Systematic Review and Meta-Analysis of MSC Exosomes in Wound Healing: Mechanisms, Efficacy, and Clinical Translation
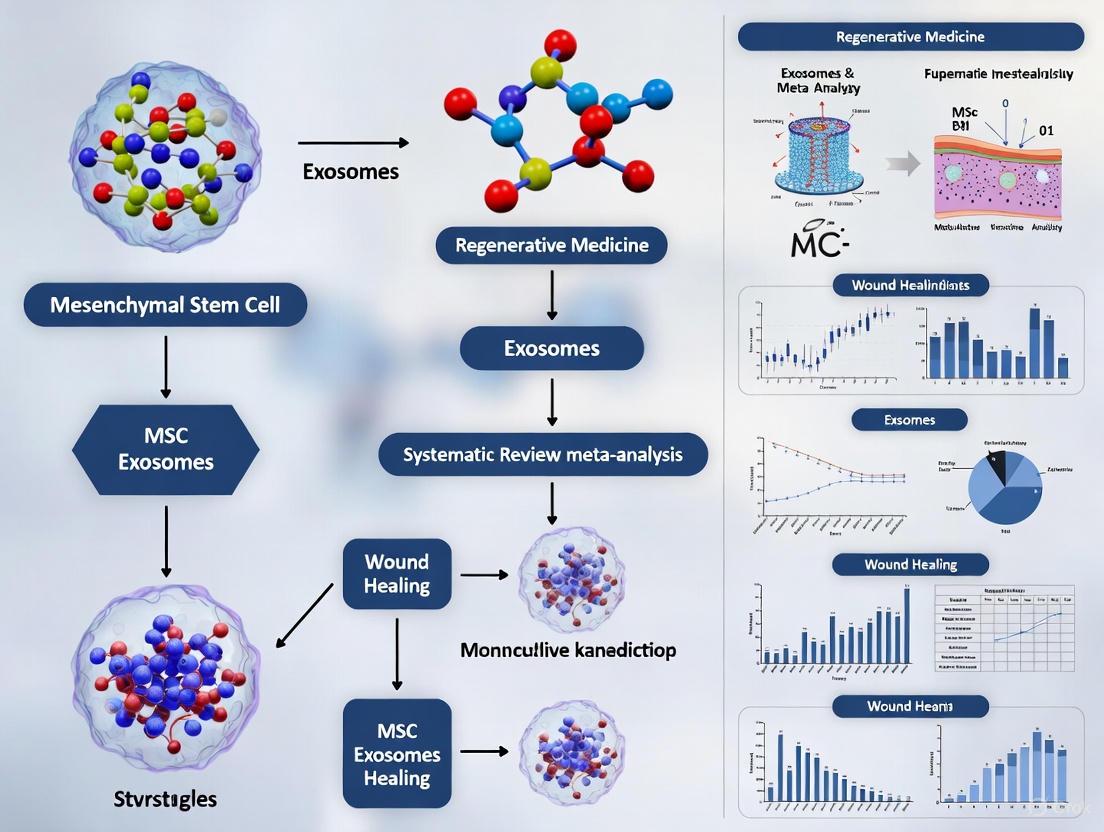
This systematic review and meta-analysis synthesizes current preclinical and clinical evidence on mesenchymal stem cell-derived exosomes (MSC-exosomes) for wound healing.
Systematic Review and Meta-Analysis of MSC Exosomes in Wound Healing: Mechanisms, Efficacy, and Clinical Translation
Abstract
This systematic review and meta-analysis synthesizes current preclinical and clinical evidence on mesenchymal stem cell-derived exosomes (MSC-exosomes) for wound healing. We examine the foundational biological mechanisms through which MSC-exosomes modulate inflammation, promote angiogenesis, and enhance tissue regeneration across various wound models, including diabetic, radiation-induced, and chronic wounds. The analysis explores methodological considerations for exosome isolation, characterization, and therapeutic application, alongside optimization strategies such as engineering and biomaterial integration. By critically evaluating comparative efficacy between MSC sources and validation through clinical trials, we address the translational challenges and future directions for developing MSC-exosome therapies as a promising cell-free treatment paradigm for enhanced wound management.
Unraveling the Mechanisms: How MSC Exosomes Orchestrate Wound Repair
Exosomes are a heterogeneous subpopulation of extracellular vesicles, typically 30–150 nm in diameter, that originate from the endosomal system and are released upon the fusion of multivesicular bodies (MVBs) with the plasma membrane [1] [2]. Since their initial description in the 1980s, exosomes have been recognized not as mere cellular waste bags but as potent mediators of intercellular communication, shuttling functional cargo—including proteins, lipids, and nucleic acids—between cells [2] [3]. This role is particularly critical in the proposed therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) for wound healing, where they modulate inflammation, promote angiogenesis, and stimulate tissue regeneration through their paracrine activity [4] [5] [6]. The efficacy of these exosomes is fundamentally governed by their molecular composition, which is determined during biogenesis by the machinery responsible for cargo sorting and ILV formation [2] [7].
The process of exosome generation is primarily governed by two overarching, and sometimes overlapping, mechanisms: the endosomal sorting complex required for transport (ESCRT)-dependent pathway and various ESCRT-independent pathways [1] [3] [7]. Understanding the nuances of these pathways is essential for researchers aiming to harness MSC-Exos for therapeutic purposes, as the specific loading of cargo directly influences their functional impact on recipient cells in the wound microenvironment [2] [6]. This guide provides a systematic comparison of these biogenesis pathways, detailing their mechanisms, key cargo, and experimental approaches for their study.
Core Machinery of Exosome Biogenesis
The biogenesis of exosomes is an intricate process that begins with the formation of early endosomes from the plasma membrane. During their maturation into late endosomes, the inward budding of the endosomal limiting membrane generates intraluminal vesicles (ILVs), transforming the structure into a multivesicular body (MVB) [1] [8]. The MVB represents a critical branch point in cellular trafficking; it can either fuse with lysosomes for degradation of its contents or fuse with the plasma membrane to release the ILVs into the extracellular space as exosomes [3] [7]. The molecular machinery that drives ILV formation and cargo selection is classified into two main categories.
The ESCRT-Dependent Pathway
The ESCRT machinery is a well-characterized, ubiquitin-dependent system comprising four protein complexes (ESCRT-0, -I, -II, and -III) that operate in concert with accessory proteins like VPS4 and Alix [1] [3]. The process is highly coordinated, as shown in Table 1.
Table 1: The Sequential Action of the ESCRT Complex in Exosome Biogenesis
| ESCRT Complex | Key Components | Primary Function in Cargo Sorting and ILV Formation |
|---|---|---|
| ESCRT-0 | HRS, STAM | Recognizes and clusters ubiquitinated cargo on the endosomal membrane; initiates pathway recruitment [1] [3]. |
| ESCRT-I & II | TSG101, VPS28 | Recruited by ESCRT-0; work together to deform the endosomal membrane, initiating bud formation [1] [2]. |
| ESCRT-III | CHMP4, CHMP3 | Forms filaments that constrict the neck of the budding vesicle, leading to membrane scission and ILV release [1] [3]. |
| Accessory Proteins | VPS4, Alix | VPS4 recycles the ESCRT machinery using ATP; Alix can provide an alternative ESCRT-III recruitment [1] [3]. |
This pathway is particularly important for sorting ubiquitinated proteins, such as endocytosed growth factor receptors [2]. Furthermore, non-canonical ESCRT-dependent pathways exist. For instance, the Syndecan-Syntenin-Alix axis sorts certain cargoes (e.g., fibroblast growth factor receptor) in a ubiquitin-independent manner. In this pathway, the transmembrane proteoglycan syndecan binds the adaptor protein syntenin, which then recruits Alix to nucleate ESCRT-III assembly and facilitate ILV formation [3].
ESCRT-Independent Pathways
Despite the central role of ESCRT, exosomes can still form upon ESCRT depletion, leading to the discovery of several ESCRT-independent mechanisms [1] [3]. These pathways often rely on the lipid composition of the endosomal membrane.
- The nSMase2-Ceramide Pathway: The enzyme neutral sphingomyelinase 2 (nSMase2) hydrolyzes sphingomyelin to generate ceramide [3]. Ceramide molecules, with their conical structure, can spontaneously induce membrane curvature and facilitate the budding of ILVs. This pathway is crucial for the sorting of specific cargoes like the proteolipid protein (PLP) in oligodendrocytes and certain RNAs in cancer cells [1] [3]. The inhibitor GW4869 is commonly used to block this pathway [3].
- Tetraspanin-Enriched Microdomains: Tetraspanins (e.g., CD9, CD63, CD81) are highly enriched in exosomes and organize membrane microdomains that facilitate the selective concentration of specific client proteins, such as β-catenin and metalloproteinases [1] [2]. For example, CD63 is involved in sorting melanosomal proteins in melanoma cells [1].
- Other Mechanisms: Additional factors contributing to ESCRT-independent biogenesis include lipid raft components (e.g., flotillins, caveolins) and the small GTPase ARF6 with its effector PLD2, which can promote ILV formation [1] [3].
Table 2: Comparative Overview of Key Exosome Biogenesis Pathways
| Feature | ESCRT-Dependent Pathway | nSMase2-Ceramide Pathway | Tetraspanin-Dependent Pathway |
|---|---|---|---|
| Key Initiator | Ubiquitinated cargo / ESCRT-0 [1] [3] | Neutral sphingomyelinase 2 (nSMase2) [3] | Tetraspanin web (e.g., CD63, CD81) [1] |
| Core Machinery | ESCRT-I, -II, -III, VPS4 [2] [3] | Ceramide [3] | Tetraspanins, associated proteins [1] |
| Model Cargo | Ubiquitinated receptors (e.g., EGFR) [2] | Proteolipid Protein (PLP) [1] [3] | Melanosomal protein (Pmel17) [1] |
| Common Inhibitors | siRNA targeting ESCRT components (e.g., TSG101) [3] | GW4869 [3] | siRNA targeting specific tetraspanins [1] |
The following diagram illustrates the coordination of these primary pathways within the endosomal system during exosome biogenesis.
Experimental Analysis of Biogenesis Pathways
Deciphering the contribution of specific biogenesis pathways requires a combination of genetic, pharmacological, and biochemical approaches. A core methodology involves isolating exosomes after perturbing a pathway of interest and analyzing the resulting changes in vesicle quantity and composition.
Key Methodologies and Reagents
Standard protocols begin with the isolation of exosomes, often via ultracentrifugation, size-exclusion chromatography (SEC), or commercial kits, from cell culture supernatants or biological fluids [8]. The following table lists essential reagents and tools for probing biogenesis mechanisms.
Table 3: Research Reagent Solutions for Studying Exosome Biogenesis
| Reagent / Tool | Function / Target | Application in Pathway Analysis |
|---|---|---|
| GW4869 | Pharmacological inhibitor of nSMase2 [3] | Inhibits the ceramide-dependent pathway; used to assess its role in cargo loading and exosome secretion. |
| siRNA/shRNA | Gene knockdown (e.g., TSG101, Alix, CD63) [3] | Silences specific components of ESCRT or tetraspanin pathways to evaluate their necessity for exosome generation. |
| VPS4 Dominant-Negative | ATPase-deficient mutant of VPS4 [3] | Blocks the disassembly of the ESCRT-III complex, thereby inhibiting the final stages of ESCRT-mediated ILV scission. |
| Antibodies for WB/IF | Detect markers (CD63, CD81, Alix, TSG101, Flotillin) [1] [8] | Characterize exosome isolates and assess the presence/absence of specific cargoes after pathway inhibition. |
| Ultracentrifugation | Isolation of exosomes via high g-force [5] [8] | Standard method for purifying exosomes from conditioned media or biological fluids for downstream analysis. |
| NTA (Nanoparticle Tracking) | Measure particle size and concentration [5] | Quantifies changes in exosome secretion levels after pharmacological or genetic perturbation. |
A typical experimental workflow to dissect these pathways is outlined below.
Illustrative Experimental Data from Wound Healing Research
Research on MSC-Exos for wound healing often characterizes the exosomes without always delineating the specific biogenesis pathway. However, the functional outcomes are direct consequences of the cargo loaded via these mechanisms. For instance, a study on umbilical cord MSC-Exos (hUCMSC-Exos) used ultracentrifugation for isolation and nanoparticle tracking analysis (NTA) and western blotting (CD63, CD81) for characterization [5]. The study demonstrated that these exosomes promoted the proliferation and migration of human skin fibroblasts (HSFs) and enhanced tube formation in human umbilical vein endothelial cells (HUVECs) in vitro. In a mouse model, they accelerated wound closure, which was associated with reduced inflammation and stimulated angiogenesis [5]. While this study did not mechanistically probe biogenesis, the pro-healing effects imply the selective packaging of specific miRNAs and proteins, likely governed by the pathways described above.
Implications for MSC Exosomes in Wound Healing
The biogenesis pathways are not merely structural mechanisms; they are fundamental regulatory checkpoints that determine the functional payload of MSC-Exos. The selective sorting of anti-inflammatory miRNAs (e.g., miR-146a, miR-223) or pro-angiogenic proteins (e.g., VEGF) into exosomes is a controlled process [6]. Dysregulation in these pathways could lead to the production of exosomes with diminished therapeutic efficacy. Therefore, a deep understanding of ESCRT-dependent and independent mechanisms provides a rational basis for engineering or preconditioning MSCs to enhance the loading of desired therapeutic molecules into exosomes, ultimately optimizing their potential for treating chronic wounds [2] [6]. Future research focused on actively modulating these pathways in MSCs will be a critical step toward developing potent and reliable exosome-based therapeutics for regenerative medicine.
Exosomes, a class of extracellular vesicles (EVs) with a diameter of 30–150 nm, have emerged as pivotal mediators of intercellular communication within the wound microenvironment [9] [10]. These lipid-bilayer enclosed vesicles are secreted by nearly all cell types and carry a diverse cargo of bioactive molecules, including microRNAs (miRNAs), proteins, and lipids, which reflect the physiological state of their parent cells [11] [6]. Upon delivery to recipient cells, these molecular players orchestrate complex biological processes essential for tissue repair, such as anti-inflammatory responses, angiogenesis, fibroblast proliferation, and extracellular matrix (ECM) remodeling [11] [12] [6]. In the context of mesenchymal stem cell (MSC)-derived exosomes, this cargo serves as an in-situ reservoir, providing tissue-specific signals on demand to accelerate wound healing [11]. This systematic analysis comprehensively compares the roles, mechanisms, and experimental evidence for these key molecular players in exosomal communication, providing a foundation for understanding their therapeutic potential in wound management.
Exosomal Biogenesis and Cargo Loading
Exosomes originate through the inward budding of the endosomal membrane, forming multivesicular bodies (MVBs) that subsequently fuse with the plasma membrane to release their contents into the extracellular space [9]. This biogenesis involves two primary pathways: the endosomal sorting complex required for transport (ESCRT)-dependent and ESCRT-independent pathways [11]. During this process, bioactive molecules are selectively packaged into the forming vesicles. Interestingly, cells selectively sort miRNAs into extracellular vesicles through mechanisms that remain partially characterized but are essential for their function [11]. Similarly, proteins and lipids are incorporated through specific sorting mechanisms that define the exosome's composition and functional properties [9]. The resulting exosomes are adorned with molecular markers (e.g., CD63, CD9, CD81) that reflect their origin and facilitate receptor-mediated recognition and cargo delivery to target cells via membrane fusion or endocytosis [11]. This precise cargo loading mechanism ensures that exosomes deliver specific signals to coordinate the wound healing process.
Table 1: Primary Exosome Isolation and Characterization Techniques
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation based on size/density | Gold standard; no reagent required | Time-consuming; may cause vesicle damage |
| Size-Based Chromatography | Size exclusion using porous matrix | High purity; preserves vesicle integrity | Limited scalability; sample dilution |
| Polymer-Based Precipitation | Reduced solubility via crowding agents | Simple protocol; high yield | Co-precipitation of contaminants |
| Immunoaffinity Capture | Antibody binding to surface markers | High specificity for subpopulations | High cost; dependent on marker expression |
MicroRNAs: Master Regulators of Gene Expression
Biogenesis and Mechanism of Action
MiRNAs are short non-coding RNAs (19–24 nucleotides) that regulate post-transcriptional gene expression through complementary binding to target mRNAs, leading to translational repression or mRNA degradation [11]. The biogenesis of miRNA begins with transcription of primary miRNAs (pri-miRNAs) from host genes, which undergo sequential processing by Drosha and Dicer enzymes to become mature miRNAs [11]. These mature miRNAs are incorporated into the RNA-induced silencing complex (RISC), where they guide the complex to partially complementary sequences primarily in the 3' untranslated region (3' UTR) of target mRNAs [11]. During exosome biogenesis, miRNAs are selectively sorted into vesicles through mechanisms that may involve specific miRNA motifs and RNA-binding proteins [11]. This selective sorting enables the packaging of functionally coordinated miRNA networks that can simultaneously regulate multiple targets in recipient cells.
Key Exosomal miRNAs in Wound Healing
Table 2: Functionally Validated Exosomal miRNAs in Wound Healing
| miRNA | Exosome Source | Validated Target/Pathway | Primary Functions in Wound Healing |
|---|---|---|---|
| miR-126 | Bone Marrow MSCs | Unknown | Increases tube formation; promotes angiogenesis [11] |
| miR-146a | MSCs | NF-κB signaling | Inhibits NF-κB; promotes M1 to M2 macrophage transition [6] |
| miR-223 | MSCs | NLRP3 inflammasome | Suppresses NLRP3 activation; reduces inflammation [6] |
| miR-21 | ADSCs | Unknown | Enhances fibroblast proliferation and migration [6] |
| miR-29a | ADSCs | Unknown | Promotes fibroblast activation; ECM remodeling [6] |
| miR-124a | Neuronal cells | GLT1 (glutamate transporter) | Regulates extracellular glutamate concentration [11] |
| let-7b | Preconditioned MSCs | Unknown | Enhances anti-inflammatory macrophage polarization [6] |
Exosomal miRNAs regulate all phases of wound healing through precise molecular interventions. During inflammation, miR-146a and miR-223 attenuate excessive inflammatory responses by targeting NF-κB signaling and NLRP3 inflammasome activation, respectively [6]. In the proliferative phase, miR-21 and miR-29a enhance fibroblast proliferation and migration, while miR-126 potently stimulates angiogenesis—a critical process for restoring blood supply to damaged tissue [11] [6]. Notably, a recent study identified 28 key miRNAs with significant pro-proliferation, anti-inflammatory, and anti-fibrosis functions that were encapsulated into synthetic exosome-like vesicles, demonstrating comparable efficacy to natural MSC exosomes in accelerating burn wound healing and reducing scarring [13]. This functional synergy among exosomal miRNAs enables coordinated regulation of the entire wound healing cascade.
Experimental Evidence and Methodologies
The therapeutic potential of exosomal miRNAs has been validated through standardized experimental approaches. In vitro functional assays include CCK-8 assays for cell proliferation, transwell migration assays, tube formation assays for angiogenesis, and gel contraction assays for fibroblast function [13]. For example, exosomes from inflammatory microenvironment-educated MSCs (EX1.25) demonstrated significantly enhanced activity (139.07 ± 5.65%) in promoting dermal fibroblast proliferation compared to control exosomes (118.14 ± 8.09%) [13]. In vivo validation typically involves diabetic or burn wound models in mice, with wound closure rates measured quantitatively. One study reported that on day 6 post-treatment, the percentage of remaining wound area was 40.16 ± 5.44% in the EX1.25 group compared to 54.31 ± 13.14% in the control exosome group [13]. miRNA profiling typically employs sequencing techniques, with bioinformatics analysis (e.g., target prediction using databases like TargetScan) to identify potential miRNA-mRNA interactions [5] [13].
Proteins: Structural and Functional Effectors
Composition and Functional Classes
Exosomal proteins encompass diverse functional classes, including transmembrane proteins, signaling molecules, growth factors, and enzymes. Tetraspanins (CD9, CD63, CD81) represent characteristic exosomal membrane proteins that facilitate cellular uptake and may participate in cargo sorting [11]. Exosomes also carry growth factors such as vascular endothelial growth factor (VEGF) and transforming growth factor-β (TGF-β), which directly stimulate angiogenesis and fibroblast activation [12]. Heat shock proteins (HSPs) within exosomes contribute to cellular stress responses and protein folding, while matrix metalloproteinases (MMPs) enable ECM remodeling by degrading matrix components [12]. The specific protein profile varies depending on the cell source and physiological conditions, with MSC-derived exosomes containing a repertoire of proteins that coordinate multiple aspects of tissue repair.
Mechanism of Action in Wound Healing
Exosomal proteins function through several complementary mechanisms. They directly activate signaling pathways in recipient cells through receptor-ligand interactions, with exosomal TGF-β and VEGF receptors capable of initiating downstream signaling cascades [12]. They also process ECM components and modify the wound microenvironment to facilitate cell migration—MMPs from exosomes degrade damaged matrix while facilitating deposition of new collagen [12]. Additionally, exosomal heat shock proteins like HSP60 contribute to quality control and cellular protection under stress conditions prevalent in chronic wounds [11]. The combined action of these proteins accelerates wound resolution by providing both structural support and regulatory signals to cells within the wound bed.
Experimental Characterization Methods
Proteomic characterization of exosomes typically involves mass spectrometry-based analysis, which identifies hundreds to thousands of proteins in a single preparation [12]. Western blotting remains the gold standard for validation of specific protein components, with antibodies against tetraspanins (CD9, CD63, CD81) serving as positive markers and proteins from nucleus, mitochondria, Golgi apparatus, and endoplasmic reticulum considered "non-exosomal" contaminants [11] [13]. Functional assays are protein-specific: angiogenesis is assessed through tube formation assays using human umbilical vein endothelial cells (HUVECs), inflammatory modulation is measured via nitric oxide (NO) synthesis and cytokine (IL-1β, TNF-α) production in macrophages, and fibrotic potential is evaluated through α-smooth muscle actin (α-SMA) expression in TGF-β1-stimulated fibroblasts [13].
Lipids: Structural Frameworks and Signaling Mediators
Lipid Composition and Biophysical Properties
The lipid bilayer of exosomes is enriched in specific lipid classes that distinguish them from parental cell membranes. Exosomal membranes particularly feature high concentrations of cholesterol, sphingomyelin, and phosphatidylserine compared to plasma membranes [9]. This unique composition contributes to membrane rigidity, stability, and protection of internal cargo from degradation. The external presentation of phosphatidylserine facilitates recognition and uptake by recipient cells, particularly immune cells like macrophages [11]. Additionally, lipid rafts—microdomains enriched in cholesterol and sphingolipids—organize signaling molecules and may participate in cargo sorting and exosome biogenesis through their role in membrane curvature [9].
Signaling Functions in Wound Repair
Beyond their structural role, exosomal lipids function as bioactive signaling molecules that influence wound healing processes. Ceramide, for instance, plays a crucial role in exosome biogenesis through the ESCRT-independent pathway and may influence apoptosis and immune responses in recipient cells [11]. Phosphatidylserine externalization contributes to the anti-inflammatory properties of some exosome populations by promoting phagocytic clearance and modulating macrophage polarization [11]. The lipid composition also determines exosome stability and cellular uptake efficiency, with specific lipid profiles potentially enhancing tissue penetration and target cell specificity—critical properties for therapeutic applications in wound healing [9].
Integrated Molecular Networks and Signaling Pathways
The therapeutic efficacy of MSC-derived exosomes emerges from the coordinated action of their molecular components working through integrated signaling networks. Experimental evidence indicates that exosomes regulate fundamental processes including inflammation, angiogenesis, and fibrosis through multi-target mechanisms [5] [13]. The diagram below illustrates the central signaling pathway through which exosomal cargo promotes wound healing.
The diagram above illustrates how exosomal molecular components collectively regulate critical wound healing processes. miRNAs such as miR-146a and miR-223 promote the transition of macrophages from pro-inflammatory M1 to anti-inflammatory M2 phenotypes, resolving chronic inflammation [6]. Simultaneously, proteins including VEGF and FGF stimulate endothelial cell sprouting and new blood vessel formation, while lipids like phosphatidylserine further support immune modulation [12] [6]. This coordinated regulation across multiple cell types and healing phases underscores the sophisticated communication network mediated by exosomal cargo.
Key signaling pathways modulated by exosomal cargo include the TGF-β/Smad pathway, which regulates fibroblast activation and scar formation [5]. NF-κB signaling represents another critical pathway, particularly in inflammation control, with exosomal miR-146a directly targeting this pathway to reduce pro-inflammatory cytokine production [6]. Additionally, hypoxia-inducible factor (HIF-1α) signaling is stimulated by hypoxic-conditioned exosomes, enhancing angiogenic responses in the wound bed [14]. The convergence of these pathways creates a synergistic effect that promotes efficient wound resolution with reduced scarring.
Therapeutic Applications and Engineering Strategies
Native Exosome Therapeutics
Native MSC-derived exosomes have demonstrated significant therapeutic potential across various wound models. In diabetic wound models, MSC exosomes have been shown to improve healing rates by 30-50%, reducing inflammation and promoting functional tissue regeneration [14] [6]. For burn wounds, exosome treatment not only accelerates closure but also ameliorates scarring through coordinated regulation of collagen synthesis and TGF-β signaling pathways [13]. The therapeutic effect stems from the ability of native exosomes to simultaneously modulate multiple aspects of the healing process, addressing the complexity of chronic wounds that often fail conventional treatments.
Engineered Exosome Platforms
To enhance their natural therapeutic properties, researchers are developing sophisticated engineering approaches for exosomes. These include modifying exosome surfaces to improve target specificity through the incorporation of homing peptides or antibodies [9]. Cargo loading techniques are being refined to enhance the packaging of therapeutic miRNAs or drugs, with one study successfully encapsulating 28 key miRNAs into synthetic exosome-like vesicles that demonstrated efficacy comparable to natural exosomes [13]. Hybrid systems combine exosomes with biomaterials such as hydrogels or microneedle patches to improve retention at the wound site and provide controlled release [15] [16] [9]. These engineering strategies address limitations of natural exosomes, including rapid clearance and batch-to-batch variability, while enhancing their therapeutic potential.
Table 3: Experimental Models for Validating Exosomal Therapeutics
| Model System | Application | Key Readouts | References |
|---|---|---|---|
| In Vitro Models | |||
| HUVEC tube formation | Angiogenesis potential | Tube length, branching points | [5] |
| Fibroblast migration assay | Cell motility | Closure rate, migration distance | [13] |
| Macrophage polarization | Immunomodulation | M1/M2 marker expression, cytokine secretion | [15] [13] |
| In Vivo Models | |||
| Diabetic mouse wound model | Chronic wound healing | Wound closure rate, angiogenesis, inflammation | [5] [6] |
| Burn wound model | Burn healing and scarring | Healing time, scar thickness, collagen organization | [13] |
| Full-thickness excision | Acute wound healing | Re-epithelialization, granulation tissue formation | [9] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Exosome Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Isolation Kits | Total Exosome Isolation Kit | Exosome purification from biofluids | Polymer-based precipitation for high yield |
| Characterization Antibodies | Anti-CD63, CD9, CD81 | Exosome identification | Detection of tetraspanin markers via WB/flow cytometry |
| miRNA Analysis Tools | miRNA sequencing kits; miRNA mimics/inhibitors | Functional miRNA studies | Profiling and functional validation of exosomal miRNAs |
| Cell Culture Reagents | MSC NutriStem XF Medium; human platelet lysate | MSC expansion and exosome production | Serum-free culture for reproducible exosome production |
| Animal Models | Diabetic (db/db) mice; burn wound models | In vivo therapeutic validation | Preclinical assessment of exosome efficacy |
| Biomaterial Scaffolds | Hyaluronic acid hydrogels; chitosan composites | Exosome delivery systems | Enhanced exosome retention and controlled release |
The molecular players within exosomes—miRNAs, proteins, and lipids—orchestrate a sophisticated intercellular communication network that coordinates the complex process of wound healing. miRNAs serve as master regulators of gene expression, proteins function as direct effectors of cellular responses, and lipids provide both structural integrity and signaling capabilities. Together, these components enable MSC-derived exosomes to simultaneously modulate inflammation, promote angiogenesis, stimulate cellular proliferation, and guide tissue remodeling. While challenges remain in standardization, scalable production, and precise delivery, the integrated action of these molecular players positions exosomal therapies as transformative tools for regenerative medicine. Future research focusing on engineering optimized exosomes and understanding their complex molecular networks will unlock further therapeutic potential for challenging wound healing scenarios.
The modulation of inflammation is a cornerstone of effective tissue repair, and the pivotal role of macrophages in this process is increasingly recognized. Macrophages, heterogeneous immune cells of the innate immune system, are not terminal effector cells but possess remarkable functional plasticity [17]. They can adopt a spectrum of activation states in response to microenvironmental cues, with the classically activated pro-inflammatory M1 phenotype and the alternatively activated anti-inflammatory, pro-reparative M2 phenotype representing polar opposites [18]. A timely transition from the M1-dominated inflammatory phase to the M2-dominated reparative phase is critical for successful wound healing [19]. Recent advances in regenerative medicine have highlighted mesenchymal stem cell-derived exosomes (MSC-exos) as powerful mediators capable of orchestrating this critical polarization shift. This review, framed within the context of a systematic analysis of MSC exosomes in wound healing research, objectively compares the mechanisms and efficacy of different therapeutic approaches in modulating the M1 to M2 transition, providing researchers and drug development professionals with a data-driven guide to this dynamic field.
Macrophage Biology and Polarization Dynamics
Origins and Subtypes of Macrophages
Macrophages populate tissues through two primary developmental pathways, which contribute to their functional diversity. Embryonically-derived macrophages originate from yolk sac progenitors and fetal liver, establishing long-lived, self-renewing populations in tissues such as the brain (microglia), liver (Kupffer cells), and skin (Langerhans cells). These cells are characterized by high expression of CX3CR1 and low expression of CCR2, functioning primarily in immune surveillance and tissue homeostasis [17]. In contrast, bone marrow (BM)-derived macrophages arise from adult hematopoietic stem cells in the bone marrow. These BM-derived Ly6Chigh monocytes circulate in the blood and are recruited to sites of injury or inflammation, where they differentiate into macrophages. This population is highly adaptable and dynamically responds to microenvironmental demands, playing a crucial role in inflammatory and reparative processes [17].
The Polarization Spectrum: M1 vs. M2 Macrophages
Macrophage polarization exists along a functional continuum, with the well-characterized M1 and M2 states representing two ends of this spectrum.
- M1 Macrophages (Pro-inflammatory): Polarization is classically induced by interferon-gamma (IFN-γ) and/or lipopolysaccharide (LPS) [18]. These macrophages are potent effector cells that mediate resistance against pathogens and contribute to tissue destruction. Their activation is associated with a specific molecular signature, including high expression of CD86 and the production of pro-inflammatory cytokines like TNF-α, IL-6, and IL-1β [19] [17]. Metabolically, M1 polarization is reprogrammed toward glycolysis and the pentose phosphate pathway [18].
- M2 Macrophages (Anti-inflammatory/Pro-reparative): Polarization is alternatively induced by cytokines such as IL-4 and IL-13 [18]. M2 macrophages are key players in the resolution of inflammation, tissue repair, angiogenesis, and fibrosis. They are characterized by high expression of surface markers like CD206 and CD163, and the production of anti-inflammatory factors including IL-10 and TGF-β [19] [17]. Metabolically, M2 polarization favors oxidative phosphorylation and fatty acid oxidation [18].
The following diagram illustrates the core macrophage polarization process and its functional outcomes.
Quantitative Comparison of Polarization Markers and Signaling
A systematic understanding of macrophage polarization requires a clear comparison of the defining markers and the signaling pathways that control their activation. The following tables summarize key experimental data and molecular features relevant for researchers designing in vitro polarization experiments or analyzing tissue samples.
Table 1: Characteristic Markers of M1 and M2 Macrophage Polarization
| Category | M1 Macrophage Markers | M2 Macrophage Markers |
|---|---|---|
| Inducing Signals | IFN-γ, LPS [18] | IL-4, IL-13 [18] |
| Cell Surface Markers | CD86 [17] | CD206, CD163 [17] |
| Gene/Protein Markers | CXCL9, CXCL10, NOS2 (iNOS) [19] [18] | MRC1, TGM2, FIZZ1, ARG1 [19] [18] |
| Secreted Cytokines | TNF-α, IL-6, IL-1β, GM-CSF [19] [18] | IL-4, IL-10, IL-13, TGF-β [19] [17] |
| Metabolic Pathways | Glycolysis, Pentose Phosphate Pathway [18] | Oxidative Phosphorylation, Fatty Acid Oxidation [18] |
Table 2: Key Signaling Pathways in Macrophage Polarization
| Signaling Pathway | Role in M1 Polarization | Role in M2 Polarization | Key Molecular Effectors |
|---|---|---|---|
| JAK-STAT | STAT1 activation by IFN-γ [17] | STAT6 activation by IL-4/IL-13 [17] | JAKs, STAT1, STAT6 |
| NF-κB | Promotes pro-inflammatory gene transcription [17] | Generally suppressed | p65, IκB |
| PI3K-AKT | Contributes to metabolic reprogramming [18] | Supports M2-associated functions [20] | PI3K, AKT, mTOR |
| MEK-ERK | Not critically involved | Critical for M2 polarization; induces PPARγ/retinoic acid signaling [18] [21] | MEK, ERK, PPARγ |
| PPARγ | Inhibited | Master regulator; promotes M2 gene program [18] | PPARγ, RXR |
The dynamic nature of polarization is evident in disease contexts. A study of periapical lesions in mice demonstrated that M1-related markers (Cxcl10, Cxcl9, Nos2) and cytokines (GM-CSF, IFN-γ, IL-6, IL-1β, TNF-α) predominated in initial periods (2-7 days). A shift toward an M2-related profile (Arg1, Fizz1, Ym1, Mrc1 and IL-4, IL-13, IL-10) was observed on day 21, indicating a repair attempt. However, by day 42, the process exacerbated, marked by a return to an M1 profile [19]. This temporal switching underscores the plasticity of macrophages and the potential for therapeutic intervention.
Molecular Mechanisms of Polarization: A Systems View
Global quantitative time-course analyses, including proteomics and phosphoproteomics, have provided unprecedented insight into the molecular machinery driving polarization. These studies reveal that M1 and M2 polarization are associated with extensive and distinct metabolic reprogramming and kinase activation patterns [18] [21].
Kinase-enrichment analysis of phosphoproteomic data has identified specific kinases that are differentially activated during M1- versus M2-type polarization. For instance, a spike in MEK signaling is a hallmark of the induction phase of M2, but not M1, polarization [18]. This finding has direct therapeutic implications, as MEK inhibitors have been shown to selectively block M2 polarization without affecting M1 polarization [18] [21]. Similarly, various histone deacetylase (HDAC) inhibitors also demonstrate a selective inhibitory effect on M2 polarization [18].
The following diagram integrates these molecular events into a coherent signaling network for M2 polarization, a key pathway amenable to therapeutic modulation.
MSC Exosomes as Modulators of Macrophage Polarization
Therapeutic Potential in Wound Healing
Within the context of wound healing, Mesenchymal Stem Cell-derived exosomes (MSC-exos) have emerged as a promising cell-free therapeutic tool. A systematic review and meta-analysis of preclinical studies demonstrates the clear potential of MSC-EVs to be developed as a therapy for wound healing and skin regeneration in both diabetic and non-diabetic animal models [22]. Compared to whole MSCs, MSC-exos offer significant advantages, including lower immunogenicity, absence of infusion toxicity, ease of storage and access, and lack of tumorigenic potential, making them an ideal candidate for biological therapy [23] [24] [20].
