Unraveling the Mechanisms of Mesenchymal Stem Cell Immunomodulation: From Basic Science to Clinical Applications
This article provides a comprehensive analysis of the molecular and cellular mechanisms underlying mesenchymal stem cell (MSC)-mediated immunomodulation, a rapidly advancing field with significant therapeutic potential.
Unraveling the Mechanisms of Mesenchymal Stem Cell Immunomodulation: From Basic Science to Clinical Applications
Abstract
This article provides a comprehensive analysis of the molecular and cellular mechanisms underlying mesenchymal stem cell (MSC)-mediated immunomodulation, a rapidly advancing field with significant therapeutic potential. Targeting researchers, scientists, and drug development professionals, we explore the foundational biology of MSC interactions with innate and adaptive immune systems, examine current methodological approaches and clinical applications in diseases like GvHD and allergic rhinitis, address key challenges in standardization and safety, and evaluate validation strategies through preclinical and clinical trials. The synthesis of these four core intents offers a roadmap for advancing MSC-based therapies from bench to bedside, highlighting emerging technologies such as engineered MSCs and exosome-based treatments that promise to enhance efficacy and safety in regenerative medicine and immunotherapy.
The Immunomodulatory Arsenal of MSCs: Decoding Cellular and Molecular Mechanisms
Mesenchymal Stem Cells (MSCs) have emerged as one of the most promising tools in cell and gene therapy, attracting considerable attention for their applications in regenerative medicine and immunomodulation [1]. However, the field has been challenged by significant heterogeneity in how these cells are defined, characterized, and reported across studies. Recognizing this critical issue, the International Society for Cellular Therapy (ISCT) established minimal criteria to standardize the definition of MSCs, aiming to enhance rigor, reproducibility, and transparency in both preclinical and clinical research [2]. These criteria serve as an essential foundation for research into MSC immunomodulation, ensuring that scientists worldwide are investigating comparable cell populations. Despite these efforts, a 2022 scoping review revealed that only 18% of published articles explicitly referred to the ISCT minimal criteria, and only 20% reported at least one functional assay [2]. This highlights the ongoing need to reinforce these standards, particularly as researchers delve deeper into the sophisticated immunomodulatory mechanisms that make MSCs biologically and therapeutically compelling.
The ISCT Minimal Defining Criteria for MSCs
The ISCT criteria, established in 2006, provide a three-part framework for defining MSCs, which distinguishes them from other cell types in the stromal compartment [3] [4].
Plastic Adherence
The primary and most fundamental criterion is that MSCs must be plastic-adherent when maintained under standard culture conditions [3] [5]. This is a functional characteristic observed during in vitro culture, where MSCs selectively attach to the surface of plastic tissue culture vessels, while hematopoietic and other non-MSC populations remain in suspension and can be removed during medium changes.
Surface Antigen Expression
MSCs must demonstrate a specific immunophenotype, characterized by the positive expression of a set of surface markers and the absence of hematopoietic markers. The expression must be ≥95% positive for positive markers and ≤2% positive for negative markers [5].
Table 1: Required Surface Marker Profile for MSCs as per ISCT Criteria
| Marker Category | Marker Examples | Requirement |
|---|---|---|
| Positive Expression | CD73, CD90, CD105 | ≥95% Positive |
| Negative Expression | CD11b, CD14, CD19, CD34, CD45, HLA-DR | ≤2% Positive |
It is important to note that beyond this core set, the panel of MSC-associated markers has expanded. Researchers often simultaneously verify additional markers such as CD29, CD44, CD146, CD166, and STRO-1 to increase confidence in cell identification, though their expression can vary depending on the tissue of origin [3]. For instance, STRO-1 is positively expressed in bone marrow and dental tissue MSCs but is negative in adipose-derived MSCs [5].
Tri-Lineage Differentiation Potential
A central defining feature of MSCs is their multipotency—the ability to differentiate into multiple cell types of the mesodermal lineage. The ISCT requires that MSCs must be able to differentiate in vitro into osteoblasts (bone), adipocytes (fat), and chondroblasts (cartilage) [3] [4]. Confirmation of this tri-lineage differentiation provides the most functional evidence for verifying MSC identity beyond surface markers.
MSCs can be isolated from a wide variety of adult and perinatal tissues. While all sources yield cells that fulfill the core ISCT criteria, significant biological differences exist in their proliferation capacity, gene expression profiles, secretory signatures, and immunomodulatory potency [4] [6]. These differences are critical to consider when selecting a cell source for specific immunomodulation research or therapy development.
Table 2: Characteristics of MSCs from Different Tissue Sources
| Tissue Source | Key Advantages | Reported Functional Differences & Notes |
|---|---|---|
| Bone Marrow (BM-MSCs) | Considered the "gold standard"; most advanced in clinical trials [4]. | Produce more VEGF and SDF-1, potentially making them more suitable for supporting angiogenesis and homing to bone marrow [4]. |
| Adipose Tissue (AT-MSCs) | Less invasive and painful collection; cells can longer retain stem cell phenotype [1]. | Some studies report more potent immunomodulatory effects than BM-MSCs [7] [6]. |
| Wharton's Jelly (WJ-MSCs) | Fetal source with high proliferation capacity; minimal risk of initiating an allogeneic immune response [7] [6]. | Higher proliferation capacity and longer telomeres than adult sources [4] [6]. WJ-MSC-CM shows a strong regenerative profile, promoting wound healing and VEGF expression in SSc fibroblasts [1]. |
| Umbilical Cord Blood (CB-MSCs) | Fetal source; ease of collection [7]. | Lower recovery rate in culture; slower to start expanding; may express less CD90 and CD105 compared to BM-/AT-MSCs [4]. |
| Placenta (PL-MSCs) | Fetal source; high proliferation capacity [4]. | Express genes for hematopoietic growth factors (LIF, SCF, TPO) and can support ex vivo expansion of hematopoietic stem cells [4]. |
The selection of a tissue source is not merely a logistical decision but a critical experimental variable. For example, a 2025 study directly comparing the secretome and functional effects of MSCs from four different sources found that WJ-MSC-conditioned medium and BM-MSC-conditioned medium showed a greater regenerative profile than those from cord blood or adipose tissue in models of skin therapy for Systemic Sclerosis. Notably, WJ-MSC-CM significantly promoted fibroblast-mediated wound healing processes and VEGF expression in SSc fibroblasts, even compared to BM-MSC-CM [1]. This underscores how the tissue source can directly influence the therapeutic mechanism of action, which is a vital consideration for immunomodulation research.
Experimental Protocols for Verifying MSC Identity
Rigorous quality control and characterization are paramount. The following methodologies are essential for confirming that a cell population meets the ISCT criteria and is suitable for research into immunomodulation.
Flow Cytometry for Surface Marker Expression
Purpose: To quantitatively assess the presence of positive and negative surface markers as defined by the ISCT. Detailed Protocol:
- Cell Preparation: Harvest MSCs at the appropriate passage (typically P2-P4) using a standard dissociation reagent like trypsin-EDTA. Wash cells with a phosphate-buffered saline (PBS) solution containing 1-5% fetal bovine serum (FBS) to block non-specific binding.
- Antibody Staining: Resuspend approximately 1x10^5 to 5x10^5 cells per tube in staining buffer. Incubate with fluorochrome-conjugated antibodies against CD73, CD90, CD105, CD34, CD45, CD14/CD11b, CD19/CD79α, and HLA-DR for 30-60 minutes on ice or at 4°C in the dark. Include appropriate isotype controls for each antibody to set fluorescence baselines.
- Analysis: Wash cells to remove unbound antibody and resuspend in staining buffer. Analyze the cells using a flow cytometer. A population is considered positive for a marker if ≥95% of cells express CD73, CD90, and CD105, and ≤2% express the hematopoietic markers [3] [5]. Multicolour flow cytometry is recommended to examine several markers simultaneously on the same cell population.
Colony-Forming Unit (CFU) Assay
Purpose: To evaluate the clonogenic and self-renewal capacity of MSCs. Detailed Protocol:
- Cell Seeding: Create a single-cell suspension of MSCs and perform serial dilution. Seed the cells at a clonogenic density of 10-100 cells per cm² in a tissue culture dish or plate. Using a low density is critical to ensure that colonies form from single cells.
- Culture: Culture the cells in standard growth medium (e.g., α-MEM or DMEM supplemented with 10% FBS) for 8-14 days, replacing the medium every 3-4 days.
- Staining and Quantification: After colonies become visible to the eye, carefully aspirate the medium, wash with PBS, and fix the cells with 4% formaldehyde or methanol. Stain with Giemsa or crystal violet for 20-30 minutes. Rinse gently with water, air dry, and count the number of colonies. A colony is typically defined as a cluster of >50 cells [3].
Tri-Lineage Differentiation Assays
Purpose: To functionally confirm the multipotent differentiation potential of MSCs into osteocytes, adipocytes, and chondrocytes. Detailed Protocol:
- Osteogenic Differentiation:
- Induction: Seed MSCs at a high density (~3x10^4 cells/cm²). Once they reach 70% confluence, replace the standard growth medium with osteogenic induction medium. This medium is typically composed of base medium supplemented with 10 mM β-glycerophosphate, 50-100 µM ascorbate-2-phosphate, and 10-100 nM dexamethasone.
- Culture and Analysis: Culture the cells for 2-4 weeks, changing the induction medium twice weekly. To confirm differentiation, fix the cells and stain with Alizarin Red S to detect calcium deposits in the mineralized extracellular matrix [3]. Alkaline phosphatase (ALP) activity can also be measured as an early marker of osteogenesis.
Adipogenic Differentiation:
- Induction: Seed MSCs at a high density (~2x10^4 cells/cm²). At 100% confluence, initiate differentiation by replacing the growth medium with adipogenic induction medium. A common cocktail includes base medium with 0.5 mM 3-isobutyl-1-methylxanthine (IBMX), 1 µM dexamethasone, 10 µM insulin, and 200 µM indomethacin.
- Culture and Analysis: Culture the cells for 1-3 weeks. The induction medium can be alternated with a maintenance medium (containing only insulin) every 2-3 days. To confirm adipogenesis, fix the cells and stain with Oil Red O to visualize the accumulated intracellular lipid droplets [3].
Chondrogenic Differentiation:
- Pellet Culture: Centrifuge 2.5x10^5 MSCs in a conical polypropylene tube to form a micromass pellet. Culture the pellet in chondrogenic induction medium, which often contains high-glucose DMEM, 1% ITS (Insulin-Transferrin-Selenium), 100 nM dexamethasone, 50 µM ascorbate-2-phosphate, and 10 ng/mL TGF-β3 (a key chondrogenic factor).
- Culture and Analysis: Culture the pellets for 3-4 weeks, changing the medium every 2-3 days. To confirm chondrogenesis, fix the pellets, embed in paraffin, section, and stain with Alcian Blue to detect the presence of sulfated glycosaminoglycans (GAGs) in the cartilage-specific extracellular matrix [3].
MSC Immunomodulation: Mechanisms and Research Workflows
The immunomodulatory capacity of MSCs is not constitutive but is primed by inflammatory factors in the microenvironment, particularly IFN-γ, often in combination with TNF-α, IL-1α, or IL-1β [8]. This licensing process triggers MSCs to employ a dual-mechanism strategy involving cell-to-cell contact and paracrine activity to suppress immune responses.
Key Immunomodulatory Mechanisms
- Cell-to-Cell Contact: MSCs directly interact with immune cells via surface molecules. The upregulation of ICAM-1 and VCAM-1 is critical for T-cell activation and recruitment [7] [6]. MSCs also express PD-L1 and PD-L2, which can inhibit T-cell proliferation by arresting the cell cycle [7]. Furthermore, galectin-1 expression on MSCs is essential for their immunomodulatory function, and its knockdown leads to a restoration of T-cell proliferation [6].
- Paracrine Activity (Soluble Factors): The licensed MSC secretome contains a plethora of immunomodulatory factors. Key among them are:
- Indoleamine 2,3-dioxygenase (IDO): Catalyzes the conversion of tryptophan to kynurenine, depleting local tryptophan and inhibiting T-cell proliferation [8] [5].
- Prostaglandin E2 (PGE2): Suppresses the proliferation and function of various immune cells, including T cells and macrophages, and can switch macrophages from a pro-inflammatory M1 to an anti-inflammatory M2 phenotype [7] [8].
- Transforming Growth Factor-β1 (TGF-β1) and Hepatocyte Growth Factor (HGF): Contribute to the suppression of T-cell proliferation and the induction of regulatory T cells (Tregs) [8].
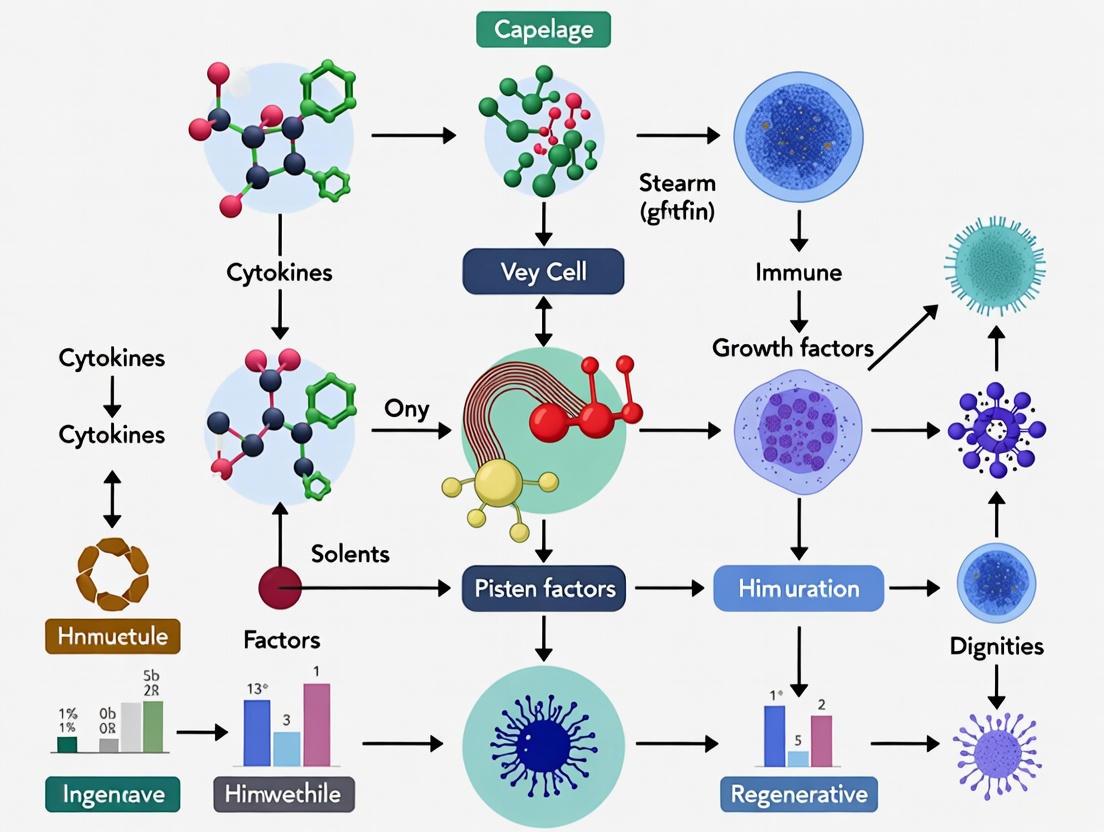
The following diagram illustrates the core immunomodulatory mechanisms and the experimental workflow for investigating them.
Diagram: MSC Immunomodulation Mechanisms & Research Workflow. The diagram illustrates how inflammatory cytokines prime MSCs, which then exert immunomodulation via cell-contact and paracrine mechanisms, leading to functional changes in immune cells. Key experimental assays for investigating these pathways are also shown.
The Scientist's Toolkit: Essential Reagents for MSC Immunomodulation Research
Table 3: Key Research Reagent Solutions for MSC Immunomodulation Studies
| Reagent / Assay | Function in Research |
|---|---|
| Flow Cytometry Antibodies | Essential for verifying MSC identity (CD73, CD90, CD105) and assessing purity by excluding hematopoietic markers (CD34, CD45). Also used to analyze immune cell populations (e.g., T-cells, B-cells) in co-cultures [3]. |
| Tri-lineage Differentiation Kits | Commercial kits provide optimized media and reagents to reliably demonstrate MSC multipotency (osteogenic, adipogenic, chondrogenic) as per ISCT criteria [3]. |
| Inflammatory Cytokines (IFN-γ, TNF-α) | Used to "license" or prime MSCs in vitro to activate their immunomodulatory functions before use in functional assays or therapeutic applications [8]. |
| Lymphocyte Proliferation Assay | Measures the ability of MSCs to suppress the proliferation of activated T-cells (e.g., using mitogens like PHA or anti-CD3/CD28 beads). A cornerstone potency assay for immunomodulation [3] [8]. |
| ELISA / Multiplex Cytokine Arrays | Quantifies the secretion of immunomodulatory factors (e.g., IDO, PGE2, TGF-β) by MSCs and measures changes in the inflammatory cytokine milieu in co-culture supernatants [1] [3]. |
| Transwell Migration Assay | Assesses the migratory and homing potential of MSCs in response to chemokines or stimuli from injured or inflamed tissues [3]. |
A rigorous adherence to the ISCT criteria is the bedrock of credible MSC research, enabling the validation of cell identity and facilitating meaningful comparisons across studies. As the field progresses, it is evident that the tissue source is a major determinant of functional potency, influencing the secretory profile and immunomodulatory mechanisms of MSCs. Future research must not only consistently apply these standards but also move towards developing more sophisticated potency assays that directly reflect the intended clinical mechanism of action. By integrating strict characterization with a nuanced understanding of source-specific biology, researchers can fully harness the potential of MSCs to develop novel and effective immunomodulatory therapies.
Mesenchymal stem cells (MSCs) have emerged as one of the most promising tools in allogeneic cell therapy due to their profound immunomodulatory capabilities [9]. These multipotent cells exert their therapeutic effects through a dual-mechanism paradigm: direct cell-cell contact and secretion of soluble factors [7]. This sophisticated dual approach enables MSCs to interact with a wide spectrum of immune cells, including T cells, B cells, natural killer (NK) cells, macrophages, monocytes, and dendritic cells, thereby modulating both innate and adaptive immunity [7]. The immunomodulatory functions of MSCs are not static but are dynamically influenced by the local tissue microenvironment, which dictates the balance and predominance of each mechanism [10]. Understanding this complex interplay is crucial for harnessing the full therapeutic potential of MSCs in treating inflammatory diseases, autoimmune disorders, and preventing transplant rejection [9] [11].
Cell-Cell Contact Mediated Immunomodulation
Direct cellular contact represents a fundamental mechanism through which MSCs communicate with and regulate immune cells. This contact-dependent signaling occurs through specialized surface molecules that facilitate precise cellular interactions.
Key Contact Molecules and Pathways
- Adhesion Molecules (ICAM-1 and VCAM-1): The upregulation of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1) on MSCs is critical for initial tethering to immune cells and subsequent suppression of T-cell activation [7]. These molecules enable the formation of the immunological synapse between MSCs and T lymphocytes, facilitating downstream signaling events.
- Immunoregulatory Ligands (PD-L1/PD-L2 and Galectin-1): Human placenta-derived MSCs (PMSCs) express high levels of programmed death-ligand 1 (PD-L1) and PD-L2, which inhibit T-cell proliferation by inducing cell cycle arrest [7]. Similarly, Galectin-1, abundantly expressed on MSCs, plays a pivotal role in modulating T-cell responses, as its knockdown results in restored CD4+ and CD8+ T-cell proliferation [7].
- Notch Signaling Pathway: The interaction between Notch receptors on T cells and their ligands on MSCs activates the Notch1/forkhead box P3 (FOXP3) pathway, increasing the percentage of CD4+CD25+FOXP3+ regulatory T cells (Tregs) [7]. This pathway represents a direct contact-mediated mechanism for expanding immunoregulatory cell populations.
The following diagram illustrates the major contact-dependent pathways MSCs use to modulate immune cell activity:
Functional Outcomes of Cellular Contact
The functional consequences of direct MSC-immune cell contact are profound. In vivo studies using syngeneic mouse models have demonstrated that contact-mediated interactions are essential for the anti-tumor effects of compact bone-derived MSCs (CB-MSCs), which involve activation of CD4+ and CD8+ T-cells while simultaneously inhibiting Tregs in the tumor microenvironment [7]. Furthermore, research has confirmed that MSCs primed by activated T cells derived from IFN-γ −/− mice exhibit a dramatically reduced ability to suppress T-cell proliferation, underscoring the non-redundant role of cell-contact mechanisms [7]. Beyond T-cells, MSCs also regulate B-cell function through contact-dependent mechanisms. Adipose-derived MSCs (A-MSCs) have been shown to increase the survival of quiescent B-cells and facilitate their differentiation independently of T-cell help [7]. These interactions are mediated through specific signaling pathways, including p38 mitogen-activated protein kinase (MAPK), which leads to cell cycle arrest of B-lymphocytes in the G0/G1 phase [7].
Soluble Factor Mediated Immunomodulation
The paracrine activity of MSCs represents the second pillar of their immunomodulatory arsenal, mediated through a diverse repertoire of secreted molecules.
Major Soluble Mediators and Their Mechanisms
- Indoleamine 2,3-Dioxygenase (IDO): This enzyme catalyzes the degradation of the essential amino acid tryptophan into kynurenine, creating a tryptophan-deficient microenvironment that suppresses T-cell proliferation and induces Treg differentiation, thereby promoting kidney allograft tolerance [7].
- Prostaglandin E2 (PGE2): MSC-secreted PGE2 plays a multifaceted role by inhibiting the differentiation of T helper 17 (Th17) cells while simultaneously promoting the switch of activated M1-like inflammatory macrophages to an M2-like anti-inflammatory phenotype [7] [11].
- Transforming Growth Factor-β (TGF-β): This potent immunoregulatory cytokine works in concert with interleukin-10 (IL-10) to inhibit T-cell activation and cytokine production through the activation of downstream Smad and STAT3 signaling pathways [11].
- Extracellular Vesicles (EVs): MSC-derived exosomes and microvesicles serve as critical vehicles for intercellular communication, transferring bioactive molecules like miRNAs to recipient cells. For instance, BM-MSC-EVs containing miR-1246 can suppress Th17-mediated pathogenesis in periodontitis by downregulating angiotensin-converting enzyme-2 expression and modulating YAP1/Hippo signaling [11].
Integrated View of Soluble Factor Signaling
The diagram below illustrates how soluble factors secreted by MSCs coordinate to regulate different immune cell populations:
Experimental Approaches for Mechanism Separation
Disentangling the contributions of cell-cell contact versus soluble factors requires specialized experimental methodologies that allow for controlled cellular interactions.
Insert Co-Culture System
The insert co-culture system represents a gold standard technique for studying paracrine signaling in the absence of direct cellular contact [12]. This system utilizes permeable membrane-based inserts that fit into multiwell tissue culture plates, allowing one cell type (e.g., MSCs) to be cultured in the insert while another cell type (e.g., immune cells) is cultured in the well below. The microporous membrane permits the free diffusion of secreted soluble factors while preventing physical contact between the two cell populations [12]. Various membrane materials are available, including polyester (PET), polycarbonate (PC), or collagen-coated polytetrafluoroethylene (PTFE), with pore sizes typically ranging from 0.4 µm to 12.0 µm, selected based on the specific experimental requirements [12].
Protocol for Insert Co-Culture Setup [12]:
- Insert Preparation: Unwrap sterile inserts from packaging and place them in an empty multiwell tissue culture plate under sterile conditions.
- Cell Seeding: Seed the first cell type (e.g., MSCs) into the inserts at the appropriate density. Simultaneously, seed the second cell type (e.g., immune cells) in the wells of the tissue culture plate.
- Assembly: Carefully place the inserts containing the first cell type into the wells containing the second cell type, ensuring no air bubbles are trapped beneath the membrane.
- Culture Conditions: Incubate the co-culture system under standard conditions (e.g., 37°C, 5% CO₂) for the desired duration, typically 24-72 hours for most immunomodulation studies.
- Analysis: Following co-culture, cells in both compartments can be harvested for functional assays (e.g., proliferation, activation status), and conditioned media can be collected for analysis of secreted factors.
Advanced Single-Cell Secretion Profiling
Recent technological advances have enabled more sophisticated analysis of cell-cell interactions through integrative single-cell secretion profiling [13]. This platform utilizes an antibody-barcode microchip that simultaneously detects various secreted factors (multiple proteins and extracellular vesicle phenotypes), spatial distances, and migration information from high-throughput paired single cells [13]. The microchip consists of a high-density microchamber array (approximately 10,000 chambers) and a glass slide patterned with spatially resolved antibodies, allowing for multiplexed detection of proteins (e.g., IL-8, IL-6, MCP-1, IL-1β) and EV markers (CD9, CD81, CD63) with high sensitivity (detection limit of 40 pg mL⁻¹ for proteins and ∼3 × 10⁴ particles µL⁻¹ for EVs) [13].
Quantitative Comparison of Immunomodulatory Mechanisms
The relative contribution of contact-dependent versus soluble factor-mediated mechanisms varies depending on the specific immune cell target and environmental context. The table below summarizes key quantitative data from studies that have dissected these dual mechanisms.
Table 1: Quantitative Comparison of Contact-Dependent vs. Soluble Factor-Mediated Immunomodulation by MSCs
| Immune Cell Target | Contact-Dependent Effects | Soluble Factor-Mediated Effects | Experimental System | Key References |
|---|---|---|---|---|
| T Cells | Upregulation of ICAM-1/VCAM-1 critical for suppression; Induction of T-cell anergy; Notch1/FOXP3 pathway activation increases CD4+CD25+FOXP3+ Tregs. | IDO-mediated tryptophan depletion inhibits proliferation; TGF-β and IL-10 suppress activation via Smad/STAT3; PGE2 inhibits Th17 differentiation. | Insert co-culture; Transwell systems; Single-cell secretion profiling | [7] [11] [13] |
| B Cells | Contact-dependent enhancement of quiescent B-cell survival; p38 MAPK-mediated cell cycle arrest in G0/G1 phase. | Conflicting reports on soluble factor effects: some studies show inhibition, others show promotion of proliferation and differentiation. | Direct co-culture vs. conditioned media experiments | [7] [11] |
| Macrophages | Phagocytosis of MSCs by monocytes induces phenotypic and functional changes. | PGE2 secretion drives switch from pro-inflammatory M1 to anti-inflammatory M2 phenotype. | Insert co-culture; In vivo tracking studies | [7] [11] |
| Tumor Microenvironment | ECM and surface proteins of normal fibroblasts mediate contact-dependent inhibition of tumor cell proliferation. | Soluble factors (GDF15, DKK1, EMAPII) in confronted conditioned media (CCM) inhibit both tumor cell proliferation and motility. | Fibroblast-tumor cell co-culture systems | [14] |
Table 2: Key Soluble Factors in MSC-Mediated Immunomodulation and Their Detection Methods
| Soluble Factor | Primary Function in Immunomodulation | Detection Method | Approximate Detection Limit |
|---|---|---|---|
| Indoleamine 2,3-dioxygenase (IDO) | Tryptophan catabolism, T-cell suppression, Treg induction | HPLC, ELISA | Varies by method |
| Prostaglandin E2 (PGE2) | M1 to M2 macrophage switch, Th17 inhibition | ELISA, Mass Spectrometry | ~15 pg/mL (ELISA) |
| Transforming Growth Factor-β (TGF-β) | T-cell suppression via Smad pathway | ELISA, Single-cell barcode chip | ~40 pg/mL (chip) |
| Extracellular Vesicles (CD9+/CD81+/CD63+) | miRNA transfer, intercellular communication | Nanoparticle tracking, Microchip immunoassay | ~3×10⁴ particles/μL (chip) |
| Interleukin-6 (IL-6) & IL-8 | Pro-inflammatory regulation in tumor microenvironment | ELISA, Single-cell barcode chip | ~40 pg/mL (chip) |
The Researcher's Toolkit: Essential Reagents and Materials
Successful investigation of MSC immunomodulatory mechanisms requires specific research tools and reagents. The following table details essential components for designing appropriate experiments.
Table 3: Essential Research Reagents for Studying MSC Immunomodulatory Mechanisms
| Reagent/Material | Primary Function | Specific Examples & Applications |
|---|---|---|
| Transwell/Insert Systems | Physically separates cell populations while allowing soluble factor exchange. | Polyester (PET), polycarbonate (PC), or collagen-coated PTFE membranes with pore sizes from 0.4-12.0 μm; used for paracrine signaling studies [12]. |
| Cell Tracking Dyes | Enables visualization and distinction of different cell populations in co-culture. | CellTracker DIO and DID membrane dyes; used for monitoring cellular interactions and migration in single-cell pairing experiments [13]. |
| Cytokine Detection Arrays | Multiplexed detection of secreted soluble factors. | Antibody-barcode microchips for proteins (IL-6, IL-8, MCP-1, IL-1β) and EV markers (CD9, CD81, CD63) [13]. |
| TLR Agonists/Antagonists | Modulates MSC polarization state for mechanistic studies. | LPS (TLR4 agonist) for pro-inflammatory MSC1 polarization; Poly(I:C) (TLR3 agonist) for immunosuppressive MSC2 polarization [10]. |
| Neutralizing Antibodies | Blocks specific ligand-receptor interactions to test molecular mechanisms. | Antibodies against ICAM-1, VCAM-1, PD-L1, Galectin-1 to inhibit contact-dependent pathways [7]. |
| Enzyme Inhibitors | Blocks specific soluble factor production or signaling. | IDO inhibitors (1-MT), COX-2 inhibitors (to block PGE2 production) for dissecting soluble mediator pathways [7] [11]. |
The dual mechanism paradigm of cell-cell contact and soluble factor secretion underpins the remarkable immunomodulatory capacity of mesenchymal stem cells. Both mechanisms work in concert, often synergistically, to achieve precise spatial and temporal regulation of immune responses. The contact-mediated pathway provides targeted, specific regulation through direct molecular interactions, while the soluble factor pathway offers broader, more diffuse modulation of the tissue microenvironment. The relative contribution of each mechanism is highly dynamic and context-dependent, influenced by factors such as the tissue type, inflammatory milieu, and specific immune cell populations involved [10] [15]. Understanding this sophisticated duality is not merely an academic exercise but is crucial for optimizing MSC-based therapies, engineering enhanced MSC products, and developing novel pharmacological approaches that mimic these natural immunoregulatory mechanisms for treating a wide spectrum of immune-mediated diseases. Future research should focus on quantitatively mapping the interplay between these pathways in specific disease contexts to enable more precise therapeutic interventions.
Within the framework of mesenchymal stem cell (MSC) immunomodulation research, a critical area of investigation involves understanding how MSCs orchestrate the functions of innate immune cells. Innate immunity serves as the body's first line of defense, comprising cells that initiate rapid responses to pathogens and abnormal cells [16]. Key cellular mediators include macrophages, dendritic cells (DCs), and natural killer (NK) cells, which participate in phagocytosis, antigen presentation, and direct cytotoxicity, respectively [17]. The immunomodulatory capabilities of MSCs significantly influence these cells, polarizing their phenotypes and altering their functional outputs to resolve inflammation and promote tissue repair [18] [19]. This whitepaper provides an in-depth technical analysis of the mechanisms by which MSCs and their derived products modulate these innate immune cells, detailing specific pathways, experimental methodologies, and key research reagents essential for advancing therapeutic development.
Mechanisms of Innate Immune Cell Modulation by MSCs
Macrophage Regulation
Macrophages demonstrate remarkable plasticity, capable of adopting pro-inflammatory (M1) or anti-inflammatory, pro-repair (M2) phenotypes. MSCs potently influence this polarization, primarily through paracrine signaling, to suppress damaging inflammation and promote tissue healing [18] [19].
Key Mechanisms:
- Soluble Factor Secretion: MSCs release anti-inflammatory molecules like TNF-α-stimulated gene/protein 6 (TSG-6) and interleukin-1 receptor antagonist (IL-1RA). TSG-6 modifies the CD44 receptor on macrophages, suppressing nuclear factor kappa-B (NF-κB) signaling and reducing the production of pro-inflammatory cytokines such as TNF-α [19]. This pathway is critical in mitigating sepsis and other hyperinflammatory conditions.
- Metabolic Reprogramming and Trained Immunity: The concept of "trained immunity" describes the long-term functional reprogramming of innate immune cells like macrophages following an initial stimulus, leading to an enhanced response to secondary challenges [20]. This process is orchestrated by distinct metabolic and epigenetic rewiring. MSCs can influence this program through the Dectin-1/Akt/mTOR/HIF1α pathway and the NOD2/NF-κB pathway. Key metabolic shifts include upregulation of glycolysis, glutaminolysis, and cholesterol synthesis, leading to accumulation of metabolites like fumarate and succinate. These metabolites act as cofactors for epigenetic enzymes such as histone demethylases, resulting in activating histone marks (e.g., H3K4me3) on promoters of pro-inflammatory genes, thereby potentiating macrophage function [20].
- Extracellular Vesicle-Mediated Communication: Mesenchymal stem cell-derived exosomes (MSCex) carry a cargo of proteins, lipids, and nucleic acids that modulate macrophage activity. These exosomes can deliver miRNAs and cytokines directly to macrophages, promoting their polarization towards the M2 phenotype and enhancing their phagocytic capacity [21].
Table 1: Mechanisms of MSC-Mediated Macrophage Modulation
| Mechanism | Key MSC-Derived Effectors | Signaling Pathways in Macrophage | Functional Outcome |
|---|---|---|---|
| Soluble Factor Secretion | TSG-6, IL-1RA, PGE2 | NF-κB suppression, STAT3 activation | Reduced pro-inflammatory cytokines (TNF-α, IL-6); Increased IL-10; M2 polarization [18] [19] |
| Metabolic Reprogramming | Influences via paracrine signals | Dectin-1/Akt/mTOR/HIF1α, NOD2/NF-κB, Glycolysis upregulation | Epigenetic rewiring (H3K4me3), enhanced cytokine production, "trained immunity" [20] |
| Extracellular Vesicles | Exosomes containing miRNAs, proteins | Transfer of bioactive cargo | M2 polarization, enhanced phagocytosis, anti-inflammatory response [21] |
Dendritic Cell Regulation
Dendritic cells are professional antigen-presenting cells that bridge innate and adaptive immunity. MSCs inhibit the maturation and antigen-presenting capacity of DCs, thereby dampening T cell activation and promoting immune tolerance [18] [22].
Key Mechanisms:
- Inhibition of Maturation: MSCs prevent the upregulation of co-stimulatory molecules (CD80, CD86) and MHC class II on DC surfaces, which is essential for effective T cell priming. This results in the generation of tolerogenic DCs that induce T cell anergy or promote the expansion of regulatory T cells (Tregs) [18] [23].
- Cell-Cell Contact and Soluble Factors: The immunomodulatory effects are mediated through both cell-cell contact, involving molecules like programmed death-ligand 1 (PD-L1), and soluble factors such as prostaglandin E2 (PGE2) and galectin-1. Knocking down galectin-1 in MSCs diminishes their capacity to suppress allogeneic T cell responses [18].
Table 2: Effects of MSCs on Dendritic Cell Phenotype and Function
| Parameter | Effect of MSC Co-Culture | Consequence |
|---|---|---|
| Maturation Markers | ↓ CD80, CD86, CD83, MHC-II [18] | Impaired antigen presentation |
| Cytokine Secretion | ↓ IL-12, ↑ IL-10 [18] | Promotion of immune tolerance |
| T cell Priming | Inhibition of naive and memory T cell activation [18] | Suppression of adaptive immune response |
| Chemotaxis | Altered migration and adhesion | Reduced homing to lymph nodes |
Natural Killer (NK) Cell Regulation
NK cells are cytotoxic lymphocytes that eliminate virus-infected and tumor cells. MSC-mediated regulation of NK cells is bidirectional, involving both suppression of proliferation and cytotoxicity and facilitation of their activation under specific conditions [24] [18].
Key Mechanisms:
- Suppression of Proliferation and Cytotoxicity: MSCs inhibit IL-2 and IL-15-induced NK cell proliferation and cytokine production (e.g., IFN-γ). They also downregulate the expression of activating receptors (e.g., NKp30, NKG2D) on NK cells, thereby blunting their cytotoxic activity. This is achieved through the release of soluble mediators like PGE2, TGF-β, and IDO [18].
- Orchestration of NK Activity: A pivotal mechanism involves the Dectin-1 receptor on dendritic cells and macrophages. Dectin-1 recognition of tumor cells expressing high levels of N-glycan structures activates the IRF5 transcription factor. This pathway is critical for inducing the full tumoricidal activity of NK cells. Mice deficient in Dectin-1 or IRF5 show exacerbated tumor growth, underscoring the importance of this cross-talk between innate immune cells for effective NK-mediated anti-tumor responses [24].
- Conditioning-Dependent Effects: The state of MSC activation influences their impact on NK cells. MSCs conditioned with peripheral blood mononuclear cells (PBMC) exhibit enhanced immunomodulatory activity, which can more effectively modulate NK cell function compared to resting MSCs [22].
(Diagram 1: Dectin-1-IRF5 Pathway in NK Cell Orchestration)
Experimental Protocols for Key Investigations
Protocol 1: Assessing Macrophage Polarization via MSC Co-Culture
Objective: To evaluate the effect of MSCs or MSC-derived exosomes on macrophage polarization from M1 to M2 phenotype.
Materials:
- Primary human monocytes isolated from PBMCs or a human monocyte cell line (e.g., THP-1).
- Human MSCs (e.g., adipose-derived or bone marrow-derived).
- Differentiation and polarization cytokines: GM-CSF, M-CSF, IFN-γ, LPS, IL-4, IL-13.
- FACS buffer and antibodies for M1/M2 markers: CD80, CD86, CD38, CD163, CD206, MHC-II.
Methodology:
- Monocyte-derived Macrophage Generation: Isolate CD14+ monocytes from PBMCs using magnetic-activated cell sorting (MACS). Differentiate monocytes into macrophages by culturing with 50 ng/mL M-CSF for 6 days.
- M1 Polarization: Polarize macrophages towards an M1 phenotype by stimulating with 100 ng/mL LPS and 20 ng/mL IFN-γ for 24-48 hours.
- Co-culture Setup: Establish a transwell co-culture system. Place M1-polarized macrophages in the lower chamber and MSCs (at a 1:5 macrophage:MSC ratio) in the upper chamber. Include control wells with M1 macrophages alone.
- Analysis:
- Flow Cytometry: After 48-72 hours of co-culture, harvest macrophages and stain for surface M1 (CD80, CD86) and M2 (CD163, CD206) markers. Analyze using flow cytometry.
- Cytokine Profiling: Collect culture supernatants and measure cytokine levels (e.g., TNF-α, IL-6 for M1; IL-10, TGF-β for M2) via ELISA or multiplex bead-based assays.
- Gene Expression: Extract RNA from macrophages and perform qRT-PCR to analyze the expression of M1 (iNOS, IL-1β) and M2 (Arg1, Ym1) marker genes [21] [18].
Protocol 2: Evaluating DC Maturation and Function
Objective: To determine the inhibitory effect of MSCs on the maturation and T cell-stimulatory capacity of dendritic cells.
Materials:
- Immature DCs (generated from monocytes with GM-CSF and IL-4).
- MSCs (resting or conditioned).
- LPS for maturation.
- CFSE-labeled allogeneic T cells.
- Antibodies: CD83, CD86, HLA-DR, CD3, CD4.
Methodology:
- DC Generation and MSC Conditioning: Differentiate CD14+ monocytes into immature DCs (imDCs) using 100 ng/mL GM-CSF and 50 ng/mL IL-4 for 5-7 days. Optionally, condition MSCs by co-culturing with PBMCs or pre-treating with IFN-γ (50 ng/mL for 24-48 hours) to enhance their immunomodulatory potency [22].
- Inhibition of Maturation: Co-culture imDCs with MSCs (e.g., 1:10 DC:MSC ratio) in a transwell system or direct contact system. Activate DC maturation by adding 100 ng/mL LPS for the final 24 hours of co-culture.
- Flow Cytometric Analysis: Harvest DCs and stain for maturation markers (CD83, CD86, HLA-DR). Analyze using flow cytometry to assess the percentage of mature DCs and the mean fluorescence intensity (MFI) of markers.
- Mixed Lymphocyte Reaction (MLR): Collect DCs from the co-culture, irradiate them to prevent proliferation, and co-culture them with CFSE-labeled allogeneic CD4+ T cells. After 5 days, analyze T cell proliferation by measuring CFSE dilution via flow cytometry. Suppressed T cell proliferation indicates impaired DC function [18] [22] [23].
Protocol 3: Analyzing NK Cell Cytotoxicity and Proliferation
Objective: To investigate the modulation of NK cell function by MSCs, focusing on proliferation, receptor expression, and cytotoxic activity.
Materials:
- Isolated human NK cells (e.g., CD56+ from PBMCs).
- MSCs (resting and PBMC-conditioned).
- Target cells (e.g., K562 erythroleukemia cell line).
- IL-2 and IL-15.
- Antibodies: CD56, CD16, NKp30, NKp46, NKG2D, Annexin V, 7-AAD.
Methodology:
- NK Cell Isolation and MSC Co-culture: Isolate NK cells from PBMCs using a negative selection kit. Co-culture purified NK cells with MSCs (e.g., 1:5 MSC:NK ratio) in the presence of 100 U/mL IL-2 and 10 ng/mL IL-15 for 48-72 hours.
- Proliferation and Phenotype Analysis: Label NK cells with CFSE prior to co-culture to track proliferation. After co-culture, analyze CFSE dilution by flow cytometry. Simultaneously, stain NK cells for activating (NKp30, NKG2D) and inhibitory receptors.
- Cytotoxicity Assay: Use a standard calcein-AM release assay or real-time cell analysis. Label K562 target cells with calcein-AM. Co-culture effector NK cells (from co-culture) with target cells at various effector-to-target (E:T) ratios (e.g., 10:1, 5:1) for 4 hours. Measure fluorescence released from lysed target cells. Calculate specific lysis percentage [24] [18].
- Dectin-1 Pathway Investigation: To study the orchestration mechanism, use a Dectin-1 agonist (e.g., β-glucan) or antagonist in a triple-culture system of DCs, MSCs, and NK cells, and assess the subsequent NK cell cytotoxicity against tumor targets.
(Diagram 2: General Workflow for MSC-Immune Cell Co-culture Studies)
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying MSC-Mediated Innate Immune Modulation
| Reagent Category | Specific Examples | Research Application | Key References |
|---|---|---|---|
| Cell Surface Markers (Flow Cytometry) | CD14, CD68, CD80 (M1 Macrophage), CD163, CD206 (M2 Macrophage), CD83, CD86 (DC Maturation), CD56, CD16, NKp30, NKp46 (NK Cells) | Phenotypic identification and functional characterization of innate immune cell subsets. | [17] |
| Cytokines & Growth Factors | M-CSF, GM-CSF, IFN-γ, IL-4, IL-13, IL-2, IL-15, TNF-α | Differentiation, polarization, and functional activation of macrophages, DCs, and NK cells. | [18] [22] |
| Inhibitors & Agonists | Rapamycin (mTOR inhibitor), Metformin, β-Glucan (Dectin-1 agonist), LPS (TLR4 agonist) | Dissecting specific signaling pathways (e.g., Dectin-1/Akt/mTOR) in trained immunity and cell activation. | [20] |
| MSC Conditioning Agents | Recombinant IFN-γ, TNF-α, Peripheral Blood Mononuclear Cells (PBMC) | Priming MSCs to enhance their immunomodulatory potency prior to functional assays. | [22] |
| Critical Assay Kits | ELISA/Multiplex Cytokine Kits (TNF-α, IL-6, IL-10, IL-12), CFSE Cell Proliferation Kit, LDH/Caspase Cytotoxicity Assays | Quantifying soluble factors, immune cell proliferation, and cytotoxic activity. | [24] [18] |
The strategic orchestration of innate immunity by mesenchymal stem cells, particularly their nuanced effects on macrophages, dendritic cells, and NK cells, represents a cornerstone of their therapeutic mechanism. This interplay, mediated by a complex network of soluble factors, cell-cell contacts, extracellular vesicles, and the induction of metabolic-epigenetic programs like trained immunity, highlights the sophistication of MSC-mediated immunomodulation. For researchers and drug development professionals, a deep understanding of these mechanisms and the associated experimental tools is paramount. The continued refinement of MSC conditioning protocols and the precise dissection of these innate immune pathways are critical for developing next-generation, cell-based therapies with enhanced efficacy for treating inflammatory, autoimmune, and oncological diseases.
