Small Extracellular Vesicles vs. Apoptotic Vesicles: A Comparative Analysis for Advanced Skin Regeneration
This article provides a comprehensive comparative analysis of two prominent classes of extracellular vesicles—small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs)—for therapeutic skin regeneration.
Small Extracellular Vesicles vs. Apoptotic Vesicles: A Comparative Analysis for Advanced Skin Regeneration
Abstract
This article provides a comprehensive comparative analysis of two prominent classes of extracellular vesicles—small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs)—for therapeutic skin regeneration. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational biology, biogenesis, and cargo. The content delves into methodological considerations for isolation and characterization, explores preclinical efficacy in diabetic and non-diabetic wound models, and directly compares therapeutic outcomes, including wound closure rates, collagen deposition, and revascularization capacity. Furthermore, it addresses critical challenges in production scalability, standardization, and clinical translation, offering a validated, evidence-based perspective to guide future research and therapeutic development in regenerative dermatology.
Decoding the Biology: Origins, Biogenesis, and Cargo of sEVs and ApoEVs
In the field of skin regeneration, extracellular vesicles (EVs) have emerged as pivotal mediators of intercellular communication, offering promising therapeutic potential. Among these, two major classes have gained significant research attention: small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs). sEVs, which include exosomes and ectosomes, are secreted by living cells and play crucial roles in maintaining tissue homeostasis. In contrast, ApoEVs are generated during programmed cell death and participate in clearance mechanisms and immune regulation. Understanding the fundamental distinctions between these vesicle types is essential for researchers and drug development professionals seeking to harness their regenerative capabilities for wound healing and skin repair. This guide provides a comprehensive comparison of their biological characteristics, functional efficacy, and experimental methodologies based on current scientific evidence.
Definitions and Key Characteristics
Classification and Biogenesis
EVs are classified based on their biogenesis pathways, size ranges, and compositional characteristics. The table below summarizes the key distinguishing features of sEVs and ApoEVs:
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Characteristic | sEVs (Small Extracellular Vesicles) | ApoEVs (Apoptotic Extracellular Vesicles) |
|---|---|---|
| Biogenesis | Secreted by living cells via endosomal pathway (exosomes) or plasma membrane budding (ectosomes) [1] [2] | Generated during apoptotic cell disassembly [2] [3] |
| Size Range | 30-200 nm (sEVs); exosomes: 30-150 nm; ectosomes: 100-1000 nm [4] | Highly heterogeneous: ApoSEVs (<1 μm), ApoBDs (1-5 μm) [5] [2] |
| Key Markers | Tetraspanins (CD9, CD63, CD81), TSG101, ALIX [4] | Phosphatidylserine exposure, histones (in ApoBDs) [2] [3] |
| Morphology | Cup-shaped (exosomes), spherical [4] | Heterogeneous; often contain organelles [2] |
| Primary Functions | Intercellular communication, signal transduction, homeostasis maintenance [6] [4] | Efferocytosis mediation, immunomodulation, "find me" and "eat me" signaling [7] [3] |
Subtype Classification
Both sEVs and ApoEVs encompass distinct subtypes that vary in their biogenesis and physical properties:
sEV Subtypes: The sEV category primarily includes exosomes (originating from multivesicular bodies) and ectosomes/microvesicles (budding directly from the plasma membrane) [1]. The International Society for Extracellular Vesicles recommends using "sEV" as an operational term for vesicles under 200nm that may include both biogenesis pathways [5] [8].
ApoEV Subtypes: ApoEVs include apoptotic small EVs (ApoSEVs, <1μm), apoptotic microvesicles (ApoMVs, 100-1000nm), and apoptotic bodies (ApoBDs, 1-5μm) [5] [3]. These subtypes differ in content and function; for instance, ApoBDs often contain intact organelles and nuclear fragments, while ApoSEVs are richer in specific signaling molecules [3].
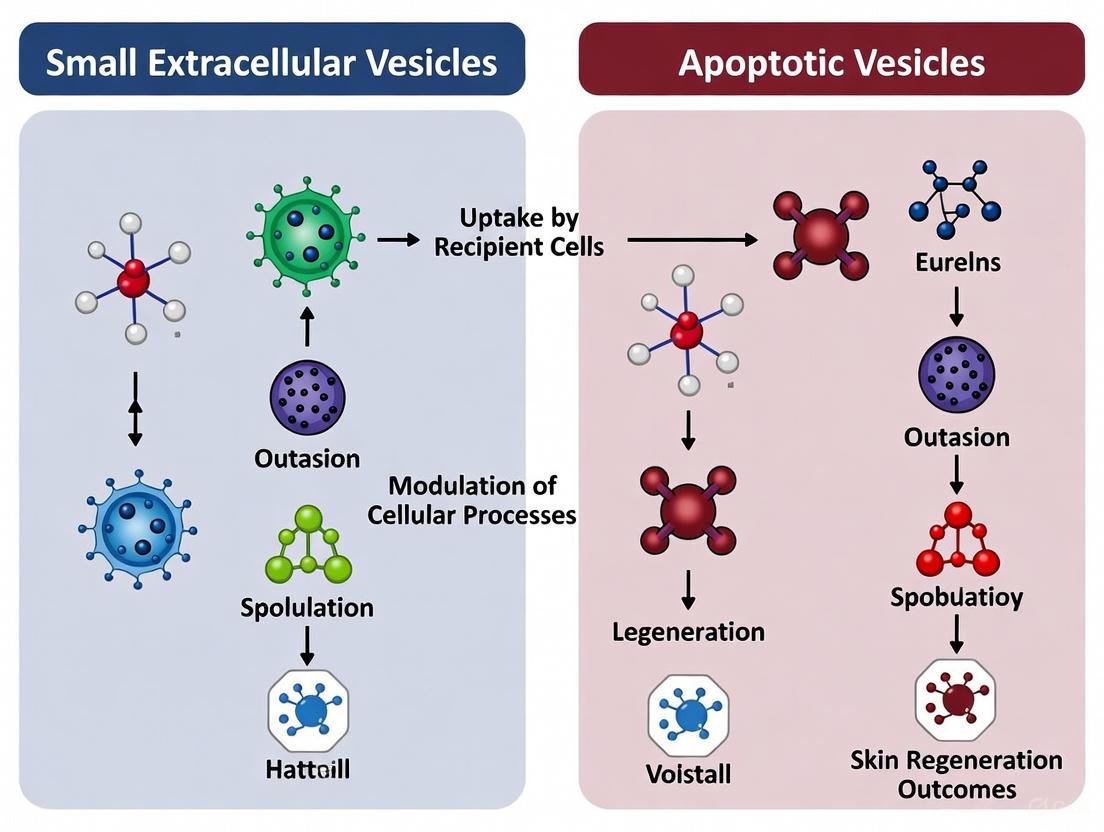
Figure 1: Biogenesis Pathways of sEVs and ApoEVs. sEVs originate from living cells via endosomal (exosomes) or plasma membrane budding (ectosomes) pathways. ApoEVs are generated during apoptotic cell disassembly through membrane blebbing and fragmentation processes.
Quantitative Therapeutic Efficacy in Skin Regeneration
Comparative Performance in Preclinical Models
Recent meta-analyses of preclinical studies provide quantitative evidence for the therapeutic potential of both sEVs and ApoEVs in wound healing and skin regeneration. The following table summarizes key efficacy metrics from animal studies:
Table 2: Therapeutic Efficacy of sEVs vs. ApoEVs in Skin Regeneration Models
| Efficacy Parameter | sEVs Performance | ApoEVs Performance | Comparative Findings |
|---|---|---|---|
| Wound Closure Rate | Significant improvement in both diabetic and non-diabetic models [8] | ApoSEVs showed better efficacy than ApoBDs and sEVs in wound closure outcome [5] | ApoSEVs > sEVs > ApoBDs |
| Collagen Deposition | Enhanced collagen fiber organization and density [8] | ApoSEVs superior to ApoBDs and sEVs in collagen deposition [5] | ApoSEVs > sEVs > ApoBDs |
| Revascularization | Promoted angiogenesis and increased blood vessel density [5] [8] | sEVs displayed better revascularization than ApoEVs [5] | sEVs > ApoEVs |
| Scar Width | Reduced scar formation in full-thickness wounds [5] | Limited comparative data available | Similar beneficial effects |
| Anti-inflammatory Effects | Modulated macrophage polarization toward M2 phenotype [8] [6] | Significant anti-inflammatory properties via immune cell regulation [7] [3] | ApoEVs may have superior immunomodulatory capacity |
Optimal Administration and Source Selection
Beyond vesicle type, administration parameters and cellular sources significantly influence therapeutic outcomes:
Administration Route: Subcutaneous injection demonstrated superior wound closure, collagen deposition, and revascularization compared to topical dressing/covering approaches [5].
MSC Source Efficacy: In sEV therapies, adipose-derived stem cells (ADSCs) showed the best effect on wound closure rate and collagen deposition, while bone marrow MSCs (BMMSCs) displayed superior revascularization potential [5].
Experimental Protocols and Methodologies
Isolation and Characterization Standards
Robust experimental protocols are essential for reliable vesicle research. The following methodologies represent current best practices:
Table 3: Standardized Methodologies for EV Research
| Experimental Step | Standard Protocol | Key Quality Controls |
|---|---|---|
| Vesicle Isolation | Differential ultracentrifugation (current gold standard) [4]; Alternative methods: ultrafiltration, size-exclusion chromatography, polymer precipitation [9] | Assessment of yield and purity; combination of methods often required for high purity [4] |
| MSC Characterization | International Society for Cell & Gene Therapy (ISCT) criteria: plastic adherence, multilineage differentiation, surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-) [5] [8] | 79.5% of studies in recent meta-analysis met all three ISCT criteria [5] |
| EV Characterization | MISEV2018/2023 guidelines: size distribution (NTA, TRPS), morphology (EM), marker detection (tetraspanins, TSG101 for sEVs; phosphatidylserine for ApoEVs) [5] [8] [9] | Protein quantification, particle concentration, assessment of contaminating proteins |
| Functional Assays | In vitro: migration, proliferation, tube formation assays; In vivo: full-thickness excisional wounds in murine models (most common) [5] [8] | Inclusion of appropriate controls; standardization of dosing (particles/wound area) |
Experimental Workflow Visualization
Figure 2: Standard Experimental Workflow for EV Skin Regeneration Studies. This diagram outlines the key steps from vesicle isolation through functional validation, highlighting critical quality control checkpoints.
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of EVs for skin regeneration requires specific reagents and methodologies. The following table catalogs essential research tools and their applications:
Table 4: Essential Research Reagents for EV Studies in Skin Regeneration
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| MSC Culture Media | MesenCult, StemMACS, DMEM/F12 with FBS/exosome-free FBS | Maintenance of MSC sources prior to EV collection [5] [10] |
| EV Isolation Kits | Total Exosome Isolation Kit, exoEasy Kit, PEG-based precipitation reagents | Alternative to ultracentrifugation for small-scale studies [4] [9] |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, ALIX (sEVs); Annexin V, Phosphatidylserine (ApoEVs) | Western blot, flow cytometry, and immuno-EM validation of EV identity [5] [3] [9] |
| Characterization Instruments | Nanoparticle Tracking Analyzer (NTA), Tunable Resistive Pulse Sensing (TRPS), Electron Microscope | Size distribution and concentration analysis [9] |
| Animal Models | C57BL/6 mice, SD rats; diabetic models (STZ-induced, db/db) | In vivo efficacy testing in physiologically relevant systems [5] [8] |
| Histological Stains | H&E, Masson's Trichrome, Picrosirius Red, CD31 immunohistochemistry | Assessment of tissue architecture, collagen deposition, and angiogenesis [5] |
sEVs and ApoEVs represent distinct classes of extracellular vesicles with unique biogenesis pathways, structural characteristics, and functional properties in skin regeneration. While both demonstrate significant therapeutic potential, current evidence suggests they may excel in different aspects of wound healing: ApoSEVs appear superior for wound closure and collagen deposition, while sEVs show enhanced revascularization capacity. These differential efficacy profiles highlight the importance of vesicle selection based on specific therapeutic objectives. For researchers pursuing EV-based skin regeneration therapies, adherence to standardized characterization protocols (MISEV guidelines), careful consideration of administration routes, and selection of appropriate cellular sources are critical factors influencing experimental outcomes and translational potential. The growing body of comparative evidence provides a foundation for rational design of EV-based therapeutics tailored to specific clinical needs in dermatology and regenerative medicine.
In the rapidly advancing field of regenerative medicine, particularly for skin regeneration, extracellular vesicles (EVs) have emerged as potent therapeutic agents. These nano-sized lipid bilayer vesicles facilitate intercellular communication by transferring functional proteins, lipids, and nucleic acids to recipient cells, thereby modulating physiological responses and promoting tissue repair [11] [12]. However, all EVs are not created equal. Their biological functions and therapeutic potential are fundamentally dictated by their distinct biogenesis pathways. This guide provides a comprehensive objective comparison between two primary EV classes: small extracellular vesicles (sEVs), which originate from the endosomal system, and apoptotic vesicles (ApoEVs), which are generated through apoptotic cell dismantling. Understanding these differences is crucial for researchers and drug development professionals selecting the optimal EV type for specific skin regeneration applications.
Defining the Vesicles: Origins and Key Identifiers
Small Extracellular Vesicles (sEVs/Exosomes)
Small Extracellular Vesicles, commonly known as exosomes, are defined by their endosomal origin. Their biogenesis begins with the inward budding of the endosomal membrane, leading to the formation of multivesicular bodies (MVBs) filled with intraluminal vesicles (ILVs) [13] [12]. These MVBs subsequently fuse with the plasma membrane, releasing the ILVs into the extracellular space as exosomes or sEVs [12]. They are typically 30-200 nm in diameter and are characterized by a specific set of protein markers reflective of their biogenesis pathway, including tetraspanins (CD63, CD81, CD9), ESCRT-related proteins (TSG101, Alix), and heat shock proteins (Hsp70, Hsp90) [13] [11] [12].
Apoptotic Vesicles (ApoEVs)
Apoptotic Vesicles are a broad category of EVs produced during the programmed cell death process of apoptosis. This process involves cytoplasmic and nuclear condensation, followed by the cell membrane contracting and splitting to enclose cellular components within membrane-bound vesicles [7]. ApoEVs can be further sub-classified based on their size and formation stage, including microvesicles (MVs, 100 nm-1 μm) and apoptotic bodies (ApoBDs, 100 nm-5 μm) [14] [7]. They display "find-me" and "eat-me" signals, such as phosphatidylserine exposure, which promote their recognition and clearance by phagocytes, a process critical for tissue homeostasis known as efferocytosis [7].
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Characteristic | Small Extracellular Vesicles (sEVs/Exosomes) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Biogenesis Origin | Endosomal system; released upon MVB fusion with plasma membrane [13] [12] | Apoptotic cell dismantling; formed through membrane blebbing and fission [7] |
| Size Range | 30-200 nm [12] | 100 nm - 5 μm [14] [7] |
| Key Morphology | Spheroid or cup-shaped [12] | Heterogeneous in size and content [7] |
| Common Markers | Tetraspanins (CD63, CD81, CD9), TSG101, Alix [13] [12] | Phosphatidylserine exposure, Caspase-cleaved products [7] |
Comparative Analysis of Biogenesis Mechanisms
The journey of a vesicle from its cellular origin to its release is a complex process governed by distinct molecular machinery. The diagrams below delineate these pathways for sEVs and ApoEVs.
sEV Biogenesis via the Endosomal System
sEV formation is a multi-step process occurring within the endosomal network. It involves the coordinated effort of various molecular complexes to create, sort, and eventually release the vesicles.
The sEV biogenesis pathway involves:
- Initiation and Cargo Sorting: Early endosomes mature into late endosomes or MVBs. The formation of ILVs within MVBs is driven primarily by the Endosomal Sorting Complex Required for Transport (ESCRT) machinery, which includes proteins like TSG101 and Alix that sort ubiquitinated cargoes [13] [12]. ESCRT-independent mechanisms also exist, often involving tetraspanin-enriched microdomains (CD9, CD63) and lipids like ceramide [13].
- MVB Fate and Vesicle Release: MVBs face one of two fates: degradation via fusion with lysosomes or secretion. For sEV release, MVBs are transported along the cytoskeleton to the plasma membrane, where they dock and fuse, a process mediated by SNARE proteins and RAB GTPases [12]. This fusion releases the ILVs into the extracellular space as sEVs [13].
ApoEV Biogenesis via Apoptotic Dismantling
The formation of ApoEVs is a hallmark of apoptosis, designed to package the dying cell's contents for efficient disposal and signaling.
The ApoEV biogenesis pathway involves:
- Apoptotic Trigger and Caspase Activation: Both intrinsic (cellular stress) and extrinsic (death ligands) pathways converge on the activation of caspases, a family of proteases that are the executioners of apoptosis [7].
- Membrane Blebbing and Vesicle Formation: Caspase activity leads to the disassembly of the cytoskeleton and activation of enzymes like ROCK I. This causes the cell membrane to bleb and fragment, pinching off into ApoEVs of various sizes [7].
- "Find-Me" and "Eat-Me" Signals: A critical step is the exposure of phosphatidylserine (PS) on the outer leaflet of the ApoEV membrane. This serves as a key "eat-me" signal for phagocytic cells like macrophages, initiating efferocytosis—the clearance of apoptotic debris [7].
Functional Outcomes in Skin Regeneration
The distinct origins of sEVs and ApoEVs endow them with different biological functions, which directly influences their therapeutic potential in skin regeneration, a process involving inflammation control, matrix remodeling, and tissue growth.
Mechanisms of sEVs in Skin Rejuvenation
sEVs, particularly those derived from mesenchymal stem cells (MSCs), have shown remarkable promise in combating skin aging and promoting repair. Their mechanisms are largely mediated by their cargo of proteins and miRNAs [11].
- Anti-Oxidative Stress: HucMSC-derived sEVs have been shown to reduce reactive oxygen species (ROS) production in skin cells exposed to UVB radiation or H₂O₂. They can activate the SIRT1-dependent antioxidant pathway and inhibit the MAPK/AP-1 pathway, thereby reducing oxidative damage and cell senescence [11].
- Promoting Matrix Synthesis: sEVs can enhance collagen production and suppress its degradation. For instance, they increase the expression of type I collagen in fibroblasts while decreasing the expression of matrix metalloproteinase-1 (MMP-1), a key enzyme that breaks down collagen. This helps restore the skin's extracellular matrix, reducing wrinkles and improving elasticity [11].
- Modulating Inflammation: sEVs from MSCs can downregulate pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6, and inhibit the NF-κB signaling pathway, creating an anti-inflammatory environment conducive to healing [11].
Mechanisms of ApoEVs in Skin Repair
ApoEVs, once considered mere waste bags, are now recognized as active regulators of tissue regeneration, primarily through their role in efferocytosis and immune modulation.
- Efferocytosis and Inflammation Resolution: The clearance of ApoEVs by macrophages via efferocytosis is not a passive process. It actively promotes the release of regenerative cytokines and drives macrophages toward an anti-inflammatory (M2) phenotype, which is crucial for resolving inflammation and initiating tissue repair [7].
- Activation of Regenerative Pathways: Studies indicate that MSC-derived ApoEVs can promote wound healing and hair growth by activating the Wnt/β-catenin pathway in skin and hair follicle stem cells [15]. This pathway is fundamental for cell proliferation and tissue regeneration.
- Direct Anti-inflammatory Action: ApoEVs possess intrinsic anti-inflammatory properties. They can polarize anti-inflammatory macrophages and suppress the activity of pro-inflammatory T helper cells (Th1, Th17), while activating regulatory T cells. This makes them a promising therapeutic tool for various inflammatory disorders [7].
Table 2: Functional Comparison in Skin Regeneration Context
| Functional Aspect | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Primary Role in Skin | Delivery of bioactive cargo (miRNA, proteins) to modulate cell activity [11] | Orchestrating immune-mediated clearance and resolution of inflammation [7] |
| Key Signaling Pathways Modulated | MAPK/AP-1, NF-κB, PI3K/Akt, SIRT1 [11] | Wnt/β-catenin, S1P/S1PR [7] [15] |
| Effect on Extracellular Matrix | ↑ Collagen I synthesis, ↓ MMP-1 expression [11] | Emerging role in tissue remodeling via efferocytosis [7] |
| Immune/Inflammatory Response | Downregulation of pro-inflammatory cytokines (TNF-α, IL-6) [11] | Induction of anti-inflammatory macrophage polarization; suppression of Th1/Th17 cells [7] |
| Therapeutic Evidence in Skin | Protection against UV-induced photoaging; enhanced fibroblast proliferation & migration [11] | Promotion of wound healing and hair growth in models [15] |
Experimental Protocols for Isolation and Characterization
Accurate isolation and characterization are paramount for conducting valid research. The following protocols are standard in the field.
Standard Isolation Workflow
The journey from biofluid or cell culture medium to purified vesicles requires careful technique to minimize cross-contamination.
Key Isolation Methods:
- Differential Ultracentrifugation: The most common method. It involves a series of increasing centrifugal forces to pellet different vesicle types sequentially. sEVs are typically pelleted at high speeds of 100,000-120,000g [13] [14].
- Density Gradient Centrifugation: Used following ultracentrifugation for further purification, separating vesicles based on their buoyant density in a sucrose or iodixanol gradient [13].
- Size-Based Filtration: Using filters with specific pore sizes to isolate vesicles within a certain diameter range [13].
- Immunoaffinity Capture: Using magnetic beads conjugated with antibodies against specific surface markers (e.g., anti-CD63 for sEVs) for highly specific isolation [13].
Essential Characterization Techniques
- Nanoparticle Tracking Analysis (NTA): Measures the size distribution and concentration of particles in a solution by tracking their Brownian motion [13].
- Transmission Electron Microscopy (TEM): Provides high-resolution images to confirm the morphology (e.g., cup-shaped for sEVs) and approximate size of the vesicles [13].
- Western Blotting: Used to detect the presence of specific protein markers associated with the vesicle type (e.g., CD63, TSG101 for sEVs) and the absence of contaminants from cellular organelles [13].
The Scientist's Toolkit: Key Research Reagents
A selection of critical reagents for studying EV biogenesis and function is listed below.
Table 3: Essential Reagents for EV Research
| Reagent / Solution | Primary Function in Research | Specific Example Targets |
|---|---|---|
| Anti-Tetraspanin Antibodies | Immunoaffinity capture and characterization of sEVs [13] | CD63, CD81, CD9 [13] [12] |
| Anti-ESCRT Protein Antibodies | Validation of sEV identity and study of biogenesis mechanism [13] [12] | TSG101, Alix [13] [12] |
| Annexin V | Detection of phosphatidylserine exposure on ApoEVs for identification and functional studies [7] | Phosphatidylserine [7] |
| Protease Inhibitors | Preservation of protein cargo integrity during vesicle isolation and processing. | Caspase inhibitors (for ApoEV studies) [7] |
| Sucrose/Iodixanol Solutions | Formation of density gradients for high-purity isolation of vesicles away from protein aggregates and other contaminants [13] | N/A |
| RAB GTPase Modulators | Investigating the molecular regulation of MVB trafficking and sEV secretion [12] | Various RAB proteins (e.g., RAB27) [12] |
| Caspase Inhibitors/Activators | To modulate or inhibit the apoptotic process, thereby controlling ApoEV production for functional studies [7] | Caspase-3, Caspase-8 [7] |
The choice between sEVs and ApoEVs for skin regeneration research is not a matter of superiority, but of strategic application. sEVs, born from the endosomal system, function as precision delivery vehicles, directly transferring miRNAs and proteins to recipient skin cells to combat oxidative stress, enhance collagen production, and modulate inflammation. In contrast, ApoEVs, products of apoptotic dismantling, serve as potent orchestrators of the immune landscape, promoting tissue repair by resolving inflammation through efferocytosis and activating regenerative pathways like Wnt/β-catenin. The decision for researchers should be guided by the specific pathological context of the target skin condition—whether the primary need is for direct cytoprotective and matrix-stimulating signals (favoring sEVs) or for immune modulation and clearance of damage to initiate healing (favoring ApoEVs). A deep understanding of these biogenesis pathways and their functional consequences is therefore the foundation for harnessing the full therapeutic potential of extracellular vesicles in regenerative dermatology.
The field of regenerative medicine is increasingly exploring cell-free therapies, with extracellular vesicles (EVs) emerging as promising candidates for skin regeneration. Among these, small extracellular vesicles (sEVs), including exosomes (30-150 nm in diameter), and apoptotic extracellular vesicles (ApoEVs), which include apoptotic small EVs (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm), are of significant interest [5] [8]. These vesicles are natural carriers of diverse biological cargo—including proteins, lipids, and microRNAs (miRNAs)—which they horizontally transfer between cells to modulate recipient cell behavior [8]. Understanding the distinct cargo profiles of sEVs and ApoEVs is crucial for evaluating their therapeutic potential, mechanisms of action, and eventual clinical application for skin repair and regeneration. This guide provides a comparative analysis of their characteristic miRNA, protein, and lipid signatures, underpinned by experimental data and methodologies relevant to skin regeneration research.
Comparative Cargo Profiles of sEVs and ApoEVs
The therapeutic efficacy of vesicles is largely dictated by their molecular cargo, which varies significantly based on the vesicle's cellular origin and biogenesis pathway.
MicroRNA (miRNA) Signatures
MiRNAs are powerful regulators of gene expression and play a central role in the therapeutic effects of EVs. Comparative analysis reveals distinct miRNA profiles between vesicles from different cellular sources.
Table 1: Characteristic miRNA Profiles of sEVs from Different Cell Sources
| Cell Source | Highly Expressed miRNAs | Putative Target Genes / Affected Pathways | Experimental Model / Functional Outcome |
|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | hsa-miR-16-5p, hsa-miR-25-3p, hsa-miR-93-5p (3 overlapping miRNAs) [16] | MAN2A1, ZNFX1, PHF19, GPR137C, ENPP5, B3GALT2, FNIP1, PKD2, FBXW7 [16] | Model: Human articular chondrocytes (hACs) [16]. Outcome: Promoted cartilage matrix formation (GAG, Col2), downregulated fibrocartilage matrix (Col1), suppressed senescence [16]. |
| Bone Marrow-MSCs (BM-MSCs) | hsa-miR-16-5p, hsa-miR-25-3p, hsa-miR-93-5p (3 overlapping miRNAs); 11 highly expressed miRNAs total [16] | Genes involved in cell growth, bone ossification, cartilage development via MAPK signalling pathway [16]. | Model: Human articular chondrocytes (hACs) [16]. Outcome: Greatest effect on maintaining hAC viability and function compared to iPSC-Exos and ADSC-Exos [16]. |
| Adipose-Derived Stem Cells (ADSCs) | hsa-miR-16-5p, hsa-miR-25-3p, hsa-miR-93-5p (3 overlapping miRNAs); 13 highly expressed miRNAs total [16] | Similar target genes as BM-MSCs, with 7 miRNAs overlapping between ADSC- and BMSC-Exos [16]. | Model: Human articular chondrocytes (hACs) [16]. Outcome: Promoted normal cartilage matrix formation and prevented senescence [16]. |
| ADSCs (in other contexts) | miR-126, miR-21, miR-146a, miR-16-5p [17] | miR-126: Activates PI3K/Akt in endothelium; miR-146a/miR-16-5p: Target TLR4/IRAK1/TRAF6 to inhibit NF-κB [17]. | Model: Lung injury, ARDS [17]. Outcome: Reduced inflammation, decreased vascular permeability, enhanced tissue regeneration [17]. |
A systematic review and meta-analysis directly compared the therapeutic efficacy of MSC-derived sEVs and ApoEVs in wound healing, indicating that ApoSEVs showed better efficacy than sEVs in wound closure outcome and collagen deposition, while sEVs displayed better performance in revascularization [5]. Furthermore, among easily accessible MSC sources, ADSCs demonstrated the best effect on wound closure rate, whereas BM-MSCs were more effective in revascularization [5].
