Strategies for Addressing Batch Variation in Autologous Cell Therapy Manufacturing
This article provides a comprehensive guide for researchers and drug development professionals on managing batch variation in autologous cell products.
Strategies for Addressing Batch Variation in Autologous Cell Therapy Manufacturing
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on managing batch variation in autologous cell products. It explores the foundational causes and impacts of batch effects, evaluates current methodological and computational correction approaches, offers troubleshooting and optimization strategies for manufacturing, and discusses validation frameworks and comparative analyses for ensuring product quality and regulatory compliance. The content synthesizes the latest research and technological advancements to address a critical challenge in scaling personalized cell therapies.
Understanding Batch Effects: Sources and Impact on Autologous Product Quality
Defining Batch Variation in the Context of Autologous Therapies
Frequently Asked Questions
What is batch variation in autologous cell therapies? Batch variation refers to the inherent differences that occur between individual production runs (batches) of autologous cell therapies. Since each batch starts with cells from a different patient, variability arises from patient-specific biological factors combined with technical manufacturing differences. This contrasts with allogeneic therapies where a single donor source is used for multiple patients [1] [2].
Why is batch variation particularly challenging for autologous therapies? Batch variation is especially problematic because each patient's cells behave differently during manufacturing. A process that works with high yield for one patient's cells may fail completely for another. This variability directly impacts patient access to treatment, as failure to manufacture a viable product can be life-threatening for patients with no alternative options [2].
What are the primary sources of batch variation?
- Patient Biological Variability: Disease severity, prior treatments (chemotherapy, radiation), age, genetic factors, and overall health status [2]
- Starting Material Collection: Differences in apheresis protocols, collection devices, operator training, and anticoagulants used [1] [2]
- Raw Materials: Variability in reagents, media, plasmids, viral vectors, and other process components [1]
- Manufacturing Process: Differences in cell growth kinetics, transduction efficiency, and handling conditions [1]
How can I detect and measure batch effects in my dataset? Several computational methods can identify batch effects in omics data:
- Visualization: PCA, t-SNE, or UMAP plots showing samples clustering by batch rather than biological source [3] [4]
- Quantitative Metrics: Normalized mutual information (NMI), adjusted rand index (ARI), kBET, or PCR_batch [3]
- Statistical Analysis: Differential expression analysis comparing batches to identify batch-correlated features [5]
Troubleshooting Guides
Problem: High Failure Rates in CAR-T Manufacturing
Symptoms: Inconsistent transduction efficiency, variable cell expansion rates, failure to meet release specifications for some patient batches.
Possible Causes and Solutions:
| Cause | Solution | Reference |
|---|---|---|
| Patient prior treatments affecting cell health | Implement stricter patient eligibility criteria or adapt process parameters | [2] |
| Variable apheresis material quality | Standardize collection protocols and operator training across sites | [2] |
| Inconsistent raw material quality | Use GMP-grade, compendial materials with quality agreements with vendors | [1] |
| Uncontrolled process parameters | Implement process analytical technologies for real-time monitoring | [2] |
Problem: Batch Effects in Single-Cell RNA Sequencing Data
Symptoms: Cells clustering by batch rather than cell type or biological condition in dimensionality reduction plots.
Detection and Correction Workflow:
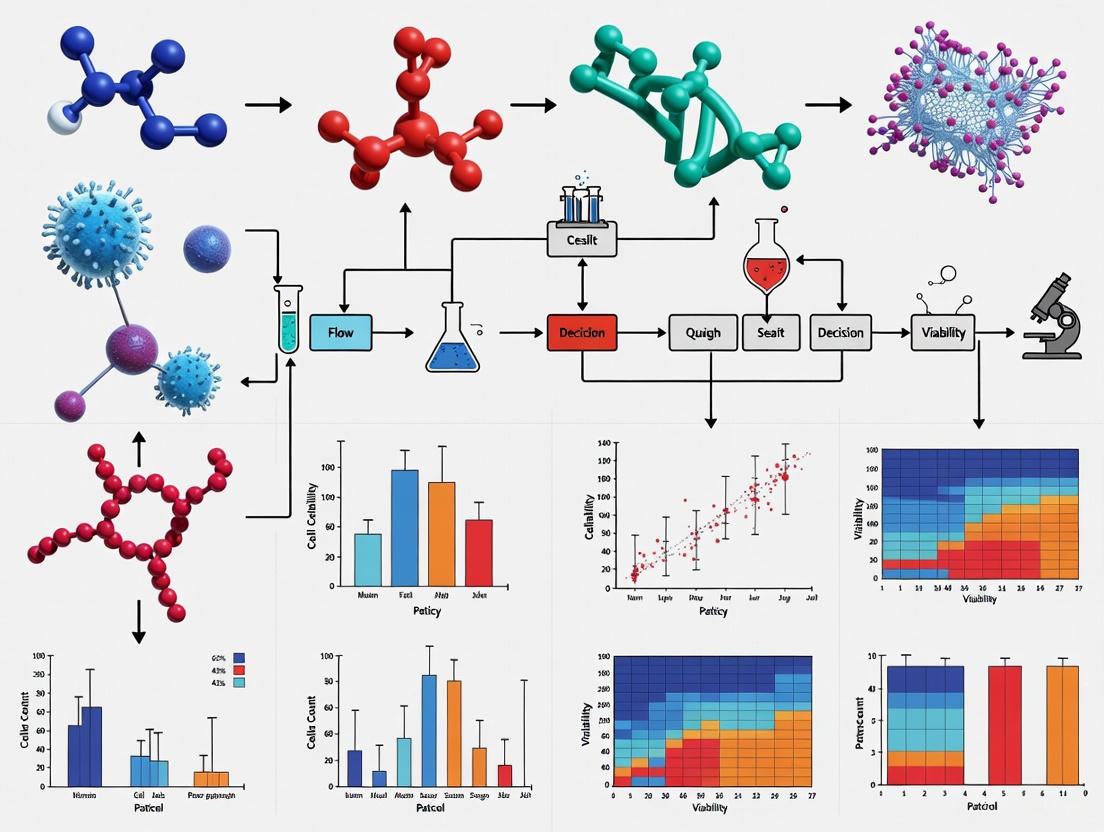
Batch Effect Analysis Workflow
Common Correction Algorithms:
| Method | Principle | Best For | |
|---|---|---|---|
| Harmony | Iterative clustering with correction factors | Large datasets, fast runtime | [3] [4] |
| Seurat CCA | Canonical correlation analysis with MNN anchoring | Well-balanced sample types | [3] [4] |
| scANVI | Variational autoencoder with Bayesian modeling | Complex batch structures | [4] |
| MNN Correct | Mutual nearest neighbors in gene expression space | Similar cell type compositions | [3] |
Avoiding Overcorrection: Monitor for these signs of overcorrection: distinct cell types clustering together, complete overlap of samples from very different conditions, and cluster-specific markers comprising ubiquitous genes like ribosomal proteins [3] [4].
Problem: Inconsistent Potency in Final Products
Symptoms: Variable functional performance in potency assays, inconsistent cytokine secretion profiles, differing target cell killing efficiency.
Quality Control Framework:
Quality Control Testing Framework
Experimental Protocols and Data Analysis
Protocol: Harmonized Quality Control Testing for Academic CAR-T Production
This protocol follows recommendations from the UNITC Consortium for standardizing QC testing [6]:
Mycoplasma Detection
- Use validated commercial nucleic acid amplification kits
- Validate detection limits for at least 10 CFU/mL
- Test both cell suspensions and culture supernatants
- Ensure compatibility with production timeline (alternative to 28-day culture method)
Endotoxin Testing
- Employ Limulus Amebocyte Lysate (LAL) or Recombinant Factor C (rFC) assays
- Validate protocols to prevent matrix interference
- Follow European Pharmacopoeia guidelines
Vector Copy Number (VCN) Quantification
- Use validated qPCR or ddPCR techniques
- Establish acceptable range per cell (balance efficacy vs. safety)
- Monitor for risk of insertional mutagenesis
Potency Assessment
- Implement IFN-γ ELISA following antigenic stimulation
- Include flow cytometry for immunophenotyping
- Perform functional assays (cytokine release, cytolytic capacity)
Quantitative Data on Batch Variation Effects
Table 1: Impact of Culture Conditions on BMSC Properties [7]
| Parameter | FBS Expansion | hPL Expansion | Significance |
|---|---|---|---|
| Proliferation Rate | Baseline | Significantly Increased | p < 0.05 |
| Gene Expression Trajectories | Distinct patterns | Different distinct patterns | Significant |
| Phenotype Markers | Canonical fibroblastic | Different signature | Significant |
| Chondrogenic Function | Decreased over time | Maintained over culture | p < 0.05 |
| Clotting Risk | Increased over time | Lower risk | p < 0.05 |
Table 2: iMSC Batch Variability in Osteoarthritis Model [8]
| Batch | Differentiation Capacity | EV Anti-inflammatory Effects | Senescence |
|---|---|---|---|
| SD1 | Variable between batches | Prolonged activity | Reduced vs. primary |
| SD2 | Variable between batches | Prolonged activity | Reduced vs. primary |
| SD3 | Variable between batches | Prolonged activity | Reduced vs. primary |
| Primary MSCs | Consistent but declines | Diminished by passage 5 | Increased over time |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Managing Batch Variation
| Material | Function | Quality Considerations |
|---|---|---|
| GMP-grade Media & Reagents | Cell culture expansion | High purity, compendial grade, produced under GMP [1] |
| Human Platelet Lysate (hPL) | FBS substitute for expansion | Standardized pooling, ABO blood group matching [7] |
| Validated QC Kits | Mycoplasma, endotoxin testing | Pharmacopoeia compliance, validated detection limits [6] |
| Clinical-grade Viral Vectors | Genetic modification | Consistent titer, purity, minimal empty capsids [9] |
| Automated, Closed Systems | Standardized manufacturing | Reduced operator variability, controlled environment [6] |
Key Risk Mitigation Strategies
Implement Flexible Processing: Design manufacturing processes that can accommodate variable growth kinetics while maintaining GMP requirements [2].
Strategic Raw Material Sourcing: Establish quality agreements with vendors, conduct incoming testing, and avoid sole-source materials when possible [1].
Comprehensive Analytics: Develop multivariate testing strategies using process analytical technologies for real-time monitoring and control [2].
Standardization Where Possible: Harmonize protocols across sites for cell collection, isolation, and processing while maintaining flexibility for patient-specific variations [6] [2].
Early Donor Variability Assessment: Intentionally introduce donor variability during process development to understand critical quality attributes [2].
This technical support center article provides troubleshooting guides and FAQs to help researchers identify and manage key sources of variability in autologous cell product manufacturing.
FAQs: Understanding and Troubleshooting Variability
1. What are the primary donor-related factors that cause variability in autologous cell therapies? The patient is the primary driver of variability. The cell product will always reflect the donor's condition at the time of collection [10]. Key factors include:
- Clinical Indication and Disease Status: Patients with different cancers (e.g., CLL, lymphoma, ALL) present with vastly different baseline blood counts and lymphocyte levels, directly impacting the starting material's cellular composition [10].
- Treatment History: Prior treatments, especially years of cytotoxic chemotherapy, can affect the quality and fitness of a patient's T cells [10].
- Patient Demographics: Age and other fixed factors can influence cell quality [10].
2. How do raw materials contribute to batch-to-batch variation? Cell culture media and other raw materials are a significant source of variability that can detrimentally affect cell growth, viability, and product quality [11]. This is due to:
- Complex Composition: Chemically defined media have many components, and minor differences in their concentrations can alter cell metabolism and function [11].
- Supply Chain Inconsistency: Variations in the production and sourcing of raw materials, including media, reagents, and cytokines, can introduce variability [12] [13].
- Mitigation Strategy: Employ rigorous raw material testing and quality control protocols. Using standardized, GMP-grade reagents helps reduce this risk [13].
3. What analytical challenges make it difficult to characterize variability? A major challenge is the lack of universal standardized assays [12]. Variability in the quality control methods themselves—such as assessments of viability, potency, and purity—can lead to differences in how cell characteristics are measured and interpreted [14]. Implementing advanced analytical techniques and process monitoring can help identify and mitigate these sources of variability [14].
4. How can the cell collection process itself introduce variability? For autologous therapies, the apheresis collection process is a key source of variation [10] [15].
- Product Contamination: Apheresis instruments have limited ability to resolve cell types. If blood flow is interrupted, the product can be contaminated with platelets, granulocytes, or red blood cells, which can inhibit T cell proliferation later in manufacturing [10].
- Lack of Standardization: Differences in equipment, collection processes, and freezing techniques across apheresis facilities contribute to variability in the starting material [14] [15].
5. Why is demonstrating comparability so challenging after process changes? Cell and gene therapies are complex living products. Even minor alterations to a manufacturing protocol can have a large impact on the final product's critical quality attributes (CQAs) [10] [16]. Regulatory bodies emphasize that demonstrating comparability requires extensive analytical characterization, stability testing, and a risk-based approach to show that process changes do not impact safety or efficacy [16] [13].
Troubleshooting Guides
Guide 1: Managing Donor-Lot Variability in Apheresis Starting Material
Problem: Significant batch-to-batch variability in the yield, purity, and cellular composition of apheresis material collected from different patients.
Investigation and Resolution:
- Step 1: Correlate with Patient Clinical Data. Review the patient's most recent complete blood count (CBC) and treatment history. Patients with lymphoma often have lymphopenia, leading to low T cell collections, while those with CLL may have lymphocytosis [10].
- Step 2: Analyze the Mononuclear Cell Product. Perform a full immunophenotype analysis (e.g., flow cytometry) on the apheresis product. Determine not just the CD3+ T cell count, but also the levels of contaminants like monocytes, B cells, and granulocytes [10].
- Step 3: Adapt the Manufacturing Process. Based on the starting material's profile, consider process adaptations. For products with high monocyte contamination, implement additional T cell enrichment or purification steps. Understand that achieving higher purity often comes at the cost of a lower yield, so find the optimal balance [10].
Guide 2: Controlling Variability from Cell Culture Media
Problem: Inconsistent cell growth, viability, or metabolic profiles between batches, suspected to be caused by media variability.
Investigation and Resolution:
- Step 1: Characterize the Media. Use advanced analytical techniques like in-depth liquid phase separations, mass spectrometry, and spectroscopic methods to characterize the media's composition and identify the root cause of variability [11].
- Step 2: Audit Your Supply Chain. Secure a reliable supply of GMP-grade raw materials and media. Implement strategic partnerships and supply chain management strategies to ensure consistency [13].
- Step 3: Implement Robust QC. Employ rigorous quality control for all incoming raw materials. This includes in-process testing and real-time release criteria to ensure the stability and reliability of the culture system [13] [11].
Table 1: Impact of Clinical Indication on Apheresis Product and Manufacturing
| Clinical Indication | Typical Peripheral Blood Profile | Impact on Apheresis Product | Downstream Manufacturing Effect |
|---|---|---|---|
| Chronic Lymphocytic Leukemia (CLL) | Lymphocytosis (increased lymphocytes) [10] | High total mononuclear cell count [10] | Requires careful purification; potential for high non-T cell contaminants [10] |
| Lymphoma | Lymphopenia (low lymphocytes) [10] | Low total mononuclear cell count; wide variation in CD3+ T cell percentage [10] | Lower manufacturing success rate; challenges in achieving target cell numbers [10] |
| Acute Lymphocytic Leukemia (ALL) | Varies by patient and disease stage | High total mononuclear cell count; wide variation in CD3+ T cell percentage [10] | Can be unpredictable; depends on specific contaminating populations [10] |
Table 2: Key Research Reagent Solutions for Variability Control
| Reagent / Material | Function | Considerations for Variability Reduction |
|---|---|---|
| Chemically-Defined Media | Provides nutrients for cell growth and expansion [11] | Use GMP-grade, high-quality lots; perform qualification assays; avoid serum to reduce unknown variables [13] [11] |
| Cell Isolation Kits (e.g., MACS, FACS) | Isolates desired cell population (e.g., T cells) from a heterogeneous mixture [15] | Standardize protocols across operators and sites; validate recovery and purity for each cell type [10] [15] |
| Recombinant Cytokines (e.g., IL-2, IL-7) | Promotes T cell expansion and can alter cell phenotype [15] | Use consistent, GMP-grade sources; carefully control concentrations and timing of supplementation [15] |
| Viral Vectors | Delivers genetic material for cell engineering (e.g., CARs) [16] [15] | Treated as a critical starting material by regulators; requires extensive testing for titer, potency, and absence of replication-competent virus [16] |
| Cryopreservation Solutions | Protects cells during freezing, transport, and storage [15] | Standardize freeze/thaw rates and cryoprotectant concentrations; monitor for transient warming events during storage [10] [15] |
Experimental Protocols and Workflows
Protocol: A Risk-Based Approach to Managing Process Changes
Purpose: To guide researchers in assessing the impact of a manufacturing process change (e.g., new media formulation, altered expansion time) on product CQAs and determining the necessary testing to demonstrate comparability [16] [13].
Workflow:
- Define the Change: Clearly document the specific change being made to the process.
- Risk Assessment: Conduct a risk assessment to identify which CQAs (e.g., potency, identity, viability) are most likely to be impacted by the change [16].
- Analytical Testing Plan: Develop a tiered testing strategy. For high-risk CQAs, employ extended characterization methods. For lower-risk attributes, release assays may suffice [16].
- Execute Study: Manufacture batches using the old and new processes.
- Compare Data: Perform a side-by-side comparison of the CQAs from both batches. Use historical data as a reference, but prioritize direct comparison data [16].
- Conclusion: Determine if the products are comparable. If significant differences are found in a critical attribute, the change may not be acceptable.
Process Change Comparability Workflow
Protocol: Characterizing Cell Culture Media Variability
Purpose: To identify and quantify the root causes of variability in cell culture media using orthogonal analytical methods [11].
Methodology:
- Sample Preparation: Acquire multiple lots of the same media formulation (both liquid and powder, if possible).
- Orthogonal Analysis: Subject the samples to a suite of analytical techniques.