The adaptive immune system, characterized by its high specificity and memory, is orchestrated primarily by T and B lymphocytes [25]. Within this system, CD4+ T helper (Th) cells play a pivotal role in directing immune responses. Their differentiation into distinct subsets—such as Th1, Th2, and Th17—is controlled by specific transcription factors and cytokine environments, while their activity is counterbalanced by immunosuppressive regulatory T cells (Tregs) [26] [27]. The precise regulation of the balance between these effector and regulatory cells is critical for maintaining immune homeostasis, preventing autoimmune reactions, and resolving inflammation. Research into mesenchymal stem cell (MSC) immunomodulation has provided profound insights into these processes. MSCs possess a remarkable capacity to suppress T-cell proliferation, shift the Th1/Th2 balance, and induce Treg formation, making them a powerful model system for studying and harnessing these mechanisms for therapeutic purposes [28] [29]. This whitepaper delves into the core mechanisms of adaptive immune regulation, framing the discussion within the context of MSC research and providing detailed experimental data and methodologies.
Core Mechanisms of T-cell Suppression
Metabolic Disruption via Tryptophan Starvation
A primary mechanism of T-cell suppression, particularly by human MSCs, involves the induction of metabolic stress through amino acid deprivation. The enzyme indoleamine 2,3-dioxygenase (IDO), produced by MSCs in response to inflammatory signals like interferon-gamma (IFN-γ), catalyzes the degradation of the essential amino acid tryptophan in the local microenvironment [30].
- Mechanism of Action: IDO consumption of tryptophan creates a local deficiency. Activated T cells, which have a high demand for tryptophan for protein synthesis and proliferation, are particularly sensitive to this deprivation. This starvation does not primarily inhibit mTOR or activate the ATF2 pathway but instead induces endoplasmic reticulum (ER) stress in the T cells, leading to a potent arrest of proliferation [30].
- Experimental Evidence: The critical role of tryptophan starvation, as opposed to the accumulation of tryptophan catabolites (kynurenines), was demonstrated by rescuing T-cell proliferation in IDO+ conditioned media through tryptophan supplementation, but not with kynurenine addition [30]. The response to tryptophan concentration is notably sharp, exhibiting a near-binary "all-or-nothing" switch over a very narrow dynamic range (a 10-fold change in concentration) [30].
Table 1: Quantitative Data on IDO-Mediated T-cell Suppression
| Experimental Condition | T-cell Proliferation (Cells/mL ± SD) | IL-2 Secretion (pg/mL ± SD) | Citation |
|---|---|---|---|
| Serum-Free Media (SFM - 21% O₂) | 5.3 × 10⁵ ± 1.8 × 10⁴ | 5305 ± 211 | [28] |
| Serum-Free Media (SFM - 2% O₂) | 5.1 × 10⁵ ± 3.0 × 10⁴ | 5347 ± 327 | [28] |
| MSC Conditioned Media (SFCM - 21% O₂) | 2.4 × 10⁵ ± 2.5 × 10⁴ | 2461 ± 178 | [28] |
| MSC Conditioned Media (SFCM - 2% O₂) | 2.2 × 10⁵ ± 5.8 × 10³ | 1625 ± 159 | [28] |
Soluble Factor-Mediated Suppression
Beyond IDO, MSCs and their secretome employ a cocktail of soluble factors to suppress T-cell activity.
- Anti-inflammatory Cytokines: The MSC secretome is rich in cytokines like IL-10, which plays a non-redundant role in immunosuppression. Neutralization of IL-10 in MSC-conditioned media restores T-cell proliferation, whereas neutralization of IL-4 or IL-13 does not, highlighting its specific and critical function [28]. Transforming Growth Factor-beta (TGF-β) is another key immunosuppressive cytokine involved in MSC-mediated T-cell inhibition [29].
- Other Mediators: In mice, which do not utilize IDO for this purpose, nitric oxide (NO) is a major mediator of T-cell suppression, ultimately also leading to the induction of cellular stress [30].
Regulation of Th1/Th2 Balance and T Helper Cell Polarization
The balance between pro-inflammatory Th1 cells and anti-inflammatory Th2 cells is a crucial determinant of immune outcome. MSCs have been demonstrated to skew the immune response away from Th1 and toward a Th2 phenotype [29].
- Th1 Differentiation: Driven by the cytokine IL-12 and the master transcription factor T-bet (Tbx21). Th1 cells typically produce IFN-γ and are critical for combating intracellular pathogens [27].
- Th2 Differentiation: Driven by the cytokine IL-4 and the master transcription factor GATA3. Th2 cells produce IL-4, IL-5, and IL-13, which are important for antibody class switching and responses to parasites, but also central to allergic inflammation [26] [27].
- MSC-Mediated Shifting: MSCs, through their secretome and interactions with antigen-presenting cells, can suppress the production of Th1-polarizing cytokines like IL-12 while promoting a Th2-favoring environment. This results in a measured shift from a pro-inflammatory Th1 to an anti-inflammatory Th2 profile, which is beneficial in contexts like autoimmune disease and allograft rejection [29].
Induction and Function of Regulatory T Cells (Tregs)
The induction of Tregs is a cornerstone of MSC-mediated immunomodulation. Tregs, characterized by the expression of the transcription factor Foxp3, are essential for maintaining peripheral tolerance and limiting immune responses [26] [29].
Mechanisms of Treg Induction
MSCs promote the generation of Tregs through multiple, synergistic pathways:
- Soluble Factors: MSC-secreted factors like TGF-β1 and IL-10 directly promote the differentiation of naive CD4+ T cells into Foxp3+ Tregs [29]. The enzyme IDO also contributes to Treg induction [29].
- Monocyte-Mediated Induction: MSCs reprogram monocytes/macrophages toward an anti-inflammatory (type 2) phenotype. These MSC-primed monocytes, in turn, produce high levels of CCL-18 and TGF-β1, which are potent inducers of Treg formation from naive CD4+ T cells [29].
- Direct Cell Contact: In some contexts, direct contact between MSCs and T cells or other immune cells can contribute to Treg induction, although the exact mechanisms are less defined [29].
The Complex Interplay Between Th2 and Treg Pathways
While Th2 cells and Tregs are distinct lineages, their developmental pathways are more intertwined than previously thought. Key Th2 components also play critical roles in Treg biology:
- IL-4: Traditionally a Th2-driver, IL-4 signaling is also vital for maintaining the immunosuppressive function of Tregs. Tregs lacking IL-4 signaling have impaired expression of regulatory molecules like IL-10, granzyme A, and granzyme B, leading to reduced suppressive capacity [27].
- Transcription Factors: The Th2 master regulator GATA3 is also expressed in a subset of Tregs and is important for their stability and function. Furthermore, the transcription factor IRF4, critical for Th2 differentiation, is induced by Foxp3 in Tregs and is specifically required for Tregs to suppress Th2-mediated responses [26] [27].
Diagram 1: Integrated Network of MSC-Mediated Immunomodulation. This diagram illustrates the synergistic actions of MSC-derived soluble factors on various immune cells, leading to T-cell suppression and Treg induction.
Experimental Models & Methodologies
In Vitro T-cell Suppression and Proliferation Assay
This is a foundational protocol for assessing the immunomodulatory capacity of MSCs or their secretome.
- Objective: To quantify the suppression of T-cell proliferation by MSC-conditioned media.
- Materials:
- Jurkat T cells or primary human CD4+ T cells isolated from peripheral blood.
- MSCs (e.g., bone marrow-derived or dental pulp-derived).
- T-cell activation reagents: Anti-CD3/CD28 antibodies.
- Cell proliferation dye: CFSE (Carboxyfluorescein succinimidyl ester).
- Serum-free media (SFM) and IFN-γ to "license" MSCs.
- IDO inhibitor: 1-Methyl-DL-tryptophan (1-MT).
- Procedure:
- Generate Conditioned Media: Culture MSCs in serum-free media with IFN-γ (e.g., 10-20 ng/mL) for 24-48 hours to generate "licensed" conditioned media (γCM). Control media is from unlicensed MSCs (CM) [30].
- Label T cells: Isolate and label CD4+ T cells with CFSE according to standard protocols.
- Activate and Culture: Activate CFSE-labeled T cells with anti-CD3/CD28 antibodies. Culture the activated T-cells in:
- 100% SFM (positive control)
- 100% γCM (test condition)
- 100% γCM + IDO inhibitor (e.g., 1-MT) or supplemental tryptophan (rescue condition) [30].
- Incubate and Analyze: Culture cells for 72-96 hours. Analyze proliferation by flow cytometry via CFSE dilution. Quantify cytokine secretion (e.g., IL-2) in supernatants by ELISA [28].
Table 2: Key Research Reagent Solutions for T-cell Immunomodulation Studies
| Reagent / Tool | Function in Experiment | Example Application |
|---|---|---|
| Anti-CD3/CD28 Antibodies | Polyclonal T-cell receptor activation. | Positive control for T-cell proliferation and IL-2 secretion [28]. |
| CFSE (Proliferation Dye) | Fluorescent cell tracing dye that dilutes with each cell division. | Quantifying the extent of T-cell proliferation inhibition by MSC secretome [30]. |
| Recombinant IFN-γ | Inflammatory cytokine to "license" or prime MSCs. | Inducing high expression of immunomodulatory genes like IDO in MSCs [30]. |
| IDO Inhibitor (1-MT) | Competitive inhibitor of the IDO enzyme. | Mechanistic studies to confirm the role of IDO in T-cell suppression [30]. |
| Neutralizing Antibodies (e.g., anti-IL-10) | Bind to and block the activity of a specific cytokine. | Identifying the specific soluble factors responsible for observed immunomodulatory effects [28]. |
Cytokine Neutralization Studies
- Objective: To identify the specific soluble factors responsible for MSC-mediated effects.
- Procedure: Co-culture activated T cells with MSC-conditioned media in the presence of neutralizing antibodies against specific cytokines (e.g., anti-IL-10, anti-IL-4, anti-IL-13, anti-TGF-β). Compare proliferation and cytokine profiles to isotype control conditions. Restoration of proliferation upon neutralization identifies a critical mediator, as demonstrated for IL-10 [28].
Diagram 2: IL-10 Mediated Suppression of T-cell Proliferation. This flowchart details the mechanism by which MSC-derived IL-10 suppresses IL-2 secretion, a critical growth factor, leading to the arrest of T-cell proliferation.
The Scientist's Toolkit: Key Research Reagent Solutions
A curated list of essential materials for studying immunomodulation, derived from the experimental protocols cited.
Table 3: The Scientist's Toolkit for Immunomodulation Research
| Reagent / Tool | Function in Experiment | Example Application |
|---|---|---|
| Anti-CD3/CD28 Antibodies | Polyclonal T-cell receptor activation. | Positive control for T-cell proliferation and IL-2 secretion [28]. |
| CFSE (Proliferation Dye) | Fluorescent cell tracing dye that dilutes with each cell division. | Quantifying the extent of T-cell proliferation inhibition by MSC secretome [30]. |
| Recombinant IFN-γ | Inflammatory cytokine to "license" or prime MSCs. | Inducing high expression of immunomodulatory genes like IDO in MSCs [30]. |
| IDO Inhibitor (1-MT) | Competitive inhibitor of the IDO enzyme. | Mechanistic studies to confirm the role of IDO in T-cell suppression [30]. |
| Neutralizing Antibodies (e.g., anti-IL-10) | Bind to and block the activity of a specific cytokine. | Identifying the specific soluble factors responsible for observed immunomodulatory effects [28]. |
The regulation of adaptive immunity through T-cell suppression, Th1/Th2 balancing, and Treg induction represents a sophisticated network of checks and balances. Research into mesenchymal stem cells has been instrumental in elucidating these mechanisms, revealing a multi-faceted strategy involving metabolic disruption (IDO), soluble factor mediation (IL-10, TGF-β), and re-education of innate immune cells to promote tolerance. The experimental data and methodologies outlined herein provide a framework for continued investigation. A deeper understanding of these principles, particularly the nuanced interplay between effector and regulatory pathways, is paramount for advancing therapeutic strategies aimed at treating autoimmune diseases, preventing transplant rejection, and managing pathological inflammation.
Mesenchymal stromal cells (MSCs) exert their potent immunomodulatory effects primarily through paracrine signaling, with soluble mediators serving as critical mechanistic components. This whitepaper provides a comprehensive technical analysis of five key soluble factors—Indoleamine 2,3-dioxygenase (IDO), Prostaglandin E2 (PGE2), Transforming Growth Factor-beta (TGF-β), Tumor Necrosis Factor-Stimulated Gene 6 (TSG-6), and Human Leukocyte Antigen-G5 (HLA-G5). Within the context of MSC research, these mediators represent promising targets for therapeutic development in autoimmune diseases, transplant medicine, and cancer. We present structured quantitative data, experimental protocols, signaling pathway visualizations, and essential research reagents to facilitate advanced research and drug development efforts.
The immunomodulatory capacity of mesenchymal stromal cells constitutes a fundamental research focus in regenerative medicine and immunotherapy. MSCs interact with both innate and adaptive immune systems through two primary mechanisms: direct cell-to-cell contact and secretion of soluble factors [29] [6]. While cell contact-dependent mechanisms involving PD-L1/PD-1 interactions and adhesion molecules are well-documented, the soluble mediator component offers broader therapeutic potential for cell-free therapies [31]. Recent research has demonstrated that the MSC secretome contains both soluble factors and extracellular vesicles, with each fraction modulating different immune pathways [32]. The complex synergy between these mediators allows MSCs to dynamically respond to inflammatory cues and restore immune homeostasis, making them promising candidates for treating autoimmune conditions, managing graft-versus-host disease, and modulating cancer immunotherapy responses [33] [6].
Comprehensive Profile of Key Soluble Mediators
Table 1: Core Functional Properties of Key Immunomodulatory Mediators
| Mediator | Full Name | Primary Cellular Source | Key Immunomodulatory Functions | Major Target Immune Cells |
|---|---|---|---|---|
| IDO | Indoleamine 2,3-dioxygenase | MSCs, Dendritic Cells, Macrophages | Tryptophan catabolism to kynurenine, T effector cell suppression, Treg differentiation | T cells, NK cells, DCs |
| PGE2 | Prostaglandin E2 | MSCs, Macrophages | Inhibition of DC maturation, macrophage polarization to M2 phenotype, T cell suppression | Macrophages, Dendritic Cells, T cells |
| TGF-β | Transforming Growth Factor-beta | MSCs, Tregs, Macrophages | Treg differentiation, suppression of T cell proliferation, B cell inhibition | T cells, B cells, Macrophages |
| TSG-6 | TNF-Stimulated Gene 6 | MSCs, Macrophages | Anti-inflammatory protein, macrophage polarization, neutrophil migration inhibition | Macrophages, Neutrophils |
| HLA-G5 | Human Leukocyte Antigen-G5 | MSCs, Placental cells | Inhibition of NK and cytotoxic T cells, Treg induction, tolerance induction | NK cells, T cells, APCs |
Table 2: Quantitative Characteristics and Experimental Detection Methods
| Mediator | Molecular Weight (kDa) | Detection Methods | Common Assays | Key Regulatory Cues |
|---|---|---|---|---|
| IDO | ~45 kDa | ELISA, Western Blot, HPLC | Kynurenine assay, IDO activity assay | IFN-γ, TNF-α, Bin1, STAT1/NF-κB pathways |
| PGE2 | 0.352 kDa | ELISA, Mass Spectrometry | Competitive EIA, PGE2 Express ELISA Kit | COX-2, TNF-α, IL-1β, cell-cell contact |
| TGF-β | 25 kDa (latent) | ELISA, Luminex, Bioassay | Bioassay with reporter cells, CAGA-luciferase | Integrins, proteases, pH changes |
| TSG-6 | ~35 kDa | ELISA, Western Blot | Hyaluronan binding assay, neutrophil migration assay | NF-κB, TNF-α, IL-1β |
| HLA-G5 | ~37 kDa (monomer) | Flow Cytometry, ELISA | Soluble HLA-G ELISA, Western Blot | Inflammation, cell stress, cytokines |
Table 3: Signaling Pathways and Downstream Effects
| Mediator | Receptor | Primary Signaling Pathways | Downstream Gene Regulation | Functional Outcomes |
|---|---|---|---|---|
| IDO | AhR (via kynurenine) | GCN2 kinase, mTOR inhibition, AhR activation | FOXP3, IL-10, IL-6 | T cell anergy, Treg differentiation, NK cell suppression |
| PGE2 | EP2/EP4 receptors | cAMP-PKA signaling, CREB activation | IL-10, TGF-β, IDO1 | DC maturation inhibition, M2 macrophage polarization |
| TGF-β | TGF-βRI/II | Smad2/3 phosphorylation, SMAD4 complex | FOXP3, CTLA-4, IL-2 inhibition | Treg differentiation, Th17 inhibition, B cell suppression |
| TSG-6 | CD44, HA receptors | NF-κB modulation, protease inhibition | TNF-α, IL-6, MMPs | Anti-inflammatory, ECM protection, macrophage reprogramming |
| HLA-G5 | ILT2/KIR2DL4 | JAK/STAT, NF-κB inhibition | Perforin, Granzyme B, IFN-γ | NK cell inhibition, cytotoxic T cell suppression, APC tolerance |
Detailed Experimental Methodologies
IDO Functional Analysis Protocol
Objective: Quantify IDO-mediated immunomodulation through kynurenine production and T cell suppression assays.
Materials:
- THP-1 dual reporter cell line (Invivogen)
- Human PBMCs from healthy donors
- IDO activity assay kit (Immusmol)
- Recombinant IFN-γ for IDO induction
- 1-Methyl-tryptophan (1-MT) as IDO inhibitor
- Ultracentrifugation equipment (150,000 × g capability)
- Flow cytometer with T cell proliferation dyes (CFSE, CellTrace Violet)
Procedure:
- MSC Priming and Supernatant Collection:
Kynurenine Quantification:
- Incubate MSC-conditioned media with 100 μM L-tryptophan for 2 hours at 37°C
- Add 30% trichloroacetic acid to terminate reaction, centrifuge at 15,000 × g
- Transfer supernatant to 96-well plate, mix with equal volume of Ehrlich's reagent
- Measure absorbance at 490 nm, calculate kynurenine concentration against standard curve
T Cell Suppression Assay:
- Isolate PBMCs from healthy donors using Ficoll density gradient
- Label CD3+ T cells with proliferation dye (CFSE, 5 μM)
- Activate T cells with anti-CD3/CD28 beads or PHA/IL-2
- Co-culture with MSC-conditioned media or IDO-knockdown MSCs as control
- After 96 hours, analyze T cell proliferation by flow cytometry
- Measure CD4+CD25+FOXP3+ Treg population using intracellular staining
PGE2 and Soluble Factor Isolation
Objective: Iscrete and quantify PGE2-mediated immunomodulation from MSC secretome.
Materials:
- Tangential Flow Filtration system with 5-100 kDa membranes
- Prostaglandin E2 Express ELISA Kit (Cayman Chemical)
- Ultracentrifugation equipment (150,000 × g)
- Bath sonicator for EV lysis
- Transwell co-culture systems
Procedure:
- Secretome Fractionation:
- Harvest MSC-conditioned media after 72-hour production phase
- Clarify through 0.45 μm filtration to remove cells/debris [32]
- Process through TFF with sequential molecular weight cutoffs (100 kDa, 30 kDa, 5 kDa)
- Validate fraction purity by nanoparticle tracking analysis and protein quantification
PGE2 Quantification:
- Lyse EV-containing fractions using bath sonication (3 × 10 min cycles) [32]
- Process samples using Prostaglandin E2 Express ELISA per manufacturer protocol
- Measure absorbance at 405-420 nm, calculate concentration from standard curve
Functional Validation:
- Use transwell systems to separate MSCs from immune cells while allowing soluble factor exchange [31]
- Treat PBMCs with resiquimod to activate NF-κB and IRF pathways
- Assess NF-κB inhibition in THP-1 dual reporter cells
- Compare immunosuppressive capacity of different secretome fractions
Diagram 1: Integrated signaling network of MSC-derived soluble mediators showing convergent immunomodulation through multiple pathways. Key interactions include IDO-mediated tryptophan metabolism and PGE2-driven macrophage polarization.
Research Reagent Solutions
Table 4: Essential Research Reagents for Soluble Mediator Studies
| Reagent/Category | Specific Product Examples | Primary Research Application | Technical Notes |
|---|---|---|---|
| IDO Inhibitors | 1-Methyl-tryptophan (1-MT), Epacadostat, INCB024360 | IDO pathway validation, control experiments | Use dose range 100-500 μM for 1-MT; monitor viability |
| PGE2 Modulators | NS-398 (COX-2 inhibitor), Misoprostol (PGE1 analog) | PGE2 pathway manipulation, signaling studies | COX-2 inhibition reduces PGE2; confirm with ELISA |
| TGF-β Neutralizers | Anti-TGF-β antibodies, SB-431542 (ALK5 inhibitor) | TGF-β pathway blockade, functional studies | Validate specificity with phospho-Smad2/3 Western |
| ELISA Kits | Prostaglandin E2 Express ELISA (Cayman), Kynurenine/Tryptophan ELISA (Immusmol) | Quantitative mediator measurement | Follow sonication protocol for EV-containing samples [32] |
| Cell Separation | MACS Pan T Cell Isolation Kit, CD4+CD25+ Treg Isolation Kit | Immune cell isolation for co-culture studies | Maintain >95% purity for reproducible results |
| EV Isolation | Tangential Flow Filtration, Ultracentrifugation | Secretome fractionation, EV isolation | TFF preserves EV integrity better than ultracentrifugation [32] |
| Reporter Cells | THP-1 Dual NF-κB/IRF reporter cells (Invivogen) | Innate immunity pathway monitoring | Measure SEAP and Lucia luciferase for NF-κB/IRF |
Diagram 2: Comprehensive experimental workflow for MSC secretome analysis, from cell culture and priming to fractionation and functional characterization of soluble mediators.
Concluding Remarks and Research Implications
The sophisticated network of soluble immunomodulatory mediators represents a promising frontier for therapeutic development. Current evidence strongly supports the cooperative nature of IDO, PGE2, TGF-β, TSG-6, and HLA-G5 in mediating MSC-driven immunomodulation, with context-dependent dominance of different factors [32] [31]. Recent findings demonstrating that soluble factors under 5 kDa target innate immune pathways while larger components regulate T cell proliferation highlight the importance of fractionation approaches in therapeutic development [32].
Future research directions should prioritize defining optimal mediator combinations for specific disease contexts, engineering MSC lines with enhanced mediator expression [34], and developing standardized potency assays for clinical translation. The continued elucidation of these soluble mediator networks will undoubtedly yield novel immunomodulatory strategies with significant impact across transplantation, autoimmunity, and cancer therapeutics.
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine and immunomodulation therapy, not as fixed-entity cells but as dynamic entities whose functional phenotypes are profoundly shaped by their microenvironment. This technical review examines the mechanisms through which physicochemical, biochemical, and cellular components of the microenvironment dictate MSC immunomodulatory plasticity. We synthesize current understanding of how factors including oxygen tension, soluble mediators, extracellular matrix, and heterotypic cell interactions direct MSC fate decisions and functional polarization through specific signaling pathways. The whitepaper provides structured quantitative data, detailed experimental methodologies, and visualization of critical mechanisms to equip researchers with tools for manipulating MSC phenotype in therapeutic contexts. Within the broader thesis of MSC immunomodulation research, this analysis underscores that targeting the microenvironment may offer more precise control over MSC function than direct cellular manipulation, potentially overcoming current limitations in clinical translation.
Mesenchymal stem cells (MSCs), multipotent stromal cells originating from various tissues, possess capabilities for self-renewal, multilineage differentiation, and extensive immunomodulation [35]. Their therapeutic potential extends across regenerative medicine, autoimmune diseases, and transplantation, primarily mediated through paracrine signaling and direct cell-cell contact. However, a fundamental characteristic complicating their clinical application is their remarkable plasticity—the ability to alter their phenotype, secretome, and functional properties in response to environmental cues [35].
The microenvironment (or niche) encompasses the complete milieu surrounding MSCs, including the extracellular matrix (ECM), neighboring cells (both homotypic and heterotypic), soluble factors (cytokines, growth factors, hormones), and physical conditions (oxygen tension, mechanical stresses) [36] [37]. The stability of this microenvironment is pivotal for maintaining normal cell proliferation, differentiation, metabolism, and functional activities. Conversely, abnormal changes in microenvironmental components can significantly disrupt MSC function [36]. This review systematically examines how specific microenvironmental elements dictate MSC immunomodulatory phenotype, providing researchers with frameworks for experimental investigation and therapeutic development.
Fundamental Mechanisms of MSC Plasticity
Defining Plasticity in MSCs
Plasticity in MSCs transcends multilineage differentiation potential. It encompasses dynamic changes in cell morphology, surface marker expression, proliferation rates, migration capacity, and immunomodulatory activity based on tissue source, disease context, and culture conditions [35]. This functional adaptability stems from the MSC's inherent responsiveness to environmental signals, allowing them to fulfill diverse physiological roles from tissue repair to immune regulation.
The plasticity manifestations observed in MSCs include:
- Morphological and Phenotypic Variations: MSCs demonstrate significant alterations in cell volume, cytoskeletal organization, and surface receptor expression under different pathological conditions [35].
- Functional Adaptations: Changes in proliferative capacity, differentiation bias, migration behavior, and paracrine secretion profiles occur in response to microenvironmental cues [35].
- Immunomodulatory Switch: MSCs can toggle between pro-inflammatory and anti-inflammatory phenotypes, particularly in response to cytokine milieus [37].
Theoretical Framework of Plasticity Regulation
The plasticity of MSCs can be understood through the concept of noise-driven differentiation dynamics [38]. Computational models represent MSC differentiation states along a continuous spectrum, with individual cells exhibiting state fluctuations influenced by environmental parameters:
Diagram: Theoretical framework of noise-driven MSC plasticity. The differentiation state (α) fluctuates randomly with environment-dependent amplitude (σ(α)), enabling reversible transitions between states. Proliferation is restricted to progenitor states (αs<α<αd).
This model predicts that at low oxygen tension, the heterogeneity of an MSC population regenerates from any selected subpopulation within approximately two days, while high oxygen tension substantially slows this regenerative plasticity [38]. The model further suggests that most functional stem cells within a pool originate from more differentiated cells through de-differentiation processes.
Microenvironmental Factors Governing MSC Immunomodulation
Soluble Biochemical Factors
The soluble component of the MSC microenvironment includes cytokines, growth factors, chemokines, and metabolic products that profoundly influence immunomodulatory phenotype through specific signaling pathways.
Table 1: Key Soluble Factors Regulating MSC Immunomodulatory Plasticity
| Soluble Factor | Source | Effect on MSC Phenotype | Resulting Immunomodulatory Function | Molecular Mechanisms |
|---|---|---|---|---|
| IFN-γ | Activated T cells, NK cells | induces immunosuppressive phenotype | enhances T-cell inhibition | Upregulates IDO, PD-L1, HLA-G [37] |
| TNF-α | Macrophages, dendritic cells | primes MSC immunomodulation | enhances anti-inflammatory secretion | activates NF-κB, increases TSG-6 production [35] |
| IL-1β | Monocytes, macrophages | pro-inflammatory priming | increases PGE2 secretion | COX-2 upregulation, PGE2 synthesis [37] |
| TGF-β | Tregs, platelets, MSCs | promotes regulatory functions | induces Treg differentiation, M2 polarization | Smad signaling, FoxP3 induction [37] |
| IL-6 | Macrophages, MSCs, T cells | context-dependent duality | both pro/anti-inflammatory effects | JAK/STAT signaling, neutrophil regulation [35] [37] |
| PGE2 | MSCs, macrophages | autocrine reinforcement | enhances M2 macrophage polarization | EP receptor signaling, cAMP activation [37] |
The context dependency of cytokine effects is particularly evident in factors like IL-6, which can exhibit both pro-inflammatory and anti-inflammatory properties based on concentration, timing, and cellular target [39]. Similarly, the presence of IFN-γ is a critical determinant for acquiring T-cell inhibitory properties through indoleamine 2,3-dioxygenase (IDO) upregulation [37].
Physicochemical Factors
Physical and chemical parameters of the microenvironment, including oxygen tension, ECM stiffness, and biomechanical forces, significantly modulate MSC immunomodulatory function.
Oxygen Tension
Oxygen concentration serves as a master regulator of MSC plasticity through hypoxia-inducible factors (HIFs) and redox-sensitive signaling pathways:
Diagram: Oxygen tension regulates MSC plasticity through state fluctuations and HIF-1α signaling. Low oxygen increases state fluctuations and plasticity rates, while high oxygen promotes differentiation.
Under low oxygen conditions (1-5% O₂), MSCs exhibit enhanced proliferation, increased plasticity, and modified paracrine secretion, including increased miR-126 in exosomes [35]. Computational models predict that low oxygen promotes faster regeneration of population heterogeneity through increased state fluctuations [38]. This has practical implications for in vitro expansion, where physiological oxygen tension (2-5% O₂) better maintains stemness compared to atmospheric oxygen (20% O₂).
Extracellular Matrix and Mechanical Cues
ECM composition, stiffness, and topography provide critical biophysical signals that influence MSC immunomodulation through mechanotransduction pathways. Higher matrix rigidity promotes osteogenic differentiation through increased integrin signaling and actin cytoskeleton tension [35], while softer matrices maintain multipotency. The tissue origin of ECM matters—MSCs proliferate better when cultured on ECM derived from their native tissue [35].
Cellular Microenvironment
The immunomodulatory functions of MSCs are significantly shaped through interactions with immune cells in their microenvironment, creating bidirectional regulatory loops.
Macrophage Interactions
MSCs promote the polarization of macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype through secretion of PGE2, TGF-β, and CCL2 [37]. In liver injury models, MSCs increase activity of the Hippo pathway, which activates NLRP3 and regulates XBP1-mediated NLRP3, leading to M2 differentiation [37]. Additionally, MSC-derived extracellular vesicles can reduce colitis in mice by inducing colonic macrophage polarization toward the M2 phenotype [37].
T-cell and B-cell Regulation
MSCs maintain macrophages and dendritic cells in an immature or anti-inflammatory state, preventing activation of effector T-cells and promoting regulatory T-cell (Treg) formation [37]. Human umbilical cord-derived MSCs specifically inhibit T lymphocyte proliferation, downregulate RORγt expression, reduce Th17 cells, and increase Treg populations in the spleen [37].
For B-cells, adipose tissue-derived MSCs inhibit plasma cell formation and promote regulatory B-cell (Breg) production [37]. These Breg cells produce IL-10, which transforms effector CD4+ T cells into Foxp3+ Tregs [37]. MSC-mediated suppression of B-cell proliferation occurs through induction of G0/G1 cell cycle arrest and secretion of Blimp-1, with intercellular communication mediated through PD-1 [37].
Experimental Approaches for Studying MSC-Microenvironment Interactions
In Vitro Modeling Protocols
Protocol 1: Cytokine Priming of MSCs for Enhanced Immunosuppression
Purpose: To pre-condition MSCs with inflammatory cytokines to enhance their immunosuppressive properties prior to therapeutic application.
Materials:
- Complete MSC culture medium (e.g., α-MEM with 10% FBS)
- Recombinant human IFN-γ, TNF-α, IL-1β
- 6-well tissue culture plates
- Phosphate buffered saline (PBS)
- Trypsin/EDTA for cell detachment
Procedure:
- Culture MSCs to 70-80% confluence in complete medium.
- Prepare cytokine cocktail containing 10-50 ng/mL IFN-γ + 10-20 ng/mL TNF-α in complete medium.
- Remove existing medium from MSC cultures and add cytokine-containing medium.
- Incubate for 24-48 hours at 37°C, 5% CO₂.
- Wash cells with PBS and harvest using standard trypsinization.
- Validate priming efficacy through IDO activity assay or PD-L1 surface expression by flow cytometry.
Technical Notes: Optimal cytokine concentrations should be determined empirically for each MSC donor source. Avoid prolonged exposure (>72 hours) to prevent senescence induction.
Protocol 2: Hypoxic Conditioning of MSCs
Purpose: To mimic physiological oxygen conditions and enhance MSC stemness and paracrine function.
Materials:
- Hypoxia chamber or tri-gas incubator
- Oxygen sensors or indicators
- Serum-free MSC collection medium
Procedure:
- Culture MSCs to 60-70% confluence under standard conditions.
- Transfer cells to hypoxia chamber pre-equilibrated to 1-5% O₂, 5% CO₂, balance N₂.
- Maintain cultures for 48-72 hours in hypoxic conditions.
- For conditioned collection, replace medium with serum-free formulation and return to hypoxia for 24 hours.
- Collect conditioned medium and analyze for secreted factors (VEGF, PGE2, miR-126).
- Assess plasticity markers (OCT4, NANOG) and differentiation potential.
Technical Notes: Monitor oxygen levels consistently. Control cells in normoxia should be handled in parallel with identical medium changes.
Analytical Methods for MSC Plasticity Assessment
Method 1: Immunophenotyping by Flow Cytometry
Purpose: To characterize MSC surface marker expression changes in response to microenvironmental manipulation.
Key Markers:
- Positive markers: CD73, CD90, CD105
- Negative markers: CD45, CD34, CD14
- Immunomodulatory markers: PD-L1, HLA-G, CD274
Procedure: Standard staining protocols with appropriate isotype controls. Analyze minimum 10,000 events per sample.
Method 2: Functional Immune Assays
Purpose: To quantify MSC immunomodulatory capacity in response to microenvironmental conditioning.
Co-culture Systems:
- MSC-PBMC co-culture with mitogen stimulation (PHA)
- MSC-macrophage co-culture with LPS/IFN-γ polarization
- Transwell systems to distinguish contact-dependent vs. soluble mediation
Readouts:
- T-cell proliferation (CFSE dilution)
- Macrophage polarization (CD86/CD206 ratio)
- Cytokine secretion multiplex (IL-10, IL-12, TNF-α, IFN-γ)
Research Reagent Solutions Toolkit
Table 2: Essential Research Reagents for MSC-Microenvironment Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Polarization Cytokines | IFN-γ, TNF-α, IL-1β, IL-4, IL-13 | MSC priming protocols | induce immunomodulatory phenotype, enhance immunosuppressive capacity |
| Hypoxia Mimetics | Dimethyloxalylglycine (DMOG), CoCl₂ | oxygen tension studies | stabilize HIF-1α, simulate hypoxic conditions |
| MSC Surface Markers | CD73, CD90, CD105, CD45, CD34 | phenotypic characterization | identify MSC population, assess purity and phenotype stability |
| Immunomodulation Markers | IDO, PD-L1, HLA-G, TSG-6 | functional assessment | quantify immunosuppressive molecule expression |
| Extracellular Vesicle Isolation | Total Exosome Isolation Kit, ultracentrifugation | paracrine mechanism studies | isolate and analyze MSC-derived vesicles for miRNA, protein content |
| 3D Culture Systems | Matrigel, collagen scaffolds, spheroid plates | microenvironment modeling | create more physiologically relevant culture conditions |
The plasticity of MSC immunomodulatory function represents both a challenge and opportunity for therapeutic development. The microenvironment serves as the central conductor orchestrating MSC phenotype through integrated biochemical, biophysical, and cellular cues. Understanding these regulatory mechanisms enables researchers to strategically manipulate MSCs for enhanced clinical efficacy.
Future research directions should focus on:
- Dynamic Monitoring: Developing real-time tracking systems for MSC plasticity changes in living tissues.
- Combinatorial Analysis: Systematic investigation of interacting microenvironmental factors rather than single-parameter studies.
- Standardization: Establishing consensus protocols for microenvironmental preconditioning to enhance therapeutic reproducibility.
- Engineering Solutions: Implementing biomaterial platforms that recapitulate critical niche components for controlled MSC delivery.
The broader thesis of MSC immunomodulation research must incorporate microenvironmental influence as a fundamental determinant of therapeutic outcome. By mastering the language of the MSC niche, researchers can more effectively harness the remarkable plasticity of these cells for advanced regenerative and immunomodulatory therapies.
Translating Mechanisms to Medicine: MSC Applications in Immune Disorders
Mesenchymal stem cells (MSCs) have emerged as one of the most promising tools in regenerative medicine and immunomodulation research due to their multipotent differentiation capacity, paracrine activity, and potent immunomodulatory functions [9] [6]. These fibroblast-like, multipotent cells can be isolated from various tissue sources, with bone marrow-derived MSCs (BM-MSCs), adipose tissue-derived MSCs (AD-MSCs), and umbilical cord-derived MSCs (UC-MSCs) representing the most extensively studied and clinically relevant populations [40] [11]. While all MSCs share fundamental characteristics—including specific surface marker expression (CD73, CD90, CD105), absence of hematopoietic markers, and trilineage differentiation capacity—they exhibit remarkable functional heterogeneity based on their tissue of origin [6] [11]. This heterogeneity manifests in their proliferative capacity, differentiation potential, secretome profiles, and particularly their immunomodulatory potency, creating a complex landscape for researchers and therapy developers to navigate [41] [11].
Within the context of immunomodulation mechanisms research, understanding these source-dependent variations is paramount. MSCs exert their immunomodulatory effects through direct cell-to-cell contact and paracrine secretion, influencing both innate and adaptive immune cells including T cells, B cells, natural killer (NK) cells, macrophages, monocytes, and dendritic cells [7] [6]. The molecular mechanisms underlying these interactions—including secreted cytokines, chemokines, growth factors, and extracellular vesicles—vary significantly among MSC sources, creating distinct functional profiles that must be matched to specific therapeutic applications [42] [41]. This technical guide provides a comprehensive, evidence-based comparison of BM-MSCs, AD-MSCs, and UC-MSCs to inform strategic tissue source selection for research and drug development programs focused on harnessing MSC immunomodulatory potential.
Basic Biological Properties and Procurement Considerations
The three primary MSC sources differ substantially in their procurement procedures, baseline biological characteristics, and practical considerations for research and therapeutic development (Table 1).
Table 1: Fundamental Characteristics of Different MSC Sources
| Characteristic | BM-MSCs | AD-MSCs | UC-MSCs |
|---|---|---|---|
| Harvesting Procedure | Invasive (bone marrow aspiration), requires general anesthesia [40] | Minimally invasive (liposuction) [40] | Non-invasive (from donated umbilical cords) [40] |
| Tissue Availability | Limited quantity [40] | Abundant source [40] | Readily available from medical waste [40] |
| Cell Yield | Low (0.001-0.01% of stromal population) [40] | High (~50% of stromal vascular fraction) [40] | Variable depending on processing method [40] |
| Effect of Donor Age | Significant decline in quantity and quality with age [40] | Decline with age [40] | Unaffected by donor age [40] |
| Immunogenicity | Low | Low [7] | Very low (minimal HLA-DR expression) [40] |
| Proliferative Capacity | Lower potential [40] [41] | Lower potential [40] | Higher potential [40] [42] |
| Expression of Pluripotency Markers | Lower (Oct-4, Nanog, Sox-2) [40] | Lower [40] | Higher [40] |
BM-MSCs, the first discovered and most historically utilized population, are obtained through invasive bone marrow aspiration, which presents practical limitations including donor discomfort and declining cell quality with advancing age [40]. AD-MSCs offer a less invasive alternative through liposuction procedures and are available in substantially higher quantities within the stromal vascular fraction of adipose tissue [40]. UC-MSCs represent the most accessible source from an ethical and logistical perspective, obtained from Wharton's jelly, cord lining, or peri-vascular regions of donated umbilical cords that would otherwise be discarded as medical waste [40]. Critically, UC-MSCs are unaffected by donor aging and exhibit higher expression of pluripotency markers, suggesting a more primitive developmental origin [40].
Functional Potency and Secretome Profiles
The functional capabilities of MSCs, particularly their immunomodulatory potency, vary significantly based on tissue source, reflected in their distinct proliferation rates, differentiation potentials, and secretome profiles (Table 2).
Table 2: Functional Characteristics and Secretome Profiles of Different MSC Sources
| Functional Aspect | BM-MSCs | AD-MSCs | UC-MSCs |
|---|---|---|---|
| Proliferation Rate | Lower [41] | Higher compared to BM-MSCs [41] | Highest [42] [40] |
| Osteogenic Potential | High [41] [43] | Lower [41] [43] | Intermediate |
| Chondrogenic Potential | High [41] [43] | Lower [41] [43] | Intermediate |
| Adipogenic Potential | Moderate [41] | High (predisposed) [40] | Lower |
| Immunomodulatory Potency | Good [40] | Potent (superior to BM-MSCs in some studies) [7] [41] | Good with unique advantages [42] [11] |
| Key Secreted Immunomodulatory Factors | TGF-β, HGF, SDF-1 [41] | CXCL1, CXCL9, CXCL10 [11] | CCL2, CCL7, CXCL2 [42] |
| Migration Toward Inflammation | Moderate | Moderate | Superior toward activated lymphocytes [42] |
| Therapeutic Specialization | Hematopoietic support, immunomodulation [11] | Angiogenic repair, metabolic regulation [11] | Immunosuppression, tissue regeneration [11] |
BM-MSCs demonstrate superior capacity for osteogenic and chondrogenic differentiation, making them particularly suitable for orthopedic applications [41] [43]. AD-MSCs show a natural predisposition toward adipogenic lineage and demonstrate potent immunomodulatory effects, with some studies indicating superior immunosuppression compared to BM-MSCs [7] [41]. UC-MSCs exhibit the highest proliferative capacity and distinct secretome profiles, with demonstrated superiority in migration toward activated lymphocytes, a critical capability for in vivo immunomodulation [42] [40].
Proteomic analyses reveal profound differences in secretome composition across MSC sources. UC-MSCs demonstrate the highest proteomic diversity, with enriched expression of immunomodulatory proteins that contribute to M2 macrophage polarization and neutrophil chemotaxis [11]. They secrete significantly higher levels of CCL2, CCL7, and CXCL2 when co-cultured with activated immune cells compared to BM-MSCs and AD-MSCs [42]. BM-MSCs produce higher levels of immunosuppressive factors like TGF-β and HGF, while AD-MSCs secrete elevated concentrations of CXCL1, CXCL9, and CXCL10 [11]. These distinct secretory profiles directly influence each MSC type's functional specialization and therapeutic potential for specific disease applications.
Experimental Methodologies for Comparative MSC Analysis
Standardized Isolation and Culture Protocols
To ensure valid comparisons across MSC sources, researchers must implement standardized isolation and culture methodologies. While specific protocols vary by tissue source, key consistent elements maintain comparability.
For BM-MSC isolation, bone marrow aspirates are typically collected with informed consent and institutional ethics approval. Mononuclear cells are separated using density gradient centrifugation (e.g., Lymphoprep) at 2,000 rpm for 30 minutes [41]. After washing, cells are plated at a density of 2×10⁵/cm² in culture flasks with appropriate medium supplementation. Non-adherent cells are removed after 2 days, and adherent cells are maintained with regular medium changes until 80-90% confluence [41].
