Stem Cell Conditioned Medium and Extracellular Vesicles: The Next Frontier in Myocardial Protection and Repair
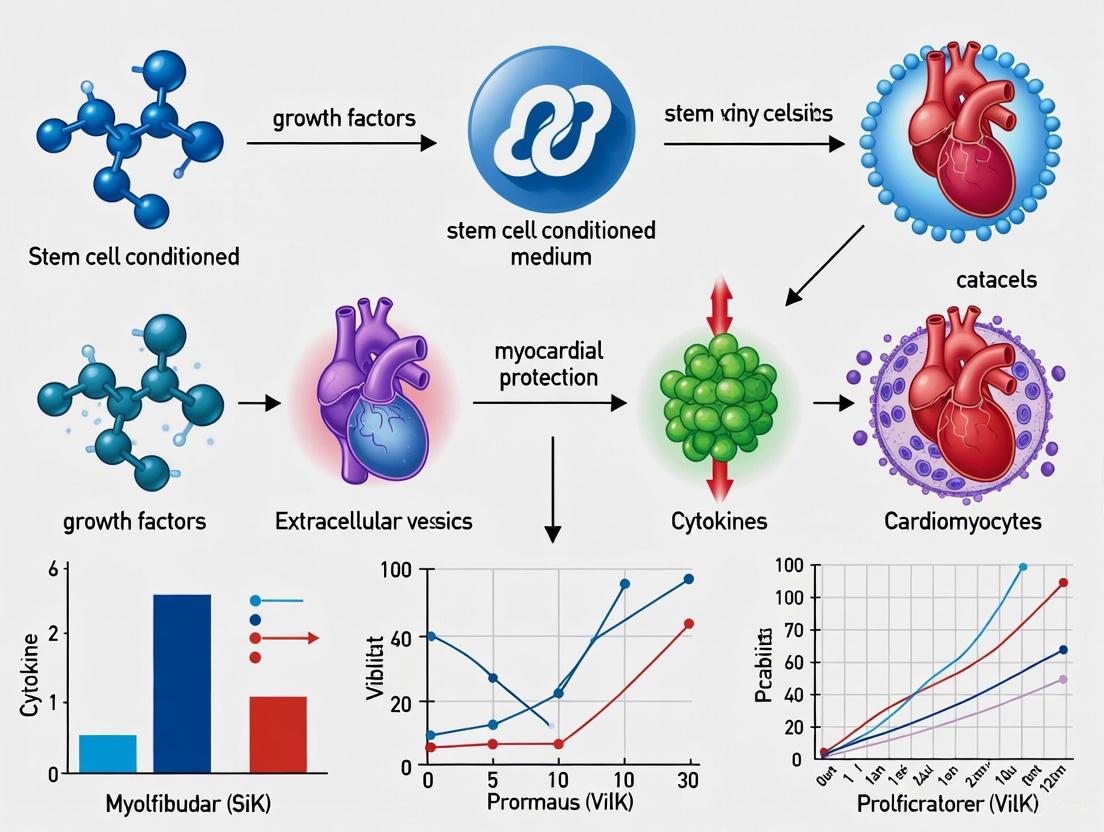
This article synthesizes current research on stem cell-conditioned medium (CM) as a novel cell-free therapy for myocardial protection.
Stem Cell Conditioned Medium and Extracellular Vesicles: The Next Frontier in Myocardial Protection and Repair
Abstract
This article synthesizes current research on stem cell-conditioned medium (CM) as a novel cell-free therapy for myocardial protection. It explores the foundational science behind CM's cardioprotective effects, primarily mediated through paracrine factors and extracellular vesicles (EVs). We detail methodological approaches for CM production and application, address key challenges in the field such as standardization and scalability, and provide a comparative analysis of CM from different mesenchymal stem cell (MSC) sources. Aimed at researchers and drug development professionals, this review highlights the significant potential of CM to overcome the limitations of direct cell transplantation, offering promising strategies for reducing infarct size, inhibiting apoptosis and fibrosis, and improving cardiac function after ischemic injury.
The Science of Secretomes: Unraveling the Paracrine Mechanisms of Cardiac Repair
Cardiovascular disease (CVD) consistently ranks as the leading cause of death worldwide, with heart failure due to ischemic myocardial infarction (MI) being a primary contributor to high CVD-associated mortality [1] [2]. Despite substantial healthcare expenditures (approximately US$43 billion in 2020 in the USA alone), the post-diagnosis 5-year survival rate for heart failure remains merely 50% [1] [2]. Current pharmacological therapies and mechanical devices primarily manage symptoms and slow disease progression but fail to address a fundamental pathological driver: the massive loss of cardiomyocytes (CMs) following MI [1] [3] [2]. The adult human heart contains about 3.2 billion CMs with an annual turnover rate of less than 1%, yet a single acute MI event can cause the death of approximately 1 billion CMs [1] [2]. This staggering cell loss creates a regenerative deficit that current treatments cannot reverse, making heart transplantation the only definitive cure for end-stage heart failure, with its associated limitations of cost, donor availability, and need for lifelong immunosuppression [1] [2].
The recognition of this fundamental therapeutic gap has driven the exploration of regenerative approaches over the past two decades. Initial enthusiasm focused on cell-based therapies using various stem cell types to directly replace lost cardiomyocytes and vasculature [1] [3] [4]. However, consistent challenges including poor cell survival, limited engraftment, arrythmogenesis, and modest functional benefits have prompted a strategic reevaluation [1] [3]. This has catalyzed a paradigm shift toward cell-free therapies that harness the paracrine secretions of therapeutic cells, particularly stem cell-derived conditioned media and extracellular vesicles, to stimulate endogenous repair mechanisms without the risks of whole-cell transplantation [1] [3] [5]. This review comprehensively examines this scientific evolution, focusing on the therapeutic potential of stem cell conditioned medium for myocardial protection and regeneration.
The Limitations of Cell-Based Cardiac Regeneration
Historical Context and Clinical Outcomes
Cell therapy for cardiac repair emerged from the compelling premise that introducing exogenous cells could directly repopulate infarcted myocardium with functional cardiomyocytes and vasculature [4]. First-generation clinical trials investigated diverse cell sources including skeletal myoblasts, endothelial cells, cardiac progenitor cells (CPCs), cardiosphere-derived cells (CDCs), and mesenchymal stem cells (MSCs) [1] [2]. Human mesenchymal stem cells (MSCs), distinguished for their proangiogenic, anti-inflammatory, and cardiogenic-differentiation potential, have been extensively investigated for cardiac repair [1] [2]. Some MSC-based clinical trials (POSEIDON, PROMETHEUS) demonstrated improved cardiac functionality without arrythmia [1] [2]. The advent of human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs) further revolutionized the landscape, offering a theoretically unlimited source of cardiomyocytes for transplantation [1] [2].
Despite promising preclinical results and initial clinical enthusiasm, meta-analyses of clinical trials reveal that cell-based therapies typically provide only marginal improvements in left ventricular ejection fraction (LVEF) of 2-5% compared to placebo [3]. Moreover, complications including cardiac arrythmias and potential graft rejections continue to present significant clinical challenges [1] [2]. The transplantation of hPSC-CMs in both murine models and human patients often leads to arrythmias and poor in vivo retention [1] [2]. These limitations fundamentally redirected scientific attention toward understanding the mechanisms underlying the observed benefits and exploring alternative therapeutic strategies.
Fundamental Challenges of Cell Therapy
Several intrinsic challenges have hampered the clinical translation of cell-based cardiac regeneration:
- Poor Cell Survival and Retention: The ischemic, inflammatory myocardial environment post-MI is profoundly hostile to transplanted cells. Quantitative studies indicate that only approximately 5% of transplanted cells remain in the heart after 2 hours, declining to a mere 1% after 20 hours [3]. This catastrophic cell loss severely limits potential direct regenerative benefits.
- Immature Phenotype of Laboratory-Grown Cardiomyocytes: In vitro-differentiated hPSC-CMs structurally and functionally resemble neonatal rather than adult cardiomyocytes, exhibiting different electrophysiological properties, calcium handling, and metabolic characteristics [1] [2]. This immaturity contributes to arrhythmogenesis and poor functional integration with host myocardium.
- Tumorigenic and Immunogenic Risks: Although MSCs exhibit immunoprivileged properties, cells derived from pluripotent sources (ESCs and iPSCs) carry a risk of teratoma formation if undifferentiated pluripotent cells remain in the population [3] [4]. Allogeneic cell transplantation also raises concerns about immune rejection, necessitating immunosuppression with its associated complications.
- Logistical and Manufacturing Hurdles: Cell-based therapies face substantial challenges in scalability, quality control, storage, transportation, and timing of administration, particularly in acute MI settings where immediate treatment is crucial [5] [4].
The Paradigm Shift: Mechanisms of Cell-Free Cardiac Repair
The Paracrine Hypothesis
The consistent observation that functional benefits from cell therapy occurred despite minimal long-term engraftment led to the formulation of the paracrine hypothesis [3] [6]. This proposes that transplanted cells exert their therapeutic effects primarily through the secretion of bioactive molecules that modulate host pathways, rather than through direct differentiation and integration [3]. These secreted factors create a regenerative microenvironment that attenuates injury pathways, promotes endogenous repair mechanisms, and modulates destructive immune responses [6] [7] [5]. This conceptual breakthrough redirected therapeutic focus from the cells themselves to their secretory products, opening the door to cell-free approaches utilizing conditioned media (CM) and extracellular vesicles (EVs) [1] [3] [5].
Key Bioactive Components of Conditioned Media
Conditioned media derived from therapeutic stem cells contains a complex mixture of bioactive factors that collectively mediate cardioprotection:
- Growth Factors: Conditioned media from various stem cell sources contains identified cardioprotective growth factors including hepatocyte growth factor (HGF), vascular endothelial growth factor (VEGF), insulin-like growth factor 1 (IGF-1), and basic fibroblast growth factor (bFGF) [6] [7] [5]. Comparative analyses reveal that HGF is significantly more highly expressed in dental pulp-derived stem cell conditioned media (SHED-CM) compared to bone marrow or adipose-derived stem cell CM, correlating with superior anti-apoptotic activity [5].
- Extracellular Vesicles: EVs are cell-derived, nano-sized, cargo-containing biomolecules that have emerged as potent alternatives to cell-based cardiac regeneration therapy [1] [3]. These membrane-enclosed particles are broadly categorized into exosomes (50-150 nm), microvesicles (150-1000 nm), and apoptotic bodies (1000-5000 nm) based on their biogenesis pathway [1] [2]. Recent guidelines suggest referring to EVs based on size (small EVs: 50-150 nm; large EVs: >200 nm) to avoid biogenesis-associated nomenclature controversies [1] [2]. Stem cell-derived EVs (Stem-EVs) carry diverse therapeutic cargoes including microRNAs, mRNAs, long non-coding RNAs, proteins, and metabolites [1]. Fractionation studies have demonstrated that the cardioprotective activity in human MSC-conditioned medium resides in the fraction containing products >1000 kDa (100-220 nm), indicating that the responsible paracrine factors are likely large complexes, potentially EVs [7].
- Anti-inflammatory Cytokines: Conditioned media contains factors that significantly suppress the expression of pro-inflammatory cytokines including TNF-α, IL-6, and IL-1β in the ischemic myocardium and in LPS-stimulated cardiomyocytes [5]. This anti-inflammatory activity contributes to reduced adverse remodeling and creates a more favorable environment for repair.
- Metabolic Modulators: Emerging evidence indicates that stem cell secretions can correct metabolic dysregulation in ischemic heart disease, including disorders of glucose metabolism, fatty acid oxidation, and branched-chain amino acid catabolism [8]. These modulations help restore energy production in stressed cardiomyocytes.
Therapeutic Effects of Conditioned Media in Experimental Models
Cardioprotection in Ischemia-Reperfusion Injury
Multiple experimental studies across different species have demonstrated the potent cardioprotective effects of stem cell conditioned media in acute ischemia-reperfusion (I/R) injury models:
- Infarct Size Reduction: In a porcine model of I/R injury, intravenous and intracoronary administration of human MSC-conditioned medium (MSC-CM) resulted in a dramatic 60% reduction in infarct size, associated with significantly improved systolic and diastolic cardiac performance assessed by echocardiography and pressure-volume loops [7]. Similarly, in a mouse I/R model, systemic delivery of SHED-CM significantly attenuated the infarct area/area at risk ratio by 55.1% compared to controls [5].
- Biomarker Improvement: SHED-CM treatment significantly reduced circulating troponin I levels, a sensitive marker of myocardial injury, at 24 hours after reperfusion [5]. This indicates reduced ongoing cardiomyocyte death following the ischemic insult.
- Functional Recovery: Echocardiographic assessment demonstrated that SHED-CM treatment significantly increased left ventricular fractional shortening in mice at 7 days after myocardial I/R compared to control-treated animals [5].
Table 1: Quantitative Cardioprotective Effects of Stem Cell Conditioned Media in Experimental Ischemia-Reperfusion Models
| Conditioned Media Source | Experimental Model | Key Protective Outcomes | Proposed Mechanisms |
|---|---|---|---|
| Human Mesenchymal Stem Cells (MSCs) [7] | Porcine I/R injury | 60% reduction in infarct size; Improved systolic/diastolic function | Reduced oxidative stress; Decreased TGF-β signaling and apoptosis |
| Stem Cells from Human Exfoliated Deciduous Teeth (SHEDs) [5] | Mouse I/R injury | 55% reduction in infarct size; Reduced troponin I; Improved fractional shortening | Suppressed apoptosis; Anti-inflammatory effects; HGF-mediated protection |
| Human Mesenchymal Stem Cells (MSCs) [6] | In vitro & ex vivo rat I/R | Reduced cell injury (LDH activity); Improved cell viability (MTT) | Paracrine activation of PI3K pathway |
| Dental Pulp Stem Cells [5] | Neonatal rat cardiomyocytes (hypoxia/serum deprivation) | 63.5% reduction in TUNEL-positive cells under hypoxia | HGF-dependent anti-apoptotic pathway |
Anti-Apoptotic and Anti-Inflammatory Actions
Conditioned media mediates powerful cytoprotective effects on cardiomyocytes exposed to ischemic stress:
- Apoptosis Suppression: In the border zone of myocardial infarction, where cardiomyocytes are at risk of delayed cell death, SHED-CM treatment significantly reduced the frequency of TUNEL-positive myocytes [5]. In vitro studies using neonatal rat cardiac myocytes subjected to hypoxia/serum-deprivation demonstrated that SHED-CM suppressed apoptosis by 63.5% under hypoxic conditions [5]. This anti-apoptotic effect was significantly stronger than that provided by bone marrow-derived or adipose-derived stem cell conditioned media [5].
- Inflammation Modulation: In the ischemic heart in vivo, SHED-CM administration attenuated the I/R-induced increases in cardiac TNF-α, IL-6, and IL-1β mRNA levels [5]. In cultured cardiac myocytes, SHED-CM pretreatment dose-dependently suppressed LPS-induced expression of these pro-inflammatory genes [5].
- Mechanistic Insights: The potent anti-apoptotic activity of SHED-CM was significantly attenuated by HGF neutralization, both in vitro and in vivo, identifying HGF as a critical mediator of this protective effect [5]. Similarly, the protection afforded by MSC-CM in vitro was significantly reduced by PI3K inhibitors (LY294002 or Wortmannin), but not by neutralizing antibodies against IGF-1 or VEGF, suggesting a central role for PI3K/Akt pathway activation in MSC-CM-mediated protection [6].
Not all conditioned media provides equivalent cardioprotection. Systematic comparisons reveal important source-dependent differences:
- Superior Efficacy of SHED-CM: In direct comparative studies, SHED-CM exhibited stronger anti-apoptotic actions and better improvement of cell viability under serum-deprived conditions compared to conditioned media from bone marrow-derived stem cells (BMSC-CM) or adipose-derived stem cells (ADSC-CM) [5].
- Cytokine Profile Variations: Cytokine antibody arrays and ELISA validation demonstrated that SHED-CM contains a significantly higher concentration of HGF than BMSC-CM and ADSC-CM, providing a mechanistic explanation for its superior anti-apoptotic potency [5].
Table 2: Comparison of Conditioned Media from Different Stem Cell Sources
| Parameter | SHED-CM | BMSC-CM | ADSC-CM |
|---|---|---|---|
| Anti-apoptotic potency [5] | Strongest (63.5% reduction under hypoxia) | Moderate | Moderate |
| Effect on cell viability (serum-deprivation) [5] | Significant improvement | No effect | No effect |
| Anti-inflammatory action [5] | Potent suppression of TNF-α, IL-6, IL-1β | Similar potency | Similar potency |
| HGF concentration [5] | Highest | Lower | Lower |
| Therapeutic infarct size reduction [5] | 55% | Not reported | Not reported |
Experimental Protocols for Conditioned Media Research
Conditioned Media Preparation Protocol
Standardized methodology for generating therapeutic conditioned media is essential for experimental reproducibility and eventual clinical translation:
- Cell Culture: Isolate and expand therapeutic stem cells (e.g., MSCs, SHEDs) under defined conditions using standard culture media. Use low passage numbers (e.g., passages 3-5) to maintain cell potency and prevent senescence-related functional decline.
- Serum Deprivation: Once cells reach 70-80% confluence, wash with phosphate-buffered saline (PBS) and replace standard growth media with serum-free basal media. Serum deprivation is critical to eliminate confounding factors from fetal bovine serum and to create a defined therapeutic product.
- Conditioning Phase: Incubate cells in serum-free media for 24-72 hours (typically 48 hours) to allow secretion of paracrine factors into the conditioned media. Maintain appropriate control conditions using serum-free media incubated without cells.
- Collection and Clarification: Collect conditioned media and remove cellular debris by centrifugation at 2,000 × g for 20 minutes followed by filtration through 0.22 µm filters.
- Concentration and Storage: Concentrate conditioned media using centrifugal filter devices (e.g., 3-5 kDa molecular weight cut-off) if desired. Aliquot and store at -80°C until use. Avoid multiple freeze-thaw cycles to preserve bioactivity.
In Vivo Myocardial Ischemia-Reperfusion Model
The efficacy of conditioned media is typically evaluated in well-established animal models of myocardial I/R injury:
- Animal Preparation: Anesthetize animals (typically mice or rats) and perform endotracheal intubation for mechanical ventilation throughout the surgical procedure.
- Thoracotomy: Perform a left thoracotomy between the fourth and fifth ribs to expose the heart.
- Coronary Artery Ligation: Identify the left anterior descending coronary artery (LAD) and ligate it temporarily using a slipknot with a piece of tubing to facilitate reperfusion. Place the suture approximately 2-3 mm from the origin of the LAD. Ischemia is confirmed by visual observation of myocardial blanching and ECG changes (ST-segment elevation).
- Reperfusion: After 30-60 minutes of ischemia (duration depends on specific model), release the ligation to allow reperfusion, confirmed by visible hyperemia in the previously ischemic territory.
- Treatment Administration: Intravenously administer conditioned media or control media (e.g., 100-200 µL for mice) 5 minutes after reperfusion initiation [5]. Alternative administration routes include intracoronary infusion [7].
- Functional and Histological Assessment: At predetermined endpoints (e.g., 24 hours for infarct size measurement, 1-4 weeks for functional assessment), evaluate outcomes using echocardiography, hemodynamic measurements, histology (TTC staining for infarct size), and molecular analyses.
In Vitro Cardioprotection Assays
Mechanistic studies utilize controlled in vitro systems to dissect specific protective pathways:
- Cardiomyocyte Culture: Isolate neonatal rat ventricular cardiomyocytes or use established cardiomyocyte cell lines. Culture under standard conditions until experiments.
- Hypoxia/Serum Deprivation Model: Replace normoxic culture media with deoxygenated, glucose-free balanced salt solutions and place cells in a hypoxic chamber (1% O₂, 5% CO₂, 94% N₂) for 6-24 hours to simulate ischemic conditions. Include serum deprivation to enhance metabolic stress.
- Conditioned Media Treatment: Add conditioned media or control media at the initiation of hypoxia or at the "reoxygenation" phase when returning to normoxic, complete media.
- Assessment of Apoptosis: Quantify apoptosis using TUNEL staining, caspase-3/7 activity assays, or Annexin V/propidium iodide flow cytometry after 24-48 hours of treatment.
- Cell Viability Measurement: Assess overall cell viability using metabolic assays such as MTT or WST-8 at 24-48 hours post-treatment [5].
- Pathway Inhibition Studies: Utilize specific pharmacological inhibitors (e.g., PI3K inhibitors LY294002 or Wortmannin [6]) or neutralizing antibodies (e.g., anti-HGF antibody [5]) to interrogate mechanistic pathways.
Experimental Workflow for Conditioned Media Research
Signaling Pathways in Conditioned Media-Mediated Cardioprotection
Conditioned media activates multiple interconnected pro-survival signaling pathways in recipient cardiomyocytes:
PI3K/Akt Pathway
The PI3K/Akt pathway emerges as a central mediator of conditioned media-induced cardioprotection. Experimental evidence demonstrates that the protective effects of MSC-CM are significantly attenuated by PI3K inhibitors (LY294002 or Wortmannin) [6]. Akt activation phosphorylates numerous downstream targets including GSK-3β, Bad, and caspase-9, collectively inhibiting mitochondrial permeability transition pore opening and apoptosis execution. This pathway integrates signals from various growth factors present in conditioned media, creating a powerful anti-apoptotic signal.
Growth Factor-Specific Signaling
Specific growth factors enriched in conditioned media activate distinct protective pathways:
- HGF/c-Met Signaling: HGF, particularly abundant in SHED-CM, activates its receptor c-Met, triggering multiple downstream pathways including PI3K/Akt, STAT3, and MAPK cascades [5]. HGF signaling promotes cardiomyocyte survival, inhibits pro-apoptotic Bcl-2 family members, and enhances cellular repair mechanisms. Neutralization studies confirm that HGF depletion significantly attenuates the anti-apoptotic actions of SHED-CM [5].
- IGF-1 Signaling: While MSC-CM protection appears independent of IGF-1 based on neutralizing antibody studies [6], IGF-1 remains a potentially important component that may activate Akt and modulate cellular metabolism and survival in other contexts.
- VEGF Signaling: Similarly, VEGF neutralization does not abolish MSC-CM protection [6], suggesting that while VEGF may contribute to angiogenic effects, it is not the primary mediator of acute cardioprotection against I/R injury.
Anti-Inflammatory Signaling
Conditioned media suppresses the activation of pro-inflammatory transcription factors including NF-κB, reducing the expression of cytokines like TNF-α, IL-6, and IL-1β [5]. This modulation of the inflammatory response limits secondary tissue damage and creates a more favorable environment for repair processes. The specific factors responsible for this immunomodulation are an active area of investigation, with HGF, TGF-β, and various EV-contained microRNAs as likely contributors.
Metabolic Modulation
Emerging evidence indicates that stem cell secretions can correct pathological metabolic remodeling in ischemic heart disease [8]. Conditioned media components may enhance glucose uptake and utilization via GLUT1/GLUT4 upregulation, modulate fatty acid oxidation through AMPK/PGC-1α signaling, and improve mitochondrial function [8]. These metabolic improvements help restore energy production in stressed cardiomyocytes, supporting contractile function and cell survival.
Signaling Pathways in Conditioned Media-Mediated Protection
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Conditioned Media Studies
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| PI3K Pathway Inhibitors | LY294002, Wortmannin [6] | Mechanistic studies of signaling pathways | Identified PI3K activation as essential for MSC-CM protection [6] |
| Growth Factor Neutralizing Antibodies | Anti-HGF, Anti-IGF-1, Anti-VEGF [6] [5] | Identification of critical bioactive factors | Established HGF as key mediator of SHED-CM anti-apoptotic effects [5] |
| Apoptosis Detection Kits | TUNEL Assay, Caspase-3/7 Activity, Annexin V/PI [5] | Quantification of cardiomyocyte death | Demonstrated 63.5% reduction in apoptosis with SHED-CM [5] |
| Cell Viability Assays | MTT, WST-8 [6] [5] | Assessment of overall cell health | Confirmed CM improves cardiomyocyte viability under stress [5] |
| Cytokine Array/Analysis | Cytokine Antibody Array, ELISA, RT-PCR [5] | Comprehensive profiling of CM components | Revealed superior HGF content in SHED-CM vs other sources [5] |
| EV Isolation Tools | Ultracentrifugation, Size-Exclusion Chromatography, Filtration [1] [7] | Separation and analysis of vesicular fractions | Identified >1000 kDa fraction as protective component [7] |
Current Challenges and Future Directions
Standardization and Manufacturing Hurdles
The transition of conditioned media therapies from research to clinical application faces several significant challenges:
- Production Standardization: Critical parameters including cell source, passage number, culture conditions, serum deprivation duration, and concentration methods require standardization to ensure batch-to-batch consistency [3] [4]. The lack of standardized protocols currently hampers reproducibility and direct comparison between studies.
- Potency and Quality Control: Developing robust potency assays that correlate with therapeutic efficacy is essential for quality control. Such assays may target specific growth factor concentrations, EV counts, or functional responses in standardized cellular assays.
- Scalable Manufacturing: Transitioning from laboratory-scale production to clinically relevant volumes under Good Manufacturing Practice (GMP) conditions presents substantial technical and regulatory challenges [3] [4].
Engineering Strategies for Enhanced Therapeutics
Future developments will likely focus on engineering approaches to enhance the therapeutic efficacy of conditioned media:
- Preconditioning Strategies: Exposing stem cells to specific environments (hypoxia, inflammatory cytokines, pharmacological agents) before conditioned media collection can enhance the potency of their secretions by upregulating beneficial factors [4].
- Engineered Extracellular Vesicles: EVs can be engineered to enhance cardiac targeting, prolong circulation half-life, and deliver specific recombinant therapeutic cargoes [1] [2]. These modifications may tilt the cardiac regeneration field further toward these novel, defined cell-free biologics.
- Biomaterial-Assisted Delivery: Incorporating conditioned media components into biomaterial scaffolds or hydrogels can create sustained-release systems that prolong therapeutic exposure at the injury site, potentially enhancing regenerative outcomes [4].
Clinical Translation Landscape
The clinical pipeline for cardiac regeneration remains dominated by cell-based approaches, but cell-free strategies are emerging. A recent analysis of ClinicalTrials.gov (August 2025) identified 23 registered interventional trials focusing on cardiac regeneration, with most being early-phase, investigator-led studies [9]. While no large-scale clinical trials exclusively testing conditioned media were identified in this analysis, the promising preclinical data summarized in this review provides a compelling rationale for such trials. The established safety profile of cell-free approaches may accelerate their clinical translation compared to cell-based therapies.
The field of cardiac regeneration has undergone a fundamental paradigm shift from cell-based to cell-free therapeutic strategies. The limitations of cell transplantation—particularly poor survival, safety concerns, and logistical complexity—have driven this transition toward harnessing the paracrine secretions of therapeutic cells. Compelling preclinical evidence demonstrates that stem cell conditioned media and its components, particularly extracellular vesicles, can significantly reduce myocardial infarct size, attenuate apoptosis, suppress inflammation, and improve cardiac function in models of ischemia-reperfusion injury. The activation of pro-survival pathways including PI3K/Akt and the involvement of specific growth factors like HGF provide mechanistic insights into these protective effects. While challenges in standardization, manufacturing, and clinical translation remain, cell-free therapies based on stem cell secretions represent a promising direction for myocardial protection and regeneration that may ultimately offer safe, effective, and clinically practical treatments for patients with ischemic heart disease.
The therapeutic paradigm for myocardial protection is shifting from whole stem cell transplantation to the use of a cell-free secretome—the complex mixture of bioactive factors released by stem cells into conditioned medium. This in-depth technical guide deconstructs the secretome's composition, production, and mechanisms of action within the context of cardiac repair. We provide a comprehensive analysis of key secretory components, detailed experimental workflows for secretome characterization, and standardized methodologies for evaluating therapeutic efficacy in cardiovascular disease models. By synthesizing current proteomic data and functional studies, this whitepaper serves as an essential resource for researchers and drug development professionals advancing next-generation cardioprotective therapies.
Stem cell-based therapy has emerged as a promising strategy for treating myocardial injury and cardiomyopathy, conditions characterized by irreversible cardiomyocyte loss and pathological remodeling that leads to heart failure [10]. While stem cells demonstrate significant therapeutic potential, their clinical application faces substantial challenges including poor survival after transplantation, limited engraftment, and potential safety concerns [10]. Consequently, research focus has pivoted toward understanding that the beneficial effects of stem cells are predominantly mediated through paracrine secretions rather than direct cell replacement [10] [11].
This secretome, composed of proteins, growth factors, cytokines, chemokines, enzymes, and extracellular vesicles containing RNA, lipids, and proteins, represents a novel "cell-free" therapeutic approach [11]. The conditioned medium (CM) containing these secretions has demonstrated significant cardioprotective capabilities, including improving cardiac function after myocardial infarction, increasing myocardial capillary density, reducing infarct size, and preserving systolic and diastolic performance [12]. In myocardial protection research, the secretome offers a promising strategy to harness the regenerative capacity of stem cells while overcoming the limitations of cell-based therapies.
Core Bioactive Components of the Secretome
The therapeutic potential of the secretome in myocardial protection is mediated through its diverse bioactive components, which act synergistically to promote cardiac repair and regeneration.
Proteinaceous Components and Growth Factors
Proteomic analyses of stem cell secretomes have identified numerous proteins critical for cardiac repair. Table 1 summarizes the key protein classes and their demonstrated functions in myocardial protection.
Table 1: Key Proteinaceous Components in Cardioprotective Secretomes
| Protein Class | Key Examples | Primary Functions in Myocardial Protection | Experimental Evidence |
|---|---|---|---|
| Growth Factors | VEGF, HGF, G-CSF, Angiopoietin | Angiogenesis, cardiomyocyte survival, anti-apoptosis | Increased capillary density (981±55 vs 645±114 capillaries/mm²; p=0.021) in MI porcine model [12] |
| Anti-inflammatory Factors | IL-10, TGF-β, PGE2 | Macrophage polarization to M2 phenotype, inflammation resolution | Enhanced M2 macrophage activation, reduced interferon-γ and IL-4 expression [10] [11] |
| Regulatory Proteins | Sirtuins, Nucleic acid metabolism proteins (376 identified), Protein modifying enzymes (292 identified) | Metabolic reprogramming, epigenetic regulation | Ferroptosis key in cardiac mesoderm; sirtuin signaling drives cardiomyocyte fate [13] |
| Metabolic Enzymes | Glycolytic enzymes, Fatty acid β-oxidation enzymes | Energy substrate switching, mitochondrial protection | Cluster analysis shows transition from glycolytic profile in iPSC-CMs to fatty acid oxidation enrichment [13] |
Extracellular Vesicles and Non-Coding RNAs
Beyond soluble proteins, the secretome contains extracellular vesicles (EVs) including exosomes and microvesicles that serve as intercellular communication vehicles. These EVs carry cargo including:
- microRNAs (e.g., anti-fibrotic miRNAs, pro-angiogenic miRNAs)
- Lipids and metabolites that influence recipient cell metabolism
- Proteins that exert enzymatic or signaling functions
These components directly target pathological processes in the injured myocardium. For instance, MSC-derived exosomes have been shown to directly target TGF-βR2, reducing Smad2 phosphorylation and exerting potent anti-inflammatory and anti-fibrotic effects both in vivo and in vitro [10]. Similarly, secretome-derived non-coding RNAs regulate multiple pro-proliferative pathways to promote cardiomyocyte proliferation [14].
Experimental Workflows for Secretome Production and Analysis
Standardized methodologies are crucial for generating reproducible, therapeutically relevant secretomes for myocardial protection research.
Secretome Production and Collection
Figure 1: Workflow for Secretome Production and Characterization
The production workflow begins with critical decisions that significantly influence secretome composition and therapeutic potency:
Cell Source Selection: Mesenchymal stem cells (MSCs) from bone marrow, adipose tissue, or umbilical cord represent the most common sources, though induced pluripotent stem cell (iPSC)-derived macrophages and other progenitors are emerging alternatives [10] [14].
Culture Method Optimization:
- 3D vs. 2D Culture: 3D culture systems more closely mimic the physiological environment and enhance anti-inflammatory, anti-angiogenic, and tissue regeneration properties. Secretomes from 3D microtissue models demonstrate enhanced mineralization capacity and homogenous distribution across scaffolds compared to 2D counterparts [11].
- Oxygen Concentration: Physiological hypoxia (1-10% O₂) maintains multipotency, enhances proliferation, and promotes regenerative/cytoprotective effects through HIF-1α upregulation, which increases production of vascularization factors (VEGF, angiotensin) [11].
- Biochemical Stimulation: Preconditioning with inflammatory factors (IFN-γ, TNF-α) increases anti-inflammatory and regenerative factors including IL-6, TGF-β, VEGF, HGF, and G-CSF, redirecting cell metabolism to the glycolytic pathway and enhancing immunomodulatory factor secretion [11].
