Stem Cell-Derived Beta Cells for Type 1 Diabetes: A Comprehensive Review of Efficacy, Clinical Applications, and Future Directions
This article provides a comprehensive analysis of the efficacy of stem cell-derived beta cells as a curative therapy for type 1 diabetes (T1D), tailored for researchers, scientists, and drug development...
Stem Cell-Derived Beta Cells for Type 1 Diabetes: A Comprehensive Review of Efficacy, Clinical Applications, and Future Directions
Abstract
This article provides a comprehensive analysis of the efficacy of stem cell-derived beta cells as a curative therapy for type 1 diabetes (T1D), tailored for researchers, scientists, and drug development professionals. It explores the foundational science establishing proof-of-concept, detailing how allogeneic stem cell-derived islets can restore endogenous insulin production and physiologic glucose control. The review examines methodological advances in cell delivery, including hepatic portal vein infusion and encapsulation devices, alongside their respective requirements for immunosuppression. It critically addresses persistent challenges in immunogenicity, scalability, and safety, evaluating troubleshooting strategies such as the development of hypoimmune cells through genetic engineering. Finally, the article presents a comparative validation of recent clinical trial outcomes, synthesizing efficacy and safety data to assess the current standing and future trajectory of this transformative therapeutic modality.
The Scientific Foundation: Establishing Proof-of-Concept for Beta Cell Replacement
For decades, the destruction of insulin-producing pancreatic beta cells has been the recognized pathophysiological cornerstone of Type 1 Diabetes (T1D), creating an absolute dependence on exogenous insulin for survival [1]. While insulin therapy is life-saving, it fails to fully mimic physiological insulin regulation, often resulting in suboptimal glycemic control and long-term complications [1] [2]. Beta cell replacement therapy emerged as a strategy to restore endogenous insulin production and achieve long-term glycemic stability. The field is now undergoing a transformative paradigm shift: moving from a reliance on scarce donor pancreatic islets toward the use of stem cell-derived beta cells as a scalable, engineered source for replacement therapy [3] [4]. This shift addresses the fundamental limitation of donor organ shortage, which has historically restricted islet transplantation to a select group of patients with severe hypoglycemic unawareness [2] [5]. This guide objectively compares the performance of traditional islet transplantation against emerging stem cell-derived beta cell therapies, providing researchers and drug development professionals with the key experimental data, protocols, and analytical tools needed to navigate this evolving landscape.
Comparative Analysis of Beta Cell Sourcing Strategies
The transition from donor-dependent to engineered cell sources represents a fundamental change in the therapeutic approach to T1D. The table below provides a direct comparison of the core characteristics of these two strategies.
Table 1: Core Characteristics of Islet Transplantation vs. Stem Cell-Derived Beta Cells
| Characteristic | Donor Islet Transplantation | Stem Cell-Derived Beta Cells |
|---|---|---|
| Cell Source | Cadaveric pancreata [2] | Human pluripotent stem cells (embryonic or induced) [1] [2] |
| Key Limitation | Severe donor organ shortage [2] [5] | Requires differentiation and potential genetic engineering [1] [6] |
| Scalability | Limited and fixed supply [4] | Theoretically unlimited, on-demand production [2] [6] |
| Standardization | High variability between donors and isolations [2] | Potential for standardized, quality-controlled cell products [3] |
| Immunosuppression | Lifelong, systemic immunosuppression required [2] [5] | Currently required for allogeneic products; strategies to obviate it are in development [3] [6] |
| Clinical Status | Established therapy for specific T1D patients [2] [5] | Late-stage clinical trials; largely experimental but rapidly advancing [1] [7] |
Efficacy and Clinical Outcomes
Recent clinical trials provide the first robust, quantitative data on the performance of stem cell-derived islets, allowing for a direct comparison with the outcomes of established donor islet transplantation.
Table 2: Comparison of Key Clinical Trial Outcomes
| Parameter | Donor Islet Transplantation (Established Protocol) | Stem Cell-Derived Islets (Zimislecel, Phase 1-2 Trial) |
|---|---|---|
| Study Reference | Shapiro et al., Edmonton Protocol [2] | Reichman et al., 2025 NEJM [3] [7] |
| Sample Size | 36 subjects [2] | 12 subjects (full-dose cohort) [7] |
| Insulin Independence (1 Year) | 44% of recipients [2] | 83% of recipients [3] [7] |
| Freedom from Severe Hypoglycemia | Significant reduction established [2] [5] | 100% of participants free from events [3] [7] |
| HbA1c Reduction | Improvement in metabolic control [2] | Mean decrease of 1.81% [3] |
| Time in Target Glucose Range | Improved stability [2] | >70% to >90% time in range (70-180 mg/dL) [3] [7] |
| C-peptide Positivity | Indicates engraftment and function | Achieved in 100% of participants post-infusion [7] |
The data indicate that stem cell-derived islets can not only meet but potentially exceed the efficacy of donor islets in key metrics, particularly in the rate of insulin independence. However, the safety profile differs. The zimislecel trial reported two deaths, one from cryptococcal meningitis linked to immunosuppression, highlighting that the reliance on chronic immunosuppression remains a significant risk with current allogeneic stem cell products [3] [7].
Technical and Experimental Protocols
Protocol 1: In Vitro Differentiation of Stem Cells into Beta-Like Cells
This protocol generates insulin-producing beta-like cells from human pluripotent stem cells (hPSCs) by mimicking in vivo pancreatic development [2].
- Definitive Endoderm Induction: Treat hPSCs with Activin A (a TGF-β family member) and Wnt3a to direct differentiation into definitive endoderm cells. This typically lasts 3 days [2].
- Primitive Gut-Tube Formation: Expose the definitive endoderm to Fibroblast Growth Factor 10 (FGF10) and KAAD-cyclopamine (a hedgehog signaling inhibitor) for several days to pattern the cells into primitive gut-tube endoderm [2].
- Pancreatic Progenitor Commitment: Further differentiate the cells using retinoic acid to promote posterior foregut fate and inhibit Sonic hedgehog (Shh) signaling to drive specification into pancreatic endoderm and endocrine precursors [2].
- Endocrine Differentiation and Maturation: Culture the pancreatic progenitors in a complex cocktail of growth factors, hormones, and signaling molecules to finalize their maturation into endocrine cells expressing insulin, glucagon, and somatostatin [2].
- In Vivo Maturation (Optional): For some protocols, cells are transplanted at the pancreatic endoderm progenitor stage into an in vivo environment (e.g., immunodeficient mice) where vascularization and other host factors support final maturation into functional, glucose-responsive beta cells [2].
Protocol 2: Generation of Hypoimmune Stem Cell-Derived Beta Cells
This protocol uses genetic engineering to create beta cells that evade immune rejection, aiming to eliminate the need for immunosuppression [3] [6].
- Base Cell Line Generation: Start with a human Pluripotent Stem Cell (hPSC) line. Using CRISPR-Cas9, create knock-out mutations in the B2M (Beta-2 Microglobulin) and CIITA (Class II Major Histocompatibility Complex Transactivator) genes. This disrupts surface expression of HLA Class I and Class II molecules, preventing T-cell recognition [6].
- "Don't Eat Me" Signal Knock-in: At the same genomic loci, knock-in genes for immune tolerogenic ligands. A common strategy is the overexpression of CD47, which ligates SIRPα on macrophages and neutrophils to inhibit phagocytosis [3] [6].
- NK Cell Inhibition Knock-in: To protect against Natural Killer (NK) cell-mediated lysis (triggered by "missing self" from HLA Class I knockout), knock-in genes for non-classical HLA molecules like HLA-E or HLA-G, which engage inhibitory receptors on NK cells [6].
- Differentiation into Beta Cells: Differentiate the engineered hypoimmune hPSC line into insulin-producing beta-like cells using a protocol similar to the one described in Section 4.1.
- Validation: Validate immune evasion through in vitro co-culture assays with human peripheral blood mononuclear cells (PBMCs) and in vivo transplantation into humanized mouse models without immunosuppression [6].
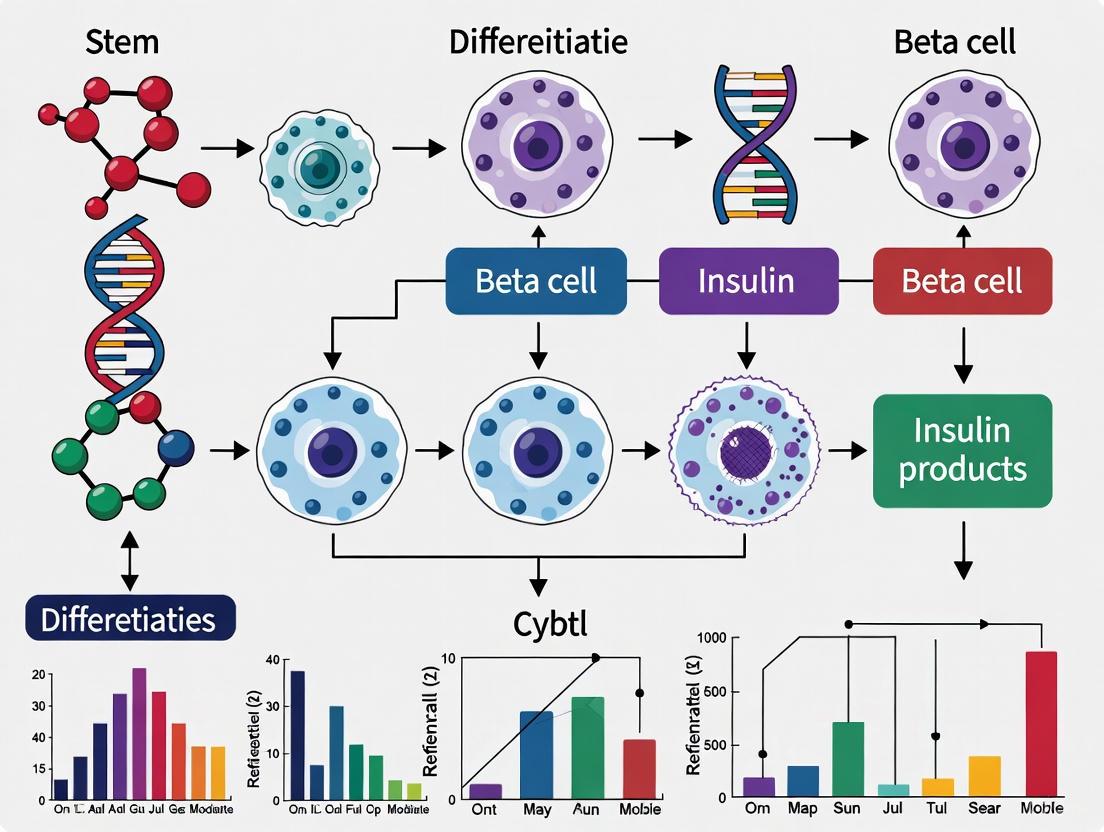
Diagram 1: Hypoimmune Beta Cell Engineering Workflow.
Signaling Pathways in Differentiation and Immune Evasion
The successful generation and transplantation of stem cell-derived beta cells hinge on the precise manipulation of key biological pathways. The diagram below illustrates the core signaling pathways involved in beta cell differentiation and the engineered pathways for immune evasion.
Diagram 2: Key Signaling Pathways in Beta Cell Differentiation and Immune Evasion.
The Scientist's Toolkit: Essential Research Reagents
Advancing research in this field requires a specific toolkit of biological reagents, assay systems, and delivery devices. The following table details key solutions and their applications for researchers developing and testing stem cell-derived beta cell therapies.
Table 3: Essential Research Reagents and Tools for Beta Cell Therapy Development
| Reagent/Tool Solution | Primary Function | Application in Research Context |
|---|---|---|
| Human Pluripotent Stem Cells (hPSCs) | Self-renewing, pluripotent starting material for differentiation [2]. | Source for generating beta-like cells; can be engineered (e.g., hypoimmune) [6]. |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific pluripotent cells reprogrammed from somatic cells [2]. | Enables autologous therapy models and disease-in-a-dish research for T1D [2]. |
| Activin A, FGF10, Retinoic Acid | Key signaling molecules for directed differentiation [2]. | Used in vitro to guide hPSCs through stages of pancreatic development. |
| CRISPR-Cas9 System | Precision gene-editing tool [6]. | Engineering hypoimmune traits (e.g., B2M KO, CD47 KI) in hPSC lines [6]. |
| Mesenchymal Stem Cells (MSCs) | Immunomodulatory and pro-angiogenic accessory cells [8] [5]. | Co-transplanted with islets to potentially enhance graft survival and function [8]. |
| Macroencapsulation Devices | Physical, semi-permeable barriers for housing islet cells [2]. | Protects transplanted cells from immune attack while allowing nutrient/insulin exchange. |
| Mixed-Meal Tolerance Test (MMTT) | Standardized challenge to stimulate insulin secretion. | Measures C-peptide levels in vivo to confirm engraftment and functional beta cell mass [7]. |
| Immunosuppressive Regimens (e.g., ATG, MMF) | Suppresses host adaptive immune system. | Required in clinical trials for allogeneic cell transplant to prevent graft rejection [1] [7]. |
The paradigm in beta cell sourcing has irrevocably shifted. Traditional islet transplantation provided critical proof-of-concept that beta cell replacement can restore physiological glucose control, but its scalability was inherently limited [2] [4]. Stem cell-derived beta cells now represent a scalable, engineered solution that has transitioned from scientific aspiration to clinical reality, demonstrating remarkable efficacy in early trials [3] [7]. The next frontier lies in resolving the dual challenges of immune rejection and scalability. Strategies like hypoimmune gene editing offer a promising path to eliminate the burdens and risks of lifelong immunosuppression [3] [6]. For the research community, the focus must now expand beyond achieving scientific feasibility to addressing the "last mile" challenges of manufacturing, cost, and accessibility to ensure these transformative therapies can reach the millions of individuals living with T1D [4].
Type 1 diabetes (T1D) is an autoimmune disorder characterized by the selective destruction of insulin-producing β-cells in the pancreatic islets of Langerhans, resulting in the inability to produce and secrete insulin in response to blood glucose levels [9]. For decades, the standard treatment has relied on exogenous insulin administration, which, while life-saving, fails to replicate the precise dynamics of physiological insulin secretion and places a significant burden on patients [9]. Stem cell-derived islets (SC-islets) have emerged as a transformative therapeutic approach aimed at providing a "functional cure" by replacing the lost β-cell mass [9]. This strategy circumvents the fundamental limitation of conventional islet transplantation—the critical shortage of donor pancreata—by offering a potentially unlimited source of insulin-producing cells [2]. This guide examines the mechanisms through which SC-islets restore endogenous insulin production, objectively comparing their performance against established alternatives and detailing the experimental methodologies used to evaluate their efficacy.
Comparative Analysis of Beta-Cell Replacement Therapies
The landscape of beta-cell replacement has evolved from solid organ pancreas transplants to cell-based therapies. The table below provides a structured comparison of the primary modalities.
Table 1: Comparison of Beta-Cell Replacement and Insulin Therapy Strategies for Type 1 Diabetes
| Therapy | Mechanism of Action | Efficacy Data | Key Limitations | Immunosuppression Requirement |
|---|---|---|---|---|
| Exogenous Insulin | Subcutaneous injection/infusion of insulin to lower blood glucose. | Maintains life but fails to fully mimic physiological control; high risk of hypoglycemia [9]. | Does not restore endogenous production; requires constant patient management [9]. | Not required. |
| Pancreas Transplant | Surgical transplantation of a whole pancreas from a deceased donor. | Restores insulin independence; considered the gold standard for glycemic control [2]. | Highly invasive surgery; significant procedural risks; limited donor availability [2]. | Lifelong immunosuppression required. |
| Donor Islet Transplant | Infusion of islets isolated from donor pancreata into the liver via the portal vein. | The Edmonton Protocol demonstrated insulin independence in all 7 patients at 1 year [9]. NIH-sponsored trials show effectiveness in reducing hypoglycemia [2]. | Requires multiple donors per recipient; limited donor availability; gradual decline in function over time [9] [2]. | Lifelong immunosuppression required. |
| Stem Cell-Derived Islets (SC-Islets) | Transplantation of in vitro-differentiated, insulin-producing islets. | Phase 1/2 trial of VX-880: 92% mean insulin use reduction; 10 of 12 patients achieved insulin independence [10]. | Challenges with post-transplant cell survival (e.g., hypoxia); potential for immune rejection [11] [12]. | Required for current non-encapsulated products; strategies for evasion in development [10] [12]. |
Mechanisms of Functional Restoration by SC-Islets
SC-islets restore glucose homeostasis by replicating the core functions of native pancreatic islets. The mechanism can be broken down into a multi-stage process.
Core Functional Mechanism
The mechanism begins with 1. Glucose Sensing. Mature SC-β cells express high levels of glucose transporters (e.g., GLUT1) and glucokinase (GK), which allow them to rapidly equilibrate intracellular glucose concentrations with the blood and initiate glycolysis, respectively [12]. This leads to 2. Metabolic Signaling, a critical stage where SC-β cells utilize oxidative phosphorylation to metabolize glucose. The nuclear receptor ERRγ has been identified as a key driver of this metabolic maturation, enhancing the capacity for mitochondrial oxidative phosphorylation [12]. This process generates ATP, increasing the ATP/ADP ratio, which in turn triggers the closure of ATP-sensitive K+ channels and membrane depolarization. This depolarization opens voltage-gated calcium channels, causing a Ca²⁺ Influx that is the key signal for 3. Insulin Secretion [12]. Finally, the synthesized insulin is released via exocytosis (4. Glucose Homeostasis), thereby restoring physiological glycemic control. The entire process is governed by the activation of a Native β-cell Network of transcription factors, including NKX6.1, PDX1, and MAFA, which are essential for establishing and maintaining β-cell identity and functional maturity [12].
Key Experimental Models and Protocols
Evaluating the in vivo functionality of SC-islets relies on standardized preclinical models and clinical assessments. The following workflow outlines a standard protocol for a diabetes reversal study in immunodeficient mice, a cornerstone experiment for validating SC-islet potency.
Preclinical Animal Model
The gold-standard protocol for assessing SC-islet function in vivo involves several key stages [2] [12]:
- Diabetes Induction: Immunodeficient mice (e.g., NOD-scid or similar) are rendered diabetic by administration of streptozotocin (STZ), a toxin that selectively destroys their endogenous insulin-producing β-cells.
- Hyperglycemia Confirmation: Mice are considered diabetic and ready for transplantation once stable hyperglycemia (blood glucose >350 mg/dL) is established.
- Transplantation: SC-islets are transplanted into a suitable site in the mouse, most commonly under the kidney capsule or via infusion into the portal vein, which leads to engraftment in the liver.
- Efficacy Monitoring: Blood glucose levels are monitored regularly. Successful engraftment and function of the SC-islets is demonstrated by a sustained return to normoglycemia (blood glucose <200 mg/dL). This is considered a "functional cure."
- Confirmation of Graft Function: To conclusively prove that the normoglycemia is due to the human SC-islet graft, the graft is surgically removed (explantation). The subsequent return to hyperglycemia confirms graft-dependent diabetes reversal.
Clinical Trial Assessment
In human trials, efficacy is measured by several key endpoints [10]:
- Stimulated C-peptide: The gold-standard metric for endogenous insulin production. Patients undergo a Mixed Meal Tolerance Test (MMTT), and the resulting C-peptide levels (a byproduct of insulin synthesis) are measured.
- Glycated Hemoglobin (A1C): Measures long-term glycemic control, with a target of <7% indicating good control.
- Time-in-Range (TIR): The percentage of time blood glucose levels remain within the target range (70-180 mg/dL), as measured by continuous glucose monitors. A TIR >70% is a key goal.
- Insulin Dose: The reduction, or complete elimination, of the need for exogenous insulin injections.
Table 2: Key Clinical Outcomes from Recent SC-Islet Trials
| Trial / Study | Patient Population | Intervention | Primary Efficacy Outcomes | Key Findings |
|---|---|---|---|---|
| FORWARD (VX-880) Phase 1/2 [10] | 12 adults with T1D and impaired hypoglycemia awareness. | Single infusion of fully differentiated SC-islets into the liver + immunosuppression. | - Stimulated C-peptide- A1C <7%- TIR >70%- Insulin use. | - Endogenous insulin restored in all 12.- 92% mean reduction in insulin use.- 10/12 patients achieved insulin independence. |
| PEC-Direct (ViaCyte) [9] | Adults with T1D (multiple sites). | Implantation of pancreatic progenitor cells (PEC-01) in a non-immune-protective device + immunosuppression. | - Meal-responsive C-peptide. | - C-peptide production detected 6-9 months post-transplant.- Grafts matured into endocrine cells in vivo. |
| Autologous CiPSC-Islets [1] [13] | A single patient with T1D for 11 years. | Transplantation of islets derived from the patient's own chemically reprogrammed stem cells. | - Insulin independence.- A1C <7%.- Safety. | - Insulin independence achieved on day 75.- Sustained A1C ≤5.7% for one year. |
The Scientist's Toolkit: Essential Research Reagents
Advancing SC-islet research requires a specific set of reagents and tools to generate, characterize, and test the cells. The following table details key solutions used in the featured experiments and the broader field.