AD-MSC isolation involves enzymatic digestion of lipoaspirate tissues using 0.2% collagenase type IV at 37°C for 30 minutes [41]. The stromal vascular fraction (SVF) is isolated by centrifugation at 300 × g, and viable cells are plated at 1×10⁶ cells per 75 cm² flask. After 2 days, unattached cells are removed by medium replacement [41].
For UC-MSC isolation, Wharton's jelly or other cord components are minced and subjected to similar enzymatic digestion or explant culture techniques. The non-invasive nature of procurement allows for easier ethical approval and larger starting material quantities [40].
Critical to contemporary MSC research is the move away from fetal bovine serum (FBS) toward human platelet lysate (hPL) supplementation, which eliminates xenogeneic immune reactions and improves clinical translation potential [41]. hPL is prepared from platelet-rich plasma standardized to approximately 1×10⁹ platelets/mL, frozen and thawed to release growth factors, then centrifuged and filtered (0.22μm) before addition to basal medium (e.g., IMDM) with heparin (2 U/mL) [41]. This standardized culture approach enables more accurate functional comparisons between MSC populations.
Assessing Immunomodulatory Potency: Key Methodologies
Migration Assay Protocol
The transwell migration assay represents a crucial methodology for evaluating MSC homing capacity toward inflammatory sites [42]. The following protocol assesses this critical functionality:
Stimulant Preparation: Activate peripheral blood mononuclear cells (PBMCs) using mitogens or specific antigens in the lower chamber of transwell plates to create a chemotactic gradient. Alternatively, use defined chemokine solutions at physiological concentrations.
MSC Preparation: Harvest test MSCs (BM-, AD-, UC-MSCs) at passage 3-5 using gentle detachment methods. Wash and resuspend in serum-free medium at standardized density (e.g., 1×10⁵ cells/mL).
Assay Setup: Add cell suspension to upper chambers (3-5μm pore size depending on MSC size). Place chambers into wells containing stimulants or control media.
Incubation and Quantification: Incubate for 6-24 hours at 37°C, 5% CO₂. Remove non-migrated cells from upper chamber with cotton swabs. Fix migrated cells on membrane underside with methanol and stain with crystal violet or calcein-AM.
Analysis: Count migrated cells in multiple predetermined fields using microscopy or measure fluorescence. Express results as migration index relative to control.
This methodology demonstrated the superior migration capacity of UC-MSCs toward activated lymphocytes in mixed lymphocyte reactions compared to BM-MSCs and AD-MSCs [42]. The assay can be modified with specific chemokine receptor inhibitors (e.g., CCR2, CXCR antagonists) or signaling pathway inhibitors to delineate precise migration mechanisms.
Immunomodulation Co-culture Assay
Direct evaluation of MSC-mediated immunomodulation employs co-culture systems with immune cells:
Immune Cell Activation: Isolate PBMCs or specific immune subsets (T cells, B cells, monocytes) from healthy donors. Activate with mitogens (e.g., PHA, ConA), anti-CD3/CD28 antibodies, or specific antigens.
Co-culture Establishment: Plate MSCs and allow adherence. Add activated immune cells at predetermined ratios (typically 1:10 to 1:100 MSC:immune cell). Include controls without MSCs.
Assessment Endpoints:
- Proliferation: Measure via ³H-thymidine incorporation or CFSE dilution by flow cytometry at 72-96 hours.
- Cytokine Profiling: Collect supernatants at 24-48 hours for multiplex cytokine analysis (IFN-γ, TNF-α, IL-10, TGF-β, etc.).
- Immune Phenotyping: Analyze regulatory T cell (CD4+CD25+FOXP3+) induction or macrophage polarization (CD206, CD80) by flow cytometry.
- Gene Expression: Evaluate immunomodulatory gene expression (IDO, PD-L1, COX-2) in MSCs using RT-qPCR.
This methodology revealed that AD-MSCs exhibit more potent immunomodulatory effects on T cell proliferation compared to BM-MSCs under standardized conditions [41], while UC-MSCs uniquely upregulate specific chemokine production when co-cultured with activated immune cells [42].
Molecular Mechanisms of Immunomodulation
Immunomodulatory Signaling Pathways
MSCs utilize complex signaling pathways to exert their immunomodulatory effects, with variations across tissue sources. The following diagram illustrates key pathways common to all MSC types and those preferentially utilized by specific sources:
Diagram 1: MSC Immunomodulatory Signaling Pathways. Key pathways common to all MSC sources (yellow), those enhanced in BM-MSCs (green), AD-MSCs (blue), and UC-MSCs (red) are shown.
The immunomodulatory functions of MSCs are not constitutive but are activated by inflammatory signals, particularly IFN-γ and TNF-α released by activated immune cells at injury or inflammation sites [6]. This licensing process triggers multiple immunosuppressive mechanisms that vary by MSC source:
BM-MSCs strongly activate the TGF-β/Smad pathway, promoting regulatory T cell (Treg) induction and inhibiting effector T cell (Teff) functions [11]. They also demonstrate robust indoleamine 2,3-dioxygenase (IDO) activation, which depletes tryptophan and generates kynurenines that suppress T cell proliferation [7].
AD-MSCs exhibit enhanced secretion of CXCL chemokines (CXCL1, CXCL9, CXCL10) that recruit specific immune subsets and promote M2 macrophage polarization [11]. They also demonstrate potent prostaglandin E2 (PGE2) production, which inhibits neutrophil and NK cell function while promoting regulatory macrophage development [7].
UC-MSCs show strong Toll-like receptor (TLR) 3 and 4 signaling, leading to NF-κB activation and context-dependent pro- or anti-inflammatory responses [6]. They uniquely upregulate CCL2, CCL7, and CXCL2 production in response to activated lymphocytes, enhancing their migratory capacity toward inflammatory sites [42].
All MSC sources utilize galectin-1 and Notch/FOXP3 pathways to varying degrees, contributing to their broad-spectrum immunomodulatory capabilities across multiple immune cell populations [6].
Cell Contact-Dependent Mechanisms
In addition to soluble factor secretion, MSCs employ direct cell contact-dependent immunomodulation through surface molecule expression:
Programmed Death Ligands (PD-L1/PD-L2): All MSC types express these T cell inhibitory ligands upon inflammatory licensing, with human placenta MSCs showing particularly high expression levels [7].
Adhesion Molecules (ICAM-1, VCAM-1): BM-MSCs upregulate these molecules to facilitate direct T cell contact, critical for their immunosuppressive capacity through non-cognate interactions [6].
CD40 Expression: Tonsil-derived MSCs utilize CD40 engagement to promote B cell proliferation via non-canonical NF-κB pathway activation, demonstrating the context-dependent nature of MSC-immune cell interactions [11].
The relative contribution of contact-dependent versus paracrine mechanisms varies among MSC sources and according to specific inflammatory microenvironments, highlighting the importance of matching MSC source to therapeutic application.
Research Reagent Solutions for MSC Immunomodulation Studies
Table 3: Essential Research Reagents for MSC Immunomodulation Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Culture Supplements | Human Platelet Lysate (hPL) [41] | Xeno-free MSC expansion | Superior to FBS for clinical translation; requires heparin supplementation |
| Recombinant IFN-γ [6] | MSC "licensing" for immunomodulation | Pre-treatment enhances immunosuppressive capacity | |
| Migration Assay Tools | Transwell plates (3-8μm pores) [42] | Migration capacity assessment | Pore size selection critical for different MSC sizes |
| Activated PBMC-conditioned medium [42] | Chemotactic gradient establishment | Provides physiologically relevant chemoattractants | |
| Immunomodulation Assessment CFSE cell proliferation dye [41] | T cell proliferation tracking | Flow cytometry-based quantification of immunosuppression | |
| Multiplex cytokine arrays [42] [41] | Secretome profiling | Enables comprehensive analysis of MSC-mediated immune modulation | |
| Signaling Pathway Tools IDO inhibitors (1-MT) [7] | Mechanism dissection | Evaluates tryptophan metabolism role in immunomodulation | |
| COX-2 inhibitors (Celecoxib) [7] | PGE2 pathway inhibition | Determines prostaglandin contribution to immunosuppression | |
| Characterization Antibodies CD73, CD90, CD105 [11] | MSC phenotype confirmation | Positive marker panel for MSC identification | |
| CD14, CD34, CD45, HLA-DR [11] | Purity assessment | Negative marker panel to exclude hematopoietic contamination |
This curated reagent toolkit enables standardized, reproducible investigation of MSC immunomodulatory mechanisms across different tissue sources. The move toward human platelet lysate as a culture supplement represents a critical advancement for clinical translation, eliminating xenogeneic components while maintaining robust MSC expansion [41]. Similarly, the inclusion of IFN-γ pre-treatment protocols mimics the inflammatory licensing that occurs in vivo, enhancing the physiological relevance of in vitro findings [6].
The comprehensive comparison of BM-MSCs, AD-MSCs, and UC-MSCs reveals a complex landscape of functional specializations that must be carefully matched to specific research and therapeutic applications. BM-MSCs demonstrate superior osteogenic and chondrogenic potential with robust immunomodulation through TGF-β and HGF pathways, making them ideal for orthopedic applications and hematopoietic support [41] [11]. AD-MSCs offer practical advantages in harvesting and expansion, with potent immunomodulatory capabilities particularly suited for angiogenic repair and metabolic regulation [40] [11]. UC-MSCs exhibit the highest proliferative capacity, primitive marker expression, and unique migratory responsiveness to activated lymphocytes, positioning them as promising candidates for allogeneic therapies and inflammatory disease applications [42] [40].
Future research directions should focus on standardized potency assays that can predict in vivo efficacy, combinatorial approaches that leverage the unique advantages of different MSC sources, and engineering strategies to enhance specific immunomodulatory functions. The growing understanding of MSC-derived extracellular vesicles as primary mediators of immunomodulation presents another promising avenue for cell-free therapies that maintain therapeutic benefits while reducing risks associated with whole-cell transplantation [6] [11]. As the field progresses, rational MSC source selection based on comprehensive functional profiling will be essential for maximizing therapeutic outcomes in specific disease contexts.
Mesenchymal stem cells (MSCs) have emerged as a groundbreaking therapeutic approach in the treatment of autoimmune diseases, representing a paradigm shift from conventional immunosuppressive strategies. These multipotent cells, characterized by their expression of CD73, CD90, and CD105 and lack of hematopoietic markers (CD45, CD34, CD14, CD19, CD11b, or HLA-DR), possess a unique capacity to modulate immune responses and promote tissue repair [7]. Their therapeutic potential extends across a spectrum of autoimmune conditions, including graft-versus-host disease (GvHD), systemic lupus erythematosus (SLE), Crohn's disease, and multiple sclerosis (MS), offering new hope for patients with treatment-refractory disease.
The immunomodulatory properties of MSCs are particularly valuable in autoimmune contexts, where they can suppress aberrant immune activation while preserving protective immunity. MSCs achieve this through complex interactions with both innate and adaptive immune cells, employing both cell-contact-dependent mechanisms and paracrine signaling [7] [8]. Their ability to respond to the local inflammatory microenvironment allows for context-dependent immunomodulation, making them ideally suited for the heterogeneous presentation of autoimmune diseases. This in-depth technical guide examines the clinical applications, mechanistic underpinnings, and experimental approaches for MSC-based therapies in autoimmune diseases, with a specific focus on GvHD, SLE, Crohn's disease, and multiple sclerosis.
Mechanisms of MSC Immunomodulation
Cell Contact-Dependent Mechanisms
MSCs mediate significant immunomodulation through direct contact with immune cells, facilitating precise control of immune responses. The interaction between MSCs and T-cells represents a cornerstone of their immunomodulatory capacity, characterized by upregulation of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), which are critical for T-cell activation and recruitment to inflammation sites [7]. Additionally, MSCs co-cultured with CD4+ T-cells activate the Notch1/FOXP3 pathway, increasing the percentage of CD4+CD25+FOXP3+ regulatory T-cells (Tregs) that are essential for maintaining immune tolerance [7].
- T-cell Regulation: Human placenta-derived MSCs (PMSCs) express high levels of programmed-death ligand 1 (PD-L1) and PD-L2, which inhibit T-cell proliferation by arresting the cell cycle [7]. This mechanism is particularly relevant in autoimmune environments where T-cell hyperactivity is a defining feature.
- B-cell Interactions: MSCs significantly impact B-cell function through contact-dependent mechanisms. Adipose-derived MSCs (A-MSCs) increase the survival of quiescent B-cells and facilitate B-cell differentiation independently of T-cells [7]. Furthermore, they inhibit Caspase 3-mediated apoptosis of B-cells by upregulating vascular endothelial growth factor (VEGF) and suppress B-lymphocyte proliferation by blocking the cell cycle in the G0/G1 phase through activation of p38 mitogen-activated protein kinase (MAPK) pathways [7].
- Innate Immune System Engagement: MSCs interact extensively with innate immune cells. Tracking studies reveal that infused umbilical cord-derived MSCs (UC-MSCs) are rapidly phagocytosed by monocytes, which subsequently undergo phenotypical and functional changes and migrate to various body sites, distributing the immunomodulatory effect systemically [7]. MSCs also modulate natural killer (NK) cell activity, with co-culture studies demonstrating that they can either suppress or induce granule polarization in different NK cell lines (KHYG-1 and NK-92) [7].
Paracrine-Mediated Immunomodulation
The secretome of MSCs comprises a diverse repertoire of multifunctional cytokines, growth factors, and chemokines that collectively modulate immune cell function. This paracrine activity represents a crucial mechanism whereby MSCs exert their therapeutic effects across considerable distances in the inflammatory microenvironment.
- Soluble Factor Production: MSCs secrete numerous immunomodulatory molecules including transforming growth factor-β1 (TGF-β1), prostaglandin E2 (PGE2), hepatocyte growth factor (HGF), indoleamine-pyrrole 2,3-dioxygenase (IDO), nitric oxide (NO), and interleukin-10 (IL-10) [7] [8]. The specific factors deployed vary depending on MSC source, target cells, and the surrounding microenvironment.
- T-cell Modulation via Soluble Factors: MSCs inhibit T helper 17 cell (Th17) differentiation by inducing production of IL-10 and PGE2 while inhibiting IL-17, IL-22, and IFN-γ [7]. MSC-secreted IDO plays a particularly important role in inducing Tregs responsible for kidney allograft tolerance [7]. Additionally, MSCs utilize the IL-25/STAT3/PD-L1 axis to suppress Th17 responses [7].
- Extracellular Vesicles: MSC-derived extracellular vesicles (MSC-EVs), including exosomes and microvesicles, encapsulate paracrine factors and display immunoregulatory functions similar to the parent MSCs [7]. These vesicles represent a promising cell-free therapeutic alternative that may reduce risks associated with whole-cell transplantation.
The diagram below illustrates the integrated mechanisms of MSC-mediated immunomodulation through both cell-contact-dependent and paracrine pathways:
Clinical Applications in Specific Autoimmune Diseases
Graft-versus-Host Disease (GvHD)
GvHD represents one of the most established clinical applications for MSC therapy, with Prochymal receiving regulatory approval for acute GvHD treatment in Canada and New Zealand [8]. MSCs demonstrate remarkable efficacy in modulating the exaggerated immune response that characterizes GvHD while promoting tissue repair in affected organs.
- Mechanism of Action: In GvHD, MSCs decrease the Th1 response and suppress T-cell proliferation through both contact-dependent mechanisms and secretion of soluble factors including PGE2, IDO, and NO [8]. They have been shown to attenuate delayed-type hypersensitivity and prevent GvHD development through mechanisms requiring TNF-α and inducible nitric oxide synthase (iNOS) [8].
- Clinical Evidence: Preclinical studies demonstrate that both allogeneic and xenogeneic MSCs can effectively treat experimental GvHD models [8]. In clinical practice, MSC administration has shown promising results in steroid-refractory acute GvHD, with response rates leading to regulatory approval in several countries.
- Protocol Considerations: MSC products for GvHD treatment are typically derived from bone marrow or adipose tissue and administered intravenously. Dosing regimens vary but often involve multiple infusions of 1-2 million cells per kilogram of recipient body weight.
Systemic Lupus Erythematosus (SLE)
SLE is a complex autoimmune disorder characterized by loss of immune tolerance and production of autoantibodies against nuclear antigens, leading to multi-organ damage through immune complex deposition [44]. MSC therapy offers a novel approach to resetting the dysregulated immune system in SLE.
- Mechanism of Action: In SLE, MSCs decrease the Th1 response and modulate the balance of autoreactive B-cells and T-cells [8]. They have been shown to reverse multiorgan dysfunction and reconstruct the bone marrow osteoblastic niche in lupus models [8].
- Clinical Evidence: Both allogeneic bone marrow-derived MSCs and xenogeneic umbilical cord blood-derived MSCs have demonstrated efficacy in delaying the development of proteinuria and improving disease outcomes in SLE patients [8]. Clinical trials have shown that MSC transplantation can lead to sustained remission in refractory SLE cases.
- Emerging Approaches: CAR T-cell therapy targeting CD19 has also shown remarkable results in SLE, with one study reporting that all five treated patients achieved durable drug-free remission, with normalized complement levels and decreased anti-dsDNA titers [45]. This approach specifically eliminates autoreactive B cells, providing a complementary strategy to MSC therapy.
Crohn's Disease
Crohn's disease is a chronic inflammatory bowel disease characterized by transmural inflammation of the gastrointestinal tract. MSC therapy has shown particular promise for the treatment of complex perianal fistulas, which are often resistant to conventional treatments [46].
- Mechanism of Action: MSCs exert immunomodulatory and regenerative effects in Crohn's disease by inhibiting T-cell alloreactivity and modulating the local inflammatory environment [46]. Their ability to migrate to sites of inflammation in a CXCR4/SDF-1 axis-dependent manner allows for targeted therapeutic effects [44].
- Clinical Evidence: Clinical trials using allogeneic adipose-derived and bone marrow-derived MSCs have demonstrated significant efficacy in achieving complete closure of complex perianal fistulas in Crohn's disease patients [46]. A phase IB/IIA clinical trial showed sustained clinical and radiographic healing at 12 months post-treatment, highlighting the durability of the MSC therapy effect [46].
- Protocol Specifications: For perianal fistulizing Crohn's disease, MSCs are typically administered via local injection directly into fistula tracts. Studies have shown that factors such as cell type, source, and dosage do not significantly alter treatment efficacy, providing flexibility in protocol design [46].
Multiple Sclerosis (MS)
Multiple sclerosis is a chronic inflammatory demyelinating disease of the central nervous system. MSC therapy offers a novel approach to modulating the autoimmune response against myelin and potentially promoting remyelination.
- Mechanism of Action: In MS, MSCs regulate immune tolerance by secreting soluble factors such as TGF-β, PGE2, and IDO, as well as exosomes enriched with regulatory miRNAs including miR-21 and miR-146a [44]. These factors suppress excessive activation of Th1 and Th17 cells while promoting the expansion of regulatory T cells (Tregs) [44].
- Clinical Evidence: Preclinical studies in experimental autoimmune encephalomyelitis (EAE) models, which mimic aspects of MS, have shown that MSCs can reduce inflammatory infiltrates and cytokines while expressing anti-inflammatory cytokines [8]. Clinical trials have demonstrated that MSC administration is safe and may stabilize or improve disease course in MS patients.
- Novel Research Directions: Recent research has identified specific patterns of autoantibody expression in MS using innovative antigen discovery technologies [47]. The Antigenome Platform, a high-throughput assay combining large-fragment cDNA libraries, phage display, and serum antibody screening, has identified 166 autoantibody targets selected by over 10% of patients' sera, providing new insights into MS pathogenesis and potential biomarkers for monitoring MSC therapy efficacy [47].
The table below summarizes key clinical trial findings for MSC therapy across these autoimmune diseases:
Table 1: Clinical Applications of MSC Therapy in Autoimmune Diseases
| Disease | Key Mechanisms | Clinical Outcomes | Notable Trials/Products |
|---|---|---|---|
| GvHD | Decreased Th1 response; T-cell suppression via PGE2, IDO, NO [8] | Improved survival in steroid-refractory acute GvHD [8] | Prochymal (approved in Canada/NZ) [8] |
| SLE | Immune tolerance restoration; Treg induction; autoreactive B-cell inhibition [8] | Delayed proteinuria; reversal of multi-organ dysfunction [8] | Allogeneic BM-MSC trials [8] |
| Crohn's Disease | T-cell alloreactivity inhibition; fistula healing; local immunomodulation [46] | Complete fistula closure; sustained healing at 12 months [46] | Allogeneic adipose-derived MSC trials [46] |
| Multiple Sclerosis | Th1/Th17 suppression; Treg expansion; miRNA-mediated regulation [44] | Reduced inflammatory activity; clinical stability [8] | Phase I/II trials with BM-MSCs and AD-MSCs [8] |
Experimental Protocols and Methodologies
MSC Isolation and Expansion
Standardized protocols for MSC isolation and expansion are critical for ensuring reproducible therapeutic outcomes in autoimmune disease applications.
- Source Materials: MSCs can be isolated from multiple tissues including bone marrow (BM-MSCs), adipose tissue (A-MSCs), umbilical cord tissue (UC-MSCs), placental tissues, dental pulp, and peripheral blood [7]. Bone marrow remains the most extensively characterized source, though umbilical cord and adipose tissue are increasingly utilized for their accessibility and potent immunomodulatory properties.
- Isolation Techniques: Density gradient centrifugation (e.g., Ficoll-Paque) is commonly employed for bone marrow and peripheral blood samples. Adipose tissue-derived MSCs typically require collagenase digestion followed by centrifugation to separate the stromal vascular fraction. Umbilical cord tissue often necessitates explant culture or enzymatic digestion to isolate MSCs.
- Expansion Media: Culture media typically consist of Dulbecco's Modified Eagle Medium (DMEM) or Alpha-MEM supplemented with 10% fetal bovine serum (FBS) or human platelet lysate, L-glutamine, and antibiotics. Basic fibroblast growth factor (bFGF) is frequently added to enhance proliferation and maintain stemness.
- Characterization: According to International Society for Cellular Therapy guidelines, MSCs must demonstrate: (1) adherence to plastic in standard culture conditions; (2) expression of CD105, CD73, and CD90 (>95%); and (3) lack of expression of CD45, CD34, CD14/CD11b, CD79a/CD19, and HLA-DR (<2%); and (4) ability to differentiate into osteoblasts, adipocytes, and chondroblasts in vitro [7].
In Vitro Immunomodulation Assays
Robust assessment of MSC immunomodulatory function is essential for quality control and potency determination prior to clinical application.
- T-cell Proliferation Assays: Peripheral blood mononuclear cells (PBMCs) are isolated from healthy donors and labeled with carboxyfluorescein succinimidyl ester (CFSE). Cells are stimulated with mitogens (e.g., phytohemagglutinin) or anti-CD3/CD28 antibodies in the presence or absence of MSCs. After 3-5 days, T-cell proliferation is measured by flow cytometry based on CFSE dilution [8].
- Mixed Lymphocyte Reaction (MLR): PBMCs from two allogeneic donors are co-cultured with or without MSCs to simulate the allogeneic immune response. Proliferation is typically measured after 5-7 days using 3H-thymidine incorporation or CFSE dilution assays [8].
- Cytokine Secretion Profiling: Supernatants from MSC-immune cell co-cultures are analyzed using multiplex ELISA or Luminex arrays to quantify pro-inflammatory (IFN-γ, TNF-α, IL-1β, IL-6, IL-17) and anti-inflammatory (IL-10, TGF-β, IL-4) cytokines [7] [8].
- IDO Activity Measurement: IDO enzymatic activity is determined by measuring the conversion of tryptophan to kynurenine using high-performance liquid chromatography (HPLC) or spectrophotometric methods, particularly after stimulation with IFN-γ [8].
The workflow for evaluating MSC immunomodulatory capacity typically follows this sequence:
In Vivo Disease Models
Animal models of autoimmune diseases provide essential platforms for evaluating MSC efficacy and mechanisms of action before clinical translation.
- Experimental Autoimmune Encephalomyelitis (EAE): The primary model for multiple sclerosis research. Mice or rats are immunized with myelin antigens (e.g., MOG35-55) emulsified in complete Freund's adjuvant, followed by pertussis toxin administration. MSCs are typically administered intravenously after disease onset, with clinical scoring of paralysis and histological analysis of CNS inflammation and demyelination [8].
- Systemic Lupus Erythematosus Models: Spontaneous models include MRL/lpr and NZB/NZW F1 mice that develop lupus-like disease with autoantibody production and glomerulonephritis. MSCs are administered at various disease stages, with monitoring of proteinuria, survival, serum autoantibodies, and renal histology [8].
- Colitis Models: For Crohn's disease research, dextran sulfate sodium (DSS)-induced colitis or trinitrobenzene sulfonic acid (TNBS)-induced colitis models are commonly used. MSCs are typically delivered intravenously or intraperitoneally, with assessment of disease activity index, colon length, histology, and inflammatory cytokine profiles [8].
- GvHD Models: Lethally irradiated mice receive allogeneic bone marrow and spleen cells to induce GvHD. MSC administration occurs at the time of transplantation or after disease manifestation, with monitoring of survival, clinical GvHD scores, and histopathology of target organs [8].
Research Reagent Solutions
The table below outlines essential research reagents and their applications in MSC immunomodulation studies for autoimmune diseases:
Table 2: Essential Research Reagents for MSC Immunomodulation Studies
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| MSC Culture Media | DMEM/F12, Alpha-MEM with FBS or human platelet lysate, bFGF [7] | MSC isolation, expansion, and maintenance | Serum-free alternatives available; platelet lysate enhances proliferation |
| Characterization Antibodies | CD73, CD90, CD105, CD45, CD34, CD14, CD19, HLA-DR [7] | Flow cytometric verification of MSC phenotype | Critical for ISCT compliance; multiple fluorochrome conjugates available |
| Immune Cell Isolation Kits | Pan T-cell, B-cell, NK cell isolation kits; CD14+ monocyte separation | Preparation of specific immune cell populations | Magnetic-activated cell sorting (MACS) or FACS methodologies |
| Cell Proliferation Assays | CFSE, 3H-thymidine, BrdU incorporation assays [8] | Quantification of immune cell proliferation | CFSE allows tracking of multiple divisions by flow cytometry |
| Cytokine Detection Assays | Multiplex ELISA, Luminex arrays, ELISpot | Comprehensive cytokine profiling | Simultaneous measurement of 20+ cytokines in small sample volumes |
| IDO Activity Assays | Tryptophan-to-kynurenine conversion kits (HPLC/spectrophotometric) [8] | Evaluation of critical immunomodulatory pathway | Requires IFN-γ pre-stimulation for optimal detection |
| Animal Model Reagents | MOG35-55 peptide, complete Freund's adjuvant, DSS, TNBS [8] | Induction of autoimmune disease models | Strain-specific susceptibility variations must be considered |
Future Directions and Concluding Remarks
The field of MSC-based therapy for autoimmune diseases continues to evolve with several promising directions emerging. Next-generation approaches include the development of engineered MSCs with enhanced immunomodulatory properties, the use of MSC-derived extracellular vesicles as cell-free therapeutics, and the exploration of allogeneic off-the-shelf MSC products to improve accessibility and reduce costs [44] [7]. Additionally, combination therapies integrating MSCs with other immunomodulatory agents or cellular therapies such as Tregs may yield synergistic effects for refractory autoimmune conditions [48] [49].
The integration of MSC therapy into the autoimmune treatment landscape represents a shift from broad immunosuppression toward targeted immunomodulation that addresses the underlying immune dysregulation while promoting tissue repair. As research continues to elucidate the precise mechanisms of MSC action and optimize delivery protocols, these innovative cellular therapies hold immense potential to transform outcomes for patients with autoimmune diseases including GvHD, SLE, Crohn's disease, and multiple sclerosis.
Mesenchymal Stem Cell-Mediated Immuno-Modulatory and Anti- Inflammatory Mechanisms in Immune and Allergic Disorders
Mesenchymal stem cells (MSCs) represent a promising therapeutic approach for immune and allergic disorders due to their potent immunomodulatory and anti-inflammatory properties. These stromal cells, present in virtually all tissues of the body, serve as the backbone of internal tissue homeostasis and possess characteristic features that make them particularly valuable for addressing the underlying immune dysregulation in allergic conditions [50]. The therapeutic potential of MSCs lies in their ability to modulate both innate and adaptive immune responses through multiple mechanisms, including direct cell-cell contact and release of soluble factors, offering a multifaceted approach to treating complex allergic diseases such as allergic rhinitis and asthma [50] [51].
The prevalence of allergic airway inflammations has increased significantly worldwide, positioning these disorders as a major health concern. Current therapies often provide symptomatic relief but fail to reinstate immune homeostasis or are restricted by specific allergens [52] [53]. MSC-based therapies demonstrate potential for overcoming these limitations by addressing the fundamental immune imbalances that characterize allergic conditions, particularly the Th1/Th2 dysregulation that drives pathophysiology in both allergic rhinitis and asthma [52] [53].
MSC Immunomodulatory Mechanisms: Multifaceted Approaches to Immune Regulation
Cell-Cell Contact Dependent Mechanisms
MSCs employ direct cellular interactions as a primary immunomodulatory strategy through surface molecule expression that enables precise regulation of immune cell function. These interactions occur via integrins (α1, α2, α3, α5, α6, αv, β1, β3, and β4), intercellular adhesion molecules (ICAM-1, ICAM-2), vascular cell adhesion molecule (VCAM-1), CD72, and CD58 (LFA-3), allowing MSCs to bind to T lymphocytes with high affinity [54]. This direct contact is essential for certain immunomodulatory functions, as demonstrated by experiments where T cell inhibition was eliminated when cells were co-cultured with BM-MSCs in Transwell systems or conditioned medium, indicating the necessity of MSC-T cell contact [54].
Table 1: Key Surface Molecules in MSC-Mediated Cell Contact Mechanisms
| Surface Molecule | Immune Cell Target | Biological Effect |
|---|---|---|
| PDL1/PDL2 | T cells (PD-1 receptor) | Inhibits T cell proliferation and cytokine production by blocking cell cycle in G0/G1 phase |
| ICOSL | ILC2 and Tregs (ICOS receptor) | Activates Tregs and inhibits Th2 responses |
| Adhesion Molecules (ICAM-1, VCAM-1) | T lymphocytes | Facilitates high-affinity binding and immune synapse formation |
| CD72, CD58 (LFA-3) | T lymphocytes | Supports stable cell-cell contact and signaling |
The PD-1/PD-L1 axis represents a particularly crucial contact-dependent mechanism. MSCs express high levels of PD-L1 and PD-L2 on their surface, which interact with the co-inhibitory receptors PD-1 and CTLA-4 on T cells [54]. These interactions trigger downstream signaling pathways that inhibit TCR-mediated activation through recruitment of SHP-1 and SHP-2 phosphatases, which dephosphorylate key signaling molecules including ZAP70 and PKCθ [54]. This leads to suppression of downstream signaling cascades, including PI3K/AKT and MAPK/ERK pathways, resulting in blocked T cell proliferation and cell cycle arrest at G0/G1 phase [54].
MSCs also modulate macrophage polarization through contact-dependent mechanisms. Studies demonstrate that MSCs increase TSG-6 production through intercellular contact with pro-inflammatory M1 macrophages, promoting their transformation into anti-inflammatory M2 macrophages in a TSG-6-dependent manner to alleviate excessive inflammation [54].
Soluble Factor-Mediated Mechanisms
The paracrine activity of MSCs constitutes a second major immunomodulatory pathway through the secretion of numerous soluble factors that coordinate immune responses. These factors include TGF-β, IL-10, PGE2, IDO, HGF, NO, TSG-6, IL-6, LIF, HLA-G5, and IL1RA [54]. The specific factors employed vary depending on the local inflammatory microenvironment, with proinflammatory cytokines like IFN-γ, TNF-α, IL-1α, and IL-1β inducing MSCs to secrete enzymes and soluble factors that mediate immunosuppressive activity [51].
Table 2: Key Soluble Factors in MSC-Mediated Immunomodulation
| Soluble Factor | Primary Mechanism | Biological Effect in Allergic Inflammation |
|---|---|---|
| TGF-β | TGF-β/Smad signaling pathway | Promotes Treg differentiation and suppresses Th2 responses |
| PGE2 | COX-2 pathway activation | Inhibits T-cell proliferation and DC maturation |
| IDO | Tryptophan to kynurenine conversion | Inhibits immune cell growth and function |
| NO | iNOS pathway | Suppresses T-cell proliferation |
| TSG-6 | Interaction with CD44 receptor | Reduces NF-κB signaling in macrophages |
The TGF-β/Smad pathway represents a pivotal mechanism for MSC-mediated immune regulation. TGF-β binds to TGF-βRII, recruiting and phosphorylating TGF-βRI to form a heterotetrameric complex [54]. This activation triggers phosphorylation of R-Smads (Smad2 and Smad3), which form a complex with Smad4 that translocates to the nucleus to regulate transcription of target genes involved in immune suppression, including FOXP3, the master regulator of Tregs [54]. Through this pathway, TGF-β promotes differentiation of naïve T cells into Tregs, essential for restoring immune tolerance in allergic conditions.
Indoleamine-pyrrole 2,3-dioxygenase represents another crucial enzyme in MSC immunomodulation. IDO catalyzes the conversion of tryptophan to kynurenine, depleting local tryptophan levels and generating immunosuppressive metabolites that inhibit T-cell responses [51]. This mechanism has been shown to inhibit allogeneic T-cell responses and induce transplant tolerance [51].
MSC Mechanisms in Allergic Rhinitis Models
Pathophysiology and Current Treatment Limitations
Allergic rhinitis affects 10-40% of the global population and is characterized by chronic inflammatory changes in the nasal mucosa driven by a dysregulated type 2 immune response to allergens [54]. Upon exposure to allergens, dendritic cells process antigens and prime naïve T cells into Th2 cells via IL-4/STAT6 signaling. Th2 cytokines (IL-4, IL-5, IL-13) then drive B cell IgE switching, eosinophil recruitment, and mast cell activation, leading to nasal inflammation, mucosal edema, and barrier dysfunction [54]. Concurrently, impaired Treg activity fails to suppress Th2 polarization, perpetuating immune imbalance [54]. Current therapies including pharmacotherapy and immunotherapy provide symptomatic relief but face limitations including drug dependency, long treatment cycles, tissue damage, and refractory symptoms in 10-20% of patients [54].
MSC Mechanisms in AR Models
Preclinical studies demonstrate that MSCs from various sources including adipose tissue, bone marrow, umbilical cord, and tonsils effectively reduce AR symptoms such as sneezing, nasal inflammation and serum IgE levels by targeting multiple aspects of the allergic response [54]. The fundamental mechanism involves correction of Th1/Th2 immune equilibrium and enhancement of Treg activity [54].
MSCs counteract AR pathophysiology through multipronged strategies: (1) TGF-β secretion restores Treg/Th2 balance; (2) PGE2 and IDO suppress DC-mediated Th2 priming; (3) Exosomal miRNAs (e.g., miR-146a-5p) directly inhibit eosinophil activation and IgE production [54]. Specific studies have shown that iPSC-MSCs and BM-MSCs inhibit proliferation of CD3 T cells isolated from peripheral blood mononuclear cells of AR patients through cell-to-cell contact and PGE2 expression, while simultaneously promoting Treg proliferation and regulating T cell phenotype to suppress Th2 responses [54].
The interaction between ICOSL on MSCs and ICOS on Tregs represents another significant mechanism. This ICOS-ICOSL interaction activates Tregs and inhibits Th2 responses [54]. Additionally, MSCs can inhibit Th2 activation by inducing Treg proliferation through the Notch1 pathway, while iPSC-MSCs can enhance Treg activation through the NF-κB signaling pathway [54].
Figure 1: MSC Mechanisms in Allergic Rhinitis. MSCs target multiple pathophysiological pathways in AR through direct and indirect immunomodulatory effects.
MSC Mechanisms in Allergic Asthma Models
Pathophysiological Features and MSC Therapeutic Targets
Asthma represents a chronic inflammatory disease characterized by complex pathophysiology involving both inflammatory processes and structural changes through tissue remodeling. Most current drugs focus on controlling inflammation but are unable to revert established tissue remodeling, leaving many patients with persistent symptoms or severe exacerbations [55]. The ideal therapy for asthma would effectively address both inflammation and airway remodeling, making MSCs particularly promising due to their demonstrated capacity to impact both processes [55].
MSC Mechanisms in Asthma Models
In experimental asthma models, MSCs demonstrate multifaceted therapeutic effects. In an immunocompetent mouse model of ovalbumin-induced allergic asthma, human adipose tissue-derived MSCs and their extracellular vesicles effectively reduced eosinophil counts in lung tissue and bronchoalveolar lavage fluid while modulating airway remodeling [55]. Both MSCs and EVs acted on static lung elastance and regulatory T cells, CD3+CD4+ T cells, and pro-inflammatory mediators including IL-4, IL-5, IL-13, and eotaxin [55]. Additionally, both treatments similarly reduced collagen fiber content in airways and lung parenchyma, levels of transforming growth factor-β in lung tissue, and CD3+CD4+ T cell counts in the thymus [55].
In mouse models of chronic or severe asthma, systemic administration of MSCs reduces allergen-specific IgE and Th2 cytokines IL-4, IL-5, and IL-13 in bronchial fluid while inhibiting airway inflammation and pathological remodeling [51]. A study by Nemeth et al. showed that BM-MSCs significantly suppressed allergic responses in a mouse model of ragweed-induced asthma through TGF-β mediated mechanisms [51]. The reduction in serum NO levels following MSC administration further demonstrates the broad impact of MSC therapy on inflammatory pathways in asthma [51].
Figure 2: MSC Therapeutic Effects in Allergic Asthma. MSCs and their extracellular vesicles target both inflammatory and remodeling pathways in experimental asthma models.
Experimental Models and Methodologies
Standardized Allergic Inflammation Models
The evaluation of MSC therapeutic potential in allergic inflammation relies on well-established animal models that replicate key features of human disease. For allergic asthma research, the ovalbumin-induced airway inflammation model in C57BL/6 mice represents a widely adopted approach [55]. In this model, mice are immunized using an adjuvant-free protocol through intraperitoneal injection of ovalbumin (100 μg in 100 μL saline) on 7 alternate days, followed forty days after the first injection by intratracheal instillation of 20 μg OVA in 20 μL sterile saline administered three times with 3-day intervals between procedures [55]. This protocol induces inflammation and remodeling of central and distal airways as well as lung parenchyma, leading to respiratory mechanical changes that mimic human asthma pathophysiology [55].
For food allergy enteritis models, researchers have employed ovalbumin-induced enteritis with similar sensitization approaches but different challenge protocols focused on gastrointestinal exposure [56]. In these models, mice typically develop significant allergic reactions including scratching around the nose and head, labored breathing, immobility, and in some cases mortality, along with increased allergic scores and diarrhea scores that can be quantitatively assessed [56].
MSC Administration and Evaluation Protocols
Therapeutic protocols typically involve administration of MSCs or their derivatives after disease establishment. In the OVA-induced asthma model, one day after the last challenge, animals receive interventions via jugular injection including saline (control), 10⁵ AD-MSCs, or extracellular vesicles released by 10⁵ AD-MSCs [55]. Evaluation occurs seven days post-treatment, with animals anesthetized for lung function assessment before tissue collection [55].
Analytical methods consistently applied across studies include:
- Lung mechanics assessment using the end-inflation occlusion method to measure static lung elastance [55]
- Histopathological analysis of lung tissues through H&E staining, toluidine blue staining, and transmission electron microscopy [55] [56]
- Bronchoalveolar lavage fluid analysis for inflammatory cell counts and differentiation [55]
- Cytokine measurement in serum and tissues using ELISA [56]
- Flow cytometric analysis of immune cell populations [55]
- Western blot analysis for protein expression [56]
- mRNA expression analysis through quantitative PCR [56]
Table 3: Quantitative Effects of MSC Therapy in Experimental Allergic Inflammation
| Parameter | Allergic Rhinitis Models | Allergic Asthma Models | Food Allergic Enteritis |
|---|---|---|---|
| IgE Levels | Significant reduction [54] | Significant reduction [51] | Significant reduction [56] |
| Eosinophil Infiltration | Marked decrease [54] | Reduced in lung tissue and BALF [55] | Not specifically reported |
| Th2 Cytokines | IL-4, IL-5, IL-13 reduction [54] | IL-4, IL-5, IL-13 reduction [55] [51] | IL-4, IL-6 reduction [56] |
| Treg Populations | Significant increase [54] | Modulation of Tregs [55] | Enhanced Treg activity [56] |
| Tissue Remodeling | Not applicable | Reduced collagen fiber content [55] | Improved epithelial barrier [56] |
| Clinical Symptoms | Reduced sneezing, nasal inflammation [54] | Improved lung function [55] | Reduced allergic scores, diarrhea [56] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for MSC Studies in Allergic Inflammation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| MSC Sources | Adipose tissue-derived MSCs, Bone marrow-derived MSCs, Umbilical cord-derived MSCs, iPSC-derived MSCs | Comparative studies of tissue-specific MSC effects; iPSC-MSCs offer unlimited expansion capacity [54] [51] |
| Characterization Antibodies | CD73, CD90, CD105 (positive); CD34, CD45, CD14/CD11b, CD79α, HLA-DR (negative) | Verification of MSC identity according to International Society for Cellular Therapy criteria [54] [56] |
| Allergens for Sensitization | Ovalbumin (chicken egg), Ragweed extract, Aspergillus hyphal extract | Induction of allergic inflammation in animal models; OVA most widely used for standardization [55] [51] |
| Cell Culture Media | Dulbecco's Modified Eagle Medium (DMEM) with fetal bovine serum (FBS) | MSC expansion and maintenance; serum-free formulations reduce xeno-contamination risks [55] |
| Extracellular Vesicle Isolation | Ultracentrifugation, Dynamic Light Scattering (DLS), Protein quantification (BCA assay) | EV characterization and standardization for comparative studies [55] |
| Cytokine Analysis | ELISA kits, Multiplex immunoassays, Quantitative PCR | Assessment of inflammatory mediators and immunomodulatory effects [55] [56] |
| Animal Models | C57BL/6 mice, BALB/c mice | In vivo evaluation of MSC therapeutic efficacy; strain selection affects immune polarization [55] [56] |
Current Challenges and Future Research Directions
Despite promising preclinical results, several significant challenges impede the clinical translation of MSC-based therapies for allergic inflammation. The field currently faces issues of heterogeneous protocols, unresolved long-term risks including potential tumorigenicity, and lack of standardized production methods [54]. Additionally, while MSCs are present in nearly all tissues, their natural concentration is limited, necessitating culture expansion that introduces variability based on specific protocols and culture conditions [50].
Future research priorities should include:
- Development of xeno-protein free culture media as alternatives to fetal bovine serum to reduce contamination risks and enhance clinical applicability [50]
- Phase I safety trials to establish preliminary safety profiles in human allergic diseases [54]
- Standardization of MSC production protocols including characterization, expansion, and quality control measures [54] [51]
- Exploration of combination strategies such as exosomes with hydrogels to improve targeting and retention [54]
- Investigation of the variable effects observed in different studies, with some failing to achieve desired results despite generally positive outcomes [50]
The immunomodulatory properties of MSCs are controlled by microenvironmental factors over which researchers currently have limited control, representing both a challenge and an opportunity for future investigation [50]. A more complete understanding of how local inflammatory environments influence MSC behavior and therapeutic efficacy will be essential for optimizing clinical applications.