The efficacy of MSC-exos is partly attributed to their ability to modulate the immune response, particularly by influencing macrophage polarization. These exosomes can "reduce oxidative stress," "promote angiogenesis," and "modulate the inflammatory response" in the wound microenvironment [23]. A key mechanism is their capacity to reduce pro-inflammatory M1 polarization while promoting anti-inflammatory M2 polarization, thereby facilitating the critical transition from the inflammatory to the proliferative phase of healing [20].
Not all MSC-exos are equivalent. Subgroup analyses from systematic reviews reveal that the therapeutic outcomes can vary depending on the cellular origin of the exosomes.
Table 3: Comparison of MSC Exosome Sources and Efficacy in Wound Healing
| MSC Source | Therapeutic Effects in Wound Healing | Key Mechanisms Related to Macrophages/Repair |
|---|---|---|
| Adipose-Derived Stem Cells (ADSCs) | Best effect on wound closure rate and collagen deposition [22]. | Regulate oxidative stress, immune cell infiltration, and inflammatory factor secretion [23]. Promote fibroblast and keratinocyte activity via AKT/HIF-1α and ERK/MAPK pathways [23]. |
| Bone Marrow-Derived MSCs (BMSCs) | Better effect on revascularization [22]. | Play active roles in all stages of wound healing; effects mediated through paracrine action of exosomes [20]. |
| Human Umbilical Cord MSCs (hUC-MSCs) | Effective in reducing clinical severity and epidermal hyperplasia in psoriasis models [24]. | Immunomodulatory and anti-inflammatory properties; key mediators of therapeutic benefits of MSCs [24]. |
| Apoptotic Small Extracellular Vesicles (ApoSEVs) | Better efficacy in wound closure outcome and collagen deposition compared to sEVs and ApoBDs [22]. | A newly appraised therapeutic potential; mechanisms under investigation [22]. |
The route of administration also influences efficacy. Subcutaneous injection of MSC-EVs demonstrated a greater improvement in wound closure, collagen deposition, and revascularization compared to topical dressing/covering [22]. Furthermore, in a meta-analysis on psoriasis, meta-regression revealed that studies using hUCMSC exosomes showed a greater improvement in clinical scores compared to other MSC sources [24].
The Scientist's Toolkit: Key Reagents and Experimental Protocols
This section provides a curated list of essential reagents and methodologies for researchers investigating macrophage polarization or developing exosome-based therapies.
Table 4: Research Reagent Solutions for Macrophage Polarization Studies
| Reagent / Tool | Function / Application | Specific Examples |
|---|---|---|
| Polarizing Cytokines | To induce specific macrophage polarization states in vitro. | M1: IFN-γ (20–50 ng/mL), LPS (10–100 ng/mL) [18]. M2: IL-4 (20–50 ng/mL), IL-13 (20–50 ng/mL) [18]. |
| Small Molecule Inhibitors | To selectively block signaling pathways and study their role in polarization. | MEK inhibitors (e.g., Trametinib, U0126) for selective M2 blockade [18] [21]. HDAC inhibitors (e.g., Trichostatin A) for selective M2 blockade [18]. |
| Surface Marker Antibodies | For identification and sorting of polarized macrophages via flow cytometry. | M1 markers: Anti-CD86 [17]. M2 markers: Anti-CD206, Anti-CD163 [17]. |
| Cytokine Quantification Kits | To measure secreted factors in supernatant or tissue lysates. | Luminex Multiplex Assays for profiling M1 (TNF-α, IL-6, IL-1β) and M2 (IL-4, IL-10, IL-13) cytokines [19]. ELISA kits for individual cytokines. |
| Exosome Isolation Kits | For purification of exosomes from MSC-conditioned media. | Ultracentrifugation (most common), Tangential Flow Filtration, or commercial kit-based methods (e.g., from System Biosciences) [25]. |
| Nanoparticle Tracking Analysis (NTA) | For determining the size distribution and concentration of isolated exosomes. | Instruments such as the ZetaView PMX 110 (Particle Metrix) [24]. |
Detailed Experimental Protocol: In Vitro Macrophage Polarization and Inhibition
The following protocol is adapted from methodologies used in key studies [18] [21] and can be used to test the effects of MSC-exos or small molecule inhibitors on polarization.
Macrophage Differentiation:
- Use the human monocytic cell line THP-1. Culture cells in RPMI-1640 medium supplemented with 10% FBS.
- Differentiate THP-1 monocytes into macrophages (M0) by treating with phorbol myristate acetate (PMA) at a concentration of 100 nM for 24 hours.
Polarization Induction:
- After PMA differentiation, wash the cells and replace with fresh medium.
- To induce M1 polarization, treat M0 macrophages with IFN-γ (50 ng/mL) and LPS (50 ng/mL).
- To induce M2 polarization, treat M0 macrophages with IL-4 (50 ng/mL).
- Maintain the polarization treatment for 24 hours to 4 days (for full polarization).
Therapeutic Intervention:
- For testing MSC-exos: Co-treat with isolated MSC-exos (e.g., (1 \times 10^8) to (1 \times 10^9) particles/mL) during the polarization induction period.
- For testing inhibitors: Pre-treat or co-treat with the inhibitor (e.g., MEK inhibitor at 1–10 µM) during the polarization induction period.
Outcome Assessment:
- Protein Analysis: Perform immunoblotting to analyze polarization markers (e.g., TGM2 and MRC1 for M2; IDO1 for M1) [18] [24].
- Gene Expression: Use qRT-PCR to measure mRNA levels of M1 (CXCL9, CXCL10, NOS2) and M2 (ARG1, FIZZ1, MRC1) markers [19].
- Functional Assays: Collect culture supernatant and use Luminex or ELISA to quantify secreted cytokines characteristic of each phenotype [19].
The strategic modulation of inflammation through the induction of a pro-reparative M2 macrophage phenotype represents a powerful therapeutic approach in wound healing and regenerative medicine. Systematic reviews and meta-analyses of preclinical data robustly support the potential of MSC-derived exosomes as a cell-free therapy to drive this transition. The efficacy of this approach is influenced by several factors, including the source of MSCs, with ADSC-exos showing particular promise for wound closure and collagen deposition, and the route of administration. The molecular underpinnings of this process involve distinct metabolic and signaling pathways, with MEK/ERK/PPARγ-driven retinoic acid signaling being a critical and druggable axis for M2 polarization. As the field advances, the standardization of exosome isolation, characterization, and application, guided by systematic evidence, will be crucial for translating these promising findings from the bench to the clinic, offering new hope for the treatment of chronic wounds and inflammatory diseases.
Chronic wounds, characterized by a failure to proceed through an orderly and timely healing process, represent a significant global health challenge. A pivotal pathophysiological feature of these wounds is a state of persistent hypoxia, which disrupts the essential process of angiogenesis—the formation of new blood vessels from pre-existing vasculature [26] [27]. Effective angiogenesis is crucial for supplying oxygen and nutrients to the healing tissue, and its impairment is a hallmark of conditions like diabetic foot ulcers [28] [29]. Within the context of a systematic review on mesenchymal stem cell (MSC) exosomes for wound healing, this article objectively compares emerging pro-angiogenic strategies. We focus on evaluating the performance of MSC-derived exosomes, gene-activated scaffolds, and other therapeutic approaches, supported by direct experimental data and detailed methodologies to aid researchers and drug development professionals.
Comparative Analysis of Pro-Angiogenic Strategies
The following table summarizes the key characteristics and experimental evidence for the primary therapeutic strategies aimed at activating angiogenesis in hypoxic wounds.
Table 1: Comparison of Pro-Angiogenic Strategies for Hypoxic Wound Healing
| Therapeutic Strategy | Key Components / Exosome Source | Primary Angiogenic Mechanisms | Reported Efficacy in Experimental Models |
|---|---|---|---|
| MSC-Derived Exosomes | ADSC-EVs, hUCMSC-Exos [26] [5] [22] | Promote endothelial cell proliferation, migration, and tube formation; modulate macrophages to resolve inflammation; carry pro-angiogenic miRNAs and proteins [26] [28] [5]. | hUCMSC-Exos significantly accelerated wound closure, reduced inflammation, and stimulated angiogenesis in vivo [5]. |
| Gene-Activated Scaffolds | Scaffold + pVEGF/GET nanoparticles (G-VEGF) [30] | Localized, sustained delivery of plasmid DNA for endogenous VEGF production; enhances endothelial cell migration and organization into vascular structures [30]. | G-VEGF scaffolds demonstrated enhanced angiogenic potential and consistently improved neurite outgrowth in vitro and ex vivo [30]. |
| Ozone Therapy | Medical-grade Ozone (O₃) [31] | Induces moderate oxidative stress, stabilizing HIF-1α and enhancing production of VEGF, NO, and PDGF to stimulate capillary formation [31]. | Strong correlation (r=0.84) between ozone exposure and increased VEGF expression in analyzed studies [31]. |
| Natural Products | Various plant-derived compounds [32] | Target endothelial cell function and cross-talk with immune cells and fibroblasts; specific mechanisms driven by unique chemical architectures [32]. | Emerging potential, with activity on angiogenic signals to restore a microenvironment favoring vascular network re-establishment [32]. |
A recent meta-analysis of preclinical studies provides robust, quantitative data on the efficacy of MSC-derived extracellular vesicles (MSC-EVs). The analysis, encompassing 83 studies, confirmed that MSC-EVs significantly enhance wound closure and tissue regeneration [22]. Subgroup analyses revealed critical insights for therapeutic development:
- EV Type: Apoptotic small extracellular vesicles (ApoSEVs) showed superior efficacy in wound closure and collagen deposition, while small EVs (sEVs/exosomes) were more effective in revascularization [22].
- Administration Route: Subcutaneous injection provided greater improvement in wound closure, collagen deposition, and revascularization compared to topical dressing/covering [22].
- MSC Source: Adipose-derived stem cells (ADSCs) demonstrated the best effect on wound closure rate, whereas bone marrow MSCs (BMMSCs) were more effective in revascularization [22].
Detailed Experimental Protocols for Key Studies
Protocol 1: Efficacy Evaluation of hUCMSC-Derived Exosomes
This protocol is adapted from the study by Frontiers in Bioengineering and Biotechnology [5].
- Objective: To investigate the therapeutic effects of human umbilical cord MSC-derived exosomes (hUCMSC-Exos) on wound healing and elucidate the underlying mechanisms.
- Methods:
- Exosome Isolation and Characterization: hUCMSC-Exos were isolated from cell culture supernatant via ultracentrifugation. They were characterized using Nanoparticle Tracking Analysis (NTA) for size/concentration, Transmission Electron Microscopy (TEM) for morphology, and Western Blot (WB) for positive (CD9, CD63) and negative (Calnexin) markers [5].
- In Vitro Angiogenesis Assay:
- Cell Culture: Human umbilical vein endothelial cells (HUVECs) and human skin fibroblasts (HSFs) were used.
- Proliferation Assay: Cell Counting Kit-8 (CCK-8) was used to assess HSF and HUVEC proliferation after hUCMSC-Exos treatment.
- Migration Assay: A scratch/wound healing assay was performed on HSFs to evaluate migration capability.
- Tube Formation Assay: HUVECs were seeded on Matrigel and observed for their ability to form capillary-like tubular structures. Tube length and number of branch points were quantified [5].
- In Vivo Wound Healing Model:
- Animal Model: A full-thickness excisional wound model was established on mice.
- Treatment: hUCMSC-Exos or a control (e.g., PBS) were administered via local injection.
- Assessment: Wound closure rate was measured over time. Harvested skin tissues were subjected to:
- Histological & Immunohistochemical Analysis: Hematoxylin and eosin (H&E) staining for general morphology and epidermal thickness; Masson's trichrome staining for collagen deposition; immunohistochemistry for CD31 (to mark blood vessels) and other inflammatory or proliferation markers [5].
- Bioinformatics Analysis: miRNA sequencing and target prediction were performed to identify potential key molecules (e.g., ULK2, COL19A1, IL6ST) involved in the repair process [5].
Protocol 2: Development and Testing of a VEGF-Activated Scaffold
This protocol is adapted from the study published in Biomaterials Science [30].
- Objective: To develop a scaffold capable of localized gene delivery to enhance both angiogenesis and nerve repair in chronic wounds.
- Methods:
- Nanoparticle Formulation: The GET peptide and plasmid DNA encoding VEGF (pVEGF) were combined at a fixed charge ratio (6:1) in OptiMEM to form self-assembling G-VEGF nanoparticles [30].
- Nanoparticle Characterization:
- Size and Zeta Potential: Analyzed using Dynamic Light Scattering (DLS) and Nanoparticle Tracking Analysis (NTA).
- Stability: Assessed via gel electrophoresis after incubation with DNase I and fetal bovine serum (FBS) to confirm protection against degradation [30].
- In Vitro Transfection and Bioactivity:
- Cell Transfection: Dermal fibroblasts were transfected with G-VEGF nanoparticles. VEGF protein expression in the supernatant was quantified using an ELISA kit.
- Cell Viability: Cytotoxicity was assessed using a metabolic activity assay (e.g., AlamarBlue).
- Endothelial Cell Migration: A scratch assay was performed with HUVECs cultured with conditioned media from transfected fibroblasts.
- Tube Formation Assay: HUVECs were seeded on Matrigel and cultured with conditioned media to observe vascular structure formation [30].
- Neurogenic Potential Assessment:
- In Vitro Neurite Outgrowth: Neural cells were cultured on the VEGF-activated scaffolds, and neurite length was measured.
- Ex Vivo Model: Dorsal root ganglia (DRG) were explanted and cultured on the scaffolds to evaluate axon extension [30].
Visualization of Signaling Pathways and Workflows
Key Angiogenic Signaling Pathways Activated by Exosomes
The following diagram illustrates the core molecular pathways through which MSC-derived exosomes promote angiogenesis in hypoxic wounds, integrating mediators from multiple studies [28] [5] [29].
Experimental Workflow for Evaluating Pro-Angiogenic Therapies
This flowchart outlines a standardized experimental pipeline for developing and testing pro-angiogenic therapies, from isolation to in vivo validation.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting research in angiogenesis and wound healing, as derived from the experimental protocols.
Table 2: Key Research Reagent Solutions for Angiogenesis Studies
| Reagent / Material | Function in Research | Specific Examples from Literature |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Cellular source for deriving exosomes and conditioned media; used to study paracrine effects. | Human Umbilical Cord MSCs (hUCMSCs), Adipose-Derived Stem Cells (ADSCs) [26] [5] [22]. |
| Extracellular Vesicle Isolation Kits | Isolate and purify exosomes and other EVs from cell culture media or biological fluids. | Ultracentrifugation protocols; Tangential Flow Filtration (TFF) systems [5] [22]. |
| Characterization Instruments | Physically characterize isolated vesicles (size, concentration, morphology). | Nanoparticle Tracking Analyzer (NTA; e.g., ZetaView, NanoSight); Transmission Electron Microscope (TEM); Dynamic Light Scattering (DLS) instrument [24] [30] [5]. |
| Endothelial Cell Culture Systems | In vitro models for studying angiogenesis mechanisms (proliferation, migration, tube formation). | Human Umbilical Vein Endothelial Cells (HUVECs); capillary formation assays using Matrigel or other ECM substitutes [30] [5]. |
| Animal Wound Models | In vivo systems to test the therapeutic efficacy of pro-angiogenic treatments. | Diabetic (e.g., db/db mice, STZ-induced) and non-diabetic murine full-thickness excisional wound models [22]. |
| Gene Delivery Vectors | Facilitate the transfer of therapeutic genes (e.g., pVEGF) into target cells. | Non-viral vectors (e.g., GET peptide system); commercial transfection reagents (e.g., lipofectamine 3000) [30]. |
| Biomaterial Scaffolds | Provide a 3D structure for cell attachment, proliferation, and localized delivery of therapeutics. | Collagen-based scaffolds; functionalized scaffolds for gene activation (Gene-Activated Scaffolds) [30]. |
| Angiogenesis Assay Kits | Quantitatively measure key angiogenic parameters in vitro and ex vivo. | Tube formation assay kits; ELISA kits for VEGF and other growth factors; immunohistochemistry kits for CD31/PECAM-1 staining [30] [5]. |
The therapeutic potential of mesenchymal stem cell (MSC)-derived exosomes represents a paradigm shift in regenerative medicine, particularly in the context of wound healing. As a cell-free alternative, these nanoscale extracellular vesicles (30-150 nm in diameter) mediate the paracrine effects of their parent cells by transferring bioactive molecules—including proteins, lipids, and nucleic acids—to recipient cells [33] [34]. A systematic review and meta-analysis of preclinical wound healing studies confirms that exosome administration significantly improves therapeutic outcomes, with the highest efficacy observed at seven days post-application (odds ratio 1.82, 95% CI [0.69, 2.95]) [25]. This review synthesizes current evidence demonstrating how MSC-derived exosomes systematically enhance keratinocyte and fibroblast function, the key cellular players in cutaneous regeneration, through defined signaling pathways and molecular mechanisms.
Comparative Efficacy of MSC Exosomes on Target Cells
Quantitative Effects on Cellular Functions
MSC-derived exosomes exert pleiotropic effects on skin cells, significantly enhancing processes critical for wound repair. The table below summarizes their differential impacts on keratinocytes and fibroblasts based on experimental data.
Table 1: Quantitative Effects of MSC-Derived Exosomes on Keratinocytes and Fibroblasts
| Cell Type | Proliferation | Migration | Key Functional Outcomes | Signaling Pathways Activated |
|---|---|---|---|---|
| Keratinocytes | Dose-dependent enhancement [35] | Accelerated re-epithelialization [36] | Enhanced epidermal barrier restoration [36] | PI3K/Akt, ERK, STAT3 [35] [36] |
| Fibroblasts | Dose-dependent enhancement [35] | Significant migration promotion [35] [5] | Increased collagen deposition [25] | Akt, ERK, STAT3 [35] |
| Endothelial Cells | Increased proliferation [5] | Enhanced tube formation [35] [5] | Improved angiogenesis [25] [5] | PI3K/Akt [36] |
Comparative Performance Against Alternative Approaches
When evaluated against other therapeutic strategies, MSC exosomes demonstrate distinct advantages in modulating cellular behavior.
Table 2: Performance Comparison of MSC Exosomes Versus Alternatives
| Therapeutic Approach | Effect on Keratinocyte Proliferation | Effect on Fibroblast Migration | Angiogenic Potential | Key Limitations |
|---|---|---|---|---|
| MSC-Derived Exosomes | Significant, dose-dependent enhancement [35] [36] | Significant, dose-dependent enhancement [35] | Promotes tube formation [35] [5] | Manufacturing standardization challenges [37] |
| Whole MSC Therapy | Enhancement observed [35] | Enhancement observed [35] | Promotes angiogenesis [35] | Risk of microvasculature occlusion, immunogenicity [34] |
| Conventional Treatments | Variable effects | Variable effects | Limited | High non-response rates in chronic wounds [35] |
| Platelet-Rich Plasma | Moderate enhancement | Moderate enhancement | Moderate | Variable composition, donor-dependent efficacy |
Experimental Data and Methodologies
Key Experimental Protocols
Exosome Isolation and Characterization
The majority of studies (64%) employ ultracentrifugation for exosome isolation, while 18% use commercial kits, and 7% combine ultracentrifugation with filtration [25]. The standard protocol involves:
- Differential Ultracentrifugation: Sequential centrifugation steps (500 ×g to remove cells, 10,000 ×g to remove debris, and 100,000-120,000 ×g for exosome pelleting) [33]
- Characterization: Multiparameter analysis using nanoparticle tracking analysis (NTA), transmission electron microscopy (TEM), and western blot for surface markers (CD63, CD9, CD81, TSG101) [25] [5]
- Quantification: Protein content determination via BCA assay [35]
In Vitro Functional Assays
- Fibroblast Migration Assay: Coculture systems with labeled MSCs and fibroblasts demonstrate enhanced migration without direct cell contact, confirming paracrine mediation [35]
- Keratinocyte Proliferation Assay: MSC exosomes internalized by keratinocytes activate proliferative pathways (Akt, ERK) [35] [36]
- Tube Formation Assay: Human umbilical vein endothelial cells (HUVECs) treated with MSC exosomes show increased tube formation, indicating enhanced angiogenic potential [35] [5]
In Vivo Wound Healing Models
- Animal Models: Rodent excisional wound models (32 mice studies, 19 rat studies) treated with topical exosome applications [25]
- Efficacy Assessment: Wound closure rate measurement, histological analysis for re-epithelialization and collagen deposition, immunohistochemical staining for cellular proliferation markers [5]
- Dosing: Optimal effects observed with multiple applications; meta-analysis supports standardized concentration guidelines [25]
Molecular Mechanisms and Signaling Pathways
Key Signaling Pathways in Keratinocyte Proliferation
MSC exosomes activate multiple interconnected signaling pathways to enhance keratinocyte function:
Diagram 1: Exosome-mediated signaling in keratinocytes (Title: Keratinocyte Signaling Pathways)
Fibroblast Activation and Matrix Remodeling
For dermal fibroblasts, MSC exosomes utilize distinct mechanisms to promote migration and extracellular matrix production:
Diagram 2: Fibroblast signaling and functional outcomes (Title: Fibroblast Signaling Pathways)
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MSC Exosome Studies
| Reagent/Technique | Function | Application Examples |
|---|---|---|
| Ultracentrifugation | Exosome isolation via sequential centrifugation | Standardized purification from conditioned media [35] [33] |
| Nanoparticle Tracking Analysis | Size distribution and concentration measurement | Characterizing exosome preparations (30-150 nm) [25] [5] |
| Transmission Electron Microscopy | Morphological visualization | Confirming cup-shaped exosome morphology [35] [25] |
| Western Blot | Protein marker confirmation | Detecting CD63, CD9, CD81, TSG101 [25] |
| PKH26 Labeling | Fluorescent exosome tracking | Cellular uptake and localization studies [35] |
| Transwell Assays | Migration quantification | Measuring fibroblast and keratinocyte migration [35] [5] |
| Tube Formation Assay | Angiogenic potential assessment | Evaluating endothelial cell function [35] [5] |
MSC-derived exosomes represent a sophisticated cell-free therapeutic platform that effectively enhances keratinocyte and fibroblast function through defined molecular mechanisms. The experimental evidence demonstrates their consistent, dose-dependent effects on cellular proliferation and migration, mediated through Akt, ERK, and STAT3 signaling pathways, along with specific miRNA-mediated regulation. While manufacturing scalability and standardization remain challenges, the compelling preclinical data and ongoing clinical translation efforts position MSC exosomes as a promising therapeutic modality in regenerative medicine. Their ability to coordinate multiple aspects of the wound healing process without the risks associated with whole-cell therapies underscores their potential to address the significant unmet needs in chronic wound management.
Cutaneous wound healing is a complex biological process aimed at restoring the skin's barrier function following injury. In adult humans, this process typically results in the replacement of damaged functional tissue with a collagen-rich patch known as a scar [38] [39]. Whereas scarring achieves rapid wound closure, it represents a compromise: scar tissue never achieves the flexibility, strength, or functionality of the original skin, with maximum tensile strength reaching only approximately 80% of uninjured skin [38]. This compromise stems primarily from aberrations in extracellular matrix (ECM) remodeling, particularly in the deposition and organization of collagen fibers [38] [40].
The ECM is not merely a structural scaffold but a dynamic, organized mesh of macromolecules that regulates cell migration, proliferation, differentiation, and growth factor bioavailability [38]. Abnormal ECM reconstruction during wound healing contributes to pathological scarring, manifesting as hypertrophic scars or keloids that cause significant physical dysfunction and psychological stress [38] [41]. Currently, there exists no satisfactory treatment for these conditions, partly due to incomplete understanding of their underlying mechanisms [38].
This review examines the delicate balance between collagen deposition and scar formation within the context of ECM remodeling, with particular emphasis on emerging therapeutic strategies involving mesenchymal stem cell (MSC)-derived exosomes. By comparing the compositional and structural differences between normal and pathological scarring, and detailing the experimental approaches used to investigate them, we aim to provide researchers and drug development professionals with a comprehensive resource for advancing regenerative therapeutics.
ECM Composition and Collagen Dynamics in Skin Repair
The Extracellular Matrix Microenvironment
The skin's extracellular matrix provides both structural integrity and biochemical signaling crucial for homeostasis and repair. The cutaneous ECM comprises a complex assortment of proteins including:
- Structural proteins (collagens, laminins, elastins)
- Proteoglycans and hyaluronan (stabilizing growth factors and hydrating the matrix)
- Glycoproteins such as integrins (regulating cell adhesion and signaling) [38]
This microenvironment interacts dynamically with local cells, particularly fibroblasts, which are the primary ECM producers [38] [42]. The ECM serves as a reservoir for growth factors like TGF-β, FGF, and VEGF, with degradation of ECM proteins during wound healing inducing local release of these factors to modulate the repair process [38].
Collagen Structure and Assembly
Collagens constitute approximately three-quarters of the dry weight of human skin, making them the most prevalent ECM component [40]. Among the 28 known collagen types, type I and type III are the main dermal collagens, constituting roughly 80-85% and 8-11% of the dermal ECM, respectively [40].
All collagens are synthesized as procollagen chains with N- and C-terminal propeptides flanking the collagen helical region [40]. The triple helix formation begins with C-terminal propeptide interactions, leading to alignment of three polypeptide chains held together by interchain hydrogen bonds in a characteristic Gly-X-Y repeat pattern (where X and Y are frequently proline and hydroxyproline) [40]. Following secretion, propeptides are cleaved, and collagen molecules assemble into fibrils through a linear staggered array stabilized by enzymatic cross-linking mediated by lysyl oxidases (LOXs) [38] [40]. This cross-linking provides fibrils with mechanical resilience and contributes to the skin's mechanical strength [40].
Table 1: Key Collagen Types in Normal Skin
| Collagen Type | % Total Skin | Location | Primary Function |
|---|---|---|---|
| I | 80-85% | Dermis | Main structural collagen providing tensile strength |
| III | 8-11% | Dermis | Provides flexibility and softness; regulates fibril diameter |
| IV | 2-4% | Basement membrane | Supports epidermal-dermal separation |
| V | <1% | Basement membrane, dermis | Bridges and stabilizes epidermal-dermal interface |
The Wound Healing Cascade and ECM Remodeling
Wound healing progresses through overlapping phases: hemostasis, inflammation, proliferation, and remodeling [43] [39]. The final remodeling phase can last up to a year or more, during which the immature scar undergoes significant ECM reorganization [38] [39].
During proliferation, fibroblasts deposit disorganized type III collagen in granulation tissue [42]. In normal remodeling, this is gradually replaced by type I collagen, and the fibrils become more organized [42] [41]. Critical to this process is the balanced activity of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs), which degrade and reorganize the ECM [38] [42]. Any disturbance in this balance can lead to either poor wound healing or excessive scarring [43].
Figure 1: The Relationship Between Wound Healing Phases and ECM Dynamics
Comparative Analysis: Normal Skin vs. Pathological Scars
Structural and Compositional Differences
Pathological scars (hypertrophic scars and keloids) demonstrate significant deviations from normal skin architecture in their collagen composition and organization. Whereas normal skin collagen fibrils form a complex network of interlaced basketweave-like fibrils with diameters averaging 110-130 nm, pathological scars show substantially thinner fibrils (~60-70 nm) despite having thicker collagen fiber bundles [40].
The collagen ratio is also altered in pathological scarring. Although the relative ratio of type III to type I collagen is reduced compared to normal skin, the expected corresponding increase in fibril diameter does not occur, suggesting additional regulatory defects [40]. Keloids in particular show irregular accumulation of both type I and type III collagen, whereas hypertrophic scars display tightly arranged type III collagen with less type I [41].
Table 2: Collagen Characteristics in Normal Skin vs. Pathological Scars
| Parameter | Normal Skin | Hypertrophic Scar | Keloid |
|---|---|---|---|
| Average fibril diameter | ~110-130 nm | ~60 nm | ~60-70 nm |
| Collagen fiber orientation | Mainly parallel to skin surface with minor out-of-plane components | Mainly parallel to epithelial surface | Random orientation to epithelial surface |
| Fiber bundle thickness | Reference thickness | Thinner than normal skin | Thicker than normal skin and hypertrophic scars |
| Fiber packing | Majority closely packed in parallel array | Loosely arrayed in wavy pattern | Packed loosely with irregular spacing |
| LOX activity | Normal baseline | Comparable to normal skin | Elevated |
Cellular Mechanisms Driving Pathological Scarring
Fibroblasts and their activated form, myofibroblasts, are key players in pathological scarring [42]. Myofibroblasts are characterized by expression of α-smooth muscle actin (α-SMA) and prominent stress fibers, granting them contractile properties [42]. These cells secrete abundant ECM components and play a major role in wound contraction and matrix maturation [42] [39].
In normal wound healing, myofibroblasts undergo apoptosis during the remodeling phase. However, in pathological scarring, they persist, leading to excessive collagen deposition and contraction [42]. The origin of these myofibroblasts may include local fibroblast activation, circulating fibrocytes, and differentiation from local mesenchymal stem cells [42].
Mechanical force has emerged as a crucial regulator of fibrotic healing. Mechanical tension activates focal adhesion kinase (FAK) pathways, leading to inflammatory signaling and fibrosis [44]. Inhibition of FAK signaling in preclinical models attenuates fibrotic scar formation while accelerating healing [44].
The Inflammation-Scarring Connection
The role of inflammation in scarring is well-established. Compared to adult wounds that heal with scars, fetal wounds that heal scarlessly have a markedly reduced inflammatory response [38]. Similarly, oral mucosa wounds heal with minimal scar formation and have lower levels of macrophage, neutrophil, and T-cell infiltration [38].
Prolonged inflammation disrupts the normal balance of MMPs and TIMPs, favoring either ECM degradation (chronic wounds) or excessive accumulation (hypertrophic scars/keloids) [43]. In chronic wounds, elevated levels of MMPs (particularly collagenase and gelatinase) excessively degrade ECM components, while in hypertrophic scars and keloids, reduced MMP activity or elevated TIMPs leads to collagen accumulation [43] [39].
MSC Exosomes: Mechanisms and Therapeutic Potential in ECM Remodeling
Biogenesis and Characteristics of MSC Exosomes
Mesenchymal stem cell-derived exosomes are nanoscale extracellular vesicles (40-150 nm in diameter) formed through the inward budding of endosomal membranes, resulting in multivesicular bodies that subsequently fuse with the plasma membrane to release their contents into the extracellular space [43] [45]. These vesicles contain proteins, lipids, mRNAs, and miRNAs, and function as key mediators of intercellular communication [43].
As therapeutic agents, MSC exosomes offer several advantages over their parent cells:
- Lower immunogenicity and reduced risk of tumorigenicity [6] [45]
- Enhanced stability and ability to cross biological barriers [6] [45]
- Easier storage and distribution without losing biological activity [45]
- No risk of vascular occlusion or ectopic tissue formation [6]
Molecular Mechanisms in Wound Healing and Scar Reduction
MSC exosomes facilitate wound healing through multiple mechanisms across all phases of repair:
Inflammation Phase: Exosomal miRNAs such as miR-146a and miR-223 inhibit NF-κB signaling and suppress NLRP3 inflammasome activation, promoting the transition from pro-inflammatory M1 to anti-inflammatory M2 macrophages [6]. This polarization is critical for resolving inflammation and preventing excessive scarring [38] [6].
Proliferation Phase: Exosomes from MSCs and adipose-derived stem cells enhance fibroblast proliferation and migration by delivering miR-21, miR-29a, and other miRNAs that optimize ECM production [6]. They also promote angiogenesis through transfer of pro-angiogenic factors [6].
Remodeling Phase: MSC exosomes help restore a more balanced collagen ratio by modulating TGF-β signaling and MMP/TIMP expression, leading to better organized ECM architecture with reduced cross-linking and collagen density characteristic of normal skin rather than scars [43] [6].
Figure 2: MSC Exosome Mechanisms in ECM Remodeling and Scar Reduction
Experimental Evidence and Comparative Efficacy
Preclinical studies demonstrate the efficacy of MSC exosomes in promoting regenerative healing. In animal models of impaired wound healing, MSC exosomes significantly accelerate wound closure, improve epithelialization, enhance angiogenesis, and reduce scar formation [43] [6]. The therapeutic effects appear comparable to MSC therapy but with improved safety profiles [6].
The source of MSCs influences exosome composition and efficacy. Exosomes derived from different sources (bone marrow, adipose tissue, umbilical cord) show variations in their miRNA profiles and regenerative properties [6] [45]. Additionally, engineering approaches to enhance exosome targeting and potency, such as preconditioning MSCs or modifying exosome content, are under active investigation [45].
Experimental Methodologies for Studying ECM Remodeling
Analytical Techniques for Collagen Characterization
Research on ECM remodeling employs sophisticated techniques to analyze collagen structure, composition, and organization:
Transmission Electron Microscopy (TEM) provides high-resolution imaging of collagen fibril ultrastructure, allowing precise measurement of fibril diameter and assessment of cross-linking patterns [40]. This technique revealed the significantly reduced fibril diameter in keloids (~76 nm) compared to normal skin (~124 nm) [40].
Scanning Electron Microscopy (SEM) enables three-dimensional visualization of collagen fiber organization and packing, demonstrating the parallel orientation in hypertrophic scars versus random orientation in keloids [40].
Histological staining techniques including Masson's Trichrome and Picrosirius Red provide qualitative and quantitative assessment of collagen content and distribution in tissue sections [40].
X-ray diffraction studies help determine the molecular arrangement of collagen fibrils and the positions of different collagen types within hybrid fibrils [40].
In Vitro and In Vivo Models
Fibroblast cultures from normal skin and pathological scars allow investigation of collagen synthesis rates, gene expression profiles, and response to therapeutic interventions [40] [41]. These models have identified differences in TGF-β responsiveness and proliferation capacity between keloid fibroblasts and normal fibroblasts [41].
Animal models of wound healing, including rodent, porcine, and rabbit models, enable assessment of scar formation and ECM remodeling in a complex physiological environment [44]. The PU.1 null mouse model, which lacks neutrophils and macrophages, has been instrumental in studying inflammation-independent healing [38] [41].
Mechanical force models apply controlled tension to healing wounds to investigate mechanotransduction pathways in fibrosis, leading to identification of FAK as a key mediator [44].