Protein and Lipid Cargo
Proteins and lipids are integral functional components of EVs, contributing to their structure, targeting, and bioactivity.
Table 2: Characteristic Protein and Lipid Profiles of EVs
| Cargo Type | Vesicle Type | Key Components | Functional Role / Experimental Context |
|---|---|---|---|
| Proteins | sEVs / Exosomes | CD9, CD63, CD81, Alix, TSG101 (characteristic markers); growth factors, cytokines, extracellular matrix components [17]. | Role: Vesicle identification, cell targeting, immunomodulation, tissue remodeling [17]. Context: Universal sEV markers used for characterization across studies [18]. |
| ApoEVs | Specific protein profiles are less defined but differ from sEVs; enriched in endoplasmic reticulum, proteasome, and mitochondrial proteins [17]. | Role: May reflect the apoptotic state of the parent cell and influence immunomodulation [17]. | |
| Lipids | sEVs / Exosomes | Higher concentration of glycolipids and free fatty acids [17]. | Role: Membrane stability, formation of lipid rafts, cellular signaling [17]. |
| ApoEVs | Enriched with ceramides and sphingomyelins [17]. | Role: Involvement in apoptotic signaling pathways [17]. | |
| Hypoxia-induced Exosomes | Increased unsaturated fatty acid-containing Lysophosphatidylcholine (LPC) [19]. | Context: Intestinal epithelial cell-derived exosomes after ischemia-reperfusion injury [19]. Outcome: Activated NF-κB pathway and inflammation in monocytes [19]. |
Experimental Protocols for Vesicle Analysis
To ensure the reliability and reproducibility of research findings, adherence to standardized experimental protocols and reporting guidelines is paramount.
Vesicle Isolation and Characterization
A. Isolation Methods:
- Ultracentrifugation (UC): The classical "gold standard" method for pelleting vesicles based on size and density. However, it can be time-consuming and may yield impure preparations [18].
- Tangential Flow Filtration (TFF): A scalable method that uses tangential flow across filters to separate vesicles based on size. Studies show TFF provides a statistically higher particle yield than UC, making it more suitable for large-scale production required for clinical translation [18].
- Polymer-Based Precipitation: Methods using solutions like ExoQuick-TC to precipitate vesicles out of solution. Useful for processing large volumes of conditioned medium [19].
B. Characterization (Adhering to MISEV Guidelines): Researchers must characterize vesicles based on size, concentration, and specific markers [5] [8].
- Nanoparticle Tracking Analysis (NTA): Determines the size distribution and concentration of particles in a solution [18].
- Transmission Electron Microscopy (TEM): Visualizes the cup-shaped morphology of sEVs/exosomes, confirming their structure [18].
- Immunoblotting: Confirms the presence of positive protein markers (e.g., CD9, CD63, CD81, TSG101 for sEVs) and the absence of negative markers (e.g., calnexin, an endoplasmic reticulum protein) [18].
Cargo Profiling and Functional Assays
A. miRNA Profiling:
- Next-Generation Sequencing (NGS): A high-throughput method used to identify and comprehensively profile the full spectrum of miRNAs in vesicle samples [16].
- Bioinformatics Analysis: Used post-sequencing to predict putative target genes of identified miRNAs and to perform enrichment analyses (e.g., Gene Ontology - GO, Kyoto Encyclopedia of Genes and Genomes - KEGG) to elucidate involved biological pathways [16].
B. Functional In Vitro Assays:
- Cell Viability and Proliferation Assays: (e.g., CCK-8, MTT). Used to assess the protective or proliferative effects of vesicles on recipient cells. Example: H₂O₂-damaged ARPE-19 cells treated with BM-MSC-sEVs showed increased viability from 37.86% to over 52% [18].
- Apoptosis Assays: (e.g., flow cytometry with Annexin V/PI staining). Used to quantify the anti-apoptotic effect of vesicles. Example: BM-MSC-sEVs significantly reduced the total percentage of apoptotic ARPE-19 cells [18].
- Reporter Assays: Used to study specific signaling pathway activation. Example: THP-1 Blue NF-κB reporter monocytes were used to demonstrate that exosomes from hypoxic IECs activate the NF-κB inflammatory pathway [19].
Signaling Pathways in Skin Regeneration Modulated by Vesicular Cargo
The therapeutic effects of sEVs and ApoEVs in skin regeneration are mediated through the regulation of key signaling pathways by their cargo, particularly miRNAs.
The diagram above summarizes the complex interplay between vesicular cargo and cellular pathways. For instance:
- miR-146a and miR-16-5p from ADSC-Exos target the TLR4/IRAK1/TRAF6 complex, leading to inhibition of NF-κB signaling, a master regulator of inflammation. This results in reduced levels of pro-inflammatory cytokines (e.g., TNF-α, IL-6), which is crucial for mitigating chronic inflammation in non-healing wounds [17].
- miR-126, also found in ADSC-Exos, activates the PI3K/Akt signaling pathway in endothelial cells. This promotes angiogenesis (revascularization), a critical process for supplying nutrients and oxygen to the regenerating tissue [17].
- Bioinformatics predictions from miRNA profiles of stem cell exosomes suggest involvement in the MAPK signaling pathway, which regulates cell growth, differentiation, and matrix formation—all vital for skin structure and function [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for EV Research in Skin Regeneration
| Item | Function / Application | Example from Search Results |
|---|---|---|
| Bovine Exosome-Depleted FBS | Used in cell culture to supplement media while preventing contamination by bovine-derived vesicles, ensuring that isolated EVs are of cellular origin. | Used in culture of hiPSCs, hBMSCs, and hADSCs for exosome collection [16]. |
| Human Platelet Lysate (hPL) | A xeno-free supplement for MSC culture, supporting cell proliferation and expansion under GMP-compliant conditions. | Used as a serum supplement in DMEM and α-MEM for BM-MSC culture [18]. |
| ExoQuick-TC | A polymer-based solution used for precipitating exosomes/EVs from conditioned cell culture medium. | Used for isolating exosomes from intestinal epithelial cell conditioned medium [19]. |
| CD9, CD63, CD81 Antibodies | Positive marker antibodies used in immunoblotting (Western Blot) or Exo-Check arrays to confirm the presence of sEVs/exosomes. | Confirmed via Western Blot as markers for BM-MSC-sEVs [18]. |
| Annexin V / Propidium Iodide (PI) | Reagents used in flow cytometry to detect and quantify apoptotic cells, used to validate anti-apoptotic effects of EVs. | Used to show BM-MSC-sEVs reduce apoptosis in ARPE-19 cells [18]. |
| THP-1 Blue NF-κB Reporter Cells | A monocytic cell line engineered to secrete alkaline phosphatase upon NF-κB activation, used to screen for pro- or anti-inflammatory effects of EV cargo. | Used to demonstrate pro-inflammatory effects of exosomes from hypoxic IECs [19]. |
| Streptozotocin (STZ) | A chemical used to induce Type 1 diabetes in animal models (e.g., rats, mice), creating a diabetic wound model for testing EV therapeutics. | Used in STZ-induced diabetic rodent wound models [5] [8]. |
sEVs and ApoEVs present distinct biological tools for skin regeneration, each with unique cargo profiles and functional strengths. The current body of evidence, including a recent meta-analysis, suggests that ApoSEVs may be superior in promoting wound closure and collagen deposition, while sEVs excel in enhancing revascularization [5]. The choice of producer cell (e.g., ADSCs for wound closure, BM-MSCs for revascularization) further fine-tunes the therapeutic outcome [5]. The characteristic cargo of miRNAs, proteins, and lipids underlies these differences by modulating key inflammatory, proliferative, and matrix-forming pathways in the skin. Future work must focus on standardizing isolation and characterization protocols, deepening our understanding of ApoEV biology, and engineering vesicles to maximize their regenerative potential for clinical translation.
The therapeutic potential of Mesenchymal Stem Cells (MSCs) in skin regeneration and wound healing represents a paradigm shift in regenerative medicine. These multipotent adult stem cells, first identified in bone marrow, possess the capacity to differentiate into multiple cell lineages, modulate immune responses, and enhance tissue repair [20]. The International Society for Cellular Therapy (ISCT) establishes three defining criteria for MSCs: adherence to plastic; specific surface antigen expression (CD73, CD90, CD105 positive; CD11b, CD14, CD19, CD34, CD45, CD79α, HLA-DR negative); and tri-lineage differentiation potential into osteoblasts, adipocytes, and chondrocytes in vitro [20]. What makes MSCs particularly valuable for therapeutic applications includes their relative ease of isolation from multiple tissue sources, reduced ethical concerns compared to embryonic stem cells, lower risk of teratoma formation than induced pluripotent stem cells, and innate ability to migrate to sites of tissue damage via chemoattraction [20].
The emergence of cell-free therapies utilizing extracellular vesicles (EVs) derived from MSCs has further accelerated research in dermatological applications. These vesicles, particularly small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs), have demonstrated remarkable efficacy in promoting skin regeneration while potentially mitigating risks associated with whole-cell transplantation [5] [8]. This review systematically compares the impact of primary MSC tissue sources on their therapeutic potential, with a specific focus on their secreted vesicles for skin regeneration outcomes, providing evidence-based guidance for researchers and therapeutic developers.
MSCs can be isolated from multiple tissue sources, each with distinct advantages and limitations for clinical translation. The table below summarizes key characteristics of major MSC sources investigated for skin regeneration applications.
Table 1: Comparison of Primary Mesenchymal Stem Cell Sources for Skin Regeneration
| Source | Relative Abundance | Isolation Complexity | Key Advantages | Documented Efficacy in Skin Regeneration |
|---|---|---|---|---|
| Adipose Tissue (AD-MSCs) | High | Moderate | Minimal morbidity; high yield; strong paracrine signaling | Superior wound closure rate and collagen deposition [5] |
| Bone Marrow (BM-MSCs) | Low | High (invasive) | Gold standard; extensive characterization | Enhanced revascularization capacity [5] |
| Umbilical Cord (UC-MSCs) | Moderate | Low (non-invasive) | Immunologically naive; high proliferation rate | Improved healing rates; reduced scarring [20] [5] |
| Induced Pluripotent Stem Cells (iMSCs) | Unlimited in vitro | High (reprogramming) | Unlimited scalability; consistent batches | Accelerated wound closure in porcine burn models [21] |
Adipose-Derived MSCs (AD-MSCs)
Adipose tissue represents a particularly abundant and accessible source of MSCs for regenerative applications. AD-MSCs demonstrate superior wound closure rates and enhanced collagen deposition compared to other sources in preclinical models, making them exceptionally promising for dermatological applications [5]. The minimally invasive harvesting procedure (via liposuction) combined with high cell yield positions AD-MSCs as a frontrunner for clinical translation in skin regeneration therapies.
Bone Marrow-Derived MSCs (BM-MSCs)
As the originally discovered MSC source, bone marrow-derived MSCs represent the most extensively characterized population. While their harvesting is more invasive and yields are lower compared to adipose tissue, BM-MSCs exhibit exceptional revascularization capacity, a critical factor in wound healing and skin regeneration [5]. This robust angiogenic potential makes BM-MSCs particularly valuable for treating chronic wounds with compromised vascularization.
Umbilical Cord-Derived MSCs (UC-MSCs)
Umbilical cord tissue, including Wharton's jelly and cord blood, provides MSCs with notable immunomodulatory properties and high proliferative capacity [20]. These cells are considered immunologically naive, making them promising candidates for allogeneic therapies. Studies indicate UC-MSCs contribute to improved healing rates with reduced scarring, potentially through modulation of inflammatory responses during wound healing [20] [5].
iPSC-Derived MSCs (iMSCs)
The differentiation of induced pluripotent stem cells into MSCs represents a innovative approach to overcome limitations of primary tissue sources. iMSCs offer theoretically unlimited scalability and batch-to-batch consistency, addressing critical manufacturing challenges for standardized therapies [21]. Recent research demonstrates that iMSCs seeded onto dermal regeneration templates significantly accelerate wound closure in porcine burn models, supporting their potential as an ideal cell source for skin regeneration [21].
MSC-Derived Vesicles: Mechanisms and Therapeutic Applications
The therapeutic effects of MSCs are increasingly attributed to their paracrine signaling via secreted extracellular vesicles rather than direct cellular engraftment. These vesicles are broadly categorized based on their biogenesis, size, and cargo.
Table 2: Characteristics of MSC-Derived Therapeutic Vesicles for Skin Regeneration
| Vesicle Type | Size Range | Biogenesis | Key Cargo | Primary Mechanisms in Skin Repair |
|---|---|---|---|---|
| Small EVs (sEVs/exosomes) | 30-200 nm | Endosomal origin; exocytosis | miRNAs, proteins, lipids | Anti-inflammatory, pro-angiogenic, fibroblast proliferation [8] |
| Apoptotic EVs (ApoEVs) | 50-5000 nm | Apoptotic cell blebbing | Nuclear fragments, organelles, miRNAs | Macrophage polarization to M2 phenotype, efferocytosis, tissue remodeling [22] [7] |
| ApoSEVs (Apoptotic Small EVs) | <1 μm | Apoptotic cell fragmentation | Specific mRNAs, phosphatidylserine | Enhanced collagen deposition, Wnt/β-catenin pathway activation [5] [15] |
Small Extracellular Vesicles (sEVs)
sEVs, including exosomes, are nano-sized vesicles (30-200 nm) formed through the endosomal pathway and released upon fusion of multivesicular bodies with the plasma membrane [8]. They carry diverse cargo including miRNAs, proteins, and lipids that mediate intercellular communication. In skin regeneration, sEVs demonstrate potent immunomodulatory effects by polarizing macrophages toward the anti-inflammatory M2 phenotype and enhancing angiogenesis through transfer of pro-angiogenic factors [20] [8]. Their small size potentially enables better tissue penetration compared to larger vesicles, though their circulation time may be limited by rapid clearance.
Apoptotic Vesicles (ApoEVs)
ApoEVs are membrane-bound vesicles released during programmed cell death, encompassing a broader size range (50-5000 nm) that includes apoptotic bodies (ApoBDs, 1-5 μm) and apoptotic small EVs (ApoSEVs, <1 μm) [22] [5]. These vesicles contain nuclear fragments, organelles, and specific genetic material from their parent cells. ApoEVs exhibit unique immunosuppressive properties and promote tissue repair primarily through efferocytosis - the process by which phagocytic cells clear apoptotic debris, leading to production of regenerative cytokines and polarization of anti-inflammatory macrophages [22] [7]. Recent evidence suggests ApoSEVs demonstrate superior collagen deposition compared to sEVs in wound healing models [5].
Comparative Efficacy in Skin Regeneration
A comprehensive meta-analysis of preclinical studies directly comparing MSC-derived vesicle types revealed distinct therapeutic advantages:
- ApoSEVs demonstrated superior efficacy in wound closure rates and collagen deposition compared to both sEVs and larger apoptotic bodies [5]
- sEVs exhibited enhanced revascularization capacity compared to ApoEVs, promoting greater blood vessel density in regenerating tissue [5]
- Administration route significantly influenced outcomes, with subcutaneous injection proving more effective than topical application for both vesicle types across multiple healing parameters [5]
These findings suggest that the optimal vesicle type may depend on the specific healing priorities - ApoSEVs for structural restoration and sEVs for vascularization - potentially enabling combination approaches targeting multiple aspects of the healing process.
Experimental Protocols and Methodologies
MSC Characterization and Vesicle Isolation
Standardized protocols for MSC characterization and vesicle isolation are critical for reproducible research and therapeutic development. The following workflow outlines key methodological steps:
Diagram 1: Experimental workflow for MSC characterization and vesicle isolation
MSC Characterization Protocol
According to ISCT guidelines, comprehensive MSC characterization must include three key assessments:
- Plastic Adherence: Confirm adherence to tissue culture plastic under standard culture conditions [5]
- Surface Marker Expression: Flow cytometric analysis demonstrating ≥95% expression of CD73, CD90, and CD105, and ≤2% expression of CD34, CD45, CD11b, CD19, and HLA-DR [20] [18]
- Tri-lineage Differentiation: Functional differentiation into osteocytes, adipocytes, and chondrocytes under appropriate induction conditions, confirmed by specific staining (Alizarin Red, Oil Red O, and Alcian Blue, respectively) [21] [18]
A recent systematic review noted that 79.5% of published studies on MSC-EVs for skin regeneration met all three ISCT characterization criteria, while 20.5% met two of the three criteria [5].
Vesicle Isolation Methods
The methodology for vesicle isolation significantly impacts yield, purity, and potentially therapeutic efficacy:
- Ultracentrifugation (UC): Traditional gold standard involving sequential centrifugation steps to separate vesicles based on size and density [18]
- Tangential Flow Filtration (TFF): Scalable method using cross-flow filtration, demonstrating significantly higher particle yields compared to UC while maintaining vesicle integrity [18]
Comparative studies indicate TFF provides statistically higher particle yields than ultracentrifugation, making it particularly suitable for large-scale therapeutic production [18].
In Vivo Assessment of Therapeutic Efficacy
Preclinical evaluation of MSC-derived vesicles for skin regeneration typically utilizes well-established animal models:
- Animal Models: Mouse (73.5%) and rat (26.5%) models predominately used; porcine models more closely mimic human skin physiology but are less common due to cost and handling complexity [5] [20]
- Wound Types: Full-thickness excisional wounds (90.4% of studies), diabetic wounds (47.0%), burn models, and photoaging models [5]
- Key Outcome Measures: Wound closure rate, scar width, blood vessel density, collagen deposition, and histopathological analysis [5]
Notably, a comprehensive meta-analysis of 83 preclinical studies demonstrated that MSC-EVs significantly promoted skin regeneration in both diabetic and non-diabetic animal models, influencing multiple facets of the healing process regardless of cell source, production protocol, or disease model [5].
Signaling Pathways in Vesicle-Mediated Skin Repair
MSC-derived vesicles exert their therapeutic effects through activation of specific signaling pathways in recipient cells. The following diagram illustrates key mechanistic pathways:
Diagram 2: Signaling pathways in vesicle-mediated skin repair
Key Mechanistic Insights
- ApoEV Internalization: Apoptotic vesicles are internalized via phosphatidylserine-dependent macropinocytosis, a mechanism distinct from classical endocytosis pathways used by sEVs [23]
- Wnt/β-catenin Activation: MSC-derived ApoEVs activate the Wnt/β-catenin pathway in skin and hair follicle stem cells, promoting wound healing and hair growth [15]
- Metabolic Regulation: Exogenous ApoEVs are partially metabolized in integumentary skin and hair follicles, with their migration enhanced by mechanical forces such as exercise [15]
- mRNA Transfer: ApoEVs carry specific functional mRNAs that are transferred to recipient cells and translated into functional proteins, enabling direct phenotypic modification [23]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC and Vesicle Studies
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Cell Culture Media | α-MEM, DMEM, Xeno-free media | MSC expansion | Optimal growth environments; α-MEM shows superior proliferation rates for BM-MSCs [18] |
| Characterization Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | MSC phenotyping | Flow cytometric verification of ISCT criteria [20] [18] |
| Differentiation Kits | Osteo-, Adipo-, Chondrogenic kits | Tri-lineage differentiation | Functional validation of MSC multipotency [21] [18] |
| Vesicle Isolation Kits | TFF systems, Ultracentrifugation | EV purification | Isolation of sEVs and ApoEVs from conditioned media [18] |
| Characterization Tools | NTA, TEM, Western Blot | EV validation | Size distribution, morphological analysis, marker confirmation (CD9, CD63, TSG101) [18] |
| Animal Models | C57BL/6 mice, SD rats, db/db mice | In vivo testing | Diabetic and non-diabetic wound healing assessment [5] |
The cellular origin of mesenchymal stem cells significantly influences their therapeutic profile for skin regeneration applications. Adipose-derived MSCs demonstrate superior wound closure and collagen deposition, bone marrow MSCs excel in revascularization, umbilical cord MSCs offer immunological advantages, and iPSC-derived MSCs provide unprecedented scalability. The emergence of vesicle-based therapeutics further refines this landscape, with apoptotic small vesicles (particularly ApoSEVs) showing enhanced efficacy in wound closure and collagen deposition, while sEVs demonstrate superior revascularization potential.
Future research directions should prioritize standardization of vesicle isolation and characterization protocols, direct comparative studies of MSC sources under consistent conditions, investigation of combination approaches leveraging complementary vesicle types, and rigorous safety profiling to facilitate clinical translation. The ongoing refinement of MSC-derived vesicle therapies holds significant promise for addressing the substantial clinical need for effective skin regeneration strategies across diverse wound etiologies.
The transition from cellular to acellular therapies in regenerative medicine has brought small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs) to the forefront of dermatological research. These nanoscale, lipid bilayer-enclosed particles, secreted by virtually all cell types including mesenchymal stem cells (MSCs), function as natural biocommunication systems that transfer functional proteins, lipids, and nucleic acids to recipient cells [24] [14]. Their inherent biocompatibility stems from their endogenous origin and natural lipid bilayer structure, while their low immunogenicity arises from evolutionary conservation and surface molecule profiles that minimize immune activation [25] [14]. This biological foundation positions both sEVs and ApoEVs as promising therapeutic agents, particularly for complex processes like skin regeneration where controlled immune activation and tissue remodeling are critical.
Comparative Analysis of sEVs and ApoEVs for Skin Regeneration
Biophysical Properties and Cargo Composition
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Parameter | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Size Range | < 200 nm [26]; typically 30-150 nm [24] | Highly heterogeneous: 0.1-5 μm [27] [7] |
| Biogenesis Origin | Endosomal pathway (exosomes) or plasma membrane (ectosomes) [24] [26] | Apoptotic cell membrane blebbing and fragmentation [7] |
| Key Markers | Tetraspanins (CD9, CD63, CD81), TSG101, ALIX [24] [26] | Phosphatidylserine exposure, DNA fragments [7] |
| Lipid Composition | Enriched in cholesterol, sphingomyelin, ceramide [24] | Similar to parent cell membrane with increased phosphatidylserine [7] |
| Nucleic Acid Cargo | miRNAs, mRNAs, circRNAs promoting proliferation and angiogenesis [24] | Genomic DNA fragments, distinct miRNA profiles [7] |
| Protein Profile | Growth factors (VEGF, TGF-β, EGF), tetraspanins [24] | Caspase-cleaved proteins, organellar components [7] |
Functional Efficacy in Skin Regeneration Models
Table 2: Therapeutic Efficacy in Preclinical Skin Regeneration Models
| Therapeutic Outcome | sEVs Performance | ApoEVs Performance | Comparative Analysis |
|---|---|---|---|
| Wound Closure Rate | Significantly enhance wound closure in diabetic and non-diabetic models [27] | Apoptotic small EVs (ApoSEVs) show superior efficacy to sEVs [27] | ApoSEVs demonstrate better wound closure outcomes [27] |
| Collagen Deposition | Promote organized collagen deposition [27] | ApoSEVs induce more effective collagen deposition [27] | ApoSEVs show superior collagen remodeling capacity [27] |
| Revascularization | Strong pro-angiogenic effects, increase blood vessel density [27] | Moderate angiogenic potential [27] | sEVs demonstrate better revascularization outcomes [27] |
| Anti-inflammatory Effects | Modulate macrophages toward anti-inflammatory phenotype [14] | Polarize anti-inflammatory macrophages, suppress inflammatory immune cells [7] | Both show significant immunomodulation via different mechanisms |
| Cellular Proliferation | Promote keratinocyte and fibroblast proliferation [24] | Stimulate proliferation through efferocytosis-linked pathways [7] | Both enhance proliferation through distinct signaling mechanisms |
Experimental Protocols for Functional Assessment
Standardized Isolation and Characterization Workflow
In Vivo Wound Healing Assessment Protocol
Animal Models:
- Diabetic Wounds: Streptozotocin (STZ)-induced diabetic mice or genetically modified db/db mice (Type 2 diabetes) [27]
- Non-Diabetic Wounds: Full-thickness excisional dorsal wounds in wild-type mice or rats [27]
- Wound Creation: 6-8mm diameter full-thickness excisional wounds [27]
Treatment Administration:
- Route: Subcutaneous injection around wound periphery vs. topical dressing/covering [27]
- Dosing: Typically 100-500 μg EV protein per application [27]
- Frequency: Multiple administrations (e.g., days 0, 2, 4, 6 post-wounding) [27]
Outcome Measures:
- Primary Endpoint: Wound closure rate measured by planimetry daily [27]
- Histological Analysis: H&E staining for re-epithelialization, Masson's trichrome for collagen deposition [27]
- Immunohistochemistry: CD31 staining for blood vessel density, α-SMA for myofibroblasts [27]
- Scar Assessment: Scar width measurement at endpoint [27]
Mechanism of Action: Signaling Pathways in Skin Regeneration
The Scientist's Toolkit: Essential Research Reagents
Table 3: Critical Reagents for EV Research in Skin Regeneration
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kits, qEV Size Exclusion Columns | Rapid isolation from cell culture media or biofluids | Enable reproducible yields with minimal equipment [26] |
| Characterization Antibodies | Anti-CD9, CD63, CD81, TSG101, ALIX, Annexin V | EV identification, quantification, and subtyping by flow cytometry, WB | MISEV guidelines recommend multiple markers [27] |
| Extracellular Matrix Proteins | Collagen I, Fibronectin, Laminin | Assessment of EV effects on fibroblast function and ECM remodeling | Critical for 3D skin equivalent models [27] |
| Cell Culture Models | Human dermal fibroblasts, HaCaT keratinocytes, HUVECs | In vitro assessment of EV bioactivity | Primary cells preferred over immortalized lines [27] |
| In Vivo Tracking Agents | DIR, DiD lipophilic dyes, GFP/RFP reporters | Biodistribution and pharmacokinetic studies | Confirm EV integrity post-labeling [25] |
| Analytical Instruments | Nanoparticle Tracking Analyzer, TEM, Western Blot | EV quantification, sizing, and characterization | Multi-method approach essential for validation [27] [26] |
Discussion: Clinical Translation Considerations
The therapeutic advantages of biocompatibility and low immunogenicity position both sEVs and ApoEVs as promising clinical candidates, yet they present distinct translational profiles. sEVs benefit from extended research history and established isolation protocols, with 64 registered clinical trials already demonstrating safety and applicability across various diseases, including complex wound healing [14]. Their nanoscale dimensions facilitate enhanced tissue penetration and biological barrier crossing, while their well-characterized pro-angiogenic properties make them particularly suitable for ischemic wound environments [27] [14].
Conversely, ApoEVs present a more complex clinical profile. Their heterogeneous size distribution may create manufacturing challenges for standardized therapeutic applications [7]. However, their superior performance in specific wound healing parameters, particularly wound closure and collagen deposition, indicates unique therapeutic value [27]. The efferocytosis-mediated mechanism of ApoEVs creates a more nuanced immunomodulatory response, potentially offering advantages in chronic inflammatory wound environments [7].
For clinical translation, administration route optimization is critical. Subcutaneous injection has demonstrated superior outcomes compared to topical application for multiple regenerative parameters, including wound closure, collagen deposition, and revascularization [27]. Additionally, source selection impacts therapeutic efficacy, with adipose-derived stem cells (ADSCs) showing particular promise for wound closure, while bone marrow MSCs excel in revascularization potential [27]. The ongoing challenge of standardization in collection conditions, separation methods, storage protocols, and dosing regimens must be addressed before widespread clinical adoption [27] [14].