Recent advances in extracellular vesicle research offer promising alternatives to whole-cell therapies. EVs derived from MSCs demonstrate similar therapeutic effects while potentially offering improved safety profiles due to reduced risks of ectopic tissue formation and embolic complications [55]. Future comparative studies examining the relative efficacy of MSCs versus their EVs across different allergic conditions will help clarify their respective niches in allergic disease treatment.
Mesenchymal stem cells represent a promising therapeutic approach for allergic rhinitis, asthma, and related allergic conditions through their multifaceted immunomodulatory mechanisms. By targeting fundamental immune dysregulations including Th1/Th2 imbalance, impaired Treg function, and persistent inflammatory signaling, MSCs offer the potential for durable remission of allergic inflammation rather than mere symptom suppression. The demonstrated efficacy of both MSCs and their extracellular vesicles in preclinical models across multiple allergic conditions underscores their therapeutic potential, while ongoing challenges in standardization and safety assessment highlight the need for continued rigorous investigation. As research advances toward clinical translation, MSC-based therapies may ultimately provide a paradigm-shifting approach to managing allergic inflammatory disorders by addressing their underlying immune pathophysiology rather than merely alleviating symptoms.
The therapeutic efficacy of mesenchymal stem cells (MSCs) is intrinsically linked to the delivery strategy employed. Within the broader context of mesenchymal stem cell immunomodulation research, selecting an administration route is a critical determinant of clinical success, influencing cell survival, homing, biodistribution, and ultimate therapeutic outcome [57]. MSCs possess a unique profile for cell therapy, including the capacity for immunomodulation, promotion of tissue repair, and migration to sites of inflammation [7] [8]. These functions are mediated through direct cell-to-cell contact and the secretion of a vast repertoire of paracrine factors, including cytokines, growth factors, and extracellular vesicles (EVs) [7] [58].
However, a significant challenge in the field is the poor engraftment and low survival rate of transplanted cells, which has led to disparate results in clinical trials [57]. To overcome these hurdles, research has focused on optimizing delivery methods, primarily categorized into systemic (e.g., intravenous) and local (e.g., direct application to the injury site) administration. This guide provides an in-depth technical analysis of these routes, summarizing key quantitative data, detailing relevant experimental protocols, and framing them within the advanced strategies that define modern MSC research.
Comparative Analysis of Administration Routes
The choice between systemic and local delivery involves a trade-off between the scope of influence and targeting precision. The table below synthesizes the core characteristics, advantages, and challenges of each primary route, providing a foundational comparison for researchers.
Table 1: Comparison of Systemic vs. Local Administration Routes for MSCs
| Feature | Systemic (Intravenous) Administration | Local Administration |
|---|---|---|
| Description | Introduction of cells into the circulatory system (e.g., via intravenous injection) [59]. | Direct application of cells to the target tissue (e.g., spinal cord injury site) or encapsulation within a scaffold [59]. |
| Key Advantages | - Broad, whole-body distribution [59].- Suitable for treating systemic or multifocal diseases (e.g., GvHD, multiple sclerosis) [8].- Minimally invasive. | - Higher local cell concentration at the injury site [59].- Avoids first-pass pulmonary entrapment [59].- Potentially enhanced engraftment and retention. |
| Major Challenges | - Significant pulmonary entrapment, reducing delivery to other sites [58].- Risk of blood vessel occlusion [58].- Limited homing to specific inflamed tissues. | - Invasiveness of the procedure.- Potential for local immune reaction or secondary injury.- Limited applicability to inaccessible organs or systemic conditions. |
| Ideal Use Cases | - Widespread inflammatory or autoimmune disorders [8].- Diseases where immunomodulation is the primary goal. | - Localized injuries (e.g., spinal cord damage, focal cartilage defects) [59].- Conditions amenable to scaffold-supported regeneration. |
Quantitative Evaluation of Route Efficacy
Empirical data is crucial for validating the comparative efficacy of administration routes. A pre-clinical study on spinal cord injury (SCI) in a rat model provides a direct, quantitative comparison of intravenous versus local delivery of MSC-derived extracellular vesicles (MSC-EVs), a key therapeutic paracrine component [59].
Table 2: Quantitative Efficacy of Intravenous vs. Local EV Administration in a Rat SCI Model [59]
| Parameter | Intravenous (IV) EV Injection | Local Fibrin-Matrix EV Application | Control (SCI, no treatment) |
|---|---|---|---|
| Locomotor Recovery (over 60 days) | Superior improvement | Improved, but less than IV | Minimal recovery |
| Therapeutic Effect | More pronounced | Less pronounced | N/A |
| Dose Dependency | Positive correlation between EV dose and recovery of motor pathways | Not specified in abstract | N/A |
| Effect on Oligodendrocytes | Maintenance of mature oligodendrocyte population | Information not specified | N/A |
This data demonstrates that in the context of SCI, systemic intravenous administration can yield superior functional recovery compared to local application, highlighting that the optimal route is highly context-dependent and not universally in favor of local delivery.
Experimental Protocol: Comparing Routes In Vivo
To facilitate the replication and further development of route-comparison studies, the following detailed methodology is adapted from the aforementioned research on spinal cord injury [59].
Title: Comparative Evaluation of MSC-EV Therapy via Intravenous vs. Local Administration in a Rat Model of Spinal Cord Injury.
Objective: To assess the efficacy of two different administration routes (IV vs. local) of MSC-derived extracellular vesicles on locomotor recovery and tissue preservation following a moderate spinal cord contusion injury.
Materials and Reagents:
- Animals: Adult female Wistar rats (250–300 g).
- MSCs: Isolated from rat adipose tissue.
- Anesthesia: Isoflurane (1.3%) and zoletil (20 mg/kg).
- Injury Device: Impact One Stereotaxic Impactor (Leica).
- EV Isolation Reagents: Dulbecco's phosphate-buffered saline (DPBS), Dulbecco's Modified Eagle Medium (DMEM), collagenase solution, cytochalasin B.
- Analysis Tools: Transmission electron microscopy (Hitachi 7700), flow cytometer (BD FACS Aria III).
Methodology:
- SCI Model Induction:
- Anesthetize rats using isoflurane and zoletil.
- Perform a laminectomy at the thoracic level (Th8).
- Induce a standardized moderate spinal cord contusion injury using an impactor with a set force (e.g., 2.5 m/s).
Experimental Groups:
- Group 1 (IV): Receives intravenous injection of MSC-EVs resuspended in saline.
- Group 2 (Local): Receives MSC-EVs encapsulated in a fibrin matrix applied directly to the injury site.
- Group 3 (Control): Receives vehicle control (saline) after SCI.
MSC and EV Preparation:
- MSC Isolation: Harvest and mince adipose tissue. Digest with 0.5% collagenase solution for 1 hour at 37°C with constant shaking. Centrifuge the homogenate and culture the cell pellet in DMEM with 10% FBS.
- EV Isolation: Culture MSCs to 90-95% confluence. Wash, trypsinize, and incubate cells in serum-free DMEM with cytochalasin B (10 μg/mL) for 30 minutes. Vigorously vortex the cell suspension and subject it to sequential centrifugation steps (500 rpm for 10 min; 700 rpm for 10 min; 12,000 rpm for 15 min) to pellet EVs. Resuspend the final EV pellet in 0.9% NaCl.
- EV Characterization: Validate EV identity and purity using transmission electron microscopy for ultrastructure and flow cytometry for surface markers (e.g., CD9, CD63, CD81).
Assessment and Endpoints:
- Functional Analysis: Monitor and score locomotor activity in an open field for a minimum of 60 days post-injury using a standardized scale (e.g., BBB scale).
- Histological Analysis: At study termination, perfuse animals and process spinal cord tissue for immunohistochemistry to assess axonal sprouting, myelin preservation, and oligodendrocyte population (e.g., staining for MBP, NF200, APC).
- Statistical Analysis: Compare results between groups using appropriate statistical tests (e.g., ANOVA with post-hoc analysis) with significance set at p < 0.05.
Advanced Formulations and Enhancement Strategies
Beyond the simple suspension of cells in saline, advanced formulations are being developed to augment the potency and durability of MSC therapies. These strategies often work in tandem with the chosen administration route.
1. Preconditioning: This involves exposing MSCs to specific stimuli prior to application to "prime" them for enhanced function. Common preconditioning agents include: - Cytokines: IFN-γ or TNF-α pretreatment upregulates the secretion of immunomodulatory molecules like PGE2, IDO, and HGF, boosting immunosuppressive capacity [57] [8]. - Hypoxia: Culturing MSCs under low oxygen tension mimics their native niche and can improve their pro-angiogenic and survival properties upon transplantation [57].
2. Genetic Manipulation: MSCs can be engineered to overexpress therapeutic factors that enhance immunomodulation or tissue repair. Targets include factors like VEGF, anti-inflammatory cytokines (e.g., IL-10), or enzymes like IDO [57] [7].
3. Cell-Derived Products and Co-Administration: - Extracellular Vesicles (EVs): As illustrated in the experimental protocol, MSC-derived EVs are emerging as a potent cell-free alternative. They recapitulate the paracrine effects of MSCs while offering improved safety, stability, and biodistribution, and can be administered both systemically and locally [59] [58]. - Supportive Biomaterials: For local delivery, MSCs (or their EVs) can be co-administered with biocompatible scaffolds (e.g., fibrin, hydrogels). These materials provide a 3D environment that improves cell retention, survival, and integration at the target site [57] [59].
The following diagram illustrates the logical workflow for selecting and enhancing an MSC delivery strategy, integrating the concepts of preconditioning, formulation, and route selection.
Diagram 1: Decision workflow for MSC delivery strategy and formulation.
The Scientist's Toolkit: Essential Reagents for MSC Delivery Research
The following table catalogues key reagents and materials essential for conducting research into MSC delivery strategies, as cited in the foundational literature.
Table 3: Key Research Reagent Solutions for MSC Delivery Studies
| Reagent / Material | Function / Application | Specific Example (from search results) |
|---|---|---|
| Pro-inflammatory Cytokines | Preconditioning agent to enhance MSC immunomodulatory potency. | IFN-γ, TNF-α, IL-1β [57]. |
| Collagenase Solution | Enzymatic digestion of tissues for the primary isolation of MSCs. | 0.5% collagenase from crab pancreas for adipose tissue digestion [59]. |
| Cytochalasin B | Chemical agent used in the generation of microvesicles/EVs from MSCs. | Incubation at 10 μg/mL to induce EV shedding [59]. |
| Fibrin Matrix | Biocompatible scaffold for the local, sustained delivery of MSCs or EVs at an injury site. | Encapsulation of MSC-EVs for application to spinal cord injury [59]. |
| Flow Cytometry Antibodies | Characterization of MSC surface markers (for identity) and EV surface markers. | CD73, CD90, CD105 (MSCs); CD9, CD63, CD81 (EVs) [59] [7]. |
| DMEM / FBS | Basal cell culture medium and serum supplement for the in vitro expansion of MSCs. | Standard culture for MSCs prior to experimentation or therapy [59]. |
The journey from laboratory discovery to clinical therapy for MSCs is paved with critical decisions, among which the choice of delivery strategy is paramount. As this guide has detailed, the selection between systemic and local administration is not a matter of one being universally superior, but rather hinges on the specific disease pathology, the desired scope of action, and the biological challenges of cell survival and engraftment. The integration of advanced formulations—such as preconditioning, biomaterial scaffolds, and the use of cell-free EVs—is pushing the boundaries of what is possible, offering solutions to traditional limitations. Future research will continue to refine these strategies, likely moving towards personalized delivery protocols that maximize the immense immunomodulatory and regenerative potential of mesenchymal stem cells.
The field of regenerative medicine is undergoing a significant transformation, moving from whole-cell therapies toward sophisticated cell-free approaches. Mesenchymal stem/stromal cells (MSCs) have long been recognized for their remarkable immunomodulatory properties and regenerative potential in treating inflammatory and autoimmune diseases [60] [61]. However, challenges related to safety, variability, and logistical constraints of living cell therapies have prompted researchers to investigate the fundamental mechanisms underlying these therapeutic effects. This exploration has revealed that a primary mechanism of MSC function occurs through paracrine secretion rather than direct cell engraftment [62] [58].
Within the secretome of MSCs, extracellular vesicles (EVs), particularly exosomes, have emerged as critical mediators of intercellular communication [60] [21]. These nanoscale vesicles transport bioactive molecules—including proteins, lipids, and nucleic acids—from parent MSCs to recipient cells, thereby modulating immune responses and promoting tissue repair [62] [63]. This technical guide comprehensively examines the current landscape of MSC-derived EV research, focusing on their immunomodulatory mechanisms, characterization methodologies, therapeutic applications, and translation challenges, providing a foundational resource for researchers and drug development professionals working within the broader context of mesenchymal stem cell immunomodulation mechanisms.
MSC-EV Biogenesis, Cargo, and Isolation
Defining Extracellular Vesicles
MSC-derived extracellular vesicles represent a heterogeneous population of membrane-enclosed particles released by cells, broadly categorized based on their biogenesis and size:
Table 1: Classification of Major Extracellular Vesicle Subtypes
| Vesicle Type | Size Range | Origin | Key Markers |
|---|---|---|---|
| Exosomes | 30-150 nm | Endosomal pathway; release upon MVB fusion with plasma membrane | CD63, CD81, CD9, TSG101, Alix |
| Microvesicles | 100-1000 nm | Outward budding and fission of the plasma membrane | Integrins, selectins, CD40 ligand |
| Apoptotic Bodies | 50-5000 nm | Cell membrane blebbing during apoptosis | Histones, phosphatidylserine |
Exosomes, the most extensively studied EV subtype, are formed through the inward budding of endosomal membranes, creating intraluminal vesicles within multivesicular bodies (MVBs) [62] [21]. These MVBs subsequently fuse with the plasma membrane, releasing exosomes into the extracellular space. This endosomal origin distinguishes exosomes from microvesicles, which are generated through direct outward budding of the plasma membrane [62].
MSC-EV Cargo and Composition
MSC-EVs encapsulate a complex molecular cargo that reflects their parental cell's biological state and mediates their therapeutic functions [62]. The contents include:
- Proteins: Tetraspanins (CD9, CD63, CD81), heat shock proteins (HSP70, HSP90), membrane transporters and fusion proteins (GTPases, annexins), and antigen-presenting molecules [64] [21].
- Nucleic Acids: miRNAs, mRNAs, and other non-coding RNAs that can modulate gene expression in recipient cells [64] [58]. MSC-EVs are enriched with immunomodulatory miRNAs such as let-7 family members, miR-21, and miR-146 [58].
- Lipids: Cholesterol, sphingomyelin, ceramide, and phosphatidylserine that contribute to membrane structure and stability [64].
The molecular composition of MSC-EVs is not static but is dynamically regulated by the microenvironment. When MSCs are exposed to inflammatory cytokines such as IFN-γ and TNF-α, their EVs become enriched with anti-inflammatory molecules including TGF-β, IL-10, PGE2, and specific miRNAs, enhancing their immunomodulatory potency [61] [65].
Figure 1: Exosome Biogenesis Pathway. This diagram illustrates the endosomal pathway of exosome formation, from early endosomes to the release of exosomes following multivesicular body fusion with the plasma membrane.
Isolation and Characterization Techniques
Isolation of high-purity EVs is crucial for both research and clinical applications. The most common isolation techniques each present distinct advantages and limitations:
Table 2: Comparison of Major EV Isolation Techniques
| Method | Principle | Advantages | Disadvantages | Common Use |
|---|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation based on size/density | Widely adopted, no reagent requirements | Time-consuming, may cause aggregation, protein contamination | Research scale |
| Size Exclusion Chromatography (SEC) | Size-based separation through porous matrix | Preserves EV integrity, good purity | Limited resolution, sample dilution | Research/Preclinical |
| Immunoaffinity Capture | Antibody binding to specific surface markers | High specificity, population isolation | Lower yield, high cost, selective capture | Analytical applications |
| Tangential Flow Filtration (TFF) | Size-based filtration with crossflow | Scalable, maintains EV function, high yield | Membrane fouling, requires optimization | Industrial scale |
For clinical translation, scalable production methods like TFF combined with SEC are increasingly adopted to maintain exosome integrity while achieving higher purity [63]. Characterization of isolated EVs typically employs multiple complementary techniques, including nanoparticle tracking analysis (NTA) for size distribution, transmission electron microscopy (TEM) for morphological assessment, and western blotting for detection of specific protein markers (CD63, CD81, CD9, TSG101) [63].
Immunomodulatory Mechanisms of MSC-Derived Exosomes
Innate Immune System Regulation
MSC-derived exosomes (MSCex) exert profound effects on innate immune cells, shifting the balance from pro-inflammatory to anti-inflammatory states:
Macrophages: MSCex promote the polarization of macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype [61] [21]. This transition is mediated through multiple mechanisms, including:
- Secretion of PGE2 which binds to EP2/EP4 receptors on macrophages, stimulating IL-10 production [61]
- Release of TNF-α-stimulated gene 6 (TSG-6) which interacts with CD44 on macrophages, suppressing NF-κβ signaling [61]
- Transfer of miRNAs like miR-182 that target TLR4 receptors, reducing inflammatory cytokine production [61]
Natural Killer (NK) Cells: MSCex inhibit NK cell proliferation, cytotoxicity, and pro-inflammatory cytokine secretion (e.g., IFN-γ) through multiple factors including PGE2, IDO, and HLA-G5 [61]. MSCex downregulate activating receptors on NK cells (NKG2D, NKp30, NKp44) and protect MSCs from NK cell-mediated lysis through IFN-γ preconditioning [61].
Dendritic Cells (DCs): MSCex impair DC differentiation, maturation, and antigen-presenting capacity by:
- Reducing expression of MHC class II molecules and costimulatory molecules (CD80, CD86) [61]
- Decreasing production of pro-inflammatory cytokines like IL-12 [61]
- Inducing a tolerogenic DC phenotype that promotes immune regulation [61]
Adaptive Immune System Modulation
MSCex similarly modulate adaptive immune responses through effects on T and B lymphocytes:
T Lymphocytes: MSCex suppress the proliferation and function of pro-inflammatory T helper cells (Th1, Th17) while promoting the expansion of regulatory T cells (Tregs) [65] [21]. In multiple sclerosis patients, MSCex significantly reduced the percentage of conventional T cells producing IFN-γ and IL-17 while increasing IL-10-producing cells [65]. This immunomodulatory effect was notably more potent than that of the parent MSCs themselves [65].
B Lymphocytes: MSCex inhibit B cell proliferation, differentiation, antibody production, and memory B cell maturation through several mechanisms:
- Internalization by activated CD19+/CD86+ B cells, suppressing their function [21]
- Downregulation of the PI3K/Akt signaling pathway via transfer of miR-155-5p [21]
- Promotion of regulatory B cells (Bregs) through delivery of TGF-β, PGE2, and IL-1RA [21]
Figure 2: MSC-Exosome Immunomodulation Network. This diagram illustrates the comprehensive immunomodulatory effects of MSC-derived exosomes on both innate and adaptive immune cells.
Experimental Protocols for MSC-EV Research
MSC Culture and EV Production
Materials:
- Human umbilical cord tissue (or bone marrow, adipose tissue)
- Collagenase IV (0.1% w/v in PBS)
- Complete DMEM/F-12 medium with 10% FBS
- Penicillin/streptomycin solution
- Phosphate Buffered Saline (PBS)
- Trypsin-EDTA (0.25%)
Protocol:
- MSC Isolation: Wash umbilical cord vein with PBS and incubate with 0.1% collagenase IV for 20 minutes at 37°C [65].
- Culture Expansion: Quench collagenase with complete DMEM/F-12, centrifuge at 500 × g for 5 minutes, and culture cells in complete medium at 37°C with 5% CO2 [65].
- EV Production: At 70-80% confluence, replace medium with EV-depleted serum and culture for 24-48 hours [65].
- Conditioned Media Collection: Collect culture supernatant and centrifuge at 2,000 × g for 20 minutes to remove cells and debris [65].
EV Isolation and Characterization
Ultracentrifugation Protocol:
- Clearing Steps: Centrifuge conditioned media at 300 × g for 10 minutes, then 2,000 × g for 20 minutes to remove cells and debris [63].
- Filtration: Filter supernatant through 0.22 μm membrane.
- High-Speed Centrifugation: Ultracentrifuge at 100,000 × g for 70 minutes at 4°C [65].
- Washing: Resuspend pellet in PBS and repeat ultracentrifugation.
- Resuspension: Resuspend final EV pellet in PBS or appropriate buffer and store at -80°C [65].
Characterization Methods:
- Nanoparticle Tracking Analysis: Dilute EVs in PBS and analyze using NTA to determine size distribution and concentration.
- Transmission Electron Microscopy: Adsorb EVs to formvar/carbon-coated grids, stain with uranyl acetate, and image.
- Western Blotting: Detect EV markers (CD63, CD81, CD9, TSG101) and absence of negative markers (calnexin, GM130).
Functional Assays for Immunomodulation
T Cell Suppression Assay:
- Isolate CD4+CD25- conventional T cells from human PBMCs using magnetic separation [65].
- Label T cells with CFSE and activate with anti-CD3/CD28 beads.
- Co-culture with MSC-EVs or MSC controls for 5 days.
- Analyze proliferation by CFSE dilution using flow cytometry [65].
- Measure cytokine production (IFN-γ, IL-17, IL-10) in supernatants by ELISA or intracellular staining.
Macrophage Polarization Assay:
- Differentiate monocytes from PBMCs into macrophages with M-CSF (50 ng/mL) for 6 days.
- Polarize toward M1 phenotype with IFN-γ (20 ng/mL) and LPS (100 ng/mL).
- Treat with MSC-EVs for 48 hours.
- Analyze surface markers (CD80, CD86 for M1; CD206, CD163 for M2) by flow cytometry.
- Measure cytokine secretion (TNF-α, IL-12, IL-10) by ELISA.
Therapeutic Applications and Delivery Strategies
Preclinical and Clinical Applications
MSC-EVs have demonstrated therapeutic efficacy across diverse disease models:
Table 3: Therapeutic Applications of MSC-Derived EVs
| Disease Category | Model System | Key Mechanisms | Outcomes |
|---|---|---|---|
| Multiple Sclerosis | EAE mouse model; RRMS patient T cells [65] | Suppression of Th1/Th17 cells; Increased Tregs and IL-10 | Reduced CNS inflammation and demyelination |
| Inflammatory Bowel Disease | Colitis animal models [21] | Macrophage polarization to M2 phenotype; T cell modulation | Reduced intestinal inflammation; Enhanced tissue repair |
| Myocardial Infarction | Ischemia-reperfusion injury models [60] [61] | miRNA transfer reducing apoptosis; Enhanced angiogenesis | Improved cardiac function; Reduced infarct size |
| Intracerebral Hemorrhage | Rat ICH model [66] | Attenuation of neuroinflammation; Modulation of MMP activity | Reduced neuronal apoptosis; Improved functional recovery |
| COVID-19/ARDS | Human patients [61] [62] | Inhibition of pro-inflammatory cytokines; Immune cell modulation | Reduced lung injury; Improved oxygenation |
Advanced Delivery Platforms
To overcome limitations of rapid clearance and enzymatic degradation of free EVs, innovative delivery systems have been developed:
3D-Printed Scaffolds for Sustained Release:
- Composition: Decellularized brain matrix (dECM), gelatin-methacryloyl (GelMA), and silk fibroin (SF) crosslinked with a photoinitiator [66].
- Fabrication: hUCMSC-exos are precisely incorporated via extrusion-based 3D bioprinting [66].
- Performance: Demonstrates sustained exosome release over 14 days, significantly promoting neural tissue regeneration while attenuating perihematomal edema in ICH models [66].
- Mechanism: Modulates pathological MMP activity and inflammatory cytokine expression, restoring extracellular matrix homeostasis and reducing neuronal apoptosis [66].
Hydrogel Encapsulation:
- Provides protective environment for EVs
- Enables localized and sustained delivery
- Maintains bioactive EV cargo integrity
- Facilitates spatial control of release kinetics
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for MSC-EV Research
| Reagent/Category | Specific Examples | Application/Function | Considerations |
|---|---|---|---|
| MSC Sources | Human umbilical cord, Bone marrow, Adipose tissue | EV production with tissue-specific characteristics | Varying immunomodulatory potency based on source |
| Isolation Kits | Ultracentrifugation, Size exclusion columns, TFF systems | EV purification from conditioned media | Balance between yield, purity, and scalability |
| Characterization Antibodies | Anti-CD63, CD81, CD9, TSG101, Alix | EV identification and quantification | Confirm presence of multiple markers for purity assessment |
| Cell Culture Media | DMEM/F-12 with EV-depleted FBS | MSC expansion and EV production | Remove contaminating bovine EVs from serum |
| Characterization Instruments | NTA, TEM, Western blot, Flow cytometry | EV physical and biochemical characterization | Multi-method approach recommended by MISEV guidelines |
| Animal Disease Models | EAE, Colitis, ICH, MI models | In vivo therapeutic efficacy assessment | Species-specific immune responses considered |
Challenges and Future Perspectives
Despite considerable progress, several challenges remain in translating MSC-EV therapies to clinical practice:
Manufacturing and Standardization:
- Scalable Production: Transition from flask-based cultures to bioreactor systems (e.g., stirred-tank reactors, hollow-fiber membranes) for industrial-scale EV production [63].
- Quality Control: Development of rigorous potency assays and release criteria to ensure batch-to-batch consistency [62] [63].
- Characterization Standards: Implementation of Minimal Information for Studies of Extracellular Vesicles (MISEV) guidelines to promote reproducibility [63].
Technical Hurdles:
- Heterogeneity: Addressing the inherent diversity in EV populations and their cargo [62].
- Optimization: Enhancing EV yield, purity, and drug loading efficiency for specific applications [63].
- Targeting: Developing engineering strategies to improve tissue-specific delivery [63] [21].
Future Directions:
- Engineering Strategies: Genetic modification of parent MSCs to enhance therapeutic cargo or incorporation of targeting ligands to improve specificity [61] [63].
- Combinatorial Approaches: Integration of EVs with biomaterial scaffolds for spatially and temporally controlled release in complex tissue environments [66].
- Personalized Medicine: Development of autologous EV therapies tailored to individual patient needs and disease states [63].
As the field advances, MSC-derived EVs represent a promising next-generation therapeutic tool that harnesses the essential immunomodulatory mechanisms of mesenchymal stem cells while overcoming critical limitations of cell-based therapies. Their ability to coordinate complex immune responses through multiple molecular pathways positions them as powerful candidates for treating inflammatory and autoimmune diseases, potentially offering enhanced safety profiles and manufacturing advantages over traditional cell therapies.
The therapeutic landscape for Mesenchymal Stem Cells (MSCs), also termed Medicinal Signaling Cells, demonstrates rapid acceleration in clinical development and regulatory approvals globally. With over 1,670 registered clinical trials and 12 approved MSC-based therapies worldwide as of 2025, these cells represent a cornerstone of advanced regenerative medicine and immunomodulation research [67]. The clinical application of MSCs leverages their unique immunoevasive properties, making them suitable for allogeneic transplantation, and their multifaceted immunomodulatory capabilities mediated through both soluble factors and cell contact-dependent mechanisms [67] [9] [8]. While approvals are concentrated in Asia and Europe, with South Korea leading with five products, no MSC-based therapeutic has yet received U.S. FDA approval, though several are under active review [67] [68]. The field is projected to grow significantly, with an anticipated 50 globally approved MSC-based products by 2040, underscoring the immense potential of these cellular therapeutics [67].
Analysis of Global Clinical Trials
The clinical investigation of MSCs is extensive and broad, covering a diverse range of disease indications and geographical locations.
Table 1: Global MSC Clinical Trial Landscape (Data sourced from ClinicalTrials.gov)
| Metric | Number | Percentage |
|---|---|---|
| Total Registered Trials | 1,670+ | 100% |
| Trials for Regenerative Medicine (RM) Products | ~1,252 | ~75% |
| Trials for Disease Modeling | ~234 | ~14% |
| Trials for Drug Discovery & Cytotoxicity Testing | ~184 | ~11% |
Disease Indication Focus
Clinical trials exploit MSC's immunomodulatory and regenerative properties for a wide spectrum of conditions. Key areas include:
- Autoimmune & Inflammatory Diseases: Graft-versus-Host Disease (GvHD), Crohn's disease, systemic lupus erythematosus (SLE), and multiple sclerosis [8] [6].
- Musculoskeletal Disorders: Degenerative arthritis, bone and cartilage repair [67] [8].
- Neurological Disorders: Spinal cord injury, Alzheimer's disease, Parkinson's disease [67].
- Cardiovascular Conditions: Myocardial infarction, cardiovascular repair [67].
- Liver Diseases: Chronic liver diseases, cirrhosis, and liver failure, where MSCs demonstrate potent anti-fibrotic and regenerative capabilities [69].
- Other Areas: Acute respiratory distress syndrome (including COVID-19), diabetes, and chronic kidney disease [6] [70].
Trial Phase Distribution and Design
The majority of registered MSC trials are in early phases, reflecting the still-maturing nature of the field. Challenges include maintaining MSC phenotype and functionality during expansion and meeting rigorous regulatory standards for consistency and safety [67]. Trials utilize both autologous (patient's own cells) and allogeneic (donor-derived cells) MSC sources, with allogeneic products from bone marrow, umbilical cord, and adipose tissue being prevalent due to their "off-the-shelf" potential [67] [70].
Approved MSC-Based Products
Despite the vast clinical trial activity, a select number of therapies have achieved market approval, highlighting the significant regulatory hurdles in the field.
Table 2: Globally Approved MSC-Based Therapies (as of 2025)
| Product Name | Approving Country/Region | Company | Primary Indication |
|---|---|---|---|
| Queencell | South Korea | Anterogen | |
| Cellgram-AMI | South Korea | Pharmicell | |
| Cupistem | South Korea | Anterogen | Anal fistula |
| Cartistem | South Korea | Medipost | Degenerative arthritis |
| NeuroNata-R | South Korea | Corestem | |
| Temcell HS | Japan | JCR Pharmaceuticals | |
| Stemirac | Japan | Nipro Corporation | |
| Holoclar | EU (EMA) | Chiesi Farmaceutici | |
| Alofisel | EU (EMA) | TiGenix/Takeda | |
| Stempeucel | India | Stempeutics | |
| MesestroCell | Iran | Cell Tech Pharmed | |
| Remestemcel-L | Australia | Mesoblast |
Key Observations:
- Geographical Concentration: Nine of the twelve approved therapies are in Asia, with South Korea being the leader with five approved products [67] [68].
- Regulatory Progress: The European Medicines Agency (EMA) has approved two products. The United States FDA has not yet approved any MSC-based therapeutic, though it is actively reviewing Mesoblast's Remestemcel-L [67].
- Diversity of Indications: Approved products target a range of conditions, including musculoskeletal disorders, anal fistula, and other inflammatory conditions [8].
Linking Clinical Applications to Immunomodulatory Mechanisms
The efficacy of MSCs in clinical trials and approved products is fundamentally rooted in their sophisticated biological mechanisms, particularly their capacity for immunomodulation.
Core Immunomodulatory Pathways
The immunomodulatory functions of MSCs are not constitutive but are "licensed" or activated by inflammatory cytokines such as IFN-γ and TNF-α in the host microenvironment [8]. The mechanisms are a synergy of two primary strategies:
Soluble Factor Secretion: Activated MSCs secrete a plethora of immunomodulatory molecules.
- Indoleamine 2,3-dioxygenase (IDO): Catalyzes the conversion of tryptophan to kynurenine, depleting a crucial amino acid required for T-cell proliferation and function [8] [7].
- Prostaglandin E2 (PGE2): Inhibits T-cell proliferation, switches macrophages from a pro-inflammatory (M1) to an anti-inflammatory (M2) phenotype, and suppresses dendritic cell maturation [8] [29].
- Transforming Growth Factor-β1 (TGF-β1) & Hepatocyte Growth Factor (HGF): These and other factors work in concert to suppress T-cell responses and promote the generation of regulatory T cells (Tregs) [8].
Cell Contact-Dependent Mechanisms: Direct interaction with immune cells is equally critical.
- Programmed Death-Ligand 1 (PD-L1): Upregulated by IFN-γ, it engages with PD-1 on T cells to inhibit their proliferation and induce apoptosis [6] [7].
- Adhesion Molecules (VCAM-1, ICAM-1): Facilitate direct contact with T cells and are crucial for immunosuppression [6].
- Galectin-1: Its knockdown abrogates the immunomodulatory effects of MSCs, underscoring its key role [6].
The following diagram illustrates the key immune cells and primary molecular mechanisms through which MSCs exert their immunomodulatory effects.
Experimental Protocols for Validating Immunomodulation
To evaluate the immunomodulatory capacity of MSCs in vitro, researchers employ a suite of standardized co-culture assays. The workflow below outlines a typical experimental design for characterizing MSC-immune cell interactions.
Detailed Methodology:
MSC Preparation and Licensing:
- Isolate MSCs from bone marrow, adipose tissue, or umbilical cord [70].
- Culture and expand MSCs, ensuring they meet the International Society for Cellular Therapy (ISCT) criteria: plastic-adherence, positive for CD73, CD90, CD105 (>95%), and negative for CD45, CD34, CD14, CD11b, CD79α, and HLA-DR (<2%) [70].
- Prior to co-culture, "license" the MSCs by treating with a cytokine cocktail (e.g., 25-50 ng/mL IFN-γ, plus TNF-α or IL-1β) for 24-72 hours to upregulate immunomodulatory genes like IDO and PD-L1 [8] [7].
Immune Cell Activation:
- Isolate Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors via density gradient centrifugation (e.g., Ficoll-Paque).
- Activate T-cells within the PBMC population using mitogens like Phytohemagglutinin (PHA) or Concanavalin A (ConA), or more specifically with anti-CD3 and anti-CD28 antibodies.
Co-culture System:
- Establish co-cultures of licensed MSCs and activated PBMCs. A common approach is to use transwell systems to distinguish between soluble factor-mediated effects (MSCs and PBMCs separated by a permeable membrane) and contact-dependent mechanisms (direct co-culture).
- A range of MSC:PBMC ratios (e.g., 1:5, 1:10, 1:50, 1:100) should be tested to establish a dose-dependent effect [8].
Readout and Analysis:
- T-cell Proliferation: Measure using CFSE dilution flow cytometry or ³H-thymidine incorporation assay. Effective MSC immunosuppression typically shows >50% inhibition of proliferation [8] [29].
- Immune Phenotyping: Use flow cytometry to quantify changes in immune cell populations, particularly the induction of CD4+CD25highFOXP3+ regulatory T cells (Tregs) [8] [6].
- Cytokine Secretion: Analyze culture supernatants via ELISA or multiplex assays (e.g., Luminex) to confirm a shift from a pro-inflammatory (high IFN-γ, TNF-α, IL-17) to an anti-inflammatory (high IL-10, TGF-β) profile [8].
The Scientist's Toolkit: Essential Research Reagents
Successful MSC research requires a suite of high-quality, standardized reagents and platforms. The following table details key materials essential for working with MSCs in an immunomodulation context.
Table 3: Essential Research Reagents for MSC Immunomodulation Studies
| Reagent / Platform | Function & Application | Key Suppliers |
|---|---|---|
| cGMP-compatible MSCs & Media Systems | Standardized, quality-assured cells and culture media for reproducible, scalable research and pre-clinical work. | RoosterBio [67] |
| Cell Isolation Kits | Immunomagnetic or column-based isolation of specific MSC populations or immune cells (T cells, monocytes) from tissue or blood. | Miltenyi Biotec, STEMCELL Technologies [67] |
| Defined MSC Culture Media | Serum-free or xeno-free media formulations that support MSC growth while maintaining phenotype and differentiation potential. | Thermo Fisher Scientific, PromoCell, Lonza [67] |
| Flow Cytometry Antibody Panels | Antibodies for characterizing MSC surface markers (CD73, CD90, CD105, CD45, HLA-DR) and immune cell phenotypes (CD4, CD8, CD25, FOXP3). | Bio-Techne (R&D Systems), BD Biosciences |
| Cytokine Priming Cocktails | Recombinant proteins (IFN-γ, TNF-α) to "license" MSCs and enhance their immunomodulatory potency prior to experimentation. | PeproTech, Bio-Techne (R&D Systems) |
| Bioreactor Systems | Scalable platforms (e.g., stirred-tank, hollow fiber) for the large-scale expansion of MSCs needed for clinical trials and eventual commercialization. | Sartorius (Xuri), Thermo Fisher Scientific [67] |
The clinical trial and regulatory approval landscape for MSCs is dynamic and promising. Future growth will be driven by several key technological and strategic advancements:
- Advanced Engineering: MSC-based gene editing is expanding, enabling the overexpression of antitumor genes and therapeutic factors to enhance potency and specificity [67].
- Manufacturing Innovation: Companies like Cynata Therapeutics are pioneering the use of induced Pluripotent Stem Cells (iPSCs) to derive MSCs (iMSCs), enabling limitless, standardized, and scalable therapeutic production [67].
- Novel Product Forms: MSC-derived products, particularly exosomes and extracellular vesicles, are emerging as cutting-edge, cell-free tools for therapeutic application, with significant investment from the cosmeceutical industry [67] [69].
- Broader Applications: The use of MSCs is expanding beyond medicine into fields like cultured meat production, leveraging their ability to differentiate into muscle and fat cells [67].
In conclusion, the robust clinical trial activity and the steady pace of new regulatory approvals underscore the transition of MSC therapies from experimental concepts to tangible clinical products. The continued elucidation of their immunomodulatory mechanisms, coupled with advancements in bioengineering and manufacturing, positions MSCs to revolutionize the treatment of inflammatory, autoimmune, and degenerative diseases in the coming decades.
Overcoming Clinical Hurdles: Standardization, Safety, and Engineering Solutions
Mesenchymal stromal cells (MSCs) represent a promising frontier in cellular therapy, with demonstrated potential in treating conditions ranging from graft-versus-host disease to Crohn's disease, multiple sclerosis, and cardiovascular disorders [71]. Their appeal lies in their multifunctional capabilities, including immunomodulation, tissue repair, and paracrine signaling. However, the transition of MSC-based Advanced Therapy Medicinal Products (ATMPs) from preclinical research to consistent clinical success has been markedly hampered by inherent heterogeneity [72]. This variability manifests across multiple dimensions—from donor characteristics and tissue sources to manufacturing protocols—resulting in therapeutic products with unpredictable potency and efficacy [71]. Understanding and addressing these sources of heterogeneity is crucial for advancing MSC therapies from promising experimental treatments to reliable clinical commodities.
The clinical implications of MSC heterogeneity are substantial. Despite encouraging preclinical outcomes in animal models, the majority of clinical trials using MSC therapy for diverse human diseases have failed to meet expectations [72]. This translation gap is partially attributable to the intrinsic and often uncontrolled variations between MSC batches. As the field progresses toward more widespread clinical application, establishing robust standardization protocols and potency assays becomes paramount for ensuring consistent product quality, predictable therapeutic outcomes, and regulatory approval [71] [73].
Biological and Donor-Based Variability
The biological foundations of MSC heterogeneity begin with their natural niches and extend to donor-specific factors that significantly influence their functional characteristics.
Tissue Source Variations: MSCs can be isolated from numerous tissues, including bone marrow (BM), adipose tissue (AT), umbilical cord tissue (UCT), dental pulp, and placental tissues [71] [74]. Each source confers distinct functional attributes to the MSCs. For instance, AT-MSCs demonstrate greater proliferative capacity than BM-MSCs, while UCT-MSCs replicate faster than both BM-MSCs and AT-MSCs [73] [74]. Differentiation potential also varies significantly by source; BM-MSCs and AT-MSCs show stronger osteogenic tendency, whereas UCT-MSCs exhibit superior chondrogenic differentiation potential but limited adipogenic capacity [74].
Donor-Specific Factors: Donor age, sex, body mass index, and underlying health conditions substantially impact MSC phenotype, morphology, differentiation potential, and function [71]. The biological age of MSC sources is particularly significant, with fetal-derived MSCs exhibiting distinct properties compared to adult-derived cells. Circulating MSC populations are abundant in fetal development but decrease dramatically after birth, reflecting fundamental differences in MSC biology across the lifespan [74].
Table 1: Functional Heterogeneity of MSCs from Different Tissue Sources
| Tissue Source | Proliferation Capacity | Differentiation Potential | Unique Functional Attributes |
|---|---|---|---|
| Bone Marrow (BM) | Moderate | Strong osteogenic, adipogenic, and chondrogenic | Most prominent immunosuppressive effect in vitro |
| Adipose Tissue (AT) | High | Strong osteogenic and adipogenic | Highest yield per gram of tissue; strong angiogenic potential |
| Umbilical Cord Tissue (UCT) | Highest | Strong chondrogenic; limited adipogenic | Faster replication rate; minimal allogeneic immune response risk |
| Dental Pulp | Variable | Neurogenic, osteogenic, chondrogenic | Neural differentiation propensity |
| Placental | High | Limited adipogenic | Superior migratory capacity |
Manufacturing-Induced Heterogeneity
The processes of isolation, expansion, and formulation introduce substantial technical variability that compounds biological heterogeneity.
Culture Conditions: The choice of culture medium supplements creates significant functional variation. While fetal bovine serum (FBS) has been traditionally used, human platelet lysate (PL) has emerged as a superior alternative that reduces batch-to-batch variability while maintaining phenotypic and functional characteristics [73] [75]. Standardized PL-based culture conditions have been shown to result in very low variability of MSC growth, revealing the true inherent characteristics of MSCs from different sources [73].
Expansion and Passage Effects: Cumulative population doublings and passage number significantly affect MSC characteristics. Single-cell RNA sequencing has identified distinct subpopulations with different functional attributes—some exhibiting greater proliferation capacity while others show enhanced differentiation potential or secretory functions [71]. Even clonally derived MSC populations become functionally heterogeneous over time through processes not fully understood [71].
Formulation and Administration Variables: Post-processing factors including cryopreservation protocols, thawing methods, cell concentration in the final product, delivery solution composition, and administration route critically impact cell viability and functionality upon administration [71]. These factors directly influence the distribution, engraftment, and ultimate therapeutic efficacy of MSC products.
Consequences of Heterogeneity on Immunomodulatory Mechanisms
Impact on Paracrine Signaling
The immunomodulatory functions of MSCs, primarily executed through their secretome, exhibit profound source-dependent variability that directly influences therapeutic outcomes.
Soluble Factor Secretion: MSCs exert immunomodulation through a diverse array of secreted factors including cytokines, chemokines, growth factors, and enzymes such as indoleamine-pyrrole 2,3-dioxygenase (IDO) and prostaglandin E2 (PGE2) [7]. The composition and concentration of these factors vary significantly between MSC sources. For instance, BM-MSCs have demonstrated more prominent immunosuppressive effects in vitro compared to other sources when cultured under standardized conditions [73]. This variation becomes critically important in clinical applications where consistent immunomodulation is required.
Extracellular Vesicle Heterogeneity: MSC-derived extracellular vesicles (EVs)—including exosomes, microvesicles, and apoptotic bodies—carry proteins, lipids, and nucleic acids that mediate intercellular communication [74]. The cargo and functionality of these EVs are heavily influenced by their parental MSC source and culture conditions. For example, EVs from BM-MSCs transfected with specific plasmids can suppress immune responses by inhibiting peripheral blood mononuclear cell proliferation and enhancing regulatory T-cell function [7]. This source-dependent variation in EV bioactivity represents a significant dimension of MSC heterogeneity with direct therapeutic implications.
Cell Contact-Dependent Mechanisms Variability
Cell-to-cell contact represents another critical mechanism of MSC immunomodulation that exhibits substantial heterogeneity across different MSC populations.