Serum-Free Conditioning: To minimize interferences from animal serum components, cells are transitioned to serum-free medium for a defined conditioning period (typically 24-72 hours) before conditioned medium collection [11].
Processing, Characterization, and Standardization
Following collection, conditioned medium undergoes processing and rigorous characterization:
Processing Methods: Ultrafiltration-based fractionation (0.2µm–50 kDa) effectively isolates fractions enriched in exosomes and proteins, preserving functionally significant secretome components while excluding larger or smaller biomolecules [15]. Concentration methods include tangential flow filtration, centrifugal concentrators, and lyophilization.
Proteomic Characterization: Multiplexed tandem mass tag (TMT)-based mass spectrometry enables comprehensive quantitative analysis. A recent study identified 4,433 unique proteins during cardiomyocyte differentiation, with 62% showing significant alterations during the differentiation process [13]. Unsupervised clustering reveals distinct protein expression patterns corresponding to key biological processes at each developmental stage.
Quality Control Metrics: Include total protein quantification, nanoparticle tracking analysis (NTA) for vesicle concentration and size distribution, electron microscopy (TEM/SEM) for vesicle morphology, and functional potency assays.
Signaling Mechanisms in Myocardial Protection
The cardioprotective effects of the secretome are mediated through complex signaling networks that target multiple pathological processes simultaneously.
Figure 2: Key Signaling Pathways in Secretome-Mediated Myocardial Protection
The molecular mechanisms through which secretome components exert cardioprotective effects include:
Anti-Fibrotic Signaling: MSC-derived exosomes directly target transforming growth factor beta receptor 2 (TGF-βR2), reducing phosphorylation of Smad2 and exerting potent anti-fibrotic activity in vitro and in vivo [10].
Angiogenic Activation: Secretome-induced HIF-1α upregulation increases production of vascular endothelial growth factor (VEGF) and angiopoietin, enhancing capillary density and myocardial perfusion after infarction [11] [12].
Anti-Apoptotic Pathways: Sirtuin signaling activation promotes cardiomyocyte survival and drives cardiomyocyte fate specification, particularly during cardiac mesoderm development [13].
Immunomodulation: Secretome components induce CCR2+ and CX3CR1+ macrophage accumulation and polarization toward the regenerative M2 phenotype, ameliorating local inflammation and improving cardiac fibroblast activity [10].
Proliferative Induction: Primitive macrophage-conditioned medium activates multiple pro-proliferative pathways in adult cardiomyocytes, promoting cell cycle re-entry and regeneration [14].
Functional Assessment in Cardiac Disease Models
Rigorous functional validation is essential to establish therapeutic efficacy. Table 2 summarizes key outcome measures and experimental findings from preclinical studies of secretome-based cardioprotection.
Table 2: Functional Assessment of Secretome Therapeutics in Cardiac Models
| Assessment Method | Key Parameters Measured | Representative Findings | Reference Model |
|---|---|---|---|
| In Vitro Cardiomyocyte Proliferation | EdU/BrdU incorporation, Ki67 staining, cytokinesis analysis | hiPM-cm promoted adult cardiomyocyte proliferation through multiple pro-proliferative pathways | Human cardiomyocytes [14] |
| Cardiac Function (Echocardiography) | LVEF, LVIDd, ±dp/dt | Significant improvements in LVEF, LVIDd, and ±dp/dt after hiPSCs-CM treatment | Myocardial infarction mice [10] |
| Histological Analysis | Capillary density, infarct size, fibrosis extent | Increased capillary density (981±55 vs 645±114 capillaries/mm²; p=0.021), reduced infarct size | Myocardial infarction porcine model [12] |
| Molecular Pathway Analysis | Phosphoprotein profiling, gene expression, pathway enrichment | Identification of 5 key proteins in hiPM-cm mediating proliferative activation; ferroptosis key in CME specification | Proteomic analysis [14] [13] |
| Metabolic Assessment | Glycolytic rates, fatty acid oxidation, mitochondrial function | Transition from glycolytic profile in iPSC-CMs to fatty acid β-oxidation enrichment in mature cardiomyocytes | Metabolic pathway analysis [13] |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for Secretome Studies in Myocardial Protection
| Reagent Category | Specific Examples | Function & Application | Technical Considerations |
|---|---|---|---|
| Stem Cell Culture Media | Human pluripotent stem cell media, Mesenchymal stem cell media, Xeno-free formulations | Maintenance, expansion, and differentiation of stem cell sources | Serum-free and xeno-free formulations essential for clinical translation; chemically defined media provide batch-to-batch consistency [16] [17] |
| Separation & Concentration Systems | Ultrafiltration devices (0.2µm–50 kDa), Tangential flow filtration, Centrifugal concentrators | Isolation of fraction enriched in exosomes and proteins | Ultrafiltration effectively captures small vesicles and mid-sized proteins while excluding larger or smaller biomolecules [15] |
| Proteomic Analysis Tools | Tandem mass tag (TMT) reagents, Nanoflow LC/ESI-MS/MS, Bioinformatics software | Quantitative proteomic profiling, pathway analysis | TMT-based mass spectrometry enabled identification of 4,433 unique proteins during cardiomyocyte differentiation [13] |
| Characterization Assays | Nanoparticle tracking analysis (NTA), ELISA, Western blot, Electron microscopy (TEM/SEM) | Quantification of vesicle concentration, protein identification, morphology assessment | Serum-containing CM exhibits significantly higher levels of total protein, non-vesicular RNA, exosomes, and nanoparticles [15] |
| Functional Assay Kits | HUVEC spheroid angiogenesis assay, Cardiomyocyte proliferation kits, Apoptosis detection assays | Validation of angiogenic, proliferative, and anti-apoptotic activities | HUVEC spheroid assays identified angiogenic properties of MSC-CM; EdU/BrdU incorporation for proliferation [14] [12] |
The systematic deconstruction of the stem cell secretome represents a transformative approach in myocardial protection research. This technical guide has synthesized current methodologies, compositional analyses, and functional validation strategies that enable researchers to harness the therapeutic potential of conditioned medium in cardiovascular applications. The standardized workflows and analytical frameworks presented here provide a foundation for advancing secretome-based therapeutics toward clinical application.
Future directions in this rapidly evolving field include the integration of AI-powered platforms for optimizing secretome formulations, which have already demonstrated 35% increases in cell proliferation rates and 28% reductions in media consumption across large-scale production batches [16]. Additionally, the development of 3D culture systems that more accurately mimic physiological environments and the implementation of real-time monitoring technologies for bioprocess control will further enhance the reproducibility and therapeutic potency of secretome products [11] [16]. As standardization improves and our understanding of mechanism deepens, secretome-based therapies offer promising avenues for addressing the significant unmet clinical needs in myocardial protection and regeneration.
The therapeutic application of stem cell conditioned medium for myocardial protection represents a paradigm shift in cardiovascular regenerative medicine. While stem cells were initially heralded for their differentiation potential, accumulating evidence now identifies their secreted factors, particularly extracellular vesicles (EVs), as the primary mediators of cardiac repair [18] [2]. These nanoscale lipid-bilayer enclosed structures serve as indispensable vehicles for intercellular communication, shuttling bioactive molecules between stem cells and compromised myocardial tissue. Within the context of ischemic heart disease, EVs execute a multifaceted therapeutic program encompassing anti-apoptotic signaling, immunomodulation, angiogenesis promotion, and metabolic reprogramming [8] [2]. This whitepaper provides a comprehensive technical examination of EV biology, mechanistic actions in myocardial protection, standardized experimental methodologies, and translational applications, specifically framed within the investigation of stem cell conditioned medium as a therapeutic agent for cardiac repair.
EV Biogenesis, Classification, and Cargo Composition
Biogenetic Pathways and Cargo Loading
Extracellular vesicles originate through distinct cellular processes that define their physical characteristics and molecular cargo. The major EV subtypes include: (1) Exosomes (30-150 nm), which form via the endosomal pathway through inward budding of multivesicular bodies (MVBs) and subsequent fusion with the plasma membrane; (2) Microvesicles (100-1000 nm), generated through direct outward budding and shedding of the plasma membrane; and (3) Apoptotic bodies (1-5 μm), released during programmed cell death [19] [20]. The biogenesis of exosomes, the most well-characterized EV population for therapeutic applications, is regulated by sophisticated molecular machinery including the ESCRT (Endosomal Sorting Complexes Required for Transport) system and various ESCRT-independent mechanisms involving tetraspanins (CD63, CD81, CD9) and ceramide [21]. Cargo loading—encompassing proteins, lipids, DNA, and diverse RNA species—occurs selectively during vesicle formation, reflecting the physiological state of the parent cell and enabling sophisticated communication with recipient cells [19] [20].
Molecular Cargo of Therapeutic EVs
Stem cell-derived EVs, particularly those from mesenchymal stem cells (MSCs), carry a rich repertoire of bioactive molecules responsible for their cardioprotective effects. The table below summarizes key cargo components identified in therapeutic EVs.
Table 1: Therapeutic Cargo in Stem Cell-Derived Extracellular Vesicles
| Cargo Category | Specific Components | Documented Functions in Myocardial Protection |
|---|---|---|
| MicroRNAs (miRNAs) | miR-21, miR-210, miR-146a, miR-1275 | Inhibit cardiomyocyte apoptosis, promote angiogenesis, modulate inflammation [22] [23] [24] |
| Growth Factors | VEGF (Vascular Endothelial Growth Factor), HGF (Hepatocyte Growth Factor), FGF (Fibroblast Growth Factor) | Stimulate angiogenesis, enhance cell survival, promote tissue repair [22] [18] |
| Proteins | IGF-1 (Insulin-like Growth Factor 1), FGF-2, HSP70 (Heat Shock Protein 70) | Promote cardiomyocyte development/survival, cardioprotective signaling [20] [19] |
| Lipids | Cholesterol, sphingomyelin, ceramide | Structural integrity, membrane signaling, microdomain organization [19] |
Mechanisms of Action: EV-Mediated Cardioprotection
Core Protective Pathways
EVs orchestrate myocardial protection through a combination of distinct yet interconnected mechanistic pathways, culminating in enhanced tissue viability and functional recovery following ischemic injury.
Figure 1: Core Cardioprotective Pathways Activated by Stem Cell-Derived EVs. EVs mediate therapeutic effects via multiple parallel mechanisms, including activation of survival signals, promotion of new blood vessels, modulation of immune responses, reprogramming of cardiac metabolism, and inhibition of scar tissue formation, ultimately leading to improved cardiac function.
The PI3K/AKT pathway is a critical survival signaling cascade activated by EV cargo. For instance, exosomal miR-1275 derived from cardiomyocytes was shown to upregulate IL-38 expression in lymphocytes, which in turn activated the PI3K/AKT pathway, leading to decreased expression of the pro-apoptotic protein Bax and increased expression of the anti-apoptotic protein Bcl-2, thereby reducing apoptosis in an LPS-induced sepsis model [24]. Furthermore, EVs modulate post-infarct immune responses by promoting polarization of macrophages toward the regenerative M2 phenotype, partly mediated by exosomal miR-132-3p, and by suppressing pro-inflammatory monocyte activation [20]. A third major mechanism involves the amelioration of metabolic disturbances in the ischemic heart. Stem cell-derived EVs can restore balance to substrate utilization by enhancing glucose uptake and oxidation, partly through upregulation of GLUT4 and PKM2, thereby improving cardiac efficiency in a low-oxygen environment [8].
Quantitative Therapeutic Outcomes
The efficacy of EV-based therapies is quantitatively demonstrated through improved functional and structural metrics in preclinical models of myocardial infarction. The following table consolidates key outcome measures from experimental studies.
Table 2: Quantitative Outcomes of EV Therapy in Preclinical Myocardial Infarction Models
| Therapy Type | Key Cargo / Feature | Reported Efficacy in Preclinical Models | Primary Mechanism |
|---|---|---|---|
| MSC-EVs | miR-21, miR-210, VEGF, HGF | Increased LVEF by 3.8%; Reduced infarct size; Enhanced angiogenesis [22] | Paracrine signaling, anti-apoptosis, angiogenesis |
| iPSC-Derived EVs | Cardiomyocyte-specific miRNAs, proteins | Improved myocardial perfusion; Reduced inflammation and apoptosis [22] [2] | Direct cytoprotection, stimulation of endogenous repair |
| Cardiac Progenitor Cell-EVs | miR-146a, miR-210, miR-132 | Promoted endothelial tube formation; Reduced cardiomyocyte apoptosis; Enhanced cardiac function [22] [23] | Angiogenesis, anti-apoptosis, intercellular communication |
| Engineered EVs (CXCR4-overexpressing) | Enhanced homing capability | Improved myocardial homing efficiency by 5.2-fold [22] | Targeted delivery to ischemic tissue |
Experimental Protocols: Isolating and Characterizing EVs from Conditioned Medium
Standardized Workflow for EV Research
The investigation of EVs from stem cell conditioned medium requires a rigorous and standardized experimental pipeline to ensure the isolation and characterization of bona fide EV populations.
Figure 2: Standardized Workflow for EV Isolation from Conditioned Medium. The critical process begins with collecting conditioned medium from stem cells grown under defined conditions, followed by sequential steps to remove non-vesicular contaminants, concentrate the vesicles, isolate them via high-purity methods, and thoroughly characterize the final EV preparation before functional testing.
Detailed Methodological Protocols
Protocol 1: Isolation of EVs from Stem Cell Conditioned Medium
- Cell Culture and Conditioned Medium Collection: Culture MSCs (or other stem cells) to 70-80% confluence. Replace growth medium with serum-free, exosome-depleted medium. After 24-48 hours, collect the conditioned medium and immediately process or store at 4°C for short periods (-80°C for long-term) [23] [24].
- Pre-Clearation Centrifugation: Centrifuge the conditioned medium at 2,000 × g for 30 minutes at 4°C to remove dead cells and large debris. Transfer the supernatant to a fresh tube and centrifuge at 10,000 × g for 45 minutes to eliminate larger vesicles and organelles [24].
- Ultracentrifugation-based Isolation: Transfer the double-cleared supernatant to ultracentrifuge tubes. Pellet EVs by ultracentrifugation at 120,000 × g for 70 minutes at 4°C. Carefully discard the supernatant and resuspend the EV pellet in a suitable buffer (e.g., sterile PBS). This step may be repeated for higher purity [24].
- Alternative Isolation Methods: For specific applications, Size-Exclusion Chromatography (SEC) provides superior purity by separating EVs from soluble proteins based on hydrodynamic radius. Alternatively, precipitation-based kits offer convenience but may co-precipitate contaminants like lipoproteins [20].
Protocol 2: Comprehensive Characterization of Isolated EVs
- Nanoparticle Tracking Analysis (NTA): Dilute the EV suspension in PBS and inject into the NTA system. This analysis determines the particle size distribution (typically 30-200 nm for exosomes) and concentration [19] [20].
- Transmission Electron Microscopy (TEM): Adhere EVs to Formvar-carbon coated grids, negative stain with uranyl acetate, and image. TEM confirms the spherical, cup-shaped morphology and membrane integrity of the vesicles [24].
- Western Blot Analysis: Lyse EVs and perform immunoblotting to detect canonical positive markers (e.g., Tetraspanins: CD63, CD81, CD9; Endosomal proteins: TSG101, Alix) and the absence of negative markers (e.g., organelle-specific proteins like Calnexin) [21] [24].
- Cargo Profiling: Extract total RNA and protein from EVs. Use qRT-PCR to profile specific miRNAs of interest (e.g., miR-21, miR-146a). For unbiased discovery, RNA-Seq or mass spectrometry-based proteomics can be employed to comprehensively map the molecular cargo [20] [24].
Protocol 3: In Vitro Validation of EV-Mediated Cardioprotection
- Model Establishment: Create an in vitro model of myocardial injury. For hypoxia, culture cardiomyocytes (e.g., H9c2 cells or primary cardiomyocytes) in a hypoxic chamber (1% O2) for 6-24 hours. For inflammatory injury, treat cells with LPS (e.g., 500 ng/mL for 3 hours) [24].
- EV Treatment and Uptake Tracking: Treat injured cardiomyocytes with isolated EVs (typical dose: 10-100 μg/mL). To confirm functional delivery, label EVs with a lipophilic dye (e.g., PKH67 or DiI) and visualize their internalization into target cells via confocal microscopy after 6-24 hours [23].
- Functional Assessment:
- Apoptosis Assay: Use an Annexin V-FITC/PI apoptosis detection kit and flow cytometry to quantify the percentage of apoptotic cells post-EV treatment.
- Cell Viability/Proliferation: Measure using a CCK-8 assay according to manufacturer protocols.
- Mechanistic Signaling Analysis: Perform Western blotting to analyze the activation of key signaling pathways, such as the phosphorylation status of PI3K and AKT, and the expression levels of apoptosis regulators like Bcl-2 and Bax [24].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents and Kits for EV Research in Myocardial Protection
| Reagent/Kits | Specific Example | Primary Function in EV Workflow |
|---|---|---|
| Serum-Free Medium | DMEM, RPMI-1640 | Production of conditioned medium without serum-derived EV contamination [24] |
| EV-Depleted FBS | Systemically depleted FBS | Supports cell growth during expansion while preventing confounding bovine EV introduction |
| Protease Inhibitors | EDTA-free cocktails | Preserves EV protein cargo integrity during isolation and processing |
| Isolation Kits | ExoQuick-TC, Total Exosome Isolation | Polymer-based precipitation for rapid EV isolation from conditioned medium |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-TSG101 | Detection of positive EV markers via Western Blot for identity validation [24] |
| Negative Marker Antibodies | Anti-Calnexin, Anti-GM130 | Confirms absence of cellular contaminants from endoplasmic reticulum/Golgi |
| EV Labeling Dyes | PKH67, DiI, DiD | Fluorescent labeling for tracking EV uptake and biodistribution in vitro and in vivo |
| RNA Isolation Kits | Trizol-based systems | Efficient extraction of high-quality RNA, including small RNAs, from EV pellets |
| qRT-PCR Assays | TaqMan MicroRNA Assays | Sensitive quantification of specific therapeutic miRNAs (e.g., miR-21, miR-146a) |
Extracellular vesicles represent the defining mechanistic link between stem cell conditioned medium and its observed therapeutic benefits in myocardial protection. Their capacity to coordinate complex reparative processes—from suppressing apoptosis and inflammation to stimulating angiogenesis and correcting metabolic imbalances—underscores their role as central mediators. The translational pathway for EV-based therapies is advancing rapidly, with ongoing efforts focusing on engineering EVs for enhanced targeting and cargo delivery. However, significant challenges related to the standardization of isolation protocols, precise functional characterization, and scalable manufacturing must be systematically addressed to fully realize the clinical potential of EVs as a primary active component in stem cell conditioned medium [2] [20]. As the field moves forward, the integration of EV biology with bioengineering and clinical cardiology promises to unlock novel, effective, and cell-free therapeutic paradigms for ischemic heart disease.
Stem cell-based therapy has emerged as a promising strategy for myocardial protection and regeneration. However, growing evidence indicates that the therapeutic benefits of mesenchymal stem cells (MSCs) are primarily mediated through paracrine factors rather than direct cell replacement [25] [10]. Conditioned medium (CM), which contains the secretory repertoire of MSCs, has demonstrated significant cardioprotective effects in various models of myocardial injury, including ischemia-reperfusion (IR) injury and myocardial infarction (MI) [25] [5]. The molecular mechanisms underlying these protective effects involve the coordinated modulation of three critical pathological processes: apoptosis, inflammation, and oxidative stress. This technical review synthesizes current experimental evidence detailing how CM mediates these effects at a molecular level, providing researchers with a comprehensive mechanistic framework and practical experimental guidelines.
Molecular Mechanisms of CM Action
Modulation of Apoptosis
CM exerts potent anti-apoptotic effects primarily through the regulation of caspase activation and the provision of pro-survival growth factors.
Caspase Pathway Inhibition: In aortic rings from brain-dead rats subjected to IR injury, CM preservation significantly lowered immunoreactivity of key apoptotic executers, including caspase-3, caspase-8, and caspase-9 [25]. Additionally, CM reduced mRNA levels of caspase-12, a mediator of endoplasmic reticulum (ER) stress-induced apoptosis, in vascular grafts from aged rats [26].
HGF-Mediated Protection: Comparative analysis revealed that CM from stem cells of human exfoliated deciduous teeth (SHEDs) contained higher concentrations of hepatocyte growth factor (HGF) than CM from bone marrow or adipose-derived stem cells [5]. Neutralization of HGF significantly attenuated the anti-apoptotic effects of SHED-CM in cardiac myocytes, establishing HGF as a critical component.
Table 1: Anti-apoptotic Effects of CM in Experimental Models
| Experimental Model | Target Molecule | Effect of CM | Quantitative Change | Citation |
|---|---|---|---|---|
| BD rat aortic rings (IR) | Caspase-3 immunoreactivity | Significant reduction | Reported as decreased | [25] |
| BD rat aortic rings (IR) | Caspase-8 immunoreactivity | Significant reduction | Reported as decreased | [25] |
| BD rat aortic rings (IR) | Caspase-9 immunoreactivity | Significant reduction | Reported as decreased | [25] |
| Aged rat vascular grafts | Caspase-12 mRNA | Significant reduction | Reported as decreased | [26] |
| Neonatal rat cardiac myocytes (hypoxia) | TUNEL-positive cells | Significant reduction | 63.5% decrease | [5] |
| SHED-CM vs. BMSC-CM | HGF concentration | significantly higher | ~2-3 fold increase (ELISA) | [5] |
Regulation of Inflammatory Responses
CM mediates significant anti-inflammatory effects, primarily through the suppression of pro-inflammatory cytokines and adhesion molecules.
Cytokine Suppression: In a mouse model of myocardial IR injury, intravenous administration of SHED-CM significantly reduced cardiac mRNA levels of pro-inflammatory cytokines TNF-α, IL-6, and IL-1β [5]. In vitro, SHED-CM pretreatment dose-dependently suppressed LPS-induced expression of these cytokines in cardiac myocytes.
Adhesion Molecule Downregulation: CM preservation of vascular grafts from brain-dead rats significantly decreased mRNA expression of vascular cell adhesion molecule (VCAM)-1 and intercellular adhesion molecule (ICAM-1), key mediators of leukocyte infiltration during inflammation [25].
Macrophage Modulation: Intracardiac injection of MSCs induced accumulation of CCR2+ and CX3CR1+ macrophages, ameliorating local inflammation and improving fibroblast activity in ischemia-reperfusion-injured hearts [10] [27].
Table 2: Anti-inflammatory Effects of CM in Experimental Models
| Experimental Model | Inflammatory Marker | Effect of CM | Quantitative Change | Citation |
|---|---|---|---|---|
| Mouse myocardial I/R | Cardiac TNF-α mRNA | Significant reduction | Reported as decreased | [5] |
| Mouse myocardial I/R | Cardiac IL-6 mRNA | Significant reduction | Reported as decreased | [5] |
| Mouse myocardial I/R | Cardiac IL-1β mRNA | Significant reduction | Reported as decreased | [5] |
| BD rat aortic rings | VCAM-1 mRNA | Significant reduction | Reported as decreased | [25] |
| BD rat aortic rings | ICAM-1 mRNA | Significant reduction | Reported as decreased | [25] |
| Ischemia-reperfused hearts | Macrophage accumulation | Induced CCR2+/CX3CR1+ macrophages | Reported as increased | [10] [27] |
Attenuation of Oxidative Stress
CM protects against oxidative damage by reducing reactive oxygen species (ROS) generation and mitigating their damaging effects on cellular components.
Reduction of Oxidative Stress Markers: CM preservation of aortic rings from brain-dead rats significantly lowered immunoreactivity of nitrotyrosine, a marker of protein nitration and peroxynitrite-mediated oxidative damage [25]. Myeloperoxidase (MPO) immunoreactivity, an indicator of neutrophil infiltration and oxidative burst, was also significantly reduced.
Antioxidant Defense Enhancement: While not directly measured in CM studies, general mechanisms against oxidative stress in cardiomyopathy include the upregulation of endogenous antioxidant systems such as superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPX) [28]. The Nrf2 pathway, a master regulator of antioxidant gene expression, represents a potential target for CM-mediated effects.
Mitochondrial Protection: CM may improve mitochondrial function and reduce ROS production at its source, as mitochondria are the primary contributors to cellular oxidative stress in cardiomyopathies [28].
Integrated Signaling Pathways
The cardioprotective effects of CM involve an integrated network of signaling pathways that coordinately regulate apoptosis, inflammation, and oxidative stress. The diagram below illustrates the key molecular targets and their interactions.
Experimental Protocols and Methodologies
CM Preparation from Bone Marrow-Derived MSCs
The following protocol details the standard methodology for obtaining CM from rat bone marrow-derived MSCs, as described in multiple studies [25] [26]:
- Isolation: Harvest femurs and tibias from 8-12-week-old male Lewis rats. Flush bones with Dulbecco's phosphate-buffered saline (DPBS) to extract bone marrow.
- Culture: Suspend cells in MSC Expansion Medium and incubate at 37°C with 5% CO₂. At 80% confluency, subculture primary cells at a 1:3 ratio.
- Expansion: Use cells at passage 3 for CM collection. At >80% confluency, wash MSCs three times with DPBS to remove serum contaminants.
- Conditioning: Add serum-free Dulbecco's modified Eagle's medium (D-MEM) and incubate for 24 hours.
- Concentration: Collect primary CM and concentrate using ultrafiltration units (4500× g for 4 hours at 4°C).
- Quality Control: Quantify protein concentration via Bradford assay (typically 0.5 mg/mL final concentration). Analyze cytokine content using antibody arrays (e.g., RayBio Biotin Label-based rat antibody array).
In Vitro Models for Assessing CM Efficacy
- Hypoxia/Serum-Deprivation in Cardiac Myocytes: Culture neonatal rat cardiac myocytes under hypoxic conditions (1% O₂) with serum deprivation for 24 hours. Add CM at the onset of hypoxia. Assess apoptosis via TUNEL staining and cell viability using WST-8 assays [5].
- Lipopolysaccharide (LPS)-Induced Inflammation: Pretreat cardiac myocytes with CM for 2 hours before adding LPS (typically 100 ng/mL). Measure pro-inflammatory cytokine (TNF-α, IL-6, IL-1β) mRNA levels using quantitative RT-PCR after 6-24 hours [5].
Ex Vivo Models of Ischemia-Reperfusion Injury
- Aortic Ring Preparation: Explain thoracic aorta from 15-month-old rats or brain-dead donors. Place in cold Krebs-Henseleit solution. Isolate and clean periadventitial fat, cut into 4-mm rings [25] [26].
- Cold Ischemic Storage: Store rings for 24 hours at 4°C in nitrogen-equilibrated tubes containing physiological saline supplemented with CM or vehicle control.
- Organ Bath Assessment: Mount rings in organ baths with Krebs-Henseleit solution at 37°C, gassed with 95% O₂-5% CO₂. Apply 2 g tension with equilibration for 60 minutes.
- Functional Measurements: Pre-contract rings with phenylephrine (10⁻⁹–10⁻⁵ M). Assess endothelium-dependent relaxation with cumulative acetylcholine (10⁻⁹–10⁻⁵ M). Evaluate endothelial-independent relaxation with sodium nitroprusside.
In Vivo Models of Myocardial Injury
- Myocardial Ischemia-Reperfusion: Subject mice to 30 minutes of myocardial ischemia followed by 24 hours of reperfusion. Administer CM intravenously 5 minutes after reperfusion [5].
- Infarct Size Measurement: After 24 hours, excise hearts. perfuse with Evans blue dye to delineate area at risk (AAR). Section and incubate with 2,3,5-triphenyltetrazolium chloride (TTC) to distinguish infarcted (pale) from viable (red) tissue. Calculate infarct area (IA) as percentage of AAR.
- Functional Assessment: Perform echocardiography at baseline and 7 days post-I/R to measure left ventricular fractional shortening and other functional parameters.
- Molecular Analysis: Collect tissue for TUNEL staining, immunohistochemistry (caspases, MPO, nitrotyrosine), and mRNA quantification of inflammatory markers.
The following workflow diagram illustrates the complete experimental pipeline from CM preparation to efficacy assessment:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CM Studies
| Reagent/Category | Specific Examples | Research Application | Function in Experimental Design |
|---|---|---|---|
| Cell Culture Media | Dulbecco's Modified Eagle Medium (D-MEM), MSC Expansion Medium | CM production, cell maintenance | Provides base medium for conditioning; supports MSC growth and factor secretion |
| Cytokine Screening Tools | RayBio Biotin Label-based Rat Antibody Array, ELISA kits | CM characterization | Identifies and quantifies specific factors (e.g., HGF, VEGF) in CM |
| Apoptosis Detection Kits | TUNEL assay, caspase activity assays, WST-8 cell viability kit | Assessment of anti-apoptotic effects | Quantifies programmed cell death and cell survival in response to CM treatment |
| Molecular Biology Reagents | qRT-PCR primers (TNF-α, IL-6, IL-1β, VCAM-1, ICAM-1, caspase-12), protein extraction kits | Gene and protein expression analysis | Measures changes in inflammatory and apoptotic markers at transcriptional level |
| Vascular Function Assessment | Acetylcholine, phenylephrine, sodium nitroprusside, organ bath system | Ex vivo vascular reactivity studies | Evaluates endothelium-dependent and independent relaxation in aortic rings |
| Animal Models | Male Lewis rats (8-12 weeks, 15 months), C57BL/6J mice, brain death models | In vivo and ex vivo disease modeling | Provides physiological context for CM efficacy in aged, brain-dead, or I/R-injured systems |
| Histological Stains | Evans blue, 2,3,5-triphenyltetrazolium chloride (TTC), hematoxylin and eosin | Infarct size measurement, tissue morphology | Delineates area at risk and infarcted tissue in myocardial I/R studies |
| Antibodies for Neutralization | Anti-HGF neutralizing antibody | Mechanistic studies | Validates contribution of specific factors to CM's protective effects |
The molecular mechanisms through which CM modulates apoptosis, inflammation, and oxidative stress involve a complex interplay of multiple factors targeting specific pathways. The coordinated inhibition of caspase activation, suppression of pro-inflammatory mediators, and reduction of oxidative damage markers collectively contribute to CM's cardioprotective efficacy. The experimental methodologies outlined provide a robust framework for researchers to investigate these mechanisms further and develop standardized protocols for CM-based therapeutic applications. Future research should focus on identifying optimal CM compositions for specific cardiac pathologies and developing engineered CM with enhanced therapeutic potential.
Stem cell conditioned medium (CM) has emerged as a promising cell-free therapeutic for myocardial protection, with its efficacy largely attributed to the paracrine release of extracellular vesicles (EVs), particularly exosomes. The therapeutic potential of these vesicles is primarily mediated by their microRNA (miRNA) cargo, which orchestrates complex protective signaling pathways in recipient cardiac cells. This technical guide synthesizes current evidence on key miRNAs—including miR-21, miR-24-3p, miR-126, and others—that are enriched in stem cell-derived EVs and demonstrates potent cardioprotective effects against myocardial ischemia-reperfusion injury. We detail the molecular mechanisms by which these miRNAs regulate apoptosis, inflammation, oxidative stress, and angiogenesis, providing comprehensive experimental protocols for profiling EV-miRNA cargo and validating functional targets. Through structured data presentation and pathway visualization, this review equips researchers with the methodological framework needed to advance the development of miRNA-based therapeutics for cardiac repair, positioning stem cell CM as a viable platform for next-generation cardiovascular regenerative medicine.
Cardiovascular disease, particularly acute myocardial infarction (MI), remains a leading cause of death worldwide despite advances in reperfusion therapies [1] [29]. The adult human heart possesses limited regenerative capacity, losing approximately one billion cardiomyocytes following an MI event, which frequently leads to heart failure [1]. While stem cell transplantation initially promised significant cardiac regeneration, growing evidence indicates that therapeutic benefits are primarily mediated through paracrine mechanisms rather than direct cell engraftment and differentiation [30].
Stem cell conditioned medium has emerged as a critical vehicle for these paracrine factors, with extracellular vesicles—especially exosomes (30-150 nm)—serving as key mediators of intercellular communication [1] [31]. EVs are membrane-bound nanoparticles that transport functional cargo including proteins, lipids, and nucleic acids, with microRNAs representing particularly potent regulators of gene expression in recipient cells [30]. These small non-coding RNAs (approximately 22 nucleotides) function as "master post-transcriptional regulators" by binding complementary sequences in target mRNAs, leading to translational repression or mRNA degradation [32].
The investigation of EV-miRNAs in myocardial protection represents a paradigm shift from cell-based to biomolecule-based therapeutics. This whitepaper comprehensively examines the miRNA cargo within stem cell-derived EVs, delineating its role in regulating protective signaling pathways against myocardial injury. By integrating current experimental evidence and methodological approaches, we aim to provide researchers with a foundational resource for advancing this promising frontier in cardiovascular medicine.
