity high, external validity often low [101] |
| RWD-Enabled Predictive Models | Moderate-High (Diverse real-world populations) [99] [104] | EHRs, claims data, registries, wearables [100] [104] | Data quality variability, confounding [100] [102] | Depression severity prediction: r=0.48-0.73 across sites [99] |
| Causal Machine Learning (CML) | High (When properly validated) [102] | Combined RCT & RWD [102] | Methodological complexity, computational demands [102] | Colorectal cancer trial emulation: 95% concordance for subgroup response [102] |
Key Experimental Evidence for RWD Model Generalizability
A multi-cohort study investigating the generalizability of clinical prediction models in mental health provides compelling evidence for RWD-enabled approaches [99]. Researchers developed a sparse machine learning model using only five easily accessible clinical variables (global functioning, extraversion, neuroticism, emotional abuse in childhood, and somatization) to predict depressive symptom severity [99]. When tested across nine external samples comprising 3,021 participants from ten European research and clinical settings, the model reliably predicted depression severity across all samples (r = 0.60, SD = 0.089, p < 0.0001) and in each individual external sample, with performance ranging from r = 0.48 in a real-world general population sample to r = 0.73 in real-world inpatients [99]. These results demonstrate that models trained on sparse clinical data can potentially predict illness severity across diverse settings.
Experimental Protocols for Generalizable Model Development
Sparse Clinical Prediction Model Development
The following workflow details the methodology used in the multi-cohort mental health prediction study [99]:
Figure 1: Experimental workflow for developing a generalizable clinical prediction model.
Key methodological details: The study used an elastic net algorithm with ten-fold cross-validation applied to develop a sparse machine learning model [99]. The cross-validation procedure randomly reshuffled the data, separated the dataset into 10 non-overlapping folds, and used 9 subsets for training, repeating the process until each subset was left out once for testing [99]. This process was repeated ten times to reduce the impact of the initial random data split, resulting in 100 total models fit to the 10 folds by 10 repeats [99]. Missing values were imputed using the median of the training set within the cross-validation procedure to preserve the independence of training and test sets [99].
Causal Machine Learning Approach
Causal machine learning integrates machine learning algorithms with causal inference principles to estimate treatment effects and counterfactual outcomes from complex, high-dimensional RWD [102]. The following workflow illustrates a typical CML analytical pipeline:
Figure 2: Causal machine learning workflow for generalizable treatment effect estimation.
Key methodological details: CML approaches use several advanced techniques to enhance generalizability. Doubly robust estimation combines propensity score and outcome models to provide unbiased effect estimates even if one model is misspecified [102]. Propensity score weighting uses machine learning methods (boosting, tree-based models, neural networks) to better handle non-linearity and complex interactions when estimating propensity scores compared to traditional logistic regression [102]. Trial emulation frameworks like the R.O.A.D. framework apply prognostic matching and cost-sensitive counterfactual models to correct biases and identify subgroups with high concordance in treatment response [102].
Table 2: Key reagents, data sources, and analytical tools for generalizable prediction modeling
| Resource Category | Specific Examples | Research Application | Generalizability Utility |
|---|---|---|---|
| Real-World Data Sources | Electronic Health Records (EHRs) [100] [104], Insurance claims data [100], Disease registries [100], Wearable devices [100] | Provides longitudinal patient journey data, treatment patterns, outcomes in diverse populations [104] | Captures broader patient diversity including elderly, comorbidities, underrepresented groups [101] |
| Analytical Frameworks | Elastic net regression [99], Causal machine learning [102], Propensity score methods [102] | Handles correlated predictors, confounding adjustment, treatment effect estimation [99] [102] | Enables transportability of findings across populations, settings [102] |
| Validation Tools | Ten-fold cross-validation [99], External validation across multiple sites [99], Synthetic control arms [100] | Internal and external validation, performance assessment across populations [99] | Directly tests generalizability across diverse settings, populations [99] |
| Software Platforms | PHOTONAI [99], Targeted learning platforms [102], Truveta Data [104] | Model development, analysis of large-scale RWD, standardized analytics [99] [104] | Facilitates multi-site collaboration, standardized analysis across datasets [104] |
Discussion and Future Directions
The expanding role of RWD and advanced analytical methods is transforming outcome prediction modeling for therapeutic response. Regulatory bodies are increasingly recognizing the value of RWE, with the FDA utilizing RWD to grant approval for new drug indications in some cases [101]. The emerging "Clinical Evidence 2030" vision emphasizes including patients at the center of evidence generation and embracing the full spectrum of data and methods, including machine learning [103]. Future directions include greater integration of large language models (LLMs) in clinical workflows [105], though current real-world adoption remains constrained by systemic, technical, and regulatory barriers [105]. Additionally, causal machine learning approaches continue to evolve, offering enhanced capabilities for estimating treatment effects that generalize across populations [102]. For researchers developing outcome prediction models for patient response to therapy, the strategic integration of RWD with robust validation across diverse populations and settings represents a critical path toward enhanced generalizability and real-world impact.
