Regenerative Pharmacology: Mechanisms of Action for Curative Therapeutics
This article explores the emerging paradigm of regenerative pharmacology, a field dedicated to developing curative therapies that restore the structure and function of damaged tissues and organs, moving beyond symptomatic...
Regenerative Pharmacology: Mechanisms of Action for Curative Therapeutics
Abstract
This article explores the emerging paradigm of regenerative pharmacology, a field dedicated to developing curative therapies that restore the structure and function of damaged tissues and organs, moving beyond symptomatic management. Aimed at researchers, scientists, and drug development professionals, it provides a comprehensive analysis of the foundational principles, key mechanisms of action, and advanced methodologies driving this discipline. The content delves into the integration of pharmacology with systems biology and regenerative medicine, examines the pharmacological toolkit for directing tissue regeneration, addresses critical translational and manufacturing challenges for Advanced Therapy Medicinal Products (ATMPs), and outlines the rigorous validation and comparative frameworks necessary for clinical success. By synthesizing current research and future directions, this article serves as a strategic guide for navigating the complexities of creating transformative regenerative pharmacotherapies.
The New Paradigm: From Symptom Management to Curative Restoration
Regenerative pharmacology represents a transformative paradigm in biomedical science, emerging from the convergence of pharmacological principles with regenerative medicine and tissue engineering. Defined operationally as "the application of pharmacological sciences to accelerate, optimize, and characterize (either in vitro or in vivo) the development, maturation, and function of bioengineered and regenerating tissues," this discipline aims to cure disease through restoration of tissue and organ function, rather than merely ameliorating symptoms [1] [2]. This strategic focus distinguishes it fundamentally from standard pharmacotherapy, which predominantly addresses symptom management rather than underlying functional restoration [1].
The field was formally coined in 2007 to describe the enormous possibilities at the interface between pharmacology, regenerative medicine, and tissue engineering [1] [2]. As a rapidly evolving multidisciplinary enterprise, regenerative pharmacology seeks to advance technologies for the repair and replacement of damaged cells, tissues, and organs, with the pharmacological sciences playing a critical role in accelerating translational progress and clinical utility [1].
Core Principles and Conceptual Framework
Foundational Principles
Regenerative pharmacology is built upon several interconnected principles that guide its research and application:
Curative Focus: Unlike conventional pharmacology that manages symptoms, regenerative pharmacology seeks to restore normal tissue and organ function through targeted interventions that promote healing and regeneration [1] [3]. This approach leverages the body's innate healing mechanisms, enhancing what the body naturally attempts to accomplish [4] [5].
Structural and Functional Restoration: The field emphasizes both the improvement of functional outcomes and the restoration of structural integrity at the tissue and organ levels [3]. This involves understanding and recapitulating the complex internal milieu that permits new functional tissue formation [1].
Multidisciplinary Integration: Success in regenerative pharmacology demands global multidisciplinary collaboration at the intersections of pharmacology, biomaterials, biomedical engineering, nanotechnology, stem cell biology, and developmental biology [1]. This integration enables a systems-level approach to therapeutic development.
Spatiotemporal Control: Effective regenerative strategies must replicate the exquisite spatiotemporal regulation characteristic of morphogen gradients in normal development, requiring sophisticated control over the delivery and presentation of bioactive compounds [1].
The Integrative and Regenerative Pharmacology (IRP) Framework
A contemporary extension of this field, termed Integrative and Regenerative Pharmacology (IRP), merges pharmacology with systems biology and regenerative medicine [3]. IRP represents a paradigm shift from traditional drug discovery models toward systems-based, healing-oriented therapeutic approaches. Its conceptual foundations include:
- Systematic investigation of drug-human interactions at molecular, cellular, organ, and system levels [3]
- Application of pharmacological rigor to regenerative medicine processes [3]
- Development of transformative curative therapeutics that improve symptomatic relief while modulating tissue formation and function [3]
Table 1: Comparison of Conventional Pharmacology and Regenerative Pharmacology
| Aspect | Conventional Pharmacology | Regenerative Pharmacology |
|---|---|---|
| Primary Goal | Symptom management, disease progression alteration | Tissue/function restoration, curative intervention |
| Therapeutic Approach | Single target, selective mechanisms | Complex mixtures, multiple pathways |
| Molecular Weight | Small molecules (<500-800 MW) | Large molecules (growth factors, 10,000->100,000 MW) |
| Temporal Focus | Chronic management | Curative outcome |
| Development Approach | Standard drug discovery pipeline | Integrated, multidisciplinary strategies |
Operational Roles in Tissue Engineering and Regenerative Medicine
Regenerative pharmacology plays both passive (characterizing) and active (directing) roles throughout the tissue engineering and regenerative medicine (TERM) process [1]. These roles can be categorized as follows:
Passive/Characterizing Roles
Functional evaluation of engineered and regenerating tissues through preclinical assessment and pharmacological characterization of tissue/organ phenotype in vitro and in vivo [1]
Mechanistic investigation of regeneration processes, including defining the mechanisms of action for stem cell-derived therapies and understanding the "basic pharmacology" controlling regenerative pathways [6]
Active/Directing Roles
Modulation of stem/progenitor cell expansion and differentiation through screening of growth factor and small molecule libraries and development of improved culture systems [1]
Development of novel drug delivery systems including biomaterials, nanomaterials, and bifunctional compounds that target active agents to specific tissue locations [1] [3]
Creation of functionalized "smart" biomaterials that serve as reservoirs for bioactive agents and cell delivery vehicles for accelerated tissue formation [1]
Pharmacological modulation of the entire regenerative process to replicate the spatiotemporal regulation characteristic of normal development [1]
Key Research Methodologies and Experimental Approaches
In Vitro Tissue Characterization Platforms
Regenerative pharmacology employs advanced in vitro systems to study and direct tissue development:
Bioreactor Technologies: Laboratory devices that recapitulate relevant aspects of the in vivo physiologic environment (stretch, flow, compression) to create advanced three-dimensional tissue constructs in vitro prior to implantation [1]. These systems allow for preclinical assessment and pharmacological characterization of tissue/organ phenotype under controlled conditions.
Bioprinting Approaches: Technologies that simultaneously deposit cells and materials in complex geometries reminiscent of native tissue architectures, providing feasible methods for the creation and assembly of 3D tissues and organs [1]. These systems enable precise spatial control over the distribution of bioactive compounds.
Organ-on-a-Chip Platforms: Microfluidic devices that emulate human organ functionality, providing sophisticated systems for drug screening and mechanistic studies in a human-relevant context [3].
Investigating the Paracrine Hypothesis
A central methodology in regenerative pharmacology involves elucidating the paracrine effect observed in cell-based therapies [6]. This hypothesis proposes that cells delivered to sites of organ injury secrete factors that have beneficial effects on tissue function through:
- Enhancement of surviving cell function
- Prevention of cell loss through activation of survival pathways
- Stimulation of resident stem cell niches
The experimental approach to investigating this hypothesis includes:
- Conditioned media analysis from therapeutic cell cultures
- Factor identification through proteomic and transcriptomic profiling
- Ligand-receptor interaction studies to identify new pharmacological targets
- Functional validation in relevant disease models
Pharmacological Modulation of Stem Cell Biology
Understanding and controlling stem cell behavior through pharmacological intervention is a critical methodology:
Directed Differentiation: Using small molecules and growth factors to steer stem cell differentiation toward specific lineages [6]. This includes modulation of complex transcription pathways involved in differentiation.
Cell Migration Control: Investigating how pharmacological agents affect stem cell homing and engraftment, such as the demonstrated inhibition of progenitor cell migration by heparin through interference with SDF-1/chemokine receptor type 4 signaling [6].
Drug-Cell Interactions: Studying how conventional medications (e.g., aspirin, COX-2 inhibitors) interact with stem cell biology, as these interactions can significantly impact the efficacy of regenerative therapies [6].
Table 2: Essential Research Reagents in Regenerative Pharmacology
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Growth Factors | FGF, EGF, VEGF, IGF, BMPs, NGF | Modulation of cell proliferation, differentiation, and tissue formation [1] |
| Stem Cell Markers | CD34+, CD105+, Muse cells | Identification, isolation, and characterization of stem cell populations [5] |
| Biomaterial Scaffolds | Gelatin sponges, atelocollagen, amnion membrane | Providing three-dimensional frameworks for tissue development [5] |
| Small Molecule Modulators | COX-2 inhibitors, Wnt/β-catenin pathway modulators | Investigation of signaling pathways controlling regeneration [6] |
| Analytical Tools | Omics technologies, biosensors, real-time monitoring systems | Characterization of tissue development and function [3] |
Signaling Pathways and Mechanistic Foundations
Understanding the signaling networks that control regeneration is fundamental to regenerative pharmacology. Several key pathways have emerged as critical regulators:
Key Regenerative Signaling Pathways
Wnt/β-catenin Signaling: This pathway plays crucial roles in stem cell proliferation and differentiation. Research has shown that aspirin inhibits mesenchymal stem cell proliferation through mechanisms involving inhibition of PGE2 formation and subsequent down-regulation of the Wnt/β-catenin signaling pathway [6]. Treatment with PGE2 increases cell proliferation and enhances activation of this pathway.
PI3K/Akt Pathway: This survival pathway has been engineered into cells to enhance their therapeutic potential through paracrine mechanisms [6]. Activation of this pathway promotes cell survival and tissue protection in injury models.
SDF-1/CXCR4 Signaling: Critical for stem cell homing and migration, this pathway can be inhibited by heparin, demonstrating how commonly used clinical agents can interfere with regenerative processes [6]. This has important implications for the choice of anticoagulants in cell therapy protocols.
Regulatory Considerations and Clinical Translation
Expedited Development Pathways
The regulatory landscape for regenerative pharmacology therapies includes special expedited programs:
RMAT Designation: The Regenerative Medicine Advanced Therapy designation was created under the 21st Century Cures Act to support development and approval of regenerative medicine products that target unmet medical needs in patients with serious conditions [7] [8]. As of September 2025, the FDA has received almost 370 RMAT designation requests and approved 184, with 13 designated products ultimately approved for marketing [8].
Accelerated Approval Pathways: The FDA encourages innovative trial designs for regenerative medicine therapies, including use of natural history data as historical controls when populations are adequately matched, and clinical trials where multiple sites participate with the intent of sharing combined data to support licensing applications [8].
Manufacturing and Quality Control Considerations
The development of regenerative pharmacology therapies faces unique manufacturing challenges:
Chemistry, Manufacturing, and Controls: Expedited clinical development timelines create challenges in aligning product development activities, potentially requiring more rapid CMC development programs [8].
Manufacturing Changes: Post-change products may no longer qualify for RMAT designation if comparability cannot be established with the pre-change product, necessitating careful risk assessment when planning manufacturing changes [8].
Long-term Safety Monitoring: Regenerative therapies likely raise unique safety considerations that benefit from long-term monitoring, including both short-term and long-term safety assessments in clinical trials [8].
Future Perspectives and Challenges
Emerging Innovations
The future of regenerative pharmacology will be shaped by several technological advances:
Advanced Biomaterials: Development of 'smart' biomaterials that can deliver bioactive compounds in a temporally controlled manner represents a key frontier [3]. Stimuli-responsive biomaterials that alter their characteristics in response to external or internal triggers represent particularly promising approaches.
Artificial Intelligence Integration: AI holds promise for transforming regenerative pharmacology by enabling more efficient targeted therapeutic development, predicting drug delivery system effectiveness, and anticipating cellular responses [3].
Personalized Approaches: Utilizing patient-specific cellular or genetic information, advanced therapies can be tailored to maximize effectiveness and minimize side effects, moving toward truly personalized regenerative treatments [3].
Implementation Challenges
Despite its promise, regenerative pharmacology faces significant translational barriers:
Investigational Obstacles: Unrepresentative preclinical animal models impact the definition of therapeutic mechanisms of action and raise questions about long-term safety and efficacy [3].
Manufacturing Issues: Scalability, automated production methods, and the need for Good Manufacturing Practice present significant hurdles [3].
Economic Factors: High manufacturing costs and reimbursement uncertainties limit accessibility, particularly in low- and middle-income countries [3].
Regulatory Complexity: Diverse regional requirements and lack of unified guidelines create challenges for global development [3].
Overcoming these challenges will require interdisciplinary collaboration between academia, industry, clinics, and regulatory authorities to establish standardized procedures and ensure consistency in therapeutic outcomes [3]. As the field continues to evolve, regenerative pharmacology holds the potential to fundamentally transform therapeutic approaches from symptomatic treatment to curative intervention, ultimately redefining how we treat degenerative diseases, injuries, and age-related tissue dysfunction.
The convergence of pharmacology, systems biology, and regenerative medicine represents a paradigm shift in biomedical science, moving beyond symptomatic treatment toward the restoration of biological structure and function. This integrated framework, termed Integrative and Regenerative Pharmacology (IRP), applies the principles of regenerative medicine and the toolkit of systems biology to drug discovery and therapeutic development [3]. IRP aims to develop transformative curative therapeutics that not only improve symptomatic relief of target organ disease but also modulate tissue formation and function, marking a fundamental departure from traditional pharmacology's focus on symptom reduction and disease course alteration [3].
The conceptual foundation of IRP rests on the systematic investigation of drug interactions with biological systems across multiple levels—from molecular and cellular to organ and system levels—while incorporating signaling pathways, bioinformatic tools, and multi-omics technologies (transcriptomics, genomics, proteomics, epigenomics, metabolomics, and microbiomics) [3]. This approach facilitates the prediction of potential targets and pathways that could inform the development of more effective therapeutics designed to repair, renew, and regenerate rather than merely block or inhibit pathological processes [3].
Core Principles and Conceptual Framework
The Triad of Integration
The integrative approach rests on three foundational pillars that create a synergistic relationship between previously distinct disciplines:
Pharmacology in Regenerative Context: Regenerative pharmacology has been defined as "the application of pharmacological sciences to accelerate, optimize, and characterize the development, maturation, and function of bioengineered and regenerating tissues" [3]. This represents the application of established pharmacological principles to cutting-edge regenerative medicine, fusing pharmacological techniques with regenerative medicine principles to develop therapies that promote the body's innate healing capacity [3].
Systems Biology as the Connective Tissue: Systems biology provides the holistic analytical framework necessary for understanding complex biological systems. It constructs comprehensive models of biological processes by incorporating data from multiple levels (molecular, cellular, organ, and organism) [9]. This multi-scale perspective enables researchers to gain deeper insights into disease mechanisms and predict how therapeutic interventions will interact with the human body [9].
Reciprocal Enhancement: The relationship between these fields is mutually reinforcing. Pharmaceutical innovations can improve the safety and efficacy of regenerative therapies, while regenerative medicine approaches offer new platforms (e.g., 3D models, organ-on-a-chip) for both drug development and testing [3]. This complementary relationship accelerates progress in both domains.
Quantitative Systems Pharmacology as a Bridge
A critical manifestation of this integration is the emergence of Quantitative Systems Pharmacology (QSP), which leverages systems biology models to simulate drug behaviors, predict patient responses, and optimize drug development strategies [9] [10]. By incorporating QSP into the drug discovery process, pharmaceutical companies can make more informed decisions, reduce development costs, and ultimately bring safer, more effective therapies to patients [9] [10]. The growing importance of QSP has stimulated collaborative industry-academia partnerships to develop educational programs that equip the next generation of scientists with the necessary multidisciplinary expertise [9] [10].
Key Methodologies and Experimental Approaches
Network Pharmacology and Multi-Omic Integration
Network pharmacology has emerged as a powerful methodological framework for implementing the integrative approach. This interdisciplinary strategy integrates systems biology, omics technologies, and computational methods to identify and analyze multi-target drug interactions, validate therapeutic mechanisms, and advance integrative drug discovery [11]. A representative workflow applied to studying traditional medicines illustrates this approach:
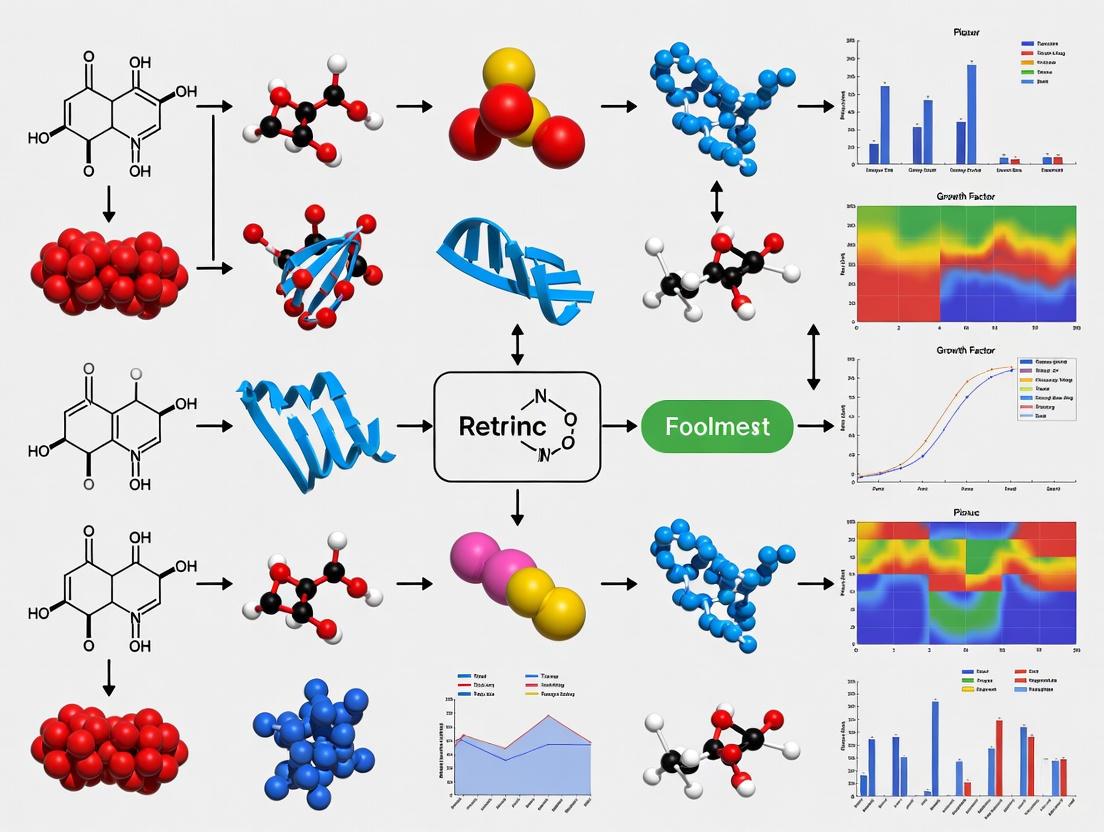
Diagram 1: Network pharmacology workflow for therapeutic mechanism elucidation.
This methodology was successfully applied to elucidate the anti-inflammatory mechanisms of Xianlinggubao (XLGB), an approved Chinese herbal remedy for osteoarthritis [12]. The study integrated bioactive compound identification from TCMSP, ETCM, and SymMap databases with target prediction through STITCH and SEA approaches, then connected these with osteoarthritis-related inflammatory targets identified through differential expression analysis of GEO datasets (GSE1919) and database mining of OMIM and GeneCards [12]. Protein-protein interaction network analysis revealed that XLGB alleviates osteoarthritis inflammation by modulating key genes including COX-2, IL-1β, TNF, IL-6, and MMP-9, with functional enrichment analysis suggesting involvement of IL-17, TNF, and NF-κB pathways [12]. These computational predictions were subsequently validated through molecular docking, dynamics simulations, RT-PCR, and immunofluorescence assays [12].
Multi-Scale Systems Biology Approaches
Advanced systems biology applications in neurodegeneration research demonstrate the power of integrative methodologies. A recent study combined an unbiased, genome-scale forward genetic screen for age-associated neurodegeneration in Drosophila with multi-omic profiling (proteomics, phosphoproteomics, and metabolomics) in Drosophila models of Alzheimer's disease [13]. This was further integrated with human Alzheimer's genetic variants that modify gene expression in disease-vulnerable neurons, using network modeling to connect these diverse data types with previously published Alzheimer's disease proteomics, lipidomics, and genomics [13].
The experimental workflow for this multi-scale integration is visually summarized below:
Diagram 2: Multi-scale systems biology approach for neurodegeneration mechanism identification.
This comprehensive approach led to the computational prediction and experimental confirmation of how HNRNPA2B1 and MEPCE enhance toxicity of the tau protein, a key pathological feature of Alzheimer's disease, and demonstrated that screen hits CSNK2A1 and NOTCH1 regulate DNA damage in both Drosophila and human stem cell-derived neural progenitor cells [13]. The study identified 198 genes that promoted age-associated neurodegeneration in Drosophila after knockdown, including orthologs of APP and presenilins (genes mutated in familial Alzheimer's disease), establishing a direct connection between the model organism screen and human disease mechanisms [13].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 1: Key Research Reagent Solutions for Integrative Pharmacology Research
| Category | Specific Reagents/Platforms | Research Application |
|---|---|---|
| Cell Models | RAW264.7 cells [12], induced Pluripotent Stem Cells (iPSCs) [13] [14], neural progenitor cells [13] | In vitro screening, toxicity assessment, disease modeling |
| Bioactive Compounds | Xianlinggubao prescription [12], small molecule reprogramming cocktails [14] | Mechanism of action studies, cellular reprogramming, therapeutic screening |
| Omics Technologies | Proteomics, phosphoproteomics, metabolomics platforms [13], RNA-sequencing [13] | Multi-omic profiling, pathway analysis, biomarker identification |
| Computational Tools | Cytoscape [12] [11], STRING [12] [11], Molecular docking (AutoDock) [12] [11], GROMACS [12] | Network construction, target identification, binding affinity assessment |
| Database Resources | TCMSP [12] [11], ETCM [12], DrugBank [11], GEO [12], OMIM [12], GeneCards [12] | Compound-target data, disease gene information, expression datasets |
| In Vivo Models | Drosophila neurodegeneration models [13], chemically-induced pluripotent stem cells (CiPSCs) [14] | Genetic screening, disease modeling, transplantation studies |
Applications and Case Studies
Neurodegenerative Disease Mechanisms
The integrative approach has generated significant insights into neurodegenerative disease mechanisms, particularly Alzheimer's disease. The genome-scale Drosophila screen followed by multi-omic integration revealed candidate pathways that could be targeted to ameliorate neurodegeneration [13]. Analysis of human orthologs of the neurodegeneration screen hits demonstrated that their expression declines with age and Alzheimer's disease in the human brain, with particularly strong associations in vulnerable regions like the hippocampus and frontal cortex [13]. This cross-species validation exemplifies how integrative approaches can bridge model organism and human studies to identify clinically relevant therapeutic targets.
Cardiovascular Drug Development
In cardiovascular medicine, integrative approaches combining AI, omics, and systems biology are helping scientists design targeted drugs for disease pathways once considered "untreatable" [15]. This innovation paradigm leverages omics approaches that provide detailed information about cellular molecules, systems biology that examines how networks of genes and proteins interact to shape disease, and AI that analyzes disease pathways to identify new drug targets and design therapeutics for specific proteins and genes [15]. The approach is particularly promising for RNA-based therapeutics, which can be designed to influence almost any gene and may be quicker to develop than conventional drugs, with early trials already demonstrating potential for cholesterol management superior to standard treatments [15].
Stem Cell-Based Regenerative Therapies
The integrative framework has accelerated the development of stem cell-based regenerative therapies. Recent advances include the generation of chemically-induced pluripotent stem cells (CiPSCs) using only small molecules, providing a new platform for cellular reprogramming [14]. Most notably, chemically-induced stem cell-derived islets (CiPSC-islets) have been transplanted into human patients, resulting in rapid reversal of diabetes [14]. This breakthrough demonstrates the clinical potential of integrating pharmacological approaches (small molecule reprogramming) with regenerative medicine (cell transplantation) for treating degenerative diseases.
Technical Protocols for Core Methodologies
Protocol 1: Network Pharmacology Analysis for Multi-Target Therapeutic Characterization
Purpose: To systematically identify the multi-target mechanisms of complex therapeutic formulations using network pharmacology.
Materials:
- Compound databases: TCMSP, ETCM, SymMap, ChEMBL
- Target prediction tools: STITCH, Similarity Ensemble Approach (SEA)
- Disease databases: OMIM, GeneCards, PubMed Gene
- Network analysis software: Cytoscape 3.7.2 with CytoHubba plugin
- Functional enrichment: ClusterProfiler package in R
- Molecular docking: AutoDock, GROMACS for dynamics simulations
Procedure:
- Bioactive Compound Screening: Retrieve all chemical components from relevant databases. Apply screening criteria (oral bioavailability ≥30%, drug-likeness ≥0.18) to identify bioactive ingredients [12].
- Target Prediction: Identify targets associated with candidate bioactive compounds using STITCH, SEA, SymMap, and ChEMBL databases with "Homo sapiens" setting. Standardize genetic data through UniProt [12].
- Disease Target Identification: Obtain disease-related targets through differential expression analysis of relevant datasets (e.g., GEO GSE1919 for osteoarthritis) using "limma" package in R (p<0.05, |log2FC|≥2). Cross-reference with inflammation-related genes from OMIM, GeneCards, and PubMed Gene [12].
- Network Construction:
- Build compound-target network linking TCM compounds to their respective targets
- Construct protein-protein interaction (PPI) network using STRING database
- Visualize interconnected network using Cytoscape 3.7.2
- Analyze topological properties through "Network Analysis" plugin [12]
- Hub Gene Identification: Use "CytoHubba" plugin to assess topological characteristics of network nodes and identify hub genes most critical to the therapeutic effect [12].
- Functional Enrichment Analysis: Perform Gene Ontology and KEGG pathway analysis of gene clusters using ClusterProfiler package in R [12].
- Experimental Validation:
- Conduct molecular docking with protein structures from PDB (e.g., PTGS2: 5F19, IL-1β: 6Y8M)
- Perform molecular dynamics simulations for 100 ns per protein-drug complex in GROMACS
- Validate key targets experimentally through RT-PCR and immunofluorescence assays [12]
Protocol 2: Multi-Omic Integration for Disease Mechanism Elucidation
Purpose: To integrate multiple omics datasets with genetic screening data for identifying novel disease mechanisms.
Materials:
- Drosophila RNAi screening: UAS-GAL4 system with elav-GAL4 driver
- Omics platforms: Proteomics, phosphoproteomics, metabolomics capabilities
- Human tissue analysis: Laser-capture microdissection system for neuron isolation
- RNA-sequencing: Bulk or single-cell RNA-seq capabilities
- Computational resources: Network modeling infrastructure, statistical analysis tools
Procedure:
- Genetic Screening:
- Perform genome-scale transgenic RNAi knockdown of target genes (e.g., 5,261 fly genes) using UAS-GAL4 system with pan-neuronal elav-GAL4 driver [13]
- Age adult flies for 30 days and assess brain integrity on tissue sections representing entire brain
- Score neuronal loss and vacuolation in blinded fashion
- Identify hits as genes causing neuronal loss or vacuolation in properly developed brains [13]
- Multi-Omic Profiling:
- Conduct proteomic, phosphoproteomic, and metabolomic analyses in disease model systems (e.g., Drosophila Alzheimer's models) [13]
- Process samples using standardized extraction protocols appropriate for each omics platform
- Human Tissue Analysis:
- Data Integration:
- Cross-Species Validation:
- Test predicted functional effects of candidate targets in original model system (e.g., Drosophila)
- Validate mechanisms in human cellular systems (e.g., iPSC-derived neural progenitor cells) [13]
- Assess conservation of pathways and mechanisms across species
Quantitative Data Synthesis
Multi-Omic Data Types in Integrative Studies
Table 2: Multi-Omic Data Types and Applications in Integrative Pharmacology
| Data Type | Key Measurements | Applications in IRP | Example Insights |
|---|---|---|---|
| Genomics | Genetic variants, mutations, polymorphisms | Identification of disease-risk genes, personalized therapy | Drosophila screen identified 198 neurodegeneration-associated genes [13] |
| Transcriptomics | Gene expression levels, RNA sequences | Pathway activity assessment, biomarker discovery | eQTL analysis in human neurons linked genetic risk to expression changes [13] |
| Proteomics | Protein expression, post-translational modifications | Target engagement assessment, mechanism elucidation | Phosphoproteomics revealed signaling alterations in disease models [13] |
| Metabolomics | Metabolite profiles, metabolic pathway fluxes | Metabolic dysfunction identification, therapeutic monitoring | Metabolic rewiring identified in neurodegenerative models [13] |
| Lipidomics | Lipid species composition and abundance | Membrane biology assessment, inflammatory mediator profiling | Integrated with genomics in Alzheimer's network models [13] |
The integrative approach merging pharmacology, systems biology, and regenerative medicine represents a fundamental transformation in therapeutic development. By combining the mechanistic rigor of pharmacology with the holistic perspective of systems biology and the regenerative capacity of regenerative medicine, this framework enables the development of transformative curative therapies that address the root causes of disease rather than merely managing symptoms. The methodologies, protocols, and applications outlined in this whitepaper provide researchers with the tools to implement this approach in their own work, accelerating progress toward truly regenerative therapeutics.
As the field advances, key areas for continued development include standardized manufacturing processes for regenerative products, improved computational models that better predict human therapeutic responses, and expanded clinical validation through rigorously designed trials. With these advances, the integrative approach promises to redefine therapeutic landscapes across neurodegenerative diseases, cardiovascular disorders, and numerous other conditions characterized by tissue degeneration and dysfunction.
Regenerative pharmacology represents a paradigm shift from conventional disease management, aiming to restore tissue structure and function by directly modulating the body's innate repair mechanisms. This in-depth technical guide focuses on the core cellular targets—stem cells, progenitor cells, and the regenerative niche—which are central to this therapeutic strategy. Stem cells are defined by their capacity for self-renewal and differentiation, while progenitor cells are more lineage-committed but retain significant regenerative potential [16]. The concept of the "niche" is critical; it is the dynamic microenvironment that houses these cells and regulates their fate through a complex interplay of cellular interactions, signaling molecules, and physical cues [17]. For researchers and drug development professionals, understanding and pharmacologically targeting these components is key to developing novel treatments for a range of intractable diseases, from degenerative disorders to impaired wound healing. This guide synthesizes current mechanistic understanding, quantitative data, and experimental approaches to illuminate the path for future therapeutic discovery.
Core Concepts and Definitions
- Stem Cells: Cells with extensive self-renewal capacity and the potential to differentiate into multiple cell types. They are categorized as:
- Embryonic Stem Cells (ESCs): Pluripotent cells derived from early-stage embryos.
- Adult Stem Cells (Somatic Stem Cells): Multipotent cells resident in specific tissues (e.g., bone marrow, skin, intestine) responsible for maintenance and repair.
- Induced Pluripotent Stem Cells (iPSCs): Adult cells that have been genetically reprogrammed to a pluripotent state, offering a patient-specific cell source without the ethical concerns of ESCs [18] [17].
- Progenitor Cells: Cells that are more lineage-committed than stem cells and have limited self-renewal capacity. They serve as an intermediate population, proliferating and differentiating to produce mature, functional cells [16].
- The Regenerative Niche: The specialized, dynamic microenvironment that hosts stem and progenitor cells. It is composed of heterologous cell types, the extracellular matrix (ECM), secreted factors, and physical parameters (e.g., oxygen tension, stiffness). The niche maintains stem cell quiescence, directs self-renewal and differentiation, and responds to injury [17]. The interaction between stem cells and their niche is reciprocal, creating a feedback loop that is essential for tissue homeostasis and regeneration [17].
Quantitative Profiling of Stem and Progenitor Cell Dynamics
Understanding the quantitative behavior of hematopoietic and other stem cell systems is fundamental for predictive toxicology and therapeutic development. The following table summarizes key quantitative parameters from recent research, including a Quantitative Systems Pharmacology (QSP) model of in vitro hematopoiesis and clinical cell therapy dosing data.
Table 1: Quantitative Parameters in Hematopoiesis and Cell Therapy
| Parameter | Value / Range | Context / System | Significance |
|---|---|---|---|
| HSC In Vitro Proliferation (Model Output) | Matches day 2-6 kinetic data [19] | Human CD34+ stem cell culture (MLTA) [19] | Validated system parameters for control (untreated) cell growth, serving as a baseline for drug perturbation studies. |
| Effective MSC:Immune Cell Ratio | 1:10 or greater [20] | In vitro immunomodulation co-culture (MSCs:PBMCs) [20] | Defines the stoichiometry required for a measurable T-cell suppressive response, a key pharmacodynamic relationship. |
| Effective Co-culture Duration | ~3 days [20] | In vitro immunomodulation co-culture (MSCs:PBMCs) [20] | The time variable required for the immunomodulation reaction, informing pharmacokinetic goals for in vivo persistence. |
| Clinical MSC Dose (Systemic) | 100–200 million cells [20] | IV infusion in a 70 kg patient (clinical trials) [20] | A typical human dose for systemic immunomodulation, highlighting the challenge of scaling from in vitro effective ratios. |
| IV-MSC Half-Life | ~24 hours [20] | Biodistribution studies in animal models [20] | Explains transient therapeutic effects; most IV-infused MSCs are rapidly cleared, primarily via lung entrapment. |
| IC90 of Granulocyte-Macrophages | Compound-specific [19] | Pre-clinical in vitro toxicity assay [19] | A historical predictor of a drug's maximum tolerated dose (MTD) in animals and humans for myelosuppressive agents. |
Experimental Protocols for Niche and Cell Analysis
Multi-Lineage Toxicity Assay (MLTA) for Myelosuppression
Purpose: To quantify the concentration-response effects of anti-cancer agents on multiple hematopoietic cell lineages simultaneously and infer mechanisms of action (anti-proliferation vs. cell-killing) [19].
Methodology:
- Cell Source: Isolate human CD34+ hematopoietic stem cells from donor tissue.
- Culture and Differentiation: Seed cells in a 96-well format and culture under conditions that support simultaneous differentiation into multiple lineages (erythroid, megakaryocyte, granulocyte, monocyte, lymphocyte).
- Drug Treatment: Expose the differentiating cultures to a range of concentrations of the drug candidate.
- Measurement: At assay endpoint, use flow cytometry with lineage-specific cell surface markers to quantify the number of viable cells in each lineage.
- Data Analysis:
- Generate dose-response curves for each cell lineage.
- Use a calibrated QSP model of in vitro hematopoiesis to deconvolute the observed net cell count decreases. The model is fit to the data to infer the magnitude and dose-dependence of drug effects (either anti-proliferation or cell-killing) on individual progenitor and mature cell populations [19].