Table 3: Experimental Models for Studying Scar Formation and ECM Remodeling
| Model Type | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Normal vs. keloid fibroblast cultures | Collagen synthesis, gene expression, drug screening | Controlled environment, mechanistic studies | Lacks tissue complexity and systemic factors |
| Rodent wound models | Initial therapeutic screening, scar assessment | Cost-effective, readily available | Healing differs from humans (more contraction) |
| Porcine wound models | Scar formation evaluation, therapeutic testing | Skin structure similar to humans | Expensive, specialized facilities required |
| PU.1 null mouse | Inflammation-scarring relationship | Genetic absence of inflammatory cells | Not representative of normal healing |
| Mechanical stress models | Mechanotransduction pathways | Clinically relevant to human scarring | Challenging to standardize |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for ECM and Scarring Investigations
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| TGF-β inhibitors | Investigate role of TGF-β signaling in fibrosis | SB-431542, neutralizing antibodies |
| FAK inhibitors | Study mechanotransduction in scarring | VS-6062 (FAK inhibitor) |
| LOX inhibitors | Assess collagen cross-linking in scarring | β-aminopropionitrile (BAPN) |
| MMP inhibitors | Probe ECM degradation balance | GM6001, TIMP overexpression |
| Collagen analysis kits | Quantify collagen content and types | Sircol assay, type-specific ELISAs |
| α-SMA antibodies | Identify myofibroblasts in tissues | Immunofluorescence, Western blot |
| MSC exosome isolation kits | Prepare therapeutic vesicles | Ultracentrifugation, commercial kits |
| Hydrogel delivery systems | Controlled release of therapeutics | Hyaluronic acid hydrogels with FAK-i |
The balance between collagen deposition and scar formation represents a central challenge in cutaneous wound healing. Current evidence confirms that pathological scarring stems from disruptions in normal ECM remodeling, characterized by aberrant collagen composition, organization, and cross-linking. The emergence of MSC exosomes as acellular therapeutics offers a promising approach to modulate this process, addressing multiple phases of wound healing simultaneously through anti-inflammatory, pro-angiogenic, and optimized regenerative mechanisms.
Future research priorities include standardizing exosome production protocols, enhancing targeted delivery to wound sites, and identifying optimal MSC sources for specific clinical applications. The integration of bioengineering approaches with biological insights—such as combining MSC exosomes with controlled-release scaffolds or mechanical tension-offloading devices—may further advance the field toward the ultimate goal of scarless regenerative healing. As our understanding of ECM biology deepens, particularly regarding fibroblast heterogeneity and mechanotransduction pathways, new therapeutic targets will undoubtedly emerge, offering hope for the millions affected by pathological scarring worldwide.
From Bench to Bedside: Isolation, Characterization and Delivery Strategies for MSC Exosomes
Within regenerative medicine, a paradigm shift is occurring from whole-cell therapies toward cell-free approaches utilizing exosomes derived from mesenchymal stem cells (MSCs). These nanoscale extracellular vesicles (30-150 nm) encapsulate the therapeutic potential of their parent cells—including proteins, lipids, and nucleic acids—while offering advantages of lower immunogenicity, easier storage, and enhanced safety profiles [23]. Among the various MSC sources, adipose tissue (ADSCs), umbilical cord (UMSCs), and bone marrow (BMSCs) have emerged as prominent contenders for exosome production. This comparative guide objectively analyzes the therapeutic performance of exosomes derived from these sources, with a specific focus on wound healing applications, to inform researchers and drug development professionals in their source selection process.
Comparative Efficacy Data in Wound Healing and Related Models
Systematic evaluation of exosomes from different MSC sources reveals distinct functional profiles and therapeutic strengths. The tables below summarize key comparative findings from direct comparison studies and individual source investigations.
Table 1: Direct Comparative Performance of MSC-derived Exosomes
| Performance Metric | ADSC-Exos | UMSC-Exos | BMSC-Exos | Experimental Context |
|---|---|---|---|---|
| Anti-inflammatory Efficacy | Moderate reduction | Superior suppression | Superior suppression | In vitro model of inflammation; reduction in NF-κB and MAPK pathway activation [46] |
| Chondroprotective Effects | Moderate enhancement | Superior protection | Superior protection | Expression of chondroprotective genes in OA models [46] |
| Cell Migration Promotion | Significant enhancement | Significant enhancement | Significant enhancement | Chondrocyte migration assay; critical for cartilage repair [46] |
| Angiogenic Capacity | Promotes angiogenesis [47] | Strongly promotes angiogenesis [48] | Promotes angiogenesis [49] | Endothelial cell tube formation assays; critical for wound healing [47] [48] [49] |
| Cytotoxicity | Low cytotoxicity | Low cytotoxicity | Low cytotoxicity | Chondrocyte viability assay at concentrations up to 1000 μg/mL [46] |
Table 2: Additional Characteristic and Preclinical Evidence
| Aspect | ADSC-Exos | UMSC-Exos | BMSC-Exos |
|---|---|---|---|
| Key Advantages | Abundant tissue source, easy harvest [47], potent immunomodulation [47] | Non-invasive sourcing, low immunogenicity [48], high proliferation capacity [46] | Extensive research history, strong tissue repair capabilities [49] |
| Documented Cargo | miR-21-5p, miR-126-3p, miR-146a (promote proliferation & angiogenesis) [23] | miRNAs targeting ULK2, COL19A1, IL6ST (potential key wound repair molecules) [48] | Varies with culture method; enhanced miRNA/protein content in 3D cultures [49] |
| In Vivo Wound Healing Evidence | Accelerates closure in diabetic mice, enhances re-epithelialization & angiogenesis [50] [23] | Significantly accelerates wound closure, reduces inflammation, stimulates angiogenesis & ECM formation [48] | Enhanced healing in rat models, promoted angiogenesis; efficacy boosted by 3D culture [49] |
Detailed Experimental Protocols for Key Assays
The comparative data presented rely on standardized, rigorous experimental methodologies. Below are detailed protocols for key assays commonly used to evaluate exosome therapeutic potential.
Exosome Isolation and Characterization
Isolation by Ultracentrifugation: Conditioned medium is collected from MSC cultures after 48 hours in exosome-depleted serum. The medium undergoes sequential centrifugation: 300 × g for 5 minutes to remove floating cells; 2,000 × g for 30 minutes at 4°C to remove cell debris; and final filtration through a 0.22 μm membrane. The supernatant is then ultracentrifuged at 100,000 × g for 70-120 minutes to pellet exosomes [48] [50].
Characterization Triad:
- Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration [46] [48].
- Transmission Electron Microscopy (TEM): Confirms the classic cup-shaped morphology and structural integrity of exosomes [46] [48].
- Western Blotting: Verifies the presence of exosomal surface markers (e.g., CD63, CD81, CD9, Alix, TSG101) and confirms the absence of negative markers [46] [48].
In Vitro Functional Assays
Cell Proliferation and Viability (CCK-8 Assay):
- Seed target cells (e.g., fibroblasts, chondrocytes) in 96-well plates.
- Treat with varying concentrations of exosomes.
- After incubation, add CCK-8 solution to each well.
- Incubate for 2 hours in the dark and measure absorbance at 450 nm. Higher absorbance indicates greater cell viability/proliferation [46].
Cell Migration Assay (Scratch/Wound Healing Assay):
- Create a confluent monolayer of target cells (e.g., human skin fibroblasts - HSFs).
- Scrape a straight line through the monolayer using a pipette tip.
- Wash away detached cells and add exosomes to the medium.
- Monitor and image the scratched area at regular intervals. The rate of gap closure quantifies cell migration capacity [48].
Tube Formation Assay (Angiogenesis):
- Plate human umbilical vein endothelial cells (HUVECs) on Matrigel.
- Treat with exosomes.
- After several hours, image the cellular networks.
- Quantify total tube length, number of branches, or meshes to assess pro-angiogenic potential [48].
In Vivo Wound Healing Model
Diabetic Mouse Model (db/db):
- Utilize genetically diabetic (e.g., db/db) mice which display impaired healing.
- Create full-thickness excisional wounds on the dorsal skin.
- Apply exosomes (often via hydrogel carrier) directly to the wound bed.
- Monitor wound closure over time by tracing wound area and calculating closure percentage.
- Harvest wound tissue for histological analysis (e.g., H&E staining for re-epithelialization, Masson's trichrome for collagen, CD31 immunohistochemistry for blood vessels) [50].
Signaling Pathways and Molecular Mechanisms
The therapeutic effects of MSC-derived exosomes are mediated through the modulation of key signaling pathways in recipient cells. The diagram below illustrates the primary molecular mechanisms involved in wound healing and anti-inflammatory responses.
The diagram above shows how exosomal cargo delivers signals that coordinately regulate multiple cellular processes. Key mechanistic insights include:
- NF-κB and MAPK Suppression: BMSC-Exos and UMSC-Exos demonstrate superior efficacy in reducing phosphorylation of p65 (NF-κB pathway) and p38/JNK/ERK (MAPK pathway), leading to significant anti-inflammatory effects [46].
- PI3K/AKT Activation: ADSC-Exos are particularly effective at activating the PI3K/AKT pathway, which promotes fibroblast and keratinocyte proliferation and migration, and enhances angiogenesis via HIF-1α [23].
- TGF-β/Smad Modulation: Exosomes from all sources, particularly UMSC-Exos and ADSC-Exos, can modulate the TGF-β/Smad pathway, which helps reduce fibrosis and scar formation during the remodeling phase of wound healing [23].
The Scientist's Toolkit: Essential Research Reagents
Successful research into MSC-derived exosomes requires specific reagents and tools for isolation, characterization, and functional testing. The following table details key solutions and their applications.
Table 3: Essential Reagents for Exosome Research
| Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| Exosome-Depleted FBS | Provides essential nutrients for cell culture without contaminating exogenous exosomes during exosome production [50]. | Prepared by ultracentrifugation (100,000-120,000 × g overnight) or commercial sources. Critical for clean exosome isolation. |
| PEG/Dextran ATPS | Aqueous Two-Phase System for isolating exosomes based on differential partitioning [46]. | An alternative to ultracentrifugation. The interfacial layer between phases enriches exosomes. |
| Lipophilic Dyes (e.g., PKH67, DiD, DiR) | Incorporate into the exosome lipid bilayer for fluorescent labeling and tracking [51] [52]. | DiR/DID are preferred for in vivo due to NIR fluorescence and lower background. Risk of dye aggregation requires controls [52]. |
| Antibodies for Surface Markers | Characterization via Western Blot or Flow Cytometry (CD63, CD81, CD9, Alix, TSG101) [46] [48]. | Confirms exosomal identity. MISEV guidelines recommend markers from multiple categories. |
| GelMA Hydrogel | A biocompatible, UV-curable hydrogel for 3D cell culture to enhance exosome yield/function and as a delivery scaffold for in vivo applications [49] [16]. | Enhances exosome secretion and angiogenic capacity compared to 2D culture. Useful for sustained release at wound site. |
| CCK-8 Assay Kit | Colorimetric assay to measure cell proliferation and cytotoxicity after exosome treatment [46] [49]. | Measures metabolic activity as a proxy for cell viability. More sensitive and safer than MTT. |
The selection of an optimal exosome source is contingent upon the specific therapeutic goals of the regenerative application. BMSC-Exos and UMSC-Exos demonstrate superior performance in modulating inflammation and protecting tissue, making them strong candidates for inflammatory phases of wound healing or applications like osteoarthritis [46]. UMSC-Exos further offer advantages in angiogenesis and proliferation, beneficial for the proliferative phase of healing, coupled with their non-invasive sourcing [48]. ADSC-Exos present a highly accessible and effective option, with strong documented results in promoting cell proliferation, migration, and angiogenesis, particularly in diabetic wound models [47] [50] [23].
Future perspectives point toward strategies for enhancing exosome potency, such as 3D culture techniques to improve BMSC-Exo yield and function [49], hypoxic preconditioning to augment ADSC-Exo efficacy [50], and bioengineering of exosomes to enrich specific cargo. The choice between ADSC, UMSC, and BMSC exosomes ultimately depends on a balanced consideration of therapeutic priorities, sourcing logistics, and scalability requirements for clinical translation.
The field of mesenchymal stem cell (MSC) exosome research has expanded exponentially in recent years, particularly in applications for wound healing and skin regeneration [22]. These small extracellular vesicles (sEVs) provide major promise for advances in therapeutics, ascribed to their distinctive cargo reflective of pathophysiological status and active involvement in intercellular communication [53]. However, the isolation of high-purity, functionally intact exosomes remains a critical challenge, with the choice of isolation technique profoundly influencing experimental outcomes and therapeutic efficacy [54]. The lack of standardization in methods for sEV isolation from cells grown in serum-containing media represents a significant bottleneck in the field [53].
Among the various isolation methods available, ultracentrifugation (UC) has traditionally been the most widely used technique, particularly for sEV isolation from cell culture conditioned media [53]. Nevertheless, problems associated with its use include disrupted structural and biological integrity of sEVs, aggregation, co-isolation of contaminating non-EV particles, and suboptimal sEV yield [53]. These limitations have driven researchers in both academia and industry to implement gentler isolation approaches with better scalability, hence the rise in the use of tangential flow filtration (TFF) and kit-based methods [53] [55].
This comprehensive guide objectively compares the performance of ultracentrifugation, tangential flow filtration, and commercial kit-based methods for MSC exosome isolation within the context of wound healing research. We summarize quantitative experimental data, provide detailed methodologies, and offer practical guidance to help researchers select the most appropriate isolation technique for their specific applications.
Technical Comparison of Isolation Techniques
Fundamental Principles and Mechanisms
Ultracentrifugation (UC) relies on differential centrifugation forces to separate vesicles based on their density, size, and shape. The process involves multiple steps of increasing centrifugal forces, typically culminating in ultracentrifugation at 100,000×g to 200,000×g to pellet exosomes [24]. The separation is based on the sedimentation rate of particles according to Stokes' law, which depends on particle size, density, and the viscosity of the medium [54].
Tangential Flow Filtration (TFF) is an advanced filtration system that concentrates and filters out particles using a cross-flow filtration principle [53]. Unlike dead-end filtration where media is applied perpendicular to the membrane, TFF applies the media parallel to the membrane, as well as through the membrane, preventing molecule accumulation and membrane fouling [53]. This method separates particles based primarily on size through membranes with specific molecular weight cut-offs (MWCO), typically enriching particles between 50 and 650 nm [55].
Kit-Based Methods encompass various commercial isolation kits that typically utilize precipitation-based techniques, affinity-based separation, or combinations thereof. These methods often involve incubating samples with proprietary solutions that precipitate exosomes or bind them to specific matrices, followed by low-speed centrifugation to collect the exosomes [54].
Comprehensive Performance Comparison
Table 1: Direct comparison of key performance metrics for exosome isolation techniques
| Performance Metric | Ultracentrifugation | Tangential Flow Filtration | Kit-Based Methods |
|---|---|---|---|
| sEV Yield | Low to moderate | Significantly higher | Variable, often high |
| Purity | Moderate, with protein contamination | High, especially when combined with SEC | Variable, often lower purity |
| Processing Time | Long (4-12 hours) | Short (2-4 hours) | Very short (30 min - 2 hours) |
| Scalability | Poor, limited by rotor capacity | Excellent, easily scalable | Moderate, limited by kit size |
| Reproducibility | Moderate, operator-dependent | High, more standardized | High, standardized protocols |
| Cost | High equipment cost, moderate per-run | Moderate equipment, low per-run | Low equipment, high per-run |
| sEV Integrity | Often compromised due to high g-forces | Better preserved | Variable |
| Technical Expertise | High | Moderate | Low |
| Suitability for Large Volumes | Poor | Excellent | Poor |
Table 2: Quantitative experimental data comparing UC and TFF from recent studies
| Parameter | Ultracentrifugation | Tangential Flow Filtration | Reference |
|---|---|---|---|
| Particle Recovery | 25-40% | 70-85% | [55] |
| Protein Contamination | High (Typical EV/protein ~3×10⁹ particles/mg) | Low (Typical EV/protein ~9×10⁹ particles/mg) | [53] |
| Processing Time for 1L sample | 6-8 hours | 2-3 hours | [53] [55] |
| Operational Consistency | Moderate (I² = 30-60%) | High (I² = 10-25%) | [53] |
| Downstream Functionality | Often impaired | Better preserved | [53] [55] |
Experimental evidence demonstrates that both ultracentrifugation and tangential flow filtration enrich consistent sEV populations, with similar size distributions of particles ranging up to 200 nm [53]. However, TFF exceeds ultracentrifugation in isolating significantly higher yields of sEVs, making it more suitable for large-scale research applications [53]. When comparing the performance of traditional ultracentrifugation and tangential flow filtration methods that had undergone further purification by size exclusion chromatography (SEC), TFF demonstrated superior capacity to separate sEVs with higher reproducibility, reduced time requirements, and lower costs [53].
The integration of size exclusion chromatography following TFF has been shown to effectively remove unbound protein contaminants, further enhancing the purity of isolated exosomes [55]. This TFF-SEC combination emerges as a scalable and superior approach for engineered EV isolation, promising significant advancements in clinical applications [55].
Experimental Protocols and Workflows
Detailed Ultracentrifugation Protocol
The following protocol is adapted from multiple studies investigating MSC exosomes for wound healing applications [24]:
Step 1: Sample Preparation
- Culture MSCs in serum-containing media with EV-depleted FBS for 48 hours
- Collect cell culture conditioned media and centrifuge at 500×g for 10 minutes to remove detached cells
- Transfer supernatant and centrifuge at 2,000×g for 30 minutes to remove apoptotic bodies
- Filter supernatant through 0.22 μm filters to remove large particle contaminants
Step 2: Ultracentrifugation
- Transfer clarified media to ultracentrifuge tubes compatible with the rotor (e.g., Thin-Walled ultracentrifuge tubes)
- Centrifuge in a preparative ultracentrifuge (e.g., Beckman Coulter Optima series) at 100,000×g at 4°C for 90-120 minutes using appropriate rotor (e.g., Type 50.2 Ti rotor, k-factor: 157.7)
- Carefully discard supernatant and resuspend crude exosome pellets in 1 mL of ice-cold PBS
- For higher purity, perform a second round of ultracentrifugation at 100,000×g at 4°C for 90-120 minutes
- Resuspend final exosome pellet in appropriate storage buffer (e.g., 0.2% BSA, 25 mM trehalose, 25 mM HEPES pH 7.0 in PBS)
Step 3: Characterization
- Determine particle concentration and size distribution using Nanoparticle Tracking Analysis (NTA)
- Confirm exosome markers (CD9, CD63, CD81, ALIX) and assess purity (calnexin negative) via immunoblotting
Detailed Tangential Flow Filtration Protocol
The following TFF protocol is adapted from studies demonstrating efficient isolation of MSC exosomes for therapeutic applications [53] [55]:
Step 1: Sample Preparation
- Culture MSCs in serum-containing media with EV-depleted FBS for 48 hours
- Collect cell culture conditioned media and centrifuge at 600×g for 30 minutes to remove cells
- Transfer supernatant and centrifuge at 2,000×g for 30 minutes to remove apoptotic bodies
Step 2: Tangential Flow Filtration
- Assemble TFF system with appropriate hollow fiber filters or flat-sheet cassettes (e.g., 500 kDa MWCO or 0.05 μm pore size)
- Filter supernatant through 0.65 μm MPES filters followed by 0.2 μm PES filters
- Concentrate the filtrate using TFF with PS filters of desired MWCO (typically 500 kDa - 0.05 μm)
- Maintain constant flow rate and transmembrane pressure according to manufacturer recommendations
- Rinse concentrated EVs with EV storage buffer
Step 3: Size Exclusion Chromatography (Optional but Recommended)
- Prepare size exclusion column (e.g., with Agarose CL-6B resin) with 10 mL bed volume
- Wash resin with 20 mL PBS before use
- Load 0.5-1 mL of concentrated EV sample to the top of the column
- Immediately collect 1 mL fractions until desired fractions have been collected
- Pool EV-rich fractions based on previous characterization
Step 4: Characterization
- Analyze particle size distribution and concentration using NTA
- Confirm exosome markers via western blot
- Assess purity by protein content (BCA assay) and ratio of particles to protein
Kit-Based Method Protocol (Generic)
While specific protocols vary by manufacturer, most kit-based methods follow this general workflow:
Step 1: Sample Preparation
- Culture MSCs and collect conditioned media as described above
- Centrifuge media at 2,000×g for 30 minutes to remove cells and debris
Step 2: Precipitation/Isolation
- Mix supernatant with proprietary precipitation solution in recommended ratio
- Incubate mixture at 4°C for recommended time (typically 30 minutes to overnight)
- Centrifuge at 1,500-10,000×g for 30-60 minutes to pellet exosomes
- Carefully discard supernatant
Step 3: Washing and Resuspension
- Resuspend pellet in PBS or appropriate buffer
- Optional: Perform additional washing steps if recommended
- Resuspend final pellet in storage buffer
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and equipment for exosome isolation and characterization
| Reagent/Equipment | Function | Examples/Specifications |
|---|---|---|
| EV-depleted FBS | Cell culture supplement for MSC exosome production | Ultracentrifuged or commercially available EV-depleted FBS |
| TFF System | Scalable exosome isolation | Hollow fiber filters (e.g., MICROKROS series) or flat-sheet cassettes |
| Ultracentrifuge | High-force centrifugation for UC method | Beckman Coulter Optima series with fixed-angle or swinging-bucket rotors |
| Size Exclusion Resin | Further purification after initial isolation | Agarose CL-6B, Sepharose CL-2B, or commercial SEC columns |
| Nanoparticle Tracking Analyzer | Particle concentration and size distribution analysis | ZetaView (Particle Metrix), NanoSight NS300 |
| Western Blot reagents | Exosome marker confirmation | Antibodies against CD9, CD63, CD81, ALIX, TSG101; calnexin for purity assessment |
| BCA Protein Assay Kit | Protein quantification for purity assessment | Pierce BCA Protein Assay Kit or equivalent |
| Exosome Storage Buffer | Preservation of exosome integrity and function | 0.2% BSA, 25 mM trehalose, 25 mM HEPES in PBS |
Implications for MSC Exosome Research in Wound Healing
The choice of isolation technique has profound implications for the therapeutic efficacy of MSC exosomes in wound healing applications. Recent meta-analyses of preclinical studies have demonstrated that MSC-derived exosomes significantly improve wound closure rates, reduce scar width, increase blood vessel density, and enhance collagen deposition [22]. However, the isolation method can influence these outcomes by affecting exosome integrity, functionality, and cargo preservation.
Studies comparing the therapeutic potential of different MSC exosome populations have revealed that apoptotic small extracellular vesicles (ApoSEVs) showed better efficacy than small extracellular vesicles (sEVs) in wound closure outcome and collagen deposition, while sEVs displayed better performance in revascularization [22]. These findings highlight the importance of selecting isolation techniques that can specifically target the desired exosome subpopulations for particular therapeutic applications.
The scalability of TFF makes it particularly suitable for producing clinical-grade MSC exosomes for wound healing applications, where consistent and large quantities of therapeutic exosomes are required. Furthermore, the combination of TFF with SEC has been shown to be effective for isolating surface-engineered extracellular vesicles, opening possibilities for customized exosome therapies for specific wound types [55].
As the field moves toward clinical translation, standardization of isolation protocols becomes increasingly critical. Current research shows high heterogeneity in collection conditions, separation methods, storage methods, modifications, treatment dose, administration route, and frequency of MSC-EVs, underscoring the urgent need for standardization in these areas [22]. Among frequently used routes of administration in wound healing studies, subcutaneous injection has displayed a greater improvement in wound closure, collagen deposition and revascularization compared to dressing/covering [22].
The systematic comparison of exosome isolation techniques presented in this guide provides researchers with evidence-based insights to select appropriate methods for their specific applications in MSC exosome research for wound healing. While ultracentrifugation remains a widely used method, its limitations in yield, scalability, and potential for exosome damage make it less suitable for large-scale therapeutic applications. Tangential flow filtration emerges as a superior approach, offering higher yields, better preservation of exosome integrity, and excellent scalability, particularly when combined with size exclusion chromatography. Kit-based methods provide convenience but may compromise on purity. The choice of isolation technique should be guided by the specific research goals, scale requirements, and intended applications, with TFF-SEC representing the most promising approach for clinical translation of MSC exosome therapies in wound healing.
The field of mesenchymal stem cell (MSC) exosome research has witnessed exponential growth, particularly in wound healing applications, yet this expansion has been accompanied by significant challenges in reproducibility and comparability across studies. The Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines, established by the International Society for Extracellular Vesicles (ISEV), provide a critical framework to address these challenges by standardizing extracellular vesicle (EV) characterization for purity and potency assessment [56]. These guidelines have evolved through multiple iterations—MISEV2014, MISEV2018, and the most recent MISEV2023—reflecting the rapidly advancing understanding of EV biology and analysis techniques [56] [57].
Within the specific context of systematic reviews and meta-analyses of MSC exosomes in wound healing, implementation of MISEV guidelines becomes paramount for generating comparable, high-quality data. The inherent complexity of exosomes as therapeutic agents, combined with methodological variability in isolation, characterization, and functional assessment, creates substantial hurdles for meaningful cross-study comparison [22] [58]. This guide examines the practical implementation of MISEV standards for establishing purity and potency benchmarks of MSC exosomes, providing researchers with a structured approach to enhance methodological rigor and translational potential in wound healing research.
Core Principles of MISEV Guidelines for MSC Exosome Characterization
Fundamental Characterization Requirements
The MISEV framework establishes foundational requirements for EV characterization that extend beyond mere compliance to ensure scientific validity. According to MISEV2023, researchers must provide:
- Quantity Assessment: Comprehensive quantification of both the starting material (cell number, fluid volume, or tissue mass) and the resulting EV preparation using at least two complementary methods, typically reporting particle number, protein amount, and potentially lipid content [56] [59].
- Marker Validation: Demonstration of presence of EV-associated components through transmembrane/lipid-bound proteins (e.g., tetraspanins CD9, CD63, CD81), cytosolic proteins (e.g., ALIX, TSG101), and absence of common contaminants from non-vesicular compartments [56] [24].
- Single-Particle Visualization: Imaging of individual EVs using electron microscopy or other high-resolution techniques to confirm morphological characteristics [59].
The MISEV guidelines intentionally avoid prescribing specific methodologies while emphasizing that chosen techniques should be "fit-for-purpose" and appropriately validated for each specific research context [56]. This flexibility allows for methodological innovation while maintaining core standardization principles essential for cross-study comparisons in systematic reviews and meta-analyses.
MISEV's Complementary Role in the Broader Standardization Landscape
MISEV guidelines do not operate in isolation but form part of an integrated ecosystem of standardization frameworks. Particularly relevant for potency assessment in wound healing applications is the integration of MISEV with the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines when analyzing nucleic acid cargo [57]. This complementary relationship ensures comprehensive quality control from EV isolation through molecular cargo analysis, addressing a critical aspect of potency assessment for MSC exosomes in regenerative applications [57].
Recent evidence highlights the necessity of this integrated approach. An umbrella review of MSC-EVs across diverse disease models, including wound healing, found that studies adhering to standardized characterization guidelines demonstrated more consistent therapeutic outcomes and enhanced reproducibility [58]. Similarly, a meta-analysis focused specifically on wound healing applications revealed that only 79.5% of included studies fully characterized their MSCs according to International Society for Cell and Gene Therapy (ISCT) criteria, while EV characterization compliance varied substantially, contributing to heterogeneity in reported outcomes [22].
Implementing MISEV Guidelines for Purity Assessment
Technical Approaches for Purity Evaluation
Purity assessment according to MISEV guidelines requires a multi-parametric approach that evaluates both presence of EV markers and absence of contaminating components. The following table summarizes the core technical requirements and methodologies:
Table 1: MISEV-Compliant Purity Assessment Techniques
| Characterization Aspect | Recommended Techniques | Specific Targets | Acceptance Criteria |
|---|---|---|---|
| Global Quantification | Nanoparticle Tracking Analysis (NTA) | Particle concentration, size distribution | Bimodal distribution with peak 30-150nm [24] [5] |
| Tunable Resistive Pulse Sensing (TRPS) | Particle concentration, size distribution | Consistent with exosome size range [59] | |
| Protein quantification (BCA, Bradford) | Total protein content | Particle-to-protein ratio >3×10^10 particles/μg [59] | |
| EV-Specific Markers | Western blot/Immunoblotting | Tetraspanins (CD9, CD63, CD81) | Clear bands at appropriate molecular weights [24] [5] |
| Flow cytometry (nanoscale) | Surface markers (CD9, CD63) | Positive population >70% [59] | |
| Electron microscopy | Morphological assessment | Cup-shaped vesicles with intact membranes [24] [5] | |
| Contaminant Assessment | Western blot/Immunoblotting | Calnexin, Apolipoproteins | Non-detectable or minimal presence [24] |
| Proteomic analysis | Albumin, other serum proteins | <5% of total protein content [59] |
Experimental Workflow for Comprehensive Purity Assessment
The following diagram illustrates a standardized workflow for purity assessment that aligns with MISEV recommendations:
This integrated approach to purity assessment ensures that MSC exosome preparations used in wound healing studies meet minimum quality standards, enabling meaningful comparisons across different research groups and experimental paradigms.
Implementing MISEV Guidelines for Potency Assessment
Defining Potency Metrics for Wound Healing Applications
While MISEV guidelines provide comprehensive direction for purity assessment, potency evaluation requires integration of functional assays specific to the intended therapeutic application. For MSC exosomes in wound healing, key potency metrics include:
- Angiogenic Potential: Ability to stimulate blood vessel formation, crucial for tissue repair and regeneration [5] [58]
- Immunomodulatory Capacity: Regulation of inflammatory responses, particularly macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotype [22] [5]
- Fibroblast Function Modulation: Enhancement of proliferation, migration, and extracellular matrix production in skin fibroblasts [5]
- Re-epithelialization Promotion: Acceleration of keratinocyte migration and proliferation for wound closure [22]
The MISEV2023 guidelines acknowledge that functional assessment must be context-specific and recommend that researchers "should provide evidence that the observed effects are due to EVs" through appropriate controls and validation experiments [56].
Experimental Approaches for Potency Assessment
Implementation of potency assessment requires standardized functional assays with clear quantification parameters:
Table 2: Functional Potency Assays for MSC Exosomes in Wound Healing
| Potency Dimension | Standard Assays | Quantification Methods | Benchmark Values |
|---|---|---|---|
| Angiogenic Potential | HUVEC tube formation assay | Tube length, junction count | >1.5-fold increase vs control [5] |
| Chick chorioallantoic membrane assay | Vessel branching points | >2-fold increase vs control [22] | |
| Immunomodulation | Macrophage polarization assay | M1/M2 marker expression (CD86/CD206) | M2/M1 ratio >2.5 [22] |
| Cytokine profiling | IL-10, TNF-α, IL-6 measurement | Anti-/pro-inflammatory cytokine ratio >3 [5] | |
| Fibroblast Function | Scratch wound assay | Closure rate over 24-48 hours | >40% increase vs control [5] |
| Proliferation assay | CCK-8, EdU incorporation | >30% increase vs control [22] | |
| Re-epithelialization | Keratinocyte migration assay | Transwell migration count | >50% increase vs control [22] |
Workflow for Integrated Potency Assessment
The following diagram illustrates a comprehensive strategy for potency assessment aligned with MISEV principles:
This multi-faceted approach to potency assessment enables researchers to establish robust correlations between MSC exosome characteristics and their functional performance in wound healing contexts, addressing a critical requirement for both preclinical studies and clinical translation.
Comparative Analysis of MSC Exosome Characterization in Wound Healing Studies
Methodological Variability and Impact on Outcomes
Recent systematic reviews and meta-analyses reveal substantial methodological heterogeneity in MSC exosome characterization for wound healing applications. Analysis of 83 preclinical studies included in a 2025 meta-analysis demonstrated that only 20% fully characterized EVs by size and at least one EV protein marker while also meeting all three ISCT criteria for MSC characterization [22]. This methodological variability directly impacts reported efficacy outcomes and contributes to the high heterogeneity observed in meta-analyses (I² > 70% in many cases) [58].
The source of MSC derivation introduces another dimension of variability. Comparative analysis reveals functional differences between exosomes derived from different tissue sources:
- Umbilical Cord MSC Exosomes: Demonstrate superior angiogenic potential and immunomodulatory capacity in wound healing models [5] [58]
- Adipose Tissue MSC Exosomes: Excel in promoting fibroblast proliferation and collagen synthesis [22]
- Bone Marrow MSC Exosomes: Show balanced performance across multiple wound healing phases [58]
These functional specializations underscore the importance of standardized characterization to identify the most appropriate exosome source for specific wound healing applications.
Efficacy Correlations with Characterization Rigor
Meta-regression analyses from recent umbrella reviews indicate that studies implementing comprehensive MISEV-guided characterization report more consistent therapeutic outcomes. Specifically, studies that employed:
- Multiple quantification methods (particle number + protein content) showed 23% higher wound closure rates with lower variance [58]
- Contaminant assessment demonstrated 31% better reproducibility in inflammatory marker reduction [22]
- Combined functional potency assays with cargo analysis had stronger correlations between specific miRNA content and angiogenic outcomes [5]
These findings highlight the tangible benefits of rigorous characterization in enhancing the predictive value of preclinical wound healing studies.
The Scientist's Toolkit: Essential Reagents and Methodologies
Successful implementation of MISEV guidelines requires specific research tools and methodologies. The following table details essential solutions for compliance:
Table 3: Essential Research Reagents and Methodologies for MISEV Compliance
| Tool Category | Specific Products/Platforms | Application in MISEV Compliance | Key Considerations |
|---|---|---|---|
| Quantification Instruments | NanoSight NS300 (NTA) | Particle concentration and size distribution | Requires appropriate dilution and camera settings [59] |
| ZetaView (Particle Metrix) | Particle counting and lipid membrane detection | Enables purity assessment via lipid staining [59] | |
| NanoFCM Flow NanoAnalyzer | Single-particle analysis and surface markers | Allows multi-parameter characterization [59] | |
| Characterization Reagents | Anti-tetraspanin antibodies (CD9, CD63, CD81) | EV-specific marker detection | Require validation for specific MSC sources [24] [5] |
| Anti-ALIX/TSG101 antibodies | Endosomal pathway marker detection | Confirms exosome biogenesis pathway [24] | |
| Anti-calnexin antibodies | Contaminant detection from endoplasmic reticulum | Validates absence of intracellular contaminants [24] | |
| Functional Assay Systems | HUVEC tube formation assay | Angiogenic potency assessment | Requires standardized matrix and serum conditions [5] |
| Scratch wound/migration assays | Fibroblast and keratinocyte function | Dependent on cell passage number and density [5] | |
| Macrophage polarization assays | Immunomodulatory potency | Requires precise M1/M2 differentiation protocols [22] |
Implementation of MISEV guidelines for purity and potency assessment represents a critical advancement in MSC exosome research for wound healing applications. The framework provided by MISEV2023 enables researchers to generate comparable, high-quality data essential for meaningful meta-analyses and systematic reviews. As the field progresses toward clinical translation, standardized characterization becomes increasingly vital for establishing robust correlations between exosome attributes and therapeutic outcomes.
The integration of purity assessment (through quantitative and marker-based analyses) with functional potency evaluation (through context-specific assays) provides a comprehensive framework for quality control. This approach not only enhances methodological rigor but also facilitates the identification of optimal exosome sources, preparation methods, and dosage regimens for specific wound healing applications. By adopting these standardized practices, the research community can accelerate the translation of MSC exosome therapies from bench to bedside while ensuring reproducible and efficacious outcomes.
Within regenerative medicine, stem cell-derived exosomes have emerged as a potent, cell-free therapeutic alternative for challenging wound types. This review objectively compares the performance of mesenchymal stem cell (MSC)-derived exosomes across three critically important animal wound models: diabetic, radiation-induced, and chronic wounds. The context is a systematic assessment of preclinical evidence informing clinical translation. MSC-exosomes mediate therapeutic effects through transfer of bioactive cargo—including proteins, lipids, and nucleic acids—to recipient cells, modulating inflammation, angiogenesis, and tissue remodeling [23] [9]. Understanding their efficacy across different wound etiologies is paramount for developing targeted therapies. This analysis synthesizes quantitative data on healing outcomes, delineates standardized experimental protocols, and deciphers underlying molecular mechanisms to provide researchers and drug development professionals with a rigorous, evidence-based comparison.