- Liquid Chromatography-Mass Spectrometry (LC-MS): For targeted and untargeted metabolomics to identify differences in nutrient and metabolite concentrations [11].
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS): To measure trace element and heavy metal contamination [11].
- Spectroscopic Methods (e.g., NMR, NIR): To provide a fingerprint of the overall media composition [11].
- Data Correlation: Correlate the analytical data from the different media lots with functional performance data from cell culture experiments (e.g., growth rate, viability, specific productivity).
Media Variability Characterization Workflow
The Profound Impact of Batch Effects on Data and Clinical Outcomes
Frequently Asked Questions
What are batch effects and why are they a critical concern in autologous cell therapy? Batch effects are technical variations in data that are unrelated to the biological questions being studied. They can be introduced at virtually any stage of research or manufacturing, from sample collection and shipping to instrument changes and reagent lots. In autologous cell therapy, where each patient's cells constitute a unique "batch," these effects are particularly concerning as they can mask true biological signals, lead to incorrect conclusions, and even compromise product quality and patient safety. One study analyzing 456 batches of autologous natural killer (NK) cells found that transit time from medical institutions to processing facilities significantly influenced the proliferative potential of primary cells in the raw material [17].
How can I identify if my data is affected by batch effects? Multiple approaches exist for detecting batch effects, ranging from simple visual checks to quantitative algorithms:
- Dimensionality Reduction: Plot samples from different batches using UMAP or t-SNE. If batches form separate "islands" or show consistent offsets, batch effects are likely present [18] [19].
- Histogram Overlays: Overlay histograms of constitutively expressed markers (e.g., CD45, CD3) across batches. Misalignment of peaks suggests technical variation [19].
- Bridge Samples: Include a consistent control sample in each batch and track its measurements over time using Levy-Jennings charts. Shifts in the control's values indicate batch effects [18].
- Variance Analysis: Calculate the variance in median marker expression or gated population percentages across files. Higher variance suggests stronger batch effects [19].
What are the most effective methods for correcting batch effects in single-cell RNA sequencing data? A 2025 benchmark study compared eight widely used batch correction methods for scRNA-seq data. The results showed that many methods introduce measurable artifacts during correction. Among the methods tested, Harmony was the only one that consistently performed well across all tests without significantly altering the data. Methods such as MNN, SCVI, and LIGER often altered the data considerably, while ComBat, ComBat-seq, BBKNN, and Seurat also introduced detectable artifacts [20].
How can I prevent batch effects when designing a longitudinal flow cytometry study? Prevention is the most effective strategy for managing batch effects:
- Standardize Procedures: Ensure all personnel follow detailed, written protocols for sample collection, processing, and staining [18].
- Reagent Titration: Titrate all antibodies correctly for the expected cell number and type [18].
- Instrument QC: Run standardized beads or controls before each acquisition to ensure consistent detector performance [18].
- Experimental Design: Randomize samples from different experimental groups across acquisition sessions instead of running all controls one day and all treatments the next [18].
- Fluorescent Cell Barcoding: Label samples with unique fluorescent tags, pool them, and stain them together in a single tube to eliminate staining and acquisition variability [18].
Troubleshooting Guides
Problem: Inconsistent Growth Rates in Autologous Cell Manufacturing
Symptoms: Variable expansion rates of patient cells, final cell products failing to meet target cell numbers.
Potential Causes and Solutions:
- Cause: Variability in raw input material due to patient health status, degree of pretreatment, or apheresis collection procedures [21] [22].
- Solution: Request complete blood count (CBC) data from apheresis centers to understand the hematological composition of incoming material [21].
- Cause: Shipping conditions and transit time affecting cell viability and potency [17].
- Solution: Standardize shipping protocols across collection sites. Monitor transit time and its impact on specific growth rates, particularly in the early culture phase [17].
- Cause: Inconsistent reagent quality, particularly between lots of critical materials like fetal bovine serum [5].
- Solution: Implement rigorous reagent qualification and establish contractual quality agreements with suppliers to address root causes of variability [21].
Table 1: Impact of Transit Time on Autologous NK Cell Manufacturing [17]
| Clinical Site | Distance to CPF | Transit Time | Average Culture Period (days) | Average Specific Growth Rate (day⁻¹) | Batches <1×10⁹ cells |
|---|---|---|---|---|---|
| Clinic A (Tokyo) | 4 km | Same day | 21 | 0.22 | 4.3% (7/164) |
| Clinic B (Fukushima) | 203 km | ~24 hours | 19 | 0.24 | 11.3% (33/292) |
Problem: Batch Effects in Multi-Omics Data Integration
Symptoms: Apparent biological differences that actually correlate with processing date, sequencing batch, or laboratory site.
Potential Causes and Solutions:
- Cause: Technical variations between library prep, sequencing runs, or analysis pipelines [23] [5].
- Solution: For large-scale studies with incomplete data profiles, consider Batch-Effect Reduction Trees (BERT), which retains significantly more numeric values compared to other methods and efficiently handles covariates [24].
- Cause: Integration of datasets from different platforms or technologies with different distributions and scales [5].
Table 2: Comparison of Batch Effect Correction Methods for Different Data Types
| Method | Best For | Key Advantages | Limitations |
|---|---|---|---|
| Harmony [20] | scRNA-seq | Consistently performs without creating artifacts; preserves biological variation | - |
| ComBat-met [25] | DNA methylation data | Beta regression framework captures unique characteristics of methylation data | May not be optimal for other data types |
| cytoNorm & cyCombine [19] | High-parameter cytometry | Reduces variance in marker expression and population percentages | Effectiveness varies across cell populations |
| BERT [24] | Incomplete multi-omics profiles | Retains up to 5 orders of magnitude more values; handles covariates | - |
Problem: High Batch-to-Batch Variability in Allogeneic Cell Products
Symptoms: Inconsistent product quality between donors, difficulty in establishing reproducible manufacturing processes.
Potential Causes and Solutions:
- Cause: Biological variability between healthy donors used as starting material [21].
- Solution: Implement rigorous donor screening and establish master cell banks from selected donors to ensure consistency [21].
- Cause: Limited ability to return to the same donor repeatedly due to health changes or availability [21].
- Solution: Maintain a pool of qualified donors with comprehensive attribute data to support sustainability [21].
Experimental Protocols
Protocol: Assessing Batch Effects Using Bridge Samples in Longitudinal Studies
Purpose: To identify and monitor technical variations across multiple batches in long-term studies.
Materials:
- Aliquots of a stable control sample (e.g., PBMCs from a large leukopak) preserved for the study duration
- Standardized staining panels and reagents
- Consistent instrument acquisition settings
Procedure:
- Preparation: In each batch of the study, thaw and prepare one aliquot of the bridge sample alongside experimental samples using identical protocols [18].
- Acquisition: Run the bridge sample each time experimental samples are acquired, maintaining consistent instrument settings and quality control procedures [18].
- Analysis: Track the expression of key markers in the bridge sample over time using Levy-Jennings charts or similar visualization tools [18].
- Monitoring: Look for sudden shifts or gradual drifts in the bridge sample measurements that may indicate batch effects requiring correction [18].
Protocol: Automated Manufacturing to Reduce Human Intervention
Purpose: To minimize variability introduced by manual processing in cell therapy manufacturing.
Materials:
- Closed, automated cell processing systems (e.g., Miltenyi Prodigy, Lonza Cocoon)
- Single-use disposable sets
- Standardized reagent kits
Procedure:
- System Setup: Implement automated systems that integrate multiple unit operations (selection, activation, expansion) rather than modular equipment requiring manual transfers [22].
- Process Validation: Establish growth curves and metabolite profiles to create automated feeding schedules that adjust based on cell growth rates [21].
- In-process Monitoring: Incorporate analytical assays (cell counts, population doublings) to guide process adjustments without manual intervention [21].
- Closed Processing: Utilize closed systems to minimize contamination risk and reduce human error [22].
Visual Guide to Batch Effect Identification and Correction
Batch Effect Identification and Correction Workflow
Table 3: Key Research Reagent Solutions for Batch Effect Management
| Resource | Function | Application Example |
|---|---|---|
| Bridge/Anchor Samples | Consistent control sample across batches | PBMCs from large leukopak aliquoted for longitudinal studies [18] |
| Fluorescent Cell Barcoding | Labels individual samples for pooled staining | Eliminates staining and acquisition variability by processing samples together [18] |
| Automated Cell Processing Systems | Integrated, closed manufacturing | Reduces human intervention and variability in cell therapy production [22] |
| Standardized Apheresis Protocols | Consistent collection of starting material | Harmonizes procedures across multiple collection sites [21] |
| Quality Control Beads | Instrument performance verification | Ensures consistent detector response across acquisitions [18] |
| Master Cell Banks | Consistent starting material for allogeneic products | Provides reproducible donor material for multiple batches [21] |
| Batch Effect Correction Algorithms | Computational removal of technical variation | Harmony for scRNA-seq, cytoNorm for cytometry, BERT for multi-omics [20] [19] [24] |
Economic and Regulatory Consequences of Irreproducibility
What are the primary economic consequences of irreproducible results in autologous cell therapy research? Irreproducible results in autologous cell therapy manufacturing lead to substantial economic burdens, including escalated production costs and clinical delays. The Cost of Goods (COGs) for autologous cell therapies like CAR-T cells typically ranges from $100,000 to $300,000 per dose [26]. Batch failures caused by irreproducibility directly contribute to these exorbitant costs. Furthermore, the financial impact extends to clinical trial delays and holds—Chemistry, Manufacturing, and Controls (CMC) issues represent a disproportionately high cause of clinical holds placed on cell therapy trials by regulatory agencies like the FDA [26]. These delays increase development costs, which average $1.94 billion to bring a cell or gene therapy to market [26], ultimately limiting patient access to these transformative treatments.
How does batch-to-batch variability affect regulatory compliance? Batch-to-batch variability poses significant regulatory challenges by compromising the consistent quality, safety, and efficacy required for approval. Regulatory bodies including the FDA and EMA mandate that manufacturing processes demonstrate robust control and reproducibility [13] [6]. Inconsistent batches fail to meet the standards for Critical Quality Attributes (CQAs), which are essential for product release [13] [26]. This variability creates substantial hurdles in compiling the consistent data packages needed for regulatory submissions. The hospital exemption pathway for Advanced Therapy Medicinal Products (ATMPs) still requires adherence to quality standards equivalent to centralized manufacturing, making standardization and harmonization of Quality Control (QC) processes across academic production sites critically important [6].
Troubleshooting Common Irreproducibility Issues
What are the main technical sources of irreproducibility in autologous cell therapy manufacturing? The main technical sources stem from variability in both the starting biological material and the complex manufacturing process itself.
- Variable Starting Material: Autologous therapies begin with cells from patients, who exhibit significant biological variation in cell quality, potency, and characteristics [13] [26]. This inherent variability is challenging to control.
- Process-Related Variability: Manual, open processing steps are common in cell therapy manufacturing and introduce risks of contamination and operator-dependent variation [27] [15]. Furthermore, raw materials, reagents, and media can vary between lots, affecting cell expansion and final product characteristics [26].
- Analytical and QC Challenges: A major hurdle is the lack of robust, standardized potency assays and other QC tests. This makes it difficult to reliably compare batches and confirm consistent product function [13] [6].
What methodologies can correct for batch effects in analytical data? For different types of biological data, specific computational batch effect correction methods have been developed. The table below summarizes recommended methodologies for DNA methylation and image-based cell profiling data, which are used for product characterization.
Table 1: Batch Effect Correction Methods for Analytical Data
| Data Type | Recommended Method | Key Principle | Considerations |
|---|---|---|---|
| DNA Methylation (β-values) | ComBat-met [28] | Uses a beta regression framework tailored for proportional data (0-1). | Accounts for over-dispersion and skewness in β-value distributions; superior to methods assuming normal distributions. |
| Image-Based Cell Profiling (e.g., Cell Painting) | Harmony or Seurat RPCA [29] | Harmony uses mixture-model based correction; Seurat RPCA uses reciprocal PCA and mutual nearest neighbors. | Effectively reduces technical variation while preserving biological signals in high-content imaging data. |
How can I implement a standardized QC strategy to minimize irreproducibility? Implementing a harmonized QC strategy is essential for batch release. The following workflow, based on recommendations from the UNITC Consortium for academic CAR-T production, outlines the critical tests and methods [6].
Detailed QC Protocols:
Mycoplasma Detection:
- Method: Use validated commercial nucleic acid amplification tests (NAAT) as an alternative to the 28-day culture method.
- Validation: Even with commercially validated kits, perform local validation to confirm detection limits (sensitivity of at least 10 CFU/mL for recommended strains) and ensure compatibility with your specific equipment and sample matrices (cell suspensions/supernatants) [6].
Endotoxin Testing:
- Method: Use Limulus Amebocyte Lysate (LAL) or Recombinant Factor C (rFC) assays.
- Protocol: Validate the test protocol to prevent matrix interference from cell culture media or other product components, which can lead to false positives or negatives [6].
Vector Copy Number (VCN) Quantification:
- Method: Use quantitative PCR (qPCR) or droplet digital PCR (ddPCR).
- Standardization: The technique must be validated to ensure accurate and reproducible quantification of the number of viral vector integrations per cell genome, a critical safety attribute [6].
Potency Assay:
- Method: A key challenge for complex products like Tregs. A common approach involves measuring IFN-γ release via ELISA after antigenic stimulation.
- Considerations: For products with multiple mechanisms of action, developing a reliable potency assay that reflects the biological function is complex and may require multi-parameter analyses [30] [6].
The Scientist's Toolkit: Key Research Reagent Solutions
Using standardized, high-quality reagents is fundamental to reducing irreproducibility. The following table lists essential materials used in the field to establish robust manufacturing and QC processes.
Table 2: Essential Research Reagent Solutions for Cell Therapy Manufacturing
| Reagent / Material | Function | Application Example |
|---|---|---|
| GMP-grade Cell Culture Media & Supplements | Provides a consistent, xeno-free environment for cell expansion, reducing variability and contamination risk from animal sera. | Expansion of T-cells, MSCs, and iPSCs [26]. |
| Cytokines (e.g., IL-2, IL-7, IL-15) | Promotes specific cell expansion, survival, and influences final product phenotype during manufacturing. | Critical for T-cell and Treg culture [15]. |
| Magnetic Cell Sorting Beads | Isolates highly pure target cell populations (e.g., CD4+/CD25+ Tregs) from a heterogeneous starting sample, ensuring a consistent input for manufacturing. | Isolation of Tregs from leukapheresis material [30]. |
| Viral Vectors (e.g., Lentivirus) | Delivers genetic material for cell engineering (e.g., introducing CARs or TCRs). Consistency in vector production is critical. | Engineering CAR-T cells and antigen-specific Tregs [30] [15]. |
| CRISPR/Cas9 Components | Enables precise gene editing for knock-in, knock-out, or gene correction in allogeneic and autologous therapies. | Engineering enhanced specificity or safety features into cell products [15]. |
| qPCR/ddPCR Reagents & Assays | Quantifies Vector Copy Number (VCN) and other genetic attributes for QC batch release. | Quality control and safety testing of genetically modified cell products [6]. |
| ELISA Kits (e.g., IFN-γ) | Measures cytokine release as a functional readout for potency assays during QC testing. | Potency assessment for T-cell based therapies [6]. |
Advanced Solutions and Future Directions
What technological innovations can help overcome scalability and reproducibility challenges? The field is moving toward increased automation and data-driven process control to enhance reproducibility.
- Automation and Closed Systems: Implementing automated, closed-system bioreactors and processing equipment reduces manual handling, minimizes contamination risk, and improves process consistency [27] [26] [15]. This is crucial for scaling up allogeneic therapies and scaling out patient-specific autologous therapies.
- Process Analytical Technologies (PAT) and AI: Integrating inline sensors and advanced analytics allows for real-time monitoring of Critical Process Parameters (CPPs). Artificial Intelligence (AI) can use this data to enable adaptive process control, automatically adjusting conditions to maintain product CQAs and manage inherent input variability [13] [12].
- Quality by Design (QbD): Adopting QbD principles early in process development involves systematically defining a target product profile, identifying CQAs, and understanding the impact of CPPs on them. This science-based approach is key to developing a robust and reproducible manufacturing process [26].
The following diagram illustrates an integrated, automated workflow that represents the future state of reproducible cell therapy manufacturing.
Benchmarking and Applying Batch Correction Methods: From Omics to Imaging
In autologous cell products research, biological variation between patients is an inherent challenge. This variability is often compounded by technical "batch effects"—non-biological differences introduced when samples are processed in different batches, at different times, or by different personnel. If not corrected, these effects can confound results, leading to incorrect biological conclusions and challenges in process reproducibility. Computational batch correction provides a set of powerful statistical and algorithmic approaches to remove these technical artifacts, allowing for clearer insight into the underlying biology and more reliable comparison of data across experimental batches.
Troubleshooting Guide: Common Batch Correction Issues
FAQ 1: My data shows clear clustering by batch even after correction. What went wrong?
Problem: Batch effect correction methods have been applied, but the data still clusters strongly by technical batch rather than biological group in the visualization.
Investigation & Solutions:
- Verify the Correct Model Specification: Ensure that the batch variable you provided to the tool correctly identifies all technical batches. A common error is mislabeling samples or including a biologically distinct group as a "batch."
- Check for Strong Covariates: A strong biological signal (e.g., major differences between cell types or disease states) might be mistaken for a batch effect. Most batch correction tools allow you to specify a "model" or "covariates" parameter. You can include known biological variables of interest in the model to ensure the correction preserves these signals while removing the technical variance. The table below outlines core reagent solutions used in computational workflows.
