Strategic Frameworks for Consistent Quality in Autologous Cell Therapy Manufacturing
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on establishing robust strategies to ensure consistent quality in autologous cell therapies.
Strategic Frameworks for Consistent Quality in Autologous Cell Therapy Manufacturing
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on establishing robust strategies to ensure consistent quality in autologous cell therapies. It explores the foundational challenges posed by patient-specific starting materials, details advanced methodological solutions like automation and decentralized manufacturing, addresses critical troubleshooting for supply chain and expansion, and outlines rigorous validation and comparability frameworks. By synthesizing current technological innovations and regulatory perspectives, this resource aims to support the scalable production of safe, efficacious, and reliable personalized cell therapies.
Understanding the Unique Quality Challenge: The Variable Nature of Autologous Starting Materials
For researchers developing autologous cell therapies, the inherent variability of patient-derived cellular starting material is a fundamental and pervasive challenge. Unlike traditional pharmaceuticals or allogeneic therapies that use controlled donor material, autologous therapies must contend with the biological reality that every patient's cells are unique. This variability, stemming from factors like the patient's disease state, prior treatments, and individual biology, directly impacts the manufacturing consistency, product quality, and ultimately, the reproducibility of experimental and clinical outcomes [1] [2].
Success in this field depends on moving from simply observing variability to actively managing it. This guide provides targeted troubleshooting advice and strategies to help you identify, quantify, and control the variability in your starting materials, thereby building a more robust foundation for your autologous therapy research.
Quantifying the Variability: Key Data for the Researcher
A critical first step is understanding the scope and scale of inherent variability. The following tables summarize key quantitative findings that illustrate this challenge, providing a benchmark for your own experimental data.
Table 1: Variability in Leukapheresis Collections from Healthy Donors
This data, derived from over 2,000 leukapheresis procedures, demonstrates the inherent variability even in starting material from healthy donors, highlighting a fundamental challenge for process development [2].
| Cell Population | Observed Range | Implication for Research & Development |
|---|---|---|
| Total White Blood Cell Yield | < 5 billion to > 30 billion cells | Impacts scale of manufacturing; may necessitate process scaling or result in insufficient yield for target dose. |
| CD3+ T Cell Percentage | High donor-to-donor variation | Affects efficiency of T-cell focused processes (e.g., CAR-T); can lead to inconsistency in initial cell input. |
| NK Cell Percentage | High donor-to-donor variation | Influences the final product's cellular composition, potentially affecting product phenotype and function. |
| B Cell Percentage | High donor-to-donor variation | Can be a critical contaminant in T-cell products; variability requires robust purification methods. |
Table 2: Impact of Variability on Critical Quality Attributes (CQAs)
Variability in the starting material can propagate through the entire manufacturing process, affecting key quality attributes of the final drug product [3] [4].
| Critical Quality Attribute (CQA) | Impact of Starting Material Variability | Common Assessment Methods |
|---|---|---|
| Cell Identity/Phenotype | Donor-specific immune cell subset ratios can shift during expansion, affecting final product composition [4]. | Flow cytometry, transcriptional fingerprinting (RNA-seq) [4]. |
| Potency/Functionality | Variations in initial T cell fitness can lead to differences in expansion potential and final cytotoxic or suppressive activity [3]. | Functional assays (e.g., tumor cell killing, suppression assays), cytokine secretion profiles [4]. |
| Viability and Expansion Capacity | Health of the patient's cells at collection can dictate maximum achievable expansion and final cell viability [3] [5]. | Cell counting (viability dyes), metabolic activity assays, cumulative population doublings. |
Troubleshooting Guides & FAQs
This section addresses specific, high-frequency problems researchers encounter due to starting material variability.
FAQ 1: How can we account for extreme donor-to-donor variability in our experimental results?
The Challenge: Your in vitro potency or expansion data shows high standard deviations, making it difficult to draw statistically significant conclusions about process changes or product efficacy.
Solution Strategy:
- Strategic Donor Sourcing: Whenever possible, utilize repeatable, recallable donor sources for your non-clinical studies. This allows you to select donors with specific biological characteristics (e.g., high CD3+ percentage) that best fit your process, improving consistency [2].
- Increase Sample Size: Power your experiments with a sufficient number of biological replicates (n) from diverse donors to adequately capture and account for expected population variability.
- Implement Robust Controls: Include a standardized control (e.g., cells from a characterized donor or cell line) in every experiment to benchmark performance and separate process-related effects from donor-related effects.
- Data Stratification: Post-experiment, stratify your data based on key starting material attributes (e.g., pre-apheresis lymphocyte count, donor age). This can reveal correlations and help define critical material specifications [2].
FAQ 2: Our cell expansion yields are inconsistent. What are the key factors to control?
The Challenge: The fold-expansion of T cells or other therapeutic cells varies significantly between batches, leading to unpredictable final cell counts.
Solution Strategy:
- Standardize Cell Activation: Ensure consistency in activation methods. The type (soluble vs. bead-bound antibodies), concentration, and timing of activation stimuli (e.g., anti-CD3/CD28) are critical. Use GMP-grade reagents to minimize batch-to-batch reagent variability [3] [6].
- Optimize Culture Media: Systemically test and qualify basal media and serum/serum-free supplements. Monitor metabolite consumption (e.g., glucose, glutamine) to understand metabolic phenotypes and optimize feeding schedules [3].
- Control Cell Density: Maintain optimal cell seeding densities throughout the culture process. High or low densities can lead to premature senescence or suboptimal growth [3].
- Monitor Starting Material Health: Assess the viability and functional status of cells immediately after collection. A poor starting point often predicts a poor expansion outcome [5].
FAQ 3: What advanced methods can ensure the identity and stability of cell products like Tregs?
The Challenge: Traditional markers like FOXP3 for Tregs may be insufficient to guarantee a stable and functional identity after extensive ex vivo manipulation and expansion [4].
Solution Strategy:
- Go Beyond Surface Phenotyping: Implement transcriptional fingerprinting via bulk or single-cell RNA-seq. This method can define a precise, multi-gene "identity fingerprint" that distinguishes your target cell type from others (e.g., Tregs from effector T cells) with high sensitivity and specificity [4].
- Develop a Stability Fingerprint: Create a second transcriptional fingerprint that characterizes the expanded state of the cells, helping to ensure the manufacturing process does not drive them toward an undesired differentiation state [4].
- Correlate with Function: Use advanced bioinformatics to correlate these molecular fingerprints with the results of your in vitro potency assays (e.g., suppression assays). This creates a more comprehensive and predictive quality control profile than any single metric alone [4].
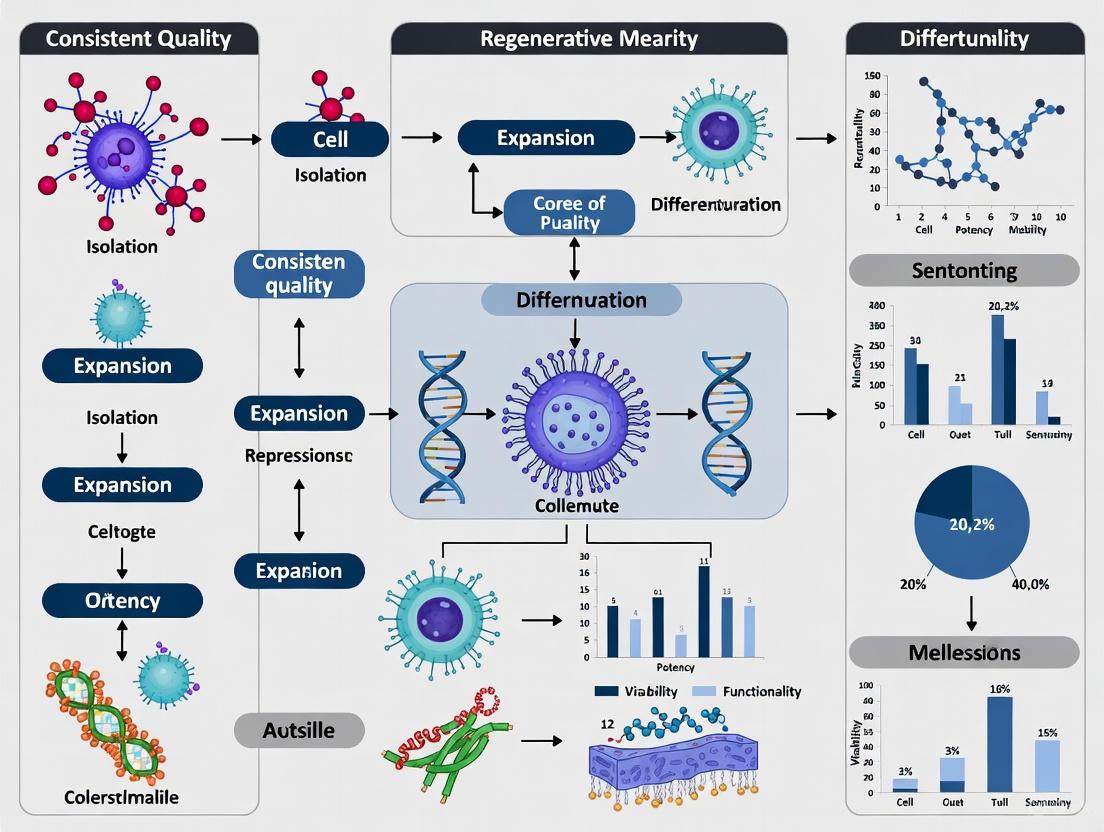
Diagram 1: A workflow for managing variability from starting material to final product, showing key control points and potential failure modes.
The Scientist's Toolkit: Essential Research Reagents & Materials
A robust research process requires high-quality, well-defined reagents. The following table details essential materials for developing autologous cell therapies, with a focus on mitigating variability.
Table 3: Key Research Reagent Solutions for Cell Therapy R&D
| Reagent/Material | Function & Application | Considerations for Reducing Variability |
|---|---|---|
| Cell Isolation Kits (e.g., MACS, FACS) | Isolate specific cell populations (e.g., CD4+ T cells, Tregs) from heterogeneous apheresis product [3]. | Use closed, automated systems to reduce contamination and operator-dependent variability. Validate recovery and purity for each cell type [6]. |
| Activation Reagents (e.g., anti-CD3/CD28 beads) | Activate T cells to initiate proliferation and enable genetic modification [3]. | Use GMP-grade, detachable beads for consistent stimulation strength and easy removal, minimizing carryover and batch effects [6]. |
| Cell Culture Media & Supplements | Provide nutrients and signaling molecules for cell survival, expansion, and differentiation [3]. | Use serum-free, xeno-free, chemically defined media to eliminate lot-to-lot variability introduced by animal sera. Pre-qualify cytokine supplements (e.g., IL-2) [3]. |
| Cryopreservation Media | Preserve cell viability and function during long-term storage and transport [3]. | Use controlled-rate freezing and standardized cryoprotectant concentrations (e.g., DMSO) to ensure consistent post-thaw recovery and functionality [3]. |
| Transcriptional Profiling Kits (RNA-seq) | Assess cell identity, purity, and stability via gene expression analysis [4]. | Implement standardized RNA extraction and library prep protocols. Use predefined gene signatures ("fingerprints") for objective quality scoring [4]. |
Experimental Protocol: Transcriptional Fingerprinting for Treg Identity
This protocol provides a detailed methodology for implementing transcriptional fingerprinting, an advanced strategy to ensure the quality of cell products like Tregs, as discussed in the troubleshooting section [4].
Objective: To molecularly characterize expanded Treg products and score them for stable identity and expansion-associated changes using bulk RNA-seq.
Materials:
- Purified Tregs (e.g., CD4+CD25hiCD127lo) and Teff cells (CD4+CD25loCD127hi) from PBMCs.
- FACS sorter.
- Cell culture reagents: CTS OpTmizer T Cell Expansion Media, anti-CD3/anti-CD28 Dynabeads.
- RNA stabilization solution and RNA extraction kit.
- Next-generation sequencing platform (e.g., Illumina).
- Computational tools for analysis (e.g., R, Python, with packages for ssGSEA or GSVA).
Methodology:
- Cell Isolation and Culture:
- Isolate PBMCs from leukapheresis product via Ficoll density gradient centrifugation.
- Sort Treg and Teff populations by FACS using defined surface markers.
- Culture sorted cells, activating them with anti-CD3/anti-CD28 Dynabeads and expanding for 14 days in optimized media.
RNA Sequencing:
- Sample Collection: Pellet at least 1x10^6 cells from both pre-expansion (D0) and post-expansion (D14) time points. Stabilize RNA immediately.
- RNA Extraction & QC: Extract total RNA. Ensure RNA Integrity Number (RIN) is ≥8.0 before proceeding.
- Library Prep & Sequencing: Construct Illumina-compatible mRNA libraries. Sequence to a minimum depth of 25 million paired-end 150bp reads per sample.
Computational Analysis & Fingerprint Scoring:
- Data Processing: Align raw sequencing reads (FASTQ) to a reference genome and generate a gene expression count matrix.
- Fingerprint Application: Apply a pre-defined, activation-independent Treg identity gene set to your data using a non-parametric algorithm (e.g., ssGSEA).
- Scoring: Generate two key scores for each sample:
- Identity Score: Measures how closely the sample's transcriptome aligns with a canonical Treg signature versus a Teff signature.
- Expansion Score: Characterizes the transcriptomic impact of the ex vivo expansion process.
- Validation: Correlate fingerprint scores with functional assay outcomes (e.g., in vitro suppression assays) to validate the biological relevance of the scores.
Diagram 2: Experimental workflow for transcriptional fingerprinting of Treg cell products.
Defining Critical Quality Attributes (CQAs) for Patient-Specific Products
FAQ: Understanding CQAs and Their Importance
What are Critical Quality Attributes (CQAs) in the context of autologous cell therapies?
Critical Quality Attributes (CQAs) are physical, chemical, biological, or microbiological properties or characteristics that must be within an appropriate limit, range, or distribution to ensure the desired product quality [7] [8]. For a living drug product like autologous cell therapy, CQAs are central to confirming the product's identity, purity, potency, safety, and viability [9]. They are defined early in the product development stage based on the desired Quality Target Product Profile (QTPP) [8].
Why is defining CQAs particularly challenging for patient-specific (autologous) products?
Unlike allogeneic (donor-derived) or conventional biopharmaceutical products, autologous therapies are manufactured starting with a patient's own cells. This presents unique challenges [7]:
- Variable Starting Material: You are "beholden to the quality of the patient cells." The patient's disease stage, previous therapies, and genetic background create inherent variability in the apheresis starting material, which is difficult to control [7] [10].
- Lack of "Fail-Safes": Cell therapies cannot undergo traditional pathogen removal steps like filtration or low pH inactivation, as these would kill the living cells. This makes in-process control and a strong understanding of CQAs even more critical for patient safety [7].
At what stages of the manufacturing process should CQAs be assessed?
Quality testing should be performed at multiple points to ensure control throughout the production journey [10]:
- Donor/Patient Testing: Medical history and infectious disease screening (though this is less critical for autologous products than allogeneic) [7] [10].
- Starting Material (Apheresis): Testing for cell concentration, viability, purity (e.g., via flow cytometry), identity, and sterility [10].
- In-Process Testing: Monitoring critical steps like cell expansion rates, transduction efficiency, and sterility during manufacturing [10] [8].
- Final Product (Lot Release) Testing: A comprehensive assessment of the final drug product against all specified CQAs, including potency, purity, identity, safety (sterility, endotoxin), and viability, before release for infusion [10] [9].
Troubleshooting Guide: Common CQA Challenges and Solutions
This guide addresses specific, frequently encountered issues when defining and measuring CQAs for autologous cell therapies.
Problem 1: High Variability in Starting Material
- Issue: The quality and composition of patient-derived apheresis material vary significantly from lot to lot, leading to inconsistent process performance and final product CQAs.
- Background: For autologous therapies, the ability to control the quality of the source material is limited. Some variability is inevitable due to the patient's disease and prior treatment history [7]. Consistency testing measures this lot-to-lot variability, which may be due to differences in the collection process or the patients themselves [10].
- Solution:
- Define Apheresis Parameters: Establish strict, specified limits for the collection procedure, including collection volume and the type of anticoagulant used [7].
- Implement Robust In-Process Controls (IPCs): Define IPC acceptance criteria for the starting material, such as minimum cell count and viability, before initiating the manufacturing process [8].
- Process Robustness: Design a manufacturing process that can tolerate a degree of input variability. Using high-quality raw materials and closed, automated processing equipment can help alleviate process variability [6].
Problem 2: Inconsistent Potency Assay Results
- Issue: The potency assay, which measures the biological activity of the product, yields inconsistent or irreproducible results, delaying product release.
- Background: Potency is a quantitative measure of the biological activity linked to the product's intended clinical effect [10]. It is one of the most important yet challenging CQAs [9]. For complex therapies like Treg cells, a single assay may be insufficient, as the product has a "poly-pharmaceutical nature" with multiple functions [11].
- Solution:
- Begin Development Early: Start developing and optimizing the potency assay well in advance, as it can take over 12 months to finalize [9].
- Use Multiple Complementary Assays: Instead of a single test, employ multiple assays that measure different product attributes associated with potency (e.g., cytolytic activity, suppressive cytokine production) [9] [11].
- Implement Controls: Always run appropriate positive and negative controls to qualify the assay performance and your sample [12].
Problem 3: Failure to Meet Viability or Purity CQAs at Final Product Release
- Issue: The final cell product has low viability or an unacceptable level of impurity cells (e.g., tumor cells in an apheresis product).
- Background: Viability and purity are critical for both safety and efficacy. Low viability may affect the dosage, while impurities can pose a patient safety risk [8]. Processes with many open, manual manipulations and shear stress from certain equipment can adversely affect cell health [7] [6].
- Solution:
- Optimize Manufacturing Equipment: Utilize low-shear, closed, and automated systems for cell processing to support high viability and minimize contamination risk [6].
- Define Purification Steps: Implement and validate robust cell isolation or enrichment techniques (e.g., magnetic bead-based selection or flow cytometry-based sorting) to ensure a pure population of the desired cell type [11].
- Establish Clear IPC Criteria: Monitor viability and purity at key in-process stages (e.g., after isolation, after expansion) to catch issues early and allow for process adjustments [8].
Problem 4: Lack of Process Understanding for Tech Transfer
- Issue: When transferring a process from research to a GMP facility or between sites, the product's CQAs change, indicating a lack of process understanding.
- Background: Translating from research-grade to clinical-grade manufacturing is challenging. A common mistake is moving too quickly without building strong GMP principles early on, which makes later tech transfer difficult and expensive [7] [8].
- Solution:
- Adopt a Quality-by-Design (QbD) Framework: Use a systematic approach early in development to link Critical Process Parameters (CPPs) to your CQAs. This builds process understanding and predictability [8].
- Utilize a GMP Simulation Unit: If available, work with a GMP simulation facility to bridge the gap between research and GMP production, allowing for process qualification and validation before full-scale GMP runs [8].
- Perform Comparability Testing: When scaling up or modifying a process, perform comparability testing to demonstrate that cells produced with the new method are equivalent to those produced with the original method in terms of critical quality attributes [10].
CQA and Process Parameter Tables for Autologous Therapy
The following tables provide a structured overview of common CQAs and their connections to the manufacturing process, using a CAR-T cell therapy as an example.