From Bench to Bedside: Production, Characterization, and Preclinical Application
Standardized Isolation and Purification Techniques
The field of regenerative medicine is increasingly focused on harnessing the therapeutic potential of extracellular vesicles (EVs), particularly for complex applications such as skin regeneration. EVs are broadly categorized based on their biogenesis, size, and content. Small extracellular vesicles (sEVs or exosomes), ranging from 30-150 nm, are of endocytic origin and formed within multivesicular bodies (MVBs) [28] [29]. In contrast, apoptotic vesicles (50-5000 nm) are generated during programmed cell death through membrane blebbing [29] [18]. The distinct biological messages carried by these vesicles—sEVs often mediate intercellular communication, while apoptotic vesicles are primarily involved in clearance of apoptotic cells—lead to dramatically different functional outcomes in skin regeneration, influencing processes like inflammation, collagen synthesis, and tissue remodeling [28] [29] [30]. However, a significant challenge complicates this promising field: the inability of standard isolation methods to perfectly separate these vesicle subtypes from complex biological fluids, leading to heterogeneous preparations and confounding research outcomes [31] [32]. This guide provides a comparative analysis of current isolation and purification techniques, presenting experimental data to help researchers select the optimal method for their specific research on skin regeneration.
Comparative Analysis of Key Isolation Method Performance
The ideal isolation method would be simple, fast, high-throughput, and yield a pure, functional vesicle population. In reality, all methods involve trade-offs between yield, purity, and practicality. The table below summarizes the quantitative performance of common methods based on recent comparative studies.
Table 1: Performance Comparison of sEV Isolation Methods from Plasma/Serum
| Isolation Method | Reported Particle Yield (Particles/mL) | Reported Size Distribution (nm) | Purity (Particle-to-Protein Ratio) | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Ultracentrifugation (UC) [32] [33] | ~1.02E+10 (Plasma) [33] | 45-335 nm [32] | High [31] [33] | Considered the "gold standard"; cost-effective consumables [29] | Time-consuming; low throughput; potential for vesicle damage/aggregation [31] [29] |
| Density Gradient UC (DGUC) [31] | Lower than UC [31] | N/A | Very High [31] | Superior purity by separating particles by density; minimal co-enrichment [31] | Cumbersome preparation; very long duration; low yield [31] [29] |
| Polymer Precipitation (e.g., TEI Kit) [32] [33] | ~1.76E+11 (Plasma) [33] | 45-535 nm (broad distribution) [32] | Low [31] [32] | Simple, fast protocol; high particle yield [32] | High co-precipitation of contaminants (e.g., lipoproteins) [31] [32] |
| Size Exclusion Chromatography (SEC) [31] [33] | Lower than precipitation [33] | Wide variation (heterogeneous) [33] | High [31] [33] | Good purity; maintains vesicle integrity and function [31] | May require sample pre-concentration; can be less effective with complex fluids [31] [33] |
| Tangential Flow Filtration (TFF) [18] | Higher than UC [18] | N/A | Moderate to High [18] | Scalable for manufacturing; gentle on vesicles [18] | Requires specialized equipment [18] |
| Affinity Capture (e.g., MagNet) [31] | Modest yield [31] | Narrowest size distribution [31] | Very High [31] | Exceptional purity and specificity (e.g., PS+ EVs) [31] | High cost; may select for subpopulations [31] |
| Combined Methods (e.g., UCT/CPF) [32] [33] | Intermediate between component methods [32] | 55-385 nm [32] | Moderate to High [32] [33] | Balances yield and purity better than single methods [32] [33] | More complex protocol [32] |
The choice of method profoundly impacts downstream proteomic analysis. A 2025 study found that despite modest yield, affinity-based methods like MagNet and MagCap provided the highest proteome coverage for plasma sEVs, while polymer-based precipitation kits, despite high particle yield, resulted in significant contamination with lipoproteins and other non-EV proteins [31]. Another study comparing UC, a precipitation kit (TEI), and a combined method (UCT) found that UC and UCT isolates from breast cancer cell lines showed higher expression of canonical sEV markers (CD9, CD63, CD81) and higher purity than TEI isolates [32].
Detailed Experimental Protocols for Key Methods
To ensure reproducibility, detailed protocols for three commonly used and contrasted methods are outlined below.
This protocol is considered the traditional benchmark for sEV isolation.
- Sample Preparation: Centrifuge thawed plasma at 3000g for 10 minutes at 4°C to remove cells and debris.
- Dilution and Initial Run: Dilute 100 µL of pre-cleared plasma with 11.9 mL of cold PBS. Transfer to an ultracentrifuge tube. Centrifuge at 150,000g for 3 hours at 4°C using a swinging-bucket rotor.
- Wash Step: Carefully aspirate the supernatant. Resuspend the pellet in 12 mL of PBS.
- Second Run: Centrifuge the resuspended solution again at 120,000g for 3 hours at 4°C.
- Resuspension: Aspirate the supernatant and resuspend the final EV pellet in 100 µL of PBS for downstream analysis.
This method enhances purity by separating particles based on density.
- Gradient Preparation: Layer solutions of iodixanol (OptiPrep) at 5%, 10%, 20%, and 40% (w/v) in PBS sequentially in a 13.2 mL ultracentrifuge tube to form a discontinuous density gradient.
- Sample Loading: Resuspend the crude EV pellet (obtained from an initial UC step) in PBS and carefully overlay it onto the top of the prepared gradient.
- Centrifugation: Centrifuge the gradient at 120,000g for 18 hours at 4°C.
- Fraction Collection: After centrifugation, collect the fraction containing the EVs (typically found within the 6 mL upper fraction).
- Washing and Concentration: Dilute the collected fraction with an equal volume of ice-cold PBS and centrifuge at 120,000g for 4 hours at 4°C to pellet the purified EVs. Resuspend the final pellet in a suitable buffer.
This hybrid method aims to balance the high yield of precipitation with the purity of other methods.
- Precipitation: Mix the biofluid (e.g., plasma, cell culture media) with a polyethylene glycol (PEG)-based precipitation solution. Incubate the mixture overnight at 4°C.
- Low-Speed Centrifugation: Centrifuge the sample at low speed (e.g., 1,500g) for 30 minutes to pellet the precipitated vesicles and contaminants.
- Resuspension: Resuspend the pellet in PBS.
- Two-Step Filtration: Pass the resuspended solution through a 0.22 µm syringe filter to remove larger particles and aggregates.
- Ultrafiltration: Use an ultrafiltration device (e.g., 10-100 kDa molecular weight cutoff) to concentrate the sEVs and remove residual soluble proteins and polymer, exchanging the buffer to PBS.
Functional Pathways in Skin Regeneration
The cargo of sEVs and apoptotic vesicles differentially regulates key signaling pathways in skin cells, leading to distinct regenerative outcomes. sEVs, particularly from mesenchymal stem cells (MSCs), promote a regenerative environment, while apoptotic vesicles can have dual roles, often resolving inflammation but potentially contributing to tissue degradation if not properly cleared.
sEVs promote skin regeneration through several key mechanisms [28] [30]:
- Activation of Regenerative Pathways: sEV cargo, including miRNAs like miR-1246 and growth factors, activates signaling pathways such as TGF-β/Smad and Wnt/β-catenin, which are crucial for tissue repair [28].
- Stimulation of Matrix Synthesis: These activated pathways lead to fibroblast proliferation and increased synthesis of essential extracellular matrix (ECM) components like Type I and III collagen and elastin, improving skin elasticity and thickness [28] [30].
- Inhibition of Matrix Degradation: sEVs can downregulate the expression of matrix metalloproteinases (MMPs) like MMP-1 and MMP-3, thereby protecting the existing collagen structure from degradation [28].
Apoptotic vesicles play a more complex role [29] [30]:
- Proper Clearance and Resolution: The efficient phagocytosis of apoptotic vesicles is critical for resolving inflammation and initiating tissue repair. This process typically promotes an anti-inflammatory environment.
- Contribution to Pathology: However, if not properly cleared, or if derived from stressed cells, their cargo can perpetuate a state of chronic inflammation (inflammaging), which is a known driver of tissue degradation and impaired regeneration, ultimately leading to collagen breakdown [28] [30].
The Scientist's Toolkit: Essential Research Reagents
Successful isolation and characterization require a suite of specific reagents and instruments. The following table details key solutions used in the experiments cited in this guide.
Table 2: Essential Reagents and Kits for EV Isolation and Characterization
| Reagent / Kit Name | Provider Examples | Primary Function in Research | Key Application in EV Studies |
|---|---|---|---|
| MagCapture Exosome Isolation Kit | Fujifilm/Wako [31] | Affinity Enrichment | Isolates phosphatidylserine-positive (PS+) EVs via Tim4 protein binding for high-purity populations. |
| Total Exosome Isolation (TEI) Kit | Invitrogen [32] | Polymer Precipitation | Rapid isolation of high-yield EVs from various biofluids by reducing solubility. |
| qEVsingle / Size Exclusion Columns | Izon Science [31] | Size Exclusion Chromatography | Separates EVs from smaller soluble proteins based on hydrodynamic radius. |
| MagResyn SAX | ReSyn Biosciences [31] | Electrostatic Interaction | Isolates negatively charged EVs using strong anion exchange magnetic resin. |
| OptiPrep Density Gradient Medium | Sigma-Aldrich [31] | Density Gradient Centrifugation | Forms iodixanol-based density gradients for high-purity EV separation in DGUC. |
| Antibodies: CD9, CD63, CD81 | Multiple (e.g., Cell Signaling, R&D Systems) [31] [32] | EV Characterization | Western Blot, Flow Cytometry: Detection of canonical EV surface markers for validation. |
| Antibodies: Apolipoprotein A1/B | R&D Systems [31] | Purity Assessment | Western Blot: Detection of common lipoprotein contaminants in plasma EV preparations. |
The selection of an isolation technique is a foundational decision that directly influences the validity and interpretation of research on vesicles in skin regeneration. No single method is superior in all aspects; the choice must be aligned with the specific research question. For discovery-phase proteomics where purity is paramount, affinity-based methods or DGUC are recommended despite their lower yield [31]. For functional cell-based assays where yield and vesicle integrity are critical, SEC or TFF may be ideal [18]. For high-throughput screening where speed and simplicity are priorities, polymer precipitation remains a popular, if less pure, option [32]. As the field advances, hybrid methods like UCT and CPF that balance multiple performance metrics are showing great promise for comprehensive translational research [32] [33]. Ultimately, rigorous characterization of the isolated vesicle population—using NTA, Western blot, and EM—is non-negotiable, and reporting the isolation methodology in detail is essential for reproducibility and scientific progress in the quest to harness vesicles for regenerative medicine.
In the rapidly advancing field of vesicle-based therapies for skin regeneration, the critical characterization of small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) forms the foundation of rigorous research and reliable therapeutic application. Accurate differentiation between these vesicle types is paramount, as their distinct biological origins and compositions directly influence their mechanistic roles and functional outcomes in wound healing, skin repair, and regeneration. This guide provides a systematic comparison of the essential characterization metrics—size, morphology, and surface markers—enabling researchers to make informed decisions when selecting vesicle types for specific dermatological applications and ensuring reproducibility across experimental studies.
Comparative Analysis of Fundamental Physical Properties
The physical properties of sEVs and ApoEVs directly reflect their different biogenesis pathways and influence their biological functions and therapeutic potential. The table below summarizes their key distinguishing characteristics.
Table 1: Comparative Physical Properties of sEVs and ApoEVs
| Characteristic | Small Extracellular Vesicles (sEVs) | Apoptotic Extracellular Vesicles (ApoEVs) |
|---|---|---|
| Size Range | 30-200 nm [26] [14] | 50-5000 nm, with subpopulations of ApoSEVs (<1 μm) and ApoBDs (1-5 μm) [5] [34] |
| Morphology | Cup-shaped, spherical; observed via Transmission Electron Microscopy (TEM) [18] [26] | Highly heterogeneous; includes spherical, irregular shapes, and complex structures [34] |
| Biogenesis Origin | Endosomal system; released upon MVB fusion with plasma membrane [6] [14] | Plasma membrane blebbing and cell fragmentation during apoptosis [35] [34] |
| Key Biogenesis Regulators | ESCRT complexes, Rab GTPases, tetraspanins (CD9, CD63, CD81) [26] | ROCK1, MLCK, caspase-mediated cleavage of structural proteins [34] |
Surface Marker Profiles and Functional Implications
Surface markers serve as essential fingerprints for vesicle identification, quality control, and functional prediction. The proteomic and lipidic landscape of sEVs and ApoEVs reveals their origins and suggests their mechanistic roles.
Table 2: Surface Marker and Cargo Profiles of sEVs and ApoEVs
| Component | Small Extracellular Vesicles (sEVs) | Apoptotic Extracellular Vesicles (ApoEVs) |
|---|---|---|
| Universal EV Markers | Tetraspanins (CD9, CD63, CD81), TSG101, Alix [18] [26] | Tetraspanins (CD9, CD63, CD81), TSG101, Alix [34] |
| Distinctive Markers | Flotillin-1, MHC classes [6] | Phosphatidylserine (PS) externalization, Caspase-3 [35] [34] |
| Lipid Composition | Enriched in cholesterol, sphingomyelin, ceramide [6] | High in phosphatidylserine; substrates for enzymes like sPLA2-X [35] |
| Characteristic Cargo | Growth factors (VEGF, TGF-β, EGF), miRNAs (e.g., miR-21-3p, miR-27b) [6] | Nuclear fragments, mitochondrial components, amplified parent cell cargo [34] |
The externalized phosphatidylserine (PS) on ApoEVs is not merely a marker but a critical functional component. It acts as an "eat-me" signal for phagocytic cells like macrophages, promoting clearance of apoptotic debris and actively modulating the immune response. This lipid also serves as a substrate for enzymes like group X secretory phospholipase A2 (sPLA2-X), generating anti-inflammatory lipid mediators such as resolvin D5 (RvD5) that accelerate cutaneous wound healing [35].
Experimental Characterization Workflows
A robust characterization pipeline is non-negotiable for definitive vesicle identification. The following workflow integrates multiple complementary techniques to confirm vesicle identity and purity.
Detailed Experimental Protocols
1. Nanoparticle Tracking Analysis (NTA)
- Principle: Tracks Brownian motion of individual particles in suspension to calculate hydrodynamic diameter and concentration.
- Protocol: Dilute purified vesicle samples in sterile, particle-free PBS to achieve an ideal concentration of 10^8-10^9 particles/mL. Load into the sample chamber of an NTA instrument (e.g., Malvern NanoSight). Capture multiple 60-second videos, ensuring particle count per frame is within the manufacturer's recommended range (20-100 particles/frame). Analyze data with built-in software to determine mean, mode, and distribution of vesicle size and concentration.
2. Transmission Electron Microscopy (TEM)
- Principle: Provides high-resolution images to assess vesicle morphology and ultrastructure.
- Protocol: Adsorb vesicles onto a Formvar/carbon-coated EM grid by floating the grid on a 10 μL drop of sample for 10-20 minutes. Fix with 2.5% glutaraldehyde, then contrast with 1-2% uranyl acetate. Alternatively, use phosphotungstic acid for negative staining. Wash gently with distilled water and air-dry thoroughly. Image using a TEM operated at 80-100 kV. The classic "cup-shape" of sEVs is a common artifact of chemical fixation and dehydration [18].
3. Western Blot Analysis
- Principle: Detects presence or absence of specific protein markers to confirm vesicle type and purity.
- Protocol: Lyse vesicles in RIPA buffer with protease inhibitors. Determine protein concentration via BCA assay. Separate 10-30 μg of protein by SDS-PAGE and transfer to a PVDF membrane. Block with 5% non-fat milk or BSA. Probe overnight at 4°C with primary antibodies against:
- Positive Markers: CD9, CD63, CD81 (tetraspanins), TSG101, Alix (ESCRT-associated) [18].
- Negative Markers: Calnexin (endoplasmic reticulum marker, indicates cellular contamination) [18].
- Apoptosis Marker: Cleaved Caspase-3 (for ApoEVs) [35]. Incubate with appropriate HRP-conjugated secondary antibodies and develop using enhanced chemiluminescence.
4. Flow Cytometry for Surface Markers
- Principle: Identifies and quantifies surface antigens on vesicles.
- Protocol: Vesicles must be captured or enlarged for detection on standard flow cytometers. Bind vesicles to aldehyde/sulfate latex beads via incubation and gentle rotation. Block unoccupied sites with BSA or glycine. Incubate bead-bound vesicles with fluorochrome-conjugated antibodies against surface markers (e.g., CD9, CD63, CD81) or Annexin V (to detect PS exposure). Include isotype controls. Analyze on a flow cytometer; high-throughput advanced flow cytometers are now capable of analyzing individual nanosized vesicles without beads.
The Scientist's Toolkit: Essential Research Reagents
Successful characterization requires a suite of reliable reagents and instruments. The table below details key solutions for comprehensive vesicle analysis.
Table 3: Essential Research Reagent Solutions for Vesicle Characterization
| Reagent/Kit | Primary Function | Application Context |
|---|---|---|
| Anti-tetraspanin Antibodies (CD9, CD63, CD81) | Immunodetection of conserved EV surface proteins | Western Blot, Flow Cytometry, Immuno-EM for general EV identification [18] [26] |
| Annexin V (FITC/APC conjugated) | Detection of phosphatidylserine (PS) exposure | Flow Cytometry to distinguish ApoEVs via PS externalization [35] [34] |
| Anti-Caspase-3 (Cleaved) Antibody | Detection of activated caspase-3, an apoptosis executor | Western Blot to confirm apoptotic origin of ApoEVs [35] |
| Particle-Free PBS/BSA | Diluent and blocking agent | Sample preparation for NTA and blocking in immunoassays to prevent non-specific binding [18] |
| Uranyl Acetate / Phosphotungstic Acid | Negative stain for electron microscopy | Enhances contrast for TEM morphological analysis [18] |
| Exosome Isolation Kits (e.g., polymer-based) | Rapid isolation of EVs from biofluids/cell media | Alternative to ultracentrifugation for fast preparation [26] |
| NTA Instrumentation (e.g., NanoSight) | High-resolution size and concentration analysis | Critical quality control for all EV preparations [18] |
Functional Correlation and Therapeutic Selection
The distinct physical and biochemical profiles of sEVs and ApoEVs translate directly to their differential performance in skin regeneration models. A systematic review and meta-analysis of preclinical studies revealed that ApoSEVs (a subtype of ApoEVs <1μm) demonstrated superior efficacy in promoting wound closure and enhancing collagen deposition compared to sEVs and larger apoptotic bodies (ApoBDs). In contrast, sEVs were more effective in promoting revascularization at the wound site [5]. This functional specialization should guide therapeutic selection: ApoSEVs may be preferred for re-epithelialization and matrix remodeling, while sEVs might be optimal for angiogenic applications.
Furthermore, the route of administration influences therapeutic outcomes. The same meta-analysis indicated that subcutaneous injection of MSC-EVs yielded better outcomes for wound closure, collagen deposition, and revascularization compared to topical dressing/covering [5]. The choice of MSC source also matters, with adipose-derived MSCs (ADSCs) showing superior effects on wound closure, while bone marrow MSCs (BMMSCs) excelled in revascularization [5].
The path to successful clinical translation of vesicle-based therapies for skin regeneration is paved with precise characterization. By systematically applying the metrics of size, morphology, and surface marker profiling, researchers can not only ensure the purity and identity of their vesicle preparations but also make informed predictions about their functional potential. The emerging consensus is that sEVs and ApoEVs are not interchangeable but rather complementary agents in the regenerative medicine toolkit, each with specialized roles dictated by their fundamental biological properties. Adherence to these critical characterization standards will accelerate the development of reproducible, safe, and effective vesicle-based therapeutics for a spectrum of dermatological conditions.
The pursuit of effective therapeutic strategies for skin regeneration has increasingly focused on extracellular vesicles (EVs) as promising cell-free alternatives to whole-cell therapies. These nano-sized and micro-sized lipid bilayer particles, capable of transferring functional proteins, lipids, and nucleic acids to recipient cells, play crucial roles in modulating wound healing processes, including inflammation, angiogenesis, and tissue remodeling [8] [6]. Among EVs, small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs) have emerged as distinct entities with significant yet different therapeutic potential. sEVs (30-200 nm), which include exosomes and small ectosomes, are derived from the endosomal system or plasma membrane of living cells and are rich in signaling molecules [26] [36]. In contrast, ApoEVs (50-5000 nm) are produced during programmed cell death and can be further classified into apoptotic small EVs (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm) [34]. The therapeutic efficacy of these vesicles is critically dependent on their delivery strategy, with administration route and dosing parameters significantly influencing their bioavailability, targeting efficiency, and ultimate regenerative outcomes. This guide objectively compares the current experimental data and methodologies for optimizing the delivery of sEVs versus ApoEVs in skin regeneration models.
Isolation and Characterization Methods: Implications for Dosing
The therapeutic potential of vesicles is fundamentally influenced by their isolation and characterization methods, which directly impact yield, purity, and biological activity. Different isolation techniques can significantly affect the particle yields and characteristics, thereby influencing subsequent dosing decisions.
Table 1: Comparison of Major Vesicle Isolation Methods
| Method | Principle | Advantages | Disadvantages | Impact on Dosing |
|---|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation at increasing speeds | Considered "gold standard"; handles large sample volumes [26] | Time-consuming; high speeds may damage vesicle integrity [26] | Lower yield may require higher starting material for therapeutic doses |
| Tangential Flow Filtration (TFF) | Size-based separation using tangential flow | Higher particle yields than UC; scalable for GMP production [18] | Requires specialized equipment; membrane fouling possible | Higher yields potentially reduce production costs for clinical dosing |
| Density Gradient Centrifugation | Separation based on buoyant density | High purity [26] | Time-consuming; may damage vesicles [26] | High purity beneficial for precise dosing but lower yield |
| Size-Exclusion Chromatography (SEC) | Separation by size through porous matrix | Preserves vesicle integrity; good reproducibility | Limited sample volume; dilution of sample | Maintains functionality but may require concentration steps before dosing |
| Polymer-Based Precipitation | Reduced solubility and dispersion of vesicles | Simple protocol; no specialized equipment needed | Co-precipitation of contaminants; lower purity [26] | Potential impurities may affect dosing accuracy and therapeutic efficacy |
Experimental data directly comparing isolation methods demonstrates that tangential flow filtration (TFF) provides statistically higher particle yields compared to ultracentrifugation (UC) when isolating BM-MSC-sEVs [18]. This yield advantage has significant implications for scaling up production for therapeutic applications where large, consistent doses are required.
The characterization of isolated vesicles is equally critical for standardizing dosing parameters. According to MISEV guidelines, characterization should include:
- Nanoparticle Tracking Analysis (NTA) for determining particle size distribution and concentration [18] [9]
- Transmission Electron Microscopy (TEM) for visualizing cup-shaped morphology [18]
- Western Blotting for detecting surface markers (CD9, CD63, CD81) and luminal proteins (TSG101, ALIX) [18] [9]
- Tunable Resistive Pulse Sensing (TRPS) for additional particle characterization [9]
Figure 1: Vesicle Isolation and Characterization Workflow for Dosing Determination
Therapeutic Efficacy Comparison: sEVs vs. ApoEVs
Direct comparative studies between sEVs and ApoEVs in skin regeneration models provide valuable insights for therapeutic optimization. A recent systematic review and meta-analysis of 83 preclinical studies revealed distinct therapeutic advantages for each vesicle type based on specific regenerative parameters [5].
Table 2: Comparative Efficacy of sEVs and ApoEVs in Skin Regeneration
| Therapeutic Outcome | sEVs Performance | ApoEVs Performance | Comparative Efficacy |
|---|---|---|---|
| Wound Closure Rate | Enhanced wound closure in diabetic and non-diabetic models [8] [5] | ApoSEVs superior to ApoBDs and sEVs [5] | ApoSEVs > sEVs > ApoBDs |
| Revascularization | Promote angiogenesis via Wnt/β-catenin, PI3K/Akt pathways [6] [5] | Moderate pro-angiogenic effects | sEVs > ApoEVs |
| Collagen Deposition | Improve collagen organization and density [5] | ApoSEVs show best outcomes [5] | ApoSEVs > sEVs > ApoBDs |
| Scar Width | Reduce scar formation [5] | Not fully characterized | sEVs demonstrated efficacy |
| Anti-inflammatory Effects | Promote M2 macrophage polarization; reduce inflammatory cytokines [8] [6] | ApoSEVs promote specific macrophage polarization [5] | Both effective; mechanisms differ |
The meta-analysis demonstrated that ApoSEVs showed better efficacy than both ApoBDs and sEVs in wound closure outcomes and collagen deposition, while sEVs displayed superior performance in revascularization [5]. These distinctions highlight the importance of matching vesicle type to therapeutic objectives when designing treatment strategies.
Mechanistically, sEVs from mesenchymal stem cells enhance healing through multiple pathways. For instance, sEVs from human umbilical cord MSCs (HUMSCs) promote angiogenesis through the Wnt4/β-catenin pathway and the PI3K/Akt signaling axis [6]. Additionally, sEV-loaded miRNAs such as miR-21-3p activate ERK1/2 signaling to enhance fibroblast function and angiogenesis [6], while miR-181c downregulates TLR4-NF-κB signaling to reduce inflammatory cytokine production [6].
Figure 2: Comparative Mechanisms of sEVs and ApoEVs in Skin Regeneration
Administration Routes and Dosing Strategies
The route of administration significantly influences the therapeutic efficacy of vesicles in skin regeneration. Current evidence from preclinical studies indicates that subcutaneous injection demonstrates superior outcomes compared to topical application (dressing/covering) across multiple regenerative parameters [5].
Administration Routes
Subcutaneous Injection: This method has shown greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering approaches [5]. The injection approach likely facilitates deeper tissue penetration and longer retention of vesicles at the wound site.
Topical Application: While convenient, topical delivery may face limitations in penetration through damaged skin barriers, potentially reducing bioavailability to target cells in the wound bed.
The choice of administration route should consider wound characteristics, with subcutaneous injection particularly advantageous for deeper wounds where targeted delivery to dermal and subcutaneous tissues is required.
Dosing Considerations
Dosing of therapeutic vesicles varies considerably across studies, reflecting differences in vesicle sources, isolation methods, and disease models. However, some general patterns emerge from the literature:
Dose Range: Effective dosing of MSC-sEVs in preclinical wound healing studies typically ranges from 10 to 100 μg per application, with 50 μg/mL demonstrating significant therapeutic effects in ARPE-19 cell protection models [18].
Dosing Frequency: Multiple administrations often yield superior results compared to single doses, supporting the need for sustained presence of vesicles throughout the healing process.
Source-Dependent Potency: The tissue origin of parent MSCs influences therapeutic potency. Research indicates that adipose-derived MSC-sEVs (ADSC-sEVs) demonstrate the best effect on wound closure rate and collagen deposition, while bone marrow MSC-sEVs (BMMSC-sEVs) show superior revascularization potential [5].
Table 3: Experimentally-Tested Dosing Regimens in Preclinical Studies
| Vesicle Type | Effective Dose | Administration Route | Frequency | Model System | Key Outcomes |
|---|---|---|---|---|---|
| BM-MSC-sEVs | 50 μg/mL | Intravitreal (ocular) | Single dose | ARPE-19 cells with H₂O₂ damage [18] | Increased cell viability from 37.86% to 54.60% |
| MSC-sEVs | 10-100 μg | Subcutaneous injection | Multiple doses | Diabetic mouse wound model [5] | Enhanced wound closure, angiogenesis, collagen deposition |
| ApoSEVs | Varies by preparation | Subcutaneous injection | Multiple doses | Mouse wound model [5] | Superior wound closure and collagen deposition vs. sEVs |
| HUMSC-sEVs | Not specified | Topical/subcutaneous | Multiple doses | Rodent wound models [6] | Promoted angiogenesis, M2 macrophage polarization |
Research Reagent Solutions and Methodological Toolkit
Standardized reagents and methodologies are crucial for ensuring reproducible research on vesicle-based therapeutics. The following toolkit outlines essential materials and their applications in vesicle research for skin regeneration.