Table 1: Key Research Reagent Solutions for Computational Batch Correction
| Item Name | Function / Explanation |
|---|---|
| pyComBat/pyComBat-Seq | A Python tool using empirical Bayes methods to adjust for batch effects in microarray (normal-distributed) and RNA-Seq (count-based) data, respectively. [31] |
| Harmony | An algorithm that iteratively corrects embeddings to integrate datasets, removing batch effects while preserving biological structure. [32] |
| Seurat Integration | A widely used toolkit in single-cell genomics that identifies "anchors" between datasets to enable integrated analysis and batch correction. [32] |
| Mutual Nearest Neighbors (MNN) | A method that identifies pairs of cells from different batches that are in a similar biological state, using them as a basis for correcting the data. [32] |
- Evaluate Alternative Methods: No single method works best for all data types. If one algorithm fails, try another. For instance, if a method designed for continuous, normalized data (like ComBat) fails on raw count data from RNA-Seq, switch to a method designed for counts (like ComBat-Seq). [31]
- Assess Data Preprocessing: Inconsistent normalization across batches can create effects that are difficult to correct. Ensure all batches were preprocessed (e.g., normalized, scaled) using the same pipeline before applying batch correction.
FAQ 2: After correction, my biological signal seems to have been removed. How can I preserve it?
Problem: The correction was too aggressive and has removed or dampened the biological variation of interest.
Investigation & Solutions:
- Use Covariates of Interest: As mentioned in FAQ 1, explicitly model the biological variable you wish to preserve (e.g.,
model = ~ biological_groupin ComBat). This instructs the algorithm to remove variance associated with the batch while protecting variance associated with your biological group. [31] - Validate with Known Biological Markers: After correction, check the expression levels of well-established biological markers for your system. If these markers no longer differentiate between groups, the correction may have been too strong.
- Choose a Less Aggressive Method: Some methods are inherently more conservative. For example, Harmony and Seurat Integration are designed to be more robust to the removal of biological signal compared to some earlier methods. [32] A study on deep learning features found ComBat successfully removed technical batch effects while retaining predictive signals for key genetic features like MSI status. [33]
FAQ 3: How do I handle multiple batch effects or complex experimental designs?
Problem: My experiment involves multiple, overlapping technical variables (e.g., different processing days and different sequencing lanes).
Investigation & Solutions:
- Consolidate Batches: If possible, define a single batch variable that is a combination of all major technical factors (e.g., "Day1Lane1", "Day1Lane2", "Day2_Lane1"). This is the simplest approach for many algorithms.
- Use Nested or Blocked Designs: Advanced users can employ more complex statistical models that can account for nested designs (e.g., sequencing lanes nested within processing days). This may require custom modeling frameworks beyond standard out-of-the-box tools.
FAQ 4: How can I quantitatively assess the success of my batch correction?
Problem: It's unclear whether the batch correction has been effective.
Investigation & Solutions:
- Visual Inspection: Use Principal Component Analysis (PCA) or t-Distributed Stochastic Neighbor Embedding (t-SNE) plots colored by batch and biological group. Successful correction is indicated by the mixing of batches while the separation of biological groups is maintained.
- Calculate Metrics: Use quantitative metrics to assess batch mixing.
- Principal Component Regression: Regress the first few principal components against the batch variable. A reduction in R-squared value post-correction indicates less variance is explained by batch.
- Local Inverse Simpson's Index (LISI): A metric that quantifies the diversity of batches within local neighborhoods of cells or samples. A higher LISI score after correction indicates better batch mixing. [32]
- Silhouette Score: Measures how similar a sample is to its own biological cluster compared to other clusters. This should be high for biological groups and low for batches after correction.
Table 2: Performance Comparison of Select Batch Correction Tools
| Tool Name | Primary Data Type | Key Methodology | Reported Performance |
|---|---|---|---|
| pyComBat (Parametric) [31] | Microarray (Normal) | Empirical Bayes | ✓ Correction efficacy similar to original ComBat✓ 4-5x faster computation time vs. R ComBat |
| pyComBat-Seq [31] | RNA-Seq (Counts) | Empirical Bayes (Negative Binomial) | ✓ Outputs identical adjusted counts to R ComBat-Seq✓ 4-5x faster computation time |
| Harmony [32] | Single-cell Genomics | Iterative clustering & integration | ✓ Effective for small sample sizes & >2 batches✓ Designed to preserve biological variance |
| Seurat Integration [32] | Single-cell Genomics | Mutual Nearest Neighbors (MNN) variant | ✓ Effective for complex single-cell datasets✓ Widely adopted with extensive community support |
Experimental Protocol: A Standard Workflow for Batch Correction with ComBat
This protocol provides a detailed methodology for applying the ComBat algorithm to a gene expression matrix, as validated in performance benchmarks. [31]
Objective: To remove technical batch effects from a combined gene expression dataset comprising multiple batches, enabling integrated downstream analysis.
Materials:
- Software: Python with the
inmoosepackage installed, or R with thesvapackage. - Input Data: A combined gene expression matrix (genes/features x samples) with associated metadata. Data should be preprocessed and normalized consistently across all batches. For microarray data, this is typically log2-transformed intensity values. For RNA-Seq raw counts, use ComBat-Seq.
Procedure:
Data Preparation and Import:
- Format your data into a single expression matrix. Ensure row names are gene identifiers and column names are sample IDs.
- Create a batch information vector where each element corresponds to the batch of the sample in the respective column of the expression matrix.
- (Optional) Create a model matrix containing any biological covariates of interest you wish to preserve.
Algorithm Execution:
In Python using
inmoose:The function will output a new, batch-corrected expression matrix of the same dimensions as the input.
Post-Correction Validation:
- Perform PCA on the corrected matrix.
- Visualize the results by plotting the first two principal components, coloring the points by both batch and biological group.
- Calculate quantitative mixing metrics like LISI or silhouette scores to compare pre- and post-correction data.
Downstream Analysis:
- Proceed with your biological analysis (e.g., differential expression, clustering) using the batch-corrected matrix.
Visualizing the Batch Correction Workflow
The following diagram illustrates the logical flow of a standard batch correction process, from raw data to validated output.
Batch Correction Process
Tool Selection Logic
Choosing the right tool is critical. The following diagram provides a logical pathway for selecting an appropriate batch correction method based on your data type and research context.
Tool Selection Guide
In the development of autologous cell products, such as Treg cell therapies, managing batch variation is a critical challenge. The manufacturing process starts with patient-specific cells, leading to inherent biological and technical variability across batches [30]. Single-cell genomics has become indispensable for characterizing these complex products, but its analysis relies heavily on computational data integration methods to separate true biological signals from unwanted technical noise. This guide benchmarks three leading tools—Harmony, Seurat, and scVI—providing practical troubleshooting advice to ensure reliable analysis in cell therapy research and development.
Independent benchmarking studies provide crucial insights for method selection. The table below summarizes key performance metrics across different data integration tasks, helping you choose the right tool for your specific challenge in autologous cell product research [34].
| Method | Best For | Batch Removal Metrics | Bio-Conservation Metrics | Scalability | Key Strengths |
|---|---|---|---|---|---|
| Harmony | simpler tasks, scATAC-seq | Good kBET, iLISI | Moderate isolated label conservation | Fast | Fast, good for simpler batch effects [34] |
| Seurat v3 | simpler tasks, multi-omics | Good on simple tasks | Good ARI, NMI | Moderate | Versatile, multiple integration options [34] [35] |
| scVI | complex atlases, large datasets | Excellent on complex tasks | Excellent trajectory conservation | Excellent for large N | Scalable, handles complex nested batches [34] [36] |
| Scanorama | complex RNA-seq tasks | High kBET & iLISI | High trajectory conservation | Good | Robust performance on complex RNA-seq [34] |
| scANVI | annotation-assisted tasks | Excellent with labels | Excellent with labels | Good | Leverages prior knowledge when available [34] |
Table 1: Benchmarking performance of major single-cell data integration methods across various integration tasks and data modalities.
Troubleshooting Common Integration Failures
FAQ 1: The integration did not remove the batch effect. Several clusters still contain cells from only one study.
Problem: Your UMAP shows distinct clusters comprised solely of cells from a single batch or study, indicating failed integration.
Solutions:
- Verify
batch_keyParameter (scVI): The batch key must correctly identify all sources of technical variation. For a complex design with multiple individuals and conditions, create a new combined batch key (e.g.,individual_condition) instead of using a single factor like 'condition' [37]. - Adjust Harmony Iterations: Increase the
max.iter.harmonyparameter beyond the default to allow the algorithm more time to converge. This addresses the "did not converge" warning [36] [38]. - Try a More Powerful Method: For large or complex datasets with strong batch effects, consider switching to a more robust method like scVI, which often handles significant technical variation better [34] [36].
- Check Preprocessing: Ensure proper normalization and high-variable gene selection before integration, as this can significantly impact the performance of most methods [34].
FAQ 2: The integration removed too much variation, and my biological signal of interest is lost.
Problem: After integration, cell types or experimental conditions that should be distinct are artificially merged, suggesting over-correction.
Solutions:
- Re-evaluate Biology vs. Batch: If your "batch" is a strong biological condition (e.g., stimulated vs. unstimulated), complete separation in UMAP may be biologically real, not a technical artifact. Do not force integration in this case [37].
- Inspect HVG Selection: Highly variable gene (HVG) selection improves integration. Re-running the analysis with a focused set of HVGs can help preserve relevant biological variance [34].
- Use a Less Aggressive Method: Methods can vary in their propensity to over-correct. If using a strong deep learning model like scVI, try a lighter method like Scanorama or Harmony, which may offer a better balance [34].
- Leverage Label-Guided Integration: If cell-type annotations are available, use a method like scANVI that can use labels to guide integration and explicitly preserve known biological structures [34].
FAQ 3: The tool is slow or fails to run due to memory issues on my large dataset.
Problem: The integration process takes an impractically long time or crashes, often with memory errors, when analyzing datasets with hundreds of thousands of cells.
Solutions:
- Utilize Scalable Methods: For very large datasets (e.g., >200,000 cells), scVI is specifically designed for scalability and is often the most efficient choice [34] [39].
- Optimize Seurat's Workflow: When using Seurat, employ the reciprocal PCA (rPCA) workflow, which is faster and more memory-efficient than the standard CCA workflow, especially for large datasets [39].
- Adjust scVI Parameters: With 700k cells, the default of 10 latent variables (n_latent) is typically sufficient. Increasing this number is not usually necessary for batch correction and will increase computational load [37].
Essential Experimental Protocols
Standardized Integration Workflow
To ensure reproducible and comparable results, follow this generalized workflow before applying any specific integration method.
Diagram 1: Standard pre-integration workflow.
Protocol: Preprocessing for Single-Cell Data Integration
Quality Control & Filtering:
- Filter out cells with high mitochondrial gene percentage (indicates low viability).
- Remove cells with an abnormally low or high number of detected genes or UMIs.
- Filter out potential doublets based on unusually high gene/UMI counts.
Normalization:
- Apply a normalization method to correct for differences in sequencing depth between cells (e.g., LogNormalize in Seurat, or SCTransform for a more advanced approach).
Feature Selection:
- Select 2,000-5,000 Highly Variable Genes (HVGs) for downstream analysis. This focuses the integration on the most biologically relevant features and improves performance for most methods [34].
Scaling and Dimensionality Reduction:
- Scale the data to regress out the influence of technical factors like UMI count (if applicable).
- Perform Principal Component Analysis (PCA) on the scaled HVGs to obtain a low-dimensional representation of the data. This PCA matrix is the direct input for many integration methods like Harmony.
Protocol: Application of Key Integration Methods
Harmony in R (Post-PCA)
Code 1: Running Harmony integration in R.
scVI in Python (Uses Raw Counts)
Code 2: Running scVI integration in Python.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key computational "reagents" and their functions in the data integration process, crucial for ensuring the consistency and quality of your analysis, much like wet-lab reagents in cell therapy manufacturing.
| Tool / Resource | Function | Role in Experimental Pipeline |
|---|---|---|
| Seurat (R) | Comprehensive toolkit for single-cell analysis. | Primary environment for data preprocessing, analysis, and visualization; runs Harmony. |
| scvi-tools (Python) | Deep learning library for single-cell omics. | Runs scVI and scANVI for scalable, powerful integration, especially on large datasets. |
| Harmony (R/Python) | Fast, linear integration algorithm. | Efficiently integrates datasets after PCA, often via Seurat's RunHarmony function. |
| Highly Variable Genes (HVGs) | A selected subset of informative genes. | Critical preprocessing step that improves integration performance by reducing noise [34]. |
| Principal Component Analysis (PCA) | Linear dimensionality reduction technique. | Creates the low-dimensional representation required as input for methods like Harmony. |
| kBET / LISI Metrics | Quantitative batch effect evaluation. | Calculates metrics to objectively assess integration quality, beyond visual inspection [34]. |
Table 2: Essential computational tools and resources for single-cell data integration.
Advanced Troubleshooting Guide
When standard fixes fail, this decision diagram helps systematically diagnose and resolve persistent integration issues.
Diagram 2: Troubleshooting workflow for failed integrations.
Applying Correction Methods to Image-Based Cell Profiling Data
In autologous cell products research, ensuring consistent and reliable data is paramount. A significant challenge in this field is batch variation, where technical differences between experiments can obscure true biological signals. This technical support center provides guides and FAQs on applying correction methods to image-based cell profiling data, a critical step for validating the quality and consistency of your autologous cell therapies.
Frequently Asked Questions (FAQs)
1. What are batch effects and why are they a problem in image-based profiling? Batch effects are technical variations in data not due to the biological variables being studied. They can arise from differences in reagent lots, processing times, equipment calibration, or experimental platforms. In image-based profiling, particularly with assays like Cell Painting, these effects severely limit the ability to integrate and interpret data collected across different laboratories and equipment, potentially leading to incorrect biological conclusions [29].
2. Which batch correction methods are most effective for Cell Painting data? Recent benchmarks using the JUMP Cell Painting dataset found that methods like Harmony and Seurat RPCA consistently rank among the top performers across various scenarios. These methods effectively reduce batch effects while conserving biological variance. The best method can depend on your specific experimental design and the complexity of the batch effects [29].
3. My CellProfiler pipeline is detecting small spots inconsistently in batch mode. What should I check? This is a common segmentation challenge. Potential solutions include:
- Fixed Coordinates: If using a crop module, use fixed coordinates for each image to ensure the same region is analyzed, provided all plates are imaged without the camera or stage moving.
- Adaptive Thresholding: Use adaptive thresholding in the IdentifyPrimaryObjects module to better detect dimmer spots, though this may also pick up some non-relevant spots.
- Image Artifacts: Check for and minimize any illuminating light that causes reflections, as this can significantly interfere with image processing [40].
4. How can I improve my profiles before applying batch correction? Data cleaning is a crucial preprocessing step. Key strategies include:
- Cell-level outlier detection: Remove outlier cells that do not show valid biological effects, often resulting from segmentation errors.
- Regress out cell area: Neutralize the effect of cell area on other features, as it is a pivotal contributor that can overly influence similarity metrics.
- Remove toxic drugs: Filter out wells with an extraordinarily low number of cells. Applying these steps can help preserve more meaningful biological information in your profiles [41].
Troubleshooting Guides
Guide 1: Benchmarking Batch Correction Methods
Problem: A researcher needs to choose an appropriate batch correction method to integrate Cell Painting data from multiple laboratories using different microscopes.
Solution: Follow this benchmarked protocol to select and apply a high-performing method.
Experimental Protocol:
- Data Preparation: Start with population-averaged well-level profiles. These are computed by mean-averaging the morphological feature vectors for all cells in a well [29].
- Method Selection: The table below summarizes high-performing methods based on a recent benchmark study. Harmony and Seurat RPCA are recommended starting points due to their consistent performance and computational efficiency [29].
- Application: Apply the chosen method using standard software packages (e.g., in R or Python). Note that methods like
fastMNN,MNN,Scanorama, andHarmonyrequire recomputing batch correction across the entire dataset when new profiles are added [29]. - Evaluation: Use a combination of metrics to evaluate success:
- Batch Effect Reduction: Assess the mixing of batches in low-dimensional embeddings.
- Biological Signal Preservation: Evaluate performance on a biological task, such as replicate retrieval (finding the replicate sample of a given compound across batches) [29].
Table 1: Benchmarking of Selected Batch Correction Methods
| Method Name | Underlying Approach | Key Requirements | Notable Characteristics |
|---|---|---|---|
| Harmony | Mixture model | Batch labels | Iterative, removes batch effects within clusters of cells; consistently high rank [29] |
| Seurat RPCA | Nearest neighbors | Batch labels | Uses reciprocal PCA; allows for dataset heterogeneity; fast for large datasets [29] |
| Combat | Linear model | Batch labels | Models batch effects as additive/multiplicative noise; can be applied to new data [29] |
| scVI | Neural network | Batch labels | Uses a variational autoencoder; does not require full recomputation for new data [29] |
| Sphering | Linear transformation | Negative controls | Computes a whitening transformation based on negative control samples [29] |
Guide 2: Preprocessing and Data Cleaning for Profile Enhancement
Problem: Morphological profiles are noisy, leading to poor performance in downstream tasks like predicting a drug's mechanism of action.
Solution: Implement a data cleaning pipeline to enhance profile quality before any downstream analysis.
Experimental Protocol:
- Illumination Correction: Apply a retrospective multi-image correction method. This builds a correction function using all images from an experiment (e.g., per plate) to recover true image intensities, which is crucial for accurate segmentation and feature measurement [42].
- Cell-level Outlier Detection: Detect and remove outlier cells using an unsupervised method like Histogram-Based Outlier Score (HBOS). This helps eliminate cells that may bias aggregated well-level profiles, for instance, due to segmentation errors creating overly large or small cells [41].
- Regress Out Cell Area: The cell area feature heavily influences many other morphological features. To capture more meaningful biological information, regress each feature against the cell area and use the residuals for downstream analysis [41].
- Filter Non-informative Compounds: Remove "outlier drugs" or compounds that do not produce a meaningful change in the features. This can be done by selecting only compounds whose median replicate correlations are greater than the 95th percentile of a null distribution formed from non-replicate correlations [41].