Table 1: Final Product Critical Quality Attributes (CQAs) and Testing Methods
| CQA Category | Specific Attribute | Justification & Impact | Common Testing Methods |
|---|---|---|---|
| Safety | Sterility, Mycoplasma, Endotoxin | Directly affects patient safety; required for release [10] [8]. | Microbial culture, PCR [10] [9]. |
| Vector Copy Number (VCN) | Addresses risk from insertional mutagenesis; affects safety [8] [9]. | ddPCR, qPCR [9]. | |
| Potency | Biological Activity (e.g., Cytolytic activity) | Confirms consistency, stability, and quality between lots; measures intended function [10] [8]. | Co-culture assays with target cells, cytokine release assays [8] [9]. |
| Purity & Identity | % Viable Cells | Low viability may affect the dosage given to the patient [8]. | Dye exclusion assays (e.g., Trypan Blue) [10]. |
| % CAR+ T-cells (Identity/Purity) | Ensures the product contains the engineered cells; affects dosage and consistency [8]. | Flow Cytometry [9]. | |
| Impurities (e.g., % Tumor Cells) | May affect patient safety and the dosage given [8]. | Flow Cytometry [8]. | |
| Quantity | Total Viable Cell Count & Dose | Determines the absolute number of cells for infusion [10]. | Automated cell counters, flow cytometry [10]. |
Table 2: Linking CQAs to Critical Process Parameters (CPPs) and In-Process Controls (IPCs)
| Critical Process Parameter (CPP) | Related CQA(s) | Justification | Recommended In-Process Control (IPC) [8] |
|---|---|---|---|
| Transduction Process | Identity (% CAR+ cells), Potency, Safety (VCN) | The efficiency of gene introduction is fundamental to product identity and function. | Transduction efficiency (e.g., Day 5), Vector Copy Number (e.g., Day 12) |
| Cell Culture Process | Viability, Potency, Purity | Culture conditions (media, duration, parameters) directly impact cell health, expansion, and function. | Cell count & viability (e.g., Day 5, Day 12), Cell morphology |
| Media Exchange / Formulation | Viability, Purity (ancillary materials) | The process of washing and formulating the final product impacts viability and removes impurities. | Viability (Final Product), Assessment of residual beads/reagents |
The Scientist's Toolkit: Essential Reagents & Materials
The following reagents and instruments are critical for developing and controlling the manufacturing process for autologous cell therapies.
Table 3: Key Research Reagent Solutions for CQA Assessment
| Reagent / Material | Function in CQA Assessment | Example & Notes |
|---|---|---|
| Cell Separation Beads | Isolation of specific cell populations (e.g., T-cells) from apheresis material to ensure purity [11]. | Magnetic beads conjugated with antibodies (e.g., anti-CD3/CD28) for activation and expansion [6]. |
| Cell Culture Media & Supplements | Supports cell expansion and maintenance of cell viability and potency during manufacturing. | Serum-free media formulations; use of supplements like rapamycin to maintain Treg phenotype during expansion [11]. |
| Viral Vectors | Genetic engineering of cells to introduce a CAR or other modifying genes, critical for product identity and potency. | Lentiviral or retroviral vectors; monitoring of transduction efficiency is a key IPC [8]. |
| Flow Cytometry Antibodies | Identity and purity testing by detecting surface and intracellular markers (e.g., CD3, CAR expression). | Essential for quantifying % CAR+ cells and characterizing cell phenotype at multiple stages [9]. |
| qPCR/ddPCR Reagents | Safety and identity testing, specifically for measuring Vector Copy Number (VCN) and sterility. | Used for quantifying genomic titer in AAV therapies or VCN in cell therapies [9]. |
Experimental Protocol: Developing a Multi-Parameter Potency Assay
Objective: To establish a robust, quantitative potency assay for an autologous CAR-T cell product that can be used for in-process and lot-release testing.
Background: A potency assay must provide a quantitative measure of the biological activity most relevant to the product's mechanism of action. Given the complexity of cell therapies, a multi-parameter approach is often necessary [9] [11].
Methodology:
- Define Mechanism of Action (MoA): Based on preclinical data, identify the key biological functions of your product. For CAR-T cells, this is typically target cell killing and cytokine secretion [9].
- Develop Individual Assay Modules:
- Cytolytic Activity Assay:
- Co-culture CAR-T cells with fluorescently labeled target cells (positive for the target antigen) at various effector-to-target (E:T) ratios.
- After a defined incubation period (e.g., 4-24 hours), measure target cell lysis using a real-time cell analyzer or by measuring fluorescence release.
- Include controls: CAR-T cells with non-target cells (negative control) and a reference CAR-T cell lot (positive control).
- Cytokine Secretion Assay:
- Following the co-culture, collect the supernatant.
- Use a multiplex ELISA or LEGENDplex assay to quantify the concentration of key cytokines (e.g., IFN-γ, IL-2, Granzyme B).
- Cytolytic Activity Assay:
- Assay Validation (Fit-for-Purpose & Beyond):
- Precision: Determine intra-assay and inter-assay variability.
- Linearity & Range: Demonstrate the assay is linear and accurate across a range of cell doses and potencies.
- Specificity: Show that the response is specific to the intended target antigen.
- Establish a Potency Index: Combine the results from the individual assay modules into a single Potency Index score. For example:
- Potency Index = (Normalized Cytolytic Activity × 0.6) + (Normalized IFN-γ Secretion × 0.4)
- The weighting of each parameter should reflect its relative importance to the MoA.
CQA Control Strategy Workflow
The following diagram illustrates the logical workflow for developing and implementing a control strategy based on CQAs, from early research through GMP manufacturing.
Regulatory Frameworks and Evolving Standards for Autologous Therapy Consistency
FAQs on Regulatory Frameworks & Quality Standards
What are the core regulatory and quality challenges in autologous cell therapy manufacturing?
The primary challenges stem from the personalized nature of the product. Each batch is for a single patient, which introduces significant variability and complicates standardization [13] [14]. Key challenges include:
- Process Complexity: The multi-step process (cell collection, genetic modification, expansion, infusion) requires precise control at each stage to ensure consistent product quality [13].
- Scalability: Expanding from single-center trials to commercial-scale production while maintaining quality is difficult [13].
- Product Consistency: Achieving lot-to-lot consistency is challenging due to variability in starting material (from different patients or the same patient at different times) and the complexity of the manufacturing process [10] [15].
- High Costs: The individualized nature of treatment, specialized facilities, and extensive quality control lead to high manufacturing costs [13] [16].
- Regulatory Compliance: Meeting stringent Good Manufacturing Practice (GMP) requirements across different regions adds a layer of complexity to the manufacturing process [13].
How do regulatory frameworks like GMP address the risk of contamination?
GMP guidelines mandate stringent controls to prevent contamination, which is critical for patient safety. This involves maintaining cleanroom facilities, using high-quality raw materials, and implementing robust quality control measures [13]. The use of closed, automated systems is central to this strategy, as it minimizes human intervention and open-process steps, thereby reducing contamination risks [13]. Furthermore, environmental controls are critical, and manufacturers must perform extensive monitoring of the production environment [14].
What is the role of potency assays in ensuring therapy consistency?
A potency assay is a quantitative measure of the biological activity of a product and is a critical release criterion for the final product [10]. It is intended to ensure that each batch of the therapy is capable of producing its intended clinical effect. The development of these assays is progressive and should be validated prior to Phase III clinical trials [10]. Potency testing is a key tool for regulators and manufacturers to ensure product consistency, stability, and comparability, especially when manufacturing processes are scaled up or modified [10] [15].
What are "comparability" and "consistency" testing, and why are they important?
These are related but distinct concepts in quality assurance:
- Consistency Testing: Measures the lot-to-lot variability of products manufactured using the same protocol. Variability can arise from differences in the starting material (donor genetics, patient health status) or from the manufacturing process itself (reagents, equipment, operator technique) [10].
- Comparability Testing: This is performed to demonstrate that products manufactured using different methods (e.g., during a scale-up of production) are comparable in terms of quality, safety, and efficacy. This is crucial for ensuring that process changes do not adversely affect the final product [10].
How is the regulatory landscape evolving to support autologous therapies?
Regulatory agencies have established specialized pathways to accelerate the development of these innovative treatments. In the US, the 21st Century Cures Act has helped accelerate development timelines [16]. The FDA's Regenerative Medicine Advanced Therapy (RMAT) designation provides expedited development and review for qualifying therapies [16]. Similarly, the European Medicines Agency (EMA) has streamlined processes through its Advanced Therapy Medicinal Products (ATMP) regulation and PRIME scheme [16].
Troubleshooting Common Experimental & Manufacturing Challenges
Challenge: High variability in cell quality and potency between batches.
- Potential Cause: Inconsistency in the starting biological material due to donor-related factors (genetics, health status, age) or variability in the collection process [10] [15].
- Solutions:
- Implement Rigorous Donor Screening: Establish strict criteria for the health status of autologous donors, though this is more challenging for patient-derived cells [10].
- Characterize Starting Material Thoroughly: Perform in-process testing on the starting material, including cell concentration, viability, purity (e.g., via flow cytometry), and identity [10].
- Use Process Controls: Establish and monitor critical control points during manufacturing. Charting the results of these controls over time helps define normal performance specifications and identify outliers [15].
Challenge: Inconsistent results from critical quality assays (e.g., cell counting, potency).
- Potential Cause: A lack of measurement assurance, where unaccounted-for variables in the assay protocol itself lead to unreliable data [15].
- Solutions:
- Apply Measurement Assurance Strategies:
- Create a Measurement Process Flow Diagram: Break down the assay into its discrete steps to identify where variability can be introduced [15].
- Use Ishikawa (Cause-and-Effect) Diagrams: Graphically identify all potential sources of variability (equipment, reagents, personnel, methods) [15].
- Employ Design of Experiments (DOE): Systematically vary assay parameters to identify which ones are most sensitive and require tightest control [15].
- Utilize Orthogonal Measurements: Using two or more different methods to measure the same attribute builds confidence if the results agree [15].
- Apply Measurement Assurance Strategies:
Challenge: Failure to meet sterility or environmental control specifications.
- Potential Cause: Breaches in aseptic technique or inadequate monitoring of the manufacturing environment.
- Solutions:
- Adopt Closed Automated Systems: Platforms like the Gibco CTS Rotea or Dynaclect systems are designed as closed systems to minimize contamination risk [13].
- Implement Rapid QC Testing: Migrate to faster, fit-for-purpose sterility and mycoplasma tests to reduce the time products are in quarantine and get results faster, which is critical for products with short shelf-lives [14].
- Enhance Environmental Monitoring: Use automated, integrated solutions to manage and data from environmental controls, which is especially important when scaling from hundreds to thousands of patient batches [14].
Challenge: Lengthy manufacturing lead times for autologous CAR-T products.
- Potential Cause: The multi-week process of cell manufacturing, coupled with time-consuming quality control testing, delays treatment for critically ill patients [14].
- Solutions:
- Process Integration and Decentralization: Streamline production and reduce transportation times by integrating processes and considering decentralized manufacturing facilities [14].
- Automate Key Unit Operations: Automation of steps like cell isolation, activation, and gene editing can enhance efficiency and reduce hands-on time [13].
- Adopt Rapid QC Methods: As mentioned above, implementing faster quality control solutions is a key strategy for reducing the overall vein-to-vein time [14].
Autologous Cell Therapy Manufacturing & Quality Data
| Metric | Value / Trend | Significance for Therapy Consistency |
|---|---|---|
| Global Market Value (2024) | USD 6.8 billion [16] | Indicates substantial investment and ongoing R&D in the field. |
| Projected Market Value (2034) | USD 18.4 billion [16] | Reflects anticipated growth and adoption, increasing need for standardized quality. |
| Compound Annual Growth Rate (CAGR) | 10.4% [16] | Highlights the rapid evolution of the field and its technologies. |
| Primary Market Driver | Rising prevalence of cancer and chronic diseases [16] | Underscores the medical need and the necessity for reliable, consistent therapies. |
| Key Technological Driver | Advancements in cell processing & automation [13] [16] | Directly addresses consistency challenges by reducing manual errors and variability. |
Table 2: Key Quality Testing Points in Autologous Therapy Production
| Testing Phase | Key Objectives | Examples of Tests Performed |
|---|---|---|
| Donor Testing | Ensure safety of starting material, protect staff. | Medical history, infectious disease testing (HIV, HBV, HCV) [10]. |
| Starting Material Testing | Confirm sufficient quantity and quality of cells collected. | Volume, cell concentration, viability (dye exclusion), purity (flow cytometry), identity (HLA, ABO), sterility [10]. |
| In-Process Testing | Monitor critical steps during manufacturing. | Cell concentration, purity, and sterility at intermediate stages [10]. |
| Final Product (Lot Release) Testing | Ensure final product meets all specifications for safety, purity, and potency before infusion. | Cell quantity, purity, viability, sterility, mycoplasma, endotoxin, and potency [10] [14]. |
Essential Experimental & Quality Control Protocols
Protocol 1: Automated Cell Processing with the Gibco CTS Rotea System
The Gibco CTS Rotea Counterflow Centrifugation System is a closed, flexible system designed for GMP-compliant cell therapy manufacturing. It helps standardize unit operations, reducing operator-induced variability [13].
Applications: Leukopak processing, PBMC separation, cell wash and concentration, buffer exchange [13]. Key Features:
- Closed System: Minimizes contamination risk.
- Low Output Volume: Ideal for autologous processes with limited cell numbers.
- High Cell Recovery and Viability: Optimized for sensitive primary cells. Methodology: The system uses counterflow centrifugation, where cells are suspended in a fluid flowing opposite to the centrifugal force. This allows for gentle and efficient separation, washing, and concentration of cells based on size, density, and sedimentation rate. The specific protocols (centrifugal speed, flow rates, buffer volumes) are programmed into the user-friendly interface and can be customized for the specific cell type and processing goal.
Protocol 2: Enzymatic Cell Dissociation for Primary Tissue
This is a common method to obtain single-cell suspensions from primary tissue, a critical step for many autologous therapies [17].
Reagents: Collagenase solution in HBSS with calcium and magnesium. Detailed Steps:
- Mince Tissue: With sterile instruments, mince tissue into 3–4 mm pieces [17].
- Wash Tissue: Wash the tissue pieces several times with HBSS containing calcium and magnesium [17].
- Enzymatic Digestion: Submerge tissue in collagenase solution (50–200 U/mL). Supplementing with 3 mM CaCl₂ can increase efficiency [17].
- Incubate: Incubate at 37°C for 4–18 hours on a rocker platform for gentle agitation [17].
- Disperse Cells: Pass the digested mixture through a sterile stainless-steel or nylon mesh (100-200 µM) to separate dispersed cells from tissue fragments [17].
- Wash Cells: Centrifuge the cell suspension and wash several times in HBSS without collagenase [17].
- Resuspend and Count: Resuspend the final cell pellet in culture medium. Determine viable cell density and percent viability using an automated cell counter or manual method [17].
Process Visualization: Workflows and Quality Systems
Autologous Therapy and Quality Control Workflow
Quality Assay Development and Validation Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Cell Processing and Quality Control
| Item | Function | Application Notes |
|---|---|---|
| Gibco CTS Rotea System | Closed, automated system for cell processing tasks like washing and concentration. | Reduces contamination risk and operator variability; GMP-compliant [13]. |
| Gibco CTS Dynaclect System | Closed, automated system for magnetic cell separation and bead removal. | Used for cell isolation (e.g., CD34+ selection) and de-beading; scalable [13]. |
| Gibco CTS Xenon System | Large-scale, modular electroporation system for non-viral genetic modification. | Enables CAR gene insertion; GMP-compliant and closed system [13]. |
| Enzymatic Dissociation Reagents (TrypLE, Collagenase) | Detach adherent cells from culture surfaces or dissociate primary tissues. | TrypLE is an animal-origin-free alternative to trypsin [17]. |
| Cell Dissociation Buffer | Non-enzymatic, gentle method for detaching lightly adherent cells. | Preserves cell surface proteins that might be damaged by enzymes [17]. |
| Automated Cell Counter | Provides rapid, consistent cell count and viability measurements. | Reduces human error in this fundamental QC step [17] [15]. |
| Flow Cytometry Assays | Measures cell purity, identity, and characterization of specific cell populations. | Critical for testing starting material, in-process samples, and final product [10]. |
| Rapid Sterility/Mycoplasma Kits | Fast microbial detection to meet tight release timelines for short-lived therapies. | Fit-for-purpose solutions are essential to reduce manufacturing lead times [14]. |
Frequently Asked Questions (FAQs)
FAQ 1: How does donor age impact the quality of cells used in autologous therapies? Donor age significantly affects the quantity and functional quality of cells. Mesenchymal stem cells (MSCs) from elderly donors exhibit a "youthful" subpopulation (approximately 8% of the total population) characterized by small cell size and positive expression of Stage-Specific Embryonic Antigen-4 (SSEA-4). However, the overall elderly MSC population shows hallmarks of aging, including [18]:
- Reduced Proliferation: Lower replication capacity and expansion potential.
- Increased Senescence: Higher concentrations of intracellular reactive oxygen species (ROS) and β-galactosidase expression.
- Impaired Energetics: Lower amounts of adenosine triphosphate (ATP). These aging effects can be mitigated by isolating the youthful subpopulation and expanding it on a supportive "young microenvironment," such as a bone marrow-derived extracellular matrix (BM-ECM) [18].
FAQ 2: Why do my autologous cell therapy validation results differ when using healthy donor cells versus patient-derived cells? Cells from patients with diseases, particularly those who have undergone prior treatments, are fundamentally different from those of healthy donors. Using only healthy donor cells for Verification and Validation (V&V) testing fails to capture the real-world biological variations present in patient-derived starting materials [19]. Key differences include [19]:
- Prior Treatments: Patients eligible for autologous therapies (like CAR-T) have often undergone multiple lines of chemotherapy or radiotherapy. These treatments can cause reduced cell production, diminished cytokine production, and altered immune cell subset populations.
- T Cell Function: Chemotherapy-exposed T cells can show diminished proliferation levels and lower viral transduction efficiency when using conventional activation methods.
- Disease Pathology: The disease state itself alters cellular biology and the microenvironment, which is not modeled by healthy cells.
FAQ 3: What specific donor factors contribute to variability in adipose-derived stem cell (ASC) therapies? The clinical efficacy of autologous fat grafting is highly variable, with retention rates ranging from 10% to 80%. This variability is strongly influenced by donor-related factors [20]:
| Donor Factor | Impact on Adipose-derived Stem Cells (ASCs) |
|---|---|
| Age | Younger donors typically have higher ASC proliferation rates and greater regenerative potential. |
| Sex | Hormonal differences between sexes can influence ASC functionality. |
| Health Status | Conditions like obesity or diabetes can impair ASC functionality. Systemic inflammation also alters the adipose tissue microenvironment. |
| Anatomical Harvest Site | Different body regions yield fat with variability in cellular composition, vascularity, and stem cell content. |
FAQ 4: Are there regulatory considerations for cell therapies related to donor variability? Yes. In the US, the FDA regulates Human Cell, Tissue, and Cellular and Tissue-Based Products (HCT/Ps) through two primary pathways based on risk. Section 361 products must meet strict criteria, including minimal manipulation and homologous use, and do not require premarket approval. Section 351 products, which often involve more than minimal manipulation (e.g., expansion, genetic modification), require an IND, clinical trials to demonstrate safety and efficacy, and must adhere to current Good Manufacturing Practices (cGMP). Managing donor variability is critical for Section 351 products to ensure product consistency, which is a key part of the regulatory review [21].
Troubleshooting Guides
Issue 1: Low Proliferation and Senescence in Cells from Elderly Donors
Problem: Cells isolated from an elderly donor show slow growth, enlarged morphology, and high senescence markers, making expansion to therapeutic doses challenging.
Solution: Implement a strategy to isolate and expand the retained youthful subpopulation.
Step-by-Step Protocol:
- Cell Isolation and Characterization: Isolate MSCs from the donor's bone marrow and characterize using standard surface markers (CD73, CD90, CD105) [18].
- Identify Youthful Subpopulation: Use Fluorescence-Activated Cell Sorting (FACS) to isolate cells based on two key parameters [18]:
- Small cell size
- Positive expression of SSEA-4
- Create a Youthful Microenvironment: Culture the isolated SSEA-4+ subpopulation on a bone marrow-derived extracellular matrix (BM-ECM) produced by young donor stromal cells. This ECM provides critical biochemical and physical cues for rejuvenation [18].
- Expand Cells: Culture the cells on the BM-ECM in standard growth medium, supplementing with 50 μM ascorbic acid during the last 8 days of culture to support ECM production and cell health [18].
Visual Guide to Isolating Youthful Cells from Elderly Donors The following workflow diagram illustrates the protocol for rescuing high-quality MSCs from an elderly donor population.