Table 3: Essential Reagents for SC-Islet Research and Development
| Research Reagent / Tool | Function | Example Usage in Protocols |
|---|---|---|
| Small Molecules & Growth Factors | Guide pluripotent stem cells through stages of pancreatic differentiation by activating/inhibiting key pathways. | Activin A (definitive endoderm), FGF10 (gut-tube endoderm), KAAD-cyclopamine (hedgehog inhibition), Retinoic Acid (pancreatic endoderm) [2] [12]. |
| Immunosuppressive Drugs | Suppress the host immune system to prevent rejection of allogeneic cell transplants in clinical trials. | Protocols often use a combination like thymoglobulin (induction) and mycophenolate mofetil (maintenance) [2] [12]. |
| EDN3 (Endothelin 3) | Protects SC-β cell identity and function under hypoxic stress post-transplantation by modulating maturation and glucose-sensing genes [11]. | Used in in vitro studies to enhance SC-islet survival and function by overexpressing EDN3 before transplantation into low-oxygen environments [11]. |
| ERRγ Agonists | Promotes metabolic maturation of SC-β cells by enhancing mitochondrial oxidative phosphorylation, which is critical for glucose-stimulated insulin secretion [12]. | Forced expression of ERRγ in SC-β cells in vitro to improve their ATP production and subsequent insulin secretion capacity before transplantation [12]. |
| Glucose-Stimulated Insulin Secretion (GSIS) Assay | In vitro functional test that measures the ability of SC-islets to secrete insulin in response to high glucose challenges, a hallmark of mature β-cell function [11]. | SC-islets are sequentially exposed to low glucose, high glucose, and then depolarizing agents (e.g., KCl) while measuring insulin in the supernatant via ELISA. |
Current Challenges and Future Directions
Despite promising results, several challenges remain. A significant hurdle is the poor survival and function of SC-islets post-transplantation due to local hypoxia (low oxygen), particularly in subcutaneous sites or within encapsulation devices [11]. Research shows that hypoxia causes SC-β cells to gradually lose their identity markers, such as insulin, and undergo a metabolic shift away from aerobic respiration, severely impairing insulin secretion [11]. Strategies to overcome this, such as overexpressing protective genes like EDN3, are under active investigation [11].
Another major focus is solving the problem of immune rejection. Current approaches require chronic immunosuppression, which carries significant risks [10] [12]. Future strategies aim to create "immune-shielded" SC-islets through:
- Encapsulation Devices: Physical barriers that protect the cells from immune attack while allowing nutrient and insulin exchange [9].
- Genetic Engineering: Modifying SC-islets to evade the immune system, for example by adding protective genes or using a "safety switch" to eliminate the cells if needed [10].
- Inducing Immune Tolerance: Innovative approaches, so far demonstrated in mice, use a combined transplant of blood stem cells and islets from the same donor to create a "hybrid" immune system that accepts the graft without long-term immunosuppression [14].
Finally, as the field progresses from proof-of-concept to widespread treatment, significant challenges in scalability, cost, and accessibility must be addressed to ensure these transformative therapies can reach the millions of patients in need [4].
In the rapidly advancing field of stem cell-derived beta cell therapy for Type 1 Diabetes (T1D), the objective assessment of therapeutic efficacy relies on a triad of critical biomarkers. The success of these innovative treatments is quantified through precise measurements of C-peptide for beta cell function, HbA1c for long-term glycemic control, and Time-in-Range (TIR) for daily glucose management. These biomarkers provide complementary insights, enabling researchers and drug development professionals to rigorously evaluate whether stem cell-based interventions can restore physiological insulin production and achieve clinically meaningful metabolic outcomes. This guide examines the technical specifications, experimental protocols, and success thresholds for each indicator, contextualized with data from recent clinical trials of stem cell-derived therapies.
C-Peptide: The Gold Standard for Beta Cell Function
Physiological Role and Clinical Significance
C-peptide (connecting peptide) is a 31-amino-acid polypeptide that is cleaved from proinsulin during insulin synthesis in pancreatic beta cells. It is secreted in equimolar amounts to endogenous insulin, serving as a direct marker of insulin production [15] [16]. Unlike insulin, C-peptide has negligible hepatic extraction and a longer half-life (20-30 minutes versus 3-5 minutes for insulin), making it a more stable and reliable measure of beta cell function, especially in insulin-treated patients where it avoids cross-reaction with exogenous insulin assays [16].
In T1D, C-peptide measurement provides crucial information about the residual beta cell function and is the primary endpoint for evaluating the success of beta cell replacement therapies. The restoration of C-peptide secretion following stem cell therapy indicates engraftment, differentiation, and functional maturation of the transplanted cells [17] [18].
Measurement Protocols and Interpretation
Table 1: C-Peptide Measurement Methods and Diagnostic Thresholds
| Method | Procedure | Advantages | Limitations | Clinical Thresholds |
|---|---|---|---|---|
| Fasting C-Peptide | Measurement after 8-10 hour fast | Easy to standardize, practical | May miss functional capacity | <0.075 nmol/L indicates severe deficiency [16] |
| Random C-Peptide | Measurement without fasting preparation | Simple, convenient for clinics | Interpretation depends on time from last meal | <0.2 nmol/L suggests insulin deficiency [16] |
| Glucagon Stimulation Test (GST) | 1 mg IV glucagon with C-peptide measurement at 0 and 6 minutes | High sensitivity and specificity, short duration | Nausea as side effect | >0.2 nmol/L post-stimulation indicates preserved function [16] |
| Mixed Meal Tolerance Test (MMTT) | Liquid meal consumption with serial measurements over 120 minutes | Physiological stimulus, research gold standard | Time-consuming, requires specialized preparation | Peak >0.2 nmol/L indicates clinically meaningful function [15] [18] |
C-Peptide in Stem Cell Therapy Trials
In recent stem cell therapy trials, C-peptide measurement has been instrumental in demonstrating efficacy:
- In a groundbreaking trial of chemically induced pluripotent stem cell-derived islets (CiPSC-islets), the patient's fasting C-peptide increased from 0 to 721.6 pmol/L (approximately 0.72 nmol/L), exceeding the normal healthy range (300-600 pmol/L) and correlating with insulin independence [17].
- In the PEC-Direct trial of encapsulated stem cell-derived pancreatic endoderm cells, three of ten patients achieved C-peptide levels ≥0.1 nmol/L by month 6, which was associated with improved continuous glucose monitoring measures and reduced insulin dosing [18].
- The threshold of ≥0.2 nmol/L after stimulation is widely considered clinically significant as it associates with fewer complications and less severe hypoglycemia [15].
HbA1c: The Long-Term Glycemic Control Marker
Biochemical Basis and Clinical Utility
Glycated hemoglobin (HbA1c) forms when hemoglobin non-enzymatically binds to glucose in the bloodstream. It reflects average blood glucose levels over the preceding 2-3 months, corresponding to the lifespan of red blood cells. HbA1c is expressed as a percentage of total hemoglobin, with lower values indicating better glycemic control [17] [19].
For T1D management, the American Diabetes Association recommends a general HbA1c target of <7.0% for most adults, with more stringent targets (<6.5%) potentially appropriate for some patients if achievable without significant hypoglycemia [17].
HbA1c in Stem Cell Therapy Efficacy Assessment
In stem cell therapy trials, HbA1c reduction demonstrates the ability of transplanted cells to provide sustained glycemic control:
- In the CiPSC-islet trial, the patient's HbA1c decreased from 7.57% to 4.76% within one year post-transplantation, well below the success threshold of >7% [17].
- Vertex Pharmaceuticals' stem cell-derived therapy (Zimislecel) reported that 10 of 12 participants who received a full dose achieved HbA1c <7% alongside insulin independence at one year [20].
- HbA1c provides crucial evidence of durable glycemic control beyond immediate post-transplant effects, making it essential for evaluating long-term therapeutic success.
Time-in-Range: The Continuous Glucose Monitoring Metric
Definition and Clinical Relevance
Time-in-Range (TIR) is a continuous glucose monitoring (CGM)-derived metric representing the percentage of time that glucose levels remain within a target range, typically 70-180 mg/dL (3.9-10.0 mmol/L). This real-world measure captures glycemic variability that may not be reflected in HbA1c [17] [18].
Complementary CGM metrics include:
- Time-Above-Range (TAR): >180 mg/dL (>10.0 mmol/L)
- Time-Below-Range (TBR): <70 mg/dL (<3.9 mmol/L)
- Glucose Management Indicator (GMI): Estimated HbA1c from CGM data [18]
TIR as a Stem Cell Therapy Outcome Measure
TIR has emerged as a critical endpoint in recent stem cell therapy trials due to its sensitivity to daily glucose fluctuations:
- In the CiPSC-islet case study, TIR improved from 43.18% at baseline to over 98% at one year post-transplantation, demonstrating remarkable restoration of physiological glucose regulation [17].
- The PEC-Direct trial reported that responders with C-peptide ≥0.1 nmol/L showed significant increases in TIR, with one patient improving from 55% to 85% by month 12 [18].
- Clinical consensus considers TIR >70% as the target for well-controlled T1D, making it a valuable benchmark for assessing stem cell therapy efficacy [18].
Integrated Success Metrics in Recent Clinical Trials
Table 2: Efficacy Outcomes from Recent Stem Cell Therapy Trials for T1D
| Trial / Therapy | C-Peptide Outcomes | HbA1c Outcomes | Time-in-Range Outcomes | Additional Efficacy Measures |
|---|---|---|---|---|
| CiPSC-Islets [17] | Increased from 0 to 721.6 pmol/L (fasting) | Decreased from 7.57% to 4.76% | Improved from 43.18% to >98% | Insulin independence achieved by day 75 |
| PEC-Direct (Encapsulated) [18] | 3/10 patients achieved ≥0.1 nmol/L (stimulated) | GMI improved in responders | Increased from 55% to 85% (best responder) | Reduced insulin dosing in responders |
| Vertex VX-880 (Zimislecel) [20] | Not specified | <7% in 10/12 patients at 1 year | >70% in 10/12 patients at 1 year | Insulin independence in 10/12 patients at 1 year |
| PEC-01 Cells [1] | Significant increase by week 26 (p=0.0026) | Not specified | Improved by 13% (p<0.001) | 20% reduction in insulin requirements (p<0.001) |
Experimental Protocols for Efficacy Assessment
Standardized Metabolic Function Tests
Mixed Meal Tolerance Test (MMTT) Protocol:
- Preparation: 10-12 hour overnight fast
- Baseline samples: Collect blood for C-peptide, glucose at t=-10 and t=0 minutes
- Stimulus administration: Liquid meal (e.g., Boost or Sustacal) consumed within 5 minutes
- Serial sampling: Collect blood at 15, 30, 60, 90, and 120 minutes post-stimulus
- Sample processing: Centrifuge within 30 minutes, freeze plasma at -20°C until analysis
- Analysis: Measure C-peptide via standardized immunoassay [15] [18]
Glucagon Stimulation Test Protocol:
- Preparation: 10-12 hour overnight fast
- Baseline sample: Collect blood for C-peptide at t=0 minutes
- Stimulus administration: Intravenous glucagon (1 mg) over 2 minutes
- Post-stimulation sample: Collect blood at t=6 minutes
- Sample processing: Centrifuge promptly, freeze plasma for analysis [16]
C-Peptide Assay Standardization Considerations
Significant variability exists between C-peptide assay methods despite common traceability to the WHO International Reference Reagent (IRR 84/510). Between-method coefficients of variation average 19.1% with manufacturers' usual calibration, improving to 7.5% after recalibration with secondary reference materials. Researchers should verify their local laboratory's assay methodology and reference ranges for consistent interpretation [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Beta Cell Function Assessment
| Reagent / Material | Function in Research | Application Examples | Technical Considerations |
|---|---|---|---|
| C-Peptide Immunoassay Kits | Quantification of C-peptide in serum/plasma/urine | Assessment of beta cell function in vitro and in vivo | Select assays with <10% proinsulin cross-reactivity; verify detection limit (<0.0025 nmol/L) [15] [16] |
| HbA1c Testing Systems | Measurement of glycated hemoglobin | Long-term glycemic control assessment | Standardize to NGSP/IFCC reference methods; account for hemoglobin variants [17] [19] |
| Continuous Glucose Monitoring Systems | Real-time interstitial glucose measurement | Time-in-Range calculation in clinical trials | Use factory-calibrated systems (e.g., Dexcom G7) with 5-minute sampling intervals [20] [18] |
| Stem Cell Differentiation Kits | Directed differentiation of pluripotent stem cells to beta cells | Generation of insulin-producing cells for transplantation | Monitor key transcription factors (PDX1, NKX6.1, NKX2.2) during differentiation [17] [1] |
| Immunosuppressive Agents | Prevention of graft rejection in allogeneic transplants | Essential for non-encapsulated cell therapies | Consider regimens including anti-thymocyte globulin, mycophenolate mofetil, tacrolimus [18] [21] |
Logical Framework for Efficacy Assessment
The following diagram illustrates the logical relationship between stem cell therapy and the key efficacy metrics, highlighting how successful engraftment leads to measurable physiological outcomes:
The comprehensive assessment of stem cell-derived beta cell therapies requires multimodal evaluation through C-peptide, HbA1c, and Time-in-Range metrics. These indicators provide complementary information: C-peptide directly measures beta cell functional capacity, HbA1c reflects long-term glycemic control, and TIR captures daily glucose variability. Recent clinical successes demonstrate that these biomarkers can collectively document the transition from exogenous insulin dependence to restored physiological glucose regulation. As stem cell therapies advance toward clinical adoption, standardized application of these efficacy metrics will be essential for validating therapeutic potential and comparing outcomes across different technological platforms.
For decades, the restoration of functional pancreatic islets in patients with type 1 diabetes (T1D) has been a primary objective of regenerative medicine. The field is now transitioning from foundational science to tangible clinical applications, with early-phase trials reporting unprecedented success in restoring endogenous insulin production. This guide compares the most recent and compelling clinical evidence for emerging stem cell-derived beta cell therapies, providing researchers and drug development professionals with a detailed analysis of experimental protocols, efficacy data, and safety profiles.
Comparative Efficacy of Leading Therapeutic Candidates
The table below summarizes key efficacy outcomes from recent landmark clinical trials and studies, highlighting the rapid advancement in this domain.
Table 1: Comparison of Efficacy Outcomes from Recent Clinical Trials of Beta-Cell Replacement Therapies
| Therapy / Candidate | Study Phase / Type | Key Efficacy Outcome(s) | Insulin Independence | C-Peptide Response | Glycemic Control (HbA1c) |
|---|---|---|---|---|---|
| Zimislecel (VX-880) [7] | Phase 1/2 Clinical Trial | 83% (10/12) of participants achieved primary endpoint; restored physiologic islet function. | 83% at Day 365 | Detected post-infusion (from undetectable at baseline) | >70% Time-in-Range (70-180 mg/dL); HbA1c <7% |
| Stem Cell-Derived Islets (Vertex) [21] | Phase 1/2 Clinical Trial (Case Report) | Insulin independence achieved in first patient by day 270. | Achieved (1/1 reported) | Restored | 5.2% |
| Hybrid Immune System (Stanford) [14] | Preclinical (Mouse Model) | Cured or prevented autoimmune diabetes in all mice; no immunosuppression required. | 100% (9/9 cured) | N/A (Preclinical) | N/A (Preclinical) |
| PEC-01 Pancreatic Endoderm Cells [21] | Phase 1/2 Clinical Trial | Meal-responsive C-peptide increased significantly by Week 26; insulin requirements reduced by 20%. | Not achieved | Significant increase | 13% improvement in Time-in-Range |
The data indicates a paradigm shift, with therapies like zimislecel demonstrating not only safety and engraftment but also a high rate of insulin independence—a previously elusive goal [7]. Simultaneously, innovative approaches targeting the underlying autoimmunity, such as the Stanford "immune system reset," show transformative potential by potentially eliminating the need for chronic immunosuppression [14].
Detailed Experimental Protocols and Methodologies
Understanding the distinct methodologies behind these breakthroughs is crucial for evaluating their mechanistic value and translational potential.
Protocol: Allogeneic Stem Cell-Derived Islet Infusion (e.g., Zimislecel)
This protocol underlies the recent Phase 1/2 results published by Vertex Pharmaceuticals [7] [21].
- Cell Product: Allogeneic stem cell-derived, fully differentiated islet cells (zimislecel).
- Dosing: A single infusion of 0.8 × 10^9 cells into the hepatic portal vein.
- Immunosuppression: Glucocorticoid-free immunosuppressive regimen administered to all participants to prevent allograft rejection.
- Primary Endpoints: Safety, freedom from severe hypoglycemic events, HbA1c <7% or reduction of ≥1 percentage point, and insulin independence between days 180 and 365.
- Engraftment Assessment: Serum C-peptide levels measured during a 4-hour mixed-meal tolerance test to confirm islet function.
Protocol: Hybrid Immune System with Combined Transplant (Stanford)
This preclinical protocol represents a novel strategy aimed at curing autoimmunity, not just replacing cells [14].
- Pre-conditioning Regimen: A "gentle" regimen involving immune-targeting antibodies, low-dose radiation, and the addition of a drug used to treat autoimmune diseases. This avoids the harsh chemotherapy typically used in bone marrow transplants.
- Transplantation: Combined infusion of blood stem cells and pancreatic islet cells from an immunologically mismatched donor.
- Mechanism of Action: Creates a chimeric or hybrid immune system comprising cells from both the donor and recipient. This resets the immune system, halting the autoimmune attack on islet cells and preventing graft-versus-host disease.
- Outcome: Animals were cured of established diabetes or protected from developing it, without the need for ongoing immune-suppressive drugs.
The core difference between these strategies is visualized below, contrasting the cell replacement approach with the immune reset strategy.
Analysis of Safety and Tolerability
The safety profiles of these therapies are critical for risk-benefit analysis and are summarized below.
Table 2: Comparison of Safety Profiles and Key Challenges
| Therapy / Candidate | Reported Adverse Events | Immunosuppression Requirement | Major Challenges & Limitations |
|---|---|---|---|
| Zimislecel (VX-880) [7] [6] | Neutropenia (3 participants); Two deaths (cryptococcal meningitis; dementia progression) - deemed unrelated to product. | Yes, lifelong | Risks associated with chronic immunosuppression (infection, malignancy); Hepatic portal vein infusion challenges. |
| Stem Cell-Derived Islets (Vertex) [21] | Data not fully published for entire cohort. | Yes | Trade-off between insulin dependence and lifelong immunosuppression. |
| Hybrid Immune System (Stanford) [14] | No graft-versus-host disease reported in preclinical models. | No | Preclinical stage; Logistical challenge of sourcing matched blood stem cells and islets from the same donor. |
| PEC-01 in Encapsulation Device [21] | Foreign body response; pericapsular fibrosis limiting efficacy. | Varies (Open device requires it) | Inconsistent cell survival due to hypoxia; device encapsulation limits nutrient exchange. |
A primary differentiator among therapies is the requirement for chronic immunosuppression. While current clinical frontrunners like zimislecel require it, leading to significant adverse events [7] [6], next-generation approaches are actively engineering solutions to this hurdle, such as hypoimmune gene editing and the immune reset strategy [14] [6].
The Scientist's Toolkit: Key Research Reagents and Materials
The development of these therapies relies on a sophisticated toolkit of biological reagents and materials.
Table 3: Essential Research Reagents for Stem Cell-Derived Beta Cell Therapy
| Reagent / Material Category | Specific Examples | Primary Function in R&D |
|---|---|---|
| Signaling Molecules & Differentiation Factors | Activin A, Wnt3a, FGF10, Retinoic Acid, KAAD-cyclopamine, T3 (Thyroid Hormone), ALK5 Inhibitors [21] [2] | To direct pluripotent stem cells through sequential stages of pancreatic development, mimicking in vivo embryogenesis. |
| Cell Lines | Human Embryonic Stem Cells (hESCs), Human Induced Pluripotent Stem Cells (hiPSCs) [21] [2] | Serve as the starting source material for generating insulin-producing cells. hiPSCs enable autologous approaches. |
| Immunosuppressive Agents | Glucocorticoid-free regimens (e.g., ATG, MMF) [7] [2] | To prevent allograft rejection in non-autologous transplantation protocols during clinical trials. |
| Encapsulation Device Materials | Semi-permeable macroencapsulation membranes (e.g., ViaCyte's devices) [21] | To physically shield transplanted cells from immune attack, potentially obviating the need for systemic immunosuppression. |
| Gene Editing Tools | CRISPR-Cas9 for creating "hypoimmune" cells (e.g., B2M−/−, CIITA−/−, HLA-E+ expression) [6] | To genetically modify stem cells to evade host immune detection, a promising strategy to eliminate immunosuppression. |
The collective evidence from early-phase trials marks a turning point, demonstrating that restored islet function and insulin independence are achievable clinical outcomes in T1D. The leading candidate, zimislecel, has set a new benchmark for efficacy [7]. However, the future landscape will likely be defined by strategies that address the dual challenge of cell replacement and autoimmunity without lifelong immunosuppression. The most promising avenues include hypoimmune gene-edited islets [6] and combined blood stem cell and islet transplants that induce immune tolerance [14]. For researchers, the immediate focus should be on refining differentiation protocols for full functional maturity, developing scalable and safe delivery platforms, and validating the long-term stability and safety of these curative approaches in diverse patient populations.
Clinical Translation: Delivery Methods, Immunosuppression, and Trial Designs
Type 1 Diabetes (T1D) results from the autoimmune destruction of insulin-producing pancreatic beta cells, leaving patients dependent on lifelong exogenous insulin therapy [1] [22]. While insulin management is the standard of care, it carries inherent risks of hypoglycemia and often fails to prevent long-term complications. Advanced cell therapies, particularly those utilizing stem-cell-derived beta cells, aim to address the underlying pathophysiology by restoring the body's ability to produce and regulate insulin physiologically [1]. The two dominant technological paradigms for delivering these curative cells are infused cell products and encapsulated cell devices. This guide provides a comparative analysis of these platforms, focusing on their operational principles, efficacy data, manufacturing considerations, and translational challenges, providing a objective resource for researchers and drug development professionals.
Infused Cell Products
Infused cell therapies involve the direct administration of stem-cell-derived pancreatic islet cells into a patient's portal vein [22]. Once infused, these cells, such as the allogeneic product Zimislecel, engraft within the liver and begin to function as endogenous islets, secreting insulin in a glucose-responsive manner [7] [22]. This platform requires the recipient to be on a chronic immunosuppressive regimen to protect the engrafted cells from host immune rejection and to prevent the recurrence of autoimmunity [22] [23]. The mechanism of action is therefore direct cell replacement and functional integration into the host's metabolic system.