Key miRNA Players in Cardioprotection
Comprehensive profiling of stem cell-derived EV cargo has identified several miRNAs that consistently demonstrate cardioprotective properties through the regulation of distinct signaling pathways. The table below summarizes the most therapeutically promising miRNAs, their regulated processes, and demonstrated functional outcomes.
Table 1: Key Cardioprotective miRNAs in Stem Cell-Derived Extracellular Vesicles
| miRNA | Primary Source | Regulated Processes | Key Validated Targets | Experimental Outcomes |
|---|---|---|---|---|
| miR-21-5p | MSC-EVs, Cardiomyocyte-CM [33] [31] | Anti-apoptosis, Anti-inflammation, Fibrosis reduction | PDCD4, PTEN [33] | ↓ Infarct size, ↓ Cardiomyocyte apoptosis (20-30%), ↑ Cardiac function [33] |
| miR-24-3p | ADSC-EVs, HUCMSC-Exos [34] [30] | Anti-apoptosis, Oxidative stress reduction | Nrf2 pathway [34] | ↓ Infarct size (∼50%), ↓ Inflammation, ↑ Antioxidant capacity [34] |
| miR-126 | EPC-EVs, Skeletal muscle-EVs [35] [31] | Angiogenesis, Endothelial function | SPRED1, VEGF pathway [31] | ↑ Capillary density, ↑ Endothelial cell proliferation/migration [35] |
| miR-29b | HUCMSC-Exos [30] | Anti-fibrosis | COL1A1, COL3A1, FBN1 [30] | ↓ Collagen deposition, ↓ Fibrosis [30] |
| miR-210 | Hypoxia-preconditioned MSC-EVs [31] | Angiogenesis, Hypoxia tolerance | Casp8ap2 [31] | ↑ Angiogenesis, ↑ Cell survival under hypoxia [31] |
| let-7 family | MSC-EVs [32] [36] | Insulin signaling, Metabolism | Multiple targets in insulin pathway [36] | Regulation of metabolic function [36] |
The miRNAs presented in Table 1 represent the most consistently identified and functionally validated species across multiple studies. Of particular note is miR-21, which is upregulated in conditioned medium from oxygen-glucose-deprived cardiomyocytes and demonstrates significant protective effects when transferred to recipient cells [33]. Depletion of miR-21 from conditioned medium substantially reduces its protective capacity against oxidative stress and fibroblast activation, confirming its functional importance [33].
Similarly, miR-24-3p has been identified as a critical component in adipose-derived stem cell nanovesicles, where it mediates cardioprotection through the Nrf2 pathway, enhancing antioxidant capability and reducing inflammatory response in injured myocardium [34]. The transfer of these miRNAs via EVs represents a sophisticated natural mechanism for coordinated regulation of cardiac repair processes across different cell types.
Experimental Protocols for miRNA Cargo Analysis
Rigorous characterization of EV-miRNA cargo and functional validation of its targets require integrated experimental approaches. Below, we detail standardized methodologies for isolation, profiling, and functional analysis of miRNAs from stem cell conditioned medium.
EV Isolation and Characterization from Conditioned Medium
Protocol 1: Sequential Ultracentrifugation for EV Isolation
- Conditioned Medium Collection: Culture stem cells (e.g., MSCs, ADSCs) to 70-80% confluence. Replace with serum-free medium for 48 hours. Collect CM and perform sequential centrifugations [33].
- Debris Removal: Centrifuge at 300 × g for 10 min at 4°C → Transfer supernatant → Centrifuge at 2,000 × g for 20 min → Transfer supernatant → Centrifuge at 10,000 × g for 30 min [37].
- EV Pellet Collection: Ultracentrifuge the resulting supernatant at 100,000 × g for 90 min at 4°C [33].
- EV Washing: Resuspend pellet in PBS → Ultracentrifuge again at 100,000 × g for 90 min [33].
- Characterization: Validate EV identity using Nanosight LM10 for size distribution (30-150 nm for exosomes), TEM for morphology, and Western blotting for markers (CD9, CD63, CD81, flotillin-1, Alix) [37].
Protocol 2: Commercial Kit Alternative
- Sample Preparation: Process CM through initial centrifugation steps as in Protocol 1 to remove cells and debris.
- EV Isolation: Use exoEasy kit (QIAGEN) per manufacturer's instructions [37].
- Quality Assessment: Quantify particle concentration (∼10^7-10^8 particles/μg protein expected) and confirm presence of EV markers [34].
miRNA Profiling and Functional Validation
Protocol 3: Small RNA Sequencing and Analysis
- RNA Isolation: Extract total RNA from isolated EVs using miRNeasy Kit (QIAGEN) with spiking of Cel-miR-39-3p as an external control [37].
- Library Preparation and Sequencing: Use platforms such as NanoString nCounter or Illumina sequencing following manufacturer protocols [32] [37].
- Bioinformatic Analysis:
Protocol 4: Functional Validation of miRNA Targets
- Gain/Loss-of-Function Studies: Transfert donor cells with miRNA mimics (20-40 nM) or inhibitors (e.g., anti-miR-21: 5'-UAGCUUAUCAGACUGAUGUUGA-3') using X-tremeGENE siRNA transfection reagent [33].
- Target Validation: Use dual-luciferase reporter assays with wild-type and mutant 3'UTR constructs of predicted targets.
- Phenotypic Assessment: Evaluate functional outcomes including:
Signaling Pathways Regulated by miRNA Cargo
The therapeutic effects of EV-miRNAs are mediated through the coordinated regulation of multiple interconnected signaling pathways. The following diagrams illustrate the principal mechanisms by which key miRNAs confer cardioprotection.
miR-21-Mediated Anti-Apoptotic and Anti-Fibrotic Signaling
Figure 1: miR-21 mediated cardioprotection. miR-21 transferred via stem cell EVs inhibits PDCD4 and PTEN, leading to reduced apoptosis and fibrosis [33] [31].
miR-24-3p Regulation of Oxidative Stress via Nrf2 Pathway
Figure 2: miR-24-3p antioxidant pathway. miR-24-3p activates Nrf2 pathway, enhancing antioxidant defense and reducing cell death [34].
Angiogenic Regulation by miR-126 and miR-210
Figure 3: Angiogenic miRNA pathways. miR-126 and miR-210 promote angiogenesis through distinct signaling pathways [31].
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of EV-miRNA function requires specific reagents and methodologies. The following table compiles essential research tools referenced across key studies.
Table 2: Essential Research Reagents for EV-miRNA Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| EV Isolation Kits | exoEasy Kit (QIAGEN) [37] | EV purification from conditioned medium | Membrane-based affinity purification of intact EVs |
| RNA Isolation Kits | miRNeasy Kit (QIAGEN) [37] | Small RNA extraction from EVs | Comprehensive recovery of miRNA species |
| miRNA Inhibitors | Anti-miR-21-5p: 5'-UAGCUUAUCAGACUGAUGUUGA-3' (Ambion AM10206) [33] | miRNA loss-of-function studies | Sequence-specific inhibition of endogenous miRNA activity |
| Transfection Reagents | X-tremeGENE siRNA Transfection Reagent (Roche) [33] | Delivery of miRNA mimics/inhibitors to cells | Efficient intracellular nucleic acid delivery with low toxicity |
| EV Characterization | Nanosight LM10 (Malvern) [37], Transmission Electron Microscope [37] | EV size and concentration analysis | Nanoparticle tracking and morphological validation |
| Sequencing Platforms | NanoString nCounter [32], Illumina Sequencers [37] | miRNA expression profiling | Multiplexed quantification of miRNA species |
| Animal MI Models | Left Coronary Artery Ligation (rat) [33], Myocardial I/R (mouse) [34] | In vivo validation of cardioprotection | Preclinical assessment of therapeutic efficacy |
The miRNA cargo within stem cell-derived extracellular vesicles represents a sophisticated endogenous system for regulating protective signaling pathways in myocardial tissue. Through coordinated modulation of apoptosis, inflammation, oxidative stress, and angiogenesis, these tiny RNA molecules exert powerful effects that belie their size. The experimental frameworks and mechanistic insights presented in this technical guide provide researchers with the foundational knowledge needed to advance this promising field.
As research progresses, several frontiers warrant particular attention: the development of engineered EVs with enhanced cardiac targeting, the optimization of scalable production methods for clinical translation, and the exploration of miRNA cocktail approaches that might surpass the efficacy of single miRNAs. With ongoing advances in EV bioengineering and miRNA delivery systems, harnessing the regulatory potential of miRNA cargo offers a promising path toward effective cell-free therapies for myocardial protection and regeneration.
From Lab to Preclinical Models: Protocols and Evidence for CM Efficacy
Mesenchymal stem cell conditioned medium (MSC-CM) has emerged as a promising cell-free therapeutic strategy in cardiovascular regenerative medicine. Within the context of myocardial protection, the beneficial effects of mesenchymal stem cells (MSCs) are primarily mediated through their paracrine activity rather than direct cell replacement [38]. The conditioned medium contains a complex mixture of bioactive factors collectively known as the secretome, which includes cytokines, chemokines, growth factors, microRNAs, and extracellular vesicles (mainly exosomes) [38]. These components present anti-inflammatory, anti-apoptotic, anti-fibrotic, and pro-angiogenic characteristics that are particularly relevant for treating ischemic myocardial injury [38] [2].
The transition toward cell-free therapies using MSC-CM offers significant advantages for clinical translation, including the potential for off-the-shelf therapies that can be collected, processed, and stored for future use [38]. This approach mitigates risks associated with direct stem cell transplantation, such as tumorigenesis, immune rejection, and microvascular complications in the lung [38]. For myocardial infarction (MI) and subsequent heart failure, MSC-CM-based therapies aim to replenish lost cardiomyocytes, reduce pathological remodeling, and restore myocardial function through enhanced paracrine signaling [22] [2].
MSC Culture Systems for Clinical-Grade Secretome Production
Source and Isolation of MSCs
The tissue source of MSCs directly influences the composition and therapeutic potential of the derived conditioned medium. MSCs can be isolated from multiple tissues including bone marrow, adipose tissue, and umbilical cord [22]. Each source presents distinct characteristics:
- Bone Marrow-derived MSCs (BM-MSCs): Historically the most studied source; demonstrated strong paracrine effects in cardiovascular disease models [22] [39].
- Adipose-derived MSCs (AD-MSCs): Contain a wider range of angiogenic factors, making them potentially superior for angiogenesis-mediated tissue regeneration [38].
- Umbilical Cord-derived MSCs: Offer high proliferative capacity and potent secretory capabilities, with fetal MSCs from umbilical cord blood considered particularly superior for anti-aging applications [40].
Culture Media and Expansion Conditions
The choice of culture medium significantly impacts MSC growth, proliferative capacity, and ultimately the composition of the conditioned medium. Studies have systematically compared different media formulations for optimizing MSC expansion:
Table: Comparison of Culture Media for MSC Expansion
| Culture Medium | Cell Population Doubling Time (Days) | Expansion Ratio | Particle Yield (Particles/Cell) | Key Findings |
|---|---|---|---|---|
| α-MEM + 10% hPL | 1.85±0.36 to 1.99±0.55 (Passage 3-6) | Higher | 4,318.72±2,110.22 | Promoted higher expansion ratio and particle yield, though not statistically significant |
| DMEM + 10% hPL | 1.90±0.45 to 2.25±0.46 (Passage 3-6) | Lower | 3,751.09±2,058.51 | Adequate for cell growth but with slightly longer doubling times |
Research indicates that BM-MSCs cultured in α-MEM showed superior morphology and proliferative capacities compared to those cultured in DMEM, although the differences were not statistically significant [39]. The expansion ratio of BM-MSCs cultured in α-MEM was higher than those cultured in DMEM, suggesting α-MEM may be preferable for clinical-grade production [39].
For clinical applications, culture systems must address challenges related to biofactor availability and environmental stressors that adversely affect cell growth and biofactor secretion [38]. The development of optimized culture systems that enhance yield and quality of MSC secretions is therefore essential [38]. This includes implementing good manufacturing practice (GMP)-compliant production using xeno-free culture media to ensure product safety and consistency [39].
Preconditioning and Priming Strategies
The secretory profile of MSCs can be significantly enhanced through preconditioning strategies that mimic the in vivo microenvironment. Cell priming represents a critical step for augmenting the therapeutic efficacy of MSC-CM for myocardial protection [38]. Priming approaches include:
- Hypoxic preconditioning: Exposing MSCs to low oxygen tension (1-5% O₂) to mimic the ischemic myocardial environment and enhance secretion of pro-angiogenic factors.
- Inflammatory cytokine priming: Incubation with cytokines like IFN-γ or TNF-α to boost immunomodulatory factor production.
- Pharmacological priming: Using compounds that modulate key signaling pathways to enhance paracrine function.
The donor's health and metabolic state significantly impact MSC secretory profiles, necessitating careful donor screening and standardization of preconditioning protocols [38]. Aging MSCs exhibit reduced proliferative capacity and altered secretome composition, highlighting the importance of controlling for donor age in clinical-grade production [38].
Protocols for MSC-CM Collection and Processing
Conditioned Medium Collection
The collection of conditioned medium requires standardized protocols to ensure consistency and therapeutic quality:
- Cell Expansion: Culture MSCs in selected medium (e.g., α-MEM with 10% hPL) under GMP-compliant conditions until passage 4-6 [39].
- Serum Deprivation: Prior to CM collection, replace growth medium with serum-free medium to eliminate confounding factors from serum proteins.
- Collection Timing: Harvest CM after 24-48 hours of incubation to ensure optimal factor concentration while avoiding nutrient depletion.
- Cell Viability Assessment: Confirm viability exceeds 90% before CM collection to minimize contamination from cellular debris [39].
- Removal of Cellular Components: Centrifuge at 2,000 × g for 20 minutes to remove cells and large debris, followed by 0.22µm filtration for sterilization.
Extraction of Secretome and Extracellular Vesicles
The secretome contains both soluble factors and extracellular vesicles (EVs), which can be isolated separately for different therapeutic applications:
Table: Comparison of EV Isolation Methods for Clinical-Grade Production
| Isolation Method | Principle | Particle Yield | Processing Time | Scalability | Key Advantages |
|---|---|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation forces | Baseline | 4-5 hours | Limited | Considered gold standard; no reagent addition |
| Tangential Flow Filtration (TFF) | Size-based separation through membranes | Significantly higher than UC | 2-3 hours | Excellent for large volumes | Gentle processing; high purity and yield |
| Size-Exclusion Chromatography | Size-based separation through porous matrix | Moderate | 1-2 hours | Moderate | High purity; minimal vesicle damage |
Studies directly comparing isolation methods have demonstrated that tangential flow filtration (TFF) provides statistically higher particle yields compared to ultracentrifugation (UC), making it more suitable for large-scale clinical production [39]. Isolated particles should be characterized using Nanoparticle Tracking Analysis (NTA), transmission electron microscopy (TEM), and Western blotting for markers CD9, CD63, and TSG101 to verify EV identity and quality [39].
The following workflow diagram illustrates the complete production process for clinical-grade MSC-CM and its derivatives:
Quality Control and Characterization of MSC-CM
Quantitative and Qualitative Assessment
Rigorous quality control is essential for clinical-grade MSC-CM production. The assessment includes both quantitative and qualitative parameters:
Quantitative Analysis:
- Particle concentration and size distribution via Nanoparticle Tracking Analysis (NTA)
- Total protein content quantification
- Specific growth factor ELISA assays (VEGF, HGF, FGF, etc.)
- Cell count and viability assessments (>90% required) [39]
Qualitative Analysis:
Potency and Functional Assays
For myocardial protection applications, MSC-CM must demonstrate functional efficacy through relevant potency assays:
- Cardioprotective Activity: Measurement of anti-apoptotic effects on cardiomyocytes under hypoxic conditions.
- Angiogenic Potential: Endothelial tube formation assays to quantify pro-angiogenic activity.
- Anti-inflammatory Effects: Inhibition of T-cell proliferation or modulation of macrophage polarization.
- Functional Recovery: In vivo assessment in myocardial infarction models measuring left ventricular ejection fraction (LVEF) improvement, infarct size reduction, and attenuation of pathological remodeling [22] [2].
Batch-to-batch consistency must be verified through these functional assays, with established specifications for release criteria based on correlation with in vivo efficacy.
Therapeutic Application in Myocardial Protection
Mechanisms of Action in Cardiac Repair
MSC-CM mediates cardioprotection through multiple parallel mechanisms that address the complex pathophysiology of myocardial infarction:
- Anti-apoptotic Effects: Secreted factors like IGF-1 and microRNAs (miR-21, miR-210) inhibit cardiomyocyte apoptosis, preserving viable tissue in the border zone of infarction [22].
- Angiogenic Induction: VEGF, FGF, and HGF promote neovascularization, restoring perfusion to ischemic myocardium [22].
- Immunomodulation: TGF-β, IL-6, and other immunomodulatory cytokines dampen excessive inflammatory responses post-MI [39].
- Anti-fibrotic Activity: Reduced expression of profibrotic factors attenuates maladaptive remodeling and scar expansion [38].
- Cardiac Repair Promotion: Factors that recruit endogenous progenitor cells and promote tissue repair through the CCL2/CCR2 axis [22].
The following diagram illustrates the key signaling pathways through which MSC-CM components mediate myocardial protection:
Administration Routes and Dosing Considerations
For myocardial protection, MSC-CM can be administered through several routes, each with distinct advantages:
- Intravenous Injection: Enables systemic distribution but may result in pulmonary first-pass effect and dilution.
- Intramyocardial Injection: Direct application to myocardial tissue during surgery or via catheter-based systems, ensuring local delivery.
- Intracoronary Infusion: Selective delivery through coronary arteries with enhanced myocardial uptake.
Clinical trials have demonstrated that intravenous infusion of bone marrow MSCs can increase left ventricular ejection fraction (LVEF) by 3.8% in heart failure patients, providing a benchmark for MSC-CM efficacy [22]. Dosing regimens must be optimized based on the concentration of bioactive factors rather than cell number, with typical doses ranging from 50-500 µg of EV protein per administration in preclinical models [39] [2].
Essential Research Reagent Solutions
The standardized production of clinical-grade MSC-CM requires specific research reagents and materials to ensure consistency, safety, and efficacy:
Table: Essential Research Reagents for Clinical-Grade MSC-CM Production
| Reagent Category | Specific Examples | Function | Quality Standards |
|---|---|---|---|
| Culture Media | α-MEM, DMEM, RPMI-1640 | Cell expansion and maintenance | GMP-grade, xeno-free |
| Serum Supplements | Human Platelet Lysate (hPL) | Provide growth factors and attachment factors | Clinical-grade, pathogen-tested |
| Dissociation Agents | Trypsin-EDTA, Accutase | Cell passaging and harvesting | GMP-grade, animal origin-free |
| Culture Vessels | Multi-layer flasks, Cell factories | Scalable cell expansion | Sterile, tissue culture-treated |
| Separation Systems | Tangential Flow Filtration systems | EV isolation and concentration | Closed-system, scalable |
| Cryopreservation Media | DMSO-based formulations | Cell banking and product storage | GMP-grade, defined composition |
| Quality Control Assays | NTA, ELISA, Flow cytometry | Product characterization and release testing | Validated, standardized |
The standardized production of clinical-grade MSC-CM represents a transformative approach for myocardial protection, offering a cell-free alternative with reduced risks and enhanced manufacturability compared to cellular therapies. Current evidence indicates that MSC-CM contains sufficient bioactive factors to elicit meaningful cardioprotective effects, including reduced inflammation, apoptosis, smaller infarct size, and improved cardiac functionality [2].
Future developments in the field will likely focus on manufacturing process optimization, including advanced bioreactor systems, improved characterization methods, and engineered EVs with enhanced cardiac targeting [2]. As the field progresses toward standardized clinical applications, addressing challenges related to variability in secretome composition, batch-to-batch variation, and the need for standardized protocols will be essential for ensuring reproducible efficacy [38]. With continued refinement of production methodologies and quality control systems, MSC-CM-based therapies hold significant promise for addressing the substantial unmet clinical need in cardiovascular disease.
Within the context of stem cell conditioned medium research for myocardial protection, the secretome—comprising all proteins, cytokines, and other factors released by cells—has emerged as a primary mediator of therapeutic effects. While cell transplantation initially showed promise for cardiac regeneration, the inconsistent long-term engraftment and functional heterogeneity of stem cells have shifted focus toward paracrine signaling as the principal mechanism of action [1] [41]. This paradigm shift positions the stem cell secretome as a critical, cell-free therapeutic biologics. Consequently, comprehensive profiling of its molecular composition is indispensable for elucidating mechanisms of cardiac repair, standardizing therapeutic preparations, and ultimately developing effective treatments for ischemic heart disease. This whitepaper provides an in-depth technical guide for researchers and drug development professionals aiming to characterize the proteomic and cytokine cargo of stem cell conditioned medium, with a specific focus on applications in myocardial protection and regeneration.
Core Analytical Methodologies for Secretome Characterization
Proteomic Profiling via Tandem Mass Tag (TMT)-Based Mass Spectrometry
In-depth quantitative proteomic analysis represents the gold standard for comprehensively characterizing the protein components of a secretome. The workflow below details the optimized protocol derived from recent stem cell and cardiac proteomics studies [13] [42].
Table 1: Key Steps in TMT-based Quantitative Proteomics Workflow
| Step | Procedure | Critical Parameters | Purpose |
|---|---|---|---|
| 1. Sample Preparation | Cell culture under serum-free conditions; protein extraction with SDS-containing lysis buffer | Use serum-free media during conditioning; include protease/phosphatase inhibitors; perform BCA assay for quantification | To collect secreted proteins without contamination; preserve protein integrity and determine concentration |
| 2. Protein Digestion | Reduction with DTT; alkylation with MMTS; digestion with Lys-C/Trypsin | Use high-purity, MS-grade enzymes; incubate at 37°C for 18 hours | To break proteins into peptides for mass spectrometry analysis |
| 3. TMT Labeling | Incubation of peptides with TMTpro 16plex reagents | Ensure pH ~8.5 during labeling; quench reaction with hydroxylamine | To differentially label samples from multiple conditions for multiplexed quantification |
| 4. Fractionation | Basic reversed-phase chromatography using high-pH solvent | Concatenate fractions to reduce analysis time; use C18 column | To reduce sample complexity and increase proteome coverage |
| 5. LC-MS/MS Analysis | Nanoflow LC separation coupled to Orbitrap mass spectrometer; MS2/MS3 for reporter ion quantification | Use data-dependent acquisition; implement dynamic exclusion; resolution ≥120,000 for MS1 | To separate peptides and obtain accurate mass and fragmentation data for identification/quantification |
| 6. Data Processing | Database search (e.g., Mascot); false discovery rate (FDR) control <1% | Use target-decoy strategy; require ≥2 unique peptides/protein; apply "match between runs" | To identify and quantify proteins with high confidence |
The experimental workflow for this multi-step proteomic analysis can be visualized as follows:
Cytokine and Growth Factor Analysis
Beyond broad proteomic coverage, targeted analysis of specific cytokines and growth factors is crucial, as these molecules often drive key therapeutic processes such as angiogenesis, anti-apoptosis, and immunomodulation. Enzyme-linked immunosorbent assays (ELISAs) provide specific, sensitive quantification of low-abundance factors. Key analytes for cardiac applications include Vascular Endothelial Growth Factor (VEGF-A), which is critical for angiogenesis, and urokinase Plasminogen Activator (uPA), involved in tissue remodeling [43]. Furthermore, multiplexed immunoassays (e.g., Luminex) enable the simultaneous quantification of dozens of cytokines from a small sample volume, providing a broader view of the secretome's immunomodulatory capacity.
Key Molecular Findings and Functional Significance
Proteomic profiling of stem cell conditioned media has revealed a complex cargo of functionally significant molecules. The following table synthesizes key protein classes and their demonstrated or putative roles in myocardial protection and repair, as identified in recent studies [13] [41] [44].
Table 2: Key Therapeutic Protein Classes in Stem Cell Conditioned Medium for Cardiac Repair
| Protein Class | Specific Examples | Therapeutic Function | Experimental Evidence |
|---|---|---|---|
| Angiogenic Factors | VEGF-A, FGF, HGF | Promote new blood vessel formation; improve perfusion of ischemic tissue | Enhanced tube formation in HUVEC assays; increased capillary density in rodent MI models [41] [43] |
| Anti-apoptotic Factors | TIMP-1, IGFBP | Inhibit cardiomyocyte apoptosis; reduce infarct size | Reduced caspase-3 activity in hypoxia-treated H9C2 cardiomyocytes; lower TUNEL+ cells in infarct border zone [41] |
| Immunomodulators | MFGE8, IL-10, TGF-β | Polarize macrophages to reparative phenotype; reduce pro-inflammatory cytokines | Lower numbers of infiltrating CD68+ macrophages in TEVG implants; modulated inflammatory response in vivo [43] |
| Metabolic Regulators | Enzymes for fatty acid oxidation, sirtuin signaling | Shift cardiomyocyte metabolism to favor survival under stress | Activated PPARα pathway; associated with improved ATP production in stressed myocardium [13] [8] |
| Proliferation-Inducing Factors | CAMP, CTNNB1, FUBP3, others from hiPM-cm | Promote adult cardiomyocyte proliferation and dedifferentiation | Increased Ki67+ and αSMA+ cardiomyocytes in vitro and in mouse hearts; improved regeneration post-MI [44] |
The functional roles of these secreted factors converge on several key signaling pathways that mediate cardiac repair. The following diagram illustrates the primary mechanistic pathways activated by the therapeutic cargo in the conditioned medium and their functional outcomes in the recipient myocardium.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful characterization of the stem cell secretome requires a carefully selected suite of reagents, materials, and instrumentation. The following table details essential components for constructing a robust profiling pipeline [13] [43] [44].
Table 3: Essential Research Reagent Solutions for Secretome Profiling
| Category / Item | Specific Example / Model | Primary Function in Workflow |
|---|---|---|
| Cell Culture | Human AD-MSCs, iPSC-derived primitive macrophages | Source of conditioned medium; ensure defined, serum-free conditions during production |
| Protein Digestion | MS-grade Trypsin/Lys-C | Specific enzymatic cleavage of proteins into peptides for LC-MS/MS analysis |
| Multiplexed Quantification | TMTpro 16plex Reagents | Isobaric labeling for simultaneous quantification of multiple samples in a single MS run |
| Chromatography | Nanoflow LC System (EASY-nLC 1200) | High-resolution separation of complex peptide mixtures prior to mass spectrometry |
| Mass Spectrometry | Orbitrap Lumos Tribrid Mass Spectrometer | High-resolution and high-mass-accuracy measurement of peptide masses and fragmentation spectra |
| Immunoassays | VEGF-A ELISA Kit, Urokinase Activity Assay | Targeted, sensitive quantification of specific, low-abundance cytokines and growth factors |
| Data Analysis | "Firmiana" Proteomic Cloud Platform, Mascot | Database search and quantitative processing of raw MS data; protein identification and quantification |
Comprehensive proteomic and cytokine profiling is not merely an analytical exercise but a fundamental prerequisite for advancing stem cell conditioned medium from a promising biological phenomenon to a standardized therapeutic product for myocardial protection. The methodologies outlined herein—from multiplexed quantitative proteomics to targeted cytokine analysis—provide researchers with a robust framework for deconstructing the complex molecular payload of the secretome. By rigorously characterizing this therapeutic cargo and understanding its mechanistic pathways, the field can progress toward optimized, consistent, and potent cell-free therapies capable of promoting angiogenesis, preventing apoptosis, modulating detrimental immune responses, and potentially even stimulating cardiomyocyte proliferation to regenerate the injured human heart.
Conditioned Medium (CM), a cocktail of bioactive secretions from stem cells, has emerged as a promising cell-free therapeutic for cardiac repair. This whitepaper consolidates evidence from recent preclinical studies demonstrating the efficacy of CM from various stem cell sources—including adipose-derived stem cells (ADSCs), menstrual blood stromal/stem cells (MenSCs), and mesenchymal stromal cells (MSCs)—in animal models of myocardial infarction (MI) and ischemia/reperfusion (I/R) injury. The documented effects encompass significant reduction in infarct size, improvement in cardiac function, and inhibition of pathological processes like apoptosis and fibrosis, primarily mediated through paracrine mechanisms. The findings herein frame the therapeutic potential of CM within the broader thesis of myocardial protection research.
Ischemic heart disease, a leading cause of global mortality, often manifests as acute myocardial infarction (MI). While reperfusion therapy is the standard treatment, it can paradoxically induce further damage, known as ischemia/reperfusion (I/R) injury [45] [46]. The quest for therapies that can protect the myocardium and repair the damage has led to the exploration of stem cell-based treatments. A paradigm shift has occurred from the initial focus on stem cell differentiation and engraftment to the recognition that their therapeutic benefits are largely mediated by paracrine factors [45] [46]. These factors, including cytokines, growth factors, and microRNAs, are secreted into the Conditioned Medium (CM) collected from stem cell cultures. This whitepaper delves into the proven efficacy of CM in animal models, providing a technical guide for researchers and drug development professionals by summarizing quantitative data, experimental protocols, and underlying mechanisms.
Quantitative Efficacy of CM in Preclinical Models
The therapeutic potential of CM has been consistently demonstrated across different animal models and stem cell sources. The tables below summarize key quantitative findings from recent studies.
Table 1: Summary of CM Efficacy on Functional Parameters in Animal Models
| CM Source | Animal Model | Key Functional Outcomes | Citation |
|---|---|---|---|
| Adipose-Derived Stem Cells (ADSCs) | Mouse, I/R | Significantly reduced infarct size; Improved ejection fraction (EF) and fractional shortening (FS) | [46] |
| Menstrual Blood Stem Cells (MenSCs) | Rat, MI | Significantly reduced scar size; Higher EF and FS compared to MI control group at day 28 | [47] |
| Human MSCs | Porcine, I/R | 60% reduction in infarct size; Marked improvement in systolic and diastolic performance | [7] |
| Cardiosphere-Derived Cells (CDCs) | Rat, I/R | High cell retention post-delivery; No significant long-term functional benefit from CM alone | [48] |
Table 2: Summary of CM Efficacy on Cellular and Molecular Parameters
| CM Source | Animal Model | Key Cellular/Molecular Outcomes | Citation |
|---|---|---|---|
| Adipose-Derived Stem Cells (ADSCs) | Mouse, I/R | Reduced apoptosis (TUNEL+ cells) and fibrosis; Downregulation of PUMA, p-p53, ETS-1, fibronectin, and collagen 3 | [46] |
| Menstrual Blood Stem Cells (MenSCs) | Rat, MI | Increased cardiomyocyte survival; Prevention of metaplasia; Mitochondrial transfer to cardiomyocytes; Down-regulation of NF-κB | [47] |
| Human MSCs | Porcine, I/R | Reduced nuclear oxidative stress (8-OHdG staining); Diminished phospho-SMAD2 and active caspase 3 expression | [7] |
| UCMSCs vs. ADMSCs | Mouse, MI | Both improved cardiac function and reduced infarction; ADMSCs showed stronger anti-apoptotic effects on residual cardiomyocytes | [41] |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear technical roadmap, this section outlines the methodologies from key cited studies.
- Animal Model: Male C57BL/6J wild-type and miR-221/222-knockout (KO) mice (8-12 weeks old) were used.
- I/R Surgery: Mice were anesthetized, and the left anterior descending (LAD) coronary artery was ligated with a suture and a silicone tube placed underneath to prevent permanent damage. After 30 minutes of occlusion, the suture was released to allow reperfusion.
- CM Administration: 25 minutes after occlusion, a total of 50 μL of ADSC-CM was uniformly injected intramuscularly into five locations in the border zone of the ischemic anterior wall.
- Assessment of Infarct Size: After 3 hours or 3 days of reperfusion, hearts were excised and sectioned. Sections were incubated with 1% Triphenyltetrazolium Chloride (TTC) at 37°C for 10 minutes. The infarct area (pale) was quantified as a percentage of the total area (red) using ImageJ software. Evans blue/TTC double staining was also used to differentiate the area at risk.
- Assessment of Cardiac Function: Cardiac function was evaluated by echocardiography under anesthesia. M-mode images were acquired to calculate Ejection Fraction (EF) and Fractional Shortening (FS).
- Histological Analysis: Apoptosis was assessed via TUNEL assay on heart sections. Fibrosis was evaluated by Masson's trichrome staining, which stains collagen fibers blue.
- Animal Model: Rats were subjected to MI by permanent ligation of the left anterior descending (LAD) coronary artery.