Issue 2: Inconsistent Performance of Patient-Derived Cells in Validation Assays
Problem: Assays used for process validation (e.g., transduction efficiency, proliferation) yield inconsistent and suboptimal results when using cells from diseased donors, despite working well with healthy donor cells.
Solution: Incorporate disease-state primary cells into your V&V testing strategy to better represent the target patient population.
Step-by-Step Protocol:
- Source Disease-State Material: Procure disease-state leukopaks or immune cell subsets from a qualified supplier that provides comprehensive clinical data (e.g., patient diagnosis, disease progression, prior treatments) [19].
- Benchmark Against Healthy Donors: Perform key assays in parallel using cells from healthy donors and disease-state donors. Essential assays include [19]:
- T Cell Proliferation Assay: Activate T cells with CD3/CD28 beads and measure proliferation over time. Expect reduced proliferation in cells from chemotherapy-treated donors [19].
- Transduction Efficiency Assay: Transduce T cells with a viral vector (e.g., for CAR-T) and measure the percentage of successfully modified cells. Chemotherapy exposure can lower transduction rates [19].
- Cytokine Production Profiling: Quantify cytokine output after activation, as this can be diminished in disease-state cells [19].
- Optimize Processes: Use the data from disease-state cells to refine manufacturing processes, media formulations, and activation methods to be more robust for the intended patient population [19].
Comparative Data: Impact of Donor Status on Key T Cell Parameters This table summarizes expected outcomes when comparing cells from healthy donors and patients pre-treated for conditions like oncology or autoimmune disorders.
| Experimental Parameter | Healthy Donor Cells | Disease-State / Pre-treated Donor Cells |
|---|---|---|
| T Cell Proliferation (post CD3/CD28 activation) | Robust proliferation | Diminished levels of proliferation [19] |
| Viral Transduction Efficiency | Standard efficiency | Can be low/reduced [19] |
| Cytokine Production | Normal profile | Diminished production [19] |
| Cell Subset Populations | Standard distribution | Fluctuations and alterations [19] |
Issue 3: High Functional Variability in Adipose-Derived Stem Cells (ASCs)
Problem: Autologous fat grafts or ASC preparations show unpredictable clinical outcomes due to underlying donor biology.
Solution: Pre-screen donors and tailor processing protocols based on donor profile.
Step-by-Step Protocol:
- Donor Profiling: Document key donor factors before the procedure: age, sex, BMI, metabolic health status (e.g., presence of diabetes), and planned anatomical harvest site [20].
- Assess ASC Quality (Optional but Recommended): If feasible, perform a small-scale test culture and quality assessment of the isolated ASCs. Key metrics include [20]:
- Proliferation Rate: Use a colony-forming unit (CFU) assay.
- Viability Staining: Use trypan blue or similar.
- Flow Cytometry: Confirm expression of typical MSC markers (CD90, CD73, CD105, CD44) and lack of hematopoietic markers (CD45, CD14) [20].
- Mitigate Variability: Based on the profile, consider strategies to enhance the graft:
- For older donors or those with compromised health, consider enriching for the stromal vascular fraction (SVF) to increase stem cell concentration [20].
- Use additives like Platelet-Rich Plasma (PRP) or specific growth factors to the graft to boost ASC survival and function [20].
- Standardize the anatomical harvest site whenever possible to reduce one source of variability.
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function / Application |
|---|---|
| Bone Marrow-derived Extracellular Matrix (BM-ECM) | A decellularized, native 3D culture system that mimics the stem cell niche. Used to rejuvenate and expand elderly MSCs while retaining stem cell properties [18]. |
| Fluorescence-Activated Cell Sorter (FACS) | An essential tool for isolating specific cell subpopulations based on markers like SSEA-4 and physical characteristics like cell size to obtain "youthful" cells from a heterogeneous elderly population [18]. |
| Disease-State Leukopaks | Peripheral blood mononuclear cells (PBMCs) collected from patients clinically diagnosed with a specific disease. Critical for representative verification and validation (V&V) testing of autologous therapies [19]. |
| Stage-Specific Embryonic Antigen-4 (SSEA-4) Antibody | A cell surface marker used to identify a potent, "youthful" subpopulation of mesenchymal stem cells within a larger, aged population for selective isolation [18]. |
| Colony-Forming Unit (CFU) Assay Kit | A functional assay to quantify the proliferation potential and clonogenicity of stem cells, such as Adipose-derived Stem Cells (ASCs), which is a key indicator of cell quality [20]. |
| Reactive Oxygen Species (ROS) Detection Kit | A fluorescent assay to measure intracellular oxidative stress levels, which are typically elevated in senescent cells from elderly donors or those with certain disease states [18]. |
Implementing Technological and Systemic Solutions for Quality Control
Leveraging Automation and Closed-System Bioreactors to Minimize Process Variability
Troubleshooting Guides
Guide 1: Addressing Contamination in Bioreactor Systems
Q: My bioreactor culture is showing signs of contamination, such as unexpected turbidity or media acidification. What are the most likely sources and immediate corrective actions?
Contamination can lead to significant losses in time and resources. Early detection and a systematic investigation are key to resolving the issue.
| Observation/Symptom | Potential Source | Corrective Action |
|---|---|---|
| Unexpected turbidity, color change (e.g., phenol red to yellow), or unusual smell [22] | Contaminated inoculum or poor inoculation technique [22] | Check the sterility of the seed train by re-plating on a rich growth medium. Review and secure inoculation procedures to avoid "aseptic pour" into open ports [22]. |
| Growth of spore-forming organisms reappearing after autoclaving [22] | Ineffective sterilization cycle or compromised vessel assembly [22] | Verify autoclave temperature with test phials. Completely disassemble the vessel and tubing. Autoclave with pauses between cycles to allow spores to germinate, then re-sterilize [22]. |
| Contamination detected post-inoculation without clear source | Failed seals, O-rings, or wet exit gas filters [22] | Inspect and replace all vessel and sensor O-rings if they are flattened, torn, or feathered (recommended every 10-20 cycles). Check reagent bottle seals and feed lines. Ensure the exit gas cooler is efficient to prevent filter wetting [22]. |
Experimental Protocol: Sterility Hold Test A critical method to confirm the success of your decontamination efforts and the sterility of your bioreactor system before use.
- Preparation: After performing the corrective actions and re-sterilizing the bioreactor, fill it with cell culture medium as you would for a normal experiment.
- Incubation: Instead of inoculating with cells, maintain the bioreactor at the standard operating conditions (e.g., 37°C, appropriate agitation) for several hours or days.
- Monitoring: Closely monitor the uninoculated medium for any signs of growth, such as turbidity or a change in pH.
- Interpretation: The absence of growth under normal operating conditions confirms that the sterilization was effective and the vessel is free of contaminants. If growth occurs, the investigation must continue [22].
Guide 2: Managing Process Variability in Autologous Cell Production
Q: How can I reduce patient-to-patient variability in my autologous CAR-T cell therapy research process?
Inherent biological variability in starting material is a major challenge for autologous therapies. Strategies focus on controlling the manufacturing process to ensure a consistent final product.
| Source of Variability | Impact on Process | Mitigation Strategy |
|---|---|---|
| Variable Input Material | Differences in patient T-cell health, count, and functionality lead to inconsistent expansion and product quality [21]. | Implement robust cell selection and purification steps early in the process. Consider automated, closed-system technologies to improve consistency in starting material quality [23]. |
| Manual Process Steps | Operator-dependent handling introduces variability in timing, cell washing, and nutrient feeding [24]. | Adopt fully automated, closed-system bioreactors (e.g., CliniMACS Prodigy, Cocoon) that integrate cell isolation, activation, expansion, and harvesting. This minimizes human intervention [25]. |
| Uncontrolled Culture Parameters | Fluctuations in dissolved oxygen, pH, and nutrient levels affect cell growth and therapeutic cell characteristics [25]. | Utilize bioreactors with advanced sensors and closed-loop control systems. These automatically adjust parameters in real-time based on continuous feedback, ensuring a consistent growth environment [25] [26]. |
| Ill-Defined Raw Materials | Lot-to-lot differences in media, cytokines, and sera can alter cell behavior and product potency [27]. | Source GMP-grade reagents and implement rigorous raw material testing and qualification protocols to ensure lot-to-lot consistency [27]. |
Experimental Protocol: Implementing a Quality-by-Design (QbD) Approach A proactive framework to understand and control the sources of variability by linking process parameters to product quality.
- Define Critical Quality Attributes (CQAs): Identify the key characteristics of your cell product that define its safety and biological function (e.g., cell viability, specific phenotype, potency) [25].
- Identify Critical Process Parameters (CPPs): Determine the process variables (e.g., activation protocol, seeding density, agitation speed, nutrient concentration) that significantly impact your CQAs [25].
- Design of Experiments (DOE): Use statistical DOE to systematically evaluate and optimize the CPPs. This establishes a "design space" where operation will consistently produce a product meeting the desired quality profile [25] [24].
- Implement Process Controls: Establish control strategies and real-time monitoring (e.g., with PAT tools) for the CPPs to ensure the process remains within the defined design space [25].
Frequently Asked Questions (FAQs)
Q: What are the key advantages of using a closed-system automated bioreactor like the CliniMACS Prodigy or Cocoon for autologous therapy research?
A: These systems offer several critical advantages for ensuring consistency:
- Integrated Automation: They combine multiple discrete processes (cell isolation, activation, transduction, expansion, formulation) into a single, automated workflow, drastically reducing manual handling and associated variability [25].
- Closed Environment: The closed-system design minimizes the risk of contamination, a significant source of batch failure [25] [23].
- Real-time Monitoring and Control: Equipped with advanced sensors, they continuously monitor parameters like pH, dissolved oxygen, and temperature, allowing for precise control of the culture environment [25].
- Scalability and GMP Compliance: These platforms are designed to be scalable from clinical research to commercial production and are built to comply with Good Manufacturing Practice (GMP) standards [25] [27].
Q: How can I effectively monitor cell growth and viability in real-time to make better process decisions?
A: Moving beyond manual sampling is key. You can implement:
- In-line Dielectric Spectroscopy: This method measures permittivity, which correlates with the viable cell biovolume. It provides continuous, real-time data on cell growth but can be less reliable during the death phase when cell size changes [26].
- Automated On-line Sampling: Systems like the Numera can be integrated with bioreactors to automatically draw samples and transfer them to analyzers like the Cedex HiRes. This provides high-frequency, reliable data on viable cell density and viability without manual intervention, reducing contamination risk and operator error [26].
Q: We are in the early research phase. When is the right time to invest in automation?
A: Financial constraints allowing, it is advisable to consider automation as early as possible. Focusing initially on the most complex, biologically modifying steps (e.g., genetic modification, cell expansion) provides greater process control early on. Automation should ideally be in place by the time pivotal clinical trials commence to ensure robust and reproducible data for regulatory submissions [23].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Solution | Function / Application |
|---|---|
| GMP-grade Media & Cytokines | Provides a consistent, defined, and high-quality nutrient base for cell culture, minimizing variability introduced by lot-to-l differences in raw materials [27]. |
| Serum-Free Media | Eliminates the high variability and unknown composition of fetal bovine serum (FBS), enhancing process consistency and product safety profiles [27]. |
| Single-Use Bioreactor Assemblies | Pre-assembled, sterile flow paths (including tubing, bags, and sensors) for single-use bioreactors. They reduce cross-contamination risk, eliminate cleaning validation, and increase operational flexibility [25] [28]. |
| Closed-System Sterile Connectors | Enable the aseptic connection of fluid pathways within a closed process, maintaining a sterile environment during additions or transfers [28]. |
| Process Analytical Technology (PAT) | A category of tools and software (e.g., Raman spectroscopy, advanced sensors) for real-time monitoring of critical process parameters to ensure process control and facilitate real-time release testing [25] [26]. |
The Role of AI and Digital Twins in Predictive Process Control and Real-Time Monitoring
Fundamental Concepts FAQ
Q1: What is a Digital Twin in the context of autologous cell therapy manufacturing? A Digital Twin is a virtual replica of a physical bioprocess, such as CAR-T cell expansion. It uses real-time data from sensors and IoT devices to mimic the behavior and performance of its real-world counterpart. This allows researchers to monitor, simulate, and analyze the entire production process in a virtual environment, enabling predictive control and optimization [29] [30] [31].
Q2: How does AI integrate with Digital Twins for predictive process control? AI, particularly machine learning (ML), analyzes the vast amounts of data generated by the Digital Twin. It identifies complex patterns to predict process outcomes, such as final cell viability or differentiation efficiency. This creates a closed-loop control system where the AI can proactively suggest or even implement adjustments to the bioprocess parameters to maintain quality and improve yield [32] [33] [30].
Q3: What are the key benefits of using these technologies for autologous therapies? The primary benefits include:
- Improved Consistency: Mitigates patient-to-patient variability in starting materials [33] [30].
- Enhanced Monitoring: Enables real-time, non-invasive monitoring of Critical Quality Attributes (CQAs) [30].
- Predictive Maintenance: Anticipates equipment failures to avoid costly downtime [29] [31].
- Accelerated Development: "In-silico" simulation experiments speed up process development and reduce raw material costs [30] [31].
Q4: What is the difference between a simulation and a Digital Twin? While both use models, a simulation typically runs predefined scenarios in a static, virtual-only environment. A Digital Twin is dynamically connected to a specific physical asset via a continuous, real-time data flow, allowing it to reflect the current state of the process and send insights back to the physical system [31].
Troubleshooting Guides
Guide 1: Addressing Data Quality and Integration Issues
Problem: The Digital Twin model produces inaccurate predictions or fails to synchronize with the physical bioreactor.
| Step | Action & Diagnosis | Solution |
|---|---|---|
| 1. Identify | Examine system logs for error messages like "Invalid input format" or "API request failed." Check for failed data transmissions [34]. | Implement comprehensive logging to capture input data, model parameters, and intermediate outputs for tracing [35]. |
| 2. Analyze | Examine the data pipeline from sensor to model. Verify the execution path and check for misconfigured triggers or conditions that pre-process the data [34]. | Use visualization tools to inspect raw sensor data for anomalies or missing values. Validate that all data sources are correctly configured and calibrated [35]. |
| 3. Test & Isolate | Run the workflow with standardized, synthetic input data with known outputs. selectively disable specific data streams to pinpoint the source of the error [34] [35]. | Break down the data pipeline into smaller components (e.g., sensor data collection, data transmission, data pre-processing) and test each one separately [34]. |
| 4. Implement Fix | If the issue is with input data, clean and re-format it to meet required standards. If the issue is a workflow misconfiguration, adjust the relevant data processing steps [34]. | For persistent model inaccuracies, retrain the AI model with corrected and validated data, or adjust its hyperparameters [34] [33]. |
| 5. Validate | Confirm the fix by running the Digital Twin with a diverse set of validation data, ensuring it now operates smoothly and produces expected outputs [34]. | |
| 6. Monitor | Continuously monitor data quality metrics and system logs to catch new issues early and ensure long-term stability [34]. |
Guide 2: Troubleshooting AI Model Performance and Drift
Problem: The AI model's predictive performance degrades over time, leading to suboptimal process control.
| Step | Action & Diagnosis | Solution |
|---|---|---|
| 1. Identify | Monitor key performance metrics like prediction error rates or drift in key output parameters. Look for unexpected or inconsistent process outputs [34] [35]. | Utilize an analytics dashboard for real-time insights into model performance and to spot trends and anomalies [35]. |
| 2. Analyze | Investigate potential causes, such as changes in raw material variability (e.g., patient cell characteristics) or shifts in the underlying process dynamics that the model was not trained on [33] [30]. | Use Explainable AI (XAI) techniques like SHAP or LIME to understand which input features the model is relying on and if these have changed [35]. |
| 3. Test & Isolate | Conduct A/B testing by running the new model in parallel with the previous stable version to isolate the impact of the change [35]. | Create a controlled simulation environment to test the model's response to edge cases and new variability patterns [33]. |
| 4. Implement Fix | Update the AI model by retraining it with recent process data that reflects the new variability. For a hybrid approach, adjust the data-driven model components while retaining the foundational mechanistic model [30]. | |
| 5. Validate | Thoroughly validate the updated model using historical and new test data to ensure it resolves the performance issue without introducing new errors [34]. | |
| 6. Monitor | Establish ongoing monitoring of model performance and data distributions to proactively detect and address future model drift [34] [35]. |
Experimental Protocols & Methodologies
Protocol 1: Developing a Hybrid Digital Twin for a Bioreactor
Aim: To create a hybrid Digital Twin for the real-time monitoring and prediction of cell density and viability in a CAR-T cell expansion process.
Methodology:
System Definition and Sensor Integration:
Model Development (Hybrid Approach):
- Mechanistic Model Component: Develop a model based on convection-diffusion equations to simulate the spatial distribution of nutrients and metabolites in the bioreactor. This component is grounded in established physical laws [30].
- Data-Driven Model Component: Use machine learning (e.g., a convolutional neural network) on the daily label-free images to generate maps highlighting live cells, local cell density, and pluripotency levels. This AI acts as a "soft sensor" for CQAs that are difficult to measure directly in real-time [33] [30].
- Integration: The outputs of both models are combined into a unified hybrid Digital Twin that provides a comprehensive view of the bioprocess.
Validation and Deployment:
- Validate the Digital Twin's predictions against offline analytical measurements (e.g., flow cytometry for cell identity, trypan blue exclusion for viability).
- Once validated, deploy the Digital Twin for real-time monitoring and use its predictions to inform a closed-loop control strategy, such as automatically adjusting perfusion rates to maintain optimal cell density [32] [30].
The following workflow diagram illustrates this hybrid modeling approach:
Protocol 2: Implementing a Closed-Loop Control System with AI
Aim: To establish an AI-driven closed-loop control system for maintaining healthy cell cultures by proactively removing unwanted cells.
Methodology:
Data Acquisition and Mapping:
- The system performs daily, label-free imaging of the entire cell culture.
- An AI algorithm analyzes these images to generate detailed maps identifying live cells, dead cells, local cell density, and pluripotency levels [33].
Analysis and Decision Making:
- The AI analyzes the maps to identify regions with unwanted cell types or unhealthy colonies that could hinder the growth of the target cell population.
- Based on predefined quality thresholds, the system decides which cells to remove.
Precision Intervention:
- The AI-generated maps guide a proprietary laser system.
- The laser precisely targets and removes unwanted cells by absorbing energy in a specialized coating beneath the cells, generating mechanical bubbles that eliminate the target cells without affecting neighboring healthy cells [33].
Validation and Iteration:
- The process is continuously validated through subsequent imaging and AI analysis.
- A multi-agent reinforcement learning model, trained in a simulated environment, can be used to optimize the cell culture management strategy, learning to manage multiple colonies within a confined space to avoid collisions and overgrowth [33].
The logical flow of this autonomous control system is shown below:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, technologies, and software solutions critical for experiments involving AI and Digital Twins in cell therapy.
| Item / Solution | Function / Application |
|---|---|
| CRISPR/Cas9 & Plasmids | Gene editing tools used for precise modification of T-cells to express Chimeric Antigen Receptors (CARs) [36]. |
| Bioreactors & Closed-System Culture Platforms | Facilitate the growth and expansion of genetically modified T-cells under controlled, automated conditions [32] [36]. |
| Flow Cytometer (e.g., CytoFLEX) | An analytical tool essential for quality control, used to confirm CAR-T cell identity and characterize cell subpopulations [32] [36]. |
| Cell Viability Analyzer (e.g., Vi-CELL BLU) | Automates cell viability and count analysis using the Trypan Blue exclusion method, a critical quality control test [36]. |
| Process Information Management System (PIMS) | Cloud-native, compliant software that creates a contextualized data backbone of all manufacturing process and quality data across batches, essential for training AI models [36]. |
| Semi-Automated Devices (e.g., Cocoon, Prodigy) | Reduce hands-on production time and risk of contamination for autologous therapy manufacturing, generating standardized process data [32]. |
| AI-powered Imaging & Analysis Software | Provides label-free, non-invasive analysis of cell cultures, generating data on cell count, viability, and morphology for the Digital Twin [33]. |
Adopting Point-of-Care and Decentralized Manufacturing Models with Centralized QMS Oversight
Point-of-care (POC) and decentralized manufacturing represent a paradigm shift in producing autologous cell therapies, moving production from large, centralized facilities to multiple, smaller sites close to the patient. This model is particularly vital for autologous cell therapies, where a patient's own cells are harvested, engineered, and reinfused. The traditional centralized approach faces significant challenges with complex logistics, cryopreservation, and lengthy "vein-to-vein" times that can exceed three weeks [37] [38] [39]. Decentralized manufacturing addresses these by locating production at or near the treatment center, drastically reducing turnaround time and simplifying cold chain logistics [37] [40].