Table 4: Essential Research Reagent Solutions for Vesicle Studies
| Reagent/Material | Function/Application | Experimental Considerations |
|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free supplement for MSC culture [18] | Supports expansion of MSCs for vesicle production under GMP conditions |
| Alpha Minimum Essential Medium (α-MEM) | Culture medium for BM-MSCs [18] | Shows higher cell proliferation and vesicle yields compared to DMEM |
| Dulbecco's Modified Eagle Medium (DMEM) | Alternative culture medium for MSCs [18] | Yields lower vesicle production compared to α-MEM |
| CD63/CD81/CD9 Antibodies | Vesicle characterization via Western blot [18] [9] | Confirm presence of tetraspanins as sEV markers |
| TSG101/ALIX Antibodies | Detection of luminal vesicle markers [9] | Additional confirmation of vesicle identity |
| Annexin V | Apoptosis detection for ApoEV studies [34] | Identifies phosphatidylserine exposure on ApoEVs |
| Nanoparticle Tracking Analyzer | Size distribution and concentration analysis [18] [9] | Essential for quantifying and characterizing vesicle preparations |
| Transmission Electron Microscope | Morphological analysis of vesicles [18] | Visualizes cup-shaped morphology of sEVs |
| Flow Cytometer | Analysis of MSC surface markers and vesicle uptake [18] [9] | Confirms MSC identity (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-) |
The optimization of delivery strategies for sEVs and ApoEVs in skin regeneration requires careful consideration of multiple interrelated factors. Current evidence indicates that ApoSEVs demonstrate superior performance in wound closure and collagen deposition, while sEVs excel in promoting revascularization. The subcutaneous route of administration appears more effective than topical applications, likely due to enhanced bioavailability to target tissues. Dosing regimens should be tailored based on vesicle type, source, and specific therapeutic objectives, with most effective protocols utilizing multiple administrations in the 10-100 μg range.
Significant challenges remain in standardizing production methods, characterizing functional cargo, and optimizing dosing regimens for clinical translation. The high heterogeneity observed in collection conditions, separation methods, storage protocols, and treatment parameters across studies underscores the urgent need for standardized guidelines [5]. Future research should focus on elucidating the precise mechanisms of vesicle uptake and signaling in skin cells, engineering vesicles for enhanced targeting and functionality, and conducting well-controlled comparative studies to establish evidence-based dosing protocols. As the field advances, vesicle-based therapies hold immense promise for addressing the growing clinical need for effective skin regeneration strategies, particularly in challenging diabetic and aged wound healing contexts.
Mechanisms of Action in Skin Regeneration
The quest for effective strategies to promote skin regeneration has led to the exploration of cell-free therapies, particularly those utilizing natural biological nanoparticles. Among these, extracellular vesicles (EVs) have emerged as promising therapeutic agents. This guide focuses on two distinct types: small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs). sEVs (30-200 nm in diameter) are primarily secreted by living cells and include exosomes and microvesicles, while ApoEVs (50-5000 nm) are generated during programmed cell death [26] [34]. Both function as intercellular communication vehicles by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating skin regeneration processes [11] [7]. Understanding their comparative mechanisms, efficacy, and optimal application is crucial for researchers and drug development professionals advancing regenerative dermatology.
sEVs and ApoEVs differ fundamentally in their biogenesis, physical characteristics, and cargo composition, which directly influences their functional roles in skin biology.
Small Extracellular Vesicles (sEVs) are predominantly released through the endosomal pathway or by direct budding from the plasma membrane of viable cells [14]. The endosomal pathway involves the formation of intraluminal vesicles within multivesicular bodies (MVBs), which subsequently fuse with the plasma membrane to release exosomes. In contrast, microvesicles bud directly from the cell surface [26]. These vesicles are characterized by the presence of tetraspanin markers (CD9, CD63, CD81) and endosomal-associated proteins like TSG101 [11] [18].
Apoptotic Extracellular Vesicles (ApoEVs) are produced during the execution phase of apoptosis through a process termed "apoptotic membrane blebbing." This process is rigorously controlled by caspase-mediated activation of kinases, including Rho-associated protein kinase 1 (ROCK1) and myosin light chain kinase (MLCK), which drive cytoskeletal contraction and membrane budding [34]. ApoEVs constitute a heterogeneous population that includes large apoptotic bodies (1-5 μm) and smaller apoptotic vesicles (ApoSEVs, <1 μm) [5] [34]. Recent research indicates that these subpopulations may have distinct and sometimes opposing biological functions in regeneration [34].
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Characteristic | Small Extracellular Vesicles (sEVs) | Apoptotic Extracellular Vesicles (ApoEVs) |
|---|---|---|
| Size Range | 30-200 nm [26] | 50-5000 nm [34] |
| Cellular Origin | Living, healthy cells [14] | Cells undergoing programmed cell death (apoptosis) [34] |
| Biogenesis Pathway | Endosomal system (exosomes) or plasma membrane budding (microvesicles) [26] [14] | Apoptotic membrane blebbing and cellular fragmentation [34] |
| Key Regulators of Formation | ESCRT complexes, Rab GTPases [26] | ROCK1, MLCK, caspases [34] |
| Common Markers | CD9, CD63, CD81, TSG101 [11] [18] | Phosphatidylserine exposure, specific markers less defined [7] |
Quantitative Comparison of Therapeutic Efficacy
Preclinical studies directly comparing the regenerative potential of MSC-derived sEVs and ApoEVs provide compelling evidence for their differential effectiveness across various wound healing parameters. A recent systematic review and meta-analysis of 83 preclinical studies offers crucial comparative data [5].
Wound Closure and Collagen Deposition: The meta-analysis revealed that apoptotic small extracellular vesicles (ApoSEVs) demonstrated superior efficacy in promoting wound closure and enhancing collagen deposition compared to both sEVs and larger apoptotic bodies (ApoBDs) [5]. This suggests that the smaller apoptotic vesicle fraction is particularly potent in stimulating re-epithelialization and extracellular matrix remodeling.
Revascularization Potential: In contrast, sEVs derived from living MSCs exhibited more robust effects on blood vessel density at the wound site compared to ApoEVs. This indicates a specialized role for sEVs in promoting angiogenesis, a critical process for supplying nutrients and oxygen to regenerating tissue [5].
Source-Dependent Variability: The cellular origin of vesicles significantly influences their therapeutic performance. For wound closure rate and collagen deposition, vesicles from adipose-derived stem cells (ADSCs) showed the best outcomes, while for revascularization, bone marrow MSC-derived vesicles were most effective [5].
Table 2: Comparative Efficacy of MSC-Derived Vesicles in Preclinical Wound Healing Models
| Therapeutic Parameter | sEVs Performance | ApoEVs Performance | Performance Notes |
|---|---|---|---|
| Wound Closure Rate | Effective | Superior (ApoSEVs) [5] | ApoSEVs outperform ApoBDs and sEVs |
| Collagen Deposition | Effective | Superior (ApoSEVs) [5] | Enhanced matrix remodeling with ApoSEVs |
| Revascularization (Blood Vessel Density) | Superior [5] | Effective | sEVs show stronger pro-angiogenic effects |
| Optimal MSC Source | Bone Marrow (for revascularization) [5] | Adipose Tissue (for closure/collagen) [5] | Source significantly impacts efficacy |
| Administration Route Efficacy | Subcutaneous injection superior to topical dressing [5] | Subcutaneous injection superior to topical dressing [5] | Injection enhances bioavailability |
Molecular Mechanisms and Signaling Pathways
The distinct regenerative outcomes of sEVs and ApoEVs stem from their differential engagement with specific molecular pathways in target skin cells, including keratinocytes, fibroblasts, and immune cells.
sEV-Mediated Signaling in Skin Regeneration
sEVs derived from mesenchymal stem cells promote skin regeneration through multiple coordinated mechanisms:
- Anti-inflammatory Signaling: sEVs modulate the NF-κB pathway, reducing the expression of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6. This creates a favorable microenvironment for regeneration [11].
- Extracellular Matrix Remodeling: sUVs inhibit the MAPK/AP-1 signaling pathway, leading to decreased expression of matrix metalloproteinases (MMPs). This reduction in MMP activity limits collagen degradation and helps preserve the extracellular matrix structure [11].
- Oxidative Stress Reduction: Through delivery of specific cargo, sEVs activate the PI3K/Akt pathway and SIRT1-dependent antioxidant pathways. This enhances cell viability under oxidative stress conditions and promotes autophagy, thereby mitigating damage from reactive oxygen species (ROS) [11].
- Promotion of Angiogenesis: sEVs transfer pro-angiogenic miRNAs and proteins that activate VEGF and HIF-1α signaling pathways, stimulating endothelial cell proliferation and new blood vessel formation [5] [14].
sEV Signaling in Skin Regeneration: This diagram illustrates how sEV cargo components modulate specific cellular pathways to promote skin regeneration through enhanced cell proliferation, reduced inflammation and oxidative stress, extracellular matrix preservation, and angiogenesis.
ApoEV-Mediated Signaling in Skin Regeneration
ApoEVs engage distinct mechanistic pathways to promote skin repair:
- Immunomodulation via Efferocytosis: ApoEVs are actively engulfed by phagocytes (particularly macrophages) through the process of efferocytosis. This clearance mechanism promotes polarization of macrophages toward an anti-inflammatory M2 phenotype, characterized by the release of regenerative cytokines such as TGF-β and IL-10, which resolve inflammation and support tissue repair [7] [34].
- T-cell Regulation: ApoEVs can directly interact with T helpers in the immune system, potentially suppressing pro-inflammatory Th1 and Th17 responses while activating regulatory T cells (Tregs). This immunomodulatory action is particularly beneficial in chronic inflammatory wound environments [7].
- Activation of Regenerative Programs: Emerging evidence suggests that ApoEVs can initiate autophagy in recipient cells, a catabolic process essential for cellular homeostasis and tissue regeneration [7].
- S1P/S1PR Signaling: ApoEVs may influence the sphingosine-1-phosphate (S1P) signaling pathway, which plays a crucial role in regulating immune cell migration, vascular integrity, and inflammatory responses [7].
ApoEV Signaling in Skin Regeneration: This diagram illustrates how ApoEVs are taken up by phagocytes through efferocytosis, leading to immunomodulation and activation of regenerative programs that resolve inflammation and promote tissue repair.
Experimental Protocols and Methodological Considerations
Robust experimental design is essential for evaluating the therapeutic potential of sEVs and ApoEVs. Below are key methodological considerations and protocols derived from recent studies.
Vesicle Isolation and Characterization
Isolation Techniques:
- Differential Ultracentrifugation: Considered the "gold standard" for sEV isolation, this method employs sequential centrifugation steps at increasing speeds (typically culminating at 100,000-120,000 × g) to pellet vesicles based on size and density [26] [18]. However, prolonged high-speed centrifugation may damage vesicle integrity.
- Tangential Flow Filtration (TFF): This scalable method uses recirculating flow across membrane filters to separate vesicles based on size. Recent comparative studies indicate TFF provides higher particle yields compared to ultracentrifugation while maintaining biological activity, making it promising for clinical translation [18].
- Density Gradient Centrifugation: This technique separates vesicles based on buoyant density, resulting in higher purity preparations by effectively contaminating proteins and lipoproteins [26].
Characterization Protocols:
- Nanoparticle Tracking Analysis (NTA): Measures the size distribution and concentration of vesicles in suspension by tracking their Brownian motion [18]. sEVs typically show a peak size distribution of 100-150 nm, while ApoEV preparations are more heterogeneous.
- Transmission Electron Microscopy (TEM): Provides high-resolution morphological assessment, revealing the characteristic cup-shaped morphology of sEVs or the more heterogeneous appearance of ApoEVs [18].
- Western Blotting: Confirms the presence of vesicle-associated markers (CD9, CD63, CD81, TSG101 for sEVs) and the absence of negative markers (e.g., calnexin, GM130) to assess preparation purity [18].
- Imaging Flow Cytometry: An emerging technology that allows for multiparametric analysis of vesicle subpopulations using specific surface markers, enabling detailed characterization of heterogeneous samples [37].
Table 3: Standard Characterization Parameters for sEVs and ApoEVs
| Characterization Method | Key Parameters | Expected Results for sEVs | Expected Results for ApoEVs |
|---|---|---|---|
| Nanoparticle Tracking Analysis | Size distribution, concentration | Peak: 100-150 nm [18] | Heterogeneous: 50-5000 nm [34] |
| Transmission Electron Microscopy | Morphology, membrane integrity | Cup-shaped vesicles [18] | Heterogeneous morphology [34] |
| Western Blotting | Protein marker expression | CD9+, CD63+, CD81+, TSG101+ [18] | Phosphatidylserine exposure [7] |
| Imaging Flow Cytometry | Surface marker profiling | CD9+, CD63+, CD81+ [37] | Variable marker expression [34] |
Functional Assessment in Skin Regeneration Models
In Vitro Models:
- Fibroblast Migration and Proliferation Assays: Scratch/wound healing assays and standardized proliferation assays (e.g., MTT, CCK-8) evaluate the potential of vesicles to promote cell movement and growth [5] [11].
- Oxidative Stress Protection Models: Pretreatment of keratinocytes or fibroblasts with vesicles followed by exposure to UV radiation or H₂O₂ to assess protective effects against oxidative damage. Cell viability is typically measured 24 hours post-insult [11] [18].
- Angiogenesis Assays: Tube formation assays using human umbilical vein endothelial cells (HUVECs) plated on Matrigel to quantify the pro-angiogenic potential of vesicles [5].
In Vivo Models:
- Full-Thickness Excisional Wounds: The most common model involves creating dorsal wounds in mice or rats, with test articles applied via subcutaneous injection or topical dressing. Wound closure is monitored planimetrically over 7-21 days [5].
- Diabetic Wound Models: Induced by streptozotocin (type 1 diabetes) or using genetically modified db/db mice (type 2 diabetes) to mimic impaired healing conditions [5].
- Histological Analysis: Harvested wound tissue is assessed for re-epithelialization, collagen deposition (Masson's trichrome or Picrosirius red staining), blood vessel density (CD31 immunohistochemistry), and immune cell infiltration [5].
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of sEV and ApoEV biology requires specific reagents and methodologies. The following table outlines key solutions for researchers in this field.
Table 4: Essential Research Reagents for EV Studies in Skin Regeneration
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Vesicle Isolation Kits | Polymer-based precipitation kits, Size-exclusion chromatography columns | Isolation of vesicles from conditioned media or biological fluids | Rapid isolation with preserved bioactivity; suitable for different sample volumes |
| Characterization Antibodies | Anti-CD9, Anti-CD63, Anti-CD81, Anti-TSG101, Anti-calnexin (negative marker) | Western blotting, Imaging flow cytometry, Immuno-EM | Verification of vesicle identity and assessment of preparation purity |
| Cell Culture Media | α-MEM, DMEM, Xeno-free media with human platelet lysate [18] | MSC expansion and vesicle production | Optimization of cell growth and vesicle yield under defined culture conditions |
| Functional Assay Kits | CCK-8 proliferation assay, Caspase-3 activity assay, ROS detection kits | In vitro assessment of vesicle bioactivity | Quantification of effects on cell viability, apoptosis, and oxidative stress |
| Animal Model Supplies | Sterile wound creation tools (biopsy punches), Hydrogel dressings, Osmotic pumps | Preclinical efficacy testing in rodent wound models | Standardized wound creation and controlled vesicle delivery in vivo |
| Engineering Tools | Electroporation systems, Transfection reagents (for parent cell modification) | Vesicle loading with therapeutic cargo | Production of engineered vesicles with enhanced regenerative capacity |
sEVs and ApoEVs represent distinct biological entities with unique mechanisms of action in skin regeneration. The current evidence suggests a complementary rather than competitive relationship: ApoSEVs excel in promoting wound closure and collagen deposition, while sEVs demonstrate superior angiogenic capacity [5]. These functional differences likely stem from their divergent cellular origins and cargo compositions.
Future research directions should focus on:
- Standardization of isolation protocols to reduce heterogeneity and improve reproducibility [5] [14]
- Engineering approaches to enhance targeting specificity and therapeutic potency [38] [34]
- Detailed cargo profiling to identify the specific molecular mediators responsible for observed regenerative effects
- Advanced delivery systems such as hydrogels and microneedles to improve vesicle retention and bioavailability in the wound environment [11] [38]
For drug development professionals, these insights suggest a potential strategic approach: ApoSEV-enriched preparations may be optimal for re-epithelialization and matrix restoration, while sEV-based products might be preferable for vascularization-deficient wounds. As the field progresses toward clinical translation, understanding these nuanced mechanistic differences will be essential for designing effective, evidence-based regenerative therapies tailored to specific patient needs and wound types.
Preclinical Efficacy in Animal Models of Wound Healing and Photoaging
The search for effective therapies in skin regeneration has increasingly focused on cell-free approaches, particularly extracellular vesicles (EVs). Among these, small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) have emerged as promising therapeutic agents with distinct biological properties and functional mechanisms. This comparison guide provides a systematic evaluation of the preclinical efficacy of sEVs versus ApoEVs based on current animal model research, focusing on their applications in wound healing and photoaging. The content is structured to assist researchers and drug development professionals in making evidence-based decisions for their therapeutic development strategies by providing direct comparative data on vesicle performance, optimized experimental protocols, and mechanistic insights.
Quantitative Efficacy Comparison in Animal Models
Comparative Therapeutic Efficacy Metrics
Table 1: Direct comparison of sEV and ApoEV therapeutic outcomes in preclinical wound healing models
| Performance Parameter | sEVs (Pooled Data) | ApoSEVs (<1 μm) | ApoBDs (1-5 μm) |
|---|---|---|---|
| Wound Closure Rate | Standard improvement | Superior efficacy | Inferior to ApoSEVs |
| Scar Width Reduction | Moderate effect | Not reported | Not reported |
| Blood Vessel Density | Significant improvement | Moderate effect | Not reported |
| Collagen Deposition | Moderate enhancement | Superior efficacy | Inhibitory effects observed |
| Macrophage Polarization | Promotes M2 phenotype | Promotes M2 phenotype | Variable effects |
Source: Meta-analysis of 83 preclinical studies [5]
Table 2: Efficacy based on administration route and vesicle source (pooled data from diabetic and non-diabetic models)
| Factor | Optimal Choice | Performance Notes |
|---|---|---|
| Administration Route | Subcutaneous injection | Superior to dressing/covering for closure, collagen deposition, and revascularization |
| sEV Source (Wound Closure) | Adipose-derived MSCs (ADSCs) | Best effect on wound closure rate |
| sEV Source (Revascularization) | Bone marrow MSCs (BMMSCs) | Superior angiogenic potential |
| Vesicle Type (Overall) | ApoSEVs | Better wound closure and collagen deposition than sEVs and ApoBDs |
Source: Subgroup analysis of preclinical studies [5]
Key Findings from Meta-Analysis
A comprehensive meta-analysis of 83 preclinical studies published between 2015-2024 revealed that both sEVs and ApoEVs demonstrate significant potential for wound healing and skin regeneration in animal models [5]. The analysis included 61 mouse models (73.5%) and 22 rat models (26.5%), with 47% focusing on diabetic wounds and 43.4% on non-diabetic wounds [5].
The data demonstrates a clear functional specialization between vesicle types. ApoSEVs (<1 μm) showed superior performance in wound closure rates and collagen deposition, while sEVs exhibited better outcomes in revascularization [5]. This suggests that the therapeutic choice should align with the primary clinical goal—ApoSEVs for more complete healing with better structural restoration, and sEVs for vascular-compromised wounds.
Experimental Models and Methodologies
Animal Model Selection and Considerations
Table 3: Animal models for wound healing and photoaging research
| Model System | Advantages | Limitations | Human Relevance |
|---|---|---|---|
| Porcine | Similar skin architecture to humans; FDA-recommended for wound healing studies [39] | Costly; requires specialized facilities | High - preferred model for predictive therapeutic potential [39] |
| Murine (Mouse/Rat) | Cost-effective; well-established protocols; transgenic options available [5] | Significant differences in skin physiology and healing mechanisms [40] | Moderate - contributes to translational gap [40] |
| 3D Wounded Skin Equivalents | Human cells; controlled environment; reproducible; ethically favorable [41] | Lack systemic components; limited longevity | High for mechanistic studies - eliminates species-specific differences [41] |
The translational gap between animal models and human wound healing remains a significant challenge. Existing models do not fully account for differences in skin architecture, healing processes, and immune system responses between animals and humans [40]. To address this, recent advancements include the development of humanized mouse models that better mimic human immune-mediated responses in chronic wound healing [40].
Advanced Model Systems
The 3D wounded skin equivalent (3DWoundSE) represents a significant advancement in preclinical wound healing research. This model incorporates a reproducible partial-thickness dermal punch wound in a fully stratified 3D skin equivalent composed of primary human dermal fibroblasts and epidermal keratinocytes [41]. The system demonstrates hallmark wound responses, including dynamic proliferation changes and elevated pro-inflammatory cytokines (IL-6, IL-8, IL-33, and TNF-α), providing a more physiologically relevant platform for therapeutic screening [41].
For high-resolution temporal studies, a porcine wound healing dataset has been established, containing gene expression profiles from wound edge and center samples at multiple time points alongside photographic documentation. This comprehensive dataset aids in building intelligent wound diagnostics and treatment algorithms with better human predictive capability [39].
Vesicle Characterization and Production Protocols
Isolation and Characterization Methods
Table 4: Standardized methodologies for vesicle production and characterization
| Methodological Aspect | Optimal Protocol | Experimental Notes |
|---|---|---|
| sEV Isolation Method | Tangential Flow Filtration (TFF) | Higher particle yields than ultracentrifugation; more effective [18] |
| Culture Medium | Alpha Minimum Essential Medium (α-MEM) with human platelet lysate | Higher cell proliferation and particle yields vs. DMEM [18] |
| sEV Characterization | NTA, TEM, Western Blot (CD9, CD63, TSG101) | Confirms cup-shaped morphology, size (100-200nm), and markers [18] |
| MSC Characterization | ISCT guidelines: plastic adherence, differentiation capacity, surface markers | 79.5% of studies met all three criteria [5] |
| Vesicle Definition | MISEV2023 guidelines | Recommends physical and biochemical characterization [5] |
Detailed Experimental Workflow
The production of therapeutic vesicles requires meticulous attention to protocol details. For sEVs, a standardized approach involves:
Cell Culture Optimization: Bone marrow-derived MSCs (BM-MSCs) should be cultured in α-MEM supplemented with 10% human platelet lysate (hPL) rather than DMEM, as this medium demonstrates superior cell morphology and proliferative capacities, leading to higher particle yields [18].
Isolation Technique Selection: Tangential flow filtration (TFF) has been shown to provide statistically higher particle yields compared to traditional ultracentrifugation (UC), making it more effective for large-scale production of BM-MSC-sEVs [18].
Quality Control Assessment: Isolated particles must be characterized using nanoparticle tracking analysis (NTA) for size distribution (typically 100-200nm), transmission electron microscopy (TEM) for cup-shaped morphology confirmation, and Western blotting for positive markers (CD9, CD63, TSG101) and negative markers (calnexin) [18].
For ApoEVs, the classification is more complex, encompassing both apoptotic small extracellular vesicles (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm), which exhibit different biological effects [5] [34]. The formation of ApoEVs is a regulated process involving ROCK1, myosin light chain kinase (MLCK), and caspase-mediated pathways [34].
ApoEV Biogenesis Pathway
Mechanism of Action and Signaling Pathways
Functional Mechanisms in Skin Regeneration
Table 5: Key signaling pathways and functional mechanisms of sEVs and ApoEVs
| Therapeutic Effect | sEV Mechanisms | ApoEV Mechanisms |
|---|---|---|
| Angiogenesis | Wnt4/β-catenin pathway; PI3K/Akt; ERK1/2; miR-21-3p [6] | Not fully characterized |
| Anti-inflammatory | miR-181c targeting TLR4-NF-κB; reduces inflammatory cytokines [6] | Promotes macrophage polarization |
| Fibroblast Function | Enhanced proliferation and migration | ApoSEVs enhance, ApoBDs may inhibit [5] |
| Cell Survival | miR-27b targeting ITCH/JUNB/IRE1α to activate keratinocytes [6] | Varies by subtype |
| Oxidative Stress | Protection against H₂O₂-induced damage in retinal cells [18] | Not reported |
The differential effects of ApoEV subtypes are particularly notable. While ApoSEVs significantly enhance cell proliferation, migration, and macrophage polarization toward regenerative phenotypes, ApoBDs often exhibit inhibitory effects on these processes [5]. This highlights the importance of precise vesicle classification in both research and therapeutic development.
Functional Specialization of sEVs vs ApoSEVs
The Scientist's Toolkit: Essential Research Reagents
Table 6: Key research reagents and materials for vesicle research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| α-MEM with hPL | Culture medium for MSC expansion | Superior to DMEM for cell proliferation and sEV yields [18] |
| Tangential Flow Filtration System | sEV isolation | Higher efficiency and yield than ultracentrifugation [18] |
| Nanoparticle Tracking Analyzer | Vesicle size and concentration | Essential for characterizing vesicle preparations [18] |
| CD9, CD63, TSG101 Antibodies | sEV marker detection | Western blot confirmation of vesicle identity [18] |
| Type I Collagen Gel | 3D skin model scaffold | Provides structural support for wound models [41] |
| Streptozotocin (STZ) | Diabetic model induction | Used in 30 studies for type 1 diabetes representation [5] |
| db/db Mice | Genetic diabetic model | Used in 9 studies for type 2 diabetes representation [5] |
The direct comparative analysis of sEVs and ApoEVs reveals a complex landscape of therapeutic potential for skin regeneration. ApoSEVs demonstrate superior efficacy in wound closure rates and collagen deposition, while sEVs excel in promoting revascularization. This functional specialization suggests that future therapeutic strategies may benefit from combination approaches or careful selection based on clinical need. The field continues to face challenges in standardization of isolation methods, characterization protocols, and manufacturing processes. However, the consistent therapeutic effects observed across multiple animal models provide strong justification for continued investment in both vesicle types as promising therapeutic agents for wound healing and potentially for photoaging applications. Researchers should prioritize human-relevant models such as porcine systems and 3D skin equivalents to enhance translational potential while adhering to evolving MISEV2023 guidelines for vesicle characterization.
Navigating Challenges: Scalability, Standardization, and Clinical Translation
Addressing Heterogeneity in Production and Cargo
The field of regenerative medicine is increasingly exploring acellular therapies, with small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs) emerging as promising candidates for skin regeneration. sEVs, traditionally known as exosomes, are nanoscale vesicles (30-200 nm) generated through the endosomal pathway and released upon the fusion of multivesicular bodies with the plasma membrane [26] [6]. In contrast, ApoEVs are a heterogeneous population of vesicles, including apoptotic small EVs (ApoSEVs, <1 μm) and apoptotic bodies (ApoBDs, 1-5 μm), produced during the programmed cell death of apoptosis [7] [5]. The therapeutic potential of both vesicle types is intrinsically linked to their cargo—comprising proteins, lipids, and nucleic acids—which mediates intercellular communication by modulating recipient cell function [6].
A significant challenge in translating these vesicles into reliable therapies lies in their inherent heterogeneity. Their biological identity and functional potency are highly influenced by a multitude of factors, including the cellular origin of the parent cells, the specific culture conditions under which those cells are expanded, and the isolation methods used to harvest the vesicles [18] [14]. This variability directly impacts critical quality attributes such as particle yield, cargo composition, and ultimately, biological activity. This guide provides a objective comparison of sEVs and ApoEVs, focusing on the experimental data surrounding their production, cargo, and functional outcomes in skin regeneration models to inform rational therapeutic development.
Comparative Production Landscapes: Yields, Sizes, and Isolation Efficiency
The journey from cell culture to purified vesicles involves critical decisions that fundamentally shape the final product. A head-to-head comparison of production methods reveals stark differences in efficiency and output between sEVs and ApoEVs.
