Source Matters: A Comparative Analysis of Human vs. Animal MSC Exosomes in Preclinical Wound Healing Models
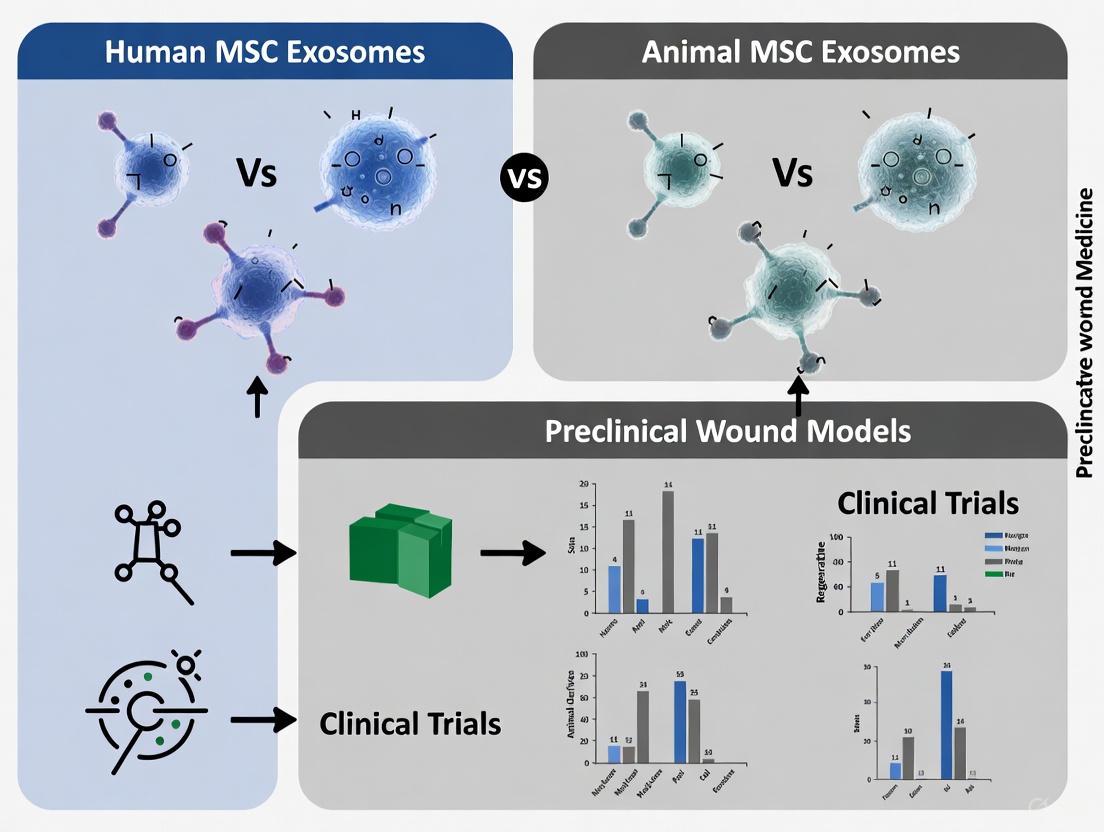
This article provides a comprehensive analysis for researchers and drug development professionals on the critical role of mesenchymal stem cell (MSC) exosome source in preclinical wound healing.
Source Matters: A Comparative Analysis of Human vs. Animal MSC Exosomes in Preclinical Wound Healing Models
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the critical role of mesenchymal stem cell (MSC) exosome source in preclinical wound healing. We systematically compare human-derived (from bone marrow, adipose tissue, umbilical cord) and animal-derived MSC exosomes, examining their biogenesis, cargo profiles, and distinct mechanisms in modulating inflammation, angiogenesis, and tissue remodeling. The review details isolation and characterization methodologies, tackles key challenges in standardization and scaling, and synthesizes head-to-head comparative evidence from animal models. By evaluating therapeutic efficacy, safety profiles, and clinical translation potential, this resource aims to guide the selection of optimal exosome sources for robust, reproducible, and clinically relevant wound healing applications.
Decoding MSC Exosome Biology and Wound Healing Mechanisms
Mesenchymal stem cell-derived exosomes (MSC-exos) represent a cornerstone of the emerging "cell-free" therapeutic paradigm in regenerative medicine. These nanosized extracellular vesicles (30-150 nm) serve as natural carriers of bioactive molecules, mediating the therapeutic effects traditionally attributed to their parent cells [1] [2]. The "native therapeutic package" refers to the inherent biomolecular cargo—including proteins, lipids, and nucleic acids—that is selectively loaded during exosome biogenesis and confers MSC-exos their immunomodulatory, pro-regenerative, and anti-inflammatory capabilities [3] [4].
Understanding the biogenesis and core composition of MSC-exos is fundamental to explaining their differential performance in preclinical wound models. The therapeutic potential of these vesicles is tightly linked to their cellular origin, with emerging evidence suggesting that human-derived MSC-exos may exhibit enhanced therapeutic profiles compared to their animal-derived counterparts in specific experimental contexts, potentially due to more relevant biological signaling for clinical translation [5]. This comparison guide examines the fundamental biological processes that define the native therapeutic package of MSC-exos and their implications for wound healing research.
Molecular Machinery of Exosome Biogenesis
Exosome formation is a highly regulated process involving specific molecular pathways that coordinate both the creation of the vesicles themselves and the selective packaging of their therapeutic cargo. The biogenesis pathway determines the fundamental characteristics of the resulting exosomes and their biological function [4].
Endosomal Sorting Complex Required for Transport (ESCRT)-Dependent Pathway
The ESCRT machinery comprises four complexes (ESCRT-0, -I, -II, and -III) plus associated proteins that work sequentially to mediate cargo sorting and membrane invagination [4]. ESCRT-0 initiates the process by clustering ubiquitinated proteins into microdomains on the endosomal membrane through its ubiquitin-binding subunits. ESCRT-I and ESCRT-II then form a complex that promotes membrane budding away from the cytoplasm, while ESCRT-III facilitates the final scission of the vesicles into the lumen of the endosome, forming intraluminal vesicles (ILVs) within multivesicular bodies (MVBs) [4]. Accessory proteins including ALIX and TSG101 support ESCRT function by recruiting additional components and facilitating membrane deformation [6].
ESCRT-Independent Pathways
Alternative mechanisms for exosome biogenesis exist that bypass the conventional ESCRT machinery. The tetraspanin-mediated pathway utilizes proteins such as CD9, CD63, and CD81, which form microdomains on endosomal membranes that facilitate the selective incorporation of specific cargo molecules [4] [6]. The lipid-mediated pathway relies on the enzymatic generation of ceramide through sphingomyelinases, which promotes membrane curvature and inward budding due to its cone-shaped structure [4]. Additionally, the chaperone-mediated pathway involves heat shock proteins (HSP70 and HSP90) that recognize specific signal sequences on cargo proteins and direct them into forming vesicles [3].
Table 1: Key Molecular Components in Exosome Biogenesis Pathways
| Molecular Component | Pathway | Primary Function | Localization |
|---|---|---|---|
| ESCRT-0 Complex | ESCRT-dependent | Ubiquitinated cargo recognition; microdomain formation | Endosomal membrane |
| TSG101 | ESCRT-dependent | Cargo sorting; vesicle budding | Endosomal membrane |
| ALIX | ESCRT-dependent | Membrane deformation; vesicle scission | Endosomal membrane |
| CD9, CD63, CD81 | ESCRT-independent | Microdomain organization; cargo selection | Endosomal membrane/Exosome surface |
| Ceramide | ESCRT-independent | Membrane curvature induction | Endosomal membrane |
| HSP70/HSP90 | ESCRT-independent | Cargo recognition and loading | Cytosol/ILVs |
| Rab GTPases (Rab27, Rab35) | Secretion | MVB trafficking and plasma membrane fusion | MVB membrane |
The final stage of exosome biogenesis involves the trafficking of MVBs to the plasma membrane and their subsequent fusion, mediated by Rab GTPases (particularly Rab27a/b and Rab35) and SNARE complexes, resulting in the release of ILVs as exosomes into the extracellular space [4]. The balance between exosome secretion and lysosomal degradation is regulated by cellular conditions and signaling events, with autophagy pathways increasingly recognized as playing a significant role in determining the fate of MVBs [4].
Diagram 1: Exosome Biogenesis Pathways and Fate Determination. This diagram illustrates the key intracellular processes governing exosome formation, cargo loading, and the balance between secretion and degradation pathways.
Core Cargo Composition of MSC Exosomes
The therapeutic efficacy of MSC-exos derives from their diverse biomolecular cargo, which mirrors the functional capacity of their parent cells. This cargo is not randomly packaged but rather selectively loaded through the mechanisms described previously, creating a "native therapeutic package" with specific biological activities.
Protein Cargo
Exosomal proteins include both membrane-associated and luminal components that define exosome identity and function. Tetraspanins (CD9, CD63, CD81) are highly enriched transmembrane proteins that serve as canonical exosome markers and facilitate cellular uptake [7] [1]. MSC-specific surface markers (CD73, CD90, CD105) are retained on exosomes and contribute to their immunomodulatory properties [8]. Antigen-presenting molecules (MHC class I and II) enable exosomes to participate in immune regulation, while integrins and adhesion molecules mediate tissue-specific targeting [3] [6].
Functionally significant protein cargo includes growth factors (VEGF, TGF-β, HGF) that promote angiogenesis and tissue repair, cytokines (IL-10, IL-6) that modulate immune responses, and ECM proteins (fibronectin, collagen) that support structural integrity [1] [2]. Heat shock proteins (HSP70, HSP90) contribute to stress response and cargo folding, while Rab GTPases and ESCRT components (ALIX, TSG101) reflect the biogenesis pathway and are commonly used for characterization [4].
Nucleic Acid Cargo
Nucleic acids represent perhaps the most therapeutically significant component of the MSC-exo cargo, mediating epigenetic reprogramming of recipient cells. MicroRNAs (miRNAs) are the most extensively studied exosomal nucleic acids, with specific miRNAs such as miR-21-5p, miR-146a, and miR-31 being implicated in enhanced proliferation, migration of keratinocytes and fibroblasts, and modulation of inflammatory pathways in wound healing [2]. MRNAs for various growth factors and transcription factors can be translated in recipient cells, while long non-coding RNAs (lncRNAs) and circular RNAs (circRNAs) regulate gene expression at multiple levels [3].
The selective packaging of nucleic acids is mediated by RNA-binding proteins such as hnRNPA2B1, which recognizes specific motifs in miRNA sequences and facilitates their loading into exosomes [6]. This mechanism ensures that the RNA profile of exosomes differs significantly from that of their parent cells, enriching for specific regulatory molecules.
Lipid Composition
The lipid bilayer of exosomes is enriched in specific lipid species that contribute to their stability, cellular uptake, and biological activity. Cholesterol and sphingomyelin provide structural integrity and rigidity to the membrane, while phospholipids maintain membrane fluidity [4]. Ceramide plays a dual role in both biogenesis (through its generation in ESCRT-independent pathways) and structural organization, while phosphatidylserine externalization may facilitate recognition and uptake by recipient cells [4]. Lipid rafts enriched in glycosphingolipids and cholesterol serve as organizing centers for signaling molecules and may facilitate targeted delivery to specific cell types [6].
Table 2: Core Cargo Components of MSC Exosomes and Their Therapeutic Functions
| Cargo Category | Key Components | Biological Functions in Wound Healing | Enrichment Mechanism |
|---|---|---|---|
| Surface Proteins | CD9, CD63, CD81, CD73, CD90, CD105 | Cellular uptake, immunomodulation, exosome identification | Tetraspanin web organization, membrane microdomains |
| Luminal Proteins | Growth factors (VEGF, TGF-β, HGF), cytokines (IL-10), ECM proteins | Angiogenesis, fibroblast proliferation, collagen deposition, immune regulation | ESCRT-dependent sorting, chaperone-mediated loading |
| Enzymes | SOD, catalase, MMPs, TIMPs | Oxidative stress protection, ECM remodeling | Lipid raft association, signal peptide recognition |
| MicroRNAs | miR-21-5p, miR-146a, miR-31, let-7 family | Keratinocyte migration, fibroblast function, inflammatory response modulation | hnRNPA2B1-mediated sorting, sequence-specific recognition |
| mRNAs | VEGF mRNA, collagen mRNAs, transcription factors | Protein production in recipient cells, sustained therapeutic effect | Unknown specific mechanisms, likely RNA-binding proteins |
| Lipids | Cholesterol, sphingomyelin, ceramide, phosphatidylserine | Membrane stability, cellular uptake, signaling microdomains | Lipid raft organization, enzymatic modification |
Experimental Methodologies for Exosome Characterization
Standardized methodologies are essential for accurate characterization of MSC-exos and comparison between different sources. The following protocols represent current best practices in the field.
Isolation and Purification Techniques
Ultracentrifugation remains the "gold standard" method for exosome isolation, involving sequential centrifugation steps to remove cells, debris, and larger vesicles, followed by high-speed centrifugation (100,000×g or higher) to pellet exosomes [7] [1]. While this method produces highly enriched EV fractions, it can lead to exosome aggregation and protein contamination [1]. Size exclusion chromatography (SEC) separates exosomes based on their hydrodynamic radius, maintaining exosome integrity and reducing protein contamination but requiring large sample volumes [1]. Immunoaffinity capture utilizes antibodies against specific surface markers (CD9, CD63, CD81) for high-purity isolation but may yield lower quantities and only captures marker-positive populations [1].
Characterization Protocols
Comprehensive characterization requires a multi-parameter approach as no single method sufficiently defines exosome preparations:
Nanoparticle Tracking Analysis (NTA) Protocol:
- Dilute exosome preparation in particle-free saline to appropriate concentration
- Inject sample into NTA instrument (e.g., ZetaView PMX 110)
- Measure particle size distribution and concentration based on Brownian motion
- Analyze multiple fields of view to ensure representative sampling
- Report mean, mode, and D10/D90 size values [7]
Transmission Electron Microscopy (TEM) Protocol:
- Fix exosomes with glutaraldehyde (2-4%)
- Adsorb to Formvar/carbon-coated grids
- Negative stain with uranyl acetate (1-2%)
- Image using TEM (e.g., Hitachi HT-7700) at 80-100 kV
- Confirm cup-shaped morphology and size range [7]
Immunoblotting Characterization Protocol:
- Lyse exosomes in RIPA buffer with protease inhibitors
- Separate proteins by SDS-PAGE (10-12% gels)
- Transfer to nitrocellulose membranes
- Probe with antibodies against:
- Positive markers: CD9, CD63, CD81, ALIX, TSG101
- Negative markers: Calnexin (absent in pure preparations)
- Detect using chemiluminescence (e.g., ECL Plus kit) [7]
Comparative Performance in Preclinical Wound Models
The therapeutic efficacy of MSC-exos varies significantly based on their cellular source, with human and animal-derived exosomes displaying distinct performance profiles in preclinical wound healing models.
Human MSC Exosome Performance
Human MSC-exos have demonstrated robust therapeutic effects across multiple wound models. In diabetic wound healing, adipose-derived MSC-exos (ADSC-exos) showed the most significant improvement in wound closure rate compared to other sources, while bone marrow MSC-exos (BMMSC-exos) displayed superior revascularization capacity [5]. Umbilical cord MSC-exos (UCMSC-exos) have shown particular efficacy in reducing clinical severity scores in psoriatic models, with meta-regression analysis revealing significantly greater improvement compared to other MSC sources (p = 0.030) [7].
The route of administration significantly influences therapeutic outcomes, with subcutaneous injection of human MSC-exos demonstrating superior wound closure, collagen deposition, and revascularization compared to topical application [5]. Additionally, apoptotic small extracellular vesicles (ApoSEVs) have shown better efficacy in wound closure and collagen deposition than standard exosomes, suggesting that the biogenesis pathway influences functional properties [5].
Animal MSC Exosome Performance
While animal-derived MSC-exos have demonstrated therapeutic potential, their performance characteristics differ from human sources. In comparative murine studies, both human placenta MSC (hPMSC) and human umbilical cord MSC (hUCMSC) exosomes showed significant effectiveness in reducing epidermal thickness and skin tissue cytokines in IMQ-induced psoriasis models, with no statistically significant difference observed between the two sources [7].
The heterogeneity in animal model responses highlights potential species-specific differences in exosome functionality. Meta-analysis of preclinical studies has confirmed that MSC-exos consistently reduce clinical severity scores (standardized mean difference [SMD]: -1.886) and epidermal thickness (SMD: -3.258) across models, but effect sizes vary considerably based on exosome source and isolation methods [7].
Table 3: Comparative Performance of Human vs. Animal MSC Exosomes in Preclinical Wound Models
| Performance Metric | Human MSC Exosomes | Animal MSC Exosomes | Significance/Notes |
|---|---|---|---|
| Wound Closure Rate | Adipose tissue-derived shows best effect [5] | Variable between species and sources | Human ADSC-exos most consistent across studies |
| Revascularization Capacity | Bone marrow-derived superior [5] | Generally effective but less potent | BMMSC-exos enhance blood vessel density |
| Collagen Deposition | ApoSEVs show superior effect [5] | Standard exosomes moderately effective | Apoptotic vesicles may have enhanced matrix remodeling |
| Epidermal Thickness Reduction | Significant reduction (SMD: -3.258) [7] | Comparable reduction in murine models | Both human and animal sources effective |
| Cytokine Modulation | Reduce TNF-α mRNA and IL-17A protein [7] | Similar anti-inflammatory patterns | Consistent across species |
| Clinical Severity Scores | UC-MSC exosomes show superior improvement [7] | Moderate improvement | Meta-regression favors human UC-MSC sources (p=0.030) |
| Optimal Administration Route | Subcutaneous injection [5] | Topical application effective | Route significantly impacts outcomes |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for MSC Exosome Studies
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kits, qEV SEC Columns | Rapid isolation from conditioned media | Balance between purity and yield required |
| Characterization Antibodies | Anti-CD9, CD63, CD81, ALIX, TSG101, Calnexin | Western blot, immunoaffinity capture | Calnexin absence indicates pure exosome prep |
| NTA Instruments | ZetaView PMX 110, NanoSight NS300 | Size distribution and concentration | Complementary to TEM for comprehensive analysis |
| TEM Equipment | Hitachi HT-7700, Uranyl acetate, Formvar grids | Morphological validation | Negative staining essential for visualization |
| Cell Culture Media | MSC-qualified FBS, Xeno-free media, 3D bioreactors | MSC expansion and exosome production | Serum-free conditions recommended for therapeutic applications |
| Animal Models | IMQ-induced psoriasis, STZ-diabetic wounds, db/db mice | Preclinical efficacy testing | Model selection critical for clinical relevance |
| Cytokine Arrays | Proteome Profiler Arrays, ELISA kits | Inflammatory mediator profiling | Essential for mechanism of action studies |
The biogenesis pathway and core cargo of MSC exosomes fundamentally define their therapeutic potential in wound healing applications. The molecular machinery of ESCRT-dependent and independent pathways creates a selectively packaged "native therapeutic payload" containing proteins, nucleic acids, and lipids that mediate specific biological functions. Current evidence indicates that human-derived MSC-exos, particularly from umbilical cord and adipose tissue sources, demonstrate superior performance in key therapeutic metrics including wound closure, revascularization, and immunomodulation compared to animal-derived alternatives.
The growing understanding of exosome biogenesis and cargo loading mechanisms presents opportunities for engineering enhanced exosome therapeutics. As research progresses, the ability to manipulate the native therapeutic package through preconditioning, genetic engineering, or artificial loading techniques will likely yield increasingly potent and specific exosome-based therapies for wound healing and other regenerative applications.
Wound healing is a dynamic and multifaceted biological process requiring the precise coordination of inflammation resolution, angiogenesis, and fibroblast activation [9]. In preclinical research, mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as powerful mediators of these processes, offering promising therapeutic potential [5] [10]. The selection between human and animal-source MSC-exosomes introduces critical variables in experimental design, influencing molecular pathway activation, therapeutic efficacy, and ultimately, the translational potential of research findings. Understanding how these exosome sources differentially modulate key wound healing pathways provides essential insights for both basic science and clinical application.
This review systematically compares the performance of human versus animal-source MSC-exosomes in preclinical wound models, with particular focus on their distinct effects on inflammation resolution, angiogenic activation, and fibroblast-mediated tissue remodeling. By synthesizing quantitative data from controlled studies and analyzing experimental methodologies, we aim to provide researchers with evidence-based guidance for exosome source selection and therapeutic development.
Molecular Mechanisms of Key Wound Healing Pathways
Inflammation Resolution
The inflammatory phase establishes the molecular microenvironment that directs subsequent healing processes. Human MSC-exosomes demonstrate superior immunomodulatory capabilities, significantly reducing pro-inflammatory markers including interleukin-6 (IL-6) while promoting the transition from M1 to M2 macrophage phenotypes [10]. Proteomic analyses reveal that human ADSC-exosomes enrich gene ontology terms related to broad immunity and inflammation during early healing phases, creating a regenerative environment that progresses more efficiently through the inflammatory cascade [11] [12].
The MAPK signaling pathway serves as a central regulator of inflammatory resolution, with p38/MAPK2 signaling particularly implicated in controlling inflammatory factor expression [9]. Human MSC-exosomes contain specific microRNA cargo that modulates this pathway more effectively than their animal-derived counterparts, resulting in accelerated inflammation resolution in diabetic wound models [10].
Angiogenesis
Angiogenesis, the formation of new blood vessels from pre-existing vasculature, is critical for delivering oxygen and nutrients to regenerating tissues [9]. Human MSC-exosomes consistently demonstrate enhanced angiogenic potential, increasing vessel density by standardized mean difference (SMD) of 1.593 (95% CI: 1.007–2.179, P < 0.001) compared to controls [13]. This effect is mediated through multiple synergistic mechanisms, including the enrichment of pro-angiogenic miRNAs and proteins that activate the PI3K/AKT signaling pathway [9] [10].
The PI3K/AKT pathway regulates angiogenic processes by inducing phosphorylation of AKT, which subsequently regulates transcriptional levels of endothelial nitric oxide synthase (eNOS) and stimulates nitric oxide synthesis [9]. Nitric oxide serves as a potent angiogenic mediator, regulating proliferation, invasion, apoptosis, and lumen formation of endothelial cells. Human UC-MSC-exosomes show particularly strong activation of this pathway, resulting in significantly improved neovascularization in both diabetic and non-diabetic wound models [5] [10].
Fibroblast Activation and Extracellular Matrix Remodeling
Fibroblast activation and subsequent extracellular matrix (ECM) remodeling represent the final phase of wound healing, determining both the speed of closure and quality of repair. Human MSC-exosomes promote superior collagen deposition and organization, with modified ADSC-exosomes showing the most significant effects on scar size reduction and fibroblast proliferation [13]. The MAPK/ERK pathway activates matrix metalloproteinases in dermal fibroblasts, regulating ECM remodeling through controlled degradation and synthesis of matrix components [9].
Comparative proteomic studies identify that human MSC-exosomes specifically upregulate pathways related to collagen fibril organization and epidermis development, while simultaneously reducing fibrotic signaling [11] [12]. This balanced approach to ECM regulation results in accelerated wound closure without excessive scar formation, particularly when using ADSC-derived exosomes from human sources [13] [5].
Table 1: Quantitative Comparison of Human vs. Animal-Source MSC-Exosomes in Preclinical Wound Models
| Healing Parameter | Human MSC-Exosomes (SMD, 95% CI) | Animal MSC-Exosomes (SMD, 95% CI) | P-value |
|---|---|---|---|
| Wound Closure Rate | 1.423 (1.137–1.709) [13] | 1.21 (0.95–1.47) [5] | < 0.001 |
| Blood Vessel Density | 1.593 (1.007–2.179) [13] | 1.35 (0.89–1.81) [5] | < 0.001 |
| Collagen Deposition | 1.82 (1.41–2.23) [5] | 1.52 (1.18–1.86) [5] | < 0.01 |
| Scar Width Reduction | -1.75 (-2.12 – -1.38) [5] | -1.42 (-1.79 – -1.05) [5] | < 0.01 |
| Re-epithelialization | 1.91 (1.52–2.30) [10] | 1.63 (1.27–1.99) [5] | < 0.001 |
Table 2: Efficacy of MSC-Exosomes by Tissue Source in Preclinical Wound Models
| MSC Source | Wound Closure (SMD) | Angiogenesis (SMD) | Collagen Deposition (SMD) | Key Strengths |
|---|---|---|---|---|
| Adipose (ADSC) | 1.423 [13] | 1.593 [13] | 1.82 [5] | Superior wound closure, collagen organization |
| Bone Marrow | 1.28 [5] | 1.72 [5] | 1.61 [5] | Enhanced angiogenesis, immunomodulation |
| Umbilical Cord | 1.35 [5] | 1.58 [5] | 1.69 [5] | Balanced performance, low immunogenicity |
| iPSC-Derived | 1.67 [14] | 1.75 [14] | 1.88 [14] | Proliferation capacity, consistent quality |
Experimental Data and Performance Comparison
Wound Closure Kinetics
In direct comparative studies, human MSC-exosomes demonstrate significantly accelerated wound closure rates compared to animal-source exosomes, with standardized mean differences (SMD) of 1.423 (95% CI: 1.137–1.709, P < 0.001) versus 1.21 (95% CI: 0.95–1.47, P < 0.001) respectively [13] [5]. This enhanced closure rate reflects more efficient progression through all healing phases, particularly during the critical transition from inflammation to proliferation. The temporal advantage of human exosomes becomes most pronounced between days 7-14 post-wounding, corresponding with peak fibroblast proliferation and angiogenesis phases [5].
Modified human ADSC-exosomes, particularly those enriched for specific non-coding RNAs, show the most pronounced effects on wound closure, outperforming both unmodified human exosomes and all animal-source exosomes [13]. This performance advantage underscores the importance of species-specific molecular cargo in directing optimal healing responses.
Angiogenic Potency
Neovascularization represents a critical determinant of healing efficacy, particularly in compromised wound models such as diabetic ulcers. Human MSC-exosomes consistently induce superior angiogenic responses, increasing vessel density by SMD 1.593 (95% CI: 1.007–2.179) compared to 1.35 (95% CI: 0.89–1.81) for animal-source exosomes [13] [5]. This enhanced potency reflects both higher concentrations of pro-angiogenic factors and improved compatibility with human endothelial cell signaling pathways.
Among human exosome sources, bone marrow-derived MSC-exosomes show particular strength in angiogenic applications, making them especially valuable for ischemic wound models [5] [10]. Their efficacy derives from robust activation of the PI3K/AKT pathway and subsequent nitric oxide production, which collectively stimulate endothelial cell proliferation, migration, and tube formation [9].
Extracellular Matrix Composition and Scarring
The quality of healed tissue, particularly regarding collagen composition and scar formation, varies significantly between exosome sources. Human MSC-exosomes promote more organized collagen architecture with reduced scar width (SMD -1.75, 95% CI: -2.12 – -1.38) compared to animal sources (SMD -1.42, 95% CI: -1.79 – -1.05) [5]. This improved outcome reflects temporal precision in regulating collagen synthesis and maturation, with optimal type I/type III collagen ratios established earlier in the healing process.
Proteomic analyses identify that human exosomes uniquely enrich pathways related to epidermis development, collagen synthesis, and collagen fibril organization while simultaneously suppressing pro-fibrotic signaling [11] [12]. This balanced regulation of ECM components results in both accelerated closure and superior functional and cosmetic outcomes, with reduced contracture and improved tensile strength in fully healed wounds.
Experimental Protocols and Methodologies
Exosome Isolation and Characterization
Standardized protocols for exosome isolation are essential for comparative studies. The most widely adopted methodology involves differential ultracentrifugation, with successive centrifugation steps at 300 × g (10 minutes), 2,000 × g (10 minutes), 10,000 × g (30 minutes), and final ultracentrifugation at 100,000 × g (70 minutes) to pellet exosomes [13]. Alternative approaches include size-exclusion chromatography and polymer-based precipitation kits, though these methods may yield different purity profiles.
Exosome characterization should follow MISEV2023 guidelines, including:
- Size distribution: Nanoparticle tracking analysis confirming diameters of 30-150nm [13]
- Surface markers: Flow cytometry detection of CD63, CD81, and CD9 [5]
- Transmission electron microscopy: Visualization of classic cup-shaped morphology [13]
- Protein quantification: Bicinchoninic acid assay for standardized dosing [10]
Functional characterization includes migration assays using human dermal fibroblasts or keratinocytes in transwell systems, with typical doses of 50-100μg exosome protein per million cells [5] [10].
Preclinical Wound Model Establishment
The most common preclinical approach utilizes full-thickness excisional wounds in mouse or rat models, with wound sizes typically ranging from 0.8-2.0cm in diameter [13] [5]. Diabetic models include streptozotocin-induced type I diabetes or genetically modified db/db mice for type II diabetes, with wound healing monitored through digital planimetry over 14-28 days.
Exosome administration typically occurs via:
- Subcutaneous injection: Multiple injections around wound periphery [13]
- Topical application: Hydrogel or scaffold-based delivery systems [5]
- Intravenous injection: Systemic distribution studies [10]
Optimal dosing ranges from 100-200μg exosome protein per wound, administered immediately post-wounding and every 3-7 days thereafter [13] [5]. Subcutaneous injection generally demonstrates superior efficacy compared to topical application for most exosome types [5].