However, distributing manufacturing across multiple locations introduces risks of process variability. A Centralized Quality Management System (QMS) is the critical framework that ensures product quality, safety, and consistency across all manufacturing sites, providing unified regulatory oversight and standardizing operations [41]. This hybrid approach—decentralized production with centralized quality control—enables wider patient access without compromising the rigorous standards required for advanced therapy medicinal products (ATMPs) [41].
Troubleshooting Guides
Common Workflow Challenges and Solutions
Table: Troubleshooting Common POC Manufacturing Challenges
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Cell Processing | Low cell viability post-thaw | Improper thawing technique; osmotic shock [42]. | Thaw cells quickly (<2 mins at 37°C); use pre-warmed medium; add medium drop-wise to dilute cryoprotectant [43] [42]. |
| Cell Processing | Poor cell attachment | Matrix coating dried; incorrect seeding density; lack of attachment factors [43] [42]. | Shorten time between coating and cell seeding; verify lot-specific seeding density; use appropriate coating matrix [43] [42]. |
| Process Control | High batch-to-batch variability | Manual, open processing steps; patient-to-patient input material variation [38] [39]. | Implement automated, closed-system bioprocessing; use standardized protocols managed by the Centralized QMS [41] [38] [39]. |
| Contamination Control | Microbial contamination in non-cleanroom settings | High microbial burden in hospital environments; open system processing [44]. | Employ isolator-based closed systems (e.g., positive pressure isolators with VHP decontamination) [44]. |
| Logistics & Timing | Short product shelf-life | Fresh cell products; prolonged QC testing [41]. | Implement rapid, real-time QC testing (e.g., inline analytics); coordinate scheduling via centralized QMS [44] [41]. |
Quality Management and Regulatory Hurdles
Table: Troubleshooting QMS and Regulatory Compliance
| Challenge | Root Cause | Corrective and Preventive Actions |
|---|---|---|
| Demonstrating product comparability across sites | Inherent facility-to-facility differences; non-identical equipment [41]. | Perform extensive process validation and analytical method qualification at each site. The Control Site must hold and maintain the POCare Master File to demonstrate consistency [41]. |
| Regulatory ambiguity for multi-site production | Evolving regulatory frameworks for decentralized models [41] [38]. | Proactively engage with regulators (FDA, EMA, MHRA) through emerging programs like the FDA's Emerging Technology Program and FRAME initiative [41]. |
| Maintaining training consistency | High staff turnover at POC sites; varying levels of GMP expertise [44] [41]. | Establish an overarching, standardized training platform managed by the Control Site. Utilize an Electronic QMS (eQMS) for training records and standard procedures [41] [45]. |
| Managing deviations and non-conformances | Paper-based QMS leading to poor traceability and delayed reporting [45]. | Implement an eQMS to centralize and automate deviation tracking, corrective actions, and change management, ensuring real-time visibility for the Quality Unit [45]. |
Frequently Asked Questions (FAQs)
Q1: What are the main technological enablers for decentralized manufacturing of autologous cell therapies? The shift to decentralized manufacturing is made feasible by several key technologies:
- Automated Closed Systems: Platforms like the
CliniMACS ProdigyorLonza Cocoonintegrate multiple manufacturing steps (isolation, activation, transduction, expansion) within a single-use, disposable kit, minimizing manual intervention and contamination risk [39]. - Isolator Technology: Sealed containment devices provide an ISO Class 5 environment within a non-classified hospital room. They use glove ports, rapid transfer ports, and vaporized hydrogen peroxide (VHP) decontamination to maintain asepsis, protecting the product from the external environment [44].
- Digital Integration: Software like
CTS Cellmationenables digital automation and data collection. When integrated with an eQMS, this allows for real-time monitoring and centralized oversight of distributed processes [37] [41].
Q2: How does a Centralized QMS (Control Site) function in a decentralized network? The Control Site acts as the regulatory and quality nexus for all decentralized manufacturing sites [41]. Its core functions include:
- Holding the single Manufacturing License and maintaining the central POCare Master File for the product.
- Serving as the primary point of contact for regulatory agencies (e.g., FDA, EMA).
- Providing overarching Quality Assurance and employing the Qualified Person (QP) responsible for batch certification and release.
- Managing a centralized eQMS for deviations, change control, and training records across the network [41] [45].
Q3: Are there real-world examples of successful decentralized CAR-T cell manufacturing?
Yes, several academic institutions and clinical trials have demonstrated the feasibility of POC CAR-T manufacturing. For instance, a study by Maschan et al. reported robust safety and efficacy in patients with B-cell malignancies treated with fresh, place-of-care manufactured anti-CD19 CAR-T cells produced at two different locations using the CliniMACS Prodigy platform, eliminating the need for cryopreservation [41]. Other studies, such as one using the ARI-0001 platform, have shown manufacturing times of 8-11 days, which is a significant reduction compared to traditional centralized models [39].
Q4: What is a key advantage of using a shortened (e.g., 24-hour) manufacturing process? Shortened processes aim to preserve a less differentiated T-cell phenotype. Research shows that CAR-T cells manufactured in 24 hours exhibit a higher proportion of T stem cell memory (TSCM) cells (CD45RA+/CCR7+), which are associated with improved long-term persistence and anti-tumor activity in vivo, compared to cells expanded over 7 days that show a more differentiated and potentially exhausted phenotype [37].
Q5: How can we ensure sterility without a full GMP cleanroom at every hospital site? Isolator-based systems are designed for this exact scenario. A positive pressure isolator creates its own critical processing environment (ISO Class 5) independently of the background room. With integrated decontamination cycles and closed processing, it provides sterility assurance equivalent to or greater than a traditional biological safety cabinet within a cleanroom, but with a smaller footprint and lower facility requirements [44].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents and Instruments for POC Cell Therapy Manufacturing
| Item Name | Function/Application | Key Feature for Decentralized Manufacturing |
|---|---|---|
| CTS Detachable Dynabeads CD3/CD28 | One-step isolation and activation of T cells [37]. | Active-release feature allows for bead removal at any point, preventing T-cell overactivation and exhaustion, which is crucial for shortened processes [37]. |
| LV-MAX Lentiviral Production System | Production of lentiviral vectors for cell transduction [37]. | Provides a consistent and scalable system for generating the viral vectors needed for genetic modification at the POC [37]. |
| CTS DynaCellect Magnetic Separation System | Automated cell separation and bead detachment [37]. | An automated, closed-system instrument that integrates with the detachable beads, reducing manual steps and variability [37]. |
| CTS Rotea Counterflow Centrifugation System | Cell washing and concentration [37]. | Provides a low-shear environment that ensures high cell recovery and viability, which is critical when working with precious patient samples [37]. |
| Gibco CTS Cellmation Software | Digital automation and process control [37]. | Enables closed, automated instrumentation and software control, reducing manual touchpoints and allowing for digital record-keeping aligned with QMS needs [37]. |
| Positive Pressure Isolator | Physical barrier for aseptic processing [44]. | Enables GMP-compliant manufacturing in a non-classified hospital room through a sealed, decontaminated environment with glove ports [44]. |
Experimental Protocols and Workflow Diagrams
Protocol: Automated 24-Hour CAR-T Cell Manufacturing Workflow
This protocol, adapted from a Thermo Fisher Scientific study, demonstrates a shortened, automated process for generating CAR-T cells [37].
One-Step Isolation & Activation:
- Load the leukapheresis product into a sterile bag or kit.
- Use the
CTS DynaCellect SystemwithCTS Detachable Dynabeads CD3/CD28to simultaneously isolate and activate T cells. This step yields a highly pure T-cell population.
Lentiviral Transduction:
- Following isolation, without delay, infect the cells with a lentiviral vector containing the CAR construct (e.g., prepared using the
LV-MAX Lentiviral Production System). - A low multiplicity of infection (MOI) can be sufficient due to the high efficiency of the process [37].
- Following isolation, without delay, infect the cells with a lentiviral vector containing the CAR construct (e.g., prepared using the
Active Debeading:
- Following transduction, actively detach the magnetic beads using
CTS Detachable Dynabeads Release Bufferon theCTS DynaCellect system. - This step is crucial for controlling the activation signal and preserving a less differentiated T-cell state.
- Following transduction, actively detach the magnetic beads using
Wash and Concentrate:
- Transfer the cells to the
CTS Rotea Counterflow Centrifugation System. - Perform a wash and concentration step to remove residual beads, buffer, and viral particles. The low-shear environment minimizes cell damage.
- Transfer the cells to the
Final Formulation & Cryopreservation:
- The final cell product is formulated in an appropriate infusion buffer.
- For the 24-hour process, the product is typically cryopreserved using a controlled-rate freezer (e.g.,
CryoMed) [37]. In a fully decentralized POC model, the product could be infused fresh after QC checks.
Diagram: Automated 24-Hour CAR-T Manufacturing Workflow
Centralized QMS Oversight Model for POC Manufacturing
This diagram illustrates the flow of information, materials, and regulatory responsibility in a decentralized network managed by a central Control Site [41].
Diagram: Centralized QMS Oversight for POC Network
Integrating Advanced Analytics and NGS for Enhanced In-Process Quality Control
For researchers and drug development professionals in autologous cell therapy, ensuring consistent product quality amidst inherent biological variability is a paramount challenge. The integration of Next-Generation Sequencing (NGS) with advanced analytics into the manufacturing process provides an unprecedented window into product characteristics, moving quality control from a retrospective to a proactive function. This technical support center is designed to help you troubleshoot key challenges in implementing these technologies, framed within the broader thesis that robust, in-process monitoring is essential for scaling consistent and effective autologous therapies [46] [10].
NGS & Analytics Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Why is accurate NGS library quantification critical for monitoring cell therapy products, and what are the limitations of common QC methods?
A1: Accurate library quantification is essential because the sequencing process relies on loading a precise amount of sample onto the flow cell. Inaccurate quantification directly impacts data quality and can lead to failed runs or misleading results when assessing critical quality attributes (e.g., vector copy number, transcriptome profiles).
- Over-clustering: If library concentration is too high, it leads to over-clustered flow cells, which increases data errors and can cause run failure [47].
- Under-clustering: If library concentration is too low, it results in under-clustered flow cells, leading to inefficient sequencing, poor data yield, and increased costs per sample [47].
- Method Limitations:
- Classic Fluorometry (e.g., Qubit): Provides concentration in ng/µL but not molarity. It inaccurately measures total nucleic acids, including non-sequenceable molecules like adapter dimers, and does not provide fragment size information [47].
- qPCR: Considered the gold standard as it quantifies only amplifiable molecules. However, it is labor-intensive, time-consuming (1-4 hours), requires separate fragment size analysis, and introduces user-user variability through multiple manual dilutions [47].
- Microfluidic Electrophoresis (e.g., Bioanalyzer): Provides size distribution and molarity but is costly, slow, and has low throughput (e.g., 11 samples per run) [47].
Q2: How can we demonstrate product comparability across multiple, decentralized manufacturing sites for the same autologous therapy?
A2: Regulatory agencies like the FDA emphasize that sponsors must demonstrate a comparable product is manufactured at each location [46]. NGS-based analytics are central to this comparability exercise.
- Strategy: Implement a standardized, controlled manufacturing platform (e.g., automated, closed-system technologies) across all sites to minimize process-driven variability [46].
- Analytical Evidence: Use NGS to profile key molecular attributes of the final product (e.g., gene expression signatures, T-cell receptor clonality, vector integration sites) across batches manufactured at different sites. Statistical comparison of these profiles provides objective evidence of product comparability [46] [10].
- Control Site Oversight: A centralized "Control Site" model, as recognized by the MHRA, can serve as the regulatory nexus, maintaining master files and ensuring analytical methods and product quality are consistent across the decentralized network [46].
Q3: What are the common causes of low sequencing yield or run failure on NGS platforms, and how can they be diagnosed?
A3: Low yield or failure can originate from several points in the workflow. A systematic diagnostic approach is key.
- Library/Template Preparation: This is a frequent source of problems. Always verify the quantity and quality of library and template preparations prior to loading on the sequencer. Inadequate or degraded material will result in poor data output [48].
- Chip Loading & Instrument Check:
- Poor Chip Loading: For Ion S5 systems, a "Low ISP Yield" alarm can indicate poor chip loading or that control particles were not added. Confirm controls were added; if so, the chip or its socket may be faulty [48].
- Chip Seating: If a "Chip Check" fails, open the clamp, ensure the chip is properly seated and undamaged, and run the check again [48].
- Connectivity: If the instrument shows "No Connectivity" alarms, disconnect and re-connect the ethernet cable and verify network operation [48].
Troubleshooting Guides
Table 1: Troubleshooting Common NGS Instrument Alarms
| Alarm / Error Message | Possible Cause | Recommended Action |
|---|---|---|
| "Low ISP Yield" (Ion S5/XL) | Poor chip loading; Control Ion Sphere Particles not added; Library/template issue [48]. | 1. Confirm control particles were added.2. Verify library/template quality and quantity.3. Re-seat or replace the chip.4. Contact Technical Support if problem persists [48]. |
| "Chip Check Failed" (Ion S5/XL) | Clamp not closed; Chip not properly seated; Damaged chip [48]. | 1. Open clamp, inspect chip for damage, replace if necessary.2. Re-seat chip, ensure clamp is fully closed.3. Run "Chip Check" again.4. Contact Technical Support if failure repeats [48]. |
| "No Connectivity to Torrent Server" | Network connectivity issue; Router problem [48]. | 1. Disconnect and re-connect the ethernet cable.2. Confirm router is operational.3. Restart the instrument if needed [48]. |
| pH Measurement Error (Ion PGM) | pH of nucleotides out of range; Minor measurement glitch [48]. | 1. Press "Start" to restart measurement.2. If error repeats, note pH values and error message.3. Contact Technical Support [48]. |
| Initialization Error (Ion Proton) | Bubbles or residue on chip surface [48]. | Rinse chip by pipetting 100 μL isopropanol into the chip, followed by 100 μL of water [48]. |
Table 2: Addressing Data Quality and Analytical Challenges
| Problem | Impact on Cell Therapy QC | Solution & Mitigation Strategy |
|---|---|---|
| High Variability in QC Results | Inconsistent product quality assessment; inability to release product; failed comparability studies. | Implement synthetic "cell mimics" as stable, reproducible controls for assays (e.g., flow cytometry, potency assays). This reduces reliance on highly variable cell lines [49]. |
| Sequencing Errors in Repetitive Regions | Misinterpretation of genetic data; false positives/negatives for critical variants. | Employ robust bioinformatics quality control (e.g., read trimming, quality scoring). Use complementary methods for validation in difficult genomic regions [50]. |
| Inconsistent Potency Assay Results | Inability to reliably measure the biological activity of the cell product, a key release criterion. | Develop and validate molecular potency assays using global gene expression analysis (e.g., RNA-Seq). Identify a signature of predictive genes correlated with biological function [10]. |
Essential Workflows and Protocols
Optimized NGS Library QC Workflow
The following diagram illustrates a streamlined workflow for NGS library quality control, integrating a novel quantification method to save time and improve accuracy.
Protocol: Streamlined NGS Library QC using Integrated Quantification
Purpose: To accurately determine the molar concentration of NGS libraries in a time- and cost-efficient manner, enabling precise normalization for high-quality sequencing data [47].
Methodology: Utilize a library preparation kit with an integrated quantification technology (e.g., NuQuant principle). This method incorporates a specific number of fluorescent labels into each library molecule during the prep stage, allowing for direct molarity measurement via fluorometry without the need for separate fragment size analysis [47].
Steps:
- Library Preparation: Perform library prep using a kit with integrated fluorescent labeling.
- Direct Quantification:
- Transfer a small volume of the final library to a plate reader-compatible microplate.
- Read the fluorescence directly.
- Use a standard curve to convert fluorescence values to nanomolar (nM) concentration.
- Normalization & Pooling: Dilute each library to the required equimolar concentration based on the results from Step 2. Combine normalized libraries into a single pool for sequencing.
Key Advantages:
- Time Savings: Workflow completes in under 6 minutes compared to 1-4 hours for qPCR [47].
- Throughput: QC all samples simultaneously, unlike methods limited to individual or small-batch processing [47].
- Accuracy & Consistency: Eliminates user-user variability from serial dilutions and provides high correlation (R = 0.97) between concentration and sequencing reads [47].
- No Sample Loss: The output plate is read directly, preserving all valuable library material [47].
NGS Data Analysis Workflow for Quality Assessment
The analysis of NGS data involves multiple steps to transform raw data into interpretable information for quality assessment.
Protocol: Key Steps in NGS Data Preprocessing and Quality Control
Purpose: To ensure the integrity of sequencing data before downstream analysis, which is critical for making reliable conclusions about cell therapy product quality [51] [52].
Steps:
- Read Trimming: Remove low-quality base calls, sequencing adapters, and other technical sequences from the raw reads using tools like Trimmomatic or Cutadapt. This improves the quality of subsequent alignment [51].
- Read Alignment: Map the filtered reads to a reference genome (for DNA-Seq) or transcriptome (for RNA-Seq) using aligners such as BWA or STAR. This step determines the genomic origin of each read [51] [52].
- Quality Scoring: Assign quality scores to reads based on their accuracy. This helps in filtering out poor-quality data and is integral to variant calling [51].
- Variant/Expression Identification:
- For DNA (Variant Calling): Use tools (e.g., GATK) to identify single nucleotide variants (SNVs), insertions/deletions (indels) from the aligned reads.
- For RNA (Expression Analysis): Use tools (e.g., DESeq2, edgeR) to quantify gene expression levels and identify differentially expressed genes [51].
- Annotation and Interpretation: Determine the biological and clinical significance of identified variants or expression changes by annotating them with information from genomic databases (e.g., consequence on protein function, association with diseases) [52].
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagent Solutions for NGS-Enhanced QC
| Item | Function in NGS & Cell Therapy QC |
|---|---|
| Synthetic Cell Mimics | Stable, reproducible synthetic particles engineered to display specific cell surface biomarkers. Used as consistent controls in flow cytometry and potency assays to standardize quality control across batches and sites, replacing highly variable biological cell lines [49]. |
| Targeted NGS Panels | A predefined set of probes or primers designed to capture and sequence dozens to hundreds of genes relevant to a specific disease (e.g., a panel for hematologic malignancies). Allows for deep sequencing of critical targets to monitor product identity, purity, and safety (e.g., oncogenic mutations) [52]. |
| Integrated Library Prep & QC Kits | Kits that combine library preparation reagents with a built-in quantification technology (e.g., fluorescent labeling). They streamline the workflow, reduce hands-on time, and provide highly accurate molar concentration measurements essential for effective library normalization [47]. |
| Automated, Closed-System Bioreactors | Hardware for scalable, sterile cell expansion. When integrated with process analytics, they minimize human error and process variability, which is a foundational requirement for generating consistent starting material for NGS analysis and final cell products [46] [53]. |
| Bioinformatics Software (e.g., DESeq2, edgeR) | Statistical software packages specifically designed for the analysis of high-dimensional NGS data. They are used to identify differentially expressed genes for potency assessment, ensure product comparability, and uncover molecular signatures of product quality [51]. |
Overcoming Scalability and Supply Chain Hurdles in Personalized Production
Frequently Asked Questions (FAQs) on Capacity Expansion
FAQ 1: What are the primary strategies for expanding manufacturing capacity for autologous cell therapies?
Expanding capacity for autologous cell therapies involves a range of strategies, from short-term optimizations to long-term infrastructure projects. These are typically categorized as follows:
- Increasing Existing Suite/Room Capacity: Optimizing the layout of already approved manufacturing space, decreasing process turnaround times, and automating processes to enhance efficiency [54].