Comparative Analysis of Wound Healing Models
The choice of animal model is critical for evaluating therapeutic efficacy, as each replicates distinct pathophysiological aspects of human wounds. Table 1 provides a systematic comparison of the primary wound models used in exosome therapy research.
Table 1: Characteristics of Key Animal Wound Healing Models
| Model Characteristic | Diabetic Wound Model | Radiation-Induced Wound Model | Chronic Wound Model |
|---|---|---|---|
| Primary Etiology | Hyperglycemia, impaired angiogenesis, persistent inflammation [60] | DNA damage, vascular injury, depletion of progenitor cells [61] | Multifactorial: ischemia, repeated trauma, bacterial biofilm [61] |
| Common Induction Methods | Genetically modified (e.g., db/db mice) or chemically induced (e.g., Streptozotocin in rodents) [61] | Local or total body irradiation followed by skin wounding [61] | Excisional wounds in ischemic or aged animals; often combined with diabetes [61] |
| Key Pathophysiological Features | - Delayed re-epithelialization- Reduced angiogenesis- M1 macrophage polarization [60] | - Failed proliferation phase- Senescent fibroblasts- Compromised tissue regeneration [61] | - Prolonged inflammatory phase- Inadequate growth factor production- Failure to re-epithelialize [61] |
| Predominant Animal Species | Mice (C57BL/6, db/db), Rats (Sprague-Dawley) [61] | Mice, Rats [61] | Mice, Rats, Rabbits [61] |
| Typical Wound Type Used | Full-thickness excisional wound (dorsal or foot) [61] | Full-thickness excisional wound following irradiation [61] | Full-thickness excisional wound, often with induction of ischemia [61] |
Quantitative Synthesis of MSC-Exosome Therapeutic Outcomes
Systematic analysis of preclinical studies reveals quantitative metrics for MSC-exosome performance. Table 2 summarizes key efficacy outcomes, providing a comparative view of therapeutic effects.
Table 2: Quantitative Efficacy Outcomes of MSC-Exosome Therapy in Animal Wounds
| Therapeutic Outcome | Diabetic Wound Model | Radiation-Induced Wound Model | Chronic Wound Model |
|---|---|---|---|
| Wound Closure Rate | Acceleration of closure by ~20-50% compared to controls [61] | Limited direct data; moderate improvement over irradiated controls [61] | Consistent improvement, though slower than in acute wounds [61] |
| Re-epithelialization | Significantly enhanced; study showed ~1.8-fold increase in epidermal thickness vs. control [5] | Delayed but improved with therapy; key hurdle in this model [61] | Promoted, but highly dependent on resolving underlying pathology [61] |
| Angiogenesis (CD31+ vessels) | Robust increase; hUCMSC-Exos promoted ~2-fold higher vessel density [5] | Critically needed; exosomes can restore some microvasculature [61] | Moderate improvement, essential for breaking the chronic cycle [61] |
| Scar Formation (Collagen I/III Ratio) | Improved collagen architecture, higher Collagen I/III ratio [23] | Not well-documented; focus typically on initial healing, not scarring [61] | Variable outcomes, influenced by prolonged inflammation [61] |
| Key Molecular Markers | Downregulation of TNF-α, IL-17; Upregulation of VEGF, TGF-β3 [24] [23] | Modulation of p53, TGF-β signaling; reduction of senescent cells [61] | Regulation of MMPs/TIMPs; shift from M1 to M2 macrophages [61] [62] |
Experimental Protocols for Model Establishment and Evaluation
Diabetic Wound Model Protocol
The diabetic wound model is one of the most extensively characterized in exosome therapy research. The following protocol is synthesized from established methodologies [61].
- Animal Selection and Diabetes Induction: Utilize 8-12 week old male C57BL/6 mice or equivalent. Induce type 1 diabetes via intraperitoneal injection of Streptozotocin (STZ, 50-60 mg/kg for 5 consecutive days). Confirm hyperglycemia (blood glucose ≥ 250 mg/dL) two weeks post-injection.
- Wound Creation: Anesthetize animals and create one or multiple full-thickness excisional wounds on the dorsal skin using a sterile biopsy punch (typically 6-10 mm diameter). The underlying panniculus carnosus should be removed.
- Exosome Treatment Application: Resolve MSC-exosomes (source-specific, e.g., hUCMSC or ADSC) in phosphate-buffered saline (PBS). Topically apply a dose ranging from 1 × 10^8 to 1 × 10^10 particles in a volume of 20-50 µL directly to the wound bed every 2-3 days. Control groups receive PBS vehicle alone.
- Outcome Assessment:
- Wound Closure: Digitally photograph wounds daily and calculate wound area as a percentage of original size using image analysis software (e.g., ImageJ).
- Histological Analysis: At euthanasia (days 7-21), harvest wound tissue. Process for H&E staining to measure epidermal thickness and Masson's Trichrome to assess collagen deposition.
- Molecular Analysis: Isulate protein or RNA from wound tissue for ELISA (e.g., for VEGF, TNF-α, IL-6) or qPCR analysis of relevant genes.
Standard Protocol for Assessing Exosome Effects on Fibroblasts In Vitro
A critical component of mechanistic studies involves evaluating the direct impact of MSC-exosomes on key skin cells, such as fibroblasts [5] [62].
- Cell Culture and Staining: Culture human dermal fibroblasts (HDFs) in standard media until 80-90% confluent. Stain purified MSC-exosomes with a fluorescent lipophilic dye (e.g., PKH67).
- Exosome Uptake and Tracing: Treat HDFs with stained exosomes (e.g., 100 µg/mL) for 24 hours. Fix cells, stain nuclei with DAPI, and visualize using fluorescence microscopy to confirm exosome internalization.
- Scratch (Migration) Assay: Create a uniform scratch in a HDF monolayer using a pipette tip. Wash away debris and treat with exosomes in serum-free media. Capture images at the scratch site at 0, 12, and 24 hours. Quantify the migration rate by measuring the reduction in the scratch area over time.
- Proliferation Assay: Seed HDFs at a low density in 96-well plates. Treat with MSC-exosomes and assess proliferation after 24-72 hours using a standard assay (e.g., CCK-8 or MTT).
- Gene/Protein Expression Analysis: Harvest treated HDFs for RNA or protein extraction. Analyze expression of genes involved in extracellular matrix synthesis (e.g., Collagen I, Collagen III, α-SMA) and degradation (e.g., MMPs) via qRT-PCR or Western Blot.
Diagram: In Vitro Fibroblast Assay Workflow - This diagram outlines the key steps for assessing the effects of MSC-exosomes on fibroblast behavior in vitro, confirming uptake and quantifying functional outcomes like migration and proliferation.
Molecular Mechanisms and Signaling Pathways
The therapeutic benefits of MSC-exosomes are mediated through the modulation of key signaling pathways in recipient cells. The following diagram and description summarize the primary molecular mechanisms involved in promoting healing across different wound models.
Diagram: MSC-Exosome Signaling in Wound Healing - This diagram visualizes the core molecular pathways activated by MSC-exosome cargo in recipient skin cells, leading to key therapeutic outcomes.
The molecular mechanisms are multifaceted. A prominent action is the activation of the PI3K/AKT signaling pathway by exosomal miRNAs like miR-21-5p and miR-126-3p. This activation promotes fibroblast and keratinocyte proliferation and migration, and stabilizes HIF-1α to drive VEGF expression and angiogenesis [23]. Furthermore, MSC-exosomes modulate the TGF-β/Smad pathway, which is crucial for balancing inflammation and ECM remodeling. They can promote a regenerative TGF-β3 signal over a fibrotic TGF-β1 signal, reducing scar formation and encouraging a shift in macrophages from the pro-inflammatory M1 to the anti-inflammatory M2 phenotype [23] [62]. Studies also indicate involvement of the Wnt/β-catenin pathway in enhancing cell proliferation and contributing to improved ECM remodeling during healing [62].
The Scientist's Toolkit: Essential Research Reagents
Successful investigation into exosome-based wound therapies requires a standardized set of reagents and materials. The following table details key solutions used in the featured experiments.
Table 3: Essential Research Reagents for MSC-Exosome Wound Healing Studies
| Reagent / Material | Function and Application in Research | Example from Literature |
|---|---|---|
| Ultracentrifugation | The gold-standard method for isolating and purifying exosomes from cell culture supernatant or biological fluids [24] [5]. | Used for isolating hUCMSC-exosomes; involves sequential centrifugation steps at high speeds (e.g., 100,000-110,000× g) [24] [5]. |
| Nanoparticle Tracking Analysis (NTA) | Characterizes the size distribution and concentration of isolated exosome particles in solution [24] [5]. | Standard characterization step post-isolation to confirm exosomes are within the 30-150 nm size range [24] [5]. |
| Transmission Electron Microscopy (TEM) | Provides high-resolution imaging to confirm the spherical, cup-shaped morphology and bilayer membrane structure of exosomes [24] [5]. | Used to visualize the typical morphology of MSC-EVs and UCB-EVs [62]. |
| Western Blot (Immunoblotting) | Detects and confirms the presence of exosome-specific marker proteins (e.g., CD9, CD63, CD81, TSG101, Alix) and absence of negative markers (e.g., Calnexin) [24] [62]. | Standard validation for exosome markers like CD63 and TSG101; calnexin used as a negative control for cell debris [24] [62]. |
| PKH67 / Fluorescent Dyes | Lipophilic dyes used to fluorescently label the membrane of exosomes, allowing for in vitro and in vivo tracking and uptake studies [62]. | Staining MSC-EVs to visualize their internalization by human dermal fibroblasts in culture [62]. |
| Streptozotocin (STZ) | A chemical agent used to induce Type 1 diabetes in rodent models by selectively destroying pancreatic β-cells, creating a hyperglycemic state for diabetic wound studies [61]. | Used in mice and rats to induce diabetes prior to wound creation, mimicking the impaired healing environment [61]. |
| Imiquimod (IMQ) Cream | A topical immune activator used to induce a psoriasiform skin inflammation in mice, useful for studying inflammatory skin conditions and healing [24]. | Topical application for 6 days to induce a psoriasis-like model for testing anti-inflammatory effects of exosomes [24]. |
| Hyaluronic Acid Hydrogel | A biomaterial used as a delivery vehicle for exosomes, providing a scaffold that prolongs exosome retention at the wound site and maintains a moist environment [16] [9]. | An injectable hydrogel used for sustained release of MSC-exosomes in chronic wound models [16]. |
Diabetic, radiation-induced, and chronic wound models each present unique pathophysiological landscapes for evaluating MSC-exosome therapy. The collective preclinical data robustly demonstrate that MSC-exosomes can significantly improve healing outcomes across these models by targeting shared and distinct molecular pathways. The most compelling evidence exists for diabetic wounds, where exosomes consistently enhance angiogenesis, modulate inflammation, and accelerate closure. For radiation-induced and complex chronic wounds, the therapy shows promise in overcoming the profound cellular damage and persistent inflammation that characterize these conditions, though more targeted research is needed. The future of this field lies in optimizing exosome sources, engineering exosomes for enhanced targeting and cargo delivery, and developing sophisticated biomaterial-based delivery systems for sustained release. As standardized protocols and rigorous molecular characterization become ubiquitous, the translation of MSC-exosome therapies from robust preclinical findings to clinical reality for patients with refractory wounds is poised to advance significantly.
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-exosomes) represents a cutting-edge frontier in regenerative medicine, particularly for wound healing and skin regeneration. The efficacy of these biological nanoparticles is profoundly influenced by the method of delivery, which affects their retention, distribution, and bioavailability at the target site. Within the context of a systematic review and meta-analysis of MSC-exosomes in wound healing research, this guide objectively compares the performance of three principal administration routes: topical application, integration into hydrogel systems, and subcutaneous injection. Supporting experimental data and methodologies from recent preclinical studies are synthesized to provide a clear comparison of these strategies for researchers and drug development professionals.
Comparative Analysis of Administration Routes
The choice of administration route is a critical determinant in the therapeutic outcome of MSC-exosome-based treatments. The table below summarizes the core characteristics, supporting evidence, and key performance metrics for the three primary routes.
Table 1: Comparative overview of MSC-exosome administration routes for skin repair
| Administration Route | Description & Rationale | Key Supporting Evidence | Performance on Meta-Analysis |
|---|---|---|---|
| Topical Application | Direct application of exosomes in a liquid, gel, or cream onto the wound surface. | Effective in psoriasis models; reduces epidermal thickness and clinical severity scores [24]. | Not specifically quantified against other routes in the included meta-analysis [22]. |
| Hydrogel Integration | Exosomes are encapsulated within an injectable hydrogel that forms a protective depot at the site. | HA-hydrogel with MSC-exosomes enhances chronic wound healing by regulating inflammation and ensuring sustained release [16]. | Not specifically quantified against other routes in the included meta-analysis [22]. |
| Subcutaneous Injection | Injection of exosome suspension directly into the tissue layer beneath the skin. | Plant-based exosome injections in rats showed significantly enhanced collagen deposition and reduced inflammation [63]. | Showed a greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering (which includes topical routes) [22]. |
Quantitative Data from Preclinical Studies
A meta-analysis of 83 preclinical studies provides high-level evidence for the comparative effectiveness of these routes, while individual animal studies offer specific quantitative outcomes.
Meta-Analysis Findings on Administration Efficacy
A 2025 systematic review and meta-analysis provided direct comparative data on administration routes, specifically for wound closure outcomes. The analysis found that subcutaneous injection demonstrated a greater improvement in wound closure rate, collagen deposition, and revascularization when compared to dressing/covering methods [22]. This quantitative synthesis of multiple studies strongly supports the superiority of injectable routes for achieving robust healing responses.
Representative Experimental Outcomes in Animal Models
Data from individual rodent studies illustrate the measurable impact of different delivery strategies.
Table 2: Experimental outcomes from key animal studies
| Study & Model | Treatment Groups | Epidermal Thickness | Collagen Deposition | Inflammatory Cell Count | Clinical Severity Score |
|---|---|---|---|---|---|
| Psoriasis Murine Model [24] | IMQ Control | Baseline for comparison | - | - | Baseline for comparison |
| IMQ + hUCMSC-Exo (Topical) | Significantly Reduced | - | - | Significantly Lower (SMD: -1.886) | |
| IMQ + hPMSC-Exo (Topical) | Significantly Reduced | - | - | Significantly Lower | |
| Rat Excisional Wound [63] | Control Incision | +25.54 µm (Day 14) | +6.95% (Day 14) | - | - |
| Subcutaneous Exosome Injection | +36.37 µm (Day 14) | +9.30% (Day 14) | - | - | |
| Rat Excisional Wound (Inflammation) [63] | Control Incision | - | - | +8.21 cells (Day 7) | - |
| Subcutaneous Exosome Injection | - | - | +6.77 cells (Day 7) | - |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for research, this section details the methodologies from key cited studies.
Protocol: Subcutaneous Injection of Exosomes
A 2025 study investigating plant-based exosomes for wound healing provides a clear protocol for subcutaneous administration [63].
- Animal Model: 18 Wistar albino rats (age- and weight-matched).
- Wound Creation: A 1-cm linear incision was made on the ventral surface of the rat's hand using a No. 15 surgical blade.
- Treatment Administration: Immediately after wound creation, the treatment group received injections of the exosome solution directly into the wound bed and along the wound edges.
- Dosage and Formulation: A standardized volume of 0.03 mL of a commercial plant-based exosome solution (Elysee Exosome PDRN Ampoule) was injected.
- Post-operative Care: No post-operative dressings, antibacterial medications, or sutures were applied.
- Outcome Assessment: Tissue samples were collected at baseline, day 7, and day 14 for histological analysis (H&E and Masson trichrome staining). Epithelial thickness, collagen fiber density, and inflammatory cell count were evaluated in a blinded manner.
Protocol: Topical Application in a Psoriasis Model
A 2025 murine study and meta-analysis detailed the topical application of MSC-exosomes for treating psoriasis [24].
- Animal and Model Induction: 8-week-old male Balb/c mice had a psoriatic phenotype induced by daily topical applications of 50 mg of IMQ (5% Aldara cream) on the shaved back skin for 6 consecutive days.
- Exosome Isolation and Characterization: Exosomes were isolated from human umbilical cord and placenta MSCs via ultracentrifugation. They were characterized for size and morphology using Nanoparticle Tracking Analysis (NTA) and Transmission Electron Microscopy (TEM), and for markers (CD9, CD63, ALIX) via immunoblotting.
- Treatment Protocol: The exosomes were dissolved in phosphate-buffered saline (PBS) and applied topically to the affected skin daily for 7 days. The dosage for both hUCMSC and hPMSC exosomes was 1 × 10^8 particles in 25 µL PBS.
- Outcome Assessment: One day after the final treatment, mice were evaluated for Psoriasis Area and Severity Index (PASI) scores. Skin tissue was then harvested for histological measurement of epidermal thickness and analysis of cytokine levels using enzyme-linked immunosorbent assays (ELISA).
Signaling Pathways and Experimental Workflows
The following diagrams visualize the logical workflow for comparing administration routes and the biological mechanisms activated by MSC-exosomes in wound healing.
Exosome Administration Route Decision Workflow
MSC-Exosome Mediated Wound Healing Pathways
The Scientist's Toolkit: Key Research Reagents and Materials
Successful research into exosome delivery routes relies on specific biological materials, characterization tools, and delivery systems. The following table details essential components for such studies.
Table 3: Essential research reagents and materials for exosome administration studies
| Category | Item | Specific Examples / Characteristics | Primary Function in Research |
|---|---|---|---|
| Biologicals | MSC Sources | Adipose Tissue (ADSCs), Umbilical Cord (hUCMSCs), Bone Marrow (BMMSCs) [22] | Source of therapeutic exosomes; different sources may have varying efficacy. |
| Exosome Types | Small EVs (sEVs), Apoptotic Small EVs (ApoSEVs) [22] | The active therapeutic agent being tested. | |
| Characterization | Characterization Antibodies | CD9, CD63, ALIX (positive markers), Calnexin (negative marker) [24] | Confirming exosome identity and purity per MISEV guidelines. |
| Analysis Instruments | Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM) [24] | Determining exosome size, concentration, and morphology. | |
| Delivery Systems | Hydrogel Polymers | Hyaluronic Acid (HA), Gelatin (Ge), Chitosan [16] [64] | Forming a protective depot for sustained exosome release. |
| Crosslinkers | N-Ethyl-N'-(3-dimethyl aminopropyl) carbodiimide (EDC) [65] | Chemically stabilizing hydrogel matrices. | |
| Animal Models | Wound Models | Full-thickness excisional dorsal wound, Diabetic (STZ/db/db) wound, Imiquimod-induced psoriasis [22] [24] | Preclinical in vivo testing of therapeutic efficacy and route performance. |
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-Exos) represents a paradigm shift in regenerative medicine, offering a cell-free alternative with significant advantages in safety and stability for wound healing [4] [66]. Unlike traditional biologics, exosomes function as sophisticated nanoscale communicators, transferring complex molecular cargoes including proteins, lipids, and nucleic acids to recipient cells [25]. However, this biological complexity introduces substantial challenges in establishing standardized dosing parameters, as therapeutic effects depend not only on particle quantity but also on cargo composition, source materials, and administration routes. This systematic analysis synthesizes current evidence from preclinical and clinical studies to establish foundational principles for MSC-Exos dosage optimization in wound healing applications, providing critical guidance for researchers and therapeutic developers navigating this emerging field.
Source-Dependent Therapeutic Profiles
MSC-Exos exhibit distinct therapeutic properties based on their tissue of origin, necessitating source-specific consideration in dosage optimization. The table below summarizes key efficacy findings for different exosome sources in wound healing and related applications:
Table 1: Therapeutic Efficacy of MSC Exosomes from Different Sources
| Source | Therapeutic Advantages | Optimal Dose Ranges (Preclinical) | Key Mechanisms |
|---|---|---|---|
| Adipose Tissue (ADSC) | Superior wound closure rate and collagen deposition [22] | 100-200 μg per application in rodent models [22] | Promotes angiogenesis, fibroblast proliferation |
| Umbilical Cord (UC-MSC) | Enhanced cartilage repair, reduced inflammation [67] | 1×10^8 particles in psoriasis models [24] | Immunomodulation, macrophage polarization |
| Bone Marrow (BM-MSC) | Superior revascularization capacity [22] | 10-100 μg in mouse models [66] | T-cell modulation, anti-inflammatory effects |
| Placenta (PMSC) | Reduced epidermal thickness in psoriasis [24] | Comparable to UC-MSC efficacy at similar doses [24] | Cytokine suppression, epidermal normalization |
Meta-analyses of preclinical studies demonstrate that adipose-derived MSC exosomes (ADSC-Exos) show particularly strong performance in wound closure rates, while bone marrow-derived exosomes (BMSC-Exos) exhibit superior capacity for revascularization [22]. For inflammatory skin conditions like psoriasis, both umbilical cord-derived (UC-MSC) and placental-derived (PMSC) exosomes significantly reduce pathological features including epidermal thickness and pro-inflammatory cytokines at doses of approximately 1×10^8 particles [24].
Temporal Efficacy Patterns
The timing of therapeutic response following MSC-Exos administration reveals important patterns for treatment frequency optimization. Systematic analysis of wound healing studies indicates peak exosome efficacy at 7 days post-administration (odds ratio 1.82, 95% CI [0.69, 2.95]), with sustained but diminished effects at 14 days (odds ratio 2.29, 95% CI [0.01, 4.56]) [25]. This temporal pattern supports treatment intervals of approximately 5-7 days for maintaining therapeutic activity throughout the wound healing process. The diminishing efficacy beyond one week suggests potential exosome clearance or degradation, highlighting the importance of repeated administration for chronic or non-healing wounds.
Administration Routes and Dose Optimization
Route-Dependent Dosing Considerations
The administration route significantly influences the effective dosage of MSC-Exos by altering biodistribution, retention, and cellular uptake efficiency. The following table compares dosing parameters across different delivery methods:
Table 2: Dose Optimization by Administration Route
| Route | Therapeutic Context | Effective Dose Range | Key Considerations |
|---|---|---|---|
| Topical/Subcutaneous | Cutaneous wound healing [22] | 100-200 μg in rodent models | Subcutaneous injection superior to topical dressing for wound closure and collagen deposition |
| Intravenous | Systemic applications (GvHD, ARDS) [66] [68] | 100-200 μg/kg in human trials [66] | Higher doses required due to pulmonary clearance; potential dose-limiting toxicity |
| Nebulized Inhalation | Respiratory diseases (ARDS, COVID-19) [69] | ~1×10^8 particles (lower than IV) | Direct delivery enhances local concentration while reducing systemic exposure |
| Intra-articular | Osteoarthritis [67] | 10-100 μg in rodent models | Local retention enables extended activity with lower systemic exposure |
Subcutaneous injection has demonstrated superior efficacy compared to topical application for wound healing, particularly for outcomes including wound closure rate, collagen deposition, and revascularization [22]. For systemic applications, intravenous administration requires higher doses due to significant pulmonary clearance and sequestration, with clinical studies demonstrating safety at doses of 100-200 μg/kg [66]. Notably, nebulization therapy achieves therapeutic effects at substantially lower doses (approximately 10^8 particles) compared to intravenous administration, highlighting the impact of route selection on dose efficiency [69].
Treatment Frequency Optimization
The frequency of MSC-Exos administration significantly influences therapeutic outcomes, with emerging evidence supporting optimized intervals for different applications. In osteoarthritis models, biweekly exosome injections demonstrate superior efficacy compared to weekly administrations for cartilage repair [67]. This enhanced effect likely reflects the maintenance of therapeutic exosome concentrations during critical repair processes, suggesting that more frequent dosing may be beneficial during active tissue remodeling phases. For wound healing, the peak efficacy observed at 7 days supports weekly application schedules, though more frequent administration (2-3 times weekly) may be advantageous during the initial inflammatory phase of healing [25].
Experimental Models and Methodologies
Murine Psoriasis Model Protocol
The imiquimod (IMQ)-induced psoriasis murine model provides a standardized methodology for evaluating dermatological applications of MSC-Exos:
Table 3: Experimental Protocol for Psoriasis Model
| Parameter | Specification | Purpose |
|---|---|---|
| Animal Model | 8-week-old male Balb/c mice [24] | Standardized immunocompetent model |
| Disease Induction | Daily topical application of 50 mg IMQ cream (5%) for 6 consecutive days [24] | Consistent psoriatic phenotype induction |
| Treatment Protocol | Topical application of 1×10^8 exosome particles in 25 μL PBS daily for 7 days starting day 4 [24] | Therapeutic intervention during active disease |
| Outcome Measures | PASI score (erythema, scaling, skin thickening), epidermal thickness, skin tissue cytokines [24] | Multi-parameter efficacy assessment |
This well-characterized model demonstrates that both UC-MSC and PMSC exosomes significantly reduce psoriasis area and severity index (PASI) scores and epidermal thickness without dose-limiting adverse effects at the tested concentration [24]. The model provides a robust platform for dose-ranging studies, with the established dose of 1×10^8 particles serving as a reference point for concentration-response investigations.
Wound Healing Model Variations
Preclinical wound healing studies employ diverse models with distinct dosing implications:
Wound Model Dosing Considerations
Full-thickness excisional wounds represent the most prevalent model (90.4% of studies), primarily utilizing dorsal wound locations in mice (73.5%) and rats (26.5%) [22]. Diabetic wound models employ either streptozotocin (STZ)-induced type 1 diabetes (30 studies) or genetically modified db/db mice representing type 2 diabetes (9 studies), with diabetic models generally requiring higher exosome doses or more frequent administration to overcome impaired healing responses [22].
Molecular Mechanisms and Signaling Pathways
Key Mechanistic Pathways in Wound Healing
MSC-Exos modulate wound healing through coordinated regulation of multiple signaling pathways across different phases of repair:
Exosome Mechanisms in Wound Healing
During the inflammatory phase, MSC-Exos promote macrophage polarization toward the regenerative M2 phenotype through secretion of TSG-6, IL-6, and PGE2 [70]. This immunomodulatory activity is further enhanced through T-cell differentiation toward Th2 and regulatory T-cell phenotypes, creating an anti-inflammatory microenvironment [70]. In the proliferation phase, exosomes directly stimulate angiogenesis and fibroblast proliferation through transfer of pro-angiogenic miRNAs (miR-126, miR-125a) and growth factors [71]. During the remodeling phase, MSC-Exos regulate collagen deposition and organization through TGF-β/Smad and MAPK signaling pathways, with placental-derived exosomes shown to inhibit p38 MAPK signaling to reduce scar formation [70].
miRNA Cargo and Dose Implications
The therapeutic activity of MSC-Exos is largely mediated by their miRNA content, which varies based on source and preconditioning:
Table 4: Key Therapeutic miRNAs in MSC-Exos
| miRNA | Function | Regulation by Preconditioning |
|---|---|---|
| miR-21-5p | Angiogenesis, fibroblast activation [71] | Enhanced by TNF-α preconditioning [71] |
| miR-146a | Anti-inflammatory, macrophage polarization [71] | Increased by TNF-α, IL-1β, LPS [71] |
| miR-126 | Endothelial cell migration, angiogenesis [71] | Modulated by hypoxia and inflammatory cues |
| miR-181a | Immunomodulation, T-cell regulation [71] | Enhanced by LPS preconditioning [71] |
| miR-222-3p | Anti-apoptotic, pro-angiogenic [71] | Upregulated by low-dose LPS (0.1 μg/mL) [71] |
Preconditioning strategies with inflammatory cytokines (TNF-α, IL-1β), hypoxia, or low-dose LPS can selectively enrich therapeutic miRNAs in MSC-Exos, potentially enhancing potency and reducing the required therapeutic dose [71]. For instance, TNF-α preconditioning at 10-20 ng/mL increases miR-146a content, enhancing immunomodulatory capacity, while low-dose LPS (0.1 μg/mL) upregulates miR-222-3p expression, enhancing angiogenic potential [71]. These preconditioning approaches represent a promising strategy for optimizing the therapeutic index of MSC-Exos preparations.
Research Reagent Solutions and Methodological Standards
Essential Research Tools
The following table outlines critical reagents and methodologies for MSC-Exos research:
Table 5: Essential Research Reagents and Methodologies
| Category | Specific Solutions | Research Application |
|---|---|---|
| Isolation Methods | Ultracentrifugation (64%), Kit-based isolation (18%), Tangential flow filtration (5%) [25] | Standardized vesicle separation |
| Characterization Tools | Nanoparticle tracking analysis (NTA), Transmission electron microscopy (TEM), Western blot [25] | Vesicle quantification and validation |
| Surface Markers | CD63, CD9, CD81, TSG101 [25] | Exosome identification and purity assessment |
| Negative Markers | Calnexin [24] | Assessment of cellular contamination |
| Preconditioning Agents | TNF-α, IL-1β, LPS, Hypoxia chambers [71] | Therapeutic potency enhancement |
Ultracentrifugation remains the most prevalent isolation method (64% of studies), though kit-based approaches offer alternatives with potential advantages for specific applications [25]. Standard characterization should include nanoparticle tracking for size distribution analysis (typically 30-150 nm for exosomes), transmission electron microscopy for morphological validation, and western blot analysis for surface marker confirmation (CD63, CD9, CD81) [24] [25]. Inclusion of negative markers such as calnexin helps assess contamination with cellular debris [24].
Dosage optimization of MSC exosomes requires integrated consideration of source material, administration route, treatment frequency, and molecular mechanisms. The established concentration-response relationships from systematic analysis of preclinical studies provide foundational guidance for therapeutic development, while emerging clinical data highlight route-dependent dosing considerations. The dynamic nature of exosome cargo and biological activity underscores the need for potency-based dosing standards rather than purely quantitative metrics. As the field advances, integration of preconditioning strategies to enhance therapeutic potential and targeted delivery approaches to improve biodistribution will further refine dosage optimization paradigms. Standardization of isolation protocols, characterization methods, and potency assays remains essential for meaningful comparison across studies and accelerated clinical translation of MSC exosome therapies for wound healing applications.
Overcoming Translational Hurdles: Engineering and Standardization of MSC Exosome Therapies
Exosomes, small extracellular vesicles (sEVs) typically ranging from 30-150 nm in diameter, have emerged as promising cell-free therapeutic agents in regenerative medicine, particularly for wound healing applications [72] [73]. These nanosized vesicles are secreted by various cells, including mesenchymal stem cells (MSCs), and play crucial roles in intercellular communication by transferring proteins, lipids, and nucleic acids to recipient cells [74] [75]. In the context of wound healing, MSC-derived exosomes have demonstrated significant potential to modulate all phases of the healing process—inflammation, proliferation, and remodeling—through their diverse molecular cargo [25]. A systematic review and meta-analysis of preclinical studies on type II diabetic cutaneous wounds revealed that MSC-sEVs significantly facilitate wound healing compared to controls (standardized mean difference [SMD]=3.16, 95% confidence interval [CI]: 2.65 to 3.66, P<0.00001) [76]. This robust therapeutic effect underscores the importance of developing precise engineering strategies to enhance exosome targeting and functionality for clinical applications.
Table 1: Key Characteristics of MSC-Derived Exosomes in Wound Healing
| Property | Description | Therapeutic Relevance in Wound Healing |
|---|---|---|
| Size Range | 30-150 nm in diameter [73] | Enables deep tissue penetration and cellular uptake |
| Membrane Composition | Lipid bilayer with tetraspanins (CD9, CD63, CD81) [72] | Provides stability and biocompatibility; can be engineered for targeting |
| Natural Cargo | Proteins, miRNAs, mRNAs, lipids [74] | Modulates inflammation, angiogenesis, and tissue remodeling |
| Source Variability | Bone marrow, adipose tissue, umbilical cord [72] | Different MSC sources yield exosomes with distinct therapeutic profiles |
| Therapeutic Mechanisms | Paracrine signaling, immunomodulation, cell proliferation [76] | Addresses multiple pathological aspects of chronic wounds |
Exosome Engineering Methodologies: Cargo Loading Strategies
Exosome engineering encompasses two primary approaches: cargo loading to modify internal contents and surface functionalization to alter targeting capabilities. Cargo loading involves incorporating therapeutic molecules such as small interfering RNAs (siRNAs), microRNAs (miRNAs), or drugs into exosomes for targeted delivery to enhance bioavailability and therapeutic efficacy while minimizing systemic side effects [75]. Multiple techniques have been developed for loading therapeutic cargo into exosomes, each with distinct advantages and limitations.
Passive and Active Loading Techniques
Passive loading methods rely on diffusion or incubation techniques where exosomes are co-incubated with therapeutic agents, allowing the cargo to permeate the lipid bilayer membrane. While simple to implement, this method often results in low loading efficiency [75]. More effective active loading methods have been developed, including:
- Electroporation: This technique uses electrical pulses to create temporary pores in the exosomal membrane, facilitating the entry of nucleic acids or drugs into the vesicles. While effective for loading siRNA and miRNA, optimization is required to prevent cargo aggregation and maintain vesicle integrity [73].
- Sonication: Ultrasound waves are applied to temporarily disrupt the exosomal membrane, enabling therapeutic molecules to enter. Sonication typically achieves higher loading efficiency than passive methods but may affect membrane integrity if parameters are not carefully controlled [75].
- Extrusion: This method involves passing exosomes and therapeutic cargo through membranes with small pores under controlled pressure, facilitating cargo encapsulation through membrane fusion and reformation [77].
- Freeze-Thaw Cycles: Repeated freezing and thawing can promote cargo loading by temporarily destabilizing the exosomal membrane, though this method may cause aggregation of exosomes [77].
Table 2: Comparison of Exosome Cargo Loading Methods
| Method | Mechanism | Optimal Cargo Type | Efficiency | Advantages | Limitations |
|---|---|---|---|---|---|
| Incubation | Passive diffusion through membrane | Hydrophobic small molecules | Low | Simple, maintains exosome integrity | Low loading efficiency |
| Electroporation | Electrical field creates temporary pores | Nucleic acids (siRNA, miRNA) | Medium-High | Suitable for charged molecules | Potential vesicle aggregation, membrane damage |
| Sonication | Ultrasound disrupts membrane | Proteins, chemical drugs | High | High loading efficiency | Potential membrane protein denaturation |
| Extrusion | Mechanical pressure through membranes | Various cargo types | Medium | Uniform size distribution | Potential loss of membrane components |
| Freeze-Thaw | Membrane destabilization through ice crystals | Proteins, nucleic acids | Medium | Simple protocol | Exosome aggregation, inconsistent loading |
Experimental Protocols for Cargo Loading
Protocol for Electroporation-Mediated siRNA Loading:
- Isolate exosomes from MSC culture supernatant using ultracentrifugation (100,000-120,000 × g for 70 minutes) or size-exclusion chromatography [78].
- Resuspend exosome pellet in electroporation buffer (e.g., PBS) to a concentration of 1-2 mg/mL protein.
- Mix exosomes with siRNA (final concentration 50-100 nM) in electroporation cuvette.
- Apply electrical pulses (parameters: 100-150 V, 5-10 ms pulse length, 3-5 pulses) using electroporation system.
- Incubate on ice for 30 minutes to allow membrane recovery.
- Remove unencapsulated siRNA using ultrafiltration or size-exclusion chromatography.
- Validate loading efficiency using fluorescence-based quantification or RT-qPCR [75].
Protocol for Sonication-Assisted Drug Loading:
- Purify exosomes as described above and resuspend in PBS or appropriate buffer.
- Add therapeutic drug (e.g., curcumin or paclitaxel) at optimized drug-to-exosome ratio.