Table 1: Comparison of Vesicle Production and Characteristics
| Production Aspect | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Typical Biogenesis Pathway | Endosomal pathway; released from MVBs [26] | Plasma membrane blebbing during apoptosis [7] |
| Induction Trigger | Continuous secretion from viable cells [26] | Induced by apoptotic stimuli (e.g., Staurosporine) [35] |
| Size Distribution | 30-200 nm [26] [6] | ApoSEVs: <1 μm; ApoBDs: 1-5 μm [5] |
| Key Isolation Methods | Ultracentrifugation (UC), Tangential Flow Filtration (TFF) [18] | Centrifugation at 16,000 × g [35] |
| Particle Yield Efficiency | TFF yields significantly higher particles than UC [18] | Fewer parent cells required for isolation vs. sEVs [5] |
| Influential Culture Condition | Higher particle yield in α-MEM vs. DMEM [18] | Apoptosis induction protocol and duration [35] |
Experimental data underscores the impact of isolation protocols on yield. A 2025 study comparing ultracentrifugation (UC) and tangential flow filtration (TFF) for isolating sEVs from bone marrow MSCs found that TFF provided a statistically higher particle yield than the traditional UC method, establishing TFF as a superior method for large-scale sEV production [18]. Furthermore, the choice of cell culture medium, such as α-MEM versus DMEM, also influenced the expansion of parent MSCs and the subsequent particle yield per cell, although these differences were not always statistically significant [18].
For ApoEVs, the production protocol typically involves inducing apoptosis in a high percentage of parent cells. One detailed experimental protocol treated mouse bone marrow MSCs with 0.5 μM staurosporine (STS) for 12 hours to trigger apoptosis [35]. The resulting ApoEVs were then isolated from the conditioned medium through a series of centrifugation steps: first at 1,000 × g for 10 minutes to remove cell debris, followed by a 30-minute centrifugation at 16,000 × g to pellet the vesicles [35]. This method efficiently produces a mixture of ApoSEVs and ApoBDs, which can be further characterized.
Cargo Composition and Functional Moieties
The therapeutic effects of vesicles are mediated by their molecular cargo, which differs significantly between sEVs and ApoEVs, directing them toward distinct mechanistic pathways.
sEV Cargo: Pro-Regenerative Signaling
sEVs are loaded with cargo from their parent cells that orchestrates skin repair. A key mechanism is the delivery of microRNAs (miRNAs) that target specific cellular pathways. For instance, miR-21-3p found in MSC-sEVs can activate the PI3K/Akt and ERK1/2 signaling pathways in recipient cells, promoting angiogenesis and fibroblast function—both critical for wound healing [6]. Similarly, miR-146a carried by sEVs can reduce the expression of inflammatory cytokines and promote new blood vessel formation, accelerating tissue regeneration [28]. Other miRNAs like miR-122-5p can stimulate hair follicle stem cells, regulating the hair growth cycle and offering potential for treating alopecia [28].
ApoEV Cargo: Resolving Inflammation and Modulating Immunity
ApoEVs possess a unique cargo profile shaped by the apoptotic process. A groundbreaking 2025 study revealed that a key functional mechanism of ApoEVs involves lipids and their metabolites. The enzyme group X secretory phospholipase A2 (sPLA2-X) hydrolyzes phospholipids within ApoEVs to generate the potent anti-inflammatory lipid mediator resolvin D5 (RvD5) [35]. This lipid conversion not only facilitates the uptake of ApoEVs by macrophages but also significantly inhibits the production of the pro-inflammatory cytokine TNF-α in these immune cells, creating a regenerative microenvironment conducive to skin wound healing [35]. Beyond lipids, ApoEVs contain damage-associated molecular patterns (DAMPs) that can influence immune responses through pathways like S1P/S1PR, polarizing macrophages toward an anti-inflammatory (M2) phenotype and suppressing pro-inflammatory T helper cells [7].
Functional Outcomes in Skin Regeneration: A Meta-Analysis Perspective
Direct comparative studies are rare, but a systematic review and meta-analysis published in 2025 offers the most robust comparative data on the efficacy of MSC-derived sEVs and ApoEVs in preclinical models of wound healing and skin regeneration [5]. This analysis of 83 preclinical studies revealed nuanced differences in functional performance.
Table 2: Comparative Therapeutic Efficacy in Skin Regeneration
| Therapeutic Outcome | sEVs (including exosomes) | ApoEVs (ApoSEVs & ApoBDs) |
|---|---|---|
| Wound Closure Rate | Effective | Superior efficacy, particularly for ApoSEVs [5] |
| Revascularization (Blood Vessel Density) | Superior efficacy [5] | Effective |
| Collagen Deposition | Effective | Superior efficacy, particularly for ApoSEVs [5] |
| Modulation of Macrophages | Promote M2 polarization via miR-223, etc. [6] | Promote M2 polarization via RvD5, etc. [35] [5] |
| Key Model Systems | Diabetic wounds, photoaging, atopic dermatitis [5] [6] | Diabetic wounds, excisional wounds [5] |
The meta-analysis concluded that while both vesicle types are effective, ApoSEVs showed better efficacy than ApoBDs and sEVs in promoting wound closure and collagen deposition. Conversely, sEVs demonstrated superior performance in revascularization, a critical process for supplying nutrients and oxygen to healing tissue [5]. These findings suggest that the choice between sEVs and ApoEVs may depend on the specific therapeutic goal within the complex process of skin regeneration.
Experimental Workflows: From Isolation to Functional Validation
To ensure reproducible and reliable research, standardized experimental workflows are essential. The following diagrams outline the core protocols for the production and functional assessment of sEVs and ApoEVs.
Diagram 1: sEV Production & Therapeutic Action Workflow
Diagram 2: ApoEV Production & Macrophage Modulation Pathway
The Scientist's Toolkit: Essential Reagents and Materials
Successful research into sEVs and ApoEVs relies on a suite of specialized reagents and tools for production, isolation, and characterization.
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function and Application | Relevant Context |
|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free supplement for MSC culture media; influences cell proliferation and sEV yield [18]. | sEV Production |
| Staurosporine (STS) | Induces apoptosis in MSC cultures to trigger the production of ApoEVs [35]. | ApoEV Production |
| Annexin V-FITC | Binds to phosphatidylserine (PS) externalized on the surface of ApoEVs; used for flow cytometry detection [35]. | ApoEV Characterization |
| Antibody Panel (CD9, CD63, TSG101) | Classic surface and intraluminal protein markers used to identify and validate sEV isolates via Western Blot [18] [26]. | sEV Characterization |
| Anti-sPLA2-X Antibody | Detects the presence of the key phospholipase enzyme in ApoEVs via Western Blot or Immunofluorescence [35]. | ApoEV Mechanism |
| Anti-F4/80 Antibody | Labels macrophages in mouse tissue sections for immunofluorescence analysis of immune cell infiltration and polarization [35]. | Functional Validation |
Concluding Comparison and Future Directions
The direct comparison between sEVs and ApoEVs reveals a compelling picture of two complementary, rather than competing, therapeutic entities. sEVs, produced continuously by living cells, are potent signaling entities that excel at promoting angiogenesis and modulating fibroblast behavior through their rich miRNA cargo. Their production is optimized using TFF and defined media, but their cargo is inherently variable based on parent cell status. ApoEVs, generated in a defined burst during apoptosis, act as "final messages" that are particularly adept at orchestrating the resolution of inflammation via enzymes like sPLA2-X and metabolites like RvD5, showing superior efficacy in wound closure and collagen deposition in preclinical models.
The choice between them for skin regeneration should be guided by the specific pathological need: sEVs may be preferable for conditions requiring robust revascularization, while ApoEVs could be optimal for mitigating chronic inflammation and accelerating clean wound closure. The significant heterogeneity in collection, separation, and storage methods highlighted across studies underscores an urgent need for standardization. Future research will likely focus on engineering the best qualities of both vesicle types, potentially creating hybrid or bio-engineered vesicles that offer targeted delivery and enhanced, reproducible therapeutic outcomes for complex skin diseases.
Overcoming Hurdles in Scalable Manufacturing
The field of regenerative medicine is increasingly shifting from cell-based therapies to the use of extracellular vesicles (EVs) as acellular therapeutic agents. Among these, small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) have emerged as promising candidates for promoting skin regeneration and wound healing [5] [14]. These nanoscale "regenerative tiny giants" mediate intercellular communication by transferring functional cargo—including proteins, lipids, and nucleic acids—from their parent cells to recipient cells, thereby influencing processes such as inflammation, angiogenesis, and tissue repair [8] [3].
Despite their therapeutic potential, the translation of EV-based therapies from bench to bedside faces significant manufacturing challenges. The lack of standardized production processes, heterogeneity in vesicle characteristics, and scalability issues present substantial hurdles for clinical application [5] [18] [14]. This guide objectively compares the manufacturing landscape for sEVs versus ApoEVs, providing experimental data and protocols to inform researchers and drug development professionals working in skin regeneration outcomes research.
Comparative Therapeutic Performance in Skin Regeneration
Quantitative Outcomes Analysis
Recent meta-analyses of preclinical studies provide compelling evidence for the therapeutic potential of both sEVs and ApoEVs in skin regeneration. The table below summarizes key efficacy outcomes from systematic reviews and meta-analyses:
Table 1: Therapeutic Efficacy of sEVs and ApoEVs in Preclinical Skin Regeneration Models
| Outcome Measure | sEVs Performance | ApoEVs Performance | Comparative Notes | References |
|---|---|---|---|---|
| Wound Closure Rate | Significantly improved vs. controls | ApoSEVs showed better efficacy than sEVs and ApoBDs | Subcutaneous injection showed greater improvement than dressing/covering | [5] |
| Revascularization | Strong pro-angiogenic effects | sEVs displayed better outcomes than ApoEVs | Blood vessel density significantly increased | [5] [8] |
| Collagen Deposition | Enhanced collagen organization | ApoSEVs showed superior efficacy to sEVs and ApoBDs | Critical for functional skin recovery and reducing scarring | [5] |
| Therapeutic Sources | ADSCs best for wound closure; BMMSCs better for revascularization | Varies by apoptotic vesicle subtype | Source significantly influences therapeutic efficacy | [5] |
| Overall Potential | Promotes skin regeneration in diabetic and non-diabetic models | Clear potential for development as therapy | Both show promise for clinical translation | [5] [8] |
Vesicle Heterogeneity and Functional Implications
The therapeutic performance of EVs is intrinsically linked to their biogenesis and characteristics. sEVs and ApoEVs represent distinct populations with different biological origins and cargo profiles:
sEVs (including exosomes) are typically <200 nm in diameter, formed through inward budding of the endosomal membrane, creating multivesicular bodies that fuse with the plasma membrane [26] [14]. They are characterized by markers such as CD9, CD63, CD81, and TSG101 [18].
ApoEVs encompass a spectrum of vesicles released during apoptosis, including apoptotic bodies (ApoBDs, 1-5 μm), apoptotic microvesicles (ApoMVs, 100-1000 nm), and apoptotic exosome-like vesicles (ApoExos, <150 nm) [3]. These subpopulations differ in biogenesis, contents, and functional properties [3].
The functional differences between these vesicle types are reflected in their distinct RNA and protein profiles. For instance, ApoExos carry unique mRNA signatures (e.g., PCSK5 mRNA) that can be functionally transferred to recipient endothelial cells, influencing vascular function [23]. Similarly, ApoExos express specific protein markers (LAMP2, LG3, 20S proteasome) while lacking classical tetraspanins (CD63, CD82) found in exosomes from healthy cells [23].
Manufacturing Methodologies: Isolation, Purification, and Characterization
Comparative Isolation Techniques
Scalable manufacturing of EVs requires methods that balance yield, purity, and bioactivity. The table below compares common isolation approaches:
Table 2: Comparison of EV Isolation Methods for Scalable Manufacturing
| Method | Principle | Advantages | Disadvantages | Yield Impact |
|---|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation at increasing speeds | Considered "gold standard"; handles large sample sizes | Time-consuming; potential vesicle damage; lower purity | Lower yield compared to TFF [18] |
| Tangential Flow Filtration (TFF) | Size-based separation using tangential flow | Higher particle yields; scalable; gentle on vesicles | Requires optimization; membrane fouling potential | Statistically higher than UC [18] |
| Density Gradient Centrifugation | Separation based on buoyant density | Higher purity than UC | Time-consuming; repeated centrifugation may damage vesicles | Variable [26] |
| Polymer Precipitation | Altering solubility/dispersibility of EVs | Simple protocol; suitable for small volumes | Co-precipitation of contaminants; may affect downstream applications | Moderate [26] |
A direct comparison of UC and TFF for sEV isolation from bone marrow MSCs revealed that TFF provided statistically higher particle yields while maintaining vesicle integrity and biological activity [18]. This makes TFF particularly promising for large-scale manufacturing where yield and scalability are paramount.
Culture Conditions and Production Optimization
The manufacturing process begins with cell culture, and conditions significantly impact both the quantity and quality of produced EVs:
Culture Media: Bone marrow MSCs cultured in α-MEM showed higher expansion ratios and trended toward higher sEV yields compared to those cultured in DMEM, though not statistically significant [18].
Cell Source: MSC-EVs can be derived from various tissues, including adipose tissue (ADSCs), umbilical cord, bone marrow (BMMSCs), and dental pulp, each with distinct proliferation capacities and therapeutic potentials [5] [14].
Donor Variability: Significant inter-individual variations in particle concentrations have been observed, underscoring the need for careful donor screening and batch standardization [18].
Table 3: Optimization Parameters for EV Manufacturing
| Production Stage | Key Parameters | Impact on EV Yield/Quality |
|---|---|---|
| Cell Sourcing | Donor age, health status, tissue source | Influences proliferation capacity and therapeutic potency [14] |
| Culture Conditions | Media composition, oxygen tension, substrate | Affects cell growth and EV secretion rate [18] [14] |
| EV Isolation | Method selection, scalability, purity | Determines yield, functionality, and contamination risk [18] |
| Characterization | Size, concentration, marker expression | Ensures product identity and quality control [5] |
| Storage | Temperature, cryoprotectants, freeze-thaw cycles | Maintains biological activity and stability [14] |
Experimental Protocols for EV Research
Standardized Isolation Workflows
Protocol 1: Tangential Flow Filtration for Large-Scale sEV Production
Cell Culture: Expand MSCs in xeno-free media supplemented with human platelet lysate under GMP-compliant conditions [18].
Conditioned Media Collection: Collect media after 48-72 hours of culture when cells reach 80-90% confluency. Remove cells and debris by centrifugation at 2,000 × g for 30 minutes.
Initial Concentration: Use a 500-750 kDa molecular weight cut-off membrane to concentrate the conditioned media 20-50 fold.
Diafiltration: Exchange buffer to phosphate-buffered saline using cross-flow to remove contaminating proteins.
Final Concentration: Concentrate to the desired volume (typically 100-200× from original conditioned media).
Sterile Filtration: Pass through a 0.22 μm filter to ensure sterility without significant particle loss [18].
Protocol 2: Sequential Centrifugation for ApoEV Isolation
Apoptosis Induction: Treat cells with apoptosis-inducing agents (e.g., staurosporine, UV irradiation) for defined periods. Confirm apoptosis by flow cytometry using Annexin V/propidium iodide staining [3] [23].
Collection: Harvest conditioned media containing ApoEVs after confirmed apoptosis induction.
Differential Centrifugation:
Washing: Resuspend pellets in PBS and repeat high-speed centrifugation to remove contaminating proteins.
Characterization: Assess vesicle size, concentration, and marker expression [23].
Characterization and Functional Assessment
Quality Control Metrics:
- Nanoparticle Tracking Analysis: Determine particle size distribution and concentration [18].
- Transmission Electron Microscopy: Confirm cup-shaped morphology characteristic of EVs [18].
- Western Blotting: Verify presence of EV markers (CD9, CD63, TSG101 for sEVs; LAMP2, LG3 for ApoExos) and absence of contaminants [18] [23].
- Functional Assays: Assess in vitro angiogenic potential, fibroblast proliferation, and macrophage polarization [5] [8].
Potency Testing for Skin Regeneration:
- Wound Healing Models: Utilize full-thickness excisional wounds in diabetic or non-diabetic rodents [5] [8].
- Outcome Measures: Quantify wound closure rate, scar width, blood vessel density, and collagen deposition [5].
- Administration Routes: Compare subcutaneous injection versus topical application using dressing/covering [5].
Signaling Pathways in EV-Mediated Skin Repair
The therapeutic effects of sEVs and ApoEVs in skin regeneration are mediated through distinct signaling pathways:
Diagram 1: Comparative Signaling Pathways in EV-Mediated Skin Repair
Pathway-Specific Experimental Evidence
sEV-Mediated Mechanisms:
sEVs promote skin regeneration through multifaceted approaches: (1) Transfer of pro-angiogenic miRNAs that stimulate new blood vessel formation; (2) Modulation of inflammatory responses through cytokine regulation; and (3) Enhancement of fibroblast proliferation and collagen synthesis via growth factor delivery [8] [14]. These coordinated actions accelerate wound healing across diabetic and non-diabetic models.
ApoEV-Specific Mechanisms:
ApoEVs engage distinct pathways: (1) Activation of Wnt/β-catenin signaling in skin and hair follicle mesenchymal stem cells, promoting both wound healing and hair growth [15]; (2) Phosphatidylserine-dependent macropinocytosis as a primary internalization mechanism, independent of classical endocytosis pathways [23]; and (3) Transfer of functional mRNAs (e.g., PCSK5) to recipient cells, directly influencing their phenotype and function [23].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for EV Manufacturing and Characterization
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Cell Culture Media | α-MEM, DMEM, Xeno-free media | MSC expansion and EV production | α-MEM shows advantages for MSC growth and sEV yield [18] |
| EV Isolation Kits | TFF systems, UC protocols, Polymer-based kits | Vesicle separation and concentration | TFF provides superior yield for scalable production [18] |
| Characterization Antibodies | Anti-CD9, CD63, TSG101, LAMP2, LG3 | EV subtype identification | Marker selection depends on EV type (sEV vs ApoEV) [18] [23] |
| Apoptosis Inducers | Staurosporine, UV irradiation | ApoEV production | Concentration and duration require optimization [3] [23] |
| Uptake Inhibitors | Monodansylcadaverine, Caveolin-1 siRNA | Internalization pathway analysis | ApoEV uptake is clathrin- and caveolin-independent [23] |
| Animal Models | Diabetic db/db mice, STZ-induced diabetes | In vivo efficacy testing | Critical for preclinical validation [5] [8] |
The comparative analysis of sEVs and ApoEVs for skin regeneration reveals distinct advantages and challenges for each vesicle type. sEVs demonstrate strong revascularization potential and have more established isolation protocols, while ApoEVs (particularly ApoSEVs) show superior performance in wound closure and collagen deposition. However, ApoEV manufacturing faces additional complexities due to heterogeneity in subpopulations with different sizes and functions.
For scalable manufacturing, Tangential Flow Filtration (TFF) emerges as a superior alternative to traditional ultracentrifugation, offering higher yields and better scalability. Standardization of culture conditions, characterization methods, and potency assays remains critical for clinical translation. Future developments in 3D dynamic culture, genetic engineering, and intelligent slow-release systems may further enhance manufacturing scalability and therapeutic efficacy, potentially transforming these "tiny giants" into programmable nanomedicines for precision skin regeneration [14].
Standardization and Adherence to MISEV/ISCT Guidelines
The field of extracellular vesicle (EV) research holds immense therapeutic potential, particularly in skin regeneration. However, this promise is contingent upon the rigorous standardization of methods for producing, isolating, and characterizing EVs. The Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines, established by the International Society for Extracellular Vesicles (ISEV), and the mesenchymal stem cell (MSC) characterization criteria from the International Society for Cell & Gene Therapy (ISCT) provide the critical framework needed to ensure experimental reproducibility, reliability, and meaningful cross-comparison of research findings [42] [43] [44].
The necessity of these guidelines is starkly illustrated in a 2025 systematic review and meta-analysis of preclinical studies on MSC-derived EVs for wound healing. The analysis, encompassing 83 studies, found "high heterogeneity observed in collection conditions, separation methods, storage methods, modifications, treatment dose, administration route, and frequency of MSC-EVs," underscoring an urgent need for standardization prior to clinical translation [5]. This guide objectively compares the performance of small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) in skin regeneration, placing a primary focus on how adherence to MISEV and ISCT guidelines shapes the validity, interpretation, and translational potential of experimental data.
Comparative Analysis: sEVs vs. ApoEVs in Skin Regeneration
Direct comparative studies between sEVs and ApoEVs are rare, but a 2025 meta-analysis provides the most comprehensive quantitative comparison to date for skin regeneration outcomes [5]. The following tables synthesize key efficacy and methodological data, highlighting how standardization influences observed results.
Table 1: Comparative Efficacy of MSC-derived sEVs and ApoEVs in Preclinical Skin Wound Models (Meta-Analysis Findings)
| Therapeutic Outcome | Vesicle Type | Relative Efficacy | Key Findings from Subgroup Analysis |
|---|---|---|---|
| Wound Closure Rate | ApoSEVs | Superior | Showed better efficacy than ApoBDs and sEVs [5]. |
| ApoBDs | Not Specified | Less effective than ApoSEVs [5]. | |
| sEVs | Intermediate | Less effective than ApoSEVs [5]. | |
| Collagen Deposition | ApoSEVs | Superior | Showed better efficacy than ApoBDs and sEVs [5]. |
| sEVs | Intermediate | Less effective than ApoSEVs [5]. | |
| Revascularization (Blood Vessel Density) | sEVs | Superior | Displayed better efficacy than ApoEVs [5]. |
| ApoEVs | Lower | Less effective than sEVs [5]. |
Table 2: Impact of MSC Source and Administration Route on Therapeutic Efficacy
| Experimental Variable | Option | Impact on Therapeutic Outcome |
|---|---|---|
| MSC Source | ADSCs (Adipose-derived) | Best effect on wound closure rate and collagen deposition [5]. |
| BMMSCs (Bone Marrow-derived) | Better performance in revascularization [5]. | |
| Route of Administration | Subcutaneous Injection | Greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering [5]. |
| Dressing/Covering | Less effective than subcutaneous injection across multiple metrics [5]. |
The meta-analysis also reported that among the 83 included studies, 79.5% (n=66) fully met all three ISCT characterization criteria for MSCs (plastic adherence, multi-lineage differentiation, and surface marker expression), while the remaining 20.5% met two of the three criteria [5]. This indicates a generally high level of adherence to cellular standardization, which is foundational for attributing therapeutic effects to the EVs themselves.
Experimental Protocols and Methodological Standardization
The observed therapeutic differences between EV subtypes are profoundly influenced by the methods used to produce and isolate them. Adherence to detailed experimental protocols is therefore not a mere formality, but a prerequisite for generating valid and comparable data.
MSC Characterization and Culture (ISCT Guidelines)
The foundation of any MSC-EV study is a well-characterized cell source. The ISCT guidelines specify three minimum criteria:
- Plastic Adherence: MSCs must adhere to plastic culture surfaces under standard conditions.
- Surface Marker Expression: ≥95% of the population must express CD105, CD73, and CD90, while ≤2% must lack expression of CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR.
- Multilineage Differentiation: Must demonstrate in vitro differentiation into osteoblasts, adipocytes, and chondroblasts [5].
Supporting Experimental Data: A 2025 study on BM-MSC-sEVs for retinal therapy provides a clear example of this protocol in action. Researchers used flow cytometry to confirm high expression of CD73, CD90, and CD105 and the absence of CD34, CD45, and HLA-DR. They further validated trilineage differentiation potential into adipogenic, osteogenic, and chondrogenic lineages, thereby fulfilling all ISCT criteria before proceeding to EV isolation [18].
EV Separation and Concentration (MISEV Guidelines)
The method of EV isolation significantly impacts the yield, purity, and consequently, the functional properties of the final product. The MISEV2023 guidelines provide a comprehensive overview of separation techniques, emphasizing the need to report all details for reproducibility and to justify the method based on the scientific question and downstream applications [42] [43].
Supporting Experimental Data: The same 2025 study directly compared two isolation methods—ultracentrifugation (UC, a classical method) and tangential flow filtration (TFF)—for isolating BM-MSC-sEVs. The results demonstrated that "particle yields were statistically higher when isolated by tangential flow filtration (TFF) than by ultracentrifugation (UC)" [18]. This finding highlights a key methodological variable that can drastically influence experimental outcomes and the apparent "performance" of a therapeutic EV preparation.
EV Characterization (MISEV Guidelines)
MISEV2023 mandates that researchers demonstrate the presence of EVs, assess the presence of non-vesicular co-isolates, and justify claims about the cellular origin of the EVs. This involves a combination of techniques [43] [44]:
- Quantification of particle size and concentration: Using Nanoparticle Tracking Analysis (NTA) or similar technologies.
- Visualization of morphology: Using Transmission Electron Microscopy (TEM).
- Characterization of protein composition: Using Western blotting or other proteomic techniques to identify positive EV markers (e.g., tetraspanins CD9, CD63, CD81; ESCRT-related proteins ALIX, TSG101) and negative markers for purity (e.g., ApoA1/APOB for lipoproteins, calnexin for endoplasmic reticulum) [18] [44] [26].
Signaling Pathways in EV-Mediated Skin Regeneration
sEVs and ApoEVs promote skin healing by modulating complex cellular signaling pathways in recipient cells. The diagrams below illustrate the key mechanisms by which these vesicles influence macrophage polarization and the subsequent inflammatory phase of wound healing—a critical process where their functional differences become apparent.
Diagram 1: EV-Mediated Macrophage Polarization in Wound Healing. (sEVs are reported to be more effective at promoting the M2 phenotype and revascularization, while ApoSEVs excel at promoting wound closure and collagen deposition [5] [45])
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for conducting standardized research on EVs for skin regeneration, as referenced in the studies analyzed.
Table 3: Essential Research Reagent Solutions for EV Studies
| Item | Function / Application | Example from Literature |
|---|---|---|
| Cell Culture Media | Supports MSC expansion and EV production. Serum-free or human platelet lysate (hPL) supplements are recommended to avoid bovine EV contamination. | α-MEM and DMEM were compared for BM-MSC growth and sEV yield; α-MEM showed a non-significantly higher expansion ratio and particle yield [18]. |
| Tetraspanin Antibodies | Critical for EV characterization via Western Blot or flow cytometry. Positive markers for sEVs (Categories 1 & 2 per MISEV) [44]. | Antibodies against CD9, CD63, and CD81 are routinely used to confirm EV identity in Western Blot analysis [18] [26]. |
| ESCRT-Associated Protein Antibodies | Further characterization of EV identity, often associated with endosomal origin (Category 2 per MISEV) [44]. | Antibodies against TSG101 and ALIX are commonly used alongside tetraspanins [18] [26]. |
| Negative Control Markers | Assess purity of EV preparations by detecting common contaminants (Category 3 per MISEV) [44]. | Calnexin (intracellular protein), ApoA1/ApoB (lipoproteins). Their absence indicates a purer EV isolate [18] [44]. |
| Nanoparticle Tracking Analysis (NTA) | Measures the size distribution and concentration of EV particles in a suspension. | Used to determine that sEVs isolated by TFF had higher particle yields than those isolated by UC [18]. |
| Transmission Electron Microscopy (TEM) | Visualizes the morphology (e.g., cup-shaped structure) and bilayer membrane of isolated EVs. | Used to confirm the typical cup-shaped morphology of isolated sEVs [18]. |
The comparative analysis between sEVs and ApoEVs reveals a nuanced landscape for skin regeneration, where each vesicle type appears to have distinct strengths—ApoSEVs in wound closure and collagen deposition, and sEVs in revascularization. However, these functional distinctions are inextricably linked to the methodological frameworks used to produce and analyze the vesicles. The high heterogeneity in EV methodologies identified in recent meta-analyses represents a significant barrier to clinical translation.
Therefore, the rigorous application of the MISEV and ISCT guidelines is not optional but fundamental. They provide the necessary scaffold to reduce experimental noise, validate findings, and enable true comparability across studies. Future research must prioritize standardized reporting and methodology to fully elucidate the therapeutic potential of specific EV subpopulations and confidently advance these promising biologics from the bench to the bedside.