Quantitative Systems Pharmacology (QSP) Model Calibration for Trispecific T-Cell Engagers
Purpose: To gain mechanistic insight into the dose-response of a novel trispecific antibody (targeting CD3, CD28, and CD38) for multiple myeloma treatment [21].
Methodology:
- Model Generation: Develop a rule-based QSP model using a model generation code. The code automatically creates ordinary differential equations (ODEs) based on predefined rules for:
- Cell types (e.g., T-cell subsets, tumor cells, PBMCs).
- Receptors (CD3, CD28, CD38).
- Synapse formation between cells based on receptor binding and collision rates.
- Intracellular processes (T-cell activation, tumor cell killing) [21].
- Staged Calibration: Optimize model parameters in stages against distinct in vitro datasets to minimize uncertainty:
- Step 1 - T-cell Activation: Optimize parameters for T-cell activation and synapse formation using data on the percentage of activated T-cells in PBMC incubations (lacking tumor cells).
- Step 2 - Tumor Killing: Optimize tumor cell killing rates and resistance parameters using data from co-cultures of pre-activated CD8+ T-cells with multiple myeloma cell lines (RPMI8226 and KMS-11).
- Step 3 - Cytokine Response: Calibrate cytokine emission parameters to data from the MIMIC assay, capturing the range of possible immune responses [21].
- Model Application: Use the qualified model to simulate complex dose-response relationships, predict "effective" receptor occupancy, and explain the superior efficacy of the trispecific format compared to bispecific engagers [21].
Diagram 1: Staged QSP model calibration workflow.
Signaling Pathways and Metabolic Regulation in the Niche
The behavior of stem and progenitor cells is intricately controlled by metabolic and redox signaling pathways that are highly sensitive to the niche. A key regulatory network involves the transcription factors HIF1α and HIF2α, which are stabilized under hypoxic conditions common in stem cell niches.
- Metabolic Programming: Pluripotent and quiescent stem cells preferentially utilize glycolysis rather than mitochondrial oxidative phosphorylation for energy production. This metabolic state minimizes the generation of reactive oxygen species (ROS), preserving stemness [16].
- Redox Regulation: ROS levels act as a critical signaling mechanism within the niche. Low ROS levels help maintain HSC quiescence, while higher, non-toxic physiological levels promote proliferation, differentiation, and mobilization [16]. Pathological ROS levels, as seen in diabetes, induce oxidative stress, leading to niche dysfunction and reduced regenerative capacity of stem/progenitor cells [16].
- Key Molecular Players: The homeodomain transcription factor Meis1 is essential for activating HIF1α and HIF2α. HIF1α upregulates glycolytic enzymes, reinforcing the glycolytic metabolic state. HIF2α upregulates antioxidant enzymes to reduce cellular ROS levels. This Meis1-HIFs axis is therefore critical for maintaining the low-ROS, glycolytic state that characterizes quiescent stem cells [16].
Diagram 2: Meis1-HIFs axis in stem cell regulation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for Stem Cell and Niche Research
| Research Tool / Reagent | Function / Application | Technical Context |
|---|---|---|
| CD34+ Stem Cells | Starting population for in vitro hematopoiesis and differentiation studies. | Sourced from human donors; used in the Multi-Lineage Toxicity Assay (MLTA) to generate multiple blood cell lineages [19]. |
| Rhosin (RhoA inhibitor) | Small molecule tool compound to investigate rejuvenation of aged hematopoietic stem cells. | Inhibits the protein RhoA, a mechanosensor that becomes highly activated with age. Treatment has been shown to reverse age-associated changes in HSCs in models [22]. |
| StemRNA Clinical iPSC Seed Clones | GMP-compliant, clinically relevant starting material for deriving consistent cell therapy products. | A master iPSC cell line; a Drug Master File (DMF) has been submitted to the FDA to streamline regulatory submissions for therapies using this platform [23]. |
| Trispecific T-Cell Engager | Research tool and therapeutic candidate for engaging T cells against tumor cells via multiple receptors. | A molecule binding CD3 (on T-cells), CD38 (on myeloma cells), and CD28 (co-stimulation on T-cells and additional tumor target). Used for QSP model development [21]. |
| Flow Cytometry with Lineage-Specific Markers | Quantification of specific cell populations in a heterogeneous mixture. | Essential for endpoint analysis in the MLTA to count cells in erythroid, megakaryocyte, granulocyte, monocyte, and lymphocyte lineages [19]. |
| 'Omics Tools (Genomics, Proteomics) | Comprehensive characterization of stem cell critical quality attributes (CQA), including identity and potency. | Used to understand stem cell biology, define mechanisms of action, and develop robust potency assays for regulatory compliance [24]. |
Clinical Translation and Regulatory Landscape
The transition from basic research to approved therapies is accelerating, with several landmark approvals and an expanding clinical trial pipeline.
- Recent FDA-Approved Stem Cell Products:
- Ryoncil (remestemcel-L): Approved in December 2024, it is the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD). It utilizes allogeneic bone marrow-derived MSCs to modulate the immune response [23].
- Omisirge (omidubicel-onlv): Approved in April 2023, it is a nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cell product. It accelerates neutrophil recovery in patients with hematologic malignancies after transplantation [23].
- Lyfgenia (lovotibeglogene autotemcel): An autologous cell-based gene therapy approved in December 2023 for sickle cell disease. It involves genetically modifying the patient's own hematopoietic stem cells to produce anti-sickling hemoglobin [23].
- Advances in Pluripotent Stem Cell (PSC) Trials: As of late 2024, the global clinical trial landscape includes 115 trials involving 83 distinct PSC-derived products. Over 1,200 patients have been dosed, with no class-wide safety concerns emerging. Key therapeutic areas include ophthalmology, neurology, and oncology [23].
- Notable FDA-Authorized Clinical Trials:
- Fertilo: The first iPSC-based therapy to receive FDA IND clearance for a U.S. Phase III trial (Feb 2025). It uses iPSC-derived ovarian support cells to assist in oocyte maturation [23].
- OpCT-001: An iPSC-derived therapy for retinal degeneration, which received IND clearance for a Phase I/IIa trial in September 2024 [23].
- iPSC-Derived Neural Progenitors: Multiple therapies for Parkinson’s disease, spinal cord injury, and ALS received FDA IND clearance in 2025 [23].
Targeting stem cells, progenitor cells, and the regenerative niche represents a powerful mechanism of action for regenerative pharmacology. The field is moving beyond simple cell transplantation towards sophisticated pharmacological manipulation of endogenous repair systems. Key future directions include the development of more precise small molecules and biologics to target niche components [17], the application of QSP modeling to deconvolute complex mechanisms and optimize dosing [19] [21], and the rigorous clinical development of iPSC-derived therapies [23]. The successful translation of these strategies requires a deep, quantitative understanding of the pharmacokinetics and pharmacodynamics of cellular interventions [20]. As our knowledge of niche biology, redox regulation [16], and cell metabolism deepens, the potential to design therapies that can rejuvenate aged tissues, overcome disease-related niche dysfunction, and precisely control regenerative outcomes will fundamentally transform the treatment of degenerative diseases and tissue injury.
The paradigm of regenerative pharmacology has shifted from a focus on stem cell differentiation to understanding their paracrine activity. Mesenchymal stem cells (MSCs) exert therapeutic effects primarily through secreted bioactive molecules—the secretome—which includes extracellular vesicles (exosomes) and growth factors. This in-depth technical guide details the mechanisms by which these paracrine effectors mediate cardiac repair following myocardial infarction (MI), highlighting their roles in cytoprotection, angiogenesis, immunomodulation, and fibrosis inhibition. We provide structured quantitative data, experimental protocols for key methodologies, standardized signaling pathway visualizations, and essential research reagent solutions to support mechanistic research and therapeutic development in regenerative pharmacology.
The therapeutic use of stem cells, particularly Mesenchymal Stem Cells (MSCs), has shown promise across diverse disease models, including myocardial infarction, Parkinson's disease, and Crohn's disease [25]. Initially, the regenerative potential was attributed to the direct differentiation of transplanted cells into target tissue phenotypes [25]. However, transient engraftment and poor cellular survival post-transplantation, coupled with observations that functional benefits often exceeded the differentiation capacity of the cells, challenged this mechanism [26] [25].
This led to the formulation of the paracrine hypothesis, which posits that stem cells facilitate repair and regeneration chiefly through the secretion of biologically active factors that modulate resident cells [25]. The MSC secretome comprises both soluble factors (growth factors, cytokines) and membrane-bound vesicles, notably exosomes, which collectively create a reparative tissue microenvironment [27]. These factors are pleiotropic, influencing multiple cell types and mechanisms in a spatiotemporal manner following injury [25]. This guide details the components, functions, and research methodologies for investigating these primary effectors.
Core Components of the Paracrine Apparatus
The MSC Secretome
The secretome is the complete set of molecules secreted by a cell, including soluble proteins and extracellular vesicles (EVs). In the context of MSCs, the secretome is "personalized" according to the local microenvironmental cues, and its therapeutic potential can be optimized through various preconditioning strategies [27]. Its composition determines its regenerative capacity, influencing processes in respiratory, hepatic, and neurological diseases [27].
Exosomes and Extracellular Vesicles
Exosomes are a specific subtype of extracellular vesicle, defined as naturally occurring nanovesicles with sizes ranging from 30 to 150 nm [26]. They are formed by the inward germination of the multivesicular body membrane and subsequent fusion with the plasma membrane [26].
Key Biometric Properties:
- Biomarkers: Tetraspanins (CD63, CD81, CD9), Alix, and heat shock proteins are widespread biomarkers [26].
- Cargo: Exosomes transport biologically active substances, including proteins, lipids, mRNAs, miRNAs, and long noncoding RNAs [26]. The Exo-Carta database has cataloged thousands of these molecules.
- Functional Advantages: Compared to their parental cells, MSC-derived exosomes (MSC-Exos) offer benefits such as long-term stability, more accessible storage, lower immunogenicity, less risk of tumorigenicity, and lower production costs. Their small size prevents capillary blockage [26].
Growth Factors and Soluble Factors
MSCs secrete a range of critical growth factors and cytokines that drive paracrine effects. Key factors include:
- Vascular Endothelial Growth Factor (VEGF)
- Basic Fibroblast Growth Factor (bFGF)
- Hepatocyte Growth Factor (HGF)
- Insulin-like Growth Factor 1 (IGF-1)
- Transforming Growth Factor-beta (TGF-β)
- Prostaglandin E2 (PGE2) [25]
Elevated levels of these proteins are found in the heart following the injection of adult stem cells and are instrumental in promoting cardiac repair [25].
Quantitative Data on Paracrine Effectors in Myocardial Repair
The following tables summarize key quantitative data on the functions of specific paracrine molecules and exosomal microRNAs in myocardial infarction models.
Table 1: Key Paracrine Factors and Their Documented Effects in Myocardial Repair
| Paracrine Factor | Source | Primary Documented Functions | Experimental Model |
|---|---|---|---|
| Secreted Frizzled Related Protein 2 (Sfrp2) | Akt1-MSCs [25] | Binds Wnt3a; inhibits caspase activity and cardiomyocyte apoptosis [25] | Rat model of MI [25] |
| Hypoxic induced Akt regulated Stem cell Factor (HASF) | MSCs [25] | Activates PKCε; reduces TUNEL+ nuclei, inhibits caspase activation and mitochondrial pore opening [25] | Mouse model of MI [25] |
| Vascular Endothelial Growth Factor (VEGF) | MSCs, BMMNCs [25] | Promotes angiogenesis; critical for neovascularization [25] | Porcine MI model [26] |
| miR-19a | hUCMSC-Exos [26] | Targets SOX6; activates AKT and inhibits JNK3/caspase-3 to reduce apoptosis [26] | In vitro model of acute MI damage [26] |
| miR-25-3p | BMMSC-Exos [26] | Downregulates pro-apoptotic genes (FasL, PTEN) to reduce apoptosis in hypoxic cardiomyocytes [26] | In vitro hypoxia model [26] |
Table 2: Exosomal MicroRNAs (miRNAs) and Their Mechanisms of Action
| Exosomal miRNA | Source | Target Pathway/Gene | Functional Outcome |
|---|---|---|---|
| miR-144 [26] | BMMSC-Exos | PTEN/PI3K/AKT pathway [26] | Inhibits apoptosis in hypoxic cardiomyocytes [26] |
| miR-486-5p [26] | BMMSC-Exos | PTEN/PI3K/AKT pathway [26] | Inhibits apoptosis in hypoxic cardiomyocytes [26] |
| miR-21 [26] | Endometrial MSC-Exos | PTEN/PI3K/AKT pathway [26] | Exerts significant antiapoptotic effects [26] |
| miR-129-5p [26] | BMMSC-Exos | TRAF3/NF-κB pathway [26] | Inhibits myocardial apoptosis and improves cardiac function in MI rats [26] |
| miR-338 [26] | BMMSC-Exos | MAP3K2/JNK signaling pathway [26] | Inhibits myocardial apoptosis and improves cardiac function [26] |
Experimental Protocols for Key Paracrine Studies
Protocol: Multicellular Calcium Imaging for Paracrine Signaling
This protocol assesses paracrine ATP signaling via mechanically induced calcium waves, adapted from studies on human lens epithelium [28].
1. Sample Preparation:
- Obtain human anterior lens capsules (LCs) during cataract surgery via continuous curvilinear capsulorhexis (5-5.5 mm circles) [28].
- Store LCs in physiological solution (in mM: NaCl 131.8, KCl 5, MgCl2 2, NaH2PO4 0.5, NaHCO3 2, CaCl2 1.8, HEPES 10, glucose 10; pH 7.24) at 37°C and 5% CO2 [28].
- Immobilize LCs in plastic glass-bottom Petri dishes, gently stretching and securing them with a harp-like grid [28].
2. Cell Loading and Dye Incubation:
- Load LCs with 2 µM Fura-2 AM (acetoxymethyl ester) dissolved in DMSO and suspended in 3 mL of physiological solution [28].
- Incubate for 30 minutes at 37°C and 5% CO2 [28].
- Wash twice for 10 minutes with fresh physiological solution [28].
3. Pharmacological Perturbation:
- Apply inhibitors to specific pathways:
- Apyrase (an ATP-hydrolyzing enzyme) to degrade extracellular ATP.
- Carbenoxolone (CBX) (a gap-junctional blocker) to inhibit direct intercellular communication [28].
4. Mechanical Stimulation and Data Acquisition:
- Induce Ca²⁺ waves via mechanical stimulation.
- Record Ca²⁺ waves using a multicellular Ca²⁺ imaging setup. Quantify the spatial extent, amplitude, duration, and propagation speed of the waves under control and treatment conditions [28].
5. Data Interpretation:
- A significant suppression of wave transmission by CBX indicates strong gap-junctional coupling.
- A reduction in wave extent or duration by apyrase indicates a role for ATP-mediated paracrine signaling [28].
- A hybrid mechanism is implicated if neither blocker alone fully abolishes propagation [28].
Protocol: Evaluating MSC-Exo Function in Vitro
1. Exosome Isolation and Characterization:
- Isolate exosomes from MSC conditioned media via ultracentrifugation, precipitation, size-exclusion chromatography, or immunoaffinity capture [26].
- Characterize isolates by nanoparticle tracking analysis for size distribution (30-150 nm) and Western blot for biomarkers (CD63, CD81, CD9, Alix) [26].
2. In Vitro Modeling of Ischemic Injury:
- Culture target cells (e.g., primary cardiomyocytes, cardiomyocyte cell lines).
- Induce injury by exposing cultures to hypoxia (e.g., 1% O₂) and/or serum starvation [26] [25].
3. Functional Assays:
- Apoptosis Assay: Treat injured cells with MSC-Exos or purified paracrine factors. Measure apoptosis via TUNEL staining or caspase-3/7 activity assays [26] [25].
- Gene Expression Analysis: Use qPCR or Western blot to assess the expression of pro-apoptotic (e.g., FasL, PTEN) and anti-apoptotic genes in treated vs. untreated cells [26].
- Pathway Analysis: Utilize specific pathway inhibitors (e.g., PI3K/AKT inhibitors) to confirm the involvement of suspected signaling pathways in the observed cytoprotection [26].
Signaling Pathways and Experimental Workflows
The following diagrams, generated using Graphviz, illustrate core paracrine signaling concepts and experimental workflows.
Paracrine Signaling in Cardiomyocyte Survival
Diagram Title: MSC-Exosome miRNA Inhibits Apoptosis
Experimental Workflow for Paracrine Mechanism Analysis
Diagram Title: Calcium Wave Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Paracrine Signaling Studies
| Research Reagent | Function/Application | Example Use Case |
|---|---|---|
| Fura-2 AM [28] | Ratiometric fluorescent calcium indicator for live-cell imaging. | Loading into human lens epithelium to visualize mechanically induced Ca²⁺ waves and paracrine signaling [28]. |
| Apyrase [28] | ATP-hydrolyzing enzyme; degrades extracellular ATP. | Pharmacological perturbation to assess the contribution of purinergic (ATP-mediated) paracrine signaling to intercellular communication [28]. |
| Carbenoxolone (CBX) [28] | Gap-junctional blocker; inhibits connexin channels. | Pharmacological perturbation to assess the contribution of direct gap-junctional communication (e.g., of IP₃) to intercellular signaling [28]. |
| CD63 / CD81 / CD9 Antibodies [26] | Tetraspanin markers for exosome characterization via Western blot, immunoaffinity capture. | Isolating and confirming the identity of exosomes isolated from MSC conditioned media [26]. |
| TUNEL Assay Kit [25] | Detects DNA fragmentation characteristic of apoptosis in cells or tissue sections. | Evaluating the cytoprotective effect of MSC secretome or specific factors (e.g., HASF) on cardiomyocytes after ischemic injury in vitro or in vivo [25]. |
| Akt1 Overexpression Construct [25] | Genetic modification to enhance the pro-survival and cytoprotective potential of MSCs. | Engineering MSCs to produce a more potent, cytoprotective secretome for therapeutic testing [25]. |
The field of regenerative medicine is undergoing a fundamental transformation, moving beyond merely managing symptoms toward achieving true tissue restoration. Central to this shift is the emerging discipline of Integrative and Regenerative Pharmacology (IRP), which unites pharmacology, systems biology, and regenerative medicine to develop transformative curative therapeutics [3]. This approach represents a significant departure from traditional pharmacology, which primarily focuses on symptom reduction and disease course alteration [3].
At the core of successful tissue regeneration lies the concept of immunomodulation – the active control of the immune response to create a microenvironment conducive to repair. The immune system is no longer seen merely as a defense mechanism but as a central director of healing processes. The therapeutic goal has evolved from simple immunosuppression to precise immune tuning, where the dynamic interactions between immune cells, signaling molecules, and tissue-specific factors are carefully balanced to support regeneration while controlling inflammation [29]. This paradigm recognizes that the inflammatory microenvironment can be either a barrier to or an essential component of successful tissue repair, depending on how effectively it is modulated.
Fundamental Mechanisms of Immune-Mediated Repair
Cellular Effectors in the Inflammatory Microenvironment
The repair microenvironment is orchestrated by a complex interplay of immune and stromal cells. Macrophages are particularly crucial, demonstrating remarkable plasticity between different functional states [30]. Inflammatory (M1) macrophages typically dominate early phases, clearing pathogens and debris, while reparative (M2) macrophages emerge later to promote tissue remodeling and angiogenesis. Successful regeneration often depends on the timely transition from pro-inflammatory to pro-resolving phenotypes, a process known as macrophage repolarization [30].
Mesenchymal Stromal Cells (MSCs) have emerged as master regulators of the repair microenvironment. Rather than functioning primarily through direct differentiation, MSCs exert their therapeutic effects largely through paracrine signaling and immunomodulation [31] [32]. They release a diverse array of bioactive molecules – including growth factors, cytokines, and extracellular vesicles – that modulate the local cellular environment [32]. MSCs interact with various immune cells, including T lymphocytes, B lymphocytes, natural killer cells, and dendritic cells, shaping the immune response toward a pro-regenerative state [33].
Molecular Pathways and Signaling Networks
Several key molecular pathways serve as critical regulators of the immune response in tissue repair:
TLR/NF-κB Signaling Pathway: This pathway functions as a core mediator of inflammation, integrating signals from various pathogen-associated and damage-associated molecular patterns. The GBOD-PF hydrogel demonstrates the therapeutic potential of targeting this pathway, effectively dampening the inflammatory cascade in chronic wound healing [30]. TLR4 activation particularly drives pro-inflammatory cytokine production, contributing to tissue degradation in conditions like osteoarthritis [31].
TLR3 Signaling: This pathway is activated by double-stranded RNA and initiates signaling cascades involving transcription factors NF-κB and IRF3, leading to production of pro-inflammatory cytokines and type I interferons [31]. In orthopedic diseases, TLR3 plays a dual role by modulating immune responses and influencing tissue repair processes, with recent studies suggesting involvement in cartilage degeneration and bone remodeling regulation [31].
Other crucial pathways include JAK/STAT signaling, inflammasome activation, and resolution-phase mediators such as specialized pro-resolving lipid mediators. The convergence of these pathways determines whether inflammation resolves appropriately or becomes chronic and tissue-destructive.
Therapeutic Strategies and Applications
Advanced Biomaterial Systems
Smart biomaterial platforms represent a frontier in immunomodulatory strategies. The GBOD-PF hydrogel is a prime example of a microenvironment self-adaptive multifunctional hydrogel dressing with intrinsic hemostasis, antimicrobial, and anti-inflammatory properties [30]. Composed of aldehyde-functionalized dextran (ODT) and gelatin (Gel) cross-linked through dynamic Schiff base bonds in the presence of borax and paeoniflorin (PF), this system exhibits remodeling and self-healing properties, enhanced adhesion strength, and biocompatibility [30].
This advanced biomaterial demonstrates broad-spectrum antibacterial activity and superior hemostasis while targeting the TLR4/NF-κB signaling pathway to dampen the inflammatory cascade [30]. In diabetic chronic wound models, it enhanced immune response, induced M1-to-M2 macrophage repolarization to establish an anti-inflammatory microenvironment, regulated MMP-9, and promoted angiogenesis, thereby inducing a pro-regenerative response [30].
Cellular Therapeutics and Their Mechanisms
Cell-based therapies harness the body's innate regenerative potential, with MSCs serving as a cornerstone approach. The therapeutic profile of MSCs is characterized by several key attributes:
- Multipotent Differentiation Capacity: MSCs can differentiate into various mesodermal lineages including osteoblasts, chondrocytes, and adipocytes [32].
- Paracrine Signaling: MSCs secrete a wide range of bioactive molecules that modulate inflammation, stimulate tissue repair, and promote regeneration [31].
- Immunomodulation: MSCs interact with various immune cells, modulating the immune response through both direct cell-cell interactions and release of immunosuppressive molecules [32].
- Trophic Support: MSCs provide growth factors and other molecules that support survival and function of resident tissue cells.
The International Society for Cell and Gene Therapy (ISCT) has established standard criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73, CD90, CD105 ≥95%; hematopoietic markers ≤2%), and tri-lineage differentiation potential [32]. These standards ensure consistent characterization across research and clinical applications.
Table 1: MSC Sources and Their Therapeutic Properties
| Source Tissue | Therapeutic Properties | Clinical Applications |
|---|---|---|
| Bone Marrow | High differentiation potential, strong immunomodulatory effects | Orthopedic injuries, graft-versus-host disease [32] |
| Adipose Tissue | Easier harvesting, higher yields, comparable therapeutic properties | Regenerative procedures, inflammatory conditions [32] |
| Umbilical Cord | Enhanced proliferation, lower immunogenicity, suitable for allogeneic transplantation | Various regenerative applications, immune disorders [32] |
| Dental Pulp | Unique regenerative properties | Dental and maxillofacial applications [32] |
Clinical Translation and Outcomes
Regenerative immunomodulation strategies have demonstrated promising results across various clinical applications:
Orthopedic Diseases: MSC-based therapies have shown safety and feasibility for conditions like osteoarthritis, with improvements in pain reduction and function observed in many cases [31]. For cartilage repair, the Matrix-induced Autologous Chondrocyte Implantation (MACI) technique has demonstrated 80-90% success rates over time [34].
Inflammatory Bowel Disease (IBD): MSCs have gained interest in IBD treatment due to their unique ability to differentiate and secrete regulatory factors, including extracellular vesicles that play crucial roles in abnormal tissue organization [35]. Various administration routes – including intraperitoneal, intravenous, and local delivery – have been explored in preclinical and clinical studies [35].
Chronic Wound Healing: Multifunctional hydrogels like GBOD-PF have demonstrated accelerated large-scale chronic wound healing in infection and diabetic models by enhancing immune response, promoting angiogenesis, and regulating the inflammatory microenvironment [30].
Table 2: Clinical Success Rates of Select Regenerative Therapies
| Therapy | Condition | Success Rate / Outcome | Key Mechanisms |
|---|---|---|---|
| MACI | Cartilage defects | 80-90% success over time [34] | Chondrocyte implantation, cartilage regeneration |
| BMAC (Stem Cells) | Osteonecrosis of hip | >90% avoided collapse after 2 years [34] | Delivery of reparative cells, growth factors, tissue modulation |
| MSC Therapy | Autoimmune conditions | ~80% success for immune modulation [34] | Anti-inflammatory cytokine secretion, immune system modulation |
| Hematopoietic Stem Cell Transplant | Blood cancers | 60-70% success for certain types [34] | Immune system reconstitution, cancer cell targeting |
Experimental Approaches and Methodologies
In Vitro Immunomodulation Assessment
Standardized in vitro approaches provide essential platforms for screening immunomodulatory therapeutics before advancing to complex in vivo models. The RAW264.7, J774A.1, THP-1, and U937 cell lines serve as ideal model systems for preliminary investigation and dose selection for in vivo studies [36]. More than 40 different assays have been standardized to investigate the immune modulatory effects of therapeutic candidates.
Key methodologies include:
- Cell Viability and Proliferation: MTT assay for metabolic activity assessment
- Phagocytic Activity: Neutral red uptake assay for macrophage function
- Inflammatory Mediator Production: Griess reaction for nitric oxide detection
- Gene Expression Analysis: PCR for evaluating expression of TLRs, COX-2, iNOS, TNF-α, IL-6, and IL-1β [36]
These in vitro systems enable researchers to dissect specific mechanisms of immunomodulation in controlled environments, providing crucial data for rational therapeutic development.
Macrophage Repolarization Assay Protocol
Objective: To evaluate compound-induced macrophage polarization from M1 to M2 phenotype.
Materials:
- RAW264.7 or primary bone marrow-derived macrophages
- Lipopolysaccharide (LPS) (100 ng/mL) and IFN-γ (20 ng/mL) for M1 polarization
- IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for M2 polarization
- Test compounds (e.g., MSC-conditioned medium, immunoceuticals)
- RNA extraction kit and qPCR reagents
- ELISA kits for TNF-α, IL-1β, IL-10, TGF-β
- Flow cytometry antibodies for CD86 (M1) and CD206 (M2)
Procedure:
- Seed macrophages in appropriate culture plates and allow to adhere overnight.
- Polarize macrophages to M1 phenotype using LPS + IFN-γ for 24 hours.
- Treat M1-polarized macrophages with test compounds for 48 hours.
- Collect supernatant for cytokine analysis by ELISA.
- Harvest cells for RNA extraction and gene expression analysis of M1 markers (iNOS, TNF-α, IL-12) and M2 markers (Arg1, Ym1, Fizz1).
- Analyze surface markers by flow cytometry for CD86 and CD206.
- Calculate repolarization efficiency based on marker expression ratios.
This protocol enables quantitative assessment of a compound's ability to shift macrophage phenotype, a crucial mechanism in resolving inflammation and promoting regeneration.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Immunomodulation Studies
| Reagent/Cell Line | Function/Application | Specific Examples |
|---|---|---|
| RAW264.7, J774A.1 | Macrophage model systems for in vitro screening | Phagocytosis, cytokine production, polarization studies [36] |
| THP-1, U937 | Monocyte/macrophage cell lines for differentiation studies | PMA-induced differentiation, inflammation models [36] |
| LPS (Lipopolysaccharide) | TLR4 agonist for M1 macrophage polarization | Inflammatory activation at 100 ng/mL [36] |
| - Flow Cytometry Antibodies | Immune cell phenotyping and polarization assessment | CD86 (M1), CD206 (M2), CD73, CD90, CD105 (MSCs) [32] |
| ELISA Kits | Cytokine and inflammatory mediator quantification | TNF-α, IL-1β, IL-6, IL-10, TGF-β measurement [36] |
| PCR Primers | Gene expression analysis of immune targets | TLRs, COX-2, iNOS, TNF-α, IL-6, IL-1β [36] |
Signaling Pathways in Immunomodulation
The following diagrams visualize key signaling pathways involved in immunomodulation for tissue repair, created using Graphviz DOT language with high color contrast for clarity.
Diagram 1: Macrophage polarization pathways and MSC-mediated immunomodulation. The diagram illustrates signaling pathways driving M1 (pro-inflammatory) and M2 (pro-reparative) macrophage polarization, along with key molecular mediators through which mesenchymal stromal cells (MSCs) influence immune cell function.
Future Perspectives and Challenges
The field of immunomodulation for regenerative pharmacology continues to evolve rapidly, with several emerging trends and persistent challenges shaping its trajectory. Artificial intelligence (AI) holds significant promise for transforming regenerative pharmacology by enabling more efficient therapeutic development, predicting drug delivery system effectiveness, and anticipating cellular responses [3]. The integration of multi-omics approaches (transcriptomics, genomics, proteomics, epigenomics, metabolomics, and microbiomics) with advanced computational methods will provide unprecedented insights into the complex networks governing immune responses in tissue repair [3].
Despite substantial progress, significant translational barriers remain. These include investigational obstacles such as unrepresentative preclinical animal models, manufacturing issues related to scalability and automated production, complex regulatory pathways with varying regional requirements, ethical considerations, and economic factors such as high manufacturing costs [3]. Additionally, the high cost of advanced therapy medicinal products (ATMPs) limits accessibility, particularly in low- and middle-income countries [3].
Future advancements will likely focus on developing increasingly sophisticated 'smart' biomaterials that can deliver bioactive compounds in a temporally and spatially controlled manner in response to specific microenvironmental cues [3]. The convergence of targeted drug delivery systems, precision immunomodulation, and patient-specific cellular and genetic information will enable truly personalized regenerative therapies that maximize effectiveness while minimizing off-target effects [3] [34]. As the field matures, long-term follow-up clinical investigations and standardized, scalable bioprocesses will be essential for widespread clinical adoption and global accessibility of these transformative therapies.
The Pharmacological Toolkit for Directing Regeneration
Smart Biomaterials and Controlled Drug Delivery Systems (DDSs) for Spatiotemporal Control
Regenerative pharmacology represents a paradigm shift in therapeutic strategy, aiming not merely to manage symptoms but to restore the physiological structure and function of damaged tissues and organs. [3] Within this innovative framework, smart biomaterials for controlled Drug Delivery Systems (DDSs) are foundational. These materials are engineered to interact dynamically with biological systems, providing precise spatiotemporal control over the release of therapeutic agents—a critical capability for orchestrating complex biological processes like tissue regeneration and immune modulation. [3] [37] By applying pharmacological rigor to regenerative medicine, these systems enable transformative curative therapeutics that move beyond palliative care. [3]
The convergence of biomaterials science with regenerative pharmacology addresses a core challenge: the need for localized, sustained, and stimulus-responsive therapeutic action. This integration is essential for developing next-generation Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies, which require precise microenvironments to function effectively. [38] Smart biomaterials act as the central platform for achieving this precise control, thereby enhancing therapeutic efficacy while minimizing systemic side effects.
Fundamental Mechanisms: Stimulus-Responsive Biomaterials
Smart biomaterials achieve spatiotemporal precision through engineered responses to specific biological or external triggers. These "stimulus switches" allow for drug release that is contingent upon the presence of a specific signal at a specific time and location. [39] The mechanisms can be broadly categorized based on the source of the stimulus.
Endogenous Stimuli
Endogenous stimuli are intrinsic to the disease microenvironment or specific physiological processes. Key triggers include:
- pH: The slightly acidic microenvironment of pathological sites like tumors or inflamed tissues can trigger the degradation of acid-labile bonds (e.g., hydrazone, acetal) in a polymer, leading to drug release. [39]
- Enzymes: Overexpressed enzymes (e.g., matrix metalloproteinases, MMPs; phosphatases) at the target site can cleave specific peptide or chemical sequences incorporated into the biomaterial, resulting in a highly specific release profile. [39]
- Redox Potential: The significant difference in redox potential between the intracellular (high glutathione, GSH) and extracellular compartments can be exploited. Biomaterials with disulfide linkages remain stable in circulation but rapidly degrade and release cargo upon cell internalization. [39]
Exogenous Stimuli
Exogenous stimuli are applied externally, offering remote control over drug release. Common modalities include:
- Light: Near-infrared (NIR) light, which has superior tissue penetration, can be used to trigger drug release. For instance, gold nanorods or other photothermal agents absorb NIR light, generating heat that melts a surrounding thermal-sensitive polymer matrix (e.g., pluronic) to release the drug. [40]
- Temperature: Mild hyperthermia induced by external sources can activate thermal-sensitive biomaterials like poly(N-isopropylacrylamide) (pNIPAM). [40]
- Magnetic Fields: Magnetic nanoparticles can be guided to a specific site using an external magnet and then activated to release drugs via heat generation (magneto-thermal effect) or mechanical force. [37]
The following diagram illustrates the logical workflow of how these stimuli trigger drug release from smart biomaterials.