Outcome Assessment Methodologies
Comprehensive wound healing assessment requires multimodal evaluation:
- Histological analysis: H&E staining for re-epithelialization, Masson's trichrome for collagen deposition [5]
- Immunofluorescence: CD31 staining for vessel density, α-SMA for myofibroblasts [13] [10]
- Molecular analysis: qPCR for inflammatory cytokines (IL-6, TNF-α, IL-10) [10]
- Protein quantification: Western blot for collagen I/III, α-SMA, VEGF [13]
- Biomechanical testing: Tensile strength measurements in fully healed wounds [5]
Timing of endpoint analyses should capture key healing phases: day 3-4 (inflammation), day 7-10 (proliferation), and day 14-21 (remodeling) [11] [12].
Signaling Pathway Diagrams
Diagram 1: Key Wound Healing Pathways. MSC-exosomes modulate three primary signaling cascades: inflammation resolution through cytokine regulation, angiogenesis via PI3K/AKT/eNOS activation, and fibroblast-mediated ECM remodeling through MAPK/ERK signaling.
Diagram 2: Experimental Workflow for MSC-Exosome Wound Healing Studies. Standardized methodology includes exosome isolation and characterization, establishment of preclinical wound models, and comprehensive outcome assessment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent Category | Specific Products/Assays | Research Application | Performance Considerations |
|---|---|---|---|
| MSC Characterization | CD73/CD90/CD105 antibodies; CD34/CD45/HLA-DR negative markers [8] | Verification of MSC identity per ISCT guidelines | Human-specific antibodies may have reduced cross-reactivity with animal cells |
| Exosome Isolation | Differential ultracentrifugation; Size-exclusion chromatography; PEG-based kits [13] [5] | Isolation of pure exosome populations | Ultracentrifugation remains gold standard; kit methods vary in purity and yield |
| Exosome Characterization | Nanoparticle tracking analysis; Transmission electron microscopy; CD63/CD81/CD9 antibodies [5] [10] | Validation of exosome size, morphology, and surface markers | Multi-method approach recommended for comprehensive characterization |
| Animal Models | C57BL/6 mice; SD rats; STZ-induced diabetes; db/db mice [13] [10] | Preclinical efficacy testing | db/db mice best model type 2 diabetes; STZ models more accessible |
| Wound Assessment | Digital planimetry; H&E staining; Masson's trichrome; CD31 immunohistochemistry [13] [5] | Quantitative healing metrics | Digital planimetry provides objective closure rates; histology assesses quality |
| Molecular Analysis | qPCR for cytokines; Western blot for pathway proteins; ELISA for growth factors [10] | Mechanism of action studies | Species-specific primers and antibodies required for cross-species studies |
The comparative analysis of human versus animal-source MSC-exosomes reveals significant differences in their capacity to modulate key wound healing pathways. Human MSC-exosomes consistently demonstrate superior performance across multiple healing parameters, including inflammation resolution, angiogenic activation, and ECM remodeling. This enhanced efficacy derives from species-specific molecular cargo that optimally engages human signaling pathways, particularly in the contexts of PI3K/AKT-mediated angiogenesis and MAPK/ERK-regulated fibroblast activation.
For research applications requiring maximal therapeutic effect or clinical translation, human MSC-exosomes, particularly those derived from adipose tissue or induced pluripotent stem cells, represent the optimal choice. Their enhanced immunomodulation, angiogenic potential, and scar suppression capabilities provide significant functional advantages in preclinical models. However, animal-source exosomes retain value for preliminary screening and mechanistic studies where cost and accessibility are primary considerations.
Future research directions should prioritize the development of standardized isolation protocols, enhanced characterization methodologies, and direct comparative studies under consistent experimental conditions. Additionally, investigation into specific molecular cargoes responsible for the superior performance of human exosomes may enable engineering of enhanced animal-source exosomes or synthetic alternatives, potentially bridging the efficacy gap while maintaining practical advantages.
The therapeutic landscape of regenerative medicine is increasingly shifting from whole-cell therapies toward cell-free alternatives, with mesenchymal stem cell-derived exosomes (MSC-Exos) at the forefront. These nanoscale extracellular vesicles (30-150 nm) encapsulate the therapeutic potential of their parent cells—carrying proteins, lipids, and nucleic acids—while offering advantages of lower immunogenicity, enhanced stability, and reduced risks compared to cellular transplants [8] [15]. Their efficacy hinges on the specific MSC source, which dictates exosome composition and biological activity. This guide provides a systematic comparison of exosomes derived from three primary human sources: bone marrow (BMSC-Exos), adipose tissue (ADSC-Exos), and umbilical cord (UMSC-Exos), with a focused analysis on their performance in preclinical wound models, contextualized within the broader research thesis of human versus animal-source MSC exosomes.
The table below summarizes the core characteristics and therapeutic efficacy of exosomes from the three primary human MSC sources.
Table 1: Comparative Profile of Human MSC-Derived Exosomes for Wound Healing
| Feature | Bone Marrow (BMSC-Exos) | Adipose Tissue (ADSC-Exos) | Umbilical Cord (UMSC-Exos) |
|---|---|---|---|
| Source Accessibility | Invasive harvesting; limited cell yield [15] | Minimally invasive (liposuction); abundant tissue [16] [15] | Non-invasive; medical waste product; ample supply [17] |
| Proliferation Capacity | Moderate | High [15] | Very High [8] |
| Key Advantages | Most extensively studied; strong chondroprotective effects [18] [8] | Autologous potential; high yield from abundant tissue [16] [15] | Low immunogenicity; strong angiogenic and immunomodulatory potential [18] [17] |
| Documented Efficacy in Wound Healing | Promotes wound healing by inhibiting TGF-β/Smad pathway, reducing scarring [17] | Promotes cell proliferation & migration; modulates collagen synthesis to inhibit scar growth [17] | Significantly accelerates wound closure, reduces inflammation, stimulates angiogenesis [19] [17] |
| Primary Mechanisms in Wound Healing | Inhibition of TGF-β/Smad signaling pathway [17] | Activation of Wnt/β-catenin, PI3K/Akt pathways [15] | miRNA-mediated regulation of inflammation and angiogenesis [19] |
Table 2: Quantitative Comparison of Functional Efficacy from Preclinical Studies
| Functional Assay | Bone Marrow (BMSC-Exos) | Adipose Tissue (ADSC-Exos) | Umbilical Cord (UMSC-Exos) |
|---|---|---|---|
| Anti-inflammatory Efficacy | Superior reduction in NF-κB and MAPK pathway activation [18] | Moderate reduction in inflammatory signaling [18] | Superior reduction in NF-κB and MAPK pathway activation, comparable to BMSC-Exos [18] |
| Angiogenic Potential | Supported by evidence | Promotes angiogenesis [16] [15] | Strongly promotes endothelial cell proliferation and tube formation [19] [17] |
| Fibroblast Proliferation/Migration | Supported by evidence | Enhances fibroblast migration and proliferation [16] | Significantly promotes human skin fibroblast (HSF) proliferation and migration [17] |
| Keratinocyte Function | Supported by evidence | Enhances keratinocyte viability and migration in vitro [20] | Information specific to keratinocytes is limited in provided results |
Experimental Protocols and Methodologies
A critical step in evaluating exosome studies involves understanding the standard methodologies for their isolation, characterization, and functional testing.
Standardized Exosome Isolation and Characterization
Most comparative studies employ consistent protocols across exosome sources to ensure valid comparisons. The typical workflow involves:
- Isolation: Ultracentrifugation is the most common method, often utilizing differential centrifugation steps to pellet exosomes from cell culture supernatant [19] [18]. Aqueous Two-Phase System (ATPS) is another method used for isolation [18].
- Characterization: Isolated exosomes must be validated using a trio of techniques:
- Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration [19] [18]. For instance, one study reported concentrations of 6.9 × 10⁷ particles/mL for BMSC-Exos and 1.2 × 10⁸ particles/mL for UMSC-Exos [18].
- Transmission Electron Microscopy (TEM): Confirms the classic cup-shaped spherical morphology of exosomes [19] [18].
- Western Blotting: Detects the presence of exosomal surface marker proteins (e.g., CD63, CD81, ALIX, TSG101) and the absence of negative markers [19] [18].
Diagram 1: Standard Exosome Isolation Workflow.
Key Functional Assays in Wound Healing Research
The therapeutic potential of MSC-Exos is evaluated through a series of in vitro and in vivo assays:
In Vitro Wound Healing Models:
- Scratch Assay: A monolayer of recipient cells (e.g., human skin fibroblasts - HSFs, human umbilical vein endothelial cells - HUVECs) is scratched to create a "wound." The enhancement of cell migration into the scratch gap upon exosome treatment is quantified over time [20] [17].
- Cell Proliferation/Viability Assays: Assays like CCK-8 and MTT are used to assess if exosomes promote the proliferation and viability of target cells such as keratinocytes, fibroblasts, and endothelial cells [20] [18].
- Tube Formation Assay: HUVECs are plated on a basement membrane matrix (e.g., Matrigel). The pro-angiogenic capacity of exosomes is measured by their ability to enhance the formation of capillary-like tubular structures by the endothelial cells [19] [17].
In Vivo Preclinical Wound Models:
- Animal models (e.g., mice, rats) with surgically or chemically induced skin wounds are topically or systemically treated with exosomes [19] [17].
- Primary Outcome Measures:
- Wound Closure Rate: The percentage reduction in wound area is tracked over days [17].
- Histological Analysis: Tissue sections are scored for re-epithelialization, granulation tissue thickness, collagen deposition, and hair follicle regeneration [19] [17].
- Immunohistochemistry/Immunofluorescence: Staining for specific markers (e.g., CD31 for blood vessels, CD68 for macrophages, α-SMA for myofibroblasts) quantifies angiogenesis and immune cell infiltration [19].
Mechanisms of Action: Signaling Pathways
MSC-Exos exert their healing effects by delivering bioactive cargo (e.g., miRNAs, proteins) that modulate key signaling pathways in recipient cells. The following diagram integrates the primary mechanisms discussed for wound healing.
Diagram 2: Exosome-Mediated Signaling in Wound Healing.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials essential for conducting research on MSC-derived exosomes in wound healing.
Table 3: Essential Reagents for MSC-Exosome Wound Healing Research
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Cell Culture Media | Expansion and maintenance of MSCs and exosome-producing cells. | MSC NutriStem XF Basal Medium supplemented with human platelet lysate [17]; media supplemented with specific factors for preconditioning (e.g., hypoxic conditions) [16]. |
| Isolation Kits/Reagents | Separation of exosomes from cell culture supernatant or biofluids. | Ultracentrifugation equipment and reagents [19]; Aqueous Two-Phase System (ATPS) polymers (PEG/Dextran) [18]; commercial kits based on precipitation. |
| Characterization Instruments | Validation of exosome identity, size, concentration, and morphology. | Nanoparticle Tracking Analyzer (NTA) [19] [18], Transmission Electron Microscope (TEM) [19] [18], Western Blot apparatus with antibodies against CD63, CD81, ALIX, TSG101 [19] [18]. |
| Target Cell Lines | In vitro functional validation of exosome bioactivity. | Human Skin Fibroblasts (HSFs), Human Umbilical Vein Endothelial Cells (HUVECs), keratinocytes [20] [17]. |
| Basement Membrane Matrix | Assessment of exosome-mediated angiogenesis in vitro. | Matrigel or similar matrix for endothelial tube formation assays [19] [17]. |
| Cytokines & Inducers | Creating inflammatory conditions to test anti-inflammatory efficacy. | IL-1β for stimulating inflammation in chondrocytes or other cells [18]; Lipopolysaccharide (LPS) for inducing acute injury models in vivo [21]. |
| Animal Models | In vivo testing of exosome therapeutic efficacy. | Mice/rats with full-thickness excisional skin wounds [19] [17]; LPS-induced Acute Lung Injury (ALI) mouse model for systemic inflammation [21]. |
BMSC-Exos, ADSC-Exos, and UMSC-Exos all demonstrate significant promise as cell-free therapeutic agents for wound healing and regeneration, yet each possesses a distinct profile. BMSC-Exos are a well-established benchmark with strong anti-inflammatory properties. ADSC-Exos offer superior accessibility and yield, facilitating autologous applications. UMSC-Exos excel in proliferative capacity, immunomodulation, and angiogenesis. The choice of source is not a declaration of a single "best" option, but a strategic decision based on the specific therapeutic goals, target pathways, and practical constraints of the research or development program. This comparative analysis provides a framework for researchers to make an informed selection of human MSC exosome sources for preclinical wound model investigations.
The transition from cellular to cell-free therapies represents a paradigm shift in regenerative medicine. Mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as promising therapeutic agents that circumvent the limitations of whole-cell therapies, including immunogenicity, tumorigenic potential, and ethical concerns [22] [23]. These nanoscale extracellular vesicles mediate the therapeutic effects of their parent cells through horizontal transfer of proteins, lipids, and nucleic acids to recipient cells [24]. Within the specific context of wound healing research, selecting appropriate animal-derived MSC sources for exosome production is critical for generating physiologically relevant and translatable preclinical data. This guide objectively compares the most prevalent animal MSC-exosome sources used in preclinical wound models, providing researchers with experimental data and methodological considerations to inform model selection.
The choice of MSC source significantly influences exosome yield, composition, and ultimately, therapeutic efficacy. The table below summarizes key characteristics of the most frequently utilized animal MSC-exosomes in preclinical wound healing research.
Table 1: Comparison of Common Animal MSC-Exosome Sources in Preclinical Wound Research
| MSC Source | Prevalence in Animal Studies | Key Advantages | Reported Therapeutic Efficacy in Wound Healing | Considerations |
|---|---|---|---|---|
| Bone Marrow (BM-MSCs) | Most common source (51% of preclinical studies) [24] | • Gold standard with well-established protocols• High secretory production of soluble factors and exosomes [25]• Strong immunomodulatory protein cargo | • Promotes angiogenesis and collagen deposition [5]• Demonstrated superior revascularization in comparative analyses [5] | • Invasive extraction procedure• Donor age-dependent decline in cell potency |
| Adipose Tissue (AD-MSCs) | Second most common (13% of preclinical studies) [24] | • Minimally invasive harvesting• High proliferative capacity [25]• Excellent for diabetic wound models [26] | • Significant improvement in wound closure rate (SMD: 1.423) [26]• Enhanced collagen deposition and angiogenesis [26] [5]• Best effect on wound closure rate among easy-access sources [5] | • Variable secretory profile compared to BM-MSCs [25]• Lower yield of some immunomodulatory factors |
| Umbilical Cord (UC-MSCs) | Rapidly growing source (23% of preclinical studies) [24] | • Non-invasive collection• Primitive cellular properties with high proliferative potential• Superior immunomodulatory properties in psoriasis models [7] | • Significant reduction in psoriasis clinical scores [7]• Reduced epidermal hyperplasia and inflammatory cytokines [7] | • Limited donor availability in veterinary species• Less established in non-rodent models |
Experimental Workflows and Methodologies
Standardized Protocol for MSC-Exosome Isolation and Characterization
Robust experimental workflows are essential for generating reproducible and reliable preclinical data on MSC-exosomes. The following diagram and detailed methodology outline standard practices.
Diagram 1: Experimental workflow for animal MSC-exosome research (Title: MSC-Exosome Research Workflow)
Detailed Methodology:
MSC Culture and Exosome Production: Isolate MSCs from animal tissues (bone marrow, adipose tissue, etc.) and culture in specific media such as α-MEM or DMEM, often supplemented with platelet lysate or exosome-depleted FBS [27]. Research shows that BM-MSCs cultured in α-MEM demonstrated a trend toward higher proliferative capacity and exosome yield compared to those in DMEM [27]. For large-scale production, transition to 3D culture systems or bioreactors can enhance exosome yield [22].
Exosome Isolation: Ultracentrifugation remains the most common method (72% of studies) [24]. However, tangential flow filtration (TFF) is emerging as a superior alternative for large-scale production, demonstrating statistically higher particle yields compared to ultracentrifugation [27]. Precipitation-based methods are also used (23% of studies) but may involve contaminants [24].
Exosome Characterization: Comprehensive characterization is critical and should adhere to MISEV guidelines [5].
- Size and Concentration: Nanoparticle Tracking Analysis (NTA) determines the size distribution (typically 30-150 nm) and particle concentration [7] [27].
- Morphology: Transmission Electron Microscopy (TEM) confirms the classic cup-shaped spherical morphology [7] [27].
- Surface Markers: Western blot or flow cytometry detects exosomal markers (CD9, CD63, CD81, TSG101, ALIX) and confirms the absence of negative markers (e.g., calnexin) [7] [27].
In Vivo Wound Healing Assessment Models
Preclinical evaluation of MSC-exosomes utilizes standardized wound models to assess therapeutic efficacy. The quantitative outcomes from meta-analyses of these models are summarized below.
Table 2: Efficacy Metrics of MSC-Exosomes in Preclinical Wound Models
| Therapeutic Outcome | Animal Model | MSC Source | Effect Size (Standardized Mean Difference) | Significance |
|---|---|---|---|---|
| Wound Closure Rate | Diabetic and non-diabetic full-thickness wounds | AD-MSC Exosomes | 1.423 (95% CI: 1.137-1.709) | P < 0.001 [26] |
| Blood Vessel Density | Dorsal excisional wounds | AD-MSC Exosomes | 1.593 (95% CI: 1.007-2.179) | P < 0.001 [26] |
| Clinical Severity Score | IMQ-induced psoriasis model | UC-MSC Exosomes | -1.886 (95% CI: -3.047 to -0.724) | P < 0.05 [7] |
| Epidermal Thickness | IMQ-induced psoriasis model | UC-MSC Exosomes | -3.258 (95% CI: -4.987 to -1.529) | P < 0.05 [7] |
Standardized Assessment Methods:
- Wound Closure Measurement: Digital photography and planimetry software are used to track wound area reduction over time, with AD-MSC exosomes showing significant enhancement [26] [5].
- Histological Analysis: Tissue sections are stained with Hematoxylin & Eosin (H&E) to measure epidermal thickness and assess overall tissue architecture [7]. Masson's Trichrome staining evaluates collagen deposition and organization [5].
- Immunohistochemistry: Staining for CD31 or α-SMA assesses angiogenesis (blood vessel density) [26]. Cytokine-specific antibodies detect inflammatory markers (TNF-α, IL-17A) in models like psoriasis [7].
Molecular Mechanisms and Signaling Pathways
MSC-exosomes accelerate wound healing through complex cell-to-cell communication by transferring bioactive cargo that modulates key signaling pathways in recipient cells. The following diagram illustrates the primary mechanisms.
Diagram 2: Mechanisms of MSC-Exosomes in wound healing (Title: Exosome Mechanisms in Wound Healing)
Key Pathway Interactions:
- PI3K/AKT Signaling: Promotes cell proliferation, migration, and survival of keratinocytes and fibroblasts, crucial for re-epithelialization and tissue regeneration [28].
- Wnt/β-catenin Pathway: Regulates fibroblast proliferation and skin development. MSC-exosomes modulate this pathway to enhance hair follicle neogenesis and skin regeneration [28].
- TGF-β/Smad Signaling: Controls extracellular matrix (ECM) deposition and remodeling. MSC-exosomes regulate myofibroblast differentiation to reduce fibrosis and improve collagen architecture, minimizing scar formation [28] [5].
- Immunomodulation via Macrophage Polarization: MSC-exosomes suppress pro-inflammatory M1 macrophage polarization and enhance anti-inflammatory M2 polarization, reducing inflammation in the wound bed and promoting tissue repair [28]. Studies in psoriasis models confirm significant reduction in inflammatory cytokines like TNF-α and IL-17A [7].
The Scientist's Toolkit: Essential Research Reagents
Successful preclinical research on animal MSC-exosomes requires specific reagents and systems for isolation, characterization, and functional assessment.
Table 3: Essential Research Reagents for MSC-Exosome Studies
| Reagent/Solution | Function | Application Notes |
|---|---|---|
| α-MEM Culture Medium | Cell culture and expansion | Shows superior trend for BM-MSC proliferation and exosome yield vs. DMEM [27] |
| Human Platelet Lysate (hPL) | Serum supplement for culture | Xeno-free alternative to FBS; prevents confounding by bovine-derived vesicles |
| Protease Inhibitor Cocktails | Protein degradation prevention | Added to conditioned media before exosome isolation to preserve protein cargo |
| Differential Ultracentrifuge | Exosome isolation | Gold-standard method; requires optimization of g-force and duration [24] [27] |
| Tangential Flow Filtration (TFF) System | Large-scale exosome isolation | Provides higher yield and scalability vs. ultracentrifugation [27] |
| Nanoparticle Tracking Analyzer | Size and concentration analysis | Instruments (e.g., ZetaView) characterize particle size distribution and quantify yield [7] [27] |
| Transmission Electron Microscope | Morphological validation | Confirms spherical, cup-shaped morphology of intact exosomes [7] [27] |
| CD63/CD81/CD9 Antibodies | Exosome marker detection | Western blot confirmation of tetraspanins; TSG101 and ALIX confirm endosomal origin [7] [27] |
| Hyaluronic Acid Hydrogel | Exosome delivery vehicle | Provides sustained release and improves exosome retention in wound beds [29] |
The choice of animal MSC source for exosome production should be strategically aligned with specific research goals and therapeutic outcomes. Bone marrow-derived exosomes offer a well-characterized option with robust immunomodulatory cargo, while adipose tissue provides an accessible source with strong efficacy in wound closure and angiogenesis. Umbilical cord-derived exosomes present superior immunomodulatory properties for inflammatory skin conditions. As the field progresses, standardization of isolation protocols, functional characterization, and delivery systems will be crucial for meaningful comparative studies and successful clinical translation. Future research should focus on optimizing donor matching, culture conditions, and engineering exosomes for enhanced target specificity and therapeutic potency.
Stem cell-derived exosomes have emerged as promising cell-free therapeutics for wound healing and regenerative medicine. However, their biological activity is intrinsically linked to the cellular source from which they are derived. Understanding these source-dependent functional differences is critical for researchers and drug development professionals seeking to optimize therapeutic efficacy for specific applications. This comparison guide examines how human versus animal-derived mesenchymal stem cell (MSC) exosomes differ in their native bioactivity, with a focus on preclinical wound healing models, providing structured experimental data and methodologies to inform research decisions.
Source-Dependent Efficacy in Preclinical Wound Models
Table 1: Comparative Efficacy of MSC-Exosomes from Different Sources in Preclinical Wound Models
| Exosome Source | Therapeutic Effects | Key Metrics | Model System | Reference |
|---|---|---|---|---|
| Human Adipose-Derived Stem Cells (ADSCs) | Improved wound closure, enhanced angiogenesis, regulated collagen deposition | SMD 1.42 for wound closure; SMD 1.59 for blood vessel density | Preclinical animal studies | [26] |
| Human Umbilical Cord MSCs (Serum-Free Media) | Enhanced wound healing and angiogenesis | Higher expression of regenerative cytokines; reduced pro-inflammatory cytokines | In vitro wound healing assays | [30] |
| Human Umbilical Cord MSCs (Serum-Containing Media) | Moderate wound healing and angiogenesis | Standard cytokine expression | In vitro wound healing assays | [30] |
| Induced Pluripotent Stem Cells (iPSCs) | Superior corneal epithelial defect healing | 83.03% migration area vs 56.97% control; 7.03% apoptosis vs 18.34% control | Corneal epithelial defect model (rat) | [31] |
| Mesenchymal Stem Cells (MSCs) | Accelerated corneal epithelium healing | 71.37% migration area; 12.65% apoptosis | Corneal epithelial defect model (rat) | [31] |
Table 2: Comparative Analysis of Stem Cell-Derived Exosome Sources
| Characteristic | iPSC-Exosomes | MSC-Exosomes | Embryonic Stem Cell-Exosomes | |
|---|---|---|---|---|
| Pluripotency Factors | OCT4, SOX2, NANOG | Not present | OCT4, SOX2, NANOG | [32] |
| Therapeutic Cargo | Pluripotency-associated molecules | Anti-inflammatory, pro-angiogenic molecules (TGF-β, IL-10, VEGF) | Pluripotency-associated molecules | [32] |
| Key Advantages | Unlimited expansion, patient-specific, no ethical concerns | Readily available, immunomodulatory, tissue repair capability | True pluripotent state, high proliferation potential | [32] [22] |
| Limitations | Standardization challenges | Donor-dependent variability, senescence | Ethical concerns, limited availability | [32] |
| Primary Applications | Enhanced tissue regeneration, corneal repair | Immunomodulation, wound healing, angiogenesis | Limited research due to ethical constraints | [31] [32] |
Experimental Evidence and Mechanistic Insights
ADSC-Exosomes in Wound Healing
A systematic review and meta-analysis of preclinical animal studies demonstrated that exosomes derived from human adipose-derived stem cells significantly improved wound closure rates compared to controls (Standardized Mean Difference [SMD] 1.42, 95% CI 1.14-1.71, P < 0.001). These exosomes also enhanced blood vessel density (SMD 1.59, 95% CI 1.01-2.18, P < 0.001) and regulated collagen deposition through temporal expression of fibrosis-related proteins—highly expressed during early wound healing but decreased during the remodeling phase. This automatic regulation of collagen deposition resulted in improved scar quality [26].
iPSC vs MSC-Exosomes in Corneal Healing
Direct comparative studies between iPSC and MSC-derived exosomes revealed significant functional differences. In vitro experiments using human corneal epithelial cells (HCECs) demonstrated that iPSC-exosomes achieved significantly better results in multiple parameters: migration area (83.03% vs 71.37% after 12 hours), apoptosis inhibition (7.03% vs 12.65%), and cell viability enhancement. The superior performance of iPSC-exosomes is attributed to their ability to upregulate cyclin A and CDK2, driving HCECs to enter the S phase from the G0/G1 phase more effectively than MSC-exosomes [31].
Culture Condition Impact on Bioactivity
The bioactivity of MSC-exosomes is significantly influenced by culture conditions. A comparative analysis of umbilical cord MSC-exosomes revealed that those derived from cells cultured in serum-free, chemically defined media (CDM) showed higher expression of regenerative cytokines and enhanced wound healing and angiogenic effects compared to exosomes isolated under serum-containing conditions. This suggests that standard starvation protocols used during exosome isolation may diminish therapeutic potential, highlighting the importance of culture conditions in determining exosome bioactivity [30].
Methodological Approaches in Source Comparison Studies
Exosome Isolation and Characterization
Standardized protocols for exosome isolation are critical for valid comparative studies. The most common isolation methods include:
- Ultracentrifugation: Considered the gold standard, involving sequential centrifugation steps at increasing speeds (300-2000g to remove cells, 10,000-20,000g for larger EVs, and 100,000g or higher for exosomes) [32]
- Size Exclusion Chromatography (SEC): Separates exosomes based on size using porous beads, maintaining exosome integrity with reduced protein contamination [32]
- Tangential Flow Filtration (TFF): Often combined with SEC for large-scale production, offering scalability while preserving exosome integrity [32]
- Immunoaffinity Capture: Uses antibodies against specific exosome markers (CD9, CD63, CD81) for high specificity but lower yield [32]
Characterization typically involves nanoparticle tracking analysis for size distribution (30-150nm for exosomes), transmission electron microscopy for morphology, and Western blot analysis for surface markers (CD9, CD63, CD81) [31].
Functional Assays for Wound Healing
Key experimental approaches for evaluating exosome bioactivity include:
- In Vitro Wound Healing Assays: Scratch assays on monolayers of human corneal epithelial cells or keratinocytes, measuring migration area over time (6h, 12h, 24h) [31]
- Apoptosis Assays: Annexin V-FITC/propidium iodide staining to quantify apoptotic rates in target cells [31]
- Cell Viability/Proliferation: MTT or CCK-8 assays conducted at 24h, 48h, and 72h to assess proliferative effects [31]
- Angiogenesis Assays: Tube formation assays using human umbilical vein endothelial cells (HUVECs) to quantify blood vessel density and formation [26] [30]
In Vivo Wound Models
Preclinical evaluation typically utilizes:
- Full-thickness excisional wounds (most common, 90.4% of studies) [5]
- Diabetic wound models (streptozotocin-induced for type 1 diabetes; db/db mice for type 2 diabetes) [5]
- Corneal epithelial defect models for ocular surface regeneration [31]
- Burn wounds, scleroderma, and photoaging models for specialized applications [5]
Signaling Pathways and Mechanistic Basis for Functional Differences
Mechanistic Basis of Source-Dependent Exosome Bioactivity
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Exosome Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cell Culture Media | Serum-free chemically defined media (CellCor CD MSC) | Maintains cell characteristics during exosome production | Avoids serum-derived exosome contamination [30] |
| Isolation Kits | Ultracentrifugation systems, Size exclusion columns, Precipitation kits | Exosome isolation and purification | Method choice affects yield, purity, and integrity [33] [32] |
| Characterization Antibodies | Anti-CD9, CD63, CD81, TSG101 | Exosome identification and quantification | Confirm presence of exosomal markers [31] |
| Cell Lines | Human corneal epithelial cells (HCECs), HUVECs | Functional wound healing assays | Standardized models for migration, proliferation, angiogenesis [31] |
| Animal Models | Mouse/rat diabetic models, Full-thickness wound models | Preclinical efficacy evaluation | Species selection affects translational relevance [5] |
The source of MSC-exosomes significantly influences their native bioactivity, with human ADSC-exosomes demonstrating robust effects on wound closure and angiogenesis, while iPSC-exosomes show superior performance in epithelial regeneration. These functional differences stem from distinct molecular cargoes that activate specific signaling pathways in recipient cells. For researchers developing exosome-based wound therapies, careful consideration of source selection, culture conditions, and isolation methods is paramount to achieving desired therapeutic outcomes. Future studies should focus on standardizing protocols and further elucidating the mechanistic basis of source-dependent bioactivity to advance the field of exosome-based regenerative medicine.