Conclusion
The development of robust outcome prediction models is a multifaceted process that extends beyond achieving high statistical performance. Success hinges on using large, representative datasets to ensure stability, rigorously validating models across diverse settings to guarantee generalizability, and proactively planning for model monitoring to combat performance decay in dynamic clinical environments. Future efforts must focus on the seamless integration of these tools into clinical workflows, the demonstration of tangible improvements in patient outcomes, and the ongoing commitment to developing fair and equitable models that serve all patient populations effectively. The convergence of larger datasets, more sophisticated yet interpretable algorithms, and a focus on real-world clinical utility will define the next generation of predictive therapeutics.
References
- 1. Machine learning approaches in the therapeutic outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12381684/]
- 2. Development of the treatment prediction model in ... [https://www.nature.com/articles/s44184-025-00136-8]
- 3. Machine learning in the prediction of treatment response ... [https://www.sciencedirect.com/science/article/pii/S0272735825000595]
- 4. Evaluating PREDICT and developing outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006220/]
- 5. Predicting Therapy Outcomes in Patients With Stress ... [https://www.researchprotocols.org/2025/1/e65790]
- 6. 8 Predictions for the Health Data Industry in 2025 [https://www.datavant.com/real-world-data-rwd/8-predictions-for-the-health-data-industry-in-2025]
- 7. Article When accurate prediction models yield harmful self ... [https://www.sciencedirect.com/science/article/pii/S2666389925000777]
- 8. Predictive Healthcare 2025: Transforming Patient Outcomes [https://www.omdena.com/blog/predictive-healthcare-2025]
- 9. FDA 真实世界证据:其真正含义是什么以及它如何发挥作用? [https://namsa.com/zh-CN/resources/blog/fda-real-world-evidence/]
- 10. 用真实世界数据助推医保价值购买 [https://www.nhsa.gov.cn/art/2025/7/21/art_14_17339.html]
- 11. 药物I期临床试验管理指导原则-2025年6月 [http://www.szsdsrmyy.com/kxyj/gjywlcsyjg/zcfg/content/post_1578652.html]
- 12. 2025年确保临床研究中的数据完整性 [https://veedalifesciences.com/zh-CN/data-integrity-in-clinical-research/]
- 13. 综述:人工智能驱动的癌症支持系统和生物标志物开发的真实 ... [https://www.ebiotrade.com/newsf/2025-5/20250509175833815.htm]
- 14. 进步,而不仅仅是预测:2025年重症监护医学对数据科学的展望 [https://www.ebiotrade.com/newsf/2025-10/20251008170839702.htm]
- 15. 數據驅動與精準醫療引領腫瘤學未來方向 [https://geneonline.news/%E6%95%B8%E6%93%9A%E9%A9%85%E5%8B%95%E8%88%87%E7%B2%BE%E6%BA%96%E9%86%AB%E7%99%82%E5%BC%95%E9%A0%98%E8%85%AB%E7%98%A4%E5%AD%B8%E6%9C%AA%E4%BE%86%E6%96%B9%E5%90%91/]
- 16. Nat Med:2025年影响医学发展的11项临床试验 [https://www.medsci.cn/article/show_article.do?id=778e858089b1]
- 17. Comparative analysis of integrative classification methods for multi-omics data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11234228/]
- 18. Integrating Clinical and Multiple Omics Data for Prognostic Assessment across Human Cancers | Scientific Reports [https://www.nature.com/articles/s41598-017-17031-8]
- 19. Multi-omics Data Integration, Interpretation, and Its Application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 20. Algorithms and tools for data-driven omics integration to achieve multilayer biological insights: a narrative review | Journal of Translational Medicine [https://link.springer.com/article/10.1186/s12967-025-06446-x]
- 21. Predicting Undesired Treatment Outcomes With Machine ... [https://medinform.jmir.org/2023/1/e44322]
- 22. An efficient patient's response predicting system using ... [https://www.nature.com/articles/s41598-025-00401-y]
- 23. Frontiers | Integration of “omics” Data and Phenotypic Data ... [https://www.frontiersin.org/articles/10.3389/fninf.2018.00091/full]
- 24. Ethical framework for responsible foundational models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128638/]
- 25. Predictive Models for Assessing Patients' Response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11001619/]
- 26. Comparison of deep learning with regression analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7676403/]
- 27. Machine learning in the prediction of treatment response ... [https://pubmed.ncbi.nlm.nih.gov/40493989/]
- 28. Comparison of deep learning with traditional models to ... [https://www.nature.com/articles/s41598-020-80856-3]
- 29. Comparing three neural networks to predict depression ... [https://www.sciencedirect.com/science/article/pii/S0005796725000749]
- 30. Establishing predictive machine learning models for drug ... [https://www.nature.com/articles/s41698-025-00937-2]