- Adding Suites/Rooms to an Existing Site: Constructing new cleanrooms or manufacturing suites within a currently operational and approved site [54].
- Expansion of Existing Sites: A significant modification of a current site, which could involve adding multiple new rooms or an entirely new manufacturing wing to an approved building [54].
- Addition of an Internal Site: Bringing a completely new, company-owned manufacturing site online, achieved through new construction, merger, or acquisition [54].
- Addition of an External CMO (Contract Manufacturing Organization): Partnering with an external contract manufacturer that does not already have regulatory approval for your specific product [54].
FAQ 2: Why is capacity validation critical, and what does it typically involve?
Capacity validation is the process of demonstrating that any changes or additions to existing manufacturing do not lead to an increase in manufacturing deviations or product quality risks [54]. For autologous therapies, where each batch is for a single patient, failing to deliver on capacity commitments can result in a loss of reputation, trust, and revenue, and can directly impact patient access to treatment [54]. The validation requirements become more rigorous as the level of expansion increases, often involving:
- Aseptic Process Simulation (APS): To demonstrate the sterility of the manufacturing process in the new or modified environment [54].
- Process Performance Qualification (PPQ): To validate that the manufacturing process consistently produces a product meeting its predefined quality attributes [54].
- Comparability Studies: To demonstrate that the product manufactured in the new or expanded capacity is comparable to the product from the previously validated process [54].
- Regulatory Filings: Depending on the nature of the change, a Prior Approval Supplement (PAS) or Changes Being Effected (CBE) filing may be required [54].
FAQ 3: How do I choose the right expansion strategy for my development stage?
The choice of strategy involves a trade-off between the urgency of need, the scale of capacity increase, capital cost, and the extent of validation required. The following table summarizes the key differentiators to guide this decision.
| Expansion Strategy | Typical Implementation Time | Key Benefit | Key Drawback | Validation & Regulatory Considerations [54] |
|---|---|---|---|---|
| Increase Existing Suite Capacity | Short-term | Quick, cost-effective | Limited throughput increase | APS, PPQ may be required; CBE filing often sufficient |
| Add Rooms to Existing Site | Short-to-medium term | Increases capacity within a known quality system | Limited by site footprint | APS re-execution; PPQ likely; CBE or PAS filing |
| Expand an Existing Site | Long-term | Substantial capacity increase at a known location | High capital cost, complex | APS, PPQ, Comparability Studies; PAS and/or PAI likely |
| Add an Internal Site | Long-term | Maximum control over a major capacity increase | Very high capital cost and lead time | APS, PPQ, Comparability Studies; PAS required |
| Add an External CMO | Long-term | Faster market entry than building; reduced initial capital | Less operational control; inflexible contracts | APS, PPQ, Comparability Studies; PAS required |
FAQ 4: What are common troubleshooting issues during capacity expansion?
- Issue: Inconsistent Product Quality Post-Expansion.
- Solution: This often indicates a failure in process comparability. Implement rigorous comparability protocols early in the expansion plan. Ensure all critical process parameters (CPPs) and critical quality attributes (CQAs) are monitored throughout the validation runs. Use a risk-based approach to focus on the most impactful parameters [54] [55].
- Issue: Failure to Meet Aseptic Process Simulation (APS) Requirements.
- Solution: Re-evaluate the environmental monitoring data and personnel aseptic technique. Review the design of the new suite for potential airflow issues or contamination risks. Ensure the APS protocol accurately simulates the full manufacturing process, including all interventions [54].
- Issue: Delays in Regulatory Approval for a New Site.
- Solution: Engage with regulatory agencies early through pre-submission meetings. Ensure all validation data (APS, PPQ) is comprehensive and follows relevant ICH and FDA guidelines. A robust and well-documented quality system that is consistent with the original site is crucial for a successful Prior Approval Supplement (PAS) [54] [55].
Experimental Protocols for Capacity Validation
Protocol 1: Process Performance Qualification (PPQ) for an Expanded Autologous CAR-T Cell Line
1.0 Objective: To demonstrate and document that the manufacturing process for an autologous CAR-T cell therapy, when conducted in the expanded capacity (new suite or site), consistently produces a drug product that meets all pre-defined quality attributes.
2.0 Materials:
- Cell Therapy Instrumentation: A closed, automated system (e.g., Thermo Fisher Scientific Gibco CTS series) for cell isolation, activation, transduction/electroporation, expansion, and washing [56].
- Analytical Equipment:
- Vi-CELL BLU Cell Viability Analyzer (Beckman Coulter) for viability [57].
- CytoFLEX Flow Cytometer (Beckman Coulter) for cell identity and phenotypic analysis [57].
- SpectraMax Multi-mode Reader (Molecular Devices) for sterility and endotoxin testing [57].
- IDBS Skyland PIMS platform for GMP-compliant data management [57].
- Reagents: GMP-grade cell culture media, cytokines, activation reagents (e.g., CTS DynaBeads), viral vector or electroporation reagent, and QC assay kits.
3.0 Methodology:
- PPQ Batch Selection: Execute a minimum of three consecutive successful PPQ batches. For autologous therapies, this may use patient-apheresis material from consenting donors or a qualified surrogate starting material that accurately represents patient variability [54] [55].
- Concurrent Manufacturing: Run the PPQ batches concurrently in the original (validated) suite and the new/expanded suite, if feasible, to generate direct comparability data.
- In-Process Testing: Monitor critical process parameters at each stage:
- T-cell Activation: Percentage of CD3+ cells and activation marker expression.
- Transduction/Efficiency: Transduction efficiency or electroporation viability and CAR expression.
- Expansion: Cell count, viability, and population doublings throughout the culture period.
- Final Formulation: Total cell count, viability, and dose.
- Final Product Release Testing: Perform full release testing on the final drug product from each PPQ batch. Key attributes are summarized in the table below.
4.0 Key Quality Attributes for PPQ (CAR-T Example):
| Quality Attribute | Target Specification | Analytical Method |
|---|---|---|
| Identity | >90% CD3+ cells; CAR expression within specified range | Flow Cytometry [57] [55] |
| Potency | Meets specified cytotoxicity and cytokine secretion in a bioassay | Cell-based functional assay [55] |
| Viability | >XX% (e.g., >70%) | Vi-CELL BLU or similar [57] |
| Purity | Minimal residual bead/vector; within spec for impurities | Flow Cytometry, PCR |
| Safety (Sterility) | No growth of aerobic/anaerobic bacteria and fungi | Automated microbial detection system [57] |
| Safety (Endotoxin) | SpectraMax Reader with LAL assay [57] | |
| Dose | Within XX% of target cell count | Automated cell counter |
5.0 Acceptance Criteria: All PPQ batches must consistently meet all pre-defined in-process controls and final product release specifications. The process must be shown to be robust and reproducible, with data comparable to the historical data from the original manufacturing process [54].
Protocol 2: Conducting a Comparability Study Following a Manufacturing Expansion
1.0 Objective: To establish confidence that the autologous cell therapy product manufactured after a capacity expansion (e.g., at a new site) is comparable to the product manufactured before the change in terms of quality, safety, and efficacy.
2.0 Study Design:
- A comparative analysis using data from the PPQ batches (post-change) and historical data from clinical batches (pre-change) that supported safety and efficacy [54] [55].
- The number of pre-change batches should provide sufficient statistical power, often 10-15 batches to account for natural patient-to-patient variability.
3.0 Analytical Characterization:
- Perform extended analytical characterization on PPQ batches and select historical batches. This goes beyond release testing and includes:
- Phenotypic Characterization: Deep immunophenotyping of T-cell subsets (e.g., naïve, central memory, effector memory) via flow cytometry, as these can impact persistence and efficacy [58].
- Functional Assays: Potency assays measuring kinetic cytotoxicity and cytokine secretion profiles.
- Molecular Characterization: If applicable, assess vector copy number and transgene expression.
4.0 Data Analysis:
- Use statistical models (e.g., equivalence testing, quality range approach) to compare the two data sets.
- The new product is considered comparable if the quality attributes of the post-change product fall within the pre-defined equivalence margin established based on the variability of the pre-change product.
Research Reagent Solutions for Expansion Validation
The following table details key materials and instruments essential for conducting robust capacity expansion and validation activities.
| Item Name | Function in Validation | Brief Explanation |
|---|---|---|
| Gibco CTS Rotea System | Cell Washing & Concentration | A closed, counterflow centrifugation system for in-process cell handling, reducing open manipulations and supporting aseptic processing [56]. |
| CTS DynaCellect System | Magnetic Cell Separation & Bead Removal | An automated, closed system for T-cell activation and subsequent bead removal, critical for standardizing a key manufacturing step [56]. |
| CTS Xenon Electroporation System | Non-Viral Genetic Modification | A closed-system electroporator for introducing CAR transgenes via RNA or DNA, offering an alternative to viral vectors [56]. |
| CytoFLEX Flow Cytometer | Identity & Phenotype | GMP-compatible flow cytometer for critical quality tests like CAR expression and T-cell subset characterization (TN, TSCM, TCM) [57] [58]. |
| Vi-CELL BLU Analyzer | Viability | Automated cell viability analyzer that provides consistent and reliable viability measurements for in-process and final product testing [57]. |
| Anatel PAT700 TOC Analyzer | Environmental Monitoring | Monifies the quality of water-for-injection (WFI) systems in the GMP facility, a key part of ensuring a controlled manufacturing environment [57]. |
| Human Platelet Lysate (HPL) / Xeno-Free Media | Cell Culture Supplement | Critical raw material for cell expansion. Moving to defined, xeno-free formulations reduces batch-to-batch variability and safety concerns [59]. |
Workflow and Signaling Pathways
Capacity Expansion Strategy Decision Flowchart
This diagram outlines the logical decision-making process for selecting a capacity expansion strategy based on the need for control, capacity increase, and resource constraints.
CAR-T Cell Kinetics Post-Infusion
Understanding the in vivo kinetics of CAR-T cells is crucial for designing potency assays and defining Critical Quality Attributes (CQAs) for comparability studies. This diagram illustrates the typical phases after patient infusion.
Technical Support Center
Troubleshooting Guides
Table 1: Common Supply Chain Challenges and Solutions
| Challenge | Root Cause | Impact | Solution |
|---|---|---|---|
| Chain of Identity (COI) Break | Lack of standardized tracking systems; manual data entry errors [60] | Potential delivery of wrong product to patient; invalidated manufacturing batch [60] | Implement automated digital COI/COC tracking systems with barcode/RFID labels [60]. |
| Temperature Excursion | Equipment failure during transport; improper packaging [60] | Loss of product viability; destroyed therapy with no replacement [60] | Deploy IoT-enabled monitoring with real-time alerts and backup storage facilities [60]. |
| CMO Communication Delay | Unreported issues at Contract Manufacturing Organizations; lack of clear communication protocols [61] | Missed clinical trial deadlines; delayed patient treatment [61] | Establish robust quality agreements with required notification timelines and hold structured weekly meetings [61]. |
| Cleanroom Contamination | Human error; ineffective cleaning agents against mold spores [61] | Shutdown of manufacturing facility; product loss [61] | Implement rigorous environmental monitoring and use sporicidal cleaning agents [61]. |
| Knowledge Loss | Staff turnover without proper documentation; toxic work environment [61] | Disruption in clinical/manufacturing phases; loss of critical process knowledge [61] | Create a digital knowledge repository with video walkthroughs and decision logs [61]. |
Table 2: Scalability and Manufacturing Bottlenecks
| Bottleneck Stage | Problem | Technical Solution |
|---|---|---|
| Patient Scheduling | Poor coordination between clinical sites and manufacturing capacity [60] | Use integrated scheduling platforms that coordinate patients, manufacturing, and logistics across time zones [60]. |
| Raw Material Management | Fragmented supply chains; dependency on single-source materials [62] | Develop risk-based approach to supplier auditing; secure multiple suppliers for critical materials [61]. |
| Process Scale-Up | Process variability when moving from lab scale to commercial production [61] | Build adaptable quality controls early; document all process changes with supporting data [61]. |
| Regulatory Compliance | Lack of cross-functional understanding of Good Clinical Practices (GCP) [61] | Provide tailored GCP training for all departments (IT, CMC, regulatory) and establish a quality review board [61]. |
| Final Product Logistics | Time-sensitive delivery constraints for viable cellular products [63] | Implement redundant transportation options and real-time shipment tracking systems [63]. |
Frequently Asked Questions (FAQs)
Q: How can we prevent catastrophic Chain of Identity breaks in our autologous therapy trials? A: The most effective approach is implementing automated digital tracking that creates immutable audit trails from patient enrollment to therapy administration. This reduces human error by 90% and cuts investigation time for discrepancies from weeks to hours. Your system should integrate barcoding or RFID at each handoff point and seamlessly connect manufacturing, logistics, and clinical partners [60].
Q: What are the critical requirements for temperature monitoring during transport? A: You need multi-layered temperature control with IoT-enabled monitoring providing real-time data and predictive analytics for equipment maintenance. Best practices include using dual-temperature loggers with GPS tracking, establishing backup storage facilities along key shipping routes, and implementing automated alert systems that trigger when temperatures approach critical thresholds [60].
Q: Our CMO often delays reporting issues, impacting our timelines. How can we improve this? A: This requires a combination of contractual and relationship management. First, establish a robust quality agreement that mandates notification within one business day of any critical deviation. Include performance metrics for batch record turnaround times. Second, maintain regular structured meetings (weekly/biweekly) covering progress, issues, and next steps. Ensure both sides have designated communication leads [61].
Q: We're struggling with cleanroom mold contamination. What specific controls should we implement? A: Beyond standard aseptic techniques, you need a targeted approach for mold. Implement a rigorous environmental monitoring program that specifically tests for mold spores, not just bacteria. Replace standard cleaning agents with sporicidal formulations designed to eliminate mold spores. Enhance staff training on aseptic techniques with a focus on mold prevention, and consider your facility's humidity control systems [61].
Q: How can we maintain process consistency when scaling from R&D to commercial manufacturing? A: Build adaptable quality controls early in process development that can accommodate necessary parameter adjustments during scale-up. Thoroughly document all process changes with supporting data. Maintain open communication with regulatory agencies about process changes, providing data to demonstrate continued product quality and consistency [61].
Q: What's the most effective way to prevent knowledge loss when key staff leave? A: Create a comprehensive knowledge transfer system that captures both formal procedures and informal knowledge. This should include a digital platform storing not just SOPs but also decision rationales, troubleshooting experiences from trial runs, and video walkthroughs of critical processes. Establish a mentorship culture where senior staff actively train newer team members, and consider using part-time consultants during transitions to maintain continuity [61].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions
| Item | Function | Application Notes |
|---|---|---|
| Viral Vectors | Delivery system for genetic material in gene therapies [62] | Critical raw material; requires multiple suppliers for security [62] [61]. |
| Cell Culture Media | Supports growth and maintenance of cellular products [62] | Quality and consistency are vital; animal-derived components pose supply chain risks [62]. |
| Cryopreservation Agents | Protects cell viability during frozen storage and transport [60] | Requires strict temperature control at -196°C for long-term storage [60]. |
| Cytokines/Growth Factors | Directs cell differentiation and expansion [62] | Batch-to-batch consistency is critical for process reproducibility. |
| Quality Control Analytics | Ensures product safety, potency, and identity [63] | Next-generation sequencing enhances characterization with limited sample volumes [63]. |
| Non-Biological Affinity Reagents | Novel analytics and purification solutions for viral vectors [62] | Rationally designed smart polymer reagents can enhance development and manufacture [62]. |
Process Visualization: Autologous Cell Therapy Journey
Autologous Cell Therapy Journey
This flowchart illustrates the complex circular supply chain of autologous cell therapy, highlighting critical control points where Chain of Identity and temperature monitoring are essential [60] [63]. The process requires seamless coordination between clinical sites, logistics providers, and manufacturing facilities to maintain product viability and patient safety.
Addressing High Costs and Logistical Delays that Jeopardize Cell Viability and Potency
For researchers and therapy developers, maintaining consistent cell quality from collection to infusion is a significant hurdle. The autologous cell therapy process, which uses a patient's own cells, is particularly vulnerable to logistical delays and high costs that can directly compromise cell viability and therapeutic potency. This technical support center provides targeted guidance to identify, troubleshoot, and prevent these critical failures, enabling the development of robust and consistent quality autologous therapies.
Troubleshooting Common Cell Viability and Logistics Issues
| Problem Area | Common Symptoms & Failures | Immediate Corrective Actions | Long-Term Preventive Strategies |
|---|---|---|---|
| Cell Processing & Logistics [64] | • Low post-thaw viability• Missed infusion timelines• Product expiration | • Standardize verification steps [64]• Optimize transport containers (dry shipper vs. liquid nitrogen dewar) [64] | • Implement closed, automated systems [65]• Map workflow to minimize thaw-to-infusion time [64] |
| Cryopreservation & Thawing [42] | • Low cell recovery post-thaw• Osmotic shock• Reduced proliferative capacity | • Use fast thawing protocols (<2 mins at 37°C) [42]• Dilute cryoprotectant drop-wise [42] | • Optimize cryopreservation solution and cell concentration [66]• Validate controlled-rate freezing |
| Cell Culture & Expansion [43] | • Poor cell attachment post-thaw• Slow proliferation• Unplanned differentiation | • Use appropriate coating matrix [42]• Verify seeding density [43]• Use ROCK inhibitor for sensitive cells [43] | • Use defined, pre-qualified media systems [43]• Establish strict confluency passaging limits [43] |
| Cost of Goods (COGs) [24] | • Unsustainable production costs• Use of expensive raw materials• High batch failure rates | • Audit and rationalize reagent use• Explore alternative media formulations | • Adopt automated manufacturing platforms [67]• Implement quality-by-design (QbD) to reduce waste [24] |
Detailed Experimental Protocols for Quality Assurance
Protocol: Post-Thaw Viability and Recovery Time-Course Assay
This protocol evaluates the impact of different cryopreservation solutions on cell stability during the critical post-thaw period before infusion [66].
- Objective: To measure cell viability, recovery, and phenotype stability over a 6-hour post-thaw period to simulate clinical infusion workflows.
- Materials:
- Method:
- Thawing: Thaw cryovials in a 37°C water bath for approximately 2 minutes [66].
- Dilution: Immediately dilute the thawed cell suspension to reduce cryoprotectant concentration:
- Cells frozen at 6 M/mL: Use a 1:1 dilution with PLA/5% HA.
- Cells frozen at 9 M/mL: Use a 1:2 dilution with PLA/5% HA to a final concentration of 3 M/mL [66].
- Time-Course Sampling: Assess cell count and viability at 0, 2, 4, and 6 hours post-thaw while keeping cells at room temperature [66].
- Viability Assessment:
- Trypan Blue Exclusion: For immediate viability count.
- Annexin V/PI Staining: Perform flow cytometry to distinguish live, early apoptotic, and dead cell populations [66].
- Recovery Calculation: Calculate viable cell recovery (%) as (Total Live Cells Counted / Number of Cells Originally Cryopreserved) × 100 [66].
- Expected Outcome: Data will identify the optimal cryopreservation solution and cell concentration that maintains >80% viability and stable phenotype over the clinically relevant 6-hour window [66].
Protocol: Immunomodulatory Potency Assay Post-Cryopreservation
This assay confirms that the cryopreservation process does not impair the critical therapeutic function of MSCs.
- Objective: To compare the immunomodulatory potency of MSCs after cryopreservation in different solutions.
- Method:
- T Cell Proliferation Inhibition: Co-culture thawed MSCs with activated peripheral blood mononuclear cells (PBMCs). Measure T cell proliferation via CFSE dilution or 3H-thymidine incorporation.
- Monocytic Phagocytosis Assay: Assess the ability of thawed MSCs to improve monocytic phagocytosis function [66].
- Interpretation: Successful cryopreservation should yield MSCs with potency comparable to fresh cultures, showing significant T cell proliferation inhibition and enhanced phagocytosis.