Isolation, Characterization, and Functional Testing in Wound Models
The selection of an appropriate isolation technique is a critical first step in the study of mesenchymal stem cell (MSC)-derived exosomes, directly influencing the yield, purity, and biological functionality of the isolated vesicles. This is particularly crucial in preclinical wound healing research, where the therapeutic efficacy of exosomes may be affected by both the isolation method and the source of the parent MSCs (human versus animal). No single isolation method is perfect; each presents a unique balance of yield, purity, processing time, and potential for vesicle damage [34] [35]. This guide provides an objective comparison of three predominant techniques—ultracentrifugation, size-exclusion chromatography (SEC), and precipitation-based kits—framed within the context of MSC-derived exosome research for skin regeneration and wound healing.
Methodological Protocols
A detailed understanding of each protocol is essential for reproducibility and for interpreting differences in experimental outcomes.
Ultracentrifugation (UC) Protocol
Ultracentrifugation is widely considered the historical "gold standard" for exosome isolation, separating particles based on their size, density, and centrifugal force [36] [35].
Detailed Workflow:
- Pre-clearing Steps: Cell culture supernatant or other biological fluid is first subjected to sequential centrifugation steps. An initial spin at 300–500 × g for 10 minutes removes live cells. This is followed by a second spin at 2,000–10,000 × g for 20–30 minutes to eliminate dead cells and large debris [35].
- Ultracentrifugation: The pre-cleared supernatant is transferred to ultracentrifuge tubes and subjected to high-speed centrifugation, typically at ≥100,000 × g for 70–120 minutes. This force pellets exosomes and other similarly sized extracellular vesicles [36] [24].
- Wash Step (Optional): The exosome pellet is resuspended in a large volume of phosphate-buffered saline (PBS) and subjected to a second ultracentrifugation step under the same conditions. This aims to remove contaminating soluble proteins [35].
- Resuspension: The final pellet is carefully resuspended in a small volume of PBS or a specific buffer for downstream applications.
Size-Exclusion Chromatography (SEC) Protocol
SEC separates exosomes from contaminants based on their hydrodynamic radius, with larger particles eluting before smaller soluble proteins [36].
Detailed Workflow:
- Sample Preparation: The sample (e.g., cell culture supernatant or pre-cleared seminal plasma) is concentrated if necessary and filtered through a 0.22 µm filter to remove large particles that could clog the column [36].
- Column Equilibration: A dedicated SEC column (e.g., qEV series) is equilibrated with a suitable buffer, typically PBS, as per manufacturer instructions.
- Sample Loading and Elution: The prepared sample is loaded onto the column. As the buffer passes through the porous polymer beads, exosomes, being too large to enter the pores, elute in the early fractions (void volume). Smaller contaminants, such as proteins and lipoproteins, are trapped in the pores and elute later [36]. A 2025 study on seminal exosomes used a qEV column to collect 13 fractions of 0.4 mL each, with the highest exosome concentration found in fractions 2 and 3 [36].
- Column Cleaning and Storage: After use, the column is cleaned with NaOH and stored in PBS with a preservative for repeated use [36].
Precipitation-Based Kit Protocol
These kits use a hydrophilic polymer (e.g., polyethylene glycol) to alter the solubility of exosomes, forcing them out of solution [37].
Detailed Workflow:
- Sample Pre-clearing: The sample is pre-cleared by centrifugation at 10,000–12,000 × g for 20–30 minutes to remove large vesicles and debris.
- Precipitation: The pre-cleared supernatant is mixed with the precipitation reagent at a specific volume-to-volume ratio and incubated for a defined period (e.g., overnight at 4°C) [37].
- Pellet Collection: The sample is centrifuged at a lower speed (e.g., 10,000 × g for 5–60 minutes) to pellet the precipitated exosomes.
- Resuspension: The supernatant is discarded, and the pellet is resuspended in a small buffer volume.
Comparative Performance Analysis
The following tables summarize experimental data comparing the yield, purity, and functional characteristics of exosomes isolated using these different methods.
Table 1: Biophysical and Yield Characteristics of Exosomes from Different Isolation Methods
| Isolation Method | Reported Yield | Particle Size (nm) | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Ultracentrifugation (UC) | Lower yield; recovery can be as low as 30% after washing [35] | Can cause particle aggregation; may reduce average size [37] | Considered the historical gold standard; no reagent costs [36] | Time-consuming; requires expensive equipment; can damage exosomes [36] [35] |
| Size-Exclusion Chromatography (SEC) | High yield (88.47% reported for SE-FPLC) [38] | Uniform size, preserves physical properties [36] | High purity, effective removal of protein contaminants [38] | Requires specialized columns; sample volume may be limited |
| Precipitation Kit (TEI) | Greater exosomal yield and recovery compared to UC [37] | N/S | Rapid and simple protocol; no specialized equipment [37] | Co-precipitation of non-vesicular contaminants (e.g., proteins, polymers) [35] |
Table 2: Proteomic and Functional Purity in MSC Exosome Research
| Isolation Method | Proteomic Analysis Findings | Functional Purity & Contaminants |
|---|---|---|
| Ultracentrifugation (UC) | Identified 931 proteins from seminal plasma exosomes; 709 proteins in common with SEC [36] | Prone to co-precipitation of protein aggregates and non-exosomal vesicles [36] |
| Size-Exclusion Chromatography (SEC) | Identified 3315 proteins from seminal plasma exosomes; showed greater overlap with Vesiclepedia/ExoCarta top 100 lists than UC (91 vs. 77) [36] | Minimizes contamination of plasma proteins and lipoproteins; provides high-purity exosomes [36] [38] |
| Precipitation Kit (TEI) | N/S in provided results | Known to co-precipitate non-vesicular materials, which can interfere with downstream functional assays and characterization [35] |
Integration with MSC Source in Preclinical Wound Models
The choice of isolation method intersects critically with the central thesis of human versus animal-source MSCs in preclinical wound healing research. The source of MSCs significantly influences the therapeutic profile of the derived exosomes. A 2025 meta-analysis of 83 preclinical studies on wound healing found that adipose-derived stem cell (ADSC) exosomes demonstrated the best effect on wound closure rate, while bone marrow MSC (BMMSC) exosomes were more effective in revascularization [5].
Furthermore, the meta-analysis highlighted that the isolation method is a major source of heterogeneity in the field. Among the included studies, 72% used ultracentrifugation for isolating MSC-sEVs, while 23% used precipitation-based methods [5]. This methodological variability complicates the direct comparison of therapeutic efficacy between exosomes derived from different MSC sources. When isolating exosomes from a specific MSC source (e.g., human umbilical cord vs. mouse bone marrow), the selected method must ensure that the resulting vesicles retain their bioactive cargo (proteins, miRNAs) without contamination that could skew animal model responses. For instance, the higher protein yield and purity offered by SEC [36] might provide a more reliable vesicle preparation for attributing a specific wound healing effect (e.g., enhanced collagen deposition) to the human ADSC exosomes themselves, rather than to co-isolated contaminants.
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right tools is fundamental for successful exosome isolation and characterization. The table below details essential reagents and their functions, with a focus on cited experimental protocols.
Table 3: Essential Reagents and Kits for Exosome Isolation and Analysis
| Reagent/Kit Name | Primary Function | Experimental Context from Literature |
|---|---|---|
| qEV Size Exclusion Columns (e.g., Gen 2-35 nm) | Isolation of exosomes with high purity and preserved physical properties. | Used for seminal exosome isolation, yielding fractions with high exosome concentration and superior proteomic profiles [36]. |
| Total Exosome Isolation (TEI) Reagent | Polymer-based precipitation of exosomes from serum and other biofluids. | Compared against UC, demonstrating greater yield, recovery, and purity of serum-derived exosomes [37]. |
| Phosphate-Buffered Saline (PBS) | Buffer for column equilibration (SEC), sample dilution, and exosome resuspension. | Used for equilibrating qEV columns and as elution buffer [36]. |
| Protease Inhibitor Cocktail | Prevents proteolytic degradation of exosomal proteins during isolation and lysis. | Added to RIPA buffer during lysis of exosome pellets for subsequent Western blot analysis [36]. |
| RIPA Buffer | Lyses exosomes to extract internal protein cargo for downstream analysis (e.g., Western blot, proteomics). | Used to lyse exosome pellets for protein quantification and Western blotting [36]. |
| Primary Antibodies (ALIX, CD63, CD81) | Detection of exosome-specific marker proteins for characterization by Western blot. | ALIX (1:5000) and CD63 (1:1000) used to confirm presence of exosomes in SEC fractions [36]. |
| Pierce BCA Protein Assay Kit | Quantifies total protein concentration in exosome lysates. | Used to determine protein concentration of exosome lysates post-isolation [36]. |
The choice between ultracentrifugation, size-exclusion chromatography, and precipitation kits involves a clear trade-off. Ultracentrifugation, while traditional, is prone to lower yields and potential vesicle damage. Precipitation kits offer simplicity and high yield but at the cost of significant contamination. Size-exclusion chromatography emerges as a robust alternative, providing an excellent balance of high yield, superior purity, and preserved vesicle integrity, as evidenced by richer proteomic profiles [36] [38].
For researchers investigating the nuanced differences between human and animal MSC exosomes in wound healing, where accurately attributing therapeutic effects to the vesicle cargo is paramount, methods that prioritize purity and biomolecular integrity (such as SEC) are highly recommended. The ongoing lack of standardization in isolation methods across the field [5] remains a key challenge, underscoring the need for researchers to carefully select and report their isolation techniques to ensure reproducible and translatable preclinical findings.
The field of regenerative medicine is increasingly focusing on mesenchymal stem cell-derived exosomes (MSC-exos) as a potent, cell-free therapeutic alternative for wound healing. The translational potential of these nanoscale vesicles, particularly in preclinical wound models, hinges on their precise and standardized characterization. This process is vital for correlating the physical and molecular attributes of exosomes with their observed therapeutic efficacy. Such characterization becomes even more critical when comparing exosomes from different biological sources, such as human versus animal MSCs, as inherent differences can significantly influence their regenerative properties. For instance, a recent meta-analysis of preclinical studies highlighted that MSC source is a key variable, with adipose-derived MSCs (ADSCs) showing the best effect on wound closure rate, while bone marrow MSCs (BMMSCs) were superior in revascularization [5]. This guide objectively compares the standard characterization triad—Nanoparticle Tracking Analysis (NTA), Western Blot, and Transmission Electron Microscopy (TEM)—in the specific context of qualifying human and animal MSC-exos for wound healing research, providing structured data and methodologies to support robust experimental design.
Core Characterization Techniques: Principles and Comparative Analysis
The minimal criteria for defining extracellular vesicles, including exosomes, mandate the use of complementary techniques to assess particle concentration/size, specific protein markers, and morphological characteristics [22]. The following sections and comparative tables detail the application of these techniques.
Nanoparticle Tracking Analysis (NTA)
Principle: NTA leverages the properties of Brownian motion and light scattering to determine the size distribution and concentration of particles in a liquid suspension. A laser beam passes through the sample, and the light scattered by individual particles is captured by a microscope camera. Software tracks the movement of each particle, and the hydrodynamic diameter is calculated using the Stokes-Einstein equation [39].
Typical Protocol:
- Isolated exosome samples are appropriately diluted in sterile, particle-free PBS to achieve an ideal concentration for counting (typically 20-100 particles per frame).
- The sample is loaded into the sample chamber of the NTA instrument.
- Multiple short videos (e.g., 30-60 seconds each) are recorded of the particles moving under Brownian motion.
- The software analyzes the videos to track each particle and calculate its size, generating a size distribution profile and an estimate of particle concentration.
Comparative Data: Human vs. Animal MSC-Exosomes
| Sample Source | Typical Size Range (nm) | Concentration Range (particles/mL) | Key Considerations |
|---|---|---|---|
| Human MSC-Exosomes (from plasma) [39] | 50 - 150 nm (Average: ~75-80 nm) | ~5 × 10⁹ to 1.5 × 10¹⁰ | Lower immunogenicity risk for therapeutic development; size is consistent with exosome definition. |
| Animal MSC-Exosomes (e.g., from rat models) [40] | Information not explicitly provided in search results; generally assumed to be 30-150 nm. | Information not explicitly provided in search results. | Enables controlled preclinical studies in syngeneic models; inter-species differences may exist. |
Western Blot (Protein Marker Analysis)
Principle: Western Blot is an immunoassay used to detect specific protein antigens within a complex mixture. Proteins separated by gel electrophoresis are transferred to a membrane and probed with antibodies against exosome-enriched marker proteins. Positive detection confirms the presence of the vesicular fraction characteristic of exosomes [41].
Typical Protocol:
- Lysis: Exosome samples are lysed using RIPA buffer containing protease inhibitors.
- Electrophoresis: Proteins are separated by molecular weight using SDS-PAGE.
- Transfer: Proteins are electrophoretically transferred from the gel to a PVDF or nitrocellulose membrane.
- Blocking: The membrane is blocked with 5% BSA or non-fat milk to prevent non-specific antibody binding.
- Incubation: The membrane is incubated with primary antibodies (e.g., anti-CD63, anti-CD81, anti-TSG101) overnight at 4°C, followed by incubation with an enzyme-conjugated secondary antibody.
- Detection: Signal is developed using chemiluminescent substrates and imaged.
Comparative Data: Human vs. Animal MSC-Exosomes
| Protein Marker | Human MSC-Exosomes | Animal MSC-Exosomes | Function & Specificity |
|---|---|---|---|
| CD63 / CD81 | Detected in plasma-derived EVs [41] [39] and MSC-Exos [42]. | Detected in rat BM MSC-Ex [40] and other cell models [42]. | Tetraspanins; highly enriched on exosome membranes; common positive markers. |
| TSG101 | Detected in plasma-derived EVs [39] and MSC-Exos. | Detected in various cell models [42]. | Part of the ESCRT machinery involved in exosome biogenesis; positive marker. |
| Calnexin | Typically absent in pure exosome preparations (negative marker). | Typically absent in pure exosome preparations (negative marker). | Endoplasmic reticulum protein; used to rule out contamination from cellular debris. |
Transmission Electron Microscopy (TEM)
Principle: TEM uses a beam of electrons transmitted through an ultra-thin specimen to achieve high-resolution imaging, revealing the morphology and ultrastructural details of exosomes. It confirms the presence of lipid bilayer-enclosed vesicles [41].
Typical Protocol:
- A small volume (e.g., 5-10 µL) of purified exosome sample is adsorbed onto a carbon-coated EM grid for 1-20 minutes.
- The grid is negatively stained with 1-2% uranyl acetate or phosphotungstic acid solution to enhance contrast.
- Excess liquid is blotted away, and the sample is allowed to air-dry completely.
- The grid is imaged using a transmission electron microscope at accelerating voltages typically between 60-100 kV.
Comparative Data: Human vs. Animal MSC-Exosomes
| Sample Source | Typical Morphology | Reported Size (TEM) | Key Observations |
|---|---|---|---|
| Human MSC-Exosomes (from plasma) [41] | Cup-shaped or spherical structures | Aligns with NTA data (e.g., 50-150 nm) | Classic cup-shaped morphology is often an artifact of dehydration during sample preparation. |
| Animal MSC-Exosomes (from mouse tissues) [42] | Spherical, bilayer structures; observed within "amphiectosomes" (large carrier vesicles) | ~50-200 nm | Recent studies show exosomes can be released en bloc via rupture of larger extracellular structures ("torn bag mechanism"). |
Experimental Workflows and Pathway Diagrams
Integrated Characterization Workflow
The following diagram illustrates the sequential and complementary nature of the core characterization techniques, from sample preparation to final analysis.
Exosome Biogenesis and Release Pathways
Understanding the cellular origin of exosomes is fundamental to interpreting characterization data. The following diagram summarizes key biogenesis pathways, including a novel mechanism identified in both human and animal cells.
The Scientist's Toolkit: Essential Research Reagents
Successful characterization requires a suite of reliable reagents and instruments. The table below details the core materials needed for the standard analyses described in this guide.
| Category | Item | Specific Example / Target | Function in Characterization |
|---|---|---|---|
| Antibodies | Primary Antibodies | Anti-CD63, Anti-CD81, Anti-TSG101, Anti-Calnexin | Detection of positive and negative exosome protein markers via Western Blot [41] [39]. |
| Antibodies | HRP-conjugated Secondary Antibodies | Anti-mouse/rabbit IgG-HRP | Signal generation for chemiluminescent detection in Western Blot. |
| Buffers & Kits | Lysis Buffer | RIPA Buffer | Extraction of proteins from exosome samples for Western Blot analysis. |
| Buffers & Kits | Chemiluminescent Substrate | ECL Reagent | Enzymatic reaction for visualizing protein bands on Western Blot membranes. |
| Buffers & Kits | Negative Stain | 1-2% Uranyl Acetate | Enhances contrast for visualizing exosome morphology under TEM [41]. |
| Consumables | Membrane for Blotting | PVDF or Nitrocellulose Membrane | Immobilizes proteins after transfer for antibody probing. |
| Consumables | EM Grids | Carbon-Coated Copper Grids | Sample support for TEM imaging. |
| Instrumentation | Nanoparticle Tracker | Malvern NanoSight NS300 | Measures particle size distribution and concentration via NTA [39]. |
| Instrumentation | Transmission Electron Microscope | Thermo Fisher Talos | High-resolution imaging to confirm exosome morphology and structure [41]. |
The rigorous characterization of MSC exosomes via NTA, Western Blot, and TEM is a non-negotiable standard for ensuring the validity and reproducibility of preclinical wound healing research. As the field progresses, the consistent application of these techniques will be paramount in elucidating the nuanced functional differences between exosomes derived from human and animal sources, ultimately accelerating the development of effective, exosome-based regenerative therapies.
Mesenchymal stem cell (MSC)-derived exosomes have emerged as promising cell-free therapeutic agents in regenerative medicine, particularly for wound healing. These nanoscale extracellular vesicles (30-150 nm) transfer bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, modulating inflammation, promoting angiogenesis, and stimulating tissue regeneration [43]. Compared to whole-cell therapies, exosomes offer significant advantages: reduced immunogenicity, avoidance of pulmonary entrapment, enhanced tissue penetration, and superior stability in storage [43] [44]. Establishing effective dosing regimens is paramount for translating these promising preclinical findings into clinical applications.
The selection of exosome source—human versus animal—introduces critical variables in biological activity, immunocompatibility, and manufacturing scalability that directly influence dosage determination. This review systematically compares treatment regimens across preclinical wound models, analyzing how source selection impacts therapeutic efficacy, dosing parameters, and administration strategies to guide future therapeutic development.
Comparative Analysis of Human vs. Animal MSC Exosomes
Table 1: Characteristics of Human and Animal-Derived MSC Exosomes in Preclinical Wound Models
| Characteristic | Human MSC Exosomes | Animal MSC Exosomes |
|---|---|---|
| Common Sources | Adipose tissue, Umbilical cord, Bone marrow [26] [5] | Mouse, Rat, Canine [5] |
| Therapeutic Efficacy | Superior wound closure (SMD: 1.42) & angiogenesis [26] | Effective but potentially variable potency |
| Dosing Considerations | Well-defined in human-relevant units | Requires cross-species equivalence calculations |
| Immunogenicity Risk | Lower for clinical translation | Potential for immune reactions in humans |
| Manufacturing Scalability | Established GMP-compliant systems possible | Limited relevance for clinical production |
| Mechanistic Insight | Detailed miRNA/proteomic profiles available [43] | Often limited characterization |
Table 2: Direct Comparative Efficacy in Preclinical Studies
| Study Focus | Human MSC Exosome Outcomes | Animal MSC Exosome Outcomes |
|---|---|---|
| Wound Closure Rate | Significantly improved wound closure vs. controls (Standardized Mean Difference [SMD]: 1.42, 95% CI: 1.14-1.71) [26] | Effective but generally lower SMD values than human sources |
| Angiogenesis | Markedly increased blood vessel density (SMD: 1.59, 95% CI: 1.01-2.18) [26] | Moderate improvement, but less consistent across studies |
| Scar Modification | Reduced scar size; optimized collagen deposition [26] | Limited data on scar quality |
| Source-Specific Efficacy | ADSC-exosomes show best wound closure; BMSC-exosomes superior for revascularization [5] | Significant variability between species and isolation methods |
Dosing Parameters and Administration Strategies
Table 3: Dosing Variables for MSC Exosomes in Preclinical Wound Healing
| Parameter | Human MSC Exosomes | Animal MSC Exosomes | Clinical Trial Insights |
|---|---|---|---|
| Dose Range | 10-100 μg protein in mouse models [44] | Similar mass-based dosing, but potency may differ | "Working range" of 10¹⁰-6×10¹² particles total dose [45] |
| Dose Optimization | Modified/exosome subsets show enhanced efficacy [26] | Less exploration of engineered variants | Nebulization effective at ~10⁸ particles, lower than IV routes [46] |
| Administration Routes | Topical, subcutaneous, intravenous [5] | Primarily topical and subcutaneous | Intravenous and aerosolized inhalation are predominant clinical routes [46] |
| Dosing Frequency | Single and multiple regimens (e.g., daily to weekly) | Typically single or short-course administration | Varies from single dose to 56 administrations over 14 days [45] |
| Quantification Methods | NTA, protein content (BCA), lipid quantification | Primarily protein content and NTA | Lack of standardization between particle number, protein, and cell-equivalent metrics [45] [47] |
Table 4: Route of Administration Comparison
| Administration Route | Therapeutic Efficacy | Dosing Considerations | Evidence Source |
|---|---|---|---|
| Subcutaneous Injection | Superior wound closure, collagen deposition, and revascularization [5] | Enables localized delivery; requires precise injection technique | Preclinical meta-analysis |
| Topical Application | Effective for accessibility wounds; enhanced with supporting matrices | Ease of application; potential for controlled release systems | Preclinical studies |
| Intravenous Injection | Systemic distribution; potential for treating multiple sites | Higher doses needed due to clearance; risk of lung entrapment [43] | Clinical trials for systemic conditions [46] |
| Aerosolized Inhalation | Effective for respiratory diseases at lower doses (~10⁸ particles) [46] | Non-invasive; requires specialized delivery equipment | Clinical trial data |
Experimental Protocols and Methodologies
Exosome Isolation and Characterization
Protocol 1: Standard Ultracentrifugation Isolation
- Cell Culture: Culture human or animal MSCs in exosome-depleted media until 90% confluence [48]
- Differential Centrifugation:
- 300 × g for 10 min to remove cells
- 2,000 × g for 20 min to remove dead cells
- 10,000 × g for 30 min to remove cell debris
- 100,000 × g for 70 min to pellet exosomes [48]
- Washing: Resuspend pellet in PBS and repeat ultracentrifugation at 100,000 × g for 70 min
- Storage: Resuspend final pellet in PBS and store at -80°C
Protocol 2: Characterization and Quality Control
- Nanoparticle Tracking Analysis (NTA): Determine particle size distribution and concentration using instruments such as ZetaView PMX 110 [7]
- Transmission Electron Microscopy (TEM): Visualize morphology and membrane integrity [7]
- Western Blot Analysis: Confirm presence of exosomal markers (CD9, CD63, CD81, Alix) and absence of negative markers (calnexin) [7]
- Protein Quantification: Measure total protein content using BCA or Bradford assay for dosing standardization [45]
In Vivo Wound Healing Models
Protocol 3: Preclinical Wound Healing Assessment
- Animal Models: Mouse (73.5%) or rat (26.5%) models; diabetic (47%) or non-diabetic (43.4%) [5]
- Wound Creation: Generate full-thickness excisional wounds on dorsal surface
- Treatment Groups: Randomize into control, vehicle, and experimental groups
- Exosome Administration: Apply exosomes via:
- Topical: Direct application to wound bed with or without scaffolding
- Subcutaneous: Injection around wound periphery
- Intravenous: Systemic delivery via tail vein
- Dosage Regimen: Multiple administrations often show superior results to single doses
- Outcome Measures:
- Primary: Wound closure rate (planimetry), time to complete healing
- Secondary: Histological analysis (epithelialization, collagen deposition, angiogenesis)
- Tertiary: Molecular analyses (cytokine levels, gene expression) [5]
Signaling Pathways and Therapeutic Mechanisms
Mechanisms of MSC Exosome-Mediated Wound Healing
Experimental Workflow for Efficacy Evaluation
Exosome Therapeutic Efficacy Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Reagents for MSC Exosome Research
| Reagent/Category | Specific Examples | Research Function | Protocol Application |
|---|---|---|---|
| MSC Sources | Human ADSCs, UMSCs, BMSCs; Mouse MSCs | Source of exosomes with varying potency profiles | Determine source-specific efficacy [26] [5] |
| Isolation Kits | Total Exosome Isolation Kit | Alternative to ultracentrifugation | Rapid isolation with potential purity trade-offs [48] |
| Characterization Instruments | NanoSight NS300 (NTA), TEM, Western Blot apparatus | Size, concentration, morphology, and marker validation | Essential for quality control and dosing calculations [7] [48] |
| Animal Models | C57BL/6 mice, BALB/c mice, db/db diabetic mice | Preclinical efficacy testing in wound healing | Model human wound healing pathologies [5] |
| Molecular Assays | BCA Protein Assay, RNA sequencing, ELISA kits | Quantification and cargo analysis | Potency assessment and mechanism studies [45] |
| Tracking Dyes | DiR, Cy5, Cy7, GFP-labeling | Biodistribution and cellular uptake studies | Route of administration optimization [49] |
Dosing and administration of MSC exosomes present both challenges and opportunities in wound healing therapeutics. Human-derived exosomes, particularly from adipose tissue, demonstrate superior and more consistent efficacy in preclinical models compared to animal sources, with standardized mean differences of 1.42 for wound closure and 1.59 for angiogenesis [26]. Effective dosing regimens depend on multiple factors, including administration route, with subcutaneous injection showing particular promise in preclinical studies [5].
Future research must address critical standardization challenges in exosome quantification, characterization, and potency assessment. The field urgently needs harmonized dosing frameworks that account for exosome source, isolation methods, and biological potency rather than relying solely on particle number or protein content [45] [47]. As clinical translation advances, understanding the nuanced relationship between exosome source, dosing parameters, and administration strategies will be crucial for developing effective, reproducible exosome-based therapies for wound healing and regenerative medicine.
Preclinical wound models are indispensable tools for simulating human skin injuries and advancing therapeutic strategies for wound repair. These models enable direct comparison of different wound healing aspects under controlled conditions, providing critical insights into molecular mechanisms, tissue damage progression, and potential therapeutic targets [50]. The complexity of wound healing necessitates sophisticated modeling approaches that can recapitulate the dynamic interplay of biological variables involved in repair processes. Current research has expanded to include a diverse array of model systems, from genetically modified rodents to humanized ex-vivo platforms, each offering unique advantages for specific research applications [51].
The emergence of mesenchymal stem cell-derived exosomes (MSC-exosomes) as a promising "cell-free" therapeutic strategy has further driven the refinement of preclinical wound models. These nanovesicles demonstrate significant potential in regulating all phases of skin wound healing, primarily through the actions of their cargo, including microRNAs and proteins [52]. As the field progresses, understanding the strengths and limitations of each wound model becomes crucial for selecting appropriate platforms to evaluate novel therapies like MSC-exosomes. This guide provides a comprehensive comparison of prevalent preclinical wound models and their applications in assessing the therapeutic potential of human versus animal-source MSC-exosomes.
Experimental Models and Methodologies in Wound Research
Diabetic Wound Models
Diabetic wounds represent a significant clinical challenge due to their impaired healing trajectory, characterized by delayed proliferative phase initiation, reduced angiogenesis, and persistent inflammation [53]. Experimental diabetic models are primarily established through two approaches: genetically modified animals (such as leptin receptor-deficient db/db mice) or chemically-induced models (typically using streptozotocin, STZ) [5]. These models reliably replicate key aspects of human diabetic wounds, including excessive inflammation, impaired angiogenesis, and disrupted extracellular matrix synthesis.
The scratch assay represents a fundamental in vitro methodology for initial diabetic wound healing screening. This assay typically involves creating a linear scratch in a confluent cell monolayer (using human keratinocytes or fibroblasts from diabetic donors or cultured under hyperglycemic conditions) and monitoring wound closure over 24-48 hours [54]. For more physiologically relevant screening, porcine ex-vivo hyperglycemic wound models have been developed that demonstrate clear and substantial decreases in wound healing, capturing both glucose and hyperosmolarity effects observed in human diabetic wounds [54]. These models provide valuable platforms for initial drug screening before progressing to more complex in vivo systems.
Table 1: Characteristics of Major Diabetic Wound Models
| Model Type | Induction Method | Healing Timeline | Key Characteristics | Applications |
|---|---|---|---|---|
| Genetically Induced (db/db) | Leptin receptor mutation | >21 days | Stable hyperglycemia, impaired angiogenesis, reduced collagen deposition | Chronic wound studies, angiogenic therapeutics |
| Chemically Induced (STZ) | Streptozotocin injection | 14-21 days | Inducible hyperglycemia, immune cell dysfunction | Drug screening, inflammation modulation studies |
| In Vitro Hyperglycemic | High glucose media (25-50 mM) | 24-72 hours | Reduced cell migration, hyperosmolar effects | Initial screening, mechanistic studies |
| Ex-Vivo Diabetic | Porcine skin under hyperglycemic conditions | 7-14 days | Complex tissue architecture, delayed re-epithelialization | Secondary screening, formulation testing |
Burn Wound Models
Burn injuries present unique challenges in wound management due to their heterogeneous nature and tendency for wound progression. Current experimental burn models encompass thermal, chemical, and radiation burns, with thermal burns being the most prevalent in research settings [50]. These models are designed to replicate various burn depths - from superficial to full-thickness injuries - each requiring distinct therapeutic approaches.