Table 2: Key Data Cleaning Steps for Profile Enhancement
| Processing Step | Function | Recommended Tool/Method |
|---|---|---|
| Illumination Correction | Corrects for uneven lighting in raw images | Retrospective multi-image method [42] |
| Outlier Cell Removal | Removes cells that are artifacts of segmentation or other errors | Histogram-Based Outlier Score (HBOS) [41] |
| Cell Area Regression | Neutralizes the dominant effect of cell size on other features | Linear regression (using residuals) [41] |
| Non-informative Compound Filtering | Filters out treatments with no discernible biological effect | Replicate correlation analysis [41] |
The following workflow diagram illustrates how these data cleaning steps integrate into a broader image-based profiling pipeline.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Image-Based Cell Profiling Experiments
| Item | Function |
|---|---|
| Cell Painting Assay Kits | Provides a standardized set of fluorescent dyes to label eight cellular components (nucleus, nucleolus, ER, Golgi, mitochondria, plasma membrane, cytoplasm, cytoskeleton), enabling rich morphological profiling [29]. |
| High-Throughput Microscopy Systems | Automated microscopes for acquiring thousands of images from multi-well plates in a time- and cost-effective manner [42]. |
| CellProfiler Software | Open-source software for automated image analysis, including illumination correction, segmentation, and feature extraction [29] [41]. |
| Negative Control (e.g., DMSO) | A vehicle-control treatment that does not induce morphological changes. Essential for normalization and for methods like Sphering that require control samples to model technical variation [29] [41]. |
| Automated Cell Counter | Provides accurate and consistent cell counts and viability assessments during cell seeding, reducing a key source of human error [43]. |
| Electronic Lab Notebook (ELN) | A platform to structure data entry, manage equipment calibration, and automate workflows, thereby reducing transcriptional and decision-making errors [44]. |
Integrating Correction into the Autologous Cell Production Workflow
Troubleshooting Guide: Addressing Common Production Issues
FAQ 1: What are the primary sources of batch-to-batch variation in autologous cell therapies, and how can they be controlled?
Batch-to-batch variation is a significant challenge in autologous cell therapy manufacturing. The main sources and their control strategies are summarized in the table below.
Table 1: Key Sources and Control Strategies for Batch-to-Batch Variation
| Source of Variability | Impact on Production | Corrective and Control Strategies |
|---|---|---|
| Patient-specific Factors (Disease severity, prior treatments, age, health status) [2] | Affects initial cell quality, quantity, and functionality; influences expansion potential and final product yield [2] [45]. | Implement stringent patient eligibility criteria [2]. Design flexible manufacturing processes that can accommodate variable growth kinetics [2] [46]. |
| Apheresis Collection (Different protocols, devices, operator training, anticoagulants) [2] | Leads to differences in the composition, viability, and purity of the starting cellular material [2] [14]. | Standardize apheresis protocols and operator training across collection sites [2]. Specify the use of a particular apheresis collection device to increase consistency [2]. |
| Raw Material Variability (Cell culture media, cytokines, activation beads) [2] [47] | Can alter cell expansion, differentiation, and final product phenotype [2]. | Implement robust quality control for raw materials [15]. Use a risk-based approach to define Critical Quality Attributes (CQAs) for starting materials [2]. |
| Manual, Open Process Steps [46] | Increases risk of contamination and human error, leading to inconsistencies and batch failures [46]. | Adopt closed and automated manufacturing systems to reduce manual touchpoints [46]. |
FAQ 2: Our process frequently generates out-of-specification (OOS) products. What steps can we take to reduce this occurrence and what are the regulatory considerations for using OOS products?
The generation of OOS products is a recognized challenge in autologous therapies, primarily due to the inherent variability of patient-derived starting materials [48]. In some cases, for patients with no alternative treatment options, OOS products may be used on compassionate grounds following a thorough risk-benefit assessment [48].
Corrective Actions to Minimize OOS Rates:
- Process Understanding: Intentionally introduce donor variability during process development to understand which CQAs are truly indicative of manufacturing outcomes [2].
- In-process Controls: Implement process analytical technologies (PATs) that provide real-time data for tighter process control [2]. Conduct in-process quality checks for quicker decision-making [2].
- Process Automation: Automate critical steps like cell isolation and expansion to enhance consistency and reduce failures caused by contamination [46].
Regulatory Considerations for OOS Use:
- In the US: OOS products may be supplied under an Expanded Access Program (EAP) following an FDA-reviewed Investigational New Drug (IND) application, IRB approval, and patient consent [48].
- In Europe: OOS Advanced Therapy Medicinal Products (ATMPs) can be provided as commercial products under exceptional circumstances. The MAH must perform a risk assessment, and the treating physician makes the final decision after informing the patient [48].
- Documentation: Meticulous documentation of the risk assessment and justification for OOS product use is mandatory [48].
Experimental Protocols for Process Control
Detailed Methodology: Conducting a Comparability Study for a Process Change
When integrating a corrective action or process improvement (e.g., new raw material, automated equipment), a comparability study is essential to demonstrate the change does not adversely impact the product [47].
Objective: To demonstrate that the cell therapy product manufactured after a process change is comparable to the product manufactured before the change in terms of critical quality attributes (CQAs), safety, and efficacy.
Protocol:
Risk Assessment and Study Design:
Sample Manufacturing:
- Manufacture multiple batches (as feasible given autologous batch size limitations) using both the old and new processes.
- Acknowledge the inherent donor variability. Use a sufficient number of donor samples representing a range of expected variability (e.g., from healthy and "exhausted" donors) to ensure the process is robust [2] [47].
Analytical Testing and Data Collection:
- Test pre- and post-change products against a panel of CQAs. The table below outlines a recommended analytical framework.
Table 2: Analytical Framework for Comparability Studies
| Quality Attribute Category | Specific Test Metrics | Brief Explanation of Function |
|---|---|---|
| Identity & Purity | Flow cytometry for cell surface markers (e.g., CD3, CD4, CD8, CAR-positive %) [15] [45] | Confirms the identity of the cell population and the proportion of successfully engineered cells. |
| Potency | In vitro cytotoxicity assays, cytokine secretion profiling [15] | Measures the biological activity and therapeutic function of the product. |
| Viability | Cell count and viability (e.g., via trypan blue exclusion) [2] [15] | Assesses the health and proportion of live cells in the final product. |
| Safety | Sterility, mycoplasma, endotoxin testing [15] | Ensures the product is free from microbial contamination. |
| Characterization | T-cell immunophenotyping (e.g., naïve, memory, effector subsets) [45] | Provides deeper insight into the cell composition, which can impact persistence and efficacy. |
- Data Analysis and Conclusion:
- Use statistical methods where appropriate to analyze the data.
- Define pre-established acceptance criteria for comparability. If the results fall within these criteria, the products are considered comparable.
- If CQAs are not comparable, a root cause investigation must be conducted, and a clinical bridging study may be required [47].
Visualization of Workflow and Correction Integration
The following diagram illustrates a standard autologous cell therapy manufacturing workflow with key decision points where corrective actions and controls should be integrated to manage variability.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and technologies used in autologous cell therapy manufacturing to ensure process consistency and control.
Table 3: Essential Reagents and Technologies for Process Control
| Item / Technology | Function in the Workflow | Key Consideration for Reducing Variation |
|---|---|---|
| Magnetic Cell Sorting(e.g., MACS Beads) | Isolation of target T-cell populations (e.g., CD4+/CD8+) from apheresis material [15] [45]. | Using consistent bead-to-cell ratios and isolation techniques improves purity and yield of the starting population, reducing downstream variability [45]. |
| Cell Activation Reagents(e.g., anti-CD3/CD28 beads) | Activates T-cells, initiating the proliferation and manufacturing process [15]. | Standardizing the source, concentration, and duration of stimulation is critical for consistent activation and expansion [15]. |
| Genetic Modification(Viral Vectors: Lentivirus, Retrovirus) | Introduces the therapeutic CAR gene into the patient's T-cells [45]. | Vector quality, titer, and transduction efficiency (MOI) are major sources of variation. Rigorous quality control of vectors is essential [47]. |
| Cell Culture Media & Cytokines(e.g., IL-2, IL-7, IL-15) | Supports ex vivo cell expansion and influences final T-cell phenotype [15] [45]. | Media formulation and cytokine cocktail can drive differentiation towards desired memory phenotypes. Sourcing from qualified suppliers and avoiding formulation changes is key [2] [45]. |
| Closed AutomatedBioreactor Systems | Provides a controlled, scalable environment for cell expansion [46]. | Replaces manual, open processes in flasks/bags, minimizing contamination risk and human error, thereby improving batch consistency [46]. |
| Cryopreservation Media(e.g., with DMSO) | Protects cells during freezing for storage and transport [15]. | Standardized freezing protocols and cryopreservation media are vital for maintaining consistent post-thaw viability and function [2] [15]. |
Troubleshooting Manufacturing Variability and Implementing Process Controls
Identifying and Mitigating Critical Process Parameters
Troubleshooting Guides
Guide 1: Addressing High Batch-to-Batch Variability in Autologous Cell Products
Problem: Significant variation in final product quality and yield between different patient batches.
Symptoms:
- Inconsistent cell expansion rates
- Fluctuations in critical quality attributes (CQAs)
- Variable potency and viability measurements
Root Causes & Solutions:
| Root Cause | Diagnostic Methods | Corrective Actions |
|---|---|---|
| Patient-to-patient variability in starting material [2] | - Pre-apheresis CD3+ cell counts- Patient treatment history analysis- Cell viability assessment | - Implement stringent donor screening [49]- Establish patient eligibility criteria [2] |
| Inconsistent apheresis collection [2] | - Review collection protocols- Analyze anticoagulant variations- Assess collection device types | - Standardize operator training [2]- Specify collection devices [2] |
| Raw material variability [49] | - Functional release assays- Lot-to-lift purity testing- Endotoxin monitoring | - Early raw material specification locking [49]- Quality secondary suppliers [49] |
Preventive Measures:
- Implement Design of Experiments (DoE) studies to clarify acceptable input variation ranges [49]
- Establish real-time phenotyping for incoming materials [49]
- Develop flexible automated systems designed to accommodate variable growth kinetics [2]
Guide 2: Managing Raw Material Variability in Autologous Therapies
Problem: Inconsistencies in raw materials leading to irreproducible process outcomes.
Symptoms:
- Irreproducible proof-of-concept data when switching to GMP-grade reagents
- Unpredictable expansion kinetics
- Batch-to-batch potency swings
Investigation Protocol:
- Material Characterization: Test multiple lots of raw materials for functional performance
- Process Robustness: Challenge your process with intentionally variable inputs [2]
- Analytical Development: Implement functional release assays rather than compositional testing alone [49]
Mitigation Strategies:
- Establish well-defined supply chain strategies early in development [49]
- Use process analytical technologies for real-time data and tighter process control [2]
- Implement a hybrid analytical matrix approach to better understand product characteristics [2]
Critical Process Parameters and Quality Attributes Monitoring
| Process Parameter Category | Specific Parameters | Monitoring Frequency | Impact on CQAs |
|---|---|---|---|
| Physiochemical Properties | pH, Dissolved Oxygen (DO) | Continuous monitoring | Cell viability, metabolic activity, differentiation potential |
| Nutrient Supply | Glucose, lactate, amino acid concentrations | Daily sampling | Cell expansion rates, volumetric productivity |
| Cultivation System | Bioreactor type, media composition, microcarrier selection | Beginning/end of process | Immunophenotype, genetic stability, purity |
| Process Control | Agitation rate, temperature, feeding strategies | Throughout expansion | Cell number, viability, batch-to-batch consistency |
| Quality Attribute Category | Specific Measurements | Acceptance Criteria | Testing Frequency |
|---|---|---|---|
| Cell Growth & Viability | Cell count, viability, doubling time | Viability >70-80% (varies by product) | Throughout process |
| Identity/Purity | Immunophenotype (CD105, CD73, CD90), lack of hematopoietic markers | Meet ISCT criteria [50] | Final product release |
| Potency | Differentiation potential, biological activity assays | Differentiation to osteoblasts, adipocytes, chondroblasts [50] | Final product and in-process |
| Safety | Sterility, mycoplasma, endotoxins, genetic stability | Sterility: no growth; Endotoxins: <5 EU/kg [51] | Final product release |
Experimental Protocols
Protocol 1: Process Characterization Using Design of Experiments (DoE)
Purpose: To systematically map critical process parameters and set defensible operating ranges [49].
Materials:
- Research-grade and GMP-grade raw materials for comparison
- Cells from multiple donors to capture variability
- Bioreactor system with monitoring capabilities
Methodology:
- Define Factors: Identify potentially critical process parameters (e.g., seeding density, media composition, feeding schedules)
- Establish Ranges: Set minimum and maximum values for each parameter based on preliminary data
- Run Experiments: Execute DoE matrix, measuring all relevant CQAs as responses
- Statistical Analysis: Identify significant factors and interactions using statistical software
- Design Space Definition: Establish proven acceptable ranges for critical parameters
Expected Outcomes: Data-driven justification for process parameter ranges in regulatory filings [49].
Purpose: To evaluate the functional potency of hematopoietic stem and progenitor cells (HSPCs) as a quality control measure.
Materials:
- MethoCult or similar methylcellulose-based media
- 35mm culture dishes
- Incubator maintained at 37°C, 5% CO₂
- Inverted microscope for colony counting
Procedure:
- Cell Preparation: Thaw cryopreserved HSPC product and perform cell count and viability assessment
- Plating: Mix cells with methylcellulose medium at appropriate concentration (typically 1-2×10⁴ cells/dish)
- Culture: Plate cells in 35mm dishes and incubate for 14-16 days
- Scoring: Identify and count colony types (BFU-E, CFU-GM, CFU-GEMM) based on morphological characteristics
- Interpretation: Calculate CFU frequency per input cell number; compare to established specifications
Quality Control: Use standardized scoring criteria and establish assay controls to minimize inter-operator variability.
Process Visualization
Diagram 1: CPP Investigation Workflow
Diagram 2: Raw Material Variability Management
Research Reagent Solutions
Table 3: Essential Materials for Cell Therapy Process Development
| Reagent Category | Specific Examples | Function in Process Development |
|---|---|---|
| Cell Culture Media | Serum-free media formulations, cytokine supplements (SCF, Flt3, TPO, IL-3, IL-6) [52] | Support cell expansion while maintaining desired phenotype and functionality |
| Genetic Modification | Lentiviral vectors, mRNA encoding nucleases (TALENs, CRISPR-Cas9) [53] | Introduce CAR constructs or edit genes (e.g., TRAC knockout) to enhance safety |
| Process Monitoring | Metabolite assays (glucose, lactate), flow cytometry antibodies, CFU assay materials [52] | Measure CPPs and CQAs throughout manufacturing process |
| Cryopreservation | DMSO, cryopreservation media, controlled-rate freezing containers | Maintain cell viability and potency during storage and transport |
| Quality Control | Sterility testing kits, endotoxin detection assays, mycoplasma testing | Ensure final product safety and regulatory compliance |
Frequently Asked Questions
Q1: What are the first steps in managing autologous cell therapy variability? Begin with a comprehensive manufacturability assessment that evaluates each unit operation from cell isolation through fill-finish [49]. Establish tight donor screening protocols and raw material specifications early [49] [2]. Most importantly, intentionally introduce variability during process development to understand which CQAs truly indicate manufacturing outcomes [2].
Q2: How can we justify process parameter ranges to regulators? Use structured DoE studies to generate data mapping how parameter variations affect CQAs [49]. This data-driven approach establishes defensible operating ranges and demonstrates process understanding. Implement continuous process verification to collect data supporting your parameter ranges [47].
Q3: What analytical methods are most critical for monitoring process consistency? For hematopoietic products, CFU assays provide critical potency data that correlates with engraftment potential [52]. For MSCs, regular immunophenotyping (CD105, CD73, CD90) and differentiation potential assays are essential [50]. Implement process analytical technologies for real-time monitoring of critical parameters [2].
Q4: How do we manage comparability when implementing process changes? Conduct risk assessment focusing on the nature and ranking of changes [47]. For higher-risk changes (e.g., critical raw materials, key culture operations), more extensive comparability studies are needed. When CQAs are not well-characterized, non-clinical and/or clinical bridging studies may be necessary [47].
Q5: What strategies help accommodate inherent raw material variability? Develop flexible automated systems that accommodate variable growth kinetics [2]. Implement modular process designs with freezing points at various stages [2]. Use detailed SOPs with instructions for handling different scenarios that might arise due to starting material variability [2].
The Role of Automation and AI in Reducing Human-Induced Variability
Technical Support Center
Troubleshooting Guides
Guide 1: Troubleshooting High Variability in Cell Expansion
Problem: Inconsistent cell growth and final yield between batches of autologous cell products.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Variable Raw Materials | Review Certificate of Analysis for incoming patient apheresis material; Check pre-apheresis patient CD3+ counts and viability data [2]. | Implement stricter incoming material specifications; Use flexible, automated media dosing to adjust for initial cell quality [2]. |
| Inconsistent Seeding Density | Audit automated cell counter calibration and nozzle function; Review logs of cell suspension mixing steps pre-seeding. | Recalibrate the automated cell counter; Standardize the cell suspension mixing protocol within the automated workflow. |
| Uncontrolled Process Parameters | Check data logs from bioreactor for temperature, pH, and dissolved O2 fluctuations; Verify sensor calibration [54]. | Adjust and validate control algorithms on the automated bioreactor system to maintain tighter environmental control [54]. |
Guide 2: Investigating Failed Automated Tests or QC Checks
Problem: An automated quality control check (e.g., for cell viability or purity) fails during a production run.
| Investigation Step | Actions | Expected Outcome |
|---|---|---|
| Confirm Failure | Run the failed automated check multiple times to see if the failure is consistent or intermittent [55]. | Determine if the issue is reproducible or a transient event. |
| Review Recent Changes | Check for any recent changes to the system under test, including software updates, reagent lot changes, or minor protocol adjustments [55]. | Identify a potential root cause linked to a specific change. |
| Verify Test Environment | Confirm that all required APIs (e.g., for data transfer) are working, test conditions (temperature) are met, and there are no OS-level conflicts [55]. | Rule out environmental and system integration issues. |
| Diagnose Check vs. System | Determine if the problem is with the automated check's code/script or with the product/process being tested [55]. | Focus the investigation on the correct domain (automation or production). |
Guide 3: Addressing Batch Effects in Analytical Data
Problem: Analysis of product CQAs shows systematic variation correlated with experimental batches (e.g., different reagent lots or analysis days), obscuring true biological signals.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Reagent Lot Variation | Perform ANOVA-based analysis to quantify variation from different reagent lots; Correlate specific lot IDs with CQA outcomes [56]. | Increase lot-to-lot quality control for critical reagents; Use larger lot sizes to minimize the frequency of changeovers. |
| Instrument/Scanner Drift | Analyze low-dimensional feature representations (e.g., from PCA) of control samples colored by processing date or instrument ID [57]. | Implement more frequent instrument calibration and standardized protocols across all equipment [57]. |
| Operator-Induced Variability | Review metadata for correlations between specific operators and out-of-specification results. | Enhance standardized operator training and leverage automation for the most sensitive process steps [2]. |
Frequently Asked Questions (FAQs)
Q1: Our autologous cell therapy process is highly manual. Which steps should we prioritize for automation to achieve the biggest reduction in variability? A: Prioritize automating the steps most sensitive to human technique. This typically includes cell seeding, where consistent density is critical for reproducible expansion; media exchanges and feeding, where precise timing and volumes are key; and final product formulation, where accurate cell concentration and volume are essential for dosing [2]. Automated systems ensure these repetitive tasks are performed identically for every batch, regardless of the originating patient material.