Stimulus-Response Logic for Smart DDSs
Advanced Platforms for Spatiotemporal Control
Recent research has yielded sophisticated biomaterial platforms that exemplify these mechanisms:
- NIR-Triggered Supramolecular Hydrogels: Yang et al. developed hydrogels incorporating MXene (a photothermal nanomaterial) complexed with doxorubicin. Upon NIR irradiation, the photothermal effect disrupts the hydrogel supramolecular network, providing excellent tumor localization and spatiotemporal control over chemotherapeutic release. [40]
- Enzyme-Responsive Bioinks: Han et al. created a cerebrovascular-specific extracellular matrix bioink for 3D bioprinting of blood-brain barrier models. The microenvironment provided by this bioink supports the self-assembly of endothelial cells and pericytes, responding to physiological and pathological enzymatic cues. [40]
- Polymer-based mRNA Delivery: Lee et al. systematically investigated how the structure and ratio of poly(ethylene glycol) (PEG)-lipids in lipid nanoparticles (LNPs) influence the efficacy and immunogenicity of repeated mRNA administrations. This work highlights the critical role of biomaterial chemistry in avoiding accelerated blood clearance, a key challenge for chronic dosing. [40]
Table 1: Summary of Key Stimulus-Responsive Mechanisms in Smart Biomaterials
| Stimulus Type | Example Trigger | Material/Biomaterial Response | Therapeutic Outcome |
|---|---|---|---|
| Endogenous / Biochemical | Low pH (e.g., tumor microenvironment) | Degradation of acid-labile bonds in polymer backbone or side chains [39] | Targeted drug release in pathological tissues |
| Overexpressed Enzymes (e.g., MMPs) | Cleavage of specific peptide sequences crosslinking the material [39] | Site-specific release and enhanced tissue penetration | |
| High Redox Potential (High GSH) | Reduction and cleavage of disulfide bonds within the material [39] | Intracellular drug delivery following endocytosis | |
| Exogenous / Physical | Near-Infrared (NIR) Light | Photothermal agent heats up, melting a thermal-sensitive polymer matrix [40] | Remote spatiotemporal control for synergistic photothermal-chemotherapy |
| Alternating Magnetic Field | Magnetic nanoparticles generate heat, triggering release from thermal-sensitive carrier [37] | Deep-tissue penetration for remote-activated release | |
| Mild Hyperthermia | Change in conformation/aggregation of thermal-sensitive polymers (e.g., pNIPAM) [40] | Enhanced drug release and potentiation of other therapies (e.g., immunotherapy) |
Experimental Methodologies for Development and Validation
The development of effective smart DDSs requires a suite of rigorous experimental protocols to validate material properties, biological efficacy, and spatiotemporal control.
Protocol: In Vitro Validation of Cytosolic Delivery Efficiency
A significant bottleneck in nanomedicine is the inefficient release of cargo from entrapping endosomes into the cell cytosol (typically only 1-2%). The following protocol, adapted from a recent breakthrough, uses a color-coded, fluorescence-based assay to quantitatively screen hundreds of nanoparticle formulations for their cytosolic delivery efficiency. [41]
1. Principle: Genetically engineered mouse cells express a fluorescent protein (Gal8-mRuby) that binds to glycans on the endosomal membrane. When a nanoparticle successfully ruptures or escapes the endosome, the membrane is compromised, recruiting Gal8-mRuby which emits an orange-red fluorescent signal. [41]
2. Workflow:
- Step 1: Cell Preparation. Seed genetically engineered cells expressing the Gal8-mRuby protein in a multi-well plate and culture until ~70% confluency.
- Step 2: Nanoparticle Treatment. Incubate the cells with the library of polymer-based nanoparticles, each carrying a model drug cargo (e.g., mRNA or a fluorescent dye).
- Step 3: Imaging and Analysis. After a set incubation period, use high-content fluorescence microscopy to capture images. A custom computer program then analyzes the images to:
- Track nanoparticle location using a red fluorescent marker.
- Quantify cytosolic delivery efficiency by measuring the amount of orange-red fluorescent light (from Gal8-mRuby) in the vicinity of each nanoparticle. [41]
3. Validation: The top-performing nanoparticle formulations from the in vitro screen are administered to living mice. The nanoparticles are loaded with mRNA encoding a reporter gene (e.g., luciferase). Successful cytosolic delivery and functional release are confirmed by bioluminescence imaging, showing expression of the reporter protein in target tissues. A high correlation between in vitro and in vivo performance validates the assay's predictive power. [41]
The following diagram outlines the key steps of this experimental workflow.
Workflow for Cytosolic Delivery Assay
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the development and testing of smart biomaterials for drug delivery, as featured in the cited research.
Table 2: Research Reagent Solutions for Smart Biomaterial Development
| Reagent / Material | Function / Explanation | Example Application |
|---|---|---|
| MXene-Doxorubicin Complexes | 2D inorganic material with high photothermal conversion efficiency; complexes with chemotherapeutics for combinational therapy. [40] | Near-infrared-triggered drug release from supramolecular hydrogels for synergistic chemo-photothermal cancer therapy. [40] |
| Gal8-mRuby Reporter Cell Line | Genetically engineered cells that fluoresce orange-red when endosomal membranes are damaged, signaling successful cytosolic delivery. [41] | High-throughput screening of nanoparticle formulations for their ability to escape endosomes and deliver cargo into the cell interior. [41] |
| Cerebrovascular-Specific ECM Bioink | A blend of brain- and vessel-derived decellularized matrices that provides a physiologically relevant microenvironment. [40] | Coaxial 3D bioprinting of perfusable blood-brain barrier models for studying neuroinflammation and drug delivery. [40] |
| PEG-Lipids of Varying Structure/Ratio | Key component of lipid nanoparticles (LNPs) that modulates stability, pharmacokinetics, and immunogenicity. [40] | Optimizing repeated administration of mRNA therapeutics by avoiding accelerated blood clearance. [40] |
| Silica-Coated Gold Nanorods (AuNR@SiO2) | Photothermal nanoparticles with improved biocompatibility and controlled heating profile. [40] | Achieving accurately controlled mild hyperthermia to enhance immune checkpoint blockade therapy in cancer. [40] |
| Low-Molecular-Weight PEGs | Acts as a cryoprotectant with reduced toxicity compared to conventional agents like DMSO. [40] | Cryopreservation of 3D stem cell spheroids while preserving cell viability, function, and morphology. [40] |
Quantitative Performance Data and Efficacy
The efficacy of smart biomaterial-based DDSs is demonstrated through quantitative improvements in therapeutic outcomes across various disease models. The following table consolidates key performance metrics from recent preclinical studies.
Table 3: Quantitative Efficacy of Selected Smart Biomaterial DDSs
| Therapeutic Platform | Disease Model | Key Efficacy Metric | Reported Outcome | Source |
|---|---|---|---|---|
| AuNR@SiO2 + Anti-PD-1 | Cancer (in vivo) | Tumor Regression & Immunological Memory | Complete tumor regression and long-term immunological memory achieved. [40] | Yun et al. |
| MSCs with High Glutathione | Osteoarthritis | Chondrocyte Rejuvenation | Secreted IGF2 promoted autophagy and matrix production, alleviating osteoarthritis. [40] | Cho et al. |
| Electrically Primed MSCs | Osteochondral Defect (Rat) | Cartilage Regeneration | Significant increase in cartilage-specific gene expression, proteoglycan deposition, and in vivo regeneration. [40] | Yi et al. |
| Bifunctional Tumor-Targeting Bioprobe | Cancer (in vivo) | Tumor-Specific Accumulation & Therapy | Combined real-time NIR imaging with synergistic photodynamic/photothermal therapy. [40] | Park et al. |
| Bone Marrow Aspirate Concentrate (BMAC) | Osteonecrosis of the Hip | Joint Collapse Prevention | >90% of treated hips avoided collapse at 2-year follow-up. [34] | Clinical Study |
| Matrix-induced Autologous Chondrocyte Implantation (MACI) | Knee Cartilage Defects | Clinical Success Rate | 80% to 90% success rate over time. [34] | Clinical Data |
Future Directions and Integration with Regenerative Pharmacology
The future of smart biomaterials in regenerative pharmacology is intrinsically linked to technological convergence. Key emerging trends include:
- Artificial Intelligence (AI) and Data-Driven Design: AI is poised to transform regenerative pharmacology by enabling the prediction of optimal biomaterial formulations, forecasting DDS effectiveness, and anticipating complex cellular responses. This helps in navigating the vast design space of chemical properties to steer nanoparticles to specific tissues and cells. [3] [41] [42]
- Advanced Manufacturing and 3D Bioprinting: The integration of smart biomaterials as bioinks is crucial for fabricating complex, physiologically relevant tissue constructs. Technologies like coaxial 3D bioprinting allow for the creation of perfusable vascular networks, which are essential for sustaining engineered tissues and modeling diseases like neuroinflammation. [40] [37]
- Overcoming Translational Barriers: For smart DDSs to become mainstream clinical tools, challenges in scalable, GMP-compliant manufacturing must be addressed. This includes automating production, establishing robust quality control (e.g., real-time release criteria), and managing complex supply chains for raw materials. [38] Furthermore, the high cost of these advanced therapies necessitates developments for improved global accessibility. [3]
The ultimate vision is a future of personalized regenerative therapies. Treatments will be tailored to a patient's unique cellular and genetic profile, using smart biomaterials as the delivery platform for patient-specific cells or genetically modified agents. This approach, central to the mission of regenerative pharmacology, promises to restore not just tissue, but full health. [3] [34]
The central paradigm of regenerative pharmacology is shifting from single-factor intervention to the orchestrated delivery of multiple bioactive compounds. This evolution stems from the recognition that natural tissue repair is not governed by solitary signals but by complex, dynamic cascades of molecular events. While individual growth factors have demonstrated promising regenerative potential in preclinical settings, their clinical translation has been hampered by several limitations. These include short half-lives, rapid diffusion from delivery sites, and dose-limiting side effects when administered at supraphysiological concentrations [43]. For instance, recombinant human Bone Morphogenetic Protein-2 (BMP-2), while approved for spinal fusion and bone regeneration, has been associated with ectopic bone formation, inflammatory complications, and other adverse effects linked to its unphysiological delivery [43].
The pleiotropic nature of growth factors further complicates their therapeutic application. A single factor, such as Transforming Growth Factor-β (TGF-β) or Epidermal Growth Factor (EGF), can drive complete limb regeneration in urodele amphibians yet promotes fibrosis and scarring in mammalian systems, including humans [44]. This functional ambiguity suggests that the regenerative outcome depends less on the presence of individual factors and more on the precise spatiotemporal context of their presentation. The evolutionary conservation of growth factor and receptor tyrosine kinase systems between species with high and low regenerative capacity indicates that the difference lies not in the molecular toolkit itself, but in how it is deployed [44]. Consequently, the next frontier in regenerative medicine involves developing strategies to recapitulate the native signaling dynamics that guide successful tissue repair, moving beyond single-factor approaches to sophisticated multi-component systems.
Clinical Landscape of Growth Factor-Based Therapies
Several growth factor-based therapies have achieved clinical approval, demonstrating the therapeutic potential of this class of molecules. These products, however, primarily rely on single growth factors delivered via biomaterial scaffolds, highlighting both the feasibility and the limitations of current approaches.
Table 1: Clinically Approved Growth Factor-Based Products
| Product Name | Growth Factor | Delivery System | Approved Indications | Regulatory Authority |
|---|---|---|---|---|
| Infuse Bone Graft | BMP-2 | Collagen sponge | Spinal fusion, bone regeneration | FDA (U.S.) |
| OP-1 Putty | BMP-7 | Bovine bone-derived collagen | Spinal fusion, bone regeneration | FDA (U.S.) |
| Regranex | PDGF-BB | Sodium carboxymethylcellulose gel | Chronic diabetic wounds | FDA (U.S.) |
| Augment Bone Graft | PDGF-BB | Beta-tricalcium phosphate | Ankle and hindfoot fusion | FDA (U.S.) |
| PELNAC | FGF-2 | Collagen sponge | Bedsores, cutaneous ulcers | PMDA (Japan) |
| REGEN-D | EGF | Cellulose gel | Diabetic foot ulcers | MFDS (South Korea) |
| Kepivance | FGF-7 (KGF) | Intravenous injection | Gastrointestinal injury | FDA (U.S.) |
| Increlex | IGF-1 | Subcutaneous injection | Primary IGF-1 deficiency | FDA (U.S.) |
Abbreviations: BMP, Bone Morphogenetic Protein; PDGF, Platelet-Derived Growth Factor; FGF, Fibroblast Growth Factor; EGF, Epidermal Growth Factor; KGF, Keratinocyte Growth Factor; IGF, Insulin-like Growth Factor; FDA, U.S. Food and Drug Administration; PMDA, Pharmaceuticals and Medical Devices Agency (Japan); MFDS, Ministry of Food and Drug Safety (South Korea). [43]
The clinical use of these agents is constrained by their inherent pharmacokinetic challenges. A critical obstacle is the short in vivo half-life of many growth factors; for example, the active form of TGF-β1 has a half-life of only 2-3 minutes, and EGF is cleared in under one minute [43]. This necessitates the use of delivery systems that maintain local concentrations, yet controlling the precise spatiotemporal release profile remains a significant engineering challenge. The development of next-generation regenerative therapies therefore focuses on overcoming these limitations through improved delivery technologies and rational factor combinations that more closely mimic the native healing cascade.
Engineering Controlled Release and Delivery Systems
A primary strategy to enhance the efficacy and safety of growth factor therapies is their incorporation into advanced delivery systems that provide localized and sustained release. These biomaterial-based systems aim to protect growth factors from degradation, reduce their rapid clearance, and decrease the need for supraphysiological, and potentially harmful, dosing [43] [45].
Covalent Immobilization Strategies
Covalent conjugation of growth factors to a biomaterial scaffold is a common method to prevent rapid diffusion. This approach often relies on chemistries such as 1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide (EDC) and N-hydroxy-succinimide (NHS) crosslinking, which form stable amide bonds. While simple and FDA-approved, EDC/NHS chemistry targets primary amines and carboxylic acids randomly throughout the protein, which can potentially occlude receptor-binding sites and reduce bioactivity [43]. More sophisticated, site-specific conjugation methods have been developed to address this limitation. One prominent example is the use of enzymatic crosslinking via transglutaminase Factor XIIIa. Growth factors can be engineered to contain a substrate sequence (e.g., the α2-plasmin inhibitor-derived sequence, α2PI1−8) that allows for specific covalent incorporation into fibrin matrices [43]. This strategy has been successfully applied to BMP-2, VEGF-A, PDGF-AB, and IGF-1. In a critical-size cranial defect model in rats, α2PI1−8-BMP-2 delivered in a fibrin matrix induced significantly higher bone formation than wild-type BMP-2 [43].
Biomaterial Scaffolds and Depot Systems
A wide range of natural and synthetic biomaterials serve as reservoirs for the controlled release of growth factors. These include:
- Hydrogels (e.g., fibrin, collagen, gelatin, hyaluronic acid): Provide a hydrated, three-dimensional environment that can be modified for tunable release kinetics [45].
- Microspheres and Nanoparticles: fabricated from polymers like PLGA (poly(lactic-co-glycolic acid)), allowing for pulsatile or sustained release profiles depending on their composition and degradation rate [45].
- Plate-Rich Plasma (PRP) and Preparation Rich in Growth Factors (PRGF): Autologous preparations that constitute a natural cocktail of multiple growth factors, including PDGF, TGF-β, VEGF, and IGF, released from platelet alpha-granules upon activation [45]. These preparations represent a readily available, multi-factor approach to stimulate healing, particularly in orthopedic and dental applications.
The design of these systems is increasingly focused on achieving sequential release to mirror the natural timeline of healing. For example, a system might be engineered to release angiogenic factors like VEGF first, to establish a blood supply, followed by osteogenic factors like BMP-2 later, to promote bone deposition [45].
Experimental Platforms for Evaluating Combinatorial Therapies
Rigorous preclinical evaluation is essential for deconvoluting the complex interactions within multi-factor regenerative therapies. Advanced experimental platforms enable researchers to systematically test combinations and quantify their effects on cellular behavior and tissue formation.
High-Throughput Screening and Protein Dynamics
Novel high-throughput platforms are transforming the capacity to study protein dynamics and signaling in response to combinatorial cues. The recent development of a high-throughput single-molecule tracking (htSMT) platform allows for the real-time measurement of protein motion and interactions in living cells at an unprecedented scale, capable of screening over 10,000 compounds and imaging more than one million cells per day [46]. This technology can determine the potency, pathway selectivity, target engagement, and mechanism of action for identified hits in a single experimental modality. For instance, applying htSMT to the estrogen receptor (ER) revealed how different ligands alter ER dynamics and identified novel kinase-mediated regulatory mechanisms. The sensitivity of this approach uncovered a correlation between ER dynamics and the efficacy of ER antagonists in suppressing cancer cell growth [46]. Such platforms are powerful for understanding how growth factor combinations integratively modulate intracellular signaling networks.
In Vivo and Preclinical Model Systems
Validating combinatorial strategies requires robust in vivo models that recapitulate key aspects of human tissue repair. The following protocols represent standardized methodologies for assessing regenerative efficacy:
Protocol: Critical-Size Bone Defect Model in Rats [43]
- Objective: To evaluate the osteoinductive capacity of growth factor combinations in a load-bearing, non-healing bone defect.
- Procedure:
- Create a segmental defect (typically >6mm in the rat femur) using an oscillating saw under general anesthesia and aseptic conditions.
- Stabilize the defect using an internal plate or external fixator.
- Implant the test article (e.g., growth factor-laden scaffold) into the defect site. The control group receives a scaffold-only implant.
- Administer post-operative analgesia and monitor animals for a predetermined period (e.g., 4-12 weeks).
- Analysis:
- Longitudinal Radiography: Assesses bone bridging and callus formation.
- Micro-Computed Tomography (μCT): Provides quantitative 3D analysis of bone volume, trabecular architecture, and mineral density.
- Histology and Immunohistochemistry: (e.g., H&E, Masson's Trichrome, osteocalcin immunostaining) evaluates tissue morphology, collagen deposition, and osteogenic differentiation at the cellular level.
Protocol: Ischemic Hind Limb Model in Rodents [43]
- Objective: To test the pro-angiogenic potential of factor combinations in tissue ischemia.
- Procedure:
- Induce unilateral hind limb ischemia by ligating and excising the femoral artery under anesthesia.
- Inject the therapeutic formulation (e.g., fibrin matrix containing engineered VEGF-A) into the ischemic muscle bed at the time of surgery or post-operatively.
- The control group receives a vehicle injection.
- Analysis:
- Laser Doppler Perfusion Imaging: Quantifies blood flow recovery over time.
- Capillary Density Analysis: Histological sections are stained with antibodies against CD31 or other endothelial markers to quantify capillary formation.
- Functional Assessment: Evaluation of limb mobility and tissue integrity.
The following diagram illustrates the logical workflow for developing and testing a combinatorial growth factor therapy, from initial concept through to preclinical validation.
The Scientist's Toolkit: Essential Research Reagents
Successful research in combinatorial regenerative pharmacology relies on a suite of specialized reagents and tools. The following table details key materials and their applications in experimental workflows.
Table 2: Key Research Reagent Solutions for Combinatorial Regeneration Studies
| Research Reagent | Function & Application in Regenerative Studies |
|---|---|
| Recombinant Growth Factors (e.g., BMP-2, VEGF, FGF, PDGF) | Purified proteins used as the active therapeutic agents in combination studies. Quality and source are critical for reproducibility. |
| Engineered Factor Variants (e.g., α2PI1−8-tagged proteins) | Growth factors engineered with specific peptide tags (e.g., for Factor XIIIa crosslinking) enable site-specific, covalent immobilization to biomaterial matrices like fibrin [43]. |
| HaloTag Fusion Proteins & JF549 Ligand | A self-labeling protein tag system. When cells express a HaloTag-fused protein of interest (e.g., a receptor), the bright, photostable JF549 dye forms a covalent bond, allowing for high-quality single-molecule tracking (SMT) of protein dynamics in live cells [46]. |
| Bioactive Scaffolds (e.g., Fibrin, Collagen, PLGA, Hyaluronic Acid) | Natural or synthetic matrices that serve as 3D delivery platforms. Their chemical and physical properties (degradation rate, stiffness, porosity) can be tuned to control growth factor release and cell infiltration. |
| Factor XIIIa (Transglutaminase) | Enzyme used to cross-link engineered growth factors (containing the α2PI1−8 sequence) into fibrin matrices, creating a stable, bioactive depot [43]. |
| EDC/NHS Crosslinker Chemistry | A zero-length crosslinking system used to covalently conjugate growth factors to biomaterials containing carboxyl or amine groups via amide bonds. A standard, though non-specific, immobilization method [43]. |
| sc-ImmuAging Clock Models | A computational tool comprising cell-type-specific transcriptomic aging clocks for immune cells (monocytes, T cells, B cells). It can predict biological age from single-cell RNA-seq data and measure transcriptome age acceleration/rejuvenation in response to therapies or disease [47]. |
Signaling Pathways and Molecular Mechanisms
The therapeutic action of combined growth factors converges on a network of intracellular signaling pathways that direct cell fate decisions. Understanding these pathways is critical for rational therapy design.
The core signaling apparatus for many growth factors is the Receptor Tyrosine Kinase (RTK)-MAPK cascade. This system, which evolved to allow multicellular organisms to integrate complex stimuli, provides the molecular basis for the pleiotropic effects of growth factors [44]. The cascade involves sequential phosphorylation events that create a short-term "memory," allowing the cell to amplify signals and integrate inputs from multiple growth factors simultaneously [44]. This explains why the context and timing of signal presentation are deterministic for cellular outcomes such as proliferation, differentiation, or apoptosis.
A key challenge in human regeneration is the balance between regeneration and fibrosis, which is governed by the interplay of multiple signaling pathways. The following diagram illustrates the signaling nodes that can be targeted by combinatorial growth factor therapies to steer this balance toward functional tissue repair.
Future Perspectives and Concluding Remarks
The field of regenerative pharmacology is advancing toward an era of increasingly sophisticated, personalized, and integrative therapies. The future of orchestrating regeneration lies in moving beyond simple combinations toward systems that are dynamically responsive to the wound environment. "Smart" biomaterials that release factors in response to specific enzymatic activity, pH changes, or mechanical stress represent a key direction [3]. Furthermore, the integration of advanced therapies medicinal products (ATMPs), such as somatic cell therapies, with controlled release systems creates opportunities for synergistic effects where engineered cells act as local, sustained factories for producing therapeutic factor combinations [38].
The convergence of artificial intelligence (AI) and systems biology is poised to accelerate discovery. AI can help predict optimal growth factor combinations and dosing schedules by modeling complex signaling networks and analyzing high-throughput screening data [3]. Meanwhile, tools like single-cell transcriptomic aging clocks (e.g., sc-ImmuAging) provide a means to quantitatively assess the biological impact of therapies, not just on tissue structure but on cellular age and function [47]. Finally, the growing emphasis on scalable, GMP-compliant manufacturing and rigorous regulatory science will be essential to translate these complex combinatorial products from the laboratory to the clinic, ultimately fulfilling their promise to restore structure and function in damaged tissues [38].
The field of regenerative pharmacology is undergoing a profound transformation, shifting from a focus on symptomatic relief to developing curative interventions that restore the physiological structure and function of damaged tissues and organs. [3] This paradigm leverages the body's innate healing mechanisms through targeted therapies, demanding more sophisticated and human-relevant testing platforms. Advanced in vitro models, particularly those employing 3D bioprinting, organoids, and organ-on-a-chip (OoC) technologies, have emerged as powerful tools to deconstruct the complex mechanisms of action (MoA) of regenerative therapies. [3] [48] These technologies enable the creation of biomimetic tissue constructs that replicate key aspects of human physiology, overcoming the limitations of traditional 2D models and animal studies, which often fail to accurately predict human clinical outcomes. [49] [48] Their integration is foundational to Integrative and Regenerative Pharmacology (IRP), a discipline that combines pharmacological sciences with systems biology and regenerative medicine to develop multi-level, holistic interventions. [3]
The passing of the FDA Modernization Act 2.0 has further accelerated the adoption of these models by reducing animal testing requirements for drug trials, marking a significant regulatory milestone. [48] This review provides an in-depth technical examination of these advanced models, their synergies, and their critical role in pioneering the next generation of regenerative pharmacotherapeutics.
Technological Foundations and Capabilities
3D Bioprinting: Engineering Biological Structures
3D bioprinting is an additive manufacturing process that enables the layer-by-layer deposition of bioinks—combinations of living cells, biomaterials, and bioactive factors—to create complex, three-dimensional tissue constructs with high spatial precision. [50] Its significance lies in its ability to produce tissue models that closely resemble their in vivo counterparts, providing a more accurate platform for studying cellular interactions, disease progression, and therapeutic responses. [50]
The table below summarizes the core bioprinting techniques, their operating principles, and key characteristics.
Table 1: Core 3D Bioprinting Techniques and Characteristics
| Technique | Working Principle | Resolution | Cell Viability | Advantages | Disadvantages |
|---|---|---|---|---|---|
| Extrusion-Based | Continuous deposition of bioink through a nozzle via pneumatic or mechanical pressure. [50] | 100 – 500 µm [50] | Moderate (subject to shear stress) [50] | Ability to print high-viscosity bioinks; suitable for large, complex structures. [50] | Shear stress can compromise cell viability. [50] |
| Inkjet-Based | Thermal or piezoelectric forces eject discrete droplets of bioink. [50] | ~100 – 500 µm [50] | High [50] | High speed and relatively low cost; good cell viability. [50] | Limited to low-viscosity bioinks; clogging can occur. [50] |
| Laser-Assisted | A focused laser pulse creates a pressure bubble that transfers bioink from a ribbon onto a substrate. [50] | < 10 µm [50] | >95% [50] | Nozzle-free, high resolution, enabling single-cell placement. [50] | High cost, complex setup, and slow for large structures. [50] |
| Stereolithography (SLA) | A laser or digital light projector crosslinks photopolymerizable bioinks in a layer-by-layer fashion. [50] | Down to 10 µm [50] | 70 – 90% [50] | Very high resolution and smooth surface finish. [50] | Limited to photopolymerizable materials; potential cytotoxicity from photoinitiators. [50] |
Bioinks are a critical component and an area of intense innovation. They are typically composed of printable polymer-based hydrogels, such as alginate-gelatin blends or decellularized extracellular matrix (dECM) bioinks, which more accurately replicate the native tissue microenvironment. [49] [50] Innovations like multi-material printing and the incorporation of iodixanol to mitigate light scattering in high-cell-density SLA printing are pushing the boundaries of resolution and biological complexity. [50]
Organoids: Self-Organizing Mini-Organs
Organoids are three-dimensional, self-assembled structures derived from stem cells (pluripotent or adult) or tissue-specific progenitor cells that recapitulate key architectural and functional features of their corresponding organ. [51] [48] They are powerful for modeling human development, disease, and patient-specific responses. For instance, bone/cartilage organoids can model disorders like osteoporosis and osteoarthritis, providing a platform for drug screening and regenerative strategy development. [51] Their self-organizing nature allows them to exhibit complex multicellular niches and microstructures that are difficult to engineer from the top down. [51]
Organ-on-a-Chip (OoC) Platforms: Mimicking Dynamic Physiology
Organ-on-a-chip systems are microfluidic devices that house engineered living tissues designed to recapitulate organ-level functions. [50] [52] These platforms incorporate continuous perfusion, which enables the delivery of nutrients, removal of waste, and application of biomechanical cues (e.g., fluid shear stress, cyclic strain), thereby creating a more physiologically relevant dynamic microenvironment. [50] The convergence of 3D bioprinting with microfluidics has revolutionized OoC development, allowing for the precise and automated fabrication of complex 3D tissue structures directly within the microfluidic chip. [50] [52] This integration facilitates the creation of intricate, perfusable vascular networks and the precise spatial arrangement of multiple cell types, which are essential for maintaining tissue viability and function in higher-throughput screening applications. [50]
Applications in Regenerative Pharmacology and Drug Development
The application of these advanced models is accelerating research across the entire spectrum of regenerative pharmacology, from basic MoA research to clinical translation.
Disease Modeling and Mechanism Deconvolution
These models provide unprecedented windows into human pathology. For example:
- Neurological Disorders: Brain organoids are used to model sporadic Alzheimer's disease, exposing the complex interplay of genetic and environmental factors. [48]
- Infectious Diseases: Human airway and nasal organoids have been critical for investigating the escalating replicative fitness of SARS-CoV-2 emerging variants. [48]
- Orthopedic Disorders: 3D-bioprinted bone/cartilage organoids offer platforms to study localized pathologies and systemic responses in osteoporosis and osteoarthritis. [51]
- Inflammatory Bowel Disease (IBD): Intestinal organoids model the complex gut mucosa environment, enabling the study of disease mechanisms and screening of anti-inflammatory compounds. [48]
Drug Screening and Toxicology
Advanced models offer more human-relevant and ethical platforms for preclinical testing. They enable high-throughput screening of compound libraries and detailed assessment of drug-induced toxicity. [49] [48] For instance, human liver organoid models have been developed to test drug-induced liver fibrosis, a major cause of drug attrition. [48] The ability to connect multiple OoCs to create multi-organ "human-on-a-chip" systems allows researchers to study complex systemic drug responses, including pharmacokinetics and toxicokinetics, such as the conversion of a prodrug into its active metabolite in one "organ" and its subsequent effect on another. [48]
Personalized and Precision Medicine
A cornerstone of regenerative pharmacology is the development of personalized therapies. Patient-derived organoids, particularly from cancer biopsies, can predict individual response to chemotherapy, guiding treatment selection. [48] In cystic fibrosis, rectal organoids have enabled personalized treatment by predicting patient-specific responses to CFTR modulator therapies. [48] The use of a patient's own cells in 3D-bioprinted constructs or organoids paves the way for autologous regenerative therapies that minimize the risk of immune rejection. [34]
Table 2: Documented Success Rates of Select Regenerative Therapies
| Therapy / Application | Condition | Reported Success / Efficacy | Key Context |
|---|---|---|---|
| Matrix-induced Autologous Chondrocyte Implantation (MACI) | Knee Cartilage Defects [34] | 80% - 90% success rate over time [34] | An example of an advanced tissue engineering approach. |
| Bone Marrow Aspirate Concentrate (BMAC) | Osteonecrosis of the Hip [34] | >90% of hips avoided collapse after 2 years (Mayo Clinic study) [34] | Demonstrates the potential of cell-based therapies to prevent joint collapse. |
| Hematopoietic Stem Cell Transplantation | Blood Cancers (e.g., Multiple Myeloma) [34] | 60% - 70% success rate; 79% 3-year survival for Multiple Myeloma [34] | A long-established and validated cell therapy. |
| Mesenchymal Stem Cell (MSC) Therapy | Autoimmune & Inflammatory Conditions [34] | ~80% success rate reported [34] | Attributed to potent immunomodulatory properties. |
| Platelet-Rich Plasma (PRP) | Knee Osteoarthritis [34] | Symptom improvement for 6+ months [34] | Effectiveness can vary; often not covered by insurance. |
Experimental Workflow and Research Toolkit
Generalized Workflow for Model Development
The following diagram outlines a generalized, iterative workflow for developing and utilizing these advanced models in a regenerative pharmacology context.
Workflow for Advanced Model Development and Use
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for constructing and utilizing these advanced models.
Table 3: Essential Research Reagents and Materials for Advanced Models
| Category / Item | Function / Purpose | Specific Examples & Notes |
|---|---|---|
| Cell Sources | ||
| Induced Pluripotent Stem Cells (iPSCs) | Provides a patient-specific, ethically favorable source for generating any cell type. [53] | Critical for personalized disease modeling and autologous therapies. [53] |
| Mesenchymal Stem Cells (MSCs) | Multipotent stem cells with immunomodulatory properties; differentiate into mesodermal lineages. [32] | Sourced from bone marrow (BM-MSC), adipose tissue (AD-MSC), or umbilical cord (UC-MSC). [32] |
| Biomaterials & Bioinks | ||
| Hydrogels | Serve as the 3D scaffold or "bioink" that mimics the native extracellular matrix (ECM). | Alginate-gelatin blends [49], PEG-based polymers, collagen, fibrin. [50] |
| Decellularized ECM (dECM) | Bioink derived from native tissues, providing tissue-specific biochemical cues. [50] | Enhances tissue-specific differentiation and function. [50] |
| Culture Components | ||
| Growth Factors & Cytokines | Direct cell differentiation, proliferation, and tissue maturation. | BMPs for bone [51], TGF-β for cartilage [51], VEGF for vasculature. |
| Small Molecule Inhibitors/Activators | Precisely control signaling pathways during differentiation and culture. | CHIR99021 (Wnt activator), SB431542 (TGF-β inhibitor). |
| Microfabrication | ||
| Photopolymerizable Resins | Used in SLA bioprinting to create high-resolution scaffolds. [50] | Must be cytocompatible; may require photoinitiators like LAP. [50] |
| PDMS | Elastomer used for rapid prototyping of microfluidic OoC devices. [50] | Properties: gas-permeable, can absorb small hydrophobic molecules. [50] |
Current Challenges and Future Directions
Despite the significant promise, the widespread adoption and clinical translation of these technologies face several hurdles.
Technical and Manufacturing Challenges: Key issues include achieving scalability and standardized, automated production, particularly for Advanced Therapy Medicinal Products (ATMPs). [3] [38] Ensuring long-term stability and vascularization of large tissue constructs remains difficult. [38] There is also a need for greater standardization of protocols, biomaterials, and cell sources to ensure reproducibility and enable cross-study comparisons. [3] [51]
Biological and Safety Concerns: A primary risk in cell-based therapies is tumorigenicity, particularly from residual undifferentiated pluripotent stem cells. [38] Sensitive in vitro assays, such as digital soft agar assays, are being developed to detect rare transformed cells. [38] The genetic instability of cells during long-term culture is another concern, necessitating rigorous karyotype testing. [38]
Regulatory and Ethical Hurdles: The regulatory pathway for ATMPs and related technologies is complex and lacks global harmonization. [3] [38] Ethical considerations, particularly regarding the use of embryonic stem cells and patient data privacy, require ongoing attention. [3]
The future of these technologies is being shaped by several promising trends. The integration of Artificial Intelligence (AI) and machine learning is poised to revolutionize bioink design, optimize bioprinting parameters, and predict tissue maturation pathways and therapeutic outcomes. [3] [38] [50] 4D bioprinting, which uses stimuli-responsive biomaterials to create dynamic structures that change shape or function over time, introduces a new temporal dimension to tissue engineering. [50] Finally, the development of 'smart' biomaterials that can release bioactive compounds in a temporally and spatially controlled manner in response to environmental triggers will be key to creating more autonomous and effective regenerative therapies. [3] The convergence of these technologies, supported by interdisciplinary collaboration, will be instrumental in realizing the ultimate goal of regenerative pharmacology: to deliver curative, transformative therapeutics to patients.