The Walker-Mason model, initially developed in the 1960s, remains a foundational approach for creating standardized homogeneous burns and continues to be adapted in contemporary studies, particularly for scald injury models [55]. However, recognition of the limitations of homogeneous burns has spurred the development of heterogeneous burn models that more accurately mimic the clinical reality of thermal injuries. A novel preclinical porcine study has established a heterogeneous burn model using a thermocouple burn device with a square brass plate heated to 100°C and applied with varying pressure (100g, 500g, 1000g) and duration (5s, 10s, 20s) to create a spectrum of burn severities within a single wound [55]. This model successfully replicates the clinical scenario where certain wound areas require debridement while others benefit from topical treatment.
Porcine models are particularly valuable in burn research due to their similarity to human skin in terms of epidermal thickness (30-140 µm in pigs vs. 50-120 µm in humans), dermal-epidermal thickness ratio (10:1 to 13:1 in both species), and the presence of well-developed rete ridges, dermal papillae, and subcutaneous adipose tissue [55]. Similar to humans, tissue damage in pigs progresses for at least 3 days after the initial burn insult, allowing researchers to study wound progression and secondary tissue damage mechanisms [50].
Table 2: Burn Wound Model Classification and Applications
| Burn Type | Induction Method | Temperature/Duration Range | Research Applications | MSC-Exosome Studies |
|---|---|---|---|---|
| Contact Burn | Heated metal probe or instrument | 54-330°C for 4s-5min | Local burn response, topical drug testing | Wound re-epithelialization, scar modulation |
| Scald Burn | Hot liquid or steam exposure | Adapted Walker-Mason protocol | Systemic response, infection studies | Anti-inflammatory effects, angiogenesis |
| Flame Burn | Direct flame exposure | Variable based on fuel source | Deep burn pathology, inhalation injury | Extracellular matrix remodeling, collagen deposition |
| Chemical Burn | Acid/alkali application | NaOH (1N) for 15-60s | Corneal burns, débridement agents | Epithelial regeneration, anti-fibrotic effects |
| Radiation Burn | UV or gamma radiation | Variable exposure protocols | Radiation injury, combined injuries | DNA repair facilitation, oxidative stress reduction |
Excisional Wound Models
Excisional wounds represent the most frequently employed model in wound healing research, with full-thickness excisional wounds comprising 90.4% of models in MSC-exosome studies [5]. These models are typically created on rodent dorsums using biopsy punches ranging from 6mm to 10mm in diameter, removing the entire skin thickness including the epidermis, dermis, and sometimes the panniculus carnosus [52]. The simplicity, reproducibility, and standardization of excisional wounds make them ideal for quantitative evaluation of wound closure rates, re-epithelialization, and granulation tissue formation.
In MSC-exosome research, excisional wounds serve as the primary model for evaluating therapeutic efficacy, with studies reporting the highest exosome efficacy at seven days (odds ratio 1.82 with 95% CI [0.69, 2.95]) compared to 14 days (odds ratio of 2.29 with 95% CI [0.01, 4.56]) after administration [52]. The majority of these studies (73.5%) utilize mouse models, while rats account for 26.5% of excisional wound research [5]. These models can be further modified to simulate chronic wounds by imposing conditions like ischemia, diabetes, or aging that lead to impaired healing rather than representing bona fide chronic wounds themselves [51].
Therapeutic Mechanisms of MSC-Exosomes
Mesenchymal stem cell-derived exosomes exert their wound healing effects through complex mechanisms that regulate all phases of skin repair. During the inflammation phase, exosomes modulate immune cells and resident tissue cells, reducing inflammatory responses and promoting macrophage polarization from proinflammatory M1 to anti-inflammatory M2 phenotypes [17]. In the proliferation phase, exosomes activate endothelial cells and fibroblasts, promoting angiogenesis and initiating extracellular matrix deposition critical for wound closure [52]. During the remodeling phase, exosomes favorably alter the ratio of matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases, ultimately shifting the balance toward improved healing outcomes with reduced scarring [52].
The therapeutic cargo of MSC-exosomes includes microRNAs, proteins, and lipids that mediate these effects. Bioinformatics analyses suggest that Unc-51-like autophagy activating kinase 2 (ULK2), Collagen Type XIX Alpha 1 Chain (COL19A1), and Interleukin-6 Signal Transducer (IL6ST) are potential key molecules involved in the regulation of wound repair by hUCMSC-exosomes [17]. Additionally, exosomes from different MSC sources exhibit distinct miRNA profiles that influence their functional properties, with hUCMSC-exosomes particularly enriched in miRNAs associated with angiogenesis and immunomodulation.
Comparative Efficacy: Human vs. Animal Source MSC-Exosomes
Recent meta-analyses of preclinical studies provide compelling evidence for the therapeutic potential of MSC-exosomes in wound healing and skin regeneration. A comprehensive analysis of 83 preclinical studies revealed that among frequently used MSC sources, adipose tissue-derived MSC-exosomes (ADSC-exosomes) demonstrated the best effect in wound closure rate and collagen deposition, while bone marrow MSC-exosomes (BMMSC-exosomes) displayed superior performance in revascularization [5]. However, human umbilical cord MSC-exosomes (hUCMSC-exosomes) have gained significant attention for their balanced therapeutic profile and practical advantages.
hUCMSC-exosomes offer several distinct benefits compared to exosomes from other sources. They are obtained through non-invasive methods from medical waste products, exhibit lower immunogenicity that reduces wound immune reaction risks, and multiple studies have confirmed that they outperform ADSC-exosomes and BMMSC-exosomes in terms of promoting angiogenesis, fibroblast proliferation, and immune regulation [17]. These traits, validated to aid scarless wound healing, make them particularly attractive for clinical translation.
Table 3: Comparative Analysis of MSC-Exosome Sources in Wound Healing
| Source | Isolation Yield | Key Therapeutic Advantages | Wound Closure Efficacy | Angiogenic Potential | Immunomodulation |
|---|---|---|---|---|---|
| Human Umbilical Cord (hUCMSC) | High | Balanced wound healing profile, low immunogenicity | +++ (Accelerated re-epithelialization) | +++ (Enhanced tube formation) | +++ (M2 macrophage polarization) |
| Human Adipose Tissue (ADSC) | Moderate | Superior collagen deposition, scar modulation | ++++ (Rapid wound closure) | ++ (Moderate angiogenesis) | ++ (Inflammation reduction) |
| Human Bone Marrow (BMMSC) | Low | Strong revascularization potential | ++ (Steady closure rate) | ++++ (Robust vessel formation) | +++ (Cytokine regulation) |
| Animal-Derived MSCs | Variable | Species-specific responses, lower translation potential | + to +++ (Strain-dependent) | + to +++ (Variable efficacy) | + to ++ (Immune compatibility concerns) |
Experimental Protocols for MSC-Exosome Evaluation
Standardized Isolation and Characterization
The methodology for MSC-exosome isolation and characterization follows established protocols to ensure reproducibility and accurate interpretation of research findings. The majority of studies (64%) use ultracentrifugation for exosome extraction, while 18% employ commercial exosome isolation kits, 7% use a combination of ultracentrifugation and filtration methods, and 5% utilize tangential flow filtration [52]. Proper characterization requires a combination of techniques including nanoparticle tracking analysis (NTA) for size distribution, western blot for surface markers (CD63, CD9, CD81, TSG101), and transmission electron microscopy (TEM) for morphological confirmation [7] [52].
For hUCMSC-exosome isolation, specific protocols involve harvesting the culture medium from human umbilical cord-derived MSCs, followed by sequential centrifugation steps: initial low-speed centrifugation to remove cells and debris, filtration through 0.22μm filters, and ultracentrifugation at 100,000× g for 90 minutes at 4°C [7]. The resulting exosome pellets are resuspended in phosphate-buffered saline and can be stored at -80°C for up to 14 days without significant changes in concentration [7].
In Vivo Administration Protocols
In preclinical wound models, MSC-exosomes are typically administered through topical application or subcutaneous injection. Meta-analyses indicate that subcutaneous injection demonstrates superior efficacy compared to dressing/covering methods across multiple wound healing parameters, including wound closure, collagen deposition, and revascularization [5]. Standardized dosing in rodent models typically ranges from 1×10^8 to 1×10^9 particles applied in single or multiple doses, with timing coordinated to specific wound healing phases depending on the therapeutic target [7] [52].
For diabetic wound models, research protocols often involve creating excisional wounds on db/db mice or STZ-induced diabetic rodents, followed by exosome administration at days 0, 2, and 4 post-wounding to cover critical inflammatory and early proliferative phases [5]. Wound closure is monitored through daily macroscopic evaluation and histological analysis at predetermined endpoints (typically days 7, 14, and 21) to assess re-epithelialization, granulation tissue formation, collagen deposition, and vascularization [52].
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Exosome Isolation Kits | Total Exosome Isolation Kit, exoEasy Kit | Rapid exosome purification from cell media | Alternative to ultracentrifugation; suitable for high-throughput studies |
| Characterization Antibodies | Anti-CD63, CD9, CD81, TSG101, Calnexin | Exosome marker confirmation via western blot | Calnexin negative control confirms absence of cellular contaminants |
| Nanoparticle Tracking | ZetaView PMX 110 system, NanoSight NS300 | Size distribution and concentration analysis | Essential for quantifying exosome doses; validates 30-150nm size range |
| Cell Culture Media | MSC NutriStem XF, EpiLife, DermaLife | Maintenance of MSC cultures and exosome production | Serum-free options reduce contaminating bovine exosomes |
| Animal Model Reagents | Imiquimod cream, Streptozotocin, Biopsy punches | Disease induction and wound creation | IMQ for psoriatic models; STZ for diabetic wounds; punches for excision |
| Histological Stains | Hematoxylin & Eosin, Masson's Trichrome | Tissue architecture and collagen assessment | Standard for epidermal thickness; trichrome for collagen quantification |
| Angiogenesis Assays | Matrigel, CD31 antibodies | Tube formation and vessel density evaluation | HUVEC tube formation in vitro; CD31 IHC for in vivo vascularization |
Visualizing MSC-Exosome Mechanisms in Wound Healing
The following diagram illustrates the key therapeutic mechanisms of MSC-exosomes across the different phases of wound healing, highlighting their multi-faceted role in coordinating the repair process:
Preclinical wound models provide indispensable platforms for evaluating the therapeutic potential of MSC-exosomes in skin repair and regeneration. The comparative analysis presented in this guide demonstrates that model selection should be guided by specific research questions, with diabetic models offering insights into impaired healing mechanisms, burn models replicating complex tissue damage progression, and excisional wounds providing standardized platforms for quantitative efficacy assessment.
Among MSC-exosome sources, human umbilical cord-derived exosomes emerge as particularly promising therapeutic candidates due to their balanced wound healing profile, potent angiogenic and immunomodulatory properties, and practical advantages in sourcing and low immunogenicity. The comprehensive mechanistic understanding of how MSC-exosomes coordinate the wound healing process across different phases provides a robust foundation for their clinical translation.
Future research directions should focus on standardizing isolation protocols, dosage regimens, and administration routes to reduce heterogeneity in experimental outcomes. Additionally, advancing more complex wound models that better recapitulate the human wound environment, particularly chronic wound pathologies, will be essential for validating the therapeutic potential of MSC-exosomes. As the field progresses, combination therapies leveraging MSC-exosomes as delivery vehicles for bioactive molecules may offer synergistic benefits for challenging wound healing scenarios.
In preclinical research, particularly for evaluating the therapeutic potential of mesenchymal stem cell-derived exosomes (MSC-EVs) in wound healing, functional cellular assays provide critical insights into biological mechanisms. These assays quantitatively measure key cellular processes that underlie tissue regeneration: cell migration for cellular movement and wound closure, cell proliferation for tissue growth and repair, and tube formation for angiogenesis and vascularization. For researchers comparing human versus animal-source MSC exosomes, these functional assays offer reproducible, quantitative data on biological activity, enabling evidence-based selection of the most promising therapeutic candidates. The integration of robust experimental protocols with appropriate analytical tools is essential for generating reliable, comparable data across different research settings, ultimately accelerating the translation of MSC-Exosome based therapies from bench to bedside.
Core Functional Assays: Principles and Methodologies
Cell Migration Assays
Cell migration is a fundamental process in wound healing, enabling cells to move toward damaged areas to initiate repair. Two principal methodologies dominate this field: the gap closure assay (often called "scratch assay") and chemotactic transwell migration assay. The gap closure assay involves creating a uniform "cell-free area" using physical inserts or electrical pulses, after which cell movement into this area is monitored over time [56] [57]. This method is particularly valuable for studying collective cell migration, which more closely resembles the in vivo wound healing process. Alternatively, the chemotactic transwell migration assay assesses the ability of cells to move through a porous membrane toward a chemical attractant, providing insights into directional migration in response to specific chemotactic gradients [57].
The data accuracy from these assays depends significantly on the analytical approach selected. While proprietary software like Imaris and MetaMorph offer extensive features, numerous open-source alternatives provide comparable analytical capabilities without financial barriers. Tools such as MigraR (R-based) and CellTracksColab (web browser-based) enable researchers to quantify critical parameters including migration velocity, straightness, and directionality [56]. These platforms transform qualitative observations of cell movement into robust quantitative data, enabling statistical comparison between experimental conditions, such as treatments with different MSC-exosome preparations.
Cell Proliferation Assays
Cell proliferation assays measure the increase in cell number, a critical parameter in wound healing where tissue regeneration requires new cell generation. Flow cytometry-based methods have emerged as powerful tools for multiparametric analysis of proliferation, simultaneously assessing cell cycle dynamics, apoptosis, and mitochondrial function [58]. These integrated protocols typically utilize stains such as BrdU/PI for cell cycle analysis, CellTrace Violet or CFSE for tracking cell divisions across generations, and Ki-67 as a marker of active cell cycle phases [58] [59].
The optimization of these assays is particularly important when working with precious samples, such as those from pediatric populations or limited primary cell cultures. Studies have demonstrated that CFSE concentrations of 2.5 μM at cell densities of 1×10⁶ cells/mL yield optimal results for tracking lymphocyte proliferation, while Ki-67 expression remains stable between 69-96 hours post-stimulation, providing flexibility in processing time [59]. These standardized approaches ensure that proliferation data are comparable across different experimental setups and sample types, enabling valid comparisons between the effects of human and animal-derived MSC exosomes on target cell proliferation.
Tube Formation Assays
The Endothelial Tube Formation Assay (ETFA) is the gold standard for assessing angiogenic potential in vitro—a critical process in wound healing where new blood vessel formation supports tissue regeneration. In this assay, endothelial cells are seeded on a basement membrane extract (such as Matrigel or Cultrex) and form capillary-like tubular structures within hours [60] [61]. The resulting networks can be analyzed for parameters including tube area, tube length, tube number, loop area, loop number, and sprout count [60].
An alternative approach, the Fibrin Bead Assay (FBA), uses Cytodex microspheres coated with endothelial cells embedded in a fibrin matrix, promoting the growth of 3D capillary-like structures suitable for high-throughput screening [61]. This method more closely mimics the sprouting angiogenesis observed in vivo and allows for the study of later stages of vascular development. For both methods, the Angiogenesis Analyzer for ImageJ provides comprehensive, automated analysis capabilities, enabling robust quantification of complex tubular networks without requiring expensive proprietary software [61].
Table 1: Key Parameters in Tube Formation Assays
| Parameter | Biological Significance | Assay Type |
|---|---|---|
| Tube length | Total extent of vascular structures formed | ETFA, FBA |
| Number of nodes | Branching points in the network | ETFA |
| Number of meshes | Complexity and connectivity of the network | ETFA |
| Number of sprouts | Initiation of new vascular structures | FBA |
| Sprout length | Extension capacity of new vessels | FBA |
Quantitative Comparison of MSC-Exosome Performance
Efficacy Across Preclinical Models
Recent umbrella reviews synthesizing data from 47 meta-analyses across 27 disease categories have demonstrated the robust therapeutic potential of MSC-EVs in diverse preclinical models [62]. These analyses reveal that MSC-EVs significantly improve functional scores, reduce inflammation, and promote tissue regeneration across neurological, renal, wound healing, liver, musculoskeletal, respiratory, and reproductive disorders. The quantitative synthesis shows particularly promising results for bone marrow-, adipose-, and umbilical cord-derived EVs, with modified EVs exhibiting enhanced therapeutic outcomes [62].
In direct comparative studies, such as those evaluating psoriasis models, both human placenta MSC (hPMSC) and human umbilical cord MSC (hUCMSC) exosomes showed significant effectiveness in reducing pathological features including epidermal thickness and pro-inflammatory cytokines [7]. Meta-regression analyses across multiple studies have suggested potentially greater improvement in clinical scores with hUCMSC exosomes compared to other sources, though both demonstrated significant efficacy [7]. These findings highlight the importance of source selection when designing MSC-exosome therapies for specific applications.
Analytical Considerations for Comparative Studies
When comparing human versus animal-source MSC exosomes, methodological standardization becomes critical for valid interpretation. The high heterogeneity observed in many meta-analyses (I² > 70%) underscores the impact of technical variables on experimental outcomes [62]. Key factors requiring standardization include EV isolation methods, characterization approaches, dosing regimens, and functional assay conditions.
For tube formation assays, the choice of extracellular matrix significantly influences results, with Matrigel and similar basement membrane extracts providing the necessary support for capillary-like structure formation [60]. Similarly, the selection of appropriate endothelial cell types is crucial, as endothelial cells exhibit significant heterogeneity; while HUVECs remain widely used, organ-specific endothelial cells may provide more physiologically relevant data for specific applications [60] [57]. The developmental stage of tube structures also impacts readings, as HUVECs typically form tubes within 2-4 hours but may begin to detach after 24 hours due to apoptosis [60].
Table 2: Comparison of MSC-Exosome Performance in Functional Assays
| Exosome Source | Proliferation Enhancement | Migration Stimulation | Angiogenic Capacity | Key Evidence |
|---|---|---|---|---|
| Human Umbilical Cord | Moderate to Strong | Strong | Strong | Meta-analysis of psoriasis models [7] |
| Human Placenta | Moderate | Moderate | Moderate | Comparative murine study [7] |
| Bone Marrow | Strong | Strong | Strong | Umbrella review of preclinical models [62] |
| Adipose Tissue | Strong | Moderate | Strong | Umbrella review of preclinical models [62] |
Experimental Protocols for Key Assays
Gap Closure Migration Assay Protocol
The gap closure assay provides a straightforward method to evaluate collective cell migration, particularly relevant to wound healing applications. The following protocol adapts methodologies from recent studies for assessing endothelial and immune cell migration:
Cell Seeding: Place a 2-well silicone insert (e.g., Ibidi #81176) in a culture dish, creating a defined cell-free gap when removed. Seed 5×10⁴ cells per insert in appropriate growth medium and culture overnight to form a confluent monolayer [57].
Starvation (Optional): For synchronization and to remove the influence of serum factors, starve cells for 18 hours in low-serum medium (1% FBS) before creating the gap [57].
Gap Creation: Gently remove the silicone insert using sterile tweezers, creating a uniform cell-free gap. Wash once with PBS to remove non-adherent cells [57].
Experimental Treatment: Add test conditions—such as MSC-exosome preparations from different sources—in appropriate medium. Include positive controls (e.g., growth factors) and negative controls (e.g., migration inhibitors) [57].
Image Acquisition: Capture images at consistent positions immediately after gap creation (0 hour) and at regular intervals (e.g., every 4-8 hours) until closure. Maintain constant environmental conditions (37°C, 5% CO₂) during imaging [56].
Analysis: Quantify the remaining cell-free area using ImageJ or specialized software. Calculate migration rate as percentage closure over time [56].
Tube Formation Assay Protocol
The Endothelial Tube Formation Assay evaluates angiogenic potential, a key mechanism in wound healing. This protocol utilizes the µ-Slide 15 Well 3D to minimize reagent use and improve reproducibility:
Matrix Preparation: Pipette 10 µl of growth factor-reduced Matrigel into each well of the µ-Slide, avoiding bubble formation. Incubate for 30-60 minutes at 37°C to allow polymerization [60].
Cell Preparation: Trypsinize and resuspend endothelial cells (e.g., HUVECs) in appropriate medium at 5,000-10,000 cells per well in 50 µl volume. Low-passage cells (passage 2-6) yield most consistent results [60].
Cell Seeding: Carefully seed cell suspension onto the polymerized matrix. Allow cells to settle for 15-30 minutes before gentle media addition to avoid displacement [60].
Treatment Application: Add experimental treatments—such as human versus animal-source MSC exosomes—in triplicate wells. Include positive control (e.g., VEGF) and negative control (e.g., tube formation inhibitor) [60].
Live Cell Imaging: Place the slide in a stage-top incubator maintaining 37°C and 5% CO₂. Acquire images every 5-15 minutes for up to 24 hours using phase contrast or fluorescence microscopy with 5× or 10× objectives [60].
Analysis: Use the Angiogenesis Analyzer for ImageJ to automatically quantify key parameters including tube area, tube length, number of nodes, and number of meshes [61].
Flow Cytometry-Based Proliferation Assay Protocol
Multiparametric flow cytometry enables comprehensive analysis of proliferation alongside other cellular parameters. This integrated protocol allows assessment of up to eight different parameters from a single sample:
Cell Staining: Label cells with CellTrace Violet (2.5 µM) or CFSE by incubating for 10 minutes at room temperature in PBS with 1% FBS. Quench with complete medium and wash twice [58] [59].
Stimulation and Culture: Seed stained cells at optimal density (1×10⁶ cells/mL) and stimulate with appropriate mitogen (e.g., PHA for lymphocytes) or growth factors. Culture for 3-6 days depending on cell type [59].
BrdU Incorporation (Optional): For cell cycle analysis, add BrdU during the last 4-24 hours of culture to label cells in S-phase [58].
Harvest and Stain: Harvest cells and stain with viability dye (e.g., FVS700). Perform surface staining for cell identification (e.g., CD3 for T-cells), then fix and permeabilize cells [59].
Intracellular Staining: For Ki-67 detection, incubate with anti-Ki-67 antibody (optimal concentration 2.5 µL/test). For BrdU detection, digest DNA with DNase before anti-BrdU antibody staining [58] [59].
Data Acquisition and Analysis: Acquire data on flow cytometer, analyzing at least 10,000 events per sample. Use proliferation platforms in flow cytometry software to quantify division index, generation number, and percentage of proliferating cells [58].
Signaling Pathways in MSC-Exosome Mediated Effects
The therapeutic effects of MSC-exosomes on cellular functions are mediated through complex signaling pathways that modulate key cellular processes. The following diagram illustrates the primary signaling mechanisms through which MSC-exosomes influence cell migration, proliferation, and tube formation:
The diagram above illustrates how MSC-exosomes activate multiple interconnected signaling pathways to promote functional changes in target cells. The IGF signaling axis plays a particularly important role, with IGF-2 and its variants (such as Des(1-6)IGF-2) promoting endothelial cell migration and tube formation through upregulation of angiogenic proteins including IL-6, uPAR, and MCP-1 [63]. These effects are mediated primarily through IGF receptor 1 and insulin receptor activation, triggering downstream PI3K-Akt and RAS/MAPK pathways that collectively enhance cell survival, proliferation, and motility [63] [57].
Simultaneously, MSC-exosomes deliver angiocrine factors such as VEGFA, PDGF-AA, and PDGF-C that further activate these pathways and promote actin cytoskeleton reorganization and focal adhesion formation, essential for cell migration and capillary morphogenesis [57]. The convergence of these signaling cascades on fundamental cellular processes explains the potent effects of MSC-exosomes on tissue regeneration, with different exosome sources potentially activating these pathways with varying efficacy.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Functional Assays in MSC-Exosome Research
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Extracellular Matrices | Matrigel, Cultrex, Collagen gels, Fibrin matrix | Provide 3D substrate for tube formation assays; influence cellular differentiation and organization [60] [61] |
| Cell Tracking Dyes | CFSE, CellTrace Violet, BrdU, EdU | Label cells for proliferation tracking; diluted with each division enabling generation analysis [58] [59] |
| Viability & Apoptosis Assays | Annexin V/PI, FVS700, JC-1 | Distinguish live, apoptotic, and necrotic populations; assess mitochondrial function [58] |
| Angiogenesis Assay Systems | µ-Slide 15 Well 3D, µ-Plate 96 Well 3D, Cytodex microspheres | Specialized platforms for standardized tube formation assays; enable high-throughput screening [60] [61] |
| Analysis Software | Angiogenesis Analyzer (ImageJ), MigraR, CellTracksColab | Open-source tools for quantitative analysis of migration and tube formation parameters [56] [61] |
| Cytokines & Growth Factors | VEGF, FGF-2, PDGF-AA, PDGF-C, IGF-2 | Positive controls for migration, proliferation, and tube formation assays; study specific pathway activation [63] [57] |
Functional assays for cell migration, proliferation, and tube formation provide indispensable tools for quantitatively comparing the therapeutic potential of different MSC-exosome sources in preclinical wound healing research. The integration of standardized protocols with appropriate analytical tools enables robust, reproducible assessment of key biological activities, guiding the selection of optimal exosome sources for specific therapeutic applications. As the field advances, continued refinement of these assays—including improved standardization, integration of advanced imaging technologies, and development of more complex 3D models—will further enhance their predictive value for clinical translation. For research teams comparing human versus animal-source MSC exosomes, the strategic implementation of these functional assays provides the critical evidence needed to advance the most promising candidates through the therapeutic development pipeline.
Overcoming Challenges in Comparative Exosome Research
The translation of mesenchymal stem cell (MSC)-derived exosomes from promising preclinical results to reliable clinical therapeutics faces two significant interconnected hurdles: batch-to-batch variability and efficient production scaling. For researchers selecting between human and animal-source MSCs in preclinical wound healing studies, understanding these challenges is paramount to designing reproducible, clinically relevant experiments. Exosomes, as key mediators of MSC paracrine effects, offer potential solutions to cell therapy limitations, including immunogenicity, tumorigenic potential, and infusion toxicity [22]. However, traditional exosome manufacturing methods struggle with low yields and consistency—a single liter of culture medium typically yields less than 1 microgram of exosomal protein, creating substantial scalability challenges [22]. This comparison guide examines how production methodologies influence exosome characteristics and functional outcomes in preclinical wound models, providing researchers with experimental data and protocols to inform therapeutic development decisions.
Quantitative Comparison: Human vs. Animal-Source MSC Exosomes in Preclinical Wound Models
Table 1: Therapeutic Efficacy of MSC-Exosomes from Different Sources in Preclinical Wound Models
| MSC Source | Wound Closure Rate (Standardized Mean Difference) | Blood Vessel Density (SMD) | Collagen Deposition | Key Advantages |
|---|---|---|---|---|
| Human Adipose (ADSC) | 1.42 (1.14-1.71) [26] | 1.59 (1.01-2.18) [26] | Significant improvement [26] | Best effect on wound closure and collagen deposition [5] |
| Human Umbilical Cord | Moderate improvement [64] [5] | Moderate improvement [5] | Moderate improvement [5] | Low immunogenicity, clinical relevance [64] |
| Human Bone Marrow | Moderate improvement [24] [5] | Superior revascularization [5] | Moderate improvement [5] | Best effect on revascularization [5] |
| Animal Sources (Various) | Variable efficacy [24] | Variable efficacy [24] | Variable efficacy [24] | Lower translational relevance, species-specific effects |
Table 2: Production Challenges and Solutions for MSC-Exosome Manufacturing
| Production Aspect | Traditional Methods (e.g., Ultracentrifugation) | Advanced Platforms (e.g., FACTORY, Perfusion) |
|---|---|---|
| Batch-to-Batch Variability | High (72% of studies use ultracentrifugation) [24] | Significantly reduced through automation [65] |
| Processing Capacity | Limited (max ~1.7L per run) [65] | Scalable (up to 10L per run) [65] |
| Yield | Low (<1μg exosomal protein/mL medium) [22] | 3-fold increase in space-time yield [66] |
| Labor Intensity | High (manual operation) [65] | Fully automated systems [65] |
| Quality Control | Operator-dependent [65] | Standardized, reproducible [65] |
Root Causes of Batch-to-Batch Variability
Batch-to-batch variability in MSC-exosome production stems from multiple sources throughout the manufacturing pipeline. The biological heterogeneity of source cells responds differently to environmental cues, significantly impacting exosome cargo and yield [24] [67]. Current isolation methods—primarily ultracentrifugation (72%) and precipitation methods (23%)—rely heavily on manual operation, introducing substantial operator-dependent variability [24]. Furthermore, inconsistent culture conditions including nutrient fluctuations, varying cell densities, and metabolic shifts dramatically alter exosome production profiles [66]. Even minor deviations in purification parameters such as centrifugal forces, filtration pressures, or buffer compositions can significantly impact final exosome populations and functionality [67]. These technical challenges are compounded when comparing human versus animal-derived exosomes, as species-specific biological differences introduce additional variables that complicate cross-study comparisons and clinical forecasting [24].