Q2: How can we use AI/ML to predict and prevent batch failure in real-time? A: Machine learning models can be trained on historical process data (e.g., cell growth rates, metabolite levels, imaging data) from both successful and failed batches. By analyzing real-time process data from a new batch against these models, the AI can flag early warning signs of potential failure, such as aberrant growth kinetics [2]. This allows for potential intervention or early decision-making, saving time and valuable patient material. Real-time data visualization is a key enabler of this approach [58].
Q3: We are implementing an automated bioreactor. What critical process parameters (CPPs) should we focus on controlling most tightly? A: For cell culture, the most critical parameters to control are temperature, pH, and dissolved oxygen [54]. Even small, manual fluctuations in these parameters can significantly impact cell growth and product quality. Automated bioreactors use integrated sensors and control algorithms to maintain these CPPs within a narrow, predefined range throughout the entire culture process, ensuring a consistent environment for every batch [54].
Q4: Our data shows high donor-to-donor variability. How can we design our processes to be more robust to this inherent variation? A: Since patient-specific variability cannot be eliminated, the strategy is to design a flexible and adaptable process. This involves:
- Intentional Variability Studies: During process development, intentionally introduce donor/cellular starting material with a wide range of qualities to understand the process boundaries [2].
- Defining a "Process Envelope": Establish the range of input material attributes (e.g., initial cell count, viability) that your process can successfully accommodate [1].
- In-Process Adjustments: Use real-time analytics to monitor growth and allow the automated system to make predefined adjustments (e.g., feeding schedule, harvest time) based on the specific batch's performance [58].
Q5: What are the key elements of a data infrastructure needed to support variability reduction? A: A robust data infrastructure is foundational. It should be capable of:
- Centralizing Data: Integrate data from disparate sources, including manufacturing execution systems (MES), logistics/courier tracking, and quality control labs [58].
- Real-Time Visualization: Provide dashboards for visualizing production, logistics, and testing data in real-time to enable rapid decision-making [58].
- Ensuring Traceability: Maintain complete batch genealogy, linking all raw materials, process parameters, and analytical results to a specific patient batch for full traceability and root cause analysis [54].
Essential Research Reagent Solutions
The following table details key materials used in automated cell therapy processes to mitigate variability.
| Item | Function | Key Consideration for Variability Reduction |
|---|---|---|
| GMP-Grade Raw Materials | Cell culture media, cytokines, growth factors, and activation reagents. | Using high-purity, compendial grade materials produced under Good Manufacturing Practice (GMP) ensures defined quality and minimal batch-to-batch variability, unlike research-grade reagents [1]. |
| Single-Use, Closed-System Consumables | Pre-sterilized bioreactor bags, tubing sets, and connection devices. | Eliminates risk of cross-contamination between batches and removes variability associated with cleaning validation of reusable equipment [1]. |
| Defined Coagulants/Anticoagulants | Citrate-based or other defined agents used during apheresis. | Standardizing the type and concentration of anticoagulant helps reduce a key source of pre-manufacturing variability in the incoming patient material [2]. |
| Characterized Cell Separation Beads | Antibody-coated magnetic beads for cell selection and activation. | Selecting beads with consistent performance and coupling them with automated separation systems (e.g., closed-system magnetic separators) reduces variability in cell purity and activation state [1]. |
This methodology allows researchers to systematically break down and quantify the different sources of variability in their data, distinguishing between technical noise (e.g., from different plates or days) and true biological signals [56].
1. Objective: To quantify the proportion of total variance in a Critical Quality Attribute (CQA) that is attributable to specific factors such as the laboratory site, experimental plate, donor, and drug/dosage.
2. Materials and Equipment:
- High-throughput screening platform or automated cell culture and assay system.
- Standardized reagents and cell culture materials.
- Data analysis software capable of performing linear modeling and ANOVA (e.g., R, Python with statsmodels).
3. Procedure:
- Step 1: Experimental Design. Design a screen where multiple cell lines (or patient samples) are treated with various compounds across multiple doses. This experiment should be replicated across different plates and, if possible, in different laboratories to introduce known technical variations [56].
- Step 2: Data Collection. Collect a robust, quantitative measurement of the CQA (e.g., cell viability, percent cell killing) for every combination of cell line, drug, dose, plate, and lab.
- Step 3: Linear Model Fitting. Fit a linear model to the data. A simplified model might look like:
CQA ~ Laboratory + Plate + Donor + Drug + Dose + (Drug:Dose)...where the(Drug:Dose)term represents the interaction effect. - Step 4: Analysis of Variance (ANOVA). Perform an ANOVA on the fitted linear model. This analysis will decompose the total sum of squares in the data into components attributed to each factor in the model [56].
- Step 5: Variance Quantification. Calculate the percentage of the total variance explained by each factor (e.g.,
Laboratory,Plate). A high percentage of variance attributed toPlatewould indicate a significant batch effect that needs correction.
Process Visualization
The following diagram illustrates a data-driven workflow for identifying and mitigating sources of human-induced variability in automated cell product manufacturing.
Understanding Batch Effects in Cell Therapy
What Are Batch Effects?
Batch effects are technical variations introduced into experimental data or products that are unrelated to the biological variables of interest. In the context of autologous cell therapy manufacturing, these are systematic, non-biological differences arising from inconsistencies in raw materials, particularly serum and viral vectors, across different production batches [5] [59].
These effects can manifest as significant variations in cell growth, transduction efficiency, viability, and ultimately, the potency and consistency of the final therapeutic product [46] [14].
Why Serum and Vector Batches Are Critical
Serum (e.g., Fetal Bovine Serum) and viral vectors are among the most variable raw materials in cell therapy production.
- Serum Batches: Different lots of serum contain varying concentrations of growth factors, hormones, lipids, and other undefined components that can dramatically alter cell expansion rates, differentiation, and functionality [5].
- Vector Batches: Variations in viral vector production can lead to differences in titer, transduction efficiency, and transgene expression levels, directly impacting the potency and consistency of genetically modified cell therapies like CAR-T cells [46].
The profound impact of batch effects is not just theoretical; they are a paramount factor contributing to irreproducibility in biomedical research, sometimes resulting in retracted articles, invalidated findings, and significant economic losses [5].
Detection and Diagnosis: Identifying Batch Effects
Key Indicators of Batch Effects
Researchers should monitor for these warning signs that may indicate batch effects:
- Sudden shifts in cell growth kinetics or viability metrics coinciding with new raw material batches
- Unexplained variations in transduction efficiency despite consistent protocols
- Changes in critical quality attributes (CQAs) such as cell phenotype or potency markers
- Statistical clustering by processing date rather than biological variables in analytical assessments [59] [18]
Systematic Detection Methods
The table below summarizes quantitative and qualitative methods for detecting batch effects in your manufacturing process:
Table: Batch Effect Detection Methodologies
| Method | Application | Key Procedure | Interpretation |
|---|---|---|---|
| Dimensionality Reduction (PCA, UMAP) | All manufacturing stages | Project high-dimensional data (e.g., cell marker expression) into 2D/3D space [59] [18] | Samples clustering by batch rather than biological group indicates batch effects |
| Bridge Samples | Longitudinal studies | Include consistent control sample in each manufacturing batch [18] | Significant shifts in bridge sample metrics across batches indicates technical variation |
| Levy-Jennings Charts | Process monitoring | Plot control sample metrics over time with control limits [18] | Points outside control limits or showing systematic trends indicate batch effects |
| Statistical Metrics (kBET, LISI) | Data analysis | Compute batch mixing scores on processed data [59] | Low scores indicate poor batch integration and presence of batch effects |
Prevention Strategies: Proactive Raw Material Management
Serum Batch Management
Table: Comprehensive Serum Batch Management Strategy
| Strategy | Protocol | Rationale |
|---|---|---|
| Rigorous Pre-qualification | Test multiple lots with relevant cell-based assays before selection | Identifies lots supporting consistent cell growth and functionality |
| Adequate Stockpiling | Purchase sufficient quantity of qualified lot for entire clinical trial | Eliminates inter-lot variability during study duration |
| Standardized Testing | Implement consistent potency assays for each new lot | Ensures comparable performance across serum batches |
| Documentation | Maintain detailed records of lot numbers and corresponding performance | Enables retrospective analysis of batch-related variations |
Vector Batch Consistency
- Centralized Vector Production: Where possible, produce large master vector banks under standardized conditions to minimize batch-to-batch variation [46]
- Comprehensive QC Testing: Perform extensive characterization of each vector batch including titer determination, transduction efficiency assessment, and sterility testing
- Standardized Transduction Protocols: Implement consistent cell density, multiplicity of infection (MOI), and incubation parameters across all batches [46]
Experimental Protocols for Batch Effect Assessment
Protocol: Serum Batch Qualification
Objective: Systematically evaluate multiple serum lots for consistent performance in cell culture.
Materials:
- Candidate serum lots
- Early-passage cell stock (e.g., T-cells, stem cells)
- Base media without serum
- Standardized culture vessels
- Cell counting equipment
- Flow cytometry reagents for phenotype analysis (as appropriate)
Procedure:
- Preparation: Thaw serum lots completely and heat-inactivate if required by your protocol
- Cell Seeding: Seed cells at standardized density in media supplemented with test serum lots
- Monitoring: Track cell density, viability, and morphology daily
- Analysis: At predetermined timepoints, assess:
- Population doubling time
- Maximum cell density
- Viability metrics
- Relevant phenotype markers (via flow cytometry)
- Functional assays (e.g., differentiation potential, activation markers)
- Selection: Choose lots supporting consistent growth and functionality across multiple replicates
Validation: Include a reference serum lot as control throughout testing [14] [18]
Protocol: Vector Batch Potency Assessment
Objective: Determine consistency of viral vector batches in transducing target cells.
Materials:
- Vector batches to be tested
- Target cells at appropriate passage
- Transduction reagents (e.g., polybrene, retronectin)
- Appropriate media
- Flow cytometry reagents for detection
Procedure:
- Cell Preparation: Seed target cells at standardized density
- Transduction: Apply vectors at multiple MOIs in technical replicates
- Analysis: After appropriate expression period, assess:
- Transduction efficiency (% positive cells)
- Transgene expression level (mean fluorescence intensity)
- Cell viability post-transduction
- Functional output (e.g., cytokine production, target cell killing)
- Comparison: Statistical comparison of potency across vector batches
Note: Include a reference vector batch as control if available [46]
Correction Methodologies: Addressing Established Batch Effects
Statistical Batch Effect Correction
When batch effects are detected in analytical data, several computational approaches can be employed:
- ComBat and Related Algorithms: Empirical Bayes frameworks that adjust for known batch variables [60] [59]
- Linear Model-Based Approaches: Methods like
removeBatchEffectfrom the limma package that use linear modeling [61] - Harmony and MNN: Advanced algorithms for integrating datasets with complex batch effects [59]
Table: Comparison of Batch Effect Correction Methods
| Method | Mechanism | Advantages | Limitations |
|---|---|---|---|
| ComBat | Empirical Bayes framework | Adjusts for known batch effects; widely used [59] | Requires known batch information; may not handle nonlinear effects [59] |
| SVA (Surrogate Variable Analysis) | Estimates hidden variation | Captures unknown batch effects [59] | Risk of removing biological signal; requires careful modeling [59] |
| limma removeBatchEffect | Linear modeling | Efficient; integrates with analysis workflows [59] | Assumes known, additive batch effect; less flexible [59] |
| Harmony | Non-linear integration | Aligns cells in shared embedding space [59] | May require parameter optimization |
Process-Based Corrections
- Process Re-standardization: When batch effects are detected, review and potentially re-optimize critical process parameters
- Bridge Normalization: Use data from consistent control samples to mathematically adjust for technical variations [18]
- Cross-validation: When possible, repeat critical experiments using alternative batches to confirm findings
The Scientist's Toolkit: Essential Reagents and Materials
Table: Research Reagent Solutions for Batch Effect Management
| Reagent/Material | Function | Batch Management Consideration |
|---|---|---|
| Master Cell Bank | Consistent cellular starting material | Extensive characterization and single source minimizes variability |
| Serum Lot Repository | Cell culture supplement | Pre-qualified, large-volume lots ensure long-term consistency |
| Vector Master Banks | Genetic modification | Single production run minimizes transduction variability |
| Reference Standards | Process controls | Qualified materials for cross-batch normalization [18] |
| Defined, Serum-free Media | Culture medium | Eliminates serum-associated variability entirely |
| Fluorescent Cell Barcoding Kits | Sample multiplexing | Enables combined processing of multiple samples [18] |
Frequently Asked Questions (FAQs)
Q1: How many batches should we test when qualifying a new serum lot? A: We recommend testing a minimum of three independent batches from the same supplier to establish consistency, plus batches from at least two alternative suppliers as backups [14].
Q2: Can we completely eliminate batch effects through statistical correction? A: No. Statistical correction should be viewed as a mitigation strategy, not a complete solution. These methods can introduce their own artifacts and may inadvertently remove biological signal if applied improperly. Robust experimental design with proper randomization and blocking remains the gold standard [5] [59].
Q3: What is the minimum number of bridge samples needed per batch? A: While even a single well-characterized bridge sample provides value, we recommend including at least three technical replicates of your bridge sample per batch to account for stochastic variation and enable statistical assessment of batch effects [18].
Q4: How do we handle situations where our qualified serum lot is discontinued? A: Maintain a strategic reserve of qualified lots and establish relationships with suppliers for advance notice of discontinuation. Always have at least one backup qualified lot available, and initiate crossover studies well before your primary lot is exhausted to ensure seamless transition [14].
Q5: What critical quality attributes (CQAs) are most sensitive to serum batch effects? A: Potency, proliferation rate, and differentiation capacity (for stem cell products) are typically most sensitive. These should be prioritized during serum qualification studies [14].
Workflow Visualization
Batch Effect Management Workflow
Effective management of serum and vector batch effects requires a comprehensive, multi-pronged approach spanning prevention, detection, and correction strategies. By implementing rigorous raw material qualification, maintaining strategic reserves, employing consistent monitoring through bridge samples, and having appropriate statistical tools ready when needed, researchers can significantly enhance the consistency and reliability of autologous cell therapy manufacturing. Remember that the goal is not just to correct batch effects when they occur, but to build robust processes that minimize their impact from the outset, ultimately ensuring the production of safe and effective cell therapies for patients.
Implementing Quality by Design (QbD) and Process Analytical Technologies (PAT)
Troubleshooting Guides
Raw Material Variability in Autologous Cell Therapies
Problem: Inconsistent quality, yield, or performance of final cell therapy products due to inherent variability in patient-derived starting materials.
Question: Why does my autologous cell therapy process work perfectly for one patient's cells but fail for another, and how can I manage this?
Root Causes:
- Patient-Specific Factors: The patient's disease severity, genetic background, prior treatments (chemotherapy, radiation), age, and overall health status significantly impact the quality and functionality of the cells collected via apheresis [2].
- Collection Process Variability: Differences in apheresis protocols, training of collection staff, types of anticoagulants used, and collection devices contribute to variability in the cellular raw material [2].
- Logistical Factors: The time between apheresis and manufacturing initiation, as well as cryopreservation and thawing methods, can affect cell viability and performance [2].
Solutions:
- Implement a Risk-Based Approach: Use risk assessment tools like Failure Mode Effects Analysis (FMEA) to define the most Critical Quality Attributes (CQAs) for your starting materials and process [62] [2].
- Introduce Donor Variability Early: Intentionally include cells from a wide range of donors (including those from the target patient population with advanced disease) during process development to build robustness into your system [2].
- Standardize and Control: Work towards standardizing apheresis protocols and operator training across collection sites. Specify the use of consistent collection devices and shipping containers [2].
- Design a Flexible Process: Create detailed Standard Operating Procedures (SOPs) that include instructions for handling different scenarios arising from starting material variability. Consider modular process designs with planned pauses (e.g., cryopreservation) to allow for in-process testing and decision-making [2].
Establishing a Effective Control Strategy with PAT
Problem: Difficulty in implementing real-time monitoring and control for complex, multi-step cell culture processes, leading to reactive quality control and batch failures.
Question: How can I move from end-product testing to real-time quality assurance for my cell culture process?
Root Causes:
- Lack of Process Understanding: Insufficient knowledge of the relationships between Critical Process Parameters (CPPs) and CQAs [62] [63].
- Technical Barriers: Nonlinear parameter interactions in complex biological systems and a lack of suitable, non-invasive analytical probes for certain CQAs [62].
- Organizational Resistance: Cultural reluctance to adopt new technologies and iterative regulatory approaches [62].
Solutions:
- Systematic Development using QbD:
- Define QTPP: Start with a clear Quality Target Product Profile (e.g., target cell count, viability, potency, purity) [62].
- Identify CQAs: Link product attributes to safety and efficacy (e.g., cell viability, identity, potency, sterility) [62].
- Link CPPs to CQAs: Use risk assessment and Design of Experiments (DoE) to understand how process parameters (e.g., feeding strategy, dissolved oxygen, pH) impact your CQAs [62] [64].