- Treatment Administration: 30 minutes after ligation, treatments were injected into the infarct border zone. The experimental groups were:
- Sham group
- MI group (control)
- CM group (MenSC-derived conditioned medium)
- MenSCs+CM group (MenSCs suspended in their own CM)
- Functional and Histological Analysis: Cardiac function (EF and FS) was measured by echocardiography on day 28 post-MI. The heart was then harvested for histological assessment of scar size and cardiomyocyte survival.
- CM Collection and Fractionation: Human MSC-CM was collected following a clinically compliant protocol. The CM was subsequently fractionated based on molecular size.
- Animal Model and Treatment: A porcine model of ischemia and reperfusion injury was used. CM or its fractions were administered via intravenous and intracoronary routes.
- Efficacy Assessment: Infarct size was measured. Cardiac performance was comprehensively assessed using echocardiography and pressure-volume loops. The study identified that the fraction containing products >1000 kDa (100-220 nm) was responsible for the cardioprotective effects, suggesting the active component is a large complex, possibly an exosome or protein aggregate.
Mechanisms of Action and Signaling Pathways
The therapeutic effects of CM are mediated through multiple interconnected mechanisms that target key pathological processes in MI and I/R injury. The diagram below illustrates the primary signaling pathways identified in the reviewed studies.
Diagram Title: Key Signaling Pathways Targeted by CM in Cardiac Protection
This diagram shows that CM acts on multiple fronts. A central mechanism involves the delivery of microRNAs like miR-221/222, which inhibit the p38/NF-κB pathway [46]. This inhibition leads to the downregulation of key executors:
- PUMA, which drives apoptosis via the p53/BCL2 axis.
- ETS-1, which promotes fibrosis by upregulating fibronectin and collagen production.
Concurrently, CM components can directly inhibit novel cell death pathways. For instance, a newly identified mechanism involves ZBP1, which forms a PANoptosome complex (ZBP1/RIPK3/CASP8/CASP6) to drive a coordinated cell death process known as PANoptosis (simultaneously involving pyroptosis, apoptosis, and necroptosis) during I/R injury [49]. CM's ability to suppress this complex contributes to reduced cardiomyocyte loss. Furthermore, CM helps in metabolic regulation by improving glucose and fatty acid oxidation in the stressed myocardium, supporting energy production and cell survival [8].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and models used in the featured experiments, providing a resource for researchers aiming to design similar studies.
Table 3: Key Research Reagents and Experimental Models
| Reagent / Model | Specifications / Example Source | Function in Research |
|---|---|---|
| ADSC-CM | Collected from human ADSCs (e.g., Lonza) in DMEM + 20% FBS [46] | Source of paracrine factors (miR-221/222) for testing anti-apoptotic and anti-fibrotic effects. |
| H9c2 Cells | Embryonic rat ventricular cardiomyocytes (ATCC) [46] | In vitro model for simulating I/R injury via Hypoxia/Reoxygenation (H/R) to study cardiomyocyte apoptosis. |
| C57BL/6J Mice | 8-12 weeks old, male [46] | Common in vivo model for myocardial I/R surgery to evaluate therapeutic efficacy in a standardized genetic background. |
| Triphenyltetrazolium Chloride (TTC) | 1-2% solution in PBS [46] | Vital stain used to differentiate metabolically active (red) from infarcted (pale) tissue in heart sections. |
| miR-221/222 KO Mice | Generated on a C57BL/6J background [46] | Genetic tool to validate the specific role of miR-221/222 in the protective mechanism of action of ADSC-CM. |
| ZBP1 Inhibitor (MSB) | Small molecule compound identified via virtual screening (KD=725 nM) [49] | Pharmacological tool to inhibit ZBP1-mediated PANoptosis, mimicking a protective effect of CM. |
| Anti-phospho-SMAD2 Antibody | Specific for immunohistochemistry/Western blot [7] | Reagent to detect and quantify TGF-β signaling activity, a pathway modulated by human MSC-CM. |
The collective evidence from diverse animal models solidifies the position of Conditioned Medium as a potent therapeutic candidate for myocardial protection. Its efficacy in reducing infarct size, improving systolic and diastolic function, and mitigating apoptosis, fibrosis, and complex cell death pathways like PANoptosis, underscores the power of stem cell paracrine signaling. The detailed protocols and mechanistic insights provided here offer a foundation for further preclinical optimization and standardization. Future research should focus on the identification and standardization of the critical active components within CM, the development of scalable GMP-production protocols, and the design of robust clinical trials to translate this promising cell-free therapy to the bedside.
The limited regenerative capacity of the adult human heart following myocardial infarction (MI) represents a fundamental challenge in cardiovascular medicine. The irreversible loss of cardiomyocytes leads to adverse remodeling, scar formation, and progressive heart failure, with a five-year survival rate of only 50% for advanced stages [8]. While conventional therapies manage symptoms, they fail to address the core issue of cardiomyocyte loss. Within this therapeutic landscape, stem cell-based approaches have emerged as promising strategies for cardiac regeneration.
A significant paradigm shift has occurred from initial focus on cell transplantation toward understanding paracrine mechanisms as primary mediators of cardiac repair. Research demonstrates that the secretome—the totality of factors secreted by stem cells—confers cardioprotective benefits without requiring direct cell engraftment [50]. This whitepaper synthesizes evidence documenting the functional outcomes achieved through stem cell conditioned medium (CM), specifically focusing on its validated effects on reducing infarct size, enhancing capillary density, and restoring cardiac performance. The transition to secretome-based therapies addresses critical limitations of cell-based approaches, including low cell survival, potential arrhythmogenicity, and ethical concerns [2] [51].
Documented Functional Outcomes of Stem Cell Conditioned Medium
Reduction of Myocardial Infarct Size
Experimental Evidence In a pivotal porcine model of ischemia and reperfusion injury, intravenous and intracoronary administration of human mesenchymal stem cell conditioned medium (MSC-CM) resulted in a significant 60% reduction in infarct size compared to controls [52] [7]. This dramatic cardioprotective effect was associated with molecular evidence of reduced oxidative stress, as determined by decreased immunostaining for 8-hydroxy-2'-deoxyguanosine, a marker of DNA damage [52]. Additionally, diminished expression of active caspase 3 and phospho-SMAD2 following CM treatment indicated suppression of apoptotic pathways and TGF-β signaling, respectively [52] [7].
Active Fraction Identification Fractionation studies revealed that cardioprotective properties resided exclusively in the >1000 kDa fraction (100-220 nm) of the conditioned medium [52]. This critical finding indicates that the therapeutic agent is likely a large macromolecular complex, potentially comprising extracellular vesicles (EVs) such as exosomes or microvesicles, rather than a single small molecule [52] [2]. These vesicles are known to carry bioactive cargoes, including miRNAs, proteins, and lipids, that modulate recipient cell responses [2].
Table 1: Documented Effects of MSC-CM on Myocardial Infarct Size
| Experimental Model | Intervention | Control | Infarct Size Reduction | Key Mechanisms |
|---|---|---|---|---|
| Porcine I/R injury [52] | IV & IC MSC-CM | Non-CM | 60% | ↓ Oxidative stress, ↓ Apoptosis (caspase 3), ↓ TGF-β signaling (p-SMAD2) |
| Mouse I/R injury [52] | >1000 kDa CM fraction | <1000 kDa fraction | Significant protection | Activity confined to large complex (100-220 nm) |
Enhancement of Myocardial Capillary Density
Quantitative Angiogenic Effects The therapeutic potential of MSC-CM extends profoundly to angiogenesis. In a porcine MI model, intravenous MSC-CM treatment significantly increased myocardial capillary density to 981 ± 55 capillaries/mm² compared to 645 ± 114 capillaries/mm² in non-CM treated controls [53]. This 52% increase in capillary density demonstrates the potent pro-angiogenic capacity of the stem cell secretome.
Mechanistic Insights Proteomic analysis of MSC-CM identified a rich composition of angiogenic factors [53]. Functional validation using in vitro HUVEC spheroid assays confirmed that MSC-CM actively promotes endothelial cell tubulogenesis, a fundamental process in new blood vessel formation [53]. The enhanced capillary network directly improves myocardial perfusion, delivering oxygen and nutrients to the ischemic tissue and supporting salvageable cardiomyocytes in the border zone [8] [53].
Table 2: Effects of MSC-CM on Capillary Density and Cardiac Function
| Parameter Assessed | Experimental Model | Intervention | Results | Statistical Significance |
|---|---|---|---|---|
| Capillary Density [53] | Porcine MI | IV MSC-CM | 981 ± 55 vs. 645 ± 114 capillaries/mm² | P = 0.021 |
| Systolic Performance [52] | Porcine I/R injury | IV & IC MSC-CM | Marked improvement (PV loops) | Significant |
| Diastolic Performance [52] | Porcine I/R injury | IV & IC MSC-CM | Marked improvement (PV loops) | Significant |
Improvement in Cardiac Performance
Functional Recovery Documentation The structural improvements in infarct size and vascularity translate directly to enhanced cardiac function. Porcine studies documented marked improvement in both systolic and diastolic performance following MSC-CM treatment, as comprehensively assessed through echocardiography and pressure-volume loops [52]. These advanced hemodynamic measurements provide robust evidence of functional recovery at the organ level.
Metabolic Correlates of Functional Improvement Emerging research suggests that stem cell secretome may also improve cardiac function by addressing metabolic dysregulation in the ischemic heart. Following MI, the heart undergoes significant metabolic remodeling, including disturbances in glucose, fatty acid, and branched-chain amino acid metabolism [8]. The secretome's potential to modulate these pathological metabolic pathways—such as enhancing glucose utilization or reducing toxic lipid accumulation—may represent an additional mechanism contributing to improved cardiac efficiency and performance [8].
Detailed Experimental Protocols
MSC-CM Preparation Protocol
Cell Culture and Conditioning
- Source: Human mesenchymal stem cells (MSCs) from bone marrow [52]
- Expansion: Culture in clinically compliant, serum-free media under Good Manufacturing Practice (GMP) guidelines [52] [50]
- Conditioning: Collect conditioned medium after 48-72 hours of culture during log-phase growth [52]
- Processing: Concentrate using tangential flow filtration or ultrafiltration [52] [50]
- Quality Control: Perform proteomic analysis to characterize secretome composition [53]
Fractionation Methodology
- Size-based Separation: Implement sequential filtration or size exclusion chromatography [52]
- Critical Fraction: Isolate >1000 kDa fraction (100-220 nm) containing large complexes [52]
- Storage: Preserve at -80°C with protein stabilizers if not used immediately [50]
In Vivo Efficacy Testing Protocol
Animal Model Establishment
- Species Selection: Porcine model for superior cardiovascular translational relevance [52] [53]
- Surgical Procedure: Perform left circumflex coronary artery ligation to induce MI [53]
- Ischemia-Reperfusion: Apply temporary occlusion (60-90 mins) followed by reperfusion [52]
Treatment Administration
- Timing: Initiate treatment at reperfusion or within 24 hours post-MI [52]
- Routes: Intravenous and intracoronary delivery [52] [7]
- Dosing: Daily administration for 7 days [53]
- Control: Use non-conditioned medium (identical base medium without MSC secretion) [52]
Endpoint Assessment
- Histological Analysis:
- Functional Assessment:
Molecular Mechanism Elucidation
Signaling Pathway Analysis
- Apoptosis Assessment: Western blot for active caspase-3 cleavage [52]
- Oxidative Stress Quantification: Immunohistochemistry for 8-OHdG [52]
- TGF-β Pathway: Phospho-SMAD2/SMAD2 ratio measurement [52]
- Metabolic Pathways: AMPK, PGC-1α, and glucose transporter analysis [8]
Pathway Integration Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for MSC-CM Investigations
| Reagent/Category | Specific Examples | Research Function | Key Applications |
|---|---|---|---|
| Stem Cell Sources | Human bone marrow MSCs [52], Umbilical cord MSCs [50], Adipose-derived MSCs [50] | Paracrine factor production | CM generation, potency comparison studies |
| Culture Media | Serum-free, clinically compliant media [52] [50] | MSC expansion under GMP-like conditions | Production of therapeutically relevant CM |
| Separation Systems | Tangential flow filtration, Size exclusion chromatography, Ultracentrifugation [52] | Fractionation by molecular size | Isolation of >1000 kDa active fraction |
| Characterization Tools | Proteomic arrays, ELISA, Nanoparticle tracking analysis [50] [53] | CM composition quantification | Quality control, biomarker identification |
| Animal Models | Porcine I/R injury [52] [53], Mouse MI model [52] | Preclinical efficacy testing | Translational validation, mechanism studies |
| Assessment Reagents | Antibodies to 8-OHdG, caspase-3, p-SMAD2, CD31 [52] [53] | Histological and molecular analysis | Quantifying oxidative stress, apoptosis, angiogenesis |
| Functional Assays | Echocardiography, Pressure-volume loops, HUVEC tubulogenesis [52] [53] | Functional outcome measurement | Cardiac performance assessment, angiogenic potential |
The comprehensive evidence presented herein substantiates that stem cell conditioned medium represents a promising therapeutic strategy for myocardial protection, with documented efficacy across three critical domains: significant reduction of infarct size, substantial enhancement of capillary density, and marked improvement in cardiac performance. The paracrine hypothesis—that stem cell secretions mediate cardioprotection—has transitioned from speculation to well-demonstrated scientific fact [52] [53] [7].
Future research directions should prioritize several key areas: First, precise identification of the active components within the >1000 kDa fraction, with extracellular vesicles representing prime candidates [52] [2]. Second, standardization of production protocols to ensure batch-to-batch consistency and compliance with regulatory requirements for clinical translation [50]. Third, exploration of combination strategies that integrate MSC-CM with metabolic modulators to address the complex pathophysiology of ischemic heart disease [8].
The transition from cell-based therapies to acellular secretome-based approaches offers distinct advantages, including improved safety profile, enhanced scalability, and simplified storage and administration [50] [2]. As research continues to elucidate the intricate mechanisms through which the stem cell secretome mediates its effects, the prospect of developing effective, clinically applicable therapies for myocardial infarction and ischemic heart failure becomes increasingly attainable.
The pursuit of effective myocardial protection and regeneration strategies represents a cornerstone of modern cardiovascular research. Within this field, stem cell-based therapies have emerged as a promising avenue for repairing damaged cardiac tissue following ischemic events such as myocardial infarction. While initial approaches focused on direct stem cell transplantation, recent investigations have revealed that the therapeutic benefits are largely mediated through paracrine mechanisms rather than direct cell engraftment and differentiation [2]. This paradigm shift has catalyzed growing interest in stem cell-conditioned medium (CM), which contains a repertoire of secreted factors—including cytokines, growth factors, and extracellular vesicles—that can elicit cardioprotective effects without the complexities of cell transplantation [53].
The efficacy of these therapeutic agents is fundamentally dependent on the delivery strategy employed to administer them to the compromised myocardium. The route of administration directly influences biodistribution, target engagement, retention, and ultimately, therapeutic outcomes [54]. This technical review provides an in-depth analysis of three principal delivery routes—intramuscular, intravenous, and intracoronary—for administering stem cell-derived conditioned medium in myocardial protection research. We examine the technical specifications, methodological considerations, and experimental evidence supporting each approach, with particular emphasis on their application in preclinical models.
Delivery Route Technical Specifications and Comparative Analysis
The selection of an appropriate delivery route requires careful consideration of multiple parameters, including targeting efficiency, retention, invasiveness, and technical feasibility. The table below provides a systematic comparison of the three primary administration strategies for cardiac-directed therapies.
Table 1: Comparative Analysis of Delivery Routes for Myocardial Therapy Administration
| Parameter | Intramuscular (IM) | Intravenous (IV) | Intracoronary (IC) |
|---|---|---|---|
| Targeting Precision | High (direct injection into myocardium) | Low (systemic distribution) | Moderate (regional coronary delivery) |
| Therapeutic Retention | High at site of injection | Low due to systemic dilution | Moderate, limited by washout |
| Invasiveness | High (requires thoracotomy or catheter-based systems) | Minimal | Moderate (requires catheterization) |
| Technical Difficulty | High | Low | Moderate to High |
| Risk Profile | Risk of arrhythmias, perforation | Systemic exposure, off-target effects | Coronary injury, no-reflow phenomenon |
| Primary Applications | Preclinical large animal studies; direct cardiac repair | Delivery of systemic-acting paracrine factors | Regional cardioprotection in acute MI |
| Model System Example | Porcine MI model via guided injection | Porcine MI model with systemic infusion | Porcine MI model during catheterization |
The intramuscular approach, also referred to as intramyocardial injection, involves the direct administration of therapeutic agents into the myocardial tissue [54]. This method can be performed either epicardially during open-chest procedures or transendocardially using catheter-based systems with electromechanical mapping guidance [54]. The key advantage of this technique is its ability to achieve high local concentrations precisely at the site of injury, thereby maximizing therapeutic engagement with the infarct and border zones while minimizing systemic exposure.
The intravenous route represents the least invasive method, involving the systemic administration of therapeutics through peripheral or central veins [54]. While technically straightforward, this approach results in widespread biodistribution and significant dilution of the therapeutic agent, with only a small fraction reaching the intended cardiac target [54]. The efficacy of intravenous delivery relies heavily on the ability of therapeutic agents to extravasate from the vasculature and penetrate the cardiac tissue, which can be limited by endothelial barriers and interstitial pressure.
The intracoronary route offers a middle ground, balancing invasiveness with targeting capability. This technique involves the infusion of therapeutic agents directly into the coronary arteries, typically during catheterization procedures [54]. The method enables first-pass cardiac exposure, allowing the therapeutic agents to perfuse through the myocardial microvasculature before systemic distribution. However, successful implementation requires careful control of infusion parameters to prevent hemodynamic compromise and ensure homogeneous distribution.
Table 2: Functional Outcomes of Different Delivery Routes in Preclinical Models
| Delivery Route | Reported Efficacy Outcomes | Experimental Model | Key Findings |
|---|---|---|---|
| Intramuscular | Improved capillary density, reduced infarct size, preserved systolic/diastolic function | Porcine LCx ligation model [53] | MSC-CM treatment increased capillary density (981 ± 55 vs 645 ± 114 capillaries/mm²) and preserved cardiac function |
| Intravenous | Modest functional improvement, systemic effects | Porcine model with daily infusions [53] | 7-day IV MSC-CM treatment improved myocardial perfusion and function |
| Intracoronary | Enhanced regional repair, reduced no-reflow | Porcine ischemia-reperfusion model [55] | Adenosine IC infusion improved LVEF recovery (ΔLVEF: 13.8 ± 7.4% vs. 12.1 ± 8.4%) |
Experimental Protocols for Delivery Route Evaluation
Intramuscular Delivery in Preclinical Porcine Model
The porcine model of myocardial infarction provides a physiologically relevant platform for evaluating intramuscular delivery of stem cell-conditioned medium, owing to its similarities to human cardiac anatomy and coronary circulation.
Surgical Procedure:
- Myocardial Infarction Induction: Anesthetize and ventilate Yorkshire swine (25-30 kg). Perform a left thoracotomy to access the heart. Identify the left circumflex (LCx) coronary artery and permanently ligate it to induce myocardial infarction [53].
- Therapeutic Administration: Following infarction, use a 29-gauge insulin syringe to perform multiple intramyocardial injections (100-200 µL per injection) into the ischemic border zone. The conditioned medium should be administered within 24 hours post-infarction for optimal efficacy.
- Endpoint Assessment: After a predetermined period (e.g., 3 weeks), euthanize animals for histological analysis. Harvest myocardial tissue from the infarct, border, and remote zones for assessment of capillary density, infarct size, and fibrotic area [53].
Key Considerations:
- Injection volume and number should be optimized to maximize distribution while minimizing tissue trauma and backflow.
- Electromechanical mapping systems can be employed in catheter-based approaches to precisely target infarct border zones.
- Inclusion of tracer particles or fluorescent labels in the injectate allows for verification of delivery accuracy and distribution.
Intravenous Delivery Protocol
The intravenous route offers simplicity but requires consideration of dosing regimens and pharmacokinetics.
Administration Procedure:
- Catheter Placement: Establish peripheral intravenous access (marginal ear vein or jugular vein) in the anesthetized porcine subject.
- Therapeutic Infusion: Administer stem cell-conditioned medium as a controlled intravenous infusion over 15-30 minutes to prevent hemodynamic instability. Studies have employed daily infusions for 7 days post-myocardial infarction to achieve therapeutic effects [53].
- Monitoring: Continuously monitor vital signs (heart rate, blood pressure, oxygen saturation) during and after infusion to detect potential adverse reactions.
Key Considerations:
- Multiple dosing regimens may be necessary to maintain therapeutic levels due to rapid clearance.
- The inclusion of plasma stability data for conditioned medium components strengthens experimental design.
- Biodistribution studies using labeled extracellular vesicles or proteins can validate cardiac homing following systemic administration.
Intracoronary Infusion Technique
Intracoronary delivery enables direct coronary perfusion of therapeutics, balancing invasiveness with targeting efficiency.
Catheterization Procedure:
- Vascular Access: Perform femoral artery puncture using the Seldinger technique under sterile conditions. Introduce a guiding catheter and advance it under fluoroscopic guidance to engage the ostium of the target coronary artery.
- Therapeutic Infusion: Dilute the conditioned medium in a physiologically compatible vehicle (e.g., saline) to a volume of 10-20 mL. Administer the solution as a slow, controlled infusion over 3-5 minutes to prevent hemodynamic compromise and ensure adequate distribution [55].
- Monitoring: Continuously monitor coronary pressure and electrocardiogram during infusion. Temporary bradycardia or hypotension may occur during right coronary artery infusions.
Key Considerations:
- Infusion pressure should be maintained below 300 mmHg to minimize endothelial injury.
- The use of a balloon catheter with distal occlusion can enhance distribution by preventing antegrade washout.
- Pre-clinical testing of infusion parameters in healthy animals is recommended before proceeding to infarcted models.
Visualization of Myocardial Delivery Pathways
The following diagram illustrates the anatomical pathways and functional relationships of the three delivery strategies for myocardial therapy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of delivery route studies requires specialized reagents and equipment. The following table details essential components for investigating stem cell-conditioned medium in myocardial protection research.
Table 3: Essential Research Reagents and Materials for Conditioned Medium Delivery Studies
| Category | Specific Reagent/Equipment | Function/Application | Technical Notes |
|---|---|---|---|
| Cell Culture | Human Mesenchymal Stem Cells (MSCs) | Source of paracrine factors for conditioned medium production | Use early passages (P3-P5); characterize with surface markers (CD73+, CD90+, CD105+) |
| Serum-free Medium | Production of conditioned medium without confounding serum factors | 48-72 hour collection period recommended; concentrate using 3-5 kDa cutoff filters | |
| Delivery Equipment | 29-Gauge Insulin Syringes | Intramuscular injections in small animal models | Precise volume delivery; minimal tissue trauma |
| Over-the-Wire Balloon Catheter | Intracoronary infusion with controlled dwell time | Prevents washout; enhances local retention | |
| Electromechanical Mapping System | Guidance for transendocardial injections | NOGA system for 3D myocardial mapping and targeted delivery | |
| Analysis Reagents | Anti-CD31 Antibody | Immunohistochemical staining for capillary density | Quantify angiogenesis in infarct border zones |
| Triphenyltetrazolium Chloride (TTC) | Histochemical assessment of infarct size | Differentiates viable (red) from necrotic (white) tissue | |
| ELISA Kits for Cytokines | Quantification of paracrine factors in conditioned medium | Validate batch-to-batch consistency (VEGF, HGF, IGF-1) | |
| Animal Models | Yorkshire Swine | Large animal model for translational delivery studies | Anatomical similarity to humans; susceptible to coronary ligation |
| Left Circumflex (LCx) Coronary Artery Ligation | Standardized myocardial infarction model | Reproducible infarct creation for therapy testing |
The selection of an appropriate delivery route represents a critical determinant in the efficacy of stem cell-conditioned medium for myocardial protection. Each administration strategy—intramuscular, intravenous, and intracoronary—offers distinct advantages and limitations that must be carefully balanced against experimental objectives and translational goals. Intramuscular delivery provides superior targeting and retention but requires invasive procedures, while intravenous administration offers simplicity but suffers from poor cardiac specificity. Intracoronary infusion represents an intermediate approach with clinical relevance for acute coronary syndromes. Future advancements in this field will likely focus on optimizing delivery parameters, developing targeted extracellular vesicles, and combining multiple administration routes to maximize therapeutic outcomes while minimizing procedural risks.
Overcoming Hurdles: Strategies to Enhance CM Potency and Clinical Translation
The therapeutic potential of mesenchymal stem cell (MSC) conditioned medium (CM) for myocardial protection is primarily mediated through its rich composition of secreted bioactive factors, including growth factors, cytokines, chemokines, and extracellular vesicles. This complex mixture, known as the secretome, demonstrates significant promise in promoting vascular repair, reducing inflammation, and enhancing tissue regeneration following ischemic injury [56]. However, the translation of MSC-CM therapies from preclinical research to clinical applications faces a substantial hurdle: significant heterogeneity in the composition and biological activity of these secretome-based products. This variability stems primarily from two key sources: the tissue origin of the MSCs and individual donor-related factors [57] [58]. Understanding and controlling these sources of variation is critical for the development of standardized, efficacious, and reproducible cell-free therapies for cardiovascular repair. The inherent diversity of MSCs, while reflecting their adaptive capacity in vivo, presents a formidable obstacle to manufacturing consistent biopharmaceuticals, necessitating rigorous investigation and protocol standardization [57].
Impact of MSC Tissue Source on Secretome Composition and Function
The biological source of MSCs is a major determinant of their secretory profile and consequent therapeutic potency. Research has demonstrated that MSCs isolated from different anatomical niches exhibit distinct paracrine signatures, leading to differential effects on target tissues, including the damaged myocardium.
A comprehensive 2024 study directly compared the reparative effects of conditioned media from umbilical cord-derived MSCs (UMSCs), adipose-derived MSCs (ADSCs), and bone marrow-derived MSCs (BMSCs) on human umbilical vein endothelial cells (HUVECs) damaged by high glucose, a model relevant to diabetic cardiovascular complications [56]. The findings revealed significant differences in both the quantity of secreted proteins and their functional capacity to promote key processes in vascular repair. The following table summarizes the key quantitative findings from this investigation.
Table 1: Comparative Analysis of MSC-CM from Different Tissue Sources on HUVEC Repair [56]
| Parameter | UMSC-CM | BMSC-CM | ADSC-CM | Notes |
|---|---|---|---|---|
| Total Protein Secretion | Highest | Intermediate | Lowest | Measured via BCA assay |
| Proliferation Repair | Superior | Superior | Moderate | Effect on HUVECs under high glucose |
| Migration Repair | Strongest | Moderate | Weaker | Evaluated via Transwell assay |
| Tube Formation | Most Pronounced | Moderate | Present | Assessed by nodes, branches, total length |
| Key Proteomic Pathways | Vasculature development, cell adhesion, tissue remodeling | Promotion of vascular development | Not specified | Identified via TMT-labeled LC-MS/MS |
Functional Implications for Myocardial Protection
The functional superiority of UMSC-CM in promoting endothelial cell migration and tube formation, as detailed in Table 1, suggests its secretome is particularly enriched with factors that facilitate angiogenesis and vascular repair [56]. This makes UMSCs a highly promising candidate for treating myocardial ischemia. The proteomic analysis further confirmed that the UMSC secretome was heavily involved in biological processes critical for healing, such as vasculature development and tissue remodeling. Conversely, while BMSC-CM also demonstrated robust pro-angiogenic capabilities, its profile was distinct, underscoring the importance of matching the MSC source to the specific therapeutic goal of myocardial protection, whether it be enhancing neovascularization, modulating inflammation, or preventing fibrosis.
Donor Variability: A Critical Factor in Secretome Consistency
Beyond tissue source, inter-individual donor variability constitutes a major and often underappreciated source of heterogeneity, potentially impacting the reliability of autologous and allogenic MSC-CM therapies.
Evidence of Intra-Individual Variability in Secretome Composition
A 2023 study meticulously analyzed the secretome of adipose-derived MSCs (adMSCs) isolated from ten different human donors, revealing striking individual variability in the secretion of key growth factors with known relevance to cardiovascular and neurological repair [58]. The study measured concentrations of factors including VEGF-A, BDNF, PDGF-AA, PDGF-AB/BB, and HGF in the conditioned medium from each donor. The results demonstrated a significant spread in the concentrations of these critical bioactive molecules, independent of the common MSC tissue source.
The functional consequences of this biochemical variability were profound. When the individual donor-derived conditioned media were applied to neuronal cultures exposed to oxygen-glucose deprivation (OGD) to simulate ischemic injury, their neuroprotective capacity was highly variable [58]. This protective effect showed a strong positive correlation with the specific concentrations of VEGF-A, BDNF, and PDGF-AA in the CM. Furthermore, the ability to promote the differentiation of oligodendrocyte precursor cells was positively correlated with PDGF-AA concentration. These findings underscore that donor-specific secretome profiles directly translate to divergent therapeutic outcomes in disease models.
Underlying Donor-Related Factors
The biological basis for this donor variability is linked to factors such as the donor's age, health status, and genetic background, which can influence the fundamental characteristics of the isolated MSCs [58]. This inherent variability presents a significant challenge for the manufacturing of standardized secretome-derived products, as the "potency" of the final product becomes inherently linked to the biological lottery of the donor cell source.
Experimental Protocols for Characterizing MSC Heterogeneity
Robust and standardized experimental methodologies are essential for quantifying and understanding MSC secretome heterogeneity. The following protocols are representative of those used to generate the data discussed in this review.
Protocol for Preparation and Functional Testing of MSC-CM
- Cell Culture and CM Collection: MSCs (UMSCs, ADSCs, BMSCs) are cultured in standard DMEM medium with 10% FBS. To produce conditioned medium, the growth medium is replaced with serum-free DMEM, and cells are cultured for 48 hours. The supernatant (CM) is then collected, centrifuged at 500 g for 3 minutes to remove cells and debris, and filtered through a 0.22 µm filter. Finally, the CM is concentrated using a 10 kDa ultrafiltration tube, and the protein concentrate is stored at -80°C [56].
- Proliferation Assay (CCK-8): HUVECs are seeded in 96-well plates and damaged using a high glucose (30 mM) medium. The damaged cells are then treated with the different MSC-CMs. After 24 hours, CCK-8 solution is added to each well. Following a 4-hour incubation, the absorbance at 450 nm is measured with a microplate reader to quantify cell proliferation [56].
- Migration Assay (Transwell): HUVECs in the logarithmic growth phase are inoculated into the upper chamber of a Transwell plate. The lower chamber is filled with MSC-CM as a chemoattractant. After 6 hours of incubation, cells that have not migrated are removed from the top surface with a cotton swab. Migrated cells on the lower surface are fixed, stained with crystal violet, and counted [56].
- Tube Formation Assay: A Matrigel matrix is polymerized in 96-well plates. HUVECs are then seeded onto the gel and treated with the various MSC-CMs. After 4-6 hours of incubation, the formation of tubular structures is observed under a microscope. Parameters such as the number of nodes, branches, and total tube length are quantified using image analysis software like ImageJ [56].
Protocol for Proteomic Analysis of MSC-CM
For a deep characterization of the secretome, quantitative proteomics can be performed.
- Protein Digestion: 100 µg of proteins from the CM are reduced, alkylated, and digested with trypsin overnight at 37°C [56].
- TMT Labeling: The resulting peptides are labeled with Tandem Mass Tag (TMT) reagents according to the manufacturer's instructions. This allows multiple samples to be pooled and analyzed simultaneously in a single LC-MS/MS run [56].
- LC-MS/MS Analysis: The labeled peptides are mixed in equal amounts, purified, and separated by liquid chromatography (LC) coupled online to a high-resolution mass spectrometer (MS/MS). The MS/MS data is used to identify the proteins and quantify their relative abundance across the different MSC-CM samples [56].
- Bioinformatic Analysis: The final protein lists are subjected to bioinformatic analysis (e.g., Gene Ontology, KEGG pathway enrichment) to identify the biological processes and pathways that are differentially regulated among the MSC sources [56].
Diagram 1: Workflow for comparative secretome analysis.
Strategies to Overcome Heterogeneity in Therapeutic Development
To translate MSC-CM from a research tool into a reliable biopharmaceutical, several strategies are being explored to mitigate the impacts of source and donor variability.
- Standardization of Manufacturing Protocols: Variations in cell culture conditions, including the choice of basal medium, duration of conditioning, cell passage number, and confluency, significantly impact the composition of the secretome [59] [57]. Adopting standardized, Good Manufacturing Practice (GMP)-compliant protocols is a fundamental step toward reducing batch-to-batch variability.
- Donor Screening and Cell Banking: Carefully characterizing MSCs from different donors and selecting those with a desirable and potent secretome profile for the creation of master cell banks can provide a more consistent starting material for production [58].