Frequently Asked Questions (FAQs)
Q: What are the key considerations for choosing a cryopreservation solution for a clinical-grade product? A: Selection must balance cell quality with regulatory and clinical needs. Key parameters include DMSO concentration (5-10%), regulatory support files (DMF, RSF), and post-thaw viability, recovery, and potency. Note that solutions with lower DMSO (e.g., 5%) may show a decreasing trend in viability and a significant (10-fold) reduction in proliferative capacity post-thaw compared to 10% DMSO formulations [66]. Always request a Regulatory Support File (RSF) from the vendor to aid your regulatory submission [68].
Q: We are experiencing low cell attachment efficiency after thawing primary cells. What should we check? A: Low attachment often stems from thawing technique or suboptimal culture conditions.
- Thawing: Ensure rapid thawing (<2 minutes at 37°C) and use of a specialized thawing medium. Do not centrifuge extremely fragile cells (e.g., primary neurons) [42].
- Handling: Use wide-bore pipette tips, mix slowly, and avoid osmotic shock by adding medium drop-wise after thawing [42].
- Culture Setup: Always use a recommended coating matrix (e.g., Geltrex, Collagen I), verify the lot-specific seeding density, and ensure proper dispersion of cells during plating [42].
Q: How can we reduce the high costs associated with autologous cell therapy manufacturing? A: Focus on streamlining processes and reducing failures.
- Automation: Implement automated, closed-system technologies (e.g., Lonza's Cocoon Platform) to lower labor costs, reduce contamination risk, and improve scale-up efficiency [67].
- Process Optimization: Use Quality by Design (QbD) and Design of Experiment (DoE) approaches to optimize media and process parameters, creating a more robust and reproducible process that reduces batch failure [24].
- Supply Chain: Work with suppliers that offer stable supply chains and regulatory documentation to mitigate risks and delays [68].
Q: Our cell therapy product has a very short infusion window post-thaw. How can we optimize the workflow? A: Short infusion windows require a highly coordinated and standardized workflow.
- Logistics: Locate the cell processing lab onsite or minimize transport time to the clinical floor. This can reduce the thaw-to-infusion time from over 40 minutes to less than 20 minutes [64].
- Standardization: Implement clear SOPs for product verification, thawing, and infusion. One study found that facilities typically perform three separate verification steps, taking about 6 minutes [64].
- Training: Ensure all staff (Cell Therapy Technologists, nurses) are cross-trained on the standardized protocols to ensure smooth execution [64].
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Solution | Primary Function | Key Considerations for Autologous Therapy |
|---|---|---|
| DMSO-based Cryopreservation Media (e.g., CryoStor, NutriFreez) | Protects cells from ice crystal damage during freezing via permeating cryoprotection [65] [66]. | • DMSO concentration (5-10%) impacts viability and potency [66].• Requires regulatory documentation (DMF/RSF) for clinical use [68]. |
| Plasmalyte-A with Human Albumin (PHD10) | An in-house clinical-ready formulation; serves as a base solution and protein source, reducing osmotic stress [66]. | • Offers a defined, xeno-free alternative.• Requires in-house formulation and quality control. |
| ROCK Inhibitor (Y-27632) | Improves survival of single cells and cryopreserved cells by inhibiting apoptosis [43]. | • Typically used for 18-24 hours post-passage or post-thaw [43].• Critical for stabilizing sensitive cell types like pluripotent stem cells. |
| Essential 8 Medium | A defined, xeno-free culture medium for the feeder-free maintenance of pluripotent stem cells [43]. | • Supports the transition of cells from other media systems.• Essential for maintaining a consistent, regulatory-compliant process. |
| Annexin V / Propidium Iodide (PI) | Flow cytometry stains to quantify viable (AV-/PI-), early apoptotic (AV+/PI-), and dead (AV+/PI+) cells [66]. | • Provides a more accurate picture of post-thaw health than trypan blue alone [66]. |
Cryopreservation Solution Performance Data
The table below summarizes key quality parameters for MSCs cryopreserved in different solutions, based on a comparative study. This data is critical for making an informed, evidence-based selection.
| Cryopreservation Solution | DMSO Concentration | Post-Thaw Viability (0-6h) | Cell Recovery | Proliferative Capacity (Post 6-day culture) | Immunomodulatory Potency |
|---|---|---|---|---|---|
| NutriFreez | 10% | Comparable to other 10% DMSO solutions [66] | Maintained up to 6h post-thaw [66] | Similar to PHD10 [66] | Comparable to PHD10; no significant difference [66] |
| PHD10 (Plasmalyte/HA/DMSO) | 10% | Comparable to other 10% DMSO solutions [66] | Maintained up to 6h post-thaw [66] | Similar to NutriFreez [66] | Comparable to NutriFreez; no significant difference [66] |
| CryoStor CS10 | 10% | Comparable to other 10% DMSO solutions [66] | Maintained up to 6h post-thaw [66] | 10-fold less at 3 & 6 M/mL [66] | Information Missing |
| CryoStor CS5 | 5% | Decreasing trend over 6h [66] | Decreasing trend [66] | 10-fold less at 3 & 6 M/mL [66] | Information Missing |
Workflow Optimization Diagram
Achieving consistent quality in autologous cell therapy research is a multifaceted challenge. By implementing standardized protocols, rigorously testing cryopreservation solutions for both viability and potency, and optimizing logistical workflows, researchers can effectively mitigate the risks that jeopardize cell viability and potency. A proactive approach to troubleshooting, grounded in a detailed Target Product Profile and quality-by-design principles, is essential for advancing robust and reliable autologous cell therapies from the bench to the clinic.
Mitigating Contamination Risks in Multi-Site and Point-of-Care Manufacturing Networks
Troubleshooting Guides
Troubleshooting Guide 1: Addressing Frequent Environmental Monitoring Failures
Problem: Multiple environmental monitoring (EM) alerts for microbial contamination are being reported across several manufacturing sites, despite adherence to manual cleaning protocols.
Investigation & Resolution:
- Step 1: Root Cause Analysis
- Review EM data to identify recurring microbial species and their locations to pinpoint contamination reservoirs.
- Audit operator gowning procedures and material transfer protocols at the points of failure.
- Validate the efficacy and shelf-life of prepared disinfectants against the isolated organisms [69].
- Step 2: Implement Corrective Actions
- Enhance cleaning procedures by rotating sporicidal and bactericidal disinfectants to break down biofilms [69].
- Transition from open biosafety cabinets to closed processing systems or isolators to create a physical barrier between the operator and the process [70].
- Consider implementing automated decontamination technologies, such as Hydrogen Peroxide Vapor, for more consistent and reliable surface disinfection between production runs [70].
Troubleshooting Guide 2: Managing Process Failures in Automated Point-of-Care Systems
Problem: A point-of-care (POC) molecular testing system, used for rapid sterility testing, is exhibiting high assay failure rates, leading to delays and potential product loss.
Investigation & Resolution:
- Step 1: System Performance Check
- Step 2: Process Refinement
- Implement immediate retesting of the original sample with a new test cartridge as a standard operating procedure for initial failures [71].
- Provide enhanced, hands-on training for POC system users, focusing on sample handling steps that most commonly cause errors.
- If a specific analyzer continues to fail at a high rate (e.g., >10%), work with the vendor to replace the instrument [71].
Frequently Asked Questions (FAQs)
FAQ 1: What is the single greatest contamination risk in a cell therapy cleanroom, and how can it be mitigated? The greatest contamination risk comes from human operators and the transfer of materials in or out of an aseptic process [70]. Mitigation strategies include rigorous gowning procedures, using closed or functionally closed systems like isolators, and employing sterile connection technologies to minimize open interventions [70].
FAQ 2: For a Phase I clinical trial, are we required to follow full GMP regulations? Regulatory expectations are phase-appropriate. In the U.S., Phase I trials are exempt from full 21 CFR 211 GMP regulations but must still be produced under a quality system that controls for safety, purity, and identity [72]. The FDA advocates a risk-based approach for Phase I GMP compliance, focusing on controls over sterility, cell viability, and safety assays [73].
FAQ 3: How can we ensure consistent quality and prevent contamination when manufacturing is decentralized across multiple regional centers? Implement an integrated platform with closed, automated, and digitally connected systems [74]. This reduces manual intervention and variability. Furthermore, use validated production processes with automated feedback loops and robust, rapid quality control measures that are standardized across all sites to ensure consistent product quality, regardless of the manufacturing location [74].
FAQ 4: Are automated decontamination systems significantly better than manual methods? Yes, automated decontamination (e.g., Hydrogen Peroxide Vapor) offers greater consistency, repeatability, and easier validation compared to manual methods, which are prone to human variability [70]. Automated systems provide better documentation and traceability, reduce downtime, and lower the health risk to operators [70].
FAQ 5: What is a key advantage of using a non-viral gene delivery system for autologous cell therapy? Non-viral systems, such as lipid nanoparticles, are considered "simple reagents." They are easily scalable, cost-effective, and do not require specialized electroporation equipment, which can compromise cell viability. This simplifies and standardizes the workflow, making it well-suited for automated, closed-system manufacturing [74].
Experimental Protocols
Protocol 1: Validation of Disinfectant Efficacy
Objective: To confirm the effectiveness of a disinfectant against common environmental isolates in your facility, following a risk-based approach [69].
Methodology:
- Surface Coupon Preparation: Use materials representative of your cleanroom (e.g., stainless steel, vinyl, plexiglass). Sterilize them before use.
- Inoculation: Inoculate coupon surfaces with a known concentration (e.g., 10^6 CFU) of challenge organisms. These should include standard test strains (e.g., Staphylococcus aureus, Pseudomonas aeruginosa) and any recurring isolates from your EM program.
- Disinfectant Application: Apply the disinfectant at its specified use concentration and contact time. Include a neutralization control to confirm that the disinfectant is effectively neutralized and does not continue to act during the recovery phase.
- Recovery and Enumeration: After the contact time, neutralize the disinfectant and recover any remaining microorganisms. Compare the log reduction in the test group to the control group (treated with a neutralizer only).
- Acceptance Criteria: A validated disinfectant should typically achieve a ≥3-log reduction for bacteria and a ≥2-log reduction for fungi and spores within the specified contact time [69].
Protocol 2: Rapid Sterility Testing at Point-of-Care
Objective: To perform a rapid, near-patient sterility test to reduce vein-to-vein time for short-shelf-life autologous therapies.
Methodology (based on POC molecular systems):
- Sample Collection: Aseptically collect a sample from the final cell therapy product. The sample volume and collection device must be compatible with the POC test system (e.g., specific swab and transport media) [71].
- Immediate Testing: Transport the sample to the POC testing instrument and analyze it immediately according to the manufacturer's instructions. This minimizes the risk of sample degradation or contamination.
- Result Interpretation: The automated system will typically provide a "Detected" (positive) or "Not Detected" (negative) result for microbial contaminants in a matter of hours, a significant improvement over the 7-14 day traditional sterility test [74] [71].
- Environmental Monitoring: Conduct weekly environmental swabbing of the POC instrument and surrounding benchtop. Test these swabs using the same POC system to monitor for potential amplicon or specimen contamination in the testing area [71].
Data Presentation
| Method | Key Advantages | Key Disadvantages |
|---|---|---|
| Hydrogen Peroxide Vapor | Excellent distribution & material compatibility; active aeration for fast cycles; low-level safety sensors. | Requires specialized equipment. |
| Aerosolized Hydrogen Peroxide | Good material compatibility. | Liquid droplets prone to gravity & "shadowing"; longer cycle times. |
| Chlorine Dioxide | Highly effective microbial kill; can be fast at high concentrations. | Highly corrosive; high consumables cost; high toxicity requires building evacuation. |
| UV Irradiation | Very fast; no need to seal enclosure. | Prone to shadowing; may not kill spores; efficacy decreases with distance. |
Visualizations
Diagram 1: Comprehensive Contamination Control Strategy
Diagram 2: Point-of-Care Sterility Test Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Contamination Control
| Reagent / Material | Primary Function in Contamination Control |
|---|---|
| Validated Disinfectants (e.g., sporicidal, bactericidal) | Used in manual and automated cleaning protocols to eliminate environmental microbes from surfaces and equipment [69] [70]. |
| LipidBrick Cell Ready Delivery System | A non-viral gene delivery reagent that simplifies workflow, reduces cost, and is well-suited for standardized, closed-system manufacturing, minimizing open manipulations [74]. |
| Environmental Monitoring Kits | Includes contact plates, swabs, and settling plates for routine monitoring of microbial and particulate contamination in cleanrooms and on equipment surfaces [70]. |
| High-Efficiency Particulate Air (HEPA) Filters | Used in cleanrooms and biosafety cabinets to prevent airborne cross-contamination by filtering particles and microorganisms from the air [75]. |
| Sterile, Single-Use Consumables | Closed-system kits and bags for cell processing (e.g., centrifugation, magnetic separation) eliminate the need for cleaning validation and reduce contamination risk during unit operations [13]. |
Demonstrating Product Comparability and Ensuring Regulatory Compliance
Designing Robust Comparability Studies for Process Changes and Multi-Site Manufacturing
Technical Support Center
Troubleshooting Guides & FAQs
This section addresses specific, high-priority challenges you might encounter when establishing comparability for autologous cell therapies.
FAQ 1: Our autologous starting material is highly variable. How can we achieve a consistent input for comparability studies?
Answer: Implementing a robust, GMP-compliant cell selection method is crucial for overcoming patient-to-patient variability in starting material. Magnetic cell selection within a closed, automated manufacturing system can be an effective strategy. This method helps ensure a highly purified and consistent cellular starting material, which is a fundamental prerequisite for a reliable comparability study. Transitioning from manual, open processes to such automated, scalable workflows enhances both consistency and commercial viability [76].
FAQ 2: What is the core regulatory standard for demonstrating comparability after a process change?
Answer: The foundational regulatory guidance is ICH Q5E. It states that the goal is not to prove the pre- and post-change products are identical, but to demonstrate they are highly similar. You must establish, through a comprehensive comparability package, that any differences in quality attributes have no adverse impact upon the product's safety or efficacy. The burden of proof lies with the manufacturer to demonstrate control over the modified process [77].
FAQ 3: We are planning a major process change in Phase 3. What is the recommended testing strategy for our comparability study?
Answer: For late-stage development, a rigorous, multi-faceted approach is required. The gold standard involves head-to-head testing of multiple batches:
- Extended Characterization: Uses orthogonal, molecule-specific methods to deeply characterize critical quality attributes (CQAs).
- Forced Degradation: Subjects pre- and post-change batches to stress conditions (e.g., thermal, pH, oxidative) to reveal and compare degradation pathways.
- Stability Studies: Includes real-time and accelerated stability studies.
- Statistical Analysis: The recommended format is 3 pre-change batches versus 3 post-change batches to provide a robust statistical comparison [77].
FAQ 4: During forced degradation, what should we do if we observe a new, unexpected degradation product?
Answer: An unexpected result requires immediate investigation. You should:
- Characterize the New Product: Use techniques like LC-MS to identify the nature of the variant.
- Assess Risk: Determine if the new pathway poses a risk to product safety or efficacy based on its structure and quantity.
- Justify and Inform: Document the finding and your scientific rationale in the comparability protocol. Proactively communicating these challenges and your mitigation plans in the study protocol can prevent difficult questions during regulatory review. Learning from these findings can also strengthen your overall control strategy [77].
Experimental Protocols & Data Presentation
Table 1: Phase-Appropriate Comparability Testing Strategy
This table outlines the evolving testing rigor required as a product moves through development.
| Development Phase | Primary Testing Components | Lot Selection Strategy | Key Objectives |
|---|---|---|---|
| Early Phase (e.g., Phase 1) | Release testing, stability, initial extended characterization using platform methods. | Single pre- and post-change batch. | Establish basic biophysical characteristics, screen forced degradation conditions. |
| Late Phase (e.g., Phase 3) | Extended characterization, forced degradation, stability, statistical analysis of historical release data. | 3 pre-change vs. 3 post-change batches (the "gold standard"). | Formally demonstrate comparability for regulatory submission; understand degradation pathways and molecule-specific CQAs. |
| Post-Approval (BLA/MAA) | As required by the specific change; often a subset of Phase 3 studies. | Batches representative of the validated commercial process. | Ensure ongoing control and demonstrate highly similar product quality after changes to the licensed process. |
Source: Adapted from information on phase-appropriate strategies [77].
Table 2: Example Extended Characterization Testing Panel for Monoclonal Antibodies
For a thorough comparability assessment, a suite of orthogonal analytical methods is used to interrogate multiple product attributes.
| Quality Attribute | Example Analytical Technique | Function in Comparability |
|---|---|---|
| Size Variants | Size Exclusion Chromatography (SEC-MALS) | Quantifies and characterizes aggregates and fragments. |
| Charge Variants | Imaged Capillary Isoelectric Focusing (iCIEF) | Profiles acidic and basic variants, including deamidation and sialylation. |
| Sequence & PTMs | Liquid Chromatography-Mass Spectrometry (LC-MS, ESI-TOF MS) | Confirms amino acid sequence and identifies post-translational modifications (e.g., glycosylation, oxidation). |
| Potency | Cell-based bioassay | Measures the biological activity of the molecule, a critical quality attribute. |
| Purity/Identity | Peptide Mapping, Sequencing Variant Analysis (SVA) | Provides a high-resolution identity test and monitors for sequence variants. |
Source: Based on example testing panels for monoclonal antibodies [77].
Table 3: Common Forced Degradation Stress Conditions
Forced degradation studies "pressure-test" the molecule to compare the stability profiles of pre- and post-change materials.
| Stress Type | Example Conditions | Typical Impact on Product |
|---|---|---|
| Thermal | 25°C - 50°C for up to 3 months | Can induce aggregation, fragmentation, and oxidation. |
| pH | Incubation at low (e.g., 3-4) and high (e.g., 8-9) pH | May cause deamidation, isomerization, aggregation, or fragmentation. |
| Oxidative | Incubation with hydrogen peroxide (e.g., 0.1%) | Can oxidize methionine and tryptophan residues. |
| Light | Exposure to UV and visible light per ICH Q1B | Can lead to photo-degradation and color changes. |
Source: Based on types of forced degradation stress used in comparability studies [77].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Key Reagents for Robust Immunostaining in Comparability
Chromogenic immunostaining is often used in characterization to assess cell-specific markers and critical quality attributes.
| Reagent / Solution | Function | Technical Notes & Troubleshooting |
|---|---|---|
| Polymer-based Detection Reagents (e.g., HRP-labeled) | High-sensitivity detection of primary antibodies. Preferred over biotin-labeled methods (e.g., ABC, LSAB) to avoid interference from endogenous biotin in tissues like liver and kidney [78] [79]. | |
| Antibody Diluent with BSA | Dilutes antibodies to working concentration while maintaining stability. | Use 1% Bovine Serum Albumin in 0.01M Phosphate-Buffered Saline (PBS), pH 7.4. Avoid repeated freezing/thawing of diluted antibodies [78]. |
| Diaminobenzidine (DAB) | Chromogenic substrate for HRP, producing a brown precipitate at the antigen site. | Standard chromogen for permanent staining. Solution contains DAB and hydrogen peroxide in Tris-HCl buffer [78]. |
| Mayer's Hematoxylin | Nuclear counterstain, providing deep blue contrast to DAB staining. | Brief counterstaining (e.g., 10 seconds) is typically sufficient [78]. |
| Glycerol-based Cryopreservative | Protects diluted antibodies during frozen storage. | Adding 25-50% glycerol to the antibody diluent prevents damage from repeated freeze-thaw cycles [78]. |
Workflow Visualization
Diagram 1: Comparability Study Workflow
This diagram outlines the logical flow and key decision points for designing and executing a comparability study.
Diagram 2: Forced Degradation Pathways
This diagram illustrates the logical relationships between different stress conditions and the potential degradation pathways they can reveal in a biologic product.
Validation Requirements for Different Capacity Expansion Models (Internal vs. CMO)
For developers of autologous cell therapies, selecting a capacity expansion model is a critical decision with profound implications for process validation, regulatory strategy, and ultimate commercial success. Whether scaling operations internally or through a Contract Manufacturing Organization (CMO), ensuring consistent product quality is paramount. This technical support center provides a structured guide to navigating the distinct validation requirements for each model, framed within the broader thesis of achieving consistent quality in autologous cell therapy research.