- Select Appropriate PAT Tools: Implement spectroscopic tools (e.g., Raman, NIR) and other sensors for in-line, on-line, or at-line monitoring of key metabolites, nutrients, and cell health indicators [65].
- Develop a Knowledge-Rich Submission: For regulatory filings, demonstrate your deep process understanding. A well-defined design space provides regulatory flexibility, allowing you to operate within proven acceptable ranges without prior approval [62] [66].
High Batch Failure Rates and Inconsistent Yield
Problem: Unacceptable levels of batch failures and inconsistent product yield during scale-up or commercial manufacturing.
Question: What strategies can I use to drastically reduce batch failure rates and improve process robustness?
Root Causes:
- Empirical Process Development: A "trial-and-error" approach that fails to systematically identify and control sources of variability [62].
- Inadequate Process Characterization: Lack of understanding of the multidimensional combination of input variables that ensure quality [62].
- Rigid Processes: Processes that are not designed to accommodate natural variations in raw materials or environmental conditions [66].
Solutions:
- Adopt a QbD Framework: A proactive QbD approach can reduce batch failures by up to 40% by building quality in from the beginning [62]. The systematic workflow is outlined below.
- Implement PAT for Real-Time Control: Use PAT to monitor CPPs and CQAs in real-time, allowing for immediate adjustments to keep the process within the design space and prevent drift towards failure [63] [66]. This enables a "right-first-time" manufacturing philosophy.
- Quantify the ROI: Studies show that PAT implementation can cut 90% of labor costs in analytical labs and reduce rework expenses by a similar percentage. When combined with Lean manufacturing, it can slash process cycle times by 50% and increase operating margins by 6% [66].
Frequently Asked Questions (FAQs)
Q1: What are the core regulatory documents that form the foundation of QbD? A: The foundation of QbD is built on the International Council for Harmonisation (ICH) guidelines:
- ICH Q8 (R2): Pharmaceutical Development - Introduces key concepts like the Quality Target Product Profile (QTPP), Critical Quality Attributes (CQAs), and Design Space [62] [63].
- ICH Q9: Quality Risk Management - Provides the principles and tools for systematic risk assessment [62] [63].
- ICH Q10: Pharmaceutical Quality System - Covers a model for an effective quality management system throughout the product lifecycle [62] [63].
Q2: In the context of autologous cell therapies, what does "the process is the product" mean? A: This phrase emphasizes that the complex, multi-step manufacturing process is intrinsically linked to the final cell product's identity, quality, and function. Even minor changes in the process (e.g., media, feeding schedule, handling) can alter the critical quality attributes of the cells, effectively creating a different product with a different safety and efficacy profile [2]. Therefore, tight process control is essential.
Q3: What are the most common PAT tools used in biopharmaceutical manufacturing, and what do they monitor? A: Common PAT tools and their applications include:
Table: Common Process Analytical Technology (PAT) Tools and Applications
| PAT Tool | Typical Mode | Key Application Examples in Manufacturing |
|---|---|---|
| Raman Spectroscopy | In-line/At-line | Monitoring culture metabolites (glucose, lactate), protein concentration, product titer, and cell culture process states [65]. |
| Near-Infrared (NIR) Spectroscopy | In-line/On-line | Analysis of moisture content, blend uniformity in powders, and raw material identification [65]. |
| Fourier Transform Infrared (FTIR) | In-line/On-line | Similar applications to Raman and NIR; used for real-time reaction monitoring [65]. |
| Nuclear Magnetic Resonance (NMR) | At-line | Determining molecular structures, identifying drug metabolites, and quantifying impurities [65]. |
| Dielectric Spectroscopy | In-line | Monitoring live cell biomass and viability in bioreactors in real-time [65]. |
Q4: How can I justify the significant investment in PAT and QbD implementation to management? A: The justification is a strong business case based on quantifiable returns:
- Cost Avoidance: Preventing a single batch failure, which can cost $250,000 to $500,000, provides a massive return [66].
- Operational Efficiency: PAT can reduce QC labor and rework costs by up to 90% [66].
- Increased Yield and Throughput: PAT and QbD can increase process robustness and yield, with some reports showing cycle time reductions of 50% and operating margin improvements of 6% [66].
- Regulatory and IP Benefits: A robust QbD submission can lead to faster approval and creates a "competitive moat" through deep process understanding and potential process patents [66].
Q5: What is a simple example of a Critical Process Parameter (CPP) and a Critical Quality Attribute (CQA)? A: In tablet manufacturing, the compression force (e.g., controlled within 10–15 kN) is a CPP because it directly impacts the tablet's hardness and dissolution rate. The dissolution rate (e.g., ≤80% API released within 30 minutes) is a CQA because it is a direct measure of the product's bioavailability and therapeutic efficacy [62].
The Scientist's Toolkit: Essential Research Reagent Solutions
For researchers developing QbD- and PAT-driven processes for cell therapies, certain tools and materials are essential. The following table details key solutions for building a robust experimental framework.
Table: Essential Research Reagent Solutions for QbD in Cell Therapy Development
| Item | Function in QbD/PAT Context |
|---|---|
| Defined Culture Media Systems | Using consistent, well-characterized media is crucial for identifying how Critical Material Attributes (CMAs) impact cell growth and CQAs. Reduces one major source of variability during DoE studies [2]. |
| Process Analytical Probes (e.g., pH, DO, Metabolite Sensors) | The hardware for PAT. These in-line probes provide the real-time data on Critical Process Parameters (CPPs) and some CQAs (e.g., metabolite levels) needed for building process models and control strategies [65]. |
| Cell Characterization Kits (Viability, Phenotype, Potency) | The analytical core for defining CQAs. Robust assays for viability (e.g., flow cytometry with viability dyes), identity (phenotyping by flow cytometry), and potency (functional assays) are non-negotiable for linking process performance to product quality [14] [2]. |
| DoE Software | Software platforms that enable the statistical design and analysis of complex multivariate experiments. Essential for efficiently mapping the design space and understanding parameter interactions [62]. |
| Cryopreservation Media | A critical CMA. Consistent, high-quality cryopreservation media are vital for ensuring high post-thaw viability and recovery, a key CQA for cellular starting materials and final products [2]. |
Experimental Protocol: A QbD-based Workflow for Optimizing a Cell Expansion Process
This protocol provides a methodology for using QbD principles to systematically understand and optimize a cell expansion step, a common bottleneck in autologous therapy manufacturing.
Objective: To define the design space for a cell expansion process by understanding the impact of key process parameters on Critical Quality Attributes (CQAs) like final cell yield and viability.
Step 1: Define the Quality Target Product Profile (QTPP)
- Prospectively define the target profile for the expanded cells. Example: "The expanded cell population must achieve a minimum yield of 1x10^9 viable cells with ≥90% viability and express specific surface markers (CDX, CDY) at ≥95%."
Step 2: Identify Critical Quality Attributes (CQAs)
- From the QTPP, list the measurable quality attributes critical to safety and efficacy. For this step, the CQAs are:
- Final Viable Cell Density (VCD)
- Final Cell Viability (%)
- Phenotype Purity (%)
Step 3: Risk Assessment & Parameter Screening
- Use an Ishikawa (fishbone) diagram or a Risk Estimation Matrix to brainstorm and rank all potential material attributes and process parameters that could impact the CQAs.
- Parameters to consider: Seeding density, basal media type, growth factor concentration, feeding strategy (frequency and volume), dissolved oxygen (DO) setpoint, pH setpoint.
- Output: A prioritized list of high-risk parameters to investigate further (e.g., growth factor concentration, feeding strategy, seeding density).
Step 4: Design of Experiments (DoE)
- Instead of a One-Factor-at-a-Time approach, use a multivariate DoE to study the high-risk parameters and their interactions efficiently.
- Example: A 2^3 full factorial design with a center point, investigating:
- Factor A: Growth Factor Concentration (low vs. high)
- Factor B: Feeding Frequency (every 24h vs. every 48h)
- Factor C: Seeding Density (low vs. high)
- Execution: Run all experiments defined by the DoE matrix in a randomized order. Monitor cell growth and metabolites daily using PAT tools (e.g., dielectric spectroscopy for biomass, bioanalyzer for metabolites). At the end of the run, measure the CQAs (VCD, viability, phenotype).
Step 5: Data Analysis and Design Space Establishment
- Use multiple linear regression to build a mathematical model linking the process parameters (A, B, C) to each CQA.
- Create contour plots or 3D response surface models to visualize the "sweet spot" where all CQAs meet their targets.
- Define the Design Space: The multidimensional combination of Growth Factor Concentration, Feeding Frequency, and Seeding Density where you can reliably expect to meet all CQAs.
Step 6: Control Strategy
- Based on the model, define the control strategy. For parameters with a large impact on CQAs (e.g., growth factor concentration), set tight controls. Implement PAT (e.g., daily metabolite monitoring) to ensure the process remains within the design space and to enable real-time release of the cell batch.
Validating Product Consistency and Comparative Analytical Assessments
Establishing Metrics for Successful Batch Effect Correction
In autologous cell products research, where each product batch originates from a unique patient donor, controlling for technical variation is paramount. Batch effects—unwanted technical variations introduced by differences in sequencing runs, reagents, equipment, or personnel—can confound true biological signals and compromise data integrity. Establishing robust metrics to evaluate the success of batch effect correction ensures that observed variations genuinely reflect biological differences rather than technical artifacts, leading to more reliable and reproducible research outcomes.
FAQs: Core Concepts and Metric Selection
What are the primary metrics used to evaluate batch effect correction?
Several established metrics quantitatively assess how well batch effects have been removed while preserving biological variation. The table below summarizes the key metrics, their measurement focus, and ideal outcomes.
| Metric Name | What It Measures | Ideal Outcome |
|---|---|---|
| kBET [67] [68] | Local batch mixing using chi-square test on k-nearest neighbors. | Low rejection rate (close to 0). |
| LISI [67] [68] | Diversity of batches in a cell's local neighborhood. | High score (close to number of batches). |
| ASW (Average Silhouette Width) [67] | Compactness of batches and separation of cell types. | High batch mixing (batch ASW ~0), high cell type separation (cell type ASW ~1). |
| ARI (Adjusted Rand Index) [67] | Similarity between clustering results before and after correction. | High score (closer to 1) for cell type clusters. |
| RBET [68] | Batch effect on stable Reference Genes; sensitive to overcorrection. | Low score indicates good correction; a U-shaped curve can indicate overcorrection. |
How do I choose the right batch correction method for my data?
The choice of method depends on your data's characteristics and computational needs. Benchmarking studies have consistently identified top-performing methods.
| Method | Key Principle | Recommended For |
|---|---|---|
| Harmony [67] [69] [70] | Iterative clustering and mixture-based correction in PCA space. | General first choice; fast runtime, handles multiple batches well. |
| Seurat (RPCA/CCA) [67] [69] | Identifies mutual nearest neighbors (anchors) in a shared low-dimensional space (RPCA or CCA). | Datasets with shared cell types; Seurat-RPCA is faster for large datasets [69]. |
| Scanorama [67] [69] | Approximate mutual nearest neighbors across all datasets in a low-dimensional space. | Large, heterogeneous datasets; relaxes assumption of common cell populations [69]. |
| LIGER [67] | Integrative non-negative matrix factorization and quantile alignment. | Situations where biological differences between batches are expected. |
| scGen [67] | Variational autoencoder (VAE) trained on a reference dataset. | Data with a well-defined reference; can model complex non-linearities. |
What are the clear signs of overcorrection?
Overcorrection occurs when a method removes not only technical batch effects but also genuine biological variation. Key signs include [70] [4]:
- Distinct cell types are incorrectly merged: On a UMAP plot, clearly separate cell types (e.g., T-cells and monocytes) appear as a single, mixed cluster after correction.
- Loss of variation in housekeeping genes: Reference genes (RGs) or housekeeping genes show a loss of expression variation after correction, which should not occur [68].
- Complete overlap of samples from different conditions: If samples from vastly different biological conditions (e.g., healthy vs. diseased) overlap entirely after correction, biological signal may have been erased.
- Cluster-specific markers are non-informative: A significant portion of the genes that define clusters after correction are generic, widely high-expressed genes (e.g., ribosomal genes) rather than specific marker genes [4].
Troubleshooting Guides
Problem: Inconsistent Cell Type Annotations After Correction
Issue: Downstream analysis, like cell type annotation, yields different or less accurate results after batch correction compared to analyzing batches separately.
Solution:
- Check for Overcorrection: Follow the steps in the "Signs of Overcorrection" section above. Generate a UMAP colored by both batch and cell type to see if biological separation has been lost.
- Re-evaluate Metric Scores: Calculate the ARI for cell type labels and the RBET score. A low ARI or a rising RBET score suggests overcorrection is degrading biological information [68].
- Adjust Method Parameters: If using a method like Seurat, try reducing the
k.anchorork.filterparameters, which control the number of neighbors used to find integration anchors. Starting with lower values can prevent over-smoothing [68]. - Try a Less Aggressive Method: Switch from a method known to be strong (like Seurat) to a potentially gentler one like Harmony or Scanorama, and re-evaluate the results [67] [4].
Problem: Poor Batch Mixing Persists After Correction
Issue: Metrics like kBET and LISI indicate that batch effects remain strong even after applying a correction method.
Solution:
- Verify Preprocessing: Ensure that data normalization and the selection of highly variable genes (HVGs) were performed correctly on the batch-corrected data (if it is a count matrix) before generating embeddings for visualization and metric calculation [67].
- Increase Correction Strength: For methods with tunable parameters, you can cautiously increase the correction strength. In Harmony, for instance, you might adjust the
thetaparameter, which dictates the diversity penalty. - Use a Different Integration Strategy: If your datasets have highly different cell type compositions, a method like Seurat-RPCA or LIGER, which are designed to handle more heterogeneity, might perform better than Seurat-CCA [69].
- Check for Sample Imbalance: If one batch has vastly more cells or different cell type proportions, it can hinder effective integration. Consider downsampling the larger batch or using methods benchmarked to handle imbalance better [4].
Experimental Protocols for Metric Evaluation
Protocol: Benchmarking Batch Effect Correction Methods
This protocol provides a step-by-step workflow to systematically evaluate different batch correction methods on a single-cell RNA sequencing dataset, helping you select the most appropriate one for your research.
Title: Batch Correction Benchmarking Workflow
Materials/Software Needed:
- R or Python: With appropriate single-cell analysis packages (Seurat, Scanpy).
- Batch Correction Tools: Harmony, Seurat, Scanorama, etc.
- Metrics Calculation Functions: For kBET, LISI, ARI, etc. (e.g., the
kBETR package,lisiR package,scikit-learnfor ARI in Python).
Procedure:
- Data Preprocessing: Begin with the raw count matrix. Perform standard normalization and log-transformation. Select the most highly variable genes (HVGs) to reduce dimensionality and noise [67].
- Method Application: Apply each batch correction method you wish to benchmark (e.g., Harmony, Seurat, Scanorama) to the preprocessed data. Adhere to the default parameters as a starting point.
- Dimensionality Reduction: For each corrected dataset, perform Principal Component Analysis (PCA) followed by UMAP to generate low-dimensional embeddings for visualization and metric calculation.
- Metric Calculation: Compute a suite of metrics on the PCA embedding of the corrected data.
- Visual Inspection: Create UMAP plots colored by batch and by cell type for each method. Visually confirm the results suggested by the quantitative metrics.
- Synthesis and Selection: Compare the results across all methods. The best method effectively mixes batches (high LISI, low kBET) while preserving biological cell type clusters (high cell type ARI and ASW, stable RBET).
Protocol: Simulating a Null Batch Effect to Test for Artifacts
This protocol tests whether a batch correction method introduces artificial structure into the data when no real batch effect exists, which is a key test of calibration [70].
Materials/Software Needed:
- A single, homogeneous scRNA-seq dataset without major batch effects.
- Batch correction software.
Procedure:
- Create Pseudobatches: Take a single, well-controlled dataset and randomly assign each cell to one of two "pseudobatches" (e.g., 'Batch A' and 'Batch B'). This creates a scenario with no true technical variation between the groups [70].
- Apply Correction: Apply the batch correction method to this dataset, providing the pseudobatch labels.
- Analyze Changes: Compare the data before and after correction.
- k-NN Graph: Check if the k-nearest neighbor graph has been significantly altered.
- Clustering: Perform clustering on the corrected data and check if new, spurious clusters have appeared that correlate with the pseudobatches.
- Differential Expression: Test for differentially expressed genes between the pseudobatches after correction. A well-calibrated method should find very few or no significant genes [70].
| Item / Resource | Function / Purpose |
|---|---|
| Reference Genes (RGs) [68] | A set of genes (e.g., housekeeping genes) with stable expression across cell types and conditions. Used in metrics like RBET to detect overcorrection by ensuring their expression pattern remains stable post-correction. |
| Universal Reference Materials [71] | Standardized control samples (e.g., the Quartet reference materials) profiled across batches and labs. Enable ratio-based correction methods and provide a ground truth for benchmarking. |
| Negative Control Samples [69] | Samples (e.g., vehicle controls) where variation is presumed to be primarily technical. Used by methods like Sphering to model and remove batch effects. |
| PCA | A foundational dimensionality reduction technique. Used by many methods (e.g., Harmony, fastMNN) as an initial step to project data into a lower-dimensional space where batch correction is performed [67] [69]. |
| UMAP/t-SNE | Non-linear dimensionality reduction algorithms. Critical for the visual assessment of batch mixing and cell type separation before and after correction [4]. |
| k-Nearest Neighbor (k-NN) Graph | A graph representing cell similarities. The preservation of its biological structure after correction is a key indicator of success and lack of artifacts [70]. |
Designing Validation Studies for Process and Product Consistency
Frequently Asked Questions (FAQs)
Q1: What are the most common sources of batch-to-batch variation in autologous cell therapies? The most common sources stem from variability in the patient-derived starting material and process-related factors [14] [2].
- Patient-Specific Variability: The disease severity, prior treatments (e.g., chemotherapy), age, and overall health of the patient can significantly impact the quality, quantity, and functionality of the cells collected via apheresis [2].