- Use of Immortalized Cell Lines: The development of immortalized monoclonal MSC lines is being investigated as a potential solution to achieve ultimate batch consistency and overcome the limitations of primary cell donors [60].
- Defining Critical Quality Attributes (CQAs): Moving away from ill-defined "secretome" products requires identifying specific, mechanistically relevant components that correlate with therapeutic potency. This involves a critical re-evaluation of assumed effectors, such as microRNAs in extracellular vesicles, and a focus on establishing robust potency assays based on verifiable mechanisms of action [60].
Diagram 2: Strategies to overcome MSC heterogeneity.
The Scientist's Toolkit: Essential Reagents and Materials
The following table compiles key reagents and their functions for conducting research on MSC conditioned medium, as derived from the cited experimental protocols.
Table 2: Research Reagent Solutions for MSC-CM Studies [56] [59] [58]
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| MSCs from Different Sources | Core biological material to investigate source-dependent variability. | Umbilical Cord (UMSC), Adipose (ADSC), Bone Marrow (BMSC). |
| Serum-Free Basal Media | Used for conditioning to produce CM, free of serum interference. | DMEM-LG, MSC NutriStem XF [59]. |
| Ultrafiltration Devices (10 kDa) | Concentration of conditioned medium to enrich for secreted factors. | Essential for proteomic and functional analysis. |
| BCA Protein Assay Kit | Quantification of total secreted protein in CM. | Standard method to compare total secretion levels. |
| Cell Proliferation Assay Kits | Functional testing of CM's effect on target cell growth. | CCK-8, MTT, WST assays. |
| Transwell / Boyden Chambers | Functional testing of CM's chemotactic and migratory effects. | Typically used with HUVECs or other relevant cell types. |
| Matrigel / Basement Membrane Matrix | Functional testing of CM's pro-angiogenic potential via tube formation. | Simulates a complex 3D environment for endothelial cells. |
| TMT / iTRAQ Reagents | Multiplexed quantitative proteomic analysis of CM composition. | Enables comparison of multiple CM samples in one MS run. |
| ELISA / Multiplex Assay Kits | Targeted quantification of specific growth factors and cytokines. | For validating proteomic data or screening donor CM (e.g., VEGF, BDNF, HGF) [58]. |
| Flow Cytometry Antibodies | Immunophenotypic characterization of MSCs to ensure quality. | CD73, CD90, CD105 (positive); CD14, CD34, CD45 (negative). |
The therapeutic promise of MSC conditioned medium for myocardial protection is undeniable, yet its clinical translation is inextricably linked to solving the heterogeneity hurdle. The tissue source of MSCs and individual donor variability are non-trivial factors that dictate the composition, potency, and functional specificity of the secretome. As evidenced by comparative studies, the selection between umbilical cord, adipose, or bone marrow MSCs can determine the efficacy of angiogenesis and vascular repair in target tissues. Furthermore, variability among donors introduces another layer of complexity, mandating rigorous donor screening and process standardization. Future progress in the field depends on a concerted shift toward GMP-compliant manufacturing, the establishment of mechanistically grounded critical quality attributes, and the development of robust potency assays. By systematically addressing these sources of heterogeneity, the scientific community can unlock the full potential of MSC secretome-derived products as reliable and effective cell-free therapies for cardiovascular disease.
Cardiovascular disease, particularly heart failure following ischemic myocardial infarction (MI), remains a leading cause of death worldwide [1]. The fundamental pathology driving this mortality is the irreversible loss of approximately one billion cardiomyocytes (CMs) after an acute MI incident, which adult human hearts cannot regenerate due to cardiomyocyte turnover rates of less than 1% per year [1]. While stem cell therapy has emerged as a promising strategy to replenish lost cardiomyocytes and recover myocardial function, clinical trials employing cell transplantation have demonstrated only marginal improvements, complicated by issues such as arrythmias, poor graft survival, and immune rejection [1] [22].
A significant paradigm shift is occurring in regenerative medicine, with attention moving from direct cell replacement to paracrine-mediated therapeutic effects [1] [22] [61]. Research indicates that transplanted stem cells exert their beneficial effects primarily through secreted bioactive factors that modulate the host environment rather than directly replacing damaged tissue [22]. This understanding has catalyzed interest in stem cell conditioned medium (CM) as a cell-free therapeutic alternative, containing a complex cocktail of therapeutic molecules including growth factors, cytokines, and extracellular vesicles [61] [62]. Within the context of myocardial protection research, optimizing the bioactive composition of CM through strategic preconditioning of stem cells before CM collection represents a promising frontier for therapeutic development.
This technical guide explores two powerful pretreatment strategies—hypoxic preconditioning and three-dimensional (3D) culture—that synergistically enhance the therapeutic potency of stem cell-derived conditioned medium for cardiac repair, providing researchers with methodologies, mechanistic insights, and practical implementation guidelines.
Scientific Rationale: How Hypoxia and 3D Culture Enhance Stem Cell Secretome
Physiological Basis for Hypoxic Preconditioning
The therapeutic application of hypoxia is founded on solid physiological principles. Mesenchymal stem cells (MSCs) naturally reside in tissues with low oxygen tension (approximately 1%-7% O₂), such as bone marrow and adipose tissue, significantly lower than the 21% O₂ typical in conventional normoxic cell culture [61]. This physiological normoxia ranges from 2%-9% O₂ across various embryonic and adult cell types, with specific niches like bone marrow functioning at ≤1% O₂ [63].
Molecular Mechanisms of Hypoxic Response The cellular response to low oxygen is primarily mediated by the hypoxia-inducible factor (HIF) pathway [63] [61]. Under normoxic conditions, HIF-1α subunits are continuously hydroxylated by prolyl hydroxylases (PHDs), leading to von Hippel-Lindau (VHL) protein-mediated ubiquitination and proteasomal degradation [63]. Under hypoxic conditions, HIF-1α stabilization occurs, allowing dimerization with HIF-1β, nuclear translocation, and activation of genes containing hypoxia-response elements (HREs) [63]. This genetic program enhances cellular survival, metabolic adaptation, and secretion of reparative factors.
Three-Dimensional Culture Advantages
The transition from conventional two-dimensional (2D) monolayers to three-dimensional (3D) culture systems represents another critical advancement in stem cell preconditioning. When cultured as 3D spheroids, stem cells recapitulate aspects of native tissue architecture and cell-cell interactions that significantly influence their secretory profile [63] [62].
In 3D spheroids, cells experience spatial heterogeneity in oxygen and nutrient availability. Cells located in the spheroid core encounter physiological hypoxia, activating HIF-mediated pathways, while peripheral cells maintain normal metabolic activity [62]. This creates a gradient of activation states within the same culture, potentially broadening the spectrum of secreted factors. Research demonstrates that hADSCs cultured as 3D spheroids secrete increased amounts of angiogenic growth factors compared to 2D-cultured cells, with VEGF expression significantly elevated in 3D formats [62].
Quantitative Evidence: Efficacy Data for Pretreatment Strategies
Enhanced Secretory Profile and Functional Outcomes
Multiple studies have quantified the enhancement in secretory profile and functional efficacy achieved through hypoxic preconditioning and 3D culture techniques. The table below summarizes key quantitative findings from recent research:
Table 1: Quantitative Enhancements from Hypoxic Preconditioning and 3D Culture
| Parameter Measured | Pretreatment Strategy | Enhancement Compared to Control | Experimental Model | Citation |
|---|---|---|---|---|
| VEGF Concentration | 3D spheroid + light irradiation | 10-fold increase vs. 2D culture; 1.4-fold vs. 3D alone | hADSC conditioned medium | [62] |
| CM Yield | Hypoxia (4% O₂) + intermittent agitation | ~1000-fold improvement | Murine iPSC differentiation in bioreactor | [64] |
| Therapeutic Efficacy | Hypoxic preconditioning (1% O₂) | Significantly enhanced reduction in lesion size and sensorimotor impairments | Neonatal HI brain injury model | [65] |
| Migratory Capacity | Hypoxic preconditioning (1% O₂) | Significantly increased migration to injured hemisphere | In vivo MSC tracking | [65] |
| Cell Survival | Hypoxic preconditioning | Increased survival under oxidative stress | BMSC transplantation in SCI model | [66] |
Synergistic Effects of Combined Approaches
The most significant enhancements occur when hypoxia and 3D culture are strategically combined. In a landmark study, combining hypoxia culture (4% O₂ tension) with intermittent agitation profile in stirred tank bioreactors resulted in an improvement of approximately 1000-fold in CM yields compared to normoxic and continuously agitated cultures [64]. Furthermore, wave-induced agitation in bioreactors enabled differentiation of iPSCs toward CMs with faster kinetics and higher yields (60 CMs/input iPSC), producing clinically relevant numbers of CMs (2.3 × 10⁹ CMs/1 L) within an 11-day differentiation protocol [64].
The combination of 3D spheroid culture with additional stimulation (such as light irradiation) demonstrates synergistic effects on secretory profiles. When hADSCs were cultured as 3D spheroids and subjected to low-level light therapy (LLLT), the expression of various angiogenic factors increased substantially, with important pro-angiogenesis factors (including Ang-1, artemin, CD105, FGFR2, IGFBP-3, CCL3, and μPA) increasing two-fold or more compared to 3D culture alone [62].
Experimental Protocols: Methodologies for Implementation
Hypoxic Preconditioning Methodology
Standardized Protocol for Hypoxic Preconditioning of MSCs:
- Cell Culture Preparation: Culture MSCs to 70-80% confluence under standard conditions (37°C, 5% CO₂, 21% O₂).
- Hypoxia Induction: Transfer cells to a specialized hypoxic chamber or incubator with controlled gas mixture (1-5% O₂, 5% CO₂, balanced N₂).
- Preconditioning Duration: Maintain cells under hypoxic conditions for 24-48 hours. Note: Exposure beyond 48 hours may induce cellular senescence and reduce therapeutic efficacy [61].
- Conditioned Medium Collection: Replace culture medium with serum-free formulation and continue hypoxia for additional 24-48 hours to accumulate secreted factors.
- CM Harvesting: Collect conditioned medium and centrifuge (2,000 × g, 10 minutes) to remove cellular debris.
- Concentration and Storage: Concentrate CM using centrifugal filters (e.g., 3-kDa cutoff) and store at -80°C for future applications [62].
Critical Optimization Parameters:
- Oxygen Concentration: Mild hypoxia (1-5% O₂) enhances therapeutic potential, while severe hypoxia (<1% O₂) promotes senescence and apoptosis [61].
- Temporal Considerations: Optimal exposure time is typically less than 48 hours to activate protective mechanisms without significant cellular damage [61].
- Cell Density: Maintain appropriate confluence (70-80%) to prevent contact inhibition or nutrient depletion.
3D Spheroid Culture Techniques
hADSC Spheroid Formation with Light Stimulation Protocol [62]:
- Cell Preparation: Harvest hADSCs at passage 3-5 using standard enzymatic dissociation.
- Spheroid Formation: Seed cells in ultra-low attachment plates at optimized density (3 × 10⁴ cells/400 μL serum-free media per well).
- Spheroid Maturation: Centrifuge plates (500 × g, 5 minutes) to promote aggregate formation and incubate for 24 hours (37°C, 5% CO₂).
- Light Stimulation: Apply low-level light therapy (LLLT) using organic light-emitting diodes (OLEDs) with wavelength 600-700 nm at appropriate energy density.
- Conditioned Medium Collection: Harvest CM after 24 hours of light stimulation, centrifuge to remove debris (2,000 × g, 10 minutes), and store at -80°C.
Bioreactor Protocol for Scalable Production [64]:
- Cell Aggregation: Inoculate murine iPSCs at 0.7 × 10⁵ cell/mL into Erlenmeyer flasks containing differentiation medium on orbital shakers (80-90 rpm).
- Bioreactor Transfer: After two days, transfer aggregates to stirred tank bioreactors at concentration of 150 aggregates/mL in 200 mL differentiation medium.
- Hypoxic Conditioning: Maintain cultures at 4% O₂ tension with intermittent agitation profile (ON: 30 s, OFF: 0 s) with direction change.
- CM Purification: Implement partial medium changes at specified intervals with selection medium to eliminate non-CMs.
Signaling Pathways and Mechanistic Insights
Molecular Mediators of Enhanced Potency
The enhanced therapeutic efficacy of conditioned medium derived from preconditioned stem cells involves multiple molecular mediators and signaling pathways:
HIF-1α Mediated Angiogenic Activation: Hypoxic preconditioning stabilizes HIF-1α, which translocates to the nucleus and activates transcription of pro-angiogenic genes including VEGF (vascular endothelial growth factor) and SDF-1α (stromal cell-derived factor 1-alpha) [61]. This enhances the angiogenic capacity of the secretome, crucial for revascularizing ischemic myocardial tissue. Research demonstrates that HIF-1α plays a central role in promoting survival of preconditioned MSCs under oxidative stress conditions, with HIF-1α inducers attenuating apoptosis even under challenging microenvironments [66].
Metabolic Reprogramming: Hypoxia induces a shift from oxidative phosphorylation to anaerobic glycolysis, enhancing glucose uptake and altering the metabolic intermediate composition of the secretome [63] [61]. This metabolic reprogramming enhances cellular survival under low-oxygen conditions and influences the bioactive cargo of extracellular vesicles.
Extracellular Vesicle (EV) Modification: Preconditioning strategies significantly alter the cargo of extracellular vesicles, particularly exosomes, which represent important mediators of paracrine effects. Stem-cell-derived extracellular vesicles (Stem-EVs) carry cardioprotective therapeutic cargos and demonstrate reduced immunogenicity compared to cell-based therapies [1]. Hypoxic preconditioning enriches EVs with miRNAs (e.g., miR-21, miR-210) that regulate cardiomyocyte apoptosis and fibrosis, enhancing their therapeutic potential for myocardial protection [22].
Enhanced Homing and Immunomodulation
Hypoxic preconditioning upregulates expression of CXCR4, the receptor for SDF-1α, enhancing migratory capacity toward injury sites [65] [61]. This improved homing efficiency is particularly valuable for targeted delivery of therapeutic factors to ischemic myocardium. Additionally, preconditioned MSCs demonstrate enhanced immunomodulatory capacity, suppressing pro-inflammatory cytokines (IL-6, IL-8) while increasing anti-inflammatory factors (IL-1ra, GM-CSF) [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Preconditioning Strategies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Hypoxia Systems | Hypoxic chambers, Tri-gas incubators | Maintain precise O₂ levels (1-5%) during preconditioning | Ensure proper calibration and monitoring |
| 3D Culture Platforms | Ultra-low attachment plates, Hanging drop plates, Bioreactors | Facilitate spheroid formation and maintenance | Select based on scalability needs |
| Extracellular Vesicle Isolation Kits | ExoQuick, Total Exosome Isolation kits | Isolate and concentrate EVs from conditioned medium | Consider yield and purity requirements |
| Angiogenesis Arrays | Proteome Profiler Angiogenesis Array | Simultaneously detect multiple angiogenic factors | Enable comprehensive secretome analysis |
| HIF Pathway Modulators | FG-4592 (HIF inducer), HIF-1α siRNA | Mechanistic studies of HIF-dependent effects | Verify specificity and optimal concentration |
| Cell Viability Assays | MTT, LDH release assays | Assess cytotoxicity and preconditioning effects | Use multiple methods for validation |
| Migration Assays | Transwell migration, Scratch wound assays | Evaluate enhanced homing capacity | Standardize serum concentration in chemoattractant |
The strategic preconditioning of stem cells through hypoxic exposure and 3D culture represents a powerful approach to enhance the therapeutic potency of conditioned medium for myocardial protection. These techniques leverage evolved cellular response mechanisms to hypoxia and tissue architecture, resulting in a secretome enriched with cardioprotective, angiogenic, and immunomodulatory factors. The quantitative evidence demonstrates substantial improvements in secretory profiles and functional outcomes, supporting continued investigation and development of these approaches.
Future research directions should focus on optimizing combination protocols that maximize synergistic effects, developing standardized production methodologies for clinical translation, and establishing comprehensive characterization of the preconditioned secretome. Additionally, exploring the potential of engineered stem cell-derived extracellular vesicles with enhanced cardiac targeting and recombinant therapeutic cargos may further advance the field toward effective cell-free biologics for cardiac repair and regeneration [1]. As these technologies mature, preconditioned conditioned medium products hold significant promise as standardized, safe, and efficacious therapeutics for myocardial protection and cardiovascular regeneration.
The therapeutic benefits of stem cell-conditioned medium for myocardial protection are now largely attributed to paracrine factors rather than direct cell engraftment [53]. Among these factors, extracellular vesicles (EVs) have emerged as potent mediators of intercellular communication, carrying a complex cargo of proteins, lipids, and nucleic acids that reflect the physiological state of their parent cells [67]. These nano-sized particles (30-150 nm) are naturally secreted by virtually all cell types and play crucial roles in cardiovascular pathophysiology [68]. In the context of stem cell conditioned medium research, EVs derived from mesenchymal stem cells (MSCs) and other progenitor cells have demonstrated remarkable cardioprotective capabilities, including reducing inflammation, inhibiting apoptosis, promoting angiogenesis, and potentially stimulating endogenous regeneration [1] [69]. The recognition that EVs convey most of the therapeutic effects of stem cell conditioned medium has shifted research focus toward engineering these natural delivery vehicles for enhanced cardiac targeting and drug delivery, creating a promising new frontier in cardiovascular therapeutics.
Native vs. Engineered EVs: Comparative Therapeutic Profiles
Native EV Cargo and Cardioprotective Mechanisms
Stem cell-derived EVs (Stem-EVs) inherently possess therapeutic properties that contribute to myocardial protection. The table below summarizes the key native cargo components and their demonstrated cardioprotective functions.
Table 1: Native Therapeutic Cargo in Stem Cell-Derived EVs and Their Cardioprotective Functions
| Cargo Type | Specific Components | Cardioprotective Functions | Mechanisms of Action |
|---|---|---|---|
| microRNAs | miR-21, miR-146a, miR-19a | Anti-fibrotic, anti-inflammatory, pro-survival | Target apoptotic pathways, reduce inflammation, inhibit fibrosis [68] [67] |
| Proteins | VEGF, bFGF, IGF-1 | Pro-angiogenic, pro-survival | Promote new blood vessel formation, enhance cardiomyocyte survival [69] |
| Growth Factors | VEGF, PGF | Angiogenesis, endothelial cell proliferation | Stimulate endothelial cell growth and migration [69] |
| Lipids | Sphingolipids, ceramides | Membrane stability, signaling | Enhance EV stability, facilitate recipient cell interactions [67] |
Limitations of Native EVs and Engineering Solutions
While native Stem-EVs demonstrate significant therapeutic potential, they face several limitations that restrict their clinical efficacy. These include lack of tissue specificity, leading to off-target distribution; rapid clearance by the mononuclear phagocyte system; limited drug loading capacity for exogenous therapeutics; and variable cargo composition depending on parent cell conditions [70] [68]. Engineering approaches directly address these limitations through strategic modifications:
- Enhanced targeting through surface ligand conjugation
- Prolonged circulation half-life via stealth coating
- Controlled cargo loading with therapeutic molecules
- Improved consistency through synthetic biology approaches
Engineering Strategies for Advanced EV Therapeutics
EV Source Selection and Characteristics
The therapeutic potential of EVs is significantly influenced by their cellular origin. Different source cells impart distinct biological properties and cargo profiles to their EVs, making source selection a critical design parameter for cardiac applications.
Table 2: EV Sources and Their Therapeutic Characteristics for Cardiac Applications
| EV Source | Therapeutic Advantages | Limitations/Considerations | Clinical Relevance |
|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Most widely used (57% of studies); strong anti-inflammatory and pro-angiogenic properties; immunomodulatory [68] | Source-dependent variability (BM, AD, UC); donor age effects | Multiple clinical trials; favorable safety profile [69] |
| Cardiac Progenitor Cells (CPCs) | Innate cardiac tropism; cardioprotective cargo (15% of studies) [68] | Limited cell availability; expansion challenges | Cardiac-specific repair mechanisms |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific origin; scalable; pluripotent differentiation capacity | Tumorigenicity concerns; need for purification | Personalized medicine approach [71] |
| Embryonic Stem Cells (ESCs) | Potent regenerative cargo; well-characterized | Ethical concerns; immunogenicity | Limited clinical translation [72] |
Exogenous Cargo Loading Methods and Applications
Engineering EVs to carry exogenous therapeutic cargo significantly expands their potential beyond native capabilities. The selection of loading method depends on the characteristics of the cargo molecule and the intended application.
Table 3: Methods for Loading Exogenous Cargo into EVs
| Loading Method | Process Description | Advantages | Limitations | Optimal Cargo Types |
|---|---|---|---|---|
| Pre-secretion (20 studies) | Genetic engineering of parent cells to express desired cargo; endogenous loading during EV biogenesis [68] | High natural loading efficiency; maintains EV integrity | Limited control over loading efficiency; potential parent cell toxicity | miRNA, proteins, reporter genes [68] |
| Post-selection (13 studies) | Direct loading into isolated EVs using physical or chemical methods | Precise control over cargo amount; versatile for diverse cargo types | Potential EV membrane damage; technical complexity | Chemical drugs, oligonucleotides, small molecules [68] |
| Incubation | Simple co-incubation of cargo with EVs | Technically simple; maintains EV structure | Low loading efficiency; passive diffusion limitation | Hydrophobic small molecules [68] |
| Electroporation | Electrical pulses create temporary pores in EV membrane | Higher efficiency for nucleic acids; controllable parameters | Cargo aggregation; membrane disruption risk | miRNA, siRNA, DNA [68] |
Surface Modification Strategies for Cardiac Targeting
Surface engineering enables EVs to specifically target cardiac tissues, dramatically enhancing delivery efficiency while reducing off-target effects. These modifications leverage molecular recognition systems to achieve tissue-specific homing.
Table 4: Surface Modification Strategies for Enhanced Cardiac Targeting
| Modification Strategy | Targeting Ligand/Moiety | Target Receptor | Cardiac Specificity | Key Findings |
|---|---|---|---|---|
| Peptide-based | Cardiac homing peptide (CHP) | Unknown cardiac cell surface protein | Ischemic myocardium | 3-fold increase in cardiac retention [68] |
| Protein-based | Anti-myosin light chain antibody | Myosin light chain | Damaged cardiomyocytes | Selective binding to injured myocardium [67] |
| Lipid-based | PEGylation | N/A | Prolonged circulation | Increased half-life from ~2 to ~12 hours [70] |
| Receptor-targeted | RGD peptide | Integrins αvβ3 | Activated endothelium | Enhanced angiogenesis in infarcted tissue [68] |
Experimental Workflows for EV Engineering and Evaluation
Integrated EV Engineering and Evaluation Workflow
The development of therapeutic EVs follows a systematic process from engineering through preclinical evaluation. The diagram below outlines the key stages in creating and validating engineered EVs for cardiac applications.
EV-Mediated Signaling Pathways in Cardiac Repair
Engineered EVs exert their therapeutic effects through multiple molecular pathways that promote cardiac repair and regeneration. The following diagram illustrates the key signaling mechanisms through which engineered EVs mediate their cardioprotective effects.
The Scientist's Toolkit: Essential Reagents and Materials
Successful development of engineered EV therapeutics requires specialized reagents and materials optimized for various stages of production, modification, and evaluation.
Table 5: Essential Research Reagents for EV Engineering and Evaluation
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| EV Isolation | Ultracentrifugation reagents; Size-exclusion chromatography columns; Polymer-based precipitation kits; Immunoaffinity beads | EV purification from conditioned medium; size-based separation; subtype isolation | Purity vs. yield trade-offs; maintenance of EV integrity; scalability [68] |
| Characterization | Antibodies to CD9, CD63, CD81; TSG101, ALIX; NTA instruments; TEM reagents; Western blot kits | EV identification and quantification; size distribution analysis; morphology assessment | MISEV2023 guidelines compliance; multi-method validation required [68] |
| Engineering | Cardiac homing peptides (CHP); PEG lipids; click chemistry reagents; electroporation buffers | Surface modification for targeting; stealth properties; cargo loading | Maintenance of EV function post-modification; loading efficiency [68] [67] |
| In Vitro Assays | HUVEC spheroids; cardiomyocyte cultures; transwell migration plates; tube formation matrices | Angiogenic potential assessment; uptake studies; functional validation | Relevance to cardiac physiology; reproducibility [53] |
| In Vivo Models | Mouse/rat MI models (LAD ligation); myocardial injection devices; imaging agents | Therapeutic efficacy evaluation; biodistribution studies; safety assessment | Clinical relevance of model; appropriate endpoints [1] [68] |
Administration Strategies and Biodistribution Enhancement
Delivery Routes and Their Efficiency Profiles
The route of administration significantly influences the distribution, retention, and ultimate efficacy of engineered EV therapeutics. The table below compares various delivery methods for cardiac applications.
Table 6: Comparison of Administration Routes for Engineered EV Therapeutics
| Administration Route | Cardiac Retention Efficiency | Advantages | Disadvantages | Best Applications |
|---|---|---|---|---|
| Intramyocardial | 15-22% retention; highest cardiac delivery | Direct delivery to target tissue; bypasses systemic clearance | Invasive procedure; potential tissue damage; limited distribution | Localized repair; chronic MI settings [68] |
| Intravenous | 2-5% retention; widespread distribution | Minimally invasive; repeatable; whole-body delivery | Rapid clearance; low cardiac specificity; potential off-target effects | Acute MI; systemic conditions [68] |
| Intracoronary | 8-12% retention; improved distribution | Catheter-based; direct coronary access; clinically familiar | First-pass clearance; embolization risk; technical complexity | Post-MI treatment; integrated with PCI [69] |
| Hydrogel-assisted | 25-40% retention; sustained release | Enhanced retention; controlled release; reduced clearance | Additional biomaterial; potential inflammation | Chronic repair; sustained release needs [68] |
Biomaterial-Enhanced EV Delivery Systems
Advanced biomaterial systems can dramatically improve EV retention and therapeutic persistence in the challenging cardiac environment. Hydrogel-based delivery platforms provide a supportive matrix that protects EVs from rapid clearance and enables sustained release kinetics [68]. These hydrophilic macromolecular networks exhibit excellent biocompatibility and mechanical properties similar to natural cardiac tissues, making them ideal for cardiac applications. Common hydrogel formulations for EV delivery include:
- Alginate-based systems: Provide gentle gelation conditions that maintain EV integrity
- Hyaluronic acid matrices: Mimic natural extracellular matrix components
- Decellularized cardiac ECM: Preserves native cardiac biochemical cues
- Thermo-responsive polymers: Enable minimally invasive injection in liquid form followed by in situ gelation
Studies demonstrate that hydrogel-encapsulated EVs can achieve 3-5 times higher retention compared to bolus injections, with sustained release profiles extending therapeutic activity from days to weeks [68]. This approach is particularly valuable for delivering multiple therapeutic cargoes or creating supportive microenvironments for tissue regeneration.
Engineering extracellular vesicles represents a paradigm shift in leveraging stem cell paracrine signaling for myocardial protection. By combining native therapeutic cargo with enhanced targeting capabilities and engineered therapeutic molecules, next-generation EVs offer unprecedented opportunities for precise cardiac repair. The integration of advanced loading techniques, surface modifications, and biomaterial-assisted delivery addresses the critical limitations of native EVs while preserving their natural biocompatibility and low immunogenicity. As the field progresses, standardized protocols for EV engineering, comprehensive safety profiling, and scalable manufacturing will be essential for clinical translation. The strategic engineering of EVs positions these natural nanotherapeutics as powerful tools for realizing the full potential of stem cell conditioned medium research in cardiovascular medicine.
The transition from whole cell-based therapies to cell-free therapies utilizing conditioned medium (CM) represents a paradigm shift in regenerative medicine, particularly for myocardial protection. CM, comprising the complex mixture of bioactive factors secreted by mesenchymal stromal cells (MSCs), offers significant therapeutic potential without the risks associated with whole cell administration [73]. However, this very complexity creates substantial standardization challenges for developing robust potency assays—defined as quantitative measures of biological activity—and definitive release criteria. The inherent variability of biological systems, combined with multifaceted mechanisms of action (MoAs), necessitates a systematic approach to ensure that CM products are consistently potent, safe, and effective for cardiovascular applications [74]. This technical guide examines these challenges and provides a framework for establishing scientifically rigorous and clinically meaningful quality control standards for CM-based therapeutics targeting myocardial protection.
The Regulatory Imperative and Current Landscape of Potency Testing
Regulatory Requirements
Regulatory agencies globally, including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA), mandate the use of a validated potency assay for the release of any biologic product, including CM [74]. Potency is considered a critical quality attribute (CQA) that must be measured to ensure product consistency and efficacy. As per regulatory guidelines, a potency assay must be "relevant, practical, reliable and ideally quantify the biological activity related to the MoA" [74]. The assessment of potency should be integrated early in product development, with data available by the time of the first clinical trial [74].
Analysis of Approved Cell Therapy Products
An analysis of potency tests for the 31 U.S. FDA-approved cell therapy products (CTPs) through 2024 provides crucial context for CM development. This analysis revealed several informative patterns [75]:
- Approved CTPs utilize an average of 3.4 potency tests per product (standard deviation 2.0).
- The most frequently used test categories are "Viability and count" (52%) and "Expression" (27%).
- Only 7% of non-redacted tests were categorized as "Bioassays" that measure functional activity, though redacted information may increase this percentage.
- A significant 84% of CTPs cite physicochemical assays (non-bioassays) as part of their potency testing [75].
Table 1: Potency Test Categories for FDA-Approved Cell Therapy Products
| Test Category | Frequency | Percentage | Examples |
|---|---|---|---|
| Viability and Count | 37 | 52% | Cell viability, total nucleated cell count |
| Expression | 19 | 27% | CAR expression, surface marker expression |
| Bioassays | 7 | 7% | Cytotoxicity, cytokine release |
| Genetic Modification | 6 | 9% | Vector copy number |
| Histology | 2 | 3% | Tissue morphology assessment |
For CM products, which lack living cells, the "Viability and count" category becomes irrelevant, shifting emphasis to "Expression" profiling of specific factors and functional "Bioassays" that can capture the complex MoA of the secretome.
Critical Challenges in CM Potency Assay Standardization
Source Material and Manufacturing Variability
The composition and biological activity of CM are profoundly influenced by multiple variables in the manufacturing process, creating a significant standardization hurdle [73]:
- MSC Source: Tissue origin (umbilical cord, bone marrow, adipose tissue) significantly impacts secretome composition.
- Donor Heterogeneity: Individual donor characteristics introduce inherent biological variability.
- Culture Conditions: Media formulation (e.g., use of fetal bovine serum vs. human platelet lysate), oxygen tension, and cell density affect factor secretion.
- Production Timeline: Cell passage number and conditioning period duration influence CM composition.
Research demonstrates that using human platelet lysate (hPL) instead of fetal bovine serum (FBS) in MSC culture not only eliminates xenogeneic risks but also provides a more standardized supplement that reduces batch-to-batch variability [73]. One optimized protocol using 5% IsoCell GROWTH hPL from a pool of 100 donors successfully generated CM with consistent compositional profiles independent of donor individuality, achieving production scales of approximately 120 liters from a single umbilical cord [73].
Mechanistic Complexity in Myocardial Protection
The development of potency assays for CM in cardiovascular applications is particularly challenging due to the multiple mechanistic pathways involved in myocardial protection and repair. The MoA is rarely unitary but rather a symphony of coordinated biological processes:
- Anti-apoptotic Effects: Prevention of cardiomyocyte cell death post-injury
- Anti-inflammatory Activity: Modulation of excessive immune responses
- Angiogenic Induction: Stimulation of new blood vessel formation
- Fibrosis Reduction: Attenuation of pathological scar tissue formation
- Metabolic Modulation: Improvement of cardiac energy metabolism
This multifaceted MoA necessitates an assay matrix approach rather than reliance on a single potency test [74]. No individual assay can adequately capture the complete therapeutic potential of CM, requiring multiple complementary tests that collectively reflect the relevant biological activities.
Analytical and Practical Limitations
The development of robust potency assays for CM faces several technical and practical constraints:
- Limited Sample Availability: Especially challenging for autologous approaches where CM quantities are restricted [74].
- Lack of Reference Standards: The field suffers from an absence of standardized reference materials for result normalization [74].
- In Vitro-In Vivo Correlation: Demonstrating meaningful correlation between in vitro potency measurements and in vivo therapeutic effects remains difficult [74].
- Stability-Indicating Challenges: Determining shelf-life and optimal storage conditions requires potency assays that can detect product degradation over time.