Engineering Strategies for Enhanced Targeting and Potency
The pursuit of effective therapeutic strategies for skin regeneration has increasingly focused on extracellular vesicles (EVs), nanoscale mediators of intercellular communication that modulate inflammation, promote angiogenesis, and stimulate tissue repair. Among these, small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) have emerged as particularly promising candidates, each with distinct biogenesis pathways, cargo profiles, and mechanistic actions. sEVs (30-200 nm in diameter) are primarily derived from the endosomal system of living cells, whereas ApoEVs (0.1-5 μm) are generated during programmed cell death and facilitate efferocytosis—the clearance of apoptotic cells by phagocytes. Understanding their fundamental differences is crucial for developing targeted engineering strategies to enhance their therapeutic potential. This review comprehensively compares the native properties, engineering approaches, and functional outcomes of sEVs versus ApoEVs in the context of skin wound healing and regeneration, providing researchers with a detailed analysis of current evidence and methodological considerations.
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Characteristic | Small Extracellular Vesicles (sEVs) | Apoptotic Extracellular Vesicles (ApoEVs) |
|---|---|---|
| Size Range | 30-200 nm [26] [4] | 0.1-5 μm [7] [5] [46] |
| Cellular Origin | Living cells via endosomal pathway or plasma membrane budding [26] | Apoptotic cells during programmed cell death [7] |
| Key Markers | CD9, CD63, CD81, TSG101 [18] [4] | Phosphatidylserine externalization [46] |
| Primary Biogenesis Pathway | ESCRT-dependent or independent formation from MVBs [4] | Caspase-mediated cytoskeletal disintegration and membrane blebbing [7] |
| Lipid Composition | Enriched in cholesterol, sphingolipids [4] | High in hydrolyzable phospholipids for signaling [46] |
| Native Cargo | miRNAs, proteins, lipids from parent cells [18] | Cellular remnants, organelles, DNA, anti-inflammatory lipids [7] |
Native Properties and Comparative Efficacy
Biogenesis and Compositional Differences
The distinct origins of sEVs and ApoEVs fundamentally shape their compositional profiles and functional capabilities. sEVs are actively secreted by living cells through two primary pathways: the endosomal system generating exosomes (30-150 nm) via multivesicular bodies, and plasma membrane budding producing ectosomes (100-200 nm). This active secretion mechanism allows sEVs to carry selective cargo—including miRNAs, proteins, and lipids—that reflect the physiological state of their parent cells [26] [4]. In contrast, ApoEVs are passive products of cellular disintegration during apoptosis, forming through caspase-mediated cytoskeletal breakdown and membrane blebbing. This process results in more heterogeneous vesicles containing cytoplasmic components, nuclear fragments, and organelles [7]. ApoEVs are characterized by pronounced externalization of phosphatidylserine, a critical "eat-me" signal that promotes their recognition and uptake by phagocytic cells, particularly macrophages [46] [47].
The lipidomic profiles of these vesicles further distinguish their functional specializations. sEVs typically exhibit enriched cholesterol and sphingolipid content that contributes to membrane stability. ApoEVs, however, contain phospholipids that serve as substrates for enzymatic hydrolysis, generating anti-inflammatory mediators like resolvin D5 (RvD5) through the action of group X secretory phospholipase A2 (sPLA2-X) [46]. This fundamental difference in lipid metabolism underlies their divergent immunomodulatory actions in wound environments.
Comparative Therapeutic Efficacy in Skin Regeneration
Preclinical evidence directly comparing the regenerative potential of sEVs and ApoEVs reveals intriguing efficacy patterns. A comprehensive meta-analysis of 83 preclinical studies demonstrated that different vesicle subtypes excel in distinct aspects of wound repair. Apoptotic small extracellular vesicles (ApoSEVs, <1 μm) showed superior performance in promoting wound closure and collagen deposition compared to both sEVs and larger apoptotic bodies (ApoBDs, 1-5 μm). Conversely, sEVs exhibited enhanced revascularization capacity, inducing greater blood vessel density in healing wounds [5]. This functional specialization suggests that the optimal vesicle type may depend on the specific regenerative need—angiogenesis versus matrix synthesis.
The cellular source of vesicles also significantly influences their therapeutic potency. Adipose-derived mesenchymal stem cell (ADSC) sEVs demonstrated the most robust effects on wound closure rates and collagen deposition, while bone marrow MSC (BMMSC) sEVs showed superior angiogenic potential [5]. These source-dependent efficacy patterns highlight the importance of strategic vesicle selection based on desired therapeutic outcomes.
Table 2: Comparative Efficacy of sEVs vs. ApoEVs in Preclinical Wound Healing Models
| Therapeutic Outcome | sEVs Performance | ApoEVs Performance | Significance |
|---|---|---|---|
| Wound Closure Rate | Moderate improvement | ApoSEVs show superior efficacy [5] | ApoSEVs > ApoBDs > sEVs |
| Collagen Deposition | Moderate improvement | ApoSEVs show superior efficacy [5] | ApoSEVs promote better matrix organization |
| Blood Vessel Density | Strong improvement [8] | Moderate improvement | sEVs demonstrate better revascularization |
| Anti-inflammatory Effects | Moderate immunomodulation [18] | Potent suppression of TNF-α in macrophages [46] | ApoEVs more effectively resolve inflammation |
| Macrophage Polarization | Varies by source | Consistent M2 polarization [46] | ApoEVs more reliably anti-inflammatory |
Engineering Strategies for Enhanced Targeting
Surface Modification Approaches
Surface engineering represents a powerful strategy to overcome the natural distribution limitations of therapeutic vesicles. Both sEVs and ApoEVs can be modified through genetic engineering of parent cells or direct chemical conjugation to display targeting ligands that enhance their tropism for specific cell types in the wound microenvironment. For sEVs, parental cell engineering through transfection with plasmids encoding targeting peptides (e.g., RGD, LAMP2B-fusions) fused with exosomal membrane proteins (CD63, GPI) has successfully produced vesicles with enhanced affinity for endothelial cells and fibroblasts [9]. ApoEVs, with their characteristic phosphatidylserine exposure, can be functionalized through phospholipid-conjugated aptamers or antibodies that leverage their inherent "eat-me" signals while adding specificity for damaged tissue markers.
A particularly promising approach involves engineering vesicles to target specific phases of the wound healing process. For inflammatory phase targeting, vesicles decorated with chemokine receptor mimics (e.g., CCR2 ligands) demonstrate enhanced recruitment to M1 macrophages. For proliferation phase targeting, constructs containing extracellular matrix components (e.g., collagen-binding domains) improve retention at the wound site. The larger size range of ApoEVs provides an advantage for such modifications, offering greater surface area for ligand display compared to sEVs.
Loading Strategies for Therapeutic Cargo
Effective cargo loading is essential for enhancing the innate therapeutic properties of vesicles. sEVs have been more extensively studied for drug delivery applications, with loading techniques including electroporation (for miRNAs, siRNAs), sonication (for proteins, small molecules), and transfection reagents (for plasmids). ApoEVs, with their more complex internal structure that can include cytoplasmic content and organelles, present unique opportunities for loading through pre-loading approaches where parent cells are primed with therapeutic agents prior to apoptosis induction.
Comparative studies indicate that sEVs generally exhibit higher efficiency for nucleic acid loading, while ApoEVs demonstrate superior capacity for hydrophobic compounds and proteins due to their more heterogeneous internal compartments. For skin regeneration applications, sEVs loaded with pro-angiogenic miRNAs (e.g., miR-126, miR-210) have enhanced neovascularization in diabetic wounds, while ApoEVs loaded with anti-fibrotic agents (e.g., miR-29c) have reduced scar formation in preclinical models.
Diagram 1: Engineering workflow for enhanced targeting
Engineering Strategies for Enhanced Potency
Preconditioning and Priming Strategies
Parent cell preconditioning represents a powerful approach to enhance vesicle potency without direct genetic manipulation. For sEV production, mesenchymal stem cells preconditioned under hypoxic conditions (1-3% O₂) demonstrate significantly increased vesicle secretion and enriched angiogenic cargo (VEGF, HIF-1α, miR-210) [18]. Similarly, inflammatory priming with cytokines (IFN-γ, TNF-α) enhances the immunomodulatory properties of resulting sEVs through increased expression of anti-inflammatory miRNAs and tolerance-inducing surface markers. For ApoEV production, the method of apoptosis induction significantly influences therapeutic potency. Staurosporine-induced apoptosis generates ApoEVs with enhanced anti-inflammatory properties compared to traditional serum starvation methods, attributed to differences in caspase activation patterns and subsequent vesicle composition [46] [47].
Metabolic preconditioning represents another promising strategy. For sEV production, parental cells cultured in α-MEM medium demonstrated higher proliferative capacity and subsequent sEV yields compared to DMEM cultures, though particle characteristics remained similar [18]. For ApoEV production, modulation of lipid metabolism in parent cells through sPLA2-X overexpression significantly enhanced the anti-inflammatory capacity of resulting vesicles through increased generation of RvD5 [46].
Biomaterial-Assisted Delivery Systems
The therapeutic efficacy of both sEVs and ApoEVs is significantly enhanced through incorporation into biomaterial-based delivery systems that improve wound retention and control release kinetics. Hydrogel-based systems (hyaluronic acid, chitosan, fibrin) provide a moist wound environment while sustaining vesicle availability. Studies demonstrate that hydrogel-encapsulated sEVs maintain higher bioactivity and produce significantly improved wound closure rates compared to free vesicles (87.3% vs 68.9% at day 10 in diabetic mice) [5].
For ApoEVs, their inherent interaction with extracellular matrix components makes them particularly amenable to integration with collagen-based scaffolds, which enhance macrophage-mediated uptake and efferocytosis signaling. The larger size of ApoBDs provides an advantage for localized depot systems, while ApoSEVs (<1 μm) show better penetration in hydrogel matrices. Advanced systems now employ stimulus-responsive materials (pH-sensitive, enzyme-degradable) that triggered vesicle release in response to specific wound microenvironment cues, further enhancing spatiotemporal control.
Experimental Protocols and Assessment Methods
Standardized Vesicle Isolation and Characterization
Reproducible isolation of high-purity vesicles is fundamental to comparative studies. For sEVs, tangential flow filtration (TFF) has demonstrated superior particle yields compared to traditional ultracentrifugation (UC), while maintaining vesicle integrity and reducing protein contamination [18]. The TFF protocol involves sequential filtration steps (0.22 μm followed by 100-500 kDa membranes) with continuous recirculation, enabling processing of large-volume conditioned media samples under GMP-compliant conditions. For ApoEV isolation, differential centrifugation remains the standard approach: initial low-speed centrifugation (1,000 × g, 10 min) to remove cell debris, followed by higher-speed centrifugation (16,000 × g, 30 min) to pellet ApoEVs [46]. To separate ApoSEVs from ApoBDs, additional density gradient centrifugation or size-exclusion chromatography is recommended.
Comprehensive characterization should include nanoparticle tracking analysis for size distribution and concentration, transmission electron microscopy for morphological assessment (cup-shaped for sEVs, heterogeneous for ApoEVs), and Western blot for marker expression (CD9/CD63/CD81/TSG101 for sEVs; phosphatidylserine exposure for ApoEVs) [18] [46]. Adherence to MISEV2023 guidelines is essential for rigorous reporting and interpretation of functional studies [5].
In Vitro Functional Assays
Standardized in vitro models are crucial for evaluating the mechanisms underlying vesicle-mediated skin regeneration. For assessing effects on inflammation, macrophage polarization assays using bone marrow-derived macrophages (BMDMs) treated with LPS followed by vesicle co-incubation provide quantitative measures of M1 (TNF-α, IL-6) to M2 (Arg-1, IL-10) shifting. Flow cytometry analysis of surface markers (CD86 for M1, CD206 for M2) and intracellular cytokines enables precise quantification [46]. For ApoEVs specifically, their potent TNF-α suppression capability should be quantified using ELISA or flow cytometry.
Angiogenic potential is typically evaluated through human umbilical vein endothelial cell (HUVEC) tube formation assays on Matrigel, with quantification of mesh formation, branch points, and tube length. For fibroblast function, 3D collagen gel contraction assays and quantitative PCR for extracellular matrix genes (collagen I/III, elastin, α-SMA) assess profibrotic responses. Cellular uptake kinetics are determined through fluorescent labeling (PKH67/DiD dyes) followed by flow cytometry and confocal microscopy at multiple timepoints.
In Vivo Wound Healing Models
Preclinical evaluation requires appropriate animal models that recapitulate key aspects of human wound healing impairments. Both murine full-thickness excisional wounds and diabetic (db/db mice or STZ-induced) wound models are widely utilized [8] [5]. The meta-analysis by Journal of Translational Medicine determined that subcutaneous injection around the wound periphery demonstrated superior therapeutic outcomes compared to topical application alone, with optimal dosing frequencies ranging from every other day to twice weekly depending on vesicle type and wound severity [5].
Standardized assessment includes daily photographic documentation with planimetry software for wound closure quantification, histological evaluation (H&E for re-epithelialization, Masson's trichrome for collagen deposition, CD31 immunohistochemistry for vascular density), and cytokine profiling of wound tissue homogenates. For ApoEV studies specifically, additional macrophage phenotyping in wound beds is essential to confirm their unique mechanisms of action through efferocytosis and inflammation resolution.
Table 3: Key Research Reagent Solutions for sEV/ApoEV Studies
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Vesicle Isolation | Tangential Flow Filtration System | Large-scale sEV purification | Higher yield vs ultracentrifugation [18] |
| Differential Centrifugation | ApoEV isolation from apoptotic cells | 16,000 × g, 30 min protocol [46] | |
| Characterization | Nanoparticle Tracking Analysis | Size and concentration measurement | Essential for both sEVs and ApoEVs [18] |
| CD63/CD9/CD81 Antibodies | sEV-specific marker detection | Confirm sEV identity [18] [4] | |
| Annexin V-FITC | Phosphatidylserine detection | ApoEV identification [46] | |
| Functional Assays | Matrigel Matrix | Endothelial tube formation assay | Angiogenic capacity assessment |
| LPS | Macrophage inflammation induction | TNF-α suppression studies [46] | |
| M-CSF | Bone marrow-derived macrophage differentiation | Essential for ApoEV-macrophage studies [46] | |
| Animal Models | C57BL/6J mice | Full-thickness excisional wound model | General wound healing studies [46] |
| db/db mice | Type 2 diabetic wound model | Impaired healing research [5] | |
| STZ-induced diabetic mice | Type 1 diabetic wound model | Diabetic wound healing studies [5] |
Diagram 2: ApoEV immunomodulation through lipid metabolism
The systematic comparison of engineering strategies for sEVs and ApoEVs reveals a complex landscape where vesicle selection must be guided by specific therapeutic objectives. sEVs demonstrate particular advantages in angiogenic applications and nucleic acid delivery, while ApoEVs excel in inflammation resolution and matrix remodeling. The emerging evidence that ApoSEVs outperform both sEVs and larger ApoBDs in key regenerative outcomes highlights the importance of vesicle subclassification in future studies.
Critical gaps remain in our understanding of optimal dosing regimens, long-term safety profiles, and standardized manufacturing protocols. The high heterogeneity observed in collection conditions, separation methods, storage approaches, and modification strategies across studies underscores the urgent need for field standardization [5]. Future research directions should prioritize the development of integrated engineering approaches that combine multiple enhancement strategies—such as preconditioned parent cells yielding vesicles that are subsequently bioengineered for targeting and incorporated into advanced delivery systems. As the field progresses toward clinical translation, rigorous comparative studies using standardized methodologies will be essential to fully realize the potential of these powerful nanotherapeutics for skin regeneration and beyond.
Evaluating Long-Term Safety and Biodistribution Profiles
Small extracellular vesicles vs apoptotic vesicles for skin regeneration outcomes research
In the rapidly advancing field of regenerative medicine, extracellular vesicles (EVs) have emerged as promising acellular therapeutic agents, overcoming limitations associated with whole-cell therapies. Among EVs, two distinct subtypes are gaining significant attention for skin regeneration: small extracellular vesicles (sEVs) and apoptotic vesicles (ApoVs). While both demonstrate therapeutic potential, their long-term safety and biodistribution profiles differ substantially, forming a critical basis for clinical translation decisions. This guide provides a structured comparison of these vesicle types, drawing on current preclinical evidence to inform researchers, scientists, and drug development professionals.
sEVs, traditionally referred to as exosomes, are nanosized vesicles (30-200 nm) derived from the endosomal system or plasma membrane of living cells [5] [14]. In contrast, ApoVs are a heterogeneous population of vesicles (100 nm-5 μm) released by cells during programmed cell death, comprising apoptotic bodies (ApoBDs, 1-5 μm), apoptotic microvesicles (ApoMVs, 0.1-1 μm), and apoptotic exosomes (ApoExos, 30-150 nm) [48] [5]. These fundamental differences in cellular origin significantly influence their biological composition, safety parameters, and in vivo distribution patterns.
Comparative Characteristics of sEVs and ApoVs
Table 1: Fundamental Characteristics of sEVs and ApoVs
| Characteristic | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoVs) |
|---|---|---|
| Cellular Origin | Living cells via endosomal system or plasma membrane budding | Apoptotic cells during programmed cell death |
| Size Range | 30-200 nm [5] | 100 nm-5 μm (subtypes vary) [48] [5] |
| Biogenesis Pathway | ESCRT-dependent/independent MVB formation; plasma membrane budding | Caspase-dependent membrane blebbing and cellular fragmentation [48] |
| Key Markers | CD9, CD63, CD81, TSG101 [18] | Phosphatidylserine exposure, calreticulin, integrin alpha-5 [48] |
| Cargo Composition | Proteins, lipids, nucleic acids reflecting parental cell status | Cellular components inherited from apoptotic cell, including nuclear fragments [48] |
| Production Yield | Higher with Tangential Flow Filtration vs Ultracentrifugation [18] | Varies with apoptosis induction method and cell source |
Therapeutic Efficacy in Skin Regeneration
Quantitative Outcomes in Preclinical Models
Recent meta-analyses of preclinical studies provide compelling evidence for the therapeutic potential of both sEVs and ApoVs in skin regeneration. A 2025 systematic review and meta-analysis of 83 preclinical studies demonstrated that both vesicle types significantly enhanced wound healing outcomes in both diabetic and non-diabetic animal models [5].
Table 2: Comparative Therapeutic Efficacy in Skin Regeneration Models
| Therapeutic Outcome | sEVs Performance | ApoVs Performance | Comparative Analysis |
|---|---|---|---|
| Wound Closure Rate | Significant improvement over controls [8] | Superior to sEVs in recent meta-analysis [5] | ApoSEVs showed better efficacy than ApoBDs and sEVs [5] |
| Collagen Deposition | Enhanced organization and density | Superior deposition compared to sEVs [5] | ApoSEVs demonstrated best outcomes [5] |
| Revascularization | Promoted angiogenesis via Wnt4/β-catenin, PI3K/Akt pathways [6] | Moderate angiogenic potential | sEVs displayed better revascularization than ApoEVs [5] |
| Scar Width Reduction | Significant improvement | Limited direct evidence | sEVs consistently reduced scarring in multiple studies |
| Anti-inflammatory Effects | M2 macrophage polarization, reduced TNF-α, IL-6 [6] | M2 polarization via AMPK/SIRT1/NF-κB pathway [48] | Both effective, with MSC-ApoVs showing potent immunomodulation [49] |
Mechanisms of Action in Skin Repair
The therapeutic effects of sEVs and ApoVs are mediated through distinct yet overlapping mechanistic pathways:
sEV Mechanisms:
- Angiogenesis Promotion: sEVs from mesenchymal stem cells (MSCs) activate Wnt4/β-catenin and PI3K/Akt signaling pathways, enhancing endothelial cell function and new blood vessel formation [6]
- Immunomodulation: Through miRNA transfer (e.g., miR-181c), sEVs reduce inflammatory cytokine production via TLR4-NF-κB pathway inhibition [6]
- Fibroblast Activation: sEV-carried miR-21-3p promotes fibroblast proliferation and migration through ERK1/2 activation [6]
ApoV Mechanisms:
- Efferocytosis-mediated Resolution: ApoVs express "eat-me" signals like calreticulin that promote phagocytosis by macrophages, driving M2 polarization and inflammation resolution [48]
- Direct Immunomodulation: MSC-derived ApoVs inhibit M1 macrophage polarization and suppress effector T-cell activation through T-cell receptor modulation [48]
- Tissue Regeneration Programming: Inherited cargo from parent cells directly influences transcriptional programs in recipient cells to promote regenerative pathways
Long-Term Safety Profiles
Comprehensive Safety Assessment
Table 3: Comparative Safety Profiles of sEVs and ApoVs
| Safety Parameter | sEVs Evidence | ApoVs Evidence | Risk Assessment |
|---|---|---|---|
| Immunogenicity | Low immunogenicity; no significant immune activation reported [14] | Relative immunological tolerance; no significant adverse events [8] [48] | Both favorable, with ApoVs potentially lower risk |
| Tumorigenicity | No replication capacity; significantly mitigates carcinogenesis risk [14] | Derived from apoptotic cells; theoretically low risk | Both lower risk than whole-cell therapies |
| Toxicity Profile | Non-cytotoxic to retinal pigment epithelium [18] | No harmful events reported in preclinical studies [8] [48] | Both demonstrate excellent safety in available studies |
| Systemic Effects | No embolism risk due to nanoscale size [14] | Systematic injection well-tolerated in septic mice [48] | sEVs may have advantage in biodistribution |
| Adverse Event Reports | Manageable adverse events in clinical trials for retinal diseases [18] | Limited clinical data; no adverse events in preclinical models | sEVs have more extensive clinical safety data |
Biodistribution Patterns
Understanding the in vivo distribution of therapeutic vesicles is crucial for evaluating both efficacy and potential off-target effects. Current evidence suggests distinct biodistribution patterns for sEVs versus ApoVs:
sEV Biodistribution:
- Enhanced Tissue Penetration: Their nanoscale size (30-200 nm) enables efficient penetration across biological barriers, including potential access to the central nervous system through the blood-brain barrier [14]
- Targeted Accumulation: sEVs naturally inherit targeting molecules from parent cells, facilitating specific tissue homing, though this varies with cell source and isolation methods
- Clearance Pathways: Primarily cleared through hepatic and renal routes, with half-life dependent on administration route and surface modifications
ApoV Biodistribution:
- Phagocyte-Mediated Clearance: ApoVs naturally express "eat-me" signals like phosphatidylserine that promote rapid uptake by phagocytic cells, particularly macrophages [48]
- Inflammation-Targeted: MSC-derived ApoVs demonstrate targeted accumulation in inflammatory sites, such as bone marrow in septic mice, through electrostatic interactions with neutrophil extracellular traps (NETs) [48]
- Size-Dependent Variability: Larger ApoBDs (1-5 μm) may have different distribution patterns compared to smaller ApoSEVs (<1 μm), with potential for more localized effects
Experimental Protocols for Safety and Biodistribution Assessment
Vesicle Isolation and Characterization
sEV Isolation Protocol:
- Tangential Flow Filtration (TFF): Superior for large-scale production with higher particle yields compared to ultracentrifugation [18]
- Ultracentrifugation: Classical method involving sequential centrifugation steps (10,000-100,000 × g) with filtration [18]
- Characterization Requirements: Nanoparticle tracking analysis (NTA) for size distribution, transmission electron microscopy (TEM) for morphology, Western blot for markers (CD9, CD63, TSG101) [18]
ApoV Isolation Protocol:
- Differential Centrifugation: 300g for 10 min (remove cells), 3,000g for 10 min (ApoBDs), 20,000g for 30 min (ApoMVs), 120,000g for 60 min (ApoExos) with appropriate filtration [48]
- Induction Methods: Serum starvation, staurosporine treatment, ultraviolet irradiation, or death receptor activation to initiate apoptosis [48]
- Characterization Requirements: NTA for size distribution, TEM for cup-shaped morphology, flow cytometry for Annexin V positivity, Western blot for specific markers (calreticulin, integrin alpha-5) [48]
Biodistribution Tracking Methodologies
- Fluorescent Labeling: Lipophilic dyes (DiR, DiD) for in vivo imaging system (IVIS) tracking
- Radiolabeling: Zirconium-89 (^89^Zr) or other isotopes for quantitative biodistribution via PET imaging
- Luciferase Tagging: Genetic engineering of parent cells to express Gaussia or Cypridina luciferase for sensitive detection
- Immunohistochemistry: Tissue section analysis using vesicle-specific markers for spatial distribution
Safety Assessment Protocols
- Repeat-Dose Toxicity Studies: Multiple administrations over 2-4 weeks in rodent models with detailed clinical pathology
- Immunogenicity Assessment: Cytokine profiling, immune cell activation assays, and antibody production monitoring
- Tumorigenicity Evaluation: Long-term studies in immunocompromised models with careful monitoring of neoplastic formation
- Local Tolerance Testing: Histopathological examination of administration sites for irritation or tissue damage
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Vesicle Safety and Biodistribution Studies
| Reagent Category | Specific Products/Tools | Research Application | Considerations |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit, qEV Size Exclusion Columns, TIM4 Affinity Beads | Vesicle purification from biological samples | Kit-based methods vary in purity and yield; validate with multiple characterization methods |
| Characterization Tools | Nanoparticle Tracking Analyzer, Tunable Resistive Pulse Sensing, NanoFCM | Size distribution and concentration analysis | NTA remains gold standard; combine with protein quantification for complete characterization |
| Tracking Agents | DiR/DiD fluorescent dyes, ^89^Zr-oxine radiolabel, Luciferase reporter systems | In vivo biodistribution monitoring | Consider label effects on vesicle properties; use multiple methods for confirmation |
| Cell Culture Media | Xeno-free media, Human Platelet Lysate supplements, Serum-free formulations | GMP-compliant vesicle production | Culture conditions significantly impact vesicle characteristics and functionality [18] |
| Analytical Standards | MISEV2018/2023 guidelines, ISCT criteria for MSCs, Reference materials | Standardization and quality control | Adherence to MISEV guidelines critical for publication and regulatory acceptance [8] [5] |
| Animal Models | Diabetic db/db mice, STZ-induced diabetic models, Full-thickness excision wounds | Preclinical efficacy and safety testing | Animal species and disease model significantly influence outcomes [8] [5] |
The comprehensive evaluation of long-term safety and biodistribution profiles reveals distinct advantages and considerations for both sEVs and ApoVs in skin regeneration applications. sEVs benefit from more extensive safety data, including early clinical trial results, and demonstrate superior revascularization capabilities. Their nanoscale size enables enhanced tissue penetration, though this may also lead to wider biodistribution. ApoVs, particularly ApoSEVs, show exceptional promise in wound closure and collagen deposition, with theoretically favorable safety profiles due to their natural resolution pathways. However, clinical data for ApoVs remains limited compared to sEVs.
For researchers selecting between these vesicle types, consideration must be given to the specific clinical application, with sEVs potentially better suited for vascular-dependent healing and ApoVs for direct tissue regeneration and inflammation resolution. Both vesicle types offer significant advantages over whole-cell therapies, including reduced risks of immunogenicity, tumorigenicity, and embolism. As the field advances, standardization of isolation protocols, characterization methods, and safety assessment frameworks will be crucial for meaningful comparison and clinical translation of both sEV and ApoV-based therapeutics.
Head-to-Head Efficacy: Meta-Analysis of Regenerative Outcomes
Comparative Analysis of Wound Closure Rates
The therapeutic potential of extracellular vesicles (EVs) derived from mesenchymal stem cells (MSCs) has emerged as a promising cell-free strategy for enhancing wound healing and skin regeneration. Among these vesicles, small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs) represent distinct subpopulations with potentially different mechanistic actions and therapeutic outcomes. This comparison guide objectively analyzes the performance of sEVs versus ApoEVs in wound closure rates, providing researchers and drug development professionals with synthesized experimental data and methodologies from current preclinical studies. Understanding the comparative efficacy of these EV subtypes is crucial for developing targeted therapies for both diabetic and non-diabetic chronic wounds, which affect millions globally and pose significant clinical challenges [50].