The Role of Bioreactors in Tissue Maturation and Functional Assessment
Regenerative pharmacology aims to cure disease through the restoration of tissue and organ function, a strategy distinct from standard pharmacotherapy which is often limited to the amelioration of symptoms [1]. The success of this endeavor hinges on the ability to create biologically relevant, mature tissues in vitro that can accurately model human physiology and disease for drug screening or be successfully implanted for functional restoration. Bioreactors are fundamental tools enabling this transition, providing the controlled, dynamic environments necessary for tissue maturation and the functional, non-destructive assessment required to characterize these tissues pre-implantation or for in vitro studies [1] [54]. By recapitulating critical aspects of the in vivo physiologic environment—such as nutrient perfusion, mechanical stimulation, and electrochemical signaling—bioreactors bridge the gap between simple cell culture and complex living systems. Within the context of regenerative pharmacology mechanisms of action research, they provide a platform to investigate how pharmacological agents direct tissue assembly, maturation, and function, thereby accelerating the development of curative therapeutics [1] [55].
This technical guide details the operational principles of advanced bioreactor systems, provides validated experimental protocols for tissue maturation and assessment, and synthesizes quantitative data on bioreactor performance, serving as a resource for researchers and drug development professionals.
Bioreactor Systems for Tissue Maturation
Operational Principles and Bioreactor Typology
Bioreactors are devices that support a biologically active environment for the cultivation of cells, tissues, or organs. They achieve this by controlling key culture parameters, including temperature, pH, dissolved oxygen, and nutrient supply, while simultaneously introducing critical biophysical cues such as fluid shear stress, compression, and stretch [54] [56]. The mode of operation is a primary classification criterion, with each type offering unique advantages for specific tissue engineering applications.
- Perfusion Bioreactors: These systems drive culture medium continuously through a scaffold or tissue construct, typically via an inlet and outlet pipe system [57]. This direct perfusion is critical for nutrient delivery and waste removal in thick, dense tissues, preventing necrotic core formation. Furthermore, the resulting fluid shear stress is a potent mechanical stimulus that promotes the maturation of endothelialized vessels and enhances the organization and function of epithelial tissues [58] [57]. Their design often includes a glass vessel and scaffolds for cell arrangement, equipped with sensors and a control unit to regulate chemical and physical parameters [57].
- Stirred-Tank Bioreactors (STBRs): STBRs employ one or multiple impellers to agitate the culture medium, creating a homogeneous suspension culture. This configuration is ideal for the large-scale expansion of stem cells, such as human pluripotent stem cells (hPSCs) and human mesenchymal stromal cells (hMSCs), which are critical raw materials for regenerative medicine [59]. These systems are well-characterized with established scale-up criteria, though shear stress from impellers must be carefully controlled to avoid detrimental effects on cell viability and phenotype [59].
- Rotating Wall Vessel Bioreactors: These bioreactors typically consist of a cylindrical vessel that rotates around a horizontal axis, suspending cell aggregates or tissue constructs in a state of constant free-fall. This setup minimizes shear stress while providing excellent mass transfer, making it suitable for the formation of 3D spheroids and organoids [54].
Table 1: Comparative Analysis of Bioreactor Types for Tissue Maturation
| Bioreactor Type | Key Operational Principle | Primary Cues Provided | Ideal Tissue Applications | Key Advantages |
|---|---|---|---|---|
| Perfusion | Continuous flow of medium through a scaffold | Fluid shear stress, enhanced nutrient/waste exchange | Vascular grafts, mammary ducts, bone tissue [58] [57] | Mimics in vivo vascular flow; prevents core necrosis |
| Stirred-Tank (STBR) | Agitation via impellers for suspension culture | Homogeneous mixing, controllable oxygen transfer | Large-scale stem cell expansion (hPSCs, hMSCs) [59] | Well-characterized, scalable, suitable for microcarriers |
| Rotating Wall | Vessel rotation suspends constructs | Low-shear environment, optimized diffusion | 3D organoid formation, spheroid culture [54] | Minimal shear forces; promotes 3D self-assembly |
Mechanisms of Tissue Maturation
Bioreactors promote tissue maturation by providing environmental cues that direct cellular processes. The following diagram illustrates the core workflow and logical relationships involved in this process.
The mechanistic pathway to tissue maturation begins with the presentation of physicochemical cues by the bioreactor. For instance, in a perfusion system, fluid flow exerts shear stress on endothelial cells, prompting their alignment and the formation of confluent, lumen-like structures [58]. Mechanical stretch and compression in specialized bioreactors can mimic the physiological loading of musculoskeletal tissues, driving stem cells towards an osteogenic or chondrogenic lineage and encouraging robust extracellular matrix (ECM) deposition [54]. Furthermore, the role of bioelectrical signaling is increasingly recognized; endogenous bioelectrical networks, mediated by ion channels and gap junctions, process morphogenetic information that controls tissue pattern formation. Targeting these networks with "electroceuticals" represents a novel pharmacological strategy to control growth and form in regenerating tissues [55].
These cues trigger downstream cellular processes that include changes in gene expression, protein synthesis, and metabolic activity. The culmination of these processes is the achievement of native-like tissue outcomes, such as the physiological organization of a mammary duct model [58], the contractile function of engineered muscle [60], or the metabolic activity indicative of a viable tissue construct [56].
Functional Assessment of Engineered Tissues
A critical advantage of advanced bioreactor systems is their capacity for integrated, non-destructive functional assessment. This allows for real-time monitoring of tissue maturation and the acquisition of pharmacological response data without compromising the construct.
Integrated Sensing Modalities
- Optical Imaging Windows: Custom-designed bioreactors increasingly incorporate transparent optical windows, enabling real-time, high-resolution imaging. A prime application is Fluorescence Lifetime Imaging Microscopy (FLIM), which can measure the fluorescence decay of endogenous metabolites like NADH. The FLIM decay curve, fitted to ( F(t) = \alpha1e^{-t/\tau1} + \alpha2e^{-t/\tau2} ), where ( \tau1 ) and ( \tau2 ) represent the lifetimes of free and protein-bound NADH respectively, serves as a sensitive readout of cellular metabolic status [56]. Shifts in the mean NADH lifetime or the relative contributions of ( \tau1 ) and ( \tau2 ) can indicate metabolic perturbations in response to drug candidates or pathogenic insults.
- Magnetic Resonance Spectroscopy (MRS): Bioreactors compatible with preclinical MRI systems allow for non-invasive metabolic monitoring via techniques like hyperpolarized 13C-pyruvate MRS. This method tracks the real-time conversion of 13C-pyruvate to 13C-lactate, providing a direct measure of lactate dehydrogenase (LDH) activity and upregulated glycolysis, a hallmark of cancer cell metabolism [56]. The combination of FLIM and MRS in a single bioreactor enables correlative analysis of metabolism at the cellular (optical) and population (MR) scales.
- Physicochemical Probes: Standard integrated probes for pH, dissolved oxygen (pO₂), and temperature provide essential data on the bulk culture environment. These parameters are crucial for maintaining tissue viability during long-term culture and for ensuring experimental reproducibility [59].
Table 2: Modalities for Functional Assessment of Engineered Tissues
| Assessment Modality | Measured Parameter | Technical Readout | Significance in Regenerative Pharmacology |
|---|---|---|---|
| FLIM | NADH fluorescence lifetime | Mean lifetime (τ), Fractional contributions (τ₁, τ₂) | Reports on cellular redox state and metabolic pathway activity; drug efficacy screening [56] |
| Hyperpolarized 13C MRS | Pyruvate-to-Lactate conversion | Lac:Pyr ratio | Measures LDH activity and glycolytic flux; key for cancer drug development [56] |
| Integrated Physicochemical Probes | pH, pO₂, Temperature | Real-time sensor data | Ensures tissue viability and quality control during long-term culture and drug exposure [59] |
| In Vivo Implantation | Physiological integration & function | Patency, Anastomosis, Host cell recruitment | Ultimate validation of functional maturity; e.g., bioprinted vessel incorporation [61] |
Experimental Protocol: Multimodal Metabolic Assessment in a Perfusion Bioreactor
The following protocol details the use of a combined FLIM-MRS bioreactor for assessing metabolic shifts in a 3D cancer model, as exemplified by studies on murine breast cancer cells (4T1) [56].
Objective: To quantify the metabolic response of 3D breast cancer organoids to glucose deprivation using correlated FLIM and hyperpolarized 13C MRS. Primary Materials: Multimodal bioreactor with optical window and MRS compatibility [56], collagen type I matrix, 4T1 murine breast cancer cells, high-glucose and glucose-free culture media, [1-13C] pyruvate for hyperpolarization, two-photon fluorescence microscope with time-correlated single photon counting (TCSPC) capability, preclinical MRI system with hyperpolarizer.
Step-by-Step Workflow:
- 3D Construct Preparation: Embed 4T1 cells at a density of 5-10 million cells/mL within a sterile collagen type I gel (e.g., 5 mg/mL concentration). Polymerize the cell-laden gel within the sterile bioreactor chamber. Perfuse with high-glucose medium (e.g., DMEM) for 24-48 hours to establish growth.
- Experimental Setup: Connect the bioreactor to the perfusion system and place within the MRI cradle. Maintain temperature at 37°C throughout the experiment. Connect the inlet tubing to reservoirs containing either the high-glucose (control) or glucose-free (test) medium.
- FLIM Data Acquisition (Pre-treatment Baseline): Place the bioreactor on the microscope stage. Using a two-photon laser tuned to 740 nm for NADH excitation, acquire FLIM data from multiple fields of view within the 3D construct. Collect data until >1000 photon counts per pixel are achieved for robust decay curve fitting.
- Metabolic Perturbation: Switch the perfusion medium to the glucose-free reservoir. Continue perfusion for a defined period (e.g., 4-6 hours).
- FLIM Data Acquisition (Post-treatment): Repeat Step 3 to acquire FLIM data under glucose-deprived conditions.
- Hyperpolarized 13C MRS Acquisition: Transfer the bioreactor to the MRI scanner. Inject a bolus of hyperpolarized [1-13C] pyruvate into the perfusion line proximal to the bioreactor inlet. Immediately acquire dynamic 13C spectra to monitor the time-resolved production of [1-13C] lactate. Calculate the Lac:Pyr area-under-the-curve ratio.
- Data Analysis:
- FLIM: Fit the fluorescence decay curves to a two-component model. Calculate the mean lifetime and the individual lifetimes (τ₁, τ₂) and their fractional contributions. A significant increase in the mean lifetime and τ₂ (bound NADH) under glucose deprivation indicates a shift toward oxidative phosphorylation [56].
- MRS: Compare the Lac:Pyr ratio between control and test conditions. A significantly lower ratio in glucose-deprived cells confirms a reduction in glycolytic flux [56].
- Correlation: Correlate the optical (FLIM) and spectroscopic (MRS) metrics to validate the multi-scale metabolic response.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting bioreactor-based tissue maturation and assessment experiments.
Table 3: Research Reagent Solutions for Bioreactor-Based Tissue Maturation
| Item | Function/Application | Specific Examples |
|---|---|---|
| Stimuli-Responsive "Smart" Polymers | 4D dynamic scaffolds that change properties (stiffness, shape) in response to stimuli (temperature, pH, light); enable controlled drug release and mimic dynamic ECM [54]. | Thermoresponsive poly(N-isopropylacrylamide); light-responsive polymers; redox-responsive hydrogels [54]. |
| Hyaluronic Acid-Based Bioink | Key component of hydrogel bioinks for 3D bioprinting; provides compression strength, hydration, and allows for cell adhesion and motility [61]. | HyStem-C Kit (Hyaluronic acid, Gelatin, PEGDA) [61]. |
| Decellularized Extracellular Matrix (dECM) | Biologically derived scaffold material that provides native tissue-specific biochemical and structural cues to enhance cell attachment, differentiation, and tissue-specific function. | Animal- or human tissue-derived dECM hydrogels. |
| Chemically Defined Media Supplements | Replace serum to ensure reproducibility, minimize batch variation, and support the expansion and differentiation of stem cells (hPSCs, hMSCs) in bioreactors [59]. | Recombinant growth factors (FGF, EGF, VEGF), lipids, and insulin. |
| Human Pluripotent Stem Cells (hPSCs) | Raw material for generating patient-specific tissues; capable of differentiating into any cell type in the body for disease modeling and regenerative therapy [59]. | Human embryonic stem cells (hESCs); human-induced pluripotent stem cells (hiPSCs). |
| Metabolic Tracer Molecules | Enable functional assessment of tissue metabolism via techniques like hyperpolarized MRS or FLIM [56]. | [1-13C] Pyruvate (for MRS); endogenous NADH (for FLIM). |
Bioreactors have evolved from simple culture vessels to sophisticated platforms that are indispensable for the maturation and functional assessment of engineered tissues. By providing controlled physicochemical and mechanical cues, they drive tissues toward a native-like state. Furthermore, through integrated sensing and imaging modalities, they enable the non-destructive, quantitative functional assessment that is a prerequisite for rigorous regenerative pharmacology research. The continued optimization of bioreactor design, coupled with the development of novel smart biomaterials and advanced sensing technologies, will further enhance their capacity to produce biologically relevant tissues for curative drug discovery and therapeutic implantation.
Harnessing AI and Multi-Omics for Target Discovery and Mechanism Prediction
The convergence of artificial intelligence (AI) and multi-omics technologies is fundamentally reshaping the landscape of target discovery and mechanism prediction, marking a pivotal shift in regenerative pharmacology. This field aims not merely to manage symptoms but to restore the physiological structure and function of tissues through targeted therapies [3]. Traditional single-omics approaches often fail to capture the complex, dynamic interactions across biological layers that characterize regenerative processes. The integration of multi-omics data—spanning genomics, transcriptomics, proteomics, metabolomics, and epigenomics—with sophisticated AI algorithms provides an unprecedented, holistic view of biological systems. This enables researchers to move beyond static snapshots to dynamic, predictive models of disease and regeneration, thereby accelerating the identification of novel therapeutic targets and the elucidation of complex mechanisms of action (MoA) for regenerative therapies [62] [63]. This technical guide explores the core methodologies, experimental protocols, and practical tools driving this transformation, framed within the specific context of advancing regenerative pharmacology.
Core AI Methodologies for Multi-Omics Integration
AI provides the essential computational scaffold for integrating disparate, high-dimensional omics datasets. The table below summarizes the key AI models and their specific applications in multi-omics analysis for regenerative target discovery.
Table 1: Key AI Models for Multi-Omics Integration in Target Discovery
| AI Model Category | Key Examples | Primary Application in Multi-Omics | Relevance to Regenerative Pharmacology |
|---|---|---|---|
| Graph Neural Networks (GNNs) | GNNBlockDTI [64] | Modeling biological networks (e.g., protein-protein interactions); substructure-aware drug-target interaction prediction. | Identifying druggable hubs in tissue repair pathways; understanding cellular crosstalk in regeneration [62]. |
| Multimodal Transformers | Unified Multimodal Molecule Encoder (UMME) [64] | Fusing molecular graphs, protein sequences, transcriptomic data, and textual descriptions. | Creating unified representations of regenerative compounds and their cellular contexts. |
| Foundation Models | ESMFold [65], Bioptimus [66] | Protein structure and function prediction; building universal multi-scale representations of biology. | Predicting structures of novel regenerative targets; simulating biological processes across scales (proteins to tissues) [66]. |
| Explainable AI (XAI) | SHapley Additive exPlanations (SHAP) [62] | Interpreting "black box" models to clarify feature contribution (e.g., which genomic variants impact a toxicity score). | Building trust in AI predictions for clinical translation; elucidating key drivers of regenerative outcomes [62]. |
These models excel at identifying non-linear patterns across high-dimensional spaces that traditional statistical methods often miss. For instance, GNNs can model how a somatic mutation perturbs a protein-protein interaction network central to wound healing, thereby prioritizing druggable hubs. Meanwhile, multimodal transformers use hierarchical attention fusion strategies to align intra- and inter-modal representations, effectively integrating chemical structure with proteomic and transcriptomic context to predict a compound's MoA in a regenerative setting [64] [62].
Experimental Workflows and Protocols
A robust experimental framework is critical for validating AI-driven discoveries. The following workflow outlines a closed-loop, multi-omics approach for target identification and mechanistic validation in regenerative pharmacology.
Diagram 1: Experimental workflow for AI-driven target discovery.
Step-by-Step Experimental Protocol
Step 1: Patient Sample Collection & Multi-Omics Profiling
- Protocol: Collect relevant tissue or biofluid samples (e.g., from damaged and healthy tissues). Perform simultaneous multi-omics profiling using:
- Whole Genome/Exome Sequencing (Genomics) to identify genetic variants.
- RNA-Seq (bulk or single-cell) (Transcriptomics) to reveal active gene expression patterns in regenerative zones.
- Mass Spectrometry-based Proteomics (e.g., TMT-LC/MS-MS) to quantify protein expression and post-translational modifications.
- LC-MS/NMR (Metabolomics) to profile small-molecule metabolites and biochemical endpoints [62] [63].
- Data Output: Raw sequencing reads (FASTQ), protein abundance matrices, metabolite concentration tables.
Step 2: AI-Driven Data Integration & Target Hypothesis Generation
- Protocol: Implement an AI pipeline for data harmonization and integration.
- Preprocessing: Perform batch effect correction (e.g., using ComBat), normalization (e.g., DESeq2 for RNA-seq), and missing data imputation (e.g., with matrix factorization or DL-based reconstruction) [62].
- Integration & Modeling: Input preprocessed data into a multimodal AI model (e.g., a transformer or GNN). Train the model to identify cross-omics features that correlate with regenerative phenotypes or outcomes. The model will output a ranked list of potential candidate targets (e.g., genes, proteins) and predict their involvement in biological pathways [64] [62].
Step 3: In Silico Validation
- Protocol: Prioritize top candidate targets for computational validation.
- Structure Prediction: For protein targets, use foundation models like ESMFold to predict 3D structure if unknown [65].
- Molecular Docking & Dynamics (MD): Dock libraries of small molecules or biologic candidates against the predicted target structure. Perform MD simulations (e.g., using GROMACS) to assess binding stability and affinity over time, as exemplified in the discovery of HPV16 E6 inhibitors [64] [42].
- Digital Twin Simulation: Where data permits, use generative AI to create patient-specific "digital twins" to simulate intervention effects in silico [62].
Step 4: Experimental Validation
- Protocol: Validate top candidates using functional assays.
- Phenotypic Screening: Use high-content imaging (e.g., Cell Painting assay) and functional genomics (e.g., Perturb-seq) on relevant cell lines or patient-derived organoids. Treat with candidate compounds or use CRISPR-based gene editing (KO/activation) to modulate the target and observe phenotypic changes relevant to regeneration (e.g., cell migration, differentiation) [67].
- Mechanistic Confirmation: Employ techniques like Western Blot, qPCR, and immunohistochemistry to confirm predicted changes in protein levels, pathway activation (e.g., phosphorylation), and gene expression.
- Multi-omics Follow-up: Re-run a focused multi-omics analysis on validated samples to confirm the AI-predicted MoA and identify biomarker signatures of target engagement [62] [67].
Integrating Phenotypic Screening with AI and Multi-Omics
A powerful emerging paradigm is the integration of phenotypic screening with multi-omics and AI, which allows for target-agnostic discovery grounded in observable biology.
- Workflow: This involves (1) conducting a high-content phenotypic screen (e.g., using Cell Painting to capture morphological changes), (2) generating multi-omics data from the same perturbed system, and (3) using AI to map the phenotypic readouts to the underlying molecular changes [67].
- AI's Role: Models like the idTRAX machine learning-based approach can backtrack from an observed phenotypic shift to identify the cancer-selective targets and MoA responsible. Platforms like Ardigen's PhenAID integrate cell morphology data with omics layers to identify patterns correlating with MoA, efficacy, or safety [67].
- Application in Regeneration: This approach is ideal for complex regenerative processes where the key molecular players are not fully known. It can uncover novel ligands or pathways that drive stem cell differentiation or tissue remodeling without presupposing a target.
The Scientist's Toolkit: Key Research Reagents and Platforms
Successful implementation of these workflows relies on a suite of specialized reagents, computational tools, and platforms.
Table 2: Essential Research Reagent Solutions and Platforms
| Tool Category | Specific Examples | Function | Application in Workflow |
|---|---|---|---|
| AI/Drug Discovery Platforms | PandaOmics, Chemistry42 (Insilico) [65], PhenAID (Ardigen) [67] | End-to-end AI platforms for target discovery (PandaOmics), compound design (Chemistry42), and phenotypic data analysis (PhenAID). | Target hypothesis generation, candidate compound screening, and MoA prediction. |
| Biomolecular Foundation Models | ESMFold [65], AlphaFold, Bioptimus [66] | AI models for protein structure prediction (ESMFold, AlphaFold) and universal biological representation (Bioptimus). | In silico target validation and structure-based drug design. |
| Specialized LLMs for Biomedicine | BioGPT [65], BioBERT [65], ChatPandaGPT [65] | Large language models trained on biomedical literature for knowledge extraction, relation extraction, and target identification from text. | Mining scientific literature and databases to build biological context for candidate targets. |
| High-Content Screening Reagents | Cell Painting Assay Kits [67] | A multiplexed fluorescence assay using up to 6 dyes to label diverse cellular components, enabling high-content morphological profiling. | Generating rich phenotypic data from in vitro models for AI integration. |
| Functional Genomics Tools | CRISPR-Cas9 Libraries (e.g., for Perturb-seq) [67] | Pooled libraries of guide RNAs for targeted gene knockout or activation, coupled with single-cell RNA sequencing readout. | Experimental validation of target function and its downstream transcriptional effects. |
Challenges and Future Directions
Despite its promise, the integration of AI and multi-omics in regenerative pharmacology faces significant hurdles. Key challenges include data harmonization (managing heterogeneity, batch effects, and missing data), infrastructure limitations (requiring advanced storage and cloud computing), model interpretability (the "black box" problem, addressed by XAI), and ethical and regulatory considerations around patient data privacy and algorithm bias [62] [63].
Future progress will be driven by several emerging trends:
- Single-Cell and Spatial Multi-Omics: These technologies will map molecular activity at the level of individual cells within their tissue context, crucial for understanding cellular heterogeneity in regenerating tissues [63].
- Federated Learning: This privacy-preserving technique allows for model training across multiple decentralized data sources without sharing raw patient data, facilitating broader collaboration [62].
- Patient-Centric "N-of-1" Models: AI will enable the creation of highly personalized models for predicting therapeutic response, aligning with the ultimate goal of regenerative and personalized medicine [62].
In conclusion, the synergy of AI and multi-omics provides a powerful, systems-level framework for deconvoluting the complex mechanisms of regeneration. By adopting the workflows, tools, and best practices outlined in this guide, researchers can accelerate the discovery of transformative therapeutic targets and bring the field of regenerative pharmacology closer to its goal of restoring, rather than just managing, health.
Navigating Translational and Manufacturing Hurdles in ATMPs
In the evolving field of regenerative pharmacology, the transition from promising laboratory discoveries to clinically available therapies represents a critical bottleneck. This challenge is particularly acute for Advanced Therapy Medicinal Products (ATMPs), where the journey from Good Laboratory Practice (GLP) non-clinical studies to Good Manufacturing Practice (GMP)-compliant production presents multifaceted hurdles [38]. Regenerative pharmacology applies pharmacological sciences to accelerate and optimize the development of bioengineered and regenerating tissues, creating a paradigm aimed at restoring physiological structure and function rather than merely managing symptoms [3]. However, the transformative potential of these therapies is often hindered by manufacturing complexities, particularly in scaling up processes while maintaining consistent product quality, safety, and efficacy.
The inherent variability of biological systems, contamination risks, and difficulties in translating manual research processes into automated, scalable manufacturing protocols present significant obstacles [38] [68]. Furthermore, demonstrating product comparability after manufacturing process changes remains one of the most critical concerns for ATMP scalability [38]. This technical guide examines these challenges within the context of regenerative pharmacology mechanisms of action research and provides a structured approach to overcoming them through technological innovation and strategic process development.
Core Challenges in GLP to GMP Translation
Fundamental Transition Barriers
The successful translation of regenerative therapies from laboratory to clinic requires implementing GMP-compliant manufacturing processes that reliably meet quality specifications defined during product development, including data from GLP-compliant non-clinical studies [38]. This transition faces several fundamental barriers:
- Raw Material Sourcing: Securing a reliable supply of GMP-grade raw materials, reagents, and critical components presents complex logistical challenges, particularly for novel or specialized products [38]
- Biological Variability: Cells derived from patients or donors exhibit significant variability in quality, potency, and stability, making reproducible manufacturing processes difficult to achieve [38]
- Scalable Expansion: Large cell volumes for clinical applications often require extensive cell expansion, which can alter cellular phenotype and functionality [38]
- Infrastructure Adaptation: Adapting existing research infrastructure to meet GMP requirements for contamination control and product integrity represents a significant undertaking [38]
- Process Validation: Extensive testing and documentation are required to validate manufacturing processes for consistent product quality, safety, and efficacy [38]
Safety and Efficacy Considerations
Safety and efficacy concerns present additional translational challenges, with tumorigenesis risk being a particularly critical consideration in regenerative medicine [38]. The potential transformation of stem cells into neoplastic cells during therapy requires robust safety testing protocols. For pluripotent stem cell (PSC)-derived products, in vivo teratoma formation assays validate pluripotency and detect residual undifferentiated PSCs [38]. For somatic cell-based therapies, tumorigenicity is assessed using in vivo studies in immunocompromised models rather than teratoma tests [38]. Genetic instability from successive cultures represents another challenge that requires monitoring through karyotype analysis and selection of genetically stable cells [38].
Demonstrating long-term clinical efficacy remains particularly challenging for ATMPs, which often target rare diseases with limited patient populations, making statistically robust data difficult to obtain [38]. Difficulties in defining and assessing mechanisms of action and potency create additional obstacles to confirming clinical effectiveness [38].
Table 1: Key Challenges in Transitioning from GLP to GMP Compliance
| Challenge Category | Specific Challenges | Potential Impacts |
|---|---|---|
| Manufacturing Process | Scalable cell expansion, accommodating biological variability, process validation | Inconsistent product quality, altered cell functionality |
| Safety & Contamination | Aseptic processing, tumorigenicity risk, genetic instability | Product contamination, patient safety concerns |
| Regulatory & Compliance | GMP facility requirements, quality control standardization, documentation | Regulatory approval delays, compliance failures |
| Efficacy Demonstration | Long-term clinical benefit assessment, limited patient populations, potency assays | Uncertain therapeutic value, limited statistical power |
Automated Bioreactor Systems: Technological Solutions
System Architectures and Platforms
Advanced bioreactor systems represent a technological cornerstone for overcoming scalability challenges in regenerative medicine manufacturing. These systems have evolved significantly from traditional manual processes to sophisticated automated platforms capable of maintaining optimal culture conditions while reducing contamination risks and production inconsistencies [68].
The Bioreactor with Expandable Culture Area (BECA) platform exemplifies this evolution, featuring a versatile design that supports both manual small-scale operation at the R&D phase (BECA-S) and functionally closed automated scaled-out operation at the manufacturing phase (BECA-Auto) [68]. This integrated approach facilitates seamless transition between manual and automated processing for autologous T cell therapy manufacturing, addressing a critical bottleneck in cell therapy production.
Single-use bioreactors (SUBs) represent another revolutionary advancement, with market forecasts projecting growth from USD 1.3 billion to USD 6.6 billion by 2035, driven by a compound annual growth rate near 15% [69]. These systems utilize pre-sterilized disposable plastic liners instead of traditional stainless-steel tanks, eliminating cleaning cycles, reducing water and chemical usage, and lowering contamination risks between batches [69]. Companies report up to 60% lower operating costs with SUBs compared to stainless-steel systems, alongside reduced utility bills, less labor, and fewer validation steps [69].
The Stratyx 250 laboratory bioreactor exemplifies modern system capabilities, offering cloud-integrated, modular design with remote monitoring and automation features [70]. This system demonstrates the industry trend toward flexible, mobile platforms that reduce operational overhead while supporting scale-up applications.
Table 2: Comparison of Automated Bioreactor Systems and Features
| System/Platform | Key Features | Scale/Volume | Automation Level | Unique Advantages |
|---|---|---|---|---|
| BECA Platform [68] | Expandable culture area, standalone operation, modular design | Not specified | Medium-High | Seamless transition from manual (BECA-S) to automated (BECA-Auto) |
| Stratyx 250 [70] | Cloud integration, mobile platform, single-use components | 250mL | High | Remote monitoring, >10-hour FTE time reduction, 30% better scale-up success |
| Single-Use Bioreactors [69] | Disposable liners, pre-sterilized, flexible configurations | Various scales (small research to commercial) | Variable | 60% lower operating costs, reduced contamination risk |
| Industry Systems [71] | Various control features, data integration, compliance support | 250mL to over 5L | Variable | Vendor-specific specializations for different applications |
Control Systems and Automation Technologies
Modern automated bioreactor systems incorporate sophisticated control technologies that enable precise regulation of critical process parameters. The BECA-Auto system exemplifies this approach with its integrated control units [68]:
- Capsule Internal Fluid Controller (CIFC): Manages fluid movement using peristaltic pumps and pinch valves, with optimized action sequences to ensure smooth flow and volume accuracy [68]
- Device for Automated Aseptic Sampling (DAAS): Enables automated, aseptic sampling through a series of peristaltic pumps and pinch valves that create an aseptic barrier, allowing small-volume samples (0.02 ml to 1 ml) to be drawn repeatedly without compromising sterility [68]
- Actuation Platform: Provides three degrees of freedom - expanding culture surface area, rocking the vessel for culture resuspension, and tilting for culture consolidation - with sensors to precisely regulate movement extent and speed [68]
- Enclosure and Climate Control: Maintains specified environmental parameters (temperature, humidity, CO2, O2) through sensors and closed-loop feedback controls that trigger appropriate system responses [68]
Industry-wide initiatives like the Automated Bioreactor workstream are developing frameworks for fully automated control of single-use perfusion bioreactors [72]. These efforts integrate real-time sensing technologies (Raman spectroscopy, capacitance, auto sampling) with feedback and feed-forward control strategies to modernize upstream operations, reduce risk, and accelerate speed to market [72].
Additional automation advancements include digital twin technology, integrated control systems, automated sampling and analysis, and smart bioreactors [73]. Process Analytical Technology (PAT) enhances monitoring at "moments of truth" where critical control points impact drug quality, safety, and efficacy [73]. Integration with manufacturing execution systems and laboratory information management systems ensures full process visibility and control.
Experimental Protocols for Scalable Process Development
Direct Process Translation Methodology
The BECA platform demonstrates an effective methodology for direct translation of manual processes to automated systems [68]. This approach utilizes identical culture vessel designs between manual (BECA-S) and automated (BECA-Auto) configurations, enabling seamless technology transfer:
Manual Process Development: Initial process parameters are established using BECA-S, a single-chamber culture vessel handled similarly to a T-flask but with an internal movable wall that expands surface area (19-102.4 cm²) as culture requirements increase [68]
System Configuration: Pre-sterilized single-use kits are assembled in a Biosafety Cabinet (BSC) to form a functionally closed flow path, which is then installed onto the Actuation Platform and coupled to DAAS and CIFC units [68]
Environmental Control: The enclosure is sealed and the Climate Control system activated to establish and maintain specified environmental parameters (typically 37°C, 90% relative humidity, 5% CO2, 20% O2) [68]
Culture Seeding: A sterile culture bag with seeding culture is connected to the Manifold Assembly via AseptiQuik connectors, after which the system executes an automated Seeding program [68]
Process Monitoring: Automated systems monitor critical parameters while DAAS extracts samples at programmed intervals for external analysis without compromising sterility [68]
This methodology demonstrates insignificant differences in culture outcomes between manual and automated operations, validating the translation approach [68].
Scalability Assessment Framework
A structured framework for scalability assessment ensures successful transition from GLP to GMP environments:
Critical Quality Attribute (CQA) Identification: Define product quality attributes that should be maintained within appropriate limits to ensure the desired product quality [38]
Process Parameter Mapping: Identify critical process parameters (CPPs) that significantly impact CQAs and define their acceptable ranges [73]
Comparative Analysis: Conduct side-by-side comparisons between manual and automated processes using standardized metrics including cell viability, expansion rates, potency markers, and functional assays [68]
Consistency Validation: Perform multiple runs to establish process consistency and determine normal operating ranges for key parameters [38]
Quality Control Integration: Implement real-time release testing protocols where possible, leveraging process analytical technology for continuous quality monitoring [73]
Essential Research Tools and Reagents
Successful implementation of scalable bioreactor systems requires specific research tools and reagents that maintain consistency across the GLP to GMP transition. The following table details essential components identified from experimental protocols.
Table 3: Essential Research Reagent Solutions for Scalable Bioprocessing
| Reagent/Material | Function/Purpose | GMP-Grade Requirement | Implementation Example |
|---|---|---|---|
| Culture Vessels | Provides sterile environment for cell growth and expansion | Single-use, pre-sterilized | BECA-S vessels with expandable culture area (19-102.4 cm²) [68] |
| Tubing Networks | Enables closed-system fluid transfer without contamination | Biocompatible, sterilizable | Manifold Assembly with AseptiQuiq connectors [68] |
| Sensors | Monitors critical parameters (pH, DO, temperature) | Calibrated, validated | Integrated sensor systems with PAT integration [73] [72] |
| Cell Culture Media | Provides nutrients for cell growth and maintenance | Chemically defined, xeno-free | Formulations supporting specific cell types (T cells, MSCs) [68] |
| Process Gases | Maintains physiological pH and oxygen levels | Medical grade, filtered | CO₂ and N₂ supplies with HEPA gas filtration [68] |
| Quality Assays | Assesses product safety, potency, identity | Validated, standardized | Tumorigenicity testing, karyotype analysis, potency assays [38] |
Regulatory and Validation Considerations
Compliance Framework
Navigating regulatory requirements represents a critical aspect of the GLP to GMP transition. Regulatory authorities in the US, EU, and Japan have issued tailored guidance (FDA 2023, EMA 2019, and MHLW 2024, respectively) to address ATMP manufacturing challenges [38]. These documents emphasize:
- Risk-based comparability assessments to evaluate process changes [38]
- Extended analytical characterization to ensure product consistency [38]
- Staged testing approaches to demonstrate that changes do not impact safety or efficacy [38]
The FDA recommends a tiered approach for reporting changes, while the EMA highlights the need to identify CQAs most susceptible to process variations [38]. However, harmonization remains limited, with regional differences in stability requirements and other technical standards [38].