T-cell Modulation: MSCs inhibit naive and memory T-cell responses through upregulation of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), which are critical for T-cell activation and leukocyte recruitment [7]. The efficiency of this suppression varies between MSC sources, with BM-MSCs demonstrating particularly potent effects on T-cell proliferation. Additionally, MSC interactions with regulatory T-cells (Tregs) through the Notch1/forkhead box P3 (FOXP3) pathway enhance immunomodulatory capacity in a source-dependent manner [7].
Innate Immune Interactions: MSCs significantly influence innate immunity through direct contact with monocytes, natural killer (NK) cells, macrophages, and neutrophils [7]. The phagocytosis of umbilical cord MSCs by monocytes induces phenotypic and functional changes that subsequently modulate adaptive immunity, distributing immunomodulatory effects systemically [7]. Adipose-derived MSCs can switch activated M1-like inflammatory macrophages to an M2-like phenotype via prostaglandin E2 (PGE2), demonstrating the tissue-specific nuances in MSC-innate immune cell interactions [7].
Table 2: Heterogeneity in MSC Immunomodulatory Mechanisms by Tissue Source
| Immunomodulatory Mechanism | BM-MSC | AT-MSC | UC-MSC |
|---|---|---|---|
| T-cell Suppression | Strong inhibition of proliferation | Moderate inhibition | Variable inhibition |
| B-cell Modulation | Cell cycle arrest in G0/G1 phase | Increased survival of quiescent B-cells | Less characterized |
| Macrophage Polarization | M2 induction via soluble factors | M2 induction via PGE2 | Efficient M2 induction |
| Monocyte Interaction | Phagocytosis-induced changes | Moderate interaction | Strong phagocytosis with functional changes |
| NK Cell Regulation | Suppression of granule polarization | Differential crosstalk | Moderate regulation |
| Treg Induction | Strong via IDO and contact | Moderate | Variable |
Standardization Strategies and Potency Testing
Current Standards and Their Limitations
The International Society for Cell and Gene Therapy (ISCT) established minimal criteria for MSC definition in 2006, including plastic adherence, specific surface marker expression (CD105, CD73, CD90 positive; CD45, CD34, CD14, CD19, HLA-DR negative), and trilineage differentiation potential [71]. However, these criteria have proven insufficient for ensuring consistent therapeutic potency. A concerning scoping review revealed that only 18% of randomly analyzed MSC studies explicitly referred to all ISCT criteria, with just 36% reporting plastic adherence, 40% performing differentiation assays, and 53% conducting complete cell marker analysis [71].
The fundamental limitation of current standards lies in their focus on identity characteristics rather than functional potency. MSC populations that satisfy all ISCT criteria can still exhibit dramatic variations in secretory profile, immunomodulatory capacity, and therapeutic efficacy [72] [71]. This gap between characterization and functionality represents a critical challenge in MSC product standardization.
Advanced Potency Testing Methodologies
Comprehensive potency testing must extend beyond basic phenotypic characterization to assess functional capacity relevant to intended therapeutic applications.
Standardized Growth Conditions: Implementing defined culture conditions with standardized human platelet lysate as a growth stimulus provides a critical foundation for meaningful potency comparisons [73] [75]. This approach minimizes variability introduced by culture supplements and reveals inherent tissue-specific and donor-specific MSC characteristics. Under such standardized conditions, research has demonstrated that AT-MSCs exhibit the highest yield per gram of initial tissue, while UCT-MSCs demonstrate superior proliferation capacity despite lower initial yield [73].
Functional Potency Assays: Robust potency testing requires disease-relevant functional assessments. For immunomodulatory applications, these should include quantitative measures of T-cell proliferation inhibition, macrophage polarization efficiency, cytokine secretion profiling, and IDO activity quantification [73] [7]. For tissue regeneration applications, differentiation efficiency, secretome analysis, and angiogenic potential require evaluation. Implementing such comprehensive testing enables correlation of specific MSC attributes with clinical outcomes.
Research Reagent Solutions for Standardization
Table 3: Essential Research Reagents for MSC Standardization
| Reagent Category | Specific Examples | Function in Standardization | Considerations |
|---|---|---|---|
| Culture Supplements | Human platelet lysate (PL) | Standardized growth stimulus replacing FBS | Reduces batch variability; xeno-free [73] [75] |
| Characterization Antibodies | CD105, CD73, CD90, CD45, CD34, CD14, HLA-DR | Phenotypic characterization per ISCT criteria | Essential for identity confirmation [71] |
| Differentiation Kits | Osteogenic, adipogenic, chondrogenic media | Trilineage differentiation potential assessment | Confirms multipotency [73] |
| Cytokine Assays | IFN-γ, TNF-α, IL-10, PGE2, IDO activity | Immunomodulatory potency assessment | Correlates with therapeutic function [7] |
| Molecular Biology Tools | scRNA-seq reagents, PCR arrays | Comprehensive functional profiling | Identifies subpopulations; predicts potency [71] |
Experimental Protocols for Assessing MSC Heterogeneity
Standardized MSC Expansion and Characterization Protocol
This protocol establishes a standardized framework for MSC expansion and initial characterization, minimizing technical variability to enable meaningful comparison across different MSC sources.
Materials and Reagents:
- Standardized human platelet lysate (PL) supplement [73] [75]
- Basal medium (e.g., α-MEM or DMEM)
- Cell culture plasticware
- Flow cytometry antibodies against CD105, CD73, CD90, CD45, CD34, CD14, HLA-DR
- Trilineage differentiation media (osteogenic, adipogenic, chondrogenic)
Procedure:
- Isolation: Process tissue samples (BM, AT, UCT) within 24 hours of collection using standardized enzymatic digestion (collagenase NB4 at 0.15 IU per gram of tissue) and mechanical dissociation protocols [75].
- Primary Culture: Seed isolated cells at standardized densities (e.g., 1×10^5 cells/cm²) in complete medium supplemented with 5-10% PL. Maintain at 37°C with 5% CO₂.
- Expansion Monitoring: Passage cells upon reaching 80-90% confluence, recording population doubling times and cumulative population doublings at each passage.
- Phenotypic Characterization: At passage 2-4, analyze surface marker expression using flow cytometry. ≥95% of cells must express CD105, CD73, and CD90, while ≤2% may express CD45, CD34, CD14, CD19, and HLA-DR [71].
- Differentiation Potential: Seed cells in specialized media for osteogenic, adipogenic, and chondrogenic differentiation. After 21 days, assess differentiation using lineage-specific stains (Alizarin Red for osteogenesis, Oil Red O for adipogenesis, Alcian Blue for chondrogenesis) [73].
Quality Control Criteria:
- Successful isolation of first-generation MSCs within 2 weeks of culture
- Consistent four-fold expansion at each passage within 1 week of culture
- Cumulative expansion from P0 to P2 of ≥35-fold within 1 month [75]
Comprehensive Immunomodulatory Potency Assay
This protocol provides a standardized approach to assess the immunomodulatory capacity of MSCs, offering critical insights into functional potency beyond basic characterization.
Materials and Reagents:
- Peripheral blood mononuclear cells (PBMCs) from healthy donors
- T-cell mitogens (e.g., phytohemagglutinin)
- Cytokine measurement kits (IFN-γ, TNF-α, IL-10, IL-17)
- IDO activity assay kit
- Transwell co-culture system
Procedure:
- Immune Cell Activation: Isolate PBMCs from donor blood using density gradient centrifugation. Activate T-cells using mitogens at predetermined optimal concentrations.
- Co-culture Establishment: Establish direct and indirect (transwell) co-culture systems with MSCs and activated PBMCs at ratios ranging from 1:1 to 1:10 (MSC:PBMC).
- Proliferation Assessment: After 72-96 hours of co-culture, measure T-cell proliferation using CFSE dilution or BrdU incorporation assays.
- Cytokine Profiling: Collect supernatant at 24, 48, and 72 hours for cytokine analysis using ELISA or multiplex assays.
- IDO Activity Measurement: Assess IDO activity through kynurenine production measurement in culture supernatants using spectrophotometric methods.
- Immune Cell Phenotyping: Analyze regulatory T-cell (CD4+CD25+FOXP3+) populations and macrophage polarization (CD86 for M1, CD206 for M2) using flow cytometry.
Interpretation and Standardization:
- Compare immunosuppressive capacity across MSC sources using dose-response curves
- Establish internal reference standards for assay validation
- Correlate specific secretory profiles (IDO activity, PGE2 production) with functional outcomes [7]
Future Perspectives and Concluding Remarks
The path toward standardized MSC-based therapies requires a multidimensional approach that acknowledges both the challenges of heterogeneity and the opportunities for innovation. Several promising strategies are emerging to address these challenges:
Manufacturing Innovations: Advanced manufacturing approaches including MSC pooling to average out donor-related variability, three-dimensional culture systems that better mimic natural niches, and closed automated bioreactor systems that minimize processing variations represent promising avenues for reducing product heterogeneity [71]. These technologies enable more controlled, scalable, and reproducible MSC expansion while potentially preserving critical functional attributes.
Advanced Characterization Technologies: Single-cell RNA sequencing and other high-resolution profiling technologies enable unprecedented dissection of MSC heterogeneity at the cellular level [71]. These approaches facilitate identification of functionally distinct subpopulations and correlation of specific molecular signatures with therapeutic outcomes. Implementation of such detailed characterization in manufacturing could enable more precise quality control and potency prediction.
Pathway-Specific Potency Engineering: Genetic engineering of MSCs to enhance specific immunomodulatory pathways offers potential for more consistent and potent products [7]. Overexpression of key immunomodulatory factors such as IDO, PD-L1, or IL-10 could create more predictable and potent MSC products, potentially overcoming the limitations of natural heterogeneity.
In conclusion, addressing MSC heterogeneity requires integrated strategies spanning from donor selection through manufacturing and quality control. While heterogeneity presents significant challenges for clinical translation, embracing this complexity through advanced characterization and standardization approaches offers the path forward. The future of MSC therapeutics lies not in eliminating heterogeneity entirely, but in understanding, controlling, and harnessing it to produce more consistent and effective therapies for patients.
The therapeutic application of Mesenchymal Stem Cells (MSCs) has emerged as a highly promising strategy in regenerative medicine and immunomodulation therapy. Expectations for MSC treatments are particularly high in the fields of sepsis, transplant medicine, and autoimmune diseases [76]. These multipotent stromal cells possess unique immunomodulatory properties that make them invaluable for repairing tissue damage caused by chronic inflammation or autoimmune disorders [8]. However, two significant challenges have tempered clinical enthusiasm: questions regarding the long-term viability of administered cells and ongoing concerns about their potential tumorigenicity [76] [77].
The discovery that MSCs exert therapeutic effects beyond direct cellular replacement has revolutionized our understanding of their mechanisms of action. Rather than depending solely on engraftment and differentiation, MSCs primarily function through paracrine signaling and immunomodulatory interactions [78]. This understanding has led to a paradigm shift in the field, with emerging evidence demonstrating that apoptotic, metabolically inactivated, or even fragmented MSCs retain significant immunomodulatory potential [76] [29]. This review examines the scientific foundation for using non-viable MSC preparations as alternatives to viable cells, focusing on their mechanisms of action, comparative efficacy, and potential for reducing tumorigenic risks.
Tumorigenicity Concerns with Living MSCs
Mechanisms of Tumor Promotion
The potential of living MSCs to promote tumor growth represents a significant safety consideration in therapeutic development. Mesenchymal stromal cells actively migrate to tumor sites and function as important cellular constituents of tumor stroma, playing an active role in tumor development [77]. The complex interactions between MSCs and cancer cells promote tumor progression by creating a favorable milieu for tumor cell proliferation, angiogenesis, motility, invasion, and metastasis [77]. The mechanisms underlying MSC-mediated tumor promotion are multifaceted and include:
- Growth Factor Secretion: MSCs release various growth-promoting signals including fibroblast growth factor (FGF), hepatocyte growth factor (HGF), monocyte chemoattractant protein-1 (MCP-1), and particularly interleukin-6 (IL-6), which activates STAT3 signaling in cancer cells [77].
- Immunosuppression: Within tumor microenvironments, MSCs are activated by pro-inflammatory cytokines (TNF-α, IFN-γ, IL-1β) and induce extensive immunosuppression through secretion of factors like indoleamine 2,3-dioxygenase (IDO), prostaglandin E2 (PGE2), and transforming growth factor beta (TGF-β) [79].
- Stemness Induction: MSCs can stimulate cancer cells to acquire stem cell-like characteristics via paracrine signaling involving IL-6, IL-8, and CCL5, thereby increasing tumor-initiating potential and supporting cancer stem cells [77].
- Extracellular Vesicle Mediation: MSC-derived extracellular vesicles transfer biological materials including miRNAs and proteins that enhance tumor growth, invasion, and chemoresistance [77].
Context-Dependent Anti-Tumor Effects
Interestingly, the relationship between MSCs and tumors is not universally promotional. Under certain circumstances, MSCs can impede tumor growth through various mechanisms, including inhibition of angiogenesis, induction of cancer cell apoptosis, and suppression of proliferation pathways [79] [77]. The critical determinants of whether MSCs support or suppress tumors appear to include the specific tumor type, microenvironmental conditions, and the state of MSC activation [79]. This complex, dual nature of MSC-tumor interactions underscores the safety concerns associated with administering viable, replicating MSCs to patients, particularly those with underlying oncological conditions.
Immunomodulatory Mechanisms of Non-Viable MSCs
Apoptotic MSC Mechanisms
The immunomodulatory capacity of apoptotic MSCs represents a fascinating aspect of MSC biology with significant therapeutic implications. Research has demonstrated that MSCs in early apoptosis stages maintain their immunosuppressive functions through mechanisms that involve phagocytosis by monocytes and subsequent immune modulation [29]. When monocytes phagocytose apoptotic MSCs, they undergo phenotypic changes toward an anti-inflammatory M2-like phenotype characterized by increased production of interleukin-10 (IL-10) and decreased secretion of pro-inflammatory cytokines like TNF-α and IL-12p70 [29].
This phenomenon aligns with the natural physiological process where apoptotic cells are cleared by phagocytes in an anti-inflammatory manner. The phagocytosis of apoptotic MSCs primarily occurs in non-classical Ly6C^low monocytes, which subsequently induce the polarization of classical CD14++CD16− monocytes toward a CD14++CD16+CD206+ immune regulatory intermediate subtype with enhanced anti-inflammatory properties and increased expression of IL-10 and programmed death ligand-1 (PD-L1) [29]. These primed monocytes can then induce the formation of CD4+CD25^hi regulatory T cells (Tregs) to a significantly greater extent than unprimed monocytes, effectively amplifying the immunomodulatory signal [29].
Fragmented MSC Mechanisms
Even more remarkably, research indicates that not only apoptotic but even fragmented MSCs retain immunomodulatory capabilities. MSC fragments, including those generated through mechanical disruption or freeze-thaw cycles, appear to maintain certain surface molecules and intracellular components that can influence immune responses [76]. The precise mechanisms remain under investigation but likely involve:
- Rapid phagocytosis of MSC fragments by antigen-presenting cells
- Release of intracellular immunomodulatory factors contained within the fragments
- Surface expression of immunomodulatory molecules that engage with immune cells
- Induction of tolerogenic dendritic cells that promote Treg differentiation
The immunomodulatory effects of fragmented MSCs may involve similar pathways to apoptotic cells, particularly in their interaction with monocytes and macrophages, though with potentially faster kinetics due to increased surface area and accessibility of intracellular components [76].
Key Molecular Pathways
Both apoptotic and fragmented MSCs engage specific molecular pathways to exert their immunomodulatory effects. While the complete signaling network remains to be fully elucidated, several key players have been identified:
- CCL18 Signaling: Macrophages that have interacted with MSCs produce CCL18, which can turn memory CD4+ T cells into CD4+CD25+Foxp3+ Tregs and differentiate dendritic cells into tolerogenic DCs [29].
- Galectin-1: This protein abundantly expressed in MSCs influences cytokine secretion and mediates immunomodulatory effects on T cells, even in non-viable MSC preparations [6].
- PD-1/PD-L1 Axis: MSC-secreted PD-1 ligands (including PD-L1 and PD-L2) exert immunosuppressive effects on T-cell proliferation, and these molecules may remain functional in fragmented MSC preparations [7].
Table 1: Comparative Immunomodulatory Mechanisms of Viable, Apoptotic, and Fragmented MSCs
| Mechanism | Viable MSCs | Apoptotic MSCs | Fragmented MSCs |
|---|---|---|---|
| Soluble Factor Secretion | Extensive (IDO, PGE2, TGF-β1, HGF) | Limited | Minimal |
| Cell-Cell Contact Dependent | Significant | Limited | Minimal |
| Phagocytosis-Dependent | Minor component | Primary mechanism | Primary mechanism |
| Treg Induction | Direct and indirect | Primarily indirect via monocytes | Primarily indirect via monocytes |
| Monocyte Polarization | Via soluble factors and direct contact | Via phagocytosis | Via phagocytosis of fragments |
| Duration of Effects | Potentially longer-lasting | Transient but significant | Potentially transient |
Comparative Analysis: Viable vs. Non-Viable MSCs
Efficacy Comparisons
The surprising finding that non-viable MSCs can exert substantial immunomodulatory effects raises questions about how their efficacy compares to viable cells. Current evidence suggests that while the magnitude of immunosuppression may be somewhat reduced with non-viable preparations, they still retain significant therapeutic potential [76]. The comparison reveals several important distinctions:
- Kinetics of Action: Viable MSCs can respond dynamically to their microenvironment, adjusting their secretory profile in response to local inflammatory signals [8]. This dynamic responsiveness is lost in non-viable preparations, which provide a more static immunomodulatory signal.
- Breadth of Effects: Viable MSCs influence a wider range of immune cells through multiple simultaneous mechanisms, including secretion of various soluble factors, direct cell-cell contact, and mitochondrial transfer [8]. Non-viable MSCs primarily operate through phagocytosis-dependent pathways, which selectively target monocyte/macrophage populations.
- Duration of Effects: The effects of viable MSCs may persist longer due to continuous secretion of immunomodulatory factors, while the impact of non-viable MSCs may be more transient but still clinically significant [76].
Advantages of Non-Viable MSC Approaches
The use of apoptotic or fragmented MSCs offers several distinct advantages from both therapeutic and manufacturing perspectives:
- Reduced Tumorigenic Risk: Without viable, replicating cells, the potential for tumor formation or promotion is substantially diminished [76].
- Elimination of Uncontrolled Proliferation: Non-viable MSC preparations cannot undergo uncontrolled expansion or ectopic tissue formation.
- Simplified Storage and Transport: Apoptotic or fragmented MSC products may have less demanding storage requirements compared to live cell products that require strict viability maintenance.
- Standardized Dosing: Non-viable products can be more easily standardized and quantified than living biological entities with variable metabolic states and potency.
- Reduced Host Immune Reactions: While MSCs are generally considered immunoprivileged, non-viable preparations further minimize any potential immune recognition issues.
Table 2: Tumorigenicity Risk Assessment of Different MSC Formulations
| Risk Factor | Viable MSCs | Apoptotic MSCs | Fragmented MSCs |
|---|---|---|---|
| Long-term Engraftment | Possible | Not possible | Not possible |
| Uncontrolled Proliferation | Potential risk | No risk | No risk |
| Support of Preexisting Tumors | Documented risk [77] | Theoretical risk only | Theoretical risk only |
| Genetic Instability | Potential risk | No risk | No risk |
| Malignant Transformation | Rare but documented | No risk | No risk |
| Angiogenesis Promotion | Significant potential | Limited potential | Limited potential |
Experimental Models and Assessment Methodologies
Induction of Apoptosis and Fragmentation
Research investigating non-viable MSCs has employed various methods to induce apoptosis or fragmentation while preserving immunomodulatory function. Standardized protocols include:
- UV Irradiation: Exposure to ultraviolet light at specific wavelengths (typically UV-C at 254 nm) for precisely controlled durations induces consistent apoptotic states. A common protocol involves 50-100 mJ/cm² followed by incubation for 4-24 hours to allow apoptotic progression [76].
- Chemical Apoptosis Inducers: Agents such as staurosporine (0.1-1 µM for 2-6 hours) or other kinase inhibitors can reliably induce apoptosis. After treatment, cells are thoroughly washed to remove the inducing agents before therapeutic use.
- Freeze-Thaw Fragmentation: Multiple rapid freeze-thaw cycles (typically 3-5 cycles between -80°C and 37°C) mechanically disrupt MSC membranes while preserving certain surface proteins and intracellular components.
- Sonication: Controlled ultrasonic energy application can fragment MSCs while preserving biologically active components. Parameters vary by equipment but typically involve short bursts (10-30 seconds) at medium intensity.
Validation of Apoptotic State
Confirming the appropriate apoptotic state is crucial for experimental consistency and therapeutic reproducibility. Standard assessment methods include:
- Annexin V/Propidium Iodide Staining: Flow cytometric analysis distinguishing early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) populations.
- Caspase Activation Assays: Measurement of executioner caspase activity (caspase-3/7) using fluorogenic substrates.
- Morphological Assessment: Characteristic apoptotic morphology (cell shrinkage, membrane blebbing, chromatin condensation) via microscopy.
- Metabolic Activity Measurement: Confirmation of reduced metabolic activity using assays like MTT or WST-1 while maintaining membrane integrity.
Functional Immunomodulation Assays
The immunomodulatory capacity of non-viable MSC preparations is typically evaluated using standardized in vitro and in vivo assays:
- Lymphocyte Proliferation Assays: Measurement of T-cell proliferation inhibition in response to mitogens or allogeneic stimulation when co-cultured with non-viable MSCs.
- Monocyte Polarization Assays: Assessment of CD14+ monocyte differentiation toward M2-like anti-inflammatory phenotypes following phagocytosis of non-viable MSCs.
- Treg Induction Assays: Quantification of CD4+CD25+FoxP3+ regulatory T cell generation in co-culture systems.
- Cytokine Secretion Profiles: Multiplex analysis of pro-inflammatory (TNF-α, IFN-γ, IL-1β, IL-6) versus anti-inflammatory (IL-10, TGF-β1) cytokine production.
- In Vivo Disease Models: Evaluation in established models such as graft-versus-host disease, experimental autoimmune encephalomyelitis, or colitis to assess therapeutic efficacy.
Diagram 1: Experimental workflow for preparing and evaluating non-viable MSC formulations, illustrating the parallel pathways for creating apoptotic versus fragmented MSC products and their subsequent validation and functional testing.
Signaling Pathways in Non-Viable MSC Immunomodulation
The immunomodulatory effects of non-viable MSCs involve specific signaling pathways that differ somewhat from those engaged by viable cells. Understanding these pathways is essential for optimizing therapeutic applications.
Phagocytosis-Mediated Pathways
The primary mechanism through which non-viable MSCs exert their effects involves phagocytosis by monocytes and macrophages, triggering intracellular signaling cascades that promote anti-inflammatory phenotypes:
- Tyro3/Axl/MerTK Receptor Signaling: Phagocytic receptors of the TAM family recognize phosphatidylserine exposed on the surface of apoptotic MSCs, initiating anti-inflammatory signaling through downstream effectors including SOCS1/3 [29].
- TGF-β1/Smad Pathway: Phagocytosis of apoptotic MSCs enhances TGF-β1 production and signaling through Smad2/3 phosphorylation, promoting FoxP3 expression and Treg differentiation [29].
- IL-10/STAT3 Pathway: Increased IL-10 secretion following phagocytosis activates STAT3 signaling in immune cells, further reinforcing anti-inflammatory responses [29].
Surface Molecule-Mediated Signaling
Even in non-viable states, MSC surface molecules can engage with receptors on immune cells to modulate their function:
- Galectin-1 Interactions: Surface-expressed galectin-1 on MSC fragments engages CD7, CD43, and CD45 on T cells, inhibiting TCR signaling and promoting apoptosis of activated T cells [6].
- PD-L1/PD-1 Engagement: Programmed death ligands preserved on MSC fragments engage PD-1 receptors on T cells, delivering inhibitory signals that suppress T-cell activation and proliferation [7].
- HLA-G-Mediated Tolerance: The non-classical MHC class I molecule HLA-G, expressed by MSCs and potentially preserved in non-viable preparations, interacts with inhibitory receptors (ILT2, ILT4) on immune cells to suppress their function [79].
Diagram 2: Key signaling pathways in non-viable MSC immunomodulation, illustrating how phagocytosis of apoptotic MSCs or fragments triggers intracellular signaling cascades in monocytes/macrophages that ultimately drive systemic immunomodulation through anti-inflammatory macrophage polarization and regulatory T cell induction.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Non-Viable MSC Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Apoptosis Inducers | Staurosporine, UV Crosslinkers, Camptothecin | Induction of controlled apoptosis in MSC cultures | Concentration and timing optimization critical; validate with Annexin V/PI staining |
| Cell Fragmentation Tools | Sonicators, French Press, Freeze-Thaw Equipment | Mechanical disruption of MSCs | Parameter standardization essential for batch consistency |
| Phagocytosis Inhibitors | Cytochalasin D, Latrunculin A | Mechanism validation studies | Confirm inhibition without non-specific cytotoxicity |
| Monocyte/Macrophage Markers | CD14, CD16, CD163, CD206, HLA-DR | Phenotypic characterization by flow cytometry | Panel design should distinguish classical, intermediate, non-classical subsets |
| Treg Analysis Reagents | CD4, CD25, FoxP3, CD127, Helios | Regulatory T cell quantification | Intracellular staining requires fixation/permeabilization |
| Cytokine Analysis | Multiplex arrays, ELISA kits for IL-10, TGF-β1, TNF-α, IL-6 | Secreted factor profiling | Consider both pro-inflammatory and anti-inflammatory mediators |
| Signaling Pathway Inhibitors | STAT3 inhibitors, TGF-βR inhibitors, SMAD inhibitors | Mechanism dissection studies | Verify specificity and use multiple inhibitors per pathway when possible |
Clinical Translation and Future Perspectives
Clinical Applications
The therapeutic application of non-viable MSCs holds particular promise for several clinical conditions where immunomodulation is desired without the risks associated with viable cell transplantation:
- Acute Inflammatory Conditions: Sepsis, acute respiratory distress syndrome (ARDS), and other hyperinflammatory states where transient immunomodulation is sufficient and long-term engraftment unnecessary.
- Autoimmune Diseases: Conditions like Crohn's disease, graft-versus-host disease (GvHD), and multiple sclerosis where current MSC trials show efficacy but safety concerns persist [8].
- Transplant Medicine: Induction of tolerance in solid organ transplantation without the risks of long-term MSC persistence in immunocompromised recipients.
- Topical Applications: Wound healing and localized inflammatory conditions where MSC fragments can be applied directly without systemic distribution concerns.
Manufacturing and Regulatory Considerations
The development of non-viable MSC therapies requires specialized manufacturing approaches and distinct regulatory considerations compared to viable cell products:
- Killing Method Validation: Rigorous demonstration that the apoptosis induction or fragmentation method consistently produces the desired non-viable product with minimal batch-to-batch variability.
- Potency Assays: Development of functional assays that correlate with clinical efficacy, likely focusing on phagocytosis-dependent immunomodulation rather than traditional MSC potency markers.
- Storage and Stability: Establishing shelf-life under various storage conditions, with potential advantages over viable cells in terms of stability and distribution logistics.
- Product Characterization: Comprehensive profiling of surface markers, residual soluble factors, and intracellular components that contribute to the mechanism of action.
Future Research Directions
While the field of non-viable MSC therapies has advanced significantly, several important research questions remain:
- Mechanism Elucidation: More precise understanding of how MSC fragments maintain immunomodulatory capacity, including the roles of specific surface molecules and intracellular components.
- Optimization of Preparation Methods: Comparative studies of different apoptosis induction or fragmentation methods to identify approaches that maximize immunomodulatory potency while minimizing variability.
- Dosing Strategies: Determination of optimal dosing regimens for non-viable MSC products, which may differ significantly from viable cell dosing based on differential pharmacokinetics and mechanisms.
- Combination Approaches: Exploration of hybrid therapies that combine non-viable MSCs with other immunomodulatory agents to enhance or prolong therapeutic effects.
The investigation of apoptotic and fragmented MSCs as alternatives to viable cells represents a promising frontier in cellular therapy that directly addresses significant safety concerns regarding tumorigenicity. The compelling evidence that non-viable MSC preparations retain substantial immunomodulatory capacity through phagocytosis-dependent mechanisms challenges traditional paradigms in cell therapy while opening new therapeutic possibilities [76] [29]. As research continues to elucidate the precise mechanisms involved and optimize preparation methods, non-viable MSC products may offer an attractive combination of efficacy and safety for a range of inflammatory and autoimmune conditions.
The successful clinical translation of these approaches will require careful attention to manufacturing consistency, appropriate potency assay development, and thoughtful clinical trial design tailored to the unique pharmacokinetics and mechanisms of non-viable cell products. With these considerations addressed, apoptotic and fragmented MSCs may soon emerge as valuable additions to the therapeutic arsenal for immune-mediated diseases.
Mesenchymal Stem Cells (MSCs) have emerged as a powerful tool in regenerative medicine and immunotherapy due to their multipotency, low immunogenicity, and potent immunomodulatory properties [80]. Unlike traditional cell therapies that rely on engraftment and differentiation, MSCs primarily function through paracrine signaling—secreting bioactive molecules like vascular endothelial growth factor (VEGF), transforming growth factor-beta (TGF-β), and exosomes that contribute to tissue repair, promote angiogenesis, and modulate immune responses in damaged or inflamed tissues [80]. Recent research has further identified mitochondrial transfer as a novel therapeutic mechanism, where MSCs donate mitochondria to injured cells, restoring their bioenergetic function in conditions such as acute respiratory distress syndrome (ARDS) and myocardial ischemia [80].
However, the transition from promising preclinical results to consistent clinical success has faced significant challenges. Clinical applications reveal that MSC-based therapy encounters major hurdles including poor migration and homing capacities, low survival rate post-transplantation, limited proliferation and differentiation potential, and donor-dependent variation [81]. Furthermore, MSC senescence during long-term culture alters their morphology, reduces stemness, changes intercellular communication, and diminishes differentiation ability, ultimately compromising their therapeutic efficacy [82]. These limitations have stimulated the development of engineering strategies to enhance MSC functionality, with genetic modification and preconditioning emerging as two pivotal approaches to augment their therapeutic potential for diverse clinical applications [83].
Genetic Modification Strategies for Enhanced MSC Function
Genetic modification involves the introduction of specific genetic sequences into MSCs using viral vectors or CRISPR/Cas9 systems to alter the expression of distinctive genes that control survival, homing, immunomodulation, and secretory profiles [83]. These strategies aim to create MSCs with enhanced and more consistent therapeutic properties.
Key Genetic Targets and Their Functional Outcomes
Table 1: Key Genetic Modification Strategies for Enhancing MSC Therapeutic Potential
| Genetic Target | Modification Approach | Functional Outcome | Potential Applications |
|---|---|---|---|
| Anti-apoptotic Genes (Bcl-2, Akt1) | Viral vector-mediated overexpression | Enhanced resistance to apoptosis in hostile microenvironments; Improved cell survival post-transplantation [83] | Myocardial infarction, Stroke |
| Homing Factors (CXCR4, SDF-1) | CRISPR/Cas9-mediated gene editing | Enhanced migration toward inflammatory chemokine gradients; Improved targeting to injury sites [83] | Tissue repair, Inflammatory diseases |
| Immunomodulatory Genes (IDO, PD-L1) | Non-viral plasmid transfection | Potentiated suppression of T-cell proliferation; Enhanced induction of regulatory T-cells [7] | Graft-versus-host disease, Autoimmune disorders |
| Trophic Factors (VEGF, HGF) | Retroviral vector transduction | Increased secretion of angiogenic and cytoprotective factors; Enhanced tissue repair and regeneration [80] | Cardiovascular diseases, Liver cirrhosis |
| Metabolic Enzymes (HO-1) | Lentiviral vector delivery | Improved antioxidant defense mechanisms; Reduced oxidative stress damage [83] | Ischemia-reperfusion injury |
Clinical Translation of Genetically Modified MSCs
The clinical application of genetically modified MSCs is progressing, with several investigations demonstrating promising results. Engineered MSCs have been evaluated in contexts ranging from cancer therapy to regenerative medicine. For instance, in a syngeneic orthotopic mouse model of ovarian cancer, compact bone-derived MSCs (CB-MSCs) genetically modified to express a fusion protein demonstrated enhanced anti-tumor effects through activation of CD4+ and CD8+ T-cells while inhibiting Tregs in the tumor microenvironment [7]. As genetic engineering technologies advance, particularly with the precision of CRISPR/Cas9 systems, and as regulatory frameworks evolve, the clinical prospects for genetically enhanced MSCs continue to expand [80] [83].
Preconditioning Strategies to Augment MSC Efficacy
Preconditioning involves exposing MSCs to sub-lethal environmental stresses or treating them with specific drugs, biomolecules, and growth factors prior to transplantation. This process activates intrinsic adaptive responses, effectively "priming" the cells to better withstand the harsh conditions they will encounter at injury sites [83].
Methodological Approaches to MSC Preconditioning
Table 2: Preconditioning Strategies to Enhance MSC Therapeutic Properties
| Preconditioning Method | Experimental Protocol | Mechanism of Action | Resulting Functional Enhancement |
|---|---|---|---|
| Hypoxia Preconditioning | Culture at 1-3% O₂ for 24-72 hours | Stabilization of HIF-1α; Activation of hypoxia-responsive pathways [81] | Improved survival, Increased angiogenic factor secretion, Enhanced mitochondrial transfer |
| Cytokine Priming | Pre-treatment with IFN-γ (10-50 ng/mL) and/or TNF-α (10-20 ng/mL) for 48 hours [82] | Upregulation of IDO and PGE2; Enhanced immunomodulatory protein expression [82] | Potentiated immunosuppressive capacity, Improved Treg induction |
| 3D Culture Systems | Spheroid formation using hanging drop or low-adhesion plates for 48-96 hours | Enhanced cell-cell interactions; Altered paracrine signaling profiles [82] | Reduced senescence, Improved secretory profile, Enhanced in vivo persistence |
| Pharmacological Preconditioning | Treatment with rapamycin (0.1-1 µM) or dexamethasone (0.1-1 µM) for 24 hours [83] | Induction of autophagy; Modulation of stress response pathways | Improved resistance to apoptosis, Enhanced anti-inflammatory activity |
| Mitochondrial Transfer Enhancement | Co-culture with damaged target cells or pre-treatment with mitochondrial stressors | Upregulation of TNT formation and intercellular communication mechanisms [80] | Improved bioenergetic rescue capacity, Enhanced tissue repair in ARDS and myocardial ischemia |
Technical Implementation of Preconditioning Protocols
For researchers implementing preconditioning strategies, specific technical details are critical for reproducibility. For hypoxia preconditioning, MSCs should be cultured in specialized chambers maintaining 1-3% oxygen tension for 24-72 hours, followed by immediate use in experiments or transplantation [81]. Cytokine priming with IFN-γ typically involves concentrations of 10-50 ng/mL for 48 hours, which significantly upregulates indoleamine 2,3-dioxygenase (IDO) expression, a key enzyme in MSC-mediated immunosuppression [82]. For 3D culture, the hanging drop method or low-adhesion plates with 10,000-20,000 cells per spheroid cultured for 48-96 hours effectively enhances cell-cell interactions and paracrine factor secretion while reducing senescence markers [82].
Integrated Workflow for Engineering Enhanced MSCs
The process of developing engineered MSCs with enhanced therapeutic potential involves a systematic approach that integrates both preconditioning and genetic modification strategies, followed by comprehensive functional validation.
Figure 1: Integrated Workflow for Engineering Enhanced MSCs. This comprehensive approach begins with therapeutic objective assessment, proceeds through strategy-specific implementation, and concludes with rigorous functional validation prior to clinical translation.
Signaling Pathways in MSC Immunomodulation
The therapeutic effects of MSCs, particularly their immunomodulatory capabilities, are mediated through complex signaling pathways that respond to environmental cues. Understanding these pathways is essential for developing effective engineering strategies.
Figure 2: Key Signaling Pathways in MSC-Mediated Immunomodulation. Inflammatory signals trigger multiple immunosuppressive mechanisms in MSCs, leading to coordinated inhibition of pro-inflammatory responses and promotion of regulatory immune cell populations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of MSC engineering strategies requires access to specific, high-quality research reagents and materials. The following table summarizes essential components for experimental workflows in this field.
Table 3: Essential Research Reagents and Materials for MSC Engineering Studies
| Reagent/Material Category | Specific Examples | Research Application | Key Suppliers |
|---|---|---|---|
| Cell Culture Media & Supplements | MesenCult, StemMACS, Fetal Bovine Serum (FBS) | Maintenance and expansion of MSC cultures while preserving multipotency [84] [85] | STEMCELL Technologies, Merck KGaA, Thermo Fisher Scientific |
| Cell Separation Products | MACS CD271 MicroBead Kit, Ficoll-Paque | Isolation and purification of MSCs from tissue sources [85] | Miltenyi Biotec, Cytiva |
| Genetic Modification Tools | Lentiviral vectors, CRISPR/Cas9 systems, Transfection reagents | Introduction of genetic modifications to enhance MSC therapeutic properties [83] | Thermo Fisher Scientific, Lonza Group |
| Cytokines & Growth Factors | Recombinant IFN-γ, TNF-α, TGF-β, HGF | Preconditioning MSCs to enhance immunomodulatory function [82] [81] | Bio-Techne, PeproTech |
| Characterization Antibodies | Anti-CD73, CD90, CD105, CD34, CD45 | Validation of MSC phenotype and purity using flow cytometry [80] [11] | BioLegend, BD Biosciences |
| 3D Culture Systems | Low attachment plates, Hanging drop plates, Hydrogels | Spheroid formation to enhance MSC paracrine activity and reduce senescence [82] | Corning, PromoCell |
| Specialized Culture Equipment | Hypoxia chambers, Bioreactors | Preconditioning under controlled oxygen tension and scalable production [81] | Thermo Fisher Scientific, Lonza Group |
The field of MSC engineering through genetic modification and preconditioning represents a promising frontier in regenerative medicine and immunotherapy. As research advances, several key areas are emerging as critical for future development. The integration of AI-driven platforms to personalize MSC therapy and optimize cell selection represents a promising direction [80]. Additionally, innovative approaches like 3D bioprinting and scalable manufacturing are paving the way for more consistent and precise therapies [80]. The growing understanding of novel mechanisms such as mitochondrial transfer further expands the therapeutic potential of engineered MSCs [80].
For clinical translation, future work must focus on establishing robust quality control and regulatory frameworks essential to translating engineered MSC therapies from bench to bedside and ensuring their reliable application in clinical practice [80]. As these advanced cellular products move through development pipelines, careful attention to both efficacy and safety parameters will be paramount. The continued refinement of engineering strategies covered in this technical guide will undoubtedly play a crucial role in realizing the full therapeutic potential of mesenchymal stem cells for treating a wide spectrum of human diseases.
Mesenchymal stem cell (MSC) therapy represents a transformative approach in regenerative medicine, leveraging the cells' innate immunomodulatory properties and multipotent differentiation potential. However, the clinical translation of MSC-based therapies faces significant hurdles, primarily centered around poor cell survival, limited retention at target sites, and unpredictable therapeutic efficacy following administration. Research indicates that after systemic infusion, an estimated >99% of administered MSCs become trapped in filter organs like the lungs, spleen, and liver, drastically reducing the quantity reaching the intended injury site [86]. Furthermore, those cells that do reach the target tissue often exhibit low survival times due to harsh microenvironments characterized by inflammation, hypoxia, and oxidative stress [87]. These limitations severely constrain the paracrine signaling and immunomodulatory functions that underpin MSCs' therapeutic mechanism, creating an urgent need for advanced delivery strategies that can protect these cells and enhance their persistence in vivo.
Hydrogel encapsulation has emerged as a powerful biomaterial-based strategy to overcome these challenges. By entrapping MSCs within a three-dimensional, hydrophilic polymer network, hydrogel systems provide a protective niche that shields cells from mechanical stress and immune clearance during transplantation and supports their subsequent survival and function [88]. This technical guide examines the fundamental principles, tuning parameters, and mechanistic insights of hydrogel encapsulation, positioning this technology within the broader context of MSC immunomodulation research for expert audiences in drug development and biomedical science.
Hydrogel Design Parameters for MSC Fate and Function
The therapeutic performance of encapsulated MSCs is profoundly influenced by multiple hydrogel properties, which can be systematically tuned to direct specific cellular responses.
Biomechanical Properties
A hydrogel's mechanical properties significantly influence MSC behavior, viability, and therapeutic potential. Stiffness, quantitatively defined by the Young's modulus, has been identified as a critical parameter. Recent research demonstrates that stiff hydrogel encapsulation directly promotes MSC proliferation and enhances in vivo persistence compared to softer formulations [89] [90]. The relationship between substrate mechanics and cell adhesion is mechanistically explained by the interaction between integrin receptors on the MSC surface and RGD (Arg-Gly-Asp) peptide sequences incorporated into the hydrogel matrix. Studies have shown that a higher Young's modulus correlates with a longer persistence time for these integrin-RGD bonds, thereby fostering stronger cell-matrix adhesion and more robust survival signaling [90].
Viscoelasticity, which defines a material's combined viscous (liquid-like) and elastic (solid-like) responses, also plays a crucial role. Hydrogels with stress-relaxing properties can better mimic the dynamic nature of native tissues, promoting improved MSC spread and potentially enhancing immunomodulatory factor secretion [88].
Table 1: Impact of Hydrogel Biomechanical Properties on MSC Behavior
| Property | Experimental Measurement | Impact on MSC Behavior | Recommended Range |
|---|---|---|---|
| Stiffness (Young's Modulus) | Atomic Force Microscopy, Rheometry | Stiffer gels promote proliferation, stemness retention, and prolonged in vivo persistence [89] [90]. | 1-50 kPa (varies by target tissue) |
| Viscoelasticity | Stress relaxation tests, Rheometry | Stress-relaxing gels facilitate cell spreading and may enhance paracrine secretion [88]. | Relaxation time constants of seconds to minutes |
| Porosity | Scanning Electron Microscopy, Micro-CT | Larger, interconnected pores facilitate nutrient waste exchange and neovascularization [88]. | Pore sizes >50 μm for vascular ingrowth |
Biochemical Composition
The chemical makeup of a hydrogel dictates its bioactivity and interactions with encapsulated MSCs.
Natural polymers, such as alginate, collagen, and chitosan, offer inherent biocompatibility and often contain native cell-adhesion motifs. Alginate, a seaweed-derived polysaccharide, is widely used due to its gentle ionic crosslinking process and high tunability; its molecular weight can be adjusted to control the mechanical properties of the resulting microcapsule [89]. Synthetic polymers, like polyethylene glycol (PEG), provide a high degree of control over mechanical properties and chemical consistency but require functionalization with adhesive peptides (e.g., RGD) to support cell adhesion [88].
Functional modifications are frequently employed to enhance biofunctionality. The incorporation of RGD peptides is a standard strategy to promote integrin-mediated MSC adhesion and survival [90]. Furthermore, hydrogels can be modified with protease-degradable crosslinkers (e.g., matrix metalloproteinase-sensitive peptides), allowing MSCs to remodel their local environment, which is crucial for migration and tissue integration [88].
Structural and Topographical Features
The physical architecture of the hydrogel scaffold is critical for mass transport and tissue integration. Porosity and pore interconnectivity are vital for the diffusion of nutrients, oxygen, and metabolic waste, directly impacting the viability of encapsulated cells. A highly interconnected porous network also facilitates host cell infiltration and vascularization post-implantation, which is essential for the long-term engraftment and function of the therapeutic construct [88]. Advances in fabrication techniques like droplet microfluidics enable the production of hydrogels with highly uniform and tunable structural features, such as core-shell microcapsules that offer optimal protection while maintaining permeability [89].