Table 2: Key Research Reagent Solutions for CM Potency Assessment
| Reagent/Category | Function | Application in Potency Testing |
|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free culture supplement | Standardized MSC expansion for consistent CM production |
| Umbilical Cord Tissue | MSC source | Provides primitive MSCs with high trophic factor production |
| Molecular Probes for Flow Cytometry | Cell surface marker detection | MSC identity verification (CD73+, CD90+, CD105+, CD45-) |
| ELISA/Multiplex Assay Kits | Protein quantification | Measurement of specific bioactive factors (VEGF, HGF, IGF-1) |
| Tube Formation Assay Kit | Angiogenic potential assessment | Functional testing of CM pro-angiogenic activity |
| Metabolic Assay Kits (e.g., ATP, ROS) | Cell viability and stress measurement | Quantification of cytoprotective effects |
Mechanism-Based Framework for Potency Assay Development
Mechanism of Action as the Foundation
The foundation of robust potency testing begins with a thorough understanding of the MoA. For CM in myocardial protection, this requires identifying the key biological processes that counteract the pathophysiological events following myocardial injury [76] [74]. The proposed framework involves:
- Define Intended Function: Clearly articulate the primary therapeutic goal (e.g., protection from ischemia-reperfusion injury, reduction of inflammatory damage, stimulation of repair).
- Identify Biological Pathways: Map the specific pathways involved in the therapeutic effect (e.g., AKT signaling for cell survival, NF-κB modulation for inflammation).
- Select Relevant Assays: Choose assays that directly measure these biological activities rather than relying on surrogate markers with uncertain relevance [76].
This approach aligns with regulatory thinking, as emphasized by the Association for the Advancement of Blood & Biotherapies (AABB), which states that "potency testing must do more than produce a number—it must tell a story about how the product works" [76].
Assay Matrix Design for Multifunctional CM
Given the multifaceted nature of CM bioactivity, a single assay cannot adequately represent potency. An assay matrix approach, employing multiple complementary tests, is essential [74]. The specific combination of assays should be tailored to the proposed MoA for myocardial protection:
Diagram 1: Mechanism-Based Potency Assay Matrix. This diagram illustrates how multiple mechanism-based assays collectively contribute to comprehensive potency assessment.
Advanced Technologies for Enhanced Potency Assessment
Emerging technologies offer unprecedented opportunities to develop more sophisticated and predictive potency assays:
- Multi-Omics Approaches: Proteomic profiling of CM provides comprehensive analysis of factor composition, while transcriptomic analysis of target cells reveals response pathways [77].
- Microphysiological Systems: Organ-on-a-chip platforms with human cardiomyocytes enable more physiologically relevant testing of CM effects on human cardiac tissue.
- High-Content Imaging: Automated microscopy with advanced image analysis can quantify multiple cellular responses simultaneously in a single assay.
- Biosensor Arrays: Real-time monitoring of cardiomyocyte function and metabolism in response to CM exposure.
These advanced approaches align with the concept of "embracing innovation thoughtfully" as recommended in recent potency testing guidelines [76].
Experimental Workflows and Methodological Considerations
Standardized CM Production Workflow
A critical prerequisite for meaningful potency testing is the consistent production of CM itself. The following optimized workflow has demonstrated success in generating reproducible, high-quality CM from Wharton's Jelly MSCs [73]:
Diagram 2: Standardized CM Production and Quality Control Workflow
This standardized protocol has demonstrated the capacity to produce approximately 120 liters of CM from a single umbilical cord, providing sufficient material for comprehensive potency assay development and industrial-scale production [73].
Key Functional Assays for Myocardial Protection
For CM intended for myocardial protection, the following functional assays provide mechanism-relevant potency measurements:
Anti-apoptotic Activity Assay
- Principle: Measure protection of cardiomyocytes from induced apoptosis
- Methodology:
- Culture H9c2 rat cardiomyocytes or human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs)
- Induce apoptosis with H₂O₂ (100-500 μM) or serum starvation
- Treat with CM (10-20% v/v) for 24 hours
- Quantify apoptosis using Caspase-3/7 activity assay or Annexin V/propidium iodide flow cytometry
- Calculate percentage protection compared to untreated controls
Angiogenic Potential Assessment
- Principle: Measure stimulation of endothelial tube formation
- Methodology:
- Seed human umbilical vein endothelial cells (HUVECs) on Matrigel-coated plates
- Treat with CM (10-50% v/v) or control media
- Incubate for 6-18 hours at 37°C
- Capture images using phase-contrast microscopy
- Quantify total tube length, number of branches, and mesh areas using image analysis software
Anti-inflammatory Activity Evaluation
- Principle: Measure modulation of inflammatory response
- Methodology:
- Culture macrophages (THP-1 cell line or primary)
- Polarize to pro-inflammatory phenotype using LPS (100 ng/mL) and IFN-γ (20 ng/mL)
- Treat with CM (10-20% v/v) for 24 hours
- Collect supernatant for cytokine profiling (TNF-α, IL-6, IL-1β) via ELISA
- Analyze anti-inflammatory markers (IL-10, Arg-1) via qPCR
Each functional assay should be validated for accuracy, precision, specificity, and linearity according to regulatory guidelines [74].
Establishing Quantitative Release Criteria and Quality Standards
Defining Acceptance Criteria
Establishing scientifically justified acceptance criteria for potency assays represents one of the most challenging aspects of CM standardization. The process should involve:
- Statistical Analysis of Manufacturing Consistency: Analyze multiple CM batches (typically 10-30) to establish normal operating ranges.
- Correlation with Preclinical Efficacy: Determine the minimum potency value that produces the desired therapeutic effect in relevant animal models.
- Stability Studies: Monitor potency decline over time to establish shelf-life and storage conditions.
For quantitative assays, results should be normalized to a reference standard and expressed in International Units (IU) whenever possible to enable cross-laboratory comparisons [74].
Comprehensive Quality Control System
A robust quality control system for CM should include both release and characterization assays, recognizing that not all tests need be performed on every batch:
Table 3: Proposed Quality Control Tests for CM for Myocardial Protection
| Test Category | Specific Test | Release Criteria | Frequency |
|---|---|---|---|
| Safety | Sterility (bacteria, fungi) | No growth | Every batch |
| Mycoplasma | Negative | Every batch | |
| Endotoxin | <5 EU/mL | Every batch | |
| Identity | Protein Fingerprinting | Similarity to reference >85% | Every batch |
| Specific Factor ELISA | Within ±3SD of historical mean | Every batch | |
| Potency | Anti-apoptotic Activity | ≥40% protection vs control | Every batch |
| Angiogenic Potential | ≥50% increase vs control | Every batch | |
| Anti-inflammatory Activity | ≥30% reduction in TNF-α | Every batch | |
| Characterization | Comprehensive Proteomics | Report profile | First in human, then annual |
| miRNA Signature | Report profile | First in human, then annual | |
| Lipidomic Analysis | Report profile | First in human, then annual |
The development of robust potency assays and release criteria for CM represents a critical milestone in advancing cell-free therapies for myocardial protection from research tools to regulated clinical products. Success in this endeavor requires collaborative efforts between researchers, manufacturers, and regulatory agencies to establish:
- Standardized Reference Materials: Well-characterized CM reference standards to enable cross-product and cross-facility comparisons.
- Mechanism-Based Assay Frameworks: Assay matrices that reflect the multifaceted MoA of CM in cardiovascular repair.
- Qualified Surrogate Assays: Practical, reproducible tests correlated with clinically relevant outcomes.
- Advanced Analytical Approaches: Implementation of multi-omics technologies for comprehensive product characterization.
By addressing these standardization challenges with scientific rigor and regulatory awareness, the field can unlock the full potential of CM-based therapies for myocardial protection, ensuring consistent product quality while maintaining the complex biological activity that makes these therapeutics so promising.
The transition of stem cell-based therapies from laboratory research to clinical application represents one of the most significant challenges in modern regenerative medicine. For myocardial protection research, stem cell conditioned medium has emerged as a promising therapeutic strategy, offering the cardioprotective benefits of cell-based therapies without the complexities of administering living cells. These secretomes, containing bioactive molecules and extracellular vesicles, have demonstrated significant potential for reducing apoptosis and fibrosis in myocardial ischemia/reperfusion injury models [46]. However, the very promise of these treatments creates a pressing manufacturing challenge: how to consistently produce these complex biological products at a scale sufficient for clinical trials and eventual widespread patient access while maintaining rigorous quality standards.
The journey from a meticulously optimized laboratory process to large-scale Good Manufacturing Practice (GMP) production is fraught with technical, regulatory, and operational hurdles. Current Good Manufacturing Practice (cGMP) regulations, enforced by agencies like the FDA and EMA, establish minimum requirements for the methods, facilities, and controls used in manufacturing, ensuring products are safe for use and possess the claimed ingredients and strength [78]. The World Health Organization emphasizes that GMP ensures medicinal products are consistently produced and controlled to quality standards appropriate for their intended use [79]. For conditioned medium production, this means establishing a robust, reproducible manufacturing process that preserves the critical quality attributes of the therapeutic secretome while meeting stringent safety requirements.
This technical guide examines the critical pathway to scalable GMP manufacturing of stem cell conditioned medium for cardiac applications, addressing fundamental principles, specific manufacturing hurdles, and practical strategies for successful scale-up, providing researchers and drug development professionals with a framework for navigating this complex landscape.
Fundamental GMP Principles for Biological Products
GMP compliance for biological products like stem cell conditioned medium extends beyond simple cleanroom requirements. It encompasses a comprehensive quality assurance system covering all aspects of production. According to WHO, GMP defines quality measures for both production and quality control and ensures that processes are clearly defined, validated, reviewed, and documented, and that personnel, premises, and materials are suitable for pharmaceutical production [79].
For conditioned medium products, several foundational principles take on particular importance. The primacy of patient welfare requires that risks to patients are minimized, with clinical testing never allowing promise for future patients to override the welfare of current research subjects [80]. Transparency in timely data sharing and social justice in distributing benefits fairly are equally crucial ethical underpinnings [80]. From a technical perspective, the integrity of the research enterprise necessitates that information obtained is trustworthy, reliable, and responsive to scientific uncertainties, maintained through independent peer review, oversight, replication, and accountability at each research stage [80].
The regulatory framework for these advanced therapies is complex and evolving. In Europe, products like mesenchymal stromal cell (MSC) secretomes are classified as Advanced Therapy Medicinal Products (ATMPs) under Regulation 1394/2007/EC and Directive 2009/120/EC [81]. The US FDA regulates these products under Title 21 of the Code of Federal Regulations, particularly parts 210, 211, and 600 for biological products [78]. Navigating this regulatory landscape requires early and continuous engagement with regulatory bodies to align development strategies with expectations.
Key Manufacturing Hurdles in Scaling Conditioned Medium Production
Process Reproducibility and Raw Material Control
The transition from research-scale to large-scale production introduces multiple variables that can compromise product consistency. Variations in mixing efficiency, heat transfer, and mass transfer often differ between small and large vessels, potentially compromising product quality and yield [82]. For conditioned medium production, this is further complicated by the biological nature of the starting material—living stem cells whose secretome composition can be influenced by subtle environmental changes.
A critical consideration is the move from research-grade to GMP-grade materials. The culture media used for stem cell expansion significantly impacts the resulting secretome. While fetal bovine serum (FBS) has been commonly used in research, its poorly defined composition and risk of inter-species contamination make it unsuitable for GMP manufacturing [81]. Alternatives include human platelet lysate (hPL) or chemically defined, xeno-free GMP-compliant media [81]. These switches are not trivial; they can influence MSC phenotype and performance, potentially altering the therapeutic profile of the conditioned medium [81] [83].
Analytical and Characterization Challenges
The complex and heterogeneous nature of conditioned medium presents significant characterization challenges. Unlike single-molecule pharmaceuticals, conditioned medium contains a diverse mixture of proteins, extracellular vesicles, lipids, and nucleic acids that collectively contribute to its therapeutic effect [84] [46]. This complexity makes it difficult to establish definitive critical quality attributes (CQAs) and potency assays.
For extracellular vesicle (EV)-enriched secretomes, characterization should follow recommendations of the Minimal Information for Studies of EV 2018 (MISEV2018) guidelines, which include specifying EV-specific markers and biochemical composition [84]. However, as noted in recent research, "the field of EV-based therapeutics is in its infancy," creating challenges in developing "a quality control (QC) release strategy which is meaningful, scientifically valid, acceptable to regulatory agencies, and ensures the manufacturing process is controlled and reproducible" [84].
Supply Chain and Raw Material Sourcing
Scaling up production places substantial strain on the supply chain. As production volumes increase, so does demand for raw materials, intermediates, and packaging [82]. Variability in the quality of these materials can disrupt manufacturing processes, while sourcing issues can delay production timelines. The situation is particularly acute for conditioned medium production, which requires consistent, high-quality starting materials for cell culture.
Supply chain fragility is a critical concern, with single suppliers for many components creating vulnerability [85]. Additionally, the ultra-cold chain logistics required for many cell therapy products add significant complexity and risk of product degradation [85]. Building strong relationships with suppliers and diversifying sourcing options can help mitigate these risks, as can implementing supply chain management tools and analytics to optimize material procurement [82].
Table 1: Key Challenges in Scaling GMP Manufacturing of Stem Cell Conditioned Medium
| Challenge Category | Specific Hurdles | Impact on Production |
|---|---|---|
| Process Design | Transition from open to closed systems; Scaling parameters; Preservation of critical quality attributes | Inconsistent product quality; Alteration of therapeutic profile; Process failures |
| Raw Materials | Moving from FBS to defined media; Sourcing GMP-grade cytokines; Supplier qualification | Changes in secretome composition; Lot-to-lot variability; Supply disruptions |
| Characterization | Defining potency assays; Quantifying active components; Establishing release criteria | Inability to demonstrate consistency; Regulatory approval delays |
| Supply Chain | Single-source reagents; Cold chain requirements; Vendor quality variability | Production bottlenecks; Increased costs; Quality failures |
Strategies for Successful Scale-Up
Quality by Design (QbD) Framework
Implementing a Quality by Design (QbD) approach is fundamental to successful scale-up. QbD involves designing processes that are robust and reliable, ensuring consistent product quality from the start [82]. This begins with identifying Critical Quality Attributes (CQAs)—the physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality [82].
For conditioned medium production, CQAs might include specific protein concentrations (e.g., cardioprotective miRNAs like miR-221/222 [46]), EV concentration and size distribution, absence of residual host cell DNA, and sterility. Once CQAs are established, Critical Process Parameters (CPPs) that significantly impact these attributes are identified and controlled. A proactive approach to compliance includes "early engagement with regulatory bodies to clarify expectations, conduct extensive documentation, and use a QbD framework" [82].
Advanced Manufacturing Technologies
Adopting innovative technologies can significantly enhance manufacturing consistency and efficiency. For EV-enriched secretome production, tangential flow filtration (TFF) has emerged as a scalable method for processing large volumes of conditioned media [84]. When integrated into a fully closed system, TFF enables uninterrupted processing from cell culture to final product, maintaining aseptic conditions essential for GMP manufacturing [84].
The adoption of single-use systems and modular infrastructure allows faster transitions from clinical to commercial scale [85]. These technologies reduce contamination risk, increase flexibility, and decrease cleaning validation requirements. Additionally, Process Analytical Technology (PAT) enables real-time monitoring of process variables, allowing manufacturers to detect deviations early and take corrective action to ensure consistent product quality [82].
Pilot-Scale Testing and Process Characterization
Conducting pilot-scale studies is critical for identifying and addressing challenges before full-scale production begins. These studies allow manufacturers to simulate real-world production conditions and assess process performance at larger scales [82]. Data gathered from pilot-scale testing informs decisions regarding process optimization, equipment selection, and risk management strategies.
For conditioned medium production, this involves systematically scaling up cell culture volumes while monitoring the impact on secretome composition and functionality. As noted in recent research, "the manufacturing process may require an upgrade from open to closed methods, and other procedural steps may likewise be changed for better manufacturability or process control at large scale" [84]. These changes can have dramatic effects on therapeutic efficacy, making thorough characterization at pilot scale essential.
Case Study: GMP Manufacturing of CPC Secretome for Cardiac Application
A recent landmark achievement demonstrates the successful translation of these principles into practice. Researchers developed a robust, reproducible large-scale GMP-compliant process for producing an EV-enriched secretome derived from cardiovascular progenitor cells (CPC) for treating heart failure [84]. This case study offers valuable insights into the practical application of scale-up principles.
The process began with human induced pluripotent stem cell (hiPSC)-derived CPCs produced under GMP-compliant conditions, providing a single, well-defined, and highly expandable cell source to minimize batch-to-batch variability [84]. The manufacturing process included CPC vesiculation, secretome purification and concentration using scaled-up tangential flow filtration (TFF), and sterilizing filtration [84]. The entire process was conducted in accordance with GMP regulations using closed methods to maintain aseptic conditions.
This approach enabled "processing of a large enough volume of conditioned media to cover the needs of QC release testing; Good Laboratory Practice (GLP) animal toxicity and tumorigenicity assessments; treatment of the patients for the whole clinical trial; and stability testing for more that 3 years" [84]. The final investigational medicinal product (IMP) was stored between –65°C and –85°C and could be easily diluted by the hospital pharmacy for patient infusion.
Quality Control Strategy
The researchers implemented a comprehensive QC strategy for in-process and release testing to guarantee quantity, safety, purity, and identity of the final product [84]. This strategy followed both MISEV2018 guidelines and European Pharmacopoeia regulations, including thorough characterization of molecular and functional parameters of mother cells before and after vesiculation, and of the final cell-free product [84].
The IMP demonstrated biological activity and was non-immunogenic in vitro, with no signs of toxicity or tumor development in vivo [84]. This comprehensive approach resulted in regulatory approval from the French National Agency for Medicines and Health (ANSM) for a Phase I clinical trial for heart failure treatment (NCT05774509) [84].
Diagram Title: GMP Manufacturing Workflow for CPC Secretome
Experimental Protocols for Characterizing Cardioprotective Secretome
In Vitro Hypoxia/Reoxygenation Model
To evaluate the cardioprotective effects of conditioned medium, researchers have established robust in vitro models that mimic myocardial ischemia/reperfusion injury. The hypoxia/reoxygenation (H/R) model using H9c2 cardiomyocytes (originally derived from embryonic rat ventricular tissue) provides a standardized system for assessing therapeutic potential [46].
Detailed Methodology:
- Cell Culture: Maintain H9c2 cells in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum and 1% penicillin at 37°C in a humid incubator (95% air and 5% CO₂) [46].
- Hypoxia Induction: Expose cells to hypoxia for 24 hours in a specialized hypoxic incubator (5% CO₂ and 1% O₂ at 37°C), with O₂ replaced by N₂ [46].
- Reoxygenation Phase: Following hypoxic exposure, transfer cells to normoxic conditions (95% air and 5% CO₂) at 37°C for 12 hours [46].
- Treatment Protocol: Apply conditioned medium during the reoxygenation phase. Include appropriate controls (untreated cells, normoxic controls, etc.).
- Assessment Endpoints: Evaluate apoptosis (Annexin V/PI flow cytometry, TUNEL assay), fibrosis (immunocytochemistry for fibronectin, collagen 3), and relevant signaling pathways (Western blot for p-p53, PUMA, ETS-1) [46].
In Vivo Myocardial Ischemia/Reperfusion Model
For in vivo validation, the murine myocardial ischemia/reperfusion model provides a physiologically relevant system for evaluating therapeutic efficacy.
Detailed Methodology:
- Animal Preparation: Use male C57BL/6J wild-type mice aged 8-12 weeks. Anesthetize with 3% isoflurane [46].
- Surgical Procedure: Perform left thoracotomy to expose the heart. Ligate the left anterior descending coronary artery (LAD) with a 7-0 nylon suture, placing a silicone tube (OD 86 mm) 1 mm below the ligation to prevent arterial damage [46].
- Ischemia Period: Maintain occlusion for 30 minutes, verified by whitening of the ventricle distal to the ligation [46].
- Treatment Administration: At 25 minutes post-occlusion, intramuscularly inject 50 μL of conditioned medium (4 μg/mL) uniformly into five locations in the border area of the anterior left ventricular wall [46].
- Reperfusion: Remove the silicone tube after 30 minutes of occlusion to allow blood reperfusion.
- Assessment: After 3 hours or 3 days of reperfusion, evaluate infarct size (Evans blue/TTC staining), cardiac function (echocardiography), apoptosis (TUNEL assay), and fibrosis (Masson's trichrome staining) [46].
Table 2: Key Analytical Methods for Characterizing Cardioprotective Secretome
| Analysis Type | Specific Methods | Parameters Measured | Significance |
|---|---|---|---|
| Potency Assays | In vitro H/R model with H9c2 cells; Annexin V/PI flow cytometry; TUNEL assay | Anti-apoptotic activity; Reduction in fibrosis markers; Pathway modulation (p-p53, PUMA, ETS-1) | Demonstrates biological activity; Links product to mechanism of action |
| Vesicle Characterization | Nanoparticle tracking analysis; Transmission electron microscopy; Tetraspanin detection (CD9, CD63, CD81) | Particle concentration and size distribution; Morphological confirmation; EV-specific markers | Confirms presence of key therapeutic vehicles; Ensures product consistency |
| Molecular Composition | miRNA profiling (e.g., miR-221/222); Proteomic analysis; Western blot for specific factors | Cargo composition; Protein content; Specific biomarker quantification | Correlates composition with efficacy; Identifies critical quality attributes |
| Safety Testing | Sterility testing; Endotoxin detection; Mycoplasma testing; In vivo tumorigenicity studies | Microbial contamination; Pyrogenic substances; Oncogenic potential | Ensures patient safety; Required for regulatory approval |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Conditioned Medium Production
| Reagent Category | Specific Examples | Function & Importance | GMP Considerations |
|---|---|---|---|
| Cell Culture Media | Xeno-free, chemically defined MSC media; Human platelet lysate (hPL) supplements | Supports cell growth and secretome production; Defined composition reduces variability | Must have Drug Master File or equivalent regulatory support; Traceability and qualification of raw materials essential |
| Cell Sources | hiPSC-derived cardiovascular progenitor cells; Bone marrow-derived MSCs; Adipose-derived stem cells (ADSCs) | Determines secretome composition; Starting material defines therapeutic potential | Comprehensive characterization and banking; Donor screening for allogeneic sources; Stability data across passages |
| Purification Systems | Tangential Flow Filtration (TFF) systems; Chromatography resins; Ultracentrifugation systems | Isulates and concentrates active components; Removes undesirable impurities | Closed-system processing preferred; Scalable technologies; Validated cleaning or single-use systems |
| Cryopreservation Solutions | DMSO-free, defined cryoprotectants; Serum-free freezing media | Maintains product stability during storage; Prevents loss of activity | Qualified for human use; Composition documented and controlled; Compatibility with administration protocol |
| Analytical Standards | Recombinant tetraspanin proteins; Synthetic miRNA standards; EV reference materials | Enables quantification and method validation; Ensures assay performance and accuracy | Certified reference materials where available; Documented traceability to recognized standards |
Molecular Mechanisms of Cardioprotective Secretome
Research has elucidated specific molecular mechanisms through which stem cell conditioned medium exerts cardioprotective effects. Adipose-derived stem cell conditioned medium (ADSC-CM) has been shown to attenuate cardiac apoptosis and fibrosis by reducing the expression of key regulators in these processes [46].
The miR-221/222/p38/NF-κB pathway has been identified as a central mechanism. Conditioned medium containing abundant miR-221/222 targets and regulates two critical proteins: PUMA (p53-upregulated modulator of apoptosis) and ETS-1 (an important mediator of cardiac fibrosis) [46]. This dual targeting enables coordinated suppression of both apoptotic and fibrotic pathways activated during ischemia/reperfusion injury.
Diagram Title: Molecular Mechanism of ADSC-CM Cardioprotection
The path to large-scale GMP manufacturing of stem cell conditioned medium for myocardial protection requires integrating scalability considerations from the earliest stages of therapeutic development. Successful translation depends on a systematic approach that addresses both technical and regulatory challenges while maintaining focus on the fundamental goal: producing a consistent, safe, and efficacious product for patients.
The remarkable success in scaling up mRNA-based COVID-19 vaccine production offers valuable lessons for the regenerative medicine field. Through the application of QbD principles, advanced bioreactor technologies, and close collaboration with regulatory agencies, manufacturers were able to rapidly scale up production without compromising product quality [82]. This achievement demonstrates that with appropriate strategies and collaboration, even the most complex manufacturing challenges can be overcome.
For myocardial protection research, the establishment of GMP-compliant processes for producing cardioprotective secretomes marks a significant milestone. As these advanced therapies progress through clinical development, continued emphasis on manufacturing innovation, quality systems, and regulatory science will be essential to realizing their full potential to transform care for patients with cardiovascular disease.
Comparative Efficacy and Future Directions: CM Versus Whole Cell Therapies
Within the evolving paradigm of cardiovascular regenerative medicine, the therapeutic use of conditioned medium (CM) derived from mesenchymal stem cells (MSCs) has emerged as a promising cell-free strategy for myocardial protection and repair. The efficacy of MSC-CM is intrinsically linked to the secretory profile of the parent cells, which varies significantly based on the tissue of origin. This technical review provides a systematic, head-to-head comparison of CM derived from three prominent MSC sources: bone marrow (BM), adipose tissue (AT), and umbilical cord tissue (UCT), with a specific focus on applications for ischemic heart disease and cardiomyopathy. As the field moves towards clinical translation, understanding these source-dependent differences is critical for rational therapy design and optimizing cardiac outcomes [22] [2] [72].
The therapeutic rationale for using CM lies in harnessing the paracrine secretome of MSCs, which includes growth factors, cytokines, and extracellular vesicles. This secretome mediates cardioprotective effects such as angiogenesis, anti-inflammation, anti-apoptosis, and anti-fibrosis, without the complexities and risks associated with whole-cell transplantation. Research indicates that most stem-cell-derived extracellular vesicles are non-immunogenic and carry cardioprotective therapeutic cargo, making them potent alternatives to cell-based therapies [2] [27]. The core thesis of this review is that the biological advantages of each MSC source must be systematically considered to select the optimal secretome for specific pathological aspects of myocardial injury.
Source-Specific Proliferation and Immunophenotype
The growth potential and surface marker profile of MSCs are fundamental to their ex vivo expansion and subsequent secretome production. Significant variations exist in the proliferation capacity of MSCs derived from different tissues, which impacts the scalability of CM production.
Table 1: Comparative Growth Kinetics of MSCs from Different Sources
| Source | Population Doubling Time (Hours) | Cumulative Population Doublings (at Passage 3) | Primary Culture Time to Confluence (Days) | References |
|---|---|---|---|---|
| Bone Marrow (BM) | 99 ± 22 | 6 ± 0.5 | 7-8 | [86] |
| Adipose Tissue (AT) | 40 ± 7 | 9.6 ± 0.4 | 7-8 | [87] [86] |
| Umbilical Cord (UCT) | 21 ± 2 | 12.3 ± 0.7 | ~13 | [88] [86] |
While all MSCs express classic positive markers (CD73, CD90, CD105) and lack hematopoietic markers (CD14, CD45, CD34), source-specific differences exist. For instance, UCT-MSCs show higher expression of CD146, while AT-MSCs may retain low levels of CD34. BM-MSCs exhibit high expression of MSCA-1 and SSEA-4, whereas UCT-MSCs are negative for MSCA-1 [86]. These immunophenotypic differences hint at underlying functional specializations.
Differentiation Potential and Implications for Secretome
The tri-lineage differentiation potential is a defining characteristic of MSCs. BM-MSCs generally demonstrate superior osteogenic and chondrogenic potential compared to AT-MSCs and UCT-MSCs [87] [89]. In contrast, AT-MSCs exhibit a more pronounced and efficient adipogenic differentiation capability [89]. These differential lineage propensities reflect the ontological programming of the cells from their native niche and are likely mirrored in their secretory profiles, tailoring them for specific regenerative tasks.
Comparative Analysis of MSC Secretome Composition
The therapeutic potency of CM is directly determined by its composition of bioactive factors. Quantitative analyses reveal significant quantitative and qualitative differences in the secretion of key paracrine factors by BM-, AT-, and UCT-MSCs.
Key Soluble Factors in Myocardial Protection
Table 2: Secretome Composition of MSCs from Different Sources
| Secreted Factor / Functional Group | Bone Marrow (BM-MSC) | Adipose Tissue (AT-MSC) | Umbilical Cord (UCT-MSC) | Primary Function in Cardiac Repair |
|---|---|---|---|---|
| Hepatocyte Growth Factor (HGF) | Lower secretion [86] | Higher secretion [87] [86] | Higher secretion [86] | Angiogenesis, anti-apoptosis, anti-fibrosis |
| Vascular Endothelial Growth Factor (VEGF) | Comparable pro-angiogenic effects [88] | Secreted [22] | Secreted [88] | Promotes angiogenesis & endothelial cell survival |
| Fibroblast Growth Factor 2 (FGF-2/bFGF) | Lower secretion [86] | Higher secretion [87] | Intermediate secretion [86] | Angiogenesis, fibroblast proliferation |
| Insulin-like Growth Factor-1 (IGF-1) | Lower secretion [87] | Higher secretion [87] | Data Insufficient | Promotes cardiomyocyte survival & hypertrophy |
| Stromal Cell-Derived Factor-1 (SDF-1/CXCL12) | Higher secretion [87] | Lower secretion [87] | Data Insufficient | Stem cell homing, angiogenesis |
| Angiopoietin-1 (Ang-1) | Expressed [88] | Expressed [22] | Expressed [88] | Stabilizes newly formed blood vessels |
| Anti-inflammatory Cytokines (e.g., IL-10, TSG-6) | Lower gene expression [88] | Potent immunomodulation [90] [87] | Higher gene expression [88] | Suppresses detrimental inflammation post-MI |
UCT-MSCs demonstrate a particularly robust secretory profile for factors critical to cardiac repair. In vitro, UCT-MSCs showed greater proliferation and expression of anti-inflammatory cytokines like IL-10 and TSG-6 compared to BM-MSCs [88]. AT-MSCs also display a strong paracrine function, with studies indicating a more potent secretion profile for certain cytokines and greater immunomodulatory effects compared to BM-MSCs [87] [89]. BM-MSCs, while having a lower proliferation rate and secretion of some factors, are notable for their high secretion of SDF-1, which is crucial for stem cell homing [87].
Functional Efficacy in Cardiac and Related Models
In Vitro Functional Assays
Functional assays provide direct evidence of CM bioactivity. In a wound healing assay using lung epithelial cells (as a model for cellular repair), cells incubated with UCT-MSC CM demonstrated better wound closure following scratch injury compared to those with BM-MSC CM [88]. Furthermore, both UCT-MSC CM and BM-MSC CM exhibited similar pro-angiogenic effects on hyperoxia-exposed pulmonary microvascular endothelial cells, suggesting shared potency in promoting vascular network formation [88]. The secretome from all three MSC sources has demonstrated a pronounced neurotrophic potential, which may contribute to regulating cardiac autonomic function, though this is more relevant in neural disorder models [86].
In Vivo Efficacy in Disease Models
Evidence from animal models of disease solidifies the therapeutic promise of MSC-CM and highlights source-specific strengths.
- Experimental Bronchopulmonary Dysplasia (BPD) Model: In a hyperoxia-induced BPD model in newborn rats, both BM-MSC and UCT-MSC administration significantly improved alveolar structure, lung angiogenesis, and vascular remodeling, and reduced lung inflammation. However, UCT-MSC treatment led to greater improvement in some morphometric measures of alveolarization and less lung macrophage infiltration compared to the BM-MSC-treated group, underscoring its potentially superior anti-inflammatory and regenerative capacity [88].
- Immunomodulation: The immunomodulatory capacity of the CM is a key mechanism for dampening post-infarction inflammation. BM-MSCs have been shown to possess the most prominent immunomodulatory activity, effectively suppressing immune cell proliferation through both cell-contact and paracrine mechanisms [86]. In co-culture studies, MSCs from all sources inhibited T cell and NK cell activation, but their effects on B cells varied, with UCT-MSCs showing no inhibitory effect under the tested conditions [90]. AT-MSCs have been reported to have more potent immunomodulatory effects than BM-MSCs in some studies [87].
Experimental Protocols for CM Evaluation
To ensure reproducibility and rigorous comparison of CM from different MSC sources, standardized experimental protocols are essential.
Protocol 1: CM Production and Collection
- Cell Culture: Culture BM-, AT-, and UCT-MSCs in a standardized, xenogeneic-free medium, such as α-MEM supplemented with 5% human platelet lysate (hPL) to ensure clinical relevance [87] [86].
- Cell Expansion: Use cells at passages 3-5 for all experiments to avoid senescence-related changes in secretome.
- Serum Starvation: Prior to CM collection, wash cells with PBS and incubate in a serum-free basal medium for 24-48 hours to eliminate interference from serum proteins.
- CM Collection: Collect the supernatant and centrifuge at 2,000 × g for 10 minutes to remove cell debris.