Encapsulated Cell Products
Encapsulated cell therapies co-house therapeutic doses of cells within semipermeable biomaterial devices, which are then implanted into sites such as the subcutaneous space [24]. These encapsulation devices are designed to act as immunoprotective barriers, allowing for the bidirectional diffusion of oxygen, nutrients, and therapeutic proteins like insulin, while simultaneously excluding hostile immune cells and antibodies [24]. The primary mechanism is the creation of a bio-hybrid organ that provides continuous, glucose-responsive insulin secretion without mandating systemic immunosuppression, as the membrane protects the cells from immune attack.
Table: Comparative Mechanism of Action and Technology Features
| Feature | Infused Products (e.g., Zimislecel) | Encapsulated Products |
|---|---|---|
| Delivery Method | Infusion into the hepatic portal vein [22] | Implantation of macrodevices (e.g., subcutaneous) [24] |
| Immunoprotection | Systemic immunosuppression [22] [23] | Device-based, via semipermeable membranes [24] |
| Proposed MOA | Direct engraftment and functional integration into host liver [7] | Function as an external, bio-hybrid organ secreting insulin [24] |
| Key Cell Source | Allogeneic stem-cell-derived, fully differentiated islets [7] [22] | Allogeneic cells or xenogeneic islets [24] |
Comparative Efficacy and Safety Data
Clinical Performance of Infused Cell Therapy
Recent Phase 1/2 trial results for Zimislecel demonstrate the substantial therapeutic potential of the infused platform. In a cohort of 12 T1D patients with impaired hypoglycemic awareness who received a full dose:
- Glycemic Control: All 12 participants achieved an HbA1c level of below 7%, with the mean HbA1c decreasing from 7.8% to 6.0% [23]. The mean Time-in-Range (TIR) on continuous glucose monitoring exceeded 93% [23].
- Insulin Independence: 83% (10 out of 12) of participants were free from exogenous insulin use at the 12-month mark [7] [22] [23].
- Hypoglycemia: Severe Hypoglycemic Events (SHEs) were eliminated from day 90 onwards [22] [23].
- Safety: The therapy was generally well-tolerated. The safety profile was consistent with the expected effects of the steroid-free immunosuppressive regimen and the infusion procedure itself. Two deaths occurred in the broader trial program but were assessed as unrelated to the cell therapy [7] [22].
Pre-clinical and Development-Stage Data for Encapsulated Therapies
Encapsulated cell therapies are largely in pre-clinical and early clinical development. Their efficacy is highly contingent on overcoming the foreign body response (FBR) and ensuring adequate oxygen and nutrient transport to the encapsulated cells [24].
- Material Science Advances: Studies using TMTD-modified alginate for microencapsulation have shown promise. In mouse models of diabetes, xenogeneic stem-cell-derived islets encapsulated in TMTD-alginate achieved diabetic reversal for over 170 days [24]. This approach has been successfully scaled to non-human primates, supporting islet survival and function for four months without immunosuppression [24].
- Key Challenge: A major hurdle is hypoxia within macrodevices, which can lead to significant cell death. Achieving therapeutic cell densities (e.g., ~10,000 islet equivalents/cm²) in a patient-friendly device size remains a significant materials and engineering challenge [24].
Table: Summary of Key Efficacy and Safety Outcomes
| Parameter | Infused Product (Zimislecel) | Encapsulated Products (Pre-clinical) |
|---|---|---|
| HbA1c Reduction | Mean reduction from 7.8% to 6.0% [23] | Demonstrated functional efficacy in animal models [24] |
| Insulin Independence | 83% (10/12) at 12 months [7] [23] | The primary goal; achieved in rodent models [24] |
| Severe Hypoglycemia | Eliminated [22] [23] | Not specifically reported |
| Key Safety Concern | Risks associated with chronic immunosuppression and infusion procedure [7] [22] | Foreign body response, fibrotic encapsulation, and hypoxia [24] |
| Immunosuppression | Required [22] [23] | Not required (Device-dependent) [24] |
Experimental Protocols and Methodologies
Protocol for Infused Cell Therapy Clinical Trials
The evaluation of Zimislecel follows a structured clinical trial protocol, as seen in the FORWARD (VX-880-101) study [7] [22].
- Patient Population: Adults with T1D, impaired hypoglycemic awareness, and a history of severe hypoglycemic events.
- Manufacturing: Zimislecel is manufactured as an allogeneic, stem-cell-derived, fully differentiated islet cell product.
- Dosing: A single infusion of a full dose (0.8 × 10^9 cells) is delivered into the hepatic portal vein [7].
- Immunosuppression: Patients receive a glucocorticoid-free immunosuppressive regimen, typically including induction and maintenance agents, to prevent rejection [7] [22].
- Endpoints:
- Functional Assessment: Engraftment and islet function are confirmed through a 4-hour Mixed-Meal Tolerance Test (MMTT) with serial measurement of C-peptide, which is undetectable at baseline in these patients [7].
Protocol for Assessing Encapsulated Device Performance
Pre-clinical assessment of encapsulated therapies focuses on material biocompatibility and in vivo function [24].
- Material Fabrication & Screening:
- Hundreds of alginate analogs are synthesized through combinatorial chemistry (e.g., modifying with triazole-thiomorpholine dioxide (TMTD)) [24].
- These materials are screened in vivo, typically in the subcutaneous space of immune-competent mice (e.g., C57BL/6 J), to identify leads that minimize fibrotic encapsulation.
- Device Implantation and Efficacy Testing:
- Lead materials are used to encapsulate stem-cell-derived islets or insulinoma cells.
- Devices are implanted into streptozotocin (STZ)-induced diabetic rodent models.
- Primary Endpoint: Reversal of diabetes, defined as the restoration of normoglycemia without exogenous insulin support.
- Secondary Endpoints: Measurement of human C-peptide in blood (for xenografts), explant histology to assess fibrosis and cell survival, and immunohistochemical analysis for markers of immune response and vascularization [24].
- Advanced Testing: Promising devices are advanced into larger animal models, such as non-human primates, to validate efficacy and biocompatibility in a physiology more relevant to humans [24].
Key Challenges and Translational Considerations
The development paths for infused and encapsulated therapies are marked by distinct challenges.
Challenges for Infused Products
- Chronic Immunosuppression: The necessity for lifelong immunosuppression exposes patients to increased risks of infection, potential organ toxicity, and other drug-related side effects [22] [25].
- Limited Cell Supply: Manufacturing a consistent and scalable supply of fully functional, stem-cell-derived islets is complex and costly.
- Durability and Rejection: The long-term durability of the graft is not yet fully established, and the potential for immune rejection or autoimmune recurrence remains a persistent risk [25].
Challenges for Encapsulated Products
- The Foreign Body Response (FBR): This is the primary barrier. The FBR leads to the formation of a dense, collagenous fibrotic capsule around the implant, which blocks the transport of oxygen and nutrients, leading to hypoxia and cell death [24].
- Hypoxia: High cell packing densities required for a therapeutic effect in a reasonably sized device can create extreme hypoxic cores, necessitating advanced materials or integrated oxygenation solutions [24].
- Material Design and Durability: Creating membranes with precise pore sizes for optimal immunoprotection, while maintaining robust mechanical properties for long-term implantation, is a significant materials science challenge.
Diagram: Key Workflows and Challenges for Cell Therapy Platforms. The infused platform's primary challenge is the need for systemic immunosuppression (red), while the encapsulated platform's key challenge is the Foreign Body Response leading to fibrosis and hypoxia (red).
The Scientist's Toolkit: Essential Research Reagents and Materials
The development of these advanced therapies relies on a suite of specialized reagents, materials, and assays.
Table: Key Research Reagent Solutions for Beta Cell Therapy Development
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Stem-Cell-Derived Islets | The foundational therapeutic agent for both platforms; insulin-producing, glucose-responsive cells. | Differentiated from human pluripotent stem cells (hPSCs) for infusion or encapsulation [1]. |
| TMTD-Modified Alginate | A lead biomaterial for microencapsulation that demonstrates reduced fibrotic encapsulation in vivo. | Used to form hydrogel capsules around islets for immunoprotection without immunosuppression [24]. |
| Zwitterionic Polymers (e.g., PCBMA) | Surface modification materials that resist protein fouling and reduce the Foreign Body Response. | Coating macroencapsulation devices to improve biocompatibility and reduce fibrosis [24]. |
| Mixed-Meal Tolerance Test (MMTT) | A key bioassay to assess the dynamic insulin secretion and functional engraftment of the transplanted cells. | Measuring C-peptide levels in patients post-infusion to confirm graft function [7] [1]. |
| Continuous Glucose Monitoring (CGM) | A wearable technology providing real-time, ambulatory glycemic data for efficacy assessment. | Used in clinical trials to calculate Time-in-Range and assess hypoglycemia risk [23]. |
| Steroid-Free Immunosuppressive Regimen | A drug combination to prevent allograft rejection without the beta-cell-toxic effects of steroids. | Administered to patients receiving infused islet products like Zimislecel [7] [22]. |
The pursuit of a functional cure for T1D is being aggressively advanced through two complementary technological paradigms: infused and encapsulated stem-cell-derived beta cell therapies. Infused products, exemplified by Zimislecel, have demonstrated compelling clinical proof-of-concept, achieving insulin independence and normoglycemia in a majority of patients in early trials, albeit with the trade-off of requiring chronic immunosuppression [7] [22] [23]. In contrast, encapsulated products offer the potential for an off-the-shelf, immunosuppression-free therapy but must overcome significant translational barriers related to the host foreign body response and device-induced hypoxia [24].
Future progress will be driven by parallel advancements. For infused therapies, the focus will be on optimizing immunosuppression regimens, validating long-term durability, and scaling manufacturing. For encapsulated therapies, the critical path forward lies in fundamental materials science—developing "superbiocompatible" materials that completely evade the FBR and engineering devices that ensure adequate oxygen supply to the encapsulated cells. As both platforms evolve, they hold the collective promise of resetting the standard of care for T1D from lifelong management to a definitive, curative treatment.
For individuals with type 1 diabetes (T1D), allogeneic beta-cell replacement represents a promising path toward restoring endogenous insulin production. The recent development of stem cell-derived islets (SC-islets) provides a potentially unlimited source of insulin-producing cells, overcoming the critical limitation of donor scarcity inherent to cadaveric islet transplantation [4]. However, the success of these revolutionary therapies is entirely dependent on effective immunosuppression protocols to protect the graft from the host immune system. Without such protection, allogeneic cells are rapidly rejected, negating any therapeutic benefit. This guide compares the current landscape of immunosuppressive strategies, from conventional pharmaceutical regimens to groundbreaking genetic and cellular approaches, providing researchers and drug development professionals with a detailed analysis of their mechanisms, efficacy, and trade-offs.
Conventional Immunosuppression in Clinical Practice
Conventional immunosuppression relies on a combination of drugs that systemically dampen the immune response to prevent graft rejection. These protocols are the current clinical standard for both solid organ and cellular transplants, including the emerging class of stem cell-derived islet products.
Key Agents and Regimens
The glucocorticoid-free immunosuppressive regimen used in a recent phase 1-2 trial of stem cell-derived islets (zimislecel) exemplifies a modern approach [7]. The trial demonstrated that this protocol could support engraftment and function, with 10 out of 12 participants achieving insulin independence at one year. However, the serious adverse events observed, including one death from cryptococcal meningitis, underscore the significant risks of systemic immunosuppression, such as increased susceptibility to opportunistic infections [7].
The selection and management of these drugs are critical. A 2025 retrospective study of patients receiving post-transplantation cyclophosphamide (PTCy) for GVHD prophylaxis found that tacrolimus or sirolimus levels ≥10 ng/mL in the first week post-transplant were associated with decreased overall survival, suggesting that lower target levels may be optimal with PTCy-based regimens [26].
Table 1: Common Immunosuppressive Agents and Their Roles in Allogeneic Graft Protection
| Agent Class | Example Drugs | Primary Mechanism of Action | Common Clinical Use |
|---|---|---|---|
| Calcineurin Inhibitors (CNI) | Tacrolimus, Cyclosporine | Inhibits T-cell activation by blocking IL-2 production | Foundation of most maintenance regimens [26] |
| Antiproliferatives | Mycophenolate Mofetil (MMF) | Inhibits lymphocyte proliferation by blocking purine synthesis | Used in combination with CNIs [26] [27] |
| mTOR Inhibitors | Sirolimus | Blocks cytokine-driven T-cell proliferation | Alternative to CNIs; part of PTCy regimens [26] |
| Biologics | Anti-thymocyte Globulin (ATG) | Depletes T-cells | Induction therapy; part of tolerance protocols [28] |
| Alkylating Agents | Cyclophosphamide (PTCy) | Eliminates alloreactive T-cells post-transplant | GVHD prophylaxis in haploidentical HCT [26] [29] |
Emerging Paradigms: Engineering Immune Evasion
To circumvent the complications of lifelong drug-based immunosuppression, significant research is focused on engineering the graft itself to evade immune detection. These "hypoimmune" strategies aim to create "off-the-shelf" cell products that do not require recipient immunosuppression.
Hypoimmunogenic Engineering of Stem Cell-Derived Islets
The core principle of hypoimmunogenic engineering is to genetically modify the donor cells to reduce their immunogenicity. This primarily involves editing the expression of human leukocyte antigen (HLA) molecules, which are the primary triggers of T-cell-mediated rejection.
- HLA Class I Deletion: Knocking out Beta-2-microglobulin (B2M) eliminates surface expression of HLA class I molecules, preventing recognition by host CD8+ T-cells [30] [6].
- Preventing NK Cell Attack: The deletion of HLA class I can trigger "missing-self" recognition and attack by natural killer (NK) cells. To counter this, strategies often include the overexpression of non-classical HLA molecules (e.g., HLA-E, HLA-G) that engage inhibitory receptors on NK cells [30] [6].
- Modulating Co-Inhibitory Signals: Overexpression of immunomodulatory ligands like PD-L1 (Programmed Death-Ligand 1) on the graft surface can engage PD-1 on host T cells, directly inducing T-cell exhaustion and tolerance [30] [6].
- CD47 Overexpression: The "don't eat me" signal provided by CD47 helps protect graft cells from phagocytosis by host macrophages [30].
A 2025 review highlighted that combining these approaches—for instance, creating B2M−/− CIITA−/− PSCs with engineered expression of HLA-G, PD-L1, and CD47—can simultaneously protect against T-cell and NK-cell-mediated rejection, creating a robustly hypoimmunogenic graft [6].
The following diagram illustrates the key genetic modifications involved in creating a hypoimmunogenic stem cell-derived islet and how they interact with the host immune system.
A Paradigm Shift: Immune System Reset and Hybrid Tolerance
Perhaps the most transformative approach is moving from suppressing or evading the immune system to fundamentally reprogramming it. This strategy, exemplified by recent work at Stanford Medicine, involves creating a "hybrid" immune system that tolerates the graft.
Protocol for Immune System Reset in Autoimmune Diabetes
This protocol combines a gentle conditioning regimen with the transplantation of allogeneic hematopoietic stem cells (HSCs) and pancreatic islets from the same donor [14]. The goal is to establish a state of mixed chimerism, where the host's immune system is partially repopulated by donor-derived immune cells, leading to mutual tolerance.
- Step 1: Gentle Conditioning: The recipient is pre-treated with a regimen of immune-targeting antibodies, low-dose radiation, and a drug used for autoimmune diseases. Unlike the myeloablative conditioning used in oncology, this "gentle" approach is designed not to eradicate the host immune system but to create a niche for donor cell engraftment [14].
- Step 2: Combined Transplant: The recipient receives an infusion of donor-derived HSCs alongside pancreatic islets. The HSCs are the key to tolerance induction.
- Step 3: Establishment of a Hybrid Immune System: The donor HSCs engraft and give rise to immune cells that coexist with the recipient's immune cells. This hybrid system "re-educates" the immune system to recognize the donor islets as "self," halting the underlying autoimmune attack on beta cells and preventing rejection of the transplanted islets [14].
In a mouse model of T1D, this approach completely prevented or cured diabetes in all animals without the use of immunosuppressive drugs and without causing graft-versus-host disease [14]. The translational potential is high, as the core components of this protocol are already used in clinical practice for other conditions.
The workflow below outlines the key steps in this innovative protocol for achieving graft tolerance through an immune system reset.
Comparative Analysis of Immunosuppression Protocols
The choice of an immunosuppression strategy involves balancing efficacy, safety, complexity, and scalability. The table below provides a direct comparison of the three main paradigms.
Table 2: Comparison of Immunosuppression Protocols for Allogeneic Grafts
| Parameter | Conventional Pharmacotherapy | Hypoimmunogenic Grafts | Immune System Reset |
|---|---|---|---|
| Mechanism | Systemic inhibition of immune cell function | Reduction of graft immunogenicity via genetic engineering | Establishment of donor-specific central tolerance |
| Graft Source | Any (Cadaveric islets, SC-islets) | Genetically engineered SC-islets only | Requires HSCs and islets from same donor |
| Immunosuppression Duration | Lifelong (chronic) | Potentially none | Transient (during conditioning) |
| Key Risks | Opportunistic infections, malignancy, drug toxicity [7] | Potential for immune escape, tumorigenicity from edits [30] | Graft-versus-host disease, conditioning toxicity [28] |
| Efficacy Evidence | Insulin independence in 83% at 1 year (Zimislecel trial) [7] | Preclinical NHP studies; early-phase human trials [30] [6] | Cured T1D in mouse models; human kidney transplant success [14] [28] |
| Scalability | High, but limited by drug cost/toxicity | Theoretically high for "off-the-shelf" products | Limited by donor availability & procedural complexity |
| Stage of Development | Clinical standard of care | Early-phase clinical trials | Preclinical/early clinical investigation |
The Scientist's Toolkit: Essential Research Reagents
Research into these advanced immunosuppression protocols relies on a suite of critical reagents and tools.
Table 3: Key Research Reagents for Investigating Graft Immunosuppression
| Reagent / Tool | Function in Research | Example Application |
|---|---|---|
| CRISPR-Cas9 Systems | Gene editing for creating knock-out (e.g., B2M, CIITA) and knock-in (e.g., CD47, HLA-G) mutations in pluripotent stem cells. | Generating hypoimmunogenic stem cell lines for differentiation into SC-islets [30] [6]. |
| Anti-Thymocyte Globulin (ATG) | Polyclonal antibody used for in vivo T-cell depletion in animal models. | Mimicking the lymphodepleting conditioning regimen used in immune reset protocols [28]. |
| Post-Transplant Cyclophosphamide (PTCy) | Alkylating agent administered after transplant to eliminate alloreactive T-cells. | Studying GVHD prophylaxis in humanized mouse models of combined HSC/islet transplantation [26] [29]. |
| Tacrolimus / Sirolimus | Pharmacologic inhibitors of T-cell activation and proliferation. | Establishing therapeutic drug level targets in preclinical transplant models and clinical trials [26] [7]. |
| Flow Cytometry Panels (Immune Cell Subsets) | High-dimensional profiling of immune cell populations (T, B, NK cells, monocytes) post-transplant. | Monitoring immune reconstitution, chimerism, and rejection responses [27]. |
The field of immunosuppression for allogeneic grafts is undergoing a rapid evolution, driven by the pressing need to make curative cell therapies for T1D both effective and safe. While conventional pharmacotherapy remains a proven, if imperfect, cornerstone, the future is leaning towards more integrated solutions. The development of hypoimmunogenic SC-islets addresses the problem at the source of immune recognition, while the immune reset strategy seeks to create a lasting state of tolerance. Each approach presents a distinct profile of advantages, risks, and developmental challenges. For researchers and drug developers, the path forward will likely involve combining elements from these strategies—for example, using a gentler conditioning regimen to support the engraftment of a partially hypoimmunogenic graft—to achieve the ultimate goal: a durable, functional cure for T1D without the burden of lifelong immunosuppression.
Clinical trials are the cornerstone of therapeutic development, providing the critical evidence required for regulatory approval and clinical adoption. For innovative therapies like stem cell-derived beta cells for Type 1 Diabetes (T1D), optimal trial design is paramount for accurately demonstrating safety and efficacy. The traditional clinical trial paradigm is undergoing significant modernization, moving away from rigid, historically-based designs toward more flexible, patient-centric, and data-driven approaches [31]. This evolution encompasses all trial elements: from how doses are selected and optimized, to how patients are chosen for participation, and what endpoints are measured to determine success. These changes are particularly relevant for complex cellular therapies targeting T1D, where the therapeutic mechanism differs fundamentally from conventional small molecules or biologics. This article examines the core components of modern trial design—dosing strategies, patient selection, and endpoint selection—within the context of T1D research, providing a framework for developing robust clinical programs for stem cell-derived beta cell therapies.
Dosing Strategies: From Maximum Tolerated Dose to Therapeutic Optimization
Dosing strategy is a foundational element that can determine the ultimate success or failure of a drug development program. The traditional approach, developed for cytotoxic chemotherapies, focuses on identifying the Maximum Tolerated Dose (MTD). This method, often using a "3+3" trial design, escalates doses in small patient cohorts until a pre-defined level of dose-limiting toxicity is observed [31]. However, for many modern therapeutics, including targeted agents and potentially cellular therapies, the MTD paradigm is often suboptimal. Studies show that nearly 50% of patients in late-stage trials of targeted therapies require dose reductions due to intolerable side effects, and the FDA has required post-marketing dose-finding studies for over 50% of recently approved cancer drugs [31]. This demonstrates the inadequacy of relying solely on short-term toxicity data to establish a dosage for long-term use.