- Subject the mixture to probe sonication (parameters: 20-40% amplitude, 30-60 seconds total in pulse mode: 5 seconds on, 2 seconds off) while keeping the sample on ice.
- Incubate the sonicated mixture at 37°C for 30-60 minutes to allow membrane recovery.
- Remove unencapsulated drug using gel filtration or dialysis.
- Characterize drug-loaded exosomes for size, concentration, and drug encapsulation efficiency [75].
Surface Modification Strategies for Targeted Delivery
Surface engineering of exosomes enhances their targeting specificity to desired tissues or cells, thereby improving therapeutic efficacy while reducing off-target effects in wound healing applications. These strategies involve modifying the exosomal membrane with targeting ligands, such as peptides, antibodies, or other homing molecules, that can recognize and bind to specific receptors at the wound site [75]. Surface modification approaches can be broadly categorized into pre-isolation methods (genetic engineering of parent cells) and post-isolation methods (direct modification of purified exosomes).
Pre-isolation Modification Strategies
Pre-isolation methods involve genetically engineering parent cells to express targeting ligands on the surface of subsequently secreted exosomes:
Genetic Engineering of Parent Cells: Parent cells (typically MSCs) are transfected with genes encoding targeting peptides or proteins fused to exosomal membrane proteins (e.g., Lamp2b, CD63, or PDGFR). The engineered cells then naturally incorporate these fusion proteins into exosomes during biogenesis [77]. For wound healing applications, targeting motifs might include RGD peptides (for integrins upregulated in angiogenesis) or specific chemokine receptors that home to inflammatory sites.
Metabolic Engineering: This approach utilizes metabolic labeling with bioorthogonal groups (e.g., azide-modified sugars) that are incorporated into exosomal glycoproteins during biogenesis. These groups can later be conjugated with targeting ligands using click chemistry after exosome isolation [77].
Cellular Preconditioning: Exosome properties can be modulated by preconditioning parent MSCs with specific microenvironments relevant to wound healing. For instance, hypoxia preconditioning enhances the angiogenic properties of MSC-derived exosomes, while inflammatory cytokine pretreatment (e.g., with TNF-α or IFN-γ) can boost their immunomodulatory capacities [72].
Post-isolation Modification Strategies
Post-isolation methods directly modify purified exosomes through various chemical and physical techniques:
Chemical Conjugation: Targeting ligands are conjugated to amine or carboxyl groups on exosomal surface proteins using crosslinkers such as NHS-PEG-Maleimide. This method provides controlled ligand density but requires optimization to prevent exosome aggregation [77].
Hydrophobic Insertion: Engineered ligands conjugated to hydrophobic molecules (e.g., phospholipids or cholesterol) can be spontaneously inserted into the exosomal membrane through incubation. While simpler than chemical conjugation, this method may have lower stability in biological environments [75].
Click Chemistry: Bioorthogonal reactions (e.g., between azide and alkyne groups) enable specific, efficient conjugation of targeting ligands to pre-labeled exosomes with minimal damage to vesicle integrity [77].
Table 3: Surface Modification Strategies for Exosome Engineering
| Strategy | Mechanism | Ligand Examples | Applications in Wound Healing | Advantages | Limitations |
|---|---|---|---|---|---|
| Genetic Engineering | Fusion of targeting peptide with exosomal membrane protein | RGD, E7, CGKRK peptides | Targeting endothelial cells, fibroblasts | Stable expression, natural incorporation | Technical complexity, potential cell toxicity |
| Metabolic Engineering | Incorporation of bioorthogonal groups for click chemistry | Azide-modified sugars | Specific conjugation after isolation | High specificity, minimal disruption | Requires specialized chemical expertise |
| Chemical Conjugation | Covalent linkage to surface functional groups | Antibodies, transferrin | Targeting specific cell receptors | Controlled ligand density | Potential vesicle aggregation |
| Hydrophobic Insertion | Spontaneous membrane insertion | Cholesterol-tagged ligands | General membrane modification | Simple protocol, rapid | Lower stability in biological fluids |
| Membrane Fusion | Fusion with functional liposomes | PEGylated lipids | Enhancing circulation time | Can incorporate multiple functionalities | May alter natural exosome properties |
Experimental Protocols for Surface Modification
Protocol for Genetic Engineering of Parent Cells:
- Design DNA construct encoding targeting peptide (e.g., RGD for angiogenesis targeting) fused to exosomal membrane protein (e.g., Lamp2b).
- Transfect MSCs with construct using appropriate method (lentiviral transduction for stable expression or lipofection for transient expression).
- Select successfully transfected cells using antibiotic resistance (e.g., puromycin) or fluorescence-activated cell sorting (FACS).
- Culture engineered MSCs in exosome-depleted medium for 48-72 hours.
- Collect conditioned medium and isolate exosomes using standard methods (ultracentrifugation or tangential flow filtration).
- Validate surface modification using western blotting for the fusion protein and immunogold electron microscopy for surface localization [77].
Protocol for Chemical Conjugation via NHS-PEG-Maleimide:
- Isolate and purify exosomes using size-exclusion chromatography to remove contaminating proteins.
- Activate targeting ligand (e.g., peptide with cysteine residue) using maleimide-PEG-NHS crosslinker (molar ratio 1:1.5, incubate 30 minutes at room temperature).
- Remove excess crosslinker using desalting column or dialysis.
- Mix activated ligand with exosomes (optimized ratio: 100-500 ligands per exosome) and incubate for 2-4 hours at room temperature with gentle agitation.
- Remove unconjugated ligand using ultrafiltration (100 kDa MWCO) or SEC.
- Characterize conjugation efficiency using fluorescence labeling or surface plasmon resonance [75].
Therapeutic Efficacy and Functional Validation in Wound Healing
Engineering exosomes for enhanced wound healing applications requires comprehensive validation of their therapeutic efficacy through in vitro and in vivo models. The meta-analysis by Frontiers in Endocrinology demonstrated that MSC-sEVs significantly improve wound closure rates in type II diabetic models (SMD=3.16, 95% CI: 2.65 to 3.66, P<0.00001) with low heterogeneity (I²=39%), supporting their therapeutic potential [76]. Engineered exosomes can further enhance these effects through improved targeting and cargo delivery.
Mechanisms of Action in Wound Healing
Engineered exosomes facilitate wound healing through multiple mechanisms:
Immunomodulation: MSC-derived exosomes transfer regulatory miRNAs (e.g., miR-21, miR-146a, miR-181) to target cells, promoting anti-inflammatory M2 macrophage polarization while suppressing pro-inflammatory M1 macrophages [72]. This helps resolve prolonged inflammation that impairs healing in chronic wounds.
Angiogenesis Promotion: Exosomes engineered to carry pro-angiogenic factors (VEGF, FGF-2) or miRNAs (miR-125a, miR-126) enhance neovascularization in wound beds, improving oxygen and nutrient supply to healing tissues [72] [25].
Re-epithelialization and Collagen Remodeling: Engineered exosomes accelerate keratinocyte migration and proliferation through activation of Wnt/β-catenin and AKT signaling pathways, while also modulating collagen synthesis and organization for improved extracellular matrix deposition [72].
Experimental Validation Protocols
In Vitro Wound Healing Assay:
- Culture target cells (human dermal fibroblasts or keratinocytes) to confluence in 24-well plates.
- Create a linear "wound" scratch using a sterile 200 μL pipette tip.
- Wash cells to remove debris and add treatments: (1) control medium, (2) native exosomes, (3) engineered exosomes.
- Capture images at 0, 12, 24, and 48 hours at predetermined locations.
- Quantify migration rate by measuring scratch closure percentage using image analysis software (e.g., ImageJ).
- For enhanced analysis, incorporate live-cell imaging to track individual cell movements [72].
In Vivo Diabetic Wound Healing Model:
- Induce type II diabetes in rodents using high-fat diet combined with low-dose streptozotocin injections (e.g., 35 mg/kg for 5 consecutive days) [76].
- Confirm diabetic state through blood glucose measurements (>300 mg/dL).
- Create full-thickness excisional wounds on dorsal skin (typically 6-8 mm diameter).
- Apply treatments: (1) vehicle control (PBS), (2) native MSC exosomes, (3) engineered MSC exosomes.
- Administer treatments via local injection around wound edges or using biomaterial scaffolds (e.g., chitosan/silk hydrogel) for sustained release [72].
- Monitor wound closure every 2-3 days using digital photography and planimetry analysis.
- Harvest tissue at predetermined endpoints (7, 14, 21 days) for histological analysis (H&E staining for re-epithelialization, Masson's trichrome for collagen deposition, CD31 immunohistochemistry for angiogenesis) [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful engineering of exosomes for wound healing applications requires specific reagents and methodologies. The following table summarizes key materials and their applications in exosome research.
Table 4: Essential Research Reagents for Exosome Engineering and Analysis
| Category | Reagent/Material | Specific Function | Application Examples |
|---|---|---|---|
| Isolation Materials | Ultracentrifuge with fixed-angle rotors | High-speed pelleting of exosomes | Differential ultracentrifugation protocol [78] |
| Size-exclusion chromatography columns | Separation by hydrodynamic radius | Pure exosome isolation with preserved functionality [78] | |
| Polymeric precipitation reagents (ExoQuick) | Volume reduction and exosome precipitation | Rapid isolation from conditioned media [78] | |
| Tangential flow filtration systems | Concentration and buffer exchange | Scalable exosome processing [79] | |
| Characterization Reagents | CD63/CD81/CD9 antibodies | Tetraspanin detection for exosome validation | Western blot, flow cytometry characterization [25] |
| TSG101 and Alix antibodies | MVB-related protein detection | Confirm exosomal identity [72] | |
| Negative stain (phosphotungstic acid) | EM contrast enhancement | Visualization of cup-shaped morphology [78] | |
| Nanoparticle Tracking Analyzer | Size distribution and concentration | Nanosight system analysis [78] | |
| Engineering Tools | NHS-PEG-Maleimide crosslinkers | Covalent surface conjugation | Chemical modification with targeting ligands [77] |
| Electroporation systems | Membrane permeabilization for cargo loading | Nucleic acid encapsulation [75] | |
| Sonication probes | Membrane disruption for drug loading | Small molecule encapsulation [75] | |
| Lentiviral vectors for membrane protein fusions | Genetic engineering of parent cells | Stable expression of targeting ligands [77] | |
| Functional Assay Materials | Matrigel basement membrane matrix | Angiogenesis tube formation assay | In vitro endothelial network formation [72] |
| Transwell migration chambers | Cell migration and invasion assays | Chemotaxis evaluation [72] | |
| ELISA kits for cytokines (IL-6, IL-10, TNF-α) | Inflammation profiling | Immunomodulatory capacity assessment [76] | |
| Click-iT EdU proliferation assay | DNA synthesis measurement | Cell proliferation quantification [72] |
Engineering strategies for precision modification of exosome cargo and surface properties represent a transformative approach in regenerative medicine, particularly for enhancing the therapeutic potential of MSC-derived exosomes in wound healing. The integration of systematic review and meta-analysis methodologies provides robust evidence for the efficacy of native MSC-sEVs in diabetic wound models, while engineering approaches offer opportunities to further optimize these natural therapeutics. As the field advances, key challenges remain in standardizing isolation protocols, scaling up production, and navigating regulatory pathways for clinical translation. Future research directions should focus on developing more precise targeting strategies, optimizing combination cargo loading, and establishing quality control standards that will enable the transition of engineered exosome therapies from bench to bedside. With continued innovation in engineering methodologies and validation approaches, exosome-based therapies hold significant promise for addressing the persistent clinical challenge of chronic wounds.
The therapeutic use of mesenchymal stem cell-derived exosomes (MSC-exos) represents a paradigm shift in regenerative medicine, particularly for wound healing. These nanoscale vesicles exert profound effects by modulating inflammation, promoting angiogenesis, and facilitating extracellular matrix (ECM) remodeling [80] [6]. However, a critical challenge hinders their clinical translation: the rapid clearance and limited retention of free exosomes at the dynamic wound site [81]. To overcome these limitations, biomaterial-based strategies have emerged as essential enabling technologies. Hydrogels, with their highly hydrated three-dimensional networks and exceptional biocompatibility, provide an ideal platform for the sustained delivery of therapeutic exosomes [82] [81] [83]. This guide systematically compares the performance of various hydrogel and scaffold systems, providing researchers with objective data and methodologies to inform the development of next-generation wound healing therapies.
Comparative Performance of Hydrogel-Exosome Systems
The efficacy of a hydrogel-exosome complex is influenced by multiple factors, including the source of the exosomes, the composition of the hydrogel, and its physical architecture. The tables below summarize key experimental findings from recent studies.
Table 1: Comparative In Vivo Wound Healing Efficacy of Different Hydrogel-Exosome Systems
| Exosome Source | Hydrogel Type | Animal Model | Wound Closure Rate (Key Time Point) | Key Histological & Molecular Outcomes |
|---|---|---|---|---|
| ucMSC-exos [84] | Recombinant Human Collagen (RHC) | Rat full-thickness wound | Best performance among compared MSC-exos | Enhanced angiogenesis, reduced inflammation, improved collagen deposition |
| ADSC-exos [84] | Recombinant Human Collagen (RHC) | Rat full-thickness wound | Effective | Promoted blood vessel formation |
| BMSC-exos [84] | Recombinant Human Collagen (RHC) | Rat full-thickness wound | Effective | Boosted cell growth and survival |
| MSC-EVs (Cord Blood) [62] | Injectable (Local Injection) | Mouse full-cut wound | Accelerated vs. control | Reduced scar width, stimulated re-epithelialization, down-regulated TGF-β, up-regulated Wnt pathway |
| "Checks" Pattern Hydrogel [85] | Silicone-based (No exosomes) | Rat skin incision | 90.4% at Day 7 (vs. 65.1% in vehicle) | Increased Col1A protein expression at Day 14 |
Table 2: Impact of Hydrogel Micro-patterning on Wound Healing Performance [85]
| Hydrogel Surface Pattern | Wound Closure Rate (Day 7) | Time Constant (τ, Days) | Interpretation of Performance |
|---|---|---|---|
| Checks | 90.4% | 2.7 | Fastest healing; minimal fluid drainage/infection |
| Lines | 76.8% | 3.8 | Good performance |
| Waves | 78.2% | 4.0 | Good performance |
| No-shape (Flat) | 70.5% | 5.8 | Moderate improvement over control |
| Vehicle (Control) | 65.1% | 6.7 | Baseline healing rate |
Experimental Protocols for Key Assays
To ensure the reproducibility of comparative studies, detailed methodologies for critical in vitro and in vivo experiments are essential.
- Objective: To evaluate the promigratory effect of MSC-exos on human dermal fibroblast-adult cells (HDF-a).
- Procedure:
- Seed 5 × 10^5 HDF-a cells per well in a 6-well plate and culture until full confluence.
- Create a scratch wound in the cell monolayer using a sterile 200 µL pipette tip.
- Wash the well with D-PBS to remove detached cells.
- Add serum-free medium containing the test substance:
- Control: 100 µL/mL D-PBS.
- Treatment: 100 µg/mL MSC-EVs or UCB-EVs.
- Incubate the plates at 37°C in a 5% CO2 incubator.
- Capture images of the scratch at 0, 12, and 24 hours post-scratching.
- Quantitative Analysis: Use image analysis software (e.g., ImageJ) to measure the initial scratch area (A0) and the remaining area at each time point (An). Calculate the migration area percentage as:
(A0 - An)/A0 × 100.
- Objective: To assess the therapeutic efficacy of exosome-loaded hydrogels in a preclinical model.
- Procedure:
- Animal: Use 6-8 week-old male BALB/c mice or specific pathogen-free (SPF) rats.
- Wound Creation: Create full-thickness or full-cut excisional wounds on the dorsum after anaesthesia and hair removal.
- Group Allocation: Randomize animals into groups (e.g., control, hydrogel only, exosome solution, exosome-loaded hydrogel).
- Treatment Application:
- Monitoring: Document wound closure by capturing digital photographs at regular intervals (e.g., days 0, 3, 7, 14).
- Wound Closure Analysis: Calculate the wound closure rate using image analysis software.
- Tissue Harvesting: At predetermined endpoints, euthanize the animals and harvest the wound tissue and surrounding skin.
- Histological Analysis: Process tissue samples for H&E staining, Masson's trichrome staining (for collagen), and immunohistochemical staining (e.g., for CD31 to assess angiogenesis, or specific cytokines).
Signaling Pathways in Exosome-Mediated Healing
MSC-exos delivered via hydrogels promote healing through coordinated modulation of key signaling pathways. The following diagram illustrates the core mechanisms involving inflammation resolution and angiogenesis.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogues critical reagents and materials used in the featured studies for developing and testing exosome-loaded hydrogels.
Table 3: Essential Reagents and Materials for Hydrogel-Exosome Research
| Item Name | Function/Application | Specific Examples from Research |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Source of therapeutic exosomes. | Human umbilical cord MSCs (hUCMSCs) [5], Bone marrow MSCs (BMSCs) [81], Adipose-derived stem cells (ADSCs) [6]. |
| Hydrogel Polymers | Form the 3D scaffold for exosome encapsulation and sustained release. | Recombinant Human Collagen (RHC) [84], Chitosan (CS) [81], Hyaluronic Acid [16], Polyvinyl Alcohol (PVA) [83], Polyethylene Glycol (PEG) [85]. |
| Crosslinking Agents | Modify mechanical properties and degradation kinetics of hydrogels. | Methacrylate anhydride (for RHCMA hydrogel) [84], UV light with photoinitiator [84]. |
| Exosome Isolation Kits | Purify exosomes from cell culture supernatant. | Ultracentrifugation (standard method) [62] [5], Ultrafiltration, Polymer-based precipitation kits. |
| Exosome Characterization Tools | Identify and validate isolated exosomes. | Nanoparticle Tracking Analysis (NTA) for size/concentration [62] [5], Transmission Electron Microscopy (TEM) for morphology [62] [5], Western Blot for markers (CD63, TSG101) [62]. |
| Cell Lines for In Vitro Assays | Model cellular responses in wound healing. | Human Dermal Fibroblasts-adult (HDF-a) [62], Human Umbilical Vein Endothelial Cells (HUVECs) [5], NIH/3T3 fibroblasts (for biocompatibility) [84]. |
| Animal Models | Preclinical in vivo evaluation of therapeutic efficacy. | BALB/c mice [62], Sprague-Dawley (SD) rats [85] [84]. |
| Fluorescent Tracers | Label exosomes for uptake and tracking studies. | PKH67 dye [62], DID lipophilic dye [84]. |
The integration of MSC-derived exosomes with advanced hydrogel scaffolds represents a powerful and promising strategy for enhancing wound healing. Objective comparison of experimental data reveals that the therapeutic outcome is highly dependent on the specific choices of exosome source and biomaterial design. Umbilical cord-derived exosomes consistently demonstrate superior performance in promoting angiogenesis and resolving inflammation [5] [84]. Furthermore, the physical architecture of the scaffold, such as micro-patterning, can significantly influence healing kinetics by modulating the wound microenvironment [85]. Future research should focus on the development of "smart," stimulus-responsive hydrogels that can dynamically interact with the wound bed to release their cargo on demand [83]. By systematically evaluating these variables using standardized experimental protocols, researchers can accelerate the translation of these sophisticated biomaterial-based therapies from the laboratory to the clinic, ultimately improving outcomes for patients with acute and chronic wounds.
The therapeutic application of mesenchymal stem cell-derived extracellular vesicles (MSC-EVs) represents a paradigm shift in regenerative medicine, particularly for complex pathologies such as chronic wounds. However, the clinical translation of MSC-EV therapies faces significant challenges, primarily concerning the insufficient yield and variable therapeutic potency of naturally secreted EVs. Preconditioning of parent MSCs prior to EV collection has emerged as a powerful strategy to overcome these limitations. By subjecting MSCs to controlled stress conditions—including hypoxia, pharmacological stimuli, or genetic modification—researchers can enhance EV biogenesis and enrich EVs with specific bioactive molecules. This guide systematically compares the experimental performance, protocols, and mechanistic basis of major preconditioning approaches, providing critical data for optimizing EV-based therapeutic development.
Comparative Analysis of Preconditioning Strategies
The table below provides a quantitative comparison of the three primary preconditioning strategies based on recent experimental findings.
Table 1: Performance Comparison of Major MSC Preconditioning Strategies
| Preconditioning Approach | Reported EV Yield Increase | Key Therapeutic Outcomes in Wound Healing | Key Molecular Mechanisms/Components |
|---|---|---|---|
| Hypoxia | 4- to 5-fold (1% O₂) [86] | • Enhanced angiogenesis [87]• Improved collagen deposition [86]• Macrophage polarization to M2 phenotype [87]• Superior early wound closure (adult ADSCs) [50] | • HIF-1α pathway activation [87]• Upregulation of pro-angiogenic miRNAs [50] [88]• Increased VEGF, CD31 [87] |
| Pharmacological (ETH Combination) | 4- to 5-fold [86] | • Superior angiogenesis & collagen deposition [86]• Enhanced regulation of inflammation [86] | • EGF: Promotes MSC proliferation [86]• TNF-α: Drives EV biogenesis [86]• Synergistic activation of multiple pathways |
| Genetic Modification (E-selectin) | Not quantified for yield | • Accelerated wound closure [89]• Enhanced angiogenic response [89]• Stronger MSC survival/viability in wounds [89] | • Membrane-bound E-selectin expression [89]• Improved progenitor cell homing [89] |
| Platelet-Supplemented Media | Not quantified for yield | • Enhanced fibroblast proliferation & angiogenesis [90]• High concentrations of KGF, VEGF-A, PDGF-BB, IL-6, IL-7, IL-8 [90] | • Enrichment of multiple growth factors and interleukins [90] |
Detailed Experimental Protocols
Hypoxia Preconditioning Methodology
The implementation of hypoxia preconditioning requires precise environmental control and standardized culture techniques.
Detailed Protocol from Recent Studies:
- Cell Culture: Human umbilical cord MSCs (HUCMSCs) are cultured to approximately 80% confluence using standard media [87].
- Hypoxic Induction: The culture environment is maintained at 3% O₂, 5% CO₂, and 92% N₂ for 48 hours using a hypoxic incubator equipped with dual flow meters and modular oxygen monitors for precise control [87].
- Alternative Oxygen Levels: Some studies employ 1% O₂ for preconditioning, demonstrating that different oxygen concentrations can be optimized for specific MSC sources [86] [50].
- EV Collection: Following the hypoxic period, culture medium is replaced with serum-free medium, and cells are incubated for an additional 48 hours under the same hypoxic conditions before EV isolation [87].
- Control Conditions: Normoxic controls are maintained at 21% O₂, 5% CO₂, and 74% N₂ for identical durations [87].
Pharmacological Preconditioning (ETH Protocol)
The ETH (EGF, TNF-α, Hypoxia) protocol represents an integrated approach that combines pharmacological and environmental stimuli.
Orthogonal Optimization Procedure:
- Stimulator Screening: MSCs are seeded in 96-well plates (3,000 cells/well) and treated individually with various stimuli including EGF, TNF-α, VEGF, PDGF, bFGF, IGF-I, LPS, and CaCl₂ at different concentrations for 24 hours [86].
- Orthogonal Design: An L9(34) orthogonal form is selected and redesigned using the quasi-level method to optimize the doses of EGF and TNF-α, along with oxygen content [86].
- Optimal Condition Identification: Through range analysis and variance analysis of EV production per cell, the optimal preconditioning condition is identified as EGF (10 ng/mL), TNF-α (50 ng/mL), and a hypoxic environment of 1% O₂ [86].
- Validation: Each treatment is performed in triplicate to ensure statistical reliability, with EV production quantified using nanoflow cytometry after labeling with wheat germ agglutinin (WGA) [86].
Genetic Modification (E-selectin Overexpression)
Genetic modification protocols utilize viral vectors to stably enhance the therapeutic properties of MSCs.
AAV-Mediated Transduction Protocol:
- Vector Production: Murine E-selectin and GFP genes are inserted into pZac vectors and packaged into adeno-associated virus serotype DJ (AAV-DJ), which demonstrates superior transduction efficiency based on pretesting of AAV variant tropisms [89].
- MSC Transduction: A total of 1×10⁶ MSCs are transduced in 100 mm cell culture plates using AAV-DJ at a multiplicity of infection of 50,000 viral particles per cell [89].
- Expression Confirmation: GFP expression is assessed via fluorescence microscopy and flow cytometry for E-selectin expression 4-5 days post-transduction [89].
- Functional Validation: Transduced MSCs are evaluated for maintenance of trilineage differentiation capability, colony-forming efficiency, and surface marker expression to confirm retention of core MSC properties [89].
Signaling Pathways and Mechanisms
The therapeutic benefits of preconditioned MSC-EVs are mediated through specific molecular pathways that enhance wound healing processes.
Diagram 1: Signaling Pathways in Preconditioning Approaches
This diagram illustrates the core signaling pathways activated by different preconditioning strategies. Hypoxia stabilizes HIF-1α, leading to upregulation of VEGF and subsequent angiogenesis [87]. EGF primarily stimulates MSC proliferation, while TNF-α promotes EV biogenesis [86]. E-selectin modification enhances cell homing capabilities [89], and hypoxia additionally promotes the polarization of macrophages from the pro-inflammatory M1 to the anti-inflammatory M2 phenotype [87].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of preconditioning strategies requires specific reagents and materials with defined functions.
Table 2: Essential Research Reagents for Preconditioning Studies
| Reagent/Material | Function in Preconditioning | Example Specifications |
|---|---|---|
| Hypoxic Chamber | Maintains precise low-oxygen environment for preconditioning | 3% O₂, 5% CO₂, 92% N₂; with oxygen monitor [87] |
| Recombinant Human EGF | Stimulates MSC proliferation in pharmacological preconditioning | 10 ng/mL working concentration [86] |
| Recombinant Human TNF-α | Enhances EV biogenesis in pharmacological preconditioning | 50 ng/mL working concentration [86] |
| AAV-DJ Viral Vector | Efficiently delivers genetic modifications to MSCs | Serotype DJ with E-selectin insert; MOI 50,000 [89] |
| Platelet-Supplemented Media | Provides rich growth factor environment for enhanced EV production | Alternative to serum-free media for growth factor enrichment [90] |
| EV-Depleted FBS | Ensures clean EV isolation without serum contamination | Prepared by filtering standard FBS through 100-kDa MWCO filters [50] |
| Nanoflow Cytometer | Quantifies EV production after preconditioning | Used with WGA labeling for particle quantification [86] |
The strategic preconditioning of parent MSCs presents a powerful approach to amplify both the yield and therapeutic efficacy of MSC-derived extracellular vesicles for wound healing applications. Hypoxia preconditioning consistently demonstrates enhanced angiogenic potential through HIF-1α pathway activation. Combined ETH preconditioning offers a synergistic effect on EV production and regenerative capacity. Genetic modification, particularly E-selectin overexpression, improves MSC retention and wound closure rates. The selection of an optimal preconditioning strategy should be guided by the specific therapeutic goals, whether prioritizing EV yield, angiogenic potential, or modulation of the wound immune environment. Future research should address standardization of protocols and exploration of combination approaches to further advance the clinical translation of preconditioned MSC-EVs.
The translation of Mesenchymal Stem Cell-derived exosomes (MSC-exosomes) from research to clinical application represents a paradigm shift in regenerative medicine, particularly for wound healing. While a growing body of evidence, including systematic reviews and meta-analyses, confirms the therapeutic efficacy of MSC-exosomes in enhancing wound closure, reducing scar width, increasing blood vessel density, and promoting collagen deposition, their widespread clinical adoption faces significant manufacturing hurdles [22]. The scalability of production is hampered substantially by persistent challenges in maintaining consistent product quality and function across manufacturing batches. This variability poses a critical barrier to the development of standardized, reliable therapies and can significantly impact the reproducibility of preclinical and clinical outcomes [91] [92]. Understanding the sources of this variability and developing strategies to mitigate it is therefore essential for advancing the field of MSC-exosome therapeutics in wound healing.
The therapeutic potency of MSC-exosomes in wound healing is well-documented, yet their functional profile is not uniform. This variability stems from multiple factors intrinsic to their biological origin and production process.
Cell Source Heterogeneity: The tissue origin of parent MSCs significantly influences exosome characteristics. Adipose tissue, bone marrow, and umbilical cord are common sources, each yielding exosomes with distinct cargo and functional properties [22]. Furthermore, the donor-specific factors such as age, health status, and genetic background contribute to inter-individual differences in MSC populations, which are subsequently reflected in their secreted exosomes [91].
Production and Culture System Differences: The method used to differentiate induced pluripotent stem cells (iPSCs) into MSCs (iMSCs) can introduce functional inconsistencies in the resulting exosome products. Independent iMSC-EV preparations have shown variances in EV-specific protein profiles, leading to batch-to-batch functional inconsistencies [91]. The composition of the culture medium, including the use of supplements like xenogeneic serum or human platelet lysate, also critically affects exosome yield, composition, and biological activity [93].
Impact of Cell Senescence and Expansion: Primary MSCs have a limited expansion capability in vitro, and prolonged culture leads to replicative senescence. This state is characterized by reduced multipotency and metabolic changes that heavily affect the restorative properties of both MSCs and their derived exosome products [94]. While iMSCs offer an expansive growth advantage over primary MSCs, they do not inherently overcome the challenge of functional variability of the resulting exosome products [91].
Table 1: Key Sources of Batch-to-Batch Variability in MSC-Exosome Production
| Variability Factor | Impact on Exosome Product | Supporting Evidence |
|---|---|---|
| Parent MSC Source | Varies cargo (proteins, miRNAs), yield, and immunomodulatory potency. | Systematic reviews note differing efficacy in wound closure and revascularization by source [22]. |
| Donor Heterogeneity | Inter-individual differences in exosome composition and function. | Studies on primary human bone marrow MSCs show variability in immunomodulatory effects [91]. |
| Culture Conditions | Alters exosome biogenesis, cargo loading, and surface marker expression. | Senescence from long-term expansion diminishes anti-inflammatory properties of EVs [94]. |
| iPSC-Derived MSCs (iMSCs) | Batch-to-batch functional inconsistencies despite expansive growth. | iMSC-EV products displayed functional inconsistencies and varying protein profiles [91]. |
A comprehensive understanding of how different MSC sources influence exosome characteristics is vital for selecting appropriate cell lines for scalable manufacturing. The table below provides a detailed comparison based on recent meta-analyses and primary studies.
Table 2: Comparative Analysis of MSC-Exosomes from Different Cell Sources for Wound Healing
| MSC Source | Proliferation & Scalability Potential | Reported Therapeutic Strengths in Wound Healing | Key Challenges & Variability Issues |
|---|---|---|---|
| Bone Marrow (BM-MSCs) | Limited proliferation, enters senescence, restricting batch size [91] [94]. | Promotes revascularization; demonstrates robust immunomodulatory effects [22]. | Donor-dependent variability; well-documented inter-batch functional differences [91] [93]. |
| Adipose Tissue (AD-MSCs) | Accessible tissue source, but primary cells have finite expansion [22]. | Best effect on wound closure rate and collagen deposition in comparative analyses [22]. | Subject to donor variability and senescence-induced changes during scale-up. |
| Umbilical Cord (UC-MSCs) | Higher proliferative capacity compared to adult tissue-derived MSCs [93]. | Favorable angiogenic potential; used in clinical trials for conditions like dry eye and GvHD [92]. | Requires a consistent supply of donor tissue; potential inter-donor differences. |
| iPSC-Derived (iMSCs) | "Enhanced expansion potential," can achieve more population doublings [91] [94]. | Prolonged anti-inflammatory effect window; scalable cell source [91] [94]. | "Batch-to-batch functional inconsistencies" and variability in differentiation outcomes [91] [94]. |
Methodological Protocols and Their Impact on Consistency
The journey from cell culture to purified exosomes involves multiple steps, each of which can introduce variability. Standardizing these protocols is a cornerstone for achieving manufacturing consistency.
Cell Culture and Exosome Production
For clinical-grade manufacturing, it is critical to use defined, xeno-free culture media. Fetal bovine serum (FBS) is a common source of contaminating exogenous exosomes and xenobiotics. Protocols have been developed using human platelet lysate that is further processed by ultracentrifugation to deplete it of endogenous EVs and fibrinogen, thereby ensuring the purity of the manufactured exosome product [93]. For iMSC generation, one documented protocol involves maintaining iPSCs in a defined medium, then inducing MSC differentiation using a medium supplemented with a WNT activator like CHIR99021 for several days, before switching to a standard MSC medium for outgrowth and expansion [91].
Exosome Isolation and Characterization
The isolation method directly impacts exosome yield, purity, and biological integrity. A meta-analysis of wound healing studies found that 64% of preclinical studies used ultracentrifugation, while other methods included commercial kits (18%), tangential flow filtration (5%), and combinations of techniques [25]. Ultracentrifugation, while common, can cause mechanical damage and co-precipitation of contaminants [92]. Tangential Flow Filtration (TFF) is increasingly recognized for its scalability and gentler processing, resulting in higher yields and reduced albumin contamination compared to ultracentrifugation [93].
Characterization must adhere to guidelines from the International Society for Extracellular Vesicles (MISEV). This typically involves using at least two complementary techniques, such as:
- Nanoparticle Tracking Analysis (NTA): For determining particle size distribution and concentration [25] [93].
- Transmission Electron Microscopy (TEM): For visualizing exosome morphology [25].
- Western Blot: For detecting protein markers positive for exosomes (e.g., CD63, CD9, CD81, TSG101) and negative for contaminants (e.g., calnexin) [25] [93].
A analysis of studies found that 45% used a combination of Western Blot and TEM for characterization, underscoring its commonality in the field [25].
Diagram Title: Workflow for MSC-Exosome Production and Quality Control
Signaling Pathways and Functional Mechanisms in Wound Healing
MSC-exosomes accelerate wound healing by coordinating all phases of the repair process through the delivery of their cargo to recipient cells in the wound environment [25].
- Inflammation Phase: Exosomes modulate immune responses, transforming pro-inflammatory cues into regulatory signals that foster a pro-regenerative milieu. They reduce the inflammatory response by affecting various immune cells and resident tissue cells [91] [25].
- Proliferation Phase: Exosomes are rich in pro-angiogenic factors (e.g., VEGF, EGFR, FGF) that activate endothelial cells, promoting new blood vessel formation (angiogenesis) [95] [93]. They also promote fibroblast proliferation and migration, initiating extracellular matrix (ECM) deposition essential for forming new tissue [25] [96].
- Remodeling Phase: Exosomes aid in tissue remodeling by altering the ratio of matrix metalloproteinases (MMPs) and their tissue inhibitors (TIMPs), favoring a balance that leads to improved collagen organization and reduced scarring [25].
The cargo responsible for these effects includes specific miRNAs, proteins, and growth factors. For instance, exosomal miRNAs are known to regulate key signaling pathways such as Akt, Erk, and Stat3, which control cell survival, proliferation, and migration [97].
Diagram Title: Exosome-Mediated Regulation of Wound Healing Phases
The Scientist's Toolkit: Key Research Reagent Solutions
To address scalability and variability challenges, researchers are employing a suite of tools and reagents designed to standardize production and ensure quality.