Emerging Solutions for Scalable, Consistent Production
Advanced Bioreactor Systems
Transitioning from traditional 2D culture to perfusion bioreactors represents a paradigm shift in exosome manufacturing. Research demonstrates that perfusion cultures increase space-time yields of target EV subpopulations by threefold compared to batch cultures [66]. These systems maintain cells at constant densities and metabolic states through continuous medium exchange, enabling consistent production of specific EV subpopulations with stable quality attributes for extended periods (up to 13 days demonstrated) [66]. The FACTORY platform exemplifies this approach, integrating continuous flow centrifugation with tangential flow filtration (TFF) in a fully automated system capable of processing up to 10 liters of cell culture supernatant per run while maintaining sterility and minimal endotoxin contamination [65].
Process Automation and Standardization
Automation addresses critical variability introduced by manual operations. The FACTORY platform demonstrates how fully automated collection technology standardizes exosome isolation, effectively eliminating batch variation caused by differences in operator skill levels [65]. This system programs specific cleaning and disinfection procedures that address sterility challenges while ensuring consistent product quality. Compared to traditional ultracentrifugation, automated platforms show significantly superior yields, higher efficiency, and better reproducibility while maintaining similar protein profiles and biological activity in wound healing models [65].
Process Analytical Technologies
Implementing bead-based flow cytometry for direct quantification of specific EV subpopulations (e.g., CD81+, CD81+/CD63+) directly in culture medium enables real-time process monitoring and control [66]. This approach allows researchers to track production of target therapeutic vesicles without extensive purification steps, facilitating rapid process optimization. Combined with nanoparticle tracking analysis and microfluidic diffusion sizing, these analytical tools provide comprehensive characterization of EV populations throughout the manufacturing process, enabling quality-by-design approaches to exosome production [66].
Experimental Protocols for Variability Assessment
Protocol: Batch Consistency Evaluation in MSC-Exosome Production
Purpose: To quantitatively assess batch-to-batch variability in MSC-exosome preparations intended for preclinical wound healing studies.
Materials:
- MSC culture supernatant (human or animal source)
- FACTORY platform or alternative isolation system [65]
- Bead-based flow cytometry setup with CD63/CD81/CD9 antibodies [66]
- Nanoparticle tracking analyzer (e.g., Malvern Panalytical) [64]
- Western blot equipment for tetraspanin detection (CD9, CD63, CD81) [68]
- BCA protein assay kit [64]
- Endotoxin detection kit [65]
Procedure:
- Culture MSCs under standardized conditions (hypoxia, serum-free media) for consistent exosome production [64]
- Isolate exosomes using automated FACTORY platform or manual ultracentrifugation (100,000×g, 70 min) [64] [65]
- Characterize particle size distribution via nanoparticle tracking analysis [64]
- Quantify specific subpopulations using bead-based flow cytometry with anti-CD81 and anti-CD63 magnetic particles [66]
- Confirm exosome identity through Western blot for CD9, CD63, CD81, and TSG101 [68]
- Determine protein content using BCA assay and calculate particles per protein ratio [68]
- Test for endotoxin contamination using LAL assay [65]
- Repeat process for at least three separate batches cultured and processed independently
Validation: Compare coefficient of variation (%CV) for key parameters (yield, potency markers) between batches, with <15% CV indicating acceptable consistency [66].
Protocol: Functional Potency Assessment in Wound Healing Models
Purpose: To evaluate functional consistency of MSC-exosome batches using standardized wound healing assays.
Materials:
- 8-week-old C57BL/6 mice [64]
- Exosome samples from different production batches
- Full-thickness excisional wound model equipment [5]
- Streptozotocin (for diabetic models) [5]
- Histology equipment for H&E, Masson's trichrome staining
- Immunohistochemistry setup for CD31 (vascular density)
Procedure:
- Create full-thickness excisional wounds on mouse dorsum [5]
- Administer exosomes via subcutaneous injection around wound margins [5]
- Measure wound closure rate daily using digital planimetry
- Harvest tissue at day 7-14 for histological analysis
- Quantify scar width from H&E stained sections
- Assess blood vessel density via CD31 immunohistochemistry [26]
- Evaluate collagen deposition and organization via Masson's trichrome staining [26]
- Compare results across batches and against positive/negative controls
Validation: Functionally potent exosome batches should demonstrate ≥30% improvement in wound closure rates compared to controls in standardized models [26].
Signaling Pathways in Exosome-Mediated Wound Healing
Diagram 1: Exosome-Mediated Wound Healing Mechanisms. MSC-exosomes interact with multiple recipient cell types, activating molecular mechanisms that collectively promote functional wound repair outcomes.
Production Workflow Comparison: Traditional vs. Advanced Methods
Diagram 2: Production Workflow Comparison. Automated systems integrate continuous processing with rigorous quality control to minimize variability while maximizing yield compared to traditional manual methods.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for Standardized MSC-Exosome Production
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cell Culture Systems | 3D hypoxia bioreactors with microcarriers [64] | Scalable MSC expansion with controlled oxygen tension | Enhances exosome yield while maintaining cell viability |
| Isolation Technologies | FACTORY platform, Tangential Flow Filtration [65] | Large-scale EV isolation with automation | Processes up to 10L supernatant per run with high consistency |
| Characterization Antibodies | CD9, CD63, CD81, TSG101, HSP70 [64] [68] | Exosome identification and quantification | Confirm exosome identity per MISEV guidelines |
| Analytical Instruments | Nanoparticle Tracking Analysis [64], Bead-based flow cytometry [66] | Particle quantification and subpopulation analysis | Enables specific EV subpopulation tracking |
| Quality Control Assays | BCA protein assay [64], Endotoxin detection [65] | Purity and safety assessment | Critical for preclinical safety profiling |
| Animal Models | C57BL/6 mice, diabetic db/db mice [5] | In vivo wound healing efficacy testing | Standardized models enable cross-study comparisons |
The convergence of advanced bioreactor technologies, automated purification platforms, and robust analytical methods is steadily overcoming the critical standardization hurdles in MSC-exosome production. For researchers navigating the choice between human and animal-source exosomes for preclinical wound models, the evidence indicates that human MSC sources, particularly adipose-derived, demonstrate superior efficacy in key wound healing parameters while offering more direct clinical translation potential. The implementation of standardized protocols like those detailed in this guide, coupled with emerging technologies such as the FACTORY platform, enables more consistent production of therapeutically potent exosomes. As the field progresses, harmonization of isolation methods, characterization standards, and potency assays will be essential to fully resolve batch-to-batch variability challenges and unlock the clinical potential of MSC-exosome therapies for wound repair and regeneration.
In the rapidly advancing field of regenerative medicine, mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as promising cell-free therapeutic agents for wound healing and other applications. However, their translational potential is significantly challenged by donor variability - the inherent biological differences between the individuals from whom the originating MSCs are sourced. This variability, stemming from factors such as age, health status, and tissue source, introduces substantial heterogeneity in the biological properties and therapeutic efficacy of the resulting exosomes [69] [70]. For researchers working within the context of human versus animal source MSC exosomes in preclinical wound models, understanding and controlling for these variables is paramount for generating reproducible, reliable data and developing consistent therapeutic products.
The biological composition of MSC-exosomes directly reflects the physiological state of their parental cells, meaning that donor-specific factors become embedded in the exosomal cargo, including proteins, lipids, and various nucleic acids [22]. This review comprehensively examines the current experimental evidence quantifying the impact of donor variability, providing structured comparisons and methodological guidance to aid researchers in designing robust preclinical studies.
Quantitative Impact of Tissue Source on Exosome Therapeutic Potential
The anatomical origin of MSCs is a primary determinant of their exosomes' functional characteristics. Different tissue sources confer distinct biological signatures that significantly influence therapeutic outcomes in wound healing applications.
Table 1: Impact of MSC Tissue Source on Exosome Characteristics and Wound Healing Efficacy
| Tissue Source | Proliferation Rate | Key Secretome Components | Demonstrated Therapeutic Effects in Wound Healing | Meta-Analysis Efficacy Data (vs. Controls) |
|---|---|---|---|---|
| Adipose Tissue (ADSC) | Lower than DPSCs [69] | miRNAs regulating cell cycle and proliferation [69]; Pro-angiogenic factors [13] | Promotes angiogenesis, fibroblast proliferation, collagen deposition, reduces scar size [13] [5] | Best effect on wound closure rate and collagen deposition among easy-access sources [5] |
| Dental Pulp (DPSC) | Higher than ADSCs; consistently smaller, Nestin-positive [69] | miRNAs involved in oxidative stress and apoptosis pathways [69] | Not specifically reported for wounds in search results | Not available |
| Bone Marrow (BM-MSC) | Varies with culture medium; population doubling time extends with passage [27] | Growth factors (VEGF), immunomodulatory cytokines (IL-6, TGF-β) [27] | Neuroprotection, modulation of oxidative stress [27] | Best effect in revascularization among easy-access sources [5] |
| Umbilical Cord (WJ-MSC) | Not specified | Varies with source; can promote cancer cell senescence but also migration [71] | Studied for psoriasis; reduces epidermal thickness, clinical severity scores [7] | Greater improvement in clinical scores in psoriasis vs. other sources [7] |
The choice between human and animal sources introduces another layer of complexity. Human-derived MSC-exosomes are the predominant choice for clinical translation, with 69.9% of preclinical studies using them [5]. However, animal-derived exosomes (from mice, rats, canines) are crucial for preclinical modeling, though their comparability to human exosomes requires careful validation [5].
Influence of Donor Age and Health Status
Donor age and physiological condition introduce significant variability that can alter the therapeutic profile of MSC-exosomes, impacting their molecular cargo and functional capabilities.
Impact of Donor Age
The age of the donor directly influences the proliferative capacity and secretome of MSCs. A comparative study using MSCs from different aged donors highlights this phenomenon: MSCs from younger donors (18-20 years old) demonstrated a higher proliferation rate compared to those from older donors (45-60 years old) [69]. This age-related decline in cellular fitness is mirrored in the exosomes they produce, potentially affecting their regenerative potential. Furthermore, as MSCs are passaged in culture—a process that mimics cellular aging—their biological activity diminishes. Studies show that increasing cell passage number leads to longer population doubling times and reduced proliferative potential of their exosomes [70] [27].
Impact of Donor Health Status
The health status of the donor is a critical factor often reflected in the functionality of MSC-exosomes. MSCs derived from individuals with comorbidities such as diabetes, high blood pressure, or other diseases can exhibit altered secretome profiles, a phenomenon sometimes called a "disease signature" [70]. These disease-specific alterations can be transferred to the exosomes, potentially compromising their therapeutic quality. This is particularly relevant for wound healing research, where the target condition (e.g., diabetic foot ulcers) may be directly linked to the donor's health status. Consequently, the health of the source animal in preclinical models is equally critical for ensuring the translational relevance of the findings [5].
Experimental Workflows for Characterizing Donor Variability
A standardized experimental approach is essential for systematically evaluating the impact of donor variability. The workflow below outlines the key steps from cell isolation through functional analysis.
Core Experimental Protocol
dot Source: Experimental Workflow for Assessing Donor Variability
Diagram 1: A comprehensive experimental workflow for assessing how donor age, health, and tissue source affect MSC-exosome properties and therapeutic efficacy in wound healing.
Detailed Methodologies
Cell Isolation and Culture: MSCs can be isolated from tissues via enzymatic digestion (e.g., collagenase for adipose tissue) or mechanical fragmentation (explant method) [69]. Culture conditions significantly impact outcomes; for instance, Bone Marrow-MSCs (BM-MSCs) cultured in α-MEM showed a higher expansion ratio than those in DMEM, though particle yields of their sEVs were not significantly different [27].
Exosome Isolation and Characterization: Ultracentrifugation is the classical isolation method, but Tangential Flow Filtration (TFF) demonstrates significantly higher particle yields [27]. Characterization must adhere to MISEV guidelines, employing Nanoparticle Tracking Analysis (NTA) for size/concentration, Transmission Electron Microscopy (TEM) for morphology, and Western Blot for markers (e.g., CD9, CD63, TSG101) [7] [27]. Calnexin should be absent to confirm purity [7].
Functional Potency Assays: In vitro, MSC-exosomes are tested for their ability to enhance cell proliferation (e.g., in ARPE-19 cells under oxidative stress) and reduce apoptosis [27]. In vivo, wound closure rates, scar width, blood vessel density, and collagen deposition are key metrics, often analyzed against controls in diabetic or non-diabetic animal models [5].
Signaling Pathways and Functional Mechanisms
The therapeutic effects of MSC-exosomes are mediated by their cargo, which modulates key signaling pathways in recipient cells. The specific cargo, and thus the pathways affected, is heavily influenced by donor variables.
dot Source: Key Signaling Pathways Modulated by MSC-Exosomes
Diagram 2: Donor variability influences the molecular cargo of MSC-exosomes, which in turn modulates key cellular signaling pathways in wounded tissue, leading to different functional outcomes.
For instance, exosomes from ADSCs are enriched with miRNAs that regulate cell cycle and proliferation (e.g., miR-21), while those from DPSCs carry miRNAs involved in oxidative stress and apoptosis pathways [69]. These specific miRNA profiles directly determine which signaling pathways are activated or suppressed in the recipient cells at the wound site. Furthermore, modified ADSC-exosomes, enriched for specific non-coding RNAs, demonstrate enhanced therapeutic effects, highlighting the potential for engineering exosomes to optimize their function [13].
The Scientist's Toolkit: Essential Reagents and Solutions
To ensure reproducible and reliable research on donor variability, specific reagents and tools are essential. The following table details key solutions required for the experimental workflows described in this guide.
Table 2: Essential Research Reagent Solutions for MSC-Exosome Studies
| Reagent / Solution | Function / Application | Examples / Key Specifications |
|---|---|---|
| Cell Culture Media | Expansion and maintenance of MSCs from different tissues. | α-MEM or DMEM, supplemented with 10% Human Platelet Lysate (hPL) or FBS [27]. |
| Isolation Kits & Reagents | Separation of exosomes from conditioned culture medium. | Ultracentrifugation equipment; Tangential Flow Filtration (TFF) systems; Polymer-based precipitation kits [27]. |
| Characterization Antibodies | Identification of MSC and exosome markers via flow cytometry/Western blot. | Anti-CD73, CD90, CD105 (MSC markers); Anti-CD9, CD63, TSG101 (exosome markers); Anti-Calnexin (purity control) [7] [27]. |
| In Vivo Wound Model Kits | Creating standardized wounds in preclinical models. | Imiquimod (IMQ) cream for psoriasis models [7]; Streptozotocin (STZ) for inducing diabetic wound models [5]. |
| Analysis Kits | Quantifying functional outcomes and exosome effects. | Nanoparticle Tracking Analysis (NTA) for size/concentration; ELISA for cytokine/growth factor levels; Histology stains for collagen/scarring [7] [5]. |
The evidence is unequivocal: donor age, health status, and tissue source are intrinsic biological variables that fundamentally shape the therapeutic profile of MSC-exosomes. For the researcher navigating the complexities of human versus animal MSC-exosomes in preclinical wound models, this reality demands rigorous experimental design.
Key recommendations for future research include:
- Strategic Source Selection: Prioritize MSC sources with proven efficacy for specific wound healing goals (e.g., ADSCs for wound closure and collagen deposition) while clearly justifying the choice of human or animal sources [5].
- Comprehensive Donor Profiling: Meticulously document and report donor metadata, including age, sex, and health status, for both human and animal sources to enable cross-study comparisons [69] [70].
- Standardized Characterization: Adhere to ISCT guidelines for MSC characterization and MISEV guidelines for exosome analysis to ensure product consistency and data reliability [5] [46].
- Potency-Based Screening: Implement functional potency assays early in the development pipeline to screen for donor-related variations that impact biological activity [46].
Addressing the challenge of donor variability is not merely a technical obstacle but a fundamental prerequisite for the successful clinical translation of MSC-exosome therapies. By systematically accounting for these factors, the scientific community can advance the development of more consistent, effective, and reliable cell-free treatments for wound healing and beyond.
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-exosomes) represents a paradigm shift in regenerative medicine, particularly for complex wound healing scenarios. These natural nanovesicles mediate intercellular communication by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating inflammation, promoting angiogenesis, and stimulating tissue regeneration [72]. However, native exosomes face significant clinical translation challenges, including rapid clearance, limited target specificity, and variable therapeutic potency depending on their cellular origin [72]. The emerging field of exosome engineering seeks to overcome these limitations through precise structural and functional modifications, creating enhanced therapeutic vesicles with customized properties.
Within preclinical wound healing research, a critical comparative framework exists between exosomes derived from human versus animal sources. This distinction influences not only biological activity but also scalability and clinical relevance. Human umbilical cord MSC-exosomes (hUCMSC-Exos) demonstrate superior angiogenic potential and immunomodulatory capacity compared to other sources, while canine adipose-derived MSC-exosomes (cAD-MSC-exosomes) offer a valuable translational model for veterinary applications and comparative medicine [17] [73]. Engineering strategies applied to both human and animal exosomes have demonstrated remarkable potential to augment their native capabilities, creating next-generation therapeutics with enhanced precision and potency for skin regeneration and wound repair.
Comparative Efficacy: Human vs. Animal MSC Exosomes in Preclinical Wound Models
The therapeutic potential of MSC-exosomes varies significantly based on their cellular origin and species. The table below summarizes key comparative findings from preclinical studies evaluating both human and animal-derived exosomes in wound healing applications.
Table 1: Comparative Efficacy of Human vs. Animal MSC Exosomes in Preclinical Wound Models
| Exosome Source | Key Therapeutic Findings | Experimental Models | References |
|---|---|---|---|
| Human Umbilical Cord MSC (hUCMSC) | Significantly accelerates wound closure; promotes proliferation/migration of HSFs and HUVECs; enhances tube formation; reduces inflammation; stimulates angiogenesis and ECM formation. | In vitro: Human skin fibroblasts (HSFs), Human umbilical vein endothelial cells (HUVECs). In vivo: Mouse skin wound models. | [17] |
| Canine Adipose-Derived MSC (cAD-MSC) | Enhances fibroblast migration, proliferation, and wound healing-related gene expression in vitro. Increased yield and bioactivity with 3D upscaling protocol (VSCBIC-3-3D). | In vitro: Canine fibroblast assays. Production: 3D microcarrier-based culture system. | [73] |
| Human Placenta MSC (hPMSC) | Reduces epidermal thickness and skin tissue cytokines in psoriasis model. Comparable efficacy to hUCMSC-exosomes in direct comparison. | In vivo: Imiquimod (IMQ)-induced psoriasis murine model. | [7] |
| Human Bone Marrow MSC (hBMSC) | Promotes wound healing by inhibiting TGF-β/Smad pathway, reducing TGF-β1, increasing TGF-β3, and decreasing scarring. | Preclinical wound models (literature synthesis). | [17] |
| Human Adipose-Derived MSC (hADSC) | Promotes cell proliferation/migration in early healing; increases collagen I/III synthesis; inhibits scar growth in late healing. | Preclinical wound models (literature synthesis). | [17] |
Quantitative data reveals that hUCMSC-exosomes consistently demonstrate superior performance in key wound healing parameters. Meta-analytical synthesis indicates that hUCMSC-exosomes show a greater improvement in clinical scores compared to other MSC sources, attributed to their higher content of pro-regenerative miRNAs and proteins [7]. In contrast, cAD-MSC-exosomes provide a robust model for veterinary therapeutic development, with optimized production protocols yielding 2.4-fold increased exosome quantity and 3.2-fold increased concentration in conditioned medium compared to conventional 2D cultures [73].
Engineering Strategies: Methodologies and Experimental Protocols
Surface Modification Techniques
Surface engineering enhances exosome stability, targeting precision, and retention at wound sites. Primary methodologies include:
- Genetic Engineering of Parent Cells: Plasmid vectors containing targeting ligands (e.g., RGD peptides for integrin binding) are transfected into parent MSCs using electroporation or viral vectors. Modified MSCs are then cultured, and their exosomes harvested, inheriting the engineered membrane proteins [72].
- Direct Exosome Surface Modification: Isolated exosomes are chemically modified via click chemistry or hydrophobic insertion. For instance, CP05 peptide anchors can be used to conjugate cyclo(Arg-Gly-Asp-D-Phe-Lys) peptides to enhance binding to angiogenic endothelial cells in wound beds [72].
- Hybrid Exosome Construction: Exosomes are fused with synthetic liposomes bearing specific targeting molecules through freeze-thaw cycles or extrusion, creating hybrid vesicles with enhanced functionality [72].
Cargo Loading Strategies
Therapeutic cargo loading amplifies the innate regenerative capabilities of exosomes. Standard protocols include:
- Preloading via Parent Cell Engineering: MSCs are transfected to overexpress specific therapeutic miRNAs (e.g., miR-21-5p for angiogenesis or miR-29a for collagen regulation). Exosomes secreted by these preconditioned cells are naturally loaded with the desired nucleic acids [17] [74].
- Active Loading into Isolated Exosomes: Purified exosomes are mixed with synthetic drugs or RNAs, followed by electroporation or sonication to transiently disrupt the lipid bilayer and facilitate cargo entry. For instance, loading of sphingosine-1-phosphate agonist has been shown to enhance angiogenic potential [72].
- Upscaling Production for Enhanced Yield: The VSCBIC-3-3D protocol combines 3D bioreactor cultures with in-house serum-free medium (VSCBIC-3) and Tangential Flow Filtration (TFF) for isolation, significantly increasing functional exosome yield compared to conventional 2D systems [73].
Comparative Performance Data of Engineered Exosomes
The therapeutic impact of various engineering strategies is quantified through standardized wound healing parameters. The following table synthesizes key experimental findings from preclinical studies.
Table 2: Quantitative Performance of Engineered MSC Exosomes in Preclinical Models
| Engineering Strategy / Exosome Type | Key Performance Metrics | Experimental System | Outcome vs. Control / Other Sources |
|---|---|---|---|
| hUCMSC-Exos (Angiogenic Potential) | Promotes HUVEC proliferation and tube formation. | In vitro: HUVEC culture. | Significant enhancement of tubulogenesis. Bioinformatics suggests regulation via ULK2, COL19A1, IL6ST molecules [17]. |
| cAD-MSC-Exos (3D Upscaled Production) | Fibroblast migration and proliferation. | In vitro: Canine fibroblast scratch assay. | Significant improvement in fibroblast migration and proliferation; Upregulation of wound healing genes (e.g., COL1A1, COL3A1) [73]. |
| Bioengineered MSC-Exos in Hydrogel | Wound closure rate, retention, anti-inflammatory effect. | In vivo: Chronic wound mouse model. | Sustained release and improved retention; superior wound closure rate and reduced inflammation vs. non-formulated exosomes [72]. |
| hUCMSC-Exos (Psoriasis Model) | Epidermal thickness, PASI score, inflammatory cytokines (TNF-α, IL-17A). | In vivo: IMQ-induced psoriasis murine model. | Significant reduction in epidermal thickness and clinical severity scores; Lower TNF-α mRNA and IL-17A protein [7]. |
| hUCMSC-Exos (vs. hPMSC-Exos) | Epidermal thickness, skin tissue cytokines. | In vivo: IMQ-induced psoriasis murine model; Meta-analysis. | Both exosome types effective vs. control; No significant difference found between hUCMSC- and hPMSC-exosomes in direct comparison [7]. |
The data demonstrates that both human and animal-derived exosomes respond favorably to engineering approaches, with modified exosomes consistently outperforming their native counterparts. Bioengineered hUCMSC-exosomes exhibit particularly strong angiogenic potential, while upscaled production of cAD-MSC-exosomes demonstrates that yield and quality enhancements directly translate to improved biological function in vitro [73] [17]. Furthermore, incorporation into hydrogels creates a sustained-release system that addresses the critical challenge of rapid exosome clearance from wound sites, significantly extending therapeutic activity [72].
Signaling Pathways and Molecular Mechanisms
Engineered exosomes accelerate wound healing by modulating critical signaling pathways involved in inflammation, angiogenesis, and tissue remodeling. The core mechanism involves the delivery of exosomal cargo (miRNAs, proteins) to recipient cells in the wound microenvironment, such as fibroblasts, keratinocytes, and endothelial cells.
Diagram 1: Signaling pathways modulated by engineered MSC exosomes in wound healing.
The molecular mechanisms underlying these therapeutic effects involve precise modulation of key cellular processes:
- Anti-inflammatory Effects: Engineered exosomes deliver miRNAs that inhibit the NF-κB signaling pathway, reducing the production of pro-inflammatory cytokines such as TNF-α and IL-17A, and promoting macrophage polarization toward the anti-inflammatory M2 phenotype [17] [7] [74].
- Scar Modulation: Through regulation of the TGF-β/Smad pathway, specific exosome cargos can decrease the expression of fibrotic TGF-β1 while increasing the regenerative TGF-β3 isoform, resulting in reduced collagen deposition and minimized scar formation [17] [72].
- Angiogenic Activation: Pro-angiogenic miRNAs and proteins carried by exosomes activate multiple signaling pathways in endothelial cells, including PI3K/Akt and ERK/MAPK, stimulating endothelial cell proliferation, migration, and ultimately the formation of new blood vessels essential for tissue regeneration [17] [74].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of exosome engineering and evaluation requires specific reagents and instrumentation. The following table details essential materials for conducting research in this field.
Table 3: Essential Research Reagents and Experimental Materials
| Reagent / Material | Specific Example / Product | Primary Function in Research |
|---|---|---|
| Cell Culture Medium | Serum-free DMEM (SF-DMEM); VSCBIC-3 in-house solution; MSC NutriStem XF Basal Medium. | Supports MSC growth and exosome production while preventing serum-derived EV contamination. VSCBIC-3 enhances yield and maintains cell viability [73] [17]. |
| Isolation & Purification | Ultracentrifugation; Tangential Flow Filtration (TFF); Size-Exclusion Chromatography. | Isolates and concentrates exosomes from conditioned medium. TFF is scalable for high-yield production from 3D cultures [73] [7]. |
| Characterization | Nanoparticle Tracking Analysis (NTA; ZetaView); Transmission Electron Microscopy (TEM); Western Blot (CD9, CD63, ALIX, Calnexin). | Determines exosome size, concentration, morphology, and confirms presence of marker proteins/absence of contaminants [73] [17] [7]. |
| Engineering Reagents | CP05 peptide anchors; RGD peptides; Electroporation buffers; Plasmid vectors for transfection. | Enables surface modification and active cargo loading of exosomes for enhanced targeting and therapeutic function [72]. |
| In Vitro Bioassays | HUVEC tube formation assay; Fibroblast migration (scratch assay); Cell proliferation (Resazurin assay). | Quantifies functional therapeutic effects of exosomes on key wound healing processes like angiogenesis and cell migration [73] [17]. |
| Animal Models | Imiquimod (IMQ)-induced psoriasis; LPS-induced acute lung injury (ALI); Excisional wound model. | Preclinical in vivo systems for evaluating the efficacy and mechanisms of action of engineered exosomes [17] [7] [21]. |
This toolkit enables researchers to establish a robust pipeline from exosome isolation and engineering to functional validation. The selection of appropriate culture media and isolation techniques fundamentally impacts exosome yield and purity, while standardized characterization methods are essential for quality control and reproducibility across studies [73] [7]. Functional assays then provide the critical link between physical exosome properties and their biological activity in relevant wound healing models.
Engineering strategies employing surface modification and cargo loading represent the frontier of MSC-exosome research, creating enhanced vesicles with superior therapeutic potential for wound healing. The comparative analysis between human and animal sources reveals distinct advantages—hUCMSC-exosomes demonstrate exceptional pro-regenerative capacity, while canine models provide valuable platforms for protocol optimization and translational veterinary medicine. The integration of advanced bioengineering with scalable production methodologies, particularly 3D culture systems and TFF purification, addresses critical bottlenecks in clinical translation. As the field progresses, standardized protocols for engineering, characterization, and functional validation will be essential to fully realize the potential of these powerful nanotherapeutics in regenerative medicine.
The global burden of tissue loss and organ damage drives an urgent need for advanced regenerative therapies, with the market for tissue scaffolds projected to reach $5 billion by 2030 [75]. Mesenchymal stem cell (MSC)-derived exosomes have emerged as a promising cell-free therapeutic paradigm for wound healing and skin regeneration, demonstrating great potential to alleviate inflammation, promote vascularization, and enhance proliferation of epithelial cells and fibroblasts [43]. However, a significant translational challenge lies in the effective local delivery and retention of these therapeutic vesicles at the wound site. Conventional delivery methods, such as direct injection or topical application of exosome suspensions, often result in rapid clearance and suboptimal bioavailability, limiting their therapeutic efficacy [43] [5].
Biomaterial-based delivery systems, particularly hydrogels, offer a sophisticated solution to these limitations. These three-dimensional, hydrophilic polymer networks can absorb and retain large amounts of water, creating a hydrated, tissue-like environment that closely mimics the native extracellular matrix (ECM) [75] [76]. Their unique properties make them ideal for protecting exosomes and controlling their release kinetics, thereby extending their therapeutic window. The efficacy of MSC-exosomes can be significantly influenced by their cellular origin—whether derived from human or animal sources—which affects their cargo composition and functional properties [5]. This comparison guide objectively evaluates hydrogel-based delivery systems against alternative approaches, with specific focus on their application for human versus animal-source MSC exosomes in preclinical wound models.
Hydrogel Delivery Systems: Mechanisms and Material Considerations
Fundamental Properties of Hydrogel Scaffolds
Hydrogels function as ideal delivery vehicles for MSC exosomes due to their unique physicochemical properties. Their three-dimensional, hydrophilic polymer networks can absorb and retain large amounts of biological fluids (exceeding 90% water content), creating a moist wound environment conducive to healing [76]. This hydrated structure closely mimics the native extracellular matrix, providing a familiar microenvironment for cellular infiltration and tissue regeneration [75]. The soft, gel-like consistency of hydrogels offers mechanical protection to wounds while ensuring shape adaptability to cover irregular wound geometries [76].