Modern Dose Optimization Frameworks
Recognizing these limitations, regulatory agencies have championed new frameworks. The FDA's Project Optimus encourages a shift from MTD to a focus on identifying doses that optimize the balance between efficacy and safety [31] [32]. This involves directly comparing multiple dosages in trials designed to assess antitumor activity, safety, and tolerability. Key modern dose-finding approaches include:
- Model-Informed Drug Development (MIDD): Utilizing mathematical models that incorporate pharmacokinetic, pharmacodynamic, and biomarker data to predict effective dosing in humans from preclinical data, often allowing for higher, more effective starting doses than traditional methods [31].
- Novel Trial Designs: Adaptive trial designs, such as the Bayesian Optimal Interval (BOIN) design, allow for more nuanced dose-escalation and de-escalation based on both efficacy and safety outcomes from preceding patient cohorts. These designs can treat more patients at potentially optimal dose levels and adapt based on accumulating data [32].
- Biomarker-Driven Dosing: The concept of the Biologically Effective Dose (BED) is crucial for modern therapies. The BED is determined using biomarkers that indicate target engagement and biological activity, which may occur at a dose lower than the MTD [32]. For stem cell-derived beta cells, this could involve imaging biomarkers or secreted factors indicating engraftment and function.
Table 1: Comparison of Traditional vs. Modern Dosing Paradigms in Oncology (as a model for other fields)
| Feature | Traditional MTD Paradigm | Modern Optimization Paradigm |
|---|---|---|
| Primary Goal | Identify maximum tolerated dose | Identify dose with optimal efficacy-safety balance |
| Key Trial Design | 3+3 dose escalation | Model-informed, adaptive designs (e.g., BOIN) |
| Data Driving Decisions | Short-term toxicity | Integrated safety, efficacy, and biomarker data |
| Role of Biomarkers | Limited | Central to establishing Biologically Effective Dose (BED) |
| Typical Outcome | Single MTD for development | Multiple doses compared for final selection |
| Post-Marketing Needs | Common (dose optimization often required) | Reduced (optimization occurs pre-approval) |
Source: Adapted from AACR Blog and FDA-AACR Workshop Summary [31] [32]
Application to Stem Cell-Derived Beta Cell Therapies
For a stem cell-derived beta cell therapy, the dosing strategy must be uniquely tailored. The therapy is not a simple drug with linear pharmacokinetics, but a living product. Dosing may be defined by the number of functional islet equivalents or cells transplanted, the transplantation procedure (e.g., single vs. multiple infusions), and the intensity of concomitant immunosuppression. A model-informed approach could use preclinical data on engraftment efficiency and function to model human dosing. An adaptive trial could then evaluate two or more cell doses, using biomarkers like circulating C-peptide or insulin independence to identify a BED, while meticulously monitoring safety signals related to the transplantation procedure and immunosuppression.
Patient Selection: Balancing Scientific Rigor with Inclusivity
Patient eligibility criteria define the study population and are essential for patient safety and data interpretability. However, excessively narrow criteria can hinder enrollment, delay trial completion, and limit the generalizability of the results to real-world patient populations [33] [34]. A meta-analysis found that 22% of potential trial participants were excluded due to restrictive eligibility criteria, a significant barrier to accrual [34].
Expanding Eligibility Criteria
A major initiative in clinical trial modernization is the expansion of eligibility criteria to be more inclusive, while maintaining scientific integrity and patient safety. Joint recommendations from the American Society of Clinical Oncology (ASCO) and Friends of Cancer Research provide a framework for broadening eligibility in key areas [33]:
- Brain Metastases: Allowing patients with stable, treated brain metastases.
- HIV/AIDS: Including patients with well-controlled HIV infection.
- Prior and Concurrent Malignancies: Enrolling patients with a history of other cancers, based on individualized risk assessment.
- Organ Dysfunction: Carefully including patients with mild to moderate renal, hepatic, or cardiac dysfunction, rather than using absolute laboratory cut-offs.
- Age: Including adolescent patients in adult trials where scientifically appropriate.
Implementing these expanded criteria in protocol templates has successfully increased the inclusiveness of trials without compromising safety [33].
Leveraging Real-World Data for Smarter Enrollment
Real-World Data (RWD), such as electronic health records (EHR) and insurance claims data, are powerful tools for designing more feasible and representative trials [35]. RWD can be applied in two key ways:
- Planning Feasible Eligibility Criteria: By analyzing RWD from large patient populations, sponsors can simulate the impact of different eligibility criteria on the potential pool of participants. This allows for the design of criteria that are broad enough for efficient recruitment but narrow enough to address the scientific question [35].
- Enhancing Recruitment: RWD can be used to identify potential participants more efficiently through direct outreach or by flagging eligible patients at the point of care, a strategy shown to improve recruitment effectiveness and efficiency [35].
Table 2: Using Real-World Data (RWD) for Patient Selection and Recruitment
| RWD Application | Description | Utility in Stem Cell-Derived Beta Cell Trials |
|---|---|---|
| EHR Data Analysis | Analyzing de-identified electronic health records to understand patient demographics, comorbidities, and treatment patterns. | Estimate the real-world population of T1D patients who would meet proposed trial criteria; identify centers with high volumes of eligible patients. |
| Claims Data Analysis | Using insurance claims to track disease codes, procedures, and medication use across healthcare systems. | Understand healthcare utilization patterns of T1D patients to design feasible visit schedules and endpoint assessments. |
| Site Identification | Using RWD to identify clinical sites with a high concentration of the target patient population. | Select high-performing clinical trial sites with access to the precise T1D patient profile needed for the study. |
| Patient Pre-screening | Using RWD platforms to identify potentially eligible patients for targeted outreach, with appropriate privacy safeguards. | Accelerate enrollment by pre-identifying patients who meet key lab or diagnostic criteria for T1D with complications. |
Source: Adapted from CTTI Recommendations on RWD [35]
For a trial of stem cell-derived beta cells, eligibility must be carefully considered. Key inclusion criteria would likely involve a confirmed diagnosis of T1D with specific autoantibodies, a disease duration range, and demonstrated C-peptide deficiency. Using RWD, sponsors could model whether adding common exclusions—such as a history of other autoimmune diseases, body mass index (BMI) limits, or specific comorbid conditions—would drastically reduce the recruitable population. The goal is to justify each criterion scientifically rather than relying on historical precedent, thereby ensuring the trial can enroll a population that is both representative and adequate to answer the research question.
Primary Endpoints: Defining and Measuring Success
The primary endpoint is the ultimate measure of a trial's success. It must be precisely defined, clinically meaningful, and reliably measurable. The choice of endpoint is dictated by the phase of the trial, the mechanism of action of the therapy, and regulatory standards.
Established Endpoints in Diabetes Trials
In T1D and related metabolic disease trials, several well-validated endpoints are commonly used:
- Glycated Hemoglobin (HbA1c): A measure of average blood glucose over the preceding 2-3 months. It is a standard primary endpoint for many glucose-lowering therapies, as seen in the SEPRA trial for semaglutide, where the proportion of participants achieving HbA1c <7.0% was the primary outcome [36].
- Urine Albumin-to-Creatinine Ratio (UACR): A key marker for kidney disease progression and cardiovascular risk, which is often a primary endpoint in trials for diabetic complications. The FINE-ONE trial for finerenone in T1D and chronic kidney disease used the relative change in UACR from baseline as its primary endpoint [37].
- Composite Endpoints: Many cardiovascular and renal outcome trials use composite endpoints to capture the overall clinical benefit. For instance, a trial might use a composite of time to first occurrence of cardiovascular death, non-fatal myocardial infarction, or hospitalization for heart failure.
Biomarkers and Surrogate Endpoints
Biomarkers are increasingly critical in early-phase trials to provide early signals of biological activity and inform go/no-go decisions [32]. They can be categorized as:
- Pharmacodynamic/Response Biomarkers: Indicate the biological activity of a therapeutic. For beta cell therapy, this would include fasting or stimulated C-peptide levels, which directly measure the function of the transplanted insulin-producing cells.
- Surrogate Endpoints: Are expected to predict clinical benefit. HbA1c is a validated surrogate endpoint for microvascular complications in diabetes.
- Predictive Biomarkers: Identify patients more likely to respond to a treatment. In the context of cellular therapy, this could involve biomarkers related to the immune system's state that predict graft acceptance or rejection.
Circulating tumor DNA (ctDNA) is a powerful example from oncology, used for patient selection, pharmacodynamic monitoring, and as an early surrogate of efficacy [32]. This illustrates the potential for novel biomarker applications in T1D trials, such as using beta cell-specific markers or immune cell profiling in a similar longitudinal manner to monitor engraftment and rejection.
Table 3: Key Endpoints and Biomarkers for Type 1 Diabetes Trials
| Endpoint/Biomarker | Type | Clinical/Functional Significance | Relevance to Stem Cell-Derived Beta Cell Trials |
|---|---|---|---|
| HbA1c | Surrogate Endpoint / Efficacy Endpoint | Long-term glycemic control; predicts risk of microvascular complications. | Primary Efficacy Endpoint: Reduction in HbA1c demonstrates improved glycemic control. |
| Stimulated C-peptide | Pharmacodynamic / Response Biomarker | Direct measure of endogenous insulin secretion from functional beta cells. | Primary Efficacy Endpoint (early phase): Directly measures functional engraftment of the cell product. |
| Urine Albumin-to-Creatinine Ratio (UACR) | Renal Endpoint | Marker of kidney damage and cardiovascular risk. | Safety/Exploratory Endpoint: To monitor potential renal effects of immunosuppression or therapy. |
| Insulin Dose | Clinical Endpoint | Daily exogenous insulin requirement. | Key Secondary Endpoint: Reduction or elimination of exogenous insulin is a direct patient benefit. |
| Time-in-Range (TIR) | Glycemic Control Endpoint | Percentage of time glucose is in target range (70-180 mg/dL), measured by CGM. | Key Secondary Endpoint: Provides a detailed picture of glycemic stability beyond HbA1c. |
| Hypoglycemia Event Rate | Safety Endpoint | Frequency of clinically significant low blood glucose events. | Critical Safety Endpoint: Must demonstrate that the therapy does not increase hypoglycemia risk. |
Source: Compiled from multiple sources including FINE-ONE and SEPRA trials [37] [36]
For a pivotal trial of stem cell-derived beta cells, a primary endpoint of change from baseline in stimulated C-peptide would be a direct, mechanism-based measure of efficacy. HbA1c reduction and insulin dose reduction would be highly clinically meaningful secondary endpoints. The trial would also need to meticulously collect safety data, particularly regarding the risks of immunosuppression and the transplantation procedure itself.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key research reagent solutions essential for conducting experiments in stem cell-derived beta cell research and related clinical trials.
Table 4: Essential Research Reagent Solutions for Beta Cell Therapy Development
| Research Reagent / Material | Function and Application | Experimental Context |
|---|---|---|
| Differentiation Kits & Media | Defined cocktails of growth factors and small molecules to direct pluripotent stem cells through pancreatic progenitor stages to mature, glucose-responsive beta cells. | In vitro generation of the cellular therapy product from stem cell banks. |
| C-peptide ELISA/EIA Kits | Quantify C-peptide levels in cell culture supernatant, serum, or plasma via immunoassay. Used as a specific marker of insulin secretion and beta cell function. | In vitro potency assays; measurement of primary endpoint in clinical trials (patient serum). |
| Flow Cytometry Antibodies | Antibodies against markers (e.g., PDX1, NGN3, NKX6.1, Insulin, C-peptide, Glucagon) to characterize differentiation efficiency and purity of stem cell-derived islet populations. | Quality control of cell product; analysis of graft composition in vivo (preclinical). |
| Glucose Stimulated Insulin Secretion (GSIS) Assay Kits | Provide reagents for in vitro functional testing of beta cells by measuring insulin/C-peptide secretion in response to low and high glucose challenges. | Critical potency assay for batch release of the cell therapy product. |
| Immunosuppressive Agents | Drugs (e.g., Tacrolimus, Sirolimus, Mycophenolate Mofetil) used to prevent immune rejection of the transplanted allogeneic cell graft. | Administration to trial participants in the peri-transplant and maintenance phases. |
| HLA Typing Kits | Molecular biology reagents to determine the human leukocyte antigen (HLA) profile of cell donors and recipients. Used for matching and immune risk assessment. | Screening of patient eligibility and selection of appropriate cell product lot. |
Integrated Trial Workflow and Signaling Pathways
The development path for a stem cell-derived beta cell therapy involves a tightly integrated sequence of preclinical and clinical activities. The workflow below illustrates the key stages from hypothesis generation to final analysis, highlighting the interconnectedness of dosing, patient selection, and endpoint strategy.
Diagram Title: Integrated Clinical Trial Workflow for Beta Cell Therapy
The core biological mechanism of action involves the engraftment and function of the transplanted cells, a process governed by key signaling pathways that can be monitored via specific biomarkers.
Diagram Title: Beta Cell Therapy Mechanism of Action
The anatomy of a clinical trial is evolving. The successful development of transformative therapies like stem cell-derived beta cells for T1D depends on a modern, integrated approach to trial design. This involves moving beyond the MTD to a dose optimization paradigm that finds the best balance of efficacy and safety using model-informed and adaptive strategies. It requires a patient selection strategy that uses real-world data to create inclusive, feasible eligibility criteria and efficient recruitment plans. Finally, it demands a thoughtful endpoint strategy that leverages validated clinical endpoints like HbA1c alongside mechanism-based biomarkers like C-peptide to convincingly demonstrate therapeutic value. By integrating these three pillars—optimized dosing, inclusive patient selection, and meaningful endpoints—researchers can design robust, efficient, and generalizable clinical trials that accelerate the delivery of new therapies to patients.
Type 1 diabetes (T1D) is a chronic autoimmune disorder characterized by the destruction of insulin-producing beta cells in the pancreas, leading to insulin deficiency and chronic hyperglycemia [2]. Current standard treatments, primarily exogenous insulin administration, fail to fully mimic physiological insulin regulation and often result in suboptimal glycemic control [2]. In recent years, stem cell-derived beta cell therapies have emerged as promising approaches to restore endogenous insulin production and potentially achieve long-term glycemic stability [2] [17]. Among the most notable clinical investigations in this field are the FORWARD trial (evaluating Vertex Pharmaceuticals' zimislecel, formerly VX-880) and the PEC-Direct trial (evaluating ViaCyte's pancreatic endoderm cells). This analysis provides a comprehensive comparison of the efficacy data and experimental protocols from these two landmark studies, offering critical insights for researchers and drug development professionals working in diabetes therapeutics.
FORWARD Trial (NCT04786262): Zimislecel (VX-880)
The FORWARD trial is a Phase 1/2 study investigating zimislecel, an allogeneic stem cell-derived islet cell therapy for T1D patients with impaired hypoglycemia awareness and severe hypoglycemic events [38]. The therapy consists of fully differentiated, insulin-producing islet cells derived from human embryonic stem cells (hESCs) [38].
Key Design Elements:
- Therapy Composition: Fully differentiated pancreatic islet cells
- Cell Source: Human embryonic stem cells (hESCs)
- Delivery Method: Hepatic portal vein infusion
- Immunosuppression: Requires chronic immunosuppressive therapy
- Primary Outcomes: HbA1c <7%, time in range >70%, insulin independence, absence of severe hypoglycemic events [38]
PEC-Direct Trial (NCT03163511): PEC-01 Pancreatic Progenitor Cells
The PEC-Direct trial evaluates the safety and efficacy of pancreatic endoderm cells (PEC-01) contained within a perforated encapsulation device that allows direct vascularization of the implanted cells [39]. The trial focuses on T1D patients who have struggled with glycemic control and are at high risk for complications [39].
Key Design Elements:
- Therapy Composition: Pancreatic progenitor cells (PEC-01)
- Cell Source: Human embryonic stem cells (hESCs)
- Delivery Method: Subcutaneous implantation of encapsulated cells
- Immunosuppression: Requires immunosuppressive therapy
- Primary Outcomes: Safety, metabolic measures (HbA1c, C-peptide), insulin independence [39]
Efficacy Outcomes and Comparative Analysis
Quantitative Efficacy Data
Table 1: Comparative Efficacy Outcomes from FORWARD and PEC-Direct Trials
| Efficacy Parameter | FORWARD Trial (Zimislecel) | PEC-Direct Trial (PEC-01) |
|---|---|---|
| Insulin Independence | 83% (10/12 patients at 1 year) [38] | Limited data; some reduction in insulin needs [39] |
| HbA1c Reduction | All patients achieved <7% [38] | Specific percentage not reported in available data |
| C-peptide Production | Detectable in all patients, indicating restored insulin production [38] | 3 of 10 patients showed C-peptide levels ≥0.1 nmol/L by month 6 [39] |
| Time in Range (TIR) | >70% in all patients [38] | Not specifically reported in available data |
| Hypoglycemic Events | Elimination of severe hypoglycemic events [38] | Not specifically reported in available data |
Safety Profiles and Adverse Events
FORWARD Trial Safety: No serious adverse events were directly tied to zimislecel, with the safety profile aligning with expectations for the immunosuppressive regimen [38]. Two unrelated deaths were reported but not attributed to the investigational therapy.
PEC-Direct Trial Safety: The trial demonstrated acceptable safety, with the main concerns being procedural risks associated with device implantation and standard immunosuppression-related complications [39]. Device fibrosis was noted as a challenge affecting long-term efficacy [39].
Experimental Protocols and Methodologies
Cell Differentiation and Manufacturing Protocols
FORWARD Trial Protocol: Zimislecel utilizes fully differentiated, insulin-producing islet cells derived from human embryonic stem cells through a multi-stage differentiation protocol [2] [38]. The process mimics in vivo pancreatic development by guiding hESCs through definitive endoderm, gut-tube endoderm, pancreatic endoderm, and endocrine precursor stages [2]. Key differentiation factors include:
- Activin A and Wnt3a to induce definitive endoderm
- Fibroblast growth factor 10 (FGF10) and KAAD-cyclopamine to inhibit hedgehog signaling
- Retinoic acid to stimulate development of posterior foregut cells Final differentiated cells express key pancreatic markers including insulin, glucagon, and somatostatin, demonstrating glucose-responsive insulin secretion [2].
PEC-Direct Trial Protocol: The PEC-Direct approach utilizes pancreatic endoderm cells (PEC-01) derived from hESCs, which are precursor cells that undergo further maturation after transplantation [39]. These progenitor cells are characterized by expression of key pancreatic transcription factors including PDX1, NKX6.1, and NKX2.2 [39]. The cells are encapsulated in a device that allows direct vascularization, facilitating nutrient exchange and supporting in vivo maturation into functional insulin-producing cells [39].
Transplantation and Delivery Methods
Diagram 1: Transplantation workflows for FORWARD and PEC-Direct trials
FORWARD Trial Delivery: Zimislecel is infused into the hepatic portal vein via percutaneous transhepatic approach [38]. This established islet transplantation site provides immediate access to blood supply and physiological cues for insulin secretion, though it carries risks including portal vein thrombosis and bleeding [5] [38].
PEC-Direct Trial Delivery: The PEC-01 cells are contained within a perforated encapsulation device implanted in the subcutaneous space [39]. This approach offers a less invasive procedure with retrievability potential, though it faces challenges with consistent vascularization and foreign body response [39].
Immunosuppression Strategies
Both trials require immunosuppression to prevent rejection of the allogeneic cells, representing a significant limitation for broad clinical application [38] [39].
FORWARD Trial Immunosuppression: Utilizes a chronic immunosuppressive regimen, though specific agents and dosages are tailored based on the patient profile [38]. The regimen is designed to balance efficacy with toxicity risks.
PEC-Direct Trial Immunosuppression: Patients receive standard immunosuppressive medications to prevent immune rejection of the implanted cells and device [39]. The encapsulation device provides some physical protection but does not eliminate the need for systemic immunosuppression due to its perforated design that allows vascular integration.
Signaling Pathways in Beta Cell Maturation and Function
Diagram 2: Key signaling pathways in beta cell development
The successful differentiation and function of stem cell-derived beta cells depends on precise regulation of multiple signaling pathways. Both the FORWARD and PEC-Direct protocols leverage these pathways, though at different maturation stages:
Pancreatic Development Pathways: Both protocols utilize retinoic acid signaling to promote pancreatic commitment and fibroblast growth factors (FGFs) for patterning pancreatic progenitors [2]. Inhibition of bone morphogenetic proteins (BMP) and Sonic hedgehog (SHH) signaling is crucial for proper pancreatic specification [2].
Beta Cell Maturation Pathways: The FORWARD trial's fully differentiated cells leverage DYRK1A inhibition pathways that enhance beta cell replication [40]. TGF-β signaling regulates beta cell maturation, while GLP-1 receptor activation enhances glucose-responsive insulin secretion [40]. Wnt/β-catenin pathway activation promotes beta cell proliferation in both progenitor and mature cell types [40].
Research Reagent Solutions for Beta Cell Therapy Development
Table 2: Essential Research Reagents for Stem Cell-Derived Beta Cell Development
| Reagent Category | Specific Examples | Research Function | Application in Trials |
|---|---|---|---|
| Differentiation Factors | Activin A, Wnt3a, FGF10, KAAD-cyclopamine, Retinoic acid [2] | Guide sequential differentiation from pluripotent stem cells to pancreatic lineage | Used in both FORWARD and PEC-Direct cell manufacturing |
| Small Molecule Inhibitors | DYRK1A inhibitors, TGF-β pathway modulators, SIK inhibitors [40] | Enhance beta cell proliferation and maturation | Particularly relevant for in vitro maturation in FORWARD |
| Cell Surface Markers | PDX1, NKX6.1, NKX2.2, C-peptide [2] [17] | Identify and purify specific pancreatic progenitor and endocrine cell populations | Quality control in both trials' manufacturing processes |
| Encapsulation Materials | Semi-permeable membranes, biocompatible polymers [39] | Protect transplanted cells from immune attack while allowing nutrient exchange | Critical component of PEC-Direct delivery system |
| Immunosuppressants | Sirolimus, Tacrolimus, T-cell depletion agents [5] | Prevent immune rejection of allogeneic cell products | Required in both trials to support graft survival |
Discussion and Future Directions
The FORWARD and PEC-Direct trials represent complementary approaches in the development of stem cell-based therapies for T1D. The FORWARD trial demonstrates impressive efficacy in achieving insulin independence with fully differentiated islet cells, representing a more mature therapeutic product [38]. In contrast, the PEC-Direct approach utilizes progenitor cells that mature in vivo, potentially offering greater flexibility but with currently more modest efficacy outcomes [39].