- Collection Process Variability: Differences in apheresis protocols, training of collection staff, types of collection devices, and anticoagulants used contribute to variability in the leukapheresis material [2].
- Manufacturing Process Variability: Inconsistent cell culture conditions, efficiency of genetic modification, and cell expansion kinetics can amplify the initial variability from the starting material [72] [14].
Q2: What is the difference between process validation and process verification? This is a critical distinction in a regulated environment [73].
- Process Validation is a proactive, forward-looking activity. It establishes documented evidence that a process is capable of consistently delivering a quality product. It asks, "Will this process consistently work in the future?" [73] [74]
- Process Verification is a reactive, backward-looking activity. It confirms that a specific batch or run of an already validated process met its predetermined specifications. It asks, "Did this specific batch work correctly?" [73]
Q3: How can a risk-based approach be applied to process validation? A risk-based approach is central to modern validation principles and helps focus efforts on what matters most for product quality [73] [75]. Key tools include:
- Failure Mode and Effects Analysis (FMEA): Used to identify and prioritize potential process failure points, their causes, and their effects on product quality [73].
- Critical Quality Attributes (CQAs): Identify the product properties that must be controlled to ensure safety and efficacy [75].
- Critical Process Parameters (CPPs): Determine the process parameters that have a direct impact on the CQAs. Validation studies then focus on demonstrating control over these CPPs [73].
Q4: What are the regulatory requirements for handling an out-of-specification (OOS) autologous product? Regulatory frameworks provide pathways for the compassionate use of OOS products when no alternatives exist [48].
- United States: An OOS product may be supplied under an Expanded Access Program (EAP). The treating physician requests the OOS product from the Marketing Authorisation Holder (MAH), who conducts a risk assessment. The MAH may then supply the product under an Investigational New Drug (IND) application after IRB approval and patient consent [48].
- Europe: OOS Advanced Therapy Medicinal Products (ATMPs) can be provided as commercial products under exceptional circumstances. The MAH performs a risk assessment, and the treating physician, upon reviewing this assessment, makes the final decision to administer the product. The MAH must notify the regulatory authorities within 48 hours [48].
Troubleshooting Guides
Issue 1: High Variability in Cell Expansion Yields
Potential Causes and Solutions:
| Cause | Investigation | Corrective & Preventive Actions |
|---|---|---|
| Variable starting material quality from different patients [2]. | Assess pre-apheresis cell counts (e.g., CD3+) and patient treatment history. Correlate with expansion data [2]. | Implement stricter patient eligibility criteria. Develop a flexible process that can accommodate a wider range of input material quality [2]. |
| Inconsistent culture conditions or media components [14]. | Review batch records for deviations in media formulation, cytokine concentrations, or feeding schedules. | Standardize raw material suppliers and implement rigorous raw material testing. Use Design of Experiments (DoE) to optimize and define robust operating ranges for culture parameters [75]. |
| Uncontrolled or open process steps leading to contamination or variability [72]. | Audit the manufacturing process for manual, open manipulations. | Implement closed processing systems and automation where possible to improve consistency and reduce human error [72]. |
Experimental Protocol: Assessing Impact of Starting Material on Expansion
- Cell Source: Collect leukapheresis products from multiple donors, ensuring a range of pre-apheresis CD3+ counts and health statuses [2].
- Isolation: Isolate CD3+ or Treg cells using a standardized, bead-based method [72].
- Culture: Culture cells in a standardized, rapamycin-supplemented medium to selectively expand Tregs [72].
- Monitoring: Monitor cell count and viability daily. Calculate population doublings and final yield at the end of the culture period.
- Analysis: Correlate the final cell yield and growth kinetics with the initial donor characteristics (e.g., pre-apheresis CD3+ count) using statistical regression analysis.
Issue 2: Inconsistent Potency of the Final Drug Product
Potential Causes and Solutions:
| Cause | Investigation | Corrective & Preventive Actions |
|---|---|---|
| Lack of a robust, quantitative potency assay that reflects the mechanism of action [76]. | Audit the potency assay method. Is it a functional cell-based assay or merely a surrogate (e.g., phenotype)? | Develop a mechanism-relevant bioassay. For a Treg product, this could be a suppression assay measuring inhibition of effector T-cell proliferation [72] [76]. |
| Loss of critical cell phenotype or function during manufacturing [72]. | Perform in-process testing for phenotype markers (e.g., FOXP3, CD25 for Tregs) and suppressive function at different stages. | Optimize the manufacturing process to maintain cell identity. This may involve using specific cytokines (e.g., IL-2) and mTOR inhibitors like rapamycin during expansion to prevent Treg conversion to effector cells [72]. |
| Genetic instability of the engineered cell product [72]. | Perform genomic analyses on the final product to check for consistency in CAR/TCR expression and genetic integrity. | Incorporate vector copy number (VCN) analysis and tests for expression consistency of the genetic modification as part of the release criteria [72]. |
Experimental Protocol: Developing a Functional Potency Assay
- Effector Cell Preparation: Isolate CD4+/CD8+ T-cells from a healthy donor and label with a fluorescent dye (e.g., CFSE).
- Stimulation: Activate the effector T-cells with anti-CD3/CD28 beads.
- Co-culture: Co-culture the activated effector cells with serial dilutions of the final Treg drug product.
- Readout: After several days, analyze the suppression of effector cell proliferation via flow cytometry (CFSE dilution) and/or measure the secretion of suppression-related cytokines (e.g., IL-10, TGF-β) via ELISA.
- Quantification: Establish a dose-response curve and define the potency of the drug product in terms of its IC50 (the concentration that causes 50% suppression).
Process Validation Lifecycle: A Framework for Consistency
The FDA's process validation lifecycle provides a structured framework for ensuring process and product consistency [73] [74]. The following diagram illustrates the three-stage approach and key activities for autologous cell therapies.
Stage 1: Process Design This stage focuses on building process knowledge and establishing a robust foundation [73] [74].
- Activities:
- Define Critical Quality Attributes (CQAs): Product characteristics critical to safety and efficacy (e.g., viability, purity, potency, identity) [73] [76].
- Identify Critical Process Parameters (CPPs): Process variables that impact CQAs (e.g., cell seeding density, cytokine concentration, transduction parameters) [73].
- Use Risk Assessment Tools like FMEA and Design of Experiments (DoE) to understand the relationship between CPPs and CQAs and define an optimal "design space" [73] [75].
- Deliverable: A well-understood and characterized process ready for qualification.
Stage 2: Process Qualification This stage confirms that the process design performs as expected in the GMP manufacturing environment [73] [74].
- Activities:
- Equipment Qualification: Execute Installation (IQ) and Operational (OQ) Qualification for all equipment.
- Process Performance Qualification (PPQ): Execute a predefined number of consecutive successful process runs using patient materials that represent expected variability. This demonstrates the process is capable of consistently producing product meeting all release specifications [77] [73].
- Deliverable: Documented evidence that the process is effective and reproducible.
Stage 3: Continued Process Verification This is an ongoing stage to ensure the process remains in a state of control during routine commercial production [73] [74].
- Activities:
- Implement a system for ongoing monitoring of CQAs and CPPs.
- Use Statistical Process Control (SPC) charts to detect trends or process shifts.
- Establish a robust change control process to manage any modifications and determine if re-validation is required.
- Deliverable: Assurance that the process remains validated over its entire lifecycle.
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials used in autologous cell therapy process development and validation.
| Item | Function & Application | Key Considerations |
|---|---|---|
| Magnetic Cell Separation Beads | Isolation of target cell populations (e.g., CD4+/CD25+ Tregs) from leukapheresis product [72]. | Antibody specificity and purity of the isolated population are critical. Can be combined with sorting for higher purity [72]. |
| Cell Culture Media & Supplements | Ex vivo expansion of isolated cells. | Use of GMP-grade, xeno-free components is critical for clinical use. Supplements like rapamycin help maintain Treg phenotype and prevent Teff contamination [72]. |
| Cryopreservation Media | Long-term storage of apheresis starting material and final drug product [2]. | Formulation (e.g., DMSO concentration) and controlled-rate freezing protocols are vital for maintaining post-thaw viability and function [2]. |
| Viral Vectors | Genetic modification of cells (e.g., lentivirus for CAR/TCR transduction) [72]. | Vector copy number (VCN), titer, and transduction efficiency are key process parameters that must be controlled and monitored [72] [76]. |
| Flow Cytometry Antibodies | Characterization of cell phenotype (identity, purity) and potency throughout the process [76]. | Panels must be designed to monitor critical markers (e.g., CD3, CD4, CD25, CD127, FOXP3 for Tregs) and detect potential contaminants [72]. |
| Cell-Based Potency Assay Kits | Quantifying the biological function of the cell product, a critical release criterion [76]. | The assay must be quantitative, robust, and reflect the product's documented mechanism of action (MoA) [76]. |
Leveraging Comparative Analytical Assessments for Biosimilarity
Comparative Analytical Assessment (CAA) serves as the scientific foundation for demonstrating that a proposed biosimilar product is highly similar to an already licensed reference biological product. For researchers working with autologous cell products, which are inherently variable due to their patient-specific nature, the principles of CAA provide a structured framework to understand, monitor, and control batch-to-batch variation, ensuring consistent product quality and performance.
FAQs: Core Principles and Regulatory Framework
Q1: What is the scientific basis for relying on Comparative Analytical Assessment (CAA) for biosimilarity? The scientific foundation rests on the principle that a comprehensive and sensitive comparative analytical assessment can detect even subtle structural and functional differences between biological products that are more sensitive than clinical efficacy studies [78]. The "Totality of the Evidence" approach, endorsed by the U.S. Food and Drug Administration (FDA), places CAA at the base of a stepwise hierarchy for demonstrating biosimilarity [79]. When CAAs show a high degree of similarity, they can form the primary evidence, potentially reducing the need for extensive comparative clinical trials [80] [81].
Q2: How has the regulatory expectation for clinical data in biosimilar development recently evolved? In a significant policy shift outlined in an October 2025 draft guidance, the FDA has stated that for many proposed biosimilars, comparative clinical efficacy studies (CES) may no longer be a default requirement [78] [81]. The agency now recognizes that for well-characterized products, an appropriately designed human pharmacokinetic (PK) study and an immunogenicity assessment, supported by a robust CAA, may be sufficient to demonstrate biosimilarity [80] [81]. This evolution is based on the FDA's growing experience and advances in analytical technologies [82].
Q3: What is a tiered approach for assessing quality attributes in a CAA? The tiered approach is a risk-based strategy for evaluating Critical Quality Attributes (CQAs) identified during analytical characterization. CQAs are classified into three tiers based on their potential impact on clinical outcomes [79]:
- Tier 1: Attributes most critical to clinical outcomes. They are evaluated using a rigorous equivalence test with a pre-defined similarity margin.
- Tier 2: Attributes with mild-to-moderate relevance. They are assessed using the quality range approach, often based on the distribution of the reference product.
- Tier 3: Attributes with lower risk. They are evaluated with simple graphical comparisons or raw data analysis.
Troubleshooting Guides for CAA
Guide 1: Addressing Inconsistencies in Higher-Order Structure (HOS) Analysis
Problem: Inconsistent results when comparing hydrodynamic size (D_h) between a proposed biosimilar and a reference product using Dynamic Light Scattering (DLS), leading to an inability to conclusively demonstrate similarity.
Investigation and Resolution:
| Step | Action | Technical Detail |
|---|---|---|
| 1 | Go beyond the signature peak. Do not rely solely on the monomer peak in its native state. The "signature peak" alone is often insufficient to show analytical similarity in D_h size distribution [83]. |
- |
| 2 | Implement a forced degradation study. Subject both the test and reference products to controlled stress conditions (e.g., thermal stress) to accelerate degradation and amplify subtle differences in stability and aggregation pathways [83]. | - |
| 3 | Develop a "Sweet Spot Method." Optimize the experimental conditions for thermal stress to find the temperature range where differences become apparent. This "sweet spot" varies from product to product [83]. | Protocol: Use a High-Throughput DLS (HT-DLS) plate reader. For monoclonal antibodies, a method with a temperature range of 50-70°C, a 3°C increment, and a 2-minute hold time at each step has proven effective [83]. |
| 4 | Apply Multivariate Data Analysis. Use Principal Component Analysis (PCA) to interpret the complex D_h size distribution data generated across the temperature gradient. PCA can clearly group products with similar degradation patterns and distinguish outliers [83]. |
- |
Guide 2: Managing High Variability in Autologous Cell Products
Problem: In autologous cell therapy research and manufacturing, the starting material (patient cells) exhibits high inherent variability, making it difficult to establish a consistent process and define critical quality attributes (CQAs).
Investigation and Resolution:
| Step | Action | Technical Detail |
|---|---|---|
| 1 | Implement Advanced Process Controls. Utilize automated, closed-system manufacturing platforms to minimize manual handling, reduce contamination risk, and improve process consistency [27] [13]. | - |
| 2 | Leverage AI and Predictive Analytics. Integrate artificial intelligence (AI) for real-time process monitoring and control. AI-powered systems can use predictive analytics to optimize cell culture conditions and improve batch-to-batch consistency [13] [84]. | - |
| 3 | Adopt a Risk-Based Comparability Framework. Follow regulatory guidance on demonstrating product comparability after process changes. Use a tiered, risk-based approach for comparability assessments, focusing extensive analytical characterization on CQAs most susceptible to process variations [13]. | - |
| 4 | Establish Robust Potency Assays. Develop and validate quantitative assays that are clinically relevant to the product's mechanism of action (MOA). This is critical for proving efficacy and defining CQAs, especially for complex cell-based products [13]. | - |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Materials for Comparative Analytical Assessment
| Item | Function in CAA | Example Application |
|---|---|---|
| Reference Product | Serves as the benchmark for all comparative analytical, non-clinical, and clinical studies. | The licensed biological product against which the proposed biosimilar is compared [85]. |
| Well-Characterized Reference Standard (e.g., NIST mAb) | Provides a control standard to validate analytical methods and instrument performance. | Used during method development to differentiate drug products and demonstrate assay suitability [83]. |
| High-Throughput Dynamic Light Scattering (HT-DLS) | Determines the hydrodynamic size distribution of particles in solution and monitors protein aggregation under stress conditions. | Used in the "Sweet Spot Method" to compare the D_h size change pattern of a biosimilar and reference product across a temperature gradient [83]. |
| Cell Lines for Bioassays | Used to develop functional assays that assess the biological activity of the product relative to the reference product. | Critical for evaluating mechanism of action (MOA) and classifying CQAs into tiers [79]. |
Experimental Protocols and Data Analysis
Protocol: HT-DLS Sweet Spot Method for HOS Similarity
Methodology: This protocol uses forced thermal degradation and HT-DLS to compare the hydrodynamic size (D_h) distribution of a proposed biosimilar and its reference product [83].
Step-by-Step Procedure:
- Sample Preparation: Use the drug products at their original concentration. If dilution is necessary, ensure the same dilution factor is applied to both the test and reference products.
- Instrument Setup: Load samples into a HT-DLS plate reader.
- Preliminary Scouting Run: Perform a temperature ramp from ~22°C to 50°C to establish a baseline where no
D_hsize change occurs. - Sweet Spot Method Run:
- Set the temperature range based on scouting data (e.g., 50°C to 70°C for mAbs).
- Configure the method with a temperature increment of 3°C and a hold time of 2 minutes at each step.
- Use the instrument's event scheduler to automate the run.
- Collect
D_hdata using both cumulants (Z-average) and regularization processing models.
- Data Analysis:
- Plot
D_hsize versus temperature for all products. - Visually inspect for similar size change patterns between the biosimilar and reference product.
- Use Principal Component Analysis (PCA) to statistically model the data and confirm grouping of similar products.
- Plot
Expected Outcomes: A proposed biosimilar that is highly similar to the reference product will show a nearly identical D_h size change pattern across the temperature gradient and will group closely with the reference product in the PCA score plot, while a different product will show a distinct pattern and separate in the PCA [83].
Data Presentation and Analysis
Table: Key Statistical Methods for Tiered Analysis of CQAs [79]
| Tier | CQA Criticality | Recommended Statistical Method | Purpose and Description |
|---|---|---|---|
| Tier 1 | Highest | Equivalence Test | To test a formal statistical hypothesis that the mean difference between the proposed and reference product is within a pre-specified equivalence margin (δ). |
| Tier 2 | Medium | Quality Range Approach | To assess whether the test product values fall within a range established based on the reference product (e.g., ± 3 standard deviations). |
| Tier 3 | Lower | Graphical Comparison / Raw Data | To provide supporting, descriptive information through visual aids like plots or by presenting the raw data directly. |
Process Visualization Diagrams
Diagram 1: Tiered Approach for CQA Assessment
Diagram 2: HT-DLS Sweet Spot Method Workflow
Navigating the Evolving Regulatory Landscape for Complex Therapies
Autologous cell therapies represent a paradigm shift in personalized medicine, manufacturing a unique drug product for each individual patient. This patient-specific nature inherently introduces significant batch-to-batch variation, which remains a central challenge for researchers and manufacturers. Variability in the cellular starting material—the patient's own cells—compounds through every step of the manufacturing process, posing difficulties for standardization, quality control, and regulatory compliance [2]. Successfully navigating this complex landscape requires a deep understanding of variation sources, strategic process design, and robust analytical methods to ensure the consistent production of safe, high-quality, and efficacious therapies.
Frequently Asked Questions (FAQs)
1. What are the primary sources of batch-to-batch variation in autologous cell therapies? Variability arises from multiple sources, creating a complex challenge for standardization.
- Patient-to-Patient Variability: The disease severity, prior treatments (e.g., chemotherapy), age, genetic background, and overall health of a patient can significantly impact the quality, quantity, and functionality of the collected cells [2].
- Collection Process Variability: Differences in apheresis protocols, collection devices, operator training, anticoagulants used, and the handling of cells post-collection contribute to variability in the starting material [2].
- Manufacturing Process Variability: The complex, multi-step processes of cell activation, genetic modification, and expansion can compound existing variability. Manual, open processes are particularly susceptible to operator-induced variation [86] [87].