Table 3: Essential Research Reagents and Tools for MSC-Exosome Studies
| Reagent/Tool | Function | Considerations for Scalability & Consistency |
|---|---|---|
| Xeno-Free Cell Culture Media | Supports MSC growth without animal-derived components. | Eliminates contaminating serum-derived EVs; critical for GMP compliance and batch-to-batch consistency [94] [93]. |
| Human Platelet Lysate (hPL) | Serum substitute for MSC culture, promotes cell proliferation. | Must be processed (e.g., ultracentrifuged) to remove endogenous EVs and fibrinogen before use [93]. |
| Tangential Flow Filtration (TFF) | Scalable method for isolating and concentrating exosomes from large volumes of conditioned media. | Gentler than ultracentrifugation; suitable for closed-system manufacturing; improves yield and reduces contamination [93]. |
| Characterization Antibodies | Detect exosomal markers (CD63, CD9, CD81, TSG101) and negative markers (Calnexin). | Essential for quality control and confirming exosome identity per MISEV guidelines across production batches [25] [93]. |
| Nanoparticle Tracking Analyzer | Measures exosome particle size and concentration. | A key tool for establishing critical quality attributes (CQAs) of the final product for lot-release criteria [93]. |
The path to clinical-grade MSC-exosome therapies for wound healing is inextricably linked to solving the dual challenges of manufacturing scalability and batch-to-batch consistency. While the therapeutic promise of MSC-exosomes is undeniable, functional variability arising from the cell source, culture conditions, and production methods remains a significant hurdle. Overcoming this requires a multi-pronged strategy: the adoption of standardized, GMP-compliant protocols from cell culture to final purification; the implementation of rigorous quality control measures and functional potency assays; and a deeper investigation into the fundamental biology that governs exosome biogenesis and cargo loading. The increasing use of scalable isolation technologies like TFF and the development of defined cell sources like iMSCs are positive steps forward. By systematically addressing these manufacturing challenges, the field can unlock the full potential of MSC-exosomes, transforming them from a promising research tool into a reliable and effective clinical treatment for wound healing.
The therapeutic application of mesenchymal stem cell-derived exosomes (MSC-exos) in wound healing represents a paradigm shift in regenerative medicine, offering a cell-free alternative with significant advantages in safety, storage, and biological activity [6] [45]. However, the translational potential of these "tiny giants of regeneration" is substantially hampered by a critical bottleneck: the profound lack of standardization in isolation methods and characterization protocols [45] [22]. This methodological heterogeneity introduces unacceptable variability in exosome quality, composition, and function, compromising experimental reproducibility and clinical outcomes.
Recent systematic reviews highlight that the field has reached a consensus on the urgent need for standardized protocols [22]. As of 2025, 64 registered clinical trials are exploring MSC-extracellular vesicle therapies, yet the absence of uniform production and characterization standards remains a fundamental barrier to clinical translation [45]. This comprehensive analysis examines the specific sources of methodological heterogeneity in MSC-exos research for wound healing, provides quantitative comparisons of experimental approaches, and outlines essential pathways toward standardization that will enable the field to progress from promising preclinical findings to reliable clinical applications.
Comparative Analysis of Isolation Methods: Yield, Purity, and Scalability
The isolation of exosomes from conditioned media represents perhaps the most significant source of methodological variability in the field. Different isolation techniques preferentially capture different subpopulations of extracellular vesicles, directly impacting downstream experimental results and therapeutic efficacy [98] [22].
Table 1: Comparative Analysis of Primary Exosome Isolation Methods
| Isolation Method | Principle | Average Particle Yield | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Ultracentrifugation (UC) | Sequential centrifugation based on size/density | 3,751-4,319 particles/cell [98] | Considered "gold standard"; widely accessible; no chemical additives [98] | Low scalability; equipment-intensive; potential particle damage [98] |
| Tangential Flow Filtration (TFF) | Size-based separation through membranes | Significantly higher than UC [98] [99] | High scalability; suitable for GMP production; gentle on vesicles [98] [99] | Membrane fouling; requires optimization [98] |
| Polymer-Based Precipitation | Polymer-induced vesicle precipitation | Variable; often higher than UC | Technical simplicity; compatible with small volumes; low equipment needs [22] | Co-precipitation of contaminants; lower purity [22] |
| Size-Exclusion Chromatography | Size-based separation in porous matrix | Moderate | High purity; preserved biological activity [22] | Sample dilution; limited loading capacity [22] |
Recent comparative studies demonstrate clear functional implications of these methodological choices. In direct comparisons, TFF has emerged as superior to ultracentrifugation for large-scale production needs, showing statistically higher particle yields while maintaining biological functionality [98]. This is particularly relevant for clinical translation, where TFF's compatibility with Good Manufacturing Practice (GMP) standards offers a significant advantage [98]. Meanwhile, research specifically focused on wound healing applications has demonstrated that isolation method selection directly impacts the therapeutic potential of the resulting exosomes, with TFF-isolated exosomes from canine adipose-derived MSCs showing enhanced capability to promote fibroblast migration and proliferation in vitro [99].
Experimental Protocols: Ultracentrifugation vs. TFF
Ultracentrifugation Protocol (as described in [98]):
- Conditioned media centrifuged at 300 × g for 10 min to remove cells
- Supernatant centrifuged at 2,000 × g for 20 min to remove dead cells
- Subsequent centrifugation at 10,000 × g for 30 min to remove cell debris
- Final ultracentrifugation at 100,000 × g for 70 min to pellet exosomes
- Exosome pellet resuspended in PBS for further analysis
Tangential Flow Filtration Protocol (as adapted from [98] [99]):
- Clarified conditioned media concentrated using TFF system with 100-500 kDa molecular weight cut-off membranes
- Diafiltration with PBS to exchange buffer and remove contaminants
- Further purification using 200 nm pore size membranes to isolate small extracellular vesicles
- Final concentration to desired volume for storage or administration
Heterogeneity in Characterization Protocols: Beyond Minimal Information Requirements
The Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines provide a framework for extracellular vesicle characterization, yet implementation varies considerably across wound healing studies, complicating cross-study comparisons and meta-analyses [22].
Table 2: Characterization Methods for MSC-Derived Exosomes in Wound Healing Research
| Characterization Parameter | Standard Techniques | Methodological Variants | Impact on Data Interpretation |
|---|---|---|---|
| Size Distribution | Nanoparticle Tracking Analysis (NTA) | Different instruments (Malvern vs. Particle Metrix); different measurement parameters [98] [99] | Affects reported exosome size ranges (typically 30-150nm) and concentration calculations [98] |
| Morphology | Transmission Electron Microscopy (TEM) | Negative staining vs. cryo-TEM; different magnification [98] | Confirms cup-shaped morphology but quality affects subjective assessment [98] |
| Surface Markers | Western Blot; Flow Cytometry | Antibody selection (CD9/CD63/CD81 combinations); detection sensitivity [98] [22] | Inconsistent marker profiles affect exosome identity verification [22] |
| Purity Assessment | Protein-to-particle ratio; contaminant markers | BCA vs. Bradford protein assays; assessment of apolipoprotein contaminants [22] | Impacts functional dose calculations and interpretation of therapeutic effects [22] |
A systematic review of 83 preclinical studies on MSC-EVs for wound healing revealed that only 79.5% fully characterized MSCs according to International Society for Cell and Gene Therapy (ISCT) criteria, while approximately 20% failed to adequately describe characterization methods for either MSCs or their secreted vesicles [22]. This characterization gap introduces significant uncertainty in meta-analyses attempting to correlate exosome properties with therapeutic outcomes.
The following diagram illustrates the current heterogeneous landscape in exosome isolation and characterization and the path toward standardization:
Pathway from Heterogeneity to Standardization in MSC Exosome Research
Impact of Culture Conditions on Exosome Heterogeneity
Beyond isolation and characterization methods, the initial culture conditions of parent MSCs significantly influence the resulting exosome profile, creating another layer of variability in wound healing studies [100] [98].
Culture Media Composition
A 2024 comparative study specifically examined how five different culture media affect the therapeutic potential of umbilical cord MSC-derived exosomes for wound healing applications [100]. The research demonstrated that while MSCs maintained similar proliferation and morphology across different media, their secreted exosomes displayed markedly different cargo profiles [100]. Notably, exosomes derived from platelet-supplemented media (DM-PLT_EXs) exhibited significantly higher concentrations of key wound-healing growth factors including keratinocyte growth factor (KGF), vascular endothelial growth factor (VEGF-A), and platelet-derived growth factor (PDGF-BB), along with elevated levels of interleukins IL-6, IL-7, and IL-8 [100]. These compositional differences directly correlated with functional superiority in promoting human skin fibroblast proliferation and stimulating angiogenesis [100].
Similar media-dependent effects were observed in studies optimizing exosome production for retinal therapies, where α-MEM medium supplemented with human platelet lysate yielded higher particle concentrations compared to DMEM-based formulations [98]. These findings collectively underscore that culture media composition represents a critical variable determining exosome efficacy in wound healing contexts.
Three-Dimensional Culture Systems
Innovative culture approaches are emerging to address scalability challenges in exosome production. Recent studies have demonstrated that transitioning from conventional two-dimensional (2D) to three-dimensional (3D) culture systems using microcarriers can increase exosome yield by 2.4-fold and concentration in conditioned medium by 3.2-fold [99]. This scalable production method yielded exosomes with enhanced purity and bioactivity, demonstrating superior capability to improve fibroblast migration, proliferation, and wound healing-related gene expression in vitro [99].
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for MSC Exosome Studies
| Reagent/Material | Function | Application Notes | References |
|---|---|---|---|
| Human Platelet Lysate | Xeno-free supplement for MSC culture | Enhances exosome production; improves wound healing factors | [100] [98] |
| Serum-Free Media Formulations | Defined culture conditions | Redances batch variability; eliminates serum-derived contaminants | [100] [99] |
| Microcarriers (3D Culture) | Scalable exosome production | Increases yield 2.4-fold; enhances bioactivity | [99] |
| TrypLE Select Enzyme | Cell passaging | Gentle cell detachment; maintains viability | [100] |
| CD9/CD63/CD81 Antibodies | Exosome characterization | Verification of exosomal identity; quality control | [98] [22] |
| TSG101 Antibody | Exosome characterization | Endosomal pathway marker; confirms biogenesis | [98] |
| Calnexin Antibody | Purity assessment | Negative marker for endoplasmic reticulum contaminants | [98] |
Standardization Pathways: Toward Reproducible Research and Clinical Translation
Overcoming the standardization barriers in MSC exosome research requires concerted efforts across multiple domains. The following workflow outlines a potential pathway for standardized exosome production and characterization specifically for wound healing applications:
Standardized Workflow for MSC Exosome Production
The standardization pathway encompasses several critical elements. First, rigorous characterization of parent MSCs according to ISCT guidelines must become mandatory, including demonstration of plastic adherence, specific surface marker expression (CD73, CD90, CD105 positive; CD45, CD34, HLA-DR negative), and trilineage differentiation potential [100] [22]. Second, implementation of MISEV2023 guidelines for exosome characterization should be universally adopted, with mandatory reporting of size distribution, morphological assessment, detection of multiple exosomal markers (CD9, CD63, CD81, TSG101), and assessment of purity through negative markers [22]. Third, functional potency assays specific to wound healing applications must be developed and standardized, including quantitative measures of fibroblast migration, angiogenesis promotion, and macrophage polarization [99] [22].
Meta-analyses of preclinical wound healing studies provide compelling evidence for the importance of standardization. These analyses reveal that specific exosome sources and administration routes yield significantly different therapeutic outcomes, with apoptotic small extracellular vesicles (ApoSEVs) showing superior wound closure outcomes compared to traditional small extracellular vesicles, and subcutaneous injection demonstrating better efficacy than topical application [22]. Without standardized protocols, however, these insights remain difficult to translate into optimized clinical applications.
The heterogeneity in isolation methods and characterization protocols represents a critical barrier hindering the progression of MSC exosome research from promising preclinical findings to reliable clinical applications in wound healing. Quantitative comparisons demonstrate that methodological choices in isolation techniques, culture conditions, and characterization approaches significantly impact both the quantity and quality of the resulting exosomes, directly influencing their therapeutic potential. The field has reached a consensus on the need for standardization, with clear pathways forward through adherence to MISEV and ISCT guidelines, adoption of scalable isolation methods like TFF, and implementation of standardized functional potency assays. Only through concerted efforts to address these standardization challenges can the full therapeutic potential of MSC-derived exosomes for wound healing be realized in consistent, reproducible, and clinically effective treatments.
The translational potential of MSC exosomes in regenerative medicine, particularly for wound healing, is profoundly influenced by storage and stability protocols. Maintaining the structural integrity, molecular cargo, and bioactivity of these nanoscale vesicles from production to administration presents a significant challenge for researchers and therapeutic developers. As evidenced by systematic reviews, high heterogeneity exists in storage methods, separation techniques, and preservation protocols across preclinical studies, underscoring the urgent need for standardization prior to clinical translation [22]. The nanoscale properties of exosomes make them exceptionally sensitive to environmental conditions, with suboptimal storage leading to particle aggregation, cargo degradation, and loss of therapeutic function [101] [102]. This guide objectively compares current preservation methodologies, evaluates their impact on bioactivity retention, and provides evidence-based protocols to ensure experimental reproducibility and therapeutic efficacy.
Impact of Storage Conditions on MSC Exosome Integrity
Temperature Considerations for Short and Long-Term Storage
Storage temperature significantly influences exosome recovery, structural integrity, and biological functionality. Evidence from systematic evaluation indicates that constant subzero temperatures at -80°C optimally preserve particle concentration, RNA content, morphology, and bioactivity for long-term preservation [101] [102]. Studies comparing temperature ranges demonstrate that exosomes from human umbilical cord mesenchymal stem cells (hUC-MSCs) maintained uniform size, integrity, and bioactivity when stored at -80°C for one month, while those stored at -20°C showed significant particle aggregation and size increases [101]. Similarly, HEK293T and MSC-derived exosomes preserved their size, concentration, morphology, and RNA/protein content better at -80°C versus -20°C for up to 26 weeks [101].
Table 1: Comparative Effects of Storage Temperatures on MSC Exosome Integrity
| Storage Temperature | Particle Concentration | Size Distribution | RNA Content | Morphology | Bioactivity |
|---|---|---|---|---|---|
| -80°C | Minimal decrease | Stable maintenance | Well-preserved | Intact membranes | High retention |
| -20°C | Moderate decrease | Significant aggregation | Partial degradation | Membrane deformation | Reduced activity |
| 4°C | Variable stability | Progressive aggregation | Rapid degradation | Structural changes | Limited retention |
| Room Temperature | Rapid decline | Substantial aggregation | Extensive degradation | Severe damage | Minimal retention |
Notably, storage at -196°C (liquid nitrogen) shows limited advantages over -80°C, with some studies reporting size reduction in exosomes from mice bone marrow MSCs stored in liquid nitrogen for one month, and less concentration loss when stored at -80°C compared to liquid nitrogen [101]. One study demonstrated membrane disruption in exosomes frozen in liquid nitrogen followed by storing at -80°C [101]. Therefore, -80°C remains the most practical and commonly recommended option for long-term exosome preservation across diverse sources, including conditioned media, biofluids, and tissue extracts.
Freeze-Thaw Cycles and Stability Implications
Multiple freeze-thaw cycles present a significant challenge to exosome integrity. Evidence consistently demonstrates that subjecting exosomes to repeated freezing and thawing decreases particle concentrations, reduces RNA content, impairs bioactivity, and increases exosome size and aggregation [101] [102]. Electron microscopy reveals vesicle enlargement, fusion, and membrane deformation after exposure to multiple freeze-thaw cycles [101]. Studies on exosomes encapsulated in microneedles (EV@MN) made of hyaluronic acid demonstrated maintained integrity through up to 10 freeze-thaw cycles, while those in PBS showed significant degradation [102]. To maximize stability, researchers should aliquot exosomes in single-use portions to avoid repeated freezing and thawing, and implement rapid freezing procedures to minimize ice crystal formation that can damage exosome membranes.
Stabilization Strategies and Cryoprotectants
Comparative Evaluation of Cryoprotectants
The addition of stabilizing agents represents a crucial strategy for maintaining exosome integrity during storage. Systematic comparisons of cryoprotectants reveal significant differences in their protective efficacy. Research evaluating sEVs and lEVs derived from Glioblastoma U87 cells stored at -80°C for 10 weeks demonstrated that trehalose (25 mM) effectively maintained exosome stability based on morphology, concentration, size, protein amount, RNA content, and drug delivery efficiency [103]. Similarly, studies incorporating trehalose and cellulose into microneedle formulations enabled exosomes to maintain count, size, and membrane integrity for 12 months at room temperature [102].
Table 2: Efficacy Comparison of Exosome Cryoprotectants and Stabilizers
| Cryoprotectant | Mechanism of Action | Concentration | Preservation Efficacy | Potential Limitations |
|---|---|---|---|---|
| Trehalose | Replaces water molecules, interacts with phospholipid head groups | 25 mM | High stability maintenance, preserves drug delivery capability | May require formulation optimization |
| DMSO | Penetrates membranes, reduces ice formation | 6% | Moderate protection | Potential cytotoxicity concerns |
| Glycerol | Penetrates intracellular structures, reduces ice formation | 30% | Variable effectiveness | May affect downstream applications |
| Hyaluronic Acid | Forms protective matrix in microneedles | Varies | Excellent bioactivity preservation | Application-specific formulation |
| PBS Alone | Standard buffer | N/A | Limited protection, rapid degradation | Not recommended for long-term storage |
The non-permeable nature of trehalose protects lipid-based particles by replacing water molecules surrounding the lipid head groups through interactions between the phospholipid head groups and the hydroxyl (OH) groups of the sugar, thereby preventing lipid particle aggregation [103]. This mechanism differs from permeable cryoprotectants like glycerol and DMSO, which penetrate the cell membrane and protect intracellular structures by reducing ice formation. Notably, storage in native biofluids offers improved stability over purified exosomes in buffers, suggesting that some native components may provide natural stabilization [101] [102].
Advanced Formulation Strategies
Innovative formulation approaches have demonstrated remarkable success in preserving exosome stability under challenging conditions. Encapsulation of exosomes in hyaluronic acid-based microneedles (EV@MN) enabled preservation at -20°C, +4°C, and +25°C for six months with negligible decrease in concentration and over 99% protein activity retention when stored at 4°C or -20°C [102]. This contrasts sharply with exosomes in PBS, which lost protein activity at any temperature within 2 weeks. The EV@MN formulation also maintained exosome functions in cell proliferation and fibroblast migration assays for up to six months [102]. Similarly, engineered exosomes loaded into microneedles supplemented with trehalose and cellulose maintained intact membranes and stability for 12 months at room temperature [102]. These advanced formulation strategies represent promising approaches for enhancing exosome shelf-life and facilitating clinical translation.
Experimental Protocols for Stability Assessment
Standardized Methodology for Stability Evaluation
Comprehensive assessment of exosome stability requires a multi-parameter approach evaluating physicochemical properties and functional characteristics. The following protocol outlines a standardized methodology for evaluating storage impact on MSC exosomes:
Sample Preparation and Storage Conditions
- Isolate MSC exosomes using preferred method (ultracentrifugation, size-exclusion chromatography, or tangential flow filtration)
- Divide into aliquots for different storage conditions: -80°C, -20°C, 4°C, and room temperature
- Prepare samples with different cryoprotectants: PBS (control), 25mM trehalose, 6% DMSO, 30% glycerol
- Implement rapid freezing procedures for subzero storage
- Avoid repeated freeze-thaw cycles by using single-use aliquots
Physicochemical Characterization
- Particle Concentration and Size Distribution: Analyze using Nanoparticle Tracking Analysis (NTA) with instruments such as ZetaView PMX 110 system [24]
- Morphological Assessment: Utilize Transmission Electron Microscopy (TEM) with negative staining to visualize membrane integrity and structural preservation [24]
- Molecular Marker Preservation: Confirm via immunoblotting assays for CD9, CD63, ALIX, and calnexin (purity indicator) [24]
- Zeta Potential Measurement: Assess surface charge and colloidal stability using Dynamic Light Scattering (DLS)
Content and Functional Integrity Assessment
- Protein Content Quantification: Perform using bicinchoninic acid (BCA) assay
- RNA Integrity Evaluation: Isolate RNA and assess quality via spectrophotometry or bioanalyzer
- Bioactivity Testing: Conduct functional assays relevant to intended application (e.g., cell proliferation, migration, angiogenesis assays for wound healing applications)
Workflow for Systematic Stability Assessment
The following diagram illustrates the comprehensive workflow for evaluating exosome stability under different storage conditions:
Implications for Wound Healing Applications
Storage Considerations for Optimal Therapeutic Outcomes
The preservation of bioactivity is particularly crucial for MSC exosomes intended for wound healing applications, where specific therapeutic mechanisms must be maintained. Systematic reviews indicate that apoptotic small extracellular vesicles (ApoSEVs) show better efficacy in wound closure outcome and collagen deposition compared to apoptotic bodies (ApoBDs) and small extracellular vesicles (sEVs), while sEVs display better performance in revascularization [22]. Among frequently used routes of administration, subcutaneous injection displayed greater improvement in wound closure, collagen deposition, and revascularization compared to dressing/covering approaches [22]. These functional specializations underscore the importance of preserving exosome subpopulations with distinct therapeutic properties through appropriate storage conditions.
For wound healing applications, maintenance of specific bioactive cargo is essential. MSC exosomes contain more than 304 proteins and 150 microRNAs that contribute to tissue recovery by maintaining and recruiting endogenous stem cells, inhibiting apoptosis, regulating the immune system, and stimulating angiogenesis [104]. The preservation of these components during storage directly correlates with therapeutic efficacy in preclinical wound models. Furthermore, among easily accessible MSC sources, ADSCs demonstrated the best effect in wound closure rate and collagen deposition, while BMMSCs displayed better performance in revascularization [22], suggesting that storage optimization may need to be tailored to specific exosome sources and intended therapeutic applications.
Pathway of Storage Impact on Wound Healing Efficacy
The following diagram illustrates how storage conditions influence the therapeutic efficacy of MSC exosomes in wound healing applications:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Exosome Storage and Stability Studies
| Reagent / Material | Function / Application | Considerations for Use |
|---|---|---|
| Trehalose | Non-permeable cryoprotectant that stabilizes lipid bilayers | Effective at 25mM concentration; interacts with phospholipid head groups |
| Dimethyl Sulfoxide (DMSO) | Permeable cryoprotectant that reduces ice crystal formation | Use at 6% concentration; potential cytotoxicity concerns |
| Glycerol | Penetrating cryoprotectant for intracellular protection | Test at 30% concentration; may impact downstream applications |
| Hyaluronic Acid | Biocompatible polymer for microneedle encapsulation | Provides protective matrix; application-specific formulation needed |
| Phosphate-Buffered Saline (PBS) | Standard suspension buffer for biological specimens | Limited protective properties alone; requires cryoprotectant additives |
| Sucrose | Disaccharide cryoprotectant for membrane stabilization | Similar mechanism to trehalose; concentration optimization needed |
| Size Exclusion Chromatography Materials | Purification of exosomes from contaminants | Improves sample purity before storage; reduces degradative enzymes |
The preservation of MSC exosome bioactivity during storage is a critical consideration for both research reproducibility and clinical translation in wound healing applications. Evidence consistently supports -80°C storage with appropriate cryoprotectants like trehalose as the current optimal approach for maintaining exosome integrity. The avoidance of multiple freeze-thaw cycles through proper aliquoting and the implementation of advanced formulation strategies such as hyaluronic acid encapsulation further enhance stability. As the field progresses toward standardized protocols, researchers should comprehensively document and report storage conditions to enable meaningful comparisons across studies and accelerate the therapeutic development of MSC exosomes for wound healing and other regenerative applications.
Evidence Synthesis and Comparative Efficacy: MSC Exosomes Versus Conventional Therapies
The therapeutic landscape of regenerative medicine has witnessed a paradigm shift from stem cell-based therapies toward the use of their secreted factors, particularly mesenchymal stem cell-derived exosomes (MSC-exosomes). As nanoscale extracellular vesicles, these exosomes mediate intercellular communication by transferring bioactive molecules like proteins, lipids, and nucleic acids, thereby orchestrating tissue repair [105]. This meta-analysis synthesizes evidence from preclinical studies to evaluate the efficacy of MSC-exosomes in improving wound closure rates and histological outcomes, providing a critical appraisal of their potential as a cell-free therapeutic alternative.
Systematic reviews and meta-analyses of controlled preclinical animal studies provide robust evidence supporting the therapeutic efficacy of MSC-exosomes in wound healing.
A systematic review of 51 rodent studies found that exosome treatment resulted in significantly higher wound closure rates, with the most substantial wound healing efficacy observed at day 7 (odds ratio: 1.82, 95% CI [0.69, 2.95]) and day 14 (odds ratio: 2.29, 95% CI [0.01, 4.56]) post-administration [25]. These exosomes were reported to regulate all phases of skin wound healing—inflammation, proliferation, and remodeling—primarily through the actions of circulating microRNA [25].
A more recent and comprehensive meta-analysis of 83 preclinical studies further quantified these benefits across multiple wound healing parameters, as summarized in Table 1 [22].
Table 1: Overall Efficacy of MSC Exosomes in Preclinical Wound Models
| Outcome Measure | Standardized Mean Difference (SMD) | 95% Confidence Interval | Number of Studies |
|---|---|---|---|
| Wound Closure Rate | -2.923 | [-3.570, -2.277] | 71 |
| Scar Width | -2.381 | [-3.352, -1.410] | 10 |
| Blood Vessel Density | 2.800 | [2.192, 3.408] | 47 |
| Collagen Deposition | 2.911 | [2.237, 3.585] | 46 |
The consistent, statistically significant SMDs across these key outcomes demonstrate that MSC-exosome treatment not only accelerates wound closure but also enhances the quality of healing by promoting angiogenesis and collagen deposition, while reducing scar formation [22].
Comparative Analysis of MSC Exosome Applications
The therapeutic efficacy of MSC-exosomes is not uniform but is influenced by factors such as the vesicle type, cellular origin of MSCs, and administration route.
Efficacy by Exosome Type
While most studies investigate small extracellular vesicles (sEVs), often termed exosomes, emerging evidence highlights the potent effects of apoptotic extracellular vesicles (ApoEVs). As shown in Table 2, ApoEVs, particularly apoptotic small EVs (ApoSEVs), demonstrate superior performance in certain aspects of wound healing compared to traditional sEVs [22].
Table 2: Comparative Efficacy of Different Extracellular Vesicle Types
| Vesicle Type | Wound Closure Outcome | Collagen Deposition | Revascularization |
|---|---|---|---|
| ApoSEVs | Best efficacy | Best efficacy | - |
| ApoBDs | Moderate efficacy | Moderate efficacy | - |
| sEVs (Exosomes) | Good efficacy | Good efficacy | Better than ApoEVs |
Efficacy by MSC Source and Administration Route
The therapeutic effect varies significantly depending on the tissue source of the parent MSCs and how the exosomes are delivered.
- MSC Source: Among commonly used sources, adipose-derived MSCs (ADSCs) demonstrated the best effect on wound closure rate and collagen deposition. Conversely, bone marrow-derived MSCs (BMMSCs) showed superior performance in revascularization [22].
- Administration Route: Subcutaneous injection of exosomes led to greater improvement in wound closure, collagen deposition, and revascularization compared to topical application via dressing or covering [22].
Experimental Data and Outcomes
Quantitative Synthesis of Wound Closure Rates
The meta-analysis of 71 studies provided a definitive quantitative synthesis, revealing a pooled SMD of -2.923 (95% CI: -3.570, -2.277) for wound closure rate favoring MSC-exosome treatment over controls [22]. This large, negative SMD indicates a significant and substantial reduction in wound size and time to closure in exosome-treated groups. The analysis included studies across both diabetic and non-diabetic animal models, demonstrating consistent therapeutic effects.
Histological and Tissue-Level Outcomes
Beyond macroscopic wound closure, MSC-exosomes significantly improve key histological parameters that define healing quality:
- Angiogenesis: A pooled SMD of 2.800 (95% CI: 2.192, 3.408) from 47 studies confirms that MSC-exosomes strongly promote the formation of new blood vessels, a critical process for delivering oxygen and nutrients to the regenerating tissue [22].
- Collagen Deposition and Organization: The meta-analysis found a pooled SMD of 2.911 (95% CI: 2.237, 3.585) for collagen deposition, indicating enhanced and more organized extracellular matrix synthesis, which contributes to improved tensile strength of healed tissue [22].
- Scar Formation: Data from 10 studies demonstrated a significant reduction in scar width with an SMD of -2.381 (95% CI: -3.352, -1.410), suggesting that exosome therapy promotes a more regenerative, less fibrotic healing process [22].
Mechanisms of Action: Signaling Pathways
MSC-exosomes orchestrate wound healing by modulating multiple cellular activities and signaling pathways across different phases of repair. The diagram below illustrates the core mechanisms through which MSC-exosomes promote skin wound healing.
Mechanistic Pathway of MSC-Exosomes in Wound Healing
The therapeutic effects are primarily mediated by exosomal cargo, especially microRNAs (miRNAs), which regulate gene expression in recipient cells [25]. During the inflammation phase, exosomes modulate immune cells to reduce the inflammatory response [25]. In the proliferation phase, they activate endothelial cells and fibroblasts to promote angiogenesis and initiate extracellular matrix (ECM) deposition [25]. During the remodeling phase, exosomes alter the ratio of matrix metalloproteinases (MMPs) to their tissue inhibitors (TIMPs), favoring improved ECM organization and reduced scarring [25].
Furthermore, the discovery of the GAS6-AXL signaling pathway, which is highly active in oral mucosa and enables scarless healing, provides a specific molecular target. Preclinical studies have shown that stimulating this pathway in skin wounds can improve healing quality [106].
Experimental Models and Methodologies
Common Preclinical Wound Models
The evidence synthesized in this analysis is derived from well-established in vivo models:
- Animal Species: The majority of studies used mice (73.5%) or rats (26.5%) [22].
- Wound Types: Full-thickness excisional wounds were the most prevalent model (90.4%), primarily created on the dorsal surface. Other models included burn wounds, diabetic foot ulcers, and scleroderma models [22].
- Diabetic Models: Both chemically-induced (streptozotocin) and genetic (db/db mice) diabetic models were utilized to simulate impaired healing, representing type 1 and type 2 diabetes, respectively [22].
Standardized Experimental Workflow
A typical preclinical study evaluating MSC-exosomes follows a standardized workflow, from vesicle preparation to outcome assessment, as illustrated below.
Preclinical Study Workflow for MSC-Exosomes
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for MSC-Exosome Wound Healing Research
| Reagent/Material | Function/Purpose | Common Examples/Specifications |
|---|---|---|
| MSC Culture Media | Expansion of mesenchymal stem cells | Serum-free media, often with defined supplements and exosome-depleted FBS |
| Isolation Kits | Extraction of exosomes from conditioned media | Commercial kits based on precipitation or size-exclusion chromatography |
| Ultracentrifuge | Gold-standard isolation method; sequential centrifugation | Requires fixed-angle or swinging-bucket rotors capable of ≥100,000× g |
| Characterization Antibodies | Detection of exosomal surface markers for validation | Anti-CD63, Anti-CD9, Anti-CD81, Anti-TSG101; Purity check: Anti-Calnexin |
| Animal Wound Model | In vivo testing platform | Mouse/rat dorsal excisional wound, diabetic (db/db or STZ-induced) models |
| Nanoparticle Tracking Analyzer | Size distribution and concentration analysis of exosomes | Instruments like ZetaView PMX 110 (Particle Metrix) |
| Histology Reagents | Assessment of tissue morphology and outcomes | H&E staining (epidermal thickness), Masson's Trichrome (collagen), CD31 (vessels) |
This meta-analysis provides compelling evidence that MSC-exosomes significantly enhance both the speed and quality of wound healing in preclinical models. The quantitative synthesis demonstrates their robust effects on wound closure rates, angiogenesis, collagen deposition, and scar reduction. The efficacy is influenced by specific experimental factors, including the type of extracellular vesicle, source of MSCs, and route of administration.
Despite the promising results, significant heterogeneity in methodologies and reporting practices exists across studies [25] [22]. Future research should prioritize standardization in exosome isolation, characterization, and dosing, alongside exploration in large animal models to better bridge the translational gap to clinical applications [107]. The mechanistic insights gained, particularly the role of exosomal miRNAs and specific pathways like GAS6-AXL, offer exciting avenues for developing targeted therapeutic strategies for impaired wound healing.
Mesenchymal stem cell-derived exosomes (MSC-Exos) have emerged as a promising cell-free therapeutic strategy in regenerative medicine, particularly for wound healing and tissue repair. These nanoscale extracellular vesicles transfer proteins, lipids, and nucleic acids from their parental cells to recipient cells, mediating complex intercellular communication. As the field progresses toward clinical translation, understanding the nuanced efficacy profiles of exosomes derived from different MSC sources—primarily adipose tissue (ADSC-Exos), umbilical cord (hUCMSC-Exos), and bone marrow (BMSC-Exos)—becomes paramount for researchers and drug development professionals. This guide provides a systematic, evidence-based comparison of these sources, highlighting their distinctive mechanistic pathways, therapeutic strengths, and appropriate experimental contexts to inform preclinical research design.
Comparative Efficacy Profiles of MSC Exosomes
The therapeutic potential of MSC exosomes varies significantly based on their tissue of origin, which influences their molecular cargo and functional properties. The table below provides a detailed comparison of the three primary MSC exosome types.
Table 1: Comprehensive Efficacy Profile of MSC Exosomes from Different Sources
| Efficacy Parameter | Adipose (ADSC-Exos) | Umbilical Cord (hUCMSC-Exos) | Bone Marrow (BMSC-Exos) |
|---|---|---|---|
| Key Strengths | Superior scar inhibition & re-epithelialization [108] | Potent angiogenic & immunomodulatory effects [5] [48] | Enhanced osteogenesis & fracture healing [109] |
| Wound Closure Rate | ≈95% (1µg dose, POD 14) [108] | Significantly accelerated [5] [48] | Primarily studied in bone healing [109] |
| Scar Formation | ↓ Scar width, ↓ epidermal thickening [108] | Inhibits scarring via TGF-β/Smad pathway [5] | Data limited for dermal scarring |
| Collagen Modulation | Promotes Type III collagen expression [108] | Promotes organized ECM formation [5] | - |
| Angiogenic Potential | Moderate | High (stimulates HUVEC tube formation) [5] [48] | Promotes vascularization in bone [109] |
| Immunomodulation | Reduces TNF-α, IL-6, promotes M1-to-M2 shift [108] | Strong anti-inflammatory, induces M2 polarization [5] [48] | Immunosuppressive properties [105] |
| Bone Regeneration | - | - | Improves fracture healing via metabolic reprogramming [109] |
| Key Mechanisms | 14-3-3 zeta-YAP-Hippo pathway, EMP in prolif KC [108] | miRNA-mediated, targets ULK2, COL19A1, IL6ST [48] | HIF-1 signaling pathway, metabolic reprogramming [109] |
| Advantages for Research | Abundant tissue source, easy isolation, minimal ethical concerns [110] | Non-invasive sourcing, low immunogenicity, high proliferative rate [5] [48] | Gold standard for osteogenic research [109] |
Detailed Experimental Protocols and Methodologies
To ensure the reproducibility of research findings, this section outlines the standard experimental workflows for evaluating MSC exosome efficacy, from isolation to functional validation.
Standardized Isolation and Characterization
Consistent exosome isolation and characterization are fundamental for comparative studies. The following workflow illustrates the core process.
Figure 1: Basic workflow for MSC exosome isolation via ultracentrifugation, the most common method for research purposes [108] [5] [109].