Validation Strategies
Comprehensive validation strategies should encompass multiple aspects of the manufacturing process:
- Process Validation: Establishing documented evidence that the process consistently produces a product meeting its predetermined specifications and quality attributes [38]
- Aseptic Processing Validation: Media fill simulations to validate the effectiveness of aseptic processing, particularly for cell-based products where traditional sterilization methods are not feasible [38]
- Environmental Monitoring: Periodic assessment of the production environment to reduce contamination risks and ensure product safety [38]
- Analytical Method Validation: Demonstrating that testing methods are suitable for their intended purpose in assessing the quality of raw materials, intermediates, and final products [38]
The successful translation of regenerative pharmacology discoveries to clinically viable treatments requires integrating scalability considerations early in the research and development process. By adopting platform approaches like the BECA system that support both manual R&D and automated manufacturing, researchers can significantly reduce technology transfer timelines and challenges [68]. The implementation of single-use technologies, cloud-integrated monitoring systems, and advanced process controls addresses critical bottlenecks in the GLP to GMP transition while maintaining the integrity of therapeutic mechanisms of action.
Future advancements in artificial intelligence, machine learning, and integrated data analytics promise to further accelerate this transition through improved process understanding and predictive modeling [38] [73]. However, realizing this potential requires continued collaboration between researchers, technology developers, and regulatory agencies to establish standardized approaches that ensure both innovation and patient safety. As regenerative pharmacology continues to evolve, building scalability into the fundamental research paradigm will be essential for delivering on the field's promise to restore biological structure and function rather than merely managing disease symptoms.
Addressing Tumorigenicity and Long-Term Safety Concerns for Cell-Based Therapies
Cell-based therapy, defined as the transfer of autologous or allogeneic cellular material into a patient for medical intervention, represents a cornerstone of regenerative medicine with remarkable therapeutic potential [74]. However, its development and clinical application require rigorous biosafety measures, with tumorigenicity evaluation standing as a critical aspect of safety assessment for these "living drugs" [74] [75]. The inherent complexity and heterogeneity of cell-based therapies introduce unique safety challenges that differ substantially from conventional pharmaceuticals. Tumorigenicity risk—the potential for administered cells to form tumors in vivo—is influenced by multiple product-specific characteristics, including cellular source, phenotype, differentiation status, proliferative capacity, ex vivo culture conditions, processing methods, and administration route [75]. For stem cell-based therapies utilizing human embryonic stem cells (hESCs) or induced pluripotent stem cells (iPSCs), the risk is particularly significant as final products may contain residual undifferentiated cells with high proliferative and differentiation potential [75].
The clinical need for robust tumorigenicity assessment is underscored by the rapid expansion of cell therapy applications. While the vast majority of FDA-approved approaches currently involve immune cell preparations (such as afamitresgene autoleucel and lifileucel for solid tumors), therapies utilizing pluripotent and tissue-specific stem cells are advancing through clinical development [74]. Promising applications include the use of mesenchymal stem/stromal cells (MSCs) in fibrin gel for inflammatory bowel disease, differentiated pancreatic endoderm cells for type I diabetes, and various tissue-specific cells for restoring damaged organs [74]. Each of these applications carries distinct tumorigenicity profiles that must be thoroughly characterized to ensure patient safety. A comprehensive biosafety assessment framework must integrate analysis of biodistribution patterns, toxicity profiles, proliferative activity, oncogenic potential, teratogenic effects, immunogenicity, cell survival rates, and rigorous confirmation of cellular product quality [74].
Tumorigenicity Risk Assessment Framework
Risk-Based Approach to Safety Evaluation
The evaluation of tumorigenicity should follow a science-driven, risk-based approach that anticipates potential safety concerns based on existing knowledge of the product type [76]. The Committee for Advanced Therapies (CAT) of the European Medicines Agency (EMA) emphasizes that risk assessment should guide the design of safety and efficacy studies, with the product's inherent characteristics dictating the specific safety concerns requiring investigation [76]. This approach acknowledges that not all cell-based products carry identical risks and allows for tailored testing strategies that address product-specific concerns while avoiding unnecessary studies. The risk-based framework considers multiple factors, including the biological properties of the cells (differentiation status, proliferative capacity, and tumorigenic potential), the manufacturing process (extent of manipulation, culture duration, and senescence), and clinical application (administration route, target population, and intended duration of effect) [76] [75].
Global regulatory agencies recognize that tumorigenicity evaluation must consider the complexity of design and multifactorial influences, though specific requirements and practices vary across regions [75]. Through analysis of marketed and development-stage products, fundamental assessment focus areas have emerged, including characterization of the cell product, in vitro and in vivo models for tumorigenicity testing, and clinical monitoring strategies. The risk assessment process should begin early in product development and iteratively refine throughout the development lifecycle. Key elements include:
- Product Characterization: Comprehensive profiling of cellular identity, purity, potency, and stability [74] [77]
- Process Controls: Evaluation of manufacturing consistency and impact on cellular behavior [76]
- Preclinical Modeling: Appropriate in vitro and in vivo models to assess tumorigenic potential [75]
- Clinical Monitoring: Strategies for long-term patient follow-up to detect delayed adverse events [74]
Risk Categorization of Cell-Based Products
Cell-based therapies can be categorized according to their inherent tumorigenicity risk, which informs the extent and type of safety studies required. Table 1 outlines a risk classification system for different cell types based on their biological characteristics and clinical evidence.
Table 1: Tumorigenicity Risk Categorization for Cell-Based Therapies
| Risk Category | Cell Types | Key Risk Factors | Recommended Testing Level |
|---|---|---|---|
| High Risk | Human embryonic stem cells (hESCs), induced pluripotent stem cells (iPSCs) | Pluripotency, potential for residual undifferentiated cells, extensive in vitro manipulation, karyotypic instability | Comprehensive in vitro and in vivo tumorigenicity studies, long-term follow-up (15+ years) |
| Medium Risk | Mesenchymal stem/stromal cells (MSCs), tissue-specific progenitor cells | Multipotenency, in vitro expansion potential, donor age and source variations, reported spontaneous transformation | Case-specific in vivo tumorigenicity studies, mid-term follow-up (5-10 years) |
| Lower Risk | Differentiated cells (chondrocytes, keratinocytes), terminally differentiated cells | Limited proliferative capacity, minimal in vitro expansion, established safety profile in clinical use | Focused in vitro studies, abbreviated in vivo testing if justified, monitoring for ectopic tissue formation |
| Variable Risk | Genetically modified cells (CAR-T, engineered receptors) | Insertional mutagenesis, transgene-related transformation, vector design, integration site analysis | Molecular characterization, genotoxicity assessment, long-term integration site monitoring |
This risk categorization provides a framework for determining the appropriate extent of tumorigenicity evaluation, with higher-risk products requiring more rigorous assessment [76] [75]. It is important to note that risk level is not static and should be re-evaluated as new safety information emerges throughout product development.
Methodologies for Tumorigenicity Evaluation
In Vitro Assessment Techniques
In vitro methods provide initial screening for tumorigenic potential and form the foundation of a comprehensive safety assessment strategy. These assays evaluate fundamental cellular characteristics associated with malignant transformation, including proliferation control, differentiation capacity, and genetic stability. The following experimental protocols represent core methodologies for in vitro tumorigenicity assessment:
Protocol 1: Soft Agar Colony Formation Assay
- Purpose: Evaluates anchorage-independent growth, a hallmark of transformation
- Methodology:
- Prepare base agar layer with 0.5-1.0% agar in complete culture medium in 6-well plates
- After solidification, prepare cell suspension layer with 0.3-0.4% agar containing 5,000-20,000 cells/mL
- Add complete culture medium as a top layer to prevent drying
- Incubate at 37°C with 5% CO₂ for 2-4 weeks, refreshing medium weekly
- Stain colonies with 0.005% Crystal Violet or INT (iodonitrotetrazolium chloride) and quantify using colony counting software
- Interpretation: Formation of colonies >50μm diameter indicates anchorage-independent growth potential
- Controls: Include known tumorigenic (positive) and non-tumorigenic (negative) cell lines
Protocol 2: Karyotypic Analysis and Genetic Stability Assessment
- Purpose: Detects chromosomal abnormalities that may predispose to malignant transformation
- Methodology:
- Culture cells to 60-70% confluence and treat with colcemid (0.1μg/mL) for 2-4 hours to arrest cells in metaphase
- Harvest cells using trypsinization, hypotonic treatment (0.075M KCl), and fix in 3:1 methanol:acetic acid
- Prepare metaphase spreads on clean glass slides and age overnight
- Perform G-banding using trypsin-Giemsa banding or spectral karyotyping (SKY)
- Analyze 20-50 metaphase spreads per sample for numerical and structural abnormalities
- Quality Control: Use cells at different passages to assess culture-induced genomic changes
- Advanced Methods: Comparative genomic hybridization (CGH) arrays or single nucleotide polymorphism (SNP) arrays for higher resolution
Protocol 3: Telomerase Activity Measurement
- Purpose: Assesses telomere maintenance mechanisms associated with immortalization
- Methodology:
- Extract protein using CHAPS lysis buffer
- Perform Telomeric Repeat Amplification Protocol (TRAP) assay
- Measure telomerase activity using quantitative PCR-based methods or ELISA-based TRAP assays
- Normalize activity to protein concentration and positive controls
- Interpretation: High telomerase activity in differentiated cells may indicate aberrant growth regulation
Protocol 4: Differentiation Capacity Assessment
- Purpose: Evaluates functional differentiation potential and detection of residual undifferentiated cells
- Methodology:
- Induce differentiation using lineage-specific media (ectodermal, mesodermal, endodermal)
- Culture for 14-21 days with medium changes every 2-3 days
- Fix cells and perform immunocytochemistry for lineage-specific markers
- Quantify differentiation efficiency using flow cytometry or high-content imaging
- Markers: Include pluripotency markers (OCT4, NANOG, SOX2) and differentiation markers (βIII-tubulin, α-SMA, AFP)
In Vivo Tumorigenicity Studies
In vivo models provide a more comprehensive assessment of tumorigenic potential by evaluating cellular behavior in a complex biological environment. These studies are particularly important for higher-risk products and should be designed to reflect the intended clinical application while addressing specific safety concerns. Key considerations include species selection, immunosuppression requirements, cell delivery method, and study duration.
Protocol 5: In Vivo Tumorigenicity Study in Immunodeficient Mice
- Animal Model: NOD-scid gamma (NSG) or similar immunocompromised mice (4-6 weeks old)
- Cell Preparation:
- Test article: Clinical candidate cells at maximum intended dose and higher multiples (e.g., 10x)
- Controls: Known tumorigenic cells (positive control) and non-tumorigenic cells (negative control)
- Experimental Groups:
- Group 1: Vehicle control (n=10)
- Group 2: Negative control cells (n=10)
- Group 3: Test article - clinical dose (n=15)
- Group 4: Test article - 10x clinical dose (n=15)
- Group 5: Positive control cells (n=10)
- Administration: Use clinical route where feasible or appropriate orthotopic site
- Study Duration: Minimum 16 weeks, extended to 6 months for slow-growing cells
- Endpoint Assessments:
- Daily clinical observations
- Weekly palpation for mass formation
- Biweekly body weight measurements
- Bioluminescent imaging (if cells are labeled) to track cell survival and distribution
- Necropsy with histopathological examination of injection site and major organs
- Statistical Analysis: Compare tumor incidence and latency between groups using appropriate statistical methods
The use of homologous products (testing analogous animal cells in immunocompetent animals) may provide valuable supplementary data, though regulatory authorities typically require testing of the actual clinical candidate [76]. When using immunosuppressed animals, it is advisable to test the clinical candidate in conjunction with homologous product studies in immunocompetent animals to enable better understanding of species-specific features [76].
Biodistribution and Long-Term Monitoring
Understanding the biodistribution pattern of administered cells is essential for tumorigenicity risk assessment, as it identifies sites of potential ectopic engraftment that might not be clinically apparent [74]. Biodistribution assessment typically involves quantitative PCR (for human-specific DNA sequences) and imaging techniques such as positron emission tomography (PET) or magnetic resonance imaging (MRI) to monitor cell fate over time [74]. The extent of biodistribution, potential for ectopic engraftment, and persistence at intended and unintended sites dictate the extent and type of additional safety studies needed [76].
Protocol 6: Biodistribution Assessment Using Quantitative PCR
- Cell Labeling: Pre-label cells with persistent markers (e.g., luciferase/GFP for imaging, DNA barcodes)
- Animal Model: Immunosuppressed rodents (additional species may be required for specific applications)
- Administration: Use clinical route of administration at intended clinical dose
- Time Points: Assess at 24-48 hours (initial distribution), 1-2 weeks (short-term engraftment), and 1-3 months (long-term persistence)
- Tissue Collection: Harvest major organs (brain, lungs, liver, spleen, kidneys, reproductive organs, bone marrow) and administration site
- DNA Extraction: Isolve total DNA from homogenized tissues using standardized protocols
- qPCR Analysis:
- Use human-specific Alu sequence or species-specific DNA probes
- Include standard curves for quantitative assessment
- Express results as genome equivalents per microgram of total DNA
- Interpretation: Compare distribution across tissues and persistence over time to establish safety profile
For long-term safety monitoring, clinical trials should incorporate extended follow-up periods specifically designed to detect delayed tumorigenic events. The recommended duration varies based on product risk category, with high-risk products requiring 15 years or more of patient monitoring [75]. This should include regular imaging, physical examinations, and laboratory assessments appropriate for the specific product and target population.
Quantitative Data and Analytical Methods
Tumorigenicity Testing Outcomes and Metrics
Table 2 summarizes quantitative data from representative tumorigenicity studies for different cell therapy product types, illustrating the range of outcomes observed across product categories.
Table 2: Comparative Tumorigenicity Assessment Data for Cell Therapy Products
| Product Type | In Vitro Transformation Frequency | Soft Agar Colony Formation | In Vivo Tumor Incidence | Latency Period | Key Risk Mitigation Strategies |
|---|---|---|---|---|---|
| iPSC-Derived Cardiomyocytes | 0.01-0.1% (residual undifferentiated cells) | 5-20 colonies/10⁴ cells (with undifferentiated cells) | 10-40% in NSG mice (with undifferentiated cells) | 12-24 weeks | Purification (≥99.9% target cells), suicide genes |
| iPSC-Derived Neural Progenitors | 0.001-0.01% | 0-5 colonies/10⁴ cells (purified population) | 0-5% in NSG mice (purified population) | 20-30 weeks | Pre-differentiation, fluorescence-activated cell sorting (FACS) |
| Bone Marrow MSCs | <0.001% (early passage) | 0-2 colonies/10⁶ cells | 0% in multiple studies (early passage) | N/A | Passage limitation (≤P5), senescence monitoring |
| Adipose-Derived MSCs | <0.001% (early passage) | 0-3 colonies/10⁶ cells | 0-2% in NSG mice | N/A | Passage limitation, genomic stability assessment |
| CAR-T Cells | N/A | N/A | 0% (no tumor formation reported) | N/A | Vector design improvements, integration site analysis |
The data reveal several important patterns: higher-risk products like iPSC-derived therapies demonstrate measurable tumorigenicity that can be mitigated through purification strategies, while adult stem cells like MSCs show minimal tumorigenic potential when properly characterized and controlled. The inclusion of undifferentiated cells in iPSC products significantly increases tumorigenicity risk, highlighting the critical importance of purification processes.
Analytical Framework for Tumorigenicity Data Interpretation
The interpretation of tumorigenicity data requires a comprehensive weight-of-evidence approach that integrates results from multiple assays and considers both quantitative metrics and qualitative observations. Statistical analysis should account for study sensitivity and power to detect rare tumorigenic events. Key analytical considerations include:
- Dose-Response Relationship: Assessment of whether tumorigenic potential increases with cell dose
- Time-to-Tumor Analysis: Evaluation of latency periods for tumor development
- Historical Control Data: Comparison with established tumorigenic and non-tumorigenic cell lines
- Integrated Risk Assessment: Synthesis of in vitro, in vivo, and biodistribution data
For quantitative risk assessment, the tumorigenic potential can be expressed as the number of tumor-forming units per million cells administered, though standardized approaches for such quantification are still evolving [75]. The field would benefit from established reference materials and standardized reporting metrics to enable cross-study comparisons and more robust safety assessments.
Essential Research Reagents and Tools
The experimental workflows for tumorigenicity assessment require specialized reagents and tools designed to evaluate specific aspects of cellular behavior associated with malignant transformation. Table 3 catalogues essential research reagent solutions for conducting comprehensive tumorigenicity evaluation.
Table 3: Essential Research Reagent Solutions for Tumorigenicity Assessment
| Reagent/Tool Category | Specific Examples | Primary Function | Key Considerations |
|---|---|---|---|
| Cell Line Controls | H9 hESCs (positive control), Human fibroblasts (negative control), HeLa (transformation control) | Benchmarking and assay validation | Use at appropriate passage numbers, verify authenticity regularly |
| Pluripotency Markers | Antibodies to OCT4, NANOG, SOX2, SSEA-4, TRA-1-60 | Detection of residual undifferentiated cells | Validate specificity, use multiple markers for comprehensive assessment |
| Senescence Assay Kits | β-galactosidase staining kits, Senescence-associated secretory phenotype (SASP) arrays | Detection of cellular senescence | Correlate with population doubling level, use as release criterion |
| Karyotyping Systems | G-banding reagents, Spectral Karyotyping (SKY) paints, mFISH platforms | Chromosomal abnormality detection | Minimum 20 metaphases analyzed, use high-resolution methods for subtle changes |
| Molecular Analysis Tools | hTERT PCR assays, Telomere length measurement kits, Oncogene mutation panels | Evaluation of immortalization and transformation markers | Establish baseline for normal cells, monitor drift over passages |
| Animal Models | NOD-scid gamma (NSG) mice, NOG mice, Humanized mouse models | In vivo tumorigenicity testing | Monitor health status, ensure appropriate immunosuppression |
| Cell Tracking Reagents | Luciferase/GFP lentivectors, DNA barcodes, Quantum dots | Biodistribution and persistence monitoring | Validate labeling does not alter cell behavior, ensure signal persistence |
| qPCR Reagents | Human-specific Alu sequence probes, Species-specific reference genes | Biodistribution quantification | Standardize tissue processing, include inhibition controls |
These reagents form the foundation of a robust tumorigenicity assessment program and should be carefully selected, validated, and implemented under appropriate quality control measures. Reagent performance should be regularly verified using appropriate controls to ensure assay reliability and reproducibility.
Tumorigenicity evaluation does not occur in isolation but must be integrated into a comprehensive safety assessment framework that includes general toxicity, immunogenicity, and administration-related risks [74]. The concept of cellular product toxicity encompasses the degree of harmful effects that cells and their components have on the recipient, requiring assessment of both acute and chronic toxicity parameters [74]. Toxicity studies should determine the maximum tolerated dose for single and repeated administration through careful monitoring of mortality rates, behavioral and physiological parameters, and comprehensive laboratory testing including complete blood count, biochemical parameters, and histopathological examination of multiple organs [74].
The immunogenicity of cell-based products represents another critical safety consideration, particularly for allogeneic approaches. Assessment should include evaluation of both innate immunity (complement activation, T- and NK-cell responses) and adaptive immune responses, with HLA typing recommended for appropriate patient matching [74]. For products with immunomodulatory properties, detailed immunotoxicity assessment including cytokine profiling, lymphocyte subset analysis, and functional immune tests is essential [74].
The relationship between mechanism of action (MOA) and safety profile deserves particular attention in cell-based therapy development. While understanding the MOA is crucial for appropriate safety assessment, regulatory documentation for many approved cell therapy products indicates that the MOA is not fully known or that potency tests do not clearly correlate with clinical efficacy [77]. This challenge underscores the importance of developing safety assessment strategies that do not exclusively rely on complete understanding of therapeutic mechanisms but instead adopt a comprehensive, risk-based approach to identifying potential harms.
Visualizing Tumorigenicity Assessment Workflows
The following diagrams illustrate key experimental workflows and decision processes in tumorigenicity assessment, created using DOT language with the specified color palette.
Tumorigenicity Risk Assessment Workflow
Integrated Tumorigenicity Testing Strategy
Mechanism of Action and Safety Relationship
The assessment of tumorigenicity and long-term safety for cell-based therapies requires a multifaceted, science-driven approach that evolves with product development and accumulating clinical experience. As the field advances, several areas warrant continued attention and development. First, standardization of assessment methodologies across regulatory jurisdictions would facilitate more efficient product development and clearer safety expectations. While regulatory requirements currently vary globally, emerging consensus on core evaluation principles provides a foundation for international harmonization [75]. Second, advanced technologies for detecting rare tumorigenic cells and predicting malignant potential in vivo will enhance the sensitivity and predictive value of safety assessments. Single-cell omics, improved imaging modalities, and sophisticated computational models offer promising avenues for more precise risk characterization [78].
Perhaps most importantly, the field must continue to develop robust correlation between preclinical safety assessments and clinical outcomes. As more cell-based therapies enter clinical use and long-term follow-up data accumulate, retrospective analysis of which preclinical findings predict clinical safety concerns will refine future testing strategies. This knowledge feedback loop is essential for validating current approaches and guiding the evolution of tumorigenicity assessment paradigms. Through continued scientific advancement, regulatory collaboration, and clinical vigilance, the field can maximize the transformative potential of cell-based therapies while ensuring the highest standards of patient safety.
In the evolving paradigm of Integrative and Regenerative Pharmacology (IRP), the primary objective is shifting from merely managing symptoms to restoring the physiological structure and function of tissues through targeted therapies [3]. This paradigm relies heavily on Advanced Therapy Medicinal Products (ATMPs), which include cell and gene therapies. For these complex, often living products, demonstrating consistent quality is a formidable scientific and regulatory challenge. Central to this challenge is potency testing—a functional assessment of a product's biological activity. A well-defined potency assay is not just a regulatory requirement; it is the cornerstone that links a product's mechanism of action (MoA) to its clinical efficacy, ensuring that every batch delivered to patients has the intended therapeutic effect [79]. Within a research thesis on regenerative pharmacology, mastering potency is fundamental to translating mechanistic insights into reliable, real-world treatments.
The convergence of systems biology and regenerative medicine has underscored that the therapeutic effects of ATMPs, such as mesenchymal stem cells (MSCs), are often mediated through complex, multi-factorial processes like the release of bioactive molecules (e.g., growth factors, cytokines, extracellular vesicles) and intricate interactions with the host immune system [3] [32]. Consequently, potency assays must evolve beyond single-parameter measurements to capture the holistic biological activity of the product, thereby validating the proposed mechanisms of action that form the core of IRP research [3].
The Critical Link Between Potency, MoA, and Consistency
Defining Potency in the Context of Regenerative Medicines
According to regulatory principles, potency is the "functional effect of an ADC on the target system to confirm its biological activity" [80]. This definition extends directly to ATMPs. It is a measure of the product's specific ability to achieve a defined biological effect [79]. For a batch of ATMPs to be released for clinical use, its potency must fall within a pre-defined, validated range that has been correlated with clinical effectiveness.
The foundation of any meaningful potency assay is a deep understanding of the product's MoA. The assay must be a bioanalytical representation of the primary biological activity responsible for the therapeutic effect [80]. For instance:
- If an MSC-based product functions primarily through immunomodulation (e.g., suppressing T-cell proliferation), the potency assay should quantitatively measure this suppression.
- If a product works via direct tissue repair through secreted factors, the assay might measure the concentration of key regenerative molecules or their functional impact on target cells in vitro.
The Imperative for Batch-to-Batch Consistency
ATMPs are inherently variable due to their biological nature. Sources of variability include:
- Donor-to-donor differences in source materials.
- Process-related variations in cell expansion, differentiation, and formulation.
A robust potency assay acts as a final, critical control point. It ensures that despite these inherent variabilities, the final product's biological activity remains consistent and predictable from batch to batch [79] [80]. This consistency is non-negotiable for establishing a reliable dose-response relationship and ensuring that clinical trial results can be replicated in commercialized products, a significant hurdle in the field [38]. Regulatory authorities mandate that specifications for potency "reflect the true batch to batch consistency of the product" [79].
Key Challenges in Developing Potency Assays for ATMPs
Developing robust, MoA-reflective potency assays for ATMPs presents several interconnected technical and logistical hurdles that can delay clinical development and regulatory approval.
Inherent Biological Variability: The living nature of ATMPs means they are more variable than traditional small-molecule drugs. Factors such as passage number, donor tissue source, and culture conditions can significantly alter the product's phenotypic and functional characteristics, making it difficult to establish a narrow and consistent potency range [38] [80].
Multifactorial Mechanisms of Action: Many ATMPs, particularly MSCs, exert their therapeutic effects through multiple parallel pathways—differentiation, paracrine signaling, and immunomodulation [32]. A single potency assay may be insufficient to capture this complexity, necessitating a panel of assays to fully characterize the product's functional profile, which is more resource-intensive [38].
Scalability and Comparability: As processes are scaled up from research and development (RD) to commercial Good Manufacturing Practice (GMP) production, demonstrating that the potency of the clinical-grade product is comparable to the material used in non-clinical studies is a major challenge. Changes in the manufacturing process require rigorous risk-based comparability assessments to ensure they do not impact the product's critical quality attributes (CQAs), with potency being a central CQA [38].
Long Development Timelines and Standardization: The field lacks universally standardized protocols for many ATMPs. This forces developers to create and validate custom assays, a process that requires extensive data collection to establish a correlation between the assay result and the clinical outcome, thereby prolonging development timelines [38] [80].
The following workflow outlines the key stages and decision points in developing and validating a robust potency assay.
Methodologies and Experimental Protocols for Potency Testing
A phase-appropriate approach is essential, where assay complexity and validation rigor increase as the product moves from preclinical research to market.
Foundational Principles and Assay Types
All potency assays, regardless of format, must be designed with four key performance parameters in mind, as per ICH Guideline Q2(R2): accuracy, precision, specificity, and linearity [80]. The choice of assay type is dictated by the product's MoA.
Cell-Based Bioassays: These are the gold standard for potency testing when a functional response can be measured in a live cell system. They provide a holistic measure of biological activity.
- Protocol Example: T-cell Proliferation Inhibition Assay (for Immunomodulatory MSCs)
- Co-culture Setup: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors. Seed them in a 96-well plate. Add the test MSC product at varying ratios (e.g., 1:10 MSC:PBMC). Activate T-cell proliferation using a mitogen like anti-CD3/CD28 antibodies.
- Controls: Include wells with PBMCs alone (negative control) and PBMCs + mitogen (positive control). A reference standard MSC batch with known potency is essential.
- Incubation: Culture for 3-5 days in a controlled environment (37°C, 5% CO₂).
- Quantification: Add a luminescent cell viability dye (e.g., ATP-based assay) for the final 4-24 hours. Measure luminescence. The potency is determined by the concentration of MSCs required to inhibit 50% of T-cell proliferation (IC50) relative to the reference standard.
- Data Analysis: Use parallel-line analysis to compare the dose-response curves of the test sample and the reference standard.
- Protocol Example: T-cell Proliferation Inhibition Assay (for Immunomodulatory MSCs)
Biomarker-Based Assays: These quantify specific molecules (e.g., growth factors, cytokines, surface receptors) crucial to the product's function. They are often more reproducible but must be rigorously correlated to the biological activity.
- Protocol Example: ELISA for Paracrine Factor Secretion
- Sample Preparation: Culture the test ATMP under standardized conditions. After a defined period, collect the conditioned medium.
- Assay Execution: Use a commercial or validated in-house ELISA kit to quantify the target biomarker (e.g., VEGF, HGF, PGE2) according to the manufacturer's protocol.
- Data Analysis: Compare the biomarker concentration in the test sample against a standard curve and pre-established specifications.
- Protocol Example: ELISA for Paracrine Factor Secretion
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials required for developing and executing robust potency assays.
Table 1: Research Reagent Solutions for Potency Assay Development
| Item | Function in Potency Testing | Key Considerations |
|---|---|---|
| Characterized Cell Banks | Provide consistent, biologically relevant systems for cell-based bioassays (e.g., reporter cell lines, primary target cells). | Ensure stable passage number, consistent receptor density, and pre-validated response to a reference standard [80]. |
| Reference Standard | Serves as the benchmark for calibrating potency and ensuring batch-to-batch consistency. | Must be well-characterized, stable, and stored in aliquots to minimize freeze-thaw cycles. Potency is assigned relative to this standard [80]. |
| Critical Assay Reagents | Antibodies, ligands, cytokines, and detection substrates (e.g., viability dyes) used in the assay. | Require strict qualification and stability testing. Inconsistent serum batches or enzyme activity can introduce significant variability [80]. |
| GMP-Compliant Culture Media & Supplements | Used in the production of the ATMP and potentially in the assay itself. | Raw materials must meet quality standards to ensure product and assay consistency. Sourcing GMP-grade materials can be a logistical challenge [38]. |
Regulatory Frameworks and Future Directions
Evolving Regulatory Expectations
Global regulatory agencies, including the FDA and EMA, require that potency assays for lot release be MoA-reflective and functionally based unless specifically justified otherwise [79] [80]. The FDA's recent draft guidance on expedited programs for regenerative medicine therapies (RMAT) emphasizes the need for robust Chemistry, Manufacturing, and Controls (CMC) information, with potency being a central element, even for accelerated pathways [8] [7]. The guidance encourages flexibility but does not waive the fundamental requirement for a quantitative potency measure.
Regulators acknowledge the challenges with ATMPs and may accept a phase-appropriate approach. Early in clinical development, a well-justified surrogate assay may be acceptable, but the assay must be refined and fully validated as the program progresses toward market approval [80]. The ultimate goal is to have a potency assay that can detect changes in product stability and ensure that the clinical performance is maintained throughout the product's shelf life.
Integrating Novel Technologies and Future Perspectives
The future of potency testing lies in embracing technological innovations to overcome current limitations.
- Artificial Intelligence (AI) and Data Integration: AI holds the promise of transforming regenerative pharmacology by integrating complex, multi-parametric data from omics technologies (transcriptomics, proteomics, metabolomics) to identify novel potency biomarkers and predict therapeutic outcomes more accurately [3] [38]. AI can also help in modeling dose-response relationships and optimizing assay conditions.
- Advanced Analytical Platforms: Technologies like live-cell imaging and high-throughput automated systems can provide dynamic, real-time insights into cell viability and function, moving beyond single endpoint measurements to capture more nuanced biological activity [80]. This enhances the characterization of the MoA and provides richer data for potency assessment.
- Standardization and Organoid Models: The development of organoid technology provides more physiologically relevant human disease models for preclinical testing and potency assessment, potentially offering better predictive power for clinical efficacy than traditional 2D cell cultures [38].
The following diagram illustrates how various technological and regulatory components integrate to form a comprehensive strategy for ensuring product consistency and efficacy.
Within the framework of regenerative pharmacology mechanisms of action research, standardization and potency testing are not mere regulatory checkboxes but are fundamental to scientific and clinical credibility. A robust, MoA-driven potency assay is the critical link that ensures the complex biological processes under investigation in the laboratory are reliably translated into a consistent, safe, and effective therapeutic product for patients. As the field advances, embracing a holistic strategy that integrates deep biological understanding, technological innovation, and proactive regulatory engagement will be essential for overcoming the current challenges and fully realizing the transformative potential of regenerative medicines.
Complex Regulatory Pathways for Gene Therapies and Combined ATMPs
The field of regenerative pharmacology is being transformed by advanced therapy medicinal products (ATMPs), a category that includes gene therapies, somatic-cell therapies, tissue-engineered products, and combined ATMPs that incorporate medical devices as integral components [81]. For researchers and drug development professionals, navigating the complex regulatory pathways for these innovative therapies presents significant challenges. The regulatory landscape for ATMPs has evolved substantially since the European Union established its foundational framework in 2007 with Regulation (EC) No 1394/2007 [81] [82] [83]. This framework recognizes three main types of ATMPs: gene therapy medicines that contain recombinant genes for therapeutic, prophylactic, or diagnostic effects; somatic-cell therapy medicines containing manipulated cells or tissues; and tissue-engineered medicines comprising cells or tissues modified to repair, regenerate, or replace human tissue [81].
In the United States, the term "ATMP" is not formally used; instead, the FDA classifies these products as cell and gene therapies or as human cells, tissues, and cellular and tissue-based products (HCT/Ps) regulated under the Public Health Service Act and the Federal Food, Drug, and Cosmetic Act [82] [84]. The fundamental distinction between regulatory approaches lies in their classification systems and specific expedited pathways, though both regions maintain rigorous standards for demonstrating safety, efficacy, and quality. Understanding these pathways is crucial for researchers aiming to translate regenerative pharmacology mechanisms from basic research to clinical applications, particularly as scientific advances in areas like CRISPR/Cas9 gene editing challenge existing regulatory paradigms [83].
Global Regulatory Landscape and Classification
European Regulatory Framework
The European Medicines Agency (EMA) operates a centralized authorization procedure for all ATMPs, with the Committee for Advanced Therapies (CAT) serving as the central scientific authority [81] [82]. The CAT provides scientific expertise for evaluating ATMPs, classifies advanced therapy products, and advises on pharmacovigilance and risk management systems [81]. The overarching regulatory framework is established in Regulation (EC) No 1394/2007, which builds upon and amends Directive 2001/83/EC and Regulation (EC) No 726/2004, with additional detailed requirements specified in Commission Directive 2009/120/EC [82].
For developers using human-derived materials, the Cell and Tissue Directive (2004/23/EC)—soon to be replaced by the Substances of Human Origin Regulation (SoHO-R) in 2027—establishes requirements for donation, procurement, collection, and testing of tissues and cells [82]. ATMPs involving genetically modified organisms (GMOs) must comply with two separate legal pathways: the Contained Use Directive (2009/41/EC) and the Deliberate Release Directive (2001/18/EC), implemented at national levels with varying requirements across Member States [82].
The EMA offers several support mechanisms to facilitate ATMP development, including the Priority Medicines (PRIME) scheme for therapies addressing unmet medical needs, the Innovation Task Force (ITF) briefing meetings for early dialogue on innovative approaches, and orphan designation programs that provide incentives for rare disease therapies [82]. A specific pilot program launched in 2022 offers dedicated regulatory support to academic and non-profit organizations developing ATMPs targeting unmet clinical needs [81].
United States Regulatory Framework
In the U.S., the Center for Biologics Evaluation and Research (CBER), a division of the FDA, regulates cellular and gene therapy products under the authority of the Public Health Service Act and the Federal Food, Drug, and Cosmetic Act [82] [84]. These products are subject to the Investigational New Drug (IND) application process before clinical testing can begin, followed by a Biologics License Application (BLA) for market approval [82].
The FDA has established several expedited programs to accelerate development and review of promising therapies. These include Fast Track designation for serious conditions with unmet needs, Breakthrough Therapy designation for treatments demonstrating substantial improvement over available therapies, Accelerated Approval based on surrogate endpoints, and Priority Review to shorten the review timeline [82]. Specifically for regenerative medicine, the Regenerative Medicine Advanced Therapy (RMAT) designation, established under the 21st Century Cures Act, provides expedited development and review pathways for regenerative medicine therapies targeting serious conditions [7].