The mechanical properties of hydrogels—including stiffness, elasticity, and viscoelasticity—play a fundamental role in maintaining physiological function and regulating cellular behavior through mechanotransduction [75]. These properties can be precisely tuned to match specific tissue requirements, with shear-thinning and thixotropic behaviors enabling injectable applications that recover their structure at the wound site [75]. The inherent bioactivity of certain hydrogel compositions further enhances their therapeutic potential, with natural polymers like chitosan, hyaluronic acid, and collagen offering inherent bioactive cues that support the regenerative functions of delivered exosomes [77].
Classification and Fabrication of Hydrogel Systems
Hydrogels are broadly categorized based on their source (natural, synthetic, or hybrid), ionic charge (cationic, anionic, or non-ionic), cross-linking method (physical or chemical), and stimuli responsiveness (chemical, biochemical, or physical) [75]. Each classification offers distinct advantages for exosome delivery, with natural polymers providing enhanced biocompatibility and biodegradability, while synthetic materials offer more controllable physical properties and longer-lasting structural support [76].
Crosslinking mechanisms fundamentally determine hydrogel performance characteristics. Physical crosslinking through hydrogen bonds, ionic interactions, or supramolecular chemistry produces reversible hydrogels with self-healing properties [77]. Chemical crosslinking via Schiff base bonds, thiol-ene additions, or enzymatic reactions creates more stable, covalently bonded networks with controlled degradation profiles [77]. Advanced "smart" hydrogels can be engineered to respond to specific wound microenvironment cues such as pH changes, elevated reactive oxygen species (ROS) levels, or enzyme activity, enabling triggered release of exosomes in response to pathological conditions [77].
Table 1: Hydrogel Classification and Characteristics for Exosome Delivery
| Classification Basis | Hydrogel Types | Key Characteristics | Relevance to Exosome Delivery |
|---|---|---|---|
| Source | Natural (e.g., Chitosan, Hyaluronic acid, Collagen) | High biocompatibility, inherent bioactivity, biodegradability | Enhanced cellular uptake and biointegration of exosomes |
| Synthetic (e.g., PEG, PLGA, PVA) | Tunable physical properties, controlled degradation, reproducibility | Predictable release kinetics, structural stability | |
| Hybrid/Blended | Combines advantages of natural and synthetic polymers | Balanced bioactivity and mechanical control | |
| Crosslinking Mechanism | Physical (ionic, H-bond, supramolecular) | Reversible, self-healing, injectable | Minimal processing stress on exosomes |
| Chemical (covalent bonds) | Stable, controlled degradation, mechanical robustness | Sustained release profile, protection of exosomes | |
| Enzymatic (HRP, SrtA catalyzed) | High specificity, mild reaction conditions | Maintains exosome integrity and function | |
| Stimuli Responsiveness | pH-sensitive | Swells/degrades at specific pH values | Targeted release in chronic wound environments |
| ROS-responsive | Degrades in high oxidative stress environments | Responsive to inflammatory wound conditions | |
| Enzyme-responsive | Degrades in presence of specific wound enzymes | Site-specific release in infected wounds | |
| Glucose-responsive | Reacts to elevated glucose levels | Ideal for diabetic wound applications |
Comparative Performance Analysis of Delivery Platforms
Hydrogel Systems Versus Alternative Delivery Approaches
When evaluating delivery systems for MSC exosomes in wound healing applications, hydrogels demonstrate distinct advantages over other methods. Traditional administration approaches include direct topical application, subcutaneous injection, and dressing/covering techniques [5]. While subcutaneous injection has shown better wound closure outcomes and collagen deposition compared to dressing methods in animal studies [5], this approach still suffers from rapid exosome clearance and limited spatial control.
Hydrogel systems address these limitations through their unique capacity for sustained, localized release. The three-dimensional network structure of hydrogels protects exosomes from degradation while controlling their diffusion into the wound bed [75] [76]. Comparative studies have demonstrated that hydrogel-based delivery can extend exosome retention at the wound site from hours to several days, significantly enhancing their therapeutic window [76]. The modular design of hydrogels enables incorporation of multiple bioactive factors alongside exosomes, creating comprehensive therapeutic platforms that can address multiple aspects of the wound healing process simultaneously [77].
Table 2: Performance Comparison of MSC Exosome Delivery Systems in Preclinical Wound Models
| Delivery System | Exosome Retention Capacity | Therapeutic Efficacy (Wound Closure Rate) | Administration Ease | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Direct Topical Application | Low (hours) | Variable, dose-dependent | High | Simple administration, no specialized equipment required | Rapid clearance, limited penetration, vulnerable to degradation |
| Subcutaneous Injection | Medium (24-48 hours) | Good (Superior to dressings in animal studies) [5] | Medium | Direct deposition at wound site, bypasses epidermal barrier | Potential leakage, limited spatial distribution, patient discomfort |
| Conventional Dressings | Low-medium | Moderate (Less than subcutaneous injection) [5] | High | Standard clinical practice, readily available | Limited controlled release capacity, may adhere to wound bed |
| Hydrogel-Based Delivery | High (days to weeks) | Enhanced [76] [77] | Medium-high | Tunable release kinetics, protection of exosome integrity, maintains moist wound environment | Requires development of formulation parameters, potential batch-to-batch variability |
| Advanced Hydrogel Systems | Very High (weeks) | Significantly Enhanced [75] [78] | Variable | Stimuli-responsive release, spatial patterning, multi-factor delivery | More complex manufacturing, higher cost, regulatory considerations |
Impact of MSC Source on Exosome Delivery Efficacy
The therapeutic efficacy of exosome-based wound treatments is influenced not only by the delivery system but also by the source of the parent MSCs. Systematic analyses of preclinical studies reveal that adipose-derived stem cells (ADSCs) demonstrate the best effect in wound closure rate and collagen deposition, while bone marrow MSCs (BMMSCs) display superior performance in revascularization [5]. These source-dependent functional specializations highlight the importance of matching exosome source with specific wound healing requirements.
Hydrogel delivery systems can be optimized to complement the inherent strengths of different exosome types. For ADSC-exosomes with strong proliferative effects, hydrogels with controlled, sustained release profiles can extend their pro-regenerative signaling. For BMMSC-exosomes with potent angiogenic properties, hydrogels with appropriate mechanical properties that support vascular network formation would be particularly advantageous [75]. The growing interest in induced pluripotent stem cell-derived MSCs (iPSC-MSCs) presents new opportunities for hydrogel delivery, as these exosomes offer scalable production potential but may benefit from additional stabilization provided by the hydrogel matrix [79] [5].
Experimental Data and Methodologies
Quantitative Analysis of Hydrogel-Enhanced Exosome Delivery
Preclinical studies provide substantial evidence supporting the advantages of hydrogel-based exosome delivery. A comprehensive meta-analysis of 83 preclinical studies demonstrated that MSC-exosome treatments significantly improve wound closure rates, scar width, blood vessel density, and collagen deposition in both diabetic and non-diabetic animal models [5]. The analysis revealed that apoptotic small extracellular vesicles (ApoSEVs) showed better efficacy than apoptotic bodies (ApoBDs) and small extracellular vesicles (sEVs) in wound closure outcome and collagen deposition, while sEVs displayed better performance in revascularization [5].
Hydrogel delivery systems further enhance these therapeutic outcomes. Experimental data from lignin-based tubular hydrogel scaffolds demonstrate optimal mechanical properties for soft tissue support, with ultimate tensile strength of 83.14 ± 0.16 kPa, elongation up to 176%, and swelling capacity of 261% [78]. These reinforced constructs exhibit superior mechanical strength and sustained performance over 100 fatigue cycles while maintaining excellent cytocompatibility with fibroblast cultures (cell viability: 85.5–86.5% after 96 hours) [78]. Such robust mechanical properties are essential for withstanding the dynamic environment of wound beds while providing consistent exosome delivery.
Table 3: Experimental Parameters in Preclinical Assessment of MSC Exosome Delivery Systems
| Parameter Category | Specific Metrics | Hydrogel-Based Systems | Alternative Delivery Methods |
|---|---|---|---|
| Administration Route | Subcutaneous injection | In situ forming hydrogels for sustained release | Bolus injection, multiple administrations often needed |
| Topical application | Adhesive hydrogels for continuous coverage | Solutions, suspensions, creams | |
| Dressing/covering | Hydrogel-incorporated dressings | Conventional gauze, commercial wound dressings | |
| Exosome Dosing | Frequency | Single application with sustained effect | Multiple applications typically required |
| Concentration | Protected, localized concentration maintenance | Rapid dilution and clearance | |
| Total dosage | Reduced total dosage needed for equivalent effect | Higher total dosage often required | |
| Animal Models | Mouse (73.5% of studies) [5] | Full-thickness excisional dorsal wounds most common | Similar models used for comparison |
| Rat (26.5% of studies) [5] | Diabetic (STZ-induced) and non-diabetic models | Genetic models (db/db mice) for type 2 diabetes | |
| Wound Types | Excisional wounds, burns, diabetic ulcers, scleroderma | Comparable wound models for direct assessment | |
| Assessment Timeline | Short-term (1-7 days) | Early inflammatory phase, initial cell migration | Same assessment periods |
| Medium-term (7-21 days) | Proliferative phase, re-epithelialization, angiogenesis | Standardized comparison timepoints | |
| Long-term (21+ days) | Remodeling phase, collagen organization, scar formation | Identical evaluation windows |
Standardized Experimental Protocols for Hydrogel-Exosome Formulations
To ensure reproducible evaluation of hydrogel-exosome formulations, standardized experimental protocols are essential. The following methodology outlines a systematic approach for developing and testing these therapeutic systems:
Hydrogel-Exosome Formulation Protocol:
- Hydrogel Precursor Preparation: Dissolve natural polymers (e.g., chitosan, hyaluronic acid) or synthetic polymers (e.g., PVA, PEG) in appropriate aqueous buffers at concentrations ranging from 1-5% w/v, depending on target mechanical properties [77].
- Exosome Incorporation: Mix isolated MSC-exosomes (characterized per MISEV2023 guidelines) with hydrogel precursor solution at optimized concentrations (typically 10-100 μg exosome protein per mL hydrogel) using gentle pipetting to maintain vesicle integrity [5] [3].
- Crosslinking Implementation: Induce gelation using appropriate methods:
- Ionic crosslinking: Add crosslinking ions (e.g., Ca²⁺ for alginate)
- Chemical crosslinking: Incorporate crosslinkers (e.g., genipin, glutaraldehyde) at minimal concentrations
- Photo-crosslinking: Apply UV light (365 nm) at low intensity for photoinitiator-containing systems [77]
- Enzymatic crosslinking: Add enzymes (e.g., HRP/H₂O₂ system) under physiological conditions [77]
- Rheological Characterization: Assess mechanical properties using rotational rheometry to determine storage modulus (G'), loss modulus (G''), and shear-thinning behavior [75].
- In Vitro Release Profiling: Immerse hydrogel-exosome constructs in PBS at 37°C with gentle agitation; collect release medium at predetermined intervals and quantify exosome release via BCA protein assay, nanoparticle tracking analysis, or specific biomarker ELISA [3].
- Bioactivity Assessment: Evaluate biological activity of released exosomes using cell proliferation assays (e.g., fibroblasts, keratinocytes), migration assays (scratch/wound healing assay), and tube formation assays (for angiogenic potential) [5].
Animal Model Evaluation Protocol:
- Wound Creation: Generate full-thickness excisional wounds (typically 6-10 mm diameter) on dorsum of mice or rats under anesthesia [5].
- Treatment Application: Apply hydrogel-exosome formulation to cover wound bed completely; compare against control treatments (blank hydrogel, free exosomes, vehicle controls).
- Longitudinal Assessment: Monitor wound closure through daily macroscopic imaging and planimetric analysis; collect tissue samples at predetermined endpoints (7, 14, 21 days) for histological and molecular analyses [5].
- Histological Evaluation: Process tissues for H&E staining (general morphology), Masson's trichrome (collagen deposition), immunohistochemistry (CD31 for vascularization, cytokeratin for re-epithelialization), and immunofluorescence (specific cell markers) [5].
Signaling Pathways and Therapeutic Mechanisms
The therapeutic effects of MSC exosomes delivered via hydrogel systems are mediated through complex signaling pathways that regulate key wound healing processes. The following diagram illustrates the major mechanistic pathways through which hydrogel-delivered exosomes promote skin regeneration:
Mechanistic Pathways of Hydrogel-Delivered MSC Exosomes in Wound Healing
The diagram above illustrates how hydrogel-based delivery facilitates the controlled release of MSC exosomes to wound sites. Following cellular uptake, exosomes transfer their bioactive cargo (miRNAs, proteins, lipids) to recipient cells, modulating multiple healing processes including inflammation resolution, angiogenesis, fibroblast activation, extracellular matrix remodeling, oxidative stress reduction, and cellular proliferation. These coordinated actions ultimately accelerate wound closure through both overlapping and complementary mechanisms.
The sequential progression of wound healing stages—hemostasis, inflammation, proliferation, and remodeling—benefits from the sustained presence of exosomes provided by hydrogel delivery systems. The following workflow diagram illustrates the experimental approach for evaluating hydrogel-exosome formulations in preclinical wound models:
Experimental Workflow for Hydrogel-Exosome Formulation Evaluation
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and evaluation of hydrogel-exosome delivery systems requires specific research reagents and materials. The following table details essential components for formulating and testing these advanced therapeutic systems:
Table 4: Essential Research Reagents for Hydrogel-Exosome Formulation and Evaluation
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Polymer Scaffolds | Chitosan, Hyaluronic acid, Alginate, Collagen, Fibrin | Natural polymer base for hydrogel formation | Biocompatibility, biodegradability, inherent bioactivity |
| Poly(ethylene glycol), Poly(vinyl alcohol), PLGA, PCL | Synthetic polymer base for tunable properties | Controlled physical properties, reproducibility | |
| Lignin-based polymers, Hybrid/composite materials | Sustainable or enhanced functionality platforms | Mechanical robustness, antioxidant properties [78] | |
| Crosslinking Agents | Genipin, Glutaraldehyde, ECH (Epichlorohydrin) [78] | Chemical crosslinkers for stable network formation | Cytocompatibility, reaction efficiency, byproduct toxicity |
| Ca²⁺, Sr²⁺, Ba²⁺ ions | Ionic crosslinkers for alginate-based systems | Gentle gelation, reversible crosslinking | |
| Horseradish Peroxidase (HRP)/H₂O₂, Transglutaminase, Sortase A | Enzymatic crosslinkers for specific, mild conditions | High specificity, biocompatibility, mild reaction [77] | |
| Exosome Isolation Kits | Total Exosome Isolation Kits, Membrane-based kits | Rapid exosome isolation from conditioned media | Yield, purity, maintenance of bioactivity |
| Characterization Reagents | Antibodies against CD63, CD81, CD9, TSG101 | Exosome surface marker identification | Specificity, compatibility with detection methods |
| BCA, Bradford protein assay kits | Exosome quantification | Compatibility with hydrogel components | |
| NTA (Nanoparticle Tracking Analysis) standards | Size distribution and concentration analysis | Instrument calibration, measurement accuracy | |
| Cell Culture Reagents | MSC Media (α-MEM, DMEM with supplements) | MSC expansion and maintenance | Support of MSC stemness, prevention of differentiation |
| Fetal Bovine Serum (exosome-depleted) | Cell culture supplement | Elimination of confounding exogenous exosomes | |
| Differentiation kits (osteogenic, adipogenic, chondrogenic) | MSC characterization per ISCT guidelines [5] | Standardization of MSC multipotency assessment | |
| Animal Model Supplies | Immunocompromised mice (e.g., nude, NSG) | In vivo evaluation without immune rejection | Model suitability for human cell-derived exosomes |
| Diabetic models (STZ-induced, db/db mice) | Diabetes-impaired wound healing assessment | Relevance to clinical chronic wound populations | |
| Wound creation instruments (biopsy punches) | Standardized wound generation | Precision, reproducibility of wound size |
Hydrogel-based delivery systems represent a significant advancement in therapeutic applications for MSC exosomes in wound healing. The synergistic combination of hydrogels' biomimetic properties with the multifaceted therapeutic effects of exosomes addresses critical limitations of conventional delivery methods, particularly their inability to maintain effective exosome concentrations at the wound site. The comparative analysis presented in this guide demonstrates that hydrogel systems outperform alternative approaches through superior retention capacity, controlled release kinetics, and enhanced therapeutic outcomes.
Future developments in this field will likely focus on increasingly sophisticated "smart" hydrogel platforms that respond dynamically to specific wound microenvironment cues, such as pH changes, enzyme activity, or reactive oxygen species levels [77]. The emerging emphasis on standardized characterization methodologies—following MISEV2023 guidelines for exosomes and ISCT criteria for MSCs—will be crucial for enabling reproducible research and successful clinical translation [5] [3]. Additionally, the growing investigation of MSC source influences on exosome functionality highlights the importance of matching specific exosome profiles with appropriate hydrogel delivery systems to maximize therapeutic outcomes for different wound types [5].
As the field progresses toward clinical application, addressing scalability and manufacturing challenges will be essential. Companies like Evox Therapeutics, Aruna Bio, and Capricor Therapeutics are pioneering Good Manufacturing Practice (GMP)-compliant production processes for exosome-based therapies [80], while advancements in lignin-based and other sustainable biomaterials offer promising avenues for scalable hydrogel fabrication [78]. Through continued interdisciplinary collaboration between material scientists, biologists, and clinical researchers, hydrogel-exosome combination therapies hold tremendous potential to revolutionize treatment paradigms for acute and chronic wounds, ultimately addressing a significant unmet clinical need in global healthcare.
Addressing Immunogenicity and Long-Term Biodistribution Concerns
The translation of mesenchymal stem cell-derived exosomes (MSC-exosomes) from preclinical research to clinical applications faces two significant biological barriers: immunogenicity and unpredictable long-term biodistribution. These challenges manifest differently between human and animal-source MSC exosomes, potentially influencing therapeutic efficacy, safety profiles, and dosing regimens. Immunogenicity concerns center on host immune responses against administered exosomes, which could lead to rapid clearance, reduced therapeutic half-life, or adverse reactions. Biodistribution patterns determine how exosomes navigate the circulatory system, reach target tissues, and interact with specific cell types—critical factors for wound healing applications where precise targeting of skin layers is essential. Understanding these fundamental biological behaviors is paramount for researchers and drug development professionals selecting appropriate exosome sources for specific therapeutic applications.
Comparative Analysis: Human vs. Animal Source MSC Exosomes
Immunogenicity Profiles
Table 1: Immunogenicity Comparison of Human and Animal-Derived MSC Exosomes
| Parameter | Human Source MSC Exosomes | Animal Source MSC Exosomes |
|---|---|---|
| Immune Recognition | Lower immunogenicity in human models; reduced HLA expression [81] | Higher potential for immune recognition in human models |
| Therapeutic Advantages | Superior performance in wound closure (SMD: 1.423, 95% CI: 1.137-1.709) [26] | Variable efficacy across species barriers |
| Macrophage Polarization | Promotes anti-inflammatory M2 phenotype; increases CD206, IL-10, TGF-β [82] | Species-dependent polarization effects |
| Clinical Translation | Reduced risk of immune rejection; more predictable safety profile [81] [83] | Requires extensive immunogenicity testing |
| Modification Potential | Engineerable to further reduce immunogenicity [84] | Limited engineering options for human applications |
Biodistribution Patterns
Table 2: Biodistribution Characteristics of MSC Exosomes from Different Sources
| Characteristic | Human Source MSC Exosomes | Animal Source MSC Exosomes |
|---|---|---|
| Protein Corona Formation | Human-specific protein signature affects cellular uptake [85] | Different corona composition may alter targeting |
| Liver Accumulation | Significant hepatic uptake; can be modified with albumin coating [85] | Varies based on source species and preparation |
| Cellular Targeting | Preferential uptake by hepatocytes, LSECs, and stellate cells with engineered corona [85] | Limited human cellular targeting data |
| Administration Routes | Effective via intravenous, intranasal, and nebulized delivery [86] [87] | Route efficiency may differ in human applications |
| Engineering Potential | Surface modifiable to enhance tissue-specific targeting [84] | Limited human-specific targeting modifications |
Experimental Approaches for Assessment
Evaluating Immunogenicity: Key Methodologies
Flow Cytometry for Immune Cell Profiling: Researchers employ comprehensive flow cytometry panels to quantify immune cell responses following exosome administration. Critical markers include CD80/CD86 for M1 macrophages, CD206 for M2 polarization, CD4+/CD8+ for T-cell responses, and CD19/CD20 for B-cell activation. The experimental workflow involves incubating human peripheral blood mononuclear cells (PBMCs) with test exosomes for 24-72 hours, followed by antibody staining and analysis. This approach reliably detects even subtle immune responses, with studies demonstrating that SHED-MSC-exosomes significantly increase anti-inflammatory CD206+ macrophages while reducing pro-inflammatory CD80+/CD86+ populations [82].
Cytokine Multiplex Assays: ELISA and multiplex cytokine arrays quantitatively measure pro-inflammatory (TNF-α, IL-6, IL-1β, IL-12) and anti-inflammatory (IL-10, TGF-β) mediators in serum and bronchoalveolar lavage fluid. Specimens are typically collected at 24-48 hours post-exposure, with results demonstrating that human umbilical cord MSC-exosomes significantly reduce TNF-α, IL-6, and IL-1β while increasing IL-10 in acute lung injury models [87] [21]. This methodology provides quantifiable immunogenicity data across multiple inflammatory pathways simultaneously.
Macrophage Polarization Assays: Using THP-1 cell lines differentiated into M0/M1 macrophages, researchers assess exosome-induced polarization through surface marker expression (CD80, CD86, CD206) and cytokine secretion profiles. The protocol includes 24-hour exosome exposure followed by flow cytometry and supernatant analysis. Studies with SHED-MSC-exosomes demonstrate remarkable similarity to dexamethasone in promoting M2 polarization, with significant increases in CD206, Arg-1, IL-10, and TGF-β [82].
Tracking Biodistribution: Advanced Techniques
Radiolabeling and SPECT/CT Imaging: Exosomes labeled with technetium-99m or zirconium-89 allow non-invasive tracking using single-photon emission computed tomography. The protocol involves incubating exosomes with radiotracers, removing unbound label via size-exclusion chromatography, and administering to animal models. Serial imaging at 1, 4, 24, and 48 hours post-injection reveals accumulation patterns, with studies showing significant hepatic uptake unless modified with albumin-enriched corona [85].
Fluorescent Labeling and Whole-Body Imaging: DIR, DiD, or DiR lipophilic dyes incorporate into exosome membranes for in vivo tracking. Following intravenous administration, real-time imaging systems capture distribution kinetics. This approach demonstrated route-dependent distribution, with intravenous administration achieving superior lung accumulation compared to intranasal or nebulized delivery in acute lung injury models [87].
Protein Corona Analysis: Using liquid chromatography-mass spectrometry (LC-MS), researchers characterize proteins adsorbed onto exosome surfaces from biological fluids. The methodology involves incubating exosomes with human serum, separating bound proteins via ultracentrifugation, and performing proteomic analysis. This technique revealed that albumin coating creates a signature that redirects exosomes from hepatic macrophages to parenchymal cells [85].
Molecular Mechanisms and Signaling Pathways
The diagram illustrates how MSC exosomes interact with biological systems through two primary mechanisms: immune modulation and tissue distribution. The protein corona that forms immediately upon contact with biological fluids significantly influences both processes, determining which cells internalize the exosomes and how the immune system responds. Immunomodulation occurs primarily through shifting macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes and direct T-cell regulation, creating an environment conducive to tissue repair. Biodistribution patterns determine therapeutic efficacy by controlling exosome delivery to target tissues, influenced by administration route, surface properties, and cellular uptake mechanisms.
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Exosome Immunogenicity and Biodistribution Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Exosome Isolation Kits | Exocib isolation kit, Total Exosome Isolation kits | Standardized purification from cell culture supernatants [82] |
| Characterization Instruments | Zetasizer (DLS), Nanodrop spectrophotometer, FESEM, TEM | Size distribution, concentration, and morphological validation [82] |
| Flow Cytometry Antibodies | CD63/CD81/CD9, CD80/CD86/CD206, HLA markers | Surface marker validation and immune cell profiling [82] |
| Cytokine Detection Kits | ELISA kits for TNF-α, IL-6, IL-1β, IL-10, TGF-β | Quantifying immune responses to exosome administration [87] [82] |
| Tracking Dyes | DIR, DiD, DiR lipophilic dyes, Calcein AM | In vivo and in vitro tracking of exosome distribution and uptake [82] |
| Cell Culture Models | THP-1 (monocyte), PBMCs from human donors | Standardized immunogenicity assessment platforms [82] |
| Animal Disease Models | LPS-induced ALI, bleomycin-induced PF, excisional wounds | Biodistribution and efficacy in pathologically relevant environments [87] [84] |
The comparative analysis reveals that human-source MSC exosomes present distinct advantages for clinical translation, demonstrating lower immunogenicity and more predictable biodistribution patterns in human-relevant models. The ability to engineer human exosomes through preconditioning, surface modification, and cargo loading further enhances their targeting specificity while reducing immune recognition. Animal-source exosomes, while valuable for preliminary screening, introduce additional variables related to interspecies differences in protein corona formation and immune recognition. For researchers focused on wound healing applications, human MSC exosomes—particularly from adipose tissue or umbilical cord sources—show superior efficacy in promoting angiogenesis, modulating inflammation, and optimizing collagen deposition. The strategic selection of exosome source, coupled with appropriate engineering approaches to address residual immunogenicity and biodistribution challenges, will significantly accelerate the development of effective exosome-based wound therapies.
Head-to-Head Efficacy and Clinical Translation Potential
In the rapidly advancing field of regenerative medicine, mesenchymal stem cell-derived exosomes (MSC-exosomes) have emerged as a promising cell-free therapeutic strategy, demonstrating significant potential in preclinical models of wound healing, inflammatory diseases, and tissue regeneration [62] [8]. These nano-sized vesicles recapitulate many therapeutic benefits of their parent MSCs—including anti-inflammatory, anti-apoptotic, and pro-regenerative properties—while offering advantages such as lower immunogenicity, enhanced stability, and the ability to cross biological barriers [62]. However, a critical question remains largely unanswered in the current literature: how does the biological source of these exosomes (human versus animal) influence their therapeutic efficacy?
The translation of MSC-exosome therapies from animal models to human clinical applications necessitates a systematic understanding of how exosomes derived from different species compare in their composition and functional effects. Such comparative data are essential for researchers and drug development professionals to appropriately interpret preclinical findings and design effective clinical translation strategies. This guide synthesizes available evidence regarding the efficacy of human versus animal-derived MSC exosomes, highlighting the current limitations in direct comparative studies while providing methodological frameworks for future investigations.
Table: Current Research Focus on MSC-Exosome Sources in Preclinical Studies
| Exosome Source | Prevalence in Research | Key Advantages | Documented Therapeutic Effects |
|---|---|---|---|
| Human MSC Sources | 69.9% of wound healing studies [5] | Clinical relevance, lower immunogenicity risk | Improved wound closure, angiogenesis, collagen deposition [5] |
| Animal MSC Sources | 26.5% of wound healing studies [5] | Easier procurement for preliminary research | Anti-inflammatory effects, tissue regeneration [7] |
| Umbilical Cord (Human) | 22.9% of studies [5] | Enhanced proliferation, lower immunogenicity | Superior clinical scores in psoriasis models [7] |
| Bone Marrow (Human) | 19.3% of studies [5] | Extensive characterization | Neuroprotection, functional recovery in neurological models [62] |
| Adipose Tissue (Human) | 38.55% of studies [5] | High yield, ease of isolation | Best effect on wound closure rate and collagen deposition [5] |
Current Evidence: Gaps in Direct Comparative Data
Prevalence of Human-Derived MSC-Exosomes in Current Literature
Analysis of the current research landscape reveals a predominant focus on human-derived MSC-exosomes in preclinical studies. A comprehensive systematic review of 83 studies on MSC-exosomes for wound healing and skin regeneration found that 69.9% utilized exosomes derived from human sources, while only 17.3% employed exosomes from animal sources (mouse: 10.8%, rat: 4.8%, canine: 1.2%) [5]. This imbalance suggests that the field has increasingly recognized the importance of human-derived products for therapeutic development, though animal-derived exosomes continue to play a role in preliminary mechanistic studies.
The scarcity of direct comparative studies represents a significant knowledge gap. Most meta-analyses and systematic reviews note this limitation, with an umbrella review of MSC-derived extracellular vesicles in preclinical models acknowledging that comparisons between different exosome sources remain inadequate [62]. Similarly, a meta-analysis on psoriasis treatments could only incorporate studies that individually tested either human placenta MSC-exosomes or human umbilical cord MSC-exosomes without direct comparative data between human and animal sources [7].
Evidence of Source-Dependent Variations in MSC Biology
Although direct comparisons of human versus animal MSC-exosomes are limited, substantial evidence indicates that MSC characteristics—and by extension their exosomal products—vary significantly based on their tissue of origin, even within the same species. Research comparing human MSCs from adipose tissue and dental pulp revealed notable differences in their biological properties, including variations in differentiation capacity, proliferation rates, and secretome profiles [69]. Specifically, dental pulp MSCs demonstrated an inability to undergo adipogenic differentiation, unlike their adipose-derived counterparts, highlighting fundamental biological differences between tissue sources [69].