Vesicle Classification and Biogenesis
Extracellular vesicles are membrane-bound nanoparticles that facilitate intercellular communication by transferring bioactive molecules such as proteins, lipids, and nucleic acids. For wound healing applications, two primary categories are clinically relevant:
- Small Extracellular Vesicles (sEVs): These vesicles, typically <200 nm in diameter, include exosomes (originating from the endosomal system) and ectosomes (budding from the plasma membrane). sEVs form a nanosized subclass that has been extensively studied for wound healing applications [27] [4].
- Apoptotic Extracellular Vesicles (ApoEVs): Generated during programmed cell death, ApoEVs comprise apoptotic bodies (ApoBDs, 1-5 μm) and apoptotic small EVs (ApoSEVs, <1 μm). These vesicles preserve contents from their parent cells and offer distinct advantages in ethical considerations, preparation methodologies, and consistency [27] [46].
The fundamental differences in biogenesis contribute to variations in cargo composition, surface markers, and ultimately, their functional effects on wound healing processes [4].
Comparative Efficacy in Wound Closure
A recent meta-analysis of 83 preclinical studies provides direct comparative data on the efficacy of different MSC-EV subtypes for wound healing applications. The findings demonstrate that various EV subtypes excel in distinct aspects of the wound healing process, as summarized in Table 1 [27].
Table 1: Comparative Efficacy of EV Subtypes in Wound Healing Parameters
| EV Subtype | Wound Closure Efficacy | Collagen Deposition | Revascularization Potential | Key Strengths |
|---|---|---|---|---|
| ApoSEVs | ++++ (Best) | ++++ (Best) | ++ | Superior wound closure and collagen deposition |
| ApoBDs | ++ | ++ | + | Moderate overall efficacy |
| sEVs | +++ | +++ | ++++ (Best) | Superior revascularization |
| ApoEVs | +++ | +++ | ++ | Balanced approach |
The meta-analysis revealed that ApoSEVs demonstrated significantly better efficacy in wound closure rates and collagen deposition compared to both ApoBDs and sEVs. Conversely, sEVs displayed superior performance in revascularization, a critical process for supplying nutrients and oxygen to healing tissue. These findings suggest that the selection of EV subtype should be guided by the specific healing deficits present in the target wound type [27].
Experimental Models and Methodologies
Animal Models and Wound Types
Preclinical studies evaluating EV efficacy have utilized standardized wound models to generate comparable data:
- Animal Species: Most studies (73.5%) used mouse models, while rats accounted for 26.5% of studies. Larger animal models, including diabetic porcine models, have been employed in some investigations to enhance translational relevance [27] [51].
- Disease Models: Research has been conducted in both non-diabetic (43.4%) and diabetic (47.0%) wound models. Diabetic models included streptozotocin (STZ)-induced type 1 diabetes (30 studies) and genetically modified db/db mice representing type 2 diabetes (9 studies) [27].
- Wound Types: Full-thickness excisional wounds were the most frequently studied model (90.4%), with dorsal wounds being predominant. Other models included burns, photoaging, atopic dermatitis, and frostbite injury [27].
Vesicle Isolation and Characterization
Standardized protocols for vesicle isolation and characterization are critical for experimental reproducibility:
- sEV Isolation: Differential ultracentrifugation remains the most widely used method, often combined with ultrafiltration or polymer precipitation to enhance purity [4].
- ApoEV Induction: Apoptotic vesicles are typically generated by treating MSCs with 0.5 μM staurosporine for 12 hours to induce apoptosis, followed by collection and purification of released vesicles [46].
- Characterization: Essential characterization includes nanoparticle tracking analysis for size distribution, transmission electron microscopy for structural assessment, and Western blotting for surface markers (CD63, syntenin for sEVs) [51].
Administration Protocols
Route and frequency of administration significantly impact therapeutic outcomes:
- Administration Routes: Subcutaneous injection around wound edges demonstrated superior improvement in wound closure, collagen deposition, and revascularization compared to topical dressing/covering approaches [27].
- Dosing Regimens: Treatment dose and frequency varied considerably across studies, highlighting the need for standardized dosing protocols in future research [27].
Mechanism of Action: Signaling Pathways
The differential effects of sEVs and ApoEVs on wound closure rates stem from their distinct mechanisms of action, which involve multiple signaling pathways and cellular processes as illustrated below:
sEVs and ApoEVs Mechanism of Action
sEV Signaling Pathways
sEVs primarily enhance wound healing through pro-angiogenic mechanisms:
- Angiogenesis Activation: sEVs promote new blood vessel formation by transferring pro-angiogenic factors to endothelial cells [52].
- VEGF Upregulation: Experimental data show sEVs restore endothelial cell migration by 35.7±5.6% and tube formation by 36.1±2.4% under hyperglycemic conditions, accompanied by increased expression of VEGF and CD31 [51].
- Cell Migration Enhancement: sEVs significantly improve fibroblast migration (31.4±4.4%) and reduce senescence (24.7±5.8%) in high-glucose-stimulated human dermal fibroblasts, facilitating re-epithelialization [51].
ApoEV Signaling Pathways
ApoEVs exert their effects through distinct mechanisms involving immunomodulation and lipid metabolism:
- Macrophage Function Modulation: ApoEVs are phagocytosed by macrophages and accelerate cutaneous wound healing by modulating macrophage function [46].
- Lipid Metabolism: Group X secretory phospholipase A2 (sPLA2-X) in ApoEVs significantly increases production of anti-inflammatory lipid mediator resolvin D5 (RvD5) through phospholipid hydrolysis [46].
- Anti-inflammatory Effects: ApoEV-mediated RvD5 production effectively inhibits tumor necrosis factor-alpha (TNF-α) expression in macrophages, creating an anti-inflammatory environment conducive to healing [46].
Source-Dependent Efficacy Variations
The therapeutic efficacy of both sEVs and ApoEVs varies significantly depending on their cellular origin. ADSC-derived vesicles demonstrated the best effect on wound closure rate and collagen deposition, while bone marrow MSC-derived vesicles showed superior performance in revascularization [27]. This source-dependent variation highlights the importance of selecting appropriate parent cells for specific therapeutic goals.
Research Reagent Solutions
Table 2 outlines essential research reagents and their applications in EV wound healing research, compiled from methodologies across multiple studies:
Table 2: Key Research Reagents for EV Wound Healing Studies
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| EV Isolation Kits | TOOLSharp exosome extraction kit | RJEV isolation from royal jelly [51] | Rapid EV purification from biological fluids |
| Apoptosis Inducers | Staurosporine (STS) | ApoEV generation from MSCs [46] | Induces programmed cell death for ApoEV production |
| Cell Line Markers | CD63, CD81, CD9, Syntenin | EV characterization [51] [4] | sEV identification and quantification |
| Angiogenesis Assays | VEGF, CD31 antibodies | Assessment of neovascularization [51] | Markers for endothelial cell function and vessel formation |
| Cytokine Analysis | IL-1β, IL-6, IL-8, TNF-α ELISA | Inflammation monitoring [51] | Quantification of pro-inflammatory mediators |
| Cell Tracking Dyes | ExoSparkler Exosome Membrane Labeling Kit | Cellular uptake studies [51] | Fluorescent EV labeling for trafficking experiments |
| Animal Model Inducers | Streptozotocin (STZ) | Diabetic wound models [27] [51] | Chemical induction of type 1 diabetes for wound studies |
The comparative analysis of wound closure rates reveals a compelling case for matching EV subtypes to specific wound healing deficits. sEVs demonstrate superior revascularization capacity, making them particularly suitable for wounds with impaired angiogenesis. In contrast, ApoSEVs excel in promoting wound closure and collagen deposition, suggesting their potential application for wounds requiring enhanced re-epithelialization and matrix restoration. The optimal therapeutic approach may involve either selecting the appropriate EV subtype based on the specific wound pathology or developing combination strategies that leverage the complementary strengths of both vesicle types. Future research should focus on standardizing isolation protocols, optimizing dosing regimens, and conducting direct comparative studies in clinically relevant wound models to accelerate translational applications.
Impact on Collagen Deposition and ECM Remodeling
The extracellular matrix (ECM) provides critical structural and biochemical support for skin tissue, with collagen deposition being a fundamental process in maintaining skin integrity and facilitating repair. In regenerative medicine, small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs) have emerged as promising cell-free therapeutic agents. These nano-sized particles facilitate intercellular communication by transferring bioactive molecules, thereby orchestrating tissue regeneration. This guide provides a objective comparison of the documented effects of sEVs versus ApoEVs on collagen deposition and ECM remodeling, synthesizing current preclinical data to inform research and development strategies.
Vesicle Characteristics and Biogenesis
Table 1: Fundamental Characteristics of sEVs and ApoEVs
| Feature | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Biogenesis | Formed via inward budding of endosomal membranes, released upon fusion of multivesicular bodies with the plasma membrane [6] | Formed via outward blebbing of the plasma membrane during the execution phase of apoptosis [7] [6] |
| Size Range | 30 - 150 nm [18] [6] | 100 - 5000 nm (includes ApoBDs: 1-5 μm; ApoSEVs: <1 μm) [7] [5] [53] |
| Common Markers | CD9, CD63, CD81, TSG101 [18] [6] | Phosphatidylserine externalization [7] |
| Primary Cargo | miRNAs, growth factors (VEGF, TGF-β), tetraspanins [18] [6] | Cellular debris, organelles, DAMPs, microRNAs [7] |
Figure 1: Vesicle Biogenesis Pathways. sEVs are generated from the endosomal system, while ApoEVs are produced during programmed cell death.
Quantitative Comparison of Therapeutic Outcomes
Table 2: Efficacy Outcomes in Preclinical Skin Regeneration Models (Meta-Analysis Data) [5]
| Outcome Measure | Vesicle Type | Model Type | Standardized Mean Difference (SMD) | Confidence Interval (CI) | Key Findings |
|---|---|---|---|---|---|
| Wound Closure Rate | ApoSEVs | Diabetic/Non-Diabetic | 1.89 | [1.21, 2.57] | Superior efficacy vs. ApoBDs & sEVs |
| sEVs | Diabetic/Non-Diabetic | 1.24 | [0.98, 1.50] | Effective, but less than ApoSEVs | |
| Collagen Deposition | ApoSEVs | Diabetic/Non-Diabetic | 1.93 | [1.19, 2.67] | Promotes more organized collagen fibers |
| sEVs | Diabetic/Non-Diabetic | 1.41 | [1.13, 1.69] | Improves collagen density & maturity | |
| Revascularization | sEVs | Diabetic/Non-Diabetic | 1.65 | [1.33, 1.97] | Promotes angiogenesis & blood vessel density |
| ApoEVs | Diabetic/Non-Diabetic | 1.21 | [0.75, 1.67] | Moderate pro-angiogenic effect | |
| Scar Width | sEVs | Non-Diabetic | -1.81 | [-2.23, -1.39] | Significant reduction in scar tissue |
Mechanisms of Action on ECM and Collagen
sEV-Mediated ECM Remodeling
sEVs promote a balanced ECM remodeling process by delivering specific microRNAs and growth factors to recipient cells like fibroblasts and keratinocytes. [6] They enhance collagen synthesis by activating the Wnt4/β-catenin and PI3K/Akt signaling pathways, which upregulate the production of collagen types I and III. [6] Furthermore, sEVs modulate the tissue microenvironment by promoting M2 macrophage polarization, a phenotype associated with anti-inflammatory responses and tissue repair. [5] [6] They also carry and regulate the activity of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs), preventing excessive ECM degradation and ensuring proper collagen maturation and organization. [54]
ApoEV-Mediated ECM Modulation
ApoEVs exert their primary effects through powerful immunomodulation. They are efficiently engulfed by phagocytes, such as macrophages, a process known as efferocytosis. [7] This process triggers a shift towards an anti-inflammatory M2 macrophage state and the release of regenerative cytokines like TGF-β, which in turn stimulates fibroblast-mediated collagen deposition. [7] [55] A specific mechanism involves the delivery of mmu-miR-21a-5p by MSC-derived ApoEVs, which downregulates pro-inflammatory pathways and drives M2 polarization, creating a favorable microenvironment for ECM reconstruction and wound healing. [55]
Figure 2: Key Signaling Pathways. sEVs act directly on ECM-producing cells, while ApoEVs work through efferocytosis and immunomodulation.
Experimental Protocols and Workflows
Vesicle Isolation and Characterization
Table 3: Standard Protocols for Vesicle Production and Isolation
| Protocol Step | sEV Workflow [18] | ApoEV Workflow [5] [55] |
|---|---|---|
| Source Cell Culture | BM-MSCs expanded in α-MEM + 10% hPL under GMP conditions [18] | MSCs induced to undergo apoptosis (e.g., via serum starvation or chemical inducers) |
| Vesicle Harvesting | Collection of conditioned medium from viable cells | Collection of medium from apoptotic cell cultures |
| Isolation Method | Tangential Flow Filtration (TFF) or Ultracentrifugation (UC); TFF yields higher particle numbers [18] | Differential centrifugation to pellet larger ApoBDs and subsequent isolation of ApoSEVs |
| Characterization | NTA (size/concentration), TEM (morphology), Western Blot (CD9, CD63, TSG101) [18] | NTA, TEM, Flow Cytometry (Annexin V for phosphatidylserine) |
Figure 3: Experimental Workflow for Vesicle Isolation. TFF is efficient for sEVs, while differential centrifugation is standard for ApoEVs.
In Vivo Model and Treatment Evaluation
A typical protocol for evaluating vesicle efficacy in skin regeneration involves:
- Animal Model: Creating full-thickness excisional wounds on the dorsum of mice or rats. Diabetic models (e.g., db/db mice or STZ-induced) are commonly used to mimic impaired healing. [5]
- Vesicle Administration: Treatment via subcutaneous injection around the wound bed or topical application using a scaffold/dressing. Meta-analysis indicates subcutaneous injection is more effective for both sEVs and ApoEVs. [5]
- Dosage: A common effective dose for sEVs is 50 µg/mL per wound, applied multiple times during the healing process. [18] [5]
- Outcome Analysis:
- Wound Closure: Digital planimetry to measure area over time.
- Collagen Analysis: Histology (Masson's Trichrome or Picrosirius Red staining) to assess collagen deposition, fiber thickness, and organization.
- Immunohistochemistry: Staining for CD31 (blood vessel density), α-SMA (myofibroblasts), and macrophage polarization markers (e.g., CD206 for M2). [5] [6]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Materials for Vesicle Research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| α-MEM with hPL | Xeno-free cell culture medium for MSC expansion | Promotes superior BM-MSC growth and sEV yield compared to DMEM [18] |
| Tangential Flow Filtration (TFF) System | Scalable, gentle isolation of sEVs from conditioned medium | Higher particle yield vs. ultracentrifugation; suitable for GMP production [18] |
| Nanoparticle Tracking Analyzer (NTA) | Measures vesicle size distribution and concentration | Essential for characterizing both sEV and ApoSEV preparations [18] |
| CD63/CD81/CD9 Antibodies | Detection of common sEV surface markers via Western Blot | Critical for confirming sEV identity per MISEV guidelines [18] [5] |
| Annexin V | Binds phosphatidylserine on the surface of ApoEVs | Key reagent for flow cytometry-based identification of ApoEVs [7] |
| Polycaprolactone (PCL) Scaffold | Biocompatible material for sustained local delivery of vesicles | Used to deliver MSC-ABs, showing efficacy in wound healing models [55] |
| Masson's Trichrome Stain | Histological staining to visualize collagen fibers (blue/green) | Standard method for quantifying collagen deposition in regenerated skin [5] |
sEVs and ApoEVs represent two distinct yet powerful biological agents for promoting skin regeneration through targeted ECM remodeling and collagen deposition. The current preclinical data, synthesized in this guide, suggests a compelling division of labor: ApoSEVs demonstrate superior efficacy in accelerating wound closure and enhancing collagen deposition, likely through potent immunomodulation. In contrast, sEVs excel in promoting revascularization and reducing scar width. The choice between vesicle types is not a matter of overall superiority but depends on the primary therapeutic goal—whether rapid wound closure and matrix synthesis or vascularization and scar quality is paramount. Future research must focus on standardizing isolation protocols, optimizing scalable production under GMP guidelines, and conducting rigorous comparative in vivo studies to fully realize the clinical potential of these sophisticated biological nanoparticles.
Angiogenic Potential and Blood Vessel Density
The therapeutic promotion of angiogenesis, the formation of new blood vessels from pre-existing vasculature, is a critical objective in regenerative medicine, particularly for skin repair where adequate blood supply determines tissue survival and regeneration outcomes. Among the most promising therapeutic agents are extracellular vesicles (EVs)—nanoscale, lipid-bilayer enclosed particles that facilitate intercellular communication by transferring bioactive cargo such as proteins, nucleic acids, and lipids. Small extracellular vesicles (sEVs) and apoptotic vesicles (ApoEVs) represent two distinct EV subpopulations with unique biogenic origins, cargo profiles, and functional activities [26] [7] [34]. This guide provides an objective, data-driven comparison of the angiogenic potential of sEVs versus ApoEVs, synthesizing current experimental evidence to inform selection for research and therapeutic development in skin regeneration. sEVs (30-200 nm), historically referred to as exosomes, are generated through the endosomal pathway and released upon the fusion of multivesicular bodies with the plasma membrane [26] [56]. In contrast, ApoEVs (50-5000 nm) are produced during the programmed cell death of apoptosis, forming as the cell membrane buds and packages cellular contents [7] [34] [3]. Their inherent differences in formation underlie significant variations in cargo, mechanisms of action, and, consequently, their ability to modulate blood vessel density.
Comparative Biophysical and Functional Profiles
The fundamental differences between sEVs and ApoEVs directly influence their respective roles in angiogenesis. The table below summarizes their core characteristics and documented effects on blood vessel formation.
Table 1: Comparative Overview of sEVs and ApoEVs in Angiogenesis
| Feature | Small Extracellular Vesicles (sEVs) | Apoptotic Vesicles (ApoEVs) |
|---|---|---|
| Biogenic Origin | Endosomal pathway; release from multivesicular bodies [26] [56] | Plasma membrane budding during apoptosis [7] [34] |
| Size Range | 30 - 200 nm [26] [57] | 50 - 5000 nm (highly heterogeneous) [34] [3] |
| Key Markers | Tetraspanins (CD9, CD63, CD81), TSG101, ALIX [26] [56] | Phosphatidylserine (PS) exposure [7] [3] |
| Primary Angiogenic Cargo | miRNA-126, miRNA-210, miRNA-135b, pro-angiogenic proteins (e.g., MMP-9) [58] [56] | "Find me" signals (S1P), "eat me" signals (PS), regulatory miRNAs [7] [3] |
| Mechanism in Angiogenesis | Transfer of pro-angiogenic miRNAs/mRNAs to endothelial cells; direct protein signaling [57] [58] | Efferocytosis-induced immune polarization; promotion of anti-inflammatory and pro-regenerative macrophage phenotypes [7] [34] |
| Reported Effects on Vessel Density | Significantly enhanced tubulogenesis, endothelial cell migration, and proliferation in vitro; improved blood perfusion in vivo [57] [58] | Promotion of tissue regeneration and resolution of inflammation, creating a conducive microenvironment for vascular repair [7] [34] |
Supporting Experimental Data and Protocols
The functional data supporting the angiogenic capabilities of these vesicles are derived from standardized in vitro and in vivo models. The following table consolidates key quantitative findings from seminal studies.
Table 2: Experimental Data on Angiogenic Potential
| Experimental Model | Vesicle Type & Source | Key Quantitative Findings | Reference |
|---|---|---|---|
| In Vitro Tube Formation (HUVECs) | Plasma sEVs (advanced-stage HNC patients) | Significantly increased tubulogenesis and endothelial cell migration compared to sEVs from healthy donors. | [57] |
| In Vitro Tube Formation (HUVECs) | Engineered sEVs from BM-MSCs overexpressing angio-miRNA | EV126 and EV135b significantly enhanced tube formation vs. control. Combination EVs (EV126+EV135b) showed superior effects. | [58] |
| In Vivo Hindlimb Ischemia (Mouse) | Engineered sEVs from BM-MSCs overexpressing angio-miRNA | Double (EV126+EV135b) and triple (EV126+EV135b+EV210) EV groups significantly improved limb perfusion and capillary density vs. single EVs or control. | [58] |
| In Vitro / In Vivo Models | ApoEVs from stem cells | Demonstrated anti-inflammatory effects, macrophage polarization, and promotion of tissue regeneration, indirectly supporting vascular repair. | [7] [34] |
Detailed Experimental Protocols
To ensure the reproducibility of angiogenic testing, researchers adhere to established protocols for vesicle isolation and functional assays.
1. Vesicle Isolation and Characterization:
- sEV Isolation via Size-Exclusion Chromatography (SEC): Cell culture supernatant or plasma is subjected to sequential centrifugation (e.g., 2,000 × g for 10 min, then 14,000 × g for 30 min) to remove cells and debris. The supernatant is then filtered (0.22 µm) and loaded onto a SEC column (e.g., Sepharose CL-2B). sEVs are eluted with phosphate-buffered saline (PBS), typically in the 4th fraction [57]. Characterization involves Nanoparticle Tracking Analysis (NTA) for size/concentration, transmission electron microscopy (TEM) for morphology, and western blot for markers (CD9, CD63, CD81, TSG101) [57].
- ApoEV Isolation via Differential Centrifugation: Apoptosis is induced in source cells (e.g., with staurosporine or UV irradiation). The conditioned medium is collected and centrifuged at low speed (e.g., 2,000 × g) to remove intact cells. ApoEVs are then pelleted by high-speed centrifugation (e.g., 10,000 - 20,000 × g). Further purification can be achieved using density gradient centrifugation [34] [3]. Characterization includes NTA, TEM, and flow cytometry for phosphatidylserine exposure [3].
2. Key Angiogenesis Assays:
- Endothelial Tube Formation Assay: Human umbilical vein endothelial cells (HUVECs) are co-cultured with test vesicles on a basement membrane matrix (e.g., Geltrex or Matrigel). After 4-24 hours, tube structures are visualized, and parameters like the number of junctions, total segment length, and total mesh area are quantified using software like ImageJ with the Angiogenesis Analyzer plugin [57] [58].
- Cell Migration/Proliferation Assays: For migration, a "scratch" wound is created in a confluent HUVEC monolayer, and closure is monitored with/without vesicle treatment. Proliferation is measured using assays like MTS, where metabolic activity correlates with cell number after vesicle treatment [57].
- In Vivo Ischemic Models: In the mouse hindlimb ischemia model, the femoral artery is ligated. Vesicles are then injected intramuscularly into the ischemic area. Blood flow recovery is tracked over time using Laser Doppler Perfusion Imaging, and capillary density in muscle tissue is quantified histologically after staining for endothelial markers (e.g., CD31) [58].
Mechanisms of sEV and ApoEV Action in Angiogenesis
The Scientist's Toolkit: Essential Research Reagents
Successful investigation into vesicle-mediated angiogenesis relies on a suite of specialized reagents and tools.
Table 3: Essential Reagents for EV Angiogenesis Research
| Reagent / Tool | Function & Application | Example Use-Case |
|---|---|---|
| Sepharose CL-2B | Size-exclusion chromatography matrix for high-purity sEV isolation from biofluids. | Isolation of sEVs from human plasma or cell culture conditioned medium [57]. |
| Differential Ultracentrifugation | The "gold standard" method for pelleting EVs based on size and density. | Sequential centrifugation to isolate ApoEVs from apoptotic cell culture supernatant [26] [34]. |
| Nanoparticle Tracking Analyzer | Instrument for determining EV particle size distribution and concentration. | Characterizing the size profile and yield of isolated sEVs/ApoEVs [57] [58]. |
| Basement Membrane Matrix | Extracellular matrix hydrogel for 3D endothelial cell culture. | Substrate for the in vitro tube formation assay with HUVECs [57] [58]. |
| Human Umbilical Vein Endothelial Cells | Primary endothelial cells used as a standard model for angiogenic studies. | Recipient cells for testing the pro-angiogenic effects of EVs in migration and tube formation assays [57] [58]. |
| Lentiviral Vectors | Tools for stable genetic modification of parent cells to engineer EV cargo. | Overexpressing specific angio-miRNAs (e.g., miR-126) in mesenchymal stem cells to produce engineered sEVs [58]. |
The choice between sEVs and ApoEVs for enhancing blood vessel density in skin regeneration is not a matter of superiority but of strategic application. sEVs, particularly those engineered from mesenchymal stromal cells, function as direct molecular tools that aggressively promote angiogenesis by delivering a concentrated payload of pro-angiogenic factors to endothelial cells, making them ideal for rapidly initiating and sustaining new blood vessel growth. In contrast, ApoEVs act as indirect orchestrators of a pro-regenerative microenvironment. By modulating immune responses and resolving inflammation, they pave the way for orderly and integrated vascular repair. The future of vesicle-based therapeutics likely lies in combination approaches, leveraging the direct angiogenic stimulatory capacity of engineered sEVs with the potent, inflammation-resolving power of ApoEVs to achieve optimal and durable skin regeneration outcomes.
Modulation of Inflammation and Scar Formation
The pursuit of optimal regenerative therapies for skin wounds has intensified the focus on two distinct types of extracellular vesicles (EVs): small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs). Both are membrane-bound nanoparticles that facilitate intercellular communication by transferring bioactive cargoes—such as proteins, lipids, and nucleic acids—from parent cells to recipient cells, thereby modulating the wound microenvironment [26] [59]. sEVs (traditionally known as exosomes) are typically smaller than 200 nm and are constitutively released by living cells via the endosomal pathway [26] [6]. In contrast, ApoEVs are a heterogeneous population of vesicles, ranging from 0.1 to 5 μm, which are shed in an ordered manner by cells undergoing programmed cell death [26] [60]. Within the context of skin repair, the therapeutic potential of mesenchymal stem cell (MSC)-derived sEVs and ApoEVs is particularly promising. They orchestrate healing by influencing key processes such as inflammation, angiogenesis, fibroblast function, and extracellular matrix (ECM) remodeling [5] [52] [50]. This guide provides a objective, data-driven comparison of their performance in modulating the critical outcomes of inflammation and scar formation.
Comparative Efficacy: Quantitative Outcomes Analysis
Direct comparative studies and meta-analyses of preclinical data provide a foundation for evaluating the relative strengths of sEVs and ApoEVs. A 2025 systematic review and meta-analysis of 83 preclinical studies offers the most comprehensive direct comparison to date [5]. The table below summarizes the key quantitative findings from this and other relevant studies.