For human cells, tissues, and cellular and tissue-based products (HCT/Ps), the FDA applies a risk-based regulatory approach under 21 CFR Part 1271 [84]. HCT/Ps that are minimally manipulated, intended for homologous use, and not combined with another article (except water, crystalloids, or sterilizing/preserving agents) are regulated solely under Section 361 of the Public Health Service Act [84]. Products that exceed these criteria—through more than minimal manipulation, non-homologous use, or combination with another article—are regulated as drugs, devices, or biologics requiring premarket approval [84].
Comparative Analysis of EU and US Regulatory Pathways
Table 1: Comparison of Key Regulatory Elements for ATMPs/Cellular & Gene Therapy Products in the EU and US
| Regulatory Element | European Union | United States |
|---|---|---|
| Central Regulatory Body | European Medicines Agency (EMA) | Food and Drug Administration (FDA) |
| Specialized Evaluating Committee | Committee for Advanced Therapies (CAT) | Center for Biologics Evaluation and Research (CBER) |
| Primary Legal Framework | Regulation (EC) No 1394/2007 | Public Health Service Act + Federal Food, Drug, and Cosmetic Act |
| Classification System | Gene Therapy, Somatic-Cell Therapy, Tissue-Engineered, Combined ATMP | Cell and Gene Therapy Products, HCT/Ps |
| Clinical Trial Authorization | Clinical Trial Application (CTA) to National Competent Authorities | Investigational New Drug (IND) Application |
| Market Authorization Application | Marketing Authorization Application (MAA) via Centralized Procedure | Biologics License Application (BLA) |
| Expedited Pathways | PRIME, Accelerated Assessment | RMAT, Fast Track, Breakthrough Therapy |
| Tissue/Cell Regulation | Cell & Tissue Directive (transitioning to SoHO Regulation) | 21 CFR Part 1271 (HCT/Ps) |
Technical Requirements and Characterization Methods
Critical Quality Attributes and Process Parameters
The development of ATMPs requires meticulous characterization of Critical Quality Attributes (CQAs)—physical, chemical, biological, or microbiological properties that must be within appropriate limits to ensure product quality [85]. Similarly, Critical Process Parameters (CPPs) that significantly impact CQAs must be identified and controlled [85]. The relationship between CQAs and CPPs is established through a Quality by Design (QbD) approach, which employs scientific, risk-based, and holistic principles to pharmaceutical development [85].
For gene therapy products, key CQAs include vector identity and titer, purity (including replication-competent viruses), potency, and identity of the genetic construct [81] [82]. For cell-based ATMPs, CQAs typically include cell viability, identity (surface marker expression), purity, potency, and safety (sterility, endotoxin, mycoplasma) [81] [84]. The design space concept—defined as the multidimensional combination and interaction of input variables and process parameters that have been demonstrated to provide assurance of quality—is fundamental to establishing control strategies for ATMPs [85].
Experimental Protocols for ATMP Characterization
Protocol for Vector Characterization in Gene Therapy Products
Objective: To characterize critical quality attributes of viral vectors used in gene therapy products.
Methodology:
- Vector Titer Determination: Perform qPCR-based titration to measure vector genome concentration using validated methods with appropriate reference standards.
- Potency Assay: Conduct in vitro transduction assays with permissive cell lines, measuring transgene expression via flow cytometry or ELISA.
- Purity Analysis: Assess empty/full capsid ratio using analytical ultracentrifugation or HPLC; test for replication-competent viruses using PCR-based methods or cell-based assays.
- Identity Confirmation: Verify genetic identity through restriction enzyme digestion and sequencing of the expression cassette; confirm vector identity using Western blot for viral proteins.
- Sterility Testing: Perform compendial sterility testing according to pharmacopeial standards; test for mycoplasma using culture-based and PCR-based methods.
Data Analysis: Establish specifications for each CQA based on manufacturing experience and clinical data. Implement statistical process control for ongoing monitoring of vector quality.
Protocol for Cell Characterization in Somatic-Cell Therapy Products
Objective: To comprehensively characterize cellular products for identity, potency, purity, and safety.
Methodology:
- Cell Viability and Count: Determine viability using dye exclusion methods (e.g., trypan blue) or automated cell counters; calculate total and viable cell numbers.
- Identity and Purity: Characterize surface marker expression using multicolor flow cytometry with antibodies specific for expected cell population markers and contaminants.
- Potency Assay: Develop mechanism-based potency assays that measure biological activity relevant to the proposed mechanism of action (e.g., differentiation potential, cytokine secretion, enzymatic activity).
- Sterility and Safety: Test for sterility, mycoplasma, and endotoxin according to compendial methods; perform adventitious agent testing as appropriate.
- Genetic Stability: Assess genetic stability through karyotyping or more sophisticated methods like comparative genomic hybridization if cells undergo extensive manipulation or culture.
Data Analysis: Establish acceptance criteria for all CQAs based on manufacturing experience and clinical correlation. Implement donor qualification and testing programs for allogeneic products.
Process Development and Manufacturing Controls
ATMP manufacturing processes require careful control and validation to ensure consistent product quality. The process characterization approach involves identifying CPPs through risk assessment and experimental design, then establishing proven acceptable ranges (PARs) for these parameters [85]. For gene therapies, this includes controlling parameters for vector production, purification, and formulation [82]. For cell therapies, critical parameters include cell culture conditions, harvest methods, cryopreservation, and storage conditions [81] [84].
The manufacturing process must demonstrate robustness—the ability to tolerate variability in process parameters without adversely affecting product quality—through appropriate challenge studies [85]. A control strategy encompassing in-process controls, release testing, and characterization assays should be implemented to ensure consistent manufacturing of ATMPs [85].
Table 2: Research Reagent Solutions for ATMP Development and Characterization
| Research Reagent | Function | Application Examples |
|---|---|---|
| Flow Cytometry Antibodies | Cell surface and intracellular marker detection | Immune phenotyping, purity assessment, identity testing |
| qPCR/qRT-PCR Reagents | Nucleic acid amplification and quantification | Vector genome titer, transgene expression, mycoplasma testing |
| ELISA Kits | Protein quantification | Cytokine measurement, transgene product detection, impurity testing |
| Cell Culture Media | Cell growth and maintenance | Expansion of cellular products, vector production |
| Viral Vector Purification Kits | Vector purification and concentration | Downstream processing of gene therapy products |
| Cell Separation Kits | Isolation of specific cell populations | Preparation of cell therapy products, removal of unwanted cells |
| Endotoxin Testing Kits | Bacterial endotoxin detection | Safety testing of final product and in-process materials |
| Sequencing Reagents | Genetic sequence determination | Identity confirmation, genetic stability assessment |
Regulatory Submission and Lifecycle Management
Clinical Trial Applications
In the EU, a Clinical Trial Application (CTA) must be submitted and approved by relevant national authorities and ethics committees before initiating clinical trials with investigational ATMPs [82]. The CTA must include detailed information on product quality, non-clinical data, clinical protocols, and controls, as outlined in the EMA's 'Guideline on quality, non-clinical and clinical requirements for investigational advanced therapy medicinal products in clinical trials' released in January 2025 [82].
In the U.S., developers must submit an Investigational New Drug (IND) application to CBER before initiating clinical trials [82] [84]. The IND must contain information on product manufacturing and characterization, preclinical proof-of-concept and safety data, and clinical trial protocols [84]. For significant risk devices that are part of combined ATMPs, an Investigational Device Exemption (IDE) may also be required [81].
Market Authorization Applications
Following successful clinical trials, a Marketing Authorization Application (MAA) is submitted to the EMA in the EU [82]. The CAT prepares a draft opinion on the quality, safety, and efficacy of the ATMP, which is then used by the Committee for Medicinal Products for Human Use (CHMP) to adopt an opinion recommending authorization to the European Commission [81]. The European Commission makes the final authorization decision [81].
In the U.S., developers submit a Biologics License Application (BLA) to CBER for market approval [82]. The BLA must contain comprehensive information demonstrating the safety, purity, and potency of the biological product, including chemistry, manufacturing, and controls data; preclinical and clinical data; and proposed labeling [82] [84].
Post-Authorization Requirements
After authorization, ATMPs are subject to ongoing pharmacovigilance requirements and additional monitoring in many cases [81]. The EMA continues to monitor the safety and efficacy of authorized ATMPs and may require post-authorization safety studies (PASS) or post-authorization efficacy studies (PAES) [81]. In the U.S., post-market requirements may include additional studies, long-term follow-up for gene therapy patients, and established pharmacovigilance systems [84].
The high cost of ATMPs—with some gene therapies priced at over €2 million per treatment—has led to the implementation of managed entry agreements (MEAs) in many countries, including risk-sharing arrangements, outcome-based agreements, and confidential discounts [86]. These mechanisms aim to balance patient access with the financial sustainability of healthcare systems while collecting additional evidence on real-world effectiveness [86].
Emerging Challenges and Future Directions
Regulatory Challenges for Innovative Therapies
The rapid pace of scientific advancement in gene editing technologies, particularly CRISPR/Cas9 systems, is challenging existing regulatory frameworks [83]. The current EU regulatory framework for ATMPs, established in 2007, is showing inherent limitations when applied to new frontiers in gene therapeutics, manufacturing technologies, and delivery systems [83]. There are ongoing discussions about enhancing classification criteria for gene therapy medicinal products (GTMPs) and rationalizing regulatory support and incentives for the most complex therapies [83].
The development of decentralized manufacturing models for ATMPs, including point-of-care manufacturing, presents additional regulatory challenges regarding quality control and standardization [84]. The FDA has begun addressing these challenges through enforcement discretion policies for certain minimally manipulated autologous therapies, such as micro-fragmented adipose tissue and bone marrow aspirate concentrate, when used in specific surgical settings [84].
Access and Equity Considerations
Significant disparities in access to approved gene therapies exist across the European Union, creating ethical challenges related to fairness, justice, and solidarity in healthcare [86]. These disparities are driven by differences in affordability (with treatments costing €1-2 million per patient), geographical location, and fragmented national healthcare systems [86]. While alternative pathways such as the Hospital Exemption and Compassionate Use Programs aim to improve access, their inconsistent implementation across Member States can exacerbate inequalities [86].
The following diagram illustrates the complex regulatory pathway for ATMPs from research to market authorization:
Diagram 1: ATMP Regulatory Pathway from Research to Market
Future Regulatory Evolution
The European Commission is exploring regulatory innovations such as Regulatory Sandboxes to create controlled environments for testing innovative gene therapies under regulatory supervision [83]. There are also proposals to decouple ATMP regulation from the production technology of the active substance to better accommodate emerging manufacturing platforms [83].
In both the EU and U.S., there is growing emphasis on real-world evidence to support regulatory decision-making and post-authorization monitoring of ATMPs [81] [84]. The integration of real-world data collection into regulatory frameworks may help address evidence gaps while facilitating patient access to promising therapies.
The development of advanced manufacturing technologies, including closed automated systems and process analytical technology (PAT), is expected to enhance the consistency and scalability of ATMP manufacturing [85]. These technological advances, combined with evolving regulatory approaches, will likely shape the future development of gene therapies and combined ATMPs within the broader context of regenerative pharmacology research.
The following workflow diagram outlines the key experimental characterization requirements for ATMPs:
Diagram 2: ATMP Critical Quality Attribute Assessment Workflow
Regenerative pharmacology represents a paradigm shift in therapeutic science, aiming to restore the physiological structure and function of damaged tissues rather than merely managing symptoms [3]. This field stands at the nexus of pharmacology, systems biology, and regenerative medicine, creating what is now termed Integrative and Regenerative Pharmacology (IRP) [3]. However, the very innovations that promise to redefine therapeutic landscapes also present a significant economic paradox: how to reconcile the extraordinary costs of development and manufacturing with the imperative for global accessibility. Advanced Therapy Medicinal Products (ATMPs), including cell therapies, gene therapies, and tissue-engineered products, embody this challenge through their complex biological nature and personalized applications [38]. The global regenerative medicine market, valued at USD 48.45 billion in 2024 and projected to skyrocket to USD 403.86 billion by 2032, demonstrates the field's immense commercial potential [87]. Yet, this growth is threatened by fundamental economic constraints that limit patient access, particularly in low- and middle-income countries. This whitepaper examines the multifaceted economic and accessibility challenges within regenerative pharmacology and provides technical strategies for overcoming these barriers without compromising therapeutic innovation or quality.
Market Landscape and Economic Significance
The economic context of regenerative medicine reveals both its transformative potential and its financial challenges. The market is experiencing unprecedented growth, with varying projections reflecting different methodological approaches but converging on the same exponential trajectory.
Table 1: Global Regenerative Medicine Market Projections
| Market Source | 2024/2025 Baseline Value | 2032/2034 Projected Value | Compound Annual Growth Rate (CAGR) |
|---|---|---|---|
| DataM Intelligence | USD 48.45 billion (2024) | USD 403.86 billion (2032) | 27.3% (2025-2032) [87] |
| Precedence Research | USD 43.80 billion (2025) | USD 212.80 billion (2034) | 19.2% (2025-2034) [88] |
| Custom Market Insights | USD 167.99 billion (2024) | USD 248.73 billion (2034) | 19.2% (2025-2034) [89] |
Regional market analysis reveals North America as the dominant force, capturing over 48% of the global market share in 2024, with the United States alone accounting for USD 21.3 billion in revenue [87] [88]. The Asia-Pacific region represents the fastest-growing market, projected to expand at a CAGR of 25% from 2025 to 2034 [88]. This growth is fueled by dramatic scientific advances, rapid commercialization of gene and cell therapies, rising prevalence of chronic diseases, and aggressive investment from biotechnology companies [87]. The industry is transforming from experimental science to commercial reality, with breakthrough approvals in CAR-T therapy, stem-cell therapy, gene-editing platforms, engineered tissues, and acellular regenerative scaffolds supporting expansion into oncology, neurology, musculoskeletal repair, dermatology, cardiovascular disorders, and rare genetic diseases [87].
Table 2: Regenerative Medicine Market Share by Therapy Type (2024)
| Therapy Type | Market Share | Market Value (USD Billion) | Primary Applications |
|---|---|---|---|
| Cell Therapy | 39% | 18.9 | Oncology, immunology [87] |
| Gene Therapy | 22% | 10.7 | Rare genetic disorders, hematological diseases [87] |
| Tissue Engineering | 18% | 8.7 | Orthopedics, burns, chronic ulcers [87] |
| Stem Cell Therapy | 17% | 8.2 | Musculoskeletal, dermatology, CNS, cardiovascular [87] |
The economic significance of regenerative pharmacology extends beyond market valuations to its potential impact on healthcare systems. These therapies offer durable and sometimes curative outcomes for conditions where conventional pharmaceuticals have limited effectiveness, such as heart failure, rare genetic disorders, spinal cord injuries, severe burns, chronic wounds, and neurodegenerative diseases [87]. This represents a shift from chronic disease management to potential cures, with profound implications for healthcare economics and patient quality of life.
Analysis of Primary Cost Drivers
The development and commercialization of regenerative pharmacology interventions face substantial cost drivers that challenge sustainable implementation and global accessibility.
Manufacturing Complexities
Manufacturing ATMPs presents unique challenges compared to conventional pharmaceuticals. These products often involve living cells with complex biological characteristics that require stringent process controls. A critical barrier is implementing Good Manufacturing Practice (GMP)-compliant manufacturing processes that reliably meet quality specifications defined during product development [38]. The transition from Good Laboratory Practice (GLP) non-clinical studies to GMP-compliant manufacturing requires extensive validation, testing, and documentation to ensure consistent product quality, safety, and efficacy [38]. Scalable cell expansion represents another significant challenge, as large cell volumes for clinical applications often require extensive expansion that can alter cellular phenotype and functionality [38]. Additionally, traditional sterilization methods are not feasible for cell-based products, necessitating expensive aseptic processing and validation through media fill simulations [90]. Tumorigenicity testing requirements further complicate manufacturing, with in vivo studies in immunocompromised models and increasingly sensitive in vitro methods like digital soft agar assays adding to timelines and costs [38].
Regulatory Hurdles and Technical Inefficiencies
The regenerative medicine market faces substantial threats from regulatory and compliance difficulties [89]. Stringent regulations from bodies like the U.S. FDA and European Medicines Agency (EMA), while essential for ensuring safety and efficacy, often create delays in approval and market access [89]. The regulatory framework for ATMPs continues to evolve, with regional differences in requirements for scaling up manufacturing processes [38]. Technical inefficiencies also hamper market growth, including operational challenges in tissue engineering procedures where cell adhesions break during tissue repair, leading to proliferation issues and incomplete colonization in scaffold external layers [88]. The absence of built-in vascularization presents another significant technical hurdle, as implanted tissues exceeding 100-200μm require separate blood vessel supplies for nutrients and oxygen, which remains challenging for tissue engineering transplantation [88]. Inefficient cell isolation and culture techniques can lead to failure in tissue growth after implantation, while external environmental conditions can reduce growth momentum and differentiation of cells [88].
Research and Development Investments
The high costs of regenerative medicine begin at the research and development stage. Global regenerative medicine funding, including public, private, and venture investments, surpassed USD 50 billion in 2024 [87]. The complex nature of these biological products necessitates extensive preclinical testing and clinical trials to demonstrate safety and efficacy. For ATMPs focused on rare diseases, limited patient populations make it challenging to gather statistically robust data, potentially requiring larger or longer trials [38]. Additionally, difficulties in clearly defining and assessing mechanism of action and potency pose obstacles to confirming clinical effectiveness [38]. Long-term follow-up clinical investigation is required to assess regenerative drugs and biologics beyond initial clinical trials, adding to overall development costs [3]. The high failure rate of experimental therapies in clinical development further contributes to the overall cost burden of successful products.
Technical Strategies for Cost Management and Enhanced Accessibility
Innovative technical approaches and strategic manufacturing evolution present promising pathways to mitigate costs while maintaining therapeutic quality.
Advanced Manufacturing Platforms
Implementing advanced manufacturing platforms is essential for reducing production costs and improving accessibility. Automated closed-system bioreactors represent a transformative technology for scalable, GMP-compliant cell expansion [38] [3]. These systems minimize manual handling, reduce contamination risks, and improve process consistency. Allogeneic "off-the-shelf" therapies offer another strategic approach, utilizing donor-derived cells that can be manufactured in large batches and distributed to multiple patients [87] [91]. This model contrasts with autologous therapies, which are patient-specific and inherently more costly and time-consuming to produce. As Frank Edenhofer from the University of Innsbruck notes, allogeneic approaches allow creation of "big batch of cells which can then be distributed to clinical centers applying this therapy to numerous patients. That is relatively cost-efficient" [91]. Modular, flexible facility and equipment designs that can be easily adapted to meet GMP requirements provide additional manufacturing efficiency [38] [92].
Process Standardization and Analytical Advances
Standardization of manufacturing processes and analytical methods is crucial for reducing costs while maintaining quality. Comprehensive process validation protocols and quality management systems help ensure product consistency and reliability [34]. Standardized cell characterization and quality control assays are essential for ensuring consistent cell product quality despite inherent biological variability [91]. Robust quality control systems, including in-process testing, real-time release criteria, and stability studies, are fundamental for ensuring the stability and reliability of the final product [92]. Strategic partnerships and supply chain management strategies help secure reliable sources of GMP-compliant raw materials and components, addressing a complex logistical challenge, especially for novel or specialized products [92]. Harmonization of regulatory requirements across regions would further streamline manufacturing processes and reduce costs associated with complying with multiple regulatory frameworks [3] [38].
Novel Cellular Reprogramming Technologies
Innovative cellular reprogramming technologies offer promising avenues for reducing costs and improving accessibility. Induced pluripotent stem cells (iPSCs) have emerged as a particularly transformative technology, addressing both ethical concerns associated with embryonic stem cells and potential immune rejection issues [91]. iPSCs are reprogrammed from adult cells to a pluripotent state, from which they can differentiate into myriad cell types [91]. Further advancements include direct reprogramming approaches that convert somatic cells directly into other cell types without transitioning through a pluripotent state. As Constantinos Chronis from the University of Illinois Chicago explains, "Using this technology, researchers could bypass iPSC generation altogether, which could reduce production time, lower manufacturing costs and potentially enhance safety" [91]. Similarly, Frank Edenhofer's team has developed a protocol to generate induced neural stem cells (iNSCs) directly from patient dermal fibroblasts or blood cells, creating a shortcut that is "four times faster" than going through iPSCs [91].
Figure 1: Cellular Reprogramming Pathways for Regenerative Therapies
Experimental Protocols for Cost-Effective Research and Development
Implementing standardized, efficient experimental protocols is essential for advancing regenerative pharmacology while managing costs.
Protocol for Induced Pluripotent Stem Cell Generation
The generation of iPSCs from somatic cells represents a foundational protocol in regenerative pharmacology research with significant implications for cost reduction and personalized medicine applications.
Table 3: Research Reagent Solutions for iPSC Generation
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Dermal Fibroblasts | Somatic cell source for reprogramming | Obtainable via minimally invasive punch biopsy; alternative sources include peripheral blood mononuclear cells [91] |
| Yamanaka Factors | Transcription factors for reprogramming (OCT4, SOX2, KLF4, c-MYC) | Can be delivered via integrating lentiviruses, non-integrating Sendai virus, or episomal plasmids [91] |
| Reprogramming Media | Supports dedifferentiation process | Typically contains supplements that enhance reprogramming efficiency and cell survival |
| Feeder Cells | Provide extracellular matrix support | Mouse embryonic fibroblasts (MEFs) traditionally used; feeder-free systems now available but more expensive |
| Stem Cell Culture Media | Maintains pluripotency of established iPSCs | Serum-free, defined formulations preferred for consistency and reducing batch-to-batch variability [89] |
Step-by-Step Methodology:
- Cell Sourcing and Expansion: Obtain patient-derived dermal fibroblasts via 3-4mm punch biopsy. Culture in fibroblast medium (DMEM supplemented with 10% FBS, 1% non-essential amino acids, and 1% GlutaMAX) for 2-3 passages to obtain sufficient cell numbers [91].
- Reprogramming Factor Delivery: Plate fibroblasts at optimal density (5×10^4 cells per well in 6-well plate). Transduce with viral vectors encoding Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) at appropriate multiplicity of infection (MOI). Alternative non-integrating methods include mRNA transfection or Sendai viral vectors [91].
- Reprogramming Culture Transition: After 48-72 hours, replace transduction medium with standard fibroblast medium for 4 days. Transition to iPSC culture medium containing bFGF on feeder layers or defined substrate [91].
- iPSC Colony Identification and Expansion: Monitor for emergence of compact, domed-shaped colonies with defined borders between days 14-21. Mechanically pick or enzymatically dissociate colonies for expansion [91].
- Quality Control and Characterization: Validate pluripotency through immunocytochemistry (OCT4, NANOG, SSEA-4), trilineage differentiation potential, and karyotype analysis to ensure genetic stability [38] [91].
Protocol for Scalable Bioreactor Culture of Therapeutic Cells
Transitioning from laboratory-scale culture to scalable manufacturing represents a critical pathway toward cost reduction.
Step-by-Step Methodology:
- Cell Bank Thawing and Expansion: Rapidly thaw working cell bank vial and transfer to pre-warmed expansion medium. Begin in traditional flask-based culture for initial recovery [38].
- Bioreactor Inoculation and Process Optimization: Transfer cells to small-scale bioreactor (e.g., 100mL working volume) with defined parameters including dissolved oxygen (40%), pH (7.2), temperature (37°C), and agitation rate (50-100rpm) [38] [3].
- Monitoring and Feeding Strategy: Implement continuous monitoring of critical quality attributes (CQAs) including glucose consumption, lactate production, and cell viability. Employ perfusion or fed-batch feeding strategies based on metabolic consumption rates [38].
- Harvest and Formulation: Upon reaching target cell density or expansion fold, harvest cells using enzymatic or mechanical dissociation methods. Formulate final product in appropriate cryopreservation medium [38].
- Quality Control Testing: Perform in-process and lot-release testing including viability, potency, identity, purity, and sterility assessments according to predetermined specifications [38] [34].
Figure 2: Comparison of Autologous vs. Allogeneic Manufacturing Models
The economic and accessibility challenges facing regenerative pharmacology are substantial but not insurmountable. Strategic approaches focusing on manufacturing innovation, process standardization, and novel cellular technologies offer promising pathways to reconcile the high costs of development with the need for global accessibility. The integration of artificial intelligence in manufacturing and research, development of more cost-effective reprogramming methodologies, and evolution toward allogeneic "off-the-shelf" therapies will be instrumental in driving down costs while maintaining therapeutic efficacy [3] [88] [91]. Furthermore, regulatory harmonization across regions and innovative reimbursement models will be essential for enabling broader patient access. As the field continues to mature, collaboration between academia, industry, clinicians, and regulatory authorities will be paramount to establishing standardized procedures, ensuring consistency in therapeutic outcomes, and ultimately developing transformative curative therapies that are accessible across global healthcare systems [3]. Without this collaborative effort, regenerative pharmacology may not fully progress from the bench to the bedside, limiting its potential to revolutionize treatment for patients worldwide. The future of regenerative pharmacology depends not only on scientific innovation but also on developing sustainable economic models that enable global reach without compromising therapeutic potential.
Establishing Efficacy and Differentiating from Conventional Therapies
Within the emerging paradigm of Integrative and Regenerative Pharmacology (IRP), the development of Advanced Therapy Medicinal Products (ATMPs) represents a transformative approach to treating disease by restoring the physiological structure and function of tissues rather than merely managing symptoms [3]. A critical challenge in this field is the rigorous quantification of biological activity for complex living therapies. Functional potency assays are essential tools that bridge this gap, providing quantitative, mechanism-based measurements of a product's biological activity linked to its intended mechanism of action (MoA) [93]. This technical guide details validated methodologies for assessing three critical therapeutic processes in regenerative pharmacology: immunomodulation, angiogenesis, and tissue formation, framing them within the required context of mechanistic research for drug development professionals.
The Role of Potency Assays in Regenerative Pharmacology
In the context of IRP, which unites pharmacology, systems biology, and regenerative medicine, potency assays are not merely quality control tests but are fundamental to understanding therapeutic MoA [3]. According to regulatory requirements, at least one assay demonstrating biological activity is required for the release of a gene-therapy vector or ATMP for commercial use [93]. These assays must provide a quantitative measure of biological activity linked to relevant biological properties and should ideally represent the product's MoA [93].
For ATMPs, demonstrating product comparability after manufacturing process changes is a critical scale-up concern, requiring robust potency assays for risk-based comparability assessments and extended analytical characterization [38]. Unlike traditional pharmacology's focus on symptom reduction, IRP aims to restore tissue structure and function, necessitating potency assays that can quantify complex processes like immunomodulation, angiogenesis, and tissue formation [3].
Validating Angiogenic Potency
Background and Significance
Angiogenesis, the formation of new blood vessels from pre-existing ones, is essential for tissue regeneration and repair, particularly in response to injuries [94]. This process is especially critical for regenerative medicine applications targeting chronic wounds and ischemic diseases [94] [95]. Dental mesenchymal stem cells (DMSCs) and other progenitor cells have demonstrated significant proangiogenic potential, making them promising candidates for clinical applications requiring vascularization [94].
Scratch Wound Healing Assay for Angiogenic Potential
Experimental Protocol
The scratch wound healing assay serves as a robust in vitro model to mimic endothelial cell migration and proliferation necessary for angiogenesis [94]. The following protocol has been validated for assessing the angiogenic potential of secretomes derived from dental mesenchymal stem cells:
- Cell Culture: Culture DMSCs (e.g., from dental pulp, periodontal ligament, gingiva) under standard conditions and collect their secretomes - the complex mixture of proteins, lipids, nucleic acids, growth factors, and cytokines they secrete [94].
- Endothelial Cell Preparation: Culture human endothelial cells to confluence in an appropriate vessel (e.g., multi-well plate).
- Scratch Formation: Create a uniform "wound" or linear scratch in the confluent endothelial cell monolayer using a sterile pipette tip or specialized instrument.
- Treatment Application: Apply the collected DMSC-derived secretomes to the scratched endothelial cell cultures. Include controls treated with standard growth medium alone.
- Migration Quantification: Observe and capture images of endothelial cell migration into the scratch area at regular intervals (e.g., 0, 24, and 48 hours). Quantify migration by measuring the reduction in scratch width over time using image analysis software [94].
Key Data Interpretation
Preliminary findings indicate that DMSC-derived secretomes, particularly from dental pulp, significantly enhance the migration of endothelial cells compared to controls, suggesting strong angiogenic potential [94]. This enhanced migration is attributed to the presence of crucial signaling molecules in the secretome, including vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and basic fibroblast growth factor (bFGF) [94].
Diagram 1: Scratch Wound Assay Workflow for Angiogenesis.
Quantitative Cell-Based Biochemical Potency Assay
Experimental Protocol
For advanced therapeutic products like gene therapies, more quantitative potency assays are required. The following validated assay for AAV2-hRPE65v2 (Luxturna) provides a template for mechanistic assays of other vectors [93]:
- Cell Transduction: Transduce modified HEK293-LRAT cells (stably expressing lecithin retinol acyltransferase) with multiple multiplicities of infection (MOIs) of the AAV2-hRPE65v2 vector.
- Lysate Preparation: Prepare lysates from the transduced cells.
- Enzymatic Reaction: Incubate cell lysates with the substrate all-trans-retinol (at-ROL). The transgene product, RPE65 protein, acts as a retinoid isomerohydrolase in the visual cycle.
- Product Quantification: Detect and quantify the reaction product, 11-cis-retinol (11-cis-ROL), using liquid chromatography with tandem mass spectrometry (LC-MS/MS). This step separates the product from the substrate and other cis-retinol isoforms [93].
Validation Parameters
This assay was validated for seven key characteristics: system and sample suitability, specificity, linearity, precision, relative accuracy, range, and robustness [93]. The validated assay can confirm the relative potency levels of different product lots in the range of 50%–150% of a reference standard, providing a quantitative measure of biological activity essential for regulatory approval and lot-to-lot consistency [93].
Assessing Immunomodulatory Potency
Background and Significance
Mesenchymal stem cells (MSCs) have emerged as pivotal agents in regenerative medicine due to their immunomodulatory, angiogenic, and anti-fibrotic properties [96] [95]. Their ability to modulate immune responses is particularly valuable for treating chronic wounds characterized by persistent inflammation [95]. MSCs from various sources, including bone marrow (BM-MSCs), adipose tissue (AT-MSCs), and umbilical cord (UC-MSCs), contribute to tissue repair partly through secretion of trophic factors that modulate inflammation [96].
Essential Research Reagent Solutions
Table 1: Key Reagents for Immunomodulation Assays
| Research Reagent | Function in Assay | Specific Application Example |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary therapeutic agent with immunomodulatory capacity | Sourced from bone marrow (BM-MSCs), adipose tissue (AT-MSCs), or umbilical cord (UC-MSCs) [96] |
| Peripheral Blood Mononuclear Cells (PBMCs) | Represent immune cell populations for co-culture studies | Used as responder cells to measure MSC-mediated immunomodulation |
| Mitogens (e.g., PHA, ConA) | Polyclonal T-cell activators to simulate immune activation | Stimulate PBMC proliferation in suppression assays |
| Flow Cytometry Antibodies | Characterize immune cell phenotypes and activation states | Target CD4, CD8, CD25, CD69, FoxP3 for T-cell analysis [94] |
| Cytokine Detection Assays | Quantify secreted immunomodulatory factors | ELISA or multiplex arrays for IFN-γ, IL-10, TGF-β, PGE2 |
T-Lymphocyte Proliferation Suppression Assay
Experimental Protocol
A cornerstone method for evaluating immunomodulatory potency measures the capacity of therapeutic cells to suppress T-cell proliferation:
- Responder Cell Preparation: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors and label with a cell division tracker such as CFSE (Carboxyfluorescein succinimidyl ester).
- Therapeutic Cell Preparation: Culture the test therapeutic cells (e.g., MSCs) to establish a monolayer. For trans-well systems, seed MSCs in inserts to separate them from responder cells while allowing soluble factor exchange.
- Co-culture Establishment: Activate the CFSE-labeled PBMCs with a mitogen (e.g., phytohemagglutinin-PHA or anti-CD3/CD28 antibodies) and co-culture them with the test therapeutic cells. Include controls of activated PBMCs alone and non-activated PBMCs.
- Incubation and Analysis: Incubate for 3-5 days, then harvest PBMCs and analyze CFSE dilution by flow cytometry to determine the percentage of proliferated T-cells [96].
Key Data Interpretation
The immunomodulatory potency is calculated as the percentage suppression of T-cell proliferation compared to activated PBMCs alone. MSCs from different sources exhibit varying efficacy; for example, UC-MSCs have been observed to show higher anti-inflammatory effects compared to other sources [96]. This suppression is mediated through both cell-contact-dependent mechanisms and soluble factors such as PGE2, IDO, and TGF-β.
Quantifying Tissue-Forming Potency
Background and Significance
The ultimate goal of many regenerative therapies is the formation of functional new tissue. This involves the coordinated processes of cell proliferation, migration, and extracellular matrix (ECM) production and remodeling [96]. Fibroblasts play a key role in the proliferative and remodeling phases of wound healing by producing ECM proteins like fibronectin, collagen, and proteoglycans that provide structural support for regenerating tissue [96].
Engineered Tissue Construct Functional Assessment
Experimental Protocol
For therapies involving tissue-engineered products, functional assessment of tissue-forming capacity is essential:
- Cell-Seeding on Scaffolds: Seed therapeutic cells (e.g., fibroblasts, MSCs, keratinocytes) onto 3D biomaterial scaffolds (e.g., collagen, hydrogels, synthetic polymers) at defined densities.
- In Vitro Maturation: Culture the cell-scaffold constructs under conditions conducive to tissue development (e.g., with ascorbate to promote collagen synthesis, or in bioreactors providing mechanical stimulation).
- Histological and Biochemical Analysis:
- Process constructs for histology and stain with Hematoxylin and Eosin (H&E) for general structure and Masson's Trichrome or Sirius Red for collagen deposition and organization.
- Quantify specific ECM components biochemically (e.g., hydroxyproline assay for total collagen content).
- Mechanical Testing: Assess the functional mechanical properties of the constructs using uniaxial tensile testing or compression testing to determine tensile strength, Young's modulus, and other relevant parameters [96].