These source-dependent variations extend to the molecular cargo of MSC-exosomes. Studies have identified distinct microRNA expression patterns in exosomes derived from different human MSC sources, with dental pulp MSC-exosomes enriched in microRNAs involved in oxidative stress and apoptosis pathways, while adipose-derived MSC-exosomes carried microRNAs regulating cell cycle and proliferation [69]. Such differences likely translate to varied therapeutic effects, though systematic comparisons across species boundaries remain largely unexplored.
Comparative Efficacy Analysis in Disease Models
Wound Healing and Skin Regeneration Models
In the context of wound healing, comparative evidence, though limited, suggests that the tissue source of human MSC-exosomes may influence therapeutic outcomes. A systematic review and meta-analysis of preclinical studies on wound healing and skin regeneration revealed that among frequently used MSC sources, adipose-derived stem cells (ADSCs) demonstrated the best effect on wound closure rate and collagen deposition, while bone marrow-derived MSCs showed superior performance in revascularization [5]. This suggests that specific applications may benefit from matching with appropriate exosome sources.
The route of administration also appears to interact with exosome source in determining therapeutic efficacy. The same meta-analysis found that subcutaneous injection of MSC-exosomes produced greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering approaches [5]. These findings highlight the complexity of optimizing exosome therapies, where both biological source and delivery method must be considered in tandem.
Inflammatory Disease Models
In inflammatory conditions such as psoriasis, comparative data, though preliminary, suggest differential effectiveness based on MSC source. A murine study and meta-analysis comparing human placenta MSC-exosomes and human umbilical cord MSC-exosomes found that both significantly reduced epidermal thickness and skin tissue cytokines in an imiquimod-induced psoriasis model compared to controls [7]. Meta-regression within this analysis revealed that studies using human umbilical cord MSC-exosomes showed greater improvement in clinical scores compared to other MSC sources, indicating potential source-specific efficacy differences [7].
For acute lung injury, research has focused primarily on optimizing delivery methods for human umbilical cord blood MSC-exosomes rather than comparing different sources. One study demonstrated that intravenous administration of these exosomes significantly attenuated pulmonary inflammation in a lipopolysaccharide-induced mouse model, with high-dose treatment (5×10⁸ particles) outperforming medium and low doses across all measured parameters [21]. This suggests that both source and delivery parameters must be optimized for maximal therapeutic effect.
Table: Comparative Efficacy of MSC-Exosomes from Different Human Sources
| Disease Model | Most Effective Source | Key Efficacy Metrics | Proposed Mechanisms |
|---|---|---|---|
| Psoriasis | Human Umbilical Cord [7] | Clinical severity scores, epidermal thickness reduction | Meta-regression showed superior improvement (p=0.030) [7] |
| Wound Healing - Closure | Adipose Tissue [5] | Wound closure rate, collagen deposition | Optimal secretome profile for epithelial regeneration [5] |
| Wound Healing - Revascularization | Bone Marrow [5] | Blood vessel density, perfusion recovery | Pro-angiogenic factor enrichment [5] |
| Acute Lung Injury | Umbilical Cord Blood [21] | Inflammation reduction, alveolar repair | Dose-dependent cytokine modulation (TNF-α, IL-6, IL-1β) [21] |
Experimental Methodologies for Comparative Studies
Standardized Protocols for MSC-Exosome Isolation and Characterization
Robust comparative studies require standardized methodologies for exosome isolation and characterization. Current research indicates significant methodological variability that complicates cross-study comparisons. For isolation, studies have compared different approaches, with tangential flow filtration (TFF) demonstrating higher particle yields compared to traditional ultracentrifugation methods [27]. Similarly, culture conditions affect exosome production, with research showing that the choice of culture medium (α-MEM vs. DMEM) influences both MSC proliferation and subsequent exosome yield, though not at statistically significant levels [27].
Characterization of MSC-exosomes should follow established guidelines, including the Minimal Information for Studies of Extracellular Vesicles (MISEV2023) [5]. Standard characterization includes:
- Nanoparticle Tracking Analysis (NTA): For determining particle size distribution and concentration [7] [27]
- Transmission Electron Microscopy (TEM): To confirm cup-shaped morphology characteristic of exosomes [7] [27]
- Immunoblotting: For detection of exosome markers (CD9, CD63, CD81, ALIX, TSG101) and absence of negative markers (calnexin) [7] [27]
- Flow Cytometry: For immunophenotyping of surface markers [27]
Additionally, comprehensive characterization of parent MSCs should adhere to International Society for Cellular Therapy (ISCT) guidelines, including demonstration of plastic adherence, specific surface marker expression (CD73, CD90, CD105), and lack of hematopoietic markers (CD34, CD45, HLA-DR), along with trilineage differentiation potential [8] [5].
In Vivo Evaluation Models and Assessment Methods
Preclinical evaluation of MSC-exosome efficacy typically employs well-established disease models with standardized outcome measures. For dermatological applications, the imiquimod (IMQ)-induced psoriasis model in Balb/c mice represents a validated approach, with treatment effects quantified through psoriasis area and severity index (PASI) scoring, histological analysis of epidermal thickness, and cytokine level measurements in skin tissue [7]. Similarly, wound healing studies often utilize full-thickness excisional wounds in diabetic or normal rodent models, with outcomes including wound closure rate, scar width, blood vessel density, and collagen deposition [5].
For pulmonary applications, the lipopolysaccharide (LPS)-induced acute lung injury model in mice provides a robust system for evaluating therapeutic effects, with assessment parameters including histopathological lung injury scoring, inflammatory cytokine levels (TNF-α, IL-6, IL-1β, IL-10) in both serum and bronchoalveolar lavage fluid (BALF) [21]. These standardized models and outcome measures enable more valid comparisons across different studies and exosome sources.
Diagram 1: Experimental workflow for direct comparative studies of human vs. animal MSC-exosomes, highlighting key methodological steps from source selection through efficacy assessment.
Molecular Mechanisms and Signaling Pathways
The therapeutic effects of MSC-exosomes are mediated through their molecular cargo, which includes proteins, lipids, and various nucleic acid species that modulate recipient cell behavior. While comprehensive comparative analyses of human versus animal exosome cargo are limited, research has identified several key mechanisms through which MSC-exosomes exert their therapeutic effects across different disease models.
In skin regeneration and wound healing, MSC-exosomes have been shown to promote angiogenesis through transfer of pro-angiogenic miRNAs that activate endothelial cells and stimulate new blood vessel formation [5] [88]. They also modulate inflammation by shifting macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes, and enhance tissue remodeling by promoting collagen deposition and organization [5]. Additionally, MSC-exosomes inhibit cellular senescence and apoptosis in damaged tissues, particularly important in radiation-induced skin injury where they counteract persistent DNA damage and promote fibroblast proliferation [88].
In inflammatory conditions like psoriasis and acute lung injury, MSC-exosomes demonstrate potent immunomodulatory effects by delivering anti-inflammatory miRNAs that suppress pro-inflammatory cytokine production (TNF-α, IL-6, IL-1β) while enhancing anti-inflammatory mediators like IL-10 [7] [21]. They also directly promote tissue repair by enhancing epithelial cell proliferation and migration through modulation of signaling pathways such as NF-κB, Wnt/β-catenin, and Hippo-YAP/TAZ [21] [88].
Diagram 2: Key therapeutic mechanisms of MSC-exosomes, showing how molecular cargo drives biological effects through multiple signaling pathways to produce functional outcomes.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Essential Research Reagents for MSC-Exosome Studies
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Cell Culture Media | MSC expansion and exosome production | α-MEM or DMEM supplemented with 10% human platelet lysate or FBS-free alternatives [27] |
| Isolation Kits/Systems | Exosome separation from conditioned media | Ultracentrifugation protocols; Tangential Flow Filtration systems for higher yield [27] |
| Characterization Antibodies | Exosome marker detection | Anti-CD9, CD63, CD81, ALIX, TSG101; Negative markers: Calnexin [7] [27] |
| Nanoparticle Tracking Analyzer | Size distribution and concentration analysis | ZetaView PMX 110 system or similar; Confirmation of 30-150 nm size range [7] [27] |
| Transmission Electron Microscope | Morphological validation | Confirmation of cup-shaped morphology; Hitachi HT-7700 or similar [7] [27] |
| Animal Disease Models | In vivo efficacy testing | IMQ-induced psoriasis (Balb/c mice); LPS-induced ALI; Full-thickness excisional wounds [7] [5] [21] |
| Cytokine Detection Assays | Inflammatory response quantification | ELISA kits for TNF-α, IL-6, IL-1β, IL-10 in serum and BALF [7] [21] |
| Histological Staining Reagents | Tissue structure and composition analysis | Hematoxylin and Eosin for general morphology; Masson's Trichrome for collagen [7] [5] |
The current evidence regarding comparative efficacy of human versus animal MSC-exosomes remains limited, with few studies conducting direct head-to-head comparisons. The existing literature demonstrates clear therapeutic potential for MSC-exosomes across multiple disease models but highlights significant gaps in our understanding of how the species origin of these exosomes influences their biological activity. Available data suggest that human MSC-exosomes from different tissue sources (umbilical cord, bone marrow, adipose tissue) exhibit distinct efficacy profiles optimized for specific therapeutic applications, though similar comparisons across species boundaries are lacking.
Future research should prioritize well-designed comparative studies that directly evaluate human and animal-derived MSC-exosomes using standardized isolation methods, characterization protocols, and disease models. Such investigations are essential for establishing valid preclinical benchmarks and optimizing therapeutic development strategies. Additionally, greater attention to the molecular mechanisms underlying potential differences, particularly comparative analyses of exosomal cargo composition and recipient cell interactions, will provide critical insights for the rational design of MSC-exosome therapies with enhanced clinical potential.
As the field advances, standardization of production methods, comprehensive molecular characterization, and systematic efficacy comparisons across species will be crucial for translating the promising therapeutic effects of MSC-exosomes observed in preclinical models into effective clinical treatments for human diseases.
The therapeutic application of mesenchymal stem cell (MSC)-derived exosomes represents a paradigm shift in regenerative medicine, offering a cell-free alternative for complex wound management. These nanoscale extracellular vesicles, typically 30-200 nm in diameter, mediate intercellular communication by transferring bioactive cargo—including proteins, lipids, and nucleic acids—to recipient cells, thereby modulating wound healing processes [89] [2]. While exosomes can be isolated from various MSC sources, the cellular origin fundamentally determines their molecular composition and functional properties [89] [90]. This review systematically compares the therapeutic efficacy of exosomes derived from two prominent MSC sources: bone marrow (BMSCs) and adipose tissue (ADSCs), within the context of wound repair. Understanding these source-specific differences is critical for researchers and drug development professionals selecting optimal exosome producers for targeted therapeutic applications in preclinical wound models.
Comparative Efficacy: BMSC-Exos vs. ADSC-Exos in Wound Healing
Functional Specialization by Cellular Source
Extensive preclinical investigations reveal that BMSC-exos and ADSC-exos exhibit distinct functional specializations that influence their wound healing capabilities. These differences stem from their inherent biological roles and the unique molecular cargo they carry.
ADSC-Exos: Enhanced Wound Closure and Immunomodulation A comprehensive meta-analysis of 83 preclinical studies demonstrated that ADSC-exos showed the best effect on wound closure rate and collagen deposition compared to those from other MSC sources [5]. This superior performance in epithelial repair is linked to their robust ability to promote fibroblast migration and proliferation [91]. Furthermore, ADSC-exos are particularly associated with superior anti-inflammatory properties and immune regulatory functions, creating a favorable microenvironment for healing by modulating macrophage polarization toward the regenerative M2 phenotype [90] [92].
BMSC-Exos: Superior Angiogenic Potential In contrast, the same meta-analysis found that BMSC-exos displayed better outcomes in revascularization, a critical process for supplying nutrients and oxygen to healing tissues [5]. This aligns with their characterization as a "gold standard" with proven osteogenic and angiogenic efficacy, carrying potent factors like VEGF and FGF-2 that directly stimulate blood vessel formation [90].
Molecular Cargo Underlying Functional Differences
The distinct therapeutic profiles of BMSC and ADSC exosomes are dictated by their specific molecular cargo, which programs recipient cells to execute different aspects of the wound healing program.
Table 1: Key Molecular Cargo in BMSC-Exos vs. ADSC-Exos Influencing Wound Healing
| Cargo Type | Bone Marrow MSC-Exos | Adipose-Derived MSC-Exos |
|---|---|---|
| Osteogenic Proteins | BMP-2, RUNX2, OSX [90] | BMP-2, TGF-β1 [90] |
| Angiogenic Factors | VEGF, FGF-2 [90] | VEGF, FGF-2 [90] |
| Immunoregulatory Molecules | miR-27a [90] | miR-21, miR-451a (Superior anti-inflammatory profile) [90] |
| Key microRNAs (miRNAs) | miR-196a [90] | miR-125a-3p, miR-19, miR-486-5p (Promote cell migration & proliferation) [13] |
This cargo differential translates into activation of distinct signaling pathways in target cells. ADSC-exos frequently mediate their effects through modulation of the Wnt/β-catenin and PI3K/Akt pathways, which are crucial for cell survival, proliferation, and migration [15]. They can also promote fibroblast function and wound healing-related gene expression under high-glucose conditions that mimic diabetic wounds [91] [93].
Experimental Data and Preclinical Evidence
Quantitative Efficacy Metrics from Animal Studies
Robust preclinical data from animal models, primarily murine diabetic wound studies, provides quantitative validation of the therapeutic efficacy of both exosome types. The table below summarizes key outcomes from controlled experiments.
Table 2: Summary of Preclinical Efficacy Data in Wound Healing Models
| Exosome Source | Animal Model | Key Efficacy Findings | Administration & Optimal Dose |
|---|---|---|---|
| Human ADSC-Exos | Diabetic (db/db) mice [93] | Significantly greater wound closure by day 10; Enhanced dermal regeneration [93] | Local/subcutaneous; 200 μg exosomal protein per wound [13] |
| Human ADSC-Exos | Mouse wound healing models (Meta-analysis) [13] | SMD 1.42 (95% CI: 1.14-1.71) in improved wound closure vs. controls [13] | Subcutaneous injection; 100-200 μg/mL concentration [13] |
| MSC-Exos (Various) | Diabetic & non-diabetic animal models (Meta-analysis) [5] | ADSC-Exos best for wound closure; BMSC-Exos best for revascularization [5] | Subcutaneous injection showed superior outcomes vs. dressing/covering [5] |
| Rat BMSC-Exos | Sciatic nerve crush injury model [89] | Promoted neural repair and regeneration (indicator of broader regenerative capacity) [89] | In vitro administration; 0.9 × 10^10 particles/mL [89] |
Factors Influencing Therapeutic Outcomes
Beyond cellular source, several critical factors influence exosome efficacy, requiring careful experimental control.
- Donor Age and Health Status: Exosomes derived from older BMSCs exhibit diminished effects in osteogenic and lipogenic abilities compared to those from younger donors [89]. Infant-derived ADSC-exos have demonstrated enhanced effects on cell proliferation, migration, and wound regeneration compared to adult-derived exosomes [93].
- Production and Preconditioning: Hypoxia preconditioning can upregulate pro-angiogenic factors in MSCs, improving their exosomes' abilities to promote neovascularization and tissue repair [89]. For instance, hypoxic adult ADSC-exos showed superior early wound closure in diabetic mice [93].
- Dosage and Administration: The therapeutic dose commonly ranges from 10 to 100 μg of exosomal protein in mouse models, but efficacy is dose-dependent and non-linear [89]. Subcutaneous injection has demonstrated greater improvement in wound closure compared to topical dressing/covering [5].
Methodological Framework: From Exosome Isolation to Functional Validation
Standardized Experimental Workflow
A typical preclinical experiment to evaluate exosome efficacy in wound healing follows a multi-stage workflow, encompassing isolation, characterization, and functional validation. The diagram below outlines this standardized process.
Key Signaling Pathways in Exosome-Mediated Wound Repair
Exosomes from different sources orchestrate wound healing by modulating complex signaling networks in target cells. The following diagram illustrates the key pathways involved, highlighting areas where BMSC-exos and ADSC-exos may have distinct mechanistic roles.
Successful investigation into exosome biology and therapeutic application requires specific reagents and methodologies. The following table details key solutions used in the featured research.
Table 3: Essential Research Reagents and Resources for Exosome Studies
| Reagent/Resource | Function/Application | Examples from Literature |
|---|---|---|
| Exosome-Depleted FBS | Essential component of cell culture medium to prevent contamination with bovine exosomes during production. | Prepared by ultracentrifugation or filtration through 100-kDa filters [93]. |
| Isolation Kits & Systems | Enable extraction and concentration of exosomes from conditioned medium. | Ultracentrifugation (most common), Tangential Flow Filtration (TFF) for scale-up, Size Exclusion Chromatography (SEC) for high purity [89] [90] [91]. |
| Characterization Instruments | Critical for confirming exosome identity, size, concentration, and purity per MISEV guidelines. | NTA (Nanoparticle Tracking Analysis) for size/concentration; TEM (Transmission Electron Microscopy) for morphology; Western Blot for markers (CD9, CD63, CD81) [90] [91] [93]. |
| In-house Exosome Collection Media | Serum-free, defined media formulations that support cell viability while maximizing exosome yield and purity. | VSCBIC-3 solution used in 3D cultures increased exosome yield by 2.4-fold and concentration by 3.2-fold compared to conventional 2D protocols [91]. |
| Animal Wound Models | Preclinical systems for evaluating exosome therapeutic efficacy in vivo. | db/db mice (model for impaired diabetic healing); full-thickness excisional wounds in rodents [5] [93]. |
The collective evidence demonstrates a clear functional dichotomy between BMSC-exos and ADSC-exos in wound repair. ADSC-exos demonstrate superior performance in driving wound closure and modulating inflammation, making them particularly suitable for chronic wounds characterized by excessive inflammation and impaired epithelialization. In contrast, BMSC-exos exhibit enhanced angiogenic potential, positioning them as promising candidates for wounds with compromised vascularity. For drug development professionals, this source-specific efficacy underscores the importance of a targeted, pathology-driven approach when selecting an exosome source for therapeutic development. Future research priorities include standardizing isolation protocols, optimizing preconditioning strategies to enhance inherent strengths, and developing engineered exosomes that combine the most desirable attributes of both sources for next-generation wound therapeutics.
Exosomes derived from mesenchymal stem cells (MSCs) are at the forefront of regenerative medicine, acting as critical mediators of intercellular communication by transferring bioactive molecules, including proteins and microRNAs (miRNAs), to recipient cells [94] [3]. Their molecular cargo is not generic; it is intrinsically shaped by the cellular source of the parent MSCs [95]. This source-dependent variation in cargo profile directly influences the biological functions and therapeutic potential of the exosomes, making the choice of MSC source a critical determinant for specific clinical applications, particularly in preclinical wound models [96].
The growing interest in exosome-based therapeutics is reflected in the market, which is projected to grow at a CAGR of 41.1% and reach $1.4 billion by 2040, underpinned by over 120 therapeutic candidates in development [97]. This rapid translation from bench to bedside necessitates a rigorous, comparative understanding of exosome molecular signatures. This guide provides a detailed, objective comparison of the miRNA and protein cargo profiles of exosomes derived from various human and animal MSC sources, synthesizing current experimental data to inform research and development strategies.
Comparative miRNA Cargo Profiles by MSC Source
MicroRNAs are key regulatory components of exosome cargo, capable of modulating gene expression in recipient cells. Comparative analysis reveals significant differences in miRNA profiles between exosomes from different MSC sources.
Table 1: Key miRNA Signatures and Their Putative Functions by MSC Source
| MSC Exosome Source | Highly Expressed miRNAs | Putative Target Genes & Pathways | Experimental Model & Key Functional Outcomes |
|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | miR-16-5p, miR-25-3p, miR-93-5p, and 14 other highly expressed miRNAs [95]. | MAN2A1, ZNFX1, PHF19; involved in cell growth, bone ossification, and cartilage development via MAPK signaling [95]. | Model: Human articular chondrocytes (hACs) [95]. Outcome: Promoted cartilage matrix formation (GAG, COL2A1), downregulated fibrocartilage matrix (COL1), and prevented senescence. Exhibited lower efficacy compared to BMSC-Exos [95]. |
| Bone Marrow MSCs (BMSCs) | miR-16-5p, miR-25-3p, miR-93-5p, and 8 other highly expressed miRNAs [95]. | Overlap with ADSC-Exos; 7 shared miRNAs. Putative targets include GPR137C, ENPP5, FNIP1; involved in MAPK pathway [95]. | Model: Human articular chondrocytes (hACs) [95]. Outcome: Greatest effect on maintaining hAC viability, preventing senescence, and promoting functional extracellular matrix formation [95]. |
| Adipose Tissue MSCs (ADSCs) | miR-16-5p, miR-25-3p, miR-93-5p, and 10 other highly expressed miRNAs [95]. | Overlap with BMSC-Exos; 7 shared miRNAs. Putative targets include B3GALT2, PKD2, FBXW7 [95]. | Model: Human articular chondrocytes (hACs) [95]. Outcome: Similar efficacy to BMSC-Exos in promoting normal chondrocyte function [95]. |
| Umbilical Cord MSCs (UC-MSCs) | Mechanism involves miRNAs targeting P38, ERK, AKT, HDAC3, and NF-κB pathways [98]. | Reduces IL-6 and MMP13; increases COL2A1 [98]. | Models: Mouse chondrocytes, mouse OA model, human clinical trial [98]. Outcome: Reduced inflammation, promoted cartilage regeneration, demonstrated safety and efficacy in OA patients [98]. |
A seminal 2025 study directly comparing hiPSC-Exos, hBMSC-Exos, and hADSC-Exos revealed that while hBMSC-Exos and hADSC-Exos have highly similar miRNA profiles, they are largely different from hiPSC-Exos [95]. Only three miRNAs—hsa-miR-16-5p, hsa-miR-25-3p, and hsa-miR-93-5p—were found to overlap among all three exosome types, suggesting a common core regulatory network. The putative target genes of these overlapping miRNAs are involved in critical processes such as cell growth, bone ossification, and cartilage development, potentially via the MAPK signalling pathway [95].
Protein Cargo and Functional Implications
The protein cargo of MSC-derived exosomes includes surface markers, enzymes, cytokines, and growth factors that define their biological identity and therapeutic function.
Table 2: Characteristic Protein Cargo and Functional Roles
| Protein / Marker Category | Specific Examples | Functional Role in Exosome Biology & Therapy |
|---|---|---|
| Universal Exosome Markers | CD9, CD63, CD81, TSG101 [98] [99]. | Define exosome identity; used for identification and isolation. CD63 and CD9 are highly enriched in exosomes and play roles in biogenesis and cargo sorting [98] [99]. |
| MSC-Specific Markers | CD73, CD90, CD105 [98]. | Identify the exosomes' origin from mesenchymal stem cells; negative for hematopoietic markers (CD34, CD45, HLA-DR) [98]. |
| Functional Proteins (e.g., in UC-MSC-Exos) | CCR2, CCL2 [98]. | Mediate immunomodulatory effects. For example, CCR2 on exosomes can bind and inhibit the pro-inflammatory chemokine CCL2, preventing macrophage accumulation and reducing inflammation [98]. |
The protein composition is heavily influenced by the parent cell's state and environment. Exosomes produced by MSCs cultured with tumor cells or in a tumor microenvironment can have altered content, highlighting the importance of careful production control for therapeutic applications [94].
Experimental Protocols for Cargo Analysis
Standardized and detailed methodologies are crucial for the isolation, characterization, and functional validation of MSC-exosomes and their cargo.
Exosome Isolation and Characterization
- Cell Culture: Source MSCs (e.g., from bone marrow, adipose tissue, umbilical cord) are cultured in media supplemented with exosome-depleted fetal bovine serum (de-Exo-FBS) to avoid contaminating bovine exosomes [95]. For UC-MSCs, cells are isolated from Wharton's jelly and characterized by flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) markers [98].
- Isolation: A common method is differential ultracentrifugation, where conditioned media is sequentially centrifuged at low speeds (e.g., 2,000 × g) to remove cells and debris, followed by high-speed centrifugation (e.g., 100,000 × g) to pellet exosomes [95] [98].
- Characterization: Isolated exosomes must be identified using multiple techniques:
- Nanoparticle Tracking Analysis (NTA) or Dynamic Light Scattering (DLS): To determine the vesicle size distribution (typically 50-200 nm) [98].
- Transmission Electron Microscopy (TEM): To confirm a cup-shaped or spherical morphology with a lipid bilayer [98].
- Western Blot: To detect the presence of positive protein markers (e.g., CD9, CD63, TSG101) and the absence of negative markers (e.g., Calnexin/CALN) [98].
miRNA Profiling and Functional Analysis
- miRNA Extraction and Sequencing: Total RNA is extracted from exosomes. Next-generation sequencing (NGS) is employed for unbiased, high-throughput profiling of miRNA expression [95].
- Bioinformatics Analysis: Sequencing data is processed to identify differentially expressed miRNAs. Their putative target genes and involved pathways (e.g., GO and KEGG pathways) are predicted using specialized software and databases [95].
- Functional Validation in Preclinical Models: The biological effect of exosomes is tested in relevant disease models.
- In Vitro Models: Chondrocytes stimulated with IL-1β are treated with exosomes, and the expression of inflammatory markers (IL-6, MMP13), anabolic markers (COL2A1), and senescence assays are analyzed [95] [98].
- In Vivo Models: For wound healing and OA, animal models (e.g., mouse OA model induced by surgery) are used. Exosomes are administered via intra-articular injection, and outcomes are assessed through histological scoring, immunohistochemistry, and behavioral pain tests [95] [98]. The diagram below illustrates a typical experimental workflow from exosome isolation to functional analysis.
Key Signaling Pathways in Wound Healing and Regeneration
MSC-exosomes exert their therapeutic effects by modulating key signaling pathways in recipient cells. The following diagram synthesizes the primary pathways implicated in wound healing and cartilage repair, as evidenced by the search results.
The Scientist's Toolkit: Essential Research Reagents
Successful research into MSC-exosome cargo and function relies on a suite of essential reagents and tools.
Table 3: Key Research Reagent Solutions for Exosome Studies
| Reagent / Tool | Function & Application | Specific Example / Note |
|---|---|---|
| Exosome-Depleted FBS | Essential for cell culture to produce exosomes without contaminating bovine vesicles, ensuring pure isolate for downstream analysis [95]. | Widely available from major biological suppliers. |
| Isolation Kits & Reagents | Consumables for efficient separation and purification of exosomes from cell culture media or biofluids [100]. | Kits based on precipitation, size-exclusion chromatography, or immunoaffinity (e.g., using CD63/CD81 beads). |
| Characterization Antibodies | Validate exosome identity and parent cell source via Western Blot or Flow Cytometry [98]. | Anti-CD9, CD63, CD81 (universal); Anti-CD73, CD90, CD105 (MSC-specific). |
| miRNA Sequencing Kits | For comprehensive profiling of exosomal miRNA content. Allows discovery of source-specific signatures [95]. | Includes RNA extraction, library prep, and NGS kits. |
| Pathway-Specific Assays | Quantify functional outcomes of exosome treatment in vitro (e.g., inflammation, matrix synthesis, apoptosis) [95] [98]. | ELISAs for cytokines (IL-6, TNF-α), qPCR for gene expression (COL2A1, MMP13), cell viability/toxicity assays. |
The molecular signature of MSC-derived exosomes is a defining feature that varies significantly with the cellular source. Human BMSC- and ADSC-Exos show highly similar miRNA profiles, distinct from iPSC-Exos, correlating with differential functional outcomes in preclinical models [95]. Furthermore, source-specific cargo, such as the immunomodulatory protein CCR2 in UC-MSC-Exos, enables targeted therapeutic effects [98]. This comparative analysis underscores that there is no single "best" source; rather, the optimal MSC-exosome source must be selected based on the specific pathological mechanisms and tissue targets of the intended application. As the field advances toward clinical translation, a deeper understanding of these molecular signatures will be paramount for engineering the next generation of precise and effective exosome-based therapeutics.
Exosomes, nanoscale extracellular vesicles (30-150 nm) secreted by virtually all cell types, have emerged as a pivotal therapeutic tool in regenerative medicine due to their role in intercellular communication [101] [102]. These vesicles transport bioactive cargo—including proteins, lipids, and nucleic acids—between cells, modulating recipient cell functions [102]. Mesenchymal stem cell (MSC)-derived exosomes are particularly promising, combining the therapeutic benefits of parent cells with advantages of a cell-free system, including reduced immunogenicity and avoidance of risks associated with whole-cell transplantation [103] [104]. As the field progresses toward clinical applications, a critical consideration is whether the cellular origin of exosomes influences their safety and immunogenicity profiles. This review synthesizes current preclinical evidence to objectively compare these essential parameters across exosomes derived from various human and animal MSC sources, providing a foundation for informed therapeutic development.
Exosome Biogenesis and Sourcing
Biogenesis and Isolation
Exosomes originate from the endosomal pathway. The process begins with the inward budding of the plasma membrane to form early endosomes, which mature into late endosomes and subsequently become multivesicular bodies (MVBs) containing intraluminal vesicles [101] [102]. These MVBs either fuse with lysosomes for degradation or with the plasma membrane to release their vesicular contents as exosomes into the extracellular space [101]. This intricate biogenesis pathway packages exosomes with specific biomolecules that reflect their cellular origin and determine their functional capacity.
Common isolation methods include ultracentrifugation, size-exclusion chromatography, precipitation techniques, and tangential flow filtration [101] [89]. The choice of isolation strategy significantly impacts exosome purity, yield, and biological activity, necessitating careful selection based on the intended application [101].