- 31. Development and comparison of machine learning models ... [https://www.sciencedirect.com/science/article/pii/S0939641124001371]
- 32. Comparison of Deep Learning With Multiple Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741413/]
- 33. Uncertainty-driven ensembles of multi-scale deep ... [https://www.sciencedirect.com/science/article/pii/S1566253522001038]
- 34. A multi model ensemble based deep convolution neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8413482/]
- 35. Multimodal CNN-DDI: using multimodal CNN for drug to ... [https://www.nature.com/articles/s41598-024-54409-x]
- 36. Multi-scale deep learning ensemble for segmentation of ... [https://link.springer.com/article/10.1007/s00521-024-09828-2]
- 37. An Ensemble Patient Graph Framework for Predictive ... [https://www.mdpi.com/2075-4418/15/6/756]
- 38. Comparison of Different Methods for Building Ensembles ... [https://www.mdpi.com/2079-9292/12/21/4428]
- 39. Machine Learning for Multi-Target Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473769/]
- 40. 团队在高维数据特征降维及可解释智能模型研究领域取得系列进展 [https://cilab.upc.edu.cn/2025/0331/c7601a262951/page.htm]
- 41. Optimizing high dimensional data classification with a ... [https://www.nature.com/articles/s41598-025-08699-4]
- 42. Optimized feature selection in high-dimensional gene ... [https://www.sciencedirect.com/science/article/pii/S1568494625006404]
- 43. 关于发布可解释、可通用的下一代人工智能方法重大研究计划 ... [https://www.nsfc.gov.cn/p1/3381/2824/66768.html]
- 44. 高维数据中特征筛选方法的思考总结——多变量分析筛选法 [https://blog.csdn.net/fjsd155/article/details/93754257]
- 45. 高维数据分析中特征选择方法及分类原创 [https://blog.csdn.net/weixin_44380645/article/details/123850135]
- 46. Feature Selection for Large Data by Optimizing the Cutoff [https://arxiv.org/html/2508.00954v1]
- 47. Q-learning enhanced differential evolution for feature ... [https://link.springer.com/article/10.1007/s44443-025-00303-z]
- 48. 预测分析模型准确度如何?2025年新增10种AI算法! [https://www.fanruan.com/blog/article/1780894/]
- 49. Future of Clinical Decision Support System (CDSS) in 2025 [https://www.champsoft.com/2025/11/06/future-of-clinical-decision-support-system-cdss-in-2025/]
- 50. Clinical Decision Support Systems (CDSS) Market to ... [https://www.towardshealthcare.com/insights/clinical-decision-support-systems-cdss-market-sizing]
- 51. Using Artificial Intelligence to Develop Clinical Decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468058/]
- 52. Patient perspective on predictive models in healthcare [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751774/]
- 53. DICOMweb | OHIF - Open Health Imaging Foundation [https://docs.ohif.org/configuration/dataSources/dicom-web]
- 54. Integrate OHIF viewer with AWS HealthImaging and ... [https://aws.amazon.com/blogs/industries/integrate-ohif-viewer-with-aws-healthimaging-and-openid-connect-authentication/]
- 55. Understanding the Role of Clinical Decision Support Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511814/]
- 56. Clinical Decision Support System Markets, 2024-2025 & ... [https://finance.yahoo.com/news/clinical-decision-support-system-markets-080500829.html]
- 57. Clinical prediction models and the multiverse of madness [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-03212-y]
- 58. Beyond Comparing Machine Learning and Logistic ... [https://www.jmir.org/2025/1/e77721]
- 59. Predicting Therapy Outcomes in Patients With Stress ... [https://pubmed.ncbi.nlm.nih.gov/40132191/]
- 60. Predictive Modelling of Depression Treatment Response ... [https://www.medrxiv.org/content/10.1101/2025.09.17.25335980v1]
- 61. Psychotherapy? Zoloft? AI can help your doctor choose [https://news.northeastern.edu/2025/09/17/northeastern-machine-learning-mental-health/]
- 62. Beyond Comparing Machine Learning and Logistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631085/]
- 63. Predicting Therapy Outcomes in Patients With Stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11979537/]
- 64. Comparison of different approaches in handling missing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11972534/]
- 65. Handling missing data in clinical research [https://www.sciencedirect.com/science/article/pii/S0895435622002189]
- 66. Dealing With Missing, Imbalanced, and Sparse Features ... [https://medinform.jmir.org/2023/1/e38590/]
- 67. Multi-Level Transfer Learning for irregular clinical time ... [https://www.sciencedirect.com/science/article/abs/pii/S0950705125008718]
- 68. Time series in healthcare: challenges and solutions ... [https://www.vanderschaar-lab.com/time-series-in-healthcare/]
- 69. Identify the most appropriate imputation method for handling ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02310-6]