The differing delivery methods present distinct advantages and challenges. Hepatic portal vein infusion provides immediate access to physiological cues but carries procedural risks [5] [38]. Subcutaneous encapsulation offers a less invasive, potentially retrievable approach but faces challenges with consistent vascularization and foreign body responses [39].
Both trials highlight the ongoing challenge of immune rejection, requiring chronic immunosuppression with associated risks including increased infection susceptibility and systemic toxicity [2] [41]. Future directions focus on developing immune-evasive cells through gene editing (e.g., CRISPR's VCTX211) [42] [38] or improved encapsulation technologies that eliminate the need for systemic immunosuppression [17] [38].
The progression of these trials marks significant milestones in beta cell replacement therapy. The FORWARD trial has advanced to Phase 3 with regulatory submission anticipated in 2026 [38], while the PEC-Direct program continues to optimize its platform. These approaches, along with other emerging technologies, hold promise for transforming T1D management from daily insulin replacement to durable biological solutions.
Overcoming Hurdles: Immunogenicity, Scalability, and Safety Optimization
Beta-cell replacement therapy represents a transformative approach for treating Type 1 Diabetes (T1D), an autoimmune condition characterized by the destruction of insulin-producing pancreatic beta cells. While stem cell-derived beta cells offer a potentially unlimited source of insulin-producing cells, immune rejection remains the most significant barrier to their clinical application [4]. The recipient's immune system recognizes transplanted allogeneic cells as foreign, triggering destructive responses that can eliminate functional grafts. This challenge has catalyzed the development of two primary strategic approaches: physical encapsulation of cells within protective barriers and genetic engineering to create "hypoimmune" cells that evade immune detection [6] [30] [43]. Both paradigms aim to achieve the same fundamental goal – protecting transplanted cells from rejection without requiring lifelong immunosuppression, which carries risks of infection, malignancy, and organ toxicity [30] [44]. This review comprehensively compares these competing strategies, examining their underlying mechanisms, experimental support, and relative advantages and limitations to inform research and development priorities.
Encapsulation Strategies: Creating a Physical Barrier
Encapsulation technology employs semi-permeable membranes to create a physical barrier between transplanted cells and the host immune system. These devices allow for the bidirectional diffusion of oxygen, nutrients, glucose, and insulin while blocking the passage of immune cells and antibodies [44].
Macroencapsulation Devices and Clinical Outcomes
Macroencapsulation devices, which house thousands of cells within a single implantable container, have advanced significantly into clinical testing. The PEC-Direct device (ViaCyte/CyteCorp) represents a prominent example of this approach, utilizing a perforated membrane that allows host blood vessels to grow into close proximity with the encapsulated pancreatic endoderm cells (PEC-01) [18].
Table 1: Clinical Outcomes from Macroencapsulation Trials (PEC-Direct)
| Clinical Parameter | Baseline (Pre-Transplant) | Post-Transplant Outcomes (Month 12) | Significance |
|---|---|---|---|
| Meal-Stimulated C-peptide | Undetectable (<0.03 nmol/L) in all patients | 3/10 patients achieved ≥0.1 nmol/L [18] | Indicates functional insulin production by grafts |
| Time-in-Range (TIR) | ~55% (Case 1) | Increased to ~85% (Case 1) [18] | Measures improved glycemic control |
| Exogenous Insulin Use | Full dependency | Significantly reduced in responders [18] | Demonstrates therapeutic effect |
| Graft Composition (at 6 months) | N/A | β-cell mass: 4% of initial load; α-cells: 16% [18] | Suggests suboptimal maturation/selective survival |
Analysis of explanted sentinel devices revealed a critical challenge: even in the most successful patient, the functional β-cell mass constituted only 4% of the initial transplanted cell load [18]. This significant cell loss, coupled with a disproportionate survival of alpha cells, highlights limitations in the encapsulation microenvironment that require further optimization.
Key Experimental Protocols in Encapsulation Research
Protocol: Preclinical Evaluation of a Novel Macroencapsulation Device
- Objective: To assess the efficacy and safety of a new device design in supporting stem cell-derived pancreatic precursor cells in an immunocompetent model.
- Cell Preparation: Human embryonic stem cells (CyT49 line) are differentiated into PEC-01 cells using a directed, multi-stage protocol [18].
- Device Loading: Cells are loaded into devices featuring a novel membrane perforation pattern designed to enhance vascular ingrowth [18].
- Implantation: Devices are implanted subcutaneously in subjects with T1D who are administered immunosuppression (Anti-thymocyte globulin induction, maintained on mycophenolate mofetil and tacrolimus) [18].
- Outcome Measures: Graft function is assessed via Mixed Meal Tolerance Tests (MMTT) measuring C-peptide, Continuous Glucose Monitoring (CGM) metrics, and daily insulin requirements. Device retrieval allows for histology and cellular composition analysis [18].
Hypoimmune Engineering: Making Cells Invisible to the Immune System
Hypoimmune engineering takes a fundamentally different approach by using genetic editing tools like CRISPR/Cas9 to modify the transplanted cells themselves, eliminating the markers that trigger immune recognition [6] [30]. This strategy aims to create universal "off-the-shelf" cell products that do not require encapsulation or systemic immunosuppression.
Key Genetic Targets and Their Immune Functions
The hypoimmune approach focuses on disrupting the complex dialogue between transplanted cells and the host's innate and adaptive immune systems.
Table 2: Major Genetic Targets for Hypoimmune Engineering of Stem Cell-Derived Beta Cells
| Genetic Target | Immune Function | Engineering Approach | Rationale & Challenge |
|---|---|---|---|
| B2M (Beta-2 Microglobulin) | Required for surface expression of HLA Class I molecules [30]. | Knockout (KO) | Prevents CD8+ T cell recognition. Risk: Triggers "missing-self" response by NK cells [6]. |
| CIITA (Class II Transactivator) | Master regulator of HLA Class II expression [30]. | Knockout (KO) | Prevents CD4+ T cell help. Mainly relevant if inflammation induces Class II on beta cells [6]. |
| CD47 | "Don't eat me" signal that inhibits phagocytosis [6]. | Overexpression | Protects cells from innate immune cells like macrophages. |
| PD-L1 (Programmed Death-Ligand 1) | Ligand for PD-1, an inhibitory receptor on T cells [30]. | Overexpression | Induces local T cell exhaustion/tolerance, acting as an "immune checkpoint" [6]. |
| HLA-G | Non-classical HLA molecule that inhibits NK and T cell activity [30]. | Overexpression | Compensates for HLA Class I KO by providing inhibitory signals to NK cells [6]. |
A leading strategy combines B2M and CIITA knockout with the overexpression of CD47 and PD-L1 [6]. This multi-pronged approach simultaneously reduces antigen presentation while actively engaging inhibitory immune pathways.
Key Experimental Protocols in Hypoimmune Research
Protocol: In Vitro Immune Challenge of Hypoimmune Cells
- Objective: To test the ability of genetically modified hypoimmune stem cell-derived beta cells to evade allogeneic immune responses.
- Cell Engineering: Pluripotent stem cells are edited using CRISPR/Cas9 to knockout B2M and CIITA. Lentiviral vectors are used to stably overexpress CD47 and PD-L1 [6].
- Differentiation: Edited clones are differentiated into insulin-producing beta-like cells using established protocols [21].
- Immune Co-culture: The resulting beta cells are co-cultured with allogeneic peripheral blood mononuclear cells (PBMCs) from mismatched donors.
- Outcome Measures: T-cell proliferation is measured (e.g., by CFSE dilution), and cytokine release (e.g., IFN-γ) is quantified via ELISA. Cytotoxicity is assessed using assays like LDH release [6]. Control groups include unedited beta cells.
Direct Comparative Analysis: Encapsulation vs. Hypoimmune Engineering
When evaluating encapsulation versus hypoimmune engineering for clinical application, distinct profiles of advantages and limitations emerge.
Table 3: Strategic Comparison of Encapsulation vs. Hypoimmune Engineering
| Parameter | Encapsulation Strategy | Hypoimmune Engineering Strategy |
|---|---|---|
| Mechanism of Action | Physical barrier blocking immune cell contact [44] | Genetic elimination of immune triggers [6] |
| Immune Protection | Broad but incomplete (may not block cytokines/antibodies) [44] | Targeted but potentially less robust against primed autoimmunity [45] |
| Graft Survival Site | Typically subcutaneous or peritoneal [18] | Potentially any site, including portal vein (standard for islets) [21] |
| Key Advantage | Device retrievability enhances safety profile [18] | Potential for "off-the-shelf" universal donor cells [30] |
| Primary Limitation | Suboptimal oxygenation and nutrient diffusion [18] [44] | Potential for unforeseen consequences of genetic edits [21] |
| Foreign Body Response | Significant concern: fibrotic encapsulation can isolate device [6] | Not applicable |
| Clinical Translation | Advanced (Phase 1/2 trials showing C-peptide production) [18] | Early stage (Preclinical and emerging first-in-human trials) [6] [30] |
| Scalability | Challenging due to device manufacturing [4] | Theoretically high via cell banking [30] |
A critical consideration for hypoimmune cells in T1D is the autoimmune environment. While these cells may evade allogeneic rejection, they might remain susceptible to the original autoimmune attack that destroyed the patient's native beta cells, as autoreactive T cells may still recognize islet antigens presented by host antigen-presenting cells [45].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in both encapsulation and hypoimmune engineering relies on a specialized set of reagents and tools.
Table 4: Essential Research Toolkit for Immune Protection Strategies
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| CRISPR/Cas9 System | Precise gene knockout (e.g., B2M, CIITA) [6] | Hypoimmune Engineering |
| Lentiviral Vectors | Stable gene overexpression (e.g., CD47, PD-L1, HLA-G) [30] | Hypoimmune Engineering |
| Semi-Permeable Membranes | Form the physical barrier of encapsulation devices [18] [44] | Encapsulation |
| PEC-01 Cells | Pancreatic endoderm cells derived from hESCs (CyT49 line) [18] | Both (as a starting cell source) |
| Allogeneic PBMCs | Source of immune effector cells for in vitro challenge assays [6] | Hypoimmune Engineering (Validation) |
| Immunosuppressants (Tacrolimus, MMF) | Suppress host immune system in pre-clinical models and clinical trials [18] | Both (Often used as a control) |
| C-peptide ELISA | Quantify human-specific insulin secretion in vitro and in vivo [18] | Both (Functional Assessment) |
| Continuous Glucose Monitors (CGM) | Measure glycemic control (Time-in-Range, HbA1c) in animal models and patients [18] | Both (Efficacy Readout) |
The quest to solve the immune challenge in beta-cell replacement therapy has bifurcated into two sophisticated, yet fundamentally different, strategies. Encapsulation offers a potentially safer, retrievable solution but is hampered by device-related limitations in nutrient exchange and foreign body responses. In contrast, hypoimmune engineering promises a more elegant, scalable "off-the-shelf" product but carries uncertainties regarding long-term safety, functional stability, and resilience against recurrent autoimmunity [6] [4] [18].
The future likely lies not in choosing one strategy over the other, but in their intelligent integration. A combined approach, utilizing mildly engineered cells within optimized encapsulation devices, could potentially lower the genetic modification burden while enhancing device performance, thereby achieving durable graft survival without the need for chronic immunosuppression. As these technologies mature, the focus must expand beyond scientific feasibility to encompass scalability, cost-effectiveness, and accessibility, ensuring that the ultimate cure for T1D reaches the millions in need [4].
Beta cell replacement therapy for type 1 diabetes (T1D) stands at a pivotal juncture. Decades of research have yielded compelling proof-of-concept that restoring endogenous insulin production can achieve long-term glycemic control, protect from severe hypoglycemia, and significantly improve quality of life [4]. The emergence of stem cell-derived beta-like cells (SC-islets) represents a paradigm shift from donor-dependent islet transplantation, offering a potentially unlimited source of insulin-producing β cells [46]. Early clinical trials have demonstrated the scientific feasibility of this approach, with participants exhibiting functional insulin secretion and, in some cases, achieving insulin independence [7] [18].
However, this journey from feasibility to widespread accessibility presents what is known as the "last mile" problem—a phase where the challenges of scaling, cost, and implementation become more complex than the initial scientific breakthroughs [4]. Without a strategic shift in development philosophy, beta cell therapy risks becoming an elite intervention, restricted by cost and infrastructure rather than medical necessity [4]. This analysis compares the current therapeutic landscape, examines the experimental evidence, and identifies the critical barriers that must be overcome to bridge this gap.
Comparative Analysis of Beta Cell Replacement Therapies
Table 1: Comparative Analysis of Beta Cell Replacement Approaches for Type 1 Diabetes
| Feature | Allogeneic Islet Transplantation | Stem Cell-Derived Islets (Unencapsulated) | Stem Cell-Derived Islets (Encapsulated) |
|---|---|---|---|
| Cell Source | Deceased organ donors [4] | Human pluripotent stem cells (hPSCs) [7] [46] | CyT49 human embryonic stem cell line [18] |
| Proof-of-Concept | Established; long-term glycemic control achieved [4] | Early clinical trials show promise [7] | Early clinical trials show promise [18] |
| Key Efficacy Data | >50% insulin independence at 5 years in responders [4] | 83% (10/12) insulin independence at Day 365 [7] | 30% (3/10) achieved C-peptide ≥0.1 nmol/L with improved glucose control [18] |
| Immunological Consideration | Requires lifelong immunosuppression [4] [18] | Requires immunosuppression [7] | Device may obviate immunosuppression; protects from immune rejection [18] |
| Major Scalability Limitation | Severe donor scarcity [4] | Manufacturing scale, cost, and immunosuppression [4] | Cell survival and function within encapsulation device [18] |
Table 2: Quantitative Outcomes from Recent Clinical Trials of Stem Cell-Derived Therapies
| Outcome Measure | Zimislecel (Vertex VX-880) [7] | Encapsulated PEC-Direct (ViaCyte) [18] |
|---|---|---|
| Participants with 12-month Data | 14 | 10 |
| Baseline C-peptide | Undetectable in all participants | Undetectable in all participants |
| Engraftment Success | 100% (14/14) showed detectable C-peptide post-infusion | 40% (4/10) showed detectable C-peptide at 6 months |
| Achievement of Metabolically Significant C-peptide (≥0.1 nmol/L) | Not explicitly stated, but 83% achieved insulin independence | 30% (3/10) |
| Insulin Independence at 1 Year | 83% (10/12 on full dose) | Not reported |
| Impact on Glucose Control | >70% time in target glucose range (70-180 mg/dL) [7] | Increased Time-in-Range from 55% to 85% in top responder [18] |
Experimental Protocols and Methodologies
Clinical Trial Design for Stem Cell-Derived Islets (Zimislecel)
The Phase 1-2 study of zimislecel employed a multi-part design to assess safety and efficacy [7]:
- Part A: Participants received a half-dose (0.4 × 10^9 cells) as a single infusion into the portal vein, with an option for a second half-dose within 2 years. The primary endpoint was safety.
- Parts B & C: Participants received a full dose (0.8 × 10^9 cells) as a single infusion. The primary efficacy endpoint for Part C was freedom from severe hypoglycemic events during days 90 through 365, coupled with a glycated hemoglobin level of less than 7% or a decrease of at least 1 percentage point from baseline.
- Immunosuppression: All participants received glucocorticoid-free immunosuppressive therapy.
- Functional Assessment: Engraftment and islet function were assessed by detecting serum C-peptide during a 4-hour mixed-meal tolerance test (MMTT).
Clinical Trial Design for Encapsulated Beta Cells (PEC-Direct)
The Phase 1/2 trial for the encapsulated PEC-Direct product focused on optimizing cell engraftment [18]:
- Cell Product & Dose: The implant consisted of 8-10 large device units, each containing approximately 75 million PEC-01 cells (pancreatic endoderm cells derived from the CyT49 cell line). Some participants also received smaller "sentinel" devices for post-retrieval analysis.
- Immunosuppression: Patients received immunosuppression induced by anti-thymocyte globulin and maintained by mycophenolate mofetil and tacrolimus.
- Endpoint Analysis: The primary endpoint was an increase in MMTT-stimulated C-peptide above the limit of detection (0.03 nmol/L) at month 6. Secondary endpoints included C-peptide >0.07 nmol/L, improvement in continuous glucose monitoring (CGM) metrics, and reduced insulin dosing over 12 months.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents and Materials for SC-Islet Research and Development
| Reagent/Material | Function in R&D | Example from Cited Research |
|---|---|---|
| Human Pluripotent Stem Cells (hPSCs) | Starting material for generating a limitless supply of insulin-producing cells. Includes both embryonic (ESC) and induced pluripotent (iPSC) lines. | CyT49 human embryonic stem cell line [18] |
| Differentiation Factors | Cytokines and small molecules that direct hPSCs through developmental stages to become pancreatic endoderm and mature β cells. | Not specified in results, but critical for protocol [46] |
| Encapsulation Devices | Physical barriers to protect transplanted cells from immune rejection and contain any off-target cells. May be "open" to allow vascularization. | PEC-Direct device with optimized membrane perforation pattern [18] |
| Immunosuppressive Regimens | Drug combinations to prevent immune rejection of allogeneic cell products, especially in unencapsulated or "open" device approaches. | Glucocorticoid-free regimen (Vertex); Anti-thymocyte globulin, mycophenolate mofetil, tacrolimus (PEC-Direct) [7] [18] |
| Functional Assays (C-peptide, MMTT) | To validate in vivo function of derived β cells and monitor graft success post-transplantation. C-peptide is a marker of endogenous insulin production. | Mixed-Meal Tolerance Test (MMTT) to stimulate and measure plasma C-peptide [7] [18] |
| Continuous Glucose Monitoring (CGM) | To assess the physiological impact of the therapy on day-to-day glucose control, measured via Time-in-Range (TIR) and other metrics. | Used to track Time-in-Range, Time-Above-Range, and Time-Below-Range [18] |
Navigating the Scalability Conundrum
The "last mile" in beta-cell replacement therapy is fraught with challenges that extend beyond the laboratory. Drawing an analogy to space exploration, while the monumental achievement of landing on the moon (scientific proof-of-concept) has been accomplished, the establishment of a sustainable lunar colony (widespread, accessible therapy) remains an entirely different level of challenge [4].
Critical Barriers to Widespread Access
- Manufacturing at Scale: Generating highly functional and well-characterized SC-islets in quantities sufficient to treat millions of individuals with T1D requires bioprocessing innovations that are only now in development [4] [46]. The current "Apollo mission" mindset, focused on bespoke production for small clinical trials, is not viable for population-level scaling [4].
- Economic Viability: The field must learn from the cautionary tales of gene and cell therapies for rare diseases, where unsustainable pricing has led to market withdrawals despite regulatory approval [4]. Therapies like fidanacogene elaparvovec for hemophilia B, priced at $3.5 million per patient, are not a replicable model for a common disease like T1D [4].
- Procedural and Infrastructure Hurdles: Even if the need for immunosuppression is overcome, the procedures themselves—dependent on skilled operators and specialized centers—are not easily automated or broadly implemented, inherently limiting patient access [4].
A Path Forward: Quality by Design
To successfully navigate the last mile, a strategic shift is imperative. A Quality by Design (QbD) approach is proposed, which emphasizes scalability, ease of use, and economic feasibility from the earliest stages of development, not as afterthoughts [4]. This means:
- Prioritizing allogeneic ("off-the-shelf") therapies over autologous (patient-specific) ones to leverage economies of scale, where a single manufacturing batch can treat multiple patients [4].
- Investing in automation and bioprocessing technologies to drive down per-patient costs without compromising quality or efficacy [4].
- Aligning corporate interests, academic research, and regulatory pathways with the overarching goal of widespread accessibility rather than niche applications [4].
The journey toward a cure for type 1 diabetes has entered its most critical phase. The demonstrated success of stem cell-derived beta cells in restoring insulin secretion and improving glycemic control marks a triumphant end to the first leg of this voyage [7] [18]. However, the path ahead—the "last mile"—presents a scalability conundrum of manufacturing, economics, and implementation that is as complex as the initial scientific challenge. The lessons from other advanced therapies are clear: without a deliberate and coordinated strategy focused on accessibility from the outset, even the most effective therapy will fail to achieve its potential to eradicate a disease. The focus must now expand from merely proving that the therapy works to ensuring that it can reach the millions who stand to benefit.
For researchers and drug development professionals working on stem cell-derived beta cells (SC-β) for type 1 diabetes (T1D), managing immune responses remains a pivotal translational challenge. T1D is characterized by autoimmune destruction of pancreatic beta cells, and any replacement therapy must overcome both allogeneic rejection and recurrent autoimmunity [12] [47]. While stem cell-derived islets offer a potentially limitless supply of insulin-producing cells, their clinical application is constrained by the necessity to protect grafts from immune destruction without causing systemic complications [6] [2]. Current strategies span conventional immunosuppression, immunomodulatory protocols, and innovative bioengineering approaches, each with distinct safety and adverse event profiles. This analysis comprehensively compares these strategies through the lens of risk management, providing critical safety data and methodological details to inform preclinical and clinical development decisions.