Core Signaling Pathways and Mechanotransduction
The encapsulation of MSCs within a hydrogel does not merely serve as a physical barrier; it actively engages in biochemical dialogue with the cells, modulating key signaling pathways that govern their survival, stemness, and immunomodulatory output.
Mechanical Signaling and Stemness Retention
The maintenance of MSC "stemness"—their multipotency and regenerative capacity—is strongly influenced by the physical cues from the hydrogel matrix. The primary mechanism involves the integrin-mediated mechanotransduction pathway. When integrins on the MSC membrane bind to ligands (e.g., RGD) in the hydrogel, they cluster to form focal adhesions. This process recruits and activates focal adhesion kinase (FAK), which initiates a downstream signaling cascade. A critical node in this cascade is the YAP/TAZ pathway. In a stiff 3D hydrogel environment, the resulting strong cytoskeletal tension prevents the phosphorylation and cytoplasmic sequestration of YAP/TAZ, allowing these transcriptional co-activators to translocate to the nucleus. There, they associate with transcription factors like TEAD to drive the expression of genes that promote proliferation, inhibit differentiation, and maintain stemness [89] [90]. Single-cell RNA sequencing has confirmed that stiff 3D hydrogel encapsulation promotes the residence of MSC subpopulations with a bipotent prechondro-osteogenic and tripotent lineage potential, while suppressing differentiation into pre-smooth muscle cells [90].
Diagram 1: Stiff hydrogel promotes MSC stemness via YAP/TAZ signaling.
Immunomodulatory Pathway Activation
The immunomodulatory functions of MSCs are not constitutive but are activated by inflammatory cues from the injury microenvironment. A key trigger is IFN-γ released by resident immune cells. Hydrogel encapsulation enhances this process by prolonging MSC survival at the site of inflammation, thereby increasing their exposure to these activating signals. Upon engagement of IFN-γ with its receptor on MSCs, the JAK-STAT1 signaling pathway is activated, leading to the transcription of key immunomodulatory mediators. The most prominent of these is Indoleamine 2,3-dioxygenase (IDO), a potent immunomodulatory enzyme. IDO catalyzes the breakdown of tryptophan into kynurenine, creating a local microenvironment that suppresses effector T-cell proliferation and function while promoting the expansion of regulatory T cells (Tregs) [91]. This mechanism is characteristic of the MSC2 phenotype, which is primed for immunosuppression. Hydrogel encapsulation thus acts as a enabling technology, fostering the MSC2 phenotype by ensuring sufficient numbers of cells are present and viable to respond to inflammatory signals and exert their therapeutic immunomodulation [91].
Diagram 2: Hydrogel encapsulation enhances MSC immunomodulation.
Advanced Experimental Protocols
Protocol: Fabrication of Alginate Hydrogel Microcapsules via Droplet Microfluidics
This protocol details the creation of monodisperse, core-shell alginate microcapsules for MSC encapsulation, a method proven to enhance in vivo persistence [89] [90].
- Objective: To generate uniform alginate hydrogel microcapsules with controlled shell stiffness for the encapsulation and sustained delivery of MSCs.
Materials:
- Sodium Alginate (varying molecular weights: low ~80 kDa and high ~250 kDa)
- MSC Culture Medium (e.g., DMEM/F12 supplemented with FBS)
- Calcium Chloride (CaCl₂) Crosslinking Solution (100 mM)
- RGD-Modified Alginate (or RGD peptide)
- Droplet Microfluidic Device (flow-focusing geometry)
- Programmable Syringe Pumps
- Sterile Connectors and Tubing
Step-by-Step Procedure:
- Cell Preparation: Harvest MSCs at 80-90% confluence using standard trypsinization. Centrifuge and resuspend cells at a high density (5-10 × 10^6 cells/mL) in a sterile, viscous solution of 1.5% (w/v) low-MW alginate.
- Hydrogel Precursor Preparation: Prepare two alginate solutions:
- Core Solution: 1.5% (w/v) low-MW alginate with suspended MSCs.
- Shell Solution: 2.0% (w/v) high-MW alginate (for stiffer shells) or low-MW alginate (for softer shells), functionalized with 1 mM RGD peptide.
- Microfluidic Setup: Load the core and shell solutions into separate syringes. Mount syringes onto precision pumps. Prime the microfluidic device and tubing with the respective solutions without bubbles.
- Droplet Generation: Set the flow rates to achieve stable jetting and droplet breakup.
- Core phase (cell suspension): 5 mL/h
- Shell phase: 10 mL/h
- Continuous oil phase (containing surfactant): 25 mL/h
- Crosslinking: Collect the emitted core-shell droplets in a bath of 100 mM CaCl₂ solution under gentle agitation for 15 minutes to ionically crosslink the alginate.
- Washing and Culture: Transfer the resulting microcapsules to a culture plate, wash thrice with PBS to remove residual oil and CaCl₂, and finally immerse in complete MSC culture medium. Culture at 37°C, 5% CO₂.
Key Quality Control:
- Size Distribution: Analyze microcapsule diameter using optical microscopy; target coefficient of variation <5%.
- Cell Viability: Assess using Live/Dead assay (e.g., Calcein-AM/EthD-1) at 24 hours post-encapsulation; expect >90% viability.
- Mechanical Properties: Characterize shell stiffness via micropipette aspiration or AFM.
Protocol: Evaluating In Vivo Persistence and Immunomodulation
This protocol describes a method to assess the survival and immune function of encapsulated MSCs in an immunocompetent animal model.
- Objective: To quantify the in vivo retention, persistence, and immunophenotype of hydrogel-encapsulated MSCs compared to free MSC injection.
Materials:
- Immunocompetent Mouse Model (e.g., C57BL/6)
- Luciferase-expressing MSCs (for bioluminescent imaging)
- In Vivo Imaging System (IVIS)
- D-Luciferin substrate
- Flow Cytometer
- Antibodies for immune cell profiling (e.g., CD4, CD25, FoxP3 for Tregs)
Step-by-Step Procedure:
- Experimental Groups:
- Group 1: Free luciferase-MSCs (suspended in PBS, injected subcutaneously or systemically).
- Group 2: Hydrogel-encapsulated luciferase-MSCs (implanted subcutaneously).
- Group 3: Empty hydrogel (sham control).
- Cell Transplantation: Implant a standardized number of MSCs (e.g., 1 × 10^6) per animal in each group.
- Longitudinal Imaging:
- At days 1, 3, 7, 14, and 28 post-transplantation, inject mice intraperitoneally with D-luciferin (150 mg/kg).
- Anesthetize mice and acquire bioluminescence images using IVIS under consistent exposure settings.
- Quantify the total flux (photons/sec) in a fixed region of interest around the implant site to track cell persistence.
- Endpoint Analysis:
- At day 7 or 14, harvest the implant site and draining lymph nodes.
- Digest the tissue to create a single-cell suspension.
- Stain cells with fluorescent antibodies and analyze by flow cytometry to quantify the infiltration of T cells (CD4+, CD8+), Tregs (CD4+CD25+FoxP3+), and macrophages (F4/80+).
- Experimental Groups:
- Expected Outcomes: The hydrogel-encapsulated MSC group is expected to show a significantly higher bioluminescence signal over time, indicating superior cell retention and survival. Flow cytometry analysis should reveal a higher proportion of Tregs and a lower proportion of pro-inflammatory T cells in the encapsulated group, confirming enhanced local immunomodulation [89] [90].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Hydrogel-based MSC Studies
| Reagent / Material | Function and Role in Experimentation | Example Application |
|---|---|---|
| Sodium Alginate (varying MW) | Forms the primary hydrogel matrix via ionic crosslinking; MW controls mechanical stiffness [89]. | Fabrication of tunable microcapsules via droplet microfluidics. |
| RGD Peptide | Promotes integrin-mediated cell adhesion to the otherwise non-adhesive hydrogel network, enhancing survival and signaling [90]. | Functionalization of alginate or PEG hydrogels. |
| Droplet Microfluidic Device | Generates highly uniform monodisperse hydrogel microcapsules with precise core-shell architectures [89]. | High-throughput production of encapsulated MSC constructs. |
| Calcium Chloride (CaCl₂) | Divalent cation source that crosslinks alginate polymers to form a stable hydrogel. | Standard crosslinking agent for alginate hydrogels. |
| Luciferase-Expressing MSCs | Enables real-time, non-invasive tracking of cell location and survival in vivo via bioluminescence imaging [90]. | Quantifying cell persistence in animal models. |
| CD9 / CD63 / CD81 Antibodies | Markers for characterizing and quantifying exosomes and extracellular vesicles derived from MSCs [92]. | Isolation and validation of MSC-derived EVs for cell-free therapy. |
| Collagen Hydrogel | Natural, bioactive scaffold that can be loaded with MSC-derived exosomes for sustained release [92]. | Creating cell-free therapeutic systems for wound healing. |
Emerging Frontiers and Clinical Translation
Cell-Free Therapeutics: Hydrogel Delivery of MSC-Derived Secretome
A paradigm shift is occurring toward cell-free therapies utilizing the MSC-derived secretome, particularly extracellular vesicles (EVs) and exosomes. These nanoscale vesicles carry a complex cargo of proteins, lipids, and nucleic acids (e.g., miRNAs) that mediate the therapeutic effects of MSCs but pose lower risks of immune rejection and tumorigenicity [86]. However, a major challenge is the rapid clearance of freely administered EVs. To address this, hydrogels are being employed as localized, sustained-release delivery systems. For instance, a collagen hydrogel loaded with calcium silicate-stimulated ADSC-derived EVs (CSEV) was developed for diabetic wound healing. The CSEV exhibited enhanced pro-angiogenic and anti-inflammatory cargo, and the collagen hydrogel provided a controlled release platform, leading to superior re-epithelialization and organized collagen deposition in vivo [92]. This approach represents a next-generation strategy for harnessing MSC immunomodulation without the complexities of live-cell transplantation.
Advanced Characterization with Single-Cell Transcriptomics
Understanding the heterogeneity of MSC populations after encapsulation is crucial for optimizing their function. The emergence of single-cell RNA sequencing (scRNA-seq) allows for the deconvolution of MSC subpopulations and their specific responses to the hydrogel microenvironment. For example, scRNA-seq analysis of MSCs encapsulated in stiff alginate hydrogels revealed a distinct transcriptomic profile favoring the maintenance of bipotent prechondro-osteogenic lineages and suppressing commitment to pre-smooth muscle cells [89] [90]. This high-resolution data provides unprecedented insights into how material properties guide stem cell fate, enabling the rational design of hydrogels to enrich for MSC subpopulations with tailored immunomodulatory or regenerative capacities.
Hydrogel encapsulation has evolved from a simple cell-delivery tool to a sophisticated technology capable of actively directing MSC fate and function. By carefully tuning biomechanical properties, biochemical composition, and structural features, researchers can create an artificial niche that enhances MSC targeting by localizing cells, improves persistence by providing mechanical and immune protection, and amplifies immunomodulation by promoting a potent, sustained paracrine response. The integration of advanced tools—from droplet microfluidics for precise fabrication to scRNA-seq for deep mechanistic insight—is pushing the field toward more predictable and potent MSC-based therapies. As research progresses, the combination of hydrogels with cell-free secretome products and gene-edited MSCs promises to further elevate the precision and efficacy of regenerative immunomodulation, ultimately accelerating the clinical translation of these powerful therapeutic platforms.
Mesenchymal stromal cells (MSCs) represent one of the most promising therapeutic agents in regenerative medicine and immunomodulation, demonstrating remarkable potential for treating conditions ranging from graft-versus-host disease (GvHD) and autoimmune disorders to tissue injury repair. Their therapeutic efficacy stems from their unique immunomodulatory characteristics, trophic activity, and high in vitro self-renewal ability [9] [8]. Unlike many other cell therapies, MSCs can be readily engineered to enhance their immunomodulatory functions and possess inherent immunomodulatory properties that affect most immune effector cells through direct contact and responses to local microenvironmental factors [9] [29].
However, the transition from laboratory success to widespread clinical application has been hampered by two significant and interrelated biological challenges: the short persistence time of MSCs after administration and their tendency to trigger the instant blood-mediated inflammatory reaction (IBMIR) [93]. These challenges collectively compromise cell survival, engraftment, and ultimate therapeutic efficacy. After systemic infusion, MSCs have a short half-life and become entrapped in lung capillaries, failing to reach target tissues in significant numbers [29] [94]. Furthermore, cryopreserved MSCs—the most practical formulation for clinical use—display impaired immunomodulatory and therapeutic properties post-thaw, with reduced responsiveness to inflammatory stimuli and impaired production of anti-inflammatory mediators [93]. This technical guide examines the mechanisms underlying these challenges and details current methodological approaches to overcome them, framed within the broader context of mesenchymal stem cell immunomodulation research.
Core Challenges: Pathophysiological Mechanisms
Short Persistence Time: Biological Basis
The therapeutic potential of MSCs relies critically on their survival and retention at target sites following administration. Unfortunately, multiple factors conspire to limit their in vivo persistence:
- Rapid Clearance After Infusion: Studies demonstrate that systemically delivered MSCs have remarkably short half-lives, with rapid clearance from the circulation. This is particularly pronounced for cryopreserved cells, which show twice the efficiency in lysis after serum exposure compared to freshly harvested cells [93].
- Lung Entrapment: Intravenously administered MSCs cannot pass through the lung capillary network, becoming physically trapped and unable to reach other target tissues [29] [94]. This pulmonary first-pass effect drastically reduces the number of cells available for therapeutic action at disease sites.
- Poor Engraftment and Survival: Even when reaching target tissues, MSCs demonstrate limited engraftment capabilities. Suboptimal encapsulation and injection approaches lead to poor survival, retention time, and engraftment, severely restricting their therapeutic potential [95].
- Passage-Dependent Viability: Clinical observations indicate a trend where fresh cells and cells of low passage demonstrate improved clinical outcomes. Patients treated with freshly harvested cells in low passage had a 100% response rate, twice the response rate of 50% observed in a comparable group treated with freeze-thawed cells at higher passage [93].
Instant Blood-Mediated Inflammatory Reaction (IBMIR)
The IBMIR represents a major thromboinflammatory response that significantly compromises MSC viability and function after administration:
- Complement Activation: Cryopreserved MSCs demonstrate a strong activation of the complement cascade compared to fresh cells, leading to opsonization and membrane attack complex formation [93].
- Coagulation Pathway Trigger: MSCs express procoagulant molecules like tissue factor (TF), triggering the extrinsic coagulation cascade and potentially leading to thromboembolic complications [94]. This procoagulant activity varies by tissue source, with lipoaspirate-derived MSCs associated with higher risks of embolic events compared to bone marrow-derived MSCs in animal models [94].
- Platelet Activation and Aggregation: While some MSC types can inhibit platelet activation via CD73-converted adenosine, others may promote platelet thrombus formation, creating a variable risk profile depending on MSC source and preparation method [94].
- Inflammatory Cell Recruitment: The IBMIR triggers rapid innate immune activation, recruiting neutrophils and monocytes that contribute to MSC clearance through phagocytosis and inflammatory mediator production [93] [29].
Table 1: Quantitative Comparison of Fresh vs. Cryopreserved MSC Properties
| Parameter | Fresh MSCs | Cryopreserved MSCs | Measurement Method |
|---|---|---|---|
| Viable cells after 1h serum exposure | 50% reduction | 80% reduction | In vitro viability assay [93] |
| Complement activation | Lower | Strong activation | Complement deposition assay [93] |
| Immunomodulatory mediator production | Normal | Impaired | ELISA for PGE2, IDO, TGF-β [93] |
| Response to inflammatory stimuli | Intact | Reduced | IFN-γ stimulation assay [93] |
| Clinical response rate | 100% (low passage) | 50% (higher passage) | Patient clinical outcomes [93] |
Experimental Models and Assessment Methodologies
In Vivo Tracking and Persistence Assays
Evaluating MSC persistence requires sophisticated tracking methodologies:
- Luciferase-Labeled MSC Tracking: Bioluminescent imaging using luciferase-labeled MSCs enables non-invasive quantification of cell retention over time. Cells are transduced with luciferase reporter genes prior to administration, and luminescent signals are tracked using IVIS imaging systems [95].
- In Vivo Residence Time Protocol:
- Transduce MSCs with luciferase reporter vector
- Administer cells via intended route (e.g., intravenous, subcutaneous)
- Image animals at predetermined time points (e.g., 1h, 24h, 72h, 1 week)
- Quantify luminescent signal intensity in regions of interest
- Calculate cell persistence half-life from signal decay curves [95]
IBMIR Evaluation Protocols
Comprehensive assessment of IBMIR activation requires multiple analytical approaches:
- Flow Cytometry for Platelet Activation:
- Prepare platelet-rich plasma (PRP) from fresh blood samples
- Incubate PRP with MSCs or MSC-conditioned medium
- Activate with TRAP-6, ADP, or U46619 (typically 5μM)
- Stain with PAC-1-FITC (activated GPIIb/IIIa), CD62P-APC (P-selectin), CD63-PE-Cy7 (LAMP-3), and CD41-PE (platelet identification)
- Analyze by flow cytometry, recording at least 10,000 events [94]
- Complement Activation Assays:
- Expose MSCs to human serum (50% in PBS)
- Incubate at 37°C for 60 minutes
- Measure complement activation products (C3a, C5a, SC5b-9) by ELISA
- Assess membrane attack complex deposition by immunofluorescence [93]
- Thrombogenicity Testing:
- Utilize thromboelastography or rotational thromboelastometry
- Measure clotting initiation, propagation, and strength parameters
- Compare MSC types from different tissue sources [94]
Diagram 1: IBMIR and Persistence Challenge Pathway
Strategic Solutions and Advanced Engineering Approaches
Biomaterial-Based Encapsulation Strategies
Material science approaches offer promising solutions to enhance MSC persistence:
- Injectable Self-Healing Hydrogels: Novel hydrogel systems composed of N,O-carboxymethyl chitosan (CS-CM) and 4-armed benzaldehyde-terminated polyethylene glycol (PEG-BA) form 3D networks via reversible Schiff-base connections, imparting self-healing capacity after injection [95].
- Enhanced Viability and Function: MSCs encapsulated in CS-CM/PEG-BA hydrogels demonstrate:
- Promoted MSC proliferation in the 3D matrix
- Increased cellular half-life in vivo compared to free cells
- Improved immunomodulatory functions including enhanced angiopoiesis promotion
- Inhibited fibrosis in disease models by modulating collagen synthesis [95]
- Minimally Invasive Application: These hydrogels are injectable through percutaneous needles (26-gauge demonstrated), enabling targeted delivery with minimal invasion [95].
MSC Preconditioning and Engineering
- Inflammatory Priming: Pre-treatment with IFN-γ, TNF-α, or IL-1β enhances MSC immunomodulatory potency by upregulating critical mediators like IDO, PGE2, and COX-2 [8] [29].
- Metabolic Optimization: Culture conditions that mimic in vivo physiological environments (e.g., hypoxia) improve MSC fitness and stress resistance post-transplantation.
- Genetic Modification: Engineering MSCs to overexpress specific immunomodulatory factors (IL-10, IDO, TGF-β) or anti-apoptotic genes (Bcl-2) enhances their survival and function [9].
Table 2: Hydrogel Encapsulation Efficacy Data
| Performance Metric | Free MSCs | Hydrogel-Encapsulated MSCs | Experimental Model |
|---|---|---|---|
| In vivo residence time | Short (hours) | Significantly extended | Subcutaneous mouse model [95] |
| Cell viability post-transplantation | Low | High (>2-fold improvement) | Live/dead staining [95] |
| Immunomodulatory capacity | Variable | Enhanced | T-cell suppression assay [95] |
| Angiogenic potential | Moderate | Significantly promoted | Tube formation assay [95] |
| Anti-fibrotic effect | Partial | Robust inhibition | Bleomycin-induced SSc model [95] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MSC Persistence and IBMIR Studies
| Reagent/Cell Type | Function/Application | Key Characteristics |
|---|---|---|
| Bone Marrow-MSCs (BM-MSCs) | Gold standard reference cells | Inhibit platelet activation via CD73/adenosine pathway [94] |
| Lipoaspirate-MSCs (LA-MSCs) | Alternative MSC source with higher yield | Variable procoagulant potential; higher embolic risk in models [94] |
| N,O-carboxymethyl chitosan (CS-CM) | Hydrogel component for encapsulation | Carbohydrate-based polymer; forms Schiff bases with PEG-BA [95] |
| 4-arm PEG-BA (PEG-BA) | Crosslinker for self-healing hydrogels | 4-armed benzaldehyde-terminated polyethylene glycol (Mw 6000) [95] |
| CD73 inhibitors (AMP-CP) | Ectonucleotidase function blockade | α,β-methyleneadenosine 5'-diphosphate; validates adenosine mechanism [94] |
| Adenosine deaminase (ADA) | Adenosine elimination | Deaminates adenosine; confirms adenosinergic pathways [94] |
| Flow antibodies panel | Platelet activation assessment | PAC-1-FITC, CD62P-APC, CD63-PE-Cy7, CD41-PE [94] |
| Luciferase reporter systems | In vivo cell tracking | Enables IVIS imaging for persistence quantification [95] |
Diagram 2: Strategic Solutions for MSC Challenges
The challenges of short persistence and IBMIR represent critical barriers in the translational pathway of MSC therapies that must be addressed within the broader context of MSC immunomodulation mechanisms. The emerging understanding that MSCs employ both cell contact-dependent mechanisms and soluble factor-mediated immunomodulation underscores why persistence time is so critical to therapeutic success [8] [29]. Similarly, the IBMIR represents not merely a delivery obstacle but a fundamental disruption of the delicate interplay between MSCs and the immune system that is essential for their therapeutic function.
Future research directions should focus on:
- Source-Specific Solutions: Recognizing that MSCs from different tissues (bone marrow, adipose, cord blood) exhibit distinct persistence and IBMIR profiles, enabling source selection based on application requirements [94].
- Combination Approaches: Integrating biomaterial encapsulation with preconditioning and genetic engineering to create synergistic improvements in MSC survival and function.
- Standardized Assessment Protocols: Developing validated, standardized assays for persistence and IBMIR potential to enable comparison across studies and cell preparation methods.
- Clinical Translation: Bridging the gap between promising preclinical solutions and clinical application through rigorous safety and efficacy testing.
Overcoming the challenges of short persistence and IBMIR will unlock the full potential of MSC-based immunomodulation therapies, enabling their successful translation from laboratory findings to clinical realities for a wide spectrum of inflammatory and autoimmune conditions.
Within the rapidly advancing field of mesenchymal stem cell (MSC) research, the development of robust quality control frameworks is paramount for successful clinical translation. The therapeutic potency of MSC-based products, defined as their specific biological function relevant to their intended clinical effect, is one of the most critical quality attributes [96]. For MSCs developed for immunomodulation, establishing mechanism-based potency assays presents unique challenges due to the complexity of their action mechanisms, which include paracrine signaling, mitochondrial transfer, and direct cell-cell interactions [80]. The fundamental principle guiding regulatory agencies worldwide is that potency must be measured to ensure manufacturing consistency, product stability, and ultimately, clinical efficacy [96]. This technical guide provides a comprehensive framework for establishing potency assays and release criteria specifically for MSC-based therapeutics, with particular emphasis on their immunomodulatory applications.
Regulatory Foundations and Definitions
The Fundamental Importance of Potency Testing
According to regulatory guidance, potency represents one of the most important parameters of a cellular therapeutic product [96]. A well-defined potency assay serves multiple essential functions in product development:
- Provides the basis for demonstrating manufacturing consistency
- Establishes product stability and shelf life
- Serves as a lot release criterion for final product administration
- Can predict product failure or toxicity due to incorrect potency levels
- Determines appropriate dosing to ensure products perform as intended [96]
For MSC-based immunomodulation products, the complexity of their mechanisms of action necessitates particularly rigorous potency assessment strategies that reflect the biological heterogeneity of these living products.
Regulatory Framework and Guidelines
The International Society for Stem Cell Research (ISSCR) regularly updates its guidelines to address evolving scientific capabilities while maintaining rigorous ethical and quality standards [97] [98]. Although not specific to potency testing, these guidelines establish the fundamental framework for responsible translation of stem cell research, emphasizing rigor, oversight, and transparency throughout development [98]. Regulatory agencies including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) classify MSCs as advanced therapy medicinal products (ATMPs) when producing systemic effects, subjecting them to stringent potency testing requirements [96].
MSC Immunomodulatory Mechanisms: Implications for Potency Assay Design
Primary and Secondary Mechanisms of Action
Table 1: Key Immunomodulatory Mechanisms of MSCs Relevant to Potency Assay Development
| Mechanism Category | Specific Mechanism | Key Effector Molecules/C Processes | Therapeutic Relevance |
|---|---|---|---|
| Paracrine Signaling | Soluble factor secretion | PGE2, IDO, VEGF, TGF-β, IL-10 [80] | GvHD, RA, IBD |
| Extracellular Vesicle Communication | sEV/miRNA transport | miRNAs, proteins (theoretical) [99] | Tissue repair, anti-inflammatory effects |
| Direct Cellular Interaction | T-cell inhibition | PD-L1 expression [80] | Autoimmune conditions |
| Immune Cell Reprogramming | Macrophage polarization | M1 to M2 conversion [80] | Inflammatory conditions |
| Novel Mechanisms | Mitochondrial transfer | Tunneling nanotube formation [80] | ARDS, myocardial ischemia |
Paradigm Shift: From Cellular Engraftment to Paracrine and Vesicular Mediators
The understanding of MSC therapeutic mechanisms has evolved significantly from initial focus on differentiation potential to recognition of paracrine dominance [80]. This shift has crucial implications for potency assay design, as assays must now measure secretory capacity rather than, or in addition to, differentiation potential. The discovery that MSC-derived small extracellular vesicles (MSC-sEVs) can recapitulate many therapeutic benefits of their parent cells further emphasizes the need to quantify vesicle-associated activities [99]. These nanosized vesicles are now widely regarded as principal therapeutic effectors of MSCs, offering superior safety, scalability, and stability profiles compared to whole-cell therapies [99].
Establishing a Comprehensive Potency Assay Strategy
Hierarchical Approach to Potency Assessment
A robust potency assessment strategy for MSC immunomodulation products should employ a hierarchical approach that progresses from general quality attributes to specific mechanistic measures.
Critical Distinction: Viability Versus Potency
A fundamental concept in MSC therapeutic development is the clear distinction between cell viability and biological potency [96]. While viability measures cellular integrity and metabolic activity, potency specifically assesses the therapeutic capacity relevant to the clinical indication. This distinction is particularly critical for immunomodulatory applications where MSC function depends on specific secretory capabilities rather than simply the presence of metabolically active cells.
Mechanism-Based Potency Assays for Immunomodulation
Quantitative Functional Assays for Immunomodulatory Capacity
Table 2: Functional Potency Assays for MSC Immunomodulatory Properties
| Assay Category | Specific Assay Type | Measured Parameters | Application in Release Criteria |
|---|---|---|---|
| T-cell Modulation | T-cell proliferation inhibition | Percentage suppression of activated T-cell growth [80] | Primary potency indicator |
| Macrophage Reprogramming | Macrophage polarization assay | M1/M2 marker expression (CD86, CD206) [80] | Mechanism-specific potency |
| Cytokine Secretion | Multiplex cytokine analysis | PGE2, IDO, TGF-β, IL-10 secretion levels [80] | Quantitative release parameter |
| Gene Expression | qRT-PCR of immunomodulatory genes | IDO, PD-L1, TSG-6 expression [80] | Complementary potency data |
| Mitochondrial Transfer | Mitochondrial transfer imaging | Tunneling nanotube formation, mitochondrial movement [80] | Novel mechanism assessment |
Secretome-Focused Potency Assessment
For MSC secretome-based products, including conditioned media and extracellular vesicle preparations, potency assay development presents unique challenges that are not fully covered by existing regulatory frameworks [100]. Specific attention should be paid to possible effects on stem cell niches, with particular consideration of how secretome components might recover or reactivate damaged or lost niche components [100]. This approach requires:
- Standardization of secretome collection conditions
- Definition of critical quality attributes (CQAs) relevant to mechanism of action
- Establishment of reference materials for assay calibration
- Demonstration of correlation between in vitro potency measures and in vivo efficacy [100]
Reevaluating miRNA as Potency Attributes
Despite initial enthusiasm regarding miRNAs as primary effectors of MSC-sEV activity, recent evidence challenges their functional relevance [99]. Critical considerations for potency assay development include:
- miRNAs are significantly underrepresented in sEVs compared to cellular content
- miRNAs occur at very low copy numbers in therapeutic sEV preparations
- MSC-sEVs lack essential components (e.g., Argonaute proteins) required for canonical RNA interference
- Efficiency of EV internalization and endosomal escape remains exceedingly low [99]
These findings necessitate a reevaluation of miRNA quantification as a standalone potency attribute and support the development of multi-parameter potency assays that incorporate protein and lipid components alongside nucleic acids.
Technical Protocols for Key Potency Assays
T-cell Suppression Assay (Gold Standard Protocol)
The T-cell suppression assay represents a cornerstone potency assessment for immunomodulatory MSCs, directly measuring a primary mechanism of action.
Materials and Reagents:
- Isolated peripheral blood mononuclear cells (PBMCs) from healthy donors
- T-cell activation reagents: Anti-CD3/CD28 antibodies or phytohemagglutinin (PHA)
- Cell culture medium: RPMI-1640 with 10% fetal bovine serum
- Flow cytometry antibodies: CD4, CD8, proliferation markers (CFSE or Ki-67)
- Cytokine detection: ELISA or multiplex array for IFN-γ, TNF-α, IL-2
Experimental Procedure:
- PBMC Isolation: Isolate PBMCs from buffy coats using Ficoll density gradient centrifugation
- T-cell Activation: Label PBMCs with CFSE (5μM, 10 minutes) and activate with anti-CD3/CD28 beads (1 bead:1 cell ratio)
- Co-culture Establishment: Plate activated PBMCs with MSCs at varying ratios (e.g., 1:1 to 10:1 PBMC:MSC ratios) in 96-well U-bottom plates
- Culture Conditions: Incubate co-cultures for 3-5 days at 37°C, 5% CO₂
- Analysis:
- Analyze T-cell proliferation by CFSE dilution via flow cytometry
- Quantify cytokine secretion in supernatant by ELISA
- Calculate percentage suppression relative to PBMC-only controls
Acceptance Criteria: Test articles should demonstrate dose-dependent suppression of T-cell proliferation, typically ≥30% suppression at 1:10 MSC:PBMC ratio for release criteria.
IDO Functional Activity Assay
Indoleamine 2,3-dioxygenase (IDO) represents a key enzymatic mechanism in MSC-mediated immunomodulation, measurable through functional assessment.
Materials and Reagents:
- L-tryptophan substrate: Prepared in PBS
- Reaction buffer: Potassium phosphate buffer with ascorbic acid and methylene blue
- Detection reagents: Trichloroacetic acid, Ehrlich's reagent
- Standard curve materials: L-kynurenine for quantification
Experimental Procedure:
- Enzyme Preparation: Lyse MSCs using freeze-thaw cycles in potassium phosphate buffer
- Reaction Setup: Incubate cell lysates with L-tryptophan (0.1-1mM) for 2-4 hours at 37°C
- Reaction Termination: Add trichloroacetic acid (30% w/v) to stop enzymatic activity
- Color Development: Mix supernatant with Ehrlich's reagent and incubate 10-30 minutes
- Quantification: Measure absorbance at 490nm and calculate kynurenine production using standard curve
Acceptance Criteria: Functional MSCs should demonstrate measurable IDO activity, typically ≥1μM kynurenine/10⁶ cells/hour under inflammatory conditions (IFN-γ stimulation).
Research Reagent Solutions for Potency Assessment
Table 3: Essential Research Reagents for MSC Potency Evaluation
| Reagent Category | Specific Examples | Function in Potency Assessment | Technical Notes |
|---|---|---|---|
| Flow Cytometry Antibodies | CD73, CD90, CD105, CD34, CD45, CD14 [80] | Identity and purity assessment | Follow ISCT minimal criteria [80] |
| Cell Activation Reagents | Anti-CD3/CD28 beads, PHA, LPS | T-cell and macrophage activation for functional assays | Standardize source and concentration |
| Cytokine Detection | IFN-γ ELISA, multiplex arrays | Quantification of secretory function | Include both pro- and anti-inflammatory panels |
| Cell Tracking Dyes | CFSE, PKH26, CellTrace dyes | Proliferation and migration assessment | Optimize concentration to avoid toxicity |
| Culture Supplements | IFN-γ, TNF-α, IL-1β | Inflammatory priming of MSCs | Standardize concentration and exposure time |
Implementation Strategy and Quality System Integration
Potency Assay Validation Framework
Implementing potency assays within a quality system requires rigorous validation demonstrating the following assay characteristics:
- Accuracy: Measure of closeness between test result and accepted reference value
- Precision: Degree of agreement among individual test results when performed repeatedly
- Specificity: Ability to measure the analyte accurately in the presence of interfering components
- Linearity: Ability to produce results proportional to analyte concentration
- Range: Interval between upper and lower levels of analyte that can be measured with precision and accuracy
- Robustness: Capacity to remain unaffected by small variations in method parameters [96]
Correlation with In Vivo Efficacy
The ultimate validation of any potency assay requires demonstration of correlation with in vivo activity [100]. This involves:
- Parallel testing of MSC batches with known in vivo efficacy
- Statistical analysis of correlation between potency assay results and therapeutic outcomes
- Establishment of potency specifications based on efficacious batches
- Ongoing monitoring of clinical outcomes to refine potency ranges
For MSC immunomodulation products, this typically involves correlation with disease-specific animal models including graft-versus-host disease, inflammatory bowel disease, or autoimmune encephalitis models.
The establishment of robust, mechanism-based potency assays represents a critical milestone in the clinical development of MSC-based immunomodulatory therapies. As the field advances toward increasingly defined products, including MSC-sEVs and genetically modified MSCs, potency assessment strategies must evolve accordingly [99] [80]. The framework presented herein provides a scientifically rigorous approach to potency assay development that aligns with regulatory expectations while addressing the biological complexity of MSC therapeutic action. Through implementation of these comprehensive quality control strategies, developers can enhance manufacturing consistency, improve clinical trial success rates, and ultimately deliver more reliable MSC-based immunomodulatory therapies to patients.
Evaluating Therapeutic Efficacy: Preclinical Models and Clinical Evidence
Preclinical models are indispensable for elucidating the mechanisms of mesenchymal stem/stromal cell (MSC) immunomodulation and advancing therapeutic development. These models span from reductionist in vitro systems to complex in vivo animal models, each offering unique insights into the multifaceted interactions between MSCs and immune cells. MSCs possess innate immunoregulatory capabilities affecting both adaptive and innate immunity through cell-cell contact, soluble mediators, and extracellular vesicles [22]. The selection of an appropriate model system depends on the specific research question, whether investigating molecular mechanisms, screening therapeutic candidates, or validating efficacy in pathophysiologically relevant contexts. This guide provides a comprehensive technical overview of current preclinical models, emphasizing their application in MSC immunomodulation research, with detailed methodologies and analytical frameworks to support researchers in designing robust experimental workflows.
Mesenchymal Stem Cell Immunomodulation: Core Mechanisms
MSCs mediate immunomodulation through interconnected cellular and molecular mechanisms that are context-dependent and influenced by the local inflammatory microenvironment. Understanding these mechanisms is prerequisite to selecting appropriate preclinical models.
Cellular Targets: MSCs directly modulate both innate and adaptive immune cells. They suppress neutrophil respiratory burst via IL-6 release, inhibit monocyte differentiation into dendritic cells, reduce natural killer cell proliferation and IFN-γ production, suppress T-cell proliferation, and modulate B-cell function [101]. Additionally, they promote the generation and expansion of regulatory T cells (Tregs), which are crucial for maintaining immune tolerance [102] [22].
Molecular Mediators: The immunomodulatory effects are mediated through soluble factors and surface molecules. Key soluble factors include prostaglandin E2 (PGE2), transforming growth factor-β (TGF-β), interleukin-10 (IL-10), indoleamine 2,3-dioxygenase (IDO), heme oxygenase-1 (HO-1), and tumor necrosis factor-inducible gene 6 protein (TSG-6) [101] [102]. Critical surface molecules involved in immune interactions include CD54 (ICAM-1) for cell adhesion, PD-L1 (CD274) for checkpoint inhibition, and CD273 [22].
Conditioning and Priming: The immunomodulatory potency of MSCs is not constitutive but requires activation by inflammatory cues. This "licensing" can be achieved through priming with pro-inflammatory cytokines like interferon-γ (IFN-γ) or, more physiologically, through co-culture with peripheral blood mononuclear cells (PBMCs). PBMC conditioning induces distinct transcriptomic and phenotypic signatures in MSCs, upregulating molecules like CD26 (DPP4), CD54, CD273, IDO1, and PTGS2 (COX-2), significantly enhancing their immunosuppressive capacity [22].
Table 1: Key Molecular Mediators of MSC Immunomodulation
| Molecule | Type | Primary Function in Immunomodulation | Key Immune Cells Affected |
|---|---|---|---|
| IDO | Enzyme | Tryptophan catabolism, inhibits T-cell proliferation | T cells, NK cells |
| PGE2 | Lipid mediator | Suppresses NK cell function, promotes M2 macrophage polarization | Macrophages, NK cells, T cells |
| TSG-6 | Protein | Anti-inflammatory, reduces NF-κB signaling in macrophages | Macrophages, dendritic cells |
| IL-10 | Cytokine | Potent anti-inflammatory cytokine, inhibits Th1 responses | Macrophages, T cells, dendritic cells |
| TGF-β | Cytokine | Suppresses T-cell activation, promotes Treg differentiation | T cells, B cells |
| CD275 (PD-L1) | Surface protein | Inhibits T-cell activation via PD-1 engagement | T cells |
| CD54 (ICAM-1) | Surface protein | Facilitates MSC-immune cell contact and signaling | T cells, monocytes |
3In VitroCo-culture Model Systems
In vitro co-culture systems provide reductionist, controlled environments for dissecting the molecular and cellular mechanisms of MSC immunomodulation with high reproducibility.
PBMC Conditioning of MSCs
Purpose: To enhance and study the activated immunomodulatory phenotype of MSCs. Detailed Protocol:
- MSC Culture: Expand human adipose-derived MSCs in αMEM medium supplemented with 5% human platelet lysate (hPL) and 2U/mL heparin. Culture at 37°C in 5% CO2 until 80-90% confluence [22].
- PBMC Isolation: Isulate PBMCs from healthy donor venous blood using density gradient centrifugation with Lymphoprep. Freeze in FBS with 10% DMSO for storage [22].
- Conditioning Co-culture: Thaw and wash PBMCs. Seed MSCs at a density of 5,000 cells/cm². Add PBMCs to the MSC culture at a recommended MSC:PBMC ratio of 1:5. Co-culture for 48-72 hours in the aforementioned medium [22].
- Harvesting cMSCs: After co-culture, carefully wash the plate to remove non-adherent PBMCs. The remaining adherent, conditioned MSCs (cMSCs) can be harvested with trypsin for subsequent functional assays or analysis [22]. Analytical Methods:
- Transcriptomics: RNA sequencing of cMSCs versus resting MSCs (rMSCs) identifies differentially expressed genes (e.g., CCL2, CCL11, DPP4, ICAM1, IL6, PDCD1LG2) [22].
- Phenotyping: Use flow or mass cytometry to validate upregulated surface (CD26, CD54, CD273) and intracellular (IDO1, PTGS2) proteins [22].
- Secretome Analysis: Profile conditioned media using multiplex cytokine arrays or proteomics to identify secreted immunomodulatory factors [22].
Diagram 1: PBMC Conditioning Workflow
Functional T-cell Suppression Assay
Purpose: To quantitatively evaluate the functional capacity of cMSCs to suppress immune cell proliferation. Detailed Protocol:
- T-cell Activation: Isolate T-cells from PBMCs using negative selection kits. Label T-cells with cell proliferation dyes such as CFSE (5-6 carboxyfluorescein diacetate succinimidyl ester) or similar dyes [22].
- Co-culture Setup: Activate the labeled T-cells using anti-CD3/CD28 antibodies or phytohemagglutinin (PHA). Seed the activated T-cells with either resting MSCs or conditioned MSCs (cMSCs) at varying MSC:T-cell ratios (e.g., 1:10, 1:50) in a multi-well plate. Include controls for maximal T-cell proliferation (no MSCs) and baseline proliferation (non-activated T-cells) [22].
- Culture and Analysis: Culture for 3-5 days. Harvest cells and analyze CFSE dilution, which indicates cell division, using flow cytometry. The percentage of proliferating T-cells in each condition is quantified and compared [22]. Analytical Methods:
- Calculate the percentage suppression of T-cell proliferation:
(1 - (% Proliferation with MSCs / % Proliferation without MSCs)) * 100[22]. - Simultaneously analyze T-cell subsets (e.g., CD4+, CD8+) and the emergence of Tregs (CD4+CD25+FOXP3+) by flow cytometry [102] [22].
Animal Disease Models for MSC Therapy Validation
Animal models provide a pathophysiological context to validate the therapeutic efficacy and mechanisms of MSC immunomodulation in vivo. The choice of model is critical and depends on the human disease being simulated.
Collagen-Induced Arthritis (CIA) Model
Purpose: A robust and widely used model for studying rheumatoid arthritis (RA) and testing MSC-based therapies [102]. Detailed Protocol:
- Animals: Use 8-12 week old male DBA/1 mice, which are genetically susceptible to CIA [102].
- Immunization: Emulsify bovine or chicken type II collagen (CII) in complete Freund's adjuvant (CFA). Inject the emulsion intradermally at the base of the tail (Day 0). A booster immunization with CII in incomplete Freund's adjuvant (IFA) is typically given on Day 21 [102].
- MSC Administration: Once arthritis is clinically evident (typically around day 25-35), administer MSCs intravenously, intraperitoneally, or intra-articularly. Common doses range from 0.5-2 x 10^6 cells per mouse [102].
- Disease Monitoring: Monitor mice 2-3 times weekly for clinical signs of arthritis. Score each paw on a scale of 0-4 based on redness, swelling, and deformity. Calculate a cumulative arthritis index for each animal [102]. Analytical Endpoints:
- Clinical: Arthritis incidence and clinical score over time [102].
- Histopathological: Upon termination, process hind paws for histology (H&E staining). Score for synovitis, pannus formation, cartilage damage, and bone erosion [102].
- Immunological: Analyze serum for anti-collagen II antibodies and cytokines (e.g., TNF-α, IL-6, IL-17). Isolate splenocytes or draining lymph node cells for ex vivo restimulation and flow cytometric analysis of T-cell subsets (Th1, Th17, Tregs) [102].
Humanized Myasthenia Gravis (MG) Model
Purpose: To test MSC efficacy in a humanized, antibody-mediated autoimmune disease context [22]. Detailed Protocol:
- Model Generation: Utilize immunodeficient NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) mice. Implant fragments of human MG thymus (obtained from thymectomy patients) subcutaneously [22].
- MSC Administration: After confirming human immune cell engraftment and/or the presence of human anti-acetylcholine receptor (AChR) antibodies, inject cMSCs intravenously (e.g., 1-2 x 10^6 cells per mouse) [22].
- Disease Monitoring: Assess mice regularly for signs of muscle weakness using standardized functional tests. A common method is the grip strength test, where a progressive decrease in strength indicates disease severity [22]. Analytical Endpoints:
- Functional: Quantitative grip strength measurements and clinical scoring of disease severity [22].