Core Characterization Techniques:
- Nanoparticle Tracking Analysis (NTA): Utilizes instruments like the ZetaView PMX 110 to determine the size distribution and concentration of exosomes in suspension, confirming a profile of ~30-150 nm [5] [24] [109].
- Transmission Electron Microscopy (TEM): Employed for morphological analysis, verifying the classic spherical, cup-shaped morphology of exosomes under high resolution [5] [24].
- Immunoblotting (Western Blot): Used to confirm the presence of positive exosome markers (e.g., CD9, CD63, CD81, Alix, TSG101) and the absence of negative markers (e.g., Calnexin, an endoplasmic reticulum protein) to ensure purity [108] [24] [109].
In Vitro Functional Assays
- Cell Proliferation/Migration (Scratch Assay): To assess the pro-regenerative effects on skin cells, a scratch is created in a confluent monolayer of human skin fibroblasts (HSFs) or other relevant cell types. The closure of this scratch, when treated with MSC-Exos, is monitored and quantified over 24-48 hours and compared to controls [5] [48].
- Tube Formation Assay: To evaluate angiogenic potential, human umbilical vein endothelial cells (HUVECs) are seeded on a basement membrane matrix (e.g., Matrigel). The promotion of tubular network structures by hUCMSC-Exos is quantified by measuring total tube length, number of branches, or junctions [5] [48].
In Vivo Wound Healing Models
- Mouse Dorsal Splint Wound Model: A full-thickness excisional wound (e.g., 10 mm in diameter) is created on the dorsum of anesthetized mice. A splint is placed around the wound to prevent contraction, favoring healing by re-epithelialization, which more closely mimics human healing [108].
- Intervention: Test groups receive topical application of PBS, positive control (e.g., aFGF), or different MSC-Exos (e.g., 1 µg in PBS) at regular intervals [108].
- Outcome Measures:
- Wound Closure Rate: Digital photography and planimetry to calculate the percentage reduction in wound area over time, typically up to Postoperative Day (POD) 14 [108].
- Histological Analysis: Harvested tissue sections are stained with Hematoxylin and Eosin (H&E) for evaluating epidermal architecture and Masson's Trichrome for collagen deposition and organization. Scar width and epidermal thickness are key quantitative metrics [108].
- Immunohistochemical (IHC) Staining: Used to localize and quantify specific proteins in wound tissue, such as Ki67 (proliferation), α-SMA (myofibroblasts), CD68 (M1 macrophages), and CD206 (M2 macrophages) [108].
Key Signaling Pathways and Mechanisms
The distinct therapeutic profiles of MSC exosomes are governed by their action on specific molecular pathways.
ADSC-Exos: Targeting Scarless Healing
hADSC-Exos promote scar-free healing by modulating epithelial-mesenchymal plasticity (EMP) in proliferating keratinocytes, a process regulated by the 14-3-3 zeta-YAP-Hippo signaling axis [108].
Figure 2: ADSC-Exos mechanism for scar inhibition via the 14-3-3 zeta-YAP-Hippo pathway [108].
hUCMSC-Exos: Orchestrating Regeneration via miRNA
hUCMSC-Exos exert their potent effects by delivering a rich cargo of microRNAs (miRNAs) to recipient cells, such as fibroblasts and endothelial cells, thereby regulating key genes involved in inflammation and angiogenesis [5] [48].
Figure 3: hUCMSC-Exos function through miRNA-mediated regulation of target genes [5] [48].
BMSC-Exos: Driving Bone Repair
BMSC-Exos facilitate fracture healing by reprogramming the metabolic landscape of recipient cells at the injury site, activating critical pathways for bone formation [109].
Figure 4: BMSC-Exos promote bone repair through metabolic reprogramming [109].
The Scientist's Toolkit: Essential Research Reagents
This table catalogs key reagents and their applications for investigating MSC exosomes, based on methodologies from the cited literature.
Table 2: Essential Reagents for MSC Exosome Research
| Reagent / Material | Primary Function in Research | Example Application |
|---|---|---|
| DMEM/F12 Medium | Culture and expansion of MSCs. | Baseline nutrient medium for cell growth [109]. |
| Fetal Bovine Serum (FBS) | Provides essential growth factors for cell culture. | Standard component of complete cell culture media [109]. |
| Exosome-Depleted FBS | Used for conditioning media for exosome production. | Prevents contamination with bovine exosomes during collection [109]. |
| Dulbecco's PBS (D-PBS) | Washing cells and diluting exosomes for application. | Buffer for in vitro and in vivo experiments [5] [24]. |
| Trypsin-EDTA | Detaching adherent cells for passaging. | Standard reagent for cell culture [109]. |
| Antibody Panel (CD73, CD90, CD105) | Confirming MSC phenotype via flow cytometry. | Positive marker identification for MSCs [108]. |
| Antibody Panel (CD9, CD63, CD81, Alix, TSG101) | Characterizing exosomes via Western Blot. | Positive marker identification for exosomes [24] [109]. |
| Anti-Calnexin Antibody | Assessing exosome purity via Western Blot. | Negative marker (checks for cellular contaminants) [24]. |
| Primary Antibodies (Ki67, α-SMA, CD68, CD206) | Immunohistochemical staining of wound tissues. | Analyzing cell proliferation, myofibroblasts, and macrophage polarization in vivo [108]. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | In vitro model for angiogenesis assays. | Tube formation assay to test pro-angiogenic effects [5] [48]. |
| Human Skin Fibroblasts (HSFs) | In vitro model for dermal repair studies. | Scratch (migration) and proliferation assays [5] [48]. |
| Balb/c or C57BL/6 Mice | In vivo model for wound healing studies. | Creating dorsal splint or other wound models [108] [24]. |
| Imiquimod (IMQ) Cream | Inducing psoriatic skin inflammation in mice. | Modeling inflammatory dermatosis for therapy testing [24]. |
This systematic comparison elucidates that ADSC-Exos, hUCMSC-Exos, and BMSC-Exos possess distinct and complementary efficacy profiles. ADSC-Exos demonstrate superior efficacy in promoting scarless wound healing by specifically modulating keratinocyte behavior. hUCMSC-Exos excel in orchestrating the inflammatory and angiogenic phases of repair, making them ideal for complex or chronic wounds. BMSC-Exos are the foremost choice for musculoskeletal regeneration, particularly in bone fracture models. The selection of an exosome source for preclinical research should be guided by the primary therapeutic target—be it fibrosis inhibition, immunomodulation, or osteogenesis—and validated using the standardized experimental frameworks outlined herein.
The pursuit of advanced therapeutic strategies for wound healing represents a critical frontier in regenerative medicine. Among the most promising candidates are mesenchymal stem cell (MSC) exosomes, which are nano-sized extracellular vesicles that mediate the paracrine effects of their parent cells. This review systematically benchmarks MSC exosomes against two established therapeutic classes—growth factors and cell-based therapies—within the context of wound healing. MSC exosomes emerge as a novel "cell-free" therapy, boasting a unique cargo of proteins, lipids, and nucleic acids that can modulate inflammation, promote angiogenesis, and stimulate tissue regeneration [111] [23]. This analysis synthesizes current preclinical and clinical evidence to objectively evaluate the comparative performance, mechanisms, and practical applications of these therapeutic modalities, providing a foundation for informed decision-making among researchers and drug development professionals.
Fundamental Concepts and Therapeutic Profiles
MSC Exosomes: The Paracrine Mediators
MSC exosomes are vesicles 30-150 nm in diameter, originating from the endosomal pathway and released upon fusion of multivesicular bodies with the plasma membrane [111]. They are defined by their specific size, lipid bilayer membrane, and characteristic surface markers (e.g., CD9, CD63, CD81) [111]. Their therapeutic utility in wound healing stems from their role as natural carriers of bioactive molecules, including growth factors, cytokines, and various genetic materials such as microRNA (miRNA) [5] [23]. These vesicles facilitate intercellular communication by transferring their cargo to recipient cells, such as fibroblasts and keratinocytes, thereby influencing key processes like cell proliferation, migration, and differentiation [112] [23]. A significant advantage of exosomes is their status as a cell-free therapeutic, which circumvents many safety concerns associated with whole-cell transplantation, such as the risk of immune rejection or tumorigenicity [111].
Growth Factors: The Signaling Proteins
Growth factors are soluble signaling proteins that bind to specific receptors on target cells, activating intracellular cascades that drive processes essential for wound healing, such as cell proliferation and migration [23]. Clinically used growth factors, like recombinant human platelet-derived growth factor (rhPDGF), function by supplementing the wound microenvironment with concentrated signals to directly stimulate tissue repair. Their mechanism is inherently ligand-receptor based, making them potent but often narrowly focused in their action.
Cell-Based Therapies: The Living Agents
Cell-based therapies, particularly those utilizing MSCs, involve the administration of living cells directly into the wound site. These cells are multipotent, capable of differentiating into various mesodermal lineages, and contribute to healing through two primary mechanisms: direct differentiation into tissue-specific cells (e.g., keratinocytes) and, predominantly, through potent paracrine signaling [113]. It is now understood that a significant portion of their therapeutic effect is mediated by the secreted factors, including exosomes [113] [23]. However, the use of whole cells introduces complexities related to cell survival, engraftment, potential immune reactions, and logistical challenges in storage and handling.
Table 1: Core Characteristics of Therapeutic Modalities for Wound Healing.
| Characteristic | MSC Exosomes | Growth Factors | Cell-Based Therapies (MSCs) |
|---|---|---|---|
| Nature | Nano-sized extracellular vesicles (30-150 nm) | Soluble signaling proteins | Living, whole cells |
| Key Mechanism | Transfer of multi-molecular cargo (proteins, lipids, miRNAs) to recipient cells | Ligand-receptor binding to activate intracellular signaling pathways | Direct differentiation and paracrine secretion of bioactive factors |
| Therapeutic Cargo | Proteins, miRNAs, mRNAs, lipids (complex, multi-faceted) | Single or defined protein mixtures (targeted) | Complex secretome (growth factors, cytokines, exosomes) |
| Production Complexity | High (involves cell culture, vesicle isolation, and purification) | Low (recombinant protein production) | Moderate to High (cell expansion, quality control) |
| Storage & Stability | Generally stable, may be lyophilized [63] | Typically require refrigeration; stability varies | Often requires cryopreservation; limited shelf-life |
| Immunogenicity | Generally low | Can be immunogenic | Low to moderate (depending on source and allo-/auto- logous nature) |
Comparative Performance and Efficacy
Preclinical Evidence in Wound Healing
Preclinical studies provide direct head-to-head and indirect comparisons of the therapeutic potential of these agents. MSC exosomes have demonstrated robust efficacy in accelerating wound closure, enhancing re-epithelialization, promoting angiogenesis, and modulating inflammation across various animal models.
A study on umbilical cord blood-derived MSC extracellular vesicles (MSC-EVs) demonstrated their ability to significantly promote the proliferation and migration of human dermal fibroblasts in vitro. In a mouse model of full-thickness skin wounds, local injection of these MSC-EVs accelerated wound closure, stimulated angiogenesis, and enhanced the formation of the extracellular matrix. Spatial transcriptomics analysis further revealed that the treatment reduced the expression of myofibroblast marker genes and modulated key pathways, namely reducing TGF-β signaling and increasing Wnt signaling, which is associated with reduced scar formation [62].
Similarly, exosomes derived from human umbilical cord MSCs (hUCMSC-Exos) were shown to be internalized by human skin fibroblasts (HSFs) and human umbilical vein endothelial cells (HUVECs), significantly promoting their proliferation and migration. In skin wound models, hUCMSC-Exos accelerated healing by reducing inflammation and stimulating angiogenesis [5].
Notably, a comparative study involving plant-derived exosomes highlighted the broader potential of exosome-based therapeutics. Injection of plant-based exosomes into rat skin wounds resulted in a significantly enhanced healing response, characterized by increased epithelial thickness, greater and more organized collagen deposition, and a substantial reduction in inflammatory cell infiltration compared to the control group [63].
Clinical and Meta-Analysis Evidence
The transition from preclinical models to clinical application is underway, with meta-analyses beginning to consolidate evidence for efficacy.
A meta-analysis focusing on chronic kidney disease (CKD) demonstrated the systemic therapeutic potential of MSC-derived exosomes (MSC-EXOs). The analysis of 15 preclinical and 6 clinical studies concluded that MSC-EXOs were effective in improving renal function, attenuating tubular injury, inflammation, apoptosis, and fibrosis. Specifically, treatment was associated with significant reductions in blood urea nitrogen (BUN) and serum creatinine (SCR) levels, underscoring their promise as a viable and secure alternative to cell-based therapies [114].
In the context of complex wound healing, a systematic review and meta-analysis evaluated MSC-based therapies for perianal fistulizing Crohn's disease. The analysis, which included 25 studies, found that local injection of MSC therapies led to a combined remission rate of 57.9% at 6 months, demonstrating a significant effect compared to placebo. The review noted that both adipose-derived stem cells (ASCs) and bone marrow-derived stem cells (BMSCs) were effective, with no clear superiority demonstrated between them [115]. This reinforces the role of the paracrine mechanism, in which exosomes are key mediators.
Table 2: Summary of Key Efficacy Outcomes from Meta-Analyses and Systematic Reviews.
| Therapeutic Agent | Disease / Condition Model | Key Reported Efficacy Outcomes | Source Type |
|---|---|---|---|
| MSC Exosomes (MSC-EXOs) | Chronic Kidney Disease | Significant improvement in renal function; reduction in BUN and SCR levels; attenuation of inflammation, apoptosis, and fibrosis. | Meta-analysis of 15 preclin. & 6 clin. studies [114] |
| MSC-Based Therapies (Cell-Based) | Perianal Fistulizing Crohn's Disease | Combined remission rate of 57.9% at 6 months; significant effect over placebo. | Meta-analysis of 25 prospective studies [115] |
| MSC-EVs / Exosomes | Skin Wound Healing | Accelerated wound closure, promoted proliferation/migration of fibroblasts/endothelial cells, stimulated angiogenesis, reduced inflammation and scar width. | Preclinical Studies [62] [5] |
Experimental Protocols and Methodologies
Standardized Workflow for MSC Exosome Research
A typical experimental protocol for evaluating MSC exosomes in wound healing involves a sequence of critical steps, from isolation to functional validation. The following diagram illustrates a generalized workflow integrating common methodologies from recent studies.
Diagram Title: Experimental Workflow for MSC Exosome Research.
1. Exosome Isolation and Purification: The most common method is ultracentrifugation. The process typically involves a series of centrifugation steps to remove cells and debris (e.g., 2,000 × g for 30 min), followed by higher-speed centrifugation to pellet larger vesicles (e.g., 10,000 × g for 45 min), and finally, high-speed ultracentrifugation (e.g., 110,000 × g for 70 min) to sediment the exosomes [62]. Alternative methods include size-exclusion chromatography (SEC), which separates vesicles based on size and preserves their integrity, and immunoaffinity capture, which uses antibodies for high-purity isolation of specific exosome subpopulations [111].
2. Exosome Characterization: Isolated vesicles must be rigorously characterized to confirm they are exosomes. This is typically a tripartite analysis:
- Nanoparticle Tracking Analysis (NTA): To determine the particle size distribution and concentration (confirming the 30-150 nm range) [62] [5].
- Transmission Electron Microscopy (TEM): To visualize the classic cup-shaped or spherical morphology of the vesicles [62] [5].
- Western Blot (WB): To detect the presence of exosome marker proteins (e.g., CD63, CD81, TSG101) and the absence of negative markers [62].
3. In Vitro Functional Assays: Before moving to animal models, the biological activity of exosomes is tested on relevant cell types.
- Cell Proliferation Assays: (e.g., CCK-8, MTT) to assess if exosomes promote the growth of fibroblasts or endothelial cells [5].
- Cell Migration/Scratch Assay: A scratch is made in a confluent cell monolayer (e.g., human dermal fibroblasts), and the rate of gap closure upon exosome treatment is measured over time (e.g., 0, 12, 24 hours) to evaluate migratory promotion [62] [5].
- Tube Formation Assay: HUVECs are seeded on a Matrigel substrate and treated with exosomes. The formation of capillary-like structures is quantified to assess the pro-angiogenic potential of the exosomes [5].
4. In Vivo Animal Models and Analysis: The efficacy of exosomes is ultimately validated in an animal wound model.
- Wound Creation and Treatment: A common model is the full-thickness excisional skin wound in mice or rats. Animals are randomly allocated into groups (e.g., control, exosome-treated). Treatments (e.g., local injection of ~100 µg exosomes or PBS control around the wound) are administered post-wounding [62] [63].
- Outcome Measurement: The primary outcome is often the wound closure rate, measured over days. After sacrifice, tissue samples are collected for:
- Histological Analysis: Using Hematoxylin and Eosin (H&E) staining to evaluate re-epithelialization and general morphology, and Masson's Trichrome staining to assess collagen deposition and organization [62] [63].
- Advanced Molecular Analysis: Techniques like spatial transcriptomics (ST) can be used to map gene expression in tissue samples, revealing effects on specific pathways (e.g., TGF-β, Wnt) and cell types (e.g., myofibroblasts) [62].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Materials and Reagents for MSC Exosome Wound Healing Research.
| Item / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| MSC Culture Medium | Expansion and maintenance of parent MSCs. | MSC NutriStem XF Basal Medium supplemented with human platelet lysate [5]. |
| Ultracentrifuge | Isolation and concentration of exosomes from conditioned medium or biofluids. | Critical for the "gold standard" isolation method [111] [62]. |
| Nanoparticle Tracking Analyzer (NTA) | Characterizing exosome size distribution and concentration. | e.g., Malvern Panalytical NS300 system [62]. |
| Transmission Electron Microscope (TEM) | Visualizing exosome morphology and ultrastructure. | Confirms the classic cup-shaped morphology [62] [5]. |
| Specific Antibodies | Identifying exosomes and parent cells via Western Blot or flow cytometry. | Anti-CD63, Anti-TSG101 (exosome markers); CD73, CD90, CD105 (MSC markers) [62] [113]. |
| Human Dermal Fibroblasts (HDF-a) | In vitro model for testing exosome effects on skin cell proliferation and migration. | Used in scratch/migration assays and proliferation assays [62]. |
| HUVECs | In vitro model for assessing exosome pro-angiogenic potential. | Used in tube formation assays [5] [23]. |
| Animal Model | In vivo validation of therapeutic efficacy. | Typically, BALB/c mice or Wistar Albino rats with full-thickness skin wounds [62] [63]. |
| PKH67 Fluorescent Dye | Labeling exosomes for cellular uptake tracking in vitro. | Labeled exosomes are incubated with cells and visualized via fluorescence microscopy [62]. |
Mechanisms of Action and Signaling Pathways
The superior and multifaceted efficacy of MSC exosomes in wound healing can be attributed to their complex cargo and its coordinated action on multiple phases of the healing process. The following diagram summarizes the key pathways and cellular processes modulated by MSC exosomes.
Diagram Title: MSC Exosome Mechanisms in Wound Healing.
Modulation of Inflammation and Angiogenesis: MSC exosomes polarize macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype, reducing the production of pro-inflammatory cytokines and increasing the secretion of IL-10 [5] [113]. They also significantly promote the proliferation and tube formation of endothelial cells (e.g., HUVECs), directly stimulating angiogenesis, a critical step in wound healing [5]. This pro-angiogenic effect can be mediated by cargo miRNAs that activate pathways like AKT/HIF-1α [23].
Activation of Fibroblasts and Keratinocytes: A key mechanism is the direct promotion of proliferation and migration in skin cells. Exosomes from sources like umbilical cord MSCs are internalized by human skin fibroblasts (HSFs) and human keratinocytes (HaCaT cells), activating pro-proliferative and pro-migratory pathways such as PI3K/AKT and ERK/MAPK [23] [5]. For instance, ADSC-derived exosomes were shown to increase the expression of N-cadherin, cyclin-1, and PCNA in fibroblasts [23].
Regulation of ECM and Scar Formation: MSC exosomes critically influence tissue remodeling by modulating the composition of the extracellular matrix (ECM). They have been shown to increase the ratio of collagen III to collagen I, which is associated with more regenerative, less scarred tissue [23]. This is achieved by regulating the TGF-β signaling pathway, a master regulator of fibrosis. Specifically, exosomes can downregulate the TGF-β1/Smad pathway while upregulating TGF-β3, thereby suppressing the differentiation of fibroblasts into pro-fibrotic myofibroblasts and reducing collagen deposition [62] [23]. Spatial transcriptomic analysis has confirmed that MSC-EVs reduce the expression of myofibroblast marker genes and the TGF-β signaling pathway while enhancing the Wnt signaling pathway, leading to reduced scar width [62].
The systematic benchmarking presented herein positions MSC exosomes as a highly competitive therapeutic modality in the wound healing landscape. They offer a unique combination of advantages: the multi-targeted, holistic mechanistic approach of cell-based therapies without the associated risks and logistical hurdles, and a more complex, information-rich cargo than single growth factors. The consolidated experimental data confirms their efficacy in promoting key wound healing processes—angiogenesis, cell proliferation, migration, and immunomodulation—while concurrently mitigating scar formation.
For researchers and drug development professionals, the future of MSC exosome therapy lies in addressing current challenges, such as standardizing isolation protocols and scaling up production. Further exploration of exosome engineering to enhance target specificity or to load specific therapeutic molecules (e.g., miRNAs) holds immense promise. As the field progresses, MSC exosomes are poised to transition from a powerful research tool to a mainstream, cell-free therapeutic, potentially setting a new benchmark for safety, efficacy, and precision in regenerative medicine.
The management of chronic wounds represents a significant and growing clinical challenge, affecting approximately 1%-2% of the population and consuming substantial healthcare resources worldwide [26]. These wounds, characterized by impaired healing processes and prolonged inflammation, fail to progress through the normal stages of tissue repair, resulting in substantial patient burden and healthcare costs [26]. Current standard treatments often focus on symptomatic management rather than rectifying the dysfunctional wound microenvironment, highlighting the pressing need for innovative therapeutic approaches [26].
Among emerging strategies, mesenchymal stem cell-derived exosomes (MSC-exosomes) have garnered considerable interest as a promising cell-free therapeutic agent for wound healing [116]. These nano-sized extracellular vesicles (30-150 nm in diameter) mediate the paracrine effects of MSCs, delivering bioactive molecules such as proteins, mRNAs, and microRNAs that modulate critical processes in wound repair [116] [5]. Compared to cell-based therapies, MSC-exosomes offer several advantages, including lower immunogenicity, no risk of tumorigenesis or thrombosis, greater stability, and easier storage [69] [116]. As key paracrine mediators, MSC-exosomes precisely modulate various cells within the wound microenvironment, including keratinocytes, macrophages, endothelial cells, and fibroblasts, promoting re-epithelialization, resolving inflammation, stimulating angiogenesis, and modulating extracellular matrix remodeling [26].
This systematic analysis examines the current clinical trial landscape for MSC-exosomes in wound healing, evaluating safety profiles, efficacy endpoints, and methodological approaches. By synthesizing evidence from registered trials and published studies, we aim to provide researchers and drug development professionals with a comprehensive understanding of this rapidly evolving field.
Current Clinical Trial Landscape
The clinical investigation of MSC-derived extracellular vesicles (MSC-EVs), including exosomes, has expanded significantly in recent years. A comprehensive review of global clinical trial registries including ClinicalTrials.gov, the Chinese Clinical Trial Registry, and the Cochrane Register of Studies identified 66 registered trials evaluating MSC-EVs and exosomes as of February 2024 [69]. These trials span diverse medical applications, with wound healing representing a substantial portion of the investigated indications.
The distribution of MSC sources in clinical trials reflects practical considerations regarding accessibility and potency. Adipose-derived stem cells (ADSCs) have been frequently utilized due to their high abundance, accessibility, and well-documented efficacy in promoting wound healing [26]. Clinical evidence indicates that ADSC transplantation effectively promotes healing across diverse chronic wound types while improving healing quality and reducing pathological scarring [26]. Umbilical cord-derived MSCs (UCMSCs) offer advantages of non-invasive sourcing, abundant supply, low immunogenicity, and demonstrated potency in promoting angiogenesis, fibroblast proliferation, and immune regulation [5]. Bone marrow-derived MSCs represent another common source, though their use in wound healing applications has been somewhat surpassed by more accessible alternatives [117].
Analysis of Trial Design and Status
A systematic review of published clinical trials investigating ADSCs in cutaneous wound healing identified 16 registered trials encompassing four distinct disease models: chronic ulcers (n=4), diabetic wounds (n=5), postoperative scar prevention (n=3), and scar revision (n=4) [26]. Most trials have been exploratory pilot studies with modest sample sizes; only two were Phase II clinical trials, and no Phase III studies have been reported to date [26].
The majority of these wound healing trials (14/16) employed local injection as the predominant route of administration, while two trials utilized allogenic ADSCs incorporated into hydrogel or gel-based carriers for topical application [26]. Although most studies reported high follow-up compliance, methodological limitations were common: only three of sixteen trials implemented double-blinding due to technical constraints, and risk-of-bias assessment revealed a high risk of bias in 14 of 16 studies [26]. These findings underscore the need for more rigorously designed, large-scale randomized controlled trials in future research.
Table 1: Characteristics of Clinical Trials for ADSC-Based Wound Therapies
| Disease/Indication | Number of Trials | Intervention | Delivery Method | Phase | Key Outcomes |
|---|---|---|---|---|---|
| Chronic leg ulcer | 4 | Autologous centrifuged adipose tissue, SVF | Intralesional injection | II (1 trial), others not specified | Accelerated healing time, pain reduction, complete re-epithelialization |
| Diabetic wounds | 5 | Autologous ADSCs, allogeneic ADSCs in hydrogel | Intralesional injection, topical application | Not specified for most | Enhanced healing rates, improved tissue quality |
| Postoperative scar prevention | 3 | Autologous SVF, ADSCs | Intralesional injection | Not specified | Reduced scar formation, improved cosmetic outcomes |
| Scar revision | 4 | Autologous fat grafting, SVF | Intralesional injection | Not specified | Improved scar quality, texture, and pliability |
Administration Routes and Dosing Considerations
The route of administration represents a critical factor in optimizing MSC-exosome therapeutics. Analysis of registered trials indicates that intravenous infusion and aerosolized inhalation are predominant methods, particularly for systemic conditions [69]. For wound healing applications, local delivery approaches including intralesional injection and topical application have been most common [26].
Notably, dose-effect relationships appear to be route-dependent. Evidence suggests that nebulization therapy achieves therapeutic effects at doses around 10⁸ particles, significantly lower than those required for intravenous routes [69]. This indicates a relatively narrow and route-dependent effective dose window that must be carefully considered in trial design. However, substantial variations in exosome characterization, dose units, and outcome measures have been observed across trials, highlighting the lack of harmonized reporting standards in the field [69].
Safety and Tolerability Profile
Clinical Safety Evidence
The safety profile of MSC-exosomes represents a critical consideration for clinical translation. Current evidence, though limited by the preliminary nature of most studies, suggests favorable safety outcomes. Among published clinical trials of ADSC-based therapies for wound healing, no serious adverse events related to the treatments have been reported [26]. This safety record extends to allogeneic ADSC transplantation, which has demonstrated comparable safety and efficacy to autologous approaches, thereby broadening clinical applicability [26].
A phase 1 open-label study specifically evaluated the safety of topical MSC-exosome ointment (PTD2021P) in ten healthy adult volunteers [118]. Subjects received topical treatment thrice daily for 20 days, with comprehensive safety monitoring throughout the study period. Results demonstrated that only one subject experienced a treatment-emergent adverse event (COVID-19 infection) assessed as moderate in severity and unlikely related to the study drug [118]. No subjects displayed clinically significant abnormalities in laboratory parameters, vital signs, or local skin reactions at the application site [118]. This study concluded that the MSC-exosome ointment was well-tolerated with no serious adverse events or treatment-related discontinuations [118].
Theoretical Safety Advantages
The favorable safety profile of MSC-exosomes aligns with their theoretical advantages over cell-based therapies. Unlike whole cell transplants, exosomes pose no risk of tumorigenesis, thrombosis, or immune rejection [69] [116]. Their nanoscale size and biological composition reduce the potential for adverse immune reactions, while their limited half-life and controlled degradation minimize long-term safety concerns [116]. These characteristics position MSC-exosomes as a promising safer alternative to stem cell therapies, though continued rigorous safety monitoring in larger trials remains essential.
Efficacy Endpoints and Mechanisms of Action
Key Efficacy Endpoints in Clinical Trials
Clinical trials of MSC-exosomes for wound healing have employed multiple efficacy endpoints to evaluate therapeutic outcomes. The most consistently reported efficacy measures include:
- Wound closure rate: Quantitative assessment of reduction in wound surface area over time [26] [5]
- Re-epithelialization: Histological evaluation of epidermal regeneration [26]
- Angiogenesis: Increased capillary density and perfusion measured through immunohistochemical analysis (e.g., CD31 staining) [5]
- Scar formation and quality: Macroscopic and microscopic evaluation of scar characteristics including collagen organization [26]
- Pain reduction: Patient-reported pain scores using standardized scales [26]
- Infection rates: Reduction in wound infection incidents and bacterial burden [119]
These efficacy endpoints correspond to the multifaceted activities of MSC-exosomes in promoting coordinated wound healing through multiple mechanistic pathways.
Molecular and Cellular Mechanisms
MSC-exosomes accelerate wound healing through precisely coordinated effects on multiple cell types and biological processes in the wound microenvironment:
The therapeutic effects illustrated in Figure 1 are mediated by specific molecular cargo within MSC-exosomes. Bioengineering approaches have been employed to enhance these natural capabilities through preconditioning strategies, genetic modification of progenitor cells, direct exosome engineering, and development of hybrid exosomes [116]. For instance, exosomes derived from MSCs cultured in platelet-supplemented media exhibit significantly higher concentrations of keratinocyte growth factor (KGF), vascular endothelial growth factor (VEGF-A), platelet-derived growth factor (PDGF-BB), and interleukins 6, 7, and 8 compared to those from standard media [120]. These enriched exosomes demonstrate superior capability to promote human skin fibroblast proliferation and stimulate angiogenesis of human umbilical vein endothelial cells [120].
Table 2: Key Molecular Mediators in MSC-Exosomes and Their Functions in Wound Healing
| Molecular Mediator | Type | Primary Functions in Wound Healing |
|---|---|---|
| Keratinocyte Growth Factor (KGF) | Protein | Stimulates keratinocyte proliferation and migration, modulates epidermal structure |
| Vascular Endothelial Growth Factor (VEGF-A) | Protein | Promotes angiogenesis, enhances endothelial cell proliferation and tube formation |
| Platelet-Derived Growth Factor (PDGF-BB) | Protein | Stimulates fibroblast proliferation, collagen synthesis, and granulation tissue formation |
| microRNA-223 | miRNA | Reduces inflammation through modulation of inflammatory pathways |
| microRNA-181c | miRNA | Suppresses excessive inflammatory response |
| Interleukins (IL-6, IL-7, IL-8) | Cytokines | Regulate immune cell recruitment and activity, modulate inflammatory phase |
| Transforming Growth Factor-β3 (TGF-β3) | Protein | Promotes regenerative healing with reduced scarring |
Experimental Protocols and Methodologies
Standardized Isolation and Characterization
The translation of MSC-exosome research to clinical applications requires standardized protocols for isolation, characterization, and quality control. The most commonly employed methodology involves:
Isolation Protocol: Ultracentrifugation remains the gold standard for exosome isolation from MSC-conditioned media [5]. This multi-step process typically involves successive centrifugation steps to remove cells and debris (300 × g for 10 min), apoptotic bodies (2,000 × g for 10 min), and microvesicles (10,000 × g for 30 min), followed by high-speed ultracentrifugation (100,000 × g for 70-120 min) to pellet exosomes [5]. Alternative methods include size-exclusion chromatography, polymer-based precipitation, and immunoaffinity capture, though these are less commonly used in clinical-grade production.
Characterization Methods: Comprehensive characterization of MSC-exosomes requires multiple complementary techniques [5]:
- Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration
- Transmission Electron Microscopy (TEM): Visualizes morphology and ultrastructural features
- Western Blotting: Confirms presence of exosomal markers (CD9, CD63, CD81, TSG101) and absence of negative markers (calnexin, GM130)
- Flow Cytometry: Analyzes surface antigen expression using antibody-conjugated beads
Functional Assessment assays
Preclinical assessment of MSC-exosome efficacy employs standardized in vitro and in vivo models that recapitulate key aspects of wound healing:
In Vitro Functional Assays:
- Cell Proliferation: Measured using MTT, CCK-8, or EdU assays on human skin fibroblasts and keratinocytes [5]
- Migration Capacity: Evaluated through scratch/wound healing assays and transwell migration chambers [5]
- Angiogenic Potential: Assessed via tube formation assay using human umbilical vein endothelial cells (HUVECs) on Matrigel [5]
- Cytokine Secretion: Quantified using ELISA or multiplex immunoassays [120]
In Vivo Wound Healing Models:
- Animal Models: Typically employ murine or porcine full-thickness excisional wound models [5]
- Treatment Protocol: Direct application of exosomes in saline (local injection) or incorporation into hydrogel carriers for sustained release [116]
- Outcome Measures: Include wound closure rate (digital planimetry), histological analysis (H&E, Masson's trichrome), immunohistochemistry (CD31 for angiogenesis, CK10 for re-epithelialization), and gene expression profiling [5]
Research Reagent Solutions
The standardization of research reagents is critical for ensuring reproducibility and comparability across MSC-exosome studies. Key reagents and their functions in experimental workflows include:
Table 3: Essential Research Reagents for MSC-Exosome Studies
| Reagent Category | Specific Examples | Primary Function | Considerations |
|---|---|---|---|
| Cell Culture Media | Serum-free media (StemPro, NutriStem), Platelet lysate-supplemented media, FBS-supplemented media | Support MSC expansion and exosome production | Platelet-supplemented media enhances growth factor content in exosomes [120] |
| Isolation Kits | Ultracentrifugation reagents, Size-exclusion chromatography columns, Polymer-based precipitation kits | Isolate and purify exosomes from conditioned media | Ultracentrifugation remains gold standard; kit methods vary in purity and yield |
| Characterization Antibodies | Anti-CD63, CD9, CD81, TSG101, Calnexin | Confirm exosomal identity and purity | Essential for quality control via Western blot and flow cytometry |
| Functional Assay Reagents | Matrigel (tube formation), CCK-8/MTT (proliferation), Transwell chambers (migration) | Evaluate biological activity of exosomes | Standardized protocols enable cross-study comparisons |
| Animal Model Materials | Hydrogel carriers (hyaluronic acid, chitosan), Wound measuring tools, Histology reagents | Facilitate in vivo efficacy assessment | Hydrogel systems improve exosome retention and stability [116] |
The clinical trial landscape for MSC-exosomes in wound healing is characterized by promising early-stage evidence with a clear need for more rigorous, large-scale investigations. Current clinical evidence supports the safety and therapeutic potential of MSC-exosome interventions, with multiple mechanisms of action targeting various phases of the wound healing process. The field has matured from proof-of-concept studies to more sophisticated approaches involving bioengineering, targeted delivery systems, and standardized manufacturing protocols.
Significant challenges remain in the clinical translation of MSC-exosome therapies, particularly regarding standardization of isolation methods, characterization protocols, dosing strategies, and potency assays. The heterogeneity in current clinical trial designs, combined with variations in exosome sources, production methods, and administration routes, complicates cross-study comparisons and meta-analyses. Future research priorities should include the establishment of harmonized standards, validation of potency biomarkers, development of scalable manufacturing processes, and execution of well-controlled Phase II and III clinical trials with standardized efficacy endpoints. As these advancements materialize, MSC-exosome therapies hold substantial promise for addressing the significant unmet clinical needs in chronic wound management.