Framework and Comparative Analysis
The foundational principles of process validation—Process Design, Process Qualification, and Continued Process Verification—apply to both internal and CMO models. However, the execution, data collection, and control strategies differ significantly [80].
Table 1: Key Comparison of Validation Requirements for Internal vs. CMO Models
| Validation Aspect | Internal Capacity Expansion | CMO Partnership |
|---|---|---|
| Primary Objective | Maintain direct control and intellectual property; build long-term internal expertise [81]. | Access specialized expertise and established infrastructure to accelerate timelines [81] [82]. |
| Process Design & Characterization | Direct control over process development and characterization studies. Easier to manage process changes. | Reliance on CMO's platform processes. Requires robust, collaborative tech transfer and clear definition of Critical Process Parameters (CPPs) [80]. |
| Process Performance Qualification (PPQ) | Execute PPQ batches using internal resources and facility. Direct oversight of all validation activities. | CMO executes PPQ. Sponsors must ensure CMO's validation protocols and acceptance criteria are pre-agreed and scientifically justified [80]. |
| Capacity & Utilization | Requires significant capital investment. Biotherapeutic developers historically show lower capacity utilization (~63%), maintaining "flex" capacity [83]. | Leverages CMO's existing capacity. CMOs often have higher utilization rates (~69%) and expertise in scaling multiple programs [83]. |
| Data Management & Control Strategy | Direct ownership of all process and analytical data. Easier integration of Continued Process Verification (CPV) data. | Sponsor must ensure right-to-audit and secure transparent, real-time data sharing from the CMO for regulatory submissions and lifecycle management [80]. |
| Handling of Process Variability | Direct ability to investigate and manage the inherent variability of autologous starting materials [82] [55]. | Must verify the CMO has validated systems to handle patient-to-patient variability, often through surrogate model validation [80]. |
| Regulatory Liaison | Sponsor has direct communication with regulatory agencies on all CMC matters. | Roles and responsibilities for regulatory interactions (e.g, who responds to CMC questions) must be clearly defined in the quality agreement. |
Table 2: Quantitative Considerations for Model Selection (Data from Industry Surveys)
| Parameter | Biotherapeutic Developers (Internal) | Contract Manufacturing Organizations (CMO) |
|---|---|---|
| Avg. Mammalian Cell Culture Capacity Utilization (2007) | 62.7% | 69.4% [83] |
| Projected Capacity Expansion (by 2012) | Varies by company | 46% average industry projection [83] |
| Organizations Experiencing Significant Constraints (2007) | 16.2% of respondents | |
| Typical Validation Approach for Autologous PPQ | Use of patient-derived materials, leading to ethical and material availability challenges [80]. | Frequent use of surrogate cells from healthy donors to enable full characterization and testing [80]. |
Experimental Protocols for Validation
A robust validation strategy is built on structured experimental stages. The following protocols outline the key activities for both internal and CMO models.
Protocol 1: Process Design and Characterization
This stage aims to define a robust manufacturing process and understand the impact of process parameters on product quality.
1. Define Target Product Profile (TPP) and Critical Quality Attributes (CQAs):
- Objective: Create a "living document" that aligns the therapy's clinical goals with its manufacturing specifications [24].
- Methodology: Assemble a cross-functional team (Process Development, Regulatory, Quality, Clinical) to define the CQAs, such as cell identity, purity, viability, potency, and safety (e.g., free from adventitious agents) [24] [55]. The TPP should specify minimal, target, and ideal ranges for each attribute.
2. Process Characterization Studies:
- Objective: Identify and link Critical Process Parameters (CPPs) to CQAs.
- Methodology:
- Design of Experiments (DoE): Use multivariate analysis to systematically evaluate the effect of multiple process parameters (e.g., cell seeding density, cytokine concentrations, media formulation, harvest time) on CQAs [24].
- Scale-Down Model Validation: Develop and qualify a representative small-scale model of the manufacturing process to enable high-throughput experimentation [80].
- Risk Analysis: Use tools like Failure Mode and Effects Analysis (FMEA) to prioritize parameters for experimentation.
CMO-Specific Consideration: During tech transfer, the sponsor must ensure the CMO fully understands the proven acceptable ranges for all CPPs and the rationale behind them, as defined in the process characterization report [80].
Protocol 2: Process Performance Qualification (PPQ)
This stage confirms the manufacturing process, as designed, can consistently produce product meeting pre-determined quality standards.
1. PPQ Protocol Design:
- Objective: Draft a statistically justified protocol with clear acceptance criteria for CQAs.
- Methodology: The protocol should specify the number of batches, sampling plans, and test methods. For autologous therapies, the limited number of batches and high variability pose a challenge [80].
2. PPQ Batch Execution:
- Objective: Generate data to demonstrate process reproducibility.
- Methodology for Internal Model: Execute consecutive PPQ batches in the GMP facility using the final process, equipment, and procedures. For autologous therapies, using actual patient materials may be limited, creating an ethical dilemma between dosing the patient and fully characterizing the product [80].
- Methodology for CMO Model: The CMO executes the PPQ batches. A common solution for autologous therapies is the use of surrogate cells from healthy donors [80]. The validation must demonstrate that the drug product made from surrogate cells is representative of that made from patient cells.
3. PPQ Report and Approval:
- Objective: Document and justify that the process is validated.
- Methodology: Compile all data against pre-defined acceptance criteria. Any deviations must be thoroughly investigated. The report serves as a cornerstone for the regulatory submission.
Protocol 3: Analytical Method Validation
Robust analytics are required to generate the data for process validation and lot release. This follows ICH Q2(R2) guidelines, with the level of validation increasing with clinical phase [55].
1. Assay Selection and Development:
- Objective: Establish product-specific methods to measure CQAs.
- Methodology: Develop methods for identity (e.g., flow cytometry), purity, viability, safety (sterility, endotoxin), and most critically, potency [55]. Potency assays are particularly challenging and should be based on the product's mechanism of action, often requiring an assay matrix rather than a single test [80] [55].
2. Assay Qualification and Validation:
- Objective: Demonstrate the assay is suitable for its intended purpose.
- Methodology: Test parameters including accuracy, precision, specificity, range, and robustness. For novel CGT methods, which often have high inherent variability, demonstrating robustness is essential [80] [55].
CMO-Specific Consideration: The sponsor must confirm that the CMO's analytical methods are appropriately validated and that the CMO can provide all required documentation and data for regulatory review.
Validation Pathway for Capacity Models
Troubleshooting Guides and FAQs
FAQ 1: We are an early-stage biotech with a promising autologous therapy. How do we justify a PPQ with only a limited number of batches, as is common in cell therapy?
- Answer: Regulatory agencies acknowledge the challenge of limited batch numbers in cell therapy. The justification should be based on a comprehensive risk-based strategy [80]. This includes:
- Leveraging all available data from clinical and pilot batches.
- Using a platform process or data from similar processes to support consistency.
- Implementing a strong Continued Process Verification (CPV) program post-approval to continuously monitor process performance [80].
- For CMOs, using well-justified surrogate models for PPQ can provide the extensive characterization data that would be ethically challenging to obtain from patient-specific batches [80].
FAQ 2: Our CMO uses a slightly different flow cytometry method for identity testing than we developed in-house. How do we ensure this doesn't impact product quality and regulatory filing?
- Answer: This is a common tech transfer issue. A comparability study is required.
- Method Bridging: Test a set of representative samples (e.g., from PPQ batches) using both the in-house and the CMO's method.
- Data Analysis: Demonstrate that the CMO's method produces equivalent or superior results, meeting all pre-defined validation parameters (precision, specificity, etc.).
- Documentation: The comparability study protocol and report must be included in the regulatory submission to justify the method change [80] [55].
FAQ 3: What are the most critical clauses to include in a quality agreement with a CMO to safeguard our validation strategy?
- Answer: The quality agreement is paramount. Key clauses must cover:
- Right-to-Audit: Unrestricted rights for the sponsor to audit the CMO's facilities and data.
- Data Ownership and Access: Clear terms that the sponsor owns all process and product data, with guaranteed real-time access for regulatory purposes.
- Change Control: A defined process where the sponsor must be notified and approve any changes to the validated process, raw materials, or analytical methods.
- Roles and Responsibilities: Explicit definition of who is responsible for investigations, deviations, regulatory queries, and CAPA implementation [80].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Cell Therapy Process Development and Validation
| Reagent / Material | Function in Process Development & Validation | Key Considerations |
|---|---|---|
| Cell Culture Media | Supports cell activation, expansion, and maintains viability [3]. | Chemically defined, xeno-free formulations are critical for regulatory compliance and reducing variability. Must be qualified for use in GMP [84] [3]. |
| Cytokines (e.g., IL-2, IL-7) | Directs cell differentiation, expansion, and functional potency [3]. | Concentration and timing are Critical Process Parameters (CPPs). Require GMP-grade for commercial manufacturing [3]. |
| Cell Isolation Reagents (MACS/FACS) | Isulates target cell population (e.g., T cells) from apheresis product [3]. | Purity and viability of the isolated fraction are key. Closed, automated systems are preferred to reduce contamination risk [82] [3]. |
| Viral Vector | Mediates genetic modification (e.g., for CAR-T therapies) [55]. | Titer, infectivity, and purity are critical quality attributes. A major cost driver; requires rigorous testing and validation [55]. |
| Cryopreservation Media | Preserves cell viability and functionality during storage and transport [3]. | Formulation with DMSO and controlled-rate freezing are essential to prevent cell damage. Must be validated for post-thaw recovery and function [3]. |
GMP-Compliant Chain of Identity System
Establishing a Control Site Model for Regulatory Oversight in Decentralized Networks
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center provides practical guidance for implementing a control site model to ensure consistent quality in autologous cell therapy research within decentralized networks. The following FAQs address specific, high-priority challenges researchers encounter.
FAQ 1: What are the core regulatory expectations for preclinical efficacy data in early-phase clinical trials?
Answer: Regulatory guidance emphasizes that preclinical studies must robustly bridge findings to clinical application. Key expectations include:
- Mechanism of Action (MoA): Your application must thoroughly describe the proposed mechanism of action, as this is a cornerstone for justifying clinical translation [85].
- Clinical Relevance: Preclinical models, intervention parameters, and outcome measures should be clinically relevant to the human condition being treated [85].
- Study Rigor: While less frequently explicitly mandated, incorporating robust study design elements like randomization and blinding into preclinical work strengthens your application and reduces bias [85].
The U.S. FDA clarifies that for biological product licensure, substantial evidence of effectiveness is required, typically from two adequate and well-controlled clinical investigations. However, for some cell and gene therapy (CGT) products, data from one adequate study paired with confirmatory evidence may be sufficient, depending on factors such as disease seriousness, the practicability of conducting a second trial, and the persuasiveness of the single study [86].
FAQ 2: How can we manage decentralized manufacturing while ensuring consistent starting material quality?
Answer: Achieving consistency with highly variable patient-derived starting material is a critical challenge in autologous therapy manufacture. A control site model should enforce standardized selection and processing methods across all nodes.
- Implement Flexible, Closed Systems: Utilize magnetically active cell selection within a flexible, closed manufacturing system to obtain highly purified cells from variable starting material. This method is crucial for delivering a consistent final product [76].
- Automate Processes: Transitioning from manual or semi-automated processes to fully automated, scalable workflows (e.g., from sample loading to harvest) enhances consistency, reduces variability, and improves commercial viability [76].
- Standardize Characterization and Release Testing: Clearly distinguish between characterization testing (which provides informational product understanding) and release testing (which is for safety, purity, and potency). Results from both must be included in IND or BLA applications, with release test results reported on the product certificate of analysis [86].
FAQ 3: What is the recommended approach for long-term safety monitoring of autologous cell therapies?
Answer: Given that CGT products are often administered as a single dose, the FDA recommends intensive safety monitoring.
- Short-Term Monitoring: Monitor patients closely for adverse effects for weeks and months after administration [86].
- Long-Term Follow-Up: Depending on the product, sponsors should observe subjects for delayed adverse effects in long-term follow-up trials for up to 15 years post-exposure [86].
FAQ 4: How should we structure an IND for an umbrella trial testing multiple product versions?
Answer: The FDA has provided guidance to streamline the IND submission process for early-phase umbrella trials, which test multiple versions of a cellular or gene therapy product under a single master protocol [87].
- Primary IND: Submit one primary IND (IND A) containing the master protocol and the complete Chemistry, Manufacturing, and Controls (CMC) and pharmacology/toxicology (P/T) information for one version of the product (Product A) [87].
- Secondary INDs: For each additional product version (B, C, D, etc.), submit secondary INDs. These need only contain the CMC and P/T information for their specific product version and can cross-reference the primary IND for the master protocol details [87].
- Defining a "Version": A change that creates a different product version requires a separate IND. For example, investigating two different mutated AAV capsids for in vivo delivery constitutes two different versions, even if the CRISPR payload is identical. A change in cell culture method (e.g., adherent to suspension) during development typically does not [87].
Experimental Protocols for Quality Control
Protocol 1: Characterization of Elderly Donor Mesenchymal Stem Cells (MSCs) for Autologous Therapy
Objective: To isolate and expand a high-quality, "youthful" subpopulation from an elderly donor's MSC population for autologous therapy.
Methodology:
Cell Isolation and Culture:
- Obtain bone marrow (BM) from elderly donors and isolate MSCs via collagenase digestion and centrifugation [18].
- Culture cells in growth media on standard tissue culture plastic (TCP) for initial expansion.
Flow Cytometry and Sorting:
- Characterize the elderly MSC population using standard surface markers (CD73, CD90, CD105) per International Society for Cellular Therapy (ISCT) criteria [18].
- Further analyze for intracellular reactive oxygen species, β-galactosidase expression, ATP content, and SSEA-4 expression [18].
- Isolate subpopulations using Fluorescence-Activated Cell Sorting (FACS) based on cell size and SSEA-4 expression [18].
"Rejuvenation" Culture:
Quality Assessment:
Troubleshooting: If the isolated subpopulation does not expand sufficiently, ensure the BM-ECM is produced correctly and that ascorbic acid is added during the matrix production phase to support ECM formation [18].
Protocol 2: Implementing a Control Site Model for Decentralized Data Governance
Objective: To establish a federated governance model that balances central oversight with local autonomy in a decentralized research network.
Methodology:
- Define a Central Governing Body: Establish a central committee with representatives from key domains (e.g., bioinformatics, regulatory affairs, clinical operations) [88].
- Develop Central Policies: This central body is responsible for defining overarching data governance policies, standards, and guidelines. This includes data quality standards, security controls, and metadata management practices [88].
- Empower Local Teams: Delegate the implementation and enforcement of these policies to individual research sites or business units. These local teams operate with a degree of autonomy but must align with the central framework [88].
- Implement a Data Catalog: Deploy a data catalog to support the governance framework by documenting data assets, lineage, and policies across all nodes, ensuring transparency and discoverability [88].
- Monitor and Coordinate: Maintain regular communication and oversight between the central body and local teams to ensure consistency, address challenges, and drive continuous improvement [88].
Troubleshooting: If consistency across sites is difficult to achieve, strengthen the communication channels and review the clarity of the central policies. The central body should provide explicit guidance while allowing flexibility for site-specific needs [88].
Workflow Visualization
Decentralized Network Governance Workflow
Autologous MSC Characterization & Rejuvenation
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and their functions for the experimental protocols cited.
| Research Reagent | Function in Experiment |
|---|---|
| Fluorescence-Activated Cell Sorter (FACS) | Isulates specific cell subpopulations based on size and surface marker expression (e.g., SSEA-4) [18]. |
| Bone Marrow-Derived Extracellular Matrix (BM-ECM) | Provides a "young microenvironment" to culture and expand MSCs, helping to restore a youthful phenotype during replication [18]. |
| Stage-Specific Embryonic Antigen-4 (SSEA-4) Antibody | A cell surface marker used to identify a potent, "youthful" subpopulation within a heterogeneous elderly MSC population [18]. |
| Plerixafor | A mobilization agent used in autologous stem cell transplantation to improve stem cell yields and reduce mobilization failure rates [89]. |
| Data Catalog | A software tool that supports data governance across decentralized models by documenting data assets, lineage, and policies for transparency and discoverability [88]. |
The development of cell therapies represents a paradigm shift in treating complex diseases, from cancer to neurodegenerative disorders. Within this field, autologous (patient-specific) and allogeneic (donor-derived) approaches present fundamentally different quality paradigms. For researchers and drug development professionals, ensuring consistent quality across these modalities requires understanding their distinct biological behaviors, manufacturing challenges, and quality control requirements. This technical support center provides targeted guidance for navigating the specific quality challenges inherent in both autologous and allogeneic cell therapy research, with particular emphasis on strategies for achieving consistency in patient-specific therapies where starting material variability presents unique obstacles.
Fundamental Comparative Analysis: Autologous vs. Allogeneic Therapies
Core Biological and Manufacturing Differences
Understanding the fundamental distinctions between autologous and allogeneic approaches is essential for establishing appropriate quality benchmarks.
Table 1: Core Characteristics of Autologous vs. Allogeneic Cell Therapies
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [90] [5] | Healthy donor(s) [91] [92] |
| Immune Compatibility | Minimal rejection risk; no GvHD [90] [91] [5] | Requires HLA matching; risk of GvHD and host rejection [91] [92] |
| Manufacturing Paradigm | Personalized, patient-specific batches [90] [93] | Off-the-shelf, scalable batches [91] [92] |
| Production Timeline | 3-5 weeks vein-to-vein [93] | Immediately available from cryostock [91] |
| Key Quality Challenges | Input material variability [94] [93]; manufacturing consistency [93] | Donor screening; controlling allo-reactivity [91] [92] |
Quantitative Comparison of Quality Attributes
Benchmarking quality requires evaluating critical quality attributes (CQAs) across both modalities. The following table summarizes key quantitative differences that impact quality assessment protocols.
Table 2: Comparative Analysis of Critical Quality Attributes
| Quality Attribute | Autologous Therapy Considerations | Allogeneic Therapy Considerations |
|---|---|---|
| Starting Material Variability | High variability due to patient health status and prior treatments [94] [93] | More consistent from healthy donors [91] |
| Product Consistency | Batch-to-batch variability; personalized products [93] | Highly consistent across doses from same master cell bank [91] |
| Potency Assays | Must account for variable T-cell fitness [90] [94] | More standardized across products [91] |
| Identity Testing | Confirmation of patient origin required [4] | Donor lineage tracking essential [91] |
| Purity Requirements | Removal of malignant cell contamination critical [94] | Elimination of alloreactive T-cells crucial [91] [92] |
Troubleshooting Common Quality Issues
FAQ: Addressing Autologous Therapy Quality Challenges
Q: How can we manage the high variability in input material quality for autologous therapies?
A: Implement rigorous pre-apheresis patient health assessment and lymphocyte counting protocols. Consider lymphocyte enrichment methods to improve starting population quality. For T-cell therapies, selection of specific T-cell subsets (e.g., CD62L+, CD4/CD8 ratio control) can reduce final product variability [94] [93]. Establish acceptance criteria for apheresis material based on viability, cell composition, and functional assays.
Q: What strategies can reduce manufacturing failure rates in autologous systems?
A: Adoption of closed, automated systems (e.g., Cocoon, Prodigy) reduces human error and contamination risk [93]. Implement process analytical technologies (PAT) for real-time monitoring of critical process parameters. Develop rapid microbial testing methods to minimize hold times. Establish robust cryopreservation protocols for apheresis material to decouple collection from manufacturing scheduling [94].
Q: How can we ensure consistent potency despite variable starting material?
A: Implement fingerprinting technologies like transcriptional profiling to define identity and expansion signatures [4]. Develop correlation models between early-process biomarkers and final product potency. Utilize functional potency assays that measure specific mechanisms of action relevant to your therapy [4].
FAQ: Addressing Allogeneic Therapy Quality Challenges
Q: What are the critical quality controls for preventing graft-versus-host disease in allogeneic products?
A: Implement efficient T-cell depletion strategies (e.g., CD34+ selection, TCR disruption) validated using sensitive mixed lymphocyte reaction assays [91]. Conduct comprehensive characterization of residual T-cell repertoire post-manipulation. Establish stringent limits for alloreactive T-cell frequency in final products.