- 70. Statistical Methods for Handling Missing Data in Long- ... [https://www.pcori.org/research-results/2013/statistical-methods-handling-missing-data-long-term-clinical-research]
- 71. TrajGPT: Irregular Time-Series Representation Learning ... [https://arxiv.org/html/2410.02133v1]
- 72. Large language models forecast patient health trajectories ... [https://www.nature.com/articles/s41746-025-02004-3]
- 73. Keeping Medical AI Healthy: A Review of Detection and ... [https://arxiv.org/html/2506.17442v1]
- 74. An integrated framework for prognosis prediction and drug ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05127-5]
- 75. Efficiency and Convergence Insights in Large-Scale ... [https://www.mdpi.com/2227-7390/13/22/3657]
- 76. A Review of Modeling Approaches to Predict Drug Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122624/]
- 77. Deep learning methods for drug response prediction in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1086097/full]
- 78. Scaling bigger, faster, cheaper data centers with smarter ... [https://www.mckinsey.com/industries/private-capital/our-insights/scaling-bigger-faster-cheaper-data-centers-with-smarter-designs]
- 79. Efficient and scalable reinforcement learning for large- ... [https://www.nature.com/articles/s42256-024-00879-7]
- 80. Advances and challenges in data-driven optimization [https://www.sciencedirect.com/science/article/pii/S295016012500004X]
- 81. Methodological guidance for the evaluation and updating of ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01801-8]
- 82. Perspectives on validation of clinical predictive algorithms [https://www.nature.com/articles/s41746-023-00832-9]
- 83. Targeted validation: validating clinical prediction models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9773429/]
- 84. Prediction models need appropriate internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578404/]
- 85. There is no such thing as a validated prediction model [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02779-w]
- 86. 3 misconceptions about external validation of clinical ... [https://www.sciencedirect.com/science/article/pii/S0895435624001422]
- 87. External validation and comparison of clinical prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482746/]
- 88. Navigating fairness aspects of clinical prediction models [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04340-3]
- 89. Reporting of Fairness Metrics in Clinical Risk Prediction ... [https://ojphi.jmir.org/2025/1/e66598]
- 90. . Machine [ Learning Analysis][ vs ] Deep Learning Deep 2025 [https://digitaldefynd.com/IQ/machine-learning-vs-deep-learning/]
- 91. Step-by-Step Guide to Deep in Learning vs Machine Learning 2025 [https://www.sobot.io/article/deep-learning-vs-machine-learning-guide-for-beginners-2025/]
- 92. 2025 Outlook: Machine Learning Applications in Healthcare [https://kms-technology.com/blog/machine-learning-applications-in-healthcare/]
- 93. AI and Deep Learning in Healthcare: Use Cases & ... [https://www.keragon.com/blog/deep-learning-in-healthcare]
- 94. Comparing Deep Learning and Conventional Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8861709/]
- 95. Frontiers | Machine approaches in the learning ... therapeutic outcome [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1588963/full]
- 96. Machine Learning and Deep Learning for Healthcare Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025807/]
- 97. A comparison between machine and deep learning models ... [https://www.nature.com/articles/s41598-024-70341-6]
- 98. A Comparative Analysis of Machine Learning and Deep ... [https://www.mdpi.com/2813-2203/4/1/5]
- 99. Generalizability of clinical prediction models in mental health [https://www.nature.com/articles/s41380-025-02950-0]
- 100. Real world data clinical trials: Essential 2025 [https://lifebit.ai/blog/real-world-data-clinical-trials/]
- 101. The Importance of Real-World Evidence in Medical ... [https://www.appliedclinicaltrialsonline.com/view/real-world-evidence-medical-research-drug-development]
- 102. Real-World Data and Causal Machine Learning to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579681/]
- 103. Parallel Progress in Artificial Intelligence and Real-World ... [https://globalforum.diaglobal.org/issue/august-2025/parallel-progress-in-artificial-intelligence-and-real-world-evidence-creates-a-new-vision-for-clinical-evidence/]
- 104. How real-world data is unlocking mental health [https://www.truveta.com/blog/data/real-world-data-mental-health]
- 105. Large language models in real-world clinical workflows [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1659134/full]