Comparative Safety Profiles of Current Immunosuppressive Strategies
Table 1: Adverse Event Profiles of Immunosuppressive Regimens in Beta Cell Therapy
| Strategy Category | Specific Regimen/Approach | Common Adverse Events | Serious Risks | Mechanistic Basis | Evidence Source |
|---|---|---|---|---|---|
| Calcineurin Inhibitor-based | Edmonton Protocol (Sirolimus, Tacrolimus) | Mouth ulceration, anemia [2] | Lymphopenia, elevated IL-7/IL-15, expansion of autoreactive CD8+ T cells, graft failure [48] | IL-2 signaling inhibition; blocks T-cell activation | Clinical trial (Phase 3) [48] |
| Lymphocyte Depletion | Anti-thymocyte globulin (ATG) | Fever, chills, cytokine release syndrome | Increased infection risk, malignancy [12] [6] | T-cell depletion | Clinical islet transplantation [6] |
| Biologics & Targeted Agents | Anti-IL-2Rα (Daclizumab), CTLA4-Ig (Abatacept) | Injection site reactions | Autoimmune complications, infection risk [48] [49] | Blocks IL-2 receptor or T-cell co-stimulation | Phase II/III trials [49] |
| Metabolic Inhibitor | Mycophenolate Mofetil (MMF) | Gastrointestinal distress, leukopenia | Teratogenicity, progressive multifocal leukoencephalopathy [6] | Inhibits purine synthesis, blocks lymphocyte proliferation | Clinical transplantation [48] [6] |
| Cell Therapy Infusion | MSC Systemic Infusion | Transient headache, nausea, fever [50] | Thromboembolism, central retinal vein occlusion (rare) [51] | Procoagulant tissue factor expression [51] | Clinical trials for various conditions [51] [50] |
| Bioengineered Grafts | Hypoimmune SC-β Cells | Procedure-related (pain at implant site) [1] | Theoretical: tumorigenicity from genetic edits, NK cell activation from "missing-self" [6] | HLA class I/II knockout with "don't-eat-me" signals (e.g., CD47) [6] | Preclinical models [6] |
The Edmonton protocol, a landmark steroid-free regimen, demonstrated that insulin independence was achievable but also revealed a critical long-term safety issue: the regimen-induced lymphopenia was associated with elevated serum levels of homeostatic cytokines IL-7 and IL-15. This environment drove the in vivo expansion of autoreactive CD8+ T cells, likely contributing to late graft failure [48]. This finding underscores a fundamental risk of broad immunosuppression—the potential to exacerbate the very autoimmune process the therapy aims to circumvent. Switching from rapamycin and tacrolimus to mycophenolate mofetil (MMF) in two patients blocked spontaneous lymphocyte proliferation despite high IL-7 levels, suggesting regimen-specific safety profiles [48].
For cell infusion procedures, particularly with mesenchymal stromal cells (MSCs), thromboembolism emerges as a predominant and dose-related serious adverse event. This is mechanistically linked to MSCs' expression of procoagulant tissue factor [51]. A systematic review noted cases of inflammatory-associated thromboembolism in kidney transplant patients following umbilical cord-derived MSC infusion [51]. Common, less severe infusion reactions include transient headache, chills, nausea, and low-grade fever, typically resolving without intervention [50].
Methodological Protocols for Safety and Efficacy Assessment
Assessing Immunosuppression-Related Lymphopenia and Autoimmunity
Experimental Objective: To evaluate whether an immunosuppressive regimen induces lymphopenia and consequent homeostatic expansion of autoreactive T cells, as observed with the Edmonton protocol [48].
Detailed Protocol:
- Patient Monitoring: Collect peripheral blood samples from trial participants pre-transplantation and at regular intervals post-transplantation and immunosuppression initiation.
- Lymphocyte Enumeration: Perform complete blood counts with differential to quantify absolute lymphocyte numbers and identify lymphopenia.
- Cytokine Measurement: Analyze serum samples for levels of homeostatic cytokines (IL-7, IL-15) using ELISA or multiplex immunoassays.
- T Cell Phenotyping:
- Use flow cytometry with fluorochrome-labeled HLA multimer (pentamer) staining specific for islet autoantigens (e.g., GAD65) to identify autoreactive CD8+ T cells.
- Co-stain for the proliferation marker Ki-67 and memory marker CD45RO to identify proliferating autoreactive memory T cells.
- Functional Assay: Isolate peripheral blood mononuclear cells (PBMCs) and culture them for 48 hours without stimulation. Measure IFN-γ production in the supernatant via ELISA to assess effector memory T cell activation.
- Drug Testing In Vitro: Culture PBMCs from patients with elevated cytokine levels. Add different immunosuppressants (e.g., MMF, rapamycin, FK506) to the cultures to assess their ability to block spontaneous proliferation (via Ki-67 staining) and IFN-γ production.
Evaluating Procoagulant Risk of Cell Infusion Products
Experimental Objective: To determine the prothrombotic potential of a stem cell-derived therapy prior to clinical infusion, mitigating thromboembolism risk [51].
Detailed Protocol:
- Tissue Factor Expression:
- Analyze the cell product for expression of tissue factor (CD142) via flow cytometry and quantitative PCR.
- Compare expression levels against primary human umbilical vein endothelial cells (HUVECs) as a reference.
- Functional Clotting Assay:
- Incubate a standardized number of cells (e.g., 1 x 10^6) with normal human plasma in vitro.
- Measure the time to fibrin clot formation using a coagulometer.
- Compare clotting times to cell-free controls and negative control cells (e.g., fibroblasts).
- In Vivo Safety Assessment:
- Utilize an immunocompromised mouse model.
- Administer the cell product via a clinically relevant route (e.g., intravenous, portal vein).
- Monitor for signs of distress and perform histopathological analysis of major organs (lungs, liver) post-sacrifice to check for microthrombi.
The following diagram illustrates the key immune pathways targeted by different immunosuppressive strategies and the associated risks of homeostatic autoimmunity.
In Vivo Assessment of Hypoimmune Edited Grafts
Experimental Objective: To test the efficacy and safety of genetically engineered hypoimmune SC-β cells in avoiding immune rejection without systemic immunosuppression [6].
Detailed Protocol:
- Genetic Engineering:
- Using CRISPR-Cas9 in human pluripotent stem cells (hPSCs), knock out Beta-2-microglobulin (B2M) to eliminate HLA class I surface expression.
- To mitigate NK cell-mediated "missing-self" lysis, simultaneously knock in genes for non-classical HLA molecules (HLA-E, HLA-G) and the "don't-eat-me" signal CD47.
- Differentiation: Differentiate the engineered hPSCs into SC-β cells using a established, multi-step protocol [12].
- In Vivo Transplantation:
- Transplant SC-β cell clusters into immunocompetent humanized mouse models.
- Include control groups: unedited SC-β cells (rejected), and edited cells in immunodeficient mice (function control).
- Efficacy & Safety Monitoring:
- Graft Function: Monitor mouse blood glucose levels to determine time to normoglycemia and perform glucose tolerance tests.
- Graft Survival: Retrieve grafts at endpoint for histology; stain for insulin and immune cell markers (CD3, CD8, CD68) to assess immune infiltration and beta cell mass.
- Safety Screening: Assess for teratoma formation and perform RNA-seq on grafts to check for unintended consequences of genetic editing.
Emerging Solutions and the Research Toolkit
Table 2: Research Reagent Solutions for Immune Safety Assessment
| Research Reagent / Tool | Primary Function in Safety Research | Example Application |
|---|---|---|
| HLA Pentamers (e.g., GAD65) | Flow cytometry-based identification of autoreactive CD8+ T cells | Tracking expansion of antigen-specific autoreactive T cells post-therapy [48] |
| Anti-Ki-67 Antibody | Marker of cell proliferation; identifies proliferating lymphocyte populations | Detecting homeostatic T-cell proliferation in lymphopenic hosts [48] |
| CRISPR-Cas9 System | Gene editing for knockout (B2M, CIITA) or knock-in (CD47, HLA-G) | Creating hypoimmune stem cell lines to evade allorejection [6] |
| CD142 (Tissue Factor) Antibody | Procoagulant risk assessment of cell therapy products | Quantifying thrombogenic potential of MSCs or SC-β cells before infusion [51] |
| Cytokine Multiplex Array (IL-7, IL-15) | Multiplexed quantification of serum homeostatic cytokines | Monitoring for cytokine changes predictive of auto-reactive expansion [48] |
| Anti-CD3/CD8/CD45RO Antibodies | Immunophenotyping of T cell populations (activation, memory) | Profiling the immune infiltrate in explanted grafts [48] [6] |
The field is rapidly moving beyond generalized immunosuppression. Promising strategies include the use of autologous regulatory T cells (Tregs) [49] [52] and the engineering of "hypoimmune" or "immune-evasive" SC-β cells [6]. These cells are genetically modified to delete classical HLA class I and II molecules, thereby reducing their visibility to the adaptive immune system. A major safety challenge for this approach is avoiding subsequent killing by natural killer (NK) cells, which are activated by "missing-self" signals. Current strategies co-express non-classical HLA molecules (HLA-E, HLA-G) and the "don't-eat-me" signal CD47 to inhibit NK cells and macrophages [6]. The first-in-human trial of genetically modified allogeneic islets has reported positive six-month results, marking a significant milestone for this technology [6].
The diagram below outlines the key genetic engineering strategy for creating these hypoimmune cells.
The management of immunosuppression and infusion risks for SC-β cell therapies is a critical determinant of their translational success. Data confirms that conventional systemic immunosuppression, while enabling initial engraftment, carries significant long-term risks, including opportunistic infections, malignancies, and the paradoxical expansion of autoreactive T cells. Infusion procedures, particularly with MSCs, require rigorous pre-clinical assessment of procoagulant activity to mitigate thromboembolic risks. The emerging generation of bioengineered, hypoimmune cell products represents a paradigm shift, aiming to achieve graft tolerance without systemic immunosuppression. For researchers, the priority must be the continued refinement of these safer, targeted strategies through robust preclinical models and carefully designed clinical trials that include comprehensive immune monitoring. The ultimate goal is a durable, safe, and effective cell replacement therapy for T1D that minimizes systemic risks while providing robust glycemic control.
The therapeutic landscape for Type 1 Diabetes (T1D) is being reshaped by two pioneering strategies: CRISPR/Cas9 gene editing and co-transplantation approaches. Both aim to overcome the critical barriers that have limited the success of stem cell-derived beta (SC-β) cell therapies—namely, immune rejection and the loss of cellular function post-transplantation. This guide provides a comparative analysis of these solutions, detailing their underlying mechanisms, experimental protocols, and quantitative performance data to inform research and development efforts.
Type 1 diabetes is an autoimmune disease characterized by the destruction of insulin-producing β-cells in the pancreas [53]. Regenerative medicine offers the potential for a functional cure through the transplantation of SC-β cells. However, the path to clinical application is fraught with two major hurdles:
- Immunogenicity: Transplanted cells face attack from the host's immune system, including both allogeneic rejection (as the cells are foreign) and recurrent autoimmunity (the original cause of the disease) [6].
- Post-Transplant Cell Fitness: A significant loss of SC-β cell function and identity occurs after transplantation, largely due to hypoxic stress before the graft becomes fully vascularized [11].
The following sections dissect how CRISPR/Cas9 engineering and co-transplantation strategies are being designed to address these obstacles.
CRISPR/Cas9-Generated Hypoimmune SC-β Cells
This strategy involves genetically engineering SC-β cells to evade immune detection, creating "hypoimmune" or "stealth" grafts that can potentially survive without long-term immunosuppression.
Core Mechanism and Signaling Pathways
The approach focuses on modulating key cell-surface ligands that regulate immune activation and inhibition. The primary genetic modifications aim to:
- Remove "Eat Me" Signals: Knock out Major Histocompatibility Complex (MHC) class I and II proteins to prevent T-cell recognition and activation.
- Express "Don't Eat Me" Signals: Introduce immunomodulatory proteins that directly inhibit immune cell activity.
The diagram below illustrates the core signaling pathways involved in immune evasion and the strategic points of CRISPR/Cas9 intervention.
Key Experimental Protocols
A standard protocol for generating hypoimmune SC-β cells involves a multi-step process of genetic modification and differentiation [6] [53]:
- Target Selection: Key genes are selected for knockout (e.g.,
B2Mfor MHC-I,CIITAfor MHC-II) and knock-in (e.g.,CD47,PD-L1,HLA-G). - gRNA Design and Complex Formation: Single-guide RNAs (sgRNAs) are designed for each target. The sgRNA forms a ribonucleoprotein (RNP) complex with the Cas9 nuclease.
- Delivery into Pluripotent Stem Cells (PSCs): The RNP complexes, along with donor DNA templates for knock-ins, are delivered into human PSCs (hPSCs) via electroporation or lipid nanoparticles (LNPs).
- Selection and Validation: Successfully edited clonal lines are selected and validated using sequencing (Sanger, NGS) and flow cytometry to confirm protein expression loss/gain.
- Directed Differentiation: The engineered hPSC clones are differentiated into SC-β cells using established multi-stage protocols involving specific growth factors and small molecules [11].
Performance and Efficacy Data
Recent preclinical and early clinical studies demonstrate the potential of this approach.
Table 1: Efficacy Data for CRISPR/Cas9-Engineered Cell Therapies in Diabetes and Related Fields
| Therapy / Model | Key Genetic Modifications | Efficacy Outcome | Source / Reference |
|---|---|---|---|
| First-in-Human Allogeneic Islet Transplant (Clinical) | Not fully detailed; edits to evade immune detection. | Insulin production for months without immunosuppressive drugs. | [54] |
| Hypoimmune PSC-derived β cells (Preclinical) | B2M/CIITA KO; HLA-E/CD47/PD-L1 KI. |
Protection against T-cell and NK cell-mediated allorejection. | [6] |
| In Vivo CRISPR (hATTR trial) | Knockout of disease gene (TTR) in liver cells. | ~90% sustained reduction in disease-related protein for 2+ years. | [55] |
Co-transplantation for Immune Reset and Graft Support
Co-transplantation involves administering SC-β cells alongside other supportive cells, such as hematopoietic stem cells (HSCs) or mesenchymal stem cells (MSCs), to create a favorable microenvironment for graft survival and function.
Core Mechanism and Workflow
This strategy aims to "re-educate" the host immune system to tolerate the graft. A groundbreaking study in mice combined blood stem cell and pancreatic islet cell transplantation from a single, immunologically mismatched donor [56]. The workflow is as follows:
Key Experimental Protocols
The protocol from the Stanford study that cured T1D in mice is detailed below [56]:
- Animal Model: Use non-obese diabetic (NOD) mice or other established autoimmune diabetes models.
- Pre-Conditioning: Treat mice with a non-myeloablative regimen including:
- Immune-targeting antibodies (e.g., anti-CD117).
- Low-dose radiation.
- An add-on drug used for autoimmune diseases (e.g., to control autoimmunity).
- Cell Sourcing and Transplantation: Isolate two cell types from a single, immunologically mismatched donor:
- Hematopoietic Stem Cells (HSCs): To reconstitute a hybrid immune system.
- Pancreatic Islet Cells: To replace lost insulin-producing capacity.
- Infuse both cell types into the conditioned host.
- Monitoring: Monitor blood glucose levels, glucose tolerance, and insulin dependence for at least six months. Assess immune cell chimerism and the absence of graft-versus-host disease (GvHD) via flow cytometry and histology.
Performance and Efficacy Data
This approach has shown remarkable success in murine models, addressing both the immune and regenerative aspects of T1D.
Table 2: Efficacy Data for Co-Transplantation Approaches in Preclinical Models
| Transplant Model | Co-Transplanted Cells | Pre-Conditioning | Efficacy Outcome | Source / Reference |
|---|---|---|---|---|
| Autoimmune Diabetic Mice | HSCs + Pancreatic Islets (mismatched donor) | Antibodies + Low-dose radiation + Autoimmune drug | 19/19 mice prevented from T1D; 9/9 mice with long-standing T1D cured. No GvHD or immunosuppression needed. | [56] |
| SC-β Cell Therapy (General) | MSCs or Regulatory T Cells (Tregs) | Varies | Aims to provide pro-angiogenic and anti-apoptotic signals; limited by uncertain survival of accessory cells. | [6] |
Direct Comparison and Research Frontiers
Comparative Analysis of Key Parameters
Table 3: Direct Comparison of CRISPR/Cas9 and Co-Transplantation Strategies
| Parameter | CRISPR/Cas9 Hypoimmune Cells | Co-Transplantation (HSC + Islets) |
|---|---|---|
| Primary Mechanism | Direct genetic modification of graft to evade immune recognition. | Immune system reset via creation of a hybrid immune system. |
| Target Challenge | Addresses immunogenicity and allorejection. | Addresses immunogenicity, autoimmunity, and provides new islets. |
| Key Advantage | Potentially universal, "off-the-shelf" product; no need for donor-recipient matching. | Addresses the root cause of autoimmunity; no complex cell engineering required. |
| Key Limitation | Risk of off-target edits; long-term safety of engineered cells is unknown. | Requires rigorous pre-conditioning; complex logistics of dual cell sourcing. |
| Clinical Stage | Early clinical trials (immune-evasive islets) [54]. | Preclinical (murine models) [56]. |
| Scalability | High, if safety is proven, as one cell line can treat many patients. | Lower, limited by donor availability for two cell types. |
Emerging Innovations and Future Directions
Both fields are advancing rapidly, aided by new technologies:
- Enhanced Delivery Systems: New nanostructures like Lipid Nanoparticle Spherical Nucleic Acids (LNP-SNAs) have been shown to triple CRISPR gene-editing efficiency and reduce toxicity compared to standard LNPs [57].
- Addressing Cellular Fitness: Research is identifying genes like
EDN3that, when overexpressed, can help preserve SC-β cell identity and function under hypoxic stress, a critical challenge post-transplantation [11]. This represents a complementary strategy that could be combined with either main approach. - Combination Therapies: The future may lie in integrating these strategies—for example, using hypoimmune SC-β cells differentiated from engineered PSCs to simplify the co-transplantation approach by eliminating the need for immune suppression.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Next-Generation SC-β Cell Research
| Reagent / Solution | Critical Function | Application Context |
|---|---|---|
| CRISPR/Cas9 RNP Complex | Induces targeted double-strand breaks in DNA for gene knockout/knock-in. | Generating hypoimmune PSC lines [6] [53]. |
| Lipid Nanoparticles (LNPs) | Delivers CRISPR machinery or mRNA in vivo; liver-tropic. | In vivo CRISPR therapies (e.g., for hATTR) [55]. |
| LNP-SNAs | Advanced nanostructure for enhanced cellular uptake and reduced toxicity of CRISPR cargo. | Next-generation delivery system for improved editing [57]. |
| hPSCs (human PSCs) | The starting cell population capable of indefinite self-renewal and differentiation into any cell type. | Source for deriving SC-β cells [6] [11]. |
| Differentiation Kits/Protocols | Contains precise combinations of growth factors and small molecules to direct hPSCs into SC-β cells. | In vitro generation of functional, glucose-responsive insulin-producing cells [11]. |
| Anti-CD117 Antibody | Depletes host HSCs to create niche for donor engraftment. | Gentle pre-conditioning for co-transplantation in murine models [56]. |
| EDN3 Expression Vector | Enforced expression helps maintain β-cell identity and function under hypoxia. | Improving post-transplant survival and function of SC-β cells [11]. |
Efficacy Validation and Comparative Analysis with Established Therapies
Type 1 diabetes (T1D) management is undergoing a transformative shift with the advancement of beta-cell replacement therapies, moving beyond traditional insulin administration to strategies aimed at restoring endogenous insulin production. Two leading approaches have emerged: allogeneic islet transplantation, recently validated by the FDA approval of Lantidra (donislecel-jujn), and stem cell-derived islet therapies, which leverage pluripotent stem cells to generate insulin-producing cells [2] [58]. This guide provides a head-to-head comparison of these modalities, focusing on efficacy outcomes, experimental methodologies, and underlying biological mechanisms for researchers and drug development professionals. Both strategies share the ultimate goal of achieving physiological glucose control but diverge significantly in cell source, manufacturing, and clinical implementation.
Efficacy Outcomes and Clinical Performance
Direct comparative randomized trials between stem cell-derived islets and allogeneic islet transplantation are not yet available. However, emerging data from recent clinical studies and trials provide critical insights into their relative performance.
Table 1: Key Efficacy Outcomes from Clinical Studies
| Therapy | Clinical Trial / Product | Insulin Independence Rate | Key Efficacy Endpoints | Duration of Follow-up |
|---|---|---|---|---|
| Allogeneic Islet Transplantation | Lantidra (FDA-approved) [59] | 21-30% of participants at 1 year | Elimination of exogenous insulin need; Reduction/elimination of severe hypoglycemic events | Benefits lasting over five years in some cases |
| Allogeneic Islet Transplantation | Japanese Multicenter Trial (2025) [60] | Primary endpoint achieved in 75% (6 of 8 recipients) | HbA1c <7.4% and absence of severe hypoglycemic events at 1 year | Median HbA1c 6.1% at 2 years (730 days) |
| Stem Cell-Derived Islets | Vertex VX-880 (Phase I/II) [61] | Nearly all participants (11 of 12) with reduction or elimination; All 3 with ≥1yr follow-up off insulin | Islet cell engraftment; Glucose-responsive insulin production (C-peptide+); Improved glycemic control | Ongoing trials; 1-year data available for initial patients |
| Stem Cell-Derived Islets | Chinese iPSC-derived islets (Case Report) [61] | 1 patient off insulin | Normal blood sugar levels (Time in Range 99%); Normalized HbA1c | 1-year follow-up |
Table 2: Safety and Practical Considerations
| Parameter | Allogeneic Islet Transplantation (Lantidra) | Stem Cell-Derived Islets (e.g., VX-880) |
|---|---|---|
| Cell Source | Deceased donor pancreata [59] [62] | Human pluripotent stem cells (ESC or iPSC) [2] [61] |
| Immunosuppression Requirement | Required (concomitant) [59] | Required in non-encapsulated protocols [61] |
| Key Safety Concerns | Complications from immunosuppression; risks from infusion procedure [59] [58] | Risks from immunosuppression; potential immune reactions to autologous iPSCs [61] |
| Scalability Challenge | Limited by deceased donor organ availability [2] | Potentially unlimited cell source [2] |
| Regulatory Status | FDA-approved (2023) [59] | Phase I/II and III clinical trials [61] |
Experimental Protocols and Methodologies
Manufacturing and Cell Processing
Allogeneic Islet Transplantation (Lantidra): The manufacturing of Lantidra begins with pancreas procurement from screened deceased donors. Islets are isolated using a collagenase-based enzymatic digestion method, fundamentally based on the Ricordi method developed in the late 1980s [2]. This process involves perfusing the pancreas with collagenase and then mechanically dissociating it in a chamber, allowing for the purification of islets with minimal damage. The critical steps include:
- Digestion: The pancreas is digested using a validated, standardized collagenase-based protocol.