Q: How do we ensure consistent product quality across multiple donations?
A: Develop extensive donor screening protocols including HLA typing, health status assessment, and cell functionality testing. Establish master cell banks with comprehensive characterization including identity, purity, potency, and stability data [91]. Implement comparability protocols for assessing products from different donors.
Experimental Protocols for Quality Assessment
Protocol: T-cell Product Transcriptional Fingerprinting
Purpose: To molecularly characterize T-cell products for identity and expansion potential using transcriptional fingerprinting [4].
Methodology:
- Cell Isolation: Isolate T-cell populations (Treg or Teff) from PBMCs by FACS sorting using CD4+/CD25hi/CD127lo for Treg and CD4+/CD25lo/CD127hi for Teff [4].
- Sample Preparation: Collect cell pellets (1×10^6 cells) for RNA extraction. Ensure RNA integrity number (RIN) ≥8 before library preparation.
- RNA Sequencing: Perform bulk RNA-seq using Illumina platforms (minimum 25M reads per sample, paired-end 150bp).
- Computational Analysis: Apply non-parametric algorithm to score samples against pre-defined identity and expansion fingerprints [4].
- Interpretation: Identity fingerprint distinguishes Treg from Teff (100% sensitivity/specificity reported). Expansion fingerprint identifies expansion history of cells [4].
Troubleshooting Tip: Low RIN scores often result from improper cell handling. Use RNase-free conditions and process samples rapidly after collection.
Protocol: Assessing Allogeneic T-cell Alloreactivity
Purpose: To evaluate residual alloreactive potential in allogeneic cell products.
Methodology:
- Responder Cell Preparation: Isolate PBMCs from multiple HLA-mismatched healthy donors (minimum n=3).
- Co-culture Establishment: Culture allogeneic test product with responder PBMCs at optimized ratios (typically 1:1 to 1:10) in RPMI-1640 with 10% FBS.
- Proliferation Assay: Measure responder cell proliferation using CFSE dilution or [3H]-thymidine incorporation after 5-7 days.
- Cytokine Analysis: Quantify IFN-γ, IL-2, TNF-α in supernatant by ELISA or multiplex assay.
- Acceptance Criteria: Establish threshold for stimulation index (SI) based on clinical safety data.
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Cell Therapy Quality Assessment
| Reagent/Category | Specific Examples | Research Application | Quality Consideration |
|---|---|---|---|
| Cell Separation | Anti-CD25 beads; Akadeum microbubble technology [90] | T-cell isolation and purification | Purity, viability, and activation state of isolated cells |
| Cell Activation | Anti-CD3/CD28 Dynabeads [4] [94] | T-cell activation and expansion | Consistency of activation; bead removal efficiency |
| Culture Media | CTS OpTmizer T Cell Expansion media [4] | Ex vivo cell expansion | Batch-to-batch consistency; impact on differentiation |
| Genetic Modification | Lentiviral/gammaretroviral vectors; electroporation systems [94] [93] | CAR insertion or gene editing | Transduction efficiency; insertional mutagenesis risk |
| Characterization | FOXP3 staining panels; TSDR methylation analysis [4] | Treg identity confirmation | Specificity for stable Treg population |
Workflow Visualization: Quality Paradigm Comparison
Diagram 1: Comparative Quality Paradigms in Cell Therapy Manufacturing
Advanced Quality Control Methodologies
Transcriptional Fingerprinting for Identity Assurance
For autologous therapies, particularly those involving regulatory T-cells (Treg), traditional markers like FOXP3 and TSDR demethylation may be insufficient for ensuring product quality [4]. Advanced transcriptional fingerprinting provides a robust framework for molecular characterization:
Implementation Strategy:
- Develop identity fingerprints that distinguish Treg from effector T-cells (Teff) regardless of activation status [4]
- Establish expansion fingerprints to characterize manufacturing impact on cellular properties [4]
- Utilize machine learning algorithms to score manufacturing products against reference fingerprints
- Correlate fingerprint scores with functional potency assays and clinical outcomes
Application Example: In Treg therapy development, identity fingerprints achieved 100% sensitivity and specificity in distinguishing Treg from Teff populations, providing superior quality assurance compared to single-marker approaches [4].
Process Analytical Technology (PAT) Implementation
Integrating PAT into cell therapy manufacturing enables real-time quality monitoring and control:
Key Implementation Areas:
- In-line monitoring of metabolic parameters (glucose, lactate, oxygen) during expansion
- At-line assessment of cell density and viability
- On-line measurement of critical quality attributes using advanced sensors
- Multivariate data analysis for predicting product quality
Successful cell therapy development requires recognizing that autologous and allogeneic therapies are not simply interchangeable approaches but represent fundamentally different quality paradigms. Autologous therapies demand strategies for managing inherent variability through robust process controls and advanced characterization methods like transcriptional fingerprinting. Allogeneic therapies require rigorous donor screening and comprehensive alloreactivity control. By implementing the troubleshooting guides, experimental protocols, and quality assessment frameworks outlined in this technical support center, researchers can advance both autologous and allogeneic cell therapies with appropriate quality benchmarks, ultimately accelerating the development of safe and effective treatments for patients.
Conclusion
Ensuring consistent quality in autologous cell therapy is not a single-step solution but a multi-faceted strategy integrating advanced technology, robust systems, and proactive regulatory planning. The convergence of automation, AI-driven analytics, and innovative decentralized models presents a viable path to standardizing these highly personalized treatments. Future success hinges on the industry's ability to further develop scalable, closed-system technologies, establish harmonized global regulatory standards for point-of-care manufacturing, and implement sophisticated digital platforms for seamless supply chain orchestration. By steadfastly addressing these areas, the field can overcome the inherent challenges of variability, unlocking the full potential of autologous cell therapies to provide consistent, life-changing treatments for a broader patient population.
References
- 1. What are the hurdles impacting patient access to cell and gene... [https://ct.catapult.org.uk/news/what-are-the-hurdles-impacting-patient-access-to-cell-and-gene-therapies-in-the-uk]
- 2. Ensuring source material consistency & continuity for... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/1501/ensuring-source-material-consistency-continuity-for-commercialization-of-advanced-therapies]
- 3. Process Steps in Cell Therapy Manufacturing [https://www.cellandgene.com/topic/cell-therapy-manufacturing]
- 4. Frontiers | Transcriptional fingerprinting of regulatory T cells : ensuring... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1602172/full]
- 5. Autologous Cell Therapy: Types, Benefits & Challenges | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/autologous-cell-therapy-overview.html]
- 6. Enhancing Speed in CAR-T Cell Manufacturing with Cell ... Therapy [https://www.thermofisher.com/blog/behindthebench/enhancing-speed-in-car-t-cell-manufacturing-with-cell-therapy-solutions/]
- 7. insights.bio/ cell -and-gene- therapy -insights/journal/article/344... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/344/understanding-the-role-of-critical-quality-attributes-along-the-commercialization-pathway]
- 8. Basics of advanced therapy medicinal product development in academic pharma and the role of a GMP simulation unit - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10772236/]
- 9. and gene Cell answers: Assessing the therapy ... critical quality [https://www.labcorp.com/education-events/articles/cell-and-gene-therapy-answers-assessing-critical-quality-attributes-challenges-and-importance-cmc]
- 10. Quality assessment of cellular therapies: the emerging role of molecular assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2983004/]
- 11. Frontiers | Treg cell manufacturability: current state of the art... therapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1604483/full]
- 12. RNAscope Troubleshooting Guide and FAQ | Troubleshooting [https://acdbio.com/technical-support/solutions]
- 13. Guide to Cell GMP Manufacturing for Therapy CAR T Autologous [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 14. of Evolution and Gene Cell and the Role of Rapid Therapies ... Quality [https://www.biomerieux.com/corp/en/blog/pharmaceutical-qc/Evolution-Cell-Gene-Therapies-Role-Rapid-Quality-Control-Solutions-Safe-Effective-Products.html]
- 15. Strategies for Achieving Measurement Assurance for Cell Therapy Products - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4878336/]
- 16. Market Size, Share & Forecast Outlook... Autologous Cell Therapy [https://www.emergenresearch.com/industry-report/autologous-cell-therapy-market]
- 17. Cell Culture Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-troubleshooting/cell-culture-troubleshooting-guide.html]
- 18. Restoring the quantity and quality of elderly human mesenchymal... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-017-0688-x]
- 19. primary Disease for verification and validation testing state cells [https://www.news-medical.net/whitepaper/20240201/Disease-State-Primary-Cells-for-Verification-and-Validation-Testing.aspx]
- 20. in adipose tissue-derived stem Donor : implications for... variability cells [https://www.explorationpub.com/Journals/em/Article/1001243]
- 21. Identifying and Managing Sources of Variability in Cell Therapy Manufacturing and Clinical Trials | Regenerative Engineering and Translational Medicine [https://link.springer.com/article/10.1007/s40883-019-00129-y]
- 22. How to troubleshoot contamination | INFORS HT bioreactor [https://infors-ht.com/en/blog/how-to-troubleshoot-bioreactor-contamination]
- 23. Automation in cell and gene bioprocessing: challenges, opportunities and what lies ahead [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/12/Automation-in-cell-and-gene-bioprocessing-challenges-opportunities-and-what-lies-ahead]
- 24. Concise Review: Process Development Considerations for Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572896/]
- 25. Innovative Bioreactor Technologies for Advanced Cell... | Preprints.org [https://www.preprints.org/manuscript/202412.2416/v1]
- 26. on-line cell culture monitoring using numera® and the... Automated [https://www.securecell.ch/insights/automated-on-line-cell-culture-monitoring-using-numera]
- 27. Concise Review: Guidance in Developing Commercializable Autologous/Patient-Specific Cell Therapy Manufacturing - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808202/]
- 28. Automation Will Dominate Single-Use Bioprocessing within the Next Five Years | Professional Education [https://professional.mit.edu/news/articles/automation-will-dominate-single-use-bioprocessing-within-next-five-years]
- 29. Digital Twins for Buildings: FAQs | Twinview [https://www.twinview.com/insights/digital-twins-for-buildings-faqs]
- 30. – An essential step towards smart ATMP processes Digital twins [https://www.antleron.com/post/digital-twins-an-essential-step-towards-smart-atmp-processes]
- 31. What Is a Digital Twin? | IBM [https://www.ibm.com/think/topics/digital-twin]
- 32. Toward Rapid, Widely Available Autologous CAR-T Cell ... Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC9207622/]
- 33. Transforming Regenerative Medicine Manufacturing with AI [https://www.linkedin.com/pulse/transforming-regenerative-medicine-manufacturing-ai-1businessworld-rzwpe]
- 34. How to Troubleshoot and Fix AI Workflows for Text Input | Copy. ai [https://www.copy.ai/guides/how-to-troubleshoot-and-fix-ai-workflows-for-text-input]
- 35. Debugging AI : Tools and Techniques for Troubleshooting ... AI [https://dev.to/ultraai/debugging-ai-tools-and-techniques-for-troubleshooting-ai-applications-3h2p]
- 36. Autologous CAR-T Cell Therapy Manufacturing | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/solutions/cell-therapy/autologous-car-t-cell-therapy.html]
- 37. with Accelerated... Decentralizing Autologous Cell Therapies [https://www.thermofisher.com/blog/behindthebench/decentralizing-autologous-cell-therapies-with-accelerated-manufacturing-workflows/]
- 38. Health Advances Insights :: Health Advances [https://www.healthadvances.com/insights/blog/breaking-barriers-the-evolution-of-decentralized-autologous-cell-therapy-manufacturing]
- 39. Promises and challenges of a decentralized CAR T- cell manufacturing... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11235344/]
- 40. - Point - of of care | imec manufacturing cell therapies [https://www.imec-int.com/en/articles/how-point-care-manufacturing-will-enable-cell-therapies-reach-patients-who-need-them]
- 41. Implementation of a quality management system for decentralized manufacturing of cell and gene therapy products - technical and regulatory considerations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361990/]
- 42. Primary Cell Culture Support—Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/primary-cell-culture-support/primary-cell-culture-support-troubleshooting.html]
- 43. Stem Cell Culture Support—Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 44. Frontiers | Isolator-based point-of-care manufacturing: a practical solution for GMP-compliant cell and extracellular vesicles therapy production [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1644318/full]
- 45. Redefining quality in cell and gene therapies: Lessons from implementing electronic QMS in academic cGMP facility - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1525001625002588]
- 46. Frontiers | Implementation of a quality management system for... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1591751/full]
- 47. How to optimize NGS library QC to improve your NGS ... - Tecan [https://www.tecan.com/blog/the-benefits-of-optimizing-ngs-library-qc]
- 48. NGS Sequencing Support-Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 49. Streamline cell therapy quality control with ‘cell mimics’ [https://www.nature.com/articles/d42473-024-00170-8]
- 50. How NGS Based Diagnostics Works — In One Simple Flow ( 2025 ) [https://www.linkedin.com/pulse/how-ngs-based-diagnostics-works-one-simple-flow-2025-mhrlf/]
- 51. in Biostatistics: A Statistical Perspective NGS [https://www.numberanalytics.com/blog/statistical-perspective-next-generation-sequencing-biostatistics]
- 52. Next-generation sequencing and its clinical application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6528456/]
- 53. How Autologous Works — In One Simple Flow ( Cell ) Therapy 2025 [https://www.linkedin.com/pulse/how-autologous-cell-therapy-works-one-simple-flow-2025-qi2qf]
- 54. Manufacturing Capacity and Validation for Expansion ... Autologous [https://www.pda.org/pda-letter-portal/home/full-article/manufacturing-capacity-expansion-and-validation-for-autologous-cell-therapies]
- 55. Manufacturing: Testing, Cell & Regulatory Insights Therapy Validation [https://www.allucent.com/resources/blog/cell-therapy-manufacturing]
- 56. Manufacturing CAR T Cell Therapies: Challenges, Insights and Solutions - Behind the Bench [https://www.thermofisher.com/blog/behindthebench/manufacturing-car-t-cell-therapies-challenges-insights-and-solutions/]
- 57. CAR-T Cell Therapy Quality Control - Release Testing Solutions | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/solutions/cell-therapy/autologous-car-t-cell-therapy/process-steps/release-testing.html]
- 58. Model‐informed drug development of autologous CAR‐T cell ... therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10681459/]
- 59. Bioprocess engineering strategies for autologous human MSC-based... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/404/Bioprocess-engineering-strategies-for-autologous-human-MSC-based-therapies-one-size-does-not-fit-all]
- 60. Gene Cell : Problems & Solutions Therapy Supply Chain 2025 [https://www.linkedin.com/pulse/copy-cell-gene-therapy-supply-chain-common-problems-practical-balaji-qk2fc]
- 61. Management in Quality and Gene Cell : An Expert Guide... Therapy [https://www.thefdagroup.com/blog/quality-management-in-cell-and-gene-therapy]
- 62. The Future of Cell and Gene Therapy : Navigating... - BioSpace [https://www.biospace.com/drug-development/the-future-of-cell-and-gene-therapy-navigating-innovation-regulation-and-manufacturing-challenges]
- 63. Solutions Autologous Cell Therapy Supply Chain [https://www.bioprocessintl.com/cell-therapies/ebook-autologous-cell-therapies-shoring-up-supply-chains-for-scalability]
- 64. Comparative analysis of cell therapy infusion workflows at clinical sites - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9013238/]
- 65. Solution in the Real World: 5 Uses You'll Actually... Cell Preservation [https://www.linkedin.com/pulse/cell-preservation-solution-real-world-5-uses-youll-tysce]
- 66. Frontiers | Key quality parameter comparison of mesenchymal stem... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1412811/full]
- 67. Market Growth & Opportunities Report Autologous Cell Therapy 2025 [https://www.thebusinessresearchcompany.com/report/autologous-cell-therapy-global-market-report]
- 68. Cell Therapy Systems (CTS) Support | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/clinical/cell-gene-therapy/cell-therapy/cell-therapy-systems/cell-therapy-systems-support.html]
- 69. Disinfectant Efficacy: Understanding the Expectations and How to... [https://pubmed.ncbi.nlm.nih.gov/31732692/]
- 70. Control Contamination | Ecolab Strategies [https://www.ecolab.com/articles/2025/04/contamination-control-strategies]
- 71. Assessment of Test Performance and Potential for Environmental... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6355544/]
- 72. Considering Cell Therapy Product “Good Manufacturing Practice” Status - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936751/]
- 73. Navigating Operational Complexities in Phase I GMP Cell Therapy Manufacturing: A Compliance Perspective [https://news.cuanschutz.edu/gates/operational-complexity-in-phase-i-gmp-cell-therapy-manufacturing]
- 74. Integrated Platforms for Autologous Cell Therapy [https://www.bioprocessintl.com/sponsored-content/autologous-cell-therapy-can-integrated-platforms-break-the-bottlenecks-]
- 75. Cell therapy: cGMP facilities and manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3666518/]
- 76. Magnetic selection for consistent starting material in... cellular [https://www.insights.bio/cell-and-gene-therapy-insights/webinars/269/magnetic-selection-for-consistent-cellular-starting-material-in-autologous-cell-therapy-manufacture]
- 77. Understanding comparability studies for biologics: Why They Matter [https://mmsholdings.com/perspectives/comparability-studies-biologics-importance/]
- 78. Pitfalls and Caveats in Applying Chromogenic Immunostaining to Histopathological Diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232789/]
- 79. Fluorescent vs. Chromogenic Detection in Immunohistochemistry – ... [https://blog.biossusa.com/blogs/iggy-the-bioss-dragon/fluorescent-vs-chromogenic-detection-ihc]
- 80. Proposed Solutions For Cell & Gene Therapy Validation Challenges [https://www.cellandgene.com/doc/proposed-solutions-for-cell-gene-therapy-validation-challenges-0001]
- 81. Top Cell Companies & How to Therapy Them (2026) CMO Compare [https://www.linkedin.com/pulse/top-cell-therapy-cmo-companies-how-aezwf]
- 82. Autologous Cell Therapy Manufacturing - Patheon pharma services [https://www.patheon.com/us/en/insights-resources/blog/autologous-cell-therapy-manufacturing-challenges-and-best-practices.html]
- 83. Trends in capacity utilization for therapeutic monoclonal antibody... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2725417/]
- 84. & Gene Cell Products to Meet Therapy GMP Guidelines [https://www.fishersci.ie/ie/en/scientific-products/publications/lab-reporter/2022/issue-2/cell-gene-therapy-to-meet-gmp-guidelines.html]
- 85. Synthesizing regulatory guidance for demonstrating preclinical efficacy and translating promising cell therapies to early phase clinical trials: a scoping review | BMC Medicine | Full Text [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-024-03690-8]
- 86. Duane Morris LLP - FDA Issues Draft Guidance Q&A on Developing Potential Cellular and Gene Therapy Products [https://www.duanemorris.com/alerts/fda_draft_guidance_q&a_developing_potential_cellular_gene_therapy_products_0125.html]
- 87. Understanding FDA Cell and Gene Therapy Guidance [https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance/]
- 88. Understand Data Governance Models : Centralized, Decentralized ... [https://www.alation.com/blog/understand-data-governance-models-centralized-decentralized-federated/]
- 89. Optimizing autologous stem cell mobilization strategies to improve... [https://pubmed.ncbi.nlm.nih.gov/24141007/]
- 90. Autologous Cell Therapy: Akadeum’s Cell Therapy Technology [https://www.akadeum.com/technology/cell-expansion/autologous/]
- 91. Advances in Stem Cell : Therapy ... Allogeneic vs Autologous [https://mtrb.org/allogeneic-vs-autologous-transplants/]
- 92. CAR T- Allogeneic Explained | AJMC vs Autologous Cell Therapy [https://www.ajmc.com/view/allogeneic-vs-autologous-car-t-cell-therapy-explained]
- 93. Autologous Cell Therapy: Key Challenges and Bioprocessing Innovations | L.E.K. Consulting [https://www.lek.com/insights/hea/us/ei/autologous-cell-therapy-key-challenges-and-bioprocessing-innovations]
- 94. Scalable Manufacturing of CAR T Cells for Cancer Immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8462122/]