2. What analytical challenges exist for characterizing autologous products? Analytical science faces unique hurdles in the autologous space. Variability in the methods used for quality control and testing can lead to differences in the assessment of critical cell characteristics like viability, potency, and purity [14]. Furthermore, the industry faces challenges with assay development, variability, and statistical analysis given the small numbers of manufacturing runs for a given patient-specific product [2].
3. How can raw material variability be controlled? While not all variability can be eliminated, several strategies can introduce control.
- Stringent Donor Eligibility: Implementing strict patient inclusion and exclusion criteria for clinical trials helps minimize initial variability [2].
- Process Standardization: Standardizing operator training, collection methods, and post-collection handling and logistics as much as possible reduces introduced variation [2].
- Risk-Based Approach: Using a risk-based approach to define the most critical starting materials and Critical Quality Attributes (CQAs) allows for focused control efforts [2].
4. What regulatory pathways exist for products that do not meet specifications? In exceptional circumstances, out-of-specification (OOS) autologous products may be used under compassionate grounds. Regulatory frameworks for this differ:
- United States: OOS products can be provided through the Expanded Access Program (EAP) after a risk assessment and under an Investigational New Drug (IND) application [48].
- Europe: EU guidelines allow the administration of OOS Advanced Therapy Medicinal Products (ATMPs) when necessary to avoid a serious risk to the patient, provided the treating physician accepts the product after a risk assessment [48].
- Japan: OOS products are currently supplied within clinical trial frameworks, which creates significant administrative burdens [48].
Technical Troubleshooting Guide
Issue: High Variability in Cell Growth and Expansion
Potential Causes and Solutions:
| Cause | Solution | Rationale |
|---|---|---|
| Variable quality of apheresis material [2] | Implement pre-screening assays for cell health and functionality. Adjust culture media and feeding schedules based on incoming cell quality. | Proactive assessment allows for process adjustments to accommodate variable growth kinetics. |
| Manual, open processing steps [86] | Integrate closed, automated systems for cell isolation, activation, and expansion (e.g., Gibco CTS Rotea System) [86]. | Automation minimizes human intervention, reduces contamination risk, and enhances process consistency. |
| Inconsistent raw materials | Use GMP-manufactured, quality-assured reagents and media from a reputable vendor to ensure a reliable supply [86]. | High-quality, consistent raw materials are foundational to a robust manufacturing process. |
Issue: Inconsistent Product Potency
Potential Causes and Solutions:
| Cause | Solution | Rationale |
|---|---|---|
| Limited understanding of Critical Quality Attributes (CQAs) [14] | Employ a multivariate analytical approach (e.g., an analytical matrix) to better understand the relationship between process parameters and product potency [2]. | A comprehensive understanding of CQAs is crucial for defining what controls product efficacy. |
| Lack of real-time process data | Implement Process Analytical Technologies (PAT) for real-time monitoring of critical process parameters [2]. | Real-time data enables timely feed rate adjustments and tighter process control. |
| Variability in genetic modification | Standardize transfection/transduction protocols and use automated, closed electroporation systems (e.g., Gibco CTS Xenon System) [86]. | Automated systems improve the consistency and efficiency of gene editing steps. |
Strategic Approaches to Minimize Variation
Process Automation and Closed Systems
Automation is central to reducing manual errors and enhancing consistency. Adopting closed, automated systems for key unit operations like cell isolation, activation, and electroporation minimizes contamination risk and operator-induced variability [86]. These systems improve process consistency and reliability by reducing hands-on time and are designed to be GMP-compliant, supporting the transition from research to clinical manufacturing [86].
Robust Data Management and Process Analytics
An integrated data model is essential for managing the complexities of autologous therapy manufacturing. Data should be collected at all stages, from apheresis to final product infusion, and converted into useful information to draw insights that improve operations [14]. Leveraging advanced analytical techniques helps identify and mitigate sources of variability early in the process [14].
Early and Proactive Regulatory Engagement
Regulatory bodies like the FDA are building capacity and launching new initiatives to support cell therapy developers.
- INTERACT Meetings: The FDA's INitial Targeted Engagement for Regulatory Advice on CBER/CDER ProducTs (INTERACT) meeting program facilitates early discussions on novel, challenging issues before IND submission [88].
- Gene Therapy Pilot Program: This program provides gene therapy developers with real-time FDA input throughout the clinical development process, potentially enabling shorter development cycles [88]. Prioritizing open communication with regulatory bodies through these channels ensures clarity and helps prevent mistakes caused by misunderstandings of complex guidelines [88].
Regulatory Pathways and Control Strategies
The regulatory landscape for complex therapies is dynamic. In the U.S., the FDA has established specialized "super offices" like the Office of Therapeutic Products (OTP) to centralize review processes and increase capacity for cell and gene therapies [88]. For autologous products, regulators recognize the unique challenges of batch variation. The focus is on demonstrating control through strategies such as Quality by Design (QbD) and implementing robust Quality Control measures rather than achieving absolute uniformity [14].
A key part of the control strategy is defining the Critical Quality Attributes (CQAs) of the final product. Given the variability in starting materials, the "process is the product" [2]. Therefore, controlling the manufacturing process itself is paramount to ensuring that the final product, even with inherent batch-to-batch differences, consistently meets the predefined CQAs for safety, identity, purity, and potency.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in Autologous Cell Therapy Research |
|---|---|
| GMP-manufactured Cell Culture Media | Provides a consistent, high-quality, and well-defined nutrient base for the expansion of patient cells, supporting cell viability and growth [86]. |
| Cell Separation Kits (e.g., for PBMCs) | Used for the initial isolation and purification of target cell populations (e.g., T-cells) from a leukapheresis product, a critical first step in manufacturing [86]. |
| Activation/Transfection Reagents | Enables the genetic modification of cells (e.g., to express a CAR). Using GMP-compliant reagents is crucial for clinical translation [86]. |
| Cryopreservation Media | Allows for the freezing and storage of both apheresis starting material and the final drug product, providing flexibility in logistics and manufacturing scheduling [87]. |
Experimental Workflow for Process Characterization
The following diagram illustrates a generalized workflow for developing and controlling an autologous cell therapy process, highlighting key points where variability can be managed.
Conclusion
Effectively addressing batch variation in autologous cell products requires an integrated, multi-faceted strategy that combines robust experimental design, advanced computational correction, and stringent process controls. The field is moving towards greater reliance on sensitive analytical methods and AI-driven automation to ensure product consistency. Future success hinges on the continued development of standardized benchmarking frameworks, the adoption of Quality by Design principles, and close collaboration with regulatory bodies to establish clear pathways for demonstrating product quality and biosimilarity, ultimately ensuring the reliable and scalable delivery of these transformative personalized medicines.
References
- 1. Addressing Variability and Meeting Quality Expectations in the ... [https://www.ncbi.nlm.nih.gov/books/NBK544021/]
- 2. Managing Raw Material Variability for Autologous Cell ... [https://www.biopharminternational.com/view/managing-raw-material-variability-for-autologous-cell-therapies]
- 3. Batch Effect in Single-cell RNA-seq: Frequently Asked ... [https://www.elucidata.io/blog/batch-effect-in-single-cell-rna-seq-frequently-asked-questions-and-answers]
- 4. 4 Handy Tips For Correcting Batch Effects | ScRNA-seq ... [https://www.pythiabio.com/post/4-handy-tips-for-correcting-batch-effects-scrna-seq-analysis-101]
- 5. Assessing and mitigating batch effects in large-scale omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447944/]
- 6. Harmonisation of quality control tests for academic ... [https://www.nature.com/articles/s41409-025-02637-8]
- 7. Batch Effects during Human Bone Marrow Stromal Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8946746/]
- 8. Batch variability and anti-inflammatory effects of iPSC ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1536843/full]
- 9. Cell and Gene Therapy Quality Control & Assurance [https://www.cellandgene.com/topic/cell-gene-therapy-qa-qc]
- 10. Addressing Variability in Donor Tissues and Cells - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK544028/]
- 11. Examining the sources of variability culture media used for... in cell [https://pubmed.ncbi.nlm.nih.gov/28940015/]
- 12. Cell and Gene Therapy Spotlights 2025 [https://www.insights.bio/cell-and-gene-therapy-insights/spotlights/year/2025]
- 13. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 14. Inside Cell Gene Live "How To Reduce Batch ... [https://www.cellandgene.com/doc/inside-cell-gene-live-how-to-reduce-batch-to-batch-variation-in-cell-therapy-manufacturing-0001]
- 15. Process Steps in Cell Therapy Manufacturing [https://www.cellandgene.com/topic/cell-therapy-manufacturing]
- 16. Manufacturing and control strategies for Cell and Gene ... [https://www.parexel.com/insights/blog/manufacturing-and-control-strategies-for-cell-and-gene-therapy-products-navigating-eu-and-us-regulatory-requirements]
- 17. Variation in the manufacturing reproducibility of autologous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6933469/]
- 18. How to Identify and Prevent Batch Effects in Longitudinal ... [https://cytekbio.com/blogs/blog/how-to-identify-and-prevent-batch-effects-in-longitudinal-flow-cytometry-research-studies]
- 19. Batch to the Future: How normalisation tools help reduce ... [https://help.omiq.ai/hc/en-us/articles/40037326944148-Batch-to-the-Future-How-normalisation-tools-help-reduce-batch-effect-in-high-parameter-cytometry]
- 20. Batch correction methods used in single-cell RNA sequencing ... [https://genome.cshlp.org/content/early/2025/07/07/gr.279886.124]
- 21. How To Promote Batch-To-Batch Consistency In CAR-T ... [https://www.cellandgene.com/doc/how-to-promote-batch-to-batch-consistency-in-car-t-therapies-0001]
- 22. Autologous Cell Therapy: Key Challenges and ... [https://www.lek.com/insights/hea/us/ei/autologous-cell-therapy-key-challenges-and-bioprocessing-innovations]
- 23. Stop Wasting Time: Correcting Batch Effects in Multi-Omics ... [https://pluto.bio/resources/Learning%20Series/batch-effects-multi-omics-data-analysis]
- 24. High performance data integration for large-scale analyses ... [https://www.nature.com/articles/s41467-025-62237-4]
- 25. ComBat-met: adjusting batch effects in DNA methylation data [https://pubmed.ncbi.nlm.nih.gov/40391088/]
- 26. Addressing Performance, Scalability, and Regulatory ... [https://www.biopharminternational.com/view/addressing-performance-scalability-and-regulatory-challenges-to-accelerate-cell-therapy-manufacturing]
- 27. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 28. ComBat-met: adjusting batch effects in DNA methylation data [https://pmc.ncbi.nlm.nih.gov/articles/PMC12086544/]
- 29. Evaluating batch correction methods for image-based cell ... [https://www.nature.com/articles/s41467-024-50613-5]
- 30. Treg cell therapy manufacturability: current state of the art, ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1604483/full]
- 31. pyComBat, a Python tool for batch effects correction in high ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05578-5]
- 32. Batch Effect Correction [https://www.10xgenomics.com/analysis-guides/introduction-batch-effect-correction]
- 33. Deep feature batch correction using ComBat for machine ... [https://www.sciencedirect.com/science/article/pii/S215335392400035X]
- 34. Benchmarking atlas-level data integration in single-cell ... [https://www.nature.com/articles/s41592-021-01336-8]
- 35. Benchmarking multi-omics integration algorithms across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10944570/]
- 36. remove batch effect [https://www.biostars.org/p/9576719/]
- 37. Failure to remove a batch_key/ effect of number of LVs [https://discourse.scverse.org/t/failure-to-remove-a-batch-key-effect-of-number-of-lvs/1973]
- 38. Getting started with harmony - davetang.github.io [https://davetang.github.io/muse/harmony.html]
- 39. Getting Started with Seurat v4 [https://satijalab.org/seurat/articles/get_started.html]
- 40. Detection issues in cell profiler - Image Analysis [https://forum.image.sc/t/detection-issues-in-cell-profiler/77612]
- 41. Image-based cell profiling enhancement via data cleaning ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0267280]
- 42. Data-analysis strategies for image-based cell profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6871000/]
- 43. Accurate Cell Counting : A Practical Guide [https://logosbio.com/accurate-cell-counting-a-practical-guide/]
- 44. Avoiding Human Errors in Experiments for Biologics [https://www.dotmatics.com/blog/avoiding-human-errors-in-experiments-for-biologics]
- 45. CAR-T cell manufacturing: Major process parameters and next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10791545/]
- 46. Addressing Cell Therapy Challenges Through a Modular ... [https://www.biopharminternational.com/view/addressing-cell-therapy-challenges-through-a-modular-closed-and-automated-manufacturing-system]
- 47. QuestionsandAnswersontheMan... [https://www.ccfdie.org/en/fgflf/webinfo/2024/12/1732613151824791.htm]
- 48. Challenges and opportunities in the compassionate use of out ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04343-0]
- 49. Managing Cell Therapy IND Timeline Risks [https://kincellbio.com/managing-cell-therapy-investigational-new-drug-ind-timeline-risks/]
- 50. Identification of critical process parameters and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408662/]
- 51. FROM AUTOLOGOUS CELL BANKING TO ALLOGENEIC ... [https://www.sciencedirect.com/science/article/pii/S1465324924003347]
- 52. Evaluating Hematopoietic Cell Therapy Product Potency [https://www.stemcell.com/cfu-cell-therapy-questions]
- 53. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 54. How Batch Processing Enhances Product Quality and ... [https://www.proconexdirect.com/blog/2025/how-batch-processing-enhances-product-quality-and-consistency/]
- 55. How do you “Investigate Failed Automated Tests”? - Archive [https://club.ministryoftesting.com/t/how-do-you-investigate-failed-automated-tests-automation-in-testing-curriculum/59820]
- 56. Analysis of variability in high throughput screening data [https://pmc.ncbi.nlm.nih.gov/articles/PMC5438608/]
- 57. Understanding and Mitigating Batch Effects in Histopathology [https://www.trillium.de/en/journals/trillium-pathology/archive/2025/tp-1/2025/computational-pathology/image-analysis-understanding-and-mitigating-batch-effects-in-histopathology.html]
- 58. Four Keys to Reducing Variability in the Cell Therapy ... [https://www.roslinct.com/insights/four-keys-to-reducing-variability-in-the-cell-therapy-process/]
- 59. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 60. Highly effective batch effect correction method for RNA-seq ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11718288/]
- 61. Chapter 1 Correcting batch effects | Multi-Sample Single- ... [https://bioconductor.org/books/3.15/OSCA.multisample/integrating-datasets.html]
- 62. Aspects and Implementation of Pharmaceutical Quality by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 63. Quality by Design and the Importance of PAT in QbD [https://www.sciencedirect.com/science/article/abs/pii/B978012375680000005X]
- 64. A Troubleshooting Guide for Topical Drug Manufacturing [https://www.pharmtech.com/view/troubleshooting-guide-topical-drug-manufacturing]
- 65. Enhancing manufacturing with process analytical ... [https://www.bruker.com/pt/news-and-events/webinars/2025/enhancing-manufacturing-with-process-analytical-technology-pat-in-2025.html]
- 66. Mastering the Generic Drug: A Strategic Blueprint ... [https://www.drugpatentwatch.com/blog/mastering-the-generic-drug-a-strategic-blueprint-for-a-profitable-future-with-pat-and-qbd/?srsltid=AfmBOoqMYtMWppjowcvUmiOwvU1PEbMWWQpEl5Vy7-mS7oQJNLaGMmB_]
- 67. A benchmark of batch - effect methods for single-cell RNA... correction [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1850-9]
- 68. Reference-informed evaluation of batch correction for ... [https://www.nature.com/articles/s42003-025-07947-7]
- 69. Evaluating batch correction methods for image-based cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11297288/]
- 70. Batch correction methods used in single-cell RNA sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315870/]
- 71. Protein-level batch - effect ... | Nature Communications correction [https://www.nature.com/articles/s41467-025-64718-y?error=cookies_not_supported&code=65014dd1-7d5a-4ea8-bf0c-a7f02a997002]
- 72. Treg cell therapy manufacturability: current state of the art ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12141221/]
- 73. Process Validation in Six Sigma: A Complete Guide [https://www.6sigma.us/process-improvement/process-validation/]
- 74. Process Validation: A Guide to Ensuring Quality and ... [https://trainual.com/manual/process-validation]
- 75. Process Development Considerations for Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572896/]
- 76. Cell Therapy Manufacturing: Testing, Validation & ... [https://www.allucent.com/resources/blog/cell-therapy-manufacturing]
- 77. Manufacturing Capacity Expansion and Validation for ... [https://www.pda.org/pda-letter-portal/home/full-article/manufacturing-capacity-expansion-and-validation-for-autologous-cell-therapies]
- 78. New FDA Guidance Aims to Simplify the Biosimilar ... [https://www.bigmoleculewatch.com/2025/11/14/new-fda-guidance-aims-to-simplify-the-biosimilar-approval-process/]
- 79. Analytical Similarity Assessment in Biosimilar Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5256601/]
- 80. Comparative Efficacy Studies No Longer a Default for ... [https://www.alston.com/en/insights/publications/2025/11/fda-comparative-efficacy-studies-biosimilars]
- 81. FDA Proposes To Eliminate Comparative Clinical ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-proposes-to-eliminate-biosimilar-comparative-studies]
- 82. Biosimilars | Science and Research [https://www.fda.gov/drugs/biosimilars/biosimilars-science-and-research]
- 83. Innovative approach to support therapeutic proteins ... [https://www.nature.com/articles/s41598-025-97377-6]
- 84. Autologous Cell Therapy Market Expand at 18.9% CAGR ... [https://www.towardshealthcare.com/insights/autologous-cell-therapy-market-sizing]
- 85. Development of Therapeutic Protein Biosimilars ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analytical-assessment-and-other-quality]
- 86. Guide to Cell Therapy GMP Manufacturing for Autologous ... [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 87. Manufacturing autologous cell therapies [https://www.patheon.com/us/en/insights-resources/blog/autologous-cell-therapy-manufacturing-challenges-and-best-practices.html]
- 88. Global Regulatory Landscape for Cell and Gene Therapies [https://www.pharmafocusamerica.com/strategy/global-regulatory-landscape]