- Purification: Islets are separated from exocrine tissue using density gradient centrifugation.
- Quality Control: The final product must meet strict cGMP standards for release criteria, including identity, purity, potency, safety, viability, and functionality [59]. The product is then cultured and transported under controlled conditions to prevent microbial contamination.
Stem Cell-Derived Islets: The generation of stem cell-derived islets employs directed differentiation protocols designed to mimic the stages of in vivo pancreatic development [2]. A representative protocol involves:
- Definitive Endoderm Induction: Human pluripotent stem cells (hPSCs), either ESCs or iPSCs, are treated with Activin A (a TGF-β family member) and Wnt3a to direct differentiation into definitive endoderm.
- Primordial Gut Tube Formation: Cells are then directed to a primitive gut-tube stage using factors like FGF10 and KAAD-cyclopamine (an inhibitor of Sonic hedgehog signaling).
- Pancreatic Progenitor Specification: Subsequent stages involve the use of retinoic acid to promote posterior foregut fate and the generation of pancreatic endoderm and endocrine precursors.
- Final Maturation: Cells are further differentiated into hormone-expressing endocrine cells. For some protocols, final maturation occurs in vivo post-transplantation, taking advantage of the host's vascularization and microenvironment [2].
Transplantation and Immunosuppression Protocols
Allogeneic Islet Transplantation: The clinical procedure involves infusing the purified islets into the recipient's portal vein, with the liver serving as the transplant site [59] [63]. Patients require concomitant immunosuppression. The foundational regimen was the Edmonton Protocol, which used a steroid-free combination of:
- Sirolimus: Inhibits mTOR to prevent T-cell proliferation.
- Tacrolimus: A calcineurin inhibitor that reduces IL-2 production and T-cell activation.
- Daclizumab: An anti-CD25 monoclonal antibody that blocks the IL-2 receptor (since withdrawn from the market) [63]. Newer regimens are exploring less toxic agents, such as Belatacept (a CTLA4-Ig that blocks CD28/B7 costimulation) [63] and engineered anti-CD40L antibodies like Tegoprubart (AT-1501) [63].
Stem Cell-Derived Islet Transplantation: In clinical trials, two primary delivery strategies are being tested:
- Intraportal Infusion with Immunosuppression: The Vertex VX-880 trial uses the same intraportal delivery route as allogeneic islets, coupled with standard immunosuppression [61].
- Encapsulation in Macrodevices: Companies like ViaCyte and Vertex are also testing devices (e.g., Encaptra) that encapsulate the stem cell-derived islets within semipermeable membranes. These devices are designed for subcutaneous implantation and aim to protect the cells from immune attack without requiring systemic immunosuppression [58].
Signaling Pathways and Mechanistic Insights
The success and failure of beta-cell replacement therapies are governed by critical immune signaling pathways. Immunosuppressive drugs target key nodes within these pathways to prevent graft rejection.
Diagram 1: Immunosuppression targets T-cell activation pathways.
The diagram above illustrates the primary signaling pathways targeted by immunosuppressive regimens in transplantation. T-cell activation requires both T-cell receptor (TCR) engagement by antigen and costimulatory signals like the CD28-B7 interaction [63]. The CD40-CD40L interaction provides a critical secondary signal between T-cells and antigen-presenting cells [63]. Upon full activation, T-cells produce IL-2, which binds to the IL-2 receptor in an autocrine and paracrine fashion, driving T-cell proliferation and clonal expansion. Modern immunosuppressive drugs specifically target these nodes: Belatacept blocks CD28 costimulation, Tacrolimus inhibits IL-2 production, Daclizumab blocks the IL-2 receptor, Sirolimus inhibits the proliferative response to IL-2, and anti-CD40L antibodies block the CD40-CD40L costimulatory pathway [63].
Diagram 2: Stem cell differentiation into functional islets.
The differentiation of stem cells into functional, glucose-responsive islet cells is a tightly controlled process that recapitulates embryonic development, as shown in Diagram 2. Protocols guide hPSCs through sequential stages using specific morphogens and signaling molecules [2]. The process begins with induction of Definitive Endoderm using Activin A and Wnt3a. Subsequent stages, involving FGF10 and hedgehog pathway inhibition (KAAD-cyclopamine), promote Gut-Tube Endoderm formation. Retinoic acid is then critical for specifying Pancreatic Endoderm and endocrine fate. Some protocols transplant cells at the progenitor stage, relying on the in vivo environment for final maturation into functional Stem Cell-Derived Islet Cells [2].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents and Materials for Beta-Cell Replacement Research
| Reagent / Material | Function in Research | Specific Examples & Applications |
|---|---|---|
| Collagenase Enzymes | Enzymatic digestion of pancreatic tissue for islet isolation from donor pancreata. | Foundation of the Ricordi method for isolating allogeneic islets for transplantation [2]. |
| Morphogens & Growth Factors | Directing stem cell differentiation through sequential developmental stages. | Activin A, Wnt3a, FGF10, Retinoic Acid used in protocols to generate SC-islets from hPSCs [2]. |
| Immunosuppressive Compounds | To prevent graft rejection in animal models and clinical trials; studying immune tolerance. | Tacrolimus, Sirolimus, Belatacept, Anti-CD40L antibodies (e.g., Tegoprubart) [63]. |
| Alginate & Encapsulation Polymers | Creating semi-permeable membranes for immunoisolation of transplanted islets/SC-islets. | Used in microencapsulation (e.g., Sigilon's spheres) and macrodevices (e.g., ViaCyte's Encaptra) [58]. |
| cGMP Manufacturing Systems | Ensuring consistent, high-quality, and safe production of cellular products for clinical use. | Critical for scaling up production of both allogeneic islets (Lantidra) and SC-islets under FDA regulations [59]. |
| Pluripotent Stem Cell Lines | Source material for generating scalable and genetically defined insulin-producing cells. | Human Embryonic Stem Cells (hESCs) and induced Pluripotent Stem Cells (iPSCs) [2] [61]. |
The head-to-head comparison reveals that allogeneic islet transplantation, solidified by the FDA approval of Lantidra, offers a proven and effective therapy for a specific, high-risk population with brittle T1D, with documented long-term efficacy [59] [62]. In contrast, stem cell-derived islet therapies, while currently less established in clinical practice, have demonstrated remarkable preliminary efficacy in trials and possess a fundamental advantage in scalability due to their freedom from donor organ limitations [2] [61]. The critical challenge for both approaches remains the management of the immune response. The future of the field lies in immunoengineering strategies that could benefit both modalities, such as advanced encapsulation devices [58], localized immunomodulation [63], and gene editing to create "immune-stealth" cells [59] [61]. For researchers, the focus should be on holistic "quality by design" in developing Advanced Medicinal Therapy Products that integrate cellular composition, delivery systems, and immune protection from the outset [61]. This integrated approach will be essential for moving beyond managing severe hypoglycemia and toward a widely accessible, durable cure for type 1 diabetes.
Type 1 diabetes (T1D) results from the autoimmune destruction of insulin-producing pancreatic beta cells, leading to a lifelong dependence on exogenous insulin therapy [22]. Despite advanced insulin delivery systems, maintaining glycemic control remains challenging, with only approximately one in four individuals with T1D globally achieving the recommended HbA1c target of below 7% [22]. This failure is associated with significant risks of both acute complications, such as severe hypoglycemic events (SHEs), and long-term micro- and macrovascular complications [22]. Stem cell-derived beta-like cell therapies represent a pioneering approach aimed at addressing the underlying pathology of T1D by replacing destroyed islet cells and restoring endogenous, glucose-responsive insulin production [1]. This guide objectively compares the emerging performance data of these therapies against established alternatives, synthesizing key efficacy outcomes at the critical 12-month benchmark.
Comparative Analysis of Therapeutic Outcomes at 12 Months
The table below synthesizes key efficacy outcomes at approximately 12 months for stem cell-derived therapies, conventional medical management, and islet transplantation.
Table 1: Comparison of Therapeutic Outcomes for Type 1 Diabetes at 12 Months
| Therapy / Intervention | Insulin Independence Rate | HbA1c <7% Achievement | Severe Hypoglycemic Events (SHEs) | Key Efficacy Endpoints |
|---|---|---|---|---|
| Stem Cell-Derived Islet Cells (Zimislecel) [22] | 83% (10/12 patients) | 100% (12/12 patients) | Eliminated from Day 90 onwards | • Mean 92% reduction in daily insulin use>70% Time-in-Range (TIR) |
| Allogeneic Islet Transplantation [1] | Reported in selected trials, specific rate not detailed in sources | Improved glycemic control reported | Reduced frequency reported | • Meal-responsive C-peptide increase at 26 weeks• 20% reduction in insulin requirements |
| Intensive Medical Management (Standard of Care) [22] | 0% | ~25% (population average) | Persistent risk | • Reliant on exogenous insulinChallenging to achieve consensus HbA1c/TIR targets |
| Adipose-Derived Stem Cells (ASC) + Vitamin D [1] | Not primary outcome (insulin dose stable) | Improved (p=0.01) | Not specifically reported | • Improved basal C-peptide (p=0.018)Prolongation of honeymoon phase |
Detailed Experimental Protocols and Methodologies
Stem Cell-Derived Islet Cell Therapy (Zimislecel)
The clinical trial for zimislecel is an ongoing study evaluating an investigational, allogeneic stem cell-derived, fully differentiated, insulin-producing islet cell therapy [22].
- Patient Population: The data summarized in Table 1 is from a cohort of patients with T1D complicated by impaired hypoglycemic awareness and severe hypoglycemia. As of the June 2025 data presentation, 12 patients who received a full dose of zimislecel as a single infusion had been followed for at least one year [22].
- Intervention Protocol: Participants received a single infusion of zimislecel into the hepatic portal vein. The therapy is manufactured from stem cells using a proprietary differentiation protocol to create fully functional, insulin-producing islet cells [22].
- Concomitant Medication: To prevent immune rejection of the allogeneic cells, all recipients were placed on a chronic immunosuppressive regimen. The safety profile of the treatment was consistent with the known effects of this immunosuppressive therapy [22].
- Outcome Assessment: Key efficacy measures included HbA1c, Time-in-Range (TIR) from continuous glucose monitoring, fasting and stimulated C-peptide levels (as a marker of endogenous insulin production), daily insulin usage, and the occurrence of severe hypoglycemic events [22].
High-Intensity Progressive Resistance Training (PRT) in Type 2 Diabetes
While not a therapy for T1D, the GREAT2DO study provides a robust methodology for a non-pharmacological intervention impacting glycemic control, measured via HbA1c.
- Study Design: A 12-month randomized, double-blind, sham-exercise controlled trial involving 103 older adults with type 2 diabetes [64].
- Training Protocol: The intervention group performed high-intensity, high-velocity progressive resistance training (PRT) three days per week using pneumatic resistance equipment. Exercises targeted large muscle groups, with intensity set at 80% of the one-repetition maximum and reassessed every 4 weeks. The sham exercise group used the same equipment with minimal, non-progressive resistance [64].
- Outcome Measures: The primary outcomes were changes in insulin resistance (HOMA2-IR) and HbA1c. Body composition was assessed using bioelectrical impedance analysis (BIA) for skeletal muscle mass and total fat mass, and computed tomography (CT) for visceral adipose tissue and mid-thigh muscle characteristics [64].
Visualizing Therapeutic Mechanisms and Research Workflows
Stem Cell Differentiation to Functional Beta Cells
The following diagram illustrates the multi-stage protocol for generating functional, insulin-producing cells from pluripotent stem cells, a core process behind therapies like zimislecel.
Pathway from Therapy to Clinical Outcomes
This flowchart outlines the causal pathway from cell transplantation to its primary physiological effects and resulting clinical outcomes in patients.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and evaluation of stem cell therapies for diabetes rely on a specific set of reagents and tools, as utilized in the cited studies.
Table 2: Key Research Reagent Solutions for Beta Cell Therapy Development
| Reagent / Material | Function in Research Context |
|---|---|
| Human Pluripotent Stem Cells (hPSCs) [1] | The starting raw material, with the potential to differentiate into any cell type, including pancreatic beta-like cells. |
| Differentiation Factor Cocktails [1] | A sequence of specific growth factors and signaling molecules (e.g., Activin A, Retinoic Acid) that direct hPSCs through the precise stages of pancreatic development. |
| Glucose Stimulation Assays | In vitro tests used to validate the functionality of derived beta-like cells by measuring insulin secretion in response to changing glucose concentrations. |
| C-peptide ELISA/EIA Kits | Essential for quantifying C-peptide levels in serum or culture medium, serving as a direct marker of endogenous insulin production in both preclinical and clinical settings [64] [1]. |
| Immunosuppressive Agents [22] | Drugs (e.g., ATG, MMF) used in clinical trials to prevent immune rejection of allogeneic cell transplants, critical for assessing the therapy's safety and efficacy balance. |
| HbA1c Clinical Assays [65] | Standardized, high-performance liquid chromatography (HPLC) or immunoassays for measuring glycated hemoglobin, the key primary endpoint for evaluating long-term glycemic control. |
Discussion and Future Directions
The 12-month data for stem cell-derived islet cell therapy demonstrates its transformative potential, with a majority of patients achieving insulin independence and all attaining excellent glycemic control [22]. This represents a significant advance over the standard of care. However, challenges remain, including the need for chronic immunosuppression, the complexity of manufacturing, and the need for longer-term efficacy and safety data from larger, more diverse cohorts [1]. Future research will focus on optimizing differentiation protocols to achieve complete beta cell maturity, developing novel encapsulation devices to avoid immunosuppression, and conducting larger Phase 3 trials to confirm these promising interim results.
The therapeutic landscape for type 1 diabetes (T1D) is evolving beyond conventional pharmacotherapy (insulin) towards two advanced, technology-driven approaches: Automated Insulin Delivery (AID) systems and beta-cell replacement therapies. The table below provides a high-level quantitative comparison of their performance based on recent clinical evidence.
| Therapeutic Approach | Key Efficacy Metric (vs. Control) | Mechanism of Action | Stage of Development | Notable Considerations |
|---|---|---|---|---|
| AID Systems (AHCL) | TIR: +24.1% (vs. pump therapy) [66] [67] [68] | Hybrid-closed loop algorithm automating insulin delivery via pump and CGM [69] [70] | Clinically available | Requires patient intervention for mealtime boluses; minimal impact on severe hypoglycemia awareness [71] |
| Stem Cell-Derived Beta Cells | C-peptide: ≥0.1 nmol/L achieved in 3 of 10 patients; TIR: 55% to 85% in top responder [18] | Subcutaneous implantation of encapsulated pancreatic endoderm cells that mature into glucose-responsive, insulin-secreting cells [18] | Phase 1/2 Clinical Trials | Requires immunosuppression; efficacy is variable and dependent on achieved functional beta cell mass [18] |
| Islet Transplantation (Allogenic) | Insulin Independence: >50% of patients at 5 years; normalizes counter-regulatory hormone response to hypoglycemia [71] | Infusion of donor-derived islets into the liver via the portal vein [71] | Established clinical therapy (limited use) | Requires lifelong immunosuppression; limited by donor organ availability [71] |
Detailed Efficacy Analysis of AID Systems
Automated Insulin Delivery (AID) systems, also known as artificial pancreas systems, combine a continuous glucose monitor (CGM), an insulin pump, and a control algorithm to automate insulin dosing. They are categorized as Hybrid Closed-Loop (HCL), which require user-input for mealtime boluses, or the more advanced Advanced HCL (AHCL) and Full Closed-Loop (FCL) systems [69] [66].
Quantitative Performance Data from Meta-Analyses
Recent large-scale meta-analyses provide robust, quantitative evidence of the efficacy of AID systems. The following table consolidates key glycemic outcomes from these comprehensive reviews.
| Glucose Metric | AID System Type | Improvement vs. Control (95% CI) | Certainty of Evidence |
|---|---|---|---|
| Time in Range (TIR)(70-180 mg/dL) | AHCL | +24.1% (18.2% to 29.9%) [66] [68] | Moderate [66] [68] |
| HCL | +19.7% (13.2% to 26.1%) [66] | Moderate [66] | |
| FCL | +25.5% (11.1% to 39.9%) [66] | High [66] | |
| All AID (Pooled) | +11.74% (9.37% to 14.12%) [69] [70] | N/A | |
| Time Above Range (TAR)(>180 mg/dL) | AHCL | -19.6% (-25.1% to -14.0%) [66] [67] | Moderate [66] |
| Time Below Range (TBR)(<70 mg/dL) | All AID | Overall effect uncertain; benefit most pronounced in patients with long disease duration (≥20 years) [69] [67] | Very Low to Low [66] |
Experimental Protocols for AID System Evaluation
The evidence in the table above is derived from outpatient randomized controlled trials (RCTs) with specific methodological standards [66] [68]:
- Population: Individuals with T1D across all age groups.
- Intervention & Comparator: AID systems (HCL, AHCL, FCL) are tested against other insulin therapies like multiple daily injections (MDI) or insulin pump therapy.
- Duration: Intervention periods are typically 3 weeks or longer.
- Primary Outcome: Percentage of Time in Range (TIR 70-180 mg/dL) measured by Continuous Glucose Monitoring (CGM).
- Data Synthesis: Network meta-analyses pool data from dozens of RCTs (e.g., 46 studies with 4,113 participants) to compare treatments, using the Cochrane Risk of Bias tool and GRADE framework to assess evidence certainty [66].
Emerging Paradigm: Stem Cell-Derived Beta Cell Replacement
Beta cell replacement therapy aims to restore the body's natural, physiological insulin secretion. While islet transplantation from deceased donors is an established but limited procedure, stem cell-derived beta cells represent a potentially unlimited source for transplantation [18] [1].
Key Clinical Trial Data and Protocols
A pivotal phase 1/2 trial (NCT03163511) investigated the safety and efficacy of encapsulated pancreatic endoderm cells (PEC-01) derived from human embryonic stem cells [18].
- Cell Source & Device: PEC-01 cells were loaded into macro-encapsulation devices with a perforated membrane to allow vascular ingrowth.
- Implantation & Immunosuppression: Devices were implanted subcutaneously. Unlike fully encapsulated cells, the perforations require recipients to be on immunosuppression (anti-thymocyte globulin, mycophenolate mofetil, and tacrolimus) [18].
- Primary Endpoint: Stimulated plasma C-peptide level ≥0.1 nmol/L at month 6, a threshold for metabolic significance.
Interim 1-Year Outcomes (N=10) [18]:
- Engraftment Success: 4 of 10 recipients had detectable C-peptide at month 6.
- Glycemic Impact: 3 of these 4 achieved C-peptide ≥0.1 nmol/L. The top responder saw TIR increase from 55% to 85% and a significant reduction in insulin dosing.
- Limitation: Quantitative analysis of a sentinel device from the top responder showed that the beta cell mass was only 4% of the initial implanted cell mass, indicating significant room for improving cell survival and maturation.
The Research Toolkit for Stem Cell-Derived Therapies
The following table details essential reagents and materials used in this cutting-edge field.
| Research Reagent / Material | Function in Development & Therapy |
|---|---|
| Human Pluripotent Stem Cells (hPSCs) | The starting raw material; can be embryonic stem cells or induced pluripotent stem cells (iPSCs) reprogrammed from adult tissues [1]. |
| PEC-01 Pancreatic Endoderm Cells | The differentiated cell product implanted; these cells are designed to further mature into insulin-producing beta cells in vivo [18]. |
| Macroencapsulation Device | A retrievable, permeable container that houses the cells, providing a physical barrier against immune attack while allowing nutrient and oxygen exchange [18]. |
| Immunosuppressive Regimen | A drug cocktail (e.g., ATG, MMF, Tacrolimus) required in some protocols to prevent rejection of the implanted cells, especially with perforated devices [18]. |
| Anti-thymocyte globulin (ATG) | An immunosuppressive drug used for induction therapy to deplete T-cells at the time of transplantation [18]. |
Critical Comparative Analysis
Mechanisms and Clinical Implications
The fundamental difference between these therapies dictates their clinical profiles. AID systems are a device-driven, external management strategy that improves upon manual insulin delivery. In contrast, cell replacement is a biologic, disease-modifying strategy that seeks to restore the body's endogenous insulin production system [71].
This distinction leads to key clinical trade-offs:
- Hypoglycemia Awareness: Islet transplantation has been shown to restore the physiological glucagon response and normalize counter-regulatory defenses against hypoglycemia, benefits that current single-hormone AID systems do not provide [71].
- Risk Profile: AID systems involve the risks of device use but avoid the significant risks associated with the immunosuppression required for most cell therapies, such as increased susceptibility to infections and drug toxicity [71].
- Accessibility & Scalability: AID systems are widely available, whereas cell therapies are limited by donor availability (islet transplants) or are still experimental (stem cell-derived cells).