Key Data Interpretation
Successful tissue formation is indicated by widespread, organized collagen deposition throughout the scaffold, significantly higher than in acellular controls. The ultimate tensile strength of the construct provides a direct functional measure of its integrity, which is critical for applications requiring mechanical resilience, such as skin or cartilage repair. Combining stem cells with bioengineered scaffolds and hydrogel matrices has been shown to significantly enhance wound contraction and collagen deposition in animal models [95].
Diagram 2: Tissue Formation Potency Assessment Workflow.
Quantitative Data from Tissue Formation Assays
Table 2: Quantitative Metrics for Tissue Formation Potency
| Assay Type | Measured Parameter | Typical Data Output | Significance in Tissue Formation |
|---|---|---|---|
| Histomorphometry | Collagen Staining Area | Percentage of field area positive for collagen-specific stain (e.g., >40% increase over control) | Indicates ECM deposition and maturation [96] |
| Hydroxyproline Assay | Total Collagen Content | μg collagen per mg tissue (e.g., 50 μg/mg in test vs. 20 μg/mg control) | Quantitative measure of major structural protein in ECM [96] |
| Tensile Testing | Ultimate Tensile Strength | MPa (e.g., 2.5 MPa in engineered construct) | Functional measure of tissue integrity and mechanical competence [96] |
| Cell Proliferation | Metabolic Activity/DNA Content | Fold-increase in fluorescence/absorbance vs. day 0 (e.g., 3.5-fold increase over 7 days) | Indicates cell growth and viability within the construct |
Integration with Regulatory Pathways
The development and validation of functional potency assays are critical for regulatory approval of ATMPs. Regulatory authorities require validated assays with defined acceptance criteria for biologics licensing [93]. The transition from Good Laboratory Practice (GLP) non-clinical studies to Good Manufacturing Practice (GMP)-compliant manufacturing processes represents a significant challenge, requiring extensive testing and documentation to ensure consistent product quality, safety, and efficacy [38].
For pluripotent stem cell (PSC)-derived products, in vivo teratoma formation assays are used to validate pluripotency of PSCs and detect residual undifferentiated PSCs in drug products [38]. For somatic cell-based therapies, tumorigenicity is assessed using in vivo studies in immunocompromised models rather than teratoma tests [38]. More sensitive in vitro methods such as digital soft agar assays or cell proliferation characterization tests are now recommended for detecting rare transformed cells in therapeutic products [38].
Functional potency assays for immunomodulation, angiogenesis, and tissue formation are indispensable tools in the translational pathway of regenerative pharmacology. By providing quantitative, mechanism-based measurements of biological activity, these assays bridge the gap between traditional pharmacology's focus on symptom management and regenerative medicine's goal of restoring tissue structure and function. As the field advances, the integration of these robust potency assessments with AI-driven analytics, advanced biomaterials, and personalized medicine approaches will be essential for realizing the full therapeutic potential of ATMPs and overcoming current challenges in manufacturing, scalability, and regulatory approval.
In the evolving landscape of regenerative medicine, Mechanism of Action (MoA) studies have transitioned from a regulatory requirement to a fundamental scientific discipline that enables the development of transformative therapies. Integrative and Regenerative Pharmacology (IRP) represents a new paradigm that unifies pharmacology, systems biology, and regenerative medicine to advance personalized therapies that restore physiological structure and function rather than merely managing symptoms [3]. Within this framework, MoA research provides the critical foundation for understanding how regenerative therapies achieve their therapeutic effects at molecular, cellular, and systems levels.
The convergence of three key aspects defines the grand challenge for IPR: (1) implementation of integrative pharmacology strategies across in vitro, ex vivo, and animal models that recapitulate human clinical conditions; (2) development of cutting-edge targeted drug delivery systems capable of localized treatment without off-target effects; and (3) leveraging these approaches to develop transformative curative therapeutics that modulate tissue formation and function [3]. MoA studies serve as the connective tissue bridging these domains, enabling researchers to deconstruct complex pharmacological interactions in regenerative therapies.
For Advanced Therapy Medicinal Products (ATMPs), including cell therapies, tissue-engineered products, and combined therapies, understanding MoA is particularly challenging due to the living nature of these products and their complex interactions with host systems [38]. This whitepaper provides an in-depth technical examination of contemporary approaches for MoA investigation specifically within the context of regenerative pharmacology, addressing both conceptual frameworks and practical methodologies for researchers, scientists, and drug development professionals.
Conceptual Foundations: Defining MoA, Potency, and Efficacy in Regenerative Context
Terminology and Interrelationships
Clear conceptual distinctions between MoA, potency, and efficacy are fundamental to rigorous research design. The following definitions adapted from regulatory guidelines and metrological principles provide essential framing [77]:
- Mechanism of Action (MoA): The specific process, often pharmacologic, through which a product produces its intended effect.
- Potency: The attribute of a product that enables it to achieve its intended mechanism of action.
- Potency Test: A test that measures the attribute of a product that enables it to achieve its intended mechanism of action.
- Efficacy: The ability of the product to have the desired effect in patients.
- Efficacy Endpoint: Attributes related to how a patient feels, functions, or survives.
- Efficacy Endpoint Test: A test that measures attributes related to how a patient feels, functions, or survives.
These relationships can be visualized through the following potency and efficacy process framework:
The Distinct Challenge for Cell Therapies and ATMPs
For cell-based regenerative therapies, the relationship between potency tests and clinical efficacy is often complex and poorly correlated. Examination of the 27 FDA-approved Cell Therapy Products (CTPs) reveals that for many, the MoA remains incompletely understood, and potency tests may not reliably predict clinical outcomes [77]. For example, the documentation for Kymriah (tisagenlecleucel) indicates that interferon-γ production varied greatly from lot-to-lot, making correlation with efficacy difficult [77]. This challenge necessitates sophisticated MoA investigation frameworks specifically designed for the unique properties of regenerative therapies.
Experimental Approaches for MoA Deconstruction in Regenerative Pharmacology
Mode of Action-Based Candidate Testing Suites
The development of mechanism-based testing suites represents a powerful approach for screening regenerative therapy candidates. Resolution Therapeutics pioneered this methodology for their Regenerative Macrophage Therapy (RTX001) for end-stage liver disease, developing a comprehensive testing suite that recapitulates both anti-inflammatory and anti-fibrotic mechanisms of action [97].
Table 1: MoA-Based Testing Suite Components for Regenerative Macrophage Therapy
| MoA Category | Test Component | Measured Parameter | Technical Approach |
|---|---|---|---|
| Anti-inflammatory | Phagocytosis assay | Engulfment of target material | Fluorescent-labeled target cells or particles |
| Monocyte recruitment | Chemotactic migration | Transwell migration assays | |
| Macrophage polarization | Phenotype switching | Surface marker and cytokine secretion profiling | |
| Anti-fibrotic | Collagen degradation | ECM remodeling | Collagen gel contraction or degradation assays |
| Myofibroblast deactivation | Reduced fibrotic activity | α-SMA expression and collagen production measurement |
This testing suite enabled the identification of IL-10+MMP9 as the optimal payload combination for RTX001, which demonstrated superior efficacy compared to non-engineered macrophages in both in vitro and in vivo models [97].
Integrative Pharmacology Strategies
Integrative pharmacology employs a systematic approach to investigating drug interactions across multiple biological scales, combining traditional pharmacology with signaling pathway analysis, bioinformatic tools, and multi-omics technologies (transcriptomics, genomics, proteomics, epigenomics, metabolomics, and microbiomics) [3]. The workflow for integrative MoA investigation involves:
Advanced Biomaterials and Delivery Systems in MoA Studies
The development of 'smart' biomaterials that enable localized, temporally controlled delivery of bioactive compounds represents a critical enabling technology for regenerative pharmacology MoA studies [3]. These advanced delivery systems facilitate more precise investigation of pharmacological mechanisms by:
- Providing controlled spatiotemporal release profiles
- Enabling real-time monitoring of physiological responses
- Minimizing off-target effects that complicate MoA interpretation
- Creating more physiologically relevant microenvironments for tissue regeneration
Stimuli-responsive biomaterials that alter their mechanical characteristics, shape, or drug release profile in response to external or internal triggers represent particularly valuable tools for decomplexing pharmacological interactions in regenerative contexts [3].
Technical and Methodological Considerations
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for MoA Studies
| Research Tool Category | Specific Examples | Function in MoA Studies | Application Context |
|---|---|---|---|
| Advanced Cell Culture Systems | 3D organoids, organ-on-chip platforms | Recapitulate tissue-level complexity and cell-cell interactions | Preclinical efficacy and safety testing |
| Multi-omic Profiling Tools | Single-cell RNA sequencing, spatial proteomics | Uncover heterogeneous responses and cellular subtypes | Biomarker identification, MoA deconvolution |
| Biosensors and Reporters | FRET-based kinase sensors, calcium indicators | Real-time monitoring of signaling pathway activation | Dynamic MoA assessment |
| Engineered Animal Models | Humanized mice, disease phenocopies | Contextualize human-relevant MoA | Translational validation |
| Computational Modeling Platforms | Systems pharmacology models, AI/ML algorithms | Predict complex interactions and dose-response relationships | MoA hypothesis generation |
Quantitative Framework for Probabilistic Dose-Response Assessment
Recent advances in MoA-based probabilistic dose-response assessment have introduced alternative fitting functions (sigmoid, hyperbolic tangent, and arctangent) that enhance the quantification of dose-response relationships in regenerative contexts [98]. This framework enables derivation of probabilistic Reference Doses (RfDs) and Reference Concentrations (RfCs) from subacute (5 weeks) and subchronic (13 weeks) data, validating that shorter-duration studies can capture dose-response behavior relevant to chronic outcomes [98].
Key findings from this approach include:
- Probabilistic Points of Departure (PODs) for Benzo[a]pyrene at 5 weeks (0.01-6.94 mg/kg) align with traditional PODs (0.06-5.2 mg/kg)
- Function form contributes more to uncertainty than exposure duration or data quality in dose-response modeling
- The framework successfully derives health-protective exposure limits from shorter-duration studies across distinct chemical classes and exposure routes
Translational Challenges and Regulatory Considerations
Manufacturing and Scalability Constraints
The transition from Good Laboratory Practice (GLP) non-clinical studies to Good Manufacturing Practice (GMP)-compliant manufacturing presents significant challenges for MoA validation in regenerative therapies [38]. Critical manufacturing considerations that impact MoA include:
- Raw material variability: Securing reliable GMP-compliant raw materials, reagents, and critical components
- Process consistency: Ensuring reproducible manufacturing despite patient/donor cell variability
- Scalable expansion: Maintaining consistent phenotype and functionality during large-scale cell expansion
- Quality control: Implementing robust in-process testing, real-time release criteria, and stability studies
These manufacturing challenges directly impact MoA through their effect on Critical Quality Attributes (CQAs) that must be maintained throughout scale-up [38].
Safety and Tumorigenicity Assessment
For cell-based regenerative therapies, comprehensive tumorigenicity assessment represents an essential component of MoA evaluation. Recommended approaches include [38]:
- Pluripotent stem cell-derived products: In vivo teratoma formation assays to validate pluripotency and detect residual undifferentiated cells
- Somatic cell-based therapies: In vivo studies in immunocompromised models (NOG/NSG mice)
- Enhanced in vitro testing: Digital soft agar assays or cell proliferation characterization tests with superior sensitivity compared to conventional methods
Regulatory Science Framework
The regulatory landscape for ATMPs continues to evolve, with agencies including the FDA (2023 guidance), EMA (2019 guidance), and MHLW (2024 guidance) issuing tailored recommendations for demonstrating product comparability after manufacturing process changes [38]. A risk-based comparability assessment approach is emphasized, with extended analytical characterization and staged testing to ensure changes do not impact safety or efficacy.
Future Perspectives: Emerging Technologies and Approaches
Artificial Intelligence and Data-Driven MoA Elucidation
Artificial intelligence (AI) holds significant promise for addressing IRP challenges and enhancing therapeutic outcomes through [3] [38]:
- Predicting drug delivery system effectiveness and cellular responses
- Enabling more efficient and targeted therapeutic development
- Facilitating comprehensive understanding of pharmacokinetic and pharmacodynamic profiles in regenerative approaches
- Addressing monitoring concerns, automation, and data management in manufacturing
Challenges in AI implementation include standardization of experimental/clinical datasets and their conversion into accurate, reliable information amenable to further investigation [3].
Advanced Biomaterials with Integrated Sensing Capabilities
The next generation of 'smart' biomaterials combining delivery and imaging capabilities will enable real-time monitoring of physiological responses to released compounds and the regeneration process itself [3]. These systems will provide unprecedented insights into in vivo MoA by allowing researchers to:
- Track therapeutic agent distribution and retention
- Monitor tissue regeneration processes longitudinally
- Correlate local pharmacokinetics with pharmacodynamic responses
- Adjust treatment parameters based on real-time feedback
Organoid and Microphysiological Systems
Organoid technology provides more accurate disease models for drug screening and personalized medicine applications, addressing significant challenges in ATMP preclinical development and modeling [38]. These systems enable more human-relevant MoA assessment by:
- Capturing patient-specific disease phenotypes
- Enabling high-throughput screening in human-derived systems
- Modeling complex tissue-level interactions
- Facilitating personalized therapy optimization
Mechanism of Action studies represent the foundational element that connects integrative pharmacology, systems biology, and regenerative medicine. As the field progresses toward increasingly sophisticated regenerative therapies, robust MoA investigation frameworks will be essential for bridging the gap between empirical observations and fundamental biological understanding. The approaches outlined in this technical guide provide researchers with methodologies for deconstructing complex pharmacological interactions in regenerative contexts, ultimately accelerating the development of transformative therapies that restore structure and function rather than merely managing symptoms. Future advances will depend on continued innovation in experimental platforms, computational modeling, and regulatory science to keep pace with the rapidly evolving landscape of regenerative pharmacology.
The emergence of regenerative medicine and one-time curative therapies, such as gene addition and gene editing, necessitates a paradigm shift in clinical trial design. Moving beyond endpoints that measure symptom relief, the field requires new frameworks for defining and validating curative endpoints. This whitepaper provides an in-depth technical guide for researchers and drug development professionals, situating these frameworks within the broader mechanistic context of regenerative pharmacology. We detail novel endpoint classifications, sophisticated statistical designs for trials targeting single-intervention cures, and specific methodologies for functional evaluation of bioengineered and regenerating tissues.
Regenerative pharmacology is defined as "the application of pharmacological sciences to accelerate, optimize, and characterize the development, maturation, and function of bioengineered and regenerating tissues" [1]. Its explicit goal is to cure disease through the restoration of tissue or organ function, a strategy distinct from standard pharmacotherapy, which is often limited to the amelioration of symptoms [1]. This curative approach is exemplified by a growing number of gene addition and gene editing therapies for monogenic diseases, such as transfusion-dependent β-thalassemia (TDT), which aim to provide a one-time functional cure [99].
A key challenge in this new era is selecting endpoints that can robustly distinguish a curative outcome from one that is merely ameliorative [99]. This requires a fundamental re-evaluation of clinical trial design, from endpoint selection and statistical powering to the creation of new functional assays that can quantify the restoration of normal biological function.
Defining Curative Endpoints in the Context of Regenerative Pharmacology
Curative endpoints must demonstrate durable and definitive restoration of normal physiological function, moving beyond transient biomarkers or symptom reduction.
Classification of Endpoint Types
The table below summarizes the critical differences between traditional and curative endpoints.
Table 1: Classification of Endpoint Types in Clinical Trials
| Endpoint Category | Definition | Traditional Example | Curative Example |
|---|---|---|---|
| Symptom Relief | Amelioration of disease-associated symptoms or signs; does not address underlying cause. | Reduction in pain score. | Not applicable for a curative claim. |
| Biomarker Surrogate | A laboratory or physical sign used as a substitute for a clinically meaningful endpoint. | HbA1c level in diabetes trials. | Not sufficient as a standalone curative endpoint. |
| Functional Cure | Durable restoration of normal function without ongoing intervention, despite possible residual sub-clinical disease markers. | Not commonly used in traditional trials. | Sustained independence from red blood cell transfusions in TDT [99]. |
| Complete Curative Endpoint | Definitive eradication of the underlying disease pathophysiology and restoration of normal homeostasis. | Not applicable in most chronic disease trials. | Normalization of erythropoiesis and iron metabolism, confirmed by functional assays and long-term follow-up [99]. |
Endpoints in Action: The Case of Transfusion-Dependent β-Thalassemia (TDT)
In TDT, the clinical hallmarks are ineffective erythropoiesis and a lifelong requirement for regular red blood cell transfusions [99]. A curative endpoint, therefore, must demonstrate freedom from this dependency.
- Transfusion Independence (TI): A primary endpoint for TDT gene therapy trials is the proportion of patients achieving TI, defined as maintaining a pre-specified hemoglobin level without transfusions for a sustained period (e.g., ≥ 12 months) [99].
- Beyond TI - Composite Curative Endpoints: A truly curative outcome requires a series of endpoints that quantify the reversal of the disease's downstream effects, forming a composite picture of restored health:
- Normalization of Hemoglobin Levels: Stable, near-normal peripheral hemoglobin levels without transfusions.
- Resolution of Ineffective Erythropoiesis: Quantified through biomarkers like erythroid marrow activity.
- Improvement in Iron Overload: Demonstrated by a reduction in serum ferritin and liver iron concentration, potentially leading to a reduction or cessation of iron chelation therapy [99].
Designing Trials for Curative Therapies: Statistical and Methodological Considerations
The one-time, transformative nature of curative therapies introduces unique complexities into trial design, requiring stringent error control and long-term follow-up strategies.
Endpoint Multiplicity and False-Positive Error Control
A trial with a single primary endpoint and a single analysis controls its false-positive (α) error rate at a pre-specified level (e.g., 5%). However, trials with multiple primary endpoints inflate the overall false-positive rate. The probability of making at least one false-positive conclusion is calculated as 1 - (1 - α)^number of tests [100]. With an α of 0.05, ten tests yield a 40% chance of a false positive. To control this, the α must be allocated ("split") across endpoints a priori [100].
Analysis of Time-to-Event Endpoints with Competing Risks
For curative therapies, endpoints like "time to treatment failure" (where failure could be relapse or need for re-treatment) are often relevant. If a subject can experience more than one event (e.g., death from an unrelated cause), standard Kaplan-Meier estimates and log-rank tests are inappropriate [100]. Instead, cumulative incidence functions and tests that account for competing risks must be employed to provide unbiased estimates of the event probability [100].
Power and Sample Size for Durable Effects
Power in trials with time-to-event endpoints is driven by the number of observed events, not just the number of subjects enrolled [100]. For curative therapies where the treatment effect is expected to be durable, event rates may be very low. This necessitates:
- Longer follow-up times to observe a sufficient number of events if the control arm event rate is high.
- Larger sample sizes if the event rate in both arms is low, to detect a statistically significant difference in durable outcomes.
Table 2: Key Statistical Considerations for Curative Trial Design
| Design Element | Traditional Consideration | Curative Trial Adaptation |
|---|---|---|
| Primary Endpoint | Often a single, symptom-based measure. | A composite of functional restoration; may require multiple co-primary endpoints. |
| α (Alpha) Splitting | May not be necessary with a single endpoint. | Critical to pre-specify alpha allocation across multiple endpoints to control false-positive rates [100]. |
| Analysis Method | Kaplan-Meier for time-to-event. | Cumulative incidence analysis to account for competing risks (e.g., death before relapse) [100]. |
| Study Power | Based on assumed event rates over a fixed period. | Requires assumptions about durability of effect; may need extended follow-up to capture sufficient events. |
| Long-Term Follow-Up | Often 1-2 years for safety. | Mandatory for 10+ years to confirm durability of cure and monitor for late-onset effects. |
The Scientist's Toolkit: Experimental Protocols for Functional Evaluation
Regenerative pharmacology requires sophisticated protocols to characterize the function of engineered tissues and cells in vitro and in vivo [1].
In Vitro Functional Maturation in a Bioreactor
Purpose: To mimic the in vivo environment and drive bioengineered tissues toward a mature, functional state prior to implantation [1]. Detailed Workflow:
- Scaffold Seeding: Seed an appropriate 3D biomaterial scaffold (e.g., decellularized matrix, synthetic polymer) with the therapeutic cell population (e.g., genetically corrected hematopoietic stem cells).
- Bioreactor Culture: Place the seeded scaffold into a bioreactor system. The bioreactor provides critical environmental cues:
- Perfusion Flow: Mimics shear stress and enhances nutrient/waste exchange, critical for vascularized tissues.
- Cyclic Mechanical Stretch: Applicable for muscle or heart tissue engineering.
- Electrical Stimulation: For neural or cardiac tissues to promote electromechanical coupling.
- Pharmacological Conditioning: Introduce specific growth factors and cytokines (e.g., VEGF, FGF, BMPs) in a spatiotemporally controlled manner to recapitulate developmental morphogen gradients and direct tissue assembly [1].
- Functional Assays: Periodically sample the medium and tissue to quantify:
- Metabolic Activity: (e.g., glucose consumption, lactate production).
- Secretome Analysis: Quantification of tissue-specific proteins (e.g., albumin for liver, insulin for pancreas).
- Structural Analysis: Histology and immunohistochemistry for marker expression and tissue architecture.
In Vivo Assessment of Physiological Integration
Purpose: To evaluate the survival, integration, and functional performance of the regenerative therapy within a living organism. Detailed Workflow (Using a Pre-Clinical Model):
- Therapy Administration: Implant the in vitro-matured construct or infuse the cell therapy product.
- Longitudinal Molecular & Cellular Tracking:
- Use non-invasive imaging (e.g., bioluminescence, MRI) to track cell location and survival.
- For gene therapies, employ droplet digital PCR (ddPCR) to quantify vector copy number in peripheral blood and target tissues.
- Functional Outcome Measures:
- Disease-Specific Function: For TDT, measure hemoglobin levels, reticulocyte counts, and, ultimately, transfusion independence.
- Target Organ Function: Perform organ-specific stress tests to assess functional reserve.
- Systemic Metabolic Correction: Measure the normalization of secondary disease pathways (e.g., iron metabolism in TDT).
- Terminal Histological Analysis: Upon study completion, perform detailed histology on explanted tissues to assess structural integration, vascularization, and the absence of pathology (e.g., tumor formation).
The following diagram illustrates the core workflow for developing and validating a curative therapy, integrating both in vitro and in vivo stages.
Research Reagent Solutions for Curative Mechanism of Action (MoA) Studies
The following table details key reagents and their applications in de-risking the development of curative therapies.
Table 3: Essential Research Reagents for Curative Therapy Development
| Research Reagent / Tool | Function / Application in MoA Research |
|---|---|
| Functionalized "Smart" Biomaterials | Serve as 3D scaffolds and local reservoirs for the controlled release of bioactive compounds (growth factors, cytokines) to direct tissue formation and function [1]. |
| Bioactive Molecule Libraries | (e.g., FGF, EGF, VEGF, BMPs). Used in high-throughput screens to identify optimal cocktails for driving stem/progenitor cell expansion and differentiation toward a target lineage [1]. |
| Lentiviral/Baculoviral Vectors | For efficient delivery of gene editing machinery (e.g., CRISPR-Cas9) or therapeutic transgenes into primary cells, including hard-to-transfect hematopoietic stem cells. |
| In Vivo Bioluminescence/Fluorescence Imaging Systems | Enable non-invasive, longitudinal tracking of cell survival, location, and proliferation in live animal models. |
| Droplet Digital PCR (ddPCR) | Provides absolute quantification of vector copy number and off-target editing events with high sensitivity and precision, critical for safety and efficacy assessment. |
A Decision Framework for Curative Endpoint Selection
Selecting the right endpoints requires a structured approach that aligns with the therapy's proposed mechanism of action. The following diagram outlines the key decision nodes.
The successful development of curative therapies hinges on a fundamental evolution in clinical trial design. This requires a collaborative, interdisciplinary effort among pharmacologists, clinical trialists, biostatisticians, and biomedical engineers. By adopting rigorous, pre-specified curative endpoints that measure the durable restoration of physiological function, controlling for statistical inflation from multiple comparisons, and implementing sophisticated functional assays, the field can robustly validate the promise of regenerative pharmacology and deliver transformative cures to patients.
Regenerative pharmacology represents a paradigm shift in therapeutic science, moving beyond the symptom-focused approach of conventional pharmacotherapy to actively restore the structure and function of damaged tissues and organs. This whitepaper provides a comprehensive technical analysis comparing the mechanisms of action, therapeutic goals, and methodological frameworks of these two disciplines. Rooted in the context of mechanisms of action research, we examine how regenerative pharmacology integrates principles of tissue engineering, stem cell biology, and advanced drug delivery to achieve curative outcomes. Through detailed experimental protocols, visualization of signaling pathways, and analysis of key research reagents, this guide serves as an essential resource for researchers and drug development professionals navigating this transformative field.
The historical division between conventional pharmacotherapy and emerging regenerative approaches reflects a fundamental evolution in how we conceptualize disease treatment. Conventional pharmacotherapy has primarily focused on developing drugs with increasingly selective mechanisms of action for symptom management, typically using small molecules (<500-800 molecular weight) to alter disease course or provide palliative relief [1]. In contrast, regenerative pharmacology represents a multidisciplinary, translational research enterprise explicitly aimed at repairing and replacing damaged cells, tissues, and organs through restoration of physiological structure and function [1]. This emerging field, sometimes termed Integrative and Regenerative Pharmacology (IRP), operates at the nexus of pharmacology, regenerative medicine, and systems biology, creating a new paradigm for therapeutic development [3].
The operational definition of regenerative pharmacology is "the application of pharmacological sciences to accelerate, optimize, and characterize (either in vitro or in vivo) the development, maturation, and function of bioengineered and regenerating tissues" [1]. This strategy is fundamentally distinct from standard pharmacotherapy, which is often limited to ameliorating symptoms without addressing underlying tissue damage or loss of function. Where conventional medicine often relies on continued medication for symptom management, regenerative approaches aim to fix the root cause of disease, potentially offering long-term benefits without requiring frequent follow-ups or medication reliance [101].
Conceptual Framework and Foundational Principles
Philosophical and Therapeutic Goals
The conceptual divergence between these approaches begins with their fundamental therapeutic goals. Conventional pharmacology traditionally focuses on developing drugs to reduce symptoms and alter disease course through single-target approaches, while regenerative pharmacology aims to restore the physiological structure and function of tissues through targeted, often combinatorial interventions [3]. This distinction represents a shift from management to cure, from symptom relief to functional restoration.
Conventional pharmacotherapy typically follows a disease management model, where therapeutic effects are maintained only while the patient remains on medication. This approach often relies on continued pharmaceutical intervention for symptom control rather than addressing the underlying pathophysiology [101]. For example, in orthopedic pain management, conventional practitioners often prescribe painkillers that work for several hours before the patient returns to the original painful state [101].
Regenerative pharmacology seeks to cure disease through restoration of tissue and organ function by leveraging the body's innate healing mechanisms. Rather than merely blocking or inhibiting pathological processes, regenerative approaches introduce pharmacological rigor into the regenerative space to promote true healing and tissue restoration [3]. This is achieved through complex mixtures of compounds including growth factors and other bioactive molecules that orchestrate complete functional regenerative responses [1].
Mechanisms of Action: Comparative Analysis
The mechanistic approaches of these two paradigms differ significantly in their scope, targets, and temporal dimensions. The table below summarizes the key distinctions:
Table 1: Comparative Mechanisms of Action: Regenerative vs. Conventional Pharmacology
| Parameter | Regenerative Pharmacology | Conventional Pharmacotherapy |
|---|---|---|
| Primary Mechanism | Uses stem cells, exosomes, platelet-rich plasma, and growth factors to promote natural healing and tissue regeneration [101] | Relies on synthetic small molecule drugs or biologics to manage symptoms [101] |
| Therapeutic Target | Fixes root cause at cellular level; aims for structural and functional restoration [101] [1] | Manages symptoms; often does not address underlying tissue damage [101] |
| Temporal Dimension | Effects continue supporting healing long after treatment; potentially curative [101] | Efficacy remains only while on medication; typically requires ongoing use [101] |
| Therapeutic Approach | Complex mixtures of compounds (growth factors, cells, biomaterials) for restoration [1] | Single selective mechanisms of action; symptom-focused [1] |
| Specificity | Targeted drug delivery systems exert local treatment without systemic side effects [3] | Often systemic exposure with off-target effects potential |
| Scientific Foundation | Integrates systems biology, tissue engineering, developmental biology [3] | Traditional pharmacology, biochemistry, molecular biology |
The diagram below illustrates the fundamental paradigm shift from conventional to regenerative therapeutic approaches:
Mechanisms of Action in Regenerative Pharmacology
Core Regenerative Mechanisms
Regenerative pharmacology employs multiple sophisticated mechanisms to achieve tissue restoration, operating across molecular, cellular, and tissue levels:
Cellular Mechanisms and Stem Cell Therapeutics: Stem cells serve as the foundation of many regenerative approaches, with different types offering distinct therapeutic capabilities. Mesenchymal Stem Cells (MSCs) found in bone marrow and adipose tissue can differentiate into bone, cartilage, or fat cells, while also targeting inflammation through immunomodulatory functions [34]. These cells are particularly valuable for pain management and orthopedic applications. Hematopoietic stem cells (HSCs), blood-forming cells from bone marrow, have been used for decades in transplants for blood cancers and disorders, with proven success rates of 60-70% for certain malignancies [34]. Induced Pluripotent Stem Cells (iPSCs) represent a more recent advancement, where adult cells are reprogrammed to an embryonic-like state, offering incredible potential for personalized medicine, though they remain primarily in research settings due to safety considerations [34].
Molecular Mechanisms and Signaling Pathways: Regenerative pharmacology leverages complex signaling networks and growth factors to direct tissue repair. Key molecular players include:
- Fibroblast Growth Factor (FGF): Promotes cell proliferation and tissue repair
- Vascular Endothelial Growth Factor (VEGF): Stimulates blood vessel formation
- Bone Morphogenic Proteins (BMPs): Direct bone and cartilage formation
- Platelet-Derived Growth Factor (PDGF): Enhances cell migration and proliferation
- Nerve Growth Factor (NGF): Supports neuronal survival and differentiation [1]
These factors work in coordinated temporal sequences to recapitulate developmental processes, orchestrating the complex cellular behaviors needed for functional tissue restoration.
Tissue Engineering and Biomaterial Integration
Beyond cellular therapies, regenerative pharmacology incorporates advanced biomaterials and engineering approaches:
Scaffolds and 3D Architecture: Biodegradable scaffolds provide critical structural templates for cells to organize into functional tissues. These biomaterials create the appropriate mechanical and biochemical microenvironment to support cell attachment, proliferation, and differentiation [1]. The emergence of 3D bioprinting technologies further advances this capability by precisely layering living cells and biomaterials to create complex tissue architectures reminiscent of native tissues [34].
Bioreactor Systems and In Vitro Maturation: Bioreactors are essential laboratory devices that recapitulate relevant aspects of the in vivo physiologic environment such as mechanical stretch, fluid flow, and compression [1]. By subjecting cell-seeded scaffolds to appropriate environmental cues in bioreactors, researchers can create more advanced three-dimensional tissue constructs in vitro prior to implantation, enhancing their functional capacity and integration potential.
Drug Delivery Systems (DDSs): Advanced drug delivery technologies represent a critical interface between conventional pharmacology and regenerative approaches. Cutting-edge DDSs capable of exerting local treatment promote healing without side or off-target effects [3]. These include 'smart' biomaterials that can deliver bioactive compounds in a temporally controlled manner and stimuli-responsive systems that alter their characteristics in response to external or internal triggers [3].
Experimental Models and Methodological Approaches
In Vitro and Ex Vivo Model Systems
Robust experimental models are essential for characterizing regenerative pharmacology mechanisms and screening candidate therapies:
Advanced 3D Culture Systems: Moving beyond traditional 2D cell culture, regenerative pharmacology utilizes sophisticated three-dimensional model systems that better recapitulate tissue architecture and cell-cell interactions. Organoid technologies provide particularly powerful models, generating "mini-organs" that mimic the structural and functional complexity of native tissues [38]. These systems enable more accurate disease modeling, drug screening, and personalized medicine approaches.
Organ-on-a-Chip Platforms: Microfluidic organ-on-a-chip systems replicate key functional units of human organs, allowing for high-content screening of regenerative compounds in a more physiologically relevant context. These platforms permit real-time monitoring of tissue responses and can be interconnected to create human-on-a-chip models for assessing systemic effects [3].
Bioreactor-Based Tissue Maturation: As previously mentioned, bioreactors provide dynamic culture environments that apply biomechanical stimuli critical for tissue development. Experimental protocols typically involve seeding cells onto biodegradable scaffolds, mounting these constructs in appropriate bioreactor systems, and applying specific regimen of mechanical conditioning (e.g., cyclic strain for musculoskeletal tissues, flow perfusion for vascularized tissues) over defined culture periods [1].
In Vivo Models and Preclinical Validation
Animal models remain essential for evaluating the functional efficacy and safety of regenerative therapies:
Disease-Specific Animal Models: Regenerative pharmacology utilizes animal models that recapitulate specific human clinical conditions, ranging from rodent models of myocardial infarction and osteoarthritis to large animal models for bone and cartilage repair [3]. Selection of appropriate models requires careful consideration of their ability to predict human responses, with emphasis on functional outcome measures rather than purely histological endpoints.
Long-Term Safety and Efficacy Assessment: Comprehensive preclinical evaluation includes long-term follow-up to assess durable functional restoration and monitor for potential adverse effects such as tumorigenesis [38]. For pluripotent stem cell-derived products, in vivo teratoma formation assays validate pluripotency and detect residual undifferentiated cells [38]. For somatic cell-based therapies, tumorigenicity is assessed using in vivo studies in immunocompromised models (e.g., NOG/NSG mice) [38].