Table 1: Comparative Efficacy of sEVs and ApoEVs in Preclinical Wound Healing Models
| Outcome Measure | sEVs Performance | ApoEVs Performance | Comparative Findings | Supporting References |
|---|---|---|---|---|
| Wound Closure Rate | Significantly improves vs. controls | Significantly improves vs. controls | ApoSEVs showed better efficacy than sEVs and ApoBDs (Apoptotic Bodies) in subgroup analysis. | [5] |
| Revascularization (Blood Vessel Density) | Promotes angiogenesis effectively | Promotes angiogenesis | sEVs displayed better outcomes than ApoEVs in subgroup analysis. | [5] |
| Collagen Deposition & Scar Width | Reduces scar width, improves collagen organization | Increases Type III/I collagen ratio, reduces scar width | ApoSEVs showed better efficacy in enhancing collagen deposition. ApoEVs promote a more regenerative collagen profile. | [61] [5] |
| Modulation of Apoptosis | Reduces total apoptotic cells in injured tissue (e.g., from 37.9% viability to 54.6%) | Information Not Specified | Demonstrated in a retinal epithelium injury model, indicating a strong anti-apoptotic function. | [18] |
| Anti-fibrotic Signaling | Inhibits TGF-β signaling pathway | Markedly inhibits Hedgehog signaling pathway; downregulates Shh and Gli1 | Both vesicle types target key pro-fibrotic pathways, but through distinct mechanisms. | [61] [62] |
Table 2: Key Mechanistic Actions of sEVs and ApoEVs in the Wound Microenvironment
| Cell Target | sEVs Actions | ApoEVs Actions |
|---|---|---|
| Macrophages | Promote polarization towards anti-inflammatory M2 phenotype [52] [6]. | Inhibit macrophage pyroptosis; promote M2 polarization [60]. |
| Fibroblasts | Promote proliferation, migration, and collagen production [62]. | Enhance mitochondrial function and OXPHOS; suppress glycolysis; inhibit aberrant ECM deposition [61]. |
| Endothelial Cells | Stimulate angiogenesis via VEGF, Wnt4/β-catenin, and PI3K/Akt pathways [52] [6]. | Promote proliferation and migration of endothelial cells, enhancing neo-angiogenesis [60]. |
| Keratinocytes | Activate and promote re-epithelialization [6]. | Information Not Specified |
Experimental Protocols and Workflows
Vesicle Isolation and Characterization
Standardized protocols are critical for the reproducible production of high-quality vesicles for research and therapy.
- Source Cell Culture: MSCs are typically isolated from tissues like human umbilical cord, adipose tissue, or bone marrow and expanded in culture flasks using media such as α-MEM supplemented with 10% human platelet lysate (hPL) or fetal bovine serum (FBS) [18] [60]. For ApoEV production, apoptosis is induced in confluent MSCs using agents like staurosporine (STS) at 0.5 μM for 16-18 hours; a TUNEL assay confirming an apoptotic rate of >90% is a common quality checkpoint [60].
- Vesicle Isolation from Conditioned Media:
- Ultracentrifugation (UC): The classical "gold standard" method. Cell culture supernatant is subjected to sequential centrifugation steps: 2,000 × g for 30 min and 10,000 × g for 45 min to remove cells and debris, followed by high-speed ultracentrifugation at 110,000 - 120,000 × g for 70 minutes to pellet vesicles [18] [62]. The pellet is resuspended in phosphate-buffered saline (PBS).
- Tangential Flow Filtration (TFF): A scalable method ideal for processing large volumes. The sample is circulated through a membrane system, separating vesicles based on size. Studies show TFF provides a statistically higher particle yield compared to UC [18].
- Vesicle Characterization:
- Nanoparticle Tracking Analysis (NTA): Used to determine the particle size distribution and concentration (particles/mL) [18] [60].
- Transmission Electron Microscopy (TEM): Confirms the cup-shaped or spherical morphology of the isolated vesicles [18] [62].
- Western Blot (WB): Verifies the presence of vesicle marker proteins (e.g., CD63, CD9, TSG101 for sEVs) and the absence of negative markers (e.g., calnexin) [18] [62].
In Vitro and In Vivo Functional Assays
- In Vitro Migration (Scratch Assay): A monolayer of recipient cells (e.g., Human Dermal Fibroblasts-adult, HDF-a) is scratched with a pipette tip. The rate of cell migration into the scratch area is measured over 24-48 hours after treatment with vesicles (typically at 50-100 μg/mL) versus a PBS control. The migration area percentage is calculated as (A0-An)/A0 × 100, where A0 is the initial scratch area and An is the remaining area [62].
- In Vivo Wound Healing Models: Full-thickness excisional wounds (e.g., 6-8 mm diameter) are created on the dorsum of mice or rats. Vesicles (e.g., 100 μg in 100 μL PBS) or a control solution are administered via local subcutaneous injection around the wound periphery. Key metrics tracked over time include:
- Wound Closure Rate: The percentage reduction in wound area over days post-injury [5] [62].
- Histological Analysis: After sacrifice, wound tissue is sectioned and stained (e.g., with H&E, Masson's Trichrome) to assess re-epithelialization, collagen deposition, blood vessel density, and scar width [62].
- Advanced Molecular Analysis:
- Spatial Transcriptomics (ST): This technique maps gene expression profiles within the context of tissue architecture. It has been used to show that MSC-EVs reduce the expression of myofibroblast marker genes and the TGF-β signaling pathway while upregulating the Wnt pathway in healed wounds, explaining the observed reduction in scarring [62].
- Flow Cytometry: Used to quantify apoptosis in recipient cells after injury and treatment, demonstrating the anti-apoptotic effects of vesicles [18].
Signaling Pathways: A Visual Synthesis
The therapeutic effects of sEVs and ApoEVs are mediated through their modulation of distinct and overlapping signaling pathways in target cells within the wound.
Figure 1: Key Signaling Pathways Modulated by sEVs and ApoEVs. sEVs primarily act through downregulation of TGF-β and activation of Wnt/PI3K pathways. ApoEVs notably inhibit the Hedgehog pathway and reprogram fibroblast metabolism. Both vesicle types promote anti-inflammatory macrophage polarization [61] [5] [6].
Experimental Workflow: From Vesicle Production to Analysis
A typical research pipeline for evaluating sEVs and ApoEVs involves sequential stages from source cell preparation to functional validation.
Figure 2: Experimental Workflow for sEV and ApoEV Research. The workflow diverges at the stage of vesicle production, where sEVs are harvested from the conditioned medium of living cells, while ApoEVs are collected following the induction of apoptosis. Subsequent isolation, characterization, and functional validation steps are broadly parallel [18] [60] [62].
The Scientist's Toolkit: Essential Research Reagents
Successful research into sEVs and ApoEVs relies on a suite of key reagents and methodologies. The following table details essential components of the experimental toolkit.
Table 3: Key Research Reagent Solutions for EV Studies
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Culture Media & Supplements | Supports the expansion and maintenance of parent MSCs. | Alpha-MEM (α-MEM); Dulbecco's Modified Eagle Medium (DMEM); Fetal Bovine Serum (FBS); Human Platelet Lysate (hPL) – a xeno-free alternative [18] [60]. |
| Apoptosis Inducers | Triggers programmed cell death for ApoEV production. | Staurosporine (STS), typically used at 0.5 μM for 16-18 hours [60]. |
| Isolation Kits & Systems | Separates vesicles from complex biological fluids or cell culture supernatant based on physical properties. | Ultracentrifugation systems (e.g., Beckman Coulter optima XPN); Tangential Flow Filtration (TFF) systems; Polymeric precipitation kits [18] [26]. |
| Characterization Instruments | Determines the physical, molecular, and morphological properties of isolated vesicles. | Nanoparticle Tracking Analyzer (NTA, e.g., ZetaView) for size/concentration; Transmission Electron Microscope (TEM) for morphology; Western Blot apparatus for protein markers (CD63, TSG101, CD81) [18] [60] [62]. |
| In Vivo Model Systems | Provides a biologically complex system to evaluate therapeutic efficacy and mechanisms. | Mouse (e.g., BALB/c, C57BL/6) or Rat (e.g., Sprague Dawley) full-thickness excisional wound models; Diabetic models (e.g., db/db mice, STZ-induced) [5] [62]. |
| Cell Tracking Dyes | Labels vesicles for uptake and trafficking studies in recipient cells. | PKH67 (green fluorescent) or PKH26 (red fluorescent) lipophilic dyes [62]. |
The accumulated data indicates that the choice between sEVs and ApoEVs is not a matter of one being universally superior, but rather depends on the primary therapeutic goal. sEVs, with their robust pro-angiogenic and anti-apoptotic properties, appear particularly suited for treating ischemic or non-healing wounds where revascularization is critical [18] [5]. Conversely, ApoEVs demonstrate exceptional promise in driving high-quality, regenerative healing with minimal fibrosis, making them strong candidates for applications where controlling scar formation and optimizing collagen architecture are the primary objectives, such as in cosmetic and functional skin repair [61] [5] [60]. Future research will undoubtedly focus on engineering these vesicles to enhance their inherent strengths, optimizing delivery strategies, and standardizing production protocols to accelerate their transition from promising research entities to mainstream clinical therapeutics.
In the evolving landscape of regenerative medicine, the therapeutic application of mesenchymal stem cells (MSCs) is increasingly shifting from whole-cell therapies to cell-free approaches utilizing their derived extracellular vesicles (EVs). These vesicles, particularly small extracellular vesicles (sEVs) and apoptotic extracellular vesicles (ApoEVs), mediate regenerative effects by transferring bioactive molecules to recipient cells, offering a promising strategy for skin regeneration [5] [28]. The efficacy of these EVs is not uniform but is significantly influenced by the tissue source of the parent MSCs. This guide provides a systematic, data-driven comparison of EVs derived from three predominant MSC sources: Adipose-Derived Stem Cells (ADSCs), Bone Marrow-Derived Mesenchymal Stem Cells (BMMSCs), and Umbilical Cord-Derived Mesenchymal Stem Cells (UMSCs). It aims to objectively inform researchers and drug development professionals about source-specific therapeutic profiles to guide experimental design and clinical translation in dermatology and wound healing.
Comparative Analysis of MSC-Source Efficacy
Extensive preclinical analyses have revealed that sEVs from different MSC sources exhibit distinct strengths across various therapeutic domains, influenced by their inherent biological characteristics and secretome profiles.
Table 1: Comparative Characteristics of MSC Sources for EV Production
| Parameter | Adipose-Derived MSCs (ADSCs) | Bone Marrow-Derived MSCs (BMMSCs) | Umbilical Cord-Derived MSCs (UMSCs) |
|---|---|---|---|
| Primary Harvest Site | Subcutaneous fat (via liposuction) [63] | Iliac crest (via bone marrow aspiration) [63] | Wharton's Jelly of umbilical cord [64] |
| Invasiveness of Harvest | Minimally invasive [63] [65] | More invasive, painful [63] [65] | Non-invasive, postnatal tissue [65] |
| Cell Yield per mL Tissue | High (~500,000–2,000,000) [63] | Low (~5,000–100,000) [63] | Variable, generally high [65] |
| Proliferation Rate | Higher [63] | Moderate [63] | High [64] |
| Key Therapeutic Strengths | Superior in wound closure & collagen deposition [5] | Strong chondrogenic differentiation; superior anti-inflammatory signaling [63] [64] | Potent immunomodulation; strong anti-inflammatory & regenerative effects [64] |
Table 2: Quantitative Efficacy of MSC-sEVs in Key Functional Assays (In Vitro/Ex Vivo)
| Functional Assay | ADSC-sEVs Performance | BMMSC-sEVs Performance | UMSC-sEVs Performance | References |
|---|---|---|---|---|
| Anti-Inflammatory (NF-κB & MAPK pathway suppression) | Moderate reduction of pp65, pp38, pJNK, pERK [64] | Superior suppression of pp65, pp38, pJNK, pERK [64] | Superior and potent suppression of inflammatory pathway phosphoproteins [64] | [64] |
| Chondroprotective & Cartilage Regeneration | Moderate efficacy [64] | Superior efficacy in upregulating chondroprotective genes [64] | Superior efficacy, comparable to BMMSC-sEVs [64] | [64] |
| Wound Closure Rate (Preclinical Models) | Superior effect compared to other sources [5] | Data not specifically superior to ADSCs | Data not specifically superior to ADSCs | [5] |
| Collagen Deposition (Preclinical Models) | Superior effect compared to other sources [5] | Data not specifically superior to ADSCs | Data not specifically superior to ADSCs | [5] |
| Angiogenesis (Blood Vessel Density) | Moderate effect [5] | Superior effect in revascularization [5] | Data not specifically superior to BMMSCs | [5] |
The data from these functional assays demonstrate a clear trend: BMMSC- and UMSC-sEVs exhibit more potent immunomodulatory capabilities, effectively downregulating key inflammatory pathways like NF-κB and MAPK, which are crucial in the early phases of wound healing [64]. In contrast, ADSC-sEVs show a distinct advantage in directly promoting wound closure and collagen deposition, processes vital for tissue integrity and regeneration [5]. Furthermore, a meta-analysis on skin regeneration confirmed that among easily accessible sources, ADSCs demonstrated the best effect on wound closure rate, while BMMSCs were more effective in promoting revascularization [5].
Experimental Protocols for EV Research
To ensure the reliability and reproducibility of comparative studies on MSC-EVs, standardized protocols for their isolation, characterization, and functional validation are paramount.
EV Isolation and Characterization
The production of high-quality EV preparations requires careful optimization from cell culture to final isolation.
Cell Culture Conditions: Studies have compared different culture media for MSC expansion. For instance, one study found that BMMSCs cultured in Alpha Minimum Essential Medium (α-MEM) supplemented with 10% human platelet lysate (hPL) showed a higher expansion ratio and yielded a higher, though not statistically significant, number of sEVs per cell compared to those cultured in Dulbecco's Modified Eagle Medium (DMEM) [18]. Culture systems (2D vs. 3D) also significantly impact the potency and identity of the produced sEVs [18].
Isolation Techniques: Multiple methods exist for sEV isolation, each with advantages and limitations.
- Ultracentrifugation (UC): This is often considered the "gold standard" method. It involves sequential centrifugation steps to remove cells, debris, and larger vesicles, followed by high-speed centrifugation to pellet sEVs. Its main drawbacks are being time-consuming and the potential for high g-forces to damage vesicles [26].
- Tangential Flow Filtration (TFF): This method is scalable and gentler. A study directly comparing TFF and UC for isolating BMMSC-sEVs found that TFF resulted in a statistically higher particle yield [18].
- Aqueous Two-Phase System (ATPS): This polymer-based separation method has been used successfully to isolate exosomes from BMMSCs, ADSCs, and UMSCs for functional comparisons, confirming the presence of exosomal markers (CD63, CD81, ALIX) and typical cup-shaped morphology [64].
Characterization Requirements: Isolated EVs must be characterized by a combination of techniques to confirm their identity and purity, as per MISEV (Minimal Information for Studies of Extracellular Vesicles) guidelines [5].
- Nanoparticle Tracking Analysis (NTA): Determines the particle size distribution and concentration [18] [64].
- Transmission Electron Microscopy (TEM): Visualizes the morphology of the vesicles (e.g., cup-shaped) [18] [64].
- Western Blotting: Confirms the presence of positive protein markers (e.g., CD9, CD63, CD81, TSG101, ALIX) and the absence of negative markers (e.g., calnexin) [18] [64].
The following workflow diagram illustrates the optimized protocol for producing and validating MSC-sEVs for functional studies:
Key Functional Assays for Skin Regeneration
To evaluate the therapeutic potential of MSC-sEVs for skin applications, the following in vitro and ex vivo assays are critical:
Anti-Inflammatory Signaling Assay:
- Protocol: Chondrocytes or dermal fibroblasts are stimulated with the pro-inflammatory cytokine IL-1β (e.g., 10 ng/mL) to create an inflammatory environment. Cells are then treated with MSC-sEVs from different sources. The suppression of inflammation is evaluated via Western Blot analysis of key signaling pathways. The reduction in phosphorylated proteins of the NF-κB pathway (e.g., p-p65) and the MAPK pathway (e.g., p-p38, p-JNK, p-ERK) is measured and compared across treatment groups [64].
Chondroprotective & Regenerative Gene Expression:
- Protocol: Using an ex vivo model of osteoarthritis (as a proxy for cartilage matrix regulation relevant to skin structure), cartilage explants are treated with MSC-sEVs. The expression of anabolic and catabolic genes is quantified using RT-qPCR. Key markers include the upregulation of chondroprotective genes (e.g., COL2A1, ACAN) and downregulation of inflammatory and matrix-degrading enzymes (e.g., MMP-13, ADAMTS-5) [64].
Wound Closure & Angiogenesis In Vivo:
- Protocol: Preclinical wound healing models (e.g., full-thickness excisional wounds in mice or rats) are used. MSC-sEVs are administered via multiple routes, with subcutaneous injection demonstrating superior outcomes for wound closure, collagen deposition, and revascularization compared to topical dressing [5]. Wound closure rate is tracked over time, and at endpoint, tissue is harvested for histological analysis (e.g., H&E for scar width, Masson's trichrome for collagen density, CD31 immunohistochemistry for blood vessel density) [5].
Signaling Pathways and Mechanisms of Action
The therapeutic effects of MSC-sEVs are mediated through the modulation of specific signaling pathways in recipient cells. The following diagram summarizes the key mechanistic pathways involved in skin regeneration, highlighting source-dependent variations in efficacy.
The differential efficacy of MSC sources can be attributed to their unique molecular cargo. For instance, BMMSC-Exos and UMSC-Exos show superior downregulation of phosphorylated p65 (NF-κB pathway) and phosphorylated p38/JNK (MAPK pathway), correlating with their stronger anti-inflammatory performance [64]. All MSC-sEVs can activate regenerative pathways like TGF-β/Smad, which enhances collagen production. Furthermore, specific exosomal microRNAs, such as miR-1246 (activating TGF-β/Smad and inhibiting apoptosis) and miR-767 (delaying aging), play critical roles in regulating fibroblast function and promoting skin regeneration [28].
The Scientist's Toolkit: Essential Research Reagents
To conduct rigorous research in this field, specific reagents and tools are essential. The following table details a core set of "Research Reagent Solutions" for the isolation, characterization, and functional testing of MSC-sEVs.
Table 3: Essential Research Reagents for MSC-sEV Studies
| Reagent / Tool | Primary Function | Specific Examples & Notes |
|---|---|---|
| Cell Culture Medium | Expansion of MSCs prior to EV collection. | Alpha-MEM (α-MEM) or DMEM, supplemented with human platelet lysate (hPL) or exosome-depleted FBS to reduce contaminating vesicles [18]. |
| Isolation Kits/Systems | Separation of sEVs from conditioned cell culture media. | Tangential Flow Filtration (TFF) systems for high-yield, scalable isolation; Ultracentrifugation protocols as a benchmark; Aqueous Two-Phase System (ATPS) kits [18] [64] [26]. |
| Characterization Antibodies | Confirmation of EV identity via Western Blot. | Antibodies against positive markers: CD9, CD63, CD81, TSG101, ALIX; negative marker: Calnexin (absent) [18] [64]. |
| Nanoparticle Tracking Analyzer | Determining particle size distribution and concentration. | Instruments like Malvern NanoSight NS300 for NTA, providing data on particle size (d.nm) and concentration (particles/mL) [18] [64]. |
| Transmission Electron Microscope | Visualizing the morphology and ultrastructure of isolated sEVs. | Used to confirm the classic cup-shaped morphology of sEVs [18] [64]. |
| Cytokine & Signaling Inducers | Creating in vitro models of inflammation for functional assays. | Recombinant Human IL-1β protein for stimulating inflammatory pathways (NF-κB, MAPK) in chondrocytes or fibroblasts [64]. |
| Pathway-Specific Antibodies | Evaluating mechanistic effects via Western Blot. | Phospho-specific antibodies for NF-κB pathway (e.g., p-p65) and MAPK pathway (e.g., p-p38, p-JNK, p-ERK) [64]. |
The choice of MSC source for deriving therapeutic extracellular vesicles is a critical determinant of efficacy in skin regeneration, with ADSCs, BMMSCs, and UMSCs each presenting a unique therapeutic profile. ADSC-EVs demonstrate superior performance in directly promoting wound closure and collagen deposition, making them a compelling choice for therapies targeting re-epithelialization and matrix restoration. In contrast, BMMSC-EVs and UMSC-EVs exhibit more potent immunomodulatory properties, effectively suppressing key inflammatory pathways like NF-κB and MAPK, which is advantageous for mitigating the inflammatory phase of wound healing. UMSC-EVs, in particular, combine strong anti-inflammatory action with high proliferative capacity.
This guide underscores that there is no single "best" source; rather, the optimal choice is dictated by the specific therapeutic goal—be it rapid wound closure, robust anti-inflammatory action, or enhanced revascularization. Future research must prioritize the standardization of EV isolation and characterization protocols, direct comparative studies within unified experiments, and the exploration of engineered EVs to maximize the therapeutic potential of these promising nanoscale therapeutics.
Conclusion
The burgeoning field of vesicle-based therapies presents sEVs and ApoEVs as powerful, cell-free tools for skin regeneration, each with distinct strengths. Meta-analyses of preclinical data suggest a nuanced picture: ApoSEVs may excel in accelerating wound closure and enhancing collagen deposition, while sEVs demonstrate superior pro-angiogenic capabilities. The choice between vesicle types is not a matter of superiority but of strategic application based on the specific regenerative need—be it rapid re-epithelialization, matrix reconstruction, or revascularization. Future progress hinges on interdisciplinary efforts to standardize production, engineer vesicles for precision targeting, and conduct rigorous clinical trials. This will ultimately pave the way for transforming these 'tiny giants' from promising laboratory entities into programmable, next-generation nanomedicines for dermatology and regenerative medicine.
References
- 1. shedding the confusion between extracellular vesicles - PubMed [https://pubmed.ncbi.nlm.nih.gov/25683921/]
- 2. Extracellular vesicles arising from apoptosis: forms, functions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10952477/]
- 3. Advances in biological functions and applications of apoptotic ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01251-9]
- 4. Small extracellular vesicles: the origins, current status, future ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04330-5]
- 5. Mesenchymal stem cells-derived small extracellular vesicles and... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 6. Extracellular Vesicles in Skin: Biological Function and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12442902/]
- 7. Therapeutic potential of apoptotic vesicles in modulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960034/]
- 8. Efficacy and safety of small extracellular vesicle interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9516230/]
- 9. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]
- 10. Restoration of Ovarian Cell Function by Primed Extracellular Vesicles [https://www.dovepress.com/primed-extracellular-vesicles-as-a-nanotherapeutic-strategy-to-enhance-peer-reviewed-fulltext-article-IJN]
- 11. Unveiling exosomes in combating skin aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395928/]
- 12. The exosome journey: from biogenesis to uptake and ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-021-00730-1]
- 13. Biogenesis of extracellular vesicles (EV): exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5533094/]
- 14. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 15. Apoptotic extracellular vesicles are metabolized regulators ... [https://www.sciencedirect.com/science/article/pii/S2452199X2200192X]
- 16. Comparisons of miRNA profiles of exosomes derived from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359900/]
- 17. Adipose-derived stem cell exosomes: multifaceted therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527763/]
- 18. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 19. Profiles of lipid, protein and microRNA expression in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0283702]
- 20. Applications of Mesenchymal Stem Cells in Skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7957487/]
- 21. Human iPSCs-derived mesenchymal stem cells promote ... [https://www.nature.com/articles/s41536-025-00427-w]
- 22. apoptotic bodies' unique anti-inflammatory potential [https://pmc.ncbi.nlm.nih.gov/articles/PMC10353199/]
- 23. Apoptotic exosome-like vesicles transfer specific and ... [https://www.nature.com/articles/s41419-023-05991-x]
- 24. in Extracellular : Biological Function and Therapeutic Po Vesicles Skin [https://www.dovepress.com/extracellular-vesicles-in-skin-biological-function-and-therapeutic-pot-peer-reviewed-fulltext-article-IJN]
- 25. in nanomedicine and Extracellular medicine... vesicles regenerative [https://pubmed.ncbi.nlm.nih.gov/38450204/]
- 26. Small extracellular vesicles: the origins, current status, future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004682/]
- 27. Mesenchymal stem cells-derived small and... extracellular vesicles [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934660/]
- 28. Effectiveness of Extracellular Vesicle Application in Skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899913/]
- 29. Efficient methods of isolation and purification of extracellular ... [https://nanoconvergencejournal.springeropen.com/articles/10.1186/s40580-025-00509-x]
- 30. Extracellular vesicles and bioactive peptides for ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725000583]
- 31. Comprehensive Comparison of Methods for Isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150312/]
- 32. Comparison Study of Small Extracellular Vesicle Isolation ... [https://www.mdpi.com/1422-0067/24/20/15462]
- 33. A simplified and efficient method for isolating small ... [https://www.nature.com/articles/s41598-025-99822-y]
- 34. Apoptotic extracellular vesicles: mechanisms, applications ... [https://link.springer.com/article/10.1007/s44258-024-00039-x]
- 35. Lipid metabolism of apoptotic vesicles accelerates cutaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11823102/]
- 36. Recent advances in extracellular vesicles for therapeutic ... [https://www.nature.com/articles/s12276-024-01201-6]
- 37. Stress type–specific small extracellular vesicle signatures ... [https://www.nature.com/articles/s41598-025-21575-5]
- 38. Extracellular vesicles in skin health and diseases [https://www.sciencedirect.com/science/article/abs/pii/S0024320525004485]
- 39. A high-resolution temporal transcriptomic and imaging ... [https://www.nature.com/articles/s41597-025-05921-w]
- 40. Comparative Analysis of Animal Models in Wound Healing ... [https://pubmed.ncbi.nlm.nih.gov/40418175/]
- 41. Engineering a 3D wounded skin equivalent to study early ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1621566/full]
- 42. Minimal Information for Studies of Extracellular Vesicles (MISEV) [https://pmc.ncbi.nlm.nih.gov/articles/PMC11597804/]
- 43. MISEV [https://www.isev.org/misev]
- 44. MISEV: extracellular vesicle research standards [https://www.cellgs.com/blog/misev-extracellular-vesicle-research-standards.html]
- 45. Comparative Analysis of Exosomes and Extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11314465/]
- 46. Lipid metabolism of apoptotic vesicles accelerates cutaneous ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03194-4]
- 47. Comparison of in-vitro immunomodulatory capacity ... [https://www.sciencedirect.com/science/article/pii/S1567576925004709]
- 48. Apoptotic Vesicles: Therapeutic Mechanisms and Critical Issues [https://pmc.ncbi.nlm.nih.gov/articles/PMC11653339/]
- 49. Mesenchymal stem cell-derived apoptotic vesicles [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03649-8]
- 50. Extracellular vesicles: innovative cell-free solutions for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1571461/full]
- 51. Royal Jelly Extracellular Vesicles Enhance Diabetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554291/]
- 52. Wound Healing: Harnessing Extracellular Vesicles Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587863/]
- 53. ECM-binding properties of extracellular vesicles [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02156-5]
- 54. Extracellular Vesicles and Matrix Remodeling Enzymes [https://pmc.ncbi.nlm.nih.gov/articles/PMC6210724/]
- 55. Fibrous scaffolds loaded with BMSC-derived apoptotic ... [https://www.sciencedirect.com/science/article/pii/S2352304224001855]
- 56. Extracellular Vesicles' Role in Angiogenesis and Altering ... [https://www.mdpi.com/2076-3271/12/1/4]
- 57. Plasma-derived small extracellular vesicles unleash the ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-023-00659-w]
- 58. Angiogenic Ability of Extracellular Vesicles Derived from ... [https://link.springer.com/article/10.1007/s13770-025-00741-w]
- 59. Extracellular vesicle-based drug overview: research ... [https://www.nature.com/articles/s41392-025-02312-w]
- 60. The Effect of Age on the Regenerative Potential of Adipose ... [https://www.medsci.org/v21p1529.htm]
- 61. Interleukin-10 Derived Apoptotic Vesicles Enhance ... [https://pubmed.ncbi.nlm.nih.gov/41077631/?utm_source=Chrome&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1lctWWIYk_QLWNappF5RPMniCCLItHFyJToY7oFLvou9bmRsrQ&fc=20200619082506&ff=20251013093523&v=2.18.0.post9+e462414]
- 62. MSC-EVs and UCB-EVs promote skin wound healing and ... [https://www.nature.com/articles/s41598-025-87592-6]
- 63. Comparative Study of Adipose-Derived and Bone Marrow ... [https://www.genesispub.org/comparative-study-of-adipose-derived-and-bone-marrow-derived-mesenchyme-stem-cells-for-intervertebral-disc-regeneration-in-patients-with-degenerative-disc-disease]
- 64. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 65. Current progress and limitations of research regarding the ... [https://link.springer.com/article/10.1007/s43994-024-00147-9]