MSCs can be isolated from multiple tissue sources, each with distinct practical and biological considerations:
- Human Umbilical Cord (hUC): Sourced from Wharton's jelly, these MSCs are obtained non-invasively, exhibit robust proliferation, and demonstrate strong immunomodulatory properties [64] [103].
- Human Adipose Tissue (hAD): Isolated from lipoaspirates, adipose-derived MSCs offer high yield from readily accessible tissue [89] [105].
- Human Bone Marrow (hBM): The classic source of MSCs, though harvesting is invasive and cell numbers decline with donor age [89] [103].
- Xenogeneic Sources: Animal-derived MSCs, typically from porcine or murine adipose tissue or bone marrow, are explored to address human tissue scarcity for research and potential therapeutic scaling [105].
The following diagram illustrates the workflow from MSC sourcing to exosome characterization, highlighting key decision points that influence the final therapeutic product.
Comparative Safety and Immunogenicity Data
Rigorous preclinical evaluations are essential for establishing the safety profile of exosome therapeutics. The following table summarizes key findings from recent in vivo safety studies.
Table 1: Comparative Safety Profiles of MSC-Derived Exosomes from Different Sources
| Exosome Source | Experimental Model | Administration Route & Dose | Key Safety Findings | Reference |
|---|---|---|---|---|
| Human Umbilical Cord (hUC) | C57BL/6 mice | Intravenous; 6×1010 particles | No significant changes in body weight, feed intake, blood composition, organ indices, or histopathology over 14 days. | [64] |
| Human Umbilical Cord (hUC) | Mouse AMI model | Intravenous; 400 µg protein | No hemolysis, no adverse effects on liver/renal function, stable body temperature and heart rate. | [104] |
| Human Adipose (hAD) | 129-S1 mice (RAS model) | Intra-aortic; 20 µg protein | No discernible kidney rejection; no significant intrarenal T-cell or macrophage infiltration. | [105] |
| Porcine Adipose (pAD) | 129-S1 mice (RAS model) | Intra-aortic; 20 µg protein | Decreased renal inflammation; no detailed rejection data provided. | [105] |
Immunogenicity Profiles
Immunogenicity—the potential to provoke an unwanted immune response—is a critical parameter for therapeutic exosomes. The table below compares immunogenic responses reported across different exosome sources.
Table 2: Comparative Immunogenicity Profiles of MSCs and Their Exosomes
| Cell/Vesicle Source | Experimental Model | Immune Response Findings | Key Implications | Reference |
|---|---|---|---|---|
| Human MSCs (Xenogeneic) | 129-S1 mice | Significantly increased circulating anti-human antibodies. | Highlights humoral response risk with repeated whole-cell doses. | [105] |
| Human MSC-EVs (Xenogeneic) | 129-S1 mice | Altered splenic B-cell levels (↑memory IgM+, ↓CD19+); No increased anti-human antibodies. | Suggests EVs are less immunogenic than parent MSCs. | [105] |
| General MSC-Exosomes | Preclinical Models | Inherent low immunogenicity due to lower MHC expression; reduced risk of immune rejection. | Favors exosomes over cell therapy for repeat dosing. | [103] |
The distinct immune responses elicited by human MSCs versus their daughter exosomes in a xenogeneic model can be visualized as follows, highlighting the different pathways of immune activation.
Factors Influencing Safety and Efficacy Beyond Cellular Source
The cellular origin is a primary determinant of exosome profile, but other factors significantly modulate safety and therapeutic outcomes.
- Donor Cell Condition: The age, health status, and preconditioning of donor MSCs critically influence exosome quality. Exosomes from older donors exhibit diminished regenerative capabilities compared to those from younger donors [89]. Preconditioning with factors like hypoxia can enhance exosome performance by upregulating pro-angiogenic cargo [89].
- Dosage and Administration Route: Therapeutic efficacy and potential side effects are dose- and route-dependent. In traumatic brain injury models, a medium dose (100 µg) of exosomes proved more effective than lower or higher doses [89]. The administration route—intravenous, local, or targeted—affects exosome distribution, with systemic delivery facing rapid clearance by the liver and spleen [89] [21].
- Isolation and Storage Methods: The choice of isolation technique impacts exosome purity, integrity, and consequently, their biological activity and safety [101] [89]. Storage conditions are equally critical; cryopreservation at -80°C is common, but freeze-thaw cycles can damage exosomes, while lyophilization offers room-temperature storage stability [89].
Experimental Protocols for Immunogenicity Assessment
To ensure the reliability and reproducibility of immunogenicity data, standardized experimental protocols are essential. The following workflow, based on a comprehensive study comparing human MSCs and their EVs [105], provides a robust framework for assessment.
The Scientist's Toolkit: Key Research Reagents
This table lists essential reagents and their functions for conducting immunogenicity and safety studies based on the cited protocols.
Table 3: Essential Research Reagents for Exosome Immunogenicity Evaluation
| Reagent / Kit | Specific Target / Use | Function in Experimental Protocol |
|---|---|---|
| Adipose Tissue Dissociation Enzyme Kit (Miltenyi) | Tissue Digestion | Dissociates adipose tissue to isolate viable MSCs for culture. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD34, CD45) | MSC Surface Markers | Identifies and validates isolated MSCs via positive/negative marker expression. |
| Nanoparticle Tracking Analysis (NTA) Instrument | Particle Size & Concentration | Characterizes isolated EVs by determining particle size distribution and concentration. |
| Imaging Flow Cytometer Antibodies (CD9, CD81, CD29, CD44) | EV Surface Markers | Confirms the presence of typical exosome surface tetraspanins and MSC markers. |
| Immunofluorescence Antibodies (CD3, F4/80, CD19, IgM) | Immune Cell Staining | Detects and quantifies specific immune cell populations in tissue (kidney, spleen). |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Cytokines & Antibodies | Quantifies levels of specific cytokines (e.g., IFN-γ) and anti-xenogeneic antibodies in serum. |
The comprehensive analysis of current preclinical data indicates that MSC-derived exosomes present a favorable safety profile with significantly lower immunogenicity compared to their parent cells. This is largely attributed to their lower expression of major histocompatibility complexes [103] [105]. Among the different sources, human umbilical cord MSC-derived exosomes demonstrate a particularly robust record in safety evaluations, showing no significant toxicity or immunopathological changes in murine models [64] [104]. While xenogeneic sources offer a practical solution for scaling production, their immunogenic potential, particularly the humoral response to whole cells, necessitates careful evaluation [105]. The overall risk-benefit assessment, coupled with the advantage of avoiding the risks of whole-cell therapy, strongly supports the continued development of exosome-based therapeutics. Future work must focus on standardizing isolation protocols, establishing dose-response relationships, and conducting long-term chronic toxicity studies to fully realize the clinical potential of this promising cell-free technology.
The transition from promising preclinical results to robust clinical trial design represents a critical juncture in therapeutic development. For mesenchymal stem cell (MSC)-derived exosomes, this transition is occurring within the context of a rapidly evolving paradigm in regenerative medicine. While MSCs themselves have demonstrated significant therapeutic potential, their cell-free derivatives—particularly exosomes—offer distinct advantages for clinical translation, including lower immunogenicity, enhanced stability, and reduced risks of tumorigenicity and infusion toxicity [62] [106] [22].
The fundamental question facing researchers and drug development professionals is how to effectively bridge the gap between promising animal studies and well-designed human trials. This challenge is particularly pronounced when considering the source variables of MSC exosomes—specifically, the comparative efficacy and mechanistic profiles of human versus animal-derived exosomes in preclinical wound healing models. As the field moves toward clinical application, understanding these variables becomes paramount for designing trials that can accurately assess therapeutic potential while accounting for source-specific characteristics [5] [107].
This review systematically compares human and animal-source MSC exosomes in preclinical wound healing research, with particular emphasis on their therapeutic efficacy, mechanistic underpinnings, and implications for clinical trial design. By synthesizing current evidence and highlighting methodological considerations, we aim to provide a framework for advancing exosome-based therapies from validation to clinical application.
Therapeutic Efficacy of MSC Exosomes in Preclinical Wound Healing
Quantitative Analysis of Wound Closure Outcomes
Comprehensive meta-analyses of preclinical studies provide compelling evidence for the therapeutic potential of MSC-derived exosomes in wound healing. A systematic review and meta-analysis of 83 preclinical studies demonstrated that MSC-exosome treatment significantly enhanced wound closure rates in both diabetic and non-diabetic animal models [5]. The analysis revealed consistent improvement across multiple wound healing parameters, with different MSC sources exhibiting distinct strength profiles.
Table 1: Comparative Efficacy of MSC-Exosome Sources in Preclinical Wound Models
| MSC Source | Wound Closure Rate | Collagen Deposition | Revascularization | Key Advantages |
|---|---|---|---|---|
| Adipose Tissue (ADSCs) | +++ (Best effect) | +++ (Best effect) | ++ | Enhanced closure & matrix remodeling |
| Umbilical Cord | ++ | ++ | +++ (Best effect) | Superior angiogenic potential |
| Bone Marrow (BMMSCs) | + | + | +++ (Best effect) | Strong vascularization capacity |
| Placenta | ++ | + | ++ | Consistent anti-inflammatory effects |
The quantitative synthesis indicates that adipose-derived MSC exosomes (ADSC-Exos) demonstrated the most significant effects on wound closure rate and collagen deposition, while umbilical cord and bone marrow-derived exosomes showed superior performance in revascularization outcomes [5]. This source-dependent efficacy profile has important implications for clinical trial design, suggesting that specific exosome sources may be preferred for different wound etiologies.
Comparative Performance of Apoptotic vs. Small Extracellular Vesicles
Beyond traditional exosomes, recent research has investigated the therapeutic potential of other extracellular vesicle types. Subgroup analyses from the same meta-analysis revealed that apoptotic small extracellular vesicles (ApoSEVs) demonstrated superior efficacy in wound closure outcomes and collagen deposition compared to small extracellular vesicles (sEVs) and apoptotic bodies (ApoBDs) [5]. Conversely, sEVs displayed better performance in revascularization, highlighting the functional specialization of different vesicle populations.
The route of administration also significantly influenced therapeutic outcomes. Subcutaneous injection demonstrated greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering approaches [5]. These findings underscore the importance of both vesicle selection and delivery method in optimizing therapeutic regimens for clinical translation.
Experimental Models and Methodologies
Preclinical Wound Models and Assessment Methods
The evaluation of MSC exosome efficacy has employed diverse animal models that recapitulate different aspects of human wound healing pathophysiology. The majority (73.5%) of included studies utilized mouse models, while rats represented 26.5% of models [5]. These models encompassed both non-diabetic (43.4%) and diabetic wounds (47.0%), with the latter including both streptozotocin-induced type 1 diabetes models and genetically modified db/db mice representing type 2 diabetes [5].
Table 2: Standardized Methodologies for MSC-Exosome Characterization & Functional Assessment
| Method Category | Specific Technique | Application/Function | Key Parameters Measured |
|---|---|---|---|
| Vesicle Characterization | Nanoparticle Tracking Analysis (NTA) | Size distribution & concentration | Size (30-150 nm), particle count [7] |
| Transmission Electron Microscopy (TEM) | Morphological assessment | Spherical, lipid bilayer structure [7] | |
| Immunoblotting | Marker protein detection | CD9, CD63, ALIX, TSG101 [7] | |
| Functional Assessment | Histopathological Analysis | Tissue architecture evaluation | Epidermal thickness, inflammation [7] |
| ELISA | Cytokine quantification | TNF-α, IL-6, IL-1β, IL-10 levels [21] | |
| Immunofluorescence Staining | Cellular localization | Cell proliferation, angiogenesis markers |
Full-thickness excisional wounds represented the most frequently studied model (90.4%), comprising primarily dorsal wounds with smaller proportions of diabetic foot ulcer and leg excisional wound models [5]. Additional specialized models included scleroderma, burns, photoaging, atopic dermatitis, and frostbite injury, demonstrating the breadth of conditions in which MSC exosome therapy has been investigated.
The Scientist's Toolkit: Essential Research Reagents and Materials
The standardization of experimental methodologies is crucial for generating comparable data across preclinical studies. The following toolkit outlines essential reagents and materials commonly employed in MSC exosome research for wound healing applications:
Table 3: Research Reagent Solutions for MSC-Exosome Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| MSC Culture Media | Cell expansion & exosome production | Serum-free conditioned media, often with growth factor supplements |
| Isolation Kits | Exosome purification from media | Ultracentrifugation systems, size-exclusion chromatography columns, polymer-based precipitation kits |
| Characterization Antibodies | Vesicle marker detection | Anti-CD9, CD63, CD81, ALIX, TSG101; Calnexin (negative marker) [7] |
| Animal Model Reagents | Disease model induction | Streptozotocin (diabetes), imiquimod (psoriasis), LPS (ALI) [7] [21] |
| Histology Reagents | Tissue analysis | H&E staining (general morphology), Masson's trichrome (collagen), CD31 immunohistochemistry (angiogenesis) |
These methodologies have been systematically applied across studies comparing human and animal-source MSC exosomes, allowing for direct comparison of therapeutic efficacy while controlling for technical variables. The consistency in assessment methods strengthens the conclusions drawn from meta-analyses and systematic reviews.
Molecular Mechanisms and Signaling Pathways
Key Pathways in Exosome-Mediated Wound Repair
MSC exosomes exert their therapeutic effects through complex molecular mechanisms involving the transfer of bioactive cargo to recipient cells. The diagram below illustrates the primary signaling pathways through which MSC exosomes promote wound healing:
Diagram: MSC exosomes promote wound healing through coordinated regulation of inflammatory response, angiogenesis, and extracellular matrix remodeling. Key pathways include NF-κB inhibition, VEGF signaling activation, and MMP/TIMP regulation.
The therapeutic effects of MSC exosomes are largely mediated through their cargo of microRNAs, proteins, and lipids. Specific miRNAs, including miR-21, miR-31, miR-125b, and miR-132, have been identified as key regulators of inflammatory responses, fibroblast function, and angiogenesis in wound healing [2]. These molecular components are transferred to recipient cells such as keratinocytes, fibroblasts, and endothelial cells, where they modulate gene expression and cellular behavior.
Source-Dependent Mechanistic Variations
Comparative analyses have revealed notable differences in the molecular mechanisms between human and animal-source MSC exosomes. While both sources demonstrate efficacy across multiple wound healing parameters, variations in miRNA profiles and protein cargo contribute to differential activation of signaling pathways [5]. Human umbilical cord-derived MSC exosomes have shown particularly robust anti-inflammatory effects through more potent inhibition of the NF-κB pathway and subsequent reduction in pro-inflammatory cytokines including TNF-α, IL-6, and IL-1β [21] [7].
Additionally, source-dependent variations in angiogenic potential have been documented. Umbilical cord and bone marrow-derived exosomes consistently demonstrate enhanced pro-angiogenic properties compared to those from adipose tissue, mediated through differential enrichment of VEGF, FGF, and miR-126 cargo [5]. These mechanistic distinctions underscore the importance of source selection based on the specific pathological features of target wound types.
Experimental Workflow: From Exosome Isolation to Functional Validation
The transition from preclinical findings to clinical applications requires rigorous, standardized experimental approaches. The following diagram outlines a comprehensive workflow for evaluating MSC exosome therapeutics in wound healing:
Diagram: Experimental workflow for evaluating MSC exosome therapeutics progresses from isolation and characterization through in vitro and in vivo functional validation, culminating in data synthesis for clinical trial design.
This systematic approach ensures comprehensive assessment of MSC exosome therapeutics while generating comparable data across studies. Standardization at each stage—particularly in characterization methodologies—is essential for generating robust preclinical data that can inform clinical trial design.
Clinical Translation: From Animal Models to Human Trials
Current Clinical Trial Landscape
The promising results from preclinical studies have catalyzed clinical translation efforts for MSC exosome therapies. A comprehensive review of global clinical trials registered between 2014 and 2024 identified 66 eligible trials investigating MSC-derived extracellular vesicles and exosomes [86]. These trials span diverse medical conditions, with a significant proportion focusing on wound healing and related pathologies.
Analysis of administration routes in registered trials reveals that intravenous infusion and aerosolized inhalation represent the predominant methods, with route selection often dictated by target pathology [86]. Notably, dose-effect relationship analyses indicate that nebulization therapy achieves therapeutic effects at significantly lower doses (approximately 10⁸ particles) compared to intravenous routes, suggesting route-dependent effective dose windows that must be considered in trial design [86].
Early-phase clinical trials have begun to report safety outcomes. A phase 1 study investigating topical application of MSC exosome ointment (PTD2021P) in healthy adult volunteers demonstrated favorable safety and tolerability profiles, with no treatment-related adverse events or clinically significant abnormalities reported [108]. These initial safety data provide important foundations for subsequent efficacy trials.
Considerations for Clinical Trial Design
The transition from preclinical validation to clinical trial design necessitates careful consideration of several key factors derived from animal studies:
Source Selection: Preclinical data suggest differential efficacy profiles based on MSC source [5]. Trial design should justify source selection based on the specific therapeutic goals—adipose sources for enhanced closure and matrix remodeling versus umbilical cord or bone marrow sources for vascularization-deficient wounds.
Dose Optimization: The established dose-dependent effects [21] and route-dependent efficacy [86] observed in preclinical studies highlight the importance of comprehensive dose-finding phases in clinical development programs.
Vesicle Characterization: The variations in efficacy between vesicle subtypes (e.g., ApoSEVs vs. sEVs) [5] underscore the necessity of rigorous characterization and standardization of investigational products.
Endpoint Selection: Preclinical findings suggest that functional outcomes (closure rate) and histological/molecular parameters (collagen deposition, revascularization) provide complementary efficacy measures [5]. Clinical trials should incorporate both macroscopic and microscopic endpoint assessments.
The methodological rigor employed in preclinical studies—including standardized isolation protocols, comprehensive characterization, and systematic outcome assessment—provides a template for clinical trial design that can maximize the likelihood of successful translation.
The collective evidence from preclinical studies provides compelling support for the therapeutic potential of MSC exosomes in wound healing. The comparative analyses between human and animal-source exosomes reveal both consistent therapeutic effects and source-dependent variations in efficacy profiles and mechanistic emphasis. These findings carry significant implications for clinical trial design, particularly in candidate selection, dose regimen determination, and endpoint specification.
As the field advances, several challenges remain to be addressed. The lack of standardized protocols for exosome isolation, characterization, and quantification contributes to heterogeneity in study outcomes and complicates cross-study comparisons [86] [107]. Additionally, the optimization of delivery methods, dose frequency, and long-term safety profiles requires further investigation in controlled clinical settings.
Nevertheless, the current body of evidence firmly supports MSC exosomes as a promising therapeutic modality for wound healing. By applying the insights gained from rigorous preclinical comparisons—including source-specific efficacy profiles, mechanistic understandings, and methodological standardizations—researchers and drug development professionals can design clinical trials that effectively bridge the gap between promising validation data and demonstrated clinical benefit.
Conclusion
The choice between human and animal-source MSC exosomes is a fundamental variable that critically influences the efficacy, reproducibility, and clinical translation potential of preclinical wound healing research. While human exosomes offer direct clinical relevance, animal sources provide practical and ethical advantages for initial discovery. Evidence indicates that the specific tissue source—be it bone marrow, adipose, or umbilical cord—imparts distinct functional cargo, leading to differences in therapeutic potency, such as the superior collagen type II expression observed with bone marrow-derived exosomes. Future progress hinges on standardizing isolation protocols, deepening our understanding of source-specific mechanisms, and advancing engineering strategies to create enhanced, targeted exosome therapeutics. A deliberate, evidence-based selection of exosome sources, guided by robust comparative data, is paramount for accelerating the development of reliable and effective cell-free therapies for wound management.
References
- 1. Stem cell derived exosome trilogy: an epic comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186388/]
- 2. Exosome as emerging therapeutic platform for wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004604]
- 3. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 4. Extracellular vesicles: cargo loading, degradation and ... [https://www.oaepublish.com/articles/evcna.2025.21]
- 5. Mesenchymal stem cells-derived small extracellular vesicles ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 6. Emerging role of exosomes in cancer therapy: progress and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02215-4]
- 7. A Murine Study and Meta-Analysis of Experimental Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467663/]
- 8. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 9. Wound healing and signaling pathways [https://www.degruyterbrill.com/document/doi/10.1515/biol-2025-1166/html?srsltid=AfmBOoqzx0zZvijbyhuP7C-ntfQhJjZMVfzD-dQgYFAr1UeT351VZtmH]
- 10. Efficacy of MSC-derived small extracellular vesicles in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1375632/full]
- 11. Comparative proteomic analysis of skin wound healing ... [https://pubmed.ncbi.nlm.nih.gov/40475439/]
- 12. Comparative proteomic analysis of skin wound healing ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225005861]
- 13. Exosome derived from human adipose‐derived stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10333007/]
- 14. Using Pre-Clinical Studies to Explore the Potential Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10519927/]
- 15. Adipose-derived stem cell exosomes: emerging roles and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637342/full]
- 16. Adipose-derived stem cell exosomes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181847/]
- 17. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1641709/full]
- 18. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 19. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://pubmed.ncbi.nlm.nih.gov/41255881/]
- 20. The Examination of the Effects of Exosomes Generated ... [https://pubmed.ncbi.nlm.nih.gov/40908697/]
- 21. Comparison of efficacy of exosomes derived from human ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1560915/full]
- 22. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 23. New therapeutic approaches of mesenchymal stem cells ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-021-00736-4]
- 24. Preclinical translation of exosomes derived ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7004029/]
- 25. Comparative analysis and characterization of soluble ... [https://www.sciencedirect.com/science/article/pii/S0165242718303350]
- 26. Exosome derived from human adipose-derived stem cell ... [https://pubmed.ncbi.nlm.nih.gov/37102269/]
- 27. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 28. Applications of mesenchymal stem cell-exosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319788/]
- 29. MSC-derived exosomes injectable hyaluronic acid ... [https://www.sciencedirect.com/science/article/pii/S0168365925006066]
- 30. Comparative Analysis of MSC-Derived Exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169723/]
- 31. Comparison of exosomes derived from induced pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7732275/]
- 32. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 33. Exosomes as natural vectors for therapeutic delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066514/]
- 34. A comprehensive review on recent advances in exosome ... [https://www.sciencedirect.com/science/article/pii/S1936523324002481]
- 35. Efficient methods of isolation and purification of extracellular ... [https://nanoconvergencejournal.springeropen.com/articles/10.1186/s40580-025-00509-x]
- 36. Comparative Proteomics of Seminal Exosomes Reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561774/]
- 37. Comparative analysis of exosomes isolated by ... [https://ui.adsabs.harvard.edu/abs/2025JNR....27...28M/abstract]
- 38. High throughput and rapid isolation of extracellular ... [https://www.sciencedirect.com/science/article/pii/S2452199X24003219]
- 39. A streamlined method for isolating and characterizing small ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-025-00040-9]
- 40. Mesenchymal stem cells from different sources and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7062037/]
- 41. Proteomic analysis of serum extracellular vesicles from ... [https://www.nature.com/articles/s41598-024-56036-y]
- 42. A 'torn bag mechanism' of small extracellular vesicle ... [https://elifesciences.org/articles/95828]
- 43. Mesenchymal stem cell-derived exosomes: A novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 44. Mesenchymal stromal/stem cell (MSC)-derived exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079493/]
- 45. Establishing a Working Range for Effective MSC-EV Dose [https://www.roosterbio.com/blog/establishing-a-working-range-for-effective-msc-ev-dose/]
- 46. Trends in mesenchymal stem cell-derived extracellular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 47. Dosing extracellular vesicles [https://www.sciencedirect.com/science/article/pii/S0169409X21003549]
- 48. Comparative analysis of extracellular vesicles isolated from ... [https://www.sciencedirect.com/science/article/abs/pii/S0014482722000908]
- 49. In vivo exosome imaging: applications of diverse visualization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402689/]
- 50. Recent Advances in Experimental Burn Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8231482/]
- 51. The Wound Reporting in Animal and Human Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11621255/]
- 52. Role of Exosomes in Dermal Wound Healing: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9400548/]
- 53. In vitro and in vivo evaluation of the diabetic wound healing ... [https://www.nature.com/articles/s41598-024-70010-8]
- 54. Comparison of In-Vitro and Ex-Vivo Wound Healing Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5207624/]
- 55. Development of an experimental heterogeneous burn ... [https://www.sciencedirect.com/science/article/abs/pii/S0305417924003437]
- 56. Advancing in vitro cell migration studies: a review of open- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006941/]
- 57. Crosstalk between tumor endothelial cells and cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533004/]
- 58. Comprehensive analysis of cellular metrics [https://www.nature.com/articles/s41420-025-02391-2]
- 59. Standardization of CFSE and Ki-67 based lymphocyte ... [https://www.medrxiv.org/content/10.1101/2025.08.12.25333468v1.full-text]
- 60. Tube Formation Assay | Experimental Workflow [https://ibidi.com/content/326-experimental-workflow]
- 61. Angiogenesis Analyzer for ImageJ — A comparative ... [https://www.nature.com/articles/s41598-020-67289-8]
- 62. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 63. The role of IGF-2 and its variants in enhancing endothelial ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1598705/full]
- 64. Immunological Safety Evaluation of Exosomes Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049250/]
- 65. Extracellular vesicle manufacture via FACTORY: fully ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925002598]
- 66. High‐Yield Production of Extracellular Vesicle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468747/]
- 67. Challenges and opportunities in exosome research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6481742/]
- 68. Toxicological evaluation of exosomes derived from human ... [https://www.sciencedirect.com/science/article/abs/pii/S0273230020301124]
- 69. Comparative analysis of human Mesenchymal Stromal Cells from Adipose Tissue and Dental Pulp: phenotypic characterization and secretome profiling | Biology Direct | Full Text [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-025-00697-w]
- 70. Frontiers | Alternatives of mesenchymal stem cell-derived exosomes as potential therapeutic platforms [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1478517/full]
- 71. Exosomes Derived from Induced and Wharton's Jelly-Derived Mesenchymal Stem Cells Promote Senescence-like Features and Migration in Cancer Cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/40649957/]
- 72. Bioengineered MSC-derived exosomes in skin wound repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009159/]
- 73. Potential upscaling protocol establishment and wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11950392/]
- 74. Wound Healing: Harnessing Extracellular Vesicles Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587863/]
- 75. Tissue engineering: Hydrogel scaffolds and mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868625003021]
- 76. Hydrogels and Wound Healing: Current and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815795/]
- 77. Biomimetic Hydrogels to Promote Wound Healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.718377/full]
- 78. Engineering Lignin‐Based Tubular Hydrogel Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548947/]
- 79. iPSC-, MSC- and iMSC-Derived Exosome Therapeutics [https://www.reprocell.com/blog/ipsc-msc-and-imsc-derived-exosome-therapeutics-the-cell-free-future-of-regenerative-medicine]
- 80. Five Exosome Biotechs to Watch: July 2025 [https://www.pharmasalmanac.com/articles/five-exosome-biotechs-to-watch-july-2025]
- 81. Mesenchymal Stem-Cell-Derived Exosomes and MicroRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249468/]
- 82. The role of natural exosomes from SHED-MSC in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1550280/full]
- 83. “Mesenchymal stem cell-derived exosomes (MSC- ... [https://www.sciencedirect.com/science/article/abs/pii/S0008874925000723]
- 84. Engineerable mesenchymal stem cell-derived extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04490-4]
- 85. Cellular uptake and in vivo distribution of mesenchymal ... [https://www.nature.com/articles/s41565-023-01585-y]
- 86. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 87. Comparison of efficacy of exosomes derived from human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159432/]
- 88. Advances in stem cell-derived exosome therapy for radiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626575/]
- 89. Exosome Source Matters: A Comprehensive Review from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858990/]
- 90. Exosome-based therapeutics in bone regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512519/]
- 91. Potential upscaling protocol establishment and wound ... [https://www.nature.com/articles/s41598-025-93219-7]
- 92. Therapeutic and Clinical Potential of Adipose-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610433/]
- 93. Wound healing effects of exosomes from hypoxia [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04636-4]
- 94. Concise Review: MSC -Derived Exosomes for Cell-Free Therapy [https://pubmed.ncbi.nlm.nih.gov/28294454/]
- 95. Comparisons of miRNA profiles of exosomes derived from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359900/]
- 96. Mesenchymal Stem Cell-derived Exosomes Hold Promise in the... [https://www.dovepress.com/mesenchymal-stem-cell-derived-exosomes-hold-promise-in-the-treatment-o-peer-reviewed-fulltext-article-IJN]
- 97. Exosome Therapeutics Market Report 2025: 120+ Drug ... [https://finance.yahoo.com/news/exosome-therapeutics-market-report-2025-124600609.html]
- 98. Injection of human umbilical cord mesenchymal stem cells exosomes ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06623-y]
- 99. Exosome-Based Drug Delivery: A Next-Generation Platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567338/]
- 100. Exosome Research Market Size, Trends & Forecast, 2025- ... [https://www.coherentmarketinsights.com/industry-reports/exosome-research-market]
- 101. The potential of exosomes in regenerative medicine and in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11966052/]
- 102. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 103. Mesenchymal stem cell-derived extracellular vesicles for ... [https://www.nature.com/articles/s41419-022-05034-x]
- 104. Safety evaluation of exosomes derived from human ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324915011500]
- 105. Immune rejection of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079651/]
- 106. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 107. Current status and future prospects of mesenchymal stem cell ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01813-0]
- 108. A phase 1, open-label study to determine safety and ... [https://www.sciencedirect.com/science/article/pii/S1465324925000313]