For researchers developing novel therapies like MSC exosomes for wound healing, navigating the U.S. Food and Drug Administration (FDA) regulatory landscape is crucial. The FDA oversees product approval and manufacturing quality through distinct but interconnected frameworks. "Novel" drugs are defined as new drugs never before approved or marketed in the U.S., which would include first-in-class exosome-based biologics [121]. The approval process involves rigorous evaluation of safety and efficacy data through various pathways, while quality control is mandated through Current Good Manufacturing Practice (CGMP) regulations that set minimum requirements for methods, facilities, and controls used in manufacturing [122].
For medical devices or combination products, the FDA has recently harmonized its Quality System Regulation (QSR) with the international standard ISO 13485:2016, creating the Quality Management System Regulation (QMSR). This final rule, effective February 2, 2026, aims to align the U.S. regulatory framework with global standards while maintaining rigorous oversight of device safety and effectiveness [123].
FDA Drug Approval Process for Novel Therapies
Novel Drug Approval Pathway
The FDA's Center for Drug Evaluation and Research (CDER) provides guidance on necessary study design elements and data requirements for drug applications. Each year, CDER approves a wide range of new drugs and biological products, including New Molecular Entities (NMEs) containing active moieties not previously approved by the FDA [124]. The approval process involves several stages:
- Preclinical Research: Extensive laboratory and animal studies to demonstrate biological activity and safety
- Investigational New Drug (IND) Application: Submission of preclinical data and proposed clinical trial protocols
- Clinical Trials: Three phases of human studies evaluating safety, efficacy, and dosage
- New Drug Application (NDA): Comprehensive submission of all research data for FDA review
- Post-Marketing Surveillance: Ongoing monitoring of safety and effectiveness after approval
Recent Novel Drug Approvals
The table below summarizes select novel drug approvals from 2025, demonstrating the diversity of therapeutic areas and molecular types that receive FDA approval [121]:
Table: Selected FDA Novel Drug Approvals in 2025
| Drug Name | Active Ingredient | Approval Date | FDA-Approved Use |
|---|---|---|---|
| Hyrnuo | sevabertinib | 11/19/2025 | Locally advanced or metastatic non-squamous non-small cell lung cancer with HER2 mutations |
| Redemplo | plozasiran | 11/18/2025 | Reduce triglycerides in adults with familial chylomicronemia syndrome |
| Komzifti | ziftomenib | 11/13/2025 | Relapsed or refractory acute myeloid leukemia with NPM1 mutation |
| Kygevvi | doxecitine and doxribtimine | 11/3/2025 | Thymidine kinase 2 deficiency in pediatric patients |
| Lynkuet | elinzanetant | 10/24/2025 | Moderate-to-severe vasomotor symptoms due to menopause |
| Jascayd | nerandomilast | 10/7/2025 | Idiopathic pulmonary fibrosis |
| Brinsupri | brensocatib | 8/12/2025 | Non-cystic fibrosis bronchiectasis |
| Vizz | aceclidine | 7/31/2025 | Treatment of presbyopia |
Quality Control Requirements
Pharmaceutical CGMP Regulations
For drug products including biologics, FDA mandates compliance with Current Good Manufacturing Practice (CGMP) regulations under 21 CFR parts 210 and 211. These regulations ensure that products are safe for use and contain the ingredients and strength they claim to have. The CGMP framework covers [122]:
- Facilities and Equipment: Appropriate design, maintenance, and cleaning
- Raw Material Controls: Testing and verification of incoming components
- Production Process Controls: Standardized procedures and documentation
- Quality Control Units: Independent oversight of manufacturing operations
- Laboratory Controls: Testing of in-process materials and finished products
- Records and Reports: Comprehensive documentation of all manufacturing activities
- Stability Testing: Ongoing assessment of product shelf life
Quality Management System Regulation (QMSR) for Devices
For medical devices, the FDA's updated Quality Management System Regulation (QMSR) incorporates by reference the international standard ISO 13485:2016. Key aspects of this harmonized framework include [123]:
- Effective Date: February 2, 2026 (two years after publication on February 2, 2024)
- Scope: Applies to medical device current good manufacturing practice (CGMP) requirements
- Key Changes: Withdrawal of the Quality System Inspection Technique (QSIT) and implementation of a new inspection process
- Record Access: FDA investigators may review management review, quality audits, and supplier audit reports previously exempt under § 820.180(c)
- Training: Comprehensive FDA staff training on the final rule and revised inspection processes
Table: Comparison of Quality System Regulation vs. Quality Management System Regulation
| Aspect | QS Regulation (Current) | QMSR (Effective 2026) |
|---|---|---|
| Basis | 21 CFR Part 820 | ISO 13485:2016 with FDA modifications |
| Inspection Approach | Quality System Inspection Technique (QSIT) | New process aligned with international standards |
| Record Access | Exceptions for internal audits, supplier audits, and management review | FDA can inspect all quality management system records |
| Harmonization | U.S.-specific requirements | Aligned with global medical device regulatory authorities |
| Training | FDA staff trained on QSIT | FDA staff trained on QMSR and new inspection processes |
MSC Exosomes in Wound Healing: Experimental Evidence
Therapeutic Mechanisms and Efficacy
Mesenchymal stem cell-derived exosomes (MSC-Exos) represent a promising "cell-free" therapeutic strategy for wound healing. These nano-sized extracellular vesicles (30-150 nm in diameter) transport proteins, lipids, mRNAs, and miRNAs that mediate regenerative functions including anti-inflammatory effects, angiogenesis promotion, and extracellular matrix remodeling [6]. Compared to their parent cells, SC-Exos offer greater stability, lower immunogenicity, absence of tumorigenic risks, and easier storage and distribution [6].
Recent research demonstrates that umbilical cord mesenchymal stem cell-derived exosomes (hUCMSC-Exos) significantly promote wound healing through multiple mechanisms [5]:
- Cellular Proliferation and Migration: hUCMSC-Exos are easily internalized by human umbilical vein endothelial cells (HUVECs) and human skin fibroblasts (HSFs), significantly promoting proliferation and migration of HSFs and tube formation of HUVECs
- Angiogenesis Stimulation: Enhanced formation of new blood vessels at wound sites
- Inflammation Reduction: Modulation of immune response and reduction of chronic inflammation
- Extracellular Matrix Formation: Promotion of organized collagen deposition and tissue remodeling
Bioinformatics analysis suggests that Unc-51-like autophagy activating kinase 2 (ULK2), Collagen Type XIX Alpha 1 Chain (COL19A1), and Interleukin-6 Signal Transducer (IL6ST) are potential key molecules involved in the regulation of wound repair by hUCMSC-Exos [5].
Table: Therapeutic Effects of Stem Cell-Derived Exosomes in Wound Healing
| Exosome Source | Key Therapeutic Effects | Proposed Mechanisms | Experimental Models |
|---|---|---|---|
| Human Umbilical Cord MSC (hUCMSC) | Accelerated wound closure, reduced scarring, improved angiogenesis | miRNA-mediated regulation of ULK2, COL19A1, IL6ST; reduction of inflammation | In vitro: HUVEC, HSF assays; In vivo: murine wound models [5] |
| Adipose-Derived MSC (ADMSC) | Enhanced cell proliferation, migration, collagen synthesis | Inhibition of TGF-β/Smad pathway; increased collagen I/III synthesis | In vitro: fibroblast assays; In vivo: rodent wound models [6] |
| Bone Marrow MSC (BMSC) | Improved healing, reduced scar formation | Inhibition of TGF-β/Smad pathway; increased TGF-β3 secretion | In vitro: keratinocyte assays; In vivo: murine burn models [6] |
| Injectable Hydrogel with MSC Exosomes | Sustained release, enhanced chronic wound healing | In situ crosslinking; prolonged exosome retention; inflammation regulation | In vitro: release kinetics; In vivo: diabetic wound models [16] |
Experimental Methodologies for MSC Exosome Research
Standardized Isolation and Characterization Protocols
For reproducible research on MSC exosomes, standardized methodologies are essential. The following protocols are commonly employed in the field [5]:
- Isolation by Ultracentrifugation: Sequential centrifugation steps to remove cells, debris, and concentrate exosomes
- Characterization Techniques:
- Nanoparticle Tracking Analysis (NTA): For size distribution and concentration measurements
- Western Blotting (WB): Detection of exosomal markers (CD9, CD63, CD81)
- Transmission Electron Microscopy (TEM): Visualization of exosome morphology and structure
- Cell Culture Conditions: Use of specialized media such as MSC NutriStem XF Basal Medium with supplements and human platelet lysate
Functional Assays for Wound Healing Applications
To evaluate the therapeutic potential of MSC exosomes for wound healing, researchers employ a range of functional assays [5]:
- In Vitro Analysis:
- Proliferation and migration assays using human skin fibroblasts (HSFs)
- Tube formation assays with human umbilical vein endothelial cells (HUVECs)
- Cellular internalization studies using fluorescent labeling
- In Vivo Assessment:
- Wound closure rate measurement in animal models
- Histological and immunohistochemical analyses of tissue samples
- Evaluation of inflammation, angiogenesis, and extracellular matrix formation
Diagram Title: Experimental Workflow for MSC Exosome Research
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagent Solutions for MSC Exosome Studies
| Reagent/Resource | Function | Example Application |
|---|---|---|
| MSC NutriStem XF Media | Serum-free culture medium for MSC expansion | Maintenance of hUCMSCs in undifferentiated state [5] |
| Human Platelet Lysate | Growth factor supplement for MSC culture | Enhanced MSC proliferation and exosome production [5] |
| Dulbecco's PBS | Buffer for washing and solution preparation | Rinsing umbilical cord tissues and cell washing [5] |
| Trypsin-EDTA Solution | Cell dissociation reagent | Subculturing of adherent MSCs [5] |
| Exosome Isolation Kits | Rapid extraction of exosomes from conditioned media | Alternative to ultracentrifugation for small samples |
| CD9/CD63/CD81 Antibodies | Exosomal marker detection | Western blot confirmation of exosome identity [5] |
| CellTracker Dyes | Fluorescent cell labeling | Tracking exosome uptake by recipient cells [5] |
| ELISA Kits | Cytokine and growth factor quantification | Analysis of exosome cargo and bioactivity |
| Matrigel | Basement membrane matrix | Endothelial tube formation assays [5] |
| RNAseq Kits | Transcriptome analysis | miRNA and mRNA profiling of exosome cargo [5] |
Signaling Pathways in MSC Exosome-Mediated Wound Healing
The therapeutic effects of MSC exosomes in wound healing are mediated through complex signaling pathways that coordinate the different phases of healing:
- Inflammation Regulation: Exosomal miRNAs (miR-146a, miR-223) inhibit NF-κB signaling and suppress NLRP3 inflammasome activation, facilitating the transition from pro-inflammatory M1 to anti-inflammatory M2 macrophages [6]
- Angiogenesis Stimulation: VEGF and FGF-2 signaling promotes endothelial cell proliferation and new blood vessel formation
- Fibroblast Activation: TGF-β1 signaling stimulates fibroblast migration, proliferation, and extracellular matrix synthesis
- Re-epithelialization: Keratinocyte migration and proliferation are enhanced through multiple growth factor pathways
Diagram Title: Key Signaling Pathways in Exosome-Mediated Wound Healing
The regulatory framework for FDA approval and quality control provides a structured pathway for translating MSC exosome research from bench to bedside. For wound healing applications, researchers must navigate both the drug approval process and appropriate quality management systems based on the product classification. The experimental evidence supporting MSC exosomes as therapeutic agents continues to grow, with standardized methodologies enabling more reproducible research across different laboratories. As the field advances, understanding both the scientific mechanisms and regulatory requirements will be essential for successfully developing effective exosome-based therapies for chronic wounds.
The field of regenerative medicine is increasingly focusing on exosome therapy as a promising, cell-free therapeutic strategy. Mesenchymal stem cell (MSC)-derived exosomes, in particular, have demonstrated significant potential in wound healing and other applications, driving both scientific and commercial interest. [125] A thorough cost-benefit analysis of their development is crucial for researchers, scientists, and drug development professionals to strategically navigate this innovative yet complex landscape. This analysis objectively compares the economic viability of exosome therapies against alternative approaches, examining development costs, market potential, and the underlying experimental data that informs their therapeutic value, all within the context of a systematic review of MSC exosomes in wound healing.
Market Outlook and Growth Drivers
The exosome therapeutics market is poised for substantial growth, with varying projections underscoring its potential. Analysts forecast the global market to reach $1.4 billion by 2040, growing at a compound annual growth rate (CAGR) of 41.1% from 2029. [126] Another projection estimates the market will be valued at $1.39 billion in 2025, growing to $3.36 billion by 2034. [127] A more conservative estimate places the 2025 market size at $928.93 thousand, expanding to $4.02 million by 2034 at a CAGR of 17.68%. [128] These variances likely reflect different definitions of market scope but consistently indicate strong growth.
This growth is fueled by several key drivers:
- Rising Demand for Targeted Therapies: Exosomes' innate ability to be engineered for precise drug delivery aligns with the shift towards personalized medicine, offering improved efficacy and reduced systemic toxicity compared to conventional drugs. [129]
- Robust R&D Pipeline: Over 120 exosome therapeutic candidates are currently in development, with more than 40% in clinical stages, indicating a rich and maturing pipeline. [126]
- Significant Investment: Venture capital and strategic investors have injected over $570 million into the sector across more than 30 funding instances, reflecting strong financial confidence. [126]
Table 1: Global Exosome Therapeutics Market Projections
| Report Source | Base Year/Value | Projection Year/Value | CAGR | Key Segments |
|---|---|---|---|---|
| ResearchAndMarkets [126] | $30M (2029) | $1.4B (2040) | 41.1% | Allogeneic, Autologous, Oncology |
| HealthE1 Analysis [127] | $1.39B (2025) | $3.36B (2034) | ~10-17% | Musculoskeletal, Neuro, Dermatology |
| Precedence Research [128] | $928.93k (2025) | $4.02M (2034) | 17.68% | MSC-derived, Oncology, Intravenous |
Cost Structure and Investment Analysis
Developing exosome-based therapies involves a high-cost structure, presenting significant financial barriers and risks.
Major Cost Components
- Research and Development: The initial stage requires extensive investment in laboratory research to isolate exosomes, optimize purification, engineer them for specific applications, and conduct rigorous pre-clinical testing on animal models. [129]
- Clinical Trials: Following successful R&D, multiple phases of human clinical trials are necessary, each stage taking years and requiring massive investments running into hundreds of millions of dollars. [129]
- Manufacturing and Quality Control: Scaling up production while maintaining consistency and quality is a key challenge. Costs include GMP-grade production facilities, donor screening, viral testing, and sophisticated purification technologies like ultrafiltration and size-exclusion chromatography. [129] [127]
Financial Risks and Mitigation
The financial risks are amplified by the low probability of a candidate successfully transitioning from the lab to the market. [129] This high failure rate necessitates a large and risky capital outlay. To mitigate these risks, leading companies are adopting several key strategies:
- Strategic Partnerships and Collaborations: Forming alliances with pharmaceutical companies, academic institutions, and biotech firms to share expertise, resources, and financial burden. [129] [128]
- Strategic Acquisitions: Larger players are acquiring specialized companies to bolster their technical expertise and product pipelines quickly. [129]
- Focus on Clinical Validation: Moving beyond platform technologies to clinically validating candidates, which de-risks investment and accelerates regulatory approval. [129]
Comparative Cost-Benefit Analysis: Exosome Therapy vs. Alternatives
A critical assessment of exosome therapy against other regenerative and conventional options reveals a distinct cost-benefit profile.
Table 2: Cost-Benefit Comparison: Exosome Therapy vs. Alternative Regenerative Therapies
| Therapy | Estimated Cost per Session | Key Benefits | Key Risks & Costs |
|---|---|---|---|
| Exosome IV Therapy | $1,500 - $3,000 [127] | Lower immunogenicity, no tumorigenic risk, off-the-shelf availability, precise targeting [24] [125] [127] | High R&D costs, complex manufacturing, uncertain reimbursement [129] |
| Live Stem-Cell Infusion | >$3,000 (Higher than Exosomes) [127] | Can synthesize extracellular matrix [127] | Risk of immune rejection, microvascular lodging, tumorigenic potential, complex storage [127] |
| Platelet-Rich Plasma (PRP) | <$1,500 (Less than Exosomes) [127] | Autologous, lower cost, uses patient's own growth factors [127] | Variable potency based on patient age/health, requires phlebotomy [127] |
The economic case for exosomes is strengthened by their "cell-free" advantages over whole-cell therapies. They eliminate risks associated with cell transplantation, such as immune rejection and tumor formation, potentially reducing long-term healthcare costs related to complication management. [24] [125] Furthermore, their off-the-shelf availability and longer shelf-life compared to live cells streamline logistics and reduce waste, contributing to better economic scalability. [129] [127]
Experimental Evidence and Therapeutic Efficacy in Wound Healing
The economic potential of MSC exosomes is underpinned by compelling and reproducible experimental evidence, particularly in wound healing, which demonstrates their mechanism of action and therapeutic superiority.
Key Methodologies in Exosome Research
Robust experimental protocols are critical for validating efficacy. Key methodologies include:
- Exosome Isolation and Purification: Ultracentrifugation is a standard method. It involves sequential centrifugation of cell culture supernatant, followed by high-speed ultracentrifugation (e.g., 100,000× g for 90 minutes) to pellet exosomes. [24] [5]
- Characterization: Isolated exosomes are characterized using:
- Nanoparticle Tracking Analysis (NTA): To determine particle size distribution and concentration. [24] [5]
- Transmission Electron Microscopy (TEM): To confirm spherical morphology and bilayer membrane structure. [24] [5]
- Immunoblotting: To detect exosome-specific surface markers (e.g., CD9, CD63, ALIX) and assess purity (e.g., absence of calnexin). [24]
- In Vitro Functional Assays:
- Proliferation Assays: (e.g., CCK-8 assay) to measure exosome-induced proliferation of human skin fibroblasts (HSFs). [5]
- Migration Assays: (e.g., scratch wound assay) to assess HSF migration capability. [5]
- Tube Formation Assays: Using human umbilical vein endothelial cells (HUVECs) to quantify angiogenesis potential. [5]
- In Vivo Efficacy Models: The imiquimod (IMQ)-induced psoriasis murine model and full-thickness skin wound models are widely used. Topical application or injection of exosomes is followed by evaluation of wound closure rate, histological analysis (e.g., H&E staining for epidermal thickness), and immunohistochemical analysis for inflammation and angiogenesis markers. [24] [5]
Diagram 1: MSC exosomes are internalized by skin cells, leading to functional changes that drive wound healing.
Supporting Data from Preclinical and Meta-Analysis Studies
A 2025 meta-analysis of MSC exosomes in IMQ-induced psoriasis models provided level-1 evidence, showing significantly lower clinical severity scores (SMD: -1.886) and reduced epidermal thickness (SMD: -3.258) in exosome-treated groups compared to controls. [24] This confirms a strong therapeutic effect at the organism level.
Specific studies on human umbilical cord MSC-derived exosomes (hUCMSC-Exos) have elucidated the mechanistic basis for this efficacy. hUCMSC-Exos are internalized by human skin fibroblasts (HSFs) and human umbilical vein endothelial cells (HUVECs), significantly promoting their proliferation and migration. [5] Crucially, they enhance the tube-forming capability of HUVECs, a key indicator of angiogenic potential. [5] In animal wound models, this translates to accelerated wound closure, stimulated angiogenesis, and promoted formation of the extracellular matrix. [5] Bioinformatic analysis suggests that exosome-derived miRNAs target genes like ULK2, COL19A1, and IL6ST, which are involved in regulating inflammation and angiogenesis. [5]
Diagram 2: A typical experimental workflow for evaluating the efficacy of exosomes in wound healing, from isolation to in vivo validation.
The Scientist's Toolkit: Key Reagents and Materials
Successful research and development in this field depend on specific, high-quality reagents and technologies.
Table 3: Essential Research Reagent Solutions for Exosome Studies
| Reagent / Material | Function in Research | Specific Example / Note |
|---|---|---|
| Mesenchymal Stem Cells | Source of therapeutic exosomes. | Sourced from umbilical cord, placenta, adipose tissue; require specific culture media. [125] [5] |
| Cell Culture Media | Supports growth and exosome production of MSCs. | Serum-free, xeno-free media like NutriStem XF are often used. [5] |
| Isolation Kits (Ultracentrifugation) | Standard method for purifying exosomes from culture supernatant. | Requires high-speed ultracentrifuge and fixed-angle rotors. [24] [5] |
| Nanoparticle Tracking Analyzer | Measures exosome size distribution and concentration. | Instruments like ZetaView PMX 110 (Particle Metrix) are used. [24] |
| Transmission Electron Microscope | Visualizes exosome morphology and membrane structure. | e.g., Hitachi HT-7700 instrument. [24] |
| Antibodies for Characterization | Identifies exosome-specific markers via immunoblotting. | Anti-CD9, anti-CD63, anti-ALIX; anti-calnexin for purity assessment. [24] |
| Animal Disease Models | For in vivo efficacy testing. | IMQ-induced psoriasis model; full-thickness excisional wound model. [24] [5] |
Regulatory Hurdles and Future Economic Opportunities
The regulatory pathway for exosome therapies remains a significant challenge. The FDA classifies them as biologics, requiring an Investigational New Drug (IND) application before clinical use. [127] As of 2025, no drug regulatory authority has issued specific technical guidelines for exosome-based drugs, creating uncertainty in development and approval processes. [125] The FDA has issued warning letters to clinics offering unauthorized exosome infractions, emphasizing strict enforcement. [127]
Despite these hurdles, significant economic opportunities exist:
- Expansion into Emerging Markets: Asia-Pacific is anticipated to be the fastest-growing market, with countries like China investing heavily in biotechnology. [126] [128] [130] This offers a huge patient population and commercialization potential.
- Technological Convergence: The integration of Artificial Intelligence (AI) is optimizing drug discovery, personalizing treatments, and accelerating exosome data analysis, which can reduce R&D costs and timelines. [128]
- Niche Applications: Near-term value is seen in neurology, musculoskeletal disorders, and dermatology, where high unmet needs and promising clinical data can support premium pricing. [127]
The cost-benefit analysis of exosome therapy development reveals a field with high upfront costs and regulatory complexity, balanced by a compelling long-term economic and therapeutic value proposition. The strong market growth forecasts, extensive R&D pipeline, and significant investment underscore the financial viability. The superior safety profile of exosomes compared to cell-based therapies and their proven efficacy in pre-clinical models, such as wound healing, provide a solid foundation for this potential. For researchers and drug developers, success will depend on navigating the regulatory landscape, forming strategic partnerships to share costs and expertise, and focusing on clinical validation to de-risk investment. As the science matures and regulatory paths become clearer, exosome therapies are poised to become a economically viable and transformative force in the treatment of degenerative, inflammatory, and traumatic conditions.
Conclusion
MSC-exosomes represent a transformative, cell-free therapeutic paradigm for wound healing, demonstrating robust efficacy across diverse preclinical models through multifaceted mechanisms of action. This systematic review confirms their potent immunomodulatory, pro-angiogenic, and regenerative capabilities, while highlighting the critical importance of source selection, isolation standardization, and delivery optimization for clinical success. Despite promising results, significant challenges remain in manufacturing scalability, regulatory approval, and clinical validation. Future research must prioritize engineered exosomes with enhanced targeting capabilities, robust clinical trials with standardized endpoints, and development of integrated biomaterial delivery systems to fully realize the therapeutic potential of MSC-exosomes in revolutionizing wound care management.
References
- 1. Inclusion Biogenesis, Methods of Isolation and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7074492/]
- 2. Regulation of cargo selection in exosome biogenesis and ... [https://www.nature.com/articles/s12276-024-01209-y]
- 3. Exosome biogenesis: machinery, regulation, and therapeutic ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01671-0]
- 4. Mesenchymal stem cell-derived exosomes: emerging ... [https://www.sciencedirect.com/science/article/pii/S2773041725000253]
- 5. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1641709/full]
- 6. Therapeutic Potential of Stem Cell-Derived Exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383377/]
- 7. Extracellular vesicles: cargo loading, degradation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540057/]
- 8. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 9. Exosome as emerging therapeutic platform for wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004604]
- 10. Extracellular vesicles: innovative cell-free solutions for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1571461/full]
- 11. Extracellular vesicle microRNA cargoes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551403/]
- 12. Exosomal peptides and proteins in wound healing and skin ... [https://pubmed.ncbi.nlm.nih.gov/40627201/]
- 13. Exosome-like vesicles encapsulated with specific microRNAs ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03337-7]
- 14. Exosomes As A Revolutionary Tool In Wound Healing And ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5678084]
- 15. Research advances in enhancing wound healing through ... [https://pubmed.ncbi.nlm.nih.gov/41075695/]
- 16. MSC-derived exosomes injectable hyaluronic acid ... [https://www.sciencedirect.com/science/article/pii/S0168365925006066]
- 17. Macrophages: Subtypes, Distribution, Polarization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290311/]
- 18. Global characterization of macrophage polarization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8783961/]
- 19. M1 and M2 macrophages markers are alternately ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296229/]
- 20. Applications of mesenchymal stem cell-exosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319788/]
- 21. Global characterization of macrophage polarization ... [https://www.sciencedirect.com/science/article/pii/S2211124721014327]
- 22. a systematic review and meta-analysis of preclinical studies [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05744-0]
- 23. emerging therapeutic opportunities for wound healing | Stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03345-0]
- 24. A Murine Study and Meta-Analysis of Experimental Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467663/]
- 25. Role of Exosomes in Dermal Wound Healing: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9400548/]
- 26. Wound Healing: Harnessing Extracellular Vesicles Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587863/]
- 27. The Role of Vascular Endothelial Growth Factor in Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2728016/]
- 28. Harnessing exosomal mediators for advanced wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0026286225000809]
- 29. Exosomes: the future of acellular nanotherapeutics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443856/]
- 30. Development of a VEGF-activated scaffold with enhanced ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01051e]
- 31. Mechanisms and therapeutic potential of ozone therapy in ... [https://link.springer.com/article/10.1007/s44337-025-00491-7]
- 32. Targeting angiogenesis in diabetic wound healing [https://www.sciencedirect.com/science/article/pii/S2095177925002928]
- 33. derived- Mesenchymal : a modern approach in... stem cell exosomes [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02622-3]
- 34. -derived Mesenchymal as a new therapeutic... stem cell exosomes [https://www.nature.com/articles/emm201763?error=cookies_not_supported&code=b22bbb6b-6420-4320-9b3d-7d545242d342]
- 35. Mesenchymal Stem Cell Exosomes Induce Proliferation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4499790/]
- 36. Advances in stem cell-derived exosome therapy for radiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626575/]
- 37. Mesenchymal Stem Cells vs Exosomes: A Comparison ... [https://celltexbank.com/mscs-vs-exosomes/]
- 38. Extracellular Matrix Reorganization During Wound Healing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4352699/]
- 39. The Role of Extracellular Matrix in Skin Wound Healing [https://pmc.ncbi.nlm.nih.gov/articles/PMC8706213/]
- 40. Mini review on collagens in normal skin and pathological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11291465/]
- 41. Scarring Skin: Mechanisms and Therapies [https://www.mdpi.com/1422-0067/25/3/1458]
- 42. Scar Formation: Cellular Mechanisms - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK586083/]
- 43. Mesenchymal stem cell-derived exosomes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8362559/]
- 44. Disrupting Mechanotransduction Pathways to Improve ... [https://gurtnerlab.arizona.edu/translational-research/disrupting-mechanotransduction-pathways-improve-wound-healing-and-prevent]
- 45. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 46. Comparative Efficacy of Exosomes Derived from Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193399/]
- 47. Adipose-derived stem cell exosomes: multifaceted therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527763/]
- 48. Umbilical cord mesenchymal stem cell-derived exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620388/]
- 49. High-yield BMSC-derived exosomes by the 3D culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041419/]
- 50. Wound healing effects of exosomes from hypoxia [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04636-4]
- 51. How to Label Exosomes? [https://www.creative-biostructure.com/how-to-label-exosomes.htm?srsltid=AfmBOopJNOs2nJXz7gaNsAHJTkUoTm9ypozxzgjX3p540xvHuoEipwq0]
- 52. Strategies for labelling of exogenous and endogenous ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01548-3]
- 53. Comparative analysis of tangential flow filtration and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9486818/]
- 54. Commonly used methods for extracellular vesicles ... [https://www.sciencedirect.com/science/article/pii/S0171933522000309]
- 55. Scalable isolation of surface-engineered extracellular vesicles ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-024-00009-0]
- 56. Minimal information for studies of extracellular vesicles ( MISEV 2023)... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850029/]
- 57. and MIQE: integrating domain-specific and general standards to... MISEV [https://www.oaepublish.com/articles/evcna.2025.68]
- 58. Umbrella review of mesenchymal stem cell-derived ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1655623/full]
- 59. From Benchmark to Airborne: MISEV Inspire... - RoosterBio Guidelines [https://www.roosterbio.com/blog/from-benchmark-to-airborne-misev-guidelines-inspire-fledgling-ev-exosome-analytics-services/]
- 60. Advances of exosomes in diabetic wound healing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836438/]
- 61. Efficacy and safety of small extracellular vesicle interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9516230/]
- 62. MSC-EVs and UCB-EVs promote skin wound healing and ... [https://www.nature.com/articles/s41598-025-87592-6]
- 63. Plant-based Exosome Injections for Skin Wound Healing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245253/]
- 64. Current and Future Prospective of Injectable Hydrogels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8948902/]
- 65. Subcutaneous Application of a Gelatin/Hyaluronic Acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10935399/]
- 66. Mesenchymal stromal/stem cell (MSC)-derived exosomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079493/]
- 67. Mesenchymal stem cell-derived exosomes for the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1588841/full]
- 68. The rise of exosome-mediated mechanisms in MSC therapy [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06747-1]
- 69. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 70. Engineering strategies to enhance the research progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220656/]
- 71. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 72. Therapeutic potential of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10907468/]
- 73. Recent advances in extracellular vesicles for therapeutic ... [https://www.nature.com/articles/s12276-024-01201-6]
- 74. Mesenchymal Stem Cell-Derived Exosomes as Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11277139/]
- 75. Recent Progress and Challenges in Exosomes for ... [https://www.sciencedirect.com/science/article/abs/pii/S3050475925007778]
- 76. Frontiers | Efficacy of MSC-derived small extracellular vesicles in treating type II diabetic cutaneous wounds: a systematic review and meta-analysis of animal models [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1375632/full]
- 77. Extracellular vesicles for targeted drug delivery: advances in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07077-y]
- 78. Comparison of isolation methods of exosomes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548045/]
- 79. Exosome-based therapeutics in bone regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512519/]
- 80. Biomimetic scaffolds loaded with mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11549779/]
- 81. Different exosomes are loaded in hydrogels for the ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1545636/full]
- 82. Innovative hydrogels in cutaneous wound healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1454903/full]
- 83. Prospects of Hydrogels in Wound Healing: Toward the ... [https://www.mdpi.com/1999-4923/17/11/1486]
- 84. Recombinant human collagen hydrogels with different stem ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03319-9]
- 85. Comparison of Wound Healing Effects of Different Micro- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12026865/]
- 86. EGF, TNF-α, and Hypoxia Preconditioning Enhances the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421495/]
- 87. Hypoxia-Induced Extracellular Vesicles Derived from ... [https://www.mdpi.com/2218-273X/15/11/1504]
- 88. Adipose-derived stem cell exosomes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181847/]
- 89. Novel Gene-Modified Mesenchymal Stem Cell Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10414148/]
- 90. Manufacturing exosomes for wound healing [https://pubmed.ncbi.nlm.nih.gov/39541412/]
- 91. EV products obtained from iPSC-derived MSCs show batch-to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10642442/]
- 92. Applications, challenges and prospects of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8478268/]
- 93. Challenges of manufacturing mesenchymal stromal cell– ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324920305673]
- 94. Batch variability and anti-inflammatory effects of iPSC ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1536843/full]
- 95. The Opportunities and Challenges of Mesenchymal Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11640604/]
- 96. Mesenchymal stem cell-derived exosomes: A novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157601/]
- 97. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 98. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 99. Potential upscaling protocol establishment and wound ... [https://www.nature.com/articles/s41598-025-93219-7]
- 100. Manufacturing exosomes for wound healing - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11563385/]
- 101. Different storage and freezing protocols for extracellular vesicles [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04005-7]
- 102. Different storage and freezing protocols for extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600612/]
- 103. Preservation of extracellular vesicles for drug delivery [https://www.sciencedirect.com/science/article/abs/pii/S1773224725002539]
- 104. Mesenchymal stem cell-derived extracellular vesicles [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399395/]
- 105. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 106. Preclinical Study Unlocks a Mystery of Rapid Mouth Healing [https://www.cedars-sinai.org/newsroom/preclinical-study-unlocks-a-mystery-of-rapid-mouth-healing/]
- 107. Mesenchymal stem cell exosomes in bone regenerative ... [https://www.sciencedirect.com/science/article/pii/S2590006420300272]
- 108. Human adipose-derived mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261776/]
- 109. Bone marrow mesenchymal stem cell exosomes improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934688/]
- 110. Adipose-derived stem cell exosomes: emerging roles and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637342/full]
- 111. Stem cell derived exosome trilogy: an epic comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186388/]
- 112. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 113. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 114. Meta-analysis study of the therapeutic impact ... [https://pubmed.ncbi.nlm.nih.gov/40524833/]
- 115. Efficacy of mesenchymal stem cell-based therapies in the ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04272-y]
- 116. Bioengineered MSC-derived exosomes in skin wound repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009159/]
- 117. Comparison of Effects Exosomes Derived from ... [https://www.traumamon.com/article_209240.html]
- 118. A phase 1, open-label study to determine safety and ... [https://www.sciencedirect.com/science/article/pii/S1465324925000313]
- 119. Reducing Infections and Improving Healing in Complex ... [https://pubmed.ncbi.nlm.nih.gov/40364268/]
- 120. Manufacturing exosomes for wound healing - Research journals [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0313697]
- 121. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 122. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 123. Quality Management System Regulation: Final Rule [https://www.fda.gov/medical-devices/quality-system-qs-regulationmedical-device-current-good-manufacturing-practices-cgmp/quality-management-system-regulation-final-rule-amending-quality-system-regulation-frequently-asked]
- 124. Novel Drug Approvals at FDA [https://www.fda.gov/drugs/development-approval-process-drugs/novel-drug-approvals-fda]
- 125. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 126. Exosome Therapeutics Market Report 2025: 120+ Drug ... [https://finance.yahoo.com/news/exosome-therapeutics-market-report-2025-124600609.html]
- 127. Exosome IV Therapy 2025: Safety, Cost, Benefits [https://healthe1medical.com/exosome-iv-therapy-2025/]
- 128. Exosome Therapeutics Market Size 2025 to 2034 [https://www.precedenceresearch.com/exosome-therapeutics-market]
- 129. Exosome Therapeutics Market Share Opportunities, 2025- ... [https://www.coherentmi.com/industry-reports/exosome-therapeutics-market]
- 130. Exosome Therapy Market Analysis Report 2025-2032 [https://www.linkedin.com/pulse/exosome-therapy-market-analysis-report-yahme]