Future Directions
Both fields are rapidly advancing. Next-generation AID systems are exploring the use of glucagon (dual-hormone systems) to better prevent hypoglycemia and fully closed-loop algorithms that may eliminate the need for meal announcements [69]. For cell therapies, the focus is on improving the survival and function of implanted cells, developing immune-protective encapsulation devices to eliminate the need for immunosuppression, and scaling up manufacturing [18].
Stem cell-derived beta cell (SC-β) therapy represents a paradigm shift in the treatment of Type 1 Diabetes (T1D), moving beyond symptomatic management with exogenous insulin toward a potential biological cure. By replacing the insulin-producing cells destroyed by autoimmunity, this approach aims to restore the body's innate glucose-responsive insulin secretion [1] [21]. Preclinical studies have demonstrated the ability of human pluripotent stem cells (hPSCs), including both embryonic and induced pluripotent stem cells, to differentiate into pancreatic progenitors and, ultimately, functional insulin-producing β-like cells [72]. These developments have paved the way for human clinical trials. However, the translation of these promising findings into reliable and safe clinical therapies is constrained by three critical limitations: significant inter-patient variability in efficacy, questions surrounding the long-term durability of the cellular implants, and substantial safety trade-offs primarily related to immunogenicity and the requirement for immunosuppression [1] [18] [21]. This critical appraisal synthesizes current clinical evidence to objectively evaluate these constraints, providing a comparative analysis for research professionals in the field.
Inter-patient Variability in Therapeutic Efficacy
A foremost challenge in SC-β cell therapy is the inconsistent engraftment and functional outcomes observed across recipients. Despite receiving comparable cell products and undergoing standardized transplantation protocols, patients exhibit a wide spectrum of metabolic responses.
Clinical Evidence of Variable Outcomes
Interim results from a phase 1/2 trial of encapsulated pancreatic endoderm cells (PEC-01) revealed stark efficacy differences among participants. In this cohort, only 4 out of 10 patients achieved the primary endpoint of detectable meal-stimulated C-peptide at 6 months post-transplant. Among these responders, only three attained C-peptide levels ≥0.1 nmol/L, a threshold considered metabolically significant, and demonstrated measurable improvements in glycemic control [18]. The patient with the best response (Case 1) achieved a C-peptide level of 0.23 nmol/L, which was associated with a dramatic increase in time-in-range (TIR) from 55% to 85%. In contrast, other recipients in the same trial showed minimal or no C-peptide production, underscoring a high degree of inter-patient variability that cannot be fully explained by baseline patient characteristics [18].
Table 1: Summary of Efficacy Outcomes from Key Clinical Trials
| Trial / Study | Cell Type / Product | Sample Size | Responders (C-peptide+) | Metabolically Significant Response (C-peptide ≥0.1 nmol/L) | Key Efficacy Notes |
|---|---|---|---|---|---|
| Schulze et al., 2024 [18] | PEC-01 (Pancreatic Endoderm Cells) in optimized device | 10 | 4/10 (40%) | 3/10 (30%) | 1 patient achieved 85% TIR; insulin dose reduced in responders. |
| Ramzy et al., 2021 [1] | PEC-01 cells | 15 | Not fully reported | Not fully reported | Meal-responsive C-peptide increased; insulin requirements reduced by 20%. |
| Wang et al., 2024 [1] | Autologous CiPSC-islets | 1 | 1/1 (100%) | 1/1 (100%) | Achieved insulin independence on day 75; HbA1c ≤ 5.7%. |
| Dantas et al., 2020 [1] | Adipose-derived Stromal/Stem Cells (ASC) + Vitamin D | 7 (ASC+Vit D) | 7/7 (100% for honeymoon phase) | Not assessed | 100% in honeymoon phase at 6 months vs. 50% in controls; improved basal C-peptide. |
Underlying Factors Contributing to Variability
The heterogeneity in patient responses is multifactorial. Analysis of explanted devices points to variable graft survival and composition as a primary driver. In one high-performing case, the functional β-cell mass at month 6 was a mere 4% of the initially implanted cell mass, and β-cells constituted only 3% of all cells within the device—a fivefold lower proportion than α-cells (16%) [18]. This suggests that inefficient final differentiation and maturation post-transplant are key limitations. Furthermore, the host foreign body response (FBR) and the degree of peri-device fibrotic encapsulation can create a hypoxic microenvironment, impairing nutrient diffusion and compromising cell viability [21]. The success of the single patient treated with autologous chemically induced iPSC-derived islets (CiPSC-islets) also hints at the significant role of allogeneic immune responses, even with immunosuppression, in contributing to variable graft outcomes [1].
Durability and Long-Term Function
The ability of SC-β cell grafts to sustain insulin production over many years is a fundamental requirement for a viable therapy, yet long-term data remains sparse and the existing evidence raises concerns.
Evidence of Waning Function
While the phase 1/2 trial of PEC-01 cells demonstrated that C-peptide production could be maintained in responders for the 12-month follow-up period, functional analysis indicated potential strain on the grafts [18]. In the top responder (Case 1), a prolonged mixed-meal tolerance test at month 12 revealed that the β-cell mass could not correct hyperglycemia. The observed progressive decline in C-peptide levels during sustained activation, coupled with an elevated proinsulin-to-insulin ratio, indicated low cellular hormone reserves—a sign of an overworked and potentially insufficient β-cell mass [18]. This suggests that the current grafts, while functional, may be operating at their maximum capacity and are vulnerable to exhaustion over time.
Challenges to Long-Term Survival
The durability of SC-β cells is threatened by several factors. Recurrence of autoimmunity is a principal theoretical risk; the new β-cells remain susceptible to the same autoimmune attack that destroyed the patient's native islets [21]. The persistent senescent and pro-fibrotic environment around the encapsulation device can gradually erode graft function. Moreover, the functional immaturity of SC-β cells compared to primary human islets, including differences in insulin content, secretory capacity, and metabolic signaling, may render them less resilient to metabolic stresses in the long run [72].
Safety Trade-offs: Immunogenicity and Device-Related Complications
The safety profile of SC-β cell therapies is defined by a trade-off between achieving metabolic control and accepting risks associated with immunosuppression or device implantation.
The Immunosuppression Dilemma
Most advanced clinical trials using allogeneic cells require concurrent immunosuppression to prevent graft rejection. The regimen often includes drugs like anti-thymocyte globulin (ATG), mycophenolate mofetil (MMF), and tacrolimus, which are associated with well-documented risks [1] [18]. These include increased susceptibility to infections, potential renal toxicity, and other metabolic side effects. In one trial, treatment-emergent serious adverse events (TESAEs) were attributable to the surgical procedure and the protocol-specified immunosuppression [18]. This creates a significant trade-off for patients, exchanging the burden of daily insulin therapy for the risks and monitoring required by long-term immunosuppression [21].
Device and Cell-Related Safety Concerns
Encapsulation devices, designed to protect cells without systemic immunosuppression, introduce their own challenges. The most common adverse event is procedural pain at the implantation site [18]. More critically, devices can provoke a foreign body response, leading to fibrotic overgrowth that limits oxygen and nutrient diffusion, ultimately starving the encapsulated cells [21]. From a cellular standpoint, the risk of teratoma formation from residual undifferentiated pluripotent cells, though a primary safety concern in preclinical development, was not observed in the reported trials [1] [18]. Other potential risks include graft overgrowth and the need for explantation.
Comparative Analysis of Therapeutic Approaches
The limitations of SC-β cell therapy are best understood in the context of existing and emerging treatments for T1D. The table below provides a direct comparison based on key parameters.
Table 2: Comparison of Therapeutic Approaches for Type 1 Diabetes
| Therapeutic Approach | Mechanism of Action | Efficacy (Glycemic Control) | Key Limitations | Immunosuppression Required? |
|---|---|---|---|---|
| Exogenous Insulin | Substitution therapy via injection/pump | Prevents DKA but often suboptimal TIR | Risk of hypoglycemia; does not prevent complications; high burden of disease management. | No |
| Whole Pancreas Transplant | Replaces entire insulin-producing organ | High; can achieve insulin independence | Highly invasive surgery; limited organ availability; significant surgical risks. | Yes |
| Donor Islet Transplantation | Replaces insulin-producing cells | High; can achieve insulin independence | Extremely limited donor supply; declining function over time. | Yes |
| SC-β Cells (Open Device) | Replaces insulin-producing cells | Variable; limited evidence of insulin independence | Inter-patient variability; potential for fibrosis; requires immunosuppression. | Yes |
| SC-β Cells (Encapsulated) | Replaces insulin-producing cells | Limited by device failure and hypoxia | Significant foreign body response; insufficient vascularization; low cell survival. | No |
| Autologous SC-β Cells | Replaces insulin-producing cells | Promising in first case report [1] | Complex, costly, and lengthy manufacturing; potential autoimmune recurrence. | No (Theoretically) |
Methodologies and Research Toolkit
Key Experimental Protocols
The progression of SC-β cell therapy from bench to bedside relies on standardized, complex protocols.
- In Vitro Differentiation of hPSCs: The most successful protocols involve a multi-stage process mimicking embryonic pancreatic development. This typically begins with definitive endoderm induction using Activin A, followed by sequential patterning into primitive gut tube, posterior foregut, pancreatic progenitor (PDX1+/NKX6.1+), and endocrine precursor stages, finally maturing into glucose-responsive β-like cells [21] [72]. This process can take from 2 to over 6 weeks in culture.
- Preclinical Animal Testing: Differentiated cells are typically transplanted into immunocompromised diabetic mouse models (e.g., SCID-beige or NSG mice rendered diabetic with streptozotocin). The gold standard for the functional assessment is the reversal of diabetes, measured by the restoration of normoglycemia. Further validation includes intraperitoneal glucose tolerance tests (IPGTTs) and the measurement of human C-peptide in the blood [72].
- Clinical Trial Endpoints: Primary endpoints in early-phase trials often focus on safety and proof-of-concept. Efficacy is measured by the emergence of meal-stimulated plasma C-peptide, changes in HbA1c, insulin requirements, and CGM metrics like Time-in-Range (TIR) [1] [18]. Insulin independence is the ultimate efficacy endpoint but is rarely achieved in initial trials.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials in SC-β Cell Research
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| Human Pluripotent Stem Cells (hPSCs) | Starting cell population capable of unlimited self-renewal and differentiation into any cell type. | hESC lines (e.g., CyT49) or patient-specific hiPSCs are used as the source for differentiation protocols [18] [72]. |
| Activin A | A TGF-β family growth factor used to direct differentiation toward definitive endoderm. | Critical first step in most differentiation protocols to establish the correct developmental lineage [72]. |
| Small Molecule Inducers | Chemicals that modulate key signaling pathways to steer cell fate. | Used to inhibit or activate pathways like BMP, TGF-β, and Retinoic Acid to pattern cells into pancreatic progenitors [72]. |
| Encapsulation Device | A physical container (e.g., macroencapsulation device) that houses the transplanted cells. | Used to protect allogeneic cells from immune attack and to allow for retrievability [18] [21]. |
| Immunosuppressive Regimen | A combination of drugs to suppress the host immune system and prevent graft rejection. | Used in trials with "open" or non-immunoprotective devices (e.g., ATG, MMF, Tacrolimus) [1] [18]. |
Visualizing the Clinical Translation Pathway
The journey from stem cell to clinical therapy involves a defined sequence of steps, each with its own challenges and decision points, as outlined below.
Stem cell-derived beta cell therapy stands at a promising but challenging crossroads. Clinical trials have unequivocally demonstrated proof-of-concept that hPSCs can be differentiated into cells capable of producing physiologically relevant insulin in humans [1] [18]. However, the widespread application of this therapy is currently hampered by the significant inter-patient variability in engraftment success, unresolved questions about the long-term durability of the grafts, and the considerable safety trade-offs posed by immunosuppression or device-related complications. Overcoming these hurdles requires a multi-pronged research strategy. Future efforts must focus on optimizing differentiation protocols to generate more mature and resilient β-cells, developing next-generation encapsulation devices that promote enhanced vascularization and minimize the foreign body response, and pioneering immune-evading or autologous cell lines to eliminate the need for lifelong immunosuppression [21] [72]. For researchers and drug developers, the path forward lies in systematically addressing these limitations through rigorous preclinical modeling and innovative clinical trial designs that prioritize long-term follow-up and detailed analysis of both responder and non-responder populations.
Conclusion
Stem cell-derived beta cell therapy has unequivocally transitioned from a scientific concept to a clinically validated intervention, with recent trials demonstrating robust efficacy in restoring insulin independence and physiologic glycemic control in T1D. However, the path to a widely accessible cure necessitates overcoming significant final-mile challenges. The foremost hurdles remain the requisite for chronic immunosuppression, the high cost and complexity of manufacturing, and ensuring long-term graft durability and safety. Future research must prioritize the development of reliable immune evasion strategies, such as hypoimmune engineering, and scalable, cost-effective production platforms. The collaborative focus for the scientific community should be on transforming this remarkable 'Apollo mission' achievement into a viable 'lunar colonization' effort, ensuring this transformative therapy can reach the millions of patients who stand to benefit.
References
- 1. Stem cell-derived pancreatic beta cells - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265369/]
- 2. Islet Cell Replacement and Regeneration for Type 1 Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906537/]
- 3. A New Era in Islet Transplantation: Stem Cell-Derived and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620690/]
- 4. The Last Mile in Beta-Cell Replacement Therapy for Type 1 ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14565/full]
- 5. Pancreatic islet transplantation: current advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1391504/full]
- 6. Engineering hypoimmune stem cell-derived beta cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04745-0]
- 7. Stem Cell-Derived, Fully Differentiated Islets for Type 1 ... [https://pubmed.ncbi.nlm.nih.gov/40544428/]
- 8. From stem cells to therapeutics: Advancing islet function ... [https://www.sciencedirect.com/science/article/pii/S1570180825001514]
- 9. Developments in stem cell-derived islet replacement therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10167558/]
- 10. Stem Cell-Derived Islet Therapies Shown to Reduce the ... [https://diabetes.org/newsroom/press-releases/stem-cell-derived-islet-therapies-shown-reduce-need-injectable-insulin]
- 11. Improving cellular fitness of human stem cell-derived islets ... [https://www.nature.com/articles/s41467-025-59924-7]
- 12. Immune Protection of Stem Cell-Derived Islet Cell Therapy ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.716625/full]
- 13. Insulin independence from stem-cell-derived islets [https://www.nature.com/articles/s41551-024-01331-2]
- 14. Type 1 diabetes cured in mice with gentle blood stem-cell and ... [https://med.stanford.edu/news/all-news/2025/11/type-1-diabetes-cure.html]
- 15. C‐peptide determination in the diagnosis of type of diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9543865/]
- 16. A Practical Review of C-Peptide Testing in Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC5446389/]
- 17. Recent advances in stem cell-based therapies for type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12499549/]
- 18. Encapsulated stem cell–derived β cells exert glucose ... [https://www.nature.com/articles/s41587-023-02055-5]
- 19. Advances and future perspectives in the treatment ... [https://www.frontiersin.org/journals/clinical-diabetes-and-healthcare/articles/10.3389/fcdhc.2025.1651061/full]
- 20. Top Type 1 Diabetes Research Breakthroughs to Watch in ... [https://www.type1strong.org/blog-post/top-type-1-diabetes-research-breakthroughs-to-watch-in-2025]
- 21. Current status of stem cell therapy for type 1 diabetes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03636-0]
- 22. Vertex Presents Positive Data for Zimislecel in Type 1 ... [https://news.vrtx.com/news-releases/news-release-details/vertex-presents-positive-data-zimislecel-type-1-diabetes]
- 23. EASD 2025: Zimislecel infusion advances insulin ... [https://www.pharmaceutical-technology.com/analyst-comment/easd-2025-zimislecel-infusion-insulin-t1d/]
- 24. Materials approaches for next-generation encapsulated ... [https://link.springer.com/article/10.1557/s43579-024-00678-6]
- 25. Methods and Approaches for Capturing Post-Approval ... [https://www.asgct.org/advocacy/policy-statements/methods-and-approaches-for-capturing-post-approval-safety-and-efficacy-data-on-cgt-products-listening-session]
- 26. Evaluation of Immunosuppression Levels and Risk of Graft ... [https://pubmed.ncbi.nlm.nih.gov/40043847/]
- 27. 462 A Comparison of Early Immune Reconstitution Post ... [https://www.sciencedirect.com/science/article/pii/S2666636725005391]
- 28. Tolerance Induction Strategies in Organ Transplantation [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14958/full]
- 29. Indications for haematopoietic cell transplantation and ... [https://www.nature.com/articles/s41409-025-02701-3]
- 30. Hypoimmune stem cells and islets: hype or a true ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492583/]
- 31. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 32. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614637/]
- 33. Expansion of clinical trial eligibility criteria - NCI [https://dctd.cancer.gov/research/research-areas/clinical-trials/modernization/criteria-expand-trial-eligibility]
- 34. The Challenge of Patient Enrollment in Clinical Trials [https://www.ncoda.org/news/the-challenge-of-patient-enrollment-in-clinical-trials/]
- 35. CTTI Recommendations: Use of Real-World Data to Plan ... [https://ctti-clinicaltrials.org/about/ctti-projects/real-world-data/ctti-recommendations-use-of-real-world-data-to-plan-eligibility-criteria-and-enhance-recruitment/]
- 36. a randomized pragmatic clinical trial [https://pubmed.ncbi.nlm.nih.gov/41093600/]
- 37. KERENDIA® (finerenone) Meets Primary Endpoint in ... [https://www.bayer.com/en/us/news-stories/kerendia-for-type-1-diabetes-and-chronic-kidney-disease]
- 38. Cell Therapy for Type 1 Diabetes: Vertex Trial Results and ... [https://news.syenza.com/zimislecel-type-1-diabetes-trial-results/]
- 39. Finally, a possible long-term treatment for type 1 diabetes [https://www.ucihealth.org/blog/2020/03/diabetes-clinical-trial]
- 40. Drug-induced regeneration of pancreatic beta cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413367/]
- 41. Stem cells differentiation into insulin-producing cells (IPCs) [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02977-y]
- 42. 2024 T1D Practical Cure Projects in Human Trials [https://www.thejdca.org/publications/report-library/archived-reports/2024-reports/2024-t1d-practical-cure-projects-in-human-trials.html]
- 43. Encapsulation vs. Naked Cell Therapy—Immune ... [https://www.adameetingnews.org/encapsulation-vs-naked-cell-therapy-immune-challenges-and-beta-cell-perspectives-in-diabetes-treatment/]
- 44. Encapsulation and Immune Protection for Type 1 Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10948298/]
- 45. Immune-evasive beta cells in type 1 diabetes [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1618086/full]
- 46. Developments in stem cell-derived islet replacement ... [https://www.sciencedirect.com/science/article/pii/S1934590923001200]
- 47. Innovative immunotherapies and emerging treatments in ... [https://www.sciencedirect.com/science/article/pii/S2666970624000519]
- 48. Immunosuppression in islet transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2323197/]
- 49. Clinical Immunologic Interventions for the Treatment of Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405831/]
- 50. Side Effects of Stem Cell Therapy [https://www.dvcstem.com/post/stem-cell-therapy-safe]
- 51. Adverse events, side effects and complications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9659480/]
- 52. Towards effective beta-cell replacement through ... [https://www.sciencedirect.com/science/article/pii/S2468498821000202]
- 53. Challenges of CRISPR/Cas-Based Cell Therapy for Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10743607/]
- 54. Hope for diabetes: CRISPR-edited cells pump out insulin in ... [https://www.nature.com/articles/d41586-025-02802-5]
- 55. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 56. New transplant approach resets the immune system to stop ... [https://www.news-medical.net/news/20251118/New-transplant-approach-resets-the-immune-system-to-stop-Type-1-diabetes.aspx]
- 57. Scientists just made CRISPR three times more effective [https://www.sciencedaily.com/releases/2025/09/250907024543.htm]
- 58. Advances and challenges of the cell-based therapies among ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05226-3]
- 59. The future of islet transplantation beyond the BLA approval [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925927/]
- 60. Efficacy and Safety of Allogeneic Islet Transplantation ... [https://pubmed.ncbi.nlm.nih.gov/39936131/]
- 61. Allogeneic Islet Transplantation: Chronicle of a Death Foretold? [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14598/full]
- 62. UI Health performs first islet cell transplant with Lantidra [https://today.uic.edu/ui-health-performs-first-islet-cell-transplant-with-lantidra/]
- 63. From Edmonton to Lantidra and beyond [https://www.frontiersin.org/journals/transplantation/articles/10.3389/frtra.2025.1514956/full]
- 64. Changes in Insulin Resistance and HbA1c Are Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3714491/]
- 65. Significance of HbA Test in Diagnosis and Prognosis of Diabetic... 1 c [https://pmc.ncbi.nlm.nih.gov/articles/PMC4933534/]
- 66. Efficacy of automated insulin delivery systems in people with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12017971/]
- 67. Type 1 Diabetes and AID Systems: Meta-Analysis Proves Eff [https://www.dzd-ev.de/en/press/press-releases/press-releases-2025/type-1-diabetes-and-aid-systems-meta-analysis-proves-eff]
- 68. Efficacy of automated insulin delivery systems in people ... [https://www.sciencedirect.com/science/article/pii/S2589537025001221]
- 69. Efficacy and Safety of Automated Insulin Delivery Systems in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960199/]
- 70. Efficacy and Safety of Automated Insulin Delivery Systems ... [http://e-dmj.org/journal/view.php?doi=10.4093/dmj.2024.0130]
- 71. Physicians debate the comparative benefits of smart insulin ... [https://www.adameetingnews.org/physicians-debate-the-comparative-benefits-of-smart-insulin-delivery-and-pancreatic-cell-transplant/]
- 72. recent advances towards stem cell-derived islets - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6925596/]