The following diagram illustrates a comprehensive workflow for regenerative therapy development:
Research Reagent Solutions and Essential Materials
The experimental toolkit for regenerative pharmacology research includes specialized reagents and materials that enable the development and characterization of regenerative therapies:
Table 2: Essential Research Reagents for Regenerative Pharmacology Investigations
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Stem Cell Sources | Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), Hematopoietic Stem Cells (HSCs) [34] | Cell therapy development, disease modeling, drug screening | Provide renewable cell sources with multilineage differentiation potential |
| Growth Factors & Cytokines | FGF, VEGF, BMPs, NGF, PDGF, IGF [1] | Directing cell differentiation, enhancing tissue repair | Act as signaling molecules to regulate cellular processes in tissue formation |
| Biomaterials & Scaffolds | Biodegradable polymers (PLA, PLGA), hydrogels, decellularized ECM [1] | 3D tissue engineering, drug delivery systems | Provide structural support and biochemical cues for tissue development |
| Characterization Tools | Flow cytometry antibodies, differentiation kits, PCR arrays | Cell phenotype verification, potency assays | Validate cell identity, purity, and functional capacity |
| Advanced Delivery Systems | Nanoparticles, microspheres, stimuli-responsive biomaterials [3] | Controlled release of bioactive factors | Spatiotemporally control presentation of therapeutic agents |
Quantitative Framework and Systems Pharmacology
The complexity of regenerative interventions demands sophisticated quantitative approaches to understand mechanisms and predict outcomes:
Quantitative Systems Pharmacology (QSP) in Regenerative Medicine
Quantitative and Systems Pharmacology (QSP) represents an innovative and integrative approach that combines physiology and pharmacology to accelerate medical research [102]. QSP provides a holistic understanding of interactions between the human body, diseases, and drugs by simultaneously considering receptor-ligand interactions of various cell types, metabolic pathways, signaling networks, and disease biomarkers [102].
In regenerative pharmacology, QSP models are particularly valuable for:
- Predicting clinical outcomes based on preclinical data
- Optimizing dosing regimens for complex biologic therapies
- Evaluating combination therapies with different mechanisms of action
- Understanding personalized responses through population variability modeling [102]
Modeling Approaches and Computational Frameworks
QSP in regenerative medicine typically employs sophisticated mathematical models, frequently represented as Ordinary Differential Equations (ODEs), to capture intricate mechanistic details of pathophysiology [102]. These models integrate knowledge across multiple scales, incorporating both "top-down" clinical perspectives (e.g., functional outcome measures) and "bottom-up" approaches (e.g., molecular signaling rates) [102].
The QSP modeling process follows a "learn and confirm" paradigm, where experimental findings are systematically integrated into the model to generate testable hypotheses, which are then refined through precise experimental designs [102]. This iterative process requires interdisciplinary collaboration among experts in pharmacology, biochemistry, genetics, mathematics, and medicine [102].
Clinical Translation and Therapeutic Applications
Success Rates Across Disease Areas
Regenerative pharmacology has demonstrated significant clinical success across multiple therapeutic areas, with varying levels of evidence and maturity:
Table 3: Regenerative Medicine Success Rates by Clinical Application
| Clinical Application | Specific Treatment | Reported Success Rates / Outcomes | Evidence Level |
|---|---|---|---|
| Orthopedic & Joint Repair | PRP for Knee Osteoarthritis | Symptom improvement for ≥6 months; often outlasts corticosteroids [34] | Established clinical use |
| BMAC for Osteonecrosis | >90% success in preventing hip collapse at 2 years [34] | Strong clinical evidence | |
| MACI for Cartilage Defects | 80-90% success rate over time [34] | Established procedure | |
| Blood Cancers | Stem Cell Transplants | 60-70% success rates for certain types; 79% 3-year survival for multiple myeloma [34] | Standard of care |
| Systemic Diseases | HSCT for Sickle Cell Disease | Only curative therapy available [34] | Established with limitations |
| MSC Therapy for Autoimmune Conditions | ~80% success rate for immune modulation [34] | Emerging evidence |
Clinical Trial Design and Endpoint Selection
Demonstrating efficacy of regenerative therapies requires specialized clinical trial methodologies distinct from conventional drug development:
Endpoint Selection: Regenerative medicine trials necessitate multidimensional endpoint assessment, including:
- Clinical Observations: Physical examination, range of motion, functional assessment
- Patient-Reported Outcomes (PROs): Validated questionnaires tracking pain, quality of life, and function
- Imaging Studies: MRI, CT, or ultrasound to visualize tissue healing and structural improvement
- Laboratory Tests: Biomarker analysis (e.g., inflammatory markers) to confirm cellular-level changes [34]
Long-Term Follow-Up: Unlike conventional drugs whose effects dissipate after discontinuation, regenerative therapies aim for durable benefits, necessitating extended follow-up periods in clinical trials to assess longevity of effect and monitor for potential late-onset adverse events [38].
Challenges and Future Directions
Current Implementation Barriers
Despite its significant promise, regenerative pharmacology faces substantial translational challenges:
Manufacturing and Scalability: Producing clinical-grade regenerative therapies consistently at scale remains a critical hurdle. Challenges include maintaining cell viability and potency during expansion, ensuring batch-to-batch consistency, and developing automated closed-system bioreactors for scalable GMP-compliant production [38].
Regulatory Complexity: The unique nature of regenerative products creates difficulties in applying existing regulatory frameworks. Advanced Therapy Medicinal Products (ATMPs) face complex regulatory pathways with different regional requirements (e.g., EMEA, FDA) and no unified international guidelines [3] [38].
Safety Concerns: Tumorigenesis risk represents a significant safety consideration, particularly for pluripotent stem cell-based therapies. Comprehensive safety assessment requires sensitive methods such as digital soft agar assays or cell proliferation characterization tests to detect rare transformed cells in therapeutic products [38].
Economic Considerations: High manufacturing costs and limited reimbursement create accessibility challenges, particularly for healthcare systems with limited resources. The high cost of ATMPs ultimately limits accessibility, especially in low- and middle-income countries [3].
Emerging Technologies and Future Perspectives
Several emerging technologies hold promise for addressing current limitations and advancing regenerative pharmacology:
Artificial Intelligence and Machine Learning: AI technologies are addressing monitoring concerns, automation, and data management in regenerative medicine [38]. Machine learning approaches can predict optimal culture conditions, identify critical quality attributes, and optimize manufacturing processes.
Gene Editing Technologies: Advanced gene-editing tools like CRISPR/Cas9 enable precise genetic modifications for both therapeutic applications and disease modeling [34]. Clinical trials using CRISPR for sickle cell disease demonstrate the therapeutic potential of these approaches.
Advanced Biomanufacturing: Innovations in bioprinting, automated bioreactor systems, and closed processing technologies aim to overcome current manufacturing limitations, enabling more reproducible and scalable production of regenerative therapies.
Personalized Medicine Approaches: The future of regenerative pharmacology lies in increasing personalization, using patient-specific cellular or genetic information to tailor therapies for maximal effectiveness and minimal side effects [34].
Regenerative pharmacology represents a fundamental paradigm shift from conventional pharmacotherapy, moving beyond symptomatic treatment to curative approaches that restore tissue structure and function. This emerging discipline integrates principles from pharmacology, systems biology, tissue engineering, and stem cell biology to develop transformative therapies that address the root causes of disease rather than merely managing symptoms.
While significant challenges remain in manufacturing, regulatory approval, and clinical adoption, the continued convergence of technological innovations across multiple disciplines promises to accelerate the development and accessibility of regenerative therapies. The ongoing evolution of regenerative pharmacology demands sustained interdisciplinary collaborations and continued methodological refinement to fully realize its potential to revolutionize therapeutic science and patient care.
The mechanistic understanding of regenerative processes will continue to deepen through advanced model systems, quantitative approaches, and rigorous clinical validation, ultimately enabling more targeted, effective, and accessible regenerative therapies for a broad range of conditions that currently lack adequate treatment options.
Functional restoration represents a paradigm shift in managing chronic conditions, moving beyond symptomatic relief to focus on holistic functional recovery. This whitepaper establishes precise benchmarks for evaluating success and long-term durability within the context of regenerative pharmacology mechanisms of action research. We synthesize evidence from clinical outcomes, define core biomarkers of durability, and present standardized experimental protocols for quantifying functional gains. For researchers and drug development professionals, this framework provides critical tools for assessing how regenerative interventions translate into sustained functional improvement, addressing a crucial gap in therapeutic development for age-related functional decline and chronic disease states.
Functional restoration (FR) is an interdisciplinary biopsychosocial approach to chronic pain and disability that focuses on restoring physical capacity and psychosocial performance, rather than merely eliminating pain [103]. Originally developed by Mayer and Gatchel, this paradigm has gained considerable attention worldwide due to its demonstrated superiority to standard care [103]. In the context of regenerative pharmacology—which aims to restore physiological structure and function through targeted therapies—functional restoration provides a critical framework for measuring therapeutic success [3].
Regenerative pharmacology represents a fundamental shift from traditional symptom-focused interventions toward therapies that promote the body's innate healing ability and restore tissue integrity [3] [42]. This emerging field applies pharmacological sciences to accelerate and characterize the development, maturation, and function of bioengineered and regenerating tissues [3]. Where traditional pharmacology often focuses on blocking or inhibiting pathologic processes, regenerative pharmacology aims to repair, renew, and regenerate, thereby addressing the root causes of functional decline [3].
The integration of functional restoration principles with regenerative pharmacology creates a powerful synergy for developing transformative curative therapeutics. This combined approach is particularly relevant for addressing the decline in regenerative capacity that occurs with aging—a process closely linked to the reduced function of stem and progenitor cells [104]. By establishing clear benchmarks for success and long-term durability, researchers can more effectively evaluate how regenerative interventions translate into meaningful functional improvements that persist over time.
Defining Functional Restoration: Core Components and Mechanisms
The Biopsychosocial Framework
Functional restoration is grounded in the biopsychosocial model which views pain and disability as complex interactions among physiologic, psychologic, and social factors that perpetuate and worsen clinical presentation [103]. This approach addresses the significant variations observed among patients with chronic conditions in terms of symptomatology and treatment response. The fundamental premise is that combined interventions administered within an integrated program produce greater effects than the sum of individual components delivered in isolation [103].
Essential Components of Functional Restoration Programs
Effective functional restoration programs incorporate several core components that work synergistically to restore function:
- Formal, repeated quantification of physical deficits: Objective measures guide, individualize, and monitor physical training progress, moving beyond subjective self-reports [103].
- Comprehensive psychosocial and socioeconomic assessment: Identifies potential barriers to recovery and monitors pain, disability, and behavioral outcomes throughout treatment [103].
- Multimodal disability management: Utilizes cognitive-behavioral therapy (CBT) approaches to address psychological barriers to recovery [103]. CBT has been identified as the most appropriate and effective modality for interdisciplinary pain management programs.
- Psychopharmacological management: Addresses medication detoxification needs and co-existing psychological conditions when present [103].
- Interdisciplinary team approach: Involves coordinated care from medical, therapeutic, and psychological professionals with formal staff meetings and frequent conferences [103].
Table: Core Components of Interdisciplinary Functional Restoration Teams
| Practitioner | Role in Functional Restoration |
|---|---|
| Medical Director | Physician with understanding of biopsychosocial philosophy and medical rehabilitation |
| Physical Therapist | Addresses physical deconditioning, educates on pain physiology, teaches body mechanics and exercise pacing |
| Occupational Therapist | Manages both physical and vocational aspects of rehabilitation, including return-to-work planning |
| Psychologist/Psychiatrist | Identifies psychosocial barriers, provides CBT for pain-related depression, anxiety, and substance abuse |
| Nurse | Serves as physician-extender, follows procedures, addresses patient needs |
| Pain Management Specialist | Provides interventional procedures such as injections and nerve blocks |
Mechanism of Action
The therapeutic benefit of functional restoration derives from enhanced communication between providers and simultaneous addressing of physical, psychological, and vocational impediments to recovery [103]. This coordinated approach creates synergy where the combined effect exceeds what would be expected from individual components delivered separately. The sports medicine approach, with its emphasis on quantified functional progress and gradual training advances, provides the philosophical foundation for physical reactivation, while CBT addresses maladaptive thought patterns and behaviors that perpetuate disability [103].
Quantitative Benchmarks for Success and Durability
Primary Outcome Measures
Establishing standardized, quantifiable benchmarks is essential for evaluating the success and durability of functional restoration interventions, particularly in the context of regenerative pharmacology research. The NIH Research Task Force (pain) impact score (PIS) has emerged as a primary outcome measure—a composite metric that incorporates average pain intensity, pain interference, and physical function [105]. The PIS ranges from 8-50, with a minimal clinically important difference (MCID) estimated at 3 points based on the MCIDs of its component measures [105].
Functional performance represents another critical benchmark, typically assessed through performance-based measures. One validated approach is the treadmill-lift-carry (TLC) battery, which assesses walking or jogging tolerance, lifting capacity (floor to waist and waist to shoulder), and carrying tolerance [105]. These measures are converted to z-scores and combined into a composite score, which is then transformed to a 0-100 T-scale score to enhance interpretability. The MCID for the TLC composite score has been determined to be an increase of 6 points [105].
Defining Long-Term Durability
Long-term durability refers to the maintenance of clinically meaningful improvements beyond the immediate post-treatment period. Research with military populations demonstrates that while mean PIS improvements may not always sustain at 6-month follow-up, functional performance gains can persist [105]. Responder analyses provide a more nuanced understanding of durability, with studies showing that 42% of participants maintain improvements exceeding MCID thresholds in either PIS or functional performance at 6 months post-treatment [105].
Table: Quantitative Benchmarks for Functional Restoration Success
| Metric | Description | Assessment Method | MCID | Sustained Response Rate |
|---|---|---|---|---|
| Pain Impact Score (PIS) | Composite of pain intensity, interference, and physical function | NIH Research Task Force metric (range: 8-50) | 3 points | Improves prediction: younger age, no neuropathic pain, less baseline disability |
| Functional Performance | Composite of treadmill, lifting, and carrying tolerances | TLC battery converted to T-scale (0-100) | 6 points | Improves prediction: more treatment hours, lower baseline pain catastrophizing |
| Overall Responder Rate | Patients maintaining MCID improvement at 6 months | Combined PIS and functional performance assessment | N/A | 42% show sustained improvement in either domain |
Predictors of Sustained Response
Identifying predictors of sustained response enables better patient selection and targeted intervention strategies. Research indicates that predictors of sustained PIS improvement include younger age, absence of neuropathic pain features, less self-rated disability, better baseline functional performance, and worse baseline PIS [105]. For sustained functional performance improvement, significant predictors include more treatment hours, lower baseline pain catastrophizing, and lower baseline functional performance [105]. These findings highlight the importance of addressing psychological factors such as pain catastrophizing and modifying programs based on baseline characteristics to enhance long-term durability.
Methodologies for Assessing Durability in Clinical Research
Experimental Design Considerations
Rigorous assessment of functional restoration durability requires methodologically sound clinical trials with extended follow-up periods. Randomized controlled trials (RCTs) represent the gold standard for establishing efficacy, with comprehensive outcome assessments at baseline, immediately post-treatment, and at multiple follow-up intervals (typically 3, 6, and 12 months) [105]. These designs should incorporate both intention-to-treat and per-protocol analyses to account for attrition and protocol deviations.
Military population studies have demonstrated the effectiveness of such methodologies, showing significantly better outcomes across psychosocial and functional performance measures compared to usual care, with maintained improvements at 6-month follow-up and reduced healthcare utilization at 1 year [105]. These findings highlight the importance of including healthcare utilization metrics as secondary durability measures.
Standardized Assessment Protocols
Comprehensive durability assessment requires multidimensional evaluation:
- Physical function quantification: Use standardized performance-based measures like the TLC battery, administered by trained physical or occupational therapists who instruct participants to continue until they experience increased pain or reach maximally safe exertion [105]. Isokinetic testing equipment (e.g., Biodex systems) provides objective, quantifiable measures of joint strength and lifting capacity [106].
- Patient-reported outcomes: Implement validated tools like the Pain Assessment Screening Tool and Outcomes Registry (PASTOR), which includes Defense and Veterans Pain Rating Scale (DVPRS) for pain intensity and Patient-Reported Outcome Measurement Information System (PROMIS) measures for pain interference, physical function, depression, anxiety, anger, sleep-related impairment, fatigue, and satisfaction with social roles [105].
- Psychological assessment: Administer targeted instruments such as the Pain Catastrophizing Scale (PCS) and Tampa Scale for Kinesiophobia (TSK-11) to evaluate psychological barriers to recovery [105].
- Biomarker integration: Incorporate emerging biomarkers of aging and biological resilience, such as epigenetic clocks (e.g., DunedinPACE, GrimAge) and proteomic profiles, to quantify physiological durability [107] [108].
Biomarker Integration in Durability Research
The integration of biomarkers provides objective, physiological indicators of treatment response and durability. Epigenetic clocks such as DunedinPACE and GrimAge have shown sensitivity to interventions in clinical trials [107]. For example, the CALERIE study demonstrated significant reduction of DunedinPACE following caloric restriction, while the DAMA trial showed GrimAge reduction in response to plant-food rich diet and exercise interventions [107].
Multi-omic biological age estimation based on the Klemera-Doubal method (KDM) applied to over 900 principal component transformed biomarkers (metabolites, proteins, genomics, and clinical measures) has been successfully commercialized for tracking biological age [107]. These biomarkers can be leveraged in regenerative pharmacology research to quantify how functional restoration interventions impact biological aging processes and contribute to long-term durability.
Table: Research Reagent Solutions for Durability Assessment
| Reagent/Instrument | Application in Durability Research | Key Function |
|---|---|---|
| Biodex System 4 | Isokinetic strength testing | Provides objective, quantifiable measures of joint strength and lifting capacity |
| PROMIS Computer Adaptive Tests | Patient-reported outcome assessment | Measures pain interference, physical function, and psychosocial domains with reduced response burden |
| DNA Methylation Kits | Epigenetic age estimation | Quantifies biological aging through epigenetic clocks (e.g., DunedinPACE, GrimAge) |
| Pain Catastrophizing Scale | Psychological assessment | Evaluates rumination, magnification, and helplessness related to pain experience |
| Treadmill-Lift-Carry Equipment | Functional performance testing | Standardized assessment of physical tolerances for composite functional score |
Regenerative Pharmacology Applications and Future Directions
Integrative and Regenerative Pharmacology Framework
Integrative and Regenerative Pharmacology (IRP) represents a state-of-the-art interdisciplinary field that bridges pharmacology, systems biology, and regenerative medicine [3]. This framework merg conventional drugs with target therapies intended to repair, renew, and regenerate rather than merely block or inhibit pathological processes [3]. IRP aims to restore physiological structure and function through multi-level, holistic interventions, positioning it ideally for enhancing functional restoration outcomes.
The convergent challenges for IRP include implementing integrative pharmacology strategies across in vitro, ex vivo, and in vivo systems; developing cutting-edge targeted drug delivery systems that promote healing without off-target effects; and leveraging these approaches to develop transformative curative therapeutics that improve symptomatic relief while modulating tissue formation and function [3]. This framework directly supports the objectives of functional restoration by addressing both biological mechanisms of tissue repair and functional outcomes.
Biomaterials and Targeted Delivery Systems
Advanced biomaterials and targeted delivery systems represent promising avenues for enhancing functional restoration durability. "Smart" biomaterials that can deliver bioactive compounds in a temporally controlled manner are expected to be key to future therapeutics [3]. Stimuli-responsive biomaterials, which alter their mechanical characteristics, shape, or drug release profile in response to external or internal triggers, represent transformative approaches for supporting tissue regeneration while restoring function.
Improved delivery systems, such as nanosystems (nanoparticles, nanofibers) and scaffold-based approaches, when combined with imaging capabilities, enable real-time monitoring of physiological response to released compounds or regeneration processes [3]. These technologies allow for more precise intervention at the site of injury or degeneration, potentially enhancing both the magnitude and durability of functional improvements.
Artificial Intelligence and Multi-Omic Integration
Artificial intelligence (AI) and multi-omic technologies hold significant promise for advancing functional restoration durability research. AI has the potential to transform regenerative pharmacology by enabling more efficient and targeted therapeutic development, predicting delivery system effectiveness, and anticipating cellular responses [3]. Machine learning approaches can integrate multi-omic data (genomics, transcriptomics, proteomics, metabolomics) with clinical outcomes to identify novel biomarkers of durability and personalize treatment approaches.
Database resources like Regeneration Roadmap—which contains over 2.38 million data entries across 11 species and 36 tissues, including regeneration-related genes, transcriptomics, epigenomics, and pharmacogenomics data—provide valuable tools for understanding conserved regeneration mechanisms [104]. Similarly, metabolomic and proteomic studies of long-lived populations have identified potential longevity-related biomarkers such as omega-3 polyunsaturated fatty acids, specific sphingolipids, and proteins including apolipoprotein E (APOE) and pleiotrophin (PTN) [108]. These resources support the identification of novel therapeutic targets for enhancing functional durability.
Clinical Translation and Future Research Priorities
To advance functional restoration durability research, three key priorities must be emphasized according to recent analyses of regenerative pharmacology [42]:
Integration Beyond Innovation: The field must focus on integrating existing technologies and knowledge rather than pursuing isolated innovations. This includes combining biomaterials, targeted delivery systems, and functional restoration protocols in coordinated therapeutic approaches.
Clinical Trial Rigor: There is an urgent need to increase the robustness and rigor of clinical trials in regenerative medicine. This requires interdisciplinary trial designs that incorporate pharmacology, bioengineering, and functional outcome measures with extended follow-up periods to assess durability.
Collaborative Ecosystems: Establishing cooperation between academia, industry, clinics, and regulatory authorities is essential for developing standardized procedures, ensuring consistency in therapeutic outcomes, and advancing transformative curative therapies [3].
Future research should prioritize longitudinal studies that integrate multi-omic biomarkers with traditional functional outcomes to identify early predictors of sustained response. Additionally, combination approaches that pair regenerative pharmacology interventions with structured functional restoration programs represent a promising avenue for enhancing both the magnitude and durability of treatment effects.
Defining benchmarks for success and long-term durability in functional restoration requires a multidimensional approach that integrates performance-based measures, patient-reported outcomes, psychological assessments, and emerging biomarkers of biological aging. The integration of regenerative pharmacology principles with functional restoration protocols creates powerful opportunities for developing transformative interventions that address both biological mechanisms of tissue repair and functional outcomes. As the field advances, standardized assessment methodologies, AI-driven analytics, and targeted delivery systems will enhance our ability to not only achieve immediate functional improvements but sustain these gains over extended periods. For researchers and drug development professionals, this integrated framework provides the tools necessary to quantify and optimize the long-term durability of interventions aimed at restoring function and quality of life in chronic conditions.
Conclusion
Regenerative pharmacology represents a fundamental shift in therapeutic design, aiming for curative outcomes through the sophisticated orchestration of biological repair processes. The key takeaways from this analysis underscore that success hinges on interdisciplinary integration, leveraging AI and smart biomaterials for precision, and rigorously validating mechanisms through advanced functional assays. The field's progression is no longer limited by conceptual feasibility but by overcoming translational challenges in manufacturing, standardization, and regulatory navigation. Future progress demands sustained collaboration between academia, industry, and regulators to establish robust, scalable, and accessible frameworks. Ultimately, by mastering the mechanisms of action that guide tissue restoration, regenerative pharmacology holds the promise to redefine treatment paradigms for a wide spectrum of degenerative, injury-related, and age-related diseases, moving medicine from lifelong management to definitive cures.
References
- 1. The Pharmacology of Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3698935/]
- 2. The pharmacology of regenerative medicine - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/23818131/]
- 3. Unifying pharmacology, systems biology, and regenerative ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1729610/full]
- 4. The 5 Basic Principles of Regenerative Medicine [https://lonestarpain.com/2021/07/19/the-5-basic-principles-of-regenerative-medicine/]
- 5. An overview of regenerative medicine: its principles and ... [https://advances.tri-kobe.org/en/the-principles-of-regenerative-medicine/52/an-overview-of-regenerative-medicine_-its-principles-and-the-scope-of-the-current-revolution.html]
- 6. The birth of 'regenerative pharmacology': a clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3651653/]
- 7. Expedited Programs for Regenerative Medicine Therapies ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/expedited-programs-regenerative-medicine-therapies-serious-conditions-0]
- 8. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 9. Bridging academia and industry: advancing systems ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1627214/full]
- 10. advancing systems biology and QSP education through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463889/]
- 11. Leveraging network pharmacology for drug discovery [https://www.sciencedirect.com/science/article/pii/S259009862500017X]
- 12. Integrated network pharmacology reveals the mechanism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108044/]
- 13. An integrative systems-biology approach defines ... [https://www.nature.com/articles/s41467-025-59654-w]
- 14. Bridging the Gap in Translational Regenerative Medicine ... [https://tts.org/46-ctrms/ctrms-education/1607-ctrms-may20-2025]
- 15. AI, omics, and systems biology could transform heart drug ... [https://www.news-medical.net/news/20251007/AI-omics-and-systems-biology-could-transform-heart-drug-development.aspx]
- 16. Redox and Metabolic Regulation of Stem/Progenitor Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4175426/]
- 17. Modulating the stem cell niche for tissue regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4422171/]
- 18. Stem Cell Research: The Future of Regenerative Medicine ... [https://www.dvcstem.com/post/stem-cell-research]
- 19. An in vitro quantitative systems pharmacology approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7402526/]
- 20. Convergence of Cell Pharmacology and Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6708059/]
- 21. Quantitative systems pharmacology modeling sheds light ... [https://www.nature.com/articles/s41598-022-14726-5]
- 22. Rhosin shown to reverse blood stem cell ageing [https://www.drugtargetreview.com/news/190920/rhosin-shown-to-reverse-blood-stem-cell-ageing/]
- 23. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 24. Stem cells characterization: OMICS reinforcing analytics [https://www.sciencedirect.com/science/article/pii/S0958166921001336]
- 25. Emerging Concepts in Paracrine Mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4874329/]
- 26. Mechanisms and Optimization Strategies of Paracrine ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10686715/]
- 27. Mesenchymal stem cell secretome for regenerative medicine [https://www.sciencedirect.com/science/article/pii/S2090123224001814]
- 28. Gap Junctional Versus Paracrine Signaling in the Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637001/]
- 29. Immunoceuticals: Harnessing Their Immunomodulatory ... [https://www.mdpi.com/2072-6643/14/19/4075]
- 30. Microenvironment self-adaptive multifunctional hydrogels ... [https://pubmed.ncbi.nlm.nih.gov/41080732/]
- 31. Advances in cell therapy for orthopedic diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567640/full]
- 32. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 33. Global scientific trends on the immunomodulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9449834/]
- 34. How successful is regenerative medicine [https://californiapain.com/how-successful-is-regenerative-medicine/]
- 35. Remodeling the intestinal immune microenvironment [https://pubmed.ncbi.nlm.nih.gov/40433382/]
- 36. Understanding immune-modulatory efficacy in vitro [https://www.sciencedirect.com/science/article/pii/S0009279721004142]
- 37. Biomaterials for Drug Delivery and Human Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10817481/]
- 38. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 39. Stimulus switches for spatial-temporal precision in ... [https://www.sciopen.com/article/10.26599/NR.2025.94907571?issn=1998-0124]
- 40. Smart Biomaterials for Delivery of Drugs and Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311304/]
- 41. Color-coded test checks if medical nanoparticles hit their target [https://www.futurity.org/color-coded-test-nanoparticles-drug-delivery-2679342/]
- 42. Interdisciplinary advances in regenerative pharmacology [https://www.sciencedirect.com/science/article/abs/pii/S0014299925006703]
- 43. Growth Factor Engineering Strategies for Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6985039/]
- 44. Growth Factors in Regeneration and Regenerative Medicine [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00384/full]
- 45. Delivering growth factors for therapeutics [https://www.sciencedirect.com/science/article/abs/pii/S016561470700260X]
- 46. A high-throughput platform for single-molecule tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717362/]
- 47. Single-cell immune aging clocks reveal inter-individual ... [https://www.nature.com/articles/s43587-025-00819-z]
- 48. Organoids and organs-on-chips: Recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S2666634025000947]
- 49. 3D Bioprinting for Engineering Organoids and Organ-on-a- ... [https://pubmed.ncbi.nlm.nih.gov/40452179/]
- 50. Advances in 3D Bioprinting and Microfluidics for Organ-on- ... [https://www.mdpi.com/2073-4360/17/22/3078]
- 51. 3D bioprinting bone/cartilage organoids: construction, ... [https://www.sciencedirect.com/science/article/pii/S2214031X2500138X]
- 52. Developing 3D bioprinting for organs-on-chips - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00769g]
- 53. Cell Therapy: Revolutionizing Regenerative Medicine (2025) [https://www.dvcstem.com/post/cell-therapy]
- 54. Bioreactor design-assisted bioprinting of stimuli-responsive ... [https://www.sciencedirect.com/science/article/abs/pii/S2405886623000684]
- 55. Morphoceuticals: Perspectives for discovery of drugs ... [https://www.sciencedirect.com/science/article/pii/S1359644623001010]
- 56. A novel bioreactor for combined magnetic resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6414270/]
- 57. Perfusion Bioreactor Technology for Organoid and Tissue ... [https://www.mdpi.com/2673-7523/5/2/17]
- 58. Development of a bioreactor and volumetric bioprinting ... [https://pubmed.ncbi.nlm.nih.gov/40300616/]
- 59. Single-Use Bioreactors for Human Pluripotent and Adult ... [https://www.mdpi.com/2306-5354/8/5/68]
- 60. Cell manufacturing for cell-based tissue engineering [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2025.1637075/full]
- 61. Development and deployment of a functional 3D-bioprinted ... [https://www.nature.com/articles/s41598-025-93276-y]
- 62. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 63. Advancing drug discovery through multiomics [https://www.ddw-online.com/advancing-drug-discovery-through-multiomics-37448-202510/]
- 64. Editorial: Advancing drug discovery with AI [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1721323/full]
- 65. Application of artificial intelligence large language models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279696/]
- 66. 2025 AI in Drug Discovery: Predictions [https://lizard.bio/knowledge-hub/2025-ai-in-drug-discovery-predictions]
- 67. The Future of Drug Discovery: Integrating Phenotypic Data ... [https://ardigen.com/the-future-of-drug-discovery-integrating-phenotypic-data-with-omics-and-ai/]
- 68. Transition from manual to automated processes for ... [https://www.nature.com/articles/s41598-025-00015-4]
- 69. Why Single-Use Bioreactors Are Revolutionizing Cell ... [https://cellculturecompany.com/why-single-use-bioreactors-are-revolutionizing-cell-culture-in-2025/]
- 70. Stratyx™ Laboratory Bioreactor System [https://www.culturebiosciences.com/stratyx]
- 71. Top Laboratory Bioreactors Companies & How to Compare ... [https://www.linkedin.com/pulse/top-laboratory-bioreactors-companies-how-compare-them-2026-gcxnf]
- 72. Automated Bioreactor [https://www.biophorum.com/workstream/automated-bioreactor/]
- 73. Progressing Toward Full Automation in Biomanufacturing [https://www.biopharminternational.com/view/progressing-toward-full-automation-in-biomanufacturing]
- 74. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 75. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 76. White Paper on How to Go Forward with Cell-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4195483/]
- 77. Mechanism of action, potency and efficacy: considerations for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05179-7]
- 78. Quantification of tumor heterogeneity: from data acquisition ... [https://www.sciencedirect.com/science/article/pii/S0167779921002675]
- 79. Setting specifications for potency assays--basic principles [https://pubmed.ncbi.nlm.nih.gov/12079184/]
- 80. Challenges in developing robust potency assays for ADCs [https://abzena.com/articles/feature-articles/robust-potency-assays-for-adcs/]
- 81. Advanced therapy medicinal products: Overview [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview]
- 82. Navigating the ATMP Regulatory Landscape ... [https://www.evotec.com/sciencepool/navigating-the-atmp-regulatory-landscape]
- 83. gene therapy: bringing the EU regulation into the future [https://www.sciencedirect.com/science/article/pii/S1359644625001370]
- 84. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 85. A New Era for Bioprocess Design and Control, Part 1 [https://www.bioprocessintl.com/process-development/a-new-era-for-bioprocess-design-and-control-part-1]
- 86. Disparities in access to gene therapy in the European Union [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481686/]
- 87. Regenerative Medicine Market to Skyrocket to USD 403.86 ... [https://www.prnewswire.com/news-releases/regenerative-medicine-market-to-skyrocket-to-usd-403-86-billion-by-2032-driven-by-cell--gene-therapy-breakthroughs-stem-cell-advancements-and-multi-indication-expansion-302624480.html]
- 88. Regenerative Medicine Market Size to Hit USD 212.80 ... [https://www.precedenceresearch.com/regenerative-medicine-market]
- 89. Global Regenerative Medicine Market 2025–2034 [https://www.custommarketinsights.com/report/regenerative-medicine-market/]
- 90. United States Regenerative Medicine Report 2025: Market ... [https://finance.yahoo.com/news/united-states-regenerative-medicine-report-142500852.html]
- 91. A new kind of stem cell is revolutionizing regenerative ... [https://www.asbmb.org/asbmb-today/science/040125/stem-cells-revolutionize-regenerative-medicine]
- 92. 10 Exciting Ways Regenerative Medicine is Changing Lives in ... [https://celmedica.com/top-10-advances-in-regenerative-medicine-in-2025/]
- 93. Validation of a quantitative cell-based relative potency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11914788/]
- 94. Enhancing angiogenesis through secretomes: Insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167018/]
- 95. Advances in Stem Cell Therapy, Growth Factor Modulation ... [https://link.springer.com/article/10.1007/s13555-025-01564-2]
- 96. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 97. Resolution Therapeutics Announces Regenerative ... - PharmiWeb.com [https://www.pharmiweb.com/press-release/2025-05-14/resolution-therapeutics-announces-regenerative-macrophage-therapy-rmt-manufacturing-process-candidate-testing-suite-at-asgct-2025]
- 98. Enhanced MOA-based probabilistic dose-response ... [https://www.sciencedirect.com/science/article/pii/S0147651325016367]
- 99. Defining curative endpoints for transfusion-dependent β ... [https://pubmed.ncbi.nlm.nih.gov/38100154/]
- 100. Clinical trials: design, endpoints and interpretation of ... [https://www.nature.com/articles/s41409-021-01542-0]
- 101. Regenerative Medicine Vs. Conventional Treatments [https://www.nexgenesishealthcare.com/regenerative-medicine-vs-conventional-treatments/]
- 102. Applying quantitative and systems pharmacology to drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11483046/]
- 103. Evidence informed management of chronic low back pain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3237293/]
- 104. Regeneration Roadmap: database resources for regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8728239/]
- 105. Predictors of Sustained Response to Functional Restoration in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10637275/]
- 106. Functional Restoration Program | Chronic Pain Rehabilitation [https://frius.com/functional-restoration-program/]
- 107. Biomarkers of Aging for the Identification and Evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11088934/]
- 108. The Biomarkers in Extreme Longevity: Insights Gained from ... [https://www.medsci.org/v21p2725.htm]