- Serological: Measure levels of human anti-AChR antibodies in mouse serum by ELISA [22].
- Cellular Analysis: Analyze human immune cell populations from mouse spleen or blood by flow cytometry to assess changes in B and T cell subsets, particularly Tregs [22].
Table 2: Summary of Key Animal Models for MSC Immunomodulation Research
| Disease Area | Model Name | Species/Strain | Key Readouts | MSC Efficacy Notes |
|---|---|---|---|---|
| Rheumatoid Arthritis | Collagen-Induced Arthritis (CIA) | DBA/1 mice | Arthritis score, paw swelling, histopathology, anti-CII antibodies, pro-inflammatory cytokines | Reduces clinical score, inflammation, and cartilage/bone damage; increases Tregs [102]. |
| Systemic Lupus | MRL/lpr mouse | MRL/MpJ-Faslpr/J mice | Proteinuria, anti-dsDNA antibodies, glomerulonephritis histology, survival | Ameliorates kidney disease, reduces autoantibody levels [102]. |
| Myasthenia Gravis | Humanized NSG-MG | NSG mice + human MG thymus | Grip strength, clinical score, human anti-AChR Ab titers | cMSCs halve disease severity; modulate T/B cell responses [22]. |
| Bone Repair/Defect | Monocortical Tibial Defect (MTD) | C57BL/6 mice | Micro-CT (bone volume, density), histology, biomechanical testing | MSCs enhance bone regeneration; most remain undifferentiated, support vascularization [103]. |
Diagram 2: Animal Model Evaluation Flow
Advanced 3D and ComplexIn VitroModels (CIVMs)
To bridge the gap between traditional in vitro systems and animal models, complex in vitro models (CIVMs) offer more physiologically relevant human-based platforms.
Organoid-Immune Co-culture Models
These models are powerful for studying human-specific tumor-immune interactions or mucosal immunity, and can be adapted for screening MSC immunomodulatory functions in a tissue-like context.
- Innate Immune Microenvironment Models: Tumor tissue-derived organoids are cultured using methods that preserve the native tumor microenvironment (TME), including autologous tumor-infiltrating lymphocytes (TILs). These organoids can be used to study the PD-1/PD-L1 axis and test immunotherapies [104].
- Immune Reconstitution Models: Tumor organoids derived from core biopsies are co-cultured with autologous peripheral blood lymphocytes. This model successfully captures the differential response to PD-1 blockade seen in patients with high versus low tumor mutational burden, demonstrating its predictive power [104].
- Protocol Workflow:
- Organoid Establishment: Generate patient-derived organoids from tissue biopsies in a 3D extracellular matrix (e.g., Matrigel or synthetic hydrogels) with optimized growth factor cocktails [104].
- Immune Cell Preparation: Isolate immune cells (TILs or PBMCs) from the same patient.
- Co-culture: Add the immune cells to the established organoid culture. Media may require T-cell stimulators like IL-2 and anti-CD3 antibody [104].
- Intervention & Readout: Add MSCs to the co-culture system. Key readouts include organoid viability/cell death (e.g., by caspase-3 activation) and immune cell phenotype/function analyzed by flow cytometry (e.g., T-cell activation markers, proliferation, cytokine production) [104].
MSC-Laden Hydrogel Systems
3D hydrogels act as bioactive delivery vehicles that can enhance MSC survival, retention, and function by mimicking the native extracellular matrix.
- Application in Regeneration: Preclinical studies show MSC-laden hydrogels enhance tissue repair in musculoskeletal, cardiovascular, dermal, and neural injuries. The 3D environment can modulate MSC paracrine signaling and differentiation [105].
- Design Principles: Hydrogels can be engineered from natural (e.g., hyaluronic acid, collagen) or synthetic (e.g., PEG) polymers. "Smart" hydrogels can be designed to respond to local physiological stimuli (e.g., enzyme activity, pH) for controlled release of cells or factors [105].
- Translation: Clinical application is facilitated by using xeno-free, GMP-compliant components like clinical-grade hPL or synthetic polymers [105].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for MSC Immunomodulation Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| MSC Culture Media | αMEM, DMEM | Base medium for MSC expansion. |
| Culture Supplements | Human Platelet Lysate (hPL), Fetal Bovine Serum (FBS) | Provides essential growth factors and adhesion proteins for cell growth. Prefer hPL for xeno-free clinical translation [22] [105]. |
| Immune Cell Isolation | Lymphoprep, Ficoll-Paque, CD3/CD19 Microbeads | Isolate PBMCs or specific immune cell subsets from blood [22]. |
| T-cell Activators | Anti-CD3/CD28 antibodies, Phytohemagglutinin (PHA) | Polyclonal activation of T-cells for functional suppression assays [22]. |
| Flow Cytometry Antibodies | Anti-human: CD73, CD90, CD105, CD45, CD34, HLA-DR, CD4, CD8, CD25, FOXP3, CD19 | Characterize MSC phenotype (ISCT criteria) and immune cell populations/subsets [101] [102] [22]. |
| Cytokine/Antibody Detection | ELISA kits, Multiplex Bead Arrays (e.g., Luminex) | Quantify soluble factors (e.g., TNF-α, IL-6, IL-10, IFN-γ) and autoantibodies in supernatants and serum [102] [22]. |
| Extracellular Matrix (ECM) | Matrigel, Synthetic Hydrogels (e.g., GelMA) | Provide 3D support for organoid culture and MSC delivery [104] [105]. |
| Animal Model Reagents | Type II Collagen, Complete Freund's Adjuvant (CFA) | Essential for inducing Collagen-Induced Arthritis (CIA) [102]. |
Technical and Methodological Considerations
Robust preclinical research requires careful attention to methodological details and potential biases.
MSC Source and Heterogeneity: MSCs can be isolated from bone marrow, adipose tissue, umbilical cord, and other tissues. These sources exhibit variable growth potential, differentiation capacity, and immunomodulatory potency, which must be reported and considered when comparing studies [101] [102]. The species of origin (e.g., human vs. murine) also leads to significant differences in marker expression and behavior [101].
Cell Tracking and Fate In Vivo: Understanding the distribution, persistence, and fate of administered MSCs is crucial. Methods include:
- Fluorescent Nanoparticles (fNPs): Allow long-term tracking of implanted MSCs without genetic manipulation, enabling spatial analysis of their location and differentiation status (e.g., SCA-1+, PRRX1+, OSX+) in tissues like bone [103].
- Pharmacokinetic Modeling: Applied to quantitative MSC detection data to predict and optimize cell distribution, persistence, and dosing regimens [106].
Addressing Model Limitations and Bias:
- Animal Model Translational Gaps: Genetically engineered animal models for rare diseases often fail to fully recapitulate human pathophysiology [107]. CIVMs can complement animal studies by providing human-relevant data.
- Preclinical Study Quality: Umbrella reviews of preclinical MSC-EV studies highlight recurring issues like high heterogeneity (I² > 70%) and risk of bias, primarily due to poor randomization, blinding, and outcome reporting [108]. Adherence to SYRCLE's risk of bias tool and CAMARADES guidelines is recommended to improve rigor [108].
The unique immunomodulatory properties of mesenchymal stem cells (MSCs) position them as a transformative therapeutic strategy for immune-related disorders, particularly graft-versus-host disease (GvHD) and other inflammatory conditions [51]. These multipotent stem cells, characterized by their capacity for self-renewal, low immunogenicity, and homing capabilities, exert profound effects on both innate and adaptive immune systems [61]. The analysis of Phase I-III clinical trial data reveals a dynamic and rapidly evolving landscape where MSC-based therapies and targeted pharmacological agents are demonstrating significant potential in managing these complex conditions. This technical guide provides an in-depth analysis of clinical trial outcomes within the broader context of mesenchymal stem cell immunomodulation research, offering methodologies and frameworks essential for researchers, scientists, and drug development professionals navigating this innovative field.
Analysis of Recent Clinical Trial Outcomes in GvHD
The GvHD therapeutic landscape has evolved significantly beyond traditional steroids and broad immunosuppressants to include targeted therapies, cellular approaches, and novel biologics [109]. Recent clinical trials have focused particularly on steroid-refractory cases, with several late-stage therapies demonstrating promising outcomes.
Table 1: Late-Stage GvHD Therapies in Clinical Development
| Therapy Name | Developer | Mechanism of Action | Indication | Trial Phase | Key Outcomes |
|---|---|---|---|---|---|
| CSL964 (Zemaira) | CSL Behring | Alpha-1 Antitrypsin (Alpha1-Proteinase Inhibitor) | Steroid-refractory aGvHD treatment and prevention in high-risk HSCT patients | Phase III | Under investigation; Phase II/III for prevention [109] |
| EQ001 (Itolizumab) | Equillium/Biocon | Anti-CD6 monoclonal antibody inhibiting pathogenic T-cell activation and migration | First-line GvHD treatment with corticosteroids | Phase III (EQUATOR) | Did not meet primary endpoints (CR/ORR at Day 29); showed statistically significant benefits in secondary endpoints (CR at Day 99, response duration, failure-free survival) [109] |
| MaaT013 | MaaT Pharma | Donor-derived, standardized microbiome ecosystem therapy (BUTYCORE consortium) | Steroid-resistant, GI-predominant aGvHD | Phase III (ARES trial) | 62% overall GI response rate by Day 28; Orphan Drug Designation from FDA and EMA [109] |
| MC0518 | medac | Mesenchymal stromal cell (MSC) therapy with immune-modulating capabilities | Steroid-refractory aGvHD in children and adolescents | Phase III (IDUNN trial) | Primary endpoint: ORR at Day 28; secondary endpoints: OS up to 24 months and FFTF within 6 months; well-tolerated in preclinical models [109] |
Table 2: FDA-Approved Therapies for Chronic GvHD
| Therapy Name | Mechanism of Action | Approval Year | Indication | Key Clinical Outcomes |
|---|---|---|---|---|
| IMBRUVICA (Ibrutinib) | Bruton tyrosine kinase inhibitor targeting B-cell signaling | 2017 | Chronic GvHD | First FDA-approved therapy for cGvHD; inhibits B-cell receptor signaling and IL-2-inducible T-cell kinase [110] |
| JAKAFI (Ruxolitinib) | JAK1/JAK2 inhibitor | 2019 | Steroid-refractory acute GvHD | REACH3 trial showed efficacy and safety through 3-year follow-up; suppresses cytokine signaling and inflammatory response [110] |
| REZUROCK (Belumosudil) | ROCK2 inhibitor targeting STAT3-dependent mechanism | 2021 | Chronic GvHD after failure of ≥2 therapies | Demonstrated clinical response in bronchiolitis obliterans syndrome; projected to achieve 10% peak market share [109] [110] |
| NIKTIMVO (Axatilimab) | CSF-1R inhibitor targeting proinflammatory myeloid cells | 2024 | Chronic GvHD | Recent approval; projected to achieve 8% market share [109] |
| RYONCIL (Remestemcel-L) | Allogeneic MSC therapy | 2024 | Pediatric steroid-refractory acute GvHD | MSC-based therapy demonstrating efficacy in pediatric population [109] |
Analysis of MSC Clinical Performance in GvHD
MSC therapies have demonstrated variable but promising outcomes across GvHD trials. The immunomodulatory effects of MSCs in GvHD are primarily mediated through paracrine signaling and direct cell contact, modulating T-cell proliferation, dendritic cell maturation, and macrophage polarization [61] [51]. Clinical studies reveal that MSCs exert their therapeutic effects without necessarily migrating to the skin or target tissues, instead functioning through systemic immunomodulation that persists long after the cells are cleared from the body (typically within one week post-infusion) [111]. This paradoxical lasting effect, observed for up to 12 months in human studies, suggests MSCs initiate sustained immunological reprogramming rather than providing temporary suppression [111].
In steroid-refractory GvHD cases, MSC therapies like MC0518 and RYONCIL have demonstrated particular promise in pediatric populations, with trial endpoints focusing on overall response rates (ORR) at Day 28 and long-term outcomes including overall survival (OS) and freedom from treatment failure (FFTF) [109]. The therapeutic efficacy appears linked to MSC-mediated inhibition of chemokine signaling (particularly CCL2, CCL3, CCL5, CCL17, and CCL22), which reduces infiltration of pathogenic T cells and macrophages into target tissues [111].
Methodologies for Analyzing MSC Immunomodulation in Clinical Trials
Experimental Protocols for Assessing MSC Immunomodulation
In Vitro Co-culture Systems for Immune Cell Function Assessment
- T-cell Proliferation Assay: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors or patients and label with CFSE. Co-culture with MSCs at ratios ranging from 1:10 to 1:100 (MSC:PBMC) in the presence of T-cell activators (e.g., anti-CD3/CD28 antibodies or phytohemagglutinin). After 3-5 days, analyze T-cell proliferation flow cytometrically via CFSE dilution. Include transwell systems to distinguish contact-dependent versus soluble factor-mediated effects [51].
- Macrophage Polarization Protocol: Isolate human monocytes using CD14+ magnetic sorting and differentiate into M1 macrophages with GM-CSF (50 ng/mL) for 6 days. Co-culture with MSCs in direct contact or transwell systems for 48 hours. Analyze M2 polarization via flow cytometry (CD206, CD163 expression) and ELISA measurement of IL-10, IL-12, TNF-α, and IL-1β in supernatants [61].
- Dendritic Cell Maturation Assay: Generate dendritic cells from CD34+ progenitors or monocyte-derived precursors with GM-CSF and IL-4. Co-culture with MSCs during LPS-induced maturation. Assess DC maturation status via flow cytometry (CD83, CD86, HLA-DR expression) and measure IL-12 production via ELISA [61].
In Vivo Models for GvHD and Inflammatory Disease
- Xenogeneic GvHD Mouse Model: Irradiate NOD-scid IL2Rγnull (NSG) mice with 200-300 cGy and inject with 5-10×10^6 human PBMCs to induce GvHD. For MSC treatment, administer 1-2×10^6 human MSCs intravenously at time of PBMC injection or after GvHD symptoms appear. Monitor mice for clinical scores (weight loss, posture, activity, fur texture), survival, and tissue histopathology [51].
- Inflammatory Skin Fibrosis Models: For sclerodermatous GvHD models, inject B10.D2 splenocytes into BALB/c recipients followed by MSC treatment. For systemic sclerosis models, use bleomycin-induced skin fibrosis. Administer MSCs intravenously at various disease stages. Assess skin thickness, collagen content (hydroxyproline assay), and immune cell infiltration (flow cytometry) [111].
Signaling Pathways in MSC-Mediated Immunomodulation
MSC Immunomodulation Pathways in GvHD and Inflammation
Analytical Approaches for Clinical Trial Data
Standardized Data Collection Frameworks Implementation of the Analysis Results Data Model (ARDM) enables "calculate once, use many times" methodology for clinical trial data analysis [112]. This approach reframes analysis targets from static representations (PDFs, tables) to structured data models that support secondary analysis and knowledge discovery. The model includes:
- Metadata tables documenting variable types, measurement units, and analysis parameters
- Intermediate data tables aggregating subject-level information to avoid repeated transformations
- Results tables storing statistical outputs in machine-readable formats for future reuse [112]
Advanced Data Visualization for Harms Assessment Clinical trial visualization tools like REACT (Real-time Analytics for Clinical Trials) and DETECT (Data Evaluation Tool for End of Clinical Trial data) provide intuitive platforms for data interpretation, enabling researchers to interact with data, view relationships between different clinical data types, and assess information over time at both patient and population levels [113].
For comprehensive harms assessment, several visualization methods have demonstrated particular value:
- Dot Plots: Two-panel displays showing incidence by treatment group alongside summary measures with confidence intervals [114]
- Volcano Plots: Bubble plots summarizing multiple harm characteristics including frequency, treatment association, statistical significance, and effect size [114]
- Stacked Bar Charts: Depict occurrence of harms across higher-order classifications with severity stratification [114]
Table 3: Key Research Reagent Solutions for MSC Immunomodulation Studies
| Reagent/Category | Specific Examples | Research Application | Function in Experimental Protocols |
|---|---|---|---|
| Cell Isolation Kits | CD14+ magnetic beads, CD34+ progenitor isolation kits, Pan T-cell isolation kits | Immune cell isolation for co-culture studies | Isolation of specific immune cell populations from PBMCs or tissue samples for MSC co-culture experiments [61] [51] |
| Cell Culture Media | MSC expansion media (serum-free defined), RPMI-1640 for immune cells, Dendritic cell differentiation media | Maintenance and differentiation of cells | Support growth and function of MSCs and various immune cell types during in vitro studies [61] [51] |
| Cytokines & Activation Reagents | IFN-γ, TNF-α, IL-1β, IL-2, IL-15, anti-CD3/CD28 antibodies, LPS, GM-CSF, IL-4 | Immune cell activation and polarization | Create inflammatory environments, activate T cells, polarize macrophages, mature dendritic cells [61] [51] |
| Flow Cytometry Antibodies | CD73, CD90, CD105 (MSC markers); CD3, CD4, CD8 (T cells); CD14, CD16 (monocytes); CD19, CD20 (B cells); CD56 (NK cells); CD83, CD86, HLA-DR (DC) | Cell phenotype characterization | Verify cell identity, assess activation status, evaluate MSC marker expression according to ISCT criteria [61] [109] |
| ELISA/Kits | PGE2 ELISA, IDO activity assays, TGF-β1 ELISA, IL-10 ELISA, TNF-α ELISA, IFN-γ ELISA | Soluble factor measurement | Quantify production of immunomodulatory factors in co-culture supernatants or patient sera [61] [51] |
| Molecular Biology Reagents | miRNA isolation kits, qRT-PCR reagents for collagen genes, Western blot reagents for signaling proteins | Mechanism investigation | Analyze molecular mechanisms of MSC action including miRNA transfer, gene expression changes, signaling pathway activation [111] |
The analysis of Phase I-III clinical trial outcomes in GvHD and inflammatory diseases reveals a rapidly advancing field where MSC-based therapies demonstrate significant potential through their multifaceted immunomodulatory capabilities. The evolving landscape includes both cellular therapies and targeted molecular agents that address specific pathways in these complex immune disorders. As research progresses, standardized methodologies for assessing MSC-immune interactions, coupled with advanced data analysis and visualization approaches, will be essential for translating preclinical findings into clinical applications. The continued investigation of MSC mechanisms—particularly their paracrine effects, cell contact-dependent regulation, and capacity for immunological reprogramming—will undoubtedly yield new insights and therapeutic strategies for managing GvHD and other inflammatory conditions.
Mesenchymal stem cells (MSCs) have emerged as one of the most promising platforms for allogeneic cell therapy, primarily due to their potent and multifaceted immunomodulatory capabilities [9] [6]. Within the broader thesis of MSC immunomodulation research, understanding the comparative effectiveness of different MSC sources, dosing strategies, and administration protocols becomes paramount for clinical translation. The therapeutic efficacy of MSCs is not merely a function of their presence but is intricately governed by their origin, preparation, and delivery parameters [115] [116]. These cells exhibit a unique capacity to modulate both innate and adaptive immune responses through direct cell-cell contact and paracrine activity, influencing T cells, B cells, natural killer (NK) cells, macrophages, monocytes, dendritic cells (DCs), and neutrophils [7] [6]. This in-depth technical guide synthesizes current evidence to provide researchers, scientists, and drug development professionals with a structured framework for optimizing MSC-based therapies, with data presentation standardized for comparative analysis across studies.
Tissue Source Considerations and Comparative Potency
MSCs can be isolated from a diverse range of adult and perinatal tissues, each with distinct immunological, proliferative, and functional characteristics that influence their therapeutic potential [116] [6]. The International Society for Cellular Therapy (ISCT) has established minimal criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73, CD90, CD105 positive; CD14, CD34, CD45, HLA-DR negative), and tri-lineage differentiation potential [116] [91]. However, beyond these defining criteria, significant functional heterogeneity exists across tissue sources.
Table 1: Comparative Analysis of Primary MSC Sources and Immunomodulatory Properties
| MSC Source | Key Immunomodulatory Mechanisms | Proliferation Capacity | Clinical Advantages | Documented Limitations |
|---|---|---|---|---|
| Bone Marrow (BM-MSCs) | - Secretion of IDO, PGE2, TGF-β [51]- T-cell suppression via cell contact [6]- Induction of Tregs [51] | Moderate [116] | - Extensive safety profile [116]- Well-documented immunomodulation [9] | - Invasive isolation procedure [116]- Age-dependent functional decline [116] |
| Adipose Tissue (AT-MSCs) | - Potent PGE2 secretion promotes M2 macrophage polarization [7]- Enhanced B-cell regulation [7]- High TSG-6 production [54] | High [116] | - Abundant tissue source [116]- Less invasive harvesting [116]- Potent cytokine secretion [7] | - Donor metabolic status affects quality [116] |
| Umbilical Cord (UC-MSCs) | - Minimal allogeneic immune response [7] [6]- Phagocytosis by monocytes amplifies immunomodulation [7]- High angiogenic factor content [116] | Very High [116] [6] | - Non-invasive collection [116]- Immune-privileged properties [7]- Consistent young donor profile [116] | - Perinatal source limitations [116] |
| Dental Pulp (DP-MSCs) | - Suppression of CD4+ T cells and IFN-γ/IL-17 secretion [6] | Moderate to High [6] | - Accessibility from medical waste [6] | - Limited study compared to other sources [6] |
Experimental Protocols for MSC Source Characterization
Standardized Isolation and Expansion Protocol:
- Tissue Processing: Minced tissue subjected to collagenase type I (1-2 mg/mL) digestion at 37°C for 45-90 minutes with agitation [116] [91]
- Culture Conditions: Resuspend cells in α-MEM or DMEM/F-12 supplemented with 10% fetal bovine serum (FBS), 1% penicillin/streptomycin, and 2 mM L-glutamine [116]
- Plastic Adherence Selection: Culture at 37°C with 5% CO₂ with first medium change at 72 hours to remove non-adherent cells, subsequent changes every 3-4 days [7] [116]
- Subculture: Harvest at 80% confluence using 0.25% trypsin/EDTA and reseed at 1,000-5,000 cells/cm² [116]
- Immunophenotyping: Passage 3-5 cells analyzed by flow cytometry for CD73, CD90, CD105 (≥95% positive) and CD14, CD34, CD45, HLA-DR (≤2% positive) [116] [91]
Functional Potency Assay - T-cell Suppression:
- MSC Preparation: Irradiate MSCs (30-40 Gy) or treat with mitomycin C (25 µg/mL for 30 minutes) to prevent proliferation [51]
- Immune Cell Co-culture: Seed MSCs in 96-well plates at varying ratios (1:1 to 1:100 MSC:peripheral blood mononuclear cells (PBMCs)) [51] [6]
- T-cell Activation: Add anti-CD3/CD28 beads or phytohemagglutinin (PHA, 2-5 µg/mL) to stimulate T-cell proliferation [51]
- Proliferation Measurement: After 72-96 hours, add ³H-thymidine (1 µCi/well) for final 16-18 hours or use CFSE dye dilution assay [51] [6]
- Cytokine Analysis: Collect supernatants for IFN-γ, TNF-α, IL-10, and IL-4 quantification by ELISA [51] [6]
MSC Immunomodulatory Mechanisms and Signaling Pathways
The immunomodulatory functions of MSCs are mediated through an intricate network of cellular interactions and secretory activities that modulate the immune response in a context-dependent manner [9] [7]. These mechanisms can be broadly categorized into cell-contact-dependent suppression and paracrine-mediated immunomodulation, with the specific mechanisms activated being heavily influenced by the local inflammatory microenvironment [51] [6].
Key Signaling Pathways in MSC Immunomodulation
Diagram 1: Inflammatory Signaling in MSC Immunomodulation. This diagram illustrates how pro-inflammatory signals prime MSCs through TLR and NF-κB pathways to activate key immunomodulatory mechanisms including IDO expression and PGE2 secretion, ultimately driving functional immune cell changes.
The immunomodulatory functions of MSCs are not constitutive but are rather licensed by inflammatory cytokines, particularly IFN-γ in combination with TNF-α, IL-1α, or IL-1β [51] [6]. This priming step triggers significant changes in MSC gene expression and secretome, inducing the production of various enzymes and soluble factors including cyclooxygenase 2 (COX-2), prostaglandin E2 (PGE2), and indoleamine-pyrrole 2,3-dioxygenase (IDO) that mediate immunosuppressive activity [51]. The specific mechanisms employed vary based on the inflammatory context and MSC tissue origin, creating a dynamic regulatory system that responds to the host immune environment.
Cell Contact-Dependent Mechanisms
Direct cell-cell contact between MSCs and immune cells plays a crucial role in immunomodulation through several receptor-ligand systems [7] [6]:
Programmed Death Ligand Systems:
- MSCs express PD-L1 and PD-L2 which interact with PD-1 on T cells [54]
- This interaction recruits SHP-1 and SHP-2 phosphatases that dephosphorylate key signaling molecules including ZAP70 and PKCθ [54]
- Downstream effects include suppression of PI3K/AKT and MAPK/ERK pathways, ultimately blocking T cell proliferation and cell cycle progression at G0/G1 phase [54]
Adhesion-Mediated Suppression:
- MSCs express high levels of ICAM-1 and VCAM-1 that support direct interaction with T cells [7] [6]
- The Notch1/FOXP3 pathway activation in CD4+ T cells increases CD4+CD25+FOXP3+ regulatory T cell populations [7] [6]
- Galectin-1 expressed on MSC surfaces is critical for T cell suppression, with knockdown resulting in loss of immunomodulatory function [7]
Experimental Protocol for Cell Contact Dependence:
- Transwell System Setup: Culture MSCs in lower chamber and activated PBMCs in upper chamber (0.4µm pore size) [51] [54]
- Contact-Dependent Condition: Seed MSCs and PBMCs together in direct contact
- Proliferation Measurement: Compare T cell proliferation between conditions using ³H-thymidine incorporation or CFSE dilution
- Inhibition Validation: Incorporate functional blocking antibodies against PD-L1, PD-L2, ICAM-1, or VCAM-1 to confirm contact-dependent mechanisms [54]
Dosing Regimens and Administration Protocols
Dosing Strategy Considerations
The therapeutic efficacy of MSCs is profoundly influenced by dosing strategies, which must account for cell source, expansion conditions, inflammatory environment, and route of administration [9] [115]. Unlike pharmaceutical compounds with straightforward pharmacokinetics, MSC dosing involves complex biological interactions that exhibit non-linear responses.
Table 2: MSC Dosing Considerations Across Disease Models
| Disease Context | Effective Cell Dose Range | Dosing Frequency | Critical Factors |
|---|---|---|---|
| Graft vs. Host Disease (GvHD) | 1-5 × 10⁶ cells/kg [115] [51] | Single or multiple doses (1-2 week intervals) [115] | - Early intervention critical [115]- HLA-mismatch tolerance [115] |
| Allergic Rhinitis Models | 1-2 × 10⁶ cells per animal [54] | Single dose | - Route of administration [54]- Timing relative to allergen challenge [54] |
| Autoimmune Encephalomyelitis | 1 × 10⁶ cells per animal [51] | Single dose | - MSC preconditioning [51]- Inflammatory priming requirement [51] |
| Clinical COVID-19 Applications | 1-10 × 10⁷ cells per patient [6] | 1-3 doses (2-4 day intervals) [6] | - Disease severity [6]- Inflammatory cytokine levels [6] |
Administration Route Optimization
The administration pathway significantly influences MSC trafficking, engraftment, and ultimate therapeutic efficacy [115] [116]. Each route offers distinct advantages and limitations that must be matched to the specific disease pathology.
Intravenous (IV) Administration:
- Protocol: Slow infusion (1-2 mL/min) of MSCs in lactated Ringer's or normal saline with 1-5% human serum albumin [116]
- Experimental Considerations: First-pass pulmonary entrapment of 50-80% of cells; rapid clearance of apoptotic MSCs by monocytes/macrophages within 24-72 hours [7] [91]
- Advantages: Systemic distribution; suitable for disseminated diseases like GvHD [115]
- Limitations: Pulmonary embolism risk at high densities; instant blood-mediated inflammatory reaction (IBMIR) [116]
Local/Topical Administration:
- Protocol: Direct injection into target tissue (joint, muscle, lesion site) under ultrasound guidance [116]
- Experimental Considerations: Enhanced retention at disease site; reduced systemic exposure [54]
- Advantages: Higher local concentration; bypasses pulmonary clearance [54]
- Limitations: Invasive procedure; potentially limited diffusion from injection site [116]
Experimental Protocol for Biodistribution Tracking:
- Cell Labeling: Label MSCs with DIR near-infrared dye (1 µM in PBS for 20 minutes at 37°C) or luciferase reporter gene [116]
- Administration: Deliver labeled cells via selected route to disease model animals
- Imaging: Perform serial IVIS imaging at 0, 4, 24, 72, and 168 hours post-administration
- Ex Vivo Validation: Euthanize animals at endpoint, harvest organs, and quantify signal intensity in each tissue
- Immunohistochemistry: Process tissues for immunohistochemical detection of human-specific antibodies (e.g., anti-human mitochondria) to confirm MSC presence [116]
Advanced Engineering and Formulation Strategies
MSC Engineering for Enhanced Potency
Genetic modification and preconditioning strategies can significantly enhance MSC immunomodulatory functions and overcome limitations of native cells [9] [91].
CRISPR/Cas9 Enhancement Protocol:
- Target Selection: Identify genes of interest (e.g., IDO1, COX-2, PD-L1) for knockout or knockin [91]
- Guide RNA Design: Design sgRNAs with minimal off-target potential using computational tools
- Delivery System: Transfect MSCs using nucleofection with CRISPR/Cas9 ribonucleoprotein complexes
- Selection and Validation: Isolate single-cell clones and validate edits by Sanger sequencing and functional assays [91]
Preconditioning Strategies:
- Inflammatory Priming: Incubate MSCs with IFN-γ (25-50 ng/mL) and TNF-α (10-20 ng/mL) for 24-48 hours before administration [51] [6]
- Hypoxic Preconditioning: Culture MSCs at 1-5% O₂ for 24-72 hours to enhance survival and paracrine function [91]
- 3D Spheroid Culture: Form spheroids using hanging drop or low-attachment plates to improve anti-inflammatory potency [91]
Cell-Free Approaches: Extracellular Vesicles and Secretomes
MSC-derived extracellular vesicles (MSC-EVs) have emerged as a promising cell-free alternative that recapitulates many therapeutic benefits of whole cells while offering enhanced safety and stability profiles [108].
MSC-EV Isolation and Characterization Protocol:
- EV Production: Culture MSCs in EV-depleted FBS medium for 48-72 hours [108]
- Collection and Processing: Collect conditioned medium and perform sequential centrifugation: 300 × g for 10 min, 2,000 × g for 20 min, 10,000 × g for 30 min [108]
- Ultracentrifugation: Pellet EVs at 100,000 × g for 70 minutes at 4°C [108]
- Purification: Resuspend pellets in PBS and filter through 0.22µm membrane [108]
- Characterization: Quantify particle size and concentration via nanoparticle tracking analysis; confirm EV markers (CD63, CD81, TSG101) by western blot [108]
Therapeutic Application of MSC-EVs:
- Dosing Considerations: 50-200 µg protein equivalent per administration in rodent models [108]
- Efficacy Evidence: Umbrella review of 47 meta-analyses demonstrated significant functional improvement across 27 disease models, with bone marrow-, adipose-, and umbilical cord-derived EVs showing highest efficacy [108]
- Engineering Potential: Modified EVs through parental cell engineering show enhanced targeting and functionality [108]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MSC Immunomodulation Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Surface Marker Antibodies | CD73, CD90, CD105 (positive); CD14, CD34, CD45, HLA-DR (negative) [116] [91] | MSC characterization and purity assessment by flow cytometry | ≥95% positive for CD73, CD90, CD105; ≤2% positive for negative markers [116] |
| Functional Assay Kits | IDO activity assay, PGE2 ELISA, T cell proliferation kits (CFSE/³H-thymidine) [51] [6] | Quantification of immunomodulatory capacity | IDO activity highly dependent on IFN-γ priming [51] |
| Cytokine Priming Cocktails | Recombinant IFN-γ, TNF-α, IL-1β [51] [6] | MSC licensing and potency enhancement | Optimal concentration and timing varies by MSC source [51] |
| EV Characterization Tools | Antibodies against CD63, CD81, TSG101; nanoparticle tracking analyzer [108] | Validation of MSC-derived extracellular vesicles | Require minimum of 3 positive EV markers per MISEV guidelines [108] |
The comparative effectiveness of MSC-based immunomodulatory therapies is influenced by a complex interplay between cell source, dosing strategy, administration route, and engineering approach. The field is progressing toward precision-designed MSC therapies that may involve combination strategies such as hydrogel-encapsulated MSCs for sustained release [54], genetically engineered MSCs with enhanced homing capacity [91], and optimized MSC-EV formulations for specific immune disorders [108]. As research continues to delineate the precise mechanisms governing MSC immunomodulation, the rational design of MSC-based therapeutics will increasingly leverage the distinctive advantages of each tissue source while implementing sophisticated engineering strategies to overcome current limitations in cell survival, engraftment, and consistent potency. The integration of single-cell technologies, spatial transcriptomics, and advanced bioengineering approaches promises to further deconvolute MSC heterogeneity and accelerate the development of next-generation immunomodulatory cell therapies [91].
Mesenchymal stem cell (MSC) therapies demonstrate significant promise for treating immune-mediated disorders, from autoimmune diseases to transplant-related complications and age-related degenerative conditions [117] [118] [29]. The foundational thesis of contemporary MSC research posits that these cells exert their therapeutic effects primarily through multifaceted immunomodulatory mechanisms rather than direct tissue regeneration alone [117]. Within this context, robust biomarker development becomes paramount for deciphering the complex interplay between administered MSCs and the host immune system. Reliable biomarkers serve as critical indicators for predicting therapeutic efficacy, optimizing treatment protocols, and ultimately correlating immunological changes with meaningful clinical outcomes.
The immunomodulatory capacity of MSCs operates through a sophisticated synergy of cell contact-dependent mechanisms and soluble factors, affecting nearly all effector cells of the immune system [9] [29]. This complexity necessitates a systematic approach to biomarker identification and validation. Furthermore, emerging evidence suggests that even apoptotic or metabolically inactivated MSCs retain immunomodulatory potential, expanding the landscape of potential biomarkers beyond those associated solely with viable cells [29]. This technical guide provides a comprehensive framework for developing, validating, and implementing biomarkers that effectively bridge immunological observations with clinical endpoints in MSC-based therapeutic interventions.
Analytical Frameworks for Immunological Biomarkers
Classification of Biomarker Types in MSC Therapy
Biomarkers in MSC immunomodulation research can be categorized based on their biological source, analytical method, and clinical application. The most informative biomarker strategies often integrate multiple categories to create a composite profile of the immunomodulatory response.
Table 1: Classification of Biomarkers in MSC Immunomodulation Research
| Category | Biomarker Examples | Analytical Methods | Clinical Correlation |
|---|---|---|---|
| Soluble Mediators | PGE2, IDO, TSG-6, IL-1RA, CCL18, sIL-2R | Multiplex immunoassays, ELISA, MSD assays | GvHD response, sepsis mortality, autoimmune disease activity |
| Cellular Immune Phenotypes | Treg frequency (CD4+CD25+FoxP3+), Monocyte polarization (CD14++CD16+), DC maturation status | Flow cytometry, mass cytometry (CyTOF), single-cell RNA sequencing | Transplant tolerance, infection risk, therapeutic responsiveness |
| Gene Expression Profiles | MHC class II mRNA, indoleamine 2,3-dioxygenase (IDO) expression, TGF-β pathway genes | RNA sequencing, RT-qPCR, nanostring analysis | MSC potency, immunogenicity upon differentiation, long-term engraftment |
| Functional Assay Readouts | T-cell proliferation suppression, monocyte phagocytic activity, TCR diversity | Mixed lymphocyte reactions, CFSE dilution assays, TCR sequencing | Overall survival, graft rejection, disease relapse |
Several critical signaling pathways underlie MSC-mediated immunomodulation and provide rich sources for biomarker development. Understanding these pathways enables researchers to select mechanistically relevant biomarkers with higher predictive value.
The Monocyte-Macrophage Polarization Pathway: MSCs promote the shift of monocytes/macrophages toward an anti-inflammatory type 2 phenotype through multiple mechanisms. This occurs via MSC-secreted factors including IL-1RA, IL-6, and hepatocyte growth factor (HGF), resulting in increased IL-10 production and decreased expression of TNF-α, IL-12p70, and IL-17 [29]. The resulting anti-inflammatory monocytes express high levels of MHC class II, CD45R, and CD11b, and can suppress T-cell activity independently of Tregs. These polarized monocytes further amplify immunomodulation by producing CCL18 and TGF-β1, which induce the formation of FoxP3+ Tregs from naïve CD4+ T cells [29].
The Phagocytosis-Dependent Regulatory Pathway: A cytokine-independent pathway has been identified wherein MSC phagocytosis by monocytes, particularly non-classical Ly6Clow monocytes, induces an immune-regulatory intermediate phenotype (CD14++CD16+CD206+) with elevated IL-10 and PD-L1 expression [29]. These primed monocytes demonstrate enhanced capacity to induce CD4+CD25hi Treg formation, creating an amplification loop for immunomodulation.
The T-cell Regulation Pathway: MSCs suppress proliferation of both CD4+ and CD8+ T cells in a dose-dependent manner and facilitate a shift from pro-inflammatory Th1 to anti-inflammatory Th2 responses [29]. Crucially, MSCs promote the formation and expansion of regulatory T cells (Tregs), which are essential for maintaining immune tolerance and have been correlated with improved clinical outcomes in graft-versus-host disease (GvHD) and autoimmune conditions [29].
Diagram 1: Key immunomodulatory pathways connecting MSC administration to clinical outcomes. These pathways provide the mechanistic basis for biomarker development.
Methodological Approaches for Biomarker Assessment
Experimental Protocols for Key Biomarker Assays
Protocol 1: Flow Cytometry Analysis of Treg and Monocyte Populations
This protocol enables quantitative assessment of critical cellular biomarkers, including regulatory T cells and monocyte subsets, which have demonstrated correlation with clinical outcomes in MSC therapy [29].
Sample Collection: Collect peripheral blood mononuclear cells (PBMCs) from patients pre-MSC infusion and at defined intervals post-infusion (e.g., 24 hours, 7 days, 30 days). Use sodium heparin or EDTA tubes, process within 4 hours of collection.
Cell Staining:
- Isolate PBMCs using Ficoll density gradient centrifugation.
- Aliquot 1×10^6 cells per staining tube.
- For surface staining: Incubate with fluorochrome-conjugated antibodies against CD3, CD4, CD25, CD14, CD16, CD45R, CD11b, and MHC class II for 20 minutes at 4°C in the dark.
- For intracellular FoxP3 staining: Fix and permeabilize cells using FoxP3/Transcription Factor Staining Buffer Set, then incubate with anti-FoxP3 antibody for 30 minutes at 4°C.
- Include appropriate isotype controls and compensation beads.
Data Acquisition and Analysis:
- Acquire data using a flow cytometer capable of detecting 8+ colors.
- Analyze using FlowJo or similar software.
- Gate on lymphocytes (by FSC/SSC) → CD3+CD4+ T cells → CD25+FoxP3+ Tregs.
- Gate on monocytes (by FSC/SSC) → CD14+CD16- (classical), CD14+CD16+ (intermediate), CD14dimCD16+ (non-classical).
- Report frequencies as percentage of parent population and absolute counts.
Protocol 2: Soluble Biomarker Quantification Using Multiplex Immunoassays
This protocol simultaneously measures multiple soluble factors implicated in MSC immunomodulation, providing a comprehensive profile of the immune response.
Sample Preparation:
- Collect serum or plasma (EDTA or heparin) pre-MSC infusion and at serial timepoints post-infusion.
- Centrifuge blood samples at 2000×g for 10 minutes, aliquot supernatant, and store at -80°C.
- Avoid freeze-thaw cycles.
Assay Procedure:
- Select a multiplex panel targeting MSC-relevant biomarkers: IL-10, TGF-β1, TNF-α, IFN-γ, IL-6, sIL-2R, CCL18, IL-12p70, IL-17, and IL-1RA.
- Thaw samples on ice and centrifuge at 10,000×g for 5 minutes.
- Follow manufacturer instructions for the specific multiplex platform (e.g., Luminex, MSD, LEGENDplex).
- Include standard curves, quality controls, and blanks in each run.
- Measure analyte concentrations using a multiplex array reader.
Data Analysis:
- Use five-parameter logistic curve fitting for standard curves.
- Normalize values to pre-infusion baseline.
- Apply appropriate statistical tests to identify significant changes correlated with clinical outcomes.
Protocol 3: Functional T-cell Suppression Assay
This assay evaluates the functional consequence of MSC immunomodulation by measuring T-cell proliferation capacity, a key biomarker for therapeutic efficacy.
Responder and Stimulator Cell Preparation:
- Isolate PBMCs from patient pre- and post-treatment as responder cells.
- Irradiate (30-50 Gy) or treat with mitomycin C (50 μg/mL for 30 minutes) PBMCs from unrelated donors as stimulator cells.
Mixed Lymphocyte Reaction (MLR):
- Co-culture responder and stimulator cells at 1:1 ratio (1×10^5 cells each) in U-bottom 96-well plates.
- Include wells with responders alone (negative control) and responders with PHA (5 μg/mL, positive control).
- Culture for 5 days at 37°C, 5% CO2.
- Add ³H-thymidine (1 μCi/well) for the final 16-18 hours of culture.
- Harvest cells onto filter mats and measure incorporated radioactivity using a beta counter.
Alternative CFSE-based Method:
- Label responder PBMCs with 5 μM CFSE for 10 minutes at 37°C before co-culture.
- After 5 days of culture, analyze CFSE dilution in CD3+ T cells by flow cytometry.
- Calculate proliferation index and percentage of divided cells using proliferation modeling software.
Biomarker Correlation with Clinical Outcomes: Quantitative Analysis
The clinical utility of immunological biomarkers depends on their consistent correlation with meaningful patient outcomes. The following table synthesizes key biomarker-clinical outcome relationships documented in the literature.
Table 2: Correlation of Immunological Biomarkers with Clinical Outcomes in MSC Therapy
| Biomarker Category | Specific Biomarker | Direction of Change | Clinical Correlation | Strength of Evidence |
|---|---|---|---|---|
| Soluble Mediators | Soluble IL-2 Receptor | Significant decline post-infusion [119] | Improved response in aGvHD [119] | Clinical study (n=31) |
| Soluble Mediators | IL-10 | Increase | Survival in sepsis models [29] | Preclinical |
| Soluble Mediators | CCL18 | Increase | Treg induction, transplant tolerance [29] | Preclinical/Mechanistic |
| Cellular Populations | Treg Frequency (CD4+CD25+FoxP3+) | Increase | Improved GvHD response, autoimmune disease improvement [29] | Multiple preclinical/clinical |
| Cellular Populations | Anti-inflammatory Monocytes (CD14++CD16+) | Increase | Immunomodulatory amplification, linked to Treg induction [29] | Mechanistic |
| Cellular Populations | Monocyte Phagocytic Activity | Increase | Clearance of apoptotic cells, immunomodulation [29] | Preclinical |
| Treatment Parameters | MSC Passage Number | Early passage (1-2) vs. late (3-4) [119] | 75% vs. 21% 1-year survival in GvHD [119] | Clinical study |
| Functional Assays | T-cell Proliferation | Suppression | In vitro correlate of immunomodulatory potency [29] | In vitro validation |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful biomarker development requires carefully selected reagents and platforms optimized for detecting immunological changes in MSC research.