- Concentration & Storage: Concentrate the CM using centrifugal filter units (e.g., 3 kDa cutoff). Aliquot and store at -80°C. Avoid multiple freeze-thaw cycles.
Protocol 2: In Vitro Wound Healing/Scratch Assay
This assay tests the capacity of CM to promote the repair of a cell monolayer.
- Cell Seeding: Seed relevant cells (e.g., cardiac fibroblasts, endothelial cells) in a 24-well plate until they form a 100% confluent monolayer.
- Scratch Creation: Use a sterile 200 μL pipette tip to create a straight "scratch" in the monolayer. Wash with PBS to remove dislodged cells.
- CM Application: Add the test CMs (from BM, AT, UCT) or control serum-free medium to the respective wells.
- Imaging and Analysis: Capture images of the scratch at 0 hours and at regular intervals (e.g., 12, 24 hours) using an inverted microscope. Quantify the percentage of wound closure using image analysis software (e.g., ImageJ).
Protocol 3: Tube Formation Assay
This assay evaluates the pro-angiogenic potential of the CM.
- Matrigel Coating: Thaw Matrigel on ice and coat a 96-well plate (50 μL/well). Incubate at 37°C for 30 minutes to allow polymerization.
- Cell Seeding and Treatment: Seed human umbilical vein endothelial cells (HUVECs) or similar on the Matrigel surface. Treat cells with the different MSCs CMs or control media.
- Incubation and Imaging: Incubate the plate at 37°C for 4-16 hours.
- Analysis: Capture images using a microscope. Quantify parameters such as total tube length, number of master junctions, and number of meshes per field using automated software.
The following workflow diagram summarizes the key experimental steps for generating and functionally testing MSC-CM:
Diagram 1: Experimental workflow for generating and testing MSC-CM, covering from cell isolation to functional and analytical characterization.
Signaling Pathways and Mechanistic Insights
The therapeutic effects of MSC-CM are mediated through the activation of multiple interconnected signaling pathways in recipient cells. The following diagram maps the key cardioprotective pathways and the bioactive molecules involved:
Diagram 2: Core signaling pathways activated by MSC-CM, leading to cardioprotective effects. Key: GFs=Growth Factors; EVs=Extracellular Vesicles.
The activation of these pathways is mediated by a complex cocktail of molecules within the CM. For instance, VEGF, FGF-2, and HGF are potent activators of the PI3K/Akt and MAPK/ERK pathways, promoting endothelial cell survival, proliferation, and angiogenesis. The anti-apoptotic effects on cardiomyocytes are largely mediated through Akt activation by factors like IGF-1 and HGF. The anti-inflammatory response is driven by cytokines such as IL-10 and TSG-6, which modulate the JAK/STAT3 and NF-κB pathways, leading to reduced production of pro-inflammatory cytokines and a shift towards a regenerative immune environment [88] [22] [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for MSC-CM Research
| Reagent / Material | Function in Research | Example Application / Note |
|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free supplement for clinical-grade MSC expansion. Promotes robust cell growth. | Replaces fetal bovine serum (FBS) to avoid xenogeneic immune reactions and conform to GMP standards [87] [86]. |
| Lymphocyte Separation Medium | Isolates mononuclear cells from bone marrow or other tissues during primary MSC isolation. | Density gradient centrifugation is a standard first step in purifying BM-MSCs [88] [87]. |
| Collagenase Type II / IV | Enzymatic digestion of tissues to isolate stromal cells. | Used for isolating MSCs from adipose tissue (Type II) [89] and umbilical cord matrix (Type II) [88]. |
| Matrigel / Geltrex | Basement membrane matrix for 3D cell culture and pro-angiogenic assays. | Essential for the in vitro tube formation assay to assess CM's angiogenic potential [91]. |
| Centrifugal Filter Units (3kDa) | Concentrates and buffer-exchanges protein-rich CM. | Allows for the removal of dilute basal medium components and concentration of the secretome for functional studies. |
| ELISA / Multiplex Assay Kits | Quantifies specific protein levels (e.g., VEGF, HGF, IL-10) in CM. | Critical for the analytical characterization and batch-to-batch consistency checking of CM preparations [87] [86]. |
| Exosome Isolation Kits | Isolates small extracellular vesicles from CM for mechanistic studies. | Enables researchers to dissect the contribution of the vesicular versus soluble fraction of the CM [2]. |
This head-to-head comparison elucidates that the choice of MSC source for generating conditioned medium is not trivial and should be guided by the specific therapeutic goals for myocardial protection. UCT-MSCs demonstrate a superior profile in terms of proliferative capacity and secretion of key anti-inflammatory and epithelial repair factors. AT-MSCs offer a strong combination of proliferation and potent immunomodulatory and pro-angiogenic secretome, with the added advantage of easy accessibility. BM-MSCs, while more challenging to expand, are highly immunomodulatory and are a potent source of homing factors like SDF-1.
Future research should focus on the systematic profiling of the complete secretome, including miRNAs and proteins, from MSCs cultured under standardized, clinically relevant conditions. Furthermore, exploring the synergistic effects of combining CM from different sources or pre-conditioning MSCs to enhance the secretion of desired factors could unlock the next level of efficacy. As the field advances, the "cell-free" therapy using optimized MSC-CM holds significant promise as a safe and effective strategy for mitigating myocardial injury and fostering a regenerative environment in the failing heart.
The pursuit of effective therapies for myocardial protection, particularly following ischemic injury, has positioned stem cell-conditioned medium (CM) as a pivotal biological therapeutic. The functional benefits of stem cell transplantation are now largely attributed to paracrine signaling, mediated by the complex cocktail of growth factors, cytokines, and extracellular vesicles secreted into the CM [1] [53]. Within this secretome, two potent biological processes—angiogenesis (the formation of new blood vessels) and anti-apoptosis (the inhibition of programmed cell death)—are considered critical for cardiac repair. However, these functionalities are not uniformly expressed across all stem cell sources. This whitepaper provides an in-depth comparative analysis of the angiogenic and anti-apoptotic potency of different mesenchymal stromal cell (MSC) sources, framing the findings within the context of developing optimized, cell-free conditioned medium therapies for myocardial protection. It synthesizes current research data, details standardized experimental protocols, and visualizes core signaling pathways to equip researchers and drug development professionals with the tools for advanced therapeutic development.
The therapeutic potential of MSCs is heavily influenced by their tissue of origin, leading to significant functional heterogeneity. The following tables consolidate quantitative data from recent studies, enabling a direct comparison of the angiogenic and anti-apoptotic capabilities of umbilical cord-derived MSCs (UCMSCs) and adipose-derived MSCs (ADMSCs).
Table 1: Comparative Angiogenic and Anti-Apoptotic Potency of MSC Sources
| MSC Source | Key Pro-Angiogenic Factors | Key Anti-Apoptotic Factors | Reported Angiogenic Potency | Reported Anti-Apoptotic Potency |
|---|---|---|---|---|
| UCMSCs | VEGF, bFGF, HGF [41] | BCL-2, Survivin [41] | Superior pro-angiogenic activity in vitro and in vivo; greater capillary density in MI models [41] | Moderate; improves cardiomyocyte survival post-MI [41] |
| ADMSCs | VEGF, bFGF (lower expression than UCMSCs) [41] | BCL-2, Survivin (higher expression than UCMSCs) [41] | Lower pro-angiogenic potential in comparative assays [41] | Superior; stronger protective effect on residual cardiomyocytes in acute MI [41] |
Table 2: Functional Outcomes in Myocardial Infarction (MI) Models
| Parameter | UCMSC Treatment | ADMSC Treatment | Control (PBS/NCM) |
|---|---|---|---|
| Capillary Density (capillaries/mm²) | ~981 ± 55 [53] | Significant improvement over control, but less than UCMSCs [41] | ~645 ± 114 [53] |
| Infarct Size Reduction | Significant reduction [41] [53] | Significant reduction, potentially greater than UCMSCs in acute MI [41] | Baseline infarct size |
| Cardiac Function (LVEF) | Improved [41] | Improved, with one study indicating better overall protection [41] | Deteriorated function |
| Primary Proposed Mechanism | Angiogenesis-led repair [41] | Anti-apoptosis-led repair, especially critical in acute phase [41] | N/A |
Decoding the Signaling Pathways
The angiogenic and anti-apoptotic effects of the CM are mediated through specific, well-characterized signaling pathways. Understanding these mechanisms is crucial for rational therapy design.
Core Angiogenic Signaling Pathway
The Vascular Endothelial Growth Factor (VEGF) pathway is a central regulator of angiogenesis in both physiological and pathological contexts, including corpus luteum formation and tumor growth [92] [93]. The pathway is initiated when VEGF ligands (e.g., VEGF-A) bind to VEGF receptors (mainly VEGFR2) on endothelial cell surfaces. This triggers a cascade of intracellular events, primarily through the MAPK/ERK and PI3K/Akt signaling branches, leading to endothelial cell proliferation, migration, and survival, and ultimately the formation of new blood vessels [92] [93]. This pathway is a primary target for pro-angiogenic therapies in ischemic disease and anti-angiogenic therapies in cancer.
Diagram 1: Core VEGF Signaling in Angiogenesis. This pathway is a key mediator of the pro-angiogenic effects of stem cell-conditioned medium.
Core Anti-Apoptotic Signaling Pathway
The mitochondrial (intrinsic) apoptosis pathway is a key regulatory node for cell survival. In the context of myocardial ischemia, stress signals converge on the BCL-2 protein family. Pro-apoptotic proteins like BAX and BAK promote mitochondrial outer membrane permeabilization (MOMP), leading to Cytochrome C release and Caspase-9 activation, which triggers the apoptotic cascade. The anti-apoptotic potency of MSC-CM is largely attributed to secreted factors that upregulate anti-apoptotic proteins like BCL-2, which directly inhibit BAX/BAK, thereby preserving mitochondrial integrity and preventing cell death [92] [41].
Diagram 2: Mitochondrial Apoptosis Pathway & MSC-Mediated Inhibition. Stem cell secretome promotes cell survival by bolstering anti-apoptotic BCL-2 to counter pro-apoptotic signals.
Standardized Experimental Protocols for Potency Assessment
To ensure reproducibility and valid comparisons between research findings, standardized protocols for quantifying angiogenic and anti-apoptotic activity are essential.
In Vitro Assessment of Angiogenic Potential
4.1.1 Endothelial Cell Tube Formation Assay
This assay is a gold-standard functional test for angiogenic potency, measuring the ability of factors in the CM to stimulate endothelial cells to form capillary-like structures.
- Workflow Diagram:
Diagram 3: Workflow for Endothelial Tube Formation Assay.
- Detailed Protocol:
- Matrigel Coating: Thaw Growth Factor Reduced Matrigel on ice. Coat each well of a 96-well plate with 50 µL of Matrigel and incubate at 37°C for 1 hour to allow polymerization.
- Cell Preparation: Harvest Human Umbilical Vein Endothelial Cells (HUVECs) at a low passage number. Resuspend the HUVECs in the conditioned medium (CM) to be tested. A negative control (basal medium) and a positive control (medium supplemented with VEGF and bFGF) must be included.
- Seeding and Incubation: Seed 20,000 HUVECs per well onto the polymerized Matrigel. Incubate the plate at 37°C with 5% CO₂ for 6 to 8 hours.
- Imaging and Quantification: After incubation, randomly capture images of the tube networks using an inverted microscope. Quantify the total tube length, number of master segments (junctions), and number of nodes using automated image analysis software such as ImageJ with the Angiogenesis Analyzer plugin [41].
In Vitro Assessment of Anti-Apoptotic Potential
4.2.1 Flow Cytometry Analysis of Apoptosis
This protocol provides a quantitative measure of the protective effect of CM against induced apoptosis in cardiomyocyte cell lines.
- Workflow Diagram:
Diagram 4: Workflow for Flow Cytometry-Based Apoptosis Assay.
- Detailed Protocol:
- Pre-treatment: Culture target cells (e.g., H9c2 rat cardiomyoblasts or HL-1 mouse cardiomyocytes) with the test MSC-CM, negative control medium, or a pro-survival positive control for 12-24 hours.
- Apoptosis Induction: Expose the cells to a defined apoptotic stimulus. For modeling ischemia, this is typically achieved by placing the cells in a hypoxic chamber (1% O₂) for 24-48 hours. Alternatively, chemical induction using hydrogen peroxide (H₂O₂, e.g., 200-500 µM) for several hours can be used.
- Cell Staining: Harvest the cells using gentle trypsinization and wash with PBS. Resuspend the cell pellet in a binding buffer and stain with fluorescently labelled Annexin V (which binds to phosphatidylserine externalized on the surface of apoptotic cells) and Propidium Iodide (PI, which stains dead cells with compromised membranes). Incubate for 15 minutes in the dark.
- Flow Cytometry and Analysis: Analyze the stained cells using a flow cytometer. A minimum of 10,000 events per sample should be acquired. The resulting data can be divided into four quadrants: viable (Annexin V⁻/PI⁻), early apoptotic (Annexin V⁺/PI⁻), late apoptotic (Annexin V⁺/PI⁺), and necrotic (Annexin V⁻/PI⁺). The percentage of total apoptotic cells (early + late) is the key metric for comparing the anti-apoptotic potency of different CM samples [41].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of the aforementioned protocols requires a defined set of high-quality reagents and models. The following table catalogues essential components for this field of research.
Table 3: Research Reagent Solutions for CM Potency Analysis
| Category | Item / Model | Specific Function / Application |
|---|---|---|
| Cell Models | Human Umbilical Vein Endothelial Cells (HUVECs) | Gold-standard in vitro model for studying angiogenesis and performing tube formation assays [41]. |
| H9c2 Rat Cardiomyoblasts / HL-1 Mouse Cardiomyocytes | Common, tractable cell lines used for in vitro assessment of anti-apoptotic effects on cardiomyocyte-like cells [41]. | |
| Key Assay Kits | Matrigel Matrix (GFR) | A basement membrane extract that provides the 3D substrate required for HUVECs to form capillary-like tube structures in vitro [41]. |
| Annexin V-FITC/PI Apoptosis Detection Kit | Standard kit for distinguishing apoptotic from necrotic cells via flow cytometry. Annexin V binds to PS, PI stains dead cells [41]. | |
| In Vivo Models | Mouse Myocardial Infarction (MI) Model (LAD Ligation) | The primary in vivo model for evaluating the therapeutic efficacy of CM on cardiac function, angiogenesis, and apoptosis post-ischemia [41] [53]. |
| Analytical Tools | ImageJ with Angiogenesis Analyzer | Open-source software and plugin for the quantitative analysis of tube formation assays (nodes, junctions, length) [41]. |
| Flow Cytometer (e.g., BD Accuri) | Instrument for quantifying the proportion of apoptotic cells in a population based on Annexin V/PI staining [41]. |
Discussion and Clinical Outlook
The comparative data clearly indicate a functional specialization between UCMSCs and ADMSCs, with UCMSCs exhibiting superior angiogenic potency and ADMSCs demonstrating stronger anti-apoptotic effects in an acute MI model [41]. This dichotomy suggests that the optimal therapeutic strategy may not be a one-size-fits-all solution but should be tailored to the specific pathophysiology of the patient's condition. For instance, a UCMSC-CM product might be ideal for promoting long-term revascularization in chronic ischemic heart failure, whereas an ADMSC-CM product could be more effective for salvaging myocardium in the acute phase of a myocardial infarction where rapid apoptosis is the dominant mechanism of cell loss [41].
The future of CM therapy lies in precision medicine. This involves screening and selecting the most appropriate MSC source based on the patient's dominant clinical need (angiogenesis vs. anti-apoptosis) [41]. Furthermore, the field is rapidly advancing beyond naive CM towards engineered CM. This includes priming MSCs during culture under specific conditions (e.g., hypoxia) to enhance their secretome, or genetically modifying MSCs to overexpress specific therapeutic factors like VEGF-A or BCL-2, thereby creating a product with targeted and heightened potency [1]. The shift towards using the purified extracellular vesicle (EV) fraction of the CM, which carries a concentrated cargo of bioactive molecules without the risks of whole cells, represents the next frontier in cell-free regenerative therapy for myocardial protection [1] [8].
Cardiovascular disease remains the leading cause of death worldwide, with heart failure due to ischemic myocardial infarction (MI) being a primary contributor to high mortality rates [1]. The significant loss of cardiomyocytes following MI represents a fundamental challenge, as these contractile cells exhibit minimal regenerative capacity in the adult human heart [1]. For decades, cell transplantation therapy has been investigated as a promising strategy to replenish lost cardiomyocytes and restore myocardial function. However, challenges including arrhythmogenesis, poor graft retention, and immunogenic rejection continue to limit its clinical translation [1].
In recent years, a paradigm shift has occurred toward cell-free therapies, with stem cell-conditioned medium (CM) emerging as a novel biological approach for myocardial protection and repair. This whitepaper provides an in-depth technical analysis of the safety and immunogenicity profile of cell-free CM compared to traditional cell transplantation, framing this discussion within the context of stem cell CM research for myocardial protection.
Cell Transplantation: Therapeutic Promise and Clinical Challenges
Cell therapy for cardiac repair has primarily investigated multiple cell sources, including mesenchymal stem cells (MSCs), cardiac progenitor cells (CPCs), cardiosphere-derived cells (CDCs), and induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) [1] [71]. These approaches have been grounded in the concept that transplanted cells can directly differentiate into functional cardiomyocytes or promote angiogenesis through structural integration.
Table 1: Cell Types Used in Cardiac Cell Therapy
| Cell Type | Origin | Key Characteristics | Major Challenges |
|---|---|---|---|
| MSCs | Bone marrow, adipose tissue, umbilical cord | Multipotent, immunomodulatory, paracrine factor secretion [94] [95] | Poor long-term survival, heterogeneous effects [95] |
| CPCs/CDCs | Cardiac tissue | Cardiac lineage commitment, endogenous repair activation | Limited quantity, arrythmias in clinical trials [1] |
| iPSC-CMs | Reprogrammed somatic cells | Patient-specific, unlimited expansion capacity | Immature phenotype, teratoma risk, arrythmias [1] [71] |
| ESCs | Blastocyst stage embryos | Pluripotent, high differentiation capacity | Ethical concerns, immunogenic rejection, teratoma formation [71] [4] |
Safety and Immunogenicity Concerns with Cell Transplantation
Immunogenic Reactions
Despite claims of immune privilege for certain stem cell types, allogeneic cell transplantation faces significant immunogenic challenges. Research has demonstrated that repeated intra-articular injections of allogeneic MSCs in animal models resulted in adverse clinical responses, indicative of allogeneic MSC immune recognition by the host [95]. While MSCs are considered to have low immunogenicity due to the absence of costimulatory molecules, their immunocompatibility remains a concern in transplantation settings.
The use of embryonic stem cells (ESCs) raises additional immunological concerns, as they express major histocompatibility complex (MHC) molecules that can trigger host immune responses [4]. Even with patient-specific induced pluripotent stem cells (iPSCs), the potential for immunogenic rejection persists due to epigenetic memory or reprogramming factors that may alter their immunogenicity profile.
Tumorigenicity and Arrythmogenesis
Pluripotent stem cells, including ESCs and iPSCs, carry inherent tumorigenic risks due to their potential for uncontrolled proliferation and teratoma formation [71] [4]. This safety concern represents a significant barrier to clinical application, necessitating rigorous purification protocols and long-term monitoring.
Clinical trials utilizing various cell types have frequently reported cardiac arrythmias as a concerning adverse effect. Transplantation of iPSC-derived cardiomyocytes in both murine MI models and human patients has been associated with arrythmias, complicating their therapeutic potential [1]. The electrical integration of transplanted cells with host myocardium remains challenging, with the potential for creating pro-arrhythmic substrates.
Procedural and Engraftment Challenges
Cell transplantation faces significant practical hurdles related to cell delivery and engraftment. Studies consistently demonstrate poor long-term survival of transplanted cells, with most being cleared within days to weeks after administration [95]. Lineage tracing experiments in murine models have shown that only a small fraction of MSCs integrate into host tissue, and these seldom retain long-term viability [95].
The heterogeneity of cell populations presents additional challenges, with variations observed between donors, tissue sources, and culture conditions [95]. This heterogeneity contributes to inconsistent therapeutic outcomes and difficulties in standardizing treatments.
Cell-Free Therapy: The Paradigm of Stem Cell Conditioned Medium
Composition and Bioactive Components
Stem cell-conditioned medium represents a cell-free approach that harnesses the paracrine factors secreted by stem cells without the risks associated with whole-cell transplantation. The therapeutic effects of CM are mediated through a complex mixture of bioactive molecules, including growth factors, cytokines, chemokines, and extracellular vesicles (EVs) [95].
Table 2: Key Bioactive Components in Stem Cell Conditioned Medium
| Component Category | Key Examples | Primary Functions |
|---|---|---|
| Extracellular Vesicles | Exosomes, microvesicles [1] | Intercellular communication, miRNA transfer, cardioprotective cargo delivery |
| Growth Factors | VEGF, FGF, HGF, IGF-1 [94] [95] | Angiogenesis promotion, cell survival, tissue repair |
| Cytokines/Chemokines | IL-10, TGF-β, SDF-1 [94] | Immunomodulation, anti-inflammatory effects, stem cell homing |
| Non-coding RNAs | miRNAs, lncRNAs [1] | Gene expression regulation, signaling pathway modulation |
Among these components, extracellular vesicles (EVs), particularly exosomes, have emerged as particularly potent mediators of cardiac repair. These nano-sized, membrane-enclosed particles carry diverse therapeutic cargo, including miRNAs, mRNAs, lncRNAs, proteins, and metabolites [1]. Recent studies demonstrate that most stem-cell-derived extracellular vesicles (Stem-EVs) are nonimmunogenic and carry cardioprotective therapeutic cargos [1].
Mechanisms of Action in Cardiac Repair
Cell-free CM exerts its therapeutic effects through multiple coordinated mechanisms:
Cardioprotective and Anti-apoptotic Effects
Administration of multiple Stem-EV types in animal models of acute MI results in reduced inflammation, apoptosis, smaller infarct size and improved cardiac functionality [1]. The CM components activate survival pathways in jeopardized cardiomyocytes, mitigating the oxidative stress and calcium overload that characterize ischemia-reperfusion injury [96] [97].
Immunomodulation
CM components such as IL-10, TGF-β, and prostaglandin E2 create an anti-inflammatory microenvironment by modulating various immune cells, including T cells, B cells, dendritic cells, and macrophages [94]. This immunomodulation occurs without triggering the aggressive immune responses associated with whole-cell transplantation.
Angiogenic and Regenerative Effects
Through the action of VEGF, FGF, and angiogenic miRNAs, CM promotes neovascularization in the ischemic myocardium, restoring perfusion to compromised areas [95]. Additionally, CM components can activate endogenous cardiac progenitor cells, potentially stimulating the heart's innate regenerative capacity.
Direct Comparative Analysis: Safety and Immunogenicity
Immunogenicity Profile
The fundamental advantage of cell-free CM lies in its reduced immunogenicity. While cell transplantation introduces foreign cell membranes, MHC complexes, and cell surface proteins that can trigger immune recognition, CM contains predominantly acellular components with lower immunogenic potential [1] [95]. Specifically, stem cell-derived extracellular vesicles have been shown to be nonimmunogenic, making them particularly attractive for allogeneic applications without matching requirements [1].
Figure 1: Comparative Immunogenicity Profiles of Cell Transplantation versus Cell-Free CM Approaches
Safety and Tumorigenicity Profile
Cell-free CM eliminates the tumorigenic risks associated with whole-cell transplantation, particularly concerning when using pluripotent stem cells [1] [71]. Without living, proliferating cells, CM cannot form teratomas or undergo uncontrolled expansion. This significantly simplifies regulatory pathways and reduces long-term safety monitoring requirements.
Additionally, CM administration avoids the arrhythmogenic risks documented with cell transplantation approaches. The electrical stability of the myocardium is preserved while still delivering therapeutic benefits [1].
Practical Safety Considerations
From a clinical translation perspective, cell-free CM offers several practical safety advantages:
- Standardized manufacturing: CM can be rigorously characterized, filtered, and standardized, overcoming the heterogeneity challenges of cell-based products [95]
- Storage and stability: CM components, particularly EVs, demonstrate better stability and longer shelf-life than living cells [1]
- Dosing control: Precise dosing is more achievable with CM than with cell transplantation, where engraftment variability affects delivered dose
- Administration safety: CM can be delivered through less invasive routes, including intravenous infusion, reducing procedural risks
Table 3: Comprehensive Safety and Immunogenicity Comparison
| Parameter | Cell Transplantation | Cell-Free Conditioned Medium |
|---|---|---|
| Immunogenic Potential | High (MHC mismatch, allogeneic recognition) [95] | Low (nonimmunogenic EVs, acellular) [1] |
| Tumorigenic Risk | Significant with pluripotent cells [71] [4] | Negligible (no living, proliferating cells) [1] |
| Arrhythmogenic Risk | Documented in clinical trials [1] | Minimal reported |
| Graft Rejection | Common, requires immunosuppression [1] | Not applicable |
| Long-term Survival | Poor, rapid clearance [95] | Not applicable |
| Manufacturing Consistency | Variable due to biological heterogeneity [95] | Highly standardizable |
| Storage Requirements | Complex cryopreservation needed | Stable, longer shelf-life |
Experimental Models and Methodologies
CM Preparation and Characterization Protocols
CM Collection and Processing
Standardized protocols for CM production begin with stem cell expansion under defined culture conditions. Upon reaching 70-80% confluence, cells are thoroughly washed and maintained in serum-free medium for 24-48 hours to collect secreted factors [94]. The conditioned medium is then sequentially processed through:
- Centrifugation at 300 × g for 10 minutes to remove cellular debris
- Filtration through 0.22 μm membranes to eliminate remaining particulates
- Concentration using ultrafiltration devices (e.g., 3-10 kDa molecular weight cutoff)
- Characterization of protein content, EV concentration, and specific biomarker expression
Extracellular Vesicle Isolation
For EV-enriched CM preparations, additional purification steps are implemented:
- Differential ultracentrifugation at 100,000 × g for 70 minutes
- Size-exclusion chromatography for high-purity EV isolation
- Characterization per MISEV2023 guidelines [1], including:
- Nanoparticle tracking analysis for size distribution
- Transmission electron microscopy for morphology
- Western blotting for EV markers (CD63, CD81, TSG101)
In Vitro and In Vivo Efficacy Assessment
In Vitro Cardioprotection Models
Hypoxia/reoxygenation models using primary cardiomyocytes or cardiac cell lines are established to simulate ischemia-reperfusion injury. Cells are pretreated with CM or EVs before subjecting to hypoxic conditions (1% O₂, 24 hours) followed by reoxygenation (normoxia, 4 hours). Assessment includes:
- Cell viability via MTT or WST-8 assays
- Apoptosis measurement through TUNEL staining and caspase-3/7 activity
- Calcium handling evaluation using fluorometric assays
- Mitochondrial function assessment via JC-1 staining and ATP measurement
In Vivo Myocardial Infarction Models
Rodent MI models generated by permanent or transient left anterior descending coronary artery ligation represent the gold standard for efficacy assessment. CM or EVs are administered via:
- Intramyocardial injection during open-chest surgery
- Intravenous infusion via tail vein
- Intracoronary delivery via catheter-based approaches
Functional assessment includes echocardiography for left ventricular ejection fraction, hemodynamic measurements for pressure-volume relationships, and histological analysis for infarct size, fibrosis, and vascular density.
Figure 2: Experimental Workflow for Evaluating Cell-Free CM Therapeutic Potential
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for CM and EV Research
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Stem Cell Sources | Human MSCs (BM, UC, AD), iPSCs [94] [95] | CM production, EV isolation | Select source based on specific research goals and availability |
| EV Isolation Kits | ExoQuick-TC, Total Exosome Isolation Kit | Rapid EV purification from CM | Balance yield against purity requirements |
| Characterization Antibodies | Anti-CD63, CD81, TSG101, Calnexin [1] | EV characterization via Western blot | Include positive and negative markers per MISEV guidelines |
| Nanoparticle Tracking | NanoSight NS300, qNano | Size distribution and concentration | Essential for pre-clinical product characterization |
| Cardiomyocyte Cells | H9c2 cells, primary rodent cardiomyocytes, iPSC-CMs | In vitro cardioprotection assays | Primary cells offer greater physiological relevance |
| MI Model Reagents | LAD ligation equipment, isoflurane, buprenorphine | In vivo efficacy studies | Strict adherence to animal welfare guidelines |
| Angiogenesis Assays | Matrigel tube formation kit, VEGF ELISA | Pro-angiogenic assessment | Combine in vitro and in vivo approaches |
| Immunomodulation Assays | T-cell proliferation kit, cytokine array | Immune response profiling | Critical for safety assessment |
Future Perspectives and Engineering Strategies
The field of cell-free cardiac therapy is rapidly evolving, with several promising engineering strategies emerging to enhance CM efficacy:
Engineered Stem-EVs
Recent developments focus on creating engineered Stem-EVs with enhanced cardiac targeting, prolonged circulation, and recombinant therapeutic cargos [1]. These modified EVs can be designed to overexpress specific cardioprotective miRNAs or proteins, maximizing their therapeutic potential while maintaining favorable safety profiles.
Preconditioning Strategies
Preconditioning of stem cells before CM collection represents another enhancement approach. Exposure to hypoxic conditions, inflammatory cytokines, or pharmacological agents can prime cells to secrete CM with enriched therapeutic factors [95]. For instance, hypoxia-preconditioned MSCs secrete higher levels of pro-angiogenic and anti-apoptotic factors.
Biomaterial-Assisted Delivery
Innovative delivery systems using hydrogels, cardiac patches, or injectable matrices can prolong CM retention in the myocardial environment, overcoming rapid clearance limitations [4]. These systems enable sustained release of therapeutic factors, potentially reducing dosing frequency and improving efficacy.
The comprehensive analysis of safety and immunogenicity profiles demonstrates clear advantages of cell-free CM approaches over traditional cell transplantation for myocardial protection and repair. The nonimmunogenic nature of therapeutic EVs, elimination of tumorigenic risks, reduced arrhythmogenic potential, and superior manufacturability position cell-free strategies as the next frontier in cardiovascular regenerative medicine. While challenges remain in standardization, optimization, and clinical translation, the compelling safety profile of cell-free CM warrants continued intensive investigation as a promising therapeutic paradigm for ischemic heart disease.
The pursuit of effective cardiac regenerative therapies has catalyzed the development of multiple innovative strategies, each occupying a distinct position in the therapeutic landscape. This whitepaper provides a technical analysis of three prominent approaches: stem cell-derived conditioned medium (CM), direct cardiac reprogramming, and cardiac stem cell transplantation. We examine their core mechanisms, therapeutic actions, and experimental evidence, with a particular focus on the paracrine-factor driven, cell-free paradigm of CM therapy. By comparing their respective advantages and challenges, this review aims to inform researchers and drug development professionals about the strategic positioning of these therapies for myocardial protection and regeneration.
Cardiovascular disease remains a leading cause of death worldwide, with myocardial infarction (MI) resulting in the catastrophic loss of cardiomyocytes that are replaced by fibrotic tissue [98] [99]. The adult human heart has limited regenerative capacity, and the loss of functional tissue often leads to progressive heart failure. Traditional interventions focus on restoring blood flow but do not address the fundamental issue of cardiomyocyte loss, creating a pressing need for regenerative strategies that can replace damaged tissue and restore cardiac function [99]. This landscape has fostered the development of several regenerative approaches, each with distinct mechanisms and therapeutic profiles, which are positioned to address different aspects of the post-infarction pathophysiology.
Conditioned Medium (CM) Therapy: A Paracrine-Factor Driven Approach
Core Concept and Mechanisms
Conditioned medium refers to the nutrient-rich fluid collected from stem cell cultures, containing a diverse array of secreted bioactive factors, including cytokines, growth factors, exosomes, and other signaling molecules [100] [101]. Rather than relying on direct cell replacement, CM therapy leverages these paracrine factors to modulate the cardiac microenvironment, promote endogenous repair mechanisms, and protect viable myocardium. The therapeutic effects are mediated through multiple coordinated mechanisms, including anti-apoptosis, angiogenesis, immunomodulation, and limited fibrotic remodeling.
The molecular composition of CM varies depending on the cell source, but typically includes factors such as vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), fibroblast growth factor (bFGF), and insulin-like growth factor (IGF-1) [100] [101]. These factors activate survival pathways in cardiomyocytes, notably the PI3K/Akt pathway, which inhibits apoptosis and promotes cellular survival in the ischemic milieu [99]. Additionally, CM promotes angiogenesis through coordinated activation of multiple pro-angiogenic signaling cascades, including VEGF/PI3K/Akt and MAPK pathways, enhancing blood vessel formation in the ischemic border zone [99].
Key Signaling Pathways Activated by CM
Table 1: Key Signaling Pathways in CM-Mediated Cardioprotection
| Pathway | Key Components | Biological Effects | Therapeutic Outcome |
|---|---|---|---|
| PI3K/Akt | PI3K, Akt/PKB, eNOS, mTOR, GSK-3β, FOXO | Inhibits apoptosis, promotes cell survival, enhances angiogenesis | Cardiomyocyte protection, improved cardiac function, reduced infarct size |
| MAPK | ERK1/2, JNK, p38 | Regulates cell growth, differentiation, survival | Angiogenesis, reduced apoptosis, tissue repair |
| JAK/STAT | JAK, STAT | Cytokine signaling, cell survival, immune regulation | Anti-inflammatory effects, cardiomyocyte protection |
Experimental Evidence and Protocols
CM has demonstrated efficacy across various disease models. In experimental autoimmune neuritis, SHED-CM (from human exfoliated deciduous teeth) significantly ameliorated clinical scores and promoted remyelination by upregulating myelin basic protein (MBP) and early growth response 2 (EGR2) while downregulating the negative regulator c-JUN [101]. In skin rejuvenation clinical studies, CM application increased skin elasticity by 27.07% and hydration by over 20% while reducing wrinkles by more than 10% [100].
Typical CM Preparation Protocol:
- Culture stem cells (e.g., mesenchymal stem cells, dental pulp stem cells) to 70-80% confluency
- Wash cells twice with PBS and once with serum-free basal medium
- Incubate with serum-free medium for 48-72 hours
- Collect supernatant and centrifuge at 1,750 × g for 10 minutes to remove cell debris
- Filter through 0.22 μm filter to eliminate remaining particulates
- Concentrate using centrifugal filters (e.g., 10 kDa Amicon Ultra filters) if needed
- Store at 4°C for short-term use or -80°C for long-term preservation [101]
Diagram 1: Mechanism of Action of Conditioned Medium Therapy. CM contains multiple bioactive factors that activate various signaling pathways to produce coordinated therapeutic effects on damaged myocardium.
Direct Cardiac Reprogramming: Lineage Conversion Strategy
Core Concept and Mechanisms
Direct cardiac reprogramming represents a groundbreaking approach that converts endogenous cardiac fibroblasts (CFs) directly into induced cardiomyocyte-like cells (iCMs) through the forced expression of specific transcription factors, bypassing the pluripotent stage [98] [102]. This technique leverages the abundant pool of fibroblasts in the heart that typically contribute to scar formation after MI, effectively converting pathological cells into functionally beneficial ones.
The pioneering work in this field identified three core cardiogenic transcription factors - Gata4, Mef2c, and Tbx5 (collectively known as GMT) - capable of initiating this conversion in mice [98]. Subsequent research has revealed that human cells require additional factors such as Mesp1 and Myocd for efficient reprogramming [98]. The process involves epigenetic remodeling that opens cardiac-specific chromatin regions while closing fibroblast-specific ones, enabling the activation of the cardiomyocyte gene program.
Key Molecular Factors in Direct Reprogramming
Table 2: Key Factors in Direct Cardiac Reprogramming
| Category | Factors | Function in Reprogramming |
|---|---|---|
| Core Transcription Factors | Gata4, Mef2c, Tbx5 (GMT) | Initiate cardiac gene program, essential for mouse fibroblast reprogramming |
| Supplementary Factors for Human Cells | Mesp1, Myocd | Required for efficient human fibroblast reprogramming |
| Efficiency Enhancers | miR-133, Hand2, Akt1 | Improve conversion efficiency and maturation of iCMs |
| Signaling Pathway Modulators | TGF-β inhibitors, Wnt inhibitors, Notch signaling inhibitors (e.g., DAPT), FGF-2, FGF-10, VEGF | Enhance reprogramming efficiency by modifying culture conditions and signaling environment |
| Epigenetic Modulators | Bmi1 (reduction), TET1 | Alter histone modifications and DNA methylation to facilitate chromatin remodeling |
Experimental Evidence and Protocols
In vivo studies in mouse models of myocardial infarction have demonstrated that direct cardiac reprogramming can improve left ventricular systolic performance by approximately 10% and significantly reduce fibrotic tissue [98] [102]. The development of polycistronic vectors that combine multiple factors on a single vector has improved reprogramming efficiency approximately two-fold compared to individual vectors [98]. Recent research has shown that in vivo cardiac reprogramming not only regenerates myocardium but also reverses fibrosis by inducing quiescence of pro-fibrotic fibroblasts, offering dual benefits in chronic MI settings [102].
Typical Direct Reprogramming Protocol (In Vivo):
- Create myocardial infarction model (e.g., by coronary artery ligation)
- Prepare viral vectors (typically retroviral or lentiviral) encoding reprogramming factors
- Directly inject vector mixture into infarction border zone
- Allow 4-8 weeks for reprogramming and maturation of iCMs
- Assess outcomes via histological analysis, functional measurements, and electrophysiological studies [98]
For in vitro reprogramming:
- Isolate cardiac fibroblasts from tissue samples
- Culture to appropriate density
- Transduce with reprogramming factors using viral vectors or non-viral methods
- Change to cardiac-supportive culture medium
- Monitor for appearance of cardiomyocyte markers (e.g., cardiac troponin T, α-actinin) over 2-4 weeks
- Assess functional maturation through electrophysiology and calcium handling [98]
Diagram 2: Direct Cardiac Reprogramming Process. Cardiac fibroblasts are converted to induced cardiomyocyte-like cells through a combination of transcription factors and various enhancers that facilitate chromatin remodeling and cardiac gene activation.
Comparative Analysis of Therapeutic Approaches
Functional and Technical Comparison
Table 3: Comparative Analysis of Cardiac Regenerative Approaches
| Parameter | Conditioned Medium | Direct Reprogramming | Cardiac Stem Cells |
|---|---|---|---|
| Mechanism of Action | Paracrine signaling, bioactive factors | Lineage conversion, transdifferentiation | Cell replacement, paracrine effects |
| Therapeutic Effects | Anti-apoptosis, angiogenesis, anti-inflammation, anti-fibrosis | Myocyte regeneration, reduced fibrosis, direct contractile improvement | Myocyte regeneration, paracrine signaling |
| Technical Complexity | Low (cell-free preparation) | High (vector design, delivery) | Moderate (cell isolation, expansion) |
| Delivery Method | Intravenous, intracardiac injection | Direct myocardial injection (viral vectors) | Intracoronary, myocardial injection |
| Onset of Action | Relatively rapid (hours-days) | Slow (weeks-months for maturation) | Intermediate (days-weeks) |
| Tumorigenic Risk | None (cell-free) | Low (non-integrating vectors) or moderate | Low with proper characterization |
| Regulatory Pathway | Biologics, less complex | Gene therapy, more complex | Cell therapy, complex |
| Key Challenges | Standardization, quantification of active components | Low efficiency, maturation of iCMs, delivery | Cell survival, engraftment, heterogeneity |
| Clinical Translation Status | Early clinical trials for some applications | Preclinical development | Mixed results in clinical trials |
Synergistic Potential and Combinatorial Approaches
The distinct mechanisms of these approaches present opportunities for combinatorial therapies that may yield synergistic benefits. CM could be utilized to create a supportive environment for directly reprogrammed iCMs or transplanted stem cells by reducing inflammation and fibrosis while promoting vascularization [100] [99]. Sequential application might involve using CM initially to modulate the hostile post-infarction environment, followed by direct reprogramming or stem cell therapy to achieve more robust regeneration.
Research has shown that factors present in CM, such as FGF-2, FGF-10, and VEGF, can enhance the efficiency of direct cardiac reprogramming [98], suggesting potential for coordinated application. Additionally, the anti-fibrotic effects of CM could complement the fibrotic reversal demonstrated by direct reprogramming in chronic MI models [102].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Cardiac Regeneration Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Reprogramming Factors | Gata4, Mef2c, Tbx5 (GMT), Mesp1, Myocd, Hand2 | Direct cardiac reprogramming, iCM induction |
| Signaling Modulators | TGF-β inhibitors, Wnt inhibitors, DAPT (Notch inhibitor), FGF-2, FGF-10, VEGF | Enhance reprogramming efficiency, modulate cardiac signaling pathways |
| Cell Culture Media | Serum-free DMEM, specialized MSC media, cardiac differentiation media | CM production, stem cell culture, cardiac cell differentiation |
| Viral Vectors | Retrovirus, lentivirus, adenovirus | Delivery of reprogramming factors for direct reprogramming |
| Characterization Antibodies | Anti-cardiac troponin T, anti-α-actinin, anti-GATA4, anti-MEF2C | Immunocytochemistry, immunohistochemistry for iCM validation |
| CM Concentration Devices | Amicon Ultra Centrifugal Filters (10 kDa) | Concentration of conditioned medium for experimental use |
| Animal Models | Myocardial infarction models (coronary ligation), EAN models | In vivo testing of therapeutic efficacy |
The therapeutic landscape for cardiac regeneration is diversifying with conditioned medium, direct reprogramming, and cardiac stem cells each offering distinct advantages and facing unique challenges. CM therapy presents as a relatively low-risk, cell-free approach that modulates the cardiac microenvironment through paracrine signaling, while direct reprogramming offers the potential for direct lineage conversion of fibroblasts into functional cardiomyocytes. Strategic positioning of these therapies will depend on further elucidation of their mechanisms, optimization of delivery methods, and careful evaluation of their safety and efficacy profiles.
Future research directions should focus on identifying the critical bioactive components in CM, improving the efficiency and maturation of directly reprogrammed iCMs, and exploring synergistic combinations of these approaches. As these fields advance, they hold the promise of fundamentally changing how we treat ischemic heart disease, moving beyond symptomatic management to true cardiac regeneration and functional restoration.
In the landscape of cardiovascular regenerative medicine, stem cell-based therapies have emerged as a promising modality to replenish lost cardiomyocytes and recover myocardial function following ischemic injury [103]. However, significant challenges including low cell survival post-transplantation, poor long-term retention, and risks of uncontrolled differentiation have hampered their clinical translation [104]. This landscape has catalyzed a paradigm shift toward cell-free approaches, particularly stem cell-conditioned medium (CM) and its derived components, which harness the therapeutic benefits of stem cell paracrine signaling without the complexities of cell transplantation [1] [105]. This whitepaper provides a critical appraisal of the preclinical evidence supporting CM therapies and evaluates their readiness for clinical application in myocardial protection, framed within the broader thesis that soluble factors and extracellular vesicles (EVs) in CM mediate cardioprotection through multimodal mechanisms.
Preclinical Evidence: Mechanisms and Efficacy of Conditioned Medium Therapy
Paracrine Factor Composition and Cardioprotective Actions
Stem cell-conditioned medium is composed of a complex mixture of secreted bioactive factors, including growth factors, cytokines, chemokines, and extracellular vesicles, which collectively mediate therapeutic effects through paracrine mechanisms [105] [106]. The table below summarizes key functional categories of paracrine factors identified in CM and their demonstrated cardioprotective actions.
Table 1: Key Paracrine Factors in Stem Cell-Conditioned Medium and Their Cardioprotective Mechanisms
| Factor Category | Specific Factors Identified | Primary Cardioprotective Actions | Experimental Models |
|---|---|---|---|
| Angiogenic Factors | VEGF, bFGF, EGF, CXCL5 [105] [106] | Stimulate endothelial cell proliferation and tubule formation; promote neovascularization | HUVEC cultures, rat sponge implantation model [106] |
| Anti-inflammatory Factors | IL-10, miR-146a [1] [106] | Suppress pro-inflammatory mediators (TNF-α, IL-1β, IL-6, IFN-γ); modulate macrophage activity | T2D rat wound model [105] |
| Anti-fibrotic & Anti-apoptotic Factors | miR-21, miR-210, GDF-11 [1] [104] | Reduce cardiomyocyte apoptosis; decrease collagen deposition and fibrosis | Murine MI models [1] [104] |
| Immune Modulators | HGF, SDF-1α, IGF-1 [104] | Inhibit T-cell activation; promote recruitment of progenitor cells | Preclinical models of myocardial infarction [104] |
Preconditioning Strategies to Enhance CM Potency
A significant advancement in the field involves preconditioning stem cells prior to CM collection to enhance the potency and specificity of its secretome. Preconditioning mimics the hostile microenvironment of the injured myocardium (e.g., hypoxia, inflammation) or uses biochemical inducers to upregulate beneficial pathways.
Table 2: Preconditioning Strategies for Enhancing CM Efficacy
| Preconditioning Method | Key Transcriptomic/Secretomic Changes | Documented Functional Outcomes |
|---|---|---|
| Butyrate Treatment [106] | Upregulation of CXCL8, SOD2, TGM2; increased secretion of IL-10, CXCL5, MMP-1 | ≈32% improvement in myocardial perfusion in rat MI model; enhanced HUVEC wound closure and in vivo angiogenesis |
| Hypoxic Conditioning [104] | Upregulation of HIF-1α target genes; increased secretion of VEGF, SDF-1 | Enhanced angiogenic potential; improved stem cell survival and homing (preclinical data) |
| Inflammatory Cytokine Exposure (e.g., TNF-α, IFN-γ) | Increased expression of IDO, PGE2, TGF-β; enhanced immunomodulatory factor secretion | Potentiated immunomodulation and improved functional recovery in rodent MI models |
Butyrate preconditioning of human adipose-derived stem cells (ASCs), for instance, resulted in a CM that significantly enhanced human umbilical vein endothelial cell (HUVEC) wound closure in vitro. When this CM was tested in a rat myocardial infarction model, single-photon emission computed tomography (SPECT/CT) imaging revealed an approximately 32% improvement in myocardial perfusion compared to controls, a critical metric of cardiac recovery [106]. This strategy demonstrates the potential of preconditioning to unlock greater therapeutic efficacy from CM.
Signaling Pathways Modulated by Conditioned Medium
The therapeutic effects of CM are mediated through the modulation of critical signaling pathways in recipient cardiac cells. Transcriptome sequencing of tissues treated with adipose-derived stem cell-conditioned medium (ACM) revealed significant downregulation of the TNF signaling pathway and chemokine signaling pathway, which are key drivers of post-injury inflammatory response [105]. Furthermore, CM rich in specific microRNAs (e.g., miR-21, miR-146a, miR-210) can regulate apoptosis and fibrosis by targeting genes within the PTEN/PI3K/Akt and NF-κB pathways [1] [104].
Diagram 1: CM modulates key signaling pathways for cardioprotection.
Critical Appraisal of Clinical Readiness
Analysis of Current Clinical Trial Evidence
The transition from preclinical models to clinical application is underway, though evidence remains limited. A phase 3 randomized clinical trial (PREVENT-TAHA8) published in 2025 investigated intracoronary infusion of Wharton's jelly-derived mesenchymal stem cells (MSCs) in 396 patients with acute myocardial infarction and weakened heart function [107]. While this trial used whole cells, its positive outcomes inform the potential of MSC-derived therapies. Over 33 months of follow-up, the cell therapy group showed significantly reduced rates of heart failure (2.77 vs. 6.48 per 100 person-years) and hospital readmission for heart failure (0.92 vs. 4.20 per 100 person-years) compared to standard care alone [107]. Furthermore, left ventricular ejection fraction (LVEF) showed significantly greater improvement at six months in the intervention group [107].
However, direct clinical evidence for conditioned medium in cardiac patients is still nascent. Most advanced clinical applications of CM are currently in related fields, such as wound healing. A study on ACM for type 2 diabetic wounds demonstrated accelerated wound closure and suppression of pro-inflammatory mediators (TNF-α, IL-1β, IL-6, COX-2) in a rat model, providing proof-of-concept for its efficacy in a complex pathological microenvironment [105].
Identified Challenges and Translational Gaps
Despite promising preclinical results, several challenges must be addressed before CM therapy can achieve widespread clinical readiness.
- Standardization and Characterization: A major hurdle is the lack of standardization in CM production. Variability in stem cell sources, culture conditions, collection methods, and preconditioning protocols leads to inconsistent CM composition and efficacy [106]. Defining critical quality attributes (CQAs) and establishing potency assays are essential next steps.
- Optimized Delivery and Dosing: Preclinical studies have not yet converged on optimal delivery routes (intravenous, intracoronary, intramyocardial), timing, or dosing regimens for CM or its derivatives like EVs [103] [1]. The optimal therapeutic window, likely between 4-14 days post-MI to avoid the initial inflammatory storm yet capitalize on homing signals, requires clinical validation [103].
- Manufacturing and Regulatory Hurdles: Scaling up the production of clinical-grade CM and EVs under Good Manufacturing Practice (GMP) conditions presents significant logistical and economic challenges [1]. Regulatory agencies have yet to establish clear pathways for approving these complex, cell-free biologics.
Experimental Protocols for CM Research
Protocol for Generating Preconditioned Adipose-Der Stem Cell CM
This protocol is adapted from studies investigating butyrate-preconditioned CM for cardiac repair [106].
Isolation and Culture of Human ASCs:
- Obtain human adipose tissue (e.g., lipoaspirate) under informed consent and ethical approval.
- Wash tissue extensively with PBS containing 1-2% antibiotics/antimycotics.
- Minced tissue is digested with 0.1% collagenase type I in a shaking water bath for 30-60 minutes at 37°C.
- Neutralize digestion with culture medium (α-MEM with 10% FBS), centrifuge, and resuspend the stromal vascular fraction (SVF).
- Culture SVF cells in T-flasks. Remove non-adherent cells after 24-48 hours. Expand adherent ASCs (P0) using standard culture conditions (37°C, 5% CO2). Use cells at passages 3-5 for experiments.
Butyrate Preconditioning and CM Collection:
- At ~80% confluence, wash ASCs with PBS to remove serum.
- Treat cells with serum-free medium containing a predetermined optimal concentration of sodium butyrate (e.g., 0.5-1 mM) for 24-48 hours [106].
- Control CM is collected from ASCs cultured in parallel with serum-free medium without butyrate.
- Collect the supernatant and centrifuge at 3,000 × g for 5-10 minutes to remove cell debris.
- Concentrate the CM using ultrafiltration (e.g., 3 kDa molecular weight cut-off membrane) [105].
- Aliquot and store the concentrated CM at -80°C. Protein concentration can be quantified using a BCA assay.
Diagram 2: Workflow for generating preconditioned ASC-CM.
In Vitro and In Vivo Functional Assays
To validate the bioactivity of generated CM, a suite of functional assays is required.
Table 3: Key Functional Assays for CM Potency Evaluation
| Assay Type | Protocol Summary | Key Readouts |
|---|---|---|
| In Vitro: Endothelial Wound Healing (Scratch Assay) [106] | Seed HUVECs in a 24-well plate. Create a scratch with a pipette tip. Wash and add CM. Image at 0, 6, 12, 24h. | Percentage of wound closure over time. |
| In Vitro: Endothelial Tube Formation Assay [105] | Coat 96-well plates with Matrigel. Seed HUVECs suspended in CM. Incubate for 4-18h. | Number of master junctions, nodes, and total tubule length. |
| In Vivo: Myocardial Infarction Model [1] [106] | Induce MI in rodents (e.g., by LAD coronary artery ligation). Administer CM/EVs via intramyocardial or intravenous injection post-MI. | SPECT/CT Imaging: Myocardial perfusion [106]. Echocardiography: LVEF, fractional shortening. Histology: Infarct size, capillary density, fibrosis. |
The Scientist's Toolkit: Key Research Reagent Solutions
The table below details essential materials and reagents used in CM research for myocardial protection, as cited in the literature.
Table 4: Essential Research Reagents for CM-Based Cardioprotection Studies
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | In vitro model for assessing angiogenic and endothelial repair potential of CM. | Used in wound healing and tube formation assays [105] [106]. |
| Sodium Butyrate | Biochemical preconditioning agent to enhance the immunomodulatory and angiogenic potency of ASC secretome. | Preconditioning at 0.5-1 mM for 24-48h [106]. |
| Matrigel Basement Membrane Matrix | Synthetic basement membrane for 3D cell culture; essential for in vitro endothelial tube formation assays. | Used to coat plates for HUVEC tubulogenesis assay [105]. |
| Tangential Flow Filtration (TFF) Capsule | For concentration and buffer exchange of collected CM; allows for processing of large volumes. | Used with a 3 kDa molecular weight cut-off membrane to concentrate CM [105]. |
| SPECT/CT Imaging with Thallium-201 | Non-invasive in vivo functional imaging to quantify myocardial perfusion and viability in animal models. | Used to assess ≈32% improvement in perfusion in rat MI model post-CM treatment [106]. |
| Cytokine/Chemokine Array | Multiplexed protein immunoassay to comprehensively characterize the secretory profile (secretome) of CM. | Used to identify increased IL-10, CXCL5, and MMP-1 in butyrate-preconditioned CM [106]. |
| RNA-sequencing | Transcriptomic analysis to identify global gene expression changes in recipient cells or preconditioned stem cells. | Used to identify ACM-mediated downregulation of TNF and chemokine signaling pathways [105]. |
The synthesis of current evidence firmly establishes the robust preclinical success of stem cell-conditioned medium as a multifaceted cardioprotective therapy. Its mechanisms, mediated by a complex cocktail of paracrine factors and EVs, converge on key pathological processes post-MI: inflammation, apoptosis, fibrosis, and impaired angiogenesis. Preconditioning strategies represent a powerful tool to further enhance CM potency.
However, clinical readiness remains a work in progress. While the therapeutic concept is sound, and early clinical trials with whole cells show promise, the path forward for CM requires a concerted effort to overcome critical translational barriers. Future research must prioritize the standardization of CM manufacturing, the rigorous characterization of active components, the validation of optimal delivery strategies in large animal models, and the initiation of well-controlled pilot clinical trials. The collective goal is to transform this compelling preclinical evidence into a standardized, efficacious, and off-the-shelf cell-free therapeutic for the millions of patients suffering from ischemic heart disease.
Conclusion
Stem cell-conditioned medium represents a transformative, cell-free paradigm for myocardial protection, with robust preclinical evidence supporting its efficacy in reducing infarct size, promoting angiogenesis, and preserving cardiac function post-MI. Its therapeutic action is predominantly mediated by a complex secretome of paracrine factors, with extracellular vesicles and their miRNA cargo, such as miR-221/222, playing a central role. While challenges related to heterogeneity, standardization, and scalable manufacturing remain, emerging strategies like cell preconditioning and EV engineering are poised to enhance therapeutic potency. The future of CM therapy lies in the development of well-defined, off-the-shelf biologics that offer the benefits of stem cell therapy without the associated risks of cell transplantation, ultimately paving the way for more effective and accessible treatments for cardiovascular diseases.
References
- 1. Cardiac repair and regeneration: cell therapy, in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586717/]
- 2. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 3. Cells Versus Cell-Derived Signals in Cardiac Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610112/]
- 4. Current status and new horizons in stem cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406451/]
- 5. Dental pulp-derived stem cell conditioned medium reduces ... [https://www.nature.com/articles/srep16295]
- 6. Mesenchymal Stem Cell Conditioned Media Attenuates in ... [https://pubmed.ncbi.nlm.nih.gov/21030271/]
- 7. Reduction of myocardial infarct size by human ... [https://www.sciencedirect.com/science/article/pii/S1873506108000056]
- 8. Metabolic regulation for the treatment of ischemic heart ... [https://www.nature.com/articles/s44325-025-00089-z]
- 9. Cardiac Regeneration Innovation in the Clinical Trial Pipeline [https://www.cardiologyresearchjournal.com/articles/cardiac-regeneration-innovation-in-the-clinical-trial-pipeline.html]
- 10. Frontiers | Stem in the treatment of cells injury-induced... myocardial [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1600604/full]
- 11. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 12. Human mesenchymal stem - cell improves... conditioned medium [https://pubmed.ncbi.nlm.nih.gov/21419744/]
- 13. Dynamic proteome profiling of differentiating human ... [https://www.nature.com/articles/s41598-025-24649-6]
- 14. Medium from human iPSC-derived primitive macrophages ... [https://pubmed.ncbi.nlm.nih.gov/40148355/]
- 15. Comparative analysis of enriched mesenchymal stem ... cells [https://nsr.jinr.int/article/51]
- 16. Stem Cell Media Market Insights & Growth Outlook 2025– ... [https://www.congruencemarketinsights.com/report/stem-cell-media-market]
- 17. Stem Cell Culture Medium Market Shifts: Strategic Analysis ... [https://www.linkedin.com/pulse/stem-cell-culture-medium-market-shifts-strategic-analysis-d90ce]
- 18. Mesenchymal Stem Cell-Based Therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6037203/]
- 19. The emerging role of extracellular vesicles in viral ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1634758/full]
- 20. Extracellular Vesicles as Diagnostic Metrics for ... [https://link.springer.com/article/10.1007/s12265-025-10629-8]
- 21. Adipose-Derived Exosomes: mediators of crosstalk between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360202/]
- 22. Stem cell therapy for myocardial infarction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512856/]
- 23. Research progress on exosomes in diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10393655/]
- 24. Exosome-derived miR-1275 mediates IL-38 upregulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415573/]
- 25. Mesenchymal stem cell-derived conditioned medium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7905634/]
- 26. Conditioned Medium from Mesenchymal Stem Cells ... [https://www.mdpi.com/2073-4409/10/5/1231]
- 27. Stem cells in the treatment of myocardial injury-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213730/]
- 28. Molecular Insights into Oxidative-Stress-Mediated ... [https://www.mdpi.com/2218-273X/15/5/670]
- 29. Pathways for Cardioprotection in Perspective: Focus on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953525/]
- 30. Therapeutic potential of human umbilical cord ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1667140/full]
- 31. Extracellular vesicles in cardiac regeneration and aging [https://www.oaepublish.com/articles/jca.2025.30]
- 32. microRNA regulation related to the protective effects of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8042572/]
- 33. MicroRNA-21 Mediates the Protective Effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6721717/]
- 34. Adipose stem cell-derived nanovesicles for cardioprotection [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006108]
- 35. Cardiovascular System is Influenced by Skeletal Muscle ... [https://www.medsci.org/v22p2382.htm]
- 36. Multi-step regulation of microRNA expression and ... [https://www.sciencedirect.com/science/article/pii/S2211124724008209]
- 37. Analysis of MicroRNA Cargo in Circulating Extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11172129/]
- 38. Updated protocols for cell lysate, secretome, and exosome ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000568]
- 39. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 40. A Comprehensive Review of Stem Cell Conditioned Media ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11416772/]
- 41. The therapeutic efficacy comparison of MSCs derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077008/]
- 42. Comparison of the proteomic landscape in experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976975/]
- 43. Mesenchymal Stem Cell-Conditioned Media-Loaded ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11428691/]
- 44. Medium from human iPSC-derived primitive macrophages ... [https://www.nature.com/articles/s41467-025-58301-8]
- 45. Stem Cell Therapy against Ischemic Heart Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011361/]
- 46. Conditioned medium from adipose-derived stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7847683/]
- 47. Higher Improvement of Cardiac Function Following ... [https://pubmed.ncbi.nlm.nih.gov/37538240/]
- 48. Safety and efficacy of global intracoronary administration ... [https://www.sciencedirect.com/science/article/pii/S1109966618305645]
- 49. ZBP1介导心肌细胞PANoptosis:缺血再灌注损伤的新机制与 ... [https://www.ebiotrade.com/newsf/2025-10/20251008004245476.htm]
- 50. The paradigm of stem cell secretome in tissue repair and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11711308/]
- 51. Assessing the Potential Benefits of Stem Cell Therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786102/]
- 52. Reduction of myocardial infarct size by human mesenchymal stem cell conditioned medium - PubMed [https://pubmed.ncbi.nlm.nih.gov/19383393/]
- 53. Human mesenchymal stem cell-conditioned medium improves cardiac function following myocardial infarction - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S187350611100002X]
- 54. Current Stem Cell Delivery Methods for Myocardial Repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC3591183/]
- 55. Impact of intracoronary adenosine on the no-reflow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595116/]
- 56. Repair effect analysis of mesenchymal stem ... cell conditioned media [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-024-09521-5]
- 57. Towards the Standardization of Mesenchymal Stem ... Cell [https://pubmed.ncbi.nlm.nih.gov/37628774/]
- 58. Intra-individual variability in the neuroprotective and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03344-1]
- 59. Conditioned Medium from Human Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6479925/]
- 60. Rethinking miRNAs in MSC -sEV therapeutics: implications for... [https://www.oaepublish.com/articles/evcna.2025.55]
- 61. unlocking the regenerative potential of secreted factors [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1609082/full]
- 62. Increasing angiogenic efficacy of conditioned medium ... [https://www.nature.com/articles/s42003-022-03838-3]
- 63. Hypoxia and Multilineage Communication in 3D Organoids ... [https://www.mdpi.com/2313-7673/10/9/624]
- 64. Combining Hypoxia and Bioreactor Hydrodynamics Boosts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4225049/]
- 65. Hypoxic Preconditioning Enhances the Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180708/]
- 66. Hypoxia preconditioning promotes bone marrow ... [https://www.nature.com/articles/s41419-019-1410-y]
- 67. Engineering extracellular vesicles for targeted therapeutics ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2024.1503830/full]
- 68. Extracellular vesicle therapeutics for cardiac repair [https://www.sciencedirect.com/science/article/abs/pii/S0022282824001950]
- 69. Therapeutic Efficacy of Mesenchymal Stem Cells for ... [https://www.mdpi.com/2392-7674/8/2/23]
- 70. Clinical insights into extracellular vesicles for targeted ... [https://pubmed.ncbi.nlm.nih.gov/40883963/]
- 71. A comprehensive review of clinical trials and progress in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001944]
- 72. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 73. An optimized procedure for preparation of conditioned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10580810/]
- 74. The Essential Need for a Validated Potency Assay for Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8599250/]
- 75. Analysis of the measurements used as potency tests for the 31 ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06253-4]
- 76. A Checklist For Mechanism-Based Potency Testing In Cell ... [https://www.cellandgene.com/doc/a-checklist-for-mechanism-based-potency-testing-in-cell-therapy-0001]
- 77. New insights on potency assays from recent advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 78. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 79. Good Manufacturing Practice (GMP) standards [https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/norms-and-standards/gmp]
- 80. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 81. Current good manufacturing practice considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934414/]
- 82. Overcoming Challenges in Scale-Up Production [https://www.worldpharmatoday.com/articles/overcoming-challenges-in-scale-up-production/]
- 83. GMP-grade Mesenchymal Stem Cell Media in the Real World [https://www.linkedin.com/pulse/gmp-grade-mesenchymal-stem-cell-media-real-gvscc/]
- 84. GMP‐Compliant Process for the Manufacturing of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365392/]
- 85. What are the most significant manufacturing hurdles in ... [https://www.pharmasalmanac.com/articles/what-are-the-most-significant-manufacturing-hurdles-in-biopharma-and-how-can-they-be-addressed]
- 86. A Comparative Analysis of Multipotent Mesenchymal ... [https://www.nature.com/articles/s41598-020-61167-z]
- 87. Comparative analysis of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4453294/]
- 88. Comparative Effects of Bone Marrow-derived Versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8929420/]
- 89. Side-by-Side Comparison of the Biological Characteristics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3722850/]
- 90. Mesenchymal stem cells from umbilical cord matrix, adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3854702/]
- 91. Injectable Stem Cell-Based Therapies for Myocardial ... [https://www.mdpi.com/2079-4983/16/5/152]
- 92. Angiogenesis and Apoptosis: Data Comparison of Similar ... [https://www.mdpi.com/2076-2615/14/7/1118]
- 93. Angiogenic signaling pathways and anti ... [https://www.nature.com/articles/s41392-023-01460-1]
- 94. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 95. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 96. Different types of cell death and their interactions in ... [https://www.nature.com/articles/s41420-025-02372-5]
- 97. Mechanisms of postischemic cardiac death and protection ... [https://www.jci.org/articles/view/184134]
- 98. Cardiac regeneration by direct reprogramming in this ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8247073/]
- 99. Signaling pathways and targeted therapy for myocardial ... [https://www.nature.com/articles/s41392-022-00925-z]
- 100. Effectiveness of regenerative medicine for skin lightening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465346/]
- 101. Therapeutic effects of conditioned medium of immortalized ... [https://www.nature.com/articles/s41598-025-22449-6]
- 102. Development of direct cardiac reprogramming for clinical ... [https://www.sciencedirect.com/science/article/pii/S0022282823000354]
- 103. Injectable Stem Cell-Based Therapies for Myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12111900/]
- 104. Stem cell therapy for myocardial infarction and atherosclerosis [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04678-8]
- 105. Mesenchymal stem cell-conditioned medium accelerates ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1659444/full]
- 106. Butyrate-preconditioned human adipose-derived stem cell ... [https://www.sciencedirect.com/science/article/pii/S2352320425002251]
- 107. Stem cells show promise in preventing post-heart attack ... [https://www.news-medical.net/news/20251030/Stem-cells-show-promise-in-preventing-post-heart-attack-heart-failure.aspx]