Table 3: Essential Research Reagent Solutions for MSC Immunomodulation Biomarker Studies
| Reagent Category | Specific Product Examples | Application in Biomarker Development | Technical Considerations |
|---|---|---|---|
| Cell Isolation Kits | Human CD4+ T Cell Isolation Kit, Pan Monocyte Isolation Kit, CD14 MicroBeads | Isolation of specific immune cell populations for functional assays or phenotyping | Consider negative selection to avoid cell activation; assess purity (>90%) and viability (>95%) |
| Flow Cytometry Antibodies | Anti-human CD3, CD4, CD25, FoxP3, CD14, CD16, CD45R, CD11b, MHC Class II, CD206 | Comprehensive immunophenotyping of T-cell, monocyte, and dendritic cell subsets | Validate antibody clones for specific applications; optimize panel with compensation controls |
| Immunoassay Kits | LEGENDplex Human Inflammation Panel, Luminex Human Cytokine Panel, IL-2R ELISA Kit | Quantification of soluble mediators in serum, plasma, or culture supernatant | Check validation for specific sample matrix; determine optimal sample dilution factor |
| Cell Culture Reagents | RPMI-1640, Fetal Bovine Serum (FBS), Penicillin-Streptomycin, L-Glutamine, HEPES | Maintenance of immune cells for functional assays (MLR, suppression assays) | Use characterized FBS lots; consider serum-free media for specific applications |
| Functional Assay Kits | CFSE Cell Division Tracker Kit, ³H-Thymidine, BrdU Assay Kit, ATP Luminescence Assay | Measurement of T-cell proliferation and metabolic activity in response to MSC co-culture | Compare methods for sensitivity and reproducibility; optimize cell numbers and culture duration |
| Molecular Biology Reagents | RNA Isolation Kits, Reverse Transcription Reagents, qPCR Probes for IDO, TGF-β, IL-10 | Gene expression analysis of immunomodulatory pathways in MSCs and immune cells | Isolate high-quality RNA (RIN >8); use validated reference genes for normalization |
Data Integration and Clinical Translation
Advanced Analytical Approaches
Correlating immunological changes with clinical outcomes requires sophisticated analytical approaches that integrate multiple data streams. Multivariate statistical models, including principal component analysis and linear discriminant analysis, can identify biomarker patterns that better predict clinical responses than single parameters. Machine learning algorithms offer powerful tools for developing predictive models from high-dimensional biomarker data, potentially identifying novel biomarker combinations with enhanced clinical utility.
Longitudinal analysis is particularly important in MSC therapy, as the immunological effects may evolve over time. Mixed-effects models can account for both within-subject and between-subject variability, providing more robust estimates of biomarker-clinical outcome relationships. Survival analysis techniques, such as Cox proportional hazards models, can evaluate how baseline biomarker levels or early post-treatment changes predict long-term clinical outcomes.
Validation and Standardization Frameworks
Before immunological biomarkers can be widely adopted in clinical practice or regulatory decision-making, they must undergo rigorous validation. The biomarker validation framework should include:
- Analytical Validation: Establishing that the biomarker assay is accurate, precise, sensitive, specific, and reproducible across multiple sites.
- Biological Validation: Confirming that the biomarker reflects biologically relevant processes in MSC immunomodulation through mechanistic studies.
- Clinical Validation: Demonstrating that the biomarker reliably predicts clinically meaningful outcomes across independent patient cohorts.
Standardization efforts should focus on key parameters that significantly impact outcomes, such as MSC passage number [119]. Development of reference standards and proficiency testing programs will facilitate comparability of biomarker data across different research centers and clinical trials.
The development of robust biomarkers that correlate immunological changes with clinical outcomes represents a critical advancement in MSC research. By implementing the comprehensive frameworks, methodologies, and tools outlined in this technical guide, researchers can systematically decipher the complex immunomodulatory mechanisms of MSCs and accelerate the development of more effective, predictable cellular therapies. The integration of multimodal biomarker data—encompassing soluble mediators, cellular phenotypes, and functional assays—provides the most promising path toward personalized MSC therapies optimized for individual patient needs and responsive to real-time immunological monitoring.
Mesenchymal stem cell (MSC) therapies represent one of the most promising and intensely pursued cellular therapeutics, with more than 800 registered clinical studies globally [120]. Their profound immunomodulatory and regenerative properties have driven extensive clinical translation, particularly for inflammatory and autoimmune conditions. While meta-analyses of first-generation MSC products have demonstrated acceptable short-term safety profiles, comprehensive long-term safety assessment remains paramount as therapeutic applications diversify [120] [121]. The established safety record of bone marrow-derived MSCs cannot be directly extrapolated to MSCs from alternative sources such as adipose or perinatal tissues, necessitating rigorous long-term tracking strategies [121]. This whitepaper examines current methodologies, findings, and challenges in long-term safety assessment of MSC therapies within the broader context of immunomodulation mechanism research.
Methodological Frameworks for Long-term Safety Assessment
Preclinical Toxicity and Distribution Studies
Comprehensive preclinical studies establish foundational safety data necessary for clinical translation. Repeat-dose toxicity studies in immunodeficient mouse models provide critical safety parameters including the no-observed-adverse-effect level (NOAEL), target organ identification, and cell distribution patterns [122].
A recent subcutaneous administration study in NOG mice implemented a robust protocol with five repeated hUC-MSC injections at doses of 2.5 × 10⁷ and 2.0 × 10⁸ cells/kg over three weeks, followed by a 6-week recovery period [122]. This study design aligned with ICH M3(R2) guidelines and incorporated detailed clinical observations, behavioral analyses, histopathology, organ weight measurements, and quantitative PCR for cell distribution tracking [122]. The established NOAEL of 2.5 × 10⁷ cells/kg provides crucial dosing guidance for clinical applications, particularly in dermatology and aesthetic medicine [122].
Table 1: Key Parameters in Preclinical Repeat-Dose Toxicity Studies
| Parameter | Assessment Method | Findings in hUC-MSC Study |
|---|---|---|
| Clinical Observations | Daily documentation of appearance, behavior, respiratory function | No abnormal effects except masses at administration site in high-dose group |
| Body Weight & Food Intake | Twice-weekly monitoring | No significant effects observed |
| Histopathology | H&E staining of major organs | Foamy cells under pleural membrane in high-dose mice |
| Cell Distribution | qPCR and immunohistochemistry | Primary colonization in skin tissues 24h post-administration |
| NOAEL | Dose-response relationship | 2.5 × 10⁷ cells/kg established |
Clinical Trial Design for Long-term Assessment
Clinical safety assessment requires carefully structured trials with extended follow-up periods to capture potential delayed effects. The long-term extension (LTE) study design represents best practice for tracking outcomes beyond initial treatment periods [123]. Pooled data from multiple randomized clinical trials followed by LTE studies provide sufficient statistical power to detect rare adverse events and evaluate sustainability of treatment effects.
Recent research in rheumatoid arthritis patients employed a comprehensive framework with initial 48-week core trials followed by extended observation periods reaching 5-7 years [123]. This approach enabled systematic assessment of long-term safety signals, including potential immunosuppression, infection risks, and tumorigenesis – all theoretical concerns with MSC therapies [123]. Safety monitoring encompassed treatment-emergent adverse events (AEs), serious AEs (SAEs), laboratory parameters, vital signs, and physical examinations, all coded using standardized medical dictionaries (MedDRA) for consistent analysis [123].
Figure 1: Long-term Extension Study Workflow
Quantitative Safety Outcomes in Long-term Studies
Adverse Event Profiles in Extended Follow-up
Long-term safety data from pooled clinical trials provide valuable insights into the real-world risk profiles of MSC therapies. In a comprehensive analysis of 110 rheumatoid arthritis patients followed for 5-7 years, exposure-adjusted event rates demonstrated favorable long-term safety profiles for both MSC monotherapy and combination treatments [123].
Table 2: Long-term Adverse Event Rates in MSC Clinical Trials
| Safety Parameter | MSC Monotherapy | MSC + IFN-γ Combination | Assessment Period |
|---|---|---|---|
| Serious AE Rate (per 100 PY) | 2.47 | 2.31 | 5 years |
| Overall AE Rate (per 100 PY) | 36.17 | 35.86 | 5 years |
| Most Frequent AEs | Decreased lymphocyte count (15.95/100 PY), COVID-19 (17.52/100 PY) | Decreased lymphocyte count (15.62/100 PY), COVID-19 (16.15/100 PY) | 5 years |
| Discontinuation Due to AEs | 5.5% | Included in combination group rate | 5 years |
| New Autoimmune Events | Not reported | 2 cases in combination group | 5 years |
Notably, no increase in adverse event rates was observed over the five-year extension period, supporting the long-term safety of MSC-based interventions [123]. The most frequently reported adverse events – decreased lymphocyte count and COVID-19 infection – reflected background population rates rather than specific treatment-related toxicities.
Manufacturing and Formulation Considerations
Long-term safety profiles of MSC products are significantly influenced by manufacturing processes and final formulation parameters [120]. Key considerations include:
- Tissue Source Impact: MSC products derived from bone marrow (BM-MSCs), adipose tissue (AT-MSCs), and perinatal tissue (PT-MSCs) demonstrate functional differences that may influence long-term safety profiles [120]
- Cryopreservation Effects: Freeze-thawed cells show transient impairment of metabolism and cellular integrity compared to fresh culture-derived cells, potentially affecting both safety and efficacy [120]
- Formulation Components: Final cell suspension composition, including additives like heparin and human albumin versus human blood type AB plasma, influences in vivo cellular pharmacodynamics [120]
- Delivery Method Consequences: Intravascularly delivered MSCs face extensive pulmonary trapping, while local delivery approaches present different distribution and clearance patterns [120]
Mechanisms Linking Immunomodulation to Safety Outcomes
Bidirectional Immune Crosstalk
The immunomodulatory mechanisms of MSCs contribute significantly to their long-term safety profile. Rather than employing a single mechanism, MSCs modulate immune responses through multiple parallel pathways including direct cell-cell contact, paracrine factor secretion, extracellular vesicle communication, and efferocytosis mechanisms [120] [7]. This multifaceted immunomodulation creates a complex safety profile that varies based on patient factors and disease context.
MSCs engage in bidirectional crosstalk with host immune cells, influencing both innate and adaptive immunity [7]. They suppress T-cell proliferation through both contact-dependent mechanisms (via ICAM-1, VCAM-1, and PD-L1) and soluble factors (including PGE2, IDO, and TGF-β) [7]. Additionally, MSCs modulate B-cell function, dendritic cell maturation, macrophage polarization, and NK cell activity [7]. These interactions create a regulatory immune environment that typically resolves inflammation without causing broad immunosuppression.
Figure 2: MSC Immunomodulation Mechanisms Influencing Safety
Cell Fate and Host Response Considerations
The in vivo persistence and fate of administered MSCs significantly influence long-term safety outcomes. Research indicates that MSCs exhibit limited long-term engraftment, with most cells cleared within days to weeks after administration [120]. This transient persistence may explain the favorable long-term safety profile observed in clinical studies, as it limits opportunities for malignant transformation or sustained unintended effects.
Apoptotic and dead MSCs continue to contribute to immunomodulation through efferocytosis mechanisms, where phagocytic cells clear cellular debris while promoting anti-inflammatory responses [120]. This phenomenon demonstrates that MSC therapeutic activity does not necessarily require long-term viability, potentially reducing safety concerns related to permanent engraftment. The host immune system plays a crucial role in processing administered MSCs, with monocytes phagocytosing MSCs and subsequently distributing immunomodulatory signals throughout the body [7].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Long-term Safety Assessment
| Reagent/Category | Specific Examples | Research Application | Safety Assessment Relevance |
|---|---|---|---|
| MSC Characterization | CD90, CD73, CD105 antibodies; CD14, CD19, CD34, CD45, HLA-DR exclusion markers | Flow cytometry phenotyping | Product characterization consistency, identity testing |
| Cell Viability Assays | Trypan blue exclusion assay; Metabolic activity probes | Viability assessment pre-administration | Potency correlation, safety specification |
| qPCR Reagents | Human-specific primers/probes; DNA extraction kits | Cell distribution and persistence studies | Biodistribution tracking, engraftment assessment |
| Histopathology Tools | H&E staining reagents; Davidson's fixative; formalin | Tissue pathology examination | Target organ toxicity identification |
| Cell Culture Media | Serum-free expansion media; differentiation induction kits | MSC expansion and functional testing | Manufacturing process validation |
| Cryopreservation Solutions | DMSO-containing cryoprotectants; controlled-rate freezing equipment | Cell banking and storage | Product consistency, post-thaw viability |
Long-term safety assessment of MSC therapies requires integrated approaches spanning preclinical toxicology, controlled clinical trials with extended follow-up periods, and mechanistic studies elucidating immunomodulatory pathways. Current evidence from studies tracking outcomes up to seven years post-treatment demonstrates favorable safety profiles, with adverse event rates comparable to background expectations [123]. The transient persistence of MSCs, coupled with their multifaceted immunomodulatory mechanisms that promote resolution rather than suppression of immune responses, contributes to this safety record [120] [7]. As MSC product diversification continues, maintaining rigorous long-term safety assessment protocols remains essential for responsible clinical translation. Future directions should include standardized potency assays, improved understanding of donor and tissue source variables, and continued development of humanized models for safety evaluation [121].
The field of mesenchymal stem cell (MSC) research is undergoing a transformative shift, driven by the integration of sophisticated validation platforms. The therapeutic potential of MSCs, particularly their immunomodulatory capabilities, has been well-documented in treating inflammatory disorders, graft-versus-host disease, and autoimmune conditions [9] [29]. However, the underlying mechanisms of action have not been fully characterized, leading to inconsistent outcomes in clinical trials [124] [29]. Emerging multi-omics approaches and advanced imaging techniques are now providing unprecedented resolution for deconstructing the complexity of MSC immunobiology, enabling more precise characterization of MSC heterogeneity, senescence, and functional potency [124] [125]. This technical guide examines these cutting-edge validation platforms within the context of MSC immunomodulation research, providing detailed methodologies and analytical frameworks for researchers and drug development professionals seeking to standardize and enhance the therapeutic application of MSCs.
Multi-omics Platforms for MSC Characterization
Integrated Single-Cell Multi-omics Approaches
Single-cell technologies have revolutionized our understanding of MSC heterogeneity and senescence, two critical factors influencing immunomodulatory potency. A 2023 study profiled single-cell transcriptomes of MSCs isolated from adipose tissue, bone marrow, placental chorionic membrane, and umbilical cord, revealing a progressive aging process that directly impacts immunosuppressive function through downregulation of PD-L1 [124].
Experimental Protocol: Integrated Single-Cell RNA Sequencing and Proteomics
- Cell Preparation: Isolate MSCs from target tissues (adipose, bone marrow, umbilical cord, placental chorionic membrane) and culture following International Society for Cellular Therapy criteria [124]. Validate surface marker expression (CD105, CD73, CD90) and absence of negative markers (CD45, CD34, CD14, CD19) via flow cytometry.
- Single-Cell RNA Sequencing: Use droplet-based scRNA-seq (10x Genomics platform). Prepare single-cell suspensions, target 10,000 cells per sample, and generate libraries using standard protocols. Sequence on Illumina platforms to achieve >50,000 reads per cell.
- Proteomic Analysis: Perform mass spectrometry-based proteomics on parallel cell aliquots. Extract proteins, digest with trypsin, and analyze by LC-MS/MS.
- Data Integration: Apply computational integration using tools such as Seurat or Monocle. Identify co-expression networks and perform trajectory analysis to reconstruct cellular senescence pathways.
- Functional Validation: Correlate transcriptional clusters with functional assays including T-cell suppression and PD-L1 surface expression by flow cytometry [124].
Table 1: Key Molecular Regulators of MSC Senescence and Immunomodulation Identified via Multi-omics
| Molecule | Expression in Senescent MSCs | Functional Impact | Validation Method |
|---|---|---|---|
| PD-L1 | Downregulated [124] | Reduced T-cell suppression capacity [124] | Flow cytometry, functional assays |
| GATA2 | Downregulated [124] | Accelerated senescence, reduced immunomodulation [124] | CRISPR inhibition/activation |
| TP53/p53 | Upregulated [124] | Cell cycle arrest, senescence induction [124] | Immunostaining, Western blot |
| CDKN1A/p21 | Upregulated [124] | Cell cycle arrest [124] | qPCR, Western blot |
| IL6 | Upregulated [124] | Senescence-associated secretory phenotype [124] | ELISA, RNA scope |
Spatial Multi-omics on Single Tissue Sections
A groundbreaking 2025 study developed an integrated workflow for spatial transcriptomics and proteomics on the same tissue section, overcoming previous limitations of spatial misalignment between adjacent sections [125].
Experimental Protocol: Co-localized Spatial Transcriptomics and Proteomics
- Sample Preparation: Use formalin-fixed paraffin-embedded (FFPE) tissue sections (5μm thickness) mounted on appropriate slides [125].
- Spatial Transcriptomics: Perform Xenium In Situ Gene Expression (10x Genomics) with a targeted gene panel (e.g., 289-gene human lung cancer panel). Follow manufacturer's protocol for hybridization, ligation, amplification, and sequencing.
- Spatial Proteomics: Following Xenium analysis, process slides for hyperplex immunohistochemistry using COMET platform (Lunaphore Technologies). Apply 40-antibody panel with cyclical staining, imaging, and elution.
- H&E Staining: After COMET, perform manual hematoxylin and eosin staining on the same section [125].
- Image Registration: Co-register DAPI images from Xenium and COMET to H&E using non-rigid spline-based algorithms in Weave software (Aspect Analytics) [125].
- Cell Segmentation: Apply CellSAM, a deep learning-based method integrating nuclear (DAPI) and membrane (pan-cytokeratin) markers for segmentation [125].
- Data Analysis: Calculate transcript counts and protein intensities per cell. Perform correlation analysis, clustering, and cell type identification.
Figure 1: Spatial Multi-omics Workflow on Single Tissue Section
Metabolomic and Transcriptomic Integration
Multi-omics approaches extend beyond transcriptomics and proteomics to include metabolomics, providing insights into MSC metabolic pathways that influence immunomodulatory function. A 2024 study on human umbilical cord-derived MSCs (HUCMSCs) demonstrated that treatment improved age-related disorders through reduction of DNA damage and modulation of gut microbiota and metabolism [126].
Experimental Protocol: Metabolomic and Transcriptomic Profiling of MSCs
- Sample Collection: Prepare MSC samples from different sources (subcutaneous, perirenal, epididymal adipose tissue) [127].
- RNA Extraction and Sequencing: Extract total RNA using standard kits. Prepare libraries for RNA-seq and sequence on Illumina platform. Identify differentially expressed genes (DEGs) with FC >2.0, FDR <0.05.
- Metabolite Extraction and Profiling: Use liquid chromatography-mass spectrometry (LC-MS) for carboxyl metabolomic profiling. Apply quality control measures including pooled quality control samples.
- Pathway Integration: Map DEGs and differential metabolites to KEGG pathways. Identify hub genes and key metabolic pathways using integrated analysis.
- Functional Correlation: Correlate transcriptomic and metabolomic findings with functional assays such as adipogenic differentiation capacity and insulin resistance [127].
Table 2: Multi-omics Analysis of Adipose-Derived MSCs from Different Tissue Origins
| MSC Type | Key Upregulated Pathways | Key Downregulated Pathways | Functional Correlations |
|---|---|---|---|
| Epididymal ASCs (EASCs) | Mitotic cell cycle, G protein-coupled receptor signaling [127] | Oncostatin M signaling via Jak-Stat [127] | Enhanced fat metabolism, insulin resistance [127] |
| Perirenal ASCs (PASCs) | Supramolecular fiber organization, cell cycle phase transition [127] | SCAP/SREBP control of cholesterol biosynthesis [127] | Association with tumors and cardiovascular disease [127] |
| Subcutaneous ASCs (SASCs) | (Reference group) | (Reference group) | Standard adipogenic potential [127] |
Advanced Imaging Techniques for MSC-Immune Cell Interactions
High-Resolution Imaging of Immune Signaling
Advanced imaging technologies provide critical insights into the spatiotemporal dynamics of MSC-mediated immunomodulation. These techniques vary in their resolution capabilities, spanning from nanometers to micrometers spatially and from microseconds to hours temporally [128].
Experimental Protocol: Visualizing MSC-Immune Cell Interactions
- Sample Preparation: Co-culture MSCs with target immune cells (T cells, monocytes) on imaging-compatible chambers. For in vivo tracking, label MSCs with fluorescent dyes or express fluorescent proteins.
- Microscopy Selection:
- Super-resolution microscopy: STORM/PALM for nanoscale localization of immune synapses (∼20 nm resolution).
- Lattice light-sheet microscopy: For rapid, high-resolution 3D imaging of living MSC-immune cell interactions with minimal phototoxicity.
- Confocal microscopy: For fixed samples and higher-throughput imaging of multiple markers.
- Image Acquisition: For immune signaling studies, acquire time-lapse images every 30-60 seconds for 30-120 minutes. For super-resolution, acquire 10,000-20,000 frames for single-molecule localization.
- Data Analysis: Track cell movements, contact times, and protein localization. Quantify fluorescence intensity at interaction sites over time [128].
Correlative Imaging and Multi-omics Integration
The integration of advanced imaging with multi-omics data creates powerful validation platforms for understanding MSC function in tissue contexts.
Experimental Protocol: Correlative Spatial Multi-omics and Imaging
- Region Selection: First, identify regions of interest (e.g., MSC-immune cell interfaces) using standard fluorescence microscopy.
- Multi-modal Registration: Apply computational registration methods to align imaging data with spatial transcriptomics/proteomics data from consecutive sections.
- Spatial Annotation: Transfer cell type annotations from omics data to imaging data based on spatial coordinates.
- Cross-validation: Validate protein expression detected by imaging with proteomic data, and transcript localization with transcriptomic data [125].
Figure 2: Multi-scale Imaging of MSC-Immune Interactions
Application to MSC Immunomodulation Research
Resolving MSC Heterogeneity and Senescence
The integration of multi-omics and advanced imaging has revealed critical insights into how MSC heterogeneity and senescence impact immunomodulatory function. Single-cell transcriptomic analysis has identified seven distinct subpopulations within in vitro-expanded MSC products, with varying proportions across tissue sources [124]. Senescent MSC subsets (C5-C7) demonstrate upregulation of TP53, CDKN1A, IL6, and SASP factors, alongside diminished proliferative capacity and stem cell features [124]. Most importantly, these senescent subsets show impaired immunomodulatory activity correlated with reduced PD-L1 expression [124].
Experimental Protocol: Assessing MSC Senescence and Immunomodulatory Capacity
- Senescence Detection: Combine multiple markers: β-galactosidase activity (GLB1), p53/p21 expression, SASP factor secretion (IL-6), and DNA damage markers (γH2AX) [124].
- Functional Correlation: Correlate senescence markers with PD-L1 expression and T-cell suppression capacity in inhibition assays.
- Source Comparison: Compare senescence profiles and immunomodulatory potency across MSC sources (umbilical cord, adipose tissue, bone marrow) [124].
- Intervention Studies: Test strategies to enhance potency, such as GATA2 overexpression to delay senescence and enhance PD-L1 expression [124].
Validating MSC Mechanisms of Action
Multi-omics and imaging platforms have elucidated both direct and indirect mechanisms of MSC-mediated immunomodulation:
- Cytokine-Mediated Effects: Omics analyses validate the role of MSC-secreted factors (PGE2, IDO, TGF-β, IL-6, HGF) in modulating immune cell function [29].
- Cell Contact-Dependent Mechanisms: Advanced imaging reveals the importance of direct MSC-immune cell contacts, particularly through PD-L1/PD-1 interactions [124].
- Apoptotic MSC Effects: Multi-omics demonstrates that apoptotic MSCs are phagocytosed by monocytes, inducing anti-inflammatory phenotypes (increased IL-10, PD-L1) and regulatory T cell formation [29].
- Metabolic Reprogramming: Metabolomic profiling shows MSC-mediated shifts in immune cell metabolism that support immunomodulation [126].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Multi-omics and Imaging Validation
| Category | Specific Products/Platforms | Key Applications in MSC Research |
|---|---|---|
| Single-Cell RNA-seq | 10x Genomics Chromium, Parse Biosciences | MSC heterogeneity analysis, senescence subpopulation identification [124] |
| Spatial Transcriptomics | 10x Genomics Xenium, NanoString CosMx | Spatial mapping of MSC interactions in tissue contexts [125] |
| Spatial Proteomics | COMET (Lunaphore), CODEX (Akoya) | High-plex protein validation in MSC-treated tissues [125] |
| Imaging Platforms | Lattice Light-Sheet, STORM/PALM | Live imaging of MSC-immune cell interactions at high resolution [128] |
| Data Integration | Weave (Aspect Analytics), Seurat | Registration and analysis of multi-omics datasets [125] |
| Cell Segmentation | CellSAM, CellPose | AI-based segmentation for multi-omics data [125] |
| Metabolomics | LC-MS platforms, Seahorse Analyzer | MSC metabolic profiling and therapy response biomarkers [126] |
Multi-omics approaches and advanced imaging techniques represent a paradigm shift in MSC validation, moving beyond traditional characterization methods to provide comprehensive, high-resolution insights into MSC biology and therapeutic mechanisms. The integration of these platforms enables researchers to deconstruct MSC heterogeneity, identify functional subpopulations, monitor spatiotemporal dynamics of MSC-immune interactions, and develop predictive biomarkers for therapeutic potency. As these technologies continue to evolve, they promise to standardize MSC-based products, enhance clinical trial design, and ultimately fulfill the therapeutic potential of mesenchymal stem cells in treating inflammatory and autoimmune diseases. For research and drug development professionals, mastery of these emerging validation platforms is becoming increasingly essential for advancing the field of MSC immunomodulation.
Conclusion
The immunomodulatory capacity of MSCs represents a paradigm shift in treating immune-mediated diseases, operating through sophisticated mechanisms that regulate both innate and adaptive immunity. The convergence of basic science discoveries with clinical applications has yielded promising results in conditions ranging from GvHD to allergic rhinitis, yet challenges in standardization, safety, and consistent efficacy remain. Future directions will likely focus on engineered MSCs with enhanced functionality, optimized delivery systems including exosome-based approaches, and improved patient stratification. The successful clinical translation of MSC therapies will depend on collaborative efforts between basic scientists and clinical researchers to address current limitations while leveraging emerging technologies. As our understanding of MSC biology deepens, these multifaceted cells continue to offer tremendous potential for developing novel immunomodulatory treatments that address the root causes of immune dysregulation rather than merely managing symptoms.
References
- 1. Frontiers | Cell -free regenerative medicine: identifying the best source ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1518412/full]
- 2. Definition and Characteristics of Mesenchymal Stromal Cells in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8895491/]
- 3. Quality Control in MSC Culture: Ensuring Purity and Viability for Cancer... [https://www.atlantisbioscience.com/blog/quality-control-in-msc-culture-ensuring-purity-and-viability-for-cancer-studies/]
- 4. – Mesenchymal and Clinical Applications - PMC Stem Cells Sources [https://pmc.ncbi.nlm.nih.gov/articles/PMC3076359/]
- 5. What are Stromal Cells ( Mesenchymal )? Stem Cells [https://www.news-medical.net/life-sciences/What-are-Stromal-Cells.aspx]
- 6. Immunomodulatory Mechanisms and Therapeutic Potential of Mesenchymal Stem Cells | Stem Cell Reviews and Reports [https://link.springer.com/article/10.1007/s12015-023-10539-9]
- 7. Mesenchymal Stem Cell Immunomodulation: Mechanisms and Therapeutic potential - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751844/]
- 8. Mesenchymal stem cells and immunomodulation: current status and future prospects | Cell Death & Disease [https://www.nature.com/articles/cddis2015327]
- 9. : Mesenchymal and... Stem Cell Immunomodulation Mechanisms [https://pubmed.ncbi.nlm.nih.gov/32709406/]
- 10. A New Mesenchymal Stem Cell (MSC) Paradigm ... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0010088]
- 11. The role and mechanism of mesenchymal in... stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04431-1]
- 12. Development of an Insert Co-culture System of Two Cellular Types in... [https://www.jove.com/t/54356/development-an-insert-co-culture-system-two-cellular-types-absence]
- 13. Deciphering Cell–Cell Interactions with Integrative Single‐Cell Secretion Profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10323649/]
- 14. Inhibition of tumor cell proliferation and motility by fibroblasts is both contact and soluble factor dependent - PubMed [https://pubmed.ncbi.nlm.nih.gov/25404301/]
- 15. – Cell communication in kidney fibrosis - PMC cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11494227/]
- 16. An introduction to immunology and immunopathology | Allergy, Asthma & Clinical Immunology | Full Text [https://aacijournal.biomedcentral.com/articles/10.1186/s13223-018-0278-1]
- 17. Markers- Innate , mast, Immunity , dendritic ... NK macrophages [https://www.bio-techne.com/research-areas/immunology/innate-immunity-cell-markers]
- 18. Immunomodulatory Mechanisms and Therapeutic Potential of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10103048/]
- 19. Immunomodulatory Functions of Mesenchymal in Tissue... Stem Cells [https://archrazi.areeo.ac.ir/article_131575.html]
- 20. The mechanisms and cross-protection of trained innate immunity [https://virologyj.biomedcentral.com/articles/10.1186/s12985-022-01937-5]
- 21. Frontiers | Mesenchymal -derived exosomes as a plausible... stem cell [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1563427/full]
- 22. stromal Mesenchymal conditioned by peripheral blood... cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04534-9]
- 23. The interaction of innate immune and adaptive immune system - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11401974/]
- 24. Recognition of tumor cells by Dectin-1 orchestrates ... innate immune [https://pubmed.ncbi.nlm.nih.gov/25149452/]
- 25. Principles and therapeutic applications of adaptive immunity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11177542/]
- 26. Regulation of the T helper cell type 2 (Th2)/T regulatory cell (Treg) balance by IL-4 and STAT6 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2872539/]
- 27. Frontiers | The Mechanisms of Effector Th Cell Responses Contribute to Treg Cell Function: New Insights into Pathogenesis and Therapy of Asthma [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.862866/full]
- 28. Human Mesenchymal Secretome Driven Stem ... Cell T Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC9658100/]
- 29. Frontiers | Immunomodulation by Mesenchymal ... Stem Cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01191/full]
- 30. inhibit Mesenchymal - stem function through... | PLOS One cells T cell [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0213170]
- 31. The Immunomodulatory mechanism and research progress of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008879/]
- 32. Size-dependent immunomodulation by MSC secretome: soluble ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04670-2]
- 33. Immune Checkpoint Inhibitors and Mesenchymal Stem/Stromal Cells Combination Therapy Might Offer a Promising Treatment Option for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10143520/]
- 34. Investigating the effects of IDO1, PTGS2, and TGF-β1 overexpression on immunomodulatory properties of hTERT-MSCs and their extracellular vesicles | Scientific Reports [https://www.nature.com/articles/s41598-021-87153-7]
- 35. Characteristics and regulation of mesenchymal stem cell plasticity by... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8843883/]
- 36. and their Mesenchymal stem cells microenvironment [https://pubmed.ncbi.nlm.nih.gov/35987711/]
- 37. and their Mesenchymal | stem ... cells microenvironment Stem Cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02985-y]
- 38. Individual fates of mesenchymal stem cells in vitro | BMC Systems... [https://bmcsystbiol.biomedcentral.com/articles/10.1186/1752-0509-4-73]
- 39. Engineering Strategies for Immunomodulatory Cytokine Therapies – Challenges and Clinical Progress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8562465/]
- 40. How are Mesenchymal Stem Cells... - Atlantis Bioscience Pte Ltd [https://www.atlantisbioscience.com/blog/how-are-mesenchymal-stem-cells-harvested-for-research-and-potential-therapies/]
- 41. Comparative analysis of human mesenchymal stem cells from bone marrow and adipose tissue under xeno-free conditions for cell therapy | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-015-0066-5]
- 42. Superior migration ability of umbilical cord-derived mesenchymal... [https://pubmed.ncbi.nlm.nih.gov/38529405/]
- 43. Frontiers | Adipose, Bone Marrow and Synovial Joint-Derived Mesenchymal Stem Cells for Cartilage Repair [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2016.00213/full]
- 44. Frontiers | Global clinical trials on stem cell therapy for autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 45. Innovations in immunotherapy for autoimmune diseases: recent breakthroughs and future directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 46. Exploring the Newest Crohn's Disease Medications (2025) [https://www.dvcstem.com/post/new-crohns-medication]
- 47. Patterns of autoantibody expression in multiple sclerosis identified through development of an autoantigen discovery technology - PubMed [https://pubmed.ncbi.nlm.nih.gov/40026247/]
- 48. Frontiers | T-regulatory cells for the treatment of autoimmune diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1511671/full]
- 49. Breaking barriers: advancing cellular therapies in autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11638217/]
- 50. Mesenchymal Stem Cell-Mediated Immuno-Modulatory and Anti... [https://pubmed.ncbi.nlm.nih.gov/32000656/]
- 51. Mesenchymal stem cells and immunomodulation: current status and... [https://www.nature.com/articles/cddis2015327?error=cookies_not_supported&code=889de2ef-77df-4f1f-96f7-d68df84addac]
- 52. Mesenchymal stem cells and allergic airway inflammation... [https://pubmed.ncbi.nlm.nih.gov/37230032/]
- 53. Immunomodulatory properties of mesenchymal stem cells: A potential therapeutic strategy for allergic rhinitis - PubMed [https://pubmed.ncbi.nlm.nih.gov/36975714/]
- 54. The Immunomodulatory mechanism and research progress of mesenchymal stem cells in the treatment of allergic rhinitis | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04333-2]
- 55. Human adipose tissue mesenchymal stromal cells and their... [https://link.springer.com/article/10.1186/s13287-017-0600-8]
- 56. Human umbilical cord-derived mesenchymal stem cells attenate histaminergic effect of intestinal mucosa through bax/bcl-2 pathway in food allergic enteritis | Scientific Reports [https://www.nature.com/articles/s41598-025-03563-x]
- 57. Functional enhancement strategies for immunomodulation of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7491075/]
- 58. Frontiers | Therapeutic Application of Mesenchymal ... Stem Cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.02663/full]
- 59. A Comparative Study of Mesenchymal -Derived... Stem Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC9775578/]
- 60. /Stromal Mesenchymal - Stem and... Cell Derived Extracellular Vesicles [https://pubmed.ncbi.nlm.nih.gov/28684664/]
- 61. Immunomodulatory Mechanisms of Mesenchymal Stem Cells and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9456387/]
- 62. - Mesenchymal for... stem cell derived extracellular vesicles [https://www.nature.com/articles/s41419-022-05034-x?error=cookies_not_supported&code=3205a36a-4a74-4b43-9974-0f4ea6d3a639]
- 63. Stem cell derived exosome trilogy: an epic comparison of human MSCs, ESCs and iPSCs | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 64. Advances in Immunomodulatory Mechanisms of Mesenchymal Stem... [https://www.dovepress.com/advances-in-immunomodulatory-mechanisms-of-mesenchymal-stem-cells-deri-peer-reviewed-fulltext-article-IJN]
- 65. Immunomodulatory Potential of Human Mesenchymal Stem Cells and... [https://apb.tbzmed.ac.ir/FullHtml/apb-30357]
- 66. Effects of 3D-printed exosome-functionalized brain acellular matrix hydrogel on neuroinflammation in rats following cerebral hemorrhage | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04332-3]
- 67. /Medicinal Signaling Mesenchymal Advances... Stem Cells Cells [https://www.businesswire.com/news/home/20251009529610/en/Mesenchymal-Stem-CellsMedicinal-Signaling-Cells-Advances-Applications-Report-2025-1670-Trials-12-Approvals-Worldwide-and-Path-to-50-Approvals-by-2040---ResearchAndMarkets.com]
- 68. Therapies Mesenchymal by Regulatory... Stem Cell Approved [https://pubmed.ncbi.nlm.nih.gov/37765141/]
- 69. therapy as a game-changer in liver diseases... Mesenchymal stem cell [https://pubmed.ncbi.nlm.nih.gov/39762946/]
- 70. Immunomodulatory effects of mesenchymal therapy in... stem cell [https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-025-04029-y]
- 71. Frontiers | The issue of heterogeneity of MSC-based advanced... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1400347/full]
- 72. Cause and consequence of heterogeneity in human mesenchymal ... [https://pubmed.ncbi.nlm.nih.gov/38870711/]
- 73. testing of Potency stromal mesenchymal growth expanded in... cell [https://pubmed.ncbi.nlm.nih.gov/27557940/]
- 74. Functional heterogeneity of mesenchymal from natural... stem cells [https://link.springer.com/article/10.1007/s00018-020-03600-0]
- 75. testing of Potency stromal mesenchymal growth expanded in... cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-016-0383-3]
- 76. by Immunomodulation ... Mesenchymal Stem Cells [https://pubmed.ncbi.nlm.nih.gov/31214172/]
- 77. Mesenchymal stromal cells as cancer promoters | Oncogene [https://www.nature.com/articles/s41388-024-03183-1]
- 78. Mesenchymal stem cells in treating human diseases: molecular mechanisms and clinical studies | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02313-9]
- 79. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines | Cellular & Molecular Biology Letters | Full Text [https://cmbl.biomedcentral.com/articles/10.1186/s11658-020-00246-5]
- 80. Frontiers | From bench to bedside: translating mesenchymal ... stem cell [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1639439/full]
- 81. Recent advances to enhance the immunomodulatory potential of mesenchymal stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9537745/]
- 82. Preventing MSC aging and enhancing immunomodulation: Novel strategies for cell-based therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124620/]
- 83. and Genetic strategies to enhance... modification preconditioning [https://pubmed.ncbi.nlm.nih.gov/37073114/]
- 84. Manufacturing Industry Stem -2033 Overview: Trends... Cell 2025 [https://www.datainsightsmarket.com/reports/stem-cell-manufacturing-industry-11299]
- 85. Global Stem Source Market Report Cell Edition, Market Size... 2025 [https://www.cognitivemarketresearch.com/stem-cell-source-market-report]
- 86. Hydrogel Encapsulation of Mesenchymal Stem Cells and Their Derived Exosomes for Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7827932/]
- 87. Hydrogel Encapsulation: Taking the Therapy of Mesenchymal Stem Cells and Their Derived Secretome to the Next Level - PubMed [https://pubmed.ncbi.nlm.nih.gov/35433656/]
- 88. Enhancing Immunomodulatory Function of Mesenchymal Stromal... [https://pubmed.ncbi.nlm.nih.gov/38334602/]
- 89. Stiff Hydrogel Encapsulation Retains Mesenchymal Stem Cell Stemness for Regenerative Medicine - PubMed [https://pubmed.ncbi.nlm.nih.gov/39553898/]
- 90. Stiff hydrogel encapsulation retains mesenchymal stem cell stemness for regenerative medicine - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2590238524003047]
- 91. Next-generation approaches for mesenchymal ... stem cell [https://www.bsmiab.org/jabet/articles/178-1749644943]
- 92. effects of collagen Immunomodulation ... hydrogel encapsulating [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03097-4]
- 93. Do cryopreserved mesenchymal stromal cells display impaired... [https://pubmed.ncbi.nlm.nih.gov/24805247/]
- 94. Human mesenchymal stromal cells inhibit platelet activation and... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0936-8]
- 95. -laden injectable self-healing hydrogel for systemic sclerosis... MSCs [https://pmc.ncbi.nlm.nih.gov/articles/PMC8964965/]
- 96. the Measuring of a Potency Therapeutic | SpringerLink Stem Cell [https://link.springer.com/protocol/10.1007/978-1-4939-1785-3_4]
- 97. The ISSCR Releases Targeted Update to the Guidelines for Stem Cell Research and Clinical Translation — International Society for Stem Cell Research [https://www.isscr.org/isscr-news/the-isscr-releases-targeted-update-to-the-guidelines-for-stem-cell-research-and-clinical-translation]
- 98. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 99. Rethinking miRNAs in MSC-sEV therapeutics: implications for... [https://www.oaepublish.com/articles/evcna.2025.55]
- 100. for Potency Stromal Assays Secretome-Based... Mesenchymal Cell [https://pubmed.ncbi.nlm.nih.gov/37298329/]
- 101. Mesenchymal stem cells: Biology, patho-physiology, translational findings, and therapeutic implications for cardiac disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3604746/]
- 102. Evaluation of the Therapeutic Potential of Mesenchymal ... Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9352490/]
- 103. Single-cell spatiotemporal analysis reveals cell fates and functions of transplanted mesenchymal stromal cells during bone repair - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9561611/]
- 104. Breakthroughs and challenges of organoid models for assessing cancer immunotherapy: a cutting-edge tool for advancing personalised treatments | Cell Death Discovery [https://www.nature.com/articles/s41420-025-02505-w]
- 105. stromal Mesenchymal -laden hydrogels in tissue... | CoLab cell [https://colab.ws/articles/10.3389%2Ffphar.2025.1670649]
- 106. Concise Review: Quantitative Detection and Modeling the In Vivo Kinetics of Therapeutic Mesenchymal Stem/Stromal Cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/29210198/]
- 107. Frontiers | Human-based complex in vitro models: their promise and potential for rare disease therapeutics [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1526306/full]
- 108. Frontiers | Umbrella review of mesenchymal -derived... stem cell [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1655623/full]
- 109. 4 Breakthrough Late-stage GvHD Drugs in Development [https://www.delveinsight.com/blog/gvhd-drugs-in-development]
- 110. FDA-approved therapies for chronic GVHD - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0006497124114735]
- 111. -based therapy for autoimmune-related fibrotic... Mesenchymal stem cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03543-w]
- 112. Rethinking clinical study data: why we should respect analysis results as data | Scientific Data [https://www.nature.com/articles/s41597-022-01789-2]
- 113. Clinical trial data visualisation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4660337/]
- 114. Comparing the Value of Data Visualization Methods for Communicating Harms in Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780120/]
- 115. and Mesenchymal : current status... stem cells immunomodulation [https://pubmed.ncbi.nlm.nih.gov/26794657/]
- 116. A Brief Overview of Global Trends in MSC-Based Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8958818/]
- 117. by Immunomodulation : a potential... mesenchymal stem cells [https://pubmed.ncbi.nlm.nih.gov/18586907/]
- 118. Frontiers | Recent progress in stem and immune cell -based... cell [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2025.1638168/full]
- 119. Long-term complications, immunologic effects, and role of passage for... [https://pubmed.ncbi.nlm.nih.gov/21820393/]
- 120. Editorial: Safety , Efficacy and Mechanisms of Action of Mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7040069/]
- 121. , Efficacy and Safety of Action of Mechanisms ... Mesenchymal Stem [https://www.frontiersin.org/research-topics/8614/safety-efficacy-and-mechanisms-of-action-of-mesenchymal-stem-cell-therapies/magazine]
- 122. Frontiers | Repeat-dose toxicity of human umbilical cord mesenchymal ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1558310/full]
- 123. combined with IFN-γ treatment versus... Mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04772-x]
- 124. Multi-omics analysis of human mesenchymal stem cells shows cell aging that alters immunomodulatory activity through the downregulation of PD-L1 | Nature Communications [https://www.nature.com/articles/s41467-023-39958-5]
- 125. Frontiers | An integrated approach for analyzing spatially resolved... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1614288/full]
- 126. Multi-omics evaluation of clinical-grade human umbilical cord-derived mesenchymal stem cells in synergistic improvement of aging related disorders in a senescence-accelerated mouse model | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03986-9]
- 127. Multi-Omics Analysis to Examine Gene Expression and Metabolites From Multisite Adipose-Derived Mesenchymal Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7930907/]
- 128. Understanding immune signaling using advanced imaging techniques - PubMed [https://pubmed.ncbi.nlm.nih